Volume 26, Number 1, January 2025



Volume 26, Number 1, January 2025
Cardiology
1 A Pilot Study Assessing Left Ventricle Diastolic Function in the Parasternal Long-axis View
Mümin Murat Yazici, Nurullah Parça, Enes Hamdioğlu, Meryem Kaçan, Özcan Yavaşi, Özlem Bilir
Critical Care
10 Association Between Fentanyl Use and Post-Intubation Mean Arterial Pressure During Rapid Sequence Intubation: Prospective Observational Study
Abdullah Bakhsh, Ahmad Bakhribah, Raghad Alshehri, Nada Alghazzawi, Jehan Alsubhi, Ebtesam Redwan, Yasmin Nour, Ahmed Nashar, Elmoiz Babekir, Mohamed Azzam
Disaster Medicine
20 Beirut Port Blast: Use of Electronic Health Record System During a Mass Casualty Event
Eveline Hitti, Dima Hadid, Miriam Saliba, Zouhair Sadek, Rima Jabbour, Rula Antoun, Mazen El Sayed
Disaster Response
30 Integrating Disaster Response Tools for Clinical Leadership
Kenneth V. Iserson
Education
40 Practice Patterns of Graduates of a Rural Emergency Medicine Training Program
Dylan S. Kellogg, Miriam S. Teixeira, Michael Witt
47 Substantial Variation Exists in Clinical Exposure to Chief Complaints Among Residents Within an Emergency Medicine Training Program
Corlin M. Jewell, Amy T. Hummel, Dann J. Hekman, Benjamin H. Schnapp
53 The Effect of Hospital Boarding on Emergency Medicine Residency Productivity
Peter Moffett, Al Best, Nathan Lewis, Stephen Miller, Grace Hickam, Hannah Kissel-Smith, Laura Barrera, Scott Huang, Joel Moll

















About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.
Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania

FOR MORE INFORMATION PLEASE CONTACT:
Heather Peffley, PHR CPRP
Penn State Health Lead Physician Recruiter hpeffley@pennstatehealth.psu.edu


Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Mark I. Langdorf, MD, MHPE, Editor-in-Chief
University of California, Irvine School of MedicineIrvine, California
University of California, Irvine School of MedicineIrvine, California
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Niels K. Rathlev, MD, Associate Editor Tufts University School of Medicine-Boston, Massachusetts
Michael Shalaby, MD, Deputy Editor Mount Sinai Medical Center
Susan R. Wilcox, MD, Associate Editor
Massachusetts General Hospital- Boston, Massachusetts
Elizabeth Burner, MD, MPH, Associate Editor
University of Southern California- Los Angeles, California
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts s
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Section Editors
Behavioral Emergencies
Leslie Zun, MD, MBA
Rosalind Franklin University of Medicine and Science
Marc L. Martel, MD Hennepin County Medical Center
Behavioral Health
Ryan Ley, MD, MBA, MS University of Nevada School of Medicine
Cardiac Care
Anthony Lucero, MD Kaweah Health Medical Center
Mary McLean, MD, FAAEM, FACEP AdventHealth East Orlando Emergency Medicine Residency
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD Carolinas Medical Center
Casey Clements, MD, PhD
Mayo Clinic
Patrick Meloy, MD Emory University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Dell Simmons, MD Geisinger Health
Joseph Shiber, MD University of Florida-College of Medicine
David Page, MD University of Alabama
Erik Melnychuk, MD Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
Andrew Milsten, MD, MS UMass Chan Medical School
Scott Goldstein, DO, FACEP, FAEMS, EMT-T/P
Jefferson Einstein
John Broach, MD, MPH, MBA, FACEP
University of Massachusetts Medical School
UMass Memorial Medical Center
Christopher Kang, MD Madigan Army Medical Center
Rick A. McPheeters, DO, Associate Editor
R. Gentry Wilkerson, MD, Associate Editor University of Maryland
Education
Asit Misra, MD, MSMEd, CHSE University of Miami
University of Colorado
ED Administration, Quality, Safety
Tehreem Rehman, MD, MPH, MBA
Mount Sinai Hospital
David C. Lee, MD
Northshore University Hospital
Gary Johnson, MD Upstate Medical University
Brian J. Yun, MD, MBA, MPH Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH
Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH
University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine University of California, Davis
Emergency Medical Services
Daniel Joseph, MD Yale University
Joshua B. Gaither, MD
University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Stephen Meldon, MD
Cleveland Clinic
Luna Ragsdale, MD, MPH Duke University Health Equity
Sara Heinert, PhD, MPH
Rutgers Robert Wood Johnson Medical School
Naomi George, MD, MPH University of New Mexico School of Medicine
Sarah Aly, DO
Yale Department of Emergency Medicine
Lauren Walter, MD, MSPH University of Alabama at Birmingham
Victor Cisneros, MD, MPH
Eisenhower Medical Center
Faith Quenzer Temecula Valley Hospital San Ysidro Health Center
University of Texas-Houston/McGovern Medical School- Houston Texa
Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Payal Modi, MD MScPH University of Massachusetts Medical Infectious Disease
Elissa Schechter-Perkins, MD, MPH Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Stephen Liang, MD, MPHS
Washington University School of Medicine
Injury Prevention
Mark Faul, PhD, MA
Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH
Prisma Health Richland
Taylor Burkholder, MD, MPH
Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Indiana University School of Medicine Statistics and Methodology
Monica Gaddis, PhD University of Missouri, Kansas City School of Medicine
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH
Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS
Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS
Neurosciences
Antonio Siniscalchi, MD
Annunziata Hospital, Cosenza, Italy
Rick Lucarelli, MD
Medical City Dallas Hospital
William D. Whetstone, MD University of California, San Francisco
Pediatric Emergency Medicine
Ronnie Waldrop, MD
University of South Alabama
Jabeen Fayyaz, MD, MCPS, FCPS, MHPE, PhD, IHP
The Hospital for Sick Children
Muhammad Waseem, MD Lincoln Medical & Mental Health Center
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
John Ashurst, DO Lehigh Valley Health Network
Tony Zitek, MD
Kendall Regional Medical Center
Erik S. Anderson, MD Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD
Henry Fo
Chris Baker, MD University of California, San Francisco rd Hospital
Phillips Perera, MD Stanford University Medical Center Trauma
Whitney K. Brown, MD, MPH, Med, CTropMed University of Cincinnati College of Medicine
Robert Flint, MD, FACEP, FAAEM University of Maryland School of Medicine
Lesley Osborn, MD University of Colorado
Kathleen Stephanos, MD University of Maryland School of Medicine
T. Andrew Windsor, MD AEMUS-FPD
University of Maryland School of Medicine
Pierre Borczuk, MD Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS Virginia Commonwealth University
University of California, Irvine Ultrasound J. Matthew Fields, MD
Robert Allen, MD Los Angeles General Medical Center
Shane Summers, MD Brooke Army Medical Center
Robert R. Ehrman
Wayne State University
Ryan C. Gibbons, MD Temple Health
Women’s Health
Marianne Haughey, MD Northwell Health
Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine


American Academy of Emergency Medicine







Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA
Integrating Emergency Care with Population Health
Integrating Emergency with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
MAAEM
Amin A. Kazzi, MD, MAAEM
Amin A. Kazzi, MD, MAAEM
Gayle Galleta, MD
Beirut,
The American University of Beirut, Lebanon
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University of Texas, Houston
Brent King, MD, MMM University Texas, Houston
Christopher E. San Miguel, MD
Ohio State University Wexner Medical Center
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Christopher E. San Miguel, Ohio State University Wexner Medical Center
Daniel J. Dire, MD
Daniel J. Dire, MD University Texas Health Sciences Center San Antonio
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Douglas Ander, MD Emory University
Douglas Ander, Emory University
Emory University
Edward Michelson, MD Texas Tech University
Edward Michelson, Texas Tech University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH South
Edward Panacek, MD, MPH University of South Alabama
Edward MD, MPH University South Alabama
Francesco
“Maggiore della Carità,” Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Elena Lopez-Gusman, JD
Elena Lopez-Gusman, JD
California ACEP
California ACEP
Elena Lopez-Gusman, JD California ACEP American College of Emergency
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Gayle Galleta, MD Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog,
Hjalti Björnsson, MD
Niels K. Rathlev, MD Tufts University School of Medicine
Tufts University School of Medicine
Niels K. Rathlev, MD Tufts University School of Medicine
Scott Zeller, MD
Scott Zeller, MD University of California, Riverside
Scott Zeller, MD University of California, Riverside
Hjalti MD Icelandic Society of Emergency Medicine
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Jaqueline Le, MD Desert Regional Medical Center
Jaqueline Le, MD Desert Medical Center
Regional
Jeffrey Love, MD
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jeffrey Love, The George Washington University School of Medicine and Health Sciences
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Katsuhiro Kanemaru, MD University of Hospital, Miyazaki, Japan
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Bell,
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Singapore
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands
Peter Sokolove, MD University of California, San Francisco
University of California, San Francisco
Wirachin Hoonpongsimanont, MD, MSBATS
Wirachin Hoonpongsimanont, MD, MSBATS
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
The George Washington University School of Medicine and Health Sciences Arizona,
Leslie Zun, MD, MBA Chicago Medical School
Leslie Zun, MD, MBA Chicago Medical School
Rachel A. Lindor, MD, JD Mayo Clinic
Rachel A. Lindor, MD, JD Mayo Clinic
Rachel A. Lindor, MD, JD
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert Suter, DO, MHA
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
University of California, Davis
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Linda S. Murphy, MLIS University of California, Irvine School of Medicine
Chicago Medical School Librarian
American College of Emergency Physicians
American College of Emergency Physicians
Jennifer Kanapicki Comer, MD FAAEM
Jennifer Kanapicki Comer, MD FAAEM
California Chapter Division of AAEM Stanford University School of Medicine
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE
DeAnna McNett, CAE
Kimberly Ang, MBA UC Irvine Health School of Medicine
American College of Osteopathic Emergency Physicians
American College of Osteopathic Emergency Physicians
Randall J. Young, MD, MMM, FACEP California ACEP
Kimberly Ang, MBA
American College of Emergency Physicians Kaiser Permanente
UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians
Kaiser Permanente
J. American College of Emergency Physicians Kaiser Permanente

Scott Rudkin, MD, MBA University of California, Irvine
Scott Rudkin, MD, MBA
Scott Rudkin, MD, MBA University of California, Irvine
Staff
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Langdorf, MAAEM, FACEP
Isabelle Nepomuceno, BS Executive Editorial Director
Isabelle Kawaguchi, BS Executive Editorial Director
June Casey, BA Copy Editor
Cassandra Saucedo, MS Executive Publishing Director
UC Irvine Health School of Medicine
UC Irvine Health School Medicine
UC Irvine Health School of Medicine
Robert Suter, DO, MHA
Robert Suter, DO, MHA American College of Osteopathic
American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Shahram Lotfipour, MD, MPH FAAEM, FACEP
UC Irvine Health School Medicine
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP
Jorge Fernandez, MD, FACEP
Ian Olliffe, BS Associate Editorial Director, WestJEM
Visha Bajaria, BS WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Visha Bajaria, BS WestJEM Editorial Director WestJEM
UC San Diego Health School of Medicine
UC San Diego Health School of Medicine
Jorge Fernandez, MD, UC San Diego Health School of Medicine
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director

and Publishing Office: JEM/Depatment of





Tran Nguyen, BS Associate Editorial Director, CPC-EM
Nicole Valenzi, BA WestJEM Publishing Director
Cassandra Saucedo, MS WestJEM Publishing Director
Sheya Aquino, BS Associate Editorial Director
June Casey, BA Copy Editor
Nancy Taki, BS Associate Editorial Director
Alyson Tsai, BS Associate Publishing Director
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine

Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org

Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
62 Preparation for Rural Practice with a Multimodal Rural Emergency Medicine Curriculum
Ashley K. Weisman, Skyler A. Lentz, Julie T. Vieth, Joseph M. Kennedy, Richard B. Bounds
66 Emergency Medicine Clerkship Grading Scheme, Grade, and Rank-List Distribution as Reported on Standardized Letters of Evaluation
Alexandra Mannix, Thomas Beardsley, Thomas Alcorn, Morgan Sweere, Michael Gottlieb
70
Leadership Perceptions, Educational Struggles and Barriers, and Effective Modalities for Teaching Vertigo and the HINTS Exam: A National Survey of Emergency Medicine Residency Program Directors
Mary McLean, Justin Stowens, Ryan Barnicle, Negar Mafi, Kaushal Shah
Emergency Department Operations
78 Characteristics and Outcomes of Implementing Emergency Department-based Intensive Care Units: A Scoping Review
Jutamas Saoraya, Liran Shechtman, Paweenuch Bootjeamjai, Khrongwong Musikatavorn, Federico Angriman
Emergency Medical Services
86 Emergency Medical Services Provider-Perceived Alzheimer’s Disease and Related Dementias in the Prehospital Setting
Esmeralda Melgoza, Valeria Cardenas, Hiram Beltrán-Sánchez
Endemic Infections
96 Self-Reported COVID-19 Vaccine Status and Barriers for Pediatric Emergency Patients and Caregivers
Amanda M. Szarzanowicz, Kendra Fabian, Maya Alexandri, Carly A. Robinson, Sonia Singh, Michael Wallace, Michelle D. Penque, Nan Nan, Changxing Ma, Bradford Z. Reynolds, Bethany W. Harvey, Heidi Suffoletto, E. Brooke Lerner
Global Health
103 Needs Assessment and Tailored Training Pilot for Emergency Care Clinicians in the Prehospital Setting in Rwanda
Naz Karim, Jeanne D’Arc Nyinawankusi, Mikaela S. Belsky, Pascal Mugemangango, Zeta Mutabazi, Catalina Gonzalez Marques, Angela Y. Zhang, Janette Baird, Jean Marie Uwitonze, Adam C. Levine
Health Equity
111 Emergency Physicians’ and Nurses’ Perspectives on Transgender, Intersexual, and Non-Binary Patients in Germany
Torben Brod, Carsten Stoetzer, Christoph Schroeder, Stephanie Stiel, Kambiz Afshar
120 Pediatric Emergency Department-based Food Insecurity Screening During the COVID-19 Pandemic
Stephanie Ruest, Lana Nguyen, Celeste Corcoran, Susan Duffy
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
129 Effectiveness of a Collaborative, Virtual Outreach Curriculum for 4th-Year EM-bound Students at a Medical School Affiliated with a Historically Black College and University
Cortlyn Brown, Richard Carter, Nicholas Hartman, Aaryn Hammond, Emily MacNeill, Lynne Holden, Ava Pierce, Linelle Campbell, Marquita Norman
Health Outcomes
135 Associations of the Need for Surgery in Emergency Department Patients with Small Bowel Obstructions
Daniel J. Berman, Alexander W. Mahler, Ryan C. Burke, Andrew E. Bennett, Nathan I. Shapiro, Leslie A. Bilello
Injury Prevention
142 Survey of Firearm Storage Practices and Preferences Among Parents and Caregivers of Children
Meredith B. Haag, Catlin H. Dennis, Steven McGaughey, Tess A. Gilbert, Susan DeFrancesco, Adrienne R. Gallardo, Benjamin D. Hoffman, Kathleen F. Carlson
Neurology
147 Electroencephalography Correlation of Ketamine-induced Clinical Excitatory Movements: A Systematic Review
Emine M. Tunc, Neil Uspal, Lindsey Morgan, Sue L. Groshong, Julie C. Brown
Patient Communication
155 #emergencymedicine: A TikTok Content Analysis of Emergency Medicine-related Content
Madison Stolly, Erika Wilt, Nathan Gembreska, Mohamad Nawras, Emily Moore, Kelly Walker, Rhonda Hercher, Mohamad Moussa
Patient Safety
161 A Machine Learning Algorithm to Predict Medical Device Recall by the Food and Drug Administration
Victor Barbosa Slivinskis, Isabela Agi Maluli, Joshua Seth Broder
Pediatrics
171 Impact of Treatment on Rate of Biphasic Reaction in Children with Anaphylaxis
William Bonadio, Connor Welsh, Brad Pradarelli, Yunfai Ng
Letters to the Editor
176 Hyperkalemia or Not? A Diagnostic Pitfall in the Emergency Department
Frank-Peter Stephan, Florian N. Riede, Luca Ünlü, Gioele Capoferri, Tito Bosia, Axel Regeniter, Roland Bingisser, Christian H. Nickel
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Albany Medical College Albany, NY
Allegheny Health Network Pittsburgh, PA
American University of Beirut Beirut, Lebanon
AMITA Health Resurrection Medical Center Chicago, IL
Arrowhead Regional Medical Center Colton, CA
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
INTEGRIS Health Oklahoma City, OK
Kaiser Permenante Medical Center San Diego, CA
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Lakeland HealthCare St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Louisiana State University Shreveport Shereveport, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maine Medical Center Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Mayo Clinic Jacksonville, FL
Mayo Clinic College of Medicine Rochester, MN
Mercy Health - Hackley Campus Muskegon, MI
Merit Health Wesley Hattiesburg, MS
Midwestern University Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program St. Paul, MN
Rhode Island Hospital Providence, RI
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
St. Luke’s University Health Network Bethlehem, PA
Spectrum Health Lakeland St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
The MetroHealth System/ Case Western Reserve University Cleveland, OH
UMass Chan Medical School Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Tucson, AZ
University of California, Davis Medical Center Sacramento, CA
University of California, Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago Chicago, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Massachusetts Amherst, MA
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Nebraska Medical Center Omaha, NE
University of Nevada, Las Vegas Las Vegas, NV
University of Southern Alabama Mobile, AL
University of Southern California Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University Winston-Salem, NC
Wake Technical Community College Raleigh, NC
Wayne State Detroit, MI
Wright State University Dayton, OH
Yale School of Medicine New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
MüminMuratYazici,MD
NurullahParça,MD
EnesHamdio ˘ glu,MD
MeryemKaçan,MD
ÖzcanYavas¸i,MD
ÖzlemBilir,MD
SectionEditor:ShaneSummers,MD
RecepTayyipErdo ˘ ganUniversityTrainingandResearchHospital,Departmentof EmergencyMedicine,Rize,Türkiye
Submissionhistory:SubmittedMay29,2024;RevisionreceivedOctober9,2024;AcceptedOctober11,2024
ElectronicallypublishedNovember21,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21272
Introduction: SpectralDopplerechocardiographyisusedtoevaluatediastolicdysfunctionoftheheart. However,itisdifficulttoassessdiastolicfunctionwiththismodalityinemergencydepartment(ED) settings.BasedonthehypothesisthatE-pointseptalseparation(EPSS)measuredbyM-modeinthe parasternallong-axis(PSLA)viewmayfacilitatetheassessmentofdiastolicfunctioninemergency patientcare,weaimedtoinvestigatewhetherEPSSmeasuredbyM-modeinthePSLAviewcorrelates withspectralDopplerassessmentinpatientswithgrade1diastolicdysfunction.
Methods: Weperformedthisprospective,observational,single-centerstudywasperformedintheEDof atertiarytrainingandresearchhospital.Allpatientswhopresentedtotheemergencycriticalcareunit withsymptomsofheartfailurewereevaluatedbythecardiologydepartment,hadgrade1diastolic dysfunctionconfirmedbythecardiologydepartment,anddidnotmeetanyofthestudy’sexclusion criteria.Thestudypopulationof40(includedrate14%)wasformedaftertheexclusioncriteriawere appliedto285patientswhomettheseconditions.Patientsincludedinthestudyunderwentspectral Dopplermeasurementsintheapicalfour-chamber(A4C)viewfollowedbyM-modemeasurementsinthe PSLAview.Wethencomparedthemeasurements.
Results: Thecorrelationbetweentheearlydiastolicvelocityofthemitralinflowtothelatediastolic velocity(E/A)ratioinspectralDopplermeasurementsandtheEPSS/A-pointseptalseparation(APSS) ratioinM-modewasstrong(correlationcoefficient0.677, P = 0.001).Similarly,thecorrelationbetweenE inspectralDopplermeasurementsandtheEPSS/APSSratioinM-modemeasurementswasalso moderatelystrong(correlationcoefficient0.557, P = 0.001).
Conclusion: AsignificantcorrelationexistsbetweentheM-modeEPSS/APSSratiomeasurementinthe PSLAviewandthespectralDopplerE/AratiomeasurementintheA4Cwindowtoevaluategrade1 diastolicdysfunction.ThisassociationsuggeststhatM-modemeasurementsinthePSLAmaybeusedin diastolicdysfunction.[WestJEmergMed.2025;26(1)1–9.]
Point-of-careultrasound(POCUS)isofvitalimportance forassessingheartfunctionsintheemergencydepartment (ED).1–3 Bedsideechocardiography,acomponentof POCUS,isanon-invasiveimagingtechniqueusedtoobtain
real-timeimagesoftheheart.Inthisway,systolicand diastoliccardiacfunctioncanbeevaluatedintheED.4,5 Althoughtherearemanyechocardiographicmethodsfor assessingsystolicfunction,theE-pointseptalseparation (EPSS)method,whichmeasuresthedistancebetweenthe
ventricularseptalwallandtheanteriorleafletofthemitral valve(MV)intheparasternallongaxis(PSLA)view,isused intheEDtoassessthesystolicfunctionoftheheart.The EPSSmethodisreliableandsimpleanddoesnotrequire specializedequipmentorcomplexcalculations.Itis particularlyusefulinemergencypatientcare.6–8
ThebedsideuseoftheAmericanSocietyof Echocardiography(ASE)andEuropeanAssociationof CardiovascularImaging(EACI)guidelinesforthe assessmentofdiastolicfunctionusingechocardiographyis difficultinintheEDsettingisdifficultandchallengingin manyrespects.9 InspectralDopplerechocardiography variousparameters,suchastheratiooftheearlydiastolic velocityofthemitralinflowtothelatediastolicvelocity (E/A),theEdecelerationtime,andtheratiooftheearly diastolicvelocityofthemitralinflowtotheearlydiastolic velocityofthemitralannulus(E/e 0 ),areevaluatedinthe apicalfour-chamberview(A4C)toassessthediastolic functionoftheheart.10,11 Evaluatingdiastolicfunctionusing thisspectralDopplermethodissimplynotpracticalin emergencypatientcare.
Variousstudieshaveexaminedtheevaluationofdiastolic dysfunctionbyemergencyphysiciansusingspectralDoppler echocardiography.12,13 Someresearchershaveobservedthat theE/Apatternevaluatedwithpulsedwave(PW)Dopplerin theA4CviewissimilartothemotionpatternoftheMV anteriorleafletseenwhenmeasuringEPSSwithM-modein thePSLAview.14,15 Basedonthehypothesisthatthis similaritymayfacilitatetheassessmentofdiastolicfunction inemergencypatientcare,weaimedtoinvestigatewhether EPSSmeasuredwithM-modeinPSLAviewcorrelateswith spectralDopplerassessmentinpatientswithgrade1 diastolicdysfunction.
StudyDesignandSetting
Thisprospective,observational,single-centerstudywas performedintheemergencydepartmentofatertiarytraining andresearchhospitalinTürkiyebetweenDecember1, 2023–March31,2024.Localethicalcommitteeapprovalwas grantedpriortocommencement(decisionno.2023/259).All patientsweplannedtoincludeinthestudyweretoldhowand forwhatpurposebedsideultrasonographywouldbe performed,andwritteninformedconsentwasobtainedfrom allpatientswhoconsentedtobeincludedinthestudy.
Allpatientswhopresentedtotheemergencycriticalcare unitwithsymptomsofheartfailurewereevaluatedbythe cardiologydepartment,hadgrade1diastolicdysfunction confirmedbycardiology,anddidnotmeetanyofthestudy’ s exclusioncriteria.Thefollowingpatientswereexcluded:two whowere <18yearsofage;75withtachycardiaor bradycardiaatpresentation;47withahistoryofmitral
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
TheuseofDopplermeasurementsinthe evaluationofdiastolicfunctionintheED isdif fi cult.Therefore,itisnecessarytoassess diastolicfunctionbyapracticalmethod.
Whatwastheresearchquestion?
DomeasurementsmadebyE-pointseptal separation(EPSS)assessmentwithM-mode inparasternallong-axis(PSLA)view correlatewiththosemadebyspectralDoppler inpatientswithgrade1diastolicdysfunction?
Whatwasthemajor findingofthestudy?
Thecorrelationbetweentheearlydiastolic velocityofmitralin fl owtolatediastolic velocity(E/A)ratioinspectralDopplerand theEPSS/A-pointseptalseparation(APSS) ratioinM-modewasstrong(correlation coef fi cient0.677,P=0.001.Thissuggests thatM-modemeasurementsinthePSLAmay beusedindiastolicdysfunction.
Howdoesthisimprovepopulationhealth?
TheabilitytouseM-modemeasurementsin PSLAfordiastolicdysf unctionenablesrapid diagnosisandprompttreatmentofpatientsin theED.
stenosisormitralregurgitation;44witharrhythmia;24with ahistoryofmitralvalvesurgery;fourwhorefuseddiagnosis andtreatment;14whodidnothaveacardiologist-approved newechocardiographyreport;29forwhomultrasound measurementscouldnotbeperformed;andsixwhowere broughttotheEDbecauseofcardiacarrest.Thestudy populationof40patients(includedrate14%)wasformed aftertheexclusioncriteriawereappliedto285patientswho mettheseconditions.Thepatient flowchartisshown in Figure1
InitialpatientevaluationsintheEDwereperformedby emergencymedicineresidents.Thestudy’spatient populationwasformedprimarilybasedongrade1diastolic dysfunctionconfirmedbyacardiologist,resultinginagroup ofstandardizedpatients.Inthenextstep,patientswitha historyofmitralstenosisormitralregurgitationandahistory ofmitralvalvesurgeryinechocardiographyresultswhodid nothaveacardiologist-approvednewechocardiography
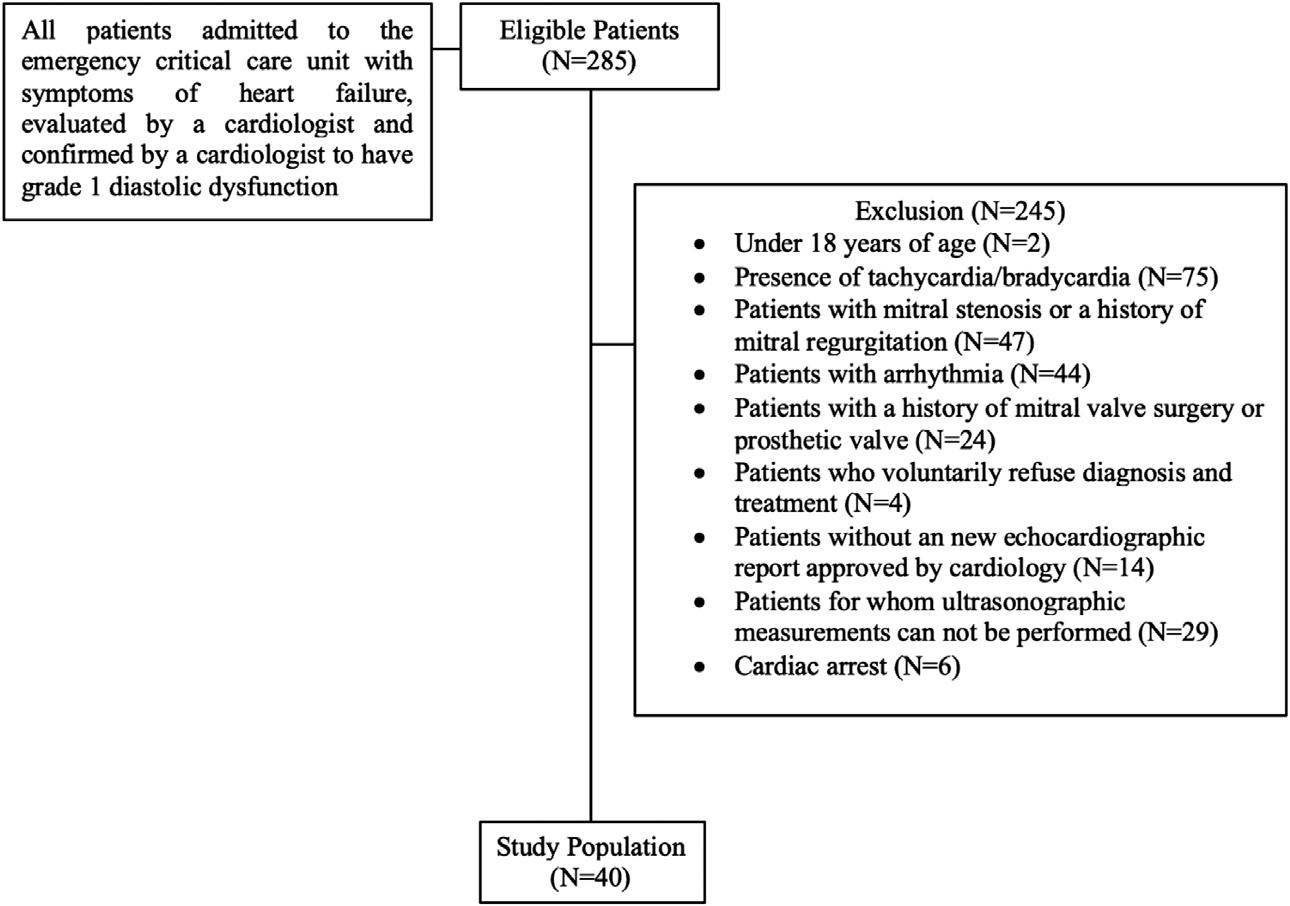
reportwereexcluded.Then,otherexclusioncriteriawere applied.Finally,weexcludedpatientsforwhom ultrasonographicmeasurementswerenotappropriateand whorefuseddiagnosisandtreatment.
Theemergencymedicineresidentperformingtheinitial evaluationrecordedallvitalandphysicalexamination findingsduringpresentation.Theresidentalsorecordedthe demographiccharacteristics,comorbiddiseases,and cardiologist-confirmedechocardiographyresultsofthe patientheincludedinthestudyviathehospital’sautomaed system.Primarydiagnosesandtreatmentsweremadeand administeredbytheemergencymedicineresidentperforming theinitialevaluation.
Twoemergencyphysicianswhohadnoresponsibilityfor thepatients’ primarycareperformedthePOCUS examinations.Bothhadparticipatedinandsuccessfully completedultrasoundcourses(basicandadvanced)that werecertifiedbyprofessionalemergencymedicine associations(fiveyearsofexperienceinPOCUSwithan averageof500ultrasoundsperyear).Theywereblindedto thestudypatients’ laboratoryparameters,vital findings, diagnoses,andtreatments.
POCUSProtocol
SonographicexaminationswereperformedonaFujifilmSonosite-FC1(FUJIFILMSonoSiteInc,Bothell,WA)2015 modelUSdevice.Allmeasurementsweremadewith1–5 megahertzsector(cardiac)probe.Thestudyprotocol includedpulsed-wave(PW)Dopplermeasurementsfor diastolicfunctionevaluationinA4Cview,followedbyMmodemeasurementsviaPSLAviewscansoftheMVanterior leaflet.Atsonographicexamination,E,A,andEdescent time(EDT)measurementswere firstperformedwithPW
DopplerinA4Cview.ThenEPSS,A-pointseptalseparation (APSS),A-pointopeninglength(APOL),andE-point openinglength(EPOL)weremeasuredwithM-mode evaluationatthelevelofthemitralvalveinthePSLAview. Theejectionfraction(EF)wascalculatedusingtheEPSS method.MeasurementtimewasrecordedforbothA4Cview measurementsandPSLAviewmeasurements.Therecording procedurecommencedoncetheultrasonographicwindows providedbytheimageswereclearlyvisible,anditwas concludedwhenthedesiredmeasurementshad finished.All measurementsaresummarizedin Figures2 and 3
Theprimaryendpointinthisstudywastoevaluatethe correlationbetweenmeasurementsperformedwithPW DopplerintheA4CviewandM-modemeasurementsinthe PSLAviewinpatientswithgrade1diastolicdysfunction. Thesecondaryoutcomepointwastocomparethetime elapsingbetweenthemeasurements.
WeperformedallanalysesusingJamoviversion1.6 statisticalsoftware(theJamoviProject2021,Sydney, Australia).Categoricaldatawereexpressedasfrequency(n) andpercentage.Normallydistributedcontinuousvariables werepresentedasmeanplusstandarddeviation,andnonnormallydistributeddataasmedianandinterquartilerange (IQR).Normalityofdistributionwasevaluatedusingthe Shapiro-Wilktest.Wecomparedcontinuousvariablesin dependentgroupsusingthepaired t -testincaseofnormal distributionandtheWilcoxontestincaseofnon-normal distribution.ThePearsoncorrelationfornormally distributedvariablesandSpearmancorrelationanalysisfor
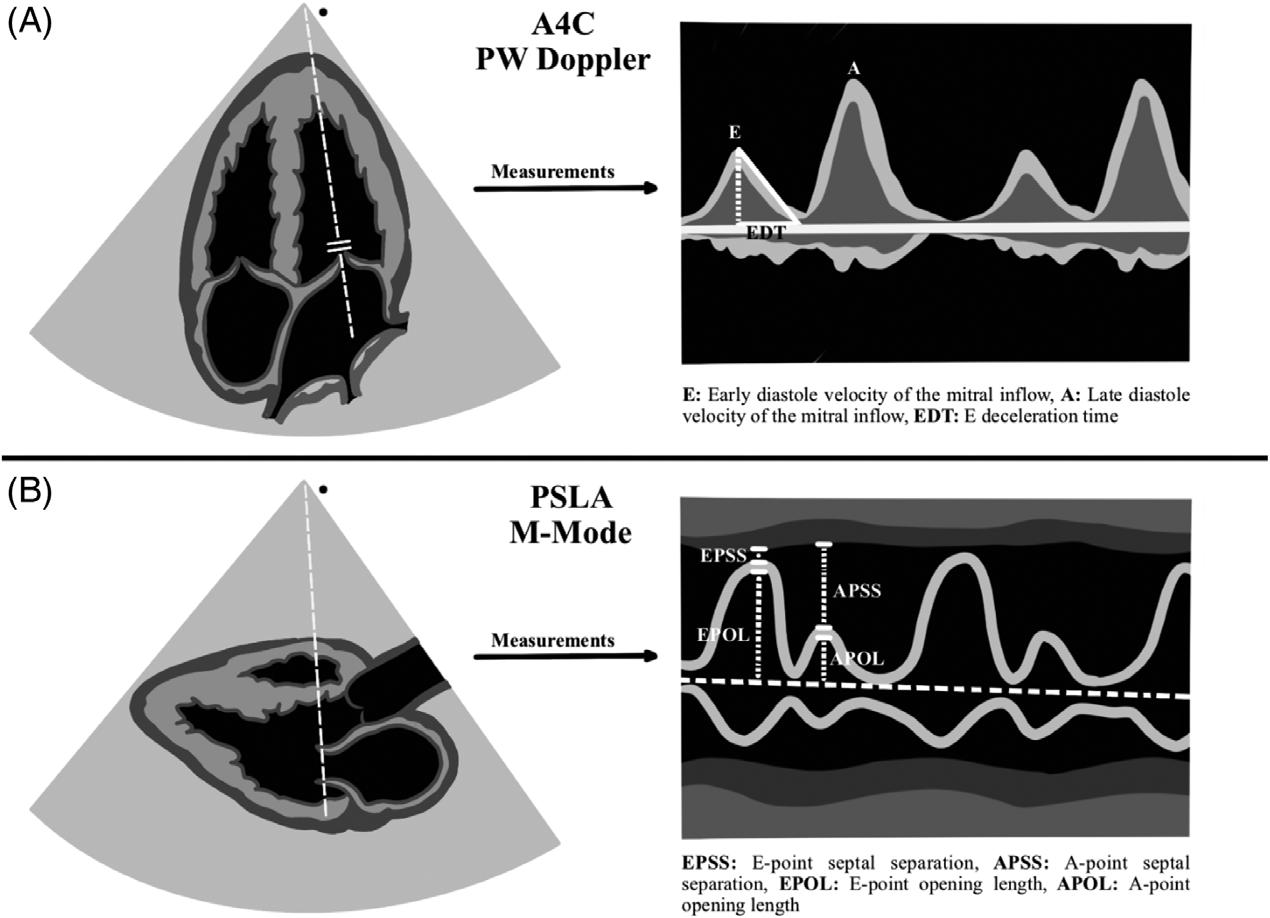
Figure2. Illustrationofmeasurements. PSLA,parasternallongaxis; A4C,apicalfour-chamber; PW,pulsedwave.
non-normallydistributedvariableswereperformedto evaluatetherelationshipsbetweenMVmeasurementsin PSLAviewandPWDopplermeasurementsinA4Cview. SincetherelationshipbetweenMVanteriorleafletM-mode
measurementsinthePSLAviewandDopplerinflowvelocity MVmeasurementshadnotyetbeendetermined,wedidot performsamplesizecalculation. P -values <0.05were consideredsignificantforallanalyses.
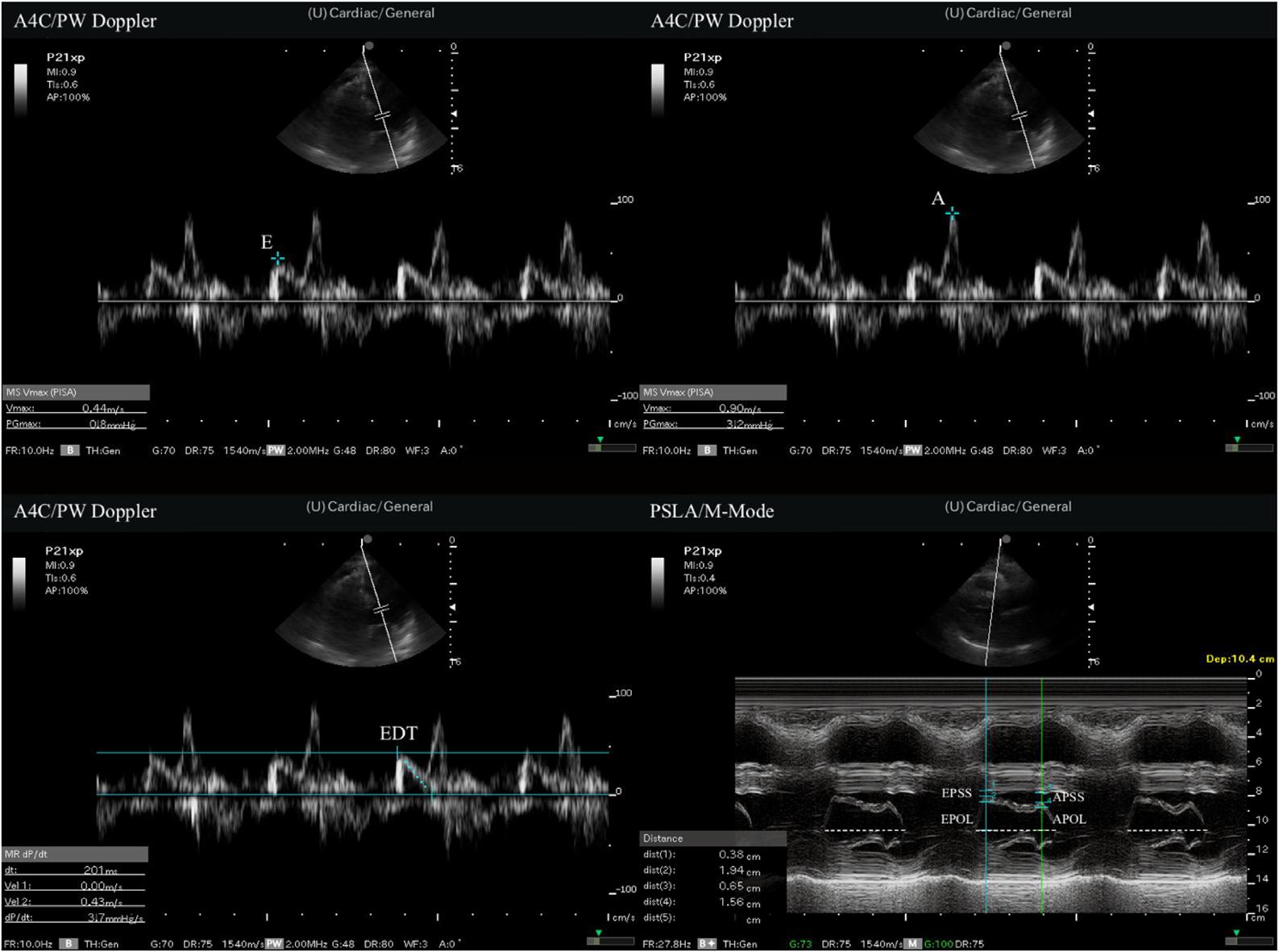
Figure3. Measurementsofpoint-of-careultrasound. A,latediastolevelocityofthemitralinflow; A4C,apical4-chamber; APOL,A-pointopeninglength; APSS,A-pointseptalseparation; E,early diastolevelocityofthemitralinflow; EDT,Edecelerationtime; EPOL,E-pointopeninglength; EPSS,E-pointseptalseparation; PSLA, parasternallongaxis; PW,pulsedwave.
Thestudypopulationof40patientswasconstituted followingapplicationoftheinclusionandexclusioncriteria. Thestudypopulationwasformedafterallexclusionsteps, andultrasonographicevaluationswereperformedonall40 patients.Considering29patientsevaluatedbycardiologists butexcludedbecauseoftheinabilitytoperform measurementsbysonographers,sonographerswereableto performmeasurementsin40of69patients(58.0%).Twentysix(65%)ofthepatientsenrolledweremen,and14(35%) werewomen.Thepatients’ meanagewas76.6years,ranging between35–97.Hypertension(HT)andcoronaryartery disease(CAD)werethemostcommonaccompanying comorbiddiseases.
AnalysisofmeasurementsusingPWDopplerintheA4C revealedamedianEvalueof0.5meterspersecond(m/s), withanIQRof0.4–0.6m/s,medianA0.7m/s,IQR 0.6–0.8m/s,andmedianEDT258m/s,IQR233–279m/s. Similarly,analysisofmeasurementstakenwithM-modein thePSLAviewrevealedamedianEPSSvalueof0.77 centimeters(cm),withanIQRof0.54–0.89cm,median APSS1.10cm,IQR0.79–1.31cm,medianEPOL1.51cm, IQR1.23–1.74cm,andmedianAPOL1.31cm,IQR 1.10–1.57cm.Measurementtimewasevaluatedforboth A4CviewmeasurementsandPSLAviewmeasurements.The A4Cviewmeasurementsmeanwas70.3 ± 5.4seconds(sec) tocomplete,whilethePSLAviewmeasurementsmeanwas 44.1 ± 3.8sectocomplete.Thepatients’ demographicdata, initialvital findings,allmeasurementdata,andmeasurement timeareshownin Table1
ThecorrelationbetweentheE/AratioinPWDoppler measurementsandtheEPSS/APSSratioinM-modewas strong(correlationcoefficient0.677, P = 0.001).Similarly, thecorrelationbetweenEinPWDopplermeasurementsand theEPSS/APSSratioinM-modemeasurementswasalso moderatelystrong(correlationcoefficient0.557, P = 0.001). Nootherstatisticallysignificantcorrelationswereobserved betweenPWandM-modemeasurements.Correlation analysisandgraphicsbetweenmeasurementsinthePSLA andA4Cviewsissummarizedin Table2 and Figure4.
Echocardiographyplaysanimportantroleinthe evaluationofthesystolicanddiastolicfunctionsoftheleft ventricle.Itis,therefore,employedintheEDforevaluating boththesystolicanddiastolicfunctionsoftheheart.12,13 It representsarapid,repeatable,andnon-invasivediagnostic toolforemergencyphysicians.
Diastolicdysfunctioncanbeseeninconditionssuchas HT,CAD,anddiabetesandcanrepresentadeterminantof morbidityandmortalityinsuchdiseases.16–18 TheASEand EACIpublishedupdatedguidelinestotheevaluationof diastolicdysfunctionin2016.10 Theguidelinesrecommended theevaluationoffourparametersforthediagnosisof
diastolicdysfunction:theE/E 0 ratio;septale 0 orlaterale 0 velocity;tricuspidregurgitationvelocity;andtheleftatrial volumeindex.Itsuggestedthatabnormalityshouldbe presentinthreeorfouroftheseparametersforadiagnosisof diastolicdysfunction.Theserecommendationsentail difficultiesfortheevaluationofpatientsintheEDsetting, oneofthesebeingthatemergencyphysiciansshouldbe trainedintheuseofPOCUS.Themeasurements recommendedintheguidelinesinvolvecomplexparameters andmeasurementsforPOCUSunderEDconditions.More practicaldiastolicdysfunctionevaluationwithE,A,and EDTmeasurementusingthePWDopplermethodis, therefore,employedintheED.11,19,20 However,itisalso difficulttoperformthesefocusedDopplermeasurements underEDconditions.
Inlightofthesedifficulties,weundertookthisstudyto investigatealternativemeasurementmethods.Adifferent measurementmethodforevaluatinggrade1diastolic dysfunctionwastriedbyapplyingM-modeevaluationof MVanteriormovementinPSLAview.Astatisticallystrong correlationwasthusobservedbetweengrade1diastolic dysfunctionpatients’ EPSS/APSSratiosfromM-mode measurementsinthePSLAviewandE/AratiosfromPW DopplermeasurementsintheA4Cview(correlation coefficient0.677, P = 0.001).These findingssuggestthat EPSSandAPSSvaluesmeasuredintheEDviaM-mode evaluationofMVanteriorleafletmovementinthePSLA viewmayrepresentapracticalapproachfordiastolic functionestimation,similarlytotheEPSSmethodusedfor systolicfunctionestimation.
ParketalevaluatedtherelationshipbetweenMVanterior leafletmotioninthePSLAviewwithM-modemeasurements andPWDopplermeasurementsintheA4Cviewinhealthy humans.Thoseauthorsdeterminedasignificantcorrelation betweentheAPSS/EPSSratioandEvalues(correlation coefficient = 0.4).Theyconcludedthatvisualevaluationof theM-modepatternontheMVanteriorleafletinthePSLA viewmightrepresentapracticalapproachtowardestimating diastolicfunctionintheED.15 Inthepresentstudywe evaluatedtherelationshipbetweenM-modemeasurements ofMVanteriorleafletmotioninthePSLAviewandPW DopplermeasurementsintheA4Cviewinpatientswith grade1diastolicdysfunction.Incontrasttothecorrelation reportedbyParketal,weobservedpositivecorrelations betweentheE/AratioandEPSS/APSSratioandbetweenE andtheEPSS/APSSratio.
Weattributethisdiscrepancytothepresenceofan oppositerelationshipintheE/Aratiobetweennormal healthyindividualsandpatientswithgrade1diastolic dysfunction.ThiscontrastmaybeduetotheE/Aratio typicallybeing >1inhealthyindividuals,whileitfallsto <1 withthedevelopmentofdiastolicdysfunction(grade1).We alsothinkthatthepositivecorrelationbetweentheE/Aratio andtheEPSS/APSSratioisassociatedwithphysiological
Table1. Thepatients’ demographicdataandbaselinecharacteristics.
Characteristics,N =
Gender
Comorbidities
Hypertension,n(%)
Dementia,n(%)
Vitalsigns
Systolicbloodpressure(mmHg),median(IQR)133(IQR130–140)
Diastolicbloodpressure(mmHg),median(IQR)80(IQR70–90)
Measurements
Measurementtimes
A,latediastolevelocityofthemitralinflow; A4C,apical4-chamber; APOL,A-pointopeninglength;APSS,A-pointseptalseparation; IQR, interquartilerange(25p,75p); CAD,coronaryarterydisease; CHF,congestiveheartfailure; E,earlydiastolevelocityofthemitralin flow; EDT, E-pointdecelerationtime; EF,ejectionfraction; EPSS,E-pointseptalseparation; EPOL,E-pointopeninglength; PSLA,parasternallongaxis.
compensationdevelopingingrade1diastolicdysfunction. Thisisbecauseingrade1diastolicdysfunction,theleft ventricular(LV)inflowvelocity(E)decreases(passive filling) inearlydiastoleduetoimpairedLVrelaxation,whichcan leadtoanincreaseinEPSSandadecreaseinEPOL.
Subsequently,duringlatediastole,theLV fillingrate(A) increases(fillingwithactivepropulsion),thuscausingan increaseintheEPSS/APSSratiobyproducingadecreasein APSS.TheEPSS/APSSratiomayhaveexhibiteda positivecorrelationwiththeE/Aratioasaresultofthis physiologicalcompensation.
Heartfailureremainsamajorcauseofmorbidityand mortality.Symptomaticheartfailureisduetosystolic dysfunctionbutisalsocommonlyduetodiastolic dysfunction.21,22 Theassessmentofdiastolicdysfunctionisof greatimportanceasitisacommoncauseofsymptomatic heartfailure.Manyemergencyphysiciansdonot findthe detailedmeasurementsincludedintheASEguidelines applicabletoPOCUSintheEDsetting.Thisisdueto multiplefactors.Forexample,ifthepatienthasdyspneaor hypoxemia,theymaynotbeabletolie flatorbeproperly positionedforthesonographertoobtainanadequatefour-
Table2. Correlationbetweenmeasurementsintheparasternallongaxisviewandmeasurementsintheapicalfour-chamberview. Correlationcoefficient(P-value)
APOL* 0.086(0.596)
0.212(0.189)0.021(0.898)0.074(0.650)
EPSS/APSS*0.557(0.001)0.090(0.581)
*Spearman’scorrelationanalysis.
0.003(0.986)0.677(0.001)
APOL,A-pointopeninglength; APSS,A-pointseptalseparation; E,earlydiastolevelocityofthemitralin flow; EDT,earlydecelerationtime; EF,ejectionfraction; EPSS, E-pointseptalseparation; EPOL, E-pointopeninglength;diastolevelocityofthemitralinflow.
chamberview.Inaddition,manyemergencyphysiciansmay nothaveadvancedechocardiographictrainingtoperform thesemeasurements.Consideringtheselimitationswe thoughtthatasimplemethodtoassessdiastolicdysfunction isimportantfortheED.
Weperformedthispilotstudytodemonstratethatarapid andpracticalmethodcanbeappliedintheED.Ourstudy includedonlypatientswithgrade1diastolicdysfunction, whichmadeitdifficulttogeneralizeourstudy.Considering thatgrade1diastolicdysfunctioncanbeeasilyaffectedby thecurrentclinicalconceptionandtreatment,amongother factors,itsuggeststhatourstudyshouldbeconductedto includeallsubgroupsofdiastolicdysfunction.Inaddition, becauseourstudyincludedonlygrade1diastolic dysfunction,itincludedasingle-groupevaluation.This makesitimpossibletocalculatethesensitivityorspecificity oftheM-modeEPSS/APSSratiomeasurement. Accordingly,moreevidenceisneededforthegeneraluseof
theM-modeEPSS/APSSratiomeasurementsforgrade1 diastolicdysfunction.
ThisstudyalsoevaluatedthetimetakenforM-mode measurementsoftheMVanteriorleafletinthePSLAview andPWDopplermeasurementsintheA4Cview.Themean timetakenformeasurementsinthePSLAviewwasshorter thanthemeantimetakenformeasurementsintheA4Cview. Adoptingthetimemeasuredaftertheimagewindowwas providedasthestartingpointeliminatedthetimedifference in findingtheappropriatewindow.TheshorterPSLA measurementtimesuggeststhatthismaybeadvantageous fordiastolicassessment.
Thereareanumberoflimitationstothisstudy.The firstis thesmallstudypopulationandthesingle-centernatureofthe research.ThesecondisthatsincetherelationshipbetweenMmodemeasurementsoftheMVanteriorleafletinthePSLA
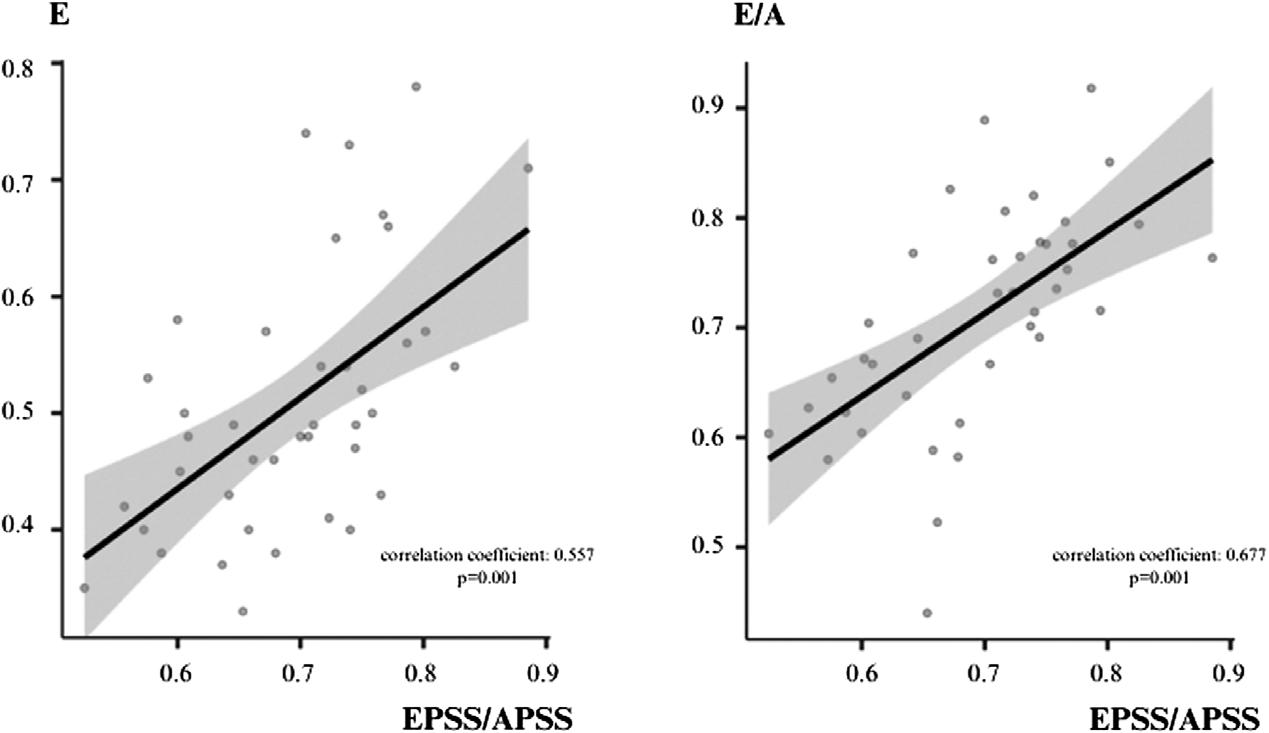
Figure4. CorrelationgraphicsbetweenmeasurementsinparasternallongaxisPSLAviewandmeasurementsinapicalfour-chamberview. APSS,A-pointseptalseparation; E,earlydiastolevelocityofthemitralinflow; E/A,earlydiastolicvelocityofthemitralinflowtothelate diastolicvelocityratio; EPSS,E-pointseptalseparation.
viewandDopplermeasurementsoftheMVinflowvelocityin theA4Cviewisstillunclear,samplesizecalculationcouldnot beperformed.Itis,therefore,difficulttogeneralizeourresults tothewiderpopulation.However,wefocusedonM-mode measurementsinthePSLAviewandE,A,andEDT measurementsintheA4Cview,whichalsopermitteda simplifiedevaluation.Despitetheadvantagesofthisapproach, itrepresentsanotherlimitationofthisstudyasitdoesnotcover theentirespectrumofdiastolicfunctionevaluation.Carewas takentoensurethattherewasnotimebetweentheUS evaluationperformedbytheemergencyphysiciansandthe echocardiographyevaluationperformedbythecardiologists forpatientselection,whichcouldhaveaffectedtheclinical parameters(eg,vitalsigns)forworsening/improvement. However,thefactthatthiswasnotevaluatedintermsoftimeis anotherlimitationofourstudy.Finally,POCUSwasapplied bytwoemergencyphysicianswithexperienceinultrasound, andinter-observeragreementwasnotevaluated.Thesefactors mayhaveaffectedourresults.Furtherstudieswithalarger population,includingtheevaluationofinterobserver agreement,areneededtoincreasethereproducibilityand reliabilityofthediastolicfunctionevaluationmethod.
Whenevaluatinggrade1diastolicdysfunction,wefounda significantcorrelationbetweentheM-modeE-pointseptal separation/A-pointseptalseparationratiomeasurementin theparasternallong-axisviewandthePWDopplerratioof theearlydiastolicvelocityofthemitralinflowtothelate diastolicvelocitymeasurementintheapicalfour-chamber window.ThisassociationsuggeststhatM-mode measurementsinthePSLAmaybeusedin diastolicdysfunction.
AddressforCorrespondence:MüminMuratYazici,MD,Recep TayyipErdoganUniversityTrainingandResearchHospital,No:74, postalcode:53020,Centre,Rize,Türkiye.Email: mmuratyazici53@ gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Yazicietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ChenLandMalekT.Point-of-careultrasonographyinemergencyand criticalcaremedicine. CritCareNursQ. 2018;41(2):94–101.
2.WhitsonMRandMayoPH.Ultrasonographyintheemergency department. CritCare. 2016;20(1):227.
3.GaberHR,MahmoudMI,CarnellJ,etal.Diagnosticaccuracy andtemporalimpactofultrasoundinpatientswithdyspnea admittedtotheemergencydepartment. ClinExEmergMed. 2019;6(3):226–34.
4.WrightJ,JarmanR,ConnollyJ,etal.Echocardiographyinthe emergencydepartment. EmergMedJ. 2009;26(2):82–6.
5.KuoDCandPeacockWF.Diagnosingandmanagingacuteheart failureintheemergencydepartment. ClinExpEmergMed. 2015;2(3):141–9.
6.MassieBM,SchillerNB,RatshinRA,etal.Mitral-septalseparation:new echocardiographicindexofleftventricularfunction. AmJCardiol. 1977;39(7):1008–16.
7.SilversteinJR,LaffelyNH,RifkinRD.Quantitativeestimationofleft ventricularejectionfractionfrommitralvalveE-pointtoseptalseparation andcomparisontomagneticresonanceimaging. AmJCardiol. 2006;97(1):137–40.
8.SeckoMA,LazarJM,SalciccioliLA,etal.Canjunioremergency physiciansuseE-pointseptalseparationtoaccuratelyestimateleft ventricularfunctioninacutelydyspneicpatients? AcadEmergMed. 2011;18(11):1223–6.
9.GreensteinYYandMayoPH.Evaluationofleftventriculardiastolic functionbytheintensivist. Chest. 2018;153(3):723–32.
10.NaguehSF,SmisethOA,AppletonCP,etal.Recommendationsforthe evaluationofleftventriculardiastolicfunctionbyechocardiography:an updatefromtheAmericanSocietyofEchocardiographyandthe EuropeanAssociationofCardiovascularImaging. JAmSoc Echocardiogr. 2016;29(4):277–314.
11.OhJK,ParkSJ,NaguehSF.Establishedandnovelclinicalapplications ofdiastolicfunctionassessmentbyechocardiography. CircCardiovasc Imaging. 2011;4(4):444–55.
12.UnluerEE,BayataS,PostaciN,etal.Limitedbedside echocardiographybyemergencyphysiciansfordiagnosisofdiastolic heartfailure. EmergMedJ. 2012;29(4):280–3.
13.EhrmanRR,RussellFM,AnsariAH,etal.Canemergency physiciansdiagnoseandcorrectlyclassifydiastolicdysfunction usingbedsideechocardiography? AmJEmergMed. 2015;33(9):1178–83.
14.KoneckeLL,FeigenbaumH,ChangS,etal.Abnormalmitralvalve motioninpatientswithelevatedleftventriculardiastolicpressures. Circulation. 1973;47(5):989–96.
15.ParkCH,YoonH,JoIJ,etal.ApilotstudyevaluatingLVdiastolic functionwithM-modemeasurementofmitralvalvemovement intheparasternallongaxisview. Diagnostics(Basel). 2023;13(14):2412.
16.VasanRS,BenjaminEJ,LevyD.Prevalence,clinicalfeaturesand prognosisofdiastolicheartfailure:anepidemiologicperspective. JAm CollCardiol. 1995;26(7):1565–74.
17.FiackCAandFarberHW.Heartfailurewithpreservedejectionfraction. NEnglJMed. 2006;355(17):1828–31.
18.OwanTE,HodgeDO,HergesRM,etal.Trendsinprevalenceand outcomeofheartfailurewithpreservedejectionfraction. NEnglJMed. 2006;355(3):251–9.
19.KingSA,SalernoA,DowningJV,etal.POCUSfordiastolicdysfunction: areviewoftheliterature. POCUSJ. 2023;8(1):88–92.
20.LiY,YinW,QinY,etal.Preliminaryexplorationofepidemiologicand hemodynamiccharacteristicsofrestrictive fillingdiastolicdysfunction basedonechocardiographyincriticallyillpatients:aretrospectivestudy. BiomedResInt. 2018;2018:5429868.
21.AbbateA,ArenaR,AbouzakiN,etal.Heartfailurewith preservedejectionfraction:refocusingondiastole. IntJCardiol. 2015;179:430–40.
22.YancyCW,LopatinM,StevensonLW,etal.Clinicalpresentation, management,andin-hospitaloutcomesofpatientsadmitted withacutedecompensatedheartfailurewithpreservedsystolic function:areportfromtheAcuteDecompensatedHeartFailure NationalRegistry(ADHERE)database. JAmCollCardiol. 2006;47(1):76–84.
AbdullahBakhsh,MBBS* AhmadBakhribah,MBBS* RaghadAlshehri,MBBS† NadaAlghazzawi,MBBS† JehanAlsubhi,MBBS† EbtesamRedwan,MBBS† YasminNour,MBBS† AhmedNashar,MBBS* ElmoizBabekir,MBBS‡ MohamedAzzam,MD,FRCP,FCCM§
SectionEditor:QuincyK.Tran,MD,PhD
*DepartmentofEmergencyMedicine,FacultyofMedicine,KingAbdulaziz University,Jeddah,SaudiArabia
† FacultyofMedicine,KingAbdulazizUniversity,Jeddah,SaudiArabia ‡ DepartmentofEmergencyMedicineandAnesthesiaCriticalCare,College ofMedicalSciences,IbnSinaNationalCollege,Jeddah,SaudiArabia
§ DepartmentofEmergencyMedicineandCriticalCare,AlHabibMedical Group,Jeddah,SaudiArabia
Submissionhistory:SubmittedAugust18,2023;RevisionreceivedJuly24,2024;AcceptedJuly31,2024
ElectronicallypublishedNovember7,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18435
Introduction: Thechoiceofmedicationsusedinrapidsequenceintubation(RSI)canresultinthe differencebetweenanacceptableoutcomeandalethalone.Whenexecutedproperly,RSIisalifesaving intervention.Nonetheless,RSImayresultinfatalcomplicationssuchasperi-intubationcardiacarrest. Theriskofperi-intubationcardiacarrestreportedlyincreasesinpatientswhoareprofoundlyhypoxicor hypotensivepriortoendotrachealintubation.MedicationchoiceforRSImayeitheroptimizeor deoptimizehemodynamicparameters,therebyimpactingpatientoutcomes.Therefore,ourstudyaimed toexaminetheassociationofchangeinmeanarterialpressure(MAP)withandwithouttheuseofa predetermineddoseof50micrograms(μg)intravenousfentanylasapretreatmentagentduringRSI.
Methods: ThisprospectiveobservationalstudyincludedpatientsundergoingRSIatanacademic emergencydepartment(ED)overathree-yearperiodbetweenJanuary1,2018–January1,2021. Averagehemodynamicparametersweremeasuredatthetimeofinduction(priortomedication administration)and10minutesafterinduction.Wecategorizedpatientsintofentanylandnon-fentanyl groupsforanalysis,andwecompareddatausingchi-squareand t-testasappropriate.Logistic regressionanalysiswasconductedtoaccountforpotentialconfoundingfactors.
Results: Atotalof278patientswereincludedintheanalysis,ofwhom160receivedfentanyland118did not.ThemajorityofthepatientsunderwentRSIbytrainees95.0%ofthetime.The first-passsuccessrate was77.7%inoursampleanddidnotdiffersignificantlybetweenthetwogroups(P = 0.84).Unadjusted analysisshowedalargerdecreaseinhemodynamicparametersinthefentanylgroupcomparedtothe non-fentanylgroup;systolicbloodpressuredecreasedby11.2%vs1.6%,diastolicbloodpressure decreasedby13.7%vs3.8%,andMAPdecreasedby12.7%vs3.2%.Afteradjustingforpotential confounders,fentanylwas2.14timesmorelikelytolowerMAPby10%.
Conclusion: Theuseof50 μgfentanylforrapidsequenceintubationinanEDisassociatedwithhigher oddsofdecreasingmeanarterialpressurebyatleast10%at10minutesfromthetimeofinduction. Therefore,itshouldbecarefullydosed,anditsuseinclinicalpracticeshouldbejustifiedtoavoid unnecessarycomplications.[WestJEmergMed.2025;26(1)10–19.]
Rapidsequenceintubation(RSI)isthecornerstoneof airwaymanagementintheemergencydepartment(ED).1 Theprocessinvolvestheadministrationofaninduction agentandaneuromuscularblockingagenttofacilitate endotrachealintubation.TheprimaryaimofRSIisto provideoptimaltrachealintubationconditionsandreduce gastricregurgitation.2 Criticallyillpatientspresentingtoan EDgenerallyhaveprofoundphysiologicalderangements, whichareoftenpairedwitharapiddecline.Thechoiceof pharmacologicalagentsmayoptimizeorexacerbatethe underlyingphysiology.Therefore,theidealtechniqueshould providerapidoptimalintubationconditions,allowingahigh rateof first-passintubationsuccesswhilereliablyattenuating excessivehemodynamicchanges.3
Whenexecutedproperly,RSIisalifesavingintervention. However,ithasbeenassociatedwithaperi-intubation cardiacarrestrateof0.9–2.7%.4,5 Inparticular,patientswith pre-intubationoxygensaturation <90%orpre-intubation systolicbloodpressure(SBP) <100millimetersofmercury (mmHg)havebeenreportedtohaveahigherlikelihoodof peri-intubationcardiacarrest.5 Factorsrelatedtopatient characteristicsandproceduretechniquehavearemarkable impactontherateofoccurrenceofadverseevents.Astute cliniciansoptimizepatientphysiologybeforeundertaking RSItolimitcomplications.
MedicationsusedforRSIhaveasignificantimpacton patientoutcomes.Fentanyl,anultra-short-acting pretreatmentagent,isusedtobluntthecatecholaminesurge dueto α-receptorstimulationfromendotrachealintubation. Thetypicaldoseis3–5microgramsperkilogram(μg/kg) administeredintravenously(IV)threeminutespriorto intubation.6 Itistraditionallyadvocatedforpatientsin whomhypertensioncanbedangerous,suchasthosewith intracranialhemorrhage,elevatedintracranialpressure, ischemicheartdisease,andaorticaneurysm/dissection.6 We couldnot findstudiesreportingtheuseoffentanylas pretreatmentduringRSIbyemergencyphysiciansfornontraumavictims.Theuseoffentanyl,however,isreportedin theanesthesiologyliteratureandlimitedtotrauma victims.7,8 Nonetheless,previousstudieshavereported thattheuseoffentanylasapretreatmentagentisassociated withanincreasedriskofadverseevents,suchaspostintubationhypotension.9,10 Infact,post-intubation hypotensionisaknownriskfactorforhigherin-hospital mortalityratesandprolongeddurationofintensivecare unitstays.11,12,13
Amulticenter,randomizedcontrolledtrialcomparedthe useoffentanylvsplacebowithketamineandrocuroniumin patientsundergoingRSIinanED.14 Thetrial’ssecondary outcomerevealedthat29%ofpatientsinthefentanylgroup hadatleastoneSBPmeasurement <100mmHgcomparedto 16%intheplacebogroup.14 Inanotherstudyresearchers
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Peri-intubationhypotensionwiththeuseof fentanylhaspreviouslybeenseenintrauma patientsandintheanesthesiologyliterature.
Whatwastheresearchquestion?
Wastheuseoffentanylasapretreatment agentduringrapidsequenceintubationinthe EDassociatedwithachangeinmeanarterial pressure(MAP)?
Whatwasthemajor findingofthestudy?
FentanylwasassociatedwithreducedMAP ( 12.7%vs 3.2%;P < 0.01),comparedto thosewithoutfentanyl.
Howdoesthisimprovepopulationhealth?
Emergencyphysiciansshouldbeawareofthe complicationsassociatedwithfentanylusein theED.Carefuldosingandclinical justi fi cationisadvised.
conductedasecondaryanalysisofdatafromamulticenter, prospectivestudyof14JapaneseEDs.Theyfoundthat patientswhoreceivedfentanylhadahigherriskofpostintubationhypotensionincomparisontothosewhodidnot receivethedrug.15 Previousstudiesinvestigatedtheuseof fentanylwithadefinedcutoffSBPvalue.Inthepresentstudy, wesoughttoexaminetheuseof50 μgofIVfentanylasa pretreatmentagentbeforeRSIanditsassociationwith percentchangeinpost-intubationmeanarterial pressure(MAP).
Thissingle-center,prospectiveobservationalstudy includedpatientsundergoingRSIatanacademicEDduring athree-yearperiodbetweenJanuary1,2018–January1, 2021.ThestudyprotocolwasapprovedbytheUnitof BiomedicalEthicsattheinstitution(reg.no.:HA-02-J-008) andwasconductedinaccordancewiththetenetsofthe DeclarationofHelsinki.Theneedforinformedconsentwas waivedduetotheobservationalnatureofthestudy.
WeconductedthestudyatanacademicEDwithan annualcensusofapproximately60,000includingadult,
pediatric,andpregnantpatients.TheEDhasanaccredited four-yearemergencymedicineresidencytrainingprogram withatotalcapacityof32residents.Uponacceptanceinto theprogram,allresidentsarerequiredtoparticipateinan airwaymanagementworkshop.Moreover,residentsrotate throughtheanesthesiadepartmentwithafocusonelective airwaymanagement.Themajorityofintubationswere performedbyEDresidentsunderthesupervisionofboardcertifiedemergencyphysicianswithexpertiseinRSI.All patientsrequiringRSIwerescreenedforeligibility.The inclusioncriteriawereasfollows:patientsaged ≥18years; thosewhowereadministeredbothinductionand neuromuscularblockades;andthosewhorequiredemergent trachealintubationatthediscretionoftheemergency physician.Patientswhodidnotreceiveneuromuscular blockades,were <18years,hadreceivedvasopressorsfor hypotensionpriortointubation,andthoseinwhom intubationwasperformedinsettingsotherthantheEDwere excludedfromthestudy.
Alltreatmentdecisionsweremadeatthediscretion ofthetreatingphysicianandwerenotinfluencedbythe study.OncethedecisiontoperformRSIwasmade, patientswerepreparedinaccordancewiththefollowing departmentalprotocol:
1.Non-invasivemonitoringofheartrate,systolic, diastolic,meanarterialbloodpressure,respiratoryrate, 3-leadelectrocardiogram,andoxygensaturationusing CARESCAPEB650(GEHealthcare,Chicago,IL) monitors.
2.Placementoftwolarge-boreIVcathetersatthelevel oftheantecubitalfossaorabove.
3.SelectionofIVfentanyl(fixeddoseof50 μg)asa pretreatmentagentwasoptionalatthediscretionof thephysician.
4.SelectionofanIVinductionagent(etomidate0.3 milligramsperkilogram(mg/kg),ketamine1mg/kg, propofol1mg/kg,ormidazolam0.3mg/kg)andan IVneuromuscularblockingagent(succinylcholine 1.5mg/kgorrocuronium1.2mg/kg)basedonthe physician’spreference.(Dosingmaybereducedin hypotensionbasedonphysiciandiscretion.)
- Allmedicationswereadministeredatthesametime usingthefollowingsequence:pretreatment – induction –neuromuscularblockade,whenpretreatmentwasgiven; andinduction – neuromuscularblockade,when pretreatmentwasnotgiven
5.Optimizationofthehemodynamicstatustoachievea SBPofatleast100mmHg.
6.Optimizationofpre-inductionoxygensaturationto atleast98%(eithervianon-rebreathermaskat15 litersperminuteorpositivepressureventilation usingbagvalvemask(BVM)whenoxygen saturationdroppedbelow90%).
7.Placementofthepatientina20–30 ° uprightposition duringpreoxygenation.
8.Preparationofasuctioncanisterwitha Yankauercatheter.
9.Preparationofanintubatingdevicebasedonthe physician’spreference(eitherdirectlaryngoscopy usingasize3or4Macintoshbladeorvideo laryngoscopyusingahyperangulatedlaryngoscope). Allendotrachealtubeswereloadedwithastylet appropriateforthedeviceused.Adjunctsand backupdeviceswerealsoprepared,including nasopharyngealairways,oropharyngealairways, laryngealmaskairways,andgum-elasticbougies.
10.Confirmationofthepositionoftheendotrachealtube usingcapnometryorcontinuouscapnography.
Uponcompletionofasuccessfulendotrachealintubation, thetreatingphysicianwasrequiredtocompleteanairway procedurenote.Atleasttworegisterednursesweretobe presentduringtheprocedure;oneperformeddocumentation, whiletheotherpreparedmedications.Ultimately,thetreating physicianwasrequiredtoenteralltheproceduredetailsinthe patient’selectronichealthrecord.Whenenteringanelectronic procedurenote,itwasmandatorythatthephysicianinclude allthedetailsoritmighthaveresultedintheinabilityto continuepatientcareviaelectronicmedicalrecordssystem. Thisledtoadatacapturerateof100%.
Anattemptwasdefinedasalaryngoscopebladeplaced intotheoropharynxregardlessofwhetheranendotracheal tubewaspassed.Whenoxygensaturationmeasurements droppedbelow90%,theoperatorremovedthelaryngoscope bladeandprovidedpositivepressureventilationviaaBVM untiloxygensaturationreachedatleast98%.Modifications insubsequentattemptsweremadeatthediscretionofthe treatingclinician.
Previousstudieshavedefinedhypotensionasanabsolute SBP <90mmHgorMAP <65mmHg.16 Itis,however, crucialtonotethatbinarydefinitionsarenotalways applicableinclinicalpractice.17 Classicalanesthesiapractice suggestsmaintainingbloodpressurewithinarelative20%of thepreoperativevalues.17 Thisisbasedonthetheorythat patientswithhypertensionrequirehigherthannormal pressuretoadequatelyperfuseorgansthatarehabituatedto highpressure.17 Infact,asystematicreview18 examinedthe definitionsofintraoperativehypotensionandfoundthatit couldbeeitherbasedonabsolutevalues(ie,MAP <50mm Hg, <55mmHg, <60mmHg, <65mmHg, <70mmHg, <75mmHg)orthresholdsrelativetobaselinepreoperative values(ie,decreaseinMAPby >10%frombaseline,decrease inMAPby >15%frombaseline,decreaseinMAPby >20% frombaseline,decreaseinMAPby >25%frombaseline, decreaseinMAP >30%frombaseline).Basedonthe
aforementioned findings,wedefinedpost-intubation hypotensionasadecreaseinMAPby >10%within10 minutesofinduction.18
OncethetreatingphysiciandecidedtoproceedwithRSI, allpatientsunderwentcontinuousmonitoringofvitalsigns (heartrate,bloodpressure,oxygensaturation,respiratory rate)vianon-invasivemeasures.Bloodpressurewas measuredusingacuffplacedaroundtheupperarmand cycledeverytwominutes.Anaverageofthreevitalsign readingswasobtainedatthetimeofinduction(immediately priortotheadministrationofpretreatmentorinduction)asa pre-inductionvalue,and10minutesaftertheadministration ofthe firstmedicationinthesequenceasapost-intubation value.Adverseeventsweredocumentediftheyoccurred within60minutesafterinduction.Anindividualwas assignedtomeasurethehemodynamicparametersandthe timeusingastopwatch.Pulmonaryaspirationwas documentedbasedonchestradiographevidenceof aspirationwithin14daysofinduction.
Wepresentcategoricalvariablesasfrequenciesand percentages,whilecontinuousvariablesarepresentedas medianandinterquartileranges.Patientswerecategorized intotwogroups:fentanylandnon-fentanyl.Weperformed comparisonsusingchi-squareforcategoricaldataand t -test forcontinuousdata.Wemeasuredpercentchangein hemodynamicparameters(atinductionand10minutesafter induction)usingthefollowingformula:[(post-intubation value pre-inductionvalue)/pre-inductionvalue] × 100.
Wecomparedpercentchangeinhemodynamic parametersbetweenthetwocategoriesusingthe t -test. Binarylogisticregressionanalysiswasperformedtoadjust forpotentialconfoundingfactors.Thedependentvariable wasatleasta10%reductioninMAP(yes/no),while independentvariablesincludedage(inyears);weight(inkg); indicationforintubation(airwayprotection[yes/no]); respiratoryfailure[yes/no]);anticipateddeterioration[yes/ no]);clinicaldiagnosis(pulmonarydiseases[yes/no]; cardiovasculardiseases[yes/no];hepaticdiseases[yes/no]; renaldiseases[yes/no];neurologicaldiseases[yes/no]; endocrinedisorders[yes/no];infectiousdiseases[yes/no]; toxicity[yes/no]);andchoiceofmedication(fentanyl[yes/ no];etomidate[yes/no];ketamine[yes/no];propofol[yes/no]; succinylcholine[yes/no];rocuronium[yes/no]).Independent variableswereselectedaprioritoavoidoverfittingthemodel.
Wecategorizedpresentingconditionsintothefollowing: pulmonarydiseases(includingacuterespiratorydistress syndrome,pulmonaryedema,pulmonaryembolism,acute asthmaexacerbation,chronicobstructivepulmonarydisease exacerbation,pneumothorax,pleuraleffusion,interstitial lungdisease,andhemoptysis);cardiovasculardiseases
(includingacutecoronarysyndrome,aorticsyndromes, dysrhythmias,andcirculatoryshockduetoanycause); hepaticdiseases(includingacuteandchronicliverfailureand hematemesisduetoliverfailure);renaldiseases(including end-stagerenaldiseaserequiringdialysisandobstructive uropathy);neurologicaldiseases(includingstatus epilepticus,hepaticencephalopathy,uremic encephalopathy,hypertensiveencephalopathy,acute ischemicstroke,intracranialhemorrhage,neuromuscular weakness,andalteredmentalstatusduetoanycause); endocrinedisorders(includingdiabeticketoacidosis, decompensatedhypothyroidism,thyroidstorm,andadrenal insufficiency);infectiousdiseases(includingmeningitis, encephalitis,cerebralabscess,pyelonephritis,pneumonia, spontaneousbacterialperitonitis,andsepsisfromanycause); andtoxicity(includingopioidtoxicity,benzodiazepine toxicity,cocainetoxicity,andalcoholintoxication).
Theprimaryendpointwasatleasta10%changeinMAP measured10minutesfromthetimeofinduction.Levelof significancewassetat P < 0.05.
Duringthethree-yearstudyperiod,wecollecteddatafrom 361intubationencounters.Ofthese,only278patientsmet ourinclusioncriteria(Figure1).Atotalof160patients receivedfentanylaspretreatment,whereas118didnot receivefentanylaspretreatmentforRSI.Baseline
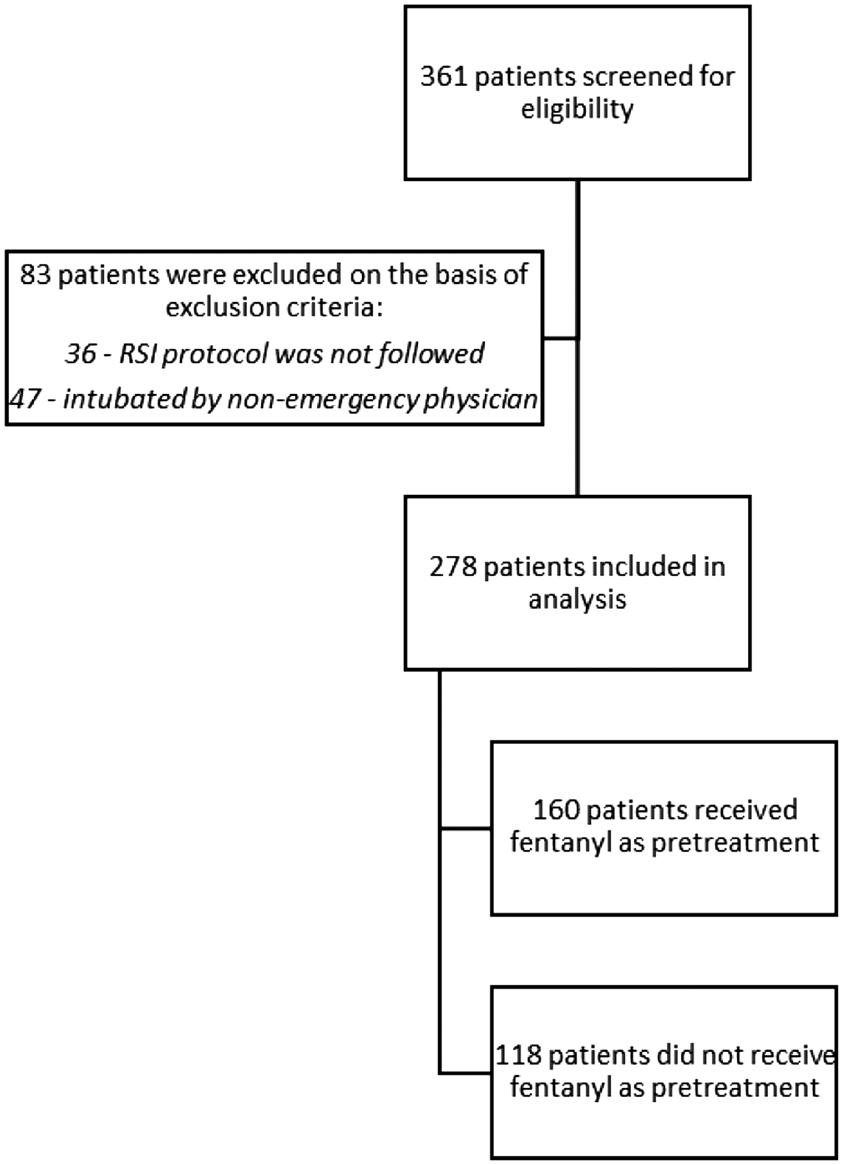
Figure1. Flowdiagramforstudyparticipants. RSI,rapidsequenceintubation.
Table1. Characteristicsofpatientsundergoingrapidsequenceintubationstrati fiedbyuseoffentanyl.
–96)82(62–92)89(77
Inductionagent
Etomidate263(94.6%)149(93.1%)114(96.6%)0.20
Ketamine14(5.0%)11(6.9%)3(2.5%)0.10
Propofol2(0.7%)1(0.6%)1(0.8%)0.82
Paralyticagent
Succinylcholine252(90.6%)142(88.8%)110(93.2%)0.20
Rocuronium26(9.4%)18(11.3%)8(6.8%)0.20
Cormack-Lehanegrade
Good235(84.5%)137(85.6%)98(83.1%)0.55
Poor43(15.5%)23(14.4%)20(16.9%)
Firstpasssuccess216(77.7%)125(78.1%)91(77.1%)0.84 (Continued onnextpage)
RSI, rapidsequenceintubation; IQR,interquartilerange; SBP,systolicbloodpressure; DBP,diastolicbloodpressure; MAP,meanarterial pressure; HR,heartrate; RR,respiratoryrate; SpO2,oxygensaturation; GCS,GlasgowComaScale.
characteristicsoftheparticipants(includingage,weight, gender,presentingcondition,pre-inductionvitalsigns, inductionagents,Cormack-Lehanegrade, first-passsuccess rates,deviceused,andpost-inductionadverseevents)were mostlysimilarbetweenthetwogroups(Table1).However, operatorsandpost-intubationhemodynamicparameters weresignificantlydifferentbetweenthetwogroups.Atotal of264(95.0%)patientsunderwentintubationbytrainees. Post-inductionmedianSBP(110mmHg[88–128]vs119mm Hg[106–129]; P = 0.01),diastolicbloodpressure(DBP) (69mmHg[49–75]vs75mmHg[60–87]); P =< 0.01),and MAP(82mmHg[62–95]vs89mmHg[77–100]); P < 0.01) weresignificantlylowerinthefentanylgroupthaninthenonfentanylgroup(Table1 and Figure2).
Uponexaminingpercentchangeinhemodynamic parametersbetweenthetwogroups(Table2),wefound significantlylargerdifferencesinthefentanylgroupinSBP ( 11.2vs 1.6%; P < 0.01),DBP( 13.7vs +3.8%; P < 0.01), MAP( 12.7%vs 3.2%; P < 0.01),andheartrate(12.2%vs +3.7%; P < 0.01).[Table2]
Weperformedlogisticregressionanalysis(Table3)to ascertaintheassociationofconfoundingfactorsonthe likelihoodthatstudyparticipantswouldsustainatleasta 10%reductioninMAP.Themodelexplained77.1% (NagelkerkeR2)ofthevarianceinpost-induction
hypotensionandcorrectlyclassified88.1%ofthecases.Our modelshowedthattheuseoffentanylwas2.14times(95% confidenceinterval[CI]1.34–4.11)morelikelytobe associatedwithatleast10%reductioninMAPpostintubation.Theremainingpredictorsdidnotrevealany association.Basedonourposthocpoweranalysis,the samplesizehad86.9%(α = 0.05) powertodetectachangein MAPofatleast10%.
Inthissingle-centerEDstudy,wefoundthatadecreasein MAPbyatleast10%wasassociatedwiththeuseof50 μgof fentanylasapretreatmentagentinRSI.Thisreductionwas alsoseeninSBPandDBP.ThereductioninMAPwas observedevenafteradjustingforpotentialconfounding factors.Inductionagentshavebeenpreviouslyreportedtobe associatedwithperi-intubationhypotension.18,19 Etomidate isleastlikelytobeassociatedwiththisoutcome.19,20,21 Fentanylisanoptionalpretreatmentagent;althoughstudies onitsusearescant,itisanavailableoptionasapretreatment agentforRSIinsomepartsoftheworldandincertain conditionssuchastrauma.8 Studiesexaminingthe associationbetweenfentanyluseandperi-intubation hypotensionarelimited.14,15 Whiletheaforementioned studiesdefinedhypotensionbasedonacutoffSBPvalue,in Table1. Continued.
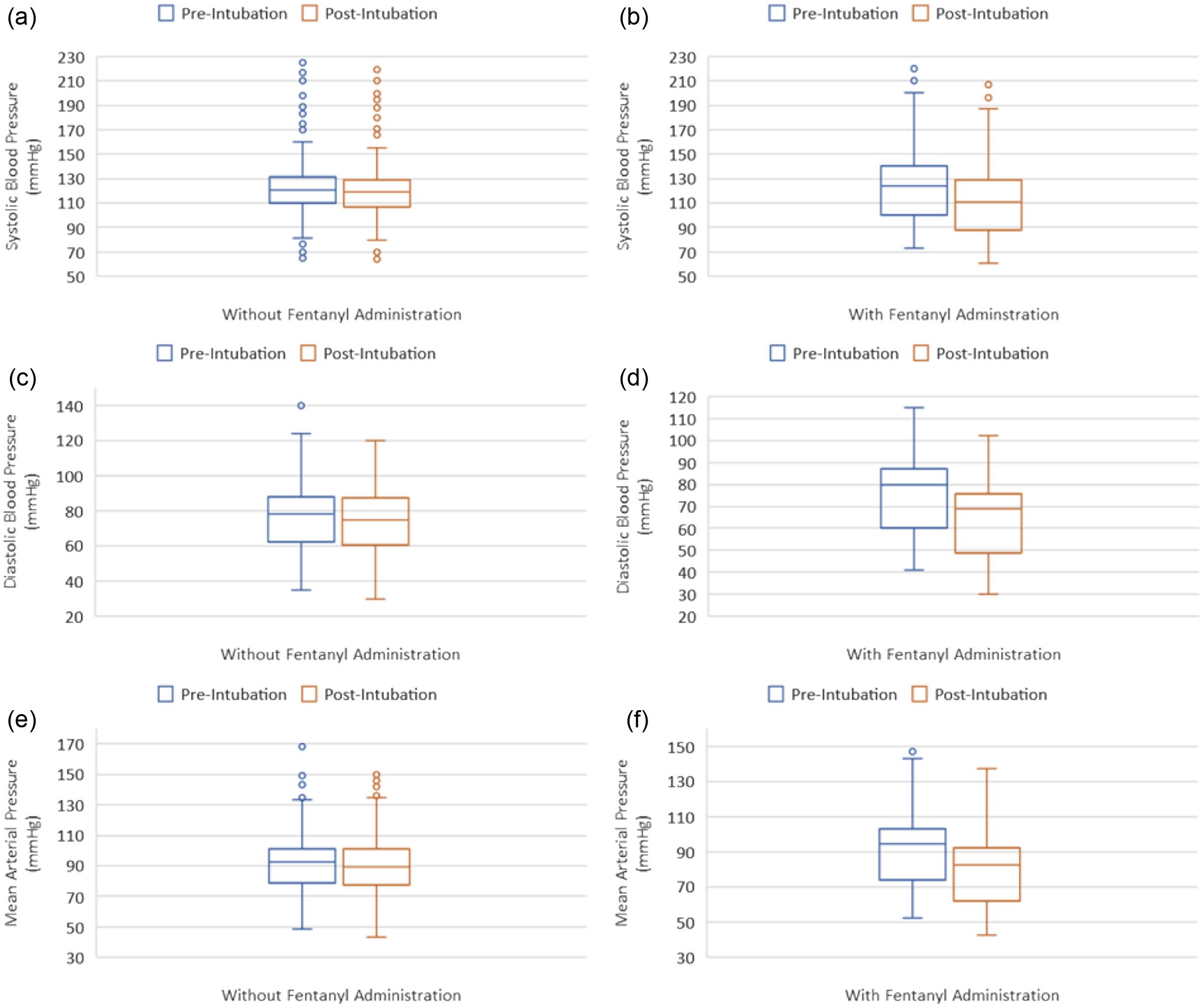
Figure2. Hemodynamicparametersatthetimeofinduction(pre-intubation)andat10minutesafterinduction(post-intubation)stratifiedby fentanyladministration:(a)changeinsystolicbloodpressure(SBP)withoutfentanyl;(b)changeinSBPwithfentanyl;(c)changeindiastolic bloodpressure(DBP)withoutfentanyl;(d)changeinDBPwithfentanyl;(e)changeinmeanarterialpressure(MAP)withoutfentanyl; (f)changeinMAPwithfentanyl.
thisstudywesoughttoexaminethechangeinhemodynamic parametersfromthetimeofinductionuntil10minutesafter inductioninrelationtotheuseoffentanyl.Thisapproach providesamoredynamicdefinitionofhypotension.Our analysisfoundatleasta10%reductioninSBP,DBP,and MAPassociatedwiththeuseoffentanyl.
Thepurposeoffentanylistobluntthesympatheticsurge inducedbylaryngoscopy;thus,dosingshouldbedecided withcaution.Whilelowerdosesmayachievefentanyl’ s purpose,higherdosesmayintroduceunwantedadverse eventssuchashypotension.Weusedastandarddoseof50 μg thatwasadministeredimmediatelybeforetheinduction agent,anditshowedanassociationwithatleast10% reductioninhemodynamicparameters.Whileinourstudy weuseddosingwellbelowwhatisdescribedintheliterature, apreviousstudythatexaminedtheimpactofdose-dependent
effectsonhemodynamicparametersdidnotreveala significantdifferencebetweenthefullandlowerdose regimens.23 Bloodpressuredecreasedanaverageof12mm Hg(95%CI7–16)inthefull-dosegroupandby6mmHg (95%CI1–11)inthereduced-dosegroup(P = 0.10).22
Althoughnotsignificantlydifferent,itiscriticaltonotethat hemodynamicparametersshowedlowertrendsinthefulldosegroup.Therefore,theuseoffentanylshouldbeclinically justifiedandcarefullydosed,especiallyforcriticallyill patientswhoaredependentontheirsympatheticdrivefor survival.Furthermore,itspreparationandadministration areadditionalstepsinamultistepprocedure.
Wefoundasignificantdifferencebetweenoperatorsin termsoftheuseoffentanyl.Whilethemajorityof intubationswereperformedbytrainees,ourstudyshowed thatattendingphysiciansusedfentanylasapretreatment
Table2. Changeinhemodynamicparameters(betweenpre-inductionandpost-intubationvalues)strati
mmHg, millimetersofmercury; BPM,beatsperminute.
agentbeforeRSImorefrequentlythantrainees.Thiscanbe attributedtoclinicalpracticesdevelopedbyattending physiciansovertheirtrainingperiod.Whilethephysicians
Table3. Factorspredicting10%reductioninmeanarterialpressure fromthetimeofpretreatment(orinduction)until10minutes afterinduction.
staffingourdepartmenthavebeentrainedinemergency medicine,themajorityweretrainedintheMiddleEastand someinNorthAmericaninstitutions.Thismaysuggestthat theuseoffentanylasapretreatmentagentforRSIisvariable basedontrainingandpractice.
Sincetheliteraturedoesnotshowastrongbenefitin outcomes,(ie,higher first-passsuccess,reducedmortality rates,reducedesophagealintubation,orreducedhypoxia), wequestiontheuseoffentanylinroutineclinicalpractice. Weemphasizetheimportanceofoptimizinghemodynamic parametersbeforeRSIandaimingfor first-passsuccess. Therefore,theselectionofinductionagentsthatattenuate peri-intubationhypotensionduringRSIisdesirable.Amajor advantageofetomidatecomparedwithotherinduction agentsisthatitpreservescardiovascularstability.Ittypically doesnotcausesignificanthypotensionuponinductionata doseof0.3 μg/kg.23,24 Thisisbecauseetomidatedoesnot significantlyinhibitsympathetictoneandpreserves autonomicreflexes.Itisthoughtthatetomidatehasthis propertybecauseitactsasanagonistatthe α-2 adrenoreceptorsresponsiblefortheperipheral vasoconstrictionresponsetohypotensiveeffects.24 However, thereareconcernswithitsuseincriticallyillpatientsbecause itisknowntoinhibitadrenalenzymesbutisclinically insignificantfromasinglebolusdose.Otherreportedside effectsincludenausea,vomiting,laryngospasm,and myoclonus,allofwhichcanbeattenuatedby neuromuscularblockade.23
CI, confidenceinterval.
Importantly,etomidatedidnotshowincreasedmortality whencomparedwithotherinductionagents.23 Ketamine maybeareasonableoptionforRSIbecauseofitsquickonset andshortdurationofaction,itspreservationofrespiratory drive,anditssympathomimeticproperties.However,in criticallyillpatientswithdepletedcatecholaminestores,
thereisconcernforhypotensionandcardiacarrest.23 Propofol,althoughhavingaquickonsetandshortduration ofaction,hasthemostprofoundeffectonbloodpressure, whichmaylimititsuseincriticallyillpatients.23 Midazolam maybelessdesirableforRSIasithasalongeronsetofaction comparedwithetomidateandketamineandisapotent venodilatoratRSIdoses.23
Takenasawhole,therewasnosignificantdifference betweenetomidateandotherinductionagentsinthemost seriousoutcome,mortality.Inaddition,moststudies demonstratedfavorableperi-intubationhemodynamicswith etomidate.Becauseetomidateisoftenreadilyavailable, clinicianshaveexperiencewithitsuse,anditscostislow,itis areasonableRSIinductionagentforcriticallyillpatients.23 However,insettingswherephysiciansmaynothave accesstohemodynamicallyneutralagentssuchas etomidateforRSI,itwouldbeprudenttooptimizepatient physiologyandhemodynamicparametersduring airwaymanagement.
Ourstudyhadafewlimitationsthatneedconsideration. First,thissingle-centerstudywasconductedintheED, whichlimitsitsgeneralizabilitytoothersettingsand institutions.Second,hemodynamicparameterswere measuredusingnon-invasivemethods,whichmighthave loweredtheaccuracyoftheresults.However,thisreflects real-worldpracticeduetolimitedtimeandresourceswhen performinganarteriallineinpatientsrequiringemergent airwayintervention.Third,ourstudylacksvaluable hemodynamicdatabeyondthe10-minutetimeframe. Fourth,thiswasanobservationalstudythatallowed physician’sdiscretion.However,adepartmentalprotocol existsforRSItostandardizetheprocedure.
Fifth,ourdepartmentprotocolallowsamaximumdoseof 50 μgofIVfentanyl.Thedoseusedinthisstudyiswellbelow thedosingdescribed(3–5 μg/kg)intheliterature.Therefore, wewereunabletodeterminetheassociationof hemodynamicparameterswithdifferentdosingstrategies. Sixth,althoughdatawascollectedinrealtime,itwas typicallyenteredmanuallyaftertheprocedure,whichmay haveresultedinrecallbias.Seventh,theinclusionof inductionagentdosinganditsassociationwithpostintubationhypotensionwouldaddvaluableinformation,but itisnotreportedinourstudyduetothevariabilityindosing betweenphysiciansandtheextremelylowuseofcertain inductionagentssuchaspropofol.Finally,whilewe performedalogisticregressionanalysistoaccountfor confoundingfactors,otherunmeasuredconfoundersmay stillexistgiventheobservationalnatureofthestudy.
Inthisprospective,single-centerEDstudy,wefoundthat theuseof50 μgfentanylisassociatedwithhigheroddsof
reductioninmeanarterialpressurebyatleast10%.While fentanylisanultra-short-actingagentthatcouldbebeneficial forcertainconditions,itshouldbecarefullydosed,anditsuse shouldbejustifiedinclinicalpracticetoavoidunnecessary complicationsarisingfrombloodpressurereduction.
AddressforCorrespondence:AbdullahBakhsh,MBBS,King AbdulazizUniversity,DepartmentofEmergencyMedicine,P.O.Box 80215,Jeddah21589,SaudiArabia.Email: aarbakhsh@kau.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy.This projectwasfundedbytheDeanshipofScientificResearch(DSR)at theKingAbdulazizUniversity,Jeddah,SaudiArabia(grantno:437140-2024).Theauthors,therefore,extendtheirappreciationtothe DSRfortheirtechnicaland financialsupport.
Copyright:©2025Bakhshetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.NattBandMosierJ.Airwaymanagementinthecriticallyillpatient. Curr AnesthesiolRep. 2021;11(2):116–27.
2.CookTM,WoodallN,FrerkC.Majorcomplicationsofairway managementintheUK:resultsofthe4th NationalAuditProjectofthe RoyalCollegeofAnaesthetistsandtheDifficultAirwaySociety.Part1: anaesthesia. BrJAnaesth. 2011;106(5):617–31.
3.LyonRM,PerkinsZB,ChatterjeeD,1074208.etal.Significant modificationoftraditionalrapidsequenceinductionimproves safetyandeffectivenessofpre-hospitaltraumaanaesthesia. CritCare. 2015;19(1):134.
4.MosierJM,SaklesJC,LawJA,etal.Trachealintubationinthecritically ill.Wherewecamefromandwhereweshouldgo. AmJRespirCritCare Med. 2020;201(7):775–88.
5.AprilMD,AranaA,ReynoldsJC,etal.Peri-intubationcardiacarrestin theemergencydepartment:aNationalEmergencyAirwayRegistry (NEAR)study. Resuscitation. 2021;162:403–11.
6.SchoferJM.Premedicationduringrapidsequenceintubation:a necessityorwasteofvaluabletime? CalJEmergMed. 2006;7(4):75–9.
7.WahlenBM,El-MenyarA,AsimM,etal.Rapidsequenceinduction(RSI) intraumapatients:insightsfromhealthcareproviders. WorldJEmerg Med. 2019;10(1):19–26.
8.SajayanA,WickerJ,UngureanuN,etal.Currentpracticeofrapid sequenceinductionofanaesthesiaintheUK:anationalsurvey. BrJAnaesth. 2016;117Suppl1:i69–74.
9.GriesdaleDEG,BosmaTL,KurthT,1074208.etal.Complications ofendotrachealintubationinthecriticallyill. IntensiveCareMed. 2008;34(10):1835–42.
10.FastingSandGisvoldSE.Seriousintraoperativeproblems:a five-year reviewof83,844anesthetics. CanJAnaesth. 2002;49(6):545–53.
11.DominoKB,PosnerKL,CaplanRA,etal.Airwayinjuryduringanesthesia: aclosedclaimsanalysis. Anesthesiology. 1999;91(6):1703–11.
12.FranklinC,SamuelJ,HuTC.Life-threateninghypotensionassociated withemergencyintubationandtheinitiationofmechanicalventilation. AmJEmergMed. 1994;12(4):425–8.
13.SchwartzDE,MatthayMA,CohenNH.Deathandothercomplicationsof emergencyairwaymanagementincriticallyilladults.Aprospective investigationof297trachealintubations. Anesthesiology. 1995;82(2):367–76.
14.FergusonI,ButtfieldA,BurnsB,etal.AustralasianCollegefor EmergencyMedicineClinicalTrialsNetwork.Fentanylversusplacebo withketamineandrocuroniumforpatientsundergoingrapidsequence intubationintheemergencydepartment:theFAKTstudy-arandomized clinicaltrial. AcadEmergMed. 2022;29(6):719–28.
15.TakahashiJ,GotoT,OkamotoH,etal.Associationoffentanylusein rapidsequenceintubationwithpost-intubationhypotension. AmJ EmergMed. 2018;36(11):2044–49.
16.SchenkJ,vanderVenWH,SchuurmansJ,etal.Definitionand incidenceofhypotensioninintensivecareunitpatients,aninternational surveyoftheEuropeanSocietyofIntensiveCareMedicine. JCritCare. 2021;65:142–8.
17.SalmasiV,MaheshwariK,YangD,etal.Relationshipbetween intraoperativehypotension,definedbyeitherreductionfrombaselineor absolutethresholds,andacutekidneyandmyocardialinjuryafter
noncardiacsurgery:aretrospectivecohortanalysis. Anesthesiology. 2017;126(1):47–65.
18.BijkerJB,vanKleiWA,KappenTH,etal.Incidenceofintraoperative hypotensionasafunctionofthechosendefinition:literaturedefinitions appliedtoaretrospectivecohortusingautomateddatacollection. Anesthesiology. 2007;107(2):213–20.
19.AprilMD,AranaA,SchauerSG,etal.Ketamineversusetomidateand peri-intubationhypotension:aNationalEmergencyAirwayRegistry study. AcadEmergMed. 2020;27(11):1106–15.
20.MohrNM,PapeSG,RundeD,etal.Etomidateuseisassociatedwithless hypotensionthanketamineforemergencydepartmentsepsisintubations: aNEARcohortstudy. AcadEmergMed. 2020;27(11):1140–9.
21.ShardaSCandBhatiaMS.Etomidatecomparedtoketaminefor inductionduringrapidsequenceintubation:asystematicreviewand meta-analysis. IndianJCritCareMed. 2022;26(1):108–13.
22.TerAvestE,RagavanD,GriggsJ,etal.Haemodynamiceffectsofa prehospitalemergencyanaesthesiaprotocolconsistingoffentanyl, ketamineandrocuroniuminpatientswithtrauma:aretrospective analysisofdatafromahelicopteremergencymedicalservice. BMJ Open. 2021;11(12):e056487.
23.AcquistoN,MosierJ,BittnerE,etal.SocietyofCriticalCareMedicine clinical practiceguidelinesforrapidsequenceintubationinthecritically illadultpatient. CritCareMed. 2023;51(10):1411–30.
24.ValkBIandStruysMMRF.Etomidateanditsanalogs:areviewof pharmacokineticsandpharmacodynamics. ClinPharmacokinet. 2021;60(10):1253–69.
EvelineHitti,MD,MBA*
DimaHadid,MAPH*†
MiriamSaliba,MPH*
ZouhairSadek,MSc*
RimaJabbour,RN*
RulaAntoun,MSc* MazenElSayed,MD,MPH*
SectionEditor:ChristopherKang,MD
*AmericanUniversityofBeirut,DepartmentofEmergencyMedicine,Beirut,Lebanon † McMasterUniversity,HealthPolicyPhDProgram,DepartmentofHealthResearch Methods,Evidence,andImpact,Hamilton,Canada
Submissionhistory:SubmittedApril29,2024;RevisionreceivedOctober18,2024;AcceptedOctober22,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20942
Introduction: Emergencydepartments(ED)playacentralroleindefiningtheeffectivenessandquality oftheoverallhospital’smasscasualtyincident(MCI)response.Theuseofelectronichealthrecords (EHR)inhospitalsettingshasbeenrapidlygrowingglobally.Thereis,however,apaucityofliteratureon theuseandperformanceofEHRduringMCIs.
Methods: InthisstudyweaimedtodescribeEHRuse,aswellasthechallengesandlessonslearntin responsetothe2020explosioninthePortofBeirut,Lebanon,duringwhichthehospitalreceivedover 360casualties.
Results: Informationtechnologysupport,reducingEHRsystemrestrictions,cross-functiontraining, focusonregistrationandpatientidentification,patient flowandtracking,mobilityandbedsideaccess, andalternatesitesofcareareallimportantareastofocusonduringemergency/disaster responseplanning.
Conclusion: Innovativesolutionsthathelpaddresslogisticalchallengesfordifferentaspectsofthe disasterresponseareneeded.[WestJEmergMed.2025;26(1)20–29.]
Emergencydepartments(ED)playacentralrolein respondingtomasscasualtyincidents(MCI)anddefinethe effectivenessandqualityoftheoverallhospitalresponse.1,2 Hospitalsmustbepreparedtorespondtoalargeinfluxof patientsandcoordinateresourcesaccordingly.Thisbecomes particularlychallenginginsystemsthatlackanationalor regionalemergencymedicalservices(EMS)plananda disasterresponseframework.
PreparednessforMCIsismultifacetedandentailsa multidisciplinaryandintegratedapproachtodevelopa responseplanthatallowsforpromptactivationofadisaster codeandnotificationofstaff,expansionoftriageandclinical areas,quickregistration,rapiddisposition,patienttracking,
resourcescoordination,crowdcontrol,efficientinternaland externalcommunication,andeffectiveleadershipand governance.NumerouspreviousstudieshaveexaminedMCI responses;however,limiteddataexistsontheperformanceof electronichealthrecords(EHR)duringMCIs.3–5
TheadoptionofEHRsbyhealthcareorganizationshas seenrapidgrowthglobally,fueledbydatasupportingtheir positiveimpactonsafety,qualityandefficiency.TheEHR offersvaluableadvantagesintermsofstrengtheningpatient trackingcapabilities,improvingclinicianefficiencythrough quickaccesstomedicalrecords,andimprovingclinical decision-makingthroughbestpracticeadvisories,aswellas empoweringhealthcaresystemswithanalyticaland reportingcapabilities.6–13 Atthesametime,somestudies
haveraisedconcernsarounddecliningthroughput,lengthy documentationrequirements,increasingcomplexityof work,andchallengeswithuser-friendliness,aswellasthe levelofavailabletechnicalsupportforclinicians.14–21 ThisisparticularlyrelevanttoEDsettingswhere timeconstraintsandcomplexprocessespose additionalchallenges.
UseofEHRsinMCIsrequiresthedevelopmentof specializeddisastermodulesthatinvolvepre-registered recordsthatcanbequicklyaccessedandactivatedina disaster.GiventhetimeconstraintsinMCIs,whereroutine processesmightnotkeepupwiththe flowofpatients, specializedworkflowsarounddocumentation, financial clearance,computerizedphysicianorderentry(CPOE), medicationmanagement,patienttracking,andadmission anddischargearerequired.12,22 Toourknowledgethereare nopeer-reviewedpublicationsdocumentingtheuseand performanceofEHRsduringliveMCIs.
OnAugust4,2020,duringtheCOVID-19pandemic, Lebanonwitnesseditslargestnon-conflict-relatedMCI,the Beirutportblast,whichleftbehind ≈200deadand6,500 injured.23 InthisstudyweaimedtodescribeEHRuseduring theMCIresponse,aswellashighlightthechallengesand lessonslearntinresponsetotheBeirutportblast,oneofthe largestnon-nuclearexplosionsinhistory.
Thisisacasereportwithareviewoftheliterature.We searchedbothPubmedandMEDLINEusingthefollowing keywords:electronicmedicalrecord;disasterplanning;mass casualtyincident;hospitalemergencypreparedness;and medicalinformatics.Thisresultedintheidentificationof threemanuscripts.Allthreeinvolvedlimiteduseof informationtechnology(IT)inaMCI,andonlyoneinvolved aliveactivation.24–26 Thesearchdidnotyieldany manuscriptsonMCIresponsewithafullyintegrated EHRsystem.
TheAmericanUniversityofBeirutMedicalCenter (AUBMC)isthelargestacademic,tertiary-carecenterin Beirutwithover57,000EDvisitsannually.Inthepast 17years,AUBMC-EDhasbeenattheforefrontof respondingtoover15MCIs.Asaresult,AUBMCregularly assessedandmodifiedbothitsEDandhospitalemergency preparednessplan(EPP).TheAUBMCestablisheditsown EPPinJuly2000.Yearlydrillsandmodificationstothe existingplanwereconductedtoensurebetter communication,coordination,andavailabilityofresources duringMCIs.In2019,AUBMCbecameanHIMSSStage6 EmergencyMedicalRecord/EHRinstitutionwiththe implementationoftheEpicEHR(EpicSystems Corporation,Verona,WI).
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
HospitalsandEDsfacemajoroperational challengesduringmasscasualtyincidents (MCI).Researchontheuseofelectronic healthrecords(EHR)duringMCIs islimited.
Whatwastheresearchquestion?
ThisstudyexaminesEHRuseduringthe Beirutportblast(August2020)and highlightschallengesandlessonslearntfrom thisMCI.
Whatwasthemajor findingofthestudy?
Opportunitiesidenti fi edforimprovedEHR useduringMCIsincludedstafftrainingand scalinguproutinework fl owstoenhance ef fi ciencyofresponse.
Howdoesthisimprovepopulationhealth?
HospitalsadoptingproposedEHRchanges canbetterrespondtoMCIs,enhancing ef fi ciencyandleadingtoimproved patientoutcomes.
OnAugust4,2020,at6:07 PM,anestimated2,750tonsof storedammoniumnitrateexplodedatthePortofBeirutless than2.5milesfromAUBMC.27 TheBeirutportblastwas reportedtobeoneofthelargestnon-nuclearexplosionsin historyleavingbehindmorethan6,500peopleinjured, approximately300,000displaced,and204fatalities.27 Casualtiesimmediately floodednearbyhospitals,whichhad alreadybeenpartlydestroyedbytheblast.
TheAUBMCEDstartedreceivingcasualtiesfromwithin theinstitutionandfromitsneighborhoodlessthanthree minutesaftertheexplosionduetoitsproximitytotheblast site.ThehighestEPPnotificationlevel “CodeD-Full Activationlevel” wasimmediatelyactivatedatAUBMC, whereallhospitalstaffwerenotifiedtorespond.Duringthe three-hourintervalfollowingtheexplosion,over360victims weretreatedintheED,ofwhom87requiredadmission(52 regularbedadmissions,19criticalcarecases,and16 immediatelyoperatedon)and12reporteddeaduponarrival.
DescriptionoftheEmergencyPreparednessPlan
ThedisasterplanatAUBMCconsistsoftwolevelsofMCI response(CodeD):partialandfullactivation.Activation usuallyfollowsanalertnotification “CodeDAlert.”
“CodeD – Partialactivation” requiresallessentialstaffto reporttotheircorrespondingdepartmentsincludingtheED. “CodeD – FullActivation” requiresallactivestafftoreportto theircorrespondingdepartments.Activationofthedisaster plananditscorrespondingresponselevelistraditionallybased onthegeographicallocationoftheincidentandonthe numberofcasualtiesexpectedtopresenttotheED.
Thehospitaldirectororadministratoroncallisinchargeof announcingthelevelofhospitalresponse.CodeDAlertis usuallyannouncedbytheEDdirector,chair,ordelegatefor MCIslocatedinapredefinedgeographicalareasurrounding AUBMC.Activationlevelsarecommunicatedthroughshort textmessage(SMS),pagingandWhatsAppmessagestopreprepareddisasterlistsofhospitalstaff.Thisensuresredundancy ofcommunicationsincecellularnetworksusuallyexperience delaysinSMSdeliveryduringMCIsduetoinfrastructure damageandcalloverloadonlandlinesandmobilenetworks.
UponactivationoftheEPP,initialstepsoftheresponse consistofquicklytransformingtheEDphysicalspaceto designatedcolorcoded “ surgeareas, ” withdeploymentofprepreparedsuppliesandmedicationcartstodifferentsections.A mobiletriageareaissetupandexistingEDpatientsare dischargedorsenttoinpatientunitstoimprovesurgecapacity andprepareforthe firstwaveofcasualties.TheMCIpatients arecolortaggeduponarrivaltotheEDanddirectedfrom triagetodesignatedareasbasedonacolor-codedtriage system.PatienttriageshiftsfromEmergencySeverityIndex scoringtothemodifiedcare-flightsystem.Adetailed descriptionoftheplanhasbeenpreviouslypublished.1
DuringtheimplementationofEpicin2018,scopingand adoptionphasesfocusedonincludingastreamlineddisaster modulebecauseofthehighfrequencyofMCIsinLebanon. ThefoundationalEpicdisastermodulethatispartofthe standardimplementationpackagewasmodifiedfor alignmentwithexistingworkflows.Finalworkflows thatwereintegratedintothedisastermodulearesummarized in Table1.WiththeimplementationoftheEHR,the responseplanshiftedfrompre-preparedmanualchartstoa fullelectronicsystemusingpre-printedbraceletscontaining pre-assignedmasscasualtyrecord(MCR)numbersand requiringbarcodescanningforactivation.TheMCR numbersareuniqueidentifiersthatallowidentification andtrackingofcasualtiesduringthedisaster responsephase.
Smartgroupsofpreferredorders(laboratory,medication, radiology,admissions,procedures,etc)werebuiltintothe disastermodulebasedonpreviousdatafromMCIs.These wouldberequestedelectronicallyinEpicwhenthedisaster moduleisactivated.Resultsareviewedelectronicallywhen available,whichwouldallowphysicianstoaccessreal-time patientdata.
Trackingandidentificationofcasualtiesalsoshiftedfrom apaper-basedsystemtoanelectronicsystemwherebystaff andcaregiverscantrackcasualtiesatanypointintimeon “disasterview” usingtheEHRdisasternavigator.Moreover, chargingand financialclearanceinthedisastermodule areperformedautomaticallyinsteadofmanually. Documentationwithinthedisastermoduleincludeda simplifiedtraumatemplate.TheEHRimplementationplan alsoincludedallocationofadditionalworkstationsonwheels thatcanbedeployedintothesurgeareasforuseby front-liners.Additionalareasweredesignatedfor workstationdeploymentandincludedtriageandthe low-acuity “ greenarea, ” aswellasthedischargearea.
AftertheMCI,severaldebriefingsessionswereheldto reviewstrengthsandareasforimprovementinourresponse protocols.Psychologicaldebriefingsessionswereconducted within72hoursoftheeventwithallteammemberswho activelyparticipatedintheincidentincludingfaculty, residents,andnursingteams.Theseinitialdebriefingswere ledbythechairofthedepartment.Theywerecarriedout immediatelyaftertheincidentforstaffwhowereinvolved directlyintheMCIresponseandfocusedonemotional support,leaningonprinciplesoutlinedintheMCICORD (CouncilofResidencyDirectorsinEmergencyMedicine) SurvivalPackageforpsychologicaldebriefs.28 The psychologicaldebriefingsessionsweresubsequentlyfollowed bytechnicaldebriefsconductedaroundthreeweekspost eventbyamultidisciplinaryteamincludingclinicalandnonclinicalstafffromtheED(chairofED,EDmedicaldirector, EDnursemanager,EDqualityofficer),surgicaldepartment (chairofsurgery,directoroftrauma),medicalinformatics team(directorofmedicalcenterapplications,andchief medicalinformationofficer),riskmanagement(directorof qualitysafetyandriskmanagement,andsafetyofficer), nursingteam(directorofnursing),andpatientregistration team(directorofpatientregistration).
Thetechnicaldebriefswereledbythedirectorofquality safetyandriskmanagementandfollowedtheafter-action reviewframework,includingareviewoftheincident,an analysisofboththesuccessesandchallengesencountered,as wellasanidentificationofrootcausesofanyshortcomings.29 Minutesofthedebriefsessionswererecordedbythequality teamandsenttoparticipantsforreview,comments,and approvalpriorto finalization.Theseminuteswerethen analyzedbytwooftheauthorsfollowingthesix-stage processforthematicanalysis.30 Thisincludeddata familiarization,initialcodegeneration,reviewingthemes, definingandnamingthemes,andcompletionofwrite-up. Throughthisprocess,weidentifiedseveralkeyfocusareas. Key findingsanddiscussionpointsraisedinourdebriefing sessionswereusedtomodifytheplanforfutureresponses. Sincethiseventwasthe firsttotesttheEHRcomponentof
Table1. Changesdonetoemergencypreparednessplanningafterintroductionofanelectronichealthrecord.
ElementsPre-EHRPost-EHR
Communicationdisplay of adisasterstatuson thedashboard
Notavailable
Registrationof casualties Registrationisperformedmanually. Pre-labeledemergencywristbandsareusedatthe triagearea.
Identi ficationof casualties
MCRnumbersareusedastheonlytracking referenceforallconcerneddepartments.The patient’sname,ifidentified,isshowninanother field visibletoEDandPAstaff.
TrackingofcasualtiesCasualtytrackingchecklistsareused.
Theseincluded:
• MCRnumber
• Chiefcomplaint
• Entry/exitto/fromthecolor-codedareas
• Comments
• Patientdisposition
DischargeprocessPre-labeleddischargeformisusedtodocument diagnosisandfollow-upinstructions.
EDnursemanagerand/orEDchargenurseand/or EDclerksactivatetheEDdepartmentstatusto “Disaster” ontheEDdashboard.
Pre-printedidentificationbraceletsavailablewiththe PAteam,areusedduringpartialand/orfullactivation ofthedisaster.
Pre-printedbraceletscontainpreassignedMCR numbersandpatienthospitalnumber. PAOsprovideeachcasualtywithabracelet,scanit, andactivatethechartinEPIC.
Oncethecasualtyisregistered,therecordappearsin theDisastersection,thetriageRNthencompletes thetriageusingtheDisasterNavigatorandassigns thecasualtytoanEDsection.
MCRnumbersaretheonlytrackingreferenceforall concerneddepartments.Patient’snamewhen identifiedisaddedtoAliasesandnottotheprimary name field.
The “disasterview” isusedtotrackcasualties’ movementsduringdisaster,usingEPIC disasternavigator.
Disasterreportsaregeneratedatanypointintime duringadisastertotrackcasualties.
FulldemographicdataarecollectedbyPAOsbefore discharge.PAOscollecttheinformationincludedin theEDdisasterdischargechecklist(MCRnumber, patienttriplenameandphonenumber),toensure thatthepatientisregisteredintheEHRandto providethepatientwiththedischargeinstructions.
DocumentationApre-labeledkitsystemisusedinthetriagearea.
Thesekitscontainpre-labeledemergencypaper chartsandpreassignedMCRnumbers.
OrderingPre-labeledemergencystudies’ requestsareusedin thecolor-codedareas.
Duringadisaster,theEHRisusedbythemedical andnursingteams.
Nursesandphysiciansuse “disasternavigator” with minimaldocumentation.
Allordersrequiredduringdisaster(laboratory, medications,radiology,procedures,admissions,etc), areorderedthroughthedisasterordersnavigator. Anadmissionorderisalsoplacedbythemedical teamforcasualtiesrequiringadmission.
RadiologyprocessPre-labeledemergencystudies’ requestsareused. Aradiologistreportsthemajor findingsofthe radiograph,orCTrequestshandwritten.
LaboratoryprocessPre-labeledemergencypaperordersareused. LabresultsarecommunicatedverballytotheED teambyphonewithreadbackorhandwrittenonthe labrequestsandsenttoEDbypneumatictube.
Allradiologystudiesareorderedthroughthedisaster ordersnavigator,andresultsarereportedonthe AGFA/EHRsystem.
RainbowdrawsareorderedbytheRNsonall patientsadmittedtoredandyellowareas,unlessthe MDalreadyplacedordersforthesepatients. EDEMTs/RNprintlabels,collectthesamplesusing rainbowdrawprocess,andsendthemtoreceiving areausingpneumatictube.
MDs,inparallel,ordertherequiredtestsusing theEHR.
Laboratorythenproceedswithtesting,andtheresults appearelectronicallyonthepatient’schart.
(Continued onnextpage)
Table1. Continued.
ElementsPre-EHRPost-EHR
Chargingand financial clearance
Charging isperformedmanually.Casualtiesare assignedaspecificguarantor(070).
AllchargingdocumentsaregivenbytheEDteam, attheendofthedisastertotheEDcashier. TheEDcashierlogsthemonthebillingsystem (AS400)afterthepatient’sdischarge.
RecoveryprocessUpondisastertermination,allcasualtiesare manuallyenteredonthedashboard,tocomplete theirregistrationonAS400,placingthenecessary charges,andadmissionorders,ifneeded,and dischargingthem.
Medicationdispensing duringdisaster
Equipment
Emergencymedicationcartsareused(Pyxis didnotexist).
Papersystem(workstationwheel[WOWs] didnotexist).
Casualtiesareautomaticallyassignedaspecific guarantor(070),therebyallowingautomaticclearance ofEDregistration.
ChargingisperformedelectronicallyusingtheEHR, duringorafterthepatient’sstay.Allchargesare clearedbythecashieronthebillingsystem(AS400).
Upondisastertermination,arecoveryprocessis initiatedtoupdateinformationabouteachcasualty intheEHR(registrationstatus,location, anddisposition).
Emergencymedicationcartsareused.Medications arealsodispensedusingtheEDPyxismachine. Pyxisisreplenishedfromthecentralpharmacy.
EDandPAOstaffuseWOWsinthetriagearea, insidetheED,andatdischarge
ED, emergencydepartment; EHR,electronichealthrecord; PA,patientaccess; PAO,patientaccessofficer; Pyxis,automatedmedication dispensingsystem; RN,registerednurse; MCR,masscasualtyrecord; CT,computedtomography; MD,medicaldoctor; EMT,emergency departmenttechnician; WOW,workstationonwheels.
theEPPplan,amajorpartofthedebriefingsfocusedon EHR-specificissuesincludingworkflowsandthe performanceoftheEHR’adifferentfeatures.
WeidentifiedseveraleffectiveelementsofEPPresponse. Theactualtreatmentareasrapidlyexpandedtodesignated “ surgeareas ” withinandoutsidetheED.Patienttriage rapidlyshiftedtothemodifiedcare-flightsystem. Non-criticalcasualtiesweredirectedtopre-designatedlowacuityorgreensurgeareaswithadequatemedicalteamsand supplycarts.Theinfluxofpatientsintermsofrateand numberpresentingtotheEDwithinthe firsthourwas, however,muchhigherthanexpectedduetheproximityof AUBMCtotheexplosionsite.Casualtiesweretreatedin hallwaysandattheEDentranceonstretchers,chairs,and floors.Treatmentofpatientsproceededinaquickmanneras inpreviousMCIswithmosthospitalstaffresponding immediatelyuponactivation.
Numerousissueswere,however,facedwiththeEHR duringtheresponse.
Aninitialdelayoccurredinactivatingthedisasterstatuson Epicsinceitneededtobeactivatedmanuallybyspecifically trainedmemberswhowerenotpresentphysicallyintheEDat thetimeoftheexplosion.Thispreventedtheappearanceofthe disasternavigatoronthedashboardanddelayedinformation relaytodifferentstakeholdersintheED.
Patientregistrationwasanothermainchallenge.TheEPP plannedfor200pre-prepareddisastere-records/wristbands. Thenumberofcasualtiesexceededthiswithinthe firsthour. Callinginadditionalregistrationstaffcauseddelayin registrationandinabilitytocapturedemographic informationforpatientswhoweredischargedearly,in additiontodelaysinorderingtestsandplacingorderson otherpatients.Creatingadditionalrecordswaslogistically challengingsinceitrequiredbothregistrationstaff andITsupport.Loadingalltherecordswithinashorttime intervalalsoslowedthesystemintermsofresponse.Back-up manualchartswere,therefore,useduntiladditional wristbandswereprintedandcorrespondingelectronic recordswerecreated.WhileMCRswereusedas uniqueidentifiers,thispreventedeasyidentificationof casualtiessinceregistrationstaffwerenotcollectingpatients’ namesordemographicdatawhenhandingout MCRbracelets.
Issueswithpatient flowandwith financialworkflowswere alsoidentified.Beyondoperationaldifficultyinmanagingthe highnumberofadmissionstohospital,thestaffexperienced additionalchallengesrelatedtocomplexworkflowsthat requiredfollowingroutineadmissionprocessforevery patient.Thisprovedtobedifficultespeciallyforphysicians respondingintheEDsincetheywerefocusedonpatientcare ratherthancompletingstepsinadmissionworkflowstoallow forpatientstotransitionelectronicallytoinpatientunits. Eighty-sevenpatientsrequiredadmission,andmostofthem werephysicallysenttoinpatientunitspriortocompletingthe extensiveadmissionelectronicprocess.Financialconstraints werealsoidentifiedforpatientsduringtheirtransitionto inpatientstatusdespitepreviousmodificationof financial
workflowsfortheEDintheEPP.Chargeswerenot automaticallywaivedintheoperatingroomorinpatientfor patients,similartowhathappenedattheleveloftheED, whichrequiredcashierstomanuallyclearchargesduring theevent.
Medicationsandsuppliesweredispatchedimmediatelyto differenttreatmentareasintheEDasplannedintheEPP. Cartsweremanagedbypharmacists,nursesandstorestaff whousedpaperlogswhilehelpingdispensedifferentitems. RoutinemedicationfromPyxis(theautomatedmedication dispensingsystem)andsuppliesworkflowswere,therefore, bypassedduringtheevent.
Patienttrackingwasalsoanotherchallengefacedduring thisMCIresponse.Severalclinicalandadministrativestaff weretrackingthenumberofcasualtiesarrivingtotheED; however,movingpatientsonthedashboardbetween differentsectionswasdelayed,whichresultedindifficultiesin trackingcasualtiesandinidentifyingtheirexact physicallocation.
Clinicaldocumentationwassuboptimalduringtheevent. Despiteintroducingastreamlinedone-page “expresslane” disaster-documentationmodule,limitedclinical documentationoccurredforcasualtiestreatedintheED. Keychallengeswererelatedtoavailableworkstations,as nearlyallareasintheEDweretransformedintoclinicalareas giventhehighnumberofcasualties.Despiteprevious training,physiciansfromotherunitswerenotfamiliar enoughwiththedocumentationprocessonEDpatients duringEPP.Manypatientsweredischargedphysicallyfrom theEDwithminimalornodocumentation.
OnceCODE-Dwasdeactivated,recoveryoperations resumed.TheseconsistedofcleanupofEDclinicalareas, reconciliationofdifferentcasualtylistsandfatality management/identification,inadditiontoresupplying essentialequipmentandrestockingEDmedications.The Epicdashboardrecoveryprocesswasnotpreviously planned;therefore,thisrequiredsettingupaclinical/IT grouptohelpcleanuptheEDdashboardandtoresolve ticketsrelatedtopatient flow,CPOE,anddisposition-related issues(Table2).
ThisreviewdescribesEHRchallengesandlessonslearned atanacademic,tertiary-carecenterinLebanonduringthe responsetotheBeirutportblast,whichwasoneofthelargest non-nuclearmodernexplosionsinhistory,andreviewsthe literatureonEHRuseinaMCI.Themainchallengesinthis
caseexperiencewererelatedtocomplexworkflows,training onEHRworkflows,andtherecoveryprocess.Translatable lessonsincludeimprovingworkflowstostreamlinepatient registration,identification,andcareduringMCIs.Crosstrainingofstaffonpatient-registrationdisastermodulesis alsoimportanttocapturethelargeinfluxofpatients.In addition,havingmembersoftheITstaffontheground addressingacuteissuesduringanMCIisanimportantpart ofEPPpreparednessusingEHRs.Whileafewstudieshave reportedontheuseoftechnologyinMCI,thesehavebeen limitedtospecificaspectsofIT,suchasradiologyorderentry andtrackingsystems.Nostudiestoourknowledgehave reportedontheuseandperformanceofacomprehensive EHRduringanMCI.
Non-EHRessentialconceptsduringMCIsfocuson externalandinternalcommunication.External communicationwithEMSagencies,commandcenters,and otherneighboringhospitalsisneededtocoordinate responseandprovidestatusupdatesoncapacityandon dynamicreadinessofhospitalstoacceptadditional casualtieswhennearadisasterevent.Mosthospitalsin Beirutwereaffectedtovaryingdegreesbytheexplosion, andsomebecamenon-functionalbecauseofthedamage. Twolargehospitalsveryclosetotheexplosionsiteneeded tocoordinatewithEMStransferoftheirpatientswhowere alreadyinpatientstootherhospitalsoutsidetheBeirutarea. Severalcasualtieswalkeddirectlyfromareasnearthe explosionsitestotheclosesthospitalsandfoundthem tobenon-functional.
Internalcommunicationwasalsokeyandusedvarious methodstonotifyallessentialstaff.Notification ofstaffand dispatchofresourcesandpersonnelwaseffective.Alertsused redundantcommunicationSMS,paging,andWhatsApp notificationsofmembersofpre-prepareddisasterlists.Asin priorevents,infrastructuredamagedelayedSMSdeliveryin Beirut;however,pagermessagesandWI-FImessaging systemsalertswerepromptlyreceived.Thisallowedfor immediatedispatchofstafftotheEDaswellastheopening ofadditionaltreatmentareaswithdistributionofprepreparedsupplyandmedicationcartstoallsections.Thisis inlinewithpreviousliteratureshowingthateffective intraorganizationalcommunicationiscriticalfor crisisplanning.31
TheEHR-specificworkflowchallengessuchaspatient registration,identification,andtrackingduringMCIremain challenging.Readybraceletswithuniqueidentifiersallowfor quickactivationofrecordsoncepatientsarrivetotheED. Theyallowforeaseofordering/resultsmanagementduring MCIs.Theycanalsohelpwithpatienttrackingandpatient flowbetweentheEDandvariousdepartments.However, patientidentificationcanbedifficultifdemographic informationisnotcollectedimmediately.Communication withsearch-and-rescueteams,media,andrelativesof casualtiesrequiredimmediateidentificationofpatientsand
Table2. Summaryofchallengesandlessonslearnedduringtheresponse.
ProcessEventsandchallengesLessonslearned
Workflow related Disaster planactivationontheEHRwasdelayedasit neededtobemanuallyactivatedbyspecifictrained members:
• Preventedtheappearanceofdisasternavigator
• DelayedinformationrelaytodifferentstakeholdersinED
DelayinPatientRegistration:
• ThenumberofcasualtiesarrivingtotheEDexceeded thenumberofpre-printeddisasterwristbands(200). Thisrequiredadditionalprintingofwristbands,which waslogisticallynon-workable.
• Callingintheregistrationstaffdelayedpatients’ registrationcauseddelayinregistrationandinabilityto capturedemographicinformationforpatientswhowere dischargedearlyinadditiontodelaysinorderingtests andplacingordersonotherpatients.
• Creatingadditionalrecordsdelayedasitrequiredboth registrationstaffandITsupport.
• UseofMCRspreventedeasyidentificationofcasualties sinceregistrationstaffwerenotcollectingpatients’ namesordemographicdatawhenhandingout MCRbracelets.
• PrintingofMCRwristbandsdelayedduetolimited numberofpatientaccessusers.
Delayinpatientadmissiononthesystem:
• Patientsweresenttoinpatientunitspriortocompleting theextensiveadmissionelectronicprocess.
Financialconstraintsidentifi edforpatientsduringtheir transitiontoinpatientstatus:
• Admission financialclearanceswerenotautomatically overriddenintheoperatingroomorinpatientforpatients, similartowhathappensattheleveloftheED,which requiredpatientaccesstomanuallycleartheadmission requestsduringtheevent.
• Readybraceletswithuniqueidentifiersallowforquick activationofrecordsoncepatientsarrivetoED.
• Improvedworkflowsonhandhelddevicestohelp streamlinepatientregistration/identi fication/careduring MCIevents.
• Alternativemethodsofhealthrecordsactivationshould beimplemented,whichincludeusingdormantrecords withuniqueidentifiersactivatedbyscanningwristbands, aswellaspre-printedbackupmanualcharts.
• Activationoftheserecordscanbedonebyregistration andbynursingstaffattriageandatbedsideifneeded untiltheregistrationstaffscaleupintermsofresponse.
• TrainingonactivatingdisasterstatusontheEHRshould bedonefordifferentEDstaffandnotlimitedtonurse managersduringMCIs.
• Allstaffshouldbecrosstrainedonperformingdifferent tasksrelatedtoEHRinterfaceduringMCIs.
• HavingmembersoftheITstaffonthegroundrelaying thetechnicalissuesbacktothecompleteITteamis moreeffective.
• Access/roleslimitationspresentinroutineworkflows shouldbeaddressedandbypassedifneededduring anMCI.
• Throughputrestrictionsrelatedto financialclearance, patientadmission/discharge/flowthroughphasesofcare shouldbereviewedandrestrictionsliftedtoallow seamlesspatienttransferacrossthehospital.
Real-time operations
Inefficientpatientstrackingduringandpostdisaster:
• Delayinpatientregistrationledtoinconsistencyinthe numberofpatientsregisteredonsystemwiththose registeredonpaper.
• Severalclinicalandadministrativestaffweretrackingthe numberofcasualtiesarrivingtotheED.Thiscaused delay inmovingpatientsondashboardbetweendifferent sectionswhichresultedindifficultiesintracking casualtiesandinidentifyingtheirexactphysicallocation.
• Triageinnon-clinicalareas,bedsideregistrationby registrationstaffandnurses,collectingandrecording information,CPOEandaccesstoresultsareallimportant functionsthatcanbedoneatbedside.
• Maximizetheuseofhandhelddevicestohelpstreamline patientcare/ flowduringMCIevents.
Training related
Recovery process
• Despiteprevioustraining,physiciansfromotherunits werenotveryfamiliarwiththedocumentationprocess onEDpatientsduringEPP.
• ManypatientsweredischargedphysicallyfromtheED withminimalornodocumentation.
• Recoveryprocesswasnotpreviously thoroughlyplanned.
• Itrequiredsettingupaclinical/ITgrouptohelpcleanup theEDdashboardandtoresolveticketsrelatedto patient flow,CPOEanddispositionrelatedissues.
• RecordingtheMCRnumbersanddemographicsfrom patientspriortothemphysicallyleavingtheEDis importanttoreconcilelists.
• Uni fiedelectronicreportsthatshowcasualtylistswith clearidentifiersanddemographicdatashouldalsobe availabletoadministrativeandclinicalstaffincharge duringtheMCIresponse.
• Assesssystemresponsiveness,addressticketsrelatedto work flows,onsitehelpwithregistration/CPOE/ reconciliationissues.
• Establishatrainedmultidisciplinaryteamtoaddress tickets/resolvependingissues.
ED, emergencydepartment; EHR,electronichealthrecord; EPP,emergencypreparednessplan; IT,informationtechnology; MCR,mass casualtyrecord; MCI,masscasualtyincident; CPOE,computerizedphysicianorderentry.
theirlocation(insidethehospitalandatotherhospitals) duringtheevent;thisprovedtobeinitiallyverydifficult especiallyforunconsciouspatientssinceidentifyingpatients wasasteppreviouslyassignedtotheinpatient/pre-discharge phaseofcare.Casualtyreportsdidnotinitiallyidentify patients,whichresultedincommunicationchallenges. Additionally,closingtheloopduringthedischargeprocess byrecordingtheMCRnumbersanddemographicsfrom patientspriortothemphysicallyleavingtheEDisimportant toreconcilelists.Unifiedelectronicreportsthatshow casualtylistswithclearidentifiersanddemographicdata shouldalsobeavailabletoadministrativeandclinicalstaffin chargeduringtheMCIresponse.Theseenhancementscan helpclosegapsinEHRadoptioninthecontextofMCIsand addresspreviouslyreporteddifficultiesinthissetting.32
AnotherEHR-relatedchallengewasmobilityduring MCIs;useofhandhelddevicescanhelpimprovemobilityof staffduringresponse.Fixedworkstationsworkduring routineoperations;however,withtheneedtoexpand treatmentareas,theinfluxofcasualtiesandmedicalstaff respondingtoevent,bedsideaccesstoEHRsiskey.Triagein non-clinicalareas,bedsideregistrationbyregistrationstaff andnurses,collectingandrecordinginformation,CPOE, andaccesstoresultsareallimportantfunctionsthatcanbe doneatbedside.Withtheincreasingnumberofcasualties, dedicatedstaffwereassignedtoaccompanyandcarefor patientsduringtheirEDstayandtohandoffessential informationtoothertreatmentteams.Suchmodelsofcare requiremaximizingtheuseofhandhelddevicestohelp streamlinepatientcare/flowduringMCIevents.Disasterrelatedplanforequipment/handhelddevicesshouldalsobe partofanemergency/disasterresponseplan.
TheEHRaccessworkflowsneedtobetailoredtotheMCI response.Addressingaccessandrolelimitationsthatare presentinroutineworkflowsfordifferentprovidertypesis alsoimportant.Routinequickregistrationandfull registrationworkflowsarenoteffectiveduringahighinflux ofpatients.Limitationsarerelatedtoimmediatelyavailable registrationstaffandtoinformationcollectionrequirements. Planningshouldbedoneforalternativemethodsofhealth recordsactivation,whichincludeusingdormantrecordswith uniqueidentifiersactivatedbyscanningwristbands,aswell aspre-printed,back-upmanualcharts.WhiletheEHRbasedresponsewithinourinstitutionhadintegratedthese features,registrationstaffweretheonlyteammembers trainedonthisstepandwerenotabletokeepup.
Cross-trainingofnursingstaffattriageandatbedsideif neededuntiltheregistrationstaffscaleupintermsof responseisessential.Moreover,trainingonactivating disasterstatusonEpicshouldbedonefordifferentEDstaff andnotlimitedtonursemanagersduringMCIs.Thisstepis keytoactivatingadisastermodulewithcorresponding disasterdocumentation.Additionally,cross-trainingallstaff onperformingdifferenttasksrelatedtoEHRinterface
duringMCIsiscrucial.Thisshouldbeaccompaniedby addressingaccess/roleslimitationspresentinroutine workflowsandbypassingthemifneededduringanMCI. Exampleswouldbetoallowphysiciansornursestoactivatea patientregistrationevent.Similarlymovingpatients electronicallyfromoneareatothenextcanbedoneby differentcliniciantypes.Thisrole fluiditycanenhance previouslysuggestedmodelstooptimizethemanagementof patient flowandmedicalresourcesduringMCIs.33
Testingadmission/flow/dischargeworkflowsinplanning forMCIsisalsokey.Throughputrestrictionsrelatedto financialclearanceandpatientadmission/discharge/flow throughphasesofcareshouldbereviewedandrestrictions liftedforallowingseamlesspatienttransferacrossthe hospital.Withthehighnumberofcomplexeventsoccurring duringanMCI,routineEHR-relatedrequiredstepsin differentunits/departmentsbecomeverycumbersomeand mayresultinunnecessarycomplications.Forexample, routinesequentialstepsdonotallowapatienttobeadmitted totheintensivecareunit(ICU)andforclinicianstoinitiate CPOEofcarebundlesintheICUbeforeaphysicianplaces anadmissionorderintheED.
TheIT-relatedactivitiesbecomeextremelycomplex duringMCIs.ScalingupquicklyintermsofIThelpdeskand supportiskeyduringanMCI.Assessingoverallsystem status,creatingnewrecords,addressingticketsrelatedto workflows,andprovidingonsitehelpwithregistration/ CPOE/reconciliationissuesareveryimportant.Settingup additionalnewtreatmentareasalsorequiresITsupport.The recoveryphasealsoentailshavingatrainedmultidisciplinary teamtoaddresstickets/resolvependingissues.Business continuityactivities(BCA)plansthatareusuallyputinplace donotaccountforoperationsduringMCIs.Duringthe Beirutportblast,theITinfrastructureremainedintact. However,intheeventwhereITinfrastructureisaffected, EHRsystemsmightbeimpacted,andinstitutionsshould resorttoalternativeBCAmeasures.LiteratureonITsupport insuchcriticalsituationsislimited.Futureresearchwillshed moreinsightsonthisaspectofMCIs.
Thisstudyhasseverallimitations.Theresultsre fl ectthe experienceofasinglecenterusingaspeci fi cEHR,limiting generalizabilityofour fi ndings.Atthesametime,thisisthe largestmedicalcenterinLebanonwithoneofthelargest catchmentareas.Inaddition,theEHRadoptedatthis centerisoneofthemostwidelyusedacrosstheUnited Stateswithagrowingpresenceglobally.34 Recallbiasof participantsduringthedebriefsandtranscribingbiases areadditionallimitationsthatmayhaveimpactedthe fi ndingsthatweredocumentedintheminutes.However, thepracticeofsendingminutestoallmeetingparticipants forcommentsandapprovalspriorto fi nalizationmitigates thelatter.
Wehaveoutlinedthechallengesofusinganelectronic healthrecordsysteminalarge-scalemasscasualtyevent.The mainimprovementopportunitieswererelatedtostaff training,failuretoaddresstherecoveryprocessintheinitial plan,andcomplexEHRworkflowsthatfailedtoeffectively scaleuptotherapidinfluxofpatients.Inparticular, streamliningEHRworkflowsrelatedtopatientregistration, patientidentification/tracking,andpatientadmissionis criticaltohandlingthescaleofpatient flowduringlarge-scale MCIs,asisstafftrainingontime-sensitiveregistration processes.Addressingthesechallengesaprioriinsettings thatrelyonEHRuseandincorporatingon-the-groundIT supportaspartoftheresponseteamisessentialtoan effectivehospitalMCIresponse.
AddressforCorrespondence:MazenElSayed,MD,MPH,American UniversityofBeirutMedicalCenter,DepartmentofEmergency Medicine,P.O.Box-11-0236RiadElSolh,Beirut,Lebanon1107 2020.Email: melsayed@aub.edu.lb
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Hittietal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
1.ElSayedM,ChamiAF,HittiE.Developingahospitaldisaster preparednessplanformasscasualtyincidents:lessonslearnedfrom thedowntownBeirutbombing. DisasterMedPublicHealthPrep. 2018;12(3):379–85.
2.HittiEA,ElSayedMJ,CheaitoMA,etal.Masscasualtymanagementin theemergencydepartment:lessonslearnedinBeirut,Lebanon-partI. MedJEmergMedAcuteCare. 2020;1(3).
3.VandenBergSLandDavidsonSB.Preparationformasscasualty incidents. CritCareNursClinNorthAm. 2015;27(2):157–66.
4.HalpernP,GoldbergSA,KengJG,etal.Principlesofemergency departmentfacilitydesignforoptimalmanagementofmass-casualty incidents. PrehospDisasterMed. 2012;27(2):204–12.
5.LandmanA,TeichJM,PruittP,etal.TheBostonMarathonbombings masscasualtyincident:oneemergencydepartment’sinformation systemschallengesandopportunities. AnnEmerMed. 2015;66(1):51–9.
6.ChenY.DocumentingtransitionalinformationinEMR.In CHI ’10: ProceedingsoftheSIGCHIConferenceonHumanFactorsin ComputingSystems(1787–96).NewYork,NewYork:Associationfor ComputingMachinery,2010.
7.DuhmJ,FleischmannR,SchmidtS,etal.Mobileelectronicmedical recordspromoteworkflow:physicians’ perspectivefromasurvey. JMIR MhealthUhealth. 2016;4(2):e5464.
8.SuttonRT,PincockD,BaumgartDC,etal.Anoverviewofclinical decisionsupportsystems:benefits,risks,andstrategiesforsuccess. NPJDigitMed. 2020;3(1):17.
9.TierneyMJ,PagelerNM,KahanaM,etal.Medicaleducationinthe electronicmedicalrecord(EMR)era:benefits,challenges,andfuture directions. AcadMed. 2013;88(6):748–52.
10.SuttonRT,ChappellKD,PincockD,etal.Theeffectofanelectronic medicalrecord-basedclinicaldecisionsupportsystemonadherenceto clinicalprotocolsininflammatoryboweldiseasecare:interruptedtime seriesstudy. JMIRMedInform. 2024;12:e55314.
11.HonavarSG.Electronicmedicalrecords-thegood,thebadandthe ugly. IndianJOphthalmol. 2020;68(3):417–8.
12.LevyG,BlumbergN,KreissY,etal.Applicationofinformation technologywithina fieldhospitaldeploymentfollowingtheJanuary2010 Haitiearthquakedisaster. JAmMedInformAssoc. 2010;17(6):626–30.
13.LeeJ,KuoY-F,GoodwinJS.Theeffectofelectronicmedicalrecord adoptiononoutcomesinUShospitals. BMCHealthServRes. 2013;13(1):39–46.
14.AldosariB,Al-MansourS,AldosariH,etal.Assessmentoffactors influencingnursesacceptanceofelectronicmedicalrecordinaSaudi Arabiahospital. InformMedUnlocked. 2018;10:82–8.
15. CheriffAD,KapurAG,QiuM,etal.Physicianproductivityandthe ambulatoryEHRinalargeacademicmulti-specialtyphysiciangroup. Int JMedInform. 2010;79(7):492–500.
16.McBrideS,DelaneyJM,TietzeM.Healthinformationtechnologyand nursing. AmJNurs. 2012;112(8):36–42.
17.AlqurainiH,AlhashemAM,ShahMA,etal.Factorsinfluencingnurses’ attitudestowardstheuseofcomputerizedhealthinformationsystemsin Kuwaitihospitals. JAdvNurs 2007;57(4):375–81.
18.NoblinA,Cortelyou-WardK,CantielloJ,etal.EHRimplementation inanewclinic:acasestudyofclinicianperceptions. JMedSyst. 2013;37(4):9955.
19.KennebeckSS,TimmN,FarrellMK,etal.Impactofelectronichealth recordimplementationonpatient flowmetricsinapediatricemergency department. JAmMedInformAssoc. 2012;19(3):443–7.
20.PerryJJ,SutherlandJ,SymingtonC,etal.Assessmentoftheimpacton timetocompletemedicalrecordusinganelectronicmedicalrecord versusapaperrecordonemergencydepartmentpatients:astudy. EmergMedJ. 2014;31(12):980–5.
21.NationalAcademyofSciences,Engineering,andMedicine,National AcademyofMedicine,Committeeonsystemsapproachestoimprove patientcarebysupportingclinicianwell-being.In: TakingActionAgainst ClinicianBurnout:ASystemsApproachtoProfessional Well-Being.Washington,DC:NationalAcademiesPress,2019.
22.ChanTC,GriswoldWG,BuonoC,etal.Impactofwirelesselectronic medicalrecordsystemonthequalityofpatientdocumentationby emergency fieldrespondersduringadisastermass-casualtyexercise. PrehospDisasterMed. 2011;26(4):268–75.
23.AbouzeidM,HabibRR,JabbourS,etal.Lebanon’shumanitariancrisis escalatesaftertheBeirutblast. Lancet. 2020;396(10260):1380–2.
24.NoordergraafGJ,BoumanJH,vandenBrinkEJ,etal.Developmentof computer-assistedpatientcontrolforuseinthehospitalsettingduring masscasualtyincidents. AmJEmergMed. 1996;14(3):257–61.
25.StanescuA,GordonPE,CopotoiuSM,etal.Movingtowardauniversal digitalerainmasscasualtyincidentsanddisasters:emergency personnel’sperspectiveinRomania. TelemedJEHealth. 2018;24(4):283–91.
26.BookmanKandZaneR.Expeditedelectronicentry:anewwayto managemass-casualtyradiologyorderworkflow. PrehospDisaster Med. 2013;28(4):391–2.
27.HajjarM,AtallahG,FaysalH,etal.The2020Beirutexplosion:a healthcareperspective. AnnBurnsFireDisasters. 2021;34(4):293.
28.DouglasC.MasscasualtyincidentCORDprogramsurvivalpacket. Availableat: https://www.cordem.org/siteassets/files/committees/
resilience/mci-cord-survival-pack-public.pdf AccessedMay31,2023.
29.TamiG,BruriaA,FabianaE,etal.Anafter-actionreviewtoolforEDs: learningfrommasscasualtyincidents. AmJEmergMed. 2013;31(5):798–802.
30.ClarkeVandBraunV.Thematicanalysis. JPositPsychol. 2017;12(3):297–8.
31.GodshallCEandBanachDB.Pandemicpreparedness. InfectDisClin NorthAm. 2021;35(4):1077–89.
32.HorahanK,MorchelH,RaheemM,etal.Electronichealthrecords accessduringadisaster. OnlineJPublicHealthInform. 2014;5(3):232.
33.TariVerdiM,Miller-HooksE,KirschT.Strategiesforimprovedhospital responsetomasscasualtyincidents. DisasterMedPublicHealthPrep. 2018;12(6):778–90.
34.ChishtieJ,SapiroN,WiebeN,etal.UseofEpicelectronichealthrecord systemforhealthcareresearch:scopingreview. JMedInternetRes. 2023;25:e51003.
KennethV.Iserson,MD,MBA TheUniversityofArizona,DepartmentofEmergencyMedicine,Tucson,Arizona
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedSeptember9,2024;RevisionreceivedSeptember27,2024;AcceptedOctober4,2024
ElectronicallypublishedNovember21,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.35390
Background: Disastroussituationsintheemergencydepartment(ED)orcommunitycanoverwhelm eventhebest-preparedteamsduetotheircomplexityanddynamicnature.Inthispaperweproposean integratedapproachtodisastermanagement,combiningsixtheoreticalandpracticalframeworksto enhancedecision-makingandoperationaleffectiveness.
Discussion: Theapproachbeginswith “ sensemaking, ” aninstinctiveprocessthathelpsleaders quicklygainsituationalawareness,acrucialfoundationfortherecognition-primeddecisionprocess (RPD).RPDenablesswift,experience-baseddecis ionswithoutexhaustiveanalysis,aligningthem withtheappropriatedomainintheCyne fi nframeworktoguidesubsequentinterventions.Inchaotic situations,rapidactionisnecessary,andtheedge-of-chaostheoryguidesleaderstobalanceorder andchaosforoptimaladaptability.Complexitytheoryaidsinmanagingtheunpredictableelements ofacrisis,highlightingtheneedfor fl exibleresponses.Finally,theIncidentCommandSystem ensureseffectiveimplementationbyprovidingastandardizedapproachtocommand,control, andcoordination.Thiscohesivestrategyequipsemergencyphysiciansandincidentcommandersto managebothinternalEDcrisesandbroadercommunitydisasterseffectively,withanemphasis ontheimportanceoftrainingintheseframeworkstoenhancetheresilienceofemergency medicalservices.
Conclusion: Thismultifacetedapproachshouldimprovedisastermanagementbybetterpreparing respondersfortheunpredictablenatureofemergencies,enablingeffectiveevaluationandmanagementof complexscenarios,andleadingtoamorerapidrestorationoforder.[WestJEmergMed.2025;26(1)30–39.]
Disasters,bothnaturalandman-made,varywidelyin scopeandscale.Theyinvolvecomplexinteractionsbetween patients,theenvironment,andhealthcaresystems.Such incidentsposesignificantchallengestotheentireemergency medicalsystem(EMS)continuum,includingemergency departments(ED),prehospitalcaresystems,anddisaster responseteams.1 Whileemergencyphysicians(EP)are preparedtomanagecrises,theirtrainingmaynotextendto situationsthatlackavailableresourcesorthatgobeyond theirknowledgeorexperiences.2
Disasterscanbeinternalorexternal.3 Healthcarefacilities mayfaceinternaldisasterwhentreatingpatientswith unusualorcomplexlifethreats,orwhentheirnormal functionsaredisrupted.Disruptionsmayresultfromtheloss ofessentialresourcessuchaswater,power,computer
systems,orstaff;asuddenincreaseinpatientnumbersor severity;orimminentthreatslike fires,bombthreats,or activeshooters.Externaldisastersoccuroutsidehealthcare facilitiesandmaybesimple typicallyshort-livedand manageableusinglocalresourcesorextended causing widespreaddamageandinjuriesthatnecessitateexternal assistancetosupportthesurvivinglocalservices,including healthcarefacilities.Widespreaddisastersarelong-term situationsarisingfrompandemics,drought,famine, andwar.4 Despitetheirdifferences,alldisastersand disorderedclinicalsituationssharecommonelementsthat caninformeffectivemanagement(Table1).Managinga disorderedsituationasanEPorasaprehospitalcareor disasterteamincidentcommander(IC)requiresa comprehensiveapproachthataddressesall theseelements.
1.Strategicplanning:Developingacomprehensiveand flexibleplantoaddressdifferenttypesofdisastersand disorderedclinicalsituations.
2.Hazardassessment:Identifyingpotentialhazardsand assessingtheirpotentialimpacttoprioritizeresourcesand developappropriateresponses.
3.Riskmanagement:Identifying,assessing,and implementingmeasurestoreducerisks.
4.Mitigation:Takingstepstoreduceadisaster’seffect.
5.Preparedness:Ensuringthatresources,systemsandstaff arereadytorespondeffectivelywhendisastersoccur.
6.Response:Takingmeasurestopromptlyevacuatepeople, providemedicalcare,andcoordinateresourcesina disastersituation.
7.Recovery:Makingprovisionstorestorenormalcyfollowing adisaster.
Problem
Thispaperaddressestheinadequacyofcurrentdisaster managementapproaches,whichoftenrelyonweakor inflexibleevaluationandmanagementtools.Whenused individually,thesetoolsareoftentoorigidtoadequately planfor,manage,andrecuperatefromthecomplexand unpredictablechallengesposedbylarge-scaledisasters.Most traditionaldisasterplanninggeneratesdetailedplansthat mayfailwhenconfrontedbyreal-worldscenarios.Since “noplansurvivescontactwiththeenemy,”7 disaster managementfailswhenleadersrigidlyfollowasingle methodorplanthatlacksthescopeand flexibilityofferedby integratingmultipleapproaches.
Educationalprogramsfordisasterpreparednesshave beenspecificallydesignedforEPs,surgeons,intensivists, anesthesiologists,andsimilarmedicalspecialties.8 These haveincludedsimulations,onlinegames,casestudies,and sharedexperienceswithseasonedprofessionals.Yetitis unclearwhethercurrentsystemstoeducateprofessionals aboutdisastermanagementprovidethemwiththeadequate toolstodealwithinternalandexternaldisasters.9–11 The integratedapproachproposedinthispaperequipsEPsand ICswithcomprehensivetoolsformanagingbothinternalED crisesandwidercommunitydisasters.Ithasthe flexibilityto enhancedecision-makinginhigh-pressuresituationsand improvetheircoordination.
Whilealreadyasmallelementofmedicaleducation,useof themethodsthatcomprisetheintegratedapproachshouldbe expandedandintegratedintoresidencyandcontinuing medicaleducationprograms,aswellasintotrainingfor potentialICsinEMSor fireservices.Throughexperiential learningandscenario-basedtraining,futureleaderscan developtheRPDskillsnecessarytonavigatethe
complexitiesofdisastermanagement,boostingtheir confidenceandagilityinemergencies.12
Inthispaperweproposecombiningsixdisasterevaluation andmanagementmethodsintoanovelintegratedapproach thatprovidesastructuredmethodologyadaptableto changingcircumstances.Thisfusionofmultipletheoretical andpracticalframeworksprovides flexibilityandenhances emergencydecision-makingandoperationaleffectiveness. Theproposedframeworkincludes,inorder,thefollowing:
1.Sensemaking
2.Recognition-primeddecision-making(RPD)
3.Cynefinframework
4.Edge-of-chaostheory
5.Complexitytheory
6.IncidentCommandSystem(ICS)
Whileseveralofthedisasterassessmentandmanagement elementsdescribedinthispaperaretaughtindividuallyin disaster-orientedcourses,others,suchastheedge-of-chaos andcomplexitytheories,haverarelybeendiscussedinthe healthcareliterature.13,14
Eachcomponentincrisismanagementisinterconnected, collectivelycontributingtotheoveralleffectivenessofthe process.Theproposedsequencebeginswithsensemaking, whichequipsleaderswiththesituationalawarenessneeded toquicklyidentifyfamiliarpatternsorcues.Thisawareness iscrucialforRPD,aprocessthatallowsleaderstodrawon pastexperiencestoswiftlydetermineacourseofaction withoutexhaustivelyanalyzingeverypossibleoption.
ThedecisionsmadethroughRPDarethenalignedwith theappropriatedomainintheCynefinframework,which helpsdeterminethemosteffectiveapproachtomanagingthe crisis.Ifasituationfallsintothechaoticdomain,leaders mustactrapidlytostabilizetheenvironment.Thisiswhere leaderscanusetheedge-of-chaostheorytorapidlyactatthe brinkofchaos,allowingforinnovationandadaptability. Complexitytheorythenallowsleaderstobetterunderstand andmanagetheunpredictableandinterconnectedelements ofacrisis.Finally,theICSensuresthatthesestrategiesare executedeffectivelybyprovidingastandardizedapproachto command,control,andcoordination.TheICSenables leaderstomanagecomplexsituationsbyorganizingteams, delegatingtasks,andensuringclearcommunication.
Eachcomponentbuildsonthepreviousone,contributing toacohesiveandadaptiveapproachtomanagingcritical, time-sensitivesituations.Theinterplaybetweenthese theoriesandframeworksallowsleaderstoevaluateand managecomplexscenarioseffectivelyincrisisanddisasters.
Thebalanceofthispaperdescribesalogicalprogressionof sixassessmentandmanagerialtoolsthatEPsandICscanuse whendealingwithill-definedproblemsunderhigh-stress conditions.Despitethepresentationofthesedecisionmakingelementsinsequentialorder,theyaredistinct componentsofatheoretical flowchartdesignedfordisaster assessmentanddecision-making.Thisstructuredpatternwill notalwaysapply,sincetherealworldisunpredictableand messy.Somestepsmayneedtobeusedsimultaneously;in othercases,previousstepswillneedtoberevisitedand adjustedasnewinformationclarifiesthesituation.
Thefollowingsectionsdescribethesixcomponentsofthis proposedsysteminmoredetail,withinformationonhow theybuildoneachothertoinfluenceoutcomes,whetherthey arecurrentlytaught,andbestwaystointroducetheminto acurriculum.
Component1:Sensemakinginemergencymedicine:initial assessmentandsituationalawareness
Inemergencymedicine(EM)anddisastersituationswhen informationisoftenincompleteorrapidlyevolving,the abilitytoquicklyinterpretconfusingorunclearsituations knownassensemaking isessential.Emergencyphysicians andICsmustswiftlycollectinformation,identifypatterns, formulateandthencontinuallyupdateplausiblenarratives basedondirectobservationsandinputsfrominitial responders.Suchinputisessentialforgraspingthenature andscaleofanevent,sinceearlymisunderstandingscanlead toineffectiveordangerousdecisions.
Sensemakingistriggeredwhenpeopleencounter unexpectedsituations,thosethatcontradicttheir expectations(eg,counterfactuals),orasignificantly ambiguouseventorissue.15 Thesesituationsmaydisrupt normalroutines,leadingindividualstoquestion fundamentalassumptionsabouthowtheyshouldact. Emergencyphysicianstypicallyengageinsensemakingwhen facedwithdiagnosticchallengeswheresymptomsmaynot clearlyindicateaspecificdisease,orindisastermanagement scenarioswhereinformationisinconsistentorincomplete. Byaskingappropriatequestions(Table2),theycanconstruct amentalmodelfromavailabledata,begintounderstandthe unfoldingsituation,evaluateavailableresources,andspecify immediategoals.12,16
Whenaleaderarrivesatanemergencysite,individuals suchasnurses,housestaff,and firstrespondersmightalready beworkingtostabilizethesituation.Theseindividualsoften haveabetterunderstandingofthecurrentcircumstances thanthenewlyarrivedleader.Itisimportantforleadersto acknowledgethevalueoftheactionsalreadyinprogressand toavoidinterruptingtheteam’smomentumbystoppingtheir activitiesfordetailedbriefings,ifpossible.12
Table2. Sensemakingquestions.Usedtoidentifykey stakeholders,evaluateavailableresources,andspecify immediategoalsinanunclearsituation.
• Whoisaffected?
• Whataretheimmediatethreatstolifeandsafety?
• Whatistheprimarygoaloftheresponseeffort(eg,rescue, evacuation,treatment)?
• Whatequipment,personnel,andsuppliesareonhand?
• Whatotherresourcesareavailable?
• Whatmoredoweneedtoknowtomoveforward? Afteraddressingthesequestions,theICcanthendecide:
• WhatdoIwanttodo?
• WhatdoIhavetodo?
• WhatcanIdo?
• WhatamItryingtoachieve?
IC,incidentcommander.
Sensemakingemphasizes flexibility,allowingleadersto navigatethedelicatebalancebetweenrigidadherenceto protocolsandtheneedforreal-timeadaptation.Akey strategywithinsensemakingistoinitiatedecision-makingin disorderedsituationswithtargetedquestionsratherthan immediatelydefaultingtoestablishedprotocolslikethe ICS.17 Thisapproachhelpsteamsbuildacoherent narrativeamidchaoticambiguity(eg,multiplepotential interpretationsofasituation)anduncertainty(eg,alackof interpretationsthatleavesindividualsunsureofthe nextsteps).
Toaddressrapidlydeterioratingsituations,leadersmust remain flexibleandunderstandthattraditionalemergency responseprotocols,whilevaluable,maybedifficulttoadapt totheunpredictablenatureofdisasters.Continuingthe sensemakingprocessenablesleaderstoshifttheirobjectives asthesituationdevelops(eg,fromresuscitationto stabilization,rescuetorecovery,searchtoevacuation). Sensemakingalsoaidsincategorizingthesituationusingthe Cynefinframework,atoolformanagingcomplexityand uncertainty(Table3).
Component2:Recognition-primeddecision-makingin emergencyanddisastermanagement
Leaderswithexperienceinemergencyanddisaster managementcanuseRPDtoquicklyassesscomplextimesensitivesituations.Theyleveragetheirstoreofexperiences andtacticsfrompreviousincidentsandtrainingtoselect effectivecoursesofaction.18,19 Instinctivelyrecognizing familiarelements,ie,sensemaking,theycanusethose insightstoconstructareasonableunderstanding ofthecrisis.19
Thispatternrecognitionenablesthemtomakeswiftinitial decisionstomitigateimmediatethreats.Whilenotalways
Table3. Progressionfromsensemakingtorecognition-primed decision-making(RPD)andtheCynefinframeworkindisasters.
• Assessthescopeandconsequencesofthedisaster, includingimmediatelife-threateningconcernsandproperty damage.
• Identifycriticaltasksanddeterminetheirpriority.
• Establishanunderstandingofthesituation,focusingon plausibilityratherthanabsoluteprecision.
• Recognizefamiliarelementswithinacomplexsituationto beginimposingorderonchaosandguidethesituation towardnormalization.
fullynuanced,thesedecisionsarecrucialforstabilizingthe situationandallowingtimeformorecomprehensivedatagathering.Thedecision-makingprocessinvolvesasking criticalquestionstoassessthedisastertype,casualty numbers,environmentalhazards,andavailableresources, whilealsoclarifyingtheprimaryobjectivesoftheresponse effort.Suchclarityisessentialfordirectingactionsand resourcestowardmeaningfuloutcomes.
finframeworkinemergency anddisastermanagement
TheCynefinframework,developedbyDaveSnowdenand MaryE.Boone,canenableEPsandICstoquicklycategorize andrespondtosituationsbasedontheircomplexityand enhancestheirabilitiestomakeswift,effectivedecisions underpressure.20 Thismodel(Figure)helpsdifferentiate amongclear/obvious,complicated/difficult,complex, chaotic,anddisarray/confusion/disordered/uncertain domains,eachofwhichnecessitatesaspecificresponse strategy(Table4)torestoreorder.Assuch,itprovidesan essentialtoolformanagingthediverseandunpredictable
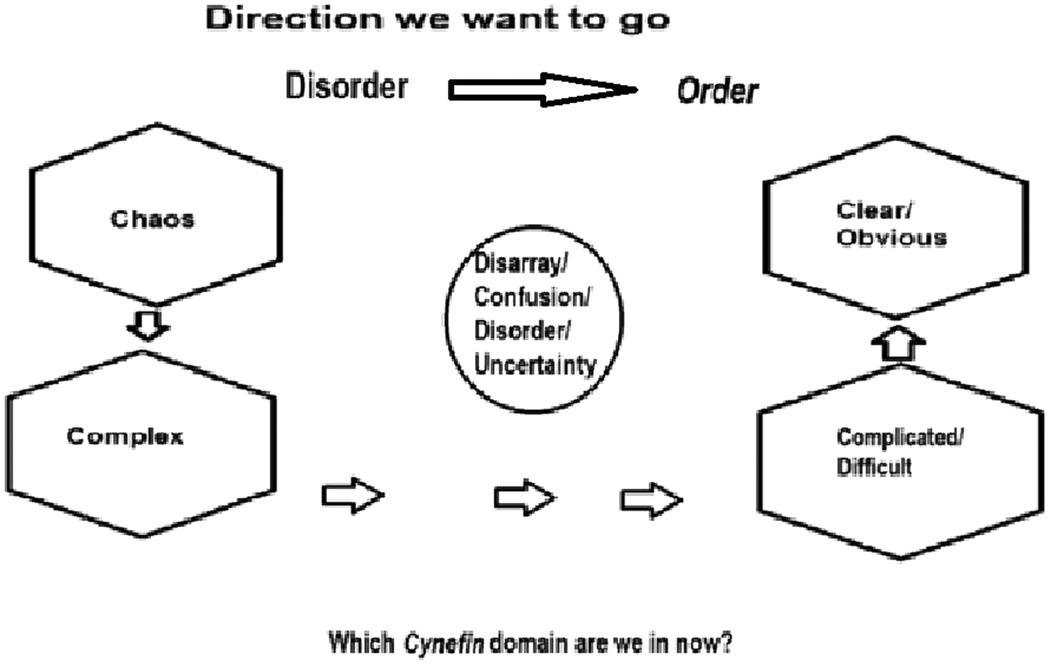
Figure. ThisCynefinmodelillustratesthedesiredmanagement flowfromdisordertoorder.Indisorderedsituations,theleader identifiesthesituation’sdomain(chaotic,complex,complicated, orclear)andusesthecorrectresponsestrategy(Table4).
Table4. Responsestrategiesfor fivedomainsinthe Cynefinframework.
• Simple/clear:Confirmrulesorprecedents,applybest practices.
• Complicated:Analyzethesituation,applyexpertknowledge.
• Complex:Experimentandadaptresponsesbasedon emergentpatterns.
• Chaotic:Actimmediatelytostabilize,seeknovelsolutions.
• Disorder:Gathermoreinformationtocategorizethesituation correctly.
natureofemergencyscenarios.Leadersinavarietyof healthcare fieldshavemodifiedthismodelfor variousscenarios.21
Originatinginthebusinessworld,theCynefinmodelhas beenadaptedtoprovideclinicianswith “ataxonomyfor categorizingthevarioustypesofuncertainty,aswellasa frameworktoapplywhennavigatinguncertaintyduring clinicalchallenges.Thesetoolscanhelpstudentsmakesense ofuncertaintyanddetermineactionsinacomplexhealth system.”22 Insituationscategorizedassimpleorclear,where therelationshipbetweencauseandeffectisstraightforward, thestrategyinvolvesmakingsenseofthesituationby gatheringdata,confirmingtheproblemhasclearrulesor precedents,andrespondingwithestablishedprotocolssuch astheICS.Suchclear,predictableproblemswithwellunderstoodsolutionsareamenabletobestpracticesand standardoperatingprocedures.Forexample,apatientwith anisolatedfracturedhumerusorminorinjuriesfromamotor vehicleaccidentwould fitintothe “simple” domain,where establishedmedicalprotocolsaredirectlyapplicable.
Morecomplexorchaoticscenariosdemandinnovative andadaptivestrategiesduetotheirunpredictabilityandthe opaquerelationshipbetweencauseandeffect.Forinstance,a patientpresentingwithararecombinationofsymptomsora catastrophiceventlikeabuildingcollapsewithmultiple casualtieswouldfallintothesedomains.Suchsituations requireexploratoryapproachesthatemphasize experimentationratherthanlinearsolutions,which oftenproveinsufficient(see Appendix).
KarlWeick,anorganizationaltheorist,emphasizesthe importanceofcategorizingunclearornovelsituationswithin theCynefinframeworktoclarifyandaddressthem effectively.Thisstructuredapproachallowspractitionersto identifythedomainasituationbelongsto beitsimple, complicated,complex,chaotic,ordisorder andtailortheir decision-makingandactionsaccordingly.Inmorecomplex orchaoticdomains,whereuncertaintyprevails,further informationgatheringisnecessarytodeterminean appropriateresponsestrategy.Here,thestrategyshifts towardmaintainingabalancebetweenstability using provenmethods and flexibility adaptingtotheunique
challengesofthesituation,assuggestedbythe edge-of-chaosparadigm.
Component4:Navigatingtheedge-of-chaosparadigmin disasterresponse
Theedgeofchaosisaconceptderivedfromcomplexity theory,whichdescribestheprecariousstateexistingbetween orderandcompleterandomness.23,24 Withinthecontextof theCynefinframework,thisconceptrepresentsaninitial stateofdisorder,confusion,anduncertainty,wherethe applicationofsensemakingandRPDiscrucial.Thisconcept canbevisualizedasaninfinitesimallythinmembrane markingthetransitionfromchaoticdisordertoanordered, manageablescenario.Insuchconditions,EPsandICsmust navigateadelicatebalancebetweenmaintainingstability (order)andadaptingtonewinformation(flexibility).The EPsandICsneedtoidentifywhenanincidentisatornearing theedgeofchaostofostereffective,adaptiveresponsesto rapidlyevolvingconditions.Theyshouldbeabletorecognize thesituationalcharacteristicsthatindicatethattheyare approachingtheedgeofchaos.Theseincludethefollowing:
Increasinginformationcomplexity
Thismayinvolvecontradictoryreports,escalating numbersofcasualties,orconflictingoperationaldirectives, allofwhichcomplicatetheresponseeffort.
Decision-makingdifficulties
Asuncertaintiesandcomplexitiesmultiply,thedecisionmakingprocessbecomesmorechallenging.Thedeclinein effectivenessofstandardprotocolsmayindicatetheneedfor adaptive,creativesolutions.
Increasedcommunicationbreakdowns
Effectivecommunicationisessentialformaintaining order.Failuresintechnologyormisunderstandingsamong teammembersthatcausecommunicationbreakdownsmay necessitateashiftinmanagementtactics.
Resourcelimitations
Adecreaseinavailableresources,whetherpersonnel, equipment,orinformation,cansignalmovementtoward chaoticconditions.Monitoringresourceusageand forecastingfutureneedsarecriticalforrecognizingand respondingtothisshift.
Theedge-of-chaosparadigmunderscoresthecomplexity ofdecision-makingunderconditionscharacterizedbytime pressure,dynamicchanges,andchallenginglogistics.It servesasabridgeacrossvariousdisasterleadership methodologies,emphasizingtheneedtomaintainabalance topreventthesituationfromtippingintochaos.This approachrequiresEPsandICstobeexceptionallyagile, usingablendofestablishedprotocolsandinnovative solutionstomanagedisasterseffectively.Byrecognizingand
respondingtothesignsoftheedgeofchaos,leaderscan preventfurtherdeteriorationofthesituationandguidetheir teamstowardrestoringorderandstability.
Component5:Complexitytheoryanditsimportancein emergencyresponse
TheEPoftenoperatesinconditionsmarkedbyhigh uncertaintyandunpredictability,conditionsthatpointtothe needforanunderstandingofcomplexitytheory.Thistheory, sometimesreferredtoas “high-dimensionalchaos,”25 is rootedinmathematics,physics,andcellularbiology,andcan helpEPs26 navigatethenatureofemergencies,facilitating betterlong-termplanningandresourceallocation.25 Itisa vitalframeworkforenhancingdecision-making,efficiency, andadaptabilityinthedynamic,unpredictableenvironments withmultipleinterconnectedcomponentstypicalof emergencyanddisasterresponses.27,28
Althoughdefiningcomplexitytheoryhasprovenelusive andhasrarelybeenappliedtohealthcare,29,30 itcanhelpEPs discernwhetherasituationiscomplicated,withclearcauseand-effectrelationships;complex,characterizedbyemergent behaviors;orchaotic,withunpredictableelements.
Thecorefeaturesofcomplexitytheoryinemergency responseincludeunpredictability,self-organization, emergentbehaviors,andfeedbackloops.
Unpredictability(nonlinearity)
Incomplexsystems,therelationshipbetweencauseand effectisnotlinear,makingoutcomeshardtopredict.Small changescantriggerdisproportionatelylargeeffects, reflectingthesystem’ssensitivitytoinitialconditions(the “butterflyeffect”).27,28,31 ThisaspectiscrucialinEM,where asmallalterationinteamdynamicsordecisionpointscan significantlyshifttheoutcome.
Self-organization
Complexsystemsexhibitacapacitytoorganize spontaneouslywithoutexternalcontrol.32 InEM,thisis observedwhenmultidisciplinaryteams(eg,a “flashmob”) rapidlyassembleinresponsetoatraumacall.Althoughtheir communications,equipment,commandstructure,andgoals maynotinitiallygel,theyquicklyaligntofunctionasasingle organicteam.Somevolunteerwildernessrescuegroupsalso worklikethis;knowingeachother’scapabilities,they automaticallyplacethemostexpertpersonateachstagein theleadrole(eg,organizingtheteam,settinguptechnical gear,medicalassessment/treatment,andevacuation)inwhat theyterma “flowingcommandsystem.” [Personal communication,fromtheSouthernArizonaRescue Association,PimaCounty,AZ;February1,2024.]
Emergentbehaviors
Thesebehaviors,whicharenotpredictablefromthe system’sinitialconditions,oftenariseincomplexsituations.
Theymaymanifestasnewpatternsofteaminteractionorthe useofinnovativeproblem-solvingapproacheswhen standardproceduresproveinsufficient.33 Ascomplex systemsself-organize,theybecomemorethanthesumof theirparts.28 Thismakesitimpossibletopreciselydetermine outcomesfrominterventions(nonlinearity).34
Feedbackisessentialforadaptingtochangingconditions withinemergencyresponses.Theseself-regulatingsystems canamplifyordampentheeffectsofthesystem’sbehavior, enhancingadaptabilityandresilience.35,36 Managing complexsituationsrequiresleaderstoknowwhich interventionshavesucceeded.Thisallowsteamstorapidly implementalternativeactionswhennecessary.Complexity theorynotonlyprovidesatheoreticalframeworkbutalso setsthestageforpracticaldecision-makinginemergency situations.Itoffersinsightsintothenatureofdisorderand remindsleadersthatunexpectedbehaviorsandoutcomesare typicalundercomplexconditions.Furthermore,thetheory underscoresthepotentialforordertoemergefromchaos throughself-organizationandresilience.
Understandingtheinteractionsamongsystem components individuals,teams,resources,and environmentalfactors iskeytomanagingoverallsystem behavior.Theseinteractionsoftengiverisetonew characteristics(ie,emergentproperties)thatcannotbe predictedfromthesystem’sindividualcomponentsalone.In essence,thesumofthepartsismorethanthewhole.This requiresmanagerstobeboth flexibleandinnovative. Includingcomplexitytheoryinemergencyresponse trainingandoperationsenhancestheabilityofEPsandICs tobettermanagedisastersbypreparingEPstoanticipateand respondtounexpectedsituations.Moreover,complexity theorysupportsthecreationofnetworksthatfoster collaborationacrossvariousagenciesanddisciplines, optimizingthecollectiveresponseeffort.Byembracinga flexible,adaptivemindsetandimplementingcontinuous learningandimprovement,emergencyprofessionalscan navigatetheevolvingdynamicsofemergenciesmore effectively(Table5).
Component6:IntegrationoftheIncidentCommandSystem inEManddisasterresponse
Afterdevastingwildfiresinthe1970s,SouthernCalifornia firefightersdevelopedtheICStorespondtodisastersina coordinatedmannerandtorequestregionalresourcesasthe situationexpanded.WhentheSeptember11attacksshowed thatcoordinatingfederalandstatewithlocalresourceswas vital,thiswasincorporatedintotheNationalIncident ManagementSystem.40 TheICSisanessentialstructured approachthatintegratessensemakingandtheCynefin frameworktomanageresourceseffectivelyacrossvarious emergencyscenarios.ThissystemprovidesEPsandICswith astandardizedmethodforincidentmanagementthat remainsconsistentregardlessofthecomplexityofthe situation beitsimple,complicated,complex,orchaotic.It ensuresclearlinesofauthority,effectivecommunication, andcoordinatedresourceallocation,makingitindispensable formanagingbothresourcesandpersonnel.
TheICSpromoteseffectivecoordinationand communicationamongallresponders,medicalpersonnel, andrescueteamsthroughitsunifiedterminology,modular organization,andclarityincommunicationchannels.These featuresarecrucial,especiallyincomplexsituations involvingmultipleagencies,whenitisnecessarytohaveall partiesalignedandinformed.Despiteitsstrengths,theICS canberestrictiveduringtheinitialphaseofdisasters.The system’srelianceonchecklistsandtasksmaylead first responderstoprioritizeproceduraladherenceovergaininga deeperunderstandingofthebroadercrisis.Thisadherenceto protocolcanlimittheabilitytoaddresschaoticsituations wherenostraightforwardguideexists,asnotedinthecritique that “Whileeveryonecanbe trainedtofollowachecklist duringlaterstagesofanevent,thereisnoexactguideforhow toworkthroughchaos.”12,17
Asscenariostransitionfromchaoticanddisorderedstates tomorecomplexorcomplicateddomains,theadvantagesof theICSbecomemoreevident.Inthesestages,thestructured natureoftheICSsupportsmethodicaldecision-making, particularlyinscenariosfamiliartoresponders.Itallowsfor deliberateactionsbasedonthoroughsituationalawareness andafactualunderstandingoftheincident.Describedasa
Rapidsetupofcoordinatedtriageareasledtoefficientpatient managementdespiteoverwhelmingnumbers.
HurricaneKatrina38 EmergenceandadaptabilityAd-hocmedicalhubsandtrainedleadersimprovedsurvivalratesamidst infrastructurecollapseandmultipleleadershipfailuresatalllevels.
COVID-19pandemic39 Allprinciplesofcomplexity theory Dynamicresponsestrategieslikeadaptablehospitalzonesandreal-time datatrackinghelpedmanagepatientloadseffectively.
Table6. Keyoutcomesofdisastermanagementtrainingforemergencyphysiciansandincidentcommanders. OutcomeDescriptionImpactonemergencycare
Enhanceddecisionmaking44
Improvedcrisis management45
Increasedsystem resilience46
Proactiveproblem solving47
Teamcohesionand dynamics48
Abilitytomakeinformeddecisionsamidstchaos.Leadstobetterpatientoutcomesandless confusionduringcrises.
Effectivemanagementofsudden,unpredictableevents.Reduceserrorsandimprovesoverallemergency responseeffectiveness.
Strengtheningoftheemergencycaresystemtowithstand pressures.
Anticipatingandaddressingcomplicationsbeforethey escalate.
Improvedteamworkunderstressthroughunderstanding ofrolesanddependencies.
military-typesystememphasizingcommand,control,and coordination,theICSisparticularlysuitedforlarge-scale operations.Itsstructuredapproachiscriticalinguiding effortsinEManddisasterresponse,especiallywhen combinedwiththeprinciplesofcomplexitytheory.This integrationacknowledgesthedynamicandmultifaceted natureofsuchenvironments,enhancingthe system’seffectiveness.
ByrecognizingthestrengthsandlimitationsoftheICS withintheframeworkofcomplexitytheory,emergency managementcanadaptthesystemtobettermeetthe demandsofdiverseemergencysituations.Thisadaptation allowsforabalancebetweentheneedforstructured responsesinfamiliarscenariosandthe flexibilityrequiredin unpredictableornovelemergencies.
Integratingeducationalmethodsforadvanced decision-makingframeworksintoEM
TrainingEPsinadvanceddecision-makingframeworks involvesastructuredapproachtounderstandingand applyingthevarioustheoriesandsystemscrucialforeffective emergencyresponse.FortheRPDmodel,scenario-based trainingisinstrumental,allowingphysicianstorapidly assimilatepastexperienceswithcurrentsituationstomake effectivedecisionsunderpressure.Integratingsensemaking intotraininginvolvesscenario-basedlearningwhere physiciansinterpretcomplexorambiguousinformationto constructacoherentunderstandingofevolving situations(Table6).41–43
Rusnacketaldescribedaworkshoptoprepareclinicians tousesensemakingandtheCynefinframeworktowork throughcomplexclinicalchallenges.Participantslearnedto categorizeproblemsintosimple,complicated,complex,or chaoticdomains,andtoapplyappropriatedecision-making strategiesbasedonthesituation’snature.39 Complexity theoryandtheedge-of-chaostheoryshouldbeintegrated intothecurriculumthroughinteractivelecturesandgroup discussionsthatexplorethedynamicsofcomplexsystems andtheirimplicationsonemergencymanagement.
Ensuressustainabilityandreliabilityofemergency medicalservices.
Decreasesincidentseverityandimprovespatient recoveryrates.
Enhancesoperationalefficiencyandstaffmorale duringemergencies.
TheICS,essentialformanagingemergencyresponses, requiresbothknowledge-basedlearningandpractical exercises.TrainingshouldincludedetailedmodulesonICS protocolsandroles,supplementedbydrillsthatsimulate multi-agencyresponsescenariostofostercoordinationand communication.Trainingthatblendstheoreticalinstruction withpracticalexercisesprovidesEPswiththeskillsneededto handleawiderangeofchallengesinemergencysituations. Thistrainingleveragesadeepunderstandingofdifferent decision-makingframeworkstoimprovetheireffectiveness andadaptabilityduringreal-worldcrises.
Thisproposaltoreformulateandintegratedisaster evaluationmethodswill,hopefully,beastimulusto emergencyanddisastermedicinetoreconsidertheir approachestocrisesbecauseitdoesthefollowing:
• Presentsaninnovativeandintegratedapproach thataddressessignificantgapsindisastermanagement.
• Enhancesdecision-making,promotescomprehensive training,andimprovesemergencyresponse effectivenessandoutcomes.
• Significantlyimprovesoutcomesbypreparing respondersfortheunpredictablenatureofemergencies. Byenhancingcoordination,decision-making,and training,itbuildsmoreresilientEMSandoptimizes resourceallocationduringcrises.
• Laysthegroundworkforfutureresearchtoevaluatethe combinedframework’seffectivenessinreal-world disasterscenarios.Bypresentingthisconcept,wecan stimulatediscussionandcollaborationamong emergencyclinicians,researchers,andpolicymakers toadvancethe fieldofdisastermanagement.
Thisexplorationofdisaster-managementtools demonstratesthatintegratingmultipletheoretical frameworksandmethodologies,suchassensemaking,the recognition-primeddecisionprocess,theCynefin
framework,theedge-of-chaostheory,complexitytheory, andtheIncidentCommandSystem,cansignificantly enhancethedecision-makingprocessandoperational efficiencyinemergencyanddisastermanagement.This synthesisoffersemergencyphysiciansandincident commandersarobusttoolsetwithwhichtonavigatethe multifacetednatureofdisastersituations whetherthese occurwithinhealthcarefacilitiesorinexternalenvironments.
Byadoptingthisintegratedapproach,emergency managementpersonnelcanbetteraddresstheinherent complexitiesofdisasterscenarios,ensuringmorerapid stabilizationofchaoticsituationsandamoreorganized transitiontorecoveryphases.Theemphasisondynamicand adaptableresponsestrategiesaidsinmanagingemergencies wheretraditional,rigidcommandstructuresmayfallshort.
Furthermore,thepaperhighlightsthecriticalroleof continuoustrainingandeducationintheseintegrated frameworks.Itarguesthatwell-preparedemergencyteams, versedintheseframeworks,arebetterequippedtomanage theunforeseenandrapidlyevolvingchallengesofdisaster scenarios.Theapplicationofthesecomprehensivestrategies notonlyenhancesthecapabilityofemergencypersonnelto performunderpressurebutalsoimprovesoverallpatient outcomesandsystemresilience.
Asdisasterscontinuetopresentuniqueandcomplex challenges,ongoingresearchandadaptationofthese frameworkswillbeessential.Theevolvingnatureofglobal threats rangingfromnaturaldisasterstotechnologicaland biologicalhazards demandsaprogressiveapproachto emergencymanagementeducationandpractice.Integrating thesediverseframeworksintoaunifiedoperationalstrategy ensuresawell-roundedresponsecapability,fosteringamore resilientandeffectiveEMS.Thispaperservesasacallto actionforemergencyresponseorganizationsandtraining institutionstoembracethismultifacetedapproach.Itisvital forenhancingthepreparednessandresponseeffectivenessin thefaceofdisasters.
AddressforCorrespondence:KennethV.Iserson,MD,MBA,The UniversityofArizona,DepartmentofEmergencyMedicine,1501N. CampbellAvenue,P.O.Box245057,Tucson,AZ85724. Email: kvi@u.arizona.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Iserson.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
1.WaldmanR.Naturalandhuman-madedisasters.In: TheCDCField EpidemiologyManual. 2018.Availableat: www.cdc.gov/eis/field-epimanual/chapters/Natural-Human-Disasters.html AccessedAugust3,2024.
2.AmericanCollegeofEmergencyPhysicians.Roleofemergency physiciansindisasterpreparednessandresponse.2021.Availableat: www.acep.org/siteassets/new-pdfs/policy-statements/roleof-emergency-physicians-in-disaster-preparedness-and-responseimpact-of-covid-pandemic.pdf.AccessedAugust3,2024.
3.SlotaM. TheJointCommission:Emergencymanagementplansand codes. 2017.Availableat: www.bmhvt.org/wp-content/uploads/ E_Mgmt_Plans_and_Codes.pdf. AccessedAugust5,2024.
4.IsersonKV. ImprovisedMedicine:ProvidingCareinExtreme Environments(6–7),2nd ed.NewYork,NY:McGraw-Hill Publishing,2016.
5.TulaneUniversity,SchoolofPublicHealthandTropicalMedicine.What isdisastermanagement?Understandingemergenciesfromprevention tomitigation.2021.Availableat: https://publichealth.tulane.edu/blog/ what-is-disaster-management/.AccessedAugust5,2024.
6.FederalEmergencyManagementAgency.Emergencymanagementin theUnitedStates.2021.Availableat: www.fema.gov/sites/ default/files/documents/nims-incident-complexity-guide.pdf AccessedAugust5,2024.
7.BarnettC. TheDesertGenerals.NewYork,NY:VikingPress,1960. Ideaoriginallyfrom:vonMoltkeH.(1871). DieThätigkeitalsChefdes GeneralstabesderArmeeimFrieden.Berlin,Germany:ErnstSiegfried MittlerundSohn.
8.KleinGA.(1993).Arecognition-primeddecision(RPD)modelofrapid decisionmaking.In:KleinGA,OrasanuJ,CalderwoodR,etal.(Eds.). DecisionMakinginAction:ModelsandMethods.Norwood,NewJersey: AblexPub,1993.
9.GowingJR,WalkerKN,ElmerSL,etal.Disasterpreparednessamong healthprofessionalsandsupportstaff:whatiseffective?Anintegrative literaturereview. PrehospDisasterMed. 2017;32(3):321–8.
10.WestmanA,KurlandL,HugeliusK.Non-technicalskillsneededby medicaldisasterresponders ascopingreview. ScandJTrauma ResuscEmergMed. 2024;2;32(1):25.
11.Khorram-ManeshA,LupescoO,FriedlT,etal.Educationindisaster management:whatdoweofferandwhatdoweneed?Proposinganew globalprogram. DisasterMedPublicHealthPrep. 2016;10(6):854–73.
12.RenaudCE. Makingsenseintheedgeofchaos:Aframeworkfor effectiveinitialresponseeffortstolarge-scaleincidents(Doctoral dissertation,Monterey,California.NavalPostgraduateSchool). Availableat: https://ahimta.org/resources/Documents/RENAUD.pdf AccessedFebruary15,2024.
13.CoetzeeC,vanNiekerkD,KrugerL.(2019).Buildingdisasterresilience ontheedgeofchaos:asystemscritiqueonmechanisticglobaldisaster reductionpolicies,frameworksandmodels.In:NewYork,NY:Springer. DisasterResearchandtheSecondEnvironmentalCrisis:Assessingthe ChallengesAhead(205–21)
14.MoeenianM,GhazinooryS,YaghmaieP.Analysingtheperformanceof ahealthinnovationecosystemintheCOVID-19crisis:complexityand chaostheoryperspective. HealthResPolicySyst,BMC. 2024;21(1):59.
15.UrquhartC,CheukB,LamL,etal.Sense-making,sensemakingand sensemaking asystematicreviewandmeta-synthesisofliteraturein informationscienceandeducation:anannualreviewofinformation scienceandtechnology(ARIST)paper. JAssocInfSciTech.Advance onlinepublication.AccessedJuly24,2024.
16.DwyerG.(2022).Learningassensemaking.In: MakingSenseof NaturalDisasters(15–42).NewYork,NY:PalgraveMacmillanCham, 2022.
17.FederalEmergencyManagementAgency.Incidentcomplexityguide: planning,preparedness,andtraining.2021.Availableat: www.fema. gov/sites/default/files/documents/nims-incident-complexity-guide.pdf AccessedFebruary20,2024.
18.ElsteinASandSchwarzA.Clinicalproblemsolvinganddiagnostic decisionmaking:selectivereviewofthecognitiveliterature. BMJ. 2002;324(7339):729–32.
19.BoinA,SternE,SundeliusB. ThePoliticsofCrisisManagement:Public LeadershipUnderPressure.Cambridge,UK:CambridgeUniversity Press,2016.
20.SnowdenDJandBooneME.Aleader’sframeworkfordecisionmaking. HarvardBusRev. 2007;85(11):68–75.
21.LanePJ,Clay-WilliamsR,JohnsonA,etal.Creatingahealthcare variantCYNEFINframeworktoimproveleadershipandurgentdecisionmakingintimesofcrisis. LeadershHealthServ. 2021;34(4):454–61.
22.RusnackF,PapanagnouD,ReopelleK,etal.Navigatinguncertaintyin clinicalpractice:aworkshoptopreparemedicalstudentstoproblemsolveduringcomplexclinicalchallenges. MedEdPORTAL. 2023;19:11334.
23.SellnowTL,SeegerMW,UlmerRR.Chaostheory,informationalneeds, andnaturaldisasters. JAppCommRes. 2002;30(4):269–92.
24.OestreicherC.Ahistoryofchaostheory. DialoguesClinNeurosci. 2007;9(3):279–89.
25.Bar-YamY.Concepts:chaosvs.complexsystems.2011. Availableat: https://necsi.edu/chaos-vs-complex-systems AccessedMarch10,2024.
26.RicklesD,HaweP,ShiellA.Asimpleguidetochaosandcomplexity. JEpidemiolCommunityHealth. 2007;61(11):933–7.
27.WeaverW.Scienceandcomplexity. AmScientist. 1948;36(4):536–44.
28.DomenicoM,BruckmannD,CarmargoC,etal.Complexityexplained. 2019.Availableat: https://complexityexplained.github.io/ AccessedMay1,2024.
29.EstradaE.Whatisacomplexsystem,afterall? FoundSci. 2023;30:1–28.
30.LitakerD,TomoloA,LiberatoreV,etal.Usingcomplexitytheorytobuild interventionsthatimprovehealthcaredeliveryinprimarycare. JGenInternalMed. 2006;21:S30–4.
31.LorenzEN.Deterministicnon-periodic flow. JAtmosphericSci. 1963;20:130–41.
32.CollinsJ.Complexityversuschaos.2014.Availableat: www.jasoncollins.blog/posts/complexity-versus-chaos AccessedFebruary12,2024.
33.IsersonKV.Informedconsentforartificialintelligence:apracticalguide. AmJEmergMed. 2024;76:225–30.
34.ChappeR.Chaostheory:complexity,emergence,andchaos.2017. Availableat: https://thebrooklyninstitute.com/items/courses/ new-york/chaos-theory-complexity-emergence-chaos/ AccessedMarch10,2024.
35.HoldenLM.Complexadaptivesystems:conceptanalysis. JAdvNurs. 2005;52(6):651–7.
36.PypeP,KrystallidouD,DeveugeleM,etal.Healthcareteamsas complexadaptivesystems:focusoninterpersonalinteraction. Patient EducCouns 2017;100(11):2028–34.
37.RiceRMandBloomfieldEF.Commemoratingdisorderinafter-action reports:rhetoricsoforganizationaltraumaaftertheLasVegasshooting. JIntCrisisRiskCommRes. 2022;5(1):87–111.
38.FarazmandA.HurricaneKatrina,thecrisisofleadership,andchaos management:timefortryingthe ‘surprisemanagementtheoryinaction.’ PublicOrgRev. 2009;9:399–412.
39.BlanchardJ,MessmanAM,BentleySK,etal.Intheirownwords: experiencesofemergencyhealthcareworkersduringtheCOVID-19 pandemic. AcadEmergMed. 2022;29(8):974–86.
40.NewburyBAandObernierR.Theincidentcommandsystem.InNew York,NY,Elsevier:CiottoneG(Ed.): Ciottone’sDisasterMedicine 3rd ed,2024.(275–80).;2024.
41.ExadaktylosA.(2021).Theimportanceofeducationandtrainingin disastermanagement:anoverview.InPikoulisEandDoucetJ(Eds.). Cham,Switzerland:Springer. EmergencyMedicine,Traumaand DisasterManagement.HotTopicsinAcuteCareSurgeryandTrauma (591–7)
42.GoniewiczK,GoniewiczM,Włoszczak-SzubzdaA,etal.The importanceofpre-traininggapanalysesandtheidentificationof competenciesandskillrequirementsofmedicalpersonnelformass casualtyincidentsanddisastertraining. BMCPublicHealth 2021;21(1):114.
43.HungMSY,LamSKK,ChowMCM,etal.Theeffectivenessofdisaster educationforundergraduatenursingstudents’ knowledge,willingness, andperceivedability:anevaluationstudy. IntJEnvironResPublic Health. 2021;18(19):10545.
44.BrooksB,CurninS,BearmanC,etal.Anassessmentofthe opportunitiestoimprovestrategicdecision-makinginemergencyand disastermanagement. AustralJEmergManag. 2016;31(4):38–43.
45.FarcasA,KoJ,ChanJ,etal.Useofincidentcommandsystemfor disasterpreparedness:amodelforanemergencydepartmentCOVID19response. DisasterMedPublicHealthPrep. 2021;15(3):e31–6.
46.JasaniG,HertelendyA,CiottoneGR.Strengtheningemergency departmentresiliency-residentdeploymentconsiderations duringamass-casualtyincident. PrehospDisasterMed. 2022;37(5):571–3.
47.FederalEmergencyManagementAgency.Decisionmaking andproblemsolvingindependentstudy.2005. https://training. fema.gov/emiweb/downloads/is241.pdf AccessedAugust17,2024.
48.ZarolaT.Theimportanceofteamcohesionandidentityforemergency preparedness.2014.Availableat: https://naru.org.uk/the-importanceof-team-cohesion-and-identity-for-emergencypreparedness/.AccessedAugust17,2024.
*†
DylanS.Kellogg,MD,MSMEd
MiriamS.Teixeira,MD,PhD‡ MichaelWitt,MD,MPH
*
SectionEditor:JeffreyDruck,MD
*ArnotOgdenMedicalCenter,DepartmentofEmergencyMedicine&Emergency MedicineResidency,Elmira,NewYork † ArnotOgdenMedicalCenter,EMSEducationProgram,Elmira,NewYork ‡ ArnotOgdenMedicalCenter,ResearchDivision,DepartmentofGraduate MedicalEducation,Elmira,NewYork
Submissionhistory:SubmittedDecember29,2023;RevisionreceivedSeptember19,2024;AcceptedOctober2,2024
ElectronicallypublishedNovember20,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18661
Introduction: Ruralcommunitiescontinuetofaceashortageofemergencyphysiciansdespitethe growingnumberofemergencymedicine(EM)residencies.Inruralareas,emergencyphysicianstendto beolder,male,andWhite,andarelesslikelytohavecompletedEMresidencytrainingorhaveboard certification.Thereisalsocurrentlyahigherrateofruralphysiciansleavingclinicalpracticethaninurban emergencydepartments(ED).Inthiscross-sectionalstudywesoughttoidentifytheworkenvironments ofgraduatesofaruralEMresidencyprogram,andthestrengthsandweaknessesofsuchaprogram.
Methods: Weconductedasurveyamong29graduatesofacommunity-basedEMprogramtoevaluate theeffectivenessofaresidencyprogramintrainingphysicianswhowillworkinruralareas.Thesurvey assessedthegraduates’ perceptionsoftheirlevelofpreparedness,furthertraining,andpracticelocation aftercompletingtheprogram.Resultsarereportedusingdescriptivestatistics.
Results: Twentyrespondentscompletedthesurvey(69%).Mostofthemidentifiedasmale(60%),White (70%),andnon-Hispanicor-Latino(80%).Seventy-fivepercentofthegraduatesworkincountieswith fewerthan1,000,000inhabitants,and70%workincommunityhospitalsandEDscaringforfewerthan 100,000patients/year.Four(20%)declaredtoworkincriticalaccesshospitals.Overall,respondentsfelt confidentintheirresidencytraining.
Conclusion: Acommunity-basedEMtrainingprogrammaybeaneffectivestrategyfor producingemergencyphysicianswhogoontoworkinruralandsmallercommunities. [WestJEmergMed.2025;26(1)40–46.]
Recentresearchhascontributedtoagreaterunderstanding ofthelandscapeoftheemergencymedicine(EM)workforce andtrainingintheUnitedStates.In2020,across-sectional studyusingtheAmericanMedicalAssociation(AMA) PhysicianMasterfiledatabasefoundthattherewere48,835 clinicallyactiveemergencyphysiciansintheUS.Among them,81%reportedhavingEMtraining,and69%wereboard certifiedinEM.Theremaining19%,whowereneitherEM trainednorcertified,weredividedamongthosewhowere familymedicine-(33%),internalmedicine-(24%),or
surgery-trained(12%)physicians.AccordingtotheUS DepartmentofAgriculture(USDA)UrbanInfluenceCodes (UIC)classification,92%workedinurbanareas,6%inlarge ruralareas,and2%insmallruralareas.Comparedtourban areas,thesurveyfoundthatlargeandsmallruralareastended tobestaffedbymales(71%vs80%and81%,respectively)and olderphysicians(50yearsofagevs58and62years, respectively),werelesslikelytohaveEMtraining(74%vs52% and37%,respectively)orboardcertification(70%vs56%and 40%,respectively),andthatthemajorityofruralemergency physicianshadgraduatedatleast20yearsbefore2020.1
Inparallel,datafromtheAMAPhysicianMasterfileand theAccreditationCouncilforGraduateMedicalEducation listingshowedanincreaseof105EMresidenciesfrom2013 to2020.Mostoftheseprogramsofferthreeyearsoftraining, withthemedianageofresidentsbeing31(29–33years)and femalesrepresenting39%ofthetrainees.Unsurprisingly,a cross-sectionaldataanalysisfoundthat98%ofthe6,993 residentsincludedinthestudywerereceivingtrainingin urbanareas,with77%beinginplaceswithover1,000,000 inhabitantsand17%inareaswithpopulationsbetween 250,000–1,000,000individuals.Lessthan2%oftheresidents weretraininginlargeruralareasand0.3%insmallrural areas(urban-ruralclassificationbasedontheUSDAUIC).2
Whilethedensityofemergencyphysiciansper100,000US populationinurbanareashasincreased1.4times,bothlarge andsmallruralareasshowedadecreaseof0.4and3.7, respectively.1 Oneoftheexplanationsforthisphenomenonis thatruralareashaveahigherrateofemergencyphysicians leavingpracticecomparedtourbanareas.3 Anotherleading causeofthisurbanpreferenceisthatresidentstendto practiceinenvironmentssimilartowheretheytrainedand staygeographicallyclosetotheirtrainingprograms,atleast inthe firstthreeyearsaftergraduation.2,4 Giventhelocations ofmosttrainingprogramsinurbancenters,thisdoesnot addresstherural-urbandisparityinemergencycare.
Inthisstudywehypothesizedthattrainingphysiciansina ruralenvironmentwillmakethemmorelikelytopracticeina ruralarea.Priorstudieshavedemonstratedtheeffectiveness ofalumnisurveysinidentifyingresidencyproblemareasto drivetargetedcurricularimprovement.5–7 However,no previousstudieshavelookedatatrainingprogram’slocation inrelationtoitsgraduates’ practicepatterns.Asasecondary outcome,wesoughttoexplorethespecificbenefitsand challengesthattrainingatacommunity-basedprogram presentedtoitsgraduates.
ThestudysiteisinthestateofNewYork.Itishometoan EMresidencytrainingprogramwitha34-bedemergency department(ED)thatseesanaverageof35,000visits peryearandservesalargelyruralpopulationof84,148 individuals.8 The firstresidencyclassbegantheirtraining in2015,andtheprogramhasgraduated29residentsin theinterveningyears.Duetothecharacteristicsofthe institutionandresidencyprogram,itsmissionistotrain physicianstoworkinruralcommunitieswithfewerthan 250,000inhabitants.
Thestudydesignwasacross-sectionalanonymous surveydeliveredthroughtheSurveyMonkeyplatform (SurveyMonkeyInc,SanMateo,CA).Theresearchprotocol wasreviewedbytheinstitution’sSystemReviewBoardand deemedexemptfrominstitutionalreviewboardapproval.
All29graduatesoftheEMresidencyprogramwere eligibleandreceivedtheinvitationtoparticipateinthesurvey
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Ruralcommunitieslackboard-certi fi ed emergencyphysicians.Residencygraduates tendtopracticeinenvironmentsliketheir trainingenvironment.
Whatwastheresearchquestion?
Dograduatesofacommunity-basedEM programinaruralareapracticeinruralareas aftercompletingtheirtraining?
Whatwasthemajor findingofthestudy?
75%ofthegraduateswerepracticingin countieswithfewerthan1millionresidents; 70%workinhospitalscaringforfewerthan 100,000patientsperyear.
Howdoesthisimprovepopulationhealth?
Acommunity-basedtrainingprogramina ruralareagraduatesemergencyphysicians whoworkinunderserved,ruralcommunities.
viaemailsretrievedfromourcontactlist.Thesurvey, consistingof23questions,wasreviewedandamendedby EMprogramfacultyandleadership.Theemailtextandthe surveycoverpageinstructedparticipantsaboutthecontent andgoalsofthestudy.Agreementtoanswerthesurvey impliedconsenttoparticipateinthestudy.Thedatacollected includedgeneraldemographics(sex,race,ethnicity,and numberofyearssincegraduation),characteristicsofthe graduate’scurrentpractices(typeofhospital,EDannual volume,county,ifcriticalaccess),additionalpostgraduate training,andadministrativeandmentoringroles.Questions abouttheresidencytrainingprogramandhowgraduatesfeel preparedfortheircurrentpracticewereelaboratedona fivepointLikertscale.Twoopen-endedquestionsaskedabout theprogram’sstrengthsandweaknesses.
Themostrelevantquestionswereplacedinthe firsthalfof thesurvey.Thesurveywasavailableforsixweeks(February andMarch2023),andthegraduatesreceivedthreeemail reminderstoencouragethemtoparticipate.
Countysizeswerereportedaccordingtothe2020US CensusBureau.8 WeusedtheUSDArural-urbancontinuum codes(RUCC)tocategorizecountiesbasedonthe populationsize,degreeofurbanization,andproximitytoa metroarea(Table1).9 TheRUCCwassuitableforthisstudy becauseithasabetterrepresentationofcountiessmallerthan
Table1. Definitionofmetro/non-metroUScountiesaccordingtothe populationsize,degreeofurbanization,andproximitytoametro area-USDepartmentofAgricultureRural-UrbanContinuumCodes (RUCC)(2023).9
Code ClassificationofUScountiesbasedon thedefinitionofmetro/non-metroareas
1Metro – countiesinmetroareasof 1millionpopulationormore
2Metro – countiesinmetroareasof 250,000to1millionpopulation
3Metro – countiesinmetroareasoffewer than250,000population
4Non-metro – urbanpopulationof20,000or more,adjacenttoametroarea
5Non-metro – urbanpopulationof20,000or more,notadjacenttoametroarea
6Non-metro – urbanpopulationof5,000to 20,000,adjacenttoametroarea
7Non-metro – urbanpopulationof5,000to 20,000,notadjacenttoametroarea
8Non-metro – urbanpopulationoffewer than5,000,adjacenttoametroarea
9Non-metro – urbanpopulationoffewer than5,000,notadjacenttoametroarea
250,000inhabitantswhencomparedtotheUSDAEconomic ResearchServiceUICusedbyotherauthors.1
Theresultsofthisstudyarereportedusingdescriptive statisticsrepresentedintablesandgraphs.TheUnitedStates
map(Figure1)wascreatedusingMapChart(Creative CommonsAttribution4.0internationallicense,Mountain View,CA)andPowerPointMicrosoft365AppsVersion 2407(MicrosoftCorp,Redmond,WA).
Twentygraduatescompletedthesurvey,correspondingto a69%responserate.Aspresentedin Table2,mostofthe respondentsidentifiedthemselvesasmale(60%),White (70%),andnon-Hispanicor-Latino(80%).Ninerespondents (45%)graduatedafter2021and11(55%)intheyearsbefore.
Overwhelmingly,respondentsself-reportedworkingin communityhospitals(14,70%),with fiveworkinginprivate hospitals(25%)andoneinauniversityhospital.Most graduatesworkinEDscaringforfewerthan100,000 patients/year(70%),andofthose,64%(9/14)workinEDs caringfor50,000orfewerpatients/year.Threerespondents whoworkincommunityhospitalsdidn’treporttheir approximateEDannualvolume.Fourgraduates(20%) workincriticalaccesshospitals,accordingtothedesignation bytheCentersforMedicareandMedicaidServices(Table3).
Accordingto2020USCensusBureaudata,75%ofthe respondentsworkincountieswithfewerthan1,000,000 inhabitants.Mostofthose(10of15)practiceincountieswith fewerthan250,000inhabitants(codes3,4,and6)andwith ruralpopulationsvaryingfrom21–73%.Forty-fivepercent (9/20)oftherespondentsliveandworkintheNortheast andarewithin90milesofthestudyinstitution(Table3),
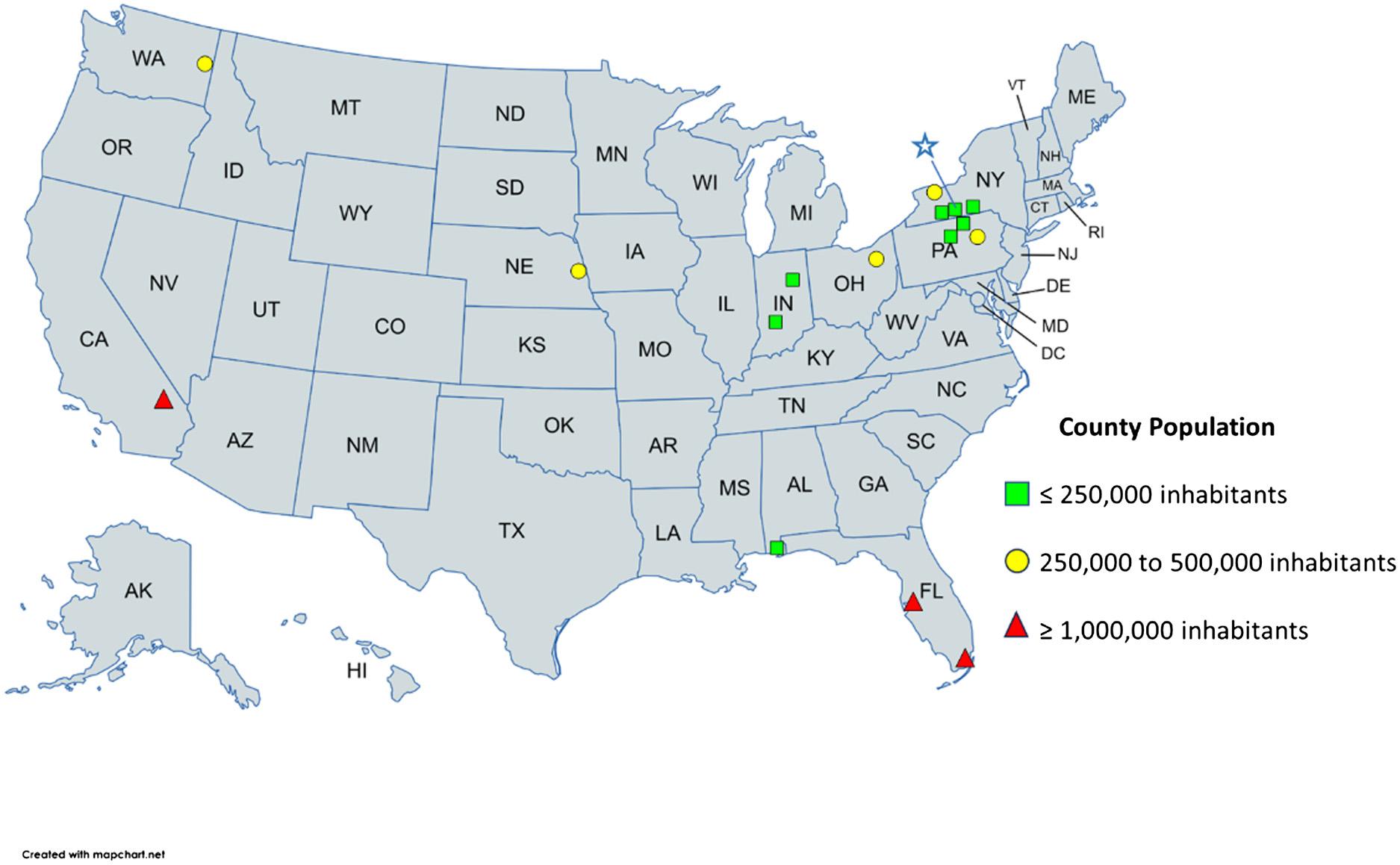
Figure1. Currentpracticesofemergencymedicinegraduatesdistributedbycountypopulationandgeographiclocation.Thebluestarinthe stateofNewYork(NY)representsthestudysitelocation.
SexFemale735%
Male1260%
Other15%
Prefernottosay00%
RaceWhite1470%
Black00%
Asian420%
NativeAmerican/Alaska Native 00%
NativeHawaiian/other PacificIslander 00%
MixedRace15%
Other15%
Prefernottosay00%
EthnicityHispanicorLatino15%
Non-Hispanicor-Latino1680%
Prefernottosay315%
Yearssince graduation 0–2945% > 21155%
andtwo-thirdsgraduatedmorethantwoyearsbefore. Thebluestarin Figure1 representsthestudysitelocationin theStateofNewYork.Onephysiciandidnotreport his/hercounty.
Respondentsdidnotdoanotherresidencyorchange specialtyareas.Three(15%)hadgoneontofurthertraining, withtwopursuingfellowshipsinaddictionmedicineandone pursuingfellowshipsinwildernessmedicineandmilitary EM,andamaster’sdegreeinpublichealth.Althoughmost respondentsdonotworkinlargeacademiccenters,allbut one(95%)reportedsomeroleinmentoringorteaching medicalstudents(75%),residents(70%),oryounger colleagues(25%)sincegraduation.Twohaveorhadan administrativepositioninthehospitalwheretheycurrently workorworkedpreviously.
Figure2 showstheresponsestothesixquestionsinLikertscaleformatabouthowpreparedgraduatesfelttotakethe boardexamsandworkasemergencyphysicians.Overall, therewerepositiveanswerstoallsixquestions.The respondentsfeltverywellpreparedtotreatcriticallyill patients,andnoneutralordisagreeingresponseswere observed.Withquestionsregardingdealingwiththe healthcaresystemandpreparednessfortheboardexams,the
responsesweremainlypositivebutwithsomeneutral answers.Uncommonly,graduatesreportedfeeling somewhatlesspreparedforproceduresnecessaryfordaily practice(1/20)anddocumentationinpatients’ charts(1/20). Theareaidentifiedasthelowestperformanceoftheprogram wasrelatedtopreparingresidentstomanagethepatient volumetheyneedtoseeroutinely,withtwoneutralsand twodisagreements.
Fromthegraduates’ pointofview,thetopthreestrengths andweaknessesoftheEMresidencyprogramwere asfollows:
• Strengths:Autonomywithlittlecompetitionfor procedures;exposuretoagoodbreadthofpathologies andcriticalcarecases;one-on-oneinteraction withattendings.
• Weaknesses:Needformoreexposuretorare procedures;moresimulations/boardpreparationand practicewithahighervolumeofpatients.
Toourknowledge,thisisthe firststudytoexaminewhether residencytraininginacommunity-basedEMprogramina ruralareaproducesgraduateswhopracticeinarural environmentaftergraduation.Theresultsofthisstudysuggest thatthisisso,althoughfutureresearchshouldexpandonthese findingstolookatthebreadthofEM-trainingprogramstosee whetherthisholdstrueacrossthecountry.Asasecondary outcome,thisstudyhighlightstheeffectivenessandlimitations ofasmall,communityEMresidencyprogramintraining emergencyphysiciansingeneralandspecificallytoworkin underservedruralenvironments.
Thedemographicsindicatethatthegraduatesofthestudy siteresidencyprogramwerepredominantlymale,White,and non-Hispanicor-Latino.Thisdistributionissimilartodata fromresidenciesaroundthecountry,regardlessofwhether theyarelargeorsmalltrainingprograms,reflectingtheneed formorediversityintheEMworkforce.1,2,10 Conscious effortsarebeingmadetorecruitresidentsandattendings fromminoritiestoincreasediversityandequityamong emergencyphysicians.
Historically,emergencyphysicianstendtopracticein environmentssimilartotheirtrainingandtoworkcloseto theirtrainingsite,atleastinthe firstthreeyearsafter graduation.1,4 Asmostresidenciesarelocatedinlargeurban areas,graduatesmayfeelrelativelyuncomfortable consideringjobsinmoreresource-limitedlocations.11 Althoughthedatapresentedhereislimited,itsuggeststhat theoppositemightalsobetrue residentstrainedinsmall communityhospitalstendtostay,andfeelcomfortable
Table3. Characteristicsofthecountiesandfacilitieswheretheresidentgraduatesarecurrentlypracticing.The “*” signalsrespondentswho declaredtoworkinmorethanonetypeofhospital. Study
workinginthatsameenvironment.Besidesincreasingthe availabilityofruralrotationsduringresidencyorgiving incentivestoattractphysicianstounderservedareas,creating newresidencyprogramsinsmallurban/ruralareasmaybe anothermeaningfulwaytoreversethetrendtowardarural EMdesertaroundthecountry.1,3,11
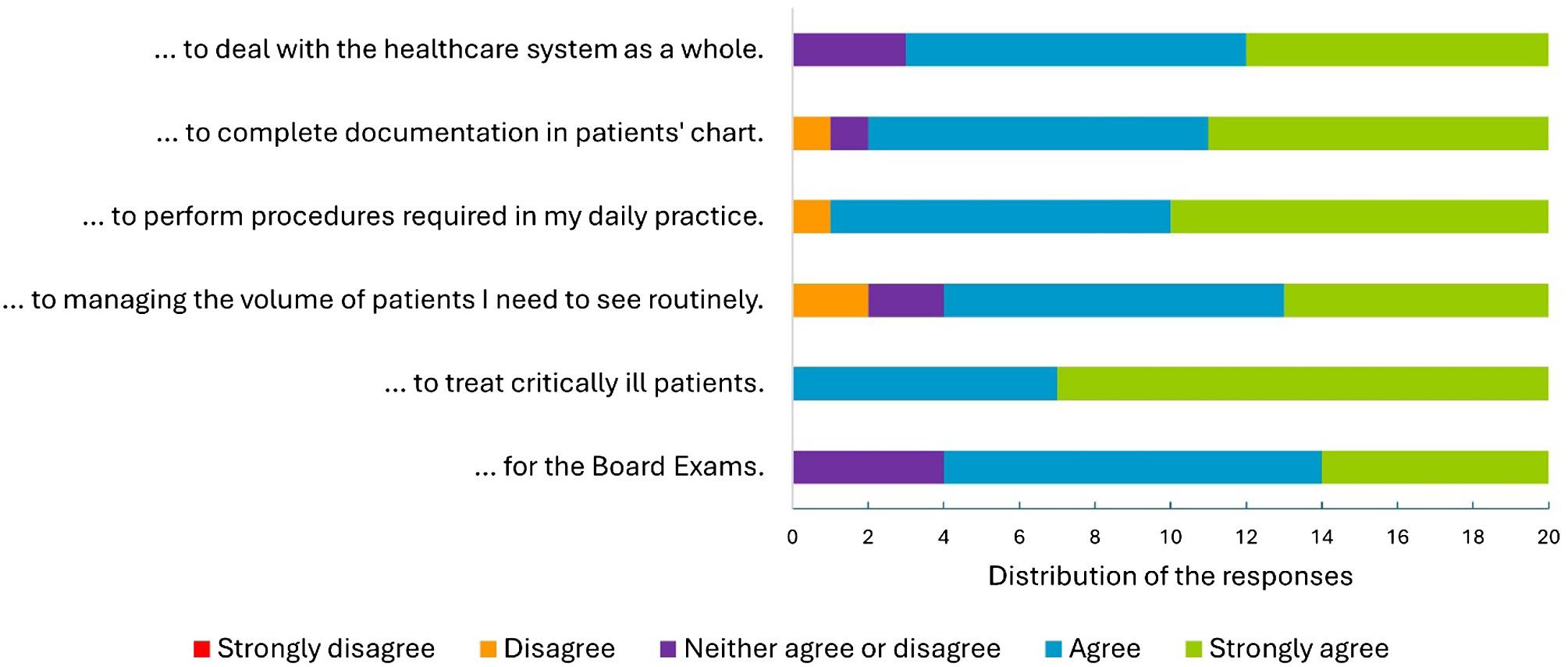
Thisgraphrepresentsthedistributionandagreementofthe20residentswhorespondedtothesurveywiththestatement, “Theemergencymedicineresidencyprogrampreparedmewell ”
Otherfactorsthatattractphysicianstoonedetermined areaarefamilyandspousalties,4 whichcanalsobe importantforthosechoosingtraininginsmallprograms.In thisstudy,wedidnotobserveatendencyofresidentswho graduatedinthepriortwoyearstoworkclosertothetraining programasdescribedbyotherauthors.Thisdeviationcould beattributedtotheuseofdifferenttimeframessince graduation,orbecauseofshiftsinthejobmarketsincethe onsetoftheCOVID-19pandemic.
Asasecondaryoutcome,thesurveyidentifiedareasfor trainingimprovementthatcouldbeaddressedthrough curriculardevelopment.Overall,respondentsfeltconfident intheirresidencytrainingatthissmallinstitution.The strengthsreportedbythegraduateswerelesscompetitionfor procedures,asenseofautonomyoverpatients,andtheclose resident-to-facultyrelationshipthathaddevelopedinasmall communityhospital.Themainconcernabouttrainingin smallEDsisthatresidentsarenotexposedtosufficient volumeandcomplexmedicalcases.However,arecentstudy comparingproceduresdonebysecond-andthird-year residentstraininginurbanvsruralcentersreportedahigher proportionofproceduresdoneinlargeruralhospitalswhen datawasstandardizedbyhoursworked.Residentswhotrain withlimitedspecialtybackuplearnvaluableskills,suchas relyingonthemselvestotreatcriticallyillcasesand stabilizingpatientswhentransfersarenecessary.12 Overall, whileitwasnottheprimarygoalofthisstudy,theresults supportthatresidentsgraduatingfromthisprogramfeltwellpreparedfortheirEMcareers.
Themostimportantlimitationofthisstudyisitssmall samplesize.The firstclassofgraduatesenteredresidencyin 2015;therefore,thestudysitetrainingprogramisrelatively
young,andthesurvey’ssamplesizeisstillsmall.However, thisstudyservesasapilotforfutureresearchintothepractice patternsofEMresidencygraduates.Welookforwardto expandingthisworkinthefuture.
Amongotherstudylimitationsarethepossibilitiesof surveyfatigue,responsebias,andnon-responsebias.The surveyhadprimarilymultiple-choicequestions,and questionsrelatedtothemaingoalofthisstudy(current practicelocations)werepresentedinthe firsthalfofthe questionnaire.Thirtypercentoftheeligibleparticipantsdid notrespondtothesurvey.Itispossiblethatthosewhodidnot respondfeltmorenegativelyabouttheirtraininganddidnot wanttosharethosereflections.Finally,itisunknowntowhat extenttheCOVID-19pandemicaffectedtheperceivedand/ orrealaspectsoftheresidency.
Thefactthat70%ofthegraduatesofaresidencyprogram locatedinaruralareanowworkincommunityhospitalswith anannualpatientvolumelowerthan100,000and75%work incountieswithfewerthan1,000,000inhabitantssuggests thatthissmallcommunity-basedtrainingprogramis succeedinginitsmission.Becausethenatureoftheprogram isemphasizedintherecruitingmaterial,itlikelydraws peoplewithapre-existinginterestinworkingawayfrom largeurbanareas.Accesstohigh-qualityemergencycareisas criticalinruralareasasitiseverywhereelseinthecountry, andthisstudysupportsthattrainingcliniciansinarural environmentfostersclinicianswhoareinvestedintheneeds ofrural,underservedcommunities.
AddressforCorrespondence:DylanS.Kellogg,MD,MSMEd,Arnot OgdenMedicalCenter,EmergencyMedicineDepartment,600Roe Ave.,Elmira,NY14905.Email: dylan.kellogg@arnothealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Kelloggetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BennettCL,SullivanAF,GindeAA,etal.Nationalstudyofthe emergencyphysicianworkforce,2020. AnnEmergMed. 2020;76(6):695–708.
2.BennettCL,ClayCE,EspinolaJA,etal.UnitedStates2020 emergencymedicineresidentworkforceanalysis. AnnEmergMed. 2022;80(1):3–11.
3.BennettCL,EspinolaJA,GindeAA,etal.Attritionfromemergency medicineclinicalpracticeintheUnitedStates,2020. AcadEmergMed. 2023;30(2):139–43.
4.HellandLC,WestfallJM,CamargoCAJr.,etal.Motivationsandbarriers forrecruitmentofnewemergencymedicineresidencygraduatestorural emergencydepartments. AnnEmergMed. 2010;56(6):668–73.
5.GaetaT,MahalingamG,PyleM,etal.Usinganalumnisurveyto targetimprovementsinanemergencymedicinetrainingprogram. EmergMedJ. 2018;35(3):189–91.
6.LüerSandAebiC.Assessmentofresidencyprogramoutcomesvia alumnisurveys. AdvMedEducPract. 2017;8:307–15.
7.RingdahlE,DelzellJEJr,KruseRL.Changingpracticepatternsoffamily medicinegraduates:acomparisonofalumnisurveysfrom1998to2004. JAmBoardFamMed. 2006;19(4):404–12.
8.UnitedStatesCensusBureau-P2urbanandruraltable.2020.Available at: https://data.census.gov/table?q=urban+and+rural&g= 050XX00US01003,06071,12057,12086,18053,18105,31055,36007, 36015,36055,36101,39153,42015,42079,42081,53063&tid= DECENNIALDHC2020.P2.AccessedAugust15,2023.
9.U.S.DepartmentofAgriculture.2023rural-urbancontinuumcodes. 2024.Availableat: https://www.ers.usda.gov/data-products/ruralurban-continuum-codes/.AccessedJuly2,2024.
10.ClevelandManchandaEC,LingAY,BottcherJL,etal.Threedecadesof demographictrendsamongacademicemergencyphysicians. JAmColl EmergPhysiciansOpen. 2022;3(4):e12781.
11.HillAD.EmergencymedicineresidenciesarefailingMainStreet America. JEmergMed. 2018;55(4):534–6.
12.CareyNI,HansrothJ,DavisH,etal.Comparingresidentprocedures inruralversusurbanemergencydepartments. Cureus. 2021;13(11):e19989.
CorlinM.Jewell,MD*
AmyT.Hummel,MD*†
DannJ.Hekman,MS*
BenjaminH.Schnapp,MD,MEd*
*UniversityofWisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,Madison,Wisconsin † EmergencyMedicineSpecialistsSC,Wauwatosa,Wisconsin
SectionEditors:DougFranzen,MDandAndrewKetterer,MD
Submissionhistory:SubmittedFebruary25,2024;RevisionreceivedSeptember27,2024;AcceptedOctober11,2024
ElectronicallypublishedNovember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20281
Introduction: Whilemanyaspectsofemergencymedicine(EM)residencytrainingarestandardized amongresidentswithinasingleresidencyprogram,thereisnostandardforthedistributionofchief complaints(CC)thatresidentsshouldseeoverthecourseofresidency.Thiscouldresultinsubstantial variabilityineachresident’sclinicalexposure.OurobjectiveinthisstudywastoexploreEMresidents’ clinicalexposuretoCCstodeterminewhethersubstantialvariationexists.Ifsuchvariationexists,this couldsuggesttheneedforcurricularreformtoaddressgapsinresidentclinicalexposureduringtraining.
Methods: ThiswasaretrospectiveobservationalstudyofEMresidentswhograduatedintheyears 2016–2021atasingle,university-affiliatedemergencydepartment(ED)inthemidwesternUnitedStates. AllpatientencounterswhereaCCwasloggedwereincludedandcategorizedinto1of20clinical domainsbasedonthe2016AmericanBoardofEmergencyMedicineModelofClinicalPractice. Wecalculateddescriptivestatisticsforthetop10mostencountereddomainsforcomparison amongresidents.
Results: Weincludedatotalof228,916patientencountersfrom69residentsintheanalysis.Residents wereinvolvedinanaverageof3,323distinctpatientencountersduringthestudyperiod.Theoverall interquartilerangeforpatientencounterswas523.ThethreeCCdomainswiththebroadestinterquartile variationwereabdominalandgastrointestinaldisorders(116),musculoskeletaldisorders(nontraumatic) (93),andtraumaticdisorders(86).
Conclusion: Withinasingle,three-yearacademicEMprogram,substantialvariationexistedamong residentswithregardtothevarietyofpatientCCsseenduringtheirresidencytraining.[WestJEmerg Med.2025;26(1)47–52.]
Medicalresidencytrainingallowsphysicianstogainthe cognitiveandproceduralskillsnecessarytopractice independently.Basedonexperientiallearningtheory,patient encountersformthefoundationuponwhichphysiciansin trainingbegintomasterthepracticeofmedicine.1 Additionally,thedevelopmentof “illnessscripts,” ormental modelsfortheclassificationofpatientpresentations,is
crucialtothedevelopmentofclinicalskillsandreasoning duringresidencytraining.2 Thesemodelsaredevelopedover timebymultipleexposurestopresentationsofsimilar diseasestates.3,4 Emergencymedicine(EM)trainees mustbeexposedtoavarietyofpatientchiefcomplaints(CC) throughoutthecourseofresidencytodevelop thesescriptsandbecomereadytobegin independentpractice.
EducatorswithinEMhaveworkedtodefinemanyaspects ofEMresidencytraining,includingoptimumnumberof shifts,on-shifteducationalgoals/practices,anddidactic content.5 Despitethis,theclinicalexperienceofanindividual residentmaybehighlyvariableandmaybepartiallydriven byself-selectionofpatientsbytheresident.Studiesin pediatricEMsuggestthatthereissignificantvariationinthe overallnumberofpatientsandrangeinacuityamong individualresidents.6,7 However,thereislittleadultEM literaturethatexploresthevariationinclinicalexperience seenbyresidentswithinamodernEMprogram.The literaturethatdoesexistinadultEMsuggeststhereis substantialvariationinclinicalexposuresamongresidents.8 Astudyfrom2006foundthatthenumberofcasesseen overallcorrelatedwithimprovedperformanceona standardizedtestdesignedtoassessclinicalcompetence. However,theeffectplateauedataround200cases.9 Prior workbyourgrouphasshownthatcasevolumeinan individualdomaindidnotcorrespondtoperformancewithin thatdomainoncorrespondingquestionsonthe in-trainingexam.10
Thesestudiessuggestthatindividualswithinasingle trainingprogrammaybegainingvariableexperiencewith certaintypesofpatientpresentationsandlackingexposure (andthereforeopportunitiestodevelopmastery)toother complaintsandpathology.However,thisvariabilityin clinicalexposureduringtraininghasnotbeenshowninadult EMforoverthreedecades.8 Sincethen,thenumberofannual visitstotheEDaswellasthecomplexityofmedicalcare providedhavesubstantiallyincreased.11,12 We,therefore, hypothesizedthatsubstantialdifferencesinclinicalexposure stillexistamongresidentsatthetimeofgraduation. Understandingthesedifferencesisofcriticalimportancefor residencyprogramsasconsiderablevariationcouldpush someresidentsbelowathresholdtodeveloprobustillness scriptssuitableforindependentpractice.
StudyDesignandSetting
Weconductedthisretrospective,observationalstudyata three-yearEMresidencyprogramsituatedwithinanurban, academicemergencydepartment(ED)intheMidwest.The EDfortheprimaryclinicalsitehasatotalof54bedsandsees anannualvolumeofapproximately60,000patientvisits. Duringthestudyperiod,theresidencyhad12 first postgraduateyearone(PGY-1)positionsavailableeach year.ThestudyEDdividesitsbedsintotwoadultclinical areasandapediatricclinicalarea.Allthreeareasare physicallyconnectedonasingle floorofthehospital. Residentsfromallthreeyearsareassignedtonine-hourshifts ineachclinicalarea.Eachshiftincludes1–2junior(PGY-1) residents,1–2senior(PGY-2orPGY-3)residents,andone attendingphysician.Anyresidentcanassignthemselvesto patientsofanyseverityregardlessofseniority.InFall2020,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Studiesfrom30yearsagoreportedvariation inthedistributionofchiefcomplaintsseenby emergencymedicineresidentsduringtraining.
Whatwastheresearchquestion?
Wehypothesizedthatsubstantialdifferences inclinicalexposurestillexistamongresidents atthetimeofgraduation.
Whatwasthemajor findingofthestudy?
Thethreechiefcomplaintdomainswiththe mostvariabilitybetweenindividualresident experience,asmeasuredbythegreatest25 – 75 interquartilerangeswereabdominaland gastrointestinaldisorders(median594 patientsperresident,IQR116), nontraumaticmusculoskeletaldisorders (median314,IQR92),andtraumatic disorders(median525,IQR86).
Howdoesthisimprovepopulationhealth?
Understandingthesedifferencesisimportant, assubstantialvariationcouldmeanthatsome residentsdonotdeveloprobustillnessscripts suitableforindependentpractice.
thestudyEDshiftedfroma “pod” modelinwhichthetwo adultclinicalareaswouldassignthemselvespredominately topatientsintheirclinicalareatoa “free-for-all” modelin whicheitheradultteamcouldassignthemselvestoanyadult patientregardlessoftheclinicalareatheywereroomedin. Duringthestudy,physicianassistantswereemployedinthe EDandwouldoccasionallytaketheplaceofaresidenton shift(particularlyduringweeklyresidentdidactics).
Residentswereeligibleforinclusioniftheyhadcompleted residencywithinthreeconsecutiveyearsandgraduatedinthe years2016–2021(therefore,thestudyperiodwasfromJune 2013–June2021).Theelectronichealthrecord(EHR)was usedtocreateadatabaseofpatientencounters;all encounterswhereeligibleEMresidentswerethe firstresident assignedtothepatientwereanalyzed.Weuseddeidentified patientencounterdata,listedby firstCC.TheCCwasusedto identifythenatureofthepatientencounterasthisdatawas availableatthetimeofpatientpresentation,oftendictates thepatient’sEDworkup,andwouldnothavebeenaffected byinformationdiscoveredduringthelaterstagesofa
patient’shospitalcourse.Thisapproachisconsistentwith priorliterature.9,13 Tomaintainanonymity,onlythesenior author,amemberoftheresidencyleadershipteam,had accesstoeachresident’sindividualizedstudy identificationnumber.
WeexcludedfromanalysisencounterswherenoCCwas listedornoresidentwasassigned.Incaseswheremultiple residentswereassignedtoasingleencounter(e.g.,apatient hadbeensignedouttoadifferentresident),weanalyzedthis encounteronlyfortheinitialresidentassigned.Thiswas doneastheyaretypicallythemostinvolvedinthecognitive workloadofdeterminingthepatient’sinitialdiagnosticand treatmentplan.TheCCforeachencounterwasselectedand enteredintotheEHRbytheprimarynursewhocaredforthe patientintheEDinitially.Atourinstitution,thisisnearly alwaysselectedfromalistofcommonCCs,althoughitcan beenteredasfreetext.EncountersinwhichmultipleCCs werelistedwereonlycodedintoasingledomainbasedonthe firstlistedCC.
AlistofcommonCCsinEMhasbeencategorizedintoa setof20contentdomainsviaaconsensusprocessbytwoEM attendingsusingthe2016AmericanBoardofEmergency Medicine(ABEM)ModelofClinicalPracticeasa framework.14 ForCCsidentifiedinourdatathatwerenot alreadycategorizedbyapreviouslydescribedmethod,13 we repeatedthesamecategorizationprocessinwhicheachCC wasassignedtoasingledomainbytwoboard-certifiedEM attendingphysiciansatourinstitution.Disagreements betweenthetworeviewerswereadjudicatedbyathirdboardcertifiedemergencyphysician.Ifasymptomwasenteredas theCC,suchas “fever” (whichcouldcorrespondtooneof multipledomains),itwaspreferentiallycategorizedintoa domainbasedonwhatthecodingphysiciansfeltwasthe
mostlikelytodictatetheEDworkup,ratherthanthe “signs, symptoms,andpresentations” domain.WeusedExcel (MicrosoftCorp,Redmond,WA)tocalculatedescriptive statisticsandcreateplotsandtables.Thetop10most encountereddomainsoverallwereanalyzed.Weexcluded lesscommondomainsgiventhelownumberoftotal encountersineacharea,whichwouldhavebeenmore vulnerabletorandom fluctuationsinwhenthesepatients presenttotheED.
Thisprojectwasdeemedexemptqualityimprovementby theUniversityofWisconsinHealthSciencesInstitutional ReviewBoard.
Atotalof315,614encounterswereinitiallyidentifiedfrom theEHR.Oftheseencounters198wereexcludedasnoCC waslisted.Afterexcludingresidentswhoseclinical experiencewasoutsidethestudyperiodandthosewhohad leftthetrainingprogrampriortograduationorhada prolongedleaveofabsence,atotalof228,916patient encountersfrom69residentswereincludedintheanalysis. Eachresidentwasassignedtoanaverageof3,323distinct patientencountersAssessmentofthetop10mostcommon clinicalexposuredomainsshowedwiderangesinthecase numbersofindividualresidents.The Table liststhemean, minimum,maximum,interquartilerange(IQR) and25thand75thpercentileforthe10mostcommon contentdomains.The Figure showstherangeof exposuretothe10mostcommondomainsin box-and-whiskerformat.
Ourdatasuggeststhatresidentswithinasingletraining programhavesubstantialvariationintheirclinical experiencesasmeasuredbythevariationinABEMcontent
Table. Mean,25th–75thpercentileranges,interquartilerange,andminimum/maximumencountersforthe10mostencountereddomains perresident.
MeanMedian25th,75th percentileIQRMinimum,maximum
