Hideaki Mori


Congress dates 10 to 12 September 2024
Pre- & postcongress 9 and 13 September 2024






Hideaki Mori


Congress dates 10 to 12 September 2024
Pre- & postcongress 9 and 13 September 2024





The medical industry is undergoing a profound transformation driven by several key advancements. Emerging trends and innovations in digital radiography are at the forefront, improving diagnostic accuracy and efficiency. By incorporating blockchain technology, patient data management becomes more secure and transparent, significantly enhancing patient satisfaction. Furthermore, the integration of human sensibility into digital healthcare ensures that technological advancements are patient-centered and compassionate.
In the Asia-Pacific region, these innovations are revolutionising healthcare delivery. The impact of cutting-edge medical devices on treatment procedures is profound, offering faster, more accurate diagnostics, and personalized treatment options. Together, these advancements are reshaping the medical industry, fostering a more efficient, secure, and patient-friendly healthcare environment.
In the cover story ‘Varian’s Mission of HopeTransforming Cancer Care in Asia’ of Asian Hospital & Healthcare Management, Hideaki Mori, President, Varian Asia Pacific & Japan writes on how the integration of advanced imaging with cutting-edge radiotherapy is pivotal in addressing the increasing burden of cancer. These technologies can streamline clinical processes and workflows, bridging the gap between imaging and treatment for greater efficiency. This shift ensures that cancer patients experience seamless, personalised
care, reducing the anxiety often associated with a cancer diagnosis.
This edition brings to light a range of compelling articles, including those exploring the evolution of sustainable practices in healthcare over the coming decade, the influence of mindfulness and resilience on patient care and clinical outcomes, and the risk factors and prognosis of early postoperative complications following pneumonectomy for lung cancer. It also features insightful expert interviews on the crucial role of mobile clinics in public health emergencies, and advancements in telehealth, telemedicine, and precision medicine.
Additionally, the book interview with the author of Digital MD: Revolutionising the Future of Healthcare will provide a fresh perspective on the integration of digital technologies in healthcare, helping readers understand how these advancements are reshaping the field.
Overall, this edition equips readers with knowledge on cutting-edge practices, emerging trends, and practical insights that are shaping the future of healthcare, fostering a deeper understanding of how innovation and expertise converge to improve health outcomes.
Medi Swetha Editor
06 The Role of Sustainable Practices Evolving in the Healthcare Industry over the Next Decade
Maria Tsiadi, Chief Executive Officer, Impacta Consulting
10 The Impact of Mindfulness and Resilience on Patient Care and Clinical Performance
Christina Foxwell, CEO & Founder, Ignite Purpose
17 Risk Factors and Prognostic Significance of Early Postoperative Complications for Patients who underwent Pneumonectomy for Lung Cancer
Dr. Güntuğ Batıhan, Associate Professor, Kafkas University
21 Gut-Brain Axis
The Connection Between Gut Health and Mental Well-Being
Tanjina Ashraf Khan Mou, CEO, Mentcouch Psychology Centre

25 Emerging Trends and Innovations in Digital Radiography: A Comprehensive Overview
James Chong, Deputy Chief Executive Officer, Columbia Asia Hospital Cheras

33 Revolutionising Healthcare in Asia-Pacific: The Impact of























































Beverly A Jensen
President/CEO
Women's Medicine Bowl, LLC
David A Shore
Adjunct Professor, Organisational Development Business School, University of Monterrey
Eiman Shafa Medical Director Spine Surgery Abbott Northwestern Hospital
Gabe Rijpma Sr. Director Health & Social Services for Asia Microsoft
Gurrit K Sethi Founder, Miindmymiind
Imelda Leslie Vargas Regional Quality Assurance Director Zuellig Pharma
K Ganapathy Director Apollo Telemedicine Networking Foundation & Apollo Tele health Services
Luzviminda Nietes
Vice-President, Business Planning & Development, Metro Manila
Nicola Pastorello Data Analytics Manager Daisee
Piyanun Yenjit Founder & Managing Director APUK Co.,Ltd.
Pradeep Chowbey Chairman
Minimal Access, Metabolic and Bariatric Surgery Centre, Sir Ganga Ram Hospital
Pradeep Kumar Ray Honorary Professor and Founder WHO Collaborating Centre on eHealth UNSW
EDITOR
Swetha M
EDITORIAL TEAM
Debi Jones
Harry Callum
Supraja B R
ART DIRECTOR
M Abdul Hannan
PRODUCT MANAGER
Jeff Kenney
SENIOR PRODUCT ASSOCIATES
Ben Johnson
David Nelson
John Milton
Peter Thomas
BUSINESS EVENTS
Sussane Vincent
PRODUCT ASSOCIATE
Ethan Wade
CIRCULATION TEAM
Sam Smith
SUBSCRIPTIONS IN-CHARGE
Vijay Kumar Gaddam
HEAD-OPERATIONS
Sivala VNR
Ochre Media Private Limited Media Resource Centre, #9-1-129/1,201, 2nd Floor, Oxford Plaza, S.D Road, Secunderabad - 500003, Telangana, INDIA, Phone: +91 40 4961 4567, Fax: +91 40 4961 4555 Email: info@ochre-media.com www.asianhhm.com | www.ochre-media.com


at the

The healthcare industry is embracing sustainable practises such as green building, waste reduction, and renewable energy. These efforts, coupled with ethical supply chains and digital transformation, will significantly reduce environmental impact and improve public health over the next decade, despite financial and regulatory challenges.
Maria Tsiadi, Chief Executive Officer, Impacta Consulting
As the global community becomes increasingly aware of the impact of climate change and environmental degradation, industries across the board are re-evaluating their practises to align with sustainability goals. The healthcare industry, traditionally focused on patient outcomes and operational efficiency, is now turning its attention to sustainability. Over the next decade, the integration of sustainable practises in healthcare will play a crucial role in reducing environmental impact, improving public health, and ensuring the long-term viability of healthcare systems. This article explores the key areas where sustainable practises are evolving in the healthcare industry and their anticipated impact.
The shift towards sustainable healthcare infrastructure is gaining momentum, with green building standards such as LEED (Leadership in Energy and

Environmental Design) becoming more prevalent. Hospitals and healthcare facilities are significant energy consumers, and the adoption of energyefficient designs can lead to substantial reductions in carbon footprints. Over the next decade, we can expect a proliferation of healthcare facilities built to these standards, incorporating renewable energy sources, efficient water use, and sustainable materials.
In addition to new constructions, existing healthcare facilities are increasingly being retrofitted to improve their sustainability. This involves upgrading HVAC systems, improving insulation, and installing energy-efficient lighting and watersaving fixtures. These retrofits not only reduce environmental impact but also result in significant cost savings over time, making them an attractive option for healthcare providers.
Medical waste is a significant environmental concern, with hospitals generating large quantities of waste daily, much of which is hazardous. Over the next decade, there will be a concerted effort to reduce medical waste through improved waste segregation, recycling programs, and the adoption of reusable medical instruments and supplies. Innovations in waste treatment technologies, such as autoclaving and microwave treatment, will further enhance the safe disposal of medical waste.
The digital transformation of healthcare also plays a crucial role in reducing waste. The shift from paper-based to electronic health records (EHRs) reduces paper waste and enhances data management efficiency. Telemedicine and remote patient monitoring, accelerated by the COVID-19 pandemic, reduce the need for physical appointments, thereby decreasing transportation - related

emissions and waste associated with traditional in-person consultations.
Healthcare facilities are increasingly exploring renewable energy sources such as solar, wind, and geothermal to power their operations. The integration of renewable energy not only reduces greenhouse gas emissions but also ensures energy resilience, particularly in regions prone to power outages. Over the next decade, we can expect more healthcare facilities to invest in on-site renewable energy generation and storage solutions.
Implementing energy efficiency measures is another critical aspect of sustainable practices in healthcare. This
includes the use of energy-efficient medical devices, smart building systems that optimize energy use, and the adoption of LED lighting. By reducing energy consumption, healthcare facilities can lower their operational costs and environmental impact.
The healthcare supply chain is complex and global, often involving multiple layers of suppliers. Ensuring the ethical sourcing of medical products and pharmaceuticals is becoming increasingly important. Over the next decade, healthcare organizations will place greater emphasis on working with suppliers who adhere to sustainable and ethical practices, such as fair labor standards and environmentally friendly manufacturing processes.
Transportation and logistics are significant contributors to the healthcare sector's carbon footprint. To address this, healthcare organizations are exploring ways to optimize their supply chains. This includes localizing procurement to reduce transportation emissions, utilizing low-emission delivery vehicles, and implementing advanced logistics technologies to improve efficiency.
Water conservation is a critical aspect of sustainability in healthcare. Hospitals use vast amounts of water for various purposes, including sanitation, cooling, and patient care. Implementing waterefficient fixtures, recycling wastewater, and utilising rainwater harvesting systems can significantly reduce water consumption. Over the next decade, water conservation strategies will become integral to the design and operation of healthcare facilities.
Pharmaceutical contamination of water sources is a growing environmental concern. Medications that are improperly disposed of can enter water systems and adversely affect aquatic life and human health. The healthcare industry is working on developing better pharmaceutical waste disposal practises and technologies to mitigate this issue.
Green chemistry involves designing chemical products and processes that reduce or eliminate the use and generation of hazardous substances. In the healthcare industry, this approach can be applied to the development of pharmaceuticals and medical devices. Over the next decade, green
chemistry principles will become more prominent in clinical care, leading to safer and more environmentally friendly medical products.
The production and disposal of pharmaceuticals have significant environmental impacts. Developing sustainable pharmaceuticals involves not only green chemistry but also innovations in drug formulation and delivery. Biodegradable drug delivery systems and pharmaceuticals with reduced environmental persistence are examples of sustainable innovations that will gain traction in the coming years.
Healthcare facilities can contribute to improved community health by reducing their own air pollution emissions. This includes minimising the use of incinerators for waste disposal and adopting cleaner energy sources. Additionally, healthcare providers can play a role in advocating for policies that address air pollution and its impact on public health.
The design of healthcare facilities can also promote healthier lifestyles and well-being. Incorporating green spaces, natural lighting, and spaces for physical activity within healthcare environments can enhance the health and recovery of patients, staff, and visitors. Over the next decade, the concept of therapeutic environments will become more integrated into healthcare facility design.
To effectively implement sustainable practises, it is essential to educate healthcare professionals about the importance of sustainability and how to incorporate it into their daily practises. Medical and nursing schools are beginning to integrate sustainability into their curricula, and this trend will continue to grow. Ongoing professional development opportunities focused on sustainability will also become more prevalent.
Healthcare organisations and professionals are uniquely positioned to advocate for policies that promote

The healthcare industry is adopting sustainable practices like green building and waste reduction to mitigate environmental impact. Innovations such as LEED-certified infrastructure and advanced waste treatment technologies will transform healthcare facilities, ensuring longterm sustainability and efficiency.
sustainability. This includes supporting legislation that addresses climate change, waste management, and renewable energy. By leveraging their expertise and influence, healthcare professionals can help drive broader societal changes towards sustainability.
Advancements in technology are paving the way for more sustainable medical devices. This includes the development of devices that are more energy-efficient, made from sustainable materials, and designed for longevity and recyclability. Over the next decade, the medical device industry will see a shift towards products that prioritise environmental considerations alongside clinical performance.
The adoption of telemedicine and remote care solutions, accelerated by the COVID-19 pandemic, will continue
to expand. These technologies reduce the need for physical travel, thereby lowering carbon emissions associated with healthcare delivery. Additionally, remote monitoring and home-based care can reduce the strain on healthcare facilities and resources.
One of the main challenges in implementing sustainable practises is the associated cost. Initial investments in green infrastructure, renewable energy, and sustainable technologies can be substantial. However, these investments often lead to long-term savings and operational efficiencies. Healthcare organisations will need to balance shortterm costs with long-term benefits and explore financing options such as green bonds and grants.
The healthcare industry is heavily regulated, and compliance with sustainability standards can be complex. Navigating these regulations while implementing sustainable practises requires careful planning and collaboration with regulatory bodies. Over the next decade, we can expect the development of more comprehensive guidelines and standards to support sustainability in healthcare.
Integrating new sustainable technologies into existing healthcare systems can be challenging. Ensuring interoperability and seamless integration with current workflows requires careful planning and investment in training and support. However, the potential benefits in terms of efficiency and sustainability make this a worthwhile endeavour.
The next decade will see significant advancements in the adoption of sustainable practises in the healthcare industry. From green building standards and energy efficiency to sustainable supply chain management and innovative clinical care, the industry is poised to make substantial contributions to environmental sustainability. While challenges remain, the opportunities for improving public health, reducing environmental impact, and ensuring the long-term viability of healthcare systems are immense. As healthcare organisations continue to embrace sustainability, they will not only enhance their own operations but also contribute to a healthier planet for future generations.
References are available at www.asianhhm.com
Mrs Maria Tsiadi is an esteemed ESG expert with over 20 years of experience. She holds a Master’s Degree in Corporate Responsibility and Risk Management from Stirling University and is currently attending a Master’s Degree on Governance and Human Rights from Leuphana University. Mrs Tsiadi is a recognised thought leader in her field, frequently speaking at global conferences and forums on ESG and D&I topics. Her extensive expertise and commitment to sustainability make her a key influencer in promoting inclusive practises at the corporate board level.


Mindfulness and resilience training significantly improve healthcare professionals' well-being, reducing burnout and enhancing patient care. Our research highlights a 30% reduction in burnout and a 25% decrease in anxiety and depression symptoms, demonstrating the transformative impact on clinical performance and job satisfaction.
In the demanding world of healthcare, professionals face immense pressures that can lead to significant stress, emotional exhaustion, and burnout. These factors not only affect the well-being of healthcare workers but also impact the quality of care provided to patients. Recent research and practical experiences have highlighted the profound impact that mindfulness and resilience training can have on addressing these challenges. This article delves into the direct benefits of such training on patient care and clinical outcomes, supported by findings from our resilience programme research and additional studies.
Christina Foxwell, CEO & Founder, Ignite Purpose
Mindfulness refers to the practice of maintaining awareness of one's thoughts, feelings, bodily sensations, and surrounding environment, often through meditation and other focused exercises. Resilience is the ability to adapt and bounce back from adversity, stress, and challenges. Both concepts are crucial in managing the high levels of stress associated with healthcare professions.
Healthcare professionals frequently operate under high-pressure conditions, managing patient loads, making critical decisions, and dealing with emotional demands. This environment often leads to burnout, characterised by emotional exhaustion, depersonalisation, and reduced personal accomplishment. The
consequences include decreased job satisfaction, lower quality of patient care, and increased turnover rates.
Our resilience programme was designed to equip healthcare professionals with the skills needed to manage stress effectively, maintain emotional balance, and enhance their overall well-being. The programme included mindfulness training, cognitive-behavioural strategies, and the development of strong support networks.
Our study employed the Connor Davidson Resilience Scale (CD-RISC) to measure changes in resilience levels among participants. The results were significant:
• Pre-Programme Average Score: 65.14
• Post-Programme Average Score: 76.43
• Average Change in Score: +11.29
Participants who completed the resilience programme reported a significant decrease in burnout levels, with a 30% reduction in burnout scores, as measured by the Maslach Burnout Inventory. Additionally, there was a 25% decrease in symptoms of anxiety and depression, which aligns with findings from other studies indicating the mental health benefits of mindfulness training (Krasner et al., 2009; West et al., 2014).
Through in-depth 30-minute interviews conducted at the end of the programme, participants shared their experiences and the impact of the training on their professional lives. Common themes included:
• Improved Coping Mechanisms: Participants reported developing better strategies for managing stress and adversity.
This article explores how mindfulness and resilience training reduce burnout and improve clinical performance among healthcare professionals. Highlighting significant reductions in anxiety and depression, the article provides practical strategies for integrating these practices into daily routines, ultimately fostering better patient outcomes and a more resilient healthcare workforce.
• Enhanced Emotional Well-Being: There was a noticeable improvement in emotional regulation and overall mental health.
• Stronger Support Networks: The programme facilitated the creation of supportive relationships among colleagues, leading to a more cohesive work environment.
One participant noted, "The mindfulness exercises and cognitivebehavioural strategies have helped me manage my stress levels and approach my work with a clearer mind. I feel more present with my patients and more connected to my colleagues."
1. Greater Self-Awareness and Emotional Intelligence
Participants reported significant shifts in self-awareness and emotional intelligence. By engaging in mindfulness practices, many healthcare workers learned to recognise their emotional triggers and manage their responses more effectively. This increased awareness not only helped them in handling stressful
situations but also improved their interactions with patients and colleagues.
One nurse shared, "Before the programme, I often reacted impulsively to stressful situations. Now, I take a moment to breathe and assess my emotions before responding, which has made a huge difference in my professional and personal life."
2. Enhanced Empathy and Compassion
Mindfulness training encouraged healthcare professionals to develop greater empathy and compassion towards themselves and others. This shift was particularly noticeable in patient care, where participants felt more connected and attentive to their patients' needs.
A physician remarked, "I've become more empathetic towards my patients. Understanding my own stress and learning to manage it has made me more compassionate and patient with others."
3. Improved Work-Life Balance
Many participants reported that the resilience programme helped them achieve a better work-life balance. By prioritising self-care and setting boundaries, healthcare professionals were able to manage their workload more effectively and reduce burnout.
One participant explained, "The programme taught me the importance of taking time for myself. I now schedule regular breaks and make sure to leave work at work, which has greatly improved my overall well-being."
4. Increased Job Satisfaction and Professional Fulfilment
As a result of the resilience training, healthcare professionals experienced higher levels of job satisfaction and professional fulfilment. By learning to manage stress and build resilience, participants felt more capable and confident in their roles, leading to a renewed sense of purpose and satisfaction in their work.
A nurse manager noted, "The resilience training reignited my passion
for nursing. I feel more equipped to handle the challenges of my job and more satisfied with my career."
1. Personal Reflection of Growth and Change
Participants provided specific examples of how the programme supported their ability to manage stress, improve patient impact, and enhance communication and connection with patients, peers, and family. One nurse stated, "The resilience programme taught me how to develop and manage stress effectively and positively. It gradually transformed me to become mindful, grateful, and more understanding, which has significantly improved my interactions with patients and colleagues."
2. Professional Development Gains
Healthcare professionals noted that the skills and techniques learned in the programme directly benefited their medical practice. For example, a doctor shared, "Through this training, I was able to understand and work out strategies to manage my emotions while dealing with patients. Prioritising self-care has increased my job satisfaction and made me more efficient."
3. Practical and Real-World Relevance
Participants highlighted how the concepts taught in the programme applied to their work and personal lives. They emphasised strategies for dealing with difficult patients, managing worklife balance, and navigating complexities in medical teamwork. One participant explained, "By accepting that there are some things I cannot control and embracing my vulnerability, I have grown positively and effectively."
4. Supportive Community and Connection Opportunities
The programme fostered a sense of community among participants, providing a supportive environment

