Volume 26, Number 2, March 2025



Volume 26, Number 2, March 2025
Cardiology
180 Critical Time Intervals in Door-to-Balloon Time Linked to One-Year Mortality in ST-Elevation
Myocardial Infarction
Shin-Ho Tsai, Yu-Ting Hsiao, Ya-Ni Yeh, Jih-Chun Lin, Shi-Quan Zhang, Ming-Jen Tsai
191 Unlocking Cardiac Insights: Displacement of Aortic Root for Calculation of Ejection Fraction in Emergency Department in India
Sudhi Manu, Gopinathan Vivek, Asanaru Kunju Sanjan, A. Ajay, S. Nisarg, Mymbilly Balakrishnan Jayaraj, T. R. Aishwarya, Mohammad Khalid, S. Chetana
Clinical Practice
200 Procedural Sedation in the Emergency Department – An Observational Study: Does Nil Per Os Status Matter?
Brendan Peterson, Amy S. Nowacki, Alexander Ulintz, Sharon E. Mace
210 Immune Checkpoint Inhibitor-associated Pneumonitis: A Narrative Review
Chang Li, Saadia A. Faiz, Megan Boysen-Osborn, Ajay Sheshadri, Monica K. Wattana
Critical Care
219 Cardiac Computed Tomography Measurements in Pulmonary Embolism Associated with Clinical Deterioration
Anthony J. Weekes, Angela M. Pikus, Parker L. Hambright, Kelly L. Goonan, Nathaniel O’Connell
Education
233 Monitoring the Evolving Match Environment in Emergency Medicine 2023
Anthony Sielicki, Brian Milman, Andrew Little, Miriam Kulkarni, James Morris, Laura Hopson, Michael Kiemeney


















About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.
Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania

FOR MORE INFORMATION PLEASE CONTACT:
Heather Peffley, PHR CPRP
Penn State Health Lead Physician Recruiter hpeffley@pennstatehealth.psu.edu


Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Mark I. Langdorf, MD, MHPE, Editor-in-Chief
University of California, Irvine School of MedicineIrvine, California
University of California, Irvine School of MedicineIrvine, California
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Niels K. Rathlev, MD, Associate Editor Tufts University School of Medicine-Boston, Massachusetts
Michael Shalaby, MD, Deputy Editor Mount Sinai Medical Center
Susan R. Wilcox, MD, Associate Editor
Massachusetts General Hospital- Boston, Massachusetts
Elizabeth Burner, MD, MPH, Associate Editor
University of Southern California- Los Angeles, California
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts s
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Section Editors
Behavioral Emergencies
Leslie Zun, MD, MBA
Rosalind Franklin University of Medicine and Science
Marc L. Martel, MD Hennepin County Medical Center
Behavioral Health
Ryan Ley, MD, MBA, MS University of Nevada School of Medicine
Cardiac Care
Anthony Lucero, MD Kaweah Health Medical Center
Mary McLean, MD, FAAEM, FACEP AdventHealth East Orlando Emergency Medicine Residency
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD Carolinas Medical Center
Casey Clements, MD, PhD
Mayo Clinic
Patrick Meloy, MD Emory University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Dell Simmons, MD Geisinger Health
Joseph Shiber, MD University of Florida-College of Medicine
David Page, MD University of Alabama
Erik Melnychuk, MD Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
Andrew Milsten, MD, MS UMass Chan Medical School
Scott Goldstein, DO, FACEP, FAEMS, EMT-T/P
Jefferson Einstein
John Broach, MD, MPH, MBA, FACEP
University of Massachusetts Medical School
UMass Memorial Medical Center
Christopher Kang, MD Madigan Army Medical Center
Rick A. McPheeters, DO, Associate Editor
R. Gentry Wilkerson, MD, Associate Editor University of Maryland
Education
Asit Misra, MD, MSMEd, CHSE University of Miami
University of Colorado
ED Administration, Quality, Safety
Tehreem Rehman, MD, MPH, MBA
Mount Sinai Hospital
David C. Lee, MD
Northshore University Hospital
Gary Johnson, MD Upstate Medical University
Brian J. Yun, MD, MBA, MPH Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH
Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH
University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine University of California, Davis
Emergency Medical Services
Daniel Joseph, MD Yale University
Joshua B. Gaither, MD
University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Stephen Meldon, MD
Cleveland Clinic
Luna Ragsdale, MD, MPH Duke University Health Equity
Sara Heinert, PhD, MPH
Rutgers Robert Wood Johnson Medical School
Naomi George, MD, MPH University of New Mexico School of Medicine
Sarah Aly, DO
Yale Department of Emergency Medicine
Lauren Walter, MD, MSPH University of Alabama at Birmingham
Victor Cisneros, MD, MPH
Eisenhower Medical Center
Faith Quenzer Temecula Valley Hospital San Ysidro Health Center
University of Texas-Houston/McGovern Medical School- Houston Texa
Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Payal Modi, MD MScPH University of Massachusetts Medical Infectious Disease
Elissa Schechter-Perkins, MD, MPH Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Stephen Liang, MD, MPHS
Washington University School of Medicine
Injury Prevention
Mark Faul, PhD, MA
Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH
Prisma Health Richland
Taylor Burkholder, MD, MPH
Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Indiana University School of Medicine Statistics and Methodology
Monica Gaddis, PhD University of Missouri, Kansas City School of Medicine
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH
Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS
Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS
Neurosciences
Antonio Siniscalchi, MD
Annunziata Hospital, Cosenza, Italy
Rick Lucarelli, MD
Medical City Dallas Hospital
William D. Whetstone, MD University of California, San Francisco
Pediatric Emergency Medicine
Ronnie Waldrop, MD
University of South Alabama
Jabeen Fayyaz, MD, MCPS, FCPS, MHPE, PhD, IHP
The Hospital for Sick Children
Muhammad Waseem, MD Lincoln Medical & Mental Health Center
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
John Ashurst, DO Lehigh Valley Health Network
Tony Zitek, MD
Kendall Regional Medical Center
Erik S. Anderson, MD Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD
Henry Fo
Chris Baker, MD University of California, San Francisco rd Hospital
Phillips Perera, MD Stanford University Medical Center Trauma
Whitney K. Brown, MD, MPH, Med, CTropMed University of Cincinnati College of Medicine
Robert Flint, MD, FACEP, FAAEM University of Maryland School of Medicine
Lesley Osborn, MD University of Colorado
Kathleen Stephanos, MD University of Maryland School of Medicine
T. Andrew Windsor, MD AEMUS-FPD
University of Maryland School of Medicine
Pierre Borczuk, MD Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS Virginia Commonwealth University
University of California, Irvine Ultrasound J. Matthew Fields, MD
Robert Allen, MD Los Angeles General Medical Center
Shane Summers, MD Brooke Army Medical Center
Robert R. Ehrman
Wayne State University
Ryan C. Gibbons, MD Temple Health
Women’s Health
Marianne Haughey, MD Northwell Health
Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine


American Academy of Emergency Medicine







Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA
Integrating Emergency with Population Health
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
MAAEM
Amin A. Kazzi, MD, MAAEM
Amin A. Kazzi, MD, MAAEM
Gayle Galleta, MD
The American University of Beirut, Lebanon
Beirut,
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University Texas, Houston
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD
Ohio State University Wexner Medical Center
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Christopher E. San Miguel, Ohio State University Wexner Medical Center
Daniel J. Dire, MD
Daniel J. Dire, MD University Texas Health Sciences Center San Antonio
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Douglas Ander, MD Emory University
Douglas Ander, Emory University
Emory University
Edward Michelson, MD Texas Tech University
Edward Michelson, Texas Tech University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH South
Edward Panacek, MD, MPH University of South Alabama
Edward MD, MPH University South Alabama
Francesco
“Maggiore della Carità,” Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Elena Lopez-Gusman, JD
Elena Lopez-Gusman, JD
California ACEP
California ACEP
Elena Lopez-Gusman, JD California ACEP American College of Emergency
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Gayle Galleta, MD Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog,
Hjalti Björnsson, MD
Niels K. Rathlev, MD Tufts University School of Medicine
Tufts University School of Medicine
Niels K. Rathlev, MD Tufts University School of Medicine
Scott Zeller, MD
Scott Zeller, MD University of California, Riverside
Scott Zeller, MD University of California, Riverside
Hjalti MD Icelandic Society of Emergency Medicine
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Jaqueline Le, MD Desert Regional Medical Center
Jaqueline Le, MD Desert Medical Center
Regional
Jeffrey Love, MD
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jeffrey Love, The George Washington University School of Medicine and Health Sciences
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Katsuhiro Kanemaru, MD University of Hospital, Miyazaki, Japan
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Bell,
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Singapore
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands
Peter Sokolove, MD University of California, San Francisco
University of California, San Francisco
Wirachin Hoonpongsimanont, MD, MSBATS
Wirachin Hoonpongsimanont, MD, MSBATS
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
The George Washington University School of Medicine and Health Sciences Arizona,
Leslie Zun, MD, MBA Chicago Medical School
Leslie Zun, MD, MBA Chicago Medical School
Rachel A. Lindor, MD, JD Mayo Clinic
Rachel A. Lindor, MD, JD Mayo Clinic
Rachel A. Lindor, MD, JD
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert Suter, DO, MHA
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
University of California, Davis
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Linda S. Murphy, MLIS University of California, Irvine School of Medicine
Chicago Medical School Librarian
American College of Emergency Physicians
American College of Emergency Physicians
Jennifer Kanapicki Comer, MD FAAEM
Jennifer Kanapicki Comer, MD FAAEM
California Chapter Division of AAEM Stanford University School of Medicine
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE
DeAnna McNett, CAE
Kimberly Ang, MBA UC Irvine Health School of Medicine
American College of Osteopathic Emergency Physicians
American College of Osteopathic Emergency Physicians
Randall J. Young, MD, MMM, FACEP California ACEP
Kimberly Ang, MBA
American College of Emergency Physicians Kaiser Permanente
UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians
Kaiser Permanente
J. American College of Emergency Physicians Kaiser Permanente

Scott Rudkin, MD, MBA University of California, Irvine
Scott Rudkin, MD, MBA
Scott Rudkin, MD, MBA University of California, Irvine
Staff
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Langdorf, MAAEM, FACEP
Isabelle Nepomuceno, BS Executive Editorial Director
Isabelle Kawaguchi, BS Executive Editorial Director
June Casey, BA Copy Editor
Cassandra Saucedo, MS Executive Publishing Director
UC Irvine Health School of Medicine
UC Irvine Health School Medicine
UC Irvine Health School of Medicine
Robert Suter, DO, MHA
Robert Suter, DO, MHA American College of Osteopathic
American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Shahram Lotfipour, MD, MPH FAAEM, FACEP
UC Irvine Health School Medicine
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP
Jorge Fernandez, MD, FACEP
Ian Olliffe, BS Associate Editorial Director, WestJEM
Visha Bajaria, BS WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Visha Bajaria, BS WestJEM Editorial Director WestJEM
UC San Diego Health School of Medicine
UC San Diego Health School of Medicine
Jorge Fernandez, MD, UC San Diego Health School of Medicine
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director

and Publishing Office: JEM/Depatment of





Tran Nguyen, BS Associate Editorial Director, CPC-EM
Nicole Valenzi, BA WestJEM Publishing Director
Cassandra Saucedo, MS WestJEM Publishing Director
Sheya Aquino, BS Associate Editorial Director
June Casey, BA Copy Editor
Nancy Taki, BS Associate Editorial Director
Alyson Tsai, BS Associate Publishing Director
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine

Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
241 Personality Traits and Burnout in Emergency Medicine Residents
Brendan Freeman, Lukasz Cygan, Laura Melville, Theodore Gaeta
246 Productivity and Efficiency Growth During Emergency Medicine Residency Training
Matthew T. Singh, David M. Austin, Stephanie C. Mullennix, Joshua C. Reynolds, J. Adam Oostema
254 Harder, Better, Faster, Stronger? Residents Seeing More Patients Per Hour See Lower Complexity
Corlin M. Jewell, Guangyu (Anthony) Bai, Dann J. Hekman, Adam M. Nicholson, Michael R. Lasarev, Roxana Alexandridis, Benjamin H. Schnapp
261 Push and Pull: What Factors Attracted Applicants to Emergency Medicine and What Factors Pushed Them Away Following the 2023 Match
Michael Kiemeney, James Morris, Lauren Lamparter, Moshe Weizberg, Andy Little, Brian Milman
271 Combining Immersive Simulation with a Collaborative Procedural Training on Local Anesthetic Systemic Toxicity and Fascia Iliaca Compartment Block: A Pilot Study
Katherine B. Griesmer, Maxwell Thompson, Briana Miller, Guihua Zhai, Jaron Raper, Andrew Bloom
279 Development of a Reliable, Valid Procedural Checklist for Assessment of Emergency Medicine Resident Performance of Emergency Cricothyrotomy
Dana E. Loke, Andrew M. Rogers, Morgan L. McCarthy, Maren K. Leibowitz, Elizabeth T. Stulpin, David H. Salzman
285 Virtual Interviews Correlate with Home and In-State Match Rates at One Emergency Medicine Program
Christine Motzkus, Casey Frey, Aloysius Humbert
Emergency Department Operations
290 Two-year Results of an Emergency Department Night Shift Buy-out Program
Charlotte W. Croteau, Joshua N. Goldstein, Lauren Nentwich, Ali S. Raja, Michael VanRooyen, Joshua J. Baugh
295 Modeling Hourly Productivity of Advanced Practice Clinicians in the Emergency Department
Bryan A. Stenson, Peter S. Antkowiak, David T. Chiu, Leon D. Sanchez, Joshua W. Joseph
Geriatrics
301 Injuries and Outcomes of Ground-level Falls Among Older Patients: A Retrospective Cohort Study
Vincent Kan, Wilson Huang, Gretta Steigauf-Regan, Jill Anderson, Ivy Dang, Chad Darling
Health Equity
307 Relationship Between Social Risk Factors and Emergency Department Use: National Health Interview Survey 2016–2018
Iraa Guleria, Jennifer A. Campbell, Abigail Thorgerson, Sanjay Bhandari, Leonard E. Egede
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
315 Associations of Individual and Neighborhood Factors with Disparities in COVID-19 Incidence and Outcomes
Margaret E. Samuels-Kalow, Rebecca E. Cash, Kori S. Zachrison, Auriole Corel Rodney Fassinou, Norman Harris II, Carlos A. Camargo Jr.
326 Food and Housing Insecurity, Resource Allocation, and Follow-up in a Pediatric Emergency Department
Raymen R. Assaf, Chloe Knudsen-Robbins, Theodore Heyming, Kellie Bacon, Shelby K. Shelton, Bharath Chakravarthy, Soheil Saadat, Jason A. Douglas, Victor Cisneros
338 Gender Disparities and Burnout Among Emergency Physicians: A Systematic Review by the World Academic Council of Emergency Medicine–Female Leadership Academy for Medical Excellence
Suman Thakur, Vivek Chauhan, Sagar Galwankar, Fatimah Lateef, Pia Daniel, Zeynep Cakir, Katia M. Lugo, Samjhana Basnet, Busra Bildik, Siham Azahaf, Sevilay Vural, Busra H. Difyeli, Lisa Moreno-Walton
Neurology
347 Use and Outcomes of Sugammadex for Neurological Examination after Neuromuscular Blockade in the Emergency Department
Stephen D. Hallisey, Christiana K. Prucnal, Annette M. Ilg, Raghu R. Seethala, Paul S. Jansson
Research Methods
353 Analysis of the Highest Altmetrics-scored Articles in Emergency Medicine Journals Başak Bayram, Murat Cetin, Önder Limon, Brit Long, Michael Gottlieb
Toxicology
364 Effort During Ethanol Breath Testing Impacts Correlation with Serum Ethanol Concentration
Samuel J. Stellpflug, William H. Menton, Bjorn C. Westgard, Ryan D. Johnsen, Alexander M. Coomes, Robert C. LeFevere, Michael D. Zwank
Trauma
367 Blood Pressure Variability and Outcome Predictors for Traumatic Brain Injury Patients with Diffuse Axonal Injury: A Retrospective Cohort Study
Christine E. Ren, Anastasia Ternovskaia, Fatima Mikdashi, Hassan Syed, Isha Vashee, Vainavi Gambhir, Natalie Chao, Jessica V. Downing, David Dreizin, Quincy K. Tran
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Albany Medical College Albany, NY
Allegheny Health Network Pittsburgh, PA
American University of Beirut Beirut, Lebanon
AMITA Health Resurrection Medical Center Chicago, IL
Arrowhead Regional Medical Center Colton, CA
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
INTEGRIS Health Oklahoma City, OK
Kaiser Permenante Medical Center San Diego, CA
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Lakeland HealthCare St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Louisiana State University Shreveport Shereveport, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maine Medical Center Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Mayo Clinic Jacksonville, FL
Mayo Clinic College of Medicine Rochester, MN
Mercy Health - Hackley Campus Muskegon, MI
Merit Health Wesley Hattiesburg, MS
Midwestern University Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program St. Paul, MN
Rhode Island Hospital Providence, RI
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
St. Luke’s University Health Network Bethlehem, PA
Spectrum Health Lakeland St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
The MetroHealth System/ Case Western Reserve University Cleveland, OH
UMass Chan Medical School Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Tucson, AZ
University of California, Davis Medical Center Sacramento, CA
University of California, Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago Chicago, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Massachusetts Amherst, MA
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Nebraska Medical Center Omaha, NE
University of Nevada, Las Vegas Las Vegas, NV
University of Southern Alabama Mobile, AL
University of Southern California Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University Winston-Salem, NC
Wake Technical Community College Raleigh, NC
Wayne State Detroit, MI
Wright State University Dayton, OH
Yale School of Medicine New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org

CriticalTimeIntervalsinDoor-to-BalloonTimeLinkedto One-YearMortalityinST-ElevationMyocardialInfarction
Shin-HoTsai,MD
Yu-TingHsiao,MD
Ya-NiYeh,MS
Jih-ChunLin,BS
Shi-QuanZhang,MD
Ming-JenTsai,MD,PhD
DitmansonMedicalFoundationChia-YiChristianHospital,DepartmentofEmergency Medicine,ChiayiCity,Taiwan
SectionEditor: CaseyM.Clements,MD,PhD
Submissionhistory:SubmittedApril11,2024;RevisionreceivedNovember5,2024;AcceptedNovember7,2024
ElectronicallypublishedJanuary30,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20779
Background: Timelyactivationofprimarypercutaneouscoronaryintervention(PCI)iscrucialfor patientswithST-segmentelevationmyocardialinfarction(STEMI).Door-to-balloon(DTB)time, representingthedurationfrompatientarrivaltoballooninflation,iscriticalforprognosis.However,the specifictimesegmentwithintheDTBthatismostassociatedwithlong-termmortalityremainsunclear. InthisstudyweaimedtoidentifythetargettimesegmentwithintheDTBthatismostassociatedwith one-yearmortalityinSTEMIpatients.
Methods: Weconductedaretrospectivecohortstudyatatertiaryteachinghospital.Allpatients diagnosedwithSTEMIandactivatedforprimaryPCIfromtheemergencydepartmentwereidentified betweenJanuary2013–December2021.Patientdemographics,medicalhistory,triageinformation, electrocardiogram,troponin-Ilevels,andcoronaryangiographyreportswereobtained.Wedividedthe DTBtimeintodoor-to-electrocardiogram(ECG),ECG-to-cardiaccatheterizationlaboratory(cathlab) activation,activation-to-cathlabarrival,andcathlabarrival-to-balloontime.WeusedKaplan-Meier survivalanalysisandmultivariableCoxproportionalhazardsmodelstodeterminetheindependent effectsofthesetimeintervalsontheriskofone-yearmortality.
Results: Atotalof732STEMIpatientswereincluded.Kaplan-Meieranalysisrevealedthatdelayed door-to-ECGtime(>10min)andcathlabarrival-to-balloontime(>30min)wereassociatedwithahigher riskofone-yearmortality(log-ranktest, P < .001and P = 0.01,respectively).InthemultivariableCox models,door-to-ECGtimewasasignificantpredictorforone-yearmortality,whetheritwasanalyzedasa dichotomized(>10minvs ≤10min)oracontinuousvariable.Thecorrespondingadjustedhazardratios (aHR)were2.81(95%confidenceinterval[CI]1.42–5.55)forthedichotomizedanalysis,and1.03(95% CI1.00–1.06)perminuteincrease,respectively.Cathlabarrival-to-balloontimealsoshowedan independenteffectonone-yearmortalitywhenanalyzedasacontinuousvariable,withanaHRof1.02 (95%CI1.00–1.04)perminuteincrease.However,ECG-to-cathlabactivationandactivation-to-cathlab arrivaltimesdidnotshowasignificantassociationwiththeriskofone-yearmortality.
Conclusion: Withinthedoor-to-ballooninterval,thetimefromdoor-to-ECGcompletionisparticularly crucialforone-yearsurvivalafterSTEMI,whilecathlabarrival-to-ballooninflationmayalsoberelevant. [WestJEmergMed.2025;26(2)180–190.]
Primarypercutaneouscoronaryintervention(PCI)stands asthecornerstonetherapyforpatientsexperiencingSTsegmentelevationmyocardialinfarction(STEMI).1–3 The promptactivationofprimaryPCIuponaSTEMIpatient’ s arrivalattheemergencydepartment(ED)iscrucialfor achievingcoronaryarteryreperfusion.1–3 Thedoor-toballoon(DTB)time,representingtheintervalfromthe patient’sEDarrivaltotheinflationofaballoonwithinthe occludedcoronaryartery,servesasapivotalmetricinthis process.1,3 ProlongedDTBtimeshaveconsistentlybeen associatedwithanelevatedriskofshort-termmortalityand majoradversecardiacevents.4–6 Consequently,DTBtime servesasaqualityindicatorforassessingtheperformanceof aPCI-capablehospital.1,7
WithintheDTBtime,severaltimesegmentscanbe delineated,includingdoor-to-electrocardiogram(ECG), ECG-to-catheterizationlaboratory(cathlab)activation, activation-to-cathlabarrival,cathlabarrival-to-needle insertion,andneedleinsertion-to-ballooninflationtime. Delaysinanyofthesetimesegmentsmayleadtoprolonged DTBtime.7–9
Previousstudieshaveexploredtherelationshipbetween DTBandshort-termmortality,suchasin-hospitaldeathor 30-daymortality.5,6 However,theimpactofDTBtimeon long-termmortalityandwhichspecifictimesegmentwithin theDTBismostlyassociatedwithlong-termoutcome remainunclear.Toaidinthedevelopmentofimprovement strategies,ourgoalinthisstudywastodeterminethetarget periodwithintheDTBthatismostassociatedwithone-year mortalityinSTEMIpatients.
StudyDesign,Setting,andParticipants
WeconductedaretrospectivecohortstudyatDitmanson MedicalFoundationChia-YiChristianHospital,a1,000bedtertiaryteachinghospitalinanurbancityofTaiwan. Thehospital’semergencydepartment(ED)handles approximately80,000patientvisitsannually.Designatedas anaccredited,advancedemergency-responsibilityhospitalin Taiwansince2013,itundergoesregularevaluationstoensure compliancewithSTEMIemergencymanagementstandards. Keyobjectivesincludeproviding24/7emergencycardiac catheterizationservices,ensuringthatover80%ofSTEMI patientsreceiveanECGexaminationwithin10minutesof EDarrival,initiatingdualantiplatelettherapyforatleast 80%ofSTEMIpatientsintheEDbeforeprimaryPCI,and achievingDTBtimesofunder90minutesforover75%of STEMIpatients.Consequently,aprotocolformanaging STEMIpatientsintheEDhasbeenimplemented (Supplementary Figure1).
Uponarrival,immediateECGisperformedforpatients withanycardiopulmonary-relatedsymptomsintriageand promptlyreviewedbyanemergencyphysician.IfSTEMIis
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Timelypercutaneouscoronaryinterventionis essentialforpatientswithST-elevation myocardialinfarction(STEMI);reducing door-to-balloon(DTB)timeimproves survivaloutcomes.
Whatwastheresearchquestion?
WhichintervalwithintheDTBtimeismost associatedwith1-yearmortalityin STEMIpatients?
Whatwasthemajor findingofthestudy?
Thetimefromdoor-to-ECGcompletion withintheDTBintervalisparticularly importantfor1-yearmortalityin STEMIpatients.
Howdoesthisimprovepopulationhealth?
IdentifyingkeyintervalswithinDTBtime associatedwithlong-termmortalityin STEMIpatientssupportsthedevelopmentof targetedimprovementstrategies.
diagnosed,aloadingdoseofdualantiplatelettherapyand anticoagulantsisadministered,andthecardiologistis immediatelyconsulted.Thecardiologistactivatesprimary PCIafterassessment.Oncethecathlabisprepared,the patientistransferredforprimaryPCIasexpeditiously aspossible.
AllpatientsdiagnosedwithSTEMIandactivatedfor primaryPCIfromtheEDareincludedinthehospital-based STEMIregistry,wheredatawasprospectivelygatheredfor qualityimprovement.Weidentifiedpatientshospitalizedfor STEMIbetweenJanuary1,2013–December31,2021,from theSTEMIregistry.FactorspotentiallyinfluencingSTEMI outcomesandDTBtime,suchasdemographicdata(age, sex,bodymassindex).10,11 timeofEDarrival,12 weekend visit,13 visitduringtheCOVID-19pandemic,4,15 modeof transportationtothehospital,16 triagelevel,17 initial troponin-Ilevels,18 comorbidities,11 findingsofECG andcoronaryangiography,10,11 anddurationof hospitalization,werecollectedfromtheregistryand electronichealthrecords.
VarioustimepointsfromEDarrivaltoballooninflation wereidentified,includingthetimeofcompletionofthe first ECG,activationofthecathlab,arrivalinthecathlab,and ballooninflation.Wedefineddoor-to-ECGtimeasthe durationfromEDarrivaltocompletionofthe firstECG,
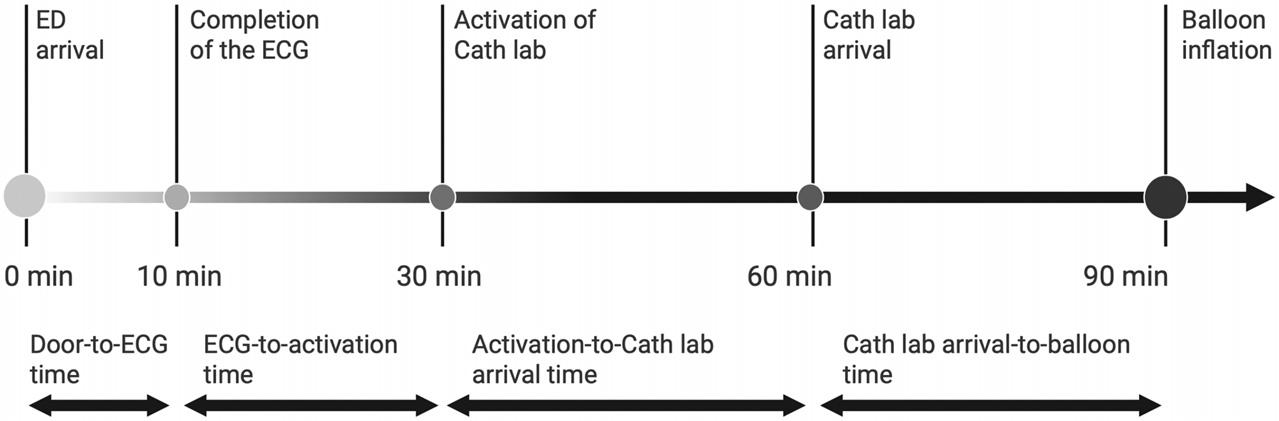
Figure1. Timesegmentswithinthedoor-to-balloontime. Cathlab,catheterizationlaboratory; ECG,electrocardiogram; ED,emergencydepartment.
ECG-to-activationtimeasthedurationfromECG completiontoactivationofthecathlab,activation-to-cath lab-arrivaltimeasthedurationfromcathlabactivationto thepatient’sarrivalinthecathlab,andcathlab-arrival-toballoontimeasthedurationfromthepatient’sarrivalinthe cathlabtoballooninflation(Figure1).1,3,7 Delaysindifferent timeintervalswithintheDTBweredefinedasfollows:doorto-ECGtime >10min;ECG-to-activationtime >20min; activation-to-cathlabarrivaltime >30min;cathlabarrivalto-balloontime >30min;andDTBtime >90min.1,5
Theprimaryoutcomeassessedinthisstudywasall-cause mortalitywithinoneyearafteradmissionforSTEMI.All STEMIpatientswerefollowedupforatleastoneyearfrom thedateofadmissiontoassessmortality.Mortalitytiming wasaccuratelydeterminedbycross-referencingstudy patientswiththeNationalCauseofDeathRegistryfrom theTaiwanNationalHealthInsurancedatabase,which documentsthetimeandcauseofdeathforalldeceased individualsinTaiwan.19 Thelastfollow-updatewas December31,2022.SinceTaiwanNationalHealth Insuranceisacompulsory,single-payerhealthcaresystem coveringnearly99.8%ofthepopulation,theoreticallyall enrolledpatientswhopassawayarerecordedintheNational CauseofDeathRegistry.19 Thus,unlessapatientwithdraws fromtheinsurancesystems,allincludedpatientscanbe trackedeitheruntilthelastfollow-updateortheirdateof death.Patientswithout-of-hospitalcardiacarrest(OHCA) andthosewithmissingdatawereexcludedfromtheanalysis.
Thiswasahealthrecordreviewstudyinwhichwe followedthemethodologicalcriteriaforhealthrecordreview studiesproposedbyWosteretal.20 AfteridentifyingSTEMI patientsfromthehospital-basedSTEMIregistry,weuseda pre-designedformwithdefinedvariablestorecordpatients’ data.Fourtrainedemergencyresidentsandnursesreviewed theelectronichealthrecordsandinputdataintotheform. Regularmeetingswereheldtoensurethecorrectnessofdata collection,andasupervisorrandomlyauditedtheaccuracy ofthedatacollected.Thedataabstractorswerenotawareof thestudy’shypothesisandwereinformedonlythattheywere
helpingtoestablishaSTEMIdatabaseforresearchpurposes. ThestudyprotocolreceivedapprovalfromtheInstitutional ReviewBoardofDitmansonMedicalFoundationChia-Yi ChristianHospital(approvalnumber:CYCH-IRB 2024010),withanexemptionfrominformedconsentowing totheretrospectivenatureofthestudy.
WecompareddatafromtheincludedSTEMIpatients betweentwogroups:thosewithandwithoutone-year mortality.Continuousvariableswereexpressedasmean ± standarddeviationormedian(interquartilerange)and assessedbetweengroupsusingtheStudent t -testorMannWhitneyUtest,respectively,basedondatadistribution.We presentcategoricalvariablesasnumber(percentage)and assessedthemusingchi-squaretest.Themortalityratewas expressedaseventsper100person-years.Toidentifythe targettimesegmentwithintheDTBmostassociatedwith one-yearmortality,weemployedKaplan-Meiersurvival analysis.Survivalcurveswereplottedforpatientsstratified intodelayvsnon-delaygroupsacrossdifferenttimeintervals withintheDTB,withdifferencesassessedusinglog-rank tests.WeusedunivariableCoxproportionalhazardsmodels toassesstheassociationbetweeneachvariableandone-year mortality.TimeintervalswithintheDTBweretreatedas eitherdichotomized(delayornon-delaygroups)or continuousvariables.Wefurtheranalyzedvariables demonstratinga P -valueoflessthan0.1intheunivariable analysisinamultivariableCoxmodelemployingforward variableselection(setat P < 0.05foradditiontothemodel) todeterminetheirindependenteffectontheriskofone-year mortality.TheSchoenfeldtestwassubsequentlyusedto verifytheassumptionofproportionalhazards.
Weconductedadditionalsensitivityanalysestoexamine theassociationbetweenvarioustimeintervalswithinthe DTBandshort-termmortalityoutcomes,suchasin-hospital and30-daymortality,aswellasone-yearmortality.These analysesusedmultivariablelogisticregressionwithaforward stepwiseWaldtest.Thevariablesincludedintheseanalyses
werethesameasthoseinthemultivariableCoxanalysis.The timeintervalswithintheDTBwereincorporatedintothe modelsseparatelyandweretreatedaseitherdichotomizedor continuousvariables.Furthermore,consideringtheextended recruitmentperiodofthisstudy(nineyears),weconducted anothersensitivityanalysistocontrolforpotential confoundingfactorsacrossdifferenttimeperiods.In additiontoadjustingforassociatedvariables,weperformed amultivariableCoxmodelincludingtheyearofpatient recruitmentasacovariate.Finally,asensitivityanalysis usingamultivariableCoxmodelwasconductedtoevaluate therelationshipbetweenDTBtimeintervalsand cardiovascular-relatedone-yearmortality.Weperformed statisticalanalysesusingStata17.0(StataCorp, CollegeStation,TX),withstatisticalsignificancesetat two-tailed <0.05.
Duringthestudyperiod,738patientswithSTEMIwere identified.AfterexcludingthosewithOHCAormissing data,732patientswere finallyincluded.Amongthem,59 patientsdiedwithinoneyearafterSTEMI(Figure2),with37 deathsattributedtocardiovascular-relatedcauses.The overallmortalityratewas9.05per100person-years (95%confidenceinterval[CI],7.02–11.69).
Table1 presentsthecharacteristicsofpatientswithand withoutmortalitywithinoneyearafterSTEMI.Patients whodiedwithinoneyearafterSTEMIwereolder(73.2 ± 13.7vs61.0 ± 12.6years, P < .001)andhadahigher proportionoffemales(35.59%vs14.56%, P < .001).They weremorelikelytobetransportedtothehospitalby ambulance(40.68%vs24.37%, P = 0.006)andhadhigher
triageacuity(triagelevel1:32.2%vs.8.92%, P < .001)and initialtroponin-Ilevels(1.72[0.12–8.52]vs0.13[0.02–2.40) nanogramspermilliliter, P < .001].Theywerealsomore likelytohavediabetesmellitus(54.24%vs38.04%, P = 0.02), hypertension(76.27%vs63.30%, P = 0.05),cerebrovascular accident(20.34%vs.6.39%, P < .001),andchronickidney disease(20.34%vs6.69%, P < .001),whilebeinglesslikelyto havehyperlipidemia(27.12%vs63.30%, P < .001).
Additionally,theyhadlongerhospitalizationdurations (6[3–14]vs5[4–6]days, P = 0.02)andlongerdoor-to-ECG (7[5–11]vs4[3–6]min, P < .001], cathlabarrival-to-balloon (25[17–40]vs22[16–28]min, P = 0.02),andDTBtimes (74[56–88]vs64[52–75]min, P < .001].Moreover,ahigher proportionofpatientshadDTBtimelongerthan90min (22.03%vs8.82%, P < .001).
Figure3 showstheKaplan-Meiercurvesformortality afteradmissionforSTEMI.Weanalyzedthemortality probabilitybetweentwogroupsbasedontheDTBtime (Figure3A).Thecumulativemortalityratewassignificantly higherinthedelayedDTBgroup(DTB > 90min)compared tothenon-delayedgroup(DTB ≤ 90min)duringtheoneyearfollow-upperiod(long-ranktest, P < .001).Next,we separatelyanalyzedforthedifferenttimesegmentswithinthe DTB.Patientswithdelayeddoor-to-ECG(Figure3B) andcathlabarrival-to-balloontimes(Figure3E)hada highermortalityriskthantheirnon-delayedcounterparts (P < .001andP = 0.007,respectively).However,no significantdifferencewasobservedbetweenpatientswithand withoutdelaysinECG-to-cathlabactivation(Figure3C) andactivation-to-cathlabarrival(Figure3D).
IntheunivariableCoxanalyses(Table2),anincreasein age,femalesex,ambulance-transportedpatients,higher
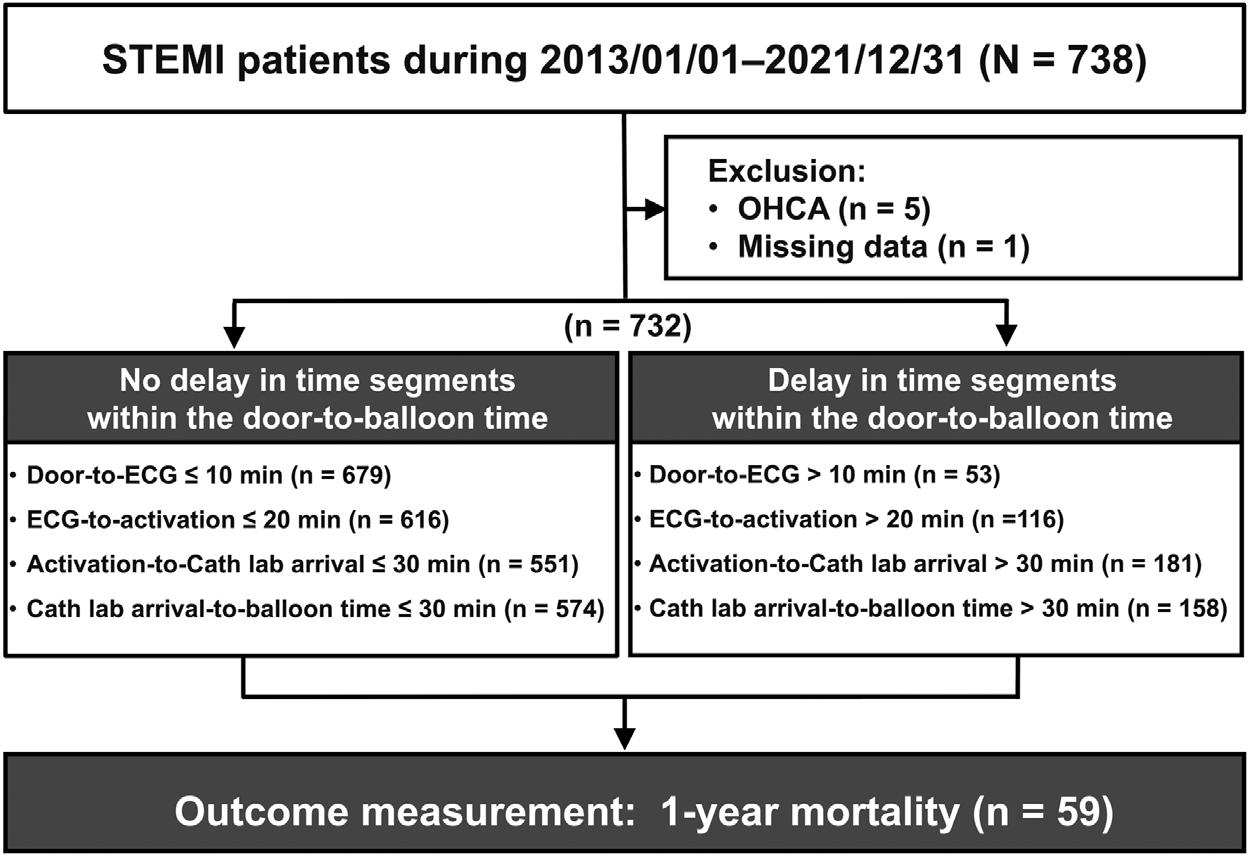
Table1. Characteristicsofpatientswithandwithoutone-yearmortalityafteradmissionforSTEMI*.
Age(year)
Characteristics1-yearsurvival(N = 673)1-yearmortality(N = 59) P-value
± 12.6
Femalesex98(14.56)21(35.59) <.001
Patientarrivaltime
Dayshift294(43.69)33(55.93)0.19
Eveningshift251(37.30)17(28.81)
Nightshift128(19.02)9(15.25)
Weekendvisit197(29.27)18(30.51)0.84
DuringCOVID-19pandemic(2020–2021)143(21.25)8(13.56)0.16
Ambulance-transportedpatient164(24.37)24(40.68)0.006
Triagelevel
160(8.92)19(32.20) <.001
2553(82.17)38(64.41)
360(8.92)2(3.39)
Laboratorytest
Medicalhistory
Diabetesmellitus256(38.04)32(54.24)0.02
Hypertension426(63.30)45(76.27)0.05
Hyperlipidemia426(63.30)16(27.12) <.001
Cerebrovascularaccident43(6.39)12(20.34) <.001
Chronickidneydisease45(6.69)12(20.34) <.001
Coronaryarterydisease92(13.67)9(15.25)0.74
COPD18(2.68)4(6.78)0.08 PAOD8(1.19)1(1.70)0.53
Smoking410(60.92)29(49.15)0.08
ECGreport
AnteriorSTEMI305(45.32)31(52.54)0.29
InferiorSTEMI340(50.67)25(42.37)0.22
LateralSTEMI23(3.43)2(3.39)1.00
PosteriorSTEMI12(1.79)0(0.00)0.61
Numbersofvesseldisease2(1–3)2(2–3)0.06
Findingsofcoronaryangiography
1vesseldisease206(30.66)14(23.73)0.23
2vesselsdisease244(36.31)18(30.51)
3vesselsdisease220(32.74)27(45.76)
Durationofhospitalization(day)5(4–6)6(3–14)0.02
Timeinterval
Door-to-ECG(min)4(3–6)7(5–11) <.001
ECG-to-activation(min)10(6–15)11(8–19)0.13
Activation-to-cathlabarrival(min)23(16–30)22(16–30)0.94
Cathlabarrival-to-balloon(min)22(16–28)25(17–40)0.02
(Continued onnextpage)
Table1. Continued.
–75)
Dataarepresentedasn(%),mean ± SD, ormedian(interquartilerange).
BMI,bodymassindex; COPD,chronicobstructivepulmonarydisease; ECG,electrocardiography; ng/mL,nanogramspermilliliter; PAOD, peripheralarterialocclusiondisease;*STEMI,ST-segmentelevationmyocardialinfarction.
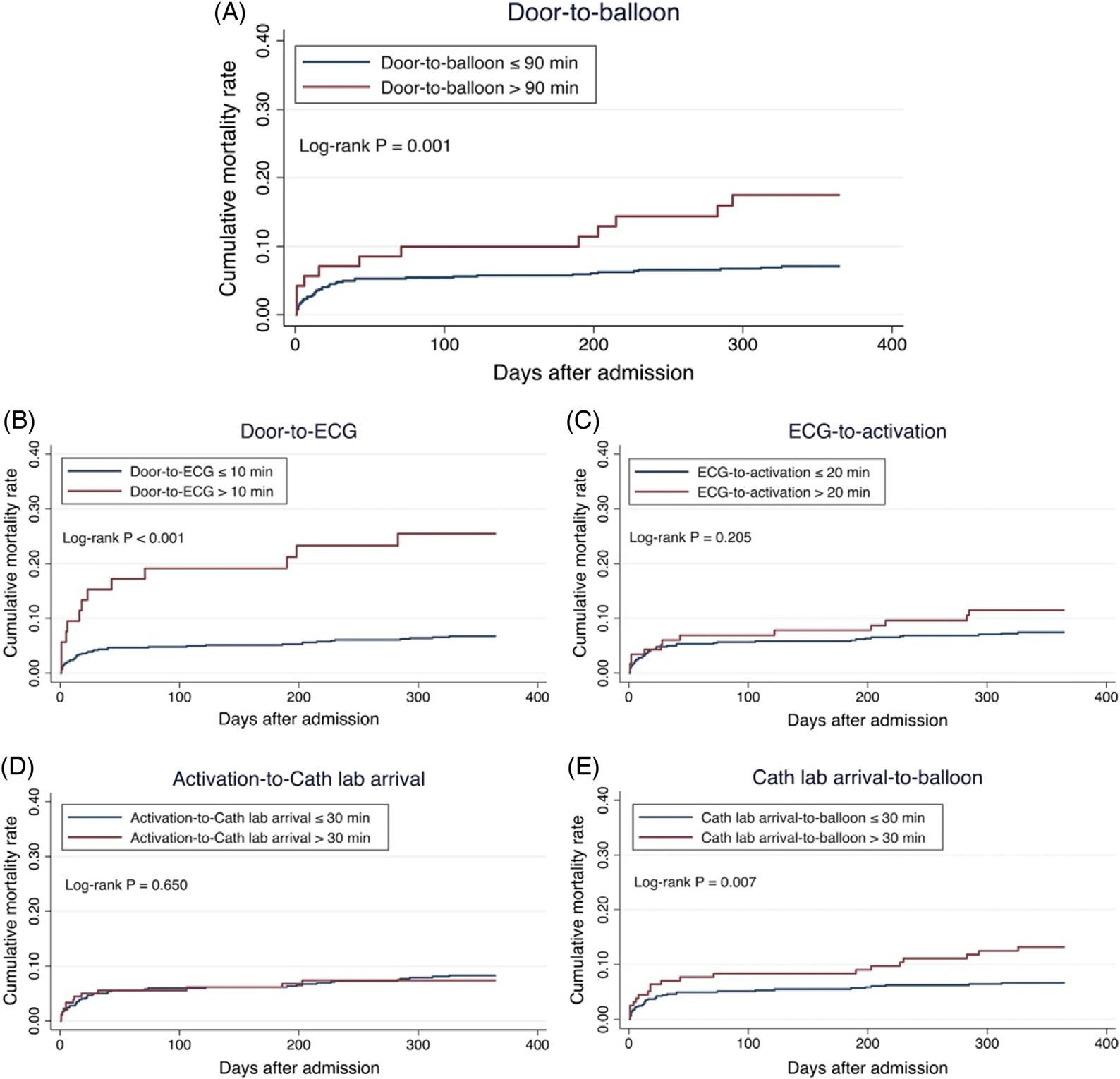
Figure3. Kaplan-Meiercurvesillustratingcumulativemortalityrateswithinaone-yearfollow-upperiodafterSTEMI*admissionfordelayand non-delaygroupsindoor-to-balloon(A),door-to-ECG(B),ECG-to-activation(C),activation-to-cathlabarrival(D),andcathlabarrival-toballoon(E)times.
*STEMI,ST-elevationmyocardialinfarction.
troponin-Ilevels,amedicalhistoryofdiabetes,hypertension, cerebrovascularaccident,orchronickidneydisease,and eachadditionaldayofhospitalizationwereassociatedwitha higherriskofone-yearmortality.Additionally,patientswith alowertriagelevelandhyperlipidemiahadalowerriskof one-yearmortality.Moreover,door-to-ECGandcathlab arrival-to-balloontimesweresignificantlyassociatedwitha higherriskofonw-yearmortalityafterSTEMI.
Table3 presentstheresultsofmultivariableCoxanalyses. Inmodel1,weanalyzedthetimeintervalsasdichotomized variables(delayvsnon-delaygroups).Afteradjustingfor associatedfactors,adelayeddoor-to-ECGtime(>10min) remainedanindependentpredictorofone-yearmortality, withanadjustedhazardratio(HR)of2.81(95%CI 1.42–5.55).Inmodel2,thetimeintervalswereanalyzedas continuousvariables.Wefoundthateachminuteincreasein
Table2. UnivariableCoxmodelsforpredictingone-yearmortality afterSTEMI*admission.
Characteristics
Age(year) 1.08(1.05–1.10) <.001
BMI 0.94(0.88–1.01)0.11
Femalesex 2.95(1.73–5.03) <.001
Patientarrivaltime
Dayshift Reference
Eveningshift 0.63(0.35–1.13)0.12
Nightshift 0.63(0.30–1.31)0.21
Weekendvisit 1.06(0.61–1.84)0.85
DuringCOVID-19 pandemic(2020–2021)
0.63(0.30–1.33)0.23
Ambulance-transported patient 2.06(1.23–3.47)0.006
Triagelevel
1 Reference
2 0.24(0.14–0.41) <.001
3 0.11(0.03–0.48)0.003
Laboratorytest
Troponin-I(ng/mL) 1.01(1.01–1.02) <.001
Medicalhistory
Diabetesmellitus 1.85(1.11–3.08)0.02
Hypertension 1.84(1.01–3.35)0.05
Hyperlipidemia 0.23(0.13–0.40) <.001
Cerebrovascularaccident3.35(1.78–6.31) <.001
Chronickidneydisease3.13(1.66–5.91) <.001
Coronaryarterydisease1.17(0.58–2.38)0.66
COPD 2.42(0.88–6.69)0.09
PAOD 1.35(0.19–9.76)0.77
Smoking 0.63(0.38–1.05)0.07
ECGreport
AnteriorSTEMI 1.36(0.81–2.26)0.24
InferiorSTEMI 0.71(0.43–1.20)0.20
LateralSTEMI 0.98(0.24–4.00)0.97
PosteriorSTEMI 4.53E-15(0–∞)1.00
Numbersofvessel disease 1.37(0.99–1.90) 0.06
Durationofhospitalization (day) 1.03(1.02–1.05) <.001
Timeinterval
Door-to-ECG >10min4.82(2.68–8.66) <.001
ECG-to-activation > 20min 1.48(0.80–2.75)0.21
Activation-to-cathlab arrival > 30min 0.87(0.47–1.61)0.65
(Continued onnextcolumn)
Table2. Continued.
Timeinterval Door-to-ECGtime(min)1.02(1.00–1.04)0.03 ECG-to-activation time(min)
Activation-to-cathlab arrivaltime(min)
Cathlabarrival-to-balloon time(min)
–1.05) <.001
BMI, bodymassindex; COPD,chronicobstructivepulmonary disease; CI,confidenceinterval; ECG,electrocardiography; HR,hazardratio; PAOD,peripheralarterialocclusiondisease; *STEMI,ST-segmentelevationmyocardialinfarction.
door-to-ECGtime(adjustedHR,1.03;95%CI1.00–1.06) andcathlabarrival-to-balloontime(adjustedHR,1.02;95% CI1.00–1.04)wereindependentlyassociatedwithone-year mortality.Furthermore,age,triagelevel,initialtroponin-I levels,andahistoryofdiabetesmellitusandhyperlipidemia wereindependentpredictorsofone-yearmortality(Table3). TheSchoenfeldtestyielded P -valuesof0.65and0.43for models1and2,respectively,indicatingnoviolationofthe proportionalhazardsassumptionfortheincludedcovariates.
Supplementary Table1 presentsthesensitivityanalysis conductedusinglogisticregressionfortheoutcomesofinhospital,30-dayandone-yearmortality.Afteradjustingfor associatedfactors,door-to-ECGtimewasconsistently identifiedasanindependentpredictorforin-hospital,30-day, andone-yearmortality,regardlessofwhetheritwasanalyzed asdichotomizedorcontinuousvariables.Moreover,cath lab-arrival-toballoontimewasidentifiedasanindependent predictorfortheone-yearmortalityoutcomewhenitwas analyzedasacontinuousvariable.Supplementary Table2 displaysanothersensitivityanalysisthatincludedtheyearof patientrecruitmentasacovariatetoaddresspotential confoundingfactorsacrossdifferenttimeperiods.Theresults weresimilartothemainanalysis.Supplementary Table3 showstheresultsofasensitivityanalysisfocusedonone-year cardiovascular-relatedmortality,whichwereconsistentwith themain findings.
Inthisstudy,weexploredspecifictimesegmentswithinthe DTBintervalassociatedwithone-yearmortalityinpatients withSTEMI.Our findingsrevealedthattheduration fromdoortoECGcompletionisparticularlyassociated withone-yearmortality,whilecathlabarrival-to-balloon inflationmayalsoberelevant.However,theintervals fromECGcompletiontocathlabactivationandfrom
Table3. MultivariableCoxmodelsforpredictingone-yearmortalityafterSTEMI*admission.
Timeinterval
Timeinterval
>30min -
**ThevariablesincludedinthemultivariableCoxmodelwithforwardselectionanalysiswereage,sex,ambulance-transportedpatient,triage level, troponinI,diabetesmellitus,hypertension,hyperlipidemia,cerebrovascularaccident,chronickidneydisease,numbersofvessel disease,durationofhospitalization,door-to-ECGtime,andcathlabarrival-to-balloontime.Thecharacteristicspresentedinthetable representthevariablesthatwereultimatelyselectedforinclusionintheCoxmodels.
ECG,electrocardiography; HR,hazardratio; ng/mL,nanogramspermilliliter;*STEMI,ST-segmentelevationmyocardialinfarction.
activation-to-cathlabarrivalwerenotsignificantly associatedwithone-yearmortality.Additionally,age,triage acuitylevel,initialtroponin-Ilevels,andahistoryofdiabetes mellitusandhyperlipidemiawereidentifiedasindependent predictorsforone-yearmortalityinSTEMIpatients.
Weobservedthatadelayindoor-to-ECGtime(>10min) wasassociatedwitha2.81-foldincreasedriskofmortality withinoneyearcomparedtothosewithoutdelay.Each minutedelayinECGacquisitionmayincreasetheriskof mortalityby3%withinoneyearafterSTEMI(Table3).This highlightstheimportanceofearlyECGacquisitionforthe long-termprognosisofSTEMI.Duringthetreatmentcourse forpatientswithSTEMI,therapeuticinterventions, suchasearlyadministrationofdualantiplateletagents, anticoagulants,andvigilantmonitoring,areinitiatedupon STEMIdiagnosis,priortoangiographicassessment (Supplementary Figure1).Currentguidelinesrecommend earlyplateletinhibitionasafundamentalcomponentof pharmacologictreatmentintheearlystagesofSTEMI,with expectedbenefitsincludingenhancedplateletinhibitionafter primaryPCIandalowerincidenceofstentthrombosis.3,21,22 Arecentsystematicreviewandmeta-analysisadditionally alsoshowstheimportanceofusingupstreamanticoagulation beforePCI,whichisassociatedwithalower30-daymortality risk,alowerincidenceofin-hospitalcardiogenicshock,and improvedreperfusionoftheinfarct-relatedartery.23 Early ECGcompletionenablespromptdiagnosisofSTEMIand timelyinitiationofantiplateletagents,anticoagulants,and
intensivecare,whicharecrucialforachievingcoronary arteryreperfusion,preventingthrombosisfollowingprimary PCI,andminimizingmyocardialdamagepostinfarction.22,23 Consequently,asobservedinthisstudy, notonlyisshort-termmortalityimproved,butlong-term mortalityaswell.Our findingsalsosupporttheimportance ofprehospitalECG,whichhasbeenshowntoreduceDTB timeandimproveshort-termmortality.24,25 Additionally, whencombinedwithprehospitaldualantiplatelettherapy, thesemeasuresmayfurtherimprovelong-termoutcomesin STEMIpatients.26
Ourstudyalsorevealedanassociationbetweencathlab arrival-to-balloontimeandone-yearmortalityfollowing STEMI,indicatingthateachminuteofdelayinthisinterval mayincreasethemortalityriskby2%withinthe firstyear (adjustedHR1.02)(Table3).Althoughtheeffectsizewas small,this findingmaybereasonable.Inadditionto pharmacologictreatmentintheinitialstagesofSTEMI, promptrestorationofblood flowintheoccludedcoronary vesselsiscritical.WhileeffortstoreduceDTBtimehasbeen explored,27 researchfocusedondecreasingthedurationfrom cathlabarrival-to-ballooninflationremainslimited.Itis essentialtoconsidervariousfactorsthatmayinfluencecath labarrival-to-balloontime,includingpatient’svascular condition,theexperienceofthecardiologist,equipment preparationandreadiness,andcathlabstaffavailability.28,29 Ongoingresearchondevelopingnewtechniquesandguiding catheterstoreducethetimefromneedleinsertiontoballoon
inflationormortalityisimperative.30 Healthcarefacilities mustassessandoptimizethesefactorstoensuretimelyand effectivedeliveryofcaretopatientsundergoingPCI proceduresforSTEMI.
ApartfromtheDTBtimeintervals,age,triageacuity level,initialtroponin-Ilevels,andahistoryofdiabetes mellitusandhyperlipidemiawereidentifiedasindependent predictorsforone-yearmortalityinSTEMIpatientsinour study.Theadverseimpactofageanddiabetesmellituson short-andlong-termmortalityinSTEMIpatientshasbeen extensivelydocumented.11 Notably,weobservedan associationbetweenahistoryofhyperlipidemiaandreduced riskofone-yearmortality(adjustedHR,0.31, P < .001in bothmodels)(Table3).Similar findingswerealsoreportedin previousresearch.31
Onepossibleexplanationforthisishowamedicalhistory ofhyperlipidemiawasdefined,basedonpatients’ prior medicalrecordsandwhethertheyreceivedlipid-lowering therapy,primarilystatins.31 IntheTaiwanNational Insuranceprogram,theprescriptionofstatinsrequiresa confirmeddiagnosisofhyperlipidemia.Therefore,we speculatethatthereducedmortalityriskobservedinpatients withahistoryofhyperlipidemiamaybebecausethese STEMIpatientswerereceivinglipid-loweringtherapy. PreviousstudieshavefoundthatpatientswithSTEMIwho weretriagedashavingloweracuitylevelswhentheyarrived atanEDexperienceddelaysinECGacquisitionand reperfusiontherapy.17,32 However,afteradjustingforDTB timeintervals,ourstudyfoundthatlowertriageacuitywas actuallyassociatedwithalowerriskofone-yearmortality. Thismaybebecausepatientwithhighertriageacuity(triage level1)oftenpresentwithunstablevitalsigns,whichare associatedwithahigherriskofmortality.
Wanamakeretalinvestigatedtherelationshipbetween troponinlevelsatpresentationandin-hospitalmortalityin STEMIpatientsundergoingPCI.Theydemonstratedthat in-hospitalmortalityincreaseswithelevatedtroponinlevels atpresentation,irrespectiveofbaselineclinicalrisk.18 Our findingsalsorevealedthatinitialtroponinlevelisan independentpredictorforone-yearmortalityinSTEMI patients.Therefore,troponinlevelsintheearlyphaseof STEMImayoffervaluablelong-termprognostic informationinpatientsundergoingprimaryPCI.
Ourstudyhasseverallimitations.Firstly,itisasinglecenterstudywithasmallsamplesize,potentiallylimitingits generalizabilitytootherpopulations.Secondly,being retrospectiveinnature,thereisapossibilityofunmeasured confoundersandselectionbiasthatcouldhaveaffectedthe results.Thirdly,thestudycoversanine-yearperiod,during whichchangesinhospitalstaff,policies,andguidelinesmay haveintroducedconfoundingfactors.However,our sensitivityanalysis,whichcontrolledfortheyearsofpatient
recruitment,yieldedsimilarresults.Nevertheless,further multicenter,prospectivestudiesarewarrantedtovalidate our findings.
WithintheDTBinterval,thetimefromdoor-to-ECG completioniscrucialforone-yearsurvivalafterSTEMI, whilecathlabarrival-to-ballooninflationmayalsobe relevant.Strategiesforimprovinglong-termoutcomesfor STEMIpatientsshouldprioritizereducingthetimefrom door-to-ECGacquisition.Thiscouldbeattributedtothe facilitationofearlyinitiationofpharmacologictreatments, suchasdualantiplateletandanticoagulationtherapy,inthe initialstagesofSTEMIprecedingPCI.
AddressforCorrespondence:Ming-JenTsai,MD,PhD,Ditmanson MedicalFoundationChia-YiChristianHospital,Departmentof EmergencyMedicine,No.539,ZhongxiaoRd.,EastDistrict,Chiayi City600,Taiwan.E-mail: tshi33@gmail.com; 07367@cych.org.tw
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Tsaietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.O’GaraPT,KushnerFG,AscheimDD,etal.2013ACCF/AHAguideline forthemanagementofST-elevationmyocardialinfarction. Circulation. 2013;127(4):e362–425.
2.LevineGN,BatesER,BlankenshipJC,etal.2015ACC/AHA/SCAI focusedupdateonprimarypercutaneouscoronaryinterventionfor patientswithST-elevationmyocardialinfarction:anupdateofthe2011 ACCF/AHA/SCAIguidelineforpercutaneouscoronaryinterventionand the2013ACCF/AHAguidelineforthemanagementofST-elevation myocardialinfarction. JAmCollCardiol. 2016;67(10):1235–50.
3.IbanezB,JamesS,AgewallS,etal.2017ESCguidelinesforthe managementofacutemyocardialinfarctioninpatientspresentingwith ST-segmentelevation:thetaskforceforthemanagementofacute myocardialinfarctioninpatientspresentingwithST-segmentelevation oftheEuropeanSocietyofCardiology(ESC). EurHeartJ. 2018;39(2):119–77.
4.TsukuiT,SakakuraK,TaniguchiY,etal.Determinantsofshortandlong door-to-balloontimeincurrentprimarypercutaneouscoronary interventions. HeartVessels. 2018;33(5):498–506.
5.MeneesDS,PetersonED,WangY,etal.Door-to-balloontimeand mortalityamongpatientsundergoingprimaryPCI. NEnglJMed. 2013;369(10):901–9.
6.FooCY,BonsuKO,NallamothuBK,etal.Coronaryinterventiondoor-toballoontimeandoutcomesinST-elevationmyocardialinfarction: ameta-analysis. Heart. 2018;104(16):1362–9.
7.BradleyEH,HerrinJ,WangY,etal.Strategiesforreducingthe door-to-balloontimeinacutemyocardialinfarction. NEnglJMed. 2006;355(22):2308–20.
8.SuH-Y,TsaiJ-L,HsuY-C,etal.Amodifiedcardiactriagestrategy reducesdoortoECGtimeinpatientswithSTelevationmyocardial infarction. SciRep. 2021;11(1):6358.
9.NoguchiM,AkoJ,MorimotoT,etal.Modifiablefactorsassociatedwith prolongeddoortoballoontimeinpatientswithST-segmentelevation myocardialinfarctionundergoingprimarypercutaneouscoronary intervention. HeartVessels. 2018;33(10):1139–48.
10.SimWJ,AngAS,TanMC,etal.Causesofdelayindoor-to-balloontime insouth-eastAsianpatientsundergoingprimarypercutaneouscoronary intervention. PLoSOne. 2017;12(9):e0185186.
11.YanF,ZhangY,PanY,etal.Prevalenceandassociatedfactorsof mortalityafterpercutaneouscoronaryinterventionforadultpatientswith ST-elevationmyocardialinfarction:asystematicreviewandmetaanalysis. JResMedSci. 2023;28:17.
12.HsiaoYT,HungJF,ZhangSQ,etal.Theimpactofemergency departmentarrivaltimeondoor-to-balloontimeinpatientswith ST-segmentelevationmyocardialinfarctionreceiving primarypercutaneouscoronaryintervention. JClinMed. 2023;12(6):2392.
13.JayawardanaS,Salas-VegaS,CornehlF,etal.Therelationship betweenoff-hoursadmissionsforprimarypercutaneouscoronary intervention,door-to-balloontimeandmortalityforpatientswith ST-elevationmyocardialinfarctioninEngland:aregistry-based prospectivenationalcohortstudy. BMJQualSaf. 2020;29(7):541–9.
14.ChewNWS,OwZGW,TeoVXY,etal.TheglobaleffectoftheCOVID-19 pandemiconSTEMIcare:asystematicreviewandmeta-analysis. CanJCardiol. 2021;37(9):1450–9.
15.DeLucaG,AlgowharyM,UguzB,etal.COVID-19pandemic, mechanicalreperfusionand30-daymortalityinSTelevationmyocardial infarction. Heart. 2022;108(6):458.
16.BansalE,DhawanR,WagmanB,etal.Importanceofhospitalentry: walk-inSTEMIandprimarypercutaneouscoronaryintervention. WestJEmergMed. 2014;15(1):81–7.
17.AtzemaCL,AustinPC,TuJV,etal.Emergencydepartmenttriageof acutemyocardialinfarctionpatientsandtheeffectonoutcomes. AnnEmergMed. 2009;53(6):736–45.
18.WanamakerBL,SethMM,SukulD,etal.Relationshipbetweentroponin onpresentationandin-hospitalmortalityinpatientswithST-segmentelevationmyocardialinfarctionundergoingprimarypercutaneous coronaryintervention. JAmHeartAssoc. 2019;8(19):e013551.
19.HsiehCY,SuCC,ShaoSC,etal.Taiwan’snationalhealthinsurance researchdatabase:pastandfuture. ClinEpidemiol. 2019;11:349–58.
20.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. AnnEmergMed. 2005;45(4):448–51.
21.LevineGN,BatesER,BittlJA,etal.2016ACC/AHAguidelinefocused updateondurationofdualantiplatelettherapyinpatientswithcoronary artery disease:areportoftheAmericanCollegeofCardiology/American HeartAssociationTaskForceonClinicalPracticeGuidelines:anupdate ofthe2011ACCF/AHA/SCAIguidelineforpercutaneouscoronary intervention,2011ACCF/AHAguidelineforcoronaryarterybypassgraft surgery,2012ACC/AHA/ACP/AATS/PCNA/SCAI/STSguidelineforthe diagnosisandmanagementofpatientswithstableischemicheart disease,2013ACCF/AHAguidelineforthemanagementof ST-elevationmyocardialinfarction,2014AHA/ACCguidelineforthe managementofpatientswithnon-ST-elevationacutecoronary syndromes,and2014ACC/AHAguidelineonperioperative cardiovascularevaluationandmanagementofpatientsundergoing noncardiacsurgery. Circulation. 2016;134(10):e123–55.
22.FabrisE,KorjianS,CollerBS,etal.Pre-hospitalantiplatelettherapyfor STEMIpatientsundergoingprimarypercutaneouscoronary intervention:whatweknowandwhatliesahead. ThrombHaemost. 2021;121(12):1562–73.
23.AlbuquerqueF,GomesDA,FerreiraJ,etal.Upstreamanticoagulationin patientswithST-segmentelevationmyocardialinfarction:asystematic reviewandmeta-analysis. ClinResCardiol. 2023;112(9):1322–30.
24.NakashimaT,HashibaK,KikuchiM,etal.Impactofprehospital12-lead electrocardiographyanddestinationhospitalnotificationonmortality inpatientswithchestpain-asystematicreview. CircRep. 2022;4(5):187–93.
25.KohashiK,NakanoM,IsshikiT,etal.Clinicalefficacyofpre-hospital electrocardiogramtransmissioninpatientsundergoingprimary percutaneouscoronaryinterventionforST-segmentelevation myocardialinfarction. IntHeartJ. 2023;64(4):535–42.
26.DanchinN,PuymiratE,CaylaG,etal.One-yearsurvivalafterSTsegment-elevationmyocardialinfarctioninrelationwithprehospital administrationofdualantiplatelettherapy. CircCardiovascInterv. 2018;11(9):e007241.
27.DeLucaG,SuryapranataH,OttervangerJP,etal.Timedelaytotreatment andmortalityinprimaryangioplastyforacutemyocardialinfarction:every minuteofdelaycounts. Circulation. 2004;109(10):1223–5.
28.MagidDJ,CalongeBN,RumsfeldJS,etal.Relationbetweenhospital primaryangioplastyvolumeandmortalityforpatientswithacuteMI treatedwithprimaryangioplastyvsthrombolytictherapy. JAMA. 2000;284(24):3131–8.
29.McGrathPD,WennbergDE,DickensJDJr,etal.Relationbetween operatorandhospitalvolumeandoutcomesfollowingpercutaneous coronaryinterventionsintheeraofthecoronarystent. JAMA. 2000;284(24):3139–44.
30.ToriiS,FujiiT,MurakamiT,etal.Impactofasingleuniversalguiding catheterondoor-to-balloontimeinprimarytransradialcoronary interventionforSTsegmentelevationmyocardialinfarction. Cardiovasc IntervTher. 2017;32(2):114–9.
31.YousufuddinM,ZhuY,AlWardR,etal.Associationofhyperlipidaemia with5-yearsurvivalafterhospitalisationforacutemyocardial infarction:apropensityscorematchedanalysis. OpenHeart. 2020;7(1):e001163.
32.TungsubutraWandNgoenjanD.Door-to-balloontimeandfactors associatedwithdelayeddoor-to-balloontimeinST-segmentelevation myocardialinfarctionatThailand’slargesttertiaryreferralcentre. JEvalClinPract. 2019;25(3):434–40.
SudhiManu,MD*
GopinathanVivek,DNB†
AsanaruKunjuSanjan,MD,DNB†
A.Ajay,MD‡
S.Nisarg,MD*
MymbillyBalakrishnanJayaraj,MD*
T.R.Aishwarya,MD§
MohammadKhalid,MD*
S.Chetana,MD*
SectionEditor: QuincyK.Tran,MD,PhD
*DepartmentofEmergencyMedicine,KasturbaMedicalCollege,Manipal, ManipalAcademyofHigherEducation,Manipal,Karnataka,India-576104 † DepartmentofEmergencyMedicine,KasturbaMedicalCollege,Mangalore, ManipalAcademyofHigherEducation,Karnataka,Manipal,576104,India ‡ DepartmentofTraumaandEmergency,AllIndiaInstituteofMedical Sciences,Nagpur,India
§ DepartmentofHospitalAdministration,KasturbaMedicalCollege,Manipal, ManipalAcademyofHigherEducation,Manipal,Karnataka,India-576104
Submissionhistory:SubmittedFebruary4,2024;RevisionreceivedNovember6,2024;AcceptedNovember8,2024
ElectronicallypublishedFebruary25,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.19394
Introduction: Assessingcardiacfunctioniscrucialformanagingacutedyspnea.Inthisstudyweaimed toevaluatedisplacementoftheaorticroot(DAR)asamethodforcalculatingejectionfraction(EF)in patientswithundifferentiateddyspneapresentingtotheemergencydepartment(ED).Theprimary objectivewastocompareEFvaluesobtainedthroughDARwiththemodifiedSimpsonmethod,whichis consideredthecriterionreference,withinanIndianacademicED.
Methods: Weconductedaprospective,cross-sectionalstudyspanningtwoyears(December 2019–December2021).Thestudyenrolled110consecutiveEDpatients ≥18yearsofage,presenting withundifferentiateddyspneaandnormalsinusrhythm.Ultrasound-trainedinvestigatorsmeasuredDAR usingM-modeultrasonography.Experiencedechocardiographers,blindedtoDAR,determinedEF usingthemodifiedSimpsonmethod.StatisticalanalysesincludedtheShapiro-Wilktest,McNemartest, andthereceiveroperatingcharacteristiccurve.
Results: ThemeanDARmeasurementwas0.781centimeters,withanaveragecalculatedEFof54.4%. TheEFcalculatedusingDARdidnotdiffersignificantlyfromEFcalculatedusingthemodifiedSimpson method.ComparativeanalysisrevealedDAR’ssuperiorsensitivity(86.21%)comparedtomitralannular planesystolicexcursion(48.28%)andend-pointseptalseparation(45.45%).TheDARmethodexhibited highaccuracy(areaunderthecurve = 0.958)withacut-offvalue0.706(sensitivity88.7%, specificity93.1%).
Conclusion: Evaluatingdisplacementoftheaorticroottocalculateejectionfractioninundifferentiated dyspneademonstratedhighaccuracy,sensitivity,andagreementwiththemodifiedSimpsonmethod, whichisconsideredthecriterionreference.Itssimplicityandnon-invasivenessmakesitavaluableinitial screeningtoolinemergencysettings,withthepotentialtoreshapecardiacassessmentapproachesand optimizepatientcarepathwaysintheED.[WestJEmergMed.2025;26(2)191–199.]
Background
Assessingcardiacfunction,particularlyejectionfraction (EF),iscrucialformanagingacutedyspnea.1–3 EchocardiographyisthecurrentstandardforcalculatingEF, butdisplacementoftheaorticroot(DAR)hasemerged asapotentialtoolforEFcalculationinpatientswith undifferentiateddyspnea.2,3 TheDARmethodquantifies alterationsinleftventricular(LV)volumethroughoutthe cardiaccycle,providingasurrogatemeasureforestimating EF.3 End-pointseptalseparation(EPSS)measurementisa relativelystraightforwardskillthatanemergencyphysician canacquirewithminimalexperience,evenwhenconfronted withregionalwallmotionabnormalities.4,5 However, measurementofLVend-systolicandend-diastolicdiameters using2DorM-modeechocardiographycanposechallenges totheemergencyphysicianinclinicalpractice.Tracingthe endocardialborderoftheheartinanechocardiogramduring diastoleandsystoleisoftendifficultandtime-consuming, especiallywherethewallispoorlydefined.6–10 Thisapproach providesclinicianswithmultipleoptionsforassessingLV systolicfunction,cateringtovaryinglevelsofexpertiseand clinicalsettings.
Mitralannularplanesystolicexcursion(MAPSE) assessesverticalmitralvalvemotionusingM-mode echocardiography,measuringannulardisplacementtowards theapex.Unlikeothermethods,MAPSEdoesn’trequire optimalendocardialdefinitionorclearLVapex visualization,enablingbroadapplicability.Diminished systolicmitralvalveexcursion,reflectedinMAPSE measurements,reliablyindicatesLVsystolicdysfunction. TheMAPSEdemonstratesstrongcorrelations,particularly innon-criticallyillpatients,offeringeffectiveLVfunction assessmenteveninchallengingimagingscenarios.11–15
EmergencyphysiciansareaccurateatvisualLVEF estimationwithoutquantitativemeasurements,butobjective measurescanbenefitearlylearnersandfacilitate communication.6 However,EFcalculationusingtheDAR methodhasnotbeendoneinanIndianpopulationintheED setting.Thishighlightstheneedforfurtherstudiesto determineDAR’sreliabilityandclinicalapplicabilityinthe contextofanIndiansetting.
GiventhecurrentlimitedresearchontheutilityofDARin IndianacademicEDsettings,withthisinvestigationwe aimedto fillthegapbyassessingDAR’sreliabilityand clinicalapplicability.Thestudyspecificallyfocuseson patientswithundifferentiateddyspnea,apopulationwhere EFestimationiscrucialforappropriatemanagement.
OurprimaryobjectivewastocalculatetheEFusingDAR andthencompareitwithEFmeasurementsobtained
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Whilethemodi fi edSimpsonmethodisthe criterionreferencetocalculateejection fraction,simplerandmorerapidtoolsare crucialforassessingleftventricular(LV) functioninemergencies.
Whatwastheresearchquestion?
Candisplacementoftheaorticroot(DAR) accuratelyestimateLVejectionfractionin theED?
Whatwasthemajor findingofthestudy?
TheDARcutoffof0.706centimetersshowed highaccuracy(AUC0.958,P < 0.001),with 88.7%sensitivityand93.1%speci fi city.
Howdoesthisimprovepopulationhealth?
TheDARmethodoffersarapid,non-invasive EFscreeningtool,enhancingtimelydiagnosis andimprovingcareforpatientswith LVdysfunction.
throughthemodifiedSimpsonmethod,definedasthe criterionreferencebytheAmericanSocietyof Echocardiography(ASE).9,16 Thesecondaryobjectivewas toidentifythecut-offforDAR,whichcouldpredictLV dysfunctionbasedonEFcalculation.Additionally,we soughttocomparetheEFcalculatedfromDARwiththose obtainedthroughEPSSandMAPSE.ByevaluatingDARin comparisontotheestablishedmethods,weaimedtoprovide insightsintoitspotentialasareliabletoolforEFestimation intheIndiansetting.
Thisprospective,cross-sectionalstudywasconducted acrossaspanoftwoyears,fromDecember2019–December 2021,withintheEDofateachinghospitalinIndia.The hospitalprovidesabroadspectrumofspecialties,andits adultEDhasapproximately37,200visitsannually.We obtainedinitialinstitutionalresearchboard/institutional ethicscommitteeapproval,withtheregistrationnumber ECR/146/Inst/KA/2013/RR-19,IEC:1057/2019,dated May8,2020,andapprovalforstudymodificationson September22,2021.Additionally,thestudyisregisteredwith theClinicalTrialsRegistry–IndiaunderthenumberCTRI/ 2020/10/028704,datedOctober28,2020.Weadheredto ethicalstandardsbyobtaininginformedconsentand
ensuringthevoluntaryparticipationandcompliance ofallsubjectsinvolvedinthestudy.WeassessedtheEF of110patientswithundifferentiateddyspneausing differentmethods.
Weenrolledpatients ≥18yearsofage,presentingwith undifferentiateddyspneaandnormalsinusrhythmbasedon aconveniencesampling.Thefollowingwereexcluded: patientsintubatedoutsideofahospital;pregnantwomen; individualswithelevatedcardiacbiomarkersatpresentation; thosewithatrial fibrillation,knownvalvularpathologyor surgery,primaryormetastaticcarcinomainthethorax; patientsforwhomthetimebetweenechocardiographyto obtainEFusingDARandthemodifiedSimpsonmethod

