Volume 25, Number 6, November 2024
Journal of Behavioral Health
858 Recent Interventions for Acute Suicidality Delivered in the Emergency Department: A Scoping Review
Alex P. Hood, Lauren M. Tibbits, Juan I. Laporta, Jennifer Carrillo, Lacee R. Adams, Stacey Young-McCaughan, Alan L. Peterson, Robert A. De Lorenzo
869 Buprenorphine-Naloxone for Opioid Use Disorder: Reduction in Mortality and Increased Remission
Krishna K. Paul, Christian G. Frey, Stanley Troung, Laura vita Q. Paglicawan, Kathryn A. Cunningham, T. Preston Hill, Lauren G. Bothwell, Georgiy Golovko, Yeoshina Pillay, Dietrich Jehle
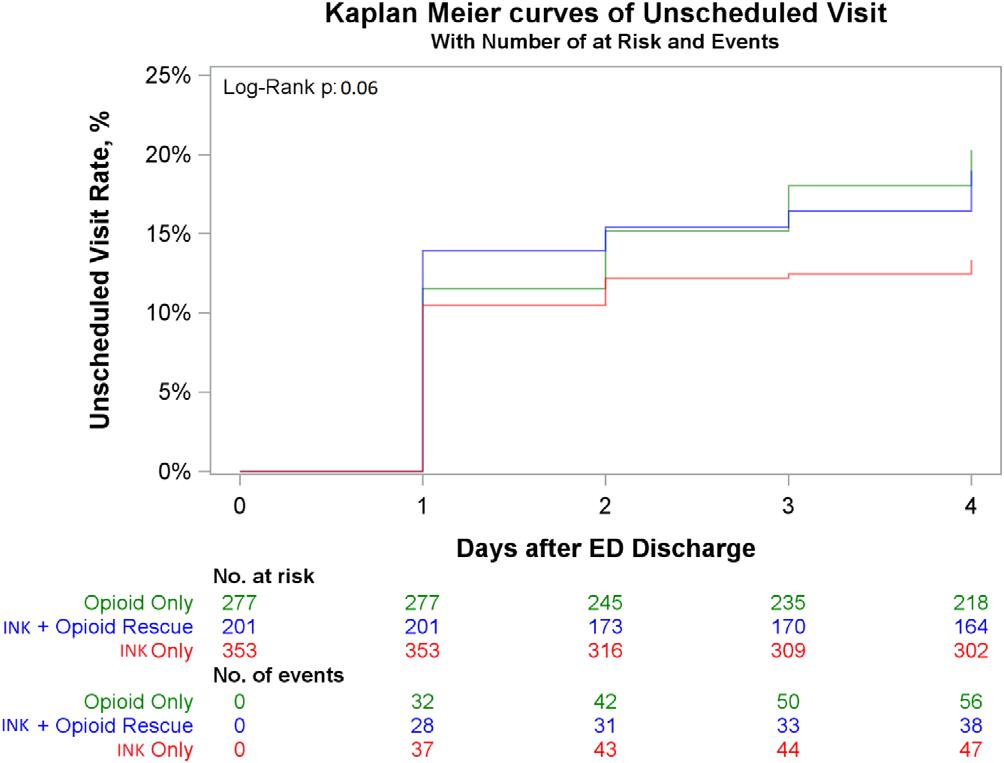
875 Opioid Treatment Is Associated with Recurrent Healthcare Visits, Increased Side Effects, and Pain
Caroline E. Freiermuth, Jenny A. Foster, Pratik Manandhar, Evangeline Arulraja, Alaattin Erkanli, Charles V. Pollack, Stephanie A. Eucker
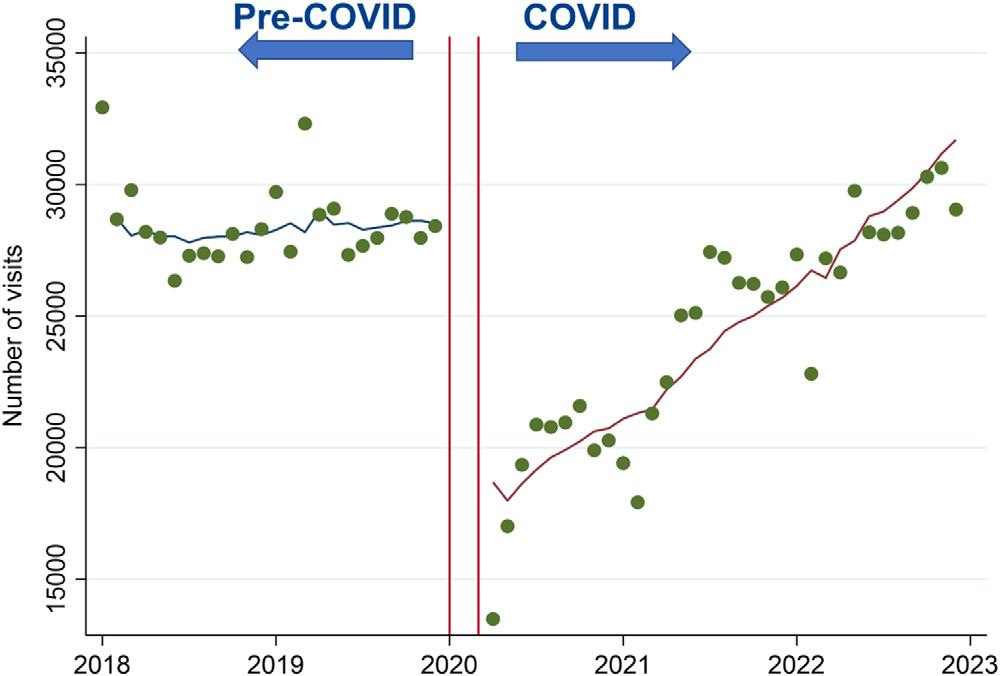
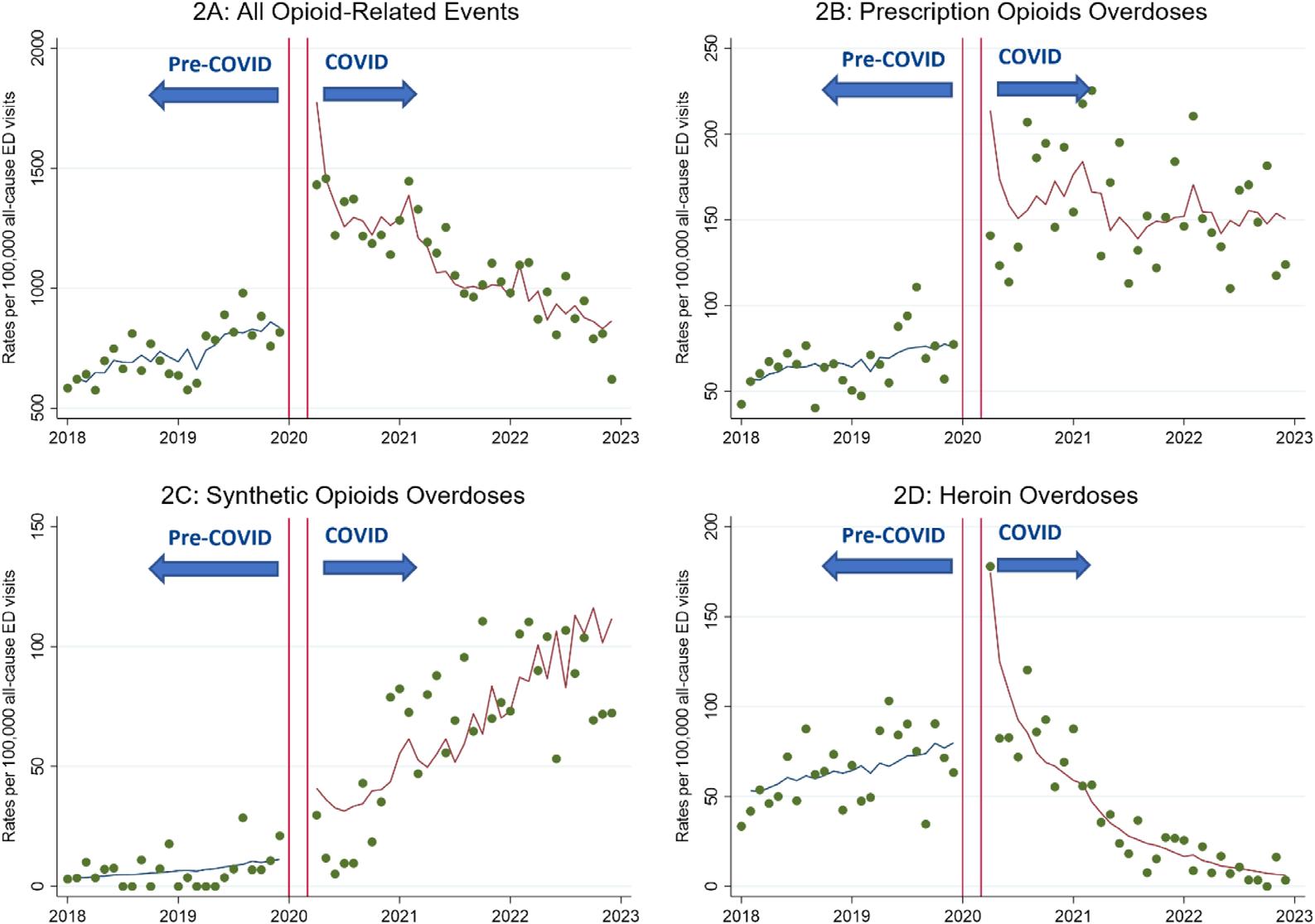
883 Impact of COVID-19 Pandemic on Emergency Department Visits for Opioid Use Disorder Across University of California Health Centers
Matthew Heshmatipour, Ding Quan Ng, Emily Yi-Wen Truong, Jianwei Zheng, Alexandre Chan, Yun Wang
Clinical Practice
890 An Assessment of the Presence of Clostridium tetani in the Soil and on Other Surfaces
Michael Shalaby, Alessandro Catenazzi, Melissa F. Smith, Robert A. Farrow II, David Farcy, Oren Mechanic, Tony Zitek
Critical Care
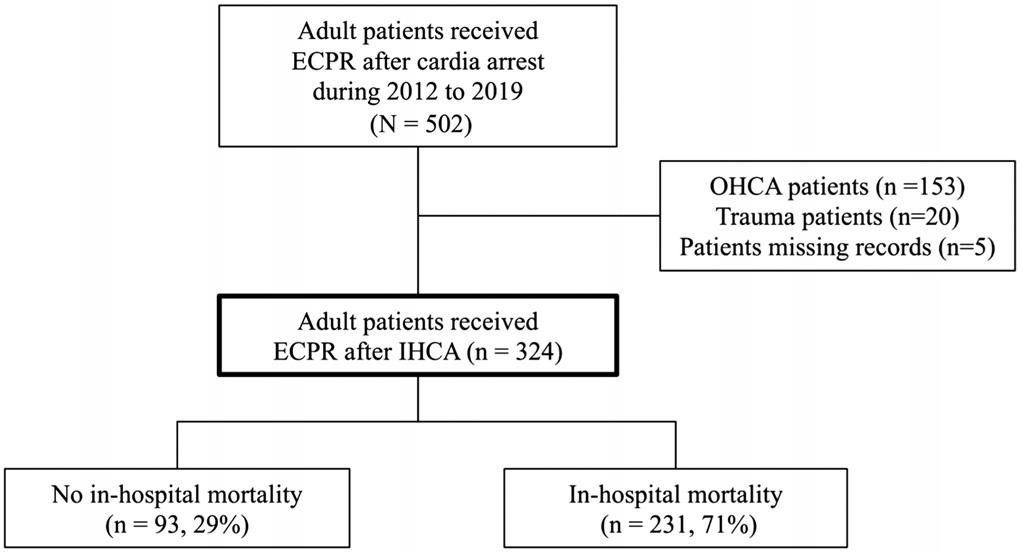
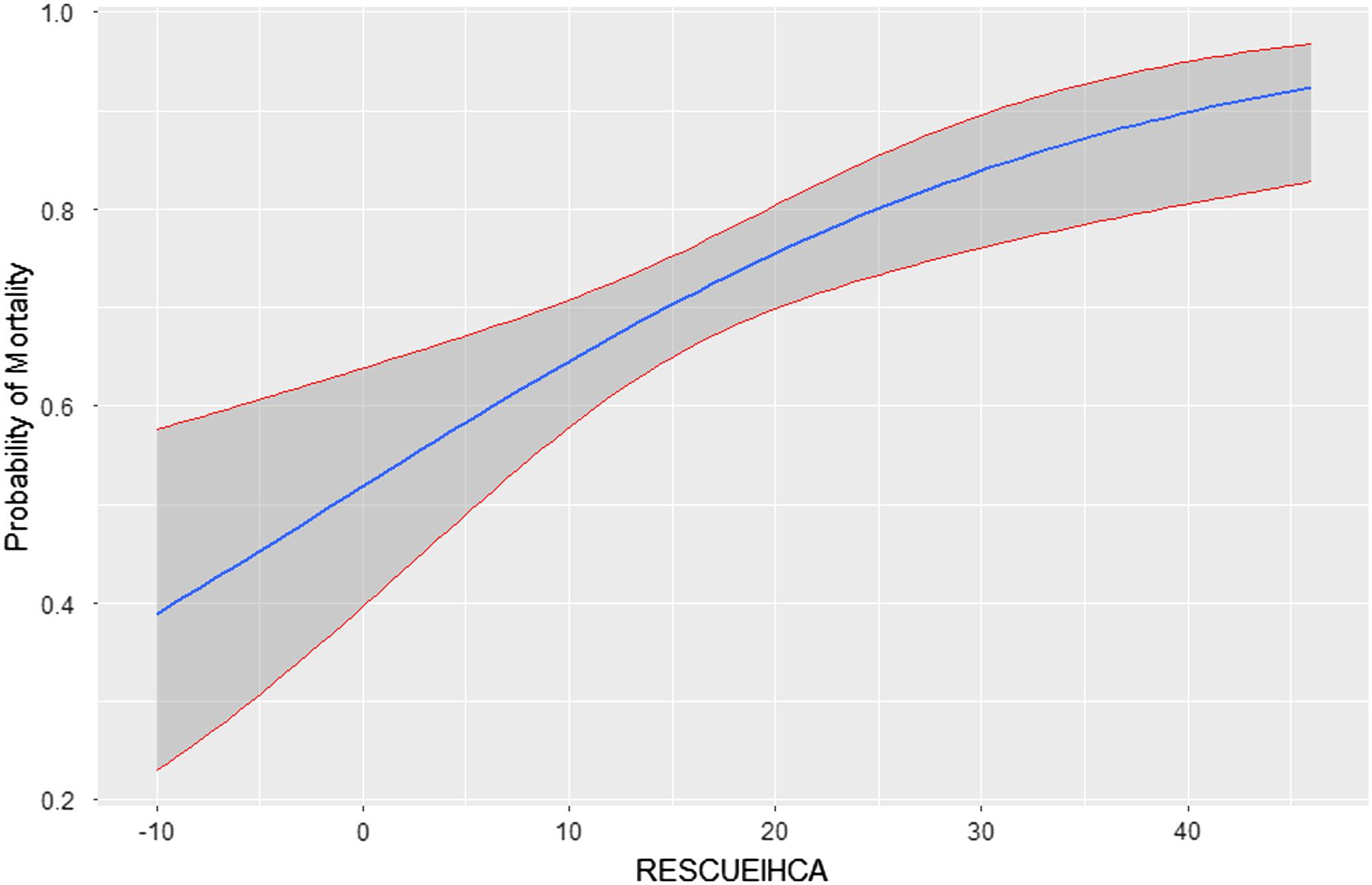
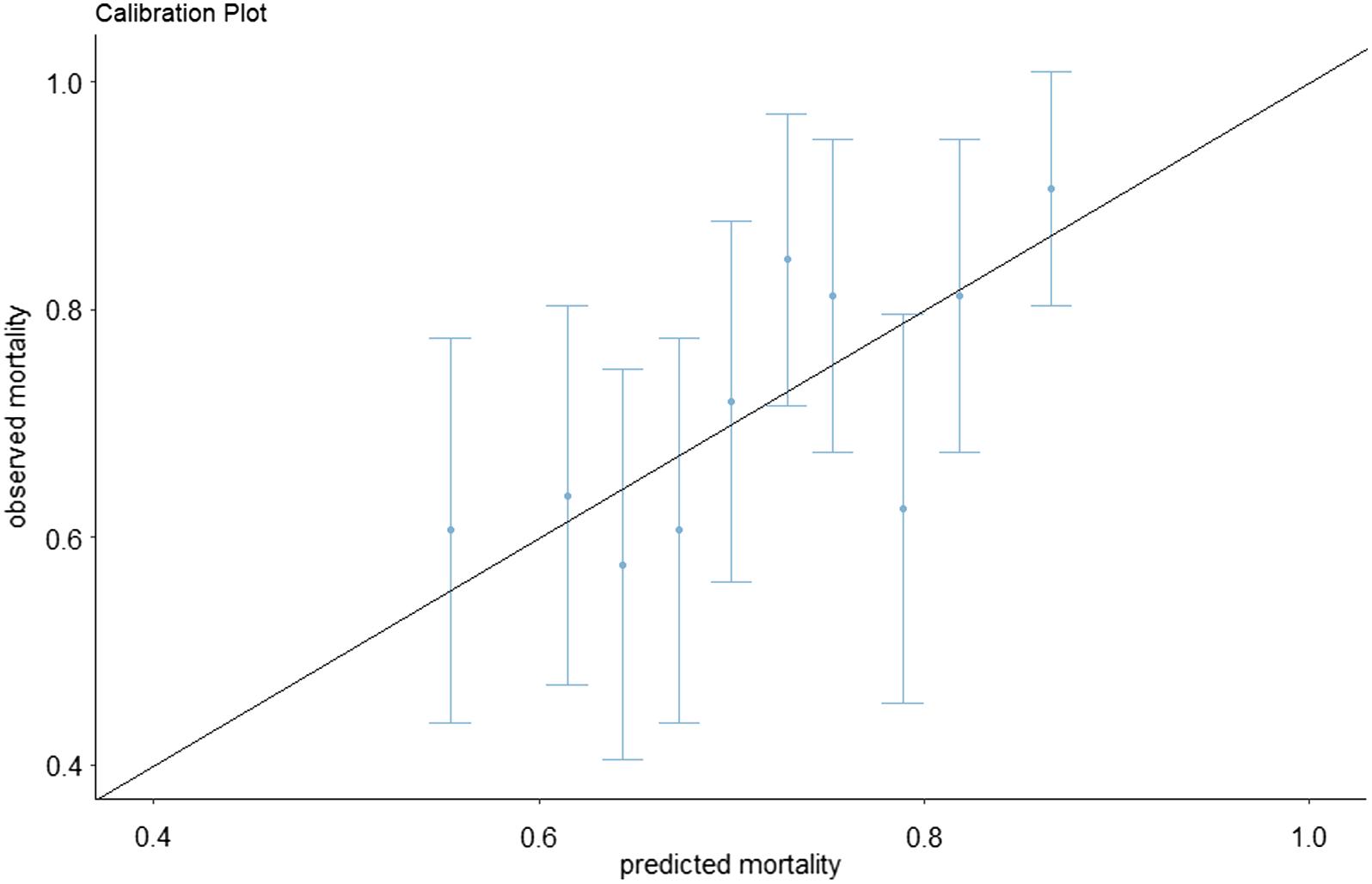
894 External Validation of the RESCUE-IHCA Score as a Predictor for In-Hospital Cardiac Arrest Patients Receiving Extracorporeal Cardiopulmonary Resuscitation
Yi-Ju Ho, Pei-I Su, Chien-Yu Chi, Min-Shan Tsai, Yih-Sharng Chen, Chien-Hua Huang
Contents continued on page iii
Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health
Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Section Editors
Behavioral Emergencies
Leslie Zun, MD, MBA
Rosalind Franklin University of Medicine and Science
Marc L. Martel, MD
Hennepin County Medical Center
Cardiac Care
Fred A. Severyn, MD University of Colorado School of Medicine
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD Carolinas Medical Center
Casey Clements, MD, PhD Mayo Clinic
Patrick Meloy, MD
Emory University
Nicholas Pettit, DO, PhD Indiana University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Gabriel Wardi, MD University of California, San Diego
Joseph Shiber, MD University of Florida-College of Medicine
Matt Prekker MD, MPH Hennepin County Medical Center
David Page, MD University of Alabama
Erik Melnychuk, MD
Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
John Broach, MD, MPH, MBA, FACEP University of Massachusetts Medical School
UMass Memorial Medical Center
Christopher Kang, MD Madigan Army Medical Center
Education
Danya Khoujah, MBBS University of Maryland School of Medicine University of Colorado
Michael Epter, DO
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of MedicineIrvine, California
University of California, Irvine School of MedicineIrvine, California
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Niels K. Rathlev, MD, Associate Editor Tufts University School of Medicine-Boston, Massachusetts
Rick A. McPheeters, DO, Associate Editor
R. Gentry Wilkerson, MD, Associate Editor University of Maryland
Maricopa Medical Center
ED Administration, Quality, Safety
Tehreem Rehman, MD, MPH, MBA Mount Sinai Hospital
David C. Lee, MD Northshore University Hospital
Gary Johnson, MD Upstate Medical University
Brian J. Yun, MD, MBA, MPH Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH
Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine University of California, Davis
Emergency Medical Services
Daniel Joseph, MD
Yale University
Joshua B. Gaither, MD University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD Yale School of Medicine
Stephen Meldon, MD
Cleveland Clinic
Luna Ragsdale, MD, MPH Duke University
Health Equity
Emily C. Manchanda, MD, MPH
Boston University School of Medicine
Faith Quenzer
Temecula Valley Hospital San Ysidro Health Center
Payal Modi, MD MScPH University of Massachusetts Medical
Infectious Disease
Elissa Schechter-Perkins, MD, MPH
Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Stephen Liang, MD, MPHS
Shadi Lahham, MD, MS, Deputy Editor Kaiser Permanente- Irvine, California
Susan R. Wilcox, MD, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Elizabeth Burner, MD, MPH, Associate Editor University of Southern California- Los Angeles, California
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston Texas
Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Washington University School of Medicine
Victor Cisneros, MD, MPH Eisenhower Medical Center
Injury Prevention
Mark Faul, PhD, MA Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS
Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH Prisma Health Richland
Taylor Burkholder, MD, MPH Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Indiana University School of Medicine
Statistics and Methodology
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH
Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS
Rick Lucarelli, MD Medical City Dallas Hospital
William D. Whetstone, MD University of California, San Francisco
Neurosciences
Antonio Siniscalchi, MD Annunziata Hospital, Cosenza, Italy
Pediatric Emergency Medicine
Paul Walsh, MD, MSc University of California, Davis
Muhammad Waseem, MD Lincoln Medical & Mental Health Center
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
Henry Ford Hospital
John Ashurst, DO Lehigh Valley Health Network
Tony Zitek, MD Kendall Regional Medical Center
Trevor Mills, MD, MPH Northern California VA Health Care
Erik S. Anderson, MD Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD Henry Ford Hospital
Phillips Perera, MD Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS Virginia Commonwealth University
University of California, Irvine
Ultrasound J. Matthew Fields, MD
Shane Summers, MD Brooke Army Medical Center
Robert R. Ehrman Wayne State University
Ryan C. Gibbons, MD Temple Health
Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine
American Academy of Emergency Medicine
Western Journal of Emergency Medicine: Western Journal of Emergency : Integrating Emergency with Population Health
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Amin A. Kazzi, MD, MAAEM
Amin A. Kazzi, MD, MAAEM
Gayle Galleta, MD
Gayle Galleta, MD
The American University of Beirut, Lebanon
Beirut,
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University of Texas, Houston
Brent King, MD, MMM University Texas, Houston
Christopher E. San Miguel, Ohio State University Wexner Medical Center
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Daniel J. Dire, MD University Texas Health Sciences Center San Antonio
Douglas Ander, Emory University
Emory University
Douglas Ander, MD Emory University
Edward Michelson, MD Texas Tech University
Edward Michelson, Texas Tech University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH South
Edward MD, MPH University South Alabama
Edward Panacek, MD, MPH University of South Alabama
Francesco
“Maggiore della Carità,” Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog,
Hjalti Björnsson, MD
Editorial Board Board
Editorial Board Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Hjalti MD Icelandic Society of Emergency Medicine
Jaqueline Le, MD Desert Regional Medical Center
Jaqueline Le, MD Desert Medical Center
Regional
Jeffrey Love, MD
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jeffrey Love, The George Washington University School of Medicine and Health Sciences
Katsuhiro Kanemaru, MD University of Hospital, Miyazaki, Japan
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Leslie Zun, MD, MBA Chicago Medical School
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine
The George Washington University School of Medicine and Health Sciences Arizona, Chicago Medical School Librarian
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Advisory Board Elena Lopez-Gusman, JD
Elena Lopez-Gusman, JD
California ACEP
Elena Lopez-Gusman, JD California ACEP
California ACEP
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Langdorf, MAAEM, FACEP
Tufts University School of Medicine
Niels K. Rathlev, Tufts University School of Medicine
Niels K. Rathlev, MD Tufts University School of Medicine
Scott Zeller, MD
Scott Zeller, MD University of California, Riverside
Scott Zeller, MD University of California, Riverside
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Bell,
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Pablo Aguilera Fuenzalida, Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter A. Bell, DO, MBA Baptist Health University
Peter Sokolove, MD University of California, Francisco
Peter Sokolove, MD University of California, San Francisco
University of California, San Francisco
Rachel A. Lindor, MD, JD
Rachel A. Lindor, MD, JD Mayo Clinic
Rachel A. Lindor, MD, JD Mayo Clinic
Robert Suter, DO, MHA
Robert Suter, DO, UT Southwestern Medical Center
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Robert W. Derlet, MD University of California, Davis
University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Scott Rudkin, MD, MBA
Scott Rudkin, MD, University of California, Irvine
Scott Rudkin, MD, MBA University of California, Irvine
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Singapore
Steven H. Lim, Changi General Hospital, Simei, Singapore
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands
Terry Mulligan, DO, MPH, FIFEM ACEP to the Netherlands Society of Emergency Physicians
Wirachin Hoonpongsimanont, MD, MSBATS
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Editorial Staff Staff Advisory Board Isabelle BS Executive Editorial Director
Isabelle Nepomuceno, BS Executive Editorial Director
American of Emergency Physicians
American College of Emergency
American College of Emergency Physicians
Jennifer Kanapicki Comer, MD FAAEM
Jennifer Kanapicki Comer, MD FAAEM
California Chapter Division of AAEM Stanford University School of Medicine
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE
Kimberly Ang, MBA
DeAnna McNett, CAE
American College of Osteopathic Emergency Physicians
American College of Osteopathic Emergency Physicians
UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP
Kimberly Ang, MBA
UC Irvine Health School of Medicine
American College of Emergency Physicians Kaiser Permanente
J. American College of Emergency Physicians Kaiser Permanente
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians Kaiser Permanente
in
UC Irvine Health School of Medicine
UC Irvine Health School of Medicine
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Shahram Lotfipour, MD, MPH FAAEM, FACEP
UC Irvine Health School of Medicine
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP
Jorge Fernandez, MD, FACEP
Jorge Fernandez, MD, FACEP
UC San Diego Health School of Medicine
UC San Diego Health School of Medicine
UC San Diego Health School of Medicine
Visha Bajaria, BS WestJEM Editorial Director
Visha Bajaria, BS WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Stephanie Burmeister, MLIS JEM Liaison
Visha Bajaria, BS WestJEM Editorial Director WestJEM
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Cassandra Saucedo, MS Executive Publishing Director
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
Cassandra Saucedo, MS WestJEM Publishing Director
Nicole Valenzi, WestJEM Publishing Director
June Casey, BA Copy Editor
June Casey, BA Copy Editor
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine
Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org
Editorial and Publishing Office: JEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA
Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
JOURNAL FOCUS Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
Table of Contents Education
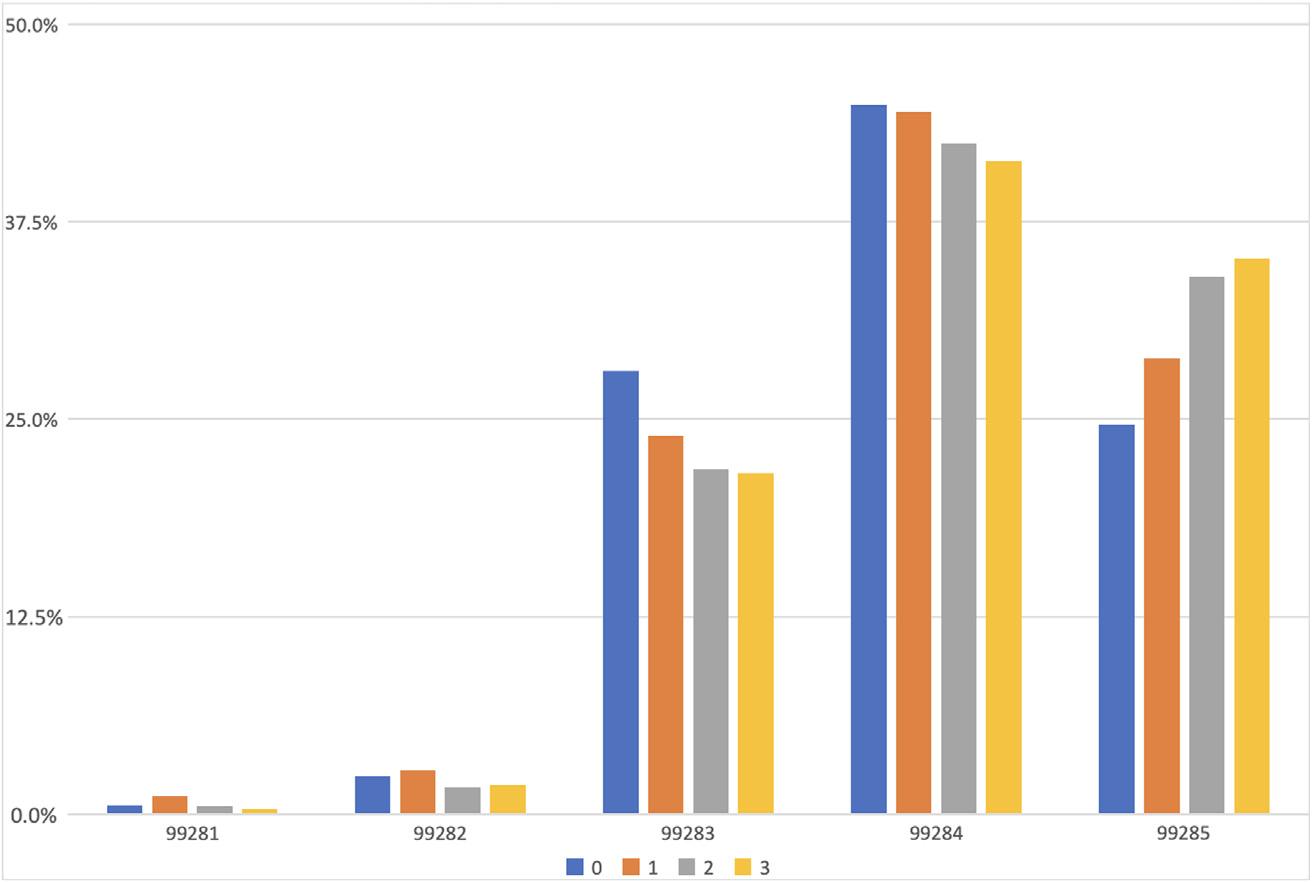
903 Teaching the New Ways: Improving Resident Documentation for the New 2023 Coding Requirements
Nathan Zapolsky, Annemarie Cardell, Riddhi Desai, Stacey Frisch, Nicholas Jobeun, Daniel Novak, Michael Silver, Arlene S. Chung
907 Telesimulation Use in Emergency Medicine Residency Programs: National Survey of Residency Simulation Leaders
Max Berger, Jack Buckanavage, Jaime Jordan, Steven Lai, Linda Regan
913 Palliative Care Boot Camp Offers Skill Building for Emergency Medicine Residents
Julie Cooper, Jenna Fredette
Emergency Department Operations
917 Improving Patient Understanding of Emergency Department Discharge Instructions
Sarah Russell, Nancy Jacobson, Ashley Pavlic
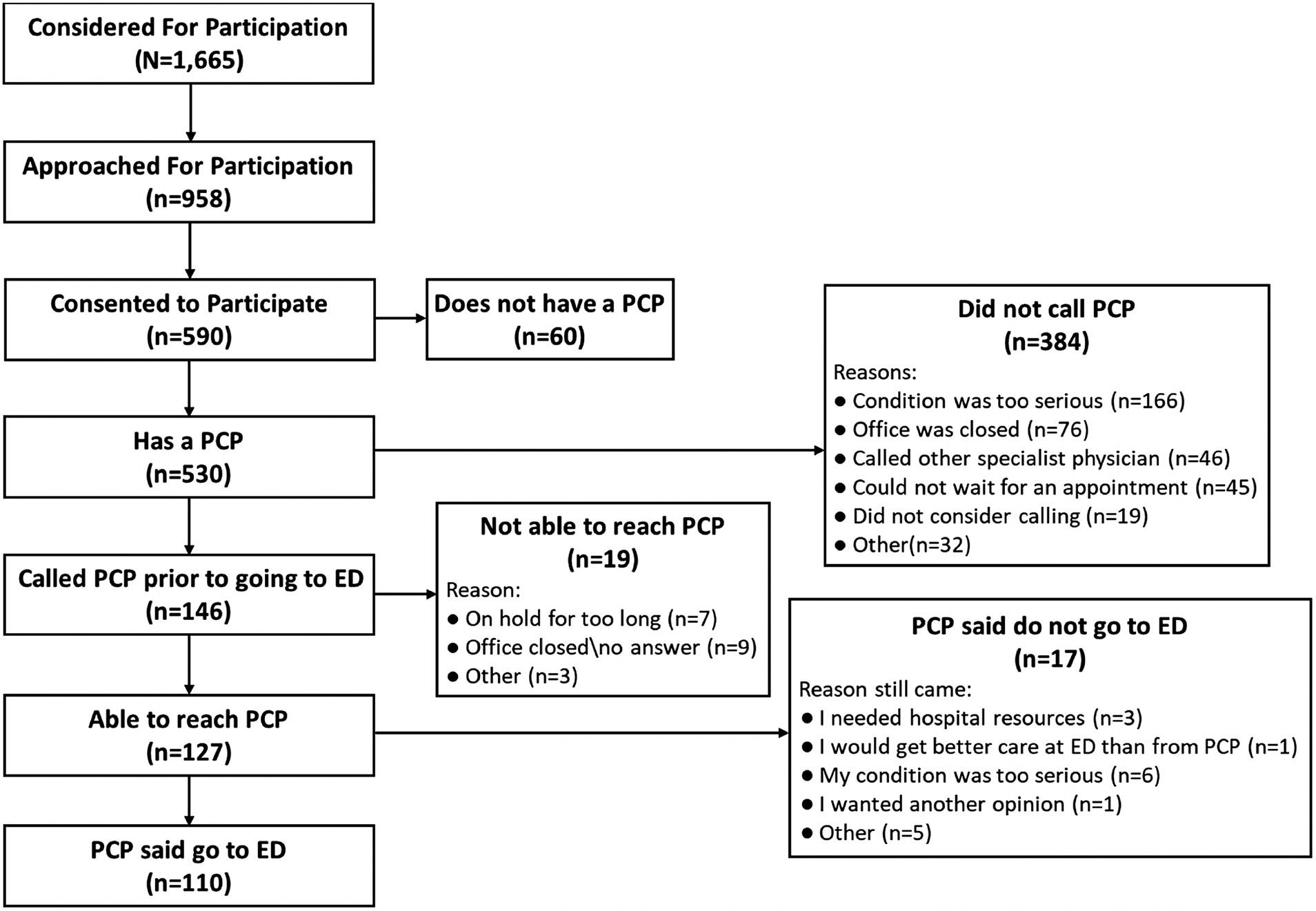
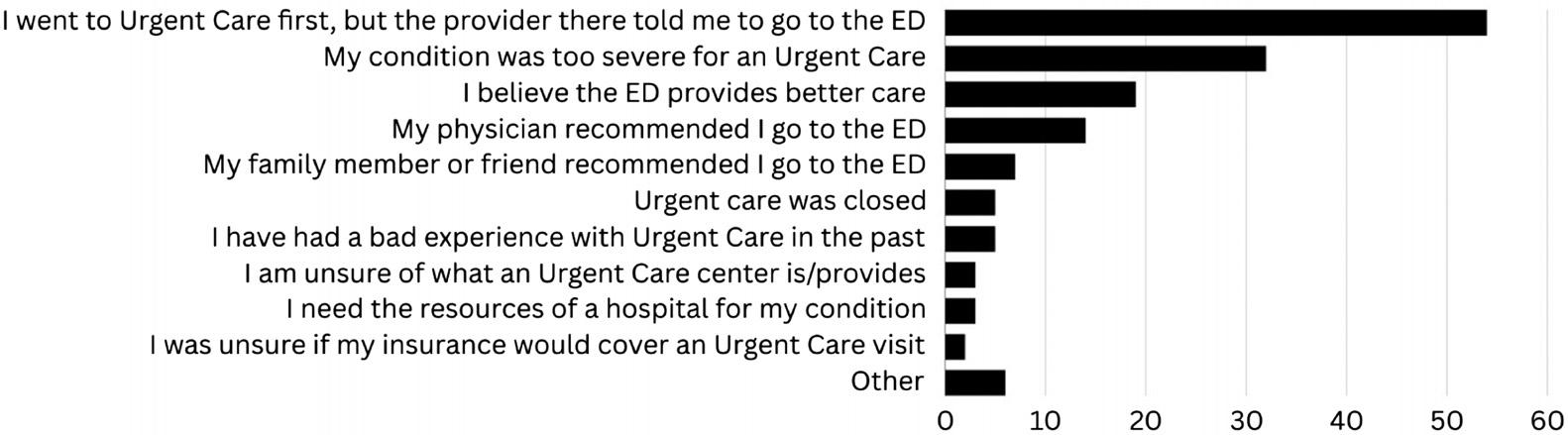
921 Why Do Patients Opt for the Emergency Department over Other Care Choices? A Multi-Hospital Analysis
Charles W. Stube, Alexander S. Ljungberg, Jason A. Borton, Kunal Chadha, Kyle J. Kelleran, E. Brooke Lerner
929 Emergency Department Patient Satisfaction Scores Are Lower for Patients Who Arrive During the Night Shift
Tony Zitek, Luke Weber, Tatiana Nuñez, Luis Puron, Adam Roitman, Claudia Corbea, Dana Sherman, Michael Shalaby, Frayda Kresch, David A. Farcy
938 Comparison of Emergency Department Disposition Times in Adult Level I and Level II Trauma Centers
Sierra Lane, Jeffry Nahmias, Michael Lekawa, John Christian Fox, Carrie Chandwani, Shahram Lotfipour, Areg Grigorian
946 Weighing In
Iyesatta M. Emeli, Patrick G. Meloy
Emergency Medical Services
949 Perceptions and Use of Automated Hospital Outcome Data by EMS Providers: A Pilot Study
Michael Kaduce, Antonio Fernandez, Scott Bourn, Dustin Calhoun, Jefferson Williams, Mallory DeLuca, Heidi Abraham, Kevin Uhl, Brian Bregenzer, Baxter Larmon, Remle P. Crowe, Alison Treichel, J. Brent Myers
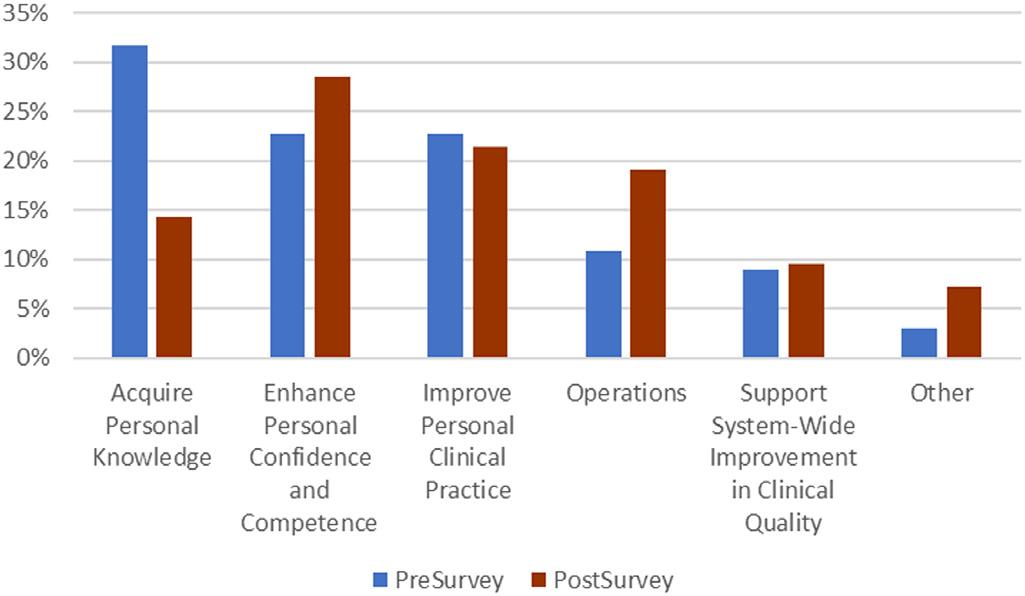
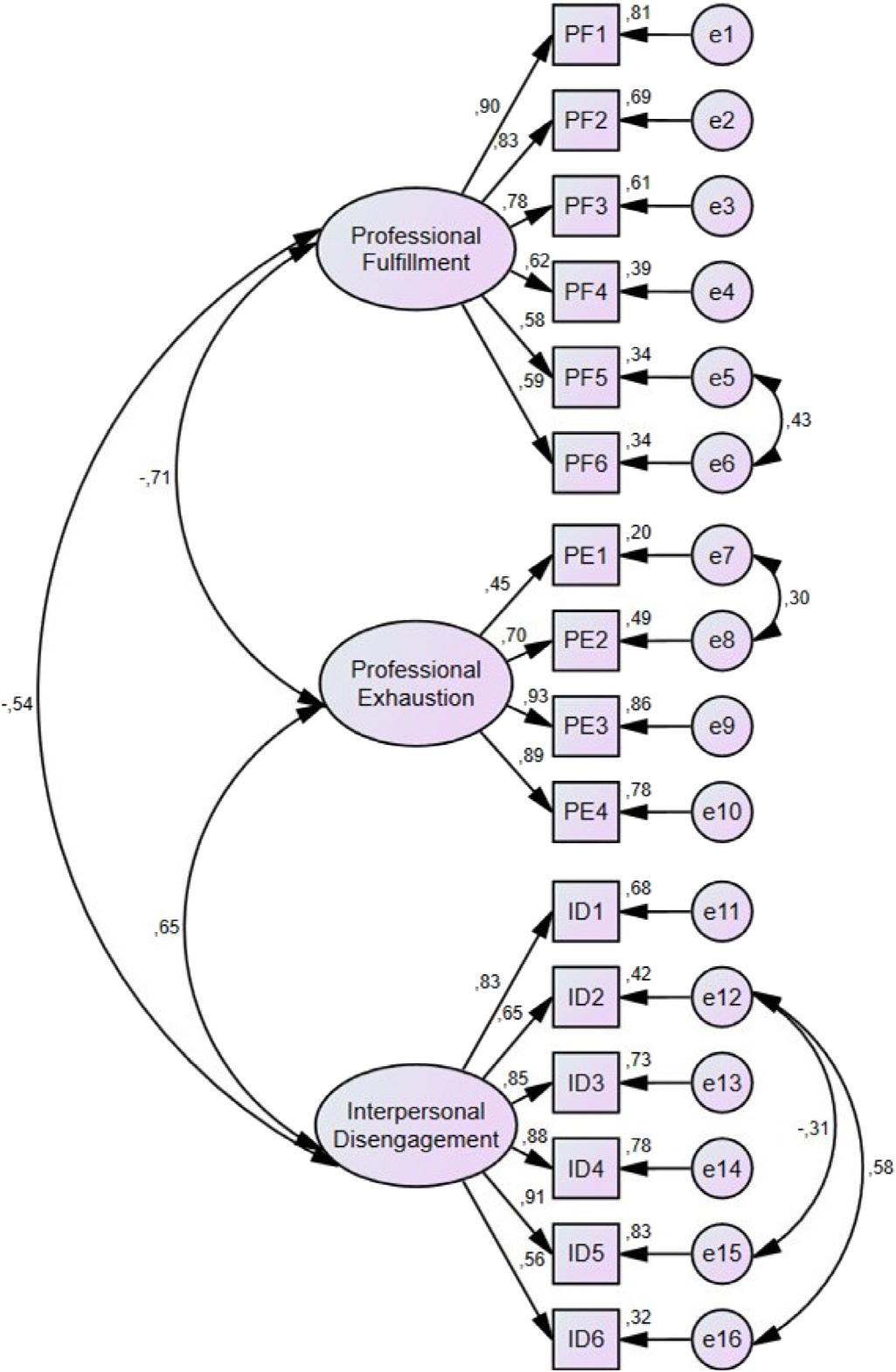
958 Validation of the Turkish Version of the Professional Fulfillment Index
Merve Eksioglu, Ayca Koca, Burcu Azapoglu Kaymak, Tuba Cimilli Ozturk, Atilla Halil Elhan
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
No. 6: November 2024
Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Table of Contents continued Endemic Infection
966 Use of Parenteral Antibiotics in Emergency Departments: Practice Patterns and Class Concordance
Megan Elli, Timothy Molinarolo, Aidan Mullan, Laura Walker
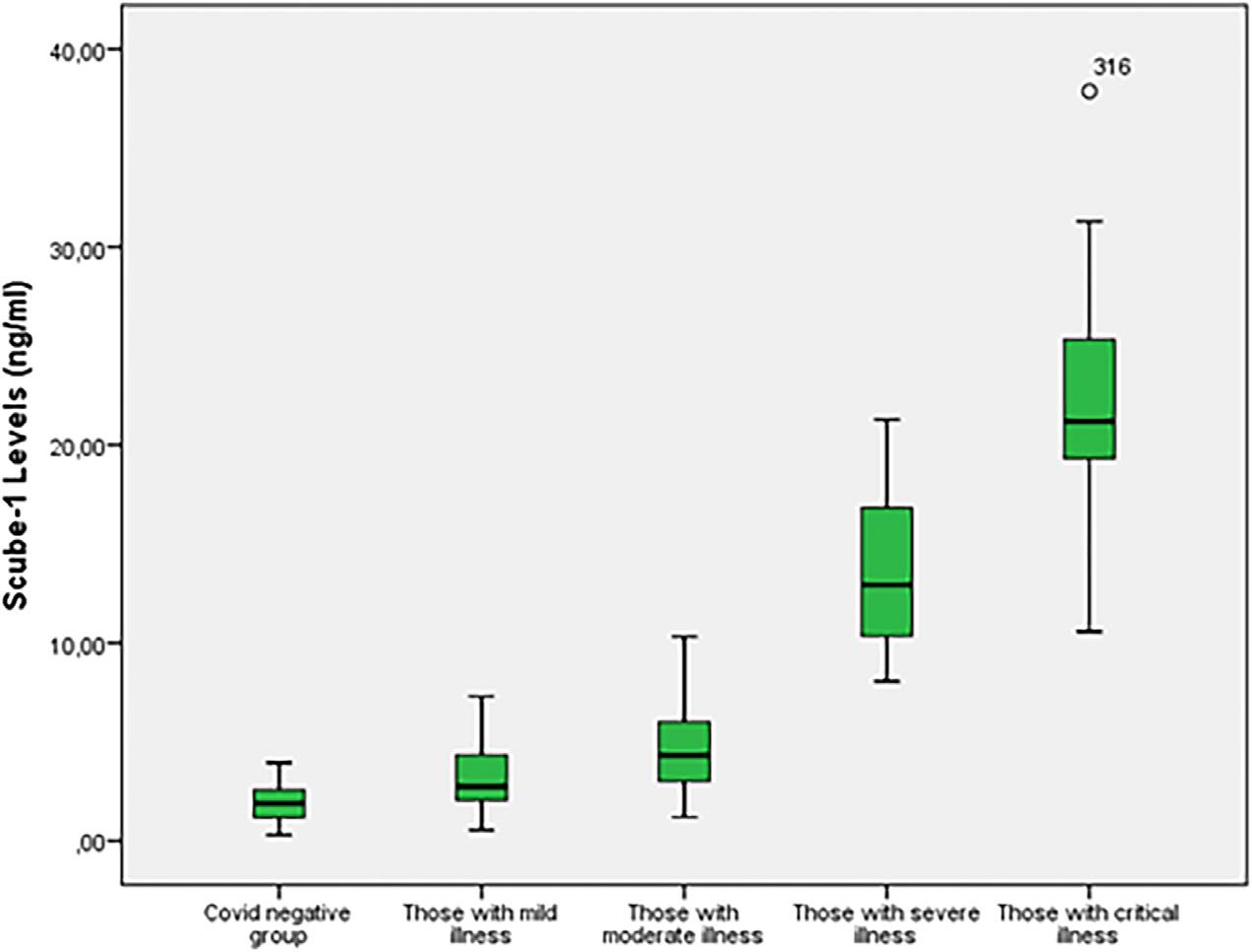
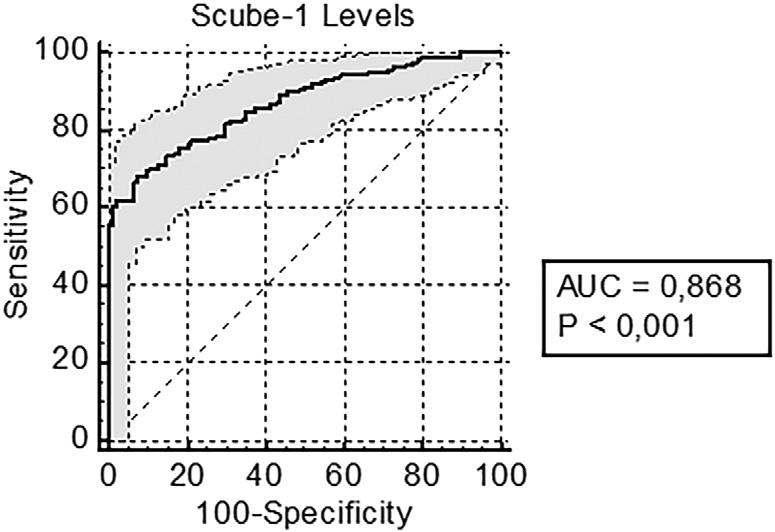
975 Diagnostic and Prognostic Value of SCUBE-1 in COVID-19 Patients
Vildan Ozer, Ozgen Gonenc Cekic, Ozlem Bulbul, Davut Aydın, Eser Bulut, Firdevs Aksoy, Mehtap Pehlivanlar Kucuk, Suleyman Caner Karahan, Ebru Emel Sozen, Esra Ozkaya, Polat Kosucu, Yunus Karaca, Suleyman Turedi
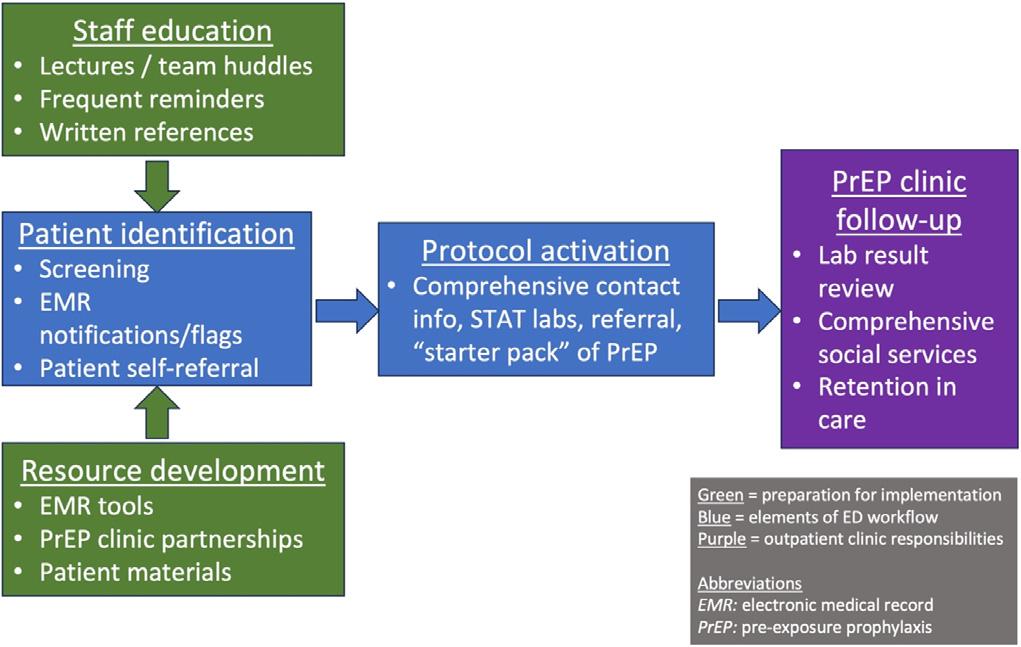
985 Feasibility of Emergency Department-Initiated HIV Pre-Exposure Prophylaxis
Ezra Bisom-Rapp, Kishan Patel, Katrin Jaradeh, Tuna C. Hayirli, Christopher R. Peabody
Health Equity
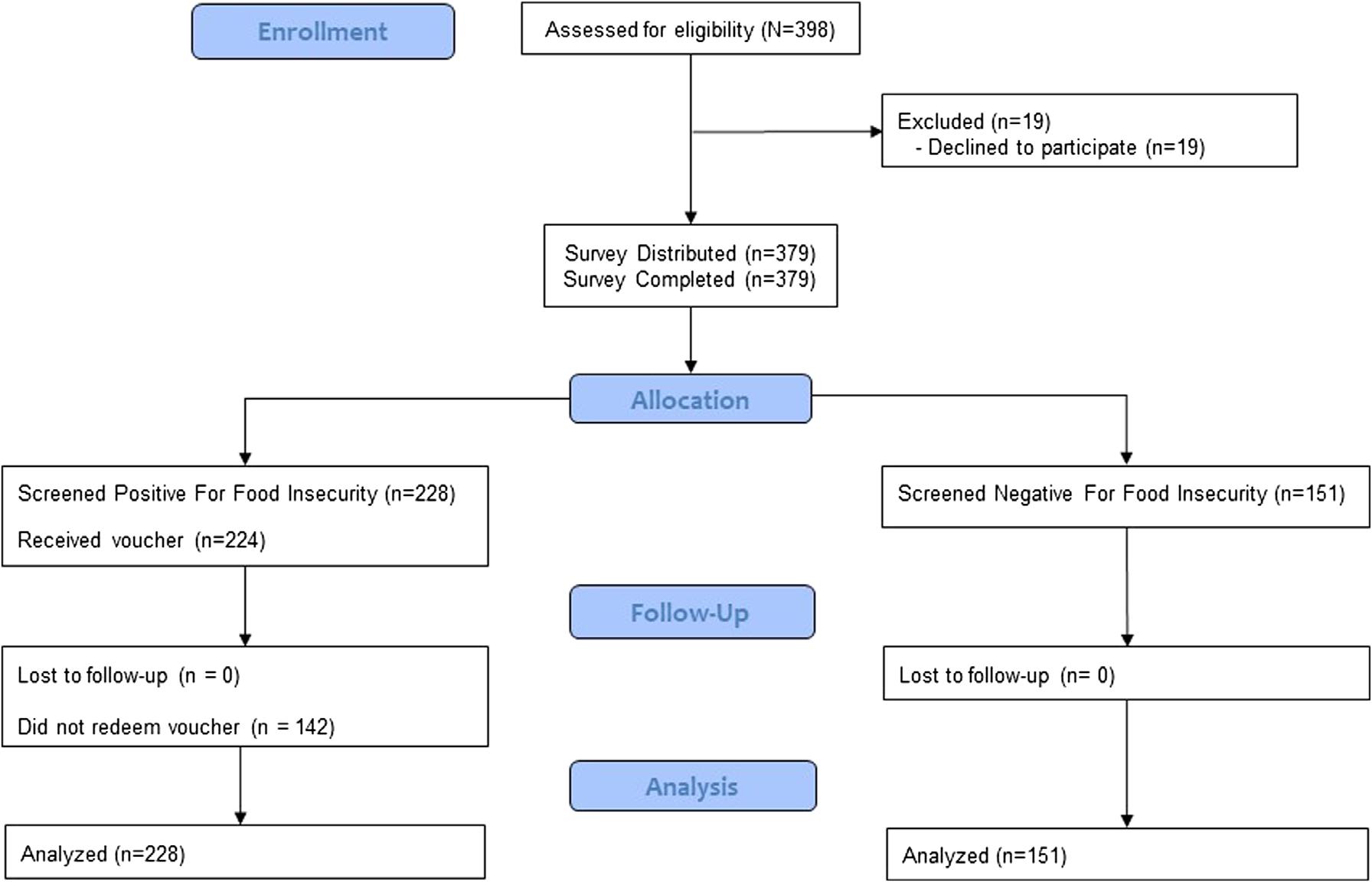
993 Emergency Department Food Insecurity Screening, Food Voucher Distribution and Utilization: A Prospective Cohort Study
Alexander J. Ulintz, Seema S. Patel, Katherine Anderson, Kevin Walters, Tyler J. Stepsis, Michael S. Lyons, Peter S. Pang
Health Policy Perspectives
1000 The California Managed Care Organization Tax and Medi-Cal Patients in the Emergency Department
Lauren Murphy, Gita Golonzka, Ellen Shank, Jorge Fernandez
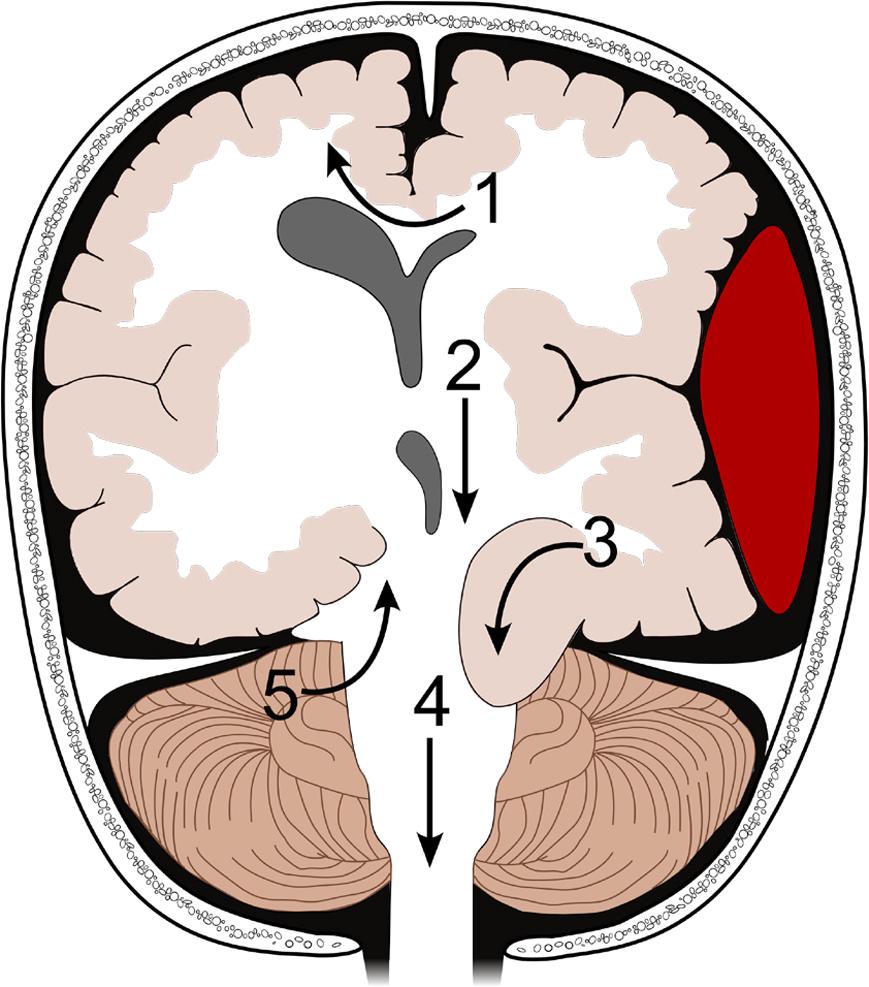
Neurology
1003 A Review of the Clinical Presentation, Causes, and Diagnostic Evaluation of Increased Intracranial Pressure in the Emergency Department
Cristiana Olaru, Sam Langberg, Nicole Streiff McCoin
Pediatrics
1011 Barriers to Adoption of a Child-Abuse Clinical Decision Support System in Emergency Departments
Alanna C. Peterson, Donald M. Yealy, Emily Heineman, Rachel P. Berger
1020 Reframing Child Protection in Emergency Medicine
Joseph P. Shapiro, Genevieve Preer, Caroline J. Kistin
Letters to the Editor
1025 Comments on “Bicarbonate and Serum Lab Markers as Predictors of Mortality in the Trauma Patient”
Patrick McGinnis, Samantha Camp, Minahil Cheema, Shriya Jaddu, Quincy Tran, Jessica Downing
Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Albany Medical College Albany, NY
Allegheny Health Network Pittsburgh, PA
American University of Beirut Beirut, Lebanon
AMITA Health Resurrection Medical Center Chicago, IL
Arrowhead Regional Medical Center Colton, CA
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
INTEGRIS Health Oklahoma City, OK
Kaiser Permenante Medical Center San Diego, CA
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Lakeland HealthCare St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Louisiana State University Shreveport Shereveport, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maine Medical Center Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Mayo Clinic Jacksonville, FL
Mayo Clinic College of Medicine Rochester, MN
Mercy Health - Hackley Campus Muskegon, MI
Merit Health Wesley Hattiesburg, MS
Midwestern University Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
25, No. 6: November 2024
Sociedad Chileno Medicina Urgencia Thai Association
Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program St. Paul, MN
Rhode Island Hospital Providence, RI
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
St. Luke’s University Health Network Bethlehem, PA
Spectrum Health Lakeland St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
The MetroHealth System/ Case Western Reserve University Cleveland, OH
UMass Chan Medical School Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Tucson, AZ
University of California, Davis Medical Center Sacramento, CA
University of California, Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago Chicago, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Massachusetts Amherst, MA
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Nebraska Medical Center Omaha, NE
University of Nevada, Las Vegas Las Vegas, NV
University of Southern Alabama Mobile, AL
University of Southern California Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University Winston-Salem, NC
Wake Technical Community College Raleigh, NC
Wayne State Detroit, MI
Wright State University Dayton, OH
Yale School of Medicine New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Sociedad Chileno Medicina Urgencia Thai Association
REVIEW RecentInterventionsforAcuteSuicidalityDeliveredinthe EmergencyDepartment:AScopingReview AlexP.Hood,BA*†
LaurenM.Tibbits,MD*
JuanI.Laporta,BS*
JenniferCarrillo,BS*
LaceeR.Adams,BS*
StaceyYoung-McCaughan,RN,PhD‡
AlanL.Peterson,PhD,ABPP‡§
RobertA.DeLorenzo,MD,MSM,MSCI*
SectionEditor:BradBobrin,MD
*UniversityofTexasHealthScienceCenteratSanAntonio, DepartmentofEmergencyMedicine,SanAntonio,Texas
† BaylorUniversity,DepartmentofPsychologyandNeuroscience, Waco,Texas
‡ UniversityofTexasHealthScienceCenteratSanAntonio,Department ofPsychiatryandBehavioralSciences,SanAntonio,Texas
§ UniversityofTexasatSanAntonio,DepartmentofPsychology, SanAntonio,Texas
Submissionhistory:SubmittedDecember21,2023;RevisionreceivedAugust12,2024;AcceptedAugust16,2024
ElectronicallypublishedOctober9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18640
Introduction: SuicidalityisagrowingproblemintheUS,andtheemergencydepartment(ED)isoften thefrontlineforthemanagementandeffectivetreatmentofacutelysuicidalpatients.Thereisadearthof interventionsthatemergencyphysiciansmayusetomanageandeffectivelytreatacutelysuicidal patients.TotheextentthatrecentlydescribedinterventionsareavailableforEDpersonnel,noreview hasbeenconductedtoidentifythem.Thisscopingreviewisintendedto fillthisgapbysystematically reviewingtheliteraturetoidentifyrecentlydescribedinterventionsthatcanbeadministeredintheEDto reducesymptomsandstabilizepatients.
Methods: WeconductedasearchofPubMed,SCOPUS,andCINAHLinJanuary2024toidentify paperspublishedbetween2013–2023fororiginalresearchtrialingrecentinterventionsfortheeffective treatmentofsuicidalityintheED.Weassessed16full-textarticlesforeligibility,andninemetinclusion criteria.Includedstudieswereevaluatedforfeaturesandcharacteristics,the fitoftheinterventiontothe EDenvironment,andinterventionalefficacy.
Results: Fourstudiesassessedtheefficacyofasingledoseoftheanesthetic/analgesicagentketamine. Threestudiesassessedtheef ficacyofabriefpsychosocialinterventiondeliveredintheED,twoofwhich pairedthisinterventionwiththeprovisionoffollow-upcare(postcardcontactandreferralassistance/ casemanagement,respectively).Theremainingtwostudiestrialedabrief,motivationalinterviewingbasedintervention.Includedstudieshadstrongexperimentaldesigns(randomizedcontrolledtrials)but smallsamplesizes(average57).Amongtheinterventionsrepresentedacrosstheseninestudies,a singledoseofketamineandthebriefpsychosocialinterventionCrisisResponsePlanning(CRP)show promiseasED-appropriateinterventionsforsuicidality.KetamineandCRPdemonstratedthestrongest fittotheEDenvironmentandmostrobustefficacy findings.
Conclusion: Thisreviewidentifiedonedrug(ketamine)andfouruniquepsychological/behavioral interventionsthathavebeenusedtotreatacutesuicidalityintheED.Thereiscurrentlyinsufficient evidencetosuggestthattheseinterventionswillproveefficaciousandwell-suitedtobedeliveredinthe EDenvironment.FuturestudiesshouldcontinuetotesttheseinterventionsintheEDsettingtodetermine theirfeasibilityandefficacy.[WestJEmergMed.2024;25(6)858–868.]
INTRODUCTION Overthepasttwodecades,thesuiciderateintheUS generalpopulationincreasedbyover33%.1 Uptohalfof suicidedecedentsvisitanemergencydepartment(ED)during theyearbeforetheirdeath,andapproximately25%visitin themonthimmediatelyprior.2,3 Theriskfordeathbysuicide amongEDpatientspresentingwithsuicidalthoughtsand behaviorsremainshighforatleastoneyearafter discharge.4,5 TheEDisoftenthe firstmedicalaccesspointfor thosewithanacutedeteriorationintheirmentalhealth; approximately10%ofallEDvisitsareformentalhealth concerns. 5–7 Newandinnovativeapproachesareneededto stemthetideofsuicidesandtohelpmitigatethecrisisof psychiatricboardinginEDs.8,9
Emergencydepartmentpersonnelhaveincreasingly voicedconcernsoverabrokensystemofmentalhealthcare thathasexacerbatedconditionsforEDpatientswith psychiatricemergencies.10 Suchserioussystemdeficiencies maycontributetotheperceptionofsuicidalEDpatientswho describeEDpersonnelaslackingempathy,andbeing brusque,irritable,andevenhostile.11 Exacerbatingthe problemisthatthenumberofstate-fundedinpatient psychiatricbedshasdroppedsubstantially,from340beds per100,000peoplein1995tounder12bedsper100,000by 2016.8,9 Conversely,thenumberofEDvisitsforpsychiatric complaintshasrisenby50%.8 Thishasledtoasituation wheremanypatientswhorequireinpatientmentalhealth caremustwaitintheEDuntilapsychiatricbedbecomes available.Thisdelayintransferringpatientstoaninpatient unitleadsto “psychiatricEDboarding.”12
Thestate-of-the-artinterventionsavailabletoemergency physiciansareorientedtowardsafelydischargingpatients homeandconnectingthemtodefinitivementalhealth services.13,14 Briefinterventionsorreferralfollowedby dischargehomearecommonforpatientspresentingwith non-life-threateningsuicidalthoughtsandbehaviors, whereaspatientspresentingwithmoderatetosevererisk behaviorsforsuicideareusuallykeptintheEDuntiltransfer toaninpatientpsychiatricfacilityispossible.15 Thissplitting ofpatientsintocategoriesofriskseverity16 meansthatthe higherapatient’sriskforsuicide,thefewerinterventionsare availabletoaddressthepatient’sparticularneeds.Notably, nopharmacologicagenthasbeenapprovedbytheUS FoodandDrugAdministrationtotreatsuicidalityinthe ED;mostmedicationsadministeredtosuicidalED patientstypicallytargetonlyagitation,notthesuicidal symptomsthemselves.16,17
Fromapsychiatricperspective,mostavailable interventionstargetsuicidalthoughtsandbehaviorsoverthe longtermasopposedtotheshort-ormediumterm17 andare thereforeill-suitedtotheacutecareenvironment. Psychopharmacologicagentssuchasantidepressants, lithium,andantipsychoticsgenerallyrequireacourseof weeksormonthstotakeeffect,14 andbeginningacourseof
antidepressanttreatmentcanparadoxicallyincrease suicidalityinsomepopulations.18 Similartimescalesare requiredforempiricallysupportedpsychotherapiessuchas cognitivebehavioraltherapyandothers,17,19 andeventhe mostabbreviatedstandardinterventionscantakeupto sixweeks.20
Whiletheimportanceofscreeningforsuicidalityiswell understood,21 thereisgrowingneedforevidence-based, rapidlyacting,effectivetreatmentoptions.15 Manyexisting toolssuitedtotheEDenvironmentthattargetsuicidality lacksupportingevidenceor,worse,are counterproductive.22,23 Onesuchinterventionisthesafety contractorno-suicideagreement.Whileatonetimethegold standardforEDanti-suicidalinterventions,thesafety contracthasbeenshowntoproduceworseoutcomesthanno interventionatall.21,24 Totheextentthatmorerecent interventionsfortheeffectivetreatmentofacutesuicidality haveemerged,therehasbeennoreviewcreatedspecificallyto identifyanddescribepotentialinterventions.
AnanalysisbyInagakiandcolleagues25 identifiedbroad classesofinterventionstopreventrepeatsuicideattemptsin patientsadmittedtoanEDbutdidnotinvestigatewhich interventionswouldbebestsuitedtotheEDenvironment. Changandcolleaguesprovidedareviewofmajordepressive disorderandsuicidalityintheEDbutdidnotofferan analysisofrecentlydescribedinterventions.21 Ina2021 review,Mannandcolleagues26 surveyedthelandscapefor evidence-basedtherapiesforsuicidalityingeneral,butthey didnotfocusspecificallyontheED.Whileotherrecent reviewshaveassessedtheavailabilityofclinician-oriented educationalinterventions,23 orinterventionsformental decompensationingeneral,27 nonehavethoroughlyassessed theliteratureforrecentlydescribedtoolsthatcliniciansmay usetotreatacutesuicidalityinthecontextoftheED. Lengvenyteandcolleagues28 publishedasystematicreview ontheimmediateandshort-termefficacyofsuicide-targeting interventionsbutdidnotfocusonrecentinterventionsused intheED.Weundertookthisreviewto fillthegapand exploretheliteraturetoidentifyanddescriberecent,patientcenteredinterventionsfortheeffectivetreatmentofacute suicidalityintheED.
Inthisreviewwefocusedonrecentlydescribed interventionsthatcanbeadministeredinthecontextofa patient’sstayintheED,namely,brieftherapiesand pharmacologicagentsthat fitwiththestandardmedical modeloftreatment.State-of-the-artpractice(ie,generally acceptedcare),definedasinterventionsforacutesuicidality, aredescribedin Rosen ’ sEmergencyMedicine:Concepts andClinicalPractice 29 or KaplanandSadock ’ s ComprehensiveTextbookofPsychiatry . 30 Theseinclude screening,jointsafetyplanning,patienteducation,lethal meanscounseling,follow-upcontacts,andtheinvolvement offriendsandfamily.29,30 Interventionslistedinor moderatelymodifiedfromthosedescribedinthesetextbooks
wereconsideredstate-of-the-artandexcludedfromthe search.Theprimaryquestionofthisreviewwasasfollows: Whatrecentlydescribedinterventionsareavailableforusein reducingsuicidalityandstabilizingpatientsduringa psychiatriccrisisintheED?
METHODS WesearchedPubMed,SCOPUS,andCINAHLon January15,2024.Thisreviewwasconductedinaccordance withbest-practicerecommendationsofthePreferred ReportingItemsforSystematicReviewsandMeta-Analysis (PRISMA)extensionforscopingreviews.31 Inclusioncriteria includedthefollowing:1)studyparticipantpatientswere presentingtotheEDwithsuicidalideation;2)thestudy assessedtheefficacyofoneormorepatient-centered intervention(s)aimedatreducingsuicidalthoughtsand behaviors;3)theinterventionbeingtestedwasadministered topatientsintheED;4)theinterventionwasadministeredby emergencyphysiciansorpersonnel;5)thestudywas availableinEnglish;and6)thestudyhadbeenpublishedin thelast10years.
DefinitionofSuicidalityandRecentInterventions Weadoptedthesuicidalitynomenclatureproposedby Silvermanandcolleagues.32 Studiesimplementingthebroad termsuicide-relatedthoughtsandbehaviors(SRTB),orany sub-categorythereof,wereconsideredeligibleforinclusion. Foraresourceonresearch-validatedscalesforthe measurementofsuicidalitywereliedonthelistcompiledby Ghasemi,Shaghaghi,andAllahverdipour.33 Wesoughtto identifyrecentlydescribed,effectivetreatmentsforthe preventionofsuicidalbehaviorthatareoutsidethestate-ofthe-art(currentstandards).Tothisend,wedefinedrecent interventionsasbeingpatient-centered,deliveredintheED, describedwithinthepast10years,andnotalreadypartof recognizedstate-of-the-artpractice.
FeaturesofEligibleStudies Weassessedstudiesforcharacteristicfeaturesoncethey wereincludedintheanalysis,andweevaluatedthe comparativestrengthsandweaknessesofstudydesign, samplesize,etc.Studiesconsideredidentifiedaspecific, recentinterventionforacutesuicidalityincontextoftheED intheprevious10years,sinceearlierinterventions wereconsideredmorelikelytobeconsistentwith state-of-the-artpractice.
Searchstrategy Weusedathree-stepsearchstrategyinconsultationwitha libraryscientist.Inthe firstphase,weconducteda preliminarysearchofPubMedtoensurerelevantresultswere retrievedfromoursearchterms.Inthesecondphase,the searchtermswereappliedtoPubMed,SCOPUS,and CINAHL.See AppendixA forthesearchtermsused.Inthe
thirdphase,wescannedtheresultsfromthesearchconducted inphasetwoforreferencesincludedinstudybibliographies thatcouldhaveprovidedadditionalarticles.Thedatabase searchstrategyissummarizedin AppendixA.Weconducted additionalsearchesofGoogletoidentifygrayliterature orpublicationsnotdiscoveredviatheabove-described searchprocess.
Studyselection Oncesearchtermsandkeywordswerenarroweddown,we removedduplicatesfromthelistofarticles.Four independentreviewersscreenedthetitlesandabstractsfor relevanceofallremainingstudies.Articlesdeterminedtobe relevantatthisstagewereretrievedinfull-textformand screenedforrelevancebytwoindependentreviewers.Apreselectedarbitersettledinconsistenciesbetweenreviewers.We recordedanddocumentedreasonsforexclusionforany article.Avisualizationofthisprocessisincludedina PRISMA flowdiagram34 in Figure1,whichalsoprovidesaa summaryofresultsinstandardPRISMAformat.
Dataextraction Data fieldscollectedfromincludedstudiesare summarizedinthedataextractiontoolgivenin AppendixB. TheprimaryauthorA.P.H.extracteddatausingthetool, andthedatawascheckedforaccuracyandcompletenessby anindependentreviewer.
RESULTS Afterduplicateswereremoved,weanalyzed1,197studies. Thereareafewreasonsforthislargenumberofresults.In keepingwithbest-practiceguidelines,andtoavoidthe
iden fied through database search (N = 1213)
iden fied in gray literature (n = 0)
a er duplicates removed (n = 1197)
iden fied via References sec ons (n = 0)
Titles/abstractsscreened (n = 1197) Records excluded (n = 1181)
Full-text ar cles assessed for eligibility (n = 16) Full-text ar cles excluded, with reasons (n = 7)
Studies included (n = 9)
Figure. PRISMA flowdiagramofstudyselection.
improperexclusionofanyrelevantarticles,weusedbroad searchtermstoreturnthemaximumnumberofpotentially relevantarticles.Additionally,noMeSHtermsspecifically aimedatexcludingscreeningandriskassessmentwereused. Thetitle/abstractreviewphasewas,therefore,acriticalstage fortheisolationofrelevantarticles,andweremoved1,181 fromfurtheranalysis.
Inthenextphaseofeligibilityscreening,twoindependent reviewersretrievedandevaluatedthefulltextsof16articles, ofwhichsevenwereexcluded.Disagreementsweresettledby anemergencyphysicianwithrelevantexpertiseinacutecare interventionsforsuicidalityR.A.D.Oftheexcludedarticles, twostudiesinvolvedinterventionsthatweretailoredtothe uniqueculturalpracticesofspecificindigenousgroupsand werethereforedeemednotgeneralizabletoallsuicidal patientspresentingtoEDs.35,36 Twoadditionalarticleswere excludedastheyusedasafetyplanningintervention operationallydefinedaspartofstate-of-the-artpractice.One articlewasexcludedbecausethestudyinterventiondidnot occurintheEDsetting.37 Finally,weexcludedtwo secondaryanalysesofarticlesthathadalreadybeen included.38,39 Oftheninearticlesincludedintheanalysis,we extracteddatausingthetoolgivenin AppendixA.Anoverviewofrelevantdatafromeachstudy ispresentedinthe Table
Fourincludedarticlesassessedtheuseofasingledoseof thepharmacologicinterventionketamine,aN-methyl-Daspartateantagonistcommonlyusedasasedative,analgesic, andanesthetic.40–43 Threestudiesassessedtheuseofan intravenous(IV)infusion,40,42,43 andoneassessedthe efficacyandtolerabilityofanintranasaladministration.41 Twooftheselectedarticlesassessedtheefficacyof interventionscenteredonmotivationalinterviewing(MI) embeddedinaninterventionalframeworkwithprovisions forfollow-upcareorreferralassistance.44,45 BothTeen OptionsforChange(TOC)45 andSuicidalTeensAccessing TreatmentAfteranEmergencyDepartmentVisit(STATED)44 targetedadolescentsamples.
Thethreeremainingincludedarticlesstudiedvarious interventionscenteredonacutepsychotherapyand/or behavioralmanagementinthepost-acuteperiod.Byfarthe largestsampleamongincludedarticleswasastudyof assertivecasemanagementforthosepresentingtotheED afterasuicideattempt.46 Whilethelengthy(18+ months) interventionunderstudyinthisarticlelargelytookplace followingdischargefromtheED,theintervention proceduresbeganwhilepatientswereintheEDandwere deliveredbypsychiatristsorothermedicalpersonnel.46
Anotherstudythatmetourcriteriainvestigatedtheefficacy ofthenovel,manualizedProblemSolvingand ComprehensiveContactIntervention(PS-CCI),whichusesa collaborativelycompletedworksheetaimedatenhancing self-efficacyandcognitive flexibilityinsuicidalEDpatients pairedwithfollow-upcare.47 Finally,astudyoftheCrisis
ResponsePlan(CRP)interventionconductedbyBryanand colleaguesinamilitaryEDmetinclusioncriteria.22 TheCRP pairsabriefhistoricalinterviewwithacollaborative identificationanddocumentationofcopingstrategiesand resourcesavailabletopatients.22
StudyFeaturesandCharacteristics Severalmeasuresofstudyfeaturesandcharacteristics weregatheredintheprocessofdataextraction.Weused PRISMAguidelinestohelpdefineelementsofquality31 includingsamplesize,studydesign,follow-uptimeframe, andmeasuresused.
Sample Thesamplesizesofthemajorityofstudiesmeeting inclusioncriteriaweresmall.Excludingtheoutlierof Kawanishietal46 withtheirrobustsampleof914,theaverage samplesizeforincludedstudieswas57,withthesmallest sample(10)collectedbyBurgerandcolleagues.40
Design Sevenofninestudiesconductedarandomizedcontrolled trial(RCT),onewasaquasi-experimentaltwo-arm prospectivelongitudinalstudy,47 andonewasanonexperimentalpilotstudydesignedtoevaluatethefeasibility andefficacyofasinglelowdoseofketaminedeliveredviaIV bolus.43 Double-blindingandrandomassignmentwere consistentlypracticedamongtheRCTsassessingtheefficacy ofketamine,andparticipantsinthecontrolconditions receivedaninactiveplaceboinjection/atomizationofnormal saline.40–42 Kawanishiandcolleagues,46 Kingetal,45 and Grupp-Phelanetal44 usedsingleblindingandacomparator conditionofenhancedusualcare(EUC).Intheirthree-arm RCT,Bryanandcolleagues22 comparedtwoversionsofCRP (standardandenhanced)tothecontrolconditionofa contractforsafety,andparticipantswereblindedtogroup assignment.Althoughthecontractforsafetywaspreviously astandardintervention,ithasmanynoteworthy shortcomings22 makingitaless-than-idealcomparison conditiontoCRP.24
Follow-upmeasuresandtimeframe Sevenoftheninestudiesincludedinthisreviewused standard,well-subscribed,psychometricallyvalidated measuresofsuicidalitytoassessoutcomevariablesof interest,aswellasevaluationsofrepeatedhospitalizations andhealthcareutilization.Themostcommonscalesused weretheColumbiaSuicideSeverityRatingScale,theBeck ScaleforSuicidalIdeation,andtheMontgomery-Asberg DepressionRatingScale.However,twostudiesevaluated onlypost-dischargesuicideattempts,suicidedeaths,and psychiatrichospitalizationrecidivismwithoutmakinguseof psychometricmeasures.46,47 Thefollow-uptimeframes
Table. Summaryofindividualstudies.
PS-CCIisfeasibleas aninterventionfor suicideintheED
3mosDidnothavethe sampleforstatistical signi fi cance,butthey appearedto fi ndthat thisinterventionwas feasibleasmeasured byacceptability, engagement, fi delity, subjectretention,and lackofAEs.
Structured worksheet manualized
AuthorsYearCountryObjective(s)InterventionMethodsN
Intervention somewhateffective shorttermandamong women,butoverall assertivecase managementdidnot outperformcontrol condition
Lowerrecurrent suicidalbehaviorat1, 3,and6mos;butat 18mostherewasno signi fi cantdifference inratesofattempted orcompletedsuicides
BriefMIwasnot usefulinthiscontext
443mos “ Clinician ” not otherwise de fi ned
Longitudinal design
2014USATodeterminethe feasibilityand acceptabilityofa novel,manualized problem-solvingand comprehensive contactintervention (PS –CCI)aimedat improvingtreatment engagementof suicidalindividuals. Manualized problem-solving and comprehensive contact intervention
Dana Alonzo
91418mos to 5years Psychiatrist, nurses,clinical psychologists, etc Case management manual, phone 18 mos-5 yrs
Two-armed RCT
Assertivecase management
2014JapanTodetermineif assertivecase managementcan reducerepeated suicideattemptsin peoplewithmental healthproblemswho hadattempted suicideandwere admittedtoEDs
Kawashini etal
None6mosMIwasnotbetter thanenhancedusual care
1592mos total Licensed socialworker
Two-armed RCT
2019USAToexaminewhether motivational interviewing(MI) increaseslinkageof adolescentsto outpatientmental healthservicesfor depressionand suiciderisk MIpluslinking tofollowup services
Grupp- Phelan etal
CRPishighly effectiveforuseinthe acutecaresettingfor acutelysuicidal patients
Indexcard6mosStandardCRPand reasonsforliving CRPwerebothmore effectivethana contractforsafetyin reducingsuicide attemptsandinpatient hospitalization.No differencebetween twoversionsofCRP
971hrCliniciannot de fi ned
CRPThree-armed RCT
Bryanetal2017USAToevaluatethe effectivenessofcrisis responseplanning (CRP)forthe preventionofsuicide attempts
IVketamineappears tobefeasibleand effectiveintheshort term (
Signi fi cantdifferences insuicidalityscores 90 –180minsafterIV ketamineinfusion. Safetyandtolerability wereexcellent.
Two weeks
IVbag,drug, 10mlsyringe, vitalsign monitoring equipment
185minsBoard-certi fi ed
EDphysician
KetamineIVPlacebo- controlled doubleblind RCT
2020USAToassessthesafety, feasibility,tolerability, andef fi cacyofa singlelow-dose intravenous(IV) ketamineinreducing suicidalideation
Domany and McCullums Smith
Table. Continued.
Ketamineshows promiseasanacute caretreatment modality,butfurther researchisneededto validatetheeffectsof thisverysmalltrial.
Groupsvaried signi fi cantlyinthe short-termduring hospitalization; however, discrepanciesin scoresontherating scalesdiminishedat thetwo-weekfollow- uppoint.
Two weeks
AuthorsYearCountryObjective(s)InterventionMethodsN
Thisintervention appearstobe promisingbutwill needtobetestedina largersample
2mosLargeeffectforthe lowingofdepression scores,moderate effectfor hopelessness,and insigni fi canteffects forsuicidalideation andalcoholuse (thoughthestudy wasn ’ tquitelarge enoughtostatistically verifythelatter fi ndings
Theauthorsnotethat ketaminedidnot showitselfasa promisingtoolto mitigateacute suicidalityintheED context,asthe reductionsin suicidalityscores werenotclinically meaningful.However, theydonotethat moreresearchis neededandthatthis resultisfarfrom de fi nitive(giventhe samplesizeandlack ofcontrolgroup).
Theketamineinfusion wasassociatedwitha bringingdownthe MADRSandSSI scoresbya statisticallysigni fi cant margin,butthe authorsnotethat,for theirpurposes,the reductioninscores wasnotclinically meaningful(e.g., belowthethreshold setforthepurposes ofthestudyofa MADRSscoreof ≤ 4). Thelargestreduction inself-reported suicidalityoccurred within40minsof ketamine administration.
( Continuedonnextpage )
105minsTrainednurseIVbag,vital sign monitoring equipment
KetamineIVDouble-blind RCT
Burgeretal2016USATocompareIV ketaminetoplacebo amongacutely suicidalpatientsina militarysetting
Handwritten followup note
Trained mentalhealth professional withminimum of40hrsof specialized training
4945mins ofMI,5 daysof follow up
RCTwith enhanced TAUas control condition
TeenOptions forChange (TOC)
Kingetal2015USAThisrandomizedtrial examinedthe effectivenessofTeen OptionsforChange (TOC),an interventionfor adolescentsseeking medicalemergency serviceswhoscreen positiveforsuicide
IVbag,vital sign- monitoring equipment 10 days
495minsNurseor attending doctor
Uncontrolled pre-test/post- test
KetamineIV bolus
2014IranThisstudywas conductedto examinetheeffects ofasingle intravenousbolusof ketamineonpatients withsuicidalideation intheED.
Kashani etal
Table. Continued.
Whilethesampleis comparativelysmall andtheoverallresults arefarfrom conclusive,thisstudy importantlyechoes previous fi ndings demonstratingthata lowdoseofketamine doesappearto transientlyreduce suicidalideationin thoseathighacute riskforsuicide.In addition,itprovides promisingevidence thatasingle, fi xed doseofketaminemay havethepotentialto reducehospital lengthsofstay,and thatintranasalisa feasiblerouteof administrationforthe acutecaresetting.
Participantswhowere administered ketaminehadnotonly amuchhigherrateof remission(roughly 80%ofthesample), butalsotypically shorterlengthsof hospitalization. Ketaminewas generallysafe;minor sideeffectswere transientandresolved within1 –2hourspost- administration. However,thelinear mixedstatistical modeldidnotshow signi fi canceon randomgroupbytime interaction.
4 weeks
PsychiatristIntranasal atomizer
AuthorsYearCountryObjective(s)InterventionMethodsN
3040mins to1hr
Double-blind RCT
Ketamine intranasal
2022USAEvaluationofsingle, fi xed-dosed intranasalketamine foracutesuicidal ideationintheED
AEs ,adverseevents; ED ,emergencydepartment; IV ,intravenous; MADRS ,MontgomeryAsbergdepressionratingscale; RCT ,randomized,controlledtrial; SSI ,BeckScalefor SuicidalIdeation; TAU ,treatmentasusual.
Domany and McCullum Smith
variedsignificantlydependingontheinterventionunder studyandaddedtotheheterogeneityofthesample.
FitofInterventiontoEmergencyDepartmentEnvironment Sinceweintendedtoanalyzerecentlydescribedtools availabletoemergencyphysiciansforuseintheacutecare setting,attentionwaspaidtotheusabilityofeach interventionintheEDsetting.Wedefinedusabilityaseaseof useand fittotheEDenvironment,andthesewereevaluated alongthedimensionsoftotaltimerequiredtoadminister,the requiredtrainingorcredentialsoftheadministering practitioner,andthetoolsandmaterialsrequiredtodeliver theintervention.
Timetoadminister Byfarthebriefestinterventionalmodalityamongthe articlesreviewedwasasingledoseofketaminedeliveredIV, which,atthemodestdosesused,averaged5–10 minutes.40,42,43 Whenadministeredintranasally,theinterval requiredtocompletetheintervention,althoughbrief(40–60 minutes),wassomewhatlonger.41 Notincludedinthe interventiondurationwasthemonitoringtimerequiredfor ketamineadministration,whichdependingonlocalprotocol canexceedseveralhours.EquivalentlybriefisCRP,which requires30–60minutestoadminister,makingitwell-suited tothedemandsofthefast-pacedEDenvironment.22 The studiesassessingMI-basedinterventionsforadolescentshad briefED-deliveredcomponents,requiringapproximately45 minutestodeliver.44,45 Thetimerequiredtoadministerthe ED-basedproblem-solvingcomponentoftheProblemSolvingandComprehensiveContactIntervention(PS-CCI) interventionwasnotspecified.47 Finally,Kawanishiand colleaguesdidnotspecifythetimecourseoftheED-based portionofassertivecasemanagement,buttheydidnotethe interventioninvolvedregularfollow-upappointments outsidetheEDoverthecourseof18months.46
Trainingrequiredtoadminister
Dueinparttovariabilityinhospitalpracticesindifferent regionsandcountries,thecredentialsofthehealthcare professionalsadministeringketaminevariedslightlyacross thefourstudiesthatinvestigateditsuse.40–43 Intravenous administrationwasconductedbyeitheranurseora physician,40,42,43 whereasthestudyusingintranasal ketaminerequiredsignificantinputfromapharmacist.41 BoththePS-CCI47 andCRP22 statedonlythatthe interventionwasdeliveredbya “clinician,” nototherwise specified.TheSTAT-EDdescribedbyGrupp-Phelanetal44 andTOCstudiedbyKingetal45 wereadministeredbya socialworkerandtrainedmentalhealthprofessional, respectively,withthelatterspecifyingthatinterventionalists wererequiredtohaveaminimumof40hoursof specializedtraining.Finally,theassertivecasemanagement interventiondescribedbyKawanishiandcolleagues46 was
conductedbycasemanagersatvariouslevelsoftraining, includingnurses,emergencyphysicians,psychiatrists,and clinicalpsychologists.
Toolsandmaterials Formostpsychosocialinterventionsunderstudyinthe presentreview,fewspecializedmaterialswererequiredfor administration.Specifically,theSTAT-EDintervention,44 CRP,22 andTOC45 requirebasicofficeequipmentsuchas copypaperandnotecards.ThePS-CCIinterventionrequires theavailabilityofastructuredworksheet,47 andtheassertive casemanagementinterventionrequiresastandardized manual,46 makingtheirresourcedemandsminimal.Aswith allnovelpharmacologicinterventions,thestudiesassessinga singledoseofketaminerequiredtheavailabilityof equipmenttomonitorvitalsigns.40–43 ThoseassessingIV ketaminerequiredIVbags,pumps,lines,andhanging apparatuses,whichareusuallyavailableinED environments,40,42,43 whilethestudyofintranasal ketaminerequiredaspecializedatomizerpreparedbya pharmacyteam.41
EfficacyFindings Theinterpretationof findingsforarticlesdescribedinthe presentreviewshouldbemoderatedbylimitationsregarding samplesize,methodologicaldiscrepancies,andevidentiary quality.Twopromisinginterventionsweidentifiedarethe variousadministrationroutesofasingle,lowdoseof ketamine,40–43 andasinglemeetingtodevelopaCRP.22 For asingledoseofketamine,threearticlesreportedpositive findingsontheshort-termreductionofself-reported suicidalityanddepression,40–42 andonereported inconclusiveresults.43 Bryanandcolleagues22 foundthat participantsrandomizedtoeitherCRPcondition(standard orenhanced)showedsignificantreductionsinacutesuicidal ideation,fewersuicideattempts,andlowerratesofinpatient hospitalizationpost-dischargethanthoseinthe comparatorgroup.
Twootherinterventionsthatwereevaluated,PS-CCIand MI,showpromise,butthereisinsufficientevidenceto supporttheirefficacy.ThePS-CCItrial47 wasnotstatistically poweredtodetermineefficacy,buttheauthorsnotethatthe interventionisfeasibletoadministerintheEDsettinggiven itshightolerability.TheTOCstudy45 andtheSTAT-ED study44 trialedsimilarMI-basedtreatmentsincomparable adolescentsamplesbutreturnedconflictingresults.The studyofassertivecasemanagementbyKawanishiand colleagues46 hadalargesamplesizebutdemonstratedno significantdifferencebetweengroupsoverthecourseof thestudy.
DISCUSSION Thepreliminaryresultsfromthefourketaminestudies includedinthisreviewecho findingsoftheuseofketamine
forsuicidalideationinoutpatientsettings.48 Therearea numberofadvantagestothisinterventionalmodality.43 First,ketamine,whenadministeredIVover5–10minutes,is byfarthebriefestinterventionnotconsideringthepostinfusionmonitoringtime.Intravenousketamineiswell suitedtothefast-pacedenvironmentoftheED.The intranasaladministrationrouteisalmostasbrief.
Intramuscular(IM)ketamineisanotheroptionbutrelatively unstudied;however,itmaybefamiliartoemergency clinicians.IfconfirmedinfullypoweredRCTs,sucharapidactinginterventionmaygiveemergencyphysicians additionaloptionsfortheplacementorevendischargeof patientswhopresentwithacutelyelevatedsuicideriskand couldserveasabridgetodefinitivementalhealthcarethat circumventstheneedforalengthydetentionintheED. Furthermore,adoseofgenericketamineisrelatively inexpensive49 andregularlystockedinmostEDs.The intranasalformofketamine,esketamine,incontrast,is moreexpensiveandlesswidelystocked.Additional researchontheefficacyofketamineforacutelysuicidalED patientsiswarranted.
ThisreviewfoundevidencethatCRPshowspromiseasan interventionwellsuitedtocombatacutesuicidalityintheED environment.Whilethereislimitedevidenceinsupportofthe efficacyofCRPintheED,thisinterventionhasseveral featuresthatmakeitwellsuitedtothespecificdemandson emergencymedicalpersonnel.First,similartoasingledose ofketamine,CRPisaninterventionalmodalitythatisbrief inadministrationandappearstorapidlydiminishacute suicidalityandimprovepatientmood.38 Additionally,CRP ismaximallyportabletoavarietyofenvironments,requires comparativelylittlespecializedtraining,toolsormaterialsto administer,and,asapsychosocialintervention,isnot contraindicatedforusewithanyconcomitantmedications. Despiteitsadvantages,theliteraturetodateontheuseof CRPintheEDcontextislimitedtoonestudy.22 Whilethe evidenceforinterventionssuchasthePS-CCI47 andTOC45 is mixed,ED-deliveredinterventionstargetingconstructsof cognitive flexibilityandadaptiveproblem-solvingappearto bearecipewithsomepromise(similartoCRP).
FutureDirections LIMITATIONS Althoughthepresentstudyhasmanynotablestrengths, someshortcomingsshouldbedelineated.First,wefocused oninterventionswithevidencesupportingtheabilitytobe performedinthechallengingEDenvironment.Itispossible thatrecentinterventionsunderstudyinotherclinical environmentsmayholdpromiseforadaptationtotheED setting.Second,asisthecasewithanyreview,itispossible thatcertaininterventionsextantintheliteraturewere erroneouslyexcludedfromouranalysisgiventhelimitations ofourMeSHsearchterms.Finally,tolimitouranalysisto onlythemostrecentinterventionswithanevidentiarybasis inthecurrentliterature,weassessedonlyarticlespublishedin theprevious10years.Itispossiblethattherearepromising, ED-basedinterventionsdescribedmorethan10yearsago thathavereceivednofurtherstudyintheinterveningtimeor havebeenstudiedexclusivelyoutsidetheEDcontextsince theirinitialdescription.
CONCLUSION Therecentlydescribedinterventionsidentifiedfor emergencyphysicianstotreatacutesuicidalityarelimitedto onedrug(ketamine)andfouruniquepsychological/ behavioralinterventions.Twoofthe fiveinterventional modalitieshavepreliminaryevidenceandmayholdpromise inmitigatingacutesuicideriskintheED:asingle,lowdose ofketamineandcrisisresponseplanning.However,thereis insufficientevidencetosupporttheirwidespreadadoption. Futureresearchshouldextendthepreliminary findings summarizedinthisreview.
AddressforCorrespondence:AlexP.Hood,BA,UniversityofTexas HealthScienceCenteratSanAntonio,DepartmentofEmergency Medicine,703FloydCurlDrive,MC7736,SanAntonio,TX78229. Email: alex_hood1@baylor.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial
Thisstudyidentifiedtwopromisinginterventionssuitedto theEDenvironment:CRPandketamine.Theevidentiary basisfortheseinterventions,particularlyinbroad-based populationsofemergentlysuicidalEDpatients,isnotfully developed.Furtherstudyisrequiredtoascertaintheextentto whichtheseinterventionsserveaseffectivetreatmentsacross presentingpsychiatricsymptoms,especiallygiventhehigh incidenceofSRTBamongpatientswithseriousmental illnessoracuteintoxicationwithasubstance,whichmay complicateeffectivetreatment.50 Giventhecrisisofboarding inEDs,additionalfundingandstudyingeneralshouldbea nationalpriority.Futurestudiesshouldalsoinvestigate ketaminedeliveredviaalternativeroutesofadministration suchasorallyandIM.WhileCRPhasdemonstrated preliminaryefficacy, 24 futureresearchshouldcompareCRP tovalidatedcurrentstandardpracticeinterventionsto properlyevaluateitseffectivenessagainsttreatmentasusual orEUC.Futurestudiesshouldalsovalidateuseofthe interventionoutsidethemilitarycontextwithparticipantsof variousbackgrounds,abilitylevels,andages.Giventhat briefMI-andCBT-basedinterventionsshowpromise,future studiesmayconsidercontinuingtohoneinterventionsthat approximatelyadheretothismodel.
relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Hoodetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.StoneDM,SimonTR,FowlerKA,etal.Vitalsigns:trendsinstate suiciderates-UnitedStates,1999–2016andcircumstances contributingtosuicide-27states,2015. MorbMortalWklyRep. 2018;67(22):617–24.
2.AhmedaniBK,SimonGE,StewartC,etal.Healthcarecontactsinthe yearbeforesuicidedeath. JGenInternMed. 2014;29(6):870–7.
