




















About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.
Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania

FOR MORE INFORMATION PLEASE CONTACT:
Heather Peffley, PHR CPRP
Penn State Health Lead Physician Recruiter hpeffley@pennstatehealth.psu.edu





Register Here: Register Here: March 2-5, 2025
A Note from the Editors:
We are excited to publish the 10th issue of the Western Journal of Emergency Medicine (WestJEM) Education Issue and first year of a rolling decision process. Ov er 10 years ago a unique relationship was formed between WestJEM, the Council of Residency Director for Emergency Medicine and the Clerkship Directors of Emergency Medicine. The idea was to promote and di sseminate educational scholarship which has been accomplished over the past decade. Senior and junior r esearchers have an opportunity to publish in the education issue because of the diverse nature of our submis sion categories, ranging from original research to brief educational advances. A successful issue requires the courage of the authors to submit their work for peer review and we do our best to provide detailed feedback reg ardless of the final decision. Publication of the issue requires the commitment and hard work of the publication staff, leadership of the organizations, editors, and peer reviewers. We want to thank them all for their efforts and professionalism. The topics of this year’s education issue likely reflect the focus of educators as we ente red a post-covid reality. Many of the topics were related to innovative curriculums and focused on the benefi ts derived. There were also several articles that were dedicated to the administrative aspects of residency and fellowships and how that has changed after COVID. We have already started to receive and review submissions for next year’s education issue. The editorial staff review every submission on a rolling basis and, once accepted, the articles are available on PubMed. There are also no processing fees when accepted to the Education Issue. This is a great opportunity to submit your educational scholarship, thereby enhancing your professional development and disseminating your work to others. We are excited that this experiment has flourished, and we look forward to seeing your work in our 11th issue.
Jeffrey Love, MD
Georgetown University School of Medicine
Co-Editor of Annual Special Issue on Education Research and Practice
Douglas Ander, MD
Emory University
Co-Editor of Annual Special Issue on Education Research and Practice
The Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health would like to thank The Clerkship Directors in Emergency Medicine (CDEM) and the Council of Residency Directors in Emergency Medicine (CORD) for helping to make this collaborative special issue possible.
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
1 Program Signaling in Emergency Medicine: The 2022–2023 Program Director Experience
AE Pelletier-Bui, T Fallon, L Smith, T Strout, M Fischer, M Olaf, E McDonough, B Barbas, M Cirone, E Barrall Werley
11 Emergency Medicine Milestones Final Ratings Are Often Subpar
DL Gorgas, KB Joldersma, FK Ankel, WA Carter, MA Barton, EJ Reisdorff
15 Emergency Department Slit Lamp Interdisciplinary Training Via Longitudinal Assessment in Medical Practice
S Hamou, S Ghiaee, C Chung, M Lloyd, K Khem, XC Zhang
25 Teaching the New Ways: Improving Resident Documentation for the New 2023 Coding Requirements
N Zapolsky, A Cardell, R Desai, S Frisch, N Jobeun, D Novak, M Silver, AS Chung
29 Telesimulation Use in Emergency Medicine Residency Programs: National Survey of Residency Simulation Leaders
M Berger, J Buckanavage, J Jordan, S Lai, L Regan
35 Substantial Variation Exists in Clinical Exposure to Chief Complaints Among Residents Within an Emergency Medicine Training Program
CM Jewell, AT Hummel, DJ Hekman, BH Schnapp
41 The Effect of Hospital Boarding on Emergency Medicine Residency Productivity
P Moffett, A Best, N Lewis, S Miller, G Hickam, H Kissel-Smith, L Barrera, S Huang, J Moll
50 Making A Difference: Launching a Multimodal, Resident-Run Social Emergency Medicine Program NP Newton, C Freeman, P Panakos
59 Palliative Care Boot Camp Offers Skill Building for Emergency Medicine Residents
J Cooper, J Fredette
63 Effectiveness of a Collaborative, Virtual Outreach Curriculum for 4th-Year EM-bound Students at a Medical School Affiliated with a Historically Black College and University
C Brown, R Carter, N Hartman, A Hammond, E MacNeill, L Holden, A Pierce, L Campbell, M Norman
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
The WestJEM Special Issue in Educational Research & Practice couldn’t exist without our many reviewers. To all, we wish to express our sincerest appreciation for their contributions to this year’s success. Each year a number of reviewers stand out for their (1) detailed reviews, (2) grasp of the tenets of education scholarship and (3) efforts to provide feedback that mentors authors on how to improve. This year’s “Gold Standard” includes:
• Dave Carlberg
• Michael Cassara
• Max Griffith/Bjorn Watsjold*
• Alana Harp/Deena Bengiamin*
• Mojibade Hassan/Kathleen White/Brad Barth*
• Heather Hechter
• Adam Heilmann/Erin Kane/John Schneider/Albert Kim*
• Corlin Jewel
• Julia Isaacson/Kerry McCabe*
• Kaitlin Lipner/Chris Merritt*
• Evie Marcolini
• Dan Mayer
• Colin McMahon/Anne Messman*
• Elspeth Pearce
• Adam Rieves
• Eric Pellegrini /Emily Rose/Aarti Jain/ Taku Taira/Jeff Riddell*
• John Priester/Richard Bounds*
• Thaddeus Schmitt
• Jeffrey Siegelman
• Jacqueline Sippel/Ashley Foreman/Erica Shaver/Chris Kiefer*
• Olivia Urbanoor/Jessica Baez/Sally Santen*
*Mentored Peer Reviews from Emergency Medicine Education Fellowship Programs
We would also like to recognize our guest consulting editors who assisted with pre-screening submissions during our initial peer-review stages. Thank you for all of your efforts and contributions.
CDEM
• Christine Stehman
• Eric Shappell
• Sharon Bord
• Andrew Golden
CORD
• Jenna Fredette
• Danielle Hart
• William Soares III
• Jamie Jordan
• Anne Messman
• Logan Weygandt
Consulting Statistician/ Psychometrician
• David Way
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Jeffrey N. Love, MD, Guest Editor
Georgetown School of Medicine- Washington, District of Columbia
Chris Merritt, MD, MPH, Associate Guest Editor Alpert Medical School of Brown University-Providence, Rhode Island
Benjamin Schnapp, MD, MEd, Associate Guest Editor University of Wisconsin-Madison, Wisconsin
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Danya Khoujah, MBBS, Associate Editor
University of Maryland School of Medicine- Baltimore, Maryland
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Resident Editors
AAEM/RSA
Tehreem Rehman, MD
Advocate Christ Medical Center
ACOEP
Justina Truong, DO Kingman Regional Medical Center
Section Editors
Behavioral Emergencies
Erin Dehon, PhD University of Mississippi Medical Center
Leslie Zun, MD, MBA Chicago Medical School
Marc L. Martel, MD Hennepin County Medical Center
Cardiac Care
Fred A. Severyn, MD University of Colorado School of Medicine
Michael C. Kurz, MD University of Alabama at Birmingham
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD
Carolinas Medical Center
Casey Clements, MD, PhD
Mayo Clinic
Patrick Meloy, MD
Emory University
Nicholas Pettit, DO, PhD
Indiana University
Eric Snoey, MD
Alameda County Medical Center
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO
Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD
University of California, San Diego
Gabriel Wardi, MD
University of California, San Diego
Joseph Shiber, MD
University of Florida-College of Medicine
Matt Prekker MD, MPH
Hennepin County Medical Center
David Page, MD
University of Alabama

Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Julianna Jung, MD, Associate Guest Editor Johns Hopkins Hospital, Baltimore, Maryland
Douglas Franzen, MD, Associate Guest Editor Harborview Medical Center, Seattle, Washington
Gentry Wilkerson, MD, Associate Editor University of Maryland
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Sara Krzyzaniak, MD Associate Guest Editor Stanford Universtiy-Palo Alto, California
Susan R. Wilcox, MD, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston, Texas
Taku Taira, MD, EDD, Associate Guest Editor LAC + USC Medical Center-Los Angeles, California
Erik Melnychuk, MD
Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
Christopher Kang, MD
Madigan Army Medical Center
Education
Danya Khoujah, MBBS University of Maryland School of Medicine
Jeffrey Druck, MD University of Colorado
John Burkhardt, MD, MA University of Michigan Medical School
Michael Epter, DO
Maricopa Medical Center
ED Administration, Quality, Safety
David C. Lee, MD
Northshore University Hospital
Gary Johnson, MD
Upstate Medical University
Brian J. Yun, MD, MBA, MPH
Harvard Medical School
Laura Walker, MD
Mayo Clinic
León D. Sánchez, MD, MPH
Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH
University of Texas Health-San Antonio
Emergency Medical Services
Daniel Joseph, MD
Yale University
Joshua B. Gaither, MD
University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH
Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD
Yale School of Medicine
Stephen Meldon, MD
Cleveland Clinic
Luna Ragsdale, MD, MPH
Duke University
Health Equity
Emily C. Manchanda, MD, MPH
Boston University School of Medicine

Douglas S. Ander, MD, Guest Editor Emory University School of Medicine-Atlanta, Georgia
Edward Ullman, MD, Associate Guest Editor Harvard University-Cambridge, Massachusetts
Abra Fant MD, MS, Associate Guest Editor
Northwestern Medicine-Chicago, Illinois
Kendra Parekh, MD, MS, Associate Guest Editor
Vanderbilt University-Nashville, Tennessee
Matthew Tews, DO, MS, Associate Guest Editor Indiana University School of Medicine, Augusta, Georgia
Rick A. McPheeters, DO, Associate Editor Kern Medical- Bakersfield, California
Niels K. Rathlev MD, MS, Associate Editor
Tufts University School of Medicine-Boston, Massachusetts
Shahram Lotfipour, MD, MPH, Managing Associate Editor University of California, Irvine School of Medicine- Irvine, California
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of Medicine- Irvine, California
Mandy J. Hill, DrPH, MPH
UT Health McGovern Medical School
Infectious Disease
Elissa Schechter-Perkins, MD, MPH
Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
Drexel University College of Medicine
Kevin Lunney, MD, MHS, PhD University of Maryland School of Medicine
Robert Derlet, MD
Founding Editor, California Journal of Emergency
Medicine
University of California, Davis
Stephen Liang, MD, MPHS
Washington University School of Medicine
Injury Prevention
Mark Faul, PhD, MA
Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS
Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH
Prisma Health Richland
Taylor Burkholder, MD, MPH
Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Melanie S. Heniff, MD, JD
Indiana University School of Medicine
Greg P. Moore, MD, JD
Madigan Army Medical Center
Statistics and Methodology
Shu B. Chan MD, MS
Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH
Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS
Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS
Pacific Northwest University
Neurosciences
Antonio Siniscalchi, MD
Annunziata Hospital, Cosenza, Italy

Rick Lucarelli, MD
Medical City Dallas Hospital
William D. Whetstone, MD University of California, San Francisco
Pediatric Emergency Medicine
Paul Walsh, MD, MSc University of California, Davis
Muhammad Waseem, MD
Lincoln Medical & Mental Health Center
Deena Berkowitz, MD, MPH
Children’s National Hospital
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
Jeremy Hess, MD, MPH University of Washington Medical Center
Jacob Manteuffel, MD
Henry Ford Hospital
John Ashurst, DO Lehigh Valley Health Network
Tony Zitek, MD
Kendall Regional Medical Center
Trevor Mills, MD, MPH Northern California VA Health Care
Erik S. Anderson, MD
Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD
Henry Ford Hospital
Phillips Perera, MD
Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS
Virginia Commonwealth University
Jeffrey R. Suchard, MD University of California, Irvine
Ultrasound
J. Matthew Fields, MD
Thomas Jefferson University
Shane Summers, MD
Brooke Army Medical Center
Robert R. Ehrman
Wayne State University
Ryan C. Gibbons, MD Temple Health

Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W Chapman Ave Ste 3200, Orange, CA 92868, USA. Office: 1-714-456-6389; Email: Editor@westjem.org.
Volume 26, Issue 1.2: January 2025
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Editorial Board
Amin A. Kazzi, MD, MAAEM
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Douglas Ander, MD Emory University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Jaqueline Le, MD Desert Regional Medical Center
Jeffrey Love, MD Georgetown School of Medicine
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Rachel A. Lindor, MD, JD Mayo Clinic
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Scott Rudkin, MD, MBA University of California, Irvine
Elena Lopez-Gusman, JD
California ACEP
American College of Emergency Physicians
Jennifer Kanapicki Comer, MD FAAEM
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett
American College of Osteopathic Emergency Physicians
Kimberly Ang, MBA UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians Kaiser Permanente
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP UC San Diego Health School of Medicine
Scott Zeller, MD University of California, Riverside
Steven H. Lim Hoon Chin, MD Changi General Hospital, Simei, Singapore
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Isabelle Nepomuceno, BS Executive Editorial Director
Ian Ollife, BS WestJEM Editorial Director
Emily Kane, BS WestJEM Editorial Director
Tran Nguyen, BS CPC-EM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
Alyson Tsai, BS CPC-EM Publishing Director
June Casey, BA Copy Editor
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine




Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 333 City Blvd, West, Rt 128-01, Orange, CA 92866, USA Office: 1-714-456-6389; Email: Editor@westjem.org
of Emergency
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians California ACEP
Academic Department of Emergency Medicine Subscriber
Alameda Health System-Highland Hospital Oakland, CA
Ascension Resurrection Chicago, IL
Arnot Ogden Medical Center Elmira, NY
Atrium Health Wake Forest Baptist Winston-Salem, NC
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Beth Israel Deaconess Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University-Rhode Island Hospital Providence, RI
Carolinas Medical Center Charlotte, NC
Cedars-Sinai Medical Center Los Angeles, CA
Cleveland Clinic Cleveland, OH
Desert Regional Medical Center Palm Springs, CA
Eisenhower Health Rancho Mirage, CA
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin Healthcare Minneapolis, MN
Henry Ford Hospital Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Howard County Department of Fire and Rescue Marriotsville, MD
Icahn School of Medicine at Mt Sinai New York, NY
Indiana University School of Medicine Indianapolis, IN
INTEGRIS Health Oklahoma City, OK
Kaweah Delta Health Care District Visalia, CA
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of AmericanAcademy of Emergency Medicine
Loma Linda University Medical Center
Loma Linda, CA
Louisiana State University Shreveport Shereveport, LA
Massachusetts General Hospital/ Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Mayo Clinic in Florida Jacksonville, FL
Mayo Clinic College of Medicine in Rochester Rochester, MN
Mayo Clinic in Arizona Phoeniz, AZ
Medical College of Wisconsin Affiliated Hospital Milwaukee, WI
Mount Sinai Medical Center Miami Beach Miami Beach, FL
Mount Sinai Morningside New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
NYC Health and Hospitals/ Jacobi New York, NY
Ochsner Medical Center New Orleans, LA
Great Lakes Chapter Division of the AmericanAcademyofEmergencyMedicine
Tennessee Chapter Division of the AmericanAcademyofEmergencyMedicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Ohio State University Wexner Medical Center Columbus, OH
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Poliklinika Drinkovic Zagreb, Croatia
Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Rush University Medical Center Chicago, IL
Rutgers Robert Wood Johnson Medical School New Brunswick, NJ
St. Luke’s University Health Network Bethlehem, PA
Southern Illinois University School of Medicine Springfield, IL
Stony Brook University Hospital Stony Brook, NY
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center
El Paso, TX
Uniformed Services Chapter Division of the American Academy of Emergency Medicine Virginia Chapter Division of the American Academy of Emergency Medicine
forEmergencyMedicine
To become a WestJEM departmental sponsor, waive article processing fee, receive print and copies for all faculty and electronic for faculty/residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California ACEP
Academic Department of Emergency Medicine Subscriber
The University of Texas Medical Branch Galveston, TX
UT Health Houston McGovern Medical School Houston, TX
Touro University College of Osteopathic Medicin Vallejo, CA
Trinity Health Muskegon Hospital Muskegon, MI
UMass Memorial Health Worcester, MA
University at Buffalo Program Buffalo, NY
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Little Rock, AR
University of Arkansas for Medical Sciences Galveston, TX
University of California, Davis Medical Center Sacramento, CA
University of California San Francisco General Hospital San Francisco, CA
University of California San Fracnsico Fresno Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida, Jacksonville Jacksonville, FL
University of Illinois at Chicago Chicago, IL
University of Iowa Hospitals and Clinics Iowa City, IA
University of Kansas Health System Kansas City, IA
University of Louisville Louisville, KY
University of Maryland School of Medicine Baltimore, MD
University of Miami Jackson Health System Miami, FL
University of Michigan Ann Arbor, MI
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Southern Alabama Mobile, AL
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine
Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Southern California Los Angeles, CA
University of Vermont Medical Cneter Burlington, VA
University of Virginia Health Charlottesville, VA
University of Washington - Harborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Medical Center Dallas, TX
Franciscan Health Olympia Fields Phoenix, AZ
WellSpan York Hospital York, PA
West Virginia University Morgantown, WV
Wright State University Boonshoft School of Medicine Fairborn, OH
Yale School of Medicine New Haven, CT
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the
American Academy of Emergency Medicine Uniformed Services Chapter Division of the
Academy of Emergency Medicine Virginia Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias Sociedad
To become a WestJEM departmental sponsor, waive article processing fee, receive print and copies for all faculty and electronic for faculty/residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
AlexisE.Pelletier-Bui,MD*
TimothyFallon,MD†
LizaSmith,MD‡
TaniaStrout,PhD,MS†
MichelleFischer,MD,MPH§
MarkOlaf,DO∥
ErinMcDonough,MD¶
BrianBarbas,MD#
MichaelCirone,MD**
ElizabethBarrallWerley,MD§
*CooperUniversityHospital/CooperMedicalSchoolofRowanUniversity, DepartmentofEmergencyMedicine,Camden,NewJersey
† MaineMedicalCenter,TuftsUniversitySchoolofMedicine,Departmentof EmergencyMedicine,Portland,Maine
‡ UniversityofMassachusettsChanSchoolofMedicine,BaystateMedicalCenter, DepartmentofEmergencyMedicine,Springfield,Massachusetts
§ PennStateCollegeofMedicine/PennStateHealthMiltonS.HersheyMedical Center,DepartmentofEmergencyMedicine,Hershey,Pennsylvania
∥ GeisingerCommonwealthSchoolofMedicine,DepartmentofEmergency Medicine,Scranton,Pennsylvania
¶ UniversityofCincinnatiCollegeofMedicine,DepartmentofEmergencyMedicine, Cincinnati,Ohio
# LoyolaUniversityChicago,StritchSchoolofMedicine,LoyolaUniversityMedical Center,DepartmentofEmergencyMedicine,Maywood,Illinois
**UniversityofIllinois,DepartmentofEmergencyMedicine,Chicago,Illinois
SectionEditors:PaulLoganWeygandt,MDandChrisMerritt,MD
Submissionhistory:SubmittedFebruary2,2024;RevisionreceivedApril22,2024;AcceptedJune3,2024
ElectronicallypublishedAugust27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.19392
Introduction: Programsignaling(PS),whichenablesresidencyapplicantstosignaltheirpreferencefora specificprogram,wasintroducedinemergencymedicine(EM)inthe2022–2023residencyapplicationcycle. InthisstudyweevaluatedEMprogramdirectors’ (PD)utilizationofPSinapplicationreviewandranking.This studyalsoexplorestherelationshipbetweenprogramcharacteristicsandnumberofsignalsreceivedaswell astherelativeimportanceandutilizationofsignalsrelatedtothenumberofsignalsreceived.
Methods: Thisisaninstitutionalreviewboard-approved,cross-sectionalstudyofPDsatAccreditation CouncilforGraduateMedicalEducation-accreditedEMresidencyprograms.Weuseddescriptive statisticstodescribethecharacteristicsofresidencyprogramsandpracticesaroundPS.Measuresof centraltendencyanddispersionsummarizedcontinuousvariables.Weusedchi-squareanalysisorthe Fisherexacttestforcomparisonsbetweengroupsforcategoricalvariables.Comparisonsforcontinuous variablesweremadeusingthe t-testforindependentsamplesoranalysisofvariance.
Results: Theresponseratewas41%(n = 113/277EMprograms).MostprogramsparticipatedinPS (n = 261/277EMprograms,94.2%).Meannumberofsignalsreceivedwas60(range2–203).Signals receivedvariedbasedonprogramcharacteristicsincludinggeographiclocationandprogramtype,duration, environment,andlongevity.MostusedPSinholisticreview(52.2%),butotherusesvariedbyproportionof applicationsthatweresignaled.TheimportanceofPSinapplicationreview(mean2.9;1–5scale,1 = not important,5 = extremelyimportant)andranklistpreparation(2.1)wasrelativelylowcomparedtoother applicationelementssuchasstandardizedlettersofevaluation(4.97forreview,4.90forranking).
Conclusion: ThestudyprovidesinsightsintoPSutilizationinEM’sinauguralyear.Wehaveidentified patternsofsignalusebasedonprogramcharacteristicsandnumberofsignalsreceivedthatcaninformsignal allocationandutilizationonanindividualapplicantandprogramlevel.Amorenuancedunderstandingof signalusecanprovidevaluableinsightasthespecialtyofEMgrappleswith fluctuationsinitsapplicant numbersandshiftingdemographicsofitsapplicantpool.[WestJEmergMed.2025;26(1.2)1–10.]
Programsignaling(PS)wasintroducedintotheresidency applicationprocessinresponsetotheincreasingnumberof applicationsreceivedbyprograms,exacerbatingthe challengeofcomprehensiveholisticreview.1 Subsequently, EMhasexperienceddrastic fluctuationsinthenumberof applicantspursuingEMandspecialtyMatchrates,aswellas unprecedentedchangestothedemographicsofits applicationpooloverthelastseveralyears.2 Evenwith variabilityinthenumberofapplicationstoemergency medicine(EM)inrecentyears,EMapplicationnumbers remainsignificantlyabovewhattheywere10yearsago.2,3 Programsignalingallowsapplicantstoassignsignalsto theirmostdesiredtrainingprograms,sothatprograms mayfocustheirholisticeffortstowardhigh-yieldinterview candidates,potentiallybenefitingbothapplicants andprograms.
ProgramsignalingwasimplementedinEMviathe ElectronicResidencyApplicationService(ERAS)inthe 2022–2023residencyapplicationcycle,allowingapplicants tosend fivesignalsatthetimeoftheirresidencyapplication submissionwithinstructiontonotsignaltheirhomeorawayrotationinstitutions.4 TheAssociationofAmericanMedical Colleges(AAMC)publishedgenericguidanceforprograms regardingtheuseofPSonlyduringtheinterview-offerphase andprogramsattestedtoacodeofconductregardingsignal usagewhenoptingintotheprocess,includingguidancenotto usePSinrankorderlist(ROL)decisions.5 Whiledatawas evaluatedbyERASacrossallparticipatingspecialties,and otherspecialtieshavereportedtheirownspecialty-specific data,opportunitiesremainedtofurtherinvestigatequestions specifictoPSwithinEM.6–18 Theuniquechallengesfacing EMcreatedanappetiteandunderscoredtheneedfor specialty-speci ficguidance.
Toprovideevidence-basedguidance,theERAS ApplicationWorkingGroup,asubsetoftheCouncilof ResidencyDirectorsinEM(CORDEM)Application ProcessImprovementCommittee,createdasurveyto addressmorenuancedEM-specificquestionsnotaskedor answeredbytheAAMCsurvey.Ourobjectiveinthisstudy wastodeterminehowEMprogramdirectors(PD)usedPSin theirapplicationreviewandrankingpracticesduringthe 2022–2023applicationcycle,particularlyinrelationtothe proportionofsignaledapplicationsreceived.Toour knowledge,nootherspecialtiesparticipatinginPShave reportedPSutilizationdatainthismanner.Wealsoexplored therelationshipbetweenprogramcharacteristicsandthe numberofsignalsreceived,includingcharacteristicsnot previouslystudiedbytheAAMCsuchasgeographic location,programlengthoftraining,programenvironment, andprogramlongevity.Lastly,weinvestigatedtherelative importanceandutilizationofsignalsincomparisontoother residencyapplicationelementsandinrelationtothenumber ofsignalsreceived.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Programsignaling(PS)wasintroducedinto theemergencymedicine(EM)residency applicationprocessin2022 – 2023viathe ElectronicResidencyApplicationService.
Whatwastheresearchquestion?
HowdidEMprogramdirectorsusePSin applicationreviewandranking?
Whatwasthemajor findingofthestudy?
52.2%ofprogramdirectorsusedPSin holisticreview.Otherusesvariedby proportionofsignaledapplications.
Howdoesthisimprovepopulationhealth? UnderstandingPSusagepatternshelps informPSallocationandusageonan individualapplicantandprogramlevel.
Weusedacross-sectionalstudydesign.Participantswere PDsinAccreditationCouncilforGraduationMedical Education(ACGME)-accreditedEMresidencyprograms participatinginthe2023NationalResidentMatching ProgramMatch.TheCORDmemberdirectory,crossreferencedwiththeACGMEAccreditationDataSystem publicsearchwebsite,wasusedtocompiletheemail distributionlist.WeeditedthelisttoreflectnewPDswhen possible(277).Thesurveywascreatedfollowingathorough literaturereviewandsynthesisofbackgroundinformation. QuestionswereiterativelyreviewedbyexpertsinEM medicaleducation.Thesurveywasfurtherrefinedafter conductingtwocognitiveinterviewswithEMresidency programleadersandthenpilotedbyseveralEMeducatorsto assessforclarityofthequestions.Datawasprimarily quantitative.Noidentifyinginformationwascollected.The studywasdesignedtotakeabout10minutestocomplete. Oursurveytoolisincludedin Appendix1.Thisstudywas approvedbytheinstitutionalreviewboardattheinstitution ofauthorsTFandTS.
Thesurveylinkwasdistributedviaemail.Wecollected datausingaconfidentialandsecureweb-based(Qualtrics, Provo,UT)surveyofEMresidencyPDsortheirdesignees. Anonymouslinkswerecreatedforeachpotentialrespondent anddistributedviaQualtrics.AsdescribedbyDillmanand
colleagues,oneweekpriortodistributionofthesurveylink, PDsreceivedabriefemailintroducingthestudyand informingthemthattheywouldreceivethestudylinkinthe comingweek.19 Participantsthenreceivedamessage containingthesurveylink.Non-respondersreceivedupto threeremindermessagesover fiveweeks.
DatawasdownloadedfromREDCap,hostedatMaine MedicalCenter,directlyintoSPSSforWindowsv27(IBM SPSSStatisticsforWindows,IBMCorp.,Armonk,NY) statisticalsoftwareforanalysis.Weuseddescriptivestatistics todescribethecharacteristicsofstudyparticipants’ residency trainingprograms.Programpracticesandexperiences aroundPSweredescribedusingnumbersandpercentagesfor eachcategoricalvariable.Wesummarizedcontinuous variablesusingmeasuresofcentraltendency(meanor median)anddispersion(standarddeviation,interquartile range[IQR]).Comparisonsbetweengroupsforcategorical variablesweremadeusingchi-squareanalysisortheFisher exacttest.Comparisonsforcontinuousvariablesweremade usingthe t -testforindependentsamplesoranalysisof variance.Weaccepteda P -valueof <0.05assignificant.We alsocomputeddifferencesbetweengroupsandtheir associated95%confidenceintervals(CI)andcreatedvisual datadisplaystoaidininterpretation.
ProgramCharacteristics
Wereceived113/277surveys(responserate41%). Participantsrepresenteddiversegeographicregions,withthe largestnumbersfromtheMiddleAtlantic,EastNorth CentralMidwest,andSouthAtlanticregions(Table1). Programsrepresentedweremostcommonlyurban, university-based,andthreeyearslengthofresidency training.Facultyatparticipatingprogramswerelargely universityorhospitalemployees,andmostprograms reportingbeingfoundedmorethan15years.
ProgramSignalingParticipationandApplicationsReceived
ThemajorityofrespondentsparticipatedinthePS componentoftheERASsupplementalapplicationduring the2022–2023residencyapplicationcycle(106,94%). Reasonsfornon-participationincludednotsigningupin time(three,2.7%),feelingthatitwouldnotcontributeto applicantrevieworinterviewofferdecisions(two,1.8%),and beinganewlyapprovedprogram(1,0.9%).Programs interviewedto fillameanandmedianof12postgraduate year(PGY)-1spots(range6–26spots,IQR8–15).The numberofsignalsreceivedbyparticipatingprogramsranged from2–203,withameanof60andmedianof50(IQR 23–86).Programsreportedreceiptofbetween283–1,400 applications(mean768,median772,IQR600–926).The proportionofapplicationsthatweresignaledranged
from0.7%to26.5%(mean7.3%,median6.5%, IQR3.9–10.1%).
Therewasamoderate,positivecorrelationbetweenthe numberofsignalsandthenumberofapplicationsreceived (r = 0.581, P < 0.001)andtheproportionofsignalsreceived increasedbaseduponthenumberofapplicationsreceived (P < 0.001)aswellastheproportionofapplicationsthat weresignaled(P < 0.001).Thenumberofsignalsreceived increasedasthenumberofPGY-1positionsincreased (P < 0.001).Fourquartilesweredeterminedforthenumber ofprogramsignalsreceived,thenumberofapplications received,andtheproportionofapplicationssignaled (SupplementalTable1)toallowforfurthercomparisonof dataassubsequentlydetailed.
Thenumberofsignalsreceiveddifferedsignificantlybased onseveralkeycharacteristics:geographiclocation,with greaternumbersofsignalsreceivedincoastalregions (P < 0.01);programduration,withfour-yearreceivingmore thanthree-yearprograms(P < 0.01);programtype,with urbanprogramsreceivingthemost(P < 0.01);program environment,withuniversity-basedprogramsreceivingthe most(P < 0.01);andlongevityofprogramswithprogramsin existence >15yearsreceivingthemost(P < 0.01). Additionaldetailisprovidedin Figures1 and 2 and SupplementalFigure1.
ProgramsmostcommonlyendorsedusingPSasone componentofholisticreview(59,52.2%).Additionalspecific waysthatsignalswereusedincludethefollowing:asa tiebreakerbetweentwoequallyqualifiedcandidates (45,39.8%);asascreeningtool(44,38.9%);tohelpprioritize theprogram’swaitlistorwaitlistorder(31,27.4%);andto sendaninterviewinvitationtoeveryapplicantwhosignaled theprogram(19,16.8%).Theproportionofapplicationsthat weresignaledappearedtoaffectthefrequencywithwhich programsendorsedusingsignalstoprioritizethewaitlist (P < 0.001),serveasatiebreaker(P < 0.001),andtosend interviewinvitationstoeverysignalingapplicant(P = 0.03) (Figure3).ParticipantsanticipatedusingPSinthe 2023–2024cyclesimilarlytotheirreporteduseinthe 2022–2023cycle,andsimilardifferenceswerealsonotedfor anticipatedusebasedontheproportionofapplicationsthat weresignaled.
Participantsratedtheimportanceofvariousapplication elementswhenconsideringinterviewinvitationsand preparingtheirprogram’srankorderlist(ROL)usinga 5-pointscale(1 = notimportantatall,5 = extremely important)(Table2).Participantsratedthestandardized letterofevaluation(SLOE)asthemostimportantelement
Table1. Characteristicsofparticipatingresidencyprogramsandsurveyrespondents.
Characteristic%(n)Comparisontoexistingprogramdata(percentageofprograms)
Professionalrole
*Programdirector100(113)
Geographicregion
MiddleAtlantic24.8(28)23.7a EastNorthCentralMidwest20.4(23)20.5a SouthAtlantic17.7(20)19.1a PacificWest11.5(13)10.6a WestSouthCentral11.5(13)9.9a NewEngland5.3(6)4.2a MountainWest4.4(5)3.9a WestNorthCentralMidwest2.7(3)3.9a EastSouthCentral1.8(2)4.2a Programlength
Threeyears77.0(87)80.6b
Fouryears23.0(26)19.4b Programenvironment
Urban63.7(72)Notavailable
Suburban30.1(34)Notavailable Rural6.2(7)Notavailable Programtype
University-based47.8(54)35.4a Community-based,university-affiliated36.3(41)46.2a Community-based15.9(18)18.4a Facultyemploymentmodel
Universityorhospital73.5(83)Notavailable Contractmanagementgroup18.6(21)Notavailable Democraticphysician-ledgroup8.0(9)Notavailable Programlongevity
<5years17.7(20)Notavailable 5–10years8.0(9)Notavailable 10–15years10.6(12)Notavailable >15years63.7(72)Notavailable *261/277EMprogramsparticipatedinPSfor2022–2023.All277programssurveyed. MiddleAtlantic = NJ,NY,PA;EastNorthCentralMidwest = IL,IN,MI,OH,WI;SouthAtlantic = DC,DE,GA,FL,MD,NC,SC,VA,WV,PR; PacificWest = AK,CA,HI,OR,WA;WestSouthCentral = AR,LA,OK,TX;NewEngland = CT,MA,ME,NH,RI,VT;MountainWest = AZ, CO,ID,MT,NM,NV,UT,WY;WestNorthCentralMidwest = IA,KS,MN,MO,ND,NE,SD;EastSouthCentral = AL,MS,KY,TN. aFellowshipandResidencyElectronicInteractiveDatabase(FREIDA), https://freida.ama-assn.org bEmergencyMedicineResidents’ Association(EMRA)MatchDatabase, https://match.emra.org/
whenreviewingapplications(mean4.97,95%CI4.93–5.00). TheSLOEs(mean4.90,95%CI4.83–4.97)andinterviewday performance(mean4.81,95%CI4.72–4.89)weremost importantwhenpreparingtheROL.Importanceofthe presenceorabsenceofaprogramsignalwhenreviewing applicationswasameanof2.9(95%CI2.67–3.13)and medianof3(2,4).Importanceofthepresenceorabsenceofa
programsignalwhenpreparingaROLwasameanof2.1 (95%CI1.87–2.32)andmedianof2(1–3).About30%of participants(28)endorsedthepresenceorabsence ofaprogramsignalasveryorextremelyimportant whenreviewingapplicationswhile11%(10)rated programsignalsasbeingequallyimportantto ROLdevelopment.

Figure1. (A)Meannumberofsignalsreceivedbygeographicregion.(B)Mediannumberofsignalsreceivedbygeographicregion. Geographicregionsinclude:EastNorthCentralMidwest(IL,IN,MI,OH,WI),EastSouthCentral(AL,MS,KY,TN),MiddleAtlantic(NJ,NY, PA),MountainWest(AZ,CO,ID,MT,NM,NV,UT,WY),NewEngland(CT,MA,ME,NH,RI,VT),Paci ficWest(AK,CA,HI,OR,WA),South Atlantic(DC,DE,GA,FL,MD,NC,SC,VA,WV,PR),WestNorthCentralMidwest(IA,KS,MN,MO,ND,NE,SD),andWestSouthCentral (AR,LA,OK,TX).
WeassessedfordifferencesinPDs’ relativeassessmentsof variousapplicationelementsbasedontheproportionof applicationsthatweresignaled(SupplementalFigure2).As theproportionofapplicationssignaledincreased,the
proportionofprogramsendorsingboardscoresas “extremelyimportant” decreased(P < 0.01).Asthe proportionofapplicationssignaledincreased,theproportion ofprogramsendorsingcommunicationbeforetheinterview
Volume26,No.1.2:January2025WesternJournal

Figure2. Meannumberofsignalsreceivedbyprogramcharacteristics.(A)Meannumberofsignalsreceivedbyprogramduration.(B)Mean numberofsignalsreceivedbyenvironmenttype.(C)Meannumberofsignalsreceivedbyprogramtype.(D)Meannumberofsignalsreceived byprogramlongevity.

