






The COVID-19 pandemic has significantly transformed lives, placing unprecedented pressure on healthcare systems worldwide. Even as hospitals and healthcare facilities faced challenges in coping with the surge in COVID-19 cases, governments and pharmaceutical companies collaborated to develop vaccines in record time, marking a remarkable achievement in medical sciences.
Travel restrictions, border closures, and lockdowns severely impacted the travel and tourism industry. This resulted in a significant decline in travel and tourism activities, causing financial losses and job cuts in the industry. The pandemic also prompted a shift towards telemedicine and virtual healthcare services. Many medical procedures and consultations have become accessible online, reducing the need for international travel for minor medical issues and follow-ups. But as the global health scenario improved and travel restrictions eased, the medical tourism industry gradually began to recover. Individuals have restarted travelling to other countries for medical treatments or services that offer value in terms of cost, quality, or accessibility.
The global medical tourism market was valued USD82 billion in 2021, a figure that is expected to grow by 121 per cent to US$ 182 billion by 2025, according to a study by Glasgow Research & Consulting.
India’s NITI Aayog estimates that the Indian economy could earn an additional US$9 billion by 2026 from Medical Value Travel (MVT) and Wellness tourism. Globally, the MVT market is projected to grow from US$ 13.98 billion in 2021 to US$ 53.51 billion in 2028 at a CAGR of 21.1 per cent.
However, this recovery required innovative solutions and strict safety measures to ensure the safety of both patients and healthcare providers. Innovation plays

a crucial role in the medical tourism industry, driving the adoption of new ideas, methods, and products to enhance patient acquisition, customer satisfaction, and overall competitiveness. Innovations in medical technology, procedures, and treatments can lead to better outcomes and patient experiences. Medical centres that invest in state-of-the-art equipment and cutting-edge treatments can attract more medical tourists seeking advanced and effective healthcare solutions. Personalised treatment plans, telemedicine consultations, and seamless coordination of travel and medical services, can significantly improve customer satisfaction.
Collaborations between medical centres, travel agencies, and government entities, leads to comprehensive medical tourism packages and seamless experiences for patients seeking healthcare abroad. Pursuing international accreditations and certifications can demonstrate a commitment to quality and safety, increasing trust and confidence among medical tourists.
The cover story in this issue on ‘Quickly Emerging, Post-COVID Market on Medical Tourism’ by David Thomas Boucher, Chief Partnerships Officer, Bumrungrad International Hospital talks about many factors that are significantly affecting medical value travel in post-COVID 2023. He also says that there is now huge pent-up demand for many types of treatments.
Keep reading!
Prasanthi Sadhu EditorMANAGEMENT
06 Employee Engagement of Generation Y Employees
Analysing the impact of talent management and responsible leadership
Uche Nwabueze, Instructional (Full) Professor, Chair of Program Assessment, Dept. of Maritime Administration,Texas A&M University
16 Healthcare Leadership
How to become a good healthcare manager and leader
Tan, Managing Director, Bagan Specialist Centre
25 Quickly Emerging, Post-COVID Market on Medical Tourism
David Thomas Boucher, Chief Partnerships Officer, Bumrungrad International Hospital
30 The Impact of Accreditation Programmes on Healthcare Manager Quality Healthcare providers’ perspectives
Abdullah Algunmeeyn, Assistant Professor of Nursing, University of Nottingham
34 Enhancing the Care of Inflammatory Bowel Disease (IBD) Patients with Precision Medicine Biomarkers
Cindy Weiss, Lead, PPI and Design, Avenna Ltd
Nina Skorytchenko, CEO, Avenna Ltd
Daryl L Fernandes, Chief Executive, Ludger Ltd; Chief Science Office, Avenna Ltd
38 Assessing the Autonomic Nervous System using ECG Recordings
Jean-Marie Grégoire, Clinical Cardiologist, Department of Cardiology, UMONS (University of Mons)
Cédric Gilon, PhD Candidate, Free University of Brussels
42 Integrating Mental Health into Primary Healthcare
Exploring the benefits and rationale for integrating mental health services into primary healthcare
Tanjina Ashraf Khan Mou, CEO & Mental Health Professional
Stella Ramette, Director, Healthcare Customer Relations and Sales, South East Asia, InterSystems

Nana Khunlertkit, Professional Services Director, South East Asia, InterSystems
44 Journey to Health
Exercise’s role in preventing and managing chronic diseases

Saint-Vil, Medical Director, Sports Medicine Department, Marietta Memorial Hospital
47 Remote Diagnosis and Tele-Treatment
Teleconsultation transforms chronic disease management
Arindam Sen, Director, i2i TeleSolutions
51 Sustainable Health and Supporting Policy
Loke Wai Chiong, Programme Lead & Senior Consultant, MOH Office for Healthcare

Transformation, Board Director and Advisor to Multiple Organisations, Nexus of health, social, environment and community
55 New Horizons of Drones
Panacea for fatal arrhythmias, delays in defibrillation and pandemic
Ozgur KARCIOGLU, Dept. of Emergency Medicine, University of Health Sciences
Canan AKMAN, Dept. of Emergency Medicine, Canakkale Onsekiz Mart University
Dogac Niyazi OZUCELIK, Dept. of Emergency Medicine, Istanbul University Cerrahpasa
57 Cybersecurity in Healthcare
Collaborating across the supply chain
Anura Fernando, Global Head of Medical Device Security, UL Solutions
60 The Future of Health Information Technology

Will hospitals disappear in 100 years?
Jong-Soo Choi, Information Technology Lead, Samsung Medical Center


Beverly A Jensen President/CEO

Women's Medicine Bowl, LLC
David A Shore Adjunct Professor, Organisational Development Business School, University of Monterrey


Eiman Shafa Medical Director
Spine Surgery Abbott Northwestern Hospital
Gabe Rijpma
Sr. Director Health & Social Services for Asia
EDITOR
Prasanthi Sadhu
EDITORIAL TEAM
Debi Jones
Grace Jones
Harry Callum
Rohith Nuguri
Swetha M
ART DIRECTOR
M Abdul Hannan
PRODUCT MANAGER
Jeff Kenney
SENIOR PRODUCT ASSOCIATES
Ben Johnson
David Nelson
Peter Thomas
Susanne Vincent
Gurrit K Sethi Founder, Miindmymiind

Imelda Leslie Vargas Regional Quality Assurance Director Zuellig Pharma


K Ganapathy Director Apollo Telemedicine Networking Foundation & Apollo Tele health Services

Luzviminda Nietes
Vice-President, Business Planning & Development, Metro Manila
Nicola Pastorello Data Analytics Manager Daisee




Microsoft Piyanun Yenjit Founder & Managing Director APUK Co.,Ltd.
Pradeep Chowbey Chairman
Minimal Access, Metabolic and Bariatric Surgery Centre, Sir Ganga Ram Hospital
Pradeep Kumar Ray Honorary Professor and Founder WHO Collaborating Centre on eHealth UNSW
Associate Partner

PRODUCT ASSOCIATE
John Milton
CIRCULATION TEAM
Sam Smith
SUBSCRIPTIONS IN-CHARGE
Vijay Kumar Gaddam
HEAD-OPERATIONS
S V Nageswara Rao
Ochre Media Private Limited Media Resource Centre, #9-1-129/1,201, 2nd Floor, Oxford Plaza, S.D Road, Secunderabad - 500003, Telangana, INDIA, Phone: +91 40 4961 4567, Fax: +91 40 4961 4555
Email: info@ochre-media.com


www.asianhhm.com | www.ochre-media.com
© Ochre Media Private Limited. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, photocopying or otherwise, without prior permission of the publisher and copyright owner. Whilst every effort has been made to ensure the accuracy of the information in this publication, the publisher accepts no responsibility for errors or omissions.
The products and services advertised are not endorsed by or connected with the publisher or its associates. The editorial opinions expressed in this publication are those of individual authors and not necessarily those of the publisher or of its associates.
Copies of Asian Hospital & Healthcare Management can be purchased at the indicated cover prices. For bulk order reprints minimum order required is 500 copies, POA.



















The aim of this study is to evaluate the impact of responsible leadership and talent management on employee engagement on gen Y employees working in the healthcare sector of the United Kingdom (UK). This study collects data using a simple random sampling technique, and 52 frontline employees are selected from 11 NHS hospitals in the United Kingdom. This study uses quantitative research methodology and collects data through a questionnaire that has been formulated using a 5-point Likert scale. Data analysis is carried out using SPSS statistical technique, and Pearson correlation and regression analysis are used to analyse the relationship between independent variables, i.e., talent management and responsible leadership, with the dependent variable, i.e., employee engagement. The findings of this study show that talent management and responsible leadership have a positive and significant relationship with employee engagement in the healthcare sector in the UK. This study contributes to the National Health Services (NHS) and explains under what conditions and how employees can be engaged. Consequently, it has both theoretical and practical implications. Lastly, the study lasted about two months and the names of the NHS hospitals and employees have been kept anonymous.
Human capital has a crucial role in any hospital system. It is widely accepted that hospital systems with the best people (doctors, nurses, etc) survive in the market for
the long term (Pandita & Ray, 2018). In parallel to this argument, the most important concerns of any hospital leader are their human capital and people resources (people, people, people).
Increasing connectivity and globalisation have enabled all organisations to stay more connected, indicating the need for robust policies for human resources management. According to Jauhari, Sehgal & Sehgal (2013), human resources (people, work environment, work conditions, and pay) have a crucial role in attaining organisational goals; organisation s must strive to support all employees to keep the quality and sustain positive attitudes and behaviour that help a company become competitive as compared to its rivalries in the marketplace. One of the most important concepts to ensuring competitiveness and relevance is employee engagement. Employee engagement is regarded as important for improving the quality of organisational human resources (Sadeli, 2015). Employee engagement is the formation of job satisfaction, employee commitment with the firm and their behaviour towards the organisation . It is further defined as a condition where employees see themselves joyous with work, feel wanted and appreciated by management and as a result become key drivers of vision, mission and purpose of the organisation (Nwabueze, 2023). Hence, scholars define employee engagement as a positive state of mind that is attributed to vigor, commitment, and absorption. Scholars provide other viewpoints and define variables that affect employee engagement like job attributes, the viewpoint of employees towards organisational support, leaders'
support, acknowledgement and support, identification with their firm and job, justice and equality provided to them in organisational procedures. All these variables have a positive relationship with employee engagement.
Scholars also describe leadership as one of the most important aspects in an organisation that has a considerable impact on employee engagement and their organisational identification (Aljunaibi, 2014). In contemporary organisation s, the emerging concept, responsible leadership is a subject of discussion due to the increasing inclination of the organisation towards ethical and moral values. Leadership is defined as the process of influencing subordinates and giving them directions to attain their optimal performance (Mousa & Ayoubi, 2019). Leadership has an important role in affecting employee engagement, and a range of scholars have developed a positive linkage between leadership and employee engagement (Hughes & Rog, 2008). As per Goestjahjanti et al. (2020), such leaders are aware of their moral values, viewpoints and understand the value of making sustainable business decisions that consider the interest of all stakeholders. O’Connor & Crowley-Henry (2019) argued that responsible leadership follows a pattern of behaviour that is inclined towards exhibiting positive ability and a positive
organisational environment. Eventually, it leads to positive self-growth and enhances confidence amongst employees. O’Connor & CrowleyHenry (2019) found that responsible leadership creates an environment of trust that keeps employees bound to each other. This specific leadership is widely acknowledged to enhance employee engagement and strengthen employee identification with the firm by
establishing positive feelings. Each firm has its leader through whom employees feel an attachment with their work and organisation . A stream of the literature shows a positive relationship between responsible leadership and employee engagement (Silzer & Dowell, 2009). Findings from Mousa & Ayoubi (2019) show that responsible leadership has a direct and positive relationship with employee engagement, which is further affirmed by Nugroho (2017) in the context of the service sector, indicating a strong and positive relationship between leadership and employee engagement.
Along with the identified variables, responsible leadership and employee engagement, talent management has an equally important role in the firm. As per Aljunaibi (2014), talent management is the firm's process to enhance its human resource management and meet its requirements. Scholars provide another understanding (e.g., Dhanalakshmi & Gurunathan, 2014) about talent management that it is a comprehensive process that aims to create the highest

Hongal & Kinange (2020) defined responsible leadership as a positive mental process in the service sector, and it provides self-awareness and a positive attitude that is governed by leaders and promote self-growth amongst employees.
potential amongst people in the firm through training and development, career growth opportunities and job enrichment that are in parallel to the firm goals and objectives. Various studies have shown that talent management affects employees’ commitment and engagement with the firm. Research carried out by Silzer & Dowell (2009) and Sadeli (2015) found that employee engagement has a positive relationship with talent management.
Talent management with its focus on employee engagement is the fastest-growing concept across firms, businesses are competing because of their talented employees and improving their operational culture. According to Taneja, Sewell & Odom (2015), talented people can perform well and have a high potential to help the firm attain its long-term objectives. Hence, talent management seems a major contributing factor in the competitive workplace and attains sustainable organisational productivity. Hence, scholars recommend that organisation s should continue fostering their strategies towards talent management with a fundamental focus on engaging the workforce daily through flexible work schedules (Doh, Stumpf & Tymon, 2011). Specifically, to generation Y that are regarded as boomers and the digital generation (born in the 1980s and early 2000) have a considerable inclination towards engagement, and scholars find enthusiasm amongst gen Y employees towards talent management and talent acquisition through development.
Generation Y employees are energetic and technology savvy and have their working styles different from previous generations (baby boomers). Such employees put considerable focus on learning and career growth opportunities while focusing on organisational values and strategic objectives. If employees from gen Y do not find such growth opportunities and inadequate organisational orientation towards ethics and morality, they switch their job and seek new career prospects
(Miska & Mendenhall, 2018). Hence, retention and engagement of such young employees are important as they are attributed to several elements like skills, knowledge, and their ability to learn in the firm (Gond et al., 2011).
Many scholars have identified the importance of talent management, responsible leadership, and employee engagement, yet recent studies identify the need to examine the role of talent management and employee engagement in the hospital sector (Fragouli & Alhaider,2020; Mwawasi, 2021). Hence, this study tends to bridge this empirical and theoretical gap in the literature and examine the influence of talent management and responsible leadership on employee engagement in the Gen Y employees.
This study has two important objectives:
• To empirically examine the linkage of talent management activities (training and development of employees, job enrichment prospects and motivation) with employee engagement (commitment, vigor and absorption) amongst Gen Y employees.
• To explore the relationship between responsible leadership (awareness towards employee requirements, moral and ethical values towards subordinates, vision, and responsibility) and employee engagement (commitment, vigor, and absorption) amongst Gen Y employees (Frangieh & Yaacoub, 2017).
This study has an important impact on the academic literature and implications for managers in the hospital sector. First, it explains the influence of talent management and responsible leadership on employee engagement and contributes to the theoretical literature to help future researchers extend their studies. Second, it bridges the empirical
gap and carries out primary research to identify the relationship between talent management, responsible leadership, and employee engagement through quantitative research methodology. Third, it tends to help the NHS have grounded theory research information about why and in which instances employees can perform better. Finally, through this paper, HR practitioners can make informed decisions and create a compelling and fun workplace.
Literature review
Talent management
Scholars put forward the description of talent management as to the set of organisational strategies for preparing and managing employees (Pandita & Ray, 2018). As per Goestjahjanti et al. (2020), talent management approaches are well-planned strategies to manage human resources so that organisation can maintain and retain its talented employees and the organisation remains productive. Talent management is a process that starts from recruiting talented people and then developing these people to retain them in the firm. In contemporary organisation s, since employees have a considerable emphasis on career growth opportunities, a talent management program is developed to facilitate its talented employees and enhance their work engagement. This study explains talent management in the following three dimensions: training and development, job enrichment, and motivation through career development opportunities. These dimensions are explained by scholars as the process of establishing talent management and offering employees clear training and development plans and enriching their job that helps them grow their skills (Lin, Huang & Huang, 2020).
According to O'Bryan & Casey (2017), responsible leadership is the process of making responsible decisions that
consider all stakeholders and their emotions, preferences. Hongal & Kinange (2020) also defined responsible leadership as a positive mental process in the service sector, and it provides selfawareness and a positive attitude that is governed by leaders and promote selfgrowth amongst employees. Responsible leaders are explained as the state of mind and positive attitude of a leader who promotes growth both in himself and in his subordinates. On the other hand, O’Connor & Crowley-Henry (2019) defined responsible leadership as the pattern of behaviour that encourages self-awareness and moral viewpoints and ethical behaviour through relational transparency. These arguments show that responsible leadership is interpreted as the positive mental state and attitude that is shown by a leader who thinks that his values and beliefs have an important role on employees. This study has used the following dimensions of responsible leadership, previously proposed by Dzimbiri & Molefakgotla (2021). The authors said that such leaders have self-awareness towards their peers and subordinates. Second, these leaders have ethical and moral values for their employees’ and exhibit responsibility for their employees. Leaders who have
this behaviour will always seek others' opinions and have values for its peers, colleagues, etc. These dimensions are used to measure responsible leadership amongst 11 NHS hospitals in the UK.
Employee engagement is about creating an engaging, enabling, and fun work environment that values, appreciates and rewards employee efforts directed at accomplishing organisational goals (Nwabueze, 2023). For Lin, Huang & Huang (2020), employee engagement is defined as a positive, fulfilling job that is linked with the state of mind and is attributed by passion, dedication, and commitment. This explanation can better explain that employee engagement illustrates employee’s connection and indulgence with an organisation through dedication and commitment. Two dimensions of employee engagement are explained by Sheehan, Grant & Garavan (2018): acknowledging the mental, physical, and cognitive energy exerted by employees and providing competitive rewards that meet the individual objectives of the employee (Sheehan et al, 2018).
Furthermore, Antony (2018), contends that employee engagement
includes three important indicators; vigor that explains a person's enthusiasm and attitude at the workplace and is attributed to a person's high level of strength and the desire to thrive at the workplace and earn even with persistent difficulties. The second variable is the commitment that is attributed to a person's feelings and is full of inspiration, pride and accepts risks in their workplace. Those who score high in this commitment are more identified with their workplace as it makes them valuable and challenging (Savanevičienė & Vilčiauskaitė, 2017). Other than that, they feel excited and proud at their workplace.
On the other hand, those who score low on commitment does not mean that they do not commit themselves with their work, but they do not have any meaningful and challenging experiences, and they are unenthusiastic about their work. The third is the absorption that is to stay preoccupied at the workplace. Employees are full of persistence, and they have a serious attitude towards their job. In their work times, they feel fast and find it very difficult to detach from their work. This study has used the following three variables, i.e., commitment, absorption, and vigor, as dimensions to explain employee engagement.
The process of talent management begins when an organisation starts its recruitment, growth and development of employees who are outstanding performance. The talent management process has a good impact on the employee engagement and results in better performance of the firm through reduced employee turnover and retains high talent (Ahsan, 2018). When the workload is provided by a firm to its employees, and it is low, employee engagement is also low. Scholars further explain this as the career development opportunities provided by the organisation to its employees. This study has also used talent management

as the employee job enrichment process and their training and firm support for their employees through motivation to attain employee engagement. Talent management activities and firm HR policies have a considerable impact on employee engagement. Talent management activities, i.e., recognition, career development opportunities and training and development, are used in this study and positively impact employee engagement. This study has focused on the significance of employees' workplace engagement and their engagement with the organisation. Thus, the following hypothesis is formulated.
H1: There is a significant and positive relationship between talent management and employee engagement.
Previous studies show that there is a positive and direct relationship between responsible leadership and employee engagement. The findings by El Masri, & Suliman (2019), showed that the relationship between responsible leadership and employee engagement is facilitated by their organisational talent management. Another study by Lin, Huang & Huang (2020) found that responsible leadership and employee engagement have insignificant relationship since awareness towards employee needs does not exhibit any relationship with employee engagement; however, other studies confirm that employees' needs have a considerable role when leaders want to exercise their responsibility and showcase their generosity towards employees. Many studies have shown that employees do not meet their leaders daily, which shows that the relationship between employees and their leaders is still not significant and needs to be proven by their role of calling as an influencer in the firm (Pandita & Ray, 2018). Hence, the second hypothesis of this study is formulated as.
H2: There is a significant and positive relationship between responsible leadership and employee engagement.
This study uses an empirical investigation with the employees working in 11 NHS hospitals. Frontline employees are the subject of the study. The population includes 11 hospitals. Data was gathered from the frontline employees. The data was gathered through questionnaires which were distributed to the employees. Such employees’ growth and development can directly affect patients and hospital productivity.
This study uses a deductive research approach, and theory is tested to accept/ reject the hypothesis. A cross-sectional time frame is used to collect the data, as this study gathers data only once from the respondents. A total of 52 sample respondents were selected using a random sampling method influenced by an earlier study conducted by O’Connor & Crowley-Henry (2019). One or two frontline desk employees were selected to take part in the study; therefore, an equal opportunity was provided to each hospital selected for this study. The response rate was 95 per cent for female participants and 5 per cent for male participants, which shows that females primarily dominate the NHS.
Moreover, a total of 45 per cent of respondents were from the age group 24 to 30 years and 35 per cent were from 31 to 36 years, and 10 per cent were from 37 to 42 years, and 10 per cent were from 43 to 47 years.
This study uses a scale that is chosen from previous studies and has used them in this study to evaluate the items of the study. The respondents of the study assessed items using a 5-point Likert scale that states 1 for strongly agree and 5 for strongly disagree. Previous studies are used to select variables of the study
and to construct questionnaires in this study. This study uses sub-variables for each selected variable of the study;
i) talent management, i.e., training and development of employees, job enrichment prospects and motivation (Hafez et al., 2017) ii) employee engagement, i.e., commitment, vigor, and absorption (Schaufeli et al., 2002).; iii) responsible leadership, i.e., awareness towards employee requirements, moral and ethical values towards subordinates, vision, and responsibility (Walumbwa et al., 2008). All these variables are assessed for the current study by making use of scales from the aforementioned studies. For employee engagement, Utrecht workplace employee engagement is used. Finally, analysis is carried out using statistical package software SPSS that helps to analyze correlation and regression tests of the study.
This study uses Pearson Correlation analysis to assess the correlation between independent variables i.e., Talent management and responsible leadership and dependent variable i.e., employee engagement. Table 1 shows the reliability test and table 2 demographic analyses, table 3 descriptive statistics and Table 4 shows Pearson correlation analysis that has been carried out in this study to evaluate the relationship between independent and dependent variables (See appendix).
This study also has shown positive statistical values of the variables and shows that there is a direct and positive association between independent and dependent variables. Furthermore, this study uses reliability analysis through Cronbach alpha that is calculated 0.887, which is greater than the rule of thumb (0.7) and a standard value used to evaluate the scale items’ reliability. The value exhibits that the scale items used in this study are all reliable and show authentic results (see appendix).
The association between talent management, responsible leadership and
employee engagement is shown using correlation analysis. The coefficient is evaluated to determine the value of beta that is used to illustrate how well the data supports the hypothesis of the study. Furthermore, this study uses beta coefficients to show the degree of changes identified in the dependent variables of
the study for their relevant independent variable. The results clearly show that the path coefficients for each variable are statistically significant at p < 0.05. Moreover, the findings show these results for the hypothesis of the study using regression analysis and identify that the dependent variable (employee
engagement) is 89 per cent explained by independent variables, i.e., talent management and responsible leadership. The results for hypothesis 1 show the following results: talent management and employee engagement =0.760, t = 17.617, p < 0.05 that exhibits a positive relationship between the variables of the study and support hypothesis 1 of this study. Hypothesis 2 is also tested for to examine the variables of the study, responsible leadership and employee engagement and shows following results; =0.347, t = 6.775, p < 0.05, and shows a positive relationship between the variables of the study. This also supports the second hypothesis of the study; hence, null hypothesis is refused.
**. Correlation is significant at the 0.01 level (2-tailed). *. Correlation is significant at the 0.05 level (2-tailed).
4: Correlation Analysis
Discussion
Given the research hypothesis, this study concludes that talent management has a significant and positive relationship with employee engagement in the NHS. The first hypothesis of the study is accepted as the value of t is greater than 1.96 and p-value is less than 0.05, which shows a significant and positive impact of talent management on employee engagement. This shows employee engagement in any organisation is increased if there is an
increased focus on talent management. These findings are in line with the studies by El Masri, & Suliman (2019) and Pandita & Ray (2018) and shows that there is a positive relationship between talent management and employee engagement. A study by Taneja, Sewell & Odom (2015), concluded that career planning and development approaches used with rewards and additional incentives could improve employer's commitment to the firm and their ability to absorb is also increased. This shows that employee engagement and commitment with the firm is enhanced. Therefore, organisation s offer

various career development programs as their strategy to enhance employee commitment with the firm. This is also supported by Pandita & Ray (2018) that talent management has a significant and positive impact on employee engagement. They further argued that the following dimensions: training and development of employees and job enrichment prospects have a positive and direct impact on employee commitment and vigor. When employees feel attached to the organisation , they are more psychologically linked to their assigned roles and duties, thus increasing overall productivity.
Silzer & Dowell (2009) also supported that talent management activities influence employee engagement where the aspects of organisation al support, and motivation influence employee engagement and improve their commitment to the firm. On the other hand, a quantitative study conducted by Miska & Mendenhall (2018) showed that talent management activities, i.e., training and development, job enrichment and recognition of employees, have positive linkage with employee engagement. Hence, this study carried out in the National Health Service (NHS) confirms previous studies and concludes that if employees are provided with adequate training, developmental opportunities, job enrichment, increased pay/rewards, personal/team recognition, their commitment and dedication to patient care is strengthened. Based on these findings, the mean viewpoint of employees towards motivational strategic
approach has a strong relationship with employee engagement, and the viewpoint of evaluating talent management attains high criteria. One of the key aspects that has the highest value is t job enrichment approaches; thus, employees feel encouraged and motivated to act well and retention is equally increased. Although a detailed analysis of this study shows that employees’ viewpoint on the items suggesting that hospital management must institute better retention strategies based on use of newer technologies like AI and flexible work schedules.
This study suggests that the British National Health service must incorporate motivational strategies regardless of whether it is the conservative or labour party that is power. A political free work environment is what the NHS needs to offer better career growth opportunities.

Given the findings of this study, and confirmation of the second hypothesis, this study affirms that responsible leadership has an important impact on employee engagement. Thus, the second hypothesis of this study is also accepted, and the null hypothesis is rejected. This shows that responsible leadership has a direct and strong association with employee engagement. A study by Frangieh & Yaacoub (2017) found that responsible leadership is directly related to employees' improved commitment to the firm. Miska & Mendenhall (2018) concluded that responsible leadership with responsibility and vision towards employees have a positive relationship with employee engagement and improve their job satisfaction, suggesting better employee performance. This study is of the view that responsible leadership has a considerable impact on employee engagement through managerial awareness of employee needs, moral and ethical values, and clearly defined organisational direction devoid of politics, but centered around patients and them, the worker bees.
A study by Lin, Huang & Huang (2020) found that responsible leadership and employee engagement have insignificant relationship since awareness towards employee needs does not exhibit any relationship with employee engagement.
The current study has several practical inferences and offers managers of the hospital systems to follow a comprehensive framework that could help them improve their HR strategies to cater to frontline employees. Hire and select leaders/managers who have a philosophical focus on employee-first mentality, ethical and moral values and a strategic and operational focus on patient care and caring.
Conclusion
This study concludes that talent management and responsible leadership have a direct, significant, and positive relationship with employee engagement in Gen Y employees working in the NHS. Since employee engagement affect employees’ decision to remain
AUTHOR BIO
in the organisation or to leave their firm; thus, through robust strategies, hospitals should attempt to enhance their relationship between their leaders and employees and create a sense of loyalty. Furthermore, it is also concluded that the HR managers can also improve their employee retention programs. Employee retention is a key challenge in contemporary organisation s when employee engagement strategy requires how a worker views their whole work experience and the treatment they get from their direct manager. People do not quit their jobs they quit their managers.
This study has certain limitations that can be used by future scholars to expand the subject of the study. First, this study uses empirical investigation and has collected data using a crosssectional research time frame; however, the longitudinal study can offer better insights and improve the understanding of the variables in this study. Second, this study has focused on the frontline employees, whereas future studies can be conducted on the mid-level employees and low-level managers. This will provide an expanded viewpoint on the wider population as compared to the current study that has focused only on the frontline employees. Finally, this study focused only on gen Y employees.
References are available at www.asianhhm.com
Uche Nwabueze received his Ph.D from Sheffield Hallam University in the United Kingdom in 1995. For 28years, Dr. Nwabueze has dedicated himself to the advancement of the theory and practice of management through research, consulting work, and teaching across four continents (North America, Europe, Asia and Africa). His students describe their classroom experience with Dr. Uche as he is fondly called; as a scholarly adventure in critical thinking, problem-solving and reflective analysis.

Preparations are in full swing as MEDICAL FAIR THAILAND makes its way to Bangkok once again in 2023. After a three-year break, the 10th edition of the exhibition will run its physical edition from 13 to 15 September at BITEC, followed by a 7-day digital extension where exhibitors and visitors can engage further online through its AI-powered businessmatching system until 22 September. This is the first time MEDICAL FAIR THAILAND will be held in a ‘phygital format’.
Highlights this year include signature showcases such as the Community Care Pavilion and Start-Up Park, and also the introduction of the Medical Manufacturing pavilion. As the region’s leading specialist trade fair for the medical and healthcare sectors for the past two decades, MEDICAL FAIR THAILAND serves the full value chain and end-to-end needs of the medical and healthcare sectors. From diagnostics, wearable technology, connected healthcare solutions, rehabilitation and therapy equipment, 3D printing technology, and now - medical technology (MedTech) components, processes and solutionsthe exhibition offers the ideal destination for medical and healthcare buyers and professionals looking to meet their sourcing objectives, gain industry insights and to share best practices.
MEDICAL FAIR THAILAND 2023 comes against a

“We have been waiting for three years so we are excited and are gearing up for a big comeback for MEDICAL FAIR THAILAND 2023. With the positive feedback, industry commitment, and almost 80% bookings received for 2023, we should be on track to reach close to pre-pandemic levels by next year. On the back of a highly successful and wellreceived phygital edition of MEDICAL FAIR ASIA that was held in Singapore earlier this year, and as we navigate further in a post-pandemic landscape, we are confident by this year the industry will be more than ready to move into high gear and Thailand will be an ideal location.”
Gernot Ringling, Managing Director, Messe Düsseldorf Asiastrengthening backdrop where Thailand continues to firm its position as a medical hub of the region with its supportive government policies and incentives, making it a model investment destination for a wide range of medical and healthcare service sectors. In line with Thailand’s 4.0 policy, the Thai government considers the healthcare industry to be a priority sector for investment, thus the staging of MEDICAL FAIR THAILAND 2023 is well-positioned.

A special themed pavilion focused on medical manufacturing processes and componentsfrom new materials, intermediate products, packaging and services, to microprocessors and nanotechnology. With Thailand’s growing reputation as a production and distribution base of medical devices both within and outside Thailand, it has become a natural market for medical devices.


According to data from the Office of Industrial Economics, Ministry of Industry (Medical Devices Intelligence Unit), there is much potential for investment opportunities in sophisticated medical devices particularly due to Thailand’s reliance on imports for this segment.

With a special spotlight on mental health with a showcase featuring digital mental health technologies, from smart medicine to therapeutic medical equipment. Its mainstay of addressing the needs of ageing societies on the back of rising chronic diseases and an ageing population, the pavilion will also feature a full suite of geriatric medicine, rehabilitative equipment, assistive technology, and mobility products.
Thailand’s proportion of citizens aged over 60 years, is forecast to be one of the highest in ASEAN by 2045, and will also exceed countries such as Europe and the United States. Thailand’s fast-increasing ageing population and the estimated more than three million Thais suffering from poor mental health, is expected to further drive the demand for related healthcare services.
A strategic platform for companies with ready-to-market healthcare solutions to meet relevant buyers and partners, industry influencers, experts, and potential investors. From innovative healthcare industry solutions, health apps and new tools for gathering and AI-supported analysis of health data, to robotic assistance systems and new approaches in diagnostics – the Start-Up Park is a must-attend for SMEs looking to scale-up their business.
The Start-Up Park plays a significant role as an enabler of the entrepreneurial ecosystem that encourages life sciences and medical and health innovation in Thailand. With the country’s vibrant start-up landscape propelled further by the government’s numerous grants and new regulations as part of Thailand’s ambitious plans to be a start-up-based country, the start-up scene has grown systematically over the years and is considered one of Asia’s hidden gems. At the last edition of MEDICAL FAIR THAILAND held in 2019, a total of 11 start-up companies participated from Singapore, Japan, South Korea, Hong Kong, Taiwan and Thailand.

Eight tips are shared on how to become a good healthcare manager and leader; from having the right mindset and attitude, to getting the right team, to being agile yet consistent, having open mind, continuously learning, and ability to carry the vision and win together.
Tan, Managing Director, Bagan Specialist Centre
Many define a good manager as being able to deliver satisfying financial results or performance outcomes of the area under their leadership. But in healthcare, being a good manager, does not mean you will be a good healthcare leader and vice versa. To be able to master both requires experience and intentional effort. Here are eight tips to consider if you want to be a good healthcare manager and leader.
Good healthcare starts from ‘heartcare’ i.e., caring from the heart about holistic care. Healthcare is not just an institution to provide medical care for detection of disease or restoration of health, or just another business to make profit. Any healthcare leader needs to start with the right mindset and attitude. When a healthcare leader leads with the right mindset and focus,
it gets reflected in the decisions and action plans. And why holistic care? Healthcare should not be transactional or provided in silo. A good healthcare is a holistic care.
No one is perfect in any management or leadership team. Hence, as a healthcare leader, it is important to gather a combination of people with different strengths and talents
to be part of the team. Find people with different talents, different strengths and different experiences to complement one another. There is a saying that goes “The eye cannot say to the hand, “I don’t need you!” And the head cannot say to the feet, “I don’t need you!” On the contrary, those parts of the body that seem to be weaker are indispensable” (The Bible, 1 Corinthians 12:20-21). Everyone is good at different things, and everyone has a different role to play. One’s strength is the other’s weakness, and one’s weakness is another’s strength, and that is how the team can work in synergy. Diversity is strength.
Healthcare is in the midst of great transformation. Digitalisation and automation will replace many traditional way of doing things. External factors such as changing national policy, ongoing public health threats from communicable and non-communicable diseases, and workforce shortage will be pressuring the healthcare delivery system to change. As a healthcare leader and manager, if one is not agile enough to know how to face challenges and when to adapt to new changes, the team and institution will be left behind. Being agile means being responsive and willing to change the usual way of doing things, change a plan that has been fixed but found not effective, or even reconsider what has been rejected.
As a leader, it is important to be consistent. Consistency in the values and principles, decision making and direction, and one’s word. This helps the team to work with peace of mind and psychological safety, knowing that the boss or supervisor is steering the ship steadily. A leader or manager that keeps changing their mind, with
no consistent value or direction, is tantamount to throwing the team into a storm in a ship without steering a wheel. How can one expect such a ship to reach its destination safely?
5. Keep Learning and growing
With the speed at which technology is being developed, and the new generation of talent is evolving, being ahead in knowledge and skills is important. An innate curiosity to want to know more and to want to be better will motivate employees to learn and grow. Passivity, indifference, and stagnancy kills. As a leader, it is like standing still while climbing a steep
Tan Hui Ling has been in healthcare leadership position for more than a decade. She is the Managing Director of Bagan Specialist Centre, Oriental Melaka Straits Medical Centre and Oriental Nilam College, Malaysia. She volunteers in Malaysia Society of Quality Healthcare and sits in the Board of Association of Private Hospitals Malaysia.

slope — not moving forward means one will be falling backward. The only way to move forward is to keep learning, keep growing and be better in what we do.
Problems happen when we do not see the problem as a problem. Having the ability to look back retrospectively and study one’s mistake or outcome of decision made, helps to refine one’s own decisionmaking skill. It is also good to regularly take stock, study retrospectively, to reassess plans to move forward. Gaining feedback and insights from peers, juniors, seniors or even competitors will help one to spot weaknesses and improve.
7. Leading with a Vision
There is a saying “people without vision perish”. A good healthcare leader should be able to not just fulfill the organisation’s mission or fulfill their duties. They should be able to envision what the organisation should be like in five or ten years. The person crafting the vision could be anyone, the manager, the founder or a predecessor. The manager needs to be interested and able to catch the vision and lead the team to run towards it.
In the dog eat dog world, many will kill to survive or kill to win. This could be a colleague that one does not see eye-toeye with or an external competitor. This mindset should have no place in healthcare. Healthcare is a common good and healthcare needs are humongous with many needs still unmet. Hence, coming together with each of their own strengths to meet the needs of the patients will ensure that everyone wins together. This means being willing to come together amidst differences to collaborate and share resources in partnership.


Digital health has embarked on a new stage in Asia. Previously, the focus was on electronic medical record systems to improve safety, efficiency and patient experience. Now, leading providers are transforming to enable new data-driven approaches. They are using AI, remote monitoring, wearable devices and mobile apps to improve medical outcomes and patient engagement while reducing costs.
While the FHIR data sharing standard has accelerated this trend, leading providers are also investing in data platforms for ease of management, data quality and advanced integration. Stella Ramette and Nana Khunlertkit from InterSystems will explain what they have learned, and how to simplify the next stage in your digital health journey.
1. How has the utilisation of AI technologies in the healthcare industry impacted medical outcomes and patient engagement on a broader scale?
STELLA: Artificial Intelligence (AI) and Machine Learning (ML) take the insights gained from data analytics and make them actionable with new predictive insights in real time. This is already having a positive impact on medical outcomes.
While AI is widely adopted for pathology and imaging interpretation, organisations have been slower to adopt its applications that offer the biggest potential for productivity improvements.
Stella Ramette, Director, Healthcare Customer Relations and Sales, South East Asia, InterSystems Nana Khunlertkit, Professional Services Director, South East Asia, InterSystemsThis is changing, however. Medical researchers like RAPIDx AI1 are now analysing data at scale and leveraging modern data platforms to provide insights into new and more effective treatments, provide evidence that they work, and integrate them into providers’ clinical workflows.
Let me give you a few other examples:
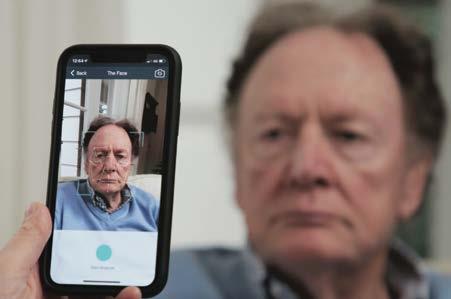
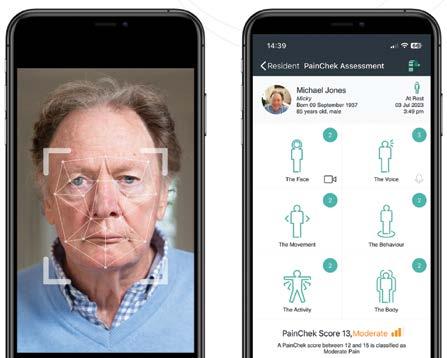
InterSystems is working with PainChek, developer of the world’s first smartphone-based pain assessment and monitoring application. PainChek’s software-as-a-service (SaaS)-based AI platform uses smart devices with cameras to evaluate patients’ pain levels accurately.

PainChek’s reliability and consistency improves care and saves time and money for healthcare providers. It also enhances the patient experience. For example, clinicians with different bedside manners may record different verbal assessments. Many patients cannot reliably describe their pain levels, are pre- or non-verbal, or are not lucid at the time.
With PainChek, a time-consuming verbal assessment and scorecard process is replaced with an AI supported digital assessment and automatically generated pain rating that is more consistent and reliable than the manual process. So, you are improving care and making it more efficient. We will see more and more digital tools like this integrated into clinical workflows, which will help to reli eve the workloads on our clinicians and make them more productive and effective.
InterSystems is working with another company, Cognetivity, which has developed an AI-powered test to detect dementia years before it would otherwise become noticeable. The test leverages the ‘food or fear’ response that human beings have developed about animals. Patients are shown images of animals, and an AI engine measures the accuracy and speed of responses and analyses the data to assess the patient’s risk of Alzheimer’s.
Because its solution is based on a data platform, Cognetivity has been able to rapidly integrate with existing healthcare systems at the NHS in the UK. In the early stages of adoption, this has allowed it to analyse existing demographic data to identify which patient cohorts would benefit most from being tested. It also expects to integrate with existing patient histories to perform more detailed analysis in the future. Within a short time, Cognetivity has been able to work with ten NHS trusts on research projects and implement commercial solutions at two of them.
NANA: Despite a global shortage of staff, clinicians could still misinterpret the purpose of AI as being their replacement and refuse to adopt these technologies. Successful implementations of these AI solutions have usually required strong commitment from organisation leaders, close engagement with clinicians, and a well developed change management process.

1 https://healthtranslationsa.org.au/projects/rapidx-ai/

STELLA: Typically, these solutions can be made possible by integrating health data from Internet-connected devices with electronic medical record (EMR) systems capable of notifying clinicians and providing alerts.
Such approaches have been proven to work. A study at Brigham and Women’s Hospital 2 in Boston, Massachusetts, found that remote monitoring technology improved outcomes and reduced costs by 40 per cent. Patients were also 70 per cent less likely to be readmitted.
2 https://www.healthline.com/health-news/being-treatedat-home-can-help-people-save-money-and-heal-faster



increased use of telemedicine, remote monitoring technology and wearable devices. And, as we discover new ways for them to support the sustainability of our healthcare systems, their importance will grow.
Telemedicine became widely used in Asia during the pandemic for urgent care, remote consultation, and following up patients with chronic conditions. Private hospitals in Thailand that were previously reliant on medical tourism, for example, switched to telemedicine to maintain a connection with their patients. More frequent telehealth follow up helped improve treatment outcomes, and lower costs have provided better value to patients.
In Singapore, COVID-19 patients were treated remotely using smartphones, tablets and Bluetoothconnected thermometers, oximeters and blood pressure meters. Hospitals in Australia also deployed monitoring devices to care for COVID-19 patients living in their homes. And in New Zealand, remote monitoring technology like ECG devices and pulse oximeters are being used to design a virtual consult service to assist vulnerable populations in South Auckland.
STELLA: Fast Healthcare Interoperability Resources (HL7® FHIR®) is not just a standardised way to share health data. It enables modern web-based technology, which was not provided by any of its predecessors, and a granular and fluid way to share and receive data. Equally important, FHIR provides curation of clean and structured data for an organisation to use for operational and clinical efficiency, analytics, mobile apps, genomics and population health. Here, the ability to ingest, cleanse and transform data is critical.
Data cleansing is not as well understood in other industries, such as retail and logistics, because typically they work with clean, real-time data. An example is a rideshare app where only real-time data about the passenger, driver and destination is managed. This is not the case with healthcare data which is complex and stored in different locations, standards and formats. To effectively make sense of the data and use it efficiently, data cleansing and harmonisation capabilities are key.
For example, there are often multiple interpretations of the same diagnosis and disparate units of measurements. One of our partners identified 58 different units strings for routine white blood cell count (WBC)! There are also several names and brands for the same drug, and multiple terms and numerical codes for a medical diagnosis. It is critical to agree on the same syntactic structure and also correct sematic data interpretation. This is the true benefit of FHIR – to enable sharing of correct information to save lives.
2. In what ways have remote monitoring and wearable devices been leveraged to improve healthcare outcomes and reduce costs industry-wide?
NANA: The COVID-19 pandemic has provided a silver lining with the
In Indonesia, for example, InterSystems is working with leading hospitals and hospital groups where the focus has evolved from digitisation and electronic medical record (EMR) systems to data-sharing and innovation. Many of these healthcare providers are adopting FHIR-based interoperability to integrate with other organisations, like insurance companies, or apps which enable closer patient engagement and involve patients in managing their own care.
Some are using FHIR and other advanced interoperability capabilities to integrate all of their clinical data into a single unified system. One customer has already deployed InterSystems IRIS to build a FHIR-based health data repository for operational analytics and a patient portal. We are currently working with them to ingest and analyse data at much higher speeds, enabling them to move to real-time clinical data analytics.
It is a sophisticated journey that needs to start ASAP. We see a similarity in the adoption of FHIR in healthcare and the adoption of the SWIFT international transfer standard in the banking industry. What was agreed as a standard to allow cross-border payments by 239 banks in 1973 became a universal standard.
NANA: Because of its capabilities and rapid adoption as a standard, FHIR has become recognised as the fastest and most cost-effective interoperability tool. Many governments in South East Asia are building healthcare data-sharing infrastructure based on FHIR, or encouraging healthcare providers to adopt FHIR so that they can participate in data-sharing initiatives.




Leading Asian healthcare providers are also looking to FHIR-based interoperability to further innovate by sharing between their own systems to
enable data analytics, AI and machine learning, for example, to further improve quality of care, patient experience and engagement, and operational efficiency.
AI and machine learning algorithms enable incredible breakthroughs in the quality and cost-effectiveness of care. But if they are not clinically tested, no one will use them. If you want to see an exciting example, look at what RAPIDx AI3 is doing to clinically test the use of AI algorithms to improve the emergency care of people with chest pain.
STELLA: Technology has advanced enormously in healthcare in recent years. We have seen a breakthrough in interoperability with the FHIR healthcare data standard. With cloud computing, we have also seen a revolution in how computer systems are deployed and scaled up to meet demand. And we have seen the advent of cloud-based data platforms, like InterSystems IRIS for Health ®, that enable interoperability, data cleansing and data analysis in the cloud.
As a result, it has never been easier or more cost-effective to exchange healthcare data between different systems, ensure it is fit for purpose, and analyse it in real time. With advances in interoperability and cloud computing, AI and ML are taking off in healthcare, encapsulating the insights gained from earlier analysis to provide predictive, actionable insights in real time.
Interoperability is not the only enabling technology that data platforms need to provide for digital health. Building the infrastructure for FHIR-based interoperability is relatively easy. The more challenging part is what you do with the data when you get it. Access to patient medical records is a great starting point. But, if the data isn’t usable at the point of care, isn’t trusted, or isn’t subject to the appropriate clinical governance, it won’t make a big enough difference.
NANA: A healthcare data platform enables these sorts of breakthroughs by connecting and translating health data sources, ensuring data quality, and delivering the data to where it needs to go, when it is needed. But a proven customer engagement and software implementation methodology, like InterSystems ARIES, is equally important for success.
ARIES includes five stage gates (starting from pre-sale to adoption sustainability) to ensure change management and system adoptions are properly planned and carefully executed to deliver the ‘biggest bang for the buck.’ We understand the danger of ‘garbage in, garbage out’ and, with ARIES, we design and implement a platform that will provide a clean and structured set of data, and can be easily sustained and support advanced analytics in the future.
STELLA: Healthcare providers must evaluate data platforms against several important criteria, depending on their objectives. These include:
3 https://healthtranslationsa.org.au/projects/rapidx-ai/
4. Can you discuss the role of data platforms in facilitating the management and analysis of large-scale healthcare data for improved decision-making?
• Does it support healthcare interoperability and data standards with deep support for FHIR, HL7 V2, IHE and other global healthcare information protocols and messaging formats to enable the integration and interoperability of health applications?
• Does it support healthcare data management with an extensible FHIR repository and comprehensive REST APIs to provide the foundation for modern healthcare application development and help seamlessly handle multiple forms of data at high speed?
• Does it support clinical research? Is it an approved platform for i2b24 (Informatics for Integrating Biology & the Bedside)?
• Does it support a healthcare analytics framework? Can you include analytics and AI in your solutions with an open analytics platform that provides a choice of embedded, standardsbased and best-of-breed analytics technologies for exploration, analysis and prediction?
• Does it complement the existing systems architecture within the organisation or is ‘rip and replace’ necessary?
NANA: Equally important, with all systems implementations healthcare providers need to understand that it is crucial to consider how planned workflow changes will affect staff members and take their existing mindsets into account with a well thought-out and implemented change management program.
End users do not always know what they need, although they can usually talk about what they want. As a vendor/implementer, our job is to encapsulate realistic long-term benefits to create a shared vision with the provider’s team to achieve them.
4 https://www.i2b2.org/
Essentially, it is to find the optimum design to fit with each provider. The optimum design does not mean endless user interface modifications to fit with end users’ expectations. But it is the most optimum design of system to be able to run operations more efficiently and effectively, and to be able to provide cleaner structured data for future analytics. With proper implementation, data management is made easy and scalable.
STELLA: The primary benefit of an advanced data platform is the ability to innovate to utilise healthcare data better. The data platform enables this by:
• The ease and speed with which healthcare organisations can acquire healthcare data, ensure it is fit for purpose and deliver it to where it is needed.
• The ease and speed with which they
can get innovative healthcare apps up and running, whether it is applications they develop themselves, or apps they integrate from third-party suppliers.
• Providing a central point of management for healthcare data and healthcare apps and ensuring that they are used according to the organisation’s governance policies.
How this support does improved care coordination and patient outcomes? Governments and healthcare providers all over Asia are grappling with a huge problem. How do they continue to broaden access to healthcare services to growing populations, while at the same time?
• The demand for healthcare is growing exponentially as populations are aging and treatments become more expensive
• There is a global shortage of clinicians to provide the care people want.
NANA: One solution is to improve healthcare outcomes AND reduce the cost of medical treatment. This is the idea behind value-based care. But first, you need to capture data about the effectiveness of outcomes and the



cost of treatment and analyse it. A platform that allows for data sharing can improve value-based care, for example, through a reduction of care duplications among multiple providers. With an open platform, care providers can have access to more accurate, timely and complete data.
Another solution, according to Gartner, is productivity improvements from a digital-first model that breaks away from traditional in-person-centred approaches to “one that prioritises digital engagement and the use of digital products and service throughout the entirety of an individual’s health journey.”
These approaches require the healthcare industry to innovate on healthcare data management, integration and interoperability. With a healthcare data platform that supports innovation, healthcare providers are better positioned to adopt new models that support better care coordination, improve patient outcomes and reduce costs.
STELLA: Privacy is always a hot topic in healthcare, and recent data breaches have put this in the spotlight. Across all industries, information security is a significant risk, and it is a challenge that all healthcare organisations face. Healthcare data sharing through systems integration or interoperability requires organisations to conduct risk assessments and tailor their security policies and measures accordingly.
InterSystems has also invested heavily in capabilities to support robust
security and privacy models within our products and partner with our customers to ensure their systems are secure. The InterSystems Global Trust program ensures the appropriate controls and measures to protect and safeguard information. InterSystems takes data security and privacy seriously and maintains a data governance framework consistent with our Data Protection, Privacy & Security Policy5
For example, InterSystems is partnering with an innovative health tech company in Singapore, Jonda Health6 that takes data privacy and security very seriously.
According to Dr Suhina Singh, Co-founder & CEO, Jonda Health: “Data privacy and security is at the heart of everything that we do. We believe that it is a fundamental human right. That’s why we not only use cryptographic endto-end security but also zero-knowledge encryption. In our patient-facing application, this ensures that only patients can decrypt their data, giving them full control of their health information.


“Given we are dealing with large amounts of unstructured data, we require massive processing capabilities. As such, we are incredibly thankful to have InterSystems as a partner to help fulfil our mission. Jonda Health leverages the InterSystems IRIS® data platform to provide the scale, speed and power we need.
“The ability to share data securely without hassle is key to creating the frictionless consumer experience that patients deserve and healthcare organisations must achieve. This also promises to eliminate treatment delays, unnecessary testing, and wasted time and money.”
which play out in many industries. Thankfully, healthcare is much better positioned to respond to ethical issues than almost any other industry. Clinical governance of new treatments and technologies is not an afterthought in healthcare. It is a core competency of all clinicians and healthcare organisations. We have years of experience working with our customers to address issues when they arise and help them configure our solutions.
For example, InterSystems global partner, PainChek, has regulatory clearance as a medical device in Australia, the UK, Europe, Singapore, Canada and New Zealand and an application to the U.S. FDA is currently in progress.
NANA: New digital technology also throws up many ethical issues,

5 https://www.intersystems.com/GTDPPS
6 https://www.jonda.health/
NANA: In a word: innovation. No one healthcare organisation can analyse all the healthcare data that it collects. But together, as an industry, we can promote innovation and share data-based solutions that all organisations can use.
In Asia, governments see the digitisation of healthcare and interoperability to enable data sharing between healthcare providers as key building blocks for data-driven healthcare. Until recently, these governments have focussed on the digitisation of healthcare. As the number of healthcare providers with EMR and other healthcare information systems
How do healthcare organisations ensure that the data collected from various sources are effectively analysed and utilised to generate meaningful insights and drive positive outcomes?
reaches critical mass, they are turning their attention to interoperability and innovation.
STELLA: Leading Asian healthcare providers are not just waiting for government-led initiatives, however. The business case for better interoperability is already becoming apparent, and the cost of providing that interoperability with standards like FHIR has never been lower.



We have also seen an innovation mindset develop around the use of data in healthcare. There is now a global ecosystem of researchers and medical start-ups pushing the boundaries in using data to improve healthcare outcomes and operational efficiencies.
InterSystems is working with startups around the world, including companies like RxPx, which supports the introduction and safe use of new medications with data-driven apps and systems, as well as Cognetivity, PainChek and Jonda Health, which I mentioned before.
NANA: Resourcing is always an issue in healthcare. Resources have traditionally been focussed on the areas of most acute need, like hospital care. On the other hand, precision medicine and preventative health has more potential to improve health and wellness but needs to be better resourced. The same is true for datadriven healthcare.
Healthcare organisations are constantly challenged when funding digital healthcare and resourcing projects.
That limits the pace of change. There is a particular challenge in creating any system-wide business case to justify the resourcing of clinical analytics and the interoperability to support it. But that is a structural issue within healthcare systems, not a technological one.
How do we overcome this going forward? In the business world, there is the concept of a growth mindset and how that promotes cultural change and innovation and disruption to existing business models. In the healthcare sector, the equivalent idea is valuebased care.
Modest investments in interoperability and analytics can enable healthcare providers to better understand the cost and the outcomes of care and provide the evidence to support changes that improve how healthcare is delivered.
Right now, that is mostly only possible within organisations or the most integrated parts of the healthcare system. But more broadly, successful value-based care initiatives can make
an enormous difference, because success is contagious.
Each successful value-based care initiative provides a model and the incentive to join up other parts of the healthcare system to get further benefits and increase the number of stakeholders who get those benefits.
In other words, there is a powerful network effect, and that has the potential to move the dial significantly in the future.
NANA: As a vendor, we are committed to leading the data-driven healthcare trend. Both InterSystems products (data platform and health information systems) and our implementation teams have been built to support the future evolution of healthcare ecosystems globally and in Asia.
Stella Ramette is Director, Healthcare Customer Relations and Sales, South East Asia for InterSystems. Based in Singapore, Stella oversees the InterSystems healthcare business in South East Asia. Stella has over 20 years of experience spanning healthcare and healthcare IT including medical imaging, medical device integration and emergency medicine. Stella worked in the digital pathology divisions of Qualcomm and Philips in Scandinavia and, in 2020, volunteered as a vaccination nurse while still working full time. Stella has also held leadership positions at Tieto, Lexmark and Atos Medical and holds both an MBA and nursing degree from Sweden.
Adjhaporn (Nana) Khunlertkit is Professional Services Director, South East Asia at InterSystems. Before joining InterSystems, Nana was Division Director, Health Information Management, Operational Analytics and Transformation at Bumrungrad International Hospital in Thailand. After receiving her PhD in Human Factors from the University of Wisconsin-Madison, she took up a position as Senior Human Factors Lead at Johns Hopkins Medicine in the U.S. In that role, Nana worked to ensure patient safety with healthcare IT, user-centred design and implementation, clinical workflow and sociotechnical systems analysis.


The COVID-19 pandemic had a monumentally negative impact on medical tourism. With borders in many countries around the world closed for traveller entry for about 18 months, many consumers dependent on crossborder medical care experienced restricted access.
There is now huge pent-up demand for many types of treatments. Many patients delayed necessary elective procedures and a significant number of patients have seen their chronic illnesses become exacerbated due
to non-treatment. With the delays in diagnosis of diseases such as cancer, patients are coming forward at a later stage of disease progression. This requires they take longer to treat and are more expensive. There are many other factors significantly affecting medical value travel in post-COVID 2023.
David Thomas Boucher, Chief Partnerships Officer, Bumrungrad International HospitalAccording to the Centers For Disease Control (CDC), USA, ‘medical tourism’ is defined as, “The travel to another country for medical care.”. To the liking of this author, this trend is now generally referred to as ‘medical value travel’ or MVT. A tourist, of course, visits a country different than their own and expects most customs to be very similar….. The tourist can become easily exasperated when they find few similarities. Conversely, a traveller visits a different country and expects most things to be different and is thrilled with the differences.

Prior to the COVID-19-plagued 2020, the countries with the highest volume of international medical travellers were Thailand, India, Turkey, Singapore, South Korea, Malaysia, Costa Rica, and the Cayman Islands. Significantly fewer patients sought care in North America — primarily Mexico and the USA.
The surgical procedures which generally lend themselves to international MVT are ones that patients can safely fly to/from, have low complication rates, relatively short lengths-of-stay (including rehabilitation), and few post-treatment follow-up protocols back home. Generally, these include orthopaedic, cardiac, general surgery, gastric bypass, cosmetic surgery, oncology, and dental procedures.
The pandemic obviously had a significant and negative impact on medical value travel. As many of us painfully recall, borders in many countries around the world were closed for traveller entry from mid-2020 through mid-2021. For people dependent on cross-border medical care, these travel prohibitions made a significant impact on their availability of care.
The results of closed borders brought significant changes to MVT in our post-pandemic world. Not surprisingly, there is now huge pent-up demand for many types of treatments. Many patients delayed necessary elective procedures and a significant number of patients have seen their chronic illnesses become exacerbated due to non-treatment (NY Times). With the delays in diagnosis of diseases such as cancer, patients are coming forward at a later stage of disease progression. This requires they take longer to treat and are more expensive.
The United Kingdom’s National Health Services (NHS) waiting list could rise to as many as 10.7 million by Spring 2024 (IMTJ). An analysis analysis of cataract surgery volumes estimated that the United States may face a backlog of over 1.6 million cataract procedures by 2023 (NIH). And according to the Canadian
Broadcasting Corporation, Ontario, Canada has a pandemic backlog of one million surgeries.
There are many other factors significantly affecting medical value travel in post-pande mic 2023. For instance, several countries are improving their in-country medical services making it more attractive and less costly for families to care locally for their own. Kuwait, the United Arab Emirates (UAE), Oman, and the Kingdom of Saudi Arabia (KSA) are good examples. Hyperinflation in 2020 in several countries quickly ratcheted up the price of medical care; Turkey is a good example, where inflation topped 85 per cent in October, 2022.
There is good news for medical travellers and for countries and hospitals which seek to attract them. In January, 2023 global air travel exceeded 2019 levels for the first time since the COVID-19 pandemic. According to Price Waterhouse Cooper (PWC), two of the top travel trends to watch this year are “Pent Up Travel Demand” and “Health”. Further, industry watchers now anticipate over 27 million medical tourists by 2023, increasing its market value from US$105 billion in 2019 to US$120 billion in 2023 (HMA).
Increasingly though, a trend of ‘medication tourism’ is blooming because patients find that necessary, often lifesaving, FDA-approved medications are either prohibitively expensive or simply not available in their home countries. The medicinal cures for Hepatitis C and Spinal Muscular Atrophy (SMA) are
excellent examples. For the former, drugs such as Harvoni and Sovaldi retail for prices over US$70,000 for a one-month course of treatment in America, but can be procured and consumed in many countries for under US$4,000.
This author has believed for many years that increasingly consumers will seek cross-border care for three (3) main reasons in this order: Safety, Service, and Savings. These become the Three Ss of Medical Value Travel.
Many consumers travel for wellness and medical care because their perception is that local care is unsafe and of low quality. In an era of increased data transparency by hospitals in countries like the United States, Great Britain, South Korea, and Malaysia (to name a few), consumers can rather quickly determine outcome measures, nosocomial infection and post-surgical infection rates, etc. through the internet. Also, internationally known brands like the Joint Commission International (JCI) and Newsweek magazine offer easy access to ‘Top Hospitals” around the world.
The second S, that of Service, continues to improve at many hospitals and medically directed wellness / antiaging centres around the globe. Today we live in an “instaculture”…… that is, as consumers most of us expect most goods and services to be produced or delivered on-demand. Think about it: We click on a computer button and we are able to watch movies, sporting events, etc. In real time, we can participate remotely in family gatherings, business meetings, and self-help groups. We can order a latte from our favourite coffee shop and have bicycle or motorcycle driver bring it so us on a park bench — all in under 10 minutes. Today’s healthcare consumer expects the same impassioned commitment to timeliness and sense of urgency. Primary care telemedicine visits need to be in near-time and on-demand. Specialist visits are expected within 24 hours. If a patient has been given a 10 AM
An analysis of cataract surgery volumes estimated that the United States may face a backlog of over 1.6 million cataract procedures by 2023 (NIH).
appointment, they reasonably expect to be in the exam room by 10 AM –baring provider emergencies with other patients. Because we, the provider community, establish the expectation in urgent care centres, patients expect door-to-door (D2D) throughput times in under 60 minutes. The consumer expectation for non-emergent patient admissions parallels that which they receive in hotels. The same expectation holds true for inpatient discharge times; once the physician tells the patient they are ready for discharge after some post-discharge nursing education, the expectation standard has been established. This is a difficult bogie to hit when there are international insurance companies involved; it can often take four hours or more to obtain final insurer approval
and payment guarantee. This lag mandates that international hospitals work closely with major insurers with which they participate.
Another factor increasing patients seeking international medical travel is patient wait times. Patient wait times for major orthopaedic surgery procedures in the United States can be as long as 6-8 months for patients who have Medicare and Medicaid. Queues

for patients in Canada and the UK are routinely much longer than this. Since there is nothing even remotely close to “on-demand” with these elongated wait times, international medical travel in a world with pent-up post-COVID demand is even more enticing.
Savings is the third “S” of the three. Medical travelers, whether domestic or international can easily save 50-85 per cent of the prices in their local areas.
So clearly, you can see that the current ‘value’ proposition in Medical Value Travel can be enormous. A consumer can go on-line to a hospital’s website, review quality indicators, select a physician, book an exam and, in most cases, be on a plane within a week and easily be home within a month. And an increased number of them are doing just that!
In the last decade, regional and global health organisations have pushed for making safety a central pillar of procurement, with a directive that cost should not be a barrier. The crucial question is: How easy is that to implement? How can a confident decision be reached that protects patients and healthcare workers without straining costs?
A Royal College of Nursing project reported that 100,000 needlestick accidents occur in the UK every year, and Bevan Brittan, a legal firm representing the

NHS, estimates the cost of needlestick injuries to each UK NHS trust to be around £500,000 each year in legal costs.1 And in the US, the initial treatment of a needle-
1 https://www.supplychain.nhs.uk/programmes/safer-sharps
stick injury (NSI) can cost between 800 - 6000 USD each2, with initial costs of medication for the Hepatitis C virus starting at around 25,000 USD3, and fines from OSHA beginning at 13,260 USD4. It should be noted that this is before associated costs are taken into consideration; staff absence interrupts the efficiency of already heavily burdened departments, and reputational damage and morale pose a considerable challenge to a sector that is struggling with staff retention. The takeaway is that indirect costs exceed the direct costs. The EU and OSHA are rigorous in their safety directives with regards to NSI, and arriving at a decision in selecting a safety device that balances costs without sacrificing safety need not be a complicated process.
An established culture of safety feeds into the selection process. But with a vast inventory of products available, how can this process be simplified? The decision should be based on the three pillars frontline
2 AOHP, 2014
3 HealthDay, 11/6/18
4 OSHA, 2018
healthcare worker input, ease of use and protecting patient safety and comfort5.
The culture of safety is in place, a short list of prospective manufacturers has been identified, fulfilling the code of conduct and sustainability criteria and the costs are clear. Should the cheapest option then be chosen? This is where a reliable supply chain can really add value in blood collection. Logistics have been transformed and optimised due to the pandemic, but still face a host of challenges; the costs of raw materials continue to increase and global events impact the availability and delivery of goods. So how does one manufacturer’s offering compare to a competitor’s?
We know that the small details of blood collection kit matter in the lab, just as much as they do on the ward. It is why every detail of our products and services are designed with that safety approach in mind. From the moment a blood sample is drawn, to the moment it becomes data.
Greiner Bio-One offers an extensive range of safety products, allowing the most suitable products to be selected for every market and customer.
The VACUETTE® QUICKSHIELD Safety Tube Holder is especially suitable for routine blood collection. There is no change to the usual collection technique, and the safety shield is activated one-handed. This product can provide the user with the simplest handling and reliable infection protection.

The VACUETTE® EVOPROTECT SAFETY Blood Collection Set is the next stage in blood collection. The semi-automatic click mechanism protects the user from the risk of needlestick injuries and makes the daily task of blood collection easier.
5 https://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-education-andresearch-center-for-occupational-safety-and-health/ce/preventing-occupational-exposurebloodborne-pathogens-healthcare


Accreditation affects healthcare management in many ways. It impacts management, leadership, and business results beyond clinical standards. Accreditation says strategic management helps hospitals adapt to market and regulatory conditions. Hospital accreditation improves resource use, service quality, and patient satisfaction. Jordan boosts health. Accreditation matters. Accreditation programmes help managers develop evidence-based practices, continuing education, and industry standards. Qualitative project. Thus, 10 nurses at various levels and 10 doctors, including specialists, from two Jordanian hospitals—one private and one public—were interviewed in person.
Promote leadership, accountability, engagement, and change. Accreditation tracks KPIs, evidence, and quality. Accreditation improves healthcare leadership and quality. Accreditation improved quality, patient satisfaction, safety, cost-effectiveness, and reputation in sampled hospitals.
Abdullah Algunmeeyn, Assistant Professor of Nursing, University of NottinghamHigh-quality care and the best possible outcomes for patients are only possible in healthcare organisations with strong management (Stern et al., 2017). Healthcare service quality can be evaluated and enhanced with the help of the accreditation programme. Accreditation has an effect on the quality of managers in healthcare organisations, but this is often disregarded despite the fact that its primary focus is on clinical standards (Algunmeeyn,A., & Mrayyan, (2022). In this article, we take a look at how accreditation programmes improve management knowledge, leadership skills, and business results as a whole (Algunmeeyn, Alrawashdeh, & Alhabashneh, (2020).
As a management philosophy, accreditation provides hospitals with a strategic way to differentiate themselves and respond to shifting market conditions and regulatory requirements (Westcott, Duffy, & Saif, 2018). Hospitals are urged to maintain a high level of performance because accreditation is based on these standards, as emphasised by Gyani (2012).
As a result, hospitals implement accreditation programmes in an effort to make better use of their resources, boost the quality of their services, and increase their patients' overall satisfaction (Oliveira & Matsuda, 2016). In turn, this improves medical standards in Jordan and cements the country's position as a leader on the Arabian Peninsula. An example of a hospital in Jordan that is dedicated to improving treatment methods is provided by Saif (2018). A'aqoulah, et al (2016) found that evaluations of Jordan's health care accreditation system found that the country's hospital management systems were created to encourage hospitals to expand their services and facilities. Additionally, these evaluations guarantee the security of healthcare services by centering on crucial administrative infrastructure (Stern et al., 2017).
For the completion of this project, a qualitative approach was utilised. Consequently, in-person interviews were conducted with ten nurses and ten doctors employed at a single public hospital in Jordan. Ten individuals from the two hospitals were interviewed for this study. The researcher interviewed ten nurses and five physicians at the public hospital. The researcher chose semi-structured (face-to-face) interviews for data collection. Two Jordanian hospitals' ethics committees approved the current research. Those who agreed to be interviewed were then sent an email form indicating their participation and permitting the researcher to schedule an interview appointment. Then, consent forms and information sheets were distributed to prospective participants based on their interest in participating in this study. The twenty interviews' data were analysed using the NVivo software for qualitative data analysis. Before data analysis, the audio-recorded interviews were transcribed word-for-word, and these transcriptions were reviewed. Later, the data were imported into the NVivo
software for qualitative data analysis in order to facilitate the linking of concepts related to the data.

Accreditation programmes in the healthcare industry provide a framework for evaluating the quality and safety of healthcare organisations (Algunmeeyn, Alrawashdeh, & Alhabashneh, (2020). These programs, which are frequently administered by independent organisations, assess various facets of patient care, including clinical processes, infrastructure, patient safety measures, and governance structures (Algunmeeyn, A., & Mrayyan, (2022). Accreditation demonstrates that a business has met predetermined quality standards and is dedicated to continuous improvement (Ali KAM, Alolayyan, 2013). Typically, accreditation programmes place an emphasis on clinical factors like patient outcomes and safety (Mansour, Boyd, Walshe, 2021 ). However, they also have a significant impact on the calibre of administrators in healthcare organisations(Raut, Narkhede, Gardas, 2017). Through effective management, clinical excellence must be translated
into efficient operations, resource optimisation, and positive patient experiences (Algunmeeyn,A., & Mrayyan, (2022).
Accreditation programmes enhance the managerial abilities of healthcare professionals. These programmes encourage managers to implement evidence-based practices, continue their education, and stay abreast of industry standards and best practices (Badr, AlFadalah, El-Jardali F, 2017) . The accreditation process exposes managers to new ideas, research findings, and innovative approaches to healthcare management. Establishing comprehensive systems for governance, leadership, and staff development is a standard requirement of accreditation programs. Managers receive education and training to bring their skills in line with accreditation standards. This training helps administrators acquire expertise in areas such as financial management, strategic planning, quality improvement, and effective communication (Mrayyan, et al, 2022).
In addition, accreditation programmes promote accountability
and quality improvement in healthcare organisations. It is strongly recommended that managers analyse data, identify performance disparities, and implement interventions supported by empirical evidence. This iterative process fosters a continuous improvement mindset among managers, thereby augmenting their decision-making and problemsolving skills. A'aqoulah, et al (2016)
In addition, accreditation programmes enhance the leadership abilities of healthcare administrators. Leadership is necessary for influencing organisational culture, motivating employees, and fostering change. (Mansour , Boyd , Walshe,2021 ). The accreditation process exposes managers to leadership models, best practices, and the significance of employee engagement.
Accreditation programmes frequently emphasise the establishment of comprehensive leadership structures, including the identification and development of future leaders (Mrayyan, et al, 2022. It is encouraged that managers participate in leadership development programs, mentoring relationships, and professional networks (Gyani (2012). These opportunities enable managers to develop their leadership skills, obtain exposure to diverse perspectives, and learn from the experiences of other leaders in their field (Mansour , Boyd , Walshe,2021 )..
In the context of accreditation programs, leadership development assists managers in becoming effective agents of change (Shaw, 2013). They are taught how to navigate complex healthcare systems, lead multidisciplinary teams, and cultivate a culture of collaboration and innovation. By encouraging leadership development, accreditation programmes contribute to the overall effectiveness and success of healthcare organisations(Mrayyan, et al, 2022).
In the healthcare industry, accreditation programmes improve organisational efficacy. Effective managers who have undergone training and development through accreditation processes are better able to align their organisations with accreditation requirements (American Society for Healthcare Risk Management, 2018). This alignment assures compliance with evidence-based practices, which leads to improved patient outcomes, fewer errors, and increased patient satisfaction (Mrayyan, et al, 2022).
Frequently, accreditation programmes mandate the implementation of quality improvement mechanisms and the monitoring of key performance indicators (Alkhenizan, & Shaw, 2011). Managers play a crucial role in the implementation of these mechanisms, the monitoring of performance data, and the promotion of improvement initiatives (Katoue MG, Somerville, Barake, 2021). Managers contribute to enhanced organisational performance by actively pursuing quality enhancement (Pomey, et al,2010).
Accreditation programmes in healthcare not only focus on clinical standards but also have a significant impact on the quality of managers within organisations. These programmes contribute to the development of managerial skills and leadership abilities, fostering a culture of continuous improvement and accountability. Effective managers, trained and developed through accreditation processes, play a crucial role in aligning organisations with accreditation standards, driving organisational performance, and improving patient outcomes. By recognizing the importance of accreditation programmes in enhancing the quality of managers, healthcare organisations can further strengthen their leadership capabilities and overall effectiveness in delivering high-quality care.
Abdullah Algunmeeyn holds a PhD degree in nursing specialised in Nursing Administration and Leadership and Quality Management graduated from University of Nottingham, UK. Currently he is working as an Assistant Professor of Nursing within the School of Nursing at Isra University. He is engaged in Nursing research and his researches mainly in the field of nursing management

Establishing comprehensive systems for governance, leadership, and staff development is a standard requirement of accreditation programs.

Current medicine for inflammatory bowel disease (IBD) is poor, characterised by misdiagnoses, late diagnoses, and guesswork. This pain arises from the lack of effective IBD biomarkers. However, this picture is changing with the development of new, reliable precision medicine biomarkers that could significantly advance the care of IBD patients.
Cindy Weiss, PPI Lead and Design, Avenna Ltd
Nina Skorytchenko, CEO, Avenna Ltd Daryl L Fernandes, Chief Executive, Ludger Ltd; Chief Science Office, Avenna LtdCaroline’s fraught IBD journey

Meet Caroline, one of our life-course models for the 5M-diagnosed IBD patients across the globe, and the additional 5M people who we estimate live with IBD, but are currently undiagnosed. Caroline is a citizen of the United Kingdom, a nation with one of the most advanced medical Care Process systems in the World. Despite this, Caroline’s health journey has been a long, painful odyssey, beset with medical mistakes. These have affected not just her, but her whole family.
Caroline’s IBD symptoms first appeared at age 13, when she suffered constant episodes of diarrhoea and experienced significant weight loss. Her general practitioner misdiagnosed her as having irritable bowel syndrome (IBS), a condition experienced by between 10 per cent to 20 per cent of the UK
population. The misdiagnosis arose because Caroline tested negative for Faecal Calprotectin (FCP). FCP is now one of the main medical assays used in primary care to identify IBD suspects, having undergone many improvements over the past decade. However, at the time that Caroline was tested, the
FCP test was insufficiently reliable. Believing that the root of her illness was psychological, Caroline’s GP referred her to a counsellor who specialised in eating disorders. This further delayed the appropriate diagnosis and treatment.

Caroline’s health did not improve significantly with the counselling. Disillusioned by conventional medicine, Caroline´s parents sought help from complementary and alternative healthcare practitioners. Over the next six years, five different practitioners diagnosed Caroline variously as having IBS, coeliac disease, and Candida overgrowth. It wasn’t until she turned 19 that Caroline tested positive for FCP. At that point her doctor, finally, referred her to a gastroenterologist for further investigation. Through the use of endoscopy and histology on her gut biopsies the specialist diagnosed Caroline as having Ulcerative Colitis (UC). This is one of the two most common forms of IBD, the other being Crohn’s Disease
(CD). The long delay in Caroline’s proper diagnosis and treatment meant that she had suffered inflammatory episodes that caused significant destruction to bowel tissue. The damage was so severe that, at age 21, Caroline had to have part of her colon surgically removed. Then, ten years later another consequence of delayed treatment became apparent — Caroline was diagnosed with colorectal cancer (CRC), which is now ranked the second leading cause of sickness and death by cancer across the globe.
IBD manifests as a series of uncontrolled fires, progressively destroying gut tissue and causing a range of distressing symptoms including severe constipation, uncontrolled diarrhoea, episodes of gut inflammation (so-called ‘IBD flares’), abdominal pain, rectal bleeding, rectal ulcers, extreme fatigue, and depression. Currently, there is no cure for IBD. Medics typically manage patients’ symptoms with antiinflammatory therapeutics and turn to
surgery to remove irreparably damaged sections of the gut. Those IBD patients with severe, long-term gut inflammation have significantly increased risk of developing CRC — so Caroline’s chances of getting cancer were greatly elevated by her late diagnosis and treatment.
Caroline’s story is relevant to the growing number of Asians at risk from IBD. Once thought to be a disease of the West, IBD is increasing across Asia – particularly in rapidly-industrialising countries such as China, which now has the highest number of prevalent IBD cases in the World. There is a further problem — Asians typically suffer from a more complex form of IBD than Caucasians, with higher levels of peri-anal complications. Our analysis is that within the next decade IBD will become a very serious health problem across continental Asia, with the most economically advanced countries suffering the highest burden of disease.
IBD patients and gastroenterologists urgently need better IBD biomarkers
Caroline is one of an estimated 10 per cent of IBD patients who were previously misdiagnosed as having IBS. Misdiagnosis is one of seven types of failure in clinical decision-making that we have identified within the patient care pathways for IBD in the UK and every other country we have investigated. The errors occur across all stages of IBD progression, spanning both primary and secondary care. We investigated why these medical mistakes are so common. Our conclusion was that they arose largely from a lack of reliable tests for the detection of changes in IBD-specific chronic inflammation (cI) that occur during disease progression. Instead of measuring cI, most inflammation markers such as hsCRP that are commonly employed by healthcare professionals to monitor IBD actually estimate levels of acute inflammation (aI). This is because aI produces large,
highly variable molecular signals that overshadow the smaller, steady signals from cI processes. To use an analogy, cI is like the climate and aI is like the weather — it’s difficult to measure climate change because the weather gets in the way.
Increases in aI signals are indirectly associated with IBD and can be caused by many conditions other than IBD. As a result, the current aI-based IBD biomarkers have low sensitivity and specificity for IBD i.e,. they are imprecise and unreliable because they measure the wrong things.
IBD is not the only condition where aI-based clinical biomarkers are being used to detect a cI-driven disease. Similar phenomena occur with other chronic inflammatory diseases. Consequently, cI in IBD and many other cIDs can increase steadily over many years, but is invisible to patients and their medics. In a significant proportion of cases, IBD-related cI only becomes noticed when the patient’s symptoms are so severe that they’re referred to a gastroenterologist. Regarding FCP, the guidance on that biomarker’s use to distinguish IBD from functional gut disorders in primary care is becoming clearer. However, the diagnosis of patients with gastrointestinal alarm symptoms and identification of IBD suspects is still complex. Given this, there’s an urgent need for better diagnostic tools for IBD.
We believe that those could be provided using a precision medicine approach.

The Human Genome Project (HGP) ushered in the age of Precision Medicine (PM). The promise was that knowledge of an individual’s genome would help us to predict what diseases they could get and how to cure them. We now know that an individual’s genome shapes their disease risk profile but does not predetermine health across their life course. Also, our ability to understand how genes relate to health outcomes is still limited. For example, around 240
gene loci are now known to be associated with IBD — but this explains at most 25 per cent of the heritability of IBD variants. There is a further complication. Studies over the past three decades show that genes interact in complex ways with many other factors to shape an individual’s health trajectory. For IBD patients, those factors include environmental parameters, the gut microbiome, food, movement, sleep, circadian and other body rhythms, and both mental and physical stress. Accordingly, today’s version of precision medicine encompasses a multidisciplinary approach to understanding the complex networks of interactions that underlie the generation and progression of chronic conditions. PM’s original promise has now turned into a premise i.e., knowledge of the aetiology (i.e. causal pathways) for a disease allows us to detect and track its progression in individuals at risk, and could also help us to identify therapeutic targets and develop effective therapies that tackle root causes, not just alleviate symptoms.
The first step in a PM approach to IBD is to realise it’s a syndrome — a collection of diseases with different aetiologies but that share common symptoms that include episodes of gut inflammation. All IBD variants are chronic inflammatory diseases — so understanding the changes in the immune system that occur with their progression over long time periods is central to PM approaches to their management. IBDXTM™, PredictSure IBD™, and GlyHealth-IBD-Escalate™ are three novel IBD PM blood biomarkers that exploit such changes.
IBDX, from GlycoMinds (https:// www.glycominds.com/), is a panel of six solid-phase enzyme-linked immunosorbent assay (ELISA) kits, each of which detects the serum level of a specific anti-glycan antibody that is a potential serological biomarker for IBD development. The kits are used in combination to probe a patient’s blood. The resulting multi-marker profiles are
Chronic inflammation (cI) is like the climate and acute inflammation (aI) is like the weather—it’s difficult to measure cI because aI gets in the way.
used (a) to aid differential diagnosis of IBD vs. non-IBD and CD vs. UC and (b) for Crohn’s disease prognosis. For CD prognosis, the number of positive IBDX antibody results correlates with the probability of Crohn’s Disease progression in the individual. For patients positive for three or more IBDX antibodies, 90 per cent are likely to have complicated disease and 80 per cent are likely to require abdominal surgery.
PredictSURE IBD, from PredictImmune (https://www. predictimmune.com), is another PM IBD biomarker for Crohn’s disease prognosis. The system is a serological test that estimates the level of CD8+ T-cell exhaustion, which correlates with the severity of the future disease course. The parameters measured are the expressions of 15 specific target genes plus 2 controls. This is performed using quantitative polymerase chain reaction with reverse transcription (RT-qPCR).
GlyHealth-IBD-Escalate (GIE) is a prognostic and predictive biomarker of IBD. The technology is being co-developed by Avenna (www.avenna. com) and Ludger (www.ludger.com) — sister companies based near Oxford in the UK — and the Translational Gastroenterology Unit at the University of Oxford. GIE is based on quantitative measurement of glycomics patterns in an IBD patient’s blood that we have shown correlate with IBD flare progression. The patterns of interest are prodromal signals of developing IBD flares i.e., they can be detected before signs of gut inflammation are visible by endoscopy. The results from retrospective clinical studies are promising, with GIE reliably predicting the likelihood that a newlydiagnosed IBD patient would need treatment escalation within 18 months of testing. Although it’s still early days, the preliminary results for GIE as a potential predictor of an IBD patient’s response to specific anti-inflammatory biologic drugs have been encouraging too. We are now preparing to test the performance of GIE in real-world
clinical settings, the first prospective study being with gastroenterologists at the IBD clinic in St. Mark’s Hospital, London which specialises in the care of patients with bowel diseases.
These new PM IBD biomarkers, and others being developed, have the potential to impact two critical areas of IBD care: (a) greatly enhancing clinical decision-making, particularly for treatment personalisation, and (b) helping to move diagnosis and treatment from late to early action. However, like most PM technologies, these have been developed in R&D labs and there are many hurdles to overcome in order to translate them into reliable, everyday medical tools for use in busy clinics. The challenges we as developers face include ensuring that: we can generate convincing evidence that the real-world performance of our biomarkers are as good as we claim; we can thoroughly test
the technologies with diverse groups of patients, including people of different ethnicities; we can meet all the regulatory hurdles for medical diagnostics; our biomarkers are straightforward to use; medics will adopt our technologies; we can manufacture and support our technologies at national scales; our technologies are demonstrably costeffective; and that healthcare payers will reimburse clinics for use of our biomarkers. Of course, these challenges also prevail for every medical technology in widespread use today — so we won’t complain. Fortunately, we can get help and advice for our technology translation journeys from precision medicine accelerator programmes and specialist organisations such as Crohn’s & Colitis Foundation. If we succeed then, in future, patients living with IBD across the globe will, we believe, have much better IBD journeys than that experienced by Caroline. References are available at www.asianhhm.com
Cindy Weiss (PPI Lead and Design, Avenna Ltd BA Product and Industrial Design). Cindy works on design and process optimisation for GIE and IF biomarkers and PPI for the IBD and AvLB PM programmes. Cindy joined Avenna in 2020 and oversees Human-Centred-Design for the commercial and medtech products.
Nina Skorytchenko (CEO, Avenna Ltd and Wellcode Life; MSc, ESCP-Business School, MA, BSc. http://linkedin.com/in/nina-skorytchenko), has a background in finance (Nomura, Bloomberg) and scientific wellness businesses. She leads the commercialisation of the GIE and the Immunofrailty assays, regulatory strategy, and development of our networks of clinical collaborators and translation partners.


Daryl L Fernandes (Chief Executive, Ludger Ltd; Chief Science Office, Avenna Ltd; D.Phil (Biochemistry, Oxon); http://uk.linkedin.com/pub/ daryl-fernandes/1/637/95) is one of the pioneers of the field of glycomics for precision medicine and is the architect of the GlyHealth programme to support the early detection, tracking, and mitigation of chronic inflammatory diseases.


Using ambulatory ECG recordings, heart rate variability measurements can analysed e the autonomic nervous system by the spontaneous behavior of successive heartbeats. All heart rate variability parameters reflect vagal modulations modified by adrenergic impulses. A more direct representation of the two branches of the autonomic nervous system can be obtained using geometric methods.
Jean-Marie Grégoire, Clinical Cardiologist, Department of Cardiology, UMONS (University of Mons) Cédric Gilon, PhD Candidate, Free University of BrusselsTraditional dogma regarding the autonomic control of cardiac function suggests that the heart is reciprocally regulated by the sympathetic and parasympathetic divisions of the autonomic nervous system (ANS), directly under the influence of the central nervous system. At the level of the heart, the regulation is done through the intrinsic cardiac nervous system. New techniques of neuromodulation of the ANS are being developed, and
it seems interesting to measure their effects. This can be done by analyzing the heart rate variability (HRV). Several methods can be used to analyse the information contained in the succession of heartbeats, which can be considered as a time series. We propose to review these methods.
Statistical methods, also called temporal, are the most obvious to use. The calculations are based on the NN complexes. The basic parameters of the HRV are estimated by the SDNN, which is the calculation of the standard deviation of the sequence of sinus intervals measured by the NN distance during a certain period. The SDNN reflects the entirety of the components responsible for HRV during the recording period. Sinus intervals should be clearly differentiated from premature intervals because the existence of premature beats distorts the results of calculations, especially if they are numerous (more than 1 per cent). HRV results in ANS assessments may
be biased if HRV is analysed without eliminating ectopic beats. Interpolation is the recommended correction method. It consists of replacing abnormal RR intervals with an interpolated RR interval. Interpolation methods include zero order, first order, spline, and nonlinear predictive interpolation.
SDANN is the standard deviation of the average NN interval calculated over short periods of time, usually 5 minutes. RMSSD (root mean square of successive differences) and pNN50 (percentage of consecutive normal sinus RR intervals greater than 50 ms) allow estimation of vagal tone.
3. Spectral analysis
Additional information contained in the sequence of RR intervals can be extracted using spectral methods. The transformation of time into frequencies allows to infer the evolution of the parasympathetic (vagal) and orthosympathetic (adrenergic) branches of the ANS and to analyse their participation in the triggering of some cardiac rhythm disorders (Figure 1 and 2).
The first use of the frequency spectrum corresponding to the oscillations of cardiac control systems was made by Sayers in a pioneering work performed to quantify the physiological origins of HRV. He showed that sinus rhythm responds to both linear and nonlinear laws and that the three main influences were the respiratory rate, blood pressure and temperature variations.
One of the keys to understanding ANS activity is the greater speed of vagal activity (on the order of 500 msec, which allows it to exert beat-to-beat control) compared to adrenergic reactivity (on the order of several seconds).
a. Spectral bands from 0.04 to 0.40 Hz
The HF and LF bands form the largest part of the signal for short recording times (of the order of a few minutes). Frequencies above 0.04 Hz are mainly due to sympathetic or parasympathetic control mechanisms.

i. The LF band: 0.04-0.15 Hz
The LF band represents at least part of the adrenergic activity. It is related to the baroreceptor reflex. Thus, a portion
of the LFs comes from vagal activity because this reflex is mediated by the vagus nerve. The vagal or adrenergic contribution to the LF band is highly variable depending on the position and activity of the subjects. Interpretation of LFs as solely representative of adrenergic activity should be avoided.
ii. The HF band: 0.15-0.40Hz
Because the sympathetic system is relatively slow, it cannot generate significant fluctuations at frequencies above 0.15-0.20Hz, and therefore all neural contributions to the HR spectra at higher frequencies are essentially
parasympathetic in origin. The HF band represents respiratory-related vagal activity, as most authors agree.
iii. The LF/HF ratio
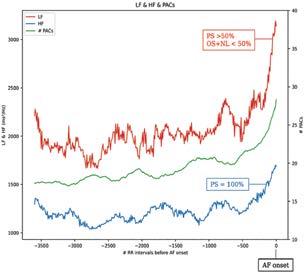
Because of the complexity of the relationship between the vagus nerve and the adrenergic system, it is hazardous to draw conclusions from this ratio alone. The terms "autonomic modulations" and "responsiveness of the ANS to various influences" should be used instead.
b. The VLF band: 0.003-0.04 Hz
The meaning of VLFs is not clear: these frequencies could correspond to slower
Figure 2: A sample of the spectral analysis corresponding to the plot in Figure 1. We can clearly see the decomposition of the spectrum into high frequencies (HF) in blue, corresponding to parasympathetic activity, and low frequencies (LF) in red, corresponding to a mixture of sympathetic (OS), parasympathetic (PS), and nonlinear (NL) activities. The green trace corresponds to premature atrial contractions (PACs). The 0 point of the abscissa corresponds to the beginning of the atrial fibrillation (AF) episode. It is easy to see that the activity of the ANS branches increases significantly just before the onset of AF.
influencing rhythms such as hormonal rhythms and thermoregulation. It could also be aliasing and artefacts due to non-stationarity of the signal over longer periods.
c. The VHF band: (0.4-0.9Hz)
The literature concerning the very high frequency (VHF) of 0.4-0.9Hz in HRV is scarce. After heart transplantation the new sinus node is completely denervated and marked VHF peaks can be observed.
4. HR turbulence (HRT)
The turbulence phenomenon is a biphasic
baroreflex-mediated HR response manifested by changes in HR in response to ventricular premature beats. It is quantified by two indices: turbulence onset, reflecting the initial HR acceleration after a premature ventricular beat, and turbulence slope, corresponding to the subsequent HR deceleration. At least 5 ventricular premature beats are required to calculate turbulence. Unlike HRV, which shows autonomic activity during sinus rhythm, HRT reflects autonomic responses to endogenous interference.
5. Deceleration capacity: phase-rectified signal averaging algorithm
Figure 3: Second Order Difference Plots: Division of SODP in 16 different regions (in red). The x-axis and y-axis values are given in milliseconds. Blue dots correspond to ∆RR values. Detailed analysis of the plots reveals the number and magnitude of accelerations and decelerations of the heart rate. The changes in rhythm reflect the pulsatile activity of the autonomic nervous system (e.g. top-right quadrants reflect decelerations, bottom-left quadrants reflect accelerations of the heart rate).
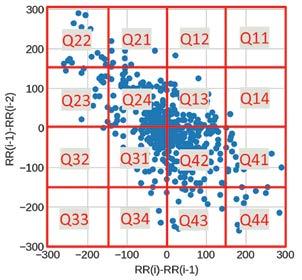
It is possible to overcome the problem of non-stationarity of long duration ECG recordings by averaging phase-rectified signals (PRSA for Bivariate phase-rectified signal averaging). This algorithm allows separate characterisation of HR deceleration and acceleration over long recording times.
The sequence of heartbeats can be considered a dynamic system that responds to linear and nonlinear laws. Although non-linear methods have contributed to the technical understanding of the
characteristics of the HRV signal, their success in developing new clinical tools remains very limited. These methods are based on the demonstration that the heart rhythm exhibits deterministic chaotic behaviour.
The bispectrum provides information on the phase relationships between frequencies. Higher order spectra (HOS) can be defined for deterministic signals but also for random processes. They can identify nonlinear systems. Their main interest lies in their ability to extract information not revealed by spectral methods. Their added clinical value has not yet been demonstrated.
The term dynamic simply refers to phenomena that evolve over time. The succession of heartbeats presents a temporal evolution and as such, follows the laws of dynamic, deterministic, non-linear systems. There are many indicators that allow us to assess the evolution and fluctuations of the heart rhythm. The entropy measures the rate of generation of new information. Detrended fluctuation analysis quantifies the short-term fractal properties of NN intervals. The Lyapunov exponent gives an idea about the predictability span of the events.
The main advantage of geometric methods is their relative insensitivity to the analytical quality of the series of intervals between heartbeats. Their implementation in an algorithm is easy and they have a low algorithmic complexity.
Those maps are indifferently called Lorenz or Poincaré plots, first return maps, recurrence graphs. They are
scatter plots showing the R-R intervals as a function of the previous R-R intervals. Their use has been suggested as a simple way to visualize HRV. These graphs allow the visualization of the global aspect of the rhythm, and their automatic recognition is likely to be used to facilitate the analysis of big data of ECG recordings acquired by mobile health applications.
The interval variation diagram second order difference plot (SODP) is constituted by the differences of the RRs compared to the previous differences (Figure 3). The different number of points in the four quadrants clearly shows that there is a heartbeat
dynamic that escapes traditional spectral analysis. SODPs can selectively measure parasympathetic activity over short duration of recordings, a difference from the PRSA algorithm which measures parasympathetic activity over longer periods of time on the order of 24 hours.
All HRV measurements essentially reflect the modulations of the vagus nerve modified by the impulses of the adrenergic system. Measurements performed over long periods provide information on individual basal autonomic status. Spectral measurements performed over short periods (usually 5 minutes) provide information on the dynamics of systems that disrupt this basal balance and may be part of the triggers of arrhythmias. Graphical methods will play an important role in e-cardiology networks, such as first return maps and difference plots, which allow rapid screening for AF. Although mathematical and computational techniques make it possible to manipulate the ECG signal to extract information and use it in predictive models, their explanatory power remains elusive. Inferences about ANS activity from these models must remain cautious.
References are available at www.asianhhm.com
Grégoire Jean-Marie, MD, PhD, is a clinical cardiologist and a researcher at IRIDIA, the artificial intelligence research laboratory of the Université Libre de Bruxelles. His area of interest is rhythmology and dynamical systems. He is currently applying neural networks to predict atrial fibrillation.

Cédric GILON is a PhD Candidate at Université Libre de Bruxelles in Belgium. His main research interest is Artificial Intelligence (AI) medical and industrial applications. His thesis explores the use of artificial intelligence models for the detection and forecast of atrial fibrillation, the most common heart arrhythmia.

One of the keys to understanding ANS activity is the greater speed of vagal activity compared to adrenergic reactivity.

Integration of mental health into primary care improves patient outcomes and makes medical practice more satisfying. Primary healthcare is intended to improve the overall health and well-being of a community.
Tanjina Ashraf Khan Mou, CEO & Mental Health ProfessionalThe main purpose of primary healthcare is to improve people's health by facilitating access to medical care. It also focuses on the individual as a whole rather than the disease of a specific organ or a particular concern. This system is intended towards improving overall health and wellbeing of a person in a community by preventing or resolving health problems that exist or may exist. It basically refers to care that is focussed on the needs of a population and can be accessed easily by a certain community. Oftentimes, the physical healthcare services like: treatment for common illnesses, cancer-related treatments, management of diabetes and heart disease and prevention of future health through advice, immunisation and awareness programmes are the basis of primary healthcare and are prioritised depending on the needs of the families. Hence, mental health, behavioral health and emotional health etc. becomes secondary or tertiary even though it is well-recommended by WHO (WHO,2001).
Mental disorders affect millions of individuals across the world and, if left untreated or unmanaged, create an enormous toll of suffering, pain and even economic loss. Concurring withNational Institute of Health (nd), persistent ailments such as cancer, heart conditions, or even diabetes might lead to psychological conditions. Despite research showing positive
results of mental health therapies, it continues to get low priority. Only a small minority of people receive even the most basic treatment. Now, this could be lack of awareness and more obviously the lack of availability within primary healthcare services. Most of the mental health services provided are limited in nature and often considered secondary or tertiary
healthcare. At primary healthcare level, there is still inadequacy that requires urgent attention.
Fully integrating mental health in primary care is the gold standard for care as it is one of the most practical and applicable means of closing the treatment gap and ensuring that every individual receive the healthcare they need as a whole. It ensures that everyone has the opportunity to address both their physical and their mental health needs as a part of primary care.
Benefits of integrating mental health services in primary healthcare
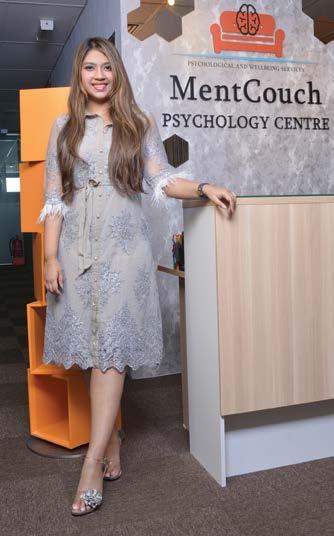
There are numerous examples of successful applications and practices where primary healthcare and mental health professionals have come together to integrate physical and mental health provision. There are several beneficial aspects that come out, some of which include:
• Having mental health professionals in the loop, provides opportunity for psychological support at an early stage, helping to secure improvements in both physical and
mental health in the initial stages. Hence, a better and faster recovery process can take place.
• A reduction in stigma related to mental health disorders can be seen when it is prioritised and made easily available as physical health services.
• Since majority of primary care related services are not related to any particular disease or conditions, stigmatisation is further diminished when looking for psychological assistance from a primary care provider, because it comes as a holistic package, making this level of care more worthy as a whole.
• Research shows that behavioural therapies help improve patients’ physical health outcomes before or after operations or therpaies. This helps patients become more resilient. This holistic support can also help patients to self-manage their long-term conditions more confidently.
• The availability of mental health therapy in primary care settings means people can expect to be treated for common conditions such as anxiety or depression at the same time with their physical health needs.
• It fulfills the promise of primary care as a holistic approach.
• Talk therapies and group discussions can be readily available and people will learn to socialise as well as self-manage in the form of sharing sessions.
• As stated in Mental Health Family Medicine Journal (nd), mental health is often comorbid with many physical health problems such as cancer, HIV/AIDS, diabetes and tuberculosis etc. When primary healthcare providers are equipped with psychological trainings, they would be able to diagnose and examine the basic issues related to mental health. Also, they would be able to better understand physical health needs of people with mental concerns along with the psychological needs of those suffering from chronic illnesses.
• Primary healthcare specialists are frontliners, making them the foremost level of contact for any individual seeking diagnosis. Preparing these workers with mental wellbeing aptitudes can advance a more all encompassing approach and guarantee better prevention as well as early detection of mental health disorders or concerns.
Tanjina Ashraf Khan Mou is an award winning, certified mental health professional, writer, entrepreneur and CEO of one of the leading private psychology centers in Kuala Lumpur, Malaysia. As an integrative therapist, she possesses a solid foundation in a wide variety of theoretical approaches and over time has developed her own way of working as a result. Tanjina specializes in positive psychology methods, resilience training, behavior analysis, mindfulness based therapies and has been actively advocating mental health and wellbeing for the past 4 years worldwide.

Exercise can have a significant role in managing chronic health issues, especially considering that most chronic ailments can only be managed by medications and not cured. By examining various health issues such as obesity, diabetes, hypertension, osteoarthritis, chronic pain, and some mental health disorders, we uncover the power of regular exercise in improving these conditions. Exercise offers a healthier and more sustainable approach to weight loss compared to medications or strict diets. It can lead to diabetes remission, reduce complications, prevent and reverse hypertension, improve joint function and pain, and even positively impact mental health disorders. Furthermore, exercise benefits brain health and lowers the risk of dementia, Parkinson’s, cancer, and more. Embracing exercise as a lifestyle change is crucial for individuals to enhance their overall well-being and pave the way for a healthier life.
Saint-Vil, Medical Director, Sports Medicine Department, Marietta Memorial HospitalAcute health issues like infectious conditions and acute trauma do not last long. Such health issues require immediate help. Though some acute issues might be life-threatening, people emerge as more resilient after recovering from these issues. However, chronic illnesses are different. They develop slowly over time and last several months or even a lifetime. In most cases, chronic health issues like osteoarthritis, diabetes, hypertension, dementia, and many more keep progressing, causing continuous pain and distress.
Modern medicine focuses much on managing acute and life-threatening illnesses. There are numerous lifesaving drugs to help. This has also helped increase the human lifespan considerably. However, despite decades of efforts in developing more effective medications
for chronic ailments, managing chronic diseases remains challenging due to limited pharmacological options for chronic illnesses. In the case of chronic diseases, modern medicine is either entirely helpless or can provide symptomatic treatment at best; it can help keep the condition more or less under control.
Since medicine cannot cure most chronic health issues like hypertension, diabetes, osteoarthritis, Parkinson’s, depression, and many others, a person has to live with these conditions for years. Therefore, chronic diseases result in a significant decline in the quality of life.
One of the reasons so many people continue to live with chronic disorders is that they keep taking medications to suppress their symptoms. However, they make little effort to overcome chronic ailments.

Overcoming chronic ailments require significant lifestyle changes, which many, if not most, fail to make. It means making significant dietary changes, sleeping well, practicing mindfulness, and above all, starting moving more beginning doing exercise. Exercise is known to benefit most chronic ailments, and below we look at some health issues that can be significantly managed with regular exercise.
One of the biggest reasons why the world is becoming unhealthier and developing so many chronic health issues is obesity. In developed nations like the US, 70 per cent of adults are either overweight or obese. And, yes, it is now regarded as a disease and not merely a risk factor for other health issues like diabetes or heart disease.

Of course, some pills help with weight loss, but you regain weight as soon as you stop taking those pills. Not to say that medications may cause much harm. A strict diet would also help, but if you go too harsh, it may cause nutritional deficiencies.
Therefore, exercise is the healthiest and most natural way for weight loss. You do not need to spend hours in a gym to lose body weight; it is crucial to get started. Even 15 minutes a day can be life-transforming. However, aim for
in the long run.
In the US, about 11-12 per cent of adults live with diabetes, and another 35 per cent are prediabetic. Of course, wrong dietary measures are among the most important causes of diabetes. However, lack of physical activity is also among the primary reasons.
There is no known drug or medication that can cure diabetes. Medications can just lower blood sugar levels and delay the development of diabetes-related complications. However, if started early enough, exercise can lead to diabetes remission. Aerobic exercise combined with some resistance training is the right way to overcome diabetes.
Not only can it help with diabetes remission, it may even help with diabetesrelated complications like neuropathies, muscle wasting, heart issues, and more. Those who exercise regularly, or at least five times a week, are highly unlikely to develop diabetes. Even if you develop diabetes, exercise is the best way to get control over it.
Need proof? Then look at the study, which says that 80 per cent of those diagnosed with type 2 diabetes may reverse it through weight loss and exercise within six months. However, regretfully, most people would prefer taking pills daily to exercise.

Exercise is your best bet whether you are at risk or living with hypertension. It is the most effective natural way to eliminate the so-called ‘silent killer.’ Doctors call it a silent killer as it does not cause many symptoms in the early stages, but it significantly increases your risk of heart disease and stroke in the long run.
Studies show that even 30 minutes of exercise five days a week prevents hypertension and even reverses mild hypertension. Combining 30 mins of aerobic exercise with three days a week of resistance training is also good. In fact, a single session of continuous exercise for 30 minutes can lower your blood pressure for about 24 hours and by about 5mmHg, and it is called post-exercise hypotension.
Globally about 16 per cent of adults are living with osteoarthritis alone. But do not forget that it is just one kind of joint disorder. More than one-fourth of adults are living with significant joint pain. Painkillers help reduce pain and inflammation. However, exercise is the only way to alter the course of these health issues. American Family Physician findings say exercise can significantly reduce pain and improve joint function.
Pain is the most common reason for people to seek medical attention. Unfortunately, millions of adults are living with chronic pain. They may have low back pain, body aches, headaches, etc. Widespread pain is making the opioid crisis worse in the US. Yet, such strong painkillers like opioids only provide temporary relief, and they do almost nothing to change the course of the disease. Therefore, if you want to get rid of chronic pain, remember that regular exercise is the best option.
Anxiety and depression are becoming all too common. Most people would experience these issues in life. Pharmacological pills can only help a bit with these mental health disorders. That is why all wise men say that money cannot buy happiness, as all that money

can afford are pills that often fail to help. However, happiness can be earned by practicing mindfulness, socializing, and exercising regularly.
Above is just an example of how exercise is the best remedy for some of the widely prevalent chronic health issues. However, remember that exercise would reduce your risk or even help overcome any chronic health issue. Exercise is also good for brain health, lowering the risk of dementia, Parkinson’s, cancer, and much more. So, to stay healthy, start moving, and begin exercising.
References are available at www.asianhhm.com
Saint-Vil is the founder of the ExerciseNow.org platform and the Medical Director of the Sports Medicine department at Marietta Memorial Hospital. He is a fellowship-trained Sports Medicine physician and a published researcher who has published countless articles promoting healthy lifestyles on Sports Medicine and fitness-related topics. He believes exercise is the best health insurance. Among his academic interests is Platelet Rich Plasma's use to regenerate tendons, ligaments, cartilage, and other soft tissues


In India, teleconsultation and tele-treatment have transformed the management of chronic diseases by overcoming the problems of healthcare accessibility and resource scarcity. This article investigates how teleconsultation affects accessibility, patient outcomes, and healthcare effectiveness. To provide patients with comprehensive care, it examines the role of tele-treatment in remote monitoring, medication management, and lifestyle coaching. The article also discusses the difficulties of managing chronic diseases in India and how teleconsultation helps. In addition to virtual consultations, virtual access to specialists, and its implications for prompt interventions and continuity of treatment, it covers the function of teleconsultation in distant diagnostics. It also examines potential developments and effects, including the use of developing technologies and AI. The article's conclusion highlights the revolutionary potential of teleconsultation while taking ethical and statutory considerations to make healthcare more patient-centric and accessible.
Arindam Sen, Director, i2i TeleSolutionsTeleconsultation, a cutting-edge field within healthcare services, offers remote consultation, diagnosis, and tele-treatment, benefiting both patients and healthcare professionals. This innovative approach provides enhanced accessibility to individuals with limited healthcare access especially in the rural parts of India, enabling them to receive necessary treatment and diagnosis without the need for travel. For individuals with chronic health conditions such as cardiac and kidney patients, this technological advancement proves invaluable by expediting their treatment processes and improving overall healthcare outcomes.
According to a 2021 World Health Organization (WHO) Report, India's healthcare system faced a substantial shortage of doctors, falling below the recommended ratio of 44.5 healthcare workers per 10,000 population in 2018 and only slightly exceeding the 2006 standard of 22.8. This significant deficit in the number of doctors required to meet the population's needs emphasises the challenge of healthcare accessibility. Teleconsultation emerges as a crucial solution, bridging the gap between doctors and patients and offering a way to overcome the healthcare accessibility challenge in India.
The Rising Relevance of Remote Diagnosis and Tele-Treatment in Chronic Disease Management:
• Chronic diseases pose significant challenges to patients and healthcare providers, requiring ongoing management and care
• Remote diagnosis and tele-treatment offer solutions to these challenges by leveraging technology to bridge the gap between patients and healthcare professionals
• The prevalence of chronic diseases and the need for long-term management make remote diagnosis and teletreatment increasingly important for improving patient outcomes.
Impact of Teleconsultation in Chronic Disease Management:
• Teleconsultation enhances accessibility, eliminating travel requirements and enabling timely diagnosis and treatment for patients with limited access to healthcare services
• Remote monitoring, medication management, and lifestyle counselling through teleconsultation improve disease management for patients with chronic conditions
• Teleconsultation saves time and costs by reducing the need for frequent hospital visits, benefiting both patients and healthcare systems
• By serving a larger number of patients efficiently, teleconsultation decreases waiting times for consultations and treatment, increasing overall healthcare efficiency
• Teleconsultation empowers patients by providing access to medical information, educational resources, and personalised care plans, fostering their active involvement and engagement in the treatment process.
The Transformation of Chronic Disease Management through TeleTreatment:
Tele-treatment is a transformative
approach that revolutionises chronic disease management by leveraging technology to remotely deliver healthcare services. It encompasses various approaches such as remote monitoring, medication management, and lifestyle counselling to provide comprehensive care to patients. The significance of tele-treatment lies in its ability to enhance disease control, reduce hospital visits, and ultimately improve patient outcomes.
Approaches in Tele-Treatment:
Remote Monitoring: Remote monitoring allows healthcare providers to track patients' health parameters from a distance using wearable devices and remote monitoring tools. This enables continuous monitoring of vital signs, blood glucose levels, or medication adherence, facilitating early detection of deviations and timely interventions.
Medication Management: Through tele-treatment, medication management utilises technology to assist with prescription management, medication reminders, and remote consultations. Patients receive timely reminders and education to ensure medication adherence and minimise errors, while healthcare providers remotely assess effectiveness and make necessary adjustments for optimised treatment outcomes.
Lifestyle Counselling: In teletreatment, lifestyle counselling offers personalised guidance and support to help patients make positive lifestyle changes. Virtual consultations provide advice on diet, exercise, stress management, and more, empowering patients to take control of their health through ongoing support and motivation from healthcare providers.
• Limitations of traditional in-person consultations: Traditional in-person consultations in India face limitations due to geographical barriers and
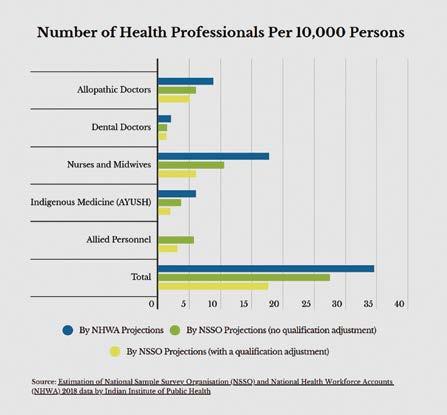
travel distances, time constraints for patients, lack of specialist availability, and challenges in follow-up and realtime monitoring of patients' health status.
• Challenges faced by healthcare providers: In India, healthcare providers face challenges of increased patient load, limiting individual consultation time, and lack of interdisciplinary care due to coordination issues among different disciplines. Additionally, limited resources and infrastructure, especially in rural areas, hinder effective chronic disease management with a shortage of specialised clinics, diagnostic equipment, and trained professionals.
• Difficulties faced by patients: Limited access to quality healthcare and specialists in remote regions,
along with a lack of awareness and education among patients, contribute to challenges in managing chronic diseases in India. Financial constraints and non-adherence to treatment plans further hinder effective management, leading to delayed diagnosis, inadequate self-care, and poor outcomes.
According to the Health Ministry's 2021 report on the Longitudinal Aging Study In India (LSAI), findings from the initial phase (2017-2018) of the world's largest study on the elderly indicate that approximately 75 million individuals aged 60 and above experience various chronic illnesses.
Furthermore, the Rural Health Statistics for 2021, issued by the health ministry, revealed a shortage of doctors in both rural and urban areas. Primary
Health Centres face a deficit of 7 per cent doctors, while Community Health Centres experience a substantial 57 per cent shortage. And according to the 2021 statistics, despite nearly two-thirds of the country's population residing in rural regions, only 33 per cent of the overall healthcare workforce and 27 per cent of doctors are available in rural areas.
Teleconsultation is essential for remote diagnosis of chronic diseases as it utilises communication technologies to connect patients with healthcare providers. This approach enables remote diagnosis and offers several benefits for patients and providers alike.
• Virtual Consultation: Through teleconsultation, patients can remotely

connect with healthcare providers using video calls, phone calls, or secure messaging platforms. This allows patients to share their symptoms, medical history, and concerns, enabling healthcare providers to assess and diagnose chronic diseases without the necessity of in-person visits.
• Remote ICU: Remote ICU in remote diagnosis enables healthcare providers to remotely monitor and diagnose ICU patients using telemedicine and advanced technology. Through video consultations, remote monitoring devices, and secure communication, critical care specialists can assess patients' condition, review vital signs, and collaborate with on-site teams, improving diagnosis and treatment decisions for patients in remote or underserved areas.
• Access to specialists: Teleconsultation bridges geographical gaps, granting patients in remote areas access to specialised healthcare professionals. This enables patients to receive expert opinions and guidance from specialists, improving the precision of diagnoses and treatment plans for complex chronic conditions.
• Improved accessibility and convenience: Teleconsultation enhances accessibility and convenience by eliminating the requirement for patients to undertake long journeys or endure crowded clinics. Healthcare services become more accessible as patients can conveniently have consultations from their homes, saving time, reducing travel costs, and minimising disruptions to their daily routines.
• Timely diagnosis and early intervention: Teleconsultation ensures prompt diagnosis and early intervention as it enables swift access to healthcare providers. Patients can promptly seek medical advice, leading to early detection and intervention for chronic diseases. This proactive approach improves treatment outcomes, reduces the risk
of disease progression, and minimises complications.
• Continuity of Care: Teleconsultation guarantees the continuity of care, particularly for patients needing regular follow-ups and monitoring. Remote consultations enable healthcare providers to evaluate patient progress, modify treatment plans, and deliver continuous support, resulting in improved disease management and patient engagement.
Additionally, teleconsultation platforms and technologies for remote diagnosis include video conferencing platforms like Zoom and Microsoft Teams, mobile health apps facilitating remote communication and health data sharing, and remote monitoring devices such as blood pressure monitors and wearable fitness trackers. Additionally, electronic health record systems provide access to patient records, test results, and informed diagnoses for healthcare providers.
The Future of Teleconsultation: Anticipated Advancements and Implications
Teleconsultation holds promise for chronic disease management by improving access to healthcare, enhancing monitoring and selfmanagement, integrating AI for personalised treatment plans, enabling
remote multidisciplinary care, and utilising advancements such as virtual reality, wearable devices, robotics, and secure data exchange. These advancements can increase efficiency, reduce costs, improve patient outcomes, address healthcare disparities, reshape the healthcare workforce, and raise ethical and legal considerations. Future teleconsultation technologies and strategies have the potential to transform healthcare systems, making them more patient-centric, efficient, and accessible while requiring careful attention to ethical and regulatory frameworks.
Teleconsultation has emerged as a transformative solution in chronic disease management. It offers remote diagnosis and tele-treatment, addressing the challenges of accessibility, limited resources, and geographical barriers faced by patients and healthcare providers. By enhancing accessibility, enabling remote monitoring, and empowering patients, teleconsultation improves healthcare outcomes for individuals with chronic conditions. However, challenges such as limited infrastructure, awareness, and adherence to treatment plans remain. Looking ahead, anticipated advancements in teleconsultation, including AI integration, remote multidisciplinary care, and emerging technologies, hold the potential to further revolutionise healthcare systems, making them more patient-centric and accessible while requiring careful consideration of ethical and regulatory aspects.
Arindam Sen is the Director at i2i Telesolutions, bringing with him two decades of experience in Healthcare Technology. Arindam holds a Bachelor's degree in Engineering from IIEST and a PG from IIM. He has actively mentored young professionals and supported initiatives that promote gender and ethnic diversity in the Health-tech industry.


Achieving sustainable health requires innovative design and effective execution of policies that address environmental, social, and governance concerns. This article highlights key principles for sustainable health policy, including prevention and health promotion, equitable access to healthcare, efficient resource allocation, environmental stewardship, and collaboration across sectors. Additionally, it emphasises the role of community development in creating resilient and socially connected communities. Furthermore, technology plays a crucial role in enhancing social and health outcomes by improving access to healthcare, providing health information and education, enabling data-driven care, supporting social connections, and facilitating proactive and personalised interventions. By integrating these principles and leveraging technology, sustainable health policies can lead to better population health, social equity, and environmental sustainability.
Attaining sustainable health requires innovative design and effective execution of the right policies. Health policy should integrate prevention, equitable access, efficient resource allocation, environmental stewardship and collaboration, to foster well-being. Technology integration enhances social and health outcomes through improved access, data-driven care, social connections, and personalised interventions, supporting sustainable health goals.
Loke Wai Chiong, Programme Lead & Senior Consultant, MOH Office for Healthcare Transformation, Board Director and Advisor to Multiple Organisations, Nexus of health, social, environment and communitySustainable health, in the context of increasing all-round attention on environment, social and governance (ESG) concerns, requires innovative design and effective execution of policy. A comprehensive approach aims to promote long-term well-being while ensuring the efficient use of resources and minimising negative impacts on society and environment. This is certainly apparent as Singapore transitions into population health and a new way of public health financing, and other countries similarly navigate their way to move their respective systems towards more value-based healthcare. Sustainable health policy recognises the interconnectedness between human health, social equity, and environmental sustainability, and could encompass the following key principles:
I. Prevention and health promotion: First and foremost, as the well-worn adage goes, “Prevention is better than cure”. And did we remember to add, “And much more costeffective too!” Emphasising preventive measures and promoting healthy lifestyles can reduce the burden of illness and improve overall population health. Policies that prioritise health education, early intervention, and access to preventive services help individuals avoid costly treatments, even as the population as a whole ages. Healthadjusted life expectancy and overall well-being is increasingly recognised as the goals to achieve beyond just improving average life expectancy.
II. Equitable access: Ensuring equitable access to quality healthcare services is essential for sustainable health. Policies should focus on reducing disparities and addressing social determinants of health, such as income, education, social-economic disparity and environment. By providing equal opportunities for all individuals to access healthcare, sustainable health policy aims to improve overall population health outcomes. On this point, the role of health-social-community integration, not just integrating health and social, will be game-changing and will be discussed in the next section of this editorial.

III. Efficient resource allocation: Optimal resource allocation and minimising waste within healthcare systems represent the greatest opportunity to curb ever up-spiralling healthcare costs. Measures include promoting evidence-based practices, adopting cost-effective interventions, and utilising health technologies efficiently. By focusing on value-based care and implementing sustainable procurement strategies, healthcare systems can reduce costs while maintaining or improving the quality of care.
IV. Environmental stewardship: Sustainable health policy recognises the importance of environmental factors in shaping health outcomes. The concept of planetary health and its impact on human health is incontrovertible. Policies should encourage environmentally friendly practices within healthcare settings, such as reducing energy consumption, minimising waste generation, and using eco-friendly materials. Additionally, promoting active transportation, green spaces, and sustainable urban planning contribute to a
healthier environment and overall wellbeing. In Singapore and many other places, government agencies, researchers, academia and private investors alike are rushing to collaborate at the intersection of urban planning and public health, to design and develop healthy cities of the future.
V. Collaboration and multi-sectoral approach: From the previous point, one can see the importance of collaboration between various sectors, including healthcare, education, built and natural environment, and social welfare. Policies that foster partnerships, information sharing, and coordinated efforts among these sectors can address complex health challenges more effectively and promote a holistic approach to well-being.
Community development plays a crucial role in achieving sustainable health and better health outcomes. As the World Health Organisation (WHO) rightly defines it, health is physical, mental and social, and all three are important. When communities build social connectedness, they are resilient and cohesive, individuals have increased access to support systems, resources, and opportunities. Indeed, communities often discover that they already have these “assets” and treasures in their midst, within neighbourhoods and place-based communities of care, and in the process of such asset-based community development (ABCD) entire communities become healthier as residents and citizens care for one another.
Community development, which creates resilient and connected communities, alongside improved quality of relationships, social support, and community engagement, therefore, leads to better population health. When individuals feel connected to their community, they are more likely to engage in healthy behaviours, seek help when needed, and have access to a network of support during challenging times. Socially connected communities have lower rates of mental health issues,
substance abuse, violent crime, and other negative health outcomes. A coordinated approach to health and social policymaking may, for example, use the appropriate and relevant levers to:
1. Promote community engagement, ownership and empowerment, strengthen social ties, build trust, and create a supportive environment that positively influences health outcomes.
2. Build social support networks through creatively designed programs and services that facilitate social support networks within communities — these may include support groups, mentoring programs, brick-and-mortar community centres or even virtual (and hybrid) chat-rooms which offer opportunities for social interaction and collaboration.
3. Increase investment in new (or optimising existing) built and natural environment features, healthpromoting infrastructure, recreational facilities and socially activated public spaces - to promote physical and mental well-being and also to foster social connections and a sense of belonging.
4. Address social determinants of health (SDOH) such as poverty, education, and housing; which have been shown repeatedly to be even more impactful on the population’s overall
well-being, morbidity and mortality, than having convenient access to the most modern hospitals or advanced therapies.
5. Facilitate collaboration and partnerships, which enable community development efforts to be most effective. Sectors include healthcare providers, government agencies, non-profit organisations, and community leaders. By working together, stakeholders can pool resources, expertise, and knowledge to implement comprehensive and sustainable interventions that promote social health.
When individuals are socially supported, engaged, and connected to their communities, they are more likely to lead healthy lifestyles, seek necessary healthcare services, and experience improved overall well-being.
Last, but certainly not least, in a publication that introduces the latest in healthcare technology and innovation, well-planned and provisioned technology development and deployment, supported by the right policy, improves social and health outcomes by enhancing connectivity, expanding access to information and services, facilitating communication, and empowering individuals and communities.
The recent pandemic has ushered in increased access to healthcare, as demonstrated in the accelerated adoption of telemedicine and telehealth solutions. In tandem, there is now the ability to reach the underserved or remote areas, and create remote access to medical expertise, consultations and follow-up care. Telemedicine can also reduce barriers to healthcare, such as transportation costs and long waiting times, leading to better health outcomes especially for those who may otherwise have difficulty seeking and receiving the care they need and deserve.
Health information and education and timely access to such resources have empowered individuals to make
Sustainable health policy recognises the interconnectedness between human health, social equity, and environmental sustainability.
informed decisions about their health. Online platforms, mobile applications, and wearable devices offer health monitoring tools and personalised health recommendations in the form of positive behavioural ‘nudges’. These enables individuals to actively manage their health, engage in preventive measures, and adopt healthier lifestyles. Whether in physical and mental health, especially with chronic lifestyle diseases like diabetes, hypertension, cardiovascular disease continually on the rise.
Technology also enables datadriven health and social care. With vast amounts of data, not limited to health but also including environmental, social and others collected in an increasingly internet of tThings (IOT) world,
new knowledge and evidence guide upcoming policies and interventions. For example, by leveraging technologies like electronic health records (EHRs) and data analytics, healthcare systems can identify trends, track population health outcomes, and target interventions to specific needs. In addition, behavioural interventions and tracking are increasingly possible through mobile applications, wearable devices, and sensors which monitor various health parameters, such as physical activity, sleep, and vital signs. Technologies can deliver real-time feedback, reminders, and personalised interventions to promote healthy behaviours and lifestyles. By fostering self-awareness and accountability,
technology encourages individuals to make positive lifestyle changes for better health.
Beyond digital health and medical technology, ‘social tech’ which support social and community building should be the next focus. Online platforms and social media networks facilitate connections among individuals facing similar health challenges, creating virtual support communities where individuals can share experiences, exchange information, and provide emotional support. Online support groups and forums are known to contribute to improved mental health outcomes and a sense of belonging, particularly for individuals with rare conditions or stigmatised health issues. Furthermore, if one takes the salutogenic approach, strengthening social connections through technology will maintain and improve health even before the onset of disease.
In planning for and building Healthy Cities and Cities of Tomorrow, data regarding environmental pollution, urban heat, space utilisation, urban transport increasingly available through IOT can be cross-analysed with data on health behaviours, resource utilisations, diseases and longer-term outcomes of the people who grow, learn, live, work and play within the defined and designed space. This offers new levers not only for proactive and personalised healthcare delivery, but also for urban planning and building design for entire populations.
In conclusion, by integrating these inter-disciplinary principles into policy, sustainable health can be achieved, creating a healthcare system that not only meets the immediate needs of individuals but also safeguards the health of future generations. A healthy population and a healthy environment are mutually reinforcing and there needs to be a balance between healthcare delivery, resource management, and social and environmental considerations.

Every minute is critical for a successful intervention in trauma and cardiac emergencies such as lifethreatening arrhythmias and airway compromise. Utilisation of drones paves the way to improve health care, especially in underserved areas. These new technological aids will enable us to transport AEDs to the patient with OHCA to save lives.
8.4 per cent . This shows that cases with VF have a better prognosis if expedient defibrillation can be accomplished.
Restoration of adequate cardiac function provides return of spontaneous circulation (ROSC). On the other hand, restoration of neurological function predicts successful resuscitation.
The most important and effective treatment in CA cases is early, appropriate, effective compression and defibrillation. This approach, defined as 'high-quality CPR', is more valuable than any medication. If we count all the positive factors:
• Witnessed arrest
• Performing CPR in the field
• Minimal interruption to compressions
• Early/immediate defibrillation
• AED use
• Administering hypothermia to comatose patients
• Avoiding hyperventilation
Time is among the most crucial aspects of health care. Many authors emphasise the “golden hour” as the critical time window for successful intervention in trauma. It is even more stringent in cardiac emergencies such as lifethreatening arrhythmias and airway compromise. Nowadays it can be contemplated that innovative measures to save lives will be an upheaval for our world.
Unmanned aerial vehicles (a.k.a. drones), appear to revolutionise prehospital medicine enabling advanced health care delivery to those in austere environments and difficult regions.

Lethal arrhythmias and subsequent sudden cardiac arrest (CA) in adults cause the death of millions of people every year all over the world. Patients with coronary artery disease and decompensated heart failure constitute approximately 80 per cent of CA cases. In 70 per cent of patients with CA, the first recorded rhythm is ventricular fibrillation (VF). This is followed by pulseless electrical activity (PEA), bradyarrhythmias, asystole, and ventricular tachycardia (VT). Survival rates, including hospital discharge, of cases with VF are between 7.7 per cent and 40 per cent , with a median value of 22 per cent (Nichol, 2008). If all CA cases are taken into account, this median rate declines to
“Quality CPR” is a prerequisite for successful resuscitation. The technical components of this are;
• 100-120 compressions per minute
• 10 breaths per minute (avoiding hyperventilation)
• Pressure depth of 5 to 6 cm
• Chest compression fraction of 80 per cent or more
• Full chest recoil
The global availability of healthcare resources based on drones stems from a need for a collaboration of a wide range of civilian and military medical forces to develop this contemporary technology for wider accessibility (Braun19). Recent years witnessed emergence of de novo strategies for defibrillation
easily accessible to thepublic, including volunteer bystander and responder programs and AED-delivery by drones (Folke23). Some researchers employed simulation-based programs to train laypersons on the operation of AEDs delivered by drones in rural and difficult regions (Gino23).
Fischer et al. designed a study with 10 paramedic personnel and 19 laypersons to face with a manikin as victims of OHCA within a field test in a difficult geography in Europe. Following a mock-call, the AEDs were brought via drones and utilised in 29 case scenarios without severe untoward events. Mean delivery times of the drones was 5.2 minutes. The paramedics applied the first shock after a mean of 12:1 ± 2:0 min and hands-off times were 50 ± 22 seconds. They postulated that the delivery and utilisation of AEDs with semi-autonomously flying vehicles (drones) in difficult regions appears to be practical (Fischer23).
The basis of drug administration within the scope of ACLS is IV administration. IO application is the first choice when necessary but not successful in 3 consecutive attempts or within 90 seconds of IV application. In cases where this is not possible, endotracheal tube (ETT) is an alternative. In this application, it is given in 2-2.5 times dose and diluted to 10 mL with saline. Then, lungs are ventilated with a bag-valve-mask (BVM) to allow it to pass through the alveolocapillary membrane to the capillaries. In IV administration, drugs are mostly infused from the arm or leg, the extremity is raised as much as possible or flushed with 20 mL IV saline. In a recent study, authors examined the association of time to treatment (drug or placebo) with survival to hospital discharge and neurologic outcome (Rahimi23). The survival rate of patients to discharge was found to be reduced as lag time to administration of the drugs is protracted, in amiodarone (OR, 0.9; per min), lidocaine (OR, 0.9). Amiodarone
resulted in more favourable survival at all times of drug administration (OR, 1.32; 95 per cent CI, 1.0-1.6). It can be considered that new advances such as drones would facilitate shorter delays in drug administration and in turn, increase the rate of survival and favourable outcomes following cardiac emergencies.

The COVID-19 pandemic spread has represented new opportunities for the drones to be beneficial in healthcare. To be more specific, in regions with difficulties to get access to developed institutions, these devices provided life-saving aids for severe and critical patients. For example, the use of drones for transportation of diagnostic samples resulted in significant shortening of the travel time taken for samples in West Africa (Sylverken 19). This opportunity can augment the potential of coping with the pandemic and other diseases affecting the globe. There have also been important advances in regard to expedite emergency blood delivery to recipients in need of these products (Ling19). Emergent need for transfusion of blood and by-products, an US–based firm, Zipline launched a drone delivery procedure in Rwanda. In 2018, Zipline initiated a more advanced genre of delivery drone, which was
faster than before. It is reported to be the fastest available commercial delivery drone. Zipline proved a higher success in its processes including the time between taking the call (order) and launching the delivery was radically diminished from 10 minutes to 1 minute. These new vehicles can now fly for almost 160 kms with up to 2 kilograms.
Matternet, another company, has successfully operated 1800 flights over Swiss cities and delivered 850 blood and pathology specimens in Swiss cities by 2019 (DDMF). Another drone-based delivery service named Flirtey from Nevada collaborates with ambulance and medical providers to deliver medications to clinics in rural areas. Flirtey has also partnered with Domino’s Pizza and 7-Eleven to deliver food, drinks, and other consumer products. The delivery took only 3 minutes, whereas vehicle delivery took 90 minutes.
Therefore, we can postulate that utilisation of drones paves the way to improve health care, especially in remote and underserved areas. These new technological aids will enable medical professionals to transport AEDs correctly to the exact location of the patient with OHCA to save lives. References are available at www.asianhhm.com
Ozgur Karcioglu has graduated from his residency in Emergency Medicine (1998). He has attended the “International Emergency Medicine” Fellowship in PSU (2005). He is the department chair of EM, Taksim Education Hospital. Five editorships and three original books were published by InTechOpen and Bentham Science, respectively.
Canan Akman received her emergency medicine specialisation from Hacettepe University Faculty of Medicine, Department of Emergency Medicine between 2006-2011. She continues to work as an associate professor at Çanakkale Onsekiz Mart University Faculty of Medicine, Department of Emergency Medicine.