to share challenges and solutions. One participant remarked, "The best part of this training is the online friends I gained. We learned from each other, supported each other, and created a special bond, making us feel not alone in our struggles."
At a major hospital in the UK, a group of emergency department physicians underwent an eight-week mindfulness training programme. Post-training assessments revealed a 30% reduction in reported stress levels and a 20% improvement in patient care quality, as measured by patient feedback and clinical performance metrics. This aligns with findings from the Journal of the American Medical Association that mindfulness training can significantly reduce symptoms of anxiety and depression (West et al., 2014).
A hospital in Australia implemented a resilience training programme for its nursing staff. Over six months, the programme included workshops on emotional regulation, mindfulness exercises, and peer support groups. Nurses reported a 35% decrease in burnout symptoms and a significant improvement in job satisfaction and
patient interaction quality. This case supports the findings of Mealer et al. (2014) in Medical Care, which highlighted the benefits of resilience training in reducing burnout among nurses.
1. Mindfulness Practices
• Daily Meditation: Short, daily meditation sessions can help healthcare professionals maintain mental clarity and emotional balance.
• Mindful Breathing: Techniques such as deep breathing can be used during high-stress situations to reduce immediate stress responses.
• Mindful Listening: Practising active listening with patients and colleagues can improve communication and relationships.
2. Resilience Building Techniques
• Cognitive Behavioural Strategies: Training in cognitive-behavioural techniques can help professionals reframe negative thoughts and build emotional resilience.
• Support Networks: Encouraging the development of strong professional support networks can provide essential emotional and professional support.
• Reflective Practices: Regular
reflection on experiences and challenges can help healthcare workers process their emotions and learn from their experiences.
Healthcare institutions can integrate mindfulness and resilience training into their ongoing professional development programmes. Offering regular workshops, providing access to mindfulness resources, and fostering a supportive work environment can significantly enhance the well-being of healthcare professionals.
Leadership plays a crucial role in promoting resilience within healthcare organisations. Leaders can set the tone by prioritising employee well-being and creating a culture that values mindfulness and resilience. This includes providing resources for resilience training, encouraging open communication about stress and burnout, and modelling resilient behaviours themselves.
1.
Research has shown that burnout and stress can lead to increased medical errors. A study in Health Affairs found that resilience training led to a 25% reduction in reported medical errors among physicians (Epstein et al., 2018). This highlights the critical importance of resilience in maintaining high standards of patient care.
The American Medical Association (AMA) conducted a survey that found physicians who engaged in resiliencebuilding activities reported a 40% increase in job satisfaction (AMA, 2019). Additionally, a study in Medical
Care found that resilience training contributed to a 25% decrease in turnover rates among nursing staff (Mealer et al., 2014).
3. Enhanced Work-Life Balance
An article in The New England Journal of Medicine highlighted that healthcare workers who practised mindfulness and resilience reported a 35% improvement in their work-life balance (Dobkin et al., 2016). This is crucial in preventing burnout and ensuring long-term career sustainability.
from Programme Participants
A Lessi, General Practitioner
"The programme has sharpened my awareness of reflex thoughts and their associated emotions, helping me handle non-traditional medical requests more calmly while adhering to evidence-based practices. This enhanced awareness has improved how I manage stress and interact with patients, peers, and family. It has also boosted my problem-solving skills by encouraging me to consider multiple perspectives, making decisionmaking less stressful and more reflective. This approach not only improves outcomes but also saves time, especially with complex social or mental health issues in patients.”
GR Costorian, Registered Nurse
"Through this training, I have learned strategies such as being calm and mindful, which have significantly improved my emotional management
Christina Foxwell, CEO of Ignite Purpose and Research Lead, is a renowned expert in human resources and organisational transformation. With over two decades of experience, she specialises in fostering resilient, high-performing workplace cultures through innovative training programs and leadership development.
while dealing with patients. I now prioritise self-care to maintain a healthy work-life balance. Practical strategies like being open to support from colleagues have increased my job satisfaction and efficiency. For example, when facing a challenging situation with a patient, I remain calm and composed, which helps in making better decisions and resolving conflicts more effectively. This training has equipped me with the tools to handle professional challenges with greater ease and confidence.”
The evidence is clear: Mindfulness and resilience training offer substantial benefits for healthcare professionals, enhancing patient care, clinical performance, and overall job satisfaction. By prioritising these practices, healthcare institutions can foster a more supportive and effective work environment, ultimately leading to better patient outcomes and a more resilient healthcare workforce. Investing in resilience is not just about improving the well-being of healthcare professionals; it's about ensuring the highest standards of patient care and creating a sustainable healthcare system for the future.
References are available at www.asianhhm.com

MEDICAL FAIR ASIA and MEDICAL MANUFACTURING ASIA 2024 11–13 September 2024 | Marina Bay Sands, Singapore

In today’s rapidly evolving healthcare landscape, driven by technological innovations and digitalisation, navigating complex markets and regulatory challenges is more crucial than ever. MEDICAL FAIR ASIA and MEDICAL MANUFACTURING ASIA 2024 stand out as Southeast Asia’s premier platforms for sourcing, business, and networking. These co-located exhibitions present the entire value chain from raw materials to final products, showcasing the latest in medical technology, equipment, systems and solutions. Mark your calendars for 11 to 13 September at Marina Bay Sands, Singapore.
Reimagining Southeast Asia's healthcare marketplace, the 15th edition of MEDICAL FAIR ASIA connects trade visitors with international manufacturers and suppliers across hospital, diagnostics, pharmaceutical, medical, and rehabilitation sectors. Since 1997, it has grown from strength to strength, and with its co-location with the 6th edition of MEDICAL MANUFACTURING ASIA, together they offer an end-to-end supply chain experience, fostering collaboration, innovation, and efficiency across all stages of medical manufacturing and supply. As healthcare systems continue to grapple with
challenges in ensuring accessibility, affordability, and quality of care, these two exhibitions are pivotal in showcasing innovation and forging partnerships that drive the industry forward.
This year, MEDICAL FAIR ASIA welcomes over 1,000 international manufacturers, suppliers, and innovative solution providers from 62 countries and 18 national and country groups. This diverse assembly caters to buyers of medical and healthcare products and services, as well as the regional healthcare community. Attendees can expect to source from a range of over 5,000 products, from diagnostics and laboratory technology, medical supplies and consumables, rehabilitation and orthopedic equipment, to medical technology and electromedicine, and IT solutions and systems.
Community Care Pavilion: Empowering Communities, Enhancing
According to the World Bank, the population aged 65
and above in Southeast Asia is projected to triple by 2050, and the Asia-Pacific region is expected to be the fastest-growing in healthcare spending, accounting for over 20 percent of global expenditure by 2030. Southeast Asia's rapid population growth, increasing aging population, and heightened health awareness further underscore this urgency. The Community Care Pavilion focuses on accessible and quality community care, highlighting the shift towards preventive health and value-based care. With an emphasis on elderly care, rehabilitation, and chronic disease management, the pavilion presents an array of healthcare solutions designed to enhance patient outcomes and streamline care processes, from assistive technologies and homecare equipment to telemedicine.
Start-Up Park: Transforming Health, One Start-Up at a Time
Experience the dynamic Start-Up Park, where innovative companies with market-ready solutions meet buyers, industry influencers, and investors. Highlights include AI-driven patient care, deep learning image processing, and cutting-edge IoT sensors. The 3-day Start-Up Podium Programme features experts from


the region discussing topics ranging from remote healthcare to cybersecurity in healthcare. For the first time this year, is the Start-Up Challenge, where companies will pitch their innovations to a panel of industry experts.
WT | Wearable Technologies Conference
| 11 Sep | *Special industry rates apply
A full-day event dedicated to cutting-edge technologies and the latest advancements in wearable tech, precision medicine, remote patient monitoring, and early detection technologies. Themes include digitalisation in healthcare, deep tech innovations, and enabling the future of healthcare, as well as healthcare, fitness, and wearables. Attendees can expect to gain insights and uncover how these innovations are transforming industries and enhancing lives. This is the region’s only dedicated WT conference and is jointly organised by German-based WT | Wearable Technologies AG and MEDICAL FAIR ASIA.
Medicine + Sports Conference
| 12 Sep | *Special industry rates apply
A multi-disciplinary full-day programme bringing together the brightest minds in sports medicine and sports science, including regional and international experts, physiotherapists and healthcare professionals, professional athletes, and sports tech visionaries. Discover innovations driving the future of sports medicine and engage in insightful dialogues on innovative approaches in performance, prevention, training, and
regeneration. Key topics include enhancing super athletes and soldiers of the future, and a shark tank of digital innovation in sports and healthcare.
3rd Paradigm Shifts in Healthcare - Ensuring the Wellbeing of Patients; Staff and the Environment
12 & 13 Sep | Admission is free
Over two half-days, distinguished speakers will discuss and present key topics, including self-care programmes for clinical staff, environmental protection strategies in operating rooms, and lessons from related industries to enhance healthcare delivery. This programme is supported by SingHealth DukeNUS Academic Medical Centre - Anaesthesiology & Perioperative Sciences, and SingHealth.
IVAM Forum: High-Tech for Medical Devices | 12 Sep | Admission is free
Brought to you by German-based IVAM Microtechnology Network, the IVAM Forum unites leading companies in medical manufacturing and devices, offering fresh perspectives from an international lineup of industry leaders. Key topics on the agenda include coating solutions for critical medical technology, importance of sterile packaging in high tech medical devices, and 360° compliance for medical devices.
SPETA Forum | 12 Sep | Admission is free
With topics such as Singapore’s MedTech regulator landscape, and emerging MedTech manufacturing technology, this forum is organised by SPETA (Singapore Precision Engineering and Technology Association) and will feature leading voices in Singapore’s medical manufacturing sectors. Learn from C-suite level speakers and gain new strategies to future-proof your organisation, navigate regulatory landscapes, and address specific industry challenges.


For more information on the exhibitions and to pre-register your free visit, go to:
www.medicalfair-asia.com
www.medmanufacturing-asia.com
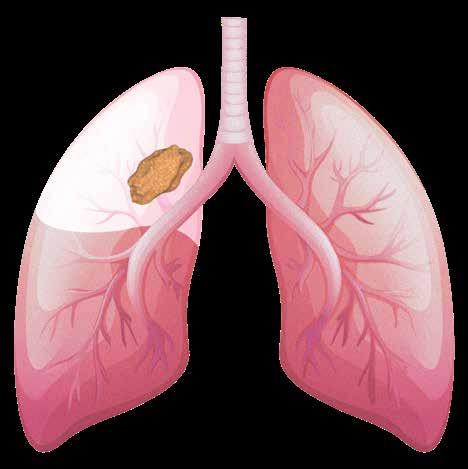
Lung cancer remains a leading cause of cancerrelated deaths globally. Lobectomy is the gold standard for early-stage non-small cell lung cancer, while pneumonectomy is necessary for advanced cases but has higher morbidity and mortality rates, highlighting the importance of careful patient selection and risk assessment.
Dr. Güntuğ Batıhan, Associate Professor, Kafkas University
Lung cancer remains a formidable challenge in oncology, being the leading cause of cancerrelated mortality worldwide (Figure 1). Surgical intervention is a cornerstone in the management of lung cancer, particularly for early-stage non-small cell lung cancer (NSCLC). Among the various surgical procedures, pneumonectomy—which involves the removal of an entire lung—plays a critical role in cases where less extensive resection is not feasible. However, pneumonectomy is associated with higher rates of postoperative morbidity
Tracheal, bronchus, and lung cancer
Colon and rectum cancer
Stomach cancer
Breast cancer
Pancreatic cancer
Esophageal cancer
Prostate cancer
Liver cancer
Cervical cancer
and mortality compared to lobectomy and segmentectomy. (Figure 1)
Previous studies have revealed morbidity rates ranging from 20% to 60%, including respiratory complications, cardiovascular issues, infections, and bronchopleural fistula. The early postoperative mortality rate is between 5% and 10%, while long-
term survival varies widely based on cancer stage, with five-year survival rates ranging from 30% to 50% (Figure 2).
Due to the high mortality and morbidity rates associated with pneumonectomy operations, studies aimed at identifying risk factors for the development of postoperative complications are of great importance.
The study conducted by Batıhan aet al. aims to explore the prognostic significance of early postoperative complications and identify risk factors that may influence patient outcomes following pneumonectomy.
The study analysed data from 136 patients who underwent pneumonectomy for NSCLC between January 2008 and May 2021. The primary objective was to evaluate the impact of early postoperative complications on overall survival (OS) and disease-free survival (DFS), as well as to identify independent risk factors associated with these complications. The findings highlight the importance of smoking history, operation side, pericardial invasion, and patient age in predicting postoperative outcomes (Figure 3 & 4).
Smoking Amount: The study found a significant association between the amount of cigarette smoking and
the incidence of early postoperative complications. Specifically, higher smoking amounts were linked to increased rates of postoperative hemorrhage. There is probably a possible indirect cause-and-effect relationship associated with increased postoperative hemorrhage. This finding is consistent with previous research indicating that smoking adversely affects respiratory function, impairs wound healing, and increases the risk of complications. However, it should be noted that this study does not contain data regarding the amount of smoking, active/passive smoking, or a cut-off value.
Operation Side: Right-sided pneumonectomy was associated with a higher risk of complications compared to left-sided procedures. This disparity is likely due to anatomical and physiological differences between the two sides of the thoracic cavity. The right lung has a larger alveolar reserve, and the left hilum is anatomically more protected, which may contribute to the higher complication rates observed in right-sided pneumonectomies. This situation necessitates that surgeons be
much more meticulous when deciding on right pneumonectomy.
Pericardial Invasion: Pericardial invasion was identified as a independent risk factor for postoperative hemorrhage. This data has been discussed by the authors as follows: In the presence of pericardial invasion, a wider dissection, including the pericardium and surrounding tissues, is necessary for the complete resection of the tumour. This situation can increase the risk of hemorrhage in the postoperative period. This finding underscores the importance of thorough preoperative assessment and surgical planning in patients with tumours involving the pericardium.
Advanced Age: Older patients were found to be more susceptible to postoperative pneumonia, the most common complication observed in the study. Age-related declines in immune function, pulmonary reserve, and overall physiological resilience likely contribute to the increased risk of pneumonia in elderly patients.
The development of early postoperative complications was found to have a
negative impact on both OS and DFS. Patients who experienced complications had significantly poorer survival outcomes compared to those without complications. This relationship highlights the critical importance of minimising postoperative complications to improve patient prognosis. The study's findings align with previous research demonstrating that postoperative complications can prolong hospital stays, delay recovery, and increase the risk of mortality.
Based on the findings of Batıhan aet al., several clinical recommendations can be made to enhance patient outcomes following pneumonectomy: Preoperative Risk Assessment: Comprehensive preoperative evaluation is essential for identifying high-risk patients. This assessment should include detailed smoking history, evaluation of potential pericardial invasion, and consideration of patient age. Advanced imaging techniques and pulmonary function tests can aid in accurately assessing the patient's suitability for pneumonectomy.
Smoking Cessation Programmes: Encouraging patients to quit smoking prior to surgery is crucial. Smoking cessation programmes should be integrated into the preoperative care pathway to reduce the risk of complications. Evidence suggests that even short-term cessation can improve postoperative outcomes.
Surgical Technique: Where feasible, less invasive surgical techniques such as video-assisted thoracoscopic surgery (VATS) should be considered. VATS has been associated with lower rates of postoperative complications and faster recovery compared to open thoracotomy. However, the choice of surgical technique should be tailored to the individual patient's anatomy and tumour characteristics.
Perioperative Management: Vigilant perioperative monitoring and early intervention are critical for
To minimize the risk of pneumonectomyrelated mortality and morbidity, the surgical team should conduct a detailed preoperative risk assessment, motivate the patient to quit smoking during the preoperative period, and ensure meticulous postoperative care.