3.GairinI,HouseA,OwensD.Attendanceattheaccidentandemergency departmentintheyearbeforesuicide:retrospectivestudy. BrJPsychiatry. 2003;183:28–33.
4.CrandallC,Fullerton-GleasonL,AgueroR,etal.Subsequentsuicide mortalityamongemergencydepartmentpatientsseenforsuicidal behavior. AcadEmergMed. 2006;13(4):435–42.
5.WeissAJ,BarrettML,HeslinKC,etal.(2006).Trendsinemergency departmentvisitsinvolvingmentalandsubstanceusedisorders, 2006–2013.In HealthcareCostandUtilizationProjectstatisticalbriefs Rockville,MD:AgencyforHealthcareResearchandQuality(US). Availableat: https://www.ncbi.nlm.nih.gov/books/NBK52651/ AccessedAugust6,2024.
6.HakenewerthAM.Emergencydepartmentvisitsbypatientswithmental healthdisorders–NorthCarolina,2008–2010. MorbMortalWklyRep. 2013;62(23):469–72.
7.OwensC,HansfordL,SharkeyS,etal.Needsandfearsofyoung peoplepresentingataccidentandemergencydepartmentfollowingan actofself-harm:secondaryanalysisofqualitativedata. BrJPsychiatry. 2016;208(3):286–91.
8.TreatmentAdvocacyCenter.Going,going,gone:trendsand consequencesofeliminatingstatepsychiatricbeds.2016.Availableat: https://www.treatmentadvocacycenter.org/reports_publications/ going-going-gone-trends-and-consequences-of-eliminatingstate-psychiatric-beds/.AccessedSeptember4,2023.
9.GoldJ.Adearthofhospitalbedsforpatientsinpsychiatriccrisis.2016. Availableat: https://kffhealthnews.org/news/a-dearth-of-hospitalbeds-for-patients-in-psychiatric-crisis/.AccessedAugust6,2024.
10.ZunL.Careofpsychiatricpatients:thechallengetoemergency physicians. WestJEmergMed. 2016;17(2):173–6.
11.FitzpatrickSJandRiverJ.Beyondthemedicalmodel:futuredirections forsuicideinterventionservices. IntJHealthServ. 2018;48(1):189–203.
12.NicksBAandMantheyDM.Theimpactofpsychiatricpatientboardingin emergencydepartments. EmergMedInt. 2012;2012:360308.
13.RihmerZPandMaurizioP.Mooddisorders:suicidalbehavior.In: SadockBJ(Ed.), KaplanandSadock’sComprehensiveTextbookof Psychiatry (3825),10thed.Philadelphia,PA:WoltersKluwer Health,2017:3825–51.
14.WassermanD.Suicide:overviewandepidemiology.In:SadockBJ(Ed.), KaplanandSadock’sComprehensiveTextbookofPsychiatry (5954). 10thed.Philadelphia,PA:WoltersKluwerHealth,2017:5954–72.
15.CapocciaLM.Caringforadultpatientswithsuiciderisk:aconsensusbasedguideforemergencydepartments.2015.Availableat: https://sprc.org/wp-content/uploads/2022/11/EDGuide_full.pdf AccessedAugust6,2024.
16.BetzJ.M.Suicide.In: Rosen’sEmergencyMedicine:Conceptsand ClinicalPractice (pagerange).9thed.Philidelphia,PA:Elsevier, Inc,2018:1366–73.
17.SudakH. Suicidetreatment.In:SadockB.J.(Ed.), KaplanandSadock’s ComprehensiveTextbookofPsychiatry (5973).10thed.Philadelphia, PA:WoltersKluwer,2017:5973–85.
18.ReevesRRandLadnerME.Antidepressant-inducedsuicidality: anupdate. CNSNeurosciTher. 2010;16(4):227–34.
19.RuddMD,BryanCJ,WertenbergerEG,etal.Briefcognitive-behavioral therapyeffectsonpost-treatmentsuicideattemptsinamilitary sample:resultsofarandomizedclinicaltrialwith2-yearfollow-up. AmJPsychiatry. 2015;172(5):441–9.
20.DavidsonKM,BrownTM,JamesV,etal.Manual-assistedcognitive therapyforself-harminpersonalitydisorderandsubstancemisuse: afeasibilitytrial. PsychiatrBull(2014). 2014;38(3):108–11.
21.ChangBP,TezanosK,GratchI,etal.Depressedandsuicidalpatientsin theemergencydepartment:anevidence-basedapproach. EmergMed Pract. 2019;21(5):1–24.
22.BryanCJ,MintzJ,ClemansTA,etal.Effectofcrisisresponseplanning vs.contractsforsafetyonsuicideriskinU.S.Armysoldiers: arandomizedclinicaltrial. JAffectDisord. 2017;212:64–72.
23.ShinHD,CassidyC,WeeksLE,etal.Interventionstochangeclinicians’ behaviorinrelationtosuicidepreventioncareintheemergencydepartment: ascopingreviewprotocol. JBIEvidSynth. 2021;19(8):2014–23.
24.RuddMD,MandrusiakM,JoinerTE.Thecaseagainstno-suicide contracts:thecommitmenttotreatmentstatementasapractice alternative. JClinPsychol. 2006;62(2):243–51.
25.InagakiM,KawashimaY,KawanishiC,etal.Interventionstoprevent repeatsuicidalbehaviorinpatientsadmittedtoanemergency departmentforasuicideattempt:ameta-analysis. JAffectDisord. 2015;175:66–78.
26.MannJJ,MichelCA,AuerbachRP.Improvingsuicideprevention throughevidence-basedstrategies:asystematicreview. AmJPsychiatry. 2021;178(7):611–24.
27.JohnstonAN,SpencerM,WallisM,etal.Reviewarticle:Interventions forpeoplepresentingtoemergencydepartmentswithamental healthproblem:asystematicscopingreview. EmergMedAustralas. 2019;31(5):715–29.
28.LengvenyteA,OliéE,StrumilaR,etal.Immediateandshort-term efficacyofsuicide-targetedinterventionsinsuicidalindividuals:a systematicreview. WorldJBiolPsychiatry. 2021;22(9):670–85.
29.MarxJA,HockbergerRS,WallsRM,etal.In: Rosen’sEmergency Medicine:ConceptsandClinicalPractice.9thed.Philadelphia,PA: Mosby/Elsevier,2018.
30.SadockBJS,AlcottV,RuizP. KaplanandSadock’sComprehensive TextbookofPsychiatry.10thed.Philadephia,PA:WoltersKluwer,2017.
31.TriccoAC,LillieE,ZarinW,etal.PRISMAextensionforscoping reviews(PRISMA-ScR):checklistandexplanation. AnnInternMed. 2018;169(7):467–73.
32.SilvermanMM,BermanAL,SanddalND,etal.RebuildingtheTowerof Babel:arevisednomenclatureforthestudyofsuicideandsuicidal behaviors.Part2:suicide-relatedideations,communications,and behaviors. SuicideLifeThreatBehav. 2007;37(3):264–77.
33.GhasemiP,ShaghaghiA,AllahverdipourH.Measurementscalesof suicidalideationandattitudes:asystematicreviewarticle. HealthPromotPerspect. 2015;5(3):156–68.
34.MoherD,LiberatiA,TetzlaffJ,etal.Preferredreportingitemsfor systematicreviewsandmeta-analyses:thePRISMAstatement. PLoSMed. 2009;6(7):e1000097.
35.CwikMF,TingeyL,LeeA,etal.Developmentandpilotingofabrief interventionforsuicidalAmericanIndianadolescents. AmIndianAlsk NativeMentHealthRes. 2016;23(1):105–24.
36.HatcherS,CoupeN,WikiriwhiK,etal.TeIraTangata:aZelen randomisedcontrolledtrialofaculturallyinformedtreatmentcompared totreatmentasusualinMaoriwhopresenttohospitalafterself-harm. SocPsychiatryPsychiatrEpidemiol. 2016;51(6):885–94.
37.MillerIW,CamargoCAJr.,AriasSA,etal.Suicidepreventioninan emergencydepartmentpopulation:theED-SAFEstudy. JAMAPsychiatry. 2017;74(6):563–70.
38.BryanCJ,MintzJ,ClemansTA,etal.Effectofcrisisresponseplanning onpatientmoodandcliniciandecisionmaking:aclinicaltrialwith suicidalU.S.soldiers. PsychiatrServ. 2018;69(1):108–11.
39.FurunoT,NakagawaM,HinoK,etal.Effectivenessofassertivecase managementonrepeatself-harminpatientsadmittedforsuicide attempt: findingsfromACTION-Jstudy. JAffectDisord. 2018;225:460–5.
40.BurgerJ,CapobiancoM,LovernR,etal.Adouble-blinded,randomized, placebo-controlledsub-dissociativedoseketaminepilotstudyinthe treatmentofacutedepressionandsuicidalityinamilitaryemergency departmentsetting. MilMed. 2016;181(10):1195–9.
41.DomanyYandMcCullumsmithCB.Single, fixed-doseintranasal ketamineforalleviationofacutesuicidalideation.Anemergency department,trans-diagnosticapproach:arandomized,double-blind,
placebo-controlled,proof-of-concepttrial. ArchSuicideRes. 2022;26(3):1250–65.
42.DomanyY,SheltonRC,McCullumSmithCB.Ketamineforacute suicidalideation.Anemergencydepartmentintervention:A randomized,double-blind,placebo-controlled,proof-of-concepttrial. DepressAnxiety. 2020;37(3):224–33.
43.KashaniP,YousefianS,AminiA,etal.Theeffectofintravenous ketamineinsuicidalideationofemergencydepartmentpatients. Emerg(Tehran). 2014;2(1):36–9.
44.Grupp-PhelanJ,StevensJ,BoydS,etal.Effectofamotivational interviewing-basedinterventiononinitiationofmentalhealthtreatment andmentalhealthafteranemergencydepartmentvisitamong suicidaladolescents:arandomizedclinicaltrial. JAMANetwOpen. 2019;2(12):e1917941.
45.KingCA,GipsonPY,HorwitzAG,etal.Teenoptionsforchange:an interventionforyoungemergencypatientswhoscreenpositivefor suiciderisk. PsychiatrServ. 2015;66(1):97–100.
46.KawanishiC,ArugaT,IshizukaN,etal.Assertivecasemanagement versusenhancedusualcareforpeoplewithmentalhealthproblemswho hadattemptedsuicideandwereadmittedtohospitalemergency departmentsinJapan(ACTION-J):amulticentre,randomisedcontrolled trial. LancetPsychiatry. 2014;1(3):193–201.
47.AlonzoD.Suicidalindividualsandmentalhealthtreatment: anovelapproachtoengagement. CommunityMentHealthJ. 2016;52(5):527–33.
48.XiongJ,LipsitzO,Chen-LiD,etal.Theacuteantisuicidaleffectsof single-doseintravenousketamineandintranasalesketaminein individualswithmajordepressionandbipolardisorders:asystematic reviewandmeta-analysis. JPsychiatrRes. 2021;134:57–68.
49.BrendleM,RobisonR,MaloneDC.Cost-effectivenessofesketamine nasalspraycomparedtointravenousketamineforpatientswith treatment-resistantdepressionintheUSutilizingclinicaltrialefficacy andreal-worldeffectivenessestimates. JAffectDisord. 2022;319:388–96.
50.RabascoA,AriasS,BenzMB,etal.Longitudinalriskofsuicide outcomesinpeoplewithseverementalillnessfollowinganemergency departmentvisitandtheeffectsofsuicidepreventiontreatment. JAffectDisord. 2024;347:477–85.
ORIGINAL RESEARCH Buprenorphine-NaloxoneforOpioidUseDisorder: ReductioninMortalityandIncreasedRemission KrishnaK.Paul,BS*
ChristianG.Frey,BS*
StanleyTroung,BA*
LauravitaQ.Paglicawan,BS*
KathrynA.Cunningham,PhD†
T.PrestonHill,MD*
LaurenG.Bothwell*
GeorgiyGolovko,PhD†
YeoshinaPillay,MD‡
DietrichJehle,MD*
SectionEditor:BradBobrin,MD
*DepartmentofEmergencyMedicine,UniversityofTexasMedicalBranch, Galveston,Texas
† DepartmentofPharmacologyandToxicology,UniversityofTexasMedical Branch,Galveston,Texas
‡ DepartmentofEmergencyMedicine,MichiganStateUniversity, EastLansing,Michigan
Submissionhistory:SubmittedDecember15,2023;RevisionreceivedJuly5,2024;AcceptedJuly11,2024
ElectronicallypublishedSeptember6,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18569
Introduction: Asfentanylhasbecomemorereadilyavailable,opioid-relatedmorbidityandmortalityin theUnitedStateshasincreaseddramatically.Preliminarystudiessuggestthathigh-affinity,partialmuopioidreceptoragonistssuchasthecombinationproductbuprenorphine-naloxonemayreducemortality fromoverdoseandpromoteremission.Withtheescalatingprevalenceofopioidusedisorder(OUD),itis essentialtoevaluatetheeffectivenessofopioidagonistslikebuprenorphine-naloxone.Thisstudy examinesmortalityandremissionratesforOUDpatientsprescribedbuprenorphine-naloxoneto determinetheef ficacyofthistreatmenttowardtheseoutcomes.
Methods: WecarriedoutaretrospectiveanalysisusingtheUSCollaborativeNetworkdatabasein TriNetX,examiningde-identifiedmedicalrecordsfromnearly92millionpatientsacross56healthcare organizations.ThestudyspannedtheyearsfromJanuary1,2017–May13,2022.Cohort1included OUDpatientswhobeganbuprenorphine-naloxonetreatmentwithinone-yearpost-diagnosis,while Cohort2,thecontrolgroup,consistedofOUDpatientswhowerenotadministeredbuprenorphine.The studymeasuredmortalityandremissionrateswithinayearoftheindexevent,incorporatingpropensity scorematchingforage,gender,andrace/ethnicity.
Results: Priortopropensitymatching,weidentifiedatotalof221,967patientswithOUD.Following exclusions,61,656patientstreatedwithbuprenorphine-naloxoneshowed34%fewerdeathswithinone yearofdiagnosiscomparedto159,061patientswhodidnotreceivebuprenorphine(2.6%vs4.0%; relativerisk[RR]0.661;95%confidenceinterval[CI]0.627–0.698; P < 0.001).Theremissionratewas approximately1.9timeshigherinthebuprenorphine-naloxonegroupcomparedtothecontrolgroup (18.8%vs10.1%;RR1.862;95%CI1.812–1.914; P < 0.001).Afterpropensitymatching,theeffecton mortalitydecreasedbutremainedstatisticallysignificant(2.6%vs3.0%;RR0.868;95%CI0.813–0.927; P < 0.001)andtheremissionrateremainedconsistent(18.8%vs10.4%;RR1.812;95%CI 1.750–1.876; P < 0.001).Numberneededtotreatforbenefitwas249fordeathand12forremission.
Conclusion: Buprenorphine-naloxonewasassociatedwithsignificantlyreducedmortalityand increasedremissionratesforpatientswithopioidusedisorderandshouldbeusedasaprimary treatment.Therecognitionandimplementationoftreatmentoptionslikebuprenorphine-naloxoneisvital inalleviatingtheimpactofOUD.[WestJEmergMed.2024;25(6)869–874.]
INTRODUCTION Background
Theincidenceandprevalenceofopioidusedisorder (OUD)isincreasingbothintheUnitedStatesandglobally. Therecentproliferationoftheillicitdrugfentanylhasonly intensifiedthepotentialforopioidabuseandraisedthe mortalityrate.1 Opioid-relateddeathshavesurgednearly four-foldsince1999,andmortalityrateshavecontinuedtheir upwardtrajectorywiththeadventofsyntheticopioids.2–4 Fentanylhasnotablybecometheprimarydriverofdrugrelatedoverdoses,withanalmost7.5-foldincreasein overdose-relateddeathsfrom2015to2021.2 However,there isarangeofUSFoodandDrugAdministration-approved medicationsavailableforOUDthatcanreduceoverdoserelatedmortalityandpromoteremission.
Partialopioidagonistmedications,suchasbuprenorphine, whichcanbefoundasamono-productformorcombinedwith naloxone(suchasbrandnameSuboxone),havedemonstrated efficacyinreducingtheriskofoverdose-relateddeath comparedtopureopioidantagonistslikenaltrexone.5–8 Buprenorphineisapartialopioidagonistthatfunctionsby bindingtothemu-opioidreceptorwithparticularlyhigh affinitywhenthereceptorisempty,therebyblockingthe bindingofotheropioidswithabusepotentialwhilealso alleviatingwithdrawalsymptomsandcravings.9 However, whenthereceptorisoccupied,buprenorphinedislodgesthe opioidfromthereceptor,thusprecipitatingwithdrawal.
Buprenorphine-naloxoneisdistinctiveinthatwhengiven asacombination,itcanbeusedtomitigatepossible inappropriateusageofbuprenorphinealone.When administeredsublingually,thenaloxonecomponenthaslittle tonoeffectduetohigh first-passhepaticmetabolism. However,ifbuprenorphine-naloxoneweretobeused intravenouslyorintranasally,thenaloxonecanprecipitate withdrawalaswellasdiminishanyperceivedeuphoria.9 This uniquecharacteristicofbuprenorphine-naloxonegreatly enhancesitspotentialtoreduceopioid-relatedoverdoses.A studyconductedovera22-yearperiod,publishedin2020, revealedthattherelativeriskofoverdose-relateddeathwas upto3.2timeshigherintheabsenceofopioidagonist therapywithbuprenorphine.8 Moreover,priorresearch demonstratespotentialindecreasingfutureillicitopioiduse followinginitiationoftreatmentwithbuprenorphinenaloxone.1 A2021studyfoundthatbuprenorphinenaloxonetherapywasassociatedwithsignificantlylower oddsoffentanylexposureovertimecomparedtomethadone orslow-releasemorphinetreatment.1 Thispositions buprenorphine-naloxoneasauniquelyeffectivecombination ofdrugsusedinthetreatmentofOUD.
Importance AstheprevalenceofOUDcontinuestorise,itisessential toidentifyatreatmentthateffectivelyreducesoverdoserelatedmortalityandincreasesremissionrates.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Opioid-relatedmorbidityandmortalityhas increasedintheUS,alongwithfentanyl use.Studiesshowbuprenorphine-naloxoneto beaneffectivetreatmentforopioiduse disorder(OUD).
Whatwastheresearchquestion?
Howarethemortalityandremissionratesof OUDpatientsaffectedbytheprescriptionof buprenorphine-naloxone?
Whatwasthemajor findingofthestudy?
Patientsprescribedbuprenorphine-naloxone had34%fewerdeaths(CI0.63 – 0.70; P < 0.001)and1.9timesmoreremission (CI1.81 – 1.91;P < 0.001).
Howdoesthisimprovepopulationhealth?
AstheincidenceofOUDandtheavailability offentanylincreases,healthcareinterventions areessential.Buprenorphine-naloxoneisan effectivetreatmentoption.
GoalsofInvestigation Inthisstudyweusedelectronichealthrecords(EHR) fromtheUnitedStatesCollaborativeNetworkinTriNetXto performananalysiscomparingpatientsprescribed buprenorphine-naloxonewithinoneyearoftheirOUD diagnosiswiththosewhodidnotuseopioidagonisttherapy. Theinvestigationexaminedmortalityandremissionrates betweenthesetwopatientcohorts.
METHODS StudyDesign TriNetXisaglobalcollaborativenetworkconsistingof de-identifiedpatientEHRdatafromaroundtheworld.All cohortandoutcomedefinitionswerebasedonthe InternationalClassificationofDiseases,10th Rev,Procedure CodingSystem,ClinicalModification(ICD-10-CM)entered intothehealthrecordsystems.Weidentifiedmedications prescribedusingRxNormcodes(Table1).RxNormisa standardizednomenclatureforclinicaldrugsanddrug deliverydevicesintheUS,developedandmaintainedbythe NationalLibraryofMedicine.UsingtheUSCollaborative NetworkofTriNetX,whichcontainsapproximately92 millionpatientsfrom56healthcareorganizations(HCO)in theUS,weestablishedtwocohorts.
Table1. InternationalClassificationofDiseasesandRxNormcodesforbuprenorphine-naloxoneandopioidusedisorder. TypeNameCodingsystemCode DiagnosisOpioiddependence,uncomplicatedICD-10-CMF11.20 DiagnosisOpioiddependence,inremissionICD-10-CMF11.21 DiagnosisOpioidabuse,inremissionICD-10-CMF11.11 DiagnosisOtherlong-term(current)drugtherapyICD-10-CMZ79.899 MedicationBuprenorphineRxNorm1819 MedicationNaloxoneRxNorm7242
ICD-10-CM,InternationalClassificationofDiseases;10th Rev,ClinicalModification; OUD,opioidusedisorder.
CohortDefinition
Cohort1includedallpatientsdiagnosedwith uncomplicatedopioiddependence(ICD-10-CM:F11.20) whoweregivenaprescriptionofbuprenorphine-naloxone (buprenorphine-RxNorm:1819 + naloxone -RxNorm:7242)withinoneyearofanyF11.20diagnosis inputintothehealthrecordsystem.Cohort2(control) consistedofpatientsdiagnosedwithuncomplicatedopioid dependencewithnocurrentorpriorprescriptionof buprenorphine.Thiswasconsideredthestartingeventor “indexevent.” Individualswhohadneverbeenprescribed buprenorphinewereselectedasthecontrolgroup,because definingthecontrolgroupasthosenothaving buprenorphine-naloxonelistedintheTriNetXdatabase couldinadvertentlyhaveexcludedpatientswhohadbeen treatedsolelywithnaloxonefollowinganoverdoseepisode. Forbothcohorts,thetimewindowwasestablishedbetween January1,2017–May13,2022.Thistimeframewaschosen asbuprenorphine-naloxonebecamewidelyaccessibleand prescribedfrom2017onward,andtheenddateof2022 ensuredtherewasatleastoneyearbetweenthedatethe patientwasseenforOUDandoneyearoffollow-up foroutcomes.
Outcomes Thetwooutcomesmeasuredinthesecohortswere mortalityandremission.Remissionwasdefinedbythe diagnosisofremissionfromopioiddependence(ICD-10CM:F11.21),remissionfromopioidabuse(ICD-10-CM: F11.11),ortheuseofotherlong-termdrugtherapy(ICD-10CM:Z79.899).Thetimewindowfortheseoutcomesranged fromonedaytooneyearfollowingtheindexevent,which wasdefinedastheusageofbuprenorphine-naloxoneornonusageofbuprenorphineforOUD.Weexcludedfromthe studypatientswithremissionpriortotheindexevent. MortalitydatawithintheTriNetXplatformwasobtained fromEHRdataandHCOs,inconjunctionwiththenational deathregistries.Thereispotentialformisseddeathevents whenapatientistreatedatanHCOnotaffiliatedwiththe TriNetXnetworkandsubsequentlyexperiencesafatal outcomeoutsidethisnetwork.However,thisrepresentsonly
aminorissue,ascurrently,94%ofHCOswithintheTriNetX networkarealsolinkedtotheUSdeathregistries.This percentageissteadilyincreasingasmoreHCOscontinueto belinkedwiththeregistries.
SecondaryAnalysisonSocioeconomicStatus Weperformedasecondaryanalysistoevaluatetheimpact ofsocioeconomicstatusontheprescriptionof buprenorphine-naloxoneandoutcomesinOUDpatients. ThepresenceoftheICD-10-codesZ56.0(Unemployment, unspecified)orZ59(Problemsrelatedtohousingand economiccircumstances)wasusedasamarkerforprior historyoflowersocioeconomicstatusandwasextracted fromeachcohort.
Apost-hocanalysiswasperformedfromJune2,2004to June2,2023,inwhichweevaluatedOUDpatientswhowere prescribedsuboxonewithinonemonthoftheOUD diagnosisandexcludedthoseonmethadoneornaltrexone. TheOUDdefinitionwasexpandedtoincludeadditional ICD09/10-codesassociatedwithopioidabuseandopioiduse aswell(SupplementaryTable1).Propensitymatchingwas slightlymorerobust,includingadditionalcovariatessuchas socialdeterminants,disordersrelatedtodrugsofabuse,and nicotine(SupplementaryTable2).
StatisticalAnalysis A1:1propensityscorematchwasproducedviaTriNetX, usinglogisticandlinearregression.Weusedgreedynearestneighbormatchingwithatoleranceof0.1andadifference betweenpropensityscoreslessthanorequalto0.1.10 Propensitymatchingwasperformedfordemographics includingageattheindexevent,race,ethnicity,andgender, usingtheBalanceCohortstoolinTriNetX.Alldemographic datawasself-reportedbypatientsandrecordedbyHCOsto HL7administrativestandards.WeusedtheMeasureof AssociationAnalysistoolinTriNetXtocalculateriskratio (RR),95%confidenceinterval(CI),and P -values(P)for outcomecomparisonsthroughunivariateanalysis.We calculatedthenumberneededtotreatforbenefit(NNTB) manuallyforeachoutcome.Patientswhomettheoutcome priortothevisitwereexcludedfromtheirrespectivecohorts
fortheoutcomeanalysistoensurethatpatientswhohadthe outcomepriortotheindexeventwereexcluded.The final datawasobtainedandanalysisconductedonMay13,2023. Statisticalsignificancewasdeterminedatatwo-sidedalpha <0.05.Becauseweusedde-identifieddatafromTriNetX,this studywasdeterminedtobeexemptbytheUniversityof TexasMedicalBranch(UTMB)IRB.TheUTMBIRB determinedthatthisprojectdidnotinvolveinterventionor interactionwithhumansubjects,andthedatawasdeidentifiedperthede-identificationstandarddefinedin Section§164.514(a)oftheHIPAAPrivacyRule.This formaldeterminationbyaqualifiedexpertrefreshedon December2020.10
RESULTS Inthisanalysis,therewereatotalof221,967patientsprior topropensitymatching,with62,041patientsinCohort1and 159,926patientsinCohort2.Regardingtheoutcomeof mortality,afterexclusions,Cohort1consistedof61,656 patients,andCohort2comprised159,061patients.Forthe outcomeofremission,therewereamuchlargernumberof patientsexcludedbecauseofpriorhistoryofremission. Cohort1included37,199patients,andCohort2contained 110,726patients.Afterpropensitymatching,Cohort1 maintainedthesamenumberofpatientsforbothoutcomes. Whenpropensitymatchingwasapplied,Cohort2included 61,746and44,284patientsfortheoutcomesofdeathand remission,respectively,afterexclusions.(Table2).
Afterpropensitymatching,OUDpatientsexperienced 13%lessdeaths(2.6%vs3.0%,RR0.87,95%CI0.81–0.93, P < 0.001)and81%greaterremissionsrates(18.8%vs10.4%,
RR1.81,95%CI1.75–1.88, P < 0.001)intheyearfollowing prescriptionofbuprenorphine-naloxonewhencomparedto thosewhowerenotprescribedbuprenorphine.Before propensitymatching,trendsweresimilar;however,theeffect ofmortalitywasmorepronounced(RR0.66)(Table3).The NNTBwas249fordeathand12forremissionwithinone yearofindexevent.
Thesecondaryanalysisfortheimpactofsocioeconomic statusshowedpatientsprescribedbuprenorphine-naloxone weremorelikelytohaveahistoryofunemploymentthan thosenotprescribedbuprenorphine(6.36%vs2.54%, P < 0.001).Similarly,patientsprescribedbuprenorphinenaloxoneweremorelikelytohavehadproblemsrelatedto housingandeconomiccircumstancesthanthosenot prescribedbuprenorphine(13.93%vs7.82%, P < 0.001).The posthocanalysisshowedthatafterpropensitymatchingfor socialdeterminantsofhealthandothersubstance-related disorders,therelativeriskofdeathinoneyearwas0.78(95% CI0.74–0.83; P < 0.001)andremissionwas2.15(95%CI 2.09–2.22; P < 0.001)forthepatientsprescribed buprenorphine-naloxonewithinonemonthofOUD diagnosis(SupplementaryTable3).Trendsweresimilar beforepropensitymatching.NNTBwas137fordeathand 12forremission.
DISCUSSION Thismulticenter,retrospectivestudyhasdemonstrated thatbuprenorphine-naloxoneusewasassocaitedwith significantlylowermortalityratesandhigherremissionrates incomparisontonotreatmentinpatientswithOUD.The utilizationoftheUnitedStatesCollaborativeNetworkin
Table2. DemographicsbeforeandafterpropensityscorematchingwithCohort1buprenorphine-naloxoneandCohort2opioiduse disordercontrols.
AI/AN564(0.91%)807(0.51%) <0.0010.05564(0.91%)412(0.66%) <0.0010.03
NHPI42(0.07%)140(0.09%) =0.140.0142(0.07%)15(0.02%) <0.0010.02
Unknownethnicity10,945(17.6%)49,014(30.6%) <0.0010.3110,945(17.6%)10,922(17.6%) =
NotHispanicorLatino47,161(76.0%)101,782(63.6%) <0.0010.2747,161(76.0%)47,249(76.2%) =0.56 <0.01 HispanicorLatino3,935(6.34%)9,130(5.71%) <0.0010.033,935(6.34%)3,870(6.24%) =0.45 <0.01
Black6,999(11.3%)22,711(14.2%) <0.0010.096,999(11.3%)6,993(11.3%) =0.96 <0.01
Asian193(0.31%)810(0.51%) <0.0010.03193(0.31%)169(0.27%) =0.21 <0.01
Unknownrace7,873(12.7%)24,643(15.4%) <0.0010.087,873(12.7%)7,916(12.8%) =0.71 <0.01
OUD,opioidusedisorder; AI/AN,AmericanIndianorAlaskanNative; NHPI,NativeHawaiianorotherPacificIslander.
Table3. OutcomesbeforeandafterpropensityscorematchingwithCohort1buprenorphine-naloxoneandCohort2opioiduse disordercontrols.
Cohort1Cohort2RR(95%CI) P-value
MortalitybeforePSM1,628(2.64%)6,352(3.99%)0.66(0.63–0.70)P < 0.001
MortalityafterPSM1,628(2.64%)1,878(3.04%)0.87(0.81–0.93)P < 0.001
RemissionbeforePSM6,984(18.78%)11,163(10.08%)1.86(1.81–1.91)P < 0.001
RemissionafterPSM6,984(18.78%)4,589(10.36%)1.81(1.75–1.88)P < 0.001
OUD,opioidusedisorder; PSM,propensityscorematching; RR,relativerisk; CI,confidenceinterval.
TriNetXprovidesthelargestsamplesizeinthecurrent literature(221,967beforepropensitymatching)comparing buprenorphine-naloxonetonointervention.Thislargedatasetapproachhasmitigatedpotentialconfounding variables,includingsocialdeterminants,thatmighthave influencedthe findingsofpreviousresearch.
The findingsofourstudyareconsistentwithother literatureexaminingoutcomesofmedicationsforOUD.The PrescriptionOpioidAddictionTreatmentStudytrial demonstratedmoresuccessfuloutcomes(abstinenceornearabstinencefromopioids)inprescriptionopioidusers maintainedonbuprenorphine-naloxonethaninthosewho weretaperedoffbuprenorphine-naloxone.11 Only7%of studyparticipantswhoweretaperedoffbuprenorphinenaloxoneachievedsuccessfuloutcomescomparedto49% whoweremaintainedonbuprenorphine-naloxone.11 This populationofprescriptionopioidusersisslightlydifferent fromourpopulationofpatientswithOUD.Otherstudies havecomparedtheuseofbuprenorphine-naloxonewith othermethods,suchasextended-releasenaltrexone,or methadone,andhavefoundeitherinterventiontobeequally safeandeffective.12–14 Patientswereevenfoundtohave greatershort-termsuccessintreatmentwithbuprenorphinenaloxonecomparedtoclonidineinasmall,multicenter, randomizedtrial.15
Anotherstudyconsiderednotreatment,inpatient detoxification,behavioralhealth,buprenorphineor methadone,naltrexone,andnon-intensivebehavioralhealth interventionsinindividualswithOUD.Onlytreatmentwith buprenorphineormethadonedemonstratedasignificantly reducedriskofoverdoseandopioid-relatedacutecareat 3-and12-monthfollow-ups.16 Ourstudyfurtherstrengthens theargumentformedicationuseintreatingOUDand demonstratestheeffectivenessofbuprenorphine-naloxone.
The findingsofthisstudycarrysignificantimplicationsfor theacutemanagementofOUD.Withtheglobalrisein OUD,exacerbatedbytheincreasedavailabilityoffentanyl, mitigatingmortalityratesforindividualswithOUDremains amajorpublichealthchallenge.17 Theseindividualsmay requiremedicalinterventionsforthetreatmentof complicationsofOUDsuchasautonomicinstability, hypoxia,endocarditis,ischemia,orcardiacarrest.18
Proactivepharmacologicmanagementisakeycomponentin preventingthelife-threateningconsequencesofOUD.
LIMITATIONS Itisimportanttoacknowledgetheinherentlimitationsof aretrospectivestudy,especiallyinthatcausationcannotbe established.Thisstudyincludedasampleof221,967patients from56HCOsbeforepropensitymatching,whichismore extensivethanpreviousstudies,therebyprovidingincreased statisticalpower.Thelargesamplesizeanduseofpropensity matchinghelpmitigatesomeoftheselimitations.Propensity matchingwasperformedforcovariatesincludingage, gender,race,andethnicity,buttheremaybeother unaccountedvariablesthatcouldhaveinfluencedthe mortalityratesorremissioninthisgroup.DuetodeidentificationandprivacypoliciesinherenttotheTriNetX database,granularandnon-codabledatasuchassocial determinantsarelimited,whilegeographicidentifierssuchas ZIPcodesareunobtainable.Moreover,thisstudydidnot takeintoaccountcomorbidmedicalconditionsor psychiatricillnesses,whichmightalsohaveimpacted theoutcomes.
Thedatabaserecordsprescriptionsinthehealthrecords butdoesnotreportthedosagesofbuprenorphine-naloxone, exacttimingofthisadjuncttherapy,orpatientadherenceto regimen.Thisomissionissignificantbecausedifferent medicationdosagesandcompliancemayaffecttheefficacy ofbuprenorphine-naloxone.Forthecontrolgroup, alternativemethodsformanagingOUDmayhavebeen presentbutwerenotconsideredintheanalysis.Additionally, withoutknowinghowlongapatientwasdrugfree,wecould notruleoutpotentialrelapsesasacausefortheindexvisitin theexcludedgroup.Furthermore,theparameterofthedata collectedrestrictsthegeneralizationofthestudyfor internationalpopulationsandlong-termresultsbeyond ayear.
Finally,thestudyevaluatedtheparametersofmortality rateandremission,butothermeasuresweren’tincluded.We didnotconsiderqualityoflifemeasures,whichcouldprovide amorecomprehensiveunderstandingoftheeffectsof buprenorphine-naloxoneonlifestyleinthosewithOUD. Futureresearchshouldfocusonotherlifeoutcomemeasures,
socialdeterminants,andthelong-termimpactsof buprenorphine-naloxoneontheindividual.
CONCLUSION Thismulticenterretrospectiveanalysisshowsthat buprenorphine-naloxoneuseisassociatedwithsignificantly improvedmortalityratescomparedtonointerventionin patientswithopioidusedisorder.Furthermore,thestudy highlightsanassociationwithhigherremissionratesinthis population.Whilethese findings,alongwithprevious studies,suggestthatbuprenorphine-naloxoneisaneffective treatmentoptionforOUD,furtherprospectivestudies comparingtoothertreatmentmodalitiesshouldbe consideredtoconfirmefficacy.
AddressforCorrespondence:KrishnaK.Paul,BS,Research Coordinator,DepartmentofEmergencyMedicine,Universityof TexasMedicalBranch,301UniversityBlvd.,Galveston,1173. Email: kkpaul@utmb.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisresearchwassupportedbythe InstituteforTranslationalSciencesatTheUniversityofTexas MedicalBranch,supportedinpartbyaClinicalandTranslational ScienceAward(UL1TR001439)fromtheNationalCenterfor AdvancingTranslationalSciencesattheNationalInstitutesofHealth (NIH).Thecontentissolelytheresponsibilityoftheauthorsanddoes notnecessarilyrepresenttheofficialviewsoftheNIH.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Pauletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.YoungS,HayashiK,GrantC,etal.Buprenorphine/naloxoneassociated withareducedoddsoffentanylexposureamongacohortofpeoplewho usedrugsinVancouver,Canada. DrugAlcoholDepend. 2021;228:109006.
2.MattsonCL,TanzLJ,QuinnK,etal.Trendsandgeographicpatternsin drugandsyntheticopioidoverdosedeaths-UnitedStates,2013–2019. MorbMortalWklyRep. 2021;70(6):202–7.
3.MartinM,HeckerJ,ClarkR,etal.Chinawhiteepidemic:aneastern UnitedStatesemergencydepartmentexperience. AnnEmergMed. 1991;20(2):158–64.
4.CentersforDiseaseControlandPrevention.Understandingtheopioid overdoseepidemic.2024.Availableat: https://www.cdc.gov/
overdose-prevention/about/understanding-the-opioid-overdoseepidemic.html.AccessedJune24,2024.
5.LarochelleMR,BernsonD,LandT,etal.Medicationforopioiduse disorderafternonfatalopioidoverdoseandassociationwithmortality: acohortstudy. AnnInternMed. 2018;169(3):137–45.
6.WattsBV,GottliebDJ,RibletNB,etal.Associationofmedication treatmentforopioidusedisorderwithsuicidemortality. AmJPsychiatry. 2022;179(4):298–304.
7.BurnsM,TangL,ChangCH,etal.Durationofmedicationtreatment foropioid-usedisorderandriskofoverdoseamongMedicaidenrollees in11states:aretrospectivecohortstudy. Addiction. 2022;117(12):3079–88.
8.PearceLA,MinJE,PiskeM,etal.Opioidagonisttreatmentandriskof mortalityduringopioidoverdosepublichealthemergency:population basedretrospectivecohortstudy. BMJ. 2020;368:m772.
9.VelanderJR.Suboxone:rationale,science,misconceptions. OchsnerJ. 2018;18(1):23–9.
10.MurphyLR,HillTP,PaulK,etal.Tenecteplaseversusalteplasefor acutestroke:mortalityandbleedingcomplications. AnnEmergMed. 2023;82(6):720–8.
11.WeissRDandRaoV.Theprescriptionopioidaddictiontreatment study:whathavewelearned. DrugAlcoholDepend. 2017;173Suppl1(Suppl1):S48–54.
12.LeeJD,NunesEVJr,NovoP,etal.Comparativeeffectivenessof extended-releasenaltrexoneversusbuprenorphine-naloxoneforopioid relapseprevention(X:BOT):amulticentre,open-label,randomised controlledtrial. Lancet. 2018;391(10118):309–18.
13.NeumannAM,BlondellRD,HoopsickRA,etal.Randomizedclinicaltrial comparingbuprenorphine/naloxoneandmethadoneforthetreatment ofpatientswithfailedbacksurgerysyndromeandopioidaddiction. JAddictDis. 2020;38(1):33–41.
14.D’OnofrioG,O’ConnorPG,PantalonMV,etal.Emergencydepartmentinitiatedbuprenorphine/naloxonetreatmentforopioiddependence:a randomizedclinicaltrial. JAMA. 2015;313(16):1636–44.
15.LingW,AmassL,ShoptawS,etal.Amulti-centerrandomizedtrialof buprenorphine-naloxoneversusclonidineforopioiddetoxification: findingsfromtheNationalInstituteonDrugAbuseClinicalTrials Network. Addiction. 2005;100(8):1090–100.[publishedcorrection appearsin Addiction.2006;101(9):1374].
16.WakemanSE,LarochelleMR,AmeliO,etal.Comparativeeffectiveness ofdifferenttreatmentpathwaysforopioidusedisorder. JAMANetw Open. 2020;3(2):e1920622.
17.RitchieH,ArriagadaP,RoserM.Opioids,cocaine,cannabisandother illicitdrugs.Ourworldindata.2022.Availableat: https://ourworldindata. org/illicit-drug-use#introduction.AccessedJuly30,2023.
18.LavonasEJandDezfulianC.Impactoftheopioidepidemic. CritCare Clin. 2020;36(4):753–69.
ORIGINAL RESEARCH OpioidTreatmentIsAssociatedwithRecurrentHealthcareVisits, IncreasedSideEffects,andPain CarolineE.Freiermuth,MD,MS*†
JennyA.Foster,BS‡
PratikManandhar,MS§
EvangelineArulraja,MD∥
AlaattinErkanli,PhD§
CharlesV.Pollack,MD,MA¶
StephanieA.Eucker,MD,PhD∥
*UniversityofCincinnati,DepartmentofEmergencyMedicine,Cincinnati,Ohio
† UniversityofCincinnatiCollegeofMedicine,CenterforAddictionResearch, Cincinnati,Ohio
‡ DukeUniversitySchoolofMedicine,Durham,NorthCarolina
§ DukeUniversity,DepartmentofBiostatisticsandBioinformatics, Durham,NorthCarolina
∥ DukeUniversity,DepartmentofEmergencyMedicine,Durham,NorthCarolina
¶ UniversityofMississippiMedicalCenter,DepartmentofEmergencyMedicine, Jackson,Mississippi
SectionEditor:PatrickMeloy,MD
Submissionhistory:SubmittedJune22,2024;RevisionreceivedJuly16,2024;AcceptedJuly16,2024
ElectronicallypublishedSeptember24,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18380
Introduction: Painisamajordriverofvisitstotheemergencydepartment(ED).Cliniciansmustconsider notonlytheefficacyoftreatmentoptionsbutalsosubsequenthealthcareutilizationandpatient-centered outcomessuchassideeffectsfromprescribedmedications.Ourgoalinthisstudywastodetermine whethertherewasanassociationbetweenacutepaintreatmentregimen(opioids,intranasal non-steroidalanti-inflammatorydrugs[NSAIDs],orboth)andunscheduledhealthcarevisitsfollowing EDdischarge.
Methods: ThisstudywasasecondaryanalysisoftheAcuteManagementofPainfromtheEmergency Department(AMPED)prospective,observationalcohortstudy.WeusedCoxproportionalhazards analysistoassesstherelationshipbetweentreatmentregimenandtimeto firstunscheduledhealthcare visit.Repeatedmeasureslogisticregressionanalyseswereusedtodeterminetherelationshipbetween treatmentregimenandanyunscheduledvisits,andtoevaluatewhetherthisrelationshipwasmediated bypainseverityand/ormedicationsideeffects.
Results: Of831totalenrolledparticipants,141(16.9%)experiencedanunplannedhealthcarevisit within fivedaysofEDdischarge.AmajorityofthesevisitshappenedonedayaftertheEDvisit.Those whoweretreatedwithintranasalNSAIDsonlywerelesslikelytohaveanunscheduledhealthcarevisit comparedtothosewhoreceivedopioidsonly,withanadjustedoddsratio(AOR)of0.63.Thehigherodds ofunscheduledhealthcarevisitswithopioidsweremediatedbyboththepresenceofsideeffectsand higherpainlevels,withAORsof2.24and1.33,respectively.
Conclusion: Opioidtreatmentforacutepainisassociatedwithincreasedunscheduledhealthcarevisits comparedtothosetreatedwithintranasalketorolac.Thisdifferencecanbeexplainedbyhigherlevelsof ongoingpainandgreatermedicationsideeffects.[WestJEmergMed.2024;25(6)875–882.]
INTRODUCTION Acutepainisthemostfrequentchiefcomplaintfor emergencydepartment(ED)visitsintheUnitedStates.1 Inadequatetreatmentofpaincontributestotheevolution
fromacutetochronicpain,whichcaninflictexcessive personalandeconomicburdensonpatients.2–4 Outsidethe limitednumberofrecommendationsguidingtreatmentofa fewspecificacuteconditions,suchaslowerbackpain,5 there
arenoevidence-basedguidelinesthataddressthe managementofacutepain,resultinginwidevariability inpractice.6–8
Inparticular,thenumberofopioidprescriptionsincreased duringthelate1990stoearly2010s,yetopioidswerenot foundtocorrelatewithimprovedpain-relatedoutcomesor patientsatisfaction.9–11 Moreover,theadventofthecurrent opioidcrisisandriseinopioid-relateddeathsmotivatednew guidelinesdiscouragingtheuseofopioidsforacuteand chronicpainmanagement.12–14 Whileopioid-prescribing ratessubsequentlybegantodeclinefrom21.5%ofpatients dischargedfromanEDin2011to8.1%in2019,thisrate remainscomparativelyhigh.15 Inaddition,opioidreductions havenotappearedtobematchedbysufficientincreasesin non-opioidprescribing.16
Inparticular,ongoingconcernsaboutthesideeffectsof alternativestoopioidssuchasnon-steroidalantiinflammatorydrugs(NSAID)havehinderedtheiruse.17 However,datashowsthateveninhigh-riskpatients,those prescribedNSAIDsdidnotexperiencehigherratesofserious adverseevents.18,19 Specifically,intranasalketorolachas beenfoundtobeaneffective,well-tolerated,andsatisfactory medicationforadultspresentingtotheEDwithacutepain, withonlyminorsideeffectssuchasnasalburningthat resolveswithinseveralminutes.20,21 Bycomparison,the adverseeffectsofopioidsoutsideopioidusedisorder-related morbidityhavereceivedrelativelylittleattention,withonly recentdatasuggestinggreatersideeffectswithopioidsthan withNSAIDs.19,22 Thus,morestudiesareneededtobetter understandtherisk-benefitcomparisonbetweenopioidsand NSAIDsforpaintreatment.
Meanwhile,therehasbeenafocusonpreventingrecurrent visitstotheED23–25 forpainaswellasothercomplaints. Revisitssubstantiallyimpactboththepatientandhealthcare systemandoftenreflectunmetpatientneeds.Recentdata suggestsopioidprescriptionsintheoutpatientsettingare associatedwithanincreasednumberofsubsequent healthcarevisits.26–29 Unplannedvisitscanresultinmissed daysofwork,30–32 disruptingthedailylivesofpatients,as wellasincreasedcosts,oftenhigherwiththerepeatthanthe initialEDvisit.33 Failuretoaddresstheinitialpresenting problemoritssequelae,aswellaslackofcommunication withpatientsregardingthetherapeuticplanand recommendedfollow-up,contributetoEDrecidivism.32,34,35 Emergencyphysiciansmustunderstandhowthetreatment theyprovideintheEDmayaffectdownstreamhealthcare utilizationtofullyconsidertheimpactoftheircareonboth patientsandhealthcaresystems.
Inthissecondaryanalysis,wesoughttodetermine whethertherewasanassociationbetweentreatmentregimen (opioidonly,intranasalNSAIDonly,orintranasalNSAID + opioid)followinganEDvisitforacutepainand subsequentdailyhealthcareutilization.Wefurther characterizedthisassociationbywhethermedicationside
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Widevariabilityinpaintreatmentinacute caresettingsisdueinparttolimitedevidence onpatientexperiencesrelatedtochoice ofmedication.
Whatwastheresearchquestion?
Whatistheassociationbetweenchoiceof acutepaintreatmentandunscheduled healthcarevisitsafterEDdischarge?
Whatwasthemajor findingofthestudy?
Comparedtoopioids,NSAIDshadalower adjustedoddsratioof0.63forpost-ED unscheduledhealthcarevisits(P=0.03,95% CI0.42 – 0.95,33.3%ofpatientsvs.39.7%).
Howdoesthisimprovepopulationhealth?
Ourstudyfurtherunderscoresand contextualizesthewidercomplexityofthe impactoftreatmentdecisions(eg,medication sideeffects,comparativeef fi cacy)on patientoutcomes.
effectsorongoingpainseveritymediatedtheeffecton healthcareutilization.
METHODS StudySettingandPopulation
Thiswasasecondaryanalysisofdataobtainedfroma multisite,prospective,observationalcohortstudy,Acute ManagementofPainfromtheEmergencyDepartment (AMPED).36 Theoriginalstudywasapprovedbythe institutionalreviewboardsatallenrollmentsites.A conveniencesampleofadultparticipants ≥18yearsoldwith acutemusculoskeletalorvisceralpainnotrequiring admissionwererecruitedfrom13EDsintheUSbetween September2012–February2014.Patientswereprescribed oneofthreetreatmentregimensfollowingEDdischarge: NSAID(intranasalketorolac)only;oralopioidonly;or both(intranasalketorolacwithopioidasarescuetherapy). Treatmentregimenwasatthediscretionofthe treatingclinician.
DataCollection Datacollectionincludedpatientdemographics, employmentstatus,paintype(visceralormusculoskeletal) andlocation,painscores(0–10numericratingscale)atED triageandEDdischarge,medicationsgivenduringtheED
visit,anddischargemedicationregimen.Patientswere contacteddailyforfourdaysfollowingEDdischargefor follow-upoutcomesincludingunplannedhealthcarevisits, medicationuse,dailyhighestandlowestpainscores,adverse eventsandsymptoms,overallqualityoflife,andoverall satisfactionwiththeprescribedpainmedication.Detailsof theunplannedhealthcarevisitswerenotrecorded,including reasonforthevisit.
StatisticalAnalysis All831patientswereincludedforanalysis.Weused descriptivestatisticstosummarizepatientdemographicsfor thosewithorwithoutunplannedhealthcarevisitsafterED discharge.Categoricalvariableswerereportedas frequencies,andcontinuousvariableswerereportedas medianvalueswithinterquartileranges(25th,75th).Fewer than fivepatientshadmissingdemographicdata.The missingdataoncategoricalvariableswereimputedtothe highestfrequencycategory,andcontinuousvariableswere imputedtomedianvalues.
Weperformedstatisticalanalysestoinvestigatewhether treatmentregimenimpactedthetimetoasubsequent unscheduledhealthcareutilizationfollowingEDdischarge andthenumberofanyunscheduledvisits,andtoevaluate possiblemediatingfactors.Thosewhoreceivedopioid-only treatmentswereusedasthereferencecategoryfortreatment regimen.Weadjustedallmodelsforage,gender,race, primaryEDdiagnosis,initialpainscore,anddischargepain score.Atwo-tailed P -valueof0.05wasusedforstatistical significance.WeperformedallanalysesusingSAS9.4(SAS InstituteInc,Cary,NC).
Toevaluatetherelationshipbetweentreatmentregimen andtimeto firstunscheduledvisitfollowingEDdischarge, weusedaCoxproportionalhazardsmodel.Unscheduled visit(UV)datawascollectedoverthefour-dayfollow-up period.The firstoccurrenceofanunscheduledvisit(UV = YES)wasusedasthedayoftheunscheduledvisit,regardless ofUV = MISSINGorUV = NOvaluesinpriordays.Ifthe UVdatawasmissingforallfourdays,thepatientwas censoredatday4.WegeneratedaKaplan-Meiercurveof unscheduledvisitwithlog-rank P -value.Toevaluatethe relationshipbetweentreatmentregimenandany unscheduledvisitsfollowingEDdischarge,weuseda repeatedmeasureslogisticregressionmodel.Missingdataon unscheduledvisitsoverthefour-dayperiodwereimputedas UV = NOvalue.Additionally,weperformedasensitivity analysiswhereallmissingdataonunscheduledvisitswere imputedasUV = YESvalue.
Toevaluateformediationoftheassociationbetween treatmentregimenandanyunscheduledvisits,weperformed threeseparaterepeatedmeasureslogisticregressionmodels toassesstheeffectof1)anymedicationsideeffect;2)daily maximumpainscores;or3)bothsideeffectsandpainscores.
RESULTS ParticipantCharacteristics Atotalof831participantswereincludedintheoriginal AMPEDstudy.Asparticipantshadtocompleteatleast threeofthefourfollow-upcallstobeincludedintheoriginal analysis,wedidnotexcludeanypatientsfromthissecondary analysis.Thedistributionofparticipantsineachdischarge treatmentregimengroupwasunevenintheoriginalstudy, withcombinationtherapy(intranasalketorolacwithopioid rescue)beingtheleastprescribedregimen.36 Asreportedin theparentstudy,characteristicsofparticipantsineach dischargetreatmentgroupwerecomparable,exceptthat participantsintheopioid-onlygroupwereslightlyolderand morelikelytohaveachronicpainhistory;participantswho hadfracturesorvisceralpainweremorelikelytoreceive opioidsaspartoftheirregimen;andparticipantsinthe intranasalketorolac-onlygrouphadslightlyloweraverage painscoresatinitialEDpresentation.36 Overall,141(16.9%) participantshadatleastoneunscheduledvisitoverthefourdayfollow-uptimeperiod.Baselineanddemographic characteristicsofparticipantsinthissub-analysisareshown byattendancetounscheduledvisits(nonevsatleastonevisit) in Table1.
ModelResults Acrossalltreatmentregimens,thehighestnumberof unscheduledvisitsoccurredonthe firstdayofthefour-day follow-upperiod(Figure1).However,afteradjustmentof thehazardratios(P > 0.05),theredidnotappeartobea statisticallysignificantassociationbetweenpainmedication prescribedandtimeto firstunscheduledvisit(Table2). Kaplan-Meiercurveofunscheduledvisitwithlog-rank P -valueisprovidedin Figure2
Whenweconsiderallunscheduledvisitsoverthefour-day follow-upperiod,participantswhoweretreatedwith intranasalketorolaconlywerelesslikelytohavean unscheduledhealthcarevisitcomparedtothosewhoreceived opioidsonly,withanadjustedoddsratioof0.63(Table3). Thesensitivityanalysisshowedthatmodeleffectswerenot meaningfullyalteredbymissingdata.Themediationanalysis demonstratedthattheassociationbetweentreatment regimenandunscheduledhealthcarevisitsiscompletely explainedbyboththepresenceofsideeffectsandtheseverity ofpain,withoddsratiosof2.24and1.33,respectively (P =<0.001),andsideeffectscontributingthelarger impact(Table4).
DISCUSSION Inthisstudyevaluatingtherelationshipbetween treatmentregimens(opioids,rapidlyactingintranasal NSAIDs,orboth)followinganEDvisitforacutepainand subsequentdailyhealthcareutilization,wefoundthat treatmentwithopioidsonlywasassociatedwithincreased subsequentunscheduledhealthcarevisitsduringthe
Table1. BaselinecharacteristicsoftheAMPED*participantsbyunscheduledvisits.
Level
Overall (N = 831)
Age(median,IQR)37.0 (27.0,48.0)
Unscheduledvisit
Nounscheduledvisit (n = 690) Atleastoneunscheduled visit(n = 141)
36.0(27.0,49.0)39.0(31.0,48.0)
Missing,n(%)1(0.1)1(0.1)0(0.0)
Treatmentregimen,n(%)Intranasalketorolaconly353(42.5)306(44.3)47(33.3)
Intranasalketorolac + opioid201(24.2)163(23.6)38(27.0)
OpioidOnly277(33.3)221(32.0)56(39.7)
Missing,n(%)0(0.0)0(0.0)0(0.0)
Employmentstatus,n(%)Other92(11.1)78(11.3)14(9.9)
Unemployed128(15.4)109(15.8)19(13.5)
Parttime129(15.5)103(14.9)26(18.4)
Fulltime481(57.9)399(57.8)82(58.2)
Missing,n(%)1(0.1)1(0.1)0(0.0)
Gender,n(%)Male434(52.2)373(54.1)61(43.3)
Female396(47.7)316(45.8)80(56.7)
Missing,n(%)1(0.1)1(0.1)0(0.0)
Race,n(%)Other169(20.3)148(21.4)21(14.9)
Caucasian251(30.2)193(28.0)58(41.1)
Black407(49.0)345(50.0)62(44.0)
Missing,n(%)4(0.5)4(0.6)0(0.0)
PrimaryEDdiagnosis,n(%)Musculoskeletal707(85.1)593(85.9)114(80.9)
Visceral124(14.9)97(14.1)27(19.1)
Missing,n(%)0(0.0)0(0.0)0(0.0)
PainscoreinED (median,IQR)
Painscoreatdischarge (median,IQR)
8.0(7.0,10.0)8.0(7.0,10.0)8.0(7.0,10.0)
Missing,n(%)1(0.1)1(0.1)0(0.0)
5.0(3.0,8.0)5.0(3.0,8.0)5.0(3.0,8.0)
Missing,n(%)1(0.1)1(0.1)0(0.0)
4-dayanysideeffect,n(%)Yes621(74.7)493(71.4)128(90.8)
No210(25.3)197(28.6)13(9.2)
Missing,n(%)0(0.0)0(0.0)0(0.0)
4-daynausea,n(%)Yes284(34.2)215(31.2)69(48.9)
No542(65.2)470(68.1)72(51.1)
Missing,n(%)5(0.6)5(0.7)0(0.0)
4-dayvomited,n(%)Yes82(9.9)57(8.3)25(17.7)
No744(89.5)628(91.0)116(82.3)
Missing,n(%)5(0.6)5(0.7)0(0.0)
4-dayconstipation,n(%)Yes272(32.7)215(31.2)57(40.4)
No554(66.7)470(68.1)84(59.6)
Missing,n(%)5(0.6)5(0.7)0(0.0)
4-daynasalirritation,n(%)Yes208(25.0)168(24.3)40(28.4)
No618(74.4)517(74.9)101(71.6)
Missing,n(%)5(0.6)5(0.7)0(0.0) (Continuedonnextpage)
Level Overall (N = 831)
Unscheduledvisit Nounscheduledvisit (n = 690) Atleastoneunscheduled visit(n = 141)
4-dayrash/hives,n(%)Yes33(4.0)17(2.5)16(11.3)
No793(95.4)668(96.8)125(88.7)
Missing,n(%)5(0.6)5(0.7)0(0.0)
4-dayabdominalpain,n(%)Yes167(20.1)122(17.7)45(31.9)
No659(79.3)563(81.6)96(68.1)
Missing,n(%)5(0.6)5(0.7)0(0.0)
4-daydrowsiness,n(%)Yes412(49.6)323(46.8)89(63.1)
No414(49.8)362(52.5)52(36.9)
Missing,n(%)5(0.6)5(0.7)0(0.0)
*AMPED,AcutePainManagementfromtheEmergencyDepartment; IQR,interquartilerange; ED,emergencydepartment.
Figure1. Dailyunscheduledvisitratesbydischarge treatmentregimen.
immediatepost-EDdischargeperiodcomparedtotreatment withintranasalketorolac.Similarassociationshavebeen reportedpreviouslybetweenopioidtreatmentforchronicpain andincreasedfrequencyofEDvisits,opioidprescriptionsand recurrentEDvisitsforlowerbackpain,aswellasopioiduse andincreasedhealthcareutilizationfollowingelectivespine surgery. 26–29 Despitethisrecentattentionontherelationship
betweentreatmentchoiceandhealthcareutilization,thereisa disconcertingpaucityofliteratureinvestigatingpossible mediatingfactors.Inparticular,severalrecentsystematic reviewshaveshownbothlowerpaintreatmentefficacyand higherratesofadverseeventswithopioidscomparedwith NSAIDs,emphasizingtheimportanceofthesefactorswhen weighingtherisksandbenefitsoftreatmentchoiceforacute painmanagement.19,22,37
Ourstudyisanimportantcontributiontotheliterature,as itisthe firsttoourknowledgetodemonstratethatthe associationbetweenpaintreatmentregimensandsubsequent healthcareutilizationpost-EDdischargeismediatedbyboth thepresenceofmedicationsideeffectsandongoing,poorly controlledpain.These findingshighlightadditionalrisksand benefitsrelatedtotheseacutepaintreatmentregimensthat mayimpactpatientoutcomes.Consideringpreviousresearch demonstratingthegreater financialburdenofrecurrent healthcareutilizationonthepatientcomparedtotheinitial visit33 aswellasthereasonspatientsreturntotheED which rangefromlackofsymptomaticimprovementtoadditional questionsorconcerns32,34,35 ourstudyservestofurther contextualizeanddemonstratethewidercomplexityofthe impactoftreatmentdecisionsonpatientoutcomes.Thus, whenchoosingapainmanagementplan,itisimportantto considertheimpactitmayhaveonmultipleaspects Table1. Continued.
Table2. Unadjustedandadjustedhazardratiosoftimeto firstunscheduledvisit.
OutcomeParameterUnadjustedHRUnadjusted
UnscheduledvisitsOpioidonly(reference)
HR,hazardratios(95%confidenceintervals).
*Adjustedforage,gender,race,primaryEDdiagnosis,painscorepriortotreatmentandpainscoreatdischarge.
Figure2. Kaplan-Meiercurveofunscheduledvisitsfortreatment regimenwithnumberofeventsandatrisk.
ofthepatient’squalityoflifeinconjunctionwith treatmentefficacy.
LIMITATIONS Studylimitationsincludethatthiswasasecondary analysisofobservationaldataand,therefore,notall potentialconfoundersmayhavebeenmeasuredor controlledfor.Additionally,thestudywasnotrandomized, whichmayhadledtoselectionbiaswithconfounding factorsthatimpactedchoiceoftreatmentregimen,which mayhaveaffectedthelikelihoodofunscheduledvisits.
Further,thedatacollectionoccurredbetweentheyears 2012–2014,whichmaylimittheapplicabilityofthese fi ndings,aspaintreatmentregimensandopioidusehave sinceevolved.
Despitethefactthatoverallrateofopioidprescriptions issuedatdischargefromtheEDdecreasedfrom14.6%in 2017to8.1%in2020,therearestillalargeoverallnumberof peoplewhoarereceivingopioids.15 Inaddition,prescribing patternsshouldnotchangetheunderlyingside-effectprofile ortheirinherentassociationswithunscheduledvisits.Itis alsoimportanttonotethatwhileour findingssupporta strongassociationbetweentreatmentregimenand unscheduledhealthcarevisitsmediatedbythepresenceof sideeffectsanddegreeofpainrelief,thereasonsfor unscheduledvisitswerenotconfirmedbypatientreport. Thus,itispossiblethatpatientssoughthealthcareforreasons unrelatedtotheiracutepain,currenttreatmentplan,orside effects.Finally,thetreatmentregimenwasnotstandardized acrossallgroupsapartfromtheintranasalketorolac;thus, thereportedsideeffectsandcomplicationsmayalsobe relatedtodifferencesinopioidtypeordosing.
CONCLUSION Outpatienttreatmentwithopioidsonlyforacutepain afteranEDvisitisassociatedwithincreasedunscheduled healthcarevisitscomparedtothosetreatedwithintranasal NSAIDsalone.Thisdifferencecanbeexplainedbyhigher levelsofongoingpainandthepresenceofmedicationside effects.Understandingtheimpactthatpainmedication choicehasonrecurrenthealthcareutilizationandthefactors
Table3. Unadjustedandadjustedoddsratiosofanyunscheduledvisit.
OR,oddsratios(95%confidenceintervals).
*Adjustedforage,gender,race,primaryEDdiagnosis,painscorepriortotreatmentandpainscoreatdischarge.
Table4. Oddsratioformediators – anysideeffectandmaximumpainscore.
thatmediatethisrelationshipaddstothebodyofknowledge regardingrisksandbenefitsofthesetreatments,allowing emergencyphysicianstomakebetterinformeddecisions.
AddressforCorrespondence:StephanieA.Eucker,MD,PhD, DepartmentofEmergencyMedicine,DukeUniversity,2301Erwin Rd.,DUMC3096,Durham,NC27710.Email: stephanie.eucker@ duke.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Freiermuthetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.CentersforDiseaseControlandPrevention(CDC).NationalHospital AmbulatoryMedicalCareSurvey:2017emergencydepartment summarytables.2017.Availableat: https://www.cdc.gov/nchs/data/ nhamcs/web_tables/2017_ed_web_tables-508.pdf AccessedJune25,2023.
2.FriedmanBW,ConwayJ,CampbellC,etal.Painoneweekafter anemergencydepartmentvisitforacutelowbackpainisassociated withpoorthree-monthoutcomes. AcadEmergMed. 2018;25(10):1138–45.
3.StevansJM,DelittoA,KhojaSS,etal.Riskfactorsassociatedwith transitionfromacutetochroniclowbackpaininUSpatientsseeking primarycare. JAMANetwOpen. 2021;4(2):e2037371.
4.CohenSP,VaseL,HootenWM.Chronicpain:anupdate onburden,bestpractices,andnewadvances. Lancet. 2021;397(10289):2082–97.
5.OliveiraCB,MaherCG,PintoRZ,etal.Clinicalpracticeguidelinesfor themanagementofnon-specificlowbackpaininprimarycare:an updatedoverview. EurSpineJ. 2018;27(11):2791–803.
6.USDepartmentofHealth.PainManagementBestPracticesInteragencyTaskForcereport:updates,gaps,inconsistencies,and recommendations.2019.Availableat: https://www.hhs.gov/sites/ default/files/pain-mgmt-best-practices-draft-final-report-05062019.pdf AccessedJune25,2023.
7.NationalAcademiesofSciences,Engineering,andMedicine. Framing OpioidPrescribingGuidelinesforAcutePain:DevelopingtheEvidence WashingtonDC:NationalAcademiesPress,2019.
8.KeatingLandSmithS.Acutepainintheemergencydepartment:the challenges. RevPain. 2011;5(3):13–7.
9.SitesBD,BeachML,DavisMA.Increasesintheuseofprescription opioidanalgesicsandthelackofimprovementindisabilitymetrics amongusers. RegAnesthPainMed. 2014;39(1):6–12.
10.NewcombP,WilsonM,BaineR,etal.Influencesonpatientsatisfaction amongpatientswhouseemergencydepartmentsfrequentlyforpainrelatedcomplaints. JEmergNurs. 2017;43(6):553–9.
11.SchwartzTM,TaiM,BabuKM,etal.LackofassociationbetweenPress Ganeyemergencydepartmentpatientsatisfactionscoresand emergencydepartmentadministrationofanalgesicmedications. AnnEmergMed. 2014;64(5):469–81.
12.ManchikantiL,HelmS,FellowsB,etal.OpioidepidemicintheUnited States. PainPhysician. 2012;15(3Suppl):ES9–38.
13.Shafi S,CollinsworthAW,CopelandLA,etal.Associationofopioidrelatedadversedrugeventswithclinicalandcostoutcomesamong surgicalpatientsinalargeintegratedhealthcaredeliverysystem. JAMASurg. 2018;153(8):757–63.
14.DowellD.CDCclinicalpracticeguidelineforprescribingopioidsfor pain UnitedStates,2022. MorbMortalWklyRecommRep 2022;71(3):1–95.
15.SantoLandSchappertSM.Opioidsprescribedtoadultsatdischarge fromemergencydepartments:UnitedStates,2017–2020. NCHSData Brief. 2023;(461):1–8.
16.GoldstickJE,GuyGP,LosbyJL,etal.Patternsinnonopioidpain medicationprescribingafterthereleaseofthe2016guidelinefor prescribingopioidsforchronicpain. JAMANetwOpen. 2022;5(6):e2216475.
17.CastellsagueJ,Riera-GuardiaN,CalingaertB,etal.IndividualNSAIDs anduppergastrointestinalcomplications:asystematicreviewand meta-analysisofobservationalstudies(theSOSproject). DrugSaf. 2012;35(12):1127–46.
18.BouckZ,MecredyGC,IversNM,etal.Frequencyandassociationsof prescriptionnonsteroidalanti-inflammatorydruguseamongpatients withamusculoskeletaldisorderandhypertension,heartfailure,or chronickidneydisease. JAMAInternMed. 2018;178(11):1516–25.
19.BusseJW,SadeghiradB,OparinY,etal.Managementofacutepain fromnon-lowback,musculoskeletalinjuries:asystematicreviewand networkmeta-analysisofrandomizedtrials. AnnInternMed. 2020;173(9):730–8.
20.GaulE,BarbourT,NowackiAS,etal.Intranasalketorolacforacute paininadultemergencydepartmentpatients. WestJNursRes. 2022;44(11):1047–56.
21.WattsK,BalzerS,DrumM,etal.Ibuprofenandacetaminophenversus intranasalketorolac(Sprix)inanuntreatedendodonticpainmodel:a randomized,double-blindinvestigation. JEndod. 2019;45(2):94–8.
22.JonesCMP,LinCWC,JamshidiM,etal.Effectivenessofopioid analgesicmedicinesprescribedinoratdischargefromemergency departmentsformusculoskeletalpain:asystematicreviewandmetaanalysis. AnnInternMed. 2022;175(11):1572–81.
23.AtzemaCLandMaclaganLC.Thetransitionofcarebetween emergencydepartmentandprimarycare:ascopingstudy. AcadEmergMed. 2017;24(2):201–15.
24.KripalaniS,TheobaldCN,AnctilB,etal.Reducinghospitalreadmission rates:currentstrategiesandfuturedirections. AnnuRevMed. 2014;65:471–85.
25.WarcholSJ,MonestimeJP,MayerRW,etal.Strategiestoreduce hospitalreadmissionratesinanon-Medicaid-expansionstate. PerspectHealthInfManag. 2019;16(Summer):1a.
26.ShergillY,RiceD,SmythC,etal.Characteristicsoffrequent usersoftheemergencydepartmentwithchronicpain. CJEM. 2020;22(3):350–8.
27.GerlachEB,PlantzMA,SwiatekPR,etal.Thedriversofpersistent opioiduseanditsimpactonhealthcareutilizationafterelectivespine surgery. GlobSpineJ. 2024;14(2):370–9.
28.GinsbergZ,GhaithS,PollockJR,etal.Relationshipbetweenpain managementmodalityandreturnratesforlowerbackpaininthe emergencydepartment. JEmergMed. 2021;61(1):49–54.
29.MegallaM,OgedegbeC,SandersAM,etal.Factorsassociatedwith repeatemergencydepartmentvisitsforlowbackpain. Cureus. 2022;14(2):e21906.
30.EuckerSA,ManandharP,ArulrajaK,etal.Higherdailypainseverity afteremergencydepartmentvisitsisassociatedwithlowerreturn-toworkrates. AmJEmergMed. 2021;45:48–53.
31.LöttersFJB,FoetsM,BurdorfA.Workandhealth,ablindspotincurative healthcare?Apilotstudy. JOccupRehabil. 2011;21(3):304–12.
32.HutchinsonCL,McCloughenA,CurtisK.Incidence,characteristicsand outcomesofpatientsthatreturntoemergencydepartments.An integrativereview. AustralasEmergCare. 2019;22(1):47–68.
33.DusejaR,BardachNS,LinGA,etal.Revisitratesandassociated costsafteranemergencydepartmentencounter:amultistateanalysis. AnnInternMed. 2015;162(11):750–6.
34.ProudMEandHowardPK.Whydopatientsreturntotheemergency department? AdvEmergNursJ. 2016;38(2):83–8.
35.NunezS,HexdallA,Aguirre-JaimeA.Unscheduledreturnstothe emergencydepartment:anoutcomeofmedicalerrors? QualSafHealth Care. 2006;15(2):102–8.
36.PollackCV,DiercksDB,ThomasSH,etal.Patient-reportedoutcomes fromanational,prospective,observationalstudyofemergency departmentacutepainmanagementwithanintranasalnonsteroidal anti-inflammatorydrug,opioids,orboth. AcadEmergMed. 2016;23(3):331–41.
37.MooreRA,DerryS,AldingtonD,etal.Singledoseoralanalgesics foracutepostoperativepaininadults-anoverviewof Cochranereviews. CochraneDatabaseSystRev. 2015;2015(9):CD008659.
ORIGINAL RESEARCH ImpactofCOVID-19PandemiconEmergencyDepartment VisitsforOpioidUseDisorderAcrossUniversityof CaliforniaHealthCenters MatthewHeshmatipour,BS* DingQuanNg,BS*
EmilyYi-WenTruong,BS† JianweiZheng,PhD‡ AlexandreChan,PharmD,MPH* YunWang,PhD‡
SectionEditor: PatrickMeloy,MD
*UniversityofCaliforniaIrvine,SchoolofPharmacyandPharmaceutical Sciences,Irvine,California
† UniversityofCaliforniaIrvine,DonaldBrenSchoolofInformationandComputer Sciences,Irvine,California
‡ ChapmanUniversity,SchoolofPharmacy,Irvine,California
Submissionhistory:SubmittedSeptember15,2023;RevisionreceivedAugust30,2024;AcceptedSeptember6,2024
ElectronicallypublishedOctober2,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18468
Introduction: Coronavirus2019(COVID-19)hashadadevastatingimpactonmentalhealthandaccess toaddictiontreatmentintheUnitedStates,includinginCalifornia,whichresultedinthehighestratesof emergencydepartmentvisits(ED)foropioidpoisoningin2020.AsCaliforniaslowlyreturnstoprepandemicnormalcy,itremainsuncertainwhethertheratesofopioid-relatedeventshavesloweddown overtime.Wehypothesizedthatthenumberofopioid-relatedEDvisitswereexacerbatedaftertheperiod oftheCOVID-19pandemicandcontinueatahighrateinthepresent.
Methods: InthisanalysiswesearchedtheUniversityofCalifornia(UC)HealthDataWarehouse a databaseofelectronichealthrecordsfromsixacademicmedicalcenters foropioidrelatedEDvisits, identifiyingusingthefollowingInternationalClassificationofDiseases,10th Ed,ClinicalModification codes:F11codes,andT40.0*,T40.1*,T40.2*,T40.3*,T40.4*,T40.6*.Opioidoverdose-associated visitswereclassifiedbytypesofopioidsinvolved:heroin(T40.1*);prescriptionopioids(T40.2*or T40.3*);andsyntheticopioids(T40.4*).Weperformedinterruptedtimeanalysistoestimatethe immediate(level)changeandchange-in-timetrend(trendchange),frombefore(January2018–October 2019)andduringthepandemic(April2020–December2022).Monthlyvisitrateswereevaluatedwith negativebinomialregressionadjustedfor first-orderautoregressionandusingall-causeEDcountsas theoffset.Wepresenteffectsizesasrateratios(RR)and95%confidenceintervals(CI),testedat α = .05.
Results: WeobservedadecreaseinoverallEDvisitsfrom28,426to25,121visitsinDecember2019and June2021,respectivelyacrossallsixUCHealthCenters.BeforeCOVID-19,wefoundthatEDvisitrates steadilyincreasedforalloutcomes(P < 0.05)exceptsyntheticopioids.Totalopioid-relatedEDvisitrates increasedby15%(RR1.15,95%CI1.02–1.29, P = 0.20)immediatelyafterMarch2020beforedecreasing by0.5%everymonth,albeitwithoutstatisticalsignificance(RR.995,95%CI.991–1.00, P = 0.06).Opioidrelatedeventsacrossthesixacademicmedicalcentersincreasefrom232inDecember2019,representing asinglemonth’stotal,andpeakedat315inJune2021.Similartrendswereobservedwithprescriptionopioid overdoses,withastepincreaseof44%(RR1.44,95%CI1.10–1.89, P = .008)beforeplateauingafterMarch 2020(RR1.01,95%CI.998–1.02, P = 0.12).Specifically,thetotalnumberofprescriptionopioid-relatedED visitsmorethandoubledbetweenDecember2019(22visits)andJune2021(49visits).AfterMarch2020, EDvisitratesforsyntheticopioidoverdoseswereincreasingsteadilyby4%everymonth(RR1.04,95%CI 1.02–1.06, P = .001),unlikewithheroin,whichwasobservedwithan8%monthlyreduction(RR.92,95%CI .90–.93, P < .001).Noimmediateincreaseinvisitrateswasobservedforeitheropioid.
Conclusion: Whileopioid-relatedEDadmissionsamongtheUChealthcentersshowedanoverall decrease,prescriptionandsyntheticopioidoverdosesremainedsignificantlyhigherthanpre-pandemic trendsasofDecember2022.Amultilevelapproachtoimproveawarenessofnewopioidhealthpolicies couldamelioratethesealarmingrisesinthepost-pandemicera.[WestJEmergMed.2024;25(6)883–889.]
INTRODUCTION Opioidsplayamajorroleinhealthcareasanimportant prescriptionmedicationforpainrelief.Opioidanalgesicsare abeneficialinterventionwhenproperlyadministered,1 thus creatingchallengeswhenregulatingtheiruseastheyhavethe potentialforlong-termadverseeffects.Althoughearlier phasesoftheopioidcrisiswerecharacterizedbythemisuseof prescriptionopioids(firstwave),recenttrendsrevealthat heroin(secondwave)andillicitsyntheticopioids(thirdwave) havebecomecrucialtocharacterizingtheopioidepidemic.2 Syntheticopioidssuchasfentanylhavebeenshowntobethe mostdevastatingcontributorstothecurrentrisingopioidrelatedcasesduetoitsassociatedpositivesupplyshock, allowingforitspricetoreducesignificantly.3 Predictedtrends overlayingscatterplots.
Beginninginearly2020,theadventofthecoronavirus 2019(COVID-19)pandemicledtoanabrupt,worldwide disruptiontosocietalfunctionsandtypicaldailylifeasstayat-homeorderswereimplementedtocurbthespreadofthe virusandpreservemedicalfacilitiesandequipmentforthe mostsevereinfections.Thesubsequentriseinunemployment ratesandsocialisolationledtoincreasedpsychological distress,4 whichwaspostulatedtohavecausedanationwide increaseinopioidoverdosecasesacrossmultiplestatesin 2020.5–8 Associetyslowlybegantoreturntopre-pandemic normalcyin2021and2022,itremainsuncertainwhetherthe ratesofopioid-relatedeventshaveslowedovertime,given thechallengesofweaningoffchronicopioiduse.Thus,a deeperexplorationintothetrendsrelatedtoopioid-related eventsin2021and2022andareviewofcurrentinterventions andsolutionsisnecessarytoallocateresourcesforenhancing ourmanagementoftheopioidepidemic.
Inthispaperwereportour findingsforemergency department(ED)visitratesassociatedwithopioid-related casesfrom2018–2022acrossthesixUniversityofCalifornia (UC)healthcenters.Wecomparedtheratesfromtheperiod beforethepandemic(January2018–December2019)with thoseduringthepandemic(April2020–December2022). AwashoutperiodbetweenJanuary–March2020was implementedduetowidespreadpublicuncertaintyregarding thenatureofthepandemicduringthattimeframe.These datestakereferencefromtheUS’ s firstconfirmedlaboratory caseonJanuary20,2020,andCalifornia’sstatewidestay-athomeorderonMarch19,2020.9 Wehypothesizedthat opioid-relatedEDvisitratescontinuedtoworsenafter
Whatdowealreadyknowaboutthisissue?
Theopioidusedisorder(OUD)epidemicand COVID-19pandemicaretwopublichealth crisesthatsigni fi cantlyincreasedEDvisitsin theUS.
Whatwastheresearchquestion?
HowdidtheCOVID-19pandemicaffect opioid-relatedEDvisitsinCalifornia?
Whatwasthemajor findingofthestudy?
Opioidprescriptionsandheroin-relatedED visitsincreasedafterthepandemicacross UChospitals.
Howdoesthisimprovepopulationhealth?
Our fi ndingsshowtrendsofopioidusein Californiaandidentifykeycommunity elementsthatcouldcontributetoOUD interventionsthroughfutureresearch.
2021andremainedhigherthanpre-pandemicratesas ofDecember2022.
MATERIALSANDMETHODS DataSource ForthisanalysisweusedtheUCHealthDataWarehouse (UCHDW),adatabaseofelectronichealthrecordsfromthe sixUCacademichealthcenters:UCDavis;UCIrvine;UC LosAngeles;UCRiverside;UCSanDiego;andUCSan Francisco.TheUCHDWcontainsclinicaldataof8.7million patientsseenataUCfacility,totalingapproximately378 millionencountersincludingofficevisits,inpatient admissions,andEDvisits.10 Alldataisorganizedbasedon theObservationalMedicalOutcomesPartnership(OMOP) commondatamodel(CDM),anopencommunitydata standardforstandardizingthestructureofreal-worldclinical dataacrossinstitutionsdespitedifferencesintheunderlying clinicaldatainfrastructure.11 AdoptingtheOMOPCDM facilitatesefficient,multicenteredstudiesandgenerationof
PopulationHealthResearchCapsule
reproducibleevidence.Institutionalreviewboard(IRB) reviewwasnotrequiredforthisdataanalysisaswedeidentifiedallaccesseddataelementspriortoreceipt.12 All dataquerieswerecompletedonFebruary8,2023.
EmergencyDepartmentVisits
FollowingthestructureoftheOMOPCDM,weidentified EDvisitsfromthe “visitoccurrence” domainusingvisit conceptidentifications(IDs)of “9203 – EmergencyRoom Visit” or “262 – EmergencyRoomandInpatientVisit.”13
Opioid-relatedEvents
TheEDvisitsassociatedwithopioid-relatedevents, labelledas “allopioid-relatedvisits,” wereidentifiedifthey hadatleastoneofthefollowingInternationalClassification ofDiseases,10th ed,ClinicalModification:F11codes,and T40.0*,T40.1*,T40.2*,T40.3*,T40.4*,T40.6*.Opioid overdose-associatedvisitswerethenfurtherclassifiedby typesofopioidsinvolved:heroin(T40.1*);prescription opioids(T40.2*orT40.3*);andsyntheticopioidsotherthan methadone(T40.4*).14
OutcomesMeasures
Wesummarizedandanalyzedtheoutcomesasmonthly EDvisitratesofopioid-relateddisordersandoverdoses(per 100,000all-causeEDvisits).Thiswasjustifiedbythelower all-causeEDvisitratesacrosstheUSduringtheCOVID-19 pandemic15 andwasimplementedinpreviouslypublished studies.8,16 WealsoplottedmonthlyEDvisitcountsacross theUChealthcentersfrom2018–2022toverifythistrend. ActualEDvisitcountsforopioid-relatedvisitswerealso maskedasperinstitutionalpolicy.
StatisticalAnalysis Weperformedinterruptedtimeanalysistoestimatethe immediate(level)changeandchange-in-timetrend(trend change)withnegativebinomialregressionwithrobust standarderrors(Huber-Whitesandwichestimator)foroverdispersedoutcomes.Themodelwasfurtheradjustedfor firstorderautoregressionusingalag-1variable(outcomevalue fromthepreviousmonth),withall-causeEDvisitcountsas theoffsetvariable.Themodelspecificationisasfollows: log EytðÞ ðÞ = β 0 + β 1
• yt wasthecountoutcomeofinterestinmonth t
• covid t wasabinarydummyvariableindicatingwhether month t wasbefore(January2018–December2019, assignedwithavalue “0”),orduring(April 2020–December2022,assignedwithavalue “1”)the COVID-19pandemic.Awashoutperiodbetween January–March2020wasimplementeddueto
widespreaduncertaintyregardingthenatureofthe pandemicduringthattimeframe.
• timet wasadiscretetimevariablecountingmonths startingfromJanuary2018,takingthevaluesof 1,2,3,etc.
• posttimet wascoded “0” fortimepointsbeforethe COVID-19pandemic(January2018–December2019) andthenbecomeadiscretetimevariablecounting monthsduringtheCOVID-19pandemic(April 2020–December2022),takingthevaluesof1,2,3,etc.
• lag 1t wasthecountoutcomeofinterestinthemonth prior(ie, yt 1 ).Thisallowscontrolofautocorrelationin atime-seriesdataset.
• offsett takesthenumberofall-causeEDvisitsinmonth t.Thisvariablewasexcludedforthetrendanalysisof all-causeEDvisitcounts.
• Thekeycoefficientsofinterestincludethefollowing:
◦ β 1 ,whichrepresentstheimmediate(level)changein log EytðÞ ðÞ duetotheCOVID-19pandemic.
◦ β 2 ,whichrepresentsthemonthlychangein log EytðÞ ðÞ beforetheCOVID-19pandemic(January 2018–December2019).
◦ β 2 + β 3 ,whichrepresentsthemonthlychangein log EytðÞ ðÞ duringtheCOVID-19pandemic(April 2020–December2022).
Effectsizesforcountandrateoutcomesarepresentedas ratiosand95%confidenceintervals(CI)viaexponentiatingthe coefficients.Predictedtrendsoverlayingscatterplotswere plottedtoillustratethetrendsinthecountandrateoutcomes permonth.Allanalysesweretestedwith α = .05andcompleted withStatav16.1(StataCorpLLC,CollegeStation,TX).
RESULTS All-CauseEDVisits AtthebaselineofDecember2019thetotalnumberofED visitswas28,426acrossthesixhealthcenters,whereasitfell slightlyto25,121visitsinJune2021.Monthlyall-causeED visitcountsremainedrelativelyconstantbeforetheCOVID19pandemic(P = 0.30).Duringthepandemic,therewasa suddendeclineby34%comparedtopre-pandemictrends (95%CI15–49%, P = 0.002)beforeincreasingby1.5%per month(95%CI0.5–2.5%, P = 0.002)(Figure1).
AllOpioid-relatedEvents AtthebaselineofDecember2019thenumberoftotal opioid-relatedEDvisitswas232acrossthesixhealthcenters, whereasitjumpedto315visitsinJune2021.TheEDvisitrates ofallopioid-relatedvisitsincreasedby1%permonthduring thepre-COVID-19period(95%CI0.6–2.0%, P < 0.001).This wasfollowedbya15%immediateincreaseduringthe pandemic,comparedtopre-pandemiclevels(95%CI2–29%, P = 0.020),andastatisticallynon-significantmonthlydecline by0.5%(95%CI 0.9to0.0%, P = 0.06)(Figure2A).
Figure1. Monthlycountsofall-causeemergency(ED)visitsfrom 2018–2022acrosssixUniversityofCaliforniahealthcenters.The periodfromJanuary2018–December2019wasdesignatedas “pre-COVID,” whiletheperiodfromApril2020–December2022 wasdesignatedas “COVID.” Awashoutperiodfrom January–March2020isrepresentedbytheredlinesinthegraph.
PrescriptionOpioidOverdoses AtthebaselineofDecember2019thenumberof prescriptionopioid-relatedEDvisitswas22acrossthesix healthcenters,whereasitjumpedto49visitsinJune2021. TheEDvisitratesofprescriptionopioidoverdosesincreased by1%everymonthbeforetheCOVID-19pandemic(95%CI
0.2–2.0%, P = 0.02).DuringCOVID-19,therewasan immediateincreaseinvisitratesof44%(95%CI10–89%, P = 0.008)andastatisticallynon-significantincreaseof1% everymonth(95%CI 0.2to2.0%, P = 0.12)(Figure2B).
SyntheticOpioidOverdoses AtthebaselineofDecember2019thenumberofsynthetic opioid-relatedEDvisitswaslessthan11acrossthesixhealth centers,whereasitjumpedslightlyto14visitsinJune2021. Countslessthan11aremaskedfollowingtheUCCenterfor Data-drivenInsightsandInnovation(CDI2)policyon limitedresearchusesusingtheUCHDW.TheEDvisitrates ofsyntheticopioidoverdosesincreased5%everymonth, albeitwithoutstatisticalsignificance(95%CI0.2–11.0%, P = 0.06),beforethepandemic.DuringCOVID-19,there wasastatisticallynon-significantincreaseof69%(95%CI 32to316%, P = 0.26)comparedtopre-pandemictrends, followedbyamonthlyincreaseof4%(95%CI2–6%, P = 0.001)(Figure2C).
HeroinOverdoses AtthebaselineofDecember2019thenumberofheroinrelatedEDvisitswas18acrossthesixhealthcenters,whereas itfellslightlytolessthan11visitsinJune2021.Aswiththe countsofsyntheticopioid-relatedEDvisits,countslessthan 11aremaskedperCDI2policy.MonthlyEDvisitratesfor
Figure2. Monthlyemergencydepartment(ED)visitratesofopioid-relateddisordersandoverdoses(per100,000all-causeEDvisits)from 2018–2022acrosssixUniversityofCaliforniaHealthcenters.TheperiodfromJanuary2018– December2019wasdesignatedas “preCOVID,” whiletheperiodfromApril2020–December2022wasdesignatedas “COVID.” AwashoutperiodfromJanuary–March2020was implementedandisrepresentedbytheredlinesinthegraph.
heroinoverdosesincreasedby2%monthlyduringthepreCOVID-19period(95%CI0.6–3.0%, P = 0.006). Subsequently,thepandemicledtoanimmediatebut statisticallynon-significantincreaseby20%(95%CI 14to 67%, P = 0.28)comparedtothepre-COVID-19period.This wasfollowedbyamonthlydeclineof8%(95%CI 10to 7%, P < 0.001)(Figure2D).
DISCUSSION TheCOVID-19pandemicbroughtlighttotheurgentneed formultilevelinnovativeapproachestoaidagainsttheopioid epidemicinCalifornia.Inparticular,thepandemichas facilitatedtheworseningoftrendsrelatedtoprescriptionand syntheticopioidoverdosesacrosstheUChealthcenters,with littlesignsofimprovementasrecentasDecember2022. Consideringthatpastresearchonthesamesubjectwasonly updatedasof2020andthatour findingsweresimilartothose papers, 5–8 ourstudymayprovidethemostrecentoutlookof thecurrentopioidcrisisacrosstheUSandreflectthatmore couldbedonetoarresttheproblem.
Interestingly,wesawadecreasingtrend,albeitnonstatisticallysignificant,inEDvisitratesrelatedtoalltypesof opioid-relatedeventsafteraninitialspikeinApril2020, whichcontrastedwiththetrendswesawwithopioid overdoses.Whilethekeyreasonscouldnotbedetermined basedontheavailabledata,wehypothesizethatthis decreasingtrendcouldbeanartifactofarecoveryinnumbers ofall-causeEDvisits.Additionally,thistrendpossibly reflectsaparadigmshiftintheseekingoftreatmentforopioid usedisorderfromEDsduringthepandemic.Akey considerationisthatopioid-relatedeventscomprisenotonly opioidoverdosecomplicationsbutalsoopioidwithdrawal episodes,andbothcanbetreatedattheEDwithlifesaving naloxoneandbuprenorphine,respectively.17
TheEDalsoprovidesthesemedicationsforopioiduse disorder(MOUD)ondischargeasstand-bymedicationsfor useasrequiredandconnectspatientswithfollow-upOUD managementinthecommunity.18,19 InCalifornia,theCA Bridgeprogramhasspearheadedthecoordinated implementationoflow-thresholdbuprenorphinetreatment foropioidwithdrawals(anapproachthatreducesasmany barriersaspossibleregardingaccesstobuprenorphine20)at EDsof52hospitals,includingfourUChealthcenters,since 2018.21 Unfortunately,theprogramreportedasteepdecline inED-initiatedbuprenorphineduringthe firstmonthsofthe pandemic.22 Ourstudymayprovidepreliminaryevidence thatthelowerratesofOUDtreatmentatEDs,especiallyfor withdrawalepisodes,havecontinuedinto2021and2022. Furtherresearch,suchasexaminingratesofadministration andprescriptionofdifferentMOUDattheED,willbe requiredtoconfirmthishypothesis.
Attheinitialstagesofthepandemic,Currieetalreported thatopioidprescriptionsacrosstheUSweregenerally maintainedamongexistingopioidusersbutdecreasedbriefly
fornewusers.23 AnotherstudybyZhengetalreporteda declineinopioidprescriptionsandprescribersbeforeand duringtheCOVID-19pandemicperiodinCalifornia.24 Therewerelittletonosignsofasuddenincreaseinopioid prescriptionsthatcouldexplainthehigherratesof prescriptionopioidoverdoseratesseeninourstudy.A multisitereportstudyingdrugusebehaviorsduringthe pandemicfoundthatCOVID-19-relatedstressors,suchas jobloss,increasedhousinginsecurity,andloneliness,were commonlycitedreasonsforincreasingdrugusebehaviors.25 Thesamestudyfurtherreportedthatsyntheticopioids, particularlyfentanyl,hadsaturatedtheillicitdrugmarket duringthistimeduetoitsinexpensivenatureandhigh accessibilitycomparedtomethamphetamineandheroin.25 Thesetrendswerefurtherverifiedinthe CaliforniaHealth CareAlmanac featureonCaliforniasubstanceuse.26 Other thanstrategizingtoreducethesupplyofillicitfentanyland fentanyl-lacedpills,improvingthementalhealthofopioid users,andtherebyreducingdemandforbothprescription andsyntheticopioids,willalsohelptomitigatetheopioid epidemicmoreeffectively.
Recentpolicychangeshavebeenmadetopurposefully bringMOUDclosertopatientsandpreventdeathsfrom fatalopioidwithdrawalsandoverdoses:1)theremovalofthe X-waiver(issuedbytheSubstanceAbuseandMentalHealth ServicesAdministrationandtheDrugEnforcement Administration)enabledphysicianstoprescribe buprenorphineinclinicswithoutadministrativebarriersand extensivecertification27,28;and2)theapprovalbytheFood andDrugAdministrationofNarcan,the firstover-thecounternaloxonenasalspray.29 However,withthe emergenceofthefourthwaveoftheopioidcrisis characterizedbyopioidandstimulantco-use,30 thewar againsttheopioidepidemicisnotyetwon,andeffective policychangeswillnecessitatekeychangesincurrent practicesandoperations.
Variscoetalidentifiedlegacybarriersinstate-level regulationsandwholesalerpolicythatcouldlimit buprenorphinesuppliesanddispensingatpharmacies.31 Educationandtheintentionaldistributiontothecommunity willberequiredtoensurethatNarcanisalwaysavailableto respondtoanopioidoverdoseevent.Finally,thereremains evidenceofhigh-riskopioidprescribinganddispensing behaviorsassociatedwithayoungerandlesseducated demographic,whichmayprecipitategreaterratesofopioidrelatedcases.32 Thereisstillmuchtodoasclinicians, researchers,andcommunityadvocatestoensurethe effectivemanagementoftheopioidepidemic,givenour availableresources.
STRENGTHSANDLIMITATIONS Onelimitationofthestudyistheuseofdeidentifieddata, whichpreventedusfromevaluatingindividual-level characteristicsthatarepredictiveofhigheropioid-related
admissionsorreadmissions.Suchdatawillneedtobe navigatedaroundexistingandnewregulatoryframeworks frommultisiteIRBsacrossmultipleUChealthcenters. Toourknowledge,thisisahurdlethathasyettobe tackledattheUC-widelevel,andwesuspectthatmore timewillbeneededtoestablishtheprocess.Onceestablished, wewillstrivetodeterminesociodemographicand geolocationfeaturesthatcouldhelpwithadvisingthe optimalallocationofresourcesinthiswaragainstthe opioidepidemic.
Regardless,thestrengthofthiscurrentstudyliesintheuse ofreal-worldEDdatatorapidlyassessthechangesinopioidrelatedEDtrendsduringtheCOVID-19crisiswhenresearch datacollectionhadbeenhaltedduetolockdownmeasures. Ourstudyhasalsodemonstratedthefeasibilityofusingthis methodologytocreateareal-timeOUDdashboard33 to facilitatethetimelydisseminationoftrenddatainopioidrelatedEDvisitsandadmissionsintheeverchanging,opioid uselandscapeinCalifornia.Additionally,wesoughtto includecommunity-basedprograms,suchasOUD-based harmreductionorganizations,asabeneficialinterventionto reducethenumberofopioid-relatedEDvisits.However,the UCHDWdidnotincludedatathatwasrelevanttothese programs,andthereisyettobearobuststudydisplaying theirsignificance.
CONCLUSION Ourdataprovidessupportthatopioid-relatedEDvisit ratesinCaliforniahaveexceededpre-pandemicratesand havecontinuedtoworsenafter2021.AlthoughtheCOVID19pandemicsawanoveralldecreasingtrendinthenumber ofopioid-relatedEDvisitsinalltheUCHealthcenters,the numberofvisitsduetoprescriptionandsyntheticopioidsrelatedoverdoseremainshigh.Moresignificantly,this increasingtrendprovidesagreatpublichealthconcern, especiallyastheUSentersthefourthwaveoftheopioid epidemic,characterizedbypolysubstanceuse.Notonlymust wereducethesupplyofillicitopioids,weshouldalsoaimto reducethedemandforprescriptionandsyntheticopioids, whichislikelythefunctionofworseningmentalhealth duringtheCOVID-19pandemic.WhiletheCOVID-19 pandemiccontinuestobecomelessnotabletothepublic, theconsequentialchanginglandscapeoftheopioid epidemicremainsanuphillbattlethatcallsformultilevel, proactive,innovative,andcollaborativeapproachesacross theUS.
ACKNOWLEDGMENTS TheauthorsthanktheCenterforData-drivenInsights andInnovationatUCHealth(CDI2; https://www.ucop.edu/ uc-health/functions/center-for-data-driven-insights-andinnovations-cdi2.html),foritsanalyticalandtechnical supportrelatedtouseoftheUCHealthDataWarehouse.
AddressesforCorrespondence:AlexandreChan,PharmD,MPH, UniversityofCaliforniaIrvine,SchoolofPharmacyand PharmaceuticalSciences,802WPeltasonDr.,Irvine,CA92697. Email: a.chan@uci.edu.YunWang,PhD,ChapmanUniversity, SchoolofPharmacy,9401JeronimoRd.,Irvine,CA92618.Email: yunwang@chapman.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Heshmatipouretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.VolkowNDandBlancoC.Thechangingopioidcrisis: development,challengesandopportunities. MolPsychiatry. 2021;26(1):218–33.
2.CiccaroneD.Thetriplewaveepidemic:supplyanddemanddriversof theUSopioidoverdosecrisis. IntJDrugPolicy. 2019;71:183–8.
3.CiccaroneD.FentanylintheUSheroinsupply:arapidlychangingrisk environment. IntJDrugPolicy. 2017;46:107–11.
4.RajA,JohnsNE,BarkerKM,etal.TimefromCOVID-19shutdown, gender-basedviolenceexposure,andmentalhealthoutcomesamonga staterepresentativesampleofCaliforniaresidents. EClinicalMedicine. 2020;26:100520.
5.RoddaLN,WestKL,LeSaintKT.Opioidoverdose-relatedemergency departmentvisitsandaccidentaldeathsduringtheCOVID-19 pandemic. JUrbanHealth. 2020;97(6):808–13.
6.HallGT,CruzDS,LankPM,etal.Opioid-relatedemergencydepartment visitsduringCOVID-19inalargehealthsystem. JAddictMed. 2021;15(4):345–8.
7.SlavovaS,RockP,BushHM,etal.Signalofincreasedopioidoverdose duringCOVID-19fromemergencymedicalservicesdata. DrugAlcohol Depend. 2020;214:108176.
8.SoaresWE,MelnickER,NathB,etal.Emergencydepartmentvisitsfor nonfatalopioidoverdoseduringtheCOVID-19pandemicacrosssixUS healthcaresystems. AnnEmergMed. 2022;79(2):158–67.
9.CentersforDiseaseControlandPrevention.CDCmuseumCOVID-19 timeline.Availableat: https://www.cdc.gov/museum/timeline/covid19. html.AccessedAugust28,2023.
10.UniversityofCaliforniaOfficeofthePresident.Centerfordata-driven insightsandinnovation(CDI2).Availableat: https://www.ucop.edu/ uc-health/departments/center-for-data-driven-insights-andinnovations-cdi2.html.AccessedAugust28,2023.
11.ObservationalHealthDataSciencesandInformatics(OHDSI). Standardizeddata:theOMOPcommondatamodel.Availableat: https:// www.ohdsi.org/data-standardization/.AccessedAugust28,2023.
12.PetersonTA,FontilV,KoliwadSK,etal.Quantifyingvariationin treatmentutilizationfortype2diabetesacross fivemajoruniversityof Californiahealthsystems. DiabetesCare. 2021;44(4):908–14.
13.ObservationalHealthDataSciencesandInformatics(OHDSI).OMOP CDMv5.3.Availableat: https://ohdsi.github.io/CommonDataModel/ cdm53.html#VISIT_OCCURRENCE.AccessedAugust28,2023.
14.DiRicoR,NambiarD,StoovéM,etal.DrugoverdoseintheED:arecord linkagestudyexaminingemergencydepartmentICD-10coding practicesinacohortofpeoplewhoinjectdrugs. BMCHealthServRes. 2018;18(1):945.
15.HartnettKP,Kite-PowellA,DeViesJ,etal.ImpactoftheCOVID-19 pandemiconemergencydepartmentvisits-UnitedStates,January1, 2019-May30,2020. MorbMortalWklyRep. 2020;69(23):699–704.