Figure1. Theprobeispositionedintheparasternallong-axis view,withthetransducerplacedperpendiculartothechestwallat thethirdorfourthintercostalspace,justtotheleftofthesternum, andtheprobemarker(blackstar)directedtowardsthepatient’s rightshoulder.
wasmorethan30minutes;andthosewhodidnotprovide consent.Thesefactorscouldhaveinfluencedtheaccuracy andreliabilityoftheEFmeasurementsobtainedthrough differentmethods.Demographicvariables,includingage andgender,wereconsideredaspotentialconfoundingfactors inthisstudy.
Afterobtainingwritteninformedconsent,theemergency clinicianconductedthebedsideultrasonographyproctored bytheexpertinpoint-of-careultrasound(POCUS).Usinga 3.6-megahertzmicro-convextransducer,theinvestigator, trainedinPOCUSduringresidencytrainingasperthe curriculum,employedaPhilipsCX50ultrasoundmachine (KoninklijkePhilipsNV,Amsterdam,Netherlands)to computetheEFusingDAR.Initially,2Dechocardiograms oftheparasternallong-axisviewwerecapturedforDAR measurement.Thisviewwasachievedbypositioningthe footprintofthetransducerperpendiculartothechestwallat thethirdorfourthintercostalspace,justtotheleftofthe sternumwiththepointertowardstherightshoulder (Figure1).17 Optimumimagerequiredclearviewofmitral valveleafletsandaorticvalves.Subsequently,M-modewas placedjustabovetheleveloftheaorticvalveandDAR recordingsweretaken.3 ThemaximumanteriorDARfrom thehorizontalaxisatend-systolewasmeasuredusingthe leading-edgetechniqueandrecordedincentimeters(cm) (Figure2A).ThecomputationofEFwasthendone,using theformula20 + 44*DAR(cm).
FollowingtheDARmeasurement,theinvestigator calculatedtheEFusingEPSSdeterminedbyEF = 75.5 –(2.5 × EPSS),andusingMAPSEcalculatedby4.8 × MAPSE (millimeters[mm]) + 5.8formenand4.2 × MAPSE(mm) + 20forwomen.5,14,18–21 Anexperiencedechocardiographer, blindedtothestudyprocedure,evaluatedLVEFusingthe ASErecommendedModifiedSimpson’sruleforthis measurement(Figure2B).9,16

Figure2. (A)Weassessedejectionfraction(EF)atthebedsideusingM-modeultrasonography,measuringthedisplacementoftheaorticroot (DAR)intheparasternallong-axisview.TherecordedDARforthispatientwas1.06cm.WecalculatedtheEFusingtheformula(EF = 20 + 44 × 1.06),whichresultedin66.6%.(B)TheechocardiographerscalculatedEFusingthemodifiedSimpsonmethod[(EDV ESV)/EDV], where[(90.2 32.7)/90.2] × 100resultedinanEFof63.7%.
Thestudysystematicallycategorizedoutcomesintotwo groups,delineating ‘normal’ EFas50%to70%and ‘lowEF’ <50%.22 Theprimaryoutcomemeasuredsignificant differenceincalculatedEFbetweentheDARandmodified Simpsonsmethods.Thesecondaryoutcomeofthestudywas todeterminecut-offvalueofDARwithhighsensitivityand specificitythroughreceiveroperatingcharacteristic(ROC) curveanalysis.Secondaryoutcomesalsoincluded comparisonofEFcalculatedfromDARwiththatcalculated fromEPSSandMAPSE.
Withadesiredmarginoferrorof10%,alphaerrorof5%, andestimatedproportionof0.5,samplesizewascalculated tobe96.Afterconsideringthedropoutrateof15%,the final samplesizewas110.
WeusedSPSSStatistics,version26.0(IBMCorp, Armonk,NY)toanalysethedata.TheShapiro-Wilktest assessednormalityforcontinuouslydistributeddata,andwe executedgroupcomparisonsinthesubsequentsteps.An exactMcNemartestwasusedtoidentifythestatistically significantchangesinEFcalculatedusingtheDARand modifiedSimpson’smethods.WecalculatedthePearson correlationcoefficienttomeasurestrengthanddirectionof thelinearrelationshipbetweentwotests.TheROCcurve playedapivotalroleindeterminingtheoptimalcut-offvalue forthevaliditymeasureofDAR.
Atotalof135patientsunderwentinitialscreeningfor participationinthestudy.BeforethePOCUSassessment,we excluded25patientsbasedonpredefinedcriteria: fivedueto externalintubation;eightwithelevatedcardiacbiomarkers; threewithabnormalrhythm;fourwithvalvularpathology; and fivewhodeclinedtoparticipate.Followingthat,a POCUSexaminationwasconductedon110patients,with10 excludedduetopoorimagequality(Figure3).The demographicandclinicalcharacteristicsof100patientswho underwentPOCUS,includingage,heartrate,meanarterial pressure,andthemeanDARvaluesinrelationtoage, gender,andcomorbiditiesaredetailedin Table1
InthisstudyweobservedameanDARmeasurementof 0.781cm(SD0.277cm)andanaveragecalculatedEFof 54.4%(SD12.2%).ThePearsoncorrelationcoefficientwas calculatedtomeasurestrengthanddirectionofthelinear relationshipbetweentwotestsandwasfoundtobe0.81, whichsuggestsastrongpositiverelationbetweentheresults. ThestudyconductedanexactMcNemartesttoidentify statisticallysignificantvariationsinabnormalandnormal EFdistributionbetweentheEFcalculatedusingDAR/ MAPSE/EPSSandtheEFmeasuredbyan
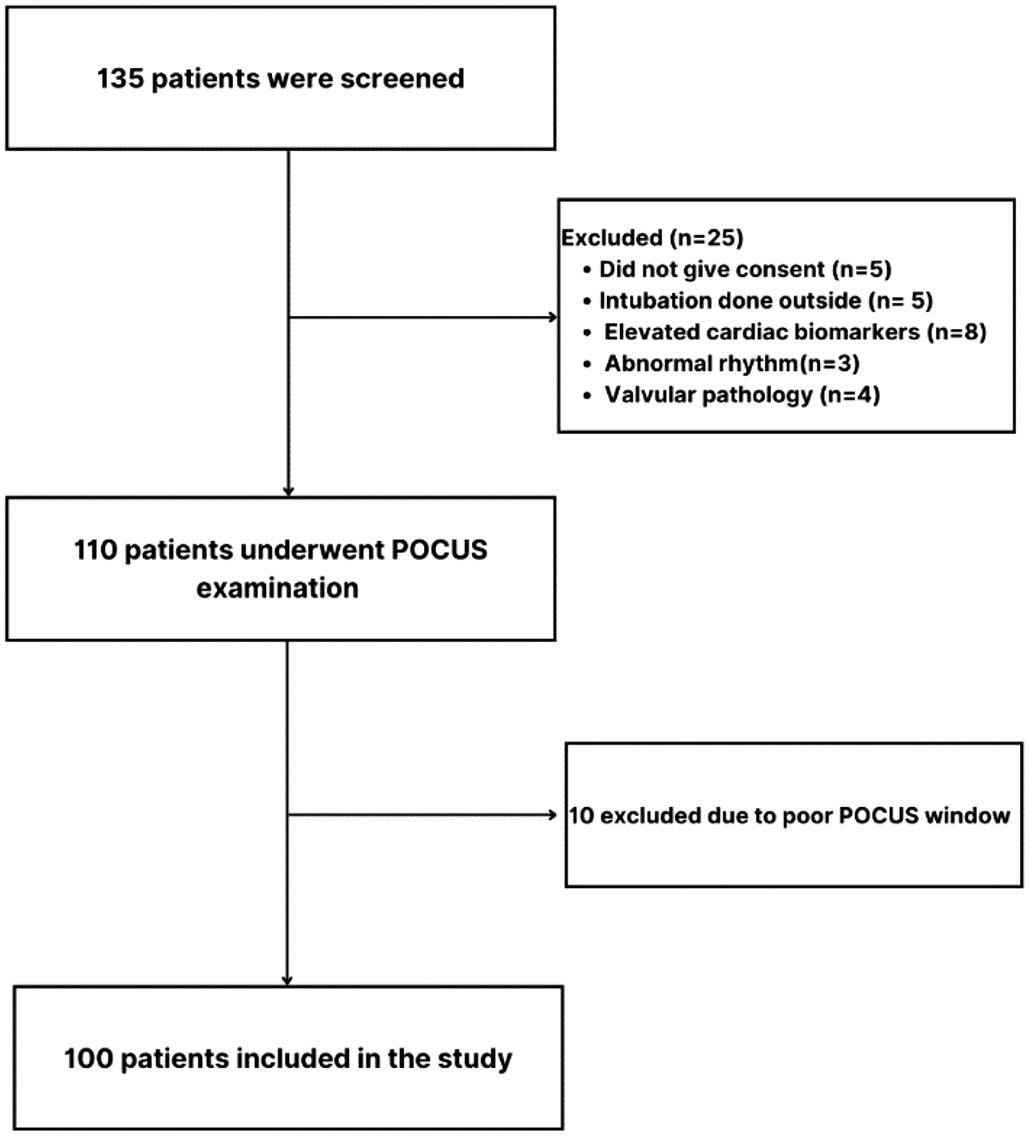
Figure3. Consortpatient flowdiagram. POCUS,point-of-careultrasound.
echocardiographer(criterionreference),asoutlinedin Table2.Thestatisticalanalysisrevealedalackofsignificant differences(P = 0.39)betweentheEFcalculatedusingDAR andtheEFmeasuredbyechocardiography.
WeconductedROCcurveanalysis,whichdemonstrated DAR’svaliditywithahighaccuracyreflectedinanarea underthecurve(AUC)of0.958(95%confidenceinterval[CI] 0.914–1.000, P < 0.001) forpredictingEF.TheoptimalcutoffpointforDARwasidentifiedas0.706,providinga sensitivityof88.7%,specificityof93.1%,LR+ (likelihood ratio)of12.86,andLR-of0.12.(Figure4).ThePearson correlationcoefficientcalculatedforEFcalculatedby MAPSEandthemodifiedSimpsonmethodwas0.54andthat ofEPSSandthemodifiedSimpsonmethodwas0.76.For calculatedEFwithMAPSE,48.3%ofpatientswere categorizedashavingabnormalEF,exhibitingastatistically significantdifferencecomparedtoEFcalculatedbythe modifiedSimpsonmethod(P = 0.01)(Table2).Similarly, calculatedEFwithEPSSdemonstratedacomparable discordance,with58.6%classifiedasabnormal,significantly differingfromEFcalculatedbythemodifiedSimpson method(P = 0.01)(Table2).
Table3 presentsacomparativeassessmentoftheefficacy ofEFmeasurementsusingMAPSE,EPSS,andDAR againstthecriterionreference.ThesensitivityofDARis notablyhigherthanMAPSEandEPSS,whichsuggests thatitisabetterscreeningtool.CalculatedEFfrom
Table1. Demographicandclinicalcharacteristicswithdisplacementofaorticrootmeanvaluesin100patientsonwhompoint-of-care ultrasoundwasperformed.
PatientcharacteristicsN = 100
Patientageinyears,mean(SD)
53.7(16.4)
Male, n(%) 73(73)
Heartrate,mean(SD) 92(17.8)
Respiratoryrate,min-max(SE) 20–36(0.31)
MAP,mean(SD),mmHg 90.6(16.7)
Symptoms
Fever,n(%) 33(33)
Cough,n(%) 33(33)
Chestpain,n(%) 14(14)
Comorbidities
TypeIIdiabetesmellitus,n(%) 36(36)
Systemichypertension,n(%) 46(46)
IHD,n(%) 16(16)
Cardiomyopathy,n(%) 2(2)
Oxygenrequirement
Nasalprongs(2L–4L),n(%) 26(26)
Facemask(6L–10L),n(%) 59(59)
Non-rebreathingmask(>10L),n(%) 14(14)
min, minimum; max,maximum; SD,standarddeviation; SE,standarderror; MAP,meanarterialpressure; IHD,ischemicheartdisease.
DARobtainedhighestnegativepredictivevalue(NPV), suggestingabetterabilitytocorrectlyidentifypatientswith normalEF.
DyspneaisacommonpresentingcomplaintintheED, accountingforapproximately5%ofallEDpresentationsin theAsia-Pacificregion.23,24 Emergencyphysicians frequentlyfacethechallengeofmakingswiftdiagnosesand developingtreatmentplansbasedonlimitedclinical information.25,26 Point-of-careultrasoundhasbecomea standardcomponentofroutineclinicalexaminationsinthe ED,enhancingthemanagementofdyspneabyfacilitating thediagnosisofitsunderlyingcauses.27 Similarly,evaluating LVEFthroughechocardiographyplaysacrucialrolein diagnosingandmanagingawiderangeofpatientsintheED,
Table2. Comparativeanalysisofejectionfraction(EF)measurementsusingDAR,MAPSE,andEPSS*againstactualEFbythemodi fied Simpsonmethod. ActualEFbymodifiedSimpsonmethod
EF, ejectionfraction;*DAR,displacementofaorticroot; MAPSE,mitralannularplanesystolicexcursion; EPSS,end-pointseptalseparation.

Figure4. TheROCcurveofthesensitivityofdisplacementofaortic rootforejectionfractionwhenthecut-offvalueis0.70centimeters. AreaundertheROCcurve = 0.958(95%confidenceinterval 0.914–1.000,P < 0.001forpredictingEF). ROC,receiver operatingcharacteristic.
furtheremphasizingtheimportanceofultrasoundin emergencycare. 28 MostresearchintheEDhasemphasized visualassessmentsofLVEFinsteadofrelyingon
calculationsderivedfrommeasuringthedimensionsofthe LVchamberacrossthecardiaccycle.29–31
Thisstudyaddressesacrucialaspectofemergencycareby exploringtheassessmentofLVfunctioninpatientswith undifferentiateddyspnea.WhilethemodifiedSimpson methodremainsthecriterionreference,investigatingthe potentialofDARasanalternativemethodopensavenuesfor expeditedandmoreaccessibleevaluationsintime-sensitive environmentsliketheED.Asanon-invasiveandeasily accessibletool,DARhasshownpromiseinaccurately predictingLVEF,makingitvaluableforidentifyingpatients atriskofLVdysfunction.3,32 TheDARmethodshowedan accuracyrateof88%incorrectlyclassifyingLVdysfunction, demonstratingitsclinicalapplicabilityinemergencysettings. ThisratesurpassestheaccuracyofMAPSEandEPSS assessmentsforLVdysfunction,includingthe75%accuracy reportedinastudybySchicketal.33
Thisstudy’srobustmethodologyandcompellingresults substantiallycontributetoestablishingthevalidityand clinicalrelevanceofDAR.TheDARmethodexhibitsgood sensitivity(86.2%)andspecificity(88.7%)andhasapositive correlationwiththevaluesofEFobtainedthroughthe modifiedSimpsonmethod.Thissensitivityandspecificityare consistentwiththe findingsofÜnlüeretal,whoreported 94.4%and94.1%,respectively.3 Theincreasedsensitivityof DARcomparedtoEPSSandMAPSEinourstudymakesita
Table3. ComparativeefficacyofejectionfractionmeasurementsusingMAPSE,EPSS,andDAR*againstthecriterionreferencewith95% confidenceintervals.
EF, ejectionfraction; MAPSE,mitralannularplanesystolicexcursion, EPSS,end-pointseptalseparation;*DAR,displacementofaorticroot; CI,confidenceinterval; PPV,positivepredictivevalue; NPV,negativepredictivevalue.
valuabletoolfortheearlydetectionofLVdysfunctionin emergencysettings.These findingsindicatethatemergency physicianscanuseDARasavaluablealternatetoolfor assessingtheLVfunctionatthebedside.33 IntheED,where rapiddecision-makingiscrucial,DARcanbeincorporated asaninitialscreeningtooltoidentifypatientswith compromisedLVfunction,guidingfurtherdiagnostic testing,management,interventionsorspecialistreferrals.
WhencomparingDARwithtraditionalmethods, MAPSEshowedasensitivityof48.3%(95%CI39.2–57.4) andspecificityof95.8%(95%CI90.3–98.4),whileEPSS exhibitedasensitivityof45.5%(95%CI36.2–54.8)and specificityof97.0%(95%CI94.4–99.4).Theseresults contrastwithpriorstudies,suchasthatbyMcKaigneyetal, whoobservedsignificantlyhigherEPSSsensitivity(83.3%) butmuchlowerspecificity(50.0%),andSchicketal,who reportedMAPSEsensitivityof42%andspecificityof 89%.18,33 Thehighersensitivity(83.3%)andlowerspecificity (50.0%)ofEPSSreportedbyMcKaigneyetalmaystemfrom theircomparisonofEPSSwithEFcalculatedusingthe Teichholzmethod.FollandetalfoundthatEFcalculated throughthemodifiedSimpsonmethoddemonstratedbetter correlationwithradionuclideventriculographythanthe Teichholzmethod,withcorrelationcoefficients(rvalues)of 0.75and0.46,respectively.Furthermore,theASEnolonger recommendstheTeichholzmethodforcalculatingLV volumes.9,34 ThehigherspecificityofMAPSEandEPSSin ourstudysuggeststhatthesemeasurementsaremore effectiveinconfirmingLVdysfunctionthanindetectingit, underscoringtheutilityofDAR’shighersensitivityfor earlyidentification.
TheDARoffersapracticaladvantageintheEDsetting duetothestraightforwardvisualizationoftheaorticroot comparedtoLVstructures,makingiteasiertomeasure underchallengingconditions.Furthermore,themotionof theaorticrootresemblestheleftatrialvolumecurve, suggestingthatitsmovement,influencedbyitsattachmentto thecardiacskeleton,mayreflectthedynamicsofleftatrial fillingandemptying.35–37 Theobservedcorrelationbetween DARandstrokevolumesuggeststhatDARmeasurements maycalculateLVEFeffectively,providingvaluableinsights intocardiacperformance.LowerDARvalueswere consistentlyassociatedwithconditionslinkedtoreduced strokevolumeandEF,highlightingDAR’srelevancein assessingpatientswithundifferentiateddyspneaand potentiallycompromisedcardiacfunction.
TheDAR’shighNPVenhancesitsreliabilityinexcluding patientswithnormalEF,whichiscrucialfordetermining appropriatenextstepsinEDcare.TheEPSSexhibitedthe highestpositivepredictivevalue,emphasizingitsrolein confirmingreducedEF.However,DAR’scombined sensitivityandNPVmakeitamorecomprehensivetoolfor initialscreening,ensuringthatpatientswithlikelynormal cardiacfunctionareappropriatelytriaged.Despiteits
advantages,DARshouldnotbeseenasareplacementforall echocardiographicassessmentsbutratherasa complementarytool,especiallyintime-limited environments.Itsheightenedsensitivitycomparedto MAPSEandEPSS,combinedwithitsrapidapplication, makesitapromisingoptionforemergencyphysicians. However,furtherresearchandvalidationarerequiredto establishDAR’sbroaderapplicabilityindiversepatient populationsandsettings.
Whiletheresultsarepromising,thisstudyhaslimitations. Itwasconductedwithinasingle-centerenvironment, potentiallylimitingthegeneralizabilityofthe findings. Amulticenterstudyinvolvingdiversepatientpopulations wouldprovidemorerobustvalidation.Additionally,the studydoesn’tdelveintothecausesofdyspnea,whichcan varywidelyandmightinfluencetheapplicabilityofDARin differentscenarios.Weexcluded9%ofpatientsfromthis studyduetoapoorPOCUSwindow.Patientsenrolledin thisstudyexhibitedexclusivelyregularcardiacrhythms. AlthougheachM-moderecordingoftheaorticroot(AR) hadthepotentialtoencompassmultiplecardiaccyclesfor DARcalculation,itiscrucialtoemphasizethattheextentof ARdisplacementconsistentlyremainsnotableacrossall cardiaccyclesinindividualswithregularheartrhythms. Whenpatientsexhibitirregularheartrhythms,apotential adaptationcouldinvolvecalculatingtheaverageDAR measurementoverthreeto fivecardiaccycles.This adjustmentcouldenhancetheaccuracyofmeasurementsin suchcohorts.Futureresearchinitiativescoulddelvedeeper intoinvestigatingandaddressingthisparticularaspect.
DARemergesasanefficientandreliablemethodforrapid EFassessment,providingemergencyphysicianswitha valuabletoolforbedsideevaluationofLVfunction, especiallywhentimeandresourcesarelimited.Thispaves thewayforintegratingDARintoemergencyprotocolsand routineemergencyclinicalpractice.Whilethese findingsare promising,weacknowledgetheneedforprospective validationinadiversepatientpopulation.
AddressforCorrespondence:SanjanAsanaruKunju,MD,DNB, DepartmentofEmergencyMedicine,KasturbaMedicalCollege, Mangalore,ManipalAcademyofHigherEducation,Karnataka, Manipal,576104,India.Email: sanjan.a@manipal.edu, sanjan. asanar@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Sudhietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KittlesonMM,PanjrathGS,AmancherlaK,etal.2023ACCexpert consensusdecisionpathwayonmanagementofheartfailurewith preservedejectionfraction:areportoftheAmericanCollegeof CardiologySolutionSetOversightCommittee. JAmCollCardiol. 2023;81(18):1835–78.
2.YamazakiY,MatsukiY,ShigemiK.Amethodforcalculatingleft ventricularejectionfractionnoninvasivelyfromleftventriculararterial coupling(Ees/Ea). BMCAnesthesiol. 2023;23(1):1–6.
3.ÜnlüerEE,KaragözA,BayataS.Analternativeapproachtothebedside assessmentofleftventricularsystolicfunctionintheemergency department:displacementoftheaorticroot. AcadEmergMed. 2013;20(4):367–73.
4.SeckoMA,LazarJM,SalciccioliLA,etal.Canjunioremergency physiciansuseE-pointseptalseparationtoaccuratelyestimateleft ventricularfunctioninacutelydyspneicpatients? AcadEmergMed. 2011;18(11):1223–6.
5.SilversteinJR,LaffelyNH,RifkinRD.Quantitativeestimationofleft ventricularejectionfractionfrommitralvalveE-pointtoseptalseparation andcomparisontomagneticresonanceimaging. AmJCardiol. 2006;97(1):137–40.
6.AlbaroudiB,HaddadM,AlbaroudiO,etal.Assessingleftventricular systolicfunctionbyemergencyphysicianusingpointofcare echocardiographycomparedtoexpert:systematicreviewandmetaanalysis. EurJEmergMed. 2022;29(1):18.
7.ChengodeS.Leftventricularglobalsystolicfunctionassessmentby echocardiography. AnnCardAnaesth. 2016;19(Suppl1):S26.
8.SchillerNB,ShahPM,CrawfordM,etal.Recommendationsfor quantitationoftheleftventriclebytwo-dimensionalechocardiography. JAmSocEchocardiogr. 1989;2(5):358–67.
9.LangRM,BadanoLP,Mor-AviV,etal.Recommendationsforcardiac chamberquantificationbyechocardiographyinadults:anupdatefrom theAmericanSocietyofEchocardiographyandtheEuropean AssociationofCardiovascularImaging. EurHeartJ-Cardiovasc Imaging. 2015;16(3):233–71.
10.BatoolS,TajIA,GhafoorM.Ejectionfractionestimationfrom echocardiogramsusingoptimalleftventriclefeatureextractionbasedon clinicalmethods. Diagnostics. 2023;13(13):2155.
11.AdelW,RoushdyAM,NabilM.Mitralannularplanesystolic excursion–derivedejectionfraction:asimpleandvalidtoolinadult maleswithleftventricularsystolicdysfunction. Echocardiography. 2016;33(2):179–84.
12.PoudelSK,MaskeyA,ShahRK,etal.Measurementofmitralannular planesystolicexcursiontoestimateleftventricularejectionfractionin patientswithleftventricularsystolicdysfunction. AsianJCardiolRes. 2022;7(2):31–7.
13.MatosJ,KronzonI,PanagopoulosG,PerkG.Mitralannularplane systolicexcursionasasurrogateforleftventricularejectionfraction. JAmSocEchocardiogr. 2012;25(9):969–74.
14.FrielingsdorfJ,SchmidtC,DebrunnerM,etal.Atrium-drivenmitral annulusmotionvelocityreflectsgloballeftventricularfunctionand pulmonarycongestionduringacutebiventricularpacing. JAmSoc Echocardiogr. 2008;21(3):288–93.
15.ShahA,NanjayyaV,IhleJ.Mitralannularplanesystolicexcursionasa predictorofleftventricularejectionfractioninmechanicallyventilated patients. AustralasJUltrasoundMed. 2019;22(2):138–42.
16.LangRM,BierigM,DevereuxRB,etal.Recommendationsforchamber quantification. EurJEchocardiogr. 2006;7(2):79–108.
17.Situ-LaCasseEandAcu ˜ naJ.Principlesofultrasoundguidance.In: The UltimateGuidetoPoint-of-CareUltrasound-GuidedProcedures(5–27). Cham,Switzerland:SpringerNature,2020,
18.McKaigneyCJ,KrantzMJ,LaRocqueCL,etal.E-pointseptal separation:abedsidetoolforemergencyphysicianassessmentofleft ventricularejectionfraction. AmJEmergMed. 2014;32(6):493–7.
19.NesserHJ,Mor-AviV,GorissenW,etal.Quantificationofleftventricular volumesusingthree-dimensionalechocardiographicspeckletracking: comparisonwithMRI. EurHeartJ. 2009;30(13):1565–73.
20.DeCaraJM,ToledoE,SalgoIS,etal.Evaluationofleftventricular systolicfunctionusingautomatedangle-independentmotiontracking ofmitralannulardisplacement. JAmSocEchocardiogr. 2005;18(12):1266–9.
21.MatosJ,KronzonI,PanagopoulosG,PerkG.Mitralannularplane systolicexcursionasasurrogateforleftventricularejectionfraction. JAmSocEchocardiogr. 2012;25(9):969–74.
22.NishimuraRA,OttoCM,BonowRO,etal.(2014).2014AHA/ACC guidelineforthemanagementofpatientswithvalvularheartdisease: executivesummary:areportoftheAmericanCollegeofCardiology/ AmericanHeartAssociationTaskForceonPracticeGuidelines. Circulation. 2014;129(23):2440–92.
23.PrekkerME,FeemsterLC,HoughCL,etal.Theepidemiologyand outcomeofprehospitalrespiratorydistress. AcadEmergMed. 2014;21(5):543–50.
24.KellyAM,KeijzersG,KlimS,etal.Anobservationalstudyofdyspneain emergencydepartments:theAsia,Australia,andNewZealand DyspneainEmergencyDepartmentsstudy(AANZDEM). AcadEmerg Med. 2017;24(3):328–36.
25.CollinsS,StorrowAB,KirkJD,etal.Beyondpulmonaryedema: diagnostic,riskstratification,andtreatmentchallengesofacuteheart failuremanagementintheemergencydepartment. AnnEmergMed. 2008;51(1):45–57.
26.LiteploAS,MarillKA,VillenT,etal.Emergencythoracicultrasoundin thedifferentiationoftheetiologyofshortnessofbreath(ETUDES): sonographicB-linesandN-terminalpro-brain-typenatriureticpeptide indiagnosingcongestiveheartfailure. AcadEmergMed. 2009;16(3):201–10.
27.GallardE,RedonnetJP,BourcierJE,etal.Diagnosticperformanceof cardiopulmonaryultrasoundperformedbytheemergencyphysician
inthemanagementofacutedyspnea. AmJEmergMed. 2015;33(3):352–8.
28.WardRP,MansourIN,LemieuxN,etal.Prospectiveevaluationofthe clinicalapplicationoftheAmericanCollegeofCardiologyFoundation/ AmericanSocietyofEchocardiographyappropriatenesscriteria fortransthoracicechocardiography. JACCCardiovascImaging. 2008;1(5):663–71.
29.GudmundssonP,RydbergE,WinterR,etal.Visuallyestimated leftventricularejectionfractionbyechocardiographyisclosely correlatedwithformalquantitativemethods. IntJCardiol. 2005;101(2):209–12.
30.WeekesAJ,TassoneHM,BabcockA,etal.Comparisonofserial qualitativeandquantitativeassessmentsofcavalindexandleft ventricularsystolicfunctionduringearly fluidresuscitationof hypotensiveemergencydepartmentpatients. AcadEmergMed. 2011;18(9):912–21.
31.HopeMD,delaPenaE,YangPC,etal.Avisualapproachforthe accuratedeterminationofechocardiographicleftventricularejection fractionbymedicalstudents. JAmSocEchocardiogr. 2003;16(8):824–31.
32.KarwatP,KlimondaZ,Styczy skiG,etal.Aorticrootmovement correlationwiththefunctionoftheleftventricle. SciRep. 2021;11(1):4473.
33.SchickAL,KaineJC,Al-SadhanNA,etal.Focusedcardiacultrasound withmitralannularplanesystolicexcursion(MAPSE)detectionofleft ventriculardysfunction. AmJEmergMed. 2023;68:52–8.
34.FollandED,ParisiAF,MoynihanPF,etal.Assessmentofleftventricular ejectionfractionandvolumesbyreal-time,two-dimensional echocardiography.acomparisonofcineangiographicandradionuclide techniques. Circulation. 1979;60(4):760–6.
35.StrunkBL,FitzgeraldJW,LiptonM,etal.Theposterioraorticwall echocardiogram.Itsrelationshiptoleftatrialvolumechange. Circulation. 1976;54(5):744–50.
36.SilvermanMEandHurstJW.Themitralcomplex.Interactionofthe anatomy,physiology,andpathologyofthemitralannulus,mitralvalve leaflets,chordaetendineae,andpapillarymuscles. AmHeartJ. 1968;76(3):399–418.
37.BurggrafGW,MathewMT,ParkerJO.Aorticrootmotiondeterminedby ultrasound:relationtocardiacperformanceinman. CathetCardiovasc Diagn. 1978;4(1):29–46.
BrendanPeterson,PharmD*
AmyS.Nowacki,PhD†‡
AlexanderUlintz,BS/BA,MD§
SharonE.Mace,MD†∥
SectionEditor: KennethScottWhitlow,DO
*OhioStateUniversity,SchoolofPharmacy,Columbus,Ohio † ClevelandClinicLernerCollegeofMedicineofCaseWesternReserveUniversity, Cleveland,Ohio ‡ LernerResearchInstitute,DepartmentofQuantitativeHealthSciences, ClevelandClinic,Cleveland,Ohio
§ OhioStateUniversity,DepartmentofEmergencyMedicine,Columbus,Ohio ∥ ClevelandClinic,DepartmentofEmergencyMedicine,Cleveland,Ohio
Submissionhistory:SubmittedDecember17,2023;RevisionreceivedOctober31,2024;AcceptedNovember1,2024
ElectronicallypublishedJanuary15,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18561
Introduction: Proceduralsedation(PS)iscommonlyperformedintheemergencydepartment(ED).Nil peros(nothingbymouth)(NPO)guidelinesextrapolatedfromstandardsforpatientsundergoingelective proceduresintheoperatingroomhavebeenappliedtoEDPSpatients.Therehasbeennolargestudyof EDPSpatientscomparingdifferencesinadverseeventsandPSsuccessratesbasedonNPOstatus.
Methods: FromacohortofconsecutiveEDPSpatientsofallagesinthe20EDsofonehospital system onequaternaryED,fourtertiaryEDs,sixcommunityhospitalEDs,oneruralED,twopediatric EDs,andsixfreestandingEDsintwostatesintheMidwestandSouth weconductedaretrospective analysisonaprospectivedatabaseover183monthsfromApril2000–June2015.Primaryoutcomewas theincidenceofsideeffectsandcomplications,whichcomprisedtheadverseeffects.Thesideeffects werenausea,vomiting,itching/rash,emergencereaction,myoclonus,paradoxicalreaction,cough,and hiccups.Complicationswereoxygendesaturation <90%,respiratorydepression(respiratoryrate <8), apnea,tachypnea,hypotension,hypertension,bradycardia,andtachycardia.Normalvitalsignswere agedependent.Secondaryoutcomewassuccessfulsedationde finedascompletionoftheprocedure. WeexaminedtheassociationbetweenadverseeventsandsuccessfulsedationwithNPOstatus.
Results: Of3,274visits,exactNPOstatuswasknownin2,643visits.ComparisonofNPO <8hoursin 1,388patientsvs ≥ 8hoursin1,255patientsrevealedsideeffects5.5%vs4.5%(P = 0.28); complications11.9%vs17.7%(P < 0.001);adverseevents16.3%vs21.5%(P < 0.001),interventions 4.1%vs4.4%(P = 0.73),andproceduralcompletions94.3%vs89.7%(P < 0.001).Afteradjustmentfor age,sex,transferstatus,AmericanSocietyofAnesthesiologyphysicalstatusclassification,race, primarysedative,multiplesedatives,sedativeplusanalgesic,andprimaryanalgesic,wefoundno associationbetweenNPOstatusandsideeffects(P = 0.68),complications(P = 0.48),oradverseeffects (P = 0.26);however,proceduralcompletionrateremainedsignificantlyhigherforNPO < 8hours (P = 0.007).
Conclusion: Anilperosstatus ≥8hoursmayhavesimilarorworseoutcomesthanNPO <8hours, whichiscontrarytomanysuggestedguidelines.StrictadherencetoNPOguidelinesinEDprocedural sedationpatientsmaynotbenecessary.[WestJEmergMed.2025;26(2)200–209.]
Emergencydepartment(ED)patientsfrequentlyundergo proceduralsedation(PS)andanalgesia,whichisdesignedto alleviatetheirpainandanxietyduringdiagnosticand/or therapeuticmedicalprocedures.1 Guidelinesregarding fastingpriortoperformingPS,promulgatedbyvarious organizationsforgeneralanesthesia,areoftenfollowedby cliniciansperformingPSintheED.1–5 Thisconcepthas recentlybeenchallenged.5 Therehasbeensomeevidencein thepediatricpopulationthatadherencetosuchguidelines doesnotresultinfeweradverseeventsduringEDPS,6–13 althoughsomeofthereportsofpediatricPShaveinvolved PSperformedinlocationsotherthantheED6,7 orinvolved onlyonesedativeinsteadofarangeofsedativeagents.8,12 SuchdataislackingforadultEDpatients.Ourgoalinthis studywastoevaluatetheeffectoffastingonPSintheEDin allagesofEDpatients,includingtheelderly.
StudiesintheliteratureontheeffectoffastingonEDPS havefocusedonthepediatricpopulation,withasurprising lackofstudiesinadults,includingtheelderly.Alarge-scale studyoftheincidenceofadverseeventsandtheneedfor interventionshasnotbeendescribed,thusrepresentinga largegapinknowledgeforacommonpractice.
GoalsofThisInvestigation
Ourgoalinthisstudywastodeterminetheimpactof fastingguidelinesonthesideeffects,complications,andneed forinterventionsduringEDPSinpatientsofallages.
StudyDesignandSetting
Thiswasacohortstudyofconsecutivepatientsofallages undergoingPSinthe20EDsofonehospitalsystem consistingofoneurban,academic,quaternaryED,four tertiaryEDs,sixcommunityhospitalEDs,oneruralED,two pediatricEDs,andsixfreestandingEDsintwostateslocated intheMidwestandtheSouth.Weperformedaretrospective analysisonaprospectivelycollecteddatabaseover183 monthsfromApril2000–June2015.Allpatientswho underwentparenteralPSintheED,performedbyattending emergencyphysicians(EP)wereincluded.Weexcluded sedationsdoneoutsidetheEDand/ornotadministered byEPs.
Amandatory,four-page,standardizedsedationform mustbecompletedbytheregisterednurse,respiratory therapist,andattendingphysicianonallpatientsundergoing PSthroughoutthehospitalincludingtheED.Thisform includespre-sedationassessment,post-sedationassessment (includingreadinessfordischarge),anddocumentationof thePSitself.DocumentationofthePSincludesthe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Proceduralsedation(PS)isacommonED procedure.Applyinganesthesiologynilperos (NPO)guidelinesforelectiveproceduresto EDPSpatientshasbeenquestioned.
Whatwastheresearchquestion?
Whatistheincidenceofadverseeventand proceduralcompletionratesforpatients meetingvsnotmeetingNPOguidelines?
Whatwasthemajor findingofthestudy?
NPO < 8vs ≥ 8hours:adverseevents16.3%vs 21.5%P < 0.001,proceduralcompletions 94.3%vs89.7%P < 0.001.
Howdoesthisimprovepopulationhealth?
NPO ≥ 8hourshassimilarorworseoutcomes thanNPO < 8hours,contrarytomany suggestedguidelines. Strictadherenceto NPOguidelinesinEDPSpatientsmaynot benecessary.
continuousmonitoringofvitalsigns:heartrate,respiratory rate,bloodpressure;pulseoximetry,cardiacrhythm, respiratorytherapyassessment,includingcapnography;and patientresponses,medicationadministration,andpatient interventions.Allsedationsincludingthesedationformsand electronichealthrecord(EHR)notesarereviewedaspartof thehospitalqualityimprovement(QI)monthlymeetingbya physician-ledcommittee.Themembersofthiscommittee werenotinvolvedinthisstudybutarepartofthehospital’ s QIprocess.
Weperformedthisretrospectivereviewwithadherence tothe12methodologiccriteriaasde fi nedbyWorsteretal.14 Dataresultedfromanelectronicpullofinformationfrom theEHR.Wedidnotuseabstractors.Therefore,criteria1, 4,5,6,7,and8accordingtoWorsteretalwerenot applicable.Theremainingcriteria(2,3,9,10,11,and12) weremet.Forcriterion2,caseselectioncriteriawere de fi nedapriori.Forcriterion3,variableswerede fi nedin themethods.Forcriterion9,thehealthrecorddatabasewas described.Forcriterion10,allpatientvisitsintheEHR meetingcriteriawereincluded.Forcriterion11,dataused waspartofamandatorystandardizedsedationform,and themissingdatawasminimal.Asdiscussedinourstudy fl owdiagram,weconductedacompletecaseanalysis.For criterion12,theinstitutionalreviewboardapproved thestudy.
Theprimaryoutcomewastheincidenceofsideeffectsand complications,whichcomprisedtheadverseeffects.Side effectswerenausea,vomiting,itching/rash,emergence reaction,myoclonus,paradoxicalreaction,cough,and hiccups.Complicationswereoxygendesaturation <90%, respiratorydepressionwitharespiratoryrate <8,apnea, tachypnea,hypotension,hypertension,bradycardia,and tachycardia.Thenormalrangeofvitalsignswasage dependent.Successfulsedationwascompletionof theprocedure.
Descriptivestatisticsofpatientdemographicsand proceduresarepresentedascount(percentage),median (Q1–Q3),orrange.Weexploredbivariableassociationsof patientdemographicsandprocedureswithNPOstatuswith eitheraWilcoxonrank-sumtestorachi-squaretest,as appropriate.TheNPOwasoriginallyrecordedasanumeric valueinpatientchartsand,thus,weexploredNPOstatus threeways:(1)classifiedasexactNPOstatusknownor unknown;(2)dichotomizedateighthourstoalignwith clinicalcareguidelines;and(3)originalscaletomaintainfull detail.WeexploredassociationsofNPOstatuswithbinary outcomemeasuresusinggeneralizedestimatingequations models,assumingacompoundsymmetrycorrelation structuretoaccommodatemultipleEDvisitsperpatient. Thiswasperformedbothunadjustedandadjustingforyear ofvisit,patientagegroup,sex,transferstatus,American
SocietyofAnesthesiology(ASA)physicalstatus classification,race,primarysedative,useofmultiple sedatives,useofsedativeplusanalgesic,andprimary analgesic.TheASAisusedtopredictoperativeriskwhere ASA1isanormalhealthypatient;ASA2isapatientwith mildsystemicdisease;andASA3isapatientwithsevere systemicdiseasethatisnotlife-threatening.TheASA4isa patientwithseveresystemicdiseasethatisaconstantthreat tolife;ASA5isamoribundpatientwhoisnotexpectedto survivewithouttheoperation.15 Reportedaretheresulting oddsratios,95%confidenceintervals,andassociated P -values.Similaranalyseswereconductedtoexplorethe associationofNPOstatuswiththeneedformedical intervention.Weusedasignificancelevelof.05.Analyses wereconductedusingSASversion9.4(SASInstitute,Cary, NC)statisticalsoftware.
CharacteristicsofPatients
Therewere3,274PSperformedintheEDon2,570 patientsofallagesbyemergencyphysiciansintheED (Figure1).Byagegrouptherewere1,177PSperformedon pediatricpatients(age ≤21years),and2,097PSperformed onadults(age >22years),ofwhom708weregeriatric (≥65yearsofage)PS.
NPOStatus:KnownvsUnknown
ThepatientswithNPOunknownweresignificantlyolder, withahigheracuityasdenotedbyhigherASAandby “ more

Figure1. StudyvisitCONSORTdiagram.
*Numberofpatientsdoesnotadduptohigherleveltotalas110patientshadmultiplevisitswithsomevisitsclassifiedasNPO <8hoursand ≥8hoursandthusthosepatientsarecountedinbothsubgroups.Numberofvisitsisinboldandinbluecolor.Numberofpatientsisinitalics andparentheses.
ED,emergecydepartment; NPO,nilperos(nothingpermouth); PS,proceduralsedation.
Table1. Patientdemographics,ASAandprocedurecharacteristics.
Ethnicity
Black 786(30%) 210(33%) 431(31%)355(28%)
White 1816(69%) 413(66%) 931(67%)885(71%)
Other 41(2%) 4(1%) 26(2%)15(1%)
ASAcategory
ASA1 952(36%) 121(19%) 589(42%)363(29%)
ASA2 667(25%) 160(25%) 353(25%)314(25%)
ASA3 904(34%) 250(40%) 391(28%)513(41%)
ASA4 115(4%) 78(12%) 54(4%)61(5%)
ASA5 5(0.2%) 22(3%) 1(0.1%)4(0.3%)
Procedure < 0.001
-100(16%)
ASA1isanormalhealthypatient.ASA2isapatientwithmildsystemicdisease.ASA3isapatientwithseveresystemicdiseasethatisnotlife threatening. ASA4isapatientwithseveresystemicdiseasethatisaconstantthreattolife.ASA5isamoribundpatientthatisnotexpectedto survivewithouttheoperation.
ASA,AmericanSocietyofAnesthesiologyphysicalstatus; NPO,nilperos(nothingbymouth); EGD,esophagogastroduodenoscopy.
critical” proceduressuchaslumbarpuncture, ventriculostomy,orcardioversioncomparedtoorthopedic proceduresorsuturing(Table1).Whenweevaluatedthe reasonsforanunlistedNPOstatustheseincludedthatthe patientwascriticalandadmittedtoanintensivecaresetting withdiagnosessuchasshockand/orrespiratorydistressor hadbeenintubatedorwasundergoingemergencysurgery. Asignificantnumberwereunabletogivereliable informationaboutwhentheyatelastduetomedicalreasons thatincludedalteredmentalstatus,dementia,autism/ developmentaldelay,andneurologicdisorders.Another largegroupofpatientswereunwillingand/orunableto
provideaccurateinformationabouttheirlastoralintakefor psychiatricreasonsincludingacutepsychiatricillnesssuchas acutemanicstateorschizophrenia,orbecausetheywere experiencingsubstanceoralcoholintoxication.Therewere alsoseveralyoungchildrenbroughtinfromdaycareor schoolbyemergencymedicalserviceswhowere unaccompanied,atleastinitially,byanadult,suchastheir daycareproviderorteacheroraparent,whocouldgive information;ortheadultwiththemhadnoinformation regardingtheirlastoralintake.Thus,youngagewithlackof abilitytotelltimewasanothercauseforanunknownNPO status.Additionally,somepatientswereonlyabletoprovide
arangeoftimesuchas “morethansixhoursago.” Intotal, therewere631visits(19.3%)wheretheexactNPOwaseither notobtainable(13.2%)ornotdocumented(6.1%).This emphasizesthefactthatPSmayneedtobedoneinanED withouttheluxuryofknowingthelastoralintakeinabout oneof fivepatientpresentations(Figure1)(Table1).
Therewasnosignificantdifferenceforsideeffects, complicationsoradverseeventsbetweenexactNPOstatus knownvsexactNPOstatusunknown(Table2).The incidenceofsideeffects,whichwasprimarilyvomiting,was greaterforNPO <8hoursat5.5%thanforNPO ≥8hoursat 4.5%,butthiswasnotstatisticallysignificant.However, whenNPOwasconsiderednumeric,itwasfoundthatas NPOtimeincreases,theriskofasideeffect,generally vomiting,significantlydecreases.Thecomplicationsand adverseeventsweresignificantlygreaterforNPO ≥8hours thanforNPO <8hoursbothwhenNPOstatuswasbinary andnumericwithcomplicationsat11.9%forNPO <8hours and17.7%forNPO ≥8hoursandadverseeventsat16.3%for
NPO <8hoursand21.5%forNPO ≥ 8hours(Table2) (Figure2).Therateofproceduralcompletionswas significantlyhigherwhenNPOstatuswasknown(92.1%vs 86.1%)andwhenNPO <8hours(94.3%vs89.7%)(Table2, Figure 2A).Wedidnot findanyinstancesofpulmonary aspirationaswerenotedinpreviousstudiesofEDPS.5 We hadoneintubationoutof3,274PS(0.03%).
LengthofNPOcategoriesislower-boundinclusive.Thus, the firstcategoryconsistsofNPOvaluesfromzerotoless thanfourhours,thesecondcategoryconsistsofNPOvalues fromfourtolessthaneight,etc.
Theneedforinterventionwasrelativelylowoverallat approximately4%.Theproportionofvisitsrequiring interventiondidnotsignificantlydifferwhentheexactNPO statuswasknown(4.2%)vsunknown(4.0%)(P = 0.70)or whenNPO <8hours(4.1%)vs ≥8hours(4.4%)(P = 0.75). Notably,therewasonlyoneintubationof3,274PS(0.03%). Thiswasanelderlyfemalewithahistoryofhypertension undergoingreductionofashoulderdislocationwhoreceived
Table2. Sideeffects,complications,adverseeventsandprocedurecompletionsaccordingtonilperosstatus.
NPO, nilperos(nothingbymouth).
NPOcategorized

Figure2. (A)Sideeffects,complications,adverseevents,and incompleteproceduresbynilperosgroup: <8hoursvs ≥8hours. (B)Sideeffects,complications,adverseevents,andincomplete proceduresbynilperos. NPO,nilperos(nothingbymouth).
propofolandhydromorphone.Sheexperiencedbradypnea. Shewasbaggedandthenintubatedforfewerthan five minutes.ShewasextubatedintheEDwithoutcomplications anddischargedhome.Atfollow-upintheofficeweekslater, shewaswellwithnoproblemsresultingfromtheintubation/ EDvisit(Table3).
Demographicandproceduralvariablesaffecting adverseevents
Accordingtomultivariateanalysis,NPOstatus,yearof visit,sex,whethertransferredornot,race,anduseofmultiple sedativeswerenotsignificantfactorsassociatedwithside effects,complications,oradverseeffects.AhigherASA classificationandolderagegroup(adult/geriatric)were significantlyassociatedwithhigherriskofcomplicationsand, thus,adverseevents(P < 0.0001)butnotsideeffects.The choiceofprimarysedativewassignificantlyassociatedwith theincidenceofsideeffects,complications,andadverse events.Comparedtopropofol,theuseofetomidate,ketamine, midazolam,orothersedativesallshowedanincreasedriskof sideeffects,primarilyvomiting;andtheuseofmethohexitalor etomidateshowedadecreasedriskofcomplications.The choiceofanalgesicwasnotassociatedwiththeincidenceof sideeffectsbutwassignificantlyassociatedwiththe
occurrenceofcomplicationsandadverseevents.Comparedto fentanyl,theuseofhydromorphone,morphine,oroxycodone showedadecreasedriskofcomplications.Usingbotha sedativeandananalgesicwasassociatedwithahigherriskof sideeffectsandadverseevents(Table4).
Sideeffects,complicationsandadverseeventsand interventionsbyfastingtime
OfinterestwastherelationshipbetweenNPOduration andpatientoutcomes,specificallysideeffects,complications, overalladverseevents,anyinterventions,respiratory interventions,andotherinterventions(non-respiratory).We exploredseveralwaysofdefiningNPOduration(Table2). First,wecomparedNPOdurationstatusknownvsunknown andfoundnosignificantdifferenceinanypatientoutcome. Next,wedichotomizedNPOdurationas <8hoursvs ≥8 hoursandfoundasignificantlyhigherrateofcomplications andoveralladverseeventsintheNPO ≥8hoursgroup.When analyzingNPOdurationasanumericvariable,wesawthat eachadditionalhourofNPOwassignificantlyassociated withadecreaseinriskofsideeffectsandanincreaseinriskof complicationsandoveralladverseevents.
Finally,wecategorizedNPOdurationintotwo-hour intervalsandcomparedeachtothereferencegroupof ≥8 hours.Therewerenosignificantdifferencesinsideeffects whencomparingthevariousNPOtimeintervals0to <2,2to <4,4to <6,and6to <8hourstoNPO ≥8hours. ComplicationsatNPO2to <4,4to <6,and6to <8hours were significantlylessthanforNPO ≥8hours.Therewere fewercomplicationsintheNPOtimeinterval0to <2hours comparedtoNPO ≥8hours,althoughthisdidnotachieve statisticalsignificance.However,itshouldbenotedthat the0to <2hoursNPOgroupcontainedonly31visits (Figure3, Table2).
StudiesregardingNPOstatusandEDPSinthepediatric populationhavefoundnoassociationbetweenNPOstatus andadverseevents.8–13 Surprisingly,toourknowledge,there havebeennoadultstudiesofNPOstatusandadverseevents inEDpatientsfromtheUnitedStatesandonlytwo internationalstudies.OnesmallAustralianstudyinpediatric andadultEDsubjectswithasomewhatatypicalpatient populationconsistingofpredominatelyASA1and2patients andanoverwhelmingmajority(84%)oforthopedicpatients withpropofolbeingtheonlysedativefounda22.4% incidenceofadverserespiratoryeventsfornot-fastedpatients vs19.5%forfastedpatientsanda33.3%incidenceof respiratoryinterventionsfornot-fastedcomparedwith 24.6%forfastedpatients.16 Ourstudyhadmorethaneight timesthenumberofpatientencountersthaninthisstudyand includedhigheracuitypatientswithhigherASAs,agreater rangeofproceduresperformed,andavarietyofsedatives andamorerobuststatisticalanalysisthatconsideredother
Table3. Interventionsbynilperosstatus.
NPO, nilperos(nothingbymouth); NPA,nasopharyngealairway; IVF,intravenous fluids.
potentialconfoundingfactors.Ourincidenceofadverse eventsof16.3%forNPO <8hoursand21.5%forthosefasted ≥8hoursiscomparabletotheAustralianstudy.16
Ouroverallincidenceofadverseevents(18.4%)compares favorablywithanotherstudy,alsofromAustralia,in pediatricandadultEDpatientsthatlookedprimarilyat adverserespiratoryeventsduringEDPS.Tayloretal reportedahigher20.8%incidenceofjustairwayeventsand foundnoassociationoffastingstatuswithvomiting.17 Our studyisconsistentwithapriorreportofelectivePSin pediatricpatientsperformedbyanelectivesedationservice regardingpredictorsofcomplicationsforpatients undergoingPSandanotherpediatricstudyofnon-emergent sedationsforresearchprocedures,whichbothreporteda higherrateofcomplicationswithhigherASA.7,18
Whencomparingbyagegroup,pediatricpatientshad significantlyfewersedation-relatedcomplicationsand adverseeventsthanadults,especiallygeriatricadults.Side effects,mostcommonlyvomiting,werehigherinpediatric patientsthanadults,whichmayatleastbepartlyexplained bythegreateruseofemetogenicsedatives,specifically ketamine,inthepediatricpatients(Table4).Ketamineasa sedativeincreasestheriskofvomitingascomparedwith othersedatives.10,11 Thespecificagegroup pediatric,nongeriatricadult,andgeriatricadult affectedtheoccurrence ofsideeffects,complications,andadverseevents.Thisage
groupfactorforEDPShasnotbeenevaluatedpreviouslyby robuststatisticalanalysis(Table4).
Wefoundinourunadjustedanalysisthatfasting ≥8hours wasassociatedwithaslightlylowerincidenceofsideeffects, mostlyvomiting,andastatisticallysignificantlygreater occurrenceofcomplicationsandadverseevents(Table2). ThisdiffersfromthepreviouspediatricEDPSstudiesthat didnot findanassociationbetweenadverseeventsandNPO status.8–13 Inonepediatricstudy,therewasanonsignificant increasedincidenceofvomitingwithincreasedfastingtime, butthecomparisonwasofthosefasted <1hourvsthose fasted ≥3hours.12 InanAustralianstudythatincluded adults,therewasnosignificantdifferenceintheincidenceof adverseprocedure-relatedeventsbasedonthetimetheylast ate/drank.17 Onevariablethatmightaccountforthevarious resultscouldbedifferentpatientpopulations:pediatricvs adultpatients,andvaryingacuityofpatients,althoughother factors,suchasmedications(sedatives,analgesics)and procedurebeingdone,couldalsoplayarole.
Ourresearchaddstothedata,primarilyinthepediatric population,indicatingthatcompliancetofastingguidelines similartothoseforelectivesurgerydoesnotsignificantly decreasetheincidenceofadverseeventsduringprocedural sedation.Ourstudydocumentsthatsuchadherencetothe recommendedfastingguidelinesmayresultinagreater incidenceofadverseeventsduringPS.Recently,graded
Table4. Multivariateanalysisofnilperosgroupandsideeffects,complications,andadverseevents.
Models fit aregeneralizedestimatingequationsassumingcompoundsymmetrycorrelationstructure.ASA1:normalhealthypatient.ASA2: mildsystemicdisease.ASA3:severesystemicdiseasebutnotlife-threatening.ASA4:patientwithseveresystemicdiseasethatisa constantthreattolife.ASA5:moribundpatientwhoisnotexpectedtosurvivewithouttheoperation.
ASA,AmericanSocietyofAnesthesiologyphysicalstatus; NPO,nilperos(nothingbymouth); CI,confidenceinterval.
fastingprecautionsbasedonvariousfactorsincluding patientcharacteristics,comorbidities,theprocedure,andthe sedationtechniquehavebeensuggested.5
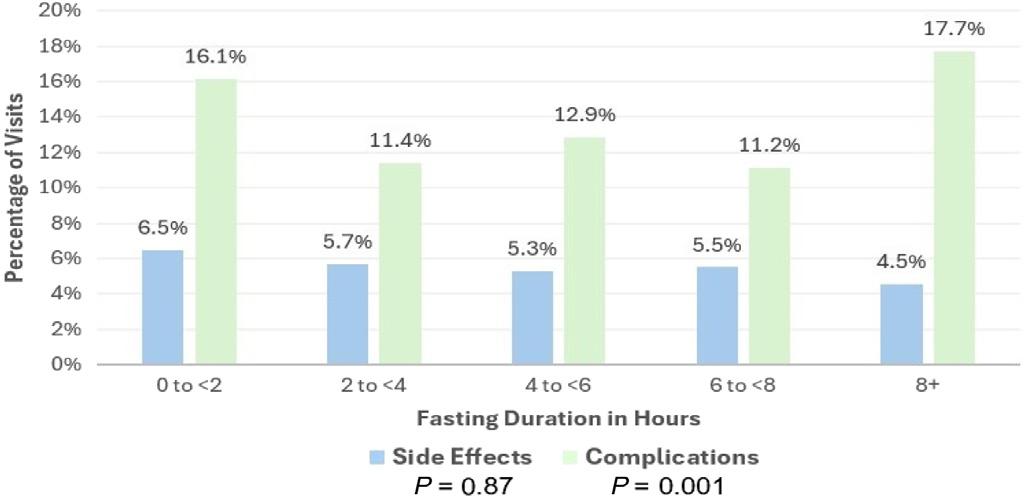
Figure3. Fastingtimeandadverseeventsbyfastingduration inhours.
Therecouldbeseveralreasonswhyfastingmayhavea negativeeffect.Hypoglycemiahasbeendescribedinanadult diabeticpatientwhowasfastingpriortoaprocedure.19 PatientsgoingwithoutPOintakemaybecomedehydrated andhypotensive.Futurestudieswouldbehelpfulin collaboratingwhetherthestatisticallysignificantnegative impactoffastingpriortoEDPSthatwefound,bothon decreasedPSsuccessratesandonanincreasedincidenceof adverseevents,isspecifictoacertainpatientpopulation, suchashigheracuityadultswithmultiplecomorbiditiesand higherASAs.
Thisstudyhasseverallimitations.Theseresultswere basedonthe findingsfromonehospitalsystem,whichmay limititsgeneralizability.However,20hospitalEDswith
manydiverselocationsinurban,suburbanandruralsettings, andvaryinggeographiclocationsintwodifferentstates,were included.Moreover,weincludedallagesofpatientswith varyingcomorbidities,ASAs,andmultiplediagnoses undergoingPSperformedbymanydifferentphysiciansover 15.25yearsusingvarioussedativesandanalgesicsandhada highnumber(over3,000)ofEDPS.
Althoughthiswasaretrospectivestudy,therecordingof datawasdoneprospectivelyatthetimeoftheEDPS primarilybythenurses,therespiratorytherapists,andthe EDattendingphysicianonastandardizedfour-pageform usedthroughoutthehospitalonwhichstaffhasbeeninservicedmultipletimesonaregularbasisaspartofthe hospital-wideQIprogram.Datasuchasvitalsignsand rhythmstripmonitoringarerecordedcontinuously throughoutallproceduralsedations,andbecausesuch informationisincludedontheformitseemshighlyunlikely thatanyadverseeventsuchashypo-orhypertension, bradypneaorapnea,oralowpulseoxygensaturationwould nothavebeenrecorded.Inaddition,theEDEHRchart completedbytheemergencyphysicianinattendanceduring thesedationandEDvisitwasalsoreviewed.Moreover,all informationwasrecordedprospectively,whichmakesit doubtfulthatanysignificantdataoroccurrencewasmissed. Hospitalpolicyrequiresthataminimumofthree personnelbepresentthroughouttheEDPS:anED registerednurse;anEDrespiratorytherapist;andanED attendingphysician.Otherssuchasaconsultantorresident areusuallypresentaswell.Thismakesitimprobablethatthis groupofindividualswouldoverlookornotrecordany adverseevent.
Fastingwasnotdocumentedinaboutone-fifthofpatients, whichcouldaffectthevalidityofthisstudy.Theprimary reasonforthiswasthecriticalconditionandhigherASAof someofourpatientsandtheemergentnatureoftheprocedural sedations(Figure1).Otherfactorsthatmayhavecontributed tomissingdataincludethetimeconstraintsfromabusyED withhighpatientvolumesand,perhaps,theimpressionthat thisdatawasnotessentialgiventhedepthofsedation anticipatedandthecontroversyoverNPOstatusforEDPS.
OurincidenceofNPOnotlistediscomparablewithother studies.OnestudyinapediatricEDhadfastingtimesnot documentedin25.4%ofcases,althoughtheyhadyounger, “healthier” patientswithfewercomorbidities,lowerASAs, andfewerdangerousproceduressuchasventriculostomyor cardioversion.13 Anotherstudyfrompediatricsedation servicesthatincludedscheduledsedationsandsedationsin non-EDsettingsreported22.4%ofNPOunknown.6
BecausetheNPOcutofftimeofeighthoursisconsistently mentionedinthevariousguidelinesandtheliterature,we usedthiseight-hourperiod,aswellasthe2-,4-,and6-hour cutofftimes 2,4,7,8,13 (Figures 2A, 3 and Tables2–4).Arecent consensusstatementdidnotmakeadistinctionbetween NPOtimeforsolids(lightmeal)vsliquids(non-humanmilk
orformula)andusedthesamecut-offtimeforallthesePO intaketypesinhealthyinfantsandchildren.5 Moreover,the guidelines/consensusstatementshavevariedwidelyovertime especiallyforliquidPOintake.Forexample,onerecent guidelinerecommendsaNPOoffourhoursforbreastmilk.2 AnotherconsensusstatementgivesnoNPOrestrictionfor breastmilkifnoriskfactors,twohoursifsomeriskfactors, andfourhoursifmoderateriskfactors.5 Anotherguideline alsodidnotdifferentiatebetweensolidsorliquidsandstated “nomilkorsolidsaftermidnight.”4 Becauseofthelackof consistentNPOtimes,2–5 basedondifferentPOintake,age, andriskfactorsovertheyears,particularlyforPOliquid intake,andthelackofdifferentiationbetweensolidsand liquidsinvariousguidelines/consensusstatements,4,5 weused NPOforanyPOintakeinouranalysis.
Observerswerenotblindedtothemedications administeredorfastingtimes,whichcouldhaveledtobias. However,observerswereunawareofthisstudy.Oursedation formhasablankforthetimeoflastPOintakebutdoesnot specifywhetherliquidsorsolidswereconsumed,although thiswasrecordedinsomeinstances.
ToourknowledgethisisthelargestEDprocedural sedationcohortthatincludedadults,particularlygeriatric patientsandhigheracuitypatients,analyzedwiththemost robuststatisticalanalysestoevaluatetheassociationamong nilperosstatusandadverseevents.Weidentifiedasignificant increaseincomplicationsandadverseeventsandincomplete proceduresforthoseNPO ≥8hoursvsNPO <8hours.These resultsindicatethatdelayingsedationtomeetestablished fastingguidelinesmayworsenoutcomesforpatientsofall ages,includingadultsintheED,andisnotindicated.
AddressforCorrespondence:SharonE.Mace,MD,Cleveland Clinic,EmergencyServicesInstitute,9500EuclidAve.,E-19, Cleveland,OH44195.Email: maces@ccf.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Petersonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GodwinSA,BurtonJH,GerardoCJ,etal.Clinicalpolicy:procedural sedationandanalgesiaintheemergencydepartment. AnnEmergMed. 2014;63(2):247–58.
2.AmericanSocietyofAnesthesiologists.Practiceguidelinesfor preoperativefastingandtheuseofpharmacologicagentstoreducethe riskofpulmonaryaspiration:applicationtohealthypatientsundergoing electiveprocedures. Anesthesiology. 2017;126(3):376–93.
3.CoteCandWilsonS.Guidelinesformonitoringandmanagementof pediatricpatientsbefore,during,andaftersedationfordiagnosticand therapeuticprocedures. Pediatrics. 2019;143(6):e20191000.
4.AmericanAcademyofPediatricsCommitteeonDrugs.Guidelinesfor theelectiveuseofconscioussedation,deepsedation,andgeneral anesthesiainpediatricpatients. Pediatrics. 1985;76(2):317–21.
5.GreenSM,LeroyPL,RobackMG,etal.Aninternational multidisciplinaryconsensusstatementonfastingbefore proceduralsedationinadultsandchildren. Anaesthesia. 2020;75(3):374–85.
6.GhafferS,HaverlandC,RamaciottiC,etal.Sedationforpediatric echocardiography:evaluationofpreprocedurefastingguidelines. JAmerSocEchocardiography. 2002;15(9):980–3.
7.BeachML,CohenDM,GallagherSM,etal.Majoradverseeventsand relationshiptonilperosstatusinpediatricsedation/anesthesiaoutside theoperatingroom. Anesthesiology. 2016;124(1):80–8.
8.BablFE,PuspitadewiA,BarnettP,etal.Preproceduralfasting stateandadverseeventsinchildrenreceivingnitrousoxidefor proceduralsedationandanalgesia. PediatrEmergCare. 2005;21(11):736–43.
9.AgrawalD,ManziSF,GuptaR,etal.Preproceduralfastingstateand adverseeventsinchildrenundergoingproceduralsedationand analgesiainapediatricemergencydepartment. AnnEmergMed. 2002;42(5):636–46.
10.BhattM,JohnsonDW,TaljaarM,etal.Associationofpreprocedural fastingwithoutcomesofemergencydepartmentsedationinchildren. JAMAPediatr. 2018;172(2):678–85.
11.ChumpitaziCE,CampEA,BhanidipatiDR,etal.Shortened preproceduralfastinginthepediatricemergencydepartment. AmJEmergMed. 2018;36(9):1577–80.
12.TrestonG.Prolongedpre-proceduralfastingtimeisunnecessarywhen usingtitratedintravenousketamineforpediatricproceduralsedation. EmergMedAustralas. 2004;16(2):145–50.
13.RobackMG,BajajL,WathenJE,etal.Preproceduralfastingand adverseeventsinproceduralsedationandanalgesiainapediatric emergencydepartment:aretheyrelated? AnnEmergMed. 2004;44(5):454–9.
14.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
15.DoyleDJ,HendrixJM,GarmonEH. AmericanSocietyofAnesthesiologists Classification.TreasureIsland,FL:StatPearlsPublishing,2024.
16.BellA,TrestonG,McNabbC,etal.Profilingadverserespiratoryevents andvomitingwhenusingpropofolforemergencydepartmentprocedural sedation. EmergMedAustralas. 2007;19(5):405–10.
17.TaylorDM,BellA,HoldgateA,etal.Riskfactorsforsedation-related eventsduringproceduralsedationintheemergencydepartment. Emerg MedAustralas. 2011;23(4):466–73.
18.KiringodaR,ThurmAE,HirschtrittBA,etal.Risksofpropofolsedation/ anesthesia forimagingstudiesinpediatricresearch. ArchPediatr AdolescMed. 2010;164(6):554–60.
19.WickerhamAL,SchultzEJ,LewineEB.Nilperosordersforimaging:a teachablemoment. JAMAInternalMed. 2017;177(11):1670–1.
ChangLi,MD*
SaadiaA.Faiz,MD†
MeganBoysen-Osborn,MD,MHPE‡
AjaySheshadri,MD†
MonicaK.Wattana,MD§
SectionEditor:CaseyM.Clements,MD,PhD
*McGovernMedicalSchoolatUniversityofTexasHealth,Divisionsof Pulmonary,CriticalCareMedicineandSleepMedicine,Houston,Texas
† TheUniversityofTexasMDAndersonCancerCenter,Departmentof PulmonaryMedicine,Houston,Texas
‡ UniversityofCaliforniaIrvineSchoolofMedicine,DepartmentofEmergency Medicine,Irvine,California
§ TheUniversityofTexasMDAndersonCancerCenter,Departmentof EmergencyMedicine,Houston,Texas
Submissionhistory:SubmittedMarch4,2024;RevisionreceivedSeptember12,2024;AcceptedDecember7,2024
ElectronicallypublishedFebruary7,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20305
Immunecheckpointinhibitors(ICI),suchaspembrolizumab,nivolumab,durvalumabandipilimumab,have significantlyenhancedsurvivalratesformultiplecancertypessuchasnon-smallcelllungcancer, melanoma,Hodgkinlymphoma,andbreastcancer,andtheyhaveemergedasanadjunctorprimary therapyformalignantdisease.Approximately40%ofpatientswithcanceronICItherapyexperienceside effectscalledimmune-relatedadverseevents(irAE).Whilenotthemostcommon,pulmonarytoxicitiescan berapidlyprogressive,potentiallyfatal,andposeathree-foldincreasedriskforrequiringintensivecare unit-levelofcare.Pneumonitisisafocalordiffuseinflammationofthelungparenchyma,andclinical manifestationsmaybehighlyvariable.Whiletheonsetisgenerallyobserved6–12weeksaftertheinitiation oftherapy,drugtoxicitycandeveloprapidlywithindaysafterthe firstinfusionormanymonthsintotherapy. Pneumonitissymptomscanbesubtleornon-specific;therefore,athoroughandsystematicevaluation consideringotherpossibleetiologiesiscrucial.Moreover,extrapulmonary findings,suchasskinlesions, colitis,orendocrinopathies,shouldraisesuspicionforirAEasdrugtoxicitycanaffectmultipleorgans simultaneously.DuetothesignificantoverlapofclinicalfeaturesbetweenICI-associatedpneumonitisand respiratoryinfections,itcanbechallengingtodifferentiatethetwoconditionsbasedonclinicalpresentation alone.AmultidisciplinaryapproachtomanagementisrecommendedforthetreatmentofICI-associated pneumonitis,andclassificationofseverityhelpstoguideinterventions.Treatmentoptionsinmoresevere casesincludesystemicimmunosuppression.GiventheincreaseduseofICIsandgreaterprobabilitythat patientswithICI-associatedpneumonitiswillbeseenintheemergencydepartment,weaimedtoprovidea comprehensiveframeworkforthediagnosisandmanagement.Inaddition,identifyingpotentialchallenges indiagnosisand/orothercontributorsofrespiratorysymptomsandradiographicmanifestationsis highlighted.[WestJEmergMed.2025;26(2)210–218.]
Patientswithcancerfrequentlyrequirecareinemergency departments(ED)owingtoacutepresentationsofmalignant disease,cancer-associatedcomplications,therapy-related adverseevents,and/orothercoexistingcomorbidities. Fortunately,mortalityhasimprovedamongmanycancer types.1,2 Inparticular,immunecheckpointinhibitors(ICI) havesignificantlyimpactedsurvivalrates,usedaloneoras
supportivetherapytoconventionalcancertreatments.3 GiventheefficacyofICIs,itislikelythatemergency physicianswillseeincreasingnumbersofcancerpatientson ICIsintheyearstocome.4
Immunecheckpointinhibitors,suchaspembrolizumab, nivolumab,andipilimumab,workbyblockingcheckpoint protein-binding.Thisinhibitorysignalremovalallows T-cellstoattackcancercells.Approximately,40%ofpatients
onICIsexperiencesideeffectscalledimmune-relatedadverse events(irAEs).5 PatientswithirAEsoftenpresentwithsubtle andnon-specificsymptomsthatmaymimicotherdiagnoses; therefore,detectionofirAEscanbechallenging. Furthermore,theycaninvolve(almost)everyorgansystem. PatientsdiagnosedwithirAEsintheEDgenerallypresent withhigher-gradetoxicities,and3.5%ofpatientswithgrade 3irAEsrequirehospitalizationandcorticosteroid treatment.6 DelaysinidentificationofirAEsmayresultin worsenedprognosisandlongerhospitallengthsofstay.6,7 Whiletoxicitiesofthepulmonarysystemarenotthemost commonirAE,theyoccurinupto10%ofpatients.8 When present,pulmonarytoxicitiescanberapidlyprogress;they arepotentiallyfatalandassociatedwithasubstantially increasedriskforrequiringintensivecareunit-ICUlevel care.9,10 Thus,promptrecognitionofICI-related pneumonitisisparamount.Inthisreviewweaimedto provideareviewoftheclinicalpresentation,riskfactors, diagnosticapproach,andmanagementofpulmonaryirAEs intheED.
Pneumonitisisfocalordiffuseinflammationofthelung parenchyma,andclinicalmanifestationsmaybehighly variable.8,11 OnsetofpneumonitisfromICIsisusually6–12 weeksaftertheinitiationoftherapy,butdrugtoxicitycan developrapidlywithindaysofthe firstinfusionormany monthsintotherapy.8,11–14 ShortertimetoonsetofirAEsis seeninpatientswithlungcancercomparedtoothertypesof malignancy,perhapsduetocomorbidpulmonarydisease, particularlyunderlyinginterstitiallungdisease.15 The severityofsymptomsassociatedwithICIpneumonitiscan rangefromasymptomaticwithonlyradiographicchangesto
life-threatening,fulminantrespiratoryfailure(Figure1). Commonsymptomsmayincludeexertionaldyspnea,cough, fatigue,anddecreasedactivitytolerance;hypoxemiamay presentacutelyorinsidiously.Feverand/orchestpain,when presentwithotherrespiratorysymptoms,shouldprompta searchforotheretiologies,includingpneumonia.
Becausethesymptomsofpneumonitiscanbesubtleor non-specific,athoroughevaluationiscrucialinreachingthe correctdiagnosis.Competingdiagnoses,suchasrespiratory infections,cardiogenicpulmonaryedema,disease progressionoftheunderlyingmalignancy,andotherdrugrelatedcomplicationsmustbeconsidered.Moreover, extrapulmonary findings,suchasskinlesions,colitis,or endocrinedisorders,shouldraisethesuspicionofirAEs,as drugtoxicitycanaffectmultipleorganssimultaneously. Additionalinformationfromcomputedtomography(CT)of thechest(Figure2)andbronchoscopyisusually incorporatedtoexcludealternativediagnoses.
Separatefrompneumonitis,infusionreactionsareadverse reactionsunrelatedtothemechanismofactionofICIs. Althoughrelativelyuncommon,theyhavebeenshownin4% ofpatientstreatedwithprogrammedcelldeath1(PD-1)or programdeath-ligand1(PD-L1)antibodiesandin2–6%of patientstreatedwithipilimumab(cytotoxicT-lymphocyte antigenorCTLA-4inhibitor).16,17 Theonsetofsymptoms canoccurwithinanytimeframeduringtheinfusionorupto onehouraftertheinfusion.Symptomsincludechest tightness,wheezing,rigors,rash,pruritus,tongueswelling, dizziness,tachycardia,hypotension/hypertension,or anaphylaxis.Infusionreactionsaretypicallymildto moderateandusuallyresolvewiththecessationofinfusion andsupportivecare.However,severereactionsuchas anaphylaxiscanoccur;therefore,premedicationwith
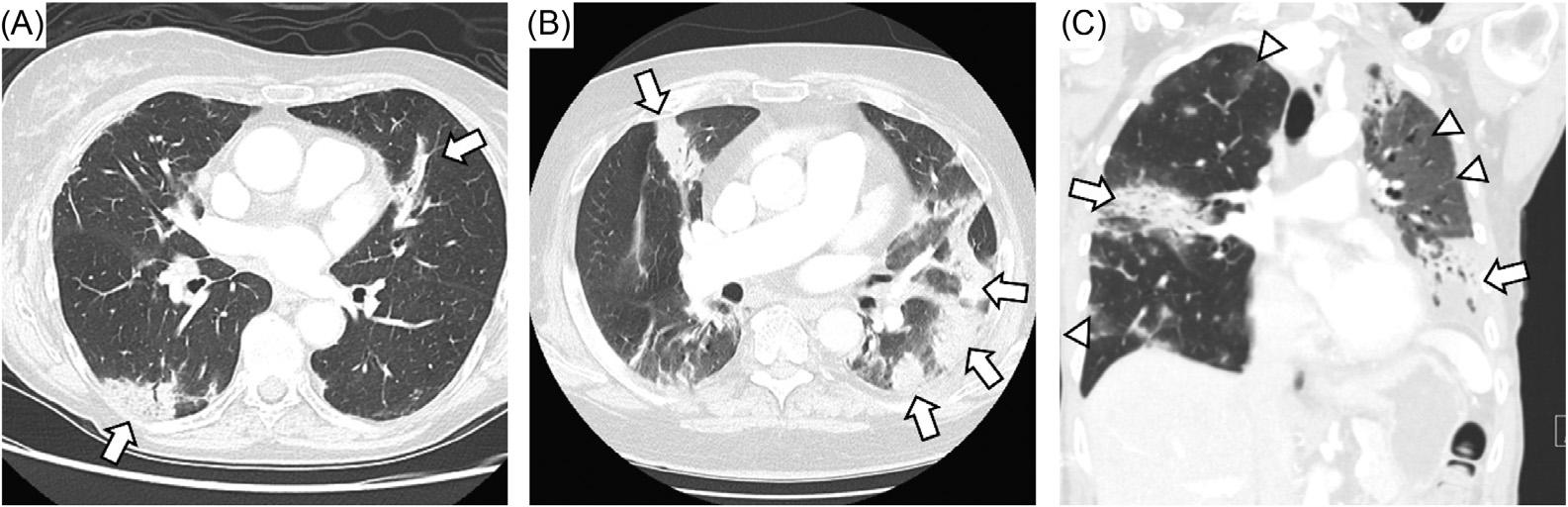
Figure1. Representativecaseofimmunecheckpointinhibitor-(ICI)associatedpneumonitis.A)Elderlywomanwithmelanomatreatedwith ICIpresentedwithpatchybilateralconsolidativeopacitieswithoutanyrespiratorysymptoms(Grade1).B)Elderlymanwithmelanoma affectingscalpunderwentsurgeryfollowedbyneoadjuvantICIpresentedwithpersistentdrycough.Computedtomographyofthechest (CTchest)revealedmultifocalconsolidativeopacities.Heunderwentbronchoscopywithbiopsyoflymphnodesandbronchoalveolarlavage withoutevidenceofmalignancyorinfection.HewasdiagnosedwithGrade2ICI-associatedpneumonitis,andheimprovedwithoralsteroids. C)Middle-agedwomanwithtriplenegativebreastcanceronICIpresentedwithcoughanddyspneawithexertionnotimprovedonoutpatient oralsteroidtherapy.Onphysicalexamshewasnotedtobetachypneicandhypoxiconroomair.CoronalCTchestrevealedconsolidative opacitiesontherightandleftalongwithground-glassinfiltratesontheleftupperlobe.ShewasadmittedandtreatedforGrade3ICIassociatedpneumonitiswithintravenousmethylprednisolone(1mg/kg)followedbyinfliximab.Sheimprovedandwasdischargedon prolongedsteroidtaper.

glucocorticoidsandantihistamineshouldbeusedwhenthe patienthashadpriorreactions.18
TheclinicalprofileofirAEsisdependentontheaffected organandtheICIagentused.Forexample,CTLA-4agents aremorelikelytocausecolitisanddermatitisthan pneumonitisorthyroiditis.19 Whilethepathophysiologyof ICI-relatedpneumonitisisnotfullyunderstood,potential riskfactorshavebeenreportedandcanbecategorizedas treatment-related,patient-related,andtumor-related factors,andthepresenceorabsenceofthemcanmodifyone’ s riskofdevelopingpneumonitisinducedbythetreatment.
Therearedifferentdegreesofpulmonarytoxicity dependingonwhetherICIsareusedasasingleagentvsin combinationwithanotherICIagent,targetedtherapy,or radiation.Ingeneral,pneumonitisoccursmorefrequentlyin patientstreatedwithPD-1inhibitors,ascomparedto patientstreatedwithPD-L1inhibitorsorwithCTLA-4 inhibitors.16,20,21 Further,PD-1andPD-L1inhibitorscause pulmonarytoxicitymoreoftenthanCTLA-4inhibitors.22
Forexample,inpatientswithadvancednon-smallcelllung cancer(NSCLC),acombinationofPD-1andCTLA-4 inhibitors(nivolumab/ipilimumab)resultedinahigher responserateandbetterprogression-freesurvivaltimethan thosereceivingchemotherapyalone.23 However, pneumonitis,particularlyhigh-gradepneumonitis,occurred moreoftenwithcombinationtherapythanICImonotherapy orchemotherapy,suggestingasynergisticeffectininducing lunginflammation.11,22,24 Furthermore,theriskof pneumonitismayincreasewhenICIsareusedin combinationwithepidermalgrowthfactorreceptor-tyrosine kinaseinhibitors(EGFR-TKI)NSCLC.Specifically, patientstreatedwithosimertinib(EGFR-TKI),followedby aPD-1oraPD-L1inhibitor,areatahighrisk ofpneumonitis.25,26
Pneumonitisafterthoracicradiationiswelldocumented, raisingtheconcernofenhancedpulmonarytoxicitywiththe combinationofICIsandradiationtherapy.27,28 Ingeneral, radiationdosescorrelatewiththeriskoflunginjury.An observationalstudyillustratedthatmorepatientsdeveloped ICI-relatedpneumonitisinthegroupthatreceivedcurative intentradiotherapythanthegroupthatreceivedpalliative intentradiotherapy.29 Otherstudieshavenotedthatmean lungdoseisasignificantriskfactorforpneumonitis,withor withoutICI.30,31 Radiation-recallpneumonitisisan inflammatoryreactionthatoccurswithinpreviously irradiated fieldsfollowingexposuretocertainchemotherapy (taxanes,anthracyclines,alkylatingagents,antimetabolites, orpyrimidineanalogs)orothermedications(tamoxifen, simvastatin,levofloxacin,orisoniazid),oftenmonthsto yearsapartfrompreviousradiationexposure.32,33 Radiation-recallpneumonitisinducedbyICIagentshasbeen reportedincasereports.34,35 Incontrasttothecommon radiographicpatternsassociatedwithICIpneumonitis, radiationrecallpneumonitisisgenerallyconfinedtoareaof priorthoracicradiation.
Chemotherapymayalsoenhanceone’sriskforICI pneumonitis.ThePACIFICstudydemonstratedstriking survivalbenefitswithdurvalumab(PD-L1inhibitor)as adjuvanttherapyafterchemoradiation.36 However,ahigher incidenceofpneumonitiswasalsofoundinthedurvalumab group(34%)comparedtotheplacebogroup(25%). Therefore,patientswithadvancedNSCLCtreatedwith concurrentchemoradiationandICIsaremuchmorelikelyto developpneumonitisthanwithconcurrentchemoradiation alone.Ingeneral,higherradiationdosesalsoincreasetherisk oflunginjury.
Pre-existinglungconditions,particularlyinterstitiallung disease(ILD),havebeenrecognizedasanindependentrisk factorforlunginjuryafterICItherapy.11,13 Patientswith ILDwerepreviouslyexcludedfromclinicaltrialsdueto
concernofpotentialexacerbationwithimmunotherapy. Therefore,theefficacyandsafetyofICIuseinpatientswith underlyinginterstitialabnormalitieshasbeenanactivearea ofinterest.Multipleretrospectivestudieshavedemonstrated thatpatientswithILDwhoreceivedICItherapyweremore likelytodevelopICIpneumonitis.PatientswithNSCLC haveahigherrateofpre-existingILDthanothersolid tumors,owingtothefactthatbothlungcancerandILDare closelyassociatedwithsmokingandotherfactorssuchas advancedage.37 PatientswithNSCLCandpre-existinglung diseasesincludingILDandchronicobstructivelungdisease (COPD),canhaveimpairedsurvivaloncepneumonitis develops.8 Theriskforpneumonitismayalsobehigherin patientswithinterstitiallungabnormalitieswithoutclinical ILD.15 ConsideringtheassociationbetweenILDandlung cancer,ICI-relatedcomplicationsareamajorconcerninthis patientpopulationgiventheshiftingparadigmfavoring ICItherapy.
Additionalpatient-relatedriskfactorstoconsiderinclude autoimmunediseasesandsmoking.Retrospectivestudies showedthatpatientswithautoimmunediseasemayhave higherratesofimmunotoxicity,including flaresoftheirpreexistingautoimmuneconditionsand/orirAEsrelatedtoICI therapy.38,39 Inamulticentercohortstudy,71%ofpatients withautoimmuneconditions,suchasrheumatoidarthritis andpsoriaticarthritis,werenotedtohave flaresorirAEs, whichweremostlymanageablewithglucocorticoids.40 WhethersmokingisdirectlyorindirectlylinkedtoICIrelatedpneumonitisisunclear,especiallywhenconsidering thecloseconnectionbetweensmoking,ILD,andlung malignancy.Inonestudy,patientswithlungcancerand
tobaccoexposuremorethan50yearshadhigherincidenceof all-gradepneumonitis.41
Certaintumortypesandhistologyareathigherriskof ICI-relatedpneumonitis.Onemeta-analysisonclinicaltrials ofICIagents(PD-1,PD-L1,andCTLA-4)from2003–2015 foundthatpneumonitiswasmorelikelytooccurinNSCLC andrenalcellcarcinomaascomparedtomelanoma.42 Anotherstudyreportedhigherratesofpneumonitisin patientswithNSCLCtreatedwithPD-1antibody.24 Additionally,squamouscellcarcinoma,asubtypeof NSCLCthatistypicallyfoundinpatientswithsmoking history,wasshowntobemoreassociatedwithpneumonitis whencomparedtoothersubtypesofNSCLC.43 However, otherstudieshavenotdemonstratedalinkbetweenNSCLC subtypeandpneumonitisrisk.8 Thisdiscrepancymaybe becausesquamouscellcancerismorecommoninpatients whosmoke,andpatientswhosmokehaveahigherrateof pneumonitisthatmaybemediatedbythepresenceof interstitiallungabnormalitiesorclinicalILD.
Evaluationofthecancerpatientwithrespiratory symptoms,feverand/orhypoxiacanbechallenging,anda broaddifferentialisneeded(Figure3).Therearemanyother conditionsthatmaybedifficulttodistinguishfromICIassociatedpneumonitisorwithwhichanirAEmaycoexist. Becausethesymptomsofpneumonitiscanbesubtleornonspecific,athoroughevaluationiscrucialinreachingthe correctdiagnosis.Competingdiagnoses,suchasrespiratory
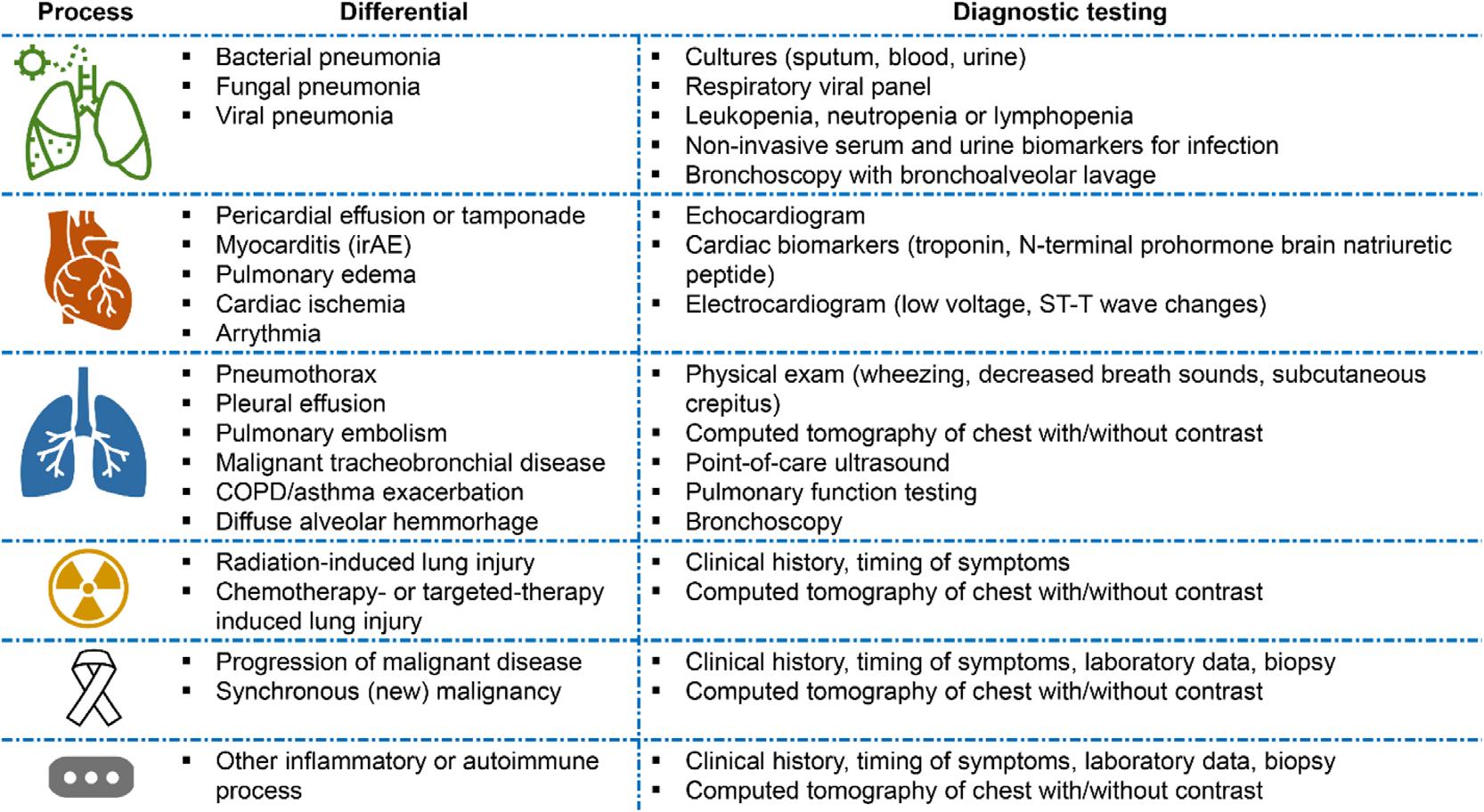
Figure3. Differentialdiagnosisforimmunecheckpointinhibitor-associatedpneumonitis. COPD,chronicobstructivepulmonarydisease; irAE,immune-relatedadverseevents.
infections,cardiogenicpulmonaryedema,disease progressionoftheunderlyingmalignancy,andotherirAE mustbeconsidered.Asmentionedpreviously, extrapulmonary findings,suchasskinlesions,colitis,or endocrinedisorders,shouldraisethesuspicionirAEasdrug toxicitycanaffectmultipleorganssimultaneously.
PneumonitisassociatedwithICIisaclinicaldiagnosis, andbothmalignantandinfectiousetiologiesshouldbe excluded.44 Physicalexam findingscanbenormalormay includerhonchiorralesonauscultation.Unfortunately, therearenopathognomonicsymptomsorradiographic findingsthatconfirmICI-associatedpneumonitis;therefore, asystematicdiagnosticapproachisneededtoexcludeother clinicalpossibilities(Figure4).45,46 Currentguidelines
recommendthoroughevaluationincludingCTchestwith (angiographyifconcernforpulmonaryembolism)or withoutcontrastandbronchoscopytoexcludealternative diagnoses.Laboratorytestsmayshowleukocytosisand/or elevatedinflammatorymarkerspotentiallysupportinga diagnosisofirAE,butthesearenon-specific.Pneumonitisis gradedbasedonradiographicand/orclinicalseverity(Table) andhelpstodirectfurthermanagement.
Duetothesignificantoverlapofclinicalfeaturesbetween ICI-associatedpneumonitisandrespiratoryinfections,itcan bechallengingtodifferentiatethetwoconditionsbasedon clinicalpresentationalone.PerAmericanSocietyofClinical Oncologyguidelines,athoroughinfectiousworkup, includingnasalswabforrespiratoryviralpathogens,sputum
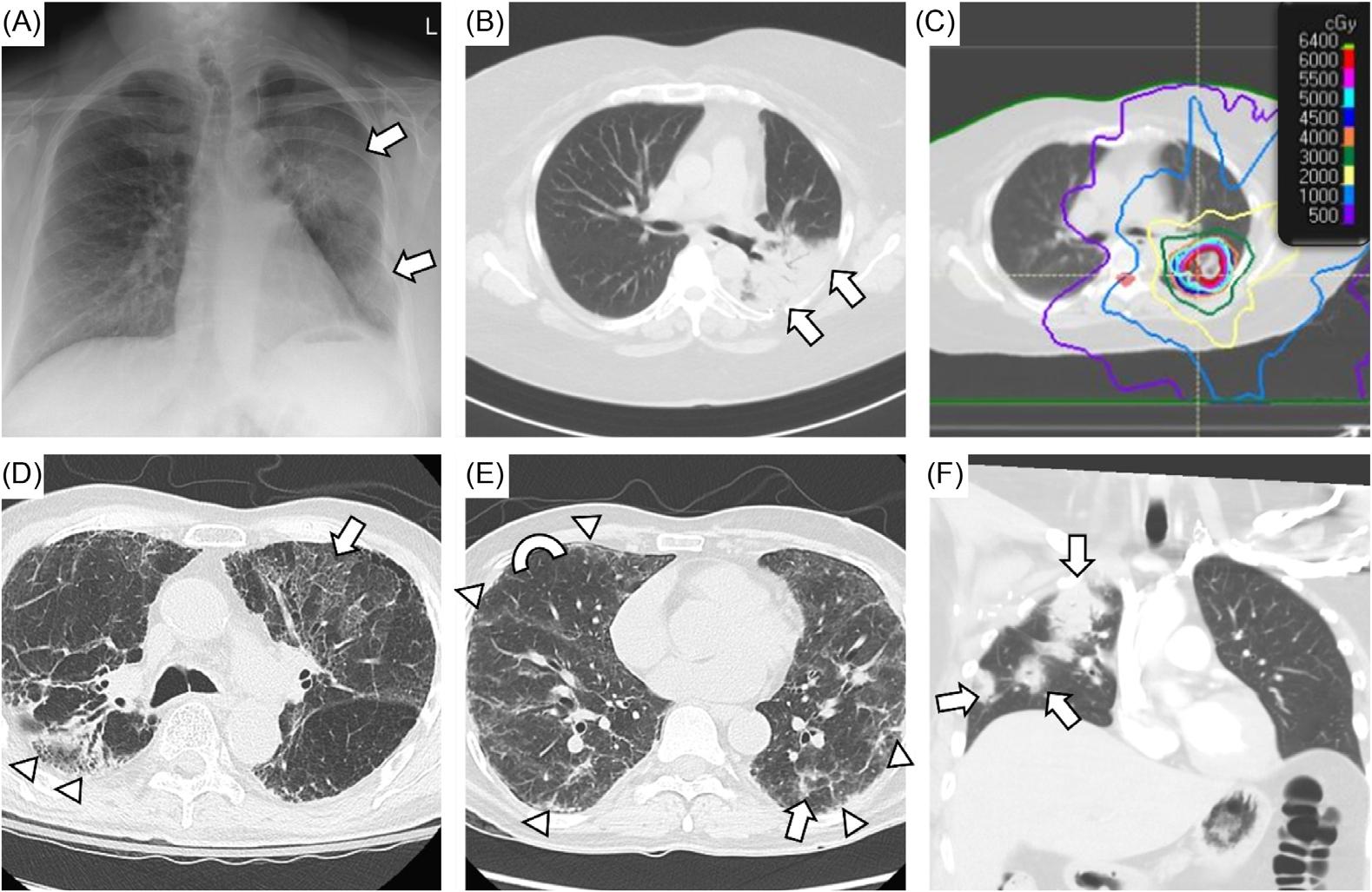
Figure4. Challengingcasesofpossibleimmunecheckpointinhibitor(ICI)pneumonitis.A-C)Middle-agedwomanwithmetastaticrenalcell carcinomatreatedwithcabozatinibandnivolumabandradiationtotheleftupperlobe.Shepresentedwithcoughanddyspneawithexertion (Grade2)sixmonthsafterradiationtherapywascompleted.Chestradiographrevealsnewinfiltratesintheleftlung(arrows),andcomputed tomographyofchest(CTchest)demonstratesdenseconsolidationintheleftupperlobewithairbronchograms(B,arrows).Herin filtrates correspondedtoradiation field(C).Shewasdiagnosedwithradiation-relatedlunginjuryandimprovedwithoralsteroid;however,ICIassociatedpneumonitiscouldhavealsocontributed.D)Elderlymanwithnon-smallcelllungcancerwhounderwentdefinitivechemoradiation therapytotherightupperlobefollowedbypembrolizumab.Hewashospitalizedafterafall,andhewasnotedtohavelowoxygensaturations. CTchestrevealedpost-treatmentchangesintherightupperlobe(arrowheads)andbilateralground-glassupperlobeinfiltrates(arrow)inthe settingofdiffuseemphysematouschanges.Hewastreatedforchronicobstructivepulmonarydisease(COPD)exacerbationwithempiric antimicrobialtherapyandoralsteroids.Hissteroidswereprolongedgivenlackofclinicalimprovement,soICI-associatedpneumonitiswas alsoaconcern.Bronchoscopywasnotfeasibleduetosignificantoxygenrequirement.E)Middle-agedmanwithpapillarythyroidcancerwho hadundergoneresectionandtreatmentwithcarboplatinandpaclitaxel.Hewassubsequentlytreatedwithpembrolizumabandpresented withcoughanddyspneawithexertion.Healsohadhistoryofvocalcorddysfunctionwithparalyzedleftvocalcordandaspirationrisk.CT chestrevealeddiffuseperipheralandsubpleuralthickening(arrowheads),ground-glassopacities(arrow),andmosaicattenuation (semicircleshowingcontrast).Heunderwentbronchoscopywithlavage,andhewastreatedempiricallyforinfectionandwithIVsteroidsfor possibledrug-relatedpneumonitis.Otherpotentialetiologiesincludedaspirationpneumonia,interstitiallungdisease,andCOPD exacerbation.F)Middle-agedwomanwithHER2-positivebreastcancertreatedwithpembrolizumabhospitalizedforfever,coughand dyspneawithexertion.CoronalCTchestrevealspatchyopacities(arrows)affectingtherightupper,middle,andlowerlobes.Bronchoscopy wasperformed,andnoobviousinfectionwasfound.ShewastreatedwithempiricantimicrobialtherapyandiIVsteroidsforpresumedICIassociatedpneumonitis.Shewasdischargedonoralsteroidstherapywith Pneumocystisjirovecii prophylaxis.
Table. Commonterminologycriteriaforadverseeventsforimmunecheckpointinhibitor-associatedpneumonitis.46
Grading Symptoms
Numberoflobes involved(onCT)
ORPercentageoflungparenchyma involved(onCT)
Grade1 – mild Asymptomatic One <25%
Grade2 – moderate Symptomatic Morethanone 25–50%
Grade3 – severe Severesymptoms Alllobes >50%
Grade4 – life-threateningLife-threateningrespiratoryfailureAlllobes >50% CT, computedtomography.
culture,bloodculture,andurineculture,isrecommendedfor grade2andabovepneumonitis.PatientsreceivingICIagents arenotnecessarilyathigherriskofinfection.Inasinglecenterstudy,patientswithlungcancertreatedwithbothICI andchemotherapyhadasimilarrateofinfection(15%)asthe controlgrouptreatedwithchemotherapyalone(22%).47 However,patientstreatedwithimmunosuppressiveagents forirAEs,suchascorticosteroidsortumornecrosisfactor (TNF)inhibitors,areathigherriskforopportunistic infectionandtuberculosisreactivation.Overall,the incidenceofinfectioninpatientswithlungcancerreceiving ICItherapyrangesbetween15–20%.47,48 Theincidenceof infectionvarieswithdifferenttumortypes.Bacterial pneumoniaisthemostcommontypeofinfectionandrisk factorsincludediabetes,COPD,andneutropenia.Prior colonizationorinfectionwith Pseudomonasaeroginosa or recentexposuretoparenteralantibioticsareindicationsto selectantimicrobialagentstargeting Pseudomonas species.49
Amultidisciplinaryapproachtomanagementis recommendedforthetreatmentofICI-associated pneumonitis,andclassificationofseverity(Table1)helpsto guideinterventions.50–52 Itisimperativetoinvolve infectious,pulmonary,and/oroncologicconsultantsearlyto determinethemostappropriatetreatment,especiallyfor complexcaseswithmultipleetiologies.Treatmentoptions generallyconsistoftemporaryICIcessationwithregular clinicalreassessment,andinmoresymptomaticcases, systemicimmunosuppressionmayberequired.53 Forgrade1 (asymptomatic)pneumonitis,ICIagentsmaybewithheld whenthereisradiographicevidenceofpneumonitis progression,butinmanycasestheICIagentcanbe continuedwithcloseclinicalandradiologicreassessmentfor developmentofrespiratorysymptoms.Ifthepatientremains asymptomatic,steroidsarenottypicallyadministered.For grade2(mildlytomoderatelysymptomatic)pneumonitis, steroids,suchasprednisoneormethylprednisolone administratedorallyorintravenously,aregivenat1–2 milligramsperkilogramperday(mg/kg/d)following infectiousworkuptoexcludeotherpotentialetiologies.If symptomsdonotimproveafter48–72hours,ahigherdoseof steroidsshouldbeconsidered.Mildgrade2casescanbe
treatedwiththelowerdoseof1mg/kgiftheresponseto treatmentisrapid.Forgrade3orhigher(severely symptomatic),prednisoneormethylprednisolonearegiven at1–2mg/kg/dwithclosemonitoring.50 Ifnoclinical improvementoccurswithin48–72hours,other immunomodulators(discussedinthe SpecialSituations sectionbelow)shouldbeconsideredtopreventfurther respiratorydecompensation.Itisrecommendedtoobtain evaluationfromconsultantsbeforeadministrationof immunosuppressants,suchassteroids,astheseagentscan havelargeimpactontheoverallclinicaloutcome.Ingeneral, casesofpneumonitisgrade3andhigherresultinpermanent ICIdiscontinuation.Dosingandtaperingcourseofsteroids forICIpneumonitisarelargelyextrapolatedfromtreatment guidelinesforhypersensitivitypneumonitisandcryptogenic organizingpneumonia.54,55 Currentguidelinesrecommenda shortcorticosteroidtaperover4–6weeks.However, retrospectivestudieshaveshownthatpneumonitismayrecur afterimprovementofsymptomsorpersistwithout improvementdespitesteroidtreatment.Shortercoursesof therapymayresultinahigherchanceofrecurrence,but optimalsteroidtaperlengthshavenotbeenstudied.
Empiricantibioticsinpatientspresentingwithrespiratory symptomswhilereceivingICItherapyisreasonablewhile furtherinvestigationisunderway.Onecaveatisthatthe humanmicrobiotaplaysanimportantroleintheresponses tocancertherapy.56 Antimicrobialuseisknowntoalterthe gut floraandhasbeenshownwithassociatednegative outcomesinpatientsreceivingICItherapy.57 Therefore,the appropriateandjudicioususeofantibioticsshouldbe consideredwhileinfectiousworkupiscarriedout.
SteroidrefractoryICI-associatedpneumonitisis characterizedbyalackofimprovement,typically,after 48hoursofcorticosteroidtreatment.Patientswhodevelop steroidrefractorypneumonitistendtohaveworseclinical outcomesduetoinfectiouscomplicationsorpneumonitis itself.WhencorticosteroidsareineffectiveintreatingICI pneumonitis,furtherimmunomodulationmayberequired. Treatmentguidelinessuggesttreatingwithagentssuchas intravenousimmunoglobulin,anti-TNFagents, mycophenolate,orcyclophosphamide.However,dataonthe
useoftheseagentsislimitedandmostlyderivedfromcase seriesorreports.58 Inthesestudies,althoughsomepatients achievedclinicalimprovementwiththeadditionof immunomodulators,theoveralloutcomewasmostly poor.59,60 Thechoiceofselectingtheseimmunomodulators intreatingsteroidrefractoryICIpneumonitisdependsonthe patient’scomorbiditiesandtheclinician’sorthecenter’ s experience.Ofnote,anegativeinterferon-gammarelease assay,suchasQuantiFERON,isoftenobtainedbefore initiatinganti-TNFagentsduetotheriskoftuberculosis reactivation.However,giventhatanti-TNFagentsare typicallygivenas1or2dosesinsteadoflong-termtherapy, theshort-termbenefitoftreatingseverepneumonitisusually greatlyoutweighsanyriskofreactivatingindolentinfections.
Ingeneral,patientswhodevelopgrade2pneumonitisand haverecovered(ie,returntograde1pneumonitis),shouldbe consideredaseligibleforreintroductionofICItherapy.Only afewstudieshaveassessedtherateofrecurrentpneumonitis afterICIreintroduction.Inacohortof107patientswho developedpneumonitis,45underwentre-challengeandof these,nine(20%)developedrecurrentpneumonitiswhile11 (24%)developedadifferentirAE.61 Inapharmacovigilance studyincluding452irAEsoccurringwithICIreintroduction inwhichrecurrencestatuswasverifiable,pneumonitis, colitis,andhepatitiswereassociatedwithanincreasedriskof recurrentirAEinadjustedanalyses.62 Whilepneumonitis grade3andhighergenerallyprecludesICIreintroduction, successfulre-challengehasbeenreported.63 Ingeneral,these casesarerare,andICIreintroductioninthisscenario requiresthatthebenefitwithICIclearlyoutweighsthehigh riskofrecurrentandpossiblyseverepneumonitis.
Insomecases,pneumonitisdoesnotresolvedespite adequatecorticosteroidtherapy.Inoneform,Naidooand associateshavesuggestedanentityofchronicpneumonitis definedasa)pneumonitisthatpersistsorworsenswith steroidtapering;andb)requiresmorethan12weeksof immunosuppressionafterICIdiscontinuation.14,64 Two percentofpatientswithNSCLCandmelanomatreatedwith anti-PD-L1agentsdevelopchronicICI-associated pneumonitis.13 Steroid-dependentpneumonitisisasub-type wherepneumonitisrecurswithoutsomeformof immunosuppression.Thereislittletoguidethetreatmentof thisformofpneumonitis,anduncertaintyexistsaboutthe optimalnon-steroidalimmunosuppression,lengthof immunosuppression,cadenceofsteroidtaper,andcancer outcomesinthisscenario.Whilethisformofpneumonitis rarelyoccurs,strategiescanincludetreatmentwithlow-dose steroidtherapyoruseofotherimmunomodulatorssuchas mycophenolatemofetilbeforeeventualattemptingtotaper.
Whileimmunecheckpointinhibitor-associated pneumonitisislesscommonthanotheradverseeffectsfrom ICIs,thepotentiallyfatalconsequencesifmissedmakes diagnosisandpromptmanagementbyemergencyphysicians crucial.Associatedriskfactorsarepatient,tumor,and/or treatmentrelated.Maintainingahighindexofsuspicionis importantwhenevaluatingpatientswithahistoryofICI treatmentpresentingwithrespiratorysymptoms.Workupin theEDinvolvesimagingandlabworktoruleoutcompeting diagnosissuchasinfectionandcardiacetiologies.Severityof ICI-pneumonitisisbasedonagradingsystemthatconsiders clinicalandradiographic findings;oncesuspected,prompt collaborationwithoncologistsandspecialistsisideal,as treatmentinvolvestheinitiationofhigh-dosesteroidsinthe EDandpossiblecessationofICItreatment.Theintegralrole oftheemergencyphysicianinthetimelydiagnosisand managementofICI-associatedpneumonitisisvitalto improvepatientoutcomes.
AddressforCorrespondence:MonicaWattana,MD,TheUniversity ofTexasMDAndersonCancerCenter,DepartmentofEmergency Medicine,Unit1462,P.O.Box301402,Houston,TX77030-1402. Email: mwattana@mdanderson.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisresearchissupportedinpartbythe NationalInstitutesofHealththroughMDAnderson’sCancerCenter SupportGrant(CA016672).Therearenootherconflictsofinterestor sourcesoffundingtodeclare.
Copyright:©2025Lietal.Thisisanopenaccessarticledistributedin accordancewiththetermsoftheCreativeCommonsAttribution(CC BY4.0)License.See: http://creativecommons.org/licenses/by/4.0/
1.SiegelRL,MillerKD,WagleNS,etal.Cancerstatistics,2023. CA CancerJClin. 2023;73(1):17–48.
2.GallawayMS,IdaikkadarN,TaiE,etal.Emergencydepartment visitsamongpeoplewithcancer:frequency,symptoms,and characteristics. JAmCollEmergPhysiciansOpen. 2021;2(3):e12438.
3.LingSP,MingLC,DhaliwalJS,etal.Roleofimmunotherapyinthe treatmentofcancer:asystematicreview. Cancers(Basel). 2022;14(21):5205.
4.RiveraDR,GallicchioL,BrownJ,etal.Trendsinadultcancer-related emergencydepartmentutilization:ananalysisofdatafromthe nationwideemergencydepartmentsample. JAMAOncol. 2017;3(10):e172450.
5.ZhengY,KimR,YuT,etal.Real-worldclinicalandeconomicoutcomes inselectedimmune-relatedadverseeventsamongpatientswithcancer
receivingimmunecheckpointinhibitors. Oncologist. 2021;26(11):e2002–12.
6.KalinichM,MurphyW,WongvibulsinS,etal.Predictionofsevere immune-relatedadverseeventsrequiringhospitaladmissioninpatients onimmunecheckpointinhibitors:studyofapopulationlevelinsurance claimsdatabasefromtheUSA. JImmunotherCancer. 2021;9(3):e001935.
7.HolsteadR,KartoloA,BaetzT.Emergencydepartmentutilizationfor patientsreceivingimmunecheckpointinhibitors:aretrospective analysisofidentificationandoutcomesforthosepresentingforimmunerelatedadverseevents. CurrOncol. 2020;28(1):52–9.
8.AltanM,SotoF,ZhongLL,etal.Incidenceandriskfactorsfor pneumonitisassociatedwithcheckpointinhibitorsinadvancednonsmallcelllungcancer:asinglecenterexperience. Oncologist. 2023;28(11):e1065–74.
9.XingP,ZhangF,WangG,etal.Incidenceratesofimmune-related adverseeventsandtheircorrelationwithresponseinadvancedsolid tumourstreatedwithNIVOorNIVO+IPI:asystematicreviewandmetaanalysis. JImmunotherCancer. 2019;7(1):341.
10.TiuBC,ZubiriL,IhekeJ,etal.Real-worldincidenceandimpactof pneumonitisinpatientswithlungcancertreatedwithimmune checkpointinhibitors:amulti-institutionalcohortstudy. JImmunother Cancer. 2022;10(6):e004670.
11.NaidooJ,WangX,WooKM,etal.Pneumonitisinpatientstreatedwith anti-programmeddeath-1/programmeddeathligand1therapy. JClin Oncol. 2017;35(7):709–17.
12.NishinoM,RamaiyaNH,AwadMM,etal.PD-1inhibitor-related pneumonitisinadvancedcancerpatients:radiographicpatternsand clinicalcourse. ClinCancerRes. 2016;22(24):6051–60.
13.ChoJY,KimJ,LeeJS,etal.Characteristics,incidence,andriskfactors ofimmunecheckpointinhibitor-relatedpneumonitisinpatientswithnonsmallcelllungcancer. LungCancer. 2018;125:150–6.
14.NaidooJ,CottrellTR,LipsonEJ,etal.Chronicimmunecheckpoint inhibitorpneumonitis. JImmunotherCancer. 2020;8(1):e000840.
15.WongA,RileyM,ZhaoS,etal.Associationbetweenpretreatmentchest imagingandimmunecheckpointinhibitorpneumonitisamong patientswithlungcancer. JNatlComprCancNetw. 2023;21(11):1164–71.e5.
16.WangY,ZhouS,YangF,etal.Treatment-relatedadverseeventsof PD-1andPD-L1inhibitorsinclinicaltrials:asystematicreviewand meta-analysis. JAMAOncol. 2019;5(7):1008–19.
17.MomtazP,ParkV,PanageasKS,etal.Safetyofinfusingipilimumab over30minutes. JClinOncol. 2015;33(30):3454–8.
18.BrahmerJR,Abu-SbeihH,AsciertoPA,etal.Societyfor ImmunotherapyofCancer(SITC)clinicalpracticeguidelineonimmune checkpointinhibitor-relatedadverseevents. JImmunotherCancer. 2021;9(6):e002435.
19.WeberJS,KahlerKC,HauschildA.Managementofimmune-related adverseeventsandkineticsofresponsewithipilimumab. JClinOncol. 2012;30(21):2691–7.
20.KhojaL,DayD,Wei-WuChenT,etal.Tumour-andclass-specific patternsofimmune-relatedadverseeventsofimmunecheckpoint inhibitors:asystematicreview. AnnOncol. 2017;28(10):2377–85.
21.KhungerM,RakshitS,PasupuletiV,etal.Incidenceofpneumonitiswith useofprogrammeddeath1andprogrammeddeath-ligand1inhibitorsin non-smallcelllungcancer:asystematicreviewandmeta-analysisof trials. Chest. 2017;152(2):271–81.
22.SuQ,ZhuEC,WuJB,etal.Riskofpneumonitisandpneumonia associatedwithimmunecheckpointinhibitorsforsolidtumors:a systematicreviewandmeta-analysis. FrontImmunol. 2019;10:108.
23.HellmannMD,CiuleanuTE,PluzanskiA,etal.Nivolumabplus ipilimumabinlungcancerwithahightumormutationalburden. NEnglJ Med. 2018;378(22):2093–104.
24.NishinoM,Giobbie-HurderA,HatabuH,etal.Incidenceofprogrammed celldeath1inhibitor-relatedpneumonitisinpatientswithadvanced cancer:asystematicreviewandmeta-analysis. JAMAOncol. 2016;2(12):1607–16.
25.OshimaY,TanimotoT,YujiK,etal.EGFR-TKI-associatedinterstitial pneumonitisinnivolumab-treatedpatientswithnon-smallcelllung cancer. JAMAOncol. 2018;4(8):1112–5.
26.SchoenfeldAJ,ArbourKC,RizviH,etal.Severeimmune-related adverseeventsarecommonwithsequentialPD-(L)1blockadeand osimertinib. AnnOncol. 2019;30(5):839–44.
27.Arroyo-HernandezM,MaldonadoF,Lozano-RuizF,etal.Radiationinducedlunginjury:currentevidence. BMCPulmMed. 2021;21(1):9.
28.BradleyJandMovsasB.Radiationpneumonitisandesophagitisin thoracicirradiation. CancerTreatRes. 2006;128:43–64.
29.VoongKR,HazellSZ,FuW,etal.Relationshipbetweenprior radiotherapyandcheckpoint-inhibitorpneumonitisinpatientswith advancednon-small-celllungcancer. ClinLungCancer. 2019;20(4):e470–9.
30.KwaSL,LebesqueJV,TheuwsJC,etal.Radiationpneumonitisasa functionofmeanlungdose:ananalysisofpooleddataof540patients. IntJRadiatOncolBiolPhys. 1998;42(1):1–9.
31.PalmaDA,SenanS,TsujinoK,etal.Predictingradiationpneumonitis afterchemoradiationtherapyforlungcancer:aninternationalindividual patientdatameta-analysis. IntJRadiatOncolBiolPhys. 2013;85(2):444–50.
32.HananiaAN,MainwaringW,GhebreYT,etal.Radiation-inducedlung injury:assessmentandmanagement. Chest. 2019;156(1):150–62.
33.FaizSA,BalachandranDD,BashouraL,etal.Pulmonaryradiation recallinducedbygemcitabine. AmJRespirCritCareMed. 2016;194(7):909–10.
34.TengF,LiM,YuJ.RadiationrecallpneumonitisinducedbyPD-1/PD-L1 blockades:mechanismsandtherapeuticimplications. BMCMed. 2020;18(1):275.
35.SchoenfeldJD,NishinoM,SevergniniM,etal.Pneumonitisresulting fromradiationandimmunecheckpointblockadeillustrates characteristicclinical,radiologicandcirculatingbiomarkerfeatures. JImmunotherCancer. 2019;7(1):112.
36.AntoniaSJ,VillegasA,DanielD,etal.Durvalumabafter chemoradiotherapyinstageIIInon-small-celllungcancer. NEnglJ Med. 2017;377(20):1919–29.
37.YamaguchiT,ShimizuJ,OyaY,etal.Riskfactorsforpneumonitisin patientswithnon-smallcelllungcancertreatedwithimmunecheckpoint inhibitorspluschemotherapy:aretrospectiveanalysis. ThoracCancer. 2022;13(5):724–31.
38.LeonardiGC,GainorJF,AltanM,etal.Safetyofprogrammeddeath-1 pathwayinhibitorsamongpatientswithnon-small-celllungcancerand preexistingautoimmunedisorders. JClinOncol. 2018;36(19):1905–12.
39.JohnsonDB,SullivanRJ,OttPA,etal.Ipilimumabtherapyinpatients withadvancedmelanomaandpreexistingautoimmunedisorders. JAMA Oncol. 2016;2(2):234–40.
40.TisonA,QuereG,MiseryL,etal.Safetyandefficacyofimmune checkpointinhibitorsinpatientswithcancerandpreexisting autoimmunedisease:anationwide,multicentercohortstudy. Arthritis Rheumatol. 2019;71(12):2100–11.
41.OkadaN,MatsuokaR,SakuradaT,etal.Riskfactorsofimmune checkpointinhibitor-relatedinterstitiallungdiseaseinpatientswith lungcancer:asingle-institutionretrospectivestudy. SciRep. 2020;10(1):13773.
42.WuJ,HongD,ZhangX,etal.PD-1inhibitorsincreasetheincidenceand riskofpneumonitisincancerpatientsinadose-independentmanner:a meta-analysis. SciRep. 2017;7:44173.
43.SureshK,VoongKR,ShankarB,etal.Pneumonitisinnon-smallcell lungcancerpatientsreceivingimmunecheckpointimmunotherapy: incidenceandriskfactors. JThoracOncol. 2018;13(12):1930–9.
44.O’KaneGM,LabbeC,DohertyMK,etal.Monitoringandmanagementof immune-relatedadverseeventsassociatedwithprogrammedcelldeath protein-1axisinhibitorsinlungcancer. Oncologist. 2017;22(1):70–80.
45.AtchleyWT,AlvarezC,Saxena-BeemS,etal.Immunecheckpoint inhibitor-relatedpneumonitisinlungcancer:real-worldincidence,risk factors,andmanagementpracticesacrosssixhealthcarecentersin NorthCarolina. Chest. 2021;160(2):731–42.
46.SchneiderBJ,NaidooJ,SantomassoBD,etal.Managementof immune-relatedadverseeventsinpatientstreatedwithimmune checkpointinhibitortherapy:ASCOguidelineupdate. JClinOncol. 2021;39(36):4073–126.
47.MalekAE,KhalilM,HachemR,etal.Impactofcheckpointinhibitor immunotherapy,primarilypembrolizumab,oninfectionriskinpatients withadvancedlungcancer:acomparativeretrospectivecohortstudy. ClinInfectDis. 2021;73(9):e2697–704.
48.FujitaK,KimYH,KanaiO,etal.Emergingconcernsofinfectious diseasesinlungcancerpatientsreceivingimmunecheckpointinhibitor therapy. RespirMed. 2019;146:66–70.
49.KalilAC,MeterskyML,KlompasM,etal.Managementofadultswith hospital-acquiredandventilator-associatedpneumonia:2016clinical practiceguidelinesbytheInfectiousDiseasesSocietyofAmericaand theAmericanThoracicSociety. ClinInfectDis. 2016;63(5):e61–111.
50.BrahmerJR,LacchettiC,SchneiderBJ,etal.Managementofimmunerelatedadverseeventsinpatientstreatedwithimmunecheckpoint
inhibitortherapy:AmericanSocietyofClinicalOncologyclinicalpractice guideline. JClinOncol. 2018;36(17):1714–68.
51. PuzanovI,DiabA,AbdallahK,etal.Managingtoxicitiesassociatedwith immunecheckpointinhibitors:consensusrecommendationsfromthe SocietyforImmunotherapyofCancer(SITC)toxicitymanagement workinggroup. JImmunotherCancer. 2017;5(1):95.
52.HaanenJ,CarbonnelF,RobertC,etal.Managementoftoxicities fromimmunotherapy:ESMOclinicalpracticeguidelinesfor diagnosis,treatmentandfollow-up. AnnOncol. 2017;28(suppl_4):iv119–42.
53.SearsCR,PeikertT,PossickJD,etal.Knowledgegapsandresearch prioritiesinimmunecheckpointinhibitor-relatedpneumonitis.anofficial AmericanThoracicSocietyresearchstatement. AmJRespirCritCare Med. 2019;200(6):e31–43.
54.HamblinM,ProschH,VasakovaM.Diagnosis,courseand managementofhypersensitivitypneumonitis. EurRespirRev. 2022;31(163):210169.
55.KingTEandLeeJS.Cryptogenicorganizingpneumonia. NEnglJMed. 2022;386(11):1058–69.
56.GopalakrishnanV,HelminkBA,SpencerCN,etal.Theinfluenceofthe gutmicrobiomeoncancer,immunity,andcancerimmunotherapy. CancerCell. 2018;33(4):570–80.
57.RoutyB,LeChatelierE,DerosaL,etal.Gutmicrobiomeinfluences efficacyofPD-1-basedimmunotherapyagainstepithelialtumors. Science. 2018;359(6371):91–7.
58.LaiKA,SheshadriA,AdrianzaAM,etal.Roleofinfliximabinimmune checkpointinhibitor-inducedpneumonitis. JImmunotherPrecisOncol. 2020;3(4):172–4.
59.PetriCR,PatellR,BataliniF,etal.Severepulmonarytoxicityfrom immunecheckpointinhibitortreatedsuccessfullywithintravenous immunoglobulin:casereportandreviewoftheliterature. RespirMed CaseRep. 2019;27:100834.
60.BeattieJ,RizviH,FuentesP,etal.Successandfailureofadditional immunemodulatorsinsteroid-refractory/resistantpneumonitisrelated toimmunecheckpointblockade. JImmunotherCancer. 2021;9(2):e001884.
61.LinX,DengH,ChuT,etal.Safetyandefficacyofimmunotherapy rechallengefollowingcheckpointinhibitor-relatedpneumonitisin advancedlungcancerpatients:aretrospectivemulti-centercohort study. TranslLungCancerRes. 2022;11(11):2289–305.
62.DolladilleC,EderhyS,SassierM,etal.Immunecheckpointinhibitor rechallengeafterimmune-relatedadverseeventsinpatientswith cancer. JAMAOncol. 2020;6(6):865–71.
63.HaanenJ,ErnstoffM,WangY,etal.Rechallengepatientswithimmune checkpointinhibitorsfollowingsevereimmune-relatedadverseevents: reviewoftheliteratureandsuggestedprophylacticstrategy. JImmunotherCancer. 2020;8(1):e000604.
64.BalajiA,HsuM,LinCT,etal.Steroid-refractoryPD-(L)1pneumonitis: incidence,clinicalfeatures,treatment,andoutcomes. JImmunother Cancer. 2021;9(1):e001731.
AnthonyJ.Weekes,MD,MSc*
AngelaM.Pikus,MD*
ParkerL.Hambright,MD*
KellyL.Goonan,MPH*
NathanielO’Connell,PhD†
SectionEditor:QuincyK.Tran,MD,PhD
*AtriumHealth’sCarolinasMedicalCenter,DepartmentofEmergencyMedicine, Charlotte,NorthCarolina
† WakeForestSchoolofMedicine,DepartmentofBiostatisticsandDataScience, Winston-Salem,NorthCarolina
Submissionhistory:SubmittedApril4,2024;RevisionreceivedOctober31,2024;AcceptedNovember1,2024
ElectronicallypublishedJanuary15,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20763
Introduction: Mostpulmonaryembolismresponseteams(PERT)usearadiologist-determinedright ventricletoleftventricleratio(RV:LV)cut-offof1.0torisk-stratifypulmonaryembolism(PE)patients. Continuousmeasurementsfromcomputedtomographypulmonaryangiograms(CTPAs)mayimprove riskstratification.WeassessedassociationsofCTPAcardiacmeasurementswithacuteclinical deteriorationanduseofadvancedPEinterventions.
Methods: ThiswasaretrospectivestudyofaPEregistryusedbyeightaffiliatedemergency departments.Weusedanartificialintelligence(AI)algorithmtomeasureRV:LVonanonymizedCTPAs fromregistrypatientsforwhomthePERTwasactivated(2018–2023)byinstitutionalguidelines.Primary outcomewasin-hospitalPE-relatedclinicaldeteriorationdefinedascardiacarrest,vasoactive medicationuseforhypotension,orrescuerespiratoryinterventions.Secondaryoutcomewasadvanced interventionuse.Weusedbivariableandmultivariableanalyses.Forthelatter,weusedleastabsolute shrinkageandselectionoperator(LASSO)andrandomforest(RF)todetermineassociationsofall candidatevariableswiththeprimaryoutcome(clinicaldeterioration),andtheYoudenindextodetermine RV:LVoptimalcut-offsforprimaryoutcome.
Results: Artificialintelligenceanalyzed1,467CTPAs,with88%agreementonRV:LVcategorization withradiologistreports(kappa0.36,95%confidenceinterval[CI]0.28–0.43).Of1,639patients,190 (11.6%)hadPE-relatedclinicaldeterioration,and314(19.2%)hadadvancedinterventions.MeanRV:LV were1.50(0.39)vs1.30(0.32)forthosewithandwithoutclinicaldeteriorationand1.62(0.33)vs1.35 (0.32)forthosewithandwithoutadvancedinterventionuse.TheRV:LVcut-offof1.0byAIand radiologistshad0.02and0.53 P-valuesforclinicaldeterioration,respectively.WithadjustedLASSO,top clinicaldeteriorationpredictorswerecardiacarrestatpresentation,lowestsystolicbloodpressure,and intensivecareunitadmission.TheRV:LVmeasurementwasatop10predictorofclinicaldeteriorationby RF.Optimalcut-offforRV:LVwas1.54withoddsratioof2.50(1.85,3.45)andareaunderthecurve 0.6(0.66,0.70).
Conclusion: Artificalintelligence-derivedRV:LVmeasurements ≥1.5oninitialCTPAhadstrong associationswithin-hospitalclinicaldeteriorationandadvancedinterventionsinalargePERTdatabase. ThisstudypointstothepotentialofcapitalizingonimmediatelyavailableCTPARV:LVmeasurementsfor gaugingPEseverityandriskstratification.[WestJEmergMed.2025;26(2)219–232.]
Establishedpulmonaryembolism(PE)risk-stratification guidelinesemploybinaryassessmentsofhemodynamic stabilityandrightventriculardysfunction(RVD)using imagingmodalitiesandtroponin.1 Themainimaging modalitiesofRVDareechocardiographyandcomputed tomographypulmonaryangiogram(CTPA).
Comprehensiveechocardiographyprovidesmultifaceted RVDassessments;however,itrarelyconfirmsdiagnosisof PEandmaynotbeimmediatelyavailable.ACTPA diagnosesPEandidentifieslimitedparametersofRVD, usuallyasrightventricle(RV)dilatation.Radiologists usuallyreportonRVDasabinaryvariableofRVtoleft ventriclediameterratio(RV:LV)usingarangeofcut-offs from0.9to1.5.2–7 RightventriculardysfunctiononCTPA, whenexpressedasacontinuousvariable,maybeabetter predictorthanitsbinaryversion.
ConsistentreportingofRVDmeasurementsmaybelabor intensiveforradiologists.Artificialintelligence(AI) algorithmshavebeendevelopedtoassistradiologists’ workflowbysimultaneouslyinterpretingpresenceof filling defectsandmeasuringcardiacchambersizes.8,9 WhileRVD byCTPAorechocardiographyisanindependentpredictor ofacuteclinicaldeterioration,10 therehavebeeninconsistent resultsregardingitsrelationshipwith30-day mortality.4,6,11–13 Echocardiographystudieshaveshownthat asRVDseverityincreases,bothriskofclinicaldeterioration anduseofadvancedinterventionsincrease.14
WeaimedtocharacterizetheassociationofAI-derived CTPAcardiacmeasurementswithin-hospitalclinical deterioration(primaryoutcome)inaregistryofpatientswith intermediate-tohigh-riskPE.Thesecondaryobjectivewas tocompareretrospectivelyderivedAImeasurementsin patientswithorwithoutuseofadvancedinterventions (secondaryoutcome).Forourexploratoryobjectives,we compared1)radiologistvsAI-derivedCTPAcategorization ofRV:LVand2)AIvsechocardiographymeasurements.If, byretrospectivestudy,weweretoshowthatAI-derived CTPAmeasurementsarestronglyassociatedwithacute clinicaldeterioration,thencapturingimmediatelyavailable CTPAcardiacmeasurementswithinclinicalworkflowcould improvePEriskstratification.15
StudySettingandDesign
Weconductedaretrospectiveanalysisofdatainour ClinicalOutcomesPulmonaryEmbolismResearchRegistry (COPERR).TheCOPERRispopulatedwithadultpatients identifiedasintermediate-orhigh-riskPEatpresentationto anyofeightAtriumHealthemergencydepartments(ED)in NorthCarolina.Weextracteddataforregistrypatientswho weretreatedbetweenJune6,2018–August31,2023.In November2023,werequestedaretrospective,remoteAI
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Pulmonaryembolism(PE)responseteams focusonpatientswithrightventricular dysfunctionusingCT fi ndingsofright ventricletoleftventricle(RV:LV)ratioof 1.0orgreater.
Whatwastheresearchquestion?
WhatCTRV:LVmeasurementsare associatedwithacuteclinicaldeterioration?
Whatwasthemajor findingofthestudy?
Theoptimalcut-offforRV:LVonCTwas 1.54withanoddsratioof2.50(1.85 – 3.45) foracuteclinicaldeterioration.
Howdoesthisimprovepopulationhealth?
ARV:LVthresholdof1.5onCTmayimprove PEriskstrati fi cationandinformuseof inpatientresources.
analysisofCTPAswithconfirmedindexPEfromthis populationofregistrypatients.
UsingtheCOPERRdatabase,weidentifiedadultpatients (≥18years)presentingtoaparticipatingEDwhohad1) acutesymptomaticPEastheprimaryEDdiagnosis(by positiveCTPA)and2)intermediate-orhigh-riskPE classification.ThePEriskwasclassifiedbyemergency cliniciansusingEuropeanSocietyofCardiology(ESC) guidelines1 andourPEresponseteam’s(PERT) “CodePE” pathway(SupplementalFigure1).Thelattershowsthe structure,function,andlogisticsofPERTactivation, triaging,multispecialtynotification,andconsiderationsfor advancedPEinterventionsbasedonPEseverityand bleedingrisk.Fortheexploratoryobjective,weincluded above-mentionedpatientswithcomprehensivetransthoracic echocardiography(TTE)andRV-focusedmeasurements completedwithin24hoursofPEdiagnosis.
Weincludedpatientswithintermediate-orhigh-riskPEat EDpresentationwithCTimagesof1-mmslicethickness availableforAIanalysisfortheprimaryobjectiveandwith anyAIanalysisforthesecondaryobjective.Weexcludedthe following:patientswithPEdiagnosedonlybyhighprobabilityventilation/perfusionnuclearimaging;those whosepoint-of-careTTE findingswerehighlysuspiciousof PEbutPEwasnotconfirmedbyCT;andthosewhoseCTPA
wasnotforindexPE.WealsoexcludedCTPAsthatcould notbeanalyzedbyAIalgorithm.
DataenteredinCOPERRandavailableforanalysis includeddemographics;clinicalpresentationfeatures (includinginitialandworstvitalsignswithinthreehoursof EDpresentation);comorbidities;PEriskfactors;criteria usedforPEriskstratification;radiologistreportofRV:LV; TTEmeasurements,dates,andtimes;PERTnotification datesandtimes;laboratorymeasurements;PE-related outcomesandinterventions;andadverseevents.14,16,17 Traineddataextractorsretrievedinformationfromthe electronichealthrecordandentereddataintheregistry.
Duringreal-timeclinicalcareofindexPEhospitalization, RV:LVwasmeasuredbyboard-certifiedradiologists,and TTEwasperformedbycertifiedcardiacsonographersfrom anechocardiographylaboratoryaccreditedbythe IntersocietalCommissionfortheAccreditationof EchocardiographyLaboratories.Giventhiswasa retrospectivestudy,theradiologistsandsonographerswere notawareofthestudyoritsobjectives.Radiologists measuredRV:LVontheminorcardiacaxisonCTPA. Measurementswereatthewidestpointsbetweentheinner freewallofeachventricletotheinnerwalloftheventricular septum.RadiologistsusedRV:LVcut-offof1.0,withless than1.0considerednegativeforRVdilatation.
SonographersusedstandardorRV-focusedapicalviews tomeasureend-diastolicRVinnerdiameteratthebase.The LVbasalend-diastolicmeasurementswereperformedinthe parasternallongaxisview.Imageswereuploadedintoa securelocalserverandportalsystemMergeCardio (MerativeLP,AnnArbor,MI[formerlyIBMWatson Health]).Board-certifiedcardiologistsinterpretedimages andmeasurementsandwereblindtostudyandclinical outcomes.Onlyinitialechocardiographymeasurementsfor indexPEhospitalizationwereusedinthisstudy.
Foreachregistrypatientincludedinthestudy,we exportedthefullyanonymizeddigitalimagingand communicationsinmedicine(DICOM) fileforeachCTPA tosharewiththeAIvendorforanalysis.Wetransferred DICOMdatafromourstudycentertotheserverofanAI operatingsystem(Aidoc,TelAviv,Israel)usingencrypted secure filetransferprotocol.Priortotransfer,alldatawere de-identifiedperthesafeharborde-identificationprotocol definedbytheHealthInsurancePortabilityand AccountabilityAct.The de-identi fi edaccessionnumber was extractedfromtheDICOMheaderofsharedstudies.The studycenterusedthekeypairof de-identi fi edaccessions and identi fi edaccessions computedatthedataanonymization steptore-identifydataforthestudy.
TheAidocPEalgorithmisFDAclearedviathe510(k) premarketnotificationpathwayrequiredofallAIsoftware medicaldevices.Aidoc’suseindetectingPEonCTPAshas
beenpreviouslyreported.8,18 TheprototypeofthePE detectionalgorithmwasdevelopedusinginputfrom anonymized,1-mmseriesofCTPAreconstructionsand basedonadeepconvolutionalneuralnetworkcomprisinga Resnetarchitectureandtrainedandvalidatedonover25,000 CTPAstakenfrommanyinstitutions.Aidocalgorithmshad specificCTPAinclusioncriteria,includingslicethickness, kernel,andcontrastphasetoallowanalysis.Aidochastwo softwarecomponents:oneforsoftwareanalysisofCTPA DICOM files,andanotherforreal-timeanalysisand reportingofinterpretationstocliniciansandradiologists. Onlythe firstcomponentwasusedinthisstudy.TheAI analysesofCTPAsandmeasurementswerenotperformed duringreal-timeclinicalcare.
EachCTPAwasanalyzedbytwoAIalgorithms independently.Forthe firstalgorithm,ifaPEwasdetected, AIdeterminedwhetherthePEwasacentralclotornot. Centralclotwasdefinedbythefollowinglocations: pulmonarytrunk;saddle(bifurcationofthemainpulmonary arterytrunk);rightorleftmainpulmonaryarteriesorlobar pulmonaryarteries.Forthesecondalgorithm,AImeasured eachRVandLVlargestdiameter(betweeninnerwalls)asa numberandcalculatedtheratioofRVtoLV.Thiswas producedinafour-stepprocess,includingventricular detection,ventricularsegmentation,interventricularseptum detection,andcaliperpositioningandmeasurements.TheAI algorithmalsoidentifiedpatientswithlargecentralPEs.Itis importanttonoteasubsegmentalPEdidnotprovidea positiveresult.ThiswasdonetoallowtheAI-augmented clinicalworkflowtoaccuratelyidentifyacutePEswithRV dilatationasnecessaryconditionsforintermediate-andhighriskPEclassification.
TheAI-basedalgorithmvariablesincludedthefollowing categoricalvalues:1)DidtheAidocalgorithmanalyzethe data(yesorno);and2)didtheCTPAcontainaPE(yesor no)?TheAI-basedcontinuousvariableswereRVbasal diameter,LVbasaldiameter,andRV:LV.Alldatafor AI-derivedCTPAvariableswerematchedtopertinentstudy IDsanduploadedintoastandardelectronicformwithin ResearchElectronicDataCapture(REDCap)toolsat ourinstitution.
TheprimaryoutcomewasPE-relatedclinical deterioration,definedasacompositeofoneormoreofthe followingclinicaldeteriorationeventswithindaysofindex PEhospitalization:death;cardiacarrest;sustained hypotensiontreatedwithvasoactivemedications;orrescue respiratoryintervention(mechanicalorpositivepressure ventilation).14 Thesecondaryoutcomewasuseofadvanced PE-specificinterventions,includingsystemicthrombolysis, catheter-directedinterventions,extracorporealmembrane oxygenation(ECMO),orsurgicalembolectomy.
Samplesizewasdeterminedbythenumberofpatients eligibleforstudyanalysis.TodetermineassociationwithPErelatedclinicaldeterioration(primaryoutcome),weused variousstatisticalmethods.Weusedbivariableanalysiswith theStudent t -testorchisquaretostratifybyprimary outcomegroups.Weconductedmultivariableanalysesfor theprimaryoutcomeintwoways.First,weusedleast absoluteshrinkageandselectionoperator(LASSO) regressiontodeveloptwomodels,onewithAIassessment variablesonlyandonewithallindependentvariables.We reportedmissingnessofeachvariableandusedcompletecase analysis.Weexpressedstrengthofassociationasoddsratios with95%confidenceintervals(CI).Second,weusedrandom forest(RF)tostatisticallyinferthestrengthoftheassociation ofallindependentvariablesinthedatasetandidentifythetop 20predictorsofPE-relatedclinicaldeterioration(primary outcome)inavariableimportanceplot.
Foreachmodel’sprognosticperformanceontheprimary outcome,wereporteddiscriminationasareaunderthecurve (AUC)andcalibrationascalibrationplotswithcalibration statistics,includingBrier,Brierscaled,interceptandslope. PerformanceforRFandLASSOlogisticmodelswasbased onout-of-bagsamplesand10-foldcrossvalidation, respectively.Finally,toaddressthetrade-offoffalse positivesandfalsenegatives,weusedtheYoudenindexto determineoptimalRV:LVcut-offsandotherAI-derived measurementsforprognosisofclinicaldeterioration.Forthe selectedoptimalRV:LVandotherAIcardiacmeasurements, wedeterminedsensitivity,specificity,likelihoodratios,and AUCwith95%CI.
Todetermineassociationwiththeuseofadvanced interventions(secondaryoutcome),weusedbivariable analysiswiththeStudent t -testorchisquaretostratifyby secondaryoutcomegroups.Tomeasurereliabilitybetween AI-derivedandradiologistCTclassificationofRV:LV ≥ 1.0 vs < 1.0,weusedtheCohenkappawithits95%CIs.Weused suggestedguidelinesofLandisandKochtodescribethe strengthofagreementforthe κ statistic:lessthan0 = poor;0to 0.20 = slight;0.021to0.40 = fair;0.41to0.60 = moderate; 0.61to0.80 = substantial;and0.81to1.00 = almostperfect.19
Wereportedmeanandstandarddeviationtimeintervals inhoursbetweenPERTnotificationandTTEforthemiddle 95%.WeusedtwomethodstoassessagreementbetweenAIderivedCTcardiacandTTEmeasurementsforRV,LV,and RV:LV.First,weusedPearsoncorrelationswith95%CIsfor continuousvariablestotestformagnitudeanddirectionof linearrelationships.20 Second,weusedBland-Altmanplots todepicttherelationshipofdifferenceandmeanforeachpair ofCTPAandTTEmeasurements.
Disclosures
Regardingtherelationshipwiththecompanythat developedandmarketstheAI-basedPEalgorithmusedin
thisstudy,wedeclarethatAidochadnoroleinthedesignof thestudy,thecollection,analysis,andinterpretationofdata, orthepreparationofthepublishedmanuscript.Wefurther declarethatwehavenotreceivedandwillnotreceiveany compensation,directorindirect,fromAidocoranyofits affiliates.Wedonotownstockinthecompany.
Figure1 showswescreened1,809patientswithCTPAconfirmedacutePEdiagnosedinED.Ofthese,1,664(92.0%) hadCTPAassociatedwithindexPEdiagnosisand anonymizedDICOM filestransferredforAIanalysis. RadiologistsprovidedcategoricalRV:LVclassificationfor 1,467of1,664(88.2%)CTPAs.TheAIvendoranalyzed 1,660ofthe1,664;fourcaseswereexcludedbecauseof inadequateCTPAslicethicknessforAIanalysis.TheAI assessmentforcentralclotwassuccessfulinall(100%) CTPAsand1,267(76.3%)werefoundtohavelargecentral PEbythealgorithm.TheAI-derivedcardiacmeasurements wereobtainedfor1,617/1,660(97.4%).TheAIfailedto analyze43CTPAsbecause1)theydidnotmeetstudy inclusioncriteria(i.e.,slicethickness,kernel,contrastphase), or2)theRV:LValgorithmwasunabletodetectappropriate landmarkstoperformRV:LVanalysis.Of1,664CTPAs,733 (44.1%)hadcomprehensiveTTEmeasurementsduringindex PEhospitalization.MeanandSDfortimeintervalbetween CTPAandTTEforthemiddle95%was13.6(11.3)hours. Wewereabletodetermineprimaryoutcomeresponsesfor 1,639uniquepatients (Table1) andsecondaryoutcomefor 1,643uniquepatients.Ofthe1,639,meanagewas63.0 ± 16years,805(49.1%)weremale,997(60.8%)wereWhite, and190(11.6%)hadoneormorecomponentsoftheprimary outcome.FourpatientshadmorethanoneEDvisitforacute PEduringthe2018–2023studyperiod.WereportedPErelatedclinicaldeterioration(primaryoutcome)for first visitonly.
Therewerenosignificantdifferencesbetweenthosewith orwithoutclinicaldeteriorationforage,gender,race,or ethnicity.Thereweresignificantdifferencesformeanvalues ofvitalsigns.PatientswhohadPE-relatedclinical deterioration(primaryoutcome)hadlowersystolicblood pressureandoxygensaturationreadingsandhigher respiratoryrateandheartratesthanpatientswithoutclinical deterioration.Therewassignificantlyincreaseduseof systemicthrombolysis,ECMO,andsurgicalembolectomyin theprimaryoutcomegroup.However,therewereno significantdifferencesinuseofcatheter-directed interventionsbetweenoutcomegroups.Forcategorical cardiacCTPAassessments, Table1 showsradiologists’ binarycategorizationofRVDusingtheRV:LVcut-off1.0 wasnotsignificantbetweenprimaryoutcomegroups.In
Not CT from index PE (N = 145 )
CT with confirmed PE from registry patients between June 2018 to August 2023, N = 1,809
Missing RV/LV ratio N = 176
Radiologist assessment of RV/LV ratio, N = 1,467 RV/LV ratio ≥ 1.0? YES (N = 1,287) NO (N = 180)
AI measurement of LV, RV and RV/LV ratio, N = 1,617 Anonymized CT from Index PE, N = 1,664
Did not meet series level criteria N = 4
Each analyses by 2 AI algorithms independently for RV/LV ratio and central clot N = 1,660
AI qualitative assessment: Presence of central clot? N = 1,660
Advanced intervention analysis, N = 1,643
Clinical information available for outcome analyses, N = 1,643
AI failed on, N = 43
Yes, n= 314 No, n= 1,329
More than one PE hospitalization, n= 4
Unique individual patient for clinical deterioration analysis, N = 1,639
(N = 1,472 ) NO (N = 145)
YES (N= 1,267) NO (N = 393 )
Acute Central PE is defined by the the following locations:
• Pulmonary trunk
• Saddle (bifurcation of the main pulmonary artery trunk)
• Right or left main pulmonary arteries
• Lobar pulmonary arteries
Figure1. Study flowdiagram*. AI,arti ficalintelligence; PE,pulmonaryembolism; CTPA,computedtomographypulmonaryangiography, RV,rightventricle; LV,leftventricle.
contrast,AI-derivedRV:LVbinarycategorizationwas significant.FormeanAI-derivedCTPAmeasurements, Table1 showssignificantdifferencesinRV:LV,RV, andLVbasaldiametersbetweenthosewithandwithout clinicaldeterioration.
Forthe733patientswithTTE,TTEmeasurementswere lessthanAI-derivedCTcardiacmeasurements.OnlyLV basaldiameterhadsignificantdifferencesbetweenthe primaryoutcomegroups.AlthoughmeanRVbasal diameterwasabovenormallimits,thedifferencewasnot statisticallysignificantforoutcome-negativeand outcome-positivegroups.
MultivariableanalyseswithunadjustedLASSOforPErelatedclinicaldeterioration(primaryoutcome)showedthe mostsignificantindependentAI-derivedpredictorswereRV: LV(19.28[3.0–109.4])andcentralclotbyAI(2.4[1.6–3.6]). BoththeadjustedLASSOandRFmodelsvettedall candidatedatabasevariables.BothRFandadjustedLASSO
prognosticmodelshadexcellentdiscriminationand calibrationmetricsforprognosticaccuracy(Supplemental Figure2):Fordiscrimination,adjustedLASSOandRFhad AUCof0.88(0.85,0.90)and0.87(0.84,0.89),respectively. BothmodelswerewellcalibratedwithBrierscoresof0.07. TheRFmodelwasslightlylesscalibratedthantheLASSO modelonothercalibrationmetrics.
Table2 and Figure2 showcardiacarrestatpresentation wasthetoppredictorofin-hospitalclinicaldeteriorationin bothmultivariablemodels(LASSOandRF).Admissionto theintensivecareunit,lowestsystolicbloodpressure,lowest oxygensaturation,andhighestheartandrespiratoryrates werealsotoppredictorsinbothmodels.TheCTPAcardiac measurementswereamongthetop11predictorsselectedby LASSO.Abnormaltroponinwasoneofthetoppredictorsby LASSObuthadalowerinfluenceonRFmodelaccuracy thanCTPAassessments.TheCTPAcardiacmeasurements and findingsofcentralclotlocationwithRV:LV ≥ 1.0were amongthetop10independentpredictorsofclinical deteriorationintheRFmodel.
Table1. Patientandimagingcharacteristicsbypulmonaryembolism-relatedclinicaldeterioration(primaryoutcome).
Race
Bodysurfacearea
PriordiagnosisofPEorDVT?
FamilyhistoryofVTE?
Recenthospitalization(in3weeks)?
Anticoagulationuse?
Currentorrecentpregnancy(ormiscarriage) within6weeks
(Continued onnextpage)
Table1. Continued.
Recentlimbimmobilization(currentorwithin3weeks)
Recenttrauma(intheprior4–6weeks)?
Surgeryrequired(mechanicalventilationorepidural) within6weeks?
Clottingdisorders(proteinC,S,factorVdeficiency)?
Hormonereplacementtherapy
Chronicpulmonarydisease
Congestiveheartfailure
TotalCharlsoncomorbidityindex
LowestsystolicBP(within3hours),mmHg
LowestO2 sat(within3hours),%
Mean(SD)93.1(5.52)85.5(16.4)92(8.00) <
Missing2(0.1%)1(0.5%)3(0.2%)
HighestHR(within3hours)
Mean(SD)106(21.2)120(22.2)108(21.8) <0.001
Median[min,max]106[11.0,198]121[62.0,178]108[11.0,198]
HighestRR(within3hours)
Mean(SD)24.4(8.64)31.3(11.1)25(9.22) <0.001
Median[min,max]23.0[14.0,200]30.0[16.0,103]23[14.0,200]
Missing4(0.3%)2(1.1%)6(0.4%) (Continued onnextpage)
Table1. Continued.
Shockindexgreaterthan1.0?
Advanced/escalatedPEintervention?
Typeofadvancedintervention: systemicthrombolysis
Catheter-directedintervention
Rightventricularassistdevice
Inferiorvenacava filterused
Computedtomography assessmentofCTbyradiologists
< 1.0
RV:LV(AI)
RV:LV ≥ 1
RV:LV < 1
RVbasalwidth,byAI,cm
LVbasalwidth,byAI,cm
RV:LVratio,byAI Mean(SD) 1.3(0.324) 1.5(0.39) 1(0.336) <0.001
26(1.6%) (Continued onnextpage)
Table1. Continued.
EchocardiographyRVbasalwidth(ECHO)
Mean (SD)
Primaryoutcome( ) (n = 1,449)
Primaryoutcome(+) (n = 190)
Total N = 1,639 P-value
4.22(0.811) 4.25(0.814) 4(0.812)0.70
Missing 640(44.2%) 110(57.9%)752(45.9%)
LVbasalwidth(ECHO)
Mean(SD)
4.1(0.811) 3.9(0.846) 4(0.817)0.004
Missing 153(10.6%) 42(22.1%)196(12.0%)
RV:LV(ECHO)
Mean(SD) 1.0(0.272) 1.1(0.332) 1(0.278)0.07
Missing 685(47.3%) 116(61.1%)1(0.278)
RV:LVcut-off = 1.0bycardiologist
RV:LV ≥ 1.0 1,155(79.7%) 147(77.4%)1,302(79.4%)0.72
RV:LV
Initialtroponin,ng/mL
Initialhigh-sensitivitytroponin,mean(SD),ng/mL195(606)
*WeusedtroponinIorhigh-sensitivitytroponinassays(Abbott,AbbottPark,IL)measuredinng/mLassay.NormalvaluesfortroponinIwere less than0.07ng/mL.Normalvaluesforhigh-sensitivitytroponinwerelessthan12forfemalesandlessthan20formales.Abnormal troponinlevelswerehigherthanabove-mentionedcut-offs.
AI,arti ficialintelligencealgorithm; CT,computedtomography; BP,bloodpressure; DVT,deepveinthrombosis; ECHO,echocardiography; ECMO, extracorporealmembraneoxygenation; HR,heartrate; ng/mL,nanogramspermilliliter; O2 sat,oxygensaturation; RR,respiratory rate; LV,leftventricle; RV,rightventricle; RV:LV,rightventricletoleftventriclediameterratio; VTE,venousthromboembolism.
Table3 showsoptimalcut-offsofAI-derivedcardiacCTPA measurementswithpredictionmetricsforPE-relatedclinical deteriorationasRV:LV1.54(OR2.5[1.85–3.45]andAUC 0.6[0.66,0.70]).Thesecut-offvalueshadhighnegative predictivevalues(NPV)butlowpositivepredictive values(PPV).
Table4 showsbivariableanalysisofcardiacassessments stratifiedbyuseofadvancedinterventions(secondary outcome).Regardlessofhowcardiacmeasurementswere derived,thereweresignificantdifferencesincardiac measurements(whethercontinuousorcategorical)between thosewithandwithoutadvancedinterventions.For example,AI-derivedCTPARV:LVmeanswithSDs were1.62(0.33)vs1.35(0.32)forthosewithandwithout advancedinterventions(secondaryoutcome),respectively. WithTTE,RV:LVmeanswere1.17(0.29)vs 1.02(0.27)forthosewithandwithoutadvanced interventions,respectively.
TherewasagreementbetweenAIandradiologistsonRV: LV ≥ 1.0for1,224casesandonRV:LV <1.0for67cases (88%overallagreement[kappa0.36,95%CI0.28–0.43],data notshown).TheRV:LVmeanswithSDswere1.48(0.31) and0.86(0.11),respectively.Therewasdisagreementfor178 (12.1%)cases.RV:LVmeanswere1.23(0.23)and0.92(0.05) whenAIreportedabnormalRV:LVvsRV:LV < 1.0, respectively.ForcomparisonofAI-derivedCTPAwithTTE measurements,PearsoncorrelationcoefficientsforRV,LV, andRV:LVwere0.47(0.42,0.52),0.58(0.53,0.62),and0.50 (0.45,0.55),respectively.Allkappaswereinterpretedas moderateagreementperLandisandKochguidelines. SupplementalFigure3showsstrongnegativebiaswith lowerTTEmeasurementsthanCTPAmeasurements atpresentation.
WefoundAI-derivedRV:LVmeasurementsonCTPA weresignificantlygreaterinPEpatientsexperiencingclinical
Table2. LASSO*regressionmodels(unadjustedandadjusted)forpulmonaryembolism-relatedclinicaldeterioration(primaryoutcome).
UnadjustedmodelwithAI-derivedCTPAassessmentsonly PE-relatedclinicaldeterioration(primaryoutcome)
PredictorsOddsratiosCon
Adjustedmodelwithallvariablesconsidered
Observations
*LASSO, leastabsoluteshrinkageandselectionoperator; PE,pulmonaryembolism; AI,artificialintelligence; CTPA,computedtomography pulmonaryangiogram; RV,rightventricle; LV,leftventricle; CPR,cardiopulmonaryresuscitation; ICU,intensivecareunit.
deteriorationorreceivingadvancedinterventionthanthose withouttheseoutcomes.Therewassignificantlyincreased useofsystemicthrombolysis,ECMO,andsurgical embolectomyintheprimaryoutcomegroup.Inourmodels, whichhadstrongdiscriminationandcalibration,AI-derived RV:LVmeasurementswereindependentpredictorsof clinicaldeterioration,alongwithabnormalvitalsignsand cardiacarrestatpresentationinoneorbothmultivariable models.TheoptimalRV:LVcut-offof1.5hadanoddsratio of2.5andAUCof0.6forPE-relatedclinicaldeterioration (primaryoutcome).TheAI-derivedRV:LVmeasurements performedbetteraspredictorsofprimaryandsecondary outcomesthanradiologists’ orAI-derivedcategorizations usingRV:LVcut-offof1.0.
Otherreportshavefocusedonoutcomessimilartoours. Beigeletal.performedastudyevaluating179intermediateriskPEpatientsforpredictorsofshort-termdeathand advancedinterventions.21 Twenty-sixpatientsrequired advancedintervention,whichwassignificantlyassociated withechocardiographicevidenceofsevereRVD(42%vs 19%, P < 0.01)orhigherRV:LVmeasurementonCTPA (1.9 ± 0.6vs1.46 ± 0.5, P < 0.001).TheRVdilatationon
TTEwasanindependentpredictorforadvanced interventions.Thisinformationfurthercorroboratesthe importanceofmeasurementstoriskstratifyPEpatients. UnlikeTTEmeasurements,cardiacCTPAmeasurements areimmediatelyavailableatthetimeofPEdiagnosisfor riskstratification.22
OtherstudiesthatassessedhowCTPAcardiac measurementsareassociatedwithclinicaloutcomeshad mixedresults.AretrospectivestudybyFoleyetal.involving 101patientswithCT-provenPEsofanyseverityatasingle centershowedstrongagreement(intraclasscorrelation0.83, [0.77–0.88])betweenradiologists’ andAI-derivedCTPA measurementsforRV:LV.15 Inthisstudy,RV:LVranged from0.67–2.43,with65%being ≥ 1.0.TheoptimalRV:LV cut-offfor30-daymortalitywas1.18.TheuseofAIanalysis inourstudyledtoachangeinriskstratificationin45%of patients.However,inalargeprospectivestudyof1,950CTconfirmedPEsbyBeenenetal.,RV:LVmeasurementsby radiologistswerenotsignificantlydifferentbetweenthose withandwithoutshort-termmortality.23 SimilartotheFoley etal.study,wefoundanelevatedRV:LVhadastrong associationwithin-hospitalclinicaldeteriorationinour

Figure2. Randomforestvariableimportanceplotforpredictingclinicaldeterioration. CTPA,computedtomographypulmonaryangiography; LV,leftventricle; RV,rightventricle; ICU,intensivecareunit.
Table3. Optimalcut-offsofartificialintelligence-derivedcardiacCTPA*measurementswithpredictionmetricsforpulmonaryembolismrelatedclinicaldeterioration(primaryoutcome).
*CTPA, computedtomographypulmonaryangiogram; AI,artificialintelligence; cm,centimeter; PPV,positivepredictivevalue; NPV,negative predictivevalue; AUC,areaunderthecurve; RV,rightventricle; LV,leftventricle.
intermediate-andhigh-riskPEcohort.OuroptimalRV:LV cut-offof1.5washigherthantheirs.
Apreviousreportshowedfairagreement(kappa0.4)for categoricalassessmentsofRVdysfunctionbetweenCTPA andTTE.22 OurstudyfoundmoderateagreementofRV:LV measurementsbyCTPAandTTE.Webelieveour findings underscoretheimportanceofusingimmediatelyavailable CTPAmeasurementsofRVDforriskstratificationand prognosis.However,atmanyinstitutions,RVmeasurements arenotroutinelyperformedorinterpretedonCTPA.One studyinalargeregionalhealthcaresystemwith21sites showedonly18.3%of1,571positiveCTPAinterpretation reportsincludedRVmeasurements.24
TheuseofAItodetectPEandanalyzeCTPAcardiac measurementsattimeofPEpresentationmayimproverisk
stratificationforPERTsandprovidequalityassuranceto enhanceradiologists’ workflow.Thediagnosticaccuracyof AIshouldincludealownumberoffalsepositivestominimize notificationfatigueandpotentialformedication mismanagement.Inaretrospectivemulticenterstudy,Cheik etal.evaluateddiagnosticperformancesoftheAidocPE algorithmonCTPAsandcomparedthemwiththoseof radiologiststodetermineimpactofAIPEdetection.18 Of 1,202patientsincluded,theAIalgorithmdetected219 suspiciousPEs,ofwhich176weretruePEs,including19true PEsmissedbyradiologists.ThehighestsensitivityandNPVs wereobtainedwithAI,whilethehighestspecificityandPPV werefoundwithradiologists.Ourretrospectivestudy focusedonlesssubtlePEdiagnoses;theAIanalysiswas specificallycreatedtofocusonnon-segmentalPE,andAI
Table4. Cardiacassessmentsgroupedbyuseofadvancedintervention(secondaryoutcome). Noadvancedintervention (n = 1,329)
= 314)
CTassessmentbyradiologist
RV:LV ≥ 1.0
RV:LV < 1.0 165(12.4%) 17(5.4%) 182(11.1%)
Missing 133(10%) 23(7.3%) 156(9.5%)
CTassessmentsbyAI
RV:LV > 1(AI)
RV:LV
RV:LV < 1
RVbasalwidth(AI)
Mean(SD)
LVbasalwidth(AI)
RV:LV(AI)
ECHOassessments
Echocardiography
LVdiameter(AI)
RVbasalwidth (ECHO)
LVbasalwidth(ECHO)
RV:LV(ECHO)
AI, arti ficialintelligencealgorithm; CT,computedtomography; ECHO,echocardiography; LV,leftventricle; RV,rightventricle; RV:LV,right ventricletoleftventriclediameterratio.
agreedthatPE findingswerepresentinallCTPAs.Artificial intelligencefurtheranalyzedventriclemeasurementson CTPAanddeterminedcentralvsnon-central fillingdefects. AlthoughourcomparisonofCTPARV:LVcategorization byAIvsradiologistshad88%agreement,thekappa0.34is interpretedasfairagreement.Agreementwasmorelikely
whenRV:LVwaswellaboveorwellbelowthe1.0cut-off;the twosourcesweremorelikelytodisagreewhenRV:LVwas closerto1.0.ItisunknownwhetherAI-derivedCTPA measurementsmight “correct” radiologistassessmentsinreal timeforthoseclosetothe1.0cut-offorwhethersucha “correction” wouldhaveclinicalsignificanceonpatientcare
andoutcomes.EvenwithanoptimalRV:LVcut-offof1.5,we notethelowPPVforPE-relatedclinicaldeterioration.So,an RV:LVcut-offof1.5isnotsufficienttobethesole determinantofdecision-makingaboutdispositionor advancedinterventions.Similartoanotherreport,ourstudy showedacombinationofCTPAparameters(centralclot locationandRV:LV)hadstrongerassociationswithclinical deteriorationthanRV:LValone(categoricalorcontinuous).22
IncorporationofCTPAcardiacmeasurementsinPErisk stratificationmayimpactlocal/regionalclinicalpracticeor guidelines.Nextstepsmayincludeprospectivestudiesthat includeCTPAmeasurementsaspredictorsofclinical outcomesandPERTriskstratification,andpragmatic comparisonsofAI-assistedworkflowvstraditionalworkflow inwhichCTPAcardiacmeasurements,clinicalmanagement metrics,andpatient-centeredoutcomesareassessed.
Ourstudyhadseverallimitations.First,weconducteda retrospective,remoteAIanalysisofCTPAwithconfirmed intermediate-andhigh-riskPE.Wedidnotstudyreal-time AIanalysesonrecentlycompletedCTPAs.Ourstudydesign andinclusioncriteria,therefore,donotlendtoany interpretationaboutdiagnosticaccuracyoftheAIplatform onCTofpatientswithloweracuityPEorwithoutPE.We cannotreportonfalsepositiveorfalsenegative interpretations,potentialimpactonPERTnotificationsor clinicalmanagement,orcomparetopreviousreportsofAI’ s diagnosticaccuracyforPE.Theoretically,wehaveshown AI-derivedmeasurementswerebetterpredictorsofacute clinicaldeteriorationthancategoricalradiologistassessment ofRV:LVcut-offof1.0.However,toshowtheimpactofAI onpatientcarebyclinicians,therewouldneedtobe pragmatic,randomizedcontrolledtrialscomparingusual carevsAI-assistedclinicalcare.Prospectivestudieswould enablereportingtimelinessofAIanalysisofCTanditseffect onradiologistworkload,physiciannotificationofpositive andsignificant findings,andimpactofmeasurementsonrisk assignment,resourceutilization,advancedinterventions, andclinicaldeterioration.
Otherlimitationsarespecifictotheexploratoryobjectives. Ourstudydidnotverifywhetheragreementsbetween radiologistandAIforRV:LV ≥ 1.0werecorrect;both interpretationscouldbeincorrect.Studydesigncouldbe improvedbyincludingacomparator,suchasareference standard(e.g.,cardiacmagneticresonanceimaging),useof anindependent,blindedradiologistforseparate measurementsortoserveasanadjudicator,orearlier contemporaneousTTEmeasurements.Forthesecond exploratoryobjective,wedidnotdeterminepresenceor absenceofinterventionsintheintervalbetweenCTandTTE. TheTTEandCTPAwereperformedatdifferenttimesand oftenmorethan12hoursapart.Therefore,thedifferences betweenthesemeasuredvariablesmaybeduetoworsening
orimprovingcardiacburdenduringthetimeintervals.Not allpatientsinthecohorthadTTE.HighmissingnessofTTE measurementswasalimitationincomparisonofthemwith theAI-derivedCTPAmeasurements.Thedifferences observedinthesemeanmeasurementsmaybedueto differentimagingmodalityortimeintervalbetweenstudies. ThesubgroupthathadTTElikelyrepresentedthosewith higheracuityatpresentation.
Rightventricle:leftventriclemeasurementsof1.5ormore ontheinitialCTpulmonaryangiogramhadstrong associationswithin-hospitalclinicaldeteriorationand advancedinterventionsinalargedatabaseofintermediateandhigh-riskpatientswithpulmonaryembolism.Thisstudy pointstothepotentialofcapitalizingonimmediately availableCTPARV:LVmeasurementsforgaugingPE severityandforriskstratification.
AddressforCorrespondence:AnthonyJ.Weekes,MD,MSc,Atrium Health’sCarolinasMedicalCenter,DepartmentofEmergency Medicine,3rdFloorMedicalEducationBuilding,1000BlytheBlvd., Charlotte,NC28203.Email: anthony.weekes@atriumhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Weekesetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KonstantinidesSV,MeyerG,BecattiniC,etal.2019ESCguidelinesfor thediagnosisandmanagementofacutepulmonaryembolism developedincollaborationwiththeEuropeanRespiratorySociety (ERS). EurHeartJ. 2020;41(4):543–603.
2.MeinelFG,NanceJWJr.,SchoepfUJ,etal.Predictivevalueof computedtomographyinacutepulmonaryembolism:systematicreview andmeta-analysis. AmJMed. 2015;128(7):747–59.e2.
3.CoutanceG,CauderlierE,EhtishamJ,etal.Theprognosticvalueof markersofrightventriculardysfunctioninpulmonaryembolism:ametaanalysis. CritCare. 2011;15(2):R103.
4.AndradeI,MehdipoorG,LeMaoR,etal.Prognosticsignificanceof computedtomography-assessedrightventricularenlargementinlowriskpatientswithpulmonaryembolism:systematicreviewandmetaanalysis. ThrombRes. 2021;197:48–55.
5.RaperJD,ThomasAM,LupezK,etal.Canrightventricular assessmentsimprovetriagingoflowriskpulmonaryembolism? Acad EmergMed. 2022;29(7):835–50.
6.BecattiniC,MarazitiG,VinsonDR,etal.Rightventricleassessmentin patientswithpulmonaryembolismatlowriskfordeathbasedonclinical models:anindividualpatientdatameta-analysis. EurHeartJ. 2021;42(33):3190–9.
7.Trujillo-SantosJ,denExterPL,GomezV,etal.Computedtomographyassessedrightventriculardysfunctionandriskstratificationofpatients withacutenon-massivepulmonaryembolism:systematicreviewand meta-analysis. JThrombHaemost. 2013;11(10):1823–32.
8.WeikertT,WinkelDJ,BremerichJ,etal.Automateddetectionof pulmonaryembolisminCTpulmonaryangiogramsusinganAI-powered algorithm. EurRadiol. 2020;30(12):6545–53.
9.KumamaruKK,HunsakerAR,KumamaruH,etal.Correlationbetween earlydirectcommunicationofpositiveCTpulmonaryangiography findingsandimprovedclinicaloutcomes. Chest. 2013;144(5):1546–54.
10.WeekesAJ,RaperJD,LupezK,etal.Developmentandvalidationofa prognostictool:pulmonaryembolismshort-termclinicaloutcomesrisk estimation(PE-SCORE). PLoSOne. 2021;16(11):e0260036.
11.JiménezD,KopecnaD,TapsonV,etal.Derivationandvalidationof multimarkerprognosticationfornormotensivepatientswithacute symptomaticpulmonaryembolism. AmJRespirCritCareMed. 2014;189(6):718–26.
12.BovaC,SanchezO,PrandoniP,etal.Identificationofintermediate-risk patientswithacutesymptomaticpulmonaryembolism. EurRespirJ. 2014;44(3):694–703.
13.ChenYL,WrightC,PietropaoliAP,etal.Rightventriculardysfunctionis superiorandsufficientforriskstratificationbyapulmonaryembolism responseteam. JThrombThrombolysis. 2020;49(1):34–41.
14.WeekesAJ,FragaDN,BelyshevV,etal.Intermediate-riskpulmonary embolism:echocardiographypredictorsofclinicaldeterioration. CritCare. 2022;26(1):160.
15.FoleyRW,Glenn-CoxS,RossdaleJ,etal.Automatedcalculationofthe rightventricletoleftventricleratioonCTfortheriskstratification ofpatientswithacutepulmonaryembolism. EurRadiol. 2021;31(8):6013–20.
16.WeekesAJ,TrautmannA,HambrightPL,etal.Comparisonoftreatment approachesandsubsequentoutcomeswithinapulmonaryembolism responseteamregistry. CritCareResPract. 2024;2024:5590805.
17.WeekesAJ,HambrightP,TrautmannA,etal.Lowstrokevolume predictsdeteriorationinintermediate-riskpulmonaryembolism: prospectivestudy. WestJEmergMed. 2024;25(4):533–47.
18.CheikhAB,GorincourG,NivetH,etal.Howartificialintelligence improvesradiologicalinterpretationinsuspectedpulmonaryembolism. EurRadiol. 2022;32(9):5831–42.
19.LandisJRandKochGG.Themeasurementofobserveragreementfor categoricaldata. Biometrics. 1977;33(1):159–74.
20. MartinBlandJandAltmanDG.Statisticsnotes:calculatingcorrelation coefficientswithrepeatedobservations:part1 correlationwithin subjects. BMJ. 1995;310(6977):446.
21.BeigelR,MazinI,GoiteinO,etal.Intermediate-riskpulmonary embolism:aimingtoimprovepatientstratification. EurJInternMed. 2019;65:32–6.
22.ErolS,GürünKayaA,ArslanF,etal.Agreementbetweentransthoracic echocardiographyandcomputedtomographypulmonaryangiography fordetectionofrightventriculardysfunctioninpulmonaryembolism. AnatolJCardiol. 2024;28(8):393–8.
23.BeenenLFM,BossuytPMM,StokerJ,etal.Prognosticvalueof cardiovascularparametersincomputedtomographypulmonary angiographyinpatientswithacutepulmonaryembolism. EurRespirJ. 2018;52(1):1702611.
24.VinsonDR,MarkDG,ChettipallyUK,etal.Increasingsafeoutpatient managementofemergencydepartmentpatientswithpulmonary embolism:acontrolledpragmatictrial. AnnInternMed. 2018;169(12):855–65.
AnthonySielicki,MD* BrianMilman,MD†
AndrewLittle,DO‡
MiriamKulkarni,MD§
JamesMorris,MD,MPH∥
LauraHopson,MD**
MichaelKiemeney,MD††
* JeffersonEinsteinHospital,DepartmentofEmergencyMedicine, Philadelphia,Pennsylvania
† UTSouthwesternMedicalCenter,DepartmentofEmergencyMedicine,Dallas,Texas ‡ AdventHealth,DepartmentofEmergencyMedicine,Orlando,Florida
§ St.John’sRiversideHospital,DepartmentofEmergencyMedicine,Yonkers,NewYork ∥ TexasTechUniversityHealthSciencesCenter,DepartmentofEmergencyMedicine, Lubbock,Texas
**UniversityofMichigan,DepartmentofEmergencyMedicine,AnnArbor,Michigan †† LomaLindaUniversityMedicalCenter,DepartmentofEmergencyMedicine, LomaLinda,California
SectionEditor:AsitMisra,MD,MSMEd
Submissionhistory:SubmittedNovember9,2023;RevisionreceivedOctober24,2024;AcceptedOctober25,2024
ElectronicallypublishedDecember31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18562
Introduction: The2023NationalResidencyMatchingProgram(NRMP)Matchinemergencymedicine (EM)left554spotsand132EMprogramsunfilled.TheCouncilofResidencyDirectorsMatchTaskForce soughttocharacterizetheprogramsthatdidanddidnot fill,learnmoreabouttheirSupplementalOffer andAcceptanceProgram(SOAP)applicants,determineresidencyprograms’ needsforfutureNRMP Matches,andinquirewhatactionsprogramleaderswouldliketoseetopromoteahealthyfuturefor traininginEM.
Methods: Weconductedaweb-basedsurveyofEMresidencyprogramleadershipduringMarchand April2023.Wegenerateddescriptivestatisticsfromthesesurveyresults.Thematicanalysiswasused forfree-textresponses.
Results: Of287programs,160(55.7%)respondedtothesurvey,including59of132programs(44.7%) thatdidnot fillintheMatch.Unfilledprogramswereoverallcontentwiththequalityofapplicantsinthe SOAP.ProgramsexpressedvaryingopinionsonwhyfewerstudentsarechoosingEM.Whilemost agreedthereareconcernsabouttheworkforce(78.1%),evenmorespreadexistsonwhatactionsshould betakentohelpsupportthefutureofresidencytraininginEM.
Conclusion: Herewepresentdataregardingthe2023MatchenvironmentforEManddescribea residencyprogram-levelneedsassessmentanddesireforaction.AnnualreviewoftheMatchdataand residencyprogramneedsshouldbecontinueduntilweseeimprovementintheMatchenvironment forEM.[WestJEmergMed.2025;26(2)233–240.]
TheNationalResidentMatchingProgram(NRMP) Matchforemergencymedicine(EM)hasevolvedoverthe pastseveralyears.Historically,EMhasbeenacompetitive specialtywithnearly100%programmatchrates.1 The2022 EMMatchrepresentedafundamentalchangecomparedto
thehistoricaldata,withover200EMpositionsandover60 residencyprogramsunfilled.2 Thistrendcontinuedinthe 2023match,with554unfilledpositionsacross132programs, althoughthistrendimprovedasofthe2024Match.3,4 Table1 displaysseveralyearsofEMmatchdata,which highlightsthegrowthofresidencyprograms,increasing
numberofpostgraduateyear-1positions,andvariable numberofapplicantstoEMresidencyprograms.5,6
Severaltheorieshavebeenproposedtoexplainwhyfewer medicalstudentsareapplyingtoEM.The2030jobsreport leftmanyconcernedthattherewouldnotbeenoughworkfor allemergencyphysicians(EP),7 whileothershavespeculated thatissueswithboarding,drugandnursingshortages, burnout,theCOVID-19pandemic,concernsforfuturenovel infectiousdiseases,andscopeofpracticeofnon-physician medicalpractitionersmaycontribute.Theseissuesare currentlyunderinvestigationbymultiplegroups,including theCouncilofResidencyDirectorsinEM(CORD).8
CORDisanorganizationcomprisedofEMresidency educatorsandprogramleadershipprovidingresourcesand developingbestpracticesforeducationinEM.InMarch 2022,CORDsurveyeditsmemberstounderstandwhatthe organizationcoulddotosupportitsmembersfollowingthe 2022Match.9 Basedonfeedbackfromthatsurvey,the CORDBoardofDirectorsconvenedtheEMMatchTask Force.Theprimaryobjectivesofthistaskforcearetocollect dataandtointervenewithregardtotheincreasednumberof unfilledEMresidencypositions.10 Theinitialgoalofthetask forcewastounderstandthefactorsthatledtotheincreased numberofunfilledspots,thequalityofapplicantstoEM,as wellasinterviewandrank-listbehaviorsofprogramsinthe 2023Match.Additionalobjectivesincludedexamining residencyleadershipopinionsontheutilityofpreference signaling,readinessofSupplementalOfferandAcceptance Program(SOAP)candidates,anddesiredactionstoimprove theEMMatchenvironment.
Consideringtheseobjectives,theCORDEMMatchTask ForcesoughttoelicittheneedsandperceptionsfromEM residencyprogramleadersasa firststeptowarddeveloping targetedinterventionstoimprovetheEMMatch environment.Inthispaper,themembersoftheCORDEM MatchTaskForcedescriberesultsofasurveyconducted followingthe2023Match.
TheCORDEMMatchTaskForcemembersdevelopeda surveyexpandingupontheworkofthe2022Muranoetal survey.Consensusmethodologybetweentaskforcemembers
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
The2023Matchforemergencymedicineleft 132residencyprogramsun fi lledand554 un fi lledspots.
Whatwastheresearchquestion?
Wesoughttodetermineresidencyprograms ’ needsforfutureMatchesandwhatactions programleadersdesiretopromoteahealthy futurefortraininginEM.
Whatwasthemajor findingofthestudy?
MostrespondentsagreedthatEMapplication numbersweredownduetoconcernsaboutthe workforce(78%),andtheleadingdesirewas tohaltopeningnewprograms(25%).
Howdoesthisimprovepopulationhealth?
These fi ndingscouldimprovepopulation healthbyensuringahealthyMatchand trainingenvironmentinEM.
wasusedtodevelopandrefinethesurvey.Thesurveywas thendistributedtoEMresidencyprogramleadership (programdirectors[PD],assistant/associateprogram directors[APD],clerkshipdirectors[CD],program coordinators[PC],chairs,andgeneralfacultymembers) duringtheCORDAcademicAssemblyinMarch2023inLas Vegas,NV.Surveyparticipationwasvoluntaryandsolicited viaQRcodeduringconferencesessions.Thesurveywasalso distributedontheCORDProgramDirectorListservtoreach programleadershipwhodidnotattendtheconference.The surveywasweb-basedandusedQualtrics(Qualtrics InternationalInc,Provo,UT)fordatacollection.
Thesurveycollectedtherespondents’ residencyprogram, theirrolewithintheprogram,anddemographicinformation abouttheprogram(ie,lengthoftraining,locationof
Table1. EmergencymedicineNationalResidentMatchProgramdata2019–2024.
EM, emergencymedicine; PGY,postgraduateyear.
program,sponsoringinstitutions).Allprogramleaderswere askedaboutthenumberandqualityofapplicantstotheir programaswellasoutcomesintheMatch.Forprograms thatdidnot fillandusedtheSOAP,weaskedquestions regardingthequalityofapplicantsintheSOAPandsought feedbackabouttheSOAPprocess.Additionally,all respondentswereaskedtoidentifywhytheythoughtfewer medicalstudentsareapplyingtoEMandwhatadditional actionstheywouldliketoseetakentoimprovetheMatch environmentinEM.ThisstudywasreviewedbytheLoma LindaUniversityInstitutionalReviewBoardandgiven exemptstatus.
WeanalyzeddatausingMicrosoftExcel365(Microsoft Corp,Redmond,WA)tocalculatedescriptivestatistics.To avoidover-weightingperspectivesfromasingleprogram,we sorteddatatoselectasingleresponseperprogram.Weused thefollowingorderofconsiderationwhenmorethanone responsewasavailableperprogram:residencyPD;PC;chair orvice/associatechair;APD;residencycorefacultymember; generalfacultymember.Free-textresponseswerecoded usingathematicanalysisbetweentwoauthors(BM,MKu) fortheSOAPqualitativedata,andbytwoauthors(BM,JM) fortheinterviewuniformity,decreasingapplicants,and futuredirectionsqualitativedata.Simultaneouscodingwas allowed.Anydisagreementsbetweencodeswereresolvedby twootherauthors(AS,MK),andifnoagreementcouldbe reachedtheresponsewasnotanalyzed.Forallquestions, onlythreeresponseswerediscardedduetonotbeingableto reachanagreement.
Intotal,245responsestothesurveywererecorded. Twelve(4.9%)wereexcludedduetoincompleteresponses, and74werediscardedduetoeitherduplicateresponsesor multipleresponsesbeingsubmittedfromdifferent representativesfromthesameresidencyprogram.There wereresponsesfrom160ofthe287EMresidencyprograms thatexistnationally,representinga55.7%responserate. Respondentsfromtheprogramsincluded109PDs(67.7%), 33APDs(20.5%),sevenCDs(4.3%),sixfacultymembers (3.7%), fivePCs(3.1%),andonevicechair(0.7%).We compareddemographicinformationofresponding programstoallknownEMprogramsbasedontheAmerican MedicalAssociation(AMA)FellowshipandResidency ElectronicInteractiveDatabaseandtheAmericanBoardof EmergencyMedicinedata,whichispresentedin Table2.11,12 Onaverage,programleadersreportedinterviewing14.9 applicantsperposition(SD4.76)inthe2022–2023 applicationcycle.Comparedtothe2021–2022application cycle,programsreportedinterviewing18.7moreapplicants total(range: 105to +185,SD40.16).Regardingcreationof arankorderlist(ROL),programsindicatedthattheyplaced ameanof13.9applicantsontheirROLperposition(SD
4.39).Comparedtothepriorapplicationcycle,programs placedameanof15.6moreapplicantsontheirROL(SD 28.4).Therewerenostatisticallysignificantdifferences between filledandunfilledprogramsintermsofnumberof applicantsinterviewedperresidencyposition(P = 0.37)or numberofapplicantsontheROLperposition(P = 0.55), usingtwo-tailed t -tests.
Comparedtothe2021–2022recruitmentseason,46/131 respondents(35.1%)indicatedthattheymadenosignificant changesintheconsiderationoftheformationoftheirROL, and47%indicatedthattheyincludedapplicantswithless desirableStandardLettersofEvaluation(SLOE)compared toprioryears.Additionally,39.7%indicatedtheyincluded thosewithmore “red flags ” ontheirapplications,suchas standardizedtestfailures,remediationofclerkships,or professionalismissues.Asimilar39.7%indicatedthatthey rankedapplicantswithalowerclassrankcomparedtoyears prior,while18.3%respondedthattheyrankedmore individualswithlessleadershiporvolunteerism,and12.9% indicatedthattheyrankedmoreofthosewhotheyfeltdidnot alignwiththemissionorvaluesoftheprogram.Five programs(3.8%)statedthattheyconsideredmore osteopathicapplicants,andanother five(3.8%)indicated thattheyconsideredmoreinternationalmedical graduates(IMG).
WhilepreferencesignalingwasnewtoEMthisyear,ithas beenusedbyotherspecialties,suchasotolaryngology,since the2020–2021applicationcycle.13 Emergencymedicine programshadvaryingwaysinwhichtheyusedpreference signalingduringthisapplicationcycle. Table3 provides detailsofhowprogramsinterpretedsignalpreferencing.
Morethanhalfofrespondentsfeltapplicantqualitywas eitheralittleworsethisyear(9.7%)orsubstantiallyworse thisyear(42.5%).Aminority(6.7%)feltapplicantquality hadimprovedthisyear.PerceptionsofMatchresultswere similartoperceptionsofapplicantquality.Morethanhalf felttheirprogram’sMatchresultswerealittleworse(39.4%) orsubstantiallyworse(19.7%)thanthepreviousyear. Notably,11.4%felttheirMatchresultswerebetterthanthe previousyear,and30%indicatedsimilarMatchresult qualitytotheprioryear.Amajorityofprogramsindicated thattheywentlowerdowntheirranklist,with75.2% indicatingthattheyeitherwentalittledeeperorsubstantially deepercomparedtoprioryears.
Ofthe132unfilledprograms,59(44.7%)oftheirprogram leadersrespondedtothissurvey.Onaverage,programshad 4.8positionsunfilled(range1–13,SD2.87)outofanaverage cohortsizeof10residentsperclass(range6–16,SD3.42), yieldingameanvacancyrateperunfilledprogramof47.8%. Oftherespondingprogramsthatdidnot fillinthe2023 Match,40.7%didnot fillinthe2021–2022applicationcycle. Programleadersreportedreceivinganaverageof257total
Table2. DemographicinformationcomparingallUSemergencymedicineprogramstothosethatrespondedtotheCouncilofResidency DirectorsMatchTaskForcesurveyregardingthe2023match. AllEMprograms (N=287)
Allrespondingprograms (n=160)
Filledresponding programs(n=101) Unfilledresponding programs(n=59)
Region
Hospitalsetting
Other(military,etc)5(1.7%)
Trainingformat
Ageofprogram
EM, emergencymedicine; PGY,postgraduateyear.
Table3. Howresidencyprogramsusedpreferencesignaling.
Morelikelytointerviewapplicants that signaled
32(23.7%)
Minorchangetointerviewselectionprocess24(17.8%)
Nochangetointerviewselectionprocess24(17.8%)
Interviewedmostbutnotallapplicants thatsignaled 13(9.6%)
Interviewedallapplicantsthatsignaled 12(8.9%)
Signalwasusedasatiebreakerbetween similarapplicants 12(8.9%)
Signalwasconsideredwheninvitingapplicants fromthewaitlist 7(5.2%)
Signalwasusedforout-of-regionapplicants6(4.4%)
Didnotoptin 5(3.7%)
SOAPapplications(SD130),or53.6applicationsper unfilledspot.Programsreportedinterviewinganaverageof 16.2applicantsperunfilledpositionintheirprogram(range 5.8–40,SD9.68);83.3%ofprogramsreportedtheywereable to fillallunfilledpositionsintheSOAP. Table4 outlines programperspectivesontheunderlyingreasonswhytheyfelt theirprogramdidnot fillintheMatch.
Table4. Topfactorsthatprogramsbelievedcontributedtonot filling inthe2023match.
Workforceconcerns 39(76.5%)
Geographic locationofprogram
Virtualinterviewsformat
Sponsoringinstitution(universityvsCMG)7(13.7%)
Programspecificfactors(wellness,curriculum changes,etc) 6(11.8%)
Socialmediaissues 4(7.8%)
Newleadership 3(5.9%)
Accreditationstatus 2(3.9%)
EM, emergencymedicine; CMG,contractmanagementgroup.
RegardingapplicantsintheSOAPandtheirpreparedness topracticeEM,35leadersofunfilledprogramsgave informationabouttheirapplicants.Eighteen(51.4%)stated thatmostapplicantshadcompletedatleastoneEMrotation butnotedthatitwasafterthetimethatERASapplications
weredue,leadingtolateconsiderationofEMastheirdesired medicalspecialty.Fiverespondents(14.3%)reportedmost applicantshadcompletedoneEMrotationbutmentionedno detailsaboutthetimingofthatrotation.Onlytwo respondents(5.7%)reportedthatthetypicalapplicanthadno orminimalexposuretoEM.Interestingly,20%ofprogram leadersmentionedthatmanyapplicantshadexposuretoEM priortostartingmedicalschool,suchasworkingasascribe orparamedic.Programleadersalsoreportedthatroughly 15%ofapplicantshadatleastoneEMSLOEavailablefor themtoreview.
Programleadersreportedtheywererelativelycontent withapplicantsavailabletothemintheSOAP,with78% respondingthattheywereeitherextremelyorsomewhat satisfiedwiththequalityofapplicants.Inaddition,80% reportedthatSOAPapplicantswereeithersignificantlyor slightlybettercomparedtothebottomquartileoftheir originalROL.
Programleaderswerealsoaskedwhatworkedwell regardingtheSOAPprocessitself.Free-textresponses underwentthematicanalysisasdescribedabovewith37 recordedresponsesevaluated.Eleven(29.7%)statedthatit wasanopportunityforcollaborationwithintheirprogram leadershipandfacultygroup.Ten(27%)mentionedthatthey thoughttheirpre-planningstrategyandorganizationduring theSOAPworkedwell.Fourrespondents(10.8%)explicitly mentionedthattheNRMPandElectronicResidency ApplicationServicetechnologyworkedwell.Additionally, 8.1%mentionedthestrongqualityofSOAPapplicants availabletothem,5.4%ofrespondentsnotedadequate supportfromCORD,andanother5.4%notedtherewas enoughtimetonavigatetheSOAPandinterviewapplicants.
Conversely,programleaderswerealsoaskedaboutthe challengestheyfacedduringtheSOAP,with49responses includedinthefollowinganalysis.Twelve(34.7%)thought thereweretoomanyapplicantsandnotenoughtimeto reviewtheirapplicationsandinterviewthem.Ten(20.4%) dislikedtheformatofSOAPoffers,notingtheirdesirefor eitheradditionalroundsorthatprogramsshouldbeableto offerspotstomorecandidates.Six(12.2%)noteddifficulties withdisingenuityfromapplicantsorviolatingNRMPSOAP rules.Threeprograms(6.1%)notedalackofqualified applicants,whiletwo(4.1%)notedconcernoverthe applicant’sinterestinacareerinEM.Finally,three programs(6.1%)respondedthattherewereissueswiththe overallnumberofunfilledprogramsandcompetition betweenprogramsforSOAPcandidates.
Thesurveyaskedopen-endedquestionsabout standardizationoftheinterviewprocess:41.2%of respondentsindicatedtheywouldliketohaveamandated returntoin-personinterviews,while11.8%preferreda requirementforvirtualinterviews.Overall,13.7%wanted
Table5. Reasonswhyprogramleadersbelievefewerstudentsare applyingtoemergencymedicine.
Workforceconcerns
107(78.1%)
Burnout 46(33.6%)
Workenvironment
COVID-19/pandemic
Boarding 36(26.8%)
CorporatizationofEM 21(15.3%)
NegativeEPmodeling 20(14.6%)
Negativepress 18(13.1%)
Advising 14(10.2%)
LackofearlyexposuretoEM 10(7.3%)
Increasedrolesofnon-physicianpractitioners6(4.4%)
Salary 5(3.6%)
EM, emergencymedicine; EP,emergencyphysician.
interviewuniformityamongprograms,and3.9%voiceda desirefor flexibilitytoallowprogramstodowhatworkedfor them.Additionally,9.8%statedtheywouldliketohave uniformcancellationstandardsforapplicants.Whenasked directly,74.3%respondedreportedtheywouldliketoseean interviewcapenforcement.Ofthe94respondentswho supportedaninterviewcapforapplicants,themean suggestedcapwas17.3interviewsperapplicant (range6–50,SD6.7).
Programleaderswerealsoaskedwhytheythoughtfewer medicalstudentswereapplyingtoEM.Themostcommon responsewasthatapplicantswereconcernedaboutthefuture oftheworkforce,which78.1%ofrespondentslistedasatop concern.Furtherresultsforthisquestionarelistedin Table5 Finally,programleaderswerealsoaskedwhatactionsthey wouldliketoseetakentohelpsupportthefutureoftraining inEM.Resultsareshownin Table6.
Thisstudybuildsupontheworkthatwasstartedby Muranoetalfollowingthe2022Match.Here,wedescribe factorsthateducationalleadersbelievecontributedtothe decreasingnumberofapplicationstoEMandtothe increasingnumberofbothunfilledprogramsandopen residencypositions.Resultsofthisstudyareconsistentwith previousstudiesidentifyinggeography,specificallylocation intheNortheasternandCentralUnitedStates,asa characteristicofunfilledprograms.14 Infact,58.8%of unfilledprogramleadersinthisstudybelievedgeographic locationwasamajorcontributingfactortotheirprogramnot fillinginthe2023Match.Anotherimportantfactoridentified byunfilledprogramleaderswastheincreasingnumberof EMspots.Therewerenostatisticallysignificantdifferences inthenumberofapplicantsinterviewedperposition,or
Table6. Actionsresidencyprogramleaderswouldliketoseetohelp supportthefutureofemergencymedicine.
HaltopeningofadditionalEMprograms 32(25%)
Increase RRCstandardsforEM 28(21.2%)
Decreasenumberofprograms 24(18.8%)
DecreasenumberoftotalEMspots 24(18.8%)
Positivemessagingcampaign 22(17.2%)
Counterworkforcestudy 16(12.5%)
CloseCMG-sponsoredprograms 8(6.25%)
Mandate4-yearprograms 5(3.9%)
Improveworkenvironment 4(3.1%)
Applicantresourcesfor findingprogrambest fit2(1.5%)
IncreaseearlyexposuretoEM 2(1.5%)
Producea “ratingsystem” ofEMprograms1(0.8%)
ExpandscopeofEM 1(0.8%)
Combatnon-physicianpractitioner scopeexpansion 1(0.8%)
Increaseresourcesforinternational medicalgraduates 1(0.8%)
EM, emergencymedicine; RRC,ResidencyReviewCommittee; CMG,contractmanagementgroup.
numberofapplicantsplacedontheROL,by filledcompared tounfilledprograms.Therefore,widespreadinterviewing andrankingofmoreapplicantsbyEMprogramswould likelynotbehelpfulinimprovingtheoverallMatchresults becauseofthedecliningapplicantpoolandexcessof trainingspots.
VirtualinterviewformathasbeensupportedbyCORD sincethebeginningoftheCOVID-19pandemic.15 Whilethis mayhelptodecreasecostsassociatedwithresidency interviewsforapplicants,lessenthecarbonfootprint associatedwithtravelforinterviews,andincreasethe amountoftimeavailabletofocusonclinicalexposurein medicalschool,itmayalsoleadtostudentsapplyingtoand interviewingwithmoreprograms.16 Inthe2023Match, studentsapplyingtoEMappliedtoamedianof69programs andinterviewedatamedianof18.5programsaccordingto NRMPChartingOutcomes.17 Comparatively,in2019the averageUSgraduateapplicantappliedto57programs.18 Thisincreasednumberofapplicationsmakesitverydifficult forprogramleaderstoknowwhichapplicantsaretruly interestedintheirprogramvsthosewhoappliedand interviewedduetotheeaseofinterviewingvirtually.This sentimentissupportedbytheresultsofthissurvey,with 45.1%ofunfilledprogramleadersstatingthatvirtual interviewswereakeycontributortowhytheywereunfilled, and41.2%ofrespondentsvoicingadesiretoreturntoinpersononlyinterviews,comparedtoonly11%whowantto continueavirtual-onlyinterviewformat.
Furthermore,amajorityofprogramleaderswereinfavor ofcappinginterviews(73.4%),withameansuggestedcapof 17interviews.However,itisnotcurrentlyknownwhetheran interviewcapispermissibleorenforceablethroughthe NRMP.Neitherisitknownwhetheraninterviewcapwould disproportionatelyharmcertainprograms,suchasmore rural,smaller,ortraditionallylesscompetitiveprograms. Interviewcaps,however,havebeenusedinotherspecialties. InresponsetovirtualinterviewsandtheCOVID-19 pandemic,ophthalmologyhasemployedinterviewcapsfor theirmatchsincethe2020–2021applicationcycleand,in fact,justloweredthecapofinterviewsfrom18to15.19 Obstetricsandgynecologyisalsoconsideringimplementing aninterviewcapand,inasimulatedenvironment,foundthat itincreasedtheoddsthatless-competitiveapplicantswould beofferedinterviews.20
Preferencesignalingwasimplementedforthe firsttimein 2023forEM,whichwasreportedasalargelydesiredchange intheMuranoetalstudy.Programsusedthesesignalsina varietyofways;however,thepluralityofprogramsstated thatreceivingasignalmadethemmorelikelytoofferan interview.Additionally,17.8%relayedthatitmadeno differenceonthedecisiontointerview,andonly3.7%of respondingprogramleadersdidnotoptintoreceive preferencesignals.Changestopreferencesignalingforthe 2023–2024match,includingtheincreasefrom fivetoseven signalsandtheintroductionofgeographicpreference signalingmayaffecthowapplicantsandprogramsuse signaling.Futureresearchwillbeneededonpreference signalingasitevolvestoincludegeographicregionsignals insteadofsignalstargetedatindividualprogramsalone.
Othergroups,suchastheEmergencyMedicineResident Association,havespeculatedastowhyfewermedical studentsarechoosingEMastheirintendedspecialty,with workforceprojections,concernforincreasingscopegivento non-physicianpractitioners,andburnouttoppingthelist.21 Theresultsofthisstudy,whichcouldbeconsideredas consensusexpertopinion,areinagreementwithseveralof thosespeculations,withover75%ofprogramleadership believingconcernforanoversupplyofEPsistheleading causeofdecliningapplicationnumbers.Othertop contributorsfromthissurveyincludeburnout,which accordingtothemostrecentAMAsurvey,placesEMasthe specialtywiththehighestrateofburnout,with62%ofEPs reportingburnout.22 Thisdegreeofburnoutandconcern overtheworkforcelikelycontributestowhyother respondentsbelievednegativeEPmodeling(14.6%)and advisingfromEPsandmedicalschooldeans(10.2%) contributestofewerstudentschoosingEM.Itisalso importanttonotethatadifficultworkenvironment(lackof neededresources,nursinganddrugshortages,difficult interactionswithadmittingteamsandconsultants),inpatientboardingintheED,andthelong-lastingstressthat COVID-19andconcernforfuturenovelinfectiousdiseases
arealsotopreasonswhyeducationleadersbelievefewer studentsarechoosingEM.
Frequently,thesituationofEMtodayiscomparedtothe expansionofresidencypositionsinanesthesiologyinthe 1980sand1990s.Duringthattime,residencyspotsnearly quadrupled,untilconcernaboutoversupplyof anesthesiologistscauseddecreasedapplicationstothe specialtyandeventualcontractionofthenumberof spots.23,24 Similarly,decreasingthenumberofEMtrainee spotswasakeythemeforrespondentswhenquestioned aboutwhatactionstheybelievedshouldbetakentoaddress theincreasingnumberofunfilledEMpositions:25% suggestednotallowinganynewprogramstoopen;and 37.6%wantedtodecreaseeitherthenumberofoverall programsorthenumberofresidencypositions.Many (21.2%)expressedthebeliefthatincreasingtheAccreditation CouncilforGraduateMedicalEducationResidencyReview CommitteestandardsforEMisawaytoaccomplishthis.
InadditiontohaltinggrowthofEMresidencyprograms anddecreasingtheoverallnumberofEMtrainees, respondentsalsovoicedadesiretobeginapositivemessaging campaignaboutEManditsfuture,whichCORDhas alreadybegunonsocialmedia.25 Anothersuggestedaction wastocountertheAmericanCollegeofEmergency Physicians2030workforcestudy(12.5%),whichseveral othershavealreadydone,mainlycitingalowattritionratein theoriginalstudy.26 Lastly,itisimportanttonotethatthe 2024MatchresultsforEMyieldedfeweropenspotsand fewerunfilledprogramscomparedto2023.TheCORDEM MatchTaskForcehasongoingworktodeterminehow programschangedtheirrecruitmentstrategiesandhowthis couldhaveaffectedtheMatchresults,orwhetherthistruly representsanimprovementintheMatchenvironment forEM.
Thiswasavoluntarysurveysubjecttoselectionbias,as thosewithstrongneedsandopinionsweremorelikelyto completethesurvey.Inaddition,becausethissurveywas distributedbothattheCORDAcademicAssemblyand throughtheCORDPDListserv,samplingwaslimitedto thoseprogramsinvolvedwithinthisorganization.However, a55.7%responseratefromallEMprogramssuggeststhat thisdatasetrepresentsabroadarrayofprogramsandideas. DatacollectionbeganinMarch2023intheweeks immediatelyfollowingtheNRMPMatchandSOAP.While thishelpedtoincreasetheresponserateandaddedtodata validity,itmayhavemademanyofthefree-textresponses regardingactionsthatshouldbetakenmore emotionallycharged.
Finally,thispaperpresentstheopinionsandvoicesof educationalleadersinEMandmaynotrepresentthereality oftheapplicantpooltoEMresidencyorthefutureof
traininginEM.Resultsreportedhereshouldnotbetakenas advicefromCORDorfromtheEMMatchTaskForce.
Herewepresentdataregardingthe2023Match environmentforEManddescribearesidencyprogram-level needsassessmentanddesireforaction.Mostprogram leadersbelievedthatthedecreasingnumberofEM applicantswasduetoconcernovertheEMworkforce, burnoutinEM,anddifficultieswiththeworkenvironment. Amajoritywereinfavorofinterviewcaps.Programleaders alsovoicedadesireforoverallfewertrainingspotsinEM, amongseveralotherideas.AnnualreviewoftheMatchdata andresidencyprogramneedsshouldbecontinueduntil improvementoccursintheMatchenvironmentforEM.
AddressforCorrespondence:AnthonySielicki,MD,Jefferson EinsteinHospital,5501OldYorkRd.,KormanResearchBuilding Suite#B-9,Philadelphia,PA19141.Email: anthony.sielicki@ jefferson.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Sielickietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.NationalResidentMatchingProgram.NationalResidentMatching Program,resultsanddata:2021mainresidencymatch.2021.Available at: https://www.nrmp.org/wp-content/uploads/2021/08/MRMResults_and-Data_2021.pdf.AccessedMarch26,2023.
2.NationalResidentMatchingProgram.NationalResidentMatching Program,resultanddata:2022NRMPmainresidencymatch.2022. Availableat: https://www.nrmp.org/wp-content/uploads/2022/05/2022Main-Match-Results-and-Data_Final.pdf. AccessedMarch26,2023.
3.NationalResidentMatchingProgram.NationalResidentMatching Program,advancedatatables:2023mainresidencymatch.2023. Availableat: https://www.nrmp.org/wp-content/uploads/2023/03/2023Advance-Data-Tables-FINAL.pdf.AccessedMarch26,2023.
4.NationalResidentMatchingProgram.NationalResidentMatching Program,advancedatatables:2024mainresidencymatch.2024. https://www.nrmp.org/wp-content/uploads/2024/03/Advance-DataTables-2024.pdf4. AccessedJune10,2024.
5.NationalResidentMatchingProgram.NationalResidentMatching Program,advancedatatables:2019mainresidencymatch.2019. Availableat: https://www.nrmp.org/wp-content/uploads/2021/07/
NRMP-Results-and-Data-2019_04112019_final.pdf AccessedJune10,2024.
6.NationalResidentMatchingProgram.Advancedatatables:2020 match.2020.Availableat: https://www.nrmp.org/wp-content/uploads/ 2021/12/MM_Results_and-Data_2020-1.pdf.AccessedJune10,2024.
7.MarcoCA,CourtneyDM,LingLJ,etal.Theemergencymedicine physicianworkforce:projectionsfor2030. AnnEmergMed. 2021;78(6):726–37.
8.AmericanCollegeofEmergencyPhysicians.Jointstatementonthe emergencymedicine2023matchresults.2023.Availableat: https:// www.acep.org/news/acep-newsroom-articles/joint-statement-match2023.AccessedMarch26,2023.
9.MurranoT,WeizbergM,BoydB,etal.Decipheringachangingmatch environmentinemergencymedicineandidentifyingresidencyprogram needs. WestJEmergMed. 2023;24(1):1–7.
10.CouncilofResidencyDirectorsinEmergencyMedicine.EMMatchTask Force.Availableat: https://www.cordem.org/involved/task-forces/emmatch-task-force.AccessedMarch26,2023.
11.AmericanMedicalAssociation.Fellowshipandresidencyelectronic interactivedatabase(FREIDA™).Availableat: https://freida.ama-assn. org/search/list?spec=42701.AccessedMarch26,2023.
12.EmergencyMedicineResidentsAssociation.EMRAmatch.Available at: https://webapps.emra.org/utils/spa/match#/search/map AccessedMarch26,2023.
13.SocietyofUniversityOtolaryngologists.Otolaryngologypreference signaling:updates.2022.Availableat: https://opdo-hns.org/mpage/ signaling-updates.AccessedMarch26,2023.
14.PreiksaitisC,KrzyzaniakS,BowersK,etal.Characteristicsof emergencymedicineresidencyprogramswithunfilledpositionsinthe 2023match. AnnEmergMed. 2023;82(5):598–607.
15.CouncilofResidencyDirectorsinEmergencyMedicine.2023CORD statementonresidencyinterviews.Availableat: https://www.cordem. org/siteassets/files/board/adv.–position-statements/2023-cordstatement-on-residency-interviews.pdf.AccessedMarch26,2023.
16.MurphyB.4reasonsvirtualresidencyinterviewsmightbeheretostay. 2023.Availableat: https://www.ama-assn.org/medical-students/
preparing-residency/4-reasons-virtual-residency-interviews-might-behere-stay.AccessedMarch26,2023.
17.NationalResidentMatchingProgram.Chartingoutcomes:applicant surveyresultsmainresidencyMatch2023.Availableat: https://www. nrmp.org/wp-content/uploads/2023/09/NRMP-2023-Applicant-Survey. pdf.AccessedOctober16,2023.
18.RamsayN.EMMatch2020bythenumbers.Availableat: https://www. emra.org/students/newsletter-articles/em-match-2020-by-thenumbers.AccessedMarch26,2023.
19.AmericanAcademyofOphthalmology.2022adviceforthe ophthalmologyresidencymatch.2022.Availableat: https://aupo.org/ sites/default/files/2022-06/2022%20Advice%20for%20the% 20Ophthalmology%20Residency%20Match%20Season%20Slides. pdf.AccessedOctober1,2023.
20.MorganHK,WinkelAF,StandifordT,etal.Thecaseforcapping residencyinterviews. JSurgEduc. 2021;78(3):755–62.
21.MurphyJA.EMresidencyapplicationsaredown.Whatdoesthismean forourfuture?EMResident.2023.Availableat: https://www.emra.org/ emresident/article/presidents-message-january-february-march-2023 AccessedOctober1,2023.
22.BergS.These6physicianspecialtieshavethemostburnout.2023. Availableat: https://www.ama-assn.org/practice-management/ physician-health/these-6-physician-specialties-have-most-burnout AccessedOctober1,2023.
23.RevesJG,RogersMC,SmithLR.ResidentworkforceinatimeofU.S. health-caresystemtransition. Anesthesiology. 1996;84(3):700–11.
24.SchubertA,EckhoutG,CooperiderT,etal.Evidenceofacurrentand lastingnationalanesthesiapersonnelshortfall:scopeandimplications. MayoClinProc. 2001;76(10):995–1010.
25.CouncilofResidencyDirectorsinEmergencyMedicine.WhyIloveEM. 2023.Availableat: https://twitter.com/CORD_EM/status/ 1706335817331863765/photo/1.AccessedOctober1,2023.
26.GettelCJ,CourtneyDM,JankeAT,etal.The2013to2019emergency medicineworkforce:clinicianentryandattritionacrosstheUS geography. AnnEmergMed. 2022;80(3):260–71.
BrendanFreeman,DO*
LukaszCygan,DO†
LauraMelville,MD,MS†
TheodoreGaeta,DO,MPH†
SectionEditor:JeffreyDruck,MD
*StatenIslandUniversityHospital|NorthwellHealth,DepartmentofEmergency Medicine,StatenIsland,NewYork † NewYork-PresbyterianBrooklynMethodistHospital,DepartmentofEmergency Medicine,Brooklyn,NewYork
Submissionhistory:SubmittedJune14,2024;RevisionreceivedNovember8,2024;AcceptedDecember16,2024
ElectronicallypublishedJanuary30,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21139
Background: Burnoutisprevalentinmedicaltraining,andsomedataindicatescertainpersonalitytypes aremoresusceptible.ThecriterionreferenceformeasurementofburnoutistheMaslachBurnout Inventory(MBI),whichscoresthreefactors:emotionalexhaustion(EE);depersonalization(DP);and personalaccomplishment(PA).Emotionalexhaustionmostcloselycorrelateswithburnout.Studies haveyettoevaluatealinkbetweenburnoutmarkersandcertainpersonalitytraitsinemergencymedicine (EM)residents.Thepersonalitytraitsofopenness,agreeableness,extraversion,conscientiousness, andneuroticismcanbemeasuredwitha50-itemInternationalPersonalityItemPool(IPIP)Big5survey. Ourgoalinthisstudywastobethe firsttoexaminetherelationshipbetweenpersonalitytraitsand burnoutamongEMresidentsandguidefutureresearchonpotentialpredictorsofburnoutandtargeted interventionsforresidentwell-being.
Methods: Thiswasanobservational,cross-sectionalstudyconductedinMarchandAprilof2023inan urban,LevelIItraumacenter,involvingallEMresidentsatathree-yearresidencyprogram.Twosurveys, theIPIPandMBI-HumanServicesSurvey,weredistributedtoallresidents,andtheirresponseswere anonymous.Wecalculatedraw/meanscoresandstandarddeviationsforeachpersonalitytrait/burnout measureandcomparedthembythePearsoncorrelationcoefficient.
Results: All38residentscompletedthesurveys.Atotalof31%ofthecohortreportedhighexhaustion, 13%reportedhighDP,and42%reportedlowPA.Twoof38(5%)residentsreportedthecombinationof highEE,highDP,andlowPA.Therewasastatisticallysignificantnegativecorrelationbetween conscientiousnessandEE(n = 38;Pearson r = 0.40, P < 0.001)andapositivecorrelationbetween conscientiousnessandPA(n = 38;Pearson r = 0.36, P = 0.03).
Conclusion: Inoursample,residentswhoweremoreconscientiousreportedexperiencinglowerlevels ofemotionalexhaustionandagreatersenseofpersonalaccomplishment.Programsmaycautiously explorethepotentialofassessingresidentpersonalitytraitsaspartofbroadereffortstoidentify predictorsofburnout,butfurtherresearchwithlarger,multicenter,longitudinalsamplesisneededto corroboratetheseresults.Thesmallsamplesizeandsingle-centerdesignmaylimitgeneralizabilityof these findings,andtheuseofself-reportedmeasuresintroducestheriskofresponsebias.[WestJ EmergMed.2025;26(2)241–245.]
Burnouthasemergedasafocalpointformanyresidency programs,givenitspervasivenessandseveritythroughoutall phasesofmedicaltraining.1–3 Duetoprolongedexposureto elevatedstresslevels,burnoutmanifeststhroughsymptoms suchasirritability,fatigue,cynicism,anddetachment.This phenomenonholdsparticularrelevancewithintherealmof emergencymedicine(EM),a fieldknowntoreportelevated levelsofburnout.TheetiologyofthisproblemwithinEMis multifacetedandrelatedtofactorssuchasworking
environment(eg,physicallayoutandconditions, administrativetasks),shiftwork,violenceintheworkplace, exposuretoinfectiousdisease,patientvolume,clinical variability,staffing,andthelife-and-deathdecision-making inherenttothespecialty.
ThepracticeofEMhingessignificantlyupon interpersonalinteractions,addinganadditionallayerof complexitytothephenomenonofburnoutintheemergency physician.BecauseofthenatureofEM,personalitytraits mayplayamoresignificantroleinpredictingburnoutthanin othersettings.Existinginvestigationsintothisassociation aresmall-scalestudiesconductedwithnon-emergency physiciansandhaveidentifiedcorrelationsofvarious measuresofpersonalitytraitswithburnoutmarkers.4–9 In general,highneuroticism,lowagreeableness,low conscientiousness,lowopenness,andlowextraversionare associatedwithburnout.10 Whilecertainpersonalitytraits mayconferresilienceorsusceptibilitytothechallenges inherentinEM,theprecisenatureofthisrelationship remainsunderexploredwithintheEMliterature.
Thegoldstandardforburnoutmeasurementisthe MaslachBurnoutInventory(MBI),whichmeasures emotionalexhaustion(EE),depersonalization(DP),and personalaccomplishment(PA).11 Amongthese,EEhas emergedasbeingmostcloselycorrelatedwiththepresenceof burnout.12,13 Variousadaptationsofthisinventoryhave beendevisedandvalidated,ofwhich,theHumanServices Survey(HSS)isthemostapplicabletohealthcareworkers.
Personalityassessmentwithinacademicstudiesoften reliesontheframeworkofthe “BigFive” traits,delineatedby Goldberg(1992).14 Thesetraitsencompassopenness, agreeableness,extraversion,conscientiousness,and neuroticism.Opennesscanbeunderstoodonascaleof inventive/curioustoconsistent/cautious.Conscientiousness rangesfromefficient/organizedtoextravagant/careless. Agreeablenessrangesfromfriendly/compassionateto critical/rational.Extraversionisdefinedasoutgoing/ energeticvssolitary/reserved.Lastly,neuroticismranges fromsensitive/nervoustoresilient/confident.Measurements ofthesetraitshavebeenadaptedandvalidatedfor numerousresearchstudies.15–19 Oneformofthisisthe 50-itemInternationalPersonalityItemPool(IPIP) representationoftheGoldbergmarkersfortheBig-Five factorstructure.20
Whilethesepersonalitytraitsexhibitrelativestabilityand maturationbytheageof30,theirpotentialprotectiveor predictiverolesinmitigatingburnoutamongresident physiciansremainunderexplored,particularlywithinthe contextofEM.21 Thescarcityofstudiesdirectlyinvestigating thisrelationshipinemergencyphysiciansunderscoresthe imperativefordedicatedresearchinitiativesaimedat elucidatingtheinterplaybetweenpersonalitytraitsand burnoutwithinthehigh-stressenvironmentcharacteristicof EM.Consequently,ourgoalwastobethe firsttoexaminethe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Innon-emergencymedicinesettings,high neuroticism,lowagreeableness,low conscientiousness,lowopenness,andlow extraversionareassociatedwithburnout.
Whatwastheresearchquestion?
Inemergencymedicineresidents,howdothe “ BigFive ” personalitytraitscorrelatewith burnoutmarkers?
Whatwasthemajor findingofthestudy?
Conscientiousnessisnegativelycorrelated withemotionalexhaustion(Pearson r = 0.40,P < 0.001,whilepositively correlatedwithpersonalachievement (r=0.36,P=0.03,N=38).
Howdoesthisimprovepopulationhealth?
Identifyingburnout-predictivetraitscould helptargetinterventionsandsupportresident well-beingandbetterpatientcare.
relationshipbetweenpersonalitytraitsandburnoutamong EMresidentsandguidefutureresearchonpotential predictorsofburnoutandtargetedinterventionsfor residentwell-being.
Thiswasanobservational,cross-sectionalstudy conductedinMarchandApril2023thatinvolvedallEM residentsinathree-yearresidencyprogramatanurban, LevelIItraumacenter.Allresidentswereofferedinclusionin thestudyviaasinglesurveyemailedtotheirworkemails.A totalof fiveemailsweresentduringthestudymonthsfor recruitment.Nootherrecruitmentmethodswereused. Subjectswereconsentedandcompletedtwosequentialonline surveysadministeredinasinglesession:the50-itemIPIP representationoftheGoldbergmarkersfortheBig-Five factorstructureandtheMBI-HSS.Theprincipal investigator(BF)selectedtheorderofthesurveysand administeredthepersonalityassessment firsttoavoidany potentialprimingeffectsfromtheburnoutinventory. Additionally,theIPIPismoretimeintensivethantheMBI and,thus,mayrequiremoreattention.Answersweresecured andanonymous.
Wecalculatedraw/meanscoresandstandarddeviations foreachpersonalitytrait/burnoutmeasureandcompared thembyPearsoncorrelationcoefficient.Resultswere
analyzedbyBFusingMicrosoftExcel(Microsoft Corporation.Redmond,WA)andPython(PythonSoftware Foundation,Wilmington,DE).Thisstudyreceived institutionalreviewboardapproval.
All38residentscompletedbothsurveys.Themean,SD, correlationcoefficientsandconfidenceintervalsarereported inthe Table. Thirty-onepercentofthecohortreportedhigh exhaustion,13%reportedhighdepersonalization,and42% reportedalowsenseofpersonalaccomplishment.Twoof38 (5%)residentsreportedthecombinationofhighEE,high DP,andlowPA.Whiletherewerenostatisticallysignificant differencesinEE,DP,orPAacrosspostgraduateyear(PGY) levels,PGY-1residentshadhigheroverallmeanscoresofEE comparedtoPGY-2residentsandhighermeanDPscores comparedtobothPGY-2andPGY-3residents.AllPGY levelsconsistentlyreportedhighlevelsofPA.
Therewasastatisticallysignificantnegativecorrelation betweenconscientiousnessandEE(Figure1, n = 38; Pearson’ s r = 0.40, P < 0.001),whichpersistedacrossall PGYlevels.Additionally,anear-significantpositive
correlationwasobservedbetweenconscientiousnessandPA (Figure2, n = 38;Pearson’ s r = 0.36, P 0.03),whichalso persistedacrossallPGYlevels.Nootherstatistically significantcorrelationswerefoundbetweenpersonalitytraits andburnoutmeasures,regardlessofPGYlevel.Forall correlations,weconsideredBonferroniadjustment (alpha < 0.003).
Thenegativecorrelationbetweenconscientiousnessand EEsuggeststhatcertainpersonalitycharacteristicsmayserve asprotectivefactorsagainstburnoutinEMresidents.This findingisconsistentwithpreviousresearchconductedin variousoccupationalsettings.21 Conscientiousindividuals tendtobediligent,organized,andachievementoriented, traitsthatmaybufferagainsttheemotionaltollof demandingworkenvironments.InthecontextofEMwhere residentsarefrequentlyexposedtohigh-stresssituationsand longhours,theabilitytomaintainorderandefficiencyin theirworkmaycontributetolowerlevelsofEE. Furthermore,eventhoughitwasnotbelowtheBonferroni adjustedalpha,therewasanear-significantpositive
Table. Correlationcoefficientmatrixwithconfidenceintervalscomparingtheburnoutfactorsofemotionalexhaustion,depersonalization,and personalaccomplishmentwith fivekeypersonalitytraits.
Valuesinsquarebracketsindicatethe95%confidence intervalforeachcorrelation.* = P < 0.05. EE,emotionalexhaustion; DP,depersonalization; PA,personalaccomplishment.
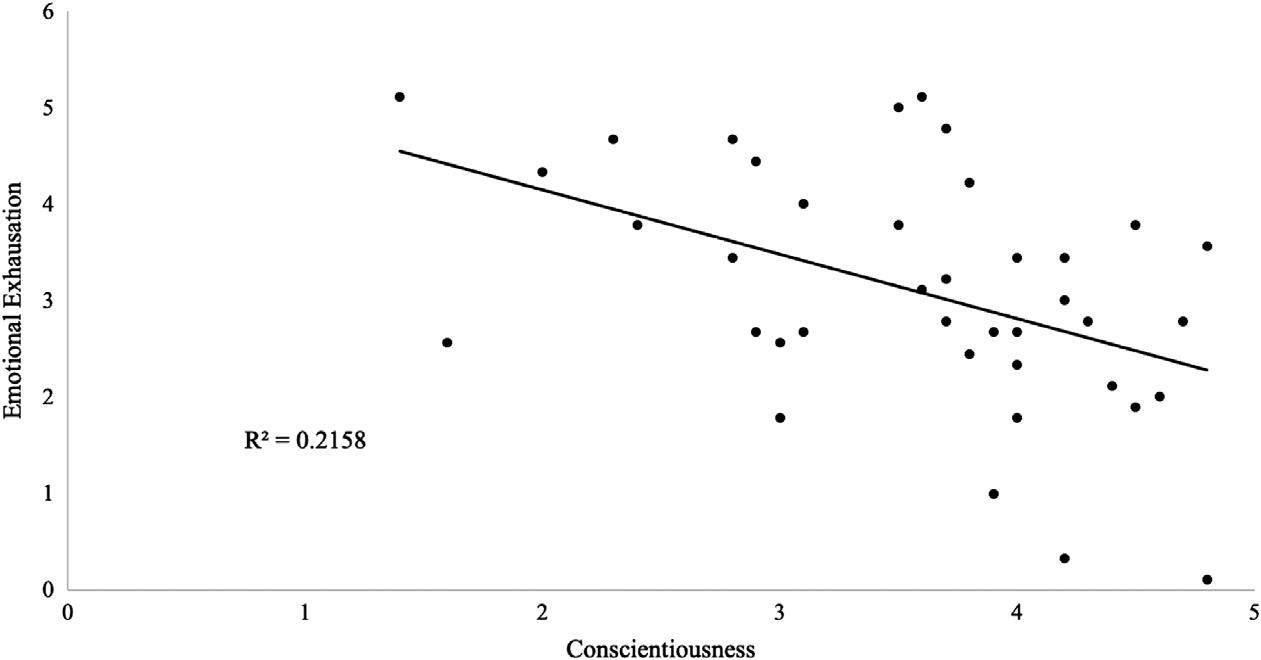
Figure1. Negativecorrelationbetweenconscientiousnessandemotionalexhaustioninemergencymedicineresidents(n = 38;Pearson’s r = 0.40, P < 0.001).
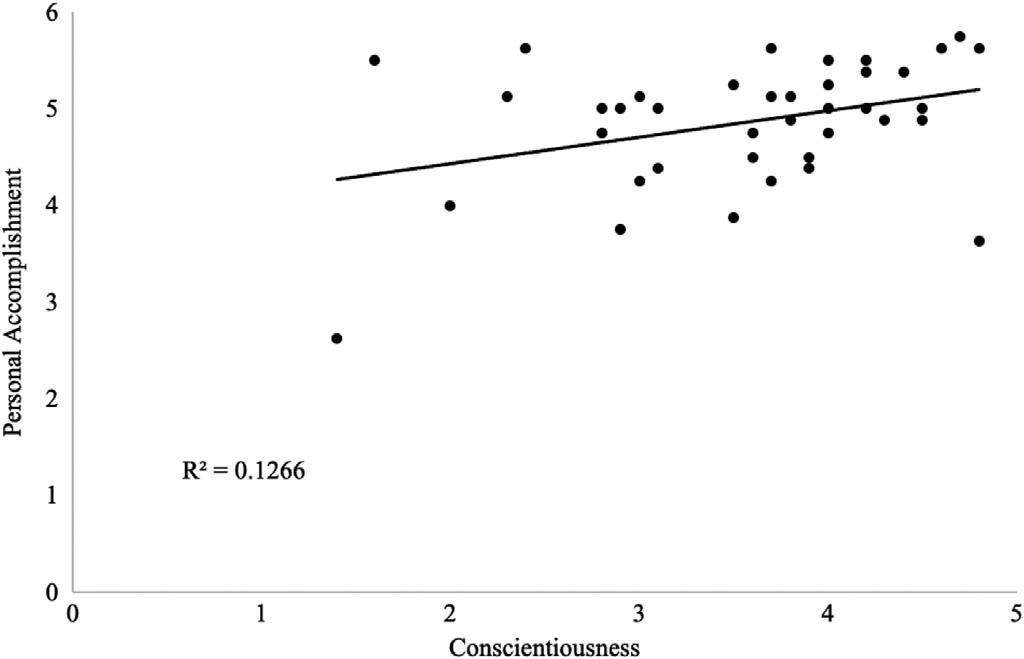
Figure2. Positivecorrelationbetweenconscientiousnessandsense ofpersonalaccomplishmentinemergencymedicineresidents (n = 38;Pearson’s r = 0.36, P = 0.03).
correlationbetweenconscientiousnessandsenseofPA, whichseemstosuggestthatcultivatingthesetraitsin residentsmayevenbeprotectiveofburnoutandcontributeto personalandprofessionalsatisfactionandcareerlongevity.
Takentogether,theseresultsofferactionableinsightsthat residencyleadershipcanleveragetosupportthewell-being andresilienceofEMresidents.Specifically,theidentification ofconscientiousnessasaprotectivefactoragainstEE suggeststhatinterventionsaimedatfosteringconscientious behaviorsamongresidentsmayhelpmitigatetheriskof burnout.Conscientiousnesshasbeenidentifiedasatraitthat canbeenhancedwithinterventionssuchasmindfulnessand life-skillstraining.22,23 Moreresearchisneededtodetermine whichinterventionsaremosteffectiveanddurable,but residencyprogramscouldconsiderincorporatingtargeted trainingsessionsorworkshopsfocusingonorganizational skills,time-managementstrategies,andstress-management techniquestocultivateconscientioustraitsamongresidents. Additionally,whileweusedanonymousdatainthisstudy, residencyleadershipmayconsiderimplementingpersonality traitassessmentsaspartofconfidentialresidentevaluations oronboardingprocesses.Occultburnoutmaypresentwith poorperformanceorevenunprofessionalbehavior.Thus, personalitytraitassessmentcouldbeusedtoinitiate conversationsaboutburnout.
Whilepersonalitytraitsmayplayaroleinshaping individuals’ susceptibilitytoburnout,organizationalfactors, workload,supportsystems,andcopingmechanismsalso exertsignificantinfluences.Futureresearchshouldaimto explorethesemultifacetedinteractionscomprehensively, incorporatinglongitudinalstudiestotrackthetrajectoriesof burnoutandpersonalitydevelopmentovertimeastheyrelate toEMresidents.Additionally,qualitativeresearchmethods couldprovidevaluableinsightsintothesubjective experiencesofresidentsandthecontextualfactorsthat contributetoburnoutinEMtrainingprograms.
Whilethisstudyprovidesvaluableinsightsintothe relationshipbetweenpersonalitytraitsandburnoutamong EMresidents,itrepresentsjustonefactoramongmany. Addressingburnoutinthispopulationrequiresa multifacetedapproachthatconsidersbothindividual characteristicsandsystemicfactorswithintheresidency educationenvironment.Bygainingadeeperunderstanding ofthesedynamics,wecandevelopmoreeffective interventionstosupportthewell-beingandresilience ofEMresidents.
Thesmallsamplesizeandsingle-centerdesignlimitthe generalizabilityofthe findingstoresidentsinothersettings, suchasruralorcommunityhospitals.Selectionbiasisalsoan importantconsiderationasresidentsmayhavechosenthis specificprogrambasedonindividualpreferences,suchas geographiclocation,whichcouldintroducevariability unrelatedtoclinicalexperienceorprogramtype.Thetiming ofthestudywaschosentoalignwitharelativelylowerperiod ofstressinourresidencyprogramacrossallPGYlevels,but theresultsmaydifferbetweentheperiodsofthesame academicyear,calendaryear,orclinicalrotations. Additionally,responsebiasisafactor,asthemeasures evaluatedhereareself-reportedandparticipants’ responses maynotaccuratelyreflecttheirtruecharacteristics.More longitudinaldatawillbeneededtofullyunderstandthe natureofthecorrelationsbetweenburnoutscoresand personalitytraitsobservedinthiscross-sectionalstudy.
Inoursample,residentswhoweremoreconscientioushad lowerlevelsofemotionalexhaustionandagreatersenseof personalaccomplishment.Programsmaycautiouslyexplore thepotentialofassessingresidentpersonalitytraitsaspartof broadereffortstoidentifypredictorsofburnout,butfurther researchwithlarger,multicenter,longitudinalsamplesis neededtocorroboratetheseresults.
AddressforCorrespondence:BrendanFreeman,DO,StatenIsland UniversityHospital|NorthwellHealth,DepartmentofEmergency Medicine,475SeaviewAvenue,StatenIsland,NY,10305.Email: bfreeman@northwell.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Freemanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GopalR,GlasheenJJ,MiyoshiTJ,etal.Burnoutandinternalmedicine residentwork-hourrestrictions. ArchInternMed. 2005;165(22):2595.
2.IsHakWW,LedererS,MandiliC,etal.Burnoutduringresidency training:aliteraturereview. JGradMedEduc. 2009;1(2):236–42.
3.OgundipeOA,OlagunjuAT,LasebikanVO,etal.Burnoutamong doctorsinresidencytraininginatertiaryhospital. AsianJPsychiatry. 2014;10:27–32.
4.AlarconG,EschlemanKJ,BowlingNA.Relationshipsbetween personalityvariablesandburnout:ameta-analysis. WorkStress. 2009;23(3):244–63.
5.BabazadehM,MolavynejadS,BereihiF,etal.Relationshipbetween personalitytraitsandburnoutinoncologynurses. JFamMedPrimCare. 2019;8(9):2898.
6.McManusIC,KeelingA,StressPaiceE.Burnoutanddoctors’ attitudes toworkaredeterminedbypersonalityandlearningstyle:atwelveyear longitudinalstudyofUKmedicalgraduates. BMCMed. 2004;2(1):29.
7.MorganBanddeBruinK.Therelationshipbetweenthebig five personalitytraitsandburnoutinSouthAfricanuniversitystudents. SAfr JPsychol. 2010;40(2):182–91.
8.RippJ,BabyatskyM,FallarR,etal.Theincidenceandpredictorsofjob burnoutin first-yearinternalmedicineresidents:a five-institutionstudy. AcadMed. 2011;86(10):1304–10.
9.LindemanB,PetrusaE,McKinleyS,etal.Associationofburnoutwith emotionalintelligenceandpersonalityinsurgicalresidents:canwe predictwhoismostatrisk? JSurgEduc. 2017;74(6):e22–30.
10.AngeliniG.BigFivemodelpersonalitytraitsandjobburnout:a systematicliteraturereview. BMCPsychol. 2023;11(1):49.
11.MaslachCandJacksonSE.Themeasurementofexperiencedburnout. JOrganBehav. 1981;2(2):99–113.
12.MaslachCandLeiterMP.Earlypredictorsofjobburnoutand engagement. JApplPsychol. 2008;93(3):498–512.
13.GarzaJA,SchneiderKM,etal.Burnoutinresidency:astatewidestudy. SouthMedJ. 2004;97(12):1171–3.
14.GoldbergLR.Thedevelopmentofmarkersforthebig-fivefactor structure. PsycholAssess. 1992;4(1):26–42.
15.GoldbergL.Internationalpersonalityitempool.2019.Availableat: https://ipip.ori.org/.AccessedJanuary10,2024.
16.EhrhartKH,RoeschSC,EhrhartMG,etal.Atestofthefactorstructure equivalenceofthe50-itemIPIP five-factormodelmeasureacross genderandethnicgroups. JPersAssess. 2008;90(5):507–16.
17.McCraeRRandJohnOP.Anintroductiontothe five-factormodelandits applications. J Pers. 1992;60(2):175–215.
18.JudgeTA,HellerD,MountMK.Five-factormodelofpersonalityandjob satisfaction:ameta-analysis. JApplPsychol. 2002;87(3):530–41.
19.KimHJ,ShinKH,SwangerN.Burnoutandengagement:acomparative analysisusingtheBigFivepersonalitydimensions. IntJHospManag. 2009;28(1):96–104.
20.AdministeringIPIPmeasures,witha50-itemsamplequestionnaire. Availableat: https://ipip.ori.org/New_IPIP-50-item-scale. htm#SampleQuestionnaire.AccessedJanuary10,2024.
21.TerraccianoA,McCraeRR,CostaPT.Intra-individualchangein personalitystabilityandage. JResPers. 2010;44(1):31–7.
22.KrasnerMS,EpsteinRM,BeckmanH,etal.Associationofan educationalprograminmindfulcommunicationwithburnout,empathy, andattitudesamongprimarycarephysicians. JAMA. 2009;302(12):1284–93.
23.RobertsBW,LuoJ,BrileyDA,etal.Asystematicreviewofpersonality traitchangethroughintervention. PsycholBull. 2017;143(2):117–41.
MatthewT.Singh,MD*†
DavidM.Austin,PhD‡
StephanieC.Mullennix,MSN†
JoshuaC.Reynolds,MD*†
J.AdamOostema,MD*†
SectionEditor:JeffreyDruck,MD
*CorewellHealth/MichiganStateUniversityCollegeofHumanMedicine, GrandRapids,Michigan
† EmergencyCareSpecialists,GrandRapids,Michigan ‡ GrandValleyStateUniversity,GrandRapids,Michigan
Submissionhistory:SubmittedMay21,2024;RevisionreceivedNovember20,2024;AcceptedNovember22,2024
ElectronicallypublishedFebruary5,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.21227
Introduction: Throughouttraining,anemergencymedicine(EM)residentisrequiredtoincrease efficiencyandproductivitytoensuresafepracticeaftergraduation.Multitaskingisoneofthe22 AccreditationCouncilforGraduateMedicalEducation(ACGME)EMmilestonesandisoftenmeasured throughevaluationsandobservation.Providingquantitativedatatobothresidentsandresidency administrationonpatientsseenperhour(PPH)andefficiencycouldimprovearesidentexperienceand traininginmanyways.Ourstudywasdesignedtoanalyzevariousthroughputmetricsandproductivity trendsusingappliedmathematicsandarobustdataset.Ourgoalsweretodefinethecurveofresident PPHovertime,adjustforrelevantconfounders,andanalyzeadditionalefficiencymetricsrelatedto throughputsuchasdoor-to-decisiontime(DTDT).
Methods: Weusedaretrospective,observationaldesigninasingle,tertiary-carecenteremergency department(ED)thatseesapproximately110,000adultpatientsperyear;ourstudyspannedtheperiod July1,2019–December31,2021.Atotalof42residentsfromanACGME-accreditedthree-year residencywereincludedintheanalysis.Weexcludedpatients <18yearsofage.Datawascollected usingasecuredatavendor,andwecreatedanexponentialregressionmodeltoassessresidentPPH data.Additionalmodelswerecreatedaccountingforpatientcovariates.
Results: Weanalyzedatotalof79,232patientsover30months.Usinganexponentialequationand adjustingforpatientcovariates,medianPPHstartedat0.898andendedat1.425PPH.ThemedianPPH bypostgraduate(PGY)yearwere1.13forPGY1;1.38forPGY2;and1.38forPGY3.MedianDTDTin minuteswasasfollows:185minutesforPGY1;171forPGY2;and166forPGY3.
Conclusion: ProductivityandefficiencymetricssuchasPPHandDTDTdataareanessentialpartof workinginanED.Ourstudyshowsthatresidentsimprovewithnumberofpatientsseenperhourover threeyearsbuttendtoplateauintheirsecondyear.Door-to-decisiontimecontinuedtoimprove throughouttheirthreeyearsoftraining.[WestJEmergMed.2025;26(2)246–253.]
Asaspecialtydedicatedtoacute,unscheduledcare,the practiceofemergencymedicine(EM)demandsthat cliniciansnotonlypracticeexceptionalmedicineaddressing awidevarietyofcomplaintsbutdosoquicklyandefficiently. Theseskillsareimportantinthesettingofincreasingpatient
volumesandillnessseverity1 aswellasthedownward pressuresonEMreimbursement.2 Initspositionstatement onemergencydepartment(ED)staffingmodels,the AmericanCollegeofEmergencyPhysiciansemphasizedthat determiningappropriateandsafestaffingmodelsrequiresan understandingofemergencyclinicianefficiency.3 Efficiency
metricsareusednotonlytoensureadequatestaffingbutalso foremergencyphysicianreimbursement.4 Despitethecentral importanceofphysicianefficiencyinclinicalpractice,EM residencyprovideslittlestructurededucationregarding efficiency,andmanyresidentbehaviorsmayaffect efficiency.5 Moreover,despitetheuseofrobusttoolstoassess EMresidentmedicalknowledge,clinicalreasoning,and interpersonalcommunication,residentefficiency assessmentsarelargelybasedonsubjectiveevaluationsfrom supervisingphysicians.6
Althoughefficiencyisanimportantaspectofpracticing EM,currentliteraturesuggeststhatthereiswidevariability inthemeasuresusedtoassessclinicianefficiency.Inarecent scopingreviewbyAnjumetal,patientvolumeand processingtimeweretwoofthemostcommonlyreported metricstoassessproductivityandefficiency,respectively.7 Providingquantitativeresidentproductivityandefficiency datamayhelpwiththeclinicalgrowthofresidentsandhelp residencyadministrationstructurestaffingandcurriculato betterprepareresidentsfortheirfuturepractice.Objective measurementsofproductivitymayallowforimplementation ofinterventionsandsupportforresidentswhoare performingbelowtheirpeersandprovidebettercustomized learningexperiencesforhigherperformingresidents.8 It couldalsohelpresidencyclinicalcompetencycommittees (CCC)toassessresidentmilestoneachievementandensure graduatingresidentsarereadyforindependentpractice.9 Finally,understandingtherangeandnormaltrajectoryof residentefficiencymetricsmaybeusefultoinformstaffing modelchangesintheEDormeasuretheimpactofefficiencyfocusedcurricula.10
Previousstudieshaveexaminedresidentefficiencywith regardtonumberofpatientsseenperhour(PPH)and relativevalueunits;however,manyofthestudieswere performedoveradecadeagobeforetheadventofaccurate electronichealthrecord(EHR)data.11,12 Thereisalackof dataregardingtheshapeofresidentproductivityand efficiencygrowthoverthecourseoftrainingandtheeffectof patientmixonefficiency.Toaddressthisknowledgegap,we usedalargeadministrativedatasettoestimateresident productivityandefficiencyoverthecourseoftrainingwith thegoalofdefiningacurveofresidentproductivityaswellas estimatingvariabilitybetweenresidentsoverthecourseof theirtraining.
StudyDesign
InthisretrospectiveobservationalstudyweestimatedEM residentproductivityandefficiencyinacohortofconsecutive adultEDpatientsoverthecourseof30monthsfrom July1,2019–December31,2021.TheSpectrumHealth InstitutionalReviewBoardexemptedthisstudyasaquality improvementproject.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencymedicine(EM)residentsare expectedtogrowinbothef fi ciencyand productivityduringtraining.
Whatwastheresearchquestion?
CanapredictivemodelofEMresident productivityandef fi ciencygrowthbede fi ned?
Whatwasthemajor findingofthestudy?
Patientsseenperhourplateaued:PGY1, 1.13;PGY2,1.38,andPGY3,1.38.Decision times(inminutes)continuedtoimprove: PGY1,185;PGY2,171;andPGY3,166.
Howdoesthisimprovepopulationhealth?
EnsuringthatEMresidentsaretrainedin bothef fi cientandproductivepatientcareis essentialtoprovidesafeandeffectivecare.
Thisstudywasconductedinasingle,regional,tertiarycarecenterED,whichisaLevelItraumacenterand comprehensivestrokecenter.Ithasanannualvolumeof approximately110,000adultpatientsperyearandregional populationofoveronemillion.Patients <18yearsofageare nottreatedinthisED;theyaretransportedtotheadjacent children’shospitalunlesstheyrequireemergentstabilization. Weexcludedfromouranalysisanypatient <18yearsofage inthedataset.ApproximatelyhalfoftheEDfootprintis staffedbyEMresidents,whopreferentiallyseehigheracuity, morecomplexcaseswithanaverageadmissionrateof42%. Theresidencyprogramisathree-yeartrainingprogram accreditedbytheAccreditationCouncilofGraduate MedicalEducation.TheEMresidentsworkanaverageof15 eight-hourshiftspermonthatthisfacility.Onshift,residents areresponsiblefordirectpatientcarewithattending oversight.Seniorresidentsdonotdirectlysupervisemore juniorresidents.Asresidentsprogressintopostgraduateyear (PGY)2andPGY3,theyareexpectedtoseehigheracuity patientsandmorecomplexity.Non-EMresidentsworkon thistrainingsitebutaccountforlessthan20%ofthetotal residentsandwerenotincludedinthisanalysis.
WeusedanadministrativedatasetthatincludesallED visitsatthestudyhospital.Thisiselectronicallyextracted fromthehospitalEHRandcontainspatient-level
demographics,limitedclinicaldata,throughputmetrics, testingdetails,disposition,andtreatingclinicians.We includedalladultpatientstreatedbyatleastoneEMresident duringanEDvisit.WeexcludedpatientencountersfornonEMresidentsorpatientswhohadnoresidentcontact.
Eachpatientinthedatasetwasassignedtothe first residentwhoprovidedtheirclinicalcare.Theprimary exposureofinterestwasresidentexperienceasmeasuredby elapsedmonthoftraining(1–36).Residentexperiencewas codedatthecaselevelforeachencounterbycalculatingthe differencebetweenthecalendarmonthofthevisitandthe calendarmonththeresidentstartedresidency.Covariates includedpatientage,sex,EmergencySeverityIndex(ESI) triageacuity,attendingofrecord,and finaldisposition (admissionvsdischarge).Theprimaryproductivityoutcome wasnumberofpatientsseenperhour(PPH).Becausethe administrativedatasetdidnotcontainresidentshiftlengths, wedefinedshiftsbygroupingconsecutivecasesseenbyeach residentuntiltherewasafour-hourgapbetweenregistration times.WecalculatedPPHbydividingthisnumberofcases bytheaverageshiftlengthforresidents(eighthours).The primaryefficiencyoutcomewasdoor-to-decisiontime (DTDT),definedasthetimeinminutesbetweenEDarrival todispositiondecision(placementofanadmissionor dischargeorder)astime-stampedintheEHR.
Weexaminedassociationsbetweenresidentmonthof trainingandthetwoprimaryoutcomesusingmixed-effects regressionmodelstoaccountfordifferencesincasemixand toquantifythevariationinPPHthatmaybeattributableto theindividualresidentsorattendings.Inthesemodels, residentexperience(inmonths),patientage,sex,ESItriage acuity,andadmissionstatusweretreatedaspatient-level fixedeffectswhiletheresidentandattendingcaringforthe patientweretreatedascrossedrandomeffects.This approachwasusedbecauseresidentsworkwithvarious attendingsandviceversa.Thesemodelsallowforestimation ofassociationsbetweenpatient-levelcharacteristicsand residentproductivityaswellasquantifyingthecontribution ofresident-andattending-levelvariabilityusingthe intraclasscorrelationcoefficient(ICC).Thisstatisticmaybe understoodastheproportionofvariationineachoutcome thatisexplainedbyapatientbeingcaredforbyanindividual residentorsupervisedbyanindividualattending.This analysiswasthenrepeatedforeachpostgraduateyearof trainingtoexaminewhethertheresident-levelvariability differedoverthecourseoftraining.Additionally,togain someunderstandingintovariabilityovertime,modelswere repeatedinsampleslimitedtoeachpostgraduateyear.
Next,usingexponentialregressionwedeveloped figures demonstratingthetrajectoryofresidentproductivity(PPH)
andefficiency(DTDT)overthecourseoftraining.Wethen developedmodelsusingresidentexperiencelevelasalone predictorvariableaswellasmodelsaccountingforpatientlevelcovariates(patientage,ESItriageacuity,andadmit status).WedevelopedexponentialmodelsusingPython’ s scriptlibrary(PythonSoftwareFoundation,Wilmington, DE)andmixed-effectsregressionmodelsusingStataversion 15(StataCorp,CollegeStation,TX).
Atotalof79,232patientsencountersthatinvolveda residentwereidentifiedover30monthsfromJuly1, 2019–December31,2021.Thesamplecontained42distinct residentswhoworkedanestimated8,378shiftsand accountedfor806resident-monthsoftraining. Characteristicsofthepatientpopulationandtheanalyzed residentsarepresentedin Table1 and Table2,respectively.
Thebivariateassociationsbetweentheexposuresand residentproductivityaswellastheresultsofmultivariable mixed-effectsregressionmodelsarepresentedin Table3 Patient-levelfactorsassociatedwithreducedPPHincluded older age,ESIacuitylevels2and3(comparedtoacuitylevel 1),andhospitaladmission.Patientfemalesexdemonstrated nostatisticallysignificantassociationwithhigherPPHin eitherunadjustedoradjustedmodels.Residentexperience waspositivelyassociatedwithPPHsuchthateachonemonth ofincreasedexperiencewasassociatedwith0.016additional patientsseenperhour(P < 0.001).Furthermore,while presenceofasupervisingattendingexplainedverylittleofthe
Table1. Characteristicsofthepatientpopulation.
PatientcharacteristicsPatientencountersN = 79,232(%)
ESItriageacuity
Level4 2,887(3.7)
Level5 270(0.3)
EDdisposition
Admit 29,734(38.9)
Discharge
ED, emergencydepartment; ESI,EmergencySeverityIndex.
Table2. Characteristicsofresidentpopulation.
–1.6)
–1.4)
–1.6) PGY-3
–1.8)
MedianresidentDTDT(minutes) 174(113–247)
PGY-1 185(123–254)
PGY-2 171(119–245)
PGY-3
–240)
PGY, postgraduateyear; PPH,patientsperhour; DTDT,door-todecisiontime.
Resultsofthebest-fitexponentialmodelofresident productivityovertimearepresentedin Figure1.Resident productivityincreasesmostrapidlyduringthe first12 monthsofresidencywithlittlemeaningfulchangebeyondthe beginningofPGY-2year.Thisrelationshipwasconsistent evenafteraccountingforpatient-levelcovariates(age,sex, ESItriageacuity).
Bivariateassociationsbetweentheexposurevariablesand DTDTandtheresultsofmultivariablemixed-effects regressionmodelsarepresentedin Table4.Aswithmodelsof residentproductivity,age >60yearsofagewasassociated withreducedefficiency(longerDTDT),aswasESItriage acuity2–4andhospitaladmission.FemalepatientshadasixminutelongerDTDTcomparedtomales(P < 0.001).When examininggroup-levelcontributionstovariabilityin DTDT,neitherattending(ICC = 0.008)norresident (ICC = 0.012)accountedforameaningfulproportionof observedvariability.
variabilityinthenumberofPPH(ICC = 0.036),residentof recordaccountedforover14%ofPPHvariability (ICC = 0.145).Resident-levelICCstatisticschangedlittle acrossmodelslimitedtoeachpostgraduateyear(ICC0.19, 0.23,and0.15forPGY1,2,and3).Whiledirectstatistical comparisonsoftheseICCswerenotpossible,PGY-2 residentsdemonstratedthenumericallygreatestbetweenresidentvariability.
Resultsforexponentialmodelsofresidentefficiency overtimearepresentedin Figure2.Therateofchange observedinDTDTwaslessthanandmoregradual thanthenumberofPPHoverthecourseofresidency
Table3. Mixed-effectsregressionmodelsdemonstratingassociationsbetweenpatientcharacteristicsandresidentproductivityasmeasured bypatientsseenperhour.
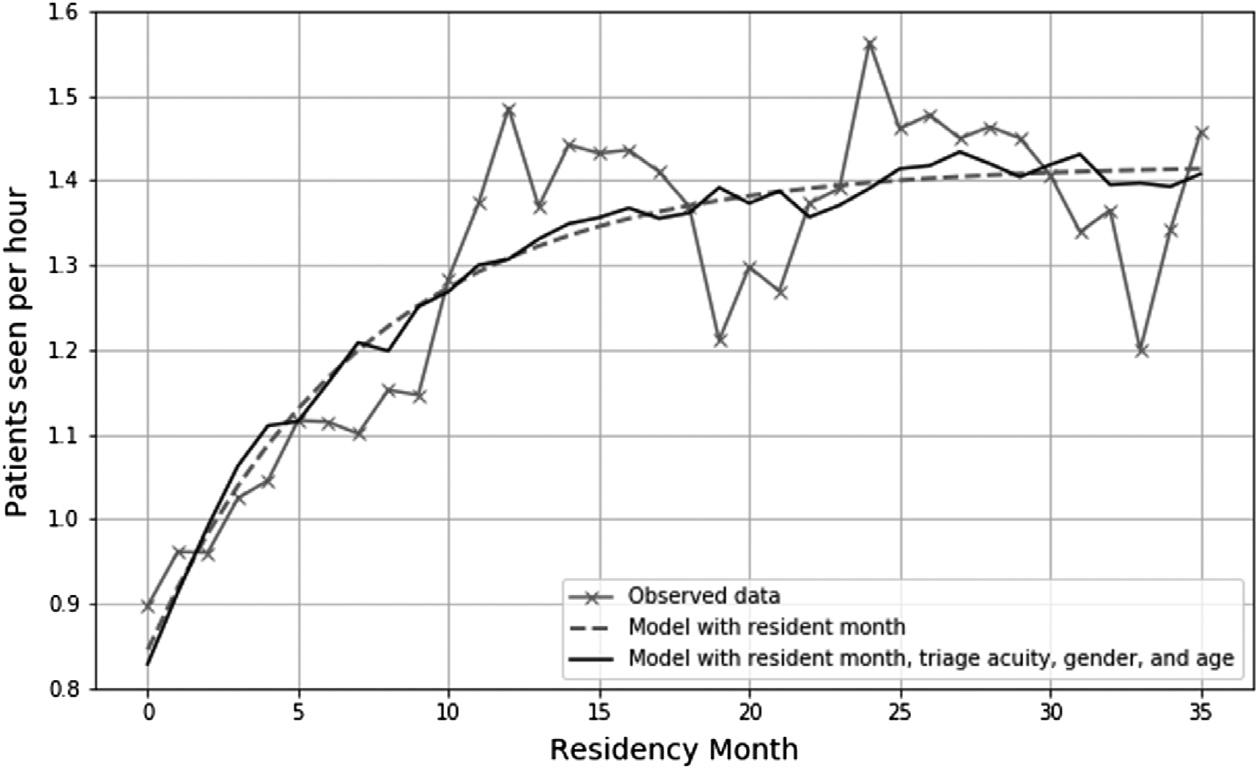
Residencyproductivitymeasuredbypatientsseenperhouroverthecourseoftraining.
training,withimprovementlevellingoffduringthe PGY-3year.
Throughouttraining,EMresidentsmustdevelopskillsin managingthecomplexneedsofmultiplepatientssuchthat theybecomebothproductiveandefficient.Theseskillsare undoubtedlyimportantandarelogicalelementstoevaluate overthecourseofresidencytraining.Nevertheless,few existingcompetenciesaddresstheseaspectsofpractice directly,andtheirassessmentisprimarilydependentupon
subjectiveevaluationbyattendingphysicians.Inthisanalysis wesoughttoquantifyresidentproductivityandefficiencyin ourinstitutionoverthecourseofresidencytrainingthrough examiningthenumberofPPHandDTDT.
Weobservedthatresidentproductivityincreases dramaticallyduringthe firstyearofresidencybutlevelsoff earlyinthePGY-2year,similartoplateausdescribedin previousstudies.12–14 Patient-levelfactorssuchasolder-age patientsrequiringhospitaladmissionwereassociatedwith lowerPPH,whilepatientstriagedaslowerESIacuity (especiallylevels4and5)wereassociatedwithhigherPPH
Table4. Mixed-effectsregressionmodelsdemonstratingassociationsbetweenpatientcharacteristicsandresidentefficiencyasmeasured bydoor-to-decisiontime.
ESI, EmergencySeverityIndex; ICC,intra-classcorrelationcoefficient.
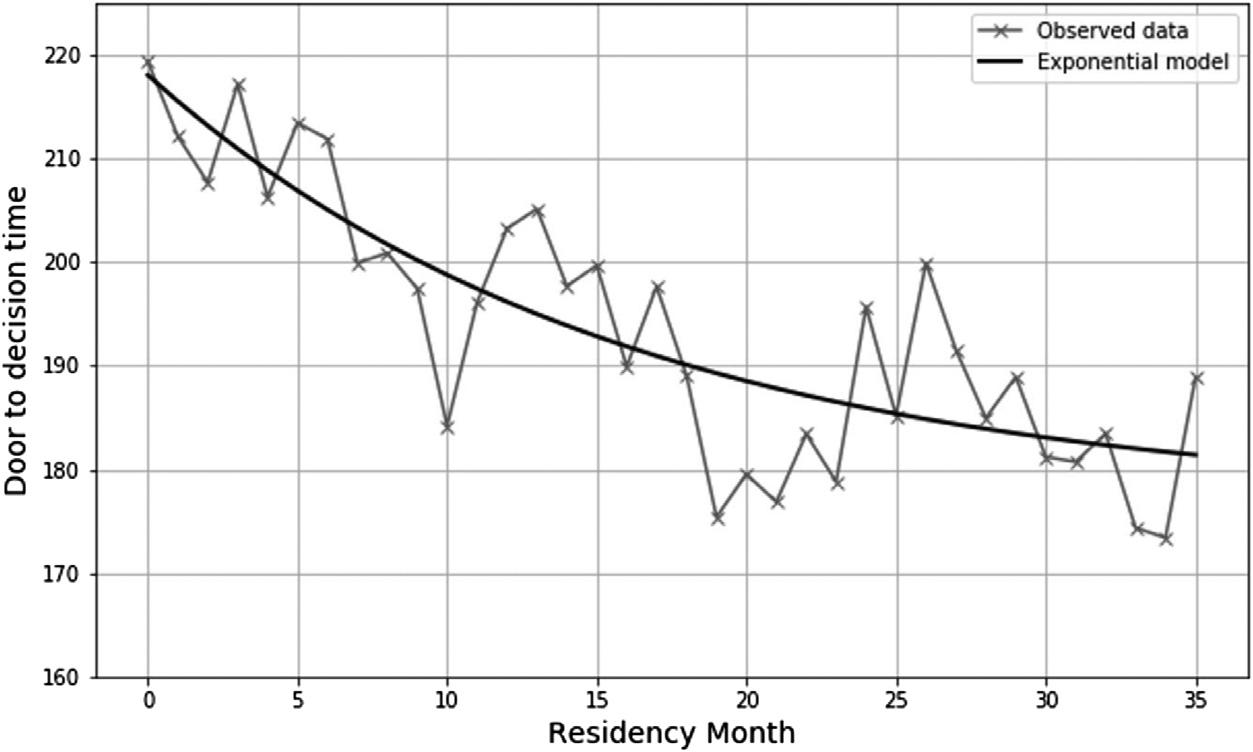
Residencyproductivitymeasuredbydoor-to-decisiontimeoverthecourseoftraining.
similartoattending-basedstudiesofPPHbyJosephetal.15 Afteraccountingfortheserelationships,theindependent associationbetweenexperienceandproductivitywas actuallystronger,suggestingthatresidentsbecomemore efficientoverthecourseoftrainingwhilealsoseeingamore difficultcasemix.
Wealsoobservedsignificantbetween-residentvariability. Overall,individualresidentsaccountedforover14%of observedvariationinPPHafteraccountingforpatient-level factors,whileattendingphysicianscontributedverylittle (3.6%).Furthermore,thedegreeofvariabilityattributableto individualresidentsafteraccountingforcasemixwashighest forPGY-2residents,butloweramongPGY-1andPGY-3 residents.Thismaysuggestthatresidentsbeginandendtheir trainingatsimilarlevelsofproductivitybutmayreachtheir plateauatdifferentpointsduringPGY2.These findings suggestthatproductivityisinpartanattributeofindividual residentsratherthancasemixorattendingstaffingpractices. Thus,theremaybearolefordesigningeducation interventionsforresidentswhodemonstratelower productivitybytheendofPGY1.Whileproductivity appearstobeanattributeofresidentsthemselves,the improvementinICCmaysuggestthatresidencytraining doeshelptoreduceperformancevariabilitytosomedegree.
Toexamineresidentefficiency,wechosetoevaluate DTDTratherthanotherthroughputmakerssuchasED lengthofstay,sinceDTDTismorelikelytoreflectresident behaviorratherthansystemfactorssuchasstaffingandED boarding.IncontrasttoPPH,thismetricdidnotplateau earlyinresidencybutrathercontinuedtoimproveoverthe courseofaresident’straining.AswithPPH,patient-level factorsweresignificantlyassociatedwithlongerDTDT, includingolderage,ESItriageacuity2and3,andadmission status.Relativetootherpatient-levelfactors,resident experiencelevelhadamoremodestrelationshipwithDTDT suchthataresident’sexperiencealoneaccountedforan
approximate15-minutereductionoverthe36monthsof training.Furthermore,incontrasttoPPH,only1%ofthe unexplainedvariationinDTDTwasattributabletothe residentprovidingcare(ICC = 0.012),andalmostnoneofit wasattributabletothesupervisingattending(ICC = 0.008). ThismaybepartiallyexplainedbythefactthatPPHisa metricthatisinherentlytiedtoresidents,resultingingreater between-residentvariation.Nevertheless,itisalsolikelytrue thatstructurallimitations(eg,timetolabresults, timetoconsultantphonecallreturn)resultingreater homogenyincompletingEDworkupsthatmayexplainthis lowerlevelofbetween-residentvariabilitywithregard toDTDT.
Usingthisdatafromthisanalysisraisesnumerous opportunitiesforresidencyadministrationandassisting residentsinmaximizingtheirperformanceandgrowth. RecognizingthatthereisaplateauinthenumberofPPH duringtrainingcouldhelpwithstaffingmodelstoensure appropriateresidentcoverageandmanageexpectations.One potentialopportunitytoleveragedatamightbeforresidency programstomonitortheirproductivitydataseveraltimes duringanacademicyeartoensurethattheirresidentsare progressingappropriatelyalongthedescribedcurve. Residentswhoarenotshowingappropriategrowthbythe endofPGY1maybenefitfromtailoredinterventionsor individualizedlearningplans.Anotherconsideration relevanttobothproductivityandefficiencymaybeto provideresidentswiththeirownperformanceonthese metricsinrelationtotheirpeers.Inourinstitution,ourCCC reviewsresidentproductivitydatasuchasPPHandDTDT twiceperyearforeachresidencyclass.Thisinformationis deidentifiedanddistributedtoeachresidenttoreviewwith theirfacultyadvisorandprogramdirector.Thisinformation isfrequentlyusedtodevelopindividualizedlearningplansto helpwiththeirpatientefficiencyandoftenusedtoadvance theirACGMEpatientcare-relatedmilestones.
Giventhatthiswasanobservationalanalysis,itis importanttoacknowledgethatthesemodelsdonotprovea causalrelationshipbetweenanyofthepotentialpredictorsof PPHorDTDTandtheirrespectiveoutcomes.WhilePPH andDTDTarerecognizedbenchmarksinmanyEDs,itis alsoimportanttorememberthatthereareotherwaysto defineproductivityandefficiency,andseveralpotential confoundersmayexistinthisdataset.16 Moreadvanced residentsmayusetheirtimeinotherwayssuchaspeer-topeerteaching,managingalargervolumeof “signed-out” patients,moreefficiencywithon-shiftdocumentation,and lesstimespentcontinuingpatientcareaftertheirshifthas ended.Thesepossibilitiesmaynottiedirectlytopatient productivitybutmayprovidevalueforboththeresidency andtheindividualizedlearner.Itiscertainlypossiblethatthe typesofpatientscaredforbyseniorresidentstendedtobe morecomplexevenafteraccountingforESItriageacuity, resultinginresidualconfounding.Furtherstudiescould evaluatesomeofthesevariablestoaccountforwhyresident efficiencytendstoplateauwithnumberofPPHintheir secondyearofresidency.
Additionally,whileourmethodofreconstructingshifts basedonpatientregistrationtimeslikelyresultsina reasonablyaccuratesummary,itremainspossiblethatsome patientswereincorrectlyassignedtoashiftresultingin under-oroverestimationofresidentproductivity.Finally, ourinstitutiondivertsloweracuitypatientstoa “fast-track” areathatisnotstaffedbyresidents.Thislikelyaccountsfor thedistributionofESItriageacuityandadmissionrates, whicharehigherthanageneralEDpopulation.Thus,the absoluteproductivitynumbersshouldbeinterpretedwith caution,anditisdifficulttoknowhowtheseresultsmay compareacrossinstitutions.
Anotherimportantconfounderthatmayreducethe generalizabilityofthisanalysisistheimpactoftheCovid-19 pandemic.Giventhatourdatasetincludesperiodsimpacted byCOVID-19,itispossiblethatthismayhaveinfluenced residentproductivityandefficiency.17 Therearemitigating factorsthatsuggestouranalysiswasnotadverselyaffected bythepandemic.First,sinceouranalysisisdefinedbymonth ofexperienceratherthancalendartime,theimpactof COVID-19wasspreadequallyamongtrainingmonths. Second,duetothemodulestructureofourdepartment,the teachingmoduleispreservedforhigher-acuitycomplaints andislessimpactedbylowEDvolumesorboardingpatients thanotherlocationsintheED.Weexaminedoverallresident patientsandPPHoverthecalendardurationofthestudy periodandfoundnomeaningfulrelationshipbetween COVID-19andnon-COVID-19periods(supplemental figure).Finally,residentswerenotrestrictedfrommanaging patientsundertheinvestigationofCOVID-19.
Lastly,itmustbeemphasizedthatproductivityand efficiency,whileimportantskillstotheemergencyclinician,
shouldnotsupplantorovershadowthemanyothercritical skillsthatrequireattentioninresidencysuchasacquisitionof medicalknowledge,effectivecommunication,andthe deliveryofcompassionate,empathetic,andequitable patientcare.
Thisanalysisconfirmsthatresidentproductivityand efficiencyimproveoverthecourseofresidencytraining. Similartothe findingsofpreviousresearch,productivityas measuredbynumberofpatientsseenperhourappearsto advancemorequicklyandreachaplateaubythePGY2year.However,efficiencyasmeasuredbydoor-to-decision timeimprovesoverthecourseoftraining.These relationshipspersistfollowingadjustmentforpotential patient-levelconfoundersand,inthecaseofPPH,are associatedwithindividualresidents.Interestingly,attending variabilityhaslittleeffectonPPH.These findingssuggest thatassessmentofthesemetricsperiodicallyduringresidency maybehelpfulintailoringeducationalinterventionstoassist residentsindevelopingtheseskills.Furtherstudyisneededto verifythese findingsanddeterminetheimpactof interventionsdesignedtomodifyresidentproductivityand efficiencyduringtraining.
AddressforCorrespondence:MatthewT.Singh,MD,Corewell Health/MichiganStateUniversity,CollegeofHumanMedicine,4100 EmbassyDrSE,Suite400,GrandRapids,MI49546.Email: matthew.singh@corewellhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Singhetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.MohrNM,WessmanBT,BassinB,etal.Boardingofcriticallyill patientsintheemergencydepartment. CritCareMed. 2020;48(8):1180–7.
2.WelchS.StrategiestohelpyourEDadapttovariablevolumesand patientneeds.2024.Availableat: https://www.acepnow.com/article/ strategies-to-help-your-ed-adapt-to-variable-volumes-and-patientneeds/
3.Staffingmodelsandtheroleoftheemergencydepartmentmedical director.2024.Availableat: https://www.acep.org/patient-care/policystatements/staffing-models-and-the-role-of-the-emergencydepartment-medical-director/
4.ACEPrespondstomajorannualMedicareproposedregulation impactingphysicianpayments.2024.Availableat: https://www.acep. org/federal-advocacy/federal-advocacy-overview/regs–eggs/regs–eggs-articles/regs–eggs september-8-2022/
5.EganHM,SwansonMB,IlkoSA,etal.High-efficiencypracticesof residentsinanacademicemergencydepartment:amixed-methods study. AEMEducTrain. 2020;5(3):e10517.
6.AmericanCollegeofEmergencyPhysicians.Emergencymedicine providerproductivity:aninformationpaper.2024.Availableat: https:// www.acep.org/siteassets/uploads/uploaded-files/acep/clinical-andpractice-management/resources/administration/ep_provider_ prod_ip_final_0909.pdf
7.AnjumO,YadavK,ChhabraS,etal.Definitionsandfactorsassociated withemergencyphysicianproductivity:ascopingreview. CJEM. 2023;25(4):314–25.
8.BeesonMS,CarterWA,ChristopherTA,etal.Thedevelopmentofthe emergencymedicinemilestones. AcadEmergMed. 2013;20(7):724–9.
9.CooneyRR,MuranoT,RingH,etal.Theemergencymedicine milestones2.0:settingthestagefor2025andbeyond. AEMEducTrain. 2021;5(3):e10640.
10.ShiberJandFontaneE.Progressionofemergencymedicineresident productivity. AcadEmergMed. 2008;15(1):107.
11.FredetteJ,KimT,McHughD,etal.Adescriptiveanalysisofemergency medicineresidentproductivityoverthecourseoftraining. AEMEduc Train. 2021;5(Suppl1):S44–8.
12.BrennanDF,SilvestriS,SunJY,etal.Progressionof emergencymedicineresidentproductivity. AcadEmergMed. 2007;14(9):790–4.
13.Turner-LawrenceDandToddBR.Monthlyprogression ofemergencymedicineresidentefficiency:whatcanwe expectofourresidentsthroughouttraining? JEmergMed. 2019;57(1):77–81.
14.JosephJW,HenningDJ,StrouseCS,etal.Modelinghourly residentproductivityintheemergencydepartment. AnnEmergMed. 2017;70(2):185–90.e6.
15.JosephJW,DavisS,WilkerEH,etal.Modellingattendingphysician productivityintheemergencydepartment:amulticentrestudy. Emerg MedJ. 2018;35(5):317–22.
16.DentonCA,SoniHC,KannampallilTG,etal.Emergencyphysicians’ perceivedinfluenceofEHRuseonclinicalworkflowandperformance metrics. ApplClinInform. 2018;9(3):725–33.
17.BoserupB,McKenneyM,ElkbuliA.TheimpactoftheCOVID-19 pandemiconemergencydepartmentvisitsandpatientsafetyinthe UnitedStates. Am JEmergMed. 2020;38(9):1732–6.
CorlinM.Jewell,MD* Guangyu(Anthony)Bai,MD†
DannJ.Hekman,MS*
AdamM.Nicholson,MD*
MichaelR.Lasarev,MS‡ RoxanaAlexandridis,PhD‡ BenjaminH.Schnapp,MD,MEd*
*UniversityofWisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,Madison,Wisconsin † IndianaUniversitySchoolofMedicine-Northwest,Gary,Indiana ‡ UniversityofWisconsinSchoolofMedicineandPublicHealth,Departmentof BiostatisticsandMedicalInformatics,Madison,Wisconsin
SectionEditors:EdUllman,MD,ChristineStehman,MD,andDougFranzen,MD
Submissionhistory:SubmittedFebruary25,2024;RevisionreceivedNovember20,2024;AcceptedNovember22,2024
ElectronicallypublishedJanuary31,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20282
Introduction: Patientsseenperhour(PPH)isapopularmetricforemergencymedicine(EM)resident efficiency,althoughitislikelyinsufficientforencapsulatingoverallefficiency.Inthisstudyweexplored therelationshipbetweenhigherpatientcomplexity,acuityonshift,andmarkersofclinicalef ficiency.
Methods: Weperformedaretrospectiveanalysisusingelectronichealthrecorddataofthepatientsseen byEMresidentsduringtheir finalyearoftrainingwhograduatedbetween2017–2020atasingle,urban, academichospital.WecomparedthenumberofPPHseenduringthethird(final)yeartopatientacuity (EmergencySeverityIndex),complexity(CurrentProceduralTerminologycodes[CPT]),propensityfor admissions,andgeneratedrelativevalueunits(RVU).
Results: Atotalof46residentswereincludedintheanalysis,representing178,037totalcases.The numberofPPHincreasedfrom firsttosecondyearofresidencyandfellslightlyduringthethirdyearof residency.Overall,foreach50%increaseintheoddsoftreatingapatientrequiringhigh-levelevaluation andmanagement(CPTcode99215),therewasa7.4%decreaseinmeanPPH.Each50%increasein oddsoftreatingacaserequiringhospitaladmissionwasassociatedwitha6.7%reduction(95% confidenceinterval[CI]0.73–12%;P = 0.03)inmeanPPH.Each0.1-pointincreaseinPPHwas associatedwitha262(95%CI157–367;P < 0.001)unitincreaseinaverageRVUsgenerated.
Conclusion: Seeingagreaternumberofpatientsperhourwasassociatedwithalower volumeofcomplexpatientsandpatientsrequiringadmissionamongEMresidents.
[WestJEmergMed.2025;26(2)254–260.]
The2019AmericanBoardofEmergencyMedicineModel ofClinicalPracticerecognizestask-switchingandmultiple patientcareascorephysiciantasks,1 andtheAccreditation CouncilforGraduateMedicalEducation(ACGME)lists multitaskingasEmergencyMedicinePatientCareMilestone 7.2 Emergencyphysicians(EP)mustefficientlyevaluateand treatahighvolumeofpatientstoeffectivelymanagecarein theemergencydepartment(ED).Variousmetricshavebeen
usedtoevaluateefficiencyandqualityofcareprovidedinthe EDbytheEDstaffaswellasindividualEPs(patientlength ofstay,EDadmissionrate,etc).3,4 Ametriccommonlyused byprogramstomeasureefficiencyinresidentsisthenumber ofpatientsseenperhour(PPH).Thismetricisenticing becauseitisbasedondatathatiseasilyretrievableand widelyapplicableacrossclinicalsites.5,6 However,itis currentlyunclearwhetherthenumberofPPHcanadequately encapsulateefficiencyinphysiciantrainees.Itisalso
uncertainhowresidencyprogramsshouldconsiderthis metricwhenassessingtheirtrainees,especiallyifnot consideredalongsideothermetrics.
Aphysician-in-trainingwhoseesmorePPHcould potentiallybeseenasmorecapableofindependently managingthehighernumberofpatientsrequiredfor independentpractice.Thismeasurementisalready commonlyusedwhenevaluatingEMresidentsandisalso frequentlyusedtoevaluateattendingEPs.5,6 However,itis unclearwhethertherearetradeoffsforresidentsthatcome withseeingahigherpatientvolume.Itislikelythatmedical traineesareonlyabletohandlea finitenumberofcognitive tasksbeforetheirperformanceisimpairedandtheyare unabletotakeonadditionaltasks.
Onemethodtoconceptualizetherelationshipbetween howpatientcomplexityandacuityimpactsotheraspectsof patientcareisthroughcognitiveloadtheory.7 Ingeneral, whencognitiveloadistoohigh,suchasincreasedextraneous loadfrommanagingmultiplepatientsorincreasedintrinsic loadfrommanagingverycomplexpatients,overallcognitive performancemaybeimpaired.Thiscoulddecreasecognitive bandwidthfornewpatient-caretasksaswellaslimitgermane loadtoallowforlearningandillness-schemecreation.7 Conversely,simple,straightforwardpatientpresentations maynotimposesuchasignificantcognitiveload,allowing cognitiveresourcestobedeployedtoseeahighervolumeof patients.8,9 Priorstudieshaveassessedresidentefficiencyin theEDintermsnumberofPPHastrainingprogresses.10 Thesestudieshavedemonstratedthatseniorresidentscansee highernumbersofpatientsperhourcomparedto postgraduateyear(PGY)-1residents,whichplateausinthe finalyearoftraining.11
Comparedtoadvancedpracticepractitioners(APP) (physicianassistants[PA]ornursepractitioners),residents seefewerPPHbutgenerateahigheramountofrelativevalue units(RVU).Thissuggestsresidentsmayseehigheracuity patientsordocumentmorethoroughly.10 TheRVUsarean objectivemeansofmeasuringtheresourcesneededto providemedicalcareasasinglemetric.12 Anothermeansof estimatingtheresourcesneededtoprovidecareareED evaluationandmanagement(E/M)CurrentProcedural Terminology(CPT)codes.Theseallowcoderstouse complexityindocumentationasasurrogatemarkerof complexityofcareprovided.WhileRVUsandCPTcodes aremeasuresassignedfollowingapatient’sED encounter,theEmergencySeverityIndex(ESI)isameansof estimatingtheacuityofthepatientintermsof priorityandresourcesallocationbasedontheir initialpresentation.
Itiscurrentlyunknownhowpatientcomplexityandacuity mayimpactmarkersofclinicalefficiencyforEDresidents. Ouraiminthisstudywastobetterevaluatethisrelationship usingmultiplemetricstoallowresidencyleaderstobetter contextualizegreaterresidentefficiencyintheED.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Patientsseenperhour(PPH)iscommonly usedbyprogramstomeasureef fi ciencyin residents.Itisunclearwhetherthisadequately encapsulatesef fi ciency.
Whatwastheresearchquestion?
Cantheuseofmultipleclinicalmetricsallow programstobettercontextualizethemeaning ofresidentef fi ciencyintheED?
Whatwasthemajor findingofthestudy?
Foreach50%increaseintheoddsoftreatinga high-complexcase,therewasa7.4% (0.79 – 13.6%;P = 0.03)decreasein meanPPH.
Howdoesthisimprovepopulationhealth?
ResidentswhoseemorePPHmaynottreatas manycomplexpatients,whichcouldhave implicationsfortheirreadinessfor independentpractice.
Thestudywasconductedatasinglethree-yearEM residencyprogramassociatedwithanurban,academicED locatedintheMidwesternUS.ThehospitalinwhichtheED issituatedisaLevelIadultandpediatrictrauma,burn, stroke,andSTEMIcenter.TheEDhas43adultbedsand seesapproximately60,000patientvisitsperyear.Duringthe studyperiod,theresidencyhad12PGY-1positions eachyear.
TheadultEDisdividedintothreeseparatetreatment areaswithtwoprimarytreatmentteams.Eachtreatment teamconsistsofasingleattendingphysiciansaswellas2–3 PAsorresidentphysicians.Shiftsareninehoursinduration. Throughoutmostofthestudyperiod,patientsweretreated bytheteamofphysiciansdesignatedtothattreatmentarea. In2019,theEDshiftedtoamodelinwhicheithertreatment teamcouldcareforanypatientineithertreatmentarea.Each treatmentteamisstaffedbyresidentsofanyPGYlevelwith atleastoneseniorresident(PGY-2orPGY-3).Allresidents wereencouragedtoassignthemselvestopatientsofany acuitylevel.Duringthestudy,PAswereemployedintheED andcouldtaketheplaceofaresidentonshift(especially duringweeklyresidentdidactics).TheAPPshadno additionalrestrictionsorprivilegescomparedtoresidentsin assigningthemselvestopatients.
Asstaffingisvariable,therearenospecificnumberof patientsthateachresidentisrequiredtoseepershift.All residentsstaffdirectlywiththeattending;noresidents superviseotherresidents.Duringexpectedpeaktimes(of patientarrival),atriageteamconsistingofasingleattending physicianandaPAisalsopresentandgenerallyseesthe lowestacuitypatients;allresidentsareassigned approximatelythesamenumberofshiftsbutmayfreely tradeshiftsamongthemselves.Whileattendingphysicians canassignthemselvestopatientsprimarily(ie,noresidentor APPassigned),thisisarareoccurrenceandtypicallyoccurs onlyduringtimesofexcessivepatientvolumeoracuity.
Wedesignedthisstudyasaretrospectiveobservational studyusingaggregated,residentcasedataextractedfromthe electronichealthrecord(EHR)(EpicSystems,Verona,WI). DataforPGY1–3residentswereextractedforfour consecutiveclassesofresidentswhograduatedbetween 2017–2020.Toremovesignificantoutliersweexcluded residentsiftheydidnotgraduatefromtheprogramwithin threeconsecutiveyears.Wecollecteddataonthe characteristicsofthepatientsseenaswellasmarkersof residencyefficiencyforallavailablepatientencounters duringthestudyperiod(Table1).Multiplemetricswereused toprovideamoreaccuratemeasureofpatientcomplexity ratherthanasinglemetricinisolation.Theresearchteam wascomposedofaseniorresident(TB)andadepartmental dataanalyst(DH),aswellasfacultyeducators(CJ,AN,BS). Wechosetheselectedmarkersastheyhavebeenusedas markersofresidentclinicalefficiencyinotherstudies.6,10
Patientcarewasattributedtothe firstassignedresident,as thisresidentistypicallythemostcognitivelyandpractically involvedinthepatient’scare.Patientswhoaresignedoutto anoncomingEDteamaresharedequallyamongall oncomingresidents.Weexcludedpediatricpatient
encounters(ie,patients <18yearsofage)aspediatriccases havesubstantialdifferencesintermsoftheresourcesand cognitiveloadrequiredtoprovideadequatecare.Therefore, itwasdeterminedthatthechosenefficiencymetricscouldnot bemeaningfullycomparedtoadultpatientencounters.13 For example,theaveragelengthofstaybetweenpediatricand adultencountersduringthestudyperiodwas219vs362 minutes.Overthecourseoftheirtraining,residentscomplete adedicatedblockofpediatricEDshiftsduringtheir firstand secondyearsandcompleteanadditional1–3pediatricED shiftsduringeachadultEDrotation.Wecalculatedthe percentageofpatientencounterscomparedtooverall patientencounters.
Giventheaggregatednatureofthedatathatdidnot containanypatientprotectedhealthinformationor identifyingresidentdata,noinformedconsentwascollected. ThedatawasextractedfromtheEHRbythedepartmental dataanalystandwasstoredonapassword-protected departmentalserveravailableonlytomembersofthestudy team.Noadditionalchartreviewwasconductedonthe includedencounters.Thisstudywasdeterminedtobequality improvementandexemptfromformalreviewbyour institutionalreviewboard.
WecalculatedthePPHforeachPGY-3residentbyusing thetotalnumberofadultpatientencountersforwhichthey werethe firstresidentassigned,dividedbythetotalnumber ofhoursworkedintheadultsectionoftheED.Residents weregroupedbasedontheyearofgraduation.Atwo-sided significancelevelof P < 0.05wasusedforallstatisticaltests. WeperformedallstatisticalanalysesandgraphicsusingR version4.1.1(RCoreTeam,RFoundationforStatistical Computing,Vienna,Austria).Weusednegativebinomial regressiontoassesstherelationshipbetweenPPHandthe oddsoftreatingapatientwhorequiredadmission,adjusted
Table1. Emergencymedicineresidentmetricsofefficiencyandthecharacteristicsofpatientsseen.
Patientcharacteristics
Emergency SeverityIndex(ESI)
Evaluationandmanagement(E/M)Current ProceduralTerminology(CPT)codes
Hospitaladmission
Efficiencymetrics
Relativevalueunits(RVU)
Patientsseenperhour
ED, emergencydepartment; PGY,postgraduateyear.
FrequencyofpatientencountersmatchingeachESIscore(1–5).Thisisameans ofestimatingtimeandresourceallocationforapatientbasedontheir initialpresentation.
FrequencyofpatientencountersreceivingeachE/MCPTcode(99281–99285). Theserepresentameansofdeterminingpatientcomplexitybasedonmeeting certaindocumentationcriteria.
Numberofpatientencountersinwhichaninpatientadmissionoccurred
TotalnumberofworkRVUsgenerated
TotalnumberofpatientsseendividedbytotalnumberofhoursworkedintheED duringPGY-3
forhoursworkedandpatientcomplexity.Allanalyseswere performedattheresidentlevel.
TodeterminetherelationshipbetweenESIandPPH,we firstdichotomizedESIintohighandlowseverity.High severityincludedencountersfromthethirdyearofresidency thatwerelabeledESI1and2andlowseverityincluded encountersthatwerelabeledESI3,4,and5.TheESI1 encounterswerenotseparatelyanalyzedastheseare relativelyrarecomparedtotheoverallnumberofpatient encounters.Wethencalculatedtheoddsoftreatingapatient withahigh-severityESI.TherelationshipbetweenCPT codesandPPHwassimilarlycalculatedbydichotomizing CPTintomoreandlesscomplex.Morecomplexincludedthe highestcomplexityCPTcode(99285),andlesscomplex includedtheremainingfourcodes(99281–99284).Wedid notconsiderCPTcode99291asonlyattendingscanbillfor criticalcare,andthereissignificantvariationwithinour attendinggroupintheuseofcriticalcarebilling.Therefore, webelievedthatthiswaslesslikelytobearesident-sensitive metric.Wesimilarlycalculatedtheoddsoftreatingapatient withamorecomplexCPT.Toassesssignificantdifferences amongPGYthatcouldintroducebias,weusedthe Kruskal-WallistestandtheNemenyiprocedurefor post-hoccomparisons.14
WeusedRVUsasaproxyforshiftcomplexityand regressedthatastheresponseinamultivariableregression modelusingPPH,PGY,andtheinteractionbetweenPPH andPGYasexplanatoryvariables.
Atotalof46residentsmetinclusioncriteria.Oneresident wasexcludedwhohadanon-consecutivetrainingperiod, andanotherresidentlefttheprogrampriortograduationat theendoftheirPGY-1year.Overall,1.6%ofthetotalpatient encounterswereassigned99291/99292CPTcodesandwere excludedfromthatanalysis.Anadditional17.6%oftotal patientencounters,consistingofpediatriccases,werealso excluded,leavingatotalof178,037patientencounters. AveragePPHdataforthefourincludedPGYscanbeseenin Table2.TheaverageESIduringthestudyperiodwas2.8.
Adjustedforclassyear,a50%increaseintheoddsof treatingacomplexcasewasassociatedwiththemeanPPH decreasing7.42%(95%confidenceinterval[CI]0.79–13.6% reductioninmeanPPH; P = 0.03).Therelationshipbetween PPHandoddsoftreatingahigh-complexitycasecanbeseen in Figure1
Each50%increaseinoddsoftreatingacaserequiring hospitalorintensivecareunit[ICU]/intermediatecareunit admissionwasassociatedwitha6.7%(95%CI0.73–12%; P = 0.03)reductioninmeanPPH.Therelationshipbetween
Table2. Patientsseenperhourdataforclassyears2017–2020. ClassyearAcademicyearMeanPPH(95%CI) 2017 2014–2015 PGY-11.20(1.13–1.28)
2015–2016PGY-21.51(1.42–1.61)
2016–2017PGY-31.52(1.43–1.62) 2018 2015–2016PGY-11.11(1.05–1.16)
2016–2017PGY-21.50(1.43–1.58)
–2018PGY-31.45(1.39–1.52)
2017PGY-11.08(1.03–1.13)
–2018PGY-21.37(1.31–1.44) 2018–2019PGY-31.26(1.21–1.32)
–2018PGY-11.01(0.96–1.05) 2018–2019PGY-21.33(1.28–1.39) 2019–2020*PGY-31.09(1.04–1.14)
*MayhavebeenimpactedbytheCOVID-19pandemic. CI, confidence interval; PPH,patientsseenperhour; PGY, postgraduateyear.

Figure1. Relationshipbetweenoddsoftreatingahigh-complex caseandmeanpatientsseenperhourduringpostgraduateyear-3, groupedbygraduationyear.Shadedregionsrepresent95% confidenceintervals. CPT,CurrentProceduralTerminology.
PPHandoddsoftreatingacaserequiringadmissioncanbe seenin Figure2.
AftercontrollingforPGY,therewasnosignificant relationshipobservedbetweenPPHandtheoddsoftreating ahighacuitycase(P = 0.30).
Themodelssuggestedthateach0.1pointincreaseinPPH isassociatedwitha262unitincrease(95%CI157–367; P < 0.001)inaverageworkRVUsgenerated,withtheassociation betweenaveragetotalRVUandPPHstableacrossthefour years.See Figure3 fortherelationshipbetweenRVUs generatedandPPH.
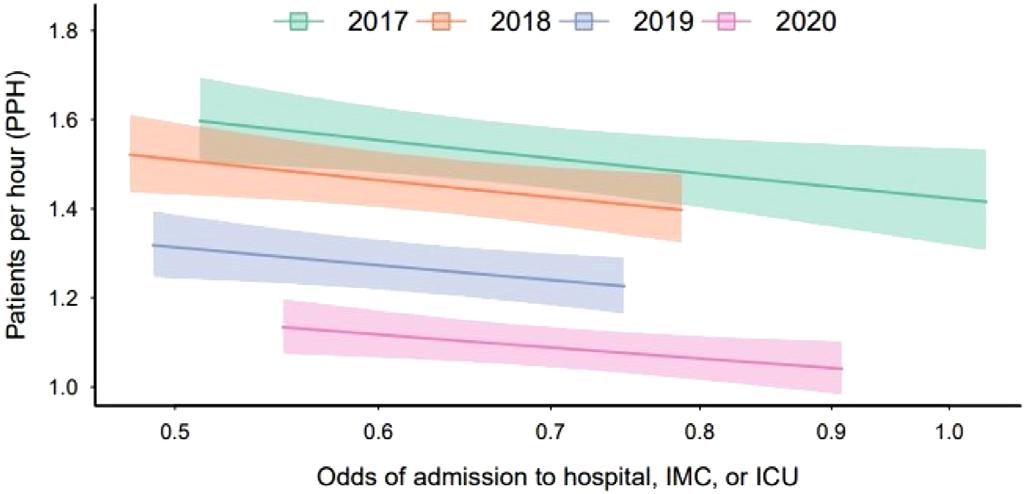
Figure2. Relationshipbetweenoddsofacaseresultingin admissionandmeanpatientsseenperhourduringpostgraduate year3,groupedbygraduationyear.Shadedregionsrepresent95% confidenceintervals.
IMC,intermediatecareunit; ICU,intensivecareunit.
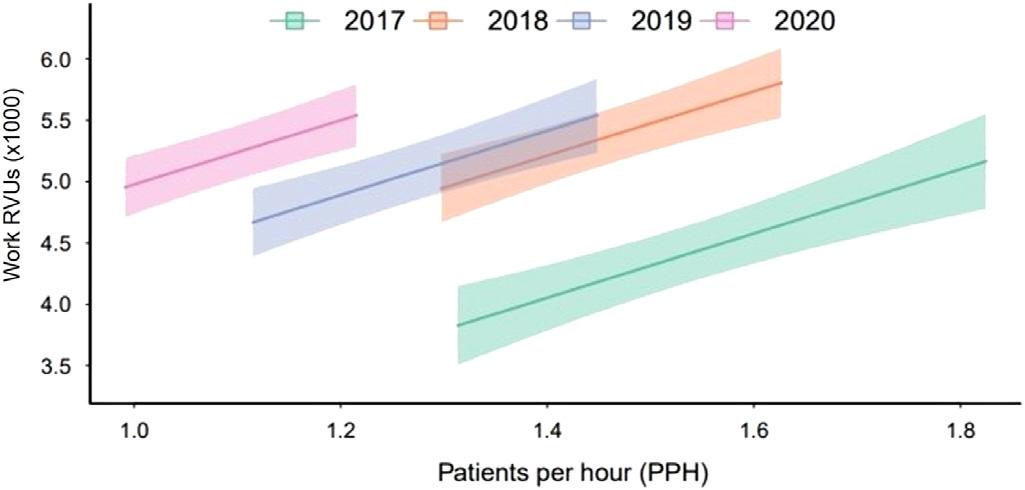
Figure3. Therelationshipbetweenrelativevalueunitsgenerated andpatientsseenperhourduringpostgraduateyear3, groupedbygraduationyear.Shadedregionsrepresent95% confidenceintervals.
RVU,relativevalueunits.
Residentsseeinghighernumbersofpatientssawfewer complexpatientsandfewerpatientsrequiringaninpatient admission.Webelievethisstudyisthe firsttoexaminethe associationofpatientcomplexityandacuityontheclinical efficiencywithwhichEMresidentsoperate.Assuggestedby cognitiveloadtheory,wefoundthatresidents’ capacityto pickupcomplexpatientsinthisstudywas finite.More complexpatientsandpatientsrequiringadmissionmay imposemoreofataskload(eg,phonecallstoconsultantsor admittingphysicians,reviewofrecords,orlongerhistorytaking)thanpatientswithloweracuity.Thisgreater cognitiveloadcouldresultinadecreaseinPPHas complexitygoesup.Thiseffectmaybemitigatedsomewhat byavarietyofeffectiveclinicalpractices,suchaspartnering withnursesorassistancefromtheirsupervisingattending. However,moreresearchisneededtodeterminewhether otherfactors,suchastheincorporationofevidence-based efficiencypracticesoraddingscribesfordocumentation,may affectresidentefficiency.
OurdatashowsthatPPHrisessharplybetweenPGY-1 and-2yearsandthenplateausbetweenthePGY-2and3years.This findingisinlinewithpreviousliterature.11 Whiletheunderlyingcauseofthis findingisultimately unknown,itmaybesecondarytochangesinfocusthatoccur betweenthelatteryearsintraining.Forexample,anyfurther increasesintheabilityofPGY-3residentstoseeadditional patientsoveraPGY-2residentmaybeoffsetbyafocuson departmental flow,instructionofjuniorlearners,orsimply succumbingto “senioritis.” Itisalsopossiblethatthemost seniorresidentspreferentiallyselectedthemostcriticallyill patientsintheEDandtheincreasedcomplexityofthese patientswerethereasonfortheplateau.
WefoundnosignificantrelationshipbetweenPPHand ESI.However,therewasanegativerelationshipwhen evaluatingPPHandCPTcodesaswellasthelikelihoodof caringforapatientwhowouldneedtobeadmitted.Thismay bebecauseESIisassignedatthebeginningofthepatient’ s treatmentcourse,whereasCPTdesignationandadmission decisionsaremadelaterinthepatient’scourse(orafterthe conclusionoftheencounterinthecaseofCPT).TheESIwas alsotreatedasabinaryvariableforanalysis,withESI3 treatedasalow-acuitypatient.However,manyofthese patientsmayhaveahigheracuityillness;itispossiblethat thisdichotomizationeliminatedatrueeffectthatwould otherwisehavebeenseen.Therefore,itcouldreflectthatESI couldnotbeusedtoaccuratelyestimatetheamountof resourcesandcognitiveeffortrequiredtocarefor thesepatients.15
Whilewedidnotanalyzetherelationshipbetweenpatient complexityandoverallgenerationofRVUs,itremainsan interestingavenueforfutureresearch.Whileitmakes intuitivesensethatthecareofasingle,morecomplexpatient wouldgeneratemoreRVUsthanasingle,lesscomplex patient,itisunknownwhetherRVUgenerationisbalanced bytheincreasedamountoftimeandcognitiveloadthese patientsoftenrequire.Thiswasnotdoneinthecurrentstudy asthiswouldalsohavedependedonhospitalcrowding, whichisaconfoundingvariablewechosenottoinclude.
Overall,ourresultssuggestthattheuseofPPHasa surrogatemeasureofpatientefficiencymaypaintan incompletepictureofresidentperformance.Whilethe currentstudydiddemonstrateastatisticallysignificant relationshipbetweenpatientcomplexityandPPH,the clinicalsignificanceisunclear.Therequirednumberof patientsseenduringtrainingrepresentsacritically unexploredareaofresidencytraining.Experientiallearning theorywouldsuggestthatseeingagreaternumberofpatients wouldresultinahigherlevelofcompetence,butthismaybe mediatedbycomplexityorotherfactors.Residency leadershipteamswhoplantoevaluatetheirresidentsontheir abilitytotaskswitchbetweenmultiplepatients(ACGME MilestonePC7)maywishtoexploretheuseofothermarkers thatmaycorrelatewithPPH.Thesemaybettercapturethe
complexityofthecareprovided,althoughfurtherstudyis requiredbeforethiscanbeconsideredbestpractice.
Animportantlimitationofthisstudyisitssingle-center design.Theresultsseenmaybeduetouniquefactorsofthe studysiteand,therefore,maynotbegeneralizabletoother sites.Forexample,thestudysitechangedfromapod-based modelin2019,whichmayhaverestrictedtheefficiencyof someresidents,toa “free-for-all” modelwhereresidents couldassignthemselvestonewpatientsassoonastheywere ready.Additionally,theremayhavebeensubtlechangesto thepatientpopulationseenbytheresidentsovertheyears,or changestotheresidency,thatwerenotassessedinthecurrent study.Forexample,the finalyearofthestudydataincludeda fewmonthsthatwereaffectedbytheCOVID-19pandemic. Thiswouldonlyhaveimpactedasmallportionofthe final yearoftrainingfortheClassof2020.However,itmayhave ledtothediscrepancyseeninPPHbetweentheClassof2020 andtheotherincludedclassesasseenin Figure3.Itis interestingthatthisdidnotresultinasubstantialchangein RVUsgenerated.Nospecificdocumentationinterventions wereimplementedduringthistimeandmaysimplyrepresent generalchangesindocumentationpractices.
Wedidnotfactorinhowpatientswhoweretakeninsignoutwouldaffecttheutilizedmetrics.Itislikelythatresidents whoweresignedoutpatientsrequiringmultipleadditional actions(suchasconsultationcalls,procedures,etc)would negativelyimpacttheirabilitytotakeonnewpatients.These caseswereexcludedbecauseitwouldhavebeenunfeasibleto accountforhowmuchadditionalworkwasrequiredfor thesepatients.Forexample,somepatients,eventhosewho werecriticallyill,maybesignedoutwhenallmajor diagnosticandtherapeuticinterventionshavealreadybeen completed,andthepatientissimplyawaitingtransfertothe hospital floor.
Wedidnotconsiderpatientswhowerespecifically admittedtoourstep-downICUunits,orthosewhowent directlytotheoperatingroom.Whiletherateofadmissionto theselocationscouldcertainlyimplyalevelofcomplexity, thewaythisisdeterminedvariesgreatlybetweeninstitutions andwouldhaveaddedasignificantlayerofcomplexitytothe currentstudy.Atourinstitution,wehavetwoaffiliated hospitalsthatwecanadmitpatientsto,eachwithdifferent levelsofcapabilitiesanddifferentcriteriaforICU/stepdown unitstatus.Thisrepresentsaninterestingavenueof futurestudy.
WealsoexcludedpatientsassignedCPTcodes99291and 99292(whichdenotecriticalcare)fromouranalysisofthe relationshipbetweenPPHandCPTcodes.Thiswasdoneas criticalcarebillingcanonlybedonebytheattending physician,anddocumentationpracticesforthisarevariable withinourattendinggroup.Theoverallpercentageof patientswhoreceived99291or99292CPTcodeswasonly
6%.However,thesepatientswerenotexcludedentirelyand wouldhavebeenincludedintheanalysisofothermetrics apartfromCPT.Asstatedearlier,theuseofmultiplemetrics inthisstudywasdesignedtoovercomelimitationsin individualmetricsalone.
Itispossiblethatthepresenceoftriagephysicianduring peakhoursofpatientarrivalmayhaveimpactedthemetrics usedinthisstudy.Whilethiswasnotspecificallycontrolled for,thetriagephysicianteamprimarilyseesonlythelowest acuitypatients(eg,simplelacerationrepairs,anklesprains, needlestickinjuries)andwasfelttonothaveabigimpacton ourchosenmetrics.Wedidnotwishtoexcludeshiftsin whichthetriagephysicianwaspresentasthistimeframe representsthehighestpatientcensusinourED.Ifanimpact occurred,thiswouldbeexpectedtodecreasethemagnitude oftherelationshipbetweenPPHandthechosen variables.Despitethis,asignificanteffectwas stilldemonstrated.
Finally,thisnumericaldatadoesnotcompletely encapsulateotherfactorsthatwouldinfluencearesident’ s overallefficiency. Thesefactorscouldincludetheirclinical abilitiesandmedicalknowledge.Becauseofthis,wecaution residencyprogramsfromlookingatthevariables investigatedinthisstudyinisolationwhenassessingtheir owntrainees.
Residentscaringforhighernumbersofpatientsperhour wereassociatedwithfewercomplexpatientsandpatients whorequiredinpatientadmission.
AddressforCorrespondence:CorlinM.Jewell,MD,Universityof WisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,800UniversityBayDr., Madison,WI53705.Email: cmjewell@medicine.wisc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Jewelletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BeesonMS,AnkelF,BhatR,etal.The2019Modelofthe ClinicalPracticeofEmergencyMedicine. JEmergMed. 2020;59(1):96–120.
2.AccreditationCouncilforGraduateMedicalEducation.ACGME CommonProgramRequirements(residency).2022.Availableat:
https://www.acgme.org/globalassets/pfassets/programrequirements/ cprresidency_2023.pdf.AccessedFebruary25,2024.
3.SørupCM,JacobsenP,ForbergJL.Evaluationofemergency departmentperformance – asystematicreviewonrecommended performanceandquality-in-caremeasures. ScandJTraumaResusc EmergMed. 2013;21:62.
4.WilerJL,WelchS,PinesJ,etal.Emergencydepartmentperformance measuresupdates:Proceedingsofthe2014EmergencyDepartment BenchmarkingAllianceConsensusSummit. AcadEmergMed. 2015;22(5):542–53.
5.JosephJW,DavisS,WilkerEH,etal.Modellingattendingphysician productivityintheemergencydepartment:amulticentrestudy. Emerg MedJ. 2018;35(5):317–22.
6.KirbyR,RobinsonRD,DibS,etal.Emergencymedicineresident efficiencyandemergencydepartmentcrowding. AEMEducTrain. 2019;3(3):209–17.
7.YoungJQ,VanMerrienboerJ,DurningS,etal.Cognitiveloadtheory: implicationsformedicaleducation:AMEEGuideNo.86. MedTeach. 2014;36(5):371–84.
8.GraberML,KissamS,PayneVL,etal.Cognitiveinterventionsto reducediagnosticerror:anarrativereview. BMJQualSaf. 2012;21(7):535–57.
9.RothschildJ,LandriganC,CroninJW,etal.Thecriticalcare safetystudy:theincidenceandnatureofadverseevents andseriousmedicalerrorsinintensivecare. CritCareMed. 2005;33(8):1694–700.
10.HamdenK,JeanmonodD,GualtieriD,etal.Comparison ofresidentandmid-levelproviderproductivityinahigh-acuity emergencydepartmentsetting. EmergMedJ. 2014;31(3):216–9.
11.DouglassA,YipK,LumanauwD,etal.Residentclinicalexperiencein theemergencydepartment:patientencountersbypostgraduateyear. AEMEducandTrain. 2019;3(3):243–50.
12.AMACPTInternational.RelativeValueUnits.Availableat: https://cpt-international.ama-assn.org/relative-value-units AccessedOctober25,2024.
13.HeatonHA,NestlerDM,JonesDD,etal.Impactofscribesonpatient throughputinadultandpediatricacademicEDs. AmJEmergMed. 2016;34(10):1982–5.
14.NemenyiP. Distribution-freeMultipleComparisons.Princeton,NJ: PrincetonUniversity,1963.
15.SaxDR,WartonEM,MarkDG,etal.Evaluationofversion4ofthe EmergencySeverityIndexinUSemergencydepartmentsfortherateof mistriage. JAMANetwOpen. 2023;6(3):e233404.
MichaelKiemeney,MD*
JamesMorris,MD,MPH†
LaurenLamparter,MD‡
MosheWeizberg,MD§
AndyLittle,DO∥
BrianMilman,MD¶
*LomaLindaUniversitySchoolofMedicine,LomaLinda,California
† TexasTechUniversityHealthSciencesCenter,Lubbock,Texas
‡ UniversityofIllinoisChicago,Chicago,Illinois
§ StatenIslandUniversity,StatenIsland,NewYork
∥ AdventHealthEastOrlando,Orlando,Florida
¶ UniversityofTexasSouthwesternMedicalCenter,Dallas,Texas
SectionEditors:MatthewTews,MD,AndrewKetterer,MD,andAndrewGolden,MD
Submissionhistory:SubmittedMay24,2024;RevisionreceivedNovember8,2024;AcceptedNovember25,2024
ElectronicallypublishedFebruary14,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21249
Introduction: Emergencymedicine(EM)historicallyenjoyedanearly100%matchrate.Arapidchange saw46%ofEMprogramswithoneormoreunfilledpositionsafterthe2023Match.Muchhasbeen discussedaboutpotentialcauses,andcharacteristicsofunfilledprogramshavebeeninvestigated.We surveyedrecentapplicantstoEMtofurtherunderstandwhatcontinuestodrawthemtoEMandwhat concernsdeterthemfromchoosingacareerinEM.
Methods: Across-sectional,mixedmethodssurveywasdistributedinthesummerof2023toa conveniencesampleofrespondentsviathelistservsofnationalEMresidentandstudentorganizations aswellasclerkshipdirectorsinEM.Wedidnotcalculateresponserateduetolistservconvenience sampling.Atotalof213responseswerereceived,representing7.7%ofthetotalnumberofEM applicants(2,765)in2023.Applicantswereaskedtorankfrom1to5theirexperienceswithEMandthe characteristicsofthespecialtythatwereimportantintheircareerdecision.Wecalculatedmeansand 95%confidenceintervalsforquantitativeresults.Weperformedqualitativeanalysisoffree-text responsestoidentifythemes.
Results: PositivefactorsforapplicantswereinteractionswithEMfaculty(4.29on1–5scale)and residents(4.42)aswellasclinicalexperiencesinthird-year(4.53)andfourth-yearclerkships(4.62). ApplicantscontinuetobedrawntoEMbythevarietyofpathologyencountered(4.66), flexiblelifestyle (4.63),andhigh-acuitypatientcare(4.43).Mostapplicants(68.5%)experiencedadvisementawayfrom EM.Ofthosewhoreceivednegativeadvisement,non-emergencyphysicianswerethemostcommon source(73.3%).FactorsnegativelyinfluencingacareerchoiceinEMwerecorporateinfluence(2.51), EDcrowding(2.52),burnout(2.59),presenceofadvancedpracticepractitioners(APP)inEM(2.63),and workforceconcerns(2.85).Jobconcernsstemmingfromthe2021EMworkforcereportwereidentifiedby respondentsastheprimaryreasonforrecentMatchresults.
Conclusion: Applicantsnotedclinicalexperiencesintheemergencydepartmentandinteractionswith EMattendingsandresidentsaspositiveexperiences.High-acuitypatientcare,varietyofpathology,and flexiblelifestylecontinuetoattractapplicants.ApplicantsidentifiedEMworkforceconcernsasthe primarycontributortorecentEMMatchresults.Corporateinfluence,EDcrowding,burnout,and presenceofAPPsintheEDwerealsosignificantissues.[WestJEmergMed.2025;26(2)261–270.]
Emergencymedicine(EM)hashistoricallyenjoyedavery competitiveoutcomeintheNationalResidencyMatching Program(NRMP,or “theMatch”)with >95%ofprograms fillingtheirspots.1 Beginningin2022,however,adramatic declineoccurredleavingmanyprogramsunfilled.2 This declinecontinuedin2023,with46%ofEMprograms remainingunfilled.3 Although79.1%ofthoseprograms filled intheSupplementalOfferandAcceptanceProgram(SOAP),4 thisrepresentsatremendouschangefrompreviousyears.
Thecauseofthischangeislikelymultifactorial,with majorcontributingfactorsbeingtheexpansionofthe numberofresidencypositions,studentperceptionsofthe futurejobmarketwithinEM,andthevirtualinterview format.5,6 Otherproposedetiologiesofthedeclineinclude thecorporatepracticeofEM(whichoccurswhenanonphysicianorcorporationexertscontroloverthemedical decision-makingorcollectsreimbursementforthemedical servicesofphysicians),7 theexpandeduseofadvanced practicepractitioners(APP)suchasphysicianassistantsand nursepractitionersintheemergencydepartment(ED),and increasedburnoutfollowingaglobalpandemic.6 Concerns regardingthejobmarketandexpandeduseofAPPsare likelyrelatedtothe2021EMworkforcereportbyMarco etal,whichproposedarangeofpotentialoutlooksbasedon variousfactorswiththemostpublicizedresultbeinga projectedoversupplyofemergencyphysiciansby2030.8
Severalfactorsaffectedwhichprogramsweremorelikely togounfilledintheMatch.Getteletalfoundthatprograms accreditedwithintheprevious fiveyears,aswellasprograms thatwereunderfor-profitownershipweremorelikelytogo unfilled.9 Anotherstudyfoundthatpredictorsofnot filling werehavingunfilledpositionsinthepreviousMatch,a smallerprogramsize,locationintheMid-AtlanticorEast NorthCentralarea,priorAmericanOsteopathicAssociation accreditation,andcorporateownershipstructure.10 Overall, programsfelttheirmatchoutcomeswereworsethanin previousyears,buttheyperceivedthequalityofapplicantsas similartopreviousyears.5
Manyfactorsinfluenceastudent’sdecisiononwhich specialtytopursueincludingrolemodels, financialincentives, gender,degreeofpatientcontact,proceduralskills,prestige, andlifestyle.11–14 Thefactorsmostassociatedwithachoiceto specializeinEMincludelifestyle,diversityofpatient presentations, flexibilityinchoosingapracticelocation,worklifebalance,andperceivedjobsatisfaction.15–19 Factors associatedwithearlierselectionofEMincludeearlyexposure tothe field,presenceofanEMresidencyprogramata student’smedicalschool,prioremploymentintheED, previousexperienceasaprehospitalpractitioner,and completionofathird-yearEMclerkship.16
InthisstudywesurveyedEMapplicantsfrom2022and 2023toidentifyfactorsdeterringorattractingthemtothe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Applicantandspecialtycharacteristics attractingapplicantstoEMhavebeen previouslydocumented.
Whatwastheresearchquestion?
Whatfactorsdeterredandattracted applicantstoEMduringthe2023Match?
Whatwasthemajor findingofthestudy?
The4th-yearclerkshipwasthemajor attractingfactor(mean4.62,95%CI 4.50 – 4.74),whilecorporatein fl uence(mean 2.51,95%CI2.33 – 2.69)wasthestrongest deterringfactor.
Howdoesthisimprovepopulationhealth?
These fi ndingsoffernewinsightsinto applicantperspectivesofEMandspecialtychoiceconsiderationsfollowingthe 2023Match.
specialtyaswellasmodifiableinfluencesimpactingtheir careerdecisions.TorestorethecompetitivenatureofEMin theMatch,itisimportanttoknowwhatmotivatesmedical studentstoselectEMasaspecialtyinthecurrent environment.Itisadditionallyimportanttofurther understandthefactorscontributingtodecreasedinterestin EM,sothatwecancontinuetoaddresstheseasaspecialty.
TheprojectwasconceivedbytheCouncilofResidency DirectorsinEmergencyMedicine(CORD)MatchTask Force,whichincludesrepresentativesfromtheAmerican AcademyofEmergencyMedicine(AAEM),American AcademyofEmergencyMedicineResidentandStudent Association(AAEM/RSA),AmericanCollegeof EmergencyPhysicians(ACEP),AmericanCollegeof OsteopathicEmergencyPhysicians(ACOEP),ACOEP ResidentandStudentOrganization(ACOEPRSO), AssociationofAcademicChairsinEmergencyMedicine (AACEM),CORD,EmergencyMedicineResidents’ Association(EMRA),theSocietyforAcademicEmergency Medicine(SAEM),andSAEMResidentsandMedical Students(SAEMRAMS).Taskforcememberscollaborated todesignthesurveyinstrument.Theconclusionsinthispaper representtheviewsandopinionsoftheindividualauthors anddonotrepresenttheviewsoftheorganizations.The
studywasapprovedbytheLomaLindaUniversityHealth InstitutionalReviewBoard.
WeperformedaliteraturereviewusingPubMedtocollect studiesinvestigatingfactorsimpactingresidencyapplicants’ specialtychoice.Questionswereadaptedfromprior publishedstudies.16,20 Currentfactorsnotpreviously investigated,suchasCOVID-19orEMworkforce projections,wereaddedfollowinganiterativeprocessof consensusdevelopmentwithintheresearchgroup.The surveywasreviewedbytheCORDMatchTaskForce membersandedited.Thesurveywasthenpilot-testedby currentmedicalstudentsandresidents.Weanalyzedthe responses,andthesurveywasrevisedforclarityandbrevity followingthebetarespondents’ feedback.
Medicalstudentswereaskedmultiple-choicequestions regardingtheirresidencyapplicationstrategyincluding whethertheyhadappliedtomorethanonespecialtyand,if so,whichspecialtiestheyappliedto.Thesurveyparticipants wereaskedtorankspecialtycharacteristicsinfluencingtheir choiceofEMasacareerona five-pointLikertscalefrom stronglypositivetostronglynegative.Theywerealsoasked toranktheimpactofpriorexperiencesontheirspecialty choiceona five-pointLikertscalefromverypositivetovery negative.Weinvestigatedtheimpactofcareeradvisement usingmultiple-choicequestionswiththeoptiontoselectup tothreeresponses.Finally,free-textresponsequestionswere askedtoassessapplicants’ opinionsaboutthecausative factorsleadingtothe2023EMMatchresults.Comment inthisspacewasoptionalandnotmeanttoreach saturationofthemes;rather,itwasmeanttoprovide participantstheopportunitytogiveadditionaldetails abouttheirexperiences.
WeusedaconveniencesampleofEM-boundmedical studentswhoappliedinboththe2022and2023Matchand thosewhoconsideredorareconsideringapplyingtoEMin upcomingMatchcycles.Surveyrespondentsweresenta web-basedsurveyviaQualtrics(QualtricsInternational,Inc, Seattle,WA)inthesummerof2023.Remindermessages weredistributedmonthlyduringthedatacollectionperiod. Thesurveywasdistributedthroughthelistservsofcurrent medicalstudentsinterestedinEMasidentifiedbytheir membershipinanEMnationalorganizationincluding AAEM/RSA,ACOEPRSO,EMRA,andSAEMRAMS. SurveyswerealsodistributedthroughtheSAEMClerkship DirectorsinEmergencyMedicine(CDEM)listservtobesent totheirrecentlymatchedapplicantswhomatchedintoEM orhadconsideredbutultimatelydecidednottopursueEM. Conveniencesamplingvialistservdistributiondidnotallow forsurveydistributionquantificationorresponse-rate calculation.Comparingthenumberofsurveyresponses (213)tothenumberofapplicantstoEMinthe2023Match (2,765)showsoursurveyresponseswereequalto7.7%ofthe totalnumberofEMapplicantsin2023.Theintendedsurvey participantsincludedmedicalstudentswho1)consideredbut
ultimatelydidnotapplytoEMresidency;2)appliedtoEM astheironlyspecialtychoice;3)dualappliedtoEMandan alternatespecialtychoice;or4)enteredEMthrough theSOAP.
A financialincentiveofa$10electronicgiftcardwasgiven tothe first160participants.Financialsupportforthestudy wasprovidedbyAAEM,AAEM/RSA,ACEP,ACOEP, AACEM,CORD,andSAEM.
WeanalyzeddatausingMicrosoftExcel365(Microsoft Corporation,Redmond,WA)tocalculatemeansand percentages.Wecalculated95%confidenceintervals(CI) usinganonlinetool.21 Aphenomenologicalapproachto qualitativeanalysiswasusedandfree-textresponseswere codedbytwoauthorswithexperienceinqualitativeanalysis (JM,BM)afterestablishingacodebookthroughaniterative processtogenerateanunderstandingofthephenomenonof theEMmatchprocessinconcertwiththequantitative questions.Anydisagreementsbetweencodeswereresolved byathirdauthor(MK).
Wereceivedresponsesfrom213individuals. Demographicsareshownin Table1.Mostrespondents (92.8%)hadappliedtoresidencyalready.Ofthose,87.2% appliedtoEMintheMatch.RespondentssecuredanEM residencypositioninthe2023Match(69.5%),2022Match (9.6%),2023SOAP(12.3%),2022SOAP(0.5%),andby othermeans(5.3%).Asmallproportionofrespondents (2.7%)werenotenteringEMresidency.
Incomparisontoapplicantssecuringapositioninthe 2023Match,oursamplewasfairlysimilarwithregardto genderbreakdown(57.2%male,39.9%femaleinoursample vs54.8%male,45.2%femaleintheMatch)butoversampled osteopathicseniors(42.7%inourstudyvs24.3%inthe Match).Regardingapplicationstrategy,70.1%appliedto onlyEMresidencies.Someindividualsappliedtomorethan onespecialtywithEMpreferred(12.3%).Themostcommon secondaryspecialtieswereinternalmedicineandfamily medicine.ApplyingtoEMasthesecondaryspecialty occurredin2.1%ofindividualswithprimaryspecialties beinganesthesiology,interventionalradiology,orthopedic surgery,andphysicalmedicineandrehabilitation. RespondentswhochosenottoapplytoEMatallmadeup 13.4%ofresponses.Thisgroupofindividualsmost commonlychosetoapplytoanesthesiology(39.1%), orthopedicsurgery(17.4%),generalsurgery(17.4%),family medicine(13.0%),internalmedicine,pathology,and preliminaryyear(each8.7%).(Responseoptionwas “Select allthatapply,” responsesum >100%).
ApplicantsmostcommonlychosetoapplytoEMinthe thirdyearofmedicalschool(33.5%)orbeforemedicalschool (33.0%).Theremainingresponseswereevenlysplitamong thepre-clinicalyearsofmedicalschool(6.8%),thefourth yearofmedicalschool(8.9%),aftermedicalschool(6.8%),
Table1. Demographicdataofsurveyrespondents.
Characteristics
Age(years)(n = 173) N(%)
25–29
35–39 13(7.5%)
40–44 2(1.2%) >44 2(1.2%)
Genderidentity(n = 173)
Male 99(57.2%)
Female 69(39.9%)
Non-binary/thirdgender 1(0.6%)
Prefernottosay 4(2.3%)
Race(n = 177)
AmericanIndian/AlaskaNative 1(0.6%)
Asian 20(11.3%)
Black/AfricanAmerican 10(5.6%)
Hawaiian/PacificIslander 0
Other 8(4.5%)
Prefernottosay 6(3.4%)
Ethnicity(n = 173)
Hispanic/Latino 18(10.4%)
NotHispanic/Latino
Prefernottosay 8(4.6%)
Medicalschoolbackground(n = 211)
MDinUS 85(40.3%)
DOinUS 90(42.7%)
UScitizenIMG 28(13.3%)
Non-UScitizenIMG 8(3.8%)
Medicalschooltype(n = 171)
Private
Public
Other 1(0.6%)
Medicalschoolgeographicregion(n = 171)
Central(IA,IL,IN,KS,MI,MN, MO,MT,ND,NE,OH,SD,WI) 43(25.1%)
Northeast(CT,DC,DE,MA, MD,ME,NH,NJ,PA,RI,VT)
29(17.0%)
South(AL,AR,FL,GA,KY,LA, OK,MS,NC,SC,TN,TX,VA,WV) 70(40.9%)
West(AK,AZ,CA,CO,HI,ID, NM,NV,OR,UT,WA,WY)
andduringSOAP(8.4%).ParticipantswereexposedtoEM intheirmedicalschoolviarequiredEMclerkshipsinthe fourthyear(42.1%),requiredclerkshipsinthethirdyear (24.0%),EMelectivesinthefourthyear(17.0%),andEM electivesinthethirdyear(11.1%). Table2 showsthedegree ofinfluenceeachfactorheldintheapplicants’ choiceofEM asacareer.Themostfrequentlycitedpositiveinfluenceswere EMresidentsonshift(4.42ona1–5scale),EMattendingson shift(4.29),thefourth-yearEMclerkship(4.62),andthirdyearEMclerkship/elective(4.53).PriorexperienceintheED inanon-physicianrole(4.43),inemergencymedicalservices (EMS)(4.52)orasascribe(4.55),wereidentifiedless frequentlybutasverypositivefactors.
Jobconcerns/workforcereport(65.8%),burnout(56.7%), increaseduseofadvancedpracticepractitioners(APP) (50.8%),andcorporateinfluenceinEM(42.5%)werethe most-citedreasonsforadvisingapplicantsawayfromEM. Emergencydepartmentcrowding(12.5%)andEM experienceduringtheCOVID-19pandemic(5.8%)wereless commonlycitedconcerns.Participantswereaskedabout advisementanditsinfluenceontheirspecialtychoice:68.5% reportedbeingadvisedagainstchoosingEMresidency training.Themostcommonsourcesofadvisementaway fromEMwereattendings/residentsinnon-EMspecialties (73.3%),peers(50.0%),socialmedia/messageboards (47.5%),andEMattendings(37.5%).Medicalschool representativesintheDean’sofficeaccountedforasmall proportionofadvisementawayfromEM(15.8%).Most participantsinoursurvey(81.8%)reportedthatadvising againstenteringEMdidnotchangetheirapplication strategy.Ofthosewhoinitiallypursuedadifferentspecialty 5.7%ultimatelyenteredEMintheSOAP,5.0%appliedto anotherspecialtyasabackuptoEM,and3.3%appliedto EMasabackupspecialty.Ofthoseapplicantswhodidnot changeapplicationstrategydespitenegativeadviceabout EM,themostcommonlycitedreasonswereperceived fitwith EM(73.7%), flexiblelifestyleofEM(64.6%),lackofinterest inotherspecialties(49.5%),anddoubtinaccuracyof workforcereport(49.5%).
Veryfewparticipantssaidtheywouldnotadviseafriend toapplytoEMforthe2024Match(2.3%).Most(75%) wouldadviseafriendtochooseEM.Mostofthosewho indicatedtheywouldadviseafriendagainstapplyingtoEM woulddosobecauseofconcernsabout fitforthespecialty (42.9%)andthejobmarket(22.9%),withcorporatizationof medicine,APPexpansion,andburnoutalsomentioned.
29(17.0%)
IMG, internationalmedicalgraduate; MD,DoctorofMedicine; DO,DoctororOsteopathicMedicine.
Mostsomewhatagreedorstronglyagreedthattheirpeers wouldbemoreinterestedinEMasacareeriftheywere exposedtoEMduringarotationinthethirdyearorearlier (82.7%).Participantswereaskedwhattheythoughtwould makeEMmoreappealingtopeerswhowereundecided
Table2. Factorsinfluencingselectionofcareerinemergencymedicine.
CI, confidenceinterval;
aboutaspecialtybutwereconsideringEM.Themost commonresponsesincludedearlyexposuretoEM(31.5%) andalleviatingconcernsaboutjobsecurityraisedbytheEM workforcereport(30.2%).Othersuggestionsincluded addressingtheexpandeduseofAPPsintheED(10.1%), improvingtheperceptionofEMamongmedicalstudents andphysicians(9.4%),andimprovingwork-lifebalanceand compensation(8.7%and8.1%,respectively).
Table3 showshowapplicantsrankeddifferentfactors whenchoosingEMasacareer.Themostimportantpositive factorswerevarietyofpatientpathology(4.66ona1–5 scale),lifestyle/flexibility(4.63),high-acuitypatientcare (4.43),lengthofresidencytraining(4.37),andfamily considerations(4.36).Participantswereaskedspecificallyif theybelievedthatEMisa “lifestylespecialty,” and60.1% respondedyes;9.0%didnotconsiderEMalifestylespecialty, while28.1%wereneutral,and2.8%wereunsure.Thefactors negativelyinfluencingacareerchoiceinEM,definedas95% CIlessthan3.0,werecorporateinfluenceinEM(2.51, 2.33–2.69),EDcrowding(2.52,2.37–2.67),burnout(2.59, 2.44–2.74),anduseofAPPsinEM(2.63,2.47–2.79).
AverageratingofconcernsaboutEMexperienceduringthe COVID-19pandemic(2.95)andworkforcereport/job securitywasnegative(2.85);however,upperlimitof95%CI waspositive,3.12and3.03,respectively.
Applicantswereaskedtoidentifythemostimportant reasoncontributingtoalarger-than-normalnumberof unfilledpositionsintheEMMatch.Theyidentifiedconcerns aboutjobsecurityandthefutureEMworkforceasthe primaryconcern(Table4).Qualitativeresponsestothe
increaseinunfilledspotsintheEMMatchpredominantly reflectedconcernsregardingtheEMworkforcereportand jobsecurity.Themesandrepresentativequotationsare includedin Table5.
ApplicantsinoursurveyweredrawntoEMbyclinical experiencesintheEDduringthethirdandfourthyearandby interactionswithEDresidentsandattendingphysiciansduring thoseexperiences.Unfortunately,onlyasmallproportionof applicantsinoursurveyhadrequiredEMclinicalexperience duringthethirdyearoftraining.Developingbestpractice recommendationsforearlyexposuretoEMduringmedical schoolmaybeanareatotargettoincreaseinterestinfuture applicants.Additionally,employmentinanEM-related field (ie,EMS,scribe)priortomedicalschoolwasalsoapositive experience.Earlyidentificationofthosestudentswithprior EM-relatedemploymentmaybeanareaformentorship effortsbyEMadvisors.
Applicantscontinuetobedrawntothehigh-acuitypatient care,diversepatientpathology,andthe flexiblelifestyleEM offers.These findingsareinlinewithpriorstudiesofEM applicantattitudesandthecornerstoneofEM’ s appeal.12–19,23 Additionalfactorsthatappealtoapplicants arethevarietyoffellowshipoptionsavailableafterEM residency,thelengthofresidencytraining,compensation, andavailabilityofjobsintheirdesiredlocation.Family considerationsareimportanttoapplicantsand,coupledwith thedesirefora flexiblelifestyle,signaladesireforwork-life balance.ShiftworkintheEDhasdownsidessuchassleep
Table3. Importanceofvariousaspectsofemergencymedicinetoapplicantsinthe2023Match. Howimportantwerethefollowing factorsinyourdecisiontoapply toEMresidency
APPs, advancedpracticepractitioners; CI,confidenceinterval; EM,emergencymedicine; ED,emergencydepartment.
transitionsassociatedwithnightshiftsandworking weekendsandholidays.However,applicantsweresignaling thoseissuesarestillfavorabletobeingoncallorworkingina
Table4. Singlemostimportantreasonforunfilledemergency medicine(EM)residencypositionsin2022and2023Match, perEMapplicants. ResponseN% Workforce/jobsecurity
Numberofresidencies
Burnout
Programs’ failuretoadapttochanging applicantpool 2(1.3%)
Note:Totalsexceed100%,asrespondentscouldindicatemorethan one item;%indicatesthepercentoftotalrespondentsendorsing achoice.
APP,advancedpracticepractitioner; EM,emergencymedicine.
clinic fivedaysaweek.Highlightingthefactorsthatresonate withapplicantsisagoodstartingpointwhenpromoting thespecialty.
WithregardtofactorspushingapplicantsawayfromEM, mostapplicantsexperiencedbadmouthingofEMand advisingawayfromthespecialty.Inpriorstudies,overthreequartersofrespondentsreportedexperiencewith badmouthingofanotherspecialtyandone-quarterchanged theirspecialtychoicebecauseofit.24–26 Whenuncertain applicantsarenarrowingtheirspecialtychoicesbetweena fewseriousoptions,contendingwithnegativityaboutyour careerchoice,bothnowandinthefuture,fromfriendsor mentorsinotherspecialtiesmaybeenoughtoswaysomeone awayfromEM.
ThemostcommonsourceofadviceagainstEMin2023 wasnotfrompeers,formalmentors,orDean’sofficesbut fromattendingsandresidentsinnon-EMspecialties. Experiencingnegativeadvisementfromatrustedmentor aboutone’sdesiredspecialtyislikelyimpactful.Inaddition, applicantsreportedreceivingnegativepressurefromtheir peersandsocialmedia.MostpeopleinvolvedinEMmedical educationsuspectedapplicantswerebeingadvisedaway fromEM.Thiswassuggestedbyourdata.Mostassumed advisorsfromtheDean’sofficewereadvisingstudentsaway fromEMtowardmoreprestigiousspecialtiesorthosewith safermatchrates.Butthatwasnotthecaseinoursurvey,as
Table5. Qualitativeanalysisthemesandrepresentativequotationsregardingthe2022and2023EMmatch.
ThemeCodeGuidelineforuse
Employment opportunities
Workforce/jobsecurity
Thiscodeisusedwhenparticipantsdiscusstheworkforcereport, jobsecurity,employmentopportunities,ordifficulty findingjobs
• There isamythgoingaroundthattherearenotenoughjobsforEMphysiciansafterresidency.Iknowalotofpeoplethatmadethis commentuponsayingIwasapplyingtoEM
• Covid,andthatdamnmemo.Yallshotyourselvesinthedamnfootwiththatboneheadmove
• Workforcereporthysteria
• Theinfamousreportpredictingacominglaborsurplus.Thetiminglinesupandittrackswithwhatfriendsinmedschoolweresaying NumberofresidenciesThiscodeisusedwhenparticipantsdiscussresidencyexpansion
• Increased amountofresidencyprogramspotscreatedbyCMGhospitals
• Toomanyresidencyprograms
• Surplusof “pop-up” programsleveragingresidentlaborwithnointentionofrealtraining
• Midlevel creep
• increasingnumberofNPs/PAs fillinginpositions
• PA/NPtakeover
This codeisusedwhenparticipantsdiscusscompetitionwith APPsforemploymentorincreaseduseofAPPsinEM
• IncreasedNP/PAreplacingjobsandthenMDlicenseonlineforanythingtheydo.Includingsigningtheircharts Practice environment Burnout
• Concern overburnout
• Fearofburnout
• Emergencydoctorsburntout
• Treatment duringCOVID-19
COVID-19
Thiscodeisusedwhenparticipantsdiscussburnout
This codeisusedwhenparticipantsdiscuss theimpactofCOVID-19
• COVID-19experiences,lackofpatientcareopportunitiesduringCOVID-19
• Highstress,especiallyduringCOVID-19
• COVID-19showedEM’struecolors
• COVID-19experiencesandfearsoffuturehealthrisks
• Corporate takeover,thusphysicianslosepowereveryday
• Corporatepracticeofmedicine
• HCAprograms!!!!!Thereareatonofnew,sketchyprograms.
This codeisusedwhenparticipantsdiscusscorporatizationof emergencymedicineorprivateequityinfluence
• Increaseinfor-profithospitalslotsavailableinTexas,Cali,andFlorida Qualityoflife,changeinpractice environment (boarding,volume,etc.)
Thiscodeisusedwhenparticipantsdiscuss negativepracticefactors
• Lack ofperceivedqualityoflife
• BadjobprospectsandEDculturehasbecometoxic
• Seeingpatientsinwaitingrooms/bedholds
• CultureofwhatEMhasbecome.Noonewantstochoosetoworkinthisoverrunenvironmentespeciallywhenthejobmarketis uncertainwhentherearespecialtieslikedermatologyandsub-specialtieswhereyoudon’thavetodealwiththechaosandpatient volumeswearenowseeingintheED.ERmedicineisatanall-timelowandneverusedtobethisoverwhelmingpre-pandemic.
Applicantor match factors Programs’ failuretoadapttochanging applicantpool
Thiscodeisusedwhenparticipantsdiscussresidencyprograms’ failuretoassesscompetitivenessorselectapplicantsefficiently
• Mismatch betweenprograms’ opinionofthemselves/howtheyareperceivedvsactualapplicantperceptionsofprograms.
• Programsbeingoverlyselectiveandnothonestlyintrospectingregardinghowapplicantsperceivetheirprogram
(Continuedonnextpage)
Table5. Continued.
This codeisusedwhenparticipantsdiscussnegativeperceptions ofemergencymedicineamongstudentsorthroughsocialmedia ormentors
• Lack ofrespecttoemergencyphysiciansandthoughtthatwearenotthatsmart
• PerceptionfromattendingsofbothEMandnon-EM
• Socialmediainfluenceandimmaturityonbehalfofapplicants
• Decreasedperceivedcompetitivenessleadingtolackofinterest
• Badreputationamongconsultantspecialties
• Jackofalltrades/EMincompetencystigma
APP,advancedpracticepractitioner; CMG,contractmanagementgroup; EM,emergencymedicine; ED,emergencydepartment; HCA,HospitalCorporationofAmerica; NP,nursepractitioner; PA,physicianassistant.
advisorsintheDean’sofficerankedasthesixthmost frequentsourceofadvisementawayfromEM.
AdditionalfactorspushingapplicantsawayfromEM werecorporateinfluenceinEM,EDcrowding,burnout,the useofAPPsinEM,theexperienceofemergencyphysicians duringCOVID-19,andconcernsregardingjobsecurity stemmingfromthe2021EMworkforcereport.Applicants arewaryofenteringaspecialtydominatedbycorporations thatplaceprofitsoverpatientcare.Residenciesatfor-profit clinicalsiteshad1.3timesgreaterriskofnot fillingin2023.9 Applicantsareshowinganaversiontotrainingatthesesites. However,spotscontinueto fillduringthetime-limitedSOAP asunmatchedapplicantsarelikelyexcitedabouttheability tosecureanytrainingposition.Furtherunderstanding applicantconcernsandtheexperiencesofresidentsin for-profitprogramsisimportantandrequiresadditional study.Likewise,understandingtheexperienceofEM residentswhoentertrainingviatheSOAPisvaluablefor futureinvestigation.
Emergencydepartmentcrowdingnotonlynegatively impactsqualityofpatientcare;italsodetersfuture emergencyphysiciansfromenteringthe field.Studentson EDrotationsseethechallengesof findingspacetoreevaluatepatients,delaysinworkup,andprolongedcareof patientsboardingintheEDwhoareawaitinginpatientbeds. Effortstoaddressboardingaswellastheimplementationof surgecapacityplansmayresultinimprovingthisfactoras studentsconsiderspecialtychoice.
Furthermore,burnoutgeneratedthelargestnumberof moderateorstronglynegativeresponses.Emergency medicineiswidelycitedasthespecialtywiththehighest ratesofburnout. 27 , 28 Requirementstopromotewell-being andcounterburnoutexistinbothundergraduate (LiaisonCommitteeonMedicalEducationstandard 12.3) 29 andgraduatemedicaleducation(Accreditation CouncilforGraduateMedicalEducationCommon ProgramRequirementsforresidencyVI.C). 30 Prior
qualitativeresearchsugg estsfacultymodelingmay in fl uenceresidents ’ careerperspectives,indicating targetingfacultyforeducationonwell-beingandburnout mayyieldsubstantialbene fi tsforbothcurrentand prospectiveresidents. 31
Applicants,additionally,haveconcernsabouttheuseof APPsintheED.Manyfree-textresponsescited “ scope creep ” ofAPPsaswellasthenegativeimpactonphysician jobavailabilityasnegativefactors.Applicantssignaledthat theyarepayingattentiontothetopicofAPPusageintheED anditisanimportantissuetothem.NationalleadersinEM areactivelyworkingtoprotectthescopeofallpractitioners intheEDandcontinuetoemphasizetheimportanceof physician-ledpatientcareteams.Furtherdisseminationof theseadvocacyeffortsandtheeffectsonourspecialtywould bebeneficialforapplicants.
Lastly,theworkforcereporthasbeenfrequently hypothesizedasamajorcontributingfactortotherapid declineinEMresidencyapplicationsoverthelasttwoyears.8 ApplicantstoEMinoursurveyconfirmedthishypothesis, citingprojectionsstemmingfromthereportasthemost importantfactorleadingtothesignificantriseinunfilledEM residencypositionsinthe2022and2023Matches. Subsequentstudieshaveaddressedworkforceconsiderations suchasphysicianattritionandgeographicdistribution.32,33 FurtherinvestigationandclarityintothefutureEM workforcewouldaidapplicantsastheyweightheir careerdecisions.
ReinforcingthepositiveaspectsofEMwhileaddressing thenegativefactorsabovewillgoalongwaytoward bolsteringtheEMapplicantpoolandfutureworkforce.The 2023EMMatchwasunprecedentedwith554unmatched positions.However,EMstillmatched2,456applicants,the fourthlargestnumberinthe2023Match.3 Oursurveyyields insightsintothepositiveaspectsofEMthatdrawapplicants tothespecialtyandidentifiesnegativefactorsfollowingthe 2023EMMatch.
Oursurveymaybeimpactedbyselectionbiasasour distributionmethoddidnotguaranteethateveryresidency applicantwhoconsideredapplyingtoEMresidencywas included.Forthisreason,surveyresponseratewasnot calculated,anditisunknowntowhatextentourresultsare representativeofallEMresidencyapplicantsinthe2022and 2023Matchcycles.Additionally,recallbiasmayalso contributeasresponsesfromapplicantswhomatchedtoEM in2022wereincluded.Aspotentialsurveyparticipantswere identifiedthroughtheirmembershipinnationalEMresident andstudentorganizations,thisstudymaynotbe representativeofindividualswhoconsideredEMearlyin theirmedicalschoolcareerandultimatelydidnotpursue EM.Theexactnumberofindividualswhoreceivedthe surveysolicitationisnotknown,makingitimpossibleto calculatearesponserate.Oursurveyresponsesrepresent 7.7%ofthetotalnumberofapplicantstoEMin2023, althoughitisunlikelythesurveyreachedallapplicantsinthe pool.Futurestudiesmaybenefitfromalongitudinal approachsolicitingEMinterest-groupparticipantsinthe firsttwoyearsofmedicalschoolandfollowing themthroughtheirrespectiveMatchyearsto improveresponserate.
Thespecialtyofemergencymedicineexperiencedasharp increaseinun fi lledpositionsinthe2022and2023matches. MostapplicantsreceivedadvisementawayfromEMwith themostcommonsourcebeingphysiciansinnon-EM specialties.Applicantsperceivecorporatein fl uenceinEM, EDcrowding,burnout,in fl uenceofadvancedpractice practitionersinEM,andworkforceconcernsasdriving forcesbehindtheEMMatchresults.Applicantscited clinicalexperiencesintheEDandinteractionswith EMattendingsandresidentsaspositivefactors.Highacuitypatientcare,diversepatientpathology,and fl exible lifestylewereseenaspositivecharacteristicsofacareer inEM.
Theauthorswouldliketothanktheboardsofdirectorsof AAEM,AAEM/RSA,ACEP,ACOEP,AACEM,CORD, andSAEMforprovidingfundsforparticipantincentives. TheauthorswouldalsoliketothankAAEM/RSA,ACOEP/ RSO,CDEM,EMRA,andSAEMRAMSforassistance withdistributingthesurveyviatheirrespectivelist-servsand tothankthemembersoftheCORDMatchTaskForcefor assistanceindevelopingthesurveytool.
AddressforCorrespondence:MichaelKiemeney,MD,LomaLinda UniversitySchoolofMedicine,11234AndersonSt,MC-A208,Loma Linda,CA92354.Email: mkiemeney@llu.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Surveyincentivesupportwasprovided byrespectiveBoardsofDirectorsforAAEM,AAEM/RSA,ACEP, ACOEP,AACEM,CORD,andSAEM.Themanuscriptrepresents theindividualauthor’sopinionsanddoesnotrepresenttheopinions oftheorganizationsproviding financialsupport.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Kiemeneyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.Nationalresidentmatchingprogram.Resultsanddata:2021main residencymatch.2021.Availableat: https://www.nrmp.org/wp-content/ uploads/2021/08/MRM-Results_and-Data_2021.pdf AccessedOctober3,2023.
2.NationalResidentMatchingProgram.2022NRMPmainresidency match:matchratesbyspecialtyandstatenationalresidentmatching program.2022.Availableat: https://www.nrmp.org/wp-content/uploads/ 2022/11/2022-Main-Match-Results-and-Data-Final-Revised.pdf AccessedOctober3,2023.
3.NationalResidentMatchingProgram.Resultsanddata:2023main residencymatch.Availableat: https://www.nrmp.org/wp-content/ uploads/2023/05/2023-Main-Match-Results-and-Data-Book-FINAL. pdf.AccessedOctober3,2023.
4.NationalResidentMatchingProgram.Resultsanddata:2023main residencymatch.Page46.Availableat: https://www.nrmp.org/wpcontent/uploads/2023/05/2023-Main-Match-Results-and-Data-BookFINAL.pdf.AccessedOctober3,2023.
5.MuranoT,WeizbergM,BurnsB,etal.Decipheringachangingmatch environmentinemergencymedicineandidentifyingresidencyprogram needs. WestJEmergMed. 2023;24(1):1–7.
6.LewisM,WilliamsK,TimpeJ,etal.The2022and2023emergency medicineresidencymatch:acautionarytale. Cureus. 2023;15(5):e38601.
7.AmericanAcademyofEmergencyMedicine.Corporatepractice. Availableat: https://www.aaem.org/publications/key-issues/corporatepractice/.AccessedOctober24,2024.
8.MarcoCA,CourtneyDM,LingLJ,etal.Theemergencymedicine physicianworkforce:projectionsfor2030. AnnEmergMed. 2021;78(6):726–37.
9.GettelCJ,BennettCL,RothenbergC,etal.Unfilledinemergency medicine:ananalysisofthe2022and2023matchbyprogram accreditation,ownership,andgeography. AEMEducTrain. 2023;7(4):e10902.
10.PreiksaitisC,KrzyzaniakS,BowersK,etal.Characteristicsof emergencymedicineresidencyprogramswithunfilledpositionsinthe 2023match. AnnEmergMed. 2023;82(5):598–607.
11.YoonJD,HamSA,ReddyST,etal.Rolemodels’ influenceonspecialty choiceforresidencytraining:anationallongitudinalstudy. JGradMed Educ. 2018;10(2):149–54.
12.DeZeeKJ,MaurerD,ColtR,etal.Effectof financialremunerationon specialtychoiceoffourth-yearU.S.medicalstudents. AcadMed. 2011;86(2):187–93.
13.LambertEMandHolmboeES.Therelationshipbetweenspecialty choiceandgenderofU.S.medicalstudents,1990–2003. AcadMed. 2005;80(9):797–802.
14.TeitelbaumHS,EhrlichN,TravisL.Factorsaffectingspecialty choiceamongosteopathicmedicalstudents. AcadMed. 2009;84(6):718–23.
15.RosenB,RosenP,SchoferJ,etal.Isemergencymedicinetheright choiceforme? JEmergMed. 2019;56(3):e35–8.
16.RayJC,HopsonLR,PetersonW,etal.Choosingemergencymedicine: influencesonmedicalstudents’ choiceofemergencymedicine. PLoS One. 2018;13(5):e0196639.
17.BoydJS,ClyneB,ReinertSE,etal.Emergencymedicinecareerchoice: aprofileoffactorsandInfluencesfromtheAssociationofAmerican MedicalColleges(AAMC)graduationquestionnaires. AcadEmergMed. 2009;16(6):544–9.
18.KeithKC,SmithE,ReddyS,etal.Lifestylefactorsandotherinfluences onmedicalstudentschoosingacareerinemergencymedicine. AEM EducTrain. 2021;5(1):37–42.
19.KazziAA,LangdorfMI,GhadishahD,etal.Motivationsforacareerin emergencymedicine:aprofileofthe1996USapplicantpool. CJEM. 2001;3(02):99–104.
20.AAMC.Graduationquestionnaire(GQ).2024.Availableat: https://www. aamc.org/data-reports/students-residents/report/graduationquestionnaire-gq.AccessedMay15,2024.
21.Caculator.net.Confidenceintervalcalculator.Availableat: https://www. calculator.net/confidence-interval-calculator.html AccessedFebruary6,2024.
22.EmergencyMedicineResidents’ Association.Consensusstatementfor theemergencymedicine2022–2023residencyapplicationcycle regardingemergencymedicineawayrotations.2022.Availableat:
https://www.emra.org/be-involved/be-an-advocate/working-for-you/ statement-for-residency-application-cycle-em-away-rotations AccessedMay7,2024.
23.MackeyC,FeldmanJ,PengC,etal.Howdoemergencymedicine applicantsevaluateresidencyprogramsinthepost-COVID-19era? AEM EducTrain. 2022;6(6):e10805.
24.AjazA,DavidR,BrownD,etal.BASH:Badmouthing,attitudesand stigmatisationinhealthcareasexperiencedbymedicalstudents. BJPsychBull. 2016;40(2):97–102.
25.HolmesD,Tumiel-BerhalterLM,ZayasLE,etal. “Bashing” ofmedical specialties:students’ experiencesandrecommendations. FamMed. 2008;40(6):400–6.
26.AlstonM,Cawse-LucasJ,HughesLS,etal.Thepersistenceofspecialty disrespect:studentperspectives. PRiMER. 2019;3:1.
27.ShanafeltTD,BooneS,TanL,etal.BurnoutandsatisfactionwithworklifebalanceamongUSphysiciansrelativetothegeneralUSpopulation. ArchInternMed. 2012;172(18):1377–85.
28.LuDW,DresdenS,McCloskeyC,etal.Impactofburnoutonselfreportedpatientcareamongemergencyphysicians. WestJEmerg Med. 2015;16(7):996–1001.
29.LiaisonCommitteeonMedicalEducation.Functionsandstructureofa medicalschool.Standardsforaccreditationofmedicaleducation programsleadingtotheMDdegree.2023.Availableat: https://lcme.org/ publications/.AccessedOctober3,2023.
30.ACGME.Commonprogramrequirementsforresidency,effective July1,2023. https://www.acgme.org/programs-and-institutions/ programs/common-program-requirements/
31.LuDW,GermannCA,NelsonSW,etal. “Pullingtheparachute”:a qualitativestudyofburnout’sinfluenceonemergencymedicineresident careerchoices. AEMEducTrain. 2020;5(3):e10535.
32.GettelCJ,CourtneyDM,JankeAT,etal.The2013to2019emergency medicineworkforce:clinicianentryandattritionacrosstheUS geography. AnnEmergMed. 2022;80(3):260–71.
33.GettelCJ,CourtneyDM,AgrawalP,etal.Emergencymedicine physicianworkforceattritiondifferencesbyageandgender. Acad EmergMed. 2023;30(11):1092–100.
KatherineB.Griesmer,MD,MPH*
MaxwellThompson,MD*
BrianaMiller,MD*
GuihuaZhai,PhD†
JaronRaper,MD*
AndrewBloom,MD*
SectionEditor: MuhammadWaseem,MD
*UniversityofAlabamaatBirminghamHeersinkSchoolofMedicine, DepartmentofEmergencyMedicine,Birmingham,Alabama † UniversityofAlabamaatBirmingham,CCTSBiostatistics,Epidemiology& ResearchDesign(BERD),Birmingham,Alabama
Submissionhistory:SubmittedJuly2,2024;RevisionreceivedOctober31,2024;AcceptedNovember1,2024
ElectronicallypublishedJanuary15,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.25020
Introduction: Readinesstoperformawidevarietyofproceduresormanagenearlyanypatient presentationremainsanessentialaspectofemergencymedicinetrainingandpractice.Often,simulation isneededtosupplementreal-lifeexposuretoprovidecomfortandknowledge,particularlywithrarer pathologyandprocedures.Asthescopeofpracticecontinuestogrow,newerprocedures,suchas ultrasound(US)-guidednerveblocks(UGNB),arebecomingintegratedintoresidenttraining,buildingon previouslyestablishedskills.Thefasciailiacacompartmentblock(FICB)isperformedonpatientswith specificfemoralfracturesandisanowacomponentofstandardmultimodalpainregimens,withUSguidancelimitingadverseevents.Giventheneedforhighvolumesoflocalanesthetictoperformthe blockitisimperativeforclinicianstounderstanddosingaswellasrecognizeandtreatlocalanesthetic systemictoxicity(LAST).Withsparseliteratureonsequentialimmersiveandproceduralsimulation involvingintertwinedtopics,thispresentsauniqueopportunityforlearners.
Methods: TostudytheperceivedknowledgeandcomfortwithFICBandLAST,apilotstudywas developedwithtwoseparatebutconcurrentone-hoursimulationscompletedencompassingoneofeach topicoveroneday.Wesurveyed19learners,consistingofresidentsrangingfrompostgraduateyears 1–3,priortoandimmediatelyfollowingcompletion,regardingtheirperceptions.WeusedtheStuartMaxwelltesttocomparesurveydata.
Results: Morethanhalfofparticipants(56%)hadnotreceivedpriorformaltrainingonFICB.Therewasa positivetrendinperceivedconfidenceandknowledgewithvisualizingrelevantanatomy(4.0[2.0–6.0]vs 9.0[7.5–10.0], P = 0.10),performingFICB(4.0[1.0–5.0]vs9.0[7.0–10.0, P = 0.08]),andperceived abilitytoteachtheirpeers(3.0[1.0–5.0]vs8.5[7.0–10.0], P = 0.20).Perceivedabilityindiagnosingand managingLASTalsoincreasedfollowingthesimulation(5.0[3.0–6.0]vs6.0[6.0–7.0], P = 0.12and 3.0[2.0–6.0]vs6.0[6.0–7.0], P = 0.08,respectively).
Conclusion: Learners’ perceptionsofthissimulationexperienceechothe findingsofpreviousstudiesin whichsimulationcanbeusedtoteachproceduresandpathology;ofnote,however,wepresenteda novelexperiencewithacombinationofimmersiveandproceduralsimulation.[WestJEmergMed. 2025;26(2)271–278.]
Toenhancepreparednesstocareforuncommonpatient presentationsandprocedures,simulationhasoftenbeenused ingraduatemedicaleducation(GME)tolaythefoundation aswellasto finetuneskills,includingresuscitations.1 Simulationhasalsobeenattheforefrontofproceduralskill acquisitionandincreasinglearner’ sconfidenceatboththe GMEandundergraduatemedicaleducationlevels,witha focusonbothhigh-acuityandlow-occurrenceprocedures.2–4 Bothinsimulationandclinicalpractice,moreproceduresare beingperformedunderultrasound(US)guidancewithtrends towardincreasedsafetyandefficacy,mostnotablyincluding placementofcentralvenouslines.5,6 Withthisincreasing incorporationofUStraininginemergencymedicine(EM) residencyprograms,thevarietyofproceduresperformedin anemergencydepartment(ED)settinghavealsoexpanded.
Regionalnerveblockswerepreviouslycompletedvia landmarkonly;however,therehasbeenprogressiontoward US-guidanceduetoreducedadverseeventsandgreater firstattemptsuccessrates.7,8 Regionalnerveblockshave increasinglyfallenunderthescopeofEMpractice, particularlywithregardtoUS-guidednerveblocks(UGNB). Manypatientsarepoorcandidatesforfrequentorhighdoses ofopioidsasaprimarypainmanagementstrategyinthe ED.9 Onestudyfoundalmost25%ofelderlypatients sufferedfromdeliriumwhilehospitalized,withthemajority ofthosereceivingpolypharmacy.10 However,UGNBisa valuabletoolformanagingpaininhipfractures,regardless ofpatientabilitytotolerateopioidandnon-opioid analgesics.Nerveblocksarenowrecommendedbythe AmericanCollegeofSurgeonsandtheAmericanAcademy ofOrthopaedicSurgeonsasastandardcomponentofa multimodalapproachtopainmanagement.11,12 The AmericanCollegeofEmergencyPhysicians(ACEP)recently statedthatUGNBsmakeupacoreskillforemergency physicians,voicingbroadsupportforitsuseandcitingits versatilityforavarietyofprocedures,fromcomplex lacerationrepairstoorthopedicreductions/splinting.7
Thefasciailiacacompartmentblock(FICB)canprovide significantanalgesia,particularlyinpopulationsthatmay havecontraindicationsorcomorbiditiesthatpreclude standardsystemicintravenousand/ororalpainregimens includingopioids,ketorolac,andotheranalgesicagents.The block,withitsdiscoveryin1989andeventualintroductionin theEMliteraturein2007,hasbeenslowtobeadopted despiteitssafetyprofileandefficacy.13,14 TheFICBcanbe usedforfemoralneckfracturesinthepre-,peri-,and postoperativestagesgiventheblockadeoffemoralnerve, localfemoralcutaneousnerve,andvariablecoverageofthe obturatornerve.8,15 ByincorporatingUSguidance,the compartmentblockisdonelateraltothefemoraltriangle (femoralnerve,artery,andvein),thusminimizingthechance ofintravascularinjection.13 Ameta-analysisofFICBhas alsobeenshowntoreducemorphinedosingrequirementand
mayevennegatetheneedforadditionalmedicationsbeyond theblock.16 Inanotherstudy,90%ofpatientshadblockade withasignificantreductioninthevisualanaloguescalefrom 7.5to2.94atthe20-minutemark.17 Withsuchcompelling dataregardingitsefficacyandthewidespreadavailabilityof USinEDs,theFICBrepresentsapowerfultoolinpain controlintheEDsettingthatiswellwithinthescopeofthe emergencyphysician.Withinourcurrentpractice,thiscould resultinincreasedpatientsatisfactionandpossiblyfreeup moreresources,includingnursing,particularlyifnot requiringconsistenttreatmentforbreakthroughpain.
Localanestheticsarecommonplacewithinthemedical fieldandespeciallywithintheEDwheretheyarearoutine componentofanyclinician’smedicalpractice.18 However, complicationsexist,particularlywhenlargequantitiesof anestheticareused,orinadvertentintravascularinjection occur,whichmaycauselocalanestheticsystemictoxicity (LAST).Elderlypatientsorthosewithorgandysfunctionare ataparticularlyhighrisk.19,20 Furthercomplicatingthe syndrome,LASThasconsiderablevariabilityinonsetand symptomatology.19 Itcanbedetrimentalthroughitseffects onboththecentralnervoussystem(CNS)and cardiovascularsystems,resultinginarrhythmias,seizures, cardiovascularcollapse,andriskofcardiacarrest.Each anestheticagenthasitsownmaximum,weight-baseddosing thatmaybeaugmentedifformulatedincombination withepinephrine.19
Previously,itwasbelievedtheagentswouldbehaveina predictable,stepwisemannerwithprecedentCNSsymptoms appearingpriortocardiacdysrhythmias;however,themore potentagentshavebeenfoundtohaveprecedingand possiblyconcomitantcardiacandCNStoxicity.20 The incidenceofLASTisvariablewithonestudyreporting occurrenceinupto25per10,000blockadesandanother specifyingoccurrencein79of10,000brachialplexus blockades.20 Regardlessofthetrueincidence,LAST occurrencehasbeenshowntobereducedwithUS-guided regionalanesthesiabyupto65%,althoughriskstillexists.21 Thus,trainingonrecognitionofthesignsandsymptoms,as wellastreatment,isimperativeforemergencyphysicians. Simulationofthisprocedureanditsmostdangerous complicationallowslearnersanopportunitytogain experiencewiththeconditionwithouteffectsonpatient outcomes.FollowingrecognitionofLAST,injectionmustbe firstdiscontinuedandinseverecasesmayrequire administrationofintralipidemulsiontherapy(ILE).The AmericanHeartAssociationalsoincludesILEinits guidelinesforcardiacarrestsecondarytoLAST.22
FollowingACEPguidelinesandexpandingonbasicsof well-knownprocedures,FICBmaybeabeneficialprocedure foremergencyphysicianstomasteralongwiththe considerationoftherisksofLASTanditsmanagement. Simulationhasbeendocumentedasbeinganeffective teachingmodality,offeringasafeenvironmentfor
learners.23,24 Ultrasound-basedtraininghasbeenpreviously showntobebeneficialwithanimprovementinconfidence andproceduralskills.23 Theliteratureissparseona combinationofsequentialimmersiveandprocedural simulationtechniquesinmedicaleducation.Whiletaking intoconsiderationthevariablepresentationsandseverityof complicationsrelatedtoLAST,aswellastherising importanceofregionalnerveblocksinEM,apaired simulationexperiencecanimproveidentificationand treatmentofthesyndrome,aswellasallowlearnersto enhancetheirskillset.HerewepresentapilotstudyonEM residents’ perceptionsandconfidencewithdiagnosingand managingLASTaswellasproceduralskillswithFICB.
Ourobjectiveinthisstudywastocreateanimmersive simulationthatteachesEMresidentstorecognizeclinical signsandsymptomsofLAST,developanappropriate treatmentalgorithm,andmanagepotentialoutcomes includingcardiacarrest.Secondaryobjectivesincluded successfulperformanceofUS-guidedFICB,troubleshooting complications,anddeterminingproperlocalanesthetic dosingtopreventLAST.Ultimately,thegoalwastodevelop asimulation-basedcurriculumtoincreaseresidentcomfort andknowledgewiththeFICBwhilerecognizingand managingitsrareandmoredangerouscomplications.
Weconductedaprospectivepilotstudy,deemedexempt bytheinstitutionalreviewboard,forbothanimmersivecase andproceduralsimulationinthefallof2023.Apresimulationquestionnairewasadministeredamonthprior withafocusonresidents’ perceivedcomfortlevelswith variousUS-guidedprocedures,alongwithuncommon causesofcardiacarrestandtheirmanagement.Anotherprequestionnairewasadministeredjustpriortotheprocedural FICBsimulationregardingcomfortandknowledgewiththe specificprocedure.
ParticipantswereEMresidentsrangingfrom postgraduateyears(PGY)1–3ataLevelItraumacenter universityhospitalsystem.Aconveniencesampleof19 residentswhowerepresentfortheconferenceday participated.Allparticipantsvoluntarilyagreedto participateintheactivitieswithinformedconsentprovided. Aspartoftheresidencycurriculum,residentsmustcomplete afour-weekrotationfocusingonUSskillsandinterpretation asPGY-1saswellasfulfilltheAccreditationCouncilfor GraduateMedicalEducation-requirednumberof resuscitations,ultrasounds,andprocedures.Anadditional fourweeksofthePGY-1yearisdevotedtotoxicologywith focusonawarenessandmanagementoftoxicologic emergencies.However,asthesessionwascompletedinthe firsthalfoftheyear,notallPGY-1shadcompleteda toxicologyand/orUSrotation.Priortothesimulations,
hands-onpracticehadonlyoccurredontheindividuallevel inthedepartmentclinicallywithnumbersascertainedprior tothesimulation.Apre-surveyhadbeen filledoutonemonth priortothesimulations.
TheLASTimmersivesimulationwasperformed firstfor eachparticipanttoavoidparticipantbiasandanchoring.For thesimulation,participantswererandomlydividedinto groupsofapproximatelythreeresidentsfora30-minute novelimmersivecasesimulationwithsubsequentstructured debriefandpost-survey.Thesimulationwasdevelopedin conjunctionwithEMsimulationfellowship-trainedfaculty. Thiscaseinvolvedascertainingahistoryandphysical,which includedarecentFICBforatraumatichipfracture.Thecase progressedwiththepatientshowingclinicalsignsand symptomsofLAST,includingseizureandsubsequent cardiacarrest.Participantsweretestedonandexpectedto developadifferentialdiagnosisforthepatient’spresentation, identifyLAST,andtreatthepatientwithintralipidtherapy aswellassupportivecare.Theteamwasinterdisciplinary withEMnursesandpharmacyresidentsalsoparticipating. Followingthesimulationduringadebriefingsession, diagnosticcriteriaandmanagementofLASTwerediscussed usinginformationprovidedbyaboard-certifiedtoxicologist. Participantsthen filledoutapost-surveyevaluatingtheir knowledgeandcomfortlevelregardingtheirrecognitionand managementofLAST.
Following completionoftheLASTimmersivesimulation, participantsweretransitionedtotheFICBprocedural simulationinaseparatelocationtoavoidcommunication withincomingparticipants.Eachgroupconsistedof approximatelysixresidentstoallowforadequatehands-on time.Apre-surveywasadministeredwithspecificquestions directedtowardresidents’ perceivedcomfortandknowledge withtheFICBprocedure.Abriefdidacticlecturefollowed withfocusonclinicalindicationsfortheprocedure,US anatomy,proceduralsetup,andlocalanesthetic specificationsanddosing.AreiterationofsignsofLASTas wellasmanagementwasincludedinthelectureaswell.A standardizedproceduralchecklistdevelopedinconjunction withboard-certifiedUSfacultywasusedbyallfacilitators (Figure1).Anotherhandoutforpracticingcalculating maximumdoseswasprovidedasacognitiveaid.
Astandardsetupofnerveblocksupplieswasused (Figure2).Theproceduralsimulationusedafasciailiaca manikin(ValkyrieSimulators,JohnsonMills,WV)for practicevisualizinganatomywithUS,andaporcine-tissue modelwasusedtopracticehydrodissectingakinto performingtheprocedureinclinicalpractice(Figure3).No manipulationsweremadetotheporcine-tissuemodel includingadditionofmocknervestructures.Following completionoftheproceduralsimulation,apost-surveywas administeredtotheresidentparticipantswithspecific questionspertainingtoconfidenceandknowledgeof proceduralindications,relevantanatomy,andperceived
Confirm patient identity using two-patient identifiers
Obtain informed consent
Perform hand hygiene and don exam gloves
Document physical exam prior to procedure including neurovascular exam
Preparing for procedure
Gatherappropriateequipment
Place patient in neutral position
Calculatemaximumdosingofanesthetic
Procedural Steps
Analyze anatomy with US including location of femoral artery
Disinfect site
Don PPE and drape field
Draw up local anesthetic and normal saline if desired in syringe
Connect spinal needle or PIV needle to connector tubing and syringe
Cover linear array with sterile probe cover
Insert with needle in-plane
Hydrodissect fascia iliaca with partner pushing syringe
Inject entire solution ensuring not to exceed maximum dose
Remove needle
Performing appropriate aftercare
Dispose of all other non-sharp materials
Remove PPE and perform hand hygiene
Clean hands usingalcohol-basedhand sanitizer or soap and water
Figure1. Learnerchecklistforfasciailiacacompartmentblock(FICB)procedure. PPE,personalprotectiveequipment; PIV,peripheralintravenous; US,ultrasound.
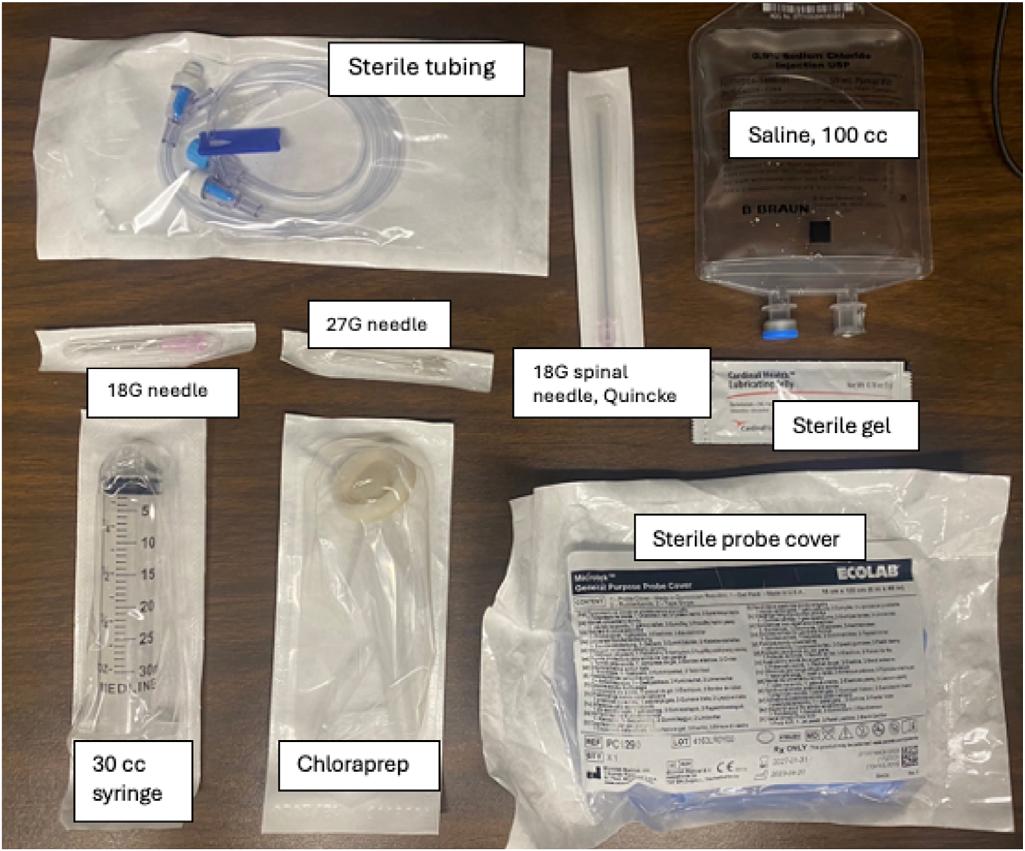
Figure2. Suppliesforfasciailiacacompartmentblockprocedure. G,gauge; cc,cubiccentimeter.
comfortinperformingtheprocedurefollowinghands-on teachingandguidance.Board-certifiedUSfacultydirected allhands-onteachingandinstruction.
Wecomparedpre-andpost-trainingsurveyresponses usingageneralizedStuart-Maxwelltesttoevaluatethe impactofthetrainingonresidents’ knowledgeandattitudes

Figure3. Simulationofhydrodissectingonporcine-tissuemodel (arrowindicatingneedletip).
towardtheprocedureandLASTtoxicity.Questionnaires includedscaleof1–10forFICBsurveysand1–7forLAST surveys,with1correspondingtostronglydisagreeandthe upperlimitsof7and10representingstronglyagree, respectively.Analphalevelof0.05wassetforallstatistical tests.WeperformedallanalysesinSAS9.4.(SASInstitute Inc,Cary,NC).25
Priortoimplementationofbothsimulations,we performedwalk-throughsessionstoanticipateandidentify anylogisticalorsystemsissues.Nursing,pharmacy,and
Table1. Groupcharacteristics.
Pre-simulationgroup characteristicsLAST(n = 19)FICB(n = 16)
PGYlevel
PGY-1
4(21.1%)3(18.8%)
PGY-2 7(36.8%)5(31.3%)
PGY-3 8(42.1%)8(50%)
Priortoworkshop:numberof previouslyperformedFICB Ihaveneverheardofit
PGY, postgraduateyear; LQ,lowerquartile; UQ,upperquartile; FICB,fasciailiacacompartmentblock; LAST,localanesthetic systemictoxicity.
simulationstaffwerealsoconsultedforinputregardingthe sessionaswellasimplementationinthedepartment.A board-certifiedtoxicologistalsoprovidedinputtoensure managementwasconsistentwiththestandardofcare.
Atotalof19EMresidentsrangingfromPGY1–3 participatedintheLASTsimulation,and16residents participatedintheFICBproceduralsimulation.The distributionamongtraininglevelsisdescribedin Table1 with askewtowardmorePGY-3s(42.1%and50%,respectively). Overall,16participants,ormorethanhalf(56%),hadnot receivedpriorformaltrainingonFICB.Halfofthe participantshadpreviouslyperformedaFICB,withthe majority(31.3%)onlyperforming1–3FICBpriortothe session(Table1).Followingsimulation,learnersreportedan improvementinconfidenceandknowledgewithperforming aFICB,withthepre-simulationimprovingfrom4.0 (1.0–5.0)to9.0(7.0–10.0)post-simulationusingthescale previouslymentionedwith10representing “stronglyagree.” Therewasalsoanincreaseintheperceptionoftheutilityof FICBintheED.LearnersfeltmoreconfidentinusingUSto visualizetherelevantanatomy(4.0[2.0–6.0]vs9.0[7.5–10.0]) andgeneralknowledgeofUGNB(5.0[2.0–7.0]vs10.0 [8.0–10.0]).Residentsfeltmoreconfidentintheirabilityto teachtheirpeerstheprocedure(3.0[1.0–5.0]vs8.5 [7.0–10.0]).Ageneralpositivetrendincomfortand knowledgewasnotedintheFICBfollowingsimulation, althoughnoresultswerestatisticallysignificant(Table2). Learnersratedsimilarperceptionincomfortwith diagnosingandmanaginguncommonconditionsbothprior toandfollowingtheLASTsimulation.Therewasanincrease incomfortinbothdiagnosingandmanagingLAST.
RecognitionofLASTincreasedfrom5.0(3.0–6.0)to6.0 (6.0–7.0)frompre-topost-simulation,respectively,with 7.0representingstrongagreementwithastatement. Perceptionregardingmanagementfollowedasimilartrend with3.0(2.0–6.0)pre-simulationto6.0(6.0–7.0)postsimulation(Table2),althoughneitherwasfoundtobe statisticallysignificant.
SimulationisakeycomponentofGME,forboth immersivecasesaswellaspracticingandmastering procedures,butthereislimitedresearchoncombiningboth approachestobettermimicreal-lifepracticeandtiein connectedtopics.SimulationoftheFICB,anditsmost seriousadverseeffect,LAST,offersauniqueopportunityfor residentsimulation.Withminimalresourcesandsetup,itis possibleforlearnerstoexperiencethemultitudeof pathologicpresentationsandneededresuscitativemeasures ofLAST.Althoughthemaingoalofbothsimulationswasto assessperceptionsinknowledgeandconfidence,theresidents werealsoabletopracticemanagementofseizures,airway, andcardiacarrestwhilealso fine-tuning US-guidanceskills. Whileourstudywaslimitedbyunderpowering,asis commoninsimulation-focusedGMEstudiesduetolimited learnernumbers,wefoundevidenceofseveralimportant trendsalthoughtheylackedstatisticalsignificance. 26 Inthe timingimmediatelyfollowingsimulation,residentsreported anincreasingtrendinconfidenceandself-perceived knowledge,withthetrendbeingmoreprofoundfortheFICB proceduralsimulation.These findingsareinlinewithprior proceduralsimulation-basedresearch,demonstratingatrend towardimprovedlearnerconfidenceandknowledge followingtheprocedure.27,28 Residentsalsonotedincreasing comfortwithteachingpeerstheprocedure.Asresident perceptionsweresurveyedimmediatelyfollowingthe simulationevents,itisunclearwhetherthosetrendspersisted beyondthedayofsimulationorwereappliedtosubsequent clinicalpractice.Futureinvestigationswouldbenefitfrom follow-upatascheduledintervalandclinicallyfocused outcomemeasures,suchasproceduralproficiencyorthe absenceofadverseevents.
Regardingtheimmersivesimulation,nosignificant impactwasseenindiagnosingandmanaginguncommon conditionsorworkinginaninterdisciplinaryteam,although therewasapositivetrendwithresidents’ abilitytodiagnose andmanageLAST.Previousstudieshavefocusedonthe impactofinterprofessionalteamsforimmersivesimulation andhavenotedapositivecorrelationwithappreciationand generalknowledgeofotherhealthcareprofessions.29 Despite resuscitationbeingamajorcomponentofEMtraining,this studymaydemonstrateaneedformoredetailedinstruction regardingrarercausesofarrest.
Overall,perceptionsofthesimulationexperiencewere alsopositivewithlearnersindicatingsupportoffuture
Table2. Pre-andpost-simulationreportedexperiences.
Meanreportedpre-andpost-simulationperceptions(FICB)(n = 16)MedianLQUQ
Perceivedknowledgeofultrasound-guidednerveblocks
PerceivedcomfortlevelwithperformingFICB
Perceivedcomfortvisualizingfasciailiacaanatomy onUS
PerceptionofFICButilityintheED
Perceivedcomfortteachingproceduretopeers
Meanreportedpre-andpost-simulationperceptions(LAST)(N = 19)
Perceivedconfidence indiagnosinguncommonconditions
Perceivedconfidenceinworkinginamulti-disciplinaryteam
PerceivedconfidenceinrecognitionofLAST
PerceivedconfidenceinmanagementofLAST
PGY, postgraduateyear; LQ,lowerquartile; UQ,upperquartile; FICB,fasciailiacacompartmentblock; LAST,localanestheticsystemic toxicity; US,ultrasound.
sessionsforotherEMresidentsandclinicians.Althoughnot statisticallysignificantandlargelysimilarpre-andpostsimulation,thecombinationofcaseswaswellreceivedby residentsinsurveycomments.Combinationcasesmay provideachanceforadeepergraspofintegratedtopicsas wellasauniqueopportunityforresidentstopracticeinan immersivesimulationenvironment.Thelimitedtime availableforresidenteducationmakesthisapproach valuable,asbothsimulationscovermultipleaspectsof medicalcare.
Limitationstothestudyincludeparticipants’ self-reported confidenceandknowledgeafterasingleencounterand,thus, mayhavebeensubjecttobiasgivenitssubjectivenature. Whiletherewasageneraltrendtowardimprovementin perceptionsofknowledgeandskillsfollowingthesimulation, thisisalsoinreferencetoshort-termrecallwithfurther studiesneededtoascertainlong-termretentionofknowledge andproceduralskills.Furtherstudieswouldalsoberequired toelucidatetheeffectsofcombinationsimulationasa
Table3. Learnerperceptionsregardingsimulationexperience. Post-simulationlearnerexperiencesurveyMedianLQUQ
Thegoalsofthesimulationwereclearlyoutlinedpriortoparticipation
Felt hadenoughsupervisionduringsimulation
Feltcomfortableaskingquestionsorforhelpduringthesimulation
Feltwasgivenadequatefeedbackduringsimulation
Simulationcomplimentedlearningstyle
ThisworkshopwouldbeusefulforfutureEDresidentsandclinicians
ED, emergencydepartment; LQ,lowerquartile; UQ,upperquartile.
learningopportunity.Neitherwereweabletomeasure translationtoreal-worldpractice,withunclearintegrationof FICBintotheparticipants’ futureclinicalpractice.An expansionofthestudywithanextendedtimelinemayshowa declineintheknowledgeandskillsacquiredinthis simulationovertime,aswellaspracticechanges. Participationwasanotherkeylimitationwitha predominanceofupper-levelresidents;andlossof participantsmaybeattributedtoschedulingdifficulties particularlywithoff-servicerotations.
Furtherlimitationsmayexistifattemptingtoreproduce thisexperienceatothersites;thissimulationisbasedon faculty’sownperceivedskillsandconfidenceinperforming, andteaching,FICB,whichmaynotbeasstrongatother sites.Thissimulationmaynotbeworthwhileatothersitesif FICBprocedurescannotbeimplementedgivenaccessibility tointralipidemulsiontherapyincaseofpossibleLAST. Althoughresearchhasalreadyshownthebenefitofusing FICBinEDsbothintheUnitedStatesandresource-limited areas,furtherstudiesshouldbeperformedonteaching modalities,particularlyforthosewithhistoricallymore limitedultrasoundteaching.13 Thehomogenousresponsesin Table3 mayreflectfurtherlimitationstothestudy,which couldreflectunderlyingbias.
Overall,thisstudycontinuestodemonstratethepositive effectregardingtheuseofsimulationinmedicaleducation, bothwithimmersiveandproceduralsimulations.Increasing exposure,evenatanintroductorylevel,ofrarerpathology, includingLAST,mayaidindiagnosisandmanagement. Residents’ perceptionoftheproceduralsimulationinthis study,whilelimitedtofasciailiacacompartmentblock procedure,alsohadapositivetrendtowardcomprehension andskillset.Althoughlimitedinthenumberofparticipants, thisstudydemonstratesthattheuseofcombination immersiveandproceduralsimulationmayprovidean excitingandworthwhileexperienceforlearners,particularly withinterconnectedtopics.
AddressforCorrespondence:KatherineB.Griesmer,MD/MPH, UniversityofAlabamaatBirminghamHeersinkSchoolofMedicine, DepartmentofEmergencyMedicine,52119thSt.,S,General ServicesBuilding,RM240,Birmingham,AL35294.
Email: kbaldwin@uabmc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Griesmeretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.RaperJD,KhouryCA,MarshallA,etal.Rapidcycledeliberatepractice trainingforsimulatedcardiopulmonaryresuscitationinresident education. WestJEmergMed. 2024;25(2):197–204.
2.ToyS,McKayRS,WalkerJL,etal.Usinglearner-centered,simulationbasedtrainingtoimprovemedicalstudents’ proceduralskills. JMed EducCurricDev. 2017;4:238212051668482.
3.HubertV,DuwatA,DeransyR,etal.Effectofsimulationtrainingon compliancewithdifficultairwaymanagementalgorithms,technical ability,andskillsretentionforemergencycricothyrotomy. Anesthesiology. 2014;120(4):999–1008.
4.BloomAD,AliottaRE,MihasA,etal.Tele-simulatedinstructionand learnerperceptionsof fiberopticintubationandnasopharyngoscopy: apilotstudy. WestJEmergMed. 2022;24(1):104–19.
5.BarrL,HatchN,RoquePJ,etal.Basicultrasound-guidedprocedures. CriticalCareClinics. 2014;30(2):275–304.
6.UltrasoundGuidelines:Emergency,point-of-careandclinicalultrasound guidelinesinmedicine. AnnEmergMed. 2017;69(5):e27–54.
7.ACEP.Policystatementultrasoundguidednerveblocks.2021. Availableat: https://www.acep.org/siteassets/new-pdfs/policystatements/ultrasound-guided-nerve-blocks.pdf AccessedDecember21,2023.
8.O’ReillyN,DesmetM,KearnsR.Fasciailiacacompartmentblock. BJAEducation. 2019;19(6):191–7.
9.HerzigSJ,StefanMS,PekowPS,etal.Riskfactorsforsevereopioidrelatedadverseeventsinanationalcohortofmedicalhospitalizations. JGenInternMed. 2019;35(2):538–45.
10.HeinC,ForguesA,PiauA,etal.Impactofpolypharmacyonoccurrence ofdeliriuminelderlyemergencypatients. JAmMedDirAssoc. 2014;15(11):850.e11–5.
11.AmericanCollegeofSurgeons.AmericanCollegeofSurgeonsbest practicesguidelinesgeriatrictraumamanagement.2023.Availableat: https://www.facs.org/media/ubyj2ubl/best-practices-guidelinesgeriatric-trauma.pdf.AccessedOctober15,2024.
12.AmericanAcademyofOrthopaedicSurgeons.AmericanAcademyof OrthopaedicSurgeonsmanagementofhipfracturesinolderadults evidence-basedclinicalpracticeguideline.2021.Availableat: https:// www.aaos.org/hipfxcpg.AccessedOctober15,2024.
13.PinsonS.Fasciailiaca(FICB)blockintheemergencydepartmentfor adultswithneckoffemurfractures:areviewoftheliterature. IntEmerg Nurs. 2015;23(4):323–8.
14.StLouisD,IsersonKV,ForgetN.Fasciailiacacompartmentblock efficacyinresource-pooremergencydepartments. ClinPractCases EmergMed. 2018;2(4):286–90.
15.ZhouY,ZhangWC,ChongH,etal.Aprospectivestudytocompare analgesiafromfemoralobturatornerveblockwithfasciailiaca compartmentblockforacutepreoperativepaininelderlypatientswith hipfracture. MedSciMonit. 2019;25:8562–70.
16.HongHandMaY.Theefficacyoffasciailiacacompartmentblockfor paincontrolafterhipfracture. Medicine. 2019;98(28):e16157.
17.KumarD.AnalgesicefficacyofultrasoundguidedFICBinpatientswith hipfracture. JClinDiagnRes. 2016;10(7):UC13–6.
18.GanzbergSandKramerKJ.Theuseoflocalanestheticagentsin medicine. DentClinNorthAm. 2010;54(4):601–10.
19.LongB,ChavezS,GottliebM,etal.Localanestheticsystemictoxicity: anarrativereviewforemergencyclinicians. AmJEmergMed. 2022;59:42–8.
20.MahajanAandDerianA.Localanesthetictoxicity.2020. Availableat: https://www.ncbi.nlm.nih.gov/books/NBK499964/ AccessedDecember22,2023.
21.El-BoghdadlyK,PawaA,ChinKJ.Localanestheticsystemictoxicity: currentperspectives. LocalRegAnesth. 2018;11:35–44.
22.LiuY,ZhangJ,YuP,etal.Mechanismsandefficacyofintravenouslipid emulsiontreatmentforsystemictoxicityfromlocalanesthetics. Front Med(Lausanne). 2021;8:756866.
23.BradleyK,QuintonA,AzizA.Determiningifsimulationiseffective fortraininginultrasound:anarrativereview. Sonography. 2019;7(1):22–32.
24. NakazatoT,CallahanZ,KuchtaK,etal.A1-daysimulation-basedboot campforincominggeneralsurgeryresidentsimprovesconfidenceand technicalskills. Surgery. 2019;166(4):572–9.
25.StuartA.Atestforhomogeneityofthemarginaldistributionsinatwowayclassification. Bimetrika. 1955;42(3–4):412–6
26.GabaDM.Historyofsimulationinmedicine:fromResusci-Annetothe present. Neurosurgery. 2013;73(Suppl1):9–14.
27.HarringtonJ,DuncanG,DAngeloK,etal.Multidisciplinarysimulation improvesresidentconfidenceforpregnantpatientsrequiringsurgical intervention. Cureus. 2022;14(3):e23454.
28.MalekniaL,BoshuizenV,CaputoH,etal.Improvingproceduralskill confidenceinpediatricresidents:alongitudinalsimulation-based workshopcurriculum. MedEdPORTAL. 2023;19:11322.
29.GuillaumeA,HarwoodC,HarwoodP,etal.Immersiveclinical simulationinundergraduatehealthcareinterprofessionaleducation: knowledgeandperceptions. ClinicalSimulationinNursing. 2014;10(4):e205–16.
DevelopmentofaReliable,ValidProceduralChecklistfor AssessmentofEmergencyMedicineResidentPerformance ofEmergencyCricothyrotomy
DanaE.Loke,MD,MS*
AndrewM.Rogers,MD,MBA†
MorganL.McCarthy,MD‡§
MarenK.Leibowitz,MD¶
ElizabethT.Stulpin,MD#
DavidH.Salzman,MD,Med‡∥
* UniversityofWisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,Madison,Wisconsin
† NorthShoreUniversityHealthSystem,DivisionofEmergencyMedicine, Evanston,Illinois
‡ NorthwesternUniversity,FeinbergSchoolofMedicine,DepartmentofEmergency Medicine,Chicago,Illinois
§ StLuke’sHospital,DepartmentofEmergencyMedicine, NewBedford,Massachusetts
¶ IcahnSchoolofMedicineatMountSinai,InstituteofCriticalCareMedicine, NewYork,NewYork
# EmoryUniversityHospital,DepartmentofEmergencyMedicine,Atlanta,Georgia
∥ NorthwesternUniversity,FeinbergSchoolofMedicine,DepartmentofMedical Education,Chicago,Illinois
SectionEditors: MatthewTews,MDandChristineStehman,MD
Submissionhistory:SubmittedJune15,2024;RevisionreceivedNovember8,2024;AcceptedNovember12,2024
ElectronicallypublishedJanuary30,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20365
Introduction: Emergencycricothyrotomyisararebutpotentiallylife-savingprocedureperformedby emergencyphysicians.Acomprehensive,dichotomousproceduralchecklistforemergency cricothyrotomyforemergencymedicine(EM)residenteducationdoesnotexist.
Objectives: Weaimedtodevelopachecklistcontainingthecriticalstepsforperforminganopen emergencycricothyrotomy,toassessperformanceofEMresidentsperforminganopenemergency cricothyrotomyusingthechecklistonasimulator,andtoevaluatethereliabilityandvalidityofthe checklistforperformingtheprocedure.
CurricularDesign: Wedevelopedapreliminarychecklistbasedonliteraturereviewandsentitto expertsinEMandtraumasurgery.AmodifiedDelphiapproachwasusedtorevisethechecklistand reachconsensusona finalversionofthechecklist.Toassessusabilityofthechecklist,weassessedEM residentsusingacricothyrotomytasktrainer.Scoresweredeterminedbythenumberofcorrectly performeditems.Wecalculatedinter-raterreliabilityusingtheCohenkappacoefficient.Validitywas assessedusingtheWelch t-testtocomparetheperformanceofresidentswhohadandhadnot performedanopenemergencycricothyrotomy,andweusedanalysisofvariancetocompare performanceofpostgraduateyear(PGY)cohorts.
Impact/Effectiveness: The final27-itemchecklistwasdevelopedafterthreeroundsofrevisions.Interraterreliabilitywasstrongoverall(κ = 0.812)withindividualchecklistitemsrangingfromslighttonearly perfectagreement.Atotalof56residentsparticipated,withanaveragescoreof14.3(52.9%). PerformancevariedsignificantlyamongPGYgroups(P < 0.001).Residentswhohadperformedan emergencycricothyrotomypreviouslyperformedsignificantlybetterthanthosewhohadnot (P = 0.005). Thedevelopedchecklist,whichcanbeusedinproceduraltrainingforopenemergencycricothyrotomy, suggeststhatimprovedtrainingapproachestoteachingandassessingemergencycricothyrotomyare neededgiventheoverallpoorperformanceofthiscohort.[WestJEmergMed.2025;26(2)279–284.]
Emergencycricothyrotomyisararebutpotentiallylifesavingprocedurethatemergencyphysicians(EP)mustbe abletocompetentlyperform.ItisperformedwhentheEPis unabletooxygenateandventilateapatientafterrapid sequenceintubationisinitiatedand,therefore,mustpursue cricothyrotomyinatime-sensitivemanner.Thus,itis essentialforEPstobeabletoperformtheprocedure correctly.Furthermore,theAccreditationCouncilfor GraduateMedicalEducationincludescricothyrotomyasa “keyprocedure” forwhichresidents “mustdemonstrate competence.”1 However,therearefewopportunitiestolearn thisprocedureintheclinicalenvironment,withonestudy demonstratingthatonly22%ofgraduatingemergency medicine(EM)residentshadtheopportunitytoperform cricothyrotomyonalivingpatient.2 Anotherstudyindicated thatevenexperiencedEPsfeltthattheylackedtrainingin performingcricothyrotomyandthatthisprocedural inexperiencecoulddirectlyaffectthesurvivalofapatientand leadtohighemotionalpressure.3 Lastly,thecritically importantnatureoftheproceduremakeslearningonshifta patientsafetyissue.
Thecombinationofcompetency-basedapproachesusing checklist-basedassessmentsandthesimulationenvironment hasdemonstratedalongtrackrecordofimprovingresident performanceonspecificproceduralskills.4–8 Whilevarious instructionalvideosandchecklistsmeantfordifferent specialtiesareavailable,astandardized,reliable,valid, comprehensive,anddichotomousproceduralchecklistfor assessmentofperformingemergencycricothyrotomyforEM residenteducationislacking.9–11 Historically,thestudysite program ’smethodforteachingtheopenemergency cricothyrotomyoccurredduringtheannual “ rare procedures” simulationlab.Thesesessionsinvolvednonstandardizedpracticewithatasktrainerorsheeplarynxthat didnotfollowacompetency-basedtrainingmodel.
RecognizingthisunmetneedinEMproceduraltraining forourlearners,wesetseveralobjectivesinthisstudy.The primaryobjectivewastodevelopachecklistcontaining thecriticalstepsforperforminganopenemergency cricothyrotomybasedoninputfromamultidisciplinary teamofexperts.Thesecondobjectivewastoevaluatethe reliabilityandvalidityofthechecklistforperformingopen emergencycricothyrotomy.Finally,thethirdobjectivewas tousethechecklisttoassessagroupofEMresidentsontheir abilitytoperformtheprocedureonasimulatorandcompare performancebytrainingyear.
ChecklistDevelopment
WeperformedaliteraturereviewinMEDLINEandthe MedEdPortaltoassesspublishedliteratureforemergency
cricothyrotomyprocedurechecklistsandcurriculums.Key phrasesforliteraturesearchesincluded “ emergency cricothyrotomycurriculum,”“emergencycricothyrotomy checklist,”“emergencycricothyrotomyprocedure,” “emergencycricothyrotomysimulation,”“ emergency cricothyrotomyresident,”“emergencycricothyrotomy residency,”“emergencycricothyrotomyeducation,” and variationsandcombinationsofthekeywords/phrases. Searchesincludedallarticlespublisheduntilthesearchdate ofNovember1,2020.AnEMproceduralskillstextbookand asurgicaltechniquetextbookwerereviewedaswell.12,13 We alsoevaluatedrelevantarticlesfromthebibliographiesofthe textbooksandincludedstudiesforinclusion.
WeusedtheStufflebeamframeworkforchecklist developmentaftertheliteraturereviewwascompleted.14 A preliminarydichotomous(“done” vs “incorrect/notdone”) checklistwasdevelopedbasedonthisliteraturereview.The initialchecklistwassenttoapanelof13expertscomprisedof emergencyphysiciansandtraumasurgeonsofvarying practicetype(academic,community,military),geographic practicelocation(withintheUnitedStates),andgender. Practicetypeincluded10academic,twocommunity,andone militaryhospital;practicelocationincluded fiveinternaland eightexternal;andbreakdownbysexwas fivefemaleand eightmale.Expertswereblindedtoeachother’sidentities andcomments.Weinformedtheexpertpanelofthe curriculum’sintendedaudienceofEMresidentswith anticipateduseforacompetency-basedcurriculum.Weused amodifiedDelphiapproachtoseriallyrefinethechecklist andreachconsensusona finalchecklist.15,16 Wethenpilottestedthechecklisttoensuretheitems,wording,and formattingwereideallyoperationalized.Finally,theexpert panelrevieweditfor finalapproval.
Thestudywasperformedatasingleurbanacademic centerwithafour-yearEMresidencytrainingprogram.Four residentswereexcludedfromthestudyduetotheir participationinthechecklistdesignandassessmentprocess. AllotherEMresidentswereincludedintheeducationaspart oftheannualsimulationcurriculum;however,participation inthestudywasvoluntary.Thestudywasreviewedbythe institutionalreviewboard(IRB)atNorthwesternUniversity, FeinbergSchoolofMedicineanddeterminedtobeexempt. Writteninformedconsentwasobtainedfromparticipants usingaconsentformapprovedbytheIRB.
Assessmentsoccurredinthesimulationcenterusinga simulationmanikin(TraumaMan,Simlab,Seattle,WA) fromAugust31–September28,2021.Performance assessmentsweredocumentedusinganelectronicversionof thechecklistinQualtrics(Qualtrics,Seattle,WA),including adichotomous “Yes” or “No” forcompletionofeachstep.
Onein-personrater(DL)wassituatedadjacenttothe simulationmanikinwiththeabilitytomoveaboutthe simulationroomtoensureidealvisualization.Audiovisual recordingoftheassessmentincludedonecameraoverhead providingadirectoverheadviewandasecondcamera situatedtoprovideaviewfromtheside.Eachparticipant assessmentwasrecordedfromstarttocompletionofthe checklist.Thedualvideofeedswithaudioweresavedasa singleside-by-sidevideorecording.Theserecordedvideos werereviewedbyasecondrateratalatertime.Weusedan onlinerandomnumberpicker(https://www.random.org/ lists/)toselect30%oftheparticipantsforscoringbythe secondrater.17 Thesecondrater(AR)scoredtherandomly selectedsampleofvideorecordingsusingthesameelectronic assessmentinstrumentinQualtrics.
Thechecklistwasanalyzedforinter-raterreliabilityand validityamongacohortofEMresidentsrangingfrom PGY1-4.Inter-raterreliabilitywascalculatedoverallandfor eachcheckliststepusingtheCohenkappacoefficient.We determinedvalidityusingtheWelch t -testtocomparethe performanceofparticipantswhohadandhadnotperformed anemergencycricothyrotomyinclinicalpracticeor simulationandalsobetweenconsecutivePGYgroups. Analysisofvariancewasusedtocompareperformance amongPGYcohorts.
Theliteraturesearchproducedatotalof394articles.After review,13articlesweredeemedsuitabletoinformchecklist development.Anadditionaltwoarticleswereidentifiedand includeduponreviewingreferencesoftheincludedarticles andthetwotextbooks.Wedevelopedapreliminary33-item dichotomouschecklistbasedonthisliteraturereview. Consensuswasachievedafterthreeroundsofrevisions, resultinginthefourthversionofthechecklistbeingthe final version.Wethentestedthe final27-itemchecklistamong ourselvesforusability.Onlyminorwordingandformatting changesweremadetoensureidealoperationalizationofthe checklist.The finalchecklistwasapprovedbytheexpert panelafterusabilitytesting,andnoadditionalrevisions weresuggested.
The table includespercentagecorrectofchecklistitems, inter-rateragreement,andCohenkappacoefficientsforeach checklistitem.Overall,inter-raterreliabilitywasstrong (κ = 0.812)withindividualchecklistitemsrangingfromfair tonearlyperfectagreement,withoneitemhavingslight agreement.Atotalof56residentsparticipated,including15 PGY-1,14PGY-2,13PGY-3,and14PGY-4residents. Whileonlyoneresidenthadperformedanemergency cricothyrotomyonalivepatient,69.6%hadpreviously performedanemergencycricothyrotomyinsimulation.The
averagechecklistscorefortheoverallresidentcohortwas 14.3(52.9%).Emergencymedicineresidentchecklist performancevariedbyPGYclass(Figure).Performance variedsignificantlyamongstPGYgroups(P < 0.001).The PGY-4sperformedbestwithanaveragescoreof16.7 (61.9%)ofchecklistitemscompletedcorrectly.They performedbetterthanPGY-3s,butnotsignificantly(61.9% vs59.5%, P = 0.21).ThePGY-3sperformedsignificantly betterthanPGY-2s(59.5%vs48.9%, P = 0.01).ThePGY-2 performancewasbetterbutnotsignificantlydifferent comparedtoPGY-1performance(48.9%vs.42.7%, P = 0.13).Theresidentswhohadpreviouslyperformedan emergencycricothyrotomyonalivepatientorinsimulation performedsignificantlybetterthanthosewhohadnot (56.8%vs.44.2%, P = 0.005).
Althoughweidentified proceduralnarrativesand checklistswithvaryingdegreesofspecificityforourlearner groupatthetimeofourliteraturereview,oursearch demonstratedalackofastandardized,validated,reliable, anddichotomousproceduralchecklistforemergency cricothyrotomyforEMresidents.Thischecklistaddsto morerecentlypublishedarticlestargetingattendings, students,and “novice” learners.Thisnewlydeveloped proceduralchecklistforemergencycricothyrotomy addressesthisunmetneedforEMresident proceduraltraining.
Theexpertpanelprovidedcriticalinsightduringthe checklistdevelopment.Ourinitialchecklistfocusedonthe classic “hookanddilator,” scalpel-basedapproachto emergencycricothyrotomy.However,weultimatelyrevised thechecklistbasedonexpertfeedbacktoincludethe additionalacceptedapproachesof “scalpelonly” and “bougie-assisted” emergencycricothyrotomy.Theinclusion ofallthreeacceptedapproachesallowedforamoreversatile checklistthatismoregeneralizabletoallresourcesettings andbetterreflectsthevariablereal-worldenvironmentand urgencyoftheprocedure.Theinclusionofmultiple techniquesalsosuggestsgeneralizabilitytootherclinical environments,suchassurgeryandotolaryngology;however, thiswasnottheintendedaudienceatthetimethechecklist wasdeveloped.Whilethereareseveralpotentialoptionsfor performinganemergencycricothyrotomy,includinga needle/wireSeldingertechnique,thischecklistreflectsthe developmentwiththeprimaryconstructofusingascalpelbasedapproach.
Thisstudy’sstrongoverallinter-raterreliabilityusingthis checklistandonein-personraterandoneremote-videorater reinforcespreviousstudiesusingasimilartechnique.18,19 Additionally,inter-raterreliabilityusingthismethodwas strongoverall,whichisconsistentwithpriorchecklist developmentstudieswithsimilarmethods.18,19 Most individualitemshadmoderatetonear-perfectinter-rater
Table. Percentcorrect,inter-rateragreement,andreliabilityforindividualchecklist-itemscoring. Checklistitem
1.Gatherssterilesupplies
2. Gathersprimarycricothyrotomyproceduresupplies
3.Gatherssecondary/supplementalcricothyrotomyproceduresupplies
4.Gatherssupplementalintubationsupplies 0%100%n/a*
5.Washeshands
6.Sterilizestheneck
7.Donspersonalprotectiveequipment
8.Proceduralistpositionsonthepatient’srightside
9.Identi fiescricothyroidmembrane(CTM)
10.Usesthumbandmiddle fingerofnon-dominanthandtostabilizeairway
11.Confirmsincisionsitewithpalpationbyindex fingerontheCTMusingnon-dominant handwhilemaintainingstabilizationusingthumbandmiddle fingerofnon-dominanthand
12.Usesscalpeltomakeverticalskinincision~2–4cminlengthovertheCTMusing dominanthand
13.DissectsdowntoCTM
14.Re-identifiesCTMbypalpationorvisualization
15.Makes~1–2cm(widthofscalpelblade)horizontalincisionthroughCTMwithdominant handandmaintainsscalpelbladeintrachea
16.Maintainspatencyoftract
17.Removesscalpel,onlyaftertrachealhook,Trousseaudilator,bougie,orsecondary scalpelhandleisinplace,maintainingpatencyofCTM
18.ProceduralistdilatesCTM
19.Insertsendotrachealtubeortrach
20.Insertsendotrachealtubeortrachtocorrectdepth
21.Inflatesthecuffwitha10-ccsyringe
22.Connectsbag-valve-masktoendotrachealtube/trachandbeginsassistedventilation92.9%94.1%0.638
23.Usescapnographytoconfirmtubelocation
24.Listensforbilateralbreathsounds
25.Securesendotrachealtube/trach
26.Orderschestradiograph
27.Documentsprocedure
*Unabletocalculatekappacoefficient duetooneorbothratersgivingthesamescoretoallscoredparticipants.
reliability,overalldemonstratingreliabilityofthechecklist.20 Theitemswiththelowestkappascoresincluded “gathers sterilesupplies” (item1), “identifiescricothyroidmembrane” (item9),and “usesscalpeltomakeverticalskinincision ~2–4cminlengthoverthecricothyroidmembraneusing dominanthand” (item12).Wesuspectthatthislikelyreflects theremotenatureofthesecondrater,asmishearingarequest forasinglepieceofequipmentorinabilitytoaccurately visualizethemembraneorexactlengthofincisionona recordedvideowouldleadraterstoscoredifferently.This couldhavebeenimprovedwithgreaterverbalizationofall stepsbythelearnerandprimaryraterorhavingasecondinpersonraterwhenable.
Theresidentswhohadperformedanemergency cricothyrotomypreviouslyperformedsignificantlybetter thanthosewhohadnot,demonstratingcriterionvalidityfor thischecklistastherewascorrelationwiththisgroup’sprior experience.Severalstudieswithsimilarmethodshavealso demonstratedcongruent findingsonchecklistvalidity.18,19 Whilenotsignificant,moreseniorPGYresidentsperformed betteraswell.Thismayhavebeenduetoincreasedclinical exposurewithseeinganemergentcricothyrotomyperformed orimprovedproceduralexperiencewithpracticeinthe simulationenvironment.However,despitethesepotential exposuresandpreviousexperiences,thiscohortonly correctlycompletedjustoverhalfofthechecklistitems.

Figure. Emergencycricothyrotomychecklistperformancebyemergencymedicineresidentpostgraduateyear.Boxlimitsrepresentthe25th and75thpercentileswiththemedianchecklistscorerepresentedbythebar. PGY,postgraduateyear.
Additionally,certainitemshadparticularlylow completionrate,including “Gatherssupplemental intubationsupplies” (item4)(0%); “Proceduralistdilates cricothyroidmembrane ” (item18)(3.6%);and “Documents procedure” (item27)(8.9%).Whilesomeofthese completionratesmaybeattributabletothesimulation environment,itisimportanttohighlightthatmerely planningforanintubationwouldnotnecessarilyensure thatallequipmentnecessaryforacricothyrotomywasalso available.Theoverallperformanceofthisresidentgroup, withresidentsonlycompletingroughly50%ofthechecklist items,suggeststhatthecurrent,non-standardized techniqueforteachingemergencycricothyrotomyinthis cohortislackingandthatacompetency-basedapproach usingawell-developedproceduralchecklistmay improveperformance.
Thisstudyhasseverallimitations.First,thesingle-site natureofthestudymaynotreflectresidentperformanceat otherinstitutions.Studyingthechecklist’suseatother residencysiteswouldhelptounderstanditsgeneralizability tootherenvironmentswithdifferentapproachestoteaching opencricothyrotomy.Second,whilewerecruitedanexpert panelincludingEMandtraumasurgeryrepresentativeswith diversityinpracticetype,practicelocation,andgender,most oftheexpertspracticedinanacademicenvironment.Despite this,thestepstoperformingtheprocedureshouldnotvaryby practiceenvironmentand,therefore,wedonotbelievethat thislimitsvalidityorgeneralizabilityofthechecklist.Expert panelreviewincludingadditionalcommunityandhybrid expertswouldhelptestthishypothesis.
Third,thechecklistandtestingwereperformedusinga bloodlesssimulationtasktrainer,whichmaynotideally representanactualpatientencounter.However,the infrequentnatureoftheprocedure,asevidencedbyonlyone residenthavingperformedanemergencycricothyrotomy duringtheirtraining,necessitatesanon-clinicalenvironment trainingsimulation.Whileemergencycricothyrotomy simulationexperiencehasbeendocumentedusingsheep larynxand3D-printedmodels,ourstudywasnotperformed usingthesemodelsandinsteadusedacommerciallyavailable trainingdevice.Therefore,wedonotknowtheinfluenceof differentsimulationmethodsonthestudyandchecklist performance,andthisremainsanareaforfuturestudy.
Wedesignedareliable,valid,dichotomousprocedural checklisttoassessEMresidents’ abilitytoperform emergencycricothyrotomy.Theoverallperformanceofthe residentstestedinthisstudysuggeststhatthecurrentmethod ofteachingemergencycricothyrotomyforthisgroupis insufficient.Giventheneedtodevelopprocedural competencyforthisrarebutpotentiallylife-saving procedure,acurriculumsuchassimulation-basedmastery learningshouldbedevelopedtoensuremasteryofthis procedureforEMresidents.Thechecklistdevelopedinthis studycouldserveasafoundationforsuchacurriculum.
AddressforCorrespondence:DanaE.Loke,MD,MS,Universityof WisconsinSchoolofMedicineandPublicHealth,BerbeeWalsh DepartmentofEmergencyMedicine,800UniversityBayDr.,Suite 310,Madison,WI,53705.Email: dloke@medicine.wisc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Lokeetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AccreditationCouncilforGraduateMedicalEducation.ACGME programrequirementsforgraduatemedicaleducationinemergency medicine.2023.Availableat: https://www.acgme.org/specialties/ emergency-medicine/program-requirements-and-faqs-andapplications/.AccessedSeptember11,2023.
2.MakowskiAL.Asurveyofgraduatingemergencymedicineresidents’ experiencewithcricothyrotomy. WestJEmergMed. 2013;14(6):654–61.
3.ZinkW,BernhardM,KeulW,etal.Invasivetechniquesinemergency medicine.I.Practice-orientedtrainingconcepttoensureadequately qualifiedemergencyphysicians. Anaesthesist. 2004;53(11):1086–92.
4.BarsukJH,CohenER,CaprioT,etal.Simulation-basededucationwith masterylearningimprovesresidents’ lumbarpunctureskills. Neurology. 2012;79(2):132–7.
5.BarsukJH,McGaghieWC,CohenER,etal.Useofsimulation-based masterylearningtoimprovethequalityofcentralvenouscatheter placementinamedicalintensivecareunit. JHospMed. 2009;4(7):397–403.
6.MillerDT,ZaidiHQ,SistaP,etal.Creationandimplementationofa masterylearningcurriculumforemergencydepartmentthoracotomy. WestJEmergMed. 2020;21(5):1258–65.
7.KleinMR,SchmitzZP,AdlerMD,etal.Simulation-basedmasterylearning improvesemergencymedicineresidents’ abilitytoperformtemporary transvenouscardiacpacing. WestJEmergMed. 2022;24(1):43–9.
8.KleinMR,LokeDE,BarsukJH,etal.Twelvetipsfordeveloping simulation-basedmasterylearningclinicalskillschecklists. MedTeach. 2024.Inpress.
9.MelchiorsJ,TodsenT,NilssonP,etal.Preparingforemergency:avalid, reliableassessmenttoolforemergencycricothyroidotomyskills. OtolaryngolHeadNeckSurg. 2015;152(2):260–5.
10.HockSM,MartinJJ,StanfieldSC,etal.Novelcricothyrotomy assessmenttoolforattendingphysicians:amulticenterstudyofanerror avoidancechecklist. AEMEducTrain. 2021;5(4):e10687.
11.IssaN,LiddyWE,SamantS,etal.Emergencycricothyrotomyduringthe COVID-19pandemic:howtosuppressaerosolization. TraumaSurg AcuteCareOpen. 2020;5(1):e000542.
12.RobertsJR,CustalowCB,ThomsenTW.Cricothyrotomyand percutaneoustranslaryngealventilation.In: ClinicalProcedures inEmergencyMedicineandAcuteCare.Philadelphia,PA: Elsevier,2020:127–141.e3.
13.Cioffi WG,AsensioJA,AdamsCA,etal.Chapter3.Surgicalairways: tracheostomyandcricothyroidotomy.In:TownsendCMandEversBM (Eds), AtlasofTrauma/EmergencySurgicalTechniques.Philadelphia, PA:Elsevier,2014:23–34.
14.StufflebeamDL.Guidelinesfordevelopingevaluationchecklists:the checklistsdevelopmentchecklist(CDC).2000.Availableat: https:// wmich.edu/sites/default/files/attachments/u350/2014/guidelines_cdc. pdf.AccessedSeptember11,2023.
15.WaggonerJ,CarlineJD,DurningSJ.Isthereaconsensuson consensusmethodology?Descriptionsandrecommendationsforfuture consensus research. AcadMed. 2016;91(5):663–8.
16.HassonF,KeeneyS,McKennaH.ResearchguidelinesfortheDelphi surveytechnique. JAdvNurs. 2000;32(4):1008–15.
17.WalterSD,EliasziwM,DonnerA.Samplesizeandoptimaldesignsfor reliabilitystudies. StatMed. 1998;17(1):101–10.
18.KleinMR,SchmitzZP,AdlerMD,etal.Developmentofarigorously designedproceduralchecklistforassessmentofemergencymedicine residentperformanceoftemporarytransvenouscardiacpacing. AEMEducTrain. 2021;5(3):e10566.
19.ZaidiHQ,DhakeSS,MillerDT,etal.Emergencydepartment thoracotomy:developmentofareliable,validatedchecklistfor proceduraltraining. AEMEducTrain. 2019;4(2):139–46.
20.McHughML.Interraterreliability:thekappastatistic. BiochemMed (Zagreb). 2012;22(3):276–82.
ChristineMotzkus,MD,PhD* CaseyFrey,MD†
AloysiusHumbert,MD*
*IndianaUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Indianapolis,Indiana † BooneCountyEmergencyMedicine,Indianapolis,Indiana
SectionEditors:JulesJung,MDandAndrewGolden,MD
Submissionhistory:SubmittedJune2,2024;RevisionreceivedNovember22,2024;AcceptedNovember26,2024
ElectronicallypublishedFebruary5,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21292
Introduction: Incorporatingvirtualinterviewsintoresidencyrecruitmentmayhelpdiversifyaccessto residencyprogramswhilereducingthecostinvolvedwithtravelandlodging.Programsmaybemore likelytorankstudentstheyhavemetinpersonataninterviewwhencomparedtounknownvirtual applicants.Ourobjectivewastocharacterizehomeinstitution,in-state,andin-regionmatchratesto emergencymedicine(EM)residencyprogramsforfourth-yearmedicalstudents.
Methods: WeusedNationalResidencyMatchingProgramdataavailabletotheprogramdirectorto identifymedicalschoolandmatchlocationoffourth-yearmedicalstudentswhointerviewedatalargeEM residencyprogramintheMidwestfrom2018–2023.Students’ medicalschoolsandultimatelymatched programsweremappedtoElectronicResidencyApplicationServicegeographicregions;subgroup analysesevaluatedallopathicandosteopathicmedicalstudentsseparately.Weusedchi-squareteststo compareproportionsofstudentsmatchingtohome,in-state,orin-regionprogramsacrossyears.
Results: Therewere1,401applicantswithmatchinformationavailable.Thepercentageofstudents matchingtoahomeinstitutionremainedstableoverthecourseofthestudy.Thepercentageofstudents matchingtoanin-stateinstitutionincreasedoverthe firsttwoyearsofvirtualinterviewsrisingfrom23.2% inthe2020matchto30.8%in-statematchesforthe2022match.Chi-squaretestsdidnotrevealany significantdifferencesamonggroupsforallapplicants.Allopathicmedicalstudentsdemonstrateda significantincreaseinmatchestohomeinstitutions.In-regionmatchesstayedrelativelystableoverthe studytimeframeregardlessofsubgroup.
Conclusion: Virtualinterviewschangedthelandscapeofresidencyinterviews.Homeinstitutionandinstatematchesmaybemorelikelyforapplicantsfromallopathicschoolswhoparticipatedinavirtual interviewasbothprogramsandapplicantsaremorefamiliarwitheachother;however,ourstudydidnot findconvincingevidenceofthispossibilityamongallapplicants.Additionalstudyisneededtodetermine ongoingeffectsofthetransitiontovirtualinterviews.[WestJEmergMed.2025;26(2)285–289.]
Interviewsareacriticalelementoftheresidencymatch processforbothresidencyprogramsandmedicalstudentsto ensureselectionofhigh-qualityapplicantsandtraining programs.UntiltheCOVID-19pandemicstruckinearly 2020,nearlyallinterviewswereconductedinperson requiringmedicalstudentstoarrangetraveltodifferent programlocations,aprocessknowntobeexpensiveand
time-consuming.1 Withtravelrestrictionsandsocial distancingconcerns,the2021Matchcyclemarkedthe first useofvirtualinterviewsforemergencymedicine(EM) residencyspots.
Thetransitiontovirtualinterviewswasmarkedwith uncertaintyfrombothstudentsandprograms.Studentswere uncertainastohowtheywouldbeabletoassessprograms whileprogramsfeltsimilarlyabouttheabilitytoassess
students,particularlythosewhohadnotcompleteda rotationattheirprogram.Programdirectorshavealsobeen notedtoreportdifficultyassessingthe fitofapplicantsdespite theincreasedconvenienceofvirtualinterviews.2 However, virtualinterviewsofferincreasedopportunitiesforstudents tocompleteadditionalinterviewsatlowercost,whichhas beennotedinsurgicalspecialtieswithatransitiontovirtual interviews.3 Programdirectorsalsoexpressedconcernsthat programswouldmatchmorestudentsfromtheirhome programs,reducingopportunitiesforprogramstobenefit fromstudentswithnon-homogenousmedicalstudent training.2 Forfellowshipapplicants,similarconcernshave beenexpressed;however,therewasnotfoundtobea significantincreaseininterviewscompletedbypediatricEM fellowshipapplicationsorachangeinfellowshipapplicants matchingwithintheirpreferredstate.4
Weevaluatedwhetherthetransitiontovirtualinterviews atonelarge,MidwesternEMprogramcorrelatedwith increasednumbersofstudentsmatchingtotheirhome programs.Additionally,weevaluatedwhetherthe transitiontovirtualinterviewscorrelatedwithincreased numbersofstudentsmatchingtoin-stateor in-regionprogram.
WeobtaineddatafromtheNationalResidentMatching Program(NRMP)forrankedmedicalstudentsfromone MidwesternEMresidencyprogramfortheyears2018–2023.
Allmedicalstudentswhointerviewedatonemidwestern universityfrom2018–2023hadtheirhomeandmatched programsrecordedaspartofroutineNRMPrecordkeeping. Alldatawasstoredonasecureserver.Thisdatawas deidentifiedbytheprogramdirectorandcodedtodetermine whethertheintervieweematchedwithaprogramfromanyof thefollowing:1)thesameinstitutionastheirmedicalschool; 2)thesamestateastheirmedicalschool;and3)thesame regionastheirmedicalschool.Regionsweredefined accordingtoElectronicResidencyApplicationService (ERAS)geographicpreferenceregions;theseregionswere designatedbeginningin2022.Intervieweeswereableto signalageographicpreferenceaccordingtotheseregions. Areasofdisagreementregardingprogramaffiliationwere discussedbetweenauthorsandresolved.AuthorAH performedtheinitialcoding,andafterreviewbyauthorCM anydiscrepancieswereresolvedbetweenaffiliationsusing resourcesincludingtheAccreditationCouncilforGraduate MedicalEducationandprogramwebsitestoverify affiliations.Weusedchi-squaredteststoassessdifferences betweengroups.5 Weconductedsubgroupanalysesto evaluatedifferencesbetweenapplicantsfromallopathic (MD)andosteopathicschools(DO).
Theprimaryoutcomeofthisstudywaspercentageof studentswhomatchedtoprogramswithintheirhome institution,state,orregion.
Thisstudywasreviewedandapprovedbytheinstitutional reviewboard.Nofundingwasobtainedforthisstudy.
Overthesixinterviewcyclesincludedinthestudyperiod, 1,401studentscontributeddatatotheNRMPandwere subsequentlycodedtohavingmatchedattheirhome programortoprogramswithinthesamestateorregion. Therewasanincreaseinthenumberofinterviewscompleted bytheprogramoverthesix-yearperiodwithanaverageof 201interviewscompletedinanin-personformatpriortoand duringthe2020pre-pandemicinterviewseason.Afterthe globalCOVID-19pandemic,beginninginthe2021 recruitmentseason,therewasaninitialincreaseinthe numberofinterviewsofferedastheformatswitchedto virtual.Virtualinterviewscontinuedthroughoutthe2022 and2023interviewseasons,butoverallnumbersof interviewsdecreasedduringthistimeframe(Table1).
Anincreasingpercentageofstudentsmatchedtotheir homeinstitutionfrom2020–2023,withthelargestincrease beingobservedoverthe2020–2021seasoncorresponding withthetransitiontovirtualinterviews;however,thistrend wasnotstatisticallysignificant.Notably,proportionsof studentsmatchingtohomeinstitutionsweresimilarin2018 and2023.Anincreasingnumberofstudentsmatchedtoinstateinstitutionsfrom2020to2021;furtherincreasesinthe percentageofin-statematcheswereobservedfrom2021to 2022beforestabilizingatapproximately30%ofin-state matchesinthe finalincludedyear,closeto2018levels.Inregionmatchesremainedroughlystableacrossthestudy periodwithslightlylessthanhalfofstudentsmatchingtoan institutionintheirhomeERASgeographicregion(Table1). Chi-squaretestsdidnotrevealanysignificantdifferences betweengroups.
Whenevaluatingthesubgroupofapplicantsfrom allopathicschools,itappearedthatanoverallincreased proportionoftheseapplicantsmatchedtotheirhome institutionsoverthecourseofthesixyearsofthestudy(P < 0.01).Thisincreasewasmostnotablein2023when31.8%of theseapplicantsmatchedtotheirhomeinstitutions,nearly doublethatofanyprioryear.Therewasalsoanincreasein MDapplicantsmatchingtoinstitutionswithinthesamestate astheirmedicalschooloverthestudyperiod(P = 0.01). Regionalinstitutionmatchesforallopathicapplicants remainedstableoverthestudyperiod.Osteopathic applicantsdidshowanincreaseinproportionofthem matchingtoin-stateorin-regioninstitutions;however,these trendswerenotstatisticallysignificant(Table2).
Wefoundnostatisticallysignificