






ACOEP stands with all emergency physicians and providers on the front line. We thank you for your tireless work and effort.
ACOEP stands with all emergency physicians and providers on the front line. We thank you for your tireless work and effort.









ACOEP stands with all emergency physicians and providers on the front line. We thank you for your tireless work and effort.
ACOEP stands with all emergency physicians and providers on the front line. We thank you for your tireless work and effort.

A Note from the Editors:
We are excited to publish the 9th issue of the Western Journal of Emergency Medicine (WestJEM) Education Issue and first year of a rolling decision process. Ov er 10 years ago a unique relationship was formed between WestJEM, the Council of Residency Director for Emergency Medicine and the Clerkship Directors of Emergency Medicine. The idea was to promote and di sseminate educational scholarship which has been accomplished over the past decade. Senior and junior r esearchers have an opportunity to publish in the education issue because of the diverse nature of our submis sion categories, ranging from original research to brief educational advances. A successful issue requires the courage of the authors to submit their work for peer review and we do our best to provide detailed feedback reg ardless of the final decision. Publication of the issue requires the commitment and hard work of the publication staff, leadership of the organizations, editors, and peer reviewers. We want to thank them all for their efforts and professionalism. The topics of this year’s education issue likely reflect the focus of educators as we ente red a post-covid reality. Many of the topics were related to innovative curriculums and focused on the benefi ts derived. There were also several articles that were dedicated to the administrative aspects of residency and fellowships and how that has changed after COVID. We have already started to receive and review submissions for next year’s education issue. The editorial staff review every submission on a rolling basis and, once accepted, the articles are available on PubMed. There are also no processing fees when accepted to the Education Issue. This is a great opportunity to submit your educational scholarship, thereby enhancing your professional development and disseminating your work to others. We are excited that this experiment has flourished, and we look forward to seeing your work in our 10th anniversary issue.
Jeffrey Love, MD
Georgetown University School of Medicine
Co-Editor of Annual Special Issue on Education Research and Practice
Douglas Ander, MD
Emory University
Co-Editor of Annual Special Issue on Education Research and Practice
The Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health would like to thank The Clerkship Directors in Emergency Medicine (CDEM) and the Council of Residency Directors in Emergency Medicine (CORD) for helping to make this collaborative special issue possible.
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
BRIEF RESEARCH REPORT
S1 Virtual Interviews and the Pediatric Emergency Medicine Match Geography: A National Survey
A Baghdassarian, JA Bailey, D Caglar, M Eckerle, A Fang, K McVety, T Ngo, JA Rose, CG Roskind, MM Tavarez, FT Benedict, J Nagler, ML Langhan
S6 Perception of Quiet Students in Emergency Medicine: An Exploration of Narratives in the Standardized Letter of Evaluation
JK Quinn, J Mongelluzzo, A Nip, J Graterol, EH Chen
S10 Changes in Residency Applicant Cancellation Patterns with Virtual Interviews: A Single-site Analysis
M Bouldin, C Eastin, R Freeze-Ramsey, A Young, M von Dohlen, L Evans, T Eastin, S Greenberger
S15 Foundations of Emergency Medicine: Impact of a Standardized, Open-access, Core Content Curriculum on In-Training Exam Scores
J Jordan, N Wheaton, ND Hartman, D Loke, N Shekem, A Osborne, PL Weygandt, K Grabow Moore
S19 Integrating Hospice and Palliative Medicine Education Within the American Board of Emergency Medicine Model
R Goett, J Lyou, LR Willoughby, DW Markwalter, DL Gorgas, LT Southerland
S27 Staffing Patterns of Non-ACGME Fellowships with 4-Year Residency Programs: A National Survey
DA Haidar, LR Hopson, RV Tucker, J Koehler, N Theyyunni, N Klekowski, CM Fung
BRIEF EDUCATIONAL ADVANCES
S33 Nudge Theory: Effectiveness in Increasing Emergency Department Faculty Completion of Residency Assessments
A Gurley, C Jenkins, T Nguyen, A Woodall, J An
S36 The Effect of a Simulation-based Intervention on Emergency Medicine Resident Management of Early Pregnancy Loss
SD Bellew, E Lowing, L Holcomb
ORIGINAL RESEARCH
S41 Integration of Geriatric Education Within the American Board of Emergency Medicine Model
LT Southerland, LR Willoughby, J Lyou, RR Goett, DW Markwalter, DL Gorgas
S51 Emergency Medicine Resident Needs Assessment and Preferences for a High-value Care Curriculum
BH Lane, SK Mand, S Wright, S Santen, B Punches
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
The WestJEM Special Issue in Educational Research & Practice couldn’t exist without our many reviewers. To all, we wish to express our sincerest appreciation for their contributions to this year’s success. Each year a number of reviewers stand out for their (1) detailed reviews, (2) grasp of the tenets of education scholarship and (3) efforts to provide feedback that mentors authors on how to improve. This year’s “Gold Standard” includes:
• Ignacio Calles/Jeffrey Riddel*
• April Choi, Kirlos Haroun, Linda Regan*
• Nathan Dreyfus/Jessie Werner*
• Eric Flounders, Samual Clarke*
• Rowan Kelner/Allie Beaulieu/Jeffrey Druck/Christine Raps*
• Andrew Kendle, Marcus Wooten, Simiao Li-Sauerwine*
• Matt Magda/Kevin Scott*
• Dan Mayer
• Joe-Ann Moser/Ben Schnapp*
• Daniela Ortiz/Tyson Pillow*
• Elspeth Pearce
• Jessica Pelletier/Albert Kim*
• Thaddeus Schmitt
• Nicole Schnabel/Laura Hopson*
• Samantha Stringer/Albert Kim*
• Olivia Urbanowicz, Edmond Irankunda, Sally Santen*
• Ivan Zvonar/Jon Ilgen*
*Mentored Peer Reviews from Emergency Medicine Education Fellowship Programs
We would also like to recognize our guest consulting editors who assisted with pre-screening submissions during our initial peer-review stages. Thank you for all of your efforts and contributions.
CDEM
• Christine Stehman
• Andrew Ketterer
• Eric Shappell
• Sharon Bord
CORD
• Jenna Fredette
• Jaime Jordan
• Anne Messman
• Kendra Parekh
• William Soares III
• Paul “Logan” Weygandt Consulting Statistician/ Psychometrician
• David Way
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Jeffrey N. Love, MD, Guest Editor
The George Washington University- Washington, District of Columbia
Danielle Hart, MD, Associate Guest Editor Hennepin County Medical Center- Minneapolis, Minnesota
Chris Merritt, MD, MPH, Associate Guest Editor
Alpert Medical School of Brown University-Providence, Rhode Island
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Resident Editors
AAEM/RSA
John J. Campo, MD Harbor-University of California, Los Angeles Medical Center
Tehreem Rehman, MD
Advocate Christ Medical Center
ACOEP
Justina Truong, DO Kingman Regional Medical Center
Section Editors
Behavioral Emergencies
Erin Dehon, PhD University of Mississippi Medical Center
Leslie Zun, MD, MBA Chicago Medical School
Marc L. Martel, MD Hennepin County Medical Center
Cardiac Care
Fred A. Severyn, MD University of Colorado School of Medicine
Michael C. Kurz, MD University of Alabama at Birmingham
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD Carolinas Medical Center
Casey Clements, MD, PhD Mayo Clinic
Patrick Meloy, MD Emory University
Nicholas Pettit, DO, PhD Indiana University
Eric Snoey, MD Alameda County Medical Center
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Gabriel Wardi, MD University of California, San Diego
Joseph Shiber, MD University of Florida-College of Medicine
Matt Prekker MD, MPH Hennepin County Medical Center
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Julianna Jung, MD, Associate Guest Editor Johns Hopkins Hospital, Baltimore, Maryland
Douglas Franzen, MD, Associate Guest Editor Harborview Medical Center, Seattle, Washington
Gentry Wilkerson, MD, Associate Editor University of Maryland
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Sara Krzyzaniak, MD Associate Guest Editor Stanford Universtiy-Palo Alto, California
Gavin Budhram, MD, Associate Editor Tufts University- Medford, Massachusetts
Susan R. Wilcox, MD, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston Texas
David Page, MD University of Alabama
Erik Melnychuk, MD Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
Christopher Kang, MD Madigan Army Medical Center
Education
Danya Khoujah, MBBS University of Maryland School of Medicine
Jeffrey Druck, MD University of Colorado
John Burkhardt, MD, MA University of Michigan Medical School
Michael Epter, DO Maricopa Medical Center
ED Administration, Quality, Safety
David C. Lee, MD Northshore University Hospital
Gary Johnson, MD
Upstate Medical University
Brian J. Yun, MD, MBA, MPH
Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH University of Texas Health-San Antonio
Emergency Medical Services
Daniel Joseph, MD Yale University
Joshua B. Gaither, MD University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD Yale School of Medicine
Stephen Meldon, MD Cleveland Clinic
Luna Ragsdale, MD, MPH
Duke University
Health Equity
Emily C. Manchanda, MD, MPH
Boston University School of Medicine
Official Journal of the California Chapter of the American College


Douglas S. Ander, MD, Guest Editor Emory University School of Medicine-Atlanta, Georgia
Edward Ullman, MD, Associate Guest Editor Harvard University-Cambridge, Massachusetts
Abra Fant, MD, Associate Guest Editor Northwestern University Feinberg School of MedicineChicago, Illinois
Matthew Tews, DO, MS, Associate Guest Editor Indiana University School of Medicine, Augusta, Georgia
Rick A. McPheeters, DO, Associate Editor Kern Medical- Bakersfield, California
Elizabeth Burner, MD, MPH, Associate Editor University of Southern California- Los Angeles, California
Shahram Lotfipour, MD, MPH, Managing Associate Editor University of California, Irvine School of Medicine- Irvine, California
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of Medicine- Irvine, California
Mandy J. Hill, DrPH, MPH
UT Health McGovern Medical School
Infectious Disease
Elissa Schechter-Perkins, MD, MPH
Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
Drexel University College of Medicine
Kevin Lunney, MD, MHS, PhD
University of Maryland School of Medicine
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine
University of California, Davis
Stephen Liang, MD, MPHS
Washington University School of Medicine
Injury Prevention
Mark Faul, PhD, MA
Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS
Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH
Prisma Health Richland
Taylor Burkholder, MD, MPH
Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Melanie S. Heniff, MD, JD
Indiana University School of Medicine
Greg P. Moore, MD, JD
Madigan Army Medical Center
Statistics and Methodology
Shu B. Chan MD, MS
Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH
Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS
Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS
Pacific Northwest University
Neurosciences
Antonio Siniscalchi, MD
Annunziata Hospital, Cosenza, Italy

Rick Lucarelli, MD
Medical City Dallas Hospital
William D. Whetstone, MD
University of California, San Francisco
Pediatric Emergency Medicine
Paul Walsh, MD, MSc
University of California, Davis
Muhammad Waseem, MD
Lincoln Medical & Mental Health Center
Deena Berkowitz, MD, MPH
Children’s National Hospital
Cristina M. Zeretzke-Bien, MD
University of Florida
Public Health
Jeremy Hess, MD, MPH
University of Washington Medical Center
Jacob Manteuffel, MD
Henry Ford Hospital
John Ashurst, DO
Lehigh Valley Health Network
Tony Zitek, MD
Kendall Regional Medical Center
Trevor Mills, MD, MPH
Northern California VA Health Care
Erik S. Anderson, MD
Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD
Henry Ford Hospital
Phillips Perera, MD
Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS
Virginia Commonwealth University
Jeffrey R. Suchard, MD
University of California, Irvine
Ultrasound
J. Matthew Fields, MD
Thomas Jefferson University
Shane Summers, MD
Brooke Army Medical Center
Robert R. Ehrman
Wayne State University
Ryan C. Gibbons, MD Temple Health

Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 333 City Blvd, West, Rt 128-01, Orange, CA 92868, USA. Office: 1-714-456-6389; Email: Editor@westjem.org.
Volume 25, Issue 4.1: May 2024
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Editorial Board
Amin A. Kazzi, MD, MAAEM
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Douglas Ander, MD Emory University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Jaqueline Le, MD Desert Regional Medical Center
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Rachel A. Lindor, MD, JD Mayo Clinic
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Scott Rudkin, MD, MBA University of California, Irvine
Scott Zeller, MD University of California, Riverside
Elena Lopez-Gusman, JD
California ACEP American College of Emergency Physicians
Jennifer Kanapicki Comer, MD FAAEM
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett
American College of Osteopathic Emergency Physicians
Kimberly Ang, MBA UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians Kaiser Permanente
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP UC San Diego Health School of Medicine
Steven H. Lim Hoon Chin, MD Changi General Hospital, Simei, Singapore
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Isabelle Nepomuceno, BS Executive Editorial Director
Emily Kane, BS WestJEM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
June Casey, BA Copy Editor
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine




Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 333 City Blvd, West, Rt 128-01, Orange, CA 92866, USA Office: 1-714-456-6389; Email: Editor@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians California ACEP
Academic Department of Emergency Medicine Subscriber
Alameda Health System-Highland Hospital Oakland, CA
Ascension Resurrection Chicago, IL
Arnot Ogden Medical Center Elmira, NY
Atrium Health Wake Forest Baptist Winston-Salem, NC
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Beth Israel Deaconess Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University-Rhode Island Hospital Providence, RI
Carolinas Medical Center Charlotte, NC
Cedars-Sinai Medical Center Los Angeles, CA
Cleveland Clinic Cleveland, OH
Desert Regional Medical Center Palm Springs, CA
Eisenhower Health Rancho Mirage, CA
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin Healthcare Minneapolis, MN
Henry Ford Hospital Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Howard County Department of Fire and Rescue Marriotsville, MD
Icahn School of Medicine at Mt Sinai New York, NY
Indiana University School of Medicine Indianapolis, IN
INTEGRIS Health Oklahoma City, OK
Kaweah Delta Health Care District Visalia, CA
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of AmericanAcademy of Emergency Medicine
Loma Linda University Medical Center
Loma Linda, CA
Louisiana State University Shreveport Shereveport, LA
Massachusetts General Hospital/ Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Mayo Clinic in Florida Jacksonville, FL
Mayo Clinic College of Medicine in Rochester Rochester, MN
Mayo Clinic in Arizona Phoeniz, AZ
Medical College of Wisconsin Affiliated Hospital Milwaukee, WI
Mount Sinai Medical Center Miami Beach Miami Beach, FL
Mount Sinai Morningside New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
NYC Health and Hospitals/ Jacobi New York, NY
Ochsner Medical Center New Orleans, LA
Great Lakes Chapter Division of the AmericanAcademyofEmergencyMedicine
Tennessee Chapter Division of the AmericanAcademyofEmergencyMedicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Ohio State University Wexner Medical Center Columbus, OH
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Poliklinika Drinkovic Zagreb, Croatia
Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Rush University Medical Center Chicago, IL
Rutgers Robert Wood Johnson Medical School New Brunswick, NJ
St. Luke’s University Health Network Bethlehem, PA
Southern Illinois University School of Medicine Springfield, IL
Stony Brook University Hospital Stony Brook, NY
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center
El Paso, TX
Uniformed Services Chapter Division of the American Academy of Emergency Medicine Virginia Chapter Division of the American Academy of Emergency Medicine
forEmergencyMedicine
To become a WestJEM departmental sponsor, waive article processing fee, receive print and copies for all faculty and electronic for faculty/residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California ACEP
Academic Department of Emergency Medicine Subscriber
The University of Texas Medical Branch Galveston, TX
UT Health Houston McGovern Medical School Houston, TX
Touro University College of Osteopathic Medicin Vallejo, CA
Trinity Health Muskegon Hospital Muskegon, MI
UMass Memorial Health Worcester, MA
University at Buffalo Program Buffalo, NY
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Little Rock, AR
University of Arkansas for Medical Sciences Galveston, TX
University of California, Davis Medical Center Sacramento, CA
University of California San Francisco General Hospital San Francisco, CA
University of California San Fracnsico Fresno Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida, Jacksonville Jacksonville, FL
University of Illinois at Chicago Chicago, IL
University of Iowa Hospitals and Clinics Iowa City, IA
University of Kansas Health System Kansas City, IA
University of Louisville Louisville, KY
University of Maryland School of Medicine Baltimore, MD
University of Miami Jackson Health System Miami, FL
University of Michigan Ann Arbor, MI
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Southern Alabama Mobile, AL
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine
Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Southern California Los Angeles, CA
University of Vermont Medical Cneter Burlington, VA
University of Virginia Health Charlottesville, VA
University of Washington - Harborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Medical Center Dallas, TX
Franciscan Health Olympia Fields Phoenix, AZ
WellSpan York Hospital York, PA
West Virginia University Morgantown, WV
Wright State University Boonshoft School of Medicine Fairborn, OH
Yale School of Medicine New Haven, CT
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the
American Academy of Emergency Medicine Uniformed Services Chapter Division of the
Academy of Emergency Medicine Virginia Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias Sociedad Chileno Medicina Urgencia Thai Association for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive print and copies for all faculty and electronic for faculty/residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
AlineBaghdassarian,MD,MPH*†
JessicaA.Bailey,MD‡
DeryaCaglar,MD§∥
MichelleEckerle,MD,MPH¶#
AndreaFang,MD**
KatherineMcVety,MD††‡‡ ThuyNgo,DO,MEd§§
JerriA.Rose,MD∥∥¶¶
CindyGanisRoskind,MD##
MelissaM.Tavarez,MD,MS***
FrancesTurcotteBenedict,MD,MPH†††‡‡‡ JoshuaNagler,MD,MHPEd§§§∥∥∥
Authorscontinuedatendofpaper
*InovaL.J.MurphyChildren'sHospital,DepartmentofPediatrics, FallsChurch,Virginia
† UniversityofVirginia,SchoolofEducation,Charlottesville,Virginia ‡ OregonHealth&ScienceUniversity,DepartmentofPediatricsand EmergencyMedicine,Portland,Oregon
§ UniversityofWashington,DepartmentofPediatrics,Seattle,Washington
∥ SeattleChildren’sHospital,DepartmentofPediatrics, Seattle,Washington
¶ UniversityofCincinnatiCollegeofMedicine,DepartmentofPediatrics, Cincinnati,Ohio
# CincinnatiChildren’sHospital,DepartmentofPediatrics,Cincinnati,Ohio
Affi liationscontinuedatendofpaper
SectionEditors:KendraParekh,MD,andChrisMerritt,MD
Submissionhistory:SubmittedNovember15,2023;RevisionreceivedFebruary10,2024;AcceptedFebruary21,2024
ElectronicallypublishedMarch14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18581
Introduction: Virtualinterviews(VI)arenowapermanentpartofpediatricemergencymedicine(PEM) recruitment,especiallygiventhecostandequityadvantages.Yetinabilitytovisitprogramsinpersoncan impactdecision-making,leadingapplicantstoapplytomoreprograms.Moreover,thecostadvantagesof VImayencourageapplicantstoapplytoprogramsfartherawaythantheymightotherwisehavebeen willingorabletotravel.Thiscouldcreateunnecessarystrainonprograms.Weconductedthisstudyto determinewhetherPEMfellowshipapplicantswouldapplytoalargernumberofprogramsandindifferent geographicpatternswithVI(2020and2021)ascomparedtoin-personinterviews(2018and2019).
Methods: WeconductedananonymousnationalsurveyofallPEMfellowscomparingtwocohorts: currentfellowswhointerviewedinperson(appliedin2018/2019)andfellowswhounderwentVIsin2020/ 2021(currentfellowsandthoserecentlymatchedin2021).ThestudytookplaceinMarch–April2022. Questionsfocusedongeographicconsiderationsduringinterviewsandthematch.Weuseddescriptive statistics,chi-squareand t-testsforanalysis.
Results: Overallresponseratewas42%(231/550);32%(n = 74)interviewedinpersonand68% (n = 157)virtually.Fellowsappliedtoamedianof4/6geographicregions(interquartilerange2,5).Most appliedforfellowshipbothinthesameregionasresidency(216,93%)andoutside(192,83%).Onlythe PacificregionsawastatisticallysignificantincreaseinapplicantsduringVI(59.9%vs43.2%, P = 0.02). Therewasnostatisticaldifferenceinthenumberofprogramsappliedtoduringin-personvsVI (meandifference(95%confidenceinterval0.72, 2.8 – 4.2).Amajoritymatchedintheirpreferred statebothduringVI(60.4%)andin-personinterviews(65.7%).Thedifferencewasnotstatistically significant(P = 0.45).
Conclusion: WhilemorePEMfellowshipapplicantsappliedoutsidethegeographicareawheretheir residencywasandtothePacificregion,therewasnooverallincreaseinthenumberofprogramsor geographicareasPEMapplicantsappliedtoduringVIascomparedtoin-personinterviewseasons.As thiswasthe firsttwoyearsofVI,ongoingdatacollectionwillfurtheridentifytrendsandtheimpactofVI. [WestJEmergMed.2024;25(4.1)1–5.]
Since2020,virtualinterviews(VI)havebeenpreferredfor traineerecruitment.1 Withthebenefitsoflowercostand greaterequity,itislikelytoremainapermanentpartof recruitment,despiteageneralpreferenceforface-to-face interviews.2–5 TheVIprocessandassociatedperceptions havebeendescribedintheliterature.2,3,6–9 Theinabilityto visitaprograminpersoncanimpactdecision-makingduring ranking,4,10–14 andanincreasednumberofapplications couldcreateunduestrainonprograms.15–17
Geographiclocation,senseof “fit,” andprogram leadershipweredescribedasmajorcontributorsto applicants’ rankpreference.18 Anationalcohortofpediatric emergencymedicineprogramdirectors(PEMPD),inajoint statement,raisedconcernthatVIcouldleadapplicantsto applytomoreprogramsandtoprogramsfartherawaythan theymaybewillingorabletotravel.10 Weconductedthis studytodeterminewhetherPEMfellowshipapplicants wouldapplytoalargernumberofprogramsandindifferent geographicpatternswithVI(2020and2021)ascomparedto in-personinterviews(2018and2019).
DesignandParticipants
Thiswasananonymous,self-administered,crosssectional,web-basedsurveyofPEMfellowsinthe UnitedStates.Participationwasvoluntary,andnoincentive wasprovidedforcompletion.Thestudywasexempted bytheinstitutionalreviewboardatYaleUniversity, withinformedconsentimpliedbycompletionofthesurvey byparticipants.
Thesurveyquestionnairewasdevelopedthroughiterative feedbackandamodifiedDelphiprocesstodetermine itemimportance.ThirteenPEMPDswithexpertisein performanceandevaluationparticipatedinmultiplerounds ofrevisionsandediting.Pilottestingwasconductedwithtwo pediatrichospitalmedicinefellowswhohadappliedtothe matchduringVIsandtwopediatricchiefresidentswhowere alsointerviewingforfellowshipsusingVI,atthelead institution.Revisionsweremadebasedonpilotfeedback (surveyprovidedin SupplementaryAppendix1).Thesurvey includedmultiple-choicequestionsaboutlocationof residency,statesappliedtoandinterviewedforfellowship, preferredlocationforfellowship,statesvisitedinpersonfor thepurposeofthematch,andstatematchedin.Italsoasked fellowstoindicatestatesofresidenceofimmediatefamily (parents,siblings,orpartners)andaboutcompellingreasons (otherthanfamily)thatmayhaveledfellowstofavorastate orregion(freetext).Geographicregionsweredefinedas Northeast,Southeast,Midwest,Southwest,Rocky Mountain,andPacificregions.19
Whatdowealreadyknowaboutthisissue?
Virtualinterviewsareapermanentpartof recruitment.Theyoffercostandequity advantageswhileposingchallengestoboth applicantsandprograms.
Whatwastheresearchquestion?
DidPEMfellowshipapplicantsapplytoa largernumberofprogramsandindifferent geographicpatternswithVIascomparedto in-personinterviews?
Whatwasthemajor findingofthestudy?
VIdidnothaveasigni fi cantimpactonthe numberofprogramsorgeographicareas applicantsappliedto.
ThesurveywasreviewedandapprovedbytheAmerican AcademyofPediatrics(AAP)SectiononEmergency Medicine(SOEM)PDsurveysubcommitteepriorto distributiononQualtrics(Qualtrics,Provo,UT)toallPEM PDs,viatheAAPSoEMPDCommitteelistserv.ThePDs forwardedthesurveylinktotheircurrentandincoming fellows(thoserecentlymatchedtostartinJuly2022).Each PDcompletedaseparatequestionnaireindicatingthetotal numberofcurrentandrecentlymatchedfellowstowhom theyforwardedthesurvey.
Participantsweredividedintotwogroups:VI(2020or 2021)andinperson(2018or2019).Weperformed descriptivestatisticsincludingfrequencies,percentages, meanswithstandarddeviations,andmedianswith interquartilerange(IQR).Chi-squaretestscompared categoricalvariablesandt-tests,continuousvariableswith 95%confidenceintervals(CI).Weconsideredatwo-tailed alphaof <0.05tobestatisticallysignificant.Weconducted analysesinIBMSPSSStatisticsversion28(IBM Corporation,Armonk,NY).
ThePDsreportedthattheyforwardedthesurveyto406 currentfellowsand144incomingfellows.Theresponserate forcurrentfellowswas35%(143/406)andforincoming fellows,61%(88/144).Overall,theresponseratewas42% (231/550).Ofthetotalrespondents,62%(143/231)were currentfellowsand38%(88/231)incoming.Twofellows (1%)didnotcompleteresidencyintheUS,and12(5%) appliedtoPEMfellowshipmorethanonce.
AllincomingfellowshadundergoneVI,whereas 48%ofthecurrentfellowshadundergoneVI(69/143). Overall,32%ofrespondents(74/231)interviewedinperson and68%(157/213)virtually.Therewasnostatistical differenceinthenumberofprogramsappliedtoduringinpersonvsVI(meandifference(95%CI):.72[ 2.8,4.2]) (Appendix2Table).
Datadescribingthegeographictrainingandlocation preferenceofparticipants arepresentedinthetablein appendix2.Fellowsappliedtoamedianoffourofthe sixgeographicregions(IQR2,5).Mostparticipantsapplied forfellowshipinthesamegeographicregionastheirresidency (216,93%)andoutsidetheirresidencyregionaswell (192,83%).OnlythePacificregionsawastatistically significantincreaseinapplicantsduringVI(59.9%vs43.2%, P = 0.02)(Table1).
Lessthanhalfofrespondentshadimmediatefamily memberslivinginthesamestateasresidency(N = 111,48%), fellowship(N = 90,39%),ortheirpreferredmatch state(N = 95,41%).Compellingreasonstoapplyto anareaincludedfamiliaritywithlocation(N = 128,55%); similarlocationtoresidency(N = 65,28%);anda desiretotraininanewarea(N = 53,23%).Partner’ s employmentwasanimportantfactorfor89(38%),salary
andcostoflivingfor76(33%),andschoolforchildren for20(9%).
OurresultsshowthatVImayallowsomecandidatesto exploreandconsiderregionstheymaynothaveotherwise duetologisticalor financialconstraints,withoutincreasing thenumberofprograms,regionsorstatestheyapplyto. Theseresultsareconsistentwiththe2021NRMPsurvey where52%reportednoimpactoftheVIonthenumberof programsappliedto.5 Residencyprogramshavereportedan increaseinmatchedinternalcandidatesduringVI.11,12,20,21 InPEM,apre-pandemicstudyofPDsshowedthat29%of fellowscompletedresidencyatthesameinstitution.22 While wedidnothavedataattheinstitutionallevel,therewasno significantincreaseinfellowsmatchingwithinthestateof theirresidencyprogramwithVI.ThissuggeststhatVIwere notasignificantdetrimenttoapplicantsrankingprograms andgeographicareas,despitetheabsenceofopportunitiesto meetinpersonandvisitprograms.Thisalsoallowsprograms tohaveaccesstoalargerandpotentiallymorediversepool ofcandidates.9
Proximitytofamilywasnotasignificantconsiderationfor mostapplicantsandwasnotimpactedbyVI.Residency
Table1. Influenceofvirtualinterviewsonapplicantbehaviorandoutcomes. In-person interviews(N = 74)
(N = 157)
ficance (P valueor95%CI)
Appliedtoregionforfellowship,N(%)
Northeast59(79.7)123(78.3)0.81
Southeast41(55.4)102(65)0.16
Midwest50(67.6)111(70.7)0.63
Southwest38(51.4)86(54.8)0.63
RockyMountains31(41.9)73(46.5)0.51
Pacific32(43.2)94(59.9)0.02
Appliedtosamegeographicregionas residency,N(%) 71(98.6)145(94.8).278
Appliedoutsidegeographicregionas residency,N(%) 56(77.8)136(88.9)0.03
Numberofregionsappliedto,mean(SD)3.4(1.8)3.8(1.8)Meandifference(95%CI):.36( .15,.89)
Numberofstatesappliedto,mean(SD)9(7.3)9.7(6.8)Meandifference(95%CI):.73( 1.2,2.7)
Numberofprogramsappliedto,mean(SD)13.3(12.8)14(12.5)Meandifference(95%CI):.72( 2.8,4.2)
Numberofprogramsinterviewedat, mean(SD) 7.2(4.7)6.9(5.2)Meandifference(95%CI): 3.1( 1.7,1.1)
Matchedinpreferredstate,N(%)46(65.7)84(60.4)0.46
Matchedinsamestateasresidency,N(%)31(42%)59(38%)0.58
Preferredtomatchinstatewithimmediate familypresent,N(%) 36(52.9)59(46.8)0.42
Wenttovisitstate/program,N(%)9(14)23(17)0.61
CI,confidenceinterval.
applicantsreportedgeography,qualityoflife,casevariety, curriculum,institutionalreputation,expertiseinareasof interest,andprogramsizeaskeyfactors.23 Applicantsto PEMhighlightedfamiliaritywiththeregionorwantingto exploreanewareaasfactorsforexploringprogramsin differentregions.
Limitationsofthisstudyincludethesmallerresponserate ofthecurrentfellowsascomparedtotheincomingfellows. Thislowresponseratelimitedthesamplesizeofthein-person cohort,impactingthestatisticalsignificanceofourresults. Thisdifferentialresponsefromtheincomingfellowsmay havebeenduetodesirabilitybiaswherethiscohortof applicantsmayhavetendedtostatethattheymatchedin theirpreferredstate.Tominimizethis,wedesignedourstudy tobefullyanonymousandself-administered,andthe questionswerewordedtoretainobjectivityoftheanswers. Respondentsmayalsohaveexperiencedrecallbiasregarding thestatesandprogramstowhichtheyapplied.Thisbias couldpotentiallyhavecontributedtothelowerresponserate amongthecurrentfellowswhohadinterviewedin2018/2019, 3–4yearspriortothesurveydate,comparedtothemore recentapplicantswhohadamorerecentrecollectionofthe questionsaskedinthesurvey.
Anotherlimitationisthatwedidn’texplicitlyaskthetotal numberoffellowsineachclasscohort;however,sincethe PEMfellowshipclasssizeintheUSdoesn’tvarysignificantly fromyeartoyear(byvirtueoftheapprovedfellowship positionsavailable),thedenominatorisexpectedtobe relativelyconstant.
Thisstudywasnotdesignedtolookattheratesof applicationstoindividualprogramsnorassessthepostmatchopinionsofprogramsandfellowsregardingthe resultsofthematch.Thisinformationwouldprovidea deeperinsightintotheimpactoftherecruitmentprocess; however,itisalsopronetobiasasfellowsonlyexperience trainingatasingleinstitution.Wealsodidnottakeinto considerationtheconcentrationofPEMprogramsby regionortheavailablefellowshipslotsperprogramor region.However,theobjectiveofthisstudywastolookat thedifferencesbeforeandduringVIs,andtherewasnota signi fi cantchangeinavailablefellowshipslotsorprograms duringtheseyears.Asthenumberofpediatricfellowship applicantsrises,furtherinvestigationintotheimpactofVIs isnecessarytogainadeeperunderstandingofits implicationsandtooptimizethisprocessbothfor applicantsandprograms. 24
WhilemorePEMfellowshipapplicantsappliedoutside thegeographicareawheretheirresidencywasandtothe Pacificregion,therewasnooverallincreaseinthenumberof
programsorgeographicareasthatPEMapplicantsapplied toduringVIduringthe firsttwoyearsofitsinstitution,as comparedtoin-personinterviewseasons.Ongoing monitoringoftheinterviewandmatchseasonswillhelp identifyfuturetrendsandimpactofVIs.
** StanfordUniversitySchoolofMedicine,Departmentof PediatricEmergencyMedicine,PaloAlto,California
††Children’sHospitalofMichigan,DepartmentofPediatrics, Detroit,Michigan
‡‡CentralMichiganUniversity,SchoolofMedicine, DepartmentofPediatrics,Detroit,Michigan
§§JohnsHopkinsUniversity,SchoolofMedicine,Department ofPediatrics,Baltimore,Maryland
∥∥
RainbowBabies&Children’sHospital,Departmentof Pediatrics,Cleveland,Ohio
¶¶CaseWesternReserveUniversity,SchoolofMedicine, DepartmentofPediatrics,Cleveland,Ohio
##ColumbiaUniversityIrvingMedicalCenter,Pediatricsin EmergencyMedicine,NewYork,NewYork
*** UniversityofPittsburgh,SchoolofMedicine,Departmentof Pediatrics,Pittsburgh,Pennsylvania
†††UniversityofMissouriofKansasCitySchoolofMedicine, DepartmentofPediatrics,KansasCity,Missouri
‡‡‡UniversityofKansasMedicalCenter,KansasCity, Missouri
§§§BostonChildren’sHospital,DepartmentofPediatricsand EmergencyMedicine,Boston,Massachusetts
∥∥∥HarvardMedicalSchool,DepartmentofPediatricsand EmergencyMedicine,Boston,Massachusetts
¶¶¶YaleUniversitySchoolofMedicine,Departmentof PediatricsandEmergencyMedicine,NewHaven, Connecticut
AddressforCorrespondence:AlineBaghdassarian,MD,MPH, InovaFairfaxL.JMurphyChildren’sHospital,3300GallowsRd., FallsChurch,VA22042-3300.Email: aline.baghdassarian@ inova.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Baghdassarianetal.Thisisanopenaccess articledistributedinaccordancewiththetermsoftheCreative CommonsAttribution(CCBY4.0)License.See: http:// creativecommons.org/licenses/by/4.0/
1.AssociationofPediatricProgramDirectors,CouncilofPediatric Subspecialties,AssociationofMedicalSchoolPediatricDepartment Chairsetal.APPD/CoPS/AMSPDC/NextGenPediatricianslettertoour pediatricscommunityaboutthefellowshiprecruitmentprocess.2021. Availableat: https://downloads.aap.org/AAP/PDF/2021_05_19_-_ Pediatric_Fellowship_Recruitment_Recommendations_Final.pdf AccessedJuly15,2022.
2.VanDerLaanL,GeorgeR,NesiamaJA,etal.Virtualinterviewingfor pediatricemergencymedicinefellowship-anationalsurvey. Pediatr EmergCare. 2022;38(4):e1207–12.
3.GuptaS,GrierArthurL,ChandlerN,etal.Isthechanginglandscapeof fellowshiprecruitmentduringCOVID-19heretostay? JPediatrSurg. 2022;57(10):445–50.
4.DasAJ,AugustinRC,CorbelliJA,etal.Residencyandfellowship programleaders’ perceptionsofvirtualrecruitmentandinterviewing. JGradMedEduc. 2022;14(6):710–3.
5.NationalResidentMatchingProgram.2021Applicantandprogram directorsurvey findings:impactofthevirtualexperienceonthetransition toresidency.2021.Availableat: https://www.nrmp.org/wp-content/ uploads/2021/08/Research-Brief-Virtual-Experience-2021-FINAL.pdf AccessedJuly15,2022.
6.WolffMandBurrowsH.Planningforvirtualinterviews:residency recruitmentduringapandemic. AcadPediatr. 2021;21(1):24–31.
7.BernsteinSA,GuA,ChretienKC,etal.Graduatemedicaleducation virtualinterviewsandrecruitmentintheeraofCOVID-19. JGradMedEduc. 2020;12(5):557–60.
8.McCainC,KempB,BaierMB,etal.Aframeworkforthevirtualmedical interviewprocess:considerationsfortheapplicantandtheinterviewer. OchsnerJournal. 2022;22(1):61–70.
9.PetersenTL,KingJC,FussellJJ,etal.Benefitsandlimitationsofvirtual recruitment:perspectivesfromsubspecialitydirectors. Pediatrics. 2022;150(4):e2022056735.
10.AllisterL,BaghdassarianA,CaglarD,etal.Pediatricemergency medicinefellowshipdirectors’ 2021collectivestatementonvirtual interviewsandsecondlooks. PediatrEmergCare. 2021;37(11):585–7.
11.EderleA,ShahriariS,WhisonantC,etal.TheimpactofCOVID-19on thedermatologymatch:anincreaseinthenumberofstudentsmatching athomeprograms. DermatolOnlineJ. 2021;27(9).
12.FaletskyA,ZitkovskyH,GuoL.TheimpactofCOVID-19on plasticsurgeryhomeprogrammatchrates. AnnPlastSurg. 2022;88(1):4–6.
13.MulcahyCF,TerhaarSJ,BoulosS,etal.Didmoreotolaryngology residencyapplicantsmatchattheirhomeinstitutionsin2021? InvestigatingtheimpactoftheCOVID-19pandemic. AnnOtolRhinol Laryngol. 2022;131(12):1375–80.
14.QuinnA,MannE,RaikinJ,etal.PD24-06Theeffectofthe COVID-19pandemiconurologymatchbylocation. JUrol. 2021;206(Suppl3):e427–8.
15.InclanPM,WoiczikMR,CummingsJ,etal.Virtualpediatricorthopaedic fellowshipinterviewsduringthepandemic:Whatdidtheapplicantsand programsthink? JPediatrOrthop. 2022;42(7):e806–10.
16.LewkowitzAK,RamseyPS,BurrellD,etal.Effectofvirtualinterviewing onapplicantapproachtoandperspectiveofthematernal-fetal medicinesubspecialtyfellowshipmatch. AmJObstetGynecolMFM. 2021;3(3):100326.
17.ReamMAandThompson-StoneR.Virtualresidencyinterview experience:thechildneurologyresidencyprogramperspective. PediatrNeurol. 2022;126:3–8.
18.DiGiustoM,LupaMC,CorridoreM,etal.TheimpactoftheCOVID-19 pandemiconthe2020pediatricanesthesiologyfellowship applicationcycle:asurveyofapplicants. PaediatrAnaesth. 2021;31(9):968–76.
19.STUDYGUIDEUSII.2cGeographyThemes.Availableat: https://www.solpass.org/7ss/standards/StudyUSII.2c.htm AccessedFebruary4,2024.
20.WhisonantCT,ShahriariSR,HarrisonJ,etal.Evaluatingtheintegrated plasticsurgeryresidencymatchduringthenovelcoronaviruspandemic. Cureus. 2021;13(8):e16988.
21.CotnerCE,MercadanteSF,SheaJA.Assessingtheimpactofthe COVID-19pandemicongeographicresidencyplacementrelativeto medicalschoollocation. JGradMedEduc. 2022;14(1)108–11.
22.BradleyT,ClingenpeelJM,PoirierM.Internalapplicantstopediatric emergencymedicinefellowshipsandcurrentuseofthenationalresident matchingprogrammatchasurveyoffellowshipdirectors. PediatrEmerg Care. 2015;31(7):487–92.
23.LoveJN,HowellJM,HegartyCB,etal.Factorsthatinfluence medicalstudentselectionofanemergencymedicineresidency program:Implicationsfortrainingprograms. AcadEmergMed. 2012;19(4):455–60.
24.TheAmericanBoardofPediatrics.Yearlygrowthinpediatricfellowsby subspecialtybydemographicsandprogramcharacteristics.Available at: https://www.abp.org/content/yearly-growth-pediatric-fellowssubspecialty-demographics-and-program-characteristics AccessedJanuary26,2023.
JohnK.Quinn,MD
JillianMongelluzzo,MD,MAEd
AlyssaNip,MD
JosephGraterol,MD
EstherH.Chen,MD
UniversityofCalifornia,SanFrancisco,DepartmentofEmergencyMedicine, SanFrancisco,California
SectionEditor:JeffreyLove,MD,MHPE,andDanielleHart,MD,MACM
Submissionhistory:SubmittedJune15,2022;RevisionreceivedMarch16,2023;AcceptedMarch17,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.57756
Introduction: TheStandardizedLetterofEvaluation(SLOE)isdesignedtoassistemergencymedicine (EM)residencyprogramsindifferentiatingapplicantsandinselectingthosetointerview.TheSLOE narrativecomponentsummarizesthestudent’sclinicalskillsaswellastheirnon-cognitiveattributes.The purposeofthisqualitativeinvestigationwastoexplorehowstudentsdescribedintheSLOEasquietare perceivedbyfacultyandtobetterunderstandhowthismayimpacttheirresidencycandidacy.
Methods: ThisretrospectivecohortstudyincludedallSLOEssubmittedtooneEMresidencyprogram duringoneapplicationcycle.WeanalyzedsentencesintheSLOEnarrativedescribingstudentsas “quiet,”“shy,” and/or “reserved.” Usinggroundedtheory,thematiccontentanalysiswithaconstructivist approach,weidentified fivemutuallyexclusivethemesthatbestcharacterizedtheusageofthese targetwords.
Results: Weidentified fivethemes:1)quiettraitsportrayedasimplied-negativeattributes(62.4%); 2)quietstudentsportrayedasovershadowedbymoreextravertedpeers(10.3%);3)quietstudents portrayedasunfitforfast-pacedclinicalsettings(3.4%);4) “quiet” portrayedasapositiveattribute (10.3%);and5) “quiet” commentsdeemeddifficulttoassessduetolackofcontext(15.6%).
Conclusion: Wefoundthatquietpersonalitytraitswereoftenportrayedasnegativeattributes.Further, commentsoftenlackedclinicalcontext,leavingthemvulnerabletomisunderstandingorbias.More researchisneededtodeterminehowquietstudentsperformcomparedtotheirnon-quietpeersandto determinewhatchangestoinstructionalpracticesmaysupportthequietstudentandhelpcreateamore inclusivelearningenvironment.[WestJEmergMed.2024;25(4.1)6–9.]
Theemergencymedicine(EM)StandardizedLetterof Evaluation(SLOE)isahigh-stakesassessmentdesignedto assistresidencyprogramsindifferentiatingapplicantsandis consideredimportantinthedecisiontointerview.1,2 The narrativecomponentsummarizesthestudent’sknowledge, clinicalskills,andnon-cognitiveattributesshowntobe predictorsofperformance.3–5 However,thenarrativemaybe difficulttointerpretduetotheuseofoverlygenerallanguage andhiddencode,bothcommoninwrittenassessment.6–9
Further,commentsaboutpersonalityoftenlackclinical context,whichreducestheirusefulnessandmakesthem vulnerabletomisinterpretationorbias.6–8 WebecameinterestedinSLOEnarrativesreferencing quietstudentsduringapplicantreviewwhenweobservedless enthusiasmforstudentsdescribedasquiet,evenforthose withstrongobjectiveapplicationdata.Whilenon-cognitive attributesareimportantcomponentsofholisticassessment, personalitytraitsshouldnotnecessarilyhinderastrong application.3–5 Nostudiesshowthatquietindividualsare
unsuitedforEMorarelesssuccessfulinEMcareers. However,inaninternalmedicinesetting, “quiet” was interpretedbyattendingsasa “red flag ” inclerkshipwritten evaluations, 9,10 andstudentsdescribedasquietintheir SLOEscoredloweronbothglobalassessmentand anticipatedranklist.11 Wefoundnootherresearch examininghowquietindividualsperformorhowthey wereperceivedinEM.Thepurposeofthisqualitative investigationwastoexplorehowquietstudentsaredescribed intheSLOEnarrativeandhowthislanguagemay impactcandidacy.
StudyDesignandPopulation
Weconductedasubgroupanalysisofaretrospective cohortstudyofallcoreEMrotationSLOEssubmitted throughtheElectronicResidencyApplicationService (ERAS)tooneEMresidencyprogramduringthe2016–2017 applicationcycle.WeexcludedSLOEsfromnon-Liaison CommitteeonMedicalEducationaccreditedschoolsand applicantswhograduatedfrommedicalschoolbeforeor duringtheapplicationcycle.Thestudywasapprovedbythe institutionalreviewboardandtheAssociationofAmerican MedicalColleges.
AuthorJMdownloadedSLOEsfromERASinto REDCap(ResearchElectronicDataCapturetoolshostedat UCSanFrancisco).andde-identifiedthempriortoanalysis. AnalysiswasperformedbyJKQ,EHC,andJM,allwith traininginmedicaleducationresearchmethodologyand educationleadershipexperience(chiefresident,associate residencydirector,andassistantresidencydirector).JKQ andEHCbrainstormedwordstypicallyusedtodescribe quietindividualsandchosethetarget-descriptorsquiet,shy, andreserved(collectivelytermed “quiet”)becausepassive, introverted,andtimidwereuncommon(3,2,and1, respectively)andalwaysco-occurredwithtarget-descriptors. Weanalyzedonlythesentencecontainingthetargetdescriptorswithoutexploringtheentirenarrative.We analyzeddatausinggroundedtheorythematiccontent analysiswithaconstructivistapproach.12 Therewasnopreexistingtheoryaboutthedatathatweaimedtoproveor disprove;instead,thegoalwastoexploreSLOEnarrativecommentsandconstructmeaningfromthemtoprovide perspectiveonhowquietstudentsareperceived.
Withoutapresetideaofhowdatawouldbesorted,JKQ andEHCindependentlybegantheinitialcodingbyreading eachcommentandconsideringhowitwasusedtodescribe thestudent.Asusagepatternsemergedtheywerecodedas like-comments.JMreadasubsetofthedata.Toestablish thatthedatasetwassufficientforthepurposeofthe investigation,wecodedthe firsthalfofthedatasetandthen determinedthatnonewpatternsemergedinthesecondhalf.
Weprogressedtoexplainingourcodingschemes,comparing them,andlookingforsimilaritiesanddifferences.Through aniterativeprocessofconstantcomparisonwecombined, deleted,andrefinedcodes,mergingthemintooverarching themes.Weusedaspreadsheettovisuallyorganizecodesand finalthemes.
Wereviewed1,582SLOEsfrom696applicants.Ofthese, 117SLOEsreferencedquietapplicantsandwereanalyzed. Theadjective “quiet” occurredin102SLOEs. “Reserved” occurredin28SLOEsandco-occurred14timeswith “quiet.” “Shy” occurredin11SLOEsandco-occurred fivetimes with “quiet.”
Initialcodingrevealedusagerelatedtointerpersonal skills,initiative,disposition,patientinteractions,leadership, medicalknowledge,responsetofeedback,workhabits,and fitnessforEM.Furtheranalysisrevealedthatmanytarget sentencesdidnot fitintothesecategories,lackedclinical context,andweredifficulttointerpret.Weeventually reachedaconsensusonaframeworkof fivemutually exclusiveoverarchingthemesthatincludedallcomments, bestrepresentedthescopeofusagepatterns,andwouldbe mostmeaningfulinaddressingourstudypurpose(Table1).
Theme1comments,62.4%describequiettraits asimplied-negativeattributes.Commentsarelabeled “implied” becausequietisnotexplicitlycallednegativebut istypicallycoupledwithacontrastingpositivetraitthat appearstobeanefforttomitigatethenegativityofthequiet comment(eg, “Quietbuthardworking”).Thestructureofthe sentencemakesitclearthatquietisnegative,butitisnot evidentinwhatwayortowhatdegreeitisnegative.Asmaller numberofcommentslinkedthequiettraitwith anotherseeminglynegativeattribute(eg, “Quietandtimidat times”).Theimpliednegativityofthesecomments coupledwiththelackofcontextmayadverselyaffectthe applicant’scandidacy.
Theme2comments(10.3%)describequietstudentsas beingovershadowedbymoreextravertedpeersandthus moredifficulttoassess.Thesecommentsalsodidnotexplain howperformancewasimpactedbythequiettrait,onlythat the studentwasnotabletodemonstratevalueasacandidate orperformattheleveloftheirpeers,whichpresumably hindersapplicantcandidacy.
Theme3comments3.4%)questionthe fitnessofquiet studentsforfast-pacedclinicalsettings.However,these commentsdidnotdetailhow,ortowhatdegree,thestudent’ s quietnessspecificallyaffectedperformance,makingthem vulnerabletomisinterpretation.Thesecommentswould likelyalsohindercandidacy,astheabilitytoperformwellin allclinicalsettingsispresumablyseenasnecessaryina successfulEMresident.
Theme4comments(10.3%) “quiet” isportrayedas apositiveattributeandtendstodescribeleadershipstyle,
Table1. Thematicanalysisof117sentencescontainingthewords
ThemeSubthemesExamples
Theme1)Impliednegative (n = 73)
Theme2)Quietstudentsmay beovershadowedbyothers (n = 12)
1A) Quietnatureismitigatedby associatingwithapositiveinterpersonal skill.
1B)Quietnatureismitigatedby associatingwithapositiveattribute unrelatedtoquietpersonality.
2A)Quietstudentsovershadowedby moreextravertedstudents.
2B)Quietstudents’ clinicalskillsdif ficult toassessduetotheirquietpersonality.
“Quietbutwasalwaysabletocommunicateeffectively.” “Somewhatreservedbutcanbeassertivewhen necessary.”
“Quietbuthardworking.”“Canbereservedattimesbut isincrediblyintelligent.”
“Quietdemeanorandpresenceof flashierstudents preventedahigherranking.”“Overshadowed,quieter thanpeers,disappearedintobackgroundmostofthe month.”
“Truncatedpresentationsandquietdemeanormakeit dif ficulttoevaluatetruepotential.”“SoquietIcouldnot judgelevelofengagement.”
Theme3)Quietstudentsmay belesssuitedforcertainclinical settings(n = 4)
3A)Quietstudentsperceivedastoo passive,slow,orunassertiveforabusy clinicalsetting.
3B)Quietstudentsperceivedasless adaptabletothedemandsofabusy clinicalsetting.
Theme4)Positivetrait(n = 12)
Theme5)Equivocal(n = 16)
ED, emergencydepartment; EM,emergencymedicine.
patientinteractions,orabilitytoperformunderpressure, ratherthandescribingstudentpersonality.Thisadditional contextmayhavecontributedtotheoverallperceptionof “quiet” asapositiveattribute.Theme5comments(15.6%) wereconsideredequivocalinthattheinvestigatorseitherdid notagreeonthepositivityornegativityoftheir interpretation,orthecommentslackedsufficientcontextto interprettheintendedmeaning(eg, “Studentwas initiallyquiet”).
Wefoundthatquiettraitswereusuallyportrayedas negativeattributesand,therefore,hadthepotentialto adverselyaffectthecandidacyofaconsiderablenumberof applicants.Theanalysisalsorevealedthatacrossthemes thequiettraitwasrarelydescribedintermsofclinical competency.Thisisconcerningbecauseanegativecomment thatlackscontextrequiresthereadertorelyoninferences orassumptionsthatmayresultinunfairlyjudgingthe applicant.Providingexamplesthatdescribeobserved behaviorandclinicalskill,ratherthanreferencing personality,willimprovethequalityandfairnessof theassessment.6,7
“Quiet,passivenaturemaynotbesuitedforhighpaced inner-cityED.”“Quietandunassumingpersonality, somenotedthistobeaconcern,particularlyinabusy countyED,othersdidn’t.”
“Calm,quiet,reserveddemeanor-somestaffquestion adaptabilitytochaoticED.”
“Soothingdemeanorandquietconfidencewillsuitquite wellthroughouttheircareer.”“Quietdemeanor,kind bedsidemannerwhichisanassetwithpatients.”
“Alittlequiet,wedonotthinkthiswillhinderabilitytobe averycapableEMresident.”“Quiet”
Our findingsthatquietstudentsaredescribedasbeing overshadowedbymoreextravertedpeers,moredifficultto assess,andless fitforfast-pacedclinicalsettingssuggestthe possibilitythatcurrentinstructionalpracticesfavormore outgoingstudents.Inaclinicalsettingwherebeingassertive isviewedfavorably,quietstudentsmaybejudgedunfairlyas beinglessknowledgeableorprepared.3,13 Changesto instructionalpracticesthatmaybetterservequietstudents includethefollowing:providingadditionalstudent observations6;usingstandardizedassessment-tools14,15; expandingassessmentcriteriatoincludestrengthsofthe introvert13;providingfacultydevelopmenttoimprove qualityofwrittenassessment7;usinggroup-writtenSLOEs thatmayreducebias1,2;andprovidingstudentmentorship.3
ThisstudywaslimitedtoSLOEsfromapplicantstoa singleinstitutionduringoneapplicationcycle.Weanalyzed onlythesentencecontainingthetarget-descriptors;reading theentirenarrativemayhaveprovidedadditionalcontext. Target-descriptorsmaybedefineddifferentlybydifferent evaluatorsandreadersandmayormaynotbeused interchangeably.Further,readersmayinterpretthe
positivityornegativityoftheusagedifferentlythanthe investigators.Thetarget-descriptorsmaynotreflectstudent personalitybutratherhowtheywereperceivedbytheir evaluatorintheclinicalsetting.Applicantsdidnotreceivea personalityinventorynordidtheyself-reporttheir personalitytype.Wedidnotidentifythegenderofapplicant ortheSLOEwriter,whichpreventedusfromdetermining whetherour findingswereaffectedbygender.Nordidwe identifythepositionorexperienceofthewriter,orwhether individualorgroupprocesswasused.Wedidnotattemptto associatequietvsnon-quietstatuswithaninvitation tointerview.
Wefoundthatquietpersonalitytraitswereoftenportrayed asnegativeattributesintheStandardizedLetterof Evaluation.Additionally,clinicalcontextwasrarely provided,leavingcommentsopentovariableinterpretation andpossiblemisunderstandingofstudentcompetency. These findingsaddtoourunderstandingaboutquietstudents inEM,butmoreresearchisneededtodeterminehow quiet-labeledstudentsperformcomparedtotheirnon-quiet peersandtodeterminewhatchangestoinstructionalpractices maysupportthequietstudentandhelpcreateamoreinclusive learningenvironmentwhereallstudentscanthrive.
AddressforCorrespondence:JohnK.Quinn,MD,Universityof California:SanFrancisco,DepartmentofEmergencyMedicine,505 ParnassusAve,SanFrancisco,CA94143.Email: john.quinn@ucsf. edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Quinnetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.LoveJN,DotyCI,SmithJL,etal.Theemergencymedicinegroup StandardizedLetterofEvaluationasaworkplace-basedassessment: ThevalidityIsinthedetail. WestJEmergMed.2020;21(3):600–9.
2.NegaardM,AssimacopoulosE,HarlandK,etal.Emergencymedicine residencyselectioncriteria:anupdateandcomparison. AEMEduc Train.2018;2(2):146–53.
3.KhanMA,MalviyaM,EnglishK,etal.Medicalstudentpersonalitytraits andclinicalgradesintheinternalmedicineclerkship. MedSciEduc 2021;31(2):637–45.
4.PinesJM,AlfarajS,BatraS,etal.FactorsImportanttotop clinicalperformanceinemergencymedicineresidency:results ofanideationsurveyandDelphipanel. AEMEducTrain 2018;2(4):269–76.
5.SobowaleK,HamSA,CurlinFA,etal.Personalitytraitsareassociated withacademicachievementinmedicalschool:anationally representativestudy. AcadPsychiatry.2018;42(3):338–45.
6.JacksonJL,KayC,JacksonWC,etal.Thequalityofwrittenfeedbackby attendingsofinternalmedicineresidents. JGenInternMed 2015;30(7):973–8.
7.LedfordR,BurgerA,LaRochelleJ,etal.Exploringperspectivesfrom internalmedicineclerkshipdirectorsintheUSAoneffectivenarrative evaluation:resultsfromtheCDIMnationalsurvey. MedSciEduc 2020;30(1):155–61.
8.LyePS,BiernatKA,BraggDS,etal.Apleasuretoworkwith–ananalysis ofwrittencommentsonstudentevaluations. AmbulPediatr 2001;1(3):128–31.
9.GinsburgS,KoganJR,GingerichA,etal.Takenoutofcontext:hazards intheinterpretationofwrittenassessmentcomments. AcadMed 2020;95(7):1082–8.
10.GinsburgS,McIlroyJ,OulanovaO,etal.Towardauthenticclinical evaluation:pitfallsinthepursuitofcompetency. AcadMed 2010;85(5):780–6.
11.QuinnJK,MongelluzzoJ,AddoN,etal.TheStandardizedLetterof Evaluation:howweperceivethequietstudent. WestJEmergMed 2023;24(2):259–63.
12.CoatesWC,JordanJ,ClarkeSO.Apracticalguideforconducting qualitativeresearchinmedicaleducation:Part2-Codingandthematic analysis. AEMEducTrain.2021;5(4):e10645.
13.DavidsonB,GilliesRA,PelletierAL.Introversionandmedicalstudent education:challengesforbothstudentsandeducators. TeachLearn Med.2015;27(1):99–104.
14.DavisKR,BankenJA.Personalitytypeandclinicalevaluationsinan obstetrics/gynecologymedicalstudentclerkship. AmJObstetGynecol 2005;193(5):1807–10.
15.SchellRM,DilorenzoAN,LiHF,etal.Anesthesiologyresident personalitytypecorrelateswithfacultyassessmentofresident performance. JClinAnesth.2012;24(7):566–72.
MeryllBouldin,MD* CarlyEastin,MD*†
RachaelFreeze-Ramsey,MD*
AmandaYoung,MD*
MeredithvonDohlen,MD*
LaurenEvans,MD*
TravisEastin,MD,MS*
SarahGreenberger,MD*
*UniversityofArkansasforMedicalSciences,DepartmentofEmergencyMedicine, LittleRock,Arkansas
† UniversityofArkansasforMedicalSciences,DepartmentofPediatrics, SectionofEmergencyMedicine,Toxicology,andPharmacology, LittleRock,Arkansas
SectionEditors:AbraFant,MD,andWilliamEdwardSoares,MD
Submissionhistory:SubmittedOctober1,2023;RevisionreceivedFebruary7,2024;AcceptedFebruary21,2024
ElectronicallypublishedMarch14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18487
Background: ResidencyprogramstransitionedtoprimarilyvirtualinterviewsduetotheCOVID-19 pandemic.Thisshiftraisedquestionsregardingexpectationsandpatternsofapplicantcancellation timeliness.Thepurposeofthisstudywastoexaminechangesinapplicantcancellationsafter transitioningtovirtualinterviews.
Methods: Thiswasaretrospectivecohortstudyofinterviewdatafromathree-yearemergencymedicine residencyatatertiary-careacademicmedicalcenter.UsingarchiveddatafromInterviewBroker,we examinedschedulingpatternsbetweenonein-person(2019–2020)andtwovirtualinterviewcohorts (2020–2021and2021–2022).Ouroutcomesweretheoverallcancellationratesrelativetointerviewslots aswellastheproportionofcancellationsthatoccurredwithin7or14daysoftheinterviewdate.
Results: Therewere453interviewslotsand568applicantsinvited.Overall,applicantscanceled17.1% ofscheduledinterviews.Comparedwithin-personinterviews,applicantscanceledsignificantlyfewer virtualinterviews(inperson:40/128(31.3%),virtualyear1:22/178(12.4%),virtualyear2:15/143 (10.5%), P = 0.001).Conversely,applicantscanceledsignificantlymorevirtualinterviewswithinboththe 14-daythreshold(inperson:8/40(20%),virtualyear1:12/22(55.5%),virtualyear2:12/15(80%), P < 0.001)andthe7-daythreshold(inperson:0/40(0%),virtualyear1:3/22(13.6%),virtualyear2:4/15 (26.7%), P = 0.004).
Conclusion: Whilelimited,atoursite,changingtoavirtualinterviewformatcorrelatedwithfewer cancellationsoverall.Theproportionofcancellationswithin14dayswasmuchhigherduring virtualinterviewseasons,withmostcancellationsoccurringduringthattimeframe.Additional studiesareneededtodeterminetheeffectsofcancellationpatternsonemergencymedicinerecruitment. [WestJEmergMed.2024;25(4.1)10–14.]
Historically,residencyapplicantstraveledtoUSprograms forin-personinterviews.In2020,theCOVID-19pandemicled theCoalitionforPhysician Accountability(COPA)to recommendthatresidencyprogramsconductonlyvirtual interviews.1 Proponentsofvirtualinterviewscitedcostand safetyaspotentialupsides,andapplicantshavereportedoverall satisfactionwithvirtualinterviewsandmoreadvantagesthan barriers.2–4 However,programshaveexpressedcontinued doubtsaboutsomeaspectsofvirtualrecruitment.2
Evenbeforethepandemic,therewerenoestablishedrules acrossspecialtiesregardinganacceptabletimeframefor interviewcancellations.Foremergencymedicine,the EmergencyMedicineResidentAssociation(EMRA) recommendedatleasttwoweeks’ noticeintheir2019 “EMRAandCORDStudentAdvisingGuide.”5 In2020,the firstyearofvirtualinterviews,emailcommunicationonthe CouncilofResidencyDirectorsinEmergencyMedicine (CORD)listservsuggestedthatprogramdirectors’ acceptablecancellationthresholdsrangedfrom48hoursto 10dayspriortotheinterviewdate.6 Ultimately,CORD statedthatsevendayswasrecommendedforapplicantsina 2020blogpostaboutinterviewingduringthepandemic, whileotherpublicationsstillrecommendedtwoweeks.7,8 Currently,the2023CORDApplicationProcess ImprovementCommitteeandthe2022–2023National ResidentMatchingProgram(NRMP)agreementhave advisedapplicantstocancelnolaterthan1–2weeksbefore theirinterviewdates.9,10
Virtualinterviewsmaybeheretostay,asevidencedby recentCOPAandAssociationofAmericanMedicalColleges (AAMC)statements,aswellasthe2023-24CORD guidelines.11–13 Understandingpatternsofvirtualinterview cancellationbehaviormayhelpprogramdirectors, applicants,andtheiradvisorsprepareforasuccessfulMatch. Tocharacterizetheeffectsofvirtualrecruitmentoninterview cancellations,wecomparedin-personinterviewcancellation patternstothoseofvirtualrecruitmentcyclesatour academicemergencymedicine(EM)residency.
Thiswasaretrospectivecohortstudyatathree-yearEM residencysponsoredbyatertiary-care,academicmedical centerinanurbansettinginthesouth-centralUnitedStates. Thisresidencyisanestablishedprogram(foundedin1984) withaclasssizeof10residentsperyear,whichincreasedto12 residentsforthe2022Match.TheUniversityofArkansasfor MedicalSciencesInstitutionalReviewBoard(IRB) approvedthisstudyinexemptstatus.
Ourprogrambeganusingtheonlineinterviewscheduling softwareInterviewBroker(TheTenthNerve,LLC,Lewes, DE;www.interviewbroker.com)inFall2019toinvite applicantstointerview.InFall2020,interviewstransitioned frominpersontovirtualandadditionalslotswereadded, withCORDcontinuingtorecommendvirtualinterviewsfor EMresidenciesinsubsequentcycles.Similartoin-person interviews,applicantsforvirtualinterviewsareinvitedina 1:1applicanttoslotratioandgiven48hourstorespond beforeanotherapplicantisinvited.
UsingarchiveddatafromInterviewBroker,weexamined schedulingpatternsbetweenthein-personinterviewcohort (2019–2020season)andtwovirtualinterviewcohorts (VirtualYear1:2020–2021andVirtualYear2:2021–2022). Unfortunately,cancellationdatapriortotheinitiationof
InterviewBrokeratoursitewasnotavailable.Asingle investigatorabstracteddatafromInterviewBrokerin aggregateformbyacademicyearusingoverallcountsof relevantvariables,includingnumberofinterviewslots,days, invitations,interviewsscheduled/unscheduled(ie,no applicantresponsereceived)/declined,cancellations,andthe timingofthosecancellationsrelativetotheinterviewdate. Wedefinedaninterviewcancellationasaninterviewthatwas scheduled,canceled,andneverrescheduled;interviewsthat wererescheduledwereconsideredcompleted.Demographic variableswerenotavailableasInterviewBrokeronlyrecords thestudent’snameandAAMCID;accessingadditional informationwouldhaverequiredqueryingtheElectronic ResidencyApplicationService,whichwasnotcoveredinour exemptIRBagreement.
Ouroutcomesweretheoverallproportionofinterview cancellationsrelativetointerviewslots,aswellasthe proportionofinterviewcancellationsthatoccurredwithin 14daysoftheinterviewdateandwithinsevendaysofthe interviewdate.Descriptivestatisticswereperformed.We performedcomparisonsusingchi-squaredortheFisherexact testassomeobservationswereuncommon.Allcomparisons weretwo-sidedwith ɑ = 0.05.Analyseswereperformedusing SPSSStatisticsforMacintoshVersion28.0(IBM Corporation,Armonk,NY).
Overthreeyears,therewere453interviewslotsand568 applicantsinvited.Mostoftheinterviewslotswerevirtual (71.7%).Overall,theprogramsentout1.25interview applicationsperslotandapplicantscanceled17.1%of scheduledinterviews(Table1).Wefoundasignificant decreaseintheproportionofoverallcancellationsrelativeto filledinterviewslots,with40/128(31.3%),22/178(12.4%), and15/143(10.5%)cancellationsforin-person,virtualyear 1,andvirtualyear2,respectively(P < 0.001).When analyzedfurtherandadjustingformultiplecomparisons,the decreasewassignificantwhencomparinginpersonvs.either virtualyear,butnotwhencomparingthetwovirtualyears. Whilefewerinterviewswerecanceled,theproportionof virtualinterviewcancellationsthatoccurredwithin14days oftheinterviewdatewassignificantlyhigher(inperson:8/40 (20%),virtualyear1:12/22(55.5%),virtualyear2:12/15 (80%), P < 0.001).Similarly,morevirtualinterviewswere canceledwithinsevendaysoftheinterviewdate(inperson:0/ 40(0%),virtualyear1:3/22(13.6%),virtualyear2:4/15 (26.7%), P = 0.004),althoughthesenumberswerelow overall.Inboththe14and7daycancellationanalyses,these dataindicatedayear-over-yearincrease,meaninginboth14 and7daycomparisonswesawasignificantincreasein cancellationsbetweeninpersonandvirtualyear1,andagain sawasignificantincreasebetweenvirtualyear1andvirtual year2.See Figures1 and 2 forgraphicalbreakdownofthe
Table1. Breakdownofin-personandvirtualinterviewcohorts;totalcountsprovidedunlessotherwisespecified.
InterviewsandCancellations
InterviewgroupInpersonVirtualyear1Virtualyear2
Numberofinterviewdays151616
Numberofinterviewslots128180145
Numberofapplicantsinvited195206167
Numberofinvitationsperinterviewslot1.521.141.15
Totalinterviewslots filled128178143
Numberofunscheduledinvitations(ie,noapplicantresponsereceived)1413
Numberwhodeclinedwithoutscheduling1356
Overallcancellations(%ofscheduled)40(31.3%)22(12.4%)15(10.5%)
Numberwhocanceled < 7days(%ofcanceled)0(0%)3(13.6%)4(26.7%)
Numberwhocanceled7–14days(%ofcanceled)8(20%)9(40.9%)8(53.3%)
Numberwhocanceled >14days(%ofcanceled)32(80%)10(45.5%)3(20.0%)
Overalldeclined,unscheduled,orcanceled(%oftotalinvited)67(34.4%)28(13.6%)24(14.3%)

overalldistributionofinvitedapplicantsandinterview cancellationrates.
Comparedwithin-personinterviews,applicantstoour programwerelesslikelytocanceltheirvirtualinterview.Of thosewhodidcancel,severalvirtualapplicantscanceled withinsevendays,andmostcancellationsoccurredwithin 14daysoftheinterviewdate.Forin-personinterviews, applicantsweretraditionallyinstructedtocancelassoonas possibleandatleasttwoweekspriortotheinterviewdate.5 Asdiscussedpreviously,recommendationsforEMvirtual interviewcancellationshaverangedfrom48hourstotwo weeks,withtheNRMPcurrentlyrecommendingatleast1–2 weeksinadvance.10 Ourresultssuggestthatshort-notice
cancellations(ie,lessthantwoweeks)bystudentsmaybe morecommoninthevirtualera.
Wearenotawareofliteratureregardingthespecifictiming ofvirtualinterviewcancellations,butour findingoffewer overallcancellationsisconsistentwithLewkowitzetal’ s findingsthatmaternal-fetalmedicinefellowshipvirtual interviewshadalowerrateofcancellationscomparedwith in-personinterviews(39.1%vs72.3%).14 Thiscouldstemfrom thereducedtimeandcostrequiredtointerviewvirtually.15,16
Unfortunately,fewerinterviewcancellationsoverallcould contributetointerviewhoardingandaninequitable distributionofinterviews.TheAAMCandsomespecialties haveexpressedconcernsabouthigherqualityapplicants receivinginvitationsforandschedulingexcessivelyhigh numbersofinterviewsandleavinglowertierstudentswith

feweroptions.15,17 WhilethishasnotbeenstudiedinEM specifically,theEmergencyMedicineConsensusStatement onthe2020–2021ResidencyApplicationprocesssuggested aninterviewlimitof17interviewsandencouragedapplicants nottointerviewattheirless-preferredprogramsloweron theirlistto “maketheseslotsavailabletootherstudents,” indicatingapotentialconcernfortheeffectsofhoardingsuch as “peersnotmatchingand/orprogramsnot filling.”18
Short-noticeinterviewcancellationsposeafewother challengesforresidencyprograms.Previously, fillinganinpersoninterviewslotrequired findingareplacementwho couldstillarrangetraveltotheinterviewlocation,whichisno longerrelevantforvirtualinterviews.Nonetheless,the NRMPrequiresthatprogramsprovidenolessthan48hours forapplicantstorespondtointerviewinvitations.10 If applicantsarecancelingonlyafewdaysbeforeaninterview, fillingtheopenspotmaybeachallengesinceprograms cannotinvitemorethanoneapplicantatatimeperspot. Short-noticecancellationscanalsobeproblematicas interviewersmayhavetoreviewcandidates’ applications wellinadvanceoftheinterviewdate.Withshort-notice cancellations,thiscouldmeanlosttimeforinterviewerswho hadalreadyreviewedthoseapplicationsorinadequatetime toreviewthereplacements.
Conversely,programdirectorswanttoavoidinterviewing applicantswhoarenotinterestedintheirprogram,anda cancellation evenonshortnotice providesan opportunitytointerviewanapplicantwithgreaterinterestin theprogram.Inourcase,wehadonlyfouropeninterview spotsoverthe firsttwovirtualyears(twounfilledperyear), indicatingthatwe filledmostcanceledspots.Therefore, whilenoofficialopinionexists,programdirectorsmaynot mindshort-noticecancellationaslongastheinterview scheduleisfull.Infact,theymaypreferfortheapplicantnot tofeelpressuredtointerviewataprograminwhichtheyare uninterestedonlybecausetheyareconcernedabout canceling,withshortnoticebeingviewedasunprofessional. Asvirtualinterviewsappeartobeheretostay,understanding cancellationpatternswillbeimportantforprograms, especiallyinbalancingthetimingcancellationswithnew
invitationssoprogramscanideallymaintainafull interviewschedule.
Thisstudywaslimitedtoonespecialtyatasingle institution,thereforethegeneralizabiltyofthese fi ndingsto otherinstitutionsorspecialtiesisunclear,especiallygiven thesmallsamplesizeandlimitedpre-postperiod.The changinglandscapeofEMresidencyrecruitmentmayalso affectthegeneralizabilityofthese fi ndings.Unfortunately, wehadonlyoneyearofin-personinterviewdataaswedid notkeeptheserecordspriortotheuseofInterviewBroker, whichcouldhaveintroducedbias.Wealsohadanincrease inresidentcomplementduringvirtualyear2,whichmay haveconfoundedtheresults.Unfortunately,wewere unabletoincludedemographicdata,whichmighthave helpedtoidentifyadditionalcancellationpatterns.Lastly, examiningtrendsinthosewhorescheduleinterviewswas notperformedinthisstudyandmaybeofvalueinfuture investigations,assomedownsidesdiscussedwithshortnoticecancellations(eg, fi llingemptyslots;havingtimeto reviewapplications)wouldstilloccurinapplicantswhoare reschedulingwithshortnotice.
Comparedwithin-personinterviewcycles,applicantsto ourresidencyprogramweresignificantlylesslikelytocancel virtualinterviews.However,themajorityofvirtual cancellationsthatdidoccurwerewithin14daysofthe interviewdateandnearlyone-fifthoccurredinunderseven days.Additionalstudies,ideallymultisitethatinclude applicantdemographicdata,areneededtodeterminehow cancellationpatternsaffectEMrecruitmentandmatch outcomesinthevirtualera.
AddressforCorrespondence:MeryllBouldin,MD,Universityof ArkansasforMedicalSciences,DepartmentofEmergency Medicine,4301WMarkhamSt.,Slot584,LittleRock,AR72205. Email: mebouldin@uams.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Bouldinetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TheCoalitionforPhysicianAccountability’sWorkGrouponMedical StudentsintheClassof2021MovingAcrossInstitutionsforPost GraduateTraining.Finalreportandrecommendationsformedical educationinstitutionsofLCME-accredited,U.S.osteopathic,andnonU.S.medicalschoolapplicants.2020.Availableat: https://www.aamc. org/system/files/2020-05/covid19_Final_Recommendations_ 05112020.pdf.AccessedMay22,2022.
2.DavisMG,HaasMRC,GottliebM,etal.Zoominginversus flyingout: virtualresidencyinterviewsintheeraofCOVID-19. AEMEducTrain. 2020;4(4):443–6.
3.DomingoA,RdesinskiRE,StensonA,etal.Virtualresidencyinterviews: applicantperceptionsregardingvirtualintervieweffectiveness, advantages,andbarriers. JGradMedEduc. 2022;14(2):224–8.
4.Li-SauerwineS,WeygandtPL,SmylieL,etal.Themorethingschange themoretheystaythesame:factorsinfluencingemergency medicineresidencyselectioninthevirtualera. AEMEducTrain. 2023;7(6):e10921.
5.EmergencyMedicineResidentsAssociationJarouZ,HillmanEA, KellogA,etal.(Eds.). EMRAandCORDStudentAdvisingGuide: AnEvidence-basedApproachtoMatchinginEM. 2019.Availableat: https://www.emra.org/books/msadvisingguide/msag AccessedJanuary19,2024.
6.EmergencyMedicineProgramDirectors.Re:interviewcancellations. CORDListservprivateemailchain.LastaccessedJanuary19,2024.
7.GorgensS.TheEMinterviewseason:pandemicedition.2020. Availableat: https://cordemblog.com/2020/09/03/the-em-interviewseason-pandemic-edition/.AccessedDecember20,2023.
8.HopsonLR,EdensMA,GoodrichM,etal.Calmingtroubledwaters:a narrativereviewofchallengesandpotentialsolutionsintheresidency interviewofferprocess. WestJEmergMed. 2020;22(1):1–6.
9.CouncilofResidencyDirectorsinEmergencyMedicine.Application ProcessImprovementCommittee(Apic):BestPracticesforthe 2023–2024ResidencyApplicationandInterviewSeason.2023.
Availableat: https://www.cordem.org/siteassets/files/match/ apic-2023-2024-application-interview-season-best-practices.pdf AccessedJuly26,2023.
10.NationalResidentMatchingProgram.MatchParticipationAgreement forPrograms.2023.Availableat: https://www.nrmp.org/wp-content/ uploads/2022/09/2023-MPA-Main-Match-Program-FINAL-3.pdf AccessedJune28,2023.
11.CouncilofResidencyDirectors.2023CORDstatementonresidency interviews.2023.Availableat: https://www.cordem.org/siteassets/files/ board/adv.–position-statements/2023-cord-statement-on-residencyinterviews.pdf.AccessedJuly26,2023.
12.AAMC.InterviewsinGME:Wheredowegofromhere?2023. Availableat: https://www.aamc.org/about-us/mission-areas/ medical-education/interviews-gme-where-do-we-go-here AccessedJuly23,2023.
13.TheCoalitionforPhysicianAccountability’sWorkGrouponMedical StudentsintheClassof2022MovingAcrossInstitutionsforInterviews forPostgraduateTraining.Recommendationson2021–22residency seasoninterviewingformedicaleducationinstitutionsconsidering applicantsfromLCME-accredited,U.S.osteopathic,andnon-U.S. medicalschools.Availableat: https://physicianaccountability.org/ wp-content/uploads/2021/08/Virtual-Rec_COVID-Only_Final.pdf AccessedJune22,2022.
14.LewkowitzAK,RamseyPS,BurrellD,etal.Effectofvirtualinterviewing onapplicantapproachtoandperspectiveofthematernal-fetal medicinesubspecialtyfellowshipmatch. AmJObstetGynecolMFM. 2021;3(3):100326.
15.BoydCJ,AnanthasekarS,VernonR,etal.Interviewhoarding: disparitiesintheintegratedplasticsurgeryapplicationcycleinthe COVID-19pandemic. AnnPlastSurg. 2021;87(1):1–2.
16.GordonAM,ConwayCA,ShethBK,etal.Howdidcoronavirus-19 impacttheexpensesformedicalstudentsapplyingtoanorthopaedic surgeryresidencyin2020to2021? ClinOrthopRelatRes. 2022;480(3):443–51.
17.WhelanA.Openletteronresidencyinterviews.2020.Availableat: https://www.aamc.org/media/50291/download?utm_source=sfmc& utm_medium=Email&utm_campaign=ERAS&utm_content=Interviews AccessedJanuary19,2024.
18.FarcyD,JungJ,AintablianH,etal.Consensusstatementonthe 2020–2021residencyapplicationprocessforUSmedicalstudents planningcareersinemergencymedicineinthemainresidency match.2020. https://www.emra.org/be-involved/be-an-advocate/ working-for-you/residency-application-process AccessedJanuary22,2024.
FoundationsofEmergencyMedicine:Impactofa Standardized,Open-access,CoreContentCurriculum onIn-TrainingExamScores
JaimeJordan,MD,MAEd*
NatashaWheaton,MD*
NicholasD.Hartman,MD,MPH† DanaLoke,MD,MS‡ NathanielShekem,MPAS§ AnwarOsborne,MD,MPM∥ P.LoganWeygandt,MD,MPH¶ KristenGrabowMoore,MD,MEd∥
SectionEditor:DanielleHart,MD
*UniversityofCaliforniaLosAngeles,DavidGeffenSchoolofMedicine, DepartmentofEmergencyMedicine,LosAngeles,California † WakeForestUniversitySchoolofMedicine,DepartmentofEmergency Medicine,Winston-Salem,NorthCarolina
‡ NorthwesternUniversityFeinbergSchoolofMedicine,Departmentof EmergencyMedicine,Chicago,Illinois
§ UniversityofIowa,DepartmentofEmergencyMedicine,IowaCity,Iowa
∥ EmoryUniversity,DepartmentofEmergencyMedicine,Atlanta,Georgia
¶ JohnsHopkinsUniversitySchoolofMedicine,Baltimore,Maryland
Submissionhistory:SubmittedJune28,2023;RevisionreceivedDecember9,2023;AcceptedJanuary12,2023
ElectronicallypublishedMarch25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18387
Introduction: Learnersfrequentlybenefitfrommodalitiessuchassmall-group,case-basedteaching andinteractivedidacticexperiencesratherthanpassivelearningmethods.Thesecontemporary techniquesarefeaturesofFoundationsofEmergencyMedicine(FoEM)curricula,andparticularlythe FoundationsI(F1)course,whichtargets first-yearresident(PGY-1)learners.TheAmericanBoardof EmergencyMedicineadministersthein-trainingexam(ITE)thatprovidesanannualassessmentofEMspecificmedicalknowledge.WesoughttoassesstheeffectofF1implementationonITEscores.
Methods: WeretrospectivelyanalyzeddatafrominternsatfourEMresidencyprogramsaccreditedbythe AccreditationCouncilforGraduateMedicalEducation.Wecollecteddatain2021.Participatingsiteswere geographicallydiverseandincludedthree-andfour-yeartrainingformats.Wecollecteddatafrominterns twoyearsbefore(controlgroup)andtwoyearsafter(interventiongroup)implementationofF1ateachsite. YearofF1implementationrangedfrom2015–2018atparticipatingsites.Weabstracteddatausinga standardformincludingprogram,ITErawscore,yearofITEadministration,USMedicalLicensingExam Step1score,Step2ClinicalKnowledge(CK)score,andgender.Weperformedunivariableand multivariablelinearregressiontoexploredifferencesbetweeninterventionandcontrolgroups.
Results: Wecollecteddatafor180PGY-1s.Step1andStep2CKscoresweresignificantpredictorsof ITEinunivariableanalyses(bothwith P < 0.001).AfteraccountingforStep1andStep2CKscores,we didnot findF1implementationtobeasignificantpredictorofITEscore, P = 0.83.
Conclusion: ImplementationofF1curriculadidnotshowsignificantchangesinperformanceontheITE aftercontrollingforimportantvariables.[WestJEmergMed.2024;25(4.1)15–18.]
Residencyprogramsprovideeducationandtrainingto developcompetentphysicians.Boardcertificationin emergencymedicine(EM)requirescompletionofan
AccreditationCouncilforGraduateMedicalEducation (ACGME)-accreditedtrainingprogramandapassingscoreon theQualifyingExamination(QE)andOralCertification Examination(OCE)administeredbytheAmericanBoardof
EmergencyMedicine(ABEM).1,2 TheABEMIn-training Examination(ITE)isanimportanttoolusedbytraining programstoassessmedicalknowledgeandprepareresidents fortheQE.1,3 TheITEisdesignedtoreflectthecontentofthe ModelofClinicalPracticeofEmergencyMedicine(EM Model)andhaspredictivevalueinestimatingthelikelihoodof individualresidentspassingtheQE.3 Priorliteraturesuggests thatclinicalexposurealoneleavessignificantgapsin fundamentalknowledgedefinedbytheEMModel.4 Residency didacticcurriculaprovideanopportunitytosupplementcore knowledge;however,thebestmethodsforproviding instructionoutsideoftheclinicalsettingandpreparingtrainees forsuccessfulperformanceontheITEareunknown.
FoundationsofEmergencyMedicine(FoEM)isa national,free,open-access,onlineEMcurriculumthathas beenwidelyadoptedintheUnitedStates.5,6 FoEMbecame availablein2015;registrationforuseofFoEMcoursesfor the2022–2023academicyearincluded237registered educationalprograms,serving6,326residentphysicians.5,6 FoEMoffersstandardized,level-specific,corecontentfor EMresidentsusinglearner-centriceducationalstrategies thathavebeenshowntobenefitlearningsuchassmall-group discussion,peerlearning,andindividualizedguidance.5–11
FoundationsI(F1)isa flippedclassroom,case-basedcourse targetingpostgraduateyear(PGY)-1residentsthatincludes a30-unit,systems-basedcurriculumoffundamentalcontent intheEMModel.5,6,12 Priorliteraturedemonstratespositive effectsofthe flippedclassroommodelonlearning outcomes.13–15 TheF1curriculumincludescuratedselfstudyresourcescalled “LearningPathways” forlearnersto reviewpriortodidacticmeetings,inwhichresidentswork throughmultipleF1caseswithaknowledgeablefacilitator providinginformationinanoral-boardsstyleformat.6 The F1summarizesessentiallearningpointsandsharesthem withlearnersto fillknowledgegapsandallowforspaced repetition.6 AlthoughtheF1curriculumisnotspecifically designedforITEreview,third-partypairedassessmentsfor eachunithavebeenavailableforusesince2017.6
LimitedoutcomedataofFoEMF1establishedquality anddemonstratedhighsatisfactionamongfacultyleaders andresidentlearners.5,6 However,therehasnotbeenan assessmentofobjectivemeasuressuchasmedicalknowledge andITEperformanceThisinformationcanprovideamore comprehensiveassessmentofthevalueofimplementingsuch aprogram.Inthisstudy,wesoughttoevaluatetheeffectof F1courseimplementationonITEperformanceinthe PGY-1year.Wehypothesizedthatimplementationofthe structuredF1curriculumwouldleadtoimproved performanceontheITE.
WeperformedaretrospectivecohortstudyofITEdata collectedfromPGY-1residentsatfourACGME-accredited EMresidencyprogramsintheUnitedStatesbeforeandafter
implementationoftheFoEMF1curriculum.Weselected participatingsitesthatweregeographicallydiverseand included3-and4-yeartrainingformats.Wecollecteddatain December2021.AllPGY-1residentsatparticipatingsites duringthestudyperiodwereeligibletoparticipate.We excludedPGY-1residentswhoweremissingdata.
Wedeterminedthattodetecta5%differenceinITEscore with80%powerandanalphaof0.05,wewouldneedto enroll81participantsineachgroup(controland intervention)foratotalof162participants.Ourcontrol groupconsistedofdatafromPGY-1residentsforthetwo yearspriortoimplementationateachsite.Ourintervention groupconsistedofdatafromPGY-1residentsforthetwo yearsafterimplementationateachsite.YearofF1 implementationrangedfrom2015–2018atparticipating sites.Theleadauthorfromeachsiteabstracteddatausinga standardformthatincludedprogram,ITErawtotalscore, yearofITEadministration,UnitedStatesMedicalLicensing Examination(USMLE)Step1score,USMLEStep2 ClinicalKnowledge(CK)score,andresidentgender.Priorto dataabstraction,theauthorgroupreadeachitemonthe formaloudandtrialedabstractingasmallportionof representativedatatoensureclarityofmeaningand consistencyinprocess.
Wecalculateddescriptivestatisticsfordemographicdata andITEperformance.Weperformedregressionanalysesto exploredifferencesbetweentheinterventionandcontrol groups.We firstperformedunivariablelinearregression analysesforvariablesincludingimplementationofF1, residencyprogram,yearofITEadministration,USMLE Step1score,USMLEStep2score,andresidentgenderwith ITErawscoreasouroutcomeofinterest.Weincluded variableswitha P -value < 0.1intheunivariableregressionin amultivariablelinearregressionwiththesameoutcome variable.Weconsideredvariableswitha P -valueof < 0.05in themultivariablemodelasstatisticallysignificant.We performedallanalysesinSPSSv27.0(IBMCorporation, Armonk,NY).
ThisstudywasapprovedbytheInstitutionalReview BoardoftheDavidGeffenSchoolofMedicineatUCLA.
Weabstracteddatafromatotalof224interns.We excluded44internswhoweremissingdata.Weanalyzed datafrom180interns(88pre-implementationand92postimplementation)whohadcompletedata.Thedemographics ofparticipantswithcompletedataareshownin Table1.The meanITErawscoreforinternsinthecontrolgroupwas 72.15 ± 6.72.ThemeanITEscoreforinternsinthe interventiongroupwas72.74 ± 7.93.Intheunivariable regressionanalyses,onlyUSMLEStep1andUSMLEStep2 CKscoresyielded P -valuesof < 0.1(Table2).Becauseour hypothesiscenteredontheimpactofimplementationofthe F1curriculumonITEscores,weforcedthisvariableasthe
Table1. Demographicdataofparticipatinginterns.
Controlgroup n(%)totaln = 88
Interventiongroup n(%)totaln = 92
Gender Male3231
Female5660
Non-binary01
MeanUSMLE
Step1score(SD)
MeanUSMLE
232(14.26)232(15.59)
Step2score(SD) 244(17.02)246(14.54)
USMLE,UnitedStatesMedicalLicensingExamination.
Table2. Resultsofunivariableregressionanalysisof recordedvariables. Variable
ImplementationofFoundationsF1curriculum0.59
Residencyprogram0.22
YearofITEadministration0.14
USMLEStep1score <0.001
USMLEStep2CKscore <0.001
Residentgender0.24
USMLE,UnitedStatesMedicalLicensingExamination; ITE, in-trainingexam; CK,clinicalknowledge.
lastvariableafterblockentryofvariablesofUSMLEStep1 scoreandUSMLEStep2CKscoreinthemultivariable regressionanalysis,despiteithavinga P -valueof0.59inthe univariableanalysis.AftercontrollingforStep1scoreand Step2CKscore,F1implementationwasnotasignificant predictorofITEscore,Rsquarechange = 0, P = 0.83.The datasatisfiedallassumptions.
OurstudydemonstratesthatbothStep1andStep2CK weresignificantpredictorsofITEscore.Thisisconsistent withpriorliteratureinmultiplespecialtiesdemonstrating associationsbetweenUSMLEscoresandITE performance.16–19 Wefoundthatourinterventiongrouphad aslightlyhigherrawITEscoreshowever,aftercontrolling forUSMLEscores,thisincreasewasnotstatistically significant,despitebeingadequatelypowered.Thiswas somewhatsurprisinggiventhatF1providesaconsistent structureandcomprehensivecoverageofcontentintheEM modelandalsoincorporatesteachingmethodsthathave beenshowntoenhancelearning.2,6–11 However,ourresults alignwithpreviousstudies,whichhavedemonstratedthat changesincurriculumwerenotassociatedwithsignificant differencesinITEperformance.20,21 Specifically,converting
anhourofsynchronousdidacticconferencetoasynchronous learning,andconvertingconferencelecturestosmallgroup, “flipped-classroom” stylelearninghavepreviouslybeen foundtohavenosignificanteffectonITEscores.20,21
ItisimportanttonotethattheobjectiveofF1isto improveEMcoreknowledgeandapplicationintheclinical environmentandisnotspecificallytargetedtowardsITEtest preparationorperformance.Additionally,performanceon theITEmaynotcomprehensivelyrepresentlearner knowledgeofEM.Thismaybeonereasonthatwedidnot findsignificantchangesinITEperformance.Additionally, variableimplementationandusageofF1atdiffering programscouldinfluencepotentialgains.Althoughthe FoEMcoursesarestandardized,participatingprograms mustaddresstheirownuniqueneedsandbarriers;thismay resultinvariabilityincourseimplementation,including variableuseof flipped-classroomstyleasynchronous resourcesandpairedassessments.Itisalsoimportanttonote thattheITEisadministeredinFebruaryofeachyear;thus, participatingPGY-1residentsinthisstudywereonly exposedtoapproximatelysevenmonthsoftheyear-longF1 curriculumpriortotheITE.
Itispossiblethatadditionalimprovementsmaybeseenwith additionaltimespentinthecurriculum.Thenonsignificant improvementseeninthisstudymaybeaugmentedwith implementationofFoundationsII(F2),whichisdesignedfor PGY-2residents,andFoundationsIII(F3),whichisdesigned forPGY-3andPGY-4residents.Theseoutcomesmeritfurther investigation.Whileourstudydidnot findasignificant increaseinITEscorescomparedtostandardcurricula,itwas notworsethanstandardpracticeandhasadditionalbenefitsof afree,standardized,pre-packaged,high-quality,adaptable formatwithuseracceptability.6
Overall,theresultsofthisstudyprovideimportant insightsforboththenumerousprogramsalreadyusing FoEMandthoseEMresidenciesconsideringincorporating itintotheirtrainingprograms.6 Inadditiontoprior feasibilityanduseracceptabilitydata,thisstudyprovidesan evaluationofobjectiveoutcomes,namelyknowledge,the firstlevelinMiller’spyramidofclinicalcompetence.6,22 Therearestillmanyunansweredquestions.Further investigationintotheeffectoftheF1curriculumonABEM QEandOCEperformanceshouldbepursued.Additionally, asFoEMisdesignedtosupportknowledgeapplicationinthe clinicalspace,futureworkcouldevaluatetheimpactof FoEMonotherdomainsofresidentperformance.
Thisstudyhaslimitations.Theremaybeconfoundersnot accountedforinouranalysisthatcouldhaveinfluenced results.WedidnotcollectdataonspecificITEpreparation curriculaatparticipatingsites,individualusageofexternal ITEpreparationmaterialsoutsideoftrainingprogram curricula,timespentusingF1curriculum,useofpaired
assessments,totalnumberofF1unitscompletedby participatingresidents,ortimespentstudyingforITEin general.However,tothebestofourknowledge,therewere noothermajorchangestothesite’sdidacticcurriculumor methodsofpreparingtraineesfortheITEduringthestudy period.AlthoughtheF1courseincludesstandardized content,participatingprogramsmustaddresstheirown uniqueneedsandvariablesthatimpacttheconsistencyof courseadministration.Theremaybedifferencesinthe personnelwhodeliverthecontent,attendancerequirements, etc,whicharenotaccountedforinourstudy.Theresultsseen inthisstudymaynottransfertoothersiteswhereadherence toimplementationguidelinesismoreorlessconsistent.
OurstudysuggeststhattheFoEMF1curriculumisnot associatedwithsignificantchangesinperformanceonthe ITEinEMtrainingprogramsaftercontrollingforimportant variables.Theseresultsmayinformtheuseand implementationofFoEMcoursesinEMtrainingprograms.
AddressforCorrespondence:JaimeJordan,MD,MAEd,University ofCaliforniaLosAngeles,DavidGeffenSchoolofMedicine, DepartmentofEmergencyMedicine,924WestwoodBlvd.,Suite 300,LosAngeles,CA90024.Email: jaimejordanmd@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Jordanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ACGME.MilestonesbySpecialty:EmergencyMedicine.Accreditation CouncilforGraduateMedicalEducation.2021.Availableat: https://www.acgme.org/globalassets/pdfs/milestones/ emergencymedicinemilestones.pdf.AccessedNovember,2022.
2.AmericanBoardofEmergencyMedicine.BecomeCertified. Availableat: https://www.abem.org/public/become-certified AccessedJune23,2023.
3.AmericanBoardofEmergencyMedicine.In-TrainingExam.Available at: https://www.abem.org/public/for-program-directors/in-trainingexamination.AccessedJune23,2023.
4.BischofJJ,EmersonG,MitzmanJ,etal.Doestheemergencymedicine in-trainingexaminationaccuratelyreflectresidents’ clinical experiences? AEMEducTrain. 2019;3(4):317–22.
5.FoundationsofEmergencyMedicine.Availableat: https:// foundationsem.com/.AccessedJune23,2023.
6.MooreKG,KettererA,WheatonN,etal.Development,implementation, andevaluationofanopenaccess,level-specific,corecontent curriculumforemergencymedicineresidents. JGradMedEduc. 2021;13(5):699–710.
7.TwengeJM.Generationalchangesandtheirimpactintheclassroom: teachingGenerationMe. MedEduc. 2009;43(5):398–405.
8.Moreno-WaltonL,BrunettP,AkhtarS,etal.Teachingacrossthe generationgap:aconsensusfromtheCouncilofEmergencyMedicine ResidencyDirectors2009AcademicAssembly. AcadEmergMed. 2009;16(Suppl2):S19–24.
9.HartDandJoingS.TheMillennialGenerationand “thelecture.” Acad EmergMed. 2011;18(11):1186–7.
10.RobertsDH,NewmanLR,SchwartzsteinRM.Twelvetipsforfacilitating Millennials’ learning. MedTeach. 2012;34(4):274–8.
11.CooperAZandRichardsJB.Lecturesforadultlearners:breakingold habitsingraduatemedicaleducation. AmJMed. 2017;130(3):376–81.
12.BeesonMS,AnkelF,BhatR,etal.The2019modeloftheClinical PracticeofEmergencyMedicine. JEmergMed. 2020;59(1):96–120.
13.KingAM,GottliebM,MitzmanJ,etal.Flippingtheclassroomingraduate medicaleducation:asystematicreview. JGradMedEduc. 2019;11(1):18–29.
14.ChenF,LuiAM,MartinelliSM.Asystematicreviewoftheeffectiveness of flippedclassroomsinmedicaleducation. MedEduc. 2017;51(6):585–97.
15.ChenKS,MonrouxeL,LuYH,etal.Academicoutcomesof flipped classroomlearning:ameta-analysis. MedEduc. 2018;52(9):910–24.
16.FeningK,HorstAV,ZirwasM.CorrelationofUSMLEStep1scoreswith performanceondermatologyin-trainingexaminations. JAmAcad Dermatol. 2011;64(1):102–6.
17.NelsonMandCalandrellaC.DoesUSMLEStep1&2scorespredict successonITEandABEMQualifyingExam:areviewofanemergency medicineresidencyprogramfromitsinception. AnnEmergMed. 2017;70(4):58–9.
18.PatzkowskiMS,HauserJM,LiuM,etal.Medicalschoolclinical knowledgeexamscores,notdemographicorotherfactors,associated withresidencyin-trainingexamperformance. MilMed. 2023;188(1-2):e388–91.
19.PerezJAJrandGreerS.CorrelationofUnitedStatesMedicalLicensing examinationandinternalmedicinein-trainingexaminationperformance. AdvHealthSciEducTheoryPract. 2009;14(5):753–8.
20.KingAM,MayerC,BarrieM,etal.Replacinglectureswithsmallgroups: theimpactof flippingtheresidencyconferenceday. WestJEmergMed. 2018;19(1):11–7.
21.WrayA,BennettK,Boysen-OsbornM,etal.Efficacyofan asynchronouselectroniccurriculuminemergencymedicineeducation intheUnitedStates. JEducEvalHealthProf. 2017;14:29.
22.MillerGE.Theassessmentofclinicalskills/competence/performance. AcadMed. 1990;65(9Suppl):S63–7.
RebeccaGoett,MD*
JasonLyou,MD†
LaurenR.Willoughby,MD†
DanielW.Markwalter,MD‡§
DianeL.Gorgas,MD†
LaurenT.Southerland,MD,MPH†
*RutgersNewJerseyMedicalSchool,DepartmentofEmergencyMedicine, Newark,NewJersey
† TheOhioStateUniversityWexnerMedicalCenter,DepartmentofEmergency Medicine,Columbus,Ohio
‡ UniversityofNorthCarolinaSchoolofMedicine,DepartmentofEmergency Medicine,ChapelHill,NorthCarolina
§ UniversityofNorthCarolinaSchoolofMedicine,UNCPalliativeCareProgram, ChapelHill,NorthCarolina
SectionEditor:ChrisMerritt,MD
Submissionhistory:SubmittedAugust29,2023;RevisionreceivedNovember20,2023;AcceptedJanuary12,2023
ElectronicallypublishedMarch25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18448
Background: Hospiceandpalliativemedicine(HPM)isaboard-certi fiedsubspecialtywithinemergency medicine(EM),butpriorstudieshaveshownthatEMresidentsdonotreceivesufficienttraininginHPM. ExpertsinHPM-EMcreatedaconsensuslistofcompetenciesforHPMtraininginEMresidency.We evaluatedhowtheHPMcompetenciesintegratewithintheAmericanBoardofEmergencyMedicine Milestones,whichincludetheModeloftheClinicalPracticeofEmergencyMedicine(EMModel)andthe knowledge,skills,andabilities(KSA)list.
Methods: ThreeemergencyphysiciansindependentlymappedtheHPM-EMcompetenciesontothe 2019EMModelitemsandthe2021KSAs.Discrepancieswereresolvedbyafourthindependent reviewer,andthe finalmappingwasreviewedbyallteammembers.
Results: TheEMModelincluded78%(18/23)oftheHPMcompetenciesasadirectmatch,andwe identifiedrecommendedareasforincorporatingtheother five.TheKSAsincluded43%(10/23).Most HPMcompetenciesincludedintheKSAsmappedontoatleastonelevelB(minimalnecessaryfor competency)KSA.ThreeHPMcompetencieswerenotclearlyincludedintheEMModelorintheKSAs (treatingend-of-lifesymptoms,caringfortheimminentlydying,andcaringforpatientsunder hospicecare).
Conclusion: ThemajorityofHPM-EMcompetenciesareincludedinthecurrentEMModelandKSAs andcorrespondtoknowledgeneededtobecompetentinEM.ProgramsrelyingontheEMMilestonesto plantheircurriculumsmaymisstraininginsymptommanagementandcareforpatientsattheendoflife orwhoareonhospice.[WestJEmergMed.2024;25(4.1)19–26.]
Athirdofadultswhodiewillreceiveemergency departmentcareinthemonthpriortotheirdeath.1 Emergencyphysiciansneedtrainingtoprovidethehighquality,goal-concordantcarethatthesepatientsdeserve. Hospiceandpalliativemedicine(HPM)isasubspecialtyof emergencymedicine(EM)thataddsanadditionalfocuson
symptommanagement,goal-concordantcare,andqualityof life,especiallyforpatientswithchronicdiseaseorlifethreateningconditions,orwhoareattheendoflife.2 Prior researchhasshownthatcurrentEMresidencytraininglacks instructioninHPM.3–7 Toaddressthis,theAmerican CollegeofEmergencyPhysiciansPalliativeMedicineSection publishedalistof23criticaldevelopmentalmilestonesin
HPMtrainingforEMresidents.8 However,itisunclearhow besttointegratetheserecommendationsintoanEM residencycurriculum.
ManyEMresidencycurriculumsarebasedonthe knowledgeneededtopasstheEMboardcertificationexams. ThisknowledgeiscodifiedintheAmericanBoardof EmergencyMedicine(ABEM)ModeloftheClinical PracticeofEmergencyMedicine(EMModel)andalistof knowledge,skills,andabilities(KSA).9,10 TheEMmodel alongwiththeKSAsarethefoundationaldocumentsusedto createtheEMMilestones,acompendiumubiquitously employedinbothEMtrainingandassessment.Ourgoalin thisstudywastodeterminewheretheHPMcompetencies fit orcould fitwithintheEMModelandKSAs.Thismapping couldhelpguidecurriculumdesignortheincorporationof theHPMcompetenciesintotestingcontent.
Thisstudywasnothumansubjectsresearchandwas deemedexemptfrominstitutionalreviewboardreview.We comparedthe2019EMModelandthe2021KSAstothe HPMcompetencies.TheHPMcompetencieswereassigned numerals.TheEMModelitemswereannotatedbytheir numberandcategory.ThenotationsfortheKSAcategories andcodeswereuseddirectlyfromthe2021document.We dividedtheKSAsintooverarchingcategories(eg,diagnosis, pharmacotherapy,reassessment)whichwethenfurther dividedintosetsofcompetencieswithinthatcategory.10 Eachcompetencywasgivenahierarchyintraining correspondingtoanalphabeticlevel(withAthemost advancedlevelofcompetencyandEtheleast).LevelAis reservedforadvancedknowledgeorskills.LevelBisthe minimalcompetencylevel,definedastheminimumskilllevel everyEMresidentshouldattaintograduate.LevelsC,D, andEareskillsinthedevelopmentofreachinglevelB.
Asthistypeofanalysishasnotbeendonebefore,weuseda sequentialapproachwithinitialindependentreviewers,a mediatorstep,andthen finalconsensusgroupdiscussion. Theconsensusgroupresultswerethenreviewedbytwo independentexternalexperts.Inthe firstphaseofconsensus mapping,tworesidents(EMpostgraduateyear(PGY)-2and EM/internalmedicine(PGY-4)andanEMattending independentlymappedpalliativecarecompetenciesusinga MicrosoftExcelspreadsheet(MicrosoftCorporation, Armonk,NY).Thethreeinitialconceptmappershad independentdatasheetsandwereblindedtoeachother’ s determinations.Acompetencycouldmapontomorethan oneareaoftheEMModel.First,keywordsfromeachHPM competencyweresearchedforintheEMModel.Ifno matcheswerefound,theEMModelwasreviewedlinebyline todeterminewhethertherewereconceptualmatches.Ifthere wasnodirectmatch,buttheHPMcompetencycouldbe incorporatedunderatopic,thiswaslistedasapotentialarea forincorporation.
Anytopicthatdidnothaveatleast2/3agreementonthe initialindependentreviewwasreviewedbyafourth emergencyphysicianwithexpertiseinEMresidenteducation andEMModeldevelopment.Shewasblindedtotheinitial reviewer’snamesbutdidhavetheirresults.Thefullgroup metandreviewedallthemappinguntilconsensuswas reached.Theconsensustableswerethenreviewed independentlybytwoadditionalexternalHPMboardcertifiedEMattendingsinvolvedinresidenteducationattwo differentEMresidencyprograms.Thesameprocesswasused formappingtheKSAs.
IncorporationintotheEmergencyMedicineModel
Fifty-oneof963EMModelitemsweretaggedinthe independent firstroundofmapping,with98.7%consensus (951/963)betweentheinitialthreeindependentreviewerson whetheranitemwasorwasnottaggedasamatch.The final reviewbytheindependentHPM-boardedEMattendingsdid notresultinadjustmentstoanyoftheexistingmappingbut didaddtothepotentialareasof fitfortheHPM competenciesthatdidnotdirectlymatchontotheEM Model. Table1 liststhecompetenciesincludedinthe2019 EMModel(18/23,78%).Manycompetencies fitinto EM Modelcategory20:OtherCoreCompetencies section, whichincludescommunicationskills,transitionsofcare, culturalcompetency,andhealthcarecoordination. Discrepancydiscussionscenteredaroundmanagementvs diagnosis.Thecompetency HPM2:Treatingdistressing symptoms(eg,nausea/vomiting,dyspnea) wasfeltto fitby keywordmatchunderEMModelcategory 1.0Signs, SymptomsandPresentations .However,thatcategorydoes notmentiontreatmentofsymptomsdirectly.Similarly, HPM18:ComplicationsofCancer couldmaptomany itemsintheEMmodel,butagainreferstopalliative managementofcancercomplicationsratherthandiagnosis.
PotentialAreasofFitintheEmergencyMedicineModel FiveHPMcompetenciesdidnot fitintotheEMModel. The firsttwo, HPM7:Treatingcommonend-of-life symptoms and HPM8:Carefortheimminentlydying (expectingdeathwithinhourstodaysorrecentlydeceased patientandtheirfamilymembers) ,couldbetaughtunder EMModelitem 20.4.4.2.2:Systems-basedPractice: Withdrawalofsupport. ThisEMModelitemcouldbe clarifiedtoensurethatitincludessymptomcontrolandendof-lifecare.Thenext, HPM11:Caringforpatientsunder hospicecare, couldbetaughtwhenteaching 20.4.4.2.3: Systems-basedPractice:HospiceReferral. However,the hospice-referralEMModelitembettermappedonto HPM 17 ,whichincludesassessingforandinitiatinghospice referrals.Theteamfeltthatidentifyingandreferringpatients tohospicewasaseparateskillsetthancaringforpatientson hospice.ThelasttwoHPMcompetencieswithoutaclear
Table1. ThehospiceandpalliativeemergencymedicineresidencyeducationcompetenciesmappedontotheAmericanBoardof EmergencyMedicineEMModel.
Hospiceand palliative competencyDescriptionEMmodelitem
1Paincontrol:a.chronicpain,b.malignant andnon-malignantpain.
19.3.1Anesthesiaandacutepain management-regionalanesthesia
19.3.2Anesthesiaandacutepain management-proceduralsedation
19.3.3Anesthesiaandacutepain management-analgesia
2Treatingdistressingsymptoms (eg,nausea/vomiting,dyspnea)
3Difficultcommunication:a.deliveryofbad news(eg,prognosisanddeathtelling) b.conflictresolution(eg,betweenfamily members
4Goalsofcarediscussions:a.assisting familieswithdecisionmaking.b.assisting patientswithdecisionmaking
1.3.32Nausea/vomiting 1.3.42Shortnessofbreath
*unclearwhethertheseEMmodelelementsreferto treatingthesesymptomsordevelopingadifferential diagnosisforthesesymptoms,butbothshould betaught.
20.1.2.2Interpersonalandcommunication skills-conflictmanagement
20.1.2.4Interpersonalandcommunicationskillsdeliveringbadnews/deathnotifications
20.4.4.1Healthcarecoordination-advancedirectives
5Caregiversupport20.3.4.6Well-beingandresilience-careforthecaregiver
6Non-initiationorstoppingofnonbeneficial interventions
19.2Resuscitation-cardiopulmonaryresuscitation
20.1.1.3Interpersonalskills-patientandfamily experienceofcare
20.4.4.2.2Healthcarecoordination-withdrawalofsupport
9Bereavementandgrieving14.2.4Mooddisordersandthought disorders-griefreaction
10Family-witnessedresuscitation19.2Resuscitation-cardiopulmonaryresuscitation
12Copingandself-care20.3.4.1Well-beingandresilience-fatigue andimpairment
20.3.4.1.1Well-beingandresilience-sleephygiene
20.3.4.3Well-beingandresilience-work/lifebalance
13End-of-lifemanagementinthemass casualtyincident/event
16Screeningforpalliativecareneeds:
a.identifyingpatientswhomaybenefit fromHPMspecialistreferral,b.identifying theimminentlydyingpatient(expected deathwithinhours-days).
17Rapidpalliativecareassessment:
a.aligningdiagnosticsandtherapeuticsto patientgoals,b.functional,psychosocial, andspiritualassessment,c.assessingfor andinitiatinghospicereferrals,d.toolkits tohelpidentifypatientneedsfor appropriatereferrals/resources, e.caregiverburden.
20.4.2.2.1Patienttriageandclassification
20.4.4.2.1Healthcarecoordination-patientidentification forpalliativecare
20.4.4.2.3Healthcarecoordination-hospicereferral
20.3.4.6Well-beingandresilience-careforthecaregiver
20.4.4.2.3Healthcarecoordination-hospicereferral
20.4.4.3.1Healthcarecoordination-activitiesofdaily living/functionalassessment (Continuedonnextpage)
Table1. Continued.
Hospiceand palliative competencyDescriptionEMmodelitem
18Complicationsofcancer:a.disease complications(eg,spinalcord compression,hypercalcemia), b.treatmentcomplications (eg,pancreatitis,tumorlysis,neutropenia, acuterenalfailure).
2.9.2.3Largebowel-radiationcolitis
2.9.2.5Largebowel-neutropenicenterocolitis/typhlitis
3.6.1Diseasesofthepericardium-pericardial tamponade
8.7Oncologicemergencies
8.7.1Oncologicemergencies-febrileneutropenia
8.7.2Oncologicemergencies-hypercalcemia ofmalignancy
8.7.3Oncologicemergencies-hyperviscositysyndrome
8.7.4Oncologicemergencies-malignant pericardialeffusion
8.7.5Oncologicemergencies-spinalcordcompression
8.7.6Oncologicemergencies-superiorvena cavasyndrome
8.7.7Oncologicemergencies-tumorhemorrhage
8.7.8Oncologicemergencies-tumorlysissyndrome
11.1.4.2Bonyabnormalities-tumor-relatedfractures
16.2.3Disordersofthepleura,mediastinum,andchest wall-pleuraleffusion
16.6.2Pulmonaryembolism/infarct-venous thromboembolism
16.6.2.1Pulmonaryembolism/infarct-massiveand submassiveembolism
19Ethical,spiritual,andculturalissues aroundend-of-lifeanddeath
20Advancedirectives:a.physicianorderfor life-sustainingtreatment(POLST), b.medicalorderforlife-sustaining treatment(MOLST),c. fivewishes.
21ethicalandlegalissues:a.decisionmakingcapacity,b.futility.
22Multidisciplinaryteamandsupport systems.(understandingteamrolesand systemresources):a.spiritualchair, b.socialchair,c.hospicecareeligibility, d.continuingcare,e.importanceoflocal andcommunitysupportsystems.
23Transitionsacrosscaresettings,eg, inpatientvshomehospice,palliative careunit
20.1.2.5Interpersonalandcommunication skills-culturalcompetency
20.4.4.1Healthcarecoordination-advancedirectives
20.3.2.4Professionalism-medicalethics
20.4.5.4Regulatory/legal-consent,capacityandrefusal ofcare-consent,capacityandrefusalofcare
20.1.1.1Interpersonalskills-inter-departmentaland medicalstaffrelations
20.1.1.2Interpersonalskills-intra-departmentalrelations, teamwork,andcollaborationskills
20.4.2.4.1EDadministration-alliedhealthprofessionals
20.4.4.2.1Healthcarecoordination-patientidentification forpalliativecare
20.4.4.2.3Healthcarecoordination-hospicereferral
associationwiththeEMModelwere HPM14:Trajectories ofdying:a.Terminalillness,b.OrganFailure,c.Frailty,d. SuddenDeath, and HPM15:Prognostication. Whilethese competenciesnecessitatehavingsoundunderstandingofthe naturalhistoryofdiseaseaswellasphysicalexaminationand clinicalworkupcomponentsinformingprognosis,theseare alsoskillsforexplainingthelikelihoodofdeathand communicatingwithpatientsandfamilies.Theteam consensuswasthatthesecouldbetaughtwithintheEM Modelitems 20.1.2.4InterpersonalandCommunication
Table2. Thepalliativeemergencymedicinecompetenciesincorporatewiththe2021AmericanBoardofEmergencyMedicineknowledge, skills,andabilities.
Hospiceandpalliative medicinecompetencyKSAcodeDescriptionLevel
3Difficultcommunicationa.deliveryofbad news(eg,prognosisanddeathtelling) b.conflictresolution (eg,betweenfamilymembers)
4Goalsofcarediscussions:a.assisting familieswithdecisionmaking.b.assisting patientswithdecisionmaking.
CS17Use flexiblecommunicationstrategiesto negotiateeffectivelywithstaff,consultants, patients,families,andotherstoprovideoptimal patientcare,recognizingandresolving interpersonalconflicts
CS3Elicitpatients’ reasonsforseekinghealthcareand theirexpectationsfromtheEDvisit
CS7Considertheexpectationsofthosewhoprovide orreceivecareintheEDandusecommunication methodsthatminimizethepotentialforstress, conflict,andmiscommunication
CS15Solicitpatientparticipationinmedicaldecisionmakingbydiscussing,risks,benefits,and alternativestocareprovided
ES15Elicitthepatient’sgoalsofcarepriortoinitiating emergencystabilization,includingevaluatingthe validityofadvanceddirectives
13End-of-lifemanagementinthemass casualtyincident/event
14Trajectoriesofdying:a.terminalillness, b.organfailure,c.frailty, d.suddendeath.
DM11Participateinamasscasualtydrilloreventinan EDinvolvingmultiplepatients,prioritizingcare, containingpotentialexposures,andappropriately assigningresources
ES6Recognizeinatimelyfashionwhenfurther clinicalinterventionisfutile
PE6Educatepatientsonthenaturalcourseoftheir diseaseandimpactofpossibletreatmentin relationtoprognosis
15PrognosticationES6Recognizeinatimelyfashionwhenfurther clinicalinterventionisfutile
ES15Elicitthepatient’sgoalsofcarepriortoinitiating emergencystabilization,includingevaluatingthe validityofadvanceddirectives
PE6Educatepatientsonthenaturalcourseoftheir diseaseandimpactofpossibletreatmentin relationtoprognosis
TC11Determine,summarize,andcommunicatethe diagnosisordiagnosticuncertainty,anticipated course,prognosis,dispositionplan,medications, futurediagnostic/therapeuticinterventions,signs andsymptomsforwhichtoseekfurthercareand follow-uptopatientorsurrogate
17Rapidpalliativecareassessment: a.aligningdiagnosticsandtherapeuticsto patientgoals,b.functional,psychosocial, andspiritualassessment,c.assessingfor andinitiatinghospicereferrals,d.toolkits tohelpidentifypatientneedsfor appropriatereferrals/resources, e.caregiverburden.
CS7Considertheexpectationsofthosewhoprovide orreceivecareintheEDandusecommunication methodsthatminimizethepotentialforstress, conflict,andmiscommunication
(Continuedonnextpage)
Table2. Continued.
Hospiceandpalliative medicinecompetencyKSAcodeDescriptionLevel
20Advancedirectives:a.physicianorderfor life-sustainingtreatment(POLST), b.medicalorderforlife-sustaining treatment(MOLST),c. fivewishes.
21Ethicalandlegalissues:a.decisionmakingcapacity,b.futility.
CS6Elicitinformationfrompatients,families,andother healthcaremembersusingverbal,nonverbal, written,andtechnologicalskills
ES15Elicitthepatient’sgoalsofcarepriortoinitiating emergencystabilization,includingevaluatingthe validityofadvanceddirectives
CS15Solicitpatientparticipationinmedicaldecisionmakingbydiscussing,risks,benefits,and alternativestocareprovided
ES6Recognizeinatimelyfashionwhenfurther clinicalinterventionisfutile
LI12Balancepatientautonomywithpatientprotection andadvocacywhenaddressingconsentand refusalofcareinaccordancewithlegaland ethicalstandards
TI9Obtaininformedconsentfromthepatientor appropriatesurrogatewhenindicated
22Multidisciplinaryteamandsupport systems.(understandingteamrolesand systemresources):a.spiritualchair, b.socialchair,c.hospicecareeligibility, d.continuingcare,e.importanceoflocal andcommunitysupportsystems.
23Transitionsacrosscaresettings, eg,inpatientvshomehospice, palliativecareunit
CS5Communicateinformationtopatientsandfamilies usingverbal,nonverbal,written,and technologicalskills,andconfirmunderstanding
CS10Communicatepertinentinformationtohealthcare colleaguesineffectiveandsafetransitions ofcare
TC11Determine,summarize,andcommunicatethe diagnosisordiagnosticuncertainty,anticipated course,prognosis,dispositionplan,medications, futurediagnostic/therapeuticinterventions,signs andsymptomsforwhichtoseekfurthercareand follow-uptopatientorsurrogate
TC15Ensuretransitionsofcareareaccuratelyand efficientlycommunicatedbetweencliniciansusing bestpractices
Skills:Deliveringbadnews/DeathNoti fi cations and 20.1.1.3InterpersonalandC ommunicationSkills:Patient andfamilyexperienceofcare.
IncorporationintotheKnowledge,SkillsandAbilities
Thirtyitemsof214weretaggedinthe firstroundwith87% consensus(187/214)betweentheinitialthreeindependent reviewersonwhetheranitemwasorwasnottaggedasa match.Tenofthe23HPMcompetencies(43%)mappedonto 16differentKSAs(Table2).Ofthe16matcheswithinthe KSAs,nonewereadvancedskills(levelA).AllbutHPM13
mappedontoatleastonelevelBskill.Atableshowingallthe HPMcompetenciesandtheirincorporationwithinthe EMModelandKSAstogetherisincludedas SupplementalDataA.
PotentialAreasofFitintotheKnowledge,Skills andAbilities
ThreeadditionalKSAswereidentifiedashavingareasof potential fitorincorporation. HPM5:Caregiversupport and HPM12:Copingandself-care couldbetaughtwhile discussing CS2:Establishrapportwithanddemonstrate
empathytowardpatientsandtheirfamilies .Finally, HPM 16:Screeningforpalliativecareneeds couldbetaughtwith TC18:Correctlydeterminetheappropriatedisposition .
ThisstudyshowedfairtogoodinclusionofHPM competencieswithinthepublishedEMKSAsandEM Model,demonstratingthattheHPMcompetenciesare representedintheMilestones.However,keytopicareaswere identifiedthatcouldimprovethefocusofEMtrainingin HPM.DemonstratingtheoverlapoftheHPMandEM contentmayhelpEMeducatorsensurethatHPMtrainingis incorporatedintotheircurriculums.Lackoftrainingon thesetopicsisaconsistent findinginnationaland internationalstudies,andeducatorsneedbetterwaysto incorporateHPM-EMtrainingintoresidency curriculums.3–7,11–13 ImprovedteachingoftheHPM-EM competencieshasthepotentialtodecreasethecaregaps seeninEDsymptommanagementandend-of-lifecare, includinglackofgoalsofcareconversationsforcritically illpatients.14,15
AlimitationoftheHPMcompetenciesisthattheyhave notbeenexternallyassessedorinvestigatedandarebasedon expertconsensus.Noneoftheinitialfourreviewerswere involvedinthedevelopmentoftheHPMcompetenciesand theyfoundthemtoalmostallmapontotheEMModelor identifiedplacesintheEMModelthatcouldbeexpandedto includethemmoreexplicitly.Additionally,theHPM competenciesthatmappedontoKSAsallmetatleastone KSAontheminimalcompetencylevel.These findingsimply thattheHPMcompetenciesareskillsthatareat residentlevel.
ThedescriptionsintheHPMcompetenciescanadddepth tothecorrespondingEMMilestonesforcurriculum developmentandsummativeevaluation.Forexample,most residenciesprovidetrainingorsimulationsofmasscasualty care.Thestudygroupenvisionedwaysinwhichend-of-life managementcouldbeaddedintothattraining(HPM13). Likewise,alectureonpost-cardiacarrestcarecould incorporatetrainingonthenon-initiationorcompassionate discontinuationofinterventionssuchasmechanical ventilation(HPM6).Summativecompetencyassessmentsat endoftrainingtogainboardcertificationcouldalso incorporatemoreHPMcompetency-basedquestions.
MuchoftheoverlapbetweentheHPMcompetenciesand theEMModelandKSAswasin Interpersonaland CommunicationSkills (EMModel)andthe CS –Communication&InterpersonalSkills (KSAs). Communicationskills,althoughchallengingtoteach,are criticalinpatient-centeredcareandwilllikelyhavean increasedemphasisasartificialintelligenceandmachine learningbecomemoreuniversallyintegratedintoclinical care.Currentmodelsforcommunicationinstructionrely heavilyonrolemodeling.16 Residentshavesuggestedthat
formaltrainingincommunicationshouldfocusongeneral communicationskillsandshouldprovidesyntaxtousein futurediscussions.17 Developingcommunicationskills requiresdeliberatepracticeoftechniques,includingNURSE statements(naming,understanding,respecting,supporting, andexploring)andAsk-Tell-Ask.17,18 Additionally, educatorsmustbecomefamiliarwithmethodsfor real-timeteachingofcommunication,suchas “CouldI addsomething?”19
Trajectoriesofdying(HPM7)andprognostication (HPM8)aretwoskillsusedtocounselpatients/familieswith seriousillnessorattheendoflifethatdidnot fitclearlywithin theEMModel.Thesearedifficultskills,andpriorstudies haveidentifiedsomediscordancebetweenwhatfamilies/ caregiversunderstandaboutaperson’sdeathandthe underlyingcausesofdeathidentifiedbythephysician-led team.20 Thus,thisskillshouldbehonedthroughouttraining. ItisourexperiencethatEMresidentsrarelyreceiveexplicit educationonprognostication,andsowerecommendits incorporationintocurriculums.Ourresultsfurthersuggest thattrainingontreatingend-of-lifesymptoms,careforthe imminentlydying,andcaringforpatientsunderhospicecare couldbeoverlookedbycurrentresidentcurriculumswith strictadherencetotheEMModel.
Alimitationofthisprojectisthateventhoughaconsensus processwasusedwithexpertsinresidencyeducationand HPM,othereducationexpertsmayinterpretthedomains andcompetenciesdifferently.Forexample,the EMModel item20.3.4.6Well-beingandResilience-Careforthe caregiver wasmatchedtoHPM5and17aboutpatient caregivers.However,thiscouldalsobeinterpretedas residentself-careasitisunderthewell-beingsection.Finally, whiletrainedHPMemergencyphysiciansreviewedallthe mapping,theinitialmappingdidincluderesidentinput.This couldbeconsideredanadvantage,astheyareexperiencing lecturesweekly,orareapotentialsourceofbias,astheyhave nothadafullEMcurriculumyet.
WeidentifiedareasofoverlapwheretheHPM-EM subspecialtycompetenciescanbeemphasizedorintegrated intoEMModel-basedresidencycurriculums.This knowledgecanbeusedforcurriculumplanningand incorporatingHPMintodefinitionsforcompetencyinEM. Thesecouldalsobereflectedin finalsummativeevaluations forcertification.
AddressforCorrespondence:LaurenT.Southerland,MD,TheOhio StateUniversityWexnerMedicalCenter,DepartmentofEmergency Medicine,725PriorHall,376W10thAve.,Columbus,OH43210. Email: Lauren.Southerland@osumc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. LaurenT.SoutherlandhasNIHgrantfundingnotpertainingtothis study.DianeL.GorgasisaboardmemberontheAmericanBoardof EmergencyMedicine.LaurenT.SoutherlandandDanielW. Markwalterhavecontributedtosomeofthefreeeducational websitesmentionedinthediscussion.Therearenootherconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Goettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ElmerJ,MikatiN,ArnoldRM,etal.Deathandend-of-lifecarein emergencydepartmentsintheUS. JAMANetwOpen. 2022;5(11):e2240399.
2.GeorgeN,BowmanJ,AaronsonE,etal.Past,present,andfutureof palliativecareinemergencymedicineintheUSA. AcuteMedSurg. 2020;7(1):e497.
3.WoodsEJ,GinsburgAD,BellolioF,etal.Palliativecareinthe emergencydepartment:asurveyassessmentofpatientandprovider perspectives. PalliatMed. 2020;34(9):1279–85.
4.MeoN,HwangU,MorrisonRS.Residentperceptionsofpalliative caretrainingintheemergencydepartment. JPalliatMed. 2011;14(5):548–55.
5.KrausCK,GreenbergMR,RayDE,etal.Palliativecareeducationin emergencymedicineresidencytraining:asurveyofprogramdirectors, associateprogramdirectors,andassistantprogramdirectors. JPain SymptomManage. 2016;51(5):898–906.
6.BaylisJ,HarrisDR,ChenC,etal.Palliativeandend-of-lifecare educationinCanadianemergencymedicineresidencyprograms: anationalcross-sectionalsurvey. CJEM. 2019;21(2):219–25.
7.AdeyemiOJ,SimanN,GoldfeldKS,etal.Emergencyproviders’ knowledgeandattitudestowardhospiceandpalliativecare:acrosssectionalanalysisacross35emergencydepartmentsintheUnited States. JPalliatMed. 2023;26(9):1252–60.
8.ShoenbergerJ,LambaS,GoettR,etal.Developmentofhospiceand palliativemedicineknowledgeandskillsforemergencymedicine
residents:usingtheAccreditationCouncilforGraduateMedical EducationMilestoneframework. AEMEducTrain. 2018;2(2):130–45.
9.AmericanBoardofEmergencyMedicine.The2019ModeloftheClinical PracticeofEmergencyMedicine.Availableat: https://www.abem.org/ public/resources/em-model.AccessedNovember3,2020.
10.AmericanBoardofEmergencyMedicine.2021Knowledge,Skills,& Abilities.Availableat: https://www.abem.org/public/resources/ emergency-medicine-milestones-ksas.AccessedNovember17,2022.
11.SandersS,CheungWJ,BakewellF,etal.Howemergencymedicine residentshaveconversationsaboutlife-sustainingtreatmentsincritical illness:aqualitativestudyusinginductivethematicanalysis. AnnEmerg Med. 2023;82(5):583–93.
12.ZengH,EugeneP,SupinoM.Wouldyoubesurprisedifthispatient diedinthenext12months?Usingthesurprisequestiontoincrease palliativecareconsultsfromtheemergencydepartment. JPalliatCare. 2020;35(4):221–5.
13.BeneschTD,MooreJE,BreyreAM,etal.Primarypalliativecare educationinemergencymedicineresidency:amixed-methodsanalysis ofayearlong,multimodalintervention. AEMEducTrain. 2022;6(6):e10823.
14.WalkerLE,StanichJA,BellolioF.Aqualitativeassessmentofaguide forgoalsofcareconversationsintheED. AmJEmergMed. 2023:75:185–7.
15.YilmazS,GrudzenCR,DurhamDD,etal.Palliativecareneedsand clinicaloutcomesofpatientswithadvancedcancerintheemergency department. JPalliatMed. 2022;25(7):1115–21.
16.OldeBekkinkM,FarrellSE,TakayesuJK.Interprofessional communicationintheemergencydepartment:residents’ perceptions andimplicationsformedicaleducation. IntJMedEduc. 2018;9:262–70.
17.RisingKL,PapanagnouD,McCarthyD,etal.Emergencymedicine residentperceptionsabouttheneedforincreasedtrainingin communicatingdiagnosticuncertainty. Cureus. 2018;10(1):e2088.
18.TalkVital.QuickGuideResources.Availableat: www.vitaltalk.org/ resources/.AccessedAugust14,2023.
19.BackAL,ArnoldRM,TulskyJA,etal. “CouldIaddsomething?”: teachingcommunicationbyinterveninginrealtimeduringaclinical encounter. AcadMed. 2010;85(6):1048–51.
20.MoonF,KissaneDW,McDermottF.Discordancebetweenthe perceptionsofcliniciansandfamiliesaboutend-of-lifetrajectories inhospitalizeddementiapatients. PalliatSupportCare. 2021;19(3):304–11.
DavidA.Haidar,MD*
LauraR.Hopson,MD*
RyanV.Tucker,MD†
RobD.Huang,MD*
JessicaKoehler,MD*
NikTheyyunni,MD*
NicoleKlekowski,MD*
ChristopherM.Fung,MD,MS*
SectionEditor:BenjaminSchnapp,MD
*UniversityofMichigan,DepartmentofEmergencyMedicine,AnnArbor,Michigan † UniversityofColorado,DepartmentofEmergencyMedicine,Aurora,Colorado
Submissionhistory:SubmittedSeptember13,2023;RevisionreceivedNovember10,2023;AcceptedDecember7,2023
ElectronicallypublishedFebruary28,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18454
Introduction: Emergencymedicine(EM)isoneoffewspecialtieswithvariabletraininglengths.Hiringa three-yeargraduatetocontinuefellowshiptraininginadepartmentthatsupportsafour-yearresidency programcanleadtoconflictsaroundresidentsupervision.Wesoughttounderstandhiringandclinical supervision,orstaffing,patternsofnon-AccreditationCouncilforGraduateMedicalEducation(ACGME) fellowshipshostedatinstitutionssupportingfour-yearresidencyprograms.
Methods: Weperformedaweb-based,cross-sectionalsurveyofnon-ACGMEfellowshipdirectors(FD) hostedatinstitutionssupportingfour-yearEMresidencyprograms.Wecalculateddescriptivestatistics. Ourprimaryoutcomewastheproportionofprogramswithfour-yearEMresidenciesthathirenonACGMEfellowsgraduatingfromthree-yearEMresidencies.
Results: Of119eligibleFDs,88(74%)completedthesurvey.SeventyFDs(80%)indicatedthattheyhire graduatesofthree-yearresidencies.Fifty-six(80%)indicatedthatthree-yeargraduatessupervise residents.MostFDs(74%)indicatednoadditionalrequirementsexisttosuperviseresidentsoutsideof beinghiredasfaculty.TheFDsciteddepartmentpolicy,concernsaboutqualityandlengthoftraining, andresidentcomplaintsasreasonsfornothiringthree-yeargraduates.Amajority(10/18,56%)noted thatnothiringfellowsfromthree-yearprogramsnegativelyimpactsrecruitmentandgivesthemaccessto asmallerapplicantpool.
Conclusion: Mostnon-ACGMEfellowshipsatinstitutionswithfour-yearEMprogramsrecruitthree-year graduatesandallowthemtosuperviseresidents.Thissurveyprovidesprogramsinformationonhow comparablefellowshipsrecruitandstafftheirdepartments,whichmayinformpoliciesthat fittheneedsof theirlearners,thefellowship,andthedepartment.[WestJEmergMed.2024;25(4.1)27–32.]
Emergencymedicine(EM)isoneoffewspecialtiesinthe UnitedStateswithvariabletraininglengths.1,2 Most residenciesimplementathree-yearmodel,whileonly20% implementafour-yearmodel.3–5 Thereislittledatato supporteithertraininglength.3–7 Somearguethatfour-year
graduateshavemoretimetogainconfidence,develop proceduralskills,developacademicinterests,andgain experiencesupervisinglearners.Advocatesofthree-year programsarguethatanextrayearasfacultywould providethesesameexperiences.1,8,9 Thesepersonal biasesmayimpactrecruitmentandhiringof
three-yeargraduatesatinstitutionssupportingfour-year residencyprograms.6,7
Whenaninstitutionhostingafour-yearresidencyhiresa three-yeargraduateintofellowshiptraining,thiscanleadto conflictsaroundclinicalsupervision,orstaffing,ofresidents relatedtoperceptionsofseniorityandqualityoftraining.1,9 Therearecurrentlynobestpracticesorguidelinestoinform programsonhowtoaddressthissituation.Thesituationis furthercomplicatedasnon-AccreditationCouncilfor MedicalEducation(ACGME)fellowshipsfrequentlylack uniformrulesthatgovernrecruitment,program requirements,andclinicalresponsibilities.10 Nostudies currentlyevaluatetheprevalenceoftheseissuesorexamine variabilityinrecruitment,hiring,andclinicalresponsibilities oftraineesatnon-ACGMEfellowships.Inthisstudy,we soughttounderstandthehiringandstaffingpatternsofnonACGMEfellowshipshostedatinstitutionswithfour-year EMresidencyprograms.
StudyDesignandParticipants
Thiswasacross-sectionalsurveyoffellowshipdirectors (FD)ofnon-ACGMEfellowshipshostedatinstitutions supportingafour-yearEMresidencyprogram.We conductedthesurveybetweenJanuary–April2023.This studywasdeemedexemptbyourinstitutionalreviewboard (HUM00221519).InNovember2022,wegeneratedalistof 54four-yearEMresidencyprogramsfromtheEmergency MedicineResidents’ Association(EMRA)Matchrosterand ElectronicResidencyApplicationServicedirectory.11–13 We identifiednon-ACGMEfellowshipsofferedusingeach program ’swebpage,theSocietyforAcademicEmergency MedicineFellowshipDirectory,andtheSocietyforClinical UltrasoundFellowshipsdirectory.14,15
WedevelopedthesurveybasedonPanacek’sgeneral surveyprinciples,literaturereview,andexpertopinionto providecontentvalidityevidence.6,16–18 Allauthorshave experiencedevelopingsurveystudies,andthegroup (includingfourcurrentorformerFDs)iterativelypilotedand revisedthesurveyforoptimalphrasing,surveylength, functionality,andappropriatemixofsuggestedand open-endedresponses,whichprovidedcontentand responseprocessvalidityevidence.18 WeusedQualtrics (QualtricsXM,Provo,UT),aweb-basedsurveyplatform,to distributethesurveyviaemailwithapersonalizedlinkfor eachFDtocollectandanalyzethedata.Wesentweekly reminderstoFDs’ institutionalemails,withanoptionto declineparticipation,foreightweeks.Wethensent personalizedweeklyreminderemailsforanadditional fourweeks.Wecollectedindividualresponsestothe surveyanonymously.
WeaskedFDstoreporttheirfellowshiptype,yearsin currentrole,anddemographicdatasuchasnumberof clinicalsites,programenvironment(academic,county, community,etc),andgeographiclocation.Ourprimary outcomewastheproportionofprogramsaffiliatedwithfouryearEMresidenciesthathirenon-ACGMEfellows graduatingfromthree-yearEMresidencies.Wealsoasked clarifyingquestionstobetterunderstandtheirstaffingmodel, andrecruiting,hiring,andclinicaloversightpolicies.The surveyincludedspaceforcommentssothattheFDscould providecontexttotheiranswers,butwedidnotanalyzethese forthemes.Thefullsurveyisavailablein AppendixA1.We analyzedthedatausingExcel365(MicrosoftCorporation, Redmond,WA)togeneratedescriptivestatisticsand analysis.Weassessedtheassociationbetweencategorical variablesusingtheFisherexacttest.Wedidnotcalculatean apriorisample-sizeestimateasweattemptedtocapturea 100%responserate.
Of54four-yearEMresidenciesintheUS,32institutions offeredatleastonenon-ACGMEfellowshipwithatotalof 128fellowshipsidentified(median3.5;range1–10).We received88responsesafterexcludingnineopt-outsandone blankresponse(88/119)foraresponserateof73.9%. ProgramandFDcharacteristicsarelistedinthe Table. Freetextresponsesareincludedin AppendixA2
Ofthe88responses,70FDs(80%)reportedhiring graduatesofthree-yearEMprogramsfortheirrespective fellowships.Fifty-sixFDs(80%)whoacceptthree-year graduatesindicatedthattheirfellowscansuperviseEM residents.Wefoundvariationinwhofellowscouldsupervise. Themostcommonpolicy(40%)wasthatfellowscan superviseEMpostgraduate-year(PGY)-3residentsand below.MostFDs(74%)indicatedthattheyhadno additionalrequirementstosuperviseresidentsoutsideof beinghiredonasfaculty.Fullsurveyresultsappearin the Figure
Programswithmultipleclinicalsitesaremorelikelytohire three-yeargraduates.Tenof23programs(57%)withone clinicalstaffingsitehiredthree-yeargraduatescomparedto 88%(57/65)ofsiteswithtwoormoreclinicalsites (P < 0.001).TheFDsreportedtheimplementationofvarious strategiestomitigatepotentialconflicts.Oneprogram hostsajointfellowshipcurriculumfortheirfellows,which incorporatesinstructiononbedsideteaching,giving feedback,andteachingvariousskills.OtherFDsreported thattheirprogramspreventedtheirfellowsfromstaffingin highacuityareasordelayworkingwithresidents.
Twenty-sevenFDs(50%)citeddepartmentpolicyasthe reasonfortheirhiringandstaffingpolicies.Selected commentsfromotherFDsincludedconcernsaboutquality andlengthoftrainingandresidentcomplaints.Others
Table. Demographicdetailsofthefellowshipsrepresentedinoursurveyoffellowshipdirectorsofnon-ACGMEfellowshipprograms. DemographicsNumberofresponses(%)
Fellowshiptype
Central(IL,IN,IA,KS,MI,MN,MO,NE,OH,WI)13(15%)
Northeast(CT,DC,DE,MA,MD,ME,NH,NJ,NY,PA,RI,VT)45(51%)
Southern(AL,AR,FL,GA,KY,LA,MS,NC,OK,PR,SC,TN,TX,VA,WV)0(0%)
Western(AZ,CA,CO,NM,NV,OR,UT,WA)30(34%)
Categoryofnon-ACGMEfellow’sprimaryclinicalsite*
Numberofclinicalsitesnon-ACGMEfellowsclinicallystaff
*Respondentscouldselectmorethanonetypeofclinicalsite.
reportedtheirclinicalenvironmentwasnotconduciveto separatingfellowsfromresidents.SevenFDsreported wantingtoavoidPGY-4fellowsstaffingPGY-4residents. OneFDindicatedthat “becausewearea4-yearprogram,we
wanttoacknowledgetoourresidentsthat4yearsiswhatwe thinkisrequiredforgraduation.” Amongtheprogramsnothiringfellowsfromthree-year programs,56%(10/18)ofFDsnotedthatthispolicy

Figure. Flowdiagramdetailingthesurveyresponsehierarchyoffellowshipdirectorsofnon-AccreditationCouncilforGraduateMedical Educationfellowshipsregardingclinicalsupervisionpatternsfor3-yearemergencymedicine(EM)residencygraduatesatinstitutionswitha 4-yearEMprogram.
EM,emergencymedicine; PGY,postgraduateyear; FPPE,focusedprofessionalpracticeevaluation.
negativelyimpactedtheirfellowshiprecruitmentandgave themaccesstoasmallerpoolofapplicants.
Toourknowledgethisstudyisthe firsttodescribestaffing patternsofnon-ACGMEfellowshipshostedatinstitutions withfour-yearEMresidencies.MostoftheFDswesurveyed hirethree-yeargraduatesasfellows,andmostprograms permitthree-yeargraduatestostaffresidentswithno additionalrequirementsbeyondbeinghired.Wealso identifiedpotentialnegativeimpactsonfellowshipsasthey restricttheirapplicantpool.OneFDindicatedthattheir fellowshipwasmostlygoingunfilledduetotheirrecruitment policy.Anotherindicatedthatthe financialsacrificeofa four-vsthree-yearresidencymayunintentionallyfavor recruitmentofthosewithout financialneedorburden, especiallysincethedebtloadofEMapplicantsisreportedly higherthanforothermedicalspecialties.1
Someprogramsoffertheirfellowsalternativeclinical sites – suchasVeteransAffairshospitals,freestandingEDs, orurgentcares.Bystaffingmultiplelocations,non-ACGME fellowscanworkwithoutaresidentpresence.This flexibility allowsprogramstohirethree-yeargraduatesandpermits fellowstointerfacewithresidentsacademicallywithout havingtosupervisethemclinically.Thisallowsforatraining
environmentconducivetotheneedsofalllearners’ growth anddevelopment.
TheFDscitedclinicalconcernsanddepartmentpolicyas themainreasonsfortheirstaffingandhiringpolicies.There isalackofobjectivedatathatfour-yeargraduates outperformthree-yeargraduatesclinicallyoronthe qualifyingwrittenboardexam,suggestingthatthismaybe rootedinbias.1,6,7 Intheabsenceofrobustdatatosupport theclinicalcapabilitiesoftraineesfromeitherthree-orfouryearprograms,theprinciplesofcompetency-basedmedical education(CBME)mayoffersolutions.19 Theprinciplesof CBMErequiredemonstrationofcompetencyanddecouple attainmentofcompetencyfromtime-in-training.19 Theuse ofCBMEtodeterminereadinessforunsupervisedpractice throughaprocessknownas “promotioninplace” hasbeen pilotedbysomeresidencyprogramsandmaybeauseful modeltoreplicateindeterminingfellowreadinessfor staffing,regardlessofPGYstatus.19,20 Ifweremovethefocus fromtime-boundedtrainingandfocusondemonstratedskill acquisition,programsmaydesignprocessestoonboard three-yeargraduatesbyfocusingondevelopingandassessing appropriateskillsforsupervisionoftrainees.
Futurestudiescouldexplorewhosetsdepartmental policiesregardingfellowstaffing,evaluatefellowand residentperceptionsofstaffingpolicies,andcompare
careeroutcomesoffellowsworkinginvarious staffingenvironments.
Wemaynothavecapturedallnon-ACGMEfellowships atfour-yearinstitutions.Wedidnotidentifyfellowship directoriesbesidesultrasound,whichmayhaveledto samplingbias.Weattemptedtomitigatethisbysearching specificprogramwebsitesforlistedfellowships.TheFDs whodidnotparticipateinourstudymayrepresentaunique populationwithdifferenthiringandstaffingpatterns.Wedid notidentifynon-ACGMEfellowshipshostedatfour-year EMprogramsinthesouthernUS,nordidwereceive responsesfromprimarilycommunityEMprograms,which couldalsohavebiasedourresults.Wedidnotsurvey ACGME-accreditedfellowships,asfellowsvaryintheway they “maintaintheirprimaryBoardskills.”21 SomeACGME fellowships(eg,criticalcare,emergencymedicalservices)do notrequireminimumclinicalhoursintheemergency department,whichleadstoaqualitativelydifferent experiencefromnon-ACGMEfellowships,wherefellowsare appointedasclinicalfaculty.2,21,22
Ourresultsindicatethatmostnon-ACGMEfellowships hostedatinstitutionswithfour-yearEMprogramsrecruit graduatesofthree-yearprogramsandallowthemto superviseresidents.Thissurveydataprovidesprogram informationonhowcomparablefellowshipprogramsrecruit andstafftheirdepartments,whichmayinformpoliciesthat fittheneedsoftheirlearners.
AddressforCorrespondence:DavidA.Haidar,MD,Universityof Michigan,DepartmentofEmergencyMedicine,1500E.Medical CenterDr.,B1-380,AnnArbor,MI48109.Email: dahaidar@med. umich.edu
Con
flictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Haidaretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.RossTM,WolfeRE,MuranoT,etal.Three-vs.four-yearemergency medicinetrainingprograms. JEmergMed. 2019;57(5):e161–5.
2.AccreditationCouncilforGraduateMedicalEducation(ACGME). ACGMEprogramrequirementsforgraduatemedicaleducationin
emergencymedicine.2023.Availableat: https://www.acgme.org/ specialties/emergency-medicine/program-requirements-and-faqsand-applications/.AccessedJanuary6,2023.
3.LotfipourS,LuuR,HaydenSR,etal.Becominganemergencymedicine resident:apracticalguideformedicalstudents. JEmergMed. 2008;35(3):339–44.
4.NelsonLS,CalderonY,AnkelFK,etal.AmericanBoardofEmergency Medicinereportonresidencyandfellowshiptraininginformation (2021–2022). AnnEmergMed. 2022;80(1):74–83.e8.
5.AccreditationCouncilforGraduateMedicalEducation(ACGME).Listof programsbyspecialty.Availableat: https://apps.acgme.org/ads/Public/ Reports/Report/1.AccessedApril29,2023.
6.HopsonL,ReganL,GisondiMA,etal.Programdirectoropiniononthe ideallengthofresidencytraininginemergencymedicine. AcadEmerg Med. 2016;23(7):823–7.
7.NikollaDA,ZocchiMS,PinesJM,etal.Four-andthree-yearemergency medicineresidencygraduatesperformsimilarlyintheir firstyearof practicecomparedtoexperiencedphysicians. AmJEmergMed. 2023;69:100–7.
8.HaydenSandPanacekE.Proceduralcompetencyinemergency medicine:thecurrentrangeofresidentexperience. AcadEmergMed. 1999;6(7):728–35.
9.WeichenthalL.Advantagesofafour-yearresidency. CalJEmergMed. 2004;5(1):18–9.
10.AccreditationCouncilforGraduateMedicalEducation(ACGME). Commonprogramrequirements(fellowship).2022.Availableat: https:// www.acgme.org/globalassets/pfassets/programrequirements/ cprfellowship_2022v3.pdf.AccessedJanuary6,2023.
11.EmergencyMedicineResidents’ Association(EMRA).Matchlist.2023. Availableat: https://webapps.acep.org/utils/spa/match#/search/list AccessedJanuary6,2023.
12.AssociationofAmericanMedicalColleges(AAMC).Electronic residencyapplicationservice(ERAS)directory.2023.Availableat: https://systems.aamc.org/eras/erasstats/par/display.cfm? NAV_ROW=PAR&SPEC_CD=110.AccessedJanuary6,2023.
13.AssociationofAmericanMedicalColleges(AAMC).Residencyexplorer tool.Availableat: https://www.residencyexplorer.org/Home/Dashboard AccessedJanuary6,2023.
14.SocietyforAcademicEmergencyMedicine(SAEM).Fellowship directory.Availableat: https://member.saem.org/SAEMIMIS/ SAEM_Directories/Fellowship_Directory/SAEM_Directories/P/ FellowshipList.aspx.AccessedJanuary6,2023.
15.SocietyofClinicalUltrasoundFellowships(SCUF).Programlist. Availableat: https://www.eusfellowships.com/programs AccessedJanuary6,2023.
16.PanacekEA.Survey-basedresearch:generalprinciples. AirMedJ. 2008;27(1):14–6.
17.AlerhandS,Situ-LacasseE,RamdinC,etal.Nationalsurveyofpoint-ofcareultrasoundscholarlytracksinemergencymedicineresidency programs. WestJEmergMed. 2021;22(5):1095–101.
18.HillJ,OgleK,GottliebM,etal.Educator’sblueprint:ahow-toguidefor collectingvalidityevidenceinsurvey-basedresearch. AEMEducTrain. 2022;6(6):e10835.
19.RyanMS,LomisKD,DeiorioNM,etal.Competency-basedmedical educationinanorm-referencedworld:arootcauseanalysisof challengestothecompetency-basedparadigminmedicalschool. AcadMed. 2023;98(11):1251–60.
20.GoldhamerMEJ,Martinez-LageM,Black-SchafferWS,etal. Reimaginingtheclinicalcompetencycommitteetoenhanceeducation andprepareforcompetency-basedtime-variableadvancement. JGenInternMed. 2022;37(9):2280–90.
21.AccreditationCouncilforGraduateMedicalEducation(ACGME). ACGMEprogramrequirementsforgraduatemedicaleducation inemergencymedicalservices.2021.Availableat: AccessedApril29,2023.
22.AccreditationCouncilforGraduateMedicalEducation(ACGME). ACGMEprogramrequirementsforgraduatemedicaleducationincritical caremedicine.2022.Availableat: https://www.acgme.org/specialties/ internal-medicine/program-requirements-and-faqs-and-applications/ AccessedApril29,2023.
AmeliaGurley,MD
ColinJenkins,MD
ThienNguyen,MD
AllisonWoodall,MD
JasonAn,MD
RiversideCommunityHospital,DepartmentofEmergencyMedicine,Riverside,California
SectionEditor:JeffreyLove,MD,MHPE
Submissionhistory:SubmittedJune14,2022;RevisionreceivedFebruary8,2023;AcceptedFebruary15,2023 ElectronicallypublishedDecember6,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.57721
Assessmentsareacorecomponentofresidencytrainingto assessdevelopmentinthegeneralcompetenciesexpectedof allphysicians.1 Manymethodsareemployedtoevaluate performance,fromcheckliststocomputer-based questionnaires,asnosinglebestpracticeexists.2 Common tomost,however,arebarrierstothecompletionof assessments.3 Forexample,residentsandfacultyoftencitea perceivedlackoftimetoperformassessments,whichmay leadtosuboptimalcomplianceincompletingassessments.3 Somemethodsofassessment,suchasprovidingnarrative feedbacktoresidentsbyfaculty,maybeseenastoo burdensome.3 Theemergencydepartmentrepresentsan especiallychallengingenvironmenttoovercomethese barriersgiventhehighcognitivedemandplacedonfaculty andresidentsbydefault.
Onepossiblestrategytoenhancefacultycompliancein completingassessmentsistoimplementbehavioralnudging intosocialandphysicalenvironments.Borrowedfrom behavioraleconomics,nudgetheoryinvolvesuseof evidence-based “nudges” thatincorporatepositive reinforcementandindirectsuggestionstoinfluencedecisions andbehavior.4 Nudgescanincludeuseofthefollowing: priming(environmentalcuestosubconsciouslydrive behavior);defaultoptions(desirableoptionsarepreselected asthedefaultchoiceandtherebyeasiestforindividualsto take);norm-basednudges(comparingindividualbehavior topeerpractice);commitment(makingapublicpromise tocompleteatask);andsalience(drawingattentiontoa particularoptionthroughcolorsoracompellingstory), amongothers.4 Forinstance,inthesurgicalintensivecare unit,handhygienecompliancewasenhancedwhen individualswereprimedwithacitrus-likefragrancethatwas dispensedintotheenvironment.5 Inanotherexample, medicalstudentassessmentswerecompletedmoreoften whenfacultywerepromptedwithelectronicformsattheend ofshifts,ratherthanrelyingonthemtocompletepaperforms
attheirowndiscretion.6 Inthisstudy,weevaluatedthe effectivenessoftwoprimingnudgesandonenorm-based nudgeinincreasingcomplianceoffacultyincompleting assessmentsofemergencymedicineresidents.
Ourprimaryobjectiveinthestudywastoassessthe effectivenessofnudgeinterventionsinincreasingthenumber ofresidentperformanceassessmentscompletedbyattending physicians.Thiswasassessedbycomparingthenumber ofassessmentscompletedduringtheyearpriorto implementationofthenudgeinterventionswiththeyears followingtheirimplementation.Oursecondaryobjectivewas toidentifywhichparticularmethodwasemployedwiththe greatestfrequency.
Thisprojectqualifiedasaresearchstudyconductedin establishedorcommonlyacceptededucationalsettings.The ResearchOversightCommitteeapprovedtheInstitutional ReviewBoardExemptReviewFormrequestforexemption. ThestudytookplaceatRiversideCommunityHospital,a tertiary-carereferralacademic/communitymedicalcenterin Riverside,California.TheresidencyprogramatRiverside CommunityHospitalisathree-yearemergencymedicine residencyaccreditedbytheAccreditationCouncilfor GraduateMedicalEducation.Eachclasshas13residentsper yearforatotalof39residents.Wehadapproximately28–30 facultyduringthestudy,and28facultyreceivedprior trainingoncompletingend-of-shiftassessments.
Wecollectedpre-interventiondatafromJuly1,2019–June 30,2020withanemaillinksenttofacultyatthebeginningof theacademicyear.Theyweresentperiodicemailreminders tocompletethesurvey.TheinterventionstartedonJuly1, 2020.Thepost-interventiondatawascollectedfromJuly1, 2020–May11,2021.
Table. Numberofassessmentscompletedovertimechartedagainsttimelineofinterventions.
Timeframe
7/1/19–6/30/20 (pre-intervention)
7/1/20–6/20/21 (post-intervention)
7/1/21–6/1/22 (post-intervention)
Numberofresponses3,6634,2434,534
Evaluationspermonth305354453
Threeprimarynudgeswereusedastheinterventionto increasethenumberofend-of-shiftassessments.Weselected thenudgesbasedonpreviousstudies,whichshowedpeople changebehaviorbasedonsocialcomparison.7 Peoplealso tendtochoosethemostvisibleoption.8 The firstnudgewas tocreateahomepageonthefacultyphonewithadirectlink totheend-of-shiftassessmentsurvey.Thesecondnudgewas aquickresponse(QR)codepostedatthefacultywork stationsthroughoutthedepartment:inthemainED;inthe rapidcare(loweracuity)zone;andinthefacultybreakroom. Thethirdnudgewasbasedonasocialproofheuristic.Atthe endofeachblockanemailwassenttoallfacultywiththe totalnumberofassessmentscompletedfortheblock,with comparisonstootherfacultymembers’ completionrateand alinktothesurvey.
Attheendofthestudyperiod,allfacultyreceivedasurvey askingwhichnudgewasusedthemostoften.Facultywere askedtorankeachintervention,fromusedmostoften (weightedscoreof3)toleastoften(weightedscoreof1). Thesurveylinkintheemailreminderwascreatedin Surveymonkey.com(Momentive,SanMateo,CA).
WecreatedtheQRcode flyeroncanva.com (SurryHills,Australia).
Webelievethattheinterventionsinthisstudycanbe replicatedatmanyotherinstitutions.TheQRcodeshouldbe postedinhighlyvisiblelocationsnearthefacultyworkspace intheED.Wediscoveredthatmanyfacultymembers requireddetailedinstructionsonhowtocreateahomepage ontheirmobiledevices.However,thefacultyreportedthat oncethehomepagewassetup,itwastheeasiestwayto completetheassessments.Theend-of-the-blocksummaryof thetotalnumberofassessmentscompletedbyfacultymaybe anadministrativeburdentosomeinstitutions.
Asshownin Table1,therewasa15.8%increaseinthe numberofassessmentscompletedintheyearafterthese interventionswereimplemented,withthenumberof completedassessmentsincreasingfrom3,663(305 assessmentspermonth)inthepre-interventionyearto4,243 (354assessmentspermonth)inthe firstpost-intervention year.Thisincreasewassustainedinthefollowingyear,with 4,534assessments(453assessmentspermonth)completedto date.Thistrendsuggeststhatour “nudge” interventionsmay havebeeneffectiveinproducingalong-termchangein facultybehaviorpatterns.
Whensurveyingthe28facultytodeterminewhichnudge wasmosteffective,therewasan85.7%(24)responserate. Oftherespondents,19(79%)indicatedthattheirmost frequentlyusednudgewasthesurveylinksavedontotheir phone,andthattheycompletedover75%oftheirassessments thisway.Thirteenrespondents(54%)reportedthatthenudge basedonsocialheuristics thelinkattheendofthemonthly emails wasthesecondmostfrequentlyused.Onlyone respondentusedtheQRcode flyersmostfrequently,and20 (83%)statedtheyneverusedtheQRcodeatall.
Fromourexperimentaldesign,welearnedthatnudgesused onlinecouldbeeffectiveinincreasingcompletionratesof assessments.Asurprisinglimitationwasthegroupingofdata intocertaintimeframes,whichcouldbedelineatedinfuture iterationstodeterminetheimpactthattimeofyearhason responserates.Wecouldalsocompareefficaciesofdifferent interventions,suchascomparingabaselinerateofusing home-screensurveylinksonlytothisbaselineplusanadded intervention,toassesstheimportanceofeachadded variableandhelpdeterminewhichinterventionstruly providebenefit.
Thisassessmentofourinterventions’ impactislimitedby severalfactors.Asthenumberandmakeupoffaculty changedduringtheintervention,itwasnotpossibleto determinewhetherastatisticallysignificantnumberof facultychangedtheirpracticeasaresultofthisintervention. Theincreaseintheassessmentcompletionratemayalsobe duenotonlytoourinterventionsbutalsotooutsidefactors suchaschanginghospitalpolicies,numberoffaculty,the impactoftheCOVID-19pandemic,overalldepartmental shiftsinattitude,ortheHawthorneeffect,anyofwhichmay haveplayedaroleininfluencingbehavior.Itisalsodifficult todistinguishwhichofthevariousinterventionsactually impactedattendingbehavior,asallwereimplemented simultaneously,andsurveyreplieswereanonymousandmay besubjecttorecallbias.Forexample,itispossiblethatthe presenceofQRcodesatworkstationswasresponsibleforthe largeincreaseinphonehome-screenassessmentcompletion.
AddressforCorrespondence:AllisonWoodall,MD,Riverside CommunityHospital,DepartmentofEmergencyMedicine, 4510BrocktonAvenue,Suite223,RiversideCA92501. Email: Allison.woodall@vituity.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived
aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Gurleyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GibbsT,BrigdenD,HellenbergD.Assessmentandevaluationin medicaleducation. SAfrFamPract.2006;48(1):5–7.
2.PerkinsSQ,DabajaA,AtiemoH.Bestapproachestoevaluationand feedbackinpost-graduatemedicaleducation. CurrUrolRep 2020;21(10):36.
3.MalikMU,DiazVossVarelaDA,StewartCM,etal.Barriersto implementingtheACGMEoutcomeproject:asystematicreviewof programdirectorsurveys. JGradMedEduc.2012;4(4):425–33.
4.YoongSL,HallA,StaceyF,etal.Nudgestrategiestoimprove healthcareproviders’ implementationofevidence-basedguidelines, policiesandpractices:asystematicreviewoftrialsincludedwithin Cochranesystematicreviews. ImplementSci.2020;15(1):50.
5.KingD,VlaevI,Everett-ThomasR,etal. “Priming” hand hygienecomplianceinclinicalenvironments. HealthPsychol 2016;35(1):96–101.
6.TewsMC,TreatRW,NanesM.IncreasingcompletionrateofanM4 emergencymedicinestudentend-of-shiftevaluationusingamobile electronicplatformandreal-timecompletion. WestJEmergMed 2016;17(4).
7.CheungTTL,KroeseFM,FennisBM,etal.TheHungerGames:using hungertopromotehealthychoicesinself-controlconflicts. Appetite 2017;116:401–9.
8.KroeseFM,MarchioriDR,deRidderDT.Nudginghealthyfoodchoices: a fieldexperimentatthetrainstation. JPublicHealth(Oxf) 2016;38(2):e133–e137.
*PrismaHealth-Upstate,UniversityofSouthCarolinaSchoolofMedicineGreenville, DepartmentofEmergencyMedicine,Greenville,SouthCarolina
†
PrismaHealth-Upstate,UniversityofSouthCarolinaSchoolofMedicineGreenville, DepartmentofObstetricsandGynecology,Greenville,SouthCarolina ‡ ClemsonUniversity,DepartmentofPublicHealthSciences,Clemson,SouthCarolina
SectionEditor:AbraFant,MD
Submissionhistory:SubmittedNovember22,2023;RevisionreceivedJanuary3,2024;AcceptedJanuary17,2024
ElectronicallypublishedMarch25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18596
Background: Theevaluationofpatientswith first-trimestervaginalbleedingandconcernforearly pregnancyloss(EPL)frequentlyoccursintheemergencydepartment(ED),accountingforapproximately 1.6%ofallEDvisits.1 Unfortunately,thesepatientsconsistentlyreportnegativeexperienceswithED care.2–8 Inadditiontoenvironmentalconcerns,suchaslongwaittimes,patientsoftendescribenegative interactionswithstaff,includingaperceivedlackofempathy,theuseofinsensitivelanguage,and inadequatecounseling.2,3 ThesepatientsandtheirpartnersoftenviewEPLasatraumaticlossoflifeand commonlyexperienceprolongedgriefreactions,includinganxietyanddepression.9–11 Poorsatisfaction withcarehasbeenassociatedwithworsementalhealthoutcomes.12 Thesecomplaintsrepresentan importantopportunityforimprovementinemergencymedicine(EM)training.13
WhilenopublishedliteraturetodatedescribestheperformanceofEMresidentsinmanaging patientspresentingwithEPL,studiessuggestthatevenobstetricsandgynecology(OB/GYN)residents findtheseinteractionschallenging.14,15 Simulation-anddidactic-basedtraininghasbeenshowntobe beneficialinimprovingOB/GYNresidentEPLcounselingandhasbeenassociatedwithimprovedpatient outcomes.16 Toourknowledge,thishasyettobereplicatedinEMresidencytraining.
Objectives: Weaimedtodevelopandevaluateasimulation-basededucationalinterventiontoimprove EMresidentmanagementofpatientspresentingwithEPL.[WestJEmergMed.2024;25(4.1)36–40.]
Theeducationalinterventionconsistedofthreephases (Figure1)andwasdesignedtooptimizelearningbasedon Kolb’slearningcycle.17,18 Residentswerepresentedwitha challengingscenario(concreteexperience)andthen promptedtoreflectonareasforimprovement(reflective observation).Theythencompletedanasynchronousmodule followedbyaninteractivegroupdiscussion(abstract conceptualization).Thelearningcyclecontinuedthrough activeexperimentationviaarepeatedopportunitytodothe simulation,followedbydebriefing.Thisformofrepetitive simulationhasbeenshowntobemoreeffectivewhen comparedwithnon-repeatedsimulation.19,20
WeimplementedtheinterventioninMay2023and conductedapre/poststudyofitsimmediateimpact,which
wasdeemedexemptbyourinstitutionalreviewboard.The interventiontookplaceatthesimulationcenterofthe affiliatedmedicalschool,duringthetwo-hourperiod typicallyallottedformonthlyresidentsimulation-based education.Postgraduateyear(PGY)1–3EMresidentswere recruitedbasedonaconveniencesampleincludingall residentsattendingsimulationthatday.Theresidents werenotinformedofthetopicoftheintervention priortothedayofthestudy,whichistypicalofour simulationcurriculum.
Sixstandardizedpatients(SP)werehiredtoportray patientsexperiencingEPL.Sixvolunteerfacultyemergency physicians(twomen,fourwomen)observedandevaluated thesimulationsandprovidedinstructionanddebriefing.One facultyOB/GYNphysicianandonefacultyemergency

Figure1. Sequenceofaneducationalinterventionforearlypregnancylosscounseling. EPL,earlypregnancyloss.
physician(bothwomen)co-facilitatedtheguidedgroup discussion-basededucation.
First,residentsparticipatedina10-minutesimulated patientencounterinwhichtheywereinstructedtocarefora SPwhoportrayedapatientwhowaseightweekspregnant andpresentedwithvaginalbleeding.Priortoevaluatingthe patient,eachresidentwasprovidedwithultrasoundresults indicatingthepregnancywasnonviable(presumably obtainedintriage).
Followingtheencounter,residentsindividuallydebriefed withanEMfacultyobserver.Residentsthenhad30minutes tocompleteanasynchronousonlineeducationalmodulethat includedcontentabouttheassessmentofearlypregnancy bleeding;diagnosingandmanagingectopicpregnancy; preventingalloimmunization;andEPLcounseling. Particularattentionwaspaidtooptimizingcaretoaddressa patient’sphysical,emotional,andcognitiveneeds,a frameworkrecommendedbyEmondetal.21 Themodulewas deliveredviaaninteractiveeducationalplatform,Rise360 Articulate(Articulate,NewYork,NY).22 Aftercompleting themodule,residentsparticipatedina15-minuteguided groupdialogwithEMandOB/GYNfaculty,discussingbest practicesandmodelingpracticalcommunicationskills. Facilitatorsgaveexamplesofhowtheywouldaddress patientsinvariousscenariostocommunicateclearlywhile alsousingsensitivelanguage.
Followingthisdiscussion,residentsrepeatedthesame 10-minutesimulatedpatientencounterfollowedby individualdebriefingwithEMfaculty.Theinterventionwas designedtoaccommodateupto24residentswiththe resourcesdescribed.
Tostudytheimmediateimpactoftheintervention, residentperformancewasevaluatedusingfourmeasures: 1)completionofcriticalactionsduringthesimulationviaan 11-itemchecklist;2)self-reportedconfidence;3)a10-item multiple-choicetestoffoundationalEPLknowledge;and4) SPperceptionsofresidentempathyduringthesimulationvia
themodifiedJeffersonScaleofEmpathy(JSE).23,24 Allfour evaluativemeasuresweredeliveredimmediatelyfollowing theinitialsimulatedencounter(Phase1)andafterthe final simulationencounter(Phase3).Inadditiontothese measures,residentswereinvitedtoparticipateinabrieffocus groupinterview,conductedbyanon-facultyfacilitator (woman),aftertheinterventiontodiscusstheirimpressions oftheintervention.
FacultyinEMandOB/GYNdevelopedthetaskchecklist toincludecriticalactionsandevidence-basedbestpractices intreatingpatientsexperiencingEPL.Thislistwasadapted fromachecklistemployedinasimilarstudyandmodifiedto reflectEDcare.25 Residentswereaskedtoratetheir perceivedconfidencelevelfromleast(1)tomost(10) confidentregardingthefollowing:knowledgeaboutthe evaluationandmanagementofpatientswith first-trimester bleeding;abilitytocommunicateinasensitiveandempathic mannerwithpatientswithEPL;andabilitytocounsela patientexperiencingEPLregardingwhattoexpectafter discharge.Theyalsocompleteda10-questionmultiplechoicetest,whichEMandOB/GYNfacultydevelopedto assessbasicobjectiveknowledge.Aftereachsimulated encounter,SPscompletedthemodifiedJSE,avalidatedtool forSPevaluationofclinicianempathyandcommunication. ThemodifiedJSEincludes fivequestionsonaseven-point Likertscalerangingfromstronglydisagree(1)tostrongly agree(7).23,24 Anoutlineofthesimulatedcase,themodule, andtheassessmenttoolsareincludedinthe supplemental material accompanyingtheonlinearticle.
Ofthe16residentswhoparticipated,75%identifiedas men,andtherewasrelativelyequalrepresentationofPGY-1 (31.3%),PGY-2(37.5%),andPGY-3(31.3%)residents. Residentsimprovedfrompre-topost-interventionacrossall fourevaluativemeasures(Table1).Beforetheintervention, fewresidentsprovidedinformationaboutwhattoexpect afterdischarge,includingthepotentialpainlevel,the likelihoodofpassingtissue,returnprecautions,andlongtermemotionalramifications.Aftertheintervention, residentsweresignificantlymorelikelytousesensitive
Table1. Residentassessmentoutcomespre-topost-intervention.
PrePostSignedrank
MeasureMaximumscoreMean(SD)Mean(SD) SP-value
Performancechecklist114.94(1.80)9.50(1.51)67.0 <.001
Self-confidence3020.06(3.38)24.69(3.50)68.0 <.001
Knowledge105.84(1.29)8.00(1.41)45.5 <.001
Empathy3521.25(6.04)28.06(5.47)65.5 <.001
Table1b. Residentchecklistperformance.
PrePost
Checklistitemn(%)n(%) P-value
1.Deliversbadnewsusingsimplelanguageandwithavoidanceof non-preferredterms(fetus,embryo)
10(62.5)16(100)0.03
2.Allowssilenceforthepatienttoabsorbthenews14(87.5)14(87.5)1.00
3.Acknowledgespatient’semotions15(93.8)15(93.8)1.00
4.Dispelsguilt15(93.8)16(100)1.00
5.Counselspatientabouttheamountofexpectedbleeding2(12.5)11(68.8)0.004
6.Counselspatientonexpectedpain1(6.3)10(62.5)0.004
7.Counselspatientonthepossibilityofpassingtissue2(12.5)12(75.0)0.006
8.Counselspatientonreturnforseverebleeding3(18.8)14(87.5)0.003
9.Counselspatientonreturnforfever2(12.5)15(93.8)0.001
10.NormalizesemotionalramificationsofEPL5(31.3)13(81.3)0.008
11.Discussesfollow-upplan10(62.5)16(100)0.030 EPL,earlypregnancyloss.
languageandtoincludeinformationaboutexpected outcomesandreturnprecautions(Table1b).
Theseresultsindicatethatfocusedtrainingresultedin immediateimprovementsinresidentperformance, particularlyregardingcounselingandcommunication. Giventhepositiveresultsofsimilarinterventionsundertaken inotherlearnerpopulations,thisimmediateimpactlikely indicatesimprovedabilitytocareforpatientsinclinical practice.Verhaegheetalpublishedtheimpactofathreehourin-situsimulationtrainingforOB/GYNresidents, whichresultedinlong-termimprovementsinpsychologic outcomesaswellasreducedneedforreturnvisits.16 As comparedtothesepreviousinterventions,ourcurriculum enhancedefficiencybyemployinganonlinetrainingmodule, whichcoveredadditionalfoundationalknowledgeofearly pregnancybleedingcare(includingectopicpregnancyand threatenedEPL).Thisefficiencyisparticularlyimportantin EMgiventhebreadthofrequiredknowledge.
Whiletheeightresidentswhoparticipatedinthefocus groupinterviewgenerallyreportedpositivefeedback,two residentsdidnotethattheywereconfusedbytheorderofthe simulationsuchthattheyhadadiagnosispriortoany interactionwiththepatient.Inthefuture,thismaybe
amelioratedbyprovidingtheresidentswithmorecontextto thecaseorsimplyrevisingthescenariosothattheultrasound reportisreceivedafteraninitialevaluationandrequestfor imaging.Additionally,thetimeallottedforthe asynchronousmodulewas30minutes,butmostresidents completeditinabout20minutes,indicatingthepossibility ofadditionalcontentorexpansionofanotheraspectof theintervention.
Thisstudydescribesresidentperformanceinasimulated patientencounter,andwecannotconcludethatthisreflects actualclinicalcare.Thisstudyonlyassessedtheimpactofthe trainingonlearning(Kirkpatricklevel2)anddidnotattempt toevaluatetheresidents’ ongoingclinicalbehaviororits effectonpatients.26 Thestudywasconductedduringone sessionand,therefore,wecannotinferinformationabout retentionoflearning.Futureworkshouldassesstheeffectof interventionssuchasthisonclinicianbehaviorandresultant patientoutcomes.Facultyevaluatorswerenotblinded duringthesimulatedpatientencounters,whichcouldhave introducedbiasintotheevaluationprovidedviathe checklist.Thisconcernissomewhataddressedbythebinary
natureofthechecklist,inwhicheitherataskwasperformed oritwasnot.Oftheassessmenttools,onlythemodifiedJSE hasbeenexternallyvalidated.CreatingandvalidatingEMspecificmeasurementtoolsforEPLcarewouldensuremore robustdatagoingforward.
“Participantsdisproportionatelyidentifiedasmen(75%), ascomparedtothenationalaverageinemergencyresidencies of62%.27 Giventhesmallpopulationfromwhichthestudy samplewasderived,wedidnotaskparticipantswhetherthey werecis-ortransgendertoavoidlossofanonymity. Similarly,wedidnotaskparticipantsaboutpersonal experienceswithEPL.Futureworkcouldexplorethe relationshipofthesecharacteristicsandexperienceswith clinicalperformance.Despitetheselimitations,theresultsof thisstudyindicateaneedforEPL-specificeducationinEM residencyandthatabrief,simulation-basedinterventionwas effectiveinproducingimmediateimprovements. Consideringtheresultsofsimilarstudiesconductedinother populations,aninterventionsuchasthismayresultin improvedclinicalcareandlong-termpatientoutcomesinthis common,butdevastating,presentation.
5.HoAL,HernandezA,RobbJM,etal.Spontaneousmiscarriage managementexperience:asystematicreview. Cureus. 2022;14(4):e24269.
6.MeluchAL.Waitingtobeseen:provider-patientcommunicationinthe emergencyroomaboutmiscarriage. HealthCommun. 2021;37(11):1452–4.
7.MillerCA,RoeAH,McAllisterA,etal.Patientexperienceswith miscarriagemanagementintheemergencyandambulatorysettings. ObstetGynecol. 2019;134(6):1285–92.
8.PunchesBE,JohnsonKD,AcquavitaSP,etal.Patientperspectivesof pregnancylossintheemergencydepartment. IntEmergNurs. 2019;43:61–6.
9.PrettymanRJ,CordleCJ,CookGD.Athree-monthfollow-upof psychologicalmorbidityafterearlymiscarriage. BrJMedPsychol. 1993;66(Pt4):363–72.
10.ZaccardiR,AbbottJ,Koziol-McLainJ.Lossandgriefreactionsafter spontaneousmiscarriageintheemergencydepartment. AnnEmerg Med. 1993;22(5):799–804.
11.BellhouseC,Temple-SmithM,WatsonS,etal. “Thelosswas traumatic somehealthcareprovidersaddedtothat”:Women’s experiencesofmiscarriage. WomenBirth. 2019;32(2):137–46.
AddressforCorrespondence:ShawnaD.Bellew,MD,MPH,Prisma Health-Upstate,UniversityofSouthCarolinaSchoolofMedicine Greenville,DepartmentofEmergencyMedicine,701GroveRoad, Greenville,SC29605.Email: Shawna.bellew@prismahealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Bellewetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.WittelsKA,PelletierAJ,BrownDF,etal.UnitedStatesemergency departmentvisitsforvaginalbleedingduringearlypregnancy, 1993–2003. AmJObstetGynecol. 2008;198(5):523.e1–6.
2.Larivière-BastienD,deMontignyF,VerdonC.Women’sexperiencesof miscarriageintheemergencydepartment. JEmergNurs. 2019;45(6):670–6.
3.MacWilliamsK,HughesJ,AstonM,etal.Understandingtheexperience ofmiscarriageintheemergencydepartment. JEmergNurs. 2016;42(6):504–12.
4.DaintyKN,SeatonMB,McLeodS,etal.Reframinghowearlypregnancy lossisviewedintheemergencydepartment. QualHealthRes. 2021;31(6):1119–28.
12.deMontignyF,VerdonC,MeunierS,etal.Women’spersistent depressiveandperinatalgriefsymptomsfollowingamiscarriage:the roleofchildlessnessandsatisfactionwithhealthcareservices. Arch WomensMentHealth. 2017;20(5):655–62.
13.EvansCS.Earlypregnancylossintheemergencydepartment:lessons learnedasaspouse,newfather,andemergencymedicineresident. Ann EmergMed. 2021;77(2):233–6.
14.BrannMandButeJJ.Communicatingtopromoteinformeddecisionsin thecontextofearlypregnancyloss. PatientEducCouns. 2017;100(12):2269–74.
15.ButeJJandBrannM.Tensionsandcontradictionsininterns’ communicationaboutunexpectedpregnancyloss. HealthCommun. 2020;35(5):529–37.
16.VerhaegheC,GicquelM,BouetPE,etal.Positiveimpactofsimulation trainingofresidentsonthepatients’ psychologicalexperience followingpregnancyloss. JGynecolObstetHumReprod. 2020;49(3):101650.
17.KolbDA. ExperientialLearning:ExperienceastheSourceofLearning andDevelopment.2nd ed.Hoboken,NJ:PearsonEducation,2015.
18.StockerM,BurmesterM,AllenM.Optimisationofsimulatedteam trainingthroughtheapplicationoflearningtheories:adebatefora conceptualframework. BMCMedEduc. 2014;14:69.
19.AuerbachM,KesslerD,FoltinJC.Repetitivepediatricsimulation resuscitationtraining. PediatrEmergCare. 2011;27(1):29–31.
20.NgC,PrimianiN,Orchanian-CheffA.Rapidcycledeliberatepracticein healthcaresimulation:ascopingreview. MedSciEduc. 2021;31(6):2105–20.
21.EmondT,deMontignyF,GuillaumieL.Exploringtheneedsof parentswhoexperiencemiscarriageintheemergencydepartment: Aqualitativestudywithparentsandnurses. JClinNurs. 2019;28(9-10):1952–65.
22.FirsttrimesterbleedingandEarlyPregnancyLoss.Availableat: https:// rise.articulate.com/share/CfDnfG-CI6UEdqU1t-FEUDtPnu_UU5mQ AccessedMay9,2023.
23.HojatM. EmpathyinHealthProfessionsEducationandPatientCare 1st ed.NewYorkCity,NY:SpringerInternationalPublishing,2016.
24.MalloryL,FloyedR,DoughtyC,etal.ValidationofamodifiedJefferson ScaleofEmpathyforobserverstoassesstrainees. AcadPediatr. 2021;21(1):165–9.
25.MarkoEK,Buery-JoynerSD,SheridanMJ,etal.Structuredteaching ofearlypregnancylosscounseling. ObstetGynecol. 2015;126(Suppl4):1s–6s.
26.JohnstonS,CoyerFM,NashR.Kirkpatrick’sevaluationofsimulation anddebriefinginhealthcareeducation:asystematicreview. JNursEduc. 2018;57(7):393–8.
27.DeFazioCR,CloudSD,VerniCM,etal.Womeninemergencymedicine residencyprograms:ananalysisofdatafromAccreditationCouncilfor GraduateMedicalEducation-approvedresidencyprograms. AEMEduc Train. 2017;1(3):175–8.
28.LeeL,MaW,DaviesS,etal.Towardoptimalemotionalcareduringthe experienceofmiscarriage:anintegrativereviewoftheperspectivesof women,partners,andhealthcareproviders. JMidwiferyWomens Health. 2023;68(1):52–61.
LaurenT.Southerland,MD,MPH*
LaurenR.Willoughby,MD*
JasonLyou,MD*
RebeccaR.Goett,MD†
DanielW.Markwalter,MD‡§
DianeL.Gorgas,MD*
*TheOhioStateUniversityWexnerMedicalCenter,DepartmentofEmergency Medicine,Columbus,Ohio
† RutgersNewJerseyMedicalSchool,DepartmentofEmergencyMedicine, Newark,NewJersey
‡ UniversityofNorthCarolinaSchoolofMedicine,DepartmentofEmergency Medicine,ChapelHill,NorthCarolina
§ UniversityofNorthCarolinaSchoolofMedicine,UNCPalliativeCareProgram, ChapelHill,NorthCarolina
SectionEditors:ChrisMerritt,MD,andJeffreyLove,MD
Submissionhistory:SubmittedMay1,2023;RevisionreceivedAugust30,2023;AcceptedNovember3,2023
ElectronicallypublishedDecember22,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.60842
Background: Emergencymedicine(EM)residenttrainingisguidedbytheAmericanBoardof EmergencyMedicineModeloftheClinicalPracticeofEmergencyMedicine(EMModel)andtheEM Milestonesasdevelopedbasedontheknowledge,skills,andabilities(KSA)list.Theseareconsensus documentsdevelopedbyacollaborativeworkinggroupofsevennationalEMorganizations.External expertsingeriatricEMalsodevelopedcompetencyrecommendationsforEMresidencyeducationin geriatrics,butthesearenotbeingtaughtinmanyresidencyprograms.Ourobjectivewastoevaluatehow thegeriatricEMcompetenciesintegrate/overlapwiththeEMModelandKSAstohelpresidency programsincludethemintheireducationalcurricula.
Methods: Trainedemergencyphysiciansindependentlymappedthegeriatricresidentcompetencies ontothe2019EMModelitemsandthe2021KSAsusingExcelspreadsheets.Discrepancieswere resolvedbyanindependentreviewerwithexperiencewiththeEMModeldevelopmentandresident education,andthe finalmappingwasreviewedbyallteammembers.
Results: TheEMModelincluded77%(20/26)ofthegeriatriccompetencies.TheKSAsincludedmostof thegeriatriccompetencies(81%,21/26).Allbutoneofthegeriatriccompetenciesmappedontoeitherthe EMModelortheKSAs.WithintheKSAs,mostofthegeriatriccompetenciesmappedontonecessary levelskills(rankedB,C,D,orE)withonly five(8%)alsomappingontoadvancedskills(rankedA).
Conclusion: AllbutoneofthegeriatricEMcompetenciesmappedtothecurrentEMModelandKSAs. ThegeriatriccompetenciescorrespondtoknowledgeatalllevelsoftrainingwithintheKSAs,from beginnertoexpertinEM.EducatorsinEMcanusethismappingtointegratethegeriatriccompetencies withintheircurriculums.[WestJEmergMed.2024;25(4.1)41–50.]
Emergencymedicine(EM)residentshave3–4yearsof trainingtolearnanextensivearrayofskills.Thisincludesthe skillsneededtocareforolderpatients,whomakeup16–20% oftheirpatients.1,2 TheAmericanBoardofEmergency Medicine(ABEM)codifiestheskillsneededforcompetency
inEMintheModeloftheClinicalPracticeofEmergency Medicine(EMModel)andthe2021knowledge,skills,and abilities(KSA).3,4 TheEMModellistsclinicalpresentations anddiseasetypesandtheKSAsarealistofskillsandabilities integraltoEMpractice.Manyresidencyprogramsbasetheir curriculumsonthesedocuments.However,itisunclearhow
besttointegrategeriatricteachingwithinthese complexcurricula.
In2010Hoganetalpublishedeightdomainswith26 competenciesofgeriatriceducationderivedfromanexpert consensuspanelthatareconsideredessentiallearningduring EMresidencyforthecareofolderadultsintheemergency department(ED).5 Thesecompetenciesarealsousedfor categorizinggeriatriccontinuingeducationforgeriatricED accreditationandhavebeenpivotaltothedevelopmentof geriatricEMasasubspecialty.6,7 Despitethisguidance, geriatricconceptsarestillonlyminimallyintegrated intoresidenteducation.8 Withoutdedicatedtraining, residentknowledgeofgeriatriccompetenciesispoor.9–11 Butthereiscurrentlynoguidanceonhowtointegrate thegeriatriccompetencieswithinanEM residencycurriculum.
OurcurriculumisbasedontheEMModelandKSAs.Our goalwastodeterminewhetherthegeriatriccompetenciescan becoveredbyanEMModel-basedcurriculum.
Thisprojectisnothumansubjectsresearchanddidnot requireinstitutionalboardreview.Thestudywasa descriptivecomparisonofthe2019EMModelandthe2021 KSAstothe2010geriatriccompetenciesusingaconsensusbasedprocess.TheKSAsincludebothadescriptionanda level.Theyaredividedintooverarchingcategories (eg,diagnosis,pharmacotherapy,reassessment)whichare thendividedintosteps.4 Eachstepisgivenahierarchyin training(withAthehighestandEthelowest).LevelAis foradvancedknowledgeorskills.LevelBistheminimal competencylevelforpassingEMresidency.LevelsC,D, andEareskillstepstoreachlevelB.
Inthe firstphaseofconsensusmapping,tworesidents (asecond-yearEMresidentandafourth-yearEM/internal medicineresident)andageriatricfellowship-trainedEM attendingindependentlymappedgeriatriccompetencies usingExcel(MicrosoftCorporation,RedmondWA).They wereinstructedto firstusethesearchbuttontolookforexact languageandthengoitembyitemthroughtheEMModel andtheKSAstomapsimilarlanguageorconcepts.For example,theconceptofdeliriumcouldbedescribedas alteredmentalstatusorencephalopathy.Aclearassociation wasdefinedbytheteamas1)akeywordmatchor 2)consensusthatitwaslikelythatanemergencyphysician lecturing/teachingontheEMModelcontentitemwould,in normalteachingpractices,teachthegeriatriccompetency.If thiswasnotthecase,butthegeriatriccompetencycouldbe incorporatedunderthistopicbysomeone intentionally teachingthecompetencies,thiswaslistedasasuggestedarea forincorporation.Reviewerswereinstructedtobegenerous withmappingduringthis firstround.
Ifallthreeor2/3agreed,thiswasconsideredinitial consensus.Anyremainingdiscrepancieswerethen
independentlyreviewedbyanotheremergencyphysician withexpertiseinresidenteducation(formerEMprogram directorandcurrentABEMexecutivecommitteemember). Thefullgroupmetandreviewedthe finaldiscrepanciesuntil consensuswasreached.Theconsensustableswerethen reviewedindependentlybytwomoreemergencyphysicians atexternalresidencyprogramsforcontentvalidity.Asimilar processwasusedformappingKSAs.Reviewerswereblinded totheKSAlevel(A-Edesignation).
Incorporationintothe2019EMModel
TheEMModelhas963items.Onthe firstround,126 items(13%ofcontent)wereidentifiedaspotentialmatches, includingallof 17.1DrugandChemicalClasses .Round1 consensuswas96.2%(927items). Table1 liststhe20geriatric competencies(77%)includedinthe2019EMModel.Key wordmatchesincludedcompetency#6: “Demonstrate abilitytorecognizepatte rnsof(physical/sexual, psychological,neglect/abandonment)thatareconsistent withelderabuse[,] ” whichmapsto “ModelContent 14.6.1.3PatternsofViolence/ Abuse/Neglect:Intrapersonal Violence:Elder . ” Otherswerematchedbyconcept,suchas competency#11: “Assessandcorrect(ifappropriate) causativefactorsinagitatedelderssuchasuntreatedpain, hypoxia,hypoglycemia,useofirritatingtethers(de fi nedas monitorleads,bloodpressurecuff,pulseoximetry, intravenousaccess,andFoleycatheter),environmental factors(light,temperature),anddisorientation[,] ” which couldbeincorporatedintoteachingon 12.14Nervous SystemDisorders:Delirium . Initialdisagreementsincludedwhethersignsand symptomsweremeanttobeusedtoformulateadifferential diagnosisforthatsymptomortodescribemanagementofthe symptoms.TherewasalsoaquestionastowhetherG11, whichdiscusses “irritatingtethers” asacauseofdelirium, shouldbemappedtoallproceduressuchas 19.4.1.4. Nasogastrictube .Thegroupdecidedthatthiswouldbe betterencompassedundertheEMModelitemfordelirium. Table2 liststhesixgeriatriccompetencieswithoutaclear fit withintheEMModelandsuggestionsfromtheteamon wheretoincludethem.
Incorporationintothe2021Knowledge,Skills,andAbilities
Theinitialindependentmappingresultedinconsensuson 84%oftheitems(179/214).Ofthegeriatriccompetencies, 216(81%)mappedontoKSAs(Table3).Themostcommon categorieswereCommunication&InterpersonalSkills (CS0),Pharmacotherapy(PT0),andTransitionsofCare (TC0).Ofthe fivecompetenciesthatdidnotmapdirectly ontotheKSAs,allhadmappingitemsintheEMModel exceptone.Theonecompetencythatdidnotmapdirectlyto anyEMModelorKSAwasEffectsofComorbidConditions (G24): “Assessanddocumentthepresenceofcomorbid
Table1. ThegeriatricteachingcompetenciesmappedontotheEmergencyMedicineModelofCare.
Geriatric competencyDescriptionEMmodelitem
G1Generateadifferentialdiagnosisrecognizingthatsignsandsymptoms suchaspainandfevermaybeabsentorlessprominentinelderswith acutecoronarysyndromes,acuteabdomens,orinfectiousprocesses.
G2Generateanage-specificdifferentialdiagnosisforelderpatients presentingtotheEDwithgeneralweakness,dizziness,falls,oraltered mentalstatus.
G3Documentconsiderationofadversereactionstomedications,including drug-druganddrug-diseaseinteractions,aspartoftheinitialdifferential diagnosis.
G4Inpatientswhohavefallen,evaluateforprecipitatingcausesoffallssuch asmedications,alcoholuse/abuse,gaitorbalanceinstability,medical illness,and/ordeteriorationofmedicalconditions.
G5Assessforgaitinstabilityinallambulatoryfallers;ifpresent,ensure appropriatedispositionandfollow-upincludingattempttoreachprimary carephysician.
G6Demonstrateabilitytorecognizepatternsoftrauma(physical/sexual, psychological,neglect/abandonment)thatareconsistentwithelder abuse.Managetheabusedpatientinaccordancewiththerulesofthe stateandinstitution.
G7Instituteappropriateearlymonitoringandtestingwiththeunderstanding thateldersmaypresentwithmutedsignsandsymptoms(eg,absentpain andneurologicchanges)andareatriskforoccultshock.
G8Assesswhetheranelderisabletogiveanaccuratehistory,participatein determiningtheplanofcare,andunderstanddischargeinstructions.
1.1Abnormalvitalsigns
1.2Pain
1.3.1General-alteredmentalstatus
1.3.4General-ataxia
1.3.19General-fatigue/malaise
1.3.28General-lightheadedness/dizziness
1.3.53General-weakness
18.3.2Multisystemtrauma-falls
1.3.55General-toxidromes
17.1Drugandchemicalclasses: entire section
1.3.4General-ataxia
1.3.53General-weakness
18.3.2Multisystemtrauma-falls
18.3.2Multisystemtrauma-falls
14.6.1.3Patternsofviolence/abuse/ neglect-elder
1.3.41General-shock
12.8.1Otherconditionsofthebraindementia
14.5.2Organicpsychoses-dementia
20.4.5.4Regulatory/legal-consent,capacity andrefusalofcare
G9Assessanddocumentcurrentmentalstatusandanychangefrom baselineineveryelder,withspecialattentiontodeterminingwhether deliriumexistsorhasbeensuperimposedondementia.
G10Emergentlyevaluateandformulateanage-specificdifferentialdiagnosis forelderswithnewcognitiveorbehavioralimpairment,includingselfneglect;initiateadiagnosticworkuptodeterminetheetiology;andinitiate treatment.
G11Assessandcorrect(ifappropriate)causativefactorsinagitatedelders suchasuntreatedpain,hypoxia,hypoglycemia,useofirritatingtethers (definedasmonitorleads,bloodpressurecuff,pulseoximetry, intravenousaccess,andFoleycatheter),environmentalfactors(light, temperature),anddisorientation.
1.3.1General-alteredmentalstatus
12.8.1Otherconditionsofthebraindementia
12.14.1Delirium-exciteddelirium syndrome
14.5.2Organicpsychoses-dementia
1.3.18General-failuretothrive
12.14.1Delirium-exciteddelirium syndrome (Continuedonnextpage)
Table1. Continued.
Geriatric competencyDescriptionEMmodelitem
G12Recommendtherapybasedontheactualbenefittoriskratio,including butnotlimitedtoacutemyocardialinfarction,stroke,andsepsis,sothat agealonedoesnotexcludeeldersfromanytherapy.
G14Prescribeappropriatedrugsanddosagesconsideringthecurrent medication,acuteandchronicdiagnoses,functionalstatus,and knowledgeofage-relatedphysiologicchanges(renalfunction,central nervoussystemsensitivity).
G15Searchforinteractionsanddocumentreasonsforusewhenprescribing drugsthatpresenthighriskeitheraloneorindrug-drugordrug-disease interactions(eg,benzodiazepines,digoxin,insulin,NSAIDs,opioids,and warfarin).
G16Explainallnewlyprescribeddrugstoeldersandcaregiversatdischarge, assuringthattheyunderstandhowandwhythedrugshouldbetaken,the possiblesideeffects,andhowandwhenthedrugshouldbestopped.
G19Withrecognitionofuniquevulnerabilitiesinelders,assessanddocument suitabilityfordischargeconsideringtheEDdiagnosis,includingcognitive function,theabilityinambulatorypatientstoambulatesafely,availability ofappropriatenutrition/socialsupport,andtheavailabilityofaccessto appropriatefollow-uptherapies.
G20Selectanddocumenttherationaleforthemostappropriateavailable disposition(home,extendedcarefacility,hospital)withtheleastriskof themanycomplicationscommonlyoccurringineldersduringinpatient hospitalizations.
G21Rapidlyestablishanddocumentanelder’sgoalsofcareforthosewitha seriousorlife-threateningconditionandmanageaccordingly.
G22AssessandprovideEDmanagementforpainandkeynon-pain symptomsbasedonthepatient’sgoalsofcare.
G23Knowhowtoaccesshospicecareandhowtomanageeldersinhospice carewhileintheED.
NSAID,non-steroidanti-in flammatorydrug; ED,emergencydepartment.
conditions(eg,pressureulcers, cognitivestatus,fallsinthe pastyear,abilitytowalkandtransfer,renalfunction,and socialsupport)andincludetheminyourmedicaldecisionmakingandplanofcare ” Incorporatingthepotential consequencesofcomorbidconditionsisincludedinKSA
PR2: “Performtheindicatedprocedureonanuncooperative patient,patientattheextremeso fage(pediatric,geriatric), multipleco-morbidities,poorlyde fi nedanatomy, hemodynamicallyunstable,highriskforpainorprocedural complications,sedationrequi red,oremergentindicationto performprocedure,andrecognizetheoutcomeand/or
12.11.1.1Stroke-intracerebralhemorrhagic stroke
12.11.1.2Stroke-subarachnoid hemorrhagicstroke
12.11.2.1Stroke-embolicischemicstroke
12.11.2.2Stroke-thromboticischemic stroke
20.4.4.1Healthcarecoordination-advance directives
17.1Drugandchemicalclasses: entire section
17.1Drugandchemicalclasses: entire section
20.1.1.3Interpersonalskills-patientand familyeducation
20.3.2.6Ethicalprinciples-careof vulnerablepopulations
20.4.4.3.1Healthcarecoordinationactivitiesofdailyliving/functional assessment
20.4.4.2.3Healthcarecoordination-hospice referral
20.4.4.1Healthcarecoordination-advance directives
20.4.4.2.1Healthcarecoordination-patient identificationforpalliativecare
19.3.3Anesthesiaandacutepain management-analgesia
20.4.4.2.3Healthcarecoordination-hospice referral
complicationsresultingfromtheprocedure ” (KSALevelB). WhilethegeriatricscompetencyaddressesmedicaldecisionmakingandtheKSAaddressdifficultprocedures,thereis someoverlapinthetrainingrequired.
Ofthe63matcheswithintheKSA, five(8%)mappedonto advancedlevelAskills(DX7,Identifyobscure,occult,or rarepatientconditions ;and TI6,Developprotocolstoavoid potentialcomplicationsofinterventions ).Abouthalf(31, 49%)mappedontorequiredcompetencyskills(LevelB),and theremaining27(43%)weredevelopingskills(LevelC,Dor E,27,43%)(Table3).
Table2. Suggestionsforteachingthegeriatriccompetenciesthatdonot fitclearlywithintheEmergencyMedicineModel.
Geriatric competencyDescription
G13Identifyandimplementmeasuresthatprotecteldersfrom developingiatrogeniccomplicationscommontotheED includinginvasivebladdercatheterization,spinal immobilization,andcentrallineplacement.
G17Documenthistoryobtainedfromskillednursingor extendedcarefacilitiesoftheacuteeventsnecessitating EDtransferincludinggoalsofvisit,medicalhistory, medications,allergies,cognitiveandfunctionalstatus, advancecareplan,andresponsiblePCP.
G18Provideskillednursingorextendedcarefacilitiesand/or PCPwithEDvisitsummaryandplanofcare,including follow-upwhenappropriate.
G24Assessanddocumentthepresenceofcomorbid conditions(eg,pressureulcers,cognitivestatus,fallsin thepastyear,abilitytowalkandtransfer,renalfunction, andsocialsupport)andincludetheminyourmedical decision-makingandplanofcare.
G25Developplansofcarethatanticipateandmonitorfor predictablecomplicationsinthepatient’scondition (eg,gastrointestinalbleedcausingischemia).
Suggestionsforteachinggeriatriccompetencies withoutaclearassociationwithEMModelitems
Couldbediscussedunder ProcedureDomain or PracticebasedLearningandImprovement:Patientsafetyand Medicalerrors
Notransitionsofcare,nursingfacility,ordispositionareas. Couldbetaughtunder InterpersonalandCommunication Skills:Intra-departmentalrelations,teamwork,and collaborationskills
Notransitionsofcare,nursingfacility,ordispositionareas. Couldbetaughtunder InterpersonalandCommunication Skills:Intra-departmentalrelations,teamwork,and collaborationskills
Whileindividualelementslistedareinthemodel (eg,ulcerativelesions:decubitus),theconceptof comorbidityinolderadultsisdistinctfromdisease-oriented items.
Couldbediscussedunder Practice-basedLearningand Improvement:PatientsafetyandMedicalErrors
G26Communicatewithpatientswithhearing/sightimpairmentCouldbediscussedunder Interpersonaland CommunicationSkills:CulturalCompetency.
ED,emergencydepartment; PCP,primarycarephysician.
ThegeriatriccompetenciesforEMresidencytraining integratewellwithintheEMModelandKSAs,with onlyonecompetencynothavingadirectmatch. Demonstratingthisoverlapbetweenthesuggested subspecialtycurriculumandtheEMmodelcanhelpEM educatorsensurethatthegeriatriccompetenciesare incorporatedintotheircurricula.Thismappingcouldalso guidethedevelopmentofboardexamquestions,lectures, orsimulationcases.
TheEMModelisverybrief,whichcanmakedirecting educationdifficult.Forinstance,trainingontheEMModel item 18.3Multi-systemTrauma:Falls isexpoundeduponin geriatriccompetency#4: “Inpatientswhohavefallen, evaluateforprecipitatingcausesoffallssuchas medications,alcoholuse/abuse,gaitorbalanceinstability, medicalillness,and/ordeteri orationofmedicalconditions . ” Oranotherexample,KSA DX1 “ Synthesizechief complaint,history,physicalexamination,andavailable medicalinformationtodevelopadifferentialdiagnosis ” can includeadiscussionofgeriatriccompetency#3 “Document considerationofadversereacti onstomedications,including drug-druganddrug-diseaseinteractions,aspartofthe initialdifferentialdiagnosis. ” Theybothdescribetheinitial generationofadifferentialdiagnosis,butthegeriatric
competencyaddspharmacologyinteractionsandadverse reactionstobeconsideredinthedifferential.
Asecond findingofthisstudywasthatthegeriatric competenciesalignwithelementsrequiredforminimalKSA competency.Thisimpliesthatdifferentaspectsofgeriatric carecan(andweargue,should)betaughtthroughouta resident’straining.Italsosuggeststhatthegeriatric competencieswerewelldevelopedfortheresidencylevelof trainingandshouldnotbeconsidered “tooadvanced” or “subspecialtytraining.” Whilepriorresearchhasevaluated separategeriatric-specificcurricula,9–11 ourworkshowsthat geriatriccompetenciescanbeintegratedthroughouta curriculumbasedontheEMModelandKSAs.Asof2021, therewereonly25geriatricfellowship-trainedemergency physicians,whichisnotenoughforeveryresidency program. 12 Programswithoutfacultywhohavenointerestor trainingingeriatricscouldalsouseexternaltraining resourcessuchastheonlinelearningmodulesat https://geri-em.com/andattheGeriatricEmergency DepartmentCollaborative(https://gedcollaborative.com/ online-learning/).
Onelimitationofthisprojectwastheconsensusdefinitions used.Wewereunableto findanyexistingmethodstohelpus
Table3. Thegeriatriccompetenciesweremappedontothe2021ABEMknowledge,skills,andabilitieslist.
Geriatric competencyDescription KSA codeDescriptionLevel
G1Generateadifferentialdiagnosisrecognizingthat signsandsymptomssuchaspainandfevermay beabsentorlessprominentinelderswithacute coronarysyndromes,acuteabdomens,or infectiousprocesses.
G2Generateanage-specificdifferentialdiagnosisfor elderpatientspresentingtotheEDwithgeneral weakness,dizziness,falls,oralteredmentalstatus.
DX1Synthesizechiefcomplaint,history,physical examination,andavailablemedicalinformationto developadifferentialdiagnosis
DX7Identifyobscure,occult,orrarepatientconditionsA
DX8Constructalistofpotentialdiagnosesbasedonthe chiefcomplaint D
DX1Synthesizechiefcomplaint,history,physical examination,andavailablemedicalinformationto developadifferentialdiagnosis
DX7Identifyobscure,occult,orrarepatientconditionsA
DX8Constructalistofpotentialdiagnosesbasedonthe chiefcomplaint D
G3Documentconsiderationofadversereactionsto medications,includingdrug-druganddrug-disease interactions,aspartoftheinitialdifferential diagnosis.
G6Demonstrateabilitytorecognizepatternsoftrauma (physical/sexual,psychological,neglect/ abandonment)thatareconsistentwithelderabuse. Managetheabusedpatientinaccordancewiththe rulesofthestateandinstitution.
DX1Synthesizechiefcomplaint,history,physical examination,andavailablemedicalinformationto developadifferentialdiagnosis
PT5Recognize,monitor,andtreatadverseeffectsof pharmacotherapy
LI8Adheretoprocessesandprocedurestoensurethat appropriateagenciesarenotifiedinsituationsthat couldposeathreattoindividualorpublichealth (eg,violenceandcommunicabledisease)in accordancewithlocallegalstandards
LI10Adheretolegalandethicalstandardstoassess andtreatpatientspresentingtotheED
LI11Advocateforpatientsvulnerabletoviolenceor abuseinaccordancewithlegalandethical standards
LI13Identifypatientsvulnerabletoabuseorand/or neglect
G7Instituteappropriateearlymonitoringandtesting withtheunderstandingthateldersmaypresent withmutedsignsandsymptoms(eg,absentpain andneurologicchanges)andareatriskforoccult shock.
G8Assesswhetheranelderisabletogivean accuratehistory,participateindeterminingtheplan ofcare,andunderstanddischargeinstructions.
DX7Identifyobscure,occult,orrarepatientconditionsA
DS1PrioritizeessentialtestingD
DS2Determinenecessityandurgencyofdiagnostic studies E
CS5Communicateinformationtopatientsandfamilies usingverbal,nonverbal,written,andtechnological skills,andconfirmunderstanding
CS15Solicitpatientparticipationinmedicaldecisionmakingbydiscussing,risks,benefits,and alternativestocareprovided
HP2Prioritizeessentialcomponentsofahistoryand physicalexaminationgivenlimited(eg,altered mentalstatus)ordynamic(eg,acutecoronary syndrome)situations
TC13Ensurepatienthasresourcesandtoolstocomply withdischargeplan,whichmayincludemodifying theplanorinvolvingadditionalresources(ie,PCP, socialwork, financialaid)tooptimizecompliance B (Continuedonnextpage)
Continued.
G9Assessanddocumentcurrentmentalstatusand anychangefrombaselineineveryelder,with specialattentiontodeterminingwhetherdelirium existsorhasbeensuperimposedondementia.
G10Emergentlyevaluateandformulateanage-specific differentialdiagnosisforelderswithnewcognitive orbehavioralimpairment,includingself-neglect; initiateadiagnosticworkuptodeterminethe etiology;andinitiatetreatment.
G12Recommendtherapybasedontheactualbenefitto riskratio,includingbutnotlimitedtoacute myocardialinfarction,stroke,andsepsis,sothat agealonedoesnotexcludeeldersfromany therapy.
TC17Explainclearlyandensurepatientunderstandingof diagnosis,dischargeinstructions,andthe importanceoffollow-upandcompliancewith treatments.
HP6Identifyrelevanthistoricalandphysical findingsto guidediagnosisandmanagementofapatient’s presentingcomplaintinthecontextoftheirbaseline condition
DX1Synthesizechiefcomplaint,history,physical examination,andavailablemedicalinformationto developadifferentialdiagnosis
HP2Prioritizeessentialcomponentsofahistoryand physicalexaminationgivenlimited(eg,altered mentalstatus)ordynamic(eg,acutecoronary syndrome)situations
CS14Communicaterisks,benefits,andalternativesto diagnosticandtherapeuticprocedures/interventions topatientsand/orappropriatesurrogates,and obtainconsentwhenindicated
DS4Reviewrisks,benefits,contraindications,and alternativestoadiagnosticstudyorprocedure
TI8Assessindications,risks,benefits,andalternatives forthetherapeuticintervention.
G13Identifyandimplementmeasuresthatprotect eldersfromdevelopingiatrogeniccomplications commontotheEDincludinginvasivebladder catheterization,spinalimmobilization,andcentral lineplacement.
DS4Reviewrisks,benefits,contraindications,and alternativestoadiagnosticstudyorprocedure
PR2Performtheindicatedprocedureonan uncooperativepatient,patientattheextremesof age(pediatric,geriatric),multiplecomorbidities, poorlydefinedanatomy,hemodynamically unstable,highriskforpainorprocedural complications,sedationrequired,oremergent indicationtoperformprocedure,andrecognizethe outcomeand/orcomplicationsresultingfromthe procedure
PR7Recognizetheindications,contraindications, alternatives,andpotentialcomplicationsfora procedure
TI8Assessindications,risks,benefits,andalternatives forthetherapeuticintervention.
G14Prescribeappropriatedrugsanddosages consideringthecurrentmedication,acuteand chronicdiagnoses,functionalstatus,and knowledgeofage-relatedphysiologicchanges (renalfunction,centralnervoussystemsensitivity).
PT2Identifyrelativeandabsolutecontraindicationsto specificpharmacotherapy
PT5Recognize,monitor,andtreatadverseeffectsof pharmacotherapy
PT6Selectandprescribeappropriatepharmaceutical agentsbasedonintendede ectandpatient allergies
(Continuedonnextpage)
Table3. Continued. Geriatric
G15Searchforinteractionsanddocumentreasonsfor usewhenprescribingdrugsthatpresenthighrisk eitheraloneorindrug-drugordrug-disease interactions(eg,benzodiazepines,digoxin,insulin, NSAIDs,opioids,andwarfarin).
PT9Select,prescribe,andbeawareofadverseeffects ofappropriatepharmaceuticalagentsbasedupon relevantconsiderationssuchasintendedeffect, financialconsiderations,possibleadverseeffects, patientpreferences,institutionalpolicies,and clinicalguidelines.
PT2Identifyrelativeandabsolutecontraindicationsto specificpharmacotherapy
PT5Recognize,monitor,andtreatadverseeffectsof pharmacotherapy
PT9Select,prescribe,andbeawareofadverseeffects ofappropriatepharmaceuticalagentsbasedupon relevantconsiderationssuchasintendedeffect, financialconsiderations,possibleadverseeffects, patientpreferences,institutionalpolicies,and clinicalguidelines.
PT10Conductfocusedmedicationreviewandidentify agentsincludingnutraceuticalsandcomplementary medicinesthatmaybecausinganadverseeffect
TI6Developprotocolstoavoidpotentialcomplications ofinterventions
TI8Assessindications,risks,benefits,andalternatives forthetherapeuticintervention.
G16Explainallnewlyprescribeddrugstoeldersand caregiversatdischarge,assuringthatthey understandhowandwhythedrugshouldbetaken, thepossiblesideeffects,andhowandwhenthe drugshouldbestopped.
G17Documenthistoryobtainedfromskillednursingor extendedcarefacilitiesoftheacuteevents necessitatingEDtransferincludinggoalsofvisit, medicalhistory,medications,allergies,cognitive andfunctionalstatus,advancecareplan,and responsiblePCP.
G18Provideskillednursingorextendedcarefacilities and/orPCPwithEDvisitsummaryandplanof care,includingfollow-upwhenappropriate.
CS5Communicateinformationtopatientsandfamilies usingverbal,nonverbal,written,andtechnological skills,andconfirmunderstanding
TC17Explainclearlyandensurepatientunderstandingof diagnosis,dischargeinstructions,andthe importanceoffollow-upandcompliancewith treatments.
CS6Elicitinformationfrompatients,families,andother healthcaremembersusingverbal,nonverbal, written,andtechnologicalskills
CS10Communicatepertinentinformationtohealthcare colleaguesineffectiveandsafetransitionsofcare
CS10Communicatepertinentinformationtohealthcare colleaguesineffectiveandsafetransitionsofcare
TC14Identifypatientswhowillrequiretransfertoa facilitythatprovidesahigherlevelofcareand coordinatethistransitionofcarebyensuring communicationwiththereceivingprovider, completionoftransferdocumentation,educationof thepatientorsurrogatethereasonsfortransfer, consentfortransfer,andarrangementof appropriatetransportation.
TC16Useappropriatetoolsfortransitionsofcare, dischargeinstructions,prescriptions,follow-up instructions,andanypendingdiagnosticstudiesto promoteeffectivecareanddecreaseerror
(Continuedonnextpage)
Table3. Continued.
Geriatric competencyDescription
G19Withrecognitionofuniquevulnerabilitiesinelders, assessanddocumentsuitabilityfordischarge consideringtheEDdiagnosis,includingcognitive function,theabilityinambulatorypatientsto ambulatesafely,availabilityofappropriatenutrition/ socialsupport,andtheavailabilityofaccessto appropriatefollow-uptherapies.
G20Selectanddocumenttherationaleforthemost appropriateavailabledisposition(home,extended carefacility,hospital)withtheleastriskofthemany complicationscommonlyoccurringineldersduring inpatienthospitalizations.
OB9Reassess,manage,andprognosticatethecourse ofpatientsinEDobservationstatustodetermine appropriatedisposition.
TC13Ensurepatienthasresourcesandtoolstocomply withdischargeplan,whichmayincludemodifying theplanorinvolvingadditionalresources(ie,PCP, socialwork, financialaid)tooptimizecompliance
TC18CorrectlydeterminetheappropriatedispositionC
CS10Communicatepertinentinformationtohealthcare colleaguesineffectiveandsafetransitionsofcare
OB1IdentifypatientsappropriateformanagementinED observationstatus
OB9Reassess,manage,andprognosticatethecourse ofpatientsinEDobservationstatustodetermine appropriatedisposition.
TC12Assignadmittedpatientstoanappropriatelevelof care
TC14Identifypatientswhowillrequiretransfertoa facilitythatprovidesahigherlevelofcareand coordinatethistransitionofcarebyensuring communicationwiththereceivingclinician, completionoftransferdocumentation,educationof thepatientorsurrogatethereasonsfortransfer, consentfortransfer,andarrangementof appropriatetransportation.
TC18CorrectlydeterminetheappropriatedispositionC
G21Rapidlyestablishanddocumentanelder’sgoalsof careforthosewithaseriousorlife-threatening conditionandmanageaccordingly.
G22AssessandprovideEDmanagementforpainand keynon-painsymptomsbasedonthepatient’s goalsofcare.
G25Developplansofcarethatanticipateandmonitor forpredictablecomplicationsinthepatient’s condition(eg,gastrointestinalbleedcausing ischemia).
G26Communicatewithpatientswithhearing/sight impairment
CS3Elicitpatients’ reasonsforseekinghealthcareand theirexpectationsfromtheEDvisit
ES15Elicitthepatient’sgoalsofcarepriortoinitiating emergencystabilization,includingevaluatingthe validityofadvanceddirectives
DS4Reviewrisks,benefits,contraindications,and alternativestoadiagnosticstudyorprocedure
TI6Developprotocolstoavoidpotentialcomplications ofinterventions
CS5Communicateinformationtopatientsandfamilies usingverbal,nonverbal,written,andtechnological skills,andconfirmunderstanding
CS7Considertheexpectationsofthosewhoprovideor receivecareintheEDandusecommunication methodsthatminimizethepotentialforstress, conflict,andmiscommunication
CS18Demonstrateinterpersonalandcommunication skillsincludingadjustmentofinteractionsto accountforfactorssuchasculture,gender,age, language,disability,thatresultintheeffective exchangeofinformationandcollaborationwith patients,families,andallotherstakeholders.
,knowledge,skills,abilities; ED,emergencydepartment; NSAID,non-steroidalanti-inflammatorydrug; PCP,primarycarephysician.
definecurricularoverlap.Whilewewerestrengthenedby havingrepresentationfrommultipleEMresidencyprograms, othereducationexpertsmayhaveadifferentinterpretationof thedomainsandcompetenciesandhowtheyaretypically taught.Additionally,thereviewerswerenotallattendingsand notallgeriatric-fellowshiptrained.Despitethis, first-round consensuswasveryhigh(84-96%),whichsuggestsshared knowledgeamongthegroup.TheEMresidentsinvolvedin thisprojecthavesincestartedfellowshipsinmedicaleducation andpalliativemedicine,demonstratingtheirpassionand additionalunderstandingintheseareas.
ThegeriatriccompetenciesareincludedwithintheEM Modelandknowledge,skills,abilitieslist.Thecompetencies providemoredetailforeducationorboardquestions. Weidentifiedareasofoverlapwherethesesubspecialty competenciescanbeemphasizedinEMresidencycurriculums.
TheauthorsthankDr.MelissaBarton,ABEMDirector ofMedicalAffairs,forheradviceindesigningthisstudy. WealsothankallthemembersoftheSocietyofAcademic EmergencyMedicine’sAcademyofGeriatric EmergencyMedicine.
AddressforCorrespondence:LaurenT.Southerland,MD,MPH,The OhioStateUniversityWexnerMedicalCenter,Departmentof EmergencyMedicine,725PriorHall,376W10thAve,Columbus, OH43210.Email: Lauren.Southerland@osumc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. DianeL.GorgasisaboardmemberoftheAmericanBoardof EmergencyMedicine.LaurenT.Southerlandhascontributedto someofthefreeeducationalwebsitesmentionedinthediscussion.
Copyright:©2024Southerlandetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KizziahMA,MillerKN,BischofJJ,etal.Emergencymedicineresident clinicalexperiencevs.in-trainingexaminationcontent:anational databasestudy. AEMEducTrain. 2022;6(2):e10729.
2.AshmanJJ,SchappertSM,SantoL.Emergencydepartmentvisits amongadultsaged60andover:UnitedStates,2014–2017. NCHSData Brief,no367.Hyattsville,MD:NationalCenterforHealthStatistics. 2020.
3.AmericanBoardofEmergencyMedicine.The2019ModeloftheClinical PracticeofEmergencyMedicine.Availableat: https://www.abem.org/ public/resources/em-model.AccessedSeptember9,2020.
4.AmericanBoardofEmergencyMedicine.2022Knowledge,Skills,& Abilities.Availableat: https://www.abem.org/public/resources/ emergency-medicine-milestones-ksas.AccessedAugust9,2022.
5.HoganTM,LosmanED,CarpenterCR,etal.Developmentofgeriatric competenciesforemergencymedicineresidentsusinganexpert consensusprocess. AcadEmergMed. 2010;17(3):316–24.
6.ACEPGeriatricEmergencyDepartmentAccreditationCriteria.Version July11,2023.Availableat: https://www.acep.org/siteassets/sites/geda/ documnets/ged-criteria.pdf.AccessedFebruary21,2023.
7.MagidsonPDandCarpenterCR.Trendsingeriatricemergency medicine. EmergMedClinNorthAm.2021;39(2):243–55.
8.RingerT,DoughertyM,McQuownC,etal.Whitepaper–geriatric emergencymedicineeducation:currentstate,challenges,and recommendationstoenhancetheemergencycareofolderadults. AEMEducTrain. 2018;2(Suppl1):S5–16.
9.HoganTM,HansotiB,ChanSB.Assessingknowledgebaseongeriatric competenciesforemergencymedicineresidents. WestJEmergMed 2014;15(4):409–13.
10.HesselinkG,SirÖ,ÖztürkE,etal.Effectsofageriatriceducation programforemergencyphysicians:amixed-methodsstudy. Health EducRes. 2020;35(3):216–27.
11.BieseKJ,RobertsE,LaMantiaM,etal.Effectofageriatriccurriculumon emergencymedicineresidentattitudes,knowledge,anddecisionmaking. AcadEmergMed.2011;18Suppl2:S92–6.
12.ThatphetP,RosenT,KayarianF,etal.Impactofgeriatricemergency fellowshiptrainingonthecareersofemergencyphysicians. Cureus. 2021;13(9):e17903.
BennettH.Lane,MD*† °
SimanjitK.Mand,MD* ° StewartWright,MD,MEd* SallySanten,MD,PhD* BrittanyPunches,PhD‡
*UniversityofCincinnatiCollegeofMedicine,DepartmentofEmergencyMedicine, Cincinnati,Ohio
† UniversityofCincinnatiHealthAirCare&MobileCare,Cincinnati,Ohio ‡ OhioStateUniversity,CollegesofNursingandMedicine,DepartmentofEmergency Medicine,Columbus,Ohio
° BennettH.LaneandSimanjitK.Mandcontributedequallytothiswork
SectionEditors: SaraKrzyzaniak,MD,andJeffreyLove,MD
Submissionhistory:SubmittedDecember13,2022;RevisionreceivedOctober3,2023;AcceptedNovember3,2023
ElectronicallypublishedDecember8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.59622
Introduction: Considerationofthecostofcareandvalueinhealthcareisnowarecognizedelementof physiciantraining.Despitetheurgencytoeducatetraineesinhigh-valuecare(HVC),educational curriculaandevaluationofthesetrainingpathsremainlimited,especiallywithrespecttoemergency medicine(EM)residents.Weaimedtocompleteaneedsassessmentandevaluatecurricular preferencesforinstructiononHVCamongEMresidents.
Methods: Thiswasaqualitative,exploratorystudyusingcontentanalysisoftwofocusgroupsincluding atotalofeightEMresidentsfromasingleMidwesternEMresidencytrainingprogram.Participantsalso completedasurveyquestionnaire.
Results: Thereweretwothemes.Withintheoverallthemeofresidentexperiencewithandperceptionof HVC,wefound fivesub-themes:1)understandingofHVCfocusesondiagnosisanddecision-making; 2)concernaboutpatientcosts,includingtheeffectsonpatients’ livesandtheirabilitytoengagewith recommendedoutpatientcare;3)conflictbetweeninternalbeliefsandexternalexpectations,including patients’ perceptionsofvalue;4)approachtoHVCchangeswithincreasingclinicalexperience;and 5)slow-moving,politicaldiscussionaroundHVC.Withintheoverallthemeofdesirededucationand curriculardesign,weidentifiedfoursub-themes:1)limitedprioreducationonHVCandhealth economics;2)motivationtoreceivetrainingonHVCandhealtheconomics;3)desirefordiscussionbasedformatforHVCcurriculum;and4)curriculumtargetedtoleveloftraining.Respondentsindicated greatestacceptabilityofinteractive,discussion-basedformats.
Discussion: WeconductedatargetedneedsassessmentforHVCamongEMresidents.Weidentified broadinterestinthetopicandlimitedself-reportedbaselineknowledge.Curricularcontentmaybenefit fromincorporatingresidentconcernsaboutpatientcostsandconflictbetweenexternalexpectationsand internalbeliefsaboutHVC.Curriculardesignmaybenefitfromafocusoninteractive,discussion-based modalitiesandtailoringtothelearner’sleveloftraining.[WestJEmergMed.2024;25(4.1)51–58.]
Arecentshifttofocuson “value” inhealthcare,often definedashealthoutcomesachievedperdollarspent,has emergedinresponsetopersistentlyrisingcostsoverdecades.1 Recenteventshavehighlightedthecostofemergencycarein thenationalspotlight,includingfederallegislationon surprisebilling,insurerdenialsofclaimsforemergency department(ED)visitswithouta finalemergentdiagnosis, andregulationsonpaymentsforairambulance transports.2–5 Consistentwiththesedevelopments,current
AccreditationCouncilforGraduateMedicalEducation (ACGME)guidelinesstatethat “residentsmustdemonstrate competencein ::: incorporatingconsiderationsofvalue, equity,costawareness,deliveryandpayment,andriskbenefitanalysisinpatientand/orpopulation-basedcare asappropriate.”6
DespitethecurrentACGMEguidelinesandincreasing demandsforhigh-valuecare(HVC),theappropriate educationalcontentandinstructionalmethodshavenotbeen clearlyestablished.Moriatesandcolleaguesdelineated21 HVCcompetencieswithbeginning,proficient,andexpert levelsthroughaniterativeprocessledbyamultidisciplinary committee.7 Whilerigorousandexpert-led,thisapproachdid notincludearesident-focusedneedsassessment,and subsequentneedsevaluationshavebeenlimitedtosurveysof internalmedicineorpediatricsresidentsatasinglesite.8–10 Similarly,evaluationofproposedinternalmedicineor pediatricsresidentcurriculahavebeenlimitedtosingle-site pre-/post-surveys,withonestudyalsoincludingpostimplementationfocusgroups.10–13
Withinemergencymedicine(EM),HVCandhealth economicseducationalresourcesarelimited,asa2010 systematicreviewofcost-effectivenesscurriculaidentified onlyasingleEMcurriculumfocusedontheOttawaankle rules.Sincethatreview,twoadditionalcontributionsthatwe areawareofinclude1)theEmergencyMedicineResidents’ Association Residents ’ AdvocacyHandbook addressing policy-relatedtopicsinatextbook-likeformatand2)acostconsciouscarecurriculumdevelopedbyLinandLaskowski atasinglesiteinNewYork(personalcommunication,L. Laskowski).14,15 Thereisapaucityofformal,residentfocusedneedsassessmentsacrossspecialties,particularly inEM.Ourobjectivewastoperformatargetedneeds assessmenttoassessEMresidents’ needsandinterests inHVCandpreferencesforinstructionalmodality.
StudyDesign
Aspartofacurriculumdevelopmentprocess,we performedaproblemidentificationandtargetedneeds assessmentforEMresidents,correspondingtoKern’ssixstepapproachtocurriculardevelopment.16 Toachieveour objective,weconductedaqualitative,exploratorystudy usingconventionalcontentanalysis.Thismethodallowedus tocriticallyexaminetheparticipantresponsestoidentify commoncategoriesandelucidatethemes.Oursecondary objectivetodeterminepreferencesforinstructionalmodality includedacollectionofrespondents’ self-assessmentsusinga surveyquestionnaire.Weobtainedinstitutionalreview board(IRB)approvalforallstudyprocedures.
ThesettingwasasingleMidwesternUnitedStatesEM residencyprogramwith56totalresidents.Twophysician
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Residenteducationguidelinesnow incorporatethetopicofvalueinhealthcare, butfewresident-focusedneedsassessments forthisconceptareavailable.
Whatwastheresearchquestion?
Forhigh-valuecare,whatareemergency medicineresidents ’ needs,interests,and preferencesforinstructionalmodality?
Whatwasthemajor findingofthestudy?
Residentsself-reportlowknowledgebutare interestedineducationonhigh-valuecare. Theypreferdiscussion-basedmodalities.
Howdoesthisimprovepopulationhealth?
Addressingcostofcarethroughgraduate medicaleducationmayhelpaddress accessibilityandaffordabilityofcare.
authorswereresidentsatthetimeofthedatacollection phaseoftheproject(BHL,SKM).Recruitmentofa conveniencesampleofeightEMresidentswasperformedvia emailbyoneoftheauthors(SKM)totheremaining54 residents.Nineresidentsresponded.(Oneresidentcouldnot participateduetoschedulingconstraints.)Noparticipant terminatedtheirparticipationduringthefocusgroup.
Weobtaineddocumentationofinformedconsentpriorto studyprocedures.Asemi-structuredinterviewguidefor focusgroupswasprimarilyauthoredbyasingleauthor (BHL)andreviewedsequentiallybyadditionalauthorsfor revisionofcontentandphrasing(SKM,BP).Theinterview guideisincludedas Appendix1.Focusgroupswereco-ledby twophysicianauthorswhowereresidentsatthetime(BHL, SKM)followingtheinterviewguide.Bothfocusgroupswere audiorecordedandsubsequentlytranscribed.No fieldnotes weremade,norweretranscriptsreturnedtoparticipantsfor comment.ThefocusgroupsoccurredduringSeptember2020 inamedicalschoolconferenceroomwithnootherperson presentasidefromfocusgroupleadersandparticipants. Afterthefocusgroupdiscussionwascomplete,participants independentlycompletedasurveyquestionnaireusingLikert scaleandrankorderquestionsonpaper(Appendix2).Each focusgroupincludedfourparticipantswithatleastone intern(postgraduateyear[PGY]1)ineachgroup.Intotal,
the firstgroupincludedonePGY-1,onePGY-2,andtwo PGY-3residents;thesecondfocusgroupincludedtwoPGY1andtwoPGY-4residents.Eachfocusgrouplastedbetween 75–85minutes.Norepeatinterviewswerecompleted. Participantsreceiveda$15giftcardforcompensation, consistentwithIRBguidelines.
Thetranscriptswerereviewedandconventionalcontent analysiswithline-by-linecodingwascompletedbytwo independentcoders(BHL,SKM).Usinganopencoding technique,importantstatementswereidentified(generally termed “the firstcut”).17 Codesweredevelopedinvivoand didnotreferencepreviousliterature.(Theyaredepictedina codingtreein Appendix3.)Significantredundancyincodes wasidentified,whichwasfelttobeconsistentwiththematic saturation.18 Theanalysisteamcametogetherwithathird reviewer(BP)tocategorize,refine,andclusterimportant statements,andsubsequentthemesanddomainsemerged. Weusedtheconsolidatedcriteriaforreportingqualitative research(COREQ)asreportingguidelines(Appendix5).19
DescriptivestatisticswereperformedinMicrosoftExcel forquestionnairedata,andweusedWord(Microsoft, Redmond,WA)fortranscriptsandcodingdocumentation. Theuseofindependentcodersandateamofthree tocategorizeanddevelopthemesenhancedcredibility, andinvestigatortriangulationaidedconfirmabilityof theresults.18
Reflexivityoftheresearchteamincludedrecognitionthat thefocusgroupleadersandcoderswereknowntothe participantsandidentifiedtheirrespectivespecificinterestsin HVC/healtheconomics(BHL)andmedicaleducation (SKM)totheparticipantsaspartoftheintroduction.The focusgroupleadersidentifiedasmale(BHL)andfemale (SKM).BHLandSKMwereresidentsatthetimeofthe study.BPprovidedtrainingtoBHLandSKMregarding techniquesinsemi-structured,focusgroupfacilitation;BHL hadlimitedpriorexperiencewithfocusgroupfacilitation.A methodologicallimitationisthatthesameresidents comprisedthefocusgroupsandcompletedsurvey questionnaires;surveyquestionnaireresultsmayhavebeen influencedbytheprecedingfocusgroupdiscussion,although allquestionnaireswerecompletedindependentlybyall participantswithoutadditionaldiscussion.
Atotalofeightresidentsparticipated.Withrespectto theimportanceofeducationaboutHVCtopics,residents endorsedtherelevanceofHVCtopicstotheresident physician(7/8,[88%])andtheimportanceofaHVC curriculum(8/8,[100%])(Appendix4,Figure2).We identifiedtwooverarchingthemes:1)experiencewithand
perceptionofHVC;and2)desirededucationandcurricular design.Foreachoverarchingtheme,componentsub-themes summarizedclustersofresidentcommentsforwhichwe includerepresentativecommentsand(ifidentified) participantrecommendations.
OverarchingTheme1:ExperiencewithandPerceptionof High-valueCare
Sub-theme1:Understandingofhigh-valuecarefocuseson diagnosisanddecision-making.
ResidentsmostfrequentlyassociatedHVCwiththe activitiesthatfacilitatediagnosisanddecision-makinginthe ED.Forexample,whenaskedwhethertheyhadageneral definitionfororhadheardofthephrase “high-valuecare,” oneresidenthighlightedusingtheEDevaluationto “appropriately fi gureoutwhatisgoingonwiththispatient anddecidewheretosendthem ” (Resident#1,PGY-1).In thisunderstanding,residentsbelievecareactivitiesarehigh valueiftheyallowthecliniciantomakeadiagnosisor disposition.Lesscommonly,otherresidentsmentioned aspectsofHVCsuchasresourceuse,stewardship(citinga specificexampleofacost-savingsinitiativerelatedtotheuse ofcombatgauze[Resident#7,PGY-4]),andtheconceptof cost-benefitanalysis: “clinicaldecisionrulesthat ::: reduce unnecessaryheadCTs,notonlyfromaradiation perspective,butalsofromacost-savingsperspective ” (Resident#8,PGY-4).
Sub-theme2:Concernaboutpatientcosts.
Inthefocusgroupdiscussion,residentsvoiceduncertainty duetovaryingpatientinsurancereimbursementofcare providedintheEDandconcernssurroundinghighpatient costs,inlargepartduetoaself-identifiedlackofknowledge. Becauseofthisknowledgegap,residentsfeltinadequately preparedtohaveconversationssurroundingcostand insurancecoveragewithpatients.Oneoftheparticipants recalledapatientencounterinwhichtheresidentfelt uninformedtoaddressthepatient’sreactionafterthe residentdisclosedthepresenceofanewmassconcerning forcancer:
Howmuchisthisgoingtocostme?HowamIgoingtopay forthis? ’ [and]Ididn ’ tknowtheanswer. It ’ dbenice ifIactuallyhadsomedata ::: likeyou ’ reuninsured,it ’ s ok,becauseit ’ sgoingtobelikethisforthe fi nancialplan, ifyou ’ reinsured,thisiswhathappens.Ihaveno clue. ” (Resident#5,PGY-3)
Otherresidentsstatedthattheywereunawareofthecosts ofcommonlyordereddiagnosticsandtherapeuticsinthe ED.Theydescribedbeingconcernedandunawareofthe financialandsocialramificationsofcareactivitieson patients’ livesoutsideofthehospital,andtheyparticularly worriedabouttheimpactonpatients’ abilitytoengagewith
recommendedoutpatientcare: “It ’ showmuchthepatient getschargedthatwouldactuallymatterfromasocial determinantsofhealthperspective ” (Resident#2,PGY-1).
Residentsparticularlycitedfeelingchallengedby shareddecision-makingdiscussionswhenpatientshad financialconcerns.
Sub-theme3:Conflictbetweeninternalbeliefsandexternal expectations.
Residentsnotedthattheremaybeaconflictbetweena physician’spersonalbeliefsandtheexternalexpectationsand pressurestheyface.Someexternalexpectations,suchas thosefromsystems-level “hurdles” placedintheelectronic healthrecord-orderinginterface,areexplicitlyidentifiable forresidents: “Itrytoorder[intravenousacetaminophen] allthetime.ITtakesyouthrough,youhavetogothroughall thesequestionsbecausethey ’ retryingtokeepmefrom ordering[it]. Iknowthey ’ retryingtokeepmefrom orderingit,butI ’ mgoingtokeeponorderingit ” (Resident #8,PGY-4).Otherexternalexpectationsareperceivedtobe implicitwithinthemedicalcommunity: “ Eventhoughwe talkaboutinanacademicsetting,orinaboardroom,it ’ sOK tohaveamissfromastatisticalperspective,Ithink culturallythat ’ snotacceptable. It ’ sjustnotplayingout intherealworld,inmyopinion,acceptingthatthereisa missrate ” (Resident#4,PGY-2).
Residentsparticularlyhighlightedthatpatientsarea sourceofexternalexpectationsandrecognizedthat patientsmayviewcost,quality,andvalueofcare differentlyfromtheemergencyphysician.Thisdifference inperceptionmayleadtoadisconnectinexpectations: “ Valuecanreallybeintheeyesofthebeholder ::: makes methinkaboutwhatIthinkmightbethebestthingforthe patientmaynotbeatallthesameaswhatthepatientvalues ” (Resident#6,PGY-3).Moreover,thecon fl ictbetween internalbeliefsandexternalexpectationscanovershadow attemptstoprioritizeHVC.Acontextcitedforthiscon fl ict wereEDvisitsofpatientswhocommonlyfrequenttheED. Forthesepatients,thelackofcommunityresourcesfor patientscanbefrustratingandrenderalearnerfeeling helplessorunabletoprovideholisticpatientcare.Forthese patients,traineesnotedfeelingadisconnectbetweenthe caretheyfeltexpectedtoprovideandthecaretheydesired toprovide.
Subtheme4:Approachtohigh-valuecarechangeswith increasingclinicalexperience.
Residentssharedanecdotesthatdemonstratehowthe definitionofandapproachtooptimizeHVCchanges withincreasingclinicalexperience.Onejuniorresident highlighted “wantingtoknow” asmotivationforordering testing: “ I ’ mascuriousas[thepatients]are,tobehonest;so Iwanttoknowthatthispatientisperhapsapresentationof
[aspeci fi cdiagnosis] ” (Resident#4,PGY-2). Similarly,as onenon-internresidentreflected:
“Andhonestly,that’ssomethingthatcomeswithtime – like ifyoutoldmeasaninternIcouldorderamillion-dollartest andgettheanswerthatIneed,Iwould100%doitbecause it’seasy,I’llberight,andIcanhelpthepatient.Butasyou practicemedicineyourealize ::: ifyouhaveamilliondollartesttoanswerifit’sGERD ::: it’snotgoingto changeyourmanagement AsI’mprogressingthrough residencyIgetmoreandmorecurious,andI’ mmore willingtoacceptinformationabout[HVC]” (Resident #5,PGY-3)
Sub-theme5:Slow-moving,politicaldiscussionaroundhighvaluecareinmedicine.
Ingeneral,residentsdescribethemselvesaslooselyaware ofthepolitical,academic, financial,andclinicalimplications ofnationaldiscussionsonHVCtopicsforfutureemergency physicians.Forexample, “Howyoudeterminevalue?I rememberbackwhenObamawasstillaroundandinof fi ce,I rememberthatwasabigdiscussion,youknow whatisreal valueandwhodeterminesthat?That ’ ssortofablackbox ” (Resident#8,PGY-4). Anotherresidentreflected,
“ Thereisalwayschatteroutthereinthe politicaland insuranceworld.AndI ’ mnotsureIknowwherelikethe landmarkpolicyor ::: guidingfoundationisforthat conversation.So,certainly,outsidethereisafeeling thatthereisalwaysthischatterhappening ” (Resident #4,PGY-2).
Whenaskedaboutproposedphysicianreimbursement modelscurrentlyundergoingfederalregulatoryreview,most residentsdidnotknowwhatthosefuturepoliciesentailed.In addition,manyresidentsreportednotbeingwellversedin currentreimbursementmodels,althoughnon-intern residentsreportedmoreinterestincurrent reimbursementinformation.
Sub-theme1:Limitedmedicaleducationonhealth economicsandhigh-valuecare.
Whenaskedabouttheirpriortraininginhealtheconomics andHVCtopics,allresidentsnotedminimaltonoprior exposureduringtheirmedicaltraining.Inthesurvey questionnaire,allparticipants(8/8[100%])eitherstrongly disagreedordisagreedwiththestatement “Ifeelconfident thatIknowthecostofthecarethatIprovidetopatientsin theemergencydepartment” (Appendix4).Muchoftheprior exposuredescribedbyresidentswascomprisedofbriefand infrequentdidactic-baseddiscussionsthatweredescribed
asleadingtolimitedinformationretentionandlimited applicationtoclinicalpractice.
Beyondthis,theyvoicedthebeliefthattherewerefew opportunitiesforknowledgeacquisitionduetolackof availableresources,particularlywithrespecttopricesand costsofhealthcareactivities.Residentswerenotfamiliar withhospital-basedornationallybasedresourcesthatcould assistwithday-to-dayclinicalhealthcarequestionssuchas patientcost: “Ithinkhospitalsaremandatedtohavesome sortoflist,masterlist,ofhowmuchthingscosts,butit ’ salso superhardto fi nd ::: IhavenoideawhereIwould fi ndthat information ” (Resident#7,PGY-4).
Sub-theme2:Motivatedtoreceivetrainingonhigh-value careandhealtheconomics.
TheEMresidentsidentifiedthemselvesasfrontline healthcareworkers.Intheirrole,theyinteractdirectlywith thecommunityandpatientswithdiversebackgrounds, particularlyindividualsfacing financialbarrierstoaccessing care.Becauseofthisuniquepositioninthemedical field, residentsbelievethat financialandinsurancepressures mayunderliepatients’ utilizationoftheEDandthat cliniciansshouldthereforeunderstandthesefactors.One residentreflected
“Ithinkwhenyou look athealthcareasagestalt, peopleareseeingprimarycar e[clinicians]lessandless andrelyingontheEDmoreforprimarycare.And assumingthatthattrendcontinues Ithinkasan emergencyphysicianitisimportanttoknowthose things[healthcareeconomicstopics]becauseofthat reason,justtheutilizationoftheEDingeneral ” (Resident#1,PGY-1).
Oneresidentalsonotedthatthelackofhealtheconomics knowledgecanputemergencyphysiciansatadisadvantage ininfluencingandleadingsystems-basedpractice:
“ Ithinknotunderstanding[HVCandhealtheconomics topics]takesawayalotofourpowertobealeaderand makesusmorepawnscarryingoutsomeoneelse ’ svision ofhowmedicineshouldbepracticed ” (Resident#6, PGY-3).
Residentsrecognizedtheimportanceofandneedfor furthertrainingonHVCtopicstounderstandtheimpact thattheirdecision-makinghasonpatientsandthe healthcaresystem.
Sub-theme3:Desirefordiscussion-basedformatforhighvaluecarecurriculum.
ResidentswereaskedwhattheoptimalformatforHVC curriculumwouldbeforresidency-levellearners,andthe majoritywereinsupportofadiscussion-basedformat.
“ Iliketheideaofthecase-based,small-groupdiscussion. Especiallywhenyouhaveattendingsthere,andyouhave variedlearnerlevels,andIkindoflikethatbecauseyou getvariedsortsofinputsandthat ’ sinteresting.AndIjust feellikethissortofstuff,thesesortsoftopics,arebest,for me,exploredverbally ” (Resident#8,PGY-4).
Oneresidentnotedthatbecausethisisnotcommon knowledgeamongemergencyclinicians,involvingacontent expertwouldbecriticaltoasuccessfulcurriculum:
“Anotherpartofincorporatingthis,iswhoisthecontent expert ::: .[HVCcareis]atopicthat ::: atypical academic[emergency]physicianwould[not]knowabout. Italmostneedstobeacollaboration [someone]with healtheconomicinterestandknowledgeandsomeonewith aneducationbackground,too,to figureouthowto incorporatethis” (Resident#7,PGY-4).
Consistentwiththisqualitativetheme,thehighest percentageofresidentsrankedmodalitieswiththe opportunityforinteractivesmall-groupdiscussionhighly, whetherasonlineappsorinperson,onthesurvey questionnaire(Figure 1).
Sub-theme4:Curriculumtargetedtotheirleveloftraining. Whilemostoftheresidentsrecognizedtheneedfora formalHVCcurriculumduringmedicaltraining,therewas variationinwhentheythoughtthiscurriculumshouldbe introducedattheresidency-traininglevel.ThePGY-1and PGY-2residentsvoiceddesiretofocusonclinicalknowledge acquisitioninlieuofhealtheconomicstopics:
“Asanintern,I’dratherbemoretowardstheclinicalaspect ofthingsrightnow ::: Idon’tthinkI’vedevelopedthatskill enoughtowanttosacrificeoneofthosejournalclubsfor healtheconomics.Ithinkasalaterresident,I’dbeon board ::: ” (Resident#1,PGY-1).
“ MyinitialthoughtwasthatIwouldwantsomething clinicallyrelevantbecaus eIfeellike[Iam]earlierin trainingandjusttryingtobuildthatfoundation ” (Resident#4,PGY-2).
Anon-internresidentnoted “ IfeellikeasI ’ mprogressing throughresidency,IgetmoreandmorecuriousandI ’ m morewillingtoacceptinformationaboutthatstuff[HVC] ” (Resident#5,PGY-3).Inreplytoaninternindicatingthe topicof “[relativevalueunits] andphysician-associated income ::: wouldn ’ tappealorapplytomerightnowwhenI wouldjustforgetit ” (Resident#3,PGY1),Resident#7 (aPGY-4)reflectedthatnon-internresidentswouldbe interestedduetopersonaldecision-making: “ Iwouldsaythe PGY-3sbecausesomeofthePGYswouldstartsigning contractsinthesummer ”

Percentageofrespondentsrankingeachinstructionalmodalityamongtoptwochoicesandmeanrankingwithineightmodality options(n = 8).
Aninterestingperspectiveraisedbyoneofthenon-intern residentswasthepotentialtonegativelyinfluencejunior learners’ practicepatternsiftopicsofHVCwereintroduced tooearlyinmedicaltraining:
“ Iwonderfromaneducationmissionside,couldyou in fl uenceearlytrainees ’ ::: practicepatternsbecauseof knowledgeofthis.AndIdon ’ twantthattohappen youneedtoseewhereyoufallinthatspectrumto developyourpracticepattern.AndIwonderifyou fi nd outthatatestcoststhisamountofmoney,maybeyou won ’ tgettofullyexplorethatspectrumanddevelop yourownpointonthatspectrum ” (Resident#7,PGY-4).
Lastly,acoupleofresidentsvoicedconcernaboutthe integrationofanovelcurriculuminanEMtrainingprogram giventhatEM’sscopeofpracticealreadyaddressesmany adjacentdisciplines:
“We’reallkindofinagreementthatabaselinelevelof understandingyoushouldhave butasfarasabout dataandliterature ::: I’dkindofreservethatforpeople thathaveaninterestinit,similartohowwedowithother things,likesportsmedicine” (Resident#3,PGY-1).
“ Youhavesomanythingstolearn.Notonlyclinically, butalsoournon-clinicalcurriculum ::: ispretty impressive,soit ’ stough[to]addawholeother curriculum ” (Resident#8,PGY-4).
ResidentsrecognizedtheimportanceoflearningHVC principlesforapplicationinbothpatientcareandtoinform systems-basedpractice;however,theyfeltinadequately trainedonthetopic.Ourneedsassessmentidentifiedtwo
mainthemestoinformEM-specificcurriculaaddressing HVCtopics:residentexperiencewithandperceptionof HVC,anddesirededucationandcurriculardesign.
Consistentwithstudiesinotherdisciplinesandsettings, theresidentsreportedlimitedconfidenceintheirknowledge ofbasicHVCprinciples,andthe financialimpactsofcostof careforindividualpatientsandthehealthcaresystemasa whole.9,10,13 Sub-themes1(understandingofHVCfocuses ondiagnosisanddecision-making)and2(residentconcerns aboutpatientcosts)inthisstudywereconsistentwiththemes fromfocusgroupscompletedwithgeneralpediatrics residentsattwocentersof “howaninterventionchanges management” and “thinkingaboutthecostasaharm.”10
Residentsstatedthatearlyonintheirtraining,HVC knowledgegapsarerelatedtopatientcosts,patientinsurance reimbursement,cost-benefitanalysis,andresource stewardship.Later,self-identifiedknowledgegapsemerging asnon-internlearnerswereprimarilyrelatedtophysician reimbursement.Areviewoftheliterature,includingprior workwithinpediatricsandinternalmedicine,suggestedno priorevidenceofresidentknowledgeorinterestvaryingby experiencelevel;ifvalidatedinadditionalsettings,such variationswithlearnerexperiencewouldprovidevaluable guidanceinthedesignofeducationalcurricula.
Theresidentparticipantsstatedtheirlackofformal traininginandbasicknowledgeofHVCwasabarrierto providinghigh-valueemergencycare.Theyalsoreported limitedawarenessofnationalhealthpolicyyetwereless interestedinadetailedunderstandingofthesetopics.This findingsuggeststhataspecializedelectivemaybebetter suitedtoeducationregardinghealthpolicytopicsthatdonot directlytieintoday-to-dayemergencycare,asintheexample describedbyGreysenandcolleagues.21 Finally,the participantsalsoindicatedtheneedformoreeducationon system-widereimbursementandHVCpolicies.Tomeetthis
need,priornational-levelsurveydatafrominternalmedicine residentsandprogramdirectorssuggeststhatinstitutional supportforbothHVCfacultydevelopmentandprovisionof physiciancost-of-careperformancedataareassociatedwith anincreaseinresidentreportsofeducationonHVC.22
UnanticipatedaspectsofHVCthatwereviewedaslearner obstaclesincludeddynamicconflictsbetweeninternallearner beliefsandexternalexpectationsandthevariabilityinvalue perceptionbetweenpatientsandclinicians.Theseissuesmay complicateresidents’ perceptionofandimplementationof HVCintheclinicalsetting;addressingtheseissueswithin HVCeducationiscriticaltoavoidunintentionalcreationof anxiety,orevenmoraldistress,inthetrainingenvironment. Inanintern-targetedcurriculumininternalmedicine,Hom andcolleaguesalsodiscussedresident-perceivedbarriers surroundingintra-team,interdisciplinary,andpatientand familydynamicsandhowtheycomplicateunderstanding andimplementationofHVCprinciplesatanearlylearner stage.14 Thus,futurecurriculawillneedtofocusbothon foundationalknowledgedisseminationandtechniqueson howtoapproachtheabovebarriers.
Anadditionalunexpectedbarrierraisedbyresidentsinthe focusgroupwastheconcernthattheexistingEMtraining curriculumdoesnothavethecapacitytoincorporateHVC; and,therefore,HVCtrainingmaynot fitasacoreelement. Whilenotaddressedinthesefocusgroups,afuturedirection forworkinthisareashouldincludeevaluationofhow residentswouldweighHVCtrainingcomparedtoother curricularelementsandwhethertherewouldbeopportunity tomakepotential “tradeoffs.”
Intermsofcurriculardesignandformat,themesemerged tooptimizenotonlyknowledgeacquisitionand understanding,butalsotimingduringtheresidencytraining program.Theresidentparticipantswereinsupportofan expert-led,discussion-basedcurriculumtolearnthe principlesofHVC,consistentwiththeexperiencesofHom andcolleagues.13 These findingsalsocoincidewiththoseof Stammenetalintheirsystematicreview,concludingthat reflectivepracticethroughfeedbackandgroupdiscussions incentivizephysicianstothinkcriticallyaboutmedical decisions.19TheresidentsalsosuggestedthatHVCtopics shouldbetargetedmoretowardnon-internresidentswho havemasteredproficiencyinbasicclinicalknowledgeand skillsandwouldbeabletoapplythesenewprincipleswith morepurposethantheirjuniorcounterparts,althoughsome earlierknowledgebasetosupplementformativeexperiential growththroughoutresidencymaybebeneficial.Theydid voiceconcernthattheintroductionofHVCtooearlyin residencycouldjeopardizeearlylearners’ practice patterndevelopment.
Thereareseverallimitationstoconsiderwithregardtoour study.First,thisstudyreflectsasampleofresidentsfroma
single-center,largeacademichospitalandmaynotbe applicabletoallacademic-andcommunity-basedtraining programs.Becauseitwasasingle-centerstudy,wecouldnot distinguishhowthree-yearprogramsorfour-yearprograms withdifferentapproachestoresidentprogressionor “seniority” woulddifferfromthe findingsidentifiedhere. Second,onlyasmallsubsetofprogramresidentsparticipated ineitherfocusgroup,leadingtothepossibilityofselection biaswithregardtotheparticipantswhovolunteeredto discusstheirthoughtsonHVC.Theseresidentsmayhave hadaparticularinterestinmedicaleducationorHVCthat maynotbeapplicabletoallEMresidentsacrossthecountry. Thesmallsubsetofparticipatingresidentsalsolikelylimited thenumberofavailableperspectivestobecollectedand informthematicsaturation.
Third,thestudyincludedamixofjuniorandsenior residents.Whilethestudyallowedforarichspectrumof experiencetoinformprevious exposuretoHVCprinciples, itmaynothavebeenasimpactfulasevaluatingthe perspectivesofthemostexperiencedresidentsina programwhohadnearlycompletedtheentireprogram curriculumandcouldidentifyareasfornuanced improvement.Fourth,whiletheuseoffocusgroups (ratherthanone-on-oneinterviews)allowedemergent discussionbetweenparticipa nts,thepresenceofpeersmay haveledsomeparticipantsto avoidmakingstatementsdue tofearofbeingperceivedascontroversial.Fifth,dueto transitionsinroles,membercheckingcouldnotbe performed.Whileourstudyaddsacriticallynecessary needsassessmenttothecurrentbodyofliterature,further andmorerigorousstudiesthatincludealargernumberof residencyprogramsandpartic ipatingresidentsareneeded toverifythese fi ndingstoaccuratelyinformfuture EMcurricula.
Ourtargetedneedsassessmentindicatesthatresidents currentlyfacegapsinknowledgeofhigh-valuecare topicspertainingtothemedicalcarethattheyprovideand maybenefitfromadditionaltrainingduringresidency. Residentsinterviewedinthisstudyidentifiedseveral perceivedbarrierstounderstandingHVC,butthey consistentlyexpressedinterestinaformalcurriculumto addressthesechallenges.Wefoundapreferencefor interactive,small-groupdiscussion-basedformats withcontentadjustedbylevelofclinicaltraining.
AddressforCorrespondence:BennettH.Lane,MD,MS,University ofCincinnatiCollegeofMedicine,DepartmentofEmergency Medicine,231AlbertSabinWayML0769,Cincinnati,OH452670769.Email: lanebt@ucmail.uc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsourcesand financialormanagementrelationshipsthatcouldbeperceivedas potentialsourcesofbias.Thisworkwassupportedbyinternal departmentalfundingfromadesignatedResidentResearchFund.No authorreportsanyrelatedconflictsofinterest.BennettH.Lanereports receivingresearchgrantsupportfromtheSocietyforAcademic EmergencyMedicineFoundationforinvestigator-initiatedworkon interhospitaltransfersbyair.BennettH.Lanealsoreportsanequity interestandconsultingfeesfromTriAxiaHealthforunrelatedwork.
Copyright:©2024Laneetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PorterME.Whatisvalueinhealthcare? NEnglJMed 2010;363(26):2477–81.
2.KliffSandSanger-KatzM.Forsurprisemedicalbills,it’sthebeginningof theend. TheNewYorkTimes.PublishedJuly1,2021.Availableat: https://www.nytimes.com/2021/07/01/upshot/surprise-medicalbills-biden.html.AccessedJuly19,2021.
3.ChouSC,GondiS,BakerO,etal.Analysisofacommercial insurancepolicytodenycoverageforemergencydepartment visitswithnonemergentdiagnoses. JAMANetwOpen 2018;1(6):e183731.
4.KellyM.Sky-highairambulanceprices. AnnEmergMed 2020;76(5):A17–A20.
5.MoleBeth.BiggesthealthinsurerplanstodenyERbillsifitdoubtsyou hadanemergency. ArsTechnica.PublishedJune10,2021.Availableat: https://arstechnica.com/science/2021/06/biggest-health-insurerplans-to-deny-er-bills-if-it-doubts-you-had-an-emergency/ AccessedJuly19,2021.
6.AccreditationCouncilforGraduateMedicalEducation.ACGME CommonProgramRequirements(Residency).PublishedonlineJuly1, 2023.Availableat: https://www.acgme.org/globalassets/pfassets/ programrequirements/cprresidency_2023.pdf AccessedOctober2,2023.
7.MoriatesC,DohanD,SpetzJ,etal.Definingcompetenciesfor educationinhealthcarevalue:recommendationsfromtheUniversityof California,SanFranciscoCenterforHealthcareValueTrainingInitiative. AcadMed.2015;90(4):421–4.
8.KohlwesRJandChouCL.Acurriculuminmedicaleconomicsfor residents. AcadMed.2002;77(5):465–6.
9.DineCJ,MillerJ,FuldA,etal.Educatingphysicians-in-trainingabout resourceutilizationandtheirownoutcomesofcareintheinpatient setting. JGradMedEduc.2010;2(2):175–80.
10.DewanM,HerrmannLE,TchouMJ,etal.Developmentandevaluation ofhigh-valuepediatrics:ahigh-valuecarepediatricresidentcurriculum. HospPediatr.2018;8(12):785–92.
11.SmithCD.Teachinghigh-value,cost-consciouscaretoresidents:the allianceforAcademicInternalMedicine–AmericanCollegeof PhysiciansCurriculum. AnnInternMed.2012;157(4):284–6.
12.MoriatesC,SoniK,LaiA,etal.Thevalueintheevidence: teachingresidentsto “choosewisely.” JAMAInternMed 2013;173(4):308–10.
13.HomJ,KumarA,EvansKH,etal.Ahighvaluecarecurriculumfor interns:adescriptionofcurriculardesign,implementationand housestafffeedback. PostgradMedJ.2017;93(1106):725–9.
14.VarkeyP,MuradMH,BraunC,etal.Areviewofcost-effectiveness, cost-containmentandeconomicscurriculaingraduatemedical education:teachingcost-effectiveness. JEvalClinPract 2010;16(6):1055–62.
15.SchlicherN,HaddockA,SolnickR,etal. EMRAEmergencyMedicine AdvocacyHandbook.5thed.EmergencyMedicineResidents’ Association;2019.
16.ThomasPA,KernDE,HughesMT,etal. CurriculumDevelopmentfor MedicalEducation:ASix-StepApproach, 3rd ed.Baltimore,MD:Johns HopkinsUniversityPress;2016.
17.PattonMQ.Qualitativeresearch.In: EncyclopediaofStatisticsin BehavioralScience;Hoboken,NJ;JohnWiley&Sons,2005.
18.LincolnYSandGubaEG. NaturalisticInquiry.ThousandOaks,CA; SagePublications,Inc.1985.
19.TongA,SainsburyP,CraigJ.Consolidatedcriteriaforreporting qualitativeresearch(COREQ):a32-itemchecklistforinterviewsand focusgroups. IntJQualHealthCare.2007;19(6):349–57.
20.StammenLA,StalmeijerRE,PaternotteE,etal.Trainingphysiciansto providehigh-value,cost-consciouscare:asystematicreview. JAMA 2015;314(22):2384–400.
21.GreysenSR,WassermannT,PayneP,etal.Teachinghealthpolicyto residents three-yearexperiencewithamulti-specialtycurriculum. JGenInternMed.2009;24(12):1322–6.
22.RyskinaKL,SmithCD,AroraVM,etal.Relationshipbetween institutionalinvestmentinhigh-valuecare(HVC)performance improvementandinternalmedicineresidents’ perceptionsofHVC training: AcadMed.2018;93(10):1517–23.
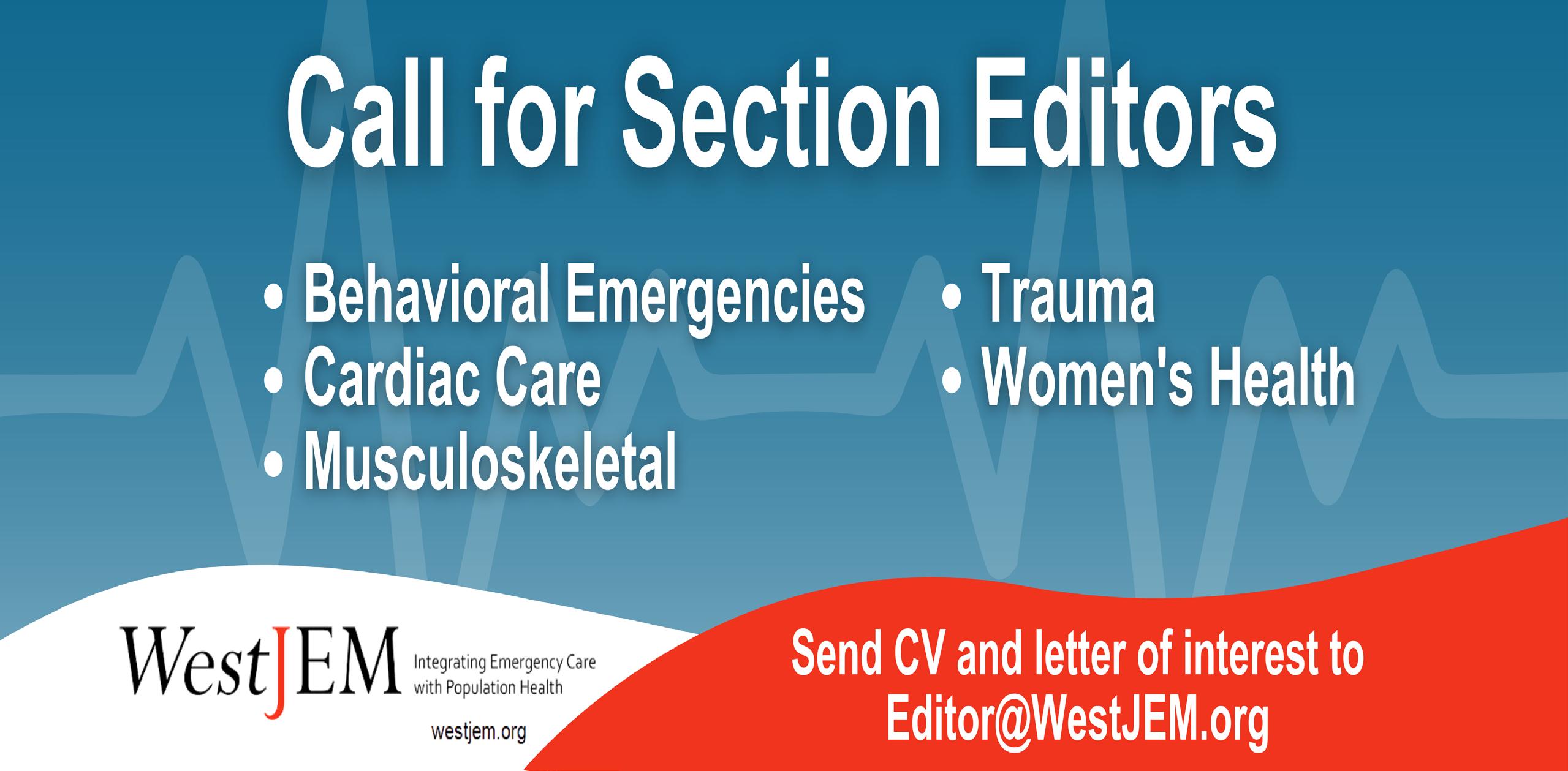







- Western Journal of Emergency Medicine Subscription - CAL/AAEM News Service email updates - Free and discounted registration to CAL/AAEM events
- And more!
CAL/AAEM NEWS SERVICE
- Healthcare industry news
- Public policy
- Government issues
- Legal cases and court decisions