16.JohnsonE,AxeenS,VosooghiA,etal.Interruptedtimeseriesanalysis: patientcharacteristicsandratesofopioid-use-disorder-related emergencydepartmentvisitsintheLosAngelesCountypublichospital systemduringCOVID-19. Healthcare(Basel). 2023;11(7):979.
17.HuhnASandDunnKE.Whyaren’tphysiciansprescribingmore buprenorphine? JSubstAbuseTreat. 2017;78:1–7.
18.HuntleyK,EinsteinE,PostmaT,etal.Advancingemergency department-initiatedbuprenorphine. JAmCollEmergPhysiciansOpen. 2021;2(3):e12451.
19.D’OnofrioG,McCormackRP,HawkK.Emergencydepartmentsa24/7/365optionforcombatingtheopioidcrisis. NEnglJMed. 2018;379(26):2487–90.
20.JakubowskiAandFoxA.Defininglow-thresholdbuprenorphine treatment. JAddictMed. 2020;14(2):95–8.
21.SnyderH,KalminMM,MoulinA,etal.Rapidadoptionoflow-threshold buprenorphinetreatmentatCaliforniaemergencydepartments participatingintheCAbridgeprogram. AnnEmergMed. 2021;78(6):759–72.
22.HerringAA,KalminM,SpeenerM,etal.Sharpdeclineinhospitaland emergencydepartmentinitiatedbuprenorphineforopioidusedisorder duringCOVID-19stateofemergencyinCalifornia. JSubstAbuseTreat. 2021;123:108260.
23.CurrieJM,SchnellMK,SchwandtH,etal.Prescribingofopioid analgesicsandbuprenorphineforopioidusedisorderduringthe COVID-19pandemic. JAMANetwOpen. 2021;4(4):e216147.
24.ZhengJ,RakovskiC,VariscoT,etal.EPH198thesustainedimpactof COVID-19onopioiddispensinginCalifornia. ValueinHealth. 2023;26(6S):S200.
25.BolinskiRS,WaltersS,Salisbury-AfsharE,etal.Theimpactof theCOVID-19pandemicondrugusebehaviors,fentanylexposure, andharmreductionservicesupportamongpeoplewhouse drugsinruralsettings. IntJEnvironResPublicHealth. 2022;19(4):2230.
26.CaliforniaHealthCareFoundation.SubstanceuseinCalifornia: prevalenceandtreatment.2022.Availableat: https://www.chcf.org/ publication/2022-edition-substance-use-california/ AccessedAugust29,2023.
27.UnitedStatesDrugEnforcementAdministration.DEAapplaudsthe repealoftheX-Waiver.2023.Availableat: https://www.dea.gov/ documents/2023/2023-01/2023-01-17/dea-applauds-repeal-x-waiver AccessedAugust28,2023.
28.HouseTW.WhiteHousehostseventtomarkremovalofbarriersto addictiontreatment.2023.Availableat: https://www.whitehouse. gov/ondcp/briefing-room/2023/01/25/white-house-hosts-event-tomark-removal-of-barriers-to-addiction-treatment/ Accessed August28,2023.
29.UnitedStatesFederalDrugAdministration.FDAapproves firstover-thecounternaloxonenasalspray.2023.Availableat: https://www.fda.gov/ news-events/press-announcements/fda-approves-first-overcounter-naloxone-nasal-spray.AccessedAugust28,2023.
30.JenkinsRA.ThefourthwaveoftheUSopioidepidemicandits implicationsfortheruralUS:afederalperspective. PrevMed. 2021;152(Pt2):106541.
31.VariscoTJ,WanatM,HillLG,etal.TheimpactoftheMainstreaming AddictionTreatmentActandassociatedlegislativeactiononpharmacy practice. JAmPharmAssoc(2003). 2023;63(4):1039–43.
32.LuH,ZhengJ,WangY.Geospatialanalysisofopioiddispensing patternsinCalifornia:a2021real-worldstudy. Healthcare(Basel). 2023;11(12):1732.
33.WuE,VillaniJ,DavisA,etal.Communitydashboardstosupport data-informeddecision-makingintheHEALingcommunitiesstudy. DrugAlcoholDepend. 2020;217:108331.
ORIGINAL RESEARCH AnAssessmentofthePresenceof Clostridiumtetani intheSoilandonOtherSurfaces MichaelShalaby,MD*†
AlessandroCatenazzi,PhD‡
MelissaF.Smith,MD†
RobertA.FarrowII,DO*†
DavidFarcy,MD*†
OrenMechanic,MD*†
TonyZitek,MD*†
SectionEditor:MarkI.Langdorf,MD,MHPE
*HerbertWertheimCollegeofMedicineatFloridaInternationalUniversity, DepartmentofEmergencyMedicineandCriticalCare,Miami,Florida † MountSinaiMedicalCenterMiamiBeach,DepartmentofEmergencyMedicine, MiamiBeach,Florida
‡ CatenazziLabatFloridaInternationalUniversity,DepartmentofBiologicalSciences, Miami,Florida
Submissionhistory:SubmittedJanuary16,2024;RevisionreceivedSeptember3,2024;AcceptedSeptember6,2024
ElectronicallypublishedOctober22,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18702
Introduction: Standardemergencymedicinepracticeincludestetanusvaccineadministrationaspartof woundcaremanagementforpatientswhoarenotfullyimmunized.Sincetherehavebeennoavailable studiesintheUnitedStatesreaffirmingtheprevalenceof Clostridiumtetani(Ctetani) since1926,we soughttoidentifyitsprevalenceinamajorurbancountyintheUS.
Methods: Wesampledsoil,rustedmetal,concrete,anddogfecestodeterminetheprevalenceof Ctetani inasinglemetropolitancountyintheUnitedStates.Soilsamplesandswabswerecollectedfrom fourlocations:thesoilofapublicparkandanelementaryschool;dogfecesfromasinglepublicdogpark; andrustedsurfaces(metalandconcrete)incommonstudentareasofauniversitycampus.The presenceof Ctetani ineachsamplewasdeterminedusingaquantitativepolymerasechainreaction.
Results: Intotal,200sampleswerecollected,ofwhich37(18.5%)testedpositivefor Ctetani DNA. Amongthe140samplestakenfromthesoil,justone(0.7%)testedpositivefor Ctetani DNA.Ofthe40 samplesofrustedmetalandconcretesurfaces,30(75%)testedpositivefor Ctetani,andsix(30%)ofthe 20samplesfromdogfecestestedpositivefor Ctetani.
Conclusion: Wefoundthat Ctetani isfrequentlypresentonrustedmetalandconcretesurfacesbutrarely insoilsamples.Minorwoundscontaminatedwithsoilmaybeconsideredlowriskfortetanus.However, futurestudiesshouldassesstheburdenof Ctetani inothersimilarurban,suburban,andruralenvironments tohelpdeterminethethreatof Ctetani moreexactly.[WestJEmergMed.2024;25(6)890–893.]
INTRODUCTION Background
Clostridiumtetani (Ctetani ),aGram-positiveobligate anaerobe,isthecausativeagentoftetanus,adisorderthat inducesuncontrollablemusclespasms(knownastetany)and carrieshighmortality.1 Itispreventedbyacommonly administeredtoxoidvaccine.1 Ctetani isthoughttoinhabit soil,mostofteninthesporeform,throughwhichitcan withstandextremetemperaturesandvolatileenvironments.2 Afterinoculationofcontaminatedwounds,thespores
proliferateandspawnvegetativebacteria,whichrelease toxinsthatprecipitatethedisease’scharacteristicsymptoms oftetany.1
Tetanusposesaconsiderableriskindevelopingcountries withlittleaccesstovaccination.In2015therewerenearly 57,000casesoftetanusreportedworldwide,with79% originatinginSouthAsiaandsub-SaharanAfrica.3 The annualincidenceoftetanusintheUnitedStates,incontrast, isverylow.Sincetheintroductionofthetetanustoxoid vaccineinthe1930s,therateofinfectionhassteadily
declinedfromapeakof500in1950tonomorethan30cases yearly.4 Documentedcasesaretypicallyininjectiondrug usersandtheelderly,whohaveahigherriskofinsufficient antibodytitersdespiteupdatedvaccinationstatus.1,4
TheUSCentersforDiseaseControlandPrevention AdvisoryCommitteeonImmunizationPractices(ACIP) recommendstetanusvaccinationaspartof “routinewound caremanagement” forpatientswhoarenotuptodatewith theirvaccinationaftersustainingawound.5 Protocolsfor woundcharacteristics(ie,abrasionvslaceration)arenot specifiedbytheACIP.6 However,theAmericanCollegeof EmergencyPhysiciansguidelinesdifferentiatebetween “minorwoundsandsuperficialburns” and “otherwounds” : minorwoundsrequireaboosterwithin10years,while “other wounds” requireaboosterwithin fiveyears. 7 Thus,tetanus toxoidisadministeredliberallyinUSemergency departments(ED)aspartofroutinewoundcare,whetherfor simpleabrasionsormorecomplexwounds.
Theprevalenceof Ctetani inthesoilhasnotbeen measuredintheUSsince1926,whenDamonetalfed culturedsoilspecimensobtainedmostlyfromfarmlandto pigsandsubsequentlymonitoredthemforsignsofdisease.8 Morerecentlyin2008,BukaretalsampledsoilinNigeria, andviaincubationofspecimenstheydemonstrateda60% incidenceof Ctetani 9 However,thesestudiesmaynotbe generalizabletomodernUSpopulations.Newer,more robustmethodsfordeterminingthepresenceof Ctetani exist today;furthermore,83%ofpeopleintheUStodayresidein urbanenvironments10 wheretheburdenof Ctetani inthe environmentmaydiffer.Thus,thetrueprevalenceof Ctetani inthemodern,urbanUSenvironmenthasyetto beelucidated.
Wesoughttodeterminethefrequencywithwhich Ctetani ispresentinthesoilascomparedtoconcrete,metal,anddog fecesinasingle,majorurbancountyintheUS.
MATERIALSANDMETHODS Weassessedenvironmentalsamplesforthepresenceof Ctetani DNAinMiami-DadeCounty,Florida,whichhasa populationofapproximately2.7millionpeople.11 Thisstudy didnotincludehumansubjectsandthuswasexemptfrom reviewbytheinstitutionalreviewboard.Thisresearch receivednooutsidefunding.
EightysoilsampleswerecollectedinsterilizedWhirl-Pak bags(FiltrationGroupCorp,Madison,WI)fromanurban publicparkandanelementaryschool.Thesesiteswerechosen basedontheirdistancefromeachotherandtheirlikelihoodto representisolatedsoil florawithinthesamecounty,butnot withincloseenoughproximitytobeexpectedtosharesimilar flora.Eachsoil-samplebagcontainedthreeseparatesamples fromwithinafewinchesofsoilusingthreeseparateplastic spoonsthatweredisposedofaftereachuse.Wecollected samplesthiswaysuchthateachbagwaslargeenoughandthat oneindividualspoonmightnot “contaminate” theothertwo
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Clostridiumtetaniisassumedtobewidely presentwithinthesoil.Thelastsoilsample studyperformedintheUnitedStateswasin 1926,whichonlyshowedonepositivesample of62collected.
Whatwastheresearchquestion?
WhatistheprevalenceofC.tetaniinthesoil, indogfeces,andonconcreteandmetal surfaceswithinasingleurbancounty?
Whatwasthemajor findingofthestudy?
Amongthe140samplestakenfromthesoil, just1(0.7%)testedpositiveforC.tetani DNA.Ofthe40samplesofrustedmetal andconcretesurfaces,30(75%)tested positive,asdid6(30%)of20samples fromdogfeces.
Howdoesthisimprovepopulationhealth?
Certainwoundtypes(ie,soilcontamination) maycarryalowerriskforCtetani,and theelevatedcostoftetanustoxoid administrationintheemergencydepartment maybeforgoneforoutpatientvaccination whichismuchcheaper.
sampleswithinthesamebag.Theothersamples,collectedby DRYSWABbrush(MedicalWire&EquipmentLtd, Corsham,UK),included20samplesofdogfecesfromonedog park,and60combinedsamplesofconcreteandrustedmetal surfaces(suchasmetalsignsandrailings,andconcrete walkways)atasinglepublicuniversity.Asubsequentsetof60 soilsamples,alsocollectedbydryswab,wereagaintakenfrom thesamelocationsastheoriginalsoilsamplesinthesterilized bags.Sampleswereimmediatelytakentotheprocessing laboratoryaftercollection.
Sampleswereanalyzedinauniversitymicrobiologylab usingquantitativepolymerasechainreaction(qPCR) followingastandardizedpreviouslydescribedmethod (Akbulutetal).12 Thisassayamplifiesa160-basepair fragmentoftheteNTgene(tetanustoxin)of Ctetani (GenBankAccessionNumberX06214,X04436).Thetipof eachswabwasremovedandplacedintoa1.5milliliter Eppendorftubecontaining50microliters(μl)PrepMan UltraSamplePreparationReagent(ThermoFisher Scientific,Waltham,MA).Thetubewasthenincubatedfor
10minutesat100°Cinadrybath,afterwhichitwas centrifugedat13,000revolutionsperminuteforthree minutes.Theinitial80soilsampleswereanalyzedwith 500milligramsofmixedsoil,whilethedryswabsweremixed withareagentintheabsenceofsignificantamountsofsoilin thesample.
Five μlofDNAwasthenextractedfromthetubeand transferredtoa0.6-milliliter(mL)qPCRtubecontaining 45 μlof1/10TEbuffer.Aftermixing,5 μlofthisdiluted DNAproductwasaddedtoanewqPCRtubealongwith 20 μlofa62.5:35.5:1:1mixtureofSYBRGreenmastermix (ThermoFisherScientific,Waltham,MA):purifiedwater: forwardprimerTeNT-F(CCTAGTTTCAAAACTTAT TGGCTTATGTAA):reverseprimerTeNT-R (CATAATTCTCCTCCTAAATCTGTTAATGAT).The qPCRwasperformedonaQuantStudioTM3Real-Time PCRInstrument(96-well0.1mLBlock)(Applied BiosystemsInc,FosterCity,CA)asfollows:twominutesat 50°C,followedbytwominutesat90°C,followedby51cycles of15secondsat95°C/1minuteat56°C,followedbya final15 secondsat95°C.OurqPCRwasspecifiedforthe first160 basepairfragmentsoftheteNTgeneof Ctetani . Theplateincludedthreedistilledwaternegativecontrols, onePrepMannegativecontrol,andthreeserialdilutionsof double-stranded,syntheticDNA(gBlock,IntegratedDNA TechnologiesInc,Coralville,IA)oftheteNTgeneof Ctetani (GenBankAccessionNumberX06214,X04436). ResultswereanalyzedinQuantStudioDesignandAnalysis Softwarev1.5.1(AppliedBiosystemsInc,FosterCity,CA). Nopowercalculationwasperformed.Withnoexternal funding,theinvestigatorsdeterminedwehadfundsforthree plates.Themaximumnumberofsamplesperplatewas82. Weanalyzed200totalsamplesfromtheenvironmentto assessforthepresenceof Ctetani DNA.Inthelaboratory setting,theassayweusedhasnearly100%sensitivityand specificityfor Ctetani DNA,butitispossiblethatin environmentalsamplesthepresenceofadditionalsubstances mayinterferewithit.Therefore,wetagged42soilsamples with Ctetani toassesstheaccuracyofourassay(thecontrol group).Wecalculatedthenumber(%)ofsamplesthatwere positivefor Ctetani overall,foreachtypeofenvironmental sample,andforthecontrolgroup.Wecomparedthethree groups(soil,concreteandmetal,anddogfeces)inapairwise fashionwithregardtothepercentageofsampleswith Ctetani DNAusingFisherexacttests.
RESULTS Overall,ofthe200samplescollectedforanalysis,37 (18.5%)testedpositivefor Ctetani DNA(Table).The first80 samplesconsistedofsoilcollectioninplasticbagsfrom publicparks.These80sampleswereallnegativefor Ctetani DNA byouranalysis.However,giventhepossibilityof interferenceofsoilhumicacidwithqPCRanalysis,13 another 60soilsampleswereobtainedviadryswabsfromthesame
Table. Swabsandsoilsampleresultsforpresenceof Clostridiumtetani
Samplelocationandtype
Allsoil:
• Park samples
• Elementaryschoolsamples
• Parkswabs
• Elementaryschoolswabs
Positive samples
1/140(0.7%)
• 0/20 (0%)
• 0/60(0%)
• 1/15(1.7%)
• 0/45(0%)
Dogparkfecesswabs 6/20(30%)
Undergraduate campus,oxidizedmetaland concreteswabs 30/40(75%)
locations(urbanparkandelementaryschool)astheoriginal 80.Repeatanalysisofthe60dryswabsofthesoilrevealed onepositivefor Ctetani DNA.Therefore,amongthe140 analyzedsoilsamples(withtwodifferentmethodsof collection),one(0.7%)wasfoundtohave Ctetani DNA.To assessthesensitivityofourassay,wetagged22samplesof soilinsterilizedplasticbagswith Ctetani DNA,and16were identifiedaspositives(72.7%).Wetagged20dryswabsofsoil with Ctetani DNA,and11(55%)werepositive.
Wecollected40swabsofcombinedpublicoxidized concreteandmetalsurfacesfromauniversitycampus,aswell as20swabsofdogfecesatasinglepublicdogpark.Ofthese, six(30%)of20dogfecessampleswerepositivefor Ctetani DNA,and30(75%)of40swabsofoxidizedconcrete andmetalwerepositive.Acontrolwascreatedandevaluated bytagging20ofthemetalandconcretesampleswith Ctetani DNA.Ofthe20controlsamples,15were positive(75%).
Therewasastatisticallysignificantdifferenceinthe percentageofsampleswith Ctetani DNAfromtheconcrete andmetalgroup(75%)ascomparedtothesoilgroup(0.7%), P < 0.001.Additionally,therewasastatisticallysignificant differenceinthepercentageofsampleswith Ctetani DNA fromthedogfecesgroup(30%)ascomparedtothesoilgroup (0.7%), P < 0.001.Finally,therewasastatisticallysignificant differenceinthepercentageofsampleswith Ctetani DNAintheconcreteandmetalgroup(75%)as comparedtothedogfecesgroups(30%), P < 0.001.
DISCUSSION Weundertookthisstudytohelpascertainthefrequency withwhich Ctetani isfoundinthesoilandonother substancesintheenvironmentinanurbanareaintheUS.Our resultssuggestthat Ctetani ismuchmorecommonon oxidizedmetalandconcrete,aswellasdogfecesthanitisin soil.OurresultsareconsistentwiththelastassessmentofUS soilfrom1926,whichdidnotstronglysuggestthat Ctetani waspresent.Withthepaucityof Ctetani isolatedinthis
sampleofUSsoilfromasinglecounty,itissuggestedthat furtherinvestigationintotheprevalenceofthebacteriumis needed.Therearebroaderimplicationstoidentifying Ctetani .Forone,thisstudyfoundthatnon-soilmediamay provideamorefavorablegrowthenvironmentfor Ctetani , andsoilitselfmaynotbeanabundantsource.Education effortsforexposuremayneedtobeconcentratedoninjuries duetorustedmetal,concrete,dogfeces,andpotentially othersourcesof Ctetani .Giventhatourstudysample wassmall,wedonotbelievethatthisdataalonemeritsa changeinEDvaccinationguidelines,especiallysincethe tetanustoxoidvaccinealsoprovidesimmunizationagainst diphtheriaandpertussis,bothofwhicharealsosignificant publichealththreats.Rather,moredatafromsimilarstudies isrequired.
LIMITATIONS Therearesomelimitationstothissmallsingle-UScounty study.Firstly, Ctetani DNAsamplesweretestedviaqPCR analysis,ratherthanincubated,andreagents,suchashumic acid,withinthesoilmayhaveinterferedwithPCRanalysis.13 Repeatanalysisofdryswabsaimedtomitigatesucherror, andsimilarresultswereproduced.Furthermore,the prevalenceof Ctetani shouldbestudiedinotherurbanareas beforepublichealthconclusionsaremade.Farmlandand non-urbanareaswerenotstudiedand,therefore,thiscannot begeneralized.Oxidizedmetalandconcretesurfaceswere analyzedtogether,andthustheextenttowhich Ctetani is presentoneithersurfacewasnotfullyassessedinthis study.Lastly,whilethisstudycontainsmoredatasamples thanprevioussimilarundertakings,200soilsamplesfrom onlyafewseparatesitesinasingle,urbancountylikely donotfullyrepresentthetrueextentofthepresenceof Ctetani inotherenvironments,suchasothersitesfrom withinthesameurbancountyandotherurban,suburban, andruralenvironments.
CONCLUSION Tetanusposesasignificantpublichealththreat.Yetits presenceinthesoilmaynotbeassignificantasiscurrently assumed,atleastnotinurbanareas,asour findingssuggest. Inourstudy,wetestedsoil,concrete,metal,anddogfecesfor Ctetani inasingleurbancounty.Theresultssuggestthat Ctetani ismoreabundantinoxidizedmetalandconcrete,as wellasindogfecesthanitisinsoil.However,several questionsabouttheprevalenceandvirulenceof Ctetani remain.Furtherstudiesshouldelucidatetheprevalenceof Ctetani inotherurban,suburban,andruralsites.
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Shalabyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.YenLMandThwaitesCL.Tetanus. Lancet(London,England). 2019;393(10181):1657–68.
2.CampbellJI,LamTMY,HuynhTL,etal.Microbiologiccharacterization andantimicrobialsusceptibilityof Clostridiumtetani isolatedfrom woundsofpatientswithclinicallydiagnosedtetanus. AmJTropMed Hyg. 2009;80(5):827–31.
3.KyuHH,MumfordJE,StanawayJD,etal.Mortalityfromtetanus between1990and2015: findingsfromtheglobalburdenofdisease study2015. BMCPublicHealth. 2017;17(1):179.
4.CentersforDiseaseControlandPrevention.Abouttetanusdisease (lockjaw).2022.Availableat: https://www.cdc.gov/tetanus/about/index. html.RetrievedApril27,2023.
5.LiangJL,TiwariT,MoroP,etal.Preventionofpertussis,tetanus, anddiphtheriawithvaccinesintheUnitedStates:recommendations oftheadvisorycommitteeonimmunizationpractices(ACIP). MMWRRecommRep. 2018;67(2):1–44.
6.HaversFP,MoroPL,HunterP,etal.Useoftetanustoxoid,reduced diphtheriatoxoid,andacellularpertussisvaccines:updated recommendationsoftheAdvisoryCommitteeonImmunizationPractices UnitedStates,2019. MorbMortalWklyRep. 2020;69(3):77–83.
7.Tetanus.Availableat: https://www.acep.org/siteassets/new-pdfs/ policy-statements/immunization-of-adults-and-children-in-theemergency-department.pdf.2020.Accessed:June12,2023.
8.DamonSRandPayabalLB.Distributionofthesporesofbacillus botulinusandbacillustetaniinthesoil:1.InMaryland, JInfectDis. 1926;39(6):491–501.
9.BukarA,MukhtarMD,AdamSA.Currenttrendinantimicrobial susceptibilitypatternof Clostridiumtetani isolatedfromsoilsamplesin Kano. BayeroJPureApplSci. 2008;1(1):112–5.
10.CenterforSustainableSystems.U.S.Citiesfactsheet.Availableat: https://css.umich.edu/publications/factsheets/built-environment/ us-cities-factsheet.Accessed:April27,2023.
11.CensusReporter.Miami-DadeCounty,FL.Availableat: http:// censusreporter.org/profiles/05000US12086-miami-dade-county-fl/ Accessed:April27,2023.
AddressforCorrespondence:MichaelShalaby,MD,Herbert WertheimCollegeofMedicine,DepartmentofEmergencyMedicine andCriticalCare,4300AltonRd.,MiamiBeach,Florida33140. Email: michael.shalaby@msmc.com
12.AkbulutD,DennisJ,GentM,etal.Woundbotulismininjectors canofdrugs:upsurgeincasesinEnglandduring2004. EuroSurveill. 2005;10(9):172–4.
13.MathesonCD,GurneyC,EsauN,etal.AssessingPCRinhibitionfrom humicsubstances. OpenEnzymInhibJ. 2010;3(1):38–45.
EDUCATIONAL SPECIAL ISSUE:ORIGINAL Yi-JuHo,MD*
Pei-ISu,MD*
Chien-YuChi,MD†
Min-ShanTsai,MD,PhD*‡
Yih-SharngChen,MD,PhD§∥
Chien-HuaHuang,MD,PhD*‡
*NationalTaiwanUniversityHospital,DepartmentofEmergencyMedicine, Taipei,Taiwan
† NationalTaiwanUniversityHospitalYun-LinBranch,DepartmentofEmergency Medicine,Yun-Lin,Taiwan
‡ NationalTaiwanUniversityHospital,DepartmentofInternalMedicine, Taipei,Taiwan
§ NationalTaiwanUniversityHospital,DepartmentofSurgery,Taipei,Taiwan
∥ NationalTaiwanUniversity,CollegeofMedicine,DepartmentofSurgery, Taipei,Taiwan
SectionEditor:EricMelnychuk,MD
Submissionhistory:SubmittedNovember28,2028;RevisionreceivedAugust1,2024;AcceptedAugust1,2024
ElectronicallypublishedOctober4,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18601
Background: Extracorporealcardiopulmonaryresuscitation(ECPR)improvestheprognosisofinhospitalcardiacarrest(IHCA).Thesix-factorRESCUE-IHCAscore(resuscitationusingECPRduring IHCA)wasdevelopedtopredictoutcomesofpost-IHCAECPR-treatedadultpatients.Ourgoalwasto validatethescoreinanAsianmedicalcenterwithahighvolumeandexperienceofECPRperformance andtocomparethedifferencesinpatientcharacteristicsbetweenthecurrentstudyandtheoriginal cohortina2022observationalstudy.
Method: Forthissingle-center,retrospectivecohortstudyweenrolled324ECPR-treatedadultIHCA patients.Theprimaryoutcomewasin-hospitalmortality.Weusedtheareaunderthereceiveroperating curve(AUROC)toexternallyvalidatetheRESCUE-IHCAscore.Thecalibrationofthemodelwastested bythedecilecalibrationplotaswellasHosmer–Lemeshowgoodness-of-fitwithanassociated P-value.
Results: Ofthe324participants,231(71%)diedbeforehospitaldischarge.Thediscriminative performanceoftheRESCUE-IHCAscorewascomparablewiththeoriginallyvalidatedcohort,withan AUCof0.63.Aprolongeddurationofcardiacarrestwasassociatedwithanincreasedriskofmortality (oddsratio[OR]1.02,95%confidenceinterval[CI]1.01–1.03, P = .006).Aninitialrhythmofventricular tachycardia(OR0.14,95%CI0.04–0.51, P = .003),ventricular fibrillation(OR0.11,95%CI0.03–0.46, P = .003),andpalpablepulse(OR0.26,95%CI0.07–0.92, P = 0.04)wereassociatedwithareduced mortalityriskcomparedtoasystoleorpulselesselectricalactivity.Incontrasttotheoriginalstudy,age (P = 0.28),resuscitationtiming(P = 0.14),diseasecategory(P = 0.18),andpre-existingrenal insufficiency(P = 0.12)werenotassociatedwithin-hospitaldeath.
Conclusion: Inexternalvalidation,theRESCUE-IHCAscoreexhibitedperformancecomparabletoits originalvalidationwithinthesingle-centerpopulation.Furtherinvestigationonhospitalexperience,timeof-dayeffect,andspecificdiseasecategoriesiswarrantedtoimprovetheselectioncriteriaforECPR candidatesduringIHCA.[WestJEmergMed.2024;25(6)894–902.]
INTRODUCTION Extracorporealcardiopulmonaryresuscitation(ECPR)is apromisingmodalitythatcombinesextracorporeal membraneoxygenation(ECMO)withtraditionalCPR techniquesforimprovingtheoutcomeaftercardiacarrest. Predictionmodelsdevelopedtoestimatethesurvival likelihoodofpatientswithrefractorycardiogenicshockor cardiacarrestwhoreceivedECPRhaverarelyfocusedon patientswhohavesustainedanin-hospitalcardiacarrest (IHCA),1,2 A2010observationalstudyshowedthatECPR leadstomorefavorableoutcomesinIHCAthaninout-ofhospitalcardiacarrest(OHCA),3 possiblyowingtothe shorterno-flowandlow-flowduration.Otherobservational studieshaveattemptedtoascertainstrongpredictorsthatcan helpidentifyIHCApatientswhowouldbenefitmost fromECPR.4,5
TheRESCUE-IHCAscoringsystem(resuscitationusing ECPRduringIHCA)wasdevelopedtopredictoutcomesof ECPR-treatedadultIHCApatientsandwasexternally validatedusingpatientdatafromtheExtracorporealLife SupportOrganization(ELSO)Registry.6 RESCUE-IHCAis asimplifiedscorethatcomprisessixvariables:1)age; 2)pre-existingrenalinsufficiency;3)timeoftheday (7 AM – 2:59 PM);4)diseasecategory(cardiac,ornon-cardiac, surgicalormedical,aspertheCurrentProcedural TerminologyandInternationalClassificationofDiseases); 5)initialrhythm;and6)thedurationofarrest,allofwhich canbeeasilycollecteduponhospitalarrival.However,inthe validationgroup,theRESCUE-IHCAscoringsystemonly demonstratedacceptablediscrimination.
Despiteitsmodestclinicalperformance,theRESCUEIHCAistheonlymodelavailableforpredictingoutcomesof ECPR-treatedIHCApatients.Therefore,furtherevaluation oftheRESCUE-IHCA’sreproducibilitybyusingexternal datasetsiswarrantedforwiderapplicationofthisscoring system.OurobjectivewastovalidatetheRESCUE-IHCA scoreusingdatafromadifferentpopulationandtoidentify potentialpredictorsthatmaydifferfromthoseintheoriginal study.Weaimedtoenhanceclinicaldecision-makingby providingmoreaccurateoutcomepredictionsforECPR initiationinIHCApatients.
METHODS StudyDesignandSetting
Thisretrospectivecohortstudywasconductedovera seven-yearperiod(January2012–December2019)ata tertiary,extracorporeallife-supportreferralmedicalcenterin Taiwan,oneofthelargestmedicalcentersinAsiawith2,600 beds,including220bedsinintensivecareunits.Mostpatients areTaiwaneseresidents,withforeignersoccasionally admittedthroughinternationaltransfer.Overthepast decade,themedicalcenterhasperformedmorethan100 ECPRproceduresannuallyundertheguidanceofcardiac surgeons. 7 Thisstudy,approvedbytheinstitutionalreview
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Extracorporealcardiopulmonary resuscitationimprovestheprognosisofinhospitalcardiacarrest.TheRESCUE-IHCA scorepredictsoutcomesforthesepatients.
Whatwastheresearchquestion?
WeaimedtovalidatetheRESCUE-IHCA scoreandtocomparedifferencesinpatient characteristicsbetweenourstudyanda2010 observationalstudy.
Whatwasthemajor findingofthestudy?
TheRESCUE-IHCAscoreshowed compromiseddiscriminationcomparedtothe originalstudy,withanAUCof0.63(95%CI 0.56 – 0.70).
Howdoesthisimprovepopulationhealth?
TheRESCUE-IHCAscoredidnotpredict outcomesbetterthantheoriginallyvalidated cohort.Methodofdiseasecategorizationmay havein fl uencedoutcomes.
board[202306052RIND],demonstratesarobustadherence tomethodologicalstandardsinhealthrecordreviewstudies.8 Therequirementofinformedconsentwaswaivedduetothe retrospectivenatureoftheresearch.Thesamplingpatients wereidentifiedthroughchartreviewofelectronic healthrecords(EHR)bymedicalandemergency physicianswhocollectedcovariatedataanddefinedthe post-IHCAoutcome.
CaseSelection BetweenJanuary2012–December2019,study participantswereenrolledbasedontheseselectioncriteria: 1)patientshadundergoneECPRfollowingIHCA;2)were aged ≥18years;and(3)hadnohistoryofOHCApriorto admission.Weusedacriticalscreeningprocesstoexclude ineligiblepatientsbasedonthefollowingcriteria:1)transfer toanotherhospitalafterreturnofspontaneouscirculation; 2)traumaticarrest;3)historyofOHCA;and4)missing outcomesintheEHR.
DataCollectionandProcessing Covariatedatafromeachmedicalchartweredefined clearlyandreviewedbyindependentphysicians,and monthlymeetingswereheldtoensureconsistencyofthe collecteddata.Tominimizepotentialbiasesorerrors,the
studydesignanddataanalysiswereundertakenbya physicianwhowasblindedtothedatacollectionprocess.We discussedanydisputesorambiguousrecordswith cardiologistsandemergencyphysicians,anddecisionswere maderegardingeachcontroversialhealthrecord.Individuals wholackedoutcomevariableswereexcludedinitially.The onlymissingdatainthecurrentcohortswasthepre-arrest laboratorydata,whichwasnotincludedinthe RESCUE-IHCAscoreorthe finalanalysis.
Variables Wecategorizedthestudyvariablesintodemographics, pre-existingdiseases,intra-arrestcharacteristics,and presumedetiologyofcardiacarrest.Demographicsincluded age,gender,bodyweight,andbodymassindex(BMI).Preexistingdiseasesincludedhypertension,diabetesmellitus, chronicobstructivepulmonarydisease,coronaryartery disease,congestiveheartfailure,chronickidneydisease, cerebralvasculardisease,andcancer,andthediagnoseswere confirmedfromtheEHRbasedonregularmedication prescriptions,treatment,andoutpatientfollow-up.Intraarrestcharacteristicsincludedinitialcardiacrhythmdefined asasystole,pulselesselectricalactivity,ventricular tachycardia(VT),ventricular fibrillation(VF),orwitha palpablepulseinitially;timeofday,durationofcardiac arrest;andintra-arresttreatmentsincludingdefibrillation andmedicationsadministered.Thepresumedetiologyof IHCAwasdeterminedbyreviewingtheEHR.We categorizedparticipantsintofourgroupsbasedon whethertheIHCAwascardiogenicornon-cardiogenic andwasrelatedtoasurgicalormedicalillness (SupplementaryTable1).
Outcomes AswiththeoutcomeoftheoriginalRESCUE-IHCA study,theprimaryoutcomeinthisstudywasin-hospital death.WecalculatedtheRESCUE-IHCAscoreinour datasetsfortheexternalvalidationprocess.
StatisticalAnalysis Continuousdatawereassessedfornormalityusingthe Kolmogorov–Smirnovtestandwereexpressedasthemean (standarddeviation)ifnormallydistributedormedian (interquartilerange[IQR])ifnon-normallydistributed.We presenteddichotomousandcategoricalvariablesasthe frequency(percentage).Wecomparedcontinuousvariables usingtheMann-Whitney U test,whereasdichotomousand categoricalvariableswereexaminedusingthechi-square test.WeusedtheHosmer-Lemeshowtesttoshowthe goodnessof fit.
TheexternalvalidationoftheRESCUE-IHCAscorewas performedinthestudycohort,andweassessed discriminatoryperformanceusingtheareaunderthereceiver operatingcharacteristiccurve(AUROC)with95%
confidenceinterval(CI).Themodelcalibrationwastested usingacalibrationplotbasedon10deciles,aswellasthe Hosmer–Lemeshowgoodness-of-fittestwithanassociated P -value.Wetestedindividualvariableswithabinarylogistic regressionmodelandadjustedtheminthemultivariate regressionmodelusingtheforce-entrymethod.Theresults werepresentedasadjustedoddsratioand95%CI.
WeperformedstatisticalanalysisusingtheStatistical PackagefortheSocialSciencesversion26.0(IBMCorp, Armonk,NY)andR4.3.0(RFoundationforStatistical Computing,Vienna,Austria).Atwo-sided P -valuelessthan 0.05wasconsideredstatisticallysignificant.
RESULTS PatientCharacteristics Duringthestudyperiod(January2012–December2019), 324eligiblepatientswhoreceivedECPRafterIHCAwere enrolledinthisstudy,andamongthem231(71%)diedbefore hospitaldischarge(Figure1). Table1 presentsthebaseline characteristicsoftheparticipants.Intheoverallcohort,121 patients(37.3%)hadaninitialshockablerhythm,and265 patients(82%)werepresumedtohaveamedicalillness. PatientswhosurvivedtodischargeafterreceivingECPRfor IHCA,whencomparedwiththenon-survivors,hadahigher frequencyofhypertension(62/93[66.7%]vs121/231[52.3%], P = 0.03),presentedmorefrequentlywithaninitial shockablerhythm(50/93[53.8%]vs71/231[30.7%], P < 0.001),hadashorterlow flowduration(28minutesvs38 minutes, P < 0.001),andthecardiacarrestwasmore frequentlypresumedtobeofamedicalcardiogenicor surgicalcardiogenicorigin(62/93[66.7%]vs125/231[54.1%]; 7/93[7.5%]vs16/231[6.9%], P = 0.03).Thedurationof ECMOsupportwasshorter(2daysvs4days, P = .002),and thetotalhospitallengthofstaywaslonger(15daysvs3days, P < .001)inthesurvivalgroup.Nosignificantintergroup differencesbetweensurvivorsandnon-survivorswere detectedintermsofage,gender,bodyweight,BMI,history ofcomorbiditiesbesideshypertension,witnessedarrest,or timeofday.
Figure1. Studyenrollment flowchart.
Table1. Comparisonofbasiccharacteristicsofin-hospitalcardiacarrestpatientsreceivingextracorporealcardiopulmonaryresuscitation withorwithoutsurvivaltodischarge.
Patientsdiedbeforedischarge(n = 231)Patientssurvivedtodischarge(n = 93) P
Pastcomorbidities
HTN121(66.1)62(33.9)0.03
DM91(67.9)43(32.1)0.27
Renalinsufficiency50(79.4)13(20.6)0.12 CVA13(81.2)3(18.8)0.57
Dichotomousvariableswerereportedasnumber(percentage)whilecontinuousvariableswerereportedasmedian(interquartilerange). BMI, bodymassindex; BW,bodyweight; CAD,coronaryarterydisease; CHF,congestiveheartfailure; CPR,cardiopulmonaryresuscitation; CVA,cerebrovascularevent; DM,diabetesmellitus; ECMO,extracorporealmembraneoxygenation; ECPR,extracorporealcardiopulmonary resuscitation; IHCA,in-hospitalcardiacarrest; IQR,interquartilerange; kg,kilograms.
ExternalValidationoftheRESCUE-IHCAScore
TheRESCUE-IHCApredictivemodelwasexternally validatedamongthe324participants.Themodel discriminationwaspoortoacceptable(areaunderthecurve 0.63[95%CI0.56–0.70]).Thepredictedprobabilityof mortalityrangedfrom38–93%accordingtotheRESCUEICHAscore(Figure2).Modelcalibrationindicatedgood fit withtheHosmer-Lemeshowgoodness-of-fittest(P = 0.91). Theobservedmortalityinthestudycohortvsthepredicted mortalitycalculatedfromtheRESCUE-IHCAscoreis
presentedin Figure3.Otherbinsizeswerelikewisetested withoutfurtherimprovementin fit.
SignificantFactorsAssociatedwithIn-HospitalDeathin theCurrentCohort
Toassesspotentialpredictivefactorsinourcohortand comparethemwiththeoriginalRESCUE-IHCAscore,we conductedunivariatelogisticregressionforallvariables, followedbymultivariateregressionforthosevariableswith P < 0.1(Table2).Theresultshowedthatthemortalityrisk
Figure2. PredictedprobabilityofdeathacrossRESCUE-IHCAscore.
waspositivelyassociatedwithlongerlow-flowduration (oddsratio[OR]1.02,95%CI1.01–1.03, P = .006),and negativelyassociatedwithaninitialcardiacrhythmofVT (OR0.14,95%CI0.04–0.51, P = .003),VF(OR0.11,95%CI 0.03–0.46, P = .003),orpalpablepulse(OR0.26,95%CI 0.07–0.92, P = 0.04).Patient’sage,pre-existingrenal insufficiency,timingofresuscitation,anddiseasecategory didnotshowsignificantassociationswithmortality.The Hosmer-Lemeshowtestresultsshowedagood fit(P = 0.66).
DISCUSSION ValidationoftheRESCUE-ICHAScore Inthepresentstudy,weperformedtemporaland geographicalexternalvalidationoftheRESCUE-IHCA scoringsysteminanAsianmedicalcenterequippedwith standardizedprotocolsforECMOinitiation.The performanceofmodeldiscrimination(AUC0.63)modestly decreasedascomparedwiththeoriginalderivationand validationcohorts(AUC0.72[95%CI0.68–0.76]and0.68
Figure3. Calibrationplotofobservedvspredictedmortalityfromvalidateddataset.
Table2. Logisticregressionmodelofriskfactorsassociatedwithin-hospitaldeath. N(%)/median(IQR)CrudeOR(95%CI) P AdjustedOR(95%CI) P
Male 227(70.1) 0.75(0.44–1.29) 0.30
Age(year)59.7(45.7–73.7)1.01(0.99–1.03)0.28
BW(kg)66.55(57.60–76.45)1.00(0.99–1.02)0.94
BMI(kg/m2)24.64(22.20–27.36)1.01(0.96–1.06)0.80
Pastcomorbidities
HTN183(56.5)0.55(0.33–0.91)0.020.70(0.41–1.20)0.19
DM134(41.4)0.76(0.47–1.23)0.26
COPD7(2.2)2.45(0.29–20.66)0.41
CAD118(36.4)0.72(0.44–1.18)0.19
CHF66(20.4)1.23(0.76–1.99)0.41
Renalinsufficiency63(19.4)1.70(0.88–3.30)0.12
CVA16(4.9)1.79(0.50–6.43)0.37
Cancer29(9)2.70(0.91–7.99)0.07
CPR
Witnessedarrest301(92.9)0.67(0.24–1.87)0.45
Presentingrhythm
Asystole42(13)referencereference
PEA19(5.9)0.29(0.06–1.45)0.130.32(0.06–1.70)0.18
VT83(25.6)0.11(0.03–0.37) <0.0010.14(0.04–0.51).003
VF34(10.5)0.10(0.03–0.38)0.0010.11(0.03–0.46).003
Pulse(+)146(45)0.24(0.07–0.81)0.020.26(0.07–0.92)0.04
Timeofday
07:00–14:59148(45.7)reference 15:00–10:59109(33.6)0.69(0.37–1.29)0.24
23:00–06:5967(20.7)1.19(0.60–2.35)0.63
Low flowduration(min)37.6(17.0–58.3)1.03(1.01–1.04)0.0011.02(1.01–1.03).006
Presumeddiseasecategory
Dichotomousvariableswerereportedasnumber(percentage)whilecontinuousvariableswerereportedasmedian(interquartilerange). Variables withP < 0.1inunivariablelogisticregressionwereadjusted. BMI,bodymassindex; BW,bodyweight; CAD,coronaryarterydisease; CHF,congestiveheartfailure; CPR,cardiopulmonaryresuscitation; CVA,cerebrovascularevent; DM,diabetesmellitus; IQR,interquartilerange; kg,kilograms; N,casenumber; OR,oddsratio; PEA,pulseless electricalactivity; VF,ventricular fibrillation; VT,ventriculartachycardia.
[95%CI0.61–0.75],respectively).Themodel’sperformance maybeattributedtothelackofsignificanceofcertain variables,includingage,timingofresuscitation,the presumeddiseasecategory,andpre-existingrenal insufficiency.Wefoundthatthelow flowdurationandthe initialcardiacrhythmserveassignificantpredictorsforthe outcome,consistentwith findingsfromprevious observationalstudiesandmeta-analyses.5,9–12,19 Despitethe single-centerfocus,thehospitalisgloballyrecognizedasthe
second-largestfacilityforECPRprocedures,managing hundredsofcaseseachyear.Thisstudyprovidesnovel insightswithinauniqueethniccontext.
IndividualPredictorsofIn-HospitalDeath Agewasnotasignificantpredictorinourstudy,possibly attributabletothesmallsamplesize.Whencomparing patientcharacteristicsbetweenstudies,weobservedasimilar agedistributionamongnon-survivorsandsurvivorsinthe
twocohorts(studycohort:63.2vs59.9;RESCUE-IHCA cohort:61vs58).
Incontrasttothenotable findingfromtheRESCUEIHCAstudy,theinfluenceoftimeofdayonsurvivalno longerpersisted.Duringlatenightandearlymorningfrom 11 PM – 5 AM,fewersurvivorswereobservedintheRESCUEIHCAcohortcomparedtothecurrentcohort(studycohort: 16/93[17.2%];RESCUE-IHCAcohort:27/306[8.8%]).The currentstudywasconductedatatertiarymedicalcenter whereECPRinitiationwasprotocolizedregardlessof timing.Whenacardiacarrestoccurs,astandardized hospital-wideemergencycallactivatesarapidresponseteam ofmedicalcardiologists,surgeons,andemergencyphysicians whopromptlydeterminetheneedforECPR.
AcomprehensivediscussiononECPRimplementation wasprovidedbyaprospectiveobservationalstudy conductedinTaiwan.7 Experiencedsurgeonsandteam memberssubsequentlyestablishECMOcannulationatthe bedsideifindicated.Despitereducedwardstaffingduringthe night,survivalrateswerenotsignificantlyaffected.Aprior studyconductedatamedicalcenterinTaiwanrevealedthat thetimeofdayhadnoimpactonthesurvivaloutcome followinganin-hospitalcardiacarrest.13 Ourstudysuggests thatanexperiencedhealthcaresystemwithtrainedcrew membersoperatinginanestablishedsystemcaneffectively mitigatetheincreasedworkloadfromdecreasedstaffing duringoff-hours.Furtherstudiesarewarrantedtodetermine theimpactofhospitalcaseloadandexperiencewhilefocusing ontheoutcomesofcardiacarrestpatientswho receiveECPR.
TheRESCUE-IHCAstudyfoundthatsurgicalcardiac, surgicalnon-cardiac,andmedical-cardiacdiseaseswere predictivefactorsforsurvival.However,theresultsofthe currentstudyonlyobservedarelationshipbetweensurgical non-cardiacdiseaseandin-hospitalmortality,althoughthis associationdidnotreachstatisticalsignificance(Table1). Thesurgicalnon-cardiacdiseasesinourstudyincluded aorticdissection,hypovolemiaorhemorrhage,and intracranialhemorrhage,whichmaypotentiallyderiveless benefitfromECPR(SupplementaryTable1).The2010 RESCUE-IHCAstudyincludedahigherproportionof surgicalpatients(610/1,075[56.7%]),whereasthecurrent studycomprisedalowerpercentageofpatientswithsurgical illnesses(59/324[18.2%]).Thediseasecategoryintheoriginal RESCUE-IHCAstudywasautomaticallyretrievedfrom CurrentProcedureTerminology(CPT)andInternational ClassificationofDiseases(ICD)codes,whereasinthisstudy wemanuallyreviewedthehealthchartstoassesstheultimate etiologyofthecardiacarrest.
Previousstudieshaveidentified “cardiacorigin” or “presumedreversiblecardiogenicetiology” ascritical selectioncriteriaforIHCApatientsreceivingECPR,without specifyingthediagnosticprocessordisease-categorization method.7–9,15,16–18 Thesedivergent findingshighlightthe
complexityofthepresumedetiologyofarrest.Concerns persistregardingthepotentialmisinterpretationof diagnoses,whichcouldresultintheinappropriateinitiation ofECPRinacutescenarios.Establishingandvalidatinga standardizeddisease-categorizationsystemforIHCA patientsreceivingECPRisacrucialchallengethatmay significantlyimproveoutcomesinthefuture.
Renalinsufficiencywasnotidentifiedasasignificant predictorformortalityinthisstudy.Ourstudyincluded fewerpatientswithpre-existingrenalinsufficiencyinboththe mortalityandsurvivalgroups(non-survivorsvssurvivorsin thestudycohort:50/231[21.6%]vs13/93[14.0%];RESCUEIHCAcohort:193/769[25.1%]vs49/306[16.0%]).Previous studiesconductedinanEastAsianpopulationexhibited similarproportionofpatientswithrenalinsufficiencytoour study.20,21 Theproportionofpatientswithrenaldisease influencestheresults;however,renalfunctionstillplaysa crucialroleinprognostication.
ApplicationoftheRESCUE-IHCAscorein real-worldscenarios
TheoverallsurvivalrateofIHCApatientstreatedwith ECPRwas28.7%inthestudy,whichapproximatestorealworldconditionsaccordingtorecentobservationalstudies andsystemicreviewswhereinreportedsurvivalratesranged from23.1–40%.22–25 Inconclusion,theperformanceofthe RESCUE-IHCAscorewasmodestlycompromisedinthis single-centercohort.Althoughasuboptimalvalidationof RESCUE-IHCAscoreinthiscohortmightnotindicateits prognosticperformanceinotherpopulationswithdifferent characteristics,suggestionsweremadeforpersonalized decisionsconsideringthepatient’sarrestetiology,clinical status,andtheinstitutionalcapacityandexperiences.
LIMITATIONS Therewereseverallimitationstothisstudy.Firstly, missingdataisacommonissueinretrospectivelycollected variables,andthisstudywasnoexception.Patientswith missingoutcomeswereexcludedfromthebeginning, compromisingthesizeofthecohort.Secondly,thesmall samplesizemayhaveledtohighervariability,whichmight notaccuratelyreflectthereal-worldsituation.Thirdly, neurologicaloutcomeswerenotassessedduetoa considerableamountofmissingdata.Furtherlarge-scale validationstudiesshouldbeperformedtoconductedto assesstheuniversalapplicabilityofthisscore.
CONCLUSION Inthecurrentstudycohort,theRESCUE-IHCAscoredid notpredictoutcomesbetterthantheoriginallyvalidated cohort,withlow flowdurationandinitialrhythmspersisting asconsistentpredictivefactors.Themethodofdisease categorizationinIHCApatientsandthedifferencesin hospitalexperiencemayhaveinfluencedtheseoutcomes.
Althoughthesix-factorscorecarriedsomeadvantages, significantlimitationswerepresent.Furtherresearchis neededtoexploretheimpactofhospitalexperienceand standardizeddiagnosticcriteriaforcardiacoriginIHCAon theECPRoutcomes.
Ethicscommitteeapproval:Thisresearchisapprovedby theInstitutionalReviewBoard(202306052RIND).The requirementforinformedconsentwaswaivedbecauseofthe retrospectivenature.
Availabilityofdataandmaterials:Thedatasetsusedor analyzedduringthecurrentstudyareavailablefromthe correspondingauthoronreasonablerequest.
Acknowledgments: Notapplicable.
AddressforCorrespondence:Chien-HuaHuang,MD,PhD,National TaiwanUniversityHospital,DepartmentofEmergencyMedicine, No.7,ZhongshanS.Rd.,ZhongzhengDist.,TaipeiCity100,Taiwan. Email: chhuang5940@ntu.edu.tw
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Hoetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
REFERENCES 1.SchmidtM,BurrellA,RobertsL,etal.PredictingsurvivalafterECMOfor refractorycardiogenicshock:thesurvivalafterveno-arterial-ECMO (SAVE)-score. EurHeartJ. 2015;36(33):2246–56.
2.OkadaY,KiguchiT,IrisawaT,etal.Developmentandvalidationofa clinicalscoretopredictneurologicaloutcomesinpatientswithout-ofhospitalcardiacarresttreatedwithextracorporealcardiopulmonary resuscitation. JAMANetworkOpen. 2020;3(11):e2022920.
3.KagawaE,InoueI,KawagoeT,etal.Assessmentofoutcomesand differencesbetweenin-andout-of-hospitalcardiacarrestpatients treatedwithcardiopulmonaryresuscitationusingextracorporeallife support. Resuscitation. 2010;81(8):968–73.
4.ShinTG,JoIJ,SimMS,etal.Two-yearsurvivalandneurological outcomeofin-hospitalcardiacarrestpatientsrescuedbyextracorporeal cardiopulmonaryresuscitation. IntJCardiol. 2013;168(4):3424–30.
5.ParkIH,YangJH,JangWJ,etal.Clinicalsignificanceoflow-flowtimein patientsundergoingextracorporealcardiopulmonaryresuscitation: resultsfromtheRESCUEregistry. JClinMed. 2020;9(11):3588.
6.TonnaJE,SelzmanCH,GirotraS,etal.ResuscitationusingECPR duringin-hospitalcardiacarrest(RESCUE-IHCA)mortalityprediction
scoreandexternalvalidation. JACCCardiovascInterv. 2022;15(3):237–47.
7.ChenYS,LinJW,YuHY,etal.Cardiopulmonaryresuscitationwith assistedextracorporeallife-supportversusconventional cardiopulmonaryresuscitationinadultswithin-hospitalcardiacarrest: anobservationalstudyandpropensityanalysis. Lancet. 2008;372(9638):554–61.
8.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
9.D’ArrigoS,CacciolaS,DennisM,etal.Predictorsoffavourable outcomeafterin-hospitalcardiacarresttreatedwithextracorporeal cardiopulmonaryresuscitation:asystematicreviewandmeta-analysis. Resuscitation. 2017;121:62–70.
10.GrandboisvanRavenhorstC,SchluepM,EndemanH,etal.Prognostic modelsforoutcomepredictionfollowingin-hospitalcardiacarrestusing pre-arrestfactors:asystematicreview,meta-analysisandcritical appraisal. CritCare. 2023;27(1):32.
11.OhbeH,TagamiT,OguraT,etal.Low-flowdurationandoutcomesof extracorporealcardiopulmonaryresuscitationinadultswithin-hospital cardiacarrest:anationwideinpatientdatabasestudy. CritCareMed. 2022;50(12):1768–77.
12.TonnaJE,SelzmanCH,GirotraS,etal.Patientandinstitutional characteristicsinfluencethedecisiontouseextracorporeal cardiopulmonaryresuscitationforin-hospitalcardiacarrest. JAmHeart Assoc. 2020;9(9):e015522.
13.ChenCT,ChiuPC,TangCY,etal.Prognosticfactorsforsurvival outcomeafterin-hospitalcardiacarrest:anobservationalstudy oftheorientalpopulationinTaiwan. JChinMedAssoc. 2016;79(1):11–6.
14.PatlollaSH,PajjuruVS,SundaragiriPR,etal.Hospital-leveldisparities inthemanagementandoutcomesofcardiacarrestcomplicatingacute myocardialinfarction. AmJCardiol. 2022;169:24–31.
15.DaubinC,BrunetJ,HuetJ,etal.Extracorporealcardiopulmonary resuscitationandsurvivalafterrefractorycardiacarrest:isECPR beneficial? AsaioJ. 2021;67(11):1232–9.
16.StubD,BernardS,PellegrinoV,etal.Refractorycardiacarresttreated withmechanicalCPR,hypothermia,ECMOandearlyreperfusion(the CHEERtrial). Resuscitation. 2015;86:88–94.
17.TonnaJE,SelzmanCH,GirotraS,etal.Patientandinstitutional characteristicsinfluencethedecisiontouseextracorporeal cardiopulmonaryresuscitationforin-hospitalcardiacarrest. JAmHeart Assoc. 2020;9(9):e015522.
18.OhbeH,OguraT,MatsuiH,etal.Extracorporealcardiopulmonary resuscitationforacuteaorticdissectionduringcardiacarrest:a nationwideretrospectiveobservationalstudy. Resuscitation. 2020;156:237–43.
19.RadeschiG,MinaA,BertaG,etal.Incidenceandoutcomeofin-hospital cardiacarrestinItaly:amulticentreobservationalstudyinthePiedmont Region. Resuscitation. 2017;119:48–55.
20.WangCH,HuangCH,ChangWT,etal.Prognosticperformanceof simplifiedout-of-hospitalcardiacarrest(OHCA)andcardiacarrest hospitalprognosis(CAHP)scoresinanEastAsianpopulation:a prospectivecohortstudy. Resuscitation. 2019;137:133–9.
21.WangCH,ChenYS,MaMH.Extracorporeallifesupport. CurrOpinCrit Care. 2013;19(3):202–7.
22.AbramsD,MacLarenG,LorussoR,etal.Extracorporeal cardiopulmonaryresuscitationinadults:evidenceandimplications. IntensiveCareMed. 2022;48(1):1–15.
23.BlumensteinJ,LeickJ,LiebetrauC,etal.Extracorporeallifesupportin cardiovascularpatientswithobservedrefractoryin-hospitalcardiac arrestisassociatedwithfavourableshortandlong-termoutcomes:
apropensity-matchedanalysis. EurHeartJAcuteCardiovascCare. 2016;5(7):13–22.
24.LasaJJ,RogersRS,LocalioR,etal.Extracorporealcardiopulmonary resuscitation(E-CPR)duringpediatricin-hospitalcardiopulmonary arrestisassociatedwithimprovedsurvivaltodischarge:a reportfromtheamericanheartassociation’sgetwiththe guidelines-resuscitation(GWTG-R)registry. Circulation. 2016;133(2):165–76.
25.GravesteijnBY,SchluepM,DisliM,etal.Neurologicaloutcomeafter extracorporealcardiopulmonaryresuscitationforin-hospital cardiacarrest:asystematicreviewandmeta-analysis. CritCare. 2020;24(1):505.
EDUCATION SPECIAL ISSUE:BRIEF EDUCATIONAL ADVANCES TeachingtheNewWays:ImprovingResidentDocumentation fortheNew2023CodingRequirements NathanZapolsky,MD*
AnnemarieCardell,MD†
RiddhiDesai,DO*
StaceyFrisch,MD,MSEd‡
NicholasJobeun,DO,MSEd§
DanielNovak,DO*
MichaelSilver,MS*
ArleneS.Chung,MD,MACM∥
*MaimonidesMedicalCenter,DepartmentofEmergencyMedicine, Brooklyn,NewYork
† EmoryUniversityHospital,DepartmentofEmergencyMedicine,Atlanta,Georgia ‡ NewYorkUniversity,GrossmanSchoolofMedicine,NewYork,NewYork
§ IcahnSchoolofMedicineatMountSinai,NewYork,NewYork
∥ UniversityofVermontMedicalCenter,Burlington,Vermont
SectionEditor: BenjaminHoldenSchnapp,MD
Submissionhistory:SubmittedJune1,2024;RevisionreceivedJune12,2024;AcceptedJuly8,2024
ElectronicallypublishedSeptember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21183
BACKGROUND InJanuary2023,significantchangestothestructureofthe CurrentProceduralTerminologyCPT(R)evaluationand management(E/M)codes(hereforwardcalledthe2023E/M changes)wereimplementedforemergencydepartment(ED) encounters.Thesemodificationsaimtolessenadministrative workloadandaccuratelymatchcodingwithcontemporary patientcarepractices.1 Theyareanticipatedtoimpact roughly85%oftherelativevalueunitsofEDcare2 and,thus, alsohavesignificant financialimplicationsforEDs. Residentsprovidefront-linecareanddocumentationfor millionsofpatientsseeninUnitedStatesEDsannually.The ModelofClinicalPracticeofEmergencyMedicine3 identifies financialprinciples,suchasbillingandcoding,toberequired corecontentforboardcertification.Furthermore,the AccreditationCouncilforGraduateMedicalEducation (ACGME)includesqualityclinicaldocumentationtobeone ofthemilestonesthatdetermineadvancementinresidency training.4 Interventionsthatalleviatedocumentationburden arealsoassociatedwithimprovedphysicianwell-beingper theexistingliterature.5 However,researchsuggeststhatmost emergencymedicine(EM)residentsdonotreceiveformal traininginbillingandcodingandhaveknowledgegapsin thisarea.6–8
Historically,documentationofencountersintheED focusedonthenumberofelementswithinhistoryofpresent illness(HPI),reviewofsystems(ROS),physicalexam(PE), andmedicaldecision-making(MDM).Thesenewcoding guidelinesshiftthefocusalmostentirelytoMDM.They emphasizedocumentationofdifferentialdiagnoses; independentinterpretationofmedicaltesting;justificationof testingnotpursued;socialdeterminantsofhealth;chronic diseases;histories;communicationwithconsultants,
ancillarystaff,andprimarycare;andreviewof externalrecords.
OBJECTIVES Wesoughttoimproveresidentunderstandingofand compliancewiththe2023E/Mchanges.Objectivesincluded identificationofthekeyelementsrequiredateachE/Mlevel, chartingandreceivingfeedbackofsampleencounters,and appreciationfortheimportanceofaccurateandhigh-quality documentation.Wesecondarilysoughttoinvestigate whetherourinterventionimprovedresidentwellness specificallyviabenefitsinconfidencetoperformaccurateand expeditiousdocumentationandcompletionofchartingina timelymanner.
CURRICULARDESIGN OurcurriculumwasdevelopedusingKern’ssix-step approachtocurriculumdesign9 asapartoftheeducational qualityimprovementprocessatasingleEMresidency programbasedatasingle,large,tertiary-care,urbanhospital withanapproximateannualEDpatientcensusof110,000 fromOctober1,2022–February28,2023.Priortostudy initiationaneedsassessmentwasperformed.Key stakeholdersindepartmentalbillingandcodingwere identifiedandinterviewed,andrelevantliteraturewas reviewed.1–10 Thisincludedthehospitalchiefmedical informationofficer,EDvicechair,andbillingandcoding leadership.Theinterviewsrevealedasharedopinionthat oftenthedocumentationtoreachtheappropriateexpected levelofservice(4or5)waslackingtosupportthatlevelof billingandmostofthatdocumentationshouldbecapturedin theMDMportionofthenote.Thus,theMDMportionof thenotewastargetedfortheintervention.
Oureducationalmethodsprimarilyusedin-person, flipped-classroomsessions.Wedecidedtousea flippedclassroomapproachforseveralreasons:1)toallowresidents togainexposuretothenewbillingcriteriapriortotheinpersonsessions;2)asamechanismtoassessresident understandingandskills,bothindividuallywithhomework responsesaswellasinagroupsetting;and3)tousefaculty’ s in-persontimeforoversightandfeedback.11 Wealsoapplied aspacedlearningapproachtomaximizeknowledge acquisitionandretention.12 Thesessionswereheldon December14,21,and28,2022.
Forpre-sessionhomeworkeachweek,allresidentswere providedasamplepatientHPI,ROS,andPEcomponents. Alllearnerswereprovidedthesamecase,andcaseswere changedeachweek.Caseswereformulatedtoinclude elementsthatcouldbeexpandeduponintheMDM, Residentswerealsoprovidedwiththe “CPTEvaluationand Management(E/M)CodeandGuidelineChanges” document.10 TheywerethenaskedtocreateanMDM sectioninaccordancewiththeabovedocument.Homework responseswerereviewedbyfaculty,andfeedbackwasgiven individuallyviaemail.Writtenfeedbackforresidentswas generatedusingatemplatebasedlargelyonthe2023E/M guidelineschanges.10 AnideallydocumentedsampleMDM sectionwasalsosuppliedforreference(Supplement1).13
Duringeach30-minutesession,residentsweredivided intosmallgroupsoffourandprovidedanexamplepatient case,whichincludedonlytheHPI,ROS,andPE components.ResidentsthencollaborativelywroteanMDM sectionforthecase.Allgroupswereprovidedthesamecase, andcaseswerechangedeachweektofocusondifferent aspectsoftheMDMsection.Eachsmallgroupofresidents sharedtheirresponsewiththelargergroupandwere providedpeerfeedbackundertheguidanceofafaculty facilitatorselectedfortheiradvancedknowledgeineither educationoroperations.Facilitatorswereprovidedin advancewithanexampleofanideallydocumentedMDM section,whichresidentswerealsoprovidedwithatthe conclusionoftheexercise.
IMPACT/EFFECTIVENESS Weemployedapre-postinterventionalstudydesignusing aconveniencesampleofresidents,inwhichgroup assignmentwasbasedonthenumberoftrainingseach residentcouldattendduetoschedulingfactorsoutsidethe scopeofthisstudy.Thisstudywasdeterminedtobeexempt bytheinstitutionalreviewboardofMaimonidesMedical Center.Participationwasvoluntaryandanonymous.We evaluatedtheimpactofourbriefeducationalinterventionon subjectivemeasuresofEMresidentknowledge,skills,and attitudesviasurveyandonobjectivemeasuresofskillsand behaviorsbyassessingaggregatechartdata.
Surveysweredevelopedthroughagroupiterativeprocess thatincludedoneauthor(ASC)withexpertiseinsurvey
designmethodology.RedCap,14,15 hostedat[Maimonides MedicalCenter]wasusedtoanonymouslydistributeboth pre-andpost-interventionsurveys.Bothsurveysconsistedof sixLikert-scalequestions,threeregardingtheirreporteduse ofdocumentationshortcuts,andthreeassessingattitudes abouttheirownunderstandingofandpredictedskillwiththe newE/Mcodingchanges.Sixadditionalmultiple-choice questionsassessedknowledgeaboutdocumentationrules.A finalquestionwasforfeedbackandrequestedideasforother E/Mbillingandcodingeducation.Thepre-intervention survey,distributedNovember30,2022,differedfromthe post-interventionsurveyofDecember28,2022, onlyinaskingtheself-reportednumberofsessions attended.(Supplement2).
Residentskillswereassessedusingactualclinical documentation.ResidentaggregateE/Mlevelswereassessed acrossthreemonthspre-intervention(October1–December 31,2022)andtwomonthspost-intervention(January 1–February28,2023).Duetovariationinresidentclinical schedules,wechosetheabovetimeperiodstocapturethe greatestproportionoftheEDencountersdocumentedby residents.WeusedtheKirkpatrickmodeltoevaluateour intervention’simpact.16 Surveyswereusedtoassessresident subjectivereactions,andobjectiveknowledgeby identificationofbillableelementsinaprovidedsample MDM.Weusedactualclinicaldocumentationtoassess changesinbehavior.Specifically,weassessedwhether traineeshadastatisticallysignificantincrease(P < 0.05)in theproportionofE/Mlevel5charts(99285)andlikewisea significantdecreaseinlevel1,2,3,and4charts(99281, 99282,99283,99284).
Weuseddescriptivestatisticsandcomparisonofmeans withtheMann-WhitneyUteststratifiedbynumberof educationalsessionsattendedtoanalyzesignificant differencesinknowledgeandattitudesbeforeandafterthe intervention.Forknowledge,thesecalculationswere summarizedwithmedianandinterquartilerange(IQR)and comparedacrosstimeperiodsusinganexactWilcoxon signed-ranktest.ABonferronicorrectionforthesignificance oftheinterventionchangesthealphato0.01667.Foreach chartlevel(99281–99285),wecreatedlogisticregression modelsusinggeneralizedestimatingequationsforindividual repeatedmeasurestoaccountforpersonalvariability.The numberofattended flipped-classroomsessionswastreatedas theindependentvariable.Zerotrainingswereconsideredto bethepre-periodforanalysis.Allanalysesconsidered alpha ≤ 0.05tobestatisticallysignificantandwereconducted usingSPSSv28.015 (SPSSStatistics,IBMCorp, Armonk,NY).
Forty-sixofthe54EMresidents(85%)eligibleforthe studycompletedbothpre-andpost-interventionsurveys.All 54residentsparticipatedinatleastonesurvey.Duetoclinical schedules,someresidentswerenotpresentatoneormoreof thethreeofferedsessions.The firstlivesessionwasattended
by33(61%)residents,thesecondby38(70%),andthethird by40(74%).Six(11%)residentsattendedonesession, 15(28%)attendedtwosessions,and25(46%)attendedthree sessions.Eight(15%)didnotattendanysessions.
Residentsdemonstratedasignificantimprovementin knowledgeregardingwhichelementsarethekeytothe MDMwithinthe2023E/Mchanges[6(5–6.5)to8(7.5–8) P < 0.001],andbycorrectlyidentifyingthenumberand complexityofproblems,complexityofdata,risklevel,and theoverallcomplexityofasampleencounter.Therewasno statisticallysignificantimprovementinidentificationofthe importantcodingelements(4[3–5]to5[3.5–5], P = 0.38). Residentsalsoendorsedgreaterconfidenceintheirability todescribe(2[1–3]to4[3–4], P < 0.005),accurately document(3[2–3]to4[3–4], P < 0.005),andbill(2[2–3]to3 [2–3] P < 0.005).Therewerenosignificantchangesintheir opinionoftheirabilitytocompletetheirchartsinatimely manner(P < 0.19,CI0.165–0.215)inthedecisiontouse dictationsoftware(P = 1),shortcuts(P = 1),orcustom preparedtextphrases(P = 1)followingtheintervention. Residentsparticipatinginanynumberof flipped-classroom sessionsshowedsignificantchangesintheirskills,including anincreaseinE/MLevel5codedcharts,andasignificant decreaseinLevel1,2,and3codedcharts(P < 0.005).The increaseinLevel5chartsanddecreaseinLevel3chartswere significantafterjustonesession(Figure).Nosignificant changewasobservedinLevel4charts.
Tothebestofourknowledge,thisisthe first studytodate todescribetheimpactofaneducationalinterventiononEM residentdocumentationknowledge,skills,andattitudes withintheframeworkofthe2023E/Mchanges.Naturally, ourexperienceandresultsatoursingleEMresidency
programbasedatalarge,urban,tertiary-carehospitalmay notbegeneralizable.Thisinterventiondataissinglecenter andpreliminary,andtheinterventionshouldundergo repetitionandcomparisonbefore firmconclusionscan bedrawn.
Wechosetocollectdataduringatimerangetiedtothe sameillnessseasontokeepthecaseacuitymixandattending/ residentstaffingcomparable.Weotherwisecouldhave comparedtothesamemonthsofthepreviousyearforpreinterventiondata,tobestmatchtheillnessseason,or alternatively,post-interventiondatacouldhavebeendrawn insteadfromthefollowingyear(2024)tohelpmitigate recencybiasintheinterventiongroup.Thatbeing said,themajordifferencesinresidentandattending staffingbetweentimesayearapartcouldalsohave confoundedresults.
Weconsideredfacultysupplementaldocumentationand itseffectondocumentationoutcomesduringourstudy designandtookapragmaticapproach.Forthedurationof thisstudytheattendingpopulationwasstable,nosignificant changestoattendingeducationwereperformedduringthis period,andattendingstaffingremainedatbaselinewithno changestoratios,shiftdurations,orstandarddistributionsof encountersthroughouttheEDcareareas.Tofurtheraddress thisconcernweattemptedanalysisoftheattending distributionbetweenthesevariousgroups.Noattendinghad agreaterthan1.4%changeintheirbillingfrompre-topostintervention,andtheirsmallcontributionstotheoverall billingforeachinterventiongroupwas,therefore,unlikelyto havebiasedthelargedifferencesseenbetweengroups. However,thedifferencesindistributionofattendingshifts betweenthegroupsvariedstatisticallysignificantly,andbias
Figure. ProportionofeachCurrentProceduralTerminologyevaluationandmanagementlevelbynumberofeducationalsessionsattended.
cannotbeassessedwithoutpatient-levelbillingrecords.This couldbeconsideredinfuturestudies.
Ourprogrammayhaveimplicationsregardingwellnessas well.Residencytrainingmustprepareemergencyphysicians forallaspectsoftheireventualprofessionalexpectations. Residentsreceivingeducationexpressedgreaterconfidence intheirabilitytodescribe,accuratelydocument,andbillfor careprovided.Businessliteraturefrequentlynoteshowalack ofclearexpectationsincreasesworkstressandharms employeewellnessandproductivity.18 However,whether thisassociationappliestoemergencyphysiciansdeserves furtherstudy.
CONCLUSION Overall,weobservedsignificantimprovementsinresident knowledge,attitudes,skills,andbehaviorsregardingclinical documentation.Wehopetoapplythesesuccessesandlessons learnedtotheformationofenduringeducationmaterialsat ourowninstitutionfordocumentationimprovementfor bothresidentsandattendings.
AddressforCorrespondence:NathanZapolsky,MD,Maimonides MedicalCenter,DepartmentofEmergencyMedicine,4802Tenth Ave.,Brooklyn,11219NY.Email: nizapo@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Zapolskyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.ThoughtLeadershipTeam.2023E/Mcodingchanges.2023.Available at: https://www.aapc.com/resources/evaluation-management-codingchanges-2023.AccessedAugust18,2023.
2.McKenzieDAandGranovskyMA.2023documentationguideline changesforEDE/Mcodes99281–99285.2022.Availableat: www. acepnow.com/article/2023-documentation-guideline-changesfor-ed-e-m-codes-99281-99285/.AccessedJanuary25,2023.
3.BeesonMS,BhatR,BroderJS,etal.The2022modelofthe clinicalpracticeofemergencymedicine. JEmergMed. 2023;64(6):659–95.
4.CooneyRR,MuranoT,RingH,etal.Theemergencymedicine milestones2.0:settingthestagefor2025andbeyond. AEMEducTrain. 2021;5(3):e10640.
5.NguyenO,JenkinsN,KhannaN,etal.Asystematicreviewof contributingfactorsofandsolutionstoelectronichealthrecord-related impactsonphysicianwell-being. JAmMedInformAssoc. 2021;28(5):974–84.
6.RomansB,NguyenE,BiddleM,etal.Billingandcoding:disparitiesin healthcareprovidertraining. JAlliedHealth. 2022;51(1):43–6.
7.DawsonB,CarterK,BrewerK,etal.Chartsmart:aneedfor documentationandbillingeducationamongemergencymedicine residents? WestJEmergMed. 2010;11(2):116–9.
8.ChinS,LiA,BouletM,HowseK,etal.Residentandfamilyphysician perspectivesonbilling:anexploratorystudy. PerspectHealthInf Manag. 2022;19(4):1g.
9.ThomasPA,KernDE,HughesMT,etal. CurriculumDevelopmentfor MedicalEducation:ASix-stepApproach,3rded.Baltimore,MD:The JohnsHopkinsUniversityPress,2015.
10.AmericanMedicalAssociation.CPT® evaluationandmanagement (E/M)codeandguidelinechanges.2022.Availableat: https://www. ama-assn.org/practice-management/cpt/cpt-evaluation-andmanagement.AccessedMarch24,2024.
11.RotellarCandCainJ.Research,perspectives,andrecommendations onimplementingthe flippedclassroom. AmJPharmEduc. 2016;80(2):34.
12.WeidmanJandBakerK.Thecognitivescienceoflearning:concepts andstrategiesfortheeducatorandlearner. AnesthAnalg. 2015;121(6):1586–99.
13.AllenA.Medicineclerkship(inpatient)H&Pexamples:H&P5.2018. Availableat: https://www.med.unc.edu/medclerk/wp-content/uploads/ sites/877/2018/10/hp5.pdf.AccessedFebruary24,2024.
14.HarrisPA,TaylorR,ThielkeR,etal.Researchelectronicdatacapture (REDCap) – ametadata-drivenmethodologyandworkflowprocessfor providingtranslationalresearchinformaticssupport, JBiomedInform. 2009;42(2):377–81.
15.HarrisPA,TaylorR,MinorBL,etal.TheREDCapconsortium:building aninternationalcommunityofsoftwarepartners, JBiomedInform. 2019;95:103208.
16.KirkpatrickDL. EvaluatingTrainingPrograms:TheFourLevels SanFrancisco,CA:Berrett-KoehlerPublishersInc,1994.
17.IBMCorp.IBMSPSSStatisticsforWindows,Version28.0.2021. Armonk,NY:IBMCorp.
18.BornsteinJ.Howalackofclearexpectationsleavesemployeesanxious andadrift.2023.Availableat: https://www.forbes.com/sites/ forbescoachescouncil/2023/06/05/how-a-lack-of-clear-expectationsleaves-employees-anxious-and-adrift/?sh=70de0f8f5983 AccessedApril23,2024.
TelesimulationUseinEmergencyMedicineResidencyPrograms: NationalSurveyofResidencySimulationLeaders MaxBerger,MD,MEHP*
JackBuckanavage,MD†
JaimeJordan,MD,MAEd*
StevenLai,MD*
LindaRegan,MD,MEd‡
*UniversityofCaliforniaLosAngeles,DavidGeffenSchoolofMedicine, DepartmentofEmergencyMedicine,LosAngeles,California
† MountSinaiSchoolofMedicine,DepartmentofEmergencyMedicine, NewYork,NewYork
‡ JohnsHopkinsUniversity,DepartmentofEmergencyMedicine,Baltimore,Maryland
SectionEditors: KendraParekh,MDandBenjaminHoldenSchnapp,MD
Submissionhistory:SubmittedJune14,2024;RevisionreceivedSeptember20,2024;AcceptedSeptember26,2024
ElectronicallypublishedOctober22,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.24863
Introduction: Coronavirus2019(COVID-19)acceleratedtheneedforvirtuallearningincluding telesimulation.Manyemergencymedicine(EM)programshaltedin-personsimulationandtrialed telesimulation,butspecificsonitsutilizationandplansforfutureuseareunknown.Telesimulationhas beendefinedas “aprocessbywhichtelecommunicationandsimulationresourcesareutilizedtoprovide education,training,and/orassessmenttolearnersatanoff-sitelocation.” Ourobjectiveinthisstudywas todescribethepatternsoftelesimulationusageinEMresidencyprogramsduringCOVID-19-induced learningrestrictionsaswellasitsanticipatedfutureutility.
Methods: WeidentifiedEMsimulationleadersviatheEMRAMatchwebsite,institutionalwebsites,or personalcontactwithresidencycoordinatorsanddirectors,andinvitedthemtoparticipatebyemail. Participantscompletedaconfidential,web-basedsurveyconsistingofmultiple-choiceitemsandone free-responsequestion,developedbyourstudyteamwithconsiderationofsurveyresearchbest practicesandMessick’svalidityframework.WecollecteddatabetweenJanuary–February2022.We calculateddescriptivestatisticsformultiple-choiceitemsandexaminedthefree-responseanswersfor commonthemes.
Results: Weobtainedcontactinformationforsimulationleadersat139EMresidencyprograms.Survey responseratewas65%(91/139).Duringin-personrestrictions,62%(56/91)ofprogramsused telesimulation.Assumingallrestrictionslifted,38%(34/90)ofrespondentsplannedtocontinuetouse telesimulation,comparedto9%(8/91)usingtelesimulationbeforeCOVID-19.Mostrespondents plannedtousetelesimulationformedicalknowledge(26/34,76%)andcommunication/teamworkfocusedcases(23/34,68%).Inresponsetothefree-responsequestionregardingexperiencewithand plansforuse,weidentifiedthreemajorthemes:1)telesimulationisavaluablealternativetoin-person learning;2)telesimulationisanoptionforlearnersunabletoparticipateinperson;and3)telesimulationis challengingforproceduraleducation.
Conclusion: DespitetherelativelylimiteduseoftelesimulationinEMresidenciespriortoCOVID-19,an increasednumberofprogramshaveplanstocontinueincorporatingtelesimulationintotheircurricula. Thisplanforcontinueduseopensopportunitiesforfurtherinnovationandscholarshipwithinsimulation education.[WestJEmergMed.2024;25(6)907–912.]
INTRODUCTION Restrictionsimposedonin-personeducationduringthe coronavirus2019(COVID-19) pandemicacceleratedtheneed forvirtuallearning,includingtelesimulation.1,2 Telesimulation hasbeendefinedas “aprocessbywhichtelecommunication andsimulationresourcesareutilizedtoprovideeducation, training,and/orassessmenttolearnersatanoff-sitelocation.”3 Initialapplicationswereinlowerresourcesettingssuchas developingcountrieswherelearnersdidnothaveaccessto simulationcentersorinstructors.4,5 Withintelesimulation, differentmodalitieshavebeendescribedthatvaryin fidelityas wellaslocationofthelearnersandinstructorsrelativetoeach otherandthesimulationcenter.6–8
Severalpublishedarticlessinceearly2020havedescribed differentinstitutions’ approachestotelesimulationsincethe pandemic.1–2,9–13 Commonthemesincludetheneedtomodify learningobjectivestovirtualenvironmentsandtoselectthe appropriatemodalityoftelesimulationbasedoninstitutional needsandresources.9–12 Differentmodalitiesoftelesimulation havebeendescribed,includingthefollowing:1)learners virtuallyobservinganddebriefingalivesimulation7; 2)learnerspresentwithamanikinwhileinstructorsfacilitate fromaseparatelocation6;3)instructorspresentwitha manikinwhilelearnersremotelyparticipate7;and 4)completelyremoteoptionwherelearnersandinstructors bothparticipateremotelyfromseparatelocations.10,11
Limiteddatacomparingtelesimulationvstraditional simulationsuggeststhatlearnersatisfactionwith telesimulationorhybridvirtualandin-personsimulationis similar,althoughthiswasnotfoundinallstudies.7,13,14
Ascopingreviewfrom2021highlightedthemixeddataon studentperceptionoftelesimulation,withsomeofthe includedstudiesindicatingremotefacilitationofsimulation beingperceivedasequallyormoreeffectivethanlive facilitation,whileothersfoundremotefacilitationtobe inferior.14 Facilitatorperceptionoftelesimulationhasnot beenwellstudied.Limitedlearningoutcomedatahas suggestedsimilarimprovementsbetweenin-person simulationandtelesimulation.8,14
Ourobjectiveinthisstudywastodescribethepatternsof telesimulationusageinemergencymedicine(EM)residency programsduringCOVID-19-induced,in-personlearning restrictionsaswellasitsanticipatedutilitymovingforward. Thisinformationiscrucialtounderstandingthevalueof telesimulationanditsutilityinmedicaleducation.
METHODS StudyDesign,Setting,andPopulation
Weconductedacross-sectionalsurveystudyoffacultyin chargeofsimulationforEMresidencyprogramsinthe UnitedStates.WecollecteddatafromJanuary–February 2022.AfteridentifyingEMresidencyprogramsandtheir websitesfromtheEMRAMatchdatabase,15 wesearched eachwebsiteforcontactinformationforthedirectorof
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
COVID-19acceleratedtheneedforvirtual learningincludingtelesimulation.
Whatwastheresearchquestion?
Towhatextendwastelesimulationusedby EMresidenciesduringCOVID-19,andwhat isitsanticipatedutilitymovingforward?
Whatwasthemajor findingofthestudy?
Only9%(8/91)ofprogramsusedtelesimulation beforeCOVID-19.DuringCOVIDrestrictions, 62%(56/91)ofprogramsusedit,whileafter limitationswerelifted,38%(34/90)plannedto continuetelesimulation.
Howdoesthisimprovepopulationhealth?
Asanadjuncttotraditionalin-person simulationcurriculum,telesimulationisa viableoptiontoimprovemedicalknowledge andcommunication-basedcompetencies.
simulationeducation.Iftherewasnodirectordesignated,we emailedeachresidency’sprogramcoordinatorand/or directoraskingforcontactinformationforthefacultyin chargeofresidencysimulation.Eachprogramwasallowed onlyonedesignatedparticipant.Thisstudywasgivenexempt statusbytheUniversityofCalifornia,LosAngeles InstitutionalReviewBoard(IRB#21-001336)andtheJohns HopkinsUniversityHomewoodIRB(HIRB00013694).
SurveyDevelopmentandDissemination Giventhelackofanypreviouslycreatedsurveyapplicable tothisconstruct,theprimaryauthor(MB)developedawebbasedsurveytoolwithconsiderationofsurveyresearchbest practicesandMessick’svalidityframework.16–19 Forcontent validityevidence,we firstperformedaliteraturereview,and theauthorgroupofexpertsimulationeducatorsandmedical educationresearchersreviewedthesurveyforclarityand relevancetotheconstruct.Wedefinedtelesimulationas includinganysimulationactivitywhere “telecommunication andsimulationresourcesareutilizedtoprovideeducation, training,and/orassessmenttolearnersatanoff-site location.”3 Wepilotedthesurveywithagroupofsimulation educatorswhowerenotincludedinthetargetsampleto gatherresponseprocessvalidityevidence.Afterpiloting,we revisedthesurveyforclarity.The finalsurveyincluded multiple-choiceitemsandonefree-textresponse item(Appendix1).
Weinvitedparticipantsbyemailandsenttwotargeted, follow-upinvitationstonon-respondersatbi-weekly intervals.WeadministeredthesurveyviaQualtrics (Qualtrics,LLC,Provo,UT).Noindividualidentifying informationwascollected.Tomaximizeresponserateand minimizeguessing,wedidnotrequireparticipantsto completeallsurveyitems.Participantswerenot compensatedforparticipatinginthestudy.
DataAnalysis Wecalculatedandreporteddescriptivestatisticsforitems withdiscreteanswers.Weconductedcalculationsusing QualtricsandMicrosoftExcelforMac(MicrosoftCorp, Redmond,WA).Weexaminedtheanswerstothefree-text responsestoidentifycommonthemesthatwouldbroadenthe reader’sunderstandingofthedata.Successivewaveanalysis wasperformedtoassesstheextentofpossiblenonresponse bias.20 Weexaminedwhetheruseoftelesimulationduringthe pandemic,plannedfutureuseoftelesimulationafterinpersonrestrictions,andrespondentprogramformat (postgraduateyears[PGY]1–3vs1–4)differedbywave. Bivariatechi-squaretestsforeachvariableofinterestby wavewereperformedusingMicrosoftExcelforMac,and P -valueslessthan0.05wereconsideredstatisticallysignificant. Weusedtheconsensus-basedchecklistforreportingofsurvey studies(CROSS)asreportingguidelines(Appendix2).23
RESULTS Of139simulationleadersweidentified,91(65%) completedthesurveywith87(63%)completingallitems.We reportdemographicdataforsurveyrespondentsin Table1, whilerespondents’ experienceandperceptionsof telesimulationareshownin Table2.PriortotheCOVID-19 pandemic,9%(8/91)ofsurveyrespondentswereusing telesimulationintheircurricula.Therewasawidevarietyof priorexperienceswithtelesimulation,withthemostcommon beingthattheyhadheardoftelesimulationbutneverbeen involved(44%).Ninety-twopercent(84/91)ofrespondents reportedthattheirinstitutionprohibitedin-personlearning activitiesatsomepointduringtheCOVID-19pandemic. Duringin-personlearningrestrictions,62%(56/91)used telesimulationinsomeform.
Whensurveyrespondentswereaskedaboutwhat format(s)oftelesimulationwereused,11%(10/90)statedthat theyonlyusedacompletelyvirtualoral-boardsstyleformat, whiletherestofthosewhousedtelesimulationreportedusing ahybridorvirtualformatinvolvingapatientmonitorand/or manikin.Thelargestpercentageofsurveyrespondentsfelt thatmedicalknowledgeandcommunication/teamworkfocusedcaseswerebestsuitedfortelesimulation(72%and 47%respectively),whilemostfeltthatproceduretraining wasnotwellsuitedfortelesimulation(62%).Thirty-eight percent(34/90)ofrespondentsstatedtheyplannedtouse telesimulationinsomeformintheircurriculummoving
Table1. Surveyrespondentdemographics. n(%)
Formatofrespondent’s current residencyprogram
PGY1–362/89(70%)
PGY1–427/89(30%)
Sizeofrespondent’scurrentresidencyprogram (totalnumberofresidentsinallyears)
≤20residents11/90(12%)
21–40residents38/90(43%)
41–60residents31/90(34%)
≥60residents10/90(11%)
Respondent’scurrentresidencyprogram primaryinstitutionsetting
University-based58/90(64%)
Community-based28/90(31%)
County-based13/90(14%)
Priorsimulationtrainingofsurveyrespondent
Fellowshiptraininginsimulation31/90(34%)
Non-fellowshiptraininginsimulation48/90(53%)
Noformaltraininginsimulation17/90(19%)
Respondentyearssinceresidencygraduation
≤522/90(24%)
6–1033/90(37%)
11–1516/90(18%)
16–208/90(9%)
≥2111/90(12%)
PGY, postgraduateyear.
forward,mostlyformedicalknowledgeandcommunication/ teamwork-focusedcases(76%and68%,respectively).
Wereceived14free-textresponses,andidentifiedthree majorthemes,describedbelowwithexemplarquotes.
1.Telesimulationisavaluablealternativeto in-personlearning: “Ithasbeenthe ‘betterthannothing’ optionbutaccepted bylearnerswhenotheroptionsarenotfeasible.” “Ithasexceededexpectationsinhowhelpfulithasbeen.”
2.Telesimulationisanoptionforlearnersunableto participateinperson:
“Wefoundthatit’sagreatoptionforresidentswith familiesorwhohaveotherextenuatingcircum-stances whytheycan’tparticipateinperson,ie,breastfeeding moms,newparents,eldercare,etc.Manyofour residentswhoarebetweennightsorbetweenmidshiftswilllogonandparticipate.”
3.Telesimulationischallengingforproceduraleducation: “Difficulttolearnmusclememoryforhighacuity,low occurrenceskills.”
Table2. Keysurveyresults. n(%)
EMresidencyprogramuseoftelesimulation
Prior toCOVID-19pandemic 8/91(9%)
Duringin-personlearningrestrictions56/91(62%)
Planneduseafterin-personrestrictionslifted34/90(38%)
DuringanypointintheCOVID-19pandemic, didyourinstitutionprohibitin-person learningactivities?
Yes 84/91(92%)
No 7/91(8%)
Experiencewithtelesimulationprior toCOVID-19
Hadneverheardoftelesimulation 17/91(19%)
Heardoftelesimulationbutneverinvolved40/91(44%)
Attendedapresentation 20/91(22%)
Participatedasaninstructor 19/91(21%)
Participatedasalearner 6/91(7%)
Conductedaresearchproject 5/91(5%)
Readapaperabouttelesimulation 16/91(18%)
Formatsoftelesimulationusedduring COVID-19restrictions
Completelyvirtual;utilizingreal-timepatient monitorand/ormanikin 21/90(23%)
Completelyvirtual;oralboardsstylecases31/90(35%)
Hybrid;instructor,learnersand/orsimtechin simcenterwhileothersremote 31/90(35%)
Whatsimulationactivitieswerebestsuited fortelesimulation?
Medicalknowledgefocusedcases 65/90(72%)
Communication/teamworkfocusedcases42/90(47%)
Procedurefocusedcases 5/90(6%)
Dedicatedproceduretraining 2/90(2%)
Proceduretrainingonhomemademodels10/90(11%)
Whatsimulationactivitieswerenotwellsuited fortelesimulation?
Medicalknowledgefocusedcases 0/87(0%)
Communication/teamworkfocusedcases18/87(21%)
Procedurefocusedcases 52/87(60%)
Dedicatedproceduretraining 54/87(62%)
Proceduretrainingonhomemademodels23/87(26%)
Percentoffuturesimulationcurriculum involvingtelesimulation
0%ofthecurriculum 56/90(62%)
1–25%ofthecurriculum 30/90(33%)
26–50%ofthecurriculum 3/90(3%)
51–75%ofthecurriculum 1/90(1%)
76–100%ofthecurriculum 0/90(0%)
(Continued onnextcolumn)
Table2. Continued. n(%)
Typesoffuturesimulationactivitiesforthose who plantocontinueusingtelesimulation
Medicalknowledge-focusedcases 26/34(76%)
Communication/teamwork-focusedcases23/34(68%)
Procedurefocusedcases 7/34(21%)
Dedicatedproceduraltraining 5/34(15%)
Proceduretrainingonhomemademodels5/34(15%)
EM, emergencymedicine.
“Proceduraltrainingwasthemostdifficulttosimulate viatelesim.”
Forthewaveanalysis,thestudyincluded91respondents, including42inwave1(46%),21inwave2(23%),and28in wave3(31%).Resultsoftheexaminedsurveyquestionsdid notstatisticallydifferbywavewithall P -values > 0.05.
(See SupplementalTable.)
DISCUSSION DespiterelativelylowuseoftelesimulationwithinEM programspriortotheCOVID-19pandemic,wefoundthat manyEMresidencyprograms(62%)quicklyadaptedtoinpersonlearningrestrictionsbyusingtelesimulation.While notallprogramsthattrialedtelesimulationplantocontinue itsuse,38%ofrespondentprogramsdoplantocontinueto usetelesimulation,comparedto9%ofprogramsusing telesimulationpriortoCOVID-19.Thisrepresentsalarge increaseintheoverallusageoftelesimulationwithinEM residencies.Ourstudyalsoshedslightonhowtelesimulation canbenefitEMprograms.Beingabletoincreaselearner participationtoincluderesidentswithfamilyobligationsor betweennightshiftscouldallowforincreasedreturnon investmentforsimulationresourcesandfacultytime.Most respondentswhoplantocontinuetousetelesimulation reportedthattheywilluseitasasmallpercentageoftheir overallsimulationcurriculum,whichhighlightsthat telesimulationisnotreplacingin-personsimulationbut augmentingthetraditionalcurriculum.Thiscouldbeina hybridformatthatallowsforincreasedparticipation,oras partofseparatetelesimulationdaysthatcouldreducethe travelburdensonlearnersandinstructors.
Therewaslargevariationinhowprogramsconducted telesimulationduringin-personrestrictions.Thisisinline withpriorliteratureandlikelyreflectsindividualprogram needs,preferences,andavailableresources.1,2,8–11,13,22 Most describedtelesimulationasbestsuitedformedicalknowledge andcommunication/teamwork-focusedcases,ratherthan forprocedureteaching.Thisisinterestinggiventhatearly descriptionsoftelesimulationintheliteraturemostly
involvedproceduralteaching.5,6 Onepossibleexplanation forthisdiscrepancyisthatthoseearlystudiesinvolved duplicatesimulatorsatremotelocations,anexpensethatis likelynotpractical,ornecessary,foraresidencyprogram giventheabilitytohostproceduretrainingaspartofthe in-personcurriculum.Whileitisapparentthatthereare increasedplansfortheuseoftelesimulationcomparedtothe pre-pandemicera,notallresidencyprogramswhoused telesimulationduringtimesofin-personrestrictionsare planningtocontinuetodoso.Thereasonsforthisare unknownbutmayrelatetotelesimulationresource availabilityorlimitedoutcomedataonitsutility.
Basedonourresults,webelievethattelesimulationcan continuetobeavaluableadditiontothetraditionalinpersonsimulationcurriculum,particularlyinallowingfor increasedparticipationoflearnersandinstructors,reducing resourcecostssuchassimulationcenterandstafftime,and allowingforaviableoptiontopracticemedicalknowledge andcommunication-basedcompetencies.Nowthat telesimulationhasbeenestablishedasaninstructional strategythatwillcontinuetobepartofmanyEMresidency curricula,itopensopportunitiesforfutureinnovationand scholarshipwithinsimulation-basedmedicaleducation. Additionalinvestigationcouldcomparedifferentmodalities oftelesimulationonobjectivelearningoutcomes.23 Itwould alsobeinterestingtoexploretheroleofvirtualand augmentedrealitywithintelesimulation.24,25
LIMITATIONS Despitemultipleattempts,wewerenotabletoobtain contactinformationforasimulationleaderfromallEM programs.However,thebreakdownofPGY1–3vsPGY1–4 programsofsurveyrespondents(70%PGY1–3vs30%PGY 1–4),approximatingtheactualdistributionoftheEM residencyprograms(81%PGY1–3vs19%PGY1–4), suggeststhatthesamplecloselyresemblesthatofthe population.8 Givenourresponserateof65%,itispossible non-responsebiasaffectedourresults,withparticipantswith lessinterestorfamiliaritywithtelesimulationbeinglesslikely torespond.However,theresultsofoursuccessivewave analysisfailedtodetectnon-responsebiasfortheselected surveyquestions.
Theremaybeotherinfluencesaffectingaprogram’suseof telesimulationthatwewerenotabletocapture,andinthis surveystudyweexaminedonlytheopinionsoffacultyand notthoseofresidentlearners.Additionally,theliteraturebaseddefinitionoftelesimulationweusedmaybeoverly broadandencompassmorethanwhattypicaleducators mightconsidertelesimulation.Finally,weacknowledgethat thesurveywasadministeredin2022within-personlearning restrictionsjuststartingtobelifted,andhowpeopleareusing telesimulationnowmaybechanging.Futureworkcould examinethisevolvinguseoftelesimulationwithinEM residencyprograms.
CONCLUSION Thisstudydescribespastandplannedfutureuseof telesimulationwithinEMresidencyprograms.Alarge proportionofEMresidenciestrialedtelesimulationduring COVID-19-inducedrestrictions.Despiterelativelylowuseof telesimulationpriortothepandemic,moreEMprograms plantoincorporatetelesimulationmovingforwardasa limitedportionoftheiroverallsimulationcurriculum. Opportunitiesforfurtherinnovationandscholarshipwithin thisareaofsimulationeducationwillbepossiblegiventhis plannedcontinueduse.
ACKNOWLEDGMENTS Thisprojectwascompletedinfulfillmentofthe requirementsfortheJohnsHopkinsUniversityMasterof EducationintheHealthProfessions.
AddressforCorrespondence:MaxBerger,MD,MEHP,Universityof CaliforniaLosAngeles,DavidGeffenSchoolofMedicine, DepartmentofEmergencyMedicine,1100GlendonAve.,Suite 1200,LosAngeles,CA90024.Email: MRBerger@mednet.ucla.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Bergeretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.PatelSM,MillerCR,SchiaviA,etal.Thesimmustgoon:adapting residenteducationtotheCOVID-19pandemicusingtelesimulation. AdvSimul.2020;5:26.
2.DiazMCGandWalshBM.Telesimulation-basededucationduring COVID-19. ClinTeach.2021;18(2):121–5.
3.McCoyCE,SayeghJ,AlrabahR,etal.Telesimulation:aninnovative toolforhealthprofessionseducation. AEMEducTrain 2017;1(2):132–6.
4.MikrogianakisA,KamA,SilverS,etal.Telesimulation:aninnovative andeffectivetoolforteachingnovelintraosseousinsertiontechniquesin developingcountries. AcadEmergMed.2011;18(4):420–7.
5.OkrainecA,HenaoO,AzzieG.Telesimulation:aneffectivemethodfor teachingthefundamentalsoflaparoscopicsurgeryinresourcerestrictedcountries. SurgEndosc.2010;24(2):417–22.
6.HaydenEM,KhatriA,KellyHR,etal.Mannequin-basedtelesimulation: increasingaccesstosimulation-basededucation. AcadEmergMed 2018;25(2):144–7.
7.McCoyCE,SayeghJ,RahmanA,etal.Prospectiverandomized crossoverstudyoftelesimulationvsstandardsimulationforteaching medicalstudentsthemanagementofcriticallyillpatients. AEMEduc Train.2017;1(4):287–292.
8.YasserNBM,TanAJQ,HarderN,etal.Telesimulationinhealthcare education:ascopingreview. NurseEduc.Today 2023;126:105805.
9.NadirNA,KimJ,CassaraM,etal.Simulation-basedemergency medicineeducationintheeraofphysicaldistancing:lessons learnedintheCOVID-19pandemic. AEMEducTrain 2021;5(3):e10586.
10.RayJM,WongAH,YangTJ,etal.Virtualtelesimulationfor medicalstudentsduringtheCOVID-19pandemic. AcadMed 2021;96(10):1431–5.
11.SanseauE,LavoieM,TayKY,etal.TeleSimBox:aperceived effectivealternativeforexperientiallearningformedicalstudent educationwithsocialdistancingrequirements. AEMEducTrain 2021;5(2):e10590.
12.ThomasA,BurnsR,SanseauE,etal.Tipsforconducting telesimulation-basedmedicaleducation. Cureus. 2021;13(1):e12479.
13.AustinA,RudolfF,FernandezJ,etal.COVID-19educational innovation:hybridin-personandvirtualsimulationforemergency medicinetrainees. AEMEducTrain. 2021;5(2):e10593.
14.HeffernanR,BrumptonK,RandlesD,etal.Acceptability,technological feasibilityandeducationalvalueofremotelyfacilitatedsimulation-based training:ascopingreview. MedEducOnline. 2021;26(1):1972506.
15.EmergencyMedicineResidents’ Association.EMRAMatch.Available at: https://webapps.emra.org/utils/spa/match#/search/map. AccessedJuly21,2021.