preventing and managing complications. Protocols for managing postoperative hemorrhage, pneumonia, and other common complications should be in place to ensure timely and effective treatment.
Postoperative Care: Ensuring optimal postoperative care is vital for enhancing patient recovery. This includes regular follow-up visits, respiratory physiotherapy, nutritional support, and vigilant monitoring for signs of complications. Early recognition and management of complications can significantly improve patient outcomes.
The study by Batıhan aet al. underscores the critical importance of early postoperative complications in determining the prognosis of patients undergoing pneumonectomy for NSCLC. Key risk factors such as smoking amount, operation side, pericardial invasion, and advanced age must be carefully considered in the preoperative assessment and perioperative management of these patients. By implementing comprehensive preoperative evaluations, smoking cessation programmes, meticulous surgical techniques, and vigilant postoperative care, healthcare providers can minimise the occurrence of complications and improve patient outcomes. Future research should focus on expanding these findings through multi-centre studies, exploring longterm outcomes, and developing targeted interventions for high-risk patients to further enhance the care of lung cancer patients undergoing pneumonectomy.
References are available at www.asianhhm.com
The Gut-Brain Axis (GBA) reveals the profound connection between gut health and mental well-being. This article explores how gut microbiota influence mood, cognitive function, and behaviour, highlighting implications for psychological interventions and future research, advocating for holistic and integrated approaches to enhance mental health treatment and overall well-being.
Tanjina Ashraf Khan Mou, CEO, Mentcouch Psychology Centre
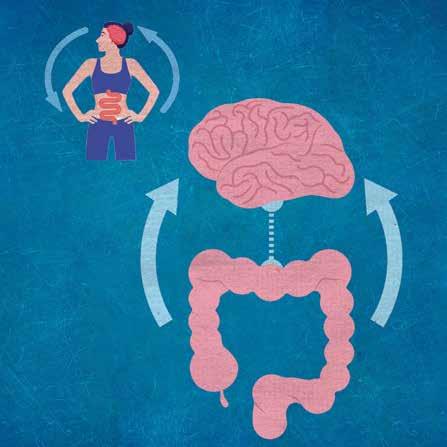
The human body is an intricate network of interconnected systems, each influencing and being influenced by the others. Among these complex interactions, the relationship between the gut and the brain, known as the Gut-Brain Axis (GBA), stands out for its profound impact on overall health. Traditionally, the brain has been considered the command centre for bodily functions and psychological states. However, emerging research reveals that the gut plays a significant role in regulating not only physical health but also mental well-being. This bidirectional communication system between the gut and the brain involves neural, hormonal, and immunological pathways that form a sophisticated network of interaction.
The gut, often referred to as the "second brain," houses an extensive network of neurons known as the enteric nervous system (ENS), which communicates directly with the
central nervous system (CNS). This communication is facilitated by the vagus nerve, a major component of the parasympathetic nervous system. Additionally, the gut is home to trillions of microorganisms collectively known as the gut microbiota. These microorganisms perform essential functions, including the synthesis of vitamins, digestion of complex carbohydrates, and modulation of the immune system.
One of the most intriguing aspects of the GBA is the production of neurotransmitters by gut microbiota. Neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA) are crucial for regulating mood, anxiety, and cognitive functions. Remarkably, about 90% of the body's serotonin is produced in the gut, emphasising the gut's significant role in mood regulation. Dysbiosis, or an imbalance in the gut microbiota, has been linked to various psychological disorders, including depression, anxiety, and irritable bowel syndrome (IBS).
The relationship between gut health and mental well-being is not merely a one-way street. Psychological stress can alter gut microbiota composition, leading to increased intestinal permeability, inflammation, and subsequent changes in brain function. This bidirectional communication suggests that maintaining gut health is crucial for mental well-being, and vice versa. The GBA thus represents a paradigm shift in understanding the etiology of mental health disorders and offers new avenues for treatment.
The implications of the GBA for mental health are vast and transformative. Traditional psychological interventions have primarily focused on cognitive and behavioural aspects of mental health, often overlooking the physiological components. However, by integrating knowledge of the GBA into mental health care, psychologists can develop
more holistic and effective treatment strategies. For instance, dietary interventions that promote a healthy gut microbiome can complement cognitive-behavioural therapy (CBT) and other psychological treatments, providing a more comprehensive approach to mental health care.
This article delves into the science behind the Gut-Brain Axis, exploring how gut microbiota influence mental health. It examines the implications of this relationship for psychological practise, highlighting the potential for integrated treatment plans that address both physical and psychological aspects of mental well-being. Additionally, the article discusses future directions
in GBA research, emphasising the need for continued interdisciplinary collaboration to fully understand and harness the therapeutic potential of the GBA. By embracing this integrative perspective, psychologists and other mental health professionals can enhance the efficacy of their interventions and contribute to a more holistic approach to mental health care.
Understanding the GBA's role in mental health provides a compelling argument for incorporating gut health into psychological interventions. The role of diet, lifestyle, and even psychobiotics in maintaining mental well-being highlights the importance of a holistic approach that considers both physical and psychological factors
As mentioned, the GBA consists of multiple pathways through which the gut and brain communicate. These include the nervous system, particularly the vagus nerve, the endocrine system, and the immune system. Central to this communication network are the gut microbiota, a diverse community of microorganisms residing in the gastrointestinal tract. These microbiota produce a variety of substances, including neurotransmitters like serotonin and dopamine, which are crucial for regulating mood and cognitive functions.
Research indicates that an imbalance in gut microbiota, known as dysbiosis, can significantly affect brain function and behaviour. This connection becomes evident in conditions such as irritable bowel syndrome (IBS), where patients often experience heightened levels of anxiety and depression. Studies also suggest that probiotics and prebiotics, which help maintain a healthy gut microbiome, can have positive effects on mental health, further supporting the link between gut health and psychological well-being.
Understanding the GBA's role in mental health provides a compelling argument for incorporating gut health into psychological interventions. Traditional psychological approaches focus primarily on cognitive and
behavioural aspects of mental health. However, recognising the physiological underpinnings of conditions like anxiety, depression, and stress related disorders allows for more comprehensive treatment plans.
For instance, dietary interventions aimed at promoting a healthy gut microbiome can be considered as complementary to cognitive behavioural therapy (CBT) and other psychological treatments. Mindfulness practises and stressreduction techniques can also benefit from an awareness of the GBA, as stress is known to alter gut microbiota composition negatively.
Mental well-being encompasses a range of positive psychological states, including happiness, resilience, and a sense of purpose. The GBA plays a critical role in maintaining these states by influencing various mental health aspects:
1. Mood Regulation: The gut microbiota produced neurotransmitters like serotonin, often referred to as the happy hormone. About 90% of serotonin is produced in the gut, underscoring the importance of gut health in mood regulation. Dysbiosis can lead to reduced serotonin levels, contributing to mood disorders such as depression and anxiety.
2. Stress response: The GBA influences the body’s stress response by modulating the hypothalamicpituitary-adrenal (HPA) axis. Chronic stress can disrupt gut microbiota balance, leading to increased inflammation and altered brain function. By maintaining a healthy gut microbiome, individuals may experience a more balanced stress response and reduced symptoms of stress-related disorders.
3. Cognitive Function: Cognitive functions such as memory, learning, and decision-making are also linked
to gut health. Emerging research suggests that gut microbiota can influence cognitive processes by producing neuroactive compounds and modulating neuroinflammation. Supporting gut health through diet and lifestyle can thus enhance cognitive well-being.
4. Sleep Quality: Gut health impacts sleep quality, which is crucial for overall mental well-being. Microbiota influence the production of sleep-regulating hormones and neurotransmitters. Dysbiosis can lead to sleep disturbances, which in turn exacerbate mental health issues. Addressing gut health can promote better sleep and improve mental resilience.
In practise, psychologists can adopt several strategies to address the GBA in their therapeutic work:
1.Nutritional Guidance: Collaborate with dietitians to provide clients with nutritional advice that supports gut health, emphasising the consumption of fibre-rich foods, probiotics, and prebiotics.
2.Psychoeducation: Educate clients about the GBA and its impact on mental health, empowering them to make informed choices about their diet and lifestyle.
3.Holistic Assessment: Include questions about digestive health and dietary habits in intake assessments to gain a fuller picture of clients’ overall well-being.
4. Integrated Treatment Plans: Work alongside medical professionals to develop integrated treatment plans that address both psychological and physiological aspects of mental health conditions.
5. Stress Management: Incorporate stress reduction techniques such as mindfulness, meditation, and yoga, which can positively affect both gut health and mental well-being.
The field of GBA research is rapidly evolving, with emerging studies continually shedding light on the complex interactions between gut health and the brain. Future research may reveal more specific mechanisms by which gut microbiota influence mental health and identify novel therapeutic targets. Psychologists should stay abreast of these developments to incorporate the latest findings into their practise effectively.
Several promising areas for future research and application include:
1. Personalised Nutrition Plans: Developing personalised nutrition plans based on individual gut microbiome profiles could enhance mental health outcomes. This approach would consider genetic, environmental, and lifestyle factors to tailor dietary recommendations that optimise gut health and, consequently, mental well-being.
2. Psychobiotics: The exploration of psychobiotics—probiotics and prebiotics that have a positive effect on mental health—holds great potential. Future research can identify specific strains of bacteria that are most beneficial for treating various psychological disorders, leading to targeted probiotic therapies.
3. Microbiome Transplants: While still experimental, fecal microbiota transplants (FMT) offer a novel approach to restoring gut health. Research into the safety, efficacy, and ethical considerations of FMT for mental health conditions could pave the way for new treatments.
4. Neuroimaging Studies: Advanced neuroimaging techniques can provide deeper insights into how changes in the gut microbiome affect brain structure and function. Longitudinal studies using these techniques could elucidate the causal pathways linking gut health and mental health.
5. Behavioural Interventions: Investigating how behavioural
interventions, such as exercise and sleep hygiene, impact the gut microbiome and mental health could inform more comprehensive treatment plans. Integrating these interventions with traditional psychological therapies might offer synergistic benefits.
6. Public Health Initiatives: Largescale public health initiatives aimed at improving gut health through diet and lifestyle changes could have widespread mental health benefits. Education campaigns and community programmes promoting gut-friendly habits could reduce the prevalence of mental health disorders.
7. Cross-Disciplinary Collaboration: Encouraging collaboration between psychologists, neuroscientists, gastroenterologists, and nutritionists can foster a more holistic understanding of the GBA. Interdisciplinary research and clinical practises can lead to more effective and integrative approaches to mental health care.
Conclusion
In conclusion, the Gut-Brain Axis offers a fascinating insight into the interconnectedness of bodily systems and their collective impact on mental health. By acknowledging and integrating this connection into psychological practise, we can enhance the efficacy of mental health interventions and promote a more holistic approach to well-being. This paradigm shift not only broadens our understanding of mental health disorders but also paves the way for innovative and integrative treatment strategies.
The potential for personalised and targeted therapies based on gut microbiome profiles opens up new avenues for treating a variety of mental health conditions. As research progresses, we may discover more specific gut microbiota profiles associated with different psychological disorders, allowing for more precise interventions. The role of diet, lifestyle, and even psychobiotics
in maintaining mental well-being highlights the importance of a holistic approach that considers both physical and psychological factors.
Moreover, the integration of GBA knowledge into public health strategies can lead to preventative measures that enhance overall societal well-being. By promoting gut health through education and community programmes, we can potentially reduce the incidence of mental health disorders and improve the quality of life for many individuals.
As we continue to explore the depths of the GBA, psychologists and other mental health professionals have a unique opportunity to expand their therapeutic toolkit, embracing a more comprehensive understanding of mental well-being that incorporates the profound influence of gut health. This integrative perspective promises a future where mental health care is more effective, personalised, and holistic, ultimately leading to better outcomes for those we serve.

AUTHOR BIO
Tanjina Ashraf Khan Mou is a distinguished mental health professional and a celebrated writer. As the CEO of one of Kuala Lumpur's premier private psychology centres, she leads with innovation and compassion. An awardwinning, certified expert in her field, Tanjina's approach as an integrative therapist is both comprehensive and unique, drawing from a rich array of theoretical frameworks to develop her own distinctive practise.
Specialising in positive psychology, resilience training, behaviour analysis, and mindfulness-based therapies, Tanjina has dedicated the past five years to advocating for mental health and well-being on a global scale. Her empathetic nature and warm personality shine through in her professional endeavours and personal passions. In her free time, she immerses herself in research on cognitive reframing, stress and expressive writing methods.
Tanjina's remarkable contributions to mental health have earned her numerous accolades and features in prestigious publications, including FORBES and COSMOPOLITAN. Her unwavering commitment to advancing mental health and her ability to inspire others make her a true leader in her field.
Digital radiography (DR) has seen remarkable advancements, driven by technological innovations and evolving healthcare needs. This article explores the top ten emerging trends in DR, highlighting their impact on medical imaging. Key advancements include improved detector technology, which enhances resolution, sensitivity, and dynamic range, and the growing adoption of wireless and portable systems, which offer flexibility and faster image acquisition. Integration with artificial intelligence (AI) is revolutionizing image reconstruction, noise reduction, and automated analysis, while dose optimization techniques prioritize patient safety without compromising image quality. Cloud-based imaging solutions facilitate secure storage, sharing, and remote access to images, enhancing collaboration among healthcare professionals.
Enhanced workflow integration with healthcare IT systems improves efficiency and reduces errors, while a focus on patient-centric care aims to enhance comfort and communication. The expansion of telemedicine and remote monitoring further underscores the importance of DR in providing timely and accessible care. Market growth is driven by the transition from analog to digital systems and the rising prevalence of chronic diseases. Additionally, DR technology is finding new applications in industrial nondestructive testing and security screening, expanding its market potential. These trends reflect the continuous evolution of digital radiography, driven by innovation, clinical advancements, and changing healthcare dynamics, positioning DR as a critical component of modern healthcare.
James Chong, Deputy Chief Executive Officer, Columbia Asia Hospital Cheras

Digital Radiography (DR) has seen remarkable progress in recent years, fueled by continuous technological advancements and the changing demands of healthcare. These innovations are revolutionizing medical imaging by enhancing diagnostic precision, improving patient outcomes, and optimizing workflow efficiency. This article explores the top ten emerging trends in digital radiography, offering an in-depth look at the latest developments and their future impact on medical imaging.
Dose optimization and radiation safety remain paramount concerns in digital radiography. The goal is to minimize patient exposure to radiation without compromising image quality. Manufacturers are developing advanced dose reduction techniques, dose monitoring tools, and image processing algorithms to address these concerns.
Innovative dose modulation algorithms adjust the radiation dose based on the specific imaging requirements and patient characteristics. These algorithms ensure that the lowest possible dose is used while maintaining diagnostic image quality. Advanced image processing techniques, such as adaptive statistical iterative reconstruction, further enhance image quality by reducing noise and improving contrast.
Advanced systems include dose reduction technologies and dose monitoring tools, ensuring optimal radiation safety while maintaining high image quality.
The demand for wireless and portable DR systems has been on the rise, particularly in point-of-care settings, mobile imaging units, and emergency departments. These systems offer unparalleled flexibility, convenience, and faster image acquisition times, which are essential for improving workflow efficiency and patient care.
Wireless and portable DR systems eliminate the need for cumbersome cables, allowing for easier maneuverability and faster setup times. This is particularly beneficial in emergency and critical care settings, where rapid and accurate imaging is crucial. Another notable development is the dual-energy mobile X-ray systems, which integrate advanced detector technology to enable simultaneous acquisition of conventional and dual-
Wireless and Portable Systems offer greater flexibility and faster image acquisition, which are critical in emergency and point-of-care settings, eliminating the need for cumbersome cables
energy images with a single exposure. This capability not only improves diagnostic accuracy but also reduces patient radiation dose and enhances workflow efficiency. Moreover, the integration of these enhanced detector technologies into wireless systems further amplifies their utility and cost-effectiveness in medical settings. Wireless detectors are designed to be compatible with both main radiography units and mobile x-ray machines, enabling seamless interchangeability across different imaging modalities within healthcare facilities.
The ability of wireless detectors to be used interchangeably between main radiography units and mobile x-ray machines streamlines workflow efficiency. Healthcare providers can utilize the same detector across various settings, reducing the need for multiple specialized devices and optimizing resource allocation.
2. Cost - Effectiveness: By eliminating the requirement for dedicated detectors for each type of imaging equipment,
healthcare facilities can achieve significant cost savings. Wireless detectors reduce equipment procurement costs and maintenance expenses associated with managing multiple devices. Additionally, they enhance operational flexibility by allowing for rapid deployment in different clinical scenarios without logistical constraints.
One of the most notable advancements in digital radiography is the continuous improvement of detector technology. Both direct and indirect conversion detectors have seen significant enhancements in resolution, sensitivity, and dynamic range. These improvements are crucial for producing higher quality images at lower radiation doses, thereby reducing patient exposure while maintaining diagnostic accuracy.
Direct conversion detectors, which convert X-rays directly into electrical signals, have benefited from materials such as amorphous selenium and cadmium telluride. These materials offer higher spatial resolution and sensitivity compared to traditional scintillatorbased detectors. On the other hand, indirect conversion detectors, which use a scintillator to convert X-rays into light before converting the light into electrical signals, have seen advancements in scintillator materials and photodiode arrays, enhancing their efficiency and image quality.
Continuous improvements in detector technology enhance resolution, sensitivity, and dynamic range, crucial for reducing radiation doses while maintaining diagnostic accuracy. The integration of advanced image processing algorithms and software solutions further complements these hardware improvements. Manufacturers are developing compact, high-resolution detectors that improve image quality and enhance workflow efficiency. For instance, the use of iterative reconstruction techniques and machine learning algorithms can
enhance image quality by reducing noise and artifacts, allowing for better visualization of anatomical structures.
The expansion of telemedicine and remote healthcare services has highlighted the importance of remote monitoring and telediagnosis in digital radiography. Remote access to DR images enables radiologists to provide timely interpretations and recommendations, particularly in underserved or remote areas.
Remote monitoring solutions allow healthcare providers to track patients’ imaging data in real-time, facilitating early detection of changes in their condition and timely intervention. These solutions are particularly valuable for managing chronic diseases and monitoring post-operative recovery, where regular imaging is required.
Telediagnosis leverages digital radiography to extend the reach of
radiology services to remote and underserved regions. By enabling radiologists to review and interpret images remotely, telediagnosis improves access to specialized care and reduces the need for patients to travel long distances for imaging services. This capability is essential for addressing healthcare disparities and improving outcomes in rural and low-resource settings.
Artificial Intelligence (AI) is revolutionizing the field of digital radiography by providing advanced tools for image reconstruction, noise reduction, artifact correction, and automated analysis. AI algorithms can assist radiologists in improving diagnostic accuracy, streamlining workflows, and enhancing overall efficiency.
AI integration in DR systems can significantly reduce the time required for image interpretation and improve diagnostic confidence. For example,

AI-powered image reconstruction algorithms can produce high-quality images from low-dose scans, reducing patient exposure to radiation. AI-based noise reduction techniques can enhance image clarity, making it easier to detect subtle abnormalities.
AI also plays a crucial role in automated analysis and decision support. AI algorithms can detect and highlight potential abnormalities, such as fractures, tumors, or pulmonary nodules, providing radiologists with a second opinion and reducing the risk of missed diagnoses. Some systems integrate AI for automated positioning and image quality enhancements, thereby reducing patient setup time and improving diagnostic accuracy.
Artificial intelligence (AI) also continues to drive innovations in digital radiography, particularly in image analysis. AI algorithms are now capable of analyzing images for patterns, anomalies, and specific diagnostic criteria with high accuracy. This capability aids radiologists in making faster and more precise diagnoses, leading to improved patient outcomes.
Seamless integration of DR systems into the broader healthcare IT ecosystem is crucial for improving workflow efficiency and enhancing communication among healthcare providers. Integration with EMR and PACS systems allows for the automatic transfer of imaging data, reducing the need for manual data entry and minimizing the risk of errors.
Enhanced workflow integration also supports the implementation of advanced imaging protocols and standardized practices. By integrating DR systems with clinical decision support tools, healthcare providers can ensure that imaging procedures are performed consistently and according to best practices. This integration facilitates the use of automated protocols for image acquisition, processing, and interpretation, improving overall
efficiency and diagnostic accuracy.
The integration of DR systems with hospital information systems (HIS) and radiology information systems (RIS) further enhances workflow efficiency. It enables the automatic scheduling of imaging procedures, realtime tracking of imaging orders, and streamlined reporting of results. These capabilities are essential for optimizing the utilization of imaging resources and ensuring timely delivery of care.
The global digital radiography market has been steadily growing, fueled by the shift from analog to digital imaging systems, the increasing prevalence of chronic diseases, and advancements in healthcare infrastructure in emerging economies. This growth is also fueled by the increasing demand for high-quality, efficient, and cost-effective imaging solutions.
The shift from analog to digital imaging is a significant driver of market growth. Digital radiography offers numerous advantages over analog systems, including faster image acquisition, improved image quality, and enhanced workflow efficiency. As healthcare facilities continue to modernize their imaging capabilities, the demand for digital radiography systems is expected to rise.
The increasing prevalence of chronic diseases, such as cardiovascular diseases, diabetes, and cancer, necessitates frequent diagnostic imaging. Digital radiography provides a reliable and efficient means of monitoring these conditions, contributing to its growing adoption in clinical practice. Additionally, advancements in healthcare infrastructure in emerging economies are expanding access to digital radiography, further driving market growth. Digital long-length imaging has advanced and increased the diagnostic confidence for chiropractic predominantly in full spine evaluations,
Artificial intelligence is enhancing image reconstruction, noise reduction, artifact correction, and automated analysis, thereby improving diagnostic accuracy and efficiency
for a wide range of imaging procedures. Pediatric digital radiography presents unique challenges due to the smaller size and higher radiation sensitivity of pediatric patients. Recent advancements focus on dose optimization techniques tailored for pediatric imaging, as well as specialized imaging protocols and ergonomic designs that prioritize patient comfort and safety.
ensuring comprehensive diagnostic capabilities and treatment planning.
To meet the growing demand for affordable imaging solutions, manufacturers are developing costeffective digital radiography systems designed for small-to-midsize imaging centers, orthopedic facilities, urgent care centers, and hospitals. These systems offer high-quality imaging and user-friendly features, making them attractive options for budget-conscious healthcare providers.
A growing emphasis on patientcentered care is reshaping the design and functionality of digital radiography systems. Manufacturers are prioritizing initiatives to enhance patient comfort during imaging procedures, minimize wait times, and improve communication of imaging results to patients.
Patient comfort is a critical consideration in the design of DR systems. Ergonomic features, such as adjustable tables and detectors, help accommodate patients of all sizes and conditions, ensuring a more comfortable and efficient imaging experience. Systems are designed with patient comfort in mind, offering compact and versatile configurations
Clear and timely communication of imaging results is also essential for patient-centered care. Advances in image processing and reporting tools enable radiologists to generate easily understandable reports and visualizations, helping patients and their families make informed decisions about their care. Patient portals and mobile applications further enhance communication by providing patients with direct access to their imaging results and educational resources.
Cloud-Based Imaging and Data Management
The adoption of cloud-based imaging solutions is transforming the way digital radiography images are stored, shared, and accessed. Cloud integration offers secure storage, seamless data exchange, and remote access to DR images, facilitating collaboration among healthcare professionals and enabling teleradiology services.
Cloud-based solutions provide several advantages over traditional on-premises storage systems. They offer scalable storage options, allowing healthcare facilities to manage large volumes of imaging data without investing in expensive hardware. Cloud platforms also enable real-time access to images from anywhere, making it easier for radiologists to provide timely interpretations and consultations.
Moreover, cloud-based imaging solutions enhance data security and compliance with regulatory standards. They offer robust encryption, access controls, and audit trails to protect
patient data and ensure compliance with privacy regulations. This level of security is essential for maintaining patient trust and safeguarding sensitive medical information.
The integration of cloud-based imaging solutions with other healthcare IT systems further streamlines workflows and improves efficiency. It enables automatic transfer of imaging data to electronic medical records (EMR) and picture archiving and communication systems (PACS), reducing manual data entry and minimizing the risk of errors.
New Applications in Various Fields
Digital radiography technology is expanding its applications beyond traditional medical imaging, encompassing industrial non-destructive testing, security screening, and other modalities. These applications expand the market potential of digital radiography and highlight its versatility in various fields.
In industrial non-destructive testing, digital radiography is used to inspect materials and structures for defects without causing damage. This application is essential for ensuring the safety and reliability of critical infrastructure, such as pipelines, bridges, and aircraft components. The ability to quickly and accurately detect defects makes digital radiography a valuable tool in quality control and maintenance processes.
In security screening, digital radiography is used to detect contraband, explosives, and other threats in baggage, cargo, and mail. The high-resolution images produced by digital radiography systems enable security personnel to identify potential threats quickly and accurately, enhancing safety and security in transportation and public venues.
Additionally, digital radiography is being utilized in veterinary medicine, forensic investigations, and research applications. The ability to capture detailed images of anatomical structures and objects makes digital radiography
Designs emphasis on patient comfort and communication, including specialized protocols for pediatric imaging, is enhancing the overall patient experience
a valuable asset in these fields, contributing to its expanding market potential.
Looking ahead, digital radiography is poised to embrace emerging technologies such as quantum detectors, photon-counting detectors, and advanced AI algorithms. These technologies promise further improvements in image quality, dose reduction, workflow automation, and diagnostic accuracy, paving the way for
personalized and precision medicine approaches.
The continuous evolution of digital radiography is driven by technological innovations, clinical advancements, and changing healthcare dynamics. Advancements in detector technology, wireless and portable systems, AI integration, dose optimization, cloudbased solutions, enhanced workflow integration, patient-centric care, remote monitoring, market growth, and new applications are shaping the future of digital radiography.
These trends reflect the growing importance of digital radiography in modern healthcare, offering significant benefits in terms of diagnostic accuracy, patient safety, workflow efficiency, and overall healthcare delivery. As digital radiography continues to advance, it will play a crucial role in improving patient outcomes, enhancing clinical workflows, and addressing the evolving needs of healthcare providers and patients alike.
References are available at www.asianhhm.com

With a
background in project management and strategic
James is dedicated to enhancing healthcare delivery and operational efficiency. His career is marked by a commitment to cost optimization and fostering key strategic partnerships.
Cover Story

Combining the power of imaging with the power of radiotherapy is key to treating the growing burden of cancer. Innovation in oncology can make healthcare more personalized, precise, predictable, and productive. However, as new innovations become available, countries in Asia are playing catch-up. Market readiness remains the most significant challenge for this revolution in cancer care, meaning companies must help their customers and governments prepare for new technologies.
Hideaki Mori, President, Varian Asia Pacific & Japan
You joined Varian APJ from Siemens Healthineers in Japan. What has stood out the most about Varian since your move?
Even before moving I could see how dedicated and passionate everyone was from Varian. Siemens Healthineers had a strategic partnership with Varian in Japan for over ten years. So, I saw firsthand how we share the same goals for innovation and bringing advanced healthcare to patients. Varian’s superpower comes from its people and the passion they have for helping to create a world without fear of cancer.
Varian sees a future where cancer can become a manageable chronic disease, like diabetes. This vision unites all of us across Varian and Siemens Healthineers. Strong progress is being made, but we are only just starting to scratch the surface of what’s possible. There are opportunities for us to build on our strong foundations in imaging and radiotherapy – namely through greater integration across the cancer patient pathway.
Together we have an expansive view of the patient's journey, so we can assess the barriers and silos that prevent patients having a seamless experience. There is a huge opportunity to drive the integration of imaging and therapeutics – but we also have the scale to innovate and do much more than any individual cancer care med-tech company in the world.
Fundamentally it’s the passion, empathy, and understanding of the patient experience that is at the core of everything we do. It fuels our pursuit to innovate and to bring the highest quality treatment to those who need it.
Integrating advanced imaging and radiotherapy is essential for improving oncology care in Asia, where a lack of market readiness prevents adoption of new technologies. Nearly half of cancer patients lack access to basic radiotherapy, with those who do often facing inconsistent care quality. The future of oncology envisions seamless collaboration among specialists through comprehensive, versatile technologies, aiming to standardize high-quality treatment across the region.
We understand that Asia accounts for half of global cancer incidences, and by 2050 the WHO estimates cases could rise over 75%. Meeting this burden will require all of us to collaborate and help tackle the universal challenges cancer care teams face – rising costs, limited resources, shortage of trained staff, and a complex care journey.
Treating cancer requires accurate diagnostics, predictive simulations, and multiple clinical disciplines. There are many stages in this journey where the transfer of data can break down, and this lack of connectivity can lead to disruptions in treatment planning and delivery.
For example, a cancer patient in a low-income country, living in a
rural area, may be referred to multiple specialists, potentially over many days. They may have to physically carry their health data to each one. It is unlikely information flows seamlessly between the specialists and there is no personalized treatment plan to speak of. The patient is effectively a bystander in their treatment, constantly asking for directions. This translates to uncertainty and delay for them, whilst also being a drain on the healthcare system.
Half of cancer patients have an experience like this. Given our comprehensive view of the patient journey, it is our responsibility to help solve these issues and put patients at the center of their care.
Our goal is that once a patient is in the system, subsequent diagnostics, imaging, and decision support can be integrated. This then provides critical insights for a multi-disciplinary team to decide the best treatment plan. All the relevant clinical information would be captured, providing a complete picture of the patient throughout the journey.
Encouraging adoption is one of the largest challenges to any medical device company. Our role is to build a greater awareness of the value of new technologies, such as how they offer more precise imaging and treatment techniques – including AI-powered software. But this requires a regulatory environment that incentivizes adoption of new technologies.
Public reimbursement, for example, has the power to incentivize new treatment techniques which can have a
significant impact on access to cancer care. Hypofractionation is a form of radiation treatment where the radiation dose (a fraction) is larger than typical doses. Treatments are given once a day or less. Adopting hypofractionated treatment in low-to-middle income countries alone is estimated to improve access to radiotherapy in Asia from 62% to 78% . However, pay-per-fraction models of reimbursement, which exist in most markets, disincentivize this course of treatment.
Patient awareness is also a barrier to adoption. All too often, the care that a patient receives is determined by their first point of interaction with the health system. If patients first see a surgeon, they will receive surgery first; if they see a radiation oncologist, the chance is higher that they will receive radiation therapy. Education, awareness, and updated clinical guidance will overcome some of the underutilization of radiotherapy that we see.
It is important for all of us to convene and build a sustainable healthcare system that can adopt treatment advances quickly. The burden of proof is ultimately on us to demonstrate the safety, efficacy, and effectiveness of our treatments. That is why Varian invests significantly in clinical research. Our role is to provide

regulators with real-world evidence to paint a realistic picture of how this is helping patient care.
We want to move away from fragmented care to a more integrated, multidisciplinary care, centered around the patient. This will ensure cancer patients have a seamless, personalized experience and help reduce some of the fear that comes with a cancer diagnosis.
To help clinicians focus more on the patient, our technologies must integrate data analytics and AI to help improve clinical processes and workflows, making the connection between imaging and treatment shorter and more efficient.
Inside the treatment room, AI can be used to alter radiotherapy treatments in real-time. Data from imaging techniques used to capture complex, high-quality images of a tumor can help physicians adapt their treatment in response to anatomical changes. This allows clinicians to safely deliver higher doses of radiation while avoiding most
Hideaki Mori joins Varian Asia Pacific and Japan as President at an important time for the business. Modern medical device companies have evolved beyond the treatment room to become crucial partners for creating a sustainable healthcare system. Leading in this era requires technical knowledge, strong communication skills, a strategic and innovative mindset, and flexibility. But it also requires a strong purpose and culture to guide the company, with a mission that reflects the value it aims to have on patients and society.
Varian, a Siemens Healthineers company, envisions a world without fear of cancer. For more than 75 years, Varian has developed, built, and delivered innovative technologies and solutions that help care providers around the globe treat millions of patients each year. It supports every step of the cancer care journey – from screening to survivorship with advanced imaging, radiation therapy, comprehensive software and services, and interventional radiology.
healthy cells, potentially leading to less time in the hospital for the patient.
This is just one example, but it will all require enhancing the clinical workforce with digital skills. Medical schools need digital components in their curriculum. Meanwhile, additional training is needed to upskill the existing workforce.
Continuous medical education programs can develop highly trained technical personnel and specialized clinicians. Varian can help customers become clinical schools for these more advanced techniques and offers additional training programs to empower workforces and ensure the long-term sustainability of the healthcare system.
There is a huge opportunity to transform cancer care in Asia. Almost half of patients currently have no access to even basic forms of radiotherapy. For those who do have access, there can be variations in the quality of care available.
Where you live shouldn’t affect if you live. Advancing cancer care for us means democratizing access to treatment across Asia – a patient in a rural part of Assam, India, should be able to receive the same standard of treatment as a patient in New York.
The future we want to create will make it easier for all the specialists involved in cancer care work together – the doctors, nurses, radiologists, medical oncologists, surgeons, and radiation oncologists. Having a better coordinated, better informed, and better-managed journey will ensure caregivers can personalize care at every stage for the patient.
To do this, we must bring comprehensive technologies that can be used by numerous disciplines across different types of markets, raising standards of care wherever we operate. This requires manufacturers, providers, and governments working together. Collectively, we can help build a world where a cancer diagnosis no longer holds the fear that it does today.
In the dynamic Asia Pacific (APAC) healthcare landscape, innovative solutions are pivotal in transforming healthcare delivery. Medical devices present opportunities to reshape the system, but successful implementation requires addressing regulatory, infrastructure, and training hurdles while prioritising patient well-being. Bijay Singh of DKSH Healthcare highlights how advancements in medical devices like remote monitoring, and self-management apps drive growth in APAC.
Bijay Singh, Global Head, Healthcare Business Unit, DKSH Healthcare
Home to 4.3 billion people (60% of the global population), the Asia Pacific (APAC) region presents a rich tapestry of cultures, languages, and socioeconomic backgrounds. From densely populated urban centres boasting stateof-the-art medical facilities, to remote rural communities facing formidable barriers to access, healthcare systems vary widely. Amidst the complexities and opportunities across this landscape, there is a demand for innovative solutions to transform the healthcare delivery system, and this is precisely where medical devices play a crucial role.
In the APAC region, a significant demographic transformation is underway –the rapid ageing of its population. By 2050, the number of individuals aged 60 and above is projected to more than double, reaching a staggering 1.3 billion or almost 25% of the population.1
This demographic trend brings with it a host of healthcare challenges, including an increased burden of age-related diseases and conditions such as cardiovascular diseases, cancer, and neurodegenerative disorders.
Alongside population ageing, there's a marked increase in the prevalence of chronic diseases. Factors contributing to this rise include sedentary lifestyles, unhealthy diets, urbanisation, and environmental factors. Healthcare systems must adapt to provide specialised care for older adults while also addressing their unique healthcare needs, including preventive care, early detection, chronic disease management, and long-term care services. As individuals age, their healthcare needs become more complex, demanding a holistic approach that addresses not just acute ailments but also the multifaceted aspects of ageing, including cognitive health, mobility issues, and social support.
Spurred by this demographic shift, the need for high-quality healthcare continues to rise in the region. This trend is further compounded by the lingering effects of the COVID-19 pandemic and existing resource shortages within healthcare systems. In navigating these healthcare challenges, medical devices play a pivotal role - from advanced monitoring technologies to assistive devices and innovative treatment modalities, medical devices reduce the burden on healthcare professionals, enabling them to deliver tailored and effective care to ageing populations and individuals battling chronic diseases. These devices facilitate early detection, remote monitoring of multiple patients, precise diagnosis, and timely intervention, ultimately improving
In the dynamic Asia Pacific (APAC) healthcare landscape, innovative solutions are pivotal in transforming healthcare delivery. Medical devices present opportunities to reshape the system, but successful implementation requires addressing regulatory, infrastructure, and training hurdles while prioritising patient well-beings
patient outcomes and enhancing the efficiency of healthcare delivery.
the
Medical devices leverage technology to deliver care safely and efficiently and help strengthen the public health infrastructure. Advanced imaging devices like MRI machines, CT scanners, and ultrasound systems have revolutionised diagnosis by providing detailed insights into internal bodily structures.
For instance, current high-resolution MRI machines enable early detection of tumours, vascular abnormalities, and neurological disorders. Moreover, robotic-assisted surgical systems have enhanced precision while minimising invasiveness. Hospitals across the region utilise these systems for procedures ranging from prostatectomies to cardiac surgeries, resulting in quicker recovery times and reduced complications.
Here's how technologically advanced devices can further contribute to this transformation:
Remote monitoring and telemedicine: Medical devices such as wearable sensors, remote monitoring devices, and telemedicine platforms enable healthcare providers to remotely monitor patients' vital signs, health status, and treatment adherence.
Point-of-care testing: Point-of-care testing devices offer rapid and convenient diagnostic capabilities outside of traditional laboratory settings. These devices can be particularly valuable in resource-limited settings or remote areas. For example, during the COVID-19 pandemic, multiple home-test kits were developed to allow the first round of testing at home. This also helped people adhere to the social distancing norms.
Self-management apps: Mobile health (mHealth) apps and devices empower patients to take an active role in managing their health and well-being. These apps enable users to track their exercise, diet, medication adherence, and vital signs, providing valuable insights into their health status and facilitating communication with healthcare providers. For instance, the Dexcom G6 continuous glucose monitoring system, now available in Singapore and Japan, allows for real-time monitoring, integrated with wearable sensors and a transmitter for the measurement of blood glucose values.
Data-driven decision-making: Medical devices generate vast amounts of patient health data, which can be leveraged to optimise resource allocation and care delivery. By analysing the data trends and patterns in patient populations, healthcare providers can identify areas for improvement, allocate resources more effectively, and implement targeted interventions to address specific healthcare needs. This data-driven approach fosters efficiency, reduces waste, and ultimately lowers healthcare costs.
Home-based care: Technological advancements have facilitated the development of medical devices designed for home use, allowing patients to
receive care in the comfort of their own homes rather than in hospitals or longterm care facilities. Home-based care reduces healthcare costs associated with hospitalisations and institutional care while promoting patient independence and quality of life. Devices such as home infusion pumps, portable oxygen concentrators, and remote monitoring systems enable patients with chronic conditions to manage their health outside of traditional healthcare settings, thereby optimising resource allocation and reducing overall healthcare expenditure. By enabling remote monitoring and telemedicine, emphasising preventive care and chronic disease management, supporting data-driven decisionmaking, and promoting home-based care, advancements in medical devices hold significant promise for optimising resource allocation and reducing longterm costs.
In 2023, the region's medical devices market reached a value of USD 111.93 billion. Projections suggest that it will further grow at a CAGR of 6.8% and reach USD 166.1 billion by 2029. This highlights the considerable potential
of the APAC region, characterised by its diverse population. APAC is experiencing strong growth in demand for medical devices, forecast to grow at 7.0% from 2018-2022, surpassing Europe to become the secondlargest market globally. Regulatory developments play a crucial role in strengthening the upward growth of this sector. One significant trend is the harmonisation of standards and regulations across key markets such as the Association of Southeast Asian Nations (ASEAN) and North Asia. This effort aims to establish consistent regulatory frameworks, streamline approval processes, and enhance market access for medical devices across borders. This creates a clearer and more consistent environment for everyone involved, from manufacturers and distributors to healthcare providers and patients.
Leveraging innovative medical devices and technologies, healthcare providers in the
healthcare delivery, such as geographical constraints, resource limitations, and workforce shortages. The interplay of technological advancements, socioeconomic conditions, and the regulatory landscape will ultimately revolutionise healthcare delivery in APAC.
However, successful implementation requires a comprehensive approach that addresses regulatory, infrastructure, reimbursement, and training challenges while ensuring patient privacy, safety, and equity. Collaboration between healthcare stakeholders, technology developers, policymakers, and regulatory authorities is essential to improve health outcomes across the region.
Given the diversity of the Asian market, medical device companies need to leverage access and in-market expertise to thrive. It is imperative for medical device companies to collaborate with trusted strategic healthcare providers who have extensive local regulatory expertise, as such partnerships are crucial for navigating the dynamic regulatory frameworks across Asia. These partnerships will ensure the efficient distribution of medical solutions, optimise resource allocation, and enhance the quality of life in communities.