(A) Programs with 03.81% (Quartile 1) of applications signaled.
(B) Programs with 3.82-6.48% (Quartile 2) of applications signaled.
(C) Programs with 6.49-10.12% (Quartile 3) of applications signaled.
(D) Programs with 10.13-26.46% (Quartile 4) of applications signaled.
Figure3. Programsignaluseinthe2022–2023academicyearbytheproportionofapplicantssignaled.* *TheAAMCCodeofConduct,whichprogramsattesttowhensigninguptoparticipateinprogramsignaling(PS),specificallyprohibitstheuse ofPSinrank-orderlistdiscussionandpreparation.
Table2. Importanceofapplicationelements.
ApplicationelementImportancewhenreviewingapplicationsImportancewhenpreparingrankorderlist
Mean(95%CI)Mean(95%CI)
SLOEs4.97(4.93–5.00)4.90(4.83–4.97)
InterviewdayinteractionsN/A4.81(4.72–4.89)
Priorworkorlifeexperiences3.61(3.42–3.80)3.52(3.32–3.72)
Boardscores3.47(3.27–3.66)3.14(2.93–3.35)
MSPE3.44(3.24–3.65)3.32(3.12–3.53)
Extracurricularinvolvement3.36(3.17–3.54)3.25(3.05–3.45)
Presenceorabsenceofaprogramsignal2.90(2.67–3.13)2.10(1.87–2.32)
Communicationbeforeinterview2.64(2.42–2.87)2.89(2.65–3.13)
Researchexperience2.46(2.27–2.64)2.43(2.24–2.62)
Lettersofrecommendation2.40(2.22–2.58)2.33(2.15–2.52)
*5pointscalewhere5 = extremelyimportantand1 = notimportantatall. CI,confidenceinterval; SLOE,standardizedletterofevaluation; MSPE,medicalstudentperformanceevaluation.
as “notimportantatall” increasedwhiletheproportion ratingthisfactor “veryimportant” decreased(P < 0.01). Extracurricularinvolvementincreasedinimportanceasthe numberofapplicationssignaledincreased,withalarger proportionofparticipantsratingthisaspectofthe application “extremelyimportant” astheproportionof applicationssignaledincreased(P = 0.04).Programswith thelowestproportionofsignalingapplicantsweremore likelytorateresearchexperienceas “notimportantatall” thanthosewhohadalargerproportionofapplications signaled(P = 0.02).
Responsestooursurveyappeartobeappropriately representativeofprogramsnationwidewithregardto geographicdistribution,programlength,andprogramtype (Table1).20,21 Rangesandmediannumbersforapplications andPSdataaresimilartoERASdata,againdemonstrating thatoursurveyrespondentsreflectedarepresentativesample ofEMprogramsthatparticipatedinPSduringthestudied applicationcycle.6
Fordataanalysis,weusedquartilesbasedonthe percentageofsignalingapplicationsaprogramreceivedto correctforthedifferencesinrawnumbersbasedonprogram size.WiththenumberofsignalsallocatedtoeachEM applicantincreasingfrom fivetosevenforthe2023–2024 academicyear,itisreasonabletopresumethattheraw numberandpercentageofsignalingapplicantsprograms receivewillalsoproportionallyincrease.Thisdiscrepancy maymakeitmoredifficultforaprogramtoaccurately identifywithagivenquartilebasedonthisyear’sapplication data,butthesedatashouldstillserveasaroughguideby whichprogramscanassessthemselves.
Understandingtherelationshipbetweenprogram characteristicsandthenumberofreceivedprogramsignals canbehelpfulforbothprogramsandapplicants.Programs candeterminetheircompetitivenesswithinthecontextof similarprograms,whichcanbeparticularlyhelpfulinthe currentEMmatchenvironmentwithachangingapplicant demographicpoolandmanyprogramsgoingunmatched overthepastfewyears.2 Providingprogramswitha barometeragainstwhichtomeasuretheirowndemographics andproportionofsignaledapplicantsearlyintheapplication cyclecanhelpguidehowtheyincorporateprogramsignals intotheirapproachandmoreeffectivelyselectapplicants whowillbehighestyieldfortheirprograms.By understandingsignalingtrendsasrelatedtoprogram characteristics,advisorsandapplicantsmaybeableto strategicallydeterminethebestapproachforallocating signalstomaximizeeachsignal’simpact.
Inourstudy,wenotedthatthePaci fi cWestandNew Englandregionsdemonstratedthehighestmeanand mediansignalnumbers.Incontrast,programsintheEast SouthCentral,Mid-Atlantic,WestSouthCentral,and WestNorthCentralMidwestreceivedfewersignals.Itis reasonabletospeculatethatmanyofthesepatternsre fl ect overallpopulationdensitypatterns,suggestinglocal preferencesthatmirrortheUSpopulation.Thishypothesis alignswithourdata,whichshowedthatmoreurban(likely morepopulation-dense)programsreceivedahigher proportionofsignals.Theonlyregionthatdoesnot fi tthis hypothesisistheMid-Atlanticregion,whichisthemost denselypopulatedinthecountry,butwesuspectthevery highEMprogramdensityinthisregionlikelycontributed toprogramsignaldilution,leadingtolowersignals perprogram.
Onaverage,four-yearprogramsreceivedahigher proportionofsignalingapplicantsthanthree-yearprograms. Whileprogramlengthitselfmaybeadriverofthis,itmay alsobeduetootherconfoundingfeaturesmorecommonly associatedwithfour-yearprograms,includingurban location,universityaffiliation,andprogramdurationand stability.Ultimately,ourdatawasunabletodiscernthis difference.Programswiththelowestproportionofsignaling applicantsweremorelikelytobesmaller,rural,andnot academicallyaffiliated.Theseprogramsweremorelikelyto rateresearchexperienceas “notimportantatall.” We suspectthatthesesmaller,morecommunity-oriented programsmaybelessresearch-focusedintheir missionsand,therefore,emphasizeresearchlessintheir applicantselection.Applicantsmaybeabletousethis informationtotargettheirsignalsdependingon theirinterests.
Itseemsintuitivethattheproportionofsignaling applicantsaprogramreceiveswouldaffecthowthat programvaluesandusesthesignal,buttoourknowledge thisisthe firstdatatodemonstratethateffect.When examiningsignalinguseamongprogramsseparatedinto quartilesbasedontheproportionofsignalingapplicants, significantdifferencesemerged.Programsthatreceived lowerproportionsofsignalingapplicantsweremorelikely toreportofferinginterviewstoallsignalingapplicants whilethosewiththehighestproportionofsignaling applicantsweremorelikelytoincorporatesignalsasa screeningtoolortohelpprioritizetheprogram’swaitlistor wait-listorder.
Byaskingprogramstoratetheimportanceofvarious applicationelements,wehopedtogainanunderstandingof therelativeimportanceofPSinrelationtointerviewoffers andROLcreation.Receivingaprogramsignalin orthopedicswasrankedamongthemostimportantfactorsin residentselectionforinterview.13 WhileasuccessfulsubinternshipatthePD’sinstitutionandlettersof recommendationwerethehighest-rankedcriteriafor residentselectionforinterviewaturologyprograms,81%of urologyPDsreportedthatalackofasignalwouldnegatively impactinterviewofferchancesforanapplicant.18 Inour study,programsignalswerenotshowntoholdasmuch weightasinorthopedicsorurology.Programsignalswere onlyratedasmoreimportantthannarrativelettersof recommendation,pre-interviewcommunication,and researchexperience.
Howanapplicantperformsclinically(SLOEs,Medical StudentPerformanceEvaluation)isunderstandablymost important,withPSintendedtobeonlyonesmallpartofthe holisticapplicationreview.22 Studentscanbereassuredthat thetraditionallyvaluedportionsoftheEMapplication retaintheirimportancewellabovethevalueofaprogram signal,andprogramsacrossallquartilesareinterviewingand rankingstudentswhodidnotsendthemasignal.
Analyzingthisdatainamoregranularfashion,wedid observesomesignificantdifferencesintherelativeimportance ofresidencyapplicationelementsbetweenquartiles.Asthe proportionofsignalingapplicantsincreased,theproportionof participantsendorsingboardscoresas “extremelyimportant” decreased.Thisdiscrepancymayspeaktotheintendedability ofPStomitigatetheuseof filteringbehavior.Programswith smallerproportionsofsignalingapplicantsmaycontinueto seekoutstrategiestostratifytheirapplicantpooltobetter allocatetheirholisticreviewefforts,suchasusingboardscore filters.Programswithahigherproportionofsignaling applicants,ontheotherhand,maynotfeelthissamepressure. Alternatively,itispossiblethathavingbeenpromptedbythe introductionofPStoinvestigateprogramsbeforeapplying, applicantsmaystrategicallyhavechosentotargettheirsignals toprogramsthatadvertisedalackofboardscorecutoffs becausetheirscorefellbelowstatedcutoffsatotherprograms orbecausetheyvaluedprogramsthatdonotemphasize standardizedtestscores.
Ourdataalsodemonstratesthatastheproportionof signalingapplicantsincreased,theproportionofrespondents ratingpre-interviewcommunicationas “extremely important” decreasedandtheproportionofrespondents ratingpre-interviewcommunicationas “notimportantat all” increased.Thistrendsuggeststhatthesignalisserving itsintendedpurposeofallowingtheapplicantto meaningfullyexpressinterest,obviatingtheneedfor additional,extra-applicationcommunication,lesseningthe burdenforbothapplicantsandprograms.Italsosuggests thatPSreducestheimpactofothercommunication fromapplicants.
TheAAMCguidancewasconsistentinitsmessagingthat programsignalswereonlytobeusedduringtheapplication reviewandinterview-offerportionoftheapplicationcycle.It isworthnotingthatdespiteallprogramshavingattestedin thecodeofconductnottousePSintheconsiderationof ROLplacement,11%ofprogramsreportedprogramsignals tobeveryimportanttotheROLdevelopmentprocess.The 2022–23AAMCPDsurveyfoundsimilarresultsamongPD respondentsfromallspecialties.6 Programdirectorsmaybe extrapolatingthatastudentwhosignaledislikelytobea higherprobabilitymatchthanastudentwhodidnotsenda signal.Thisusepresumesthatstudentpreferencewillnotbe significantlyaffectedbytheirexperiencesengagingwith programsthroughouttheinterviewseasonandisatriskof being flawedlogic.However,itisimportantthatapplicants beawarethatsignalsmaybeusedbyPDsinthismannerand shouldtakethisintoconsiderationwhenchoosingwhere tosignal.
ParticipationofEMprogramsinPSremainedrobust forthe2023–2024cycle,with278of279programs participatingand97.5%ofapplicantsparticipating(email communicationfromAAMCERASPilotAdministration Director,JaymeBograd,January2024).24 Wehopethat
thisdatahelpsinformprogramsandapplicantsona morenuancedapproachtoPSintheEMresidency applicationprocess.
Respondents(113)comparedtothetotalnumberof ACGME-accreditedEMresidencyprograms(277)was limited.ThePDswhochosetorespondmaydifferfrom thosewhodidnotconcerningtheirPSexperience.Forty-six percentofEMprogramsdidnot fi llinthe2023Main ResidencyMatch. 25 Oursurveywasdistributedintheweeks thatfollowed.ThePDsexperiencingadif fi cultMatchcycle mayhavebeenmoreorlessinclinedto fi lloutasurvey regardingtheresidencyapplicationprocess.Universitybasedprogramswereover-represented.Community-based, university-af fi liatedprogramswereunder-represented. The11%ofprogramsthatreportedusingsignalsaspartof theirROLdiscussionsmaybeanunderestimateasother programsmaynothavebeencomfortabledisclosing behaviorthatwasknowinglyinviolationofthecode ofconduct.
Thisstudyprovidesdetaileddataandpatternsofsignaluse yieldinginsightsintoprogramsignalinginEM’sinaugural yearforbothprogramsandapplicants.Ourdataprovidesa morenuancedunderstandingofsignalutilizationacrossa spectrumofEMprogramsinawaythatallowsindividual programstogobeyondthegeneralAAMCrecommendations andcomparetheirapproachtothatofprogramswithsimilar characteristics.Identifyingpatternsofsignalusebasedon programcharacteristicscanalsoinformadvisingfor studentsdecidingonhowtobestallocatetheirsignals. AsEMcontinuestonavigate fluctuationsinitsapplicant numbersandshiftingdemographicsofitsapplicantpool, providinginsighttoguidesignaluseandutilization canhelppaveapathforwardforthespecialtytowardthegoal ofmoreefficiently findingtherightapplicantforthe rightprogram.
Copyright:©2024Pelletier-Buietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.Pelletier-BuiAE,SchnappBH,SmithLG,etal.Makingourpreference known:preferencesignalingintheemergencymedicineresidency application. WestJEmergMed. 2021;23(1):72–5.
2.AssociationofAmericanMedicalColleges.ERASpreliminarydataasof January3eachseason.2024.Availableat: https://www.aamc.org/ media/6231/download?attachment.AccessedApril20,2024.
3.RamsayN.EMmatch2020bythenumbers.2020.Availableat: https:// www.emra.org/students/newsletter-articles/em-match-2020-bythe-numbers/.AccessedApril20,2024.
4.Pelletier-BuiA,WerleyE,CamejoM.EMRAhangouts-preference signaling101.2022.Availableat: https://www.emra.org/be-involved/ events–activities/emra-hangouts/20220721-preference-signaling AccessedApril20,2024.
5.AssociationofAmericanMedicalColleges.SupplementalERAS® application:guideforresidencyprograms.2022.Availableat: https://www.aamc.org/media/56451/download/ AccessedApril20,2024.
6.AssociationofAmericanMedicalColleges.SupplementalERAS® 2022–2023applicationcycle:evaluationofprogramsignaling.2023. Availableat: https://www.aamc.org/media/64591/download AccessedApril20,2024.
7.AssociationofAmericanMedicalColleges.SupplementalERAS® 2022–2023applicationcycle:resultsoftheprogramdirectorreaction survey.2023.Availableat: https://www.aamc.org/media/64996/ download.AccessedApril20,2024.
8.LaFeminaJ,RosmanIS,WallachSL,etal.Therelationshipbetween programandapplicantcharacteristicswithapplicantprogramsignalsin the2022residencyrecruitmentcycle: findingsfrom3specialties. AcadMed. 2024;99(4):430–6.
9.RosenblattAE,LaFeminaJ,SoodL,etal.Impactofpreferencesignals oninterviewselectionacrossmultipleresidencyspecialtiesand programs. JGradMedEduc. 2023;15(6):702–10.
10.BanksE,WinkelAF,MorganHK,etal.Programsignalinginobstetrics andgynecologyresidencyapplications. ObstetGynecol. 2024;143(2):281–3.
AddressforCorrespondence:AlexisPelletier-Bui,MD,Cooper MedicalSchoolofRowanUniversity/CooperUniversityHospital, DepartmentofEmergencyMedicine,401HaddonAve.,Education& ResearchBuilding,2ndFloor,CamdenNJ08103. Email: pelletier-bui-alexis@cooperhealth.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
11.BenjaminWJ,LenzeNR,BohmLA,etal.Impactofapplicants’ characteristicsandgeographicconnectionstoresidencyprogramson preferencesignalingoutcomesinthematch. AcadMed. 2024;99(4):437–44.
12.SergesketterAR,SongE,ShammasRL,etal.Preferencesignaling andtheintegratedplasticsurgerymatch:anationalsurveystudy. JSurgEduc. 2024;81(5):662–70.
13.SureshKV,CovarrubiasO,MunF,etal.Preferencesignalingsurvey ofprogramdirectors-afterthematch. JAmAcadOrthopSurg. 2024;32(5):220–7.
14.KotlierJL,MihalicAP,PetriglianoFA,etal.Understanding thematch:theeffectofsignaling,demographics,andapplicant characteristicsonmatchsuccessintheorthopaedic residencyapplicationprocess. JAmAcadOrthopSurg. 2024;32(5):e231–9.
15.CaiF,SouthworthE,SantiagoS,etal.Thegoldentickets:impactof preferencesignalingonobstetricsandgynecologyresidency applicants. AmJObstetGynecol. 2024;230(2):262.e1–9.
16.GrauerR,RantiD,GreeneK,etal.Characterizationofapplicant preferencesignals,invitationsforinterviews,andinclusiononmatch listsforresidencypositionsinurology[publishedcorrectionappears inJAMANetwOpen.2023;6(2):e233305]. JAMANetwOpen. 2023;6(1):e2250974.
17.ChangCWD,ThorneMC,MalekzadehS,etal.Two-yearinterviewand matchoutcomesofotolaryngologypreferencesignaling. Otolaryngol HeadNeckSurg. 2023;168(3):377–83.
18.Rodriguez-AlvarezJS,Munoz-LopezC,HarwoodSJr.,etal.Urology residencyapplicantselection:programdirectors’ newcriteria. Urology. 2024;S0090–4295(24):00141–9.
19.DillmanDA. MailandInternetusrveys:TheTailoredDesignMethod: 2007withNewInternet,VisualandMixed-ModeGuide.2nded. Hoboken,NJ:JohnWiley&Sons,2007.
20.AmericanMedicalAssociation.Fellowshipandresidencyelectronic interactivedatabase(FREIDA™).Availableat: https://freida.ama-assn. org.AccessedApril20,2024.
21.EmergencyMedicineResidents’ Association(EMRA).EMRAmatch database.Availableat: https://match.emra.org/ AccessedApril20,2024.
22.NationalResidentMatchingProgram.Resultsofthe2021NRMP programdirectorsurvey.2021.Availableat: https://www.nrmp.org/wpcontent/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf AccessedApril20,2024.
23.AssociationofAmericanMedicalColleges.Residencyprograms participatinginprogramsignaling.2023.Availableat: https://studentsresidents.aamc.org/applying-residencies-eras/residencyprograms-participating-program-signaling.AccessedApril20,2024.
24.AssociationofAmericanMedicalColleges.Exploringtherelationship betweenprogramsignaling&interviewinvitationsacrossspecialties: 2024ERASpreliminaryanalysis.2024.Availableat: https://www.aamc. org/media/74811/download?attachment.AccessedApril20,2024.
25.NationalResidentMatchingProgram.Resultsanddata:2023main residencymatch.2023.Availableat: https://www.nrmp.org/wp-content/ uploads/2023/05/2023-Main-Match-Results-and-Data-Book-FINAL. pdf.AccessedApril20,2024.
DianeL.Gorgas,MD*
KevinB.Joldersma,PhD†
FelixK.Ankel,MD‡
WallaceA.Carter,MD§
MelissaA.Barton,MD†
EarlJ.Reisdorff,MD†
*OhioStateUniversityWexnerMedicalCenter,DepartmentofEmergencyMedicine, Columbus,Ohio
† AmericanBoardofEmergencyMedicine,EastLansing,Michigan ‡ RegionsHospital,DepartmentofEmergencyMedicine,St.Paul,Minnesota
§ WeillCornellMedicine,DepartmentofEmergencyMedicine,NewYork,NewYork
SectionEditors:KendraParekh,MDandAbraFant,MD
Submissionhistory:SubmittedJanuary16,2024;RevisionreceivedJune14,2024;AcceptedJuly8,2024
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18703
Background: Theemergencymedicine(EM)milestonesareobjectivebehaviorsthatarecategorized intothematicdomainscalled “subcompetencies” (eg,emergencystabilization).Thescaleforrating milestonesispredicatedontheassumptionthatarating(level)of1.0correspondstoanincomingEM-1 residentandaratingof4.0isthe “targetrating” (albeitnotanexpectation)foragraduatingresident.Our aiminthisstudywastodeterminethefrequencywithwhichgraduatingresidentsreceivedthetarget milestoneratings.
Methods: Thisretrospective,cross-sectionalstudywasasecondaryanalysisofadatasetusedinaprior studybutwasnotreportedpreviously.WeanalyzedmilestonesubcompetencyratingsfromApril 25–June24,2022forcategoricalEMresidentsintheir finalyearoftraining.Ratingsweredichotomized asmeetingtheexpectedlevelatthetimeofprogramcompletion(ratingsof ≥3.5)andnotmeetingthe expectedlevelatthetimeofprogramcompletion(ratingsof ≤3.0).Wecalculatedthenumberofresidents whodidnotachievetargetratingsforeachofthesubcompetencies.
Results: InSpring2022,ofthe2,637residentsinthespringoftheirlastyearoftraining,1,613(61.2%) achievedaratingof ≥3.5oneverysubcompetencyand1,024(38.8%)failedtoachievethatratingonat leastonesubcompetency.Therewere250residents(9.5%)whofailedtoachievehalfoftheirexpected subcompetencyratingsand105(4.0%)whofailedtoachievetheexpectedrating(ie,ratingwas ≤3.0)on everysubcompetency.
Conclusion: WhenusinganEMmilestoneratingthresholdof3.5,only61.2%ofphysiciansachievedthe targetratingsforprogramgraduation;4.0%ofphysiciansfailedtoachievetargetratingsforany milestonesubcompetency;and9.5%ofphysiciansfailedtoachievethetargetratingsforgraduating residentsinhalfofthesubcompetencies.[WestJEmergMed.2025;26(1.2)11–14.]
WiththeadventoftheNextAccreditationSystem(NAS), theAccreditationCouncilforGraduateMedicalEducation (ACGME)introducedanewassessmentprocesscalledthe “milestones.”1 Themilestonesareobjectivebehaviorsthat reflectelementsofthemajorcompetencies(eg,patientcare, systems-basedpractice)inthematicdomainscalled “subcompetencies” (eg,emergencystabilization,patientandfamily-centeredcommunication).Themilestonescale
usesnineratingsfrom1.0,1.5,2.0,2.5,etc,to5.0.Thescaleis predicatedontheassumptionthatarating(level)of1.0 correspondstoanincomingemergencymedicine(EM)-1 residentandaratingof4.0isthegraduation “target,” albeit notagraduationexpectationorrequirement.Accordingto theACGME: “Level4isdesignedasagraduation goal but doesnot representagraduation requirement . ”2 TheEM milestoneshavebeenusedexclusivelyasaformative assessmentbytheACGME.Likewise,aphysician’sEM
milestoneratingsarenotconsideredwhendetermining theeligibilityofaphysiciantotaketheAmerican BoardofEmergencyMedicine(ABEM)written qualifyingexamination.
TheEMmilestoneswereintroducedin2012,andthe first ratingswerereportedin2013.3 TheEMmilestoneswere revisedin2021,resultingin22subcompetencies.Since2012, substantialvalidityevidencefortheEMmilestoneshasbeen accumulated.4–10 Aresident’smilestoneratingsareusually assignedbyclinicalcompetencycommittees(CCCs).Some subcompetencyratingsarebelowtargetlevels.Often,the subcompetencyratingsassignedbytheCCCsarelowerthan theratingsthatresidentsgivethemselves.11 Themilestones wereinitiallydesignedtohavearatingof4.0asthetargetfor aresidentcompletinganEMresidency.9 AggregateEM milestonesarereportedannuallybytheACGME.12 These dataandotherreportssuggestthatasubstantialnumberof graduatingresidentsarenotachievingalevel4ratingin manymilestonesubcompetencies.
Weundertookthisstudytodeterminethefrequency withwhichgraduatingresidentsreceivedthetarget milestonerating.
Thisretrospectivecross-sectionalstudywasasecondary analysisofanalreadyde-identifieddatasetusedinaprior study.13 Ourcurrentstudywasdeemedexemptfromhuman subjectresearchbytheWestern-CopernicusGroup InstitutionalReviewBoard.Thedatasetavailabletothe investigatorsdidnotincludephysicianorprogram characteristicsthatwouldallowamoredetailedanalysis.
Weanalyzedmilestonesubcompetencyratingsfrom Spring2022forcategoricalEMresidentsintheir finalyearof training.Thesemilestoneratingsweresubmittedbetween April25–June24.ThisratingsreportusedEMMilestones 2.0,whichincluded22subcompetencies.Thedatasethad beenprovidedearliertoABEMbytheACGMEaspartof theroutineEMmilestonessecuredata-sharingprocess.
Theprimarymeasurewasthenumberofsubcompetencies forwhichphysiciansfailedtoachieveatargetratingof3.5at thetimethattheSpringmilestoneratingsweresubmittedto theACGME.Becausetheratingsweresubmittedbetween AprilandJunepriortoresidencycompletion,andtheCCC couldhavedeterminedtheratingsevenearlierthanthat,an expectedratingforpurposesofthestudywasmodifiedtobe 3.5ratherthan4.0.Doingsoassumedthattheresidentwould achievearatingof4.0overtheremainingweekstomonthsof residencytraining.Wedeterminedthenumberofphysicians
whodidnotachievethetargetratingforthesubcompetencies (from0subcompetenciestoall22subcompetencies).
Ratingsweredichotomizedasmeetingthetargetlevelat thetimeofprogramcompletion(≥3.5)andnotmeetingthe targetlevelatthetimeofprogramcompletion(≤3.0).We calculatedthenumberofcompetenciesforwhichatarget ratingwasnotachieved.
InSpring2022,thereweremilestoneratingsfor2,637 residentsintheSpringoftheirlastyearoftrainingin279EM residencies.Therewere1,613residents(61.2%)whoachieved aratingof ≥3.5oneverysubcompetencyand1,024residents (38.8%)whofailedtoachievearatingof ≥ 3.5onatleastone subcompetency.Therewere250physicians(9.5%)whofailed tomeethalfoftheirtargetsubcompetencyratings.There were105residents(4.0%)whofailedtomeetthetargetrating (ie,ratingwas ≤3.0)oneverysubcompetency(Table).
Table. Thefrequencyofemergencymedicineresidentsreceiving targetmilestonesratingslowerthat3.5inSpring2022(n = 2,637). Numberofratings
First,theactuallevelofsubcompetencyachievementat graduationwasimpreciselyknown.Wechosearatingof ≥3.5torepresenttheperformancetarget,giventhatthe milestoneratingswereprovidedpriortothecompletionof theprogram.Usingaratingof4.0tobeassignedtwomonths priortograduationwouldlikelyunderestimate subcompetencyachievementandascoreof3.5attwo monthspriortoprogramcompletionwouldlikely overestimatesubcompetencyachievement.Anticipatingthat allresidentswitharatingof3.5wouldachievearatingof4.0 withinweekswasabenevolentassumption.Second, demographicdataonresidents(eg,gender)andprogram characteristics(eg,durationoftraining)wereunavailableto theinvestigators.Althoughthislackofadditional informationlimitedourabilitytodeterminefactors associatedwiththeratings,webelievethatthe findings aresufficientlysignificantontheirmeritandwarrant additionalinvestigation.
Third,wedidnotcorrelatepoorsubcompetencyratings withprogramextensionorremediation,thuslimitingthe opportunitytogatheranyevidenceofpredictiveor consequentialvalidity.Itispossiblethatnearlyevery physicianwhodidnotachievearatingof ≥3.5onnearlyhalf ofthemilestonesubcompetenciesunderwentremediation. Fourth,theratingsareassignedbyCCCs.Thestructuresof, andinformationusedbyCCCs,varybyEMresidency.14,15 Wedidnotattempttodeterminethereliabilityoraccuracyof theindividualratings.Moreover,wedidnotexaminethe potentialimpactofbiasintheratings.Priorstudiessuggested thatwomenwereassignedlowerperformanceratings.16,17 Sixth,theratingsusedforthisstudywerefromthe firstyear oftheEMMilestones2.0.Althoughtherewasadegreeof acclimationindevelopingfacilitywiththeEMMilestones 1.0,itislikelythatthesamedegreeofunfamiliaritywouldbe lesswiththemostrecentversion.Thedegreetowhichthe continueduseofEMMilestones2.0willchangeratingtrends isunknown.
Thisstudyisthe firstinEMtodemonstratethedegreeto whichphysicianscompletingEMresidenciesarenot achievingtargetsubcompetencyratings.Thesedatashowed thatofthe2,637residentsintheirlastyearoftraining,nearly oneintenfailedtomeettargetratingsforhalfoftheEM subcompetencies.Asimilar findingwasreportedfor physicianscompletingpediatricEMfellowships.18 However, thatreportusedatargetratingof4.0,not3.5asinourstudy. Consequently,67%ofpediatricEMfellowsdidnotattaina ratingofatleast4.0foratleastonesubcompetency.
Aphysicianshouldbeabletograduatefromresidency withoutscoring4.0onall22subcompetencies.Infact,all4.0 ratings(astraight-linescore)wouldbehighlyimprobable.19 Considerthehypotheticalsituationthatwouldresultfrom
themilestonesbeingusedinasummativemannerto determineABEMboardeligibility.Ifresidentswererequired tohavenomorethansixsubpar(ie, <3.5)milestoneratings (morethanone-fourthofthesubcompetencies),then353 residents(13.4%)intheir finalyearoftrainingwouldnotbe eligibletotaketheABEMwrittenqualifyingexamination. Giventheintentofthemilestonesasaformativeinstrument, ABEMmaintainsthepositionthatthemilestonesshouldnot beusedasasummativedeterminantofboardeligibility.
Therateofprogramextensionbyphysiciansbeyonda scheduledgraduationdatehasbeenreportedtobe approximately8.5%.13 Theseextensionsincludephysicians undergoingacademicremediation,aswellasprogram extensionsduetoapersonalleaveofabsence.Theprevalence ofphysiciansnotmeetinghalfofthetargetsubcompetency ratingswas9.5%.Basedonthese findings,therewere physicianswhofailedtomeetatleasthalfoftheEM milestonesubcompetenciesyetweredeemedcompetentto practiceautonomouslyasattestedbytheprogramdirector. Thislikelihooddoesnotchallengetheconstructvalidityof themilestones,nordoesitsuggestthatthetargetistoohigh. Inafact,apriorvaliditystudybyKorteetalusedprogram directorsurveydatatoverifytheappropriatenessofthe targetratings.9
Inthisstudywedidnotanalyzetheimpactoftraining length(EM1-3vsEM1-4).However,areviewofmeanscores wasundertakeninapriorinvestigationthatusedthesame studyperiod.13 ThescoressuggestthatresidentsinEM1-3 programstendedtohavehigherscoresthroughthe postgraduateyears(PGY)1–3.Forexample,inthePGY3year,residentsfromEM1-3programshadameanratingof 3.51(95%confidenceinterval[CI]3.50–3.53)andresidents fromEM1-4programshadameanratingof3.07(95%CI 3.05–3.09),whileEM4residentshadameanratingof3.67 (95%CI3.65–3.69).
Thisanalysisisaninitialexplorationintoamorethorough investigationofthe finalmilestonesratingthatanEM residentreceives.Thecurrentstudydoesnotidentifyvariable impactwithindemographicgroups,nordoesitprovideany indicesofpredictivevalidity.Giventhe findingsofthis analysis,amorethoroughanalysisofthemilestonesshould beundertakentodeterminetheirpsychometricqualitiesand subsequentutilityinthe field.Giventheuseofthemilestones asaformativeevaluationsystem,itshouldnotbeusedto makesummativedecisionssuchasthedeterminationof ABEMboardeligibility.Amorestructured,valid,and reliableprocessformakingthesummativedetermination thataphysicianhasdemonstratedthenecessary competenciestopracticesafelyandindependentlyis advisable.Moreover,suchadetailedsummativeprocess couldalsobeusedtomakeaconfidentdeterminationthata physicianiseligibleforboardcertification.Thisprocess wouldbeeasilyaccommodatedinamodelofcompetencybasedmedicaleducation.
ManyphysicianscompleteanEMresidencywithout meetingatargetratingforagraduatingresidentinuptohalf oftheEMmilestones.Someresidents(4%)didnotmeeta targetratinginanymilestone.These findingssupportthe continueduseofthemilestonesasaformativeinstrument, ratherthanatooltodetermineboardeligibility.
AddressforCorrespondence:DianeL.Gorgas,MD,American BoardofEmergencyMedicine,3000CoolidgeRoad,EastLansing, MI48823.Email: diane.gorgas@osumc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Drs.Gorgas,Ankel,andCarterare membersoftheAmericanBoardofEmergencyMedicine(ABEM), BoardofDirectors.Drs.Joldersma,Barton,andReisdorffare employeesofABEM.ABEMreceivesnorevenuefromEmergency MedicineMilestonesreporting.Therearenootherconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Gorgasetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.NascaTJ,PhilibertI,BrighamT,etal.ThenextGMEaccreditation system–rationaleandbenefits. NEnglJMed. 2012;366(11):1051–6.
2.EmergencyMedicineMilestones.TheAccreditationCouncilfor GraduateMedicalEducation.2021.Availableat: https://www.acgme. org/globalassets/PDFs/milestones/emergencymedicinemilestones.pdf AccessedAugust4,2023.
3.BeesonMS,CarterWA,ChristopherTA,etal.Emergencymedicine milestones. JGradMedEduc. 2013;5(1Suppl1):5–13.
4.BeesonMS,CarterWA,ChristopherTA,etal.Thedevelopmentofthe emergencymedicinemilestones. AcadEmergMed. 2013;20(7):724–9.
5.BeesonMS,HolmboeES,KorteRC,etal.Initialvalidityanalysis oftheemergencymedicinemilestones. AcadEmergMed. 2015;22(7):838–44.
6.HamstraSJ,CuddyMM,JurichD,etal.Exploringtheassociation betweenUSMLEscoresandACGMEmilestoneratings:avalidity studyusingnationaldatafromemergencymedicine. AcadMed. 2021;96(9):1324–31.
7.HamstraSJ,YamazakiK,BartonMA,etal.Anationalstudyof longitudinalconsistencyinACGMEmilestoneratingsbyclinical competencycommittees:exploringanaspectofvalidityinthe assessmentofresidents’ competence. AcadMed. 2019;94(10):1522–31.
8.HolmboeES,YamazakiK,NascaTJ,etal.Usinglongitudinal milestonesdataandlearninganalyticstofacilitatetheprofessional developmentofresidents:earlylessonsfromthreespecialties. AcadMed. 2020;95(1):97–103.
9.KorteRC,BeesonMS,RussCM,etal.Theemergencymedicine milestones:avalidationstudy. AcadEmergMed. 2013;20(7):730–5.
10.PeckTC,DuboshN,RosenC,etal.Practicingemergencyphysicians reportperformingwellonmostemergencymedicinemilestones. JEmergMed. 2014;47(4):432–40.
11.GoldflamK,BodJ,Della-GiustinaD,etal.Emergencymedicine residentsconsistentlyratethemselveshigherthanattending assessmentsonACGMEmilestones. WestJEmergMed. 2015;16(6):931–5.
12.EdgarLaura,HoganSO,HolmboeES,etal.Milestones:National Report.2022. https://www.acgme.org/globalassets/pdfs/milestones/ 1160-ACGME-Milestones-Report-2022-R22.pdf AccessedAugust4,2023.
13.BeesonMS,BartonMA,ReisdorffEJ,etal.Comparisonofperformance databetweenemergencymedicine1–3and1–4programformats. JAmCollEmergPhysicians.Open 2023;4(3):e12991.
14.DotyCI,RoppoloLP,AsherS,etal.Howdoemergencymedicine residencyprogramsstructuretheirclinicalcompetencycommittees? Asurvey. AcadEmergMed. 2015;22(11):1351–4.
15.GoyalN,FoltJ,JaskulkaB,etal.Assessmentmethodsandresource requirementsformilestonereportingbyanemergencymedicineclinical competencycommittee. MedEducOnline. 2018;23(1):1538925.
16.SantenSA,YamazakiK,HolmboeES,etal.Comparisonofmaleand femaleresidentmilestoneassessmentsduringemergencymedicine residencytraining:Anationalstudy. AcadMed. 2020;95(2):263–8.
17.DayalA,O’ConnorDM,QadriU,etal.Comparisonofmalevsfemale residentmilestoneevaluationsbyfacultyduringemergencymedicine residencytraining. JAMAInternMed. 2017;177(5):651–7.
18.RoskindCG,LeonardK,BaghdassarianA,etal.Pediatricemergency medicinefellows’ milestoneevaluations:dotheyallmeetthetargetsfor graduation? AEMEducTrain. 2021;5(3):e10620.
19.BeesonMS,HamstraSJ,BartonMA,etal.Straightlinescoringby clinicalcompetencycommitteesusingemergencymedicinemilestones. JGradMedEduc. 2017;9(6):716–20.
SamaraHamou,BA*
ShayanGhiaee,MD,MS†
ChristineChung,MD‡
MaureenLloyd,MD‡
KellyKhem,MD§
XiaoChiZhang,MD,MS§
*SidneyKimmelMedicalCollege,Philadelphia,Pennsylvania † DepartmentofEmergencyMedicine,EmoryUniversity,Atlanta,Georgia ‡ DepartmentofOphthalmology,WillsEyeHospital,Philadelphia,Pennsylvania § DepartmentofEmergencyMedicine,ThomasJeffersonUniversity, Philadelphia,Pennsylvania
SectionEditors:JulesJung,MDandAndrewKetterer,MD
Submissionhistory:SubmittedOctober20,2023;RevisionreceivedMarch21,2024;AcceptedJune7,2024
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18514
Introduction: Eyeemergenciesmakeupnearly3%ofUSemergencydepartment(ED)visits.While emergencyphysicians(EP)shoulddiagnoseandtreattheseophthalmologicemergencies,many traineesreportlimitedocularexposureandinsufficienttrainingthroughouttheirresidencytoconfidently conductathoroughslit-lampexam.
Methods: Wecreatedaninterdisciplinary,simulation-basedmasterylearning(SBML)curriculumto teachemergencyattendingphysicianshowtooperatetheslitlampwithmultimodallearning methodologyatatertiaryacademiccenter.TheEPs firstdemonstratetheirinitialslit-lampcompetency witha20-itemchecklist,andtheythenreviewthenecessarycurricularcontenttopasstheirindependent readinesstestbeforecompletingtheirin-personteachinganddemonstrationsessionwithan ophthalmologyattendingtodemonstrateproceduralmastery(minimalpassingscore >90%).
Results: FifteenEPswereenrolled;allcompletedthe finalexamofthecurriculum.Thepre-andpostcurriculumchecklistscoresincreasedbyanaverageofsevenpoints(P = .002);86.7%ofEPsfelt confidentincompletingaslit-lampexamafterthecurriculum,comparedto20%atthebeginning.Fiveof 15reportedteachinglearnerswithinthetwo-monthpost-curricularperiod,rangingfrom5–30students. Thehands-onteachingwasthemostpositivelyreviewedelementofthecurriculum.
Conclusion: TheSBMLprogramsuccessfullytrainedEPsonperformingacomprehensiveslit-lamp examwithpromisingresultsofdownstreameducationtojuniorlearners.Weencourageotherinstitutions toleverageSBMLasateachingmodalityforprocedural-basedtrainingandadvocatecross-discipline educationinitiatives.[WestJEmergMed.2025;26(1.2)15–24.]
Theslit-lamp1 (Figure1A)isamicroscopethatallowsfor adetailedexaminationoftheanterioreyesegmentusinglight beammanipulation.Theslit-lampenablesphysiciansto diagnoseanteriorophthalmicpathologiessuchascorneal injuries,iritis,hyphema,hypopyon,andforeignbodies2; furthermore,itisessentialforperformingdetailed ophthalmologicexamtechniquessuchaslideversion, fluoresceinexamination,andforeignbodyremoval.3 The Wood’slamp4 (Figure1B),incontrast,isahandhelddevice oftenusedtocharacterizeskinpigmentation,dermal infections,andmacroscopicinfectionswithabuilt-in magnifyinglensandultraviolet(UV)light.TheUV capabilitiescanhighlight fluoresceinstainingduringexternal ocularexamstoassesscornealpathologiesatlower magnification.WhiletheWood’slampoffersalessdetailed examinationthantheslitlamp,itisamoreportable diagnostictoolforlargerocularlesions,foreignbodies,or
specificreactionto fluoresceinstainingandmeetstheneedsof theemergencyphysician(EP)undercertainsituations.
Eyeemergenciesmakeupnearly3%ofUSemergency department(ED)visits,themostcommonofwhichare traumatic.5,6 Themostcommoneyeinjuryevaluatedinthe EDiscornealabrasion(superficialinjurytothecornea)and eyelidlaceration.Suchinjuriesarebestviewedunderhighfieldmagnifiedviewingusingtheslitlamptoassessfor concomitantinjuriesorco-infectionssuchascornealulcers, hypopyon/endophthalmitis,retainedforeignbody,full thicknesscorneallaceration,globeruptures,andseidel testing.7 Ocularemergenciessuchastraumaticgloberupture, ocularforeignbody,closed-angleglaucoma,and endophthalmitisarevisibleonlyusingtheslitlamp,andfall withintheEP’sscopeofpracticefordiagnosis,triaging,and management.8 Mismanagedophthalmicemergenciescan resultininappropriateconsultation,excessivetesting, financialburden,andevenirreversiblevisionloss.9 Despite thesignificanceandfrequencyofocularemergenciesacross theUS,manyEPsarenotconfidentperformingadetailed ophthalmicexam.10
PreviousliteraturehasfoundEPsreceivefewerthan10 hoursofophthalmiceducationduringresidencywithlow confidenceinperformingacomprehensiveophthalmicslitlampexam.11 Ophthalmiceducationthroughclerkshipsand didacticsinmedicalschoolisalsoindecline,leadingtothe unpreparednessofincomingresidentsbeforeanyformal residencytraining.11,12 However,itisimportantthatEPsbe confidentinusingtheslitlamptoappropriatelytriageand manageocularemergenciesaspartoftheAccreditation CouncilforGraduateMedicalEducation(ACGME) EmergencyMedicine(EM)MilestonesPatientCaredomain (PC8) – GeneralApproachtoProcedures,whichdesignatesa setofsequentialmilestonesforoverallprocedural competency,notfocusingonaspecificlistofprocedures.13
Theoptimallearningenvironmentforadultlearnersto performatechnicallychallengingprocedureshould incorporateelementsfromboththemasterylearningmodel andrapidcycledeliberatepractice(RCDP).Themastery
learningmodelensuresthatstudentscanmasteratopicif theyreceiveunlimitedtimeandsupportinlearningand reviewingmaterialuntilmasteryproficiencyisreached. Meanwhile,theRCDPmodelensureslearnerscanpractice skillsrepetitivelywhilereceivingbrief,interspersedfeedback toachieveadesignatedproficiencylevelbeforeproceedingto thenexttask.14,15–17 Withinmedicaleducation,simulationbasedmasterylearning(SBML)modelshavebeen successfullyimplementedacrossvariousspecialties,suchas emergencymedicine,generalsurgery,criticalcare,and gastroenterology.18,19,20 Inlightofsuccessful,smallerscaled studiesontheeffectivenessofslit-lamptrainingwithin undergraduatemedicaleducation,weproposeaSBML proceduraltrainingcurriculumthatcanenableadultlearners toconductdeliberateperformancesofintendedcognitiveor psychomotorskillsinsequentialorderwitharepetitiveskills assessment.15,21,22 Specific,informativefeedbackwillenable sustainedperformanceimprovementtoachieveslit-lamp mastery.23 Ourgoalwastodesignapilotinterdisciplinary coursethatcouldteachEPstocompleteacomprehensiveslitlampexamindiagnosingcommonanterioreyepathology.
Ourstudy,EmergencyDepartmentSlitLamp InterdisciplinaryTrainingviaLongitudinalAssessmentin MedicalPractice(EDSLITLAMP),isamulticentered, collaborativeprojectthatleveragestheconceptual frameworksofthemasterylearningmodelandRCDPto ensureproficiencyinconductingacomprehensiveslitlamp exam.Italsoservesasascaffoldfordeconstructingbarriers intraditionalsiloedmedicalpracticesandleadstoimproved patientcare,knowledgesynthesis,andresourceutilizationof ourconsultingservices.ThestudywasconductedatThomas JeffersonUniversity(TJUH)andtheWillsEyeHospital (WEH)from2021– 2023.Thehospitalswiththeirrespective EDs,are0.2milesapart,withstafffromeachinstitution workingasconsultantsattheother;WEHresidentsfunction asophthalmologyconsultationfortheTJUHED,while TJUHEPsfunctionasovernightmedicalemergency