16.RickardsG,MageeC,ArtinoAR,Jr.Youcan’t fixbyanalysiswhat you’vespoiledbydesign:developingsurveyinstrumentsandcollecting validityevidence. JGradMedEduc.2012;4(4):407–10.
17.GehlbachHandArtinoAR,Jr.Thesurveychecklist(manifesto). AcadMed.2018;93(3):360–66.
18.ArtinoAR,Jr.,DurningSJ,SklarDP.Guidelinesforreportingsurveybasedresearchsubmittedtoacademicmedicine. AcadMed 2018;93(3):337–40.
19.MessickS.Validity.In:LinnR.L,editor. EducationalMeasurement 3rd ed.NewYork,NY:Macmillan;1989:13–103.
20.DuszynskiTJ,FadelW,DixonBE,etal.Successivewaveanalysisto assessnonresponsebiasinastatewiderandomsampletesting studyforSARS-CoV-2. JPublicHealthManagPract. 2022;28(4):E685–91.
21.SharmaA,MinhDucNT,LuuLamThangT,etal.Aconsensus-based checklistforreportingofsurveystudies(CROSS). JGenInternMed. 2021;36(10):3179–87.
22.LevineM,SinghM,RestivoA,etal.Recommendationsforoptimizing virtualsimulation:atrialanderrorprocessfromtheCOVID-19 pandemic. JGradMedEduc.2022;14(1):18–21.
23.KirkpatrickJDandKirkpatrickWK. Kirkpatrick’sFourLevelsofTraining Evaluation.Alexandria,VA:ATDPress;2016.
24.MistryD,BrockCA,LindseyT.Thepresentandfutureofvirtual realityinmedicaleducation:anarrativereview. Cureus. 2023;15(12):e51124.
25.PallaviciniF,PepeA,ClericiM,etal.Virtualrealityapplicationsin medicineduringtheCOVID-19pandemic:systematicreview. JMIRSeriousGames. 2022Oct25;10(4):35000.
EDUCATIONAL SPECIAL ISSUE:BRIEF PalliativeCareBootCampOffersSkillBuildingfor EmergencyMedicineResidents JulieCooper,MD* JennaFredette,MD†
*UniversityofPennsylvania,DepartmentofEmergencyMedicine,Philadelphia,Pennsylvania † ChristianaCare,DepartmentofEmergencyMedicine,Newark,Delaware
SectionEditors:PaulLoganWeygandt,MDandBenjaminHoldenSchnapp,MD
Submissionhistory:SubmittedJune22,2023;RevisionreceivedMarch3,2024;AcceptedMay30,2024
ElectronicallypublishedSeptember6,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18381
BACKGROUND Emergencymedicine(EM)residentsroutinelycarefor criticallyillpatientsinboththeemergencydepartment(ED) andintensivecareunits.1 Proficiencyinprimarypalliative careskillsisessentialforallemergencyclinicians.2,3 However,asignificantnumberofresidentslackexposureto formaleducationandtraininginpalliativecare.4,5 Moreover,educationandtraininginpalliativecare encompassesseveralAccreditationCouncilforGraduate MedicalEducation(ACGME)competenciesincluding systemnavigationforpatient-centeredcare,understanding thephysician’sroleinthehealthcaresystem,patient-and family-centeredcommunication,andinterprofessionaland teamcommunication.6
Currentcurriculaaddressingprimarypalliativecareskills inEMarenotablylimited.7–12 Historically,ourresidency experiencedinconsistenciesintheteachingofprimary palliativecareskills.Theyweresporadicallycoveredduring regularconferencesorlefttodeveloporganicallyovertime. Furthermore,postgraduateyear-2(PGY-2)residents,who primarilymanageseriouslyillpatients,foundthemselves engaginginchallengingserious-illnessconversationswith patientsandfamilieswithlittletonotraining.Recognizing theimperativeformorecomprehensiveeducation,we introducedafour-week,intensiveprimarypalliativecare curriculumspecificallytailoredforEMPGY-2residentsthat wasentitled “PalliativeCareBootcamp.”
OBJECTIVES Theoverallobjectiveofthebootcampwastointroduce andstrengthenprimarypalliativecareskillsamongPGY-2 residentsatanindependentacademicmedicalcenter.Atthe endofthecurriculum,residentswouldbeableto1)definethe scopeofhospiceandpalliativemedicine;2)understandwhat primarypalliativecareskillsarefornon-specialtytrained physicians;3)recognizeEDpatientswithpalliativecare needs;4)implementahospiceevaluation;5)understandhow interdisciplinaryteamsareinvolvedinthecareofseriouslyill patients;and6)buildcommunicationskillsfordiscussing goalsofcare(GOC).
CURRICULARDESIGN Thecurriculumandassessmentwereexemptfromthe institutionalreviewboard.UsingKern’ssix-stepapproachto curriculumdevelopment,wecreatedanintroductory primarypalliativecarecurriculum.AnEMfacultymember withaninterestinpalliativecareandresidencyleadership collaboratedtodevelopthecurriculum.Theresidency programendorsedthecurriculumasitalignedwitha curriculumredesigntoincludemorePGY-specificeducation.
Thecurriculumwasinitiallydevelopedin2017.The interdisciplinarypalliativecareteamatthestudyinstitution servedascontentexperts.Theteamperformedabroad reviewoftheresidencycurriculumandprioritizedhigh-yield topicstailoredtothelocalcontext.Sessionswere scheduledduringweeklyconferenceandspannedfour consecutiveweeks.Thisscheduleallowedforanintensive experienceandallowedforrapidskilldevelopment.The curriculumisstrategicallydeliveredearlyinthePGY-2year toleverageresidents’ existingexperienceincaringfor seriouslyillpatientsandfacilitatemeaningfulreflection andinquiry.
Thecurriculumisstructuredintwophases(Table1).The firstphasespansthreeweeksandconsistsofthreetwo-hour sessions.Thesesessionsarededicatedtoprimarypalliative carefundamentalssuchasanintroductiontopalliativecare, prognosisandtrajectory,andnon-painsymptom management.SessionfacilitatorsincludedtheEMfaculty contentexpertaswellasmembersoftheinstitutional palliativecareteam,thedirectorofchaplaincywho specializedinfamilysupport,thedirectorofpalliativecare, andthepalliativecarefellow.Eachsessionencompasseda didacticsegment,interactivecase-baseddiscussionsusing scenariospreparedbyfacilitatorsorcontributedbyresidents, andopportunitiesforresidentquestions.
Inthe finalweek,residentsengagedinafour-hoursession inthesimulationcenter.ThissessionwasledbytheEM contentexpertwhoisatrainedfacilitatorwithVitalTalk,a nationalnon-profitthatpromotesevidence-basededucation inserious-illnesscommunication.13 Thissessioninvolves usingastandardizedpatient.Residentsareassignedtoa
Table1. Thebreakdownofpalliativecarebootcampsessionsbyhourdetailingthetopic,learningobjectives,mappingtoACGME* competencies,andtheformatofthesession.
HourTopicObjectives
1Introtoprimarypalliative care inemergency medicine
Defineprimarypalliativecareandidentify commonEDpresentationsofpatientswith unmetpalliativecareneeds.
Defineadvancecareplanning,goalsofcare, codestatusandtreatmentlimitationsand describehowthesearecodifiedinlegaland medicaldocuments
InterpretaPOLST(PhysicianOrdersforLife SustainingTreatment)formanddescribeits useinacutecaresettings
2PrognosisandtrajectoryDescribefourcommontrajectoriesoflifelimitingillness
Defineprognosisanddescribe3strategiesto assessprognosisinEDpatientswithserious illness
ACGME competenciesFormat/facilitator
Systemnavigationfor patientcenteredcare
Physicianrolein healthcaresystems
Lecture – EMfaculty contentexpert
Diagnosis,treatment, andclinicalreasoning
Case-basedlearning –EMcontentexpert
3Chaplainchat
4Non-painsymptom management
5Askaconsultant
6Introtohospice
7–10Seriousillness communicationworkshop (VitalTalk)
Describetheroleofthechaplaininthe interdisciplinarycareofseriouslyillpatients intheED
Chooseappropriate first-andsecond-line treatmentforseriouslyillpatientsexperiencing nauseaandvomitingintheED
Chooseappropriate first-andsecond-line treatmentforseriouslyillpatientsexperiencing dyspneaintheED
Chooseappropriate first-andsecond-line treatmentforseriouslyillpatientsexperiencing constipationintheED
DescribetheroleoftheHPMclinicianinthe careofseriouslyillpatientsinthehospital
UnderstandtheroleofHPMconsultationin theemergencydepartment
Describethescopeofhospiceservicesand thesettingswhereitcantakeplace
Identifypatientswhomayqualifyforhospice andhowtogetthemevaluated
Providegoalconcordantcaretopatients enrolledinhospicewhopresenttotheED
Practiceskillsassociatedwithgoalsofcare conversationswithasimulatedpatient.
Systemnavigationfor patient-centeredcare
Interprofessionaland teamcommunication
Pharmacotherapy
Diagnosis,treatment, andclinicalreasoning
Case-based learning – chaplain
Case-basedlearning –hospitalpalliative carespecialist
Interprofessionaland teamcommunication
Systemnavigationfor patient-centeredcare
Physicianrolein healthcaresystems
Patient-andfamilycentered communication
Case-basedlearning –hospitalpalliative carespecialist
Lecture – community hospicemedicaldirector
Simulationand standardizedpatient skills-basedpractice –EMcontentexpert
*ACGME, AccreditationCouncilforGraduateMedicalEducation; ED,emergencydepartment; EM,emergencymedicine; HPM,hospiceand palliativemedicine.
smallgroupandtheyrole-playdeliveringseriousnewswith EM-basedscenarios.Thissessionbuildsskillsaround deliveringseriousnews.
Thecurriculumunderwentiterativeadjustmentsinformed byinformalfeedbackfrombothfacilitatorsandresidents.
Modificationsweremadebasedonfacilitatoravailability andinterest,resultingintheinclusionormodificationof topics,whilecertainsubjects,suchasopioidpain management,wereremovedduetoredundancyinother educationalsettings.
SURVEYDEVELOPMENT Beforeimplementingthecurriculum,wecreatedabrief, pre-bootcampsurveytoassessresidents’ priorexposureand familiaritywithpalliativecare.Subsequently,twopostsurveyswereusedtogaugeresidents’ perceptionsregarding theachievementofsession-specificgoals.Wedevelopedthe firstsurveytoevaluatethe firstthreeweeksofthebootcamp. Theinitialdevelopmentcollectedallpotentialsurveyitems thatwererefinedthroughexpertconsultation.Thesurvey useda five-pointLikertscalerangingfrom1(strongly disagree)to5(stronglyagree).Thesurveyitemshadbeen pilottestedandrefinedinprecedingyearstoensurequestion clarity(Appendix1).
Asecondsurvey,whichwasusedforthesimulation-based session,promptedresidentstoratetheirself-assessed confidencesurroundingthespecificskillsonconducting GOCconversationscoveredinthesession(Appendix2).The surveyusesa five-pointLikertscalerangingfrom1(notvery confident)to5(veryconfident).
IMPACT/EFFECTIVENESS Thecurriculumevaluationtookplaceduringthe2022 bootcamp.Eachsessionhadanaverageof8–10PGY-2 residents,ofatotal17potentialparticipants.Attendance variedfromweektoweekduetoexcusedabsences. Participationinbothpre-andpost-surveyswasvoluntary.Of theeligibleresidents,nine(52%)completedthepre-survey, revealingthatallbutoneresidenthadpriorexposuretoa palliativecarerotationduringmedicalschool,and7of9 respondents(77%)reportedpreviouscommunicationskills trainingduringtheirPGY-1year.
Post-interventionsurveyswerecollectedaftereach session,withcompletionratesrangingfrom25%(2/8 participants)to70%(7/10participants)persession.Notably, allrespondentsindicatedagreementorstrongagreement withtheachievementofeachsession’sobjectives.Forthe simulation-basedcommunicationsession,88%(8/9)reported increasedconfidenceoverall,88%(8/9)ofresidentsreported increasedconfidenceinrespondingtostrongemotions,and 100%(9/9)reportedenhancedconfidenceinelicitingpatient goalsandvalues.
TIPSFORSUCCESS/CHALLENGES/LESSONS LEARNED Severalkeythemesemergedregardingthe implementationofabootcampcurriculuminprimary palliativecareforEMresidents.Onenotableadvantageof thiscurriculumisitslongitudinalformat,spanningfour consecutiveweekswithshortintervalsbetweensessions.This structureaffordsresidentstheopportunitytopracticenewly acquiredskillswhileactivelyworkinginclinicalsettings, fosteringcontinuousreflectionandrefinementoftheir abilities.Additionally,thecurriculumisadaptableand
enablesitsimplementationinprogramslackingEM palliativecare-trainedfaculty.Programscanuselocal resourcessuchasinstitutionalpalliativespecialists, interdisciplinarypalliativeteams,orseveralpublicly availableonlineresources.9,10,14
However,despiteitsstrengths,ourcurriculumfaces severalchallenges.Notably,residentsunabletoattend sessionsriskmissingvaluableeducationalopportunities,as thecurriculumisnotrepeatedduringtheacademicyear. Moreover,limitedopportunitiesforongoingskillacquisition andfeedbackoutsidescheduledsessionsmayhinder residents’ abilitytofullyintegratepalliativecareprinciples intotheirpractice.Furthermore,individualprogramsmay beunwillingtoinvest10hoursofcurriculumtothisspecific topicandskillset.Lastly,whiletherewasnocostforthe simulationtimeandstandardizedpatientsatthestudy institution,theremaybecostassociatedwiththisinother programsandthismustbeconsidered.
Furthermore,whileparticipantsexpressedsatisfactionwith thecurriculum,theoutcomesdatalacktherigornecessaryto definitivelyestablishitssuccess.Theimpactofthiscurriculum onlong-termknowledgeorclinicalbehaviorwithintheED remainsuncertain.Itwillbeimportanttoconductmore formalassessmentsofthecurriculumobjectivesandto evaluateitsapplicationintheclinicalsetting.
CONCLUSION Astheroleofprimarypalliativecareinemergency medicinecontinuestoevolve,thereisagrowingneedto integratetheseessentialskillsandconceptsintoallEM residencies.Thebootcampformathasproventobea valuableeducationaltoolinourprogram,andits effectivenesswarrantsfurtherexplorationanddissemination withinthebroaderEMcommunity.
AddressforCorrespondence:JulieCooper,MD,Universityof Pennsylvania,DepartmentofEmergencyMedicine,3400Spruce St.,Philadelphia,PA19104.Email: julie.cooper@pennmedicine. upenn.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Cooperetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.SmithAK,McCarthyE,WeberE,etal.HalfofolderAmericansseenin emergencydepartmentinlastmonthoflife;mostadmittedtohospital, andmanydiethere. HealthAffairs. 2012;31(6):1277–85.
2.ShoenbergerJ,LambaS,GoettR,etal.Developmentofhospiceand palliativemedicineknowledgeandskillsforemergencymedicine residents:usingtheAccreditationCouncilforGraduateMedical Educationmilestoneframework. AEMEducTrain. 2018;2(2):130–45.
3.QuillTEandAbernethyAP.Generalistplusspecialistpalliative care creatingamoresustainablemodel. NEnglJMed. 2013;368(13):1173–5.
4.BackAL,FrommeEK,MeierDE.Trainingclinicianswithcommunication skillsneededtomatchmedicaltreatmentstopatientvalues. JAmerican GeriatricsSociety. 2019;67(S2):S435–41.
5.BaylisJ,HarrisDR,ChenC,etal.Palliativeandend-of-lifecare educationinCanadianemergencymedicineresidencyprograms:a nationalcross-sectionalsurvey. CJEM. 2019;21(2):219–25.
6.AccreditationCouncilforGraduateMedicalEducation.Emergency medicinemilestones.2021.Availableat: https://www.acgme.org/ specialties/emergency-medicine/milestones/ AccessedFebruary7,2024.
7.LoffredoAJ,ChanGK,WangDH,etal.UnitedStatesbestpractice guidelinesforprimarypalliativecareintheemergencydepartment. Ann EmergMed. 2021;78(5):658–69.
8.KrausCK,GreenbergMR,RayDE,etal.Palliativecareeducationin emergencymedicineresidencytraining:asurveyofprogramdirectors, associateprogramdirectors,andassistantprogramdirectors. JPain SymptomManage. 2016;51(5):898–906.
9.NorthwesternMedicine.EPEC:Educationinpalliativeandend-of-lifecare.Availableat: https://www.bioethics.northwestern.edu/programs/ epec/index.html.AccessedFebruary7,2024.
10.NguyenDandMateseT.Assessingtheeffectofahospiceandpalliative medicinecurriculumonemergencymedicineresidents’ knowledge. AmJHospPalliatCare. 2023;40(5):462–7.
11.StanichJ,SungaK,Loprinzi-BrauerC,etal.Teachingpalliativecareto emergencymedicineresidentsusinggamifieddeliberatepracticebasedsimulation:palliativegamingsimulationstudy. JMIRMedEduc. 2023;9:e43710.
12.BeneschTD,MooreJE,BreyreAM,etal.Primarypalliativecare educationinemergencymedicineresidency:amixed-methodsanalysis ofayearlong,multimodalintervention. AEMEducTrain. 2022;6(6):e10823.
13.VitalTalk.VitalTalk.Availableat: https://www.vitaltalk.org/. AccessedFebruary21,2024.
14.CentertoAdvancePalliativeCare.CAPCclinicaltraining. Availableat: https://www.capc.org/clinical-training/ AccessedFebruary7,2024.
ORIGINAL RESEARCH ImprovingPatientUnderstandingofEmergencyDepartment DischargeInstructions SarahRussell,MD
NancyJacobson,MD
AshleyPavlic,MD,MA
MedicalCollegeofWisconsin,DepartmentofEmergencyMedicine,Milwaukee,Wisconsin
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedNovember14,2023;RevisionreceivedMay30,2024;AcceptedJune12,2024
ElectronicallypublishedSeptember24,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18579
Introduction: Previousstudieshaveshownthatpatientsintheemergencydepartment(ED)are frequentlygivenincompletedischargeinstructionsthatarewrittenatleastfourgradelevelsabovethe recommendedsixth-gradereadinglevel,leadingtopoorunderstanding.Ouraimsinthisstudywereto implementstandardizeddischargeinstructionscontainingsixkeycomponentswrittenatamore appropriatereadinglevelforcommonemergencydepartment(ED)diagnosestoimprove patientunderstanding.
Methods: Weconductedthisstudyina20-bedEDatanurbanVeteran’sAdministrationhospital.Data wascollectedviain-personpatientandclinicianinterviews.Patientinterviewswereconductedafter patientsreceivedtheirdischargeinstructions.Wecomparedpatientresponsestoclinicianresponses andmarkedthemasincorrect,partiallycorrect,orcorrectwithascoreof0,0.5,or1,respectively.The maximumpossiblescoreforeachinterviewwassix.Sixkeycomponentsofdischargeinstructionswere askedabout:diagnosis;newmedications;at-homecare;durationofillness;reasonstoreturn;and follow-up.Therewere25patientsinthepre-interventiongroupand20intheinterventiongroupwiththe standardizedsetofinstructions.WeperformedaMann-WhitneyUtestonthetotalinterviewscoresinthe controlandinterventiongroupsandconductedasub-analysisontheindividualscoresforeachofthesix keycomponents.
Results: Thepatientsintheinterventiondemonstratedastatisticallysignificantincreaseinpatientcliniciancorrelationwhencomparedtothepatientsinthepre-interventiongroupoverall(P < 0.05),and twoofthesixkeycomponentsofthedischargeinstructionsindividuallyshowedstatisticallysignificant increaseinpatient-cliniciancorrelationwhenstandardizeddischargeinstructionswereused.
Conclusion: Patientswhoreceivedthestandardizeddischargeinstructionshadimproved understandingoftheirdischargeinstructions.Futureopportunitiesextendingoffthispilotstudyinclude expandingthenumberofdiagnosesforwhichstandardizedinstructionsareusedandinvestigating patient-centeredoutcomesrelatedtotheseinstructions.[WestJEmergMed.2024;25(6)917–920.]
INTRODUCTION Severalstudieshaveanalyzedtheeffectivenessof dischargeinstructionsgiventoemergencydepartment(ED) patientsatthetimeofdischargeandhaveidentifiedareasfor improvement.1 Thesestudiesrecommendthatkey componentsofdischargeinstructionsincludediagnosis, expecteddurationofillness,at-homecare,return
precautions,andfollow-upplan.Nonetheless,manyED patientsdonotreceivedischargeinstructionsthatincludeall thesecomponents.2,3 Inadditiontobeingincomplete, dischargeinstructionsareoftendifficulttoread.4,5 Infact, dischargeinformationgiventotraumapatientsatone institutionwaswrittenatleastfourgradelevelshigheron averagethantheNationalInstitutesofHealth-recommended
sixthgradereadinglevel.Theynotedthatafterimproving readabilitybybreakingupcomplexsentences,usingsimple words,andusingbulletpointsandsubheadings,therewasa significantdecreaseinpost-dischargereturnphonecallsand readmissions.5 Additionally,havingagoodunderstandingof one ’sdischargeinstructionscanhelppromoteoptimalhealth andrecoveryfollowinganEDvisit.Patientsmayalsohave fewerunnecessaryreturnvisitstotheEDiftheybetter understandtheirdischargeinstructions.6
Currently,dischargeinstructionsatthisurbanVeteran’ s Administration(VA)hospitalincludeasectionatthe beginningoftheinstructionswhereclinicianscanfreetext anyspecificinstructionstheyhaveforthepatient.This sectionmayalsobekeptblank.Thereisalsostandardized informationaboutthedischargediagnosis,whichisincluded inallinstructions.Inthispilotstudyweaimedtodetermine whetherimplementingdischargeinstructionsthatare standardizedatanappropriatereadingleveland includekeycomponentswouldimprovepatient understandingofdischargeinstructions(measuredby patient-cliniciancorrelation).
METHODS Weconductedthispilotstudyata20-bedEDurbanVA hospital.Thisstudydidnotcollectanypersonalpatientdata andthuswasdeemedbytheVAinternalreviewboardoffice tobeinstitutionalreviewboard-exempt.Studyparticipants wereapproachedbynursingstaff,clinicians,orstudystaff andaskedwhethertheywouldbewillingtoparticipateina shortinterviewtohelpaqualityimprovementproject focusedondischargeinstructions.Ifthepatientagreed,they wereinterviewedbystudystaffregardingthekey componentsofdischargeinstructions.Theywereaskedto statetheirdiagnosis,what(ifany)newmedicationswere prescribed,whattheyneededtodoathometotakecareof theirillness,expecteddurationofillness,reasonstoreturnto theED,andwhotofollowupwith.Studystaffrecordedtheir answers.Patientswerepermittedtolookattheirdischarge instructionsatanytimeduringtheinterviewtohelpanswer thequestionsandwereremindedofthisatthestartofthe interview.Studystaffthenaskedtheclinician(physicianor advancedpracticepractioner[APP])thesamequestions.
Fortheinitialcontrolgroup,clinicianswerefreeto includewhatevertheywantedinthefree-textportionofthe dischargeinstructions.Thisgroupof25patientshadthe followingdischargediagnoses:edema;motorvehicle collision;concussion;strain;acutepsychosis;constipation; fracture;shingles;hyperglycemia;cysticacne;cervical radiculopathy;oralmucosallesions;conjunctivitis; sinusitis;pneumonia;earinfection;cellulitis;fatigue; diarrhea;chestpain;backpain;balanoposthitis;chronic obstructivepulmonarydisease(COPD);anddehydration. Theclinicianstreatingthisgroupincluded10physiciansand twoAPPs.Datawasagaincollectedbystudystaff(Russell)
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
PatientunderstandingofEDdischarge instructionsisimportantforpatientcare, outcomes,andexperience.
Whatwastheresearchquestion?
Doesimplementingstandardizeddischarge instructiontemplatesimprovepatient understandingattimeofdischarge?
Whatwasthemajor findingofthestudy?
Theinterventiongroupdemonstrateda statisticallysigni fi cantincrease inunderstandingoftheir instructions(P < 0.05).
Howdoesthisimprovepopulationhealth?
GoodunderstandingofEDdischarge instructionsisvitaltopatienthealthand empowerspatientsbyallowingthemtobetter understandtheirdiseaseanditscourse.
intheformofin-personinterviewsandaddressedthesix keycomponents.
Asetofstandardizeddischargeinstructionswere developedfor12commonEDdiagnosesandeditedto containsixkeycomponents.Thesetemplateswerecreated withsubheadingsandbulletpointstomaketheinstructions easiertofollowandunderstand(AppendixA).Thedischarge diagnosesaddressedinthisgroupincludedmanyofthemost commonemergencydepartmentdiagnoses:abdominalpain; backpain;cellulitis;chestpain;congestiveheartfailure; COPD;concussion;fracture;headache;nofracture(sprain/ strain);ribfracture;andvertigo.Thesedischargeinstruction templateswerereviewedforaccuracyandcompletenessby threeboard-certi fiedemergencyphysicians,includingone studystaff,onedirectorofEDoperations,andone educationaldirector.
Aconveniencesampleofemergencyclinicians,including bothboard-certifiedphysiciansandphysicianassistants, voluntarilyparticipatedinthepost-standardized interventionphase.Volunteerclinicianshadthestandardized dischargeinstructionsuploadedintotheirdictationsoftware Dragon(NuanceCommunications,Inc,Burlington,MA) andusedthesestandardizedinstructionswhenstudystaff wasonsitetoconductinterviews.Thestudystaffthen collecteddataviain-personinterviewsfortheseclinicians andforthe20patientsforwhomthestandardizeddischarge instructionswereused.
Inbothgroups,patientresponseswerecomparedtotheir ownclinician’sresponsesandmarkedandcodedasincorrect (0),partiallycorrect(0.5),orcorrect(1)withamaximum totalscoreofsix.Resultswerescoredbyeachmemberofthe studyteamindependentlyaswellasbyathird,boardcertifiedemergencyphysicianswhowasthedirectorofED operations.WeperformedaMann-WhitneyUtestonthe totalinterviewscoresinthecontrolandinterventiongroups andconductedasub-analysisontheindividualscoresfor eachofthesixkeycomponents.
RESULTS Demographics:Thetreatmentcliniciansforthepatientsin thebaselinegroupincluded10physiciansandtwoAPPs.The treatmentcliniciansinthepost-standardizedintervention groupincludedthreephysiciansandtwoAPPs.Notethat someclinicianswereinvolvedinbothgroups.
Patientsinthepre-standardizationgroupalreadyshowed highlevelsofunderstandinginthreeareas(above.75):their diagnosis;newmedications;andwhotofollowupwith.The patientsinthepost-standardizedgroupoveralldemonstrated astatisticallysignificantincreaseinpatient-clinician concordancewhencomparedtothepatientsinthebaseline group(P < 0.05)(Figure),andtwoofthethreelow understandingareas durationofillnessandreasonsto return hadstatisticallysignificantincreasesinpatientclinicianconcordanceinthebaselinevspoststandardizedgroup.
DISCUSSION Thedatafromthispilotstudysuggeststhatimplementing dischargeinstructionsstandardizedtoincreasereadability andincludekeycomponentsimprovedpatient understandingcomparedtodischargeinstructionsenteredin viafreetextbytheclinician.Likeotherstudies,ourstudy demonstratedthatreasonstoreturnwereamongthemost poorlyunderstood.7 AsseenintheFigure,thereisclear improvementinthisareawiththeimplementationof
standardizedinstructions.Thisisessentialtopatientcarein theED.Transitionsofcarehavebeenidentifiedascritically importanttimesfortransferofinformation.8 Thisis especiallytruewhenpatientsaretransitioningfromhospitalbasedcareintheEDtohome.Indeed,patientunderstanding ofdischargeinstructionshasbeenshowntoimprovehealth outcomesincludingminimizingreturnvisits,increasing follow-up,andenablingimprovedat-homecompliancewith theirclinician’splanofcare.6
Further,institutionssuchastheCentersforMedicareand MedicaidServiceshaveidentifiedpatientunderstandingof dischargeinstructionsasakeydomainofpatientexperience, andpatientsareaskedhowwelltheywereabletounderstand thedischargeinstructionsprovidedduringtheirEDvisiton theEDConsumerAssessmentofHealthcareProvidersand SystemsSurvey.Onerecentstudyimplementedamnemonic “DCHOME” (dischargediagnosis,carerendered,health andlifestylemodifications,obstaclesafterdischarge, prescribedmedications,andexpectations)andformalized educationregardingitsimplementationamongresident physicians,whichdemonstratedsuccessinbothinclusionof thesecomponentsandpatientsatisfaction.9 Thisintervention includedseveralofthecomponentsweincludedinour standardizedwritteninstructions.
Havingagoodunderstandingofone’sdischarge instructionsisimportantformanyreasons,includingthat patientscanhaveoptimalhealthandrecoveryfollowingtheir EDvisit.Betterunderstandingofdischargeinstructionscan alsodecreaseunnecessaryreturnvisitstotheEDby empoweringpatientswiththeinformationtheyneedtomake appropriatefollow-upappointmentsandtobetter understandtheexpectedcourseoftheirillness,whichmay decreasetheunnecessarycostofanadditionalEDvisitfor thepatient.
LIMITATIONS Onelimitationofthisstudyisthatinter-raterreliability wasnotassessedwithinthedatacollectionandstatistical analysis.Wedidnotcollectthisdataand,therefore,itis unclearhowcloselythedoctors’ ratingscorrelatedtoone another.Futureanalysisandinterventionswouldbenefit fromtwodoctorsratingtheunderstandingandthen performingkappastatisticstomeasurethelevelofagreement betweenthetwodoctors.Anadditionallimitationofthis studyisitssmallsamplesizes.Weusedsmallsamplesizesas thiswasapilotstudywiththegoalofassessingsignificant impactaswellasfeasibilityofimplementation.Asthispilot demonstratesstatisticalsignificanceandclearbeneficial impacttopatientunderstanding,wenowhaveafoundation forfutureexpansionandadditionalresearchwithinthisarea.
Basedonthispilotstudywerecognizeseveralfuture opportunities.Whilethisstudywasfocusedonstandardizing 12commondischargediagnoses,afutureworkcouldexpand thenumberofdiagnosesaswellasthenumberofclinicians.
Thereisanopportunitytoexaminepatient-centered outcomesincludingfollowingpatientsafterdischargeto assessknowledgeretention,returnEDvisits,andadherence withrecommendedfollow-up.Thispilotstudydemonstrates a firststepinbetterunderstandingthesepatientcentered outcomespotentiallyimpactedbydischargeinstructions. Further,nursingstaffweretheprimaryindividuals distributingthewrittendischargeinstructionstothepatients andexplainingthemone finaltimepriortodischarge.There iscurrentlywidelyvariablepracticeonhownursingstaff provideanddiscusstheseinstructionswiththepatients.This studydidnotaddressthisvariabilityasourgoalwasto evaluatehowchangingthesinglevariableofthewritten dischargeinstructionswouldaffectpatientunderstanding. Futureworkmayincludestandardizinghowcliniciansor nursingstaffprovidedischargeinstructionsasthishas alsobeenshowntoimpactpatientunderstanding andsatisfaction.9
CONCLUSION Overall,thiscrucialpilotstudysuggeststhatstandardized dischargeinstructionssignificantlyimprovepatients’ understandingoftheirinstructionsoveralland,specifically, theexpecteddurationofillnessandreasonstoreturn.This interventioniseasytoimplement,costeffective,empowers patientstobetterunderstandtheirhealthcondition,impacts coreEDqualitymeasures,andshouldbefurtherstudied.
aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Russelletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.CareyA,StarkweatherA,BaiA,etal.Beneciuk,emergencydepartment dischargeteachinginterventions:ascopingreview, JEmergNurs. 2024;50(3):444–62.
2.NavanandanN,SchmidtSK,CabreraN,etal.Thecaregiverperspective onunscheduled72-hourreturnvisitstopediatricacutecaresites:a focusondischargeprocesses. AcadPediatr. 2017;17(7):755–61.
3.SheikhH,BrezarA,DzwonekA,etal.Patientunderstandingof dischargeinstructionsintheemergencydepartment:dodifferent patientsneeddifferentapproaches? IntJEmergMed. 2018;11(1):5.
4.AlbertiTLandNanniniA.Patientcomprehensionofdischarge instructionsfromtheemergencydepartment:aliteraturereview. JAANP. 2012;25(4):186–94.
5.ChoudhryAJ,YounisM,Ray-ZackMD,etal.Enhancedreadabilityof dischargesummariesdecreasesprovidertelephonecallsandpatient readmissionsintheposthospitalsetting. Surgery. 2018;165(4):789–94.
6.DeSaiC,JanowiakK,SecheliB,etal.Empoweringpatients:simplifying dischargeinstructions. BMJOpenQuality. 2021;10(3):e001419.
7.EngelKG,BuckleyBA,ForthVE,etal.Patientunderstandingof emergencydepartmentdischargeinstructions:whereareknowledge deficitsgreatest? AcadEmergMed. 2012;19(9):E1035–44.
AddressforCorrespondence:SarahRussell,MD,MedicalCollege ofWisconsin,DepartmentofEmergencyMedicine,Hubfor CollaborativeMedicine,8701WatertownPlankRd.,Milwaukee, WI53226.Email: srussell@mcw.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived
8.FriesenMA,WhiteSV,ByersJF.(2008).Handoffs:implicationsfor nurses.In:HughesRG(Ed.), PatientSafetyandQuality:AnEvidenceBasedHandbookforNurses.Rockville,MD:AgencyforHealthcare ResearchandQuality,2008.
9.DalleyMT,BacaMJ,RazaC,etal.Doesastandardizeddischarge communicationtoolimproveresidentperformanceandoverallpatient satisfaction? WestJEmergMed. 2020;22(1):52–9.
ORIGINAL RESEARCH WhyDoPatientsOptfortheEmergencyDepartmentoverOther CareChoices?AMulti-HospitalAnalysis CharlesW.Stube,MS*
AlexanderS.Ljungberg,DO*
JasonA.Borton,MD*
KunalChadha,MD†
KyleJ.Kelleran,PhD*
E.BrookeLerner,PhD*†°
SectionEditor:DavidThompson,MD
*UniversityatBuffalo,DepartmentofEmergencyMedicine,Buffalo,NewYork † UniversityatBuffalo,DepartmentofPediatrics,Buffalo,NewYork ° PosthumousAuthorship
Submissionhistory:SubmittedDecember21,2023;RevisionreceivedJuly5,2024;AcceptedAugust1,2024
ElectronicallypublishedSeptember25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18647
Introduction: Thereareseveraloptionsforreceivingacutecarebesidesemergencydepartments(ED), suchasprimarycarephysician(PCP)offices,urgentcarecenters(UCC),andtelehealthservices.Itis unknownwhetherthesealternativemodesofcarehavedecreasedthenumberofEDvisitsforpatientsor whethertheyareconsideredbeforevisitingtheED.Acomprehensivestudyconsideringallpotential methodsofcareisneededtoaddresstheevolvinglandscapeofhealthcare.Ourgoalwastoidentifyany factorsorbarriersthatmayhaveinfluencedapatient’schoicetovisittheEDasopposedtoaUCC,PCP, anotherlocalED,orusetelehealthservices.
Methods: WesurveyedEDpatientsbetweenthreehospitalsitesinthegreaterBuffalo,NY,area.The surveyconsistedofquestionsregardingthepatients’ reasonsandrationaleforchoosingtheEDoverthe alternativecareoptions.Thestudyalsoinvolvedahealthrecordreviewofthepatients’ diagnoses,tests/ procedures,consults,and finaldispositionaftercompletionofthesurvey.
Results: Ofthe590patientsconsentedandsurveyed,152(25.7%)consideredseekingcareataUCC, 18(3.1%)consideredtelehealthservices,and146(24.7%)attemptedtocontacttheirPCP.Onthe recommendationoftheirPCP,patientspresentedtotheED110(20.7%)timesandonthe recommendationoftheclinicianattheUCC54(9.2%)times.Patients’ perceivedseriousnessoftheir conditionwasthemostcommonreasonfortheirselectedmodeoftransporttotheEDandreasonfor choosingtheEDasopposedtoalternativecaresites(PCP,UCC,telehealth).Basedoncriteriaforan avoidableEDvisit,83(14.1%)EDpatientsmetthesecriteria.
Conclusion: Individualsprioritizetheperceivedseverityoftheirconditionwhendecidingwheretoseek emergencycare.Whilesomeconsideredalternatives(PCP,UCC,telehealthservices),uncertainties abouttheirconditionandrecommendationsfromothercliniciansledmanytooptforEDcare.Our findings suggestapotentialgapinunderstandingtheseverityofsymptomsanddeterminingthemostsuitableplace toseekmedicalcarefortheseparticularconditions.[WestJEmergMed.2024;25(6)921–928.]
Keywords: emergencydepartment;urgentcarecenter;primarycarephysician;telehealth; hospitalutilization.
INTRODUCTION Emergencydepartments(ED)havebecomeahavenfor patientsseekingurgentmedicalattention.Asrequiredby federallaw,EDscannotrefuseevaluationandemergency treatment,regardlessofthepatient’sabilitytopay.1 A1996 studyrevealedthat11.3%ofambulancetransportswere consideredunnecessary,highlightingapositivecorrelation betweenthesevisitstotheEDandlimitedtransportation options.2 Giventheincreasedavailabilityofalternative transportationchoicestodaycomparedwith1996,including publictransportationandride-sharingservices,this correlationmayhaveshifted.Thecurrentmedicallandscape alsoprovidesvariousalternativesformanagingemergent medicalconditions,includingseeingprimarycarephysicians (PCP),visitingurgentcarecenters(UCC),andusing telehealthservices.
Theriseofalternativemedicalcareoptionsraises questionsabouttheirimpactonreducingEDvisitsfor conditionstreatablethroughPCPs,UCCs,ortelehealth services.Recentstudieshaveexaminedwhypatientsoptfor theEDoverothermedicaltreatmentfacilities,citingfactors suchaslimitedaccesstoorconfidenceinprimarycare, perceivedurgency,convenience,recommendationsfrom otherphysicians,friends,orfamily,andthebeliefthattheir conditionnecessitatedresourcesprovidedbyhospital-based emergencycare. 3–11
Despitethe findingthat13.7–27.1%ofallEDvisitscould beevaluatedandtreatedatUCCsorretailclinicswithlower cost,patientsstillfrequentlychooseEDsfornonemergent care.7,12 Anothercommonoccurrenceamongpatients visitingtheEDwithloweracuityconditionsisunnecessary referralfromaPCPorUCC.13,14 Onestudyfoundthatthere weresignificantlymoreavoidablereferralsfromPCPs (13.9%)thanUCCs(7.9%).13 Ziteketalfound that35.9%ofthepatientsenrolledintheirstudywho transferredfromaUCCtotheEDwereconsideredan unnecessarytransfer.14
Limitedresearchhasexaminedpatientdecision-making whenchoosingbetweentheEDandUCC.A2018study highlightedpatients’ uncertaintyaboutwhatconstituted urgentcare,focusingonpsychologicalfactorsratherthan societalorphysicaldeterminants.15 Mukameletal(2019) addressedthesefactors,emphasizingout-of-pocketcostsand waittimesforseveralmedicalconditionsandcarechoices.8 Their findingsrevealedthatlowerout-of-pocketcostswere prioritizedoverwaittimeforconditionslowerinseverityor acuity,whereaswaittimegainedimportanceforconditions perceivedtobemoreurgent.8
Thecurrentstudyprovidesacomprehensiveassessmentof EDpatients’ choicesforcareandexploresthefactorsand obstaclesimpactingpatients’ choicesofaparticularEDover aPCP,UCC,telehealthservice,oranothernearbyED. Additionally,wewantedtoassesshowavoidable someoftheseEDvisitscouldbebyexaminingpatients’
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Traditionally,patientsoptfortheemergency department(ED)overothermedicaloptions duetomanyfactorsincludingaccess limitations,perceivedurgency,convenience, andrecommendationsfromothers.
Whatwastheresearchquestion?
Giventheirincreasedavailability,doED patientsconsiderusingalternativecare optionspriortoreportingtotheED?
Whatwasthemajor findingofthestudy?
AmongEDpatients,14.1%mettheavoidable visitcriteria,providinganopportunityto improveresourceallocation.
Howdoesthisimprovepopulationhealth?
Asasafetynetformedicineandsociety,EDs canbecomeoverburdened.Alternativecare optionsfornon-emergentcasesmayhelp alleviatetheloadonEDs,tofocusonthe sickestpatients.
perceptionsofPCPs’,UCCs’,andtelehealthservices’ abilitiestocareforthemedicalconditionsthatcaused themtoseekcareintheEDandtounderstandthe selectionpatternswithinthisgroup.Understandingthe location,size,clientele,andspecializedcareoftheEDsmay provideinsightastowhyindividualsoptforone medicalcareoptionoveranother.Athoroughexamination ofpatients’ choicescouldoffervaluableinsightsinto enhancingtheavailabilityandaccessibilityof variousmedicalcareoptionsforindividualswith urgentconditions.
METHODS StudyDesign Thisstudyconsistedofamulti-hospitalsurveyand electronichealthchartreview.Researchassociates(RA) administeredthesurveytopatientsseekingcareatthree separatehospitalEDs.Surveyswereadministeredduring normalbusinesshourswhenmostothercareoptionswould beopenandavailable.Participantsprovidedwrittenconsent attheirbedsidepriortocompletingthesurvey.Thesurvey includedgeneraldemographicquestionsandseveral questionsregardingtheirdecisiontoseekcareinthespecific EDinwhichtheywereapproached,asopposedtousinga PCP,UCC,telehealthservice,oranotherlocalED.We
Table1. Hospitalsiteinformationandstatistics.17–20
HospitalsHospitaltypeBedsLocationSpecializationEDpatientsperyear
Site1County573UrbanFullservice,regionalLevelItraumacenter70,000
Site2Notforprofit484UrbanFullservice,regionalstrokeandSTEMIcenter64,000
Site3Notforprofit265SuburbanFullservice50,000 ED,emergencydepartment; STEMI,ST-ElevationMyocardialInfarction.
conductedasubsequenthealthchartreviewfordiagnoses, tests/procedures,consults,and finaldispositionforeach participatingpatient.Thesurveywasdevelopedfroma previousstudyconductedlocally,2 adaptedto fitcurrent standardsandmedicalcareoptions,anditwasreviewedbya groupoflocalemergencyphysicians.13,16 Thisstudywas approvedbytheinstitutionalreviewboardattheUniversity atBuffalo.
Setting Thesurveywasconductedatthreelocalhospitalsites locatedinasinglecounty.Twoareinthecenterofa metropolitanareaandoneinacitysuburb(Table1).Sites2 and3arepartofthesamehospitalsystem.TheEDsatall threesitesarestaffedbythesamephysiciangroup.The populationofthelocalcountyisabout950,000asof2021 andincludesthecitywithapopulationofabout277,000.
DataCollection EachRAwastrainedbythestudycoordinatoratSites1 and2ontheproperproceduresforreviewingtheconsent form,administeringthesurvey,andcollectingthe finaldata outcomes.AllenrollmentsatSite3weredonesolelybythe studycoordinator.Enrollmentforthisstudybeganon January3,2023,andconcludedonMay1,2023.Data collectiontookplaceatallthreesitesbetween10 AM – 10 PM, Sunday-Saturday.Subjectswereincludediftheywereatleast 18yearsold,readandspokeEnglish,andhadthecapacityto provideconsenttoparticipate.TheRAsateachhospitalthen consultedwiththepatient’sclinicianstodeterminewhether thepatientwasabletogiveconsenttoparticipateinthe survey.TheRAsdidnotapproachpatientsiftheywere altered,toosicktoparticipate,mentallyincapable,nonEnglishspeaking,sleeping,potentiallyinfectious,receiving care, >89yearsold,orreportedbystaffasbeingtooagitated orupsettoparticipate.Additionally,prisonerswerenot consideredforthisstudyasthelocationoftheircareis arrangedwithouttheirinput.Ifpatientswereunableto beapproachedforthesereasons,theywererecorded asineligible.
Afterwrittenconsentwasreceived,thesurveywas administeredverbally,andeveryanswerwasrecordedonan iPadusingREDCap10.3.3(ResearchElectronicData CaptureVanderbiltUniversity,Nashville,TN)data managementplatformsoftwarehostedatUniversityat
Buffalo.Allquestionsfromthesurveywereaskedtothe patientsasopen-ended,buttheRAswhoaskedthequestion wouldcategorizetheanswerbasedonthesurveyoptions. TheRAsweretrainedonhowtocategorizeeachresponseby thestudycoordinator.Iftheresponsedidnot fitanyofthe providedcategories,itwouldbelabeledas “other,” andthe RAwoulddescribetheansweronREDCapviaablank textbox.
Aftereachparticipatingpatientwasdischarged,admitted, ortransferredfromtheED,RAsrecordedtheirdischarge diagnosis,anytestsandproceduresdone,anyspecialists consulted,andthe finaldisposition.Weusedthisinformation todeterminewhetherthepatient’svisittotheEDcouldbe categorizedasavoidable.WedefinedanEDvisitas avoidableifthepatientdidnothaveahigh-acuitytriage categoryoflevel1(resuscitation)orlevel2(emergent),was notadmittedtothehospitalortransferred,hadnoadvanced imaging,hadnospecialistconsultationwhileintheED,and didnothaveadischargediagnosisofchestpainorsyncope. Wedefinedadvancedimagingasanyimagingotherthana radiograph(eg,computedtomography,magneticresonance imaging,orultrasound).Thesecriteriawerebasedon previousresearchcoupledwithaconsensusfromlocal emergencyphysiciansto fitregionalstandards.2,13,16
Analysis Weanalyzedthedataobtainedfromthesurveysusing SPSSStatisticalSoftwarev27(IBMCorporation,Armonk, NY)afteritwasexportedfromREDCap.Descriptive statisticswereusedtoanalyzetheresponsestothesurveyand presentthedata.
RESULTS Acrossthethreehospitals,52,246patientsreportedtothe EDduringthestudyperiod.Ofthe1,665peopleconsidered forparticipation,958(57%)wereapproachedand590 (35.4%)consentedtoparticipateinthesurvey,resultingina 1.1%studysampleofthetotalpatientpopulationduringthe collectionperiod(Table2).Mostparticipantswerefemale (60.6%)andWhite(75.8%)(Table3).
Themostcommonmethodsoftransportationreported werehavingafamilymemberorfrienddrivethem(43.9%), followedbyambulancetransport(28.3%)anddriving themselvestothehospital(19.7%).Ofthosepatientswhohad afamilymemberorfrienddrivethem,mostofthem
Table2. Studysamplerepresentationofemergencydepartment population.EmergencySeverityIndex.
Studypatients Hospitals
Patients surveyed
TotalEDpatients duringstudyperiod
Average triageESI score ED patients seen Average triageESI score
Site11982.5218,0412.75
Site21972.7518,1222.85
Site31952.8816,0832.88
Total:5902.7152,2462.82
ED,emergencydepartment; ESI,emergencyseverityindex.
describedthereasonasbeingtoosicktodrivethemselves (67.2%).Ofthosepatientswhocameinanambulance, aroundhalfofthemexplainedthattheyfelttheyneeded immediatemedicalattention(48.5%).Additionally,mostof thosewhoarrivedbyambulancestatedtheyeithercalledthe ambulancethemselves(32.9%),orafamilymemberorfriend calledoneforthem(37.1%).
Ofthe590patients,530(89.8%)reportedhavingaPCP. Only146(27.5%)ofthose530attemptedtoreachouttotheir PCP,with127(24.0%)makingcontact.Amongthose127 patientswhosuccessfullycontactedtheirPCP,110(86.6%) statedthattheirphysicianadvisedvisitingtheED(Figure1). Ofthose110patients,75(68.2%)hadatriagecategoryof3 and30(27.3%)hadatriagecategoryof2(Table4).Among the152(25.7%)patientswhoconsideredvisitingaUCC,135 (88.8%)hadusedaUCCinthepast,148(97.4%)wereaware ofaUCCintheirarea,and140(92.1%)saidtheywould considerusingaUCCinthefuture.Whenaskedwhythey chosetheEDoveraUCC,54(35.5%)patientsreportedthey wenttoaUCC first,buttheUCCclinicianrecommended theygototheED.Thesecondmostcommonanswerwasthe patientbelievedtheirconditionwastooseriousforaUCC, 33(22.4%)(Figure2).
Only18patients(3.1%)consideredusingtelehealth services.Ofthose18,12(66.7%)soughtcarethrougha telehealthservicevisitinthepast,16(88.9%)wouldconsider usingtelehealthservicesinthefuture,and10(55.6%)stated theybelievedtheyneededtheresourcesofahospital,whichis whytheychosetheEDoveratelehealthservicevisit.
ThemainreasonswhypatientschosetheirrespectiveEDs overotherlocalEDsincludedprioruseofhealthcareservices atthathospital(23.9%),livingneartheED(21.2%),andthe beliefthatthehospitalofferedthespecializedservicesthey needed(18.1%).Therewere190(32.2%)patientswitha triagecategoryof1or2.Atotalof254(43.1%)patientswere admittedtothehospital,325(55.1%)hadadvancedimaging, and150(25.4%)hadaspecialistconsultation.Atdischarge, 125(21.2%)patientshadadiagnosisofchestpainorsyncope.
Table3. Demographicsofconsentedparticipants.
Total(N = 590)
Gender
Male228(38.5%)
Female359(60.6%)
Other3(0.5%)
Prefernottoanswer0(0.0%)
Age
MeanYears51.15
SD17.82
Race
Black113(19.1%)
Asian/PacificIslander10(1.7%)
White449(75.8%)
NativeAmerican11(1.9%)
Other19(3.2%)
Prefernottoanswer2(0.3)
Hispanic/LatinX
Yes46(7.8%)
No544(91.9%)
Highestlevelofeducation
Nohighschool2(0.3%)
Somehighschool38(6.4%)
Highschoolgraduate153(25.8%)
Somecollege121(20.4%)
Associate’sdegree78(13.2%)
Bachelor’sdegree113(19.1%)
Postgraduatedegree78(13.2%)
Trade/technicaltraining7(1.2%)
Other0(0.0%)
Typeofhealthinsurance
Private374(63.4%)
Medicare112(19.0%)
Medicaid88(14.9%)
Uninsured13(2.2%)
Military3(0.5%)
Other0(0.0%)
Ofthe590patientssurveyed,only83(14.1%)patientsmet ourcriteriaforbeinganavoidablevisit.
DISCUSSION Patients’ perceivedseriousnessoftheirconditionwasthe mostcommonreasonforseekingcareattheEDinsteadof alternativesourcesofcare(Figures1 and 2).Previousstudies suggestthatmanypeoplechoosetotakeanambulance becausesomeoneelsecalledtheambulanceforthemor
Descriptionofinvolvementofprimarycarephysician(PCP)indecisiontogototheED.
Reasonswhypatientschosetheemergencydepartment(ED)insteadofurgentcarecenter(UCC).
becauseoftheperceivedurgencyoruncertaintyabouttheir medicalconditions.21,22 Thisalignedwithour findings because,ofthe167patientswhopresentedtotheEDby ambulance,81(48.5%)statedthattheyneededimmediate medicalassistanceand29(17.4%)statedthattheyweretoo sickorintoomuchpaintodrivethemselves.Furthermore,of thepatientswhohadafamilymemberorfrienddrivethemto theED,thereasonofbeingtoosicktodrivethemselveswas farmorecommonthantheotherpossiblereasons(67.2%).
Ofthe590patientssurveyed,384(65.1%)didnotattempt tocontactaPCPpriortogoingtotheEDdespite530(89.8%) reportingthattheyhadaPCP.Previousresearchcites
patientsfavoringtheEDduetoperceivedurgency,limited accesstoPCPs,andtheconvenienceofreadilyavailabletests intheED.6,11,23,24 Anotherstudyfoundtheprimaryreason patientschosetheEDinsteadofaPCPwastheperceptionof speedandconvenience.However,this findingmaybe contradictorybecauseofprolongedEDwaittimesthatmay occurwithlessacuteconditions.25 SimilartoGorodetzeretal (2020),wefoundmorethandoublethenumberofreferrals fromPCPscomparedtoUCCs(110vs54,respectively).13
MostpatientswhodidnotcalltheirPCP’sofficestatedthat theybelievedtheirconditionwastoourgent,whichis comparabletopreviousstudies.5,11,24,26
Figure1.
Figure2.
Table4. Triagecategorycomparedtorecommendationfromprimarycarephysician(N = 127).
TriageCategory
1:Resuscitation2:Emergent3:Urgent4:Lessurgent5:Nonurgent
DoctorrecommendedgoingtoED(n = 110)2(1.8%)30(27.3%)75(68.2%)3(2.7%)0(0%)
DoctordidNOTrecommendgoingtoED(n = 17)0(0%)5(29.4%)11(64.7%)1(5.9%)0(0%)
PCP,primarycarephysician; ED,emergencydepartment.
Additionally,forthosepatientswhowenttotheED againsttheadviceoftheirPCP,56.3%statedthatthey believedtheirconditionwastooseriousorthattheythought theyneededtheresourcesofahospitalfortheircondition (Figure1),whichalignswithpreviousresearch.11 Notably,of thepatientswhowenttotheEDdespitenotbeingadvisedto dosobytheirPCP,29.4%hadatriageacuityof2and64.7% hadatriageacuityof3(Table4),indicatingthatsome patients’ self-referralmayhavebeenmoreadvantageous thaniftheyhadnotchosentovisittheED.Althoughthis mayidentifyanareaforimprovementforpatients’ PCPs,itis difficulttoaccuratelyinterpretsituationsbecausethisstudy didnotrecordwhetherpatientscalledorphysicallyvisited theirPCPs’ officesortowhompatientsmayhavespoken tothere.
OfthepatientswhoconsideredvisitingaUCC,mostof themreportedusingaUCCinthepast,knewofaUCCin theirarea,andsaidtheywouldconsiderusingaUCCinthe future.Thisinformationcontraststhe findingsofPopeetal, suggestingthatpeopleintheUnitedStatesmighthavemore ofageneralawarenessofwhataUCCisandtheservicesthey mayprovide.15 Inthisstudy,patientswhostatedthatthey didnotconsiderUCCswerenotaskedwhy.Addingthis questiontothesurveymayprovideabetterindicationofthe psychological,societal,andphysicaldeterminantsastowhy patientschoosetheEDoverUCCssuchascosts,waittimes, andlackofunderstandingofUCCservices,asprevious literaturesuggests.8,15
Toourknowledge,thisisoneofthe firststudiesto investigatepatientchoicesbetweenEDandtelehealth services.Althoughithasbeenshownthattelehealthservice usedecreasedEDvolumesduringtheearlydaysofthe COVID-19pandemicin2020,thecurrentstudywas conductedJanuary–May2023anddidnotreceivemany responses(18,3.1%)pertainingtotheconsiderationof telehealthservicesinthispopulation.9 Tenparticipants (55.6%)ofthe18whoconsideredtelehealthstatedtheychose theEDovertelehealthservicesbecauseoftheperceivedneed forhospitalresources,similartothereasoningbehind choosingtheEDoverPCPofficesorUCCs.Furthermore, whenthissurveywasconducted,notallhealthinsurances policiescoveredtelehealthservices,potentiallylimiting theirimpact.
Understandingthesignificantdecision-makingbehavior andfutureconsiderationsforthesepatientsischallenging,
giventhatonly14.1%ofthepatientsmetourcriteriafor avoidablevisits.Additionally,severalstudieshaveattempted tolabela “non-urgent” EDvisitinthepast,eachwith differentcriteria,samplesize,studydesign,andresults.8,12–14 Thiscomplicatesdistinguishingbetweenthosewhotruly requiredEDcareandthosewhomightnothaveneededit, creatingaconvolutedandambiguousprocess.
LIMITATIONS Forprivacy,surveyswereconductedafterpatientswere assignedandmovedtoanEDroom.Patientswhowere treatedinnon-privateareassuchasfasttrack,hallwaybed, orwaitingroom-adjacentareaswerenotincluded;thesemay representagroupwithagreaterratioofavoidablevisits. Additionally,RAswereunableinterviewpatientswho presentedtotheEDandleftbeforereceivingtreatment.
TherequirementforRAstoreviewaconsentformand obtainasignaturefromthepatientmayhaveresultedin reluctanceorhesitationforparticipationandsubsequent declinationtoparticipatefrom109patientsformultiple reasons.First,intheirreviewoftheconsentform,RAswere requiredtoexplainthatthestudyteamwouldbeobtaining basicinformationfromthepatient’shealthrecordafterthe patientcompletedthesurvey,whichmayhavebeen perceivedasapotentialbreachofconfidentiality.Next, reviewingtheconsentdocumenttookapproximatelyfour minutes,whichcouldhavebeenenoughtimeforthe prospectivesubjectstoloseinterest,potentiallyfeeltooillto participate,orforacliniciantointerveneduringthe enrollmentprocess.Lastly,theregulatoryrequirementof obtainingwrittenconsentmayhavedecreasedthepotential numberofpatientsthatcouldhavebeenenrolledinthisstudy andmayhaveintroducedbiasintoour findings.
DiscussingandansweringquestionsabouttheirEDvisits maybeanemotionalorsensitivetopicforpatients.Although theRAsweretrainedtoaskthequestionsinanonjudgmentalandwelcomingtone,somepatientsmayhave beendisinclinedtoprovidehonestorcompleteresponses. Additionally,goingtotheEDforsomemaybeconsidereda traumaticexperience,regardlessoftriageacuity, whichmayhavereducedwillingnesstoparticipate.Finally, patientswhoweretoosick,intoxicated,orincapacitated werenotapproachedtoparticipateduetotheir condition.Thesepatientswerepresumedtobean
unavoidableEDvisit;thus,omittingtheirdatamay impactedtheresults.
Futurestudiesshouldfocusonincludingruralhospitals comparedtosuburbanandurbanhospitals.Inclusionofa ruralsettingmaycontributemoredatasurroundingpatients’ useoftelehealthservices.Additionally,includingthose patientsseeninfasttrackorotherloweracuityareas wouldprovidemoreinformationonavoidableEDvisits. Previousstudiesalsofoundthatthereisahighnumberof avoidablepediatricpatientvisitstotheED.14 Incorporating pediatricpatientsandthedecision-makingoftheir accompanyingadult(s)infutureworkcouldalso shedlightonhowpeopledecidewheretogofortheir emergencycare.
CONCLUSION Perour findings,individualsprimarilyrelyontheir perceptionoftheseverityoftheirconditionwhenmaking decisionsaboutseekingemergencycare.Whileseveral patientscontemplatedalternativeoptionssuchasscheduling avisittoaPCP’soffice,visitingaUCC,oraccessing healthcarethroughtelemedicineservices,theuncertainty surroundingtheirmedicalcondition,recommendationsfrom otherhealthcareprofessionals,andtheperceivedqualityof caresignificantlyinfluencedtheirchoiceindirectingthemto theED.Non-emergentpatientsreporttotheEDformany reasonsincludingadiscrepancyinbothunderstandingthe severityofsymptomsanddeterminingthemostsuitable placetoseekmedicalcare.
AddressforCorrespondence:AlexanderS.Ljungberg,DO, UniversityatBuffalo,DepartmentofEmergencyMedicine, 77GoodellSt.Ste.340,Buffalo,NY14203. Email: ajs36@buffalo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Stubeetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.AmericanCollegeofEmergencyPhysicians.UnderstandingEMTALA. Availableat: https://www.acep.org/life-as-a-physician/ethics–legal/ emtala/emtala-fact-sheet.AccessedMarch15,2023.
2.BillittierAJ,MoscatiR,JanickeD,etal.Amultisitesurveyoffactors contributingtomedicallyunnecessaryambulancetransports. Acad EmergMed. 1996;3(11):1046–50.
3.CosterJE,TurnerJK,BradburyD,etal.Whydopeoplechoose emergencyandurgentcareservices?Arapidreviewutilizinga systematicliteraturesearchandnarrativesynthesis. AcadEmergMed. 2017;24(9):1137–49.
4.AllenL,CummingsJR,HockenberryJM.Theimpactofurgentcare centersonnonemergentemergencydepartmentvisits. HealthServ Res. 2021;56(4):721–30.
5.AlmulhimN,AlmulhimF,AlGharashA,etal.Preferenceforvisiting emergencydepartmentoverprimaryhealthcarecenteramong populationinsaudiarabia. Cureus. 2021;13(12):1–9.
6.KorczakV,YakubuK,AngellB,etal.Understandingpatientpreferences foremergencycareforlowertriageacuitypresentationsduringgphours: aqualitativestudyinAustralia. BMCHealthServRes. 2022;22(1):1442–52.
7.MontalbanoA,RodeanJ,KangasJ,etal.Urgentcareandemergency departmentvisitsinthepediatricMedicaidpopulation. Pediatrics. 2016;137(4):1–6.
8.MukamelDB,LaddH,AminA,etal.Patients’ preferencesovercaresettings forminorillnessesandinjuries. HealthServRes. 2019;54(4):827–38.
9.RenoEM,LiBH,EutermoserM,etal.Temporalassociationsbetween emergencydepartmentandtelehealthvolumesduringtheCOVID-19 pandemic:atime-seriesanalysisfrom2academicmedicalcenters. Am JEmergMed. 2022;54(1):238–41.
10.TapiaAD,HowardJT,BeboNL,etal.Aretrospectivereviewof emergencydepartmentvisitsthatmaybeappropriateformanagement innon-emergencysettings. MilMed. 2022;187(9–10):1153–9.
11.VogelJA,RisingKL,JonesJ,etal.Reasonspatientschoosethe emergencydepartmentoverprimarycare:aqualitativemetasynthesis. J GenInternMed. 2019;34(11):2610–9.
12.WeinickRM,BurnsRM,MehrotraA.Howmanyemergencydepartment visitscouldbemanagedaturgentcarecentersandretailclinics? Health Aff. 2010;29(9):1630–6.
13.GorodetzerR,AlpertEA,OrrZ,etal.Lessonslearnedfroman evaluationofreferralstotheemergencydepartment. IsrJHealthPolicy Res. 2020;9(18):1–8.
14.ZitekT,TanoneI,RamosA,etal.Mosttransfersfromurgentcare centerstoemergencydepartmentsaredischargedandmanyare unnecessary. JEmergMed. 2018;54(6):882–8.
15.PopeC,McKennaG,TurnbullJ,etal.Navigatingandmakingsenseof urgentandemergencycareprocessesandprovision. HealthExpect. 2019;22(3):435–43.
16.Uscher-PinesL,PinesJ,KellermannA,etal.Decidingtovisitthe emergencydepartmentfornon-urgentconditions:asystematicreview oftheliterature. AmJManagCare. 2013;19(1):47–59.
17.BuffaloGeneralMedicalCenter/GatesVascularInstitute.Emergency departmentcare&treatment.Availableat: https://www.buffalogeneral. org/care/Emergency-Department.AccessedMarch15,2023.
18.BuffaloGeneralMedicalCenter/GatesVascularInstitute.StrokeCare CenteratGatesVascularInstitute|care&treatment.Availableat: https://www.buffalogeneral.org/care/Stroke-Care-Centerat-Gates-Vascular-Institute.AccessedMarch15,2023.
19.ErieCountyMedicalCenter.Emergencydepartment-trauma& emergencycare.Availableat: https://www.ecmc.edu/ health-services-and-doctors/trauma-and-emergency-care/ emergency-department/.AccessedMarch15,2023.
20.MillardFillmoreSuburbanHospital.Emergencydepartmentcare& treatment.Availableat: https://www.millardfillmoresuburban.org/care/ Emergency-Department.AccessedMarch15,2023.
21.BookerMJ,PurdyS,BarnesR,etal.Ambulanceusefor ‘primarycare’ problems:anethnographicstudyofseekingandprovidinghelpinauk ambulanceservice. BMJOpen. 2019;9(10):e033037.
22.YarrisLM,MorenoR,SchmidtTA,etal.Reasonswhypatientschoose anambulanceandwillingnesstoconsideralternatives. AcadEmerg Med. 2006;13(4):401–5.
23.O’CathainA,SimpsonR,PhillipsM,etal.Tendencytocallan ambulanceorattendanemergencydepartmentforminorornon-urgent problems:avignette-basedpopulationsurveyinbritain. EmergMedJ. 2022;39(6):436–42.
24.RocovichCandPatelT.Emergencydepartmentvisits:whyadults choosetheemergencyroomoveraprimarycarephysicianvisitduring regularofficehours? WorldJEmergMed. 2012;3(2):91–7.
25.LinD,PatrickJ,LabeauF.Estimatingthewaitingtimeofmulti-priority emergencypatientswithdownstreamblocking. HealthCareManagSci. 2014;17(1):88–99.
26.BakerDW,StevensCD,BrookRH.Determinantsofemergency departmentusebyambulatorypatientsatanurbanpublichospital. AnnEmergMed. 1995;25(3):311–6.
ORIGINAL RESEARCH EmergencyDepartmentPatientSatisfactionScoresAreLowerfor PatientsWhoArriveDuringtheNightShift TonyZitek,MD*†
LukeWeber,MD*
TatianaNunez,MD*
LuisPuron,DO*
AdamRoitman,BS†
ClaudiaCorbea,BS†
DanaSherman,DNP*†
MichaelShalaby,MD*†
FraydaKresch,MD*
DavidA.Farcy,MD*†
SectionEditor: LauraWalker,MD
*MountSinaiMedicalCenter,DepartmentofEmergencyMedicine,MiamiBeach,Florida † FloridaInternationalUniversity,HerbertWertheimCollegeofMedicine,Miami,Florida
Submissionhistory:SubmittedMarch11,2024;RevisionreceivedAugust29,2024;AcceptedAugust30,2024
ElectronicallypublishedOctober2,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20326
Background: Increasingly,patientsatisfactionscoresarebeingusedtoassessemergencyphysicians. Wesoughttodeterminewhetherthepatientsatisfactionscorescollectedbyourhospitalsystemare lowerforpatientswhoaretreatedintheemergencydepartment(ED)onnightshiftsascomparedtothose treatedondayshifts.
Methods: Weperformedacross-sectionalanalysisofpatientsatisfactionscoresfromthreeEDsin Florida.WeobtainedsatisfactiondatafromNRCHealth(thecompanythatprovidesoursurveys)usinga randomsampleof1,000completedsurveysfrompatientstreatedin2022;wealsoperformedmanual chartreviewtoobtainclinicaldata.Thesatisfactionsurveysaskedpatientshowlikelytheywouldbeto recommendthefacility(from0–10).Patientswhoprovidedascoreof9or10wereconsidered “promoters.” Forourprimaryanalysis,wecomparedthepercentageofpromotersforthedayshift encounters(7 AM to7 PM)tothenightshiftencounters(7 PM to7 AM).Wealsoperformedamultivariable logisticregressionanalysisusingseveraldemographicandclinicalvariablestofurtherassessthe associationbetweennightshiftarrivalandsatisfactionscores.
Results: Ofthe1,000surveysanalyzed,66.3%ofpatientsarrivedduringthedayshift,and33.7% arrivedduringthenightshift.Ofthosewhoarrivedduringthedayshift,525(79.2%)werepromoters comparedto228(67.7%)ofthosewhoarrivedduringthenightshift,adifferenceof11.5%(95% confidenceinterval[CI]5.7–17.4%), P < 0.001.Onmultivariableanalysis,nightshiftarrivalwas associatedwithalowerchanceofapatientbeingapromoter,withadjustedoddsratio0.60(95%CI 0.43–0.84), P = 0.003.
Conclusion: PatientswhopresentedtotheEDduringthenightshiftwerelesslikelytobe promotersthanpatientswhoarrivedduringthedayshift.Assessmentsofpatientsatisfaction datashouldaccountfortimeofvisitandotherfacility-relatedandoperationalcharacteristics.
[WestJEmergMed.2024;25(6)929–937.]
INTRODUCTION Withemergencydepartments(ED)open24/7,most emergencyphysiciansworksomenightshifts. Unfortunately,priordatahasshownthatnightshiftworkis associatedwithincreasedriskofavarietyofmedical conditions1–5 andmotorvehiclecollisionsafterthoseshifts.6 Additionally,emergencyphysiciansworkingatnightmay havetodealwithreducedsupportstaff,tiredpatients,and feweravailableconsultants.Moreover,multiplepriorstudies havedemonstratedthatwhileonnightshift,cognitive performancedeclines.7,8
Despitetheuniquechallengesofnightshifts,emergency physiciansaregenerallyheldtothesamestandardsonnight shiftsastheyareondayshifts,andonewaytheyarenow assessedisbypatientsatisfactionscores.Indeed,patient satisfactionhasbecomeanincreasinglyimportantpartof healthcareinlargepartbecauseoftheincentivesinitiatedby theAffordableCareActin20109;now,bothinstitutionand physicianpaymentaresometimesbasedonpatient satisfactionscores.10
Priorstudieshaveshownthatcertainfactorsincluding shorterEDlengthofstay(LOS),11–13 olderpatientage,14 and goodcommunication15 areassociatedwithbetterED patientsatisfactionscores.Twopriorstudieshave investigatedtherelationshipbetweentreatmentduringnight shiftsandpatientsatisfactionscores.14,16 Onefoundno statisticallysignificantassociation,14 whileanotherfound thatphysicianswhoworkedfewernightshiftshadhigher patientsatisfactionscores.16 Giventheconflictingevidence todateandtheincreasingemphasisonpatientsatisfaction, wefeltthatadditionalstudywaswarrantedtoassessthe relationshipbetweennightshiftworkintheEDand patientsatisfaction.
Ourprimaryobjectiveinthisstudywastodetermine whetherpatientswhoarecaredforduringnightshifts providelowerpatientsatisfactionscoresthanthosecaredfor duringdayshifts,usingthereal-worldsatisfactiondata. Secondarily,wesoughttodeterminewhetherother demographicandclinicalcharacteristicsareassociatedwith EDpatientsatisfactionscores.
METHODS StudyDesignandSetting
Weperformedacross-sectionalanalysisofEDpatient satisfactionscoresfrompatientswhopresentedtoasingle hospitalsystemintheStateofFloridainthesoutheastern UnitedStatesfromJanuary1–December31,2022. Specifically,weperformedasecondaryanalysisofa previouslycollecteddatasetofsatisfactionscores,andwe performedachartreviewtosupplementthatdata.We followedtheStrengtheningtheReportingofObservational StudiesinEpidemiology(STROBE)guidelines.Thestudywas approvedbytheMountSinaiMedicalCenterInstitutional ReviewBoard.Thisstudyreceivednoexternalfunding.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Physiciansarejudgedbasedonpatient satisfactionscores.Priordatafoundthat certainpatientandfacilitycharacteristicsare associatedwithsatisfactionscores.
Whatwastheresearchquestion?
DopatientswhopresenttotheEDatnight providelowersatisfactionscoresthanpatients whopresentduringthedaytime?
Whatwasthemajor findingofthestudy?
Ofdayshiftpatients,79.2%were “promoters” vs 67.7%ofnightshiftpatients(difference11.5% [95%CI5.7–17.4%]),P < 0.001.
Howdoesthisimprovepopulationhealth?
Thisdatahelpsusbetterinterpretpatient satisfactiondata,whichmayhelpimproveour abilitytoprovidepatient-centeredcare.
Ourhospitalsystemhasatertiarycare,community teachinghospitallocatedinMiamiBeach,Florida,aswellas afreestandingEDlocatedinHialeah,Florida,(freestanding ED#1)andafreestandingEDlocatedinAventura,Florida, (freestandingED#2).Themainhospital’sEDhad56,005 visitsduring2022,whilefreestandingED#1had37,932 visitsandfreestandingED#2had19,635visits.Emergency medicineresidentsworkshiftsonlyatthemainhospital’ s ED.Advancedpracticepractitioners(APP)workshiftsatall threefacilities.Shifttimesareshownin Table1.In2022, threeemergencyphysiciansonlyworkedonlynightshifts, andonephysicianworkedonlydayshifts.Someattending physiciansandAPPsonlyworkedatonefacility;others workedattwoorallthree.
SelectionofParticipants In2022,NRCHealth(Lincoln,NE)administeredour patientsatisfactionsurveysandtrackedsatisfactiondata. Surveysweresentbybothtextmessageandemailtoall patientswholefttheED.Allpatientswhocompletedthe NRCHealthEDpatientsatisfactionsurveyin2022were eligibleforinclusioninthisstudy.Admittedpatientswerenot sentsurveysandwereexcludedfromanalysis.
Measurements NRCHealthkeepsadatabasewiththeresponsesfrom satisfactionsurveysanddemographicinformationaboutthe
Table1. Emergencydepartmentstaffshifttimesin2022.
patientswhocompletethesurveys.Inourhospitalsystem, currently,individualphysician-levelpatientsatisfaction scoresaretrackedandassessedusingthesedata,but compensationisnotdependentuponthem.Wegenerateda reportfromNRCHealth’sdataforallpatientswho completedasatisfactionsurveyduring2022andthenuseda randomnumbergeneratortocreateasampleof1,000patient encountersforanalysis.Foreachofthesepatientencounters, twomedicalstudentstransferredpatientresponsesand availabledemographicinformationintoaspreadsheetin MicrosoftExcelv16.79.1(MicrosoftCorp,Redmond,WA). Inparticular,NRCHealthprovideduswiththefollowing dataforeachencounter:thedateofthevisit;thefacility;the nameofthephysicianorAPP;methodofpatientresponse (emailortextmessage);andthepatient’ sage,sex,race, medicalrecordnumber,address,maritalstatus,and preferredlanguage.Thetwomedicalstudentswho abstractedthesedatapointshadnoroleintheabstractionof theotherdatadiscussedbelow.
Next,wecreatedaseparatespreadsheetwithadditional clinicalinformationforeachofthe1.000patientencounters usingourelectronichealthrecordsystem(EHR)(Epic SystemsCorporation,Madison,WI).Sixabstractors(three emergencymedicineresidents,twoemergencyattendings, andonenursepractitioner)performedmanualchartreview todeterminethepatient’sethnicity,modeofarrivaltothe ED,timesofarrivalanddeparture,EmergencySeverity Index(ESI)score,17 disposition,clinicianwhodischargedthe patient(andtheirsupervisingattending,ifapplicable),and whetherornoteachofthefollowingwasperformedduring thepatientencounter:residentparticipation;sign-out;blood test;advancedimaging;in-personconsultantevaluation, consultationbyphone(only);opioidpainmedicine administration;andprescriptionprovided.
Ingeneral,manualchartreviewfollowedthemethods suggestedbyKajietal.18 Theabstractorswhoperformed
manualchartreviewwereblindedfromthesatisfactiondata. Noneoftheabstractorsorinvestigatorshavebeena nocturnist.Theabstractors filledin15columnsinthe spreadsheetwiththedatapointsabove.Theyweretrainedon properdataabstractionbytheprincipalinvestigator(TZ), andtheyfollowedadatadictionarythatexplicitlydefinedthe variablesandexplainedwhereto findthemintheEHR.The datadictionaryisincludedasan appendix,whichprovides detaileddefinitionsofallvariables.Thedefinitionsofafew importantvariablesarealsodefinedhereasfollows: Weconsideredpatientstohavearrivedduringtheday shiftiftheyarrivedintheEDbetween7 AM–7 PM andtothe nightshiftiftheyarrivedbetween7 PM–7 AM.Wechosethese definitionsbecausemanyphysicianandnursingshiftsfollow thesetimeschedulesinoursystem(Table1).Wealsodivided patientsintothetimeofyeartheycametotheEDby standardquarters.
Thetypeofclinician(physicianorAPP)whoevaluated thepatientprimarilywasdeterminedbasedonthenameof theclinicianonthesurveyasperNRCHealthdata.For example,apatientwasconsideredtohavebeenseen primarilybyanAPPiftheAPPwasthepersonlistedonthe satisfactionsurvey.Asmentionedabove,wealsomanually recordedthenameoftheclinician(andtheirsupervising attending)whodischargedthepatientforeachpatient encounter.Forpatientswhowerenotsignedout,the dischargingclinician(orsupervisingattending)wasfully consistentwiththelistednameonthesurveys.However,for patientswhoweresignedout,sometimestheinitialclinician whotreatedthepatientwaslistedonthesurveyand sometimesasubsequentonewas.Sinceadministratorsassess thesatisfactiondatabasedonthenameoftheclinicianonthe surveys,weusedthenameoftheclinicianonthesurveyasthe primarytreatingclinician.
PatientswholefttheEDbeforebeingevaluatedbya physicianorAPPcouldstillbeincludedinthestudyifthey
completedasatisfactionsurveybutwereconsideredtohave notbeenseenbyaphysicianorAPP.Allsixabstractors obtainedthedataforagroupofthesame50patientstoallow foranassessmentoftheinter-raterreliability.Wecalculated thefree-marginalkappaforthetwovariablesthatwe consideredtobethemostdifficulttoabstract:sign-out,and in-personevaluationbyconsultant.
Aftercompletingdatacollection,theprincipal investigator(TZ)mergedthespreadsheetswiththe satisfactiondataandtheclinicaldata,andthedatawas analyzedasdescribedbelow.
Outcomes In2022,ouradministrationconsideredthemost importantquestiononthesatisfactionsurveystobe: “How likelyisitthatyouwouldrecommend[facilityname]toa friendorcolleague?” (from0–10).Apatientwhoprovideda scoreof9or10wasconsideredtobea “promoter”;ascoreof 7or8wasconsidered “passive”;andascoreof0–6was consideredtobea “detractor.” Thepercentageofpromoters minusthepercentageofdetractorsisdeemedthe “net promoterscore,” whichisusedtomeasureoverall satisfactioninhealthcareaswellasinotherbusinesses.19,20 Ourprimaryoutcomewasthepercentageofcompleted patientsatisfactionsurveysthatqualifiedaspromoters. Secondarily,wedeterminedthenetpromoterscoreandthe adjustedoddsratiosforbeingapromoterforseveral demographicandclinicalvariables.
Analysis BasedonapreliminaryanalysisofNRCHealthdata,we anticipatedthattherewouldbeapproximatelytwiceasmany completedsurveysfrompatientswhoarrivedduringtheday shiftvsthenight.Additionally,weknewthatapproximately 75%ofourcompletedsurveysin2022qualifiedaspromoters. Basedongestalt,wehypothesizedthatthepercentageof promotersfromthedayshiftwouldbeeightpointshigher thanthenightshift.Totestourhypothesiswithanalphaof 0.05andpower0.8,werequiredresponsesfrom957patients. Weroundedthisupto1,000andchosethatasour samplesize.
Forourprimaryanalysis,wecomparedthepercentageof promotersforpatientencountersinwhichthepatientarrived duringthedayshiftcomparedtonightshift.Wemadethe unadjustedcomparisonourprimaryanalysissincethatis howpatientsatisfactionscoresarebeingusedtoassess emergencyphysiciansinourhospitalsystem.Wealso comparedthedemographicandclinicalcharacteristicsofthe patientencountersforthetwogroups.Wedetermined normalitywiththeShapiro-Wilktest.Fornormal distributions,wecomparedthemeansofgroupsusing t -tests. Fornon-normaldistributions,wecomparedmediansusing themediantest.WeusedtheFisherexacttesttocompare categoricalvariables.
Secondarily,giventhatapatientwhoarrivesduringthe endofadayshiftmightbemostlytreatedbythenightstaff (orviceversa),wealsoanalyzedpatientsbasedonthetimeof EDdeparture.Inotherwords,weconsiderednightshift patientstobethosewhodepartedbetween7 PM – 7 AM. Lastly,tofurtherisolatethenight-timehourswhenpeople aregenerallysleeping,wedividedpatientsbyarrivaltime intothreeeight-hourepochs:6 AM – 2 PM (day),2 PM – 10 PM (swing),and10 PM – 6 AM (night).
Lastly,weperformedamultivariablelogisticregression analysiswith “promoter” (yesorno)asthedependent variable.Basedonpriordata,11–14,16,21–23 weincludedthe followingvariablesinourmodel:EDLOS(continuous);ED site(categorical);elderly(age > 65)(binary);pediatric (binary);race(Whiteornot);ethnicity(HispanicornonHispanic),healthinsurancetype(noinsurance,commercial, orgovernment/other);non-Englishspeaking(binary); EmergencySeverityIndex(ESI)(2or3vs4or5);and advancedimagingperformed(binary).Basedoninvestigator hypothesis,wealsochosetoincludethefollowingas covariates:quarteroftheyear(1,2,3,or4);married(binary); seenbyaresident(binary);seenprimarilybyanAPP (binary);arrivalbyambulance(binary);andbloodtest performed(binary).Wealsohypothesizedthatconsultant evaluationswouldbeassociatedwithbettersatisfaction
113,572ED visits during 2022:
56,005visits to the main hospitalED
19,635visits to Freestanding ED #1
37,932visits to Freestanding ED #2
87,885patient encounters in which patient departed from the hospital.
Excluded 25,687admissions.
1,381 patients not sent surveys from January 1-4.
86,504patient encounters in which patient was sent a satisfaction survey.
80,129surveys not completed.
6,375(7.4%) patientencounters for which satisfaction surveywas completed.
1,000 patient surveys randomly selected. 663 arrived between 7 AM and 7 PM (day shift).
arrived between 7 PM and 7 AM (night shift).
Figure. Flowofpatientencounters.
Table2. Characteristicsofpatientvisitsforpatientswhoarrivedduringthedayshift(7 AM to7 PM)ascomparedtothosewhoarrivedduringthe nightshift(7 PM to7 AM).
Day-shiftarrival (n = 663)
Night-shift arrival(n = 337)
Patientdemographics
Meanage(SD)49.3(22.2)43.0(23.4)6.3(3.2to9.3) <0.001*
Pediatric(< 18years),n(%)60(9.0)46(13.7)4.7(0.3to8.9)0.03*
Elderly(> 65years),n(%)203(30.6)78(23.2)7.4(1.8to13.2)0.01*
Male,n(%)273(41.2)147(43.6)2.4( 4.0to8.9)0.46
RaceWhite,n(%)530(79.9)248(73.6)6.3(0.7to12.0)0.02
RaceBlack,n(%)53(8.0)31(9.2)1.2( 2.5to4.9)0.52
Hispanic,n(%)365(55.1)205(60.8)5.8( 0.7to12.2)0.08
Commercialhealthinsurance,n(%)391(59.0)203(60.2)1.2( 5.2to7.7)0.70
Nohealthinsurance,n(%)53(8.0)48(14.2)6.3(2.0to10.5)0.002*
Married,n(%)267(40.8)99(29.6)11.1(5.0to17.3) <0.001*
Non-Englishspeaking,n(%)228(34.4)114(33.8)0.6( 5.7to6.8)0.86
Fromoutofstate,n(%)41(6.2)23(6.8)0.6( 2.6to3.9)0.70
Timeofyearofvisit
Quarter1,n(%)155(23.4)82(24.3)1.0( 4.7to6.6)0.74
Quarter2,n(%)186(28.1)87(25.8)2.2( 3.6to8.0)0.75
Quarter3,n(%)157(23.7)83(4.6)1.0( 4.7to6.6)0.74 Quarter4,n(%)165(24.9)85(25.2)0.3( 5.4to6.0)0.91
Clinicianandfacilitycharacteristics
Mainhospital388(58.5)204(60.5)2.0( 4.4to8.4)0.54
FreestandingED#1160(24.1)67(19.9)4.3( 1.1to9.6)0.13 FreestandingED#2115(17.4)66(19.6)2.2( 2.9to7.4)0.38
Residentparticipated,n(%)217(32.7)179(53.1)20.4(14.0to26.8) <0.001* Advancedpracticepractitioner,n(%)171(25.8)36(10.7)15.1(10.4to19.8) <0.001* Sign-out,n(%)24(3.6)30(8.9)5.3(1.9to8.6) <0.001*
Clinicalcharacteristics
ESIa 2,n(%)20(3.0)13(3.9)0.9( 1.6to3.3)0.48
ESI3,n(%)401(60.5)229(68.0)7.5(1.3to13.7)0.02*
ESI4,n(%)239(36.1)93(27.6)8.5(2.4to14.5)0.007*
ESI5,n(%)3(0.5)2(0.6)0.1( 0.8to1.1)0.77
Arrivedbyambulance,n(%)24(3.6)22(6.5)2.9(0.0to5.9)0.04*
Bloodtestperformed,n(%)287(43.3)126(37.4)5.9( 0.5to12.3)0.07 Advancedimagingperformed,n(%)228(34.4)90(26.7)7.7(1.7to13.6)0.01*
In-personconsultantevaluation,n(%)20(3.0)8(2.4)0.7( 1.4to2.7)0.56
Phone(only)consultation,n(%)23(3.5)2(0.6)2.9(1.3to4.5)0.006*
Opioidpainmedicinegiven,n(%)72(10.9)36(10.7)0.2( 3.9to4.2)0.93
Givenprescription,n(%)374(56.4)170(50.4)6.0( 0.6to12.5)0.07
Medianlengthofstay(IQR),min194(123–259)184(123–265)10( 7to28)0.28
AMA,eloped,orLBTb,n(%)18(2.7)17(5.0)2.3( 0.3to5.0)0.06
aEmergencySeverityIndex.TherewerenopatientswithanESIof1. bAllotherpatientsweredischargedexceptfortwowhoweretransferredtootherhospitals. *Indicatesastatisticallysignificantdifferencebetweengroups.
AMA,againstmedicaladvice; CI,confidenceinterval; ED,emergencydepartment; ESI,EmergencySeverityIndex; IQR,interquartilerange; LBT,leftbeforetreatment.
Volume25,No.6:November2024WesternJournal
scores,buttheseoccurredtoorarelyinourdatasettobe includedintheregressionanalysis.WeusedtheHosmerLemeshowstatistictoassessgoodnessof fitofthe regressionmodel.
DatawasaggregatedinExcelandanalyzedinRStudio v2023.03.0(RStudioPBC,Boston,MA).Usingtwo-sided hypothesistests,weconsidered P < 0.05tobe statisticallysignificant.
MissingData Inafewcases,raceandethnicitywerenotrecorded.This washandledasfollows:Patientswhoweredocumentedas havingWhiteorCaucasianracewereconsideredtobe “White.” PatientswhoweredocumentedasBlackorAfrican Americanwereconsideredtobe “Black.” Patients documentedasAsian,AmericanIndian,multiracial,other, orforwhomracewasnotdocumentedwereconsidered neitherWhitenorBlack.Similarly,ifapatientwas documentedas “Hispanic,” theirethnicitywasconsideredto be “Hispanic.” Iftheyweredocumentedtobenon-Hispanic oriftheirethnicitywasnotdocumented,theywere considered “non-Hispanic.”
RESULTS Overall
Asshowninthe Figure,6,375satisfactionsurveyswere completedin2022,andwerandomlyselected1,000for analysis.Ofthese,824patientsrespondedbytextmessageand 176respondedbyemail.Ourdataincludedsurveysevaluating 44differentattendingphysiciansand18APPs.Therewereno missingdatapoints,exceptfor fivepatientsforwhomnorace andethnicitywererecorded.Inter-raterreliabilityforthetwo assessedvariableswasalmostperfectwithfree-marginal kappa0.98(95%confidenceinterval[CI]0.94–1.0)forsignoutand0.98(95%CI0.9–1.0)forin-personevaluationbya consultant.Overall,75.3%ofpatientencountersqualifiedas promoters,andnetpromoterscorewas57.8.
NightvsDayShifts Intotal,663(66.3%)patientsarrivedduringthedayshift, and337(33.7%)arrivedduringthenightshift. Table2 shows
acomparisonofcharacteristicsofthesetwogroups.Notably, thegroupswerenotbalancedonseveralcharacteristics includingage,race,maritalstatus,insurance,typeof cliniciansinvolved,ESI,andadvancedimagingperformed. Regardingtheprimaryoutcome,525(79.2%)ofthosewho arrivedduringthedayshiftwerepromoterscomparedto228 (67.7%)ofthosewhoarrivedduringthenightshift,an absolutedifferencebetweengroupsof11.5%(95%CI 5.7–17.4%), P < 0.001.Thenetpromoterscorefortheday shiftwas64.9and44.0forthenightshift.Datastratifiedby facilityareshownin Table3.
Whenredefiningdayshiftbydeparturetime,therewere 492day-shiftpatientsand508night-shiftpatients.Ofthose, 396(80.5%)and357(70.3%)werepromotersforthedayand nightshift,respectively,adifferenceof10.2%(95%CI 4.9–15.6%), P < 0.001.
Whenanalyzingthedatabyeight-hourepochs,307 (80.2%)of383patientswhoarrivedbetween6 AM–2 PM were promoters.Meanwhile,339(75.5%)of449patientswho arrivedbetween2 PM–10 PM werepromoters,and107(63.7%) of168whoarrivedbetween10 PM–6 AM werepromoters. Combiningtheeight-hourdayandswingshiftstogether, 77.6%ofsurveyswerepromoters,whichis13.9% (95%CI6.2–21.8%)higherthantheeight-hournightshift group, P < 0.001.
Nineteencompletedsurveyscamefrompatientsseenby oneofourthreenocturnists.Ofthose,12(63.2%)were promoters.Additionally,theonephysicianwhoonlyworked dayshiftshad24completedsurveys,ofwhich21(87.5%) werepromoters.Excludingthecombined43encountersfrom thatphysicianandthethreenocturnistsmadeitsuchthat 78.8%ofpatientswhoarrivedbetween7 AM–7 PM were promotersand68.2%ofthepatientswhoarrivedbetween7 PM–7 AM werepromoters,adifferenceof10.6%(95%CI 4.6–16.6%), P =< 0.001.
MultivariableRegressionAnalysis Onmultivariableanalysis,arrivalduringthenightshift hadastatisticallysignificantassociationwithalower chancethatthepatientwouldbeapromoter,withadjusted oddsratio0.60(95%CI0.43–0.84), P = 0.003.Other
Table3. Thepercentageofcompletedsatisfactionsurveysconsideredpromotersoverallandateachofthethreeemergencydepartments, comparingpatientswhoarrivedondayshiftvsnightshift.
Overall(N = 1,000)525(79.2)228(67.7)11.5(5.7to17.4) <
Mainhospital(n = 592)304(78.4)137(67.2)11.2(3.6to18.8)*0.003*
FreestandingED#1(n = 227)160(85.0)47(70.2)14.8(2.6to27.1)*0.01*
FreestandingED#2(n = 181)85(73.9)44(66.7)7.2( 6.7to21.2)0.30
*Indicatesastatisticallysignificantdifference. CI,confidenceinterval; ED,emergencydepartment.
Table4. Theadjustedoddsratiosofvariousdemographicandclinicalvariablesandtheirassociationwithbeinga “promoter” (apatientwho giveshighratingstoaphysicianonpatientsatisfactionsurveys).
CharacteristicAdjustedoddsratioforbeingapromoter(95%CI)
Demographics
Elderly(age > 65)(n = 281)2.62(1.72–4.08)*
Pediatric(age < 18)(n = 106)0.80(0.48–1.34)
Whiterace(n = 778)
0.91(0.62–1.31)
Hispanicethnicity(n = 570)0.86(0.59–1.26)
HealthInsurance
Commercial(n = 594)
0.78(0.53–1.14)
Governmentorother Reference
Noinsurance(n = 101)
Married(n = 366)
0.83(0.47–1.46)
0.98(0.70–1.40)
Non-Englishspeaking(n = 341) 1.82(1.18–2.82)*
Timeofyearofvisit
Quarter1(n = 237)
0.93(0.60–1.43)
Quarter2(n = 273) 0.84(0.55–1.28)
Quarter3(n = 240) 1.29(0.82–2.03)
Quarter4(n = 250) Reference
Facility
MainED(n = 592) Reference
FreestandingED#1(n = 227)0.91(0.38–1.08)
FreestandingED#2(n = 181)0.65(0.51–1.60)
Cliniciancharacteristics
Seenbyaresident(n = 397)0.81(0.51–1.27)
APPprimarily(n = 207) 0.78(0.51–1.19)
Sign-out(n = 54) 1.08(0.54–2.28)
Clinicalcharacteristics
Emergencyseverityindex
ESIlevel2or3(n = 663) Reference
ESIlevel4or5(n = 337)0.97(0.67–1.41)
Arrivedbyambulance(n = 46)0.54(0.28–1.09)
Bloodtestperformed(n = 413)1.11(0.76–1.64)
AdvancedImagingperformed(n = 318)1.38(0.92–2.09)
Opioidpainmedicinegiven(n = 108)1.01(0.60–1.73)
Prescriptiongiven(n = 543)1.15(0.84–1.59)
EDlengthofstay(for1-hincrease)0.94(0.84–1.04)
Arrivalduringnightshift(n = 337)0.60(0.43–0.84)*
*Indicatesastatisticallysignificantassociation.
APP,advancedpracticepractitioner; CI,confidenceinterval; ED,emergencydepartment; ESI,EmergencySeverityIndex.
thannight-shiftarrival,noothervariableswereassociated withareducedchanceofbeingapromoter.Ontheother hand,elderlypatients(age > 65)andnon-Englishspeaking patientshadpositiveassociationswithbeinga promoter(Table4).
DISCUSSION Inthiscross-sectionalstudy,wefoundthatEDpatients whoarriveordepartduringnightshiftarelesslikelytobe promotersascomparedtoday-shiftpatients.Notably,the patientpopulationthatcompletedthesatisfactionsurveys
andarrivedduringanightshiftwassubstantiallydifferent thanthosepatientswhoarrivedduringdayshift.Considering thisandotherintuitivechallengesofnightshifts,unadjusted comparisonsofphysicianswhoworkdifferentratiosofday andnightshiftsonanynumberofmetricsarelikelytobe compromised.However,inourstudyevenafteradjustingfor severaldifferencesbetweendayandnightshifts,westill foundanassociationbetweennight-shiftarrivalandlower patientsatisfactionscores.
Priordataonthissubjecthasbeenmixed.Onepriorstudy evaluatedtherelationshipbetweennightshiftsandED patientsatisfactionscoresusingdatafrom2009–2013froma singleEDanddidnotshowasignificantassociation.14 On theotherhand,apriorlargestudyusingdatafrom42 facilitiesfrom2012–2015foundthatphysicianswhoworked fewernightshiftshadhigherpatientsatisfactionscores.16
Bothofthesestudiesattemptedtoassessalargenumberof physician,facility,andoperationalfactorsthatmightaffect patientsatisfactionscores.Arelativestrengthofourstudy wasthatitwasamoretargetedandgranularassessment specificallyofnight-vsday-shiftpatientsatisfactionscores.
Ourstudywasnotdesignedtospecificallyassessthe associationsofothervariableswithpatientsatisfaction scores,butwewillbrieflyreviewthesecondary findings.In thisregard,ourresultswerelargelyconsistentwithprevious work,includingour findingsthatelderlypatientsandnonEnglishspeakingpatientsaremorelikelytoprovidehigh satisfactionscores.14,22 Priordatahasbeenmixedwith regardtotheassociationofLOSandpatient satisfaction.11–13,16,24,25 Wefailedto findanassociation betweenEDLOSandpatientsatisfaction(Table4),whichis consistentwithpreviousworkthathasreportedthat perceivedLOSismoreimportantthanactualLOS.24,25
Overall,althoughempathyandcommunicationare importantcontributorstopatientsatisfaction15,22,24 thatan emergencycliniciancanmostlycontrol,therearemany factorsthattheycannot.Ourdataandpreviousdemonstrate thatnightshiftwork,thepatientpopulation,14 andthe facility16,23 allinfluencepatientsatisfactionscores. ConsideringalsothattheresponserateforEDsatisfaction surveysissolow(<10%inoursystemandsimilarinmany others26)andthatonlydischargedpatientsaresentsurveys, werecommendagainsttheuseofpatientsatisfactionscores todeterminepaymentforemergencyclinicians.
LIMITATIONS Thisstudyhadseverallimitations.First,ourdatacomes fromasinglehospitalsystemthathasfairlyhighpatient satisfactionscores;so,ourresultsmaynotbeapplicableto otherEDs.Additionally,giventheretrospectiveand observationalnatureofthestudy,therecouldhavebeen someunmeasuredconfoundersthatcouldexplainthe differencesinpatientsatisfactionbetweenthedayandnight shifts.Namely,whilephysiciansusuallyworkbothdayand
nightshifts,nursingstaffandsupportstaffmoretypically workonlydaysoronlynights.Therefore,differencesin staffingmightexplainthedifferencesinsatisfactionscores. Moreover,priorstudieshavedemonstratedthat communicationisanimportantfactorinEDpatient satisfactionscores,22,27 butgiventhedesignofthisstudy,it wasnotpossibletoassessthequalityofcommunication. Next,ourdatadidnothavethegranularitytoadjustfor patientvolumeforeachshift,whichcouldhaveimpacted patientsatisfaction.However,giventhatthemedianED LOSwassimilarintheday-andnight-shiftgroups,wedoubt thatdifferencesinpatientvolumewouldexplainthelower satisfactionscoresbynight-shiftpatients.Lastly,thelow responseratetopatientsatisfactionsurveysisalimitationin thatsurveyresponsesarelikelysubstantiallyinfluencedby selectionbias,butwedonotconsiderthisalimitationspecific toourstudybecauseourgoalwastocomparethereal-world patientsatisfactionscoresfromday-vsnight-shiftpatients (withcurrentsurveytechniques).Ourresultsthusprovidea comparisonofthedatathatisactuallybeingusedtoassess clinicians’ performanceonpatientsatisfaction.
CONCLUSION Inthiscross-sectionalstudy,night-shiftarrivaltotheED wasassociatedwithastatisticallysignificantlowerchance thatthepatientwouldbeapromoteronsatisfactionsurveys. Giventhis findingandpreviousdatasuggestingthatother issuesbeyondthephysician’scontrolheavilyinfluence satisfactionscores,facilityfactors,patientcharacteristics, andoperationalfactors(includingthetimeoftheED visit)shouldbeconsideredwhenassessingpatient satisfactionscores.
AddressforCorrespondence:TonyZitek,MD,MountSinaiMedical Center,DepartmentofEmergencyMedicine,4300AltonRd.,Miami Beach,FL33140.Email: zitek10@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Ziteketal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.VetterC,DashtiHS,LaneJM,etal.Nightshiftwork,geneticrisk,and type2diabetesintheUKbiobank. DiabetesCare. 2018;41(4):762–9.
2.VetterC,DevoreEE,WegrzynLR,etal.Associationbetweenrotating nightshiftworkandriskofcoronaryheartdiseaseamongwomen. JAMA. 2016;315(16):1726–34.
3.MaidstoneRJ,TurnerJ,VetterC,etal.Nightshiftworkisassociated withanincreasedriskofasthma. Thorax. 2021;76(1):53–60.
4.Fagundo-RiveraJ,G´omez-SalgadoJ,García-IglesiasJJ,etal. Relationshipbetweennightshiftsandriskofbreastcanceramong nurses:asystematicreview. Medicina(Kaunas). 2020;56(12):680.
5.BrownDL,FeskanichD,SanchezBN,etal.Rotatingnightshiftworkand theriskofischemicstroke. AmJEpidemiol. 2009;169(11):1370–7.
6.SteeleMT,MaOJ,WatsonWA,etal.Theoccupationalriskofmotor vehiclecollisionsforemergencymedicineresidents. AcadEmergMed. 1999;6(10):1050–3.
7.DulaDJ,DulaNL,HamrickC,etal.Theeffectofworkingserialnight shiftsonthecognitivefunctioningofemergencyphysicians. AnnEmerg Med. 2001;38(2):152–5.
8.Smith-CogginsR,RosekindMR,HurdS.Relationshipofdayversus nightsleeptophysicianperformanceandmood. AnnEmergMed. 1994;24(5):928–34.
9.HealthCare.gov.ReadtheAffordableCareAct.Availableat: https:// www.healthcare.gov/where-can-i-read-the-affordable-care-act/ AccessedAugust16,2024.
10.FinkelsteinJ,LiftonJ,CaponeC.Redesigningphysiciancompensation andimprovingEDperformance. HealthcFinancManage. 2011:65(6).114–7.