Bijay Singh, with over 25 years in the healthcare industry, joined DKSH in 2015 as VP of Business Development for Healthcare. In 2017, he became Head of Business Unit Healthcare and joined the Executive Committee. Prior to DKSH, he held senior positions at Novartis and Eli Lilly.

This article explores how blockchain technology can revolutionise patient satisfaction by enhancing data security, streamlining administrative processes, increasing transparency, and incentivising patient engagement through tokenomics. The framework provided demonstrates how these improvements can address healthcare challenges and significantly improve patient experiences and outcomes.
Patient satisfaction is at the heart of compassionate healthcare. It goes beyond medical outcomes, encompassing the entire patient experience, from the first interaction to ongoing support. Understanding that each patient is a unique individual with specific needs and fears is crucial. A warm smile, a gentle touch, and a listening ear can make a world of difference in alleviating anxiety and building trust.
Compassionate care involves respecting patients' dignity, valuing their input, and involving them in decision-making. Clear, empathetic communication helps demystify complex medical information, empowering patients to participate actively in their care. It’s about creating an environment where patients feel heard, understood, and respected. Moreover, addressing the emotional and psychological needs of patients is paramount. Offering support and comfort during vulnerable times, ensuring privacy, and being sensitive to their cultural and personal backgrounds all contribute to a positive experience. A satisfied patient feels cared for beyond their physical ailments.
Ultimately, compassionate care fosters healing and well-being, enhancing patient satisfaction. It’s a commitment to seeing patients as whole individuals, deserving of empathy and kindness. In the journey of healthcare, compassion is the bridge that connects medical expertise with the human touch, ensuring patients not
only receive the best treatment but also feel genuinely cared for.
Technology has revolutionised patient satisfaction, moving beyond traditional methods like Press Ganey surveys to more dynamic and responsive tools. Here’s how:
By integrating Blockchain technology, healthcare providers can deliver more personalised, efficient, and accessible care, leading to higher patient satisfaction. The focus shifts from merely measuring satisfaction to actively enhancing it through continuous, technology-driven improvements.
Patient satisfaction is a pivotal metric in the healthcare industry, influencing everything from patient retention to clinical outcomes and reimbursement rates. In recent years, technological advancements have provided new avenues to improve patient experiences and satisfaction levels. Among these innovations, blockchain technology stands out for its potential to revolutionise various aspects of healthcare delivery and management. By leveraging blockchain’s inherent features of transparency, security, and decentralisation, healthcare providers can address several pain points in the patient journey, thus significantly enhancing patient satisfaction.
Blockchain is a distributed ledger technology that allows data to be stored across a network of computers in a manner that is secure, transparent, and immutable. Each block in the blockchain contains a list of transactions, and these blocks are linked together in a chronological order, forming a chain.
Key features of blockchain include:
1. Decentralisation: Data is not stored in a single location but distributed across a network, reducing the risk of data breaches.
2. Transparency: All transactions are visible to participants in the network, enhancing trust and accountability.
3. Immutability: Once data is recorded,
Blockchain technology is revolutionizing healthcare by enhancing patient satisfaction through improved data security, transparency, and interoperability. Discover how innovative solutions are empowering patients with control over their health records, leading to better-coordinated care and personalized treatment.
it cannot be altered or deleted, ensuring the integrity of the information.
4. Security: Advanced cryptographic techniques are used to secure data, making it highly resistant to unauthorised access.
To appreciate how blockchain can enhance patient satisfaction, it's crucial to understand the current challenges patients face:
1. Data Privacy and Security: Patients are often concerned about the security of their personal and medical information. Data breaches can lead to loss of trust and legal ramifications.
2. Administrative Inefficiencies: The healthcare system is plagued with bureaucratic delays, redundant paperwork, and inefficiencies that frustrate patients.
3. Lack of Transparency: Patients frequently find it difficult to access their medical records and understand the billing process, leading to confusion and dissatisfaction.
4. Inconsistent Care Coordination:
Poor communication between different healthcare providers can result in fragmented care, negatively impacting patient outcomes.
5. Limited Patient Engagement:
Traditional healthcare models often fail to actively involve patients in their care, leading to lower adherence to treatment plans and poorer health outcomes.
Blockchain technology can address these challenges through several mechanisms:
1. Enhanced Data Security and Privacy
Blockchain’s decentralised nature and use of encryption ensure that patient data is secure and accessible only to authorised individuals. Patients have control over their data and can grant or revoke access as needed.
2. Streamlined Administrative Processes
Smart contracts, self-executing contracts with the terms of the agreement directly written into code, can automate various administrative tasks such as billing, insurance claims, and patient consent management, reducing delays and errors.
3. Improved Transparency
Blockchain provides a transparent and tamper-proof record of all transactions, including medical records and billing information. Patients can easily access their records and understand their treatment and billing history.
4. Better Care Coordination
A blockchain-based system can facilitate seamless sharing of medical records among different healthcare providers, ensuring that all parties have access to up-to-date patient information. This leads to more coordinated and effective care.

5. Incentivising
Tokenomics, the use of digital tokens to create an economic system, can be integrated into blockchain-based healthcare platforms to incentivise patient behaviours that lead to better health outcomes. Patients can earn tokens for actions such as attending appointments, adhering to treatment plans, and engaging in preventive health activities.
To implement blockchain technology effectively for enhancing patient satisfaction, a structured framework is necessary. The following framework outlines the key components and steps involved:
• Secure Storage: Implement a
blockchain-based system for secure storage of patient data.
• Access Control: Allow patients to control who has access to their data.
• Audit Trails: Provide immutable audit trails for all data accesses and modifications.
• Automated Billing and Claims: Use smart contracts to automate billing processes and insurance claims.
• Patient Consent Management: Implement smart contracts to manage patient consent for treatments and data sharing.
• Appointment Scheduling: Automate appointment scheduling and reminders through smart contracts.
• Medical Records: Ensure that all medical records are recorded on the
blockchain, accessible to both patients and healthcare providers.
• Billing Transparency: Record all billing transactions on the blockchain to provide clear and transparent billing information.
• Interoperability: Develop interoperability standards to enable seamless sharing of data between different blockchain systems and healthcare providers.
• Provider Collaboration: Facilitate collaboration between different healthcare providers through shared access to patient data.
• Incentive Programmes: Develop token-based incentive programmes to reward patients for healthy behaviours and adherence to treatment plans.
• Health Milestones: Reward patients with tokens for achieving health milestones such as weight loss, smoking cessation, and regular exercise.
• Token Redemption: Allow patients to redeem tokens for healthcare services, discounts, or other rewards.
To illustrate the practical application of this framework, let's consider a use case model that incorporates tokenomics to enhance patient satisfaction.
• Objective: Enhance patient satisfaction by incentivising healthy behaviours, streamlining administrative processes, and ensuring better care coordination.
Components:
1. Blockchain Network: A secure and decentralised blockchain network to store patient data and facilitate transactions.
2. Digital Tokens (HealthCoins):
Digital tokens used to reward patients for positive health behaviours and engagement.
3. Smart Contracts: Smart contracts to automate administrative tasks such as billing, claims, and consent management.
4. Mobile App: A user-friendly mobile app for patients to manage their health records, track their health activities, and earn tokens.
Process:
1. Patient Registration and Data Management:
• Patients register on the HealthyLife platform and create a secure digital identity.
• Patients’ medical records are stored on the blockchain, accessible through the mobile app.
2. Incentive Programme:
• Patients earn HealthCoins for completing health-related activities such as attending appointments, adhering to medication schedules, and participating in preventive health programmes.
• Health milestones such as achieving weight loss goals or quitting smoking are rewarded with additional tokens.
3. Token Redemption:
• Patients can redeem HealthCoins for healthcare services, discounts on medical bills, or wellness products available on the platform.
4. Smart Contracts for Administrative Efficiency:
• Billing and insurance claims are processed automatically through smart contracts, reducing administrative delays and errors.
• Patients grant consent for treatments and data sharing through smart contracts, ensuring transparency and compliance.
5. Care Coordination:
• Healthcare providers on the platform
have access to up-to-date patient data, facilitating coordinated and effective care.
• Providers collaborate seamlessly through shared access to patient records, improving care outcomes.
1. Increased Patient Engagement:
• Patients are more engaged in their healthcare due to the incentive programme, leading to better health outcomes and higher satisfaction levels.
2. Enhanced Data Security and Privacy:
• Blockchain’s security features ensure that patient data is secure and only accessible to authorised individuals.
3. Administrative Efficiency:
• Automation of billing and claims processes reduces administrative burdens and errors, leading to faster and more accurate transactions.
4. Transparency and Trust:
• Patients have clear and transparent access to their medical records and billing information, increasing trust in the healthcare system.
5. Improved Care Coordination:
• Seamless sharing of patient data among healthcare providers ensures coordinated and effective care, enhancing patient outcomes.
• Some of the use cases of blockchain technology currently in use around the world to address the issue of patient satisfaction
Decentralised Healthcare Information Ecosyste
1. Ecosystem
Location: South Korea
Overview: This system creates a decentralised healthcare information ecosystem for patients, healthcare providers, and researchers using blockchain technology.
Legacy healthcare providers risk falling behind by not adopting blockchain technology. Discover how blockchain is revolutionizing patient satisfaction, data security, and care coordination, and why ignoring these innovations could jeopardize their competitive edge and patient trust
How It Enhances Patient Satisfaction: Patients gain control over their medical records, ensuring data security and privacy. They can share their records with different healthcare providers without the risk of data tampering or loss, leading to better-coordinated care and improved health outcomes.
2. Secure Electronic Health Records
Location: United Kingdom
Overview: A blockchain-based solution for creating secure, decentralised electronic health records.
How It Enhances Patient Satisfaction: Patients have full control over who accesses their medical data, building trust between patients and healthcare providers. They can grant temporary access to their records to different healthcare providers, facilitating better diagnosis and treatment.
3. National Health System Data Security
• Location: Estonia
• Overview: A data security system using blockchain technology within a national health system.
• How It Enhances Patient Satisfaction: This system ensures the integrity of patient data, protecting it from cyber threats and building patient confidence in the security of their personal health information. It also streamlines administrative processes, reducing wait times and improving overall patient experience.
4. Healthcare Administration Platform
Location: United States
Overview: A blockchain-based healthcare administration platform that coordinates care, manages benefits, and streamlines payments.
How It Enhances Patient Satisfaction: The platform improves transparency and accountability in healthcare administration. Patients can track the status of their care and understand their benefits and payments better. It also reduces administrative overhead, leading to more efficient and timely patient care.
5. Interoperability of Healthcare Data
Location: United States
Overview: A blockchain network aimed at improving the interoperability of healthcare data across different systems. How It Enhances Patient Satisfaction: By ensuring healthcare data is easily accessible and shareable across different platforms and providers, patients receive more accurate and timely care. This improved data flow reduces errors and duplicative tests, enhancing patient experience and satisfaction.
• Location: United States
• Overview: A blockchain-based platform that combines data from different sources into a single, secure patient record.
• How It Enhances Patient Satisfaction: Patients benefit from having their
health data integrated into one comprehensive record, which can be securely shared with healthcare providers. This integration facilitates personalised treatment plans and better health outcomes, directly impacting patient satisfaction.
• Location: United States
• Overview: A blockchain-based solution for storing and managing electronic medical records.
• How It Enhances Patient Satisfaction: This system provides patients with secure, easy access to their health records. They can manage and share their data with healthcare providers, leading to better-informed healthcare decisions and a more personalised care experience.
These examples demonstrate the potential of blockchain technology to transform patient satisfaction by enhancing data security, transparency,
interoperability, and patient control over personal health information. By addressing these key areas, blockchain solutions are paving the way for a more efficient, patient-centred healthcare system.
Blockchain technology, with its unique features of decentralisation, transparency, and security, holds significant promise for enhancing patient satisfaction in healthcare. By addressing key challenges such as data privacy, administrative inefficiencies, and lack of patient engagement, blockchain can transform the patient experience. The integration of tokenomics further amplifies this potential by incentivising positive health behaviours and active patient participation. As healthcare continues to evolve, embracing innovative technologies like blockchain will be crucial in creating a more patient-centred and satisfaction-driven healthcare ecosystem.

Arnab Paul, Founder & CEO of Patient Planet, has over 20 years in healthcare leadership, focusing on homecare and digital health. A WHO expert in digital health, he’s an awarded entrepreneur, Hurst Fellow, Saltire Scholar, and Strategic Advisor to FarmaTrust, a Pharma Blockchain Company. He’s also a keynote speaker at the African Blockchain Development Call.
Digital healthcare innovations promise improved patient care and efficiency. However, balancing these advancements with human empathy is essential. This article explores the integration of human sensibility in digital healthcare, with a strong emphasis on patientcentred communication. This approach values the patient's perspective, ensuring they feel integral to the healthcare process. It also underscores the importance of ethical considerations, emotional support, and cultural sensitivity to create a truly patient-centred system.
Vaikuntam Rajaratnam, Program Director, National Healthcare Group