Totalencounters33233086,36095232595,4053
Abdominalandgastrointestinaldisorders583594528,644116416,721
Traumaticdisorders529525484,57086370,725
Cardiovasculardisorders327330302,35654233,429
Nervoussystemdisorders319319301,34039226,402
Musculoskeletaldisorders(non-traumatic)314314269,36192179,460
Thoracic-respiratorydisorders280281246,31367178,383
Systemicinfectiousdisorders165169149,17930115,219
Head,ear,eye,nose,andthroatdisorders150151136,1652996,196
Signs,symptoms,andpresentations129130120,1422288,170
Psycho-behavioraldisorders126128106,1393467,211
IQR,interquartilerange.
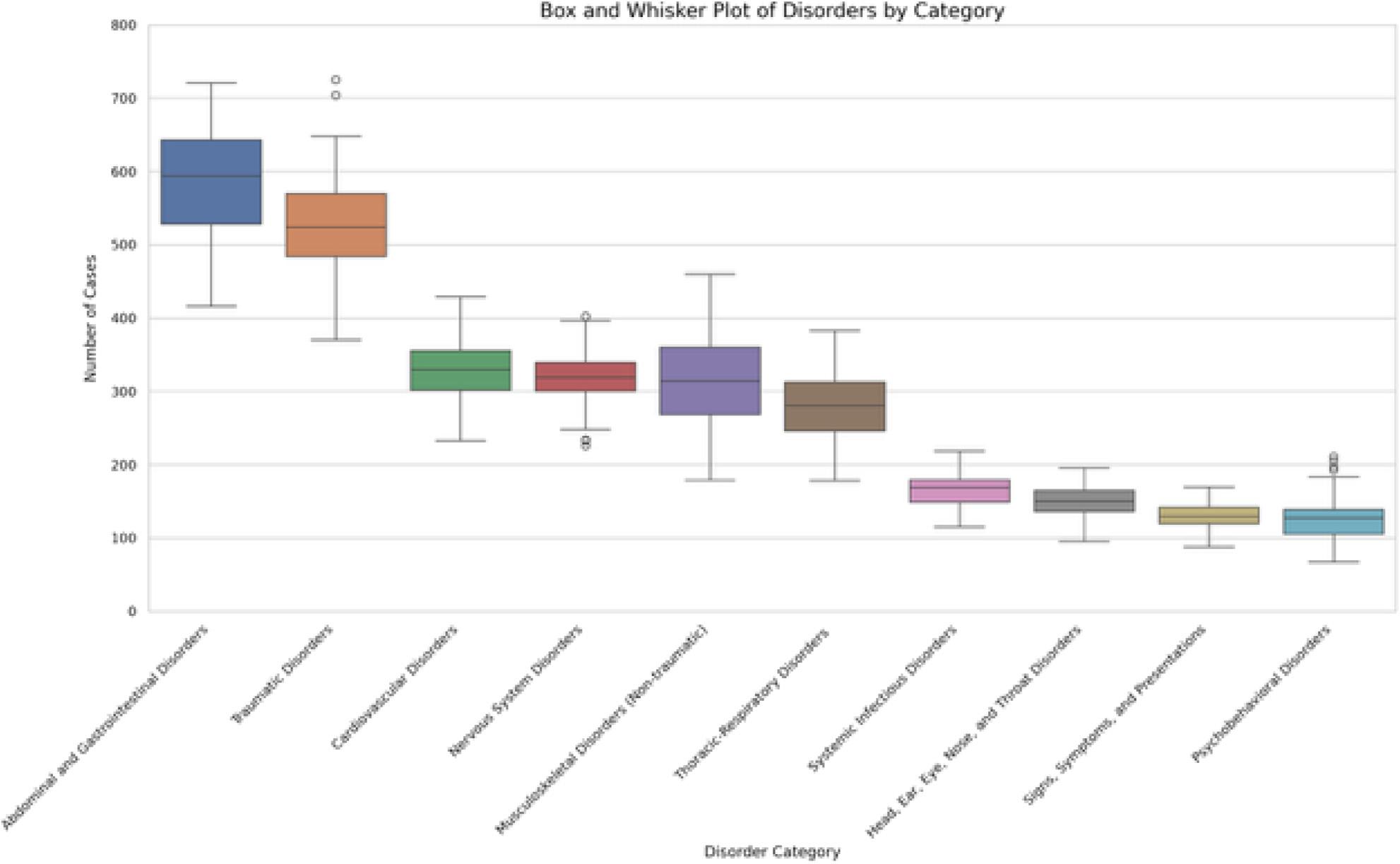
Figure. Top10mostcommonclinicalexposuredomainsseenbygraduationperresident.Boxesillustratethe25th–75thpercentileofnumber ofclinicalexposuresbyresidentsineachdomain,withwhiskersrepresentingtheminima,maxima,andoutliers.
domainsseenbyindividualresidents.Thisissimilartowhat wasdescribedbyLangdorfetal.in1990,despitetheprevious studybeingperformedoverthreedecadesagoandthe substantialsubsequentdifferencesintheutilizationofthe ED.8 Wefoundwideinterquartilerangesbetweenthe maximumandminimumnumberofencountersamong residents,suggestingthatsomeresidentssawsubstantially morepatientswithinparticulardomainsthanothers.
Themagnitudeoftheeducationalsignificanceofthe exposurevariabilityofresidentsisunclear.Itispossiblethat aresidentwhoseestwiceasmanymusculoskeletalchief complaintsasanotherresidentbygraduationissignificantly morecompetentinthatdomain.Alternatively,itisalso possiblethattheyhavebothattainedtheminimallevelof exposuretocompetentlymanagemusculoskeletal complaintsindependently.Theeffectsofclinicalexposureon clinicalcompetence,includingtheminimalnumberof encountersrequiredtodemonstratecompetencyina particulardomain,isanopenquestionandanavenuefor furtherresearch.However,theformationofillnessscriptsis continuallymodifiedbysubsequentpatientencounters.3,4 Therefore,theidentificationofhighdegreesofvariation amongresidentsmaypromptprogramleadershiptoinstitute changesinthecurriculumorsupplementclinicalexposure withindividualizedlearningplans.Thisislikelymore importantfordomainsthatareencounteredlessfrequently
overall,suchaspsycho-behavioraldisorders,wherelarger relativedifferencesinexposurecouldresultingreaterdeficits inillnessscriptformation.
Inadditiontopromptingchangesmadebytheprogram, identificationofhighvariabilityinclinicalexposuremay enhanceresidentself-assessment.Asdemonstrated previously,self-assessmentwhendoneinisolation,isan imperfectmeansofdrivingimprovementbutcanbe enhancedgreatlywheninformedbyadditionalinformation fromavarietyofsources.15 Understandingthedistribution ofthepatientencountersresidentshaveduringtraining,and thepotentialgapsintheirclinicalexposure,couldbea potentialmeansofallowingforinformedself-assessmentfor aresident’sclinicalskills.Thiscouldbepotentiallyfurther enhancediffacilitatedunderthesupervisionoffaculty coacheswithintheprogram,amethodthathasbecome increasinglypopularinmedicaleducation.16,17 Futurework couldfollowacohortofresidentswhoareabletotracktheir ownpatientvolumesmoreregularlythanwaspossibleinthe currentstudyandcomparethemselvestotheirpeers throughouttrainingandevaluatewhetheranydifferencesin clinicalcompetenceareidentified.Thiscouldalsoallow programstodeterminetheperceivedvalueofthis informationtoresidents.Finally,residentscould usethisdatatodrivetheirpatientselectionwhile workingintheED.
Beyondthepotentialforshapingresidentselfassessments,clinicalexposuredatamayhaveimportant implicationsforresidencyprogramleadershipaswemove towardaneraofcompetency-basedmedicaleducation (CBME).TwoofthepillarsofCBME, “teachingtailoredto competencies” and “effectiveprogrammaticassessment,”18 lendthemselveswelltotheidentificationofprogramclinical weaknessesaswellastothecreationofnewcurricular experiencesdesignedtoaddressareasoflimitedclinical exposureidentifiedbyresidentCCdata.Theseexperiences couldpotentiallytaketheformoftargetedreadingsor simulationsessionsdesignedtosupplementlowerfrequency clinicalencounters.
Thiswasasingle-centerstudyinanurban,academicED, and findingsmaynotbegeneralizabletotrainingprograms indifferentenvironments.Additionally,thedatawas retrospective,makingtheeducationalutilityofthis informationoranypotentialcausesofvariationdifficult todetermine.
UseofaCCtocategorizeeachpatientencounterintoa clinicaldomainhasanelementofsubjectivityandmayhave ledtosomeencountersbeingmiscategorizedwithrespectto theworkupdoneor finaldiagnosis.Someadditional subjectivitymayhavebeenintroducedbyhowweclassified CCsthatcouldpotentiallyhavebeencategorizedinto multipledifferentdomains(suchas “fever” or “ingestion”). Thiswasdonebasedonwhatwasdeterminedtobemost likelytodrivetheinitialworkupinthedepartment.For example,althoughaCCof “chestpain” couldrepresenta cardiacorpulmonaryetiology,inalmostallcases,acardiac etiologymustbeexcluded.Therefore,itwasfeltthatthis wouldinfluencetheformationandmodificationofthe resident’sillnessscriptmostheavily.Itisalsopossiblethat encountersweremischaracterizedduetoonlyusingthe first CClistedandnotconsideringtheothersifmultipleCCswere listed.Likethepriorlimitation,itwasfeltthatthe firstCC wasmostlikelytodictatetheinitialEDworkup.Using dischargeor finaldiagnosesinsteadwasconsideredforthis study,butitwasfeltthattheCCismorelikelytodrivethe initialdifferentialanddiagnosticworkupforthepatient.
Additionally,ABEMdomainsmaybetoobroadto captureimportantdifferencesinexposure(e.g.,tworesidents withthesameexposureto “respiratorydisorders” couldhave seenlargenumbersofpneumoniapatientsor,alternatively, manypatientswithasthma).Trainingisinherentlyvariable astheEMenvironmentdiffersbyclinicalsite,day,shift,or evenseason.Therefore,theremayhavebeenslight differencesinwhenindividualresidentswereintheED clinicallyorthenumber/typeofoverallEDshiftsworked.It isimportanttonotethatsomeoftheincludedresidents’ trainingoccurredduringtheCOVID-19pandemic,which mayhavehadaneffectonboththevarietyandnumberof
clinicalexposuresseenbytheseresidents.Futureworkcould alsoexploreexposurebasedonsub-domainsfromthe ABEMmodeltogetamoregranularlookatindividual residentclinicalexperiencesratherthanrelyingonthe relativelybroaddomains.
Otherclinicalvariablesmayalsohaveaneffectona resident’sclinicalexposure,includingthetimingofmonths rotatingintheED.However,theEDdidnotundergomajor changesinthestaffingmodelofphysicians(including residents)duringthisperiod.Also,whileitislikelythatmore seniorresidentsassignthemselvestocriticallyillpatients,this wasfelttobeunlikelytomeaningfullyimpactourresults giventhatdatawasobtainedatthetimeofgraduation. Therefore,eachresidentwouldhaveactedinaseniorrolefor thesameamountoftime.Finally,ouruseoftheEHRatthe mainclinicaltrainingsiteoftheresidencytogeneratethe datadidnotcapturetheclinicalexperienceattwoother trainingsitesfortheresidencythatuseadifferentEHR.This mayhaveservedtomoderateorexacerbatethedifferences seenamongresidents.However,clinicalexperiencesatthese othersitescomprisedatotalofonlyfourmonthsofthe36monthcurriculum,andsoitislikelythatouroverall findings wouldnothavebeensubstantiallyaffected.
Withinasingle,three-yearacademicemergencymedicine program,therewassubstantialvariationamongresidents regardingthevarietyofpatientchiefcomplaintsseen throughoutresidencywhenmappedtoABEM’sModelof ClinicalPractice.
AddressforCorrespondence:CorlinM.Jewell,MD,Universityof WisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,800UniversityBayDr., Madison,WI53705.Email: cmjewell@medicine.wisc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Jewelletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TeunissenPW,ScheeleF,ScherpbierAJ,etal.Howresidentslearn: qualitativeevidenceforthepivotalroleofclinicalactivities. MedEduc. 2007;41(8):763–70.
2.BowenJL.Educationalstrategiestopromoteclinicaldiagnostic reasoning. NEnglJMed. 2006;355(21):2217–25.
3.CustersEJ,RegehrG,NormanGR.Mentalrepresentationsofmedical diagnosticknowledge:areview. AcadMed. 1996;71(10Suppl):S55–61.
4.HatalaR,NormalGR,BrooksLR.Influenceofasingleexampleon subsequentelectrocardiominterpretation. TeachingandLearningin Medicine. 1999;11(2):110–7.
5.StahmerSandKuhnG.Optimizingresidenttraining:resultsand recommendationsofthe2009CouncilofResidencyDirectors ConsensusConference. AcadEmergMed. 2010;17Suppl2:S78–86.
6.LiJ,RooseveltG,McCabeK,etal.Pediatriccaseexposureduring emergencymedicineresidency. AEMEducTrain. 2018;2(4):317–27.
7.ChenEH,ChoCS,ShoferFS,etal.Residentexposuretocritical patientsinapediatricemergencydepartment. PediatrEmergCare. 2007;23(11):774–8.
8.LangdorfMI,StrangeG,MacneilP.Computerizedtrackingof emergencymedicineresidentclinicalexperience. AnnEmergMed. 1990;19(7):764–73.
9.KernMW,JewellCM,HekmanDJ,etal.Numberofpatientencountersin emergencymedicineresidencydoesnotcorrelatewithin-trainingexam domainscores. WestJEmergMed. 2022;24(1):114–8.
10.HayashinoY,FukuharaS,MatsuiK,etal.Qualityofcareassociated withnumberofcasesseenandself-reportsofclinicalcompetencefor Japanesephysicians-in-trainingininternalmedicine. BMCMedEduc. 2006;6:33.
11.StrangeGRandChenEH.Useofemergencydepartmentsby elderpatients:a five-yearfollow-upstudy. AcadEmergMed. 1998;5(12):1157–62.
12.CairnsCandKangK.NationalHospitalAmbulatoryMedicalCare Survey:2021emergencydepartmentsummarytables.2023. Availableat: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/ Dataset_Documentation/NHAMCS/doc21-ed-508.pdf AccessedSeptember21,2024.
13.BischofJJ,EmersonG,MitzmanJ,etal.Doestheemergencymedicine in-trainingexaminationaccuratelyreflectresidents’ clinical experiences? AEMEducTrain. 2019;3(4):317–22.
14.CounselmanFL,BabuK,EdensMA,etal.The2016modeloftheclinical practiceofemergencymedicine. JEmergMed. 2017;52(6):846–9.
15.WolffM,SantenSA,HopsonLR,etal.What’stheevidence:selfassessmentimplicationsforlife-longlearninginemergencymedicine. JEmergMed. 2017;53(1):116–20.
16.DeiorioNM,MooreM,SantenSA,etal.Coachingmodels,theories,and structures:anoverviewforteachingfacultyintheemergency departmentandeducatorsintheoffices. AEMEducTrain. 2022;6(5):e10801.
17.SargeantJ,LockyerJ,MannK,etal.Facilitatedreflective performancefeedback:developinganevidence-andtheory-based modelthatbuildsrelationship,exploresreactionsandcontent, andcoachesforperformancechange(R2C2). AcadMed. 2015;90(12):1698–706.
18.VanMelleE,FrankJR,HolmboeES,etal.Acorecomponents frameworkforevaluatingimplementationofcompetency-basedmedical educationprograms. AcadMed. 2019;94(7):1002–9.
PeterMoffett,MD
AlBest,PhD
NathanLewis,MD
StephenMiller,DO
GraceHickam,MD
HannahKissel-Smith,MD
LauraBarrera,MD
ScottHuang,MD
JoelMoll,MD
DepartmentofEmergencyMedicine,VirginiaCommonwealthUniversitySchoolof Medicine,Richmond,Virginia
SectionEditors:AbraFant,MDandWilliamEdwardSoares,MD
Submissionhistory:SubmittedJuly21,2024;RevisionreceivedOctober7,2024;AcceptedOctober11,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.31064
Introduction: Emergencydepartmentboardinghasescalatedtoacrisis,impactingpatientcare, hospital finances,andphysicianburnout,andcontributingtoerror.Nopriorstudieshaveexaminedthe effectsofboardinghoursonresidentproductivity.Ifboardingreducesproductivity,itmayhavenegative educationalimpacts.Weinvestigatedtheeffectofboardingonresidentproductivityasmeasuredby patientsperhourandhypothesizedthatincreasedboardingleadstodecreasedproductivity.
Methods: Thiswasaretrospectivestudyataquaternary,urban,academicLevelItraumacenterfrom 2017–2021withathree-yearemergencymedicineresidencyof10–12residentsperyearandannual volumesof80,000–101,000.Boardingwasdefinedasthetimebetweenanadmissionorderandthe patientleavingtheED.Wecreatedamultivariablemixedmodelwith fixedcovariatesforyear,month,day ofweek,residentexperience,shiftduration,totaldailyEDpatients,andwithresidentsasrepeated measures.Theeffectofboardingwasestimatedaftercovaryingoutallotherfactors.
Results: Allvariablesincludedinthemodelweresignificantlyassociatedwithchangesinproductivity. Residentexperiencehasthelargesteffectsuchthatforeachmonthofresidencyexperience,aresident adds0.012patientsperhour(95%confidenceinterval[CI]0.010–0.014).Isolatingtheeffectofboarding demonstratedthatforeveryadditional100hoursofboarding,aresident’sproductivitydecreasedby 0.022patientsperhour(95%CI0.016–0.028).Inthestudy,themediandailyboardingwas261hours;if thiswereeliminated(assumingaresidentcompletes10010-hourshiftsannually),aresidentcouldbe expectedtosee56.9morepatientsperyear(95%CI40.7–73.1).
Conclusion: Hospitalboardingsignificantlyreducesresidentproductivityasmeasuredbypatients perhour.Furtherstudiesarewarrantedtodeterminetheeducationalimpact.[WestJEmergMed. 2025;26(1)53–61.]
Emergencydepartment(ED)boarding(definedas patientsadmittedtothehospitalbutremainingintheED) hasreachedcriticallevelsandhasbeendeclaredacrisisby theAmericanCollegeofEmergencyPhysicians.1 Thescope ofthecrisisisdauntingwitheffectsonpatientcare,errors, physicianburnout,hospitaleconomicstress,andambulance diversion.2 IncreasedEDboardingalsoleadstoincreasesin
medicationerrors,timetoantibiotics,timetopercutaneous coronaryinterventionforpatientswithmyocardial infarction,timetocareforpatientswithacutestroke,patient mortality,andrisk-adjustedhospitalspending,andhas effectsonalllevelsofacuity.3–10
Withinthecontextofboarding,EDsmustalsoprovide soundeducationaltraininginvolvingbothqualityand quantityofpatientexperiences.Residencyprogramsseekto improveefficiencyandproductivityintheirresidents throughouttheirtraining.Manyvariableshavebeen associatedwithresidentproductivityincludingtimeofshift, shiftlength,andresidentexperience.11–13 Thereare, however,fewstudiesthatevaluatetheeffectofEDcrowding andboardingtimeontheeffectofemergencymedicine(EM) residentproductivity.14 Ifboardingdecreasesthenumberof patientsseenduringaresidency,theremaybeanimpacton residenteducation.
Inthisstudyweaimedtoinvestigatetheeffectofboarding onEMresidentproductivityasmeasuredbypatientsper hour.Wehypothesizedthatincreasedhospitalboarding wouldresultindecreasedresidentproductivity.
ThiswasaretrospectivestudyconductedattheVirginia CommonwealthUniversityHealthSystem,theonly comprehensiveLevelItraumacenterinRichmond,VA. DuringthestudyperiodfromJanuary2017–June2021,the totalpatientvolumesrangedfrom80,000–101,000peryear. Onaverage,30%ofpatientswereadmittedtothehospital,of whom5%wenttotheintensivecareunit.Patients <18years ofageconstituted22%ofthetotalvolume.Thedepartmentis staffedwithboard-certifiedemergencyphysicians,and duringthestudyperiod81%ofpatientswereseenbya resident.Theremainingnon-residentcaseswereseenby advancedpracticepractitioners(APP)inalow-acuityareaof theEDorbyattendingphysiciansandwerenotincludedin thestudy.Throughoutthestudytherewasnochangeinthis staffingmodelsuchthatAPPswerenevercompetingforthe samepatientsasresidents.Thedepartmenthas76bedswith 35inanacutearea,10intrauma/resuscitation,10inamidtrackarea,16inapediatricdepartment,and fiveina fast-trackzone.
Ourresidencyprogramisthreeyearsinlength,andclass sizesrangedfrom10residentsin2017to12residentsin2021. Duringpostgraduateyears(PGY)-1,2,and3,residentswork intheEDfor26weeks,29weeks,and35weeks,respectively. Residentshiftlengthsvariedfrom9–12hourswiththemost typicalshiftbeing10hours.Onaverage,each24-hourperiod hadatotalof137hoursofresidentcoverageinoverlapping shifts.TheEMresidentssawpatientsinallEmergency SeverityIndex(ESI)categoriesandweretheprimary physiciansforallemergentpatients(ESI1and2).Residents caredforpatientsinallareasoftheEDotherthanthe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencydepartmentboardingnegatively impactspatientcare,hospitalef fi ciency,and physicianwell-being.
Whatwastheresearchquestion?
DoesincreasedEDboardingreduce emergencymedicineresidentproductivity, asmeasuredbypatientsperhour?
Whatwasthemajor findingofthestudy?
Foreveryadditional100hoursofED boarding,aresident ’ sproductivitydecreased by0.022patientsperhour(95%CI 0.016 – 0.028);aresidentsees57fewer patientsperyearduetoboarding.
Howdoesthisimprovepopulationhealth?
Understandingthenegativeeffectsof boardingonproductivitymayhelppolicy makers fi ndsolutionstoimprovepatient fl ow, patientcare,residenteducation,andoverall healthoutcomes.
low-acuityarea.Allresidentsstaffpatientsdirectlywithan attendingphysicianwithoutoversightbyamoresenior resident;therefore,theproductivitynumbers forresidentsinallthreeyearsoftrainingareindependent. ThestudywasgrantedexemptstatusbytheVirginia CommonwealthUniversityInstitutionalReview Board(HM20024717).
DatafromallpatientsevaluatedbyanEMresidentwas capturedinadatabase,andinconjunctionwithscheduling dataitwasusedtodeterminetheaveragenumberofpatients perhour.OnlyEMresidentswereincluded.Thestudyperiod wasselectedasthiswasthemaximumamountoftimefor whichdatawasavailablepriortothehospitalswitchingtoa newelectronichealthrecord.Asthedatabasewasinitially createdtoprovidefeedbacktoresidents,certaindatawas removedandnotavailabletousforanalysis.Information fromthe firstmonthofEMforeachresidentwasnot provided,andduetoinitialeffectsfromtheCOVID-19 pandemic,datafromApril–July2020wasnotincluded.
Wecombinedthreedatabasesforanalysis:thepatient databaseofallEDencounters;theresidentscheduling database;andthehospitalboardingdatabase.
Duringthestudyperiod,theEMresidencyprogram receivedmonthly,system-generatedreportslistingthe uniquepatientidentifier,nameoftheresidentassignedto careforthepatient,theESIacuitylevel,thedate/timeof first contactandcheckout,andthedisposition.Theresident assignmentwasderivedfromtrackingboarddata,andin scenarioswheremultipleresidentswereassignedtoapatient encounter,onlythe firstresidentassignedwascreditedfor eachuniquepatientencounter.TheEMresidentswere scheduledfor9-hour,10-hour,or12-hourshiftsduringthe studyperiod.Allnon-EMresidentsandstaffwereexcluded fromthepatientdatabase.
Boardingdatawasreporteddailyfromhospitalanalytics. Thenumberofhoursofboardingwasdefinedasthetime betweenanadmissionorderandwhenthepatientlefttheED. Boardinghourswasselectedasthiswasthevariableavailable tousfromthehospitalanalyticsdatabase.
WedesignedamodeltoisolatetheeffectsofEDboarding onresidentproductivityasmeasuredbypatientsperhour. Patientsperhourwasdefinedasthetotalnumberofnew patientsseenduringtheshiftdividedbythedurationofthe shiftinhours.Thecovariateswerechosenfromthosefound inpreviousstudiestoberelatedtoresident productivity.11,13,15,16 Theseincludedyear,month,dayofthe week,cumulativeresidencymonthsintraining,shift duration,totalpatientsperday,andboarding.Monthsin trainingwaschosenasacontinuouscovariatetodelineate residentexperienceratherthantheroughclassificationof PGY-1,-2,or-3basedontheobservationthatresident productivitybeginslowinthePGY-1year,increasesinthe PGY-2year,andthenplateaus.Thismonthlyexperience variablewasmodeledusingcubicregression.
Wedescribedthedatausingcountsandpercentages. Patientsperhourwasmodeledusingamultivariablemixed model,withcovariatesdefinedas fixedeffectsandresidents asrepeatedmeasures.Weusedanautoregressive(AR1) covariancestructuretoaccountforthedependencebetween repeatedmeasures.The fixedeffectswereyear(reference = 2019),month(reference = 12),dayoftheweek(reference = Thursday),residentmonthintraining(centeredon18),total patientsperday/100,shiftduration,anddailyboarding hours/100.Wechosetheyear2019asareferenceasitwasthe lastfullyearofdatapriortothestartoftheCOVID-19 pandemic.Decemberwaschosenasitalignswiththe18th monthofresidency,whichiswhenproductivityplateauedin ourmodel.Thursdaywasselectedasitisthoughttorepresent thedaywiththemostideal flowsinceitavoidsweekends, Monday,andFridaypatientsurges,aswellasWednesday morningdidacticswhenEMresidentsarenotworking clinically.Thetotalpatientsperday,shiftduration,and
boardinghourswerereferencedatthemedianvaluesin ourdataset.
Weestimatedtheeffectofboardingfromthemarginal regressionmodelaftercovaryingoutallotherfactors. Estimatesaredescribedusing95%confidenceintervals.All datamanagementandanalysiswereperformedusingSAS software(version9.4andJMPProversion17.2(SAS InstituteInc,Cary,NC).
Duringthestudyperiod,263,058patientswereseeninthe EDby601cliniciansincludingthe80EMresidentsstudied. Duringthe49monthsstudiedbetween2017–2021,EM residentswerescheduledto16,949shiftsandwereassigned 188,685patients(Table1).Totaldailypatientvolumevaried considerablyduringthistime(mean177,SD26,range
Table1. Characteristicsoftheemergencydepartmentresidents’ shiftsandpatientsevaluated(January2017–June2021).
CharacteristicShiftsNPatientsN(%) Total16,949188,685 Year
20173,49644,119(23) 20183,95547,569(25) 2019(11months)*4,05347,035(25) 2020(8months)† 3,10129,191(15) 2021(6months)2,34420,771(11) Month
1-January1,90921,052(11) 2-February1,57618,004(10) 3-March1,68018,901(10)
4†-April1,30215,229(8)
5†-May1,37116,385(9)
6†-June1,33715,191(8)
7†-July82010,129(5) 8-August1,56015,543(8) 9-September1,37614,741(8) 10-October1,43115,299(8) 11*-November1,06211,639(6) 12-December1,52516,572(9) Dayofweek Sunday2,24925,887(14) Monday2,67929,099(15) Tuesday2,75629,504(16) Wednesday‡ 1,98921,970(12) Thursday2,60127,874(15) (Continuedonnextpage)
Table1. Continued.
CharacteristicShiftsNPatientsN(%)
Friday2,52528,785(15)
Saturday2,15025,566(14)
Shift
7 AM to5 PM 1,68816,332(9)
7 AM to7 PM 1802,512(1)
9 AM to7 PM 2,54628,306(15)
12 PM to10 PM 3,38638,586(20)
2 PM to12 AM 2,47028,631(15)
3 PM to12 AM 3,55341,138(22)
9 PM to7 AM 3,12633,180(18)
PGY
PGY-1§ 5,16244,817(24)
PGY-24,75657,447(30)
PGY-37,03186,421(46)
Disposition
Admitted74,663(40)
Discharged114,022(60)
*November2019wasexcludedasthehospitalinformation managementsystemwasdown.
†April2020throughJuly2020wasexcludedduetoCOVID-19and hospitalchanges.
‡Wednesdaysmorningsareresidentdidactics.
§The firstmonthofaresidencywasexcluded(orientationmonth). ESI,EmergencySeverityIndex; PGY,postgraduateyear.
88–263).Asindicatedinthetable,theEDexperienceda patientcountvariabilitythatchangedacrossyears,months, daysoftheweek,shifts,andPGYlevel.Ofall188,167 patientsseenbyEMresidents,40%wereadmitted.
Boardinghoursperdayvariedconsiderably(mean281, SD127,range50.8–914.4; Figure1).Thehospital informationsystemcalculatedboardinghoursdaily; however,acrossthe1,490daysstudied,thereweresix impossible(negative)valuesandnineverylowvalues.Low valueswereidentifiedbylargeresidualsinthemultiple regressionmodel.Ratherthantreatingtheseasmissing values,weusedamultipleregressionmodeltoimputethe 15valuesinquestion.
Allthefactorsintherepeated-measuresmixed-model weresignificant(P < 0.001). Table2 showstheestimated effectofeachterminthemodel.Thejointeffectofallthe factorsonresidentproductivityisshownin Figure2.These profileplotsshowthemarginalmodelpredictedvalueof residentproductivityontheverticalaxisacrossallthe covariatesontheseparatehorizontalaxes.Theimportance
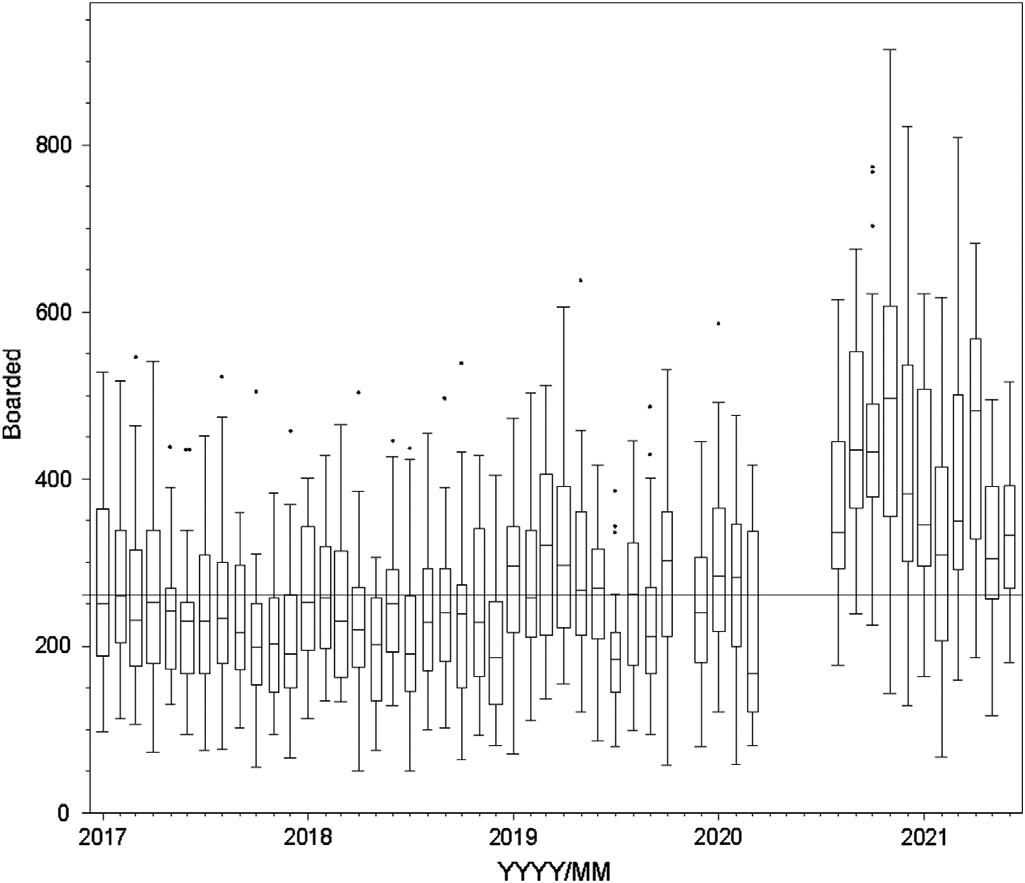
Figure1. Boardingacrossstudyyears.
Linesetatmedianboardinghoursacrosstheentirestudyperiod (261hours/day).
Eachboxplotrepresentsamonth(line = median,box = 25th to75th quartile,whiskers = typicalextremes,circles = outliers).
Note:April2020–July2020hoursarenotavailableasthey correspondtothebeginningoftheCOVID-19pandemic.
ofafactorisvisualizedbythesteepnessofthe predictiontrace.
Isolatingtheeffectofboardingdemonstratedthatfor everyadditional100hoursofdailydepartmentalboarding, individualresidentproductivitydecreasedby0.022patients perhour(95%confidenceinterval[CI]0.016–0.028, Table2). Inthereferencestandardscenario,aresidentcouldbe expectedtosee1.10patientsperhourwithboardingatthe dailymedian(261hours)butcouldsee1.15patientsperhour ifboardingwereeliminated(Figure2,PanelC). Table3 showshowresidentproductivitywasdegradedbyboarding acrosstherangeofvaluesseenatourinstitution.Aresident wouldsee1.14patientsperhourwhenboardingwasatthe lowestinthestudycomparedto0.95patientsperhouratthe maximumlevelofboardingseeninthestudy,whichisa differenceof0.19patientsperhour(95%CI0.15–0.22). Assumingaresidentcompletesapproximately100shiftsa yearthatareof10hoursdurationandboardingwas eliminated,thenaresidentcouldbeexpectedtosee56.9more patientsperyear(95%CI40.7–73.1).Thiswouldrepresenta 5%increaseinpatientvolumeperresidentannually. Residentexperiencehasthelargesteffectonresident productivity.Residentproductivitywaslowinitiallyat0.5 patientsperhour(95%CI0.46–0.54)bythesecondmonthof training(Figure2).Improvementwasinitiallyrapidto0.75 patientsperhouratsevenmonths,thenplateauednearthe 18-monthpoint(1.10patientsperhour)to finallyreach1.12 patientsperhourattheendofthe36months(95%CI 1.08–1.17).WhenevaluatingourdatabyPGYlevel,our
Table2. Multipleregressionresultspredictingnewpatientsperhourperresidentforeachvariable.
EffectEstimatednewpatientsperhourStandarderror95%CI
Intercept1.09570.01731.0618to1.1297
Year
20170.15010.01220.1262to0.1740 20180.08370.01170.0608to0.1065
2019[reference]
2020 0.06410.0137 0.0909to 0.0373 2021
Month
1-January0.06350.01720.0298to0.0972
2-February0.07760.01820.0420to0.1133
3-March0.04980.01810.0144to0.0852
4-April0.08400.01970.0453to0.1227
5-May0.07500.01960.0366to0.1133
6-June0.05850.02010.0191to0.0979
7-July
8-August0.05500.01850.0188to0.0912
9-September0.06540.01870.0288to0.1021
10-October0.04870.01840.0127to0.0847
11-November0.04860.01990.0095to0.0876
12-December[reference]
Dayoftheweek
Sunday0.05870.01180.0357to0.0818
Monday
0.03120.0118
Tuesday0.01220.01100.0094to0.0338
Wednesday0.10940.01230.0854to0.1334
Thursday[reference]
Friday0.04750.01090.0261to0.0688
Saturday0.11820.01200.0948to0.1417
Residentmonths(linear)*0.01220.00100.0101to0.0142 (quadratic)
0.0012to 0.0010 (cubic)0.000030.000010.00002to0.00004
Totalpatientsperday(per100patients)*0.40210.01650.3697to0.4344
Shiftduration*
Themixed-modelalsoincludedresidentasarepeated-effectwithanAR(1)covariancestructure. *Continuouscovariateswerereferencedtothemedianvalue.Medianresidentmonth = 18,totalpatientsperday/100 = 1.77, shiftduration = 10hours,boardedhours/100 = 2.61. CI,confidenceinterval.
PGY-1residentssaw0.75perhour,PGY-2residentssaw 1.10patientsperhour,andPGY-3residentssaw1.12 patientsperhour.
TotalpatientsperdaypresentingtotheEDwasthenext mostimportantfactorinresidentproductivity.Forevery100 newpatientspresentingtotheED,anindividualresident
wouldbeexpectedtoadd0.40patientsperhour(95%CI 0.37–0.43).Themedianvaluefordailytotalpatientvolume was177patientsperday,butalow-volumedayatthe10th percentile(143totalpatients)resultedinacorresponding decreaseinresidentproductivityto0.96patientsperhour (95%CI0.92–1.00).Forahigh-volumedayatthe90th
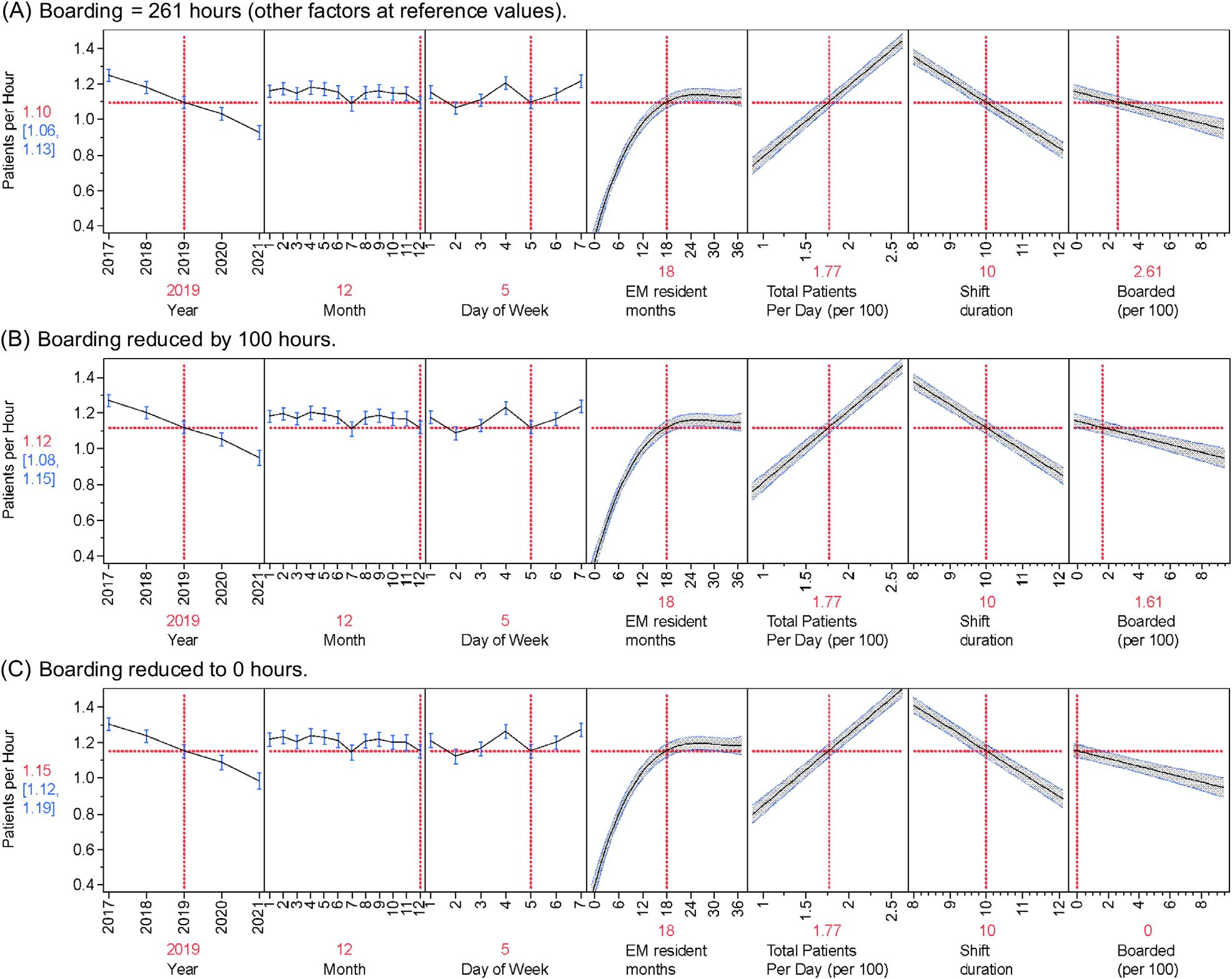
Figure2. Multipleregressionresultspredictingnewpatientsperhourperresidentforeachvariable. Allvalues(year,month,dayofweek,EMresidentmonths,totalpatients,shiftduration)inmodelheldatreferencestandardswithadjustments toboarding(lastpanelofeachgraph).ExpectedpatientsperhourineachscenarioisindicatedbytherednumberintheYaxiswith95% confidenceintervalsinblue.Asboardedhourschange(lastpanelofeachgraph)sodopatientsperhour(rednumbertoleftofeachgraph)in eachofthethreescenarios(A:Medianboardingof261hours.B:Reducingboardingby100hours.C:Eliminatingboardinghours.)
percentile(210patients),residentproductivityincreasedto 1.23patientsperhour(95%CI1.19–1.26).
Residentproductivityalsochangedbasedonthe year,shiftduration,anddayoftheweek.Resident
Table3. Estimatedresidentproductivitybyboardinghours.
productivitywashighestin2017at1.25patientsperhour (95%CI1.21–1.28)andsteadilydecreasedtothe0.93 patientsperhourseenin2021.Residentproductivityfora nine-hourshiftwaspredictedtobe1.21patientsperhour
CutoffBoarded(hours)EstimatedpatientsperhourStandarderror95%CI
Marginalestimatesfromthemixedmodelwiththefollowingfactorsheldconstant:year = 2019,month = 12,dayoftheweek = 5(Thursday), residentmonthintraining = 18,totalpatientsperday/100 = 1.77,shiftduration = 10hours. CI,confidenceinterval.
(95%CI1.19–1.26),whereasfora12-hourshiftitwas predictedtobe0.84patientsperhour(95%CI0.80–0.89). SaturdaysandWednesdaysaveragedapproximately1.21 patientsperhour,Sundays,andFridaysapproximately1.15 perhour,andMondays,Tuesdays,andThursdays1.10 patientsperhour.
Month-to-monthvariabilityhadthesmallesteffecton residentproductivity.Comparedwiththeothermonths,July andDecemberhadlowerresidentproductivity(1.09vs1.16 patientsperhour).
Toourknowledge,thisisthe firststudytodemonstrate thatthereisasignificantreductioninresidentproductivity (measuredaspatientsperhour)duetohospitalboardingin theED.Inourmodel,thisresultedinadecreaseof0.022 patientsperhour(95%CI0.016–0.028)forevery100hours ofdailyboarding.Whileperformedatasingleinstitution, ourdatasetbroadlyalignswithmultiplestudiespreviously completedregardingresidentproductivity.Inourstudy,we analyzedresidentexperienceasthenumberofmonthsin trainingratherthandividedintoPGYlevel.Thiswasbased onourobservationthatproductivityrapidlyincreased duringthePGY-1yearandthenplateauedinthemiddleof thePGY-2year.
WhenevaluatingourdatabyPGYlevel,ourPGY-1 residentssaw0.75patientsperhour,PGY-2residentssaw 1.10patientsperhour,andPGY-3residentssaw1.12 patientsperhour.Priorstudieshavedemonstratedsimilar patternswithPGY-1to-3residentsseeingbetween0.79–0.81 patientsperhour,1.05–1.2patientsperhour,and1.22–1.27 patientsperhour,respectively.17–19 AstudybyHenningetal showedrapidprogressionfromPGY-1toPGY-2yearand thengradualprogressioninPGY-3yearbutwasbasedon patientsperday.20 Similarly,astudybyTurner-Lawrence andToddsawincreasingproductivityfrom1.2patientsper hourto1.5patientsperhourto1.6patientsperhourby PGY-1to-3residents,respectively.13 Whilethese productivitynumbersarehigherthanthoseinourstudy,the authorsdidnotadjustforadditionalvariables.
Inamorecomparablestudy,Kirbyetalreportedthe efficiencyofEMresidentsduringEDcrowding.14 The authorsusedtheNationalEmergencyDepartment OvercrowdingStudy(NEDOCS)scoringsystemto categorizestatesintheEDasnotcrowded,crowded,and overcrowded.Theyfoundthatresidentproductivity measuredasnewpatientsperhourincreasedinitiallyinall yeargroupsastheEDtransitionedfromnotcrowdedto crowded,butthenremainedstablewhentransitioningfrom crowdedtoovercrowded.WhiletheNEDOCSscoreusesa measureofEDboarding(thewaitingtimeofthelongest admittedpatient),itdoesnotincludetotalpatientboarding hoursasinourstudy.Ourstudymoredirectlyexaminesthe effectofboarding(oneelementofcrowding)onresident
productivity.Theparadoxicalincreaseinresident productivityintheKirbystudymayhavebeenduetoan increasednumberofpatientspresentingtotheED,which couldhaveincreasedtheNEDOCSscore.Ourstudy demonstratedthatresidentproductivityincreasedwith higherpatientvolumes,andincludingthisinourmodel allowedustobetterisolatetheeffectofboarding.
AccordingtoastudybytheAcademyofAdministrators inAcademicEmergencyMedicineandtheAssociationof AcademicChairsofEmergencyannualbenchmarksurvey, boardingtimeshavedramaticallyincreasedsincethe COVID-19pandemic.21 Bytheendoftheirstudyperiod,the mediannumberofboardinghourspermonthwas11,480, whichapproximatesto382hoursofdailyboarding.Inour study,whichincludesapre-pandemicperiod,themedian dailyboardingwas261hours,suggestingthatboardingis likelyworseningovertimeandisaproblematmany academicmedicalcenters.
Theeducationalimpactofdecreasedpatientvolumes causedbyboardingisuncertain.Itisreasonabletoexpect thatresidentsseeingfewercasesmaylosevaluablelearning opportunities,butthishasnotbeenwellstudiedandno firm numbersexisttosuggestathresholdatwhicheducation suffers.Priorauthorshavesurveyedresidentsregardinga perceiveddecreaseineducationduringcrowding.22,23 These studiesconcludedthatresidentsdidnotperceiveadifference ineducationduringthesetimes,buttheyuseddiffering measuresofcrowding,weresurvey-based,and underpowered.Educatorsmayswitchtodifferentmodelsof teachingduringperiodsofhighboarding,leadingto residentsperceivingalessdeleteriouseffect.24
OthershavepostulatedaneducationalStarlingeffect wherebysomeboardingallowssupervisingphysiciansmore timetoteach,butatsomepointtherearediminishedreturns asfewernewpatientsbecomeavailabletodiscuss.25 Amore recentstudywasconductedduringthecurrentboarding epidemic;theauthorssurveyedEMprogramdirectors regardingtheirperceptionsoftheimpactofboardingon residenttraining.26 Inthisstudy,80%oftherespondentsfelt thatboardingnegativelyaffectedresidenteducation, especiallyinthedomainsofmanagingdepartment throughputandmanaginghighvolumesofpatientsper resident.Whilesurvey-basedinnature,thestudyresults broadlyalignswiththepriorstudiesinthisarea.
Theoretically,residentswhoseefewercasesmaylose valuablelearningopportunities.Whilethecomponentsof Bloom’sdomainsofeducationalactivitiescanbelearnedvia differentmodalitiesofinstructionaltechniques,clinical experienceallowsforthelinkingofknowledgetoskillsand thentoattitudes/emotions.27 Bydecreasingalearner’ s exposuretopatients,onecouldarguethatresidentsmaylose valuableexperientiallearningopportunities.Whilesomeof thesecanbereplicatedinsimulationorcase-based discussion,otherskillscannotandarebestlearnedviahands-
on,experientiallearningencounters.Experientiallearning theory,asdescribedbyKolb,highlightstheimportanceof real-lifeexperienceandtheinfluencethishasonlearning.28 Unliketraditionallearningandinstructionalmethodology thatfocusesonrotememorization,experientiallearningisan activeprocesswhereresidentsareengagedinconcept transformationthroughactionaswellasreflectionontheir experiencesandpatientencounters.
Thislearningtheoryalsoemphasizesprinciplesofadult educationinwhichpriorlearningexperiencescanbe leveragedtocreatemoremeaningfulandrelevant educationalexperiences.29 Additionally,decreasingpatient interactionmayalsoaffectresidents’ applicationand translationofknowledgeintopractice.Behaviorallearning theoryemphasizeslearningthroughinteractionswiththe environmentwherereinforcementandfeedbackcan encouragemodificationofbehaviors.Byincorporating behaviorallearningstrategies,medicaleducationcanfoster notonlytechnicalcompetenciesbutalsothedevelopmentof professionalhabitssuchaseffectivecommunicationbetween teammembersandpatients.30
Thisstudyhasseverallimitations.Thiswasasingle-center studythattookplaceinahighacuity,quaternary-carecenter thatalsoexperienceshighlevelsofboarding,whichmaylimit generalizabilitytoothercenters.Thedatabasethatcaptured theresidentpatientassignmentwasbasedontrackingboard dataandmayhaveoccasionallymiscreditedaresidentwitha patientencounter;however,asthedatasetwaslargeand involvedmultipleyearswithcompletedatasetsforthreefull classesofresidentsthisisunlikelytohavegreatlyinfluenced thedata.Ourresidentclasssizedidincreaseduringthe 2021yearandthuscouldtheoreticallyhavedecreasedthe numberofpatientsavailableperresident.Whilewedidnot studythatdirectly,itisunlikelytohaveimpactedthedata greatlyastheadditionalresidentsallowedforthecreationof anoutsiderotationatafree-standingemergencycenterand, therefore,residentstaffinghoursstayedgenerallyconsistent atthestudysite.
Ourmodeldidnotincludeameasureofpatientacuityasa covariate.WhiletheESIcategoryanddispositionwere recordedforeachpatient,wedidnotfeeltherewasareliable waytoconvertthisdataintoameaningfulmeasureofhourly acuitythatinfluencedtheamountoftimearesidentmight dedicatetowardpatientcare.Forexample,anESI-1patient whoisadmittedforanST-segmentelevationmyocardial infarctionmaystayinthedepartmentfor15minutesleaving thebedopenforanewpatient,whileanESI-3patient requiringaworkupforabdominalpainincludingimaging whoisdischargedmayoccupyaroomandaresidentfor multiplehours.Sinceourdatasetwaslarge,itwasassumed thatallresidentswouldbeexposedequallytothesamemixof acuitiesonindividualshifts,bytheendoftheirresidency
andthuslimittheeffectonthedata.Additionally,recent studieshavecalledintoquestiontheaccuracyofthe ESI.26,27 Apriorstudyonresidentproductivitydidnot showacorrelationbetweenESIandclinician dispositiontimes.14
OurstudyalsoincludeddatafromtheCOVID-19 pandemic,whichaffectedpatientvolumesandEDboarding. Thedatasetweusedwasinitiallymeantforreporting individualresidents’ productivitymeasures,sodatafromthe firstfewmonthsofthepandemicwasnotavailableforour currentstudy.Thislikelyservedtodecreasetheeffectofthe initialpandemicresponseonourdata.Justpriortothe pandemicourEDhadseenagrowthinpatientvolumesfrom 87,000patientsperyeartoapeakof101,000patientsper year,whichwasfollowedbyarapiddeclineto83,000ayear inthe2021–2022year.Thevolumesdidslowlyriseafterthe studyperiod.Thismayhaveinfluencedsomeofthedata fromourlaterresident-yeargroupsandservedto decreaseproductivity.
Ourmeasureofboardingmayalsohavelimitations.Total boardinghoursperdaywasthevariableavailablefromour hospitalanalyticsdepartment.Thenumberofboarded patientsperdaymayhaveprovideddifferentdata.For example,inourmodelasinglebehavioralhealthpatient boardingfor20hoursfromonedaywouldbe indistinguishablefrom20patientsboardingin20 individualroomsforasinglehoureach.Asthedatasetis large,andallresidentswereexposedtothesameconditions throughouttheirtime,itisunlikelyanyoneresident’sdata (orthetrend)wouldbeaffectedbasedonthesetypes ofoutliers.
Wefoundasignificantreductioninresidentproductivity asmeasuredbypatientsperhourduringperiodsofincreased boarding.Furtherstudiesarewarrantedtodeterminethe educationalimpactofthese findings.
AddressforCorrespondence:PeterMoffett,MD,Virginia CommonwealthUniversity,DepartmentofEmergencyMedicine, 1250EMarshallStreet,Suite600,RichmondVA23298.Email: peter.moffett@vcuhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Moffettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AmericanCollegeofEmergencyPhysicians.Emergencydepartment boardingandcrowding.Availableat: https://www.acep.org/ administration/crowding–boarding/.AccessedDecember29,2022.
2.KelenGD,WolfeR,D’OnofrioG,etal.Emergencydepartment crowding:thecanaryinthehealthcaresystem. NEJMCatalyst InnovationsinCareDelivery. 2021.Availableat: https://catalyst.nejm. org/doi/full/10.1056/CAT.21.0217.AccessedApril4,2022.
3.KulstadEB,SikkaR,SweisRT,etal.EDovercrowdingisassociated withanincreasedfrequencyofmedicationerrors. AmJEmergMed. 2010;28(3):304–9.
4.ChatterjeeP,CucchiaraBL,LazarciucN,etal.Emergencydepartment crowdingandtimetocareinpatientswithacutestroke. Stroke. 2011;42(4):1074–80.
5.KulstadEBandKelleyKM.Overcrowdingisassociatedwithdelaysin percutaneouscoronaryinterventionforacutemyocardialinfarction. IntJ EmergMed. 2009;2(3):149–54.
6.FeeC,WeberEJ,MaakCA,etal.Effectofemergencydepartment crowdingontimetoantibioticsinpatientsadmittedwithcommunityacquiredpneumonia. AnnEmergMed. 2007;50(5):501–9,509.e1.
7.BaloescuC,KinsmanJ,RaviS,etal.Thecostofwaiting:associationof EDboardingwithhospitalizationcosts. AmJEmergMed. 2021;40:169–72.
8.RichardsonDB.Increaseinpatientmortalityat10daysassociated withemergencydepartmentovercrowding. MedJAustral. 2006;184(5):213–6.
9.McCarthyML,ZegerSL,DingR,etal.Crowdingdelaystreatmentand lengthensemergencydepartmentlengthofstay,evenamong high-acuitypatients. AnnEmergMed. 2009;54(4):492–503.e4.
10.WhiteBA,BiddingerPD,ChangY,etal.Boardinginpatientsinthe emergencydepartmentincreasesdischargedpatientlengthofstay. JEmergMed. 2013;44(1):230–5.
11.JosephJW,HenningDJ,StrouseCS,etal.Modelinghourlyresident productivityintheemergencydepartment. AnnEmergMed. 2017;70(2):185–90.e6.
12.JeanmonodR,JeanmonodD,NgiamR.Residentproductivity:does shiftlengthmatter? AmJEmergMed. 2008;26(7):789–91.
13.Turner-LawrenceDandToddBR.Monthlyprogressionofemergency medicineresidentefficiency:whatcanweexpectofourresidents throughouttraining? JEmergMed. 2019;57(1):77–81.
14.KirbyR,RobinsonRD,DibS,etal.Emergencymedicineresident efficiencyandemergencydepartmentcrowding. AEMEducTrain. 2019;3(3):209–17.
15.JeanmonodR,BrookC,WintherM,etal.Residentproductivityasa functionofemergencydepartmentvolume,shifttimeofday,and cumulativetimeintheemergencydepartment. AmJEmergMed. 2009;27(3):313–9.
16.JosephJW,DavisS,WilkerEH,etal.Modellingattendingphysician productivityintheemergencydepartment:amulticentrestudy. Emerg MedJ. 2018;35(5):317–22.
17.DeBehnkeD,O’BrienS,LeschkeR.Emergencymedicineresidentwork productivityinanacademicemergencydepartment. AcadEmergMed. 2000;7(1):90–2.
18.FredetteJ,KimT,McHughD,etal.Adescriptiveanalysisofemergency medicineresidentproductivityoverthecourseoftraining. AEM EducationandTraining. 2021;5(S1):S44–8.
19.JeanmonodR,DamewoodS,BrookC.Residentproductivity:trends overconsecutiveshifts. IntJEmergMed. 2009;2(2):107–10.
20.HenningDJ,McGillicuddyDC,SanchezLD.Evaluatingtheeffectof emergencyresidencytrainingonproductivityintheemergency department. JEmergMed. 2013;45(3):414–8.
21.KilaruAS,ScheulenJJ,HarbertsonCA,etal.BoardinginUSacademic emergencydepartmentsduringtheCOVID-19pandemic. AnnEmerg Med. 2023;82(3):247–54.
22.MahlerSA,McCartneyJR,SwobodaTK,etal.Theimpactofemergency departmentovercrowdingonresidenteducation. JEmergMed. 2012;42(1):69–73.
23.PinesJM,PrabhuA,McCuskerCM,etal.TheeffectofEDcrowdingon education. AmJEmergMed. 2010;28(2):217–20.
24.AtzemaC,BandieraG,SchullMJ,etal.Emergencydepartment crowding:theeffectonresidenteducation. AnnEmergMed. 2005;45(3):276–81.
25.ShayneP,LinM,UfbergJW,etal.Theeffectofemergencydepartment crowdingoneducation:blessingorcurse? AcadEmergMed. 2009;16(1):76–82.
26.GoldflamK,BradbyC,CoughlinRF,etal.Isboardingcompromisingour residents’ education?Anationalsurveyofemergencymedicine programdirectors. AEMEducTrain. 2024;8(2):e10973.
27.BloomBS,EngelhartMD,FurstEJ,etal. TaxonomyofEducational Objectives:CognitiveandAffectiveDomains.NewYork,NewYork: DavidMcKayCompany,Inc,1956.
28.KolbDA. ExperientialLearning:ExperienceastheSourceofLearning andDevelopment.EnglewoodCliffs,NJ:Prentice-Hall;1984.
29.SchultzK,McEwenL,GriffithsJ.ApplyingKolb’slearningcycleto competency-basedresidencyeducation. AcadMed. 2014;91(2):284.
30.MerriamS. AdultLearning:LinkingTheoryandPractice.SanFrancisco, CA:Jossey-Bass;2013.
31.SaxDR,WartonEM,MarkDG,etal.Evaluationoftheemergency severityindexinUSemergencydepartmentsfortherateofmistriage. JAMANetwOpen. 2023;6(3):e233404.
32.MistryB,StewartDeRamirezS,KelenG,etal.Accuracyandreliability ofemergencydepartmenttriageusingtheemergencyseverity index:aninternationalmulticenterassessment. AnnEmergMed. 2018;71(5):581–7.e3.
AshleyK.Weisman,MD
SkylerA.Lentz,MD
JulieT.Vieth,MBChB
JosephM.Kennedy,MD
RichardB.Bounds,MD
SectionEditor: JeffreyDruck,MD
UVMHealthNetwork,TheRobertLarnerM.D.CollegeofMedicineattheUniversityof Vermont,DepartmentofEmergencyMedicine,Burlington,Vermont
Submissionhistory:SubmittedNovember13,2023;RevisionreceivedJuly16,2024;AcceptedJuly17,2024
ElectronicallypublishedNovember18,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18573
Ruralregionsfaceemergencyphysicianshortages.Most trainingprogramsarelocatedincitiesandlackruralclinical experiences,didactics,andmentorshiptoexciteandprepare residentsforruralemergencymedicine(EM)practice.There islimiteddataonoptimaltrainingmethodsforpreparing residentsforruralpractice.ToaddressthisneedforruralEM trainingandworkforce,wedevelopedaruralEMcurriculum forasingleEMresidencyprogramintheUnitedStates.We beganwithatwo-yearcasereviewfromcriticalaccess emergencydepartments.RuralEMskillsweredefinedand taughtusinglectures,simulationcases,andclinicalrotations. Weobtainedquantitativeandqualitativefeedbackfromthe first10residentsparticipatinginthecurriculum. Qualitatively,10/10residentsgainednewskillsandfound theseexperiencesvaluabletotheirtrainingandcareerchoice, with100%expressinginterestinruralpracticeand70% choosingaruralpractice.Quantitatively,residentsmanaged awidevarietyofpatientacuityandvolumeandperformed newprocedurescomparedtotheiracademiccenterrotations, allwhilegaininguniqueskillsfromthechallengesofarural environment.FocusedruralEMclinicalexperiencesand nonclinicalteachingduringresidencyareapromising approachtobridgethegapbetweenurban,tertiary-care trainingprogramsandruralemergencycareneeds.
Ruralregionsfacesignificantemergencyphysician(EP) shortages.1,2 Asruralpatientsageandfaceevengreater disparitiesandbarrierstocare,3–6 theneedforskilled,rural EPspreparedtopracticefullspectrumemergencymedicine (EM)withlimitedresourcesisparamount.RecentEM workforcestudiesdemonstratethatthecriticalneedforrural EPsislikelytoworsenratherthanimproveforseveral reasons. 7–10 Thereisasignificantmismatchinthe distributionofEPsthroughouttheUnitedStates,witha surplusofEPsinurbanareasandadeficitinruralareas.9 Ruralareashavelowerratesofphysicianentry,anolder
workforce,andhigherratesofattrition.10 Mostimportant forthefutureoftheruralEMworkforce,EMtraining programscontinuetoproliferateinurbanareas,withvery fewprogramsinruralareaswithrural-focusedtraining.7,8 Severaltrainingprogramshavesoughttoencouragerural practicebyincorporatingruralclinicalelectivesand publishedguidelinesfordevelopingruralclinical experiences.11,12 Additionalresearchdemonstratesthatrural rotationsareeducationallyvaluableandincludegreateror similarnumbersofprocedurestourbantertiaryrotations.13 Despitetheseefforts,asignificanteducationalgapremains formostresidents.ThereisnorequirementforruralEM clinicalornonclinicaleducationwithintheAccreditation CouncilforGraduateMedicalEducationcorecompetencies forEMandnostandardizedruralEMcurriculumfor residenciestoreference.Thereisalsoverylimiteddata onoptimaltrainingmethodsforpreparingresidentsfor ruralpractice.
OurteamofruralEMclinician-educatorsiswellversedin thestaffingneedsandclinicaldemandsofruralEMpractice. Weaimedtoleverageourunique,rural-academichealth networkandaddressthiseducationalchallenge.Our objectiveswereto1)deliveramultimodal(didactic, simulation,andclinical)ruralEMcurriculumthatprepares traineestoindependentlyworkinruralemergency departments(ED)atgraduation;and2)evaluateour programquantitativelyandqualitativelytoassessthe opportunitiesandlimitationsofruraltraining.
Todevelopourcurriculumcontent,ruralEMneededtobe defined:Whataretherural-specificskillsthatEPsneedto deliverexcellentcarethatarenotpartofatypicaltertiarycareresidencycurriculum?Toanswerthisquestion,we conductedatwo-yearcasereviewofalladmissions,transfers,
andgreaterthansix-hourlength-of-stay(LOS)casesfrom theEDsoftworuralcriticalaccesshospitals(CAH)inour network.Tobedesignated “criticalaccess,” ahospitalmust belocatedinaruralareamorethan35milesfromanother hospital,provide24/7emergencycare,andhave25orfewer inpatientbeds.14 ThetwoCAHEDsinourstudyeachsee 6,000patientsannuallywithbasicEMresourcesincluding lab,plainradiographs,computedtomography,andpoint-ofcareultrasound,withasolocoverageEPstaffingmodel. Thereisnospecialtyback-up,nooperatingroom,no obstetricalservices,nobloodbank,norespiratorytherapy, andlimitedpharmacistcoverage.
Wefocusedoncasesrequiringcriticalcare,transfer, specialtyconsultation,andgreaterthansix-hourLOS, becausethesecasespushedourattendinggrouptothink harder,reviewaprocedureorpathology,oruseskills typicalofnotonlyanEP,butalsoarespiratorytherapist, pharmacist,and/orspecialist.Thisallowedustoidentifya libraryofchallengingruralEMcases.Wealsocreateda 15-memberruralEMfacultyworkinggroupofacademic physicianswhoroutinelypracticeinruralenvironments. OurruralCAHcasereviewwascombinedwithinput fromourruralEMworkinggrouptocreatealistof knowledgeandskillsessentialtoruralEMpracticeyet missingfromourexistingteaching( Figure ).Inparallel,we developedaselectionofEMclinicalrotationsatour network ’ sCAHsandatpartnerruralsitesthroughout thecountry.
Tenresidentscompletedapilottwo-weekorfour-week ruralEMrotationand18monthsoftheruralnonclinical curriculumfromJuly2021–August2023.These10home residentswerethe first10residentstochoosethisrural rotationintheirsecondorthirdyearaspartofanew residencyprogram.Duringthestudyperiod,eightother homeresidentschosealternativeelectiverotations.All18 homeresidentscompletedtheruralnonclinicalcurriculum. Duringthestudyperiod,wealsoopenedourruralEM rotationtovisitingresidents.Fourvisitingresidentsfrom threeurbanresidencyprogramscompletedtheclinical
rotationbutdidnotparticipateinthenonclinicalcurriculum. Zeroresidentsenteredourruralcurriculumwithanexplicit commitmenttofutureruralpractice.Onehomeresidentin eachgroupandtwovisitingresidentsgrewupinarural area definedasaUnitedStatescensus-designatedplace withapopulationlessthan2,500.15
Qualitativeandquantitativefeedbackontherural rotationwassolicitedfromhomeandvisitingresidents. Residentscompletedavoluntarysurveythataskedthe following:1)Wastherotationbeneficialtoyourclinical training;2)describeanynewskillsanduniqueexperiences; 3)discussanylimitationsoflearninginaruralenvironment; 4)areyouinterestedinruralpractice;and5)wherewillyou practiceupongraduating?Wealsocollecteddataonpatient volume,patientacuity(discharged,admitted,or transferred),andproceduresperformedfromApril 2022–August2023.PriortoApril2022,ourelectronichealth recorddidnotconsistentlyenableresidentdocumentation, preventingaccuratechartreview.Thisqualityimprovement andeducationprojectusingresearchmethodswassubmitted toourinstitutionalreviewboard(IRB);itdidnotmeetthe definitionforhumansubjectsresearchandwasexemptfrom IRBreviewandapproval.
TheruralEMcurriculumhasprovensuccessfuloverthe firstthreeyearsandcontinuestoevolve.Atotalof10of10 homeresidentsandfouroffourvisitingresidentswho completedtheclinicalrotationreportedgainingnewskills andconfidence.Intheirfree-textresponses,residentsstated thatprovidingrespiratorysupportwithoutarespiratory therapist,managingmultiplecriticalpatients,providing solo-coveragetraumacare,anddeliveringorthopediccare werehighlightedskillsoftherotation.Comparedwith academic,tertiary-caresites,residentsseepatientvolumes thataremorevariableatruralsiteswithmoreextremepeaks (sixpatientsperhour)andtroughs(zeropatientsperhour) consistentwithsolocoverageEMpractice.Acuityis
Respiratory support without a respiratory therapistAdult respiratory distress from HFNC to NIV to MV
How to size up your resources on your first rural shift
Infant bronchiolitis from HFNC to NIV to MV
Critical care pharmacy basicsCritical access neuro critical care
Rural EMS operations and medical directionRural pediatric crashing asthma
EMTALA and transfer logisticsSolo-coverage two-patient trauma
Rural obstetricsTriple patient transfer logistics and telemedicine
Rural point of care ultrasound applications
You are the OB: delivery with PPH
Rapid rural procedures for solo coverageYou are the NICU: neonatal resuscitation
Rural pediatric critical care pearlsYou are the intensivist: code on the floor
Rural orthopedics: Solo coverage tips and tricks
You are the ENT: fiberoptic airway assessment
Teaching cases from critical access EMYou are the RN: key nurse tasks for rural docs
Figure. Nonclinicalruralcurriculumcomponents.
EMS,emergencymedicalservices; EMTALA,EmergencyMedicineTreatmentandLaborAct; HFNC,high-flownasalcannula; NIV,non-invasiveventilation; MV,mechanicalventilation; IO,intraosseous; OB,obstetrician; PPH,post-partumhemorrhage; NICU,neonatalintensivecareunit; ENT,earnoseandthroat; RN,registerednurse. Volume26,No.1:January2025WesternJournal
Table. Ruralemergencymedicinecurriculumparticipationandresidentjobchoice. ResidentgroupNumberofresidentsRuralcurriculumcompletedRuralpractice Homeresident,pilot10Clinicalandnonclinical70%(7/10) Homeresident,otherelective8Nonclinical75%(6/8) Visitingresident4Clinical25%(1/4)
similarlymorevariablethanatacademicsitesonagiven shift,buthigh-acuitycaseswerenotedtobesomeofthe highestyieldlearningexperienceswithresidentsperforming full-spectrumemergencycare.Residentsperformedagreater varietyofproceduresthanattheirtertiarysiteandmorenew procedures.Thesewereprocedurestheyoftendeferredto specialistsonbusyshiftsincludingfracture-dislocation reductions,arthrocentesis,complexlacerationrepair, priapismreduction,andregionalanesthesia.Atotalof100% ofhomeandvisitingresidentsreportedinterestinfuturerural practice,and70%ofhomeresidentswhocompletedthe clinicalandnonclinicalruralcurriculumsignedacontract witharuralCAHorsolecommunityhospital16 foraportion oftheirpracticeongraduation(Table).Additionally,75%of homeresidentswhocompletedthenonclinicalcurriculum onlyalsochosearuralpractice.
Asof2024,thiscurriculumcontinuestoevolvebasedon residentandfacultyfeedback.Datacollectionontheimpact ofruralEMeducationinourprogramisongoing.
Thissingle-centerpilotstudyofanewcurriculumwithina ruralhealthnetworkcomeswithinherentlimitations.For measuringimpact,nocomparisongroupwasavailable.Asa newresidencyprogram,therearenopriorclassesofresidents tocompareoutcomespre-andpost-ruralcurriculum.All homeresidentscompletedtheruralnonclinicalcurriculum andreceivedmentorshipfromruralfaculty.Additionally, fiveoftheeightresidentswhodidnotchoosethepre-designed ruralEMrotationscreatedtheirownrural/austererotation. Thus,ourstudydoesnotisolateclinicalornonclinical componentstodeterminewhichmightbemorestrongly associatedwithourresidents’ highrateofruralpractice followinggraduation.
Forgeneralizability,manyprogramsmaylackeasyaccess toruralclinicalsites,mentorshipfromruralfaculty,orrural lecture/simulationresources.Withinnovationand collaboration,however,ruralclinicalandnonclinical educationshouldbefeasibleforanyprogram.Allprograms havedidactictime,accesstosimulationtraining,andpatients receivedintransferfromruralsitesintheirregion.Clinical experiencescouldbecreatedthroughpartnershipswithother programsifnotavailablelocally.Tosupportother programs ’ rural-focusededucation,wearedevelopingafree, open-access “RuralEMResource” website
(ruralemresource.us)toshareourlectures,simulationcases, andtemplateforbuildingruralclinicalrotations.
Amultimodal,ruralcurriculumrepresentsafeasible approachtopreparingresidentsforindependentpractice inruralsettings.Innovativeruralcurriculashouldbe sharedbroadly,andurbanresidencyprogramsshould partnerwithruralclinicalsitestoprovideexpanded trainingopportunities.Thistypeoffocusedruralclinical andnonclinicalcurriculumdevelopmentrepresentsa promisingapproachtobridgingthegapbetweenurban, tertiary-caretrainingprogramsandruralemergency careneeds.
AddressforCorrespondence:AshleyWeisman,MD,Universityof Vermont,DepartmentofEmergencyMedicine,111ColchesterAve., EC2-206,Burlington,VT05401.Email: ashley.weisman@ uvmhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Weismanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BarretoT,JettyA,EdenAR,etal.Distributionofphysicianspecialtiesby rurality. JRuralHealth. 2021;37(4):714–22.
2.ClayCE,SullivanAF,BennettCL,etal.Supplyanddemandof emergencymedicineboard-certifiedemergencyphysiciansbyU.S. state,2017. AcadEmergMed. 2021;28(1):98–106.
3.PalusoN,CrollZ,ThayerD,etal.Residentialsettingsandhealthcare useoftherural “oldestold” Medicarepopulation.2018. Available at: https://digitalcommons.usm.maine.edu/longterm_care/8/ AccessedJune21,2023.
4.RuralHealthInformationHub.RuralHealthDataExplorer.Availableat: https://www.ruralhealthinfo.org/data-explorer?id=192 AccessedJune21,2023.
5.TheCecilGShepsCenterforHealthServicesResearch.195rural hospitalclosuresandconversions:January2005-present.2014. Availableat: https://www.shepscenter.unc.edu/programs-projects/ rural-health/rural-hospital-closures/.AccessedonJune21,2023.
6.Greenwood-EricksenMBandKocherK.Trendsinemergency departmentusebyruralandurbanpopulationsintheUnitedStates. JAMANetwOpen. 2019;2(4):e191919.
7.BennettCL,ClayCE,EspinolaJA,etal.UnitedStates2020emergency medicineresidentworkforceanalysis. AnnEmergMed. 2022;80(1):3–11.
8.TalleyBE,AnnMooreS,CamargoCAJr.,etal.Availabilityandpotential effectofruralrotationsinemergencymedicineresidencyprograms. AcadEmergMed. 2011;18(3):297–300.
9.HallMK,BurnsK,CariusM,etal.Stateofthenationalemergency departmentworkforce:whoprovidescarewhere? AnnEmergMed. 2018;72(3):302–7.
10.GettelCJ,CourtneyDM,JankeAT,etal.The2013to2019emergency medicineworkforce:clinicianentryandattritionacrosstheUS geography. AnnEmergMed. 2022;80(3):260–71.
11.WadmanMC,ClarkTR,KupasDF,etal.Ruralclinicalexperiencesfor emergencymedicineresidents:acurriculumtemplate. AcadEmerg Med. 2012;19(11):1287–93.
12.CasalettoJJ,WadmanMC,AnkelFK,etal.Emergencymedicine ruralrotations:aprogramdirector’sguide. AnnEmergMed. 2013;61(5):578–83.
13.CareyNI,HansrothJ,DavisH,etal.Comparingresidentprocedures inruralversusurbanemergencydepartments. Cureus. 2021;13(11):e19989.
14.CentersforMedicareandMedicaidServices.Criticalaccesshospitals. Availableat: https://www.cms.gov/medicare/health-safety-standards/ certification-compliance/critical-access-hospitals AccessedonMarch19,2024.
15.EconomicResourceService,UnitedStatesDepartmentof Agriculture.Vermont:threeruraldefinitionsbasedoncensus places.Availableat:~https://www.ers.usda.gov/webdocs/ DataFiles/53180/25600_VT.pdf?v=0#:~:text=Rural% 20locations%20are%20those%20outside,Outside%20Census% 20Places%20%3E%3D%202%2C500%20people AccessedonApril5,2024.
16.HealthResourcesandServicesAdministration.340Beligibility hospitals:solecommunityhospitals.2024.Availableat: https://www. hrsa.gov/opa/eligibility-and-registration/hospitals/sole-communityhospitals.AccessedonApril5,2024.
AlexandraMannix,MD*
ThomasBeardsley,MD*
ThomasAlcorn,MD†
MorganSweere,MD*
MichaelGottlieb,MD†
*UniversityofFloridaCollegeofMedicine – Jacksonville,DepartmentofEmergency Medicine,Jacksonville,Florida † RushUniversityMedicalCenter,DepartmentofEmergencyMedicine,Chicago,Illinois
SectionEditor: AsirMisraMD,MSMEd,CHSE
Submissionhistory:SubmittedJanuary8,2024;RevisionreceivedSeptember18,2024;AcceptedSeptember26,2024
ElectronicallypublishedOctober29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18687
Background: TheStandardizedLetterofEvaluation(SLOE)isacrucialcomponentoftheemergency medicine(EM)applicationprocess.GiventhecriticalroleoftheSLOE,weattemptedtobetter understandthegradingscalesused,aswellasthedistributionofgradesandrank-listpositions.
Objectives: Ourprimaryobjectiveinthisstudywastodeterminethedistributionofgradingformats, gradesgiven,andrank-listpositionsacrossEMclerkshipsusingtheSLOE.
Methods: Weperformedacross-sectionalstudyofthegradingformats,gradesgiven,andranking distributionsasreportedontheSLOEduringthe2022–23applicationcycle.WeobtaineddataonSLOEs fromEMresidencyprogramsaccreditedbytheAccreditationCouncilforGraduateMedicalEducationby reviewingallapplicantswhoappliedtoeitheroftwoEMresidencyprogramsingeographicallydifferent regions.Trainedabstractorsrecordedthefollowingdata:numberofstudentsrotatingintheprioryear; gradingformatused;andgradeandrankdistributionamongstudents.
Results: Weincluded264programsinour finalanalysis,after13programsmetexclusioncriteria.The majorityofprograms(72.2%)useanHonors/HighPass/Pass/Failgradingscheme.Wedeterminedthe meanpercentofeachgrade:Honors/A27.6%;HighPass/B31.1%;Pass/C40.8%;LowPass/D0.2%; andFail/F0.3%.Finally,wedeterminedthemeanpercentforeachrank-listposition:top10%was17.6%; topthird36.5%;midthird34.1%;andlowthird11.8%.
Conclusion: Wedeterminedthegradingschemesandgradeandrank-listdistributionsforEMprograms duringthe2022–2023academicyear.MostprogramsusedaHonors/HighPass/Pass/Failgrading scheme,withthemajorityofstudentsreceivingHonorsorHighPass,while0.3%failedtheirrotation. Bothgradesandranklistdemonstratedevidenceofaskeweddistributiontowardhighergradesand rank-listposition.[WestJEmergMed.2025;26(1)66–69.]
TheStandardizedLetterofEvaluation(SLOE)isacrucial partoftheNationalResidentMatchingProgram(Match) processintoemergencymedicine(EM)residenciesinthe UnitedStatessinceitreplacedthenarrativeletterof recommendationinthe1990s.1 TheSLOEusesevaluations fromEMrotationstocomparemedicalstudentsina standardized,objectivemannerfortheMatch.TheSLOEs havebecomeuniversallyadoptedafterbeingdeemedareliable toolinstratifyingEMresidencycandidates,makingitakey
portionoftheapplicationprocess,especiallyconsidering recentchangestoqualifyingboardexamsmovingtopass/fail.2
Thetopthreefacetsoftheapplicationusedbyprogram directorsoverallarecoreclerkshipgrades,EMclerkship grades,andlettersofrecommendation.2 TheEMclerkship gradingisirregular,withnostandardizationbetween programsregardingtheassignmentofgrades.3 Schoolshave anumberofdifferentgradingsystemsaswellasrequirements tomeeteachgradelevel,makingitmoredifficulttocompare studentsfromdifferentmedicalschools.Theclerkship gradingisconsideredtobenotasfruitfulaboutthe applicant’soverallperformanceastheglobalassessment sectionoftheSLOE.4 Infact,theinitialcreationoftheSLOE wasspurredpartiallytocombatspeculatedgradeinflation amongprograms.Evenso,theCouncilofResidency DirectorsinEmergencyMedicine(CORD)TaskForce foundthatgradeinflationwasstillalimitingfactorofthe SLOE,withsomeimprovementinrank-listinflationnoted between2012and2017.2,4
ManySLOEwritershaveindicatedthattheydidnot receiveformaltraininginhowtoproperly fillouttheSLOE andoftendonotaccesstheCORDguidelinesfordoingso.5 ThecreationoftheeSLOEin2016contributedtoanoverall improvementintherankingdistributionofstudents; however,thesystemisstillinconsistent.4 Thereisalso variabilityintheinterpretationoftheSLOE,witha significantnumberofprogramdirectorsagreeingthattheir interpretationofthedataisimpactedbywhotheletterwriter is.6 Speculationexistsregardingthevalidityofthese evaluationlettersbecauseofthisinconsistency,even extendingtootherspecialties.7
ConsideringthecriticalroleoftheSLOEasatoolfor rank-listdetermination,thereisaneedtobetterunderstand distributionofgradesandrank-listpositions.Ourprimary objectiveinthisstudywastodeterminethedistributionof gradescheme,grade,andrank-listpositionsacrossEM programsusingtheSLOE.
StudyDesign
Weperformedacross-sectionalstudyofthegradingand rankingdistributionsofEMmedicalstudentclerkshipsas reportedontheSLOEduringthe2022–23applicationcycle. TheSLOEswereevaluatedforthereportedclerkshipgrading andrank-listpositionsfromthepreviousyear,arequired componentoftheSLOE.Wedidnotreviewthegradesand rank-listpositionsthatweregiventocurrentapplicantswho appliedtoourprograms.Thisstudywasdeemedexemptby theinstitutionalreviewboardsattheUniversityofFlorida –Jacksonville,andRushUniversityMedicalCenter.
StudyProtocol
WeincludedallEMresidencyprogramsacrosstheUnited StatesthatwereaccreditedbytheAccreditationCouncilfor
GraduateMedicalEducation.ToobtainSLOEsfromeach EMUSresidency-basedclerkship,wereviewedSLOEsfrom allapplicantsduringthe2022–23cyclewhoappliedtoeither oftwoEMresidencyprogramsthatarelocatedindifferent geographicregions.TheUniversityofFlorida – Jacksonville isathree-year,countyEMprogramlocatedinJacksonville, FL.RushUniversityMedicalCenterisathree-year, academicEMprograminChicago,IL.Weincludedall clerkshipSLOEsfromprogramsthathadanaffiliatedEM residencyprogramandhadreportedeithergradedistribution orrankdistributionfromtheprioryear.Weexcluded programswithoutarotationtheprecedingyear,programs withoutreporteddatafortheprecedingyear,orprogramsfor whichwedidnothaveaccesstoaSLOE.
Trainedabstractorsfromeachinstitutioncollecteddata usingapre-pilotedstandardizeddata-abstractiontool.The abstractorsrecordedthefollowingdata:numberofstudents rotatingintheprioryear;gradingformatused(eg,Honors/ HighPass/Pass/Fail[H/HP/P/F];A/B/C/D/F;P/F;other); prioryeargradedistribution;andprioryearrank distribution(top10%/topthird/middlethird/bottomthird). Weperformeddualextractionforallprogramswithatleast twoSLOEsavailable.
Descriptivestatisticsarereportedforthetypeofgrading formatanddistribution.Wereportthemeanwithstandard deviationandmedianwithinterquartilerange(IQR)foreach gradeandrankdistributionattherotationlevel.Wealso reporttheoverallreportednumberandreportedpercentage oftotalapplicantsreceivingeachcategoryacrossall combineddata.Reportednumberwasdefinedasthetotal numberofstudentsreceivingaspecificgradeorrankbya givenprogram.Wedefinedreportedpercentageasthe percentageofthetotalstudentsinagivenprogramreceiving aspecificgradeorrank.Allanalyseswereperformed usingMicrosoftExcel2018(MicrosoftCorporation, Redmond,WA).
Of277programsidentified,weincluded264(95.3%)EM residency-basedclerkshipsinouranalysis.Thirteen clerkshipsmetexclusioncriteria(twothathadnorotationthe prioryear,onethatdidnotreportdataduetonewSLOE format,and10withnoSLOEavailableinourset).We identifiedamedianof21(IQR15–30)SLOEswritten perprogram.
Themajorityofprograms,72.2%(190/263),usedan H/HP/P/Fgradingscheme,followedbyP/F17.5%(46/263), A/B/C/D/F2.7%(7/263),andother7.6%(20/263).Theother gradingschemesareincludedin Appendix1.Oneprogram didnotprovideagradingscheme.Whenevaluatinggrade
Table1. Numberandpercentagedistributionofstudentsforeachgradeforvariousgradingformatsatnon-pass/failandpass/failprograms. Non-pass/failprograms (N = 13,599)n(%)
Pass/failprograms (N = 1,964)n(%)
Allprograms (N = 15,563)n(%)
Honors/A4,296(31.6%)4,296(27.6%)
Highpass/B4,837(35.6%)4,837(31.1%)
Pass/C4,380(32.2%)1,963(99.9%)6,343(40.8%)
Lowpass/D37(0.3%)37(0.2%)
Fail/F48(0.4%)1(<0.1%)48(0.3%)
Table2. Themeanandmediannumberofstudentsandmeanandmedianpercentageofstudents’ gradesonStandardizedLettersof Evaluation(SLOE)foreachprogram.(Medianof21[interquartilerange15–30]SLOEsperprogram.)
Meannumber* (SD)Mediannumber* (IQR)Meanpercentage** (SD)Medianpercentage** (IQR)
Honors/A16.4(22.7)9.0(2.0–20.9)26.9%(0.2%)23.0%(8%–40%)
Highpass/B18.5(23.0)12.1(1.9–24.8)30.7%(0.2%)33.0%(8%–40%)
Pass/C24.2(32.8)12.0(3.3–33.3)41.7%(0.4%)35.0%(10%–70%)
Lowpass/D0.1(1.4)0.0(0–0)0.2%(0.0%)0%(0%–0%)
Fail/F0.2(0.7)0.0(0–0)0.3%(0.0%)0%(0%–0%)
*Thetotalnumberofstudentsreceivingagivengradebyeachprogram.
**Thepercentageofstudentsreceivingagivengradebyeachprogram. IQR, interquartilerange.
Table3. Themeanandmediannumberofstudentsandmeanandmedianpercentageofstudents’ rank-listpositionsonStandardized LettersofEvaluation(SLOE)foreachprogram.(Medianof21[IQR15–30]SLOEsperprogram.)
Meannumber* (SD)Mediannumber*
*Thetotalnumberofstudentsreceivingagivengradebyeachprogram.
**Thepercentageofstudentsreceivingagivengradebyeachprogram. IQR, interquartilerange.
distribution,wedeterminedthemeanpercentageofeach gradeforall14,562students:Honors/A27.6%(4,296);High Pass/B31.1%(4,837);Pass/C40.8%(5,343);LowPass/D 0.2%(37);andFail/F0.3%(49).Gradedistributionswere thendividedintonon-P/Fprograms,andP/Fprograms,and presentedin Table1
Whenevaluatingrank-listdistribution,wedeterminedthe meanpercentageforeachrank-listpositionforallstudents acrossallprograms.Themeanpercentagesofstudents (6,221)foreachrank-listpositionwereasfollows:inthetop 10%therewere1,094students(17.6%);inthetopthirdthere were2,271students(36.5%);inthemidthird2,123students (34.1%);andinthelowthird733students(11.8%).
Finally,toassessprogram-leveldifferences,we determinedthenumberandpercentageofstudentsreceiving
agivengradeandrankbyeachprogram.Wethencalculated themeanandmediannumberandmeanandmedian percentageacrossprograms.Themeanpercentageof studentsgivenHonorsacrossprogramswas26.9%,followed by30.7%whoweregivenHighPass,and41.7%Pass (Table2).Themeanpercentageofstudentsrankedinthetop 10%byprogramswas19.8%,followedby37.1%inthetop third,32.3%inthemidthird,and10.8%inthelow third(Table3).
Thisstudyprovidesanupdatedrepresentationofnational trendsinEMSLOEgradeandrankdistribution. Historically,significantemphasishasbeenplacedonthe SLOEgradeandranklist.CurrentissueswiththeSLOE
writingsystemincludeconcernsrangingfrominexperienced authorsandnon-standardizedgradingschemestosystematic gradeinflation.
Withthecontinueduseofnon-standardizedgrading schemes,itmayappearthiselementoftheSLOEprovides littlevalue.Ourresultsshowthatwhileamajorityof programsusedtheH/HP/P/Fscheme,nearly30%of programsfavoredotherformats.OfthoseSLOEsusingthe P/Fsystem,ofwhichtherewerenearly2,000gradedstudents, onlyonerecordedafailinggrade.Withsuchan overwhelmingpredominanceofpassinggrades,theremaybe moresignificanceforafailinggradethanapassinggrade. Resultsfromnon-P/Fprogramsshowanearlyequal distributionofgradesbetweenHonors/A,HighPass/B,and Pass/C(31.6%,35.6%,and32.3%,respectively)withlessthan 1%receivingagradeoflowpassorfail.
WhileSLOE2.0nolongercontainsaglobalassessment, theranklistremainsavaluedtoolfordifferentiating applicants.Previousstudieshavedemonstratedanimproved spreadofdistributionoverthepastdecade2,4;however,that trendmayhavebecomestagnant.Ourdatashowsanearly identicalrank-listdistributiontothatofthe2016–2017 SLOEdataset,inwhichthetop10%contained18%,thetop thirdcontained37%,themidthirdcontained35%,andthe lowthirdcontained10%,respectively(withourresults showing17.6%,36.5%,54.1%,and11.8%,respectively).4 Whetherthisisacoincidenceorevidencethatthedistribution oftheranklisthastrulystagnatedremainsunclear. Evaluatorscontinuetorankveryfewapplicantsinthelow third,representinganoverlyfavorableevaluationoftheir rotatingstudents.
Thereareseverallimitationsthatwarrantconsideration. First,thisstudywaslimitedtoasingleyear;futurework shouldevaluatedifferencesingradingtrendsovertime. Additionally,thedatawaslimitedtoself-report,anditis possiblethatsomeprogramsmaynothaveaccurately reportedtheirgradeandrankdistributionfortheprioryear. WhilethemajorityofprogramsusedtheH/HP/P/Fscale, someprogramsusedalternatescales,whichmaynotfullymap tothemorecommonH/HP/P/Fscale.Moreover,wewere limitedtoapplicantswhoappliedonlytoourtwoprograms. Despitethislimitation,wehadaveryhighresponserateand onlymissed10programsnationally.Finally,therank-list reportsperceivedrank-listpositionbutmaynothavereflected students’ actualpositionontheranklist.
Wedeterminedthegradingformatsandgrade,andranklistdistributionsforEMprogramsduringthe2022–2023 academicyear.MostprogramsusedtheHonors/HighPass/ Pass/Failgradingscheme,withthemajorityofstudents receivingHonorsandHighPass,while0.3%failedtheir
rotation.Bothgradesandranklistdemonstratedevidence ofskeweddistributiontowardhighergradesand rank-listposition.
TheauthorswishtothanktheDiversityInclusion ResearchandEducationCollaborationTeam(DIRECT).
AddressforCorrespondence:AlexandraMannix,MD,University ofFloridaCollegeofMedicine-Jacksonville,Departmentof EmergencyMedicine,655W8thStreetJacksonvilleFL32209. Email: ALMannix@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Mannixetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KeimSM,ReinJA,ChisholmC,etal.Astandardizedletterof recommendationforresidencyapplication. AcadEmergMed 1999;6(11):1141–6.
2.LoveJN,DeiorioNM,Ronan-BentleS,etal.Characterizationofthe CouncilofEmergencyMedicineResidencyDirectors’ standardized letterofrecommendationin2011–2012. AcadEmergMed 2013;20(9):926–32.
3.FaganR,HarkinE,WuK,etal.Thelackofstandardizationofallopathic andosteopathicmedicalschoolgradingsystemsandtranscripts. JSurgEduc 2020;77(1):69–73.
4.JacksonJS,BondM,LoveJN,etal.Emergencymedicinestandardized letterofevaluation(SLOE): findingsfromthenewelectronicSLOE format. JGradMedEduc 2019;11(2):182–6.
5.HegartyCB,LaneDR,LoveJN,etal.CouncilofEmergencyMedicine ResidencyDirectorsstandardizedletterofrecommendationwriters’ questionnaire. JGradMedEduc 2014;6(2):301–6.
6.LoveJN,SmithJ,WeizbergM,etal.CouncilofEmergencyMedicine ResidencyDirectors’ standardizedletterofrecommendation:the programdirector’sperspective. AcadEmergMed 2014;21(6):680–7.
7.InclanPM,CoopersteinAA,PowersA,etal.When(almost)everyoneis aboveaverage:acriticalanalysisofAmericanOrthopaedicAssociation CommitteeofResidencyDirectorsstandardizedlettersof recommendation. JBJSOpenAccess[Internet] 2020;5(3):e20.00013. Availablefrom: http://dx.doi.org/10.2106/JBJS.OA.20.00013. AccessedAugust26,2024.
MaryMcLean,MD*
JustinStowens,MD†
RyanBarnicle,MD,MSEd‡
NegarMafi,MD§
KaushalShah,MD∥
*AdventHealthEastOrlando,DepartmentofEmergencyMedicine,Orlando,Florida
† ChristianaCareHealthSystem,DepartmentofEmergencyMedicine, Newark,Delaware
‡ TheWarrenAlpertMedicalSchoolofBrownUniversity,DepartmentofEmergency Medicine,Providence,RhodeIsland
§ SanJoaquinGeneralHospital,DepartmentofEmergencyMedicine, FrenchCamp,California
∥ WeillCornellMedicine,DepartmentofEmergencyMedicine,NewYork,NewYork
SectionEditors: JulesJung,MDandSharonBord,MD
Submissionhistory:SubmittedApril11,2024;RevisionreceivedNovember18,2024;AcceptedNovember19,2024
ElectronicallypublishedDecember31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20787
Introduction: Theutilityofthethree-partbedsideoculomotorexamHINTS(headimpulsetest, nystagmus,testofskew)inthehandsofemergencyphysiciansremainsunderdebatedespitebeing supportedbythemostrecentliterature.Educatorshistoricallylackconsensusonhowspecificallyto teachthisskilltoemergencymedicine(EM)residents,anditisunknownwhetherandhowEMresidency programshavebeguntoimplementHINTStrainingintotheircurricula.Weaimedtocharacterizethe stateofHINTSeducationinEMresidencyanddevelopaneedsassessment.
Methods: Inthiscross-sectionalstudy,weadministeredasurveytoEMresidencydirectors,thethemes ofwhichcenteredaroundHINTSeducationperceptions,practices,resources,andneeds.Weanalyzed Likertscaleswithmeansand95%confidenceintervalsfornormallydistributeddata,andwithmedians andinterquartilerangesfornon-normallydistributeddata.Frequencydistributions,means,andstandard deviationswereusedinallotheranalyses.
Results: Of250eligibleparticipants,201(80.4%)respondedandconsented.Ofthe192respondents providingusabledata,149/191(78.0%)believedtheHINTSexamisvaluabletoteach;124/192(64.6%) reportedHINTSeducationalofferingsinconference;and148/192(77.1%)reportedclinicalbedside teachingbyfaculty.Themost-effectiveeducationalmodalitieswereclinicalbedsideteaching,online videos,andsimulation.SubtopicteachingstruggleswithregardtoHINTSwereheadimpulsetestand test-of-skewconductionandinterpretation,selectionofthecorrectpatients,andoverallHINTS interpretation.Teachingbarrierscenteredaroundlackoffacultyexpertise,concernforpoorHINTS reproducibility,andlackofresources.Leadershipwoulddedicateameanof2.0hours/year(SD1.3 hours/year)toimplementingaformal,standardizedHINTScurriculum.
Conclusion: Despitecontroversysurroundingtheutilityof theHINTSexaminEM,mostresidencydirectors believeitisimportanttoteach.Thisneedsassessmentcanguidedevelopmentofformaleducationaland simulationcurriculafocusingonresidencydirectors’ citedHINTSexameducationalstruggles,barriers,and reportedmost-effectiveteachingmodalities.[WestJEmergMed.2025;26(1)70–77.]
Background
Posteriorstrokepresentingwithdizzinessismisdiagnosed byemergencyphysicians(EP)in35%ofcases,1 whichcan leadtoseveredebilitationandsometimesdeath.2 Paradoxically,ofpatientsdischargedfromtheemergency department(ED)withadiagnosisofdizzinessorvertigo, only1in500isdiagnosedwithastrokewithinthe first month.3 Withadvancesinstroketreatmentmodalities,it makessensethatthereisheightenedemphasisondetection. In2013,theannualcostofimagingforacutedizzinessin UnitedStatesEDswasnearly$4billion.4 Muchofthiscostis duetoutilizationofnon-contrastcomputedtomography (CT)ofthehead5 despiteitslowsensitivityfordetecting posteriorfossastroke(mean41.8%,95%confidenceinterval 30.1–54.4%)6 andthelowlifetimecost-effectiveness comparedtomagneticresonanceimaging(MRI).7 Specifically,itisestimatedthatover$1billionperyearis wastedoninappropriateCTimagingforpatientswith dizziness/vertigo.8
AworldwidesurveyofEPspublishedin2008foundthat thedevelopmentofabetterclinicaldecisionrulefor identificationofcentralvertigowasthesecondhighest clinicalpriorityforparticipants.9 Managementofdizziness andvertigoisincludedintheJointTaskForceEmergency MedicineModelofClinicalPractice,10 andEPsareexpected todiagnoseandmanagepatientswiththesechiefcomplaints. Itis,therefore,incumbentuponEMresidencyprogramsto provideadequateeducationandtrainingondizzinessand vertigo.However,a2005studyfoundthatonly35%ofEM residencyprogramsrequiredaclinicalneurologyor neurosurgeryrotation,andanannualmeanof12hours(of 280totaldidacticeducationhours)wasdedicatedto neurologicemergencies.11 Itisunknownhowmuchofthis timeisdevotedspecificallytodizzinessandvertigo,or exactlywhatisbeingtaughtregardingappropriatehistory, physical,anddiagnosticworkuprecommendations.
TheclinicalHINTSexam(headimpulsetest,nystagmus, testofskew)12 isathree-partbedsideoculomotorexamwith diagnosticaccuracyforcentralvertigosimilartothatofMRI. A2023CochraneReviewof12studiesand1,890participants foundtheclinicalHINTSexamtobe94%sensitiveand87% specific. 13 ThisexammaybeappealingtotheEPbecauseitis purportedtobearapidandlow-costbedsideevaluation. However,literaturesuggeststhatitsdiagnosticaccuracyhas fallenshortforEPsusingtheHINTSexaminclinicalpractice, with findingssuggestingthatthereasonsareapplicationto inappropriatepatients(eg,thosewithoutacutevestibular syndromeandnystagmus)anddifficultyininterpretinghead impulsetest(HIT)results.14,15 Inaddition,theliteraturehas shownpoorinter-raterreliabilityamongEPsusingthe HINTSexam.16 Withtheseconcernsinmind,twoother clinicaldecisiontoolshavesincebuiltonHINTSprinciples. The firstistheHINTS “plus” tool,whichaddsahearingtest
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Whenproperlyused,theHINTSexamhashigh diagnosticaccuracyforcentralcausesindizzy patients,butthestateofHINTSeducationin (EM)isinadequatelycharacterized.
Whatwastheresearchquestion?
Whatareprogramleadershipperceptions, educationalpractices,andbarriersto teachingHINTSinEMresidencies?
Whatwasthemajor findingofthestudy?
78.0%ofprogramleadersbelievethe3-part oculomotorexamisvaluabletoteach, and64.6%offerformalHINTS educationsessions.
Howdoesthisimprovepopulationhealth?
TeachingHINTStoEMresidentsrequires improvedcurricula,resources,andfaculty expertise.Bettereducationmayhelptranslate promisingHINTSliteratureinto clinicalpractice.
(95.3%sensitiveand72.9%specific).13 Thesecondisthe STANDING(spontaneousnystagmus,direction,head impulsetest)algorithm,whichusestwopartsoftheHINTS examandadditionalphysicalexammaneuvers(93–100% sensitiveand72–94%specific).17–19
The2023AmericanCollegeofEmergencyPhysicians (ACEP)ClinicalPracticeGuidelineoffersspecificHINTS examrecommendationsandcautions: “Beforeemployinga maneuversuchasHINTS,physiciansshouldhavesufficient educationtoperformthetechnique;notusingtoolssuchas HINTSmayleadtoexcessivetestingandadmission;and incorrectimplementationmayleadtoanincreasedriskof misdiagnosis.”20 InadditiontoACEP’srecommendations, in2023,theSocietyforAcademicEmergencyMedicine releasedGuidelinesforReasonableandAppropriateCarein theEmergencyDepartment(GRACE-3):AcuteDizziness andVertigointheEmergencyDepartment.Theyhadsimilar recommendationsthatEPeducationshouldinvolvethe following: “receivetrainingintheHINTSexam;usethe HINTSexam(onceproperlytrained)inpatientswith nystagmus;andconsidertheHINTSexamasthe first-line testoverMRI(ifaHINTS-trainedclinicianis available).”21,22 TheauthorsofGRACE-3also acknowledgedadiscordanceinthatmostEPshavenot receivedspecialtrainingintheuseoftheHINTSexam.This
lackofspecialtrainingmayhaveledtotheHINTStesting inaccuraciesreportedintherecentliterature.14,15 Thisbegs thequestionofwhich,ifany,educationaltacticshave beeneffective.
FromtherecentGRACE-3guidelines21 andreleasesby EMsocieties,10,20 thereisaclearcallforEMHINTS educationandHINTSexamintegrationintotheEMclinical arena.However,thecurrentstateofHINTSexam acceptance,education,andtrainingisunclear.IfHINTS curricularimplementationhasoccurred,informationabout theneeds,barriers,teachingstruggles,andeducator perspectivesmayaddfurtherweighttotheargumentforour specialty’soverallacceptanceoftheHINTSexam.
ThestandardofcarefortheEDevaluationofdizzy patientsmaybeevolvingtoembracetheHINTSexam,but translationoftheliteraturetoclinicalpracticeremains unclear.ItisalsounclearwhatproportionofEPshavebeen adequatelytrainedintheuseoftheHINTSexam. Furthermore,residencyprogramsmaylackthefaculty expertise,timeandfundingtoaddnewitemssuchasHINTS educationtotheircurricula.Programsthathaveadoptedthe societalguidelinesaddressingtheHINTSexammayhave alreadyadjustedtheirdidacticandsimulationcontent. SupportersoftheHINTSexamwillrecognizethe importanceofaneedsassessmentwithregardtoresidency effortsandperceivedchallengesandbarrierstodizziness evaluationandHINTSeducation.Skepticswill findthe knowledgeofcurrentHINTSteachingparadigmsusefulto determinetheirownpracticeandthepotentiallyevolving standardofcare.
Whilerecentresearchsupportsaneedforchangeinour EDclinicalpractice,ithasyettobeassessedwhetherthese ideasarecurrentlybeingtaughtwithinEMresidency programs,andifso,howtheyarebeingtaught.Ourgoalin thisinvestigationwastoassessthecurrentUnitedStatesEM residencyprogramleadershipperspectives,teaching paradigms,teachingbarriers,andfutureneedsfor implementingeducationalcurriculaonassessmentofthe dizzypatient,withaparticularfocusontheHINTSexam. Theresultsofthiseducationalneedsassessmentcanserveto guideandrefinetheconstructionofeducationalresources includingdidacticandsimulationmodalities.
Thiswasacross-sectionalobservationalstudyinavirtual setting.Participantswereofferednoincentives,therewasno funding,andthestudywasinstitutionalreviewboardapprovedasexempt.Anelectronicsurveywasadministered toEMresidencydirectorsbetweenApril6–July13,2023.
ThestudywasconductedincompliancewithSTROBE (StrengtheningtheReportingofObservationalstudiesin Epidemiology)cross-sectionalreportingguidelines.23
Includedwerecurrentprogramdirectorsforcategorical EMresidencyprogramsintheUS.Excludedwereprogram directorsfromresidencyprogramsthatreceivedinitial accreditationfromtheAccreditationCouncilforGraduate MedicalEducationonorafterJanuary1,2020.Therationale forthisexclusionwasthatnewprogramswerelesslikelyto haveadministeredanentireeducationalcurriculumcycle. Thetargetpopulationincluded250programleaders(one fromeacheligibleprogram).Programdirectorcontact informationwasobtainedfrommedicalsocietydatabases andresidencyprogramwebsites.Whilebothworkand personalemailswereoftenpubliclyavailable,weprioritized makingcontactviaworkemails.SeeAppendixAforthe participantrecruitmentmessage.
Thesurveyinstrumentwasdeveloped,tested,and validatedusingarigorousprocesswithcloseguidanceand leadershipfromseasonednationalmedicaleducationexperts viaaformalMedicalEducationResearchCertification programthroughtheCouncilofResidencyDirectorsin EmergencyMedicine.Wefollowedthesystematic,sevenstepprotocolfordevelopingmedicaleducationresearch questionnairesdescribedbyArtinoetal.24 Formalfocus groupswereusedtopropose,discuss,andreworksurvey itemsusinganiterativeprocessuntilconsensuswasreached regardingfacevalidityandinternalconsistency.Thesurvey waspilotedbyagroupof20membersofthenonprofit medicaleducationallianceALLNYCEM(consistingofEP medicaleducators,residencyleadershipmembers,and residenteducationfellows)forfeedbackonclarityand usability.Thesoleconsensusrecommendationwasto shortenthesurvey,whichwasdonepriortonational distribution.Finalsurveyitemsincludedprogram/institution demographicsandquestionsaboutperceptionsandpractices regardingdizziness,vertigo,andHINTSexameducation withineachresidencyprogram.SeeAppendixBforacopyof thecompletesurveytool.
WeusedtheelectronicplatformSurveyMonkey (SurveyMonkeyEnterprise,SanMateo,CA)todistribute thesurveyandcollectdata.The250programdirectorswere initiallycontactedindividuallyviaemailwiththerecruitment messageandtheirpersonalizedsurveylink.Subsequent contactattempts(requiredfor235programdirectors)were madefornon-responsesorincompletesurveys.Attheendof thedatacollectionperiod,allcompleteandpartialsurveys wereincludedinanalysisiftheparticipantprovideddata
beyondtheinformedconsentquestion.Exceptforthe informedconsentquestion,nosurveyquestionwasrequired. Thisallowedparticipantstooptoutofansweringspecific questionsiftheywishedwhilestillenablingthemto participate.Missingdatafromparticipantswhooptedoutof aquestionwasnotincludedinthecalculationsfor subsequentstatisticalanalysisforthatitem.
Intendedoutcomescenteredaroundresidencydirectors’ HINTSexamperceptionsaswellascurrentHINTS educationalpracticeswithinresidencyprograms,resources available,andcurricularneeds.Thepurposeofgathering informationontheseoutcomeswastogenerateaneeds assessmentfordizzinessandHINTSexamcurriculain EMresidencies.
WeanalyzeddatausingRversion4.3.2forMacOS(R FoundationforStatisticalComputing,Vienna,Austria). Likert-scaledatawasanalyzedusingmediansand interquartilerangesfornon-normaldatadistributionsor usingmeansand95%confidenceintervals(CI)fornormal datadistributions.Wetestednormalityofdatadistributions byexaminingestimatesofskewnessandkurtosisforeach scale,aswellasbyplottinghistogramsandcomparing distributionstothenormalcurve.Normalitywasconcluded onlyifallestimatesofskewnessandkurtosisfellbelowthe thresholdsof2and7,respectively,andallhistogramsaligned closelywiththenormalcurve.25 WeusedtheWilsonscore statisticforcalculationof95%CIsforbinomialproportion items(yes/noitemswithananswerof “ yes ” definedasa positiveresult).26,27 Frequencydistributionswereusedto analyzequestionsaboutstrugglesandbarrierstoteaching theHINTSexam.Weuseddescriptivestatistics(meansand standarddeviationsforallotherquantitativedata.As participantswerepermittedtoskipanyquestion,missing datawasomittedfromitem-levelanalyses.SeeAppendixC fordetailsonmissingdataanditem-levelresponserates.
Of250eligibleprograms,leadershipfrom204openedthe surveyand201providedinformedconsentforanoverall surveyresponserateof80.4%.Amongconsenting respondents,192programsprovidedusefuldatabeyondthe initialinformedconsentquestion.SeeAppendixDforthe enrollment flowsheet.Participatingprogramdemographic characteristicswerewellrepresentativeofthepopulationof alleligibleprograms(seeAppendixE).
Programleadershipreportedperceptionsthattheir residencygraduateswere,onaverage,moreconfidentand competentthantheirfacultymembersatperformanceand interpretationoftheHINTSexam.Theyalsoreported perceptionsthat,forbothresidencygraduatesandfaculty members,confidencewashigherthancompetence.However, noneofthesepatternsreachedstatisticalsignificance.
SeeAppendixF.
ThemostfrequentlycitedHINTSsubtopicteaching strugglescenteredaroundtheHIT,testofskew,HINTS applicationtocorrectpatients,andoverallHINTS interpretation.See Figure2.Themostfrequentlycited HINTSteachingbarrierscenteredaroundlackoffaculty expertise,concernforpoorHINTSexamreproducibility, andlackofresources.See Figure3.Lastly,program leadershipindicatedthattheywoulddedicateameanof2.0 hours/year(SD1.3hours/year)toimplementingaformal, standardizedHINTSexamcurriculumifsuchacurriculum werewidelyavailable.