consultantsattheWEHED.Thegeographicand relationshipproximitycreatedidealconditionstodevelop andpilotaproceduralskillcompetenceSBMLcurriculum.
Emergencyphysicianswereselectedasideallearnersdue totheirleveloftraininganduniqueteachingresponsibilities. UsingtheTJUHEDlistservwerecruitedeligible participantsandofferedstaggered financialincentives.For thispilotstudy,werequiredaminimumof12participantsto meet5%type1errorand80%powerbasedonscore improvementfrombaselinetestingtopost-testing,as referencedbyMilleratal.24 TheEDSLITLAMPstudy leveragedtalentsfromcontentandeducationexpertsfrom bothinstitutionstocreateaninterdisciplinaryprocedural teachingcurriculum.ThesuccessofatraditionalSBML curriculumislinkedtothelearners’ skillacquisition.Our studyexpandsthismeasuretoincludeinterdisciplinary collaboration,demonstratingthesuccessfulalignment betweeneducationalandpatient-centeredgoalsthatbenefit bothdepartments.Toevaluatethecurriculum,weemployed allfourlevelsoftheKirkpatrickmodel.Usingpre-andposttestLikertscalequestionnaires,ourmeasurementofsuccess includedimprovedlearnerconfidence(level1),knowledge acquisition(level2),willingnessoflearnerstoincorporate theirskillsetinclinicalpractice(level3),anddisseminationof thisknowledgetojuniorlearners(level4).Anycurricular feedbackandimprovementswereextractedforfuture curriculariterations.
Aneeds-basedanalysisconductedatTJUHEDrevealed EPsdesiredhands-onslit-lampeducationandtrainingon identifyinganteriorsegmentophthalmiccomplaints.Since ophthalmologyisarecognizedcomponentoftheAmerican BoardofEmergencyMedicineexamcontent,weconstructed thepre-testclinicalcontentbasedoncriticalandcommon oculardiagnoses,themostcommonWEHED ophthalmologydischargediagnoses,andclinical identificationsdeemed “ can ’tmiss” bytheEDand ophthalmologydepartment.
Allcurricularcontents(lecturematerials,videorecording, pre-post-postassessments,studysurveys,masterylearning checklist)werecreatedbytheprincipalinvestigator[XCZ] withophthalmologyco-investigatorsconsultation[CC, MEL]basedontargetedneedsassessment.Thesematerials underwentsequentialreviewbyselectexpertsatWEHand weremodifiedsequentiallyuntilaconsensuswasreached. Theminimalpassingchecklistscorewasdeterminedtobe 90%,basedoncombineddeterminationfrom ophthalmologistexpertsatWEHandsimilarthreshold determinedbyMilleretal.24 Eachcurriculumassessment (AppendixA)wasconstructedtomirrorthenatural knowledge,skills,andattitudeprogressionfromthe ACGMEEMMilestonesPatientCareDomain(PC8).Due tothemultifacetednatureofEM,thereisnospecific proceduralmilestoneforperformingaslit-lampexam,as describedindetailintheACGMEOphthalmologyPC1:
DataAcquisition-BasicOphthalmologyExamandTesting (Level1).13 However,theEMPC8milestonesprovide structuredlanguageapplicabletomanyEDproceduresand advanceddevice-assistedmedicalexaminations(ie,slit-lamp exam).Pleasesee Table1 forthecorrelationbetweentheEM milestoneandEDSLITLAMPassessments.
Thelongitudinalcurriculumincludedfouruniquetime points(Time0–3)ofinterventionstaggeredoversixmonths (AppendixA, AppendixB).AtTime0,participants completedanin-personbaselineslit-lampexamthatwas video-recordedandreviewedbytwoindependent investigators[XCZ][MEL].AtTime1,theparticipants gainedaccesstoanasynchronouslearningpacketthat consistedofaPowerPointpresentationoncommonEDeye complaints,digitallibrarylinkstotheWEHManual,slitlampchecklist,andavideorecordingofacomprehensiveslitlampexamination.25 Theparticipantsalsogainedaccessto anindependentreadinessassessment(IRAT),whichwas requiredtobecompletedwithin30dayswithaminimum scoreof90%beforeproceedingtothenextin-personphaseof thestudy(AppendixA).
UponachievingthepassingIRATscore,theywereinvited toparticipateintheTime2(in-person)SBMLportionofthe studywheretheyweretocompleteanin-person demonstrationofacomprehensiveslit-lampexambya board-certifiedophthalmologist[CC]onastandardized patientvolunteer.Followingthedemonstration,participants weregivenunlimitedtimeforRCDPwithbrief,interspersed feedbackundertheobservationandteachingfromthe ophthalmologist.Participantswererequiredtocompletea minimum18of20checklistitemstoachievemastery (AppendixB).Uponcompletingthe finalchecklist,the participantswereaskedtocompleteacourseevaluationand learnerconfidencesurvey(AppendixC)withLikertscaling, subjectivecommentary,andavalidated5-itemCritical IncidenceQuestionnaire(CIQ)forcurricularimprovement. Giventheunpredictabilitynatureofthe “unlimited attempts” atTime2,allparticipantswerescheduledattwohourintervalstoallowfordevicepreparation,onetotworeattempts,debriefing,surveycompletion,andgeneral troubleshooting.AtTime3,participantscompleteda60-day post-examinationsurvey,assessingtheirocularknowledge, slit-lampconfidence,clinicalteachingopportunities,and relevantinterprofessionalrelationships.
WeusedaWilcoxonsigned-ranktesttodifferentiatethe checklistscoresbetweenthecurricularinterventionby incorporatingcollectedpaireddatabeforeandafterthe training,medianandinterquartilerangevaluesofsubtotal scoresattwo-timepoints.26 WeusedMcNemar’stestto comparingeachcategoricalsub-score(Yes/No)bytime pointsandcorresponding P -valuewithinthesame population.27 Thedescriptivesummariesofsurveyquestions atTime0,Time2,andthree-monthfollow-upwereanalyzed usingBonferroniadjusted P -values(multiplying P -value
Table1. Correspondingemergencydepartmentslit-lampassessmentstoACGMEEM*milestonegeneralapproachtoprocedures. ACGME
EMmilestonePC8BoldedPC8elementsrelatabletoperformingaslitlampexam CorrelatingEDSLITLAMP assessments
Level1Identifiesindicationsforaprocedureandpertinentanatomyand physiology.Performsbasictherapeuticprocedures (eg,suturing,splinting)
Level2Assessesindications,risks,benefits,andalternativesandobtains informedconsentinlow-tomoderate-risksituations.Performsand interpretsbasicprocedures,withassistance.Recognizes commoncomplications
Level3Assessesindications,risks,andbenefitsandweighsalternativesin high-risksituations.Performsandinterpretsadvancedprocedures, withguidance.Managescommoncomplications
Level4Actstomitigatemodifiableriskfactorsinhigh-risksituations. Independentlyperformsandinterpretsadvancedprocedures. Independentlyrecognizesandmanagescomplexand uncommoncomplications
Level5Teachesadvancedproceduresandindependentlyperformsrare, time-sensitiveprocedures. Performsproceduralpeerreview
AppendixA–PartII(clinical imageexamination)
AppendixB–PartI(slitlamp technical) AppendixB (finalchecklist)
AppendixA–PartIII(ophthalmology exammix-n-match
AppendixB (finalchecklist)
AppendixC–EDSLITLAMP surveys
*ACGMEEM,AccreditationCouncilforGraduateMedicalEducationEmergencyMedicine; PC,patientcare; EDSLITLAMP,Emergency DepartmentSlitLampInterdisciplinaryTraining.
fromWilcoxonsigned-ranktestbythenumberofmultiple tests,doublingthe P -values),whichwasdirectlycomparedto thepre-specified5%significancelevel.Allstatisticalanalyses wereperformedusingR4.1.2(RFoundationforStatistical Computing,Vienna,Austria).28
Thisstudywasapprovedbytheinstitutionalreviewboard atThomasJeffersonUniversityHospital(TJUH)in Philadelphia,PA.Informedconsentwasobtainedfrom participatingphysicians.Thisstudywasfundedbythe CenterforFacultyDevelopmentandNexusLearning PedagogyGrantatThomasJeffersonUniversity.
FifteenEPs(sixfemalesandninemales)wereenrolledin EDSLITLAMPduringthetwo-yearperiod;nonewerelost tofollow-up.Allparticipantswereboard-certifiedEPswith anaverageclinicalexperienceof7.8yearspost-residency graduation.AllEPscompletedthe finalexamofthe curriculuminoneattemptandallunder60minutes.
Table2 liststhe20stepsoftheslit-lampexamcurriculum checklist,comparingparticipantresultsfromrecordedslitlampattempts(Time0)tothe finalin-personassessment (Time2).Theintra-classcorrelationintestscoresbetween EPsandophthalmologistsatTime0(2raters)was0.98.We foundasignificantincreasebetweenthechecklist scoresbeforeandaftertheeducationinitiative, 12.0to19.0, P = 0.002.
Themostnotabledifferencesbetweenthepre-andpostcurricularinterventionwereasfollows:1)instructingthe patienttoclosetheireyeswhilepoweringupandpositioning
thepatientintheslitlampwiththeforeheadtouchingthe horizontalbarandchininthechinrest(P < 0.001); 2)adjustingthemicroscope90degreestofacialplanewith illuminationsetata45-degreeangle(P = 0.008); 3)performingananteriorchamberevaluation(P = 0.002); 4)lookingforcellsand flare(P = 0.021);and5)placing fluoresceinintheinferiorfornixoftheeye(P = 0.031).The mostmissedstepsatthebaselineexamwere:1)applyinga transparentfaceshield(26.7%);2)instructingpatientsto closetheireyeswhenthemachinewasturnedon(26.7%); 3)lookingforcellsand flare(26.7%).
Figures2 and 3 illustratelearners’ confidencein performingandteachingtheslit-lampexamatthebeginning ofthestudy(Time0),immediatelyafterachievingprocedural mastery(Time2),andtwomonthslater(Time3). Figure4 illustratesthelearners’ likelihoodinteachingtheslit-lamp examatTime0andTime2.Beforeparticipatingintheslitlampcurriculum,73%ofEPsalsoreportedrarelyornever performingaslit-lampexam,while80%ofEPsreported sometimesoroftenusingaWood’slampforocular complaints.Only20%ofEPsreportedfeelingconfidentin performingandteachingacomprehensiveslit-lampexam, while67%ofEPsreportedfeelingconfidentinusingand teachingWood’slampforocularexamination.
Aftercompletingtheslit-lampcurriculum(Time2),86.7% ofEPsreportedfeelingconfidentperforminga comprehensiveslit-lampexamforocularcomplaints,and 73.3%weremoreconfidentinteachingresidentshowto performaslit-lampexam.MostEPsstronglyagreedthatthe EDSLITLAMPcurriculumhelpedthemperforman
Table2. Descriptivesummaryofchecklistevaluationatpre-andpost-curricularandcomparisonbetweentimepoints.
ChecklistitemPerformed
Time0,N(%) (N = 15)
Time2,N(%) (N = 15)
P-valuefrom exactMcNemar’s test
1-Identifyslitlampanatomy.Yes13(86.7%)15(100%)0.50
2-Applytransparentfaceshieldovertheslitlamp(COVID).Yes4(26.7%)15(100%) <0.001
3-Sanitizeforeheadandchinrestforthepatient.Yes5(33.3%)14(93.3%)0.004
4-Applytopicaltetracaine/proparacaineonpatient’seyes.Yes8(53.3%)12(80.0%)0.22
5-Unlockinstrumentbaseandshiftbypullingtowardyou.Yes15(100%)15(100%)NA
6-Adjusteyepiecesforyourinterpupillarydistanceand refractiveerror.
7-Adjusttableheightand/orchair(s)-neitherpatientnorexaminer shouldbehunchedover.
8-Instructpatienttocloseeyeswhileyoupowerupbyturningon thelightsourceatlowvoltagesettingandfocusonrighteyelid. Positionpatientinslitlampwithforeheadtouchingthehorizontal barandchininthechinrest.
9-Setmagnificationonlowestsettings(10xto12x),illuminationat largestapertureandwidestslitbeam.
10-Adjustchinrestsothepatientissittingcomfortablywiththeir chinonthechinrestandtheirforeheadagainsttheheadrest.
11-Practicemacroandmicroadjustmentsoftheslidingbase withjoystick.
12-Adjustmicroscope90° tofacialplanewithilluminationset at45° angle(angleleftforpatient’srighteye,andrightfor lefteye).
Yes10(66.7%)14(93.3%)0.22
Yes12(80.0%)14(93.3%)0.50
<0.001
Yes12(80.0%)15(100%)0.25
Yes14(93.3%)15(100%)1.00
Yes7(46.7%)15(100%)0.008
13-Performouterstructureevaluation.Yes14(93.3%)15(100%)1.00
14-Performanteriorchamberevaluation.Yes5(33.3%)15(100%)0.002
15-Lookforcellsand flare.Yes4(26.7%)12(80.0%)0.02
16-Placeadropoftetracaine/proparacaineonasterile fluoresceinstrip.
17-Placethe fluoresceinintheinferiorfornixoftheeyebypulling downonthelowerlidandgentlytouchingthebulbar conjunctivawiththe fluoresceinstrip.
18-Adjustcobaltblue filterondiaphragmwheelatmaximumbeam heightandmediumwidthslitsettingfor fluoresceinevaluation.
19-Focustheslitbeamat9:00positiononlimbus.Moveacross thecorneatothe3:00positionbytiltingjoysticklaterally.
20-Pullinstrumentbasetowardyouwhen finishedandlockin position.Turnoff.
Yes15(100%)15(100%)NA
Yes9(60.0%)15(100%)0.03
Yes14(93.3%)15(100%)1.00
Yes12(80.0%)15(100%)0.25
Yes4(26.7%)13(86.7%)0.004
Time0, median[IQR] Time2, median[IQR] P-valuefrom Wilcoxonsigned ranktest
Subtotalscore12.0[10,16]19.0[19,20]0.002 IQR,interquartilerange.
independentslit-lampexamandidentifycritical findingsfor commonocularcomplaints(80%),enhancingtheirlearning morethantraditionallecturesandreadingalone(86.7%).Of theasynchronousmaterials,thevideodemonstrationwasthe mostused(53%usedit “alot” ora “greatdeal”);the
PowerPointlectureandWEHManualweretheleastused.At twomonthspost-EDSLITLAMP(Time3),73%and67%of participantsexpressedextremeconfidenceinperformingand teachingaresidenthowtoperformaslit-lampexam.Fivetof 15EPsreportedteachinglearnerswithinthetwo-month

Figure2. Learnerconfidenceinperformingtheslit-lampexamatTime0(pre-curricular),Time2(immediatepost-SBMLcurriculum),and Time3(2-monthpost-SBMLcurriculum).

Figure3. Learnerconfidenceinteachingtheslit-lampexamatTime0(pre-curricular),Time2(immediatepost-SBMLcurriculum),Time3 (2-monthspost-SBMLcurriculum).
post-curricularperiod,rangingfrom5–30studentsper EPparticipant.
Table4summarizesthestatisticallysignificant findings fromthesurveyresponsesbasedonthethreetimeframes. Therewasastatisticallysignificantincreaseinself-reported confidencein1)performingacomprehensiveslitlampexam and2)teachingresidentstoperformthisexambetweenTime 0toTime2andTime0toTime3(P < 0.001).Therewasno differenceinrelianceonophthalmologyconsultationto modifyorreinforceatreatmentplanforocularcomplaints whencomparingTime0toTime3(P = 0.70, P = 0.814). Therewasalsonostatisticaldifferenceinthenumberof patientswithocularcomplaintsevaluatedbythestudy
participantsattheTJUHEDandWEHEDthroughoutthe study(P = 0.14, P = 1.00).
TheEDSLITLAMPcurriculumallowedEPstoincrease theiruseandconfidenceinperformingslit-lampexamsinthe ED.TheimpetusfortheprojectarosefromEPs’ intrinsic motivationtoprovidebetterpatientcare.Ourparticipant populationconsistedprimarilyofjuniorfacultywhowere initiallyuncomfortableperformingorteachingslit-lamp examsandpreferredusingtheWood’slamp.Upon completingthecurriculum,theEPsnotedasignificant increaseinself-reportedconfidenceinusingslit-lamps

Learnerlikelihoodinteachingtheslit-lampexamatTime0(pre-curriculuar)andTime2(immediatepost-SBMLcurriculum).
andwereteachingmultiplejuniorlearnersduringtheir studyenrollment.
Theimprovementbetweenthepre-andpost-curricular proceduralcompetencyalsodemonstratestheimportanceof understandingthetechnicalnuancesoftheslit-lampexam andpracticingcriticaldevicemovement,suchascareful patientpositioning,adjustingofthechinstraps,changingthe microscopeangulation,andadjustingvaryingslit-lamp beamlengthsandwidthsfordiagnosingawiderangeof anteriorophthalmicpathologies.Theseskillsaredrastically differentthanthoserequiredtooperateaWood’slamp, whichactsprimarilyasamagnifyingglasswith UVcapabilities.
OurcurriculumachievedthreeofthefourKirkpatrick goals.Themajorityoftheparticipants(over80%)reported positivereactiontothecurriculum(thecurriculumhelped themperformaslit-lampexam,evaluateforcommon pathologies,andofferedmorethantraditionallectures) (Level1);alloftheparticipantsdemonstratedprocedural masteryatTime2(Level2);upwardsof50learnersreceived instructionsfromthestudyparticipantsonhowtousetheslit lampatTime3(Level3).Whiletherelianceon ophthalmologyconsultationdidnotrevealstatistically significantchanges,wepositthatimprovedprocedural acumenresultedinmoretargetedconsultationquestioning andimprovedrapportbetweenthemedicaldisciplines.
Sinceourparticipantswereboard-certifiedEPswith limitedavailabilities,themostvaluedcomponentofthe curriculumwasthein-personRCDPsessionwiththe ophthalmologist(Time2).Thiswasreflectedinalmostevery CIQitem,withspecificmentionofdirectguidancein positioningthebeamtolookforcellsand flare.Themost surprisingelementtomanyparticipantswashowmany oculardiagnosesrequiredtheslit-lampexamandthat learningtheprocedurewasnotascomplicatedastheyhad
initiallyanticipated.Incontrast,manyoftheparticipantsfelt mostdistancedorremovedfromthecurriculuminreviewing theasynchronouslearningmaterials.
Wewereunsurprisedtoseetheconfidencelevelsinusing Wood’slampunchangedbetweenthethreedifferenttime frames.Whiletheslitlampoffersasuperiorandin-depth evaluationoftheanteriorsegmentoftheeye,we acknowledgethatacomprehensiveslit-lampexamistimeandresource-consumingandmaynotaffecttheclinician’ s managementifthesuspectedpathologyinvolveslarger lesions,foreignbodies,orspecificreactionto fluorescein staining.TheWood’slampremainsaneasierand moreportablediagnostictoolforsomeocularpathologies, anditsuseintheclinicalarenaisstillacceptablein certainsituations.
Thisstudywasconductedatasingle,large,tertiary academiccenterwithanaffiliatedophthalmologyhospital andsupportedwithinternalgrantfunding.Whiletheresults werepositive,multiplefactorsciykdpreventthisstudyfrom beingreplicated,especiallyatcommunitysiteswithouta closerelationshipwithophthalmology.Oneofthemost significantchallengesisschedulingin-personevaluationsin thepre-curricularsession,aswellasthe finalin-person trainingandexamination.Weencounteredsignificant logisticalchallengesincreatingaschedulethatwasamenable totheophthalmologists,EPs(withunpredictableshift schedules),andresearchinvestigators,aswellas findinga consistentspaceintheWEHandWEHEDthathadaccess toanattached-observerscopetoensuretheparticipantswere focusingonthecorrectanatomicstructureduringtheir proceduraldemonstration.Thiswasfurtherexacerbated whenaccountingforthe “unlimitedattempts” forRCDP. Asthiswasourpilotstudywithadvancedlearners,we
Table3. Statisticalanalysisofsurveyquestionsbetweenthethreedifferentstudytimeframes.
Surveyquestion
Slitlamp
Basedonyourcurrentpracticepatterns:how confidentareyouin:performingacomprehensiveslit lampexamforocularcomplaints?
Basedonyourcurrentpracticepatterns,how confidentareyouin:teachingresidentstoperforma comprehensiveslitlampexamforocularcomplaints
Howoftendoyou:performanindependentslit lampexamforocularcomplaints?
Wood’slamp
Basedonyourcurrentpracticepatterns,how confidentareyouin:performingacomprehensive Wood’slampexamforocularcomplaints?
Basedonyourcurrentpracticepatterns,how confidentareyouin:teachingresidentstoperforma comprehensiveWood’slampexam(withaccesstoa slitlamp)forocularcomplaints?
Howoftendoyou:useawoodlamp(withaccess toaslitlamp)forocularcomplaints?
Ophthalmologyconsultationhabits
Howconfidentareyouinidentifyingcommon ocularpathologyseeninyourmainworksite(CC, MHD,UrgentCare)?
Onaverage,howmanyeyepathologiesdoyou seeatthemainworksite?
Onaverage,howmanyeyepathologiesdoyou seeatotherfacilities?
Howoftendoyourelyonophthalmology consultationto:helpmodifyyourtreatmentplanfor ocularcomplaints?
Howoftendoyourelyonophthalmology consultationto:reinforceyourtreatmentandplanfor ocularcomplaints?
Howoftendoyourelyonophthalmology consultationto:provideadditionalinformationand guidancetoyourtreatmentandplanforocular complaints?
Bonferroni adjusted Pvaluefrom Wilcoxon signedranktest time0vs.time2 Bonferroni adjusted Pvaluefrom Wilcoxon signedranktest time0vs.time3
2[1,2.5]n/a*3[3,3]n/a*0.064
4[2,4]4[4,5]4[3,5]0.0160.03
4[2,4]4[4,5]4[3,5]0.030.08
3[3,4]n/a*3[3,3]n/a*1.00
2[2,3]n/a*3[3,4]n/a*0.018
10[4,15]n/a*5[3,12.5]n/a*0.14
12[0,40]n/a*37.5[13.5,50]n/a*1.00
3[3,3]n/a*3[2.5,3]n/a*0.70
3[2,3]n/a*3[2,3]n/a*0.814
3[3,4]n/a*3[3,3.5]n/a*1.00
Confidencelevels:1 = Notatallconfident,5 = Extremelyconfident
Frequencylevels:1 = Never,5 = Always
aTime0 = pre-curricularevaluation.
bTime2 = immediatepostSBMLexam.FrequencyofslitlampandWood’slampusewereintentionallyomittedforTime2duetotheclose proximitybetweenTime0andTime2,thusresultingin ‘n/a’ forsomecalculations.
cTime3 = threemonthsafterSBMLexam.
CC,JeffersonHospitalinCenterCityPhiladelphia; MHD,JeffersonMethodistHospital; IQR,interquartilerange.
over-budgetedatwo-hourtemplateforeachlearner,which drasticallylimitedthenumberofparticipantswecould scheduleforthe finalin-personexam.
Duetothelongitudinalnatureofthisstudyandseveralinpersoncomponents,maintainingparticipantrecruitment andengagementwasalsodifficult.Ofthe50eligibleboardcertifiedTJUHEPs,only15EPsvolunteeredtoparticipate. Theprimarydeterrence,whendiscussedwithnonparticipants,wastimerestraintsandcommutingintothecity forin-personevaluationsandexaminations.Wesuggest implementingdedicatedteachingdays(ie,conferencedaysor facultymeetings)forlargerparticipantrecruitmentand subsequentfollow-upandexamination.
Thisstudywasfundedbyaninternalgrantthatprovided minor financialincentivesfortheparticipantsand standardizedpatientvolunteers.Whileourneeds-based analysisrevealedparticipantsweremorefocusedon promotingbetterpatientcare,manyoftheparticipants expressedappreciationforthestaggeredgiftcards,which alsoincentivizedthemtocompleteeachtimeline-specific survey.Allotherinvestigators’ efforts,incontrast,wereinkindandrequireddedicatednon-academicandnon-clinical timetoenrollparticipants,recordalltheinteractions,and provideunrestrictedtimeavailabilitiesforthe finalmastery assessment.Thisstudywasalsounanimouslysupportedby bothdepartmentalleadershipstopromoteabettercollegial relationshipandinterdisciplinaryeducationopportunity betweenorganizationswiththetwoprincipalinvestigators holdinguniqueleadershippositions,ophthalmology consultingdirector[CC]andEMclerkshipdirector[XCZ]. Wesuspectthatalsopositivelyaffectedourrecruitment processandthesuccessofthisinterdisciplinarytraining curriculum.Asthisstudywasconductedatanacademic hospitalinanurbansetting,ithasbeensuggestedthat academiccenterslikelyoverestimateEPcomfortand confidenceinthediagnosisandmanagementofophthalmic emergencies.9 Furthermore,theproximitybetweenbothEDs mayskewthedata,astheseEPsarelikelyexposedtofewer ophthalmicemergenciesthanhospitalswithoutanearbyeyefocusedED.
Ultimately,thebiggestlimitationtothispilotstudywas thelackofin-personskillassessmentatthe60-dayfollow-up duetolimitedstaffingandschedulingchallenges.Inlieuofan objectivecompetencyscore,weleveragedself-reported confidenceatthe60-daymarkasanapproximate measurementoftheskillretention.Werecognizethat learnersarepooratgaugingtheirownabilities,bothoverandunderestimatingtheirskillsbasedonavarietyoffactors. Itisnotablethat80%ofourlearnerswereinitially “not confident” incompletingacomprehensiveslit-lampexam priortotheSBMLcurriculumandscoredanaverage checklistscoreof60%.AtTime2,almost87%ofresponders were “ confident” incompletingacomprehensiveslit-lamp examafterreceivinganaveragechecklistscoreof95%.
Unfortunately,thereisnoassociationbetweenlearners’ confidenceandpassingrate(score >18)atTime0(Pearson chi-square3.46, P = 0.17)andTime2(Pearsonchi-square 0.833, P = 0.66),respectively.Whileweareunabletopredict howtheselearnerswouldhaveperformedontheirslit-lamp examtestatday60,weareencouragedtoseethenumberof studyparticipantswhocontinuedtoteachslit-lampexamfor juniorlearners.Weposittheseparticipantswilllikelyhave improvedsustainedcompetenceanddecreasedskilldecayby activelyteachingothers.Futurestudiesshouldbeconsidered toadda finalexamination(procedureormultiple-choice question)tovalidateourresults.
Emergencyphysiciansareexpectedtodiagnoseand manageocularcomplaintsaspartoftheirtrainingand clinicalpractice.Ourprimaryfocuswastocreatearigorous methodologictrainingcurriculum(slit-lampexam)fora specialty-focusedskillsetthatcouldresultindownstream teaching.Thisprojecthighlightedasignificantneedforslitlampexamtrainingwithinourinstitutionthatledtoa successfultransdisciplinarysimulation-basedmastery learningcurriculumandimprovedourEPs’ confidencein performingandteachingslit-lampexamstofutureclinicians. Furthermore,thisstudydemonstratesthatadultlearners, especiallyattendingphysicianvaluedirectinteractionwith clinicalinstructorswhenlearninganewskillsetandare intrinsicallymotivatedtohonetheirskillsetandteachitto futurelearnerswhentheyhaveachievedthismastery. WeencourageotherinstitutionstoleverageSBMLasa teachingmodalityforprocedural-basedtrainingand advocatecross-disciplineeducationinitiatives.Future investigationcouldincludecreatingamulticenterstudyto implementthiscurriculumatotheracademicinstitutionsand potentiallyincludeitinEMresidencytraining.
WewanttothanktheThomasJeffersonUniversityCenter forFacultyDevelopmentandNexusLearning(CFDNL)for theirgeneroussupportandgrantfundingincompleting thisstudy.
AddressforCorrespondence:XiaoChiZhang,MD,Thomas JeffersonUniversity,DepartmentofEmergencyMedicine,1020 SansomSt.,ThompsonBldg,Suite239,Philadelphia,PA19107. Email: Xiaochi.zhang@jefferson.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudyreceivedgrantfundingfrom theCenterforFacultyDevelopmentandNexusLearning(CFDNL) Pedagogy,ThomasJeffersonUniversity.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Hamouetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.User:OKJaguar.File:slitlampandbinocularmicroscope.2019. Availableat: https://commons.wikimedia.org/wiki/File: Slit_lamp_and_binocular_microscope.jpg.AccessedAugust26,2023.
2.KnoopK.Ophthalmologicproceduresintheemergencydepartment partIII:slitlampuseandforeignbodies. AcadEmergMed. 1995;2(3):224–30.
3.SeolSH,ChoJ,LeeWJ,ChoiSC.Useofaslit-lampmicroscopefor treatingimpactedfacialforeignbodiesintheemergencydepartment. ClinExpEmergMed. 2015;2(3):188–92.
4.User:Seawind60.File:Wood’sUVlamp.2013.Availableat: https:// commons.wikimedia.org/wiki/File:Wood%27s_UV_lamp.JPG AccessedAugust26,2023.
5.BabineauMandSanchezL.Ophthalmologicproceduresin theemergencydepartment. EmergMedClinNorthAm. 2008;26(1):17–34.
6.CheungCA,Rogers-MartelM,GolasL,etal.Hospital-basedocular emergencies:epidemiology,treatment,andvisualoutcomes. AmJ EmergMed. 2014;32(3):221–4.
7.OwensPLandMutterR.(2011).Statisticalbrief#112:Emergency departmentvisitsrelatedtoeyeinjuries,2008.In Healthcarecostand utilizationproject(HCUP)statisticalbriefs.Rockville,MD:Agencyfor HealthcareResearchandQuality.
8.TheWillsEyeEmergencyDepartment.Alleyes,allthetime. EyeLevel. 2021.Availableat: https://www.willseye.org/wp-content/uploads/2021/ 05/WEB_3009-Eye-Level-Spring-2021.pdf.AccessedOctober17, 2023.
9.UhrJH,GovernatoriNJ,ZhangQE,etal.Traininginandcomfortwith diagnosisandmanagementofophthalmicemergencies amongemergencymedicinephysiciansintheUnitedStates. Eye. 2020;34(9):1504–11.
10.DruckJ,ValleyMA,LowensteinSR.Proceduralskillstrainingduring emergencymedicineresidency:areweteachingtherightthings? WestJ EmergMed. 2009;10(3):152–6.
11.GelstonCDandPatnaikJL.Ophthalmologytrainingandcompetency levelsincareofpatientswithophthalmiccomplaintsinUnitedStates internalmedicine,emergencymedicineandfamilymedicineresidents. J EducEvalHealthProf. 2019;16:25.
12.GraubartEB,WaxmanEL,ForsterSH,etal.Ophthalmologyobjectives formedicalstudents:revisitingwhateverygraduatingmedicalstudent shouldknow. Ophthalmology. 2018;125(12):1842–3.
13.AccreditationCouncilforGraduateMedicalEducation(ACGME). Emergencymedicinemilestones.2023.Availableat: https://www. acgme-i.org/globalassets/acgme-international/milestones-2.0/ emergencymedicinemilestones2.0int.pdf.AccessedOctober17,2023.
14.Griswold-TheodorsonS,PonnuruS,DongC,etal.Beyondthe simulationlaboratory:arealistsynthesisreviewofclinical outcomesofsimulation-basedmasterylearning. AcadMed. 2015;90(11):1553–60.
15.ChanceyRJ,SampayoEM,LemkeDS,etal.Learners’ experiences duringrapidcycledeliberatepracticesimulations:aqualitativeanalysis. SimulHealthc. 2019;14(1):18–28.
16.LemkeDS,FielderEK,HsuDC,etal.Improvedteamperformance duringpediatricresuscitationsafterrapidcycledeliberatepractice comparedwithtraditionaldebriefing:apilotstudy. PediatrEmergCare. 2019;35(7):480–6.
17.MavisSC,KreofskyBL,OukMY,etal.Trainingfellowsinneonatalteleresuscitationusingasimulation-basedmasterylearningmodel. ResuscitationPlus. 2021;8:100172.
18.ZendejasB,CookDA,BingenerJ,etal.Simulation-basedmastery learningimprovespatientoutcomesinlaparoscopicinguinalhernia repair:arandomizedcontrolledtrial. AnnSurg. 2011;254(3):502–9; discussion509–11.
19.FranklinBR,PlacekSB,GardnerAK,etal.PreparingfortheAmerican BoardofSurgery flexibleendoscopycurriculum:developmentofmultiinstitutionalproficiency-basedtrainingstandardsandpilottestingofa simulation-basedmasterylearningcurriculumfortheendoscopy trainingsystem. AmJSurg. 2018;216(1):167–73.
20.BarsukJH,McGaghieWC,CohenER,etal.Useofsimulation-based masterylearningtoimprovethequalityofcentralvenouscatheter placementinamedicalintensivecareunit. JHospMed. 2009;4(7):397–403.
21.QureshiN.InternationalperspectivefromSaudiArabiaon “procedural skillstrainingduringemergencymedicineresidency:areweteaching therightthings?” WestJEmergMed. 2009;10(3):157–8.
22.HoonpongsimanontW,NguyenK,DengW,etal.Effectivenessof a40-minuteophthalmologicexaminationteachingsessiononmedical studentlearning. WestJEmergMed. 2015;16(5):721–6.
23.Siddaiah-SubramanyaM,SmithS,LonieJ.Masterylearning: howisithelpful?Ananalyticalreview. AdvMedEducPract. 2017;8:269–75.
24.MillerDT,ZaidiHQ,SistaP,etal.Creationandimplementationofa masterylearningcurriculumforemergencydepartmentthoracotomy. WestJEmergMed. 2020;21(5):1258–65.
25.RutledgeBK.Thewillseyemanual:Officeandemergency roomdiagnosisandtreatmentofeyedisease. ArchOphthalmol. 1996;114(1):112.
26.McNemarQ.Noteonthesamplingerrorofthedifference betweencorrelatedproportionsorpercentages. Psychometrika. 1947;12(2):153–7.
27.ConoverWJ. PracticalNonparametricStatistics.Hoboken,NJ:John Wiley&Sons.1999.
28.R:TheRProjectforStatisticalComputing.June11,2023.Accessed August8,2023. https://www.r-project.org/
NathanZapolsky,MD*
AnnemarieCardell,MD†
RiddhiDesai,DO*
StaceyFrisch,MD,MSEd‡
NicholasJobeun,DO,MSEd§
DanielNovak,DO*
MichaelSilver,MS*
ArleneS.Chung,MD,MACM∥
*MaimonidesMedicalCenter,DepartmentofEmergencyMedicine, Brooklyn,NewYork
† EmoryUniversityHospital,DepartmentofEmergencyMedicine,Atlanta,Georgia ‡ NewYorkUniversity,GrossmanSchoolofMedicine,NewYork,NewYork
§ IcahnSchoolofMedicineatMountSinai,NewYork,NewYork
∥ UniversityofVermontMedicalCenter,Burlington,Vermont
SectionEditor:BenjaminHoldenSchnapp,MD
Submissionhistory:SubmittedJune1,2024;RevisionreceivedJune12,2024;AcceptedJuly8,2024
ElectronicallypublishedSeptember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21183
InJanuary2023,significantchangestothestructureofthe CurrentProceduralTerminologyCPT(R)evaluationand management(E/M)codes(hereforwardcalledthe2023E/M changes)wereimplementedforemergencydepartment(ED) encounters.Thesemodificationsaimtolessenadministrative workloadandaccuratelymatchcodingwithcontemporary patientcarepractices.1 Theyareanticipatedtoimpact roughly85%oftherelativevalueunitsofEDcare2 and,thus, alsohavesignificant financialimplicationsforEDs. Residentsprovidefront-linecareanddocumentationfor millionsofpatientsseeninUnitedStatesEDsannually.The ModelofClinicalPracticeofEmergencyMedicine3 identifies financialprinciples,suchasbillingandcoding,toberequired corecontentforboardcertification.Furthermore,the AccreditationCouncilforGraduateMedicalEducation (ACGME)includesqualityclinicaldocumentationtobeone ofthemilestonesthatdetermineadvancementinresidency training.4 Interventionsthatalleviatedocumentationburden arealsoassociatedwithimprovedphysicianwell-beingper theexistingliterature.5 However,researchsuggeststhatmost emergencymedicine(EM)residentsdonotreceiveformal traininginbillingandcodingandhaveknowledgegapsin thisarea.6–8
Historically,documentationofencountersintheED focusedonthenumberofelementswithinhistoryofpresent illness(HPI),reviewofsystems(ROS),physicalexam(PE), andmedicaldecision-making(MDM).Thesenewcoding guidelinesshiftthefocusalmostentirelytoMDM.They emphasizedocumentationofdifferentialdiagnoses; independentinterpretationofmedicaltesting;justificationof testingnotpursued;socialdeterminantsofhealth;chronic diseases;histories;communicationwithconsultants,
ancillarystaff,andprimarycare;andreviewof externalrecords.
Wesoughttoimproveresidentunderstandingofand compliancewiththe2023E/Mchanges.Objectivesincluded identificationofthekeyelementsrequiredateachE/Mlevel, chartingandreceivingfeedbackofsampleencounters,and appreciationfortheimportanceofaccurateandhigh-quality documentation.Wesecondarilysoughttoinvestigate whetherourinterventionimprovedresidentwellness specificallyviabenefitsinconfidencetoperformaccurateand expeditiousdocumentationandcompletionofchartingina timelymanner.
OurcurriculumwasdevelopedusingKern’ssix-step approachtocurriculumdesign9 asapartoftheeducational qualityimprovementprocessatasingleEMresidency programbasedatasingle,large,tertiary-care,urbanhospital withanapproximateannualEDpatientcensusof110,000 fromOctober1,2022–February28,2023.Priortostudy initiationaneedsassessmentwasperformed.Key stakeholdersindepartmentalbillingandcodingwere identifiedandinterviewed,andrelevantliteraturewas reviewed.1–10 Thisincludedthehospitalchiefmedical informationofficer,EDvicechair,andbillingandcoding leadership.Theinterviewsrevealedasharedopinionthat oftenthedocumentationtoreachtheappropriateexpected levelofservice(4or5)waslackingtosupportthatlevelof billingandmostofthatdocumentationshouldbecapturedin theMDMportionofthenote.Thus,theMDMportionof thenotewastargetedfortheintervention.
Oureducationalmethodsprimarilyusedin-person, flipped-classroomsessions.Wedecidedtousea flippedclassroomapproachforseveralreasons:1)toallowresidents togainexposuretothenewbillingcriteriapriortotheinpersonsessions;2)asamechanismtoassessresident understandingandskills,bothindividuallywithhomework responsesaswellasinagroupsetting;and3)tousefaculty’ s in-persontimeforoversightandfeedback.11 Wealsoapplied aspacedlearningapproachtomaximizeknowledge acquisitionandretention.12 Thesessionswereheldon December14,21,and28,2022.
Forpre-sessionhomeworkeachweek,allresidentswere providedasamplepatientHPI,ROS,andPEcomponents. Alllearnerswereprovidedthesamecase,andcaseswere changedeachweek.Caseswereformulatedtoinclude elementsthatcouldbeexpandeduponintheMDM, Residentswerealsoprovidedwiththe “CPTEvaluationand Management(E/M)CodeandGuidelineChanges” document.10 TheywerethenaskedtocreateanMDM sectioninaccordancewiththeabovedocument.Homework responseswerereviewedbyfaculty,andfeedbackwasgiven individuallyviaemail.Writtenfeedbackforresidentswas generatedusingatemplatebasedlargelyonthe2023E/M guidelineschanges.10 AnideallydocumentedsampleMDM sectionwasalsosuppliedforreference(Supplement1).13
Duringeach30-minutesession,residentsweredivided intosmallgroupsoffourandprovidedanexamplepatient case,whichincludedonlytheHPI,ROS,andPE components.ResidentsthencollaborativelywroteanMDM sectionforthecase.Allgroupswereprovidedthesamecase, andcaseswerechangedeachweektofocusondifferent aspectsoftheMDMsection.Eachsmallgroupofresidents sharedtheirresponsewiththelargergroupandwere providedpeerfeedbackundertheguidanceofafaculty facilitatorselectedfortheiradvancedknowledgeineither educationoroperations.Facilitatorswereprovidedin advancewithanexampleofanideallydocumentedMDM section,whichresidentswerealsoprovidedwithatthe conclusionoftheexercise.
Weemployedapre-postinterventionalstudydesignusing aconveniencesampleofresidents,inwhichgroup assignmentwasbasedonthenumberoftrainingseach residentcouldattendduetoschedulingfactorsoutsidethe scopeofthisstudy.Thisstudywasdeterminedtobeexempt bytheinstitutionalreviewboardofMaimonidesMedical Center.Participationwasvoluntaryandanonymous.We evaluatedtheimpactofourbriefeducationalinterventionon subjectivemeasuresofEMresidentknowledge,skills,and attitudesviasurveyandonobjectivemeasuresofskillsand behaviorsbyassessingaggregatechartdata.
Surveysweredevelopedthroughagroupiterativeprocess thatincludedoneauthor(ASC)withexpertiseinsurvey
designmethodology.RedCap,14,15 hostedat[Maimonides MedicalCenter]wasusedtoanonymouslydistributeboth pre-andpost-interventionsurveys.Bothsurveysconsistedof sixLikert-scalequestions,threeregardingtheirreporteduse ofdocumentationshortcuts,andthreeassessingattitudes abouttheirownunderstandingofandpredictedskillwiththe newE/Mcodingchanges.Sixadditionalmultiple-choice questionsassessedknowledgeaboutdocumentationrules.A finalquestionwasforfeedbackandrequestedideasforother E/Mbillingandcodingeducation.Thepre-intervention survey,distributedNovember30,2022,differedfromthe post-interventionsurveyofDecember28,2022, onlyinaskingtheself-reportednumberofsessions attended.(Supplement2).
Residentskillswereassessedusingactualclinical documentation.ResidentaggregateE/Mlevelswereassessed acrossthreemonthspre-intervention(October1–December 31,2022)andtwomonthspost-intervention(January 1–February28,2023).Duetovariationinresidentclinical schedules,wechosetheabovetimeperiodstocapturethe greatestproportionoftheEDencountersdocumentedby residents.WeusedtheKirkpatrickmodeltoevaluateour intervention’simpact.16 Surveyswereusedtoassessresident subjectivereactions,andobjectiveknowledgeby identificationofbillableelementsinaprovidedsample MDM.Weusedactualclinicaldocumentationtoassess changesinbehavior.Specifically,weassessedwhether traineeshadastatisticallysignificantincrease(P < 0.05)in theproportionofE/Mlevel5charts(99285)andlikewisea significantdecreaseinlevel1,2,3,and4charts(99281, 99282,99283,99284).
Weuseddescriptivestatisticsandcomparisonofmeans withtheMann-WhitneyUteststratifiedbynumberof educationalsessionsattendedtoanalyzesignificant differencesinknowledgeandattitudesbeforeandafterthe intervention.Forknowledge,thesecalculationswere summarizedwithmedianandinterquartilerange(IQR)and comparedacrosstimeperiodsusinganexactWilcoxon signed-ranktest.ABonferronicorrectionforthesignificance oftheinterventionchangesthealphato0.01667.Foreach chartlevel(99281–99285),wecreatedlogisticregression modelsusinggeneralizedestimatingequationsforindividual repeatedmeasurestoaccountforpersonalvariability.The numberofattended flipped-classroomsessionswastreatedas theindependentvariable.Zerotrainingswereconsideredto bethepre-periodforanalysis.Allanalysesconsidered alpha ≤ 0.05tobestatisticallysignificantandwereconducted usingSPSSv28.015 (SPSSStatistics,IBMCorp, Armonk,NY).
Forty-sixofthe54EMresidents(85%)eligibleforthe studycompletedbothpre-andpost-interventionsurveys.All 54residentsparticipatedinatleastonesurvey.Duetoclinical schedules,someresidentswerenotpresentatoneormoreof thethreeofferedsessions.The firstlivesessionwasattended

by33(61%)residents,thesecondby38(70%),andthethird by40(74%).Six(11%)residentsattendedonesession, 15(28%)attendedtwosessions,and25(46%)attendedthree sessions.Eight(15%)didnotattendanysessions.
Residentsdemonstratedasignificantimprovementin knowledgeregardingwhichelementsarethekeytothe MDMwithinthe2023E/Mchanges[6(5–6.5)to8(7.5–8) P < 0.001],andbycorrectlyidentifyingthenumberand complexityofproblems,complexityofdata,risklevel,and theoverallcomplexityofasampleencounter.Therewasno statisticallysignificantimprovementinidentificationofthe importantcodingelements(4[3–5]to5[3.5–5], P = 0.38). Residentsalsoendorsedgreaterconfidenceintheirability todescribe(2[1–3]to4[3–4], P < 0.005),accurately document(3[2–3]to4[3–4], P < 0.005),andbill(2[2–3]to3 [2–3] P < 0.005).Therewerenosignificantchangesintheir opinionoftheirabilitytocompletetheirchartsinatimely manner(P < 0.19,CI0.165–0.215)inthedecisiontouse dictationsoftware(P = 1),shortcuts(P = 1),orcustom preparedtextphrases(P = 1)followingtheintervention. Residentsparticipatinginanynumberof flipped-classroom sessionsshowedsignificantchangesintheirskills,including anincreaseinE/MLevel5codedcharts,andasignificant decreaseinLevel1,2,and3codedcharts(P < 0.005).The increaseinLevel5chartsanddecreaseinLevel3chartswere significantafterjustonesession(Figure).Nosignificant changewasobservedinLevel4charts.
Tothebestofourknowledge,thisisthe firststudytodate todescribetheimpactofaneducationalinterventiononEM residentdocumentationknowledge,skills,andattitudes withintheframeworkofthe2023E/Mchanges.Naturally, ourexperienceandresultsatoursingleEMresidency
programbasedatalarge,urban,tertiary-carehospitalmay notbegeneralizable.Thisinterventiondataissinglecenter andpreliminary,andtheinterventionshouldundergo repetitionandcomparisonbefore firmconclusionscan bedrawn.
Wechosetocollectdataduringatimerangetiedtothe sameillnessseasontokeepthecaseacuitymixandattending/ residentstaffingcomparable.Weotherwisecouldhave comparedtothesamemonthsofthepreviousyearforpreinterventiondata,tobestmatchtheillnessseason,or alternatively,post-interventiondatacouldhavebeendrawn insteadfromthefollowingyear(2024)tohelpmitigate recencybiasintheinterventiongroup.Thatbeing said,themajordifferencesinresidentandattending staffingbetweentimesayearapartcouldalsohave confoundedresults.
Weconsideredfacultysupplementaldocumentationand itseffectondocumentationoutcomesduringourstudy designandtookapragmaticapproach.Forthedurationof thisstudytheattendingpopulationwasstable,nosignificant changestoattendingeducationwereperformedduringthis period,andattendingstaffingremainedatbaselinewithno changestoratios,shiftdurations,orstandarddistributionsof encountersthroughouttheEDcareareas.Tofurtheraddress thisconcernweattemptedanalysisoftheattending distributionbetweenthesevariousgroups.Noattendinghad agreaterthan1.4%changeintheirbillingfrompre-topostintervention,andtheirsmallcontributionstotheoverall billingforeachinterventiongroupwas,therefore,unlikelyto havebiasedthelargedifferencesseenbetweengroups. However,thedifferencesindistributionofattendingshifts betweenthegroupsvariedstatisticallysignificantly,andbias
cannotbeassessedwithoutpatient-levelbillingrecords.This couldbeconsideredinfuturestudies.
Ourprogrammayhaveimplicationsregardingwellnessas well.Residencytrainingmustprepareemergencyphysicians forallaspectsoftheireventualprofessionalexpectations. Residentsreceivingeducationexpressedgreaterconfidence intheirabilitytodescribe,accuratelydocument,andbillfor careprovided.Businessliteraturefrequentlynoteshowalack ofclearexpectationsincreasesworkstressandharms employeewellnessandproductivity.18 However,whether thisassociationappliestoemergencyphysiciansdeserves furtherstudy.
Overall,weobservedsignificantimprovementsinresident knowledge,attitudes,skills,andbehaviorsregardingclinical documentation.Wehopetoapplythesesuccessesandlessons learnedtotheformationofenduringeducationmaterialsat ourowninstitutionfordocumentationimprovementfor bothresidentsandattendings.
AddressforCorrespondence:NathanZapolsky,MD,Maimonides MedicalCenter,DepartmentofEmergencyMedicine,4802Tenth Ave.,Brooklyn,11219NY.Email: nizapo@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Zapolskyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ThoughtLeadershipTeam.2023E/Mcodingchanges.2023.Available at: https://www.aapc.com/resources/evaluation-management-codingchanges-2023.AccessedAugust18,2023.
2.McKenzieDAandGranovskyMA.2023documentationguideline changesforEDE/Mcodes99281–99285.2022.Availableat: www. acepnow.com/article/2023-documentation-guideline-changesfor-ed-e-m-codes-99281-99285/.AccessedJanuary25,2023.
3.BeesonMS,BhatR,BroderJS,etal.The2022modelofthe clinicalpracticeofemergencymedicine. JEmergMed. 2023;64(6):659–95.
4.CooneyRR,MuranoT,RingH,etal.Theemergencymedicine milestones2.0:settingthestagefor2025andbeyond. AEMEducTrain. 2021;5(3):e10640.
5.NguyenO,JenkinsN,KhannaN,etal.Asystematicreviewof contributingfactorsofandsolutionstoelectronichealthrecord-related impactsonphysicianwell-being. JAmMedInformAssoc. 2021;28(5):974–84.
6.RomansB,NguyenE,BiddleM,etal.Billingandcoding:disparitiesin healthcareprovidertraining. JAlliedHealth. 2022;51(1):43–6.
7.DawsonB,CarterK,BrewerK,etal.Chartsmart:aneedfor documentationandbillingeducationamongemergencymedicine residents? WestJEmergMed. 2010;11(2):116–9.
8.ChinS,LiA,BouletM,HowseK,etal.Residentandfamilyphysician perspectivesonbilling:anexploratorystudy. PerspectHealthInf Manag. 2022;19(4):1g.
9.ThomasPA,KernDE,HughesMT,etal. CurriculumDevelopmentfor MedicalEducation:ASix-stepApproach,3rded.Baltimore,MD:The JohnsHopkinsUniversityPress,2015.
10.AmericanMedicalAssociation.CPT® evaluationandmanagement (E/M)codeandguidelinechanges.2022.Availableat: https://www. ama-assn.org/practice-management/cpt/cpt-evaluation-andmanagement.AccessedMarch24,2024.
11.RotellarCandCainJ.Research,perspectives,andrecommendations onimplementingthe flippedclassroom. AmJPharmEduc. 2016;80(2):34.
12.WeidmanJandBakerK.Thecognitivescienceoflearning:concepts andstrategiesfortheeducatorandlearner. AnesthAnalg. 2015;121(6):1586–99.
13.AllenA.Medicineclerkship(inpatient)H&Pexamples:H&P5.2018. Availableat: https://www.med.unc.edu/medclerk/wp-content/uploads/ sites/877/2018/10/hp5.pdf.AccessedFebruary24,2024.
14.HarrisPA,TaylorR,ThielkeR,etal.Researchelectronicdatacapture (REDCap) – ametadata-drivenmethodologyandworkflowprocessfor providingtranslationalresearchinformaticssupport, JBiomedInform. 2009;42(2):377–81.
15.HarrisPA,TaylorR,MinorBL,etal.TheREDCapconsortium:building aninternationalcommunityofsoftwarepartners, JBiomedInform. 2019;95:103208.
16.KirkpatrickDL. EvaluatingTrainingPrograms:TheFourLevels SanFrancisco,CA:Berrett-KoehlerPublishersInc,1994.
17.IBMCorp.IBMSPSSStatisticsforWindows,Version28.0.2021. Armonk,NY:IBMCorp.
18.BornsteinJ.Howalackofclearexpectationsleavesemployeesanxious andadrift.2023.Availableat: https://www.forbes.com/sites/ forbescoachescouncil/2023/06/05/how-a-lack-of-clear-expectationsleaves-employees-anxious-and-adrift/?sh=70de0f8f5983 AccessedApril23,2024.
MaxBerger,MD,MEHP*
JackBuckanavage,MD†
JaimeJordan,MD,MAEd*
StevenLai,MD*
LindaRegan,MD,MEd‡
*UniversityofCaliforniaLosAngeles,DavidGeffenSchoolofMedicine, DepartmentofEmergencyMedicine,LosAngeles,California
† MountSinaiSchoolofMedicine,DepartmentofEmergencyMedicine, NewYork,NewYork
‡ JohnsHopkinsUniversity,DepartmentofEmergencyMedicine,Baltimore,Maryland
SectionEditors:KendraParekh,MDandBenjaminHoldenSchnapp,MD
Submissionhistory:SubmittedJune14,2024;RevisionreceivedSeptember20,2024;AcceptedSeptember26,2024
ElectronicallypublishedOctober22,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.24863
Introduction: Coronavirus2019(COVID-19)acceleratedtheneedforvirtuallearningincluding telesimulation.Manyemergencymedicine(EM)programshaltedin-personsimulationandtrialed telesimulation,butspecificsonitsutilizationandplansforfutureuseareunknown.Telesimulationhas beendefinedas “aprocessbywhichtelecommunicationandsimulationresourcesareutilizedtoprovide education,training,and/orassessmenttolearnersatanoff-sitelocation.” Ourobjectiveinthisstudywas todescribethepatternsoftelesimulationusageinEMresidencyprogramsduringCOVID-19-induced learningrestrictionsaswellasitsanticipatedfutureutility.
Methods: WeidentifiedEMsimulationleadersviatheEMRAMatchwebsite,institutionalwebsites,or personalcontactwithresidencycoordinatorsanddirectors,andinvitedthemtoparticipatebyemail. Participantscompletedaconfidential,web-basedsurveyconsistingofmultiple-choiceitemsandone free-responsequestion,developedbyourstudyteamwithconsiderationofsurveyresearchbest practicesandMessick’svalidityframework.WecollecteddatabetweenJanuary–February2022.We calculateddescriptivestatisticsformultiple-choiceitemsandexaminedthefree-responseanswersfor commonthemes.
Results: Weobtainedcontactinformationforsimulationleadersat139EMresidencyprograms.Survey responseratewas65%(91/139).Duringin-personrestrictions,62%(56/91)ofprogramsused telesimulation.Assumingallrestrictionslifted,38%(34/90)ofrespondentsplannedtocontinuetouse telesimulation,comparedto9%(8/91)usingtelesimulationbeforeCOVID-19.Mostrespondents plannedtousetelesimulationformedicalknowledge(26/34,76%)andcommunication/teamworkfocusedcases(23/34,68%).Inresponsetothefree-responsequestionregardingexperiencewithand plansforuse,weidentifiedthreemajorthemes:1)telesimulationisavaluablealternativetoin-person learning;2)telesimulationisanoptionforlearnersunabletoparticipateinperson;and3)telesimulationis challengingforproceduraleducation.
Conclusion: DespitetherelativelylimiteduseoftelesimulationinEMresidenciespriortoCOVID-19,an increasednumberofprogramshaveplanstocontinueincorporatingtelesimulationintotheircurricula. Thisplanforcontinueduseopensopportunitiesforfurtherinnovationandscholarshipwithinsimulation education.[WestJEmergMed.2025;26(1.2)42–47.]
Restrictionsimposedonin-personeducationduringthe coronavirus2019(COVID-19) pandemicacceleratedtheneed forvirtuallearning,includingtelesimulation.1,2 Telesimulation hasbeendefinedas “aprocessbywhichtelecommunication andsimulationresourcesareutilizedtoprovideeducation, training,and/orassessmenttolearnersatanoff-sitelocation.”3 Initialapplicationswereinlowerresourcesettingssuchas developingcountrieswherelearnersdidnothaveaccessto simulationcentersorinstructors.4,5 Withintelesimulation, differentmodalitieshavebeendescribedthatvaryin fidelityas wellaslocationofthelearnersandinstructorsrelativetoeach otherandthesimulationcenter.6–8
Severalpublishedarticlessinceearly2020havedescribed differentinstitutions’ approachestotelesimulationsincethe pandemic.1–2,9–13 Commonthemesincludetheneedtomodify learningobjectivestovirtualenvironmentsandtoselectthe appropriatemodalityoftelesimulationbasedoninstitutional needsandresources.9–12 Differentmodalitiesoftelesimulation havebeendescribed,includingthefollowing:1)learners virtuallyobservinganddebriefingalivesimulation7; 2)learnerspresentwithamanikinwhileinstructorsfacilitate fromaseparatelocation6;3)instructorspresentwitha manikinwhilelearnersremotelyparticipate7;and 4)completelyremoteoptionwherelearnersandinstructors bothparticipateremotelyfromseparatelocations.10,11
Limiteddatacomparingtelesimulationvstraditional simulationsuggeststhatlearnersatisfactionwith telesimulationorhybridvirtualandin-personsimulationis similar,althoughthiswasnotfoundinallstudies.7,13,14
Ascopingreviewfrom2021highlightedthemixeddataon studentperceptionoftelesimulation,withsomeofthe includedstudiesindicatingremotefacilitationofsimulation beingperceivedasequallyormoreeffectivethanlive facilitation,whileothersfoundremotefacilitationtobe inferior.14 Facilitatorperceptionoftelesimulationhasnot beenwellstudied.Limitedlearningoutcomedatahas suggestedsimilarimprovementsbetweenin-person simulationandtelesimulation.8,14
Ourobjectiveinthisstudywastodescribethepatternsof telesimulationusageinemergencymedicine(EM)residency programsduringCOVID-19-induced,in-personlearning restrictionsaswellasitsanticipatedutilitymovingforward. Thisinformationiscrucialtounderstandingthevalueof telesimulationanditsutilityinmedicaleducation.
StudyDesign,Setting,andPopulation
Weconductedacross-sectionalsurveystudyoffacultyin chargeofsimulationforEMresidencyprogramsinthe UnitedStates.WecollecteddatafromJanuary–February 2022.AfteridentifyingEMresidencyprogramsandtheir websitesfromtheEMRAMatchdatabase,15 wesearched eachwebsiteforcontactinformationforthedirectorof
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
COVID-19acceleratedtheneedforvirtual learningincludingtelesimulation.
Whatwastheresearchquestion?
Towhatextendwastelesimulationusedby EMresidenciesduringCOVID-19,andwhat isitsanticipatedutilitymovingforward?
Whatwasthemajor findingofthestudy?
Only9%(8/91)ofprogramsusedtelesimulation beforeCOVID-19.DuringCOVIDrestrictions, 62%(56/91)ofprogramsusedit,whileafter limitationswerelifted,38%(34/90)plannedto continuetelesimulation.
Howdoesthisimprovepopulationhealth?
Asanadjuncttotraditionalin-person simulationcurriculum,telesimulationisa viableoptiontoimprovemedicalknowledge andcommunication-basedcompetencies.
simulationeducation.Iftherewasnodirectordesignated,we emailedeachresidency’sprogramcoordinatorand/or directoraskingforcontactinformationforthefacultyin chargeofresidencysimulation.Eachprogramwasallowed onlyonedesignatedparticipant.Thisstudywasgivenexempt statusbytheUniversityofCalifornia,LosAngeles InstitutionalReviewBoard(IRB#21-001336)andtheJohns HopkinsUniversityHomewoodIRB(HIRB00013694).
Giventhelackofanypreviouslycreatedsurveyapplicable tothisconstruct,theprimaryauthor(MB)developedawebbasedsurveytoolwithconsiderationofsurveyresearchbest practicesandMessick’svalidityframework.16–19 Forcontent validityevidence,we firstperformedaliteraturereview,and theauthorgroupofexpertsimulationeducatorsandmedical educationresearchersreviewedthesurveyforclarityand relevancetotheconstruct.Wedefinedtelesimulationas includinganysimulationactivitywhere “telecommunication andsimulationresourcesareutilizedtoprovideeducation, training,and/orassessmenttolearnersatanoff-site location.”3 Wepilotedthesurveywithagroupofsimulation educatorswhowerenotincludedinthetargetsampleto gatherresponseprocessvalidityevidence.Afterpiloting,we revisedthesurveyforclarity.The finalsurveyincluded multiple-choiceitemsandonefree-textresponse item(Appendix1).
Weinvitedparticipantsbyemailandsenttwotargeted, follow-upinvitationstonon-respondersatbi-weekly intervals.WeadministeredthesurveyviaQualtrics (Qualtrics,LLC,Provo,UT).Noindividualidentifying informationwascollected.Tomaximizeresponserateand minimizeguessing,wedidnotrequireparticipantsto completeallsurveyitems.Participantswerenot compensatedforparticipatinginthestudy.
Wecalculatedandreporteddescriptivestatisticsforitems withdiscreteanswers.Weconductedcalculationsusing QualtricsandMicrosoftExcelforMac(MicrosoftCorp, Redmond,WA).Weexaminedtheanswerstothefree-text responsestoidentifycommonthemesthatwouldbroadenthe reader’sunderstandingofthedata.Successivewaveanalysis wasperformedtoassesstheextentofpossiblenonresponse bias.20 Weexaminedwhetheruseoftelesimulationduringthe pandemic,plannedfutureuseoftelesimulationafterinpersonrestrictions,andrespondentprogramformat (postgraduateyears[PGY]1–3vs1–4)differedbywave. Bivariatechi-squaretestsforeachvariableofinterestby wavewereperformedusingMicrosoftExcelforMac,and P -valueslessthan0.05wereconsideredstatisticallysignificant. Weusedtheconsensus-basedchecklistforreportingofsurvey studies(CROSS)asreportingguidelines(Appendix2).23
Of139simulationleadersweidentified,91(65%) completedthesurveywith87(63%)completingallitems.We reportdemographicdataforsurveyrespondentsin Table1, whilerespondents’ experienceandperceptionsof telesimulationareshownin Table2.PriortotheCOVID-19 pandemic,9%(8/91)ofsurveyrespondentswereusing telesimulationintheircurricula.Therewasawidevarietyof priorexperienceswithtelesimulation,withthemostcommon beingthattheyhadheardoftelesimulationbutneverbeen involved(44%).Ninety-twopercent(84/91)ofrespondents reportedthattheirinstitutionprohibitedin-personlearning activitiesatsomepointduringtheCOVID-19pandemic. Duringin-personlearningrestrictions,62%(56/91)used telesimulationinsomeform.
Whensurveyrespondentswereaskedaboutwhat format(s)oftelesimulationwereused,11%(10/90)statedthat theyonlyusedacompletelyvirtualoral-boardsstyleformat, whiletherestofthosewhousedtelesimulationreportedusing ahybridorvirtualformatinvolvingapatientmonitorand/or manikin.Thelargestpercentageofsurveyrespondentsfelt thatmedicalknowledgeandcommunication/teamworkfocusedcaseswerebestsuitedfortelesimulation(72%and 47%respectively),whilemostfeltthatproceduretraining wasnotwellsuitedfortelesimulation(62%).Thirty-eight percent(34/90)ofrespondentsstatedtheyplannedtouse telesimulationinsomeformintheircurriculummoving
Table1. Surveyrespondentdemographics. n(%)
Formatofrespondent’scurrent residencyprogram
PGY1–362/89(70%)
PGY1–427/89(30%)
Sizeofrespondent’scurrentresidencyprogram (totalnumberofresidentsinallyears)
≤20residents11/90(12%)
21–40residents38/90(43%)
41–60residents31/90(34%)
≥60residents10/90(11%)
Respondent’scurrentresidencyprogram primaryinstitutionsetting
University-based58/90(64%)
Community-based28/90(31%)
County-based13/90(14%)
Priorsimulationtrainingofsurveyrespondent
Fellowshiptraininginsimulation31/90(34%)
Non-fellowshiptraininginsimulation48/90(53%)
Noformaltraininginsimulation17/90(19%)
Respondentyearssinceresidencygraduation
≤522/90(24%)
6–1033/90(37%)
11–1516/90(18%)
16–208/90(9%)
≥2111/90(12%)
PGY,postgraduateyear.
forward,mostlyformedicalknowledgeandcommunication/ teamwork-focusedcases(76%and68%,respectively).
Wereceived14free-textresponses,andidentifiedthree majorthemes,describedbelowwithexemplarquotes.
1.Telesimulationisavaluablealternativeto in-personlearning: “Ithasbeenthe ‘betterthannothing’ optionbutaccepted bylearnerswhenotheroptionsarenotfeasible.” “Ithasexceededexpectationsinhowhelpfulithasbeen.”
2.Telesimulationisanoptionforlearnersunableto participateinperson:
“Wefoundthatit’sagreatoptionforresidentswith familiesorwhohaveotherextenuatingcircum-stances whytheycan’tparticipateinperson,ie,breastfeeding moms,newparents,eldercare,etc.Manyofour residentswhoarebetweennightsorbetweenmidshiftswilllogonandparticipate.”
3.Telesimulationischallengingforproceduraleducation: “Difficulttolearnmusclememoryforhighacuity,low occurrenceskills.”
Table2. Keysurveyresults.
EMresidencyprogramuseoftelesimulation
PriortoCOVID-19pandemic8/91(9%)
Duringin-personlearningrestrictions56/91(62%)
Planneduseafterin-personrestrictionslifted34/90(38%)
DuringanypointintheCOVID-19pandemic, didyourinstitutionprohibitin-person learningactivities?
Yes84/91(92%)
No7/91(8%)
Experiencewithtelesimulationprior toCOVID-19
Hadneverheardoftelesimulation17/91(19%)
Heardoftelesimulationbutneverinvolved40/91(44%)
Attendedapresentation20/91(22%)
Participatedasaninstructor19/91(21%)
Participatedasalearner6/91(7%)
Conductedaresearchproject5/91(5%)
Readapaperabouttelesimulation16/91(18%)
Formatsoftelesimulationusedduring COVID-19restrictions
Completelyvirtual;utilizingreal-timepatient monitorand/ormanikin 21/90(23%)
Completelyvirtual;oralboardsstylecases31/90(35%)
Hybrid;instructor,learnersand/orsimtechin simcenterwhileothersremote 31/90(35%)
Whatsimulationactivitieswerebestsuited fortelesimulation?
Medicalknowledgefocusedcases65/90(72%)
Communication/teamworkfocusedcases42/90(47%)
Procedurefocusedcases5/90(6%)
Dedicatedproceduretraining2/90(2%)
Proceduretrainingonhomemademodels10/90(11%)
Whatsimulationactivitieswerenotwellsuited fortelesimulation?
Medicalknowledgefocusedcases0/87(0%)
Communication/teamworkfocusedcases18/87(21%)
Procedurefocusedcases52/87(60%)
Dedicatedproceduretraining54/87(62%)
Proceduretrainingonhomemademodels23/87(26%)
Percentoffuturesimulationcurriculum involvingtelesimulation
0%ofthecurriculum56/90(62%)
1–25%ofthecurriculum30/90(33%)
26–50%ofthecurriculum3/90(3%)
51–75%ofthecurriculum1/90(1%)
76–100%ofthecurriculum0/90(0%)
(Continuedonnextcolumn)
Table2. Continued. n(%)
Typesoffuturesimulationactivitiesforthose whoplantocontinueusingtelesimulation
Medicalknowledge-focusedcases26/34(76%)
Communication/teamwork-focusedcases23/34(68%)
Procedurefocusedcases7/34(21%)
Dedicatedproceduraltraining5/34(15%)
Proceduretrainingonhomemademodels5/34(15%)
EM,emergencymedicine.
“Proceduraltrainingwasthemostdifficulttosimulate viatelesim.”
Forthewaveanalysis,thestudyincluded91respondents, including42inwave1(46%),21inwave2(23%),and28in wave3(31%).Resultsoftheexaminedsurveyquestionsdid notstatisticallydifferbywavewithall P -values > 0.05.
(See SupplementalTable.)
DespiterelativelylowuseoftelesimulationwithinEM programspriortotheCOVID-19pandemic,wefoundthat manyEMresidencyprograms(62%)quicklyadaptedtoinpersonlearningrestrictionsbyusingtelesimulation.While notallprogramsthattrialedtelesimulationplantocontinue itsuse,38%ofrespondentprogramsdoplantocontinueto usetelesimulation,comparedto9%ofprogramsusing telesimulationpriortoCOVID-19.Thisrepresentsalarge increaseintheoverallusageoftelesimulationwithinEM residencies.Ourstudyalsoshedslightonhowtelesimulation canbenefitEMprograms.Beingabletoincreaselearner participationtoincluderesidentswithfamilyobligationsor betweennightshiftscouldallowforincreasedreturnon investmentforsimulationresourcesandfacultytime.Most respondentswhoplantocontinuetousetelesimulation reportedthattheywilluseitasasmallpercentageoftheir overallsimulationcurriculum,whichhighlightsthat telesimulationisnotreplacingin-personsimulationbut augmentingthetraditionalcurriculum.Thiscouldbeina hybridformatthatallowsforincreasedparticipation,oras partofseparatetelesimulationdaysthatcouldreducethe travelburdensonlearnersandinstructors.
Therewaslargevariationinhowprogramsconducted telesimulationduringin-personrestrictions.Thisisinline withpriorliteratureandlikelyreflectsindividualprogram needs,preferences,andavailableresources.1,2,8–11,13,22 Most describedtelesimulationasbestsuitedformedicalknowledge andcommunication/teamwork-focusedcases,ratherthan forprocedureteaching.Thisisinterestinggiventhatearly descriptionsoftelesimulationintheliteraturemostly
involvedproceduralteaching.5,6 Onepossibleexplanation forthisdiscrepancyisthatthoseearlystudiesinvolved duplicatesimulatorsatremotelocations,anexpensethatis likelynotpractical,ornecessary,foraresidencyprogram giventheabilitytohostproceduretrainingaspartofthe in-personcurriculum.Whileitisapparentthatthereare increasedplansfortheuseoftelesimulationcomparedtothe pre-pandemicera,notallresidencyprogramswhoused telesimulationduringtimesofin-personrestrictionsare planningtocontinuetodoso.Thereasonsforthisare unknownbutmayrelatetotelesimulationresource availabilityorlimitedoutcomedataonitsutility.
Basedonourresults,webelievethattelesimulationcan continuetobeavaluableadditiontothetraditionalinpersonsimulationcurriculum,particularlyinallowingfor increasedparticipationoflearnersandinstructors,reducing resourcecostssuchassimulationcenterandstafftime,and allowingforaviableoptiontopracticemedicalknowledge andcommunication-basedcompetencies.Nowthat telesimulationhasbeenestablishedasaninstructional strategythatwillcontinuetobepartofmanyEMresidency curricula,itopensopportunitiesforfutureinnovationand scholarshipwithinsimulation-basedmedicaleducation. Additionalinvestigationcouldcomparedifferentmodalities oftelesimulationonobjectivelearningoutcomes.23 Itwould alsobeinterestingtoexploretheroleofvirtualand augmentedrealitywithintelesimulation.24,25
Despitemultipleattempts,wewerenotabletoobtain contactinformationforasimulationleaderfromallEM programs.However,thebreakdownofPGY1–3vsPGY1–4 programsofsurveyrespondents(70%PGY1–3vs30%PGY 1–4),approximatingtheactualdistributionoftheEM residencyprograms(81%PGY1–3vs19%PGY1–4), suggeststhatthesamplecloselyresemblesthatofthe population.8 Givenourresponserateof65%,itispossible non-responsebiasaffectedourresults,withparticipantswith lessinterestorfamiliaritywithtelesimulationbeinglesslikely torespond.However,theresultsofoursuccessivewave analysisfailedtodetectnon-responsebiasfortheselected surveyquestions.
Theremaybeotherinfluencesaffectingaprogram’suseof telesimulationthatwewerenotabletocapture,andinthis surveystudyweexaminedonlytheopinionsoffacultyand notthoseofresidentlearners.Additionally,theliteraturebaseddefinitionoftelesimulationweusedmaybeoverly broadandencompassmorethanwhattypicaleducators mightconsidertelesimulation.Finally,weacknowledgethat thesurveywasadministeredin2022within-personlearning restrictionsjuststartingtobelifted,andhowpeopleareusing telesimulationnowmaybechanging.Futureworkcould examinethisevolvinguseoftelesimulationwithinEM residencyprograms.
Thisstudydescribespastandplannedfutureuseof telesimulationwithinEMresidencyprograms.Alarge proportionofEMresidenciestrialedtelesimulationduring COVID-19-inducedrestrictions.Despiterelativelylowuseof telesimulationpriortothepandemic,moreEMprograms plantoincorporatetelesimulationmovingforwardasa limitedportionoftheiroverallsimulationcurriculum. Opportunitiesforfurtherinnovationandscholarshipwithin thisareaofsimulationeducationwillbepossiblegiventhis plannedcontinueduse.
Thisprojectwascompletedinfulfillmentofthe requirementsfortheJohnsHopkinsUniversityMasterof EducationintheHealthProfessions.
AddressforCorrespondence:MaxBerger,MD,MEHP,Universityof CaliforniaLosAngeles,DavidGeffenSchoolofMedicine, DepartmentofEmergencyMedicine,1100GlendonAve.,Suite 1200,LosAngeles,CA90024.Email: MRBerger@mednet.ucla.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Bergeretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PatelSM,MillerCR,SchiaviA,etal.Thesimmustgoon:adapting residenteducationtotheCOVID-19pandemicusingtelesimulation. AdvSimul.2020;5:26.
2.DiazMCGandWalshBM.Telesimulation-basededucationduring COVID-19. ClinTeach.2021;18(2):121–5.
3.McCoyCE,SayeghJ,AlrabahR,etal.Telesimulation:aninnovative toolforhealthprofessionseducation. AEMEducTrain 2017;1(2):132–6.
4.MikrogianakisA,KamA,SilverS,etal.Telesimulation:aninnovative andeffectivetoolforteachingnovelintraosseousinsertiontechniquesin developingcountries. AcadEmergMed.2011;18(4):420–7.
5.OkrainecA,HenaoO,AzzieG.Telesimulation:aneffectivemethodfor teachingthefundamentalsoflaparoscopicsurgeryinresourcerestrictedcountries. SurgEndosc.2010;24(2):417–22.
6.HaydenEM,KhatriA,KellyHR,etal.Mannequin-basedtelesimulation: increasingaccesstosimulation-basededucation. AcadEmergMed 2018;25(2):144–7.
7.McCoyCE,SayeghJ,RahmanA,etal.Prospectiverandomized crossoverstudyoftelesimulationvsstandardsimulationforteaching medicalstudentsthemanagementofcriticallyillpatients. AEMEduc Train.2017;1(4):287–292.
8.YasserNBM,TanAJQ,HarderN,etal.Telesimulationinhealthcare education:ascopingreview. NurseEduc.Today 2023;126:105805.
9.NadirNA,KimJ,CassaraM,etal.Simulation-basedemergency medicineeducationintheeraofphysicaldistancing:lessons learnedintheCOVID-19pandemic. AEMEducTrain 2021;5(3):e10586.
10.RayJM,WongAH,YangTJ,etal.Virtualtelesimulationfor medicalstudentsduringtheCOVID-19pandemic. AcadMed 2021;96(10):1431–5.
11.SanseauE,LavoieM,TayKY,etal.TeleSimBox:aperceived effectivealternativeforexperientiallearningformedicalstudent educationwithsocialdistancingrequirements. AEMEducTrain 2021;5(2):e10590.
12.ThomasA,BurnsR,SanseauE,etal.Tipsforconducting telesimulation-basedmedicaleducation. Cureus. 2021;13(1):e12479.
13.AustinA,RudolfF,FernandezJ,etal.COVID-19educational innovation:hybridin-personandvirtualsimulationforemergency medicinetrainees. AEMEducTrain. 2021;5(2):e10593.
14.HeffernanR,BrumptonK,RandlesD,etal.Acceptability,technological feasibilityandeducationalvalueofremotelyfacilitatedsimulation-based training:ascopingreview. MedEducOnline. 2021;26(1):1972506.
15.EmergencyMedicineResidents’ Association.EMRAMatch.Available at: https://webapps.emra.org/utils/spa/match#/search/map. AccessedJuly21,2021.
16.RickardsG,MageeC,ArtinoAR,Jr.Youcan’t fixbyanalysiswhat you’vespoiledbydesign:developingsurveyinstrumentsandcollecting validityevidence. JGradMedEduc.2012;4(4):407–10.
17.GehlbachHandArtinoAR,Jr.Thesurveychecklist(manifesto). AcadMed.2018;93(3):360–66.
18.ArtinoAR,Jr.,DurningSJ,SklarDP.Guidelinesforreportingsurveybasedresearchsubmittedtoacademicmedicine. AcadMed 2018;93(3):337–40.
19.MessickS.Validity.In:LinnR.L,editor. EducationalMeasurement 3rd ed.NewYork,NY:Macmillan;1989:13–103.
20.DuszynskiTJ,FadelW,DixonBE,etal.Successivewaveanalysisto assessnonresponsebiasinastatewiderandomsampletesting studyforSARS-CoV-2. JPublicHealthManagPract. 2022;28(4):E685–91.
21.SharmaA,MinhDucNT,LuuLamThangT,etal.Aconsensus-based checklistforreportingofsurveystudies(CROSS). JGenInternMed. 2021;36(10):3179–87.
22.LevineM,SinghM,RestivoA,etal.Recommendationsforoptimizing virtualsimulation:atrialanderrorprocessfromtheCOVID-19 pandemic. JGradMedEduc.2022;14(1):18–21.
23.KirkpatrickJDandKirkpatrickWK. Kirkpatrick’sFourLevelsofTraining Evaluation.Alexandria,VA:ATDPress;2016.
24.MistryD,BrockCA,LindseyT.Thepresentandfutureofvirtual realityinmedicaleducation:anarrativereview. Cureus. 2023;15(12):e51124.
25.PallaviciniF,PepeA,ClericiM,etal.Virtualrealityapplicationsin medicineduringtheCOVID-19pandemic:systematicreview. JMIRSeriousGames. 2022Oct25;10(4):35000.
CorlinM.Jewell,MD*
AmyT.Hummel,MD*†
DannJ.Hekman,MS*
BenjaminH.Schnapp,MD,MEd*
*UniversityofWisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,Madison,Wisconsin † EmergencyMedicineSpecialistsSC,Wauwatosa,Wisconsin
SectionEditors:DougFranzen,MDandAndrewKetterer,MD
Submissionhistory:SubmittedFebruary25,2024;RevisionreceivedSeptember27,2024;AcceptedOctober11,2024
ElectronicallypublishedNovember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20281
Introduction: Whilemanyaspectsofemergencymedicine(EM)residencytrainingarestandardized amongresidentswithinasingleresidencyprogram,thereisnostandardforthedistributionofchief complaints(CC)thatresidentsshouldseeoverthecourseofresidency.Thiscouldresultinsubstantial variabilityineachresident’sclinicalexposure.OurobjectiveinthisstudywastoexploreEMresidents’ clinicalexposuretoCCstodeterminewhethersubstantialvariationexists.Ifsuchvariationexists,this couldsuggesttheneedforcurricularreformtoaddressgapsinresidentclinicalexposureduringtraining.
Methods: ThiswasaretrospectiveobservationalstudyofEMresidentswhograduatedintheyears 2016–2021atasingle,university-affiliatedemergencydepartment(ED)inthemidwesternUnitedStates. AllpatientencounterswhereaCCwasloggedwereincludedandcategorizedinto1of20clinical domainsbasedonthe2016AmericanBoardofEmergencyMedicineModelofClinicalPractice. Wecalculateddescriptivestatisticsforthetop10mostencountereddomainsforcomparison amongresidents.
Results: Weincludedatotalof228,916patientencountersfrom69residentsintheanalysis.Residents wereinvolvedinanaverageof3,323distinctpatientencountersduringthestudyperiod.Theoverall interquartilerangeforpatientencounterswas523.ThethreeCCdomainswiththebroadestinterquartile variationwereabdominalandgastrointestinaldisorders(116),musculoskeletaldisorders(nontraumatic) (93),andtraumaticdisorders(86).
Conclusion: Withinasingle,three-yearacademicEMprogram,substantialvariationexistedamong residentswithregardtothevarietyofpatientCCsseenduringtheirresidencytraining.[WestJEmerg Med.2025;26(1.2)48–53.]
Medicalresidencytrainingallowsphysicianstogainthe cognitiveandproceduralskillsnecessarytopractice independently.Basedonexperientiallearningtheory,patient encountersformthefoundationuponwhichphysiciansin trainingbegintomasterthepracticeofmedicine.1 Additionally,thedevelopmentof “illnessscripts,” ormental modelsfortheclassificationofpatientpresentations,is
crucialtothedevelopmentofclinicalskillsandreasoning duringresidencytraining.2 Thesemodelsaredevelopedover timebymultipleexposurestopresentationsofsimilar diseasestates.3,4 Emergencymedicine(EM)trainees mustbeexposedtoavarietyofpatientchiefcomplaints(CC) throughoutthecourseofresidencytodevelop thesescriptsandbecomereadytobegin independentpractice.
EducatorswithinEMhaveworkedtodefinemanyaspects ofEMresidencytraining,includingoptimumnumberof shifts,on-shifteducationalgoals/practices,anddidactic content.5 Despitethis,theclinicalexperienceofanindividual residentmaybehighlyvariableandmaybepartiallydriven byself-selectionofpatientsbytheresident.Studiesin pediatricEMsuggestthatthereissignificantvariationinthe overallnumberofpatientsandrangeinacuityamong individualresidents.6,7 However,thereislittleadultEM literaturethatexploresthevariationinclinicalexperience seenbyresidentswithinamodernEMprogram.The literaturethatdoesexistinadultEMsuggeststhereis substantialvariationinclinicalexposuresamongresidents.8 Astudyfrom2006foundthatthenumberofcasesseen overallcorrelatedwithimprovedperformanceona standardizedtestdesignedtoassessclinicalcompetence. However,theeffectplateauedataround200cases.9 Prior workbyourgrouphasshownthatcasevolumeinan individualdomaindidnotcorrespondtoperformancewithin thatdomainoncorrespondingquestionsonthe in-trainingexam.10
Thesestudiessuggestthatindividualswithinasingle trainingprogrammaybegainingvariableexperiencewith certaintypesofpatientpresentationsandlackingexposure (andthereforeopportunitiestodevelopmastery)toother complaintsandpathology.However,thisvariabilityin clinicalexposureduringtraininghasnotbeenshowninadult EMforoverthreedecades.8 Sincethen,thenumberofannual visitstotheEDaswellasthecomplexityofmedicalcare providedhavesubstantiallyincreased.11,12 We,therefore, hypothesizedthatsubstantialdifferencesinclinicalexposure stillexistamongresidentsatthetimeofgraduation. Understandingthesedifferencesisofcriticalimportancefor residencyprogramsasconsiderablevariationcouldpush someresidentsbelowathresholdtodeveloprobustillness scriptssuitableforindependentpractice.
StudyDesignandSetting
Weconductedthisretrospective,observationalstudyata three-yearEMresidencyprogramsituatedwithinanurban, academicemergencydepartment(ED)intheMidwest.The EDfortheprimaryclinicalsitehasatotalof54bedsandsees anannualvolumeofapproximately60,000patientvisits. Duringthestudyperiod,theresidencyhad12 first postgraduateyearone(PGY-1)positionsavailableeach year.ThestudyEDdividesitsbedsintotwoadultclinical areasandapediatricclinicalarea.Allthreeareasare physicallyconnectedonasingle floorofthehospital. Residentsfromallthreeyearsareassignedtonine-hourshifts ineachclinicalarea.Eachshiftincludes1–2junior(PGY-1) residents,1–2senior(PGY-2orPGY-3)residents,andone attendingphysician.Anyresidentcanassignthemselvesto patientsofanyseverityregardlessofseniority.InFall2020,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Studiesfrom30yearsagoreportedvariation inthedistributionofchiefcomplaintsseenby emergencymedicineresidentsduringtraining.
Whatwastheresearchquestion?
Wehypothesizedthatsubstantialdifferences inclinicalexposurestillexistamongresidents atthetimeofgraduation.
Whatwasthemajor findingofthestudy?
Thethreechiefcomplaintdomainswiththe mostvariabilitybetweenindividualresident experience,asmeasuredbythegreatest25 – 75 interquartilerangeswereabdominaland gastrointestinaldisorders(median594 patientsperresident,IQR116), nontraumaticmusculoskeletaldisorders (median314,IQR92),andtraumatic disorders(median525,IQR86).
Howdoesthisimprovepopulationhealth?
Understandingthesedifferencesisimportant, assubstantialvariationcouldmeanthatsome residentsdonotdeveloprobustillnessscripts suitableforindependentpractice.
thestudyEDshiftedfroma “pod” modelinwhichthetwo adultclinicalareaswouldassignthemselvespredominately topatientsintheirclinicalareatoa “free-for-all” modelin whicheitheradultteamcouldassignthemselvestoanyadult patientregardlessoftheclinicalareatheywereroomedin. Duringthestudy,physicianassistantswereemployedinthe EDandwouldoccasionallytaketheplaceofaresidenton shift(particularlyduringweeklyresidentdidactics).
Residentswereeligibleforinclusioniftheyhadcompleted residencywithinthreeconsecutiveyearsandgraduatedinthe years2016–2021(therefore,thestudyperiodwasfromJune 2013–June2021).Theelectronichealthrecord(EHR)was usedtocreateadatabaseofpatientencounters;all encounterswhereeligibleEMresidentswerethe firstresident assignedtothepatientwereanalyzed.Weuseddeidentified patientencounterdata,listedby firstCC.TheCCwasusedto identifythenatureofthepatientencounterasthisdatawas availableatthetimeofpatientpresentation,oftendictates thepatient’sEDworkup,andwouldnothavebeenaffected byinformationdiscoveredduringthelaterstagesofa
patient’shospitalcourse.Thisapproachisconsistentwith priorliterature.9,13 Tomaintainanonymity,onlythesenior author,amemberoftheresidencyleadershipteam,had accesstoeachresident’sindividualizedstudy identificationnumber.
WeexcludedfromanalysisencounterswherenoCCwas listedornoresidentwasassigned.Incaseswheremultiple residentswereassignedtoasingleencounter(e.g.,apatient hadbeensignedouttoadifferentresident),weanalyzedthis encounteronlyfortheinitialresidentassigned.Thiswas doneastheyaretypicallythemostinvolvedinthecognitive workloadofdeterminingthepatient’sinitialdiagnosticand treatmentplan.TheCCforeachencounterwasselectedand enteredintotheEHRbytheprimarynursewhocaredforthe patientintheEDinitially.Atourinstitution,thisisnearly alwaysselectedfromalistofcommonCCs,althoughitcan beenteredasfreetext.EncountersinwhichmultipleCCs werelistedwereonlycodedintoasingledomainbasedonthe firstlistedCC.
AlistofcommonCCsinEMhasbeencategorizedintoa setof20contentdomainsviaaconsensusprocessbytwoEM attendingsusingthe2016AmericanBoardofEmergency Medicine(ABEM)ModelofClinicalPracticeasa framework.14 ForCCsidentifiedinourdatathatwerenot alreadycategorizedbyapreviouslydescribedmethod,13 we repeatedthesamecategorizationprocessinwhicheachCC wasassignedtoasingledomainbytwoboard-certifiedEM attendingphysiciansatourinstitution.Disagreements betweenthetworeviewerswereadjudicatedbyathirdboardcertifiedemergencyphysician.Ifasymptomwasenteredas theCC,suchas “fever” (whichcouldcorrespondtooneof multipledomains),itwaspreferentiallycategorizedintoa domainbasedonwhatthecodingphysiciansfeltwasthe
mostlikelytodictatetheEDworkup,ratherthanthe “signs, symptoms,andpresentations” domain.WeusedExcel (MicrosoftCorp,Redmond,WA)tocalculatedescriptive statisticsandcreateplotsandtables.Thetop10most encountereddomainsoverallwereanalyzed.Weexcluded lesscommondomainsgiventhelownumberoftotal encountersineacharea,whichwouldhavebeenmore vulnerabletorandom fluctuationsinwhenthesepatients presenttotheED.
Thisprojectwasdeemedexemptqualityimprovementby theUniversityofWisconsinHealthSciencesInstitutional ReviewBoard.
Atotalof315,614encounterswereinitiallyidentifiedfrom theEHR.Oftheseencounters198wereexcludedasnoCC waslisted.Afterexcludingresidentswhoseclinical experiencewasoutsidethestudyperiodandthosewhohad leftthetrainingprogrampriortograduationorhada prolongedleaveofabsence,atotalof228,916patient encountersfrom69residentswereincludedintheanalysis. Eachresidentwasassignedtoanaverageof3,323distinct patientencountersAssessmentofthetop10mostcommon clinicalexposuredomainsshowedwiderangesinthecase numbersofindividualresidents.The Table liststhemean, minimum,maximum,interquartilerange(IQR) and25thand75thpercentileforthe10mostcommon contentdomains.The Figure showstherangeof exposuretothe10mostcommondomainsin box-and-whiskerformat.
Ourdatasuggeststhatresidentswithinasingletraining programhavesubstantialvariationintheirclinical experiencesasmeasuredbythevariationinABEMcontent
Table. Mean,25th–75thpercentileranges,interquartilerange,andminimum/maximumencountersforthe10mostencountereddomains perresident.
MeanMedian25th,75th percentileIQRMinimum,maximum
Totalencounters33233086,36095232595,4053
Abdominalandgastrointestinaldisorders583594528,644116416,721
Traumaticdisorders529525484,57086370,725
Cardiovasculardisorders327330302,35654233,429
Nervoussystemdisorders319319301,34039226,402
Musculoskeletaldisorders(non-traumatic)314314269,36192179,460
Thoracic-respiratorydisorders280281246,31367178,383
Systemicinfectiousdisorders165169149,17930115,219
Head,ear,eye,nose,andthroatdisorders150151136,1652996,196
Signs,symptoms,andpresentations129130120,1422288,170
Psycho-behavioraldisorders126128106,1393467,211
IQR,interquartilerange.
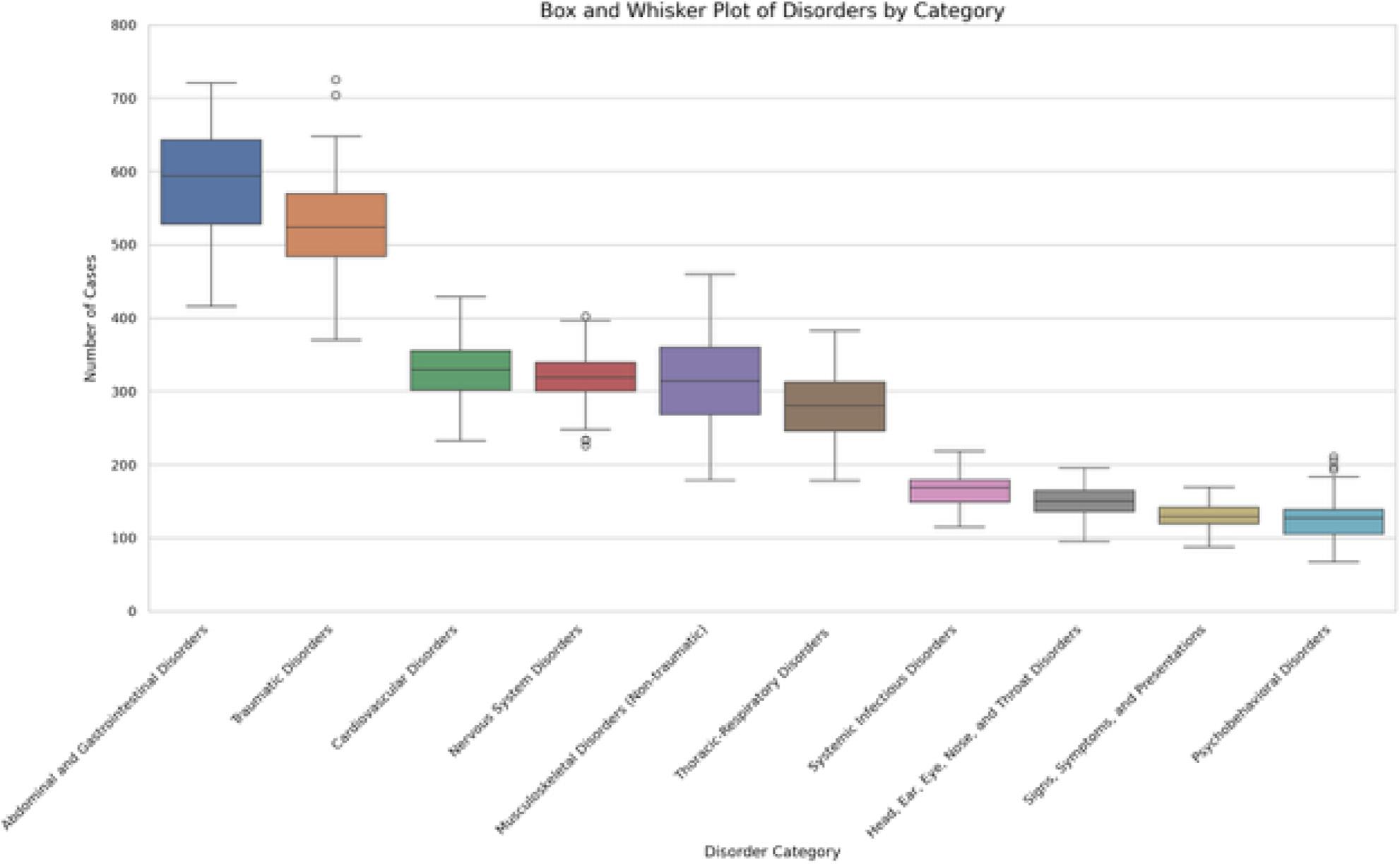
Figure. Top10mostcommonclinicalexposuredomainsseenbygraduationperresident.Boxesillustratethe25th–75thpercentileofnumber ofclinicalexposuresbyresidentsineachdomain,withwhiskersrepresentingtheminima,maxima,andoutliers.
domainsseenbyindividualresidents.Thisissimilartowhat wasdescribedbyLangdorfetal.in1990,despitetheprevious studybeingperformedoverthreedecadesagoandthe substantialsubsequentdifferencesintheutilizationofthe ED.8 Wefoundwideinterquartilerangesbetweenthe maximumandminimumnumberofencountersamong residents,suggestingthatsomeresidentssawsubstantially morepatientswithinparticulardomainsthanothers.
Themagnitudeoftheeducationalsignificanceofthe exposurevariabilityofresidentsisunclear.Itispossiblethat aresidentwhoseestwiceasmanymusculoskeletalchief complaintsasanotherresidentbygraduationissignificantly morecompetentinthatdomain.Alternatively,itisalso possiblethattheyhavebothattainedtheminimallevelof exposuretocompetentlymanagemusculoskeletal complaintsindependently.Theeffectsofclinicalexposureon clinicalcompetence,includingtheminimalnumberof encountersrequiredtodemonstratecompetencyina particulardomain,isanopenquestionandanavenuefor furtherresearch.However,theformationofillnessscriptsis continuallymodifiedbysubsequentpatientencounters.3,4 Therefore,theidentificationofhighdegreesofvariation amongresidentsmaypromptprogramleadershiptoinstitute changesinthecurriculumorsupplementclinicalexposure withindividualizedlearningplans.Thisislikelymore importantfordomainsthatareencounteredlessfrequently
overall,suchaspsycho-behavioraldisorders,wherelarger relativedifferencesinexposurecouldresultingreaterdeficits inillnessscriptformation.
Inadditiontopromptingchangesmadebytheprogram, identificationofhighvariabilityinclinicalexposuremay enhanceresidentself-assessment.Asdemonstrated previously,self-assessmentwhendoneinisolation,isan imperfectmeansofdrivingimprovementbutcanbe enhancedgreatlywheninformedbyadditionalinformation fromavarietyofsources.15 Understandingthedistribution ofthepatientencountersresidentshaveduringtraining,and thepotentialgapsintheirclinicalexposure,couldbea potentialmeansofallowingforinformedself-assessmentfor aresident’sclinicalskills.Thiscouldbepotentiallyfurther enhancediffacilitatedunderthesupervisionoffaculty coacheswithintheprogram,amethodthathasbecome increasinglypopularinmedicaleducation.16,17 Futurework couldfollowacohortofresidentswhoareabletotracktheir ownpatientvolumesmoreregularlythanwaspossibleinthe currentstudyandcomparethemselvestotheirpeers throughouttrainingandevaluatewhetheranydifferencesin clinicalcompetenceareidentified.Thiscouldalsoallow programstodeterminetheperceivedvalueofthis informationtoresidents.Finally,residentscould usethisdatatodrivetheirpatientselectionwhile workingintheED.
Beyondthepotentialforshapingresidentselfassessments,clinicalexposuredatamayhaveimportant implicationsforresidencyprogramleadershipaswemove towardaneraofcompetency-basedmedicaleducation (CBME).TwoofthepillarsofCBME, “teachingtailoredto competencies” and “effectiveprogrammaticassessment,”18 lendthemselveswelltotheidentificationofprogramclinical weaknessesaswellastothecreationofnewcurricular experiencesdesignedtoaddressareasoflimitedclinical exposureidentifiedbyresidentCCdata.Theseexperiences couldpotentiallytaketheformoftargetedreadingsor simulationsessionsdesignedtosupplementlowerfrequency clinicalencounters.
Thiswasasingle-centerstudyinanurban,academicED, and findingsmaynotbegeneralizabletotrainingprograms indifferentenvironments.Additionally,thedatawas retrospective,makingtheeducationalutilityofthis informationoranypotentialcausesofvariationdifficult todetermine.
UseofaCCtocategorizeeachpatientencounterintoa clinicaldomainhasanelementofsubjectivityandmayhave ledtosomeencountersbeingmiscategorizedwithrespectto theworkupdoneor finaldiagnosis.Someadditional subjectivitymayhavebeenintroducedbyhowweclassified CCsthatcouldpotentiallyhavebeencategorizedinto multipledifferentdomains(suchas “fever” or “ingestion”). Thiswasdonebasedonwhatwasdeterminedtobemost likelytodrivetheinitialworkupinthedepartment.For example,althoughaCCof “chestpain” couldrepresenta cardiacorpulmonaryetiology,inalmostallcases,acardiac etiologymustbeexcluded.Therefore,itwasfeltthatthis wouldinfluencetheformationandmodificationofthe resident’sillnessscriptmostheavily.Itisalsopossiblethat encountersweremischaracterizedduetoonlyusingthe first CClistedandnotconsideringtheothersifmultipleCCswere listed.Likethepriorlimitation,itwasfeltthatthe firstCC wasmostlikelytodictatetheinitialEDworkup.Using dischargeor finaldiagnosesinsteadwasconsideredforthis study,butitwasfeltthattheCCismorelikelytodrivethe initialdifferentialanddiagnosticworkupforthepatient.
Additionally,ABEMdomainsmaybetoobroadto captureimportantdifferencesinexposure(e.g.,tworesidents withthesameexposureto “respiratorydisorders” couldhave seenlargenumbersofpneumoniapatientsor,alternatively, manypatientswithasthma).Trainingisinherentlyvariable astheEMenvironmentdiffersbyclinicalsite,day,shift,or evenseason.Therefore,theremayhavebeenslight differencesinwhenindividualresidentswereintheED clinicallyorthenumber/typeofoverallEDshiftsworked.It isimportanttonotethatsomeoftheincludedresidents’ trainingoccurredduringtheCOVID-19pandemic,which mayhavehadaneffectonboththevarietyandnumberof
clinicalexposuresseenbytheseresidents.Futureworkcould alsoexploreexposurebasedonsub-domainsfromthe ABEMmodeltogetamoregranularlookatindividual residentclinicalexperiencesratherthanrelyingonthe relativelybroaddomains.
Otherclinicalvariablesmayalsohaveaneffectona resident’sclinicalexposure,includingthetimingofmonths rotatingintheED.However,theEDdidnotundergomajor changesinthestaffingmodelofphysicians(including residents)duringthisperiod.Also,whileitislikelythatmore seniorresidentsassignthemselvestocriticallyillpatients,this wasfelttobeunlikelytomeaningfullyimpactourresults giventhatdatawasobtainedatthetimeofgraduation. Therefore,eachresidentwouldhaveactedinaseniorrolefor thesameamountoftime.Finally,ouruseoftheEHRatthe mainclinicaltrainingsiteoftheresidencytogeneratethe datadidnotcapturetheclinicalexperienceattwoother trainingsitesfortheresidencythatuseadifferentEHR.This mayhaveservedtomoderateorexacerbatethedifferences seenamongresidents.However,clinicalexperiencesatthese othersitescomprisedatotalofonlyfourmonthsofthe36monthcurriculum,andsoitislikelythatouroverall findings wouldnothavebeensubstantiallyaffected.
Withinasingle,three-yearacademicemergencymedicine program,therewassubstantialvariationamongresidents regardingthevarietyofpatientchiefcomplaintsseen throughoutresidencywhenmappedtoABEM’sModelof ClinicalPractice.
AddressforCorrespondence:CorlinM.Jewell,MD,Universityof WisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,800UniversityBayDr., Madison,WI53705.Email: cmjewell@medicine.wisc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Jewelletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TeunissenPW,ScheeleF,ScherpbierAJ,etal.Howresidentslearn: qualitativeevidenceforthepivotalroleofclinicalactivities. MedEduc. 2007;41(8):763–70.
2.BowenJL.Educationalstrategiestopromoteclinicaldiagnostic reasoning. NEnglJMed. 2006;355(21):2217–25.
3.CustersEJ,RegehrG,NormanGR.Mentalrepresentationsofmedical diagnosticknowledge:areview. AcadMed. 1996;71(10Suppl):S55–61.
4.HatalaR,NormalGR,BrooksLR.Influenceofasingleexampleon subsequentelectrocardiominterpretation. TeachingandLearningin Medicine. 1999;11(2):110–7.
5.StahmerSandKuhnG.Optimizingresidenttraining:resultsand recommendationsofthe2009CouncilofResidencyDirectors ConsensusConference. AcadEmergMed. 2010;17Suppl2:S78–86.
6.LiJ,RooseveltG,McCabeK,etal.Pediatriccaseexposureduring emergencymedicineresidency. AEMEducTrain. 2018;2(4):317–27.
7.ChenEH,ChoCS,ShoferFS,etal.Residentexposuretocritical patientsinapediatricemergencydepartment. PediatrEmergCare. 2007;23(11):774–8.
8.LangdorfMI,StrangeG,MacneilP.Computerizedtrackingof emergencymedicineresidentclinicalexperience. AnnEmergMed. 1990;19(7):764–73.
9.KernMW,JewellCM,HekmanDJ,etal.Numberofpatientencountersin emergencymedicineresidencydoesnotcorrelatewithin-trainingexam domainscores. WestJEmergMed. 2022;24(1):114–8.
10.HayashinoY,FukuharaS,MatsuiK,etal.Qualityofcareassociated withnumberofcasesseenandself-reportsofclinicalcompetencefor Japanesephysicians-in-trainingininternalmedicine. BMCMedEduc. 2006;6:33.
11.StrangeGRandChenEH.Useofemergencydepartmentsby elderpatients:a five-yearfollow-upstudy. AcadEmergMed. 1998;5(12):1157–62.
12.CairnsCandKangK.NationalHospitalAmbulatoryMedicalCare Survey:2021emergencydepartmentsummarytables.2023. Availableat: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/ Dataset_Documentation/NHAMCS/doc21-ed-508.pdf AccessedSeptember21,2024.
13.BischofJJ,EmersonG,MitzmanJ,etal.Doestheemergencymedicine in-trainingexaminationaccuratelyreflectresidents’ clinical experiences? AEMEducTrain. 2019;3(4):317–22.
14.CounselmanFL,BabuK,EdensMA,etal.The2016modeloftheclinical practiceofemergencymedicine. JEmergMed. 2017;52(6):846–9.
15.WolffM,SantenSA,HopsonLR,etal.What’stheevidence:selfassessmentimplicationsforlife-longlearninginemergencymedicine. JEmergMed. 2017;53(1):116–20.
16.DeiorioNM,MooreM,SantenSA,etal.Coachingmodels,theories,and structures:anoverviewforteachingfacultyintheemergency departmentandeducatorsintheoffices. AEMEducTrain. 2022;6(5):e10801.
17.SargeantJ,LockyerJ,MannK,etal.Facilitatedreflective performancefeedback:developinganevidence-andtheory-based modelthatbuildsrelationship,exploresreactionsandcontent, andcoachesforperformancechange(R2C2). AcadMed. 2015;90(12):1698–706.
18.VanMelleE,FrankJR,HolmboeES,etal.Acorecomponents frameworkforevaluatingimplementationofcompetency-basedmedical educationprograms. AcadMed. 2019;94(7):1002–9.
PeterMoffett,MD
AlBest,PhD
NathanLewis,MD
StephenMiller,DO
GraceHickam,MD
HannahKissel-Smith,MD
LauraBarrera,MD
ScottHuang,MD
JoelMoll,MD
DepartmentofEmergencyMedicine,VirginiaCommonwealthUniversitySchoolof Medicine,Richmond,Virginia
SectionEditors:AbraFant,MDandWilliamEdwardSoares,MD
Submissionhistory:SubmittedJuly21,2024;RevisionreceivedOctober7,2024;AcceptedOctober11,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.31064
Introduction: Emergencydepartmentboardinghasescalatedtoacrisis,impactingpatientcare, hospital finances,andphysicianburnout,andcontributingtoerror.Nopriorstudieshaveexaminedthe effectsofboardinghoursonresidentproductivity.Ifboardingreducesproductivity,itmayhavenegative educationalimpacts.Weinvestigatedtheeffectofboardingonresidentproductivityasmeasuredby patientsperhourandhypothesizedthatincreasedboardingleadstodecreasedproductivity.
Methods: Thiswasaretrospectivestudyataquaternary,urban,academicLevelItraumacenterfrom 2017–2021withathree-yearemergencymedicineresidencyof10–12residentsperyearandannual volumesof80,000–101,000.Boardingwasdefinedasthetimebetweenanadmissionorderandthe patientleavingtheED.Wecreatedamultivariablemixedmodelwith fixedcovariatesforyear,month,day ofweek,residentexperience,shiftduration,totaldailyEDpatients,andwithresidentsasrepeated measures.Theeffectofboardingwasestimatedaftercovaryingoutallotherfactors.
Results: Allvariablesincludedinthemodelweresignificantlyassociatedwithchangesinproductivity. Residentexperiencehasthelargesteffectsuchthatforeachmonthofresidencyexperience,aresident adds0.012patientsperhour(95%confidenceinterval[CI]0.010–0.014).Isolatingtheeffectofboarding demonstratedthatforeveryadditional100hoursofboarding,aresident’sproductivitydecreasedby 0.022patientsperhour(95%CI0.016–0.028).Inthestudy,themediandailyboardingwas261hours;if thiswereeliminated(assumingaresidentcompletes10010-hourshiftsannually),aresidentcouldbe expectedtosee56.9morepatientsperyear(95%CI40.7–73.1).
Conclusion: Hospitalboardingsignificantlyreducesresidentproductivityasmeasuredbypatients perhour.Furtherstudiesarewarrantedtodeterminetheeducationalimpact.[WestJEmergMed. 2025;26(1.2)54–62.]
Emergencydepartment(ED)boarding(definedas patientsadmittedtothehospitalbutremainingintheED) hasreachedcriticallevelsandhasbeendeclaredacrisisby theAmericanCollegeofEmergencyPhysicians.1 Thescope ofthecrisisisdauntingwitheffectsonpatientcare,errors, physicianburnout,hospitaleconomicstress,andambulance diversion.2 IncreasedEDboardingalsoleadstoincreasesin
medicationerrors,timetoantibiotics,timetopercutaneous coronaryinterventionforpatientswithmyocardial infarction,timetocareforpatientswithacutestroke,patient mortality,andrisk-adjustedhospitalspending,andhas effectsonalllevelsofacuity.3–10
Withinthecontextofboarding,EDsmustalsoprovide soundeducationaltraininginvolvingbothqualityand quantityofpatientexperiences.Residencyprogramsseekto improveefficiencyandproductivityintheirresidents throughouttheirtraining.Manyvariableshavebeen associatedwithresidentproductivityincludingtimeofshift, shiftlength,andresidentexperience.11–13 Thereare, however,fewstudiesthatevaluatetheeffectofEDcrowding andboardingtimeontheeffectofemergencymedicine(EM) residentproductivity.14 Ifboardingdecreasesthenumberof patientsseenduringaresidency,theremaybeanimpacton residenteducation.
Inthisstudyweaimedtoinvestigatetheeffectofboarding onEMresidentproductivityasmeasuredbypatientsper hour.Wehypothesizedthatincreasedhospitalboarding wouldresultindecreasedresidentproductivity.
ThiswasaretrospectivestudyconductedattheVirginia CommonwealthUniversityHealthSystem,theonly comprehensiveLevelItraumacenterinRichmond,VA. DuringthestudyperiodfromJanuary2017–June2021,the totalpatientvolumesrangedfrom80,000–101,000peryear. Onaverage,30%ofpatientswereadmittedtothehospital,of whom5%wenttotheintensivecareunit.Patients <18years ofageconstituted22%ofthetotalvolume.Thedepartmentis staffedwithboard-certifiedemergencyphysicians,and duringthestudyperiod81%ofpatientswereseenbya resident.Theremainingnon-residentcaseswereseenby advancedpracticepractitioners(APP)inalow-acuityareaof theEDorbyattendingphysiciansandwerenotincludedin thestudy.Throughoutthestudytherewasnochangeinthis staffingmodelsuchthatAPPswerenevercompetingforthe samepatientsasresidents.Thedepartmenthas76bedswith 35inanacutearea,10intrauma/resuscitation,10inamidtrackarea,16inapediatricdepartment,and fiveina fast-trackzone.
Ourresidencyprogramisthreeyearsinlength,andclass sizesrangedfrom10residentsin2017to12residentsin2021. Duringpostgraduateyears(PGY)-1,2,and3,residentswork intheEDfor26weeks,29weeks,and35weeks,respectively. Residentshiftlengthsvariedfrom9–12hourswiththemost typicalshiftbeing10hours.Onaverage,each24-hourperiod hadatotalof137hoursofresidentcoverageinoverlapping shifts.TheEMresidentssawpatientsinallEmergency SeverityIndex(ESI)categoriesandweretheprimary physiciansforallemergentpatients(ESI1and2).Residents caredforpatientsinallareasoftheEDotherthanthe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencydepartmentboardingnegatively impactspatientcare,hospitalef fi ciency,and physicianwell-being.
Whatwastheresearchquestion?
DoesincreasedEDboardingreduce emergencymedicineresidentproductivity, asmeasuredbypatientsperhour?
Whatwasthemajor findingofthestudy?
Foreveryadditional100hoursofED boarding,aresident ’ sproductivitydecreased by0.022patientsperhour(95%CI 0.016 – 0.028);aresidentsees57fewer patientsperyearduetoboarding.
Howdoesthisimprovepopulationhealth?
Understandingthenegativeeffectsof boardingonproductivitymayhelppolicy makers fi ndsolutionstoimprovepatient fl ow, patientcare,residenteducation,andoverall healthoutcomes.
low-acuityarea.Allresidentsstaffpatientsdirectlywithan attendingphysicianwithoutoversightbyamoresenior resident;therefore,theproductivitynumbers forresidentsinallthreeyearsoftrainingareindependent. ThestudywasgrantedexemptstatusbytheVirginia CommonwealthUniversityInstitutionalReview Board(HM20024717).
DatafromallpatientsevaluatedbyanEMresidentwas capturedinadatabase,andinconjunctionwithscheduling dataitwasusedtodeterminetheaveragenumberofpatients perhour.OnlyEMresidentswereincluded.Thestudyperiod wasselectedasthiswasthemaximumamountoftimefor whichdatawasavailablepriortothehospitalswitchingtoa newelectronichealthrecord.Asthedatabasewasinitially createdtoprovidefeedbacktoresidents,certaindatawas removedandnotavailabletousforanalysis.Information fromthe firstmonthofEMforeachresidentwasnot provided,andduetoinitialeffectsfromtheCOVID-19 pandemic,datafromApril–July2020wasnotincluded.
Wecombinedthreedatabasesforanalysis:thepatient databaseofallEDencounters;theresidentscheduling database;andthehospitalboardingdatabase.
Duringthestudyperiod,theEMresidencyprogram receivedmonthly,system-generatedreportslistingthe uniquepatientidentifier,nameoftheresidentassignedto careforthepatient,theESIacuitylevel,thedate/timeof first contactandcheckout,andthedisposition.Theresident assignmentwasderivedfromtrackingboarddata,andin scenarioswheremultipleresidentswereassignedtoapatient encounter,onlythe firstresidentassignedwascreditedfor eachuniquepatientencounter.TheEMresidentswere scheduledfor9-hour,10-hour,or12-hourshiftsduringthe studyperiod.Allnon-EMresidentsandstaffwereexcluded fromthepatientdatabase.
Boardingdatawasreporteddailyfromhospitalanalytics. Thenumberofhoursofboardingwasdefinedasthetime betweenanadmissionorderandwhenthepatientlefttheED. Boardinghourswasselectedasthiswasthevariableavailable tousfromthehospitalanalyticsdatabase.
WedesignedamodeltoisolatetheeffectsofEDboarding onresidentproductivityasmeasuredbypatientsperhour. Patientsperhourwasdefinedasthetotalnumberofnew patientsseenduringtheshiftdividedbythedurationofthe shiftinhours.Thecovariateswerechosenfromthosefound inpreviousstudiestoberelatedtoresident productivity.11,13,15,16 Theseincludedyear,month,dayofthe week,cumulativeresidencymonthsintraining,shift duration,totalpatientsperday,andboarding.Monthsin trainingwaschosenasacontinuouscovariatetodelineate residentexperienceratherthantheroughclassificationof PGY-1,-2,or-3basedontheobservationthatresident productivitybeginslowinthePGY-1year,increasesinthe PGY-2year,andthenplateaus.Thismonthlyexperience variablewasmodeledusingcubicregression.
Wedescribedthedatausingcountsandpercentages. Patientsperhourwasmodeledusingamultivariablemixed model,withcovariatesdefinedas fixedeffectsandresidents asrepeatedmeasures.Weusedanautoregressive(AR1) covariancestructuretoaccountforthedependencebetween repeatedmeasures.The fixedeffectswereyear(reference = 2019),month(reference = 12),dayoftheweek(reference = Thursday),residentmonthintraining(centeredon18),total patientsperday/100,shiftduration,anddailyboarding hours/100.Wechosetheyear2019asareferenceasitwasthe lastfullyearofdatapriortothestartoftheCOVID-19 pandemic.Decemberwaschosenasitalignswiththe18th monthofresidency,whichiswhenproductivityplateauedin ourmodel.Thursdaywasselectedasitisthoughttorepresent thedaywiththemostideal flowsinceitavoidsweekends, Monday,andFridaypatientsurges,aswellasWednesday morningdidacticswhenEMresidentsarenotworking clinically.Thetotalpatientsperday,shiftduration,and
boardinghourswerereferencedatthemedianvaluesin ourdataset.
Weestimatedtheeffectofboardingfromthemarginal regressionmodelaftercovaryingoutallotherfactors. Estimatesaredescribedusing95%confidenceintervals.All datamanagementandanalysiswereperformedusingSAS software(version9.4andJMPProversion17.2(SAS InstituteInc,Cary,NC).
Duringthestudyperiod,263,058patientswereseeninthe EDby601cliniciansincludingthe80EMresidentsstudied. Duringthe49monthsstudiedbetween2017–2021,EM residentswerescheduledto16,949shiftsandwereassigned 188,685patients(Table1).Totaldailypatientvolumevaried considerablyduringthistime(mean177,SD26,range
Table1. Characteristicsoftheemergencydepartmentresidents’ shiftsandpatientsevaluated(January2017–June2021).
CharacteristicShiftsNPatientsN(%) Total16,949188,685 Year
20173,49644,119(23) 20183,95547,569(25) 2019(11months)*4,05347,035(25) 2020(8months)† 3,10129,191(15) 2021(6months)2,34420,771(11) Month
1-January1,90921,052(11) 2-February1,57618,004(10) 3-March1,68018,901(10)
4†-April1,30215,229(8)
5†-May1,37116,385(9)
6†-June1,33715,191(8)
7†-July82010,129(5) 8-August1,56015,543(8) 9-September1,37614,741(8) 10-October1,43115,299(8) 11*-November1,06211,639(6) 12-December1,52516,572(9) Dayofweek Sunday2,24925,887(14) Monday2,67929,099(15) Tuesday2,75629,504(16) Wednesday‡ 1,98921,970(12) Thursday2,60127,874(15) (Continuedonnextpage)
Table1. Continued.
CharacteristicShiftsNPatientsN(%)
Friday2,52528,785(15)
Saturday2,15025,566(14)
Shift
7 AM to5 PM 1,68816,332(9)
7 AM to7 PM 1802,512(1)
9 AM to7 PM 2,54628,306(15)
12 PM to10 PM 3,38638,586(20)
2 PM to12 AM 2,47028,631(15)
3 PM to12 AM 3,55341,138(22)
9 PM to7 AM 3,12633,180(18)
PGY
PGY-1§ 5,16244,817(24)
PGY-24,75657,447(30)
PGY-37,03186,421(46)
Disposition
Admitted74,663(40)
Discharged114,022(60)
*November2019wasexcludedasthehospitalinformation managementsystemwasdown.
†April2020throughJuly2020wasexcludedduetoCOVID-19and hospitalchanges.
‡Wednesdaysmorningsareresidentdidactics.
§The firstmonthofaresidencywasexcluded(orientationmonth). ESI,EmergencySeverityIndex; PGY,postgraduateyear.
88–263).Asindicatedinthetable,theEDexperienceda patientcountvariabilitythatchangedacrossyears,months, daysoftheweek,shifts,andPGYlevel.Ofall188,167 patientsseenbyEMresidents,40%wereadmitted.
Boardinghoursperdayvariedconsiderably(mean281, SD127,range50.8–914.4; Figure1).Thehospital informationsystemcalculatedboardinghoursdaily; however,acrossthe1,490daysstudied,thereweresix impossible(negative)valuesandnineverylowvalues.Low valueswereidentifiedbylargeresidualsinthemultiple regressionmodel.Ratherthantreatingtheseasmissing values,weusedamultipleregressionmodeltoimputethe 15valuesinquestion.
Allthefactorsintherepeated-measuresmixed-model weresignificant(P < 0.001). Table2 showstheestimated effectofeachterminthemodel.Thejointeffectofallthe factorsonresidentproductivityisshownin Figure2.These profileplotsshowthemarginalmodelpredictedvalueof residentproductivityontheverticalaxisacrossallthe covariatesontheseparatehorizontalaxes.Theimportance
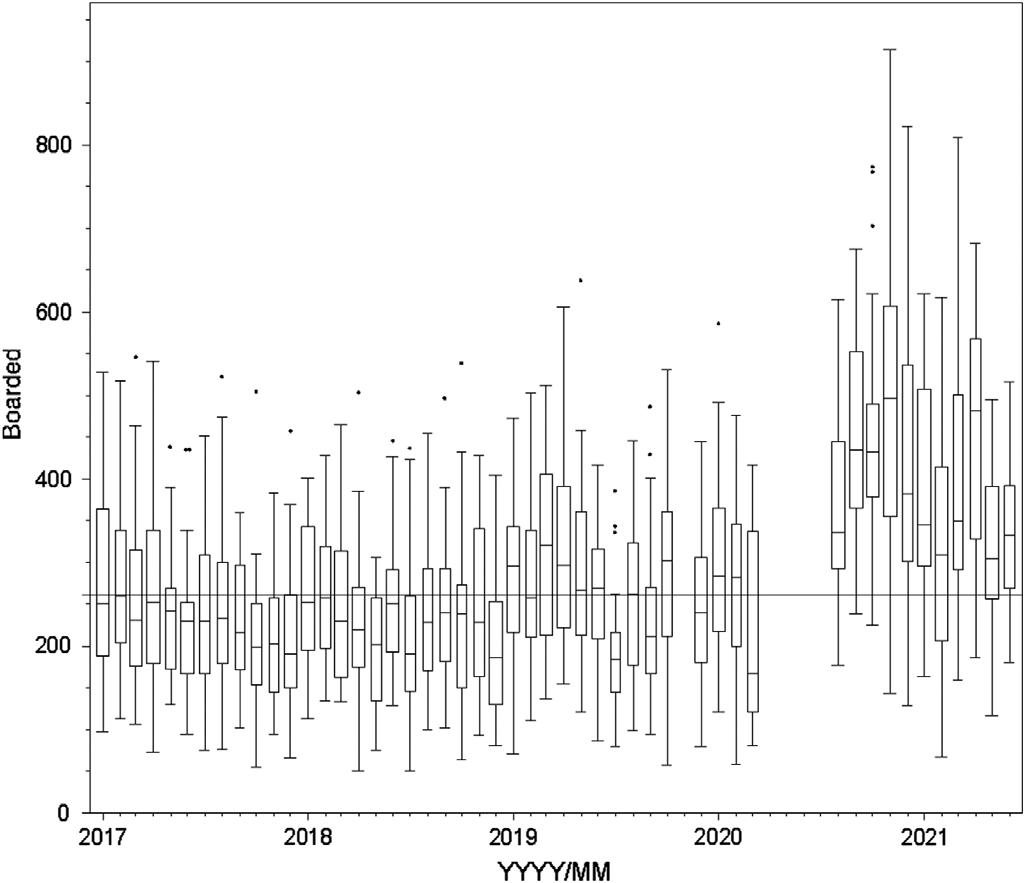
Figure1. Boardingacrossstudyyears.
Linesetatmedianboardinghoursacrosstheentirestudyperiod (261hours/day).
Eachboxplotrepresentsamonth(line = median,box = 25th to75th quartile,whiskers = typicalextremes,circles = outliers).
Note:April2020–July2020hoursarenotavailableasthey correspondtothebeginningoftheCOVID-19pandemic.
ofafactorisvisualizedbythesteepnessofthe predictiontrace.
Isolatingtheeffectofboardingdemonstratedthatfor everyadditional100hoursofdailydepartmentalboarding, individualresidentproductivitydecreasedby0.022patients perhour(95%confidenceinterval[CI]0.016–0.028, Table2). Inthereferencestandardscenario,aresidentcouldbe expectedtosee1.10patientsperhourwithboardingatthe dailymedian(261hours)butcouldsee1.15patientsperhour ifboardingwereeliminated(Figure2,PanelC). Table3 showshowresidentproductivitywasdegradedbyboarding acrosstherangeofvaluesseenatourinstitution.Aresident wouldsee1.14patientsperhourwhenboardingwasatthe lowestinthestudycomparedto0.95patientsperhouratthe maximumlevelofboardingseeninthestudy,whichisa differenceof0.19patientsperhour(95%CI0.15–0.22). Assumingaresidentcompletesapproximately100shiftsa yearthatareof10hoursdurationandboardingwas eliminated,thenaresidentcouldbeexpectedtosee56.9more patientsperyear(95%CI40.7–73.1).Thiswouldrepresenta 5%increaseinpatientvolumeperresidentannually. Residentexperiencehasthelargesteffectonresident productivity.Residentproductivitywaslowinitiallyat0.5 patientsperhour(95%CI0.46–0.54)bythesecondmonthof training(Figure2).Improvementwasinitiallyrapidto0.75 patientsperhouratsevenmonths,thenplateauednearthe 18-monthpoint(1.10patientsperhour)to finallyreach1.12 patientsperhourattheendofthe36months(95%CI 1.08–1.17).WhenevaluatingourdatabyPGYlevel,our
Table2. Multipleregressionresultspredictingnewpatientsperhourperresidentforeachvariable.
EffectEstimatednewpatientsperhourStandarderror95%CI
Intercept1.09570.01731.0618to1.1297
Year
20170.15010.01220.1262to0.1740 20180.08370.01170.0608to0.1065
2019[reference]
2020 0.06410.0137 0.0909to 0.0373 2021
Month
1-January0.06350.01720.0298to0.0972
2-February0.07760.01820.0420to0.1133
3-March0.04980.01810.0144to0.0852
4-April0.08400.01970.0453to0.1227
5-May0.07500.01960.0366to0.1133
6-June0.05850.02010.0191to0.0979
7-July
8-August0.05500.01850.0188to0.0912
9-September0.06540.01870.0288to0.1021
10-October0.04870.01840.0127to0.0847
11-November0.04860.01990.0095to0.0876
12-December[reference]
Dayoftheweek
Sunday0.05870.01180.0357to0.0818
Monday
0.03120.0118
Tuesday0.01220.01100.0094to0.0338
Wednesday0.10940.01230.0854to0.1334
Thursday[reference]
Friday0.04750.01090.0261to0.0688
Saturday0.11820.01200.0948to0.1417
Residentmonths(linear)*0.01220.00100.0101to0.0142 (quadratic)
0.0012to 0.0010 (cubic)0.000030.000010.00002to0.00004
Totalpatientsperday(per100patients)*0.40210.01650.3697to0.4344
Shiftduration*
Themixed-modelalsoincludedresidentasarepeated-effectwithanAR(1)covariancestructure. *Continuouscovariateswerereferencedtothemedianvalue.Medianresidentmonth = 18,totalpatientsperday/100 = 1.77, shiftduration = 10hours,boardedhours/100 = 2.61. CI,confidenceinterval.
PGY-1residentssaw0.75perhour,PGY-2residentssaw 1.10patientsperhour,andPGY-3residentssaw1.12 patientsperhour.
TotalpatientsperdaypresentingtotheEDwasthenext mostimportantfactorinresidentproductivity.Forevery100 newpatientspresentingtotheED,anindividualresident
wouldbeexpectedtoadd0.40patientsperhour(95%CI 0.37–0.43).Themedianvaluefordailytotalpatientvolume was177patientsperday,butalow-volumedayatthe10th percentile(143totalpatients)resultedinacorresponding decreaseinresidentproductivityto0.96patientsperhour (95%CI0.92–1.00).Forahigh-volumedayatthe90th

Figure2. Multipleregressionresultspredictingnewpatientsperhourperresidentforeachvariable. Allvalues(year,month,dayofweek,EMresidentmonths,totalpatients,shiftduration)inmodelheldatreferencestandardswithadjustments toboarding(lastpanelofeachgraph).ExpectedpatientsperhourineachscenarioisindicatedbytherednumberintheYaxiswith95% confidenceintervalsinblue.Asboardedhourschange(lastpanelofeachgraph)sodopatientsperhour(rednumbertoleftofeachgraph)in eachofthethreescenarios(A:Medianboardingof261hours.B:Reducingboardingby100hours.C:Eliminatingboardinghours.)
percentile(210patients),residentproductivityincreasedto 1.23patientsperhour(95%CI1.19–1.26).
Residentproductivityalsochangedbasedonthe year,shiftduration,anddayoftheweek.Resident
Table3. Estimatedresidentproductivitybyboardinghours.
productivitywashighestin2017at1.25patientsperhour (95%CI1.21–1.28)andsteadilydecreasedtothe0.93 patientsperhourseenin2021.Residentproductivityfora nine-hourshiftwaspredictedtobe1.21patientsperhour
CutoffBoarded(hours)EstimatedpatientsperhourStandarderror95%CI
Marginalestimatesfromthemixedmodelwiththefollowingfactorsheldconstant:year = 2019,month = 12,dayoftheweek = 5(Thursday), residentmonthintraining = 18,totalpatientsperday/100 = 1.77,shiftduration = 10hours. CI,confidenceinterval.
(95%CI1.19–1.26),whereasfora12-hourshiftitwas predictedtobe0.84patientsperhour(95%CI0.80–0.89). SaturdaysandWednesdaysaveragedapproximately1.21 patientsperhour,Sundays,andFridaysapproximately1.15 perhour,andMondays,Tuesdays,andThursdays1.10 patientsperhour.
Month-to-monthvariabilityhadthesmallesteffecton residentproductivity.Comparedwiththeothermonths,July andDecemberhadlowerresidentproductivity(1.09vs1.16 patientsperhour).
Toourknowledge,thisisthe firststudytodemonstrate thatthereisasignificantreductioninresidentproductivity (measuredaspatientsperhour)duetohospitalboardingin theED.Inourmodel,thisresultedinadecreaseof0.022 patientsperhour(95%CI0.016–0.028)forevery100hours ofdailyboarding.Whileperformedatasingleinstitution, ourdatasetbroadlyalignswithmultiplestudiespreviously completedregardingresidentproductivity.Inourstudy,we analyzedresidentexperienceasthenumberofmonthsin trainingratherthandividedintoPGYlevel.Thiswasbased onourobservationthatproductivityrapidlyincreased duringthePGY-1yearandthenplateauedinthemiddleof thePGY-2year.
WhenevaluatingourdatabyPGYlevel,ourPGY-1 residentssaw0.75patientsperhour,PGY-2residentssaw 1.10patientsperhour,andPGY-3residentssaw1.12 patientsperhour.Priorstudieshavedemonstratedsimilar patternswithPGY-1to-3residentsseeingbetween0.79–0.81 patientsperhour,1.05–1.2patientsperhour,and1.22–1.27 patientsperhour,respectively.17–19 AstudybyHenningetal showedrapidprogressionfromPGY-1toPGY-2yearand thengradualprogressioninPGY-3yearbutwasbasedon patientsperday.20 Similarly,astudybyTurner-Lawrence andToddsawincreasingproductivityfrom1.2patientsper hourto1.5patientsperhourto1.6patientsperhourby PGY-1to-3residents,respectively.13 Whilethese productivitynumbersarehigherthanthoseinourstudy,the authorsdidnotadjustforadditionalvariables.
Inamorecomparablestudy,Kirbyetalreportedthe efficiencyofEMresidentsduringEDcrowding.14 The authorsusedtheNationalEmergencyDepartment OvercrowdingStudy(NEDOCS)scoringsystemto categorizestatesintheEDasnotcrowded,crowded,and overcrowded.Theyfoundthatresidentproductivity measuredasnewpatientsperhourincreasedinitiallyinall yeargroupsastheEDtransitionedfromnotcrowdedto crowded,butthenremainedstablewhentransitioningfrom crowdedtoovercrowded.WhiletheNEDOCSscoreusesa measureofEDboarding(thewaitingtimeofthelongest admittedpatient),itdoesnotincludetotalpatientboarding hoursasinourstudy.Ourstudymoredirectlyexaminesthe effectofboarding(oneelementofcrowding)onresident
productivity.Theparadoxicalincreaseinresident productivityintheKirbystudymayhavebeenduetoan increasednumberofpatientspresentingtotheED,which couldhaveincreasedtheNEDOCSscore.Ourstudy demonstratedthatresidentproductivityincreasedwith higherpatientvolumes,andincludingthisinourmodel allowedustobetterisolatetheeffectofboarding.
AccordingtoastudybytheAcademyofAdministrators inAcademicEmergencyMedicineandtheAssociationof AcademicChairsofEmergencyannualbenchmarksurvey, boardingtimeshavedramaticallyincreasedsincethe COVID-19pandemic.21 Bytheendoftheirstudyperiod,the mediannumberofboardinghourspermonthwas11,480, whichapproximatesto382hoursofdailyboarding.Inour study,whichincludesapre-pandemicperiod,themedian dailyboardingwas261hours,suggestingthatboardingis likelyworseningovertimeandisaproblematmany academicmedicalcenters.
Theeducationalimpactofdecreasedpatientvolumes causedbyboardingisuncertain.Itisreasonabletoexpect thatresidentsseeingfewercasesmaylosevaluablelearning opportunities,butthishasnotbeenwellstudiedandno firm numbersexisttosuggestathresholdatwhicheducation suffers.Priorauthorshavesurveyedresidentsregardinga perceiveddecreaseineducationduringcrowding.22,23 These studiesconcludedthatresidentsdidnotperceiveadifference ineducationduringthesetimes,buttheyuseddiffering measuresofcrowding,weresurvey-based,and underpowered.Educatorsmayswitchtodifferentmodelsof teachingduringperiodsofhighboarding,leadingto residentsperceivingalessdeleteriouseffect.24
OthershavepostulatedaneducationalStarlingeffect wherebysomeboardingallowssupervisingphysiciansmore timetoteach,butatsomepointtherearediminishedreturns asfewernewpatientsbecomeavailabletodiscuss.25 Amore recentstudywasconductedduringthecurrentboarding epidemic;theauthorssurveyedEMprogramdirectors regardingtheirperceptionsoftheimpactofboardingon residenttraining.26 Inthisstudy,80%oftherespondentsfelt thatboardingnegativelyaffectedresidenteducation, especiallyinthedomainsofmanagingdepartment throughputandmanaginghighvolumesofpatientsper resident.Whilesurvey-basedinnature,thestudyresults broadlyalignswiththepriorstudiesinthisarea.
Theoretically,residentswhoseefewercasesmaylose valuablelearningopportunities.Whilethecomponentsof Bloom’sdomainsofeducationalactivitiescanbelearnedvia differentmodalitiesofinstructionaltechniques,clinical experienceallowsforthelinkingofknowledgetoskillsand thentoattitudes/emotions.27 Bydecreasingalearner’ s exposuretopatients,onecouldarguethatresidentsmaylose valuableexperientiallearningopportunities.Whilesomeof thesecanbereplicatedinsimulationorcase-based discussion,otherskillscannotandarebestlearnedviahands-
on,experientiallearningencounters.Experientiallearning theory,asdescribedbyKolb,highlightstheimportanceof real-lifeexperienceandtheinfluencethishasonlearning.28 Unliketraditionallearningandinstructionalmethodology thatfocusesonrotememorization,experientiallearningisan activeprocesswhereresidentsareengagedinconcept transformationthroughactionaswellasreflectionontheir experiencesandpatientencounters.
Thislearningtheoryalsoemphasizesprinciplesofadult educationinwhichpriorlearningexperiencescanbe leveragedtocreatemoremeaningfulandrelevant educationalexperiences.29 Additionally,decreasingpatient interactionmayalsoaffectresidents’ applicationand translationofknowledgeintopractice.Behaviorallearning theoryemphasizeslearningthroughinteractionswiththe environmentwherereinforcementandfeedbackcan encouragemodificationofbehaviors.Byincorporating behaviorallearningstrategies,medicaleducationcanfoster notonlytechnicalcompetenciesbutalsothedevelopmentof professionalhabitssuchaseffectivecommunicationbetween teammembersandpatients.30
Thisstudyhasseverallimitations.Thiswasasingle-center studythattookplaceinahighacuity,quaternary-carecenter thatalsoexperienceshighlevelsofboarding,whichmaylimit generalizabilitytoothercenters.Thedatabasethatcaptured theresidentpatientassignmentwasbasedontrackingboard dataandmayhaveoccasionallymiscreditedaresidentwitha patientencounter;however,asthedatasetwaslargeand involvedmultipleyearswithcompletedatasetsforthreefull classesofresidentsthisisunlikelytohavegreatlyinfluenced thedata.Ourresidentclasssizedidincreaseduringthe 2021yearandthuscouldtheoreticallyhavedecreasedthe numberofpatientsavailableperresident.Whilewedidnot studythatdirectly,itisunlikelytohaveimpactedthedata greatlyastheadditionalresidentsallowedforthecreationof anoutsiderotationatafree-standingemergencycenterand, therefore,residentstaffinghoursstayedgenerallyconsistent atthestudysite.
Ourmodeldidnotincludeameasureofpatientacuityasa covariate.WhiletheESIcategoryanddispositionwere recordedforeachpatient,wedidnotfeeltherewasareliable waytoconvertthisdataintoameaningfulmeasureofhourly acuitythatinfluencedtheamountoftimearesidentmight dedicatetowardpatientcare.Forexample,anESI-1patient whoisadmittedforanST-segmentelevationmyocardial infarctionmaystayinthedepartmentfor15minutesleaving thebedopenforanewpatient,whileanESI-3patient requiringaworkupforabdominalpainincludingimaging whoisdischargedmayoccupyaroomandaresidentfor multiplehours.Sinceourdatasetwaslarge,itwasassumed thatallresidentswouldbeexposedequallytothesamemixof acuitiesonindividualshifts,bytheendoftheirresidency
andthuslimittheeffectonthedata.Additionally,recent studieshavecalledintoquestiontheaccuracyofthe ESI.26,27 Apriorstudyonresidentproductivitydidnot showacorrelationbetweenESIandclinician dispositiontimes.14
OurstudyalsoincludeddatafromtheCOVID-19 pandemic,whichaffectedpatientvolumesandEDboarding. Thedatasetweusedwasinitiallymeantforreporting individualresidents’ productivitymeasures,sodatafromthe firstfewmonthsofthepandemicwasnotavailableforour currentstudy.Thislikelyservedtodecreasetheeffectofthe initialpandemicresponseonourdata.Justpriortothe pandemicourEDhadseenagrowthinpatientvolumesfrom 87,000patientsperyeartoapeakof101,000patientsper year,whichwasfollowedbyarapiddeclineto83,000ayear inthe2021–2022year.Thevolumesdidslowlyriseafterthe studyperiod.Thismayhaveinfluencedsomeofthedata fromourlaterresident-yeargroupsandservedto decreaseproductivity.
Ourmeasureofboardingmayalsohavelimitations.Total boardinghoursperdaywasthevariableavailablefromour hospitalanalyticsdepartment.Thenumberofboarded patientsperdaymayhaveprovideddifferentdata.For example,inourmodelasinglebehavioralhealthpatient boardingfor20hoursfromonedaywouldbe indistinguishablefrom20patientsboardingin20 individualroomsforasinglehoureach.Asthedatasetis large,andallresidentswereexposedtothesameconditions throughouttheirtime,itisunlikelyanyoneresident’sdata (orthetrend)wouldbeaffectedbasedonthesetypes ofoutliers.
Wefoundasignificantreductioninresidentproductivity asmeasuredbypatientsperhourduringperiodsofincreased boarding.Furtherstudiesarewarrantedtodeterminethe educationalimpactofthese findings.
AddressforCorrespondence:PeterMoffett,MD,Virginia CommonwealthUniversity,DepartmentofEmergencyMedicine, 1250EMarshallStreet,Suite600,RichmondVA23298.Email: peter.moffett@vcuhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Moffettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AmericanCollegeofEmergencyPhysicians.Emergencydepartment boardingandcrowding.Availableat: https://www.acep.org/ administration/crowding–boarding/.AccessedDecember29,2022.
2.KelenGD,WolfeR,D’OnofrioG,etal.Emergencydepartment crowding:thecanaryinthehealthcaresystem. NEJMCatalyst InnovationsinCareDelivery. 2021.Availableat: https://catalyst.nejm. org/doi/full/10.1056/CAT.21.0217.AccessedApril4,2022.
3.KulstadEB,SikkaR,SweisRT,etal.EDovercrowdingisassociated withanincreasedfrequencyofmedicationerrors. AmJEmergMed. 2010;28(3):304–9.
4.ChatterjeeP,CucchiaraBL,LazarciucN,etal.Emergencydepartment crowdingandtimetocareinpatientswithacutestroke. Stroke. 2011;42(4):1074–80.
5.KulstadEBandKelleyKM.Overcrowdingisassociatedwithdelaysin percutaneouscoronaryinterventionforacutemyocardialinfarction. IntJ EmergMed. 2009;2(3):149–54.
6.FeeC,WeberEJ,MaakCA,etal.Effectofemergencydepartment crowdingontimetoantibioticsinpatientsadmittedwithcommunityacquiredpneumonia. AnnEmergMed. 2007;50(5):501–9,509.e1.
7.BaloescuC,KinsmanJ,RaviS,etal.Thecostofwaiting:associationof EDboardingwithhospitalizationcosts. AmJEmergMed. 2021;40:169–72.
8.RichardsonDB.Increaseinpatientmortalityat10daysassociated withemergencydepartmentovercrowding. MedJAustral. 2006;184(5):213–6.
9.McCarthyML,ZegerSL,DingR,etal.Crowdingdelaystreatmentand lengthensemergencydepartmentlengthofstay,evenamong high-acuitypatients. AnnEmergMed. 2009;54(4):492–503.e4.
10.WhiteBA,BiddingerPD,ChangY,etal.Boardinginpatientsinthe emergencydepartmentincreasesdischargedpatientlengthofstay. JEmergMed. 2013;44(1):230–5.
11.JosephJW,HenningDJ,StrouseCS,etal.Modelinghourlyresident productivityintheemergencydepartment. AnnEmergMed. 2017;70(2):185–90.e6.
12.JeanmonodR,JeanmonodD,NgiamR.Residentproductivity:does shiftlengthmatter? AmJEmergMed. 2008;26(7):789–91.
13.Turner-LawrenceDandToddBR.Monthlyprogressionofemergency medicineresidentefficiency:whatcanweexpectofourresidents throughouttraining? JEmergMed. 2019;57(1):77–81.
14.KirbyR,RobinsonRD,DibS,etal.Emergencymedicineresident efficiencyandemergencydepartmentcrowding. AEMEducTrain. 2019;3(3):209–17.
15.JeanmonodR,BrookC,WintherM,etal.Residentproductivityasa functionofemergencydepartmentvolume,shifttimeofday,and cumulativetimeintheemergencydepartment. AmJEmergMed. 2009;27(3):313–9.
16.JosephJW,DavisS,WilkerEH,etal.Modellingattendingphysician productivityintheemergencydepartment:amulticentrestudy. Emerg MedJ. 2018;35(5):317–22.
17.DeBehnkeD,O’BrienS,LeschkeR.Emergencymedicineresidentwork productivityinanacademicemergencydepartment. AcadEmergMed. 2000;7(1):90–2.
18.FredetteJ,KimT,McHughD,etal.Adescriptiveanalysisofemergency medicineresidentproductivityoverthecourseoftraining. AEM EducationandTraining. 2021;5(S1):S44–8.
19.JeanmonodR,DamewoodS,BrookC.Residentproductivity:trends overconsecutiveshifts. IntJEmergMed. 2009;2(2):107–10.
20.HenningDJ,McGillicuddyDC,SanchezLD.Evaluatingtheeffectof emergencyresidencytrainingonproductivityintheemergency department. JEmergMed. 2013;45(3):414–8.
21.KilaruAS,ScheulenJJ,HarbertsonCA,etal.BoardinginUSacademic emergencydepartmentsduringtheCOVID-19pandemic. AnnEmerg Med. 2023;82(3):247–54.
22.MahlerSA,McCartneyJR,SwobodaTK,etal.Theimpactofemergency departmentovercrowdingonresidenteducation. JEmergMed. 2012;42(1):69–73.
23.PinesJM,PrabhuA,McCuskerCM,etal.TheeffectofEDcrowdingon education. AmJEmergMed. 2010;28(2):217–20.
24.AtzemaC,BandieraG,SchullMJ,etal.Emergencydepartment crowding:theeffectonresidenteducation. AnnEmergMed. 2005;45(3):276–81.
25.ShayneP,LinM,UfbergJW,etal.Theeffectofemergencydepartment crowdingoneducation:blessingorcurse? AcadEmergMed. 2009;16(1):76–82.
26.GoldflamK,BradbyC,CoughlinRF,etal.Isboardingcompromisingour residents’ education?Anationalsurveyofemergencymedicine programdirectors. AEMEducTrain. 2024;8(2):e10973.
27.BloomBS,EngelhartMD,FurstEJ,etal. TaxonomyofEducational Objectives:CognitiveandAffectiveDomains.NewYork,NewYork: DavidMcKayCompany,Inc,1956.
28.KolbDA. ExperientialLearning:ExperienceastheSourceofLearning andDevelopment.EnglewoodCliffs,NJ:Prentice-Hall;1984.
29.SchultzK,McEwenL,GriffithsJ.ApplyingKolb’slearningcycleto competency-basedresidencyeducation. AcadMed. 2014;91(2):284.
30.MerriamS. AdultLearning:LinkingTheoryandPractice.SanFrancisco, CA:Jossey-Bass;2013.
31.SaxDR,WartonEM,MarkDG,etal.Evaluationoftheemergency severityindexinUSemergencydepartmentsfortherateofmistriage. JAMANetwOpen. 2023;6(3):e233404.
32.MistryB,StewartDeRamirezS,KelenG,etal.Accuracyandreliability ofemergencydepartmenttriageusingtheemergencyseverity index:aninternationalmulticenterassessment. AnnEmergMed. 2018;71(5):581–7.e3.
JulieCooper,MD* JennaFredette,MD†
*UniversityofPennsylvania,DepartmentofEmergencyMedicine,Philadelphia,Pennsylvania † ChristianaCare,DepartmentofEmergencyMedicine,Newark,Delaware
SectionEditors:PaulLoganWeygandt,MDandBenjaminHoldenSchnapp,MD
Submissionhistory:SubmittedJune22,2023;RevisionreceivedMarch3,2024;AcceptedMay30,2024
ElectronicallypublishedSeptember6,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18381
Emergencymedicine(EM)residentsroutinelycarefor criticallyillpatientsinboththeemergencydepartment(ED) andintensivecareunits.1 Proficiencyinprimarypalliative careskillsisessentialforallemergencyclinicians.2,3 However,asignificantnumberofresidentslackexposureto formaleducationandtraininginpalliativecare.4,5 Moreover,educationandtraininginpalliativecare encompassesseveralAccreditationCouncilforGraduate MedicalEducation(ACGME)competenciesincluding systemnavigationforpatient-centeredcare,understanding thephysician’sroleinthehealthcaresystem,patient-and family-centeredcommunication,andinterprofessionaland teamcommunication.6
Currentcurriculaaddressingprimarypalliativecareskills inEMarenotablylimited.7–12 Historically,ourresidency experiencedinconsistenciesintheteachingofprimary palliativecareskills.Theyweresporadicallycoveredduring regularconferencesorlefttodeveloporganicallyovertime. Furthermore,postgraduateyear-2(PGY-2)residents,who primarilymanageseriouslyillpatients,foundthemselves engaginginchallengingserious-illnessconversationswith patientsandfamilieswithlittletonotraining.Recognizing theimperativeformorecomprehensiveeducation,we introducedafour-week,intensiveprimarypalliativecare curriculumspecificallytailoredforEMPGY-2residentsthat wasentitled “PalliativeCareBootcamp.”
Theoverallobjectiveofthebootcampwastointroduce andstrengthenprimarypalliativecareskillsamongPGY-2 residentsatanindependentacademicmedicalcenter.Atthe endofthecurriculum,residentswouldbeableto1)definethe scopeofhospiceandpalliativemedicine;2)understandwhat primarypalliativecareskillsarefornon-specialtytrained physicians;3)recognizeEDpatientswithpalliativecare needs;4)implementahospiceevaluation;5)understandhow interdisciplinaryteamsareinvolvedinthecareofseriouslyill patients;and6)buildcommunicationskillsfordiscussing goalsofcare(GOC).
Thecurriculumandassessmentwereexemptfromthe institutionalreviewboard.UsingKern’ssix-stepapproachto curriculumdevelopment,wecreatedanintroductory primarypalliativecarecurriculum.AnEMfacultymember withaninterestinpalliativecareandresidencyleadership collaboratedtodevelopthecurriculum.Theresidency programendorsedthecurriculumasitalignedwitha curriculumredesigntoincludemorePGY-specificeducation.
Thecurriculumwasinitiallydevelopedin2017.The interdisciplinarypalliativecareteamatthestudyinstitution servedascontentexperts.Theteamperformedabroad reviewoftheresidencycurriculumandprioritizedhigh-yield topicstailoredtothelocalcontext.Sessionswere scheduledduringweeklyconferenceandspannedfour consecutiveweeks.Thisscheduleallowedforanintensive experienceandallowedforrapidskilldevelopment.The curriculumisstrategicallydeliveredearlyinthePGY-2year toleverageresidents’ existingexperienceincaringfor seriouslyillpatientsandfacilitatemeaningfulreflection andinquiry.
Thecurriculumisstructuredintwophases(Table1).The firstphasespansthreeweeksandconsistsofthreetwo-hour sessions.Thesesessionsarededicatedtoprimarypalliative carefundamentalssuchasanintroductiontopalliativecare, prognosisandtrajectory,andnon-painsymptom management.SessionfacilitatorsincludedtheEMfaculty contentexpertaswellasmembersoftheinstitutional palliativecareteam,thedirectorofchaplaincywho specializedinfamilysupport,thedirectorofpalliativecare, andthepalliativecarefellow.Eachsessionencompasseda didacticsegment,interactivecase-baseddiscussionsusing scenariospreparedbyfacilitatorsorcontributedbyresidents, andopportunitiesforresidentquestions.
Inthe finalweek,residentsengagedinafour-hoursession inthesimulationcenter.ThissessionwasledbytheEM contentexpertwhoisatrainedfacilitatorwithVitalTalk,a nationalnon-profitthatpromotesevidence-basededucation inserious-illnesscommunication.13 Thissessioninvolves usingastandardizedpatient.Residentsareassignedtoa
Table1. Thebreakdownofpalliativecarebootcampsessionsbyhourdetailingthetopic,learningobjectives,mappingtoACGME* competencies,andtheformatofthesession.
HourTopicObjectives
1Introtoprimarypalliative careinemergency medicine
Defineprimarypalliativecareandidentify commonEDpresentationsofpatientswith unmetpalliativecareneeds.
Defineadvancecareplanning,goalsofcare, codestatusandtreatmentlimitationsand describehowthesearecodifiedinlegaland medicaldocuments
InterpretaPOLST(PhysicianOrdersforLife SustainingTreatment)formanddescribeits useinacutecaresettings
2PrognosisandtrajectoryDescribefourcommontrajectoriesoflifelimitingillness
Defineprognosisanddescribe3strategiesto assessprognosisinEDpatientswithserious illness
3ChaplainchatDescribetheroleofthechaplaininthe interdisciplinarycareofseriouslyillpatients intheED
4Non-painsymptom management
Chooseappropriate first-andsecond-line treatmentforseriouslyillpatientsexperiencing nauseaandvomitingintheED
Chooseappropriate first-andsecond-line treatmentforseriouslyillpatientsexperiencing dyspneaintheED
Chooseappropriate first-andsecond-line treatmentforseriouslyillpatientsexperiencing constipationintheED
5AskaconsultantDescribetheroleoftheHPMclinicianinthe careofseriouslyillpatientsinthehospital
UnderstandtheroleofHPMconsultationin theemergencydepartment
6IntrotohospiceDescribethescopeofhospiceservicesand thesettingswhereitcantakeplace
Identifypatientswhomayqualifyforhospice andhowtogetthemevaluated
Providegoalconcordantcaretopatients enrolledinhospicewhopresenttotheED
ACGME competenciesFormat/facilitator
Systemnavigationfor patientcenteredcare
Physicianrolein healthcaresystems
Lecture – EMfaculty contentexpert
7–10Seriousillness communicationworkshop (VitalTalk)
Practiceskillsassociatedwithgoalsofcare conversationswithasimulatedpatient.
Diagnosis,treatment, andclinicalreasoning
Case-basedlearning –EMcontentexpert
Systemnavigationfor patient-centeredcare
Interprofessionaland teamcommunication
Pharmacotherapy
Diagnosis,treatment, andclinicalreasoning
Case-based learning – chaplain
Case-basedlearning –hospitalpalliative carespecialist
Interprofessionaland teamcommunication
Systemnavigationfor patient-centeredcare
Physicianrolein healthcaresystems
Patient-andfamilycentered communication
Case-basedlearning –hospitalpalliative carespecialist
Lecture – community hospicemedicaldirector
Simulationand standardizedpatient skills-basedpractice –EMcontentexpert
*ACGME,AccreditationCouncilforGraduateMedicalEducation; ED,emergencydepartment; EM,emergencymedicine; HPM,hospiceand palliativemedicine.
smallgroupandtheyrole-playdeliveringseriousnewswith EM-basedscenarios.Thissessionbuildsskillsaround deliveringseriousnews.
Thecurriculumunderwentiterativeadjustmentsinformed byinformalfeedbackfrombothfacilitatorsandresidents.
Modificationsweremadebasedonfacilitatoravailability andinterest,resultingintheinclusionormodificationof topics,whilecertainsubjects,suchasopioidpain management,wereremovedduetoredundancyinother educationalsettings.
Beforeimplementingthecurriculum,wecreatedabrief, pre-bootcampsurveytoassessresidents’ priorexposureand familiaritywithpalliativecare.Subsequently,twopostsurveyswereusedtogaugeresidents’ perceptionsregarding theachievementofsession-specificgoals.Wedevelopedthe firstsurveytoevaluatethe firstthreeweeksofthebootcamp. Theinitialdevelopmentcollectedallpotentialsurveyitems thatwererefinedthroughexpertconsultation.Thesurvey useda five-pointLikertscalerangingfrom1(strongly disagree)to5(stronglyagree).Thesurveyitemshadbeen pilottestedandrefinedinprecedingyearstoensurequestion clarity(Appendix1).
Asecondsurvey,whichwasusedforthesimulation-based session,promptedresidentstoratetheirself-assessed confidencesurroundingthespecificskillsonconducting GOCconversationscoveredinthesession(Appendix2).The surveyusesa five-pointLikertscalerangingfrom1(notvery confident)to5(veryconfident).
Thecurriculumevaluationtookplaceduringthe2022 bootcamp.Eachsessionhadanaverageof8–10PGY-2 residents,ofatotal17potentialparticipants.Attendance variedfromweektoweekduetoexcusedabsences. Participationinbothpre-andpost-surveyswasvoluntary.Of theeligibleresidents,nine(52%)completedthepre-survey, revealingthatallbutoneresidenthadpriorexposuretoa palliativecarerotationduringmedicalschool,and7of9 respondents(77%)reportedpreviouscommunicationskills trainingduringtheirPGY-1year.
Post-interventionsurveyswerecollectedaftereach session,withcompletionratesrangingfrom25%(2/8 participants)to70%(7/10participants)persession.Notably, allrespondentsindicatedagreementorstrongagreement withtheachievementofeachsession’sobjectives.Forthe simulation-basedcommunicationsession,88%(8/9)reported increasedconfidenceoverall,88%(8/9)ofresidentsreported increasedconfidenceinrespondingtostrongemotions,and 100%(9/9)reportedenhancedconfidenceinelicitingpatient goalsandvalues.
Severalkeythemesemergedregardingthe implementationofabootcampcurriculuminprimary palliativecareforEMresidents.Onenotableadvantageof thiscurriculumisitslongitudinalformat,spanningfour consecutiveweekswithshortintervalsbetweensessions.This structureaffordsresidentstheopportunitytopracticenewly acquiredskillswhileactivelyworkinginclinicalsettings, fosteringcontinuousreflectionandrefinementoftheir abilities.Additionally,thecurriculumisadaptableand
enablesitsimplementationinprogramslackingEM palliativecare-trainedfaculty.Programscanuselocal resourcessuchasinstitutionalpalliativespecialists, interdisciplinarypalliativeteams,orseveralpublicly availableonlineresources.9,10,14
However,despiteitsstrengths,ourcurriculumfaces severalchallenges.Notably,residentsunabletoattend sessionsriskmissingvaluableeducationalopportunities,as thecurriculumisnotrepeatedduringtheacademicyear. Moreover,limitedopportunitiesforongoingskillacquisition andfeedbackoutsidescheduledsessionsmayhinder residents’ abilitytofullyintegratepalliativecareprinciples intotheirpractice.Furthermore,individualprogramsmay beunwillingtoinvest10hoursofcurriculumtothisspecific topicandskillset.Lastly,whiletherewasnocostforthe simulationtimeandstandardizedpatientsatthestudy institution,theremaybecostassociatedwiththisinother programsandthismustbeconsidered.
Furthermore,whileparticipantsexpressedsatisfactionwith thecurriculum,theoutcomesdatalacktherigornecessaryto definitivelyestablishitssuccess.Theimpactofthiscurriculum onlong-termknowledgeorclinicalbehaviorwithintheED remainsuncertain.Itwillbeimportanttoconductmore formalassessmentsofthecurriculumobjectivesandto evaluateitsapplicationintheclinicalsetting.
Astheroleofprimarypalliativecareinemergency medicinecontinuestoevolve,thereisagrowingneedto integratetheseessentialskillsandconceptsintoallEM residencies.Thebootcampformathasproventobea valuableeducationaltoolinourprogram,andits effectivenesswarrantsfurtherexplorationanddissemination withinthebroaderEMcommunity.
AddressforCorrespondence:JulieCooper,MD,Universityof Pennsylvania,DepartmentofEmergencyMedicine,3400Spruce St.,Philadelphia,PA19104.Email: julie.cooper@pennmedicine. upenn.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Cooperetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SmithAK,McCarthyE,WeberE,etal.HalfofolderAmericansseenin emergencydepartmentinlastmonthoflife;mostadmittedtohospital, andmanydiethere. HealthAffairs. 2012;31(6):1277–85.
2.ShoenbergerJ,LambaS,GoettR,etal.Developmentofhospiceand palliativemedicineknowledgeandskillsforemergencymedicine residents:usingtheAccreditationCouncilforGraduateMedical Educationmilestoneframework. AEMEducTrain. 2018;2(2):130–45.
3.QuillTEandAbernethyAP.Generalistplusspecialistpalliative care creatingamoresustainablemodel. NEnglJMed. 2013;368(13):1173–5.
4.BackAL,FrommeEK,MeierDE.Trainingclinicianswithcommunication skillsneededtomatchmedicaltreatmentstopatientvalues. JAmerican GeriatricsSociety. 2019;67(S2):S435–41.
5.BaylisJ,HarrisDR,ChenC,etal.Palliativeandend-of-lifecare educationinCanadianemergencymedicineresidencyprograms:a nationalcross-sectionalsurvey. CJEM. 2019;21(2):219–25.
6.AccreditationCouncilforGraduateMedicalEducation.Emergency medicinemilestones.2021.Availableat: https://www.acgme.org/ specialties/emergency-medicine/milestones/ AccessedFebruary7,2024.
7.LoffredoAJ,ChanGK,WangDH,etal.UnitedStatesbestpractice guidelinesforprimarypalliativecareintheemergencydepartment. Ann EmergMed. 2021;78(5):658–69.
8.KrausCK,GreenbergMR,RayDE,etal.Palliativecareeducationin emergencymedicineresidencytraining:asurveyofprogramdirectors, associateprogramdirectors,andassistantprogramdirectors. JPain SymptomManage. 2016;51(5):898–906.
9.NorthwesternMedicine.EPEC:Educationinpalliativeandend-of-lifecare.Availableat: https://www.bioethics.northwestern.edu/programs/ epec/index.html.AccessedFebruary7,2024.
10.NguyenDandMateseT.Assessingtheeffectofahospiceandpalliative medicinecurriculumonemergencymedicineresidents’ knowledge. AmJHospPalliatCare. 2023;40(5):462–7.
11.StanichJ,SungaK,Loprinzi-BrauerC,etal.Teachingpalliativecareto emergencymedicineresidentsusinggamifieddeliberatepracticebasedsimulation:palliativegamingsimulationstudy. JMIRMedEduc. 2023;9:e43710.
12.BeneschTD,MooreJE,BreyreAM,etal.Primarypalliativecare educationinemergencymedicineresidency:amixed-methodsanalysis ofayearlong,multimodalintervention. AEMEducTrain. 2022;6(6):e10823.
13.VitalTalk.VitalTalk.Availableat: https://www.vitaltalk.org/. AccessedFebruary21,2024.
14.CentertoAdvancePalliativeCare.CAPCclinicaltraining. Availableat: https://www.capc.org/clinical-training/ AccessedFebruary7,2024.
NaomiP.Newton,MD* ChristopherFreeman,MD†
PatriciaPanakos,MD†
SectionEditor:PaulLoganWeygandt,MD
*EmoryUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Atlanta,Georgia
† JacksonHealthSystem,DepartmentofEmergencyMedicine,Miami,Florida
Submissionhistory:SubmittedOctober17,2023;RevisionreceivedApril28,2024;AcceptedMay30,2024
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18509
Introduction: Socialmedicineseekstoincorporatepatients’ socialcontextsintotheirmedicalcare. Emergencyphysiciansareuniquelypositionedtoaddresssocialdeterminantsofhealth(SDoH)onthe frontlinesofthehealthcaresystem.Miami-DadeCounty(MDC)isadiverseandsociallyvulnerablearea. In2020,theUniversityofMiami-JacksonHealthSystem(UM-JHS)emergencymedicine(EM)residency programlaunchedamultimodal,resident-ledSocialEMprogramtoidentifyandaddressSDoHinthe emergencydepartment(ED).
Methods: Weuseafour-pillarapproachtoSDoHintheED:CurriculumIntegration;Community Outreach;AccesstoCare;andSocialJustice.ResidentsgraduatewithaknowledgeofSocialEM principlesthroughan18-monthcurriculum,anelective,andalongitudinaltrack.Wedeveloped sustainableinitiativesthroughinterdepartmentalandcommunity-basedpartnerships,includingaNarcan distributioninitiative,anED-basedprogramlinkinguninsuredpatientstofollow-upcare,ahuman traffickingeducationinitiative,andaqualityimprovementinitiativeforincarceratedpatients.
Results: Giventhatthe18-monthcurriculumwaslaunchedin2022,afullrotationofthecurriculumhad notbeencompletedasofthiswriting,anddatacollectionandanalysisisanongoingprocess.Theinitial pretestandpost-testsurveydatashowimprovementinknowledgeandconfidenceinmanagingSocial EMtopics.TheNarcaninitiativehasscreened1,188patients,ofwhom144havereceivedNarcan.The ED-basedpatientnavigationprogramhasenrolled31patientstodate,18ofwhomobtainedoutpatient care.Analysisoftheimpact/effectivenessoftheprogram’sotherinitiativesisongoing.
Conclusion: Toourknowledge,thisisoneofthemostrobustsocialEMprogramstodate,asmanyother programsprimarilyfocusonserviceopportunities.RootedintherevisedprinciplesofBloom’staxonomy ofcognitivelearning,thisprogrammovesbeyondunderstandingSocialEMtenetstogenerating solutionstoaddressSDoHinandoutsidetheED.[WestJEmergMed.2025;26(1.2)5–13.]
Socialmedicine,ortheincorporationofpatients’ social contextsintotheirmedicalcare,hasbecomeavibrant, interdisciplinarymovementthathasgainedtractionin medicalschools,residencies,andatthenationallevel.Social medicineemphasizestheimportanceofsocialdeterminants ofhealth(SDoH),or “theconditionsintheenvironments wherepeopleareborn,live,learn,work,play,worship,and agethataffectawiderangeofhealth,functioning,and
quality-of-lifeoutcomesandrisks.”1 TheUSDepartmentof HealthandHumanServiceslists fivecoreSDoHtoconsider duringpatientcare:economicstability;educationaccessand quality;healthcareaccessandquality;neighborhoodand builtenvironment;andsocialandcommunitycontext.1
AlthoughSDoHcanbeappliedtoallspecialties,theyare perhapsmostrelevanttoemergencymedicine(EM).Passage oftheEmergencyMedicalTreatmentandLaborAct (EMTALA)in19862 wasacknowledgmentthatemergency
physiciansareoftentheonlylinktothehealthcaresystemfor patientswith financiallimitations.Emergencyphysiciansare estimatedtoprovidetwo-thirdsofacutecareforall uninsuredpatientsandhalfofacutecareforallMedicaid patients.3 WhethertheyarerushingapatienttoCT,leading theirteamduringaresuscitation,orevaluatingpatientsina crowdedhallway,emergencyphysiciansareimmersedin longstanding,complexsocialissues:trauma;poverty; homelessness;mentalhealthdisorders;etc.Therefore, recognizingtheeffectsofSDoHonpatientcareiscriticalin theED.
JacksonMemorialHospital(JMH)istheprimarytraining sitefortheUniversityofMiami-JacksonHealthSystem (UM-JHS)EMresidencyprogram.Itisalsothethirdlargest publichospitalinthecountry.TheUM-JHSocialEM programwaslaunchedin2020toimprovetheincorporation ofpatients’ socialcontextsintotheircare.
WhendesigningaSocialEMprogram,keepingthe residency’slocationandpatientpopulationinmindis important.LikemostEDsacrossthenation,theJMHEDis aplaceofrefugeforpatientswhoseSDoHmaypreventthem fromobtainingcareelsewhere.Asasafety-nethospitalinthe seventhmostpopulouscountyinthenation,4 JMHservesa particularlydiversepatientpopulationwithstriking socioeconomicneeds.TheUMhealthsystemconducted formalneedsassessmentsofMiami-DadeCounty(MDC) from2019–2022,andtheUM-JHSSocialEMprogramwas designedtoreflecttheseneeds.4,5
TheUM-JHSSocialEMprogramwasdesignedtoensure thatallresidentsgraduatewiththeabilitytoincorporate theirpatients’ SDoHintoEDcareregardlessoftheir ultimatepracticelocations.However,certainaspectsofthis programweredesignedtoaddresstheuniqueneedsof MDC a “minority-majority” communitythatexperiences challengeswithEnglishproficiency,andinwhich20%ofthe populationlivesbelowthepovertylevel.4,5
Bloom’staxonomyofcognitivelearningobjectives outlinessixlevelsinthecognitivedomain:knowledge; comprehension;application;analysis;synthesis;and evaluation.6 Overtime,scholarshavesoughttorevisethis frameworkand,whentakenasawhole,theserevisionsplace lessemphasisonalinearprogressionthrougheachlevel.6 Instead,thereisanincreasedfocusongeneratingnew hypothesesanddevelopingprojectsthatuseandexpand upontheacquiredknowledge.6 Therefore,theUM-JHS SocialEMprogramseekstoshiftitsparticipantsfrompurely understandingSDoHastheypertaintoEM,togenerating effectivesolutionsforaddressingtheseSDoHinandoutside theED.TheSocialEMprogramoutlinessixgoalsforits residents,whoarethentaskedwithgeneratingeffective
solutionsanddesigningtheirownmeasurableoutcomesfor eachgoal.Uponsuccessfulcompletionofthisprogram, residentsshouldbeableto:
1.DefineandidentifySDoHintheEDandapplythese principlestobedsidecare.
2.EngagewithMDCoutsidetheEDandaddressits socialandmedicalneedsthroughlongitudinal involvementinlocaloutreachinitiatives.
3.Solidifyandshareacquiredknowledgethroughan 18-month,multimodalcurriculum.
4.Identifyandseektoaddressbarrierstomedicalcare experiencedbypatientswhousetheEDastheirmain sourceofhealthcare.
5.Identifyandseektoaddressrecurrentsocialjustice issuesencounteredintheED.
6.Enactpositivechangethroughadvocacyandquality improvementinitiativesathospital-wide,local,and/or nationallevels.
Sinceitslaunchin2020,theprogramhasbeendividedinto fourpillarsthataddresscoreareaswithinSocialEM: CurriculumIntegration;CommunityOutreach;Accessto Care;andSocialJustice(Figure1).Initiativeswithineach pillarwillbediscussedinaseparatesection.Anyone affiliatedwiththeUM-JHSEDcanparticipateininitiatives acrossallfourpillars.Manyoftheseinitiativesare longitudinal,allowingforvaryinglevelsofparticipation throughoutresidency.Additionally,thisprogramalsooffers leadership,peerteaching,andscholarlyopportunitiesthat maycounttowardexistingresidencyrequirements.
TheUM-JHShasathree-yearEMresidencyprogram, andeachofitsclasses(postgraduateyears[PGY]1–3)is comprisedof14–15residents.EMresidentsarenotrequired toparticipateintheSocialEMprogrambutareencouraged todoso.Theymaychoosetoserveasprogramleaders (Figure1),participateinthelongitudinaltrackand/ortwoweekelective(discussedindetailinsubsequentsections below),ortoparticipateinindividualinitiativesastheir schedulesallow.However,SocialEMprogramleadership developedaformalcurriculumtoensurethatallresidents graduatewithasolidunderstandingofcoreSocialEM principles,regardlessoftheirlevelofinvolvementwiththe program;thiswillbediscussedinaseparatesection.
Thisprogramwasdesignedtobeexecutedbyresidentsin collaborationwithfaculty,medicalstudents,andstaff.The programwasstructuredintoacoreleadershiphierarchyto appropriatelydividethelaborofdesigningandlaunching initiativesthatpertaintoeachpillar,whileensuringthat residentscompletetheirexistingclinicalandacademic




Figure1. Socialemergencymedicineprogramorganizationanddivisionoflabor.Programdirectorsconsistofonefacultydirectorand1–4 residentdirectors(EMresidentsselectedviaaformalapplicationprocess).Programdirectorsoverseeinitiativesacrossallfourpillarsbut spendadditionaltimeleadingCurriculumIntegrationinitiativestoensureaseamlessincorporationofSocialEMprinciplesintoresidency training.PillarleadersareEMresidentswhoareselectedbyprogramdirectorsviaaformalapplicationprocess;theydesignandoversee initiativesintheirassignedpillars.FacultymentorsaregenerallycorefacultyintheEMdepartmentwithexpertiseintheirassignedpillar. However,facultyinotherspecialtiesatUM-JHSmayalsoserveasmentorsiftheycurrentlyoverseeacommunityorhospital-basedinitiative thatcollaborateswiththeSocialEMprogram.(Forexample,afacultymentorfromthefamilymedicinedepartmentoverseestheIDEANeedle ExchangeClinic.)AnyoneaffiliatedwiththeEMdepartmentmayserveasateammember.Teammembersworkdirectlywiththeirassigned residentleadersanddividethetasksrequiredtolaunchandpublicizeinitiatives.
requirements(Figure1).Thisleadershiphierarchyorganizes, executes,andpublicizestheprogramanditsinitiatives.
Afacultydirectorandatleastoneresidentdirector overseetheprogramtogether(Figure1).Theoriginal directors,PatriciaPanakos,MD,andNaomiNewton,MD, authoredthispaperandconceptualizedtheprogram togetherinFall2020.ThecollaborationbetweenDrs. PanakosandNewtonwasbornefromasharedpassionfor socialmedicineandadesiretoimplementanEMresidencybasedprogramtoaddresstheSDoHofpatientsinMDC.Dr. PanakosistheassociateprogramdirectorfortheUM-JHS EMresidencyandhasundergoneformaltrainingin curriculumdevelopment.ShehasalsodevelopedED-based publichealthinitiativesatJHS,suchasauniversalscreening programforcommunicablediseases,includingHIV, hepatitisC,andsyphilis.Dr.Panakoscontinuesherroleas facultydirectorforthesocialEMprogram.Dr.Newtonisan alumnaoftheUM-JHSEMresidencyandservedaschief residentduringher finalyearoftraining.Sheassumedthe roleofthesocialEMprogram’sresidentdirectorasaPGY-1 andtransitionedherpositionuponhergraduationin2023. ShehasalsocollaboratedwithDr.Panakosonpublichealth
initiatives,includingauniversalHIVscreeninginitiativein JHS’spediatricED.Dr.Newtoniscurrentlypursuing atwo-yearfellowshipinhealthpolicyandadvocacyat EmoryUniversity.
Giventhattherewasnoprecedenceforsuchaprogramat UM-JHS,Drs.PanakosandNewtonworkedalmostdailyto createtheprogramandmaintainitssustainability,whilealso completingtheirexistingclinicalandacademic responsibilities.Drs.PanakosandNewtondesignedthe program ’soverallstructure,createdaformalselection processforpillarleaders,andidentifiedcommunitypartners andfacultymentorswithexpertiseinSocialEM.They presentedaformalproposalthatwasapprovedbyboththe chairoftheEDatJMHandtheUM-JHSEMresidency programdirectorinOctober2020.Theyalsodesignedand launchedthe18-monthcurriculum,two-weekelective,and longitudinaltrack,whicharedescribedinsubsequent sectionsofthispaper.Toaccountforcontinuedprogram growth,theoriginaldirectorsselectedfournewresident directorsforthe2023–2024academicyearviaaformal applicationprocess(Figure1).
Directorsapproveproposedinitiativesacrossallpillars andworkdirectlywithpillarleaderstotrackprogressand troubleshootchallenges.Theycheckinremotelywithpillar
leadersatleastbi-monthlytoensuretimelyproject completion.Theyalsopromotetheprogramata departmentalandhospital-widelevelandhelppillarleaders identifyfacultyandcommunitypartners(Figure1).Resident directorsarerecognizedwithaSocialEMleadershipaward upontheirgraduation.
AnaverageoftwoPGY-1orPGY-2EMresidentslead eachpillar.Interestedresidentsapplyforthispositionviaa briefelectronicapplication(GoogleSurvey)atthestartofthe academicyearandareselectedbythedirectors.Residents generallydonotserveasleadersofmorethanonepillar,as thispositionmustbebalancedwithexistingresidency obligations.Residentleadersreportdirectlytothedirectors anddedicateanaverageoftwotofourhoursperweekto theirroles.Asleadersprogressthroughtraining,theymay eitherremainintheirleadershiprolesortransitiontheirroles toincomingPGY-1sandPGY-2s.Allresidentleaderswho haveservedforatleastoneyeararerecognizedwithaspecial awardupongraduationfromresidency.
Leadersfocusondesigninginitiativesthatpertaintothe goalsoftheirassignedpillar.Theyidentifyappropriate partnerswithinJHSandMDCtoaidindevelopingand launchingtheseinitiatives(Figure1).PartnersincludeJHS faculty(includingthoseinnon-EMspecialties),local outreachorganizations(manyofwhichalreadyhad establishedrelationshipswithUM-JHSthroughmedical studentinvolvement),andotherJHS-affiliatedresidency programs(eg,pediatrics,internalmedicine,family medicine).Interdisciplinarycollaborationpreventsthe SocialEMprogramfrom “re-inventingthewheel” andhelps initiativesachievesuccesswithfewerfunding,resource,and logisticalrestrictions.Residentleadersdelegateday-to-day taskstoaninterdisciplinaryteamtodividethelaborof executingtheseinitiatives.Leadersarerequiredtocheckin remotelywiththeirteammembersatleastmonthlytodiscuss progressonpillarinitiatives.
Teammembersdividethetasksrequiredtolaunch initiativeswithintheirassignedpillar.Theyarerequiredto dedicateaminimumofonetotwohoursperweekonthese tasksandcheckinregularlywiththeirpillarleadersas previouslydiscussed.Thosewhodesiretodosomay participateinmorethanonepillarteam.Participationina pillarteamisopentoanyoneintheUM-JHSED.However, duringthe firstthreeyearsoftheprogram,teamswere primarilycomprisedofEM-boundUMmedicaland pharmacystudents,JHSclinicalpharmacyresidents,and hospitalstaff(eg,nursesandsocialworkers).
Inthefollowingsection,weprovideabroadoverviewof eachpillar’sobjectivesandhighlightseveralkeyinitiatives withineachpillar.Whenrelevant,pleaseseethe correspondingappendicesforadditionaldetails.
ThispillarincorporatesthetenetsofSocialEMinto residencytrainingtoempowerfuturegenerationsof emergencyphysicianstoapplySocialEMprinciplestotheir care.ThisistheonlypillarthatrequiresallEMresidentsto participatebecauseitsinitiativeshavebeenincorporatedinto theexistingresidencycurriculum.Doingsoensuresthatall EMresidentsgraduatewithanunderstandingofSDoHand theprinciplesofSocialEM,regardlessoftheirlevelof involvementinotherpillars.Ofnote,approvalfromthe institutionalreviewboardwasnotrequiredforthe developmentofthiscurriculum.
Wedevelopedandlaunchedamultimodal,18-month SocialEMcurriculumthathasbeenincorporatedintothe existing18-monthresidencydidacticschedule(AppendixA). Thecurriculumcovers18coresocialEMtopics(Table1)and includesjournalclubs,simulationcases,lectures,problembasedlearning,andinteractivegroupdiscussions.The curriculumisledbyfacultyandresidentswithexpertiseor
Table1. 18coreareasofstudywerechosentobecoveredmonthlyduringthe18-monthSocialEMcurriculum.Thiscurriculumisintegrated intostandardresidencydidacticschedule,whichrepeatsevery18months.Usingamultimodallearningformat,topicscanbepresentedas traditionallectures,case-baseddiscussionsandjournalclubs(“Cases”),orsimulations.Theinitialmodalitiesforeachtopicarelistedbelow; themodalitiesusedforeachtopicwillchangeevery18months(eg,thepediatrichealthlecturewouldbepresentedaseitheracaseor simulation18monthslater).Additionaldetailsregardinglogisticsandimplementationcanbefoundin AppendixA
1.Socialdeterminantsofhealth7.Implicitbias/racism13.Humantraffickinganddomesticviolence
2.Healthcarecoverageandaccess8.Homelessness14.Substanceabuseandharmreduction
3.Financialstability9.Healthliteracy15.Caringforincarceratedpatients
4.FrequentEDutilizers10.Immigration16.Highlycommunicablediseases/STIepidemics
5.Women’shealth11.Resourceinsecurity17.Languageandculturalbarrierstohealthcare
6.Pediatrichealth12.Trauma-informedcare18.Genderidentity
ED,emergencydepartment; STI,sexuallytransmittedinfection.
interestinthecoretopics.SocialEMleadershipassists presentersinidentifyinglearningobjectivesforeachsession, selectingtopics,anddevelopingcontent.Allconference attendeesparticipateinpre-andpost-surveystoassesstheir baselineknowledgeandtheeffectivenessofeachdidactic session.ResidentsarealsoaskedtoevaluatetheSocialEM curriculumduringtheannualresidencyprogramevaluation. SurveysandresultsarediscussedfurtherintheImpact/ Effectivenesssectionofthismanuscript.
In2022,welaunchedthetwo-weekSocialEMelectivefor residentswhodesireamorein-depthexperiencewiththe program(AppendixB).ThiselectiveisopentoPGY-2EM residentsduringtheirelectiveblockandiscomprisedof serviceopportunities,self-directedstudy,peerteaching,and initiativeparticipationacrossallpillars.ThePGY-2rotation scheduleisdesignedsothatonlyoneresidentcompletesan electiveinanygivenmonth.Therefore,theexperienceis personalizedforeachparticipatingresident.SocialEM directorsworkwiththeresidentaheadoftimetodesignan electiveschedulethatensuresparticipationacrossallpillars butallowsthemtoengagemoredeeplywithintheirpillar(s) ofinterest(AppendixB).
Wealsodesignedalongitudinaltrackthatwaslaunched the2023–2024academicyear.Trackparticipantsengageina
setnumberofoutreachevents,qualityimprovement initiatives,peerteaching,andself-directedstudyover18 months.Therequirementsarebasedonapointsystemthat ensuresengagementwithallpillarsbutallowsfordeeper explorationinareasofindividualinterest.Residentsmust reachaminimumof30pointstocompletethetrack (Figure2).Requirementsincludealongitudinalscholarly activitythatculminatesinapresentationatthelocal, regional,ornationallevels(eg,developingaprojectto addressfoodinsecurity).Theymustalsoparticipateinthe SocialEMdidacticcurriculumthroughpeerteaching, developingnewelementstothecurriculum,andmentoring medicalstudents.Participantslogtheirprogressviaanonline formandmustattendaminimumofninemonthlytrack meetingswiththeSocialEMdirectorsoveran18-month period.Upongraduation,residentswhocompletethetrack willreceiveaDistinctioninSocialEM.
Thispillarwasdesignedtoestablishameaningfulpresence inMDCbeyondbedsidecareandtoaddresssocialissues throughpartnershipswithlocalorganizations.Forexample, throughapartnershipwithMiamiStreetMedicine, participantsjoinaninterdisciplinaryteaminproviding

Figure2. Pointsystemforthe18-monthlongitudinaltrack.Notethatopportunitiesineachpillarmayvaryovertime.This figurelists opportunitiesfromthefallof2023.
regularmedicalcareatlocationscommonlyoccupiedby Miami’shomelesspopulation.Throughapartnershipwith theStoptheBleedCampaign,participantsundergoformal trainingtoserveaslocalinstructors.Participantsthenlead workshopsthatteachnon-medicalcommunitymembersto performbystandercardiopulmonaryresuscitationand stabilizevictimsofviolenceuntil firstrespondersarrive. ParticipantsmayserveasinstructorsforStoptheBleed eventsthroughoutMDC,astheirschedulesallow.
ThispillarlaunchedaNarcanprograminJuly2022,in partnershipwiththeUMIDEA(InfectiousDisease EliminationAct)NeedleExchangeClinicandtheUM MichaelWolfsonDepartmentofCommunityService (DOCS).ThisprogramseekstoaddressSouthFlorida’ s opioidepidemicandisinkeepingwiththestatewide EmergencyTreatmentforSuspectedOpioidOverdoseAct.7 Atcommunityhealthfairs,participantsprovidefreeopioid usedisorder(OUD)screening,basedonDiagnosticand StatisticalManualofMentalDisorders,5th ed,criteria.8 Narcanissubsequentlydistributedtothoseidentifiedtobeat highriskforlife-threateningoverdoses,andadditionalOUD counselingandtrainingonsafelyadministeringNarcan areprovided.9
AccesstoCare
Thispillarlinkschronicallyillpatients,highEDutilizers, andtheuninsuredtooutpatientcare.Italsoseeksto centralizeexistingsocialsupportresourceswithinUM-JHS andefficientlyaddressSDoHatthebedside.Througha partnershipwithDOCS,uninsuredpatientspresentingtothe EDwithchroniccomplaintsarepairedwithlong-term patientnavigators,whohelpthemsecureaffordable outpatientcareupondischarge.
TheHighUtilizersInitiativeaimstostreamlinethecareof patientswhofrequentlyvisittheED.Participantsconduct chartreviewsofindividuals flaggedasfrequentutilizersinthe electronichealthrecordandcreatepatientcarebriefsthat auto-populateintheircharts.Thesepatientsoftenpresentto theEDnumeroustimesaweekandreceivecarefrom differentclinicianseachtime.Byconsolidatingtheir pertinentmedicalinformation,thesebriefsallowforbetter, morestreamlinedpatientcarewithlessrepetitionoftestsand procedures.Thebriefsalsolessenthecognitiveloadofthe clinician,decreasingthetimespentonchartreviewsand helpingguidefuturecare.
ManypatientspresenttotheEDwithconditionsthatare exacerbatedbyalackofbasicresources.Itischallengingto addressthesecomplexSDoHamidstthetimeconstraintsof EDcare,andEDscannolongerrelyheavilyonsocial workersforassistance,duetothenationwidesocialworker shortage.10 ThispillarpartneredwithMiamiStreetMedicine andtheJMHPharmacyDepartmenttocreateresource guidesforpatientsandcliniciansinresponsetothisneed. Communityresourceguides(inEnglish,Spanish,and
HaitianCreole)provideinformationforaffordable outpatientclinics,prescriptions,mentalhealthservices, temporaryhousing,mealprograms,andsubstanceuse treatmentcenters,aswellasresourcesforpregnantpatients andvictimsofdomesticviolence.Clinicianresourcesinclude referralinformationforresident-runsubspecialtyclinics, instructionsforinitiatingbuprenorphineintheEDand referringpatientstomedication-assistedtreatmentclinics, andalgorithmsforhumantraffickingscreening.
Thispillartackleshealthinequityandinjusticeissues throughinterdisciplinaryeducationandquality improvementinitiatives.TheHumanTraffickingEducation Ambassadorprogram,inpartnershipwithJMH’sRape TreatmentCenter,teachesclinicianstoscreenforandtreat victimsofhumantrafficking.Floridahasthethirdhighest numberofhumantraffickingcasesinthenation,andMDC is,sadly,aknowntraffickinghub.11 Trainedresidentslead interactiveseminars,sharingHIPAA-complianttrafficking casesandteachingclinicianstoidentifyandaddressred flags fortrafficking.
Thispillaralsoseekstoimprovecareforincarcerated patientsintheED,particularlyconcerningpatientprivacy andexaminationsinthepresenceoflawenforcement. Initiativesincludearecentlypublishedreviewonthebarriers tocaringforthispopulationandrecommendationsto improvetheirdeliveryofcare.12 Wealsoimplementeda simulationsessiononcaringforincarceratedpatientsinto residencydidactics.
SocialEMleadershipisintheprocessofcompletinga formalimpactassessmentofthecurriculumintegrationpillar oftheprogramviaasingle-group,pretest-posttestdesign.6 Briefpre-andpost-didacticsessionsurveysaredesignedfor eachSocialEMtopicinthe18-monthcurriculum.Surveys aredesignedtoassessbaselineknowledgeofthetopicandthe changesinthisbaselineknowledgeafterthesession.Survey questionsalsoaddressrelevantepidemiologicalstatisticsand usefulcommunityresourcesforaddressingthetopicin MDC.Eachpost-surveyendswithablanksectionfor participantstowriteinanyadditionalfeedback,which SocialEMprogramleadershipusesforsubsequent didacticsessions.
Forconvenience,thesesurveysareadministeredvia electronicforms;conferenceattendeesscanQRcodestothe formsbeforeandafterthesession.Allresidents,faculty, students,andstaffinattendanceareeligibleforparticipation inthesurveys.However,thusfar,surveyparticipationhas generallybeenlimitedtoresidentattendees,asfaculty,staff, andstudentattendanceislessconsistent.Hospitalbadge
numbersareusedtocompareindividuals’ changesinpreandpost-sessionresponses.
Sincethe18-monthcurriculumwaslaunchedin2022,a fullrotationofthecurriculumhasnotbeencompletedasof thiswriting,anddatacollectionandanalysisisongoing. However,thusfar,thecurriculumtopicshavebeenwellreceived,withresidentsindicatinganimprovedconfidencein theirabilitytorecognizeandaddresstheseSocialEMissues atthebedside.Forexample, Figure3 showskeyresultsfrom thepre-andpost-surveysadministeredduringthe first sessionoftheformalcurriculumin2022 asimulation sessiononhighlycommunicablediseases/sexuallytransmittedinfection(STI)epidemics(Table1).Theseresults suggestefficacyinimprovingbaselineknowledgeand confidencewiththetopicofacuteHIVintheED,including epidemiology,communityresources,andinitiatingeither highlyactiveantiretroviraltherapyorpre-exposure prophylaxiswhenindicated.
Animpactassessmentofthetwo-weekelectiveispending, asonlyonePGY-2residenthadcompletedatthetimeofthis manuscript’sdevelopment.
Itischallengingtoconcretelyassesstheimpactofthe CommunityOutreachpillar,asitsservice-driveninitiatives aregenerallyqualitativeinnature.However,initialdata
fromtheNarcanInitiativehighlightsitsimpactonMDC.As ofMay2023,theprogramscreened1,188patientsacross MDC,ofwhom144receivedNarcan.Inrecognitionofthe NarcanInitiative’scurrentimpactandcontinuedgrowth, JMH’sDepartmentofEmergencyMedicinereceivedthe 2023UniversityofMiamiMitchellWolfsonSr.Department ofCommunityServiceaward.
Wearecurrentlyintheearlystagesofdatacollectionto analyzethesuccessoftheAccesstoCareinitiatives.Thusfar, thepatientnavigationprogramhasenrolled31EDpatients. Ofthesepatients,18wereabletosuccessfullycompletetheir navigationgoalsandobtainoutpatientcare.Thisprogram hasparticularlybenefittednon-English-speakingpatients, whoselanguagebarrierscanhindertheirabilitytonavigatea complexsystem.Forexample,navigatorswereable tolinkaSpanish-speakingpatienttooutpatientoncologic careforheruntreatedgynecologiccancer.Recently,a homeless,uninsuredpatientlivingattheMiamiRescue Mission(MRM)wastreatedforanacuteulcerative colitis flareintheED.Afterhewasdischarged,the navigatorsensuredthatheobtainedtimelyfollow-upatan MRM-affiliatedgastroenterologyclinic,astudent-runclinic staffedbyUMfaculty.Wearecontinuingtopublicize thisprogramandencourageemergencyclinicians

Figure3. Comparisonofkeypre-andpost-surveyresultsafterasimulationsessiononhighlycommunicablediseases/STIepidemics;30 residentscompletedthesurveys.Afterthesession,residentsindicatedanincreasedconfidenceintheirabilitytorecognizeacuteHIVand initiateHighlyActiveAntiretroviralTherapy(HAART)orPre-ExposureProphylaxis(PrEP)treatmentwhenindicated.Mostresidentsfound thesessionbeneficialinlearningaboutcommunityresourcesforEDpatientswithHIV,aswellasprescribingHAARTandPrEP.
toenrolltheirpatientsduringtheirshifts.Weare stillinthedatacollectionphaseoftheHigh Utilizersinitiative.
TheSocialJusticepillarinitiativesexperiencedseveral launchdelaysduetoCOVID-19pandemicrestrictionsand facultyturnover.Initiativeswereofficiallylaunched inthe2022–2023academicyear,anddataregardingtheir impactandeffectivenessispending.Thusfar,human traffickingeducationambassadorshavegiven well-receivedlecturestoJHS-affiliatedclinicsand toJMH’sfamilymedicine,pediatrics,andinternal medicineresidencies.
Sincetheprogramisunderthedirectguidanceofacurrent residencyassociateprogramdirector,thereiscontinual communicationbetweenSocialEMdirectorsandEM residencyleadership.Residencyleadershipactivelyengages withandprovidesinsightsintopillarinitiatives,leadingto timelychangestotheprogramwhendeemednecessary.For example,previousfeedbackledtothedevelopmentofthe electiveandlongitudinaltracks.ResidentsinthecoreSocial EMleadershipteamalsoobtainregularqualitativefeedback fromtheirpeersandsharethisfeedbackwiththeSocialEM directors.Thisprogramisalsoreviewedduringtheannual residencyprogramevaluationcommitteemeeting.This programhasfullEMdepartmentalsupport.
Overall,thisrobust,multimodal,resident-ledSocialEM programhasrapidlygrownoverthelastthreeyears,despite theCOVID-19pandemic.In2023,sixofthe14PGY-3 residentsgraduatedwithaSocialEMdistinction.The program ’sinterdisciplinarynatureensureditssuccess,as multipleinitiativeswerelaunchedwithoutsignificant fundingoradministrativerestrictions.Theprogramis receivingincreasingrecognition.Inadditiontothe previouslymentionedcommunityserviceawardforthe NarcanInitiative,theMDCchapteroftheStoptheBleed Campaignreceiveda2021awardfromthemayorforits educationinitiativesinlocalhighschools.In2023,wewere alsohonoredtoreceivethe2023ACEPSocialEMSection DistinguishedProgramAward.
Residents’ availabilityoftenlimitsconsistentparticipation inSocialEM.Residentshavemultipleclinicalandacademic responsibilities,andastheyprogressthroughtraining,their timeisfurtherlimitedbysearchingforjobsandapplyingfor fellowships.Inresponsetothislimitation,theelectiveand longitudinaltrackweredevelopedtoallowfor flexiblebut regularparticipation,asmanyrequirementscanbe
completedduringlighterrotations.Thedidacticcurriculum alsoensuresthatallresidentswillgraduatewiththesame baselineknowledgeofSocialEMtenets.Additionally,the SocialEMleadershipwilltransitioneverytwoyears, allowingjuniorresidentswithleadershiprolestopasson theirdutiestoincomingresidentsastheybecome seniorresidents.
Certainaspectsofthisprogramweredesignedtoaddress someofthesocialissuesthatareparticularlyprevalentin MDCandmaynotbegeneralizabletootherEMresidency programsintheUnitedStates.Otherresidencyprograms seekingtodeveloptheirownSocialEMinitiativesshould considertheuniqueneedsoftheirpatientpopulationswhen doingso.
Theprogram’ s firstthreeyearswerededicatedtooverall development,garneringparticipants, findingcommunity partners,andlaunchinginitiativesineachpillar.Therefore, datacollectiontoformallyassesstheprogram’simpactand effectivenessisstillinprocessandiscurrentlylimitedto initialdata(unblindedpre-andpost-testscompletedby residentparticipants)fromthelaunchofthe18-month didacticcurriculum.Thisdatamayalsobesubjectto selectionbias,asmostresidents,faculty,students,andstaff areexcitedabouttheSocialEMprogramandwant ittosucceed.
TheUniversityofMiami-JacksonHealthSystemSocial EMprogramwaslaunchedin2020toaddresstheSDoHof patientsinMiami-DadeCounty anareaofsigni fi cant medicalandsocialneed.Ittargetscriticalsocialissues throughfourpillars:CurriculumIntegration;Community Outreach;AccesstoCare;andSocialJustice.This multimodal,resident-runprogramachievedrapidsuccess inthreeyearsbydevelopingsustainableinitiativesin partnershipwithlocalorganizationsand otherUM-JHSdepartments.Ratherthanfocusing solelyonserviceopportunities,thisprogramenhances residents ’ knowledgeofSDoH,fostersthedevelopmentof qualityimprovementinitiatives,andprovides opportunitiestocreatemeaningfulchangeintheED andthecommunity.Thisprogramalsoprovidesresidents withleadershipandscholarlyopportunities.Wehope thatthisarticlewillinspireotherresidenciestodevelop similarprograms.
TheUniversityofMiami-JacksonHealthSystemSocial EmergencyMedicineprogramwouldnothavebeenpossible withouttheingenuity,dedication,andpassionofthe followingindividualsandorganizations.Thankyoufor everythingthatyouhavedoneandcontinuetodotocreate
positivechange:RachelArmstrong,MD;TatianaBarriga, MD;KelleyBenck;DanielBergholtz,MD;EmilyBrauer, MD;SandraCabrera,MD;DanielleCohen,MD;Emily Dawra,MD;LuisDeLaRosa,RN;ShaheenEmami; JoshuaGoldstein,MD;JamieHarris;Kristopher Hendershot,MD;ArmenHenderson,MD,MBA;Brooke Hensley,MD;SarahJabre,MD;JacksonHealthSystem ClinicalPharmacyResidency;JohnnatanMarin,MD;Julia Martinez,MD;ElizabethMay-Smith,MD;KellyMedwid, MD;MiamiStreetMedicine;VictoriaMcKee;Samantha Mosle;LienMorcate;KalebMorris;JudithOriental-Pierre, MD;RoxcyBoltonRapeTreatmentCenter;StoptheBleed; UniversityofMiamiIDEANeedleExchangeClinic; UniversityofMiami,MichaelWolfsonDepartmentof CommunityService;andMelissaVelasquez,MD.
AddressforCorrespondence:NaomiP.Newton,MD,Emory UniversityHospital,531AsburyCircle,AnnexSuiteN340,Atlanta,GA 30322.Email: naomi.newton@emory.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Newtonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.U.S.DepartmentofHealthandHumanServices.Healthypeople2030socialdeterminantsofhealth.Availableat: https://health.gov/ healthypeople/priority-areas/social-determinants-health AccessedMay2,2023.
2.ZibulewskyJ.TheEmergencyMedicalTreatmentandActiveLaborAct (EMTALA):whatitisandwhatitmeansforphysicians. Proc(BaylUniv MedCent). 2001;14(4):339–46.
3.AmericanCollegeofEmergencyPhysicians.UnderstandingEMTALA. Availableat: https://www.acep.org/life-as-a-physician/ethics–legal/ emtala/emtala-fact-sheet/.AccessedMay30,2023.
4.U-Health-UniversityofMiamiHealthSystem.Communityhealthneeds assessment2019–2021.Availableat: https://umiamihealth.org/-/media/ uhealth/chna/umhc-2019-community-health-needs-assessment.ashx AccessedMay15,2023.
5.FloridaDepartmentofHealthinMiami-DadeCounty.2022Community healthassessment.2022.Availableat: https://www.floridahealth.gov/ _media/miami-dade/community-reports/miamidade-cha.pdf AccessedMay15,2023.
6.ThomasPA,KernDE,HughesMT,etal.(Eds.),(2016).Goalsand objectives.In: CurriculumDevelopmentforMedicalEducation (53–56;130–133).3rded.Baltimore,MD:JohnsHopkinsUniversity Press,2016.
7.EmergencyTreatmentforSuspectedOpioidOverdose. Chapter381 Section887–2021FloridaStatutes,StateofFlorida2021Legislative Statutes,1Jan.2021.
8.AmericanPsychiatricAssociation.(2013). DiagnosticandStatistical ManualofMentalDisorders,5thed.(541–542).Washington,DC: AmericanPsychiatricAssociation.
9.BenkKN,GoldsteinJ,NewtonN,etal.Socialemergencymedicine: naloxoneoutoftheED&intothecommunity.2022.Availableat: https:// fcep.org/social-emergency-medicine-naloxone-out-of-the-ed-andinto-the-community/.AccessedFebruary3,2022.
10.LinVW,LinJ,ZhangX.USsocialworkerworkforcereportcard: forecastingnationwideshortages. SocWork. 2016;61(1):7–15.
11.Miami-DadeStateAttorney’sOffice.Floridafactsregardinghuman trafficking.Availableat: https://humantrafficking.miamisao.com/ human-trafficking.AccessedJune3,2023.
12.ArmstrongRE,HendershotKA,NewtonNP,etal.Addressing emergencydepartmentcareforpatientsexperiencingincarceration:a narrativereview. WestJEmergMed. 2023;24(4):654–61.
EffectivenessofaCollaborative,VirtualOutreachCurriculumfor 4th-YearEM-boundStudentsataMedicalSchoolAf filiatedwitha HistoricallyBlackCollegeandUniversity
CortlynBrown,MD,MCSO* RichardCarter,MD† NicholasHartman,MD,MPH‡ AarynHammond,MD‡ EmilyMacNeill,MD* LynneHolden,MD§ AvaPierce,MD∥ LinelleCampbell,MD§ MarquitaNorman,MD,MBA∥
*AtriumHealthCarolinasMedicalCenter,DepartmentofEmergencyMedicine, Charlotte,NorthCarolina
† HowardUniversity,CollegeofMedicine,Washington,DC ‡ WakeForestUniversity,SchoolofMedicine,Winston-Salem,NorthCarolina
§ AlbertEinsteinCollegeofMedicine,MontefioreMedicalCenter,Bronx,NewYork
∥ UTSouthwesternMedicalCenter,Dallas,Texas
SectionEditors:MatthewTews,MDandChristineStehman,MD
Submissionhistory:SubmittedJanuary24,2024;RevisionreceivedOctober9,2024;AcceptedOctober17,2024
ElectronicallypublishedDecember16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18748
Background: Diversitywithinthephysicianworkforceisassociatedwithimprovedclinicaloutcomesand patientsatisfaction.Despitethis,theUSphysicianworkforce,particularlyinemergencymedicine(EM), remainsrelativelyhomogeneous.OfallBlackmedicalschoolstudentsintheUS,14%attendthefour HistoricallyBlackCollegesandUniversities(HBCU)thathaveamedicalschool.Unfortunately,noneof theseschoolsareaffiliatedwithanacademicEMprogram.Becauseofthis,thereislessprofessional mentorshipfocusedonobtainingacareerinEMandpotentiallylessformalcurriculaforseniormedical studentsdoingtheirhomesub-internshipinEM.
Objectives: Ourobjectivewasto fillthegapleftbytheabsenceofanacademicEMdepartmentat HowardUniversityCollegeofMedicine(HUCOM)bycreatingacollaborativeeducationalexperiencefor fourth-yearmedicalstudentsduringtheirhomeEMsub-internship.Thecurricularobjectiveswereto teachcoreprinciplesofEM,buildrelationshipswithstudents,andpreparethemforpursuingEM residencytraining.
CurricularDesign: FourEMacademicdepartmentscollaboratedtocreateandimplementavirtual curriculumusingthesix-stepapproachtocurriculardevelopment.
Impact/Effectiveness: Aftercompletionofthecourse, fivestudents(100%)reportedstronglyagreeing withthefollowingstatements.Thesesessions1)helpedmelearntheapproachtocoreEMtopicsmore thanIwouldhavebeenabletodoonmyown;2)helpedmelearnkeyskillsforexcellinginanEMrotation morethanIwouldhavebeenabletodoonmyown;and3)allowedmetoconnectwithfacultyand residentmentorstolearnmoreaboutthe fieldofEM.Ofthese fivestudents,80%and20%reported stronglyagreeingandagreeing,respectively,thatthesesessionshelpedthemlearnabouttheprocessof applyingtoandselectinganEMresidencyprogram.[WestJEmergMed.2025;26(1.2)63–68.]
NeedforInnovation
Medicalstudentsinterestedinemergencymedicine(EM) whoattendahistoricallyBlackcollegeoruniversity(HBCU) donothavetheteachingandmentorshipthatoccurswhena medicalschoolisaffiliatedwithanacademicEMprogram. Weformedacollaborativeprogramamongfouracademic EMdepartmentstohelp fillthisneedforEM-boundstudents atHowardUniversityCollegeofMedicine(HUCOM).To ourknowledge,thisisthe firstsuchprogramtobereportedin theliterature.
Adiversephysicianworkforceisassociatedwithincreased accesstoandutilizationofthehealthcaresystem,improved healthoutcomesandpatientexperience,andimproved fiscal marginsforhospitals.1–4,4–6 Despitethis,themedical fieldas awholehasmademinimaladvancesinincreasingphysician diversity.In2008thepercentageofBlackorHispanicUS physiciansfromallspecialtieswas6.3%and5.5%, respectively.By2018,however,thosepercentageswereonly 5.0%and5.8%,respectively.Evenmoreconcerninggiventhe diversepatientpopulationthattheemergencydepartment (ED)serves,EMremainsamongthemedicalspecialtieswith thelowestnumberofphysiciansfrombackgroundsunderrepresentedinmedicine(URiM).Between2008–2018,the percentageofemergencyphysicianswhoidentifiedasBlack decreasedfrom5.0%to4.5%,andstayedconstantat5.3% forHispanic/Latinos.7
Whensurveyed,35%ofEMprogramdirectorsreported thatthesmallnumberofURiMresidencyapplicantswasthe greatestbarriertoobtainingadiverseresidencyclass.8 Ofall BlackmedicalschoolstudentsintheUS,14%attendfour HBCUswithamedicalschool.Becausenoneoftheseschools areaffiliatedwithanacademicEMprogram,theirmedical studentshavedecreasedexposuretoEMinthepre-clinical years,lessprofessionalmentorshipfocusedonobtaininga careerinEM,andfewerformalcurriculaforseniormedical studentsdoingtheirhomesub-internship(sub-I)inEM.This lackofmentorshiphasbeenidentifiedasacriticalbarrierfor URiMstudentsacrossvariousspecialties,contributingto lowerapplicationratesandresidencyplacement.Studies suggestthatmentorshipincreasesbothcareersatisfaction andinclusivityandthelikelihoodofthesestudentsentering andsucceedingincompetitive fieldslikeEM.9,10 Inaddition, anationalsurveyofclerkshipdirectorsfoundthathavinga structured,standardizedsub-Icurriculumsignificantly improvedthepreparednessofstudentsforresidency, especiallywhentheserotationswereaffiliatedwith residencyprograms.11
TheEmoryUniversityDepartmentofEmergency MedicinecreatedaprogramwithMorehouseSchoolof Medicinetoprovideguidancetomedicalstudentsinterested inEM.Atotalof115MorehousestudentscompletedanEM
clerkshipatEmory,and62.6%successfullymatchedinto EM.12 Whilethisprogramwassuccessful,studentstypically relyontheirhomesub-Itoprepareformandatoryaway rotations.Thisabsenceofsupportfromanacademic departmentpriortoawayrotationsmaycausethestudentsto findthemselveslesspreparedandatacompetitive disadvantagewhentheybegintheirawayrotations. Furthermore,manyEMresidenciesarenotinproximitytoa HBCU,requiringstudentstobearthe financialburdenof travelingtoothercitiesandstatesfortheirawayrotations.
AtHUCOM,theEMsub-Ireliedheavilyonanolder, recordedonlinelectureseriesfromanexternalinstitution, supplementedbybedsideteachingfromcommunity attendingsatonesite,HowardHospital.Studentsnotedthat theabsenceofformaleducationalcomponents,suchas weeklydidactics,journalclubs,andsimulation,resultedin limitedexposureto “cutting-edge” EMpractices.Moreover, thelackofinteractionwithacademicattendingswhoare dedicatedtomedicalstudenteducation,alongwiththe absenceofresidents whorepresentthenextstepincareer progression leftstudentswithoutaccesstocritical mentorshipandguidance.Thisgaphinderedstudents’ ability tovisualizetheirownprogressionandreceivepractical advicefromindividualsatasimilarstageintraining,further limitingtheirconnectiontothebroaderEMcommunity.
Tohelpovercomethatbarrier,wecreatedacollaboration betweenfouracademicEDsandHUCOMinanattemptto augmentcurricularofferingsforEM-interestedstudentson theirHUCOMfourth-yearEMhomerotation.The collaborationbetweenfouracademicEDsbroadensthe exposurestudentsreceivetodifferentteachingstyles, institutionalcultures,andclinicalperspectives.Thisvariety providesamorecomprehensiveeducationalexperiencethan whatcanbeofferedbyasingleinstitutionalone.
WeaimedtoaddresstheabsenceofanacademicEDat HUCOMbydevelopingacollaborativeeducational experience.ThisprogramfocusesoncoreprinciplesofEM andresidencypreparationandwasdesignedspecificallyfor fourth-yearmedicalstudentsduringtheirhomeEMsub-Iat HUCOM.Weobtainedinstitutionalboardreviewapproval fromWakeForestUniversitySchoolofMedicine.
Weusedthesix-stepapproachtocurriculardevelopment. All finalcurriculardesignandcontentwasagreeduponby thefacultyrepresentativesateachofthefourparticipating residencysites.13,14 1) Problemidenti fi cationandgeneral needsassessment. Unliketraditionalcurriculum developmentwheretheneedassessmentisbasedonaspecific healthproblem,ourneedsassessmentwasbasedontheneed toincreasethediversityofemergencycliniciansbyhelping prepareunder-representedstudentstosucceedinaway
rotationsandthematch.2) Determiningandprioritizing content. Whileindividualsateachparticipatinginstitution wereinvolvedwithteachingattheirowninstitution,the needsoftheHUCOMstudentswereunique.Therefore, educationalobjectivesweredevelopedinconjunctionwith thefacultyadvisortothefourth-yearEMrotationat HUCOMwhoconductedstakeholderinterviewswith five currentmedicalstudentsand fivealumniwhohadrecently graduatedandwerecurrentlyinEMresidenciesacrossthe country.Itwasdecidedthatcurricularcontentwouldinclude amixofcoreEMtopics(asdeterminedfromstakeholder interviews)andadvisingsessions.
Afterallsessions,studentswereprovidedwiththecontact informationforthefacultylecturersandwereencouragedto reachout.3) Goalsandobjectives .Broadcurriculargoals weredeveloped.Theseweretoa)teachtheapproachtocore complaintsinEM;b)teachkeyskillsinEM;c)demystifythe processofapplyingtoanEMresidencyprogram;andd) connectstudentswithresidentsandfacultyinthe fieldofEM. Afterthis,specificmeasurablelecturegoalsweredeveloped basedoncognitive,affective,andpsychomotorobjectivesfor thelearner.4) Educationalstrategies .Wecreatedanentirely virtual,four-weekdidacticprogram,withcontentorganized intoweeklyfour-hourblocks,eachledbyadifferent academicED,onaninteractiveplatformthatallowedfor case-baseddiscussions,small-groupdiscussions,and standardlectureformat.Sinceimplementationin2022,the programhasbeenmandatoryforallstudentscompleting theirfourth-yearEMsub-IatHUCOM.
Eachweek,thesessionsrequiredtheparticipationoffour to fivefacultymemberswhovolunteeredtheirtime,withthe majorityoflecturesdeliveredbyasinglefacultymember. However,selectsessions,suchasthe “Applicationand InterviewingProcess,” wereco-ledbyadynamicteam consistingoftheassistantprogramdirector,program director,andchiefresidents,providingawell-rounded perspectiveandvaluableinsightsfortheparticipants. Contentwasmappedandcoordinated,andpre-readingwas assignedfromtheAcademyforDiversityandInclusionin EmergencyMedicinewebinarseries “HowtoBeaSuccessful
Didacticsessionone
Institutionone
EMApplicant” andtheClerkshipDirectorsinEmergency Medicine/SocietyofAcademicEmergecyMedicineM4 curriculum.Eachdayincludedamixofclinicaltopicsand “advising” sessions(Table1).5) Implementation. Approval fromtheEMdirectorwasobtained,andthecurriculawas implemented.6) Evaluationandfeedback .Aftereachblock ofcontent,evaluationsforeachindividualsession(including thepresenter)weresenttoparticipatingstudentsvia REDCap(ResearchElectronicDataCapture,hosted atHowardUniversitySchoolofMedicine.
Theseevaluationsconsistedofonequestionforeach session: “Pleaseratetheeffectivenessofthefollowingsession inaccomplishingitslearningobjectives: Session,Presenter . ” Attheendofthemonth-longprogram,anoverallevaluation oftheprogramwassenttoparticipatingstudents,alsovia RedCap.Theprogramevaluationsurveytool,includingfour multiple-choicequestionsregardingtheoveralllearning objectives,isreflectedin Figure1.Thetoolalsoincludedtwo free-responsequestions:1) “Whichpartsofthecurriculum wereofmostvaluetoyou?”;and2) “Whichpartsofthe curriculumcouldbeimproved?” Werefinedthecurricula eachyearduringanend-of-yeardebrief.
Priortothe firstsession,studentswereprovideda spreadsheetwithpre-sessionwork,curriculumtopics, presentingfacultyandresidents,datesandtimes,andlinksto accesstheweeklyvirtualsessions.EachEMprogram providedfourhoursofinteractivedidacticstothestudents accordingtothescheduleddatesandtimes.
Apost-curricularsurveyfounduniversalagreementfrom studentsthatthecurriculumwaseffectiveinmeetingthe abovegoals.Ofthe fivestudents,100%reportedstrongly agreeingwiththefollowingstatements.Thesesessions1) helpedmelearntheapproachtocoreEMtopicsmorethanI wouldhavebeenabletodoonmyown;2)helpedmelearn keyskillsforexcellinginanEMrotationmorethanIwould havebeenabletodoonmyown;and3)allowedmeto
Didacticsessiontwo Institutiontwo
Didacticsessionthree Institutionthree
Didacticsessionfour Institutionfour LecturetopicsPersonalstatementPresentationskillsHowtochoosetheright programforyou Applicationandinterviewing process
ChestpainAlteredmentalstatusToxicologyoverviewHeadache ShortnessofbreathAbdominalpainShockandsepsisGynecologicandurologic emergencies
RadiographsElectrocardiogram introduction VaginalbleedingEndocrineandelectrolytes
SocialemergencymedicineUltrasoundbasicsAdvancedtraumalife support Advancedcardiaclifesupport, basiclifesupport
Session:
Presenter:
Please rate the effectiveness of the following session in accomplishing its learning objectiveson a scale from 1 (not effective) to 5 (very effective)
Questions These sessions helped me learn the approach to core emergency medicine topics (abdominal pain, chest pain, headache, etc.) more so than I would have been able to do on my own.
These sessions helped me learn key skills for excelling in an emergency medicine rotation including oral presentations, EKG interpretation, xray interpretation and ultrasound, more so than I would have been able to do on my own.
These sessions helped me learn about the process of applying to and selecting an EM residency program. These sessions allowed me to connect with faculty and resident mentors to learn more about the field of emergency medicine.
Response Options
Strongly agree, agree, neutral, disagree, strongly disagree
Strongly agree, agree, neutral, disagree, strongly disagree
Strongly agree, agree, neutral, disagree, strongly disagree
Strongly agree, agree, neutral, disagree, strongly disagree Response
Which parts of the curriculum were of most value to you?
Which parts of the curriculum could be improved?
connectwithfacultyandresidentmentorstolearnmore aboutthe fieldofEM.Ofthe fivestudents,80%and20% reportedstronglyagreeingandagreeing,respectively,that thesesessionshelpedthemlearnabouttheprocessof applyingtoandselectinganEMresidencyprogram.
Narrativefeedback,suchasthequotesbelow,from studentshighlightedthevalueofmeetingwithfacultyand residentsfromdifferentprograms.fromgoingthroughcases inrealtime.
MeetingthefacultyandprogramdirectorsatvariousEM programsreallywasthehighlightofthecurriculum.Itwas greattogetaninsidelookateachprogramandlearnmore abouttheirculture,approach,andthepeoplethere.
Ireallyenjoyedhearingtheresidents’ perspectiveonhow tonavigatetheapplicationprocess.
Narrativefeedback,suchasthequotesbelow,also emphasizedthevalueofthecurriculum’sinteractivenature andhowtraditionallyin-persontopicswereeffectively adaptedforvirtuallearning.
Myfavoritepartwasparticipatinginreal-timecases.Being involvedasthecaseunfoldedfeltlikehands-onpractice.
Itwasincredibletohavethemechanismsofultrasound explainedinsuchdetail.Breakingitdowntothebasics reallyhelpedmeunderstandultrasoundforthe firsttime.
Successfulimplementationrequiredactiveengagement fromHUCOM,specificallytheclerkshipdirectorand administrativestaff,whoservedasleadcontacts.Control overrotationschedulingwasessentialtoensureallstudents werefullyengagedinthesessions.Inaddition,as participatinginstitutionsusedvariousonlineplatformsto communicateanddisseminatecurriculamaterials,suchas Tintinalli ’ sEmergencyMedicine ,withtheirstudents,itwas necessarytohaveHUCOMmanageacentral communications-andvideo-conferencingplatform thatwasaccessibletoalllecturinginstitutionsand participatingstudents.
Recruitingfacultyandresidentsforeachinstitution’ s weekwaschallenging,buthavingrepresentativeswithstrong connectionsinmedicaleducationmadeasignificant difference.Theserelationshipsallowedthemtoquicklyand effectivelyrecruitlecturers,leveragingtheirnetworksto secureindividualswhowerebothwillingandenthusiasticto participate.Thishighlightsthevalueofhavinginstitutional leadswithestablishedtiestotheireducationalinfrastructure, streamliningtherecruitmentprocess.
Thesuccessofthisprojectinvolvedahighdegreeoftrust asmanyoftheinstitutionalrepresentativeshadnotworked together.Todevelopthistrust,wefollowedtheframeworkof engaging,listening,framing,envisioning,andcommitting.15 Thepowerofthisprogramistrulyinthecollectiverather thantheindividual.Whilestudentscouldlearnaboutatrial fibrillationfromoneinstitution,thereallearningoccurs whentheyseethecollaboration,getasenseofthescopeof EMasaprofessional field,andareabletointeractwith variedinstitutionsthathavedifferentapproachestoteaching andthepracticeofmedicine.
UnliketraditionalEMrotationsthatattractstudentsfrom acrossthecountry,ourprogramhadasmallcohort comprisedsolelyofHUCOMstudents,astherewasno affiliatedresidency.Thissmallgroupsizemeantthatifone studentmissedasessionduetointerviews,illness, orotherreasons,itnoticeablyimpactedthelearning environment,limitinggroupdynamicsand peer-to-peerlearning.
Virtuallearningposedchallengesforteachinginteractive skillssuchasultrasound.Weaddressedthisbyincorporating case-basedlearningwithcuratedimagelibrariesand real-timefeedback.Tofurtherenhancethelearning experience,futureiterationsshouldexploretheintegration ofultrasoundsimulationsoftwaretobettermimic hands-onscenarios.
AlthoughinitiallydesignedforHUCOMstudents,this modelcouldbeexpandedtoothermedicalschoolswithout academicEDs,especiallythosewithahighproportionof URiMstudents.WiththeopeningofadditionalHBCU medicalschools,thereisanevengreaterneedforprograms thatincreaseaccesstoEMeducation.
Studylimitationsincludethesmallsamplesizeaswellas lackofacomparisongroup.Futureanalyseswilladdress
theselimitationsandincludeevaluationofmatchoutcomes aswellasotherlearner-centeredtargetssuchasperformance inStandardizedLettersofEvaluationorsubsequent rotationsandinternyearperformance.
AddressforCorrespondence:CortlynBrown,MD,MCSO,Atrium HealthCarolinas,DepartmentofEmergencyMedicine,1000Blythe Blvd.,Charlotte,NC28203.Email: Cortlyn.Brown@atriumhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Brownetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KomaromyM,GrumbachK,DrakeM,etal.TheroleofBlackand Hispanicphysiciansinprovidinghealthcareforunderserved populations. NEnglJMed. 1996;334(20):1305–10.
2.MarrastLM,ZallmanL,WoolhandlerS,etal.Minorityphysicians’ rolein thecareofunderservedpatients:diversifyingthephysicianworkforce maybekeyinaddressinghealthdisparities. JAMAInternMed. 2014;174(2):289.
3.GomezLEandBernetP.Diversityimprovesperformanceand outcomes. JNatlMedAssoc. 2019;111(4):383–92.
4.SahaS,KomaromyM,KoepsellTD,etal.Patient-physicianracial concordanceandtheperceivedqualityanduseofhealthcare. Arch InternMed. 1999;159(9):997.
5.TakeshitaJ,WangS,LorenAW,etal.Associationofracial/ethnic andgenderconcordancebetweenpatientsandphysicianswithpatient experienceratings. JAMANetwOpen. 2020;3(11):e2024583.
6.ShenMJ,PetersonEB,Costas-MunizR,etal.Theeffectsofraceand racialconcordanceonpatient-physiciancommunication:asystematic reviewoftheliterature. JRacialEthnHealthDisparities. 2018;5(1):117–40.
7.GarrickJF,PerezB,AnaebereTC,etal.Thediversitysnowballeffect: thequesttoincreasediversityinemergencymedicine.Acasestudyof Highland’semergencymedicineresidencyprogram. AnnEmergMed. 2019;73(6):639–47.
8.BoatrightD,TunsonJ,CarusoE,etal.Theimpactofthe2008Councilof EmergencyResidencyDirectors(CORD)panelonemergencymedicine residentdiversity. JEmergMed. 2016;51(5):576–83.
9.MabezaRM,ChristophersB,EderaineSA,etal.Interventions associatedwithracialandethnicdiversityinUSgraduatemedical education:ascopingreview. JAMANetwOpen. 2023;6(1):e2249335.
10.MartinezJ,MieresJH,RoswellRO,URiM(underrepresented inmedicine)learnerandfacultymentoring.In:FornariAandShahDT
(Eds.), MentoringinHealthProfessionsEducation(34–43).IAMSE manuals.Cham,Switzerland:SpringerInternationalPublishing,2021.
11.DeLaCruzMSD,SairenjiT,StumbarSE,etal.Curricular recommendationsforanationalfamilymedicinesubinternship: aqualitativeanalysisfrommultiplestakeholders. FamMed. 2021;53(10):835–42.
12.GoinesJ,IledareE,AnderD,etal.Amodelpartnership:mentoring underrepresentedstudentsinmedicine(URiM)inemergencymedicine. WestJEmergMed. 2021;22(2):213–7.
13.SweetLandPalazziD.ApplicationofKern’ssix-stepapproachto curriculumdevelopmentbyglobalhealthresidents. EducHealth. 2015;28(2):138.
14.ThomasPA,KernDE,HughesMT,etal.(Eds.). CurriculumDevelopmentforMedicalEducation:aSix-step Approach.3rd Ed.Baltimore,Maryland:JohnsHopkinsUniversity Press,2016.
15.MaisterD,GreenC,GaifordR. TheTrustedAdvisor.NewYorkNew York:Simon&Schuster,20th AnniversaryEd.,2021.












- Western Journal of Emergency Medicine Subscription
- CAL/AAEM News Service email updates
- Free and discounted registration to CAL/AAEM events
- And more!
CAL/AAEM NEWS SERVICE
- Healthcare industry news
- Public policy
- Government issues
- Legal cases and court decisions