Digital technologies are reshaping how we diagnose, treat, and manage patient care. The potential benefits of these innovations are immense, from telemedicine and electronic health records (EHRs) to artificial intelligence (AI) and wearable health monitors. However, as we embrace these technological advancements,
ensuring that human sensibility remains at the forefront of healthcare delivery is crucial. This balance is essential for fostering a patient-centred approach that combines technological efficiency with empathy and understanding.
Digital healthcare uses digital technologies to enhance health outcomes, streamline healthcare
delivery, and improve patient experiences. It encompasses many tools and applications, including telehealth services, mobile health apps, electronic health records, and AI-driven diagnostic tools. These technologies offer significant benefits, such as increased accessibility, improved efficiency, personalised care, and cost-effectiveness.
Human sensibility in digital healthcare involves integrating human factors, emotions, and sensory experiences into designing and implementing digital health technologies. It ensures that technological solutions are functional, empathetic, patient-centred, and culturally sensitive. This integration is necessary for creating compelling and humane healthcare solutions.
The intersection of human sensibility and digital healthcare advancements is a critical area of exploration. Integrating human factors and sensory experiences into digital health technologies is not merely an enhancement but a necessity. It's a call to action for all healthcare professionals, researchers, and policymakers to contribute to the creation of compelling and empathetic healthcare solutions. The shift from traditional paternalistic models to patient-centred approaches, augmented by technology, represents a significant cultural transformation in healthcare.
A crucial concept emerging from the current body of knowledge (see References) is digital empathy, which is essential for achieving positive health outcomes. Digital empathy involves understanding and addressing patients' emotional and psychological needs through technological interfaces.
Telehealth Services:
Improved accessibility
Convenience and comfort
Expanded specialist access.
Electronic Health
Records (EHRs): Streamlined Patient
Information Management
Quick and Accurate Data
Retrieval
Improved Care Coordination
Mobile Health Apps:
Convenient Health Information
Personalized Health Tracking
Virtual Care and Reminders.
Automated
Administrative Tasks:
Automated Administrative Tasks
Increased Focus on Patient Care
Improved Efficiency
Reduced Wait Times
Implementing an emotive sensory web in virtual healthcare highlights the challenges and ethical issues that must be addressed to make digital health interventions genuinely supportive and humane.
Integrating human senses with digital sensors, particularly in telemedicine, emphasises the importance of sensory judgements in medical practise. Sensory skills, such as visual, tactile, auditory, and olfactory abilities, remain critical for accurate diagnosis and effective patient care. These skills ensure that technology enhances rather than replaces the nuanced understanding and empathetic touch that healthcare professionals provide.
Overall, a more human-centred approach to digital health is essential. This approach considers the complex interplay between technology, human factors, and healthcare delivery, ensuring that advancements in digital healthcare are both innovative and empathetic. By prioritising the integration of human
Wearable Health Monitors:
Health Metric Tracking
Personalized Treatment Plans
Early Health Issue Detection
Al-Driven Analytics:
Health Data Analysis
Personalised Insights Tailored Treatments.
sensibility into digital health, we can create a healthcare system that leverages technology while preserving the essential human touch, ultimately leading to improved patient outcomes and experiences.
Digital health transforms healthcare by enhancing accessibility, efficiency, personalised care, and cost-effectiveness. Technologies such as telehealth services, electronic health records (EHRs), AI-driven diagnostics, and wearable health monitors are revolutionising patient care. These innovations offer significant benefits, including more accessible access to specialist care, streamlined management of patient information, continuous health monitoring, and reduced healthcare costs. Digital health promotes preventive care and optimises resource allocation, improving patient outcomes and a more efficient healthcare system (Figure 1).
Preventive Care:
Early Chronic Condition Detection
Proactive Health Monitoring
Reduced Emergency Interventions
Reduced Hospitalizations.
Resource Optimization:
Efficient Healthcare Resource Use
Reduced Operational Costs
Lower Overhead Costs
The future of digital health promises even more revolutionary changes with advancements in artificial intelligence, blockchain technology, the Internet of Medical Things (IoMT), and genomics. AI will enhance predictive analytics and diagnostics, while blockchain will ensure secure and transparent data management. IoMT will connect medical devices for real-time monitoring and smart hospital development, and genomics will enable precision medicine with personalised treatments. Emerging technologies like virtual reality (VR), augmented reality (AR), and robotics will further evolve telemedicine and automated caregiving. Embracing these advancements while focusing on human sensibility will ensure that healthcare remains compassionate, effective, and patient-centred (Figure 2).
Despite the numerous advantages of digital healthcare, the rapid integration of these technologies presents challenges
Artificial Intelligence and Machine Learning:
Blockchain Technology:
Internet of Medical Things (IoMT):
Telemedicine Evolution:
Genomics and Precision Medicine:
Robotics and Automation:
• Predictive Analytics
• Al in Diagnostics
• Secure Data Management
• Transparent Transactions
• Connected Devices
• Smart Hospitals
• Virtual Reality (VR) and Augmented Reality (AR)
• Enhanced Telehealth Platforms
• Personalized Genomic
• Data Targeted Therapies
• Surgical Robots
• Automated Caregiving.
that require a thoughtful and empathetic approach. Human sensibility involves considering healthcare's emotional, psychological, and social dimensions. The following areas highlight the importance of maintaining human sensibility in digital healthcare: Digital tools should enhance, not replace, human interaction in healthcare.
Providers must use technology to facilitate meaningful patient conversations, ensuring their concerns and preferences are heard and respected. For instance, while telehealth consultations offer convenience, they should allow patients to express their feelings and ask questions. The development and implementation of AI and machine learning algorithms
must be transparent and fair. Ensuring these systems do not perpetuate biases and respecting patient privacy are paramount. AI-driven diagnostic tools, for example, should be designed with diverse datasets to avoid reinforcing health disparities.
Healthcare providers should recognise the emotional impact of digital health interventions. Virtual consultations and remote monitoring should include elements of empathy and reassurance to help patients feel supported, especially those dealing with chronic conditions or mental health issues. Additionally, digital health technologies should be adaptable to diverse cultural contexts. Understanding cultural nuances and patient backgrounds can enhance the effectiveness of digital health interventions. For example, telehealth platforms should be designed to accommodate language differences and cultural preferences in healthcare delivery.
Integrating Human Sensibility into Digital Healthcare
Interdisciplinary Collaboration:
• Collaboration among all stakeholders in healthcare
• Transdisciplinary approach
Patient Involvement:
• Understand and learn from experiences and preferences
• Provide valuable insights#
• Patient advisory boards
Figure 3 Integrating Human Sensibility into Digital Healthcare
Training and Education:
• Clinicians integrating digital tools while maintaining compassionate care.
• Patients should be educated on the use and benefits of these technologies.
Continuous Feedback:
• Establishing feedback mechanisms
• Regular surveys and feedback sessions
Several strategies can be employed to successfully infuse human sensibility into digital healthcare advancements (Figure 3). Collaboration among healthcare professionals, technologists, ethicists, and patients is essential for designing and implementing digital health solutions. This interdisciplinary approach ensures that technologies are user-friendly, ethical, and responsive to patient needs. For instance, involving patients in the development process can provide valuable insights into their experiences and preferences. Clinicians should receive training on effectively integrating digital tools into their practise while maintaining compassionate care. Similarly, patients should be educated on the use and benefits of these technologies. This dual approach ensures that providers and patients are comfortable with digital health interventions.
Involving patients in developing and evaluating digital health solutions
can provide valuable insights into their experiences and preferences, leading to more patient-centred innovations. For example, patient advisory boards can offer feedback on new technologies and suggest improvements based on their firsthand experiences. Establishing mechanisms for continuous feedback from patients and healthcare providers can help identify areas for improvement and ensure that digital tools remain aligned with human sensibility. Regular
surveys and feedback sessions can provide ongoing insights into the effectiveness and usability of digital health solutions. (Figure 3)
While integrating human sensibility into digital healthcare has shown promise, several challenges remain. Addressing these challenges is crucial for advancing patient-centred digital health solutions. Ensuring the privacy and security of
Data Privacy and Security Robust Data Protection Measures
Transparent Data Governance
patient data is a significant concern in digital healthcare. Robust data protection measures and transparent data governance policies are essential to maintain patient trust. Bridging the digital divide and ensuring equitable access to digital health technologies is critical. Efforts must be made to provide access to underserved populations and address barriers such as internet connectivity and digital literacy.
Developing comprehensive
Implement strong encryption, secure storage, and access control measures; regularly update security protocols.
Develop transparent data governance frameworks; ensure transparency in data collection, storage, use, and sharing practices.
Equitable Access Bridging the Digital Divide Improve internet connectivity in underserved areas; enhance digital literacy through targeted education programs.
Affordable Access
Regulatory and Ethical Frameworks
Addressing Algorithmic Bias
Data Ownership and Consent
Patient-Centred Communication Enhancing Human Interaction
Training and Education
Emotional Support and Cultural Sensitivity Integrating Empathy in Digital Health
Culturally Adaptable Technologies
Continuous Feedback and Improvement Mechanisms for Feedback
Patient Involvement in Development
Sustainability Long-term Investment
Environmental Considerations
Provide subsidies or financial support for low-income populations; develop affordable pricing models for digital health tools.
Mandate diverse datasets in AI development; conduct regular audits to detect and mitigate biases.
Clearly define patient data ownership rights; ensure informed consent processes are rigorous and comprehensible.
Design digital tools to facilitate meaningful patient-provider interactions; include features in telehealth platforms that support in-depth conversations.
Require healthcare professionals to be trained in integrating digital tools with compassionate care; educate patients on the benefits and proper use of technologies.
Design digital health interventions that include empathy and emotional support; prioritize the needs of patients with chronic conditions or mental health issues.
Ensure digital health technologies can be customized to meet diverse cultural and linguistic needs; develop user interfaces that accommodate cultural preferences.
Establish regular feedback mechanisms from patients and healthcare providers; use surveys and feedback sessions to gather insights on digital health solutions.
Involve patients in the design and evaluation of digital health technologies; create patient advisory boards for ongoing input and suggestions.
Promote ongoing investment in digital health research, development, and infrastructure; secure funding for innovative projects and maintenance of systems.
Encourage the development of environmentally sustainable digital health technologies; minimize the carbon footprint and resource usage of digital health solutions.
regulatory and ethical frameworks for digital health technologies is essential. These frameworks should address issues such as algorithmic bias, data ownership, and informed consent. Ensuring the sustainability of digital health solutions requires ongoing investment in research, development, and infrastructure. Long-term planning and funding are necessary to support digital healthcare's continued growth and integration. By tackling these challenges, we can ensure that digital health technologies are innovative, effective, equitable, secure, and sustainable.
The available literature recommends several essential policy guidelines to ensure the successful integration of human sensibility into digital healthcare (See References). First, addressing data privacy and security is paramount (Table 1). Robust data protection measures, including strong encryption, secure storage, and transparent data governance policies, are essential to maintaining patient trust. Ensuring equitable access to digital health technologies is also critical, requiring efforts to improve internet connectivity and digital literacy in underserved populations. Affordable access should be promoted through subsidies or financial support for low-income groups.
Developing comprehensive regulatory and ethical frameworks is vital for the responsible deployment of digital health technologies. These frameworks should address algorithmic bias, clearly define patient data ownership rights, and ensure rigorous and understandable informed consent processes. Enhancing patient-centred communication through digital tools that facilitate meaningful interactions between healthcare providers and patients is crucial. Training programmes for healthcare professionals and patient education on digital health technologies' benefits and proper use should be mandated.
Continuous feedback mechanisms
Integrating empathy and cultural sensitivity into digital healthcare innovations enhances patient-centred care. This approach balances technological efficiency with emotional and psychological support, ensuring ethical standards and human sensibility remain at the forefront. Future digital health solutions must prioritise patient involvement and continuous feedback to improve healthcare outcomes.
from patients and healthcare providers are essential for ongoing improvement and alignment of digital health solutions with human sensibility. Establishing patient advisory boards and regular feedback sessions can provide valuable insights. The sustainability of digital health solutions requires a long-term investment in research, development,

and infrastructure, alongside environmental considerations, to minimise these technologies' carbon footprint and resource usage. By implementing these policy guidelines, we can create a healthcare system that effectively integrates technological advancements with human empathy and ethical standards (Table 1).
Integrating digital technologies in healthcare holds immense potential to revolutionise patient care and operational efficiency. Yet, the true success of these advancements hinges on their ability to complement and elevate human sensibility. By prioritising patient-centred communication, upholding ethical standards, providing emotional support, and embracing cultural sensitivity, we can forge a healthcare system that harnesses technological innovation while preserving the vital human touch.
We must adopt a collaborative and empathetic approach to navigating this exciting frontier. By doing so, we ensure that the full benefits of digital healthcare innovations are realised, creating a future where technology and humanity coexist harmoniously to deliver outstanding healthcare experiences and outcomes. This balanced integration will drive progress and inspire trust and confidence among patients and healthcare providers alike, paving the way for a brighter, more compassionate healthcare landscape.
Dr Vaikunthan Rajaratnam is a seasoned academic and healthcare professional with over 40 years of experience in surgery, medical education, instructional design and integrating AI into healthcare practice. As a UNESCO Chair partner, he is committed to advancing digital healthcare while maintaining a patientcentred approach.

During public health crises, mobile clinics play a crucial role in reducing disparities by delivering essential medical services directly to marginalised and underserved communities. These clinics ensure that vulnerable populations receive timely care, bridging the gap in healthcare access and addressing inequities that are often exacerbated during emergencies.
Preet Kukreja, MBA, MHA, FAPM, Director, Population Health Initiatives
1. Can you share a brief overview of your journey and experiences in public health, particularly in relation to mobile clinics and their role during public health emergencies?
Thank you for this opportunity to discuss my journey in public health. My career has been driven by a passion for advancing health equity and improving healthcare access, particularly in underserved communities. As Director of Population Health Initiatives, I have led efforts to utilise both traditional and innovative delivery models, including mobile clinics, to expand access to essential services like vaccinations during the COVID-19 pandemic and other health crises.
Mobile clinics have been integral in reaching populations typically underserved due to geographic or socioeconomic barriers. For example, during the COVID-19 pandemic, we used mobile clinics to overcome accessibility challenges in medically underserved areas by securing significant grants that enabled these clinics to provide timely vaccinations and other essential healthcare services directly to
these communities. Our clinics offered services at no cost and during nontraditional hours to accommodate the schedules of working adults and families, significantly improving vaccination rates and building community trust. Looking forward, I envision mobile clinics continuing to play a vital role not only in emergency responses but also in regular healthcare provisioning, especially in managing chronic diseases and preventive care in remote or underserved areas. This reflects a broader need for healthcare systems to adapt and innovate in ways that meet the people where they are in their healthcare journeys.
2. What inspired the implementation of mobile clinics in public health strategies, and how do these clinics address the gaps in healthcare access during emergencies?
Implementing mobile clinics was inspired by the necessity to overcome traditional healthcare delivery barriers and close gaps in healthcare access, particularly in remote, rural, and underserved urban areas. These gaps
became starkly evident during public health emergencies like the COVID-19 pandemic, when the need for swift and widespread medical services was critical but often obstructed by geographic isolation and socio-economic factors. Mobile clinics have proven to be versatile and strategic tools, offering rapid deployment, direct access to communities, and the flexibility crucial during emergencies. They not only deliver healthcare but also play a key role in health education and outreach, effectively addressing misinformation and tailoring services to communityspecific needs. By consistently reaching out to marginalised communities, mobile clinics build trust and facilitate greater engagement with health systems, making healthcare more inclusive, responsive, and adaptable to all populations, especially during crises. The success of mobile clinics in recent emergencies underscores their value and is shaping future public health strategies and emergency preparedness.
3. How have mobile clinics proven to be effective during recent public health emergencies, such as the COVID-19 pandemic?
Mobile clinics have been exceptionally effective during the COVID-19 pandemic, serving as a pivotal element in our crisis management strategy, particularly in regions where healthcare services were limited or overwhelmed. Their success is rooted in several key aspects of their design and implementation. Firstly, their rapid deployment capability allowed us to quickly respond to highdemand areas, adapting to the evolving outbreak by providing crucial testing
and vaccination services where needed most. Secondly, these clinics greatly expanded testing and vaccination coverage, reaching communities with limited access to permanent healthcare facilities and ensuring a direct, efficient administration of health services. Additionally, mobile clinics displayed great versatility, not only offering vaccinations and testing but also distributing personal protective equipment and vital public health information.
Critically, mobile clinics addressed healthcare disparities by delivering services to underserved and vulnerable communities, ensuring that those most at risk during health emergencies received timely medical attention. They also played a significant role in building community trust and engagement; regular visits by culturally competent staff improved perceptions of the healthcare system and increased public compliance with health advisories.
4. Can you elaborate on how mobile clinics specifically serve marginalised and underserved communities, and what unique challenges these populations face during public health crises?
Mobile clinics are essential in our strategy to ensure equitable healthcare, especially during public health emergencies when traditional healthcare systems can become overwhelmed. These clinics directly address healthcare accessibility by bringing necessary medical services to marginalised and underserved areas. They are staffed by culturally competent providers, offering services at no or low cost, which is crucial in overcoming the economic and cultural barriers that these communities often face. Mobile clinics also play a critical role in educating populations about health practises, enhancing their ability to make informed
decisions. However, the challenges such as ensuring adequate resources, overcoming communication barriers, and building trust within these communities are significant. By deploying mobile clinics, we prioritise inclusivity and equity, ensuring that every community has the support it needs during crises. This not only mitigates immediate health issues but also strengthens community resilience, preparing them better for future public health challenges
5. What are some of the operational challenges faced by mobile clinics during public health emergencies, and how have these challenges been addressed?
Operating mobile clinics during public health emergencies involves complex challenges such as logistical coordination, supply chain management,
Mobile clinics have transformed the landscape of public health by reaching the underserved and marginalized, proving their value time and again during crises like the COVID-19 pandemic. As we look to the future, these clinics will continue to innovate and expand, leveraging technology and community partnerships to ensure that healthcare is accessible to all, regardless of location or circumstance.
workforce stability, and ensuring patient safety and community trust. To tackle these issues, we employ advanced logistical planning and real-time data to deploy resources efficiently. We maintain robust supply chains and buffer stocks to deal with supply disruptions. Our staff undergo specialised training to enhance their adaptability and resilience, supported by programmes aimed at preventing burnout. Additionally, we prioritise patient safety through strict adherence to medical protocols and engage local communities to build trust, using multilingual communication and culturally sensitive approaches. These strategic measures ensure that our mobile clinics can effectively respond to crises and contribute to broader public health resilience.
6. How important are collaborations and partnerships with local communities, governments, and other organisations in the success of mobile clinics?
Collaborations and partnerships are essential to the success of mobile clinics, particularly during public health emergencies. Engaging with local communities ensures that our services are culturally attuned and widely accepted, fostering trust and enhancing service uptake. Strategic partnerships with government agencies are crucial for securing the necessary support, including regulatory guidance, funding, and integration into wider public health strategies. Additionally, alliances with non-profits, healthcare providers, and private sectors bring added resources and expertise that bolster our operational capabilities. Such collaborative efforts not only amplify the impact of our mobile clinics but also ensure their sustainability and relevance in addressing the nuanced public health needs of diverse communities. This integrated approach maximises the
7. In what ways have technological advancements been integrated into mobile clinics to enhance their efficiency and effectiveness in public health emergencies?
Technological advancements have significantly enhanced the efficiency and effectiveness of mobile clinics, particularly during public health emergencies. We have incorporated telehealth capabilities, allowing for real-time consultations with specialists, thus broadening the scope of services available on-site. Electronic Health Records (EHRs) are integral, improving data accuracy and accessibility, which is crucial for effective patient management and continuity of care. Portable diagnostic tools, including ultrasound and rapid test kits, enable immediate diagnostics, reducing the need for referrals and expediting treatment. Geographic Information Systems (GIS) optimise the deployment of our clinics to areas most impacted by health crises, ensuring targeted and efficient care delivery. Additionally, sophisticated data analytics help in monitoring health trends and evaluating the impact of our interventions, while automated inventory systems ensure that essential medical supplies are well-managed and stocked. Together, these technologies streamline clinic operations, enhance patient care, and ensure that our mobile clinics can respond swiftly and effectively to the dynamic needs of public health emergencies.
effectiveness of our interventions and lays a foundation for long-term public health resilience.
8. What kind of training and support do the staff and volunteers of mobile clinics receive to prepare them for responding to public health emergencies?
Training and support for staff and volunteers at our mobile clinics are comprehensive, designed to ensure preparedness and effective response during public health emergencies. This includes foundational medical training, specialised instruction in handling emergency scenarios, and training in cultural competence to effectively communicate and serve diverse communities. We also emphasise technological proficiency to maximise the use of our advanced
health systems, such as electronic health records and telehealth. Recognising the stresses associated with emergency responses, we support our team with mental health resources, stress management workshops, and regular debriefings to maintain high morale and prevent burnout. Continuous education is a staple, keeping our team updated with the latest in healthcare advancements and best practises, ensuring our readiness and efficacy in meeting public health challenges.
9. How do mobile clinics collect and utilise data to improve their services and respond better to the needs of the communities they serve?
Mobile clinics are integral to our datadriven approach, efficiently collecting and analysing health data to refine
our services and better address community needs. Each patient visit generates data, recorded securely in electronic health records, detailing demographics, health conditions, and services provided. This data is analysed to identify trends and adjust services accordingly, enhancing targeted interventions and resource allocation. We also use geographic information systems (GIS) to strategically deploy clinics based on these insights, ensuring we reach underserved areas effectively. Regularly analysed, this data informs continuous improvement, supports reporting to stakeholders, and guides our proactive engagement with the communities we serve, making our healthcare delivery more adaptive and impactful.
10. What role do policies and advocacy play in the deployment and operation of mobile clinics, and what improvements are needed in this area?
Policies and advocacy are foundational to the success of mobile clinics, influencing regulatory environments, funding, and the scope of services. Effective policies ensure mobile clinics operate on a solid legal basis, facilitating efficient healthcare delivery. Advocacy is crucial for highlighting the value of mobile clinics to policymakers and the public, thereby enhancing resource allocation and supportive legislation. Currently, there is a need for more uniform regulations to ease operational burdens and enhance scalability. Advocacy should also focus on securing increased funding by demonstrating the cost-effectiveness and positive health outcomes of mobile clinics. Furthermore, policies should promote better integration of mobile clinics within the broader healthcare system to ensure continuity of care
and seamless patient data integration. Streamlining these aspects will make healthcare more accessible, particularly for those in remote or marginalised communities.
11. Can you share any success storeys or significant impacts that mobile clinics have had on communities during public health emergencies?
One of the most notable success storeys of our mobile clinics was during the COVID-19 pandemic, where we secured close to $3 million in grants from the NYC Department of Health. This substantial funding allowed us to dramatically scale up our operations and effectively double our vaccination rates. By deploying mobile clinics strategically across New York City, particularly in areas where access to healthcare was limited, we
were able to reach a wider segment of the population. Our efforts led to a 100% increase in vaccination rates in these targeted areas, significantly contributing to the city’s overall public health response to the pandemic. Another impactful storey involves our response to the Monkeypox outbreak. We received an emergency grant to address this emergent health crisis, which enabled us to quickly mobilise our resources. The mobile clinics were crucial in providing accessible, timely, and effective healthcare interventions. Our clinics played a vital role in community education and awareness. We launched informational campaigns through these mobile units, which helped demystify the disease and informed the public about prevention strategies, reducing panic and misinformation.
12. What innovations or future developments do you
foresee for mobile clinics in enhancing their role in public health emergencies?
Looking ahead, significant advancements are planned for mobile clinics to enhance their effectiveness in public health emergencies. Key innovations include integrating advanced telemedicine to provide remote access to specialist care, and utilising artificial intelligence for predictive analytics and operational efficiency. We also aim to enhance the digital integration with health systems for seamless data sharing and to extend services beyond emergency response to include preventive care and chronic disease management. Importantly, we are focusing on improving reimbursement processes to ensure these clinics are financially sustainable and can expand their reach without financial constraints. Additionally, developing environmentally sustainable mobile clinics powered by renewable