Figure1. Box-and-whiskerplotofleadership-perceivededucational modalityeffectivenessforteachingtheHINTS*examination:188 participantsprovidedusabledataonthisitem(item-levelresponse rate75.2%).Likert-scaleratingsfromleast(1)tomost(7)effective wereused.Dataforoneofthe12modalities(clinicalbedside teaching)wasnotnormallydistributedandthusmediansand interquartileranges(IQR)wereusedforallanalyses.Mediansare representedbythickverticallines,IQRsarerepresentedbygray boxes,whiskersrepresent1.5*IQR,andoutlierdataisrepresented byblackdots,withtheareaofeachdotproportionaltothe answerfrequency.
Overall,149/191(78.0%)believedtheHINTSexamis valuabletoteach,16/191(8.4%)believeditisnot,and25/191 (13.1%)wereunsure.Onsubgroupanalysesoftheseand otherkeysurveyitems,programdemographicfactors (programlength,setting,type,andregion)wereofno statisticalsignificanceaftercontrollingformultiple comparisons.Themosteffectiveeducationalmodalitiesfor teachingtheHINTSexamwerereportedtobeclinical bedsideteaching,videocasts/onlinevideos,andsimulation. Perceptionsofmodalityeffectivenessvariedwidely. See Figure1
HINTS*,headimpulsetest,nystagmus,testofskew.
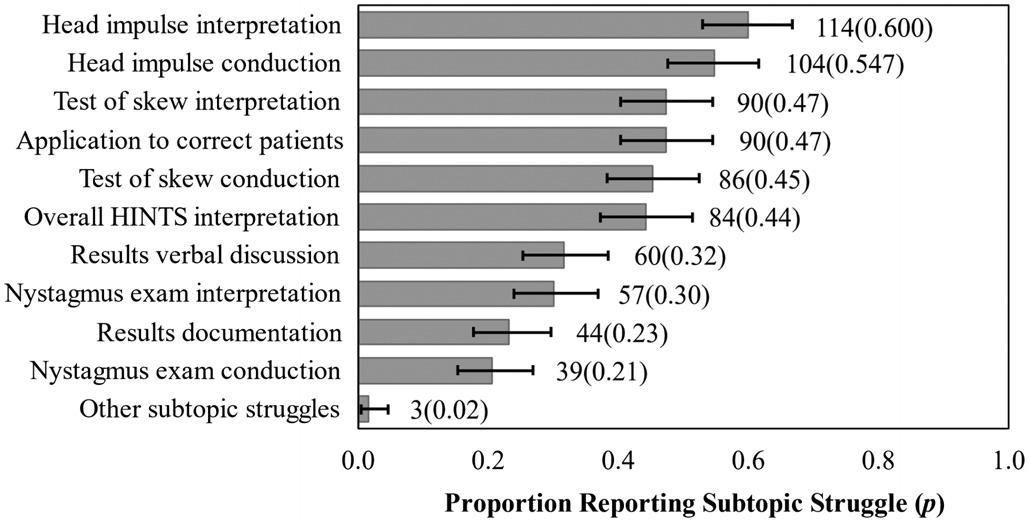
Figure2. Frequencyofresidencyprogramdirector-reportedHINTS examsubtopicteachingstruggles:190participantsprovided useabledataonthisitem(item-levelresponserate76.0%).Error barsrepresentthe95%confidenceintervalforthesebinomial proportionitemsusingtheWilsonstatistic.
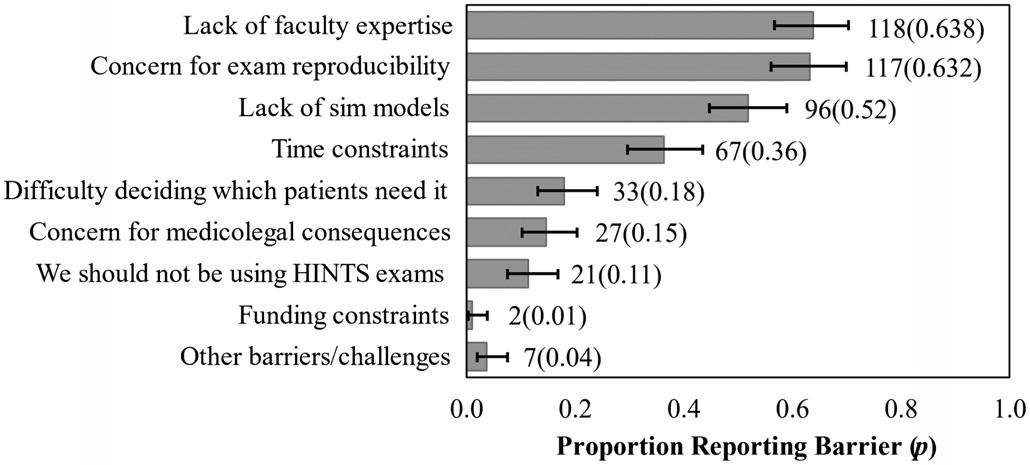
Figure3. Frequencyofresidencyprogramdirector-reportedbarriers toteachingtheHINTS*examination.185participantsprovided useabledataonthisitem(item-levelresponserate74.0%).Error barsrepresentthe95%confidenceintervalforthesebinomial proportionitemsusingtheWilsonstatistic. *HINTS,headimpulsetest,nystagmus,testofskew.
DISCUSSION
Our findingsmayreflectunderlyingcausesforthe difficultiesEPshaveteachingandusingtheHINTSexam. Facultymembersmayhesitatetoteachitiftheyexhibit discomfortwiththeirownHINTSexamskills.Inour findings, programleadershipexpressedlackoffacultyexpertiseasan educationalbarrier,andtheyalsoperceivedtheirresidency graduatestobemorecompetentwiththisskillthantheir facultymembers(althoughthis findingdidnotreachstatistical significance).Additionally,programdirectors’ citedbarrierof concernforpoorHINTSexamreproducibilitymaypoint towardphysicians’ innatedesirefordiagnosticcertaintyand theperceptionthattheHINTSexamisfallible.Our respondentsreportedthatHINTSisvaluabletoteach,but theylessoftenreportedHINTSofferingsinconferences.The citedreasonsforthisdiscordancecenteredaroundlackof time,resources,andfacultyexpertise.
IthasbeenshownintheoriginalHINTSliteratureand subsequentresearchreleasedfromneurologyandEM collaborationeffortsthatitispossibletoeffectivelylearnthis
skill,13,21 yetourresultsdonotdescribewidespreadskill acquisitionamongEPs.Itispossiblethateducational collaborationbetweenthespecialtiescouldpositivelyimpact EPs’ proficiencyintheexamitselfandinoptimaleducational methods.Regardless,oursurveyresultssupportadesireto addressthelackoffacultyexpertise.Muchcollaborationis alreadyoccurring,asevidencedbyrecentdizzinessand vertigoliteratureauthoredbyteamsincludingmembersof bothspecialties,21,28–30 aswellasresearchwithmixedcohorts frombothspecialties.1
Ourresultsshowthatsimulationwasperceivedasoneof themosteffectivemodalitiesforHINTSeducation,butlackof simulationmodelswasalsocitedasatopeducationalbarrier. TheHINTSeducationliteraturefromneurologyandneurosubspecialtieshasproposedsomeinnovativesimulation adjuncts.Forexample,onestudyfoundthatneurology trainees’ utilizationofvideo-oculography(VOG)technology insimulationcorrelatedwithsignificantimprovementsinHIT performance.31 Twostudiesusedvirtualreality-enhanced manikintasktrainersforHINTSsimulation,demonstrating examsensitivityandspecificityimprovements,including amongEPcohorts.32,33 Whilesuch “partialtasktrainers” may haveutility,oursurveysuggeststheyarenotwidelyusedor commerciallyavailable.TheVOGdevicesarecommercially availableandhavequalityassurance(QA)featurestoassist examiners’ HITperformanceviafeedbackonmaneuver anglesandvelocities.ArecentstudyusedtheseQAfeaturesin EMresidentHITsimulationandreportedsignificant improvementinHITmaneuverperformance.34
Therearenopublishedparametersfromtheneurologyor subspecialtyliteratureregardingtheoptimalHINTS curriculumtrainingdurations.However,a2022systematic reviewofHINTSandSTANDINGeducationreportedon fiveinstitutions’ EMeducationalpractices.Theyfoundwide curricularvariabilityindidactictime(1–5hours),workshop time(1–8hours),neurologyexposure(clinicalrotations),and proctoredexams(upto15)overeachresident’sdurationin theprogram.35 Ourparticipantsindicatedtheywould dedicateameanof2.0hours/yeartoHINTSeducation, andoverthecourseofathree-orfour-yearresidency,this wouldbeadequatetimefortheparametersdescribed.35 Despitewillingnesstocommitthistime,otherliterature suggeststhattheexamapplicationandmaneuversmaybe morecomplexthanourspecialtyrecognizes.14 Asreflectedin ourresults,programleadershipperceivedhigherconfidence thancompetenceamonggraduatesandfacultyalike (althoughthisdidnotreachstatisticalsignificance).This phenomenon theDunning-Krugereffect ispresentin medicine,andexistingliteraturesuggeststhatassessmentsby examinersfrommultipledisciplinesarerequiredtoensure proficiencyinsuchhigh-levelskills.36,37 Thiswould potentiallyaddmoretimetoaHINTScurriculum. Ourresultscontributetoagrowingdescriptionofthe HINTSeducationalmodalitiesinuse,buteachmodalityhas
prosandconsbeyondthetraininghoursrequired.Clinical bedsideteaching(thehighest-ratedmodalityinoursurvey) providesthehighest-fidelityandreal-lifeexperiencebutis dependentoncaseconvenience(dizzy/vertiginouspatients presenting)andeducatoravailabilityonshift.The opportunitycostofbedsidetrainingmustbeconsideredas well.Thesurveydoesnotexplorethehypotheticalon-shift facultytimespentandassociatedopportunitycost,which wouldbeausefultopicforfutureresearch.
Simulationtiedforsecondplaceasthehighest-rated HINTSeducationalmodality.Itmitigatesthecase convenienceissuebyprovidingon-demandpatientcasesina controlledsetting,butitalsopresentsafacultyopportunity/ costissuebyincreasingtrainingtimeinthesimulationcenter. Hands-onskillsimulationrequiressmall-grouporindividual instruction,whichusesmorefacultytimeandtheuseof simulationmodels,andpossiblyothersimulationadjuncts. OursurveydidnotaskaboutspecificHINTSsimulation equipmentortechniquesbeingusedatEMresidency programsintheUS,butevenifaggressivecost-ofimplementationestimatesaremade,thereturnoninvestment wouldmakeHINTSeducationalinitiatives financially worthwhile.Thenationwidecapitalexpenditures (specifically,VOGdevicesforsimulation)costabout$9.76 million,whichamountsto1%oftheestimated$1billion/year spentoninappropriateCTimagingforpatientswith dizziness/vertigointheUS.8 Theestimatednationalyearly costaftercapitalinvestment(specifically,thecostoffaculty time)isabout$331,883inadditiontocostsforany equipmentrepairornewdevices/adjuncts.SeeAppendixG forthecost-of-implementationanalysis.34,38–41
Notably,HINTSmanikin “partialtasktrainers” have beendevelopedandtested,butnonearewidelyavailable.32,33 The2023ACEPClinicalPolicyrecommendedincorporation oftechnologysuchasFrenzelgogglesandoculartracking softwareintraining.20 TheVOGdevicesarecommercially availablefor$12,000–40,000perdeviceandhaveshown promiseinthesimulationenvironment.31,34,38,42
Todescribetheeffectivenessofmanyeducationaloptions (includingthoseamenabletoasynchronousandlarge-group sessions),weaskedaboutseveralothermodalitiesin additiontoclinicalbedsideteachingandHINTSsimulation. Onlinevideosandvideocastsweretiedwithsimulationfor thesecondhighest-ratedteachingmodalityamong participants.Contrarytobedsideandsimulationteaching, thismodalityrequiresnofacultytimeorsupervisionandis free.OnlineHINTSeducationalvideoscanbeusedasan asynchronoussupplementtoclinicalbedsideteachingand simulation,butwatchingvideosisapassivelearning techniquewithnohands-onpracticeoropportunityfor acquisitionofmusclememory.However,recentstudies suggestthatachievingHINTSexamskills(particularly HITskills)doesrequireahands-oncomponentformotor skillsacquisition.34
Overall,moretime,effort,funding,andeducational researchcouldbetargetedtowardcreatingHINTScurricula andsimulationmodalities,andonmakingtheseresources widelyavailabletoimproveEMresidencyHINTS educationaloptions.Thevariabilityinoursurveyresults showsthatmultipleeducationmodalitiesarelikelybeing employedacrosstheresidencytrainingprogramsintheUS butwithsomeconsensusaboutthemostusefulmodalities.In suchasituationwheremultiplemodalitiesarebeing employedtothesameend,furtherresearchtoward developmentofastandardizedtrainingplanisneeded.
Toachieveadequateresponseratesfromoursurvey,the lengthofthesurveywaslimitedattherecommendationsof theexpertpilottestgroup.Additionally,variabilityofthe questiondesignwasemployedtoholdparticipants’ interest andincreaseresponserates.Asaresult,somequestionswere askedinabinary “yes/no” formatinsteadofLikertscalesor rankings,potentiallysacrificingsomedepthofresponse interpretation.Anotherconcernwithoursurveydesignwas responsebias.Whileallowingquestionsonthesurveytobe leftunansweredsupportsoverallincreasedresponserates, biasmayhavebeenintroducedviarespondent-allocated missingdata.Itispossiblethatprogramleaderswho answeredfewerquestionshadmorepassiveopinionsabout theHINTSexam,exhibitingneutralresponsebiaswherein, forexample,theyselected “neutral” or “noopinion” on classicLikert-scalequestions.Theoppositeisalsopossible whereinthesurveyresultsarebiasedtowardthoseinstrongly infavoroforstronglyagainsttheHINTSexam(extreme responsebias).Fortunately,ouroverallhighresponserates andwidevariabilityofresponsessuggeststheselimitations areminimal.
SurveyswereinitiallysenttoEMresidencyprogram directorswhohadtheoptionofeithercompletingit themselvesorassigningtheresponsibilitytoanassociate programdirector,ortothefacultyleaderoftheresidency’ s curricularcontent.Thereis,thus,apossibilitythatanswers varieddependingontheroleofthesurvey-takerforeach program,whichwasnotrecorded.
Emergencymedicineresidencyprogramsandmedical educatorsshouldfocustheirHINTSeducationalpriorities ondevelopmentofaformalizedcurriculumwithadequate resources.Programswillalsoneedtoaddressthebarrierof lackoffacultyexpertise.
AddressforCorrespondence:MaryMcLean,MD,AdventHealth EastOrlando,DepartmentofEmergencyMedicine,7727Lake UnderhillRd.,Orlando,FL32822.Email: Mary.McLean.MD@ AdventHealth.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025McLeanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KerberKA,BrownDL,LisabethLD,etal.Strokeamongpatientswith dizziness,vertigo,andimbalanceintheemergencydepartment: apopulation-basedstudy. Stroke. 2006;37(10):2484–7.
2.SavitzSI,CaplanLR,EdlowJA.Pitfallsinthediagnosisofcerebellar infarction. AcadEmergMed. 2007;14(1):63–8.
3.KimAS,FullertonHJ,JohnstonSC.Riskofvasculareventsin emergencydepartmentpatientsdischargedhomewithdiagnosisof dizzinessorvertigo. AnnEmergMed. 2011;57(1):34–41.
4.AhsanSF,SyamalMN,YaremchukK,etal.Thecostsandutilityof imaginginevaluatingdizzypatientsintheemergencyroom. Laryngoscope. 2013;123(9):2250–3.
5.SaberTehraniAS,CoughlanD,HsiehYH,etal.Risingannualcostsof dizzinesspresentationstoU.S.emergencydepartments. AcadEmerg Med. 2013;20(7):689–96.
6.HwangDY,SilvaGS,FurieKL,etal.Comparativesensitivityof computedtomographyvs.magneticresonanceimagingfordetecting acuteposteriorfossainfarct. JEmergMed. 2012;42(5):559–65.
7.TuLH,MelnickE,VenkateshAK,etal.Cost-effectivenessofCT,CTA, MRI,andspecializedMRIforevaluationofpatientspresentingtothe emergencydepartmentwithdizziness. AJRAmJRoentgenol. 2024;222(2):e2330060.
8.KeitaM,NasseryN,SebestyenK,etal.Diagnosticerrors,harms,and wasteinevaluatingdizzinessandvertigoinambulatorycaresettings acrosstheUnitedStates[abstract].DiagnosticErrorinMedicine11th InternationalConference.November4–6,2018;NewOrleans,Louisiana.
9.EaglesD,StiellIG,ClementCM,etal.Internationalsurveyof emergencyphysicians’ prioritiesforclinicaldecisionrules. AcadEmerg Med. 2008;15(2):177–82.
10.BeesonMS,AnkelF,BhatR,etal.The2019modeloftheclinical practiceofemergencymedicine. JEmergMed. 2020;59(1):96–120.
11.StettlerBA,JauchEC,KisselaB,etal.Neurologiceducationin emergencymedicinetrainingprograms. AcadEmergMed. 2005;12(9):909–11.
12.KattahJC,TalkadAV,WangDZ,etal.HINTStodiagnosestrokeinthe acutevestibularsyndrome:three-stepbedsideoculomotorexamination moresensitivethanearlyMRIdiffusion-weightedimaging. Stroke. 2009;40(11):3504–10.
13.GottliebM,PeksaGD,CarlsonJN.Headimpulse,nystagmus,andtest ofskewexaminationfordiagnosingcentralcausesofacutevestibular syndrome. CochraneDatabaseSystRev. 2023;(11):CD015089.
14.DmitriewC,RegisA,BodundeO,etal.Diagnosticaccuracyofthe HINTSexaminanemergencydepartment:aretrospectivechartreview. AcadEmergMed. 2021;28(4):387–93.
15.OhleR,MontpellierRA,MarchadierV,etal.Canemergencyphysicians accuratelyruleoutacentralcauseofvertigousingtheHINTS examination?Asystematicreviewandmeta-analysis. AcadEmerg Med. 2020;27(9):887–96.
16.HenriksenACandHallasP.Inter-ratervariabilityintheinterpretationof theheadimpulsetestresults. ClinExpEmergMed. 2018;5(1):69–70.
17.GerlierC,HoarauM,FelsA,etal.Differentiatingcentralfromperipheral causesofacutevertigoinanemergencysettingwiththeHINTS, STANDING,andABCD2tests:adiagnosticcohortstudy. AcadEmerg Med. 2021;28(12):1368–78.
18.VanniS,PecciR,EdlowJA,etal.Differentialdiagnosisofvertigointhe emergencydepartment:aprospectivevalidationstudyofthe STANDINGalgorithm. FrontNeurol. 2017;8:590.
19.VanniS,NazerianP,PecciR,etal.Timingfornystagmusevaluationby STANDINGorHINTSinpatientswithvertigo/dizzinessinthe emergencydepartment. AcadEmergMed. 2023;30(5):592–4.
20.AmericanCollegeofEmergencyPhysiciansClinicalPolicies Subcommittee(WritingCommittee)onAcuteIschemicStroke.LoBM, CarpenterCR,etal.Clinicalpolicy:criticalissuesinthemanagementof adultpatientspresentingtotheemergencydepartmentwithacute ischemicstroke. AnnEmergMed. 2023;82(2):e17–64.
21.EdlowJA,CarpenterC,AkhterM,etal.Guidelinesforreasonableand appropriatecareintheemergencydepartment3(GRACE-3):acute dizzinessandvertigointheemergencydepartment. AcadEmergMed. 2023;30(5):442–86.
22.ShahVP,OliveiraJESilvaL,FarahW,etal.Diagnosticaccuracyofthe physicalexaminationinemergencydepartmentpatientswithacute vertigoordizziness:asystematicreviewandmeta-analysisfor GRACE-3. AcadEmergMed. 2023;30(5):552–78.
23.vonElmE,AltmanDG,EggerM,etal.Thestrengtheningthereportingof observationalstudiesinepidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. PLoSMed. 2007;4(10):e296.
24.ArtinoARJr,LaRochelleJS,DezeeKJ,etal.Developingquestionnaires foreducationalresearch:AMEEguideno.87. MedTeach. 2014;36(6):463–74.
25.FidellLSandTabachnickBG.Preparatorydataanalysis.In:SchinkaJA &VelicerWF(Eds.) HandbookofPsychology:ResearchMethods inPsychology(115–141),Vol.2.Hoboken,NJ:JohnWiley& Sons,Inc,2003.
26.AgrestiAandCoullBA.Approximateisbetterthan “exact” forinterval estimationofbinomialproportions. AmStat. 1998;52(2):119–26.
27.BrownLDandCaiTT,DasGuptaA.Intervalestimationforabinomial proportion. StatSci. 2001;16(2):101–17.
28.EdlowJA,GurleyKL,Newman-TokerDE.Anewdiagnosticapproachto theadultpatientwithacutedizziness. JEmergMed. 2018;54(4):469–83.
29.Newman-TokerDE,PetersonSM,BadihianS,etal.(2022). Diagnostic errorsintheemergencydepartment:asystematicreview.Rockville, MD:AgencyforHealthcareResearchandQuality(US).
30.PuissantMM,GiampalmoS,WiraCRIII,etal.Approachtoacute dizziness/vertigointheemergencydepartment:selected controversiesregardingspecialtyconsultation. Stroke. 2024;55(10):2584–8.
31.KordaA,SauterTC,CaversaccioMD,etal.Quantifyingalearning curveforvideoheadimpulsetest:pitfallsandpearls. FrontNeurol. 2021;11:615651.
32.Charlery-AdèleA,GuigouC,RyardJ,etal.Effectsofsaccadedelay, sideofdeficit,andtrainingondetectionofcatch-upsaccadesduring head-impulsetestinvirtual-reality-enhancedmannequin. SciRep. 2023;13(1):2718.
33.UrsatG,CordaM,RyardJ,etal.Virtual-reality-enhancedmannequinto trainemergencyphysicianstoexaminedizzypatientsusingtheHINTS method. FrontNeurol. 2024;14:1335121.
34.LenningJC,MessmanAM,KlineJA.Applicationofmotorlearning theorytoteachtheheadimpulsetesttoemergencymedicineresident physicians. AEMEducTrain. 2024;8(1):e10936.
35.NakatsukaMandMolloyEE.TheHINTSexaminationandSTANDING algorithminacutevestibularsyndrome:asystematicreviewandmetaanalysisinvolvingfrontlinepoint-of-careemergencyphysicians. PLoSOne. 2022;17(5):e0266252.
36.KrugerJandDunningD.Unskilledandunawareofit:howdifficultiesin recognizingone’sownincompetenceleadtoinflatedself-assessments. JPersSocPsychol. 1999;77(6):1121–34.
37.BarnsleyL,LyonPM,RalstonSJ,etal.Clinicalskillsinjuniormedical officers:acomparisonofself-reportedconfidenceandobserved competence. MedEduc. 2004;38(4):358–67.
38.BastaniPB,BadihianS,PhillipsV,etal.Smartphonesversusgoggles forvideo-oculography:currentstatusandfuturedirection. ResVestib Sci. 2024;23(3):63–70.
39.KovalML.Medscapeemergencymedicinephysiciancompensation report2024:biggerchecks,yetmanydoctorsstillseeanunderpaid profession.2024.Availableat: https://www.medscape.com/ slideshow/2024-compensation-emergency-medicine-6017136 AccessedOctober1,2024.
40.AssociationofAmericanMedicalColleges.Reportonresidents.2023. Availableat: https://www.aamc.org/data-reports/students-residents/ report/report-residents.AccessedOctober1,2024.
41.LenioR.Emergencymedicineannualworkedhours:marketnormsvary widely.2023.Availableat: https://www.ajg.com/us/news-and-insights/ 2023/mar/emergency-medicine-annual-worked-hours-market-normsvary-widely/.AccessedOctober1,2024.
42.Newman-TokerDE,SaberTehraniAS,MantokoudisG,etal.Quantitative video-oculographytohelpdiagnosestrokeinacutevertigoanddizziness: towardanECGfortheeyes. Stroke. 2013;44(4):1158–61.
JutamasSaoraya,MD,PhD*†‡§
LiranShechtman,MD§∥
PaweenuchBootjeamjai,MD¶ KhrongwongMusikatavorn,MD†‡#
FedericoAngriman,MD,MPH,PhD§∥
*ChulalongkornUniversity,FacultyofMedicine,DivisionofAcademic Affairs,Bangkok,Thailand
† ChulalongkornUniversity,FacultyofMedicine,DepartmentofEmergency Medicine,Bangkok,Thailand
‡ KingChulalongkornMemorialHospital,ThaiRedCrossSociety, Bangkok,Thailand
§ UniversityofToronto,InterdepartmentalDivisionofCriticalCareMedicine, Toronto,Canada
∥ SunnybrookHealthSciencesCentre,DepartmentofCriticalCare Medicine,Toronto,Canada
¶ ChulalongkornUniversity,DepartmentofAnesthesiology, Bangkok,Thailand
# ChulalongkornUniversity,FacultyofMedicine,DepartmentofMedicine, Bangkok,Thailand
SectionEditor:ChristopherR.Tainter,MD
Submissionhistory:SubmittedJune17,2024;RevisionreceivedOctober9,2024;AcceptedOctober15,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.24874
Introduction: Theprolongedstayofcriticallyillpatientsintheemergencydepartment(ED)mayleadto worseclinicaloutcomes.Anemergencydepartment(ED)-basedintensivecareunit(ICU)isoneofthe proposedsolutionstodelivercriticalcareintheED.WethusaimedtocharacterizeexistentED-ICU modelsandtheirreportedassociationwithclinicaloutcomesincriticallyilladultpatients.
Methods: WesearchedtheOvidMEDLINEdatabasefrominceptiontoOctober2,2023.Weincluded studiesthatreportanED-ICUstructure,definedasaspacecapableofprovidingICU-levelcarewithinor adjacenttotheED,anditscharacteristics.Weexcludedpersonnel-focusedintervention(withoutthe presenceofaseparatedspace)oraspacewithoutICU-levelcarecapability.Wecollectedinformationon processmeasures,patient-relatedoutcomes,andcost-relatedoutcomes.
Results: Wescreened2,824studies,ofwhich125full-textarticleswereassessedforeligibilityand31 studieswereincludedinthisscopingreview.Studiesreportedon14ED-ICUsacrosssevencountries, withcapacitiesrangingfrom3–17beds.AllED-ICUsservedearlyandongoingcriticalcareneedsinthe ED,includingthreedistinctthemes:short-stay;palliativecare;anddisaster-responseICUs. ImplementingtheED-ICUwasassociatedwithdecreasedtimetoICU-levelcareandreducednumberof inpatientICUadmissions,butitwasnotconsistentlyassociatedwithimprovedsurvival.
Conclusion: SeveralED-ICUshavebeenestablishedaroundtheworldwithdifferentcharacteristics dependingonlocalneeds.ImplementationoftheED-ICUmaybeassociatedwithimprovedclinical outcomesandpatient flow.[WestJEmergMed.2025;26(1)78–85.]
Emergencydepartment(ED)crowdingisarecognized globalhealthproblem.1 Crowdingcanmanifestasprolonged boardingofcriticallyillpatientsintheED.2 Inturn,delayed admissiontotheintensivecareunit(ICU)mayleadto clinicallyworseoutcomes,includingincreasedhospitalstay andall-causemortality.3,4 Onestrategytomitigatethis problemistoprovidecriticalcareintheED.Severalstudies haveidentifieddifferentmodelsofprovidingcriticalcarein theED,includinggeography-basedandpersonnel-focused models.5 Thepersonnel-focusedmodelhighlightstheneedto haveearlycriticalcareconsultation,whilethegeographybasedmodelinvolvestheexpansionofICUbeds,eitherinthe existinginpatientICUorintheED(thelatterisgenerally calledtheED-basedICUortheED-ICUmodel).5
Theoretically,theED-ICUmodelcouldprovidetimely criticalcaretopatientsinneed;establishingit,therefore, representsapromisingstrategytodealwithEDcrowding.6–8 Despiteitspromisingnature,thespecificcharacteristicsof differentED-ICUsacrosstheworldhavenotbeendescribed. ItisalsouncertainwhethertheapplicationofthisED-ICU modeltoanexisting,operatingEDaffectsitsprocessesand clinicaloutcomes,inadditiontocosts.
Inthisscopingreviewweaimedtoexplorethe characteristics(eg,capacity,staffing,andutilization)of implementedED-ICUmodels.Wefurthersoughttoexplore howED-ICUsaffectprocessmeasures,inadditionto clinicallyrelevantoutcomesandhealthcare-associatedcosts.
DataSources
WesearchedtheOvidMEDLINEdatabasefrom inceptionuntilOctober2,2023usingasearchstrategy developedwithanexperiencedmedicallibrarian(see Supplementary TableS1).Wespecificallychosetolimitthe OvidMEDLINEsearchsinceweexpectedthatthisdatabase wouldresultinthehighestyieldofarticlesforthetopicof interest.Keywordsforthesearchstrategyincluded emergencydepartment,intensivecareunit,andEDICU. Therewerenolanguageorstudydesignrestrictions.We screenedthereferencesoftheincludedstudiesandmanually searchedthemtoidentifyadditionaleligiblepapers.
WeincludedallstudiesthatreportedanED-ICUmodel structure,definedasadedicatedphysicalspacewithintensive carecapacitywithinoradjacenttotheED,andits characteristicsoroutcomes.Wecapturedinformationon reportedcharacteristicssuchasnumberofICUbeds, staffing,reasonsforED-ICUinitiation,andadmission criteria.Informationonreportedoutcomesincludingprocess measures,patient-relatedoutcomes,andcost-related outcomeswasalsocollected.Weexcludedstudiesthat reportedonlyonpersonnel-focusedmodelsofcriticalcare
deliveryintheED(ie,withoutadedicatedphysicalarea),ora physicalspacethatcouldnotprovideorgansupport measuresthatarecoretoanICU-levelcare(eg,invasive mechanicalventilationorvasopressorsupport).Twoauthors independentlyscreenedabstractsandfulltexts(JS,LS,or PB).Conflictswereresolvedbyconsensusthrough discussionsheldinavirtualmeeting.
Specificdataextractedfromtheincludedfulltexts includedthenameoftheED-ICUmodel,country, institution,yearofestablishment(andreason),numberof beds,typeofstaffing,admissioncriteria,yearlycensusofthe correspondingED,utilizationofED-ICU,ED-ICUlength ofstay(LOS),ED-ICUreportedmortality,descriptionof processmeasures,patient-relatedorcost-relatedoutcomes, firstauthorandyearofpublication,studydesign,funding, andpotentialconflictofinterests.Datawasextracted independentlyintoapre-piloteddataabstractionformby twoauthors(JS,LS,orPB).Conflictswereresolvedby consensusthroughdiscussionsheldinavirtualmeeting.We summarizedthecharacteristicsofeachICUusingdescriptive statisticsasfeasible,andweidentifiedthemesofutilizationof theED-ICU.Thereportedoutcomesweregroupedintothree categories:1)processmeasures;2)patient-relatedclinical outcomes;and3)cost-relatedconsiderations.
Theprotocolofthisscopingreviewwasregisteredandcan beaccessedonOpenScienceFramework(OSF)website (registrationDOI: https://doi.org/10.17605/OSF.IO/ MEVQB).ThisreportfollowsthePRISMAextensionfor scopingreviews.9
Wescreened2,824studiesandassessed125full-text articlesforeligibility,ofwhich31wereincludedinthe presentscopingreview(Figure1).Ofthe31includedstudies, therewasoneprospectivecohortstudy,10 23retrospective cohortstudies,6–8,11–30 onesystematicreview,31 four narrativereviews,2,5,32,33 onereport,34 andone commentary.5 Thesestudiesreportedon14differentEDICUs. Table1 providesthecharacteristicsofthese14EDICUs.Supplementary TableS2 and S3 providefurther detailsofED-ICUsandeachstudy.
TheED-ICUsaredescribedusingdifferentnamesor abbreviations,suchasemergencydepartmentintensivecare unit(withtheabbreviationsEDICU,EDICU,orED-ICU), emergencyICU(EICU),emergencycriticalcarecenter (EC3),resuscitationandcriticalcareunit(ResCCU), resuscitationandacutecriticalcareunit(RACC),orshock room.TheidentifiedED-ICUsweredeployedinseven countries:sixintheUnitedStates;threeinTaiwan;andone eachinKorea,France,Belgium,Turkey,andBrazil.While
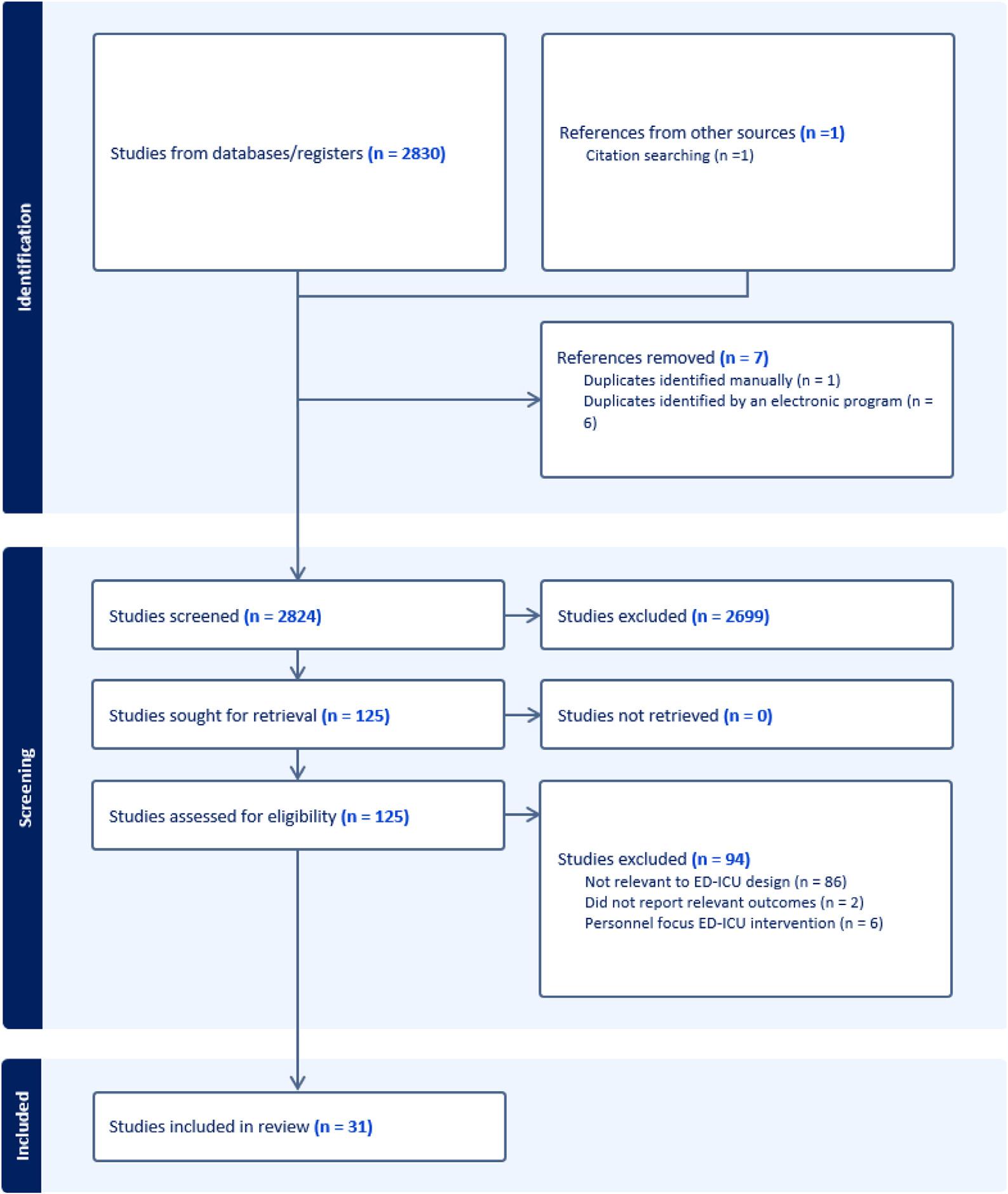
Figure. PRISMAchartforscopingreviewimpactofintensivecareunitswithinemergencydepartments. ED-ICU,emergencydepartment-basedintensivecareunit.
mostED-ICUshadoneortwostudiesthatreportedontheir overallstructures,theEC3intheUShad18related articles.2,5,6,18–22,25–33,35 Bedcapacityrangedfrom3–17beds withamedianof10beds(interquartilerange7–13).SixEDICUswerereportedtonotbeabletoadmitpatientswhen inpatientICUswereavailable,butthreewerereportedtodo so(see Table1).Severalcommonstaffingpatternswere observedintheseED-ICUs;forexample,thepresenceof1) emergencyphysicians,withorwithouttrainingincritical caremedicine,2)registerednurseswithanurse-to-patient ratioofapproximately1:2,and3)interdisciplinaryteam members,includingrespiratorytherapistsorpharmacists. OneED-ICUoperatedonlyonweekdays.8,17,23
Threethemesemergedfromreviewingtheunique utilizationoftheseED-ICUs:namelytheED-ICUasa short-stay,palliativecare,ordisaster-responseICU.First, ED-ICUscouldprovideshort-stayintensivecarefor criticallyillpatientswhowereexpectedtorecoverquickly afteraperiodofintensiveobservationortreatment(eg, patientswithacutepoisoning,uppergastrointestinal[GI] bleeding,diabeticketoacidosis[DKA],orminor intracranialhemorrhage).17,18,22,23 ,26 Second,when inpatientICUbedsarefull,patientswhoareunlikelyto survivecouldbealternativelyadmittedtotheED-ICUs. SuchED-ICUs,thusservingasapalliative-careICU,could
Table. Characteristicsofemergencydepartment-basedintensivecareunits.
NameCountryInstitution
Emergencycritical carecenter (EC3)2,5,6,18–22,25–33,35 UnitedStatesUniversityofMichiganEDboardingofICU
Resuscitationand criticalcareunit (ResCCU)2,5,8,17,23,32
Resuscitationand acutecriticalcareunit (RACC)2,5,32,33
EDintensivecareunit (EDICU)10,31
ED,emergencydepartment; EM,emergencymedicine; EP,emergencyphysician; CCM,criticalcaremedicine; COVID-19,coronavirus disease2019; ICU,intensivecareunit.
beaplacewherephysiciansinitiateend-of-lifecare discussionsandpalliativecareconsultations.10,15,24 Third, ED-ICUswereusedfordisasterresponse.Forexample,in theeventofahurricaneorthecoronavirusdisease2019 pandemic,temporaryED-ICUsweresetuptoincrease hospital-bedcapacity. 13, 34
TheED-ICUshavebeenshowntopotentiallyimprove severalprocessmeasures,includingdecreasedtimefromED presentationtodeploymentofICU-levelcare.6,7,17,18,26 Aretrospectivecohortof349,310EDvisitsrevealedthat criticallyillpatientsreceiveICU-levelcarewithamedianof
1.9hoursearlierafteropeninganED-ICUcomparedto beforeopening.6 CriticallyillpatientsadmittedtoanEDICUhad27.5%shorterboardingtimethanpatientsadmitted tootherICUs.7 ImplementingtheED-ICUmodelresultedin anincreaseinthenumberofpatientswhoreceivedevidencebasedcriticalcareintheED.14,27 Forexample,inpatients presentingwithacuteischemicstroke,thepresenceofanEDICUwasassociatedwithanincreaseinthrombolysisrate.14 Furthermore,amongintubatedpatientsintheED, establishinganED-ICUincreasedthenumberofpatients receivingalungprotectiveventilationstrategyatthetimeof EDdeparture(65.8%vs43.1%).27
Moreover,anED-ICUmodelcouldfacilitatethe reductionofinpatientICUadmissionandpreserveinpatient ICUcapacity.OpeninganED-ICUwasassociatedwitha reductionintheoddsofoveralladmissiontoaninpatient ICU(adjustedoddsratio[aOR]0.80;95%confidence interval[CI],0.76–0.83).6 Furthermore,reducedinpatient ICUadmissionswerefoundincohortsofpatientswithDKA orupperGIbleedingaftertheED-ICUimplementation.18,26 Inanothersetting,astudyshowedthattheopeningofanEDICUwasassociatedwithadecreaseinICUadmissioninthe firstmonthafteropeningamongadultpatientswithsepsis.8
Overall,thereportedLOSofpatientsintheED-ICUs variedwidely.TheED-ICUsthatadmittedpatientswith acutepoisoning,DKA,orminorintracranialhemorrhage reportedtheirED-ICULOSasfollows:72%ofpatientswith acutepoisoninghadanLOSoflessthan24hours23;themean LOSforDKAwas18.1hours18;andthemedianLOSfor minorintracranialhemorrhagewas15.7hours.22 Incontrast, theothertwoED-ICUsthatadmittedpatientswithaworse overallprognosisreportedamedianED-LOSof120hours (interquartilerange[IQR]4hours-49days),10 andamedian of3.2days(IQR1.9–5.9days).15 Similarly,awiderangeof mortalityrateswerealsoobserved,fromlessthan1%to ≈75%.DispositionsofpatientsinED-ICUsvaried;they couldbesubsequentlytransferredtoinpatientICUs, transferredtogeneralwards,ordischargedhome.
WefoundconflictingdataontheassociationofanEDICUmodelimplementationwithpatient-relatedoutcomes. Forexample,somestudiesshowedthatanED-ICUwas associatedwithimprovedclinicaloutcomes.6,14,25 Inan adjustedanalysisofconsecutiveEDvisits,implementationof theED-ICUwasassociatedwithreduced30-daymortality (aOR0.85,95%CI0.80–0.90).6 Further,inamatchedcohort fromthesameinstitution,theopeningofanED-ICUwas associatedwithlower60-daymortality(hazardratio0.84, 95%CI0.70–0.99).25 Whenfocusingonpatientswithacute stroke,thenumberofpatientswithfavorableclinical outcomesincreasedaftertheopeningofanED-ICU.14
Conversely,severalotherstudieshighlightedthatcreating anED-ICUdidnotnecessarilytranslatetoimproved
survival.8,12,26,30 Whenanalyzedusingdifferentsubgroups (ie,subgroupsofpatientswithupperGIbleedingor decompensatingpatients),thedatafromtheED-ICUthat previouslyexhibitedsurvivalbenefitdidnotshowdifferences inmortalitybetweenthepre-orpost-implementation cohorts.26,30 Amongpatientswithacuterespiratoryfailureor sepsis,theimplementationofanED-ICUwasnotassociated within-hospitalsurvival.8 Finally,astudyshowedincreased mortalityamongpatientsadmittedtotheED-ICU comparedwithpatientsadmittedtootherinpatientICUs. Thiscouldbeduetoahigherproportionofpatientswitha higherburdenofcomorbidconditionsorhigherseverityof diseaseadmittedtotheED-ICU(comparedtothe inpatientICU).12
OnestudyexploredtheassociationofED-ICUandcostrelatedoutcomes.EstablishingtheED-ICUwasassociated withincreasedinflation-adjustednetrevenueperencounter: 7%(95%CI,3.5–10.6%)andwithoutincreasedinflationadjustedcost.29
Inthisscopingreview,weidentifiedthatseveralED-ICUs havebeenestablishedaroundtheworldwithbothuniqueand sharedcharacteristics.Overall,theseED-ICUsare characterizedbytheprovisionofearlyandcontinuedICUlevelcareandaregenerallystaffedbyemergencyphysicians, nurses,andinterdisciplinaryteammembers.Implementing anED-ICUmodelmaybeassociatedwithtimelyICU-level care,aswellasreductionsininpatientICUadmissionrates withoutcompromisingclinicalpatientoutcomes.
Importantly,despitesharingseveralcharacteristics,both LOSandmortalityriskvariedgreatlyacrossreportedEDICUs.Thisvariabilitycouldbeduetodifferentutilizationof ED-ICUsanddifferentcasemix(eg,higherLOSassociated withthecareofpatientswhohaveahigherdegreeofseverity atbaseline,whileshorterLOSmaybeassociatedwithlower overallseverityortransitioningtopalliativecare).Notably, weidentifiedED-ICUsasbeingpredominantlya1)shortstayICU;2)apalliative-careICU;ora3)disaster-response ICU.Thelattertypewasfueledbylackofappropriate resourcesinthetimeofadisaster,whereastheshort-stayand palliative-careICUsweremostlyinitiatedduetoalackof inpatientICUbeds.Asshort-stayICUadmissionsgenerally compriseahighproportionofallICUadmissions,diverting thesepatientstoanED-ICUmodelcouldpreserveimportant inpatientICUcapacity.36 Thepotentialdiagnosesthatcould beservedunderashort-stayED-ICUadmissionmodelmay includeacutepoisoning,intoxication,upperGIbleeding, DKA,minorstrokes,andtransientcerebral ischemia.17,18,22,23,26,36,37 Ontheotherendofthespectrum, patientswhoareunlikelytobenefitfromaprolongedtrialof invasive,life-sustaininginterventionscouldalsobeassessed
andcaredforunderanED-ICUmodelthatcanthenserveas atransitiontoadifferentpathwaysuchasapalliative-care approach.Suchimplementationscouldpotentiallyexplain thehighmortalityrateobservedinsomeoftheseED-ICUs whereterminallyillpatientsareadmitted.10,12
Inthisreview,weidentifiedthatestablishinganED-ICU waspotentiallyassociatedwithimprovementinseveral processmeasures,includingtimetoICU-levelcare, reductionofinpatientICUadmissionrates,andincreased deliveryofevidence-basedtreatments.However,whether thistranslatestoclinicallyrelevantpatient-relatedoutcomes remainsuncleargiventhat1)studiesreportconflictingdata onpatient-relatedoutcomesand2)thehighlikelihoodof confoundingbyindication.38 Forexample,thehigher mortalityrateobservedwithinsomeED-ICUsmightbedue toconfoundingduetobaselineseverity;patientswithhigher burdenofcomorbidconditionsandseverityatbaseline(who areathigherriskofin-hospitaldeath)mightbeselectively admittedtotheED-ICUs.10,12 Moreover,whetherthe implementationofanED-ICUmodelcanbeexpectedto impactclinicaloutcomesbeyondprocessmeasures (comparedtotimelyICU-levelcaredeliveryelsewhere) remainsunclear.39
AlthoughestablishinganED-ICUmodelmayleadto improvedtimelyICU-levelcareandpreservationofinpatient ICUcapacity,adoptinganED-ICUmodelrequiresmultiple considerations.First,institutionalneedsassessmentshould beperformedbyfocusingonidentifyingkeystakeholders, evaluatingEDthroughput,anddeterminingbedcapacity andavailabilityofresources.5 Second,the financingand staffingmodelshouldnotbeneglected.Finally,healthcare leadersshouldalsoconsideralternativesolutionstoanEDICUmodel,includingimprovedinstitutionalpolicy, personnel-focusedintervention,orincreasednumberof inpatientICUbeds.
Severallimitationsneedtobeconsideredwhenevaluating our findings.First,itislikelythatmanymoreED-ICUsexist thanthosereportedintheliterature.Forexample,therewere atleastthreemoreED-ICUsintheUSthanwasreportedin theindexedliterature.40 Itremainsunknownwhetherthe reportedED-ICUmodelsrepresentthelatter,unreported group.Additionally,wedidnotincludeacommonlycited ED-ICUimplementationbecauseitdidnotmeetour definitionofanED-ICUmodel,asitwaslocatedfarther awayfromtheEDandspecificallydesignedtoacceptcritical caretransfersfromotherhospitals.41,42 Second,mostofthe reportedoutcomesassociatedwithED-ICUoperationwere fromonesite(with18relatedstudies)oftheidentified31 papers.Thiscouldpotentiallylimitthegeneralizabilityofour findings.Third,thereportedoutcomeswerelargelyobtained fromretrospectivecohorts,withseverallimitationsintheir design;moststudiesdidnotprovidesample-size
determination,andweresubjecttounmeasuredandresidual confoundingaswellasoutcomemisclassification.Fourth, ideally,thedatafromeachstudyshouldbepooledand analyzedcollectively.However,duetothesignificant heterogeneityindatareporting,patientinclusion,and severityofdiseaseacrossstudies,summarystatisticswerenot calculatedforallreporteddata.
SeveralED-ICUshavebeenestablishedaroundtheworld withdifferentcharacteristicsdependingonlocalneeds. ImplementationoftheED-ICUmaybeassociatedwith improvedprocessmeasures;however,itsimpactonclinical outcomesremainsnotfullycharacterized.Importantly, futureresearchshouldfocusonhowtheestablishmentofan ED-ICUcouldbeusefulindifferentcontextsand geographicalareas,alongsideitsrelatedsuccessfactors. Furthermore,cost-relatedoutcomesshouldbefurther explored,astheyareimportantconsiderationsfor stakeholdersinadoptinganED-ICUmodel.
AddressforCorrespondence:JutamasSaoraya,MDPhD, ChulalongkornUniversity,FacultyofMedicine,DivisionofAcademic Affairs,1873RamaIVRoad,Pathumwan,Bangkok10330Thailand. Email: jutamas.sa@chula.ac.th
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Saorayaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KelenGD,WolfeR,D’OnofrioG,etal.Emergencydepartment crowding:thecanaryinthehealthcaresystem. NEJMCatalInnovCare Deliv. 2021;2(5):7.
2.MohrNM,WessmanBT,BassinB,etal.Boardingofcriticallyillpatients intheemergencydepartment. CritCareMed.Aug2020;48(8):1180–7.
3.ChalfinDB,TrzeciakS,LikourezosA,etal.Impactofdelayedtransferof criticallyillpatientsfromtheemergencydepartmenttotheintensivecare unit. CritCareMed. 2007;35(6):1477–83.
4.HsiehCC,LeeCC,HsuHC,etal.Impactofdelayedadmissionto intensivecareunitsonpatientswithacuterespiratoryfailure. AmJEmergMed.Jan2017;35(1):39–44.
5.JayaprakashN,Pflaum-CarlsonJ,Gardner-GrayJ,etal.Criticalcare deliverysolutionsintheemergencydepartment:evolvingmodelsin caringforICUboarders. AnnEmergMed. 2020;76(6):709–16.
6.GunnersonKJ,BassinBS,HaveyRA,etal.Associationofan emergencydepartment-basedintensivecareunitwithsurvivaland inpatientintensivecareunitadmissions. JAMANetwOpen. 2019;2(7):e197584.
7.JeongH,JungYS,SuhGJ,etal.Emergencyphysician-basedintensive careunitforcriticallyillpatientsvisitingemergencydepartment. AmJEmergMed. 2020;38(11):2277–82.
8.AnesiGL,ChelluriJ,QasimZA,etal.Associationofanemergency department-embeddedcriticalcareunitwithhospitaloutcomesand intensivecareunituse. AnnAmThoracSoc. 2020;17(12):1599–609.
9.TriccoAC,LillieE,ZarinW,etal.PRISMAextensionforscopingreviews (PRISMA-ScR):checklistandexplanation. AnnInternMed. 2018;169(7):467–73.
10.AslanerMA,AkkasM,ErogluS,etal.Admissionsofcriticallyill patientstotheEDintensivecareunit. AmJEmergMed. 2015;33(4):501–5.
11.PiagnerelliM,VanNuffelenM,MaetensY,etal.A'shockroom’ for earlymanagementoftheacutelyill. AnaesthIntensiveCare. 2009;37(3):426–31.
12.TsengJ-C,LiC-H,ChenK-F,etal.Outcomesofanemergency departmentintensivecareunitinatertiarymedicalcenterinTaiwan: anobservationalstudy. JCritCare. 2015;30(3):444–8.
13.SmithSW,JaminCT,MalikS,etal.Freestandingemergencycritical careduringtheaftermathofHurricaneSandy:implicationsfordisaster preparednessandresponse. DisasterMedPublicHealthPrep. 2016;10(3):496–502.
14.PuyL,LamyC,CanapleS,etal.Creationofanintensivecareunitand organizationalchangesinanadultemergencydepartment:impacton acutestrokemanagement. AmJEmergMed. 2017;35(5):716–9.
15.CorreadaCostaRibeiroS,TavaresdeCarvalhoR,AparecidaRochaJ, etal.Criterionvalidityandinter-raterreliabilityofapalliativecare screeningtoolforpatientsadmittedtoanemergencydepartment intensivecareunit. PalliatSupportCare. 2018;16(6):685–91.
16.WangA-Y,MaH-P,KaoW-F,etal.Characteristicsandoutcomesof “donotresuscitate” patientsadmittedtotheemergencydepartmentIntensivecareunit. JFormosMedAssoc. 2019;118(1Pt2):223–9.
17.ZhouVL,ShoferFS,DesaiNG,etal.Predictorsofshortintensivecare unitstayforpatientswithdiabeticketoacidosisusinganovelemergency department-basedresuscitationandcriticalcareunit. JEmergMed. 2019;56(2):127–34.
18.HaasNL,WhitmoreSP,CranfordJA,etal.Anemergencydepartmentbasedintensivecareunitisassociatedwithdecreasedhospitaland intensivecareunitutilizationfordiabeticketoacidosis. JEmergMed. 2020;58(4):620–6.
19.HaasNL,LarabellP,SchaefferW,etal.Descriptiveanalysisof extubationsperformedinanemergencydepartment-basedintensive careunit. WestJEmergMed. 2020;21(3):532–7.
20.HaasNL,PulsHA,AdanAJ,etal.Emergencydepartment-based intensivecareunitusepeaksnearemergencydepartmentshift turnover. WestJEmergMed. 2020;21(4):866–70.
21.LeithTB,HaasNL,HarveyCE,etal.Deliveryofend-of-lifecareinan emergencydepartment-basedintensivecareunit. JACEPOpen. 2020;1(6):1500–4.
22.JosephJR,HaasNL,JosephJR,etal.Utilizationofaresuscitativecare unitforinitialtriage,management,anddispositionofminorintracranial hemorrhage. CritCareExplor. 2020;2(4):e0097.
23.MudanA,LoveJS,GreenwoodJC,etal.Themanagementofthe poisonedpatientusinganovelemergencydepartment-based resuscitationandcriticalcareunit(ResCCU). AmJEmergMed. 2020;38(10):2070–3.
24.ChangJC-Y,YangC,LaiL-L,etal.Differencesincharacteristics, hospitalcare,andoutcomesbetweenacutecriticallyillemergency departmentpatientsreceivingpalliativecareandusualcare. IntJ EnvironResPublicHealth. 2021;18(23):12546.
25.DuJ,GunnersonKJ,BassinBS,etal.Effectofanemergency departmentintensivecareunitonmedicalintensiveunitadmissionsand care:aretrospectivecohortstudy. AmJEmergMed. 2021;46:27–33.
26.HaasNL,MedlinRPJr.,CranfordJA,etal.Anemergencydepartmentbasedintensivecareunitisassociatedwithdecreasedhospitallengthof stayforuppergastrointestinalbleeding. AmJEmergMed. 2021;50(aa2,8309942):173–7.
27.HarveyCE,HaasNL,ChenCM,etal.Initiationofalungprotective ventilationstrategyintheemergencydepartment:doesanemergency department-basedICUmakeadifference? CritCareExplor. 2022;4(2):e0632.
28.PulsHA,HaasNL,CranfordJA,etal.Emergencydepartmentlengthof stayandoutcomesofemergencydepartment-basedintensivecareunit patients. JACEPOpen. 2022;3(1):e12684.
29.BassinBS,HaasNL,SefaN,etal.Cost-effectivenessofanemergency department-basedintensivecareunit. JAMANetwOpen. 2022;5(9):e2233649.
30.DoanJ,PerezS,BassinBS,etal.Impactofemergencydepartmentbasedintensivecareunitonoutcomesofdecompensatingboarding emergencydepartmentpatients. JACEPOpen. 2023;4(5):e13036.
31.McDowaldK,DirektorS,HynesEA,etal.Effectivenessofcollaboration betweenemergencydepartmentandintensivecareunitteamson mortalityratesofpatientspresentingwithcriticalillness:asystematic review. JBIDatabaseSystemRevImplementRep. 2017;15(9):2365–89.
32.LeibnerE,SpiegelR,HsuCH,etal.Anatomyofresuscitativecareunit: expandingthebordersoftraditionalintensivecareunits. EmergMedJ. 2019;36(6):364–8.
33.MermiriM,MavrovounisG,ChatzisD,etal.Criticalemergencymedicine andtheresuscitativecareunit. AcuteCritCare. 2021;36(1):22–8.
34.HickeyS,MathewsKS,SillerJ,etal.Rapiddeploymentofan emergencydepartment-intensivecareunitfortheCOVID-19pandemic. ClinExpEmergMed. 2020;7(4):319–25.
35.KurzMCandHessEP.Qualityisnottheonlypartoftheemergency department-basedintensivecareunitvalueequation. JAMANetw Open. 2019;2(7):e197570.
36.ChidiOO,PermanSM,GindeAA.Characteristicsofshort-staycritical careadmissionsfromemergencydepartmentsinMaryland. Acad EmergMed. 2017;24(10):1204–11.
37.KriegerJA,HernandezMA,SheehanJC,etal.Adescriptionof mechanicallyventilatedpatientsadmittedfromtheemergency departmentwithashortcriticalcarestay. JEmergMed. May2023;64(5):574–83.
38.LedererDJ,BellSC,BransonRD,etal.Controlofconfoundingand reportingofresultsincausalinferencestudies.Guidanceforauthors fromeditorsofrespiratory,sleep,andcriticalcarejournals. AnnAm ThoracSoc. 2019;16(1):22–8.
39.ParastL,DoyleB,DambergCL,etal.Challengesinassessing theprocess-outcomelinkinpractice. JGenInternMed. 2015;30(3):359–64.
40.WeingartS.Emergencymedicinecriticalcare,EDintensivists,andED intensivecareunits(EDICUs).2023.Availableat: https://emcrit.org/ squirt/edicu/.AccessedDecember11,2023.
41.ScaleaTM,RubinsonL,TranQ,etal.Criticalcareresuscitationunit:an innovativesolutiontoexpeditetransferofpatientswithtime-sensitive criticalillness. JAmCollSurg. 2016;222(4):614–21.
42.ShiberJ.Emergencydepartmentcriticalcareboarding. CritCareMed. 2021;49(1):e118–9.
EsmeraldaMelgoza,PhD,MPH,CHES *†‡ ValeriaCardenas,PhD§ HiramBeltrán-Sánchez,PhD
*‡
*UniversityofCaliforniaLosAngeles,JonathanandKarinFielding SchoolofPublicHealth,LosAngeles,California
† UniversityofCaliforniaLosAngeles,LatinoPolicyandPoliticsInstitute, LosAngeles,California
‡ UniversityofCaliforniaLosAngeles,CaliforniaCenterforPopulation Research,LosAngeles,California
§ UniversityofSouthernCalifornia,LeonardDavisSchoolof Gerontology,LosAngeles,California
SectionEditor:LunaRagsdale,MD,MPH
Submissionhistory:SubmittedNovember20,2023;RevisionreceivedSeptember20,2024;AcceptedOctober3,2024
ElectronicallypublishedNovember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18593
Objective: Ourgoalwastoassessemergencymedicalservices(EMS)provider-perceivedAlzheimer’s diseaseandrelateddementias(ADRD)bypatientsociodemographiccharacteristicsandZIPcode tabulationareas(ZCTA)intheprehospitalsetting.
Methods: WeconductedaretrospectivedescriptiveanalysisofEMScallswithpatientcontactforadults ≥ 65yearsofagewhowereprovidedprehospitalcarebetweenFebruary1,2020andJanuary31,2022, usingdatafromtheSanFranciscoDepartmentofEmergencyManagementandthe2021American CommunitySurvey.LogisticregressionmodelsassessedtheassociatedbetweenEMSproviderperceivedADRDandpatientsociodemographiccharacteristics,includingage,race/ethnicity,incident location,andZCTA-levelsocioeconomicstatus.
Results: Atotalof55,129patientencounterswererecorded,withEMSprovider-perceivedADRD recordedin4,112(7.5%).AmongcaseswithEMSprovider-perceivedADRD,themostcommonprimary impressionswerementaldisorders(17.1%),weakness(17.0%),injury(15.7%),andpain(13.1%). IncreasingagewasassociatedwithhigheroddsofEMSprovider-perceivedADRDamongbothsexes. Amongfemales,EMSprovider-perceivedADRDwashigheramongHispanics(oddsratio[OR]1.30, 95%confidenceinterval[CI]1.11–1.52),Blacks(OR1.20,95%CI1.03–1.40),Asians(OR1.18,95% CI1.06–1.31),andNativeHawaiianandPacificIslanders(OR1.48,95%CI1.05–2.08]),whileamong males,onlyAsians(OR87,95%CI.76–.99)hadlowerodds,allcomparedtoWhites.Femalesinlowandmedium-incomeZCTAshadloweroddsofEMSprovider-perceivedADRDrelativetohigh-income ZCTAs,withnosignificant findingsinmales.
Conclusion: Our findingssuggestahigherprevalenceofEMSprovider-perceivedAlzheimer’sdisease andrelateddementiasamongminoritizedandsocioeconomicallydisadvantagedpopulations,including theoldestadults,andracialandethnicminoritycommunities.Futureresearchandmoreprecisedata collectionisneededtoensureequityforolderadultswhoaccessemergencycareintheprehospital setting.[WestJEmergMed.2025;26(1)86–95.]
Alzheimer’sdiseaseandrelateddementia(ADRD)cases amongadults ≥65yearsofageintheUnitedStatesare projectedtoincreasefrom6.7millionto13.8millionbetween 2023and2060.1 TheprojectedincreaseinADRDcasesis partiallyattributedtotheincreasingpopulationofadults ≥65yearsofage,whichisexpectedtorisefrom58millionto 88millionbetween2021and2050.1 Althougholderagedoes notdirectlycauseADRD,itisasignificantriskfactorfor diseasedevelopment.2 TheestimatedADRDprevalenceis 5%forages65to74,13.1%forages75to84,and33.3%for ages ≥85,indicatingaheighteneddiseaseburdenwith increasingage.1
Existingliteratureprovidesevidenceofthepresenceof healthdisparitiesinADRDincidenceandprevalencebased onsex,race,ethnicity,andsocioeconomicstatus.3
Alzheimer’sdiseaseandrelateddementiasaremore prevalentinolderadultwomenthanmen.1,3 Whilewomen, onaverage,havelongerlifeexpectanciesatage65thanmen, this findingdoesnotfullyaccountfortheirincreasedADRD risk.1,3 Amongolderadults,BlackandHispanicsare2and 1.5timesmorelikely,respectively,tohaveADRDcompared toWhites.3 Dementiaincidence,includingADRD,ishighest amongBlacksandAmericanIndianorAlaskaNatives (AIAN),intermediateforHispanics,NativeHawaiianand otherPacificIslanders(NHOPI),andWhites,andlowest amongAsian-Americans.4 Lowereducationisassociated withanincreasedriskofADRD,whichsuggests socioeconomicdisparities.5
Theexistingliteraturesuggeststhattherearehealth disparitiesinADRDdetection,treatment,and research.3,6,7–9 HispanicandBlackolderadultsreportworse cognitivefunctionandmorefunctionallimitationsatADRD diagnosiscomparedtoWhites,suggestingdetectionatalater stageofthedisease.6 RacialandethnicdisparitiesinADRDtargetedtreatmentaremixed.6,7 Non-adherenceand discontinuationratesofADRDmedicationsarehigher amongHispanicandBlackolderadultscomparedtoWhites, partiallyduetochallengeswithaccessandcostof healthcare.6,7 Thegeneralizability ofADRDresearchisalsolimitedduetotheunderrepresentationofcertainracialandethnicgroups,including Hispanicolderadultsinclinicaltrials.8,9 Giventherobust literaturesuggestingracialandethnicdisparitiesinADRD detection,treatment,andresearch,assessinghealthcare servicesprovidedtopersonswithADRDintheUS emergencycaresystemiscritical.
PreviousstudiessuggestthattheUSemergencycare systemservesasanentrypointforolderadultswith ADRD.10,11 Mostresearch,however,focusesonin-hospital emergencycareprovidedintheemergencydepartment (ED).11 OlderadultswithADRDhavehigherratesofED
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Alzheimer ’ sdiseaseandrelateddementias (ADRD)inolderadultsisprojectedto increasefrom6.7to13.8millioncases between2023and2060.
Whatwastheresearchquestion?
HowdoesEMSprovider-perceivedADRD amongolderadultsvarybysociodemographic characteristicsandgeography?
Whatwasthemajor findingofthestudy?
Infemales,perceivedADRDwashigherin minorities,includingHispanics(OR1.30, 95%CI1.11 – 1.52],P =< .05),compared toWhites.
Howdoesthisimprovepopulationhealth?
Revealingsociodemo graphicandgeographic variationsamongsubpopulationsofolder adultsadvancesourunderstandingof EMSprovider-perceivedADRDinthe prehospitalsetting,.
visits,30-dayEDrevisits,andinpatientadmissions comparedtoolderadultswithoutADRD.11 IntheED,40% to64%ofvisitsbyolderadultswithADRDresultinan inpatienthospitaladmission,averagingastayof6.5days.11 AmongolderadultswithADRD,themostcommon reasonsforEDvisitsincludeaccidentsandbehavioral disturbances.12 OlderadultswithADRDwhoarefemale, ≥85yearsofage,andwhohavemultiplemedical comorbiditiesaremorelikelytousetheED.12
WhilestudiessuggestthatolderadultswithADRDare morelikelytousein-hospitalemergencyservices,including theED,fewstudieshaveexaminedtheprovisionof emergencymedicalservices(EMS)toolderadultswith suspectedorconfirmedADRD.10–12 Onestudythatassessed theprovisionofEMStoolderadultswithADRDreported moreambulancetransportstoanEDforthispopulation, comparedtoolderadultswithoutADRD.13 Inthisstudy,we aimedto1)assessthemostcommonprimaryandsecondary EMS-providerimpressionslistedintheprehospitalsetting forpersonswithEMSprovider-perceivedADRD;and2) analyzeEMSprovider-perceivedADRDbypatient sociodemographiccharacteristicsandZIPcodetabulation areas(ZCTA).
Weused9-1-1EMSdatafromtheconsolidatedcitycountyofSanFrancisco,CA.SanFranciscoisoneof58 countiesinCaliforniawithapopulationof815,201asof 2021.14 SanFranciscohas46.9squaremilesofland,making itthesmallestcountyinthestateintermsofsquaremileage butthemostdenselypopulatedwith18,629peoplepersquare mile.14 SanFranciscoisoneofthemostraciallyand ethnicallydiversecountiesinthestate,witharacial compositionof49.9%White,39.8%Asian,15.7%Hispanic, 6.7%Black,1.7%,AIAN,0.9%NHOPI,and14.2%twoor moreraces. 14 Adults ≥65yearsofageandoldercomprise 17.5%ofthecounty’spopulation,anestimatethatis projectedtoincreaseoverthenextthreedecades.14,15
Inthisretrospectivedescriptiveanalysisweuseddatafrom theSanFranciscoDepartmentofEmergencyManagement andthe2021AmericanCommunitySurvey five-year estimates.TheSanFranciscoDepartmentofEmergency Managementdatasetcontainspatientsociodemographic characteristics(eg,age,race,ethnicity,sex),incidentZIP code,providerprimaryandsecondaryimpressions,and EMSprovider-perceivedADRDforallpatientencounters. The2021AmericanCommunitySurvey five-yearestimates includeZCTA-levelestimatesandmedianhousehold income.16 Thisstudyisexemptfrominstitutionalreview boardreview.
TheEMSdatafromtheSanFranciscoDepartmentof EmergencyManagementincludesallpatientencounters submittedbytheSanFranciscoFireDepartment,King AmericanAmbulanceCompany,andAmericanMedical Response,Inc.These9-1-1agenciesincludebothmunicipal andprivateentities.TheEMSdatasetincludesallpatient encounterswithadults ≥65yearsofagewhohadanincident inSanFranciscobetweenFebruary1,2020–January31, 2022.ThestudytimeframebeganonFebruary1,2020, becausethisisthedatewhentheCaliforniadatarepository begantoreliablypopulateelectronicpatientcarereportdata afterachangeintheiranalyticservice.
Apatientencounterisdefinedasa9-1-1callwherethereis anencounterbetweenapatientandanEMSprovider.A singlepersonmayhavemultiplepatientencountersduring thestudyperiod.Althoughallpatientencountersinvolvean EMSresponse,notallEMSresponsesresultinapatient encounter.TheEMSresponseswithoutapatientencounter areexcludedfromthisstudy,astheirassociatedelectronic patientcarereportslackdetailsonkeyvariables,including patientsociodemographiccharacteristics,provider impressions,andEMSprovider-perceivedADRD. ExamplesofEMSresponseswithoutapatientencounter includecanceledcallsorinstanceswherepatientswerenot foundatthescene.Thisstudyalsoexcludesinterfacility
transports,concentratinginsteadonEMSproviderperceivedADRDamongnon-institutionalizedolderadults inthecommunity.
TheAmericanCommunitySurveyisanongoingnational surveyconductedbytheUSCensusBureauonarandom sampleofthepopulation.16 Thesurveyisadministered annually,withover3.5millionhouseholdscontactedevery yeartoparticipate.16 Selectedhouseholdscompletethe surveyviamail,telephone,orin-personinterviews,providing dataonarangeofsocial,economic,demographic,and housingtopicsacrossseveralgeographics.16 Forsmaller geographics,includingZCTAs, five-yearestimatesare publishedtoincreasestatisticaldatareliabilityand confidentiality.Inthisstudyweusedmedianhousehold incomeacrossZCTAsfromthe2021AmericanCommunity Survey five-yearestimates.
Thedependentvariableispresence(coded1)orabsence (coded0)ofEMSprovider-perceivedADRD.Thisoutcome isacombinationofADRDdiagnosesdisclosuresbypatients andcaregivers,andperceivedADRDbytheEMSprovider. Itisimpossible,however,todisentangleconfirmedwith perceivedADRDfromthedataintheelectronicpatientcare reports,althoughthisiscurrentlythebestsourceofdata availableintheprehospitalsetting.Fiveindependent variablesincludingage,sex,race/ethnicity,ZCTA-level medianhouseholdincome,andincidentZIPcode,are includedbasedonpreviousliterature.17–19 Patient sociodemographiccharacteristicsandincidentZIPcodeare recordedbyEMSprovidersintheelectronicpatientcare reports.Themethodusedtocollectsociodemographic informationforeachpatientencounterisnotavailableinthe dataset,althoughitislikelythatthisdataisobtainedthrough acombinationofpatientself-reportandproviderreport.
Ageiscodedusingthefollowingcategories:65–69 (referencegroup),70–74,75–79,80–84,85–89,90–94,and 95+.Genderiscoded1forfemaleand0formale.Therace andethnicityvariableiscoded1to6withthefollowing categories:White(referencegroup);Black;Asian;NHOPI; AIAN;andHispanic.Medianhouseholdincomeiscoded intothreegroups:$0–$104,299;$104,400–$146,999;and ≥$147,000(reference).Amongthe27ZIPcodesinSan Francisco,seven(94104,94105,94108,94111,94129,94130, and94158)hadlessthan40EMSprovider-perceivedADRD cases.Thesewerepooledforreliablecoefficientestimatesin thestatisticalmodels.ZIPcodeswithover40incidentswere sequentiallycodedfrom1to20:94102,94103,94107,94109, 94110,94112,94114to94118,94121to94124,94127,and 94131to94134.Primaryandsecondaryproviderimpressions intheelectronicpatientcarereportsarebasedonthe InternationalClassificationofDiseases,10th Revision,codes andareavailabletoEMSprovidersapriori.
The firstobjectiveassesseshowEMSprovider-perceived ADRDisrecordedintheprehospitalsetting,withafocuson themostcommonprimaryandsecondaryprovider impressions.ThesecondobjectiveanalyzesEMSproviderperceivedADRDbypatientsociodemographic characteristicsandZCTAs.
Wecalculateddescriptivestatisticsofthemostcommon primaryandsecondaryproviderimpressionsforpatient encounterswithEMSprovider-perceivedADRD.Bivariate analyseswereperformedtoassesstheassociationsbetween theindependentvariablesandtheoutcomevariable (presenceorabsenceofEMSprovider-perceivedADRD). Weusedchi-squaretestsforcategoricalvariables,while continuousvariableswereanalyzedusingStudent t -tests. Stepwiselogisticregressionwasusedtoidentifythe independentassociationsbetweenthe fiveindependent variables(age,sex,race/ethnicity,incidentZIPcode,and medianhouseholdincome)andtheoutcomevariable.(See WebAppendices Table1.)Theseregressionmodelsshow statisticallysignificantdifferencesbysexintheoddsofEMS provider-perceivedADRD,andwethusproceededto estimatestratifiedmodelsbysex.(SeeWebAppendices Tables2 and 3.)Forthisstudy,wecalculated95%confidence intervals(CI),anda P -valueof <.05wasusedtorepresent statisticalsignificance.WeusedSTATAv17.0(StataCorp, CollegeStation,TX)forstatisticalanalyses.20
Inconductingthisretrospectivedescriptiveanalysis,we adheredtoseveralbestpracticesforretrospectivechart reviewassuggestedbyWorsterandBledsoe.21 Specifically, weclearlydefinedthedependentandindependentvariables, withthedependentvariablebeingthepresenceorabsenceof EMSprovider-perceivedADRDandtheindependent variablesincludingage,sex,race/ethnicity,ZCTA-level medianhouseholdincome,andincidentZIPcode. Additionally,ourstudy’sdesignanddataanalysiswere meticulouslyplannedanddetailedtoensurearigorousand systematicanalysisofthedata.
Atotalof55,129EMSpatientencounterswere documentedamongpersons ≥65yearsofageinSan Francisco,CA,betweenFebruary1,2020–January31,2022. Ofthesepatientencounters,51,017(92.5%)didnotindicate EMSprovider-perceivedADRD.Theremaining4,112 (7.5%)didindicateEMSprovider-perceivedADRD (Table1).Amongpatientencountersthatindicatedthe presenceofEMSprovider-perceivedADRD,the sociodemographiccompositionwasmajorityfemale(60.4% femaleand39.6%male),increasedwithage,exceptfora declinestartingat90years,andwasmostlyWhite(42.7%) andAsian(32.3%),withsmallerfractionsofBlack(13.5%),
Hispanic(9.3%),NHOPI(1.4%),andAIAN(0.8%). FemaleshadahigherproportionofEMSprovider-perceived ADRDacrossallages,comparedtomales,withwidening sexdifferencesstartingatage85(Figure).Thedistributionof patientencountersshowedahigherpercentageofEMS provider-perceivedADRDinthefollowingZIPcodes: 94112,94109,and94115.OftheseZIPcodes,twoarelocated inthenorth(94109and94115)andoneislocatedinthe south(94112).
The firstobjectiveexaminesthemostcommonprimary andsecondaryproviderimpressionsamongpatient encounterswhereEMSprovider-perceivedADRDwas recorded.Aproviderprimaryimpressionisdefinedas “the EMSpersonnel’simpressionofthepatient’sprimary problemormostsignificantconditionwhichledtothe managementgiventothepatient(eg,treatments, medications,orprocedures).”22 Similarly,asecondary providerimpressionisdefinedas “theEMSpersonnel’ s impressionofthepatient’ssecondaryproblemormost significantconditionwhichledtothemanagementgivento thepatient.”22 Table2 showsthetop10mostcommon providerprimaryandsecondaryimpressionsrecordedfor patientencounterswithEMSprovider-perceivedADRD. Themostcommonprimaryimpressionsweremental disorders/alteredmentalstatus(17.1%),weakness(17.0%), andinjury(15.7%),whiletheleadingsecondaryimpressions weregeneralmedicalexamwithoutabnormal findings (57.9%),followedbyweakness(9.8%),andmentaldisorder/ alteredmentalstatus(5.4%).However,lesscommon outcomes(eg,gastrointestinalandcardiac)arelistedin similarproportionsandrankinginboththeprimaryand secondaryproviderimpressions.
OursecondobjectivewastoanalyzeEMSproviderperceivedADRDbypatientsociodemographic characteristicsandZCTAs.Thestepwiselogisticregression modelspresentedinWebAppendices Table1, 2,and 3 providedetailedanalysesofmalesandfemalestogetherand separately. Table3 showsanabridgedversionofthelasttwo modelsfromWebAppendices Table2 and 3,stratifiedbysex andcontrollingforallcovariates,includingage,race/ ethnicity,medianhouseholdincome,andincidentZIPcode. Amongmalesandfemales,theoddsofEMSproviderperceivedADRDwerehigherwithincreasingage,exceptfor aslightdeclineamongmales ≥95years,atrendthatwas likelyinfluencedbymortalityselection.Amongfemales,the oddsofEMSprovider-perceivedwereconsistentlyhigherfor Hispanics,Blacks,Asians,andNHOPIrelativetoWhites.In contrast,formales,onlyAsiansshowedsignificantlylower oddsofEMSprovider-perceivedADRDrelativetoWhites, withnosignificantdifferencesamongotherracialand ethnicgroups.
Table1. Patientencounters1 forpersons ≥65yearsofagewithandwithoutEMSprovider-perceiveddementiainSanFrancisco,CA, betweenFebruary1,2020–January31,2022.
AbsenceofEMS-provider perceivedADRD(n = 51,017)
PresenceofEMS-provider perceivedADRD(n = 4,112)
Totalsamplesize(presence andabsenceofEMSproviderperceivedADRD)(N = 55,129)
(Continued onnextpage)
Table1. Continued.
AbsenceofEMS-provider perceivedADRD(n = 51,017)
PresenceofEMS-provider perceivedADRD(n = 4,112)
Totalsamplesize(presence andabsenceofEMSproviderperceivedADRD)(N = 55,129)
94104,94105, 94108, 94111, 94129,94130, 941584
1PatientencountersaredefinedasaninteractionbetweenapatientandanEMSprovider.AsinglepatientmayhaveactivatedEMSmultiple timesduringthestudyperiod.The findingsrepresentthenumberofencounters,notdistinctindividuals.
2NHOPIreferstoNativeHawaiianorotherPacificIslander.
3AIANreferstoAmericanIndianorAlaskaNative.
4TheseZIPcodeseachhadlessthan40suspectedADRDcases,sotheywereaggregatedtoaddressproblemswithsmallsamplesizes. ADRD,Alzheimer’sdiseasesandrelateddementia; EMS,emergencymedicalservices.
Table2. Top10mostcommonEMSproviderimpressionsforpatientencounters1 withEMSprovider-perceivedAlzheimer’sdiseaseand relateddementias(N = 4,112).
1PatientencountersaredefinedasaninteractionbetweenapatientandanEMSprovider.AsinglepatientmayhaveactivatedEMSmultiple timesduringthestudyperiod.The findingsrepresentthenumberofencounters,notdistinctindividuals. EMS,emergencymedicalservices.
Amongfemales,ZCTAswithalow($0–$104,399)and medium($104,400–$146,999)medianhouseholdincome showedsignificantlyloweroddsofEMSprovider-perceived ADRD,comparedtoZCTAswithahighmedianhousehold income(≥$147,000).Incontrast,formales,nostatistically significantdifferencesweredetectedbymedianhousehold income.Amongfemales,theracebymedianhousehold incomeinteractionsuggestedthatHispanicsinlow(predictedprobability = .11,95%CI0.09–.144)andmediumincomeZCTAs(predictedprobability = .11,95%CI 0.95–0.12)hadahigherpredictedprobabilityofEMS provider-perceivedADRDrelativetoWhitesinhigh-income
ZCTAs(predictedprobability = .07,95%CI0.06–0.08). Amongmales,non-statisticallysignificant findingswere foundforHispanicsinlow-incomeZCTAsrelativetoWhites inhigh-incomeZCTAs,althoughHispanicsinmediumincomeZCTAs(predictedprobability = .07,95%CI 0.06–0.09)hadahigherpredictedprobabilityofEMS provider-perceivedADRDcomparedtoWhitesinhigh incomeZCTAs(predictedprobability = .04,95%CI 0.04–0.05).Our findingsunderscoretheimportanceof patientsociodemographiccharacteristics(eg,sex,race, ethnicity,age,medianhouseholdincome),geospatial features(eg,ZCTAs),andtheinterplayofthesefactorsin
Table3. Logisticregressionmodels1 forpresenceofEMSproviderperceivedADRDamongmalesandfemalesbypredictorspeci
Age(ref = 65–69)
Race/ethnicity(ref = White)
= $147000+)
***P < 0.001, **P < 0.01,*P < .05. Note:BlackcorrespondstoBlackorAfricanAmerican. 1AllmodelscontrolforincidentZIPcode.
2P-valuefortheoveralljointsignificanceofallrace-by-genderinteractions. AIAN, AmericanIndianorAlaskaNative;AIC,Akaikeinformationcriterion; BIC,Bayesianinformationcriterion; EMS,emergencymedical services; NHOPI, NativeHawaiianandotherPacificIslanders.
EMSprovider-perceivedADRDinolderadultsinthe prehospitalsetting.
Thisstudyadvancesourunderstandingoftheprovisionof prehospitalcareforolderadultswithEMSprovider-
perceivedADRD.Ourstudyhighlightsthecriticalrolethat EMSproviders’ perceptionandrecord-keepingpractices mayhaveonpatients’ trajectoriesthroughothersectorsof theUShealthcaresystem.Ourstudysuggeststhatthemost commonproviderimpressionsrecordedforolderadultswith EMSprovider-perceivedADRDarementaldisorders,
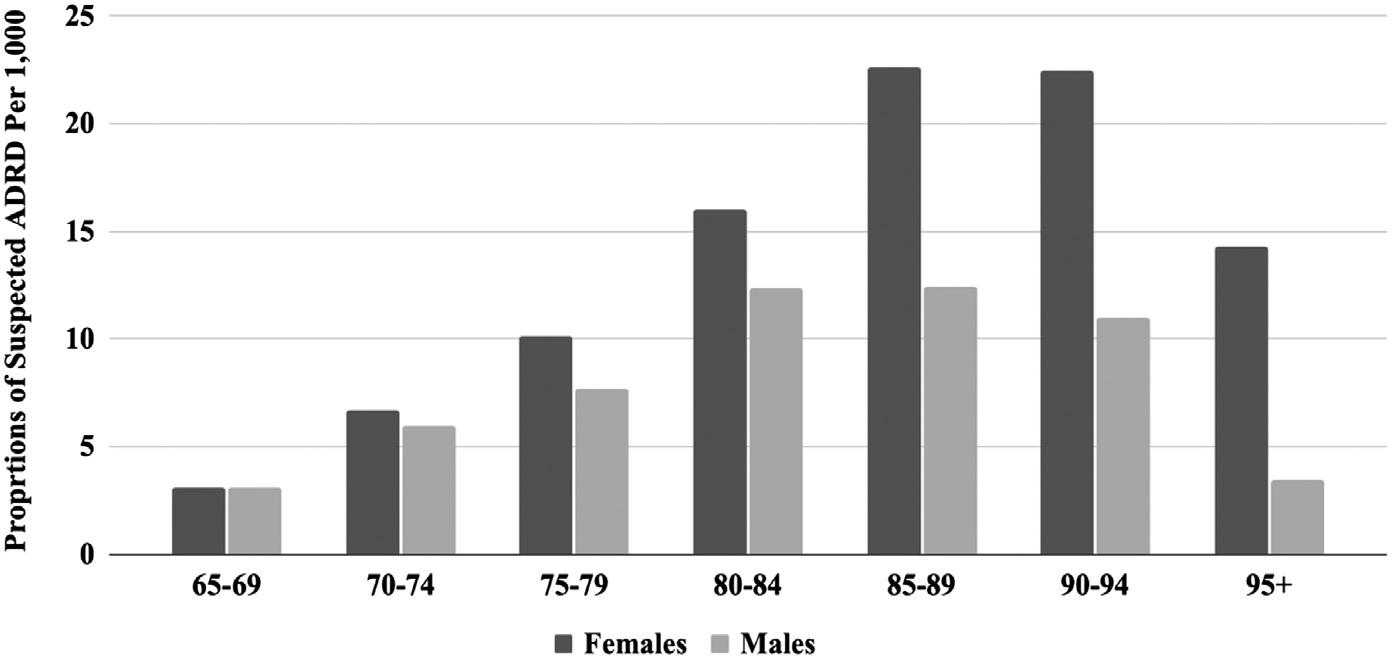
Figure. Emergencymedicalservicesprovider-perceivedAlzheimer’sdiseaseandrelateddementiasbypatientageandsexinSan Francisco,CA,betweenFebruary1,2020–January31,2022. ADRD,Alzheimer’sdiseaseandrelateddementias.
weakness,andinjury.These findingsalignwithprevious literaturethatsuggeststhataccidentsandbehavioral disturbancesarethemostcommonreasonsforEDvisits amongolderadultswithADRD.12
DespitetheinsightsfromthisstudyonEMSrecord-keeping practices,therearechallengesintheidentificationofADRDin theprehospitalsetting.Itisimpossibletodifferentiatebetween confirmedandperceivedADRDusingdocumentationfrom theprehospitalsetting,andwedidnothaveaccesstothe electronichealthrecordsfromtherecipienthospitals. Furthermore,the findingsfromseveralstudiessuggestthat theuseofstandardizedcognitiveassessments,whichare commonlyusedinthein-hospitalsetting,maynotbeas effectiveintheout-of-hospitalsetting.23–25 Thechallengesin identifyingADRDintheprehospitalsettinghighlighttheneed forenhancedEMSprovidertrainingtoimprovedetection, emphasizetheimportanceofdevelopingmoreprecise assessmenttools,andunderscoretheneedforbetterrecordkeepingpractices.TheeffortsbySanFranciscotocollect ADRD-relateddataintheprehospitalsettingcanalsoinform futureeffortsbyotherEMSagenciestoimprovethecareof personswithADRDalongtheemergencycontinuum.
The findingsfromthisstudysuggestahigherprevalenceof EMSprovider-perceivedADRDinmarginalizedand socioeconomicallydisadvantagedpopulations,includingthe oldestadults,andBlack,Hispanic,andAsiancommunities. (SeeWebAppendices Tables1, 2,and 3).Theseresults suggestthattheremaybehealthdisparitiesinEMSproviderperceivedADRD.Futureresearchisneededatthe intersectionofEMSandADRDtoensureequitablecarefor olderadultswhoaccessemergencycareintheprehospital setting.AlthoughthisstudyisbasedonEMSproviderperceivedADRDintheprehospitalsetting,the findingsare consistentwithpreviousstudiesintheED.Forexample,one studyreportedthatolderagegroupsandfemaleswith ADRDweremorelikelytousetheED.12 Inthecurrent
study,EMSprovider-perceivedADRDwasalsohigher amongolderagegroupsandfemales(Table3 andWeb Appendix Table1).PreviousworksuggeststhatHispanic andBlackolderadultsare1.5and2timesmorelikely, respectively,tohaveADRDthanWhites.3 Ourstudy supportsthese findings,indicatingHispanicsandBlackolder adultshaveahigherlikelihoodofhavingEMSproviderperceivedADRDintheirelectronicpatientcarereport, suggesstingapotentialhigherrelianceonEMSfortheir healthcareneeds.
Futureresearchshouldcontinuetoexaminethepossible impactsofintersectionalidentitiesonemergencycare providedinboththeprehospitalandin-hospitalemergency settings.Delvingdeeperintosuchinteractionscouldprovide moreinsightsforEMStrainingandinterventions,addressing potentialbiasesattheintersectionofmultiplefactorssuchas race,ethnicity,sex,socioeconomicstatus,age,language,and neighborhood.Futurestudiesshouldconsiderincorporating variedmethodologiestoassesswhetherotherfactors,suchas knowledgeofADRD,ageism,andpatient-provider languagebarriers,affectEMSproviders’ perceptionofthe presenceofADRD.
LeveragingEMS-EDlinkeddatacouldalsohelpcompare EMSprovider-perceivedADRDintheprehospitalsetting withclinicallydiagnosedADRDintheED.TheseEMS-ED datalinkagesareanovelapproachusedtostudyhealth outcomesintheemergencysector,includingcardiac emergencies,opioidoverdoses,andinjuries.26–28 TheADRD researchcanbenefitfromEMS-EDdatalinkagesbystudying theprovisionofemergencycaretoolderadultsacrossthe emergencycontinuum.Furthermore,futurestudiesshould assesstheroleofEMS-providedinterfacilitytransportsto olderadultswithADRDwhoresideinlong-termcare facilities.TheEMS-providedinterfacilitytransportsfor olderadultswithADRDisalsoanunderstudiedareawithin theUShealthcaresystem.
Thisstudyhasseverallimitations.First,weexamined EMSprovider-perceivedADRDintheprehospitalsetting, whichisacombinationofADRD-confirmeddiagnosis disclosuresbypatientsandcaregivers,andperceivedADRD. Itisimpossible,however,todisentangleconfirmedand perceivedADRDfromtheEMSdocumentation,andwe wereunabletoassessthepresenceorabsenceofthishealth outcomeintheelectronichealthrecordsoftherecipient hospitals.RecordingthepresenceofADRD,whether confirmedorperceived,isimportantbecauseitmayimpact thecourseoftreatmentprovidedintheprehospitalandinhospitalemergencysettingsandinfluenceapatient’ s trajectorythroughthehealthcaresystem.Futurestudies shouldreviewelectronicpatientcarereportnarrativesto betterunderstandtheprovisionofemergencycarefor suspectedanddiagnosedADRDcases.
ThesecondstudylimitationisthattheEMSdataset consistsofpatientencounters,notindividualpatients.A personmayberepresentedmorethanonceinthedatasetif thereweremultiple9-1-1calls(althoughthislimitationis presentinmostEMSdatasets).Thethirdstudylimitationis thesmallsamplesizeofEMSprovider-perceivedADRD acrossseveralZIPcodes(94104,94105,94108,94111,94129, 94130,94158).Toaddresssmallsamplesizes,obtainreliable statisticalestimates,andmaintainconfidentialitywe aggregatedthesevenZIPcodeswithfewerthan40EMS provider-perceivedADRDcases.Afourthstudylimitationis therelianceonincidentZIPcodesandZCTAsasthe geographicunitsofanalysis;whilenotexactlycomparable, theyarethemostcloselyalignedgeographicunitsavailable. A fifthlimitationistherelianceontheelectronicpatientcare reportsfromtheSanFranciscoDepartmentofEmergency Management,whichlimitsthegeneralizabilityofthestudy resultstoothercitiesorcounties.
ThisstudyadvancesourunderstandingofEMSproviderperceivedAlzheimer’sdiseaseandrelateddimentiasinthe prehospitalsetting,revealingsociodemographicand geographicdifferencesamongsubpopulationsofolder adults.The findingsfromthisstudyalsoemphasizethe importanceofmoreprecisedatacollectionintheprehospital setting,especiallywithafocusonADRD.
AddressforCorrespondence:EsmeraldaMelgoza,PhDCandidate, MPH,CHES,UCLAFieldingSchoolofPublicHealthBox 951772,Suite36-071CHS,LosAngeles,CA90095. Email: esmeucla@g.ucla.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsourcesand financialormanagementrelationshipsthatcouldbeperceivedas potentialsourcesofbias.EsmeraldaMelgozaisfundedbythe
NationalInstituteonAgingoftheNationalInstitutesofHealth(NIH) underawardnumber1R36AG087312-01.ValeriaCardenasis supportedbytheNationalInstituteonAgingoftheNIHunderaward numberT32AG000037.HiramBeltrán-Sánchezissupportedbythe NationalInstituteofChildHealthandHumanDevelopment(P2CHD041022)totheCaliforniaCenterforPopulationResearchatUCLA. Therearenootherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Melgozaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.Alzheimer’sAssociation.2023Alzheimer’sdiseasefactsand figures. AlzheimersDement. 2023;19(4):1598–695.
2.NationalInstituteonAging.WhatcausesAlzheimer’sdisease.Available at: https://www.nia.nih.gov/health/what-causes-alzheimers-disease. AccessedSeptember5,2023.
3.LyketsosCG,RobertsSB,SwiftEK,etal.Standardizingelectronic healthrecorddataonAD/ADRDtoacceleratehealthequityin prevention,detection,andtreatment. JPrevAlzheimersDis. 2022;9(3):556–60.
4.MayedaER,GlymourMM,QuesenberryCP,etal.Inequalitiesin dementiaincidencebetweensixracialandethnicgroupsover14years. AlzheimersDement. 2016;12(3):216–24.
5.SharpESandGatzM.Therelationshipbetweeneducationand dementiaanupdatedsystematicreview. AlzheimerDisAssocDisord. 2011;25(4):289.
6.OlchanskiN,DalyAT,ZhuY,etal.Alzheimer’sdiseasemedicationuse andadherencepatternsbyraceandethnicity. AlzheimersDement. 2023;19(4):1184–93.
7.ThorpeCT,FowlerNR,HarriganK,etal.Racialandethnicdifferencesin initiationanddiscontinuationofantidementiadrugsbyMedicare beneficiaries. JAmGeriatrSoc. 2016;64(9):1806–14.
8.ArandaMP,MarquezDX,Gallagher-ThompsonD,etal.Acallto addressstructuralbarrierstoHispanic/Latinorepresentationinclinical trialsonAlzheimer’sdiseaseandrelateddementias:amicro-mesomacroperspective. AlzheimersDementTranslResClinInterv. 2023;9(2):e12389.
9.MassettHA,MitchellAK,AlleyL,etal.Facilitators,challenges,and messagingstrategiesforHispanic/Latinopopulationsparticipatingin Alzheimer’sdiseaseandrelateddementiasclinicalresearch:aliterature review. JAlzheimersDis. 2021;82(1):107–27.
10.HuntLJ,RitchieCS,CataldoJK,etal.Painandemergencydepartment useinthelastmonthoflifeamongolderadultswithdementia. JPain SymptomManage. 2018;56(6):871–7.
11.HillJD,SchmuckerAM,SimanN,etal.Emergencyandpost-emergency careofolderadultswithAlzheimer’sdisease/Alzheimer’sdisease relateddementias. JAmGeriatrSoc. 2022;70(9):2582–91.
12.GerlachLB,MartindaleJ,BynumJP,etal.Characteristicsofemergency departmentvisitsamongolderadultswithdementia. JAMANeurol. 2023;80(9):1002–4.
13.HanchateAD,Paasche-OrlowMK,DyerKS,etal.Geographicvariation inuseofambulancetransporttotheemergencydepartment. AnnEmerg Med. 2017;70(4):533–43.
14.U.S.CensusBureau.QuickFacts:SanFranciscocounty,California. 2022.Availableat: https://www.census.gov/quickfacts/fact/table/ sanfranciscocountycalifornia/POP010220 AccessedSeptember5,2023.
15.CaliforniaDepartmentofAging.FactsaboutCalifornia’selderly. Availableat: https://aging.ca.gov/Data_and_Reports/ Facts_About_California%27s_Elderly/.AccessedSeptember5,2023.
16.AmericanCommunitySurvey5-YearData(2009–2021).Availableat: https://www.census.gov/data/developers/data-sets/acs-5year.html AccessedSeptember15,2023.
17.ShahMN,BazarianJJ,LernerEB,etal.Theepidemiologyofemergency medicalservicesusebyolderadults:ananalysisoftheNational HospitalAmbulatoryMedicalCareSurvey. AcadEmergMed. 2007;14(5):441–7.
18.MelgozaE,Beltrán-SánchezH,BustamanteAV.Emergencymedical serviceuseamonglatinosaged50andolderinCaliforniacounties, exceptLosAngeles,duringtheearlyCOVID-19pandemicperiod. FrontPublicHealth. 2021;9:660289.
19.JonesCM,WassermanEB,LiT,etal.TheeffectofolderageonEMS usefortransportationtoanemergencydepartment. PrehospDisaster Med. 2017;32(3):261–8.
20.StataCorp. Statastatisticalsoftware:Release17.CollegeStation,TX: StataCorpLLC;2021.
21.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. AnnEmergMed. 2005;45(4):448–51.
22.NationalEMSInformationSystem(NEMSIS).NEMSISdatadictionary. Availableat: https://nemsis.org/media/nemsis_v3/release-3.5.0/ DataDictionary/PDFHTML/EMSDEMSTATE/NEMSISDataDictionary. pdf.AccessedSeptember29,2023.
23.ShahMN,KaruzaJ,RueckmannE,etal.Reliabilityandvalidityof prehospitalcase findingfordepressionandcognitiveimpairment. JAmGeriatrSoc. 2009;57(4):697–702.
24.LordB.Paramedicassessmentofpaininthecognitivelyimpairedadult patient. BMCEmergMed. 2009;9:20.
25.ChoonaraEandWilliamsJ.Whatfactorsaffectparamedics’ involvementofpeoplewithdementiaindecisionsabouttheircare? Aqualitativestudy. BrParamedJ. 2021;5(4):1–8.
26.Zegre-HemseyJK,Asafu-AdjeiJ,FernandezA,etal.(2019). CharacteristicsofprehospitalelectrocardiogramuseinNorthCarolina usinganovellinkageofemergencymedicalservicesandemergency departmentdata. PrehospEmergCare.23(6):772–9.
27.FixJ,IsingAI,ProescholdbellSK,etal.Linkingemergencymedical servicesandemergencydepartmentdatatoimproveoverdose surveillanceinNorthCarolina. PublicHealthRep. 2021;136(1_suppl):54S–61S.
28.EdelmanLS,CookL,SaffleJR.Usingprobabilisticlinkageofmultiple databasestodescribeburninjuriesinUtah. JBurnCareRes 30(6):983–92.
AmandaM.Szarzanowicz,BS* KendraFabian,MD†
MayaAlexandri,MD‡ CarlyA.Robinson,BS§
SoniaSingh,MD,MPH,MBA,PhD§ MichaelWallace,MD‡ MichelleD.Penque,MD∥
NanNan,MA,PhD** ChangxingMa,PhD** BradfordZ.Reynolds,MD‡ BethanyW.Harvey,MD†† HeidiSuffoletto,MD*‡‡ E.BrookeLerner,PhD*∥a
SectionEditor:RonnieDellWaldrop,MD
*StateUniversityofNewYorkatBuffalo,JacobsSchoolofMedicineand BiomedicalSciences,DepartmentofEmergencyMedicine,Buffalo,NewYork † UniversityofWisconsin-Madison,SchoolofMedicineandPublicHealth, BerbeeWalshDepartmentofEmergencyMedicine,Madison,Wisconsin ‡ MedicalCollegeofGeorgiaatAugustaUniversity,DepartmentofEmergency Medicine,Augusta,Georgia
§ UniversityofCaliforniaDavisSchoolofMedicine,DepartmentofEmergency Medicine,Sacramento,California
∥ StateUniversityofNewYorkatBuffalo,JacobsSchoolofMedicineand BiomedicalSciences,DepartmentofPediatrics,Buffalo,NewYork
**StateUniversityofNewYorkatBuffalo,SchoolofPublicHealthandHealth Professions,DepartmentofBiostatistics,Buffalo,NewYork
†† StateUniversityofNewYorkatBuffalo,JacobsSchoolofMedicineand BiomedicalSciences,DepartmentofSurgery,Buffalo,NewYork
‡‡ StateUniversityofNewYorkatBuffalo,JacobsSchoolofMedicineand BiomedicalSciences,DepartmentofOrthopedics,Buffalo,NewYork a Posthumousauthor
Submissionhistory:SubmittedAugust2,2023;RevisionreceivedFebruary14,2024;AcceptedMay6,2024
ElectronicallypublishedOctober29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18417
Objective: Thisstudydeterminedifthecaregiversofchildrenintheemergencydepartment(ED) havethesameCOVID-19vaccinationstatusasthechild,thereasonstheychosetonotvaccinate thechild,andself-identifiedbarrierstovaccinationtodetermineiftheEDisappropriatefor vaccinationintervention.
Methods: AsurveywasadministeredtocaregiversofpediatricEDpatientsatfourChildren’sHospitals in:Augusta,GA,Buffalo,NY,Madison,WI,andSacramento,CA.Participantswereaskedabouttheir andthechild’sdemographics,vaccinationstatus,andbarrierstovaccination.Weuseddescriptive statistics,Cohen'skappa,andlogisticregressiontoanalyzeresponses.
Results: 941caregiverswereconsideredforenrollment,and800consentedtoparticipation. Participantswere75%womenwithameanageof40.9 ± 8.9years.51%(409)ofthepediatricED patientswereCOVID-19vaccinated,aswere74%(591)ofthecaregivers.Therewasvariationacross sites,butoverall,15%ofcaregiversofunvaccinatedchildrenwantedthechildtobevaccinatedwiththe mostcommonbarrierstovaccinationidentifiedassafetydata(25%),timeavailability(20%),andabilityto obtainanappointment(13%).ThemostcommonreasonfornotwantingthechildCOVID-19vaccinated wasconcernthevaccinedidn’tworkorhadtoomanysideeffects.
Conclusion: AsmallbutclinicallyimportantgroupofpediatricEDpatientsarenotCOVID-19vaccinated buttheircaregiverswantthemtobevaccinated,indicatingthatconsiderationshouldbegiventooffering vaccinationintheED.ReasonsforavoidingCOVID-19vaccinationwereprimarilyconcernswithefficacy andsideeffects.[WestJEmergMed.2025;26(1)96–102.]
Vaccinationhasbeenakeyinterventioninreducingthe burdenofCOVID-19onsocietyandthehealthcaresystem. VaccinationprovidesprotectionagainstCOVID-19andits short-andlong-termcomplications,includingpreventing multisysteminflammatorysyndromeinchildrenaftera COVID-19infection.1 TheCOVID-19vaccinationalso mitigatestheriskofchildrenactingasdiseasevectorsforhighriskpopulationsandreducestheburdenplacedonfamilies whenaninfectedchildneedstobequarantinedfromchildcare orschool.2 TheCOVID-19vaccinewasapprovedfor emergencyuseinchildrenages5–17andasofAugust2022, 38%ofUSchildrenaged5–11and70%ofchildrenaged12–17 havereceivedatleastonedoseofaCOVID-19vaccine.3 In contrast,57%ofUSchildrenaged5–12and48.1%ofchildren 13–17receivedthe fluvaccineforthe2021–2022season.4
Theuseoftheemergencydepartment(ED)todeliver vaccinesliketheCOVID-19vaccinemaybeawaytoincrease vaccinationrates,especiallyduringapandemicwheninpersonprimarycarevisitsarelimited.Afterrecognizingthe needformoretargetedeffortstovaccinatethosewhohadnot yetsoughtthevaccine,orremainedhesitant,andthepotential roleoftheEDasahealthcaresafetynetduringapandemic,a surveywasconductedofadultspresentingtoanEDin Buffalo,NYtoidentifyvaccinationratesamongEDpatients andbarrierstovaccination.Theauthorsofthatstudyfound thatadultEDpatientswerevaccinatedataslightlylowerrate thanthegeneralpopulationandthatasmallbutsignificant portionofthosewhowereunvaccinateddesiredtobe vaccinated,suggestingthattheEDmaybeasuitablelocation tovaccinateadultsagainstCOVID-19.5 Thestudydidnot considerchildren,apopulationinwhichvaccinationhesitancy hashistoricallybeenheightenedstemmingfromfalseclaims thatautismspectrumdisordermaybeattributedtochildhood vaccinationsinthe1998paperpublishedin TheLancet , 6 whichwassubsequentlydiscreditedandtheprincipalauthor AndrewWakefieldstruckfromtheUnitedKingdommedical register.Studieshaveshownthatprovidingtheinfluenza vaccineinapediatricED(PED)canincreasevaccinationrates andovercomehesitancy.7,8
VaccinationratesforCOVID-19amongchildreninthe USvarygreatlybetweenstates.3 Forthisreasonwechoseto surveyfourdifferentregionsofthecountry.Littleisknown aboutthevaccinationrateofthePEDpopulation.Inthis studyweaimedtodeterminewhethertheadultcompanions ofchildrenintheEDhadthesamevaccinationstatusasthe childtheywereaccompanying,thereasonstheychosenotto vaccinatethechildtheywerewith,andanyself-identified barrierstovaccinationofthechild.
Weconductedaresearcher-administeredsurveyinfour EDsprovidingpediatricemergencycareingeographically
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Vaccinationisausefulinterventionin epidemicsbypromotingherdimmunity.The EDisoftenusedasasafetynettoprovide primarycareforunderservedpopulations.
Whatwastheresearchquestion?
ShouldtheCOVID-19vaccinebeofferedin thepediatricED?
Whatwasthemajor findingofthestudy?
Atfourchildren ’ shospitals,themajority (73%)ofadultsaccompanyingchildrentothe EDhadthesamevaccinationstatusagainst COVID-19asthepediatricpatient.However, 15%ofcaregiverswantedtohavetheir unvaccinatedchildvaccinated.
Howdoesthisimprovepopulationhealth?
ThepediatricEDmaybeanadequatesitefor COVID-19vaccinationasasignificantportion oftheadultcompanionsofunvaccinated pediatricpatientsdesiredvaccinationfor theirchild.
diverseareasoftheUnitedStates.Thesurveywasconducted fromJune15–October28,2022withsitesstartingenrollment atdifferenttimesbasedonwhentheyreceivedinstitutional reviewboard(IRB)approval.Thesurveyswereconducted whenresearchassistants(RA)wereavailableintheEDwith thegoalofcollecting200surveysateachsite.Thisstudywas approvedbytheIRBsateachsite:AugustaUniversityin Augusta,GA;StateUniversityofNewYorkatBuffaloin Buffalo,NY;UniversityofCaliforniaDavisinSacramento, CA;andUniversityofWisconsinMadisoninMadison,WI. Eachparticipantprovidedverbalconsenttoparticipatein thesurvey.
Thesurveywasconductedatfourpediatricspecialty hospitalsintheUS.InAugusta,GA,thesitewastheregion’ s onlychildren’shospital,whichseesapproximately30,000 EDvisitsperyear.ThehospitalisinRichmondCountywith apopulationjustover200,000people.InBuffalo,NY,the sitewastheregion’sonlychildren’shospital,whichsees 45,000visitsperyear.ThehospitalisinErieCountywitha populationofjustover950,000people.InMadison,WI,the sitewastheregion’sonlychildren’shospital,whichsees 18,000visitsperyear.ThehospitalisinDaneCountywitha
populationjustunder270,000people.InSacramento,CA, thesiteisoneofthreechildren’shospitals,whichsees10,000 visitsperyear.ThehospitalisinSacramentoCountywitha populationjustover1.5millionpeople.
Allpatientsbetween5–17yearsofagewhopresentedtoa participatingEDwereconsideredforenrollmentinthe study.Triagecategory,chiefcomplaint,andpatient demographicswererecordedfromthepatient’schart.The RAthenapproachedthepatient’scliniciantodetermine whethertheadultaccompanyingthepatientcouldbe approachedforthesurvey.Reasonsthattheadult accompanyingthepatientwasnotabletobeapproached includedinfectiousprecautionsforthepatient,patientwas tooill,patientwasactivelyreceivingmedicalcare,theadult didnotspeakEnglish,thepatientwassleeping,orthe clinicianidentifiedthatitwasnotappropriateforthemtobe approachedatthattime.Ifthepatient’sadultcompanion couldbeapproachedforthesurvey,theRAenteredtheroom andobtainedverbalconsent.
Afterconsentwasobtained,thesurveywasverbally administeredtotheadultcompanionofthepatientandthe answerswererecordedusingREDCap10.3.3(Research ElectronicDataCapture,VanderbiltUniversity,Nashville, TN)(hostedatJacobsSchoolofMedicineandBiomedical Sciences)onaniPad(AppleInc.,Cupertino,CA).Thesurvey questionsareavailablein Appendix1.PediatricED(PED) patientandadultcompaniondemographiccharacteristics collectedincludedageatpresentation,race,ethnicity,and gender.Wealsocollectededucationlevel,insurancetype, andwheretherespondentreportedobtainingtheir informationonCOVID-19.
Pediatricpatientsandadultcompanionswereclassifiedas COVID-19vaccinatediftheyhadreceivedatleastonedose ofthevaccine.Thosewhowerenotvaccinatedweredivided intothosewhowantedtogetthevaccineandthosewhodid notwanttogetthevaccine.Forqueriesregardingbarriersto care,thequestionwasreadexactlytotheparticipant,but answerchoiceswerenotprovided.Instead,astheparticipant statedtheirresponse,theRAcategorizedtheresponseor recordeditas “other,” andwrotedownwhattheparticipant hadstated.Forresponsesthatdidnot fitoneofthegiven categories,RAsdocumentedthemandoneauthor(EBL) thenclassifiedthem.Iftheresponsecouldnotbeclassified,it wasdefinedas “other” foranalysis.
Oncedatacollectionwascompleted,itwasexportedfrom REDCapandanalyzedusingSAS9.4(SASInstituteInc, Cary,NC).Weuseddescriptivestatistics,Cohen’skappa, andlogisticregressiontoanalyzethesurveyresponses.We excludedcasesfromfurtheranalysisifdatawasmissing.We developedtwologisticregressionmodelstoassesstheeffects ofdemographicfactorsontheadultcompanion’sCOVID-19 vaccinationstatusandPEDpatient’sCOVID-19vaccination statusseparately,whereadultcompanionandchild’ s COVID-19vaccinationstatuswerebothabinaryresponse (vaccinated,notvaccinated),anddifferentfactorswereused intwoseparate,logisticmodels.Onelogisticmodelwas developedtoassesstheeffectsofadultclinicalsiteonthe adultcompanion’sCOVID-19vaccinationstatus.Webuilta secondlogisticregressionmodeltoinvestigatetheeffectsof thestudysiteonthePEDpatient’sCOVID-19vaccination status.Weexcludedcaseswithmissingdatafromthese models.Finally,weusedCohen’skappatomeasurethe agreementbetweenCOVID-19vaccinationstatusofadult companionandPEDpatient.
Table1. Individualsconsideredforenrollmentandenrolledinthestudycomparedbysite.
TotalBuffalo,NYDavis,CAMadison,WIAugusta,GA
Consideredforenrollment941261230241209
Staffagreedtoletresearch assistantapproach 904249219230206
Reasonnotapproached*4-patientsleeping
2-adultdidnot speakEnglish 2-patient/adultnot presentinroom 4-staffnotasked
1-patientsleeping 1-adultdidnot speakEnglish 1-patient/adultnot presentinroom
1-adulttooupset 1-unknown 6-staffnotasked
3-adultdidnot speakEnglish 1-patientreceiving medicalcare
2-adulttooupset 1-infectious precautions 4-staffnotasked
2-patientreceiving medicalcare
Consentedtoparticipate800200200200200
Note:In13casesstaffwerenotasked first,butpatientconsented(3Buffalo,6Davis,3Madison,1Augusta).
Table2. Descriptionoftheincludedsubjectscomparedbysite.
TotalN = 800Buffalon = 200Davisn = 200Madisonn = 200Augustan = 200
GenderofparticipantMale22%(174)22%(44)29%(57)22%(43)15%(30)
Female75%(600)77%(154)71%(141)78%(155)75%(150)
Otherormissing3%(26)1%(2)1%(2)1%(2)10%(20)
GenderofpatientMale49%(394)49%(97)42%(83)55%(109)53%(105)
Female50%(402)52%(103)59%(117)44%(88)47%(94)
Otherormissing1%(4)0%(0)0%(0)1%(3) <1%(1)
AgeofparticipantMeanyears(SD)40.9(8.9)40.4(8.9)41.3(8.8)41.5(6.6)40.2(10.6)
AgeofpatientMeanyears(SD)11.2(5.1)11.7(7.4)10.6(4.0)11.6(4.0)10.8(4.3)
COVID-19vaccination statusparticipant
Receivedanyvaccine74%(591)80%(159)74%(148)82%(163)61%(121)
COVID-19vaccination statuspatient Receivedanyvaccine51%(409)56%(111)47%(94)70%(140)32%(64)
Table3. Self-reportedbarrierstovaccinationinunvaccinatedbydesiretoobtainvaccine.
Reasondon’t wantvaccine forthemselves (N = 189)
Wantvaccinefor themselves;reason theyhaven’tgottenit (n = 13)
Reasondon’t wantvaccine forchildpatient (n = 318)
Wantvaccineforchild patient;reasonthey haven’tgottenit (n = 56)
Afraid1%(2)-1%(2)2%(1)
AlreadyhadCOVID-195%(10)8%(1)5%(15)7%(4)
Can’tgetanappointment/noappointmentat desiredlocation -15%(2)-13%(7)
Childdoesn’twantvaccine--1%(4)5%(3)
Don’tthinkI/childiseligibletogetvaccine/not surewhentogetit -8%(1)1%(4)5%(3)
Donothavetransportationtovaccinesite-8%(1)--
Don’tthinkvaccineworks37%(70)18%(1)27%(87)2%(1) Underlyinghealthcondition1%(1)-1%(3)7%(4)
Letothersgetvaccine first1%(1)-3%(9)Noreason/unsure1%(1)-1%(2)Itisnotnecessarytobevaccinated4%(8)-4%(13)-
Otherreason:notcategorizedorblank2%(4)-3%(11)4%(2)
Otherfamilymemberdoesn’twantchild togetvaccine --2%(5)7%(4)
Peoplelikeme/thechilddon’tget severeCOVID-19
3%(5)-2%(6)-
Personalreasons5%(10)-1%(4)-
Pregnant,planningtogetpregnant, orbreastfeeding 1%(2)---
Religiousreasons3%(5)-2%(7)-
Thesideeffects/risksassociatedwith thevaccine
20%(38)-24%(77)2%(1)
Waitingformoresafetydataonthevaccine16%(30)54%(7)19%(62)25%(14)
Waitingtoreceivephysicianapproval forvaccine --1%(2)2%(1)
Workorfamilycommitments/lackoftime1%(2)-2%(5)20%(11)
Betweenthefourstudysites,941adultcompanionswere consideredforenrollment,and800(85%)wereabletobe approachedandconsentedtoparticipate(Table1).Ofthe participants,75%werewomenandthemeanagewas40.9 ± 8.9years.Incontrast,thePEDpatientswere50%female. Whencomparedacrossstudysites,thereweredifferencesin demographicsthatgenerallyalignedwiththeparticipating hospitals’ catchmentareas(Table2).Approximatelyhalfof thePEDpatientsandthree-quartersoftheiradultcompanions werevaccinatedagainstCOVID-19.Therewasvariation acrossthesites,butfor15%(56)ofthePEDpatientswhowere notCOVID-19vaccinated,therespondentstatedthatthey wantedthechildtobevaccinated.These56casesrepresented 7%ofthetotalinterviewedsample.Further,92%(375)ofthe vaccinatedPEDpatientsand97%(571)ofthevaccinated adultcompanionsreportedreceivingtherecommended secondCOVID-19vaccinedoseorthesingledoseiftheyhad receivedtheJohnson&Johnsonvaccine.
OftheadultcompanionswhowerenotCOVID-19 vaccinatedandgavereasonsfornotgettingthemselvesorthe PEDpatientCOVID-19vaccinated,themostcommon reasonswerefeelingthatthevaccinedidn’tworkorhadtoo manysideeffects(Table3).Whenlookingatthevaccination statusofthePEDpatientandtheiradultcompanion,we foundthatfor49%bothwereCOVID-19vaccinated,andfor 24%neitherwasvaccinated.Itwasmorecommonforjustthe adultcompaniontobeCOVID-19vaccinated(25%)than justthePEDpatient(3%).Thekappaestimatewas0.44(95% confidenceinterval0.38–0.50),significantlydifferentfrom zero,indicatingmoderateagreementbetweenCOVID-19 vaccinationstatusoftheadultcompanionandPEDpatient. Weexcluded fiveobservationsfromcomparisondueto missingeithertheadultcompanion’sorPEDpatient’ s COVID-19vaccinationstatus.
Figure1 showsresultsofdemographicfactorsassociated withadultcompanionbeingCOVID-19vaccinated.Theodds ofbeingCOVID-19vaccinatedforadultcompanionsin
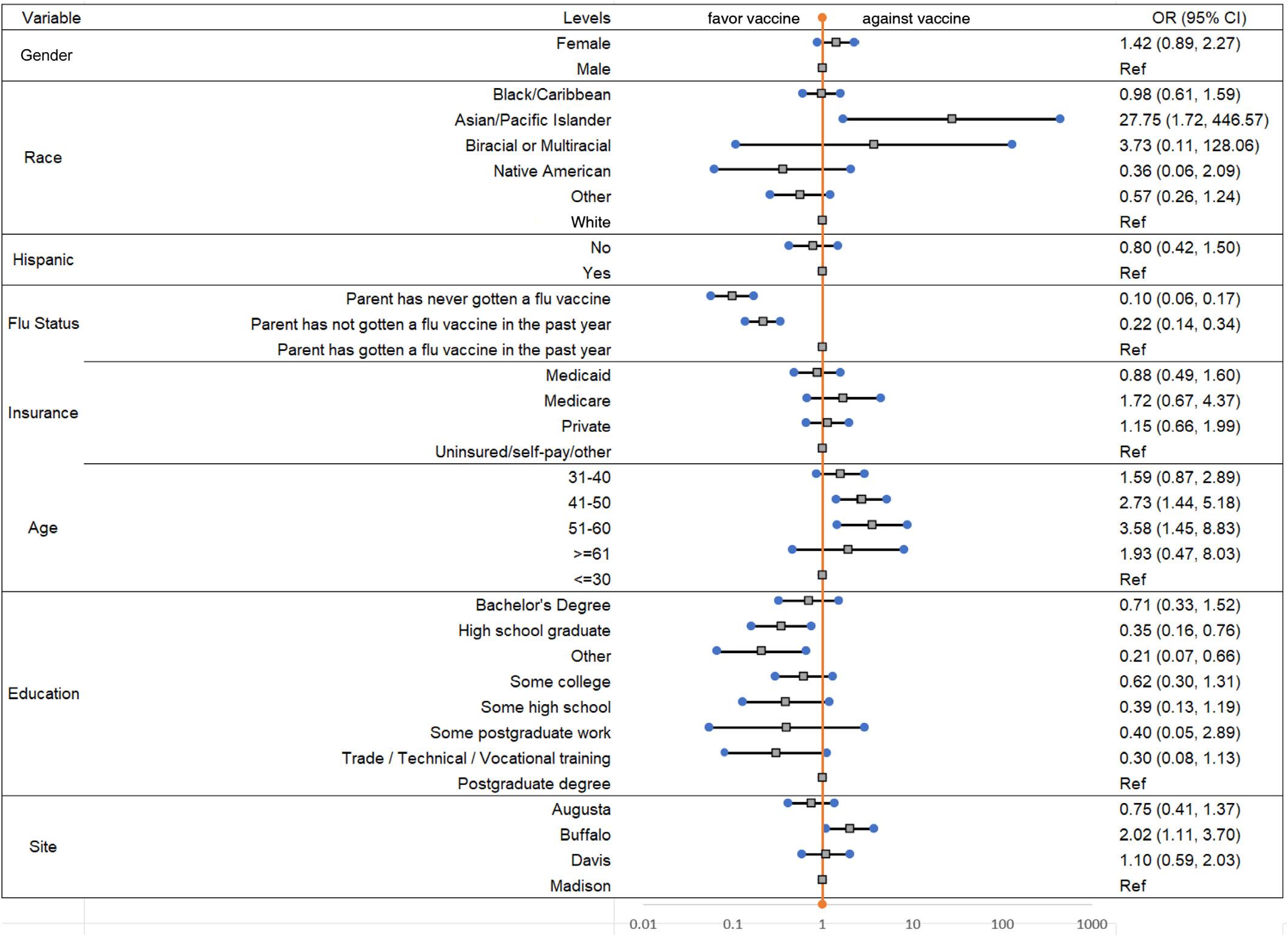
Figure1. Theoddsratios(OR)and95%confidenceintervals(CI)forparentcompanionvaccinatedfordifferentdemographiccharacteristics. Note:OddsratioforparentcompanionwereestimatedusingFirth’spenalizedlikelihoodapproach.

Theoddsratios(OR)and95%confidenceintervals(CI)forchildpatientvaccinatedfordifferentdemographiccharacteristics.
Buffalowas2.02timesthatoftheMadisonsite.Theresultsof demographicfactorsassociatedwiththePEDpatientbeing COVID-19vaccinatedisshownin Figure2.Theoddsofbeing COVID-19vaccinatedamongPEDpatientsattheAugusta sitewas0.42timesthatofPEDpatientsattheMadisonsite. ThelogisticregressionmodelsforadultcompanionsandPED patientswerebuilton738and775of800participants, respectively.Theremainingcasesweremissingdata.
Inthisstudywedeterminedthatthemajority(71.9%)of adultcompanionsofchildreninthePEDhadthesame COVID-19vaccinationstatusasthechildtheywere accompanying.OfthosewithdifferentCOVID-19 vaccinationstatus,inmostcases(90%)theadultcompanion hadbeenvaccinatedbutnotthechildtheywere accompanying.This findingmayreflectthehesitancy associatedwithchildvaccines,particularlytheCOVID-19 vaccine.9 Itmayalsobetheresultofvaccinerequirements thatwereplacedonadultsatthispointinthepandemic:for example,therequirementthatallfederalemployees, contractors,internationaltravelers,HeadStarteducation centers,andCentersforMedicare&MedicaidServicescertifiedfacilityemployeesbeCOVID-19vaccinated, whichwasrescindedin2023.10 Toourknowledgetherewere nofederalorlocalrequirementsatourstudysitesto
vaccinatechildren,whichmayhavecontributedto this finding.
Overall,49%ofthePEDpatientswerenotvaccinated. Similartotheresultsofthesurveystudyofbarriersto vaccinationofadultspresentingtotheED,5 asmallbut significantnumber(15%)ofadultcompanionsofunvaccinated childrenfromacrossallsitesreportedwantingthevaccinefor thePEDpatientbuthadnotyetreceivedit.Thispopulation shouldbeconsideredaprimarytargetforincreasingthe COVID-19vaccinerateinthepediatricpopulation.Ofthese cases,one-thirdidentifiedpracticalissuesastheprimarybarrier tovaccinationofthechild.This findingwassupportedbythe WorldHealthOrganization(WHO)StrategicAdvisoryGroup ofExpertsWorkingonGroupVaccineHesitancy.They identifiedpracticalissuesassignificantfactorswhen consideringvaccination,whichincludedavailability, affordability,easeofaccess,servicequality,andrespectfrom healthworkers.11 Theotherreasonsfornotvaccinatingthese childrenwererelatedtowhattheWHOreportdescribedas “thinkingandfeeling” issuesrelatedtoriskandvaccine confidenceand “socialprocesses” relatedtosocialnormsand healthworkerrecommendations.Manyoftheseissuesmight beabletobeaddressedthroughpatient/adultcompanion educationthatcanbeprovidedintheED.Evenifvaccinesare notofferedintheED,itmaybeadvantageoustousetheEDas asiteforprovidingaccurateinformationontherisksand benefitsofCOVID-19vaccination.
Thisstudymayhavebeenlimitedbythepatientswho declinedparticipationafterbeingapproached.AsCOVID19vaccinationcanbeconsideredcontroversial,some individualsmayhavefeltuncomfortablesharingtheirviews anddeclinedparticipation.Itispossiblethatthisgroupwas morelikelytonothavebeenvaccinated.Additionally,the surveywasreadaloudtothepatientsandtheirverbal responseswererecorded,whichmayhaveskewedresultsas peoplemayhavebeenashamedtovoicetheirviewsorfear judgmentfrommedicalprofessionals.Further,wedidnot studyarepresentativesampleoftheEDpatientpopulation sincewewouldnothaveapproachedthosewithseriousor life-threateningillnesses.However,itislikelythatanyED vaccinationprogramwouldfocusonthissamesubsetof patients.Wealsowereunabletointerviewadultcompanions whodidnotspeakEnglish.Finally,weassumedthatthe accompanyingadultwasaprimarycaregiverofthePED patient.TherelationshipbetweenthePEDpatientandthe adultcompanionwasnotdeterminedorlimitedtojust parentstoensurethestudyincludednon-traditionalfamilies.
AsmallbutclinicallyimportantgroupofpediatricED patientswerenotCOVID-19vaccinated,buttheiradult companionswantedthemtobevaccinated,indicatingthat considerationshouldbegiventoofferingvaccinationinthe EDsetting.Mostadultsaccompanyingchildrenhadthe samevaccinationstatusasthepediatricEDpatientbut, interestingly,forthemajorityofthosewithdiffering vaccinestatustheadultwasvaccinatedbutnotthechild. ReasonsforavoidingCOVID-19vaccinationseemedto centerprimarilyonconcernswithefficacyandsideeffects. Futurestudiescouldlookathowpatientdemographics impactvaccinationstatusandtheintentiontoreceive vaccinationtotargeteducationandCOVID-19 vaccinationinitiatives.
AddressforCorrespondence:AmandaM.Szarzanowicz,BS, JacobsSchoolofMedicineandBiomedicalSciences,955MainSt., Buffalo,NY14203.Email: amszarza@buffalo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Szarzanowiczetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ZambranoLD,NewhamsMM,OlsonSM,etal.BNT162b2mRNA vaccinationagainstcoronavirusdisease2019isassociatedwitha decreasedlikelihoodofmultisysteminflammatorysyndromeinchildren aged5–18years-UnitedStates,July2021–April2022. ClinInfectDis. 2023;76(3):e90–100.
2.VitielloA,FerraraF,TroianoV,etal.COVID-19vaccinesanddecreased transmissionofSARS-CoV-2. Inflammopharmacology. 2021;29(5):1357–60.
3.CentersforDiseaseControlandPrevention.COVIDdatatracker.2024. Availableat: https://covid.cdc.gov/covid-data-tracker/#datatrackerhome.AccessedJuly21,2023.
4.CentersforDiseaseControlandPrevention.Influenzavaccination coverage,children6monthsthrough17years,UnitedStates.2024. Availableat: https://www.cdc.gov/ flu/fluvaxview/dashboard/ vaccination-coverage-race.html.AccessedJuly21,2023.
5.HarveyBW,KelleranKJ,SuffolettoH,etal.Emergencydepartment patients’ COVID-19vaccinationstatusandself-reportedbarriers. WestJ EmergMed. 2022;23(3):292–301.
6.WakefieldAJ.MMRvaccinationandautism. Lancet. 1999;354(9182):949–50.
7.Baumer-MouradianSH,KleinschmidtA,ServiA,etal.Vaccinatinginthe emergencydepartment,anovelapproachtoimproveinfluenza vaccinationratesviaaqualityimprovementinitiative. PediatrQualSaf. 2020;5(4):e322.
8.Baumer-MouradianSH,ServiA,KleinschmidtA,etal.Vaccinatinginthe emergencydepartment,amodeltoovercomeinfluenzavaccine hesitancy. PediatrQualSaf. 2021;6(2):e430.
9.MacDonaldNE,SAGEWorkingGrouponVaccineHesitancy. Vaccinehesitancy:definition,scopeanddeterminants. Vaccine. 2015;33(34):4161–4.
10.TheWhiteHouse.TheBiden-HarrisadministrationwillendCOVID-19 vaccinationrequirementsforfederalemployees,contractors, internationaltravelers,headstarteducators,andCMS-certified facilities.2023.Availableat: https://www.whitehouse.gov/briefing-room/ statements-releases/2023/05/01/the-biden-administration-willend-covid-19-vaccination-requirements-for-federal-employeescontractors-international-travelers-head-start-educators-and-cmscertified-facilities/.AccessedJuly22,2023.
11.WorldHealthOrganization.Understandingthebehaviouralandsocial driversofvaccineuptake.WHOPositionPaper. WklyEpidemiolRec. 2022;97(20):209–24.
NazKarim,MD,MHA,MPH*
JeanneD’ArcNyinawankusi,MSc†
MikaelaS.Belsky,MPhil‡ PascalMugemangango,MD§ ZetaMutabazi,MD,Msc∥
CatalinaGonzalezMarques,MD¶ AngelaY.Zhang,MD#
JanetteBaird,PhD* JeanMarieUwitonze,MSc† AdamC.Levine,MD,MPH*
SectionEditor: ChristopherN.MillsMD,MPH
*BrownUniversityAlpertMedicalSchool,DepartmentofEmergency Medicine,Providence,RhodeIsland
† Serviced’AideMédicaleUrgente,Kigali,Rwanda
‡ NYUGrossmanSchoolofMedicine,NewYork,NewYork
§ UniversityTeachingHospital,Kigali,Rwanda
∥ UniversityofRwanda,DepartmentofAnaesthesia,EmergencyMedicineand CriticalCare,Kigali,Rwanda
¶ BrighamandWomen’sHospital,DepartmentofGlobalEmergencyCareand HumanitarianStudies,Boston,Massachusetts
# UniversityofWashington,DepartmentofPediatrics,Seattle,Washington
Submissionhistory:SubmittedJanuary1,2024;RevisionreceivedAugust23,2024;AcceptedSeptember26,2024
ElectronicallypublishedNovember20,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18698
Background: Inlow-andmiddle-incomecountries(LMIC),45%ofdeathscouldbeaddressedby implementationofanemergencymedicalservices(EMS)system.Prehospitalcareisacritical componentofEMSworldwide,andbasic,affordabletraininghasbeenshowntoimproveEMSsystems. However,patientoutcomeimpactisunclear.Inthisstudyweaimedtoassessthecurrentstateof prehospitalcareinKigali,Rwanda,throughaneedsassessment,focusedtrainingintervention,and analysisofcurrentpracticesandpatientoutcomes.
Methods: Weidentified30cliniciansthroughtheprehospitalmedicalcommandofficeandincludedthem inthestudy.Aprospective,nonrandomized,interruptedtime-seriesapproachwasused.Datacollected throughclosed-andopen-endedquestionnairesincludedage,sex,training,andknowledge assessment.Weusedthedatatocreateatailored,18-hourtrainingafterwhichimmediateand11-month post-testswereadministered.Linkedprehospitalandhospitalcaredatasetsallowedforevaluationof patientoutcomesandprehospitalprocessindicatorsthatincludedtrainingskillapplication,airway intervention,intravenous fluidadministration,andglucoseadministration.
Results: Of30clinicians,18(60%)werefemale,19werenurses,and11werenurseanaesthetists.Median agewas36,andmedianyearsprovidingcarewas10(IQR7–11).Twenty-four(80%)participantscompleted immediateandpost-testassessments.Meanknowledgeacross12coreskillssignificantlyimprovedfroma pre-testmeanof59.7%(95%confidenceinterval[CI]42.2–77.20)toapost-testmeanof87.8%(95%CI 74.7–100).At11monthspost-training,thescoreimprovementmaintained,withameanscoreof77.6% (95%CI59.2–96.8).Forpatientoutcomes,thetotalsamplesizewas572patients;324ofthesepatients weretransportedtotheEDduringthepre-trainingperiod(56.4%),while248weretransportedpost-training. Prehospitaloxygenadministrationforpatientswithasaturationlevelof <95%significantlyincreasedpre-to post-training(66.7%to71.7%; Δ = 5.0%; Δ95%CI1.9, 8.1%).Nosignificantchangeswerenotedinpatient treatmentoutcomesorotherprocessindicatorsduetosmallsamplesizes.
Conclusion: ThisstudyprovidesinsightsonRwandanEMSanddemonstratesthatatailored interventiontargetingeducationonprehospitalprocessindicatorshaspositiveimpactsonclinician knowledgeandpractice.[WestJEmergMed.2025;26(1)103–110.]
Keywords: trauma;training;emergency;prehospital;education.
Background
Emergencymedicalsystems(EMS)providepopulations withacutecareforadiversesetofdiseasesspanningthe spectrumofcommunicableinfections,non-communicable diseases,obstetricandpaediatricemergencies,aswellas traumaticinjuries.1 The2003WorldHealthReportdrew attentiontotheincreasingburdenofnon-communicable disease,chronicdiseases,andtraumainlow-andmiddleincomecountries(LMIC)2 andhascalledfor “rapidand sustainableexpansionofemergencytreatments” globally.3 Severalstudies,supplementedbyreportsfromtheWorld HealthOrganization(WHO),emphasizetheimportanceof improvingaccesstoemergencyhealthservicestoreduce morbidityandmortalityspecificallyinLMICs.1–11 An estimated45%ofdeathsand36%ofdisability-adjustedlife years(DALY)inLMICscouldbeaddressedbythe implementationofemergencycaresystems.4,5,6
Prehospitalcareisacriticalcomponentofemergencycare worldwide1.AsystematicreviewoftraumasystemsbyMann etalshowedconsistentsurvivalbenefitsfollowinginexpensive interventions,suchasorganizationandtraumasystem planning.7 Survivalbenefitsfromadditionofbasicand affordabletrainingtoEMShavealsobeennotedbyhealth experts.12,13 Inresource-limitedsettings,prehospitaltraining hasshownsuccessinimprovingclinicianknowledge,although impactonclinicianpracticeandpatientoutcomesis unclear.14,15 Researchonin-hospitalemergencymedicine traininginLMICsismorerobust,showingfeasibilityforsuch programstoimprovepatientandclinicaloutcomesaswellas clinicianknowledge.16,17 Still,evenforin-hospitalprograms, thereremainsaneedforfurtherresearchregardingtheir impact.16 Further,existingliteratureonprehospitaltrainingin LMICsmostoftenfocuseson firstresponderswhomaynot haveformaltraumaandemergentcaretrainingorwhodonot solelyworkintheprehospitalsetting.18–21
InRwanda,theMinistryofHealth(MOH)hasmade greatstridesinprovidingaccesstohealthcarebyrebuilding itshealthinfrastructureintheaftermathofthe1994 genocide.Toaddressprehospitalcareaccess,theMOH implementedanemergencymedicalambulancesystemin 2007,namedServiced’AideMedicaleUrgente(SAMU).22 TheSAMUprehospitalprofessionalsattheCentre HospitalierUniversitairedeKigali(CHUK)arethesole providersofprehospitalemergencycareinRwanda. Ambulancesareequippedwithoxygentanks,intravenous fluids,suppliesforperipherallineplacement,medications, anddefibrillators,andarestaffedbynursesandnurse anaesthetists.A1registerednurseswithanadvanceddiploma havecompletedthreeyearsofpost-secondaryeducation whileA0nurseshaveabachelor’sdegreewithfour yearsofpost-secondaryeducationandarecapableof intubatingpatients.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Inlow-andmiddle-incomecountries, 45%ofdeathscouldbeaddressedby emergencymedicalservice(EMS) systemimplementation
Whatwastheresearchquestion?
HowdoesamEMStrainingintervention impactcurrentpracticesand patientoutcomes?
Whatwasthemajor findingofthestudy?
Theuseofoxygenforpatientsshoweda signi fi cantincreasepost-trainingintervention (pre66.7%,post71.7%; Δ = 5.0%; Δ 95% CI1.9 – 8.1%).
Howdoesthisimprovepopulationhealth?
BasicandaffordableEMStraining interventionscanimproveclinicalmedical knowledgeandclinicalprocesses.
Alongwithinexpensivetrainingandtraumaplanning interventions,survivalbenefitsassociatedwithEMSare basedlargelyontheidentificationofkeyperformance indicatorstoimprovethequalityofpatientcare.1,13,23 Thus, theRwandanHumanResourcesforHealthStrategicPlan recognizedtheneedfornursetrainingprogramsthatdevelop prehospitalskills,whilealsostrengtheningongoing mentoringandmonitoring,especiallyasthestandard nursingcurriculumonlyoffersin-hospitalcaretraining.22 DespitetheincreasedcapacityoftheRwandanprehospital system,thereisapaucityofinformationabouttheneedsof prehospitalprofessionaltrainingaswellaslimited informationaboutcurrentpracticesofprehospital managementanditsrelationshiptopatientoutcomes.Toour knowledgethisisthe firststudythataimstounderstandthe needsofprehospitalcareprofessionals,andtheimpactofa novelprehospitalprofessionaltrainingonclinical responsivenessandpatientoutcomes.
Thestudywasconductedinmultiplephases.Inthe first phaseweanalysedprehospitalcareneedsandemergency careknowledge.Thesecondphasewasatraining interventiondesignedfromtheresultsofphase1.Inthethird phaseweassesseddataonprehospitalprocessindicatorsand patientoutcomesbeforeandafterthetrainingintervention,
aswellasprehospitalprofessionals’ pre-andpost-testscores, toevaluatetheimpactofthetraining,usingaprospective, quasi-experimental,non-randomized,interruptedtime seriesdesign.
ThetraininginterventionwasheldattheKigaliInstitute ofScienceandTechnology(KIST)inMay2017.andweused datafromtheprehospitaldatabaseattheUniversity TeachingHospitalinKigali(UTH-K)toanalyseprehospital processindicatorsandpatientoutcomes.Thestudywas approvedbytheLifespanInstitutionalReviewBoardand theInstitutionalReviewBoardandEthicsCommittee ofUTH-K.
All30prehospitalcareprofessionalsattheUTH-Kwere includedintheneedsassessmentandtrainingintervention. Weidentifiedthestudypopulationbyalistofprehospital professionalsasreportedbythehumanresourcesdepartment andconfirmedwiththedirectoroftheambulanceservices. Anon-randomizedapproachwastakentominimize interruptioninparticipantworkflow.Weexcluded ambulancedriversaswellasEMSadministrativestaffat thecallcentresnotdirectlyinvolvedinpatientcare.
Weidentifiedthepatientstudypopulationsamplethrough paper,prehospitalambulancerecords.Atrainedresearch assistantlinkedprehospitalpaperrunsheetstoemergency department(ED)healthrecords.Thelinkagewasperformed throughqueryingOpenClinic,anopen-source,integrated hospitalinformationmanagementsystem(OpenClinicGA, SanDiego,CA).Patientnames,dateofbirth,andaddresses foundinOpenClinicwerematchedtotheSAMUdatabaseto confirmidentity.Theeligibleanalyticalsampleincludedall patientstransportedtotheUTH-KEDbySAMUbetween December1,2017–June30,2018.Thesedatesareinclusiveof fourmonthsofpre-trainingandthreemonthspost-training. Weexcludedpaediatricpatientswithmedicalchief complaintsandobstetricpatientsastheyaretransferredto theirrespectiveemergencycentres.
Theneedsassessmentandpre-testdatawerecollected usingaclosed-andopen-endedquestionnaire.Thesurvey consistedofthreeparts:1)demographicdata,includingage, sex,preferredlanguage,andinformationaboutprehospital professionalbackground;2)needsassessmentonprior12 monthstrainingreceivedon12coreclinicalskills;and3)pretestquestionsassessingclinicalknowledgeaboutand confidenceinperformingthese12skills.Weusedthe informationcollectedfromthisinstrumentforthecreationof aneducationalinterventiondeemedtobelocallyappropriate andbasedontheregion’sprehospitalneeds.
TheEMSprofessionalsattendeda17-houreducational interventionadministeredovertwodays.Atwo-daycourse waspreferredbythelocalteamtolimitinterruptionofcareto patients.Thecoursestructureincludeddidacticlectures, teamdiscussions,simulationexercises,andpre-andposttestsattheKISTsimulationcentre.Thetrainingintervention focusedonpre-identifiedskillsforimprovement,basedon theneedsassessment.Theseskillsare,therefore,inclusiveof patientpresentationsthatmostoftengounrecognizedor untreatedinaprehospitalsetting,aswellasclinical interventionsthatareassociatedwithdecreasedprehospital professionalconfidence.Theefficacyofthetraining interventionwasevaluatedbyanimmediatepost-testand 11-monthpost-testdeterminingtheknowledgegainand changeinreportofconfidenceinperforming12coreclinical skills(Table1).
Tocollectdataregardingimplementationoftheselearned skills,weusedarestrictivesamplingframe.Keyprocess indicatorswereselectedbasedonelementsofEMScarethat arebothresponsivetosystemimprovementsandachievable inlow-resourcesettings.Anemphasiswasplacedon interventionswithahighprobabilityofdecreasingmedically preventabledeathordisabilityduetotrauma.Outcomes foranalysisthusincludedthefollowing:useofIV fluid resuscitationforhypotensivepatients(bloodpressureless than90/60millimetersofmercury)orpatientswithburn injury;administrationofoxygentohypoxicpatients(oxygen lessthan95%);andadministrationofglucoseto hypoglycaemicpatients(glucoselessthan60milligrams perdecilitermg/dl).
Patientoutcomedataextractedfromhospitalrecords includedinitialvitalsigns,diagnosis,hospitallengthofstay, andconditionupondischarge.TheextracteddatawasdeidentifiedandenteredintoasecuredRedCapdatabase (ResearchElectronicDataCapture,VanderbiltUniversity, Nashville,TN)hostedatLifespaninProvidence, RhodeIsland.
Weanalyzedpre-andpost-testsforchangeinknowledge. Descriptiveandinferentialstatisticswereconducted,with medianvaluesandinterquartilerange(IQR)reported. ConductedstatisticaltestsincludedtheFisherexacttestfor differencesinproportions,theWilcoxonranksumtestfor testsofmedians,andpaired t -testsfordifferencesin knowledgeandconfidence.Yesandnobinaryvariablesfor prehospitalclinicalprocessindicatorswerecodedas1or0, respectively.Theoutcomesfor fluidadministrationfor patientswithburnsandthosewithhypotensionwere combined,duetothesmallnumbersofpatients(seven)with burns.Additionally,EDpatientcareoutcomespre-and post-traininginterventionwereanalysed.Weconducted statisticalanalysiswasconductedusingSASstatistical softwarev9.4(SASInstituteInc,Cary,NC).
Table1. Prior12-monthcoreskilltrainingexperienceofprehospitalprofessionalsinRwanda.
Idonotknowwhatthis
Coreskill
Morethan11hours n(%)
a.Takingvitalsigns019(65.5)3(10.4)1(3.4)6(20.7)
b.PlacinganIntravenousline019(65.5)2(6.9)1(3.4)7(24.1)
c.PlacinganIntraosseousaccess027(93.1)01(3.4)1(3.4)
d.Checkingglucose015(57.7)3(11.5)1(3.9)7(26.9)
e.PerformingthetraumaABCevaluation1(3.5)10(34.5)3(10.3)6(20.7)9(31.0)
f.Intubation011(64.7)1(5.9)1(5.8)4(23.5)
g.Immobilizingatraumapatient012(44.4)2(7.4)5(18.5)8(29.6)
h.Performingneedledecompression018(64.3)4(14.3)4(14.3)2(7.2)
i.PerformingCPR03(15.8)06(31.6)10(52.6)
j.Performingdefibrillation018(64.3)2(7.1)3(10.7)5(17.9)
k.Splintingafracture016(59.3)3(11.1)08(29.6)
l.Injectingaubcutaneousepinephrine021(72.4)4(13.8)1(3.5)3(10.3)
CPR,cardiopulmonaryresuscitation.
Ofthe30prehospitalclinicians,18(60%)werefemale,19 werenurses,and11werenurseanaesthetists.Themedianage was36yearsandmediantimeprovidingcarewas10years (interquartileratio7–11).Twenty-fourparticipants(80%) completedthetraininginterventionandanimmediateposttest.Sixteenparticipants(53.3%)completedboththe immediateand11-monthpost-tests.
Aneedsassessmentwasconductedpriortotraining. Table1 showsthefrequencyofpriorpast-yeartraining reportedbyparticipants.Acrossthe12coreskills, ‘ no training’ wasmostfrequentlyreportedforplacingan intraosseousaccess(IO)(93.1%),injectingsubcutaneous epinephrine(72.4%),takingvitalsigns(65.5%),andplacing anIVline(65.5%).Morethan11hoursoftrainingwasmost oftenreportedforperformingcardiopulmonary resuscitation(52.6%),performingtraumaABCevaluation (31%),immobilizingatraumapatient(29.6%),andsplinting afracture(29.6%).Pre-intervention,15participants(50%) reportedwantingmoretrainingontraumaskills(bleeding control,IVandIOlineplacement,useofoxygenmasks, understandingvitalsigns).
Correspondingly,medianconfidenceinperformingthese 12coreskillsvariedatthepre-trainingneedsassessment (Table2).UsingtheWilcoxonrank-sumtestwithpaired comparisonsbetweenthethreeassessmentsofconfidence,we foundthereweresignificantincreasesinmedianconfidence inplacinganIO(pretoimmediatepost P = .02;pre to3-monthpost P < .01);andperformingneedle
decompression(pretoimmediatepost P = 0.0002,preto 11-monthpost P = 0.003).
Themeanpre-testcorrectknowledgescorewas59.7% (95%confidenceinterval[CI]42.2–77.20).Theimmediate post-testmeanscorewas87.8%(95%CI74.7–100),and11 monthsaftertrainingthemeantestscorewas77.6%(95%CI 59.2–96.8).Therewasa56%(95%CI36.2–75.8)relative increaseinmeanknowledgescorethatwasmaintained betweentheimmediateand11-monthpost-test.Therewasa significantgaininknowledgebetweenpre-interventionand immediatepost-test(P < .001),andthisdifferencewas significantbetweenpreand11-monthpost-test(P < 0.001) usingpairedt-testscomparingthesurveyadministrations. Thegainwassignificantlyhigherintheimmediatepost-test comparedtothe11-monthpost-test(P = .02).Scoresinthe categoriesofpatientassessment,respiratoryintervention, and fluidtherapyimprovedby8%,21%and8%,respectively. Allrespondentsreportedthatthetraininghadbothincreased theirmedicalknowledgeandimprovedpatientcare,andall respondentsrequestedfurthertraining.
Intotal,572patientsweretransportedtotheED forcareduringthestudy;324(56.4%)weretransported duringthepre-trainingperiod.Theaveragepatientage was37years(SD15.8,range15–96),and148(25.7%) werefemale,withnosigni fi cantdifferenceinaverage age(P = .08)orsex( P = .14)proportionpre-and post-training. Table3 showsthefrequencyofclinical conditionsofinterestpre-andpost-trainingandclinical
Table2. Prehospitalprofessionals’ confidenceonLikertscaleof1–5performingcoreskills.
Confidenceinperforming coreskill
Median(IQR) pretraining(1)
Median(IQR)post trainingimmediate(2)
Median(IQR)post training11months(3) Statistical comparison
a.Takingvitalsigns5(5,5)5(5,5)5(5,5)1vs.2 = ns
1vs.3 = ns
2vs.3 = ns
b.Placinganintravenousline5(5,5)5(5,5)5(5,5)1vs.2 = ns 1vs.3 = ns
2vs.3 = ns
c.Placinganintraosseousaccess2(2,3)3(2,4)4(3,4)1vs.2 = 0.02
= 0.002 2vs.3 = ns
d.Checkingglucose5(5,5)5(5,5)5(5,5)1vs.2 = ns
1vs.3 = ns 2vs.3 = ns
e.Performingthetrauma ABCevaluation 5(4,5)5(5,5)5(5,5)1vs.2 = ns
1vs.3 = 0.05 2vs.3 = ns
f.Intubation3(3,5)4(3,5)5(4,5)1vs.2 = ns 1vs.3 = ns 2vs.3 = ns
g.Immobilizingatraumapatient5(5,5)5(5,5)5(5,5)1vs.2 = ns
1vs.3 = ns 2vs.3 = ns
h.Performingneedledecompression3(3,4)4(4,5)4(4,5)1vs.2 =
= ns
i.PerformingCPR5(4,5)5(4,5)5(5,5)1vs.2 = ns
= 0.04
2vs.3 = ns
j.Performingdefibrillation4(3,4)4(3,4)5(4,5)1vs.2 = ns 1vs.3 = 0.03
2vs.3 = 0.05
k.Splintingafracture5(5,5)5(5,5)5(5,5)1vs.2 = ns
1vs.3 = ns
2vs.3 = ns
l.Injectingsubcutaneousepinephrine4(4,5)5(3,5)5(4,5)1vs.2 = ns
1vs.3 = ns 2vs.3 = ns
ge;1 = pretraining,2 = immediateposttraining,3 = 11monthsaftertraining. CPR,cardiopulmonaryresuscitation; IQR,interquartilerange.
outcomes.Usingchi-squaretests,wefoundnosigni fi cant differencespre-topost-trainingacrossthethreetypes ofclinicalpresentationofinterest(P = .68),EDdisposition ( P = .24),medianhoursspentintheED ( P = .64),ormedianlength-of-hospitalstayforthose admitted( P = .85).
Table4 detailsthefrequencyofprehospitalclinical interventionsbeforeandafterthetrainingintervention.A reviewofdatashowedthatIV fluidresuscitationwasgivento allindicatedpatientspre-andpost-intervention,andthatthe
useofoxygenforpatientswithasaturationlevelof < 95% showedasignificantincreaseinproportionpre-topostintervention(pre = 66.7%,post = 71.7%; Δ = 5.0%; Δ 95% CI1.9–8.1%),asthe95%CIaroundthe Δ doesnotinclude0. Table4 alsoshowsthissignificantchangeinadministration ofoxygenforhypoxicpatientsoverthepre-andpostinterventionperiod.
Thisstudynotonlydemonstratesstatisticallysignificant testimprovementsforaneedsassessment-based,contextappropriateeducationintervention,butalsoexplores
Table3. Emergencydepartmentpatientputcomes.
Clinicalpresentationn(%)Pretrainingn = 324Posttrainingn = 248
Burn5(1.5)2(0.80)
Hypotension15(4.7)13(5.4)
Hypoxia75(23.2)52(20.7)
Hypoglycaemia1(0.30)0
Clinicaloutcomes
EDdispositionAdmit = 154(73.3)
Transfer = 9(4.3)
Discharged = 39(18.6)
DiedinED = 8(3.8)
Diedafteradmission = 18(12.1)
Admit =142(79.3)
Transfer = 2(1.1)
Discharged = 33(16.7)
DiedinED = 5(2.8)
Diedafteradmission = 15(10.6)
LengthofstayinED(hours)
Median(IQR) 24(24,48)24(24,48)
Lengthofstayifadmitted(days)
Median(IQR) 3(1,10)3(2,10)
ED,emergencydepartment; IQR,interquartileratio.
Table4. Prehospitalclinicalprocessindicators(prehospitalprofessionals’ responsiveness).
ClinicalpresentationExpectedclinicalintervention Frequencyadministered pretraining(%) Frequencyadministered posttraining(%)
Burnand/orhypotensionUseofintravenous fluidresuscitation20(100)15(100)
Hypoxia(SpO2 < 95%)Oxygengiven50(66.7)38(71.7)
HypoglycaemiaGlucoseadministered00
prehospitalprocessindicatorsandpatientoutcomes.The pre-topost-testimprovements,especiallyregardingpatient assessment,respiratoryintervention,and fluidtherapy, remainedsignificantatthe11-monthpost-test, demonstratinglong-termknowledgeretention.Importantly, significantpre-topost-testincreaseinhypoxia responsivenessdemonstratesactualimplementationof learnedskills.Theseconcretepositiveresultsarebolsteredby statisticallysignificantincreasesinprehospitalclinical confidence,whichoccurredacrossmultipleskills.These improvementsareimportant,asself-confidencehasbeen showntoenhanceclinicalcompetencyandeffectiveclinical decision-making.24 Additionally,participantsnotedpositive responsestothetrainingmodulesandevenrequested additionaltraining,speakingtodesirabilityandfeasibilityof suchprehospitaltrainingmodulesinsimilarcontexts.
Itisimportanttonotethatmostprehospitalprofessionals inthisregionarewomen,assexmayimpactlearningstyles, clinicalconfidence,andotherrelevantvariables.25,26 Future studiesareneededtoassesstheimpactofgenderonlearning styles.Itisalsoimportanttonotethatthedatadidnot supportanysignificantchangeinmeasuredpatient outcomes.Thismaybebecausemeasuredoutcomeswere moreimpactedbyissuesinEDoperations,suchasstaff
boardingdifficultiesaswellaslimitedcapacityandresources. Also,therewasasmalldecreaseinEDandin-hospital mortalitypost-training,althoughthesamplesizewastoo smalltodetectanysignificantdifference,andother interventionsmayhaveconfoundedtheresult.
Directobservation,prospectiveanalysis,and improvementinmethodsareneededaftersuchatraining interventiontoassessfuturepatientoutcomes.Overall,the promisingassociationbetweenatailoredtrainingcurriculum andimprovedpost-testindicatorsinvarioustraumatopics, aswellastheacceptabilityofmodulesamongstparticipants, establishestheusefulnessforsuchtrainingsamongst prehospitalprofessionals.Furthertrainingshouldbe consideredforothergroupsincludinggraduating medicalstudentsandgeneralpractitionerspracticing emergencymedicine.
Mostimportantly,thisstudyissettingthestagefora longerterm,comprehensive,andlocallyrunemergencycare trainingtosustainablyestablishknowledgeretentionand improveclinicalprocessindicators.16
CHUKisatertiary-carehospital,withmultiple subspecialtytrainingprogramsthatwereintheirinfancyat
thetimeofthisstudy.Othertrainingprogramscould haveintroducedbiasintotheknowledgeretention assessmentandpatientoutcomeanalysis.Thus,theseresults maynotbegeneralizabletoothercontexts.Training-specific limitationsincludeinterruptionsinpost-testadministration duetoleavesofabsenceoftrainingstaff,aswellaslossof participantsduetotheneedforstaffingambulancesin criticalneed.Asaresult,theirpatientoutcomedata werenotincludedinthestudy.The11-monthpostinterventionanalysisresultsdidnothaveacontrolgroup, asequitabletrainingwasanecessaryneedatthetime. Morelongitudinalstudiesevaluatingtheimpactoftailored trainingsonclinicianretentionandclinicaleffectiveness areneeded.
Finally,processindicatorstoassessprehospital responsivenessdidnotencompassallskillsfromthetraining. Namely,thetrainingimprovedprehospitalprofessionals’ patientassessmentskills,butclinicalcasescenarios encompassedmuchmorethanwhatcouldbemeasuredfrom thepredefinedprehospitalprocessindicatorrunsheet. Quantityof fluidadministrationcouldnotbeanalysedasthis wasnotdocumented,andtheimpactofthetrainingon prehospitalresponsivenesstopatientswithburninjury,as wellashypoglycaemia,couldnotbeaccuratelymeasureddue tolimiteddataavailableforthispatientpopulation.
Thestudydemonstratedthatabasiccoursetailoredtoa groupofprehospitalEMSprofessionalsinRwandacould leadtoimprovementinemergencycareknowledge, con fi dence,andanappropriateresponsetohypoxia.Itis importanttonotethatmostprehospitalprofessionalsinthis regionarewomen.Context-driveneducationonprehospital emergencycareisneededtoappropriatelyaddressspecifi c needsinLMICsandoffersEMSprofessionalsgreater con fi denceintheirknowledgeandskills.Theresearch contributestothegeneralizableknowledgeonprehospital careinresource-limitedsettingsandservesasafoundation forthedevelopmentofprotocolsthatwillimprove patientcareandstrengthentheRwandanhealthcare system.Furtherstudiesareneededtoevaluatesuch trainingsinsimilarcontexts,toinvestigatetheimpact onclinicaloutcomes.
Theresultsfromthisstudyweredisseminatedto stakeholdersincludingprehospitalEMSprofessionals,the MinistryofHealth,andhospitalstaff.
AddressforCorrespondence:NazKarimMD,MHA,MPH,Brown UniversityAlpertMedicalSchool,DepartmentofEmergency Medicine,55ClaverickSt.ProvidenceRI02903. Email: NazKarim5@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy.This articlewassupportedbyfundingfromGoFundMeandtheEMF EmergencyMedicineFoundation.
Copyright:©2025Karimetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KobusingyeOC,HyderAA,BishaiD,etal.Emergencymedicalsystems inlow-andmiddle-incomecountries:recommendationsforaction. BullWorldHealthOrgan. 2005;83(8):626–31.
2.RazzakJAandKellermannAL.Emergencymedicalcarein developingcountries:isitworthwhile? BullWorldHealthOrgan. 2002;80(11):900–5.
3.WaltG.WHO’sWorldHealthReport2003.2004;328(7430):6.
4.ReynoldsTA,MfinangaJA,SaweHR,etal.Emergencycarecapacityin Africa:aclinicalandeducationalinitiativeinTanzania. JPublicHealth Policy. 2012;33(S1):S126–37.
5.KobusingyeOC,HyderAA,BishaiD,1074208,etal.Emergency medicalservices.In:JamisonDT,BremanJG,MeashamAR,etal. DiseaseControlPrioritiesinDevelopingCountries[Internet].2nded. Washington,DC:WorldBank;2006.Availableat: http://www.ncbi.nlm. nih.gov/books/NBK11744/.AccessedJuly7,2022.
6.JacobST,BanuraP,BaetenJM,etal.Theimpactofearlymonitored managementonsurvivalinhospitalizedadultUgandanpatientswith severesepsis:aprospectiveinterventionstudy. CritCareMed. 2012;40(7):2050–8.
7.MannNC,MullinsRJ,MacKenzieEJ,etal.Systematicreviewof publishedevidenceregardingtraumasystemeffectiveness. JTrauma AcuteCareSurg. 1999;47(3Suppl):S25–33.
8.MillerS,LesterF,HensleighP.Preventionandtreatmentofpostpartum hemorrhage:newadvancesforlow-resourcesettings. JMidwifery WomensHealth. 2004;49(4):283–92.
9.ErsdalHL,MdumaE,SvensenE,etal.Earlyinitiationofbasic resuscitationinterventionsincludingfacemaskventilationmay reducebirthasphyxiarelatedmortalityinlow-incomecountries: aprospectivedescriptiveobservationalstudy. Resuscitation. 2012;83(7):869–73.
10.HusumH,GilbertM,WisborgT,etal.Ruralprehospitaltrauma systemsimprovetraumaoutcomeinlow-incomecountries: aprospectivestudyfromNorthIraqandCambodia. JTrauma. 2003;54(6):1188–96.
11.AndersonPD,SuterRE,MulliganT,etal.WorldHealthAssembly Resolution60.22anditsimportanceasahealthcarepolicytoolfor improvingemergencycareaccessandavailabilityglobally. AnnEmerg Med. 2012;60(1):35–44.e3.
12.LibermanM,MulderD,LavoieA,etal.MulticenterCanadianstudyof prehospitaltraumacare. AnnSurg. 2003;237(2):153–60.
13.MockCN,JurkovichGJ,nii-Amon-KoteiD,etal.Traumamortality patternsinthreenationsatdifferenteconomiclevels:implications forglobaltraumasystemdevelopment. JTrauma. 1998;44(5):804–12.
14.RosenbergA,KabagemaI,AsayB,etal.Developingsustainable prehospitaltraumaeducationinRwanda. AfrJEmergMed. 2020;10(4):234–8.
15.KosokoAA,GlombNW,LabaB,etal.Evaluatinganovelsimulation courseforprehospitalclinicianresuscitationtraininginBotswana. WestJEmergMed. 2019;20(5):731–9.
16.RybarczykMM,LudmerN,BroccoliMC,etal.Emergencymedicine trainingprogramsinlow-andmiddle-incomecountries:asystematic review. AnnGlobHealth. 2020;86(1):60.
17.PetrozeRT,ByiringiroJC,NtakiyirutaG,etal.Canfocusedtrauma educationinitiativesreducemortalityorimproveresourceutilizationina low-resourcesetting? WorldJSurg. 2015;39(4):926–33.
18.MerchantA,OuthayM,Gonzaléz-CalvoL,etal.Traininglaypersons andhospitalpersonnelinbasicresuscitationtechniques:anapproach toimpacttheglobaltraumaburdeninMozambique. WorldJSurg. 2015;39(6):1433–7.
19.SaweHR,MfinangaJA,KisakeniS,etal.Developmentand implementationofshortcoursestosupporttheestablishmentofa
prehospitalsysteminSub-SaharanAfrica:lessonslearnedfrom Tanzania. EmergMedInt. 2019;2019:3160562.
20.PigogaJL,CunninghamC,KafwamfwaM,etal.Adaptingthe emergency firstaidrespondercourseforZambiathroughcurriculum mappingandblueprinting. BMJOpen. 2017;7(12):e018389.
21.CalleseTE,RichardsCT,ShawP,etal.Laypersontraumatrainingin low-andmiddle-incomecountries:areview. JSurgRes. 2014Jul;190(1):104–10.
22.SeziberaR.MinistryofHealthRwanda.Availableat: https://moh.prod. risa.rw/fileadmin/user_upload/Moh/Publications/Strategic_Plan/ EMS_Strategic_Plan_2018-min.pdf
23.JuillardCJ,MockC,GoosenJ,etal.Establishingtheevidencebasefor traumaqualityimprovement:acollaborativeWHO-IATSICReview. WorldJSurg. 2009;33(5):1075–86.
24.FryMandMacGregorC.Confidenceandimpactonclinicaldecisionmakingandbehaviourintheemergencydepartment. AUEC. 2014;17(3):91–7.
25.MangoldK,KunzeKL,QuinonezMM,etal.Learningstyle preferencesofpracticingnurses. JNursesProfDev. 2018;34(4):212–8.
26.NomuraK,YanoE,FukuiT.Genderdifferencesinclinicalconfidence: anationwidesurveyofresidentphysiciansinJapan. AcadMed. 2010;85(4):647–53.
TorbenBrod,MD*
CarstenStoetzer,MD†
ChristophSchroeder,MD*
StephanieStiel,PhD† °
KambizAfshar,MD† °
SectionEditor: PayalModi,MD,MScPH
*HannoverMedicalSchool,DepartmentofEmergencyMedicine,Hannover,Germany † HannoverMedicalSchool,InstituteforGeneralPracticeandPalliativeCare, Hannover,Germany ° Theseauthorscontributedequally.
Submissionhistory:SubmittedApril19,2024;RevisionreceivedSeptember11,2024;AcceptedSeptember25,2024
ElectronicallypublishedOctober29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.20919
Introduction: Providingappropriatehealthcarefortransgender,intersexualandnon-binary(TIN) individualsremainsasignificantchallenge,asthisgroupexperienceshigherratesofhealthinequalities, discrimination,andbarrierstoaccessingcare.Emergencyphysicians(EP)oftenlackformaltrainingand knowledgeaboutcaringforTINpatients,whilecomparativelylessevidenceisavailableforother healthcareprofessionals,includingemergencynurses(EN).Therefore,ourgoalinthisstudywasto exploretheexperiences,knowledge,andattitudesaswellaseducation/trainingneedsofbothENsand EPsinGermanyregardingthecareofTINpatients.
Methods: InFebruary2023,weelectronicallysurveyedEPsandENsfromemergencydepartments (ED)acrossGermany.Thesurvey,developedthroughliteraturereviewandcollaborationwithexperts andmembersoftheTINcommunity,consistedof15closed-endeditemsdividedintothreesections: experiencesandknowledge;attitudes;andeducation/trainingneeds.Weusedstandarddescriptive statisticsandtestedforgroupdifferencesusingthechi-squaretest.
Results: Oftheapproximately1,665EPsandENscontacted,502completedthesurveyandwere eligibleforfurtheranalysis(30%responserate).Oftherespondents,233(46%)wereEPsand269(54%) wereENs,withENsbeingsignificantlyyoungerandwithfeweryearsinpractice.Morethanhalfreported experiencecaringforTINpatients(71%ofENsvs61%ofEPs; P = 0.002),butthereweresignificant gapsinmedicalandnon-medicalknowledge.AttitudestowardTINpatientsweregenerallypositive,but differencesincommunicationapproacheswerenoted,withENssignificantlymorelikelythanEPstolimit theircommunicationwithTINpatientstowhatwasnecessary(25%ofENsvs17%ofEPs; P = 0.006). Mostrespondents(55%ofENsand58%ofEPs)hadnotraininginthemanagementofTINpatients,with only8%ofEPsand17%ofENshavingreceivedsuchtrainingduringtheirmedical/nursingschool education(P = 0.01).Bothgroupsagreedthatthereisanurgentneedtoincreaseawarenessof emergencymedicalcareforTINpatientsamongEDstaff.
Conclusion: BothemergencyphysiciansandnursesinGermanydemonstrateddeficitsinknowledgeof andclinicalpreparednesstocareforpatientsintheEDwhoidentifyastransgender,intersexualandnonbinary,indicatingaclearneedforenhancededucation,training,andinstitutionalsupporttoimprove emergencycareforthisvulnerablepatientpopulation.[WestJEmergMed.2025;26(1)111–119.]
Providingappropriatehealthcaretopeoplewith transgender,intersexual,andnon-binary(TIN)identities remainsasignificantchallengeinmanyhealthcaresystems, includinginGermany.1 IntheUnitedStatesandEurope, approximately0.6%oftheadultpopulationidentifiesas TIN,whereastheprevalenceamongadolescentsisestimated tobeapproximately1.4–4.1%.2,3,4 Whilemuchofthe relevantliteraturefocusesonLGBTQ+ (lesbian,gay, bisexual,transgender,questioning/queer)patientsingeneral anddoesnotdistinguishbetweensexualminorities(eg,LGB) andgenderminorities(eg,trans),studieshaveconsistently shownthatTINindividualsinparticularexperiencehealth inequalities,includinghigherratesofsubstanceusedisorder, disability,andmentalillness.5,6
Theirlifetimeriskofattemptingsuicideismorethan 10timeshigherthanthatofthegeneralpopulation (54%vs5%).7 IndividualsidentifyingasTINarealso disproportionatelyaffectedbyhomelessness, underemployment,andextremepoverty.8,9 Thesechallenges arecompoundedbybarrierstoaccessinghealthcareinboth theUSandEurope,asdemonstratedforGermanyinthe InTraHealthstudy.Duetofearofdiscriminationorpast negativeexperiences,manyTINindividualsavoid interactionswithhealthcareprofessionals,whichcanleadto delayedpresentation,diagnosis,andtherapy.6,10
ArecentstudybySamuelsetalfoundthatnearlyhalfof transandnon-binaryindividualssurveyedavoidedcarein theemergencydepartment(ED)duetoanticipated discrimination,fearofmistreatment,andlongwaittimes.11 Deficitsinknowledgeandclinicalpreparednesshavebeen demonstratedforemergencyphysicians(EP)andresidentsin theUSandCanada.WhilemostEPs(88%)providecareto membersofthispopulation,few(27.5%)havehadformal trainingand,therefore,lackclinicalknowledgeabout importantaspectsofcaringforTINpatients.12 Similar deficiencieshavebeendemonstratedamongemergency medicine(EM)andpediatricresidents.13,14 Thespecific situationinEuropeandespeciallyinGermanyremains largelyunexamined.
Littleevidenceisavailableforotherhealthcare professionals,includingregisterednurses.15 Emergency nurses(EN)areoftenthe firsttoencounterthesepatientsand toobtainrelevantdata,includinggender.Receiving reassuringcareatthebeginningofemergencycareiscrucial tothepatient’ssenseoftrustandsafetyandmaymitigate negativefeelingsduetopossiblepastmistreatment.While nursesappeartohaveawiderangeofattitudes,knowledge, andbeliefsthataffectthecaretheyprovidetosexualandgender-minoritypatientsingeneral,theyoftenlack LGBTQ+ educationspecifictotheneedsofthis population.16 AsofMarch2024,tothebestofour knowledge,therehasbeennopublisheddataonENsand theirattitudestowardTINpatientsspecifically.Despite
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Transgender,intersexualandnon-binary (TIN)individualsfacesigni fi canthealth disparitiesandbarrierstocareinmultiple settings,includingEDs.
Whatwastheresearchquestion?
Toexploretheknowledgeandattitudesof emergencynurses(EN)andphysicians(EP) inGermanyregardingthecareof TINpatients.
Whatwasthemajor findingofthestudy?
ENsandEPsinGermanylackedkey knowledgeaboutTINemergencycareand haddifferentapproachestocommunication withthesepatients
Howdoesthisimprovepopulationhealth?
Recognizingtheneedtoimproveeducation andtrainingforEPsandENsregardingthe careofTINpatientscouldleadtomore equitableandrespectfulemergencycare.
increasingawarenessandadvocacyforsexualandgender minorities,untilrecentlymanyhealthprofessionalcurricula (eg,medicalschool,nursingschool)providedlittleformal instruction,presumablyleadingtotheobservedgapsin clinicalandculturalcompetency.17,18
MostofthecurrentliteratureonTINemergencycare comesfromtheUSandCanada,withcomparativelyless researchinEuropeandnodataavailablefromGermany. Nevertheless,theperceptionthatemergencycare professionalsknowlittleaboutTINindividualsandtheir specifichealthcareneedsisalsowidespreadamongtheTIN communityinEurope;thisisaconcernforbothhealthcare professionalsandpatients.4,19 Therefore,ouraiminthis studywastoassesstheknowledgeandattitudesaswellas educationandtrainingneedsofbothEPsandENsin GermanyregardingthecareofTINpatients.
Weconductedacross-sectionalstudyofstaffmembersof EDsinGermanyusingaweb-basedsurvey.Thesurveywas distributedto70randomlyselectedEDsofallsizesacross Germany.BothEPsandENswereconsideredeligible toparticipate.TheEthicsCommitteeoftheHannover
MedicalSchoolapprovedthestudy(01/17/2023; No.10706_B0_K_2023).
Weconductedaliteraturereviewofhealthcare professionals’ experienceswithTINpatientsandthe healthcareneedsofthispopulation.Basedonexistingstudies andappliedquestionnaires,wedevelopedasurveyconsisting ofbothnewandpreviouslyuseditemstoassessEPs’ and ENs’ experiences,attitudes,educationandtrainingneeds relatedtocaringforTINpatients.12,20,21 Forthispurpose, previouslyuseditemsfromtheliteraturewereprioritizedand adaptedforcontent,structure,andlanguageincollaboration withaninterdisciplinarygroupofexpertsinquestionnaire development.Inaddition,weworkedwithmembersofthe TINcommunitytodevelopnewitemstobetteraddressthe specificneedsandconcernsofthispopulationwithregardto emergencycare.
Wepre-testedallselecteditemsinoursurveyforclarity withsixEPsand fiveENs,similartotheintendedstudy populationandpilotedthesameelectronicdeliverymethod asplannedforwidersurveydistributionusingananonymous onlinesurvey(SoSciSurveyGmbH,Munich,Germany).22
The finalsurveyconsistedof15closed-endeditemsequally dividedintothreethematiccategories:1) fivequestionsabout thehealthcareprofessionals’ experiencesandknowledge;2) fiveregardingtheirattitudes;and3) fivequestionsrelatedto education/trainingneeds,withresponseoptionspresentedas eithersinglechoiceor4-pointLikertscales(stronglyagree –somewhatagree – somewhatdisagree – stronglydisagree). Studyparticipants’ demographicparameterswerecollected beforethesurveybegan,followingconsentfordatause. Theanonymous,self-administeredonlinesurveywas availableforcompletionduringafour-weekperiodin February2023.Invitationsweresentviae-mailtoED medicaldirectorswiththerequesttodistributethelinktothe surveytotheirstaffmembers,asnopubliclyavailable mailinglistexistedthatallowedadirectinvitationofEPsand ENsintheseEDs.WeestimatedthenumberofEPsworking inthe70EDstobeapproximately742andthenumber ofENstobe ≈923,accordingtopublichealthdatafor EDsinGermanyandrecommendationsofGermanEM societies.23,24 Noremindersweresent.Allparticipantswho mettheinclusioncriteriaandcompletedatleastthe demographicparametersandthecontentcategoryon experiencewereincludedinthe finalanalysis.
WeextractedrawdatafromSoSciSurveyintoIBMSPSS Statisticsversion27(IBMCorp,Armonk,NY)and calculatedstandarddescriptivestatistics,including frequencies.Thechi-squaretestwasappliedforgroup comparison.Weconsidered P < 0.05tobesignificant.The effectsizeoftheCramerVisinterpretedashigh(V = 0.5), moderate(V = 0.3),andlow(V = 0.1).
Duringthestudyperiod,536surveyswerereturned,of which502wereeligibleforfurtheranalysis.Ofthose,34had tobeexcludedbecausetherespondentsdidnotcompleteat leastthedemographicparametersandthecontentcategory onexperience.Ninety-fivepercentofrespondentscompleted all15items.Theoverallresponseratewas30%,with approximately923ENs(responserate29%)and742EPs (responserate31%)contactedbytheirrespectiveEDmedical directorstoparticipateinthestudy.Oftherespondents,233 (46%)wereEPsand269(54%)wereENs.Therewere significantintergroupdifferencesinalldemographic variablesanalyzed(sex,age,yearsofworkexperience), exceptforthesizeofthecitywheretheirEDwaslocated.In particular,ENsweresignificantlyyounger(39%ofENs ≤ 30 yearsvs23%ofEPs ≤ 30years, P = 0.001;V = 0.196)and hadfeweryearsofworkexperiencethanEPs. Table1 summarizesthecharacteristicsoftherespondents.
Morethanhalfoftherespondentsreportedexperience incaringforTINpatientsintheEDinthepriortwo years.ComparedwithEPs,ahigherproportionofENs reportedthisexperience(71%vs61%; P = 0.002; V = 0.155)(Figure1).
BothEPsandENslackedmedicalknowledgeand knowledgeofnon-medicalsupportservicesfortransgender, intersexualandnon-binary(TIN)individuals.While24%of ENsand19%ofEPswereawareofnon-medicalsupport servicesorcontactpointsforTINindividualstowhichthey couldreferthesepatients,only9%ofENsand11%ofEPs couldnamespecificmedicationregimensusedaspartof genderreassignmenttreatment.Intheirworkenvironment, almostallENs(92%)andEPs(95%)reportedalackof officialrecommendationsortheirownlimitedawareness,of suchrecommendationsfordealingwithTINpatientsinthe emergencydepartment.
Mostrespondentsinbothgroupsagreedthatbothgender identityandbiologicalsexatbirthshouldbedocumented whencollectingpersonalinformationofpatientspresenting totheED(73%ofENsand74%ofEPs)(Figure2). Correspondingly,77%ofENsand80%ofEPsfelt comfortableaskingTINpatientsfortheircorrectformof address.ThereweresignificantdifferencesbetweenENsand
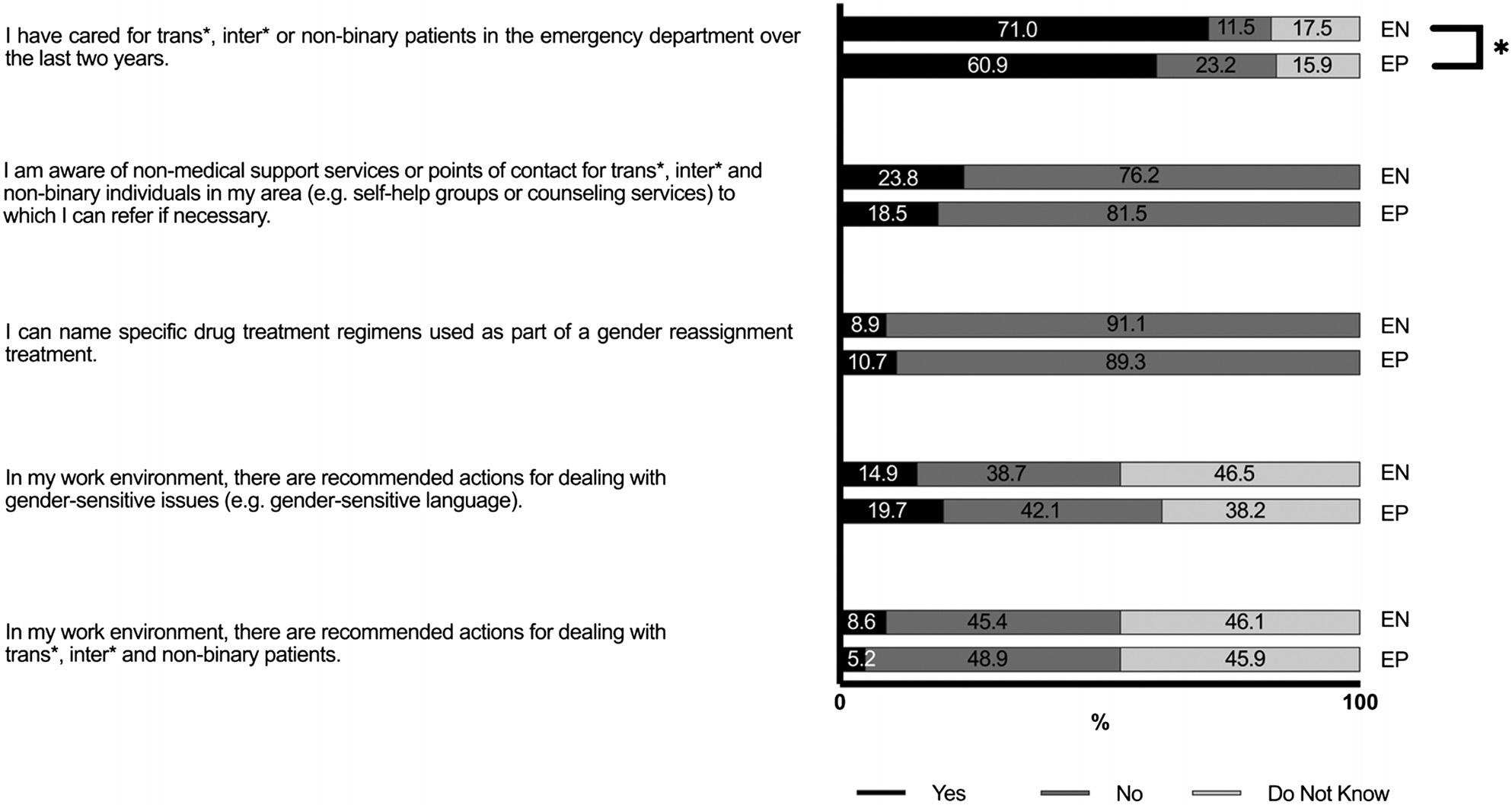
Figure1. ExperienceandknowledgeofemergencyphysiciansandnursesinGermanyincaringfortransgender,intersexualand non-binarypatients.
* = P < 0.05.
EP,emergencyphysician; EN,emergencynurse.
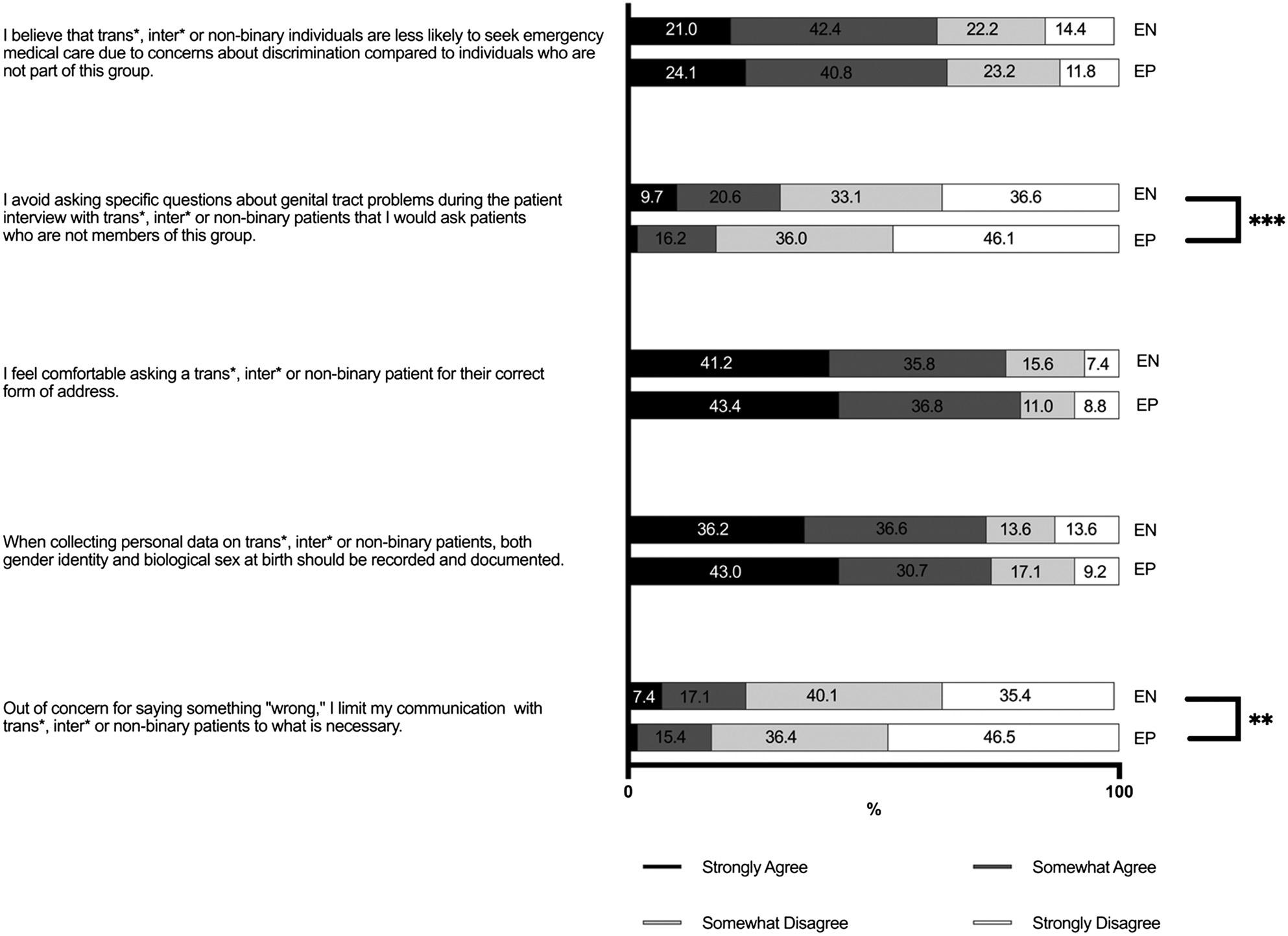
Figure2. AttitudesofemergencyphysiciansandnursesinGermanyregardingtransgender,intersexualandnon-binarypatients.
** = P < 0.01,*** = P < 0.001. EP,emergencyphysician; EN,emergencynurse.
EPsastowhethertheylimitedtheircommunicationwith TINpatientstowhatwasnecessaryoutofconcernforsaying somethingwrong(25%ofENsvs17%ofEPs; P = 0.006; V = 0.160).TheEPswerealsolesslikelytoagreethat,when interviewingTINpatients,theyavoidedaskingquestions aboutgenitaltractproblemsthattheywouldasknon-TIN patients(30%ofENsvs.18%ofEPs; P = 0.001V = 0.187). Intermsofoppressionawareness,themajorityofboth groupsagreedthattheybelievedTINindividualswereless likelytoseekemergencymedicalcarethannon-TIN individualsbecauseofconcernsaboutdiscrimination (62%ofENsand65%ofEPs).
Themajorityofrespondentsreportedthattheyhadnot receivedanytrainingintheappropriatemanagementofTIN patients(55%ofENsand58%ofEPs).Specifically,only8% ofEPsreceivedsuchtrainingduringtheirundergraduate education(medicalschool)orpostgraduate(residency/ fellowship)training,while17%ofENsreceivedformal training(P = 0.01;V = 0.151).Wefoundthat28%ofENs
and34%ofEPsreportedlearningaboutthistopicontheir own(Figure3).
BothEPs(68%)andENs(74%)agreedthattherewasa needtoincreaseEDstaffawarenessofemergencymedical careforTINpatients,andthatthisshouldbepartofmedical education/professionaltraining(78%ofENsand76%of EPs).Correspondingly,themajorityofbothgroupsbelieve thatcontinuingmedicaleducation(CME)regardingthe appropriatemanagementofTINpatientswasuseful(77%of ENsand74%ofEPs)andthattheywouldparticipateinsuch CMEwhenoffered(96%ofENsand92%ofEPs)(Figure4).
Inthiscross-sectionalstudy,wefoundthatbothEPsand ENsinGermanylackedknowledgeaboutimportantaspects ofemergencycareofTINpatientsandshoweddifferencesin attitudestowardcommunicationpractices.Therewas consensusontheneedforincreasededucationandtrainingin themanagementofsuchpatients,withamajorityagreeing ontheimportanceofintegratingthistrainingintomedical educationandCME.