Dogac Niyazi OZUCELIK received his emergency medicine specialisation from Dokuz Eylul University Faculty of Medicine, Department of Emergency Medicine between 1997-2001 and docentship from Hacettepe University Faculty of Medicine. He is especially involved in disaster management, preparedness, ambulance systems, trauma systems and resuscitation

Cybersecurity is a shared responsibility — this sentiment has resounded within healthcare circles around the world over the past decade. But what does it really mean for different groups to share the responsibility for cybersecurity in healthcare?

If you represent a healthcare delivery organisation (HDO), it might mean that you understand your organisation can’t fully control the cybersecurity posture of the devices that you acquire and plan to deploy within your hospital IT networks.
If you’re a medical device manufacturer, it might mean that you need to make certain assumptions about the network environment into which your product could be placed and then design the product accordingly.
One common approach is for the HDO to try to get the device manufacturers to make all technical details about the product available to them.
There are certainly some pros to this approach, such as:
• The opportunity to have fine-grained control over device deployment in a hospital IT network based on product design details
• The ability to compensate for residual risk remaining at the endpoint (medical device), based on a detailed understanding of technical debt and risk at the product level
• The potential to reduce the security burden on hospital network infrastructure by relying on product level security controls. However, there are also some cons, such as:
• Device manufacturers may not be comfortable releasing their sensitive design details and other intellectual property (IP) outside of the security controls of their organisation . The compromise of such IP could be crippling to the business of a medical device manufacturer if it leads to industrial espionage or low-priced counterfeit products
Device patches generally need to be validated by the manufacturers to maintain safety, effectiveness and security before being deployed within a clinical network
• HDOs may not always have the technical expertise in-house to fully utilize such information, even if it is freely shared.
Another approach is to structure hospital IT networks in a way that allows for the safe and secure integration of ‘untrusted’ devices. This approach offers some pros, including:
• A consistent baseline of security capabilities based on network architecture alone
• A single point of control when dealing with security events or new threats
• The possibility to treat vetted devicelevel security controls as “backup” controls in case of network compromise, as appropriate.
However, just like with the devicecentric approach to security, the network-centric (‘zero trust’) approach also has cons, such as:
• The need to hire and maintain in-demand and difficult-to-find cybersecurity experts
• The potentially high initial investment needed for tools for intrusion detection and protection, vulnerability scanning, asset management, etc.
• The reduced flexibility when network reconfiguration is needed.
A hybrid approach, leveraging both the network security posture and product security, can be advantageous in providing the best of both worlds. To overcome some of the challenges of each, using third-party attestations or certifications to technical product security standards in conjunction with standards’ compliant, defensively designed hospital IT network architectures can be an ideal middle ground.
Reputable third parties that operate testing and certification programs are typically accredited to and conform to standards such as ISO 17065 – “Conformity assessment — Requirements for bodies certifying products, processes and services”,
ISO 17025 – “Testing and calibration laboratories,” and ISO 17024 –“Conformity assessment — General requirements for bodies operating certification of persons.” Such accreditations help demonstrate the competency, consistency, and impartiality of the third-party and a baseline of independently assessed trustworthiness or quality when leveraging the testing, inspection and certification services of such a third-party.
One significant benefit of having an independent third party as part of this ecosystem is that sensitive information can be shared by different supply chain stakeholders with the third party while maintaining the confidence that such information will be handled and maintained as confidential, remaining subject to strong technical and procedural security controls. This level of rigor in handling sensitive data allows medical device manufacturers to share very detailed information about product design with an accredited thirdparty while also allowing healthcare delivery organisations to share information such as personally identifiable information (PII) and protected health information (PHI) with the same third party as needed for system evaluation. Thus trusted third-parties can serve as a technology transfer and claim verification bridge between supply chain stakeholders.
Third-party testing, inspection and certification organisations are also required, per their own accreditations, to establish and maintain the necessary technical competencies and properly calibrated and managed equipment to effectively and consistently deliver any services (including cybersecurity) that they offer. The existence of such third-parties can help medical device manufacturers and HDOs overcome the workforce shortages in areas like cybersecurity that we see today. Having such quality attributes can also make the delivery of support services measur-
Identify an accountable top management representative. If no one is accountable, tasks are less likely to get done, so this is a good first step.
able, repeatable and reproducible. Additionally, this means that supply chain relationships can establish metrics for continuous improvement. There can be standardisation of practices and procedures, and when problems or anomalies arise, they can be tracked and reproduced to support remediation.
For example, when following the ANSI/CAN/UL 2900 cybersecurity standards, many security concerns can be addressed through compliance. These include:
• Establishing that manufacturers have characterised and documented the technologies used in their products that could constitute an ‘attack’ surface
• Requiring threat modeling based on intended use and relative exposure
• Demonstrating the effective implementation of security controls protecting both sensitive data (e.g., PII or PHI) and assets, such as command and control data
• Providing objective evidence that software weaknesses and vulnerabilities have been appropriately dispositioned and further verified via penetration testing
• Promoting defensive design (e.g., defense-in-depth, partitioning, etc.)
• Helping ensure system robustness (e.g., fuzz testing/malformed input testing)
• Supporting monitoring of security events
• Addressing logging of security events
• Defining approach for managing security logs
• Covering updating of software to address safety, essential performance and security issues
• Requiring the handling of failures in the software update process (e.g., roll-back).
• Controlling component purchasing
• Helping with management of sensitive data (including passwords and cryptographic keys)
• Facilitating remote product management

• Examining decommissioning (e.g., purging of PII/PHI).
There are many options when it comes to standards, certifications, third-party cybersecurity service providers, implementation strategies, testing approaches, etc. But some basic concepts need to be applied no matter what options you choose:
1. Identify an accountable top management representative. If no one is accountable, tasks are less likely to get done, so this is a good first step
2. Make security part of the company culture. Security is often opposed
to usability. This tends to contribute to a common perception that cybersecurity is an added cost and complication, sometimes an annoyance, and in some cases, even a hazard. For example, what could happen if you had to enter a 13-character password before being allowed to use an Automated External Defibrillator (AED)?
3. Establish cybersecurity policies and procedures as part of a quality management system
4. Perform pre- and post-deployment cybersecurity risk assessments, which include having cybersecurity as part of the procurement process and the decommissioning or service termination process. There are many aspects to cover between those two lifecycle endpoints, such as threat modeling, determination of necessary security controls, verification and validation, coordinated vulnerability disclosure, problem resolution, change management, etc.
Many best practice guidelines and standards are available in the healthcare ecosystem that can help. All UL Standards are freely available to the public online, and all NIST standards are also available for free. Organisations like the Healthcare Sector Coordinating Council provide free tools and resources to help improve the global cybersecurity posture of critical healthcare infrastructure.
Anura Fernando is the global head of medical device security at UL Solutions. He has twenty-five years of experience at UL Solutions with safety critical software and control systems certification and safety research across multiple application domains. He has contributed to research and industry publications in Predictive Modeling and Risk analysis, cybersecurity, Systems of Systems, Health IT, and medical device safety and security. Anura has participated in project collaboration with numerous Fortune 500 companies and has contributed to the development of several domestic and international consensus standards for software, security, and functional safety. His current focus looks at the intersection of cybersecurity and safe medical device interoperability.

Transformation is not something that can be observed based on day-to-day basis. It may not require an extensive amount of time like the evolution of species, but I believe it will take at least several decades or even centuries to unfold and shape our future. Therefore, I would like to examine the healthcare digital transformation that lies ahead and share my thoughts on what we need to prepare for, drawing on my experience in Healthcare Information Technology over the past 30 years.
Jong-Soo Choi, Information Technology Lead, Samsung Medical Center
Health Information Technology (HIT) refers to the application of computer hardware, software, and systems in healthcare to store, retrieve, share, and analyse health information. It plays a critical role in managing health data across different computerised systems and enabling secure information exchange among patients, practitioners, healthcare providers, researchers, government entities, insurance companies, quality monitors, and regulatory bodies. HIT is essential for improving medical care, facilitating communication and decision-making, and meeting the diverse needs of stakeholders in the healthcare industry.
There are many types of HIT. However, the followings seven are considered to encompass the overall
meaningful aspects of HIT.
1. Electronic Health Records (EHRs) serve as the central component of the HIT infrastructure. EHRs are digital health records shared among multiple healthcare providers and agencies. They contain comprehensive information about patients' health history, diagnoses, medications, treatments, and other relevant data. EHRs facilitate information exchange between healthcare providers and ensure continuity of care. The most critical component of EHRs is Electronic Prescribing (E-prescribing), which eliminates the need for paper prescriptions by enabling direct communication between healthcare providers and pharmacies. It streamlines the process of medication ordering and pickup, reducing the chances
of errors or misplaced prescriptions. E-prescribing systems also provide alerts and reminders for drug interactions, dosage instructions, and formulary compliance.
2. Personal Health Records (PHRs) are self-maintained health records controlled by patients themselves. They allow individuals to manage and track their health information, including data from doctor visits and personal health metrics such as diet, exercise, and blood pressure. PHRs can be integrated with EHRs, enabling seamless data exchange and providing patients with a comprehensive view of their health information.
Picture Archiving and Communication Systems (PACS) and Vendor-Neutral Archives (VNAs) are types of HIT used for storing and
Will hospitals disappear in 100 years?
managing medical images, such as X-rays, MRIs, and CT scans. These systems allow healthcare professionals to store, access, and share images within a hospital or healthcare system. PACS and VNAs integrate radiology and other specialties into the main hospital workflow, improving accessibility and collaboration among healthcare providers.
3. Health Information Exchange (HIE) refers to the electronic sharing of health information between different healthcare organisations and systems. It enables the secure exchange of patient data, including EHRs, laboratory results, imaging reports, and other relevant information. HIE facilitates care coordination, reduces redundant tests and procedures, and improves patient outcomes.
4. Telemedicine and Patient Portals are technologies that enhance access to healthcare services and improve patient engagement. Telemedicine involves the use of technology to provide remote healthcare services, including video consultations between patients and healthcare providers. Patient portals, on the other hand, allow individuals to access their health information, communicate with healthcare providers, schedule appointments, view test results, and perform other tasks securely online.
5. Data Analytics and Artificial Intelligence (AI) play a crucial role in analysing large amounts of patient data to derive insights and support clinical decision-making. AI and machine learning algorithms are utilised to identify patterns, predict outcomes,

and assist in diagnosis and treatment planning. These technologies contribute to population health management, value-based healthcare, and personalised medicine.
6. Privacy and Security are essential aspects of HIT systems. These systems incorporate measures to enhance the privacy and security of health information. Consequently, HIT systems implemented encryption of electronic data, access controls, audit trails to track data access, and compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA). Privacy and security measures are crucial to protect patient confidentiality and prevent unauthorised access or data breaches.
HIT offers numerous benefits for both healthcare providers and patients. Among them, the most significant benefit is the improved quality/effectiveness of care. HIT enables healthcare providers to access accurate and complete patient health information, leading to better diagnoses and care decisions. It also supports care coordination, secure information sharing with patients and their families, early diagnosis of health problems, and reduced medical errors. Essentially, HIT provides increased efficiency. HIT systems streamline administrative and clinical processes, reducing the time and effort spent on managing daily operations and paperwork. This allows healthcare organisations to focus more on patient treatment and health. Examples of efficiency improvements include faster prescriptions, improved information sharing, reduced paperwork, and better follow-up. In terms of economic impact, there is decreased healthcare costs. HIT is seen as a means to decrease healthcare costs by improving operational efficiencies, patient safety, and chronic disease management. Digital data transfer, improved communication, and
standardised software standards aim to reshape administrative structure and enhance cost-effectiveness.
From the perspectives of healthcare providers and patients, HIT enables healthcare providers to have secure and complete access to patient information, better coordination of care, secure information sharing with patients, improved diagnostics, reduced medical errors, and lower costs. It also facilitates the efficient tracking of patient health information, even outside of regular office hours. Moreover, HIT empowers patients by giving them control over their health information. Patients can access and modify their data, share information with clinicians, request e-prescriptions, and receive secure electronic summaries of office visits. HIT tools and applications also enable patients to set and achieve health goals, monitor lifestyle factors, and participate in online communities for support.
The journey of HIT can be traced back to the early 20th century when basic information processing systems were first introduced in healthcare settings. While different countries may have distinct histories, the United States' history of HIT is the most generally applicable worldwide. Therefore, this section will describe the history of HIT in the United States.
In the 1950s and 1960s, computers began to be used for administrative tasks such as billing and scheduling. These early computer systems laid the foundation for digitising health records and gradually transitioning from paperbased documentation to electronic formats.
The 1970s witnessed the emergence of Hospital Information Systems (HIS) aimed at streamlining administrative processes within healthcare facilities. These systems encompassed patient registration, inventory management, and basic data storage but had limited functionality and lacked interoperability.
With the advent of personal computers in the 1980s, healthcare professionals gained access to more powerful tools for data processing and analysis. During this era, Electronic Medical Record (EMR) systems were developed, enabling the digital capture, storage, and retrieval of patient health information within a single healthcare organisation.
The 1990s marked a significant milestone in HIT with the introduction of standards for health data exchange. The Health Level Seven (HL7) protocol and the creation of the Clinical Document Architecture (CDA) provided a framework for interoperability, facilitating seamless sharing of health information between different systems and organisations. This era also saw the utilisation of internet technology and telemedicine applications to improve healthcare connectivity and access to specialised care.
The early 2000s brought a renewed push for HIT adoption, driven by various initiatives and legislation. The Institute of Medicine's (IoM) call for electronic prescribing systems in 2001 and the President's HIT Plan in 2004
emphasised the importance of digitising medical records and improving care efficiency. The American Recovery and Reinvestment Act of 2009 allocated significant funding for the implementation of EHRs through the Meaningful Use program, accelerating the adoption of HIT across the United States.
In recent years, HIT has experienced rapid advancements fueled by technological innovations. Cloud computing, mobile applications, and wearable devices have expanded the capabilities of HIT, enabling remote patient monitoring, telehealth services, and personalised healthcare solutions. Moreover, the integration of artificial intelligence and machine learning algorithms has opened new avenues for data analysis, clinical decision support, and population health management.
The historical journey of HIT reflects a gradual shift from basic information processing systems to advanced, interconnected networks that revolutionise how health information is managed, shared, and utilised. The ongoing advancements in HIT promise to reshape the healthcare landscape, enhancing patient care, improving outcomes, and driving innovation in the pursuit of a healthier future.
It is evident that HIT has experienced remarkable growth in recent years. However, there have been some disappointments . Despite the potential benefits and advancements in digital innovation, the healthcare industry has been slow in adopting advanced technologies compared to other industries. The COVID-19 pandemic accelerated the digital transformation of health and care services in certain areas, such as the rapid uptake of remote consultations. However, poor interoperability, privacy concerns, and difficulties in real-time data flow are persistent barriers that hinder the effective utilisation of HIT for policy
The integration of genomic data, the Internet of Medical Things (IoMT), and blockchain technology holds immense potential for transforming healthcare delivery and empowering individuals to play a more active role in their own well-being.
and planning purposes. One area that exemplifies the lackluster progress is genomics. Despite significant advancements in human genomics over the past two decades, the integration of genomic research into routine patient care has been limited. Although millions of genomes have been sequenced, translating genomic data into clinical practice remains a challenge. While single nucleotide polymorphism (SNP) arrays have been used to determine polygenic risk scores for common conditions, their implementation in clinical practice has been restricted. The availability of lower-cost whole genome sequencing holds promise for wider implementation, but challenges persist in presenting complex genomic data in a user-friendly manner and addressing the shortage of medical geneticists and genetic counselors. Efforts are needed to overcome these barriers and effectively incorporate genomics into patient care, as routine medical practice has yet to fully realise its potential.
Looking ahead, the future of HIT is marked by the evolution of data interoperability, patient engagement, and cybersecurity. The integration of genomic data, the Internet of Medical Things (IoMT), and blockchain technology holds immense potential for transforming healthcare delivery and empowering individuals to play a
more active role in their own well-being. Experts predict that integrated healthcare data, coupled with AI-driven research, will enable personalised and precise care based on genetics, proteomics, and environmental factors. Robotics will assist in surgical procedures, rehabilitation, and elderly care.
The shift from hospitals to homebased care will become more prevalent, as healthcare embraces personalised and home-based approaches. Patients will receive care in the comfort of their own homes, supported by technology and remote monitoring. Technology advancements, including AI and avatar therapists, will make healthcare more convenient and accessible, enhancing patient outcomes while preserving the doctor-patient relationship.
Efforts will be made to democratise healthcare knowledge and access through automation and technology. The aim is to ensure equitable access to high-quality care for all, addressing disparities and ensuring that healthcare advancements benefit everyone. The focus of healthcare will shift towards preventive care, leveraging AI and emerging technologies. The possibility of fully sequencing individuals at birth will enable early disease detection and emphasise disease prevention.
Promoting digital inclusivity is crucial to ensure equal access to healthcare services and HIT systems. Steps should be taken to bridge the digital divide, address disparities in technology access, and promote health literacy across all populations.
Jong-Soo

In summary, the future of HIT holds great promise, with personalised care, home-based healthcare, democratised access to knowledge, a focus on preventive care, and efforts towards digital inclusivity. These advancements, driven by technology and collaboration, will revolutionise healthcare and improve the well-being of individuals.
While recent advancements in medicine and engineering have shown promising progress, predicting the exact future of healthcare 100 years from now is challenging. Experts highlight key developments that could shape healthcare in the future, such as personalised engineering, regenerative medicine using technologies like 3D printing, and the integration of AI-driven robots with AR/ VR. However, these advancements come with significant challenges that need to be addressed, including equity issues, genomics utilisation, privacy concerns, and data protection.
Although there is a vision of hospitals undergoing innovative transformations and potentially disappearing in the future, the current state of genomics utilisation and the need for advancements in patient-centered approaches like Web 3.0 present additional obstacles. Healthcare information technology plays a central role in this transformative process, despite progress being gradual. Achieving a patient-centered approach and successfully integrating technology require careful consideration and continuous efforts.
Overcoming these challenges is essential to create a future healthcare system that prioritises patient wellbeing and provides a safer and more comfortable environment. While the ultimate outcome is uncertain, it is crucial to strive for a patient-centric future and embrace the potential of healthcare information technology.
References are available at www.asianhhm.com
To receive more information on products & services advertised in this issue, please fill up the "Info Request Form" provided with the magazine and fax it.
: Inside Front Cover 2.IBC: Inside Back Cover 3.OBC: Outside Back Cover

Grow your audience with increased reach, impact and user-friendliness
Rise above geographical boundaries
Generate new business
Gain the strong web presence differentiating yourself from competitors
Connect and engage with your target audience

Give more exposure to industry specific people
Increase your brand profile and share your capabilities with leading industry professionals