energy is a priority, which will reduce our environmental impact while increasing our operational capabilities. These advancements will transform mobile clinics into even more vital resources within our public health infrastructure, fully equipped to address both current and future health challenges effectively.
13. How do the roles and challenges of mobile clinics differ in various parts of the world, and what can be learnt from the global perspective?
The roles and challenges of mobile clinics vary significantly across the globe, shaped by local healthcare infrastructure, cultural norms, and socioeconomic conditions. In developing regions, mobile clinics often serve as primary healthcare providers due to the absence of permanent facilities, facing challenges such as harsh terrains and limited resources. In contrast, in developed urban areas, these clinics primarily address gaps in healthcare accessibility for underserved populations, focusing on issues like urban poverty and mental health. Key global lessons include the importance of adaptability to local needs, cultural competence, innovative resourcefulness, and the power of partnerships. For instance, innovations like using solar power for vaccine storage in Africa demonstrate resourcefulness that can be adapted worldwide. Additionally, integrating advanced technologies such as telemedicine has proven to enhance service delivery, making mobile clinics more effective. These insights underscore the need for global collaboration to share strategies and improve the functionality and impact of mobile clinics universally.

14. What drives your passion for public health and mobile clinics, and what is your vision for the future of healthcare accessibility through these initiatives?
My passion for public health and particularly for mobile clinics stems from a deep commitment to equity in healthcare. Witnessing firsthand the disparities in health access and outcomes across different communities has driven me to seek innovative solutions that bridge these gaps effectively. Mobile clinics, with their unique ability to reach underserved and isolated populations, embody the potential to transform healthcare delivery by making it truly accessible to all, regardless of geographic location or socio-economic status.
What excites me most about mobile clinics is their versatility and responsiveness. They can be rapidly deployed to
Preet is a distinguished Public Health Leader with expertise in addressing public health emergencies, community health needs, health disparities, and social determinants of health. She is passionate about serving medically underserved, and marginalized communities through implementation of public health programs to advance health equity. Her work has been recognized by the New York City Department of Health and Mental Hygiene for advancing health equity and preventing COVID-19 in New York City through the Public Health Corps. She has also been recognized as one of the Top 25 Emerging Leaders by Modern Healthcare for significant contributions to the culture of innovation and transformation in the field of healthcare.
disaster sites, rural areas, and urban centres alike, providing essential services from preventative care to emergency responses. This adaptability not only helps in immediate health crises but also in the routine management of chronic diseases and community health education, which are critical for long-term public health improvement.
Looking forward, I envision a future where mobile clinics are an integral part of a global health system that is proactive rather than reactive. I see them equipped with the latest in telehealth technologies, artificial intelligence, and data analytics tools to not only provide care but also predict and prevent health issues before they become crises. Furthermore, I believe in a future where policies and funding are aligned to support the expansion of mobile clinics, recognising them as vital to achieving health equity.
With social media, artificial intelligence, smart devices, and the possibilities of telemedicine becoming Key players in the daily existence of the modern population, the healthcare field is on the precipice of a revolution. Heralded as a marginal service just a couple of decades ago, telemedicine is today part of the modern healthcare core – it changes how patients obtain and care providers deliver healthcare services. Telemedicine is not just a way of having consultations via the Internet; it is changing the approach to patients, making healthcare more accessible.

1. Can you briefly explain what telemedicine is and how it has evolved over the past few years?
Telemedicine, which began in the late 1950s, uses technology to deliver healthcare services remotely, including consultations, diagnostics, and treatments through various communication tools like video calls, phone calls, and messaging platforms. Interestingly, both telemedicine and AI emerged around the same time. While AI is still catching up in terms of adoption, telemedicine has become a widely accepted practise, especially after the pandemic, which significantly boosted its use.
2. What are the most significant trends in telemedicine right now, and how has COVID-19 impacted them?
The pandemic indeed accelerated telemedicine adoption, as physical consultations were restricted. However, it’s crucial to note that many big players in telehealth, like Teladoc & Amwell, are struggling post-pandemic. The key trend now is integrating telemedicine into a holistic healthcare approach rather than relying solely on it. Margins in telehealth are low, and the software is easy to replicate. The real innovation lies in combining telehealth with other healthcare services.
3. How are artificial intelligence and machine learning being integrated into telemedicine platforms?
AI and machine learning are becoming integral to telemedicine. For example, AI can analyse consultations, summarise them, and save time for physicians. It can also perform preliminary diagnostics, analyse patient data from different medical devices, and provide recommendations. These integrations enhance efficiency and patient care, making telehealth more effective.
4. What are the key regulatory challenges facing telemedicine today?
Different regions face various regulatory challenges. For instance, in the US, there is a need to ensure that software is HIPAA compliant, while in Europe, GDPR regulations have to be mastered. There will be new security issues arising as a result of AI that require continuous monitoring and enhancements.
The changing regulatory environment is one of the biggest hurdles faced by healthcare providers. Staying up-to-date and being compliant can
be an overwhelming task due to frequent changes in rules and guidelines. During the COVID-19 pandemic, telehealth became crucial for longdistance medical care; hence its usage skyrocketed. Although telemedicine consultations together with electronic health records (EHRs) or digital patient portals enhance accessibility as well as efficiency, they also give rise to considerable threats to data privacy and security.
Recording and archiving patient consultations should abide by definite rules. Recording features are available on many unified communication platforms such as Microsoft Teams or Zoom but their own solutions often do not fit relevant regulations. It is possible to ensure compliance through some specialised apps.
Creating awareness among healthcare workers about compliance is critical considering new technologies and channels of communication that have emerged as a consequence. Regular training regarding the most recent laws along with appropriate management of patients’ information can alleviate risks
of data breaches or non-compliance. Moreover, these technologies can challenge the level of trust patients place in their healthcare providers.
Ensuring telehealth platforms comply with regulations is crucial. It is essential to have secure and encrypted communication channels to safeguard patient information and adhere to the Health Insurance Portability and Accountability Act (HIPAA). Failure to comply with HIPAA can lead to serious legal and financial repercussions. Between 2020 and 2022, fines for HIPAA violations amounted to around $21.6 million. Moreover, ensuring privacy law compliance comes with significant expenses, with the American Hospital Association revealing an annual expenditure of $39 billion on compliance. Non-compliance can damage an organisation's reputation, affecting its credibility and ability to deliver care.
New regulations are constantly emerging, necessitating the healthcare sector to adjust. This involves grasping the intricacies of state, federal, and international laws, particularly for organisations operating across Lisa Voronkova, bioengineer and CEO of OVA Solutions, has over a decade’s experience in the field of healthcare and medical device development. She strives to extend medical advances and to develop latest technologies that would enhance patients’ quality of life.

multiple regions. For instance, the Centres for Medicare and Medicaid Services (CMS) introduced a rule mandating all Third-Party Marketing Organisations to record all marketing calls with beneficiaries and securely store them in a HIPAA-compliant manner for at least a decade. This has resulted in increased operational costs for the companies affected.
Utilising technology, especially artificial intelligence, can aid in ensuring compliance. Automated solutions like Recording Insights monitor communications and identify potential compliance issues, enabling healthcare organisations to stay proactive. These solutions offer various features such as omni-channel recording, encryption, redundant recording and storage, flexible recording rules, robust search capabilities, easy replay with stringent access control, emotion detection, keyword identification, and automated compliance screening and alerting.
Thus, the monitoring of customer communication is nearly impossible without setting automated processes and intelligent software. It becomes apparent that using traditional methods, companies are able to track only a tiny percentage of customers’ communications, which leaves a high level of potential non-compliance. Thus, using artificial intelligence, all customer communication can be potentially recorded and scouted for potential threats while extracting maximum insight into customers’ needs.
Disclaimers can be verified, calls can be automatically classified as regulated or non-regulated ones, the presence of personal data in the call can be detected, and consulting ignored by the crew can be disclosed. The use of AI such as Azure Open AI helps in summarising the conversation and extracting the sentiment of the conversation, Microsoft Azure security feature enables data security within the Azure network and safe keeping of patients’ conversation.
5. How has telemedicine impacted patient satisfaction and healthcare outcomes? Can you share a case study from your experience?
For people who dwell in areas with little or no health facilities as is the case with rural areas where there is no access to a physical hospital, it is very convenient to get medical care through the phone and this makes telemedicine a very useful technology which provides solutions to this issue. Telemedicine enables the patients to interact with the healthcare providers through the use of technology hence bringing medical advice as well as support regardless of the region. Of special interest is an example of our Ukrainian work on telemedicine. To solve the problem, we created a telehealth platform where we diagnose thousands of Ukrainians that would not normally receive any health care because of a war that has significantly impacted the sector. Many hospitals have been harmed or destroyed while many healthcare personnel has lost their shelters or are completely stretched to the limit or infrastructure by the sudden influx of patients. The patients’ enrolment enables the booking of appointments with medical doctors who are kindly contributing voluntary medical advisory services online. This intervention has proved viable in refugee centres and other affected regions where it is dangerous, or rather impossible to visit a physical hospital; rather than enduring long journeys during such moments of crisis, one can simply talk to an online doctor.
6: How is telemedicine being integrated with traditional in-person healthcare? Any successful cases?
Telemedicine is being incorporated with usual care procedures, especially when it comes to patients’ subsequent checkups. For example, rather than making the patients come for more diagnosis and consultations in the hospital, they can meet with the doctors online. Besides, this not only saves time and cuts expenses on transportation but also optimises the process of caring for patients. Overall, what has been ascertained from the literature review is that by incorporating virtual consultations as a part of the patient care delivery model, healthcare professionals are better placed to cut on the time they
would have otherwise spent attending to patients’ intractate and thus increase immensely patient satisfaction. It has already found application in a great number of cases, thus showing how telemedicine might further enhance and enrich conventional methods of healthcare.
7. What do you foresee as the future of telemedicine in the next 5-10 years?
Telemedicine will increasingly become part of a broader, integrated healthcare system. Technological advancements, especially in AI, will enhance telehealth services, making them more efficient and effective. However, telemedicine should be viewed as a complementary service rather than a standalone solution.
8. What unique advantages does telemedicine offer for mental health care?
Telemedicine is most effective in organising the provision of mental health care in the country. Today, a significant number of psychologists participate in online conferences or appointments, so people suffering from mental disorders can receive help. It remained fairly stable for some time, but it is also expected to grow in the future as more and more people and providers embrace telemedicine.
Earlier, people experienced a range of challenges including distance, transportation problems, social disgrace that come with going to a mental clinic to seek a certain service. Telemedicine addresses these issues in the following ways through telecommunication systems enabling patients to have therapy sessions from the comfort of their homes.
For instance, one can think of a groundbreaking telehealth application. Some of the mental health services include and have availed online coun-
Telemedicine is being incorporated with usual care procedures, especially when it comes to patients’ subsequent checkups. For example, rather than making the patients come for more follow-ups and check-ups in the hospital, they can meet with the doctors online. Besides, this not only saves time and cuts expenses on transportation but also optimizes the process of caring for patients
selling and online therapy services from this platform through affiliated therapists. I can bring storeys when one patient from a remote rural area with almost no access to mental health professionals

Alex Koshykov is an entrepreneur and executive with a background in software and hardware development, particularly in the digital health and MedTech sectors. He co-founded a pioneering company in 2016 and has since expanded his influence to a startup hub, contributing his expertise to the growth of innovative products and businesses.
was able to speak to a licenced therapist through this application. Because of the easily accessible arrangements of the virtual sessions and no faceto-face contact with other people in a struggling state, she has agreed to do it and, as a result, her mental condition has improved drastically.
Furthermore, telemedicine has been proven to be useful during the COVID-19 outbreak since it helped in continuing with appointments while physical ones were impossible. This model proved to be popular among mental health providers and they began to rely on secure video conference platforms to carry out sessions. This not only ensures the continuity of the patient-doctor bonds but also brings treatment to those who may have otherwise not sought it due to transportrelated issues. The advantages of telemedicine also include the possibility of flexible appointments because the utilisation of telemedicine does not require patients to take time off work or rearrange their daily schedules. Such flexibility makes it easier for patients to adhere to treatment schedules and enables regular follow up which in turn leads to improved client outcomes.
Thus, as far as I know, with the further growth of the field, telemedicine is expected to increase its connection with mental health. Technologies like AI and Machine Learning are in use in telehealth solutions for diagnosis and the enhancement of treatments. For example, AI applications can help therapists review patients’ data to see the patterns and potential mental issues before they escalate.
9. What cost benefits does telemedicine provide for both patients and healthcare providers?
Telemedicine reduces costs for both. Patients save on travel expenses and time, while providers can manage more consultations efficiently.

10. What advice would you give to healthcare providers looking to incorporate telemedicine into their practise? Are there any specific skills or training programmes you would recommend for practitioners new to telemedicine?
While telemedicine has become one of the main trends in the modern healthcare industry, many primary care physicians fear that incorporation of this technology into their already packed practises will be both time-consuming and difficult. Though, those who have implemented telemedicine well, stress the fact that one does not have to be a millionaire, or have to revamp the whole system to notice improvements.
The healthcare industry is set to undergo a major change in the near future. A global telemedicine market research study conducted by BIS Research in September 2021 estimated the market to be worth $21 billion, world-
wide reaching $55 billion in 2019 and owing to a CAGR of 17% it is estimated to reach $123 billion by the year 2030. 66%. As it is seen, the utilisation of telehealth solutions constitutes one of the key strategies critical for healthcare practises regardless of their size.
The kind of telemedicine that any practise wants to implement must adhere to certain federal regulations from institutions like the FDA and CMS. This means that providers have to be careful to confirm with the laws of their home state and the state where the patients are. Also, each physician involved has to be credentialed and privileged to perform the services at any of the included hospitals.
As patients’ records go digital, it becomes necessary to adhere to the rules of HIPAA and other similar laws. This entails the firm adopting effective security measures as well as putting into place effective and secure technology.
Therefore, it is very important that a new model has to be found for operating telemedicine by including telemedicine practises in the current procedure
and training all the staff of the medical centres. Telemedicine equipment should not only be utilised but also integrated into the staff members’ daily routines. Training should include every process; from managing registration, billing, and patient follow-up in the process of telehealth.
However, proper choice of technology is also crucial. The chosen telehealth system shall therefore be able to complement the existing work routines, EMRs, EHRs and lab systems. The technology should be of high flexibility in the sense that it can be applied universally in the departments as well as in different facilities. The provider’s telehealth partner should be able to explain where the technology fits into the current environment or what changes would be required.
It is well understood that the aspects of billing in telemedicine are quite intricate the roles and responsibilities of the healthcare facility, telemedicine providers and associated specialists should be well defined, particularly with references to facility charges and professional charges. It is necessary for providers to decide on the billing codes and make equal payments in the meantime to all the relevant actors. Otherwise, there is a question of how to address the inequality of pay rates for providers in different areas because the reimbursement process is frequently tied to the patient’s address.
One must note that despite all the aforementioned advantages of telemedicine there can be certain patients who will be reluctant to engage in its use. The introduction of telemedicine to the patients should be done through showing rather than telling; short activities like taking a few minutes to explain to the patients how the telemedicine is easy to use and comes with advantages can go a long way. Generalising telemedicine into primary care requires some work, though not necessarily a lot of work.
Precision medicine is a personalised treatment that analyses your makeup (genes), the determinants of health, and lifestyle to tailor targeted therapies and preventive measures to fight disease more effectively and precisely. AI plays a central role in analysing vast datasets of genetic information, medical records, and lifestyle factors for targeted treatments.
Manthiry, CEO, InfoMed
1. How do you define precision medicine, and why is it considered a game-changer in modern healthcare?
Precision medicine is the future of healthcare. It would empower our providers with precise information and data to offer consultation, counselling, and treatment personalised and targeted to the person based on their unique genetic makeup, lifestyle, and environment. It opens a totally new avenue for providers to shift from the traditional one-size-fits-all approach towards a more personalised and preventive model of care.
Precision medicine is opening the floodgates in modern medicine to empower patients, personalising prevention, offering effective treatments, and, most importantly,
reducing healthcare costs by being efficient and targeted, thus minimising wastage and potentially avoiding unnecessary treatments and hospitalisations.
2. What role does AI play in the development and implementation of precision medicine?
AI is the premium enabler and the engine powering the development and implementation of precision medicine. Precision medicine depends on big data analytics and algorithms to analyse the vast amount of complex genetic data, medical records, personal history, and determinants of health to lead to more personalised and effective treatments ultimately. With AI and the power of computing, we can now dive deep with speed to analyse drug discovery and development in clinical trials and medical imaging offerings, which are all the developing prospects of AI in precision medicine. Now, with Generative AI enveloping the transformation at breakneck speed, we are previewing the further offerings of a powerful new force in precision medicine, adding another exciting intelligence layer to the already transformative role of AI in this field. Generative AI is poised to be a game-changer in precision medicine, potentially and significantly revolutionising healthcare delivery and checking the rising cost by improving efficiency and accuracy.
3. Can you discuss some of the key benefits of precision medicine for patients compared to traditional treatment methods?
By using precision medicine for treatments, the treatment protocol shifts from the "one-size-fits-all" traditional approach, which could lead to treatments that may be ineffective or even harmful for some patients. Precision
medicine minimises the risk of side effects, improving the overall treatment outcome by allowing the treating doctor to provide precise information about the patient, which was not available in the traditional space. It is also a patientcentric approach that personalises the treatment.
4. How does the integration of genetic information, medical records, and lifestyle factors contribute to the success of precision medicine?
Patient-centric medicine should be practised for the optimum benefit of the patient, and that should be value-based. Its success depends on comprehensive personal history (lifestyle factors), including family history and review of past medical records. Integrating genetic information is the icing on the cake for precision medicine, which takes a whole new holistic approach in tailoring the treatment to the individual.
5. What challenges do healthcare providers face when implementing precision medicine, and how can they be overcome?
Costs are a major challenge for healthcare providers when practising precision medicine. Precision medicine is driven by technological innovations, including the availability of genetic screenings and analytics to empower it. As precision medicine is in the developmental stage that is making unsurmountable progress, precision medicine treatments can be expensive and not available or accessible. To overcome these challenges, the initial stage would be for the government and public policymakers to invest in research and development of affordable precision medicine therapies and diagnosis, focusing initially on non-communicable diseases that consume almost 70% of the healthcare budgets globally.

6. Can you share some success storeys or case studies where precision medicine has significantly improved patient outcomes?
Cancer care has been at the forefront of offering precision medicine, and one good example is the discovery of the HER2 gene mutation, which led to the development of Herceptin. This targeted therapy has significantly improved survival rates for women with this specific form of breast cancer. In my experience working with doctors on genetic screening results for patients, we could precisely diagnose and offer treatment plans with supplements and lifestyle modification with targeted nutrition regimes to treat the conditions.
7. How do you see the role of precision medicine evolving in the next five to ten years, particularly in Malaysia?
I believe precision medicine will become a mainstream treatment protocol in Malaysia in the next five to ten years, a parallel development globally. Oncologists from several leading hospitals in Malaysia have been at the forefront in the last ten to fifteen years, offering precision medicine as targeted therapies as part of their cancer treatment options.
Cancer Research Malaysia is at the forefront, the first in Asia to collaborate with geneticists, gynaecologists, and oncologists to complete a study that began in 2017 for mainstream genetic counselling for genetic testing of BRCA1 and BRCA2 in ovarian cancer patients in Malaysia. The study has had a positive impact and has proven feasible for addressing the increasing need for genetic services in Malaysia and other Asian countries.
Many private companies in Malaysia are already offering genetic screenings,
Precision medicine is key to a sustainable healthcare system that will empower individuals to prevent diseases and optimize treatments for maximum impact
uncertainty and hinder the integration and adopting of new technologies like AI and genomics into mainstream healthcare.
The initial steps should be geared towards supporting the private sector's initiatives in developing precision medicine to empower healthcare professionals. I am reemphasising the importance of education and training, which does not consume big budgets. Only having healthcare professionals onboard would be the next step in implementing precision medicine as the treatment protocol for all providers.
This is the future of healthcare, and it promises to address many of its challenges. Thus, policies and strategies to cultivate a workforce of healthcare professionals with the knowledge and enthusiasm to embrace precision medicine will pave the way for its wider adoption and integration into standard treatment protocols, ultimately improving healthcare delivery for all.
and the awareness among medical professionals is growing, especially with wellness and functional medicine clinics. This augurs well for precision medicine's growth in Malaysia as it takes its position in mainstream medicine practise. Moving forward, Malaysia needs greater participation from the public sector, especially to enhance primary and preventive care.
8. How can healthcare policies and regulations support the advancement of precision medicine?
Foremost, we must educate healthcare students and healthcare professionals on the latest developments in precision medicine. This requires funding as the government initiative to support the development and implementation of the training programmes. Technological advancement, especially in AI, greatly outpaces government-supported policies and regulations. This can create
9. What are the ethical considerations involved in precision medicine, especially regarding genetic data privacy?
As with any digital and data item, it raises ethical questions, particularly regarding genetic data privacy. The primary concern is who owns your genetic data and how it is stored and secured. The many recent data compromises, even from the highsecurity digital chambers, raise many concerns among healthcare professionals and patients. Data privacy is a work in progress that will continue and should be supported. However, it should not hinder or slow the adoption of precision medicine and implementation as the benefits to the population are overwhelmingly positive and are the pathway to improving the current disease burden and challenges.
Genetic information can imply potential discrimination, such as
denying insurance coverage or employment opportunities. It could also result in social stigma, knowing your genetic predisposition for diseases, and result in psychological distress. While one standard solution commonly practised would be to strengthen the data privacy laws, a more engaging approach will be to raise public awareness about genetic privacy rights and empower individuals to make informed decisions about their data. We should address these ethical concerns to build trust and ensure responsible and equitable development of precision medicine.
10. How can healthcare providers ensure that precision medicine is accessible and affordable for all patients, regardless of their socioeconomic status?
This is a very challenging situation. It is only applicable to healthcare providers from the public sector. Private healthcare is driven as a business, sometimes with very minimal social elements infused. Thus, public policy should be in place for patients from lower socioeconomic status to gradually introduce precision medicine with the appropriate budget. In the long-term, investing in precision medicine will reap the benefits of better healthcare and reduce the cost of healthcare for severe chronic diseases that consume a major part of the budget. For providers in the private sector, where most patients are insured, it is timely for insurers to consider the importance of precision medicine positively as the pathway to manage increasing healthcare costs. One potential model is shifting healthcare reimbursement towards rewarding positive patient outcomes (value-based). This will incentivise cost-effective treatments, including patients receiving precision medicine that improves patients' health and reduces long-term costs.
Precision medicine is evolving very fast, and the costs are reducing. With more healthcare providers adopting it (volume), the cost will decrease further and make it affordable for all categories of patients irrespective of their social status. Technology in areas like gene sequencing and AI analysis is improving rapidly, which will impact the overall cost of precision medicine. Let's hope this will come forth faster than we anticipate to move closer to a future where personalised healthcare is the norm for all.
11. In what ways can precision medicine contribute to preventive healthcare and the early detection of diseases?
I am glad we are in the era witnessing the groundbreaking developments in genomics. All of us are born with unique genetic makeup, our building block that predisposes us to certain diseases. Having this knowledge from the early stages of our lives gives us the opportunity to understand our health disposition and plan our lifestyles to focus on preventive health and wellness.
It is important to note that understanding your unique genetic profile helps the individual process this information and make informed decisions. Thus, precision medicine is an enabler to kick-start your journey to "take charge of your health" and plan for optimal health and well-being.
12. How can education and training programmes for healthcare professionals be adapted to include the principles and practises of precision medicine?
The principles and practise of precision medicine should be brought into the mainstream of medical schools'
curriculum immediately. With the pace at which this future of medicine is evolving, medical students should be exposed in-depth to genomics, precision medicine principles, and ethical considerations of using patient data. Future healthcare professionals should be equipped with basic skills in interpreting genetic results using AI-powered tools to provide consultation and counselling. They should be prepared to embrace precision medicine in their practise for treatment.
For practising healthcare professionals, tailored training programmes on precision medicine should become a mainstream subject in seminars, workshops, and conferences as a continuous learning module. By integrating these training strategies, we can equip healthcare professionals with the knowledge and skills needed to deliver personalised and effective care using the tools of precision medicine. We empower the professionals, leading to better patient outcomes and a more efficient patient-centred healthcare system.

Mohan Manthiry, CEO of InfoMed, is active in the Malaysian healthcare industry due to his work as a healthcare thought leader and founder of the premier healthcare media, InfoMed. His professional role and key areas of interest are focused on improving the delivery of quality, evidence-based healthcare, aiming for affordability and sustainability.
Digital MD is a groundbreaking exploration of the technology-healthcare interface. Through a deep dive into the digital health ecosystem, this work provides a timely and comprehensive guide to the ever-evolving landscape of patient care. This timely resource explores the seamless fusion of human minds with machines, making it the right book for the right time in advancing healthcare. It showcases the complexity of healthcare while providing a landscape analysis and road map for the coming wave of digital solutions that will break over fortress medicine.
1. Dr. Kwo, “Digital MD: Revolutionising the Future of Healthcare” delves into the rapid digital transformation in the healthcare sector. Can you elaborate on the most critical changes you foresee in the next decade due to this digital revolution? In the next decade, the healthcare sector will experience transformative changes driven by digital technologies. Key changes include: Personalised Medicine: Advances in genomics and data analytics will enable tailored treatment plans based on individual genetic profiles and health data. Telemedicine and Virtual Care: The adoption of telehealth will continue to grow, providing patients with convenient access to care and reducing the need for in-person visits. AI and Machine Learning: These technologies will enhance diagnostic accuracy, predict patient outcomes, and person-
Dr. Liz Kwo
Liz Kwo, Chief Medical Officer, Everly Health
alise treatment plans. Wearable Devices: Continuous health monitoring through wearables will empower patients to manage chronic conditions and engage in preventative care. Interoperability and Data Sharing: Improved interoperability standards will facilitate seamless data exchange between different healthcare systems, enhancing coordination of care. Digital Therapeutics: Software-based interventions
will complement or replace traditional treatments for various conditions, improving patient outcomes and reducing healthcare costs.
2. Given your extensive background in both clinical practise and health technology, how do you see the role of digital health companies like Everly Health evolving to meet the needs of an increasingly techsavvy patient population?
Everly Health will play a pivotal role in meeting the needs of tech-savvy patients by: Offering Comprehensive Virtual Diagnostics: Providing accessible and accurate at-home diagnostic testing to monitor health conditions. Enhancing Patient Engagement: Using mobile apps and platforms to engage patients in their healthcare journey, offering personalised health insights and recommendations. Integrating AI and Machine Learning: Leveraging these technologies to offer predictive analytics, personalised health plans, and early detection of health issues. Expanding Telehealth Services: Integrating virtual care with diagnostic services to offer endto-end healthcare solutions. Ensuring Data Security and Privacy: Implementing robust cybersecurity measures to protect patient data and build trust.
3. In “Digital MD,” you highlight the perspectives of various stakeholders in the healthcare ecosystem, including providers, payers, and employers. How can these groups better collaborate to foster innovation and improve patient outcomes?
Establishing Shared Goals: Aligning on common objectives such as improving patient outcomes, reducing costs, and enhancing patient satisfaction. Leveraging Technology Platforms: Using integrated platforms to facilitate data sharing and communication across the healthcare ecosystem. Creating Incentive Structures: Developing value-based payment models that reward collaboration and improved patient outcomes. Encouraging Cross-Sector Partnerships: Forming alliances between healthcare providers, technology companies, and research institutions to drive innovation.
4. The book discusses the challenges and myths surrounding the funding of new health technologies. What are some of the most
common misconceptions you encounter, and how can stakeholders address these to ensure successful implementation of digital health solutions?
High Initial Costs: Many believe that digital health technologies are prohibitively expensive. Stakeholders can address this by demonstrating the long-term cost savings and improved outcomes these technologies offer. Complex Integration: There is a misconception that integrating new technologies into existing systems is too complex. Clear implementation plans and robust interoperability standards can ease this transition.
5. With your experience in modernising disease management and care delivery, particularly for large populations, what are the key data analytics strategies that can be employed to enhance health outcomes at scale?
Predictive Analytics: Using historical data to predict and prevent adverse health events. Population Health Management: Analysing population data to identify health trends and target interventions for at-risk groups. Personalised Health Insights: Providing tailored recommendations based on individual health data and behaviour.
6. “Digital MD” provides insights into building partnerships within the healthcare industry. What are the most effective strategies for healthcare innovators and corporate leaders to create impactful and sustainable collaborations?
Aligning on Mission and Goals: Ensuring all partners share a common vision and objectives. Fostering Open Communication: Maintaining transparent and frequent communication to build trust and address challenges collaboratively. Leveraging Complementary Strengths: Identifying and utilising each partner's unique capabilities and resources.
7. As someone who has founded several venture-backed companies, what advice would you give to aspiring healthcare entrepreneurs looking to navigate the complex landscape of digital health?
Advice for aspiring healthcare entrepreneurs includes: Understand the Market: Deeply research the healthcare landscape, including regulatory requirements and market needs. Focus on User-Centric Design: Develop solutions that are user-friendly and meet the needs of patients and providers. Build Strong Teams: Assemble a team with diverse expertise in healthcare, technology, and business.
8. The book emphasises the importance of understanding the factors, pitfalls, and major players in the digital health technology landscape. Could you share some key lessons learnt from your journey that can help others avoid common pitfalls?
Emphasise Interoperability: Ensure your solutions can integrate with existing healthcare systems to enhance usability and adoption. Stay Agile: Be prepared to pivot and adapt based on feedback and changing market conditions. Focus on Evidence-Based Solutions: Develop technologies that are backed by robust clinical evidence to gain trust and regulatory approval. Engage Stakeholders Early: Involve patients, providers, and payers in the development process to ensure your solutions meet their needs.
9. In your role at Everly Health, how do you balance the need for rapid innovation with the stringent regulatory and compliance requirements in the healthcare industry?
Establishing a Robust Compliance Framework: Integrate regulatory considerations into the innovation process from the beginning. Iterative Development: Use agile methodologies to iterate on innovations, allowing for continuous improvement and compliance cheques.
10. “Digital MD” aims to unleash the healthcare innovator within each reader. What are the essential skills and mindsets that you believe are necessary for driving innovation in the healthcare sector?
Curiosity and Lifelong Learning: Continuously seek knowledge and stay updated on industry trends. Collaboration and Teamwork: Work effectively with diverse teams and stakeholders. Patient-Centric Focus: Always prioritise patient outcomes and experiences.
11. Considering your experience as a faculty lecturer at Harvard Medical School, how do you integrate academic insights with practical applications in your work with digital health technologies?
Translating Research into Practise: Apply evidence-based findings to develop practical solutions. Bridging Academia and Industry: Foster partnerships between academic institutions and industry to facilitate knowledge transfer. Teaching and Mentorship: Share practical applications with students and colleagues to bridge the gap between theory and practise.
12. What role do you see artificial intelligence and machine learning playing in the future of digital health, and how can these technologies be harnessed to improve patient care and operational efficiency?
Optimising Operations: Streamlining administrative tasks, reducing costs, and improving efficiency in healthcare delivery. Supporting Decision-Making: Providing data-driven insights to support clinical decisions. Predicting Outcomes: Identifying risk factors and predicting patient outcomes to enable proactive interventions.
13. Reflecting on your career, what have been the most significant challenges you faced while modernising care delivery, and how did you overcome them? Significant challenges are resistance to change.
Dr. Liz Kwo is the Chief Commercial Officer of Everly Health, a digital health company focused on modern diagnostics. Dr. Kwo authored “DIGITAL MD: Revolutionizing the Future of Care” and served as Deputy Chief Clinical Officer for Elevance, a health insurance company dedicated to modernizing care for 43 million Americans, leveraging advanced data analytics in clinical management. Prior to this, Dr. Kwo was CEO and co-founder of InfiniteMD, a technologyenabled platform for international medical second opinions, which was acquired by Consumer Medical. She was also co-founder and President of New Pathway Education and Technology Group, which was acquired by EIC Education.


Every issue of AHHM magazine is a powerful dose of information and knowledge – filled with original and undiluted content. Written by the best brains in hospital and healthcare industry, the magazine offers timely business insights and articles on cutting-edge technologies.
Subscribe now to get your doses regularly.
Email: subscriptions@asianhhm.com
Tel: +91 40 4961 4567
Fax +91 40 4961 4555
www.asianhhm.com


Use the webinar as a platform to launch new products and services
Grow your audience with increased reach, impact and user-friendliness
Rise above geographical boundaries
Generate new business
Gain the strong web presence differentiating yourself from competitors
Connect and engage with your target audience
Give more exposure to industry specific people
Increase your brand profile and share your capabilities with leading industry professionals