* = P < 0.05.
EP,emergencyphysician; EN,emergencynurse.
Althoughmorethanhalfoftherespondentsreported encounterswithTINpatientsintheED,therewasaclear knowledgegap,demonstratedbyalackofawarenessofnonmedicalsupportservicesandspecificmedicalregimens relatedtogendertransition.Chisolm-Strakeretalreported similar findingsintheirsurveyofEPsintheUS,showingthat themajorityoftheEPshadseentransgenderandgender nonconformingpatients,butfewhadreceivedtrainingin caringforthispopulationandmosthadinaccurate knowledgeofimportantaspectsoftransgenderandgender nonconformingcare.12 StewardandO’Reillypointedout thatbothnursesandmidwiveshaveawiderangeofattitudes, knowledge,andbeliefsthataffectthecaretheyprovideto LGBTQ+ patientsingeneral,andmanyissuesofinadequate careappeartobeduetoalackofeducationaboutLGBTQ health.16 InasurveyinpediatricEDsinIreland,Kelleher etalshowedthatEPs,ENs,andotherhealthcareworkers heldpositiveattitudestowardsLGBTQ+ youngpeople; however,theywerelessconfidentintheirknowledgeof specifichealthissuesandself-reportedlowlevelsofclinical
preparedness.14 Thislackofknowledge,asdemonstratedin studiesthatincludedbothEPsandENs,mayleadto suboptimalcareandincreaseddiscomfortforthegrowing globalcommunityofTINpatientsaswellashealthcare professionalsintheED.Furthermore,thelackofofficial recommendationsforaddressinggender-sensitiveissuesin EDsmaycontributetodisparitiesinemergencycare experiencedbyTINpatients.
Severalstudieshaveexaminedtheexperiencesof transgenderandgendernonconformingpatientsin emergencycareanddemonstratedthatmorethanhalfof thesepatientsavoidEDs,mostlyduetolackofclinicianor nursesensitivity,anticipateddiscrimination,andfearof mistreatment.11,25 Focusingspecificallyontransgender patients,aSwedishstudybyCarlströmetalhighlightedthe importanceofrecognizingTINpatients’ vulnerabilityto violationsofdignity,acceptingtheiridentity,andfocusing ontheirhealthcareneedstorestoreandmaintaintheirtrust inhealthcare.26 Contrarytothesepatientreports,andsimilar tothe findingsofChisolm-Strakeretalandothers,the
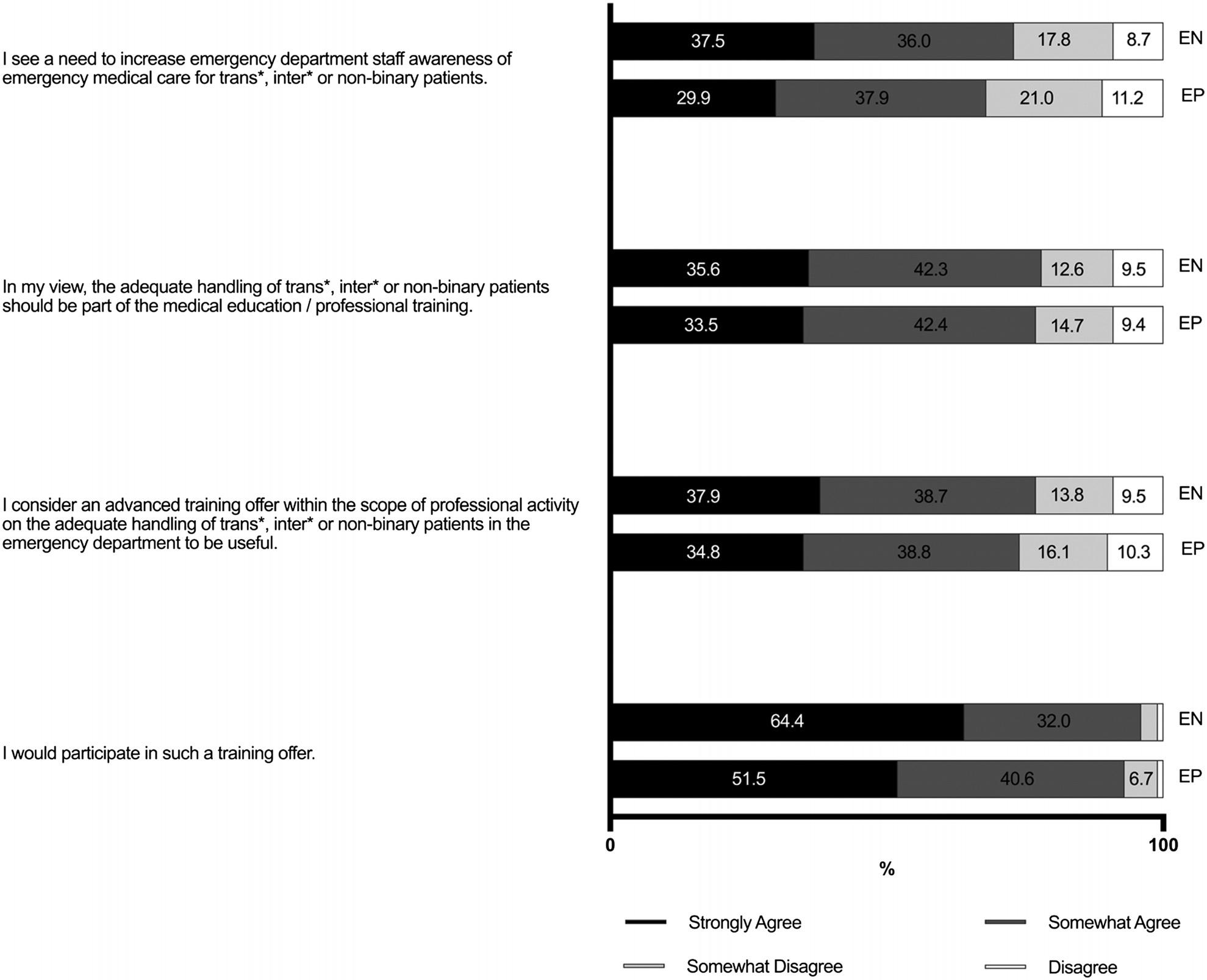
EP,emergencyphysician; EN,emergencynurse.
majorityofrespondentsinthisstudy(bothEPsandENs) expressedcomfortinaskingTINpatientsfortheircorrect formofaddressandagreedwiththeimportanceof documentingbothgenderidentityandbiologicalsexat birth.11,12,13 Thereasonsforthesediscrepanciesbetween patients’ experiencesandEPs/ENs’ perspectivesarenot entirelyclearandrequirefurtherinvestigation.
Theremaybeadiscrepancybetweenthecomfortlevelof askingTINpatientsforthecorrectformofaddressandthe useofthecorrectpronounintheactualpatientencounter.In addition,mostoftheparticipantsinthisstudywereyounger professionalsworkingandlivinginlargecitiesinGermany, whomaybemoreopentodiverseidentitiesand,therefore, moreaccustomedtoaddressingsuchissuesintheir professionalpractice(see Table1).Theartofcommunication alsorequiresfurtherattention,especiallyregardingthe correctuseofgender-sensitivelanguageandrespectful communicationpractices,whichshouldbetrainedregularly.
ThemajorityofEPsandENsinthisstudywereawarethat TINindividualsarelesslikelytoseekemergencymedical carethannon-TINindividualsduetoconcernsabout discrimination,indicatinganawarenessofoppression amongEPsandENs.Thisempathicawarenessofthe existenceandimpactofoppressionagainstTINpeopleis crucialtoremovingbarrierstohealthcareaccessfor theseindividuals.27
ComparingthetwogroupsofEPsandENs,wefound notabledifferencesinexistingattitudestoward communicationwithTINpatients.TheENsweremore likelythanEPstolimittheircommunicationwithTIN patientstowhatwasnecessary,outofconcernaboutsaying somethingwrong,andtoavoidaskingTINpatients questionsaboutgenitaltractproblems.Thesedifferences mayre fl ectdifferentrolesinpatientcarebutmayalso re fl ectdifferentlevelsofcon fi denceincommunicating withTINpatients,highlightingtheimportanceof
targetededucationandtrainingprogramsforbothEPs andENs.
Inaccordancewiththis finding,mostrespondentsinboth groupsreportedalackofformaltrainingintheappropriate managementofTINpatients,withonlyasmallpercentage havingreceivedsuchtrainingduringtheirundergraduateor postgraduateeducation.These findingsareinlinewith previouslypublishedstudiesfromboththeUSandEurope, highlightingtheimportanceofintegratingTIN-specific contentintomedicalandnursingschoolcurriculaand providingongoingCMEopportunitiesforpracticing healthcareprofessionals.28,29,30 InGermany,the InTraHealthself-learningplatformforhealthprofessionals hasbeenavailableonlinesinceApril2023,offeringguidance onaddressingandpreventingdiscriminationagainstTIN individualsinhealthcaresettings.31 However,itisnot specificallytailoredtoEPsandENs.Similarinitiativesand programsexistintheUSandCanadabutarealsooften limitedtosingle-sessioninterventionsthatfocusprimarilyon attitudesandawarenessratherthanthedevelopmentof clinicalcompetencies.32 Encouragingly,thisstudyrevealsa strongdesireamongEPsandENsformoreeducationand trainingtoincreaseEDstaffawarenessofemergencymedical careforTINpatients.
Weusedanovel,non-validatedsurveyinstrumentthat reliedonself-reporteddatafromEPsandENs,whichmay havebeensubjecttoresponsebias,includingsocial desirabilitybias.Inaddition,noinformationwasavailable onnon-responders,whichintroducedthepotentialfor positiveselectionbias.Emergencydepartmentdirectors, EPs,andENswithgreaterinterestorcomfortwiththetopic mayhavebeenmorelikelytoforwardtheinvitationtotheir teammembersorparticipateinthestudy,whereas discomfortorlackoffamiliaritywithcaringforTINpatients mayhaveactedaspotentialbarrierstoparticipation.In addition,thelackofareminderforthestudyinvitationmay havecontributedtoalowerresponserate,whichcouldaffect thegeneralizabilityofthe findings.Finally,thesamplewas limitedtoEPsandENsinGermany,whichcouldlimitthe generalizabilityofthe findingstoothercountriesor healthcaresystems.
Thisstudyaddstothegrowingbodyofevidencethat emergencyphysicianshavedeficitsinknowledgeandclinical preparednesstocareforTINpatients.Foremergencynurses, similardeficitsseemtoexist,exacerbatedbygreater uncertaintyaboutcommunicatingwithpatientswhoidentify astransgender,intersexual,andnon-binary.Thisstudy indicatestheneedforenhancededucation,training,and institutionalsupporttoimprovetheemergencycareofTIN patientsinGermany.Thisincludesbothknowledgeof
specifictreatmentsandtraininginsensitive,respectful communication,aswellasanunderstandingofthewider socialchallengesfacedbyTINindividuals.Byaddressing thesechallengesbothinmedical/nursingschoolsandbeyond, wecanstrivetoensurethatTINindividualsreceiveequitable andrespectfulmedicalcare.
AddressforCorrespondence:TorbenBrod,MD,HannoverMedical School,DepartmentofEmergencyMedicine,Carl-Neuberg-Strasse 1,Hannover,Germany30625.E-mail: brod.torben@mh-hannover.de
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Brodetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KruseMI,BighamBL,VoloshinD,etal.Careofsexualandgender minoritiesintheemergencydepartment:ascopingreview. AnnEmerg Med. 2022;79(2):196–212.
2.BonifacioJH,MaserC,StadelmanK,etal.Managementofgender dysphoriainadolescentsinprimarycare. CMAJ. 2019;191(3):E69–75.
3.HowmanyadultsandyouthidentifyastransgenderintheUnited States?WilliamsInstitute.July10,2023.Availableat: https:// williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/ AccessedJanuary10,2024.
4.KahlK,KurzC,MartinaM.Genderdiversity:ensuringsupplyfor everyone. DtschArztebl. 2022;119(38):A-1566/B-1312.
5.ReisnerSL,PoteatT,KeatleyJ,etal.Globalhealthburdenandneedsof transgenderpopulations:areview. Lancet. 2016;388(10042):412–36.
6.BauerGR,ScheimAI,DeutschMB,etal.Reportedemergency departmentavoidance,use,andexperiencesoftransgenderpersonsin Ontario,Canada:resultsfromarespondent-drivensamplingsurvey. AnnEmergMed. 2014;63(6):713–20.e1.
7.TestaRJ,MichaelsMS,BlissW,etal.Suicidalideationintransgender people:genderminoritystressandinterpersonaltheoryfactors. JAbnormPsychol. 2017;126(1):125–36.
8.GrantJM,MottetLA,TanisJ,etal.Injusticeateveryturn:areportofthe NationalTransgenderDiscriminationsurvey.Availableat: https:// www.thetaskforce.org/app/uploads/2019/07/ntds_full.pdf AccessedJanuary4,2024.
9.CochranBN,StewartAJ,GinzlerJA,etal.Challengesfacedby homelesssexualminorities:comparisonofgay,lesbian,bisexual,and transgenderhomelessadolescentswiththeirheterosexual counterparts. AmJPublicHealth. 2002;92(5):773–7.
10.Verbesserungdeszugangszurgesundheitsversorgungfürinterund transmenschendurchabbauvondiskriminierungalsversorgerseitiger zugangsbarriere(InTraHealth).Availableat: https://www. bundesgesundheitsministerium.de/fileadmin/Dateien/5_Publikationen/ Gesundheit/Berichte/Abschlussbericht_IntraHealth.pdf AccessedAugust26,2024.
11.SamuelsEA,TapeC,GarberN,etal. “Sometimesyoufeellikethefreak show”:aqualitativeassessmentofemergencycareexperiencesamong transgenderandgender-nonconformingpatients. AnnEmergMed. 2018;71(2):170–82.e1.
12.Chisolm-StrakerM,WillgingC,DaulAD,etal.Transgenderandgendernonconformingpatientsintheemergencydepartment:whatphysicians know,think,anddo. AnnEmergMed. 2018;71(2):183–8.e1.
13.LienK,VujcicB,NgV.Attitudes,behaviour,andcomfortof Canadianemergencymedicineresidentsandphysiciansincaringfor 2SLGBTQI+ patients. CJEM. 2021;23(5):617–25.
14.KelleherST,BarrettMJ,DurninS,etal.Staffcompetenceincaringfor LGBTQ+ patientsinthepaediatricemergencydepartment. ArchDisChild. 2023;108(7):525–9.
15.BristolS,KostelecT,MacDonaldR.Improvingemergencyhealthcare workers’ knowledge,competency,andattitudestowardlesbian,gay, bisexual,andtransgenderpatientsthroughinterdisciplinarycultural competencytraining. JEmergNurs. 2018;44(6):632–9.
16.StewartKandO’ReillyP.Exploringtheattitudes,knowledgeandbeliefs ofnursesandmidwivesofthehealthcareneedsoftheLGBTQ population:anintegrativereview. NurseEducToday. 2017;53:67–77.
17.Obedin-MaliverJ,GoldsmithES,StewartL,etal.Lesbian,gay, bisexual,andtransgender-relatedcontentinundergraduatemedical education. JAMA. 2011;306(9):971–7.
18.MollJ,VennardD,NotoR,etal.Theprevalenceoflesbian,gay, bisexual,andtransgenderhealtheducationandtraininginemergency medicineresidencyprograms:wherearewenow? AEMEducTrain. 2021;5(2):e10580.
19.McGlynnN,BrowneK,SherriffN,etal.Healthcareprofessionals’ assumptionsasbarrierstoLGBTIhealthcare. CultHealthSex. 2020;22(8):954–70.
20.MollJ,KriegerP,HeronSL,etal.Attitudes,behavior,andcomfortof emergencymedicineresidentsincaringforLGBTpatients:whatdowe know? AEMEducTrain. 2019;3:129–35.
21.JonesKN,BrewsterME,JonesJA.Thecreationandvalidation oftheLGBTAllyIdentityMeasure. PsycholSexOrientatGendDivers. 2014;1(2):181–95.
22.LeinerDJ.(2021).SoScisurvey(Version3.4.42)[Computer software].Availableat: https://www.soscisurvey.de AccessedSeptember10,2024.
23.vonStillfriedDandMangiapaneS.Emergencycare:needforreform fromanoutpatientperspective. InnereMedizin 2022;63(9):905–13.
24.BehringerW,GraeffI,Dietz-WittstockM,etal.Recommendationsofthe emergencymedicalsocietiesDGINA,AAEM,SGNOR,DIVI,DGAIand DGIINfornursestaffinginemergencydepartments. Notfall Rettungsmed 2019;22:330–3.
25.Chisolm-StrakerM,JardineL,BennounaC,etal.Transgenderand gendernonconforminginemergencydepartments:aqualitativereport ofpatientexperiences. TransgendHealth. 2017;2(1):8–16.
26.CarlströmR,EkS,GabrielssonS. ‘Treatmewithrespect’:transgender persons’ experiencesofencounterswithhealthcarestaff. ScandJ CaringSci. 2021;35(2):600–7.
27.StotzerR.L.Straightallies:supportiveattitudestowardlesbians, gaymen,andbisexualsinacollegesample. SexRoles. 2009;60(1–2):67–80.
28.ArthurS,JamiesonA,CrossH,etal.Medicalstudents’ awarenessof healthissues,attitudes,andconfidenceaboutcaringforlesbian,gay, bisexualandtransgenderpatients:across-sectionalsurvey. BMCMed Educ. 2021;21(1):56.
29.ParameshwaranV,CockbainBC,HillyardM,etal.Isthelackofspecific lesbian,gay,bisexual,transgenderandqueer/questioning(LGBTQ) healthcareeducationinmedicalschoolacauseforconcern?Evidence fromasurveyofknowledgeandpracticeamongUKmedicalatudents. JHomosex. 2017;64(3):367–81.
30.CollinsCA.Pediatricnursepractitioners’ attitudes/beliefsand knowledge/perceivedcompetenceincaringfortransgenderand gender-nonconformingyouth. JSpecPediatrNurs. 2021;26(2):e12321.
31.LernplattformIntrahealth.Inter*undtransmenschenimfokus derallgemeinengesundheitsversorgung.Availableat: https://intrahealth.de/.AccessedAugust26,2024.
32.DubinSN,NolanIT,StreedCGJr.,etal.Transgenderhealthcare: improvingmedicalstudents’ andresidents’ trainingandawareness. AdvMedEducPract. 2018;9:377–91.
StephanieRuest,MD,MPH* LanaNguyen,BS†
CelesteCorcoran,MD‡ SusanDuffy,MD*
*HasbroChildren’sHospital,DivisionofPediatricEmergencyMedicine,WarrenAlpert BrownUniversitySchoolofMedicine,Providence,RhodeIsland † BrownUniversity,Providence,RhodeIsland ‡ HasbroChildren’sHospital,DepartmentofPediatrics,Providence,RhodeIsland
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedFebruary23,2024;RevisionreceivedSeptember20,2024;AcceptedOctober4,2024
ElectronicallypublishedNovember21,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.19488
Introduction: Theemergencydepartment(ED)isasafetynet,caringforfamilieswholackadequate accesstofoodandotherbasicneeds.TheCOVID-19pandemiccausedadramaticriseinfoodinsecurity (FI)nationally;however,littleisknownabouttheprevalenceofFIamongfamiliesseeninpediatricEDs (PED).InthisstudyweaimedtodeterminetheprevalenceofFI,aswellasawarenessandutilizationof supplementalfoodservices,amongfamiliesseeninanurbanPEDduringtheCOVID-19pandemicusing anelectronicscreeningsurvey.
Methods: Thiswasacross-sectionalsurveyoffamiliesscreenedforFIinanurbanPED.Anelectronic surveywasadvertisedtoallfamiliesviapostersplacedinpatientroomsandotherlocationsinthePED betweenFebruary–October2022.SurveysinEnglishandSpanishwereaccessedonpersonalelectronic devicesviaQRcodes.SixvalidatedUSDepartmentofAgriculturehouseholdfoodsecurityquestionsand sociodemographicquestionswereincluded.Wecalculatedrespondents’ foodsecurityandperformed descriptiveandbivariateanalysesofpatientsociodemographicsandresponsestoFIquestions.
Results: Of42,697PEDvisits,612surveyswerecompletedandanalyzed(1.4%).Nearly50%of respondentsidentifiedasWhiteandnon-Hispanic,withapproximately80%female.Thirtypercenthada householdincomeof <$25,000and32%between$25,000–<50,000.Amongsurveyrespondents, 56.7%demonstratedFI:25%withlowfoodsecurity,and31.7%withverylowfoodsecurity.Weidentified statisticallysignificantdifferencesinawarenessanduseofsupplementalfoodservicesbyFIstatus, householdincome,andprimarylanguagespoken.
Conclusions: Nearly60%ofsurveyparticipantsinanurbanpediatricEDduringtheCOVID-19 pandemicexperiencedfoodinsecurity,substantiallyhigherthanpreviousreports.Theseresultssupport theED’scontributoryroleinFIscreening,particularlyduringtimesofapublichealthcrisis,andhighlights theneedfortargetedoutreachinthissetting.[WestJEmergMed.2025;26(1)120–128.]
Foodinsecurity(FI)isasignificantpublichealthissue, dramaticallyworsenedbytheCOVID-19pandemic.1,2 Pre-COVID-19,anestimated1in7childrenintheUS livedinhouseholdswithFI.Thisstrikinglyincreasedto nearly 1in4 householdswithchildrenduringtheearly COVID-19pandemic,1,2 withapproximately6.4million childrenlivinginFIhouseholdsin2022.2 Asurvey
performedonemonthintotheCOVID-19lockdowns demonstratedFIamongmorethan40%ofhouseholdsof motherswithchildren ≤12yearsofage.3 Althoughchildren maybeshieldedfromdirectlyexperiencingFIbytheir caregivers,2,4 anationwidesurveyofmotherswithyoung childrenidentifiedthatinalmost20%ofhouseholdswith children <12yearsofage,thechildrendirectly experiencedFI.3
Giventhemyriadofphysicalandmentalhealth implicationsofFIamongchildren,5 theAmericanAcademy ofPediatrics(AAP)PromotingFoodSecurityforAll Childrenpolicystatementadvisesthatpediatricians “playa centralrole” inbothscreeningandadvocacyforFIamong theirpatients.5 TheEDservesasasafetynetforfamilies experiencingpovertyandbarrierstoresourceaccessand utilizationandwhoareathighestriskofFIandinadequately meetingbasicneeds.Ithaspreviouslybeenreportedthat childrenwithFIhavehigheroddsofvisitinganEDthan thosewhodonot.6,7 Thus,pediatriciansandotherclinicians seeingtheseat-riskpatientsintheEDhaveacritical opportunitytoprovidetherecommendedscreening. Previouspre-COVID-19studieshavedemonstratedthe feasibilityofpediatricemergencydepartment(PED)-based FIscreening,7–10 withacaregiverpreferenceforelectronicbasedscreeningtools.7,11
Althoughstudiesinthegeneralpopulationhave demonstratedmarkedincreasesinFIduringtheCOVID-19 pandemic,theprevalenceofFIamongfamiliesinPEDsis notwellunderstood.Thus,weaimedtodescribethe prevalenceofFIamongfamiliesinanurbanPEDduringthe COVID-19pandemicwithanelectronicFIscreening programusingvalidatedUSDepartmentofAgriculture (USDA)FIscreeningquestions,andtodescribethe associatedsociodemographicsandcaregiverawarenessand useofsupplementalfoodresources.
StudyPopulationandDesign
ThissurveywasperformedintheHasbroChildren’ s HospitalPED,theonlychildren’shospital,PED,andLevel1 traumacenterinthestateofRhodeIsland.Theinstitutional PEDcaresforover55,000childrenannuallyfromRhode IslandaswellasneighboringareasofMassachusettsand Connecticut,servingasasafetynetforaregioncomprisinga broadspectrumofrural,suburban,andurbancommunities. Approximately48%ofpatientsseenintheinstitutionalPED annuallyarefemale,47%identifyasWhite,14%Black,and nearly40%Hispanic.Over55%ofpatientshavegovernment insurance.Additionally,approximately83%ofpatients reportEnglishasthepreferredlanguagewith15% reportingSpanish.
RecruitmentposterswithsurveyQRcodes,displayedin bothpatientroomsandpublicwaitingareaswithinthePED, invitedparentsandcaregivers >18yearsofagetoanswer questionsabouttheirfamilydemographicsandaccessto foodviaanelectronicsurvey(QualtricsLLC,Provo,UT). Recruitmentposterswerenotavailableinroomsdedicatedto psychiatricevaluationsandcriticalcare,orinroomsusedfor after-hoursurgentcareoverflowpatientsseenbyPED cliniciansinnon-PEDlocations.Toaccommodatepotential languagechallenges,posterswerewritteninEnglishand SpanishwithbasicinstructionstoscantheQRcodewitha
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
TheCOVID-19pandemiccauseddramatic increasesinfoodinsecurity(FI),affecting 1in4familiesnationally.
Whatwastheresearchquestion?
WhatwastheprevalenceofFIanduseof supplementalfoodprogramsamongfamilies seeninapediatricEDduringthepandemic?
Whatwasthemajor findingofthestudy?
56.7%ofrespondentshadFI;25%had lowfoodsecurity(95%CI21.6 – 28.4) and31.7%hadverylowfoodsecurity (95%CI28.0 – 35.6).
Howdoesthisimprovepopulationhealth?
GiventhehighprevalenceofFIinthis population,EDshavebecomeimportant locationsforFIscreening.
smartphone.SurveysweredisplayedbetweenFebruary–October2022basedonthegrantfundingperiodand availabilityoftrainedstudystaff.Nodirectassistancewas providedduringtheenrollmentprocess.Responseswere collectedanonymously.Allrespondentsweregiventhe optionofprovidingcontactinformationtobeeligiblefora smallincentive,agrocerygiftcard.Allrespondents, regardlessoffoodsecuritystatus,werealsogiventheoption ofprovidingtheircontactinformationtobecontactedbya hospitalresourceadvocateaftertheEDvisitforassistance withenrollmentinfoodresourceprograms.
Thesurveyincludedsociodemographicquestions pertainingtotherespondentandthechildcurrentlybeing seeninthePED(age,sex,race,ethnicity,primarylanguage, householdsizeandincome,employmentstatus,education, housing,respondent’srelationshiptothechildintheED, insurancestatus,andthechild’saccesstopediatricprimary care),andsixquestionsfromavalidatedUSDAHousehold FoodSecuritySurveyModule(Figure).12 Respondentswere alsoaskediftheyhadever “heardof” and/orwerecurrently usingsupplementalfoodservices(Women,Infants,& ChildrenProgram[WIC],SupplementalNutrition AssistanceProgram[SNAP],localfoodbanks,andfree school-lunchprograms),hereafterreferredtoas “ awareness ” and “utilization.”
WeassignedeachofthesixUSDAscreeningquestionsan individualscorebasedontheresponses,andwethen calculatedaFI “ rawscore ” bythesumoftheindividual
Prompt: Some people have made the following statement about their food situation. Please answer whether the statements were often, sometimes, or never true for you and your household in the last 12 months. Additional options for “I don’t know” and “Prefer not to answer” were provided.
Q1: The food we bought just didn’t last and we didn’t have money to get more
Q2: We couldn’t afford to eat balanced meals
Q3: Did you or anyone in your household ever cut the size of your meals or skip meals because there wasn’t enough money for food? Yes, no, I do not know, prefer not to answer
Q3b: If yes, then how often did this happen? Almost every month, some months but not every month, one or two months
Q4: In the last 12 months, did you or anyone in your household evereat less than you felt you should because there wasn’t enough money for food? Yes, no, I do not know, prefer not to answer
Q5: In the last 12 months, were you or anyone in your household hungry but didn’t eat because there wasn’t enough money for food? Yes, no, I do not know, prefer not to answer
Figure. UnitedStatesDepartmentofAgriculturefoodinsecurityscreeningquestions.a aFoodinsecurityrawscoreiscalculatedasfollows:Answersof “often” or “sometimes” forquestions1and2, “yes” onquestions3,4,and5, and “almosteverymonth” or “somemonthsbutnoteverymonth” onQ3bareallcodedasaffirmative(yes).Thesumoftheaffirmativeanswers tothese6questionsareusedtocalculatearawscore.Scoreof0–1denoteshighormarginalfoodsecurity,2–4denoteslowfoodsecurity, and5–6denotesverylowfoodsecurity.
questionscoresforeachoftheFIscreeningquestions, accordingtotheUSDAscoringguide.12 Wecalculatedthe FIrawscoreasfollows:answersof “often” or “sometimes” forquestions1and2, “ yes ” onquestions3,4,and5,and “almosteverymonth” or “somemonthsbutnotevery month” onQ3bareallcodedasaffirmative(yes).Thesumof theaffirmativeanswerstothesesixquestionswasthenused tocalculatetherawscore.Scoreof0–1denoteshighor marginalfoodsecurity,2–4denoteslowfoodsecurity,and 5–6denotesverylowfoodsecurity.Lowfoodsecurity indicatesthatthehousehold “obtainedenoughfoodtoavoid substantiallydisruptingtheireatingpatternsorreducing foodintakebyusingavarietyofcopingstrategies,suchas eatinglessvarieddiets,participatinginfederalfood assistanceprograms,orgettingfoodfromcommunityfood pantries.”2 Verylowfoodsecurityindicatesthathousehold membersreducedtheirfoodintakebecauseofinadequate moneyorresourcesforfood.2,4
Wetranslatedrespondents’ foodsecurityrawscoresinto oneofthethreefoodsecuritycategories.Respondentswere providedtheoptiontoanswer “Idonotknow” or “Iprefer nottoanswer” foreachofthesixscreeningquestions.If respondentschoseoneoftheseoptionsfor ≥1screening questionandaminimumscoreof2couldbecalculated,the FIrawscorewascategorizedas “lowfoodsecurity” (raw score2–4).Ifarawscoreof <2ornoscorewascalculated basedontheseincompleteresponses,therespondent’sFI statuswascategorizedas “unabletocalculate.”
Thisstudywasapprovedbytheinstitutionalreviewboard andwassupportedthroughgrantfundingprovidedbya2021 AAPCommunityAccesstoChildHealth ImplementationGrant.
WecollectedalldatathroughQualtrics,supportedby BrownUniversity.DatawasexportedintoExcel(Microsoft
Corporation,Redmond,WA)forcoding,andanalysiswas performedusingSASversion9.4(SASInstitute,Inc,Cary, NC).AllquestionsleftunansweredinQualtricswerecoded asmissing.Weperformeddescriptivestatisticalanalysesand reportedtheresultsasfrequenciesandproportions,with medianandinterquartileranges(IQR)calculated.Bivariate analysiswasperformedtoestablishassociationsbetween respondents’ foodsecuritystatusandvarious sociodemographicfactors,withreportof95%confidence intervals(CI).Weperformedchi-squaretestsandWilcoxon rank-sumtestsforcomparativeanalyses,whenappropriate.
BetweenFebruary–October2022,therewere42,697visits tothePED;thenumberofpatientscaredforinrooms/areas whererecruitmentposterswerenotavailableisunknown. Atotalof846visitswereassociatedwithinitiatedsurveys (2%oftotalvisits).Weexcluded234responses(27.7%of initiatedsurveys)fromtheanalysisduetolackofconsent ormissingresponsestoallsixUSDAscreeningquestions, leaving612surveys(72.3%ofinitiatedsurveysand1.4% oftotalvisits)foranalysis.
Mostofthesurveys(75.5%)werecompletedinEnglishby respondentswhoidentifiedEnglishastheirpreferred language,7.8%werecompletedinEnglishbyrespondents whoidentifiedSpanishastheirpreferredlanguage,and 15.7%werecompletedinSpanishbyrespondentswho identifiedSpanishastheirpreferredlanguage.Nearly50% ofrespondentsidentifiedasWhiteandnon-Hispanic, respectively,withapproximately80%identifyingasfemale (Table1).Nearly90%ofrespondentswerethebiological parentofthePEDpatient.
Themeannumberofhouseholdfamilymembersfor respondentswas4.1(IQR3–5,SD1.4),with62%livingin rentedhousesorapartmentsand31.3%inownedhouses
Table1. Surveyrespondents’ sociodemographicsandfoodsecurity status,N = 612.
N(%)a
Surveylanguage
English516(84.3)
Spanish96(15.7)
Primarylanguage
English437(71.4)
Spanish136(22.2)
Other/missing39(6.4)
Sex
Male94(15.4)
Female482(78.8)
Non-binary4(0.7)
Missing/prefernottoanswer32(5.2)
Race
Black51(8.3)
White304(49.7)
Otherb 189(30.9)
Missing68(11.1)
Ethnicity
Hispanic271(44.3)
Non-Hispanic294(48.0)
Prefernottoanswer18(2.9)
Missing29(4.7)
Householdannualincome
Under$15,000120(19.6)
$15,000–$24,99963(10.3)
$25,000–$34,999132(21.6)
$35,000–$49,99965(10.6)
$50,000–$74,99969(11.3)
Morethan$75,000100(16.3)
Unsure/prefernottoanswer51(8.4)
Missing12(2.0)
Housingc
House/apartmentowned188(30.7)
House/apartmentrented372(60.8)
Other24(3.9)
Temporary/nohousing8(1.3)
Prefernottoanswer8(1.3)
Missing12(2.0)
Employmentstatus
Unemployed185(30.2)
Full-time271(44.3)
Part-time102(16.7)
Other/prefernottoanswer/missing54(8.8) (Continuedonnextcolumn)
Table1. Continued. N(%)a Insurancetyped
Privateinsurance312(51.0)
Governmentinsurance217(35.5)
Other10(1.6)
None17(2.8)
Missing/prefernottoanswer/notsure56(9.2) aPercentmaynotequal100duetorounding. bOthercategoryincludesAmericanIndian,AlaskaNative,Asian, NativeHawaiian,and “other.” cOthercategoryincludesrentedroom/boardinghouse,mobilehome/ trailer,and “other.” dPrivateinsuranceincludesAetna(N = 8,1.3%);BlueCrossBlue Shield(N = 98,16.0%);BlueChip(N = 67,10.9%);Tufts(N = 67, 10.7%);UnitedHealthcare(N = 72,11.8%).Government insuranceincludesNeighborhoodHealthPlan,stateMedicaid (N = 174,28.4%);Medicaidplannototherwisespecified(N = 29, 4.7%);Medicare(N = 8,1.3%);RiteCare(N = 3,0.5%);TriCare –Military(N = 3,0.5%). “Other” insurancecategoryisanonspecifiedinsurance(N = 10,1.6%).
(Table1).Amongrespondents,29.9%hadannualhousehold incomes <$25,000,witha2022federalpovertylevel(FPL) forafamilyof4of$27,750.13 Anadditional32.2%had annualhouseholdincomesbetween$25,000–<$50,000, 15.7%between$50,000–<$100,000,11.9% >$100,000,and 10.3%notreported.Full-orpart-timeemploymentwas reportedby61%ofrespondentsandover88%hadhealth insurance(Table1).Additionally,271respondents(44.3%) had ≤ ahighschooldegreeorgeneralequivalencydiploma, 114(18.6%)hadabusinessortradecertificateortwo-year collegedegree,and126(20.6%)hadafour-yearcollegeor graduatedegree.Morethanone-thirdofrespondents(226, 36.9%)deniedhavingapartnerorspouseinthehome. Respondentsreportedthat83%ofthechildrenthatthey accompaniedtotheEDhadaccesstopediatricprimarycare.
Foodinsecuritywasdemonstratedby56.7%ofthe respondents(Table2),highormarginalfoodsecuritywas demonstratedin35.3%,and8%wereunabletobe categorizedbasedon “Idonotknow” and “prefernotto answer ” responsestothesurveyquestions.Additionally, 13.9%,65.4%,and89.2%ofrespondentsinthehigh,low,and verylowfoodsecuritygroups,respectively,reportedthat theirfamilyhadtochoosebetweenfoodandotherneeds, suchaspayingforhousing,utilities,and/orclothing,within theprior12months.
Bivariateanalysesrevealedstatisticallysignificant differencesinawarenessandutilizationofsupplementalfood servicesbasedonrespondents’ householdfoodsecurity
Table2. Surveyrespondents’ foodsecuritystatus.
USDAfoodinsecuritycategory(N = 612)
N(%)a 95%CIofPercentage
Highormarginalfoodsecurity216(35.3)31.5,39.2
Lowfoodsecurity153(25.0)21.6,28.4
Verylowfoodsecurity194(31.7)28.0,35.6
Unabletobecalculatedbasedonresponses49(8.0)6.0,10.5
Choosingbetweenfoodandotherneeds,byfoodsecuritystatusb (N = 563)
Highormarginalfoodsecurity(n = 216)30(13.9)9.6,19.2
Lowfoodsecurity(n = 153)100(65.4)57.3,72.9
Verylowfoodsecurity(n = 194)173(89.2)83.9,93.2
aPercentmaynotequal100duetorounding. bRespondentswerespecificallyaskediftheyhadtochoosebetweenspendingmoneyonfoodorotherneeds,includingrent,utilities,medical care,etc.,withinthelast12months.Affirmativeresponsesarereportedhere. CI,confidenceinterval; USDA,UnitedStatesDepartmentofAgriculture.
status,householdincome,andprimarylanguage(Table3). Overall,respondentsreportedhighestawarenessofSNAP comparedtoWIC,foodbanks,andfreelunchprograms.The mostusedserviceoverallwasSNAP.Thelowestproportion ofawarenessandutilizationamongrespondentswasforlocal foodbanks.ExceptforSNAP,householdswithhighfood securityandwithhouseholdincomes >$50,000annuallyhad statisticallysignificantlyhigherproportionsofawarenessof allsupplementalfoodservices,despitethelowestutilization oftheseservices(Table3).Notably,therewasnostatistically significantdifferenceintheproportionofrespondentswith high,low,orverylowfoodsecuritywhousedfreeschool lunches(P = 0.90),norwasthereastatisticallysignificant differenceinutilizationoffreeschoolbasedonprimary language(P = 0.19).Despitenosignificantdifferenceinthe proportionofrespondentswithEnglishvsSpanishastheir primarylanguagewhousedmostsupplementalfoodservices, therewerestatisticallysignificantdifferencesinawarenessof alltheseservicesbasedonprimarylanguage(Table3).
Finally,148respondents(24.2%)requestedfollow-upwith aresourceadvocateforassistancewithfoodresources, including74respondentswithverylowfoodsecurity (51.4%),46withlowfoodsecurity(31.9%),21withhighfood security(14.6%),andseven(4.9%)forwhomthesecurity statuswasunabletobecalculated.
TheCOVID-19pandemichadtremendouseffectson families,withpreviouslyreportedincreasesinFIamong surveysperformedingeneralpopulations.1–4 The anonymous,electronicFIsurveycontaining sociodemographicquestionsandsixvalidatedUSDAFI screeningquestionsrevealedthat56.7%ofrespondents surveyedinanurban,tertiary,PEDhadsomedegreeof householdFI.AlthoughbaselineFIdataamongpatients
seeninthePEDisunknown,thisprevalenceismarkedly higherthantheproportionofhouseholdsinthestudystate withchildren <18yearsofagereportingFIin2021(25%)and 2022(41%).14 TheprevalenceofFIinthispopulationisalso notablyhigherthanpre-COVID-19reportsinPEDs,7,8 as wellashigherthanreportsofgeneralpopulationscollected duringthepandemicnationally.1–4 Thisstudytookplacetwo yearsintotheCOVID-19pandemic,aftermanyfederaland statelegislativechangeshadoccurredthatmayhave impactedfoodsecurity.Ithasbeensuggestedthatthe observedincreasesinFIduringthistimewasinpartdueto inflationanddiscontinuationofsomeCOVID-19relief programsthatmitigatedFI.15
Despiteastate-wideincreaseinFIamonghouseholdswith children <18yearsofage,14 anevenhigherprevalencewas seeninthePEDsettingandislikelymultifactorial.First,the EDservesahigh-riskpopulation,withincreasedratesofED visitsamongFIfamiliescomparedtothosewhoarenotFI.6,7 Thus,thepatientpopulationislikelytoexperienceanoverall higherprevalenceofFI.Second,theanonymityofthe electronicscreeningtoolmayhavesupportedrespondents’ willingnesstoprovideaccurateinformationabouttheir family’sfoodsecurity.Whileourstudy’shigherprevalenceof FIalignswithreportsofincreasedFIduringtheCOVID-19 pandemic,selectionbiasmayhaveplayedaroleduetothe voluntarynatureofourenrollmentviapostersandelectronic surveys.Thismethodcouldhaveledtoanoverrepresentationoffamiliesfacinggreaterfood-related hardshipsand/orthosewithaccesstoandcomfortwithusing smartphonetechnology.However,GayleetalandGonzalez etalhavedemonstratedthatmostcaregiverspreferredan electronicscreeningmodalityoververbal/face-to-face screeningforsocialdeterminantsofhealth,7,11 andamong thosewhorespondelectronically,ahigherprevalenceofFI wasfound.7
Table3. Awarenessa vsutilizationofsupplementalfoodservicesbyfoodsecuritystatus,annualhouseholdincome,andprimarylanguage.
3a.Foodsecuritystatus
Highfoodsecurity (n = 216) Lowfoodsecurity (n = 153)
(n = 194)
Awareness
WIC167(77.3)87(57.2)110(56.7)
SNAP177(81.9)123(80.9)163(84.0)0.67
Foodbanks144(66.7)65(42.8)83(42.8)
Freelunch154(71.3)71(46.7)83(42.8)
Utilization
.001
WIC33(15.3)43(28.1)52(26.9) <.001
SNAP47(21.8)57(37.3)75(38.9)
Foodbanks13(6.0)20(13.1)33(17.1)
.001
Freelunch44(20.4)32(20.9)43(22.3)0.90
3b.Annualhouseholdincome
Awareness
WIC101(55.2)128(65.3)69(71.9)57(78.1) <.01
SNAP155(84.7)161(82.1)76(79.2)58(79.5)0.63
Foodbanks70(38.3)93(47.5)71(74.0)54(74.0) <.001
Freelunch78(42.6)95(48.5)68(70.8)58(79.5) <.001
Utilization
WIC53(29.1)58(29.6)5(5.2)2(2.7) <.001
SNAP109(59.9)56(28.6)7(7.3)2(2.7) <.001
Foodbanks26(14.3)28(14.3)10(10.4)0(0) <.01
Freelunch40(22.0)52(26.5)17(17.7)7(9.6)0.02
3c.Primarylanguagespoken
English(n = 437)Spanish(n = 136) P-value
Awareness
WIC307(70.3)65(47.8) <.001
SNAP379(86.7)94(69.1) <.001
Foodbanks257(58.8)39(26.7) <.001
Freelunch274(62.7)42(30.9) <.001
Utilization
WIC84(19.2)48(35.3) <.001
SNAP136(31.1)49(36.0)0.14
Foodbanks47(10.8)20(14.7)0.43
Freelunch97(22.2)23(16.9)0.19
aRespondentswereaskediftheyhad “everheardof” thefoodservices. WIC,Women,Infants&ChildrenProgram; SNAP,SupplementalNutritionAssistanceProgram.
Foodinsecurityismultifactorial,andhouseholdincome doesnotnecessarilyreflectthe financialneedsandhardships offamilies.Althoughfamiliesmayhavehouseholdincomes exceedingtheFPL,thehighcostofliving,utilities,andother expensesmaylimittheavailabilityoffundsforadequate food,resultinginhigherratesofFIthanratesofpoverty.One reportnotesthatone-thirdofhouseholdswithFIreporteda householdincomebetween100–200%oftheFPL,withan additionalthirdreportingover200%theFPL.16 Similarlyin thiscohort,169respondents(27.6)hadanannualhousehold
income >$50,000,approachingorexceeding200%ofthe FPLforafamilyoffour($55,000in2022),13 andyet41 (24.2%)intheseincomecategoriesstillwerecategorizedasFI basedontheirresponses.Additionallyhighlightingthe complexitiesoffoodsecurityinthesettingofotherhousehold necessities,nearly90%ofrespondentsinthissurveywithvery lowfoodsecurity,65%withlowfoodsecurity,and14%with highfoodsecurityreportedhavinghadtochoosebetween foodandothernecessitiesinthepreceding12months. Furthermore,nearly15%oftherespondentswhorequested follow-upfromaresourceadvocatewerecategorizedas havinghighfoodsecuritybasedonsurveyresponses.This couldbeduetoongoingneedsdespitecurrentlynotmeeting thescreeningthresholdforFI,notansweringallFIquestions truthfully(thusnotcapturingtheiraccuratefoodsecurity status),orotherreasons.
Therewerealsonotabledifferencesinrespondents’ awarenessandutilizationoffederalandlocalsupplemental foodserviceswhenanalyzedbyFIstatus,primarylanguage, andhouseholdincome,demonstratingkeygapswithinthis high-riskpopulation.Despite83%ofrespondentsreporting thattheirchildrenhadaccesstopediatricprimarycare, wherethemajorityofFIscreeningandinterventiongenerally takesplace,lessthanhalfofhouseholdswithlowandvery lowfoodsecurityreportedawarenessoflocalfoodbanksand freeschoollunches.Approximately60%hadheardofWIC, and84%hadheardofSNAP,withevenlowerutilizationof theseservices.Similarly,Coleman-Jensonetalpreviously reportedthatonly55%ofeligibleFIhouseholdsparticipated inWIC,SNAP,and/orfreeschool-lunchprograms.4 Some familieswhodoidentifyprimarycarephysiciansmayhave limitedavailabilitytoaccessroutinecareduringregular businesshours,thusmissingopportunitiesforscreeningand intervention,andalternativelyseekingcareinurgent careorEDswherescreeningisnotthestandardofcare. Additionally,dependingonin-officescreeningmethods(eg, paper,verbal,electronic)andlimitationsintimeallottedfor officevisitsandresourceavailability,primarycareoffices maynotidentifyallFIfamiliesand/orbeabletomeetthe needsofallitspatients.Furthermore,primarycareoffice staffmaynotbeawareofallavailablelocal,statewide, andfederalresourcesandeligibilitycriteriaforpatientswho mayqualify.Acycleofpooraccess,poorscreening, inadequateguidance,andnegativehealthoutcomes subsequentlydevelops.
Theproportionofrespondentsinthehighfoodsecurity categoryaswellasthosewithhouseholdincomes >$50,000 whoreportedawarenessofallthesupplementalfoodservices wassignificantlyhigherthantheproportionofrespondents withlowandverylowfoodsecurityandhouseholdincomes <$50,000.Highresourceawarenessamongfoodsecure familiesandgreaterannualhouseholdincomescouldbedue tooverallhighereducationandknowledgeofsocialservices evenwhentheyarenotneeded,awarenessbecauseofpastor
currentutilization,orotherreasons.Inthiscohort, respondentswiththeoverallhighestawarenessof supplementalfoodserviceshadtheoveralllowestutilization ofserviceswhenstratifiedbyhouseholdincomeandfood securitystatus.Basedonthese findings,thosewiththehighest knowledgearenotnecessarilythosewhoareinneed.This datasuggeststhatfamilieswhoarefoodsecuremaynot necessarilybefoodsecurebecauseofutilizationofservices; however,additionalstudiesneedtobedonetofurther elucidatereasonsforthese findings.
Anothernotable findingisthattheproportionof respondentswhousedfreeschoolluncheswasnot statisticallysignificantregardlessoffoodsecuritystatus.This islikelyduetolegislationincludingtheFamiliesFirst CoronavirusResponseActthatwasputinplaceduringthe COVID-19pandemictoallowaccesstofreeschoollunches forallchildrenregardlessofincome.17 Unfortunately, despiteuniversalaccessibilitytofreeschoollunches, approximately25%orfewerchildreninhouseholdswith incomes <$50,000annuallyandinthelowandverylow foodsecuritycategories,regardlessofprimarylanguage, participatedinthisservice.Significantstigmaaroundusing freeschoolmealscanleadtochildrennotparticipatinginthe programdespitequalifying,18 whichmayplayaroleinthese findings.Consideringlegislativechangesmadeduringthe pandemictoprovideaccesstofreeschoolmealsuniversally, additionalstudiesarerequiredtounderstandtheimpactof theseprogrammaticchangesovertime.
Whileitispossiblethatrespondentsmisunderstoodor incorrectlyansweredquestionsrelatedtoawarenessand utilizationordidnotknowoftheseprogramsbyname,these findingswarrantfurtherexploration.Barrierstoawareness andutilizationarewellknown,includingEnglish-language proficiency,difficultynavigatingthecomplexapplication processesviaphone,online,orinperson,andlackof transportationandaccesstogovernmentofficesand/orlocal foodresourcesparticularlyduringregularbusinesshours, amongotherfactors.Familiesareoftennotawareof eligibilitycriteria,particularlyiftheyarenotprovidedthis informationathealthcarevisits,inschools,andthrough communityoutreachprograms.Althoughundocumented familiesmayqualifyforstateandfederalassistanceservices, theymaybereluctanttoidentifythemselvestogovernment programs.Althoughdetailsofimmigrationstatus,exact householdincome,priorutilizationofservices,thestatusof pendingimmigrationapplications,andbarrierstoaccessare unknownamongthisstudycohort,thedifferencesin awarenessandutilizationarestriking,andreiteratetheneed forfurtheroutreachandinterventionamongthemost vulnerablepopulations.
Thereareimportantlimitationstothisstudytoconsider. The firstismissingdata.Whileover800respondentsinitiated
thestudy,manydidnotcompletetheUSDAscreening questions,thusexcludingthemfromanalysis.Amongthose whodidcompletethescreeningquestions,notallcompleted thesociodemographic,awareness,andutilizationquestions, potentiallyimpactingtheresultsofouranalyses.Secondis selectionbias,whichmayhavebeeninfluencedbyfactors suchasrespondentinterestinthesurvey,lackofdirect recruitment,generalandmedicalliteracy,andaccessto smartphonestocompletethesurvey.Becausetherewasno directrecruitment,respondentswithlimitedliteracyand/or thosewhospokealanguageotherthanEnglishandSpanish alsoweremissed,potentiallyintroducingadditionalselection biasandlimitinggeneralizability.
Therecruitmentposterspecificallyexcludedthewords “foodinsecurity” withtheintentoftryingtorecruit respondentsfromallsocioeconomicbackgrounds.Because therewasasmallgift-cardincentiveofferedforparticipationin thesurvey,somedegreeofselectionbiaslikelyremained,with thosewithhigherneedsprimarilyresponding.However,itis notablethatover16%ofrespondentsreportedahousehold incomeabove$75,000peryear, >250%oftheFPL.13 Further, approximately1.4%oftheannualPEDvolumecompleted surveys,whichmaynotberepresentativeofthegeneralPED populationatthestudysiteor inotherEDsettings,limiting broadergeneralizability.However,theproportionsurveyedis comparabletothatofotherstudieswithsimilarmethodology (1.8%8 and0.5%10)anddemonstratedsimilarincreasesinFI reportedduringthepandemic.1,2
Otherpotentialbiasesareimportanttoacknowledge, includingthepossibilityofmiscalculationbias,as respondents’ answersmaynothavebeenaccurateiftheydid notremembercircumstancescorrectlyoriftheywerenot familiarwiththenamesofsupplementalfoodservices, amongotherreasons.Theremayhavebeenacontributionof socialdesirabilitybias,withrespondentsnotaccurately reportingtheirincome,awareness,andutilizationofservices. Theabilitytotakethesurveyanonymouslymayhave mitigatedthisbias,however.
Amongrespondentswhoprovidedcontactinformationto receiveanincentivegiftcard,therewerenoduplicatenamesor addressesprovided.However,apotentiallimitationincludes repeatenrollmentatsubsequentvisitsamongindividualswho didnotprovidecontactinformation.Anadditionallimitation isthatthesixquestionsusedareaimedatassessing household FIandresponsesmaynotdirectlyreflectthefoodsecurity statusofthechildrenlivinginthehomes.Althoughchildren maynotdirectlyexperiencehouseholdFI,understandingthe householddynamicsandneedsisstillcriticaltoidentifying disparitiesandpopulationsinneedandidentifying opportunitiesforinterventionsbeforechildrenareimpacted.
TheCOVID-19pandemichadsignificantimpactson families,withanincreaseinfoodinsecuritynationally.This
study,alignedwithpriorpublishedresearch,demonstrates thattheEDisanimportantlocationforFIscreening.Given thehighneedsofthepatientpopulationseenintheEDand thisstudy’sstriking findingthatmorethanoneintwo householdsscreenedhadsomedegreeofFI,additional studiesmustbedonetooptimizeFIscreening,including determiningthebestscreeningmodalityandinterventions forthishigh-riskpopulation.
AddressforCorrespondence:StephanieRuest,MD,MPH,Hasbro Children’sHospital,DivisionofPediatricEmergencyMedicine,Warren AlpertBrownUniversitySchoolofMedicine,55ClaverickSt.,2nd Floor,Providence,RI02903.Email: Stephanie_Ruest@Brown.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudyreceivedfundingfromthe AmericanAcademyofPediatricsCommunityAccesstoChildHealth (CATCH)ImplementationGrant,2021.Thecontentissolelythe responsibilityoftheauthors,anddoesnotnecessarilyrepresentthe officialviewsoftheAmericanAcademyofPediatrics.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Ruestetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AmericanAcademyofPediatrics,FoodResearch&ActionCenter. Screenandintervene:atoolkitforpediatricianstoaddressfood insecurity.Availableat: https://frac.org/aaptoolkit AccessedNovember21,2023.
2.U.S.DepartmentofAgriculture.EconomicResearchService.Food securityintheU.S.keystatistics&graphics.Availableat: https://www. ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/ key-statistics-graphics/.AccessedNovember21,2023.
3.BauerL.TheCOVID-19crisishasalreadylefttoomanychildrenhungry inAmerica.2020.Availableat: https://www.hamiltonproject.org/ publication/post/the-covid-19-crisis-has-already-left-too-manychildren-hungry-in-america/#_ftn1.AccessedNovember21,2023.
4.Coleman-JensenA,RabbittMP,GregoryCA,etal.Householdfood securityintheUnitedStatesin2020,ERR-298.September2021. Availableat: https://www.ers.usda.gov/webdocs/publications/102076/ err-298.pdf?v=2067.1.AccessedNovember21,2023.
5.CouncilonCommunityPediatrics;CommitteeonNutrition.Promoting foodsecurityforallchildren. Pediatr. 2015;136(5):e1431–8.
6.PeltzAandGargA.Foodinsecurityandhealthcareuse. Pediatrics 2019;144(4):e20190347.
7.GonzalezJV,HartfordEA,MooreJ,etal.Foodinsecurityinapediatric emergencydepartmentandthefeasibilityofuniversalscreening. WestJEmergMed. 2021;22(6):1295–1300.
8.CullenD,WoodfordA,FeinJ.Foodforthought:arandomizedtrialof foodinsecurityscreeningintheemergencydepartment. AcadPediatr. 2019;19(6):646–51.
9.GattuRK,PaikG,WangY,etal.Thehungervitalsignidentifies householdfoodinsecurityamongchildreninemergencydepartments andprimarycare. Children(Basel). 2019;6(10):107.
10.PabalanL,DunnR,GregoriK,etal.Assessmentoffoodinsecurityin Children’sHospitalofWisconsin’semergencydepartment. WMJ. 2015;114(4):148–51.
11.GayleT,LawA,StokesS,etal.Parentpreferencesonscreeningfor socialdeterminantsofhealthinhospitalizedchildren. HospPediatr. 2023;13(7):623–35.
12.U.S.DepartmentofAgriculture.FoodsecurityintheU.S.surveytools. U.S.householdfoodsecuritysurveymodule,six-itemshortform.Available at: https://www.ers.usda.gov/topics/food-nutrition-assistance/foodsecurity-in-the-u-s/survey-tools/#six.AccessedNovember21,2023.
13.HealthCare.gov.Federalpovertylevel.Availableat: https://www. healthcare.gov/glossary/federal-poverty-level-fpl/ AccessedNovember21,2023.
14.RhodeIslandCommunityFoodBank.Hungerfacts.Availableat: https:// rifoodbank.org/wp-content/uploads/2023/07/2022-RICFBStatusReport-final-web.pdf.AccessedNovember21,2023.
15.RIFoodPolicyCouncil.Datadashboard:foodaccessandsecurity. https://rifoodcouncil.org/data-dashboard/food-access-and-security/ AccessedDecember19,2023.
16.WhitmoreSchanzenbachD,BaurL,NantzG.Twelvefactsaboutfood securityandSNAP.2016.Availableat: https://www.hamiltonproject.org/ publication/economic-fact/twelve-facts-about-food-security-and-snap/. AccessedNovember21,2023.
17.116thCongress(2019–2020).H.R.6201– FamiliesFirst CoronavirusResponseAct.2020.Availableat: https://www. congress.gov/bill/116th-congress/house-bill/6201 AccessedDecember18,2023.
18.CohenJ,GoslinerW,HechtC,etal.Researchbrief:impactof Massachusetts’ healthyschoolmealsforallpolicyonfamilies.2023. Availableat: https://www.childnourishlab.org/healthy-schoolmeals-for-all. AccessedDecember19,2023.
EffectivenessofaCollaborative,VirtualOutreachCurriculumfor 4th-YearEM-boundStudentsataMedicalSchoolAf filiatedwitha HistoricallyBlackCollegeandUniversity
CortlynBrown,MD,MCSO* RichardCarter,MD† NicholasHartman,MD,MPH‡ AarynHammond,MD‡ EmilyMacNeill,MD* LynneHolden,MD§ AvaPierce,MD∥ LinelleCampbell,MD§ MarquitaNorman,MD,MBA∥
*AtriumHealthCarolinasMedicalCenter,DepartmentofEmergencyMedicine, Charlotte,NorthCarolina
† HowardUniversity,CollegeofMedicine,Washington,DC ‡ WakeForestUniversity,SchoolofMedicine,Winston-Salem,NorthCarolina
§ AlbertEinsteinCollegeofMedicine,MontefioreMedicalCenter,Bronx,NewYork
∥ UTSouthwesternMedicalCenter,Dallas,Texas
SectionEditors:MatthewTews,MDandChristineStehman,MD
Submissionhistory:SubmittedJanuary24,2024;RevisionreceivedOctober9,2024;AcceptedOctober17,2024
ElectronicallypublishedDecember16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18748
Background: Diversitywithinthephysicianworkforceisassociatedwithimprovedclinicaloutcomesand patientsatisfaction.Despitethis,theUSphysicianworkforce,particularlyinemergencymedicine(EM), remainsrelativelyhomogeneous.OfallBlackmedicalschoolstudentsintheUS,14%attendthefour HistoricallyBlackCollegesandUniversities(HBCU)thathaveamedicalschool.Unfortunately,noneof theseschoolsareaffiliatedwithanacademicEMprogram.Becauseofthis,thereislessprofessional mentorshipfocusedonobtainingacareerinEMandpotentiallylessformalcurriculaforseniormedical studentsdoingtheirhomesub-internshipinEM.
Objectives: Ourobjectivewasto fillthegapleftbytheabsenceofanacademicEMdepartmentat HowardUniversityCollegeofMedicine(HUCOM)bycreatingacollaborativeeducationalexperiencefor fourth-yearmedicalstudentsduringtheirhomeEMsub-internship.Thecurricularobjectiveswereto teachcoreprinciplesofEM,buildrelationshipswithstudents,andpreparethemforpursuingEM residencytraining.
CurricularDesign: FourEMacademicdepartmentscollaboratedtocreateandimplementavirtual curriculumusingthesix-stepapproachtocurriculardevelopment.
Impact/Effectiveness: Aftercompletionofthecourse, fivestudents(100%)reportedstronglyagreeing withthefollowingstatements.Thesesessions1)helpedmelearntheapproachtocoreEMtopicsmore thanIwouldhavebeenabletodoonmyown;2)helpedmelearnkeyskillsforexcellinginanEMrotation morethanIwouldhavebeenabletodoonmyown;and3)allowedmetoconnectwithfacultyand residentmentorstolearnmoreaboutthe fieldofEM.Ofthese fivestudents,80%and20%reported stronglyagreeingandagreeing,respectively,thatthesesessionshelpedthemlearnabouttheprocessof applyingtoandselectinganEMresidencyprogram.[WestJEmergMed.2025;26(1)129–134.]
NeedforInnovation
Medicalstudentsinterestedinemergencymedicine(EM) whoattendahistoricallyBlackcollegeoruniversity(HBCU) donothavetheteachingandmentorshipthatoccurswhena medicalschoolisaffiliatedwithanacademicEMprogram. Weformedacollaborativeprogramamongfouracademic EMdepartmentstohelp fillthisneedforEM-boundstudents atHowardUniversityCollegeofMedicine(HUCOM).To ourknowledge,thisisthe firstsuchprogramtobereportedin theliterature.
Adiversephysicianworkforceisassociatedwithincreased accesstoandutilizationofthehealthcaresystem,improved healthoutcomesandpatientexperience,andimproved fiscal marginsforhospitals.1–4,4–6 Despitethis,themedical fieldas awholehasmademinimaladvancesinincreasingphysician diversity.In2008thepercentageofBlackorHispanicUS physiciansfromallspecialtieswas6.3%and5.5%, respectively.By2018,however,thosepercentageswereonly 5.0%and5.8%,respectively.Evenmoreconcerninggiventhe diversepatientpopulationthattheemergencydepartment (ED)serves,EMremainsamongthemedicalspecialtieswith thelowestnumberofphysiciansfrombackgroundsunderrepresentedinmedicine(URiM).Between2008–2018,the percentageofemergencyphysicianswhoidentifiedasBlack decreasedfrom5.0%to4.5%,andstayedconstantat5.3% forHispanic/Latinos.7
Whensurveyed,35%ofEMprogramdirectorsreported thatthesmallnumberofURiMresidencyapplicantswasthe greatestbarriertoobtainingadiverseresidencyclass.8 Ofall BlackmedicalschoolstudentsintheUS,14%attendfour HBCUswithamedicalschool.Becausenoneoftheseschools areaffiliatedwithanacademicEMprogram,theirmedical studentshavedecreasedexposuretoEMinthepre-clinical years,lessprofessionalmentorshipfocusedonobtaininga careerinEM,andfewerformalcurriculaforseniormedical studentsdoingtheirhomesub-internship(sub-I)inEM.This lackofmentorshiphasbeenidentifiedasacriticalbarrierfor URiMstudentsacrossvariousspecialties,contributingto lowerapplicationratesandresidencyplacement.Studies suggestthatmentorshipincreasesbothcareersatisfaction andinclusivityandthelikelihoodofthesestudentsentering andsucceedingincompetitive fieldslikeEM.9,10 Inaddition, anationalsurveyofclerkshipdirectorsfoundthathavinga structured,standardizedsub-Icurriculumsignificantly improvedthepreparednessofstudentsforresidency, especiallywhentheserotationswereaffiliatedwith residencyprograms.11
TheEmoryUniversityDepartmentofEmergency MedicinecreatedaprogramwithMorehouseSchoolof Medicinetoprovideguidancetomedicalstudentsinterested inEM.Atotalof115MorehousestudentscompletedanEM
clerkshipatEmory,and62.6%successfullymatchedinto EM.12 Whilethisprogramwassuccessful,studentstypically relyontheirhomesub-Itoprepareformandatoryaway rotations.Thisabsenceofsupportfromanacademic departmentpriortoawayrotationsmaycausethestudentsto findthemselveslesspreparedandatacompetitive disadvantagewhentheybegintheirawayrotations. Furthermore,manyEMresidenciesarenotinproximitytoa HBCU,requiringstudentstobearthe financialburdenof travelingtoothercitiesandstatesfortheirawayrotations.
AtHUCOM,theEMsub-Ireliedheavilyonanolder, recordedonlinelectureseriesfromanexternalinstitution, supplementedbybedsideteachingfromcommunity attendingsatonesite,HowardHospital.Studentsnotedthat theabsenceofformaleducationalcomponents,suchas weeklydidactics,journalclubs,andsimulation,resultedin limitedexposureto “cutting-edge” EMpractices.Moreover, thelackofinteractionwithacademicattendingswhoare dedicatedtomedicalstudenteducation,alongwiththe absenceofresidents whorepresentthenextstepincareer progression leftstudentswithoutaccesstocritical mentorshipandguidance.Thisgaphinderedstudents’ ability tovisualizetheirownprogressionandreceivepractical advicefromindividualsatasimilarstageintraining,further limitingtheirconnectiontothebroaderEMcommunity.
Tohelpovercomethatbarrier,wecreatedacollaboration betweenfouracademicEDsandHUCOMinanattemptto augmentcurricularofferingsforEM-interestedstudentson theirHUCOMfourth-yearEMhomerotation.The collaborationbetweenfouracademicEDsbroadensthe exposurestudentsreceivetodifferentteachingstyles, institutionalcultures,andclinicalperspectives.Thisvariety providesamorecomprehensiveeducationalexperiencethan whatcanbeofferedbyasingleinstitutionalone.
WeaimedtoaddresstheabsenceofanacademicEDat HUCOMbydevelopingacollaborativeeducational experience.ThisprogramfocusesoncoreprinciplesofEM andresidencypreparationandwasdesignedspecificallyfor fourth-yearmedicalstudentsduringtheirhomeEMsub-Iat HUCOM.Weobtainedinstitutionalboardreviewapproval fromWakeForestUniversitySchoolofMedicine.
Weusedthesix-stepapproachtocurriculardevelopment. All finalcurriculardesignandcontentwasagreeduponby thefacultyrepresentativesateachofthefourparticipating residencysites.13,14 1) Problemidenti fi cationandgeneral needsassessment. Unliketraditionalcurriculum developmentwheretheneedassessmentisbasedonaspecific healthproblem,ourneedsassessmentwasbasedontheneed toincreasethediversityofemergencycliniciansbyhelping prepareunder-representedstudentstosucceedinaway
rotationsandthematch.2) Determiningandprioritizing content. Whileindividualsateachparticipatinginstitution wereinvolvedwithteachingattheirowninstitution,the needsoftheHUCOMstudentswereunique.Therefore, educationalobjectivesweredevelopedinconjunctionwith thefacultyadvisortothefourth-yearEMrotationat HUCOMwhoconductedstakeholderinterviewswith five currentmedicalstudentsand fivealumniwhohadrecently graduatedandwerecurrentlyinEMresidenciesacrossthe country.Itwasdecidedthatcurricularcontentwouldinclude amixofcoreEMtopics(asdeterminedfromstakeholder interviews)andadvisingsessions.
Afterallsessions,studentswereprovidedwiththecontact informationforthefacultylecturersandwereencouragedto reachout.3) Goalsandobjectives .Broadcurriculargoals weredeveloped.Theseweretoa)teachtheapproachtocore complaintsinEM;b)teachkeyskillsinEM;c)demystifythe processofapplyingtoanEMresidencyprogram;andd) connectstudentswithresidentsandfacultyinthe fieldofEM. Afterthis,specificmeasurablelecturegoalsweredeveloped basedoncognitive,affective,andpsychomotorobjectivesfor thelearner.4) Educationalstrategies .Wecreatedanentirely virtual,four-weekdidacticprogram,withcontentorganized intoweeklyfour-hourblocks,eachledbyadifferent academicED,onaninteractiveplatformthatallowedfor case-baseddiscussions,small-groupdiscussions,and standardlectureformat.Sinceimplementationin2022,the programhasbeenmandatoryforallstudentscompleting theirfourth-yearEMsub-IatHUCOM.
Eachweek,thesessionsrequiredtheparticipationoffour to fivefacultymemberswhovolunteeredtheirtime,withthe majorityoflecturesdeliveredbyasinglefacultymember. However,selectsessions,suchasthe “Applicationand InterviewingProcess,” wereco-ledbyadynamicteam consistingoftheassistantprogramdirector,program director,andchiefresidents,providingawell-rounded perspectiveandvaluableinsightsfortheparticipants. Contentwasmappedandcoordinated,andpre-readingwas assignedfromtheAcademyforDiversityandInclusionin EmergencyMedicinewebinarseries “HowtoBeaSuccessful
Didacticsessionone
Institutionone
EMApplicant” andtheClerkshipDirectorsinEmergency Medicine/SocietyofAcademicEmergecyMedicineM4 curriculum.Eachdayincludedamixofclinicaltopicsand “advising” sessions(Table1).5) Implementation. Approval fromtheEMdirectorwasobtained,andthecurriculawas implemented.6) Evaluationandfeedback .Aftereachblock ofcontent,evaluationsforeachindividualsession(including thepresenter)weresenttoparticipatingstudentsvia REDCap(ResearchElectronicDataCapture,hosted atHowardUniversitySchoolofMedicine.
Theseevaluationsconsistedofonequestionforeach session: “Pleaseratetheeffectivenessofthefollowingsession inaccomplishingitslearningobjectives: Session,Presenter . ” Attheendofthemonth-longprogram,anoverallevaluation oftheprogramwassenttoparticipatingstudents,alsovia RedCap.Theprogramevaluationsurveytool,includingfour multiple-choicequestionsregardingtheoveralllearning objectives,isreflectedin Figure1.Thetoolalsoincludedtwo free-responsequestions:1) “Whichpartsofthecurriculum wereofmostvaluetoyou?”;and2) “Whichpartsofthe curriculumcouldbeimproved?” Werefinedthecurricula eachyearduringanend-of-yeardebrief.
Priortothe firstsession,studentswereprovideda spreadsheetwithpre-sessionwork,curriculumtopics, presentingfacultyandresidents,datesandtimes,andlinksto accesstheweeklyvirtualsessions.EachEMprogram providedfourhoursofinteractivedidacticstothestudents accordingtothescheduleddatesandtimes.
Apost-curricularsurveyfounduniversalagreementfrom studentsthatthecurriculumwaseffectiveinmeetingthe abovegoals.Ofthe fivestudents,100%reportedstrongly agreeingwiththefollowingstatements.Thesesessions1) helpedmelearntheapproachtocoreEMtopicsmorethanI wouldhavebeenabletodoonmyown;2)helpedmelearn keyskillsforexcellinginanEMrotationmorethanIwould havebeenabletodoonmyown;and3)allowedmeto
Didacticsessiontwo Institutiontwo
Didacticsessionthree Institutionthree
Didacticsessionfour Institutionfour LecturetopicsPersonalstatementPresentationskillsHowtochoosetheright programforyou Applicationandinterviewing process
ChestpainAlteredmentalstatusToxicologyoverviewHeadache ShortnessofbreathAbdominalpainShockandsepsisGynecologicandurologic emergencies
RadiographsElectrocardiogram introduction VaginalbleedingEndocrineandelectrolytes
SocialemergencymedicineUltrasoundbasicsAdvancedtraumalife support Advancedcardiaclifesupport, basiclifesupport
Session:
Presenter:
Please rate the effectiveness of the following session in accomplishing its learning objectiveson a scale from 1 (not effective) to 5 (very effective)
Questions These sessions helped me learn the approach to core emergency medicine topics (abdominal pain, chest pain, headache, etc.) more so than I would have been able to do on my own.
These sessions helped me learn key skills for excelling in an emergency medicine rotation including oral presentations, EKG interpretation, xray interpretation and ultrasound, more so than I would have been able to do on my own.
These sessions helped me learn about the process of applying to and selecting an EM residency program. These sessions allowed me to connect with faculty and resident mentors to learn more about the field of emergency medicine.
Response Options
Strongly agree, agree, neutral, disagree, strongly disagree
Strongly agree, agree, neutral, disagree, strongly disagree
Strongly agree, agree, neutral, disagree, strongly disagree
Strongly agree, agree, neutral, disagree, strongly disagree Response
Which parts of the curriculum were of most value to you?
Which parts of the curriculum could be improved?
connectwithfacultyandresidentmentorstolearnmore aboutthe fieldofEM.Ofthe fivestudents,80%and20% reportedstronglyagreeingandagreeing,respectively,that thesesessionshelpedthemlearnabouttheprocessof applyingtoandselectinganEMresidencyprogram.
Narrativefeedback,suchasthequotesbelow,from studentshighlightedthevalueofmeetingwithfacultyand residentsfromdifferentprograms.fromgoingthroughcases inrealtime.
MeetingthefacultyandprogramdirectorsatvariousEM programsreallywasthehighlightofthecurriculum.Itwas greattogetaninsidelookateachprogramandlearnmore abouttheirculture,approach,andthepeoplethere.
Ireallyenjoyedhearingtheresidents’ perspectiveonhow tonavigatetheapplicationprocess.
Narrativefeedback,suchasthequotesbelow,also emphasizedthevalueofthecurriculum’sinteractivenature andhowtraditionallyin-persontopicswereeffectively adaptedforvirtuallearning.
Myfavoritepartwasparticipatinginreal-timecases.Being involvedasthecaseunfoldedfeltlikehands-onpractice.
Itwasincredibletohavethemechanismsofultrasound explainedinsuchdetail.Breakingitdowntothebasics reallyhelpedmeunderstandultrasoundforthe firsttime.
Successfulimplementationrequiredactiveengagement fromHUCOM,specificallytheclerkshipdirectorand administrativestaff,whoservedasleadcontacts.Control overrotationschedulingwasessentialtoensureallstudents werefullyengagedinthesessions.Inaddition,as participatinginstitutionsusedvariousonlineplatformsto communicateanddisseminatecurriculamaterials,suchas Tintinalli ’ sEmergencyMedicine ,withtheirstudents,itwas necessarytohaveHUCOMmanageacentral communications-andvideo-conferencingplatform thatwasaccessibletoalllecturinginstitutionsand participatingstudents.
Recruitingfacultyandresidentsforeachinstitution’ s weekwaschallenging,buthavingrepresentativeswithstrong connectionsinmedicaleducationmadeasignificant difference.Theserelationshipsallowedthemtoquicklyand effectivelyrecruitlecturers,leveragingtheirnetworksto secureindividualswhowerebothwillingandenthusiasticto participate.Thishighlightsthevalueofhavinginstitutional leadswithestablishedtiestotheireducationalinfrastructure, streamliningtherecruitmentprocess.
Thesuccessofthisprojectinvolvedahighdegreeoftrust asmanyoftheinstitutionalrepresentativeshadnotworked together.Todevelopthistrust,wefollowedtheframeworkof engaging,listening,framing,envisioning,andcommitting.15 Thepowerofthisprogramistrulyinthecollectiverather thantheindividual.Whilestudentscouldlearnaboutatrial fibrillationfromoneinstitution,thereallearningoccurs whentheyseethecollaboration,getasenseofthescopeof EMasaprofessional field,andareabletointeractwith variedinstitutionsthathavedifferentapproachestoteaching andthepracticeofmedicine.
UnliketraditionalEMrotationsthatattractstudentsfrom acrossthecountry,ourprogramhadasmallcohort comprisedsolelyofHUCOMstudents,astherewasno affiliatedresidency.Thissmallgroupsizemeantthatifone studentmissedasessionduetointerviews,illness, orotherreasons,itnoticeablyimpactedthelearning environment,limitinggroupdynamicsand peer-to-peerlearning.
Virtuallearningposedchallengesforteachinginteractive skillssuchasultrasound.Weaddressedthisbyincorporating case-basedlearningwithcuratedimagelibrariesand real-timefeedback.Tofurtherenhancethelearning experience,futureiterationsshouldexploretheintegration ofultrasoundsimulationsoftwaretobettermimic hands-onscenarios.
AlthoughinitiallydesignedforHUCOMstudents,this modelcouldbeexpandedtoothermedicalschoolswithout academicEDs,especiallythosewithahighproportionof URiMstudents.WiththeopeningofadditionalHBCU medicalschools,thereisanevengreaterneedforprograms thatincreaseaccesstoEMeducation.
Studylimitationsincludethesmallsamplesizeaswellas lackofacomparisongroup.Futureanalyseswilladdress
theselimitationsandincludeevaluationofmatchoutcomes aswellasotherlearner-centeredtargetssuchasperformance inStandardizedLettersofEvaluationorsubsequent rotationsandinternyearperformance.
AddressforCorrespondence:CortlynBrown,MD,MCSO,Atrium HealthCarolinas,DepartmentofEmergencyMedicine,1000Blythe Blvd.,Charlotte,NC28203.Email: Cortlyn.Brown@atriumhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Brownetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KomaromyM,GrumbachK,DrakeM,etal.TheroleofBlackand Hispanicphysiciansinprovidinghealthcareforunderserved populations. NEnglJMed. 1996;334(20):1305–10.
2.MarrastLM,ZallmanL,WoolhandlerS,etal.Minorityphysicians’ rolein thecareofunderservedpatients:diversifyingthephysicianworkforce maybekeyinaddressinghealthdisparities. JAMAInternMed. 2014;174(2):289.
3.GomezLEandBernetP.Diversityimprovesperformanceand outcomes. JNatlMedAssoc. 2019;111(4):383–92.
4.SahaS,KomaromyM,KoepsellTD,etal.Patient-physicianracial concordanceandtheperceivedqualityanduseofhealthcare. Arch InternMed. 1999;159(9):997.
5.TakeshitaJ,WangS,LorenAW,etal.Associationofracial/ethnic andgenderconcordancebetweenpatientsandphysicianswithpatient experienceratings. JAMANetwOpen. 2020;3(11):e2024583.
6.ShenMJ,PetersonEB,Costas-MunizR,etal.Theeffectsofraceand racialconcordanceonpatient-physiciancommunication:asystematic reviewoftheliterature. JRacialEthnHealthDisparities. 2018;5(1):117–40.
7.GarrickJF,PerezB,AnaebereTC,etal.Thediversitysnowballeffect: thequesttoincreasediversityinemergencymedicine.Acasestudyof Highland’semergencymedicineresidencyprogram. AnnEmergMed. 2019;73(6):639–47.
8.BoatrightD,TunsonJ,CarusoE,etal.Theimpactofthe2008Councilof EmergencyResidencyDirectors(CORD)panelonemergencymedicine residentdiversity. JEmergMed. 2016;51(5):576–83.
9.MabezaRM,ChristophersB,EderaineSA,etal.Interventions associatedwithracialandethnicdiversityinUSgraduatemedical education:ascopingreview. JAMANetwOpen. 2023;6(1):e2249335.
10.MartinezJ,MieresJH,RoswellRO,URiM(underrepresented inmedicine)learnerandfacultymentoring.In:FornariAandShahDT
(Eds.), MentoringinHealthProfessionsEducation(34–43).IAMSE manuals.Cham,Switzerland:SpringerInternationalPublishing,2021.
11.DeLaCruzMSD,SairenjiT,StumbarSE,etal.Curricular recommendationsforanationalfamilymedicinesubinternship: aqualitativeanalysisfrommultiplestakeholders. FamMed. 2021;53(10):835–42.
12.GoinesJ,IledareE,AnderD,etal.Amodelpartnership:mentoring underrepresentedstudentsinmedicine(URiM)inemergencymedicine. WestJEmergMed. 2021;22(2):213–7.
13.SweetLandPalazziD.ApplicationofKern’ssix-stepapproachto curriculumdevelopmentbyglobalhealthresidents. EducHealth. 2015;28(2):138.
14.ThomasPA,KernDE,HughesMT,etal.(Eds.). CurriculumDevelopmentforMedicalEducation:aSix-step Approach.3rd Ed.Baltimore,Maryland:JohnsHopkinsUniversity Press,2016.
15.MaisterD,GreenC,GaifordR. TheTrustedAdvisor.NewYorkNew York:Simon&Schuster,20th AnniversaryEd.,2021.
DanielJ.Berman,MD*∘
AlexanderW.Mahler,MD†∘
RyanC.Burke,PhD,MPH†
AndrewE.Bennett,MD,PhD†
NathanI.Shapiro,MD,MPH†
LeslieA.Bilello,MD†
SectionEditor(s):DavidThompson,MD
*BethIsraelDeaconessMedicalCenter,DepartmentofEmergencyMedicine, Boston,Massachusetts † UniversityofSouthernDenmark,Odense,Denmark ∘ Co- firstauthors
Submissionhistory:SubmittedSeptember8,2023;RevisionreceivedMarch5,2024;AcceptedMarch11,2024
ElectronicallypublishedNovember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18455
Objectives: Managementstrategiesforsmallbowelobstruction(SBO)varyfromconservative approachestosurgicalintervention.Aknowncomplicationofsurgeryisthesubsequentadhesions thatcancauserecurrentSBOs,longerhospitalstays,andhighertreatmentcosts.Ourprimary outcomewastoidentifyindependentriskfactorsthatareassociatedwiththedecisionforsurgical intervention,andoursecondaryoutcomewastodescribecharacteristicsofvisitsassociated withcomplications.
Methods: Thisstudywasasingle-center,retrospectivechartreviewfromalarge,urbanuniversity hospital.Weincludedadultpatientsadmittedtotheemergencydepartment(ED)withtheInternational ClassificationofDiseases,10th Rev,codesforsmallbowelobstructionfromJune1,2017– May30,2019. Eligiblecovariatesweredemographics,radiological findings,clinicalpresentation,pastmedicalhistory, andresultsofradiologictesting.Weidentifiedunivariateassociationsofoutcomeandthenperformeda multivariatelogisticregressiontoidentifyindependentassociationsofeachoutcome.Finally,a backwardsselectionwasusedtodeterminethe finalmodel.Wecalculatedoddsratios(OR)and95% confidenceintervals(CI)alongwiththeareaunderthecurve(AUC),asappropriate.
Results: Atotalof530patientsmetthestudycriteria;148(27.9%)underwentsurgeryofwhom35(6.6%) hadcomplications.Weidentifiedsevenindependentassociationsforthedecisionofsurgery:abdominal distension(OR0.27,95%CI0.10–0.62);gastrografin(OR0.41,95%CI0.20–0.81);previousSBO(OR 0.42,95%CI0.26–0.66);higherCharlsonComorbidityIndexscore(OR0.87,95%CI0.80–0.95); nasogastricdecompression(OR2.04,95%CI1.25–3.39),initialsystolicbloodpressure <100mmHg (OR2.65,95%CI1.05–6.53);free fluidorvolvulus/closed-loopobstructiononcomputedtomography (OR7.95,95%CI4.25–15.39),withtheAUCforthepredictivemodelequaling0.73.
Conclusion: WeidentifiedsevenindependentassociationspresentintheEDassociated withthedecisionforsurgery.Theseassociationsareasteptowardbuildingbetterprediction modelsandimprovingdecision-makingintheED,allowingforamoreadequatetreatmentplan.[WestJ EmergMed.2025;26(1)135–141.]
INTRODUCTION
Thereiscurrentlyashiftfromthetraditionaldogma, “Neverletthesunriseorsetonsmallbowelobstruction, ”
whichimpliesurgentsurgicalintervention,towardnonoperativemanagementwhenclinicallyindicated.1 Thisisan importantshiftbecausenon-operativemanagementmay
havelessassociatedriskandhelpdecreaseresource utilizationwhenappropriate.2–4 Thedecisionregarding smallbowelobstruction(SBO)treatmentandinterventionis notalwaysclear.Whilesomestudieshavetriedtoelucidate waystohelpmanageourclinicaldecisions,thereareno uniformlyacceptedclinicaldecisionrules,andtheapproach islargelylefttoindividualclinicaljudgment.
WhenevaluatingapatientwithasuspectedSBO,itis importanttounderstandthedegreeofobstructionand associatedcomplicationssuchasbowelischemia, perforation,peritonitis,herniastrangulation,and anticipatedcourse.5,6 Theseconsiderationsareimportantas surgeryitselfcarriesriskssuchasinfection,bleeding,and complicationsfromgeneralanesthesia.Alsoconcerningis theriskofadditionaladhesionsleadingtorecurrentSBOs,as post-surgicaladhesionsareresponsibleforroughly70%ofall SBOsintheUnitedStates.2,3,7,8 Conversely,itisimperative todiscusstheriskofdelayedinterventioninSBOpatients whorequiresurgery.Examplesincludecomplicationssuchas bowelresection,prolongedpostoperativelengthofstay,and death.9 ThemanagementforeachSBOpatientshouldbe tailoredtothedegreeofobstruction,associated characteristics,andanticipatedcoursewhileevaluatingthe risksandbenefitsofconservativemanagement versussurgicalintervention.
Ourgoalinthisstudywastoidentifyclinicalassociations thatidentifypatientslikelytoprogresstoasurgical intervention.Wecollecteddataonpatientdemographics, physicalexam findings,vitalsignabnormalities,laboratory testresults,andradiographic findingsassociatedwith SBOsdiagnosedintheED.Ourprimaryoutcomewasto identifyindependentriskfactorsassociatedwiththe decisionforsurgicalintervention,andoursecondary outcomewastoidentifyindependentfactorsassociated withcomplications.
Weperformedaretrospectivechartreviewofpatients presentingtotheED(annualEDvolumeis55,000adult patients)ofanurban,tertiary-care,academicmedicalcenter fromJune1,2017–May30,2019.Ourstudywasreviewed andapprovedbytheinstitutionalreviewboard.Wefollowed allthebestpracticesforchartreviewasdescribedinWorst andBledsoewiththeexceptionofone,asourabstractors werenotblindtothehypothesis.10
ThestudypopulationconsistedofEDpatients ≥18years withanInternationalClassificationofDiseases,10th Rev. (ICD-10)codeconsistentwithSBO(ICD-10K56x,K91.3x, Q41.9,Q42.9,Q42.8,andQ43.1).Weexcludedpatientswho hadadvanceddirectivestoavoidsurgicalintervention(ie,if thepatientwasasurgicalcandidatebutelectednottohave
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Therearevaryingmanagementstrategiesfor smallbowelobstructions(SBO),butitisnot clearwhichpatientswouldmostbene fi tfrom surgicalintervention.
Whatwastheresearchquestion?
Arethereindependentriskfactorsassociated withsurgicalinterventionforpatientswith SBO?Andwhichpatientsdeveloped complicationsduringtheir inpatientadmission?
Whatwasthemajor findingofthestudy?
Sevenfactorswereassociatedwithdecision forsurgery:abdominaldistension(OR0.27, 95%CI0.10 – 0.62);gastrogra fi nuse(OR 0.41,0.20 – 0.81);previousSBO(0.42, 0.26 – 0.66);higherCharlsonComorbidity Index(0.87,0.80 – 0.95);nasogastrictube (2.04,1.25 – 3.39);systolicbloodpressure < 100mmHg(2.65,1.05 – 6.53);free fl uidor volvulus/closed-loopobstructiononCT(7.95, 4.25 – 15.39).
Howdoesthisimprovepopulationhealth?
These fi ndingscanhelpcliniciansidentify patientswhomightbeabettercandidatefor surgicalinterventionvsconservativetherapy tosafelymanageSBOs.
surgery)andpatientswithalargebowelobstruction identifiedbyattendingradiologistinterpretationon computedtomography(CT).
Weabstracteddataviachartreviewbytrainedreviewers compilingdatafromtheinitialpresentationwithout knowledgeofthesubsequenthospitalcourse.The parametersinvestigatedincludeddemographics,elementsof theclinicalpresentation,pastmedicalhistory,vitalsigns, physicalexam findings,andradiographicimaging.Specific demographicsandpatientdataincludedage,gender,dateof admission,andlengthofstay.Pertinentpastmedicalhistory includedpreviousSBOs,inflammatoryboweldisorders,past abdominalsurgeries,anatomicalanomalies,and malignancies.Wealsoincludedparametersthatcomprisethe CharlsonComorbidityIndex(CCI),whileexcluding connectivetissuediseases.Wehadoneattendingemergency
radiologistreviewallCTimagestoidentifythefollowing features:presenceofatransitionpoint;freeintraperitoneal fluid;debrisandgasbubbleswithinthedilatedsmallbowel lumen(smallbowelfecessign);mesentericedema;and closed-loopobstructionorvolvulustoensureconsistent wordingthroughouttheradiographicreports.We additionallynotedwhetheroral,water-solubleradiological contrast,specificallygastrografin,hadbeenusedduringtheir hospitalizations.Wecodedfornon-operativesurgical management,aswellascomplicationssuchassepsis, intubation,vasopressor-dependentshock,anatomicsurgical alterations,andbowelperforation.
ThesedatapointswereabstractedfromEDrecords, inpatienthospitalrecords,anddischargesummaries.A trained,experiencedresearcherunderwentrigoroustraining onourexplicitprotocol,includingclearlydefinedvariables andstandardizedcodingmethods,andperformedthe systematicdataabstraction.Theabstractor flagged ambiguouschartsforadditionalreviewbyanemergency medicineseniorresidentphysicianandaboard-certified emergencyattendingphysician.
Theprimaryoutcomewassurgicalintervention,definedas surgeryduringinitialhospitaladmission.Thesecondary outcomewasSBO-relatedcomplicationsduringinitial hospitaladmission.Complicationswerealsolookedforafter 90daysafterdischargebutusingsolelyourhospitalsystem
healthrecords.Complicationsincludedsepsis,intubation, vasopressor-dependentshock,anatomicsurgicalalterations, andbowelperforation.
Weemployedchi-squaretestsforcategorialvariablesand t -testsforcontinuousvariablestoidentifyunivariate associationsofoutcomes.TheFisherexacttestwasused insteadofchi-squaretestwhenthesamplenumberwaslow. Factorsassociatedwithsurgicalinterventionwere determinedwithamultivariatelogisticregressionmodel. Weemployedamultistageprocesstodeterminethe covariatestoincludeinthemodel.Possibleassociationswere includedinthemodelifthe P -valuefortheunivariate analysiswas <0.10andtheprevalencewassufficientlyhighto allowformodelconvergence.Finally,backwards selectionwasusedtodeterminethe finalmodel,withanalpha forexitof0.05.Theoddsratios(OR),95%confidence intervals(CI),andareaunderthecurve(AUC) werecalculated.
Therewere690patientsidentifiedandreviewedfor eligibility.Atotalof530patients(76.8%)mettheinclusion criteriaandwereincludedinthestudy.Thepatient populationtendedtobeolder,hadahistoryofabdominal surgeries,andpreviouslydiagnosedSBOs(Table1).Ofthe 530eligiblepatients,148(27.9%)underwentsurgeryunder
Table1. Baselinecharacteristicsofthepatientsincludedinthestudy,overallandbyoutcomes.
CharacteristicOverall(N
Demographics
Age,mean(SD)63.9(15.9)65.1(15.2)63.4(16.2)0.2866.5(14.8)63.7(16.0)0.32
Female,n(%)297(56%)89(60.1%)208(54.5%)0.2418(51.4%)279(56.4%)0.57
Symptomsreported
Constipation,n(%)34(6.4%)11(7.4%)23(6.0%)0.550(0.0%)34(6.9%)0.15*
Abdominalpain,n(%)496(93.6%)136(91.9%)360(94.2%)0.3232(91.4%)464(93.7%)0.48*
Abdominaldistension,n(%)68(12.8%)9(6.1%)59(15.5%)0.0043(8.6%)65(13.1%)0.60*
Nausea,n(%)325(61.3%)88(59.5%)237(62.0%)0.5823(65.7%)302(61.0%)0.58
Fever,n(%)16(3.0%)4(2.7%)12(3.1%)1.0000*3(8.6%)13(2.6%)0.08*
Vomiting,n(%)357(67.4%)87(58.8%)270(70.7%)0.0125(71.4%)332(67.1%)0.60
Medicalhistory
CCIscore,mean(SD)4.2(3.1)3.7(2.8)4.5(3.2)0.015.3(3.4)4.2(3.0)0.04
PreviousSBO,n(%)263(49.6%)52(35.1%)211(55.2%) <0.000110(28.6%)253(51.1%)0.01
Crohn’sdisease,n(%)53(10.0%)7(4.8%)46(12.0%)0.012(5.9%)51(10.3%)0.56*
Ulcerativecolitis,n(%)42(7.9%)9(6.1%)33(8.6%)0.340(0.0%)42(8.5%)0.10*
Intestinalcancer,n(%)67(12.6%)9(6.1%)58(15.2%)0.0053(8.6%)64(12.9%)0.60* (Continuedonnextpage) Volume26,No.1:January2025WesternJournal
Table1. Continued.
CharacteristicOverall(N = 530)
Yes(n = 148)No(n = 382) P-valueYes(n = 35)No(n = 495) P-value
Solidtumormalignancy,n(%)195(36.8%)37(25.0%)158(41.4%)0.000515(42.9%)180(36.4%)0.44
Previousabdominopelvic surgeries,n(%)
444(83.8%)117(79.1%)327(85.6%)0.0720(57.1%)424(85.7%) <0.0001
Anatomicdifferences,n(%)389(73.5%)95(64.6%)294(77.0%)0.00417(48.6%)372(75.3%)0.001
Diabetes,n(%)92(17.4%)32(21.6%)60(15.7%)0.116(17.1%)86(17.4%)0.97
Moderatetoseverekidney disease,n(%)
25(4.7%)5(3.4%)20(5.2%)0.374(11.4%)21(4.2%)0.07*
Leukemiaorlymphoma,n(%)16(3.0%)3(2.0%)13(3.4%)0.57*3(8.6%)13(2.6%)0.08*
Pepticulcerdisease,n(%)18(3.4%)5(3.4%)13(3.4%)0.990(0.0%)18(3.6%)0.62*
Visitmeasures
Triageheartrate >110bpm, n(%) 42(8.0%)16(10.9%)26(6.8%)0.124(11.4%)38(7.7%)0.51*
Triagerespiratoryrate >20, n(%) 23(4.4%)5(3.4%)18(4.7%)0.506(17.1%)17(3.5%)0.003*
TriageSBP <100mmHg, n(%)
28(5.3%)12(8.1%)16(4.2%)0.073(8.6%)25(5.1%)0.42*
Triagetemp >100.4 °F,n(%)4(0.8%)3(2.1%)1(0.3%)0.07*1(3.0%)3(0.6%)0.23*
TriageO2 <90%,n(%)10(1.9%)4(2.7%)6(1.6%)0.48*2(5.7%)8(1.6%)0.14* Nasogastricdecompression, n(%)
342(64.5%)106(71.6%)236(61.8%)0.0324(68.6%)318(64.2%)0.60
Gastrografinadministration, n(%) 83(15.7%)14(9.5%)69(18.1%)0.017(20.0%)76(15.4%)0.46
Focaltendernesson examination,n(%)
206(38.9%)57(38.5%)149(39.0%)0.5513(37.1%)193(39.0%)0.97
Reboundtenderness/ peritonitisonexamination, n(%) 13(2.5%)3(2.0%)10(2.6%)0.900(0.0%)13(2.6%)0.14
Distensiononexamination, n(%)
Diffusetendernesson examination,n(%)
CT findings
Presenceofatransitionpoint onCT,n(%)
Presenceoffree intraperitoneal fluidonCT, n(%)
Debrisandgasbubbleswithin thedilatedsmallbowellumen onCT,n(%)
228(43.0%)62(41.9%)166(43.5%)0.3919(54.3%)209(42.2%)0.24
277(52.3%)73(49.3%)204(53.4%)0.1416(45.7%)261(52.7%)0.64
475(95.0%)134(97.1%)341(94.2%)0.1830(88.2%)445(95.5%)0.08
278(55.5%)80(57.6%)198(54.7%)0.5622(64.7%)256(54.8%)0.26
174(35.2%)37(27.4%)137(38.2%)0.038(23.5%)166(36.1%)0.13
MesentericedemaonCT, n(%) 183(36.8%)53(38.4%)130(36.1%)0.6311(32.4%)172(37.1%)0.58
Volvulusorclosed-loop obstructiononCT,n(%) 61(12.2%)42(30.4%)19(5.2%) <0.00015(14.7%)56(12.0%)0.59*
*P-valuecalculatedbytheFisherexacttest. CCI,CharlsonCoborbidityIndex; SBO,smallbowelobstruction; CT,computedtomography; bpm,beatsperminute; SBP,systolicblood pressure; mmHg,millimetersofmercury; O2,oxygensaturation.
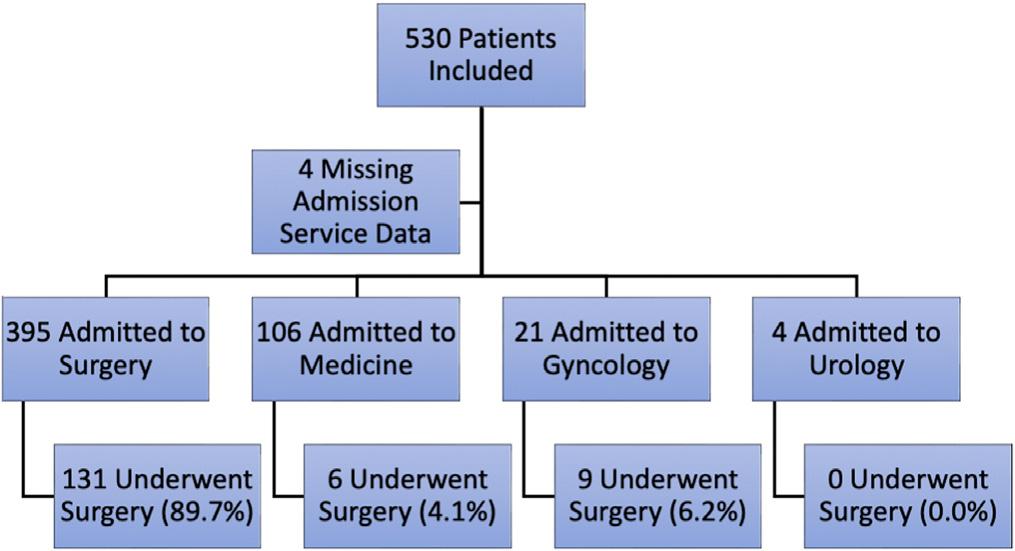
variousadmittingservices(Figure1)and35(6.6%)hadat leastonecomplication(Table2).
Weidentifiedunivariateassociationsofthedecisionfor surgicalintervention(Table1).Inourmultivariableanalysis, weidentifiedthreeindependentfactorsassociatedwitha higheroddofsurgicalintervention: fluidorvolvulus/closedloopobstructiononCT(OR7.95,95%CI4.25–15.39), nasogastricdecompression(OR2.04,95%CI1.25–3.39), andinitialsystolicbloodpressure <100millimetersof mercury(OR2.65,95%CI1.05–6.53)(Table3).Fourfactors
Table2. Occurrenceofoutcomes.
OutcomeN(%)
Surgery148(27.9%)
Complication35(6.6%)
Sepsis16(3.0%)
Intubation12(2.2%)
Vasopressordependentshock11(2.0%)
Anatomicsurgicalalteration1(0.2%)
Bowelperforation8(1.5%)
Table3. Resultsofmultivariablelogisticregressionanalysisfor decisionforsurgery.
Variable
Oddsratio (95%CI)
Historyofabdominaldistension0.27(0.10–0.62)
Gastrogra fin0.41(0.20–0.81)
PreviousSBO0.42(0.26–0.66)
HigherCCIscore0.87(0.80–0.95)
Nasogastricdecompression2.04(1.25–3.39)
Initialsystolicbloodpressure <100mmHg2.65(1.05–6.53)
Free fluidorvolvulus/closed-loopobstruction onCT 7.95(4.25–15.39)
CI,confidenceinterval; SBO,smallbowelobstruction; CCI,Charlson ComorbidityIndex; mmHG,millimetersofmercury; CT,computedtomography.
wereassociatedwithloweroddsofsurgicalintervention: HigherCCIscore(OR0.87,95%CI0.80–0.95),abdominal distensioninhistory(OR0.27,95%CI0.10–0.62),previous SBO(OR0.42,95%CI0.26–0.66),andgastrografin administration(OR0.41,95%CI0.20–0.81).TheAUCfor thelogisticregressionwas0.73.
ThegeneraltreatmentmethodofSBOsisshiftingtoward non-operativemanagement.Whiletherehavebeenattempts toconstructbetterguidelinessuchastheBolognaguidelines, thereisstillnodefinitiveconsensus.5 Weproposethatthese clinicaldecisionalgorithmscanbestrengthenedby incorporatingspecificfactors.Anexampleofasimple predictormodelisseenintheretrospectivestudybyKomatsu etal,wheretheycreatedafour-pointsystemscoringtherisk forsurgeryinpatientsundergoingconservativestrategywith theirthreevariables.11 Paststudiesregardingsurgical associationsforSBOshavemixedresults.Free fluidonCT wasfoundasapositivepredictorforsurgeryinsome studies.3,6,12 However,alaterprospectivevalidationstudy foundthatfree fluidwasnotapredictor.13
Ourresultsdemonstratedthatfree fluidorvolvulus/ closed-loopobstructionwaspositivelyassociatedwithan ORof7.95(95%CI4.25–15.39).Itisimportanttonotethat ourresultisacombinationoftwodistinctvariables;we foundthatonewasfoundtobecompletelypredictiveofthe otherand,therefore,wemergedthetwovariables.Another CT finding,namelymesentericedemahaspreviouslybeen attributedasapositivepredictor.13 Ourresults,however,did notidentifymesentericedemaassignificantintheunivariant analysisandwasnotincludedinthemultivariantmodel. Interestingly,wefoundpriorSBOtobeanindependent association,whichisprotectiveforthedecisionforsurgery withanORof0.42(95%CI0.26–0.66).InbothZielinskietal studiespriorSBOswereseenasprotectiveforoperative managementintheirunivariateanalysis,butitwasnot significantintheirregressionmodels.3,13 PriorSBOwasalso foundtobesignificantinthebivariateanalysesintheO’Daly etalstudybutwasnotsignificantintheirregressionmodel.12 Thisisincontrasttotheresultsofanotherstudythatdidnot findpriorSBOstobesignificantintheirunivariateanalysis witha P -valueof0.93.6 Apossibleexplanationforwhyprior SBOsisprotectiveinthedecisionforsurgeryisthatthere mightbeahigherriskofrecurrenceinpatientswhoreceived conservativetreatment,whiletheneedforsurgicalreinterventionwasnotdifferentbetweennon-surgicaland surgicalmanagement.7 Thiscoupledwithapossiblebiason theclinician’spartthatifapreviousmanagementworkedthe clinicianmightfavoritagain,wouldinfluencethenumberof patientswhoreceivedconservativetreatmentinourstudy timeframe.Therewillsimplybemorepatientswithprevious SBOsthathavebeentreatedconservativelyinthat giventime.
GastrografinhasrecentlybeenincludedinsomeevidencebasedpapersregardingSBOmanagementanddecisionmaking.5,14 Itisahyperosmolarwater-solublecontrast mediumshowntohaveadiagnosticandprognostic,aswell asapotentialtherapeutic,effectforpatientswithSBO.15–17 Theprognosticandtherapeuticpropertiesofgastrografin havebeenappreciatedduringagastrografinchallenge,when thepatientingestsgastrografineitherorallyorthrougha nasogastrictube,andmultipleradiographsaretakeninthe spanof24hourstoassesspassageofcontrast.Threelarge systematicreviewsandmeta-analyseshavedeterminedwhen gastrografinhaspassedthroughthepatient’sgastrointestinal tractandreachedthecolonwithin24hours,thepatientmost likelydoesnotneedsurgeryandcan,therefore,betreated conservatively.Additionally,allthreestudiesfoundthatthe admissionofgastrografinshortenedtheduration ofhospitalization.15–17
Wefoundthatgastrografinwasanindependentnegative associationforsurgery(OR0.41,95%CI0.20–0.81).While theremaybeselectionbiasforlessacutelyillpatients,itis hypothesizedthatthereisatherapeuticeffectofgastrografin, whichmaydecreasetheneedforsurgery.Alargesystematic reviewandmeta-analysisinvolving1,216patientsfrom12 studiesfoundtheORforsurgeryinterventionafter gastrografinadministrationtobe0.55(95%CI0.32–0.37, P = 0.003)15.Thisisinlinewithanothersystematicreview andmeta-analysis findingtheORtobe0.62(95%CI 0.44–0.88, P = 0.007)16
Theprimarylimitationtoourstudyisitsretrospective, single-centerdesign,whichleftusopentoselectionbias. Anotherlimitationisthatsurgeonpracticevariabilitymay notbegeneralizabletootherinstitutions.Inaddition,our chartreviewmethodologytocollectingdatainherentlymade ussusceptibletomisclassificationbias.Itisalsopossiblethat patientsmayhavere-presentedtoanotherhospitalwithout ourknowledgeandthosepotentialcomplicationsand outcomeswerelosttofollow-up.Ourstudyisfurtherlimited byoursmallsamplesize,andwewereunabletoincorporate allvariablesandcomplicationswefoundsignificantintothe multivariantmodel.Additionally,byusingsurgeryasan endpoint,wemayhavecapturedpatientswhoreceived surgerybutdidnotunequivocallyneedsurgery.Finally,we didnotclassifywhichpatientswereadmittedtoasurgical serviceasthatmayhaveimpactedthedecisiontoperform surgeryiftheywerenotonasurgicalservice.
Wefoundsevenindependentfactorsassociatedwith surgery.Webelievethatthesemayhelpcliniciansdetermine whichEDpatientsrequiresurgicalintervention.Thereare conflictingresultsinthecurrentliteratureandfurther researchisneededtodeterminemoreaccuratealgorithms
andpatientmanagementofpatientswithsmallbowel obstruction.Webelieveourlargerretrospectivestudy providesanimportantadvancementinpotentially formulatingbetterpredictionmodelstopreventunnecessary surgery.Thisresearchisimperativeforthemanagementof SBOs,asunnecessarysurgeryyieldsahigher resourceutilizationandcanleadto furthercomplications.2–4,7
Futurestudiesshouldincludelarge,prospective,multiinstitutionalstudiesencompassingawiderangeofvariables andCTparameters,ascurrentliteratureislimited.Additional predictionmodelsandalgorithmsshouldbetestedin combinationwiththeadministrationofgastrografintobuilda comprehensivemanagementplanforpatientswithSBO.
AddressforCorrespondence:DanielJ.Berman,MD,BethIsrael DeaconessMedicalCenter,EmergencyDepartment,1Deaconess Rd.,Boston,MA02215.Email: daniel.berman25@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Bermanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.MatsushimaK,SabourA,ParkC,etal.Managementofadhesivesmall bowelobstruction:adistinctparadigmshiftintheUnitedStates. J TraumaAcuteCareSurg. 2019;86(3):383–91.
2.MillerG,BomanJ,ShrierI,etal.Etiologyofsmallbowelobstruction. Am JSurg. 2000;180(1):33–6.
3.ZielinskiMD,EikenPW,BannonMP,etal.Smallbowelobstruction whoneedsanoperation?Amultivariatepredictionmodel. WorldJSurg. 2010;34(5):910–9.
4.KrielenP,vandenBeukelBA,StommelMWJ,etal.In-hospitalcostsof anadmissionforadhesivesmallbowelobstruction. WorldJEmergSurg. 2016;11:49.
5.TenBroekRPG,KrielenP,DiSaverioS,etal.Bolognaguidelinesfor diagnosisandmanagementofadhesivesmallbowelobstruction(Asbo): 2017updateoftheevidence-basedguidelinesfromtheWorldSocietyof EmergencySurgeryASBOworkinggroup. WorldJEmergSurg. 2018;13:24.
6.KulvatunyouN,PanditV,MoutamnS,etal.Amulti-institution prospectiveobservationalstudyofsmallbowelobstruction: clinicalandcomputerizedtomographypredictorsofwhich patientsmayrequireearlysurgery. JTraumaAcuteCareSurg. 2015;79(3):393–8.
7.HajibandehS,HajibandehS,PandaN,etal.Operativeversusnonoperativemanagementofadhesivesmallbowelobstruction:a systematicreviewandmeta-analysis. IntJSurg. 2017;45:58–66.
8.TaylorMRandLalaniN.Adultsmallbowelobstruction. AcadEmerg Med. 2013;20(6):528–44.
9.SchraufnagelD,RajaeeS,MillhamFH.Howmanysunsets?Timingof surgeryinadhesivesmallbowelobstruction:astudyofthenationwide inpatientsample. JTraumaAcuteCareSurg. 2013;74(1):181–7; discussion187–9.
10.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
11.KomatsuI,TokudaY,ShimadaG,etal.Developmentofasimplemodel forpredictingneedforsurgeryinpatientswhoinitiallyundergo conservativemanagementforadhesivesmallbowelobstruction. AmJ Surg. 2010;200(2):215–23.
12.O’DalyBJ,RidgwayPF,KeenanN,etal.Detectedperitoneal fluidin smallbowelobstructionisassociatedwiththeneedforsurgical intervention. CanJSurg. 2009;52(3):201–6.
13.ZielinskiMD,EikenPW,HellerSF,etal.Prospective,observational validationofamultivariatesmall-bowelobstructionmodelto predicttheneedforoperativeintervention. JAmCollSurg. 2011;212(6):1068–76.
14.AzaguryD,LiuRC,MorganA,etal.Smallbowelobstruction:apractical step-by-stepevidence-basedapproachtoevaluation,decision making,andmanagement. JTraumaAcuteCareSurg. 2015;79(4):661–8.
15.CeresoliM,CoccoliniF,CatenaF,etal.Water-solublecontrastagentin adhesivesmallbowelobstruction:asystematicreviewand meta-analysisofdiagnosticandtherapeuticvalue. AmJSurg. 2016;211(6):1114–25.
16.BrancoBC,BarmparasG,SchnürigerB,etal.DemetriadesD. Systematicreviewandmeta-analysisofthediagnosticandtherapeutic roleofwater-solublecontrastagentinadhesivesmallbowelobstruction. BrJSurg. 2010;97(4):470–8.
17.AbbasSM,BissettIP,ParryBR.Meta-analysisoforalwater-soluble contrastagentinthemanagementofadhesivesmallbowelobstruction. BrJSurg. 2007;94(4):404–11.
MeredithB.Haag,MD,MPH*°
CatlinH.Dennis,MPH*†°
StevenMcGaughey,MD,MCI‡
TessA.Gilbert,MHS†
SusanDeFrancesco,JD,MPH†
AdrienneR.Gallardo,MA*
BenjaminD.Hoffman,MD*
KathleenF.Carlson,MS,PhD†
SectionEditor:MarkI.Langdorf,MD,MHPE
*DoernbecherChildren’sHospital,OregonHealthandScienceUniversity,School ofMedicine,andDoernbecherInjuryPreventionProgramTomSargentSafety Center,DepartmentofPediatrics,Portland,Oregon
† OregonHealthandScienceUniversity-PortlandStateUniversity,SchoolofPublic Health,Portland,Oregon
‡ OregonHealthandScienceUniversity,DepartmentofEmergencyMedicine, Portland,Oregon
° Authorsareco-primaryauthors
Submissionhistory:SubmittedMay16,2024;RevisionreceivedOctober4,2024;AcceptedOctober10,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21205
Introduction: TheAmericanCollegeofEmergencyPhysicianssupportscommunity-andhospitalbasedprogramsthatintervenetoprevent firearm-relatedinjury.Tothisend,thedistributionof firearm locksorstoragedevicesintheemergencydepartment(ED)mayhelpachievethistarget.Toinform secure firearmstorageprogramsforhouseholdswithchildrenand firearms,weexamined firearm storagepractices,devicepreferences,andcosttoleranceamongparents/caregiversofchildren.
Methods: BetweenApril2018–November2019,weconductedandanalyzedanin-personsurveyof294 caregivers,aged ≥18,withbothchildrenand firearmsinthehome.Surveysassessedreasonsfor firearm ownership,storagepracticesanddevicepreferencesamong fivestorage-deviceoptions,andprices participantswerewillingtopayfordevices.Practicesandpreferenceswereexaminedbyparticipant characteristics.Weusedlogisticregressiontoestimateoddsratiosand95%confidenceintervalsfor associationsofinterest.
Results: Mostparticipants(73%)reportedpersonalprotectionasareasonforowning firearms,and nearly80%ownedatleastone firearmstoragedevice.Overhalf(55%)ownedcablelocks,butonly36% ofownersreportedregularlyusingthem.Rapid-accessdevices(electronicandbiometriclockboxes) werelesscommonlyowned(26%)butmorelikelytoberegularlyused(73%).Themosthighlyrated storagedevicefeatureswerethefollowing:theabilitytostorethe firearmunloaded(87.3%);theabilityto storethe firearmloaded(79.1%);anddeviceaffordability(65%).Mostparticipants(78%)preferredrapidaccessdevicesoverotheroptions.Participantswerewillingtopaymoreforproductsthataffordedrapid accesstothe firearm.Participantsreportedtheywouldpayamedianof$100forapushbuttonrapidaccessproduct($80retail),and$150forabiometriclockbox($210retail).
Conclusion: Understandingthestoragepracticesandpreferencesamong firearm-owninghouseholds withchildrencanhelpinformEDinjury-preventionscreeningand firearmsafetypracticeimplementation. Ourresultssuggestthatrapid-accessdevicesmaybethemostpreferable firearmstoragedevicesfor distributionbysecurestorageprograms,andcostsarelikelyminimalgivenparental/caregiver willingnesstopay.[WestJEmergMed.2025;26(1)142–146.]
Firearminjuriesarethesingleleadingcauseofdeathfor childrenintheUnitedStates.1 Despitetheirinherentrisk, firearmsremainaccessibletomanychildren:estimates suggestthatoneinthreeUShomeshaveatleastone firearm, themajorityofwhicharenotstoredsecurely.2,3 The AmericanCollegeofEmergencyPhysicians(ACEP) supportscommunity-andhospital-basedprogramsthat intervenetoprevent firearm-relatedinjury.Tothisend,the distributionof firearmlocksorstoragedevicesinthe emergencydepartment(ED)maybeeffective.4 However, underutilizationofthesedevicessuggeststhatcurrent distributionstrategiesdonotmeettheneedsof firearmowners. 5–7
Currently,thereislimitedknowledgeabout firearm storagepreferencesamongcaregiversofchildren.While priorliteraturehasindicatedthatthecostsof firearmsafes canbeadeterrenttotheiruse,toourknowledgethereisno publishedresearchregarding firearmowners ’ willingnessto payforothertypesofstoragedevicesorlocks.8,9 Thisis criticaltounderstandthecostsandfeasibilityof implementationof firearminjurypreventionprograms.Our aimwastodescribecaregiver firearmowners ’ preferences for,currentuseof,andwillingnesstopayforstoragedevices toinformpreventionstrategies.
Weconductedanin-person,cross-sectionalsurveyof firearm-owningparents/caregiversofchildrenbetweenApril 2018–February2019.Wesurveyedaconveniencesampleof caregiversofchildrenat10communitysites.Thesesiteswere geographicallyclusteredintwomajormetropolitanareas withparticipantsdrawingmainlyfromtwowesternstates. Sitesincludedanoutdoorsportingactivitiesfair,regional firearmshow,academicchildren’shospitalsafetycenter event,andmultiplelargecommunityeventsacrosstwo metropolitanareas.Eligibilitycriteriaforcaregivers includedthefollowing:1)aged ≥ 18years;2)having children(aged < 18years)spendingtimeinthehome; 3)currentornear-futurepossessionof firearm(s);and 4)Englishlanguageproficiency.Approvalforthe studywasobtainedfromourlocalinstitutionalreview board(IRB#00017762).
Procedures
Participantswererecruitedbytabling,andallsurveys wereconductedinpersonbymembersoftheresearchteam. Interestedparents/caregivers,ofwhom294meteligibility criteria,completedanonlineconsentformandanonymous surveyelectronicallyoronpaper,whichwerestoredvia ResearchElectronicDataCapture(REDCap),hosted atOregonHealth&ScienceUniversity.10,11
Surveymeasureswereadaptedfromaninstrumentusedin a firearmstoragepreferencesurveyatanotherinstitution.7 Thesurveyassessedparticipants’ sociodemographic characteristics, firearmownership, firearmandammunition storagepractices,andtheirstoragedevicepreferencesand featuresthatinfluencedtheirpreference.Thesurveyasked participantstoconsider fivedifferent firearmstoragedevices: 1)cablelock;2)LifeJackettriggerlock;3)lockboxwith combinationaccess;4)electronicpushbutton-access lockbox;and4)biometric-access(fingerprint)lockbox. Participantswereaskedtoratetheimportanceofdevice features.Theamountofmoneyparticipantswould bewillingtopayforeachdevicewasthenelicitedusinga slidingscale.
Usingdescriptiveanalyses,weexaminedparticipants’ storagepractices,devicepreferences,andwillingnesstopay bytheirsociodemographiccharacteristicsandreasonsfor firearmownership.Mediansarereportedforthe nonparametricwillingness-to-paydata.Bivariablelogistic regressionanalyseswereperformedtoestimateassociations betweenparticipantcharacteristicsandlikelihoodofthe following:1)storing firearmslocked;2)storing firearms unloaded;and3)storingammunitionlockedseparatelyatall times.Associationsarereportedasoddsratios(OR)with 95%confidenceintervals(CI).
Participantspredominantlywereaged25–34(40.3%), White(81.1%)andownedbothhandgunsandlongguns (68.3%).Socioeconomicfactorsincludingincomeand educationlevelwerenotstatisticallydifferentamongtabling sites(Table1).Amongthosewhorespondedtotheopenendedquestionassessingprimaryreasonfor firearm ownership,most(72.7%)reportedpersonal/homeprotection, whilehunting/recreationwastheexclusivereasonfora minority(20.2%).Weestimatea15%responserateofall eventparticipantsand40%ofparticipantswho wereapproached.12
Nearly80%ofparticipantsreportedowningoneormore ofthe fivedisplayed firearmstoragedevices(Table2).The mostfrequentlyowneddevicewasacablelock(55.3%);fewer ownedrapid-accesspushbuttonorbiometricstoragedevices (26.5%and24.5%,respectively).Only36.3%ofcablelock ownersreportedalwaysusingtheirdevice,whereas73.4% and73.3%ofpushbuttonandbiometriclockboxowners, respectively,reportedalwaysusingtheirdevices.Only28.5% ofparticipantsreportedcompliancewithAmerican
Table1. Characteristicsof259surveyparticipants,bymostpreferred firearmstoragedevice. Preferredstoragedevice
Totala N(%) Cablelock n(%) Lifejacket n(%) Combination lockboxn(%)
Pushbutton lockboxn(%)
Biometric lockboxn(%)
Total259(100)13(5.0)7(2.7)12(4.6)48(18.5)152(59.1)-
Age------0.06
18–2415(6.3)2(13.3)1(6.7)2(13.3)010(66.7)-
25–
3496(40.3)5(5.4)5(5.4)2(2.2)24(26.1)56(60.9)-
35–4481(34.0)4(5.2)05(6.5)13(16.9)55(71.4)-
45+ 46(19.3)1(2.4)1(2.4)2(4.9)10(24.4)27(65.9)-
Sex------ 0.05
Female141(56.9)9(6.9)7(5.3)8(6.1)28(21.4)79(60.3)-
Male107(43.2)3(3.0)04(4.0)20(19.8)74(73.3)-
Race------0.25
White201(81.1)8(4.3)6(3.2)12(6.4)37(19.7)125(66.5)OtherthanWhite47(19.0)4(9.1)1(2.3)011(25.0)28(63.6)-
Education------0.39
Highschoolorless34(13.8)3(10.3)1(3.5)4(13.8)2(6.9)19(65.5)Vocationalschool/some college 70(28.3)3(4.5)2(3.0)1(1.5)14(20.9)47(70.2)-
College97(39.3)4(4.4)3(3.3)4(4.4)23(25.0)58(63.0)Graduate/professional school 46(18.6)2(4.7)1(2.3)3(7.0)9(20.9)28(65.1)-
Income------0.94
$49,999orless59(22.8)4(7.4)1(1.9)3(5.6)11(20.4)35(64.8)$50,000ormore200(77.2)9(5.0)6(3.4)9(5.0)37(20.7)118(65.9)-
Militaryorlawenforcement inhome ------0.62
Yes53(22.4)3(4.2)1(1.4)3(4.2)19(26.4)46(63.9)No184(77.6)8(5.2)6(3.9)9(5.8)28(18.2)103(66.9)Reasonfor firearm ownership ------0.70
Personalprotectiononly83(41.9)3(4.0)3(4.0)3(4.0)18(24.0)48(64.0)Hunting/recreationonly40(20.2)3(7.9)1(2.6)2(5.3)7(18.4)25(65.8)Both61(30.8)2(3.4)1(1.7)3(5.1)11(18.6)42(71.2)Other14(7.1)2(14.3)1(1.7)1(7.1)4(28.6)6(42.9)aTotalnmaynotequalsumofpreferredstoragedeviceselectionsduetomissingresponses. bAll P-valuesbasedonFisherexacttest. Boldfaceindicatesstatisticalsignificance(P ≤ 0.05).
AcademyofPediatrics(AAP)recommendations,storing firearmsunloadedandlocked,andwithammunition lockedseparately.Thosereporting firearmownershipfor personalprotectionandthosewithahousehold memberwithcurrent/pastmilitary/lawenforcementservice werelesslikelytopracticesecurestorage(OR0.4, 95%CI0.2–0.7)and(OR0.5,95%CI0.3–0.9), respectively(Table1).
Thelargestproportionsofparticipantsendorsed biometric(59.1%)andpushbuttonrapid-access(18.5%) lockboxesastheirmostpreferredstoragedevices(Table1). Themosthighlyratedstoragedevicefeatures with >60%ofthesampleindicatingtheywereeither “ very important” or “absolutelyessential” weretheabilityto storethe firearmunloaded(87.3%),theabilityto
Table2. Firearmstoragedeviceownership,use,andwillingnesstopaythresholds.
CablelockLifejacketCombinationlockboxPushbuttonlockboxBiometriclockbox n(%)n(%)n(%)n(%)n(%) Owndevice136(55.3)19(7.6)92(37.1)66(26.5)61(24.5)
Useallthetimea 49(36.3)6(33.3)49(53.3)47(73.4)44(73.3)
Pricewillingtopay
Median(IQR)$20(5–30)$30(15–50)$50(40–95)$100(60–120)$150(100–150) %Retailcost133%67%200%125%71%
aAmongthosewhoownrespectivedevice. IQR,interquartilerange.
storethe firearmloaded(79.1%),anddevice affordability(65.0%).
Acrossdemographicgroups,participantswerewillingto paymorethanretailpriceforcombinationlockboxes (medianwillingnesstopay = $50,vs$25actualretailcost) andpushbuttonrapid-accesslockboxes(median = $100,vs $80retail; Table2).Forthemostdesiredstorageoption, biometriclockboxes,surveyparticipantsindicated thehighestwillingness-to-paydollaramount ($150vs$210retail).
Thisstudyexamines firearmstorage-devicepreferences among firearm-owningparents/caregiversofchildren, describeshowstoragepracticesvarywiththeirreasonsfor firearmownership,andreportspricestheyarewillingtopay forthesedevices.Thisuniquedataaddsimportantcontextto interventionsfocusedontheprovisionof firearmstorage devicestofamilies.Previousinterventionshaveprimarily focusedondistributingcablelocks,likelyduetocost.4,5,7 However,thereislimiteddatademonstratingsustained behaviorchangeafterdistributionofcablelocks,andsurveys of firearmownersondevicepreferencesuggesttheyare undesirable.6,9,13,14 Resultsofourstudysuggestthatmost parents/caregiverswhoown firearmsdosoforreasonsof personalprotection,andthatstorageoptionsthatprovide rapidaccessmaybemostdesirable.
Ourstudycontinuestohighlighttheneedforimproved firearmstorageinhomeswithchildren.Although73.1%of respondentsendorsedstoringall firearmslocked,adherence toothercomponentsoftheAAPrecommendationswaslow, withfewerthanone-thirdofparents/caregiversinourstudy meetingallrecommendations.
Firearmownershipamongourparticipantswas motivatedbyconcernsaboutpersonalandfamilysafety, consistentwithpriorstudies.15 Morethanhalfofthesample (53.6%)identifiedtheabilitytostorea firearmloadedas “absolutelyessential.” Thus,itisnotsurprisingthat,while cablelockswerethemostfrequentlyowneddevice,only
one-thirdofcablelockownersreportedregularlyusingthem. Incontrast,amongrapid-accessdeviceowners,nearlythreefourthsreportedregularuse.Rapid-accessdevicesoffer parents/caregiversanopportunitytosecurelystoretheir firearmswhennotinuse,whichmayleadtoahigher prevalenceoflocked firearmsand,potentially,reducedrisk tochildreninthesehomes.
Topreventunintendedaccessof firearmsbychildren/ youthinahome,preferredsecurestorageoptionsmustbe financiallyattainable.Whilerapid-accessdevicesaremore expensivethanothermodalities,ourrespondentsplaced greatervalueonthem,asdemonstratedbythemedian amounttheywerewillingtopay:$100forpush-button lockboxesand$150forthebiometriclockboxes.Sinceour surveycollection,marketforceshavedrivendowncosts,with biometriclockboxesroutinelybeingsoldforlessthan$100. Thisdatahasinformedourinstitution’ sown firearmstorage deviceofferingsbystockingbiometricandrapid-access lockboxes.Futurestudiesshouldfocusonidentifyinggroups thatmaybenefitmostfromeducationongunsafetydevices. Thisincludesinvestigatingtherelationshipbetweenchildage andmotivationtousestoragedevicesandexpandingthe surveyintomoregeographically,racially,and socioeconomicallydiversecommunities.
TheACEPstatesthat “emergencyphysiciansshould advocateforevidence-basedinjurypreventionpolicies.” Our datasuggeststhatrapid-accessstoragedevicesareadesired andvaluedpreventionstrategythatcanbeemployedbyEDs. Integratedintoastandardintakeprocess,non-partisan discussionaround firearmstorageandprovidingaccessto thesedevicescouldbeameaningfulmethodforEDstomeet advocacygoals.
Thereareseverallimitationsofthisresearch.First,this descriptivestudyinvolvedaconveniencesampleof individualsattendinghealthcareappointmentsor communityeventsinapredominantlyurbanarea.However, wecollecteddatafromawidevarietyofeventstoincreasethe diversityofparticipants.Second,oursmallsamplesize limitedtheprecisionofourestimates.Third,social
desirabilitymayhaveinfluencedparticipants’ responses.We mitigatedthislimitationbyconductinganonymoussurveys, whichwasemphasizedduringsurveyprocedures.Lastly,our estimatedresponserateswerelow.Thiswasmitigated byemployingashortsurveyandofferinga$5giftcard uponcompletion.
Existing firearmstorage-devicedistributionprogramsand practicesmaynotmeettheneedsofall firearmowners. Parents/caregiverswhoown firearmsmaymostprefer,and bemostlikelytouse,rapid-accessoptions.Whilethese deviceshavehighercosts,theyaremorelikelytohave sustaineduseandtheircostsarealignedwithperceivedvalue. WeadvocatethatED firearminterventionprogramsfocus ondevicesthatalignwithfamilies’ priorities,whichmay improvesustaineduseand,ultimately,helpdecreasetherates of firearm-relatedmortalityandmorbidityamongchildren.
AddressforCorrespondence:StevenMcGaughey,MD,MCI, OregonHealthandScienceUniversity,department,3181SWSam JacksonParkRd.,MailCode:CDW-EMPortland,OR97239.Email: mcgaughe@ohsu.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisworkwaspartiallyfundedbygrants totheDoernbecherTomSargentSafetyCenterfromtheInjuryFree CoalitionforKids,andbyatraininggranttoCatDennisfromthe NorthwestCenterforPublicHealthPractice(Region10),University ofWashington(June2018).Thisworkwasalsosupportedbythe NationalCenterforAdvancingTranslationalSciencesoftheNational InstitutesofHealthunderawardnumberUL1TR0002369toOregon HealthandScienceUniversity.Nostudysponsorshadaroleinstudy design,collection,analysis,datainterpretation,writingofthereport, orthedecisiontosubmitthereportforpublication.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Haagetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CentersforDiseaseControlandPrevention.Web-basedinjurystatistics queryandreportingsystem(WISQARS).2024.Availablefrom https:// wisqars.cdc.gov/.AccessedMay1,2024.
2.AzraelD,CohenJ,SalhiC,etal.Firearmstorageingun-owning householdswithchildren:resultsofa2015nationalsurvey. JUrban Health. 2018;95(3):295–304.
3.JohnsonRM,Coyne-BeasleyT,RunyanCW.Firearmownershipand storagepractices,U.S.households,1992–2002.Asystematicreview. AmJPrevMed. 2004;27(2):173–82.
4.Rowhani-RahbarA,SimonettiJA,RivaraFP.Effectivenessof interventionstopromotesafe firearmstorage. EpidemiolRev. 2016;38(1):111–24.
5.BarkinSL,FinchSA,IpEH,etal.Isoffice-basedcounselingabout mediause,timeouts,and firearmstorageeffective?Resultsfroma cluster-randomized,controlledtrial. Pediatrics. 2008;122(1):e15–25.
6.HornA,GrossmanDC,JonesW,etal.Communitybased programtoimprove firearmstoragepracticesinruralAlaska. InjPrev. 2003;9(3):231–4.
7.SimonettiJA,SimeonaC,GallagherC,etal.Preferencesfor firearm lockingdevicesanddevicefeaturesamongparticipantsina firearm safetyevent. WestJEmergMed. 2019;20(4):552–6.
8.GaffleyM,RauhJL,GardnerA,etal.Storagepractices,devices,and presenceofchildrenamongownersof firearms:informingpediatric firearmsafety. AmSurg. 2023;89(12):5891–6.
9.AnestisMD,Moceri-BrooksJ,JohnsonRL,etal.Assessmentof firearmstoragepracticesintheUS,2022. JAMANetwOpen. 2023;6(3):e231447.
10.HarrisPA,TaylorR,MinorBL,etal.TheREDCapconsortium:building aninternationalcommunityofsoftwareplatformpartners. JBiomed Inform. 2019;95:103208.
11.HarrisPA,TaylorR,ThielkeR,etal.Researchelectronicdatacapture (REDCap)–ametadata-drivenmethodologyandworkflowprocessfor providingtranslationalresearchinformaticssupport. JBiomedInform. 2009;42(2):377–81.
12.HalpernS,AschD,ShakedA,etal.Standarddefinitions: final dispositionsofcasecodesandoutcomeratesforsurveys. AmJTransplant. 2005;5(6):1319–25.
13.KingA,SimonettiJ,BennettE,etal.Firearmstoragepracticesin householdswithchildren:asurveyofcommunity-based firearmsafety eventparticipants. PrevMed. 2020;131:105952.
14.SimonettiJA,SimeonaC,GallagherC,etal.Preferencesfor firearm lockingdevicesanddevicefeaturesamongparticipantsina firearm safetyevent. WestJEmergMed, 2019;20(4):552–6.
15.ClevelandEC,AzraelD,SimonettiJA,etal.Firearmownershipamong Americanveterans: findingsfromthe2015NationalFirearmSurvey. Inj Epidemiol. 2017;4(1):33.
16.Buck-AtkinsonJ,McCarthyM,StanleyIH,etal.Firearmlockingdevice preferencesamong firearmownersintheUSA:asystematicreview. Inj Epidemiol. 2023;10(1):33.
17.NationalAcademiesofSciences,Engineering,andMedicine. Integrating firearminjurypreventionintohealthcare:proceedingsofa jointworkshopoftheNationalAcademiesofSciences,Engineering,and Medicine;NorthwellHealth;andPEACEInitiative.Washington,DC:The NationalAcademiesPress;2022.
EmineM.Tunc,MD* NeilUspal,MD†
LindseyMorgan,MD‡
SueL.Groshong,MLIS§
JulieC.Brown,MDCM,MPH†
*UniversityofTexasSouthwestern,DepartmentofPediatrics,Divisionof EmergencyMedicine,Dallas,Texas
† UniversityofWashington,DepartmentofPediatrics,DivisionofEmergency Medicine,Seattle,Washington
‡ UniversityofWashington,DepartmentofPediatrics,DivisionofNeurology, Seattle,Washington
§ SeattleChildren’sHospitalandResearchInstitute,LibraryandInformation Commons,Seattle,Washington
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedDecember1,2023;RevisionreceivedSeptember27,2024;AcceptedOctober8,2024
ElectronicallypublishedNovember21,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18611
Background: Thisisasystematicreviewinvestigatingthecorrelationbetweenseizuresidentifiableon electroencephalogram(EEG),clinicalexcitatorymovements(CEM),andketamineadministrationfor proceduralsedation.
Methods: WesearchedMEDLINE,EMBASE,CochraneCENTRAL,andWebofScienceinApril2021. Searchtermsincludedvariationsforketamine,myoclonus,seizures,statusepilepticus,and electroencephalography.Twoindependentreviewersassessedpapersbasedoneligibilitycriteria, whichincludedhumanstudieswhereEEGrecordingswereobtainedduringketamineadministration.
Results: Eightpaperswereeligibleforinclusionwith141subjects(24children).Sevenstudies(133 subjects)reportedepilepsyhistory;70%(94/133)ofthesesubjectshadapre-existingepilepsy diagnosis.No(0/39)subjectswithoutepilepsyand28%(26/94)ofsubjectswithepilepsyhad electrographicseizuresafterketamineadministration.Infourstudieswherepediatricandadultsubjects couldbeseparated,childrenwithepilepsyhadelectrographicseizuresin60%(3/5)ofcasescompared to28%(6/33)ofcasesofadultswithepilepsy.Ofthesubjectswithepilepsy,14%(10/74)hadCEMsvs 5%(1/21)insubjectswithoutepilepsy.MostCEMs(9/11)weretemporallycorrelatedwith electrographicseizures.
Conclusions: Our findingsindicatethatinsubjectswithepilepsy,electrographicseizureswere frequentlyseenwithketamineadministrationandwerecorrelatedwithCEMs.Noseizureactivityafter ketaminewasseeninsubjectswithoutepilepsy.Whiletheclinicalsignificanceofthese findingsneeds furtherinvestigation,cliniciansmaywanttoconsiderpatients’ seizurehistorywhenprovidingcounseling ontherisksandbenefitsofketaminesedation.[WestJEmergMed.2025;26(1)147–154.]
Background Ketamineisoneofthemostusedanestheticmedications forproceduralsedation.Inchildren,ketamineisthesedative ofchoiceinupto80%ofchildrenintheemergency department(ED),1 whileinadultsketamineisgaining
increasingfavorbasedonitsdesirablesafetyprofile.2 Itisadissociativeanestheticthatcreatesaperceptionof detachmentfromenvironmentandself.3 Lowratesof respiratoryandcardiovascularadverseeventsmake ketamineafavorablepreferredforproceduralsedation comparedtootherpopularanestheticmedications.1,2
Oneoftheassociatedsideeffectsofketamine,recognized sinceitwas firstdiscoveredin1960s,areexcitatory movementssuchastwitchingandhypertonicity.4 In2009, basedontheconsensusguidelinesonreportingadverse eventsduringproceduralsedation,thesemovementswere termedasclinicalexcitatorymovements(CEM)and classifiedintothreegroups:myoclonus;musclerigidity;and generalizedmotorseizures.5 MostCEMsareofshort duration,butevenwhenself-limitedthesemovementsmay causedistresstocaregiversorstaffastheyresembleseizures. ItisunclearwhetherCEMsareepilepticorareunrelatedto seizureactivity.Giventhisambiguity,itisimportantto understandtheriskofseizureswithketamineadministration suchthatclinicianscanbetterweightherisksandbenefitsof thismedication.
TheunderlyingetiologiesofCEMsareunknown.To determinewhetherCEMsareseizurerelated,aconcurrent electroencephalogram(EEG)isnecessary,particularlyas sedationmayalterdistinguishingepilepticfeaturessuchas pupillarychangesoreyemovements(ie,nystagmus), alterationsinmentation,ormotormanifestations.6 Weconductedasystematicreviewtoanswertwo questions:1)Doesketamineinduceelectrographicseizures; and2)areketamine-inducedCEMsassociatedwith electrographicseizureswithspecialattentionto pediatricsubjects?
METHODS
StudyDesign
WefollowedthePreferredReportingItemsforSystematic ReviewsandMeta-Analyses(PRISMA)guidelinesforthis systematicreview.7 Asearchstrategywasdevelopedin conjunctionwithamedicallibrarian.WesearchedOvid MEDLINE(1946toApril27,2021),ElsevierEMBASE (1974toApril2021),CochraneCentralRegisterof ControlledTrials(CENTRAL)(TheCochraneLibrary , Issue3of12,March2021)andWebofScienceCore Collection,ScienceCitationIndex(1985toApril2021).The MEDLINEsearchwasperformedusingMedicalSubject Headingsandtextwordsforketamine,myoclonus,seizures, statusepilepticus,andEEG.TheMEDLINEstrategywas adaptedtosearchtheotherdatabases.Resultswerelimited toEnglish-languagepublications.Inclusioncriteriawerethe useofhumanstudysubjectsandtheuseofEEG testingduringketamineadministration.Weexcludedstudies usingketamineforpatientswithongoingseizures. Comments,editorials,letters,notes,andconference abstractswereexcludedinMEDLINEandEMBASE. Thedetailsofthesearchstrategycanbeaccessed in Supplement1.
Recordswerescreenedbytitleandabstract,andall potentiallyrelevantpaperswereobtainedforfull-textreview. Full-textpaperswereincludedbasedontheinclusion criteria.Weincludedadditionalreportsbasedonreviewof
includedpapercitations.Eachmanuscriptwasabstractedby investigatorsETandNUindependently,anddiscrepancies wereresolvedbyconsensus.
Thereweretwoprimaryoutcomes:1)thefrequencyof electrographicseizuresrecordedonsurfaceand/ordeep electrodesfollowingketamineadministration(excluding studiesusingketamineforpatientswithongoingseizures) and2)theprevalenceofconcurrenceofketamine-induced CEMswithelectrographicseizures.
WeidentifiedelectrographicseizuresasEEGrecordings withconcurrentelectrographicseizureactivity,asdefinedby theEEGdefinitionatthetimeofthepaperpublication.The EEGrecordingswererarelyavailableinthemanuscripts and,whenavailable,onlyincludedafewsecondsofthe recording.Thus,EEGswereconsideredpositivefor seizuresbasedontheauthors’ report.Avarietyof ketamine-inducedCEMswerereportedthatincluded twitching,myoclonicjerks,extremitytonicmovements, generalizedtonic-clonicmovements,andmajormotor convulsions.Increasedmuscletoneororofacialdyskinesias (nystagmus,tonguefasciculations)werenot consideredCEMs.
Wedefinedsubjectsaschildrenyoungerthan18years ofage.
Theinitialliteraturesearchresultedin583individual records.Afterreviewingtitlesandabstracts,20potentially eligiblepapersqualifiedforfull-textreview.Reviewofthe citationsforthe20reviewedpapersresultedinanadditional fivepotentiallyeligiblepapers,whichwerealsoretrievedfor fulltextreview.Afterthereviewofall25full-textpapers, eight8–15 wereincludedinthestudy(Figure).
Theseeightstudiesencompassed141subjects,including 24children.Infour8–10,14 ofthestudies(involving12adults and24children)ketaminewasusedforproceduralsedation; inthree12,13,15 studies(involving56adultsand40subjects whosesexwasnotspecified),ketaminewasadministeredto volunteersforresearchpurposesonly,andinone11 studyof 30adults,thepurposewasnotexplicitlystated.Sixofeight studieswerespecificallydesignedtoassessketamine’seffect onelectrographicseizures.8,9,12–15 Allstudiesused conventionalEEGwithsurfaceelectrodes.Surface electrodeswereplacedtotheskullintheinternational10–20 EEGdistribution.Inonestudywithnineepilepticsubjectsin additiontosurfaceelectrodes,deepelectrodesweresurgically implanted “bilaterallytolimbicregion(amygdala), hippocampus(anterior,middleandposteriorpes), andhippocampalgyrus(anterior,middleandposterior
Records identified from Ovid MEDLINE (n = 184)
EMBASE (n = 486)
Web of Science (n = 18)
Cochrane Central Register of Controlled Trials (n = 155)
Records screened with titles and abstracts (n = 583)
Full -text papers sought for retrieval (n = 20)
Full text papers assessed for eligibility (n = 25)
Studies included in review (n = 8) Included
Figure. FlowofstudyselectionreportedaccordingtoPRISMA2020guidelines.
gyrus).” Thedeepelectrodesrecordedelectrographic seizuresinallsubjectsreceivingmorethan2milligrams perkilogram(mg/kg)ketamine;however,this activitydidnotspreadtothecortex,assurface electrodesdidnotrecordanyelectrographic seizures9 (Table1).
Fourstudiesprovidedagedatasuchthatpediatric(16in threestudies)andadultsubjects(63infourstudies)couldbe reportedseparately.9–12 Theagerangeforpediatricsubjects inthesestudieswas3–17years.
Dataonelectrographicseizureswerereportedforall subjects.Allbutonestudy14 providedinformationon subjects’ epilepsystatus(Table1).Seventypercentofthe subjects(94/133)hadadiagnosisofepilepsy.Onlysubjects withepilepsy(28%,26/94)hadelectrographicseizures.This wasobservedforbothadultandpediatricsubjects(Table2). Onefourthofthoseseizures(7/26)wererecordedondeep electrodeswheresimultaneoussurfaceEEGdidnotshow electrographicseizures.Durationofelectrographic seizureswasseldomreported,butinthe fivecasesin whichdurationwasprovideditrangedfrom20seconds to3.5minutes.9,15
Records removed before screening: Duplicate records removed (n = 260)
Records excluded due to lack of relevant discussion in title and/or abstract (n = 542)
Reports included from additional literature search (n = 5)
Reports excluded: Due to lack of relevant discussion in text (n = 17)
ThepresenceorabsenceofCEMswasreportedfor94 subjects(66.7%).TheCEMsweremorecommoninsubjects withepilepsy(14%10/24)thansubjectswithoutepilepsy (5%,1/21).ThesubjectswhohadbothCEMsand electrographicseizureswerereviewedforthetype,duration, andqualityoftheirevents(Tables3 and 4).TypesofCEMs wereeitherfocalmotormovementsorgeneralizedtonicclonicmotoractivity,andrarelymyoclonusorjerking movements.Inthe11subjectswithCEMs,9hadtemporally correlatingelectrographicseizures,andallthesepatientshad ahistoryofepilepsy.Fouroftheaforementionedpatients withelectrographicseizureswereidentifiedondeep-electrode recordingsonly,andnotonthesimultaneousrecordingwith surfaceelectrodes.Onlyonepatientwithoutepilepsywas describedashavingCEMs,andtheywerenotassociatedwith epileptiformdischargesontheEEGrecording.Fortheone remainingpatientwithCEM,therewasn’tinformationon correlationwithEEGseizure.
Thereweresomebehavioralchangesreportedintwo studiesthatwerenotincludedasCEMsinoursystematic reviewgiventheywerenotassociatedwithrhythmic movements.Venkataramanetalreportedincreased “muscle tone” in24and “orofacialdyskinesias” in22of30patients.
Table1. Characteristicsofstudysubjects.
Clinical excitatory movements
Electrographic seizures (n/total)
Number ofdosesEEGtype
Dose(mg/ kgper dose)
Indication ofketamineRoute
Subjects with epilepsy (%)
Pediatric subjects (%)
Age range (years)
Total subjects (n)
Author,year
Corssen,1969 8 113 –131000Elective surgery IV2.22Surface0/111/11
0/3at ≤ 1mg/kg 2/4 a at2mg/kg 1/2 a at4mg/kg
Initial IM, then IV IM- 6.5 –13 IV-1 –4.5
Bennett,1973 9 85 –2750100Dental procedure
Surface electrodes: 0/9 deepelectrodes with0.5mg/kg:1/1 with1mg/kg:0/2 with >= 2mg/kg: 6/6
1Surface deep (simultaneously recorded)
1to6Surface3/82/8 a Ferrer-Allado, 1973 10 917 –3711100Localization ofseizure focus IV1/9 –0.5 2/9 1 4/9 –2 2/9 –4
Unknown
Schwartz, 1974 11 918 –5600UnknownIV22Surface0/9Unknown Corssen, 1974 12 3019 –68070ResearchIV2.21SurfaceWithepilepsy: 1/21increased frombaseline withoutepilepsy: 0/9
Surface8/26 (15/26subjects hadwhileasleep) 1/26
Celesia,1975 13 2617 –58Unknown100UnknownIV4pts-0.5 followed by1 22pts-2 4pts2 22pts1
Rosen,1976 14 b 8Unknown100UnknownProcedural sedation IM5 –151Surface1/8Unknown
2SurfaceWithepilepsy: 8/30 withoutepilepsy: 0/10 4/30 a with epilepsy
Venkataraman, 1983 15 40UnknownUnknown75ResearchIV2followed by1
a Clinicalexcitatorymovementsassociatedwithelectroencephalographyseizures. b Notincludedin Table2 duetounknownepilepsystatus. EEG ,electroencephalography; IM ,intramuscular; IV ,intravenous; mg/kg ,milligramsperkilogram.
Table2. Summaryofelectrographicseizures.
Subjects withepilepsy
Subjectswithout epilepsy
Allsubjects
Numberofsubjects9439
Electrographicseizures26(28%)0
Adultsubjectsa
Numberofsubjects3330
Electrographicseizure6(28%)0
Pediatricsubjectsb
Numberofsubjects511
Electrographicseizures3(60%)0
EEG,electroencephalography.
aIncludedpapers:Bennett1973,9 Ferrer1973,10 Schwartz1974,11 Corssen1974.12
bIncludedpapers:Corssen1969,8 Bennett1973,9 Ferrer1973.10
Celesiaetalreported “unusualpostures” in12and “motor hyperactivity” in5of26patients.Thepresenceof electrographicseizuresincorrelationwiththesemovements werenotspecifiedinthesestudies.
Table3. Summaryofclinicalexcitatorymovements.
Subjectswith epilepsy
Allsubjects
Subjectswithout epilepsy
Numberofsubjects7321
Clinicalexcitatory movements
Positive10a (14%)1(0.5%)
Negative63(86%)20(99.5%)
Adultsubjectsb
Numberofsubjects1212
Clinicalexcitatory movements
Positive3d (25%)0
Negative9(75%)12(100%)
Pediatricsubjectsc
Numberofsubjects511
Clinicalexcitatory movements
Positive2d (40%)1(9%)
Negative3(60%)10(81%)
aNinesubjectsalsohadelectrographicseizures. bIncludedpapers:Bennett1973,9 Ferrer1973.10
cIncludedpapers:Corssen1969,8 Bennett1973,9 Ferrer1973.10
dClinicalexcitatorymovementsassociatedwith electroencephalographyseizures.
Wefoundthatinsubjectswithepilepsythereissome evidenceofketamineprovokingelectrographicseizures.In subjectswithoutepilepsy,noelectrographicseizureswere seenwithketamineadministration.Mostofthesubjectswho hadCEMsalsohadtemporallycorrelatedelectrographic seizures.Giventheinfrequencyofmyoclonicjerksobserved inthisstudy,itremainsunclearwhetherthisactivitymaybe epileptiform.Thisrelationshipbetweenketamineand electrographicseizuresmaybedosedependent.InFerrerAlladoetalthepatientswithelectrographicseizureswere givenhigherdoses(2and4mg/kg)ofketamineratherthan themoretypicalinductiondosesof1–2mg/kgusedatthe startofproceduralsedation.10,16,17
Thereisagrowingbodyofliteratureontheuseof ketamineforrefractorystatusepilepticus(RSE)inadultsand children.Ketaminehasareportedefficacyinstopping seizuresofupto73%foradultand74%forpediatric patients.18 Althoughthemechanismofactionisnotexactly known,itishypothesizedthatketamineasanon-competitive antagonistofN-methyl-D-aspartate(NMDA)receptorscan deactivateNMDAreceptorsthatareactivatedbyglutamate overflowduringRSE.Consideringketamine’sdocumented antiseizureeffects,itwouldbeunexpectedforketamine toadditionallybeassociatedwithepileptogenicactivity.Our primaryoutcomewastoevaluateEEGchanges followingketamineadministrationduringtheneutralstateof thebrain.
Onecouldspeculatethataneutral/non-excitatorystateof thebrainmayrespondtoketaminedifferentlythanthebrain intheexcitatorystatethatisseenduringRSE.Thereis evidenceinanimalstudiesthatasseizuresprolong,numbers ofNMDAreceptorsincrease,andgamma-aminobutyric acidreceptorsdecreaseonthepostsynapticsurface.This changingcellularstructuremightplayaroleinthe effectivenessofketamine,anNMDAreceptorantagonist,in haltingRSE.19 Anotherpossibleexplanationisthatobserved electrographicseizuresinsubjectswithepilepsyduring ketaminemaybeconfoundedbythefrequencyof electrographicseizuresatbaselineinthesesubjects. However,describedelectrographicseizureswithketamine werenotalwaysidenticalwithbaselineepileptiform discharges,whichmaysuggestthatthesewere separateelectrographicseizuresprovoked byketamine.9,10,12
Theassociationofseizuresanddecreasedcognitive functionhaslongbeenrecognized.20 Theseeffectshave mainlybeenshownwithprolongedseizuresorepilepsy disorders.20,21 Theeffectsofasingleseizureoncognitionin childrenseemtobeinsignificant,whereaseffectsinadultsare unclear.22,23 Furthermore,forelectrographic-onlyseizures, datasuggeststhathighseizureburdenisrequiredtocause clinicalimpact.22 Thus,eventhoughthereissomeevidence thatketaminemaybeprovokingbriefelectrographic
Volume26,No.1:January2025WesternJournal
Table4. Subjectswithclinicalexcitatorymovements.
Age
Corssen,19698
Electrographicseizures immediatelyafterketamine administrationTypeofCEMBaselineEEG
NoID <13NoneTwitchingofthearms andlegs
Bennett,19739
Case227Polyspikeandwave discharges,maximaloverthe leftanteriortemporalregion (increaseinbaselineEEG discharges)*
Case717Righttemporalfocal discharges(differentthan baselinedischarges)*
Ferrer-Allado,197310
Briefclonicmovementsof therighthandandface followedby1minuteright tonic[adversive]seizure
Lefttonic[adversive] seizure
Baseline seizure semiology
N/ANone
Slowposteriorrhythms, decreasedamplitudeoverleft temporalarea,left frontotemporalspikesand sharpandslowwaves
Lefttemporalspikeandslow waveswithsecondary synchrony,slowposterior rhythms
Focaland generalized motor seizures
Generalized motor seizures
Subject117Seizureactivityindeep electrodes* Tonic-clonicmotoractivityUnknownUnknown type
Subject720Seizureactivityindeep electrodes* Tonic-clonicmotoractivityUnknownUnknown type
Subject833Seizureactivityindeep electrodes* Jerkingmotor movements,clonicmotor activity
Celesia,197513
NoIDUnknownUnknownifthesamesubject hadelectrographicseizures
UnknownUnknown type
SporadicmyoclonicjerksUnknownPsychomotor seizures Venkataraman,198315
NoIDUnknownSeizuredischarges*Tonic-clonicmotoractivity lasting3min
UnknownUnknown type
NoIDUnknownSeizuredischarges*Tonic-clonicmotoractivity lasting3min UnknownUnknown type
NoIDUnknownSeizuredischarges*Tonic-clonicmotoractivity lasting3min UnknownUnknown type
NoIDUnknownIncreasedseizure dischargesfrombaseline* ClinicalseizureGeneralizedspike andwavedischarges Unknown type
[]oldterminology
*CEMcorrelatedwithelectrographicseizures. CEM,clinicalexcitatorymovement; EEG,electroencephalography; ID,identity; N/A,notapplicable.
seizures,theeffectoftheseseizuresoncognitionislikelynot clinicallysignificant.
Sevenof26subjectswhohadelectrographicseizureswere recordedviadeepelectrodesthatwerenotcapturedby surfaceelectrodes.Similarly,studiesusingdeepelectrodesin animalswithepilepsyhavealsoshownelectrographic seizuresduringketamineadministration,24,25 whereas animalswithouthistoryofepilepsydidnotshowany electrographicseizures.26 Theinvolvementofsubcortical structuresinmodulationandpropagationofseizureshas beendescribed;however,theincidenceandclinical
significanceofthedeepelectrographicseizuresisunknown comparedtosurfaceelectrographicseizures.27
Thereareseverallimitationsofthissystematicreview. BecausethisstudywaslimitedtoEnglish-languagestudies, wecouldhavemissedstudiesinotherlanguages.Thenumber ofsubjectsineachstudywassmall,andthereweredifferences indesignandpatientpopulationsbetweenstudies.Inonly threeofthestudieswasketamineusedforprocedural sedation;intheotherstudiesketaminewasadministeredto
volunteers,whichmaylimitgeneralizationtoketamine useinproceduralsedation.Theeligiblestudieswere performedbetween40–50yearsagowhenEEG capabilitieswerelessadvancedthantoday.28,29 Finally,most oftheEEGrecordingsdescribedinthestudieswerenot availableforreview.TheCEMsweredescribedin generalizedterms,andexactsemiologyoften wasnotdescribed.
Thisisthe firstsystematicreviewtodocumentthe relationshipbetweenketamineandclinicalexcitatory movements.Thelimitedavailabledataisinsufficienttomake strongconclusionsontheriskandclinicalsignificanceof seizureswithketamine,andthecorrelationofCEMswith electrographicseizure.Allobservedseizureswerebrief, withnonemeetingthedefinitionofstatusepilepticus.30 WhileCEMscorrespondtoelectrographicseizurein patientswithahistoryofseizures,itisunclearwhether thisisclinicallyimportant.Basedonour findings,we recommendthatclinicianswhoadministersedation askaboutapatient’shistoryofepilepsyduringtheir pre-sedationassessmenttoinformtheirassessmentofthe risksandbenefitsofketaminesedationanddiscuss thepotentialriskofincreasedelectrographicseizures. Furtherstudies,especiallywithvideo-EEGmonitoring duringketaminesedationinepilepsypatients, areneeded.
AddressforCorrespondence:EmineM.Tunc,MD,Universityof TexasSouthwestern,DepartmentofPediatrics,Divisionof EmergencyMedicine,1935MedicalDistrictDr.,Dallas,TX75235. Email: Emine.tunc@utsouthwestern.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Tuncetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BhattM,JohnsonDW,ChanJ,etal.Riskfactorsforadverseeventsin emergencydepartmentproceduralsedationforchildren. JAMAPediatr. 2017;171(10):957.
2.KhanMT,KhanAR,RohailS,etal.Safetyofproceduralsedationin emergencydepartmentsettingsamongtheadultpopulation:a systematicreviewandmeta-analysisofrandomizedcontrolledtrials. InternEmergMed. 2024;19(5):1385–403.
3.GitlinJ,ChamadiaS,LocascioJJ,etal.Thedissociativeandanalgesic propertiesofketamineareindependent. Anesthesiology. 2020;133(5):1021.
4.GreenSMandJohnsonNE.Ketaminesedationforpediatric procedures:part2,reviewandimplications. AnnEmergMed. 1990;19(9):1033–46.
5.BhattM,KennedyRM,OsmondMH,etal.Consensuspanelonsedation researchofpediatricemergencyresearchCanada(PERC)andthe pediatricemergencycareappliedresearchnetwork(PECARN). Consensus-basedrecommendationsforstandardizingterminology andreportingadverseeventsforemergencydepartment proceduralsedationandanalgesiainchildren. AnnEmergMed. 2009;53(4):426–35.e4.
6.LeibetsederA,EisermannM,LaFranceWC,etal.Howtodistinguish seizuresfromnon-epilepticmanifestations. EpilepticDisord. 2020;22(6):716–38.
7.PageMJ,McKenzieJE,BossuytPM,etal.ThePRISMA2020 statement:anupdatedguidelineforreportingsystematicreviews. BMJ. 2021;372:n71.
8.CorssenG,DominoEF,BreeRL.Electroencephalographiceffectsof ketamineanesthesiainchildren. AnesthAnalg. 1969;48(1):141–7.
9.BennettD,MadsenJ,JordanW,etal.Ketamineanesthesiainbraindamagedepileptics.Electroencephalographicandclinical observations. Neurology. 1973;23(5):449–60.
10.Ferrer-AlladoT,BrechnerVL,DymondA,etal.Ketamine-induced electroconvulsivephenomenainthehumanlimbicandthalamicregions. Anesthesiology. 1973;38(4):333–44.
11.SchwartzMS,VirdenS,ScottDF.Effectsofketamineonthe electroencephalograph. Anaesthesia. 1974;29(2):135–40.
12.CorssenG,KittleS,TavakoliM.Ketamineandepilepsy. AnesthAnalg. 1974;53(2):319–33.
13.CelesiaGG,ChenRC,BamforthBJ.Effectsofketamineinepilepsy. Neurology. 1975;25(2):169.
14.RosénIandHägerdalM.Electroencephalographicstudyof childrenduringketamineanesthesia. ActaAnaesthesiolScand. 1976;20(1):32–9.
15.VenkataramanS,VijayanG,SuriY,etal.Ketamineanaesthesiain epileptics. NeurolIndia. 1983;31(3):29–35.
16.DallimoreD,HerdDW,ShortT,etal.Dosingketamineforpediatric proceduralsedationintheemergencydepartment. PediatrEmergCare. 2008;24(8):529–33.
17.KannikeswaranN,Lieh-LaiM,MalianM,etal.Optimaldosingof intravenousketamineforproceduralsedationinchildrenintheED a randomizedcontrolledtrial. AmJEmergMed. 2016;34(8):1347–53.
18.RosatiA,DeMasiS,GuerriniR.Ketamineforrefractorystatus epilepticus:asystematicreview. CNSDrugs. 2018;32(11):997–1009.
19.MoghaddamB,AdamsB,VermaA,etal.Activationof glutamatergicneurotransmissionbyketamine:anovelstepinthe pathwayfromNMDAreceptorblockadetodopaminergicand cognitivedisruptionsassociatedwiththeprefrontalcortex. JNeurosci. 1997;17(8):2921–7.
20.Lenck-SantiniPPandScottRC.Mechanismsresponsiblefor cognitiveimpairmentinepilepsy. ColdSpringHarbPerspectMed. 2015;5(10):a022772.
21.PayneET,ZhaoXY,FrndovaH,etal.Seizureburdenisindependently associatedwithshorttermoutcomeincriticallyillchildren. Brain. 2014;137(Pt5):1429–38.
22.SogawaY,MasurD,O’DellC,etal.Cognitiveoutcomesinchildrenwho presentwitha firstunprovokedseizure. Epilepsia. 2010;51(12):2432–9.
23.AniolVG,GuekhtA,GulyaevaN.Singleseizureandcognition: clinicalandtranslationalimplications. ARCJournalofNeuroscience. 2016;1(2):4–18.
24.GowdaSandSzab´oCÁ.EffectsofketamineonEEGin baboonswithgeneticgeneralizedepilepsy. EpilepsyRes. 2019;154:50–4.
25.BlackJA,GoldenGT,FarielloRG.Ketamineactivationofexperimental corticoreticularepilepsy. Neurology. 1980;30(3):315–8.
26.NicolAUandMortonAJ.CharacteristicpatternsofEEGoscillationsin sheep(Ovisaries)inducedbyketaminemayexplainthepsychotropic effectsseeninhumans. SciRep. 2020;10(1):9440.
27.BadawyRAB,LaiA,VogrinSJ,etal.Subcorticalepilepsy? Neurology. 2013;80(20):1901–7.
28.PatelAC,ThorntonRC,MitchellTN,etal.AdvancesinEEG:home videotelemetry,highfrequencyoscillationsandelectricalsource imaging. JNeurol. 2016;263(10):2139–44.
29.FrauscherB,BénarCG,EngelJJ,etal.Neurophysiology, neuropsychology,andepilepsy,in2022:hillswehaveclimbedandhills ahead.Neurophysiologyinepilepsy. EpilepsyBehav. 2023;143:109221.
30.TrinkaE,CockH,HesdorfferD,etal.Adefinitionandclassificationof statusepilepticus-reportoftheILAEtaskforceonclassificationof statusepilepticus. Epilepsia. 2015;56(10):1515–23.
MadisonStolly,BS*
ErikaWilt,BS*
NathanGembreska,BS*
MohamadNawras,BS*
EmilyMoore,BS*
KellyWalker,BS*
RhondaHercher,MD†
MohamadMoussa,MD†
SectionEditor:JeffreyDruck,MD
*UniversityofToledoCollegeofMedicineandLifeSciences,Toledo,Ohio † DepartmentofEmergencyMedicine,UniversityofToledoCollegeofMedicineandLife Sciences,Toledo,Ohio
Submissionhistory:SubmittedFebruary20,2024;RevisionreceivedSeptember18,2024;AcceptedSeptember30,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.19466
Background: TikTokhasrapidlybecomeoneofthemostextensivelydownloadedandusedsocial mediaplatformsworldwide.Ourfocusonemergencymedicine(EM)-relatedcontentonTikTokisto identifywhatspecificvideocharacteristicsresultinhigherdegreesofaudienceengagement,definedin thisstudyasatotalofvideolikes,comments,andshares.
Methods: Fivesecond-yearmedicalstudentsusingnewlycreatedTikTokaccountsindependently downloadedthe first100videostoappearusingthehashtag#emergencymedicine.Thevideoswere reviewedfor52variables.Weperformedamultiplelinearregressionanalysistoexaminetherelationship betweenthevariablesandvideoengagement.
Results: Oftheexaminedvideos,45.8%(222/484)wereproducedbyphysicians(MDorDO). Approximatelyhalf,50.0%(242/484),hadaneducationalcomponent,while55.4%(268/484)ofvideos werejudgedtohaveanentertainmentcomponent.Preliminary findingsindicatethatamongTikTok videosfeaturing#emergencymedicine,astatisticallysignificantpositivecorrelationexistsbetweenvideo engagementandthepresenceofahealthcareidentifier,(ie,individualswearingwhitecoatsorscrubs). Nosignificantcorrelationwasobservedbetweenvideoengagementandvideocreators’ selfidentificationasahealthcareprofessional,useofentertainment,oruseofeducation.Anotablenegative correlationwasidentifiedbetweenvideoengagementandtheinclusionofmusic.
Conclusion: Weidentifiedqualitiesassociatedwithnegativeandpositivecorrelationwithvideo engagement.Forthe100videos,onlyhealthcareattire,suchaswearingawhitecoatorscrubs,showed asignificantpositivecorrelationwithengagement,whilethosewithbackgroundmusicshoweda negativecorrelation.OurstudyoffersinsightintohowEMprofessionalscaneffectivelyuse characteristicsassociatedwithhigherengagementratestorelayinformationtoawideraudienceon TikTok.[WestJEmergMed.2025;26(1)155–160.]
Inthepastseveraldecades,socialmediahasbecomean integralpartofsociety,withitsprominencecontinuingto grow.Consequently,thepublichasstartedtousesocial
mediaasaresourceforobtainingmedicalinformation regardingone’sownhealth,detailsonaspecificcondition, howtodevelophealthylifestyles,etc.1 Giventherelativeease ofsearchingforinformationonlineoronsocialmediaand
theamountofinformationavailable,over80%ofpeople withinternetaccessnowseekhealthcareinformationonline.2 Theworldofhealthcareinformationhasgrowntobealarge presenceintheonlineworld,butasthemodalitiesofonline informationcontinuetochangeandgrow,thequestion remainshowtoeffectivelydisseminateinformationonthese variousplatforms.Recently,researchersfortheRoyal CollegeofPhysiciansusingeducationtheoryexplored therisksandbenefitsofusingsocialmediaformedical educationandascertaineditsuseaspositive and “heretostay.”3
TikTokhasrapidlyemergedasthefastest-growingsocial mediaplatformcurrentlyinuse.Withavailabilityinover150 countriesandovertwobilliondownloads,itsuperseded Facebook,Twitter,andInstagramin2018and2019asthe mostfrequentlydownloadedapplication.4 Currently,12%of theglobalpopulationusestheappmonthly.5 TikTok operatesonthepremiseofshort-formvideocontentwhere userscancreateandsharevideos,whichtypicallylast between15–60seconds,coveringawiderangeoftopics,from entertainmentandhumortoeducationandcreativity.6 The app ’salgorithmemploysarecommendationsystemthat analyzesuserbehavior,suchasthevideostheylike,share, andcommenton,tocurateapersonalized “ForYouPage” (FYP).7 ThisFYPshowcasescontenttailoredtoeachuser’ s interests,ensuringahighlyengagingexperienceasit constantlyintroducesuserstonewandrelevantcontentfrom creatorsworldwide.TikTokalsohasavarietyofcreator tools,including filters,effects,andsoundtracks,thatallows creatorstoproducevisuallyappealingandentertaining contentinmultipleforms.Theplatform’semphasison discoverabilityand “goingviral” hasledtotherapidriseof internetsensationsandtrends,makingTikTokadynamic andinfluentialforceintheworldofsocialmedia.8 Limited researchhasbeenconductedonthepotentialroleitwillplay inhealthcareinformation.
Whileprioranalysesofsocialmediahealthcampaigns primarilyfocusedonFacebookorTwitter,younger generationshavebeguntouseimage-andvideo-based platformssuchasInstagram,Snapchat,orTikTok.9 Very littledatahasbeengatheredpertainingtotheeffectivenessof engagementandaccuracyofusingthesenovelplatformsto communicatehealthinformationtothegeneralpopulation. TheuseofTikTokhasproventobeasourceofsomehealth information,suchassexeducation,10 butnostudieshave beendirectedtowardemergencymedicine(EM)specifically. AstudydirectedtowardthevalidityofTikTokvideosabout diabeteseducationfoundthevideostobeofanacceptable levelofaccuracy.11 However,neitherofthesestudies addressedwhatmadeanengagingvideo.Arecentstudyby Kassamalietal12 foundthatvideoscontainingon-screen text,music,andhealthcareattireshowedthehighestratesof engagementonTikTokvideosrelatedtodermatology. Additionally,Bartaetalinvestigatedinfluencercontenton
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
TikTokisarapidlygrowingsocialmedia platform.Healthcareinformation increasinglypermeatesonlinemedia.
Whatwastheresearchquestion?
Whichspeci fi ccharacteristicsofTikTok videosleadtoincreasedengagement(total likes,comments,andshares)?
Whatwasthemajor findingofthestudy?
Therewasapositivecorrelationwith engagementandhealthcareidenti fi erssuchas whitecoatsorscrubs,andanegative correlationwithengagementand music,P < 0.05.
Howdoesthisimprovepopulationhealth?
OurstudyprovidesinsightsintohowEM professionalscanuseengagement-driving featurestoeffectivelyreachabroader audienceonTikTok.
TikTok,andtheirstudysuggestedthathumor,originality, quality,andquantityofvideoscorrelatedwithincreased ratesofengagement.13
Withnearly72%ofAmericansusingsomeformofsocial media,14 andwithTikTokvideosbeingsoshortandeasyto view,TikTokisapotentialvehicleforEMeducation especiallyintheacutesetting.Recentresearchhasexplored theconceptofmicrolearning,whichinvolvesbreakingdown informationintosmall,manageablesegmentsthatallow learnerstoabsorbknowledgeattheirownpace.Preliminary findingsindicatethatmicrolearningenhancesbothlearning outcomesandlong-termmemoryretentioncomparedto traditionallearningmethods.Giventheconcisenatureof TikTokvideos,thisplatformcouldpotentiallybeusedto facilitatemicrolearning.15 Whilethereisagrowingpresence ofphysiciansusingsocialmedia,veryfewusethemasa publicplatformtomakeeducationalvideos.16 Withsomany differentvariablesinvideocharacteristics,thequestion raisediswhethercertainvideoscreatedbyhealthcarecontent creatorshaveahigherimpactonthegeneralpublic.Such informationcouldallowfortheuseofTikToktobecomean effectiveeducationalplatformforlearnersandpatientsalike togainvaluableknowledgeaboutmedical-relatedmattersin atimelymanner.Inthisstudywesoughttoinvestigate whetherspecificfactorspresentinTikTokvideos relatedtoEMcorrelatewithhigherlevelsoflikes,comments,
andshares,therebyreinforcingstrategiesforenhancing engagementanddisseminatingcontentto thepublic.
Datausedinthisanalysiswasusedforqualitativeresearch andwascollectedonDecember4,2022,at8 PM by five separatemedicalstudentsusingnewlycreatedTikTok accountstominimizethevariationduetotheTikTok algorithm.Videosweredownloadedonthesamedateand timetoensuretheleastamountofvariabilityofcontent available.Eachaccountsearched “#emergencymedicine” anddownloadedthe first100videosthatwerelisted.This createdasamplesizeof500videostoanalyze.Despitethese beingnewaccountsandhavingnopriorinteraction,there wasvariationamongthevideosthatweredownloaded. Videoswereexcludedfromthesampleiflikes,comments,or shareswerenotavailable.Thisreducedthetotalsamplesize to484videos.Thesevideosweresavedindependentlyfor laterreviewandrecord,andallvideosweresavedwiththe watermarkincludingviews,likesandshareswhichwas locatedontheleftsideofthevideo,andusernameofthe originalcontentcreator.Oncetheyweredownloaded, studentsreviewedthespreadsheettogetherandassessed severalsampleTikTokvideostogethertoensureeachvideo wouldbeanalyzedsimilarlytoreducevariabilityindata collection.EachstudentusedanExcelspreadsheet (MicrosoftCorp,Redmond,WA)tocollecttherequired information;thiswassentforstatisticalanalysis oncecomplete.
Foreachvideo,52characteristicswererecordedbasedon themethodsusedbyRaberetal17 whostudiedTikTok contentrelatedto#mediterraneandiet.Theseincluded descriptivecharacteristicsincludinguploaddate,numberof likes,numberofcomments,numberofshares,totallengthof video,andotherhashtagsincludedinthevideodescription. Creatorinformationwascollectedandrecordedusing informationfromthecreator’sTikTokpageorlinkedsocial media.Creatorcharacteristicsrecordedincludedposter name,username,numberoffollowers,accountdescription ortagline,accounttype(private,sponsored,company), hyperlinkstoothersocialmediaorstorefronts,andany medicalorprofessionalcredentials.Aftercollection,the contentofeachTikTokwasassessedseparatelyandscored bythestudentusinganumericsystemwith0representing “ no ” and1representing “ yes. ” Generalcharacteristics assessedincludeduseofmusic,useofhumor,textoverlay, presenceofinfographics,presenceofeducational information,attempttodirectlysellaproductorservice,and presenceofanypromotionforaserviceorcompany.All contentwasalsoratedbasedoninclusionofpersonal
anecdotes,conspiracytheories,thecreatorhavingMD/DO credentials,orstudy/datausage.
Somecategoriesdidnot fitintotheabovecodingstyleand haddistinctnumericscalessuchasmainmessageofthevideo (educational,entertainment,other),videostructure(original content,stitch,responsetocomment,orother),videostyle (talkingtocamera,role-playing,dancing,emergency department(ED)withnohost,orother),andwhethera specificacuteorchronicdiseasewasmentionedinthevideo. The finalpartofthecodingforeachvideoincludedassessing whethertherewasanyeducationalorentertainmentaspectto thevideo.PerthespreadsheetbasedonRaberetal’ s methods,wedefinededucationalvideosasvideothat primarilycontainsamedicallyeducationalaspect,orcontent offersmedicalinformation,toincludeaspectsspecifictoEM; thisincludedbutwasnotlimitedtodefiningwhathappensin theEDordefiningamedicalcondition.Wedefined entertainmentvideosasincludinghumor,makingjokes aboutmedicine,dancing,orasong.Thesewere discussedwiththeratersaheadoftimetoprevent confusion.Ratersthentypedabriefdescriptionin thespreadsheet.
Thedataforeachofthespreadsheetswascombinedina masterspreadsheetandanalyzedusingamultipleregression modelwithSPSSsoftwareversion28.0.1.1(SPSSStatistics, IBMCorp,ArmonkNY).Wecomparedallusing P -value <0.05.Theindependentvariableforeachvideowasthesum oflikes,comments,andsharesrecordedinthespreadsheet, referredtoastheaveragetotalengagementforthatvideo. Thedependentvariablesincludedinthisanalysiswerethe presenceofbackgroundmusic,videocreatorattire, identificationasahealthcareprofessional,account designationofhealthcareprofessional,messageofthevideo (educationorentertainment),humor,andthepresenceof textoverlays.
Resultsoftheaverageengagement(ie,totallikes, comments,andshares)areshowninthe Table and Figure. Thesewereseparatedintothepresenceorabsenceof healthcareattire,entertainment,education,music,in-video credentials,humor,accountdesignationofMD/DO,and textoverlayforfurtherevaluationthroughlinear regressionanalysis.
Anelevatedlevelofvideoengagementexhibitedadirect positivecorrelationwithvideosfeaturingcreatorswearing healthcareidentifierssuchasawhitecoatorscrubs,witha statisticallysignificant P -valueoflessthan0.02.Moreover, theanalysisindicatedadecreaseinvideoengagementwhen backgroundmusicwaspresent,witha P -valueoflessthan 0.03.Conversely,therewasalackofcompellingevidence supportingthenotionthatindicatorssuchasthecreator’ s
Table. Averageengagementlevels(likes,comments,shares)of TikTokusersbasedonvariousvideocharacteristics.
PresentAbsent
Healthcareattire*130,725.0049,262.05
Entertainmentcomponent93,574.84120,774.50
Music**68,745.16145,558.08
In-videocredentials93,988.79123,699.12
Humor120,769.5692,047.63
AccountdesignationofMD/DO125,201.3389,126.45
Textoverlay110,236.07107,255.79
*Positivecorrelationwithcreatorswearingwhitecoats/scrubs. **Negativecorrelationwithbackgroundmusic.
age,explicitself-identificationasahealthcareprofessional withinthevideo,ortheaccount’sdesignationasahealthcarerelatedprofilehadasignificantimpactonoverallvideo engagement.Furthermore,nostatisticallysignificant correlationswereobservedbetweenanincreasedamountof engagementandvariousotherfactorsincludingthepresence ofeducation,entertainment,humor,orthepresence oftextoverlays.
Asinthe fieldofmedicine,thelandscapeofsocialmediais inaconstantstateofevolution,continuouslyintroducing andexpandingnovelinformationdistributionmethods.This studyhasprovidedvaluableinsightsintotheutilityof TikTokanditseffectiveapplicationinincreasing engagementinvideospertainingtoEM.Bycreatingnew accounts,theinvestigationtriedtomimicaFYPfreeof healthcarecontentbiastofurtherunderstandwhatageneral usermayseeontheirpagebysearchingthehashtag, #emergencymedicine.Furthermore,theresearchdelvedinto thestrategiesavailabletoemergencyhealthcare professionalsforleveragingTikTokasamediumto disseminateeducationalcontenttothegeneralpublic. Interestingly,itwasdiscoveredthattheprimaryfactor influencingtheengagementofaTikTokvideoisneitherthe credentialsnorthemessageofthecontent,butratherthe attireofthevideocreator.Therewasnobenefittothecreator statingwhethertheywerealicensedprofessional.Further, therewasnodiscernableinclinationtowardeither educationalorentertainingcontent.Thissuggeststhat usersareopenlyreceptivetodigestingeducationaland entertainingmedicalcontentontheplatform.Thisoffers guidanceonhowtoengageeffectivelywiththebroader
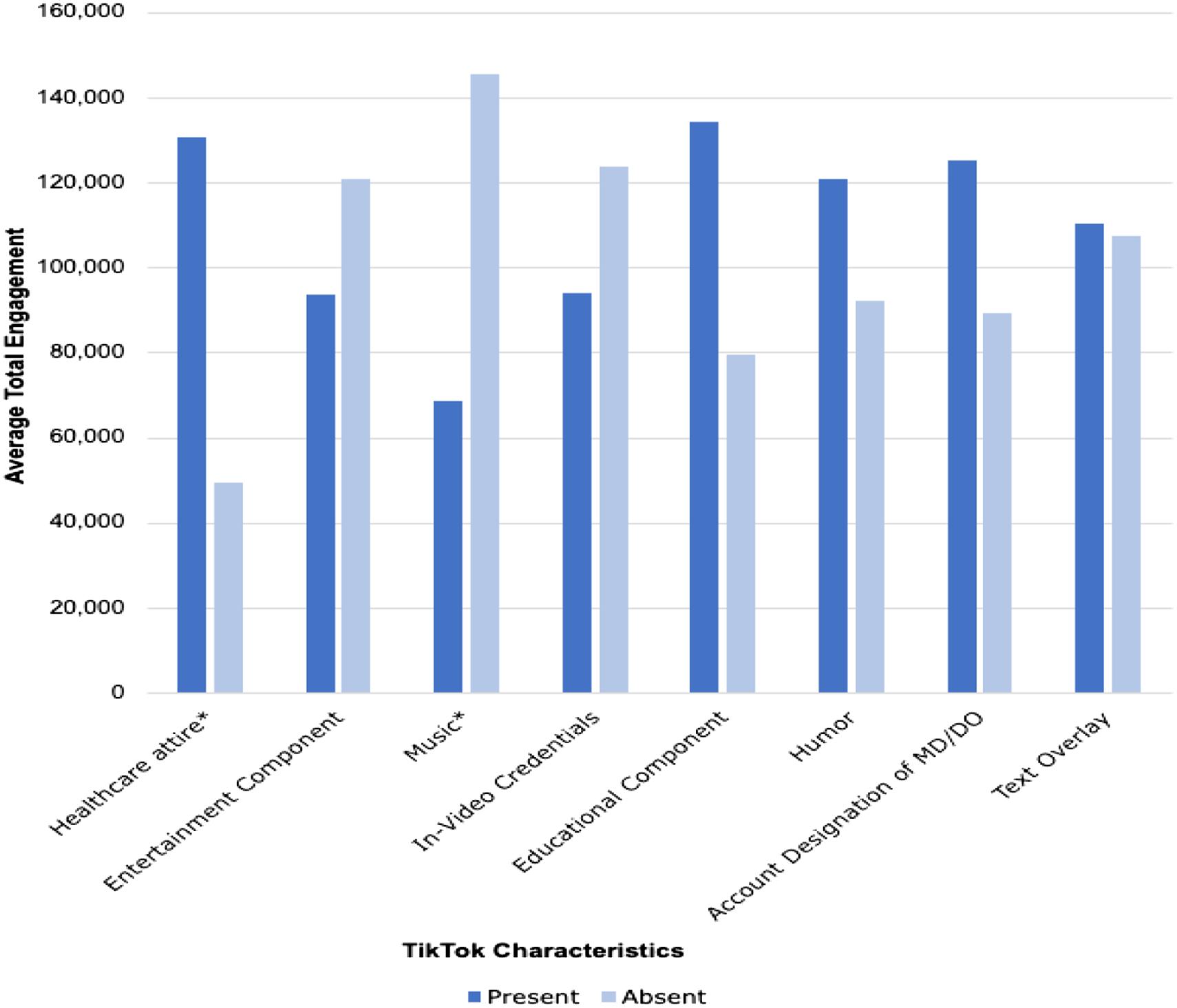
Figure. TotalAverageengagementofTikTokcontentbasedonthepresenceorabsenceofspecificvideocharacteristics.
audienceinthemedicaldomainthroughutilizationofthe FYP.Italsounderscorestheuniquenatureofcontemporary socialmediaplatforms,whererapid,split-secondjudgments playacriticalrole,emphasizingtheneedtocaptureviewers’ attentionswiftlytoachieveengagement.
ThelevelofengagementofTikTokvideosmayprovetobe contentdependentonwhichvariablesmattermostinlevels ofengagement.Forinstance,Bartaetaldiscoveredthat incorporatinghumorwasadvantageousincreatingvideosto beasuccessfulinfluencer. 13 However,whenassessing engagementspecificallywithinthesubjectmatterofEM, humordidnotdemonstrateanybeneficialimpactwhen addedtothevideos.Our findingsfurthersupportthestudy donein2021byKassamalietalastheyinvestigatedthe “virality” ofTikToksrelatingtodermatologyeducation videosandfoundthatmedicalattirewaspositivelycorrelated withoverallvirality.12 Additionally,thestudysuggested increasedengagementwithvideosthatcontainedmusicin theTikTokvideo.
Conversely,the findingsinthisstudysuggestthatTikTok videosrelatedtoEMwithbackgroundmusicactedas deterrentsforviewers,implyingeducatorsmightachieve greatereffectivenessbyspeakingdirectlytothecamera. Consequently,someaspectsofTikTokvideosmaybe content-dependentevenwithinthehealthcare field.One pioneeringaspectofsocialmediaistheabilitytoconnect ideas.Asidefromcontentcreatorsaccessingtheirintended audiences,italsoallowsforcontentcreatorstoconnectwith oneanother,collaboratingforthebestoutcome.Thus, creatorscanshareideasnotonlyregardingtheircontentbut alsohowtobestengagegeneralaudiences.
Accordingtorecentdata,42%ofallusersarebetweenthe agesof18–24,followedbyusersbetweentheagesof13–17 (27%).8 Inlightofthecontinuedsurgeinpopularityofthis socialmediaplatform,itbecomesincreasinglyimperativeto refineapproachesaimedateffectivelyengagingTikTok’ s diverseaudience.GiventhatthemajorityofTikTokusers fallwithintheagerangeof13–24,itpresentsadistinctiveand valuableopportunitytoconnectwiththisdemographicinthe realmofhealthengagement.Usingawidelyadopted communicationmedium,EMprofessionalscouldeffectively employthisplatformtodisseminateinstructiveinformation tothepopulation.Thisresearchhasopenedthedoortomany ofthepossiblemeritsofsocialmediainmedicalacademia andoutreach.Thisresearchhasdemonstratedwhatelements toincorporateandavoidwhencreatingcontentwiththe goaltoencourageengagement.Ithasillustratedwhich characteristicsofcontentwithinEMaremostlikelytodraw significantengagement.Notably,wearinghealthcare attireappearstoenhancethelikelihoodofthepublic encounteringthevideo.Thisprovedtobemore advantageouscomparedtootherfactorspresumedtobe influentialsuchasexplicitlystatingone’shealthcare profession,incorporatingentertainmentelements,or
displayingprofessionalcredentialssuchasMDorDOnext toone’ sname.
Ourresearchopensthedoorformanynewavenuesofthe intersectionofsocialmediaandmedicine,specifically medicalcontentandhowgeneralpublicuserscaninteract withit.Furtheranalysiscouldbedeterminedtoseewhat makessocialmediavideosnotonlyengagingbuteffective teachingtools.Otherpotentialresearchcouldinclude assessingthemedicalcontentofothersocialmediasitessuch asInstagramandTwitter,giventheirlargepresence.Other metricsofmedicalvideosonsocialmediacouldbeanalyzed aswell,includinganexplorationoftheuserdemographics thatengagewithvarioustypesofEMcontent.Additionally, thiscouldincludevideoaccuracy,potentiallylookingat morespecificmedicalconditions,procedures,orquality improvement.Generally,ourresearchgoalistoreachoutto awidegroupofpeople,supportingaccurateEMcontentand encouragingactiveparticipationinatechnologycenteredworld.
Forthisresearchstudyweengaged fiveautonomous assessors,eachequippedwithnewlyestablishedaccounts,to evaluatecontentsimultaneouslyonaspecificday.Theaim wastomanipulateanimpartialsearch,recognizingthatthe TikTokalgorithmdynamicallyaltersthecontentpresented toviewers,contingentontheirpreviouslyindicated preferencesandtheprevailingtimeoftheyear.Byemploying thismethodology,wesoughttomitigatetheinfluenceof personalizeduserhistoryandseasonalvariations,thereby facilitatingamoreunbiasedassessmentoftheplatform’ s contentdisseminationmechanisms.Nonetheless,thestudy encounteredcertainlimitations.
Duetofeasibilitypurposes,thestudyreliedonmedical studentstocollectthedata.Therelianceonarelativelysmall cohortofonly fiveassessors,whosemedicaleducationlevel wasatthesecondorthirdyear,mayhaveimposed constraintsontheirabilitytoaccuratelyinterpretthe informationpresented,giventheirtraininghadyettobefully comprehensiveandspecifictotheEDdomain.Further,there wasnotananalysisperformedontheraters’ inter-rater reliabilityinperformingtheanalysisofthevideos.Secondly, theevaluationofmerely100videosperassessorraisesthe possibilityofpotentialoverlapinthevideosamples observed,whichcouldinadvertentlyhaveaffectedthe diversityofthedatapool.Thestudyalsoreviewedonly videosthatused#emergencymedicine,assumingthecontent usersappropriatelyusedthehashtagforcontentrelevantto EM,andthatitisthepreferredhashtagused.Lastly,an inherentin-groupbiasmighthavebeenintroduced,asthe assessorsmayhavetendedtoperceivethevideosastargeted towardotherhealthcareprofessionals,despitetheirintended audiencebeingthepublic.Theselimitationswarrantcareful considerationwheninterpretingthe findingsandunderscore
thenecessityforprudentlyaddressingtheminfutureresearch inthisdomain.
TikTokisaplatformthatusesvideostorelaymessagesin arestrictedamountoftime,emphasizinghowimportantitis forcontentcreatorstousetimeandvideocharacteristics wiselytoengagetheaudiencebeforetheirattentionmaybe divertedelsewhere.Thissuggestsvideoscontainingaquality thatsignificantlyincreasestotalengagementmaybeusedto shareinformationtoagreateraudience.Inaddition, avoidingcharacteristicsassociatedwithnegative engagementcancontributetoreachingawideraudience. Basedonour findings,wearinghealthcare-relatedattire,such asawhitecoatorscrubs,showedastatisticallysignificant increaseintotalengagement.Conversely,backgroundmusic inthevideosdecreasedthetotalengagement.Webelieve theseresultssuggestEMprofessionalscancreatevideos usingcertainapproaches,suchaswearinghealthcareattire, tosharehealthcareinformationtoagreaternumberof individualsontheTikTokplatform.Whileitmaynotbe immediatelyclearhowTikTokcanbeusedtodisseminate healthcareinformation,our findingsprovidesomemuchneededinsightintothecurrentrelationshipbetweenTikTok and#emergencymedicine.
AddressforCorrespondence:MohamadMoussa,MD,University ofToledoCollegeofMedicineandLifeSciences,Department ofEmergencyMedicine,DowlingHall2457,MailStop1088, 3000ArlingtonAve.,Toledo,Ohio43614-2598. Email: mohamad.moussa@utoledo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Stollyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AntheunisM,TatesK,NieboerT.Patients’ andhealthprofessionals’ use ofsocialmediainhealthcare:motives,barriersandexpectations. PatientEducCouns. 2013;92(3):426–31.
2.BakerL,WagnerTH,SingerS,etal.Useoftheinternetande-mail forhealthcareinformation:resultsfromanationalsurvey. JAMA. 2003;289(18):2400–6.
3.D’souzaF,ShahS,OkiO,etal.Socialmedia:medicaleducation’s double-edgedsword. FutureHealthcJ. 2021Jul;8(2):e307–10.
4.LiY,GuanM,HammondP,etal.CommunicatingCOVID-19information onTikTok:acontentanalysisofTikTokvideosfromofficialaccounts featuredintheCOVID-19informationhub. HealthEducRes. 2021;36(3):261–71.
5.McLachlanS.50+ importantTikTokstatsmarketersneedtoknowin 2023.Availableat: https://blog.hootsuite.com/tiktok-stats/. Accessed February12,2024.
6.ZhuC,XuX,ZhangW,etal.HowhealthcommunicationviaTikTok makesadifference:acontentanalysisofTikTokaccountsrunby Chineseprovincialhealthcommittees. IntJEnvironResPublicHealth. 2019;17(1):192.
7.GuL,GaoX,LiY.WhatdrivesmetouseTikTok:alatentprofileanalysis ofusers’ motives. FrontPsychol. 2022;13:992824.
8.BaschC,HillyerG,JaimeC.COVID-19onTikTok:harnessingan emergingsocialmediaplatformtoconveyimportantpublichealth messages. IntJAdolescMedHealth. 2022;34(5):367–9.
9.LimMSC,MolenaarA,BrennanL,etal.Youngadults’ useofdifferent socialmediaplatformsforhealthinformation:insightsfromweb-based conversations. JMedInternetRes. 2022;24(1):e23656.
10.FowlerLR,SchoenL,SmithHS,etal.SexeducationonTikTok:a contentanalysisofthemes. HealthPromotPract. 2022;23(5):739–42.
11.KongW,SongS,ZhaoYC,etal.TikTokasahealthinformationsource: assessmentofthequalityofinformationindiabetes-relatedvideos. JMedInternetRes. 2021;23(9):e30409.
12.KassamaliB,Villa-RuizC,MazoriD,etal.Characterizingtop educationalTikTokvideosbydermatologistsinresponseto “TikTokanddermatology:anopportunityforpublichealthengagement.” 2021;85(1):e27–8.
13.BartaS,BelancheD,FernandezA,etal.Influencermarketingon TikTok:theeffectivenessofhumorandfollowers’ hedonicexperience. JRetaiConsumServ. 2023;70:103149.
14.CompG,DyerS,GottliebM.IsTikTokthenextsocialmediafrontierfor medicine? AEMEducTrain. 2020;5(3):10.1002/aet2.10532
15.SirwanMohammedG,WakilK,SirwanNawrolyS.Theeffectivenessof microlearningtoimprovestudents’ learningability. InternatJEducRes Rev. 2018;3(3):32–8.
16.HameedI,OakleyCT,AhmedA,etal.Analysisofphysicianuseofsocial media. JAMANetwOpen. 2021;4(7):e2118213.
17.RaberM,AllenH,HuangS,etal.#mediterraneandiet:acontentanalysis ofmediterraneandiet-relatedinformationonTikTok. CurrDevelopNutr. 2022;6(1):391.
VictorBarbosaSlivinskis* IsabelaAgiMaluli†
JoshuaSethBroder,MD‡
*DukeUniversity,PrattSchoolofEngineering,DepartmentofBiomedicalEngineering, Durham,NorthCarolina
† DukeUniversity,TrinityCollegeofArtsandSciences,DepartmentofChemistry, Durham,NorthCarolina
‡ DukeUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Durham,NorthCarolina
SectionEditor:ChrisBaker,MD
Submissionhistory:SubmittedMay22,2024;RevisionreceivedOctober21,2024;AcceptedOctober23,2024
ElectronicallypublishedNovember21,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21238
Introduction: Medicaldevicerecallsareimportanttothepracticeofemergencymedicine,asunsafe devicesincludemanyubiquitousitemsinemergencycare,suchasvascularaccessdevices,ventilators, infusionpumps,videolaryngoscopes,pulseoximetrysensors,andimplantablecardioverter defibrillators.Identificationofdangerousmedicaldevicesasearlyaspossibleisnecessarytominimize patientharmswhileavoidingfalsepositivestopreventremovalofsafedevicesfromuse.Whilethe UnitedStatesFoodandDrugAdministration(FDA)employsanadverseeventreportingprogram (MedWatch)anddatabase(MAUDE),otherdatasourcesandmethodsmighthaveutilitytoidentify potentiallydangerousmedicaldevices.Ourobjectivewastoevaluatethesensitivity,specificity,and accuracyofamachinelearning(ML)algorithmusingpubliclyavailabledatatopredictmedicaldevice recallsbytheFDA.
Methods: Weidentifiedrecalledmedicaldevices(RMD)andnon-recalledmedicaldevices(NRMD) usingtheFDA’swebsiteandonlinedatabase.WeconstructedanMLalgorithm(randomforest regressor)thatautomaticallysearchedGoogleTrendsandPubMedfortheRMDsandNRMDs.The algorithmwastrainedusing400randomlyselecteddevicesandthentestedusing100uniquerandom devices.Thealgorithmoutputacontinuousvalue(0–1)forrecallprobabilityforeachdevice,whichwere roundedfordichotomousanalysis.Wedeterminedsensitivity,specificity,andaccuracyforeachofthree timeperiodspriortorecall(T-3,6,or12months),usingFDArecallstatusasthereferencestandard. ThestudyadheredtorelevantitemsoftheStandardsforReportingDiagnosticaccuracystudies (STARD)guidelines.
Results: Usingaroundingthresholdof0.5,sensitivitiesforT-3,T-6,andT-12were89%(95% confidenceinterval[CI]69–97),90%(95%CI70–97),and75%(95%CI53–89).Specificitywas100% (95%CI95–100)forallthreetimeperiods.Accuracywas98%(95%CI93–99)forT-3andT-6,and95% (95%CI89–99)forT-12.Usingtailoredthresholdsyieldedsimilarresults.
Conclusion: AnMLalgorithmaccuratelypredictedmedicaldevicerecallstatusbytheFDAwithlead timesasgreatas12months.Futureresearchcouldincorporatelongerleadtimesanddata sourcesincludingFDAreportsandprospectivelytesttheabilityofMLalgorithmstopredictFDArecall. [WestJEmergMed.2025;26(1)161–170.]
Inourinstitutionwehaveencounteredmultiplesafety eventsassociatedwithmedicaldevicesincludingchesttubes andvascularcatheters,whichwereportedtothe manufacturersandtheUSFoodandDrugAdministration (FDA).1–3 Ourexperienceinspiredaninterestin understandingtheFDArecallprocessanddeveloping methodstoimprovetheefficiencyofpost-market,device safetyevaluation.Medicaldevicerecallsareimportanttothe practiceofemergencymedicine,astheyaffectpatients, emergencyphysiciansandotherpractitioners,health systems,andmanufacturers.Unsafedevicesandrecalls includemanyubiquitousitemsinemergencycare,suchas vascularaccessdevices,ventilators,infusionpumps,video laryngoscopes,pulseoximetrysensors,andimplantable cardioverterdefibrillators.4
Appropriaterecallofdangerousdevicesattheearliest possibletimelimitsfurtherpatientharm,whilefailingto recallanunsafedeviceexposespatientstopotentialinjuryor death.Inappropriateorexcessivelyconservativedevice recallsharmpatientsbydeprivingthemofdevicebenefits; evenappropriaterecallsmayleavenoclinicalalternative, creatingpotentialharm.Productrecallsimposea considerableburdenonhealthsystemsandmanufacturersby incurringcostsofinvestigationsforpotentialrecalls, recallingthosedevices,anddevelopingandbuyingsubstitute devicesto fillapost-recallvacuum.Regulatoryagenciesface thechallengesofinvestigativecostswith finiteresources, ongoingharmspriortorecall(orevenpost-recall,assome productssuchasimplanteddevicesmaystillbeinuse),and costsrelatedtoremovingthosedevicesandevaluatingand approvingalternatives.Therefore,developingand investigatingautomatedmethodstopredictsuchrecallsarea crucialareaofstudy.
Anoptimalmonitoringandrecallsystemwouldidentify alldangerousdeviceswithouterrors(ie,nofalsepositivesor negatives)asearlyaspossible,withhumanintervention requiredonlytovalidatethe findings.IntheUnitedStates, theFDAapprovesmedicaldevicesandconductsrecallsof unsafedevices.4 Currently,theFDAhasapassive,postmarketapprovalsystem(MedWatch)wherepatients, clinicians(includingemergencyphysicians),andhealthcare systemscansubmitreportsofmedicaldevice-associated adverseevents,andapubliclyavailable,searchable monitoringdatabaseMAUDE(ManufacturerandUser FacilityDeviceExperience),wherereportsarelogged.5,6 The FDAacknowledgesthattheaccuracyofsubmitteddataand causalrelationshipsareunknown.7 Mostdevicerecallsoccur voluntarilybymanufacturersandaregovernedbyTitle21of theCodeofFederalRegulations(CFR)7.8
TheFDAalsoevaluatesmedicaldevicerecallsthrough21 CFR810and21CFR806.9 Part810outlinestherecall process,includingevaluatinghealthrisksanddefiningthe recall’sextent.Thissectiondesignatesdevicesintothree
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Identi fi cationofdangerousmedicaldevicesby theUSFoodandDrugAdministrationis essentialtominimizepatientharmswhile avoidingunnecessaryrecalls.
Whatwastheresearchquestion?
Weevaluatedtheperformanceofamachine learningalgorithmtopredictrecallsusing publiclyavailabledata.
Whatwasthemajor findingofthestudy?
Sensitivityforrecallwas75%(95%CI 53 – 89)withspeci fi city100%(95%CI 95 – 100)witha12-monthleadtime.
Howdoesthisimprovepopulationhealth?
MachinelearningalgorithmsmightriskstratifydevicesforfurtherFDAinvestigation, improvingresourceallocationwhileallowing safedevicestoremaininuse.
classesbasedonpotentialriskseverity.ClassIincludes devicesthathavethepotentialtocauseseriousrisksofharm ordeath;IIdesignatesthosethatmaycausetemporaryor reversiblerisksandposeaslightchanceofmoreseriousharm ordeath;andIIIincludesdevicesnotlikelytocausehealth problemsorinjury.Part806focusesonreporting requirementsformanufacturersinitiatingarecallor correction.Manufacturersmustreportanydevicecorrection orremovaltoreducehealthrisks,includingthereasonforthe recallandthetotalquantityproduced.Together,21CFR7, 810,and806provideaframeworkforidentifyingand rectifyingissues,withthegoalofensuringmedicaldevices’ ongoingsafetyandeffectivenessinthemarketplace.The FDAconsiderationsincludethenatureandpotentialhealth riskofthedevice,theextentandcauseofthedefect,the likelihoodofoccurrence,themanufacturer’srecallstrategy, thenumberofaffectedproducts,thedistributionpattern, andthelevelofhazardpresentedtopatients.
From2018–2023,theFDAapprovedorclearedmore than250medicaldevices.10 TheFDAreceives approximatelyonemillionreportsannuallythroughthe MedWatchandMAUDEsystems.7 FromSeptember 2018–September2023,234seriousdevicerecallswereissued bytheFDA,withthousandsofadditionalrecallsduringthat period.4,11 Amongdevicesreachingthemarketbetween 2008–2017,10.7%ofdeviceswith510(k)clearance (FDApre-marketreviewprocess)and27.1%ofthosewith
pre-marketapprovalwererecalled.12 Toaddressrecallsand itsothermissions,theFDAhasapproximately18,000 employees,including1,887employedbytheCenterfor DevicesandRadiologicalHealthin2020.13,14 Safety monitoringisthusalogisticalchallengebecauseofthe disparitybetweenresourcesanddevicestobemonitored,as wellasthelabor-intensivejobofevaluatingeachdevice’ s meritforrecall.
Anautomatedtooltoassistindeviceriskstratification wouldbeinvaluable,andmachinelearning(ML)couldbe employedforthispurpose.Machinelearningisa fieldof artificialintelligenceinwhichlargedatasetsareusedtotrain analgorithmtocategorizeoranalyzenewdata.MLfollows twosequentialphases.Intheinitialtrainingphase,labeled dataissuppliedtoenablethealgorithmtolearnto differentiatebetweenrelevantclasses(eg, “thisisadog,thisis acat,” or “thisisadangerousmedicaldevice,thisisnot”).In asubsequenttestingphase,thealgorithmispresentedwith new,unlabeleddataandaskedtodifferentiatebetween classes(eg, “isthisacatorisitadog?” ; “willthismedical deviceberecalledornot?”).
LargedatasourcesexternaltotheFDAsystemmight provideusefulsignalsofdevicedangersforuseinML algorithms.PubMedisafreedatabasewithmorethan 37millioncitationsofbiomedicalandlifescienceliterature, developedandmaintainedbytheNationalCenterfor BiotechnologyInformation;reportsofadverseevents involvingmedicaldevicesmightbereportedhere.15 Google Trendsisafreetoolthatquantifiesthefrequencyofsearch termsonGoogleSearch,YouTube,GoogleNews,Google Shopping,andGoogleImagesovertime.16 TheFDAitself providesalistofapprovedandrecalledmedicaldevices.4
WedevelopedandevaluatedanMLalgorithmtopredict medicaldevicerecallsbytheFDAusingpubliclyavailable data.Wediscussitspotentialvalueforpatientsafetyaswell aschallengesandlimitationsofusingMLforrisk stratificationofmedicaldevices.
Weconductedaretrospective,diagnosticcase-control study.ActualFDA-recallstatusofdeviceswasdetermined fromFDAsourcesasdescribedbelow.AnMLalgorithm wasthentrainedtopredicttheprobabilityofFDArecall usingdatafromPubMedandGoogleTrends.Inthetesting phase,thealgorithmwasblindedtotheFDArecallstatusof devicesandproducedapredictionofprobabilityofrecall, whichwasthencomparedtoactualrecallstatus.Wetested theabilityofthealgorithmtopredictrecallwithleadtimesof three,six,and12monthsbeforeanactualrecallbylimiting thealgorithm’saccesstosearchdataforthecorresponding timeperiod.Ourmethodswereconsistentwithrelevant elementsoftheStandardsforReportingDiagnostic AccuracyStudies(STARD)guidelines,suchasdefinitions oftheindextestandreferencestandard,estimatesof
diagnosticaccuracyandprecision,analysesofvariabilityin diagnosticaccuracy,blinding,andpotentialsourcesof bias(Appendix1).17
DeviceDefinitionsandIdentification
Twocategoriesweredefined:recalledmedicaldevices (RMD)(“ cases ”)andnon-recalledmedicaldevices(NRMD) (“controls”).WeidentifiedRMDthroughtheFDA’ s webpagelistingseriousrecalls.4 TheNRMDwereidentified bybeinginthemedicalmarketwithoutbeingrecalledby checkingagainsttheFDAlistforRMD.Deviceswere selectedfromJanuary1,2019–September17,2023, excludingrepeateddevicesorsevereacuterespiratory syndrome-relatedcoronavirus-2(SARS-CoV-2)tests.We excludedSARS-CoV-2testsastheywereinthemarketfor veryfewyearsandcouldproduceanomalousGoogleTrends andPubMeddataduetotheirassociationwithCOVID-19. Alldevicesincludedinthestudywererandomlyselected fromthepoolsofidentifiedRMDandNRMD.
RecognizingthattheFDAinvestigationsandother processesculminatinginadevicerecallmayrequireaperiod ofmonthsoryearstocompletefollowingthe firstreportsof potentialharm,wesoughttodevelopaforecastingtoolthat couldpredictrecallsupto12monthsbeforetheiroccurrence. Weexploreddatainthreedifferentsets,eachlasting five yearsandendingmonthspriortotheactualFDArecall: threemonthsbeforerecall(T-3);sixmonthsbeforerecall (T-6);and12monthsbeforerecall(T-12).Eachofthethree setsthusincluded fiveyearsofdata.
ForeachRMDandNRMDidentifiedintheFDA webpage,PubMedandGoogleTrendswereautomatically searchedbytheMLalgorithmusingthedevicenames (Appendix2)andthethreedaterangesdescribedabove(T-3, T-6,T-12)relativetothedateofrecall.Weincludedqueries withoutGoogleTrendsorPubMeddatainthetrainingand testingdatasettoavoidselectionbias.
WebuiltanMLalgorithmonPython3.8.5(Python SoftwareFoundation,Wilmington,DE)usingrandomforest regressor,anopen-sourcealgorithm.18–20 Thistypeof algorithmisusedforlarge-volume,multivariabledataandis suitableforsetswithmissingvalues,noisydata,andoutliers. Randomforestregressortypicallyuses80%ofdatafor trainingand20%fortesting.21 Aregressoralgorithmoutputs acontinuousdecimalvaluebetween0and1;inour application,0represents0%likelihoodofrecall,and1 represents100%likelihoodofrecall.Wechosearegressor overanalternativealgorithmtype,aclassifier.Aclassifier sortstheoutputofanalgorithmintocategoriessuchas
“recalled” and “notrecalled.” Thecontinuousvalueoutputs ofaregressorcanbeconvertedintodiscreteclassificationsby applicationofthresholdvalues,allowingadditionalanalysis. Incontrast,ifaclassifierhadbeenapplied,discretedata couldnotbeconvertedintocontinuousvalues.
Forthisstudy,weperformedatrainingphase,wherethe algorithmlearnedtodifferentiatebetweenRMDand NRMDwith400randomlyselectedtrainingdata(T-3:81 RMD,319NRMD;T-6andT-12:80RMD,320NRMD), withdeviceslabeledforthealgorithmasRMDorNRMD. Inthetestingphase,100randomlyselectedtestingdata(T-3: 19RMD,81NRMD;T-6andT-12:20RMD,80NRMD) wereprovidedtothetrainedMLalgorithmtoassessits performanceindifferentiatingtheunlabeleddevices. Trainingandtestingdataweretwouniquesetswithno overlap. Figure1 outlinesthetrainingandtestingphases.
Weconvertedcontinuousdecimalpredictionoutputsofthe MLalgorithmfromthetestingphasetodichotomousvalues ofzerooroneusingtwopreviouslypublishedstrategies22:
1.Pre-specified:Roundingusingathresholdof0.5,where allvalues < 0.5wereroundedtozeroandallvalues ≥ 0.5wereroundedtoone.Thisapproachgroups validbutpotentiallyindeterminatevalues(closeto 0.5)withpositive(1)andnegative(0)results.22
2.Exploratory:Roundingusingthresholdsdetermined fromtheMLalgorithmoutputofthetrainingdata, describedbelow.Thisapproachaddressesvalues verycloseto0.5thatmighthavelittlepredictive
valueandmightbebettertreatedasuninterpretable orinconclusive.Tocalculatethesethresholds, trainingdatawasprocessedbythetrainedML algorithmtoyieldcontinuousdecimalpredictions, whichwerethenanalyzedbytheiractualFDArecall status(RMDorNRMD).Usingthemeansandone standarddeviationinthisfashionwouldbe anticipatedtoencompass84%ofthedataofa normallydistributeddataset,excludingvaluesclose to0.5(forNRMD,50%fromdatabelowthemean and34%fromdataoneSDabovethemean;for RMD,50%fromdataabovethemeanand34% fromoneSDbelowthemean).
a.TherangeofNRMDtesting wasdefinedaszerotoone SDabovethemeanoutputvaluesofNRMDtraining (0to[meanNRMDtraining + SDNRMDtraining]).Thus, inthetestingphase,outputvalues ≤ (meanNRMDtraining + SDNRMDtraining)wererounded tozero.
b.TherangeofRMDtesting wasdefinedasoneSD belowthemeanofthepredictionsforRMDtraining toone([meanRMDtraining SDRMDtraining]to1). Thus,inthetestingphase,outputvalues ≥ (meanRMDtraining SDRMDtraining)wererounded toone.
c.Intermediatevaluesbetween(meanNRMDtraining + SDNRMDtraining)and(meanRMDtraining SDRMDtraining)wereassignedtoathirdcategory, “indeterminate.” Thesewerenotroundedand werenotincludedincalculationsrequiring dichotomousoutcomes.22
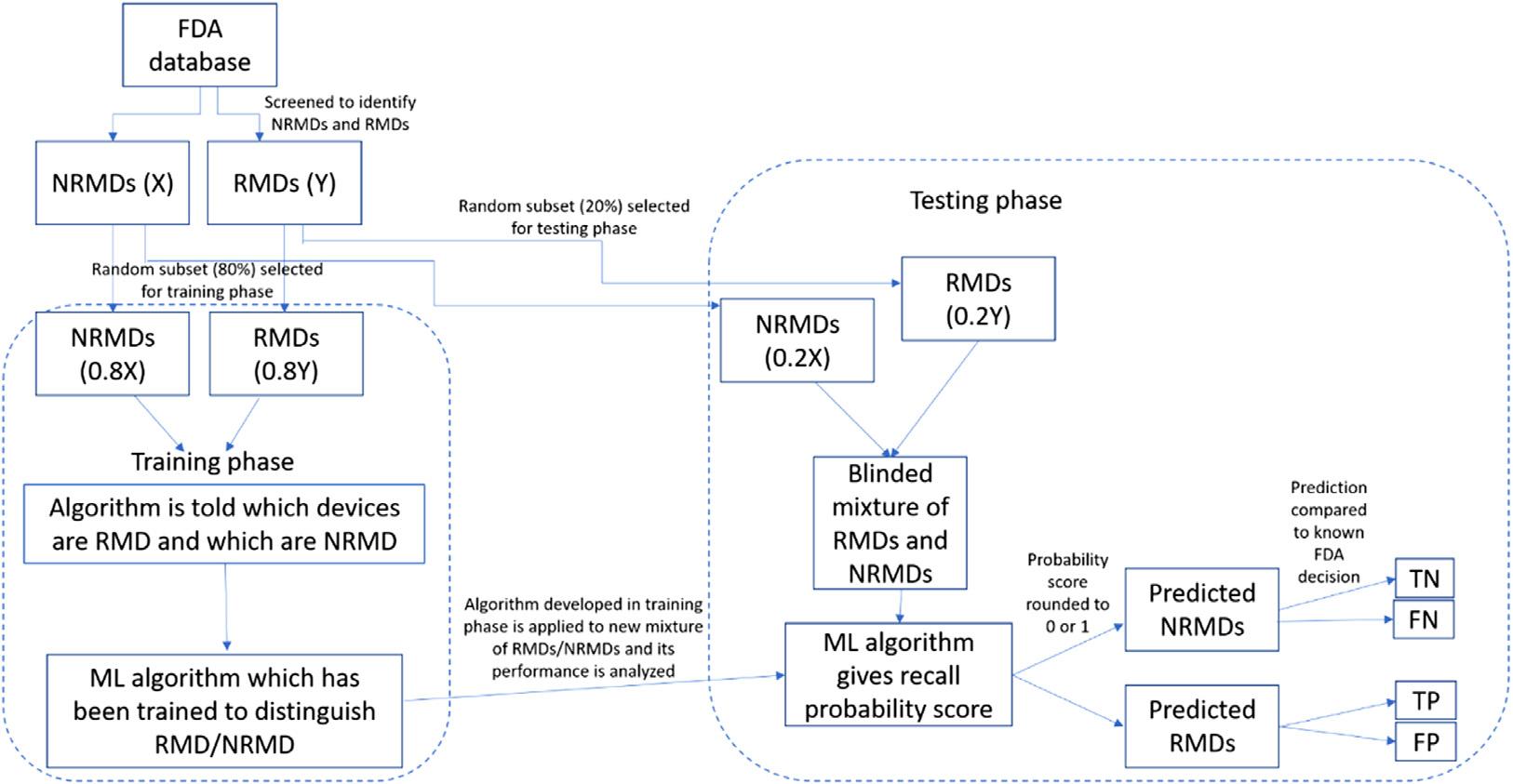
Figure1. Flowchartfortrainingandtestingphasesofthemachinelearningalgorithm.Trainingandtestingdataweretwouniquesetswith nooverlap.
FDA,USFoodandDrugAdministration; FN,falsenegative; FP,falsepositive; ML,machinelearning; NRMD,non-recalledmedicaldevices; RMD,recalledmedicaldevices; TN,truenegative; TP,truepositive.
WerecordedML-algorithm-generatedprobabilityof recallandactualrecallstatusaspre-specifiedoutcomes.We calculatedsensitivity,specificity,andaccuracyasprespecifiedoutcomes,usingpre-specifiedandexploratory thresholdvaluesasdescribedabove.Atruepositivewas consideredadevicepredictedbytheMLalgorithmtobe recalled,whichwasactuallyrecalledbytheFDA.Atrue negativewasconsideredadevicepredictedbytheML algorithmnottoberecalled,whichtheFDAdidnotactually recall.Afalsepositivewasconsideredadevicepredictedby theMLalgorithmtoberecalled,whichtheFDAdidnot actuallyrecall.Afalsenegativewasconsideredadevice predictedbytheMLalgorithmnottoberecalled,whichthe FDAactuallyrecalled.Wedefinedaccuracyas(true positives + truenegatives)dividedbytotaldevices.Testyield wasdefinedasthefractionoftestresultsincludedin calculationofbinaryoutcomes(sensitivity,specificity, accuracy)afterexclusionofindeterminateresults.22
Becausewewereinvestigatinganovelapplicationand datasourcesforanMLalgorithm,wehadnopriordatafor powerorsample-sizecalculations.GivenlimitedFDA
resources,highspecificitywasprioritizedtoavoidwasteful investigationofdevicesthatare,infact,safe.Foratarget specificitypointestimateof100%,80NRMDinthetesting phasewouldyielda95%confidenceinterval(CI) 0.95–1.0.23,24 Thealgorithm’sfocuswasto flagpotential devicesthatshouldberecalledinaseaofmedicaldevices, mostofwhichdonotneedtoberecalled.Therefore,more NRMDthanRMDwererequired,andweselecteda4:1 ratio.Asdescribedabove,theMLalgorithmpartitioned20% ofthesampletothetestingphaseand80%tothetraining phase.Thisyieldedatotalsamplesizeof400NRMDand 100RMD.
TheMLalgorithmcontinuouspredictionvaluesforeach devicefromtestingdataareplottedin Figure2, superimposedonthresholdrangesdeterminedfromtraining data.Theperformanceofthealgorithmusingarounding thresholdforrecallprobabilityof0.5isshownin Figure3 and Table1.Theperformanceofthealgorithmusing roundingthresholdsforrecallprobabilitydeterminedfrom trainingdataisshownin Figure4 and Table2.Weexcluded devicesintheindeterminate(yellow)zone(Figure2)from thisanalysis,withtestyieldreported.22
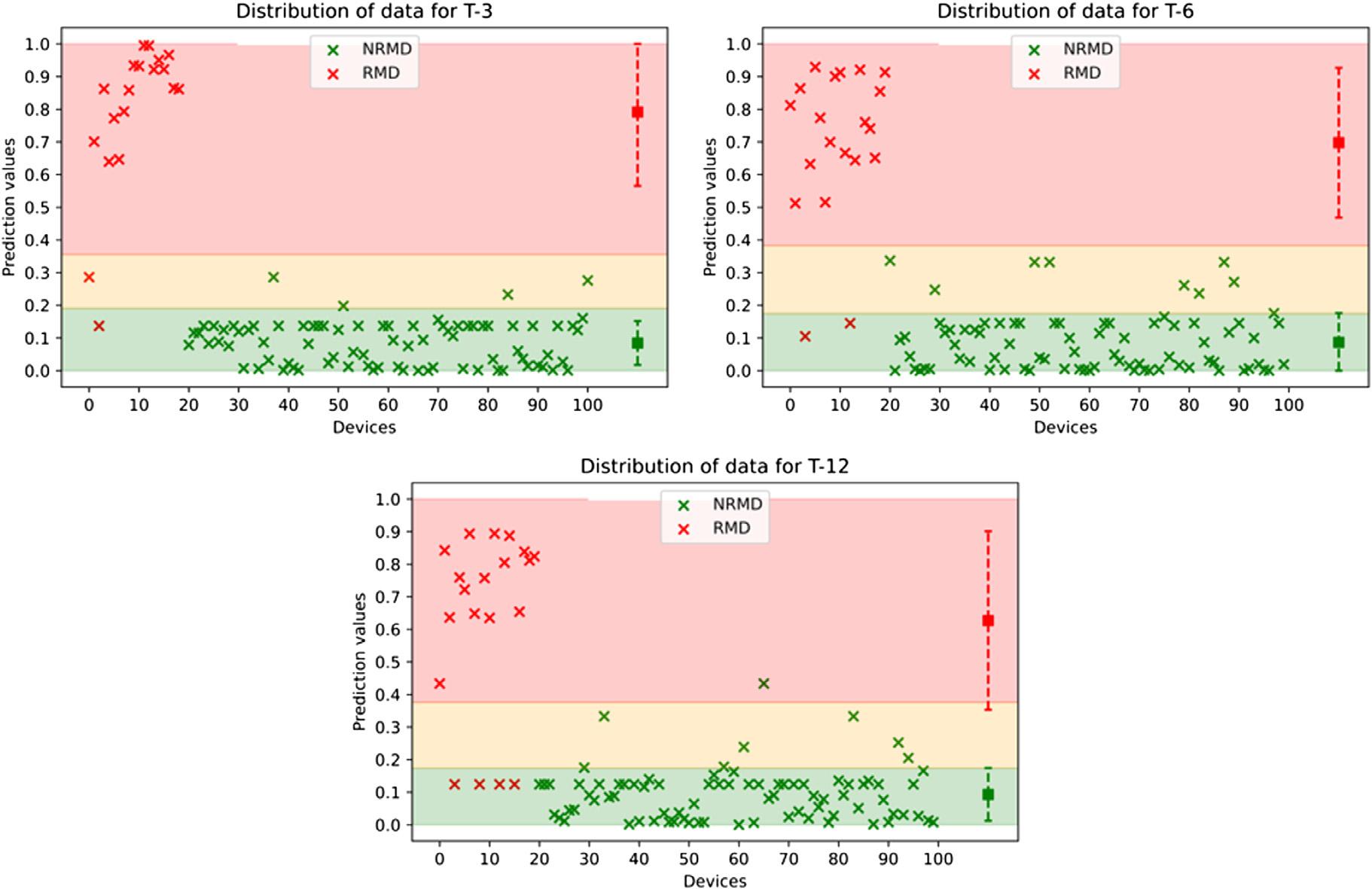
Figure2. ThedistributionofdevicesinthetestingdatasetthatwereeitherrecalledornotrecalledbytheUSFoodandDrugAdministration withleadtimesof3,6,and12months.Redx’srepresentrecalledmedicaldevices(RMD)andgreenx’srepresentnon-recalledmedical devices(NRMD).Thecoloredregionsrepresentrangesdeterminedfromtrainingdatapredictions.Thus,greenx’sinthegreenzonearetrue negatives;redx’sintheredzonearetruepositives;greenx’sintheredzonearefalsepositives;andredx’sinthegreenzonearefalse negatives.Thesquarerepresentsthemeanofeachcategory;theerrorbarsspan +/ onestandarddeviationforthetestingresults.
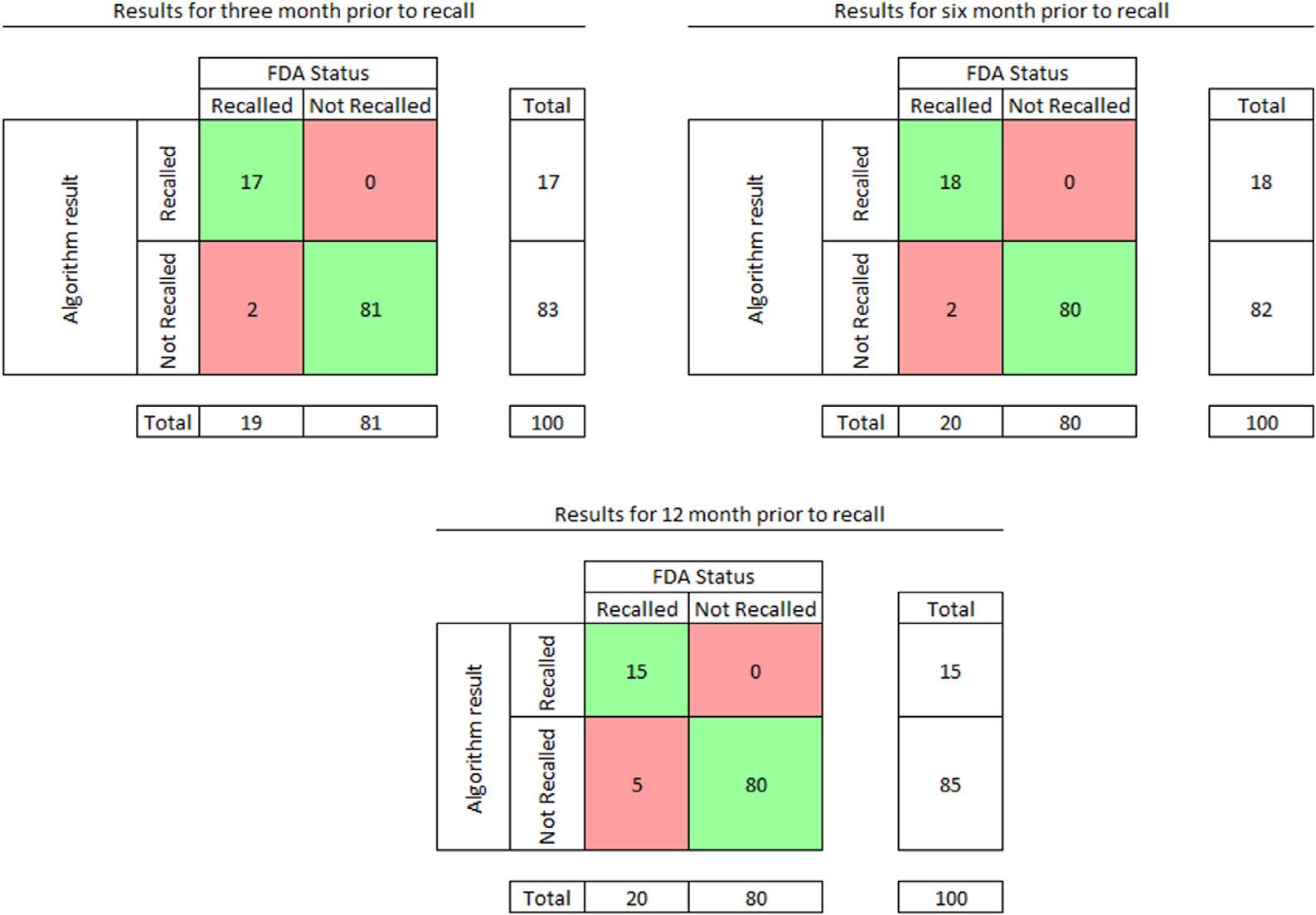
Figure3. Resultsofthetestingphasewhenroundingusing0.5,wheregreenindicatestruepositiveandtruenegative,redindicatesfalse positivesandfalsenegatives.Zerofalse-positiveresultswereencounteredduringthetestedtimeperiodsending3,6,or12monthsbefore USFoodandDrugAdministration(FDA)recall.Falsenegativeresultswereuncommoninallthreetimeperiods.Alldevicesandrecall predictionsareincludedintheanalysis.
Table1. Performanceofthemachinelearningalgorithmwithleadtimesof3,6,and12monthspriortoactualrecallwhenroundingrecall probabilityof0.5andaboveto1,otherwiseto0.
T-389(95%CI69–97)100(95%CI95–100)98(95%CI93–99)
T-690(95%CI70–97)100(95%CI95–100)98(95%CI93–99)
T-1275(95%CI53–89)100(95%CI95–100)95(95%CI89–98)
T-3,3monthsbeforerecall; T-6,6monthsbeforerecall; T-12,12monthsbeforerecall; CI,confidenceinterval.
OurdevelopmentofanMLrisk-stratificationtoolwas motivatedbyourexperiencewithrepeatedsafetyeventswith pigtailcathetersandlarge,vascularaccessdevices.1–3 We reportedthesetomanufacturersandtheFDA.Toour knowledge,theFDAresponseswerelimitedtowritten acknowledgmentsofourreports,withsomeofoursuggested modificationsincorporatedbymanufacturersasdescribed below.GiventhevolumeofreportsannuallytoFDA,we conceivedthatbetter,automatedmethodsforrisk stratificationmightbeneeded.
OurstudydemonstratesthepotentialofanMLalgorithm usingpubliclyavailable,largedatasetstopredictmedical devicerecallswithhighsensitivity,specificity,andaccuracy withleadtimesofthree,six,and12months(Tables1 and 2).
Thehighspecificity(ie,lackoffalsepositives)withnarrow
confidenceintervalsasearlyas12monthsbeforerecall indicatesthatdevices flaggedforrecallarelikelytobetruepositiveunsafedevices,worthyoffurtherFDAinvestigation. Thealgorithmisunlikelyto flagnon-recalleddevicesfor recall(falsepositive),animportantfeaturewhenscreeninga largedevicepoolconsistingprimarilyofsafedevices. Alowfalse-positiveratemayavoidunnecessarycostsand resourceutilization.
Thehighsensitivitywithleadtimesofthreeandsix monthssuggeststhatdangerousdevicesarelikelytobe identifiedbythealgorithm;sodevicesthatareratedas “not recalled” arelikelysafeandmaynotgenerallydeserve additionalFDAscrutinywithoutspecificsuspicionor concern(eg,reportsofsevereadverseeventsinMAUDE). Thesensitivityof75%witha12-monthleadtimeislessthan wehadhopedforbutmaybeacceptablebecauseofthehigh

Figure4. Resultsofthetestingphasewhenremovingthedataintheindeterminatezoneandthenroundingalldatainthegreenzoneto0and alldataintheredzoneto1.Greenindicatestruepositiveandtruenegative;redindicatesfalsepositivesandfalsenegatives.Zerofalsepositiveresultswereencounteredduringthetestedtimeperiods(T)ending3,6,or12monthsbeforeFDArecall.Falsenegativeresultswere uncommoninallthreetimeperiods.Testyield(thefractionofalltestresultsusedincalculatingbinaryoutcomesafterremovalof indeterminatevalues)22 was95%atT-3,91%atT-6,and93%atT-12months.
Table2. Performanceofthemachinelearningalgorithmwithleadtimesof3,6,and12monthspriortoactualrecallwhenremoving indeterminatedevicesandroundingallvaluesthatwereingreento0andallvaluesthatwereinredto1. LeadtimeSensitivitySpeci
T-394(95%CI74–99)100(95%CI95–100)99(95%CI92–100)
T-690(95%CI70–97)100(95%CI95–100)97(95%CI91–99)
T-1275(95%CI53–89)100(95%CI95–100)94(95%CI86–98)
T-3,3monthsbeforerecall; T-6,6monthsbeforerecall; T-12,12monthsbeforerecall; CI,confidenceinterval.
specificity(100%).Eventhoughonlythree-quartersof eventually-recalleddeviceswere flaggedbythealgorithmat thisearlytime-point,all flaggeddevicesweretruepositives andthereforewebelievewouldbeappropriateforfurther FDAinvestigation.
TheprobabilityofrecalloutputsofourMLalgorithm werecontinuousvalues(Figure2).Wecollapsedtheseinto binarycategoriesforcalculationofsensitivityandspecificity, acommonpracticefordiagnostictests.Continuousvariables oftenresultinvalidbutindeterminateresults,whichcanbe addressedbyvariousstrategies,eachwithbenefitsand costs andwithnosingleagreed-uponsolution.22,25 For clinicaldiagnostictests,different “rulein” and “ruleout” thresholdsareoftenused,with anindeterminatezoneoftest resultsrecognized.Examplesincludebrain-typenatriuretic peptide,procalcitonin,andestimatedglomerular filtrationrate.
Weappliedtwocommonlyusedapproachesasameansof sensitivityanalysis:combiningindeterminateresultsinto positiveandnegativecategories(Figure3, Table1),and removingindeterminateresults(Figure4, Table2).
Exclusionofindeterminateresultscanoverestimatetest performance,whilecombininginconclusiveresultscan underestimateaccuracyandmaynotbesensibleinthe intendedapplication.22 Forexample,characterizingadevice witha51%predictedprobabilityofrecallasanRMDwould potentiallyresultinwastefulexpenditureofFDAresources forinvestigation.Representingadevicewitha49%recall probabilityasanNRMDmightimplygreatersafetythan warranted.Inourpresentstudy,wefoundnostatistically significantdifferenceintestperformancebyexcluding indeterminateresults(95%CIforallmeasuresoverlapforthe twoanalyses),andwepresentbothanalysesfor transparency.Thetestyield22 wasgreaterthan90%forall timeperiods,indicatingthataminorityofresultswere excludedasindeterminatevalues.
Devicerecallscanhavesubstantialimpactsinthepractice ofemergencymedicine(andotherspecialties),evenwhen appropriate.Furtherillustratingthesediverseimpactsand validatingtheneedforenhancedtoolsforriskstratificationis thataftertheinitiationofourworkonMLalgorithmswe
encounteredanotherhazardousdeviceinourinstitution.An arterialcatheterusedroutinelyinouremergency departments,operatingrooms,andintensivecareunitswas notedtocreateariskofarterialembolizationofcatheter fragments.Removingthedevicefromcirculation,replacing itwithaviablealternative,andretraininghundredsof healthcareworkersoccurredoveraperiodofapproximately sixmonths beforeamanufacturerurgentrecallwasissued onMay19,2023,andanFDAClassIrecall(themostserious type)followed.26,27 Bythedateoftherecall,thedevicehad beenindistributionfor4.5years(October26,2018–May10, 2023)duringwhichtimethemanufacturerhadreceived83 complaintsofrelateddevicemalfunctionsand18injuries.A totalof262,016deviceswererecalledintheUS.OtherFDA medicaldevicerecallsrelevanttoemergencymedicine practicein2023includedangiographycatheters(forfailure toundergosterilization),infusionpumps(forfailuretodetect airinline),videolaryngoscopes(forstolendefective products),pulseoximetrysensors(forinaccuratereadings andinterferencewithdefibrillators),implantable cardioverterdefibrillators(forlowornoenergyoutput),and ventilators(forshortcircuitsandstoppingwithoutnotice).4
Additionalliteraturehasrecentlyexploredtheimpactof medicaldevicerecallsonpatientsandhealthcaresystems.In 2021,PhilipsRespironicsrecalledairwaypressuredevicesfor carcinogenicchemicalemissionsandsignificantadverse effectsincludingrespiratorydistress,inflammation,hypoxia, andhypercarbia.28 Approximately16milliondomesticand internationalpatientswereaffectedbytherecall,resultingin organizations,includingtheMayoClinic,developingnovel protocolstoensurecentralizedawarenessofdevicerecalls, aidstaffinvisualizingtheirproactiveapproachestothe situation,andefficientlycommunicatewheninforming patientsabouttherecall.
Medicaldevicerecallsinvolvecostsandeffortsfor multiplestakeholders(includingpatients,physicians,health systems,manufacturers,insurers,andregulators),from removingrecalleddevicestodevelopingalternativesto integratethemintothemarketeffectively.Theestimated meandevelopmentcostforanovelcomplexmedicaldeviceis $60million(95%CI,$27million–$209million)after accountingforpost-approvalstudies.Accountingforcostof capitalandfaileddevices,theestimatedmeancostper approveddeviceisnearly10-foldhigher:$526million(95% CI,$207million–$3396million).Fromnonclinicaltrialsto FDAapproval,theestimateddevelopmenttimeofnovel devicesis157months(13years).29 Assessingtheeconomic impactofmedicaldevicerecallsinthebroaderhealthcare ecosystemposesmanychallengesduetofactorsincluding regulatoryconditions,theroleofdeviceintegrationinto medicalprocedures,andthetemporalvariationsinfactors influencingdeviceperformance.30 Althoughindividual devicesaremostoftenproprietaryintellectualproperty, becauseofthetimeandexpensesbornebydiverse
stakeholders,complexmedicaldevicescanbeconsidereda sharedcommons,andachievingappropriatemedicalrecalls isakeysharedgoal.
Solutionstomitigatedevicerisksarenotlimitedto removalfromthemarket,withallthepotentialdetrimentsof suchaction.Somedevicescanberenderedsafe(orsafer)by morenuancedchangessuchasimprovedlabeling,warnings, instructionsforuse,softwareupdates,componentredesign, oralterationsinpowersource.Forexample,afterwe reportedadeviceriskassociatedwithaHeimlichvalve componentofachesttubekit,themanufactureradopted verbatimoursuggestionforasafetylabel.1 Afterwereported riskofaretainedobturatorcomponent,themanufacturer alsoincorporatedrevisedinstructions(abanneremphasizing removaloftheobturator)inanEnglish-languagetraining video(2minute33secondmark),althoughnotinthe Spanish,Italian,orGerman-languagevideos.2,31 Such interventionsmaybereasonablecompromisesgiventhecosts (economicandother)tovariousstakeholdersofoutright removalofadevicefromthemarket.
AriskstratificationMLalgorithmcouldassistin identifyingdevicesforsuchmodifications,ratherthan completeproductrecall.TheimplementationofanML approachandnewdatasources,concurrentlywiththe techniquesalreadyemployedbytheFDA,mightbeacrucial aidindecreasingtheintensiveresourcesrequiredforrecall investigations,allowingtheFDAtoeitherinvestigateawider breadthofdevicesortofocusmoreresourcesondevicesthat haveahigherrisk,thuspotentiallyincreasingtheoverall safetyofthehealth field.Giventhecomplexityofthemedical deviceecosystemandtheearlystageofourMLalgorithm, wearenotrecommendingthatFDArecalldevicesbe identifiedbyanalgorithm;rather,anMLalgorithmcouldbe usedaspartofalargerarmamentariumtoaddressrisk.
Futureworkcouldcharacterizethepredictive performanceofanMLalgorithmwithevengreaterlead times,usingadditionaldatasourcessuchastheFDA MAUDEdatabase,andwithprospectivepredictionsfor(asyet)unrecalleddevices.Evenanalgorithmthatdoesnot providegreaterleadtimethancurrentFDAprocessesmight increaseefficiencyandresourceutilizationofrecall processes.ComparisonofanMLalgorithm’swarning performancewithexistingFDAprocesses,accuracy,and resourceutilizationwouldbemeaningfulnextsteps.The additionofanMLalgorithmtoexistingFDAprocesses (ratherthanreplacementofextantprocesses)isanother potentiallyusefulapplication.
Despitepromisingresults,ourstudyrevealedseveral limitationsandchallengesofusingMLinhealthcare.The algorithmreliesonGoogleTrendsandPubMedfootprintsto increaseitsaccuracy,meaningitisseverelylimitedtodevices withasignificantonlinepresence.Futureiterationsofthe
algorithmmightincludeotherfreeonlineinformation,such astheinformationintheMAUDEdatabase,whichwasnot incorporatedintothecurrentMLsystem.Thelackof interpretabilityofMLalgorithmsmakesitdifficultto understandtheunderlyingmechanismsbehindtheir predictions,posingchallengesinassessingtheirreliability andvalidity.Anexampleisthatwhilethealgorithmcan predicttheFDArecalls,itisunclearwhetheritcandetermine ifthedeviceisdangerousforpatientsorwillberecalledfor otherreasons.Anotherareathatfurtherchallengesthe reliabilityandvalidityisthecontentofPubMedorGoogle Trendssearches.Authorscouldhaveonlybrieflymentioned adevice;however,asearchstillyieldsit.Additionally, currentlythereisnotawaytodistinguishwhetherthe mentionsregardingadevicearepositiveornegative,anarea forfutureMLdevelopment.
Therelativelysmalldatasetof500devicesmaylimitthe generalizabilityofthealgorithmandleadtoawideCI regardingbothsensitivityandspecificity.Futurestudies shouldconsiderusinglargerandmorediversedatasetsto trainandevaluatetheMLalgorithm.Additionally,the algorithmappliesFDAdeterminationsasthereference standard.Itremainstobeproventhatthissourceisthebest comparatorfortheoutputprovidedbythealgorithmsince theFDAmightberecallingdevicesunnecessarilyorfailing torecalldangerousdevices.Althoughitdidnotoccur commonlyinoursample,analgorithmwouldbejudgedas failingifitdidnotmatchtheFDA,evenifintruthitwere superiortotheFDAprocessinrecognizingdangerous devices.Ourstudyonlyfocusedonpredictingmedicaldevice recallsanddidnotevaluatetheclinicaleffectivenessorsafety ofthedevicesthemselves.Wedidnotcompareouralgorithm performancetocurrentFDAprocesses.Additionally,given howcloselytheMLalgorithmperformancematchesthatof theFDA,theFDAmayalreadybeusingMLalgorithmsor similarprocesses.
AmachinelearningalgorithmusingPubMedandGoogle TrendsdatapredictedmedicaldevicerecallsbytheFDA withhighsensitivity,specificity,andaccuracywithleadtimes asgreatas12months.AnMLalgorithmmightimprove patientsafetybyenhancingtheearlydetectionand preventionofmedicaldevicerecalls.Furtherresearchis neededtoimprovesensitivity,extendtheforecasting window,andpromotethedevelopmentofMLalgorithmsin otherhealthcaresegments,suchasfoodanddrugsafety.
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Slivinskisetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BroderJS,FoxJW,MilneJ,etal.Heimlichvalveorientationerror leadingtoradiographictensionpneumothorax:analysisofanerroranda callforeducation,deviceredesignandregulatoryaction. EmergMedJ. 2016;33(4):260–7.
2.BroderJS,Al-JaraniB,LananB,etal.Pigtailcatheterinsertionerror: rootcauseanalysisandrecommendationsforpatientsafety. JEmerg Med. 2020;58(3):464–72.
3.BroderJ,RobertsonJ,PetersonT,etal.Adangerouscaseofthe “Goldilockseffect”:experimentaldemonstrationofpotentialvascular injurymechanismwithcentralvenouscatheterinsertion[abstractonly]. AnnEmergMed. 2022;80(4):S158–9.
4.UnitedStatesFoodandDrugAdministration.Medicaldevicerecalls. 2024.Availableat: https://www.fda.gov/medical-devices/medicaldevice-safety/medical-device-recalls.AccessedFebruary20,2024.
5.UnitedStatesFoodandDrugAdministration.MedWatch:TheFDA safetyinformationandadverseeventreportingprogram.Availableat: https://www.fda.gov/safety/medwatch-fda-safety-information-andadverse-event-reporting-program.AccessedOctober22,2023.
6.UnitedStatesFoodandDrugAdministration.MAUDE-manufacturer anduserfacilitydeviceexperience.Availableat: https://www. accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/search.cfm AccessedSeptember12,2023.
7.UnitedStatesFoodandDrugAdminstration.Aboutmanufacturerand userfacilitydeviceexperience(MAUDE).Availableat: https://www. fda.gov/medical-devices/mandatory-reporting-requirementsmanufacturers-importers-and-device-user-facilities/aboutmanufacturer-and-user-facility-device-experience-maudedatabase.AccessedOctober22,2023.
8.UnitedStatesFoodandDrugAdministration.Recalls,correctionsand removals(devices).Availableat: https://www.fda.gov/medical-devices/ postmarket-requirements-devices/recalls-corrections-and-removalsdevices.AccessedOctober22,2023.
9.UnitedStatesFoodandDrugAdministration.CFR-Codeoffederal regulationstitle21.2023.Availableat: https://www.ecfr.gov/on/202410-21/title-21.AccessedOctober21,2024.
AddressforCorrespondence:JoshuaSethBroder,MD,Duke UniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Box3096,Durham,NC27710.Email: joshua.broder@duke.edu
10.UnitedStatesFoodandDrugAdministration.Recentlyapproved devices.Availableat: https://www.fda.gov/medical-devices/deviceapprovals-denials-and-clearances/recently-approved-devices AccessedOctober18,2023.
11.UnitedStatesFoodandDrugAdministration.Medicaldevicerecalls (onlinedatabase).Availableat: https://www.accessdata.fda.gov/scripts/ cdrh/cfdocs/cfres/res.cfm.AccessedOctober24,2023.
12.DubinJR,SimonSD,NorrellK,etal.Riskofrecallamongmedical devicesundergoingUSFoodandDrugAdministration510(k)clearance andpremarketapproval,2008–2017. JAMANetwOpen. 2021;4(5):e217274.
13.UnitedStatesFoodandDrugAdministration.Howmanypeopleare employedbyFDAandinwhatareasdotheywork?Availableat: https://www.fda.gov/about-fda/fda-basics/how-many-people-areemployed-fda-and-what-areas-do-they-work AccessedOctober18,2023.
14.UnitedStatesFoodandDrugAdministration.Detailoffull-time equivalents.Availableat: https://www.fda.gov/media/132813/ download?attachment.AccessedOctober18,2023.
15.NationalLibraryofMedicine.PubMedoverview.Availableat: https:// pubmed.ncbi.nlm.nih.gov/about/.AccessedMay22,2024.
16.Google.Googletrends.Availableat: https://trends.google.com/trends/ AccessedMay22,2024.
17.CohenJF,KorevaarDA,AltmanDG,etal.STARD2015guidelinesfor reportingdiagnosticaccuracystudies:explanationandelaboration. BMJOpen. 2016;6(11):e012799.
18.PedregosaF,VaroquauxG,GramfortA,etal.Scikit-learn:machine learninginPython. JMachLearnRes. 2011;12(85):2825–30.
19.HoTK.Randomdecisionforests. ProcIntConfDocAnalRecognit 1995;1:278–82.
20.BeheshtiN.Randomforestregression:abasicexplanationanduse casein7minutes.Availableat: https://towardsdatascience.com/ random-forest-regression-5f605132d19d.AccessedMarch2,2022.
21.Google.Trainingandtestsets:splittingdata.Availableat: https:// developers.google.com/machine-learning/crash-course/overfitting/ dividing-datasets.AccessedMay22,2024.
22.ShinkinsB,ThompsonM,MallettS,etal.Diagnosticaccuracy studies:howtoreportandanalyseinconclusivetestresults. BMJ. 2013;346:f2778.
23.LowryR.Theconfidenceintervalofaproportion.Availableat: http:// www.vassarstats.net/prop1.html.AccessedSeptember15,2024.
24.AkogluH.User’sguidetosamplesizeestimationindiagnosticaccuracy studies. TurkJEmergMed. 2022;22(4):177–85.
25.SimelDL,FeussnerJR,DeLongER,etal.Intermediate,indeterminate, anduninterpretablediagnostictestresults. MedDecisMaking. 1987;7(2):107–14.
26.TeleflexArrowInternational.UrgentmedicaldevicerecallArrow Endurance™ extendeddwellperipheralcathetersystem. Availableat: https://www.teleflex.com/usa/en/product-areas/vascularaccess/EIF-000538-FSN-US.pdf AccessedFebruary20,2024.
27.UnitedStatesFoodandDrugAdministration.Teleflex,andArrow International,recallARROWenduranceextendeddwellperipheral cathetersystemforriskofcatheterseparationandleakage. Availableat: https://www.fda.gov/medical-devices/medicaldevice-recalls/teleflex-and-arrow-international-recall-arrowendurance-extended-dwell-peripheral-catheter-system AccessedFebruary20,2024.
28.UnitedStatesFoodandDrugAdministration.FAQsonPhilips Respironicsventilator,BiPAPmachine,andCPAPmachinerecalls. Availableat: https://www.fda.gov/medical-devices/safetycommunications/faqs-philips-respironics-ventilator-bipap-machineand-cpap-machine-recalls.AccessedMay22,2024.
29.SertkayaA,DeVriesR,JessupA,etal.Estimatedcostofdevelopinga therapeuticcomplexmedicaldeviceintheUS. JAMANetwOpen. 2022;5(9):e2231609.
30.KirisitsAandRedekopWK.Theeconomicevaluationofmedical devices:challengesahead. ApplHealthEconHealthPolicy. 2013;11(1):15–26.
31.CookMedical.WaynePneumothoraxSet(Seldinger)proceduralvideo. Availableat: https://www.cookmedical.eu/critical-care/waynepneumothorax-set-seldinger-procedural-video/ AccessedSeptember17,2024.
WilliamBonadio,MD
ConnorWelsh,MD
BradPradarelli,MD
YunfaiNg,MD
SectionEditor: MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedNovember7,2023;RevisionreceivedSeptember11,2024;AcceptedSeptember25,2024
ElectronicallypublishedOctober29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18555
Objective: Ourgoalwastocharacterizealargegroupofchildrenpresentingtotheemergency department(ED)withacuteanaphylaxis,treatedwithintramuscularepinephrine(IMEPI)anda corticosteroid(CS),andtodeterminetheimpactofpharmacologicinterventionontherateandtimingof biphasicreactions(BPR).
Methods: WereviewedconsecutivechildrendiagnosedwithacuteanaphylaxismanagedinthreeEDs duringasix-yearperiod.AllreceivedIMEPIandCS,followedbymonitoringfor4–6hoursposttreatment.WeanalyzedtherateandtimingofBPR,comparingtheintervalsof0–4vs4–48hoursafter initiatingtherapy.
Results: Duringthestudyperiod,therewere371casesofanaphylaxis,ofwhich357(94%) receivedbothIMEPIandCS.Ofthese,49(14%)manifestedBPR[84%hadreceivedprehospitalIMEPI] requiringatleastoneadditionaldoseofIMEPI[14%required ≥2additionaldoses].AllBPR episodesoccurredwithinthe0–4hourintervalafterinitiatingtherapy,whereasnopatient manifestedaBPRrequiringanadditionaldoseofIMEPIduringthe4–48hoursafterinitiatingtherapy (P =<0.001,95%CI0–1.3%).NopatientreturnedtotheEDwithrecurrenceofanaphylaxissymptoms within48hoursafterdischarge.
Conclusion: Approximately1in7childrenwithanaphylaxisexperienceabiphasicreactionafter receivingintramuscularepinephrine.Childrenwithanaphylaxiswhoexhibitsymptomaticresolutionfour hoursfollowinginitiationoftherapyhavealowriskforsubsequentlydevelopingBPR.MostBPRcases requiredonlyoneadditionaldoseofIMEPItoeffectresolution.TherateofBPRinthosereceivingIMEPI andacorticosteroidissignificantlylower >4hoursvs <4hoursafterinitiatingtherapy.[WestJEmerg Med.2025;26(1)171–175.]
Anaphylaxisisacommonandpotentiallysevere,even lethal,systemicallergicreactionthatisincreasingin frequency.1 Inthosepatientswhoexperiencethiscondition andclinicallyimproveafterreceivingmedication,thereis potentialforabiphasicreaction(BPR)tomanifestas symptomaticrecurrence/exacerbation.Priorresearchhas documentedratesofBPRassociatedwithanaphylaxis widelyrangingfrom1–23%.1
Somehaverecommendedagainstroutinelytreatingacute anaphylaxiswithcorticosteroids(CS)duetolackofproven efficacy.2,3 Yetitisplausiblethattheanti-inflammatory qualitiesofthismedicationcouldpotentiallyamelioratethe IgE-mediatedanaphylaxisprocess.4,5 Sincetheeffectof intramuscularepinephrine(IMEPI)isshort-lived,lasting briefly(t½of2–3minutes),andCShasclinicalonset approximately >4hoursfollowingadministration,lasting beyond24hours,itislikelythatafter >4hourstheIMEPI
effectwanesandanyongoinganti-allergyeffectislikelydue toCS.TheBPRhasbeenshowntopotentiallymanifestat anytimeduringthesubsequent48hoursafteronset(median time18.5hoursinonestudy6);so,itshouldbetherapeutically advantageoustoadministeralongeractinganti-allergy medicationlikeCStohelppreventthiscomplication.
Thepurposeofthisstudywastoanalyzealargenumberof pediatriccasesofanaphylaxistreatedwithIMEPIand CStodeterminewhetheracorrelationexistsbetween pharmacologicinterventionandtherateandtimingofBPR.
Weconductedaretrospectivecohortstudyofconsecutive childrenaged <19yearsmanagedinthreeEDsattheMount SinaiMedicalCenterinNewYorkbetweenJanuary 2015–December2022,inclusive;twoarededicatedpediatric EDs,andoneisageneralEDalsomanagingchildren (combinedyearlypediatriccensus55,000child-visits).Our templatedelectronichealthrecord(EHR)(EpicSystems CorporationVerona,WI)stereotypicallyqueriesan extensiverosterofpotentialanaphylaxissymptoms, involvingdermal,cardiovascular,earnosethroat, pulmonary,neurologic,andgastrointestinalsystems.The EHRalsodocumentssubsequentmedicalvisitsthroughout otherareahospitals/clinics.Anaphylaxiswasdiagnosed,per previouslypublishedcriteria,7 withacuteonsetofmultiple symptomsfollowingexposuretoallergentriggerinvolvingat leasttwoorgansystems(Table1).
WedefinedBPRasarecurrence/exacerbationof symptomsfollowingadministrationofIMEPI,afteraperiod ofpartialorcompleterecovery,withoutre-exposuretothe trigger,indicativeofanaphylaxisorgeneralizedallergic reactionofsufficientseveritytorequireatleastone additionaldoseofepinephrine.
TheEDmanagementofanaphylaxiswasnearly unanimousamongallclinicians,consistingofIMEPI andCSin96%ofcases.TheCSmedicationsincluded dexamethasone,methylprednisolone,prednisolone,or prednisone(intravenouslyororally)onthedayof presentation.AllpatientswithanaphylaxisreceivedED monitoringfor4–6hourspost-therapyinitiationforBPR. Ourtemplateddischargeinstructionsfor “anaphylaxis” statespatientsshouldseekpromptmedicalattentionifanyof thefollowingoccur:1)worseningofsymptoms;2)trouble
• Skin/mucosa:urticaria,pruritis, flushing,facial/ mucosalangioedema
• Respiratory:wheezing,cough,stridor,dyspnea
• Cardiovascular:tachycardia,hypotension
• Gastrointestinal:nausea,vomiting,diarrhea,abdominalpain
• Oropharynx:throatswelling,oralpruritis
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
TheoptimalintervalofEDobservationfor treatedchildrenwithanaphylaxis,andthe impactofcorticosteroidsinmodifyingriskfor biphasicreaction(BPR),areunknown.
Whatwastheresearchquestion?
Howdoesepinephrineandcorticosteroid therapyimpacttherateandtimingofBPR?
Whatwasthemajor findingofthestudy?
AllBPRepisodesoccurred < 4hrsafter initiatingtherapy;noBPRcaserequired parenteralepinephrineduring4 – 48hrs afterinitiatingtherapy(P < 0.001, 95%CI0 – 1.3%).
Howdoesthisimprovepopulationhealth?
Theseresultshelptode fi neoptimal monitoringperiodfortreatedchildrenwith anaphylaxisandshedlightoncorticosteroid impactonBPRrecurrencerate.
breathingorswallowing;3)swellingofmouthorface;4) chestpain;and5)dizziness,weaknessorfainting.
WealsosurveyedthesubsequentEHRdocumentationto determinewhetherarepeatvisittoanEDorotheroutpatient facilityoccurredwithin48hoursofdischarge.Inpatients withanaphylaxiswhoreceivedbothIMEPIandCS,the primaryoutcomemeasurewastodetermine1)therateof BPR,and2)thecomparativeratesofBPRin0–4and4–48 hourspostreceivingIMEPI.Thesecondaryoutcome measurewastodeterminetherateofEDreturnvisitforBPR within48hoursofEDdischarge.
Categoricaldataaredescribedintermsoffrequency(%) andcomparedusing κ coefficients.Wecalculatedasampleof 280casestoallowfor80%power(alpha0.05)todetermineat leasta10%differenceinBPRratesbetweenintervalsof <4 hours(15%)vs >4hours(5%)afterCSadministration.1,8 To determineinter-rateragreementincollatingresults,30cases (15%oftotal)wererandomlyselectedandeightvariables comparedbetweenreviewers;thekappawas0.84,indicative ofsubstantialagreement.Sincetherewerefewerthan five patientsinonecell,weperformedaFisherexacttest comparingratesofBPRduringthe0–4vs >4hoursposttreatmentintervals.Wecalculatedbinomialprobability95% confidenceinterval(CI)forthosewhoreceivedIMEPIand
CSwithnoBPRoccurrence,usingtheClopper-Pearson exactmethod(CI77–84%).Thestudywasapprovedbythe IcahnSchoolofMedicineInvestigationalReviewBoard.
Duringthestudyperiod,therewere371consecutivecases ofanaphylaxisinvolving280patients;in357cases(94%) bothIMEPIandCSwereadministered.Eachrecordinthe studycohorthadacompletedattending-levelphysiciannote reviewinghistoryofpresentillness,reviewofsymptoms,
Table2. Patientcharacteristics:357casesofanaphylaxistreated withintramuscularepinephrineandcorticosteroid.
VariableN[%]
Patientagerange3months–19 years
Patientagemedian9.2years
Patientsex
• Male181[50.7%]
• Female176[49.3%]
EDlengthofstay(median)4.7hours
EDlengthofstay(range)3.5–6.2hours
Anaphylaxistrigger
• Foodexposure328[93%]
• Unknown20[5.0%]
• Environmentalexposure4[1.0%]
• Drug-related5[1.0%]
Managementreceived – allcases:
• IMEPI357[100%]
• PrehospitalIMEPI193[54%]
• CS357[100%]
• H1and/orH2receptorantagonist*344[96%]
Biphasicreactioncases^
• Total49[14%]
• received >1doseofIMEPI49[14%]
• received >2dosesofIMEPI8+ [2%]
• receivedprehospitalIMEPI41[84%]
• duringtheinitial4hoursafterinitiating therapy 49[100%]#
• duringtheinterval4–48hoursafter initiatingtherapy
Inpatienthospitalization11[3%]
Deaths0
*ReceptorantagonistH1 = diphenhydramine;H2 = famotidine. ^Within48hoursafterinitialpresentation.
+AlldosesofIMEPIweregivenduringtheinitial0–4hoursafter initiatingEDtherapy.
#P-valuecomparingratesis P < 0.001. BPR,biphasicreaction; CS,corticosteroid; ED,emergency department; IMEPI,intramuscularepinephrine.
physicalexam,andmedicaldecision-making.The demographicprofileofthiscohortisgivenin Table2.Atotal of49patients(14%)manifestedBPRrequiringatleastone additionaldoseofIMEPI[14%required ≥2additional doses];41[84%]hadreceivedprehospitaladministrationof IMEPI.AllBPReventsoccurredduringtheinitialfour hoursafterinitiatingtherapy,whereasnopatientmanifested BPRrequiringanadditionaldoseofIMEPIduringthelatter 4–48hourintervalafterinitiatingtherapy(P =<0.001).No patientwasdocumentedtoreturntotheEDwithrecurrence orexacerbationofanaphylaxissymptomswithin48hours afterdischarge.
Inouranalysiswesoughttoreviewalargenumberof pediatricanaphylaxiscasestreatedwithIMEPIandCSto determinethesubsequentrateandtimingofBPR.Our approachtomanagementwasnearlyunanimous,as96%of casesreceivedIMEPIandCS.The14%observedrateof BPR,andpredominanceoffoodallergentriggers,are consistentwithpriorpediatricreports.9,10 Themajority (84%)ofBPRcasesrequiredonlyoneadditionaldoseofIM EPItoeffectresolution.
Usingourinstitutionalapproach,the0%BPRrate achievedduringthe4–48hourintervalafterinitiating therapyislowerthanhasbeenpreviouslyreportedinthe literature;severalofthoseanalysesfoundnosignificant differenceinreturnratesbetweenthosewhodidvsthosewho didnotreceiveCS.11,12 Thefactoroftimedelayfromentry intomedicalcaretoinitialdoseofIMEPIimpactingBPR ratewasminimizedinourcohort,as84%ofpatients developingthiscomplicationhadreceivedrapiddeployment ofaninitialdoseofIMEPIintheprehospitalphaseof management.Recentreviewarticlesonpediatric anaphylaxisrecommendagainstCStreatment,duetolackof provenefficacy.2,3 One13 implicatedCStreatmentas increasing “thelikelihoodofabiphasicreactioninchildren byasmuchas50%” (nostudycitationgiven).Aforeign retrospectivestudysurveyingalargedatabasecomparing anaphylaxistreatmentwithandwithoutCSfoundno significantdifferenceinBPRratesyetdidnotspecifically correlateonsetofBPRwithtimingofCSadministration.14
TheexactpathogenesisofanaphylacticBPRisunclear; potentialtheoriesincludeasecondwaveofmastcell degranulation,delayedongoingabsorptionofoffending antigen(especiallyoralantigenicexposures),orthewaning effectoftherapy.15 Asanextensionoftreatmentforother atopicconditions,CStherapyisexpectedtoexertabeneficial effectinmodulatingtheIgE-mediatedprocessof anaphylaxis.Thisclassofdrugshasprovenefficacyin amelioratingotherallergic-mediatedconditionssuchas urticariaandasthma.ThereisevidencethatCScaninhibit mastcells,whicharestronglyimplicatedintheanaphylaxis cascade,bydown-regulatingpro-inflammatorycytokine
transcription,regulatingmultipleadaptorandsignaling molecules,andrapidlydecreasingcellhistaminerelease.4,5 ThesecharacteristicssupportthebiologicalplausibilityofCS affectingBPRprevention.Consistentwiththis,aprior study12 ofpediatricanaphylaxisshowedearlyCStherapy wasinverselyassociatedwithprolongedlengthofstayand subsequentIMEPIrequirementamongthosehospitalized.
Therearenopublishedprospectiverandomized,placebocontrolledstudiesassessingCSeffectintreatinganaphylaxis. Whilesuchstudiesandtheirdatawouldbeanimportantstep towardamorecompleteunderstandingofBPRin anaphylaxis,thedesignofsuchastudywouldbe problematic.Obtaininginformedconsenttorandomize treatmentwouldbeprohibitiveforthepotentiallylethal medicalconditionofacuteanaphylaxis,inwhichdelayin therapeuticinterventionmeasuredinminutescanbecrucial indeterminingoutcome.Duetoethicalconsiderations,such astudywouldmandatetreatmentofallpatientswithIMEPI andthencompareagrouptreatedwithCSvsplacebo.The intervalsofanalysiscomparedwouldbepriortovsafterCS therapeuticonset,likelyatthefour-hourpost-administration mark.Ourmethodologylargelysimulatesthisscheme;yet anyanalysisincludingIMEPItreatmentofallpatientsstill leavesunansweredthequestionofwhethertheinitialIMEPI doseactually “resolves” anaphylaxisvsmerelyprovidinga temporizingsuppressionofthereaction withCSexertinga furthereffectinBPRprevention.
Our findingsmayshedlightonapotentialCStherapeutic impactonrateofBPRrecurrence.Sinceinallinstancesboth IMEPIandCSwereadministered,wenotedasignificant differenceinBPRrateswhenpartitioningclinicalcourse basedonmedicationpharmacokinetics.TheIMEPIeffectis rapidinonset,lastingbriefly(t½of2–3minutes),whereasCS hasclinicalonsetapproximately >4hoursfollowing administration,lastingbeyond24hours.16–18 Itislikelythat afterfourhourstheIMEPIeffectwanes,andanyongoing anti-allergyeffectislikelyduetoCS.Withinthiscontext, wefoundtherateofBPRrequiringrepeatIMEPI administrationwassignificantlylower4–48hoursvs 0–4hoursafterinitiatingtherapy.
Aswithanyobservationalstudy,datagatheringwas limitedbyinformationpresent.Welargelyavoidedthis deficiency,inthatnearlyallourpractitionersmanaged patientsandthoroughlydocumentedmanagementina stereotypedmanner.Wedidnothavesufficientdatato analyzetimefromonsetofanaphylaxissymptomsto receivingIMEPIanditspotentialimpactonBPRrate.
Approximately1in7childrenwithanaphylaxis experienceabiphasicreactionafterreceivingintramuscular epinephrine.Childrenwithanaphylaxiswhoexhibit
symptomaticresolution4–6hoursfollowinginitiationof therapyhavealowriskforsubsequentlydevelopingBPR. ThemajorityofBPRcasesrequireoneadditionaldoseofIM EPItoeffectresolution.TherateofBPRinthosereceiving IMEPIandcorticosteroidsissignificantlylower4–48hours vs0–4hoursafterinitiatingtherapy.
AddressforCorrespondence:WilliamBonadioMD,MountSinai MorningsideMedicalCenter,20E84thSt.,NewYork,NY10028. Email: william.bonadio@mountsinai.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Bonadioetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PatekP,OwdaD,MenochM.Anaphyl-crisis:risingratesofpediatric anaphylaxis. PediatrEmergCare 2022;38(9):e1529–32.
2.AlqurashiWandEllisAK.Docorticosteroidspreventbiphasic anaphylaxis? AllergyClinImmunolPract 2017;5(5):1194–1205.
3.ChooKJL,SimonsE,SheikhA.Glucocorticoidsforthetreatment ofanaphylaxis:Cochranesystematicreview. Allergy 2010;65(10):1205–11.
4.CaslinHL,KiwanukaKN,HaqueTT,etal.Controllingmastcell activationandhomeostasis:workinfluencedbyBillPaulthatcontinues today. FrontImmunol 2018;9:868.
5.OppongE,FlinkN,CatoACB.Molecularmechanismsofglucocorticoid actioninmastcells. MolCellEndocrinol 2013;380:119–26.
6.AlqurashiW,StiellI,ChanK,etal.Epidemiologyandclinicalpredictors ofbiphasicreactionsinchildrenwithanaphylaxis. AnnAllergyAsthma Immunol 2015;115:217–23.e2.
7.CardonaV,AnsoteguiIJ,EbisawaM,etal.WorldAllergyOrganization anaphylaxisguidance2020. WorldAllergyOrganJ 2020;30;13(10):100472.
8.Tarczo I,Cichocka-JaroszE,KnappA,etal.The2020updateon anaphylaxisinpediatricpopulation. PostepyDermatolAlergol 2022;39(1):13–9.
9.SampsonHA,Munoz-FurlongA,CampbellRL,etal.Second symposiumonthedefinitionandmanagementofanaphylaxis:summary report SecondNationalInstituteofAllergyandInfectiousDisease/ FoodAllergyandAnaphylaxisNetworkSymposium. JAllergyClin Immunol 2006;117(2):391–7.
10.TejedorA,MoroM,GarcíaM.Epidemiologyofanaphylaxis. ClinExp Allergy 2015;45:1027–39.
11.LiyangeCK,GalappathyP,SenevirSL.Corticosteroidsinmanagement ofanaphylaxis;asystematicreviewofevidence. EurAnnAllergyClin Immunol 2017;49(5):196–207.
12.MichelsonKA,MonuteauxMC,NeumanMI.Glucocorticoidsand hospitallengthofstayforchildrenwithanaphylaxis:aretrospective study. JPediatr 2015;167(3):719–24.e1–3.
13.TanverdiMS,WiersmaA,KimKM,etal.Anaphylaxisinchildren. PediatrEmergCare 2022;38:456–61.
14.NagataS,OhbeH,JoT,etal.Glucocorticoidsandratesof biphasicreactionsinpatientswithadrenaline-treatedanaphylaxis: apropensityscorematchinganalysis. IntArchAllergyImmunol 2022;183(9):939–45.
15.LeeS,BellolioMF,HessEP,etal.Timeofonsetand predictorsofbiphasicanaphylacticreactions:asystematic reviewandmeta-analysis. JAllergyClinImmunolPract. 2015;3(3):408–16.
16.SamuelS,NguyenT,ChoiA.Pharmacologiccharacteristicsof corticosteroids. JNeurocritCare 2017;10:53–9.
17.DreborgSandKimH.Thepharmacokineticsofepinephrine/adrenaline auto-injectors. AllergyAsthmaClinImmunol. 2021;25.
18.ShakerM,WallaceD,GoldenD,etal.Anaphylaxis:a2020practice parameterupdate,systematicreview,andgradingofrecommendations, assessment,developmentandevaluation(GRADE)analysis. JAllergy ClinImmunol. 2020;145(4):1082–123.
Frank-PeterStephan,MD†
FlorianN.Riede,MD‡
LucaÜnlü,MD*§
GioeleCapoferri,MD*
TitoBosia,MD∥
AxelRegeniter,MD¶
RolandBingisser,MD*
ChristianH.Nickel,MD*
*UniversityHospitalBasel,EmergencyDepartment,Basel,BaselStadt,Switzerland
† BürgerspitalSolothurn,DepartmentofCardiology,Solothurn,Solothurn,Switzerland
‡ KantonsspitalAarau,DepartmentofCardiology,Aarau,Aarau,Switzerland
§ KarlLandsteinerUniversityofHealthSciences,KremsanderDonau, LowerAustria,Austria
∥ LeCentreHospitalierUniversitaireVaudois(CHUV),Lausanne, Lausanne,Switzerland
¶ MEDICAMedicalLaboratories,Zürich,Zürich,Switzerland
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedSeptember5,2024;RevisionreceivedOctober9,2024;AcceptedOctober17,2024
ElectronicallypublishedNovember27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.35286
Introduction: Hyperkalemia,apotentiallylife-threateningelectrolytedisturbance,iscommonly encounteredintheEmergencyDepartment(ED).However,thefrequencyoffactitioushyperkalemia,an artificiallyelevatedpotassiumlevelinhyperkalemicEDpatients,isunknown.Thisstudyaimstodetect therateoffactitioushyperkalemiaamongpatientswithapotassiumconcentrationof ≥5.0mmol/linan all-comerEDpopulation.
Methods: Thisretrospective,monocentricchartreviewanalyzeddataof2,440EDpatientswho presentedwithapotassiumconcentrationof ≥5.0mmol/Lintheirinitialwholebloodorplasmasample, whoalsounderwentarepeatpotassiummeasurementonthesameday.Twogroupswereestablished basedonpotassiumlevelsintheinitialandrepeatbloodtests:1)Truehyperkalemia,characterizedby consistentlyelevatedpotassiumlevelsinboththeinitialandrepeatsamples;and2)Factitious hyperkalemia,definedbyanelevatedinitialpotassiumlevelwhiletherepeatbloodtestshowedanormal potassiumlevel.Asubsetoffactitioushyperkalemiawasspurioushyperkalemia.Inspurious hyperkalemia,theinitialbloodsampleshowedanelevatedpotassiumlevelwithevidenceofhemolysis, butarepeattestrevealedanormalpotassiumlevelwithoutevidenceofhemolysis.
Results: Ofthe2,440patients,1,576(65%)hadtruehyperkalemiaand864(35%)factitious hyperkalemia.Amongthe864patientswithfactitioushyperkalemia,597(69%)displayedhemolysisin theirinitialbloodsample,indicatingspurioushyperkalemiaduetoin-vitrohemolysis.
Conclusion: ThesedatashowthataboutonethirdofallhyperkalemicbloodsamplesdrawnintheED wereduetofactitioushyperkalemia.Theleadingcauseoffactitioushyperkalemiawasspurious hyperkalemiaduetoin-vitrohemolysis.[WestJEmergMed.2025;26(1)176–179.]
Hyperkalemiaisapotentiallylife-threateningand commonlyencounteredelectrolytedisorderinthe emergencydepartment(ED).Elevatedpotassium concentrationsareassociatedwithincreasedmortalityand, hence,requirerapidinitiationofpotassium-lowering therapy.1 However,unnecessarytreatmentofhyperkalemia duetofactitioushyperkalemiaisnotwithoutrisks.2, 3 Surprisingly,thefrequencyoffactitioushyperkalemiain hyperkalemicEDpatientshasnotbeendetermined.
Therefore,ourgoalinthisstudywastodeterminethe prevalenceoffactitioushyperkalemiaamongpatients withapotassiumconcentrationof ≥5.0millimolesperliter (mmol/L)inanall-comerEDpopulation(the primaryoutcome).
Thisretrospective,monocentric,chart-reviewstudywas approvedbytheethicsoversightcommittee(EKNZ identifier:159/13).Weevaluated2,440patientsoveraperiod ofthreeyearsinwhoma firstwholebloodorplasmasample showedapotassiumconcentrationof ≥5.0mmol/LatED presentationandforwhomarepeat(wholebloodorplasma) labtestwasorderedinthesamepatient(determinedbya patientID)onthesamedaybythetreatingphysician.We adheredto8of12chartreviewcriteria.4 Ourprotocolomits performancemonitoring,hypothesisblinding,and interobserverreliability(IRR)tests,asabstractorswere involvedindesigningthestudy,andIRRtestsdidnotalign withthestudyaim.Bloodsamplingandanalysiswas performedinthesamemannerfortheinitialandrepeat bloodtest.
Bloodwascollectedusingperipheralvenouscatheters (VasofixSafetyCannula,B.BraunAG,Melsungen, Germany)withadual-useS-Monovettesystemallowing eitheraspiration-orvacuum-basedbloodsampling(Sarstedt AG,Nümbrecht,Germany).Plasmapotassium concentrationwasanalyzedusingaCobas8000analyzer (RocheDiagnostics,Basel,Switzerland),andwholeblood sampleswereanalyzedaspartofabloodgasanalysiswithan ABL800analyzer(Radiometer,Copenhagen,Denmark). Strongagreementwasfoundbetweenthepotassium measurementsoftheRocheCobas8000analyzers.5 All scheduledcalibrationsforbothdeviceswerecompletedat
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Factitioushyperkalemia,anarti fi cially elevatedpotassiumlevel,shouldberuled-out beforetreatmentofhyperkalemiaisinitiated, asunnecessarytreatmentisnotwithoutrisks.
Whatwastheresearchquestion?
Whatistherateoffactitioushyperkalemia amongpatientswithhyperkalemiainanallcomerEDpopulation?
Whatwasthemajor findingofthestudy?
Among2,440patients,factitious hyperkalemiaoccurredin35%of hyperkalemicbloodsamplesdrawnintheED.
Howdoesthisimprovepopulationhealth?
Factitioushyperkalemiaisadiagnostic pitfallthatcanpotentiallyleadto unnecessarytreatment.
24-hourintervalsinaccordancewithmanufacturer requirements.Thepresenceofhemolysiswaseither photometricallyorvisuallyassessed.
Asthereisnocommonlyaccepteddefinitionoffactitious hyperkalemia,thetermspseudo-hyperkalemia,spurious hyperkalemia,andfactitioushyperkalemiaareoftenused interchangeably.3,6–10 Tocategorizeourhyperkalemia findings,weestablishedtwodistinctgroups(see Figure1):
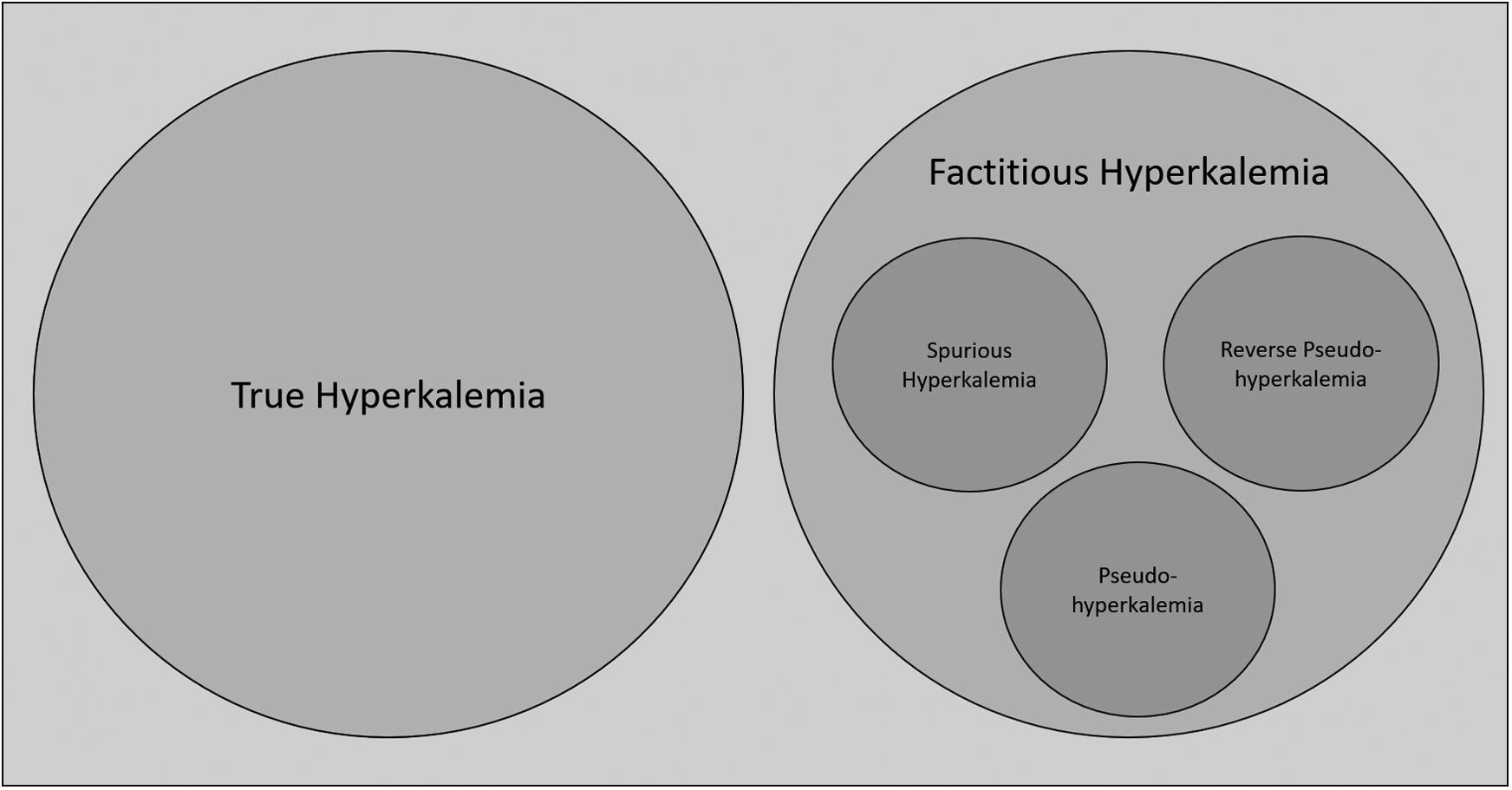
Figure1. Venndiagramillustratingdefinitionsoftruehyperkalemiaandfactitioushyperkalemia.Factitioushyperkalemiaisanumbrellaterm thatencompassesvarioussubcategoriesoffalselyelevatedpotassiumlevels.Theseincludereversepseudohyperkalemia(inleukemic patients),pseudohyperkalemia(duetothrombocytosisorerythrocytosis),andspurioushyperkalemia(duetoin-vitrohemolysis).
truehyperkalemia,characterizedbyconsistentlyelevated bloodpotassiumconcentrationsinboththeinitialandrepeat bloodtest;and factitioushyperkalemia,whichshowed elevatedbloodpotassiumconcentrationsinthe firstsample whiletherepeatbloodtestshowedanormalpotassiumlevel. Factitioushyperkalemiaisanumbrellatermforallsubentitiesoffalselyelevatedpotassiumlevels,asitdoesnot differentiatebetweenintrinsic(eg,hematologicdisorders) andextrinsiccauses(eg,bloodsamplingtechnique).
Examplesarereversepseudohyperkalemiainleukemic patientsorpseudohyperkalemiaduetothrombocytosisor erythrocytosis.Anothersubsetoffactitioushyperkalemiais spurioushyperkalemia,inwhichanelevatedpotassium concentrationwithevidenceofhemolysiswasfoundinthe firstsampleandanormalpotassiumintherepeatbloodtest. Spurioushyperkalemiaistheresultofhemolysisdueto preanalyticalerrorsduringsamplingorsamplehandling (ie,duetoextrinsiccauses).6
Weincluded2,440patientswithapotassium concentrationof ≥5.0mmol/Lintheinitialbloodsample takenonthedayofEDpresentation.Patientswithfactitious hyperkalemiahadamedianageof69years,and53%were female.Potassiumlevelsofthefactitioushyperkalemia grouprangedfrom5.0–29.9mmol/L;medianpotassium concentrationwas5.4mmol/L.Aboutone-thirdofthe864 hyperkalemiapatients(35%)metthedefinitionoffactitious hyperkalemia,and1,576(65%)ofthepatientswith hyperkalemiahadtruehyperkalemia(see Figure2).
Ofthe864patientswithfactitioushyperkalemia,blood sampleswereratedashemolyticin597cases(69%), indicatingspurioushyperkalemiaastheunderlyingetiology. Intheremaining267of864cases(31%),theetiologyof factitioushyperkalemiaisunclear.Patientswithtrue hyperkalemiahadamedianageof75years,and41%were female.Potassiumlevelsofthetruehyperkalemiagroup rangedfrom5.0–10.3mmol/L;medianpotassium concentrationwas5.4mmol/L.
Thisstudyshowsthatfactitioushyperkalemiacanbe observedinaboutone-thirdofhyperkalemicbloodsamples drawnunderreal-lifeconditionsintheED.Spurious hyperkalemiaduetopreanalyticalerrorsduringblood samplingortransportleadingto in-vitrohemolysisappearsto bethemaincauseoffalselyelevatedpotassiumlevelsinthis study.However,incritically illpatientsmanyfactorscan influenceonesamplemeasurement(eg,transientacidosisor hypoinsulinemiawithhypotension).Thus,itisunclearwhether a firsthyperkalemicmeasurement,whichresolvedinasecond measurement,isfactitious,orsimplytransientandquickly resolved.Ontheotherhand,itisconceivablethatthereistrue hyperkalemiainthecasesthatweclassifiedasfactitious hyperkalemiaasthereisalsothephenomenonof pseudonormokalemia(ie,therepeatbloodtestisfalselylow).11
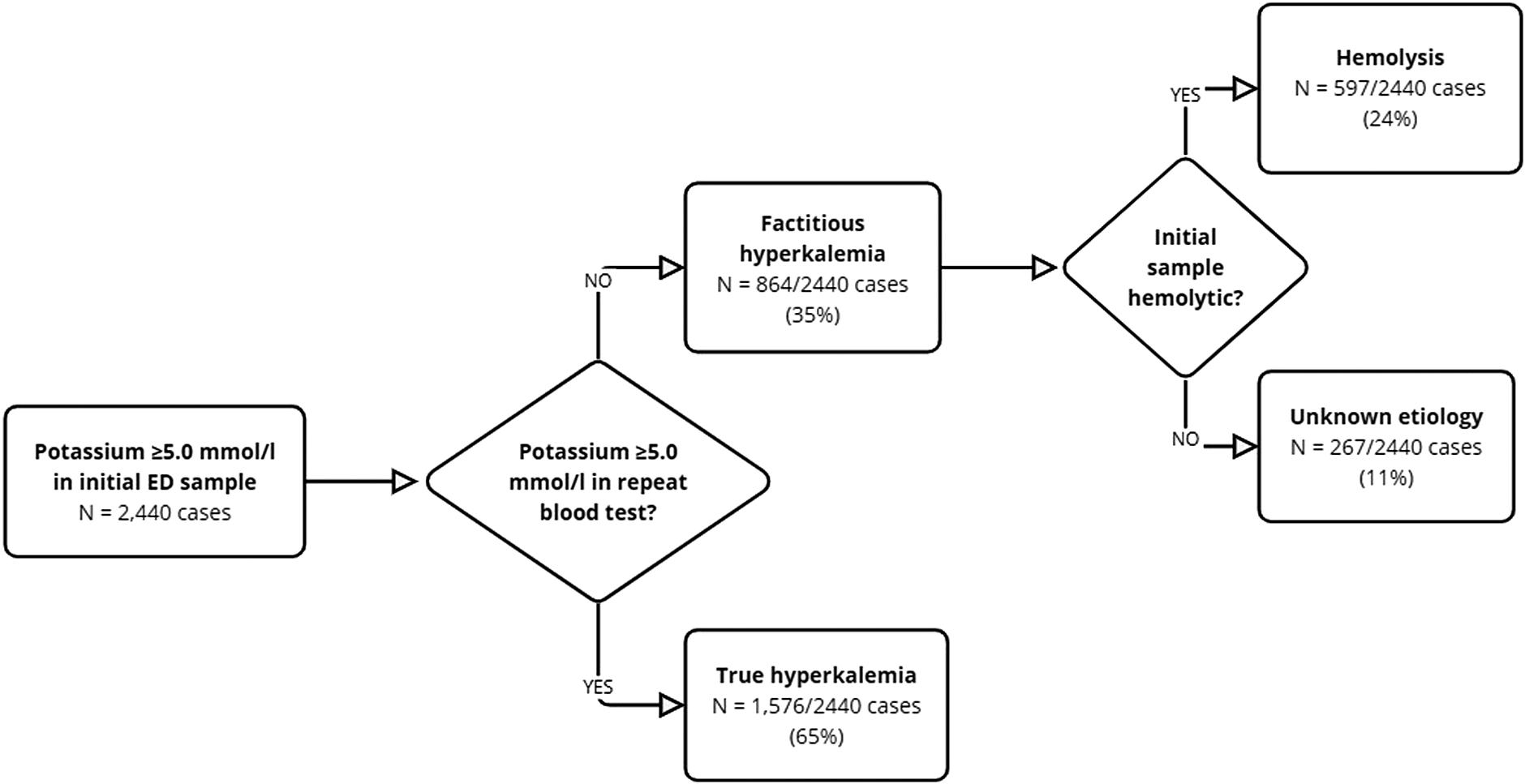
Figure2. Proportionsofpatientsthathadtrue,factitious,andspurioushyperkalemia.Of2,440caseswithapotassiumof ≥5.0millimolesper liter,1,576(65%)hadpersistenthyperkalemiainasame-dayrepeatbloodtest,(ie,theyhadtruehyperkalemia);and864(35%)didnotshow hyperkalemiainasame-dayrepeatbloodtest;hence,thesepatientshadfactitioushyperkalemia.Ofthose864cases,597(69%)showed evidenceofhemolysisintheirinitialbloodtest;thus,thesepatientshadspurioushyperkalemiaduetoin-vitrohemolysis.In267ofthe864 casesoffactitioushyperkalemia(31%),noevidenceofhemolysiswasobserved.Thereasonfortheoccurrenceoffactitioushyperkalemiain thesecasesremainsunclear. mmol/L,millimolesperliter.
Intheprocessofanalyzingtheresultsofthisstudy,we observedthattheliteratureusesavarietyoftermstodescribe factitioushyperkalemia.3,6–10 Incasesoffactitious hyperkalemiatheunderlyingcauseisoftennotconsidered, whichmightcauseconfusion.Surprisingly,thishasnotyet beenacknowledgedinhyperkalemiamanagement guidelines.3,10,12,13 Whileourstudyshowsthatspurious hyperkalemiaisamajorcontributortofactitious hyperkalemiaintheED,italsobecameapparentthatthe commonassumptionamongcliniciansthatfalselyelevated potassiumlevelsaresolelyduetohemolysisresultingfrom inadequateblood-drawingtechniquesisfalse.Thereare numerousothersignificantunderlyingpathological processesthatcanleadtofalselyelevatedpotassiumlevels (eg,thrombocytosis).Whilewecannotdifferentiatebetween alltheseunderlyingpathologicalprocessesintheED, emergencyphysiciansshouldbeawareoftheconceptsof spurious,pseudo-andreversepseudohyperkalemia,as potentiallyunnecessarytreatmentcouldbeassociated withrisks.2,3
Thisdatashowsthatone-thirdofallhyperkalemicblood samplesdrawnintheEDareduetofactitioushyperkalemia. Theleadingcauseoffactitioushyperkalemiaisspurious hyperkalemiaduetoin-vitrohemolysis.
WethankLloydG.Cantley,MDforhelpfuldiscussions.
AddressforCorrespondence:ChristianNickel,MD,University HospitalBasel,EmergencyDepartment,Petersgraben2,4031 Basel,Basel,Switzerland.Email: Christian.Nickel@usb.ch
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisworkwassupportedbyscientific fundsoftheEmergencyDepartmentoftheUniversityHospitalBasel. Therearenootherconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2025Stephanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons
Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CollinsAJ,PittB,ReavenN,etal.Associationofserumpotassium withall-causemortalityinpatientswithandwithoutheartfailure, chronickidneydisease,and/ordiabetes. AmJNephrol. 2017;46(3):213–21.
2.GuptaAA,SelfM,MuellerM,etal.Dispellingmythsandmisconceptions aboutthetreatmentofacutehyperkalemia. AmJEmergMed. 2022;52:85–91.
3.RafiqueZ,PeacockF,ArmsteadT,etal.Hyperkalemiamanagementin theemergencydepartment:anexpertpanelconsensus. JAmColl EmergPhysiciansOpen. 2021;2(5):e12572.
4.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. AnnEmergMed. 2005;45(4):448–51.
5.vonEckardsteinA,RothHJ,JonesG,etal.Cobas8000modular analyzerseriesevaluatedunderroutine-likeconditionsat14sitesin Australia,Europe,andtheUnitedStates. JLabAutom. 2013;18(4):306–27.
6.WiederkehrMRandMoeOW.Factitioushyperkalemia. AmJKidney Dis. 2000;36(5):1049–53.
7.LábadiÁ,NagyÁ,SzomorÁ,etal.Factitioushyperkalemiain hematologicdisorders. ScandJClinLab. 2017;77(1):66–72.
8.WhitfieldJB.Spurioushyperkalaemiaandhyponatraemiainapatient withthrombocythaemia. JClinPathol. 1966;19(5):496–7.
9.Saleh-AnarakiK,JainA,WilcoxCS,etal.Pseudohyperkalemia:three casesandareviewofliterature. AmJMed. 2022;135(7):e150–4.
10.LindnerG,BurdmannEA,ClaseCM,etal.Acutehyperkalemia intheemergencydepartment:asummaryfromaKidneyDisease: ImprovingGlobalOutcomesconference. EurJEmergMed. 2020;27(5):329–37.
11.FriedmanP,ScottC,BaileyK,etal.Errorsofclassificationwith potassiumbloodtesting:thevariabilityandrepeatabilityofcriticalclinical tests. MayoClinProc. 2018;93(5):566–72.
12.PalmerBF,CarreroJJ,CleggDJ,etal.Clinicalmanagementof hyperkalemia. MayoClinProc. 2021;96(3):744–62.
13.YapDYH,MaRCW,WongECK,etal.Consensusstatementonthe managementofhyperkalaemia anAsia–Pacificperspective. Nephrology. 2024;29(6):311–24.