11.ParkerBTandMarcoC.Emergencydepartmentlengthofstay: accuracyofpatientestimates. WestJEmergMed. 2014;15(2):170–5.
12.ChangAM,LinA,FuR,etal.Associationsofemergencydepartment lengthofstaywithpubliclyreportedquality-of-caremeasures. Acad EmergMed. 2017;24(2):246–50.
13.WalshMandKnottJC.Satisfactionwiththeemergencydepartment environmentdecreaseswithlengthofstay. EmergMedJ. 2010;27(11):821–8.
14.HandelDA,FrenchLK,NicholJ,etal.Associationsbetweenpatient andemergencydepartmentoperationalcharacteristicsandpatient satisfactionscoresinanadultpopulation. AnnEmergMed. 2014;64(6):604–8.
15.SonisJD,AaronsonEL,LeeRY,etal.Emergencydepartmentpatient experience. JPatientExp. 2018;5(2):101–6.
16.PinesJM,PennintiP,AlfarajS,etal.Measurementunderthe microscope:highvariabilityandlimitedconstructvalidityinemergency departmentpatient-experiencescores. AnnEmergMed. 2018;71(5):545–54.e6.
17.WuerzRC,TraversD,GilboyN,etal.Implementationandrefinementof theemergencyseverityindex. AcadEmergMed. 2001;8(2):170–6.
18.KajiA,SchrigerD,GreenS.Lookingthroughtheretrospectoscope: reducingbiasinemergencymedicinechartreviewstudies. AnnEmerg Med. 2014;64(3):292–8.
19.ReichheldFF.Theonenumberyouneedtogrow. HarvBusRev. 2003;81(124):46–54.
20.LiyakasaK.Customerexperienceiscriticalinnetpromoter benchmarks.2012.Availableat: http://www.destinationcrm.com/ Articles/Columns-Departments/Insight/Customer-Experience-IsCritical-in-Net-Promoter-Benchmarks-82569.aspx AccessedNovember29,2023.
21.BoudreauxED,FriedmanJ,ChanskyME,etal.Emergencydepartment patientsatisfaction:examiningtheroleofacuity. AcadEmergMed. 2004;11(2):162–8.
22.SunBC,AdamsJ,OravEJ,etal.Determinantsofpatientsatisfaction andwillingnesstoreturnwithemergencycare. AnnEmergMed. 2000;35(5):426–34.
23.BendeskyBS,HunterK,KirchhoffMA,etal.Samephysician,different location,differentpatientsatisfactionscores. AnnEmergMed. 2016;68(5):531–5.
24.NicholJR,FuR,FrenchK,etal.Associationbetweenpatientand emergencydepartmentoperationalcharacteristicsandpatient satisfactionscoresinapediatricpopulation. PediatrEmergCare. 2016;32(3):139–41.
25.BoudreauxEDandO’HeaL.Patientsatisfactionintheemergency department:areviewoftheliteratureandimplicationsforpractice. JEmergMed. 2004;26(1):13–26.
26.JaquisWp,DesRochersLR,EnguidanosER,etal.Patientsatisfaction. 2011.Availableat: https://www.acep.org/patientsatisfaction/.Accessed September24,2017.
27.TomaG,TrinerW,McNuttLA.Patientsatisfactionasafunctionof emergencydepartmentprevisitexpectations. AnnEmergMed. 2009;54(3):360–7.e6.
ORIGINAL RESEARCH ComparisonofEmergencyDepartmentDispositionTimesinAdult LevelIandLevelIITraumaCenters SierraLane,BS*
JeffryNahmias,MD,MHPE*
MichaelLekawa,MD*
JohnChristianFox,MD†
CarrieChandwani,MD†
ShahramLot fipour,MD,MPH† AregGrigorian,MD*
SectionEditor: GaryJohnson,MD
*UniversityofCalifornia,Irvine,DepartmentofSurgery,DivisionofTrauma, BurnsandSurgicalCriticalCare,Orange,California † UniversityofCalifornia,Irvine,DepartmentofEmergencyMedicine, Orange,California
Submissionhistory:SubmittedMarch25,2024;RevisionreceivedSeptember6,2024;AcceptedSeptember10,2024
ElectronicallypublishedOctober22,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20523
Introduction: Theef ficientutilizationofresourcesisacrucialaspectofhealthcare,particularlyinboth LevelIandLevelIIAmericanCollegeofSurgeons(ACS)-verifiedtraumacenters.Theeffectofresource allocationonemergencydepartmentlengthofstay(ED-LOS)oftraumapatientshasremainedunderinvestigated.AsEDcrowdinghasbecomemoreprevalent,especiallyatquaternarycarecenters,an evaluationofthepotentialdisparitiesinED-LOSbetweenLevelIandLevelIItraumacentersis warranted.WehypothesizedalongerED-LOSatLevelIcenterscomparedtoLevelIIcenters.
Methods: Wequeriedthe2017–2021TraumaQualityImprovementProcess(TQIP)databasefor traumapatients ≥18yearsofagepresentingtoeitheraLevel-Ior-IIcenter.TheTQIPdefinesED-LOSas thetimefromarrivaluntilthetimeanEDdisposition(admissionordischarge)orderiswritten.We excludedtransferredpatientsandthosewithmissingdataregardingACStraumacenterverification level.Weperformedbivariateanalyses,aswellassubgroupanalysesbasedonlocationofdisposition.
Results: Of2,225,067traumapatients,59.3%(1,318,497)receivedtreatmentatLevelIcenters.No significantdifferenceswerefoundinInjurySeverityScoresbetweenpatientsadmittedtotheoperating roomornon-intensivecareunit(ICU)locations,ordischargedhomefromLevel-Iand-IIcenters(all P < 0.05).TheED-LOSfortraumapatientswaslongeratLevel-Icentersforallpatientcategories:overall (198vs145minutes[min], P < 0.001),dischargedhome(286vs160min, P < 0.001),non-ICU admissions(234vs164min, P < 0.001),andthoserequiringsurgery(126vs101min, P < 0.001).
Conclusion: Evenwhentreatingpatientswithsimilarinjuryseverity,traumapatientsatLevelItrauma centershadlongerED-LOScomparedtoLevelIIcenters,irrespectiveofthepatients’ finaldisposition (surgery,non-ICUadmission,ordischarge).TooptimizeresourceutilizationandalleviateEDsaturation, furtherresearchmustdelveintotheunderlyingcausesofthesediscrepanciestoidentifybestpractices andsolutions.[WestJEmergMed.2024;25(6)938–945.]
INTRODUCTION Traumacontinuestoposeasignificantpublichealth challengethatplacessubstantialdemandsonhealthcare systems.Since2010,traumahasconsistentlybeentheleading causeofdeathforyoungadults.1 TheCoalitionforNational
TraumaResearchreportsthattraumaaccountsfor approximately41millionemergencydepartment(ED)visits eachyearaswellastwomillionhospitaladmissions annually.2 Inthiscontext,thelengthofstay(LOS)intheED actsasakeymetric,reflectingtheefficiencyandeffectiveness
ofpatientcare.ProlongedED-LOSisassociatedwith adverseclinicaloutcomes,includingincreasedriskof hospital-acquiredinfections,delaysintheadministrationof criticalmedications,andincreasedmortality,which highlightstheimportanceofrapidandwell-coordinated emergencycare. 3–10 Existingliteraturehighlightsdisparities inED-LOSacrossvariousmedicalcenters;however,thereis asignificantlackofdatafocusingontraumacenters.11
TraumacentersaredesignatedbytheAmericanCollegeof Surgeons(ACS)basedonpatientvolume,staffing,resources, injuryprevention,andeducation.12 Thistieredstructurehas enabledashiftfromtraditional,hospital-centricmodelstoa moreintegrated,regionalizedsystemoftraumacare.13 Despiteexistingstudieshighlightingthecomplexitiesof traumacasesandtheimpactofprolongedED-LOS,there remainsasubstantialgapinresearchconcerninghow resourceallocationaffectsED-LOSfortraumapatients, particularlybetweenvariouslevelsoftraumacenters.14–18 Theselevelsmaydifferintermsofresourcesandcapabilities intheED,withLevelItraumacenters(L1TC)typically handlingmorecomplexcasesandhavingmore comprehensiveresourcescomparedtoLevelIItrauma centers(L2TC).
TheimportanceofinvestigatingED-LOSdifferences betweenL1TCsandL2TCshasbecomemorepronouncedin thewakeoftheCOVID-19pandemic.Thepandemic affectedtraumamechanismsandoutcomesincluding exacerbatedEDcrowding,alongstandingissuein healthcare,andposeduniquechallengestotraumacare, particularlyinhigherleveltraumacenters,whichoftenserve asquaternarycarefacilities.19–24 Crowdingleadstodelaysin careandabidirectionalimpactonbothtraumaandnontraumapatients.TheinfluxoftraumapatientstotheED reallocatesstaffandresourcesfromotherpatients undergoingsimultaneousevaluationandtreatment, increasingtheirED-LOS.25,26
InthisstudyweaimedtoanalyzealargeUnitedStates traumadatabasetocompareED-LOSbetweenadulttrauma patientsatL1TCsandL2TCs.Wehypothesizedanincreased ED-LOSatL1TCscomparedtoL2TCs.Thisresearchmay helpimprovepatientexperienceandqualityofhealthcareas EDcrowdingcontinuestoimpacthospitalsnationwide.
METHODS Thisstudywasdeemedexemptfrominstitutionalboard review,andawaiverofconsentwasgrantedforuseofadeidentifiednationaldatabase.Weperformedaretrospective analysisoftheTraumaQualityImprovementProgram (TQIP)databasefrom2017–2021.Patients ≥18yearsofage presentingtoeitheranACS-verifiedL1TCorL2TCwere included.Weexcludedallpatientstransferredfromanother facilityaswellasthosewithmissingdataregardingACS traumacenter-verificationlevel.Ourprimaryfocuswasto accuratelyassessED-LOSfortraumapatients.Including
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
ProlongedEDlengthofstay(LOS)islinked toadverseclinicaloutcomesandhighlights theimportanceofrapidandwell-coordinated emergencycare.
Whatwastheresearchquestion?
HowdoesED-LOSfortraumapatientsdiffer betweenLevelIandLevelIItraumacenters?
Whatwasthemajor findingofthestudy?
TheED-LOSfortraumapatientsatLevelI centerswaslongeroverall(198vs145 minutes,P < 0.001)comparedto LevelIIcenters.
Howdoesthisimprovepopulationhealth?
Thisresearchenhancesourunderstandingof patientexperienceandqualityofhealthcare byaddressingEDcrowding,alongstanding issuenationwide.
transferpatientswouldhaveintroducedconfoundingfactors thatcouldhavesignificantlyskewedouranalysis.Trauma transferpatientsmayhavealreadyundergoneextensive evaluationsandimagingattheinitialhospital,whichcan artificiallyshortentheirED-LOSatthereceivinghospital. Additionally,someofthesepatientsmayhavebeenpreacceptedbythetraumateam,resultinginamoreexpedited admissionprocesscomparedtonon-transferpatients. Therefore,includingtransferpatientswouldnotprovidean accuraterepresentationofED-LOSfortraumapatients.We comparedtwogroups:adulttraumapatientstreatedat L1TCsvsL2TCs.Thisincludedacomparisonofallpatients regardlessoflevelofcare.
Wecollectedpatientdemographicvariablesincludingage andprehospitalcomorbiditiessuchasdiabetesmellitus, hypertension,anticoagulanttherapy,mentalorpersonality disorder,smokingstatus,houselessness,andsubstanceuse. TheinjuryprofileincludedtheInjurySeverityScore(ISS), andtheAbbreviatedInjuryScale(AIS)ofthehead, abdomen,andthorax.Wealsocollectedvitalsonarrival includinghypotension(systolicbloodpressure ≤ 90 millimetersofmercury),tachycardia(heartrate > 120beats perminute),andtachypnea(respiratoryrate > 22breathsper minute).TheprimaryoutcomemeasuredwasED-LOS. Additionally,wecollectedpatientdispositionfromtheED, includingadmissiontothegeneralhospital floor,intensive careunit(ICU),operatingroom(OR),ordischargetohome.
Wealsoanalyzedinpatientcomplications,suchasacute kidneyinjury,cardiacarrest,unplannedintubation, ventilator-acquiredpneumonia,anddeepveinthrombosis. Wecontrastedpatientcharacteristics,injuryprofiles, complications,anddispositionsbetweenadultpatients treatedatL1TCsandL2TCs.
WeperformedbivariateanalysesusingaMann-Whitney Utesttocomparecontinuousvariablesandchi-squareto comparecategoricalvariables.Wereportcategoricaldataas percentagesandcontinuousdataasmedianswith interquartilerange(IQR)orasmeanswithstandard deviation.Amultivariablelogisticregressionanalysiswas alsoperformedtodeterminetheassociatedriskofmortality andcomplications.Eachmodelincludedknownriskfactors formortalityandinhospitalcomplicationsfortrauma patientsincludingage,vitalsonadmission,mechanism,ISS, andthepresenceoftraumaticbraininjury.27–30 These covariatesweredeterminedbyco-authorconsensusand reviewoftheliterature.All P -valuesweretwo-sidedwitha statisticalsignificancelevelof <0.05.Weperformedall analyseswithSPSSStatisticsforWindowsv29(IBMCorp,
Armonk,NY).TheStrengtheningtheReportingof ObservationalStudiesinEpidemiology(STROBE)checklist wasusedtoensureadherencewithestablishedguidelinesfor reportingobservationalstudies.31
RESULTS Demographics,Characteristics,andInjuriesofPatientsat Level-IvsII-TraumaCenters
Of2,225,067patients,59.3%(1,318,497)received treatmentataL1TCand40.7%(906,570)ataL2TC. PatientsatL1TCsweregenerallyyounger(median50vs 58years, P < 0.001)thanatL2TCs.TheL1TCandL2TC patientshadasimilarmedianISSof9.However,patientsat L2TCshadhigherratesofthefollowingprehospital comorbidities:anticoagulanttherapy(12.1%vs8.8%, P < 0.001);diabetesmellitus(15.2%vs13.5%, P < 0.001),and hypertension(37.2%vs31.9%, P < 0.001).PatientsatL1TCs weremoreoftenhouseless(1.6%vs1.2%, P < 0.001);more oftenunderwentbloodtransfusionscomparedtoL2TCs (5.9%vs3.6%, P < 0.001),andhadhigherratesofsubstance usedisorder(9.0%vs6.3%, P < 0.001)(Table1).Patients
Table1. Demographics,comorbidities,andvitalsignsofadulttraumapatientstreatedatlevelIvslevelIItraumacenters.
Age,year,median(IQR)50(32,68)58(39,77)
Comorbidities,n(%)
Alcoholusedisorder92,090(7.1%)54,266(6.1%)
Houselessness*4,834(1.6%)2,383(1.2%)
Congestiveheartfailure48,149(3.7%)40,712(4.5%)
Currentsmoker306,022(23.5%)168,447(18.8%) <
Chronicrenalfailure20,982(1.6%)15,992(1.8%) <0.001
Cerebrovascularaccident32,748(2.5%)25,637(2.9%) <0.001
Diabetesmellitus175,825(13.5%)135,779(15.2%) <0.001
Hypertension416,425(31.9%)334,025(37.2%) <0.001
Chronicobstructivepulmonarydisease76,547(5.9%)65,353(7.3%) <0.001
Cirrhosis15,868(1.2%)9,301(1.0%) <0.001
Dementia53,592(4.1%)53,164(5.9%) <0.001
Anticoagulanttherapy114,428(8.8%)108,082(12.1%) <0.001
Anginapectoris1,872(0.1%)2,137(0.2%) <0.001
Myocardialinfarction7,609(0.6%)5,833(0.7%) <0.001
Peripheralarterialdisease10,938(0.8%)9,362(1.0%) <0.001
Substanceusedisorder117,680(9.0%)56,160(6.3%) <0.001
Vitalsonadmission,n(%)
Hypotension(SBP < 90)59,051(4.6%)29,024(3.3%) <0.001
Tachycardia(HR > 120)99,388(7.7%)55,816(6.3%) <0.001
Tachypnea(RR > 22)223,774(17.6%)136,745(15.5%) <
Bloodtransfusion,n(%)78,273(5.9%)32,230(3.6%) <0.001
*Onlyincludes2021data. IQR;interquartilerange; HR,heartrate; RR,respiratoryrate; SBP,systolicbloodpressure.
treatedatL1TCsalsohadincreasedratesofhigh-grade injuries(AIS > 3)tothehead(14.4%vs14.2%, P < 0.002), abdomen(4.8%vs.3.5%, P < 0.001),andthorax(15.8%vs. 13.1%, P < 0.001)(Table2).
ED-LOSofL1TCandL2TC PatientsatL1TCswereadmittedathigherratestothe ICU(19.3%vs17.6%, P < 0.001)anddirectlytotheOR (13.7%vs10.6%, P < 0.001),whilepatientsatL2TCswere admittedathigherratestothegeneralhospital floor/ward (57.1%vs55.4%, P < 0.001)anddischargedhome(9.8%vs 7.9%, P < 0.001).TheL1TCpatientshadincreasedmedian ED-LOSforalldispositionswhencomparedtoL2TC patients:overall(198vs145minutes[min], P < 0.001); dischargedhome(286vs160min P < 0.001);non-ICU admissions(234vs164min, P < 0.001),ICUadmissions(123 vs108min, P < 0.001),anddirecttransporttotheOR(126vs 101min, P < 0.001)(Table3).
OtherMeasuredOutcomesofLevelI-and II-TraumaCenters WhencomparedwithL2TCs,theoccurrenceofan inhospitalcomplicationwashigheratL1TCs(5.8%vs4.4%, P < 0.001).Thisincludedincreasedratesofunplanned intubation(1.1%vs0.8%, P < 0.001),ventilator-acquired pneumonia(0.5%vs0.3%, P < 0.001),anddeepvein thrombosis(0.7%vs0.5%, P < 0.001)atL1TCs.Increased ratesofunplannedICUadmissions(1.6%vs1.3%, P < 0.001)andunplannedreturnstotheOR(0.7%vs0.5%, P < 0.001)alsooccurredmorecommonlyatL1TCs(Table4).
Afteradjustingforconfounders,L1TCpatientscontinuedto exhibitahigherassociatedriskofcomplications(oddsratio [OR]1.22,confidenceinterval[CI]1.20–1.24, P < 0.001). ComparedwithL2TCpatients,L1TCpatientsexhibiteda higherrateofmortality(4.8%vs3.8%, P < 0.001) (Table4).However,thistrenddidnotpersistwhen controllingforknownriskfactorsofmortality(OR0.99, CI0.97–1.01, P = 0.09).
DISCUSSION Thiscomprehensive five-yearretrospectivenational analysisrevealedthatdespitecomparableinjuryburdens, patientstreatedatL1TCsexperiencedalongerassociated ED-LOSacrossalldispositioncategories,alongwitha higherrateandassociatedriskofcomplications,compared tothoseatL2TCs.Interestingly,theassociatedriskof mortalityremainedsimilarbetweenthetwolevelsoftrauma centerdesignations.
Emergencydepartmentcrowdingremainsaprominent issue,representingapervasivechallengeassociatedwith delayedtreatment,reducedpatientsatisfaction,and increasedmortality.32,33 Thissituationoccurswhenthe demandforemergencycaresurpassestheavailableresources intheED,hospital,orboth.34 Despitevariationsin definitionsandmeasurementsofcrowdingamonghospitals, itsrepercussionswillalmostalwaysresultinalongerEDLOS.35 Whiteetal’sstudy,focusingondischargedpatients, corroboratesthiscorrelationbyrevealinga10%increasein ED-LOSforpatientsseenduringperiodsofEDcrowding.36 Crowdingoftenleadstoabottleneckeffectinpatient flow,
Characteristic,n(%)LevelI(n
Bluntmechanism,n(%)1,107,121(84.0%)810,732(89.4%)
AISgrade > 3,n(%)
Head189,248(14.4%)128,778(14.2%)
Abdomen63,011(4.8%)31,659(3.5%)
Thorax208,098(15.8%)118,421(13.1%)
Injury,n(%)
Brain221,032(16.8%)134,573(14.8%) <0.001
Liver43,616(3.3%)18,070(2.0%) <0.001
Smallintestine17,861(1.4%)6,904(0.8%) <0.001
Colon16,162(1.2%)5,979(0.7%) <0.001
Rectum2,072(0.2%)675(0.1%) <0.001
Kidney20,043(1.5%)9,370(1.0%) <0.001
Spleen36,477(2.8%)17,827(2.0%) <0.001
Pancreas4,756(0.4%)1,687(0.2%) <0.001
Stomach5,138(0.4%)1,723(0.2%) <0.001
AIS,AbbreviatedInjuryScale; IQR,interquartilerange; ISS,InjurySeverityScale.
Table2. InjuriesforadulttraumapatientstreatedatlevelIvslevelIItraumacenter.
Table3. DispositionofadulttraumapatientstreatedatalevelIvslevelIItraumacenter.
DispositionfromED,n(%)
Admitto floor731,039(55.4%)517,613(57.1%) <0.001
AdmittoICU254,892(19.3%)159,987(17.6%) <0.001
DirecttoOR180,479(13.7%)95,952(10.6%) <0.001
Dischargedhome103,779(7.9%)88,399(9.8%) <0.001
EDLOS,minutes,median(IQR)
Allpatients198(233)145(138) <0.001
Admitto floor234(230)164(140) <0.001
AdmittoICU123(163)108(108) <0.001
DirecttoOR126(196)101(117) <0.001
Dischargedhome286(283)160(139) <0.001
ED,emergencydepartment; ICU,intensivecareunit; IQR,interquartilerange; LOS,lengthofstay; OR,operatingroom.
wherepatientsawaitingadmissionoccupyEDbeds,thus limitingtheavailabilityfornewpatients.Thisscenariois furtherexacerbatedduringpeaktimesorpublichealthcrises, liketheCOVID-19pandemic,whereaninfluxofpatientscan overwhelmEDresources.Prolongedwaittimescanleadto patientdiscomfortanddissatisfaction.37 Pinesetalobserved thatextendedED-LOSwaslinkedtoadiminished probabilityofpatientsrecommendingthehospitaltoothers, coupledwithalowerperceptionofeffectiveteamwork amonghospitalstaff.38
Thedynamicsofresourceutilizationattraumacenters requiresfurtherinvestigationtouncovertheunderlying reasonsfortheobservedprolongedED-LOSatL1TCs.For instance,thesecentersarewidelyacknowledgedfor managinghighpatientvolumesandcateringtomore complexcasesthatmighthinderthe flowofpatientsthrough theED.39 Thisissupportedbyourstudydemonstratingthat L1TCsmoreoftentreatpatientswithsevereinjuriestothe head,abdomen,andthorax,comparedtoL2TCs.Thismay necessitatemorecomprehensivediagnosticevaluations, specializedinterventions,and/orcoordinationamong varioussurgicalspecialties,allofwhichcontributetolonger LOSintheED.Additionally,L1TCsoftenhostresidency programsandfrequentlyinvolveresidentsandhousestaffin patientcare,afeaturelesscommonlyfoundatL2TCs.40 The involvementoftraineesmaycontributetoalongerED-LOS, asresidentsandhousestaffmayneedtoconsultwith attendingphysiciansandsupervisorstodiscusstreatment plans,whichmayleadtoincreaseddeliberationanddecisionmakingtime.41–43 Understandingtheimpactofeducational programsonED-LOSisnecessaryforoptimizingresource allocationandenhancingefficiencyoftraumacaredelivery withindifferentlevelsofresourcecenters.
IncreasedED-LOSmayresultinworsenedclinical outcomes.Wedidnot findahigherriskofmortalityfor patientstreatedatL1TCs;however,wedid findahigher associatedriskofinhospitalcomplications.Thispattern suggestssuboptimalutilizationoravailabilityofimportant resources,potentiallyleadingtothedecompensationof patients.Insupportofthishypothesis,wefoundthatpatients atL1TCshadhigherratesofunplannedintubation,ICU admission,andreturntotheOR.WhiletheTQIPdatabaseis notgranularenoughtodeterminewhetherthese complicationsweretheresultofincreasedED-LOS,itdoes highlighttheneedforenhancedmanagementstrategiesto ensurethatpatientsreceivetimelyandeffectivecare, particularlyinhigh-acuitysettingswherethemarginforerror isminimal.
EfficientlyaddressingthechallengeofED-LOSinvolvesa multifacetedapproach,integratingbothstrategiccapacity managementandinnovativepatientcarepractices.Key strategiesincludeoptimizinginpatientbeduse,expanding EDcapacitythroughadditionalbedsorstaffing,andearly
PatientsatL1TCswerealsomorefrequentlyimpactedby socialdeterminantsofhealthincludinghouselessnessand substanceusedisorder.OurstudyrevealedthatL1TCsmore oftencaredforhouselesspatientsandthosesufferingfrom substanceusedisorder.Unhousedpatientstendtoexperience longerED-LOSsincedispositionplanningandarrangements provetobemorecomplicatedforpatientslackingstable housingwhiletheirmedicalneedsarebeingaddressed.44–46 Moreover,houselesspatientsfacemarkedlyhigheroddsof hospitaladmissioncomparedtotheirhousedcounterparts,a disparitylikelyinfluencedbyclinicians’ concernsoverthe risksandsafetyofdischargingindividualsbacktothe streets.47,48 Thepronouncedpresenceofsocialdeterminants ofhealthamongpatientsatL1TCshighlightsthecomplex interplaybetweenhealthcaredeliveryandsocietalissues, emphasizingtheneedforfurtherinvestigationinto healthcaredisparities.
Table4. OutcomesforadulttraumapatientstreatedatlevelIvslevelIItraumacenters.
Characteristic,n(%)LevelI(n
Anycomplication76,217(5.8%)39,600(4.4%) <
Cardiacarrest12,623(1.0%)6,782(0.7%) <
Catheter-associatedUTI2,329(0.2%)1,073(0.1%) <0.001
DeepSSI1,863(0.1%)646(0.1%) <0.001
OrganspaceSSI1,432(0.1%)392(<0.1%) <0.001
SuperficialSSI1,360(0.1%)635(0.1%) <0.001
Deepveinthrombosis8,802(0.7%)4,647(0.5%) <0.001
Pulmonaryembolism4,890(0.4%)2,016(0.2%) <0.001
Unplannedintubation13,927(1.1%)7,400(0.8%) <0.001
Acutekidneyinjury7,296(0.6%)3,971(0.4%) <0.001
Pressureulcer6,036(0.5%)2,948(0.3%) <0.001
Acuterespiratorydistresssyndrome3,884(0.3%)1,822(0.2%) <0.001
UnplannedreturntoOR8,784(0.7%)4,126(0.5%) <0.001
Sepsis4,107(0.3%)1,968(0.2%) <0.001
Stroke3,581(0.3%)1,931(0.2%) <0.001
UnplannedICUadmission21,417(1.6%)11,540(1.3%) <0.001
Ventilator-associatedPNA7,027(0.5%)2,654(0.3%) <0.001
Mortalityrate,n(%)63,347(4.8%)34,067(3.8%) <0.001
ICU,intensivecareunit; OR,operatingroom; PNA,pneumonia; SSI,surgicalsiteinfection; UTI,urinarytractinfection.
physicianassessmentstoexpeditedecision-making,thereby reducingEDcrowdingandprolongedED-LOS.49 Proven interventionssuchasthefast-trackprocess,whichnotably reducedED-LOSforlow-acuitypatientsby25%,andrevised triageapproachesinL1TCshavedemonstratedsuccessin expeditingcareandreducingED-LOS.50 Anotherexample ofeffectivetriage-systemredesigninvolvesestablishing specializedunitsspecificallyforlessseverecases,alongwith theinclusionofadvancedpracticepractitioners.This approachhassuccessfullyledtoareductioninED-LOSby morethan30minutes.51
LIMITATIONS Thisstudyislimitedbypotentialreportingandselection biases,codingerrors,andmissingdatainherentindatabase studies.Wedidnotconsiderawidearrayofexternalfactors thatcouldinfluenceED-LOS,suchas fluctuationsinED volumepercenter,disproportionateincreasesincenters approved,andvariationsinhospitalandEDoccupancy. Additionally,ourstudycontainsconstraintsinidentifying specifictreatmentlocationswithinthehospital,whetherthat beadedicatedtraumaareaorthegeneralED.Afurther limitationisourinabilitytocontrolforcompetingLOS factors.Specifically,wewereunabletoaccountforfactors includingresidentstaffing,consultmanagement,andthe differingpracticepatternsforemergentandnon-emergent carebetweentheEDandotherhospitalsettings.
Geographicaldifferencesbetweentraumacenterswere notconsidered,whichmightimpactED-LOSdueto variationsinregionalhealthcarepolicies,patient demographics,andresourceavailability.TheTQIPdatabase doesnotprovidegranulardetailsonspecificinterventions anddecision-makingprocessesintheED,whichcouldaffect LOS.Furthermore,wedidnotincludepatient socioeconomicfactorsintheanalysis,whichcouldhave impactedED-LOSandpatientoutcomes.Finally,aswithall databasestudies,wecannotconcludeanydefinitivecausality statementregardingtraumacenterlevelandED-LOS. Despitetheselimitations,our findingscontribute significantlytothediscourseonED-LOS,layinga foundationforfutureresearchaimedatoptimizingresource allocationandimprovingtraumacaredeliveryinL1TCs andL2TCs.
CONCLUSION Thiscomprehensiveanalysishighlightsasignificant observeddisparityinEDlengthofstaybetweenLevelIand LevelIItraumacenters.LevelItraumacentersconsistently reportedlongerassociatedED-LOSacrossvariouspatient dispositions,aswellasahigherriskofcomplications,despite treatingsimilarlyinjuredpatients.Factorsleadingtothese findingscouldrangefromoperationalprotocolsandresource managementtopatientcasecomplexityandinstitutional policies.DuetolimitationsoftheTraumaQuality
ImprovementProgramdatabase,wewereunabletoattribute theobserveddifferencesinED-LOStoanysinglefactor,as theassociationsobservedinourstudyarebasedondatafrom alargenationaldatabase,whichenhancesthe generalizabilityofour findingsacrossdiversesettings.This broadscopereducestheinfluenceofregionalpoliciesand allowsourresultstobeapplicableonawiderscale.However, addressingtheseunderlyingcausesisessentialnotonly forenhancingtheefficiencyofpatient flowthroughthe hospitalbutalsoforimprovingtheoverallqualityofcare providedtotraumapatients.Toeffectivelytacklethisissue, furtherprospectiveresearchisneededtodelveintothe specificsofwhythesediscrepanciesexist.Thisincludes examininghospitaloperationalstrategies,patient flow processes,staffingmodels,andtheuseoftechnologyin patientmanagement.
AddressforCorrespondence:AregGrigorian,MD,Universityof California,Irvine,DepartmentofSurgery,DivisionofTrauma,Burns andSurgicalCriticalCare,333TheCityBlvd.West,Suite1600, Orange,CA.Email: agrigori@uci.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Laneetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.TheAmericanAssociationfortheSurgeryofTrauma.Traumafactsand links.2020.Availableat: https://www.aast.org/resources/trauma-facts AccessedFebruary24,2024.
2.HickersonB.MissionoftheCoalitionforNationalTraumaResearch. Availableat: https://www.nattrauma.org/who-we-are/mission/ AccessedDecember26,2023.
3.LauqueD,KhalemskyA,BoudiZ,etal.Length-of-stayintheemergency departmentandin-hospitalmortality:asystematicreviewandmetaanalysis. JClinMed. 2022;12(1):32.
4.MoweryNT,DoughertyS,HildrethA,etal.Emergencydepartment lengthofstayisanindependentpredictorofhospitalmortalityintrauma activationpatients. JTraumaAcuteCareSurg. 2011;70(6):1317–25.
5.PinesJM,LocalioAR,HollanderJE,etal.Theimpactofemergency departmentcrowdingmeasuresontimetoantibioticsforpatientswith community-acquiredpneumonia. AnnEmergMed. 2007;50(5):510–6.
6.CarrBG,KayeAJ,WiebeDJ,etal.Emergencydepartmentlengthof stay:amajorriskfactorforpneumoniainintubatedblunttrauma patients. JTraumaAcuteCareSurg. 2007;63(1):9–12.
7.SchullMJ,VermeulenM,SlaughterG,etal.Emergencydepartment crowdingandthrombolysisdelaysinacutemyocardialinfarction. Ann EmergMed. 2004;44(6):577–85.
8.SinghN,RobinsonRD,DuaneTM,etal.RoleofEDcrowdingrelativeto traumaqualitycareinalevel1traumacenter. AmJEmergMed. 2019;37(4):579–84.
9.ChalfinDB,TrzeciakS,LikourezosA,etal.Impactofdelayedtransferof criticallyillpatientsfromtheemergencydepartmenttotheintensivecare unit. CritCareMed. 2007;35(6):1477–83.
10.SingerAJ,ThodeHC,ViccelioP,etal.Theassociationbetweenlength ofemergencydepartmentboardingandmortality. AcadEmergMed. 2011;18(12):1324–9.
11.ReznekM,MichaelS,HarbertsonC,etal.Clinicaloperationsof academicversusnon-academicemergencydepartments:adescriptive comparisonoftwolargeemergencydepartmentoperationssurveys. BMCEmergMed. 2019;19(1):72.
12.AmericanCollegeofSurgeons.Resourcesforoptimalcareofthe injured.2022.Availableat: https://www.facs.org/media/1qumyf4b/ 2022_vrc_injured-patient-standardsmanual_final.pdf AccessedDecember26,2023.
13.GlanceLG,OslerTM,MukamelD,etal.Impactoftraumacenter designationonoutcomes:isthereadifferencebetweenlevelIand levelIItraumacenters? JAmCollSurg. 2012;215(3):372–8.
14.KrasnoffCC,GrigorianA,ChinT,etal.Pediatricburn-traumapatients haveincreasedlengthofstaycomparedtotrauma-onlypatients:a propensitymatchedanalysis. Burns. 2021;47(1):78–83.
15.DuanD,DengH,ChenY,etal.Associatedpredictorsofprolonged lengthofstayinpatientssurvivingextensiveburns:alargemulticenter retrospectivestudy. Burns. 2024;50(2):413–23.
16.MejaddamAY,ElmerJ,SiderisAC,etal.Prolongedemergency departmentlengthofstayisnotassociatedwithworseoutcomesin traumaticbraininjury. JEmergMed. 2013;45(3):384–91.
17.ElmerJ,PallinDJ,LiuS,etal.Prolongedemergencydepartmentlength ofstayisnotassociatedwithworseneurologicoutcomesinpatientswith intracerebralhemorrhage. NeurocritCare. 2012;17(3):334–42.
18.BurgessL,Ray-BarruelG,KynochK.Associationbetweenemergency departmentlengthofstayandpatientoutcomes:asystematicreview. ResNursHealth. 2022;45(1):59–93.
19.LuceroA,SokolK,HyunJ,etal.Worseningofemergencydepartment lengthofstayduringtheCOVID-19pandemic. JAmCollEmerg PhysiciansOpen. 2021;2(3):e12489.
20.ClarkDEandRyanLM.Concurrentpredictionofhospitalmortality andlengthofstayfromriskfactorsonadmission. HealthServRes. 2002;37(3):631–45.
21.YeatesEO,GrigorianA,BarriosC,etal.Changesintraumatic mechanismsofinjuryinSouthernCaliforniarelatedtoCOVID-19: penetratingtraumaasasecondpandemic. JTraumaAcuteCareSurg. 2021;90(4):714–21.
22.YeatesEO,GrigorianA,SchellenbergM,etal.COVID-19intrauma:a propensity-matchedanalysisofCOVIDandnon-COVIDtrauma patients. EurJTraumaEmergSurg. 2021;47(5):1335–42.
23.YeatesEO,GrigorianA,SchellenbergM,etal.Decreasedhospital lengthofstayandintensivecareunitadmissionsfornon-COVID blunttraumapatientsduringtheCOVID-19pandemic. AmJSurg. 2022;224(1):90–5.
24.OskvarekJJ,ZocchiM,BlackBS,etal.Emergencydepartmentvolume, severity,andcrowdingsincetheonsetofthecoronavirusdisease2019 pandemic. AnnEmergMed. 2023;82(6):650–60.
25.SmithDC,ChapitalA,UperesaBMB,etal.Traumaactivationsandtheir effectsonnon-traumapatients. JEmergMed. 2011;41(1):90–4.
26.AryaR,DossantosF,Ohman-StricklandP,etal.Impactoftrauma activationontheEDlengthofstayfornontraumaticpatients. AmJEmergMed. 2012;30(2):311–6.
27.AlbitarO,BallouzeR,OoiJP,etal.Riskfactorsformortalityamong COVID-19patients. DiabetesResClinPract. 2020;166:108293.
28.BattleC,CarterK,NeweyL,etal.Riskfactorsthatpredictmortalityin patientswithbluntchestwalltrauma:anupdatedsystematicreviewand meta-analysis. EmergMedJ. 2023;40(5):369–78.
29.ClementND,HallAJ,MakaramNS,etal.IMPACT-restart:theinfluence ofCOVID-19onpostoperativemortalityandriskfactorsassociatedwith SARS-CoV-2infectionafterorthopaedicandtraumasurgery. BoneJoint J. 2020;102(12):1774–81.
30.YadavK,LampronJ,NadjR,etal.Predictorsofmortalityamongolder majortraumapatients. CJEM. 2023;25(11):865–72.
31.vonElmE,AltmanDG,EggerM,etal.Thestrengtheningthe reportingofobservationalstudiesinepidemiology(STROBE) statement:guidelinesforreportingobservationalstudies. BMJ. 2007;335(7624):806–8.
32.ChangAM,LinA,FuR,etal.Associationsofemergencydepartment lengthofstaywithpubliclyreportedquality-of-caremeasures. AcadEmergMed. 2017;24(2):246–50.
33.JohnsonKDandWinkelmanC.Theeffectofemergencydepartment crowdingonpatientoutcomes:aliteraturereview. AdvEmergNursJ. 2011;33(1):39–54.
34.AmericanCollegeofEmergencyPhysicians.Crowdingpolicy statements.2019.Availableat: https://www.acep.org/siteassets/newpdfs/policy-statements/crowding.pdf.AccessedDecember31,2023.
35.McCarthyML,DingR,PinesJM,etal.Comparisonofmethodsfor measuringcrowdinganditseffectsonlengthofstayintheemergency department. AcadEmergMed. 2011;18(12):1269–77.
36.WhiteBA,BiddingerPD,ChangY,etal.Boardinginpatientsinthe emergencydepartmentincreasesdischargedpatientlengthofstay. JEmergMed. 2013;44(1):230–5.
37.LizanaFG,BotaDP,DeCubberM,etal.Long-termoutcomein ICUpatients:whataboutqualityoflife? IntensiveCareMed. 2003;29(8):1286–93.
38.PinesJM,IyerS,DisbotM,etal.Effectofemergencydepartment crowdingonpatientsatisfactionforadmittedpatients. AcadEmergMed. 2008;15(9):825–31.
39.TrzeciakSandRiversEP.Emergencydepartmentovercrowdinginthe UnitedStates:anemergingthreattopatientsafetyandpublichealth. EmergMedJ. 2003;20(5):402–5.
40.MadayagRM,SercyE,BergGM,etal.Aretraumaresearchprogramsin academicandnon-academiccentersmeasuredbyequalstandards?A surveyof137levelItraumacentersintheUnitedStates. PatientSaf Surg. 2021;15(1):34.
41.DeLaneyM,ZimmermanKD,StroutTD,etal.Theeffectofmedical studentsandresidentsonmeasuresofefficiencyandtimelinessinan academicmedicalcenteremergencydepartment. AcadMed. 2013;88(11):1723–31.
42.JamesC,HarperM,JohnstonP,etal.Effectoftraineesonlengthof stayinthepediatricemergencydepartment. AcadEmergMed. 2009;16(9):859–65.
43.LammersRL,RoigerM,RiceL,etal.Theeffectofanewemergency medicineresidencyprogramonpatientlengthofstayina communityhospitalemergencydepartment. AcadEmergMed. 2003;10(7):725–30.
44.KramerCB,GibranNS,HeimbachDM,etal.Assaultandsubstance abusecharacterizeburninjuriesinhomelesspatients. JBurnCareRes. 2008;29(3):461–7.
45.Kowal-VernAandLatenserBA.Demographicsofthehomelessinan urbanburnunit. JBurnCareRes. 2007;28(1):105–10.
46.FerradaP,AnandRJ,AboutanosM.Theuninsured,thehomeless,and theundocumentedimmigranttraumapatient.Revealinghealth-care disparityatalevel1traumacenter. AmSurg. 2016;82(1):E1–2.
47.SilverCM,ThomasAC,ReddyS,etal.Injurypatternsandhospital admissionaftertraumaamongpeopleexperiencinghomelessness. JAMANetwOpen. 2023;6(6):e2320862.
48.TrinhT,ElferganiA,BannM.Qualitativeanalysisofdispositiondecision makingforpatientsreferredforadmissionfromtheemergency departmentwithoutdefinitemedicalacuity. BMJOpen. 2021;11(7):e046598.
49.MorleyC,UnwinM,PetersonGM,etal.Emergencydepartment crowding:asystematicreviewofcauses,consequencesandsolutions. PLoSOne. 2018;13(8):e0203316.
50.MercerMP,SinghMK,KanzariaHK.Reducingemergencydepartment lengthofstay. JAMA. 2019;321(14):1402–3.
51.GardnerRM,FriedmanNA,CarlsonM,etal.Impactofrevisedtriageto improvethroughputinanEDwithlimitedtraditionalfasttrackpopulation. AmJEmergMed. 2018;36(1):124–7.
IyesattaM.Emeli,MD,MPH PatrickG.Meloy,MD
SectionEditor:CortlynBrown,MD
COMMENTARY WeighingIn EmoryUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Atlanta,Georgia
Submissionhistory:SubmittedJanuary10,2024;RevisionreceivedMay13,2024;AcceptedAugust15,2024
ElectronicallypublishedOctober4,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18690
“Whatisyourpatient’sbiggestproblem?”
Thissimplequestionwasposedtwodecadesagobyan attendingphysiciantoamedicalstudentrotatinginafamily medicineclinic.Thepatienthadthecommontrioofdiabetes, hypertension,andhyperlipidemia,andthestudentwent throughthislistofconditions.Thestudent’sattending, however,remainedunconvinced. “Obesity,” theattending finallysaid. “Obesityisthispatient’sbiggestproblem.” The patientwasoverweight,yes,butinthatcomfortablewaythat weoverlookinourfamilymembers,inourfriends,andin ourselves.Thatwasthe firsttimeinthatmedicalstudent’ s trainingthatanyclinicianhadputweightonparwith,and indeedabove,otherestablishedchronicmedicalconditions. Itwasalsothelasttime.
Thisvignettehighlightsourlackofroutine acknowledgmentofobesityasadisease.
Obesityisadisease,1,2 justasdiabetes,hypertension,and hyperlipidemiaarediseases.Obesityisalsoapublichealth crisis,bothlocallyandglobally.3 IntheUnitedStates,upto oneinthreeadultsandoneinsixchildrenareaffected,and theincidenceandprevalencehasbeenincreasingsteadily overthepast20years.3 Theincreaseinmorbidityand mortalityduetoobesitycannotbeunderstated:obeseadults havelowerlifeexpectancy,lowerqualityoflife,and substantialincreasesinhealthcarecosts.3 Additionally, obesityincreasestheriskofbeingdiagnosedwithother lifelongdiseasessuchasdiabetes,hypertension,coronary arterydisease,myocardialinfarction,andstroke.4 In addition,thecombinationofobesityandothercomorbid conditions,eg,smoking,canincreasetheriskofdeathbyup to11timesthatofanon-obese,non-smoker.5 Itisthrough theselensesthatpublichealthofficialshaverecognized obesityasanalarmingdiseaseprocessthatthreatensthe livesofbothyoungandoldandisincreasinglyprevalentin UShealthcare.
Asemergencyphysicians,wedonot,forthemostpart, havelong-termrelationshipswithourpatients.Weexpect primarycarephysiciansandthosewhoprovideongoingcare tomakeittheirbusinesstocounselonweightloss. Unfortunately,thedatasaysotherwise.AccordingtotheUS CentersforDiseaseControlandPrevention(CDC),evenin
physicianvisitsmadespecificallyforobesity,weight-related healtheducationwasonlyofferedhalfofthetime.6
Emergencydepartments(ED)arethesafetynetsoftheUS healthcaresystem,caringforacute,unscheduledpatients regardlessofabilitytopay.WhilemanyEDvisitsare subsequentlydeemedtobenon-emergent,theystillrequirea timelyevaluationandinvolvesome,albeitnotas comprehensive,preventativecareinterventions.Wetellour patientstoquitsmoking,practicesafesex,takeseizure precautions,weartheirseatbeltsandbicyclehelmets,andget theirCOVID-19shots.Chartsarelitteredwith “dotphrases” suchasthefollowing: “Patientiscounseledfortobacco cessation” ; “WilladmitforTIArule-outandinitiatestatin therapy” ; “Patientistreatedempiricallyforurethritisandis counseledonsafesexualpractices” ;or “Patientisgiven informationonlow-saltdietforcongestiveheartfailure.” However,adviceonproperdietandexerciseisuncommon;in ourclinicalexperience,wetendtoaddressobesityonlywhen itismorbidandwhenitdisruptsourintendedcareplan;for example,whenthepatientistoooverweightforastretcher,a scanner,oraprocedure.Shouldwebetalkingaboutweight intheED?Iftheanswerisyes,thenwhatisthebestwayto havesuchdiscussions?
Thequestionofthemedicalcommunity’sapproachto obesityisimportantfortworeasons.The firstiswhatthe COVID-19pandemictaughtusaboutobesity.TheCOVID19pandemicbroughtmanyofthefailuresinUShealthcare intosharpfocus,andtheobesityepidemicwasoneofthem. Ourcollectivepersonalexperienceofclinicalmedicine duringthepandemicmadeitclear:COVID-19andobesity makecatastrophicbedfellows.Ofthe2.5millionCOVID-19 deathsreportedbyFebruary2021,2.2millionoccurredin countrieswheremorethanhalfthepopulationhadabody massindexover25.7 Additionally,theCDCreportedthat obesitytripledtherateofhospitalizationforCOVID-19.8 Thesecondreasonthistopicistimelyisbecauseofthe increasingmovetonormalizeobesity,9 amovethatmakesit lesslikelyforphysiciansandpatientsaliketorecognize obesityforwhatitis:adisease.Thistypeofnormalization threatenstomakeouropeningvignettethe continuedstandard.
Ofcourse,theissueofobesityiscomplex.Obesity’ scauses aremultifactorial,andanytreatmentmust,assuch,bemultileveled.10 Inpreventativehealth,thesocialecologymodel (SEM) aframeworkforhealthpromotionthatusesa multitieredapproachtoaddresstheinterplaybetween multiplefactorsthatinfluenceagivenproblem wouldbe employedtotackleobesityatthepopulationlevel.TheSEM postulatesthatconditionssuchasobesityareshapedat severallevels:theindividual,interpersonal,organizational, community,andpublicpolicylevels.11 TheSEMpivotsaway fromanisolatedattentivenessonindividualbehaviortoa moreencompassingunderstandingoftiersofinfluence.The SEMpromotesinterventionsonthesocialdeterminantsof health,theforcesandsystemsthatshapethewell-beingofa population.Thismeansnotonlysupportingindividual effortstowardhealthydietandregularphysicalactivitybut alsochangingthecontextinwhichbehaviorsariseandare sustained.Thus,publichealthofficialscanincludetransfat eliminationinprocessedfoods,communityinfrastructure thatpromotesgreaterphysicalactivity,improvingaccessto healthyfoods,etc,aspotentialinterventions.
Givenallthis,onemightdecidethatobesityistoocomplex todealwithintheED.Nopatienttoourknowledgehasever signedintoanEDwithachiefcomplaintof “Iam overweight”;thatistosay,apatient’sweightisneverthe reasontheychoosetocometotheED.So,whytrytodiscuss whatmanyconsiderasensitivematterandriskjeopardizing one ’srapportwithapatient?WebelievetheED,while certainlynottheend-all-be-all,isstillanimportanttierof influence;so,suchdiscussionsdohaveaplacethere.
Howthencanwetalktoourpatientsaboutobesityinthe ED?Thereareguidelinesandpracticalapproachespublished inthemedicalliteraturethatprovideaframeworkinthe primarycaresettingforengagingwithpatientsabouttheir weight.12,13 TheCanadianObesityNetworkdevelopedthe “5As” ofobesitycounseling;ask,assess,advise,agreeand assist.14 GiventhebrevityoftheEDencounter,wesuggest theEDapproachshouldbeanabbreviatedversionofthe 5As,perhapsbettertermedthe3As.Itwouldinvolve first asking permissiontodiscussthepatient’shealthrisk,onerisk beingthattheyarewellaboveidealbodyweight.Sensitivity andnon-judgmentallanguageareparamount.Ifthepatient isopentoaconversation,onecouldgoonto advise themon howtheirobesitycanhurtthem.Finally,itwouldbe importantto assist thepatientbyprovidingresourcesfor outpatientfollow-upandmanagement.Thisisnotunlike whatwealreadydowhenweprovidebriefcounselingto patientsforotherhealthconcerns.Thedifferenceisthat otherhealthconcernsarerecognizedbybothpatientsand cliniciansasaddressableissues,whilethereisapervasivelack ofrecognitionofobesityasadisease.
Butobesityisadisease.Itbehoovesusnow,morethan ever,toaddressitassuch.
AddressforCorrespondence:IyesattaM.Emeli,MD,MPH,Emory UniversitySchoolofMedicine,DepartmentofEmergencyMedicine, 531AsburyCir.,AnnexBuildingSuiteN340,Atlanta,GA30322. Email: imassaq@emory.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Emelietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.Obesity:Preventingandmanagingtheglobalepidemic.Reportofa WHOconsultation. WorldHealthOrganTechRepSer. 2000;894:1–253.
2.AmericanMedicalAssociationHouseofDelegates.Resolution420. Recognitionofobesityasadisease.2013.Availableat: https://www. ama-assn.org/house-delegates/annual-meeting/proceedings-2013annual-meeting-house-delegates.AccessedNovember27,2023.
3.TiwariAandBalasundaramP.Publichealthconsiderationsregarding obesity.In: StatPearls[Internet].TreasureIsland,FL:StatPearls Publishing,2023.Availableat: https://www.ncbi.nlm.nih.gov/books/ NBK572122/. AccessedNovember27,2023.
4.Pi-SunyerX.Themedicalrisksofobesity. PostgradMed. 2009;121(6):21–33.
5.FreedmanDM,SigurdsonAJ,RajaramanP,etal.Themortality riskofsmokingandobesitycombined. AmJPrevMed. 2006;31(5):355–62.
6.TalwalkarAandMcCartyF.Characteristicsofphysicianofficevisitsfor obesitybyadultsaged20andover:UnitedStates,2012. NCHSData Brief. 2016;(237):1–8.
7.WiseJ.Covid-19:Highestdeathratesseenincountrieswithmost overweightpopulations. BMJ. 2021;372:n623.
8.KompaniyetsL,GoodmanAB,BelayB,etal.Bodymassindexandrisk forCOVID-19– relatedhospitalization,intensivecareunitadmission, invasivemechanicalventilation,anddeath UnitedStates, March–December2020.(2021). MMWRMorbMortalWklyRep. 2021;70(10):355–61.
9.HarleyZ,KelloggV,MandelT,etal. AnEcologicalApproachtoObesity andEatingDisorders.Montreal,Canada:Pressbooks,2020.
10.AtkinsonRL.Etiologiesofobesity.In:GoldsteinDJ(Ed.), The ManagementofEatingDisordersandObesity (105–18).2nded. Totowa,NJ:HumanaPress.2015.
11.GlanzKandBishopD.Theroleofbehavioralsciencetheoryin developmentandimplementationofpublichealthinterventions. AnnRevPublicHealth. 2010;31:399–418.
12.VallisM,Piccinini-VallisH,SharmaAM,etal.Clinicalreview:modified5 as:minimalinterventionforobesitycounselinginprimarycare. CanFam Physician. 2013;59(1):27–31.
13.McGowanBM.Apracticalguidetoengagingindividualswithobesity. ObesFacts. 2016;9(3):182–92.
14.Rueda-ClausenCF,BenterudE,BondT,etal.Effectof implementingthe5Asofobesitymanagementframework onprovider-patientinteractionsinprimarycare. ClinObes. 2014;4(1):39–44.
MichaelKaduce,MPS*
AntonioFernandez,PhD†
ScottBourn,PhD†
DustinCalhoun,MD‡ JeffersonWilliams,MD§
MalloryDeLuca,BS,NRP§ HeidiAbraham,MD∥
KevinUhl¶
BrianBregenzer,LP∥
BaxterLarmon,PhD# RemleP.Crowe,PhD†
AlisonTreichel,MPH† J.BrentMyers,MD†
SectionEditor:JoshuaGaither,MD
ORIGINAL RESEARCH EMSProviders:APilotStudy *FalckHealthInstitute,Orange,California
† ESO,Austin,Texas
‡ UniversityofCincinnati,Cincinnati,Ohio
§ WakeCountyEmergencyMedicalServices,WakeCounty,NorthCarolina
∥ Austin-TravisCountyEmergencyMedicalServices,Austin,Texas
¶ CincinnatiFireDepartment,Cincinnati,Ohio
# UniversityofCaliforniaLosAngeles,DavidGeffenSchoolofMedicine, LosAngeles,California
Submissionhistory:SubmittedMay9,2024;RevisionreceivedAugust9,2024;AcceptedAugust12,2024
ElectronicallypublishedOctober1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21175
Background: Ourprimaryobjectiveevaluatedtheperceptionofemergencymedicalservice(EMS) providers’ reviewofautomatedhospitaloutcomedata.Secondarily,weassessedparticipationin outcomereviewasameansofmicrolearningtoobtaincontinuingeducation(CE).
Methods: FromOctober–December2023,threehigh-volumeEMSsystemsparticipatedinathree-part interventionwithresultsevaluatedusingamixed-methodsapproach.First,EMSproviders(emergency medicaltechniciansandparamedics)wereinvited,viatheirelectronichealthrecord(EHR),tocompletea presurveyevaluatingtheirperceptionsofreviewingoutcomes.Then,EMSproviderswerenotifiedabout theopportunitytoearnCEviaamicrolearningintervention,offeringCommissiononAccreditationfor Pre-HospitalContinuingEducation(CAPCE)-approvedCEhoursforcompletionofoutcomereviewsand associatedlearningmodules.Finally,EMSproviderswereinvitedtocompleteapost-surveymirroring thepre-survey.Qualitativeanalysesidentifiedthemesamongopen-endedresponses.Quantitative analysesexaminedperceptionsbetweenpre-andpost-surveys.
Results: Of843providerscontacted,217respondedtothepre-survey(25.7%).Themostendorsed rationaleforreviewingoutcomesincludedimprovingclinicalknowledge(95%),improvingpatientcare (94%),andknowingwhethercaremadeadifference(93%).Nearlyall(91%)reportedbeingmorelikelyto reviewoutcomesifCEwereawarded.Amongthe67whocompletedtheopen-endeditems,thethree dominantthemesincludedenhancepersonalconfidenceandcompetence(43%);acquirepersonal knowledge(39%);andoperations(21%).Of211providerswhoparticipatedintheintervention,56(27%) wereawardedCE.Atotalof152providersrespondedtothepost-survey,andthepercentagewho agreedthatreviewingoutcomesimprovesjobsatisfactionrosefrom89%to95%betweenpre-andpostsurveys(P = 0.05).
Conclusion: EMSproviderssupportedthepersonalandprofessionaldevelopmentandpatientcare improvementofreviewingpatients’ outcomeswithassociatedCE.Furtherstudyiswarrantedtoevaluatethe generalizabilityofthese findingsandthebestuserexperience.[WestJEmergMed.2024;25(6)949–957.]
BACKGROUND Emergencymedicalservices(EMS)providersprovidethe majorityofprehospitalmedicalcareintheUnitedStatesand serveasacrucialcomponentofthenation’shealthcare deliverysystem.ForEMSproviderstomaintaintheirlicense, everystatehasuniquecontinuingeducation(CE) requirements,typicallyinthefashionofrequiredhours,for licensurerenewal.TheNationalRegistryofEmergency MedicalTechniciansalsomaintainsanhourandtopic requirementforrecertification.Thishourmodelhasbeen usedtoensurethecontinualcompetencyofEMSproviders,1 asithasbeenhistoricallyacceptedthatcompetencycanbe maintainedthroughCEhourrequirementsdespitealackof empiricalevidence.2
Incontinuingmedicaleducation(CME),abroader conceptofcontinuedprofessionaldevelopment(CPD),is emerging.Continuedprofessionaldevelopmentincludes educationfocusedonproblemidentificationandsolution development,allowingthehealthcareprofessionaltotailor thelearningprocesstotheirindividualneeds.3 Theprocessof CPDrecognizesaone-size-fits-allapproach,whichisnot specificenoughforeachlearner.TheInstituteofMedicine recommendsaCPDsystemthatincludespatient-centered care,interprofessionalteamwork,qualityimprovement application,andclinicaloutcomedatautilizationfor individual,team,andinstitutionalassessment.2,4 Feedback hasalsobeendemonstratedtoimprovesystemperformance andpatientoutcomes.5 Verypublicvoices,includingthe EMSAgenda2050,haveincludedcallsforEMSsystemsand providerstoreceivefeedback,includingpatientoutcomes,in realtime,asameansforcontinuousqualityimprovement, thusmovingtowardaCPDapproachtocompetency.6 The NationalAssociationofEMSPhysicianshasalsocalledfor continualmonitoringofairwayperformancedataanditsuse inthecontinuedcredentialingprocessandquality managementactivitieswithlarge-scalebidirectional informationsharedbetweenEMSandreceivingfacilitiesin theirpositionpaperonairwaymanagementandtraining.7
DespitethisdesiredtransitiontoCPD,providingpatientspecificoutcomestoEMSprovidershaslongbeena challenge.BidirectionaldatasharingbetweenEMSand hospitalshasraisedconcernsaboutpatientprivacyand technologicalchallenges8,9 Fortunately,thistrendis improving,basedontheprovisionofoutcomeelementsasa partoftheNationalEmergencyMedicalServices InformationSystemdatasetandtheclarificationthatsuch data-sharingisconsistentwiththeHealthInsurance PortabilityandAccountabilityActguidelines.10–12 When surveyed,EMSprovidersreportedadesireforpatientspecificoutcomes.Theyevenreportedusinginformal networksorgoingaroundthesystemtoobtainpatient outcomeinformation,assistingthemtodevelopclinical skills.7 Thislackofinsight,specificallycenteredaround
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
EMSprovidersreceivelimitedformalclinical feedbackormicrolearningcontinuing education(CE)followingthetreatmentand transferoftheirpatients.
Whatwastheresearchquestion?
WhataretheperceptionsofEMSproviders ’ reviewofautomatedhospitaloutcomedata andassociatedCEcredit?
Whatwasthemajor findingofthestudy?
FollowingoutcomereviewandCE opportunities,surveysdemonstrated jobsatisfactionrosefrom89%to 95%(P = 0.05).
Howdoesthisimprovepopulationhealth?
EMSreviewofpatientoutcomesimprovesjob satisfactionandclinicalknowledge,thus providingameansforcontinuedcompetency ofahighlytrainedEMSworkforce.
patientoutcomesandEMSproviderdiagnosisaccuracy,has beenreportedtoimpactprovidermentalhealth.13
TheEMSproviderisinterestedinincludingpatient outcomedataasameansofprofessionaldevelopmentsimilar totheircolleaguesinmedicine.14,15 Physicians’ continued medicaleducationhasincludedelectronichealthrecords (EHR)toassessthequalityofcareandhasbeenusedto suggestareasforimprovementthroughtheuseofCME.16 Similarly,medicaldatabaseshavefoundwaystohelp physiciansreceiveCMEwithroutineclinicalquestionsand problem-solvingintheirdailypractice.17 Graduatemedical educationalsoenvisionsasysteminwhichpatienthealth recordsandoutcomedatacanbeincorporatedintothe curriculum.Thisframeworkincludesmentorsorinstructors usingtheoutcomedatatoassess,supervise,andteach, creatingamature,professionalcommunitywhereeveryone receivesandprovidesfeedback.18 TheAccreditation CouncilforGraduateMedicalEducationsimilarlyrequires programstoconnectresident-physicianeducationto patientoutcomes.19
Usingpatientoutcomedataasfeedbackcontinuestobe calledforand,onasmallscale,hasbeendemonstratedtobe aneffectivepartofCPDprogramsforEMSproviders.In fact,theEHRservesasavaluableresourceforCPDin providingpatient-specificoutcomes.20 WhenevaluatingCE
inpediatricemergencies,briefandfrequentCEprogramsare recommendedasameanstoproviderepetitionwith immediatefeedbackanderrorcorrection.21 Whilefeedback followingacallisoutsidetheproposedtheoretical frameworkforclinicaljudgmentinEMS,ithasbeennotedas importantinthedevelopmentofEMSprovidersandallows forimprovementinperformance.22 Post-resuscitation providerfeedbackforpatientswhohavesufferedcardiac arrestandheartattackshasledtoimprovementsintimeand treatment.23,24 Sammuelandcolleaguesconductedascoping reviewoftheeffectsofCPDonhealthcareprofessionals’ performanceandpatientoutcomesandwerealsoableto demonstratechangesinproviders’ behaviorand patientoutcomes.25
DespitecallsfromleadingnationalEMSorganizations andotherhealthcareprofessionstoincorporatepatient outcomesintoCE,littleisknownaboutEMSproviders’ perceptionsofautomatedpatientoutcomedatanoritsuseas microlearningtoobtaincontinuingeducation.Ourprimary objectiveinthisstudywastoevaluateEMSproviders’ perceptionsoftheutilityofautomatedhospitaloutcomedata forprofessionaldevelopment.Secondarily,weevaluated theirparticipationinoutcomereviewasameansof microlearningtoobtainCE.
METHODS StudyDesignandPopulation
Inthismixed-methodsstudyweuedquantitativeand qualitativemethodstounderstandEMSprovider perceptionsregardingtheuseofanautomatedsystem enablingthemtoobtainCommissiononAccreditationfor Pre-HospitalContinuingEducation(CAPCE)-approvedCE byreviewingpatientoutcomesandcompletingassociated learningmodules.TheCAPCEisanaccreditingbody chargedwiththereviewandaccreditationofEMSCE.26 The studywasconductedfromOctober–December2023inthree high-volumeurbanEMSsystems.TheEMSproviderswere certifiedattheemergencymedicaltechnicianthroughthe paramediclevelandwerecontinuouslyprovided100%of theirrequiredCEhoursthroughtheiremployer.
Atthebeginningofthestudy,EMSprovidersineach systemreceivedapromptinvitingthemtoanonymously participateinthispilotstudywhentheyloggedintotheir EHR(ESO,AustinTX).Eachparticipatingagencyusesa systemthatallowsEMSproviderstoautomaticallyreceive outcomedatafromthehospital,specifictopatientsthey encounteredintheprehospitalsetting.AllCEactivitieswere completedinasingleonlinelearningplatform.
Forthosewhoagreedtoparticipateinthe firstphaseofthe pilotstudy,participantswereaskedtovoluntarilycompletea pre-survey.Theywerealsoinformedthattheywouldbe eligibletoreceiveCEhours,approvedbyCAPCE,upon completionofoutcomereviews,associatedvideos,and outcomereviewassessments.Aprompttoreviewoutcomes
aspartofthisstudywasreceivedbyparticipantswhenthey loggedintotheEHRandnavigatedtotheoutcomereview section.TheCEphasewasopenforatleasttwoweeks.This wasfollowedbyanotherinvitationintheEHRtocomplete thepost-surveythatmirroredthepre-survey.Participants wererequiredtospecificallyoptintoeachsurveyandtheCE phaseofthestudy.
CAPCE-ApprovedContinuingEducation DuringtheCEphase,participantswereprovidedalink fromtheoutcomereviewpagethatdirectedthemtologinto thelearningplatform.Twoprerequisitevideosprovided backgroundinformationanddescribedthetypesofoutcome informationavailable:InternationalClassificationof DiseasesdiagnosiscodesandCentersforMedicareand MedicaidServicesdisposition(eg,dischargetohome, dischargetoskillnursing,transfer,death,etc).Upon completionoftheseprerequisites,participantswereableto reviewtheirpatient-specificoutcomesandansweraseriesof questionsregardingeachreview.
DataAnalysis Weusedquantitativeanalysestoexamineperceptions betweenpre-andpost-surveysusingchi-squaretestsor Fisherexacttests,asappropriate.Likert-scaleresponse options(agreevsdisagree)anddemographics(Level: paramedicvsother;Role:patientcareprovidervsother; yearsofexperience:0–4years,5–10years,11–20years, ≥21years;previousfrequencyofoutcomesreview:very frequently/frequentlyvsoccasionally/rarely/never)were collapsed,asneededandwhereappropriate,duetocellsize. ParticipationintheCAPCECEphaseofthestudywasalso quantified.Dataisreportedaspercentagesandfrequencies. P -valuesofstatisticaltestsarealsoincluded.Weperformed quantitativeanalysisusingSTATAMPversion18.0 (StataCorpLLC;CollegeStation,TX).
Qualitativeanalysesidentifiedthemesamongopen-ended responses.Weusedconventionalcontentanalysisas describedbyHsiehandShannon(2005).Aninductive approachwasusedtoextractmeaningandthemesfrom responses.Allcodesweregeneratedfromthecontentdirectly withoutapriorithemes.Oncecodeswereidentified,weused adeductiveapproachtodeterminethefrequencyand distributionofthemesaswellasanyrelationshipsthat existedbetweenthemesandrespondentcharacteristics. QualitativeanalysiswasassistedusingtheQDA MinerLite3.0(ProvalisResearch;Montreal,Quebec) softwarepackage.
ThisstudywasdeemedexemptbytheUniversityof CaliforniaLosAngelesInstitutionalReviewBoard.
RESULTS Duringthestudyperiod,843EMSprovidersfromthe participatingagenciesloggedintotheEHRandwere
thereforeeligibletoparticipate.Atotalof217(25.7%)EMS providersanonymouslyrespondedtothepre-surveywhileon duty,and152(18.0%)anonymouslyrespondedtothepostsurveywhileonduty.Demographicsweresimilaramong thosethatrespondedtothepre-andpost-survey(Table1).
Overall,responsesweresimilarwhencomparingthose whorespondedtothepre-surveyandthosewhorespondedto thepost-survey(Table2).Notably,89%inthepre-surveyvs 95%inthepost-surveyindicatedagreementthatoutcomes reviewenhancedjobsatisfaction(P = 0.05).When evaluatingonlythosewithaparamediccertification,wesaw astatisticallysignificantincrease(P = 0.03)inthepercentage ofthoseindicatingtheyreviewoutcomestoimproveclinical knowledgewhencomparingpre-surveyrespondentstopostsurveyrespondents(94%vs99%,respectively).Wealso notedthatpre-andpost-surveydifferenceswithrespectto improvementsinjobsatisfactionremainedsignificantwhen onlyevaluatingparamedics.Nostatisticallysignificant differencewasnotedamongpre-andpost-surveyrespondents ofthosewithothercertificationlevels(TableS1).When
examiningyearsofEMSexperienceorroleintheEMS system,responsesbetweenpre-andpost-surveyrespondents weresimilarregardlessofhowmanyyearstheindividualhad workedinEMS(TableS2).
Thereweretwosignificantdifferenceswhencomparing thosewhorespondedtothepre-surveyandthosewho respondedtothepost-surveywhenstratifiedbyhistorical frequencyofoutcomesreview.Amongthosewhoindicated thattheyreviewpatientoutcomesfrequentlyorvery frequently,wesawasignificantlyhigherpercentageofpostsurveyrespondentsindicatingthattheyreviewedpatient outcomestoobtainclosure(90%vs98%, P = 0.01, respectively)andthatreviewingpatientoutcomesimproves jobsatisfaction(92%vs99%, P = 0.02,respectively) (TableS3).
CAPCE-ApprovedContinuingEducation Atotalof211individualsfromthethreeparticipating EMSsystemsoptedintotheCAPCECEphaseofthispilot study.Amongthose,63%(133/211)successfullyloggedinto
%(n)Pre-survey(N = 217)Post-survey(N = 152)
Certi ficationlevel
Emergencymedicaltechnician(EMT)14.8%(32)11.2%(17)
Advancedemergencymedicaltechnician(AEMT)2.3%(5)3.3%(5)
Paramedic77.9%(169)82.9%(126)
Other1.8%(4)0.0%(0)
None3.2%(7)2.6%(4)
Rolewithintheorganization
Patientcareprofessional61.2%(131)71.3%(107)
First-linesupervisor20.6%(44)18.0%(27)
Administrator/manager4.7%(10)1.3%(2)
Preceptor3.7%(8)3.3%(5)
Educator0.9%(2)0.7%(1)
Other8.9%(19)5.3%(8)
Yearsofexperience(4categories)
0–4years18.1%(39)18.4%(28)
5–10years28.2%(61)28.9%(44)
11–20years31.5%(68)28.9%(44)
≥21years22.2%(48)23.7%(36)
Frequencyofpatientoutcomesreview
Veryfrequently(morethanonceperweek)38.8%(83)36.2%(55) Frequently(aboutonceperweek)32.2%(69)33.6%(51) Occasionally(aboutonceortwicepermonth)19.2%(41)25.7%(39)
Rarely(aboutonceortwiceperyear)3.3%(7)2.0%(3) Veryrarely(lessthanonceperyear)2.8%(6)2.6%(4)
Never(Ihaveneverviewedanoutcome)3.7%(8)0.0%(0)
Table1. Participantcharacteristics.
Table2. Pre-surveyandpost-surveyoverallresponses.
Pre-surveyPost-survey
%(n)DisagreeAgreeDisagreeAgree P-value
IreviewoutcomestoimprovethecareIprovidetopatients.6.0%(12)94.0%(188)4.1%(6)95.9%(141)0.43
Ireviewoutcomestoimprovemyclinicalknowledge.5.5%(11)94.5%(188)2.1%(3)97.9%(140)0.17
Ireviewoutcomestoknowwhethermycaremadeadifference.7.0%(14)93.0%(186)4.1%(6)95.9%(140)0.26
IreviewoutcomestoknowwhetherIprovidedtherightcare.6.9%(14)93.1%(188)2.8%(4)97.2%(141)0.09
Ireviewoutcomestoobtainclosureonpatientencounters.14.0%(28)86.0%(172)8.9%(13)91.1%(133)0.15
Reviewinghospitaloutcomedatathroughthepatientoutcomes featurehelpsimprovemyjobsatisfaction. 11.3%(24)88.7%(188)5.3%(8)94.7%(142)0.05
Reviewinghospitaloutcomedatathroughthepatientoutcomes featurehelpsimprovemyclinicalknowledge. 6.8%(14)93.2%(192)6.9%(10)93.1%(135)0.97
IfIwereprovided15minutesofapprovedcontinuingeducation creditforeachpatientoutcomeIreviewed,Iwouldbemorelikely toreviewmypatientoutcomesinthepatientoutcomesfeature.
theESOlearningplatform.Ofthosewhosuccessfullylogged in,74%(98/133)completedtheirrequiredprofile.The prerequisiteswerecompletedby70%(64/98)ofthosewitha completedprofile,and88%(56/64)ofthosecompletedat leastoneCEactivity.AmongthosewhocompletedanyCE, 88%(35/64)completedmorethanoneCEactivityandless than10%(4/64)completedallavailableCEactivities (Figure1).Atotalof287outcomeswerereviewed,and responsesfollowingtheoutcomereviewactivityarelisted in Table3.
QualitativeAnalysis Therewere72pre-surveyparticipantswhoansweredthe free-textquestionthatasked, “Pleasedescribeanyother reasonsyoureviewoutcomes.” Free-textresponseswere uploadedintoQDADataMinerforanalysis.Allcodingwas performedbyasingleresearcher(SB)andreviewedbyAF andMK.Mostinitialcodesrelatedtoreasonsrespondents reviewedtheoutcomesorbenefitsgainedbydoingso.The mostcommoncodeidentifiedwas improveunderstandingof patientsI ’ veseen, whichwasidentified14times(13%ofall codes).Thesecondmostidentifiedcodewasaf fi rming(that mydiagnosisandtreatmentwerecorrect), identifiedeight times(7%ofallcodes).Weexcludedfromfurtheranalysis10 respondentswhoseonlytextcontentwascodedas “donot reviewoutcomes” or “wishlist” (acodeforentriesthat describedfeaturestheywantedtoseeinthefuture).
Wegroupedthecodesintothemesorganizedbycommon attributes.Theseinitialcodeswereorganizedbybeneficiary ofpatientoutcomereviewCE:therespondent;thepatient encounter;andtheEMSoperation(FigureS1).Notably, unknown, agroupcreatedforcodesthatdidn’tseemto fitany oftheidentifiedthemes,comprised17%ofallcodes.Asa result,weperformedasecondthematicanalysisinanattempt tointegrate “unknown” codesandidentifyhigherlevel
meaningsbehindthecodes.Theresultingthemesrepresented broaderpersonal,operational,andsystem-relatedbenefitsto reviewingpatientoutcomes.Theserevisedthemesandtheir associatedcodeswerereviewedbyAFandMKwithminor revisionsrecommendedandintegrated.
Opted in to CAPCE CE Phase (211)
Successfully Logged into ESO ODL (133)
Created Profile with CAPCE required information (98)
Completed all Prerequisites (64)
Did not log into ESO ODL (78) Incomplete Profile (35) Incomplete Prerequisites (34) CE activities incomplete (8)
Completed at least 1 outcome review and earned CE (56)
Figure1. CAPCECEoptionalparticipation. CAPCE,CommissiononAccreditationforPre-Hospital ContinuingEducation; CE,continuingeducation.
Table3. Continuingeducationactivityreviewquestions andresponses.
Allcontinuingeducationreviews
Goalsofyouroutcomereview(selectallthatapply):
Obtaincontinuingeducationcreditfor licensurerenewal.
Increasemyknowledgeregardingtheclinical conditionofthepatient.
Determinewhethermyassessmentand treatmentswereappropriate.
Determinewhethermy fieldimpressionaligns withthehospitaldiagnosis.
Basedonthisreview:
22%(224)
25%(247)
26%(258)
27%(267)
Iwouldprovidethesametreatment.84%(242)
Ineedmoreinformation.6%(17)
Iwouldmodifymytreatment.10%(28)
Indicatehowstronglyyouagreeordisagreewith thefollowing:Myuseofoutcomesreinforcesor increasesmyclinicalknowledge.
4 – stronglyagree52%(149)
3 – agree46%(132)
2 – disagree0%(1)
1 – stronglydisagree2%(5)
Indicatehowstronglyyouagreeordisagreewith thefollowing:Myuseofoutcomesimprovesthe qualityofcareIprovidetomypatients.
4 – stronglyagree50%(142)
3 – agree49%(139)
2 – disagree1%(3)
1 – stronglydisagree1%(2)
Indicatehowstronglyyouagreeordisagreewith thefollowing:IfIwereprovidedadditionalonline continuingeducationopportunitiesrelatedtothis patientoutcome,Iwouldcompletethetraining.
4 – stronglyagree44%(127)
3 – agree55%(156)
2 – disagree0%(1)
1 – stronglydisagree1%(2)
Therewereshiftsintheperceivedvalueofpatientoutcome reviewbetweenthepre-andpost-surveyperiodsandacross individualswithdifferentbackgroundsandexperience (Figure2).Thoserespondentswhoindicatedtheydidnot providedirectpatientcareplacedthemostvalueon operationsandsystemwidequality.Fortheremainderof respondents,pre-surveyresultsfoundthatthepredominant valueidentifiedwasrelatedto acquiringpersonalknowledge, with enhancingpersonalcon fi denceandcompetence, and improvingpersonalclinicalpractice following nearly10% lower.Duringthepost-survey, acquiringpersonal knowledge felltothefourthposition,with enhancing personalcon fi denceandcompetence thepredominant theme,followedby improvingpersonalclinicalpractice and operations. Inthepost-surveypopulation, acquiring personalknowledge remainedvaluedbyEMTsand individualswith0–4yearsofexperiencebutwasnotvaluedat allinthosewith ≥21yearsofexperience.
DISCUSSION EnhancePersonalConfidence/CompetenceandImprove PatientCare Whensurveyedanonymously,EMSprovidersfavored viewingtheirpatientoutcomes.Qualitativeanalysisofpresurveyresultsrevealedthatthemajorityofcertified personnelfelttheprimarybenefitwouldbeincreasesin personalknowledge;thisattitudewasparticularlyprevalent forEMTsandindividualswhohadlimitedexperience.In post-surveyresults,providersfoundthatreviewingpatient outcomeswasmorerelevanttogainingconfidenceand competenceratherthanknowledgeacquisition.McGuire andcolleaguesevaluatedfeedbackrequestsreceivedfrom EMSprovidersandfoundthemostcommonrequestwasfor the finaldiagnosisandoutcome/disposition.28 This enhancementiscommonlyreflectedinEMSproviderswho assessandcarefortheirpatientsbutarelimitedtoonlythe beginningofthepatient’sexperience,notthe finaloutcome. Providingthemwiththeoutcomeoftheirpatientallowsthem toeitherincreaseconfidenceintheirassessmentand diagnosisorparticipateinanopportunityforcontinued learning.This findingrepresentstheworkforce’sdesireforan outcome-centriccontinuedcompetencemodelover traditionalformsofCE.
The finalthemesandcodegroupingscanbefoundin FigureS2.Webelievethesecodesandthemesaccurately reflectsurveyresponses,andweusedthemforanalysisofthe post-survey,free-textquestionusingthesamemethod.
Table4 providesanoverviewofthethemes,dominantcodes, andkeyquotesforpre-andpost-surveygroups.Inaddition, wecomparedthematicfrequencyreportsbetweentheentire surveygroupandvariousdemographicgroupsby respondentlevel,experience,andfrequencyofoutcome review.Theseresultscanbefoundin TableS1–S4.
Providersalsoperceivedimprovedpatientcarebyviewing theirhospitaloutcomedata,whichpreviousworkhas demonstratedisbeneficialtothelearningprocessandcan improvepatientoutcomes.Thequalitativereviewofpostsurveyresultsrevealedanincreaseintheemphasison enhancingpersonalconfidenceandcompetenceand improvingpersonalclinicalpractice,suggestingthat providersseethepotentialforthiseducationtoimprovetheir clinicalpracticeratherthanjustprovidingknowledge.Postresuscitationfeedbackhasalsobeendemonstratedto improvethequalityofAdvancedLifeSupport,specificallyin
Table4. Overviewofthemes,codes,andkeyquotesfromthepre-andpost-survey.
ThemeDescriptionDominantcodespre-surveyDominantcodespost-survey
Acquirepersonal knowledge
Enhancepersonal confidenceand competence
Codesthatreflectlearningaboutclinical presentations,medicalknowledge,and hospitalrelatedtopatientsseen.
• Improvemyunderstandingof patientsI’veseen
• Furtherclinicalknowledge
• Improvemyunderstandingof patientsI’veseen
Keyquote: Tofollowuponpatientencountersandunderstandthecarethepatientlaterreceived
CodesthataffirmthatEMSdiagnosis andcarewereappropriate,reflectonthe impactofEMScareonpatientoutcome, andcontributetoselfQA/QI.
• Affirming
• SelfQA/QI
• Affirming
Improvepersonal clinicalpractice
Keyquote: Ireviewchartstoreviewmy findingsandQA/QImyselfforfuturepatients
Codesthatreflectimprovementin personalclinicalpracticeincluding informingfuturediagnosisandtreatment ofrecurringpatients.
• Futurebetterment
• Informfuturedifferential diagnosis
• Informfuturevisitsto samepatient
• Futurebettermentto improvecare
Keyquote: Helpsprioritizefollow-upsandwhatresourcesshouldbebroughttobearforourclients
OperationsCodesreflectingimpactonoperational tasksincludingdocumentation,followupsservicesandtraining.
• It’smyjob
• Researchbillinginquiry
SupportsystemwideQI
• Training/reinforcement fortrainees
• Informfollow-up postdischarge
Keyquote: Ireviewoutcomedatawith employees ithelpsuslearntogether,buildingtheeducationalsafetyamong ourgroup
Codesreflectingcollaboration,cultureof learningandeducation,andorganization wideQA/QI.
• Organization-widecompares crewmedicaldecisionmaking, protocolutilizationtopatient diagnosisandoutcome
• SystemQA/QI
• SystemQA/QI
• Createacultureoflearning andeducation
Keyquote: Ithelpscreateacultureinwhichlearningandeducationarethefocus,noterrorsormissteps
EMS,emergencymedicalservices; QA,qualityassurance; QI,qualityimprovement.
Figure2. Comparisonofthemespre-topost-survey.
survivaluntilhospitaldischargeandfavorableneurological outcomesandiswhyreal-life,post-resuscitationfeedbackis recommended.23 Timetotreatmentinheartattackvictims hasalsobeenshowntodecreasefollowingthe implementationofdatafeedbacktoEMSproviders,evenin asystemthatwasalreadyachievinginternationally establishedgoals.24 Sammuelandcolleaguesconducteda scopingreviewoftheeffectsofCPDonhealthprofessionals’ performanceandpatientoutcomesanddemonstrated changesinproviders’ behaviorandpatientoutcomes.25 SurveyresultspublishedbyPollardandBlackfoundthat afterreceivingpatientoutcomedata,mostEMSproviders reflectedonthecallanddidfurtherreading.29
EMSProviderJobSatisfaction Studyparticipantsfeltthatlearningtheirpatient-speci fic hospitaloutcomesimprovedjobsatisfaction.Similarresults havedemonstratedthatwhenasked,EMSproviders anticipatepatientoutcomefeedbackbenefitingtheirwellbeingandworkengagement.14 Providingpatientoutcomes helpsbringEMSprovidersfurtherintothehealthcare continuum,anddoingsoreducesthecausesofburnoutfor them.30 Thisisanimportant findingasagenciesfacea workforceshortageandtheUSseesfewerandfewerEMTs andparamedics.31
Microlearning TheCAPCE-approvedCEwaspresentedtoEMS providersintheformofmicrolearning.Microlearning consistsofsmalldosesofcontentintheformoflesson modulesorshort-termactivities.Thismethodallowslearners tocontrolallaspectsoftheirlearning,includingthetimein whichtheyreview,thepace,andthemethodbywhichthey completetheactivity.Providersreportedbeingmorelikelyto completethereviewiftheywereprovidedwithameanstouse ittocompletecertificationrenewal;thus,ifanagency providespatientoutcomestoproviders,itisbesttoincludeit asameansforcertificationrenewal.
Thispatientoutcome-specificeducationdescribesanew methodofCEforEMSprovidersandalignswiththegoalsof CPD.Additionally,patientoutcome-lededucationhasbeen demonstratedtoimproveprovidercompetencyandimprove patientoutcomes.Morestudyisneededonawiderscaleto determinewhetherthistypeofeducationdeliveryensures morecompetencythananhour-basedmodel.Thistypeof learningmayalsobeappealingfromanoperational perspective,providing flexibilitywithrespecttoscheduling educationalofferingsandreducingthetimethatEMS providersarerequiredtospendinaclassroom.
LIMITATIONS Thesamplesizeisspecifictothesethreeagencies (conveniencesample)andthosewhochosetocompletethe survey;assuchitmaynotbegeneralizabletotheentireEMS workforce.Thewindowforcompletingthesurveywasopen fortwoweeks;thus,theremayhavebeensomeproviderswho didnotworkinthatperiodandcouldnotcompletethe survey.Additionally,therequesttocompletethesurvey occurredduringoperationalhours;so,participationmay havebeenlimitedduetoother,moreurgenttasks.Byits nature,qualitativeanalysisisheavilydependentonthe backgroundandskillsoftheresearcherandmaybe influencedbypersonalbiases.
AlowproportionofproviderswhobegantheCEprocess actuallygainedCEcredits,indicatingthestepsorprocess maybetoodifficultorcumbersome.Itisalsopossiblethat participantsdidnotneedtheCEcredits,aseachofthe participatingagenciesprovides100%oftherequiredhours.
Additionalresearchisneededtodeterminehowtobest integratethislearningmethodwithexistingworkpatterns andCEprograms.
CONCLUSION Emergencymedicalservicesproviderssupportedthe personalandprofessionaldevelopmentandpatientcare improvementvalueofreviewingpatientoutcomes, includingmicrolearningactivities.Participation intherequiredactivitiestoobtaincontinuingeducationwas low.However,subjectswhodidparticipatedemonstrateda shiftinperceivedvaluefrommereacquisitionof knowledgetodevelopmentofimprovedpersonaland systemwideclinicalpractice.Furtherstudyiswarrantedto evaluatethegeneralizabilityofthese findingsandthe bestuserexperiencetofacilitatethecompletion ofCE.
AddressforCorrespondence:MichaelKaduce,MPS,FalckHealth Institute,1517W.BradenCt.,Orange,CA92868.Email: Michael. Kaduce@falck.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.AntonioFernan,ScottBourn,RemleP. Crowe,AlisonTreichel,andJ.BrentMyersareemployeesofESO. Therearenootherconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2024Kaduceetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.TerryM,PowellJ,GilmoreWS,etal.Derivingnationalcontinued competencyprioritiesforemergencymedicalservicesclinicians. PrehospEmergCare. 2023;27(4):439–48.
2.StudnekJR,FernandezAR,MargolisGS.Assessingcontinued cognitivecompetenceamongruralemergencymedicaltechnicians. PrehospEmergCare. 2009;13(3):357–63.
3.DeSiletsLD.TheInstituteofMedicine’sredesigningcontinuing educationinthehealthprofessions. JContinEducNurs. 2010;41(8):340–1.
4.BalmerJT.Thetransformationofcontinuingmedicaleducation(CME)in theUnitedStates. AdvMedEducPract. 2013;4:171–82.
5.IversN,JamtvedtG,FlottorpS,etal.Auditandfeedback:effectson professionalpracticeandhealthcareoutcomes. CochraneDatabase SystRev. 2012;(6):CD000259.
6.(2019).EMSAgenda2050TechnicalExpertPanel,NationalHighway TrafficSafetyAdministration,DepartmentofTranportation.EMS Agenda2050:apeople-centeredvisionforthefutureofemergency
medicalservices,reportNo.DOTHS812664.Washington,DC: NationalHighwayTrafficSafetyAdministration.
7.DorsettM,PanchalAR,StephensC,etal.Prehospitalairway managementtrainingandeducation:anNAEMSPpositionstatement andresourcedocument. PrehospEmergCare. 2022;26(sup1):3–13.
8.RedlenerM,OlivieriP,LooGT,etal.Nationalassessmentofquality programsinemergencymedicalservices. PrehospEmergCare. 2018;22(3):370–8.
9.DelbridgeTR,BaileyB,ChewJLJr.,etal.EMSagendaforthe future:whereweare wherewewanttobe. PrehospEmergCare. 1998;2(1):1–12.
10.ChahineS,KulasegaramKM,WrightS,etal.Acalltoinvestigatethe relationshipbetweeneducationandhealthoutcomesusingbigdata. AcadMed. 2018;93(6):829–32.
11.VithalaniV,SondheimS,CorneliusA,etal.Qualitymanagementof prehospitalairwayprograms:anNAEMSPpositionstatementand resourcedocument. PrehopEmergCare. 2022;26(sup1):14–22.
12.Page,Wolfberg&Wirth.Animaginarybarrier:howHIPAApromotes bidirectionalpatientdataexchangewithemergencymedicalservices. 2019.Availableat: https://nemsis.org/wp-content/uploads/2020/07/ HIPAA_An-Imaginary-Barrier-to-Data-Exchange.pdf AccessedJuly21,2024.
13.MorrisonL,CassidyL,WelsfordM,etal.Clinicalperformancefeedback toparamedics:whattheyreceiveandwhattheyneed. AEMEducTrain. 2017;1(2):87–97.
14.Eaton-WilliamsP,MoldF,MagnussonC.Exploringparamedic perceptionsoffeedbackusingaphenomenologicalapproach. Br ParamedJ. 2020;5(1):7–14.
15.O’HaraR,JohnsonM,SiriwardenaAN,etal.Aqualitativestudyof systemicinfluencesonparamedicdecisionmaking:caretransitionsand patientsafety. JHealthServResPolicy. 2015;20(1Suppl):45–53.
16.CampbellEGandRosenthalM.Reformofcontinuingmedical education:investmentsinphysicianhumancapital. JAMA. 2009;302(16):1807–8.
17.WoltersKluwer.ContinuingmedicaleducationwithUpToDate.2024. Availableat: https://www.wolterskluwer.com/en/solutions/uptodate/ about/continuing-medical-education.AccessedJuly21,2024.
18.CateOTandCarraccioC.Envisioningatruecontinuumofcompetencybasedmedicaleducation,training,andpractice. AcadMed. 2019;94(9):1283–8.
19.ZafarMA,DiersT,SchauerDP,etal.Connectingresidenteducationto patientoutcomes:theevolutionofaqualityimprovementcurriculumin aninternalmedicineresidency. AcadMed. 2014;89(10):1341–7.
20.KleinD,StaplesJ,PittmanC,etal.Usingelectronicclinicalpractice auditsasneedsassessmenttoproduceeffectivecontinuingmedical educationprogramming. MedTeach. 2012;34(2):151–4.
21.LammersRL,Willoughby-ByrwaMJ,VosDG,etal.Comparisonoffour methodsofparamediccontinuingeducationinthemanagementof pediatricemergencies. PrehospEmergCare. 2022;26(4):463–75.
22.GugiuMR,McKennaKD,PlattTE,etal.Aproposedtheoretical frameworkforclinicaljudgmentinEMS. PrehospEmergCare. 2023;27(4):427–31.
23.HubnerP,LobmeyrE,WallmullerC,etal.Improvementsinthequalityof advancedlifesupportandpatientoutcomeafterimplementationofa standardizedreal-lifepost-resuscitationfeedbacksystem. Resuscitation. 2017;120:38–44.
24.ScholzKH,HilgersR,AhlersmannD,etal.Contact-to-balloontimeand door-to-balloontimeafterinitiationofaformalizeddatafeedbackin patientswithacuteST-elevationmyocardialinfarction. AmJCardiol. 2008;101(1):46–52.
25.SamuelA,CerveroRM,DurningSJ,etal.Effectofcontinuing professionaldevelopmentonhealthprofessionals’ performanceand patientoutcomes:ascopingreviewofknowledgesyntheses. AcadMed. 2021;96(6):913–23.
26.CommissiononAccreditationforPre-HospitalContinuingEducation. AboutCAPCE.Availableat: https://www.capce.org/Home/About AccessedApril2024.
27.HsiehHFandShannonSE.Threeapproachestoqualitativecontent analysis. QualHealthRes. 2005;15(9):1277–88.
28.McGuireS,LukeA,KlassenA,etal.11Whatmedicswant:analysisof feedbackandpatientfollow-uprequestsfromout-of-hospitalproviders atanacademicemergencydepartment. AnnEmergMed. 2021;78(4):S5.
29.PollardJandBlackS.Doparamedics finditbenefecialtolearnthe diagnosisgiventotheirpatientsintheemergencydepartment? Emerg MedJ. 2015;32(5):421–1.
30.TorresAJandMcCoyRG.HowtobettervalueEMScliniciansaskey careteammembers. AMAJEthics. 2022;24(9):E898–905.
31.CashRE,RivardMK,ChrzanK,etal.Comparisonofvolunteerandpaid EMSprofessionalsintheUnitedStates. PrehospEmergCare. 2021;25(2):205–12.
32.JanssenA,CogginsA,TadrosJ,etal.Deliveringadaptiveonline learningusingelectronichealthdata:afeasibilityandacceptabilitystudy withemergencytrainees. ResSq. 2023.Availableat: https://doi.org/10. 21203/rs.3.rs-2395367/v1
ORIGINAL RESEARCH ValidationoftheTurkishVersionoftheProfessional FulfillmentIndex MerveEksioglu,MD*
AycaKoca,MD†
BurcuAzapogluKaymak,MD*
TubaCimilliOzturk,MD*
AtillaHalilElhan,PhD‡
SectionEditor:TehreemRehman,MD,MPH
*UniversityofHealthSciencesFatihSultanMehmetEducationandResearch Hospital,DepartmentofEmergencyMedicine,Istanbul,Turkey
† AnkaraUniversityFacultyofMedicine,DepartmentofEmergencyMedicine, Ankara,Turkey
‡ AnkaraUniversityFacultyofMedicine,DepartmentofBiostatistics, Ankara,Turkey
Submissionhistory:SubmittedMay14,2024;RevisionreceivedApril15,2024;AcceptedAugust16,2024
ElectronicallypublishedSeptember25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21199
Introduction: Clinicianburnoutrepresentsasignificantoccupationalhazardamongphysicians,witha notablyhighprevalenceamongemergencyphysicians.TheStanfordProfessionalFulfillmentIndex (PFI)wasdevelopedtocomprehensivelyassessvariousaspectsofdoctors’ workexperiences,including professionalfulfillment.InthisstudyweaimedtovalidatetheTurkishversionofthePFI(T-PFI),a16-item instrumentdesignedtomeasurephysicians’ professionalfulfillmentandburnout.
Methods: Inthiscross-sectionalstudy,wevalidatedtheT-PFIintwophases.Theinitialphaseinvolved translatingandculturallyadaptingtheoriginalPFIintoTurkish.Weevaluatedthecontentvalidityofthe translatedversionusingitemandscalecontentvalidityindices(I-CVIandS-CVI,respectively).The validatedT-PFIwasthendistributedamongabroadcohortofemergencyphysiciansviaanonlinesurvey tofurtherassessitsreliabilityandvalidity.TheassessmenttoolsincludedCronbach α,confirmatory factoranalysis,andcontentvalidityindices.
Results: Of1,434physicianswhoweresentthesurvey,425fullycompletedit(29.6%).Therewasan almostequaldistributionof215femalesand210males.Only9.6%oftheparticipantsreportedhigh levelsofprofessionalfulfillment,whereasasignificantmajority(79.1%)weresusceptibletoburnout. TheCronbach α valuesfortheprofessionalfulfillmentandoverallburnoutscaleswere0.87and 0.90,respectively.ThecontentvaliditywasconfirmedbyI-CVIvaluesexceeding0.80andan S-CVI/averagerelevanceof0.92.Theconfirmatoryfactoranalysisdemonstratedanacceptablemodel fit afteradjustments.
Conclusion: TheT-PFIisareliableandvalidtoolforassessingprofessionalfulfillmentandburnout amongemergencyphysiciansinTurkey.Effectiveinterventionstomitigateburnoutareessentialto improvephysicianwell-beinginTurkishhealthcaresettings.[WestJEmergMed.2024;25(6)958–965.]
INTRODUCTION Burnoutisasyndromeresultingfromchronicworkplace stressandoverload.1 Itischaracterizedbythreedimensions: emotionalexhaustion;depersonalization;andreduced personalaccomplishment.2 Studieshaveshownthat physiciansexperiencehigherratesofburnoutand lowersatisfactionwithwork-lifeintegrationcompared
tothegeneralpopulation.3 Emergencyphysicians,in particular,arehighlysusceptibletoburnout,withrates surpassingthoseseeninothermedicalspecialties.3 Researchontheworkexperiencesofemergencyphysicians haslargelyfocusedonindividualandworkplacefactors contributingtoburnout.4,5 Burnoutnotonlyaffects clinicians’ healthbutalsonegativelyimpactspatient
careoutcomesandtheoverallfunctioningof healthcaresystems.6,7
Toeffectivelymeasureburnoutamonghealthcare professionals,itiscrucialtoassessnotonlythenegative aspects,suchasemotionalexhaustionand depersonalization,butalsothepositiveaspectssuchas professionalsatisfaction,well-being,andoccupational fulfillment.8–11 Unliketraditionalburnoutscales,the StanfordProfessionalFulfillmentIndex(PFI)wasdeveloped toprovideacomprehensiveassessmentofphysicians’ work experiences.10 ThePFIisaconcisetoolspecificallydesigned forphysicians,offeringvaluableinsightsintotheirwellbeing,qualityoflife,andproductivity.Ithelpshealthcare organizationsevaluatebothburnoutandprofessional satisfactionlevels,enablingthedevelopmentofprogramsto enhancejobsatisfactionandoverallwell-being.However, forthePFItobeeffectiveacrossdifferentculturalcontexts, itmustbetranslatedandadaptedtoensureitsvalidity andrelevance.ThePFIhasbeensuccessfullyadapted incountriessuchasBrazilandJapan,butfurthervalidation isneededtoconfirmitspsychometricstrengthand culturalapplicability.12,13
InthisstudyweaimedtodevelopandvalidatetheTurkish PFI(T-PFI)toassesstheprofessionalfulfillmentand burnoutlevelsofemergencyphysiciansinTurkey.The T-PFIisbasedontheStanfordPFIandhasbeentranslated andadaptedto fitthespecificculturalandhealthcarecontext ofTurkey.Wethenevaluatedthepsychometricpropertiesof theT-PFItoensureitsreliabilityandvalidity.Ourgoalwas toprovidearobusttoolforaccuratelyassessingand monitoringtheprofessionalwell-beingofemergency physiciansinTurkey.
METHODS Participants
Theresearchteamcollaboratedwiththeheadsofhighvolumeemergencydepartments(ED)inprominent healthcareinstitutionsacrossTurkeytorecruitparticipants. Recognizingthepotentialforalowresponserateduetothe demandingschedulesofemergencyphysicians,weemployed severalstrategiesrecommendedbytheliteraturetoimprove responseratesandmitigatenon-responsebias.14 These strategiesincludedsendingmultipleremindersandusing variouscommunicationplatformstodistributethe surveylink.
Weinvitedemergencyphysiciansaffiliatedwiththese organizationsthroughemails,socialmediagroups,and internalcommunicationplatforms,suchasonlinemessaging systems.Toensureclarityforpotentialparticipants,we providedadetailedexplanationofthestudy’spurposeand objectives.Eligibleparticipantsincludedphysiciansactively workinginEDs.Whileourprimaryaimwastoidentify burnoutamongthesehealthcareprofessionals,weexpanded thestudytoincluderesidents,attendingphysicians,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencyphysiciansexperiencehighrates ofburnout,negativelyimpactingtheirwellbeingandpatientcare.
Whatwastheresearchquestion?
IstheTurkishversionoftheProfessional Ful fi llmentIndex(T-PFI)validandreliable?
Whatwasthemajor findingofthestudy?
TheT-PFIshowedstronginternalconsistency (Cronbach α :0.87forPF,0.90forburnout).
Howdoesthisimprovepopulationhealth?
TheT-PFIoffersareliablemeasureof professionalful fi llmentandburnout,enabling healthcareorganizationstomonitor physicianwell-being.
consultantphysicians,andfacultymembers.Withthis broaderscopeweaimedtocaptureadiverserangeof perspectives,ensuringcomprehensiverepresentationof healthcareprofessionalswithinemergencymedicine(EM).
Wesentthesurveyto1,434medicaldoctors.Participants providedelectronicinformedconsentbeforecompletingthe survey,confirmingtheirvoluntaryparticipationand understandingofthestudy’sobjectivesandprocedures.To protecttheirprivacyandencouragecandidresponses,we designedthesurveytobeanonymous.Weincludedonlyfully completedquestionnairesinthestatisticalanalysis,resulting inaresponserateof29.6%.
Procedure Weconductedthiscross-sectionalstudyintwophasesto validatetheT-PFI.Inthe firstphase,wetranslatedand culturallyadaptedtheoriginalPFIintoTurkish,adheringto WorldHealthOrganizationguidelinesforlinguisticaccuracy andculturalrelevance.15 Twobilingualemergency physiciansperformedtheforwardtranslationofthePFI fromEnglishtoTurkish.Apanelofexperts,includingthree facultymembers(oneprofessorandtwoassociateprofessors) andtwoemergencyphysicianswithaspecialinterestin physicianwell-being,reviewedandrevisedthetranslationto improveitsculturalrelevance.
ToassessthecontentvalidityofthetranslatedPFI,we calculateditemandscalecontentvalidityindices(I-CVIand S-CVI).Tenindependentexpertsrateditemrelevanceona four-pointscale,with1or2indicatingnorelevanceand3or4 indicatingrelevance.WesetacceptablethresholdsatI-CVI
>0.78andS-CVI >0.90,basedonguidelinesforexpertpanels of6–10members.16
Inthepre-testphase,weobtainedfeedbackfrom fivemale and fivefemaleemergencyphysiciansworkingincrowded EDs.Basedonthisfeedback,werefinedtheinstrument, resultinginthe finalversionoftheT-PFI(AppendixA).We thendistributedthevalidatedTurkishversiontoabroader cohortofrespondentsinEDsforfurthervalidation.The InstitutionalReviewBoardoftheUniversityofHealth SciencesFatihSultanMehmetEducationandResearch Hospitalapprovedallprocedures.
Measures ThePFI,developedbyTrockeletal,assessesprofessional fulfillmentandburnoutamongphysicians.10 Theoriginal PFIcomprises16itemscategorizedintotwoscales:the ProfessionalFulfillment(PF)scale(sixitems)andtheOverall Burnoutscale(10items),measuringthreedimensions: professionalfulfillment;professionalexhaustion,and interpersonaldisengagement.Eachitemisevaluatedusinga five-pointLikertscale(0to4).HigherscoresonthePFscale (7.5orgreater)indicatehigherprofessionalfulfillment,while scoresexceeding3.325ontheburnoutscalesuggestpotential burnout.ThePFI,validatedin2018,evaluatesemotional exhaustion,interpersonaldisengagement,andprofessional achievement,expandingbeyondtraditionalburnout dimensionstoincludeintrinsicworkcomponentssuchas happiness,meaning,self-esteem,andsatisfaction.10
DataAnalysis Wecomputeddescriptivestatisticsfordemographic characteristicsandT-PFIscores.Meanscoresforeachitem anddimensionwerecalculatedaccordingtoTrockel’ s instructions.10 WeevaluatedthereliabilityoftheT-PFI throughinternalconsistency,whichestimatestheextentto whichtheconstituentitemsofthescaleareinterrelated.The Cronbach α coefficientwasusedtoassessinternal consistency,withvaluesabove0.70indicating acceptability.17,18 Weevaluatedconstructvaliditythrough confirmatoryfactoranalysis(CFA)ofresponsestoall16 items,aimingtoassessmodel fit.Factorloadingswere calculatedusingmaximumlikelihoodestimation.To evaluatethemodel’sgoodnessof fit,weconsideredseveral indices,includingthechi-squarestatistic(χ2),rootmean squareerrorofapproximation(RMSEA),comparative fit index(CFI),andtheTucker-Lewisindex(TLI).The thresholdsfortheseindiceswereasfollows:TLI >0.90 (acceptable), >0.95(excellent);CFI >0.90(acceptable), >0.95(excellent);RMSEA <0.08(acceptable), <0.05 (excellent);andchi-squarestatisticdividedbythedegreeof freedom(<3acceptable).19,20 Erroritemswereonly correlatediftheybelongedtothesameconstruct. Forvalidationstudies,itisrecommendedtohavea minimumof50respondentsforeachcriterionandconstruct
validationstudiesthatinvolvecalculatingcorrelation coefficients.However,largersamplesizesexceeding100are preferredtoenhancetherobustnessofthe findings.21
RESULTS Wesentthesurveyto1,434medicaldoctors,and425fully completedit,resultinginaresponserateof29.6%.Among therespondents,215(50.6%)werefemaleand210(49.4%) weremale.Oftheparticipants,193(45.4%)identifiedas emergencyphysicians,156(36.7%)asEMresidents,and76 (17.9%)asmedicaldoctorswithoutaspecialty.Additionally,
Table1. Characteristicsofthestudygroup.
Sociodemographicvariablesn(%)
Sex
Male215(50.6)
Female210(49.4)
Profession
Emergencyphysician193(45.4)
EMresident156(36.7)
Medicaldoctor76(17.9)
Title
Facultymembers38(9.0) Academicstaff156(36.6) Non-academicstaff231(54.4) Workexperience(years)
<283(19.5) 2–5109(25.6)
6–10111(26.1) 11–1561(14.4) >1561(14.4)
Institution
Privatehospital13(3.1)
Statehospital122(28.7)
Cityhospital45(10.6)
Universityhospital85(20.0)
Educationalandresearchhospital160(37.5)
Weeklyhoursofwork <4023(5.4) 40–72330(77.6) >7272(16.9)
Thistablepresentsthedistributionofsociodemographicvariables amongemergencyphysicianswhoparticipatedinthestudy.The dataincludesinformationonsex,professionalrole,academictitle, yearsofworkexperience,typeofinstitutionwheretheyare employed,andtheirweeklyworkinghours.Eachcategoryand subcategoryisprovidedwiththenumberofindividualsandthe correspondingpercentageofthetotalparticipantpool. ED,emergencydepartment; EM,emergencymedicine.
38participantsheldanacademictitle.Themajority(94.5%) ofrespondentsreportedworkingmorethan40hoursper week. Table1 summarizesthedescriptivesociodemographic statisticsofthestudypopulation.
WeusedTrockel’scutpointstoanalyzetheresponses, whichindicatedthatonly9.6%ofrespondentswere consideredprofessionallyfulfilled.Conversely,asignificant 79.1%ofrespondentsreportedexperiencingburnout.The contentvalidityassessment,whichemployedbothI-CVI indexvaluesandtheS-CVI/averagerelevance(Ave),yielded excellentcontentvalidity.AllitemsdemonstratedanI-CVI valueexceeding0.80,withtheS-CVI/Avereaching0.92.The meanscores(standarddeviation)fortheitemsrangedfrom 3.34(2.94)to6.47(2.62),asshownin Table2.TheCronbach α scorefortheprofessionalfulfillmentscaleandtheoverall burnoutscalewere0.87and0.90,respectively.The Cronbach α valuesforeachdimensionarepresented in Table3.
TheCFArunontheinitialmodelwiththreefactorsand16 items(Model1)demonstratedlowCFIandTLIanddidnot meetcriteriaforgoodnessof fit.Factorloadingsofallitems weregreaterthan0.40;therefore,noitemwasremovedfrom theinitialmodel.Allfactorloadingsforeachitemare presentedin Table4.IndexmodificationssuggestedbyCFA wereappliedsubsequentlytoimprovethemodel fit.After
indexmodifications,Model2wassignificantlyimproved withacceptableCFI,TLIandRMSEA(Table5, Figure).
DISCUSSION TheT-PFIhasdemonstrateditselftobearobustand reliablemeasurementtoolamongemergencyphysiciansin Turkey.OurstudyevaluatedtheT-PFI’sreliabilityand validity,revealinghighinternalconsistency,strongfactor loadings,andCFAresultsthatalignwithinternational standards.11 ThisissignificantgiventhatpreviouscrossculturaladaptationstudiesofthePFIwereconductedin BrazilandJapan,butnotinTurkey.12,13 Ourdiverse participantgroup,consistingofphysicianswithvarious demographiccharacteristicsandprofessionalroles,enhances thegeneralizabilityofour findings.Thisdiversityprovides valuableinsightsintotheexperiencesofemergency physicians,similartostudiesconductedinother contexts.Forinstance,Asaokaetalincludedhealthcare professionalsfromdisastermedicalassistanceteamsin Japan,whileSilva-Junioretalfocusedonworkplace physiciansinBrazil.12,13
Inourstudy,weachievedaresponserateof29.6%. Variousfactors,suchasthehighworkloadofemergency physicians,mayhavecontributedtothisresponserate. AccordingtoPhillipsetal,responseratesinsurveysofhealth
Table2. Meanscoresandstandarddeviationsofthesurveytoolitems.
4.Ifeelincontrolwhendealingwithdif ficultproblemsatwork4.11(2.90)
5.Myworkismeaningfultome 5.74(3.10)
6.I’mcontributingprofessionallyinthewaysIvaluemost4.94(3.10)
Overallburnout 5.26(2.18)
Burnout:professionalexhaustion 5.98(2.28)
1.AsenseofdreadwhenIthinkabouttheworkIhavetodo4.92(2.90)
2.Physicallyexhaustedatwork
6.47(2.62)
3.Lackinginenthusiasmatwork 6.42(2.92)
4.Emotionallyexhaustedatwork 6.12(3.06)
Burnout:interpersonaldisengagement 4.78(2.48)
1.Lessempatheticwithmypatients 4.74(2.89)
2.Lessempatheticwithmycolleagues 3.92(2.92)
3.Lesssensitivetoothers’ feelings/emotions 5.04(2.98)
4.Lessinterestedintalkingwithmypatients 5.43(3.05)
5.Lessconnectedwithmypatients 5.38(3.04)
6.Lessconnectedwithmycolleagues 4.20(3.10)
ThistablepresentsthemeanscoresandSDsforitemsrelatedtoprofessionalfulfillmentandburnoutasassessedbytheTurkishProfessional FulfillmentIndex.
Table3. InternalconsistencyofthedimensionoftheTurkishProfessionalFulfillmentIndex. Cronbach α
ScaleThisstudyOriginalJapanesestudy
Professionalfulfillment0.870.910.91
Overallburnout0.900.92NA Professionalexhaustion0.840.860.80
Interpersonaldisengagement0.910.920.90
ThetabledisplaystheinternalconsistencyofthedimensionsoftheTurkishProfessionalFulfillmentIndexinthisstudy,measuredbythe Cronbach α,incomparisontotheoriginalscaleandresultsfromtheJapanesestudy.TheresultsoftheBrazilianstudyarenotincludedinthis tablesinceonlyglobalCronbach α ofthePFI(0.95)wascitedbySilva-Junioretal.13 NA:notapplicable(TheJapanesestudydidnotprovide theCronbach’s α ofoverallburnout).
Table4. FactorloadingsforeachitemoftheTurkishProfessionalFulfillmentIndex.
Standardizedfactor loadings
Professionalfulfillment1.Ifeelhappyatwork0.890.90 2.Ifeelworthwhileatwork0.820.83
3.Myworkissatisfyingtome0.780.78
4.Ifeelincontrolwhendealingwithdifficultproblemsatwork0.630.63
5.Myworkismeaningfultome0.610.58
6.IamcontributingprofessionallyinthewaysIvaluemost0.620.59
Burnout:professionalexhaustion1.AsenseofdreadwhenIthinkaboutwork,Ihavetodo0.480.45
2.Physicallyexhaustedatwork0.710.70
3.Lackinginenthusiasmatwork0.920.93
4.Emotionallyexhaustedatwork0.890.89
Burnout:interpersonaldisengagement1.Lessempatheticwithmypatients0.820.83
2.Lessempatheticwithmycolleagues0.640.65
3.Lesssensitivetoothers’ feelings/emotions0.860.86
4.Lessinterestedintalkingwithmypatients0.880.88
5.Lessconnectedwithmypatients0.900.91
6.Lessconnectedwithmycolleagues0.590.56
ThistablepresentsthestandardizedfactorloadingsforeachitemoftheTurkishProfessionalFulfillmentIndex,asmeasuredintwodifferent models(Model1andModel2).Model1:beforemodificationindex;andModel2:aftermodificationindex.
professionstraineesvarywidely,rangingfrom26.6–100%, withmulti-institutionalsurveystypicallyhavinglower responseratescomparedtosingle-institutionsurveys.22 Our study,beingmulti-institutional,alsofacedthischallenge.To improvetheresponserate,weemployedmultiplemethods, includingemails,socialmediagroups,andinternal communicationplatforms,suchasonlinemessagingsystems, andwesentreminderstoparticipants.Byemployingthese strategies,weaimedtomaximizeparticipationandreduce non-responsebias,ensuringthatour findingsaccurately reflecttheperspectivesofabroadrangeofhealthcare professionalswithinEM.
Basedonoursurveyresults,wefoundthatemergency physiciansinTurkeyexperiencehighlevelsofburnout.Only
9.6%ofparticipantsreportedprofessionalfulfillment,while 79.1%werelikelyexperiencingburnoutbasedonTrockel’ s cut-offpoints.This findingisconsistentwithprevious researchthathaslinkedthe fieldofEMtohighratesof burnout,attributedtothechallengingnatureofthe specialty.3–5,23–29 Forinstance,ameta-analysisonburnout prevalenceandriskfactorsamongemergencyhealthcare workersfoundthatTurkeyhasthehighestprevalenceofhigh emotionalexhaustion.25
Across-sectionalsurveystudyconductedamongfaculty membersoftheAcademicEmergencyMedicineAssociation, whichalsousedthePFIscale,yieldedintriguingresults.30 In thatstudy,38.7%ofparticipantsreportedfeelingsatisfied withtheiroccupation,while39.1%reportedexperiencing
Table5. Confirmatoryfactoranalysis:models’ goodnessof fitoftheTurkishProfessionalFulfillmentIndexandotherversions. #ofitems χ2/df P CFITLIRMSEAAIC
Model1165.963 <0.0010.8900.8690.108672.301
Model2162.894 <0.0010.9600.9500.067358.761
Brazilianversion163.498 <0.0010.9500.08
Japaneseversion16 <0.0010.8970.9090.085
Thistablesummarizestheresultsoftheconfirmatoryfactoranalysis(CFA)conductedtoassessthegoodnessof fitforvariousmodelsofthe TurkishProfessionalFul fillmentIndexanditscomparisonswithotherinternationalversions. χ2/df:chi-square/degreeoffreedom.
AIC,Akaikeinformationcriterion; CFI,comparative fitindex;Model1,beforemodificationindex;Model2,aftermodificationindex; RMSEA,rootmeansquareerrorofapproximation; TLI,Tucker-LewisIndex.
Figure. Con firmatoryfactoranalysisoftheTurkishProfessional FulfillmentIndex,Model2(aftermodificationindex). This figurepresentstheconfirmatoryfactoranalysisfortheTurkish ProfessionalFulfillmentIndex.Themodeldepictsthe interrelationshipsbetweenthreelatentconstructs.Theobserved variablesassociatedwiththeconstructsofprofessionalful fillment (PF),professionalexhaustion(PE),andinterpersonal disengagement(ID)arepresented.
burnout.Theseresultsindicatealowerprevalenceofburnout comparedtoourstudy.Thediscrepancymaybeattributedto thefactthatthesampleincludedsolelyEDfacultymembers, whereasourstudygroupconsistedofaheterogeneous representationofemergencyphysicians,includingresidents andattendingphysicians.Consequently,our findingsare moregeneralizableduetothediversityofparticipants, providingvaluableinsightsintotheexperiencesofclinicians inEDs.
TheinternalconsistencyoftheT-PFIwasrobust,withthe Cronbach α forprofessionalfulfillmentat0.87andfor overallburnoutat0.90.Thesevaluesarecomparabletothose reportedintheoriginalUSvalidationstudyandtheJapanese study.10,12 IntheBrazilianvalidationstudy,onlyaglobal Cronbach α of0.95wasreported,indicatinghighreliability acrossdifferentculturalcontexts.13
TheinitialCFAfortheT-PFIindicatedlowCFIandTLI, whichdidnotmeetthecriteriaforgoodnessof fit.After applyingindexmodifications,the fitindicessignificantly improved,withModel2achievingaCFIof0.960andan RMSEAof0.067.Theseresultsalignwiththoseofthe Japanesestudy,whichalsodemonstratedacceptable fit indicesaftermodifications.12 TheBrazilianstudysimilarly reportedaCFIof0.950andRMSEAof0.08,underscoring themodel’srobustnessacrossdifferentpopulations.13 Inthe Japanesevalidationstudy,theCFAmodel fitwasmodest, andexploratoryfactoranalysisconfirmedathree-factor structuresimilartotheoriginalscale.Ourstudy’sfactor loadingsrangedfrom0.45–0.93,confirmingtheT-PFI’ s structuralvalidity.
Althoughwedidnotassessconvergentvaliditywith externalmeasures,the findingsfromtheJapanesestudyof thePFIdemonstratedsignificantpositivecorrelations betweenprofessionalfulfillmentandqualityoflife,aswellas betweenburnoutsubscalesanddepressivesymptoms.12 This alignswithliteraturesuggestingthathigherlevelsof professionalfulfillmentareassociatedwithbetterqualityof life,whilehigherlevelsofburnoutarelinkedtoincreased depressivesymptoms.10
Volume25,No.6:November2024WesternJournal
TheuseofthePFIindifferenthealthcaresettings, includingpharmacistsandphysicians,hasdemonstratedits versatilityandreliability.31,32 Forinstance,astudyonUS pharmacistsfoundthatprofessionalfulfillmentwas associatedwithdemographicsandworksettings,with communitypharmacistsreportingthelowestfulfillmentand highestburnout.32 Thispatternissimilartoour findings, whereemergencyphysiciansexposedtohighstressandlong workinghoursreportedsignificantburnoutandlow professionalfulfillment.
Theresultsofthisstudyhavesignificantimplicationsfor bothclinicalpracticeandhealthcarepolicy.Thehigh prevalenceofburnoutamongemergencyphysiciansin Turkeyhighlightstheurgentneedforsystematic interventions.Healthcareadministratorsshouldintegrate theT-PFIintoregularevaluationstomonitorphysician well-beingproactively.Thiscouldleadtoearly identificationofburnoutsymptoms,allowingfortimely interventions.Forinstance,BodenheimerandSinsky emphasizetheimportanceofthequadrupleaim,which includesimprovingclinicians’ worklifeasacrucial componentofenhancingpatientcare.9 Additionally, Shanafeltetalfoundthataddressingphysicianburnoutcan significantlyimprovepatientcarequalityandreduce healthcarecosts.3,7
The findingsofthisstudycaninformpolicy decisionsatbothorganizationalandgovernmentallevels. Policiesdesignedtoreduceworkhours,provide mentalhealthresources,andcreateasupportivework environmentarejustifiedbythedataindicatinghighburnout levels.Futureresearchshouldinvestigatethelongitudinal impactofburnoutandprofessionalfulfillmenton careerlongevityandpatientcarequalityamong emergencyphysicians.Collaborativeeffortsacross countriescouldfurtherrefinetheT-PFI,making itaglobalstandardforassessing physicianwell-being.
LIMITATIONS Anotablelimitationofthisstudyisitsfocusonemergency physicians,whichmaylimitthegeneralizabilityofthe findingstoothermedicalspecialtiesordepartments.Future researchshouldincludeabroaderrangeofhealthcare professionalsacrossvariousspecialtiestoenhancethe comprehensivenessofthe findings.Additionally,wedidnot comparethedemographiccharacteristicsofrespondentsand non-respondents.Futurestudiesmightbenefitfromsuch comparisonstobetteraddressnon-responsebias. Longitudinalstudiesarealsorecommendedtounderstand thetemporaldynamicsofprofessionalfulfillmentand burnout.Investigatingorganizationalfactorscouldprovide deeperinsightsintocreatinghealthierworkenvironments forphysicians.
CONCLUSION Inthisstudywesuccessfullytranslated,adapted,and validatedtheTurkishProfessionalFulfillmentIndex, establishingitsreliabilityasatoolforassessingprofessional fulfillmentandburnoutamongmedicaldoctorsinTurkish EDs.The findingshighlightasignificantprevalenceof burnout,emphasizingtheneedfortargetedinterventionsto enhancephysicianwell-beinginTurkishhealthcaresettings. Byprovidingareliablemeasureofprofessionalfulfillment andburnout,theT-PFIcanguidehealthcareorganizations indevelopingprogramstoimprovephysicians’ job satisfactionandoverallwell-being.
AddressforCorrespondence:MerveEksioglu,MD,Departmentof EmergencyMedicine,UniversityofHealthSciences,FatihSultan MehmetEducationandResearchHospital,HastaneSokakNo:1/9, Içerenköy,Ata ¸ sehir34752Istanbul,Turkey.Atasehir-Istanbul, Turkey.Email: mervekoyunoglu@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Eksiogluetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.PetersDandRajasingamD.Burnoutinhealthcare:medicaleducators’ role. BMJ. 2019;366:l5570.
2.MaslachC,SchaufeliWB,LeiterMP.Jobburnout. AnnuRevPsychol. 2001;52:397–422.
3.ShanafeltTD,WestCP,SinskyC,etal.Changesinburnoutand satisfactionwithwork-lifeintegrationinphysiciansandthegeneral USworkingpopulationbetween2011and2017. MayoClinProc. 2019;94(9):1681–94.
4.AroraM,AshaS,ChinnappaJ,etal.Reviewarticle:burnoutinemergency medicinephysicians. EmergMedAustralas. 2013;25(6):491–5.
5.BoutouA,PitsiouG,SourlaE,etal.Burnoutsyndromeamong emergencymedicinephysicians:anupdateonitsprevalenceandrisk factors. EurRevMedPharmacolSci. 2019;23(20):9058–65.
6.WestCP,DyrbyeLN,ShanafeltTD.Physicianburnout:contributors, consequencesandsolutions. JInternMed. 2018;283(6):516–29.
7.HanS,ShanafeltTD,SinskyCA,etal.Estimatingtheattributablecostof physicianburnoutintheUnitedStates. AnnInternMed. 2019;170(11):784–90.
8.TawfikDS,ScheidA,ProfitJ,etal.Evidencerelatinghealthcare providerburnoutandqualityofcare:asystematicreviewandmetaanalysis. AnnInternMed. 2019;171(8):555–67.
9.BodenheimerTandSinskyC.Fromtripletoquadrupleaim:careofthe patientrequirescareoftheprovider. AnnFamMed. 2014;12(6):573–6.
10.TrockelM,BohmanB,LesureE,etal.Abriefinstrumenttoassessboth burnoutandprofessionalfulfillmentinphysicians:reliabilityandvalidity, includingcorrelationwithself-reportedmedicalerrors, inasampleofresidentandpracticingphysicians. AcadPsychiatry. 2018;42(1):11–24.
11.WallaceJE,LemaireJB,GhaliWA.Physicianwellness:amissing qualityindicator. Lancet. 2009;374(9702):1714–21.
12.AsaokaH,SasakiN,KoidoY,etal.Reliabilityandvalidityofthe JapaneseversionoftheProfessionalFulfillmentIndexamong healthcareprofessionals:avalidationstudy. JOccupHealth. 2023;65(1):e12422.
13.Silva-JuniorJS,NiitumaOgataAJ,ScarpelliniBC,etal.Validity evidenceofBrazilianPortugueseversionoftheProfessionalFulfillment Index. AmJHealthPromot. 2022;36(7):1112–22.
14.PhillipsAW,ReddyS,DurningSJ.Improvingresponseratesand evaluatingnonresponsebiasinsurveys:AMEEguideno.102. Med Teach. 2016;38(3):217–28.
15.WorldHealthOrganization. ProcessofTranslationandAdaptationof Instruments.Geneva,Switzerland:WorldHealthOrganization,2005.
16.PolitDFandBeckCT.Thecontentvalidityindex:areyousureyouknow what’sbeingreported?Critiqueandrecommendations. ResNurs Health. 2006;29(5):489–97.
17.BlandJMandAltmanDG.Cronbach’salpha. BMJ. 1997;314(7080):572.
18.TavakolMandDennickR.MakingsenseofCronbach’salpha. IntJMed Educ. 2011;2:53–5.
19.XiaYandYangY.RMSEA,CFI,andTLIinstructuralequationmodeling withorderedcategoricaldata:thestorytheytelldependsonthe estimationmethods. BehavResMethods. 2019;51(1):409–28.
20.RoseM,BjornerJB,BeckerJ,etal.Evaluationofapreliminaryphysical functionitembanksupportedtheexpectedadvantagesofthePatientReportedOutcomesMeasurementInformationSystem(PROMIS). JClinEpidemiol. 2008;61(1):17–33.
21.deVetHCW,TerweeCB,MokkinkLB,etal.(2011). Measurementin Medicine:APracticalGuide.PracticalGuidestoBiostatisticsand Epidemiology.Cambridge,UK:CambridgeUniversityPress,2011.
22.PhillipsAW,FriedmanBT,UtrankarA,etal.Surveysofhealth professionstrainees:prevalence,responserates,andpredictivefactors toguideresearchers. AcadMed. 2017;92(2):222–8.
23.ZhangQ,MuMC,HeY,etal.Burnoutinemergencymedicine physicians:ameta-analysisandsystematicreview. Medicine (Baltimore). 2020;99(32):e21462.
24.SakamotoJT,LeeJ,LuDW,etal.Factorsdrivingburnoutand professionalfulfillmentamongemergencymedicineresidents:a nationalwellnesssurveybytheSocietyforAcademicEmergency Medicine. AEMEducTrain. 2022;6(Suppl1):S5–12.
25.AlanazyARMandAlruwailiA.Theglobalprevalenceandassociated factorsofburnoutamongemergencydepartmenthealthcareworkers andtheimpactoftheCOVID-19pandemic:asystematicreviewand meta-analysis. Healthcare(Basel). 2023;11(15):2220.
26.MoukarzelA,MicheletP,DurandAC,etal.Burnoutsyndromeamong emergencydepartmentstaff:prevalenceandassociatedfactors. BiomedResInt. 2019;2019:6462472.
27.KimoTakayesuJ,RamoskaEA,ClarkTR,etal.Factorsassociatedwith burnoutduringemergencymedicineresidency. AcadEmergMed. 2014;21(9):1031–5.
28.StehmanCR,TestoZ,GershawRS,etal.Burnout,dropout,suicide: physicianlossinemergencymedicine,part1. WestJEmergMed. 2019;20(3):485–94.[publishedcorrectionappearsin WestJEmerg Med.2019;20(5):840–1].
29.SonmezLOandGulM.Occupationalburnout,jobsatisfactionand anxietyamongemergencymedicinedoctorsinTurkey. PakJMedSci. 2021;37(3):757–63.
30.LuDW,LeeJ,AlvarezA,etal.Driversofprofessionalfulfillmentand burnoutamongemergencymedicinefaculty:anationalwellnesssurvey bytheSocietyforAcademicEmergencyMedicine. AcadEmergMed. 2022;29(8):987–98.
31.GustafsonKA,BatesB,ClineKM,etal.Concurrentvalidityofthe ProfessionalFulfillmentIndexinasampleofpharmacyresidentsand preceptors. AmJHealthSystPharm. 2023;80(11):678–86.
32.FadareOO,DoucetteWR,GaitherCA,etal.UseoftheProfessional FulfillmentIndexinpharmacists:aconfirmatoryfactoranalysis. Pharmacy(Basel). 2021;9(4):158.
ORIGINAL RESEARCH UseofParenteralAntibioticsinEmergencyDepartments:Practice PatternsandClassConcordance *
MeganElli,MS
TimothyMolinarolo,PharmD*†
AidanMullan,MA‡
LauraWalker,MD,MBA*
SectionEditor:ShahramLotfipour,MD,MPH
*MayoClinic,DepartmentofEmergencyMedicine,Rochester,Minnesota † MayoClinic,DepartmentofPharmacy,Rochester,Minnesota ‡ MayoClinic,DepartmentofQuantitativeHealthSciences,Rochester,Minnesota
Submissionhistory:SubmittedApril9,2023;RevisionreceivedMay29,2024;AcceptedJune11,2024
ElectronicallypublishedSeptember6,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.17998
Introduction: Weaimedtoassessantibioticstewardshipbyquantifyingtheuseof first-doseintravenous (IV)vsoral-onlyantibioticsandthefrequencywithwhichantibioticclasswaschangedfordischarged patients.Secondaryaimsincludedthefollowing:evaluationoftherelativelengthofstay(LOS); differencesinprescribingpatternsbetweencliniciantypes;differencesbetweenacademicand communitysettings;assessmentofprescribingpatternsamongemergencydepartment(ED)diagnoses; andfrequencyofreturnvisitsforpatientsineachgroup.
Methods: ThiswasaretrospectivecohortstudyincludingpatientspresentingtoEDswithinfectionswho weredischargedfromourMidwesthealthcaresystemconsistingof17communityhospitalsandone academiccenter.Weincludedinfectiontype,antibioticclassandrouteofadministration,typeof infection,LOS,returnvisitwithintwoweeks,cliniciantype,anddemographics.Datawerecollected betweenJune1,2018–December31,2021andanalyzedusingdescriptivestatistics.
Results: Wehad77,204EDvisitsforpatientswithinfectionsduringthestudyperiod,ofwhom3,812 receivedIVantibioticsduringtheirvisit.Thereweremorewomen(62.4%)thanmenincluded.Ofthe 3,812patientswhoreceivedIVantibiotics,1,026(34.3%)weredischargedonadifferentclassof antibioticsthantheyreceived.ThemostcommonchangeswerefromIVcephalosporintooralquinolone orpenicillin.PatientstreatedwithIVantibioticspriortodischargehadalongerLOSintheED(median differenceof102minuteslongerforthosewhoreceivedIVantibiotics).Therewasnotasignificant differenceintheuseofIVantibioticsbetweentheacademiccenterandcommunitysitesincludedin thestudy.
Conclusion: AdministeringIVantibioticsasa firstdosepriortooralprescriptionsupondischargeis common,asisshiftingclassesfromtheIVdosetotheoralprescription.Thisoffersanopportunityfor interventiontoimproveantibioticstewardshipforEDpatientsaswellasreducecostandlengthofstay. [WestJEmergMed.2024;25(6)966–974.]
INTRODUCTION Background
Acuteinfectionsareacommonreasonforpatientsto presenttotheemergencydepartment(ED).Therewere approximately130millionEDvisitsin2018withinthe UnitedStates.Acuteinfectionsaccountforapproximately 15millionvisitstotheEDannually.1,2 Acuterespiratory
infections,skininfections(eg,cellulitisandsubcutaneous abscess),andurinarytractinfections(UTI)areamongthe mostcommoninfectionsevaluatedintheEDin recentyears.3
Priorworkhasaddressedinpatientconcernsabout transitioningfromintravenous(IV)tooralantibiotics,some ofwhichareapplicabletotheEDsetting.Theseinclude
concernsfornoclearbenefit;reducedbioavailability; inapplicabilityofbioavailabilitystudiesperformedon healthyindividuals;improvedclinicaloutcomeswithIV therapy;andconcernthatanoralrouteofadministration maycontributetoaninfectionlingering.Theseconcernsare systematicallyaddressedandincludecommentaryonthe bioavailabilityofmostantibiotics,whichisgreaterthan90%. Manyoftheclassescanachieveaserumconcentrationthatis thesameviaoralorIVroutes.TreatmentwithIVantibiotics comparedwithoralantibioticshasbeennotedtobemore expensivethanoralantibioticsalone,andIVantibioticsalso havetheriskofpossiblecomplicationsassociatedwith IV-lineinsertionanduse.4 Cephalosporinsareanotable exceptionandhavebeenstudiedinthesettingof pyelonephritiswithrecommendationsforasingleIVdosein theEDpriortodismissal(Guptaetal,below).However,the serumconcentrationachievableviaoraladministrationis adequatetotreatmildandmoderateinfections,5 aswewould expecttoseeinapatientwhoisdischargedhome.
Importance Antibioticstewardshipisincreasinglyimportantdueto therisingratesofantibioticresistanceincludingmethicillinresistant Staphylococcusaureus andmultidrugresistant bacteriainthesettingofpneumoniaandUTIs.6–8 Thereare alsorisksofantibiotic-relatedcomplicationssuchas Clostridioidesdif fi cile colitis.Itis,therefore,imperativethat antibioticsbeadministeredfortheshortestduration required,throughanappropriateroute,andprescribedonly whennecessary.9 Thereisscantinformationregardingthe concordancebetween firstdoseofIVantibioticsand subsequentprescriptionfromtheED.Therearedifferences inthe financialburdenandtimeassociatedwiththe administrationrouteofantibiotics.Oralantibioticsaremore costeffectivethanIVantibioticsandoftenprovidesimilar microbialcoverage.4 Multiplestudieshavecomparedoral andIVantibioticswhentreatingUTIs,cellulitis,or pneumoniaseparately,butstudiesarelackingthatevaluate oralandIVantibioticsfortreatinginfectionsinabroader sense. 10–12 Inmanycases,oralantibioticsmaybe appropriateandasefficaciousasIVantibiotics,providing moretime-efficientandcost-effectivecareforpatientswho aredischargedfromtheED.
GoalsofThisInvestigation Ourprimaryaimwastodeterminewhetherweadhereto bestpracticesinprescribingantibioticsforcommon infectiousconditionsbeingtreatedonanoutpatientbasis afteranEDvisit.Thisincludestherouteofadministration andconcordancebetweenanydosesgivenintheEDand subsequentprescriptions.Secondaryaimsincludedthe following:evaluationoftherelativelengthofstay(LOS)for patientsreceivingadoseofIVantibioticswhoare subsequentlydischargedcomparedtothosegivenoral
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Antibioticstewardshipisimperativedueto risingratesofantibiotic-relatedinfections andresistance;itiscrucialthatantibioticsbe prescribedappropriately.
Whatwastheresearchquestion?
Wequanti fi edtheuseof fi rst-doseIVvsoralonlyantibioticsandthefrequencythat antibioticclasswaschanged.
Whatwasthemajor findingofthestudy?
Of3,812patients(4.9%,95%CI4.8 – 5.1%) whoreceivedIVantibioticsintheED,1,273 (33.4%,95%CI31.9 – 34.9%)were prescribedadifferentantibioticclass whendischarged.
Howdoesthisimprovepopulationhealth?
Byrecognizinginconsistenciesinpatients treatedwithantibioticsintheEDpriorto discharge,thispresentsfutureopportunities toimproveuponantibioticstewardship.
antibioticsonly;differencesinprescribingpatternsbetween cliniciantypes(physician,physicianassistant/nurse practitioner)andinacademicvscommunitysettings; assessmentofprescribingpatternsamongEDdiagnoses(eg, skin/softtissue,urinary,pulmonary);andpatternsofreturn visitsforpatientsreceivingadoseofparenteralvsoral antibioticsonly.
METHODS StudyDesignandSetting
ThisstudyadherestotheSTROBEguidelinesfor reportingobservationalstudies.13 Thiswasamulticenter retrospectivecohortstudy.Weincludedpatientsinasingle academiccenterand17communityEDsaffiliatedwithour institutionlocatedthroughouttheMidwest.
SelectionofParticipants Weincludedpatientswhowereevaluatedanddischarged fromtheEDwithadiagnosisofinfection,basedon InternationalClassificationofDiseases(ICD-10)codes,and wereprescribedoralantibioticsupondischargefromtheED. SomepatientsreceivedoralantibioticsfollowingadoseofIV antibioticsprovidedpriortodischarge.Patientswhowere admittedtothehospitalorplacedinEDobservationduring their firstEDvisitwereexcludedfromouranalysis.
Measurements Ourdatasetincludedthefollowing:visitidentifier;legal gender;genderidentify;primarylanguage;ageatvisit; antibioticsgiveninED(yes/no);allergies;EDlocation;ED arrivaltime;EDdeparturetime;chiefcomplaint;primary diagnosis;diagnosislist; finaldisposition; firstattending,last attending,resident,advancedpracticepractitioner(APP), primarynurse;returnvisitidentifier;returnvisitlocation; daysbetweenreturnvisits;returnvisitarrivaltime;return visitdeparturetime;returnvisitchiefcomplaint;returnvisit primarydiagnosis;returnvisitdisposition;antibioticorder identification;outpatientantibioticorderdate;outpatient antibioticprescription;andoutpatientantibioticprescriber andspecialty.
Wecategorizedantibioticsbytheirrouteof administration(parenteralvsoral)andbypharmacologic class(aminoglycoside,carbapenem,cephalosporin,epoxide, glycopeptide,lincomycin,macrolide,nitrofurantoin, nitroimidazole,penicillin,quinolone,sulfa,ortetracycline). Topicalisincludedamongtheclassesofantibioticsduetoits distinctuse.Antibioticswereconsideredconcordantifthe antibioticprovidedparenterallywasinthesameclassasthe oralantibioticprescribedupondischarge.Prescribing patternswereevaluatedbasedoncredentialswithsubgroups ofphysicians(MD/DO/MBBS)andadvancedpractice providers(nursepractitioner[NP]/physicianassistant[PA]). Practicesettingsweredefinedasanacademiccenterthat includesanemergencymedicineresidencyprogramand community-basedsettings.TheICD-10diagnoseswere groupedbasedonorgansystemwithpresumedbacterial etiology(urinary,skin/softtissue,pulmonary, gastrointestinal,otolaryngological,animalbite,insectbite, dental,orthopedic,ophthalmologic,osteomyelitis)and/or organismtype(fungalandparasitic)andcategoriesforfever ofunknownorigin,postoperativeinfections,prophylaxis, andotherinfections,whichisacatch-allforuncommon diagnoses.AcompletelistoftheICD-10associated diagnosesincludedwithinthestudyisavailablein AppendixA.Lengthofstay(LOS)ismeasuredintime elapsedfrompresentationtotheEDuntilthetimeof discharge.Returnvisitswereconsideredpotentiallyrelated totheindexvisitforinfectioniftheyoccurredwithin twoweeks.
Outcomes Theprimaryoutcomewastherouteofadministrationof antibioticsforadiagnosedinfectionandconcordanceof prescriptionoralantibioticswithanyparenteraltreatment given.SecondaryoutcomesincludedLOSwithintheED, differencesinprescribingIVororalantibioticsbetween physiciansandAPPs,differencesbetweenacademicand communitysetting,andassociationbetweentreatmentand EDreturnvisits.
Analysis Wesummarizedcontinuousfeaturesweresummarized withmeanswithstandarddeviations,aswellasmedianswith interquartileranges;categoricalfeaturesweresummarized withfrequencycountsandpercentages.Wecalculated confidenceintervals(CI)forpercentagesusinganexact binomialdistribution.Demographicsandvisit characteristicswerecomparedbetweenpatientswhoreceived IVantibioticsandpatientswhodidnot,usingWilcoxon rank-sumtestsandchi-squaredtests.
Forthemainoutcomesofinterest,wecomparedtherates oftreatmentwithIVantibioticsbyEDpracticeandclinician typeusingchi-squaredtests.Similarly,therateoftwo-week EDreturnswascomparedbetweenpatientstreatedwithboth IVandprescriptionantibioticsandpatientstreatedonlywith prescriptionantibiotics,usingchi-squaredtests.We comparedEDLOSbetweenpatientsreceivingIVantibiotics intheEDandpatientsnottreatedwithIVantibiotics,using Wilcoxonrank-sumtests.Testresultswerereportedwiththe mediandifferenceinLOStimesalongwith95%CIs calculatedbybootstrapresampling.Alltestsweretwo-sided and P -valueslessthan0.05wereconsideredsignificant. AnalysiswasperformedusingRversion4.1.2(RFoundation forStatisticalComputing,Vienna,Austria).14
RESULTS CharacteristicsofStudySubjects Patientdemographicsandvisitcharacteristicsare summarizedin Table1.Ofnote,thereweresignificantly morefemalethanmalesubjects(62.4%vs37.6%).The medianageofpatientswasdifferentbetweenpatientswho didanddidnotreceiveIVantibiotics.Therewasamedian ageof50.0yearsforthosewhodidnotreceiveIVantibiotics comparedtoamedianageof55.5yearsforthosewhodid. Themajorityofthepatientsincludedwithinthestudywere Englishspeaking(97.2%).
MainResults Atotalof77,204EDvisitsforpatientswithinfections occurredbetweenJune1,2018–December31,2021among allsitesandwereincludedforanalysis.Therewere3,812 patients(4.9%,95%CI4.8–5.1%)whoreceivedIV antibioticsintheED.NearlyallthepatientswhoreceivedIV antibioticswithintheEDreceivedcephalosporins(3,637 patients,95.4%),withpenicillins(114patients,3.0%)and glycopeptides(32patients,0.8%)beingthenextmost common.Theprimaryinfectiousdiagnosesaresummarized within Table2.PatientsdiagnosedwithaUTIwerethe largestgrouptreatedwithIVantibiotics(63.3%).When comparingpyelonephritiswithotherUTIs,pyelonephritis wasmuchmorelikelytobetreatedwithIVantibioticsthan allotherUTIs(28.3%vs6.5%, P < 0.001).Insectbites(0.2%) andbitewounds(33of4,047visits,0.8%)receivedIV antibioticstheleastoften.
Table1. Demographicsandvisitcharacteristics.
Patientgender
Female(n = 48,157)45,600(62.1%)2,557(67.1%)
Male(n = 29,045)27,790(37.9%)1,255(32.9%)
Unknown2(0.0%)0(0.0%)
Patientage < 0.001
Mean(SD)49.2(24.5)53.4(23.6)
Median(Q1,Q3)50.0(29.0,69.0)55.5(33.0,73.0)
Primarylanguage < 0.001
English71,389(97.3%)3,686(96.7%)
Non-English1,918(2.6%)121(3.2%)
Unknown/didnotdisclose85(0.1%)5(0.1%)
EDpracticetype 0.14
Academiccenter22,591(30.8%)1,130(29.6%)
Communitypractice50,801(69.2%)2,682(70.4%)
Cliniciantype
NP/PA28,976(39.5%)1,231(32.3%)
Physician44,314(60.5%)2,578(67.7%)
EDlengthofstay < 0.001
Mean(SD)164.3(128.8)278.3(183.6)
Median(Q1,Q3)139.0(76.0,219.0)241.0(180.0,314.0)
Changeinantibioticclass
NoIVantibiotics73,392(100.0%) –
Changedantibiotics0(0.0%)1,273(33.4%)
Sameantibiotics0(0.0%)2,539(66.6%)
IV,intravenous; Abx,antibiotics; ED,emergencydepartment; Q1, firstquartile; Q3,thirdquartile; NP/PA,nursepractitioneror physicianassistant.
Table3 comparestheIVantibioticadministeredintheED tooralantibioticprescribedupondischarge.Themost commonchangesinantibioticclasswerefromIV cephalosporintooralquinolone(304visits,23.9%of changes)andfromIVcephalosporintooralpenicillin(231 visits,18.1%ofchanges).Themostcommonoralantibiotic classprescribedatdischargefromtheEDwascephalosporin. Themostcommonlyprescribedtopicalantibioticwaswithin theclassofcephalosporinsaswell.Thetypeofantibiotic prescribedtopatientstreatedparenterallywasdifferentfrom thethoseprescribedfororal-onlytreatment(P < 0.001). AmongthepatientstreatedwithIVantibiotics,1,273(33.4%, 95%CI31.9–34.9%)receivedaprescriptionforadifferent antibioticclassatdischarge.
Secondaryoutcomes Foroursecondaryendpoints,wefoundthatpatients treatedwithIVantibioticspriortodischargehadalonger LOSwithintheED(mediandifference102minuteslonger
forthosewhoreceivedIVantibiotics;95%CI97–106 minutes; P < 0.001).Physiciansweremorelikelytotreat patientswithIVantibioticscomparedtoAPPS(5.5%vs 4.1%; P < 0.001).Whilethisisstatisticallysignificant,the overallpercentagedifferenceissmall.Therewasno significantdifferenceintheuseofIVantibiotics betweentheacademiccenterandcommunitysites (4.8%vs5.0%; P = 0.14).
Whenweassesseddiagnosis-basedpatterns,wefoundthat amongpatientsgivenIVantibioticsduringtheEDvisit,the groupmostlikelytobeprescribedadifferentclassof antibioticwasthosewithpulmonaryinfections(279of361 visits,77.3%)followedbygastrointestinal(54of87visits, 62.1%).Therewasonepatientwithanophthalmologic infection,andtheclassofantibioticswaschangedupon dismissal(Table4).PatientstreatedwithIVantibioticsfor UTIswereleastlikelytochangeantibioticclassatdismissal (20.7%of391visits).TheIVandoralantibioticsclass administeredbasedontheinfectiontypeissummarized
Table2. Summaryofantibiotic,antifungal,antiparasitictreatmenttypeforemergencydepartmentinfections.
PrimaryEDdiagnosis
IVAbxintheED (N = 2,989)
NoIVAbxintheED (N = 56,289)
Percentofdiagnosed withIVAbxintheED
UTIsnotdiagnosedaspyelonephritis1,145(38.3%)16,591(29.5%)6.5%
Pyelonephritis747(25.0%)1,888(3.35%)28.3%
Skin/softtissueinfection540(18.1%)20,109(35.7%)2.6%
Pulmonaryinfection361(12.1%)6,708(11.9%)5.1%
Gastrointestinalinfection87(2.9%)4,211(7.5%)2.0%
ENTinfection36(1.2%)667(1.2%)5.1%
Bitewound33(1.1%)4,014(7.1%)0.8%
FUO15(0.5%)207(0.4%)6.8%
Otherinfection10(0.3%)66(0.1%)13.2%
Dentalinfection9(0.3%)454(0.8%)1.9%
Insectbite2(0.1%)1,096(1.9%)0.2%
Orthopedicinfection2(0.1%)62(0.1%)3.1%
Ophthalmologicinfection1(0.0%)68(0.1%)1.4%
Fungalinfection1(0.0%)61(0.1%)1.6%
Prophylaxis0(0.0%)52(0.1%)0%
Post-opinfection0(0.0%)22(0.0%)0%
Parasiticinfection0(0.0%)8(0.0%)0%
Osteomyelitis0(0.0%)4(0.0%)0%
IV,intravenous; Abx,antibiotic/antifungal/antiparasitic; ED,emergencydepartment; UTI,urinarytractinfection; ENT,otolaryngological; FUO,feverofunknownorigin.
Table3. Comparisonofintravenousandprescriptionantibiotics,antifungals,andantiparasiticagents.
IVantibioticclassadministeredintheED
Oralantibiotic class prescribedat discharge
Aminoglycoside (N = 2)
Carbapenem (N = 6)
Cephalosporin (N = 3,637)
Glycopeptide (N = 32) Lincomycin (N = 1) PCN (N = 114)
Sulfa (N = 1)
19)
Aminoglycoside0(0%)0(0%)1(0.0%)0(0%)0(0%)0(0%)0(0%)0(0%)
Carbapenem0(0%)3(50%)0(0%)0(0%)0(0%)0(0%)0(0%)0(0%)
Cephalosporin0(0%)0(0%)2,431(66.8%)6(19%)0(0%)4(3.5%)0(0%)3(16%)
Epoxide0(0%)1(17%)1(0.0%)0(0%)0(0%)0(0%)0(0%)0(0%)
Glycopeptide0(0%)0(0%)2(0.1%)0(0%)0(0%)0(0%)0(0%)0(0%)
Lincomycin0(0%)0(0%)25(0.7%)6(19%)1(100%)5(4.4%)0(0%)0(0%)
Macrolide0(0%)0(0%)172(4.7%)0(0%)0(0%)4(3.5%)0(0%)0(0%)
Nitrofuran1(50%)0(0%)86(2.4%)0(0%)0(0%)0(0%)0(0%)0(0%)
Nitroimidazole0(0%)0(0%)50(1.4%)0(0%)0(0%)1(0.9%)0(0%)1(5.3%)
PCN0(0%)0(0%)231(6.4%)2(6%)0(0%)88(77.2%)0(0%)0(0%)
Quinolone0(0%)2(33%)304(8.4%)3(9%)0(0%)5(1.8%)0(0%)0(0%)
Sulfa1(50%)0(0%)179(4.9%)8(25%)0(0%)2(1.8%)1(100%)0(0%)
Tetracycline0(0%)0(0%)153(4.2%)6(19%)0(0%)4(3.5%)0(0%)15(79%)
Topical0(0%)0(0%)2(0.1%)1(3%)0(0%)1(0.9%)0(0%)0(0%)
Shadedcellsindicateconcordantintravenousandprescriptionantibioticclass. IV,intravenous; ED,emergencydepartment; PCN,penicillin.
Tetracycline (N =
Table4. Changeinantibioticsandantifungalsbyinfectiondiagnosis. PrimarydiagnosisChangedantibiotics(N = 1,026)Sameantibiotics(N = 1,963)
Ophthalmologicinfection1(100%)0(0.0%)
Pulmonaryinfection279(77.3%)82(22.7%)
Gastrointestinalinfection54(62.1%)33(37.9%)
ENTinfection21(58.3%)15(41.7%)
Insectbite1(50.0%)1(50.0%)
Otherinfection5(50.0%)5(50.0%)
Orthopedicinfection1(50.0%)1(50.0%)
Skin/softtissueinfection256(47.4%)284(52.6%)
Dentalinfection4(44.4%)5(55.6%)
FUO6(40.0%)9(60.0%)
Bitewound7(21.2%)26(78.8%)
Urinaryinfection391(20.7%)1,501(79.3%)
Fungalinfection0(0.0%)1(100%)
Prophylaxis0(0.0%)0(0.0%)
Post-opinfection0(0.0%)0(0.0%)
Parasiticinfection0(0.0%)0(0.0%)
Osteomyelitis0(0.0%)0(0.0%)
1Percentagesarecalculatedrow-wise,relativetothetotalnumberofpatientswithineachprimarydiagnosisgroup. ENT,otolaryngological; FUO,feverofunknownorigin.
within Table5.Amongthe3,812patientswhoreceived parenteralantibioticsduringtheirEDvisit,749(19.6%),had areturnvisitwithintwoweekscomparedto11,601 (15.8%)of73,392patientswhoreceivedonlyoral antibiotics(P < 0.001).
DISCUSSION OuranalysisofEDvisitsbypatientswithcommon infectiousdiseaseswhoweretreatedwithantibioticsrevealed thatthereareopportunitiesforimprovementinselectionof antibioticsintermsofadministrationrouteandhome-going prescriptionsinourhospitalsystem.Recommendationsfrom theInfectiousDiseaseSocietyofAmerica(IDSA)are availableforthethreemostcommonareasofinfection amongourpatients:urinary;skin;andpulmonarysources. TheIDSAguidelinesregardingtreatmentforUTIs recommendoraltreatmentforuncomplicatedcystitis,and whileoralantibioticsarealsoappropriateforacute pyelonephritis,thereisanoptiontoprovideaone-timeIV doseofantibiotics,suchasalong-actingcephalosporin,prior toinitiationoforaltherapy.15 Forskininfections,theIDSA guidelinesuseamild,moderate,andseveregradingfor cellulitis.Onlymildiscategorizedasappropriatefororal therapy;moderateandseverearerecommendedtoreceiveIV antibiotics.TherearemultipleappropriateoralandIV optionsfortreatmentofbitewounds.16 First-linetreatment optionsforoutpatientcommunity-acquiredpneumonia includeoralamoxicillin,macrolides,anddoxycyclinefor
patientswithfewriskfactors,andamoxicillin-clavulanatein conjunctionwithatypicalcoverage.17 Healthcare-associated pneumoniatreatmentrecommendationsofteninclude multiplemedicationstypicallyincludingarequiredIVagent, suchasvancomycin,precludingdischarge.18
PatientswhopresenttotheEDforcareareoftencomplex; clinicalassessmentofmultiplefactorsincludingclinical gestalt,inadditiontolaboratoryandimaging findings,may cueacliniciantohaveahighersuspicionforasevere infection,thuspromptingthemtoprovideIVtreatment. Additionally,therecouldbesomediagnosticuncertainty promptingadesiretoinitiateempirictreatmentpriorto attainingadefinitivediagnosis.Patientsoftenimprovewhile underourcare,anditispossiblethatapatientisexpectedto beadmittedtothehospitalandprovidedIVantibioticsand eitherimprovesenoughfordismissal,orperhapstheydonot wanttobeadmitted.Thenumberofscenariosisnearly limitless.Thereisnoclearanswerastohowdecisionsare madetodeviatefromrecommendations,anditmaybean arearipeforadditionalresearchtounderstand thebasis.
WeidentifiedthatforUTIs,wehadthehighest concordanceratewhenanIVdoseofantibioticsis prescribed.Thisisanopportunitytoexploretherelativecost ofIVvsoraltherapies.Usingdrugs.com,wefoundthatanIV doseof1gramceftriaxonecostsapproximately$11.47,prior toreconstitution.Adoseoforalcefdinircostsunder$2.In additiontothecostofthemedications,thereareadditional
Table5. Intravenousantibioticsandantifungalsadministeredbyinfectiontype. IVantibioticsintheED
Primarydiagnosis
= 2,830)
= 103)
= 29)
(N = 17)
FUO15(100%)0(0%)0(0%)0(0%)0(0%)
Otherinfection10(100%)0(0%)0(0%)0(0%)0(0%)
Orthopedicinfection2(100%)0(0%)0(0%)0(0%)0(0%)
Insectbite2(100%)0(0.0%)0(0%)0(0%)0(0%)
Fungalinfection1(100%)0(0%)0(0%)0(0%)0(0%)
Urinaryinfection1,879(99.3%)4(0.2%)2(0.1%)0(0%)7(0.4%)
Pulmonaryinfection354(98.1%)5(1.4%)0(0%)2(0.6%)0(0%)
GIinfection74(85.1%)12(13.8%)0(0%)0(0%)1(1.1%)
Skin/softtissue
Infection
462(82.6%)38(7.0%)26(4.8%)13(2.4%)1(0.2%)
ENTinfection22(61.1%)13(36.1%)0(0%)0(0%)1(2.8%)
Dentalinfection2(22.2%)6(66.7%)1(11.1%)0(0%)0(0%)
Bitewound7(21.2%)24(72.7%)0(0%)2(6.1%)0(0%)
Ophthalmologic infection 0(0%)1(100%)0(0%)0(0%)0(0%)
1Percentagesarecalculatedrow-wise,relativetothetotalnumberofpatientswithineachprimarydiagnosisgroup. IV,intravenous; ED,emergencydepartment; GI,gastrointestinal; ENT,otolaryngological; FUO,feverofunknownorigin; Abx,antibiotics.
chargesassociatedwithIVcatheterplacementand medicationadministration.19
Useofasingle-doseglycopeptide(vancomycin)isoneof themoreproblematicexampleswithinourstudy. Unsurprisingly,wefoundthattherewerenoepisodesof concordancebetweenIVandoraladministrationfor vancomycin.Thecostforvancomycinisapproximately$200 forIVsolution.19 Inadditiontothecostforthemedication andadministration,thecostoftimeincreaseswith vancomycin,givenitslongeradministrationtimecompared tootherIVantibioticsororal-onlytherapy.
Ourstudyshowedthatthereisasignificantdifferencein LOS,whichimpactsEDthroughputandcrowding,aswellas patientqualityoflife.Wecannotattributethisdifference solelytotheprovisionofIVantibiotics,anditmaybedueto otherconfoundingfactors.However,inatimeinwhichED crowdingandpromptthroughputisamatterofpatient safety,itshouldnotbeneglected.Thereisanadditionalcost totheinstitutionfortheoccupancyofabedintheED. SchreyeretalcalculatedthepersonnelcostforasinglebedhourintheEDtobe$58.20.20 Whileover3,000patientswho receivedIVantibioticshaveanaverageLOSof100minutes greaterthanthepatientstreatedwithoralantibiotics,we find asubstantial financialimpactinadditiontoa quality-of-careeffect.20
Wefoundnodifferenceinprescribingpatternsbetween communityandacademicsettingsandonlyasmalldifference betweenphysicianandAPPs.Thismayreflectpractice
patternsestablishedbyinstitutionalnorms,training programsthatperpetuateasimilarculturebeingpassedon fromsupervisortotrainee,orsimplycommonpracticesin emergencymedicine.
The finaloutcomeweexaminedwasthelikelihoodtohave asecondvisitwithintwoweeksandwhethertherewasa differenceintheIV-oralvsoral-onlygroups(19.6%vs 15.8%).Weweresurprisedto findthatthepatientswho receivedIVantibioticsweremorelikelytoreturn.Thiscould havebeenrelatedtodiscordancebetweenIVantibiotics administeredwithintheEDandoralantibioticsthatpatients receivedupondischarge.Oritmayreflectamoresevere diseasethanwasappreciatedbythetreatingteam,resulting intheadministrationofIVantibiotics,orpatientswho declinedadmission.Furtherinvestigationintothecourseof thesepatientsmayshedadditionallightontheclinical decision-makingaroundmedicationadministration, prescription,andanticipatedtrajectoryoftheirillness.
Anadditional findingthatwediscoveredwasthe predominanceofwomenasrecipientsofIVantibiotics.This isconsistentwiththehigherincidenceofUTIsinwomenas comparedtomen,21 whichincombinationwiththehigh numbersofpatientswhoreceivedIVantibioticswithUTI/ pyelonephritiscouldaccountforthis finding.Giventhe highercostofcareduetoIVmedicationadministrationand longerdurationoftimespentintheED,itisimportantto considerthedisparitiesindownstreameffectsoftreatment betweengenders.
FutureOpportunities Opportunitiesforfurtherresearchincludeinvestigating anyvariationinaveragedurationofillness,costofcare,or patientsatisfactionbetweenpatientswhoreceiveoral antibioticsalonecomparedwithpatientswhoinitiallyreceive IVantibiotics.EvaluatingthereasonsforadministeringIV antibioticsinitiallyandthereasonforchangingfromone classofIVantibioticstoanotherclassoforalantibioticsin theEDsettingisworthfurtherinquiryaswell.Identifyingthe underlyingcauseforprescribingbehaviorsthatarenot adherenttorecommendedbestpracticeswillreveal opportunitiesforeducationandintervention.Providing educationregardingoralbioavailabilityandefficacyof appropriateantibioticsmaybehelpful.Thesemayinclude educationonpharmacokinetics,implementationof electronichealthrecorddecisionsupport,processesfor prescriberandpharmacistcollaboration,andmore. Additionally,clarificationoftheIDSAguidelinesaround first-linetreatmentmayresultinimprovedLOSintheED andotherpatient-orientedoutcomes.Inparticular,theuseof anIVdoseofvancomycinpriortodismissalonotheragents isaprimeareaforinterventionwithitsassociatedcostsand durationofadministration.
LIMITATIONS Thiswasaretrospectivecohortstudy,whichhasthe associatedlimitationsrelatedtobias.Ourstudysamplewas foundtobeskewedtowardfemalegendercomparedtothe generalpopulation.Additionally,thelargenumberof primaryEnglish-speakingpatientsmaybeanindicatorthat thisstudyisnotgeneralizabletoEDsinmorediversesettings. Ourdatawasnotabletodetecttheclinicalsignificance relatedtothereturnvisits.MorepatientswhoreceivedIV antibioticsreturnedtotheED,butitisnotclearwhetherthis wasrelatedtotheunderlyinginfection,whetherIV antibioticswereprescribedduetoaclinicaljudgmentthatthe patientappearedmoreillandwasathigherriskofdisease progression,orwhetherotherfactorsinfluencedthis trajectory.Nosurrogatesforpatientacuitywereincludedin ouranalysis.Inclusionofanillnessseverityscorecould improvetheabilitytounderstandthedecisiontoprovide parenteralantibiotics,aswellasinformthecontextregarding returnvisitsandprovideadditionalunderstandingofthe differenceinLOS.Whencomparingprescribingdifferences betweenphysiciansandAPPswedidnotcontrolforpractice setting,whichrangesfromaNP/PAwithindependent practiceatacriticalaccesshospitalorwithinanacademic EDandmayormaynotincludedirecton-sitesupervision. NeitherdidwecontrolforthepresenceofanED-based pharmacisttoassistwithprescribingrecommendations.
CONCLUSION Wefoundthatpatientswithinouranalysiswhowere treatedwithintravenousantibioticsintheEDoftenreceived
adifferentclassoforalantibioticsupondischarge.Wealso foundthatadministeringIVantibioticsasa firstdosepriorto anoralantibioticbeingprescribedupondischargefromthe EDwascommonbutmaynotbenecessary.Byrecognizing theseinconsistencies,therearefutureopportunitiesto improveuponantibioticstewardshipandadherencefor prescribingoralantibioticsthatareconcordantwithIV antibioticsthatareadministered.
AddressforCorrespondence:MeganElli,MS,MayoClinic, DepartmentofEmergencyMedicine,1216SecondStreet Southwest,Rochester,MN55902,GeneroseG410. Email: Zellmer.Megan@mayo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Ellietal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
REFERENCES 1.CairnsC,AshmanJJ,KangK.Emergencydepartmentvisitratesby selectedcharacteristics:UnitedStates,2018. NCHSDataBrief. 2021;401:1–8.
2.SocietyforAcademicEmergencyMedicine(SAEM).Challengesin diagnosinginfectioninED.Availableat: https://www.saem.org/ education/industry-sponsored-education/challenges-in-diagnosinginfection-in-the-ed.AccessedMay22,2024.
3.CairnsC,KangK,SantoL.NationalHospitalAmbulatoryMedicalCare Survey:2018emergencydepartmentsummarytables.Availableat: https://www.cdc.gov/nchs/data/nhamcs/web_tables/ 2018-ed-web-tables-508.pdf.AccessedMay22,2024.
4.ScarboroughM,LiHK,RombachI.Oralversusintravenousantibiotics forboneandjointinfections:theOVIVAnon-inferiorityRCT. Health TechnolAssess. 2019;23(38):1–92.
5.BeiqueLandZvonarR.Addressingconcernsaboutchangingtheroute ofantimicrobialadministrationfromintravenoustooralinadult inpatients. CanJHospPharm. 2015;68(4):318–26.
6.BreyreAandFrazeeBW.Skinandsofttissueinfectionsinthe emergencydepartment. EmergMedClinNorthAm. 2018;36(4):723–50.
7.RiderACandFrazeeBW.Community-acquiredpneumonia. Emerg MedClinNorthAm. 2018;36(4):665–83.
8.KhoshnoodS,HeidaryM,MirnejadR,etal.Drug-resistantgramnegativeuropathogens:areview. BiomedPharmacother. 2017;94:982–94.
9.ShresthaJ,ZahraF,CannadyP. AntimicrobialStewardship.Treasure Island,FL:StatPearlsPublishing,2023.
10.PohX-E,WuK-H,ChenC-C,etal.Outcomesforpatientswithurinary tractinfectionafteraninitialintravenousantibioticsdose beforeemergencydepartmentdischarge. InfectDisTher. 2021;10(3):1479–89.
11.BrindleR,WilliamsOM,BartonE,etal.Assessmentofantibiotic treatmentofcellulitisanderysipelas:asystematicreviewandmetaanalysis. JAMADermatol. 2019;155(9):1033–40.
12.KimuraT,ItoM,OnozawaS.Switchingfromintravenoustooral antibioticsinhospitalizedpatientswithcommunity-acquiredpneumonia: areal-worldanalysis2010–2018. JInfectChemother. 2020;26(7):706–14.
13.vonElmE,AltmanD,EggerM.Thestrengtheningreportingof observationalstudiesinepidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. AnnInternMed. 2007;147(8):573–7.
14.RCoreTeam.(2021). R:Alanguageandenvironmentforstatistical computing.Vienna,Austria:RFoundationforStatistical Computing.
15.GuptaK,HootonTM,NaberKG,etal.Internationalclinicalpractice guidelinesforthetreatmentofacuteuncomplicatedcystitisand pyelonephritisinwomen:a2010updatebytheInfectiousDiseases
SocietyofAmericaandtheEuropeanSocietyforMicrobiologyand InfectiousDiseases. ClinInfectDis. 2011;52(5):e103–20.
16.StevensDL,BisnoAL,ChambersHF,etal.Practiceguidelinesforthe diagnosisandmanagementofskinandsofttissueinfections:2014 updatebytheInfectiousDiseasesSocietyofAmerica. ClinInfectDis. 2014;59(2):147–59.
17.MetlayJP,WatererGW,LongAC,etal.Diagnosisandtreatmentof adultswithcommunity-acquiredpneumonia.Anofficialclinical practiceguidelineoftheAmericanThoracicSocietyandInfectious DiseasesSocietyofAmerica. AmJRespirCritCareMed. 2019;200(7):e45–67.
18.KalilAC,MeterskyML,KlompasM,etal.Managementofadultswith hospital-acquiredandventilator-associatedpneumonia:2016 clinicalpracticeguidelinesbytheInfectiousDiseasesSocietyof AmericaandtheAmericanThoracicSociety. ClinInfectDis. 2016;63(5):e61–111.
19.Drugs.com.Availableat: http://drugs.com.AccessedMay22,2024.
20.SchreyerKEandMartinR.Theeconomicsofanadmissionsholding unit. WestJEmergMed. 2017;18(4):553–8.
21.GeerlingsSE.Clinicalpresentationsandepidemiologyofurinarytract infections. MicrobiolSpectr. 2016;4(5).
ORIGINAL RESEARCH DiagnosticandPrognosticValueofSCUBE-1 inCOVID-19Patients VildanOzer,MD*
OzgenGonencCekic,MD†
OzlemBulbul,MD*
DavutAydın,MD‡
EserBulut,MD§
FirdevsAksoy,MD∥
MehtapPehlivanlarKucuk,MD¶ SuleymanCanerKarahan,MD# EbruEmelSozen,MD**
EsraOzkaya,MD††
Authorscontinuedatendofpaper
SectionEditor: JosephR.Shiber,MD
*KaradenizTechnicalUniversity,SchoolofMedicine,DepartmentofEmergency Medicine,Trabzon,Türkiye
† SBUKanuniTrainingandResearchHospital,DepartmentofEmergency Medicine,Trabzon,Türkiye
‡ SBUKanuniTrainingandResearchHospital,DepartmentofChestDiseases, DivisionofIntensiveCareMedicine,Trabzon,Türkiye
§ SBUKanuniTrainingandResearchHospital,DepartmentofRadiology, Trabzon,Türkiye
∥ KaradenizTechnicalUniversity,SchoolofMedicine,DepartmentofInfectious DiseasesandClinicalMicrobiology,Trabzon,Türkiye
Af filiationscontinuedatendofpaper
Submissionhistory:SubmittedNovember17,2023;RevisionreceivedAugust23,2024;AcceptedAugust26,2024
ElectronicallypublishedOctober2,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18586
Introduction: Theworkloadofphysiciansincreasedduetothenumberofpatientspresentingwith suspicionofcoronavirus2019(COVID-19)andtheprolongedwaittimesintheemergencydepartment duringtheCOVID-19pandemic.Signalpeptide-CUB-EGFdomain-containingprotein1(SCUBE-1)isa proteinpresentinplateletsandendothelialcells;itisactivatedbyinflammationfromCOVID-19andmay beassociatedwithCOVID-19’sknownthromboticrisk.WeaimedtodeterminewhetherSCUBE-1levels arediagnosticallycorrelatedinsuspectedCOVID-19patients,andwhetherSCUBE-1correlatedwith severityofdiseaseand,therefore,mightbeusefultoguidehospitalization/dischargedecisions.
Methods: ThesuspectedCOVID-19patientscaredforattertiaryhealthcareinstitutionsforoneyear betweenMay2021–May2022wereexaminedinthisstudy.ThesubjectswerebothsuspectedCOVID19patientsnotultimatelyfoundtohaveCOVID-19andthosewhowerediagnosedwithCOVID-19.By modifyingthediseaseseverityscoringsystemspresentinCOVID-19guidelinesin2021,theCOVID-19positivepatientgroupwasclassifiedasmild,moderate,severe,andcritical,andcomparedusingthe SCUBE-1levels.Moreover,SCUBE-1levelswerecomparedbetweentheCOVID-19positivegroupand theCOVID-19negativegroup.
Results: Atotalof507patientswereconsideredforthepresentstudy.Afterexcluding175patientsfor incompletedataandalternatecomorbidorganfailure.wereporton332patients(65.5%).Ofthese332 patients,80(24.0%)wereCOVID-19negative,and252(76.0%)wereCOVID-19positive.Of252(100%) patientsdiagnosedwithCOVID-19,74(29.4%)wereclassifiedasmild,95(37.7%)moderate,45(17.8%) severe,and38(15.1%)critical.TheSCUBE-1levelswerestatisticallydifferentbetweenCOVID-19 positive(8.48 ± 7.42nanogramspermilliliter[ng/mL])andCOVID-19negative(1.86 ± 0.92ng/mL) patients(P < 0.001).IntheCOVID-19positivegroup,SCUBE-1levelsincreasedwithdiseaseseverity (mild = 3.20 ± 1.65ng/mL,moderate = 4.78 ± 2.26ng/mL,severe = 13.68 ± 3.95ng/mL,andcritical = 21.87 ± 5.39ng/mL)(P < 0.001).TheinitialSCUBE-1levelsofdischargedpatientsweresignificantly lowerthanthoserequiringhospitalization(discharged = 2.89ng/mL[0.55–8.60ng/mL];wardadmitted = 7.13ng/mL[1.38–21.29ng/mL],andICUadmitted = 21.19ng/mL[10.58–37.86ng/mL])(P < 0.001).
Conclusion: TheSCUBE-1levelswerefoundtobedifferentiatedbetweenpatientswithandwithout COVID-19andtobecorrelatedwiththeseverityofillness.[WestJEmergMed.2024;25(6)975–984.]
INTRODUCTION Thecoronavirus2019(COVID-19)pandemichashada hugeimpact1,2 withmorethan770millionconfirmedcases andmorethan6.9milliondeathsreportedworldwideasof September2023.3 Althoughhospitalandemergency department(ED)admissionratesdecreasedinthe firstperiod oftheCOVID-19pandemic,theseratesreturnedtoprepandemiclevelsovertime.Previousstudiesshowedthatthe durationoftimespentbypatientsintheEDincreasedduring thepandemicperiod.4,5 ThisledtoEDcrowding,whichin turncontributedtoincreasedinhospitalmortality.6 Forthis reason,itwouldbeusefultodeterminewhichpatientscanbe managedasoutpatients,andwhichneedadmissionandto whatlevelofcare.Itisalsocrucialtopromptlydiagnoseand providetreatmentforthispatientgrouptomanagediseaserelatedprognosisbecausethemortalityrateofpatientswho visithospitalswithCOVID-19andrequireintensivecare admissionishigh.7
Asamemberofthesignalpeptide-CUB-epidermalgrowth factordomain-containingprotein(SCUBE)genefamily, SCUBE-1isacellsurfaceglycoproteinpredominantlylocated inplateletsand,toalesserextent,inendothelialcells.The SCUBE-1isstoredinthealphagranulesofinactiveplatelets andmigratestotheplateletsurfaceafteractivationby thrombinandreleasedassmallsolubleparticlesthatare incorporatedintothethrombus.Unlikeothermembersofthe SCUBEgenefamily,SCUBE-1tendstocauseinflammation andthrombosisandcanbeevaluatedasaprognosticfactorin plateletactivationandthromboticdiseases.8,9 Infectionwith COVID-19predisposespatientstovenousandarterial thromboembolismsduetoexcessiveinflammation,hypoxia, immobilization,anddisseminatedintravascular coagulation.10 Previousstudieshaveshownthatthe thromboticcomplicationrateincreaseswithincreasing severityofthedisease.1,2,11,12
WeaimedtodeterminewhetherSCUBE-1levelsare diagnosticallycorrelatedinsuspectedCOVID-19casesand todeterminewhetherSCUBE-1correlatedwithseverityof diseaseand,therefore,mightbeusefultoguide hospitalization/dischargedecisions.
METHODS StudyDesign Thestudyhadaprospectiveandobservationalcohort designandrecruitedpatientswithsuspectedCOVID-19who visitedtertiaryhealthcareinstitutionsthatmanagedpatients withCOVID-19,foroneyearbetweenMay2021–May2022. ThepatientsintheCOVID-19(+)groupweresuspectedof havingCOVID-19andwerediagnosedwithCOVID-19by laboratorytests,imaging,andreal-timepolymerasechain reaction(RT-PCR)testing.TheCOVID-19( )groupwere thosepatientswhohadsymptomsbutdidnothaveCOVID19andweredischarged.Patientexclusioncriteriawereas
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Duringthepandemic,theincreaseinthe lengthoftimethatpatientsspentinthe EDandtheresultantcrowdingledto highermortality.
Whatwastheresearchquestion?
CanSCUBE-1levelsserveasadiagnostic markerinCOVID-19andbecorrelatedwith theseverityofthedisease?
Whatwasthemajor findingofthestudy?
SCUBE-1levelswerehigherinCOVID-19 positivepatients(P < 0.001)andincreased withdiseaseseverity(P < 0.001).
Howdoesthisimprovepopulationhealth?
UsingSCUBE-1asabiomarkerenables timelydiagnosisofCOVID-19andseverity assessmentwhenRT-PCRresults aredelayed.
follows:incompletedatarecords;lackofconsent;aged <18years;andconditionsthatmayalterSCUBE-1levelsdue topredispositiontothrombosis,includingpregnancy,acute renalfailure,acutemyocardialinfarction,acuteischemic cerebrovasculardisease,acutemesentericischemiaatthe timeofdiagnosis,peripheralarterialdisease,liverfailure, heartfailure,ormalignancy.
ThediseaseseverityofpatientsintheCOVID-19(+) groupwasdeterminedinJune2020usingtheclassification introducedinguidelinespublishedbytheUSNational CenterforImmunizationandRespiratoryDiseases,Division ofViralDiseases.13 Usingtheseguidelines,patientsare classifiedas,1-mildtomoderate,2-severe,or3-critical.To determinewhethertherewasadifferencebetween “mild” and “moderate,” patientsinthe “mildtomoderate” group basedontheSCUBE-1levelwereclassifiedfurtheras “mild” vs “moderate” inJuly2023byfollowingthe “COVID-19 TreatmentGuide” publishedbytheUSNationalInstitutes ofHealth.14
Asourgoalinthisstudywastodeterminewhetherthere weredifferencesintheSCUBE-1level,basedonseverityof disease,wemadeseveralmodificationstothescoringsystems fromtheguidelinesandclassifiedpatientsas1-mild, 2-moderate,3-severe,or4-critical.Accordingly,takinginto accounttheclinicalsymptomsandradiographic findingsof
thepatients,theCOVID-19(+)groupwasclassifiedas “mild” (individualswhohadanyofthesignsorsymptomsof COVID-19[eg,fever,cough,sorethroat,malaise,headache, musclepain,nausea,vomiting,diarrhea,lossoftasteand smell]butnoshortnessofbreath,dyspnea,orabnormalchest imaging); “moderate” (individualswhoshowedevidenceof lowerrespiratorydiseaseduringclinicalassessmentor imagingandwhohadanoxygensaturationmeasuredby pulseoximetry[SpO2]of94%orhigheronroomairatsea level); “ severe ” (individualswhohadSpO2 <94%,respiration rate >30breathsperminute,or >50%lunginvolvementon imaging);and “critical” (individualswhohadrespiratory failure,septicshock,and/ormultipleorgandysfunction).13,14
Patientswhohad “mild” disease,weretobedischargedso thattheirtreatmentwouldcontinueathome.Forthosewho had “moderate” disease,treatmentwastobeathomeorin hospital.Forthosewith “ severe ” disease,treatmentwas plannedasadmissiontotheCOVID-19ward,andforthose with “critical” disease,treatmentwasplannedasadmission totheCOVID-19intensivecareunit(ICU).Hospitallength ofstay,ICUstay,requirementformechanicalventilation, high-flowoxygen,positiveinotropicsupport,andoutcomes wererecordedduringhospitalizationofthepatientsadmitted tothewardortheICU.
Forthepresentstudy,basedonG*Poweranalysis,itwas determinedthattheCOVID-19( )groupwouldhave100 participantsandtheCOVID-19(+)groupwouldhave280 patients.ThepatientsintheCOVID-19(+)groupwere dividedintofourgroupsbasedondiseaseseverity,with70in eachgroup.Beforethestudycommenced,ethicalapproval wasreceived(ApprovalNo:2021/137).
BiochemicalMeasurements Bloodsamples
Afterconsentforparticipationinthestudywasobtained, bloodsampleswerecollectedinbiochemistrytubeswith separatorgelsandroutinebloodtests(completebloodcount, urea,creatinine,sodium,potassium,aspartate aminotransferase,alaninetransaminase,totalbilirubin, lactatedehydrogenase[LDH],creatininephosphokinase, D-dimer,ferritin,troponin,andC-reactiveprotein[CRP]) wereperformed.TomeasuretheSCUBE-1level,thetubes werecentrifugedat1800 × gfor10minutesafterclottingat roomtemperaturefor20minutes,andserumportionswere carefullytransferredto1.5-milliliter(mL)cappedtubes,and storedat 80°Cuntilanalyzed.
DeterminationoftheSCUBE-1Level Inhumansera,theSCUBE-1levelwasdeterminedusing anenzyme-linkedimmunosorbentassay(ELISA)kit (Elabscience,Wuhan,Hubei,China;CatNo:E-EL-H5405, Lot:UPJ28DN4SW),accordingtothe manufacturer’srecommendations.
TransferringtheSamplestoELISAPlatesandPreparing forMeasurements Serumsamplesstoredat 80°Cwerethawedatroom temperature.TheSCUBE-1standardswereprepared followingthekitprocedures,and100-microliter(μL)samples wereaddedtothewellsandtothetestserumsamples.The platewascoveredwithfoilandincubatedonashakerat37°C for90minutes.Aftertheliquidintheplatewasremoved,100 μLofbiotinylated-Ab/AgSCUBE-1solutionwasaddedto eachwell.Theplatewasthencoveredwithfoilandincubated onashakerat37°Cfor60minutes.Afterincubation,the liquidwasremoved,andtheplatewaswashedthreetimes withbufferusingaplatewasher.Then,100 μLof streptavidin-HRPsolutionwasaddedtoeachwell.After incubation,theliquidwasremoved,andtheplatewas washed fivetimeswithbufferusingaplatewasher.
StainingofSamplesandMeasurements Forstaining,90 μLofsubstratesolutionwasaddedto eachwellandincubatedfor15minutesinadark environmentat37°C.Then,50 μLofcounter-staining solutionwasaddedtoeachwell,andtransformationtothe coloryellowwasobservedineachsampleandthestandards. Theabsorbanceofthesampleswasmeasuredat450 nanometersonaVERSAmicroplatereader(Molecular Devices,LLC,SanJose,CA),andtheresultswererecorded innanograms(ng)permL.
StatisticalAnalysis WeusedtheStatisticalPackageforSocialSciences23.0 (SPSSStatistics,IBMCorp,Armonk,NY)fordataanalysis. Categoricaldataarepresentedasnumbersandpercentages. TheKolmogorov-Smirnovtestdeterminednormalityofthe numericaldatadistributions.Datawithanormal distributionareshownasmean ± standarddeviation,and non-normallydistributeddataareshownwithmedianand quartilevalues.Weusedthechi-squaretestintheanalysisof categoricaldata.Intheanalysisofnumericaldata conformingtonormaldistribution,theStudent t -testwas usedtocomparetwogroups.Intheanalysisofnon-normally distributednumericaldata,weusedtheMann-WhitneyU testfortwo-groupcomparisonsandtheKruskal-Wallistest withBonferronicorrectionformultiple-groupcomparisons. ThediagnosticvalueoftheSCUBE-1levelwasexamined usingreceiveroperatingcurve(ROC)analysis.
RESULTS Atotalof507patientswereconsideredforthisstudy. Afterexcluding175patients(23withincompletedata,two whowithdrew,fourwithacutemyocardialinfarction,eight withacutestroke,35withacutekidneyfailure,onewith peripheralarterydisease,twowithliverfailure,48withheart failure,48withmalignancy,two <18years,andtwo pregnantpatients),wecompletedthestudywith332patients.
Amongthese332patients,80wereCOVID-19( )and252 wereCOVID-19(+).Amongthe252patientsdiagnosedwith COVID-19,74(29.4%)wereclassifiedasmild,95(37.7%)as moderate,45(17.8%)assevere,and38(15.1%)ascritical. Demographicandclinicalcharacteristics,vaccinationstatus, laboratoryresults,andcomparisonsbetweenCOVID-19( ) andCOVID-19(+)patientsareshownin Table1
ThecomparisonoftheSCUBE-1levelbetweenthe COVID-19( )andCOVID-19(+)groupsispresentedin Table2.Therewasasignificantdifferenceinthediagnostic valueofSCUBE-1forCOVID-19betweentheCOVID-19 ( )andCOVID-19(+)groups(P < 0.001).TheCOVID-19 (+)patients(8.48 ± 7.42)hadahighermeanSCUBE-1level thanCOVID-19( )patients(1.86 ± 0.92)(Table2).The ROCanalysisandinitialSCUBE-1levelcut-offvaluesfor COVID-19diagnosis(areaunderthecurve[AUC]0.891, confidenceinterval[CI]0.852–0.922, P < 0.001)areshownin Figure1 and Table3.FortheCOVID-19(+)group(n = 252) theSCUBE-1levelincreasedwithanincreaseindisease severity(P < 0.001).ComparisonsbetweenSCUBE-1levels forCOVID-19(+)patients,classifiedaccordingtodisease severity,areshownin Table2 and Figure2.
Amongthe252patientsintheCOVID-19(+)group, 118wereadmittedtotheCOVID-19wardand38tothe COVID-19ICU,inlinewithcurrentguidelinesandthe protocolpublishedbytheRepublicofTürkiyeMinistryof Health.Ninety-sixpatients,whowereCOVID-19(+)anddid notrequirehospitalizationbasedontheclinicaland laboratoryexaminations,weredischarged.Thirteenofthe96 dischargedpatients(13.5%)returnedtotheEDwithin14days afterdischarge,butonlytwoofthese13werehospitalized. Thesetwopatientswereaddedtothehospitalizedpatient groupforthestatisticalanalysis.Therefore,although94 patientsweredischarged,120patientswereconsideredtobe hospitalizedbecauseofCOVID-19.ThemeanSCUBE-1level ofthedischargedpatientswassignificantlylowerthanthatof patientsrequiringhospitalization(P < 0.001).TheCOVID-19 (+)patientsweredividedintothreegroupsbasedontheir outcomes:discharged;admittedtotheward;andadmittedto theICU.TheSCUBE-1levelsandcomparisonsbypatient outcomesarepresentedin Table2.Thecut-offvaluesforthe safedischargeofpatientsweredeterminedwithROCanalysis (AUC0.868,CI0.820–0.907, P < 0.001)(Figure3).TheROC curvesandoptimalcut-offvaluesareshownin Table4 and Figure3.
DISCUSSION TheresultsfromthisstudyshowthatthemeanSCUBE-1 levelofCOVID-19(+)patientswashigherthanforCOVID19( )patientsandthattheSCUBE-1levelincreaseswith severityofthedisease.Moreover,therewasasignificant differencebetweenpatientsrequiringhospitalization outcomes,suchasdischarged,admittedtotheward, admittedtotheICU,andtheSCUBE-1level.
Manystudieshaveexaminedthediagnosticand prognosticeffectivenessofreversetranscription-polymerase chainreaction(RT-PCR)usingimmunological, biochemical,andhematologicalparametersinpatientswith COVID-19,anddifferencesbetweenstudieshavebeen reported.AlthoughRT-PCRisknownasthegoldstandard diagnosticmethodtodiagnoseCOVID-19,ithassome drawbacks,15,16 suchasincorrectsamplecollectionandlow viralloads,whichmaycausefalsenegativeresults.15 Another studyreportedthat3%ofpatientspresentingwithCOVID19symptomshadCOVID-19-relatedtomography findings; however,whileRT-PCRtestresultsforthesepatientswere negative,serialRT-PCRtestsduringfollow-upofthese patientswerepositive.17 Consideringthattheaveragesix-day incubationperiodofthesevereacuterespiratorycoronavirus 2(SARS-CoV2),RT-PCRresultsintheearlysymptomatic periodorduringtherecoveryperiodmayyieldnegative results.18 Inbothcases,itmaybecomedifficulttocontrolthe infectionandpreventapandemicbecausecontagiousness continues,whichmaycausedelayedtreatmentinpatients.19 Moreover,thediagnosisrequiresalongerperiod,andserial testingisexpensive.Therefore,simplerdiagnostictestsare requiredinresource-limitedregionswhereRT-PCRcyclers andhighlytrainedtechniciansarenotemployed.
TheeffectivenessofIgMandIgGantibodiesdetectionin thediagnosisofCOVID-19hasbeeninvestigatedpreviously, anditwasshowninserology-basedteststhatsensitivity increasedasthetimefromsymptomonsetincreased,and sensitivitywasrelativelylowerbeforesevendays.20–23 Furthermore,thediagnosticvalueofbiochemicaland hematologicalbiomarkers(eg,D-dimer,CRP, procalcitonin,LDH,ferritin,lymphocytecount,and leukocytecount)wasexaminedforCOVID-19,andthese biomarkerswereshowntohavelowdiagnosticefficiencyand higherprognosticvaluethandiagnosticvalue.24–31 Thedata obtainedsuggeststhatlow-cost,easy-to-obtain,andeasy-tousebiomarkersthatprovideresultsinashorttimeandoffer highdiagnosticefficiencyarerequired.
TheSCUBE-1ishighlyexpressedinvascularendothelial cellsandplateletsandisknowntoincreaseinthrombotic diseaseswithplateletandendothelialactivation.32,33 Therefore,SCUBE-1hasbeenusedfordiagnosticor prognosticevaluationofmanythromboticdiseases.Ina previousstudy,theSCUBE-1levelinpatientsdiagnosed withpulmonaryembolismwashigherthaninthecontrol group,anditwasstatedthattheSCUBE-1levelcouldbe usedforthediagnosisofpulmonaryembolismatacut-off pointof >46ng/mLwith82%sensitivityand91% specificity.34 Similarly,XiaoetalreportedthatSCUBE-1 maybeapotentialbiomarkerforthediagnosisofpulmonary embolism.35 Cakiretaldeterminedthediagnosticvalueof SCUBE-1inaorticdissectionandreportedthatitcouldbe usedforthediagnosisofaorticdissectioninpatientswith aorticdissectionatlevels >19.75ngperdeciliterwith95%
Table1. Thedemographic,clinical,andbiochemicalcharacteristicsofCOVID-19negativeandCOVID-19positivegroups.
Variables COVID-19negative (n:80,%24.1) COVID-19positive (n:252,%75.9)
Demographics
Age,years65.0(24.0–95.0)63.0(18.0–92.0)0.73
Sex,male,n(%)36(45.0)104(41.3)0.56
Medicalhistory
Diabetesmellitus,n(%)20(25.0)55(21.8)0.55
Hypertension,n(%)37(46.3)114(45.2)0.87
CVA,n(%)7(8.8)12(4.8)0.18
CAD,n(%)6(7.5)31(12.3)0.23
Asthma/COPD,n(%)19(23.8)34(13.5)0.03
Smoking,n(%)13(16.3)38(15.1)0.80
Symptoms
Fever,n(%)18(22.5)54(21.4)0.84
Cough,n(%)28(35.0)165(65.5) <0.001
Dyspnea,n(%)33(41.3)153(60.7)0.002
Runnynose,n(%)5(6.3)7(2.8)0.15
Anorexia,n(%)9(11.3)48(19.0)0.11
Lossoftaste,n(%)0(0.0)6(2.4)0.16
Lossofsmell,n(%)0(0.0)1(0.4)0.57
Myalgia,n(%)24(30.0)93(36.9)0.26
Fatigue,n(%)38(47.5)143(56.7)0.15
Headache,n(%)19(23.8)52(20.6)0.55
Nausea/vomiting,n(%)18(22.5)45(17.9)0.36
Diarrhea,n(%)14(17.5)7(2.8) <0.001
Vaccination, n(%)51(63.7)161(63.9)0.98
Laboratoryresults Creatinine,(mg/dL)1.07
Valuesareexpressedasmean ± SD,n(%)ormedian(interquartilerange)unlessotherwisestated. CAD,coronaryarterydisease; COPD,chronicobstructivepulmonarydisease; CRP,C-reactiveprotein; CVA,cerebrovascularaccident; LDH,lactatedehydrogenase; N/L ratio,neutrophil/lymphocyteratio; PCT,procalcitonin; WBC,whitebloodcell.
Table2. TheSCUBE-1*levelsofCOVID-19negativeandCOVID-19positivegroupsaccordingtodiseaseseverityandpatientoutcomes.
COVID-19( ),(n = 80)1.86 ± 0.92 <0.001*
COVID-19(+),(n = 252)8.48 ± 7.42
COVID-19(+)(n = 252)Mild,(n = 74)3.20 ± 1.65 <0.001¥
Moderate,(n = 95)4.78 ± 2.26
Severe,(n = 45)13.68 ± 3.95
Critical,(n = 38)21.87 ± 5.39
COVID-19(+)(n = 252)Discharged,(n = 94)2.89(0.55–8.60) <0.001¥
Ward-admitted,(n = 120)7.13(1.38–21.29)
ICU-admitted,(n = 38)21.19(10.58–37.86)
*Mann-WhitneyUtest.
¥Kruskal-WallistestwithMann-Whitneycorrection,resultsachievedfromthecomparisonofthethreegroupswerestatisticallysignificant.
*SCUBE-1,signalpeptide-CUB-EGFdomain-containingprotein1.
Figure1. TheinitialSCUBE-1*levelcut-offandconfidence intervalvaluesforCOVID-19diagnosis.
*SCUBE-1,signalpeptide-CUB-EGFdomain-containing protein1.
AUC,areaunderthecurve; NPV,negativepredictivevalue.
sensitivityand76%specificity.36 Furthermore,Daietal concludedintheirstudythattheSCUBE-1levelmayhave diagnosticvalueinpatientswithacutecoronarysyndrome andacuteischemicstroke.37
Studiesthatexaminedthediagnosticeffectivenessof SCUBE-1werebasedontherelationshipbetweenSCUBE-1 andthrombusformationduetoendothelialdysfunction. SARS-CoV-2doesnotpossessprocoagulant
characteristics,32,38 butvascularendothelialcelldamage occursduetoanexcessiveinflammatoryresponsetriggered byCOVID-19.Thediagnosticrelationshipbetween SCUBE-1andCOVID-19wasdeterminedinthepresent studybecausehypercoagulability,plateletactivation,and endothelialdysfunctionmaydevelopwiththeresulting vasculopathy.34,39,40 Oneofthemainresultsofthisstudywas thattheSCUBE-1levelwashigherinCOVID-19(+)patients thaninCOVID-19( )patients.Inthiscontextitshowedthat theSCUBE-1levelisaneffectivebiomarkerforthediagnosis ofCOVID-19,anditcanbeusedtodiagnoseCOVID-19in EDs.However,thecurrentassaystudiedhereiscomplicated andlaborintensiveandwouldtakeatleast210minutesto perform,evenunderoptimumconditions.41
Clinicalsignsandsymptoms(eg,cough,dyspnea,fever, diarrhea,nausea,vomiting,lossoftasteandsmell, respiratoryrate,saturation,andradiographic fi ndings) wereusedtodeterminetheseverityofCOVID-19. 12 Many biochemicalparameters(eg,elevatedCRP, thrombocytopenia,andanelevatedferritinlevel)arepoor prognosticfactorsinCOVID-19,andtheyhavenotbeen usedtode fi nediseaseseverityperthecurrentliterature.42–44 Inthiscontext,determiningthediseaseseverityofpatients atthetimeofadmissionbyusingabiochemicalparameter, suchastheSCUBE-1level(withorwithoutthepresent
Table3. SCUBE-1*cut-offvalueofCOVID-19negativeandCOVID-19positivegroups.
SensitivitySpecificityPPVNPV
SCUBE-1cut-offvalue(ng/mL)(%)(95%CI)(%)(95%CI)(%)(95%CI)(%)(95%CI)
*SCUBE-1,signalpeptide-CUB-EGFdomain-containingprotein1. CI,confidenceinterval; NPV,negativepredictivevalue; PPV,positivepredictivevalue.
Figure2. *SCUBE-1levelsofCOVID-19patients.All P-values <0.001. *SCUBE-1,signalpeptide-CUB-EGFdomain-containingprotein1.
Figure3. Thecut-offandconfidenceintervalvaluesforthesafe dischargeofCOVID-19(+)patientsaccordingtoROCanalysis. ROC,receiveroperatingcharacteristiccurve; SCUBE-1,signal peptide-CUB-EGFdomain-containingprotein1.
scoringsystems),canbeusedatanearlystagetodistinguish betweensevereandcriticalpatientswithCOVID-19to reducemortalityandenabletimelytreatment. Microvascularandmacrovascularthrombotic
complicationsmaydevelopinarterial,venous,and capillaryvascularbedsbecausethromboin fl ammatory processesintensifyduringCOVID-19,particularlywith increasingseverityofthedisease.39, 45 Ina2022study conductedbyTopraketal,anelevatedSCUBE-1levelwas associatedwiththromboticcomplications,diseaseseverity, andinhospitalmortalityinpatientswithCOVID-19. 46 In thepresentstudy,theSCUBE-1levelwaselevatedin patientswithCOVID-19,andastheseverityofthedisease increasedtheSCUBE-1levelalsoincreased.
ThestudyconductedbyCaliketalreportedalow mortalityrateofpatientswhopresentedearlytohospitaland receivedearlyantiviraltreatment.47 Earlydiagnosis, appropriatetriage,andearlytreatmentofpatientswho presenttohealthcareinstitutionswithsymptomsofCOVID19andareconsideredCOVID-19(+)maypreventtheriskof contamination,reducetheneedforintensivecare,andreduce theneedforhospitalizationbyenablingrapiddecisionmakinginthebestinterestsofpatients.Fromthis perspective,biomarkersarerequiredtoguidecliniciansin
Table4. OptimalSCUBE-1*cut-offvaluesofCOVID-19positivepatientsaccordingtopatientsrequiringhospitalizationoutcomes.
Patientsrequiring hospitalizationoutcome
*SCUBE-1,signalpeptide-CUB-EGFdomain-containingprotein1. CI,confidenceinterval; ICU,intensivecareunit; NPV,negativepredictivevalue; PPV,positivepredictivevalue.
hospitalization/dischargedecisionsandward/intensivecare unitadmissionofpatientsdiagnosedwithCOVID-19.48,49 Suchabiomarkermaycontributetobetterdecision-making attheEDordischargestageandEDoccupancybyreducing patientwaittimes.
Inthepresentstudy,whentheEDoutcomesofthe patientsweregroupedasdischarge,wardadmission,or intensivecareadmission,andwhentheSCUBE-1levelswere compared,theSCUBE-1levelofdischargedpatientswas lowerthanthatofpatientswhorequiredhospitalization, andtheSCUBE-1levelofpatientswhorequiredICU admissionwashigherthanfortheothergroups.Giventhese results,itcanbearguedthattheSCUBE-1levelmayassist clinicianstopredictdiseaseseverityandassistinmaking decisionsregardinghospitalizationordischarge.Inaddition, becauseoftheriskofmicro-andmacrovascularthrombosis, ahighSCUBE-1levelmeasuredintheearlystages ofthediseasemayindicatetherequirementformore intensiveantithrombotictreatmenttoprevent thromboticcomplications.
TheRT-PCRisthegoldstandardforconfirmingthe presenceofSARS-CoV2,andthetimetoobtaintheresultfor asingletestisapproximatelytwohours.50 However,samples collectedinhospitalsweretransportedtospecificlaboratories becausePCRtestscouldnotbeperformedineverylaboratory duringthepandemicperiod,51,52 whichresultedindelaysin receivingthetestresults.Previousstudieshaveshownthatthe confirmationtimeoftheSARS-CoV-2virususingRT-PCR was6–48hoursduringthepandemicperiod.53,54 Inaddition, testssuchastheRT-PCRonlyidentifySARS-CoV2anddo notprovidedataontheseverityofCOVID-19.Considering theselimitations,theuseofRT-PCRkitsforsurveillanceor screeningpatients,preventingincreasedpatientdensityin healthcareinstitutions,andreducingpatientwaittimesmaybe difficult.53 Therefore,thereisaneedfornovelbiomarkersto enabletherapiddetectionofindividualswithCOVID-19, eveninprimaryhealthcareinstitutionsandtoguidephysicians regardingthedischargeorhospitalizationofpatients accordingtocut-offvalues.
ThetesttimeofSCUBE-1isapproximately3.5hours,and thesampleiseasytoobtainfromabloodsample,which enablestherapididentificationofpatientswithCOVID-19.41 ThepresentstudyalsorevealedthattheSCUBE-1levelis associatedwiththeseverityofdisease,whichfacilitates decision-makingregardingdischargeoradmissiontothe wardortheICU,whichmayassistinreducingpatient densityinhealthcareinstitutions,reducepatientwaittimes, andeffectivelyimprovepatientmanagement.
LIMITATIONS Thereweresomelimitationstothisstudy.First,the targetednumberofpatientswasnotrecruitedowingtothe decreasedseverityandincidenceofCOVID-19worldwide. Second,becausethenumberofSCUBE-1kitswaslimited,
SCUBE-1measurementswerelimitedtoasingleplasma sample.SerialSCUBE-1measurementsduringpatient treatmentmayhavealteredthecorrelationbetweenthe SCUBE-1levelanddiseaseseverity.
CONCLUSION EventhoughRT-PCRtestingusuallyproducesa diagnosisofCOVID-19inashorttime,theexcessivesample loadaccumulatedinlaboratoriesduringthepandemic increasedthetimetocompletionandincreasedpatientwait times.Inthepresentstudy,wefoundthattheSCUBE-1level differsbetweenpatientswithandwithoutCOVID-19andit wascorrelatedwiththeseverityofthedisease.Accordingly, besidesguidingphysiciansregardingthediagnosisof COVID-19andtheseverityofthediseaseamongpatients whopresentathealthfacilitiesduringpandemicperiods whereresultsofRT-PCRtestsmaybedelayed,SCUBE-1 mayassistcliniciansinmanaginginflammatorydiseasesthat predisposetothrombosis.
AUTHORSANDAFFILIATIONSCONTINUED PolatKosucu,MD‡‡ YunusKaraca,MD* SuleymanTuredi,MD ¶KaradenizTechnicalUniversity,SchoolofMedicine, DepartmentofChestDiseases,DivisionofIntensiveCare Medicine,Trabzon,Türkiye
#KaradenizTechnicalUniversity,SchoolofMedicine, DepartmentofBiochemistry,Trabzon,Türkiye
** SBUKanuniTrainingandResearchHospital,Departmentof InfectiousDiseasesandClinicalMicrobiology, Trabzon,Türkiye
††KaradenizTechnicalUniversity,SchoolofMedicine, DepartmentofMedicalMicrobiology,Trabzon,Türkiye ‡‡KaradenizTechnicalUniversity,SchoolofMedicine, DepartmentofRadiology,Trabzon,Türkiye
AddressforCorrespondence:VildanOzer,MD,KaradenizTechnical University,SchoolofMedicine,DepartmentofEmergencyMedicine, FarabiStreetNo.64,Ortahisar,Trabzon,Türkiye61080. Email: vildan.ozer@ktu.edu.tr
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisprojectwassupportedby KaradenizTechnicalUniversityScientificResearchProjects CoordinationUnit.ProjectNumberTHD-2021-9753.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Ozeretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.BajemaKL,OsterAM,McGovernOL,etal.Personsevaluatedfor2019 novelcoronavirus. MorbMortalWklyRep. 2020;69(6):166–70.
2.ZhuW,XieK,LuH,etal.Initialclinicalfeaturesofsuspectedcoronavirus disease2019intwoemergencydepartmentsoutsideofHubei,China. J MedVirol. 2020;92(9):1525–32.
3.WorldHealthOrganization.COVID-19weeklyepidemiological update.2023.Availableat: https://covid19.who.int/ AccessedSeptember27,2023.
4.LuceroA,SokolK,HyunJ,etal.Worseningofemergencydepartment lengthofstayduringtheCOVID-19pandemic. JAmCollEmerg PhysiciansOpen. 2021;2(3):e12489.
5.GriffinG,KrizoJ,MangiraC,etal.TheimpactofCOVID-19on emergencydepartmentboardingandin-hospitalmortality. AmJEmerg Med. 2023;67:5–9.
6.JankeAT,MelnickER,VenkateshAK.Hospitaloccupancyand emergencydepartmentboardingduringtheCOVID-19pandemic. JAMANetwOpen. 2022;5(9):e2233964.
7.PetrilliCM,JonesSA,YangJ,etal.Factorsassociatedwithhospital admissionandcriticalillnessamong5279peoplewithcoronavirus disease2019inNewYorkCity:prospectivecohortstudy. BMJ. 2020;369:m1966.
8.TuCF,SuYH,HuangYN,etal.Localizationandcharacterizationofa novelsecretedproteinSCUBE1inhumanplatelets. CardiovascRes. 2006;71(3):486–95.
9.TurkmenS,MenteseS,MenteseA,etal.ThevalueofsignalpeptideCUB-EGFdomain-containingprotein1andoxidativestressparameters inthediagnosisofacutemesentericischemia. AcadEmergMed. 2013;20(3):257–64.
10.YangRB,NgCKD,WassermanSM,etal.Identificationofanovelfamily ofcell-surfaceproteinsexpressedinhumanvascularendothelium. JBiolChem. 2002;277(48):46364–73.
11.PatelA,JerniganDB,AbdirizakF,etal.Initialpublichealthresponse andinterimclinicalguidanceforthe2019novelcoronavirusoutbreakUnitedStates. MorbMortalWklyRep. 2020;69(5):140–6.
12.FanaroffACandLopesRD.COVID-19thromboticcomplicationsand therapeuticstrategies. AnnuRevMed. 2023;74:15–30.
13.NationalCenterforImmunizationandRespiratoryDiseases(U.S.). DivisionofViralDiseases.Interimclinicalguidanceformanagementof patientswithconfirmedcoronavirusdisease(COVID-19).2020. Availableat: https://stacks.cdc.gov/view/cdc/89980 AccessedSeptember27,2023.
14.NationalInstitutesofHealth.Coronavirusdisease2019(COVID-19) treatmentguidelines.2023.Availableat: https://www. covid19treatmentguidelines.nih.gov/.AccessedSeptember26,2023.
15.HarahwaTA,YauTHL,Lim-CookeMS,etal.Theoptimaldiagnostic methodsforCOVID-19. Diagnosis. 2020;7(4):349–56.
16.MittalR,ChourasiaN,BhartiVK,etal.Blood-basedbiomarkersfor diagnosis,prognosis,andseveritypredictionofCOVID-19: opportunitiesandchallenges. JFamilyMedPrimCare. 2022;11(8):4330–41.
17.XieX,ZhongZ,ZhaoW,etal.ChestCTfortypicalcoronavirusdisease 2019(COVID-19)pneumonia:relationshiptonegativeRT-PCRtesting. Radiology. 2020;296(2):E41–5.
18.FraterJL,ZiniG,d’OnofrioG,etal.COVID-19andtheclinical hematologylaboratory. IntJLabHematol. 2020;42(Suppl1):11–8.
19.GuneysuF,YurumezY,GucluE,etal.Thediagnosticprocessof COVID-19intheemergencydepartment:laboratoryandimaging methods. RevAssocMedBras. 2020;66(Suppl2):58–64.
20.LiuL,LiuW,ZhengY,etal.Apreliminarystudyonserological assayforsevereacuterespiratorysyndromecoronavirus2 (SARS-CoV-2)in238admittedhospitalpatients. MicrobesInfect. 2020;22(4–5):206–11.
21.GuoL,RenL,YangS,etal.Profilingearlyhumoralresponseto diagnosenovelcoronavirusdisease(COVID-19). ClinInfectDis. 2020;71(15):778–85.
22.ZhaoJ,YuanQ,WangH,etal.AntibodyresponsestoSARS-CoV-2in patientswithnovelcoronavirusdisease2019. ClinInfectDis. 2020;71(16):2027–34.
23.CassanitiI,NovazziF,GiardinaF,etal.PerformanceofVivaDiag COVID-19IgM/IgGrapidtestisinadequatefordiagnosisofCOVID-19in acutepatientsreferringtoemergencyroomdepartment. JMedVirol. 2020;92(10):1724–7.
24.BattagliniD,Lopes-PachecoM,Castro-Faria-NetoHC,etal.Laboratory biomarkersfordiagnosisandprognosisinCOVID-19. FrontImmunol. 2022;13:857573.
25.IwamuraAPD,SilvaMRT,HümmelgenAL,etal.Immunityand inflammatorybiomarkersinCOVID-19:asystematicreview. RevMedVirol. 2021;31(4):e2199.
26.ShenY,ChengC,ZhengX,etal.Elevatedprocalcitoninispositively associatedwiththeseverityofCOVID-19:ameta-analysisbasedon10 cohortstudies. Medicina. 2021;57(6):594.
27.MesaAM,CesarEC,MontanezEM,etal.Acutelunginjurybiomarkers inthepredictionofCOVID-19severity:totalthiol,ferritinandlactate dehydrogenase. Antioxidants. 2021;10(8):1221.
28.ToppG,BouyeaM,CaggianoNC,etal.Biomarkerspredictive ofextubationandsurvivalofCOVID-19patients. Cureus. 2021;13(6):e15462.
29.BergerJS,KunichoffD,AdhikariS,etal.PrevalenceandoutcomesofDdimerelevationinhospitalizedpatientswithCOVID-19. Arterioscler ThrombVascBiol. 2020;40(10):2539–47.
30.SmilowitzNR,KunichoffD,GarshickM,etal.C-reactiveprotein andclinicaloutcomesinpatientswithCOVID-19. EurheartJ. 2021;42(23):2270–9.
31.AliA,MohamedS,ElkhidirI,etal.Theassociationoflymphocyte count,CRP,D-dimer,andLDHwithseverecoronavirus disease2019(COVID-19):ameta-analysis. SudanJMedSci. 2020;15(5):9–19.
32.WoolGDandMillerJL.TheimpactofCOVID-19diseaseonplatelets andcoagulation. Pathobiology. 2021;88(1):15–27.
33.ConnorsJMandLevyJH.COVID-19anditsimplicationsforthrombosis andanticoagulation. Blood. 2020;135(23):2033–40.
34.TurkmenS,SahinA,GunaydinM,etal.ThevalueofsignalpeptideCUB-EGFdomain-containingprotein-1(SCUBE1)inthediagnosisof pulmonaryembolism:apreliminarystudy. AcadEmergMed. 2015;22(8):922–6.
35.XiaoL,WangM,YangS,etal.Thediagnosticpotentialofplasma SCUBE-1concentrationforpulmonaryembolism:apilotstudy. ClinRespirJ. 2023;17(4):263–9.
36.CakırA,PayzaU,AksunS,etal.Validityofsignalpeptide-CUB-EGF domain-containingprotein-1(SCUBE-1)inthediagnosisofaortic dissection. SignaVitae. 2020;17(1):112–6.
37.DaiDF,ThajebP,TuCF,etal.PlasmaconcentrationofSCUBE1,a novelplateletprotein,iselevatedinpatientswithacutecoronary syndromeandischemicstroke. JACC. 2008;51(22):2173–80.
38.Gomez-MesaJE,Galindo-CoralS,MontesMC,etal.Thrombosisand coagulopathyinCOVID-19. CurrProbCardiol. 2021;46(3):100742.
39.VargaZ,FlammerAJ,SteigerP,etal.Endothelialcellinfectionand endotheliitisinCOVID-19. Lancet. 2020;395(10234):1417–8.
40.PanigadaM,BottinoN,TagliabueP,etal.HypercoagulabilityofCOVID19patientsinintensivecareunit:areportofthromboelastography findingsandotherparametersofhemostasis. JThrombHaemost. 2020;18(7):1738–42.
41.Elabscience.HumanSCUBE1(signalpeptide,CUBandEGF-like domain-containingprotein1)ELISAkit.Availableat: https://www. elabscience.com/p-human_scube1_signal_peptide_cub_and_ egf_like_domain_containing_protein_1_elisa_kit-19928.html AccessedNovember27,2023.
42.StringerD,BraudeP,MyintPK,etal.TheroleofC-reactiveproteinasa prognosticmarkerinCOVID-19. IntJEpidemiol. 2021;50(2):420–9.
43.PranataR,LimMA,YonasE,etal.Thrombocytopeniaasaprognostic markerinCOVID-19patients:diagnostictestaccuracymeta-analysis. EpidemiolInfect. 2021;149:e40.
44.ParaO,CarusoL,PestelliG,etal.Ferritinasprognosticmarkerin COVID-19:theFerVidstudy. PostgradMed. 2022;134(1):58–63.
45.ThachilJ,CushmanM,SrivastavaA.AproposalforstagingCOVID-19 coagulopathy. ResPractThrombHaemost. 2020;4(5):731–6.
46.ToprakK,KaplangorayM,PaliceA,etal.SCUBE1isassociatedwith thromboticcomplications,diseaseseverity,andin-hospitalmortalityin COVID-19patients. ThrombRes. 2022;220:100–6.
47.Ba ¸ saranNC,UyarogluOA,DizmanGT,etal.Outcomeof noncriticalCOVID-19patientswithearlyhospitalizationand earlyantiviraltreatmentoutsidetheICU. TurkJMedSci. 2021;51(2):411–20.
48.ErtekinB,Yortanlı M,OzelbaykalO,etal.Theperformanceofrisk scoringsystemsusedforsevereCOVID-19casesintheemergency department. PhnxMedJ. 2022;4(3):123–8.
49.ScheideggerD,FumeauxT,SchaffertB,etal.COVID-19pandemic: triageforintensive-caretreatmentunderresourcescarcity. SwissMed Wkly. 2020;150:w20229.
50.YuCY,ChanKG,YeanCY,etal.Nucleicacid-baseddiagnostictests forthedetectionSARS-CoV-2:anupdate. Diagnostics(Basel). 2021;11(1):53.
51.ArulebaRT,AdekiyaTA,AyaweiN,etal.COVID-19diagnosis:areview ofrapidantigen,RT-PCRandartificialintelligencemethods. Bioengineering. 2022;9(4):153.
52.YüceM,FiliztekinE,ÖzkayaKG.COVID-19diagnosis-areviewof currentmethods. BiosensBioelectron. 2021;172:112752.
53.MeiX,LeeHC,KyDiao,etal.Artificialintelligence-enabledrapid diagnosisofpatientswithCOVID-19. NatMed. 2020;26(8):1224–8.
54.ChaimayoC,KaewnaphanB,TanliengN,etal.RapidSARS-CoV-2 antigendetectionassayincomparisonwithreal-timeRT-PCRassay forlaboratorydiagnosisofCOVID-19inThailand. VirolJ. 2020;17(1):177.
ORIGINAL RESEARCH FeasibilityofEmergencyDepartment-InitiatedHIV Pre-ExposureProphylaxis EzraBisom-Rapp,BS*
KishanPatel,MD†‡
KatrinJaradeh,MD*†‡
TunaC.Hayirli,MD,PhD§
ChristopherR.Peabody,MD,MPH†‡
SectionEditor: IoannisKoutroulis,MD,MBA,PhD
*UniversityofCalifornia,SanFranciscoSchoolofMedicine, SanFrancisco,California
† UniversityofCaliforniaSanFrancisco,DepartmentofEmergencyMedicine, SanFrancisco,California
‡ ZuckerbergSanFranciscoGeneralHospitalandTraumaCenter, DepartmentofEmergencyMedicine,SanFrancisco,California
§ HarvardMedicalSchool,Boston,Massachusetts
Submissionhistory:SubmittedAugust13,2024;RevisionreceivedSeptember6,2024;AcceptedSeptember10,2024
ElectronicallypublishedOctober22,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.33611
Introduction: Pre-exposureprophylaxis(PrEP)forHIV usingantiretroviralmedicationinnon-infected individualstopreventHIV hasimmensepotentialtoslowthespreadofthevirus.However,uptakehas beeninsufficient,andstarkracialdisparitiesexistinbothHIVacquisitionandPrEPusage,makingPrEP accessahealthequityissue.Apromisingvenuetoengagehigh-riskpopulationsinPrEPcareisthe emergencydepartment(ED);however,existingEDPrEPinitiativeshavebeencostlyorhavehadlimited success.Wehypothesizethattwostrategiescouldovercomethesebarriers:prescribingPrEPduringan EDvisitandprovidingpatientswithaninitialsupplyofPrEPmedicationintheED.Here,wedescribethe resultsofaqualitativestudyexploringmultidisciplinaryemergencycliniciansandHIVclinicians’ needs andviewsaboutthefeasibilityofsuchaninitiative.
Methods: Weconducted22semi-structuredinterviewswithmultidisciplinarycliniciansfromanurban, safety-netmedicalcenterintheEDandtheon-siteHIVclinicthatprovidesPrEPservices.Weperformed thematicanalysistosummarizechallengesandpotentialsolutionsdescribedbyparticipants.
Results: Participants’ responsesfellintothreethematiccategories:operationalchallenges;patient-level considerations;andpotentialimpacts.OperationalchallengeshighlightedthedifficultyofPrEPinitiation inabusyEDandcliniciansupportneeds.Patient-levelconsiderationsincludedthecomplex psychosocialneedsofEDpatientswhocouldbenefitfromPrEP.Finally,participantsanticipatedthatan ED-basedPrEPinitiationprogramcouldpositivelyimpactbothindividualpatientsandpublichealth.
Conclusion: InterviewswithemergencydepartmentandHIVclinicstaffrevealedimportant considerationsandpotentialsolutionsforED-initiatedPrEPworkflows.Cliniciansinbothspecialties wereenthusiasticaboutsuchaninitiative,whichcouldfacilitateitssuccess.Thisstudylaysthe groundworkforthefuturedesignofanefficientandinnovativeworkflowtoleveragetheEDasan essentialentrypointintoHIVpreventionservices.[WestJEmergMed.2024;25(6)985–992.]
INTRODUCTION Despitesubstantialprogressinunderstandingand managinghumanimmunodeficiencyvirus(HIV),thevirus remainsapressingconcernintheUnitedStatesduetoits persistentprevalence,associatedmultisystemichealth impacts,andcoststothehealthcaresystem.1–4 This underscorestheneedforinnovativeapproachesto prevention.HIVpre-exposureprophylaxis(PrEP) theuse ofantiretroviralmedicationinnon-infectedindividualsto preventHIVacquisition hasemergedasagroundbreaking
strategythatdrasticallyreducestheriskofcontractingHIV andhasreceivedaGradeArecommendationfromtheUS PreventativeServicesTaskForce.5,6
WhilePrEPisasafeandeffectiveHIVpreventiontool, challengespersistthathavelimiteditsreal-worldimpacton theHIVepidemic.Uptakehasbeenpoor:just36%ofpeople atriskforHIVwithaPrEPindicationwereprescribedthe medicationin2022.7 Wideracialandsocioeconomic disparitiesexistinbothHIVacquisitionandPrEPuptakein theUS,8–10 leavingvulnerablepopulations disproportionatelyexposedtotheriskofHIVinfection. Addressingthesedisparitiesnecessitatesinnovative approachesthatextendbeyondtraditionalsexualhealth clinicsettings.Emergencydepartments(ED)areoftenthe onlyhealthcareaccesspointforunderservedpopulationsand havebeenidentifiedasapromisingvenuetoengagehigh-risk populationsinHIVpreventionservices.11 Researchinan urban,county-runEDestimatesthatatleast1in20ED patientsarePrEP-eligible,andofthePrEP-eligible participantswhohadpreviouslyheardofPrEP,75%were willingtostartatthatvisit.12 Otherstudieshavesimilarly demonstratedPrEP’sacceptabilityamongEDpatients.13,14 WhilemanyEDpatientscouldbenefitfromPrEP, connectingthemtolongitudinalcareatPrEPclinicsremains challenging.Astudyinahigh-volumeurbanEDshowedthat while68.6%ofpatientswhocompletedanHIVrisk assessmentwereinterestedinPrEP,11%ofthoseinterested wereabletostartPrEPmedicationafterspeakingwitha PrEPeducator,and3%ofinterestedpatientswhowere providedwithinformationaboutdrop-inPrEPclinichours receivedaprescription.14 OtherEDshavesimilarly implementedED-basedPrEPeducatorsornavigatorswith varyingdegreesofsuccess.15,16 However,thisstrategymay becost-prohibitiveformanysafety-netEDs,astheymaynot beabletofundorstaffPrEP-specificpositionstoassistwith linkages.Moreworkisneededtodeterminehowtoaddress lowPrEPinitiationrates,whileleveragingexistingresources andinterdisciplinarypersonneltoprovideequitable,highvaluecare.
Wehaveidentifiedtwostrategiesstudiedinothercontexts thatcouldbeadaptedtoaddressbarriersfacedbypreviously reportedED-basedPrEPprograms.First,researchindropinsexualhealthclinicsshowsthatprescribingPrEPduringa patient’sinitialvisit(“same-dayPrEPinitiation”),before receivingalllabresults,increasesthelikelihoodofPrEP initiationandcontinuationwithoutcompromisingpatient safety,comparedtothestandardmodelofrequiringmultiple visitsfortestingandcounselingbeforeprescribingPrEP medication.17 Second,providinga14-daysupplyof antiretroviralmedication “starterpacks” topatientswhotest positiveforHIVintheEDhasbeenshowntoincreasethe likelihoodofengagementinfollow-upHIVcare,compared topatientswhodidnotreceivemedicationstarterpacks.18 Wehypothesizethatadaptingbothofthesestrategiesto
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Theemergencydepartmentisapromising venuefortheinitiationofHIVpreexposureprophylaxis(PrEP)for underservedpopulations.
Whatwastheresearchquestion?
Whatchallengesandfacilitatorsexistforthe creationofanED-basedPrEPinitiationand carelinkageprogram?
Whatwasthemajor findingofthestudy?
BusyEDswithlimitedcliniciansupportand patients ’ complexpsychosocialneedsare factorstoconsiderinthecreationofan ED-basedPrEPinitiative.
Howdoesthisimprovepopulationhealth?
PrescribingPrEPduringapatient ’ sinitial EDvisitbeforereceivi ngalllabresultscould increasethelikelihoodofPrEPinitiationand continuationinmarginalizedcommunities.
createaworkflowthatemploys “same-dayPrEPinitiation” withintheinitialEDvisitandPrEP “starterpacks” could overcomechallengesand financialbarriersfacedby previouslydescribedprogramssolelyfocusedoncounseling andreferraltoservices.However,thefeasibilityand acceptabilityofsuchaworkflowamongEDandHIVclinic staffisunknown.
Inthispaper,wepresentaqualitativestudyinvestigating thefeasibilityof,andidentifyingbarriersandfacilitatorsto, theimplementationofasame-dayPrEPinitiationworkflow intheEDviathematicanalysisofinterviewsconductedwith multidisciplinarycliniciansfromanurbanEDandasafetynetHIVclinicthatprovidescomprehensivePrEPservices. Thisexploratorystudylaysthegroundworkforcreationand evaluationofsuchaworkflow.
METHODS StudyDesignandParticipantSelection Weconducted22half-hourinterviewsatalarge,urban, safety-netmedicalcenterinamajorCaliforniacitywith15 multidisciplinarycliniciansintheEDandsevenintheon-site HIVclinicbetweenMay25–July12,2023andJuly15–July 24,2024.Wechosethissitebecauseitisacounty-run,safetynetinstitutionthathasbothanEDandHIVcliniconthe samecampusandservesmainlypubliclyinsuredand uninsuredpatients.Moreover,manyofthiscenter’spatients
experiencepsychosociallycomplexcircumstancessuchas houselessnessorsubstanceusedisordersandareathighrisk forHIVfromsharinginjectiondrugequipment,engagingin sexwork,orhavingcondomlessanalsexwithmultiple partners.Weidentifiedparticipantsbypurposivesampling, collaborativelydraftingalistofpotentialsubjectsto representadiversearrayofprofessionalexperiences, yearsofpractice,anddegreeofpastinvolvementinharm reductioninitiatives.
Weintentionallyrecruitedsubjectswhoserveinavariety ofclinicalrolestoidentifyopportunitiesforinterprofessional collaborationandstaffingefficiency.Additionally, participantswereidentifiedbysnowballsamplingbyasking participantstoreferadditionalstaffmemberswhocouldadd auniqueperspectivetothedataset.Recruitmentcontinued iterativelyinthiswayuntilthematicsaturationwasreached, meaningthatinterviewersagreedthatinterviewswere yieldingsimilardata.Participantsreceived$25giftcardsfor theirparticipation.Ourinstitution’sinstitutionalreview boarddeterminedthisstudytobeexempt.
Interventions Interviewsweresemi-structured,usinganinterviewguide createdcollaborativelybyauthorsEBRandKJanditeratively modifiedbyallauthors(SupplementalTable1).Theinterview guideinvitedparticipantstodiscusstheirroleintheED, previousexperiencewithED-basedHIVprevention interventions,perceivedneedforHIVprevention interventionsamongtheirpatientpopulation,andanticipated barriersandsolutionsforsuccessfulPrEPinitiationand linkagetocare.Allparticipantsprovidedverbalconsentto participateinthestudy(SupplementalTable2).Besidesrole, noidentifyinginformationwascollected.Allinterviewers (EBR,KP,andKJ)haveexperiencecreatingcurriculumor workflowsformedicalprofessionalsandstudentsontopics relatedtotheneedsofmarginalizedpopulations.We consideredhowinterviewerpositionalitycouldpotentially impactparticipants’ responses;noissueswerefound,andnone oftheinterviewershadsupervisorialresponsibilitiesoverthe participantstheyinterviewed.EBRconducted14interviews; KPconductedsixinterviews,andKJconductedtwo interviews.Interviewswererecordedandtranscribedusing Zoomteleconferencingsoftwarev5.13.11(ZoomVideo Communications,Inc,SanJose,CA),andtranscriptswere reviewedforaccuracybyEBR.Recordingsandtranscripts werestoredsecurelywithinourinstitution’sapprovedsecure, enterprise,cloud-based filecollaborationsoftware.Sampling andinterviewswereconducteduntilnonewinformationwas generated,indicatingthatthematicsaturationwasreached.
Analysis Weperformedinductivethematicanalysisofinterview transcriptsaftercompletinginterviewsfollowingthe groundedtheoryapproach.Allowingparticipants’ responses
toguidethemedevelopmentenabledustoprioritizeproblem areasnotalreadyexploredintheliterature.19 Analysiswas conductedfromJuly15–August15,2023andJuly 25–August2,2024.Attheinitialstage,authorsEBR,KP, andKJinductivelydevelopedapreliminarycodebookby reflectingoninterviewsandanalyzingonefulltranscript together.Thiscodebookwasiterativelyrevisedduring codingindiscussionwiththeresearchteam.EBRcoded12 interviewsandKPcoded10interviewsusingATLAS.tiweb softwarev5.11.0-2023-08-02)(ATLAS.tiGmbH,Berlin, Germany).Afterindependentlyreviewingeachother’ s codes,EBRandKPreconciledanydiscrepanciesby discussingthemwithinthecontextofthefullinterview transcript,andKJarbitrateddisagreements.Therewasa highdegreeofconcordancebetweencoders,andcomplete agreementregardingcodesandthemeswasreached. Throughoutthisprocess,higherorderthemeswere developedthroughiterativediscussionsamongtheresearch team.Frequentmeetingsateachanalyticstepenhanced consistencyofcodingandanalysis.Fundersdidnot participateinanyportionofdatacollectionoranalysis.
Inthispaper,weuse “HIVclinic” todescribethestudysite atwhichinterviewstookplace,and “PrEPclinic” toindicate anyclinicthatcouldformpartnershipswithEDstofacilitate follow-upPrEPcare.
RESULTS Oursampleincludedeightattendingphysicians(fiveinthe EDandthreeintheHIVclinic);fourresidentphysiciansand fellows(threeintheEDandoneintheHIVclinic);onenurse practitionerintheED; fiveregisterednurses(threeintheED andtwointheHIVclinic);twosocialworkersintheED; andtwopharmacystaff(oneintheED,andoneintheHIV clinic)(Table1).
Participantsself-identifiedtheirexperiencewithdelivering PrEPas “ none, ”“limited,” or “extensive.”“Limited” PrEP experienceisdefinedasnotwithinthehealthcare professional’susualscopeofpractice,buttheyhavebeen involvedinconnectingEDpatientstoPrEPatleastonce. “Extensive” PrEPexperienceindicatesthattheyhavebeen involvedinED-prescribedPrEPmultipletimesandare comfortableinthispractice.Thirteenparticipantshadno experiencedeliveringPrEP(nineintheEDandfourinthe HIVclinic);sixhadlimitedexperience(fiveintheEDand oneintheHIVclinic);andthreehadextensiveexperience (oneintheEDandtwointheHIVclinic).Themesdiscussed byparticipantsfellintothreedistinctcategories:operational challenges;patient-levelconsiderations;andpotential impactsofanED-initiatedPrEPworkflow.
OperationalChallenges OperationalchallengestoimplementinganED-based PrEPinitiationworkflowwerereportedconsistentlyby participantsfromboththeEDandtheHIVclinic(Table2).
Table1. Participantdemographicsamong22healthcare professionalsfromtheemergencydepartment(ED)andHIVclinicat ZuckerbergSanFranciscoGeneralHospital,anurbansafety-net medicalcenter.
*LimitedPrEPexperienceisdefined as “notwithintheclinician’s usualscopeofpractice,buttheyhavebeeninvolvedinconnecting EDpatientstoPrEPatleastonce.”
**ExtensivePrEPexperienceisdefinedashavingbeen “involved inED-prescribedPrEPmultipletimesandiscomfortablein thispractice.” ED,emergencydepartment; PrEP,pre-exposureprophylaxis.
Themainconcernsparticipantsidentifiedweretime, capacity,andresourceconstraintsintheED.Emergency clinicianswerewaryofinitiatingconversationsabout preventativehealthunrelatedtothepatient’schiefconcern, asdoingsocouldextendEDlengthofstayandimpedeED operations.Oneemergencyphysicianexpressedtrepidation aboutclinicians’ abilitytohave “meaningfulconversations [aboutsexualhealthandHIVrisk]whiletryingtocarefor [many]peopleinthewaitingroomatthesametime” Needingtoconductlengthysearchesforclinicalguidelines frommultiplesourceswasalsoarecurringfactor.
Tocircumventthesetimeandcapacityconstraints,nearly allparticipantsdiscussedelectronichealthrecord(EHR) toolsorelectronicallyaccessibleworkflowsasfactorsthat couldfacilitaterapidPrEPprescriptionanddecreasethe “knowledgebaseneeded[tocorrectlyprescribePrEP]” (HIV Clinicphysician).TheEHRtoolsincludedpremadeorder setstofacilitateorderingofallrequiredlabs,prescription formulations,andreferrals;achecklistoftopicstoreview withpatientsintegratedintomedicalnotetemplates;andprewrittennotesanddischargeinstructions.Integratingthese toolsintoonepageintheEHRorelectronicallyaccessible workflowsystemcouldallayconcernsoverthecognitive burdenofimplementingthisworkflowthatsomeemergency cliniciansconsideredtobeoutsidetheirroutinescope ofpractice.
Interdisciplinarycollaborationswerecommonly discussed.Theemergencyphysicianshighlightedthe importanceofinterdisciplinarycollaborationsbetween physicians,nurses,pharmacists,socialworkers,andpatient navigators, “sothattheburdenisn’tsolelyon[oneclinician] toexplaineverythingtothepatient” (emergencymedicine resident).Manyfeltthatthiscouldeasethetimeandcapacity constraintsfeltbyphysiciansintheirdailypractice.This
Table2. Representativequotesfromparticipantinterviewsillustratingoperationalchallengestoimplementinganemergencydepartmentinitiatedpre-exposureprophylaxisworkflow.
Sub-themeswithinoperationalchallengesAssociatedquotations
TimeandcapacityconstraintsforPrEPcare within theED
Challengesassociatedwithequitably identifyinghigh-needPrEPcandidates
Needforstaffeducation
“Thisproposedprojectiscomingata nationalcrisisofEDcrowding sothere’s reallylittleexcesscapacityanywherein,inandoutsidetheEDforadditionaltasks, withoutmoreresources.” (EDMD-01)
“We’reusuallyshortstaffed,andthere’s ::: competingprioritiesusuallyduringthe shift,andsomethinglikethiswillprobablyfalltothewaysideintermsofprioritylist, butnottosayit’snotimportant.” (EDRN-3)
“Ineed[clinicians]toofferthistopeople,butnotjustthosewho[m]youassumeare atrisk,because ::: wehavealotofpatientswhoaresexworkers,andtheydon’t necessarilytellusthey’resexworkers.” (EDNP-01)
“IthinkIwouldjustneedabitmoreinformationmyself Ihavenorealexpertisein thisarea.Andso,Iwoulddefinitelywanttohaveabetterunderstandingof ::: whatI waslookingfor ::: ThenIwouldfeelprettycomfortablehavingaconversationas longas Iwaseducatedenough.” (EDSW-02)
ED, emergencydepartment; EDMD,emergencyphysician; EDRN,registerednurseintheED; EDSW,EDsocialworker; PrEP,pre-exposureprophylaxis.
sentimentwassimilarlyechoedbythenurses,pharmacists, andsocialworkersinterviewedwhofelttheirparticipation couldstrengthentheprogram.Onenursenotedthat, althoughdischargeplanningiscoordinatedbyprescribers, theseplanssometimesresult “fromtheadvocacyofbedside nurses ” (EDnurse);formalizingandencouraging interdisciplinarycollaborationcouldincreasepatient identificationandlinkage.However,anothernursenoted thatputtingtoomuchburdenonalreadybusynursingstaff wouldlimitthesuccessoftheprogram.
Participantsanticipatedchallengesinidentifyingpatients whowouldbeidealPrEPcandidates.Someworriedabout thepotential “biasofwho[clinicians]thinkisatrisk” (ED nursepractitioner),reinforcingstereotypes,orincomplete identificationofneedbasedonpatientreluctancetodisclose riskybehaviors.However,manyhadmixedfeelingsabout thesolutionstheyidentified.Whilemanyparticipants suggestedautomatedEHRpop-upreminderstriggeredby certainchiefconcernsorchartedriskfactors,they anticipatedthattheseremindersmaybeignoredbyclinicians inundatedbyaburgeoningnumberofsimilaralerts.Some suggesteduniversalscreeningforHIVriskfactorstoavoid biasedPrEPofferingbutanticipatedfeasibilityandprivacy issues.Finally,manysuggestedpostersencouragingpatients toself-identifyasPrEPcandidates,butothersfeltthis strategywouldmisshigh-needpatientswithlimitedhealth literacyorreluctancetodiscloseriskfactors.
Participantsemphasizedtheimportanceofstaff education,withmanyreportingthattheircomfortwiththe programwouldbecontingentonadequatestafftraining. Therewasnoconsensusonideallengthandmodalityof educationalsession,andsomeemphasizedtheneedfora varietyoftrainingformats livelectures,teamhuddles, emails,posters tomeettheneedsofstaffwithavariety oflearningstylesandschedules.Withregardtotraining content,emergencycliniciansdesiredmoreinformation aboutthepotentialharmthatPrEPtherapycould causepatients,particularlyrelatedtoliverandkidney health.However,HIVclinicstaffconsistentlyemphasized thatEDstafftrainingshouldhighlightthatPrEPcarries
alowriskforsevereinjuryifcliniciansadhereto prescriberguidelines.
Patient-LevelConsiderations Inadditiontooperationalconcerns,participants frequentlyreportedthatanED-basedPrEPinitiation programmustaddressfactorsthatinfluencepatients’ ability toenterandmaintainengagementwithlongitudinalPrEP care(Table3).Theneedformechanismsforreliable connectiontofollow-upcare,includingplansforpatients whopresentafterbusinesshours,wasdiscussedubiquitously. MultipleHIVclinicparticipantsemphasizedcollecting alternateformsofcontactinformationthatmightnotusually beaskedaboutduringtriage,includingemailaddresses, friends’ orcaseworkers’ contactinformation,andcampsite locationsforunhousedpatients.ManyfromboththeEDand HIVclinicemphasizedtheimportanceofhavingaclearly definedfollow-upstructureorspecificpersontoconduct outreachtopatientswithabnormallabresultsthatresulted afterdischargefromtheED.
Patientnavigatorswerediscussedasanessentialresource tofacilitateconnectiontocare.Multipleparticipantsfrom theHIVclinicmentionedthevalueofhavinganavigator basedattheHIVclinicmeetthepatientintheED,as opposedtorelyingonED-basedsupportstaffforconnection tocare.Theyfeltthatthiscouldbuildtherapeuticrapport, decreasepatientanxietyassociatedwithseekingservicesina newhealthcaresettingas “theiceisalreadybroken” (HIV Clinicphysician),andincreaselikelihoodofretentionincare.
Duetothepsychosocialcomplexityofthetargetpatient population,participantsproposedthreecomponentsofa PrEPinitiationworkflowthatareessentialforsuccess.First, manyparticipantsdiscussedtheneedtoprovidepatientsan initialsupplyofPrEPintheED,asopposedtosendingthe prescriptiontoapharmacyforthepatienttopickupafter discharge.Participantsreportedhavingexperiencedgreater successindischargemedicationinitiationwhenthisstrategy wasemployedinsimilarinitiatives.Second,participants emphasizedtheimportanceofEDspartneringwithPrEP clinicsthatcouldmeetadditionalpsychosocialneeds “that
Table3. Representativequotesfromparticipantinterviewsillustratingpatient-levelconsiderationswhenimplementinganemergency department-initiatedpre-exposureprophylaxisworkflow.
Sub-themeswithinpatient-level considerationsAssociatedquotations
Ensuringadequatefollow-up
Anticipatedbarrierstoaccessingand adheringtomedications
“In termsofobtaininggoodcontactinformationfrompeople andIdon’tjustmeanphone numbersbythat.So,itcouldbecampsites,placestheyfrequent,friends’ contactnumbers ifsomebodydoesn’thaveareliablemeansofcommunication,becausewecertainlydon’t wanttocreatebarriersforthepeoplewhoneedPrEPthemost.” (IDMD-03)
“IdoworrythatmanypatientswhoareatriskforHIVmaynothavethefacultiestobe abletotakeadailymedication.” (EDMD-05)
EDMD, emergencyphysician; IDMD,infectiousdiseasesphysician; PrEP,pre-exposureprophylaxis.
arereallyattheforefrontof[thepatient’s]life” (HIVClinic nurse).Forexample,manyparticipantsfromboththeED andHIVclinicanticipatedthataPrEPclinicthatprovides substanceusedisordersupportandwrap-aroundservices couldbetteraddressbarrierstoadherenceinhigh-risk patientsthanaclinicthatonlyoffersbasicsexualhealthcare. Third,participantsdiscussedtheimportanceoflanguageinclusivepatienteducationmaterialsandstaffforpatients withlimitedEnglishproficiency,aswellaspatienteducation materialsthatusesimplelanguage.
PotentialImpacts Participantsnearuniversallyanticipatedahighneed foranED-basedPrEPinitiationwork fl ow,andthe majoritywerenoticeablyexcitedforthepotentialrolloutof suchaninitiative( Table4 ).Participantsstatedthatthis initiativecouldhaveasigni fi cantimpactonpatientswho areathighriskforHIVinfectionandhavehighlevelsof psychosocialcomplexity,especiallyunhousedpatientsand thosewithsubstanceusedisorders.Furthermore, participantsanticipatedthatthisprogramcouldhave positiveimplicationsonpopulation-levelhealthdisparities inHIVacquisitionbyreachinghigh-riskgroupsthat currentHIVpreventionini tiativeshavenotbeenable toengage.
Participantshaddifferingviewsontheeffectthatthis programcouldhaveonEDstaffandoperations.BothED andPrEPclinicparticipantsworriedthatemergency clinicianswouldresisttheadditionaltasksrequiredforthis programand finditincompatiblewithanacutecaresetting. Oneemergencyattendingphysician,speakingtoherprevious experienceleadinganED-basedharmreductioninitiative,
notedthatconsiderableeducationalinterventionswere neededto “changethe[ED]cultureandmake[prescribing harmreductionmedication]somethingthatwaswithinthe purviewoftheemergencyteam.” However,manyEDstaff anticipatedthattheircolleagueswould findfulfillmentinthe opportunitytoengagepatientsinpreventativemedicineasa respitefrommanagingfrequentacutecrises.Additionally, someEDparticipantsviewedthisproposedworkflowaspart ofalargerperceivedcultureshiftinEDstoconsider upstreamfactorsthatcausepatientstoseekoutacutecare, evenfulfillingamoralobligation: “Weoweittoour communitytobeabletoprovide[PrEPintheED]” (emergencymedicineresident).
DISCUSSION Thisstudydemonstratedthatstaffatbothabusy,urban medicalcenterEDandsafety-netHIVclinicseetheneedfor HIVpreventionservicesamongEDpatientsandare amenabletothecreationofaworkflowtoengageat-risk patientsincarewhileintheED,assumingthatdescribed challengesareaddressed.Weintegratedthemesthatarose intoacohesiveframeworkthatcouldbeusedtoguide workflowdevelopment(Figure).
Ourdataprovidesvaluableinsightintopotential interventionstoprepareandprimeEDstafftoconsiderPrEP asanoptionforpatients.Forexample,discordantviewson PrEPsafetyandsideeffectsbetweenEDandHIVclinicstaff demonstratetheneedforeducationalinterventionstargeted atthissubject.Furthermore,theperspectivesofEDstaff excitedaboutthepotentialworkflow suchas finding fulfillmentinconnectingpatientswithPrEPorevokinga moralobligationamongstaff couldbeincorporatedinto
Table4. Representativequotesillustratingparticipant-reportedpotentialimpactsofanemergencydepartment-initiatedpre-exposure prophylaxisworkflow.
Sub-themeswithinPotentialImpactsAssociatedquotations
Individualandpublichealthbenefits ofengagingatriskpopulationsinHIVpreventionservices
Impactsonstaff
DifferingviewsontheED’sevolvingroleinthe healthcaresystem
“Alotofpeoplecometoouremergencydepartment,Isaysometimesasa lastresort,butalsoasa firstresort,becausetheydon’tknowwhereelseto go andIthinkthatitwilltouchalotmorepeoplethanIthinkwethinkitwill atthispoint.” (EDRN-01)
“Ithinkthat[clinicians]aregoingtolovebeingabletoprovidepeoplewitha wellnessactinsteadofmeetingpeopleintheirmomentofcrisis.Because that’swhatwedoallthetime.Sohowgreatisitthatwecanactuallyhelp peoplethatwanttohelpthemselvestostayhealthy.” (EDRN-01)
“Somepeopleliterallydon’tseethisastheroleoftheER,andit’sgoingto takesome,like,armtwisting.” (EDNP-01)
“Andespeciallyherethecontextof acommunityhospital, alotof peoplewhochoosetoworkhereknowthat[communityprotectionis]partof ouremergencydepartmentjob.” (EDRN-02)
“Ithinkmostpeopleinemergencymedicinerecognizethatourroleas emergencyphysiciansisconstantlyexpandingandcontractinginrelationship towhatishappeningintheworld.” (EDMD-04)
ED, emergencydepartment; EDMD,emergencyphysician; EDNP,nursepractitionerintheED; EDRN,registerednurseintheED.
Figure. Themesintegratedintoacohesiveframeworktoguidethe creationandimplementationofanemergencydepartment-based PrEPinitiationworkflow.
ED,emergencydepartment; EHR,electronichealthrecord; PrEP,pre-exposureprophylaxis.
interventionsdesignedtoshiftEDculturetobemore amenabletoprescribingPrEP.
Inourinterviews,EHRtoolssurfacedasapromising interventiontoaddressclinicianconcerns.Cliniciansfeltthat ordersetsandtemplatescoulddecreasetheamountoftime requiredforcliniciansto findandfollowup-to-date guidelines.Indeed,EHRtemplateshavebeenshownto improveclinicalguidelineadherenceforotherhealth issues.20,21 Electronicplatformsthatallowcliniciansto accessstandardizedworkflowsquickly,whichemergency clinicianscommonlyrequested,couldfurthersupplement thesetoolstoincreaseclinicianconfidencewith theprogram.22
Additionally,clinicians’ concernsoverequitable identificationofPrEPcandidates,aswellastrepidation aboutEHR-basedpop-upHIVriskalerts,arereflectedin research.Astudyconductedinalarge,managedcarehealth systemshowedthatanEHR-basedHIVriskpredictive modelbasedsolelyonPrEPguidelinesfromtheCentersfor DiseaseControlandPrevention(CDC)waslesssensitivein identifyingHIVriskinBlackpatientscomparedtoWhite patients,whereasamultivariablealgorithmgenerated throughmachinelearningwasequallysensitiveamong races. 23 ThisdemonstratesthepotentialforEHRtoolsto ameliorateracialdisparitiesinPrEPofferrate,aswellasthe needforthoughtfuldesignofthesetoolstoavoid exacerbatinghealthdisparities.
WhereaspreviousstudiesaboutPrEPintheEDfocused onlyonreferraltoservices,11,14 EDandHIVclinicstaffboth anticipatedthatimmediatePrEPinitiationwithastarter packprovidedintheEDwouldincreasechancesoffollowup.Thispredictionissupportedbyexistingliterature; immediatePrEPinitiationatthepatient’ s firstvisithasbeen showntofacilitateincreasedPrEPuptakeandpersistencein drop-insexualhealthclinicsettingsandisdescribedasatool
toaddressPrEPaccessbarriersinthe2021CDCPrEP guidelines.5,17 Thisstrategymeritsfurtherinvestigationfor adaptationtoanacutecaresetting.
Furthermore,ourdatasupportsapartnershipmodel betweentheEDandasingleoutpatientclinic.Thiscould streamlinethereferralprocessanddecreasecostsby removingtheneedforanED-basedPrEPnavigatorsor educatorstoguidepatientsthroughcomplexhealthcare systems.Direct “warmhandoffs” toPrEPclinicbasednavigatorscouldalsofacilitatetheearlydevelopment oftherapeuticrapportwithpatientsandpromote retentionincare,addressingthelow-yieldofprograms basedonprovidingresourcesheetswithPrEP clinicinformation.
Asnotedbyparticipants,theservicesofthepartnering PrEPclinicshouldmatchtheneedsofthetargetpopulation servedbytheED,includingtreatmentforsubstanceuse disorderinlocalitiesdisproportionatelyaffectedbythe opioidepidemic.Additionally,EDsmustequiptheir partneringPrEPclinicswiththeinformationneededto facilitatesuccessfulconnectiontothespecificservices providedbythatPrEPclinic.Forexample,PrEPclinicsthat performoutreachtotheunhousedmayneedinformation suchasthelocationofpatients’ encampments,whereas clinicsthatdonotoffertheseoutreachservicesmay not findthisinformationuseful.Thelocalcontextof bothservicesneededandservicesavailableshouldbetaken intoconsiderationwhendesigninganED-initiated PrEPprogram.
LIMITATIONS Toourknowledge,thisexploratorystudyistheonlyone ofitskindtoevaluatetheneedsandviewpointsof multidisciplinarycliniciansregardinganED-initiatedPrEP workflow.However,ourstudydoesnotcapturethepatient perspectiveonaprograminwhichapatientwouldinitiate PrEPintheED,animportanttopicforfutureresearch. Additionally,thisstudywasconductedatalargemedical centerinacitywitharobustsocialsafetynetandmaynotbe generalizabletosmallercommunityhospitals.
CONCLUSION Ourstudydescribesanticipatedchallengesandfacilitators ofinitiatingofapre-exposureprophylaxisworkflowinthe EDfromtheperspectiveofmultidisciplinaryemergencyand HIV-clinicclinicians.Theperspectivesofthe multidisciplinaryparticipantsinterviewedareessentialfor developingacomprehensive,successfulworkflow. Recommendationsdescribedhereprovideaframeworkfor thecreationofanovelPrEPinitiationprogram. CollaborationsbetweentheEDandpreventativemedicine programsmayhaveprofoundimplicationsforhealthequity asacutecarefacilitiesexpandtheirroleinthecommunityto
facilitateaccesstopreventativecaretothosewhohaveno othersourcefortheseservices.
LatinoMSMages21–30inSanAntonio,TX. JHIVAIDSSocServ. 2019;18(2):206–11.
10.RansomeY,BogartLM,KawachiI,etal.Area-levelHIVriskand socioeconomicfactorsassociatedwithwillingnesstousePrEPamong BlackpeopleintheU.S.South. AnnEpidemiol. 2020;42:33–41.
AddressforCorrespondence:ChristopherR.Peabody,MD,MPH, UniversityofCaliforniaSanFrancisco,DepartmentofEmergency Medicine,521ParnassusAve.,SanFrancisco,CA94143.Email: christopher.peabody@ucsf.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ChristopherR.Peabodyisaconsultant forFujiFilm – SonoSite.Thispublicationreceivedfundingfromthe UCSFInquiryFundingOfficeMedicalStudent “SummerExplore” ResearchFellowship,securedbyEzraBisom-Rapp.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Bisom-Rappetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.FarnhamPGP,HoltgraveDRP,SansomSLP,etal.Medicalcosts avertedbyHIVpreventioneffortsintheUnitedStates,1991–2006. JAIDS. 2010;54(5):565–7.
2.DeAnda-DuranI,KimbroughAD,BazzanoLA.HIVandhypertension epidemiology. CurrOpinCardiol. 2023;38(4):297–303.
3.NgDK,JacobsonLP,BrownTT,etal.HIVtherapy,metabolicand cardiovascularhealthareassociatedwithglomerularhyperfiltration amongmenwithandwithoutHIVinfection. AIDS. 2014;28(3):377–86.
4.NanniMG,CarusoR,MitchellAJ,etal.DepressioninHIVinfected patients:areview. CurrPsychiatryRep. 2015;17(1):1–11.
5.CentersforDiseaseControlandPrevention.USPublicHealthService: preexposureprophylaxisforthepreventionofHIVinfectionintheUnited States 2021update:aclinicalpracticeguideline.2021.Availableat: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021. pdf.AccessedAugust19,2024.
6.USPreventiveServicesTaskForce.Preexposureprophylaxisforthe preventionofHIVinfection:USpreventiveservicestaskforce recommendationstatement. JAMA. 2019;321(22):2203–13.
7.FanfairRNandMerminJH.Dearcolleague:preliminarydataonpreexposureprophylaxiscoveragereleased.2023.Availableat: https:// www.cdc.gov/hiv/policies/dear-colleague/dcl/20231017.html AccessedAugust15,2024.
8.HuangYA,ZhuW,SmithDK,etal.HIVpreexposureprophylaxis,by raceandethnicity UnitedStates,2014–2016. MMWRMorbMortal WklyRep. 2018;67(41):1147–50.
9.GarciaMandSawG.Socioeconomicdisparitiesassociatedwith awareness,access,andusageofpre-exposureprophylaxisamong
11.ShullJA,AttysJM,Amutah-OnukaghaNN,etal.Utilizingemergency departmentsforpre-exposureprophylaxis(PrEP). JACEPOpen. 2020;1(6):1427–35.
12.HaukoosJS,WhiteDAE,RowanSE,etal.HIVriskandpre-exposure prophylaxiseligibilityamongemergencydepartmentpatients. AIDS PatientCareSTDS. 2021;35(6):211–9.
13.AronsonB,KulieP,CastelAD,etal.Evaluatingpatientperceptionson PrEPscreeningandreferralintheacutecaresetting. AIDSBehav. 2023;27(3):1024–9.
14.RidgwayJP,AlmirolEA,BenderA,etal.Whichpatientsinthe emergencydepartmentshouldreceivepreexposureprophylaxis? Implementationofapredictiveanalyticsapproach. AIDSPatientCare STDS. 2018;32(5):202–7.
15. MahalJ,DeccyS,SeuR.Linkingemergencydepartmentpatientsatrisk forhumanimmunodeficiencyvirustopre-exposureprophylaxis. AmJ EmergMed. 2022;54:87–90.
16.ZhaoZ,JonesJ,Arrington-SandersR,etal.Emergencydepartmentbasedhumanimmunodeficiencyviruspreexposureprophylaxisreferral program-usingemergencydepartmentsasaportalforpreexposure prophylaxisservices. SexTransmDis. 2021;48(8):E102–4.
17.KamisKF,MarxGE,ScottKA,etal.Same-dayHIVpre-exposure prophylaxis(PrEP)initiationduringdrop-insexuallytransmitted diseasesclinicappointmentsisahighlyacceptable,feasible,andsafe modelthatengagesindividualsatriskforHIVintoPrEPcare. Open ForumInfectDis. 2019;6(7):ofz310.
18.WhiteDAE,JewettM,BurnsM,etal.Implementingarapidantiretroviral therapyprogramusingstarterpacksforemergencydepartment patientsdiagnosedwithHIVinfection. OpenForumInfectDis. 2023;10(7):ofad292.
19.KigerMEandVarpioL.Thematicanalysisofqualitativedata:AMEE guideno.131. MedTeach. 2020;42(8):846–54.
20.GrotellLA,BrysonL,FlorenceAM,etal.Postpartumnotetemplate implementationdemonstratesadherencetorecommendedcounseling guidelines. JMedSyst. 2021;45(1):14.
21.ChoudharyD,BrownB,KhawarN,etal.Implementationofelectronic medicalrecordtemplateimprovesscreeningforcomplicationsin childrenwithtype1diabetesmellitus. PediatricHealthMedTher. 2020;11:219–23.
22.SchwartzHEM,StarkNR,SowaCS,etal.Buildingbackbetter:applying lessonsfromtheCOVID-19pandemictoexpandcriticalinformation access. JEmergMed. 2021;61(5):607–14.
23.MarcusJL,HurleyLB,KrakowerDS,etal.Useofelectronichealth recorddataandmachinelearningtoidentifycandidatesforHIV pre-exposureprophylaxis:amodellingstudy. LancetHIV. 2019;6(10):e688–95.
ORIGINAL RESEARCH DistributionandUtilization:AProspectiveCohortStudy AlexanderJ.Ulintz,MD*
SeemaS.Patel,MD†
KatherineAnderson,MD†
KevinWalters,MD†
TylerJ.Stepsis,MD†
MichaelS.Lyons,MD,MPH*
PeterS.Pang,MD,MS†
SectionEditor:FaithQuenzer,DO,MPH
*TheOhioStateUniversityCollegeofMedicine,DepartmentofEmergencyMedicine, Columbus,Ohio
† IndianaUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Indianapolis,Indiana
Submissionhistory:SubmittedOctober27,2023;RevisionreceivedJune12,2024;AcceptedAugust15,2024
ElectronicallypublishedSeptember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18513
Objective: Foodinsecurityisaprevalentsocialriskamongemergencydepartment(ED)patients. PatientswhomaybenefitfromfoodinsecurityresourcesmaybeidentifiedviaED-basedscreening; however,manypatientsexperiencedifficultyaccessingresourcesafterdischarge.Co-locating resourcesinorneartheEDmayimproveutilizationbypatients,butthisapproachremainslargely unstudied.Thisstudycharacterizedtheacceptanceanduseofafoodvoucherredeemableatahospital foodmarketforpatientswhoscreenedpositiveforfoodinsecurityduringtheirEDvisit.
Methods: Thisprospectivecohortstudy,conductedatasinglecounty-fundedED,includedconsecutive adultpatientswhopresentedonweekdaysbetween8 AM–8 PM fromJuly–October2022andconsentedto researchparticipation.Weexcludedpatientswhorequiredresuscitationonarrivalorcouldnotprovide writteninformedconsentinEnglish.Studyparticipantscompletedapaperversionofthetwo-question HungerVitalSignscreeningtool,administeredbyresearchstaff.Participantswhoscreenedpositive receivedauniquelynumbered$30foodvoucherredeemableatthehospital’sco-locatedfoodmarket. Voucherredemptionwasquantifiedthroughregularevaluationofmarketreceiptrecordsat30-day intervals.Theprimaryoutcomewastheproportionofredeemedvouchers.Secondaryoutcomes includedtheproportionofparticipantsscreeningpositiveforfoodinsecurity,proportionofparticipants acceptingvouchers,andassociateddescriptivestatistics.
Results: Ofthe396eligibleindividualsapproached,377(95.2%)consentedandcompletedfood insecurityscreening.Mostweremiddle-aged(median53years,interquartilerange30–58years),191 werefemale(50.4%),242wereBlack(63.9%),and343werenon-Hispanic(91.0%).Oftheparticipants, 228(60.2%)screenedpositiveforfoodinsecurityand224receivedvouchers(98.2%),ofwhich86were redeemed(38.4%)amedianofninedaysaftertheEDvisit.
Conclusion: Ahighproportionofparticipantsscreenedpositiveforfoodinsecurityandacceptedfood vouchers;however,lessthanhalfofallvoucherswereredeemedattheco-locatedfoodmarket.These resultsimplyEDfoodvoucherdistributionforfoodinsecurityisfeasible,butco-locationofresources alonemaybeinsufficientinaddressingthesocialriskandalludestoalimitedunderstandingoffacilitators andbarrierstoresourceutilizationfollowingED-basedsocialneedsscreening.[WestJEmergMed. 2024;25(6)993–999.]
INTRODUCTION Socialrisks,definedasadversesocialconditions associatedwithpoorhealth,arecommonamongemergency department(ED)patientsandinfluencetheirhealth outcomes.1,2 Foodinsecurityisoneprevalentsocialrisk amongEDpatientsthatisassociatedwithprogressionand exacerbationofchronicdisease,frequentacutecareuse,and increasedall-causemortality.3–10 PreviousstudiesofEDbasedfoodinsecurityscreeningandreferraltoresources identifiedpatientswiththissocialrisk;however,many patientswhoreceivedresourcereferralshaddifficulty connectingtotheseresourcesafterdischarge.11,12 ColocatingresourcesinorneartheEDforpatientswhoscreen positiveforfoodinsecurityrepresentsonepotentialsolution thatdirectlyconnectspatientstotargetedresources; however,littleevidencesupportsthismodel.
Withinthecontextoffoodinsecurityresourceco-location, casereportsdescribea “foodbagprogram” pilotedduring theCOVID-19pandemic,whichprovidedanydischarged EDpatientwitha1–2daysupplyofshelf-stablefood.13 However,thiswasprimarilyanoperationalprojectthat prioritizedfooddistributionandwaslimitedinits conclusionsregardingfoodinsecurityscreeningandresource uptakeduetoco-location.13 Thus,itremainspoorly understoodwhetherco-locatingresourcesinorneartheED toaddressthissocialriskleadtoincreasedresource acceptanceorutilization.Inthisstudywesoughtto characterizetheacceptanceanduseofa$30foodvoucher redeemableatahospitalfoodmarketbystudyparticipants whoscreenedpositiveforfoodinsecurityduringtheir EDvisit.
METHODS StudyDesign,Setting,andParticipants
Thisprospectivecohortstudyscreenedconsecutive consentingpatientspresentingtotheEDforfoodinsecurity andprovidedafoodvouchertoparticipantswhoscreened positive.ThisstudywasapprovedbytheIndianaUniversity SchoolofMedicineInstitutionalReviewBoard(IRB #13829).Thestudysitewasa95-roomcounty-fundedED withover100,000annualvisits.Allpatientsarrivingtothe EDare firsttriagedinthewaitingroomorambulancebayby anurse;patientswhodonotrequireemergentstabilization basedonappearanceandchiefcomplaintareevaluatedin oneof24intakerooms.Intakeroomsareprivaterooms whereacompletenursingevaluationandthe firstpatientphysicianinteractiontakesplace.
ThisstudyincludedEDpatientsaged ≥18yearswho presentedonweekdaysbetween8 AM–8 PM fromJuly1–October31,2022andwereevaluatedinanintakeroom duringtheirEDvisit.Thestudyprotocolexcludedpatients whowereminors,wereplacedinanon-intakeroom(dueto requiringimmediateresuscitationora1:1nursing intervention),orwhowereunabletoprovideinformed
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
FoodinsecurityiscommonamongED patients.Screeningidenti fi esindividuals withthissocialrisk,butlittleevidence guidesreferral.
Whatwastheresearchquestion?
Willpatientswhoscreenedpositiveforfood insecurityintheEDaccepta$30foodvoucher redeemableataco-locatedhospitalmarket?
Whatwasthemajor findingofthestudy?
98.2%ofpatientswhoscreenedpositivefor foodinsecurityacceptedavoucher,butonly 38.4%hadredeemedthematamedianofnine dayslater.
Howdoesthisimprovepopulationhealth?
Referraltoco-locatedresourcesforfood insecurityisfeasible,butprogramsshould consideraccessibilityandpatientpreferences inaddressingsocialrisksidenti fi edintheED.
consentinEnglish.Researchassistantsusedtheelectronic healthrecordtoassesspatientsforeligibilityupontheir arrivalintriageandapproachedeligibleparticipantsfor consentoncemovedtoaprivateintakeroom.Eligible participantsweremadeawareofthepurposeofthestudyand thattheirsurveyresponsescouldmakethemeligiblefora foodvoucheratthehospitalfoodmarket.
ScreeningToolDistributionandScreeningDataCollection ConsentedparticipantsreceivedapaperversionoftheUS DepartmentofAgriculturebinaryquestionHungerVital Signscreeningtool(“Withinthepast12monthsweworried whetherourfoodwouldrunoutbeforewegotmoneytobuy more, ” and “Withinthepast12monthsthefoodwebought justdidn’tlastandwedidn’thavemoneytogetmore”).14 Participantsusedaprovidedwritinginstrumenttocheckyes ornotoeachscreeningtoolquestion.Apaperversionwas chosenbasedonpriorworkbyGonzalesetal(2021),which demonstratedthat75%ofpatientspreferredfoodinsecurity screeningviapaperasopposedtoverbalresponses;however, theconsentprocessdidnotifyparticipantsthatiftheycould notreadorwrite,theresearchassistant(RA)couldreadthe screeningtoquestionstothem.15 Ifthepatientdeclined assistanceinreadingor fillingoutthescreeningtool,theRA lefttheroomfor10minutesandreturnedtocollectthe completedscreeningtool.TheRAdirectlyenteredscreening
toolresultsintoapredefineddatacollectioninstrument, REDCap.Wecollectedandmanagedstudydatausing REDCapelectronicdatacapturetoolshostedatIndiana University,whichincludedthepatient’shealthrecord numberforlongitudinaltracking.Paperscreeningtoolswere thendestroyedviathehospital’ sconfidential-document disposalsystem.
Intervention Iftheparticipantscreenednegativeforfoodinsecurity,no furtherinterventionwasperformed.Iffoodinsecuritywas identifiedonthescreeningtool,theparticipantreceiveda$30 foodvoucherredeemableatthehospital’sco-locatedfood market.16 The “FreshforYou” hospital-basedmarketwas designedbythehealthsystemtoaddressfoodinsecurityby providingpatients,visitors,andstaffeasyaccesstofresh produce,preparedfoods,healthysnacks,convenience ingredients,kitchenutensils,andpantrystaplesataffordable pricesandinaconvenientlocation.17 Thefoodmarketis openweekdaysfrom10:30 AM–6 PM andislocated approximately600feetfromtheEDentrance,positioned nearabusstopandtheparkinggarage.Priortothisstudy,a similarscreeningtoolandvoucherreferralsystemhadbeen usedinselectoutpatientpractices;thevalueofthevoucher waschosenasitwassimilartotheoutpatientpractices.Each foodvoucherhadarandomthree-digitcodeontheback,and thiswasrecordedintheRedCapdatabasepriorto distributionbytheresearchstaff.Inadditiontothefood voucher(studyintervention),participantsscreeningpositive forfoodinsecurityalsoreceivedresourcesthatwerestandard ofcarepriortothisstudy,whichincludedprintedcommunity resourcesforfoodinsecurity.Ifafoodvoucherwas redeemed,itwasmarkedwiththedateandtimeof redemptionbymarketstaff.At30-dayintervals,thestudy teamqueriedhospitalfood-marketreceiptrecordsto determinewhetheravoucherhadbeenredeemedand secondarilyperformedpatientchartreviewforprimarycare follow-upvisits.
Outcomes Theprimaryoutcomewastheproportionoffood vouchersredeemedbyparticipantswhoscreenedpositivefor foodinsecurity.Secondaryoutcomesincludedthe proportionofparticipantsscreeningpositiveforfood insecurity,proportionofindividualswithoutpatientfollowupaftertheirEDvisit,anddemographicdescriptionsof thesegroups.
StatisticalMethods Theanalysisplanincludeddescriptivedataanalysiswith frequencies,proportions,andmedianswithinterquartile range(IQR).Wedidnotcalculateanapriorisamplesizedue toenrollmentbeinglimitedbythenumberofavailable vouchers.Aposthocpowercalculationfordetecting
differencesbetweenparticipantswhoredeemedordidnot redeemafoodvoucherdemonstratedlessthan80%power; thus,statisticalcomparisonwasnotperformed,andonly descriptivestatisticsarereported.Allstatisticalanalyses wereperformedusingSTATAICversion17(StataCorp, LLC;CollegeStation,TX).
RESULTS Researchassistantsapproached396eligibleindividuals, ofwhom379consentedandcompletedthefoodinsecurity screeningtool(Figure1).Noindividualwasscreenedmore thanonceduringthestudyperiod.Mostparticipantswere middle-aged(median53years,IQR30–58years);191 identifiedasfemale(50.4%);242asBlack(63.9%);and343as non-Hispanic,(91.0%);234reportedhavingaprimarycare physician(61.7%).Mostparticipants(228)screenedpositive forfoodinsecurity(60.2%)(Table1).Ofthese,194 participants(51.2%)worriedaboutfoodrunningoutbefore havingmoneytobuymore,207respondents(54.6%) reportedfoodnotlastinglongenoughandnothavingmoney formore,and175respondents(46.2%)reportedboth concerns.(Table2).
TheRAsdistributed224vouchers(98.2%ofparticipants whoscreenedpositive)andobserved86(38.4%)redemptions within30daysofdistribution(Figure2).Themediantimeto voucherredemptionwasninedays(IQR9–19days).Of participantsscreeningpositiveforfoodinsecurity,98(43.0%) hadprimarycarefollow-upwithin90daysoftheED visit.Themediantimetoprimarycarefollow-upwas41days (IQR21–67days).Ofnote,39participants(17.1%of thosewhoscreenedpositiveforfoodinsecurity)neither redeemedafoodvouchernorattendedprimarycare follow-up(Table3).
Demographicdescriptionsdidnotvarygreatlybetween participantswhoredeemedavouchercomparedtothosewho didnot.However,foodvoucherredemptionwasaffectedby dischargetime:participantsdischargedduringmarket operatinghourshadahigherproportionofvoucher redemption66,41.5%)comparedtoparticipantsdischarged whenthemarketwasclosed(20,30.8%)(Appendix1).
DISCUSSION Inthisprospectivecohortstudyofadultpatientsseenata countyED,ahighproportionofrespondentsscreened positiveforfoodinsecurityandacceptedfoodvouchers; however,theredemptionrateoffoodvouchersatthe hospital’sco-locatedfoodmarketwaslowandoften occurredgreaterthanoneweekaftervoucherdistribution.
Theobservedproportionofparticipantsscreening positiveforfoodinsecurityinthisstudy(61%)isgreaterthan inpriorstudiesofEDpatients,whichhistoricallyranged from16–51%.6,9,15,18–21 Evenwhenaccountingfortheeffect oftheCOVID-19pandemic,theobservedproportionof participantsscreeningpositiveforfoodinsecurityinthis
StudyCONSORTdiagram.
Table1. Demographicdescriptionofenrolledparticipants,stratifiedbypresenceorabsenceoffoodinsecurity.
Variable
Gender, n(column%)
Allparticipants (N = 379)
Foodinsecuritypresent (n = 228)
Foodinsecurityabsent (n = 151)
Male188(49.6)106(46.5)82(54.3)
Female191(50.4)122(53.5)69(45.7)
Age, median(IQR) 53(30–58)45(32–57)40(29–59)
Race, n(column%)
Black242(63.9)149(65.4)93(61.6)
NativeHawaiian/PacificIslander1(0.2)1(0.4)0
White133(35.1)78(34.2)55(36.4)
Missing3(0.8)03
Ethnicity, n(column%)
HispanicorLatino/a34(9.0)20(8.8)14(9.4)
Non-Hispanic343(91.0)208(91.2)135(90.6)
Missing202
Accesstocare, n(column%)
PCPpriortostudy234(61.7)141(62.4)93(61.6)
IQR,interquartilerange; PCP,primarycarephysician.
studywashigherthanotherstudiesduringthisperiod, includinganidenticalscreeningprocessimplementedin outpatientclinicsatthestudysite(30–37%).4,16 Participant acceptanceofavoucherwasalsohigherthanthe65%
acceptancerateinAylmard’s2021studyandBottinoetal’ s 2017studyacceptancerateof17%.18,22 However,participant useofthefoodvoucherresourcewassimilartoprior acceptanceratesforsocialservicesreferralsandshows
Figure1.
Table2. HungerVitalSignsquestionresponsesandscreening results(N = 379).
Questionresponsen(%)
“Withinthepast12monthsweworriedwhetherour foodwouldrunoutbeforewegotmoneyto buymore” 194(51.2)
“Withinthepast12monthsthefoodweboughtjust didn’tlastandwedidn’thavemoneytogetmore
ScreeningResult
Screenedpositiveforfoodinsecurity228(60.2)
Answeredyestoonlyonequestion51(22.4)
Answeredyestobothquestions175(76.8)
Screenednegativeforfoodinsecurity151(39.8)
Table3. Foodinsecurityafterdistribution,voucherredemption,and primarycarephysicianfollow-up(n = 228).
Variablen(%)
Foodvoucher
Vouchersdistributed224(98.2) Vouchersredeemed86(38.4)
Time-to-redemption, median(IQR) 9days(9–19)
Follow-up
PCPappointmentwithin90days98(43.3)
Time-to-appointment, median(IQR) 41days(21–67)
FoodvoucherandPCPfollowup
Bothused12(5.3) Neitherused39(17.3) IQR,interquartilerange; PCP,primarycarephysician.
ofothercookingitems(eg,cookingsprayorutensils),ifthose wereneededmorethanfooditems.Additionally,thestudy protocolalloweddistributionofperishablefood,whichhas rarelybeenofferedinsimilarED-basedprograms.These differenceshighlightkeytradeoffsbetweentwodifferent approaches:theeaseofpre-made,ED-distributedfoodbags vsthecustomizabilityofapatientsshoppingforthemselves. Futureworkshouldfurthercharacterizepatientpreferences betweenthesestrategiestoprovidecriticalinsightsintothe circumstancesinwhichoneispreferredovertheotherby patientswithsocialneeds.
Figure2. Frequencyofscreeningtoolcompletion,positive screeningforfoodinsecurity,voucheracceptancebypatient, andvoucherredemption.
similarutilizationofsummerfoodprogramsthataddressed foodinsecurityatachildren’sED.18,23
ThisstudybuildsupontheworkofJahnesetal(2020), whichaddressedasimilarproblemthroughadifferent approach:theauthorsimplementedaprograminwhich patientsweregivenabagoffoodatthetimeofdischarge withoutexaminationofeligibilitycriteriaorfurther documentation.Bagsincludedshelf-stablefoodaswellas “no-cookbags” forindividualswithoutcooking infrastructure.The firstnotabledifferenceinresultsisthat 3,000foodbagsweredistributedbyJahnesetalasopposed to226foodvouchersinthisstudy.Whilethemonetaryvalue ofeachfoodbaginJahnesetalisnotknown,evenifone assumedacostof$10perbag,morefoodwasdistributedin anoperationalprogramfocusedonfooddistributionrather thaninthisresearchstudy.Thesecondnotabledifference wasthatthisstudy’sapproachallowedparticipantstochoose whatoptionsbestservedtheirneeds,includingthepurchase
Itwasunexpectedthatdespitehighacceptanceratesof foodvouchers,lessthanhalfofallparticipantsredeemeda voucherattheco-locatedhospitalfoodmarket.Aconceptual explanationofthisdiscrepancycouldbesocialriskvssocial need;whilethescreeningidentifiedasocialrisk(ie,an adversesocialconditionassociatedwithpoorhealth)and providedresourcesdirectedatreducingasocialrisk, participantsmaynothaveperceivedfoodasasocialneed (ie,anadversesocialdeterminantofhealthforwhichthey wouldhavelikedassistanceandviewedasapriority).24
However,thisisconsideredlesslikelyduetothemedian redemptiontimeoffoodvouchersofninedays,suggesting thatusingthevoucherwasimportantenoughtoreturnfor redemption.Apragmaticexplanationoftheobserved discrepancyisthatthefoodmarketwasinitiallydesignedfor afoodinsecurityscreeningandinterventionintheoutpatient primarycaresetting(ie,weekdays,daytimehours),rather thantheEDsetting(ie,alldaysandhours).The misalignmentbetweenEDscreeningtimesandmarkethours appearstohavemodifiedtheeffectoffoodvoucher distributiononredemptionrates.Theoverallredemption ratewas38.9%;redemptionrateforindividualsdischarged duringmarkethourswas41.5%,whiletheredemptionrate forindividualsdischargedaftermarkethourswas30.8%). Theseresultsshouldpromptfurtherconsiderationofunique
aspectsofEDoperationswhendesigningfuturefood insecurityinterventionswithinahospitalsystem.
Itwasalsosurprisingthatnearly60%ofparticipants experiencingfoodinsecurityhadanestablishedprimarycare doctorpriortotheirEDevaluation.This findingcontrasts withRobinsonetal’s2018study,whichfoundfoodinsecurity wasassociatedwithlackofprimarycare.3 Whilethisstudy wasnotdesignedtodeterminewhetherpreviousprimarycare appointmentshadscreenedfororaddressedfoodinsecurity, participantwillingnesstodiscloseasocialriskduringtheED encounteralignswithCullenetal’s2019study,whichfound thatfamiliesweremorecomfortablewithsocialdeterminants screeningintheEDratherthantheprimarycaresettingand supportsongoingeffortstoscreenforsocialneedsintheED.25 Theobservedfollow-uprateoflessthan50%andtimeto primarycareappointmentexceedingonemonthareconsistent withpriorobservationsbyLooetal(2013),Wallaceetal (2021),andZuetal(2006).11,12,19
These findingsalsohighlighttheimportantroleoftheED inaddressingsocialrisksthatareidentifiedduringED screening.Ifscreenedrisksarenotaddressed(andinstead referredtooutpatientphysicians),follow-upmaynotoccur foruptoonemonth.Oneconceptualquestionthatremains unanswerediswhatservices(eg,primarycare,socialwork, casemanagement,nutrition/dietetics,communityagencies, ormultidisciplinaryteamseitherinpersonorvirtually)are mostappropriatetoreferpatientstoaftertheyscreenpositive forasocialneed,suchasfoodinsecurity,intheED.The studyprotocoloptedtoreferparticipantsbacktotheir primarycarephysicianbecausefoodinsecuritywouldlikely requireamorecomprehensivesocialneedsassessment,but researchersinfuturestudiesmaywishtoconsideralternative strategiestoaddressthisquestion.
LIMITATIONS Thestudydesignwasatriskofselectionbias,participation bias,andcontaminationbias.Selectionbiasoccurredduring inclusion/exclusionwhereinindividualsarrivingoutsidethe studyhours,individualswithpsychiatricillness,patients presentinginextremis,minors,andindividualswhocould notprovidewrittenconsentinEnglishwereexcluded. Althoughsubsequentqualityimprovementprojectshave addressedthesepopulations,theresearchresultspresented herearenotgeneralizabletopatientsoutsidethestudy population.Participationbiasmayhaveoccurredduetothe ethicsrequirementtodisclosetherisksandbenefitsofstudy participation,includingafoodvoucherwithmonetaryvalue; thismayalsoexplainthehigher-than-expectedproportionof participantsscreeningpositiveforfoodinsecurityamongthe studypopulation.Additionally,participationbiasmayhave occurredusingawrittenscreeningtoolthatmayhavemade individualswithlowliteracylesslikelytoparticipate,even thoughtheRAprotocolincludedofferingthatthescreening questionsbereadaloud.
Thesingle-centerstudydesignwithoutlongitudinal contactwithstudyparticipantslimitsourabilitytocomment oncontaminationbias;itispossiblethatpatientsobtained connectiontocarefromexternalresourcesratherthanthe study’svoucherprogramandprintedresourcesanddidnot usetheprovidedvoucherforthisreason.Thelowredemption rateoffoodvoucherswasunexpected,andthestudydesign andinformedconsentdidnotallowfurtherinvestigationinto thereasonsforthelowproportionofvoucherredemption; thus,conclusionsaboutthecausesofthis findingarelimited. Finally,theuniqueaspectsofprojectfundingandmarket locationlimitthisstudy’sgeneralizabilitytosimilarhealth systemswithsimilaravailableresources.
CONCLUSION Ahighproportionofstudyparticipantsscreenedpositive forfoodinsecurityandacceptedafoodvoucherforacolocatedresourceaddressingthissocialrisk;however,voucher redemptionrateswerelowandoccurredgreaterthanone weekfollowingdistribution.Theseresultsimplythatfood insecurityscreeningandvoucherdistributionarefeasible, butthatco-locationofresourcesalonemaynotcompletely addressthesocialriskandshouldpromptconsiderationof resourceaccessibility(bothlocationandhours), customizability,andpatientpreferencesintreatingsocial needsidentifiedintheemergencydepartment.
AddressforCorrespondence:AlexanderJ.Ulintz,MD,TheOhio StateUniversityCollegeofMedicine,DepartmentofEmergency Medicine,750PriorHall,376W10th Avenue,Columbus,Ohio 43210.Email: alexander.ulintz@osumc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudywasfundedbyaninternal grantwithintheIndianaUniversitySchoolofMedicineDepartmentof EmergencyMedicine.Theauthorsreporttherearenocompeting intereststodeclare.Therearenootherconflictsofinterestorsources offundingtodeclare.
Copyright:©2024Ulintzetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.AlderwickHandGottliebLM.Meaningsandmisunderstandings:a socialdeterminantsofhealthlexiconforhealthcaresystems. MilbankQ. 2019;97(2):407–19.
2.GordonJA.Thehospitalemergencydepartmentasasocialwelfare institution. AnnEmergMed.Mar1999;33(3):321–5.
3.RobinsonT,BryanL,JohnsonV,etal.Hunger:amissedopportunityfor screeninginthepediatricemergencydepartment. ClinPediatr(Phila). 2018;57(11):1318–25.
4.EnayatiD,ChanV,KoenigG,etal.ImpactofCOVID-19pandemicon foodinsecurityinanurbanemergencydepartmentpatientpopulation. WestJEmergMed. 2023;24(2):127–34.
5.KerseyMA,BeranMS,McGovernPG,etal.Theprevalenceandeffects ofhungerinanemergencydepartmentpatientpopulation. AcadEmerg Med. 1999;6(11):1109–14.
6.BirosMH,HoffmanPL,ReschK.Theprevalenceandperceivedhealth consequencesofhungerinemergencydepartmentpatientpopulations. AcadEmergMed. 2005;12(4):310–7.
7.NhoungHK,GoyalM,CacciapuotiM,etal.Foodinsecurityandinsulin useinhyperglycemicpatientspresentingtotheemergencydepartment. WestJEmergMed. 2020;21(4):959–63.
8.MenF,UrquiaML,TarasukV.Pain-drivenemergencydepartmentvisits andfoodinsecurity:across-sectionalstudylinkingCanadiansurveyand healthadministrativedata. CMAJOpen. 2022;10(1):E8–E18.
9.EstrellaA,ScheidellJ,KhanM,etal.Cross-sectionalanalysisoffood insecurityandfrequentemergencydepartmentuse. WestJEmergMed. 2021;22(4):911–8.
10.WalkerRJ,ChawlaA,GaracciE,etal.Assessingtherelationship betweenfoodinsecurityandmortalityamongU.S.adults. AnnEpidemiol. 2019;32:43–8.
11.WallaceAS,LutherBL,SislerSM,etal.Integratingsocialdeterminants ofhealthscreeningandreferralduringroutineemergencydepartment care:evaluationofreachandimplementationchallenges. ImplementSci Commun. 2021;2(1):114.
12.ZunLSandDowneyL.Adulthealthscreeningandreferralinthe emergencydepartment. SouthMedJ. 2006;99(9):940–8.
13.JahnesK,HopkinsK,FooteE,etal.(2020).Foodbagprogramto addresstheimmediatefoodneedsofpatientsduringtheCOVID-19 crisis.In: COVID-19:AnnFamMed[Preprint].Availableat: https://deepblue.lib.umich.edu/handle/2027.42/156010 AccessedAugust31,2023.
14.HagerE,QuiggA,BlackM,etal.Developmentandvalidationofa 2-itemscreentoidentifyfamiliesatriskforfoodinsecurity. Pediatrics. 2009;126(1):26–32.
15.GonzalezJV,HartfordEA,MooreJ,etal.Foodinsecurityinapediatric emergencydepartmentandthefeasibilityofuniversalscreening. WestJ EmergMed. 2021;22(6):1295–300.
16.ReinosoD,HautD,ClaffeyS,etal.Addressingfoodinsecurity:lessons learnedfromco-locatingafoodpantrywithafederallyqualifiedhealth center. IntJIntegrCare. 2022;22(3):24.
17.HealthE.Freshforyoumarketprovideseskenazihealthfrontline staffaccesstogroceryitems.2020.Availableat: https://www. eskenazihealth.edu/news/fresh-for-you-market-provides-eskenazihealth-frontline-staff-access-to-grocery-items AccessedAugust29,2022.
18.AylwardAF,EngelbergAndersonJ,MorrisA,etal.Usingmalnutrition andfoodinsecurityscreeningtoidentifybroaderhealth-relatedsocial needsamongstolderadultsreceivingemergencydepartmentcarein theSoutheasternUnitedStates:across-sectionalstudy. HealthSoc CareCommunity. 2021;29(6):e420–30.
19.LooS,AndersonE,LinJG,etal.Evaluatingasocialriskscreeningand referralprograminanurbansafety-nethospitalemergencydepartment. JAmCollEmergPhysiciansOpen. 2023;4(1):e12883.
20.MinerJR,WestgardB,OlivesTD,etal.Hungerandfoodinsecurity amongpatientsinanurbanemergencydepartment. WestJEmergMed. 2013;14(3):253–62.
21.ShararehN,WallaceAS,BrintzBJ,etal.Associatedfactorswithpatientreportedunmetfoodneedsamongemergencydepartmentadult patients-Asocialneedperspective. PrevMedRep. 2022;29:101974.
22.BottinoCJ,RhodesET,KreatsoulasC,etal.Foodinsecurityscreening inpediatricprimarycare:Canofferingreferralshelpidentifyfamiliesin need? AcadPediatr. 2017;17(5):497–503.
23.CullenD,BlauchA,MirthM,etal.Completeeats:Summermeals offeredbytheemergencydepartmentforfoodinsecurity. Pediatrics. 2019;144(4):e20190201.
24.MolinaMF,LiCN,ManchandaEC,etal.Prevalenceofemergency departmentsocialriskandsocialneeds. WestJEmergMed. 2020;21(6):152–61.
25.CullenD,WoodfordA,FeinJ.Foodforthought:aRandomizedtrialof foodinsecurityscreeningintheemergencydepartment. AcadPediatr. 2019;19(6):646–51.
TheCaliforniaManagedCareOrganizationTaxandMedi-Cal PatientsintheEmergencyDepartment LaurenMurphy,MS*†
GitaGolonzka,BS‡
EllenShank,MD§ JorgeFernandez,MD†
*CaliforniaStateUniversity,Chico,Chico,California † CaliforniaChapteroftheAmericanCollegeofEmergencyPhysicians, Sacramento,California ‡ UniversityofCaliforniaSanDiego,SchoolofMedicine,LaJolla,California § UniversityofCaliforniaDavisHealth,DepartmentofEmergencyMedicine, Sacramento,California
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedSeptember1,2024;RevisionreceivedSeptember4,2024;AcceptedSeptember6,2024
ElectronicallypublishedSeptember19,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.35257
Lastweek,Timothy*,a60-year-oldunhousedgentleman, presentedtotheEDrequestingmedicalclearance.When askedwhy,heexplainedthathewasstayingatawarming centerandhadbeenseparatedfromhiswifeandquarantined inaseparatesleepingspaceduetoconcernsthathewas infectious.Hethendoffedhisbeaniecaptoreveala10 × 10centimeterfungatingsquamouscellcarcinomathathadbeen thrivingonhisscalpforthepasttwoyears.Hehadmoved countiesafewyearsbackandsincethenhadhaddifficulty reestablishingandunderstandinghiscoveragewithina geographicallymanagedcaresystem.Hewasonthewaiting listtoseeadermatologistwhoacceptedMedi-Cal (California’sversionofUSMedicaidhealthinsuranceforthe poor).Furtherchartreviewrevealedthat,followingatleast threeEDvisits,hehadbeenreferredtohealthnavigatorsto trytosecureadermatologistappointment;buthehadbeen waitingoverayearandnowwassimplyrequestingmedical clearancetobereunitedwithhiswife.Thiscasewasastark exampleofthearduousbarrierssomepatientsinCalifornia mustovercometoreceivecareandthehurdlesthat emergencyphysicians(EP)mustsurmounttohelpthese coveredpatientsaccessthefollow-upcaretheyrequire.
HISTORYOFTHEMANAGEDCARE ORGANIZATION(MCO)TAX Medi-Calisfundedthroughstateandfederaldollars.The federalgovernmentusestheFederalMedicaidMatching RatetocalculatehowtomatchstatespendingonMedicaid programs.ForeverydollarspentonMedicaid,astatecan receiveatleast$1inMedicaidfederal financialparticipation (FFP)funding.Becausemanystatesstruggledtogenerate enoughrevenuetocovertheirshareofMedicaidcosts,in 1985theHealthCareFinancingAdministrationallowed statestoacceptdonationsfromprivatemedicalcare providersanddeemedthesedonationseligibleforFFP matching.1 In2006,Congressgavestatestheauthoritytotax
providers,includingmanagedcareorganizations(MCO),to meettheirshareofMedicaidspending.2 Accordingtothe MedicaidandChildren’sHealthInsuranceProgram PaymentandAccessCommission,49statesusedsomeform ofprovidertaxtofundtheirMedicaidprogramsin2019.3
CaliforniahasusedanMCOtaxforover20yearsto receivefederalFFPmatchingfunds.Thetaxmustbe authorizedbythelegislatureandissubjecttofederal approval.Theauthorizinglegislationincludesanenddate forthetax,requiringittobereauthorizedperiodically. Historically,Californiahasusedthemoniesgenerated byFFPdollarstobackfilltheGeneralFunddeficitor tofundanarrayofpublicservicesandsystemsoutsidethe Medi-Calprogram.4
2023MANAGEDCARETAXAGREEMENT WhentheauthorizinglegislationforthepreviousMCOtax wasnearingitssunsetdate,acoalitionofprovidersand healthcarefacilitiescametogethertonegotiateanewMCO taxagreement.Theproposalbythecoalitionwastodedicate theadditionalfundstoprovideaMedi-Calrateincreasefora varietyofhealthcareproviders.Theincreasewasproposedto rolloutoveraseriesofyears.Inthe first fiscalyear2023–24,a subsetofprimarycareclinicians,reproductivehealthservices, andsomeoutpatientmentalhealthserviceswouldreceive increaseseffectiveJanuary1,2024.Italsoproposedto appropriate$1.28billionforprimarycarerateincreasesand $1.15billioninspecialtyrateincreaseseffectiveJanuary1, 2025.5 Therewereadditionalfundsallocatedforfacilitiesand transport,reproductivehealth,andmentalhealththatwould alsotakeeffectin2025.ThecoalitionarguedthatCalifornia’ s Medi-Calreimbursementrateswereobjectionablylow, forcingclinicianstolimitthenumberofMedi-Calpatients theysee,therebylimitingpatientaccesstocare.
AstheLegislaturewasconsideringthecoalitionproposal, theCaliforniaChapteroftheAmericanCollegeof
EmergencyPhysician(CalACEP)advocacyteamlobbied foraspecificpooloffundingexclusivelyforEPs,arguingthat thefundingwasnecessaryduetotheirexclusionfrom previousMedi-Calphysicianincreasesandtheir disproportionatecarefortheMedi-Calpopulationrelativeto otherclinicians.Asaresultofitsadvocacy,a$200million statebudgetlineitemwasincludedtobringEMMedi-Cal ratesto87.5%ofMedicare.6
MAYREVISIONANDFINALBUDGET Theagreementbetweenthecoalition,CalACEP,andthe CaliforniaLegislaturewascodifiedinlegislationin2023and wasscheduledtotakeeffectJanuary1,2025.However, becausethestatebudgetisonlyaone-yeardocumentandthe Legislaturedoesnothavethesolepowertocreatethestate’ s budget,theMCOtaxagreementforthe2024–25 fiscalyear wassubjecttonegotiationonceagainbetweenthe Legislatureandthegovernor.GovernorNewsomincluded theagreedrateincreasesinhisproposedbudgetreleasedin January2024,buthisrevisedbudgetreleasedinMay removedtherateincreaseentirelyandusedtheMCOtax surplustobackfillCalifornia’sGeneralFunddeficit.7
TheCalACEPadvocacyteamusedavarietyofstrategiesto lobbylegislatorstorestorethe$200millionforEPrate increases.StafflobbiedmembersoftheBudgetSubcommittees inpersonforeachhouseoftheLegislaturetoexplainthe impactoflowreimbursementonemergencymedicinepractice andhowiteffectsaccesstocareforpatients.Staffalso coordinatedatargetedsocialmediacampaignthatfocusedon theSacramentoareatokeeptheissueinthemindsof stakeholders.MembersoftheCalACEPExecutiveCommittee wroteletterstotheeditorsofmajornewsorganizations throughoutthestate.Finally,CalACEPcoordinateda grassrootscampaigntoencourageEPstocontactlegislators directlyandtellpersonalstoriesabouttheirpatientsandMediCalaccess.Ultimately,the$200millionforEPrateincreases were includedinthebudgetthatGovernorNewsomsignedon June29,2024.However,noneoftheotherpreviouslypromised rateincreasesforotherspecialties,whichhadbeenscheduledto takeeffectJanuary1,2025,wereincluded.
PROPOSITION35 WhileEPswereabletogettheirincreaserestored,other physicianswerenotsofortunate.TheCaliforniaMedical Association,withthesupportoforganizationsthatwerea partofthe2023MCOcoalition,qualifiedaninitiativeforthe 2024CaliforniaStateBallotthat,ifpassedbyCalifornia voters,wouldpermanentlyenshrinetheagreementreached bytheCoalitionandtheLegislaturein2023intolaw. Proposition35wouldrequirethestatetousetheMCOtax revenuestofundincreasesfortheMedi-Calprogramforthe durationofthecurrentMCOtaxauthorization.Thiswould restoretherevokedMedi-Calrateincreasesforother cliniciansandprotecttheEPincreaseforyearstocome,
withouthavingtorenegotiatewiththeLegislatureand governoreveryyear,asistypicallyrequiredbytheannual budgetprocess.AsofAugust2024,thepropositionseemsto havebroadbipartisansupport.Numeroushealthcare organizationsincludingtheCaliforniaMedicalAssociation, PlannedParenthood,theCaliforniaHospitalAssociation, andCalACEPformallysupporttheproposition.Other supportersincludetheCaliforniaHawaiiStateConference NationalAssociationfortheAdvancementofColored People,theInsuretheUninsuredProject,theCalifornia DemocraticParty,andtheCaliforniaRepublicanParty.8
Thepropositionhasnoregisteredopposition,but GovernorNewsomhasexpressedseriousconcernsinthe pressabouttheimpactthepropositionwillhaveonthe abilityoftheLegislatureandgovernortodeliverabalanced budgetinthefuture.9
IMPACTONPATIENTSANDCLINICIANS Emergencydepartments(ED)areuniquelypoisedto sufferthestrainofinsufficientMedi-Calfunding,aspatients coveredbyMedi-CalseekcareintheEDathigherratesthan patientswithothertypesofinsurance.Since2019,oneof threeCaliforniansarecoveredbyMedi-Cal,10 but42%of visitstotheEDarebyMedi-Calpatients.11 Thisdiscrepancy islargelydrivenbylowphysicianparticipationinMedi-Cal. California’slowMedi-Calreimbursementratesfor physiciansresultinveryfewprimarycarephysiciansand specialistswhoacceptpatientswithMedi-Calandlongwait times.12 Thisoftenleavesthesickestandmostvulnerable patientswithnowheretogoexcepttheED.Emergency physiciansoperateundertheEmergencyMedicalTreatment andLaborAct,enactedin1986,whichensuresthatall patientsarrivingintheEDwillreceivetreatmentregardless ofinsurancestatusorabilitytopay.Giventhecurrentstate ofMedi-Calfunding,EPsareforcedtonavigatenotonly direlysickandurgentcases,butto fillgapsforpreventiveand specialtycare.Thisleavesthemscramblingto findand coordinatefollow-upcare.Italsoleavesthemwiththemoral injuryofshowinguptoshiftsdayinanddayoutwithout beingabletogettheirpatientsthetransferandfollow-upcare theyneed.ThisistakingatollonpatientsandEPsalike. WhileEPsareproudtohelppatientswhentheyneedit most,thecurrentfundingconditionsareunsustainable. DespitethenumberofEDpatientsincreasing,underfunded departmentsaredecreasingthenumberofEPsworking,and insomecasesareemployingmorephysicianassistantsand nursepractitioners.13 Inturn,Californiafacesdifficultyin hiringandretainingwell-qualifiedandexperiencedEPs, particularlyinhistoricallyunder-resourcedareas.14 These changesimpactallEDpatientsintheformoflongerwait timesand,intheworstcases,poorpatientoutcomes. TheimpactofMedi-Calunderfundingreverberatesfar beyondemergencyservices,especiallyasMedi-Caleligibility criteriaexpands.Underthecurrentfundingscheme,an
increasingnumberofpatientscoveredbyMedi-Calin California’shealthcaresystemwillresultindeeperinequity, asmoreMedi-Calpatientsarecompetingforthesamefew spotsfromalimitednumberofphysicians.Aproportional increaseinaccesstophysiciansisneeded,andthismustcome intheformofincreasedfunding,suchastheMedi-Calrate increasesoutlinedinProposition35.
Emergencyphysiciansneedasufficientnetworkof primarycareandspecialtyphysicianswillingtoacceptMediCaltoprovidecomprehensiveandtimelycaretopatients. AdequatenetworkswouldenablepatientslikeTimothyto receivethecaretheyneed,whentheyneedit,asopposedto thecurrentsystemofbacklogandwaiting.Increasing reimbursementtomorecloselymatchthecostofcare,and protectingdedicatedfunds,willimproveefficiencyand equityinthehealthcaresystem,ultimatelyimprovingthe qualityofcareforallCalifornians.
*Patientnamehasbeenchangedtoprotectconfidentiality.
AddressforCorrespondence:LaurenMurphy,MS,PublicHealth& HealthServicesAdministration,400W.FirstSt.,Chico,CA95929. Email: LAMurphy@csuchico.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.LaurenMurphyisapaidemployeeof CalACEP.EllenShankisaHealthPolicyfellowatUCDavisandnonvotingmemberoftheCalACEPboardofdirectors.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Murphyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.KuLandCoughlinTA.1995.Medicaiddisproportionateshareandother special financingprograms. HealthCareFinancRev. 1995;16(3):27–54.
2.109thCongress.2006.S.1932-DeficitReductionActof2005.
3.MACPAC.Healthcare-relatedtaxesinMedicaid.2021.Availableat: https://www.macpac.gov/wp-content/uploads/2020/01/HealthCare-Related-Taxes-in-Medicaid.pdf .AccessedAugust21,2024.
4.CaliforniaLegislativeAnalyst’sOffice.TheMCOtaxpackageatMay revision.2024.Availableat: https://lao.ca.gov/Publications/Report/ 4905.AccessedAugust21,2024.
5.CaliforniaDepartmentofFinance.2024enactmentbudget summary-HealthandHumanServices.2024a.Availableat: https:// ebudget.ca.gov/2024-25/pdf/BudgetSummary/ HealthandHumanServices.pdf.AccessedAugust21,2024.
6.CaliforniaDepartmentofFinance.Budgetsummary.2024c. Availableat: https://ebudget.ca.gov/2024-25/pdf/Enacted/ BudgetSummary/HealthandHumanServices.pdf AccessedAugust21,2024.
7.CaliforniaDepartmentofFinance.2024–25Mayrevisionbudget summary.2024.Availableat: https://ebudget.ca.gov/2024-25/pdf/ Revised/BudgetSummary/FullBudgetSummary.pdf AccessedAugust21,2024.
8.CaliforniaSecretaryofState.Officialvoterinformationguide. 2024.Availableat: https://voterguide.sos.ca.gov/ AccessedAugust21,2024.
9.LaL.NewsomsoundsoffonCAballotmeasuresoncrime,health insurance.2024.Availableat: https://calmatters.org/newsletter/ newsom-ballot-measures/.AccessedAugust21,2024.
10.McConvilleS,DanielsonC,HsiaR.Emergencydepartmentusein California:demographics,trends,andtheimpactoftheACA.2022. Availableat: https://www.ppic.org/publication/emergency-departmentuse-in-california-demographics-trends-and-the-impact-of-the-aca/ AccessedAugust21,2024.
11.CaliforniaHealthCareFoundation.Californiaemergencydepartments: acriticalsourceofcare.2021.Availableat: https://www.chcf.org/ wp-content/uploads/2021/12/EmergencyDepartmentsAlmanac2021. pdf.AccessedAugust21,2024.
12.IbarraA.CaliforniawantstoincreasepayforsomeMedi-Calproviders. Howitmighthelppatientsaccesscare.2023.Availableat: https://laist. com/news/health/california-wants-to-increase-pay-for-some-medi-calproviders-how-it-might-help-patients-access-care AccessedAugust21,2024.
13.WuFandDarracqMA.Comparingphysicianassistantandnurse practitionerpracticeinU.S.emergencydepartments,2010–2017. WestJEM. 2021;22(5):1150–5.
14.PreiksaitisC,KrzyzaniaketS,BowersK,etal.Characteristicsof emergencymedicineresidencyprogramswithunfilledpositionsinthe 2023match. AnnEmergMed. 2023;82(5):598–607.
AReviewoftheClinicalPresentation,Causes,andDiagnostic EvaluationofIncreasedIntracranialPressureinthe EmergencyDepartment CristianaOlaru,MD,MSCE
SamLangberg,MD
NicoleStreiffMcCoin,MD
SectionEditors:RichardLucarelli,MD
OchsnerHealth,DepartmentofEmergencyMedicine,NewOrleans,Louisiana
Submissionhistory:SubmittedOctober8,2023;RevisionreceivedFebruary6,2024;AcceptedMay6,2024
ElectronicallypublishedSeptember6,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18500
Increasedintracranialpressure(ICP)isencounteredinnumeroustraumaticandnon-traumaticmedical situations,anditrequiresimmediaterecognitionandattention.Clinically,ICPtypicallypresentswitha headachethatismostsevereinthemorning,aggravatedbyValsalva-likemaneuvers,andassociated withnauseaorvomiting.Papilledemaisawell-recognizedsignofincreasedICP;however,emergency physiciansoften finditdifficulttovisualizetheopticdiscusingophthalmoscopyortoaccuratelyinterpret digitalfundusphotographswhenusinganon-mydriaticretinalcamera.
Emergencyultrasoundcanevaluatetheopticnervesheathdiameter(ONSD)andopticdiscelevation todeterminewhetherincreasedICPispresent,however,thestudieshavebeensmallwithdifferent definitionsandmeasurementsoftheONSD.TheONSDthresholdvaluesforincreasedICPhavebeen reportedanywherefrom4.8to6.3millimeters.
Neuroimagingisthenextstepintheevaluationofpatientswithpapilledemaorhighclinicalsuspicion ofincreasedICP,asitcanidentifymoststructuralcausesortypicalradiologicalpatternsofincreased ICP.NeuroradiographicsignsofincreasedICPcanbehelpfulinsuggestingidiopathicintracranial hypertension(IIH),especiallywhenpapilledemaisabsent.
Patientswithpapilledemaandnormalneuroimagingmayundergolumbarpunctureaspartoftheir clinicalworkup.Thecerebrospinal fluid(CSF)openingpressureremainsoneofthemostimportant investigationstoestablishthediagnosisofIIH.ACSFevaluationisalsorequiredtoexcludeotheretiologies ofelevatedICPsuchasinfectious,inflammatory,andneoplasticmeningitis.InvasiveICPmeasurement remainsthestandardtomeasureandmonitorthiscondition.[WestJEmergMed.2024;25(6)1003–1010.]
INTRODUCTION Increasedintracranialpressure(ICP),regardlessof etiology,isalife-threateningconditionthatrequiresprompt diagnosisandtreatment.Itcanleadtodecreasedcerebral perfusionpressurewithsubsequentcerebralischemiaand herniation,andthuspotentialdisabilityandincreased mortality.1 RecognitionofelevatedICPisofutmost importanceintheemergencydepartment(ED).Knowledge oftheclinicalpresentation(whichcanhelpdifferentiatenot onlybetweenmultiplecausesofheadacheandalteredmental statusbutalsobetweencausesofelevatedICP)and diagnosticoptionsandtheiraccuracyisparamountfor correctdiagnosisandrapidtreatment.
TheMonro-Kelliehypothesisstatesthatthesumofthe intracranialvolumeofblood,brain,cerebrospinal fl uid (CSF),andothercomponents(eg,tumor,hematoma)is constant.Theskullisarigidcontainer;hence,anincreasein oneoftheintracranialcomponentswillcauseadecreasein thevolumeofoneormoreoftheothercomponents. Intracranialblood(especiallyinthevenouscompartment) andCSFarethetwocomponentswhosevolumecan adaptmosteasilytoaccommodateanincreaseinthe volumeofintracranialcontents.Whenthecompensatory capacityisexhausted,theICPbeginstorise,compromising cerebralperfusionandcausingcerebralischemiaor herniation.NormalICPis7–15millimetersofmercury
(mmHg)or10–20centimetersofwater(cmH 2O) inadults. 1, 2
CerebralperfusionpressureCPPðÞ = MeanarterialpressureMAPðÞ intracranialpressureICPðÞ
CAUSESANDCLINICALPRESENTATION IncreasedICPiscausedbyavarietyofdiseaseprocesses suchasspace-occupyinglesions(eg,mass,hemorrhage); obstructivehydrocephalus;communicatinghydrocephalus (eg,inadequatereabsorptionofCSFsuchasseenin subarachnoidhemorrhagesecondarytohypersecretionof CSFand fibrosisofarachnoidgranulations);venousoutflow obstruction(eg,cerebralvenoussinusthrombosis);diffuse cerebraledema(eg,vasogenic,asseenintumors;cytotoxic, asseenintraumaticbraininjuryorstroke;interstitial,asseen inhydrocephalusormeningitis;orosmotic,suchasseenin hyponatremia,diabeticketoacidosis);increasedCSF secretion(eg,choroidplexustumor);andidiopathiccauses (eg,idiopathicintracranialhypertension[IIH]).3,4,5
Thecombinationofheadache,papilledema,andvomiting isconsideredindicativeofincreasedICP,althoughthereisno consistentrelationbetweenseverityofsymptomsandthe degreeofelevatedICP.2 Headacheisacommoncomplaintin theED,representing2.6%ofEDvisits,andthesixthmost commonreasonforpresentationtotheED.6 Theheadache relatedtoincreasedICPistypicallyaglobalheadache commonlydescribedasthrobbingorbursting,ismostsevere inthemorning,oftenaggravatedbymaneuversthatincrease ICP(eg,Valsalva-likemaneuvers,coughing,sneezing, recumbency),andisassociatedwithnauseaorvomiting.3
OthersignsandsymptomsofincreasedICPincludechangesin behaviorsuchasirritabilityandrestlessness,visualchanges (eg,diplopia,visual fielddeficits),pupillarychanges(dilated unreactive,mid-position fixed,pinpointpupils),bilateral ptosis,impairedupwardgaze,focalneurologicdeficits, depressedconsciousness,seizures,andtheominous findingsof decorticateordecerebrateposturingandCushingtriad (bradycardia,hypertension,andrespiratorydepression).
Aprogressivedeteriorationinlevelofconsciousnesscan beseenwithworseningincreasedICP(exceptforIIH,which ischaracterizedbynormalmentalstatus).2 Brainherniation leadstofurtherbraininjuryandischemia,compressionof vesselsandcranialnerves,andobstructionofthenormal circulationofCSFproducinghydrocephalus.(See Figure1 fortypesofbrainherniation.)Owingtoitslocation, eachtypeofherniationisassociatedwithspecific neurologic findings.7
Subfalcineherniation,alsoknownasmidlineshiftor cingulateherniation,isthemostcommontypeofherniation. Itisusuallycausedbymasseffectthatpushestheipsilateral cingulategyrusdownandunderthefalxcerebri.The
Figure1. Typesofbrainherniation11:1)subfalcineherniation; 2)centraldescendingtranstentorialherniation;3)lateral descendingtranstentorialherniation;4)tonsillarherniation;and 5)ascendingcerebellartranstentorialherniation.
AdaptedfromUser:Delldot,CCBY-SA3.0 <http:// creativecommons.org/licenses/by-sa/3.0/>,version21:08, 5March2008viaWikimediaCommons.
quantificationofthemidlineshiftismadebymeasuringthe deviationoftheseptumpellucidumcomparedtomidlineat theleveloftheforamenofMonro.Thismeasurementisused forprognosiswithlessthan5millimeters(mm)ofdeviation associatedwithgoodprognosisandgreaterthan15mm associatedwithpoorprognosis.Itcanpresentwith hypobulia,apathy,andindifference.Iftheanteriorcerebral arteryiscompressed,itwillmanifestwithcontralateralor bilaterallegweaknessandacuteurinaryretention.7
Descendingtranstentorialherniationisthesecondmost commontypeofcerebralherniation.Itoccurswhenbrain tissueisdisplaceddownwardthroughthetentorialnotchand maybelateral(anteriorandposterior)orcentral.Lateral herniasinvolvethemedialtemporallobe;anteriorhernias involvetheuncus(alsocalleduncalherniation);and posteriorherniasinvolvetheparahippocampalgyrus.Inthe centralhernia,thereisdescentofthediencephalon, midbrain,andpons.7
Anteriordescendingtranstentorial(uncal)herniation leadstocompressionoftheparasympathetic fibersrunning withthethirdcranialnerve,causinganipsilateral fixedand dilatedpupil.Compressionoftheipsilateralcerebral pedunclewillcausecontralateralmotorparalysissincethe motortract fiberscrossbelowthislevel;however,the contralateralcerebralpedunclecanbecompressedagainst theedgeofthetentoriumcausingafalselocalizingsignwith ipsilateralhemiparesis.8 Posteriordescendingtranstentorial
herniationisduetoherniationoftheparahipoccampalgyrus, presentingwithsymptomsofParinaudsyndrome(vertical gazepalsy,lossofpupillaryreflextolightwithpreservation ofpupillaryconstrictionwithconvergence,uppereyelid retraction,convergence-retractionnystagmus).9,10 Central descendingtranstentorialherniationisduetoherniationof thethalamusandmidbrainthroughthetentorialnotchand themedullathoughtheforamenmagnum.Itcausesacute obstructivehydrocephalusandposteriorcerebralartery injury,clinicallypresentingwithagitationfollowedby obtundation,bilaterallypoorlyreactiveorpotentially midpoint fixedpupils,andthendecorticatefollowedby decerebrateposturing,Cushingtriad,coma,anddeath.9
Ascendingcerebellartranstentorialherniationisdueto cerebellarherniationsuperiorlythroughthetentorialnotch. Itpresentswithsymptomsofpontomedullarycompression: obtundation;cardiorespiratoryinstability;severe bradycardia;arrhythmia;abdpinpointpupils.9 Tonsillar herniationinvolvesherniationofthetonsilsofthecerebellum throughtheforamenmagnumintotheupperspinalcanal, compressingthemedulla.Thismayresultin cardiorespiratoryimpairment,hypertension,highpulse pressure,andCheyne-Stokerespiration.Thecombinationof bradycardia,hypertension,andirregularrespirationsis knownasCushing’ sreflexandoccursinapproximatelyone thirdofcasesoftonsillarherniation.2 Itmayalsocause pinpointpupils, flaccidparalysis,andsuddendeath.
Idiopathicintracranialhypertension,formallyknownas pseudotumorcerebriorbenignintracranialhypertension, deservesspecialattentionasithasauniquepresentation.Itis asyndromeofincreasedICPofunclearetiologythatoccurs mostofteninobesewomenofchildbearingage(averageage 28years).Itoccurslessofteninmen(approximately9%)who areusuallyobeseandaverage37yearsofageatdiagnosis.12
Itisusuallyadiagnosisofexclusionthatischaracterizedby signsandsymptomsofincreasedICP,normalmentalstatus, andabsenceoffocalneurologicsigns(althoughitcanbe associatedwithsixthandseventhnervepalsies).
NeuroimagingmightshowsignsofelevatedCSFpressure butwithoutobstructionordeformityoftheventriclesand withoutidentifiablecauseoftheincreasedICP.TheCSF evaluationwillhaveopeningpressuregreaterthan25 cmH2ObutwithnormalCSFcomposition.3
CommonsymptomsofIIHareheadache,visual disturbances,andpulsatiletinnitus.Themostcommon presentingsymptomofIIHisheadache,whichisfoundin 84%ofthepatients.Theheadacheisconstant,non-pulsating, exacerbatedbycoughingorValsalvamaneuver,andithasa progressivecourse.Thesecondmostfrequentsymptomof IIHisvisualdisturbancesuchasvariable,visual fielddefects thatcommonlygounnoticedbythepatientuntilsevere; transientvisualobscurations(transientunilateralorbilateral visuallosslastinglessthanoneminuteandoftenprecipitated byposturalchanges,withfullrapidvisualrecoveryto
baseline);enlargingblindspots;diminishedvisualacuityin patientswithadvanceddisease;diplopia,especiallyinthe horizontalplanegenerallyduetosixthcranialnervepalsy;or blurryvisionduetoshorteningoftheglobesecondaryto increasedICP.Tinnitus,anothercommonsymptominIIH, ismoreoftenbilateral,pulsatile,synchronouswithheartrate, andcanoccurwithvariablefrequencyfromdailyto monthly.3,12 Idiopathicintracranialhypertensionis characterizedbynormalmentalstatus;however,itcancause disablingheadachesandblindness.
DIAGNOSTICEVALUATION Papilledema Thepresenceofopticnerveheadedema(ONHE)in patientswithheadachesignifiesasecondarycauseforthe headacheandtheneedforfurtherurgentevaluation.13 This conditioniscommonlyencounteredinpapilledema(optic discswellingduetoincreasedICP);opticneuropathy(optic neuritis,ischemicopticneuropathy);andpseudopapilledema (discelevationwithoutnerve fiberlayeredema).The distinctionbetweenthethreemajorcausesofdiscswellingis basedonhistory,eyeexaminationincludingfundoscopy,and ancillarytesting.Othercausesofopticdiscswellingare centralretinalveinocclusion,diabeticpapillopathy,uveitis, opticdisctumors,malignanthypertension,andopticnerve infiltration(suchasseeninsarcoidosis,lymphoma,and leukemia).14 Opticneuropathiesleadtoamoreseverevisual lossandareusuallysudden,unilateral,andassociatedwith afferentpupillarydefectandimpairedcolorvision.14
Pseudopapilledemaisassociatedwithopticnervevariants thatmimicpapilledemaophthalmoscopically,suchas congenitalabnormalities;crowdedhyperopicdisc;opticdisc hamartomas;oropticnerveheaddrusen.Visuallossmay occur,butitismoreindolent,painless,andfrequently unnoticedbythepatient.Pseudopapilledemaisstableover timecomparedtountreatedpapilledema,whichwillchange andprogressintime.Therearealsoophthalmoscopic findingsthatwillhelpdifferentiatepapilledemafrom pseudopapilledema.14 Opticdiscdrusenareacellular depositslocatedintheopticnervehead.Inchildren,theoptic discdrusenarenotcalcified;theyresemblepapilledemawith opticnerveheadswellingandcanbedifficulttodiagnoseon opthalmoscopy.15 Withage,theopticdiscdrusenbecome calcifiedandeasiertodiagnoseonophthalmoscopyand ultrasound,asopticdiscdrusenarehyperechoicwith posterioracousticshadowing.15
TheFrisénclassificationisthemostfrequentlyused papilledemagradingsystemanddescribesstagesofopticdisc swelling(grades0–5);however,ithaspoorinter-rater reliability.Therefore,moredescriptiveterminologyisoften usedtodescribepapilledema(eg,mildvshighgrade).14,16,17 Papilledemaisusuallybilateralandsymmetrical;however,it canbeasymmetricaland,rarely,itcanbeunilateraloreven absent.12,18 Papilledemaisthoughttobesecondarytoeither
axoplasmicstasisthatcausesaxonalswellingordueto enlargementofthesubarachnoidspace.Usually,the developmentofpapilledemarequiresatleast1–5daysof persistentlyelevatedICP;however,ithasalsobeenfoundto developrapidly,inhours,insubarachnoidand intraparenchymalhemorrhages.IftheelevatedICPis treated,papilledemausuallyresolvesoverweeks tomonths.14
Non-expertcliniciansoften finditdifficulttoproperly viewtheopticdiscusingophthalmoscopy.19 PhaseIofthe FOTO-EDstudyfoundthatdirectophthalmoscopywas rarelyandinadequatelyperformedbyemergencyphysicians (EP)inalargeacademicmedicalcenterwhereEPsfailedto diagnoseanycasesofoptic-nerveheadedemausingdirect ophthalmoscopy.20 PhaseIIoftheFOTO-EDstudyfound thatnon-mydriaticretinalphotographyintheEDwas superiortodirectophthalmoscopyperformedbyEPs; however,EPsdonotcommonlyperformthisandidentified only16of35relevant findings(sensitivity46%).21 Sachdeva etal13 performedacross-sectionalanalysisofpatientswith ONHEintheprospectiveFOTO-EDstudyandfoundthat 2.6%ofpatientspresentingtotheEDwithachiefcomplaint ofheadache,acutevisionloss,focalneurologicdeficit,ora diastolicbloodpressure ≥120mmHghadONHE.Themost common finaldiagnoseswereIIH(19/37),CSFshunt malfunction/infection(3/37),andopticneuritis(3/37),thus reiteratingtheimportanceofocularfundusexaminationin thesepatients.13
EmergencyUltrasoundEvaluationforIncreased IntracranialPressure
Emergencyultrasoundisaneasy-to-use,noninvasive methodofincreasedICPassessmentbyevaluatingtheoptic nervesheathdiameter(ONSD)andtheopticdiscelevation (ODE).Theopticnervecanbethoughtofasanoutpouching ofintactbraintissuewiththeintraorbitalcomponentCSF and fluctuatesinsizebasedonchangesinICP.IncreasedICP causesenlargementofthesubarachnoidspaceandincrease oftheONSD.Thebulbousportionoftheopticnerve, approximately3mmposteriortotheglobe,appearstobethe mostdistensibleandsensitivetochangesinICP.22 On ultrasound,theglobeappearsasaround,anechoicstructure. Theopticnervepresentsasahypoechoicstructureposterior totheglobe(see Figure2).
Opticdiscelevation
Opticdiscelevationreferstotheheightofelevationofthe opticdiscfromthelaminacribrosa(theareathroughthe sclerawheretheopticnerveaxonspass).23 Themeasurement isperformedwiththeopticnerveinthehorizontalplane,and theviewwiththemaximumdiscelevationisselected.Disc elevationismeasuredfromtheuppermostpartoftheswollen disctothestronglyreflectinglinerepresentingthelamina cribrosa(see Figure3).24 Teismannetal25 determinedthata
Figure3. Opticdiscelevation(ODE)measurementbetweenthe topoftheswollenopticdiscandthelaminacribrosa.Inthis figure, ODEof0.13cmsuggestsopticdiscedema.
cutoffvalueof0.6mmforopticdiscelevation,asmeasured byultrasound,predictedthepresenceofopticdiscedema notedonfundoscopicexamwithasensitivityof82%(95% confidenceinterval[CI]48–98%)andaspecificityof76%(95% CI50–93%).Acutoffvalueof1.0mmyieldedasensitivityof
Figure2. Opticnerveappearanceonultrasound.
73%(95%CI39–94%)andspecificityof100%(95%CI 81–100%).Inthisstudy,mostpatientshadIIHcausingdisc swellingduetoelevatedICP;however,discswellingcanalso befoundinpatientswithmultiplesclerosis,infiltrative processessuchassarcoidosisorlymphoma,infectionsdirectly affectingtheopticnerve,andmicrovascularinfarctioncaused bymalignantsystemichypertension.
Opticnervesheathdiameter TheONSDismeasured3mmdeeptotheglobewhereit appearstobethemostdistensibleandsensitivetochangesin ICP.22 Threepossiblepositionsfordepthmarkershavebeen describedinstudies:1)locationwhereimaginarynerve midlineintersectsthecontouroftheretina;2)hyperechoic reflectioncorrespondingtothelaminacribrosa;and3)topof thehypoechoicstructurecorrespondingtotheopticnerve(see Figure4).However,thesediscrepanciesdidnotaffectONSD values,mostlikelybecausethedistancebetweenthedifferent anatomicallandmarksusedislessthan1mmresultingin comparableONSDvalues.Stevensetal26 recommendsusing thepapillaasreferenceforthe3-mmdepthassessment.
Theopticnerveitselfhasadiameterof3mm,andtheoptic nervesheathhasathicknessofapproximately1mm.From theinsideout,thesheathconsistsofpiamater,the subarachnoidspace,thearachnoidmater,andthedura mater.Whenstudieswerereviewed,twotypesofimageswith differentechoiccharacteristicsoftheopticnervesheathwere described.Onegroupofimagesshowedtwohyperechoic, stripedbandsbetweenthehyperechoicretrobulbarfat(see Figure5a),whiletheothergroupshowedasingledarklinear structuresurroundedbyhyperechoicretrobulbarfat (see Figure5b).26
Figure5. (a)Opticnerve(betweenCcalipers)asoneanechoic bandsurroundedbytwohyperechoicstripedbands(betweenC andBcalipersoneachsideoftheopticnerve)betweenthe hyperechoicretrobulbarfat(Acalipers).(b)Opticnervewithone singleanechoicbandrepresentingtheopticnerveanditssheath, Dcalipersattheborderbetweentheopticnervesheathandthe retrobulbarfat.
Thestripedbandshavebeeninterpretedtorepresenteither thepia,bothpiaandduramater,orthesubarachnoidspace. Stevensetal26 foundthatCcaliperpositionwastheleast sensitivetochangesintheICPandcorrespondstotheoutline oftheopticnerveitself.Bcalipermeasurementincreasesin patientswithelevatedICP;hence,itincorporatesthe arachnoidspace,anditlikelycorrespondstotheouteredge ofthesubarachnoidspace.Bcaliperpositionandcalipers measuringasingledarklinearstructure(Dcalipers)were foundtobeequallysensitivetochangesinICPandwere recommendedasreliableONSDmeasurements.26
TheONSDthresholdvaluesthatoptimizedsensitivityand specificityforelevatedICPvariedinstudiesfrom4.8mm (Rajajeeetal27)to6.3mm(delSaz-Saucedoetal28).The studiesonONSDhavebeensmallandheterogeneous,and thesestudieshavedonethefollowing:
• useddifferentdefinitionsandmeasurements ofONSD26
• useddifferentplanestomeasureONSD:only transverseplanes27–32;transverseandsagittal planes33–35;transverseandcoronal36
Figure4.
• predominantlyusedmeanvaluesoftheONSD measurementsobtainedfrombotheyes,withAgrawal etal36 identifyingthehighesttransversemeasurement andRajajeeetal27 studyingeachindividual transversemeasurement
• enrolleddifferentpatientpopulations,withmultiple studiesenrollingneurocriticalcarepatientswith traumaticandnon-traumaticbraininjury,andsome studiesenrollingclinicpatientswithIIH28,32
• useddifferentconfirmationsofelevatedICPincluding computedtomography(CT),37,38 lumbarpuncture (LP),28,32 orexternalventriculardrain(EVD)and intraparenchymalcatheter33,36
• definedelevatedICPaseither20mmHgor25cmH2O (20mmHg = 27cmH2O39).
Inameta-analysisincluding18prospectivestudiesthat hadICPmeasuredbyEVDorintraparenchymalcatheter (LPmeasurementsexcluded),Aletrebyetal40 demonstrated thatONSDshowedreasonableaccuracyindiagnosingraised ICP.ThehighestsensitivitywasachievedusinganONSD cutoffofmorethan6mm.40 WhileONSDof <5mm correlateswithnormalICP,thecutoffONSDforelevated ICPvariesfromstudytostudywith >6mmdemonstratinga highsensitivityforelevatedICP.AnODE >0.6mmcanalso behelpfulindeterminingpapilledema;however,ODEcanbe seeninmultipleothermedicalconditions.WhileONSDand ODEcanbehelpfulinscreeningforpapilledema,larger studieswithstandardizedONSDmeasurementsanda consistentICPcutoffarestillneeded.Itisalsoknownthat papilledemacanbeasymmetrical;hence,eacheyeONSD measurementsshouldbestudiedindependently.
Neuroimaging IntheevaluationofapatientwithincreasedICP, neuroimaginghastwomainpurposes:toexcludestructural causes;andtoidentifytypicalradiographicpatternsof elevatedICP.Non-enhancedCTiscommonlyusedasthe firsttestforevaluationofsecondaryheadachesandaltered mentalstatusintheemergencysetting,anditisthestandard imagingmodalityinacuteheadtrauma.Computed tomographyiswidelyavailable,hasshorteracquisitiontime, andislessexpensivethanbrainmagneticresonanceimaging (MRI).Intheemergencysetting,CTisregularlyperformed toreadilyidentifyconditionsthatrequiresurgical intervention.7 ACTcanidentifybrainedema,tumors, hydrocephalus,intracranialhemorrhage,andsignsof cerebralherniation.ACTmayalsodetectsignsofincreased ICP,suchasventricularorsulcaleffacement,compressionof thebasalCSFcisterns,herniation,ormidlineshift.However, ICPcanbeelevatedeveninthesettingofanormalCT. ComparedtoCT,MRIprovidesbettertissue characterization,especiallyforposteriorfossadisease,andis requiredforevaluationofunderlyingbrainlesions.Brain
MRIwithcontrastcanidentifymoststructuralcausesof increasedICP,andmagneticresonancevenography(MRV) withcontrastwillexcludecerebralvenoussinusthrombosis.3 InIIH,brainMRIandMRVareimportanttoexclude secondarycausesofelevatedICP.Additionally,emptysella turcica,posterior flatteningoftheglobe,enlargementofthe periopticsubarachnoidspace,opticnervemidportion tortuosity,hyperintensityoftheopticnerveandopticdisc, andbilateraltransversesinusstenosishavebeenfoundtobe associatedwithIIH;andthesensitivityandspecificity improvewithacombinationoftheseneuroimaging signs.12,41 Slit-likeventricles,tightsubarachnoidspace,and inferiorpositionofthecerebellartonsilsshowslowsensitivity butgoodspecificityof90–97%forIIH.12
IntracranialPressureMeasurement Patientswithpapilledemaandnormalneuroimaging couldundergoLPaspartoftheirclinicalworkuptomeasure theICPinsearchforetiologiessuchasIIH.TheCSFopening pressureremainsoneofthemostimportant findingsto establishadiagnosisofIIH.TheCSFpressuremayvary considerablywithtime;thus,thepossibilitytorepeatLPor performamoreinvasiveICPmonitoringshouldbe consideredifclinicalsuspicionishigh.12 ACSFevaluationis alsorequiredtoexcludeotheretiologiesofelevatedICPsuch asinfectious,inflammatory,orneoplasticmeningitis.3 The LPisobtainedinlateralrecumbentposition,whiletheCSF openingpressureshouldbemeasuredwiththelegsextended, headinneutralposition,andthepatientbreathingnormally. ThenormalCSFopeningpressureinadultsis10–20cmH2O andisconsideredhighifgreaterthan25cmH2O.ACSF openingpressureof20–25cmH2Oisconsideredborderline, anditisinterpretedintheclinicalcontext.3
Idiopathicintracranialhemorrhagewithoutpapilledema iswellrecognized.Thesepatientstendtohaveloweropening pressurelevelsthanthosewhopresentwithpapilledema.In theabsenceofpapilledema,theothercriteriashouldbemet, withtheadditionalsymptomofunilateralorbilateral abducensnervepalsies.Ifthereisnoabducensnervepalsy, threeofthefollowingneuroimagingcriteriashouldbemet:1) emptysella;2) flatteningoftheposterioraspectoftheglobe; 3)distentionofthesubarachnoidspacewithorwithouta tortuousopticnerve;and4)transversesinusstenosis.A normalopeningpressureleveldoesnotexcludethediagnosis ofIIHwhenthepatienthasothertypicalsymptoms. Conversely,anincreasedopeningpressurelevelwithout appropriatesymptomsshouldnotbeinterpretedasIIH.42
ALPcarriesnoriskofherniationifthereisnobrainshift, whetherCSFpressureisraisedornotandwhether papilledemaispresentornot.ACTisusedtodiagnosebrain shiftseeninspace-occupyinglesionsanddiffusebrain swelling.FindingsofbrainshiftonCTmaydemonstratethe following:displacementofbrainstructures;lossof differentiationbetweengrayandwhitematter; flattenedgyri;
effacementofCSFspaces(suchassulci,Sylvian fissures, ventriclesandbasalcisterns);dilatedventricles (inobstructivepathology);andinadvancedstagesherniation (displacementofbrainfromoneintracranial compartmenttoanother).43
AninvasiveICPmeasurementdevicesuchasexternal ventriculardrainorintraparenchymaldeviceremainsthe standardtodeterminethepressureinthecranialvault.The necessityforICPmeasurementiseitherdeducedbya pathologicalCToraconsciousnessimpairmentscoreof ≤8ontheGlasgowComaScale.44
CONCLUSION Increasedintracranialpressurerepresentsalifethreateningdiagnosis.Idiopathicintracranialhemorrhage, whilenotlife-threatening,cancauseirreversiblevisualloss anddisablingheadaches.Clinicalpresentationrequires immediaterecognitionandinvestigation.Whilepapilledema isimportanttodiagnoseintheED,emergencyphysicians havefounditdifficulttodiagnosebydirect ophthalmoscopy.20 Ocularultrasound(opticnervesheath diameterandopticdiscelevation)iscommonlyusedto screenforincreasedICP;however,thereisneedforfurther researchusingstandardizedONSDmeasurements. Neuroimagingremainsthe firststepininvestigatingelevated ICPasitexcludesstructuralcausesandidentifiestypical radiologicalpatternsofelevatedICP.InvasiveICP measurementremainsthestandardtomeasureand monitorICP.
ACKNOWLEDGMENTS Drs.OlaruandMcCoinwereaffiliatedwithOchsner Healthduringthecreationofthispaper.Currently,Dr. OlaruisaffiliatedwithUniversityofColoradoinAurora, Colorado,andDr.McCoiniscurrentlyaffiliatedwith UniversityofKentuckyCollegeofMedicinein Lexington,Kentucky.
AddressforCorrespondence:SamLangberg,MD,Divisionof EmergencyUltrasound,OchsnerHealth,DepartmentofEmergency Medicine,1514JeffersonHwy,NewOrleans,LA70121.Email: samlangberg@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Olaruetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.CanacN,JalaleddiniK,ThorpeSG,etal.Review:pathophysiologyof intracranialhypertensionandnoninvasiveintracranialpressure monitoring. FluidsBarriersCNS. 2020;17(1):40.
2.DunnLT.Raisedintracranialpressure. JNeurolNeurosurgPsychiatry. 2002;73(suppl1):i23–7.
3.ThurtellMJ.Idiopathicintracranialhypertension. Continuum(Minneap Minn). 2019;25(5):1289–1309.
4.ChenS,LuoJ,ReisC,etal.Hydrocephalusaftersubarachnoid hemorrhage:pathophysiology,diagnosis,andtreatment. BiomedRes Int. 2017;2017:8584753.
5.NehringSM,TadiP,TennyS.Cerebraledema.In: StatPearls[Internet] TreasureIsland,FL:StatPearlsPublishing,2022.Availableat: https:// www.ncbi.nlm.nih.gov/books/NBK537272/.AccessedSeptember8, 2023.
6.CairnsCandKangK.NationalHospitalAmbulatoryMedicalCare Survey:2019emergencydepartmentsummarytables.2022. Availableat: https://www.cdc.gov/nchs/data/nhamcs/web_ tables/2019-nhamcs-ed-web-tables-508.pdf.AccessedSeptember8, 2023.
7.RiverosGilardiB,Mu ˜ nozL´opezJI,HernándezVillegasAC,etal.Types ofcerebralherniationandtheirimagingfeatures. RadioGraphics. 2019;39(6):1598–610.
8.NayakLandDeangelisLM.Clinicalfeaturesofbraintumors.In: Blue BooksofNeurology,vol36.(54–70).Amsterdam,TheNetherlands: Elsevier,2010.
9.TadevosyanAandKornbluthJ.Brainherniationandintracranial hypertension. NeurolClin. 2021;39(2):293–318.
10.PrakashE,KuhtHJ,HarieaswarS,etal.Dorsalmidbrain(Parinaud) syndrome. PractNeurol. 2021;21(6):550–1.
11.Delldot.Brainherniationtypes.2008.Availableat: https://upload. wikimedia.org/wikipedia/commons/archive/c/cb/20090916112024% 21Brain_herniation_types.svg.AccessedDecember29,2023.
12.ToscanoS,LoFermoS,ReggioE,etal.Anupdateonidiopathic intracranialhypertensioninadults:alookatpathophysiology, diagnosticapproachandmanagement. JNeurol. 2021;268(9):3249–68.
13.SachdevaV,VasseneixC,HageR,etal.Opticnerveheadedema amongpatientspresentingtotheemergencydepartment. Neurology. 2018;90(5):e373–9.
14.LiuGT,VolpeNJ,GalettaSL. Liu,Volpe,andGaletta’s Neuro-Ophthalmology:DiagnosisandManagement, 3rded. Amsterdam,TheNetherlands:Elsevier,2019.
15.HamannS,MalmqvistL,CostelloF.Opticdiscdrusen:understanding anoldproblemfromanewperspective. ActaOphthalmol(Copenh). 2018;96(7):673–84.
16.SinclairAJ,BurdonMA,NightingalePG,etal.Ratingpapilloedema:an evaluationoftheFrisénclassificationinidiopathicintracranial hypertension. JNeurol. 2012;259(7):1406–12.
17.FrisénL.Swellingoftheopticnervehead:astagingscheme. J Neurol NeurosurgPsychiatry. 1982;45(1):13–8.
18.SwinkinE,JabehdarMaralaniP,SundaramAN.Unilateralpapilledema inidiopathicintracranialhypertension:acaseseries. CanJNeurolSci. 2022;49(2):278–81.
19.KardonR.Opticalcoherencetomographyinpapilledema:whatamI missing? JNeuroophthalmol. 2014;34Suppl:S10–7.
20.BruceBB,LamirelC,BiousseV,etal.Feasibilityofnonmydriaticocular fundusphotographyintheemergencydepartment:phaseIoftheFOTOEDstudy:feasibilityofnonmydriaticocularfundusphotography. Acad EmergMed. 2011;18(9):928–33.
21.BruceBB,ThulasiP,FraserCL,etal.Diagnosticaccuracyand useofnonmydriaticocularfundusphotographybyemergency physicians:phaseIIoftheFOTO-EDstudy. AnnEmergMed. 2013;62(1):28–33.e1.
22.RichardsE,MunakomiS,MathewD.Opticnervesheathultrasound.In: StatPearls[Internet].TreasureIsland,FL:StatPearlsPublishing,2022. Availableat: https://www.ncbi.nlm.nih.gov/books/NBK554479/ AccessedSeptember8,2023.
23.ElkingtonAR,InmanCBE,SteartPV,etal.Thestructureofthelamina cribrosaofthehumaneye:animmunocytochemicalandelectron microscopicalstudy. Eye. 1990;4(1):42–57.
24.ErtlM,GamulescuMA,SchlachetzkiF.(2012).Applicationoforbital sonographyinneurology.In:ThoirsK(Ed), Sonography.InTechOpen, 2012.Availableat: http://www.intechopen.com/books/sonography/ application-of-orbital-sonography-in-neurology AccessedSeptember8,2023.
25.TeismannN,LenaghanP,NolanR,etal.Point-of-careocular ultrasoundtodetectopticdiscswelling. AcadEmergMed. 2013;20(9):920–5.
26.StevensRRF,GommerED,AriesMJH,etal.Opticnervesheath diameterassessmentbyneurosonology:areviewofmethodologic discrepancies. JNeuroimaging. 2021;31(5):814–25.
27.RajajeeV,VanamanM,FletcherJJ,etal.Opticnerveultrasound forthedetectionofraisedintracranialpressure. NeurocritCare. 2011;15(3):506–15.
28.delSaz-SaucedoP,Redondo-GonzálezO,Mateu-MateuÁ,etal. Sonographicassessmentoftheopticnervesheathdiameterinthe diagnosisofidiopathicintracranialhypertension. JNeurolSci. 2016;361:122–7.
29.KimberlyHH,ShahS,MarillK,etal.Correlationofopticnervesheath diameterwithdirectmeasurementofintracranialpressure. AcadEmerg Med. 2008;15(2):201–4.
30.JeonJP,LeeSU,KimSE,etal.Correlationofopticnervesheath diameterwithdirectlymeasuredintracranialpressureinKoreanadults usingbedsideultrasonography. PLoSOne. 2017;12(9):e0183170.
31.RaffizMandAbdullahJM.Opticnervesheathdiametermeasurement:a meansofdetectingraisedICPinadulttraumaticandnon-traumatic neurosurgicalpatients. AmJEmergMed. 2017;35(1):150–3.
32.KorsbækJJ,HagenSM,SchytzHW,etal.Transorbitalsonography:a non-invasivebedsidescreeningtoolfordetectionofpseudotumor cerebrisyndrome. Cephalalgia. 2022;42(11-12):1116–26.
33.GeeraertsT,MerceronS,BenhamouD,etal.Non-invasiveassessment ofintracranialpressureusingocularsonographyinneurocriticalcare patients. IntensiveCareMed. 2008;34(11):2062–7.
34.MorettiRandPizziB.Opticnerveultrasoundfordetectionofintracranial hypertensioninintracranialhemorrhagepatients:confirmationof previous findingsinadifferentpatientpopulation. JNeurosurg Anesthesiol. 2009;21(1):16–20.
35.RobbaC,CardimD,TajsicT,etal.Ultrasoundnon-invasive measurementofintracranialpressureinneurointensivecare:a prospectiveobservationalstudy. PLoSMed. 2017;14(7):e1002356.
36.AgrawalA,ChengR,TangJ,etal.Comparisonoftwotechniquesto measureopticnervesheathdiameterinpatientsatriskforincreased intracranialpressure. CritCareMed. 2019;47(6):e495–501.
37.BlaivasM,TheodoroD,SierzenskiPR.Elevatedintracranialpressure detectedbybedsideemergencyultrasonographyoftheopticnerve sheath. AcadEmergMed. 2003;10(4):376–81.
38.TayalVS,NeulanderM,NortonHJ,etal.Emergencydepartment sonographicmeasurementofopticnervesheathdiametertodetect findingsofincreasedintracranialpressureinadultheadinjurypatients. AnnEmergMed. 2007;49(4):508–14.
39.HeifermanDM,JackMM,JohnsonKD,etal.Mercuryvs.water:an analysisofmulti-institutionalsurveydataassessingintracranial pressureunitofmeasureawareness. WorldNeurosurg. 2019;129:e657–62.
40.AletrebyW,AlharthyA,BrindleyPG,etal.Opticnervesheathdiameter ultrasoundforraisedintracranialpressure:aliteraturereviewand meta-analysisofitsdiagnosticaccuracy. JUltrasoundMed. 2022;41(3):585–95.
41.BarkatullahAF,LeishangthemL,MossHE.MRI findingsasmarkers ofidiopathicintracranialhypertension. CurrOpinNeurol. 2021;34(1):75–83.
42.GuryildirimM,KontzialisM,OzenM,etal.Acuteheadacheinthe emergencysetting. Radiographics. 2019;39(6):1739–59.
43.vanCrevelH,HijdraA,deGansJ.Lumbarpunctureandtherisk ofherniation:whenshouldwe firstperformCT? JNeurol. 2002;249(2):129–37.
44.SchürerL,WolfS,LumentaCB.1074208Intracranialhypertension.In: LumentaCB,DiRoccoC,HaaseJ,MooijJJA(Eds.), Neurosurgery (605–10).BerlinHeidelberg,Germany:Springer,2010.
BarrierstoAdoptionofaChild-AbuseClinicalDecisionSupport SysteminEmergencyDepartments AlannaC.Peterson,MD*
DonaldM.Yealy,MD†
EmilyHeineman,MA‡
RachelP.Berger,MD,MPH‡§
*UniversityofPittsburghMedicalCenter,Pittsburgh,Pennsylvania
† UniversityofPittsburgh,DepartmentofEmergencyMedicine, Pittsburgh,Pennsylvania
‡ UniversityofPittsburgh,UPMCChildren’sHospitalofPittsburgh,DivisionofChild Advocacy,DepartmentofPediatrics,Pittsburgh,Pennsylvania
§ PennsylvaniaOfficeofChildren,YouthandFamilies,Harrisburg,Pennsylvania
SectionEditor:NikhilGoyal,MD
Submissionhistory:SubmittedOctober17,2023;RevisionreceivedJuly15,2024;AcceptedAugust12,2024
ElectronicallypublishedOctober14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18501
Introduction: Childabuseisaleadingcauseofmorbidityandmortalityinchildren.Therateofmissed childabuseingeneralemergencydepartments(ED),where85%ofchildrenareevaluated,ishigherthan inpediatricEDs.Wesoughttoevaluatetheimpactofanelectronichealthrecord(EHR)-embeddedchildabuseclinicaldecisionsupportsystem(CA-CDSS)intheidentificationandevaluationofchild maltreatmentinanetworkofEDsthreeyearsafterimplementation.
Methods: Weanonymouslysurveyedall196EDattendingphysiciansandadvancedpractice practitioners(APP)intheUniversityofPittsburghMedicalCenternetwork.Thesurveyevaluated practitionerawarenessof,attitudestoward,andchangesinclinicalpracticepromptedbytheCA-CDSS. Wealsoassessedpractitionerrecognitionandevaluationofsentinelinjuries.
Results: Ofthe71practitioners(36%)whorespondedtothesurvey,75%feltthetoolraisedchildabuse awareness,and72%hadaface-to-facediscussionwiththechild’snurseafterreceivingaCA-CDSS alert.AmongAPPs,72%consultedwiththeattendingphysicianafterreceivinganalert.Many practitionerswereunawareofatleastonefunctionoftheCA-CDSS;38%didnotknowwhocompleted thechildabusescreen(CAS);54%wereunawarethattheycouldviewtheresultsoftheCASintheEHR, and69%didnotrecognizetheclinicaldecisionsupportdashboardicon.Slightlyover20%of respondentsfeltthattheCA-CDSSlimitedautonomy;and4.5%disagreedwiththerecommendationsin thephysicalabuseorderset,whichreflectsAmericanAcademyofPediatrics(AAP)guidelines.Greater than90%ofrespondentscorrectlyidentifiedanintraoralinjuryandtorsobruiseinaninfantassentinel injuriesrequiringanevaluationforabuse.
Conclusion: Achild-abuseclinicaldecisionsupportsystemembeddedintheelectronichealthrecord wasassociatedwithcommunicationamongpractitionersandwasoverallperceivedasimprovingchild abuseawarenessinoursystem.Practitionerscorrectlyrecognizedinjuriesconcerningforabuse. BarrierstoimprovingidentificationandevaluationofabuseincludegapsinknowledgeabouttheCACDSSandthepresenceofpractitionerswhodisagreewiththeAAPrecommendationsforphysicalabuse evaluationand/orfeltthatclinicaldecisionsupportingenerallimitedtheirclinicalautonomy.[WestJ EmergMed.2024;25(6)1011–1019.]
INTRODUCTION Childmaltreatmentcausessignificantmorbidityand mortalityintheUnitedStates,especiallyforchildrenunder fouryearsofage.Overthreemillionchildreneachyearare reportedtochildprotectiveservices(CPS),and1,600 childrendieatthehandsofcaregiversduetomaltreatment,1 anumbergreaterthanchildrenwhodiedfromCOVID-19 duringthe first2½yearsofthepandemic.2 Thenumberof childrendyingfrommaltreatmenthasbeenincreasing;there wasa10%increaseinfatalitiesfrom2016–2021.1,3 Between 20–25%ofchildrenwhoareultimatelydiagnosedwith physicalchildabusehavebeenpreviouslyseenbyamedical practitionerwhofailedtoidentifytheabuse.4–7 Appropriate recognitionandevaluationofphysicalchildabuseingeneral emergencydepartments(ED),wheremostchildrenreceive emergencycare,iscrucial.
Toimprovethequalityofidentification,evaluation,and reportingofchildmaltreatmentintheUniversityof PittsburghMedicalCenter(UPMC)generalEDs,we developedanddeployedachild-abuseclinicaldecision supportsystem(CA-CDSS)inourelectronichealthrecord (EHR)startingin2016.8–10 Atthattimetherewere13 generalEDswiththehospitalmanagementsoftwareCerner (CernerCorp,KansasCity,MO)intheUPMCsystem;they wentlivewiththeCA-CDSSsystembetween January–March2016.Asthehospitalsystemacquired additionalEDs(oneeachinJune2017andApril2019,and fourinSeptember2019),theywereaddedtotheCA-CDSS.
Priortothego-liveateachsite,trainingoccurredforboth EDnursesandpractitioners.Nursescompletedan interactiveonlinelearningmodule,whichremainspartofthe onboardingprocessforEDnursesandhasbecomean educationrequirementeverytwoyears.Practitioner educationwasdonethroughtheEDmedicaldirectors.Prior tothego-liveateachhospital,eachEDmedicaldirector receivedanonboardingpacketthatincludedgeneralchild abuseeducation,screenshotsofallpartsoftheCA-CDSS, caseexamples,andawayforpractitionerstoreachoutwith questions.EachEDmedicaldirectoralsometwithoneofthe authors(RB)whoreviewedtheonboardingpacketand answeredquestions.Themedicaldirectorswere,and continuetobe,responsiblefordisseminatingeducationto theirpractitioners.Inadditiontotheinitialtraining,ongoing trainingincludesfeedbacktopractitionersaboutcasesfrom themedicaldirectorofeachEDsite-specifictrainingsat standingpractitionermeetingsinindividualEDsandbimonthlysystemwideconferencecalls,whichusecase examplesasaspringboardfordiscussingspecificchildabuserelatedtopics.Thesecallsprovidecontinuingmedical educationcreditforpractitioners.
Thefeaturesofthistoolincludeasetoftriggersincludinga childabusescreen(CAS)completedbytheprimarynurse,an alertthatpractitionersreceivewhenapatienthastriggered theCA-CDSS,andaphysicalabuseordersettoassist
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Earlydiagnosisofchildabuseiscriticalto decreasemorbidityandmortality.Abuse identi fi cationingeneralEDsmaybeassisted byclinicaldecisionsupport.
Whatwastheresearchquestion?
Whatarethebene fi tsofandchallengesto sustainabilityofachildabuseclinicaldecision supportsystem(CA-CDSS)embeddedinthe electronichealthrecord(EHR)?
Whatwasthemajor findingofthestudy?
Three-quartersofpractitionersreportedthe CA-CDSSincreasedchildabuseawareness andpromptedinterdisciplinaryinteractions.
Howdoesthisimprovepopulationhealth?
UsinganEHR-embeddedCA-CDSSmaybe oneapproachtoimprovingchildabuse awarenessingeneralEDs,therebydecreasing abuse-relatedmorbidityandmortality.
practitionersinorderingthecorrecttestingbasedonpatient ageandinjury.8,9 Inaddition,triggeringtheCA-CDSS resultsinaniconappearingonthemainEDdashboardnext tothepatient’sname.Whenprovidingfeedbackto practitionersaboutcasesinwhichthephysicalabuseorder setwasn’tusedwhenitwasindicated,oneoftheco-authors (AP),whoisalsothedirectorofoneofthegeneralEDs, notedthatsomepractitionersreportedthattheydidnotagree withtherecommendationsintheordersetandpreferredto useclinicaljudgment.
Wesoughttounderstandthebarrierstocompliancewith theordersetrecommendations,assesstheimpactofthe CA-CDSS,andidentifyopportunitiestoimprovethe CA-CDSSwiththegoalofincreasingengagementwiththe CA-CDSSoverall.
METHODS Setting The19generalEDsintheUPMChospitalsystemoperate inurbanandruralsettingsandincludecommunityhospitals andacademiccenters.Theprimaryacademiccentersarein thecityofPittsburgh,PA.TheremainderareEDsaffiliated withcommunityhospitalsacrossmuchofPennsylvaniaand withindividualsitesinNewYork.Annualpractitioner turnoveratthese19generalEDsforfull-timeemployees averages6.8%forAPPsand3.6%forphysicians.Thereisa
totalof~30,000EDvisitsforchildren <13yearsofage(the ageincludedintheCA-CDSS)atthe19EDsannually;the proportionofallEDvisitsinvolvingchildrenrangesfrom 1–3%attheacademicsitesandupto12%inthe communitysites.
Survey InFebruary2020,ourteam(ageneralemergency physicianwhoisthedirectorofoneofthehospitalsystem’ s EDs[AP]andachildabusepediatrician[RB]fromthe affiliatedchildren’shospitalthatwasnotoneofthe19 includedhospitals)emailedasurveytoall196attending physiciansandadvancedpracticepractitioners(APP)atthe 19UPMCEDs.Theemailprovidedananonymouslinktoa 25-question,web-basedsurvey(QualtricsLLC,Seattle,WA) thatusedskiplogic,meaningcliniciansreceivedonly questionsthatwererelevantbasedonpreviousresponses (AppendixA).Self-reporteddemographicdataincluded yearsinpractice,hospitalaffiliation(s),andpractitionertype (physicianorAPP).Thesurveyaimedtoassessthe practitioner’s1)knowledgeabouttheCA-CDSSandits associatedfunctionality;2)engagementwithandattitudes towardtheCA-CDSS;3)recognitionofsentinelinjuries minorinjuriesthatnecessitateanevaluationforphysical abuse;and4)reasonsfornotusingthephysicalabuseorder setevenwhenitwasindicated.Thesurveywasdesignedso thatpractitionerswouldlearnabouttheCA-CDSSasthey completedthequestions.
StatisticalAnalysis/Measures Weuseddescriptiveanalysestomeasuretheproportionof surveyscompleted,knowledgeofpractitionersaboutthe CA-CDSS,attitudestowardtheCA-CDSS,recognitionof
Demographiccharacteristics ofsurveyrespondents
Practitionertype
injuriesthatshouldraiseconcernforphysicalabuse,and barrierstoevaluatingandreportingsuspectedabuse.
EthicalConsideration/Approval TheUPMCQualityImprovementCommitteeapproved thisproject.Therewasnoformalethicsreview,andno potentialconflictsofinterestwereidentified.
RESULTS ResponseRateandPractitionerCharacteristics Therewasa43%(84/196)initialresponserate,with13 surveysexcludedforlackofcompleteness,leaving71surveys (36%)foranalysis.Ofthe13incompletesurveys,one practitionerwasn’teligibleand10oftheremaining12 incompletesurveyshadfewerthan35%ofthequestions answered.Asaresult,wechosetoexcludethementirely. Mostrespondentswerephysicianswhoworkedin communityEDsandhadmorethan15yearsof experience(Table1).
PractitionerKnowledgeAbouttheCA-CDSSandIts AssociatedFunctionality Thechildabusescreen(CAS)
Ofthe71respondents,27(38%)didnotknowwho completestheCAS,and54%(38/71)wereunawarethatthey couldseethecompletedCAS(vssimplybeingalertedwhenit waspositive).
Thealert
Thesameproportionofpractitioners(27/71)didnotrecall everseeinganalert,and69%(49/71)ofpractitionersdidnot knowthatthelightbulbiconontheEDdashboardmeant thatthepatienthadtriggeredtheCA-CDSS.
#(%)ofrespondentswithcompleted surveys(N = 71)
Characteristicsofsurveyed population(n = 196)
Yearsofexperience >15yearsinpractice30(42.3%)Notavailable^ 6–15yearsinpractice27(38.0%)Notavailable 0–5yearsinpractice14(19.7%)Notavailable
*Twodeclinedtostate.
^Yearsofexperiencewascollectedaspartofthesurveyand,therefore,wasnotavailableforpractitionerswhodidnotcompletethesurvey. APP,advancedpracticepractitioner.
Table1. Demographiccharacteristicsofsurveyrespondents.
PractitionerEngagementwithandAttitudesToward theCA-CDSS
Thealert
Ofthepractitionerswhorememberedseeingthe alert,68%(30/44)reportedthattheyalwaysapproachedthe child’snurseforfurtherdetails,and86%(12/14)ofthe remainingpractitionersreportedthattheysometimes approachedthenurse;twocouldnotrecallwhether theyhaddoneso.Ofthe11practitionerswhowere APPsandrecalledseeingthealert,78%(8/11)reportedthat theyalwaysapproachedtheattendingphysician todiscussthecase,andtheotherthreereportedthey sometimesdid.
Theemergencydepartmentchildphysicalabuseorderset
Forty-twopercent(30/71)ofrespondentsreportedhaving usedthephysicalabuseorderset.Ofthe58%whodidnot reportusingit,34%(14/41)indicatedtheywereunawareofit, 54%(22/41)believedtheordersetwasnotrelevantforthe patient(s)theyweretreating,and5%(2/41)wereunableto findit.Onepractitionermadeabroadcommentaboutnot usinganyordersetsbecausehewantedto “usemybrain” and notfollowrecommendations.Half(33/66)ofrespondents indicatedtheyagreedwiththerecommendationscontained intheorderset,45%(30/66)wereneutral,and4.5%(3/66) disagreedwiththerecommendations.
Attitudes OverallattitudesabouttheCA-CDSSwerepositive,with 79%ofpractitionersagreeingorstronglyagreeingwiththe statement, “TheCA-CDSSincreasesmyawarenessofthe potentialriskforchildabuse” (Figure1a).Twenty-two percentofrespondentsfeltthattheCA-CDSSalertand physicalabuseordersetlimitedtheirabilitytomake independentdecisions(Figure1b).Morethan75%of respondentsfeltthatthealertwasclear(Figure2a), thatthealertandorderset fitwellintopractitioner workflow(Figure2b),andthatitsaved time(Figure2c).
Recognitionofinjuriesthatdoanddonotnecessitatea physicalabuseevaluation
Case1describeda13-day-oldwithasubconjunctival hemorrhageclearlydocumentedatbirth.Thiscasewasan exampleofaninfantwhodidnotneedachildabuse evaluation.Almost40%ofrespondents(26/71)incorrectly statedthatthisrequiredachildabuseevaluation.
Cases2and3describeda4-month-oldand2-month-old withanintraorallacerationandtorsobruise,respectively. Thesecaseswereusedtodemonstrateinfantswhorequirea childabuseevaluation.Inthesescenarios,91%(56/61)of practitionersincase2and97%(69/71)incase3correctly notedtheneedforachildabuseevaluation.
Figure1. Practitionerattitudesaboutthealert’seffectonclinical decision-making:a)Practitionerresponsestothestatement, “TheCA-CDSSincreasesmyawarenessofthepotentialriskfor childabuse,” (n = 70);b)Practitionerresponsestothestatement, “TheCA-CDSSpop-upalertandEDphysicalabuseordersetlimit myabilitytomakeindependentdecisions,” (n = 68)andc) Practitionerresponsestothestatement, “Iagreewiththe suggestedevaluations/workupintheEDphysicalabuseorder set.” (n = 66).
CA-CDSS,child-abuseclinicaldecisionsupportsystem; ED,emergencydepartment.
Barrierstoevaluatingandreportingsuspected physicalabuse
Ofrespondents,89%(60/71)expresseduncertainty regardingtheirabilitytorecognizechildabuse,with52% reportingatleastmoderateamountofuncertaintyin recognition(Figure3a).Whenaskedaboutpursuingthe appropriateevaluationforchildabuse,65%(46/71) expresseduncertaintyastowhichtestswereindicated (Figure3b).Lackofasocialworkerorancillarysupportin theEDwasidentifiedasabarrierby54%(38/70)of respondents.Toomuchtimeneededfortheworkupwas identifiedasabarrierfor16%(11/71)ofrespondents.Lastly, concernaboutbeingcalledtocourttotestifywasidentifiedas abarrierby10%(7/71)ofrespondents.
Free-textresponsesregardingthechildabuse-clinical decisionsupportsystem
The finalquestionallowedforrespondentstoprovidefreetextcommentsand/orsuggestionsabouttheCA-CDSS.
Figure2. Practitionerattitudesaboutthealertandorderset:a) Likertscalepractitionerresponsestothestatement “Thepop-up alertIreceivefromtheCA-CDSSisclearlyworded,” reportedasa percentageof70respondents(1declinedtostate);b)Likertscale practitionerresponsestothestatement “UsingtheEDphysical abuseorderset fitswellinmyclinicalworkflow,” Reportedasa percentageof69respondents(twodeclinedtostate);andc) Likertscalepractitionerresponsestothestatement “TheED physicalabuseordersetsavestimewhenevaluatingpatients,” reportedasapercentageof68respondents.(Threedeclined tostate.)
CA-CDSS,Child-abuseclinicaldecisionsupportsystem; ED,emergencydepartment.
Atotalof18(25%)respondentsenteredafree-textresponse. Acommonresponserelatedtothesubtletiesinthesetypesof casesandthedesiretohavetheabilitytoconsultapediatric and/orchildabusespecialistwhilethepatientisintheED.As discussedbelow,practitionersdohavethisaccessbutwere unawareofit.
SometimesIhavetroublechoosinganordersetbecause thesituationdoesnot fitinthelistprovided .
[Practitoner]uncertaintyaroundthespecifics/subtleties relatedtoaspecificcasecanbeabigfactorinchoosing tofullyutilizetheordersetand/orto fileareport.I think[practitioners]/patients/familieswouldgreatly benefitbymoredirectinvolvementwiththechild advocacyteam[while]thepatientisintheemergency department.
Figure3. Practitionerself-reportingaboutbarriersinchildabuse recognitionandevaluation:a)Lackofcertaintyaboutwhentobe concernedforabuse;b)Lackofcertaintyaboutwhattestsare indicated;c)Lackofsocialworkerorancillarysupport;andd) concernaboutbeingcalledtocourt.
Raiseawarenessto[practitioners]sothattheycan consultpediatricspecialistsincludingpeds[emergency] physiciansforfurtherassistancewithsuspectedchild abusecases.
AsecondthemewasnotrelatedspecificallytotheCACDSSbuttothemoregeneralissuesofpop-upfatigue” (ie, alertfatigue):
Morepop-upscauseclickfatigue.Thishasdestroyed medicine.
Wesufferfrompop-upfatigueandthiscanjustbe onemore.
Athirdsetofcommentswererelatedtothedesiretolearn moreabouttheCA-CDSSitself:
Iwasnotawareofthistool,sopleasesendoutanemail describingit.
Makecliniciansawareofthistool.
morewebinarsorcollaborationwith expertswould begreat.
Ifthereareroutinefreerecordedlecturesforusonclassic regionalcases ::: .Iwouldbeinterestedintakingthem :::
DISCUSSION Thisisthe firstpapertoevaluatethelong-termeffectofan EHR-embeddedCA-CDSSonpatientcareinanetworkof generalEDs.Themostencouragingobservationisthatthe CA-CDSSappearstofacilitateinterdisciplinary communicationbetweennurses,physicians,andAPPs.One oftheconcernsabouttransitioningtheCASfromapaper form thewayinwhichitwasoriginallystudiedand validated11 toanelectronicformatwasthat multidisciplinarycommunicationwouldnolongerbe requiredand,therefore,wouldnotoccur.
Thefactthat91%and97%ofpractitioners,respectively, correctlyidentifiedanintraoralinjuryandabruiseassentinel injuriesandrecognizedtheneedforachildabuseevaluation isencouraginggiventheliteraturesuggestingthat practitionersoftendonotrecognizethesemoresubtleforms ofabuse.12–14 Itisnotpossibletoknowwhetherthis knowledgeisrelatedtothepresenceoftheCA-CDSSorthe practitionereducationthathassupplementedtheCA-CDSS.
Over90%ofpractitionersstatedthatconcernaboutbeing calledtocourthadlittleornoimpactontheirdecisionto report/evaluateforabuse.Thisisencouraging;inalandmark studybyFlahertyandcolleagues,15 “Clinicianspentmany hoursincourttestifying” wasoneofthepractitioner characteristicsidentifiedinasignificantproportionofthe practitionerswhodidnotreporttoCPSdespitehaving concernformaltreatment.Eachoftheauthorsofthecurrent manuscripthaspersonallyspokenwithpractitionerswho havesaidthattheydonotwanttogetinvolvedinthelegal system.Ourdatasuggeststhat,overall,thisconcernisnot drivingdecision-makingaboutwhetherornottomakea reporttoCPSinourgeneralEDs.
Ourresultsalsounderscoretheneedforusabilityofthe CA-CDSS;practitionersfeltthealertandorderssuggested wereclearanduseful, fitwellintoworkflow,andsavedtime. Theimportanceofusabilitycannotbeoveremphasized:if thisispoorthenitisunlikelythatpractitionerswillusethe tool.16 However,asotherresponsestooursurveyseemto demonstrate,usabilityisnecessary,butnotsufficient,for
practitionerengagementwiththeCA-CDSS.Thenumberof practitionersunawareofdifferentaspectsoftheCA-CDSS includingtheicon,thealert,andtheordersetdemonstrates thechallengesineducationaboutalow-frequencyeventfor anygivenpractitionerinalargehospitalsystem,evenwitha relativelylowpractitioner-turnoverrate.
ImprovingtheknowledgeofpractitionersabouttheCACDSSitselfislikelytobechallenging.Therearemultiple studiesevaluatingtheeffectivenessofdifferenttraining modalities,includinghands-ontraininginalaboratory setting,requiredtraining,useof “ superusers ” toassistothers inlearning,anduseof “just-in-time” training.17–20 Butall theseapproachesarechallengingwhentheyaimtoaddressa relativelyrareevent.Whilechildabuseisacommoncauseof morbidityandmortalityoverall,itisnotcommonlyseenor recognizedbymostindividualpractitioners.Multiple trainingapproachesaswellasindividualizedfollow-upand ongoingtraininghaveallbeenshowntosustainengagement; theseareapproacheswehaveusedandcontinuetouse.17
Despitetheseapproaches,manyofthefree-textresponses notedanunawarenessoftheexistingresources(eg,accessto pediatricexpertsandongoingavailableeducation).We hypothesizethatsomeofthislackofawarenessmaybe relatedtotheincreaseintheuseoflocumtenensand temporarilyorcasuallyemployedpractitioners,whichwas rarepriortoCOVID-19butincreasedsignificantlyduring thepandemicandhascontinued.Thesepractitionersrarelyif everattendtheeducationsessionsanddonotreceive onboardinglikeotherpractitioners,bothofwhichcanlimit therealutilityofresourcespositionedtoaidwithknowledge andcare.
Itisconcerningthatoneofthemostcommonfree-text responsesrelatedtothedesiretohavereal-timeaccesstoa pediatricand/orchildabusespecialistwhilethepatientisin theED.EmergencycliniciansinallthegeneralEDsinthe hospitalsystemalreadyhavethisaccess.Thereisaphone numbertheycancall24/7,whichprovidesconsultationwith apediatricianatthetertiary-carepediatrichospitalinthe hospitalsystem.Ifthepediatricpractitionerisunableto answerachildabuse-specificquestion,thechildabuse specialistoncallispaged.Thelackofknowledgeaboutthis phonenumberreflectsamoregenerallackofknowledge abouthospitalresources.Asaresultofthissurvey,anemail waswidelydistributedtomakepractitionersawareofthis phonenumber,anditisnowincludedon flowsheetsin multipleEDs.
Manyofthefree-textresponsestargetedCDStoolsin generalratherthanspecificallytheCA-CDSS.Alertfatigue wasmentionedinthefree-textresponsesregardingtheCDS toolandareconsistentwithpriorstudies,which demonstratedthatinterruptivealerts(eg,pop-ups)adversely affectpractitioneruseofrecommendationsfromCDS.21–24 Bothfree-textcommentsrelatedtothealert(“Morepop-ups causeclickfatigue.Thishasdestroyedmedicine,” and “We
sufferfrompop-upfatigueandthiscanjustbeonemore”)are consistentwiththebroaderissueofalertfatigue.Whilethe lowtriggerratefortheCA-CDSSishighlyunlikelytobea majorcontributingfactortoalertfatigue,itmayexacerbate pre-existingfrustrationwiththealerts/pop-upsingeneral.
Reportedsuccessfulinterventionstocombatalertfatigue includethepersistentpresenceofthepop-uponthechart untilitisacknowledged,asopposedtohavingmultiplealerts forthesameclinicalconcern.24 Whileapersistentalert wasn ’tapossibilityinourEHRatthetimetheCA-CDSS wasdeveloped,wedesignedthesystemsothateach practitioneronlyreceivesonealertinresponsetothespecific concernoftryingtoalleviatealertfatigue.Interestingly, someoftheearlyfeedbackaboutthesystemwasthatsome practitionerswantedtobealertedrepeatedlyuntilthey decidedwhethertoevaluateforabuse,atwhichpointthey wantedtobeabletosilencethealert.Itisnotpossibleforthe currentEHRsystemtocustomizealertingrulesfordifferent practitioners;whendesigninganygivenCDSsystem,a decisionmustbemadeaboutthetimingandfrequencyof alertsthatappliestoallpractitioners.Addressingtheissueof alertfatigueischallengingbecauseitisthesumofallalerts ratherthanthealertfromanysinglesystemthatimpacts adoptionratesforallCDS.Asaresult,developingasolution requiresahospital/hospitalsystemtoholisticallyevaluateall theCDSsystemsinuse.
Multipleconversationswithpractitionersdisplayedlittle agreementaboutwhenintheworkflowandhowoftenthe alertsshouldbeprovided.Somepractitionerswantedto knowat firstchartopenthattheyshouldbeconcernedabout abuse,sothattheyhavethisinmindwhentheyexaminethe childandspeakwiththefamily,whileotherpractitioners wanttheinformationlaterinthevisitwhentheyare formulatingadifferentialdiagnosis.Somepractitioners wantedtobealertedonlyonce,whileotherspreferredtobe alertedrepeatedlyuntiltheydecidedwhethertoevaluate forabuse.
The findingthatover20%ofpractitionersperceiveCDS asathreattophysicianautonomylikelyhasasignificant impactonengagementandacceptanceofanyCDS.The concernaboutCDSimpactingpractitionerautonomyisnot specifictochildabuseCDS;ratheritisamajorbarrierto CDSingeneral.21,25–27 Interestingly,andperhaps surprisingly,thecharacteristicsofthe15clinicianswhofelt thatCDSwasathreattophysicianautonomywerenot differentfromtheclinicianswhodidnothavethissentiment intermsoftheirresponsetothequestionsabouthowoften lackofcertaintyaboutwhentobeconcernedaboutabuseor lackofcertaintyaboutwhatteststodoinfluencedtheir decisionaboutwhethertodoaphysicalchildabuseworkup. Neitherdidtheydifferfromotherpractitionersintermsof theproportionwhocorrectlyansweredthethreescenarios relatedtosentinelinjuries.Whileitisdifficulttointerpretthis datagiventhesmallnumbers,itsuggeststhatthereisaneed
tobetterunderstandhowthesepractitionerswouldpreferto receiveassistancemakinghigh-quality,evidence-based decisionssincetheyrecognizethattheyareuncertainand thatthisimpactstheirclinicaldecision-making,butthey don’tseeCDSasasolution.
Behavioraleconomics(BE),anevolving fieldrootedin economicandpsychology,maybeoneapproachtoenhance physicianengagementwiththeCA-CDSS.Behavioral economicsisbasedonrecognitionthathumansarenot rationaldecisionmakersandrarelybehaveasthe conventionaleconomicstheorywouldpredict.Interventions informedbyBEattempttochangephysicianpracticeusinga “nudge,” aninterventionthatpredictablychangeshuman behaviorwithoutsignificantlylimitingfreechoiceor changing financialincentives.Changingdefaultsettingsand providingsocialreferencepoints(eg,peercomparison)are mostconsistentlyeffectiveinterventionsinimproving physicianpracticeasitrelatestofollowingevidence-based practice.28–30 AsitrelatestoaCA-CDSS,BEmaybeableto beusedtonudgepractitionerstofollowAAP recommendationsforphysicalabuse,forexample,by providingfeedbackabouttheirperformancecomparedto theirpeers.28–30 Importantly,BEfocusesonthesubsetof practitionerswhoareamenableto “nudging,”31 whichis generallyonlyasubsetofpractitioners.Onewouldnot expectapractitionerwhohasanegativeviewofCDS(ie, feelsthatitlimitsautonomyanddoesnotimprovepatient care)tobeamenabletonudging,butitmaystilloffersome abilitytoimproveengagement.
Perhapsthemostconcerningandconfusing findingwas howmanypractitionerseitherhaveaneutralornegative opinionoftheevidence-basedAAPrecommendationsfor childphysicalabuseevaluation.Thisobservationoccurred alongside65%expressinguncertaintyabouthowtoevaluate forphysicalabuseandmorethan90%recognizingthat sentinelinjuriesrequireaphysicalabuseevaluation. Requiringausertoselectareasonfornotfollowing recommendationsprovidedwithinthealert(eg,tofollowthe recommendationsinthephysicalabuseorderset)can increasecompliancewithrecommendations32 andmay provideinsightintotheseseeminglyinconsistentresponses. Implementationofarequiredresponseneedstobeweighed againstthepossibilityofgeneratingnegativeattitudes towardthetoolandperceivedimpairmentofworkflow. AnotherwaytopotentiallyincreaseadherencetoAAP recommendationsistoensurethatpractitionersunderstand howtheCA-CDSSfunctionsandensurethatpractitioners understandthesourcefortheelectronictool recommendation27;wecurrentlydothisduringbi-monthly educationsessionswithpractitioners.
LIMITATIONS Thereareseverallimitationstothestudy.Theresponse ratewasrelativelylow,andthosewhochosetorespondmay
notberepresentativeofallpractitioners.Theonly demographicdataavailableforallpractitionerswaswhether theywereaphysicianorAPPandthetypeofhospitalthey practicedin;forthesecharacteristics,respondentsandnonrespondentslookedsimilar.Wefeltitwasimportantforthe surveytobeanonymoussothatrespondentswouldbe comfortableprovidinghonestfeedback;thisapproach meanswecouldnottargetnon-respondentstoimprovethe responserate.Itisalsopossiblethattherespondentshaving particularlystrongfeelings positiveornegative aboutthe CA-CDSSweremostlikelytorespondtothesurvey.Because ofthelownumberofpractitionerswhorespondedtothe surveyfromanysinglehospitalandbecausepractitionerscan workatmorethanonehospitalwithinthe19-hospital network,itwasnotpossibletodeterminewhethertherewere site-specificvariationsintheopinionsofpractitionersabout theCA-CDSS.Finally,theresponsestothesurveymaynot reflectactualpracticeandinsteadmayreflectwhat practitionersknowtheyshoulddo.Forexample, practitionersmaysaytheyspeakwiththenursewhenachild hasapositiveCAS,butitisnotpossibletoknowifthis actuallyoccurs.
CONCLUSION Insummary,ourdatasuggeststhatachild-abuseclinical decisionsupportsystemembeddedintheelectronichealth recordhasyieldedpositiveresultsinbothinterdisciplinary communicationandpractitionerattitudestowardthetool, includingperceivingthetoolasincreasingchildabuse awareness.However,thereremaingapsinknowledgeofthe CA-CDSSfunctionalityandincompliancewiththe recommendations.Commentssuggestthatpractitioner dislikeofCDStoolsingeneral,andspecificallyalerts deliveredinpop-upform,maycontributetopooradherence. WhilelimitationsoftheEHRlimitthetypeofalert, CA-CDSSeducationaleffortscouldbeaugmentedto specificallyaddressperceivedbarrierstoautonomyand possiblytoincludebehavioraleconomicstechniques, suchaspeercomparisonortestimonials,33–35 toimprove compliancewithAmericanAcademyofPediatrics recommendations.Furtherresearchshouldfocusonthe effectivenessoftheseinterventionsaswecontinuetoimprove careforarareeventthatcarriessignificantmorbidity andmortality.
AddressforCorrespondence:RachelBergerMD,MPH,UPMC Children’sHospitalofPittsburgh,DivisionofChildAdvocacy, DepartmentofPediatrics,4427PennAve.,Pittsburgh,PA15224. Email: rachel.berger@chp.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial
relationshipswithanycompaniesthatarerelevanttothisstudy.The statementsinthisarticlearesolelytheresponsibilityoftheauthors anddonotnecessarilyrepresenttheviewsofthePennsylvania OfficeofChildren,YouthandFamilies.Therearenoconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Petersonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.U.S.DepartmentofHealthandHumanServices,Administrationfor ChildrenandFamilies,AdministrationonChildren,YouthandFamilies, Children’sBureau.2023.Childmaltreatment2021.Availableat: https:// www.acf.hhs.gov/cb/report/child-maltreatment-2021 AccessedAugust5,2024.
2.CentersforDiseaseControlandPrevention.2021.Deathsinvolving coronavirusdisease2019(COVID-19)amongages0–18yearsinthe UnitedStates.Secondarydeathsinvolvingcoronavirusdisease2019 (COVID-19)amongages0–18yearsintheUnitedStates.Availableat: http://data.cdc.gov/browse.AccessedAugust5,2024.
3.U.S.DepartmentofHealthandHumanServices,Administrationfor ChildrenandFamilies,AdministrationonChildren,YouthandFamilies, Children’sBureau.2018.Childmaltreatment2016.Availableat: https:// www.acf.hhs.gov/cb/report/child-maltreatment-2016 AccessedAugust5,2024.
4.RavichandiranN,SchuhS,BejukM,etal.Delayedidentificationof pediatricabuse-relatedfractures. Pediatrics. 2010;125(1):60–6.
5.JennyC,HymelKP,RitzenA,etal.Analysisofmissedcasesofabusive headtrauma. JAMA. 1999;281(7):621–6.
6.ThorpeEL,ZuckerbraunNS,WolfordJE,etal.Missedopportunitiesto diagnosechildphysicalabuse. PediatrEmergCare. 2014;30(11):771–6.
7.LetsonMM,CooperJN,DeansKJ,etal.Prioropportunitiestoidentify abuseinchildrenwithabusiveheadtrauma. ChildAbuseNegl. 2016;60:36–45.
8.Rumball-SmithJ,FromkinJ,RosenthalB,etal.Implementation ofroutineelectronichealthrecord-basedchildabusescreening ingeneralemergencydepartments. ChildAbuseNegl. 2018;85:58–67.
9.RosenthalB,SkrbinJ,FromkinJ,etal.Integrationofphysicalabuse clinicaldecisionsupportat2generalemergencydepartments. JAm MedInformAssoc. 2019;26(10):1020–9.
10.Patient-CenteredOutcomesResearchInstitute(PCORI).2020. Expandingtheuseofachildabusealertsystemtoimprovedetection andreporting.Availableat: https://www.pcori.org/research-results/ 2017/expanding-use-child-abuse-alert-system-improve-detectionand-reporting.AccessedAugust5,2024.
11.LouwersEC,AffourtitMJ,MollHA,etal.Screeningforchildabuse atemergencydepartments:asystematicreview. ArchDisChild. 2010;95(3):214–8.
12.TrokelM,WadimmbaA,GriffithJ,etal.Variationinthediagnosisofchild abuseinseverelyinjuredinfants. Pediatrics. 2006;117(3):722–8.
13.PierceMC,KaczorK,AckerD,etal.History,injury,andpsychosocial riskfactorcommonalitiesamongcasesoffatalandnear-fatalphysical childabuse. ChildAbuseNegl. 2017;69:263–77.
14.TiyyaguraG,GawelM,KozielJR,etal.Barriersandfacilitatorsto detectingchildabuseandneglectingeneralemergencydepartments. AnnEmergMed. 2015;66(5):447–54.
15.FlahertyEG,SegeRD,GriffithJ,etal.Fromsuspicionofphysicalchild abusetoreporting:primarycarecliniciandecision-making. Pediatrics. 2008;122(3):611–9.
16.BatesDW,KupermanGJ,WangS,etal.Tencommandmentsfor effectiveclinicaldecisionsupport:makingthepracticeofevidencebasedmedicineareality. JAmMedInformAssoc. 2003;10(6):523–30.
17.KealeyE,Leckman-WestinE,FinnertyMT.Impactoffourtraining conditionsonphysicianuseofaweb-basedclinicaldecisionsupport system. ArtifIntellMed. 2013;59(1):39–44.
18.KoskelaT,SandstromS,MakinenJ,etal.Userperspectivesonan electronicdecision-supporttoolperformingcomprehensivemedication reviews:afocusgroupstudywithphysiciansandnurses. BMCMed InformDecisMak. 2016;16:6.
19.FossumM,EhnforsM,FruhlingA,etal.Theexperiencesofusinga computerizeddecisionsupportsystem. NI2012(2012). 2012;113_5: eCollection2012.
20.FossumM,EhnforsM,FruhlingA,etal.Anevaluationoftheusabilityofa computerizeddecisionsupportsystemfornursinghomes. ApplClin Inform. 2011;2(4):420–36.
21.LugtenbergM,WeeninkJW,vanderWeijdenT,etal.Implementationof multiple-domaincoveringcomputerizeddecisionsupportsystemsin primarycare:afocusgroupstudyonperceivedbarriers. BMCMed InformDecisMak. 2015;15:82.
22.MillerA,MoonB,AndersS,etal.Integratingcomputerizedclinical decisionsupportsystemsintoclinicalwork:ameta-synthesisof qualitativeresearch. IntJMedInform. 2015;84(12):1009–18.
23.GurwitzJH,FieldTS,RochonP,etal.Effectofcomputerizedprovider orderentrywithclinicaldecisionsupportonadversedrugeventsinthe long-termcaresetting. JAmGeriatrSoc. 2008;56(12):2225–33.
24.Scheepers-HoeksAM,GroulsRJ,NeefC,etal.Physicians’ responses toclinicaldecisionsupportonanintensivecareunit–comparisonoffour differentalertingmethods. ArtifIntellMed. 2013;59(1):33–8.
25.VanDortBA,ZhengWY,BaysariMT.Prescriberperceptionsof medication-relatedcomputerizeddecisionsupportsystemsinhospitals: asynthesisofqualitativeresearch. IntJMedInform. 2019;129:285–95.
26.EsmaeilzadehP,SambasivanM,KumarN,etal.Adoptionofclinical decisionsupportsystemsinadevelopingcountry:antecedentsand outcomesofphysician’sthreattoperceivedprofessionalautonomy. IntJ MedInform. 2015;84(8):548–60.
27.LiberatiEG,RuggieroF,GaluppoL,etal.Whathinderstheuptakeof computerizeddecisionsupportsystemsinhospitals?Aqualitativestudy andframeworkforimplementation. ImplementSci. 2017;12(1):113.
28.StevensJ.Topicalreview:Behavioraleconomicsasapromising frameworkforpromotingtreatmentadherencetopediatricregimens. J PediatrPsychol 2014;39(10):1097–103.
29.StevensJandBerlanED.Applyingprinciplesfrombehavioral economicstopromotelong-actingreversiblecontraceptive(LARC) methods. PerspectSexualReprodHealth. 2014;46(3):165–70.
30.WangSYandGroeneO.Theeffectivenessofbehavioraleconomicsinformedinterventionsonphysicianbehavioralchange:asystematic literaturereview. PLoSOne. 2020;15(6):e0234149.
31.PatelMS,VolppKG,AschDA.Nudgeunitstoimprovethedeliveryof healthcare. NEnglJMed. 2018;378(3):214–6.
32.RoshanovPS,FernandesN,WilczynskiJM,etal.Featuresofeffective computerisedclinicaldecisionsupportsystems:meta-regressionof162 randomisedtrials. BMJ. 2013;346:f657.
33.JabbariJ,RollS,BufeS,etal. “Takemywordforit”:grouptextsand testimonialsenhancestateandfederalstudentaidapplications. JBehav ExpEcon. 2022;98:101864.
34.Apolinario-HagenJ,FritscheL,WoppererJ,etal.Investigatingthe persuasiveeffectsoftestimonialsontheacceptanceofdigitalstress managementtrainingsamonguniversitystudentsandunderlying mechanisms:arandomizedcontrolledtrial. FrontPsychol. 2021;12:738950.
35.ShenJ,PangS,SchwebelDC.Evaluationofadrowningprevention programbasedontestimonialvideos:arandomizedcontrolledtrial. J PediatrPsychol. 2016;41(5):555–65.
COMMENTARY ReframingChildProtectioninEmergencyMedicine JosephP.Shapiro,MD* GenevievePreer,MD†‡
CarolineJ.Kistin,MD,MSc§
*Children’sNationalHospital,DepartmentofEmergencyMedicineandTrauma, WashingtonDC
† BostonUniversityChobanian&AvedisianSchoolofMedicine, Boston,Massachusetts
‡ BostonMedicalCenter,Boston,Massachusetts
§ BrownUniversity,SchoolofPublicHealth,HassenfeldChildHealthandInnovation Institute,DepartmentofHealthServices,Policy,andPractice, Providence,RhodeIsland
SectionEditor:MuhammadWaseem,MD
Submissionhistory:SubmittedSeptember26,2023;RevisionreceivedApril11,2024;AcceptedMay10,2024
ElectronicallypublishedOctober1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18481
ChildmaltreatmentremainsaconcerningsourceofmorbidityandmortalityintheUnitedStates,where morethan600,000childrenarevictimsofabuseeachyear,withwell-described,long-term consequencesforphysicalandmentalhealth.
However,theUSchildwelfaresystemischaracterizedbysystemicracismandinequity.Blackand NativeAmericanchildrenaremorelikelytobeevaluatedandreportedforsuspectedabusedespite evidencethatracedoesnotindependentlychangetheirriskofbeingabused.Oncereportedtochild protectiveservices(CPS),thesechildrenaremorelikelytoberemovedfromtheirhomesandlesslikely tobereunitedwiththeirfamiliesthanWhitechildren.
Muchoftheinequityinthissystemstartsatthefrontdoor,whereagrowingbodyofresearch demonstratesthatbiasregularlyinfiltratesdecision-makingintheinitialclinicalevaluationand managementofsuspectedabuse.Minoritychildrenpresentingtoemergencydepartments(ED)are morelikelytoreceivediagnostictestingandaremorelikelytobereferredtoCPS.
Inthiseditorial,wearguefortheapplicationofanequitylenstochildprotectionintheED.We discusshowemergencyphysicianscanbalanceeffortstoprotectchildrenfromabusewiththe imperativetoprotectchildrenandfamiliesfromtheharmsofaninequitablechildwelfaresystem.Our discussionconcludeswithconcreterecommendationsforemergencyclinicianstoparticipateinactive biasmitigationandthoughtfullynavigatetheirresponsibilitiesasmandatedreporters.[WestJEmerg Med.2024;25(6)1020–1024.]
Childmaltreatmentremainsaconcerningcauseof morbidityandmortalityintheUnitedStates,wheregreater than600,000childrenarevictimsofsubstantiatedabuseeach yearwithlong-termconsequencesforphysicalandmental health.1 TheUSchildwelfaresystem,however,is characterizedbymarkedinequity.2,3 BlackandNative Americanchildrenaremorelikelytobeevaluatedand reportedforsuspectedabusedespiteevidencethatracedoes notindependentlychangetheirriskofbeingabused.4,5
Inyearspast,typicalclinicaldecision-makingmighthave dictatedthatevenasmallsuspicionofchildabusemeantan automaticreporttochildprotectiveservices(CPS).However,
withthegrowingrecognitionoftheracialinequitywithinthe childwelfaresystemanditsadverseeffectsoncommunitiesof color,emergencyphysiciansnowmustreconsidertheir approach.6–8 Asfrontlinecarecliniciansforinjuredchildren, emergencyphysiciansshouldseektostrikeabalancebetween safeguardingchildrenfromabuseandshieldingfamiliesfrom unnecessaryexposuretothechildwelfaresystem.
Inasystematicreview,Cenatetalcompiled36studiesof proportionalityinchildwelfaresystemsandfoundthat27of thesestudiesshowBlackyouthareover-representedinthese systems.2 Thisdisproportionalityispresentateachphaseof thechildprotectionprocessbeginningwithreporting.
Nationally,Blackchildrenrepresent15%ofthegeneral populationbutaccountfor25%ofCPSinvestigations.9 Separatestate-levelanalysesofpublicrecordsin Washington,Colorado,Missouri,Wisconsin,Texas,and NorthCarolinashowthatBlackchildrenareatleasttwiceas likelyasWhitechildrentobereportedtoCPS.10–15
Onceaninvestigationisinitiated,BlackandNative Americanchildrenaremorelikelytoberemovedfromtheir homesandlesslikelytobereunitedwiththeirfamiliesthan Whitechildren.16 Inarecordreviewof4,000children referredtoCPSinCalifornia,Luetalfoundthatin comparisontoWhitechildren,Blackchildrenwere23.4% morelikelytobeplacedinout-of-homecareand11.7%less likelytobereunifiedwiththeirfamiliesifremovedfromthe home.17 AsimilarreviewbytheCenterfortheStudyof SocialPolicyfoundthatBlackvictimsofmaltreatmentwere 36%morelikelythanWhitevictimstoberemovedfrom theirhomes.18
TheburdenofchildwelfareinvolvementonBlackfamilies andcommunitiesissubstantial.ResearchbyKimetal indicatesthatover50%ofBlackchildrenwillundergoaCPS investigationwithintheirfamilybeforeturning18.19 SociologistDorothyRobertsandacoalitionofacademics andcommunityadvocatesleadanintellectualmovement thatcharacterizesthechildwelfaresystemasaformof “familypolicing.” Througharobustbodyofqualitativeand narrativeresearchtheyhighlighthowthesystemdisrupts parentalauthority,hinderschildren’srelationship development,fostersdistrustamongneighbors,andharms maternalmentalhealth.7,20–21 Thereislittleevidencethat contactwiththechildwelfaresystemcanimproveoutcomes forchildrenorfamilies.22
Theroleofemergencyphysiciansasmandatedreporters andprovidersoffrontlinecaretoinjuredchildrenmakesthem defactogatekeeperstothisunequalsystem.MostCPS referralsinhospitalsareforpatientswhosecarestartsinthe emergencydepartment(ED).23 Bothgeneralemergency physiciansandpediatricemergencyphysicianscarefor childrenwhomayhavebeenthevictimsofphysicalorsexual abuse,orwhomaybeexperiencingoneofmultipletypesof neglect(physical,supervisory,medical,educational,and emotional).Agrowingbodyofresearchdemonstratesthatbias regularlyinfiltratesdecision-makingintheinitialclinical evaluationandmanagementofsuspectedabuse.Ina secondaryanalysisofCPSreportsconductedatanacademic tertiaryhospital,CortetalfoundBlackandHispanicpediatric patientswerefourtimesmore likelythanWhitepediatric patientstobereportedtoCPSbymedicalpersonnel.24
Laneetaldemonstratedinaretrospectivecohortstudy thatBlackandLatinxchildrenseenforfractureswereeight timesmorelikelythanWhitechildrentoreceiveaskeletal surveyandfourtimesmorelikelytobereportedtoCPS, regardlessofinsurancestatus(poverty)orlikelihoodofan abusiveinjury.5 Inastudyofpediatricpatientsadmittedfor
traumaticbraininjuryat39hospitals,Woodetalobserved thatfewerskeletalsurveysareperformedamongWhite infants(67.8%)thanBlackinfants(84%).25 Inacrosssectionalanalysisfrom18sitesinthePediatricBrainInjury ResearchNetwork,Hymeletalfoundthatamongacutely head-injuredpatientshospitalizedforintensivecare, minoritypatientsweretwiceaslikelytobeevaluatedand reportedforabusethanWhitepatients.Thisdisparitywas seenmostinpatientswhohadalowestimatedriskofabusive headtraumaattheoutsetoftheencounter.26 Mostrecently, Rebbeetalshowedthatamonghospitalizedpatients,Asian andNativeAmericanchildrenweremorelikelythanWhite childrentohavetheirencountercodedwithamaltreatmentrelateddiagnosticcodeandtobereportedtoCPS.27 Itisin partbecausebiasfactorsintochildmaltreatmentreporting thatemergencyphysicianshavesuchameaningfulrole toplay.
Itisnotourintentiontoencouragephysicianstoshirk mandatedreportingrequirements.Physicianswitha “reasonablesuspicion” ofchildmaltreatmentshouldreport theirconcernstotheappropriateauthorities.Thisremains thelegalstandardinmostjurisdictionsacrosstheUnited States.Thatsaid,itmustbeacknowledgedthatconsiderate, well-trainedpeopledisagreeonwhatconstitutes “reasonable suspicion.” Thetermisplaguedbyindeterminacyintheory andpractice.28 Surveystudiesconsistentlyshowwide variationamongphysiciansattemptingtodefinereasonable suspicionandreachconsensusonthethresholdfor reporting.29 Inonestudy,clinicianschosetoreportonly73% ofchildrentheyconsidered “likely” or “verylikely” tohave beenabused,30 whileinaseparatestudynearlyhalfof respondentssaidtheywouldreportcaseswhereabusewas fifthorlowerontheirlistofpotentialdifferential diagnoses.31 Inmanycases,itcannotbeassumedthatany twomandatedreportersagreeontheneedfora CPSreport.
Inthesettingofthisindeterminacy,theburdenfallstothe individualclinician,anditisarguablyanethicalonemore thanalegalone.UnnecessaryreportstoCPSstandindirect conflictwiththeprinciplesofnon-maleficenceandjustice. Reasonablepeoplemaydisagreeonthethresholdfor reportingpotentialabuse,butallcliniciansshouldconsider thefullscopeofharmsandbenefitsanytimethey contemplatea filing.
Optimistically,thischallengeisalsoanopportunity.There isagrowingenthusiasmforremedyingthechildwelfare systemamongpediatrichealthcarecliniciansinmany settings.4,6 Emergencyandpediatricemergencyphysicians areperfectlypositionedtojointhismovementandmake positivechangesinanunjustsystem.Inthe recommendationsthatfollow,wedrawontheworkof expertsinchildprotectionandimplicitbiastosuggest interventionsforemergencyphysiciansattheintrapersonal andinterpersonallevels.
1.Stayabreastofcurrentevidenceand recommendations.Theevidencebaseforchildabuse pediatricsisrapidlyevolving.Itisincreasingly understoodwhichmechanismsarefeasible explanationsforcertaininjuries,makingitpossible toaccuratelyidentifythe findingsmostindicativeof abuse.Agoodunderstandingofthisevidencebase allowsclinicianstoavoidunnecessaryworkupsand referrals.TheAmericanAcademyofPediatrics providesclinicalpracticeguidelinesthatsummarize currentrecommendationsfortheevaluationof physicalabuse.32,33 Goingastepfurther,physicians canusetheirknowledgeofevidence-basedpractice toimplementstandardizationwithintheir departments.Limitedstudiesshowthatclinical practiceguidelinescanimprovedisproportionalityin childmaltreatmentevaluation.34 Thisshouldbe donecarefully.Standardscreeningguidelinesmay improveproportionality,butstandardizedreferral guidelinesriskoverexposingchildrenandfamiliesof allracestothechildwelfaresystem.
2.Useamultidisciplinaryapproachtochildprotection. Athoroughprotectiveassessmentbyaskilledsocial workerisaninvaluabletoolfordeterminingwhether aCPS filingisnecessary.Inadditiontotheinjury historytypicallyobtainedbythemedicalteam,social workersoftenhavetheopportunitytolearnmore aboutfamilydynamics,housingstatus,caretaking responsibilities,protectivefactors,orpriorCPS involvement.Allthisinformationcanbeusedto makeaholisticassessmentofprotectiveconcerns andinformdialoguetomitigatebias.
3.Consultchildabusepediatricianswheneverpossible. Childabusepediatriciansaresubspecialistswith extensivetrainingandexpertiseinallaspectsofchild protection.Theycanrecommenddiagnosticworkups, commentonwhetherinjuriesareconsistentwithstated mechanisms,andhelpphysiciansnavigatethe reportingprocess.Thereisevidencethatconsultation withachildabusepediatriciancanreduceunnecessary referralstoCPS.35
4.UnderstandyourlocalCPSandmakereferralsin accordancewiththeircapabilities.Agoodemergency roomphysiciandoesnotorderatestortreatment withoutknowledgeofitslimitations.Thesameshould applytoareporttoCPS.Whattypesofconcernsdo investigatorshavetheexpertisetoinvestigate?What supportscantheyoffertofamilies?Cantheyhelpwith childcare,housing,transportation,oremployment?It isacommonmisconceptionamongcliniciansthata reporttoCPSbenefitsfamiliesbyhelpingthemto accessadditionalresources.36,37 Inpractice,itis uncommonforCPStoprovidesocialsupportsthat couldnothavebeenmadeavailablebyahospital
socialworkerorprimarypediatrician.Ithasbeen questionedwhetherCPShasanimpactatallon modifiableriskfactorsforabuse.Inamulticenter cohortstudyof595childrenbetween4–8yearsold judgedtobeatriskofabuse,Campbelletalfoundno associationbetweenCPSinvestigationandsubsequent socialsupport,familyfunction,poverty,maternal education,orchildbehavioralproblems.38
5.Becarefulaboutlanguageandinformationsharing. Whencommunicatingaboutacasewithcolleaguesor CPS,avoiddiscussingunnecessarydemographic details(race,employmentstatus),orsharing subjectivejudgments(“lovelyfamily”).Themore communicationislimitedtoessentialinformation andneutrallanguage,themorewecanminimizethe effectofbias.
Emergencyclinicianscanplayanessentialrolein decreasingsystemicinequityinchildwelfarebymitigating implicitandexplicitbiasandtakingathoughtfulapproachto mandatedreporting.
AddressforCorrespondence:JosephP.Shapiro,MD,Children’s NationalHospital,DepartmentofEmergencyMedicineandTrauma, 111MichiganAvenueNW,WashingtonDC,20010.Email: Joseph. shapiro@childrensnational.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Shapiroetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.U.S.DepartmentofHealth&HumanServices,Administrationfor ChildrenandFamilies,AdministrationonChildren,YouthandFamilies, Children’sBureau.Childmaltreatment2019.2021.Availableat: https:// www.acf.hhs.gov/cb/research-data-technology/statistics-research/ child-maltreatment.AccessedApril1,2023.
2.CénatJM,McInteeSE,MukunziJN,etal.Overrepresentation ofBlackchildreninthechildwelfaresystem:asystematic reviewtounderstandandbetteract. ChildrenYouthServRev. 2021;120:105714.
3.DettlaffAJ.(2014).Theevolvingunderstandingofdisproportionalityand disparitiesinchildwelfare.In:KorbinJEandKrugmanRD(Eds.), HandbookofChildMaltreatment (149–68).Dordrecht,TheNetherlands: Springer;2014.
4.PalusciVJandBotashAS.Raceandbiasinchildmaltreatment diagnosisandreporting. Pediatrics. 2021;148(1):e2020049625.
5.LaneWG,RubinDM,MonteithR,etal.Racialdifferencesinthe evaluationofpediatricfracturesforphysicalabuse. JAMA. 2002;288(13):1603–9.
6.RosenthalCM,ParkerDM,ThompsonLA.Racialdisparitiesinchild abusemedicine. JAMAPediatrics. 2021;176(2):119–20.
7.FongK.Gettingeyesinthehome:childprotectiveservices investigationsandstatesurveillanceoffamilylife. AmSociolRev. 2020;85(4):610–38.
8.FreisthlerB.Wehavemoretoolstosupportat-riskfamiliesthanjustchild protectiveserviceswithmandatedreporting. JAMAPediatrics. 2024;178(1):96.
9.TheAnnieE.CaseyFoundation. TheKidsCountDataBook. 2019. Availableat: https://www.aecf.org/resources/2019-kids-count-databook.AccessedApril1,2023.
10.WashingtonStateRacialDisproportionalityAdvisoryCommittee. (2010).RacialdisproportionalityinWashingtonStatereporttothe legislature.In: Lawsof2007(SHB1472).Olympia,WA:Washington StateDepartmentofSocialandHealthServices.
11.NeedellB,WebsterD,ArmijoM,etal.Childwelfareservicesreportsfor California.Availableat: http://cssr.berkeley.edu/ucb_childwelfare AccessedAugust31,2023.
12.DrakeB,LeeSM,Jonson-ReidM.Raceandchildmaltreatment reporting:areBlacksoverrepresented? ChildrenYouthServRev. 2009;31(3):309–16.
13.ReadL,O’RourkeCM,HoferL,etal.Racialdisproportionalityin Wisconsin’schildwelfaresystem.2009.Availableat: https://minds. wisconsin.edu/handle/1793/36539.AccessedApril1,2023.
14.TexasHealthandHumanServicesCommission,DepartmentofFamily andProtectiveServices.Disproportionalityinchildprotectiveservices: statewidereformeffortbeginswithexaminationoftheproblem.2006. Availableat: https://www.dfps.texas.gov/Child_Protection/ Disproportionality/documents/2006-01-02_Disproportionality.pdf AccessedApril1,2023.
15.HillRB.Synthesisofresearchondisproportionalityinchildwelfare:an update.2006.Availableat: https://www.aecf.org/resources/ synthesis-of-research-on-disproportionality-in-child-welfare-an-update AccessedApril1,2023.
16.YiY,EdwardsFR,WildemanC.Cumulativeprevalenceof confirmedmaltreatmentandfostercareplacementforUS childrenbyrace/ethnicity,2011-2016. AmJPublicHealth. 2020;110(5):704–9.
17.LuYE,LandsverkJ,Ellis-MacleodM,etal.Race,ethnicity,and caseoutcomesinchildprotectiveservices. ChildrenYouthServRev. 2004;26(5):447–61.
18.HillRB.Ananalysisofracial/ethnicdisproportionalityanddisparityatthe national,state,andcountylevels.2007.Availableat: https://www.aecf. org/resources/an-analysis-of-racial-ethnic-disproportionality-anddisparity-at-the-nation.AccessedApril1,2023.
19.KimH,WildemanC,Jonson-ReidM,etal.Lifetimeprevalenceof investigatingchildmaltreatmentamongUSchildren. AmJPublic Health. 2017;107(2):274–80.
20.RobertsDE. ShatteredBonds:TheColorofChildWelfare.NewYork, NY:BasicBooks,2002.
21. LeeT. CatchingaCase:InequalityandFearinNewYorkCity’s ChildWelfareSystem.NewBrunswick,NJ:RutgersUniversity Press,2016.
22.EvangelistM,ThomasMMC,WaldfogelJ.Childprotectiveservices contactandyouthoutcomes. ChildAbuseNegl. 2023;136:105994.
23.RoviS,ChenPH,JohnsonMS.Theeconomicburdenof hospitalizationsassociatedwithchildabuseandneglect. AmJPublic Health. 2004;94(4):586–90.
24.CortNA,CerulliC,HeH.Investigatinghealthdisparitiesand disproportionalityinchildmaltreatmentreporting:2002–2006. JPublic HealthManagPract. 2010;16(4):329–36.
25.WoodJN,HallM,SchillingS,etal.Disparitiesintheevaluationand diagnosisofabuseamonginfantswithtraumaticbraininjury. Pediatrics. 2010;126(3):408–14.
26.HHymelKP,LaskeyAL,CrowellKR,etal.Racialandethnicdisparities andbiasintheevaluationandreportingofabusiveheadtrauma. J Pediatr. 2018;198:137–43.e1.
27.RebbeR,SattlerKM,MienkoJA.Theassociationofrace,ethnicity,and povertywithchildmaltreatmentreporting. Pediatrics. 2022;150(2):e2021053346.
28.LeviBHandLoebenG.Indexofsuspicion:feelingnotbelieving. Theor MedBioeth. 2004;25(4):277–310.
29.LeviBHandBrownG.Reasonablesuspicion:astudyof Pennsylvaniapediatriciansregardingchildabuse. Pediatrics. 2005;116(1):e5–12.
30.FlahertyEG,SegeRD,GriffithJ,etal.Fromsuspicionofphysicalchild abusetoreporting:primarycarecliniciandecision-making. Pediatrics. 2008;122(3):611–9.
31.LeviBHandBrownG.Reasonablesuspicion:astudyof Pennsylvaniapediatriciansregardingchildabuse. Pediatrics. 2005;116(1):e5–12.
32.ChristianCW,CommitteeonChildAbuseandNeglect,American AcademyofPediatrics.Theevaluationofsuspectedchildphysical abuse. Pediatrics. 2015;135(5):e1337–54.
33.SectiononRadiology,AmericanAcademyofPediatrics.Diagnostic imagingofchildabuse. Pediatrics. 2009;123(5):1430–5.
34.RangelEL,CookBS,BennettBL,etal.Eliminatingdisparityin evaluationforabuseininfantswithheadinjury:useofascreening guideline. JournalofPediatricSurgery. 2009;44(6):1229–34; discussion1234–5.
35.RazM,Gupta-KaganJ,AsnesAG.Usingchildabusespecialiststo reduceunnecessarychildprotectiveservicesreportsand investigations. JAMAPediatr. 2023;177(12):1249–50.
36.JonesR,FlahertyEG,BinnsHJ,etal.Clinicians’ descriptionoffactors influencing theirreportingofsuspectedchildabuse:reportoftheChild
AbuseReportingExperienceStudyResearchGroup. Pediatrics. 2008;122(2):259–66.
37.FeldmanKW,MonasterskyC,FeldmanGK.Whenischildhood drowningneglect? ChildAbuseNeglt. 1993;17(3):329–36.
38.CampbellKA,CookLJ,LaFleurBJ,etal.Household,family,andchild riskfactorsafteraninvestigationforsuspectedchildmaltreatment:a missedopportunityforprevention. ArchPediatrAdolescMed. 2010;164(10):943–9.
LETTERSTOTHE EDITOR Commentson “BicarbonateandSerumLabMarkersasPredictors ofMortalityintheTraumaPatient” PatrickMcGinnis,BS*
SamanthaCamp,BS*
MinahilCheema,BS*
ShriyaJaddu*
QuincyTran,MD,PhD†
JessicaDowning,MD†
*UniversityofMarylandSchoolofMedicine,Baltimore,Maryland † UniversityofMarylandMedicalCenter,Baltimore,Maryland
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedJuly17,2024;RevisionreceivedJuly25,2024;AcceptedJuly29,2024
ElectronicallypublishedSeptember25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.31021
DearEditor:
Wereadwithgreatenthusiasmthearticle “Bicarbonate andSerumLabMarkersasPredictorsofMortalityinthe TraumaPatient” byTalbottetal,1 whichwasrecently publishedinthe WesternJournalofEmergencyMedicine TalbottetalutilizedtheTriNetXdatabasetoexplore associationsbetweenserumlaboratorymarkers (bicarbonate,lactate,andbaseexcess)and30-daymortality. Despitethenoveltyoftheir findings,wehaveafewcomments aboutthemethodologyandresultsthatmaynotsupport theirconclusions.
Our firstcommentiswithregardtothelackof stratificationofanatomicallocationandtraumatype.While itiscommendabletoemploylargesamplesizestoimprove generalizability,itislesshelpfulforclinicianswhomanage varioustypesoftraumas.Forinstance,patientswhosustain gunshotwoundstothethighmaysufferhemorrhagicshock andmetabolicacidosisproducingelevatedlactatevalues,2 yettheyhaveahigherchanceofsurvivalifresuscitationis prompt.3 Severalstudieshaveshownlactatelevelsfrom patientswithblunttraumaticbraininjuryare indistinguishablefromhealthycontrols,yetthesepatients’ riskofmortalityisincreasedduetothelocationofinjury.4 Thesepatientsactivatedifferenttreatmentalgorithms, makingconclusionsabout “trauma” patientstoobroadfor clinicalutility.
Moreover,themethodologyforpatientselectioncouldbe morenarrowlydefined.TheauthorsusedtheInternational ClassificationofDiseases,10th Revision,Clinical Modification(ICD)codeICD10CM:T14Injurytoany unspecifiedbodyregion,whichincludesanyinjuryfroma superficialinjurytotraumaticamputation.Thisposesawide spectrumoftreatmentsandsurvivability,asinjurylocation impactsthetriageprocessandmobilizationofstaff andresources.
WereplicatedTalbott’sanalysiswithanarrower anatomicallocationusingICD10CM:S06Intracranial injuryincludingsubarachnoidandsubduralhemorrhage, bothofwhichraisesuspicionforelevatedlactate.Weagree higherlactatevaluesareassociatedwithincreasedriskof mortality;however,specifyingthelocationofinjury (intracranial)strengthenedthisassociationbeyondthe Talbottetalanalysis.Afterstratifyinglactatebyincrements of2wefoundthattheriskofmortalitywas1.06%,3.42%. 13.3%,27.4%,38.1%,and57.0%forlactaterangesof <2, 2–4,4–6,6–8,8–10,and10–12millimolesperliter, respectively.Theseresultsillustratehowspecifyingan injurytypeandanatomicallocationprovidesnarrower,more usefulassociationsbetweenserumlabmarkersand 30-daymortality.
Finally,Talbottetalused “sameday” lactatelevels. Althoughlactateatarrivalmayhaveprognosticvalue, persistentlyelevatedlevelafter20hoursofinjuryportends differentprognoses.5 Whenprovidingguidancetoclinicians treatingtraumapatients,thisgranularityaidsin understandingapatient’sclinicalcondition,asoutcomesfor patientswithelevatedarrivallactatethatisclearedafterfour hoursvsthosewithpersistentlyelevatedlactateat24hours arevastlydifferent.6 Nonetheless,wecommendthe workofTalbottetalandareexcitedaboutthemagnitudeof thisstudy.Werecommendthatcliniciansbe prudentininterpretingthestudy’sresultandinapplying themtotheirclinicalpractice.
AddressforCorrespondence:PatrickJohnMcGinnis,Universityof MarylandSchoolofMedicine,108NGreeneSt.,BaltimoreMD 21201.Email: pmcginnis@som.umaryland.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources
and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024McGinnisetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES 1.TalbottMM,WaguespackAN,ArmstrongPA,etal.Bicarbonateand serumlabmarkersaspredictorsofmortalityinthetraumapatient. West JEmergMed. 2024;25(4):661–7.
2.KrishnaU,JoshiSP,ModhM.Anevaluationofserialbloodlactate measurementasanearlypredictorofshockanditsoutcomeinpatients oftraumaorsepsis. IndianJCritCareMed. 2009;13(2):66–73.
3.KrauszMM.Initialresuscitationofhemorrhagicshock. WorldJEmerg Surg. 2006;1:14.
4.GlennTC,MartinNA,HorningMA,etal.Lactate:brainfuelinhuman traumaticbraininjury:acomparisonwithnormalhealthycontrol subjects. JNeurotrauma. 2015;32(11):820–32.
5.GewirtzRJ,DhillonHS,GoesSE,etal.Lactateandfreefatty acidsaftersubarachnoidhemorrhage. BrainRes. 1999;840(1–2):84–91.
6.DezmanZDW,ComerAC,SmithGS,etal.Repeatlactatelevel predictsmortalitybetterthanrateofclearance. AmJEmergMed. 2018;36(11):2005–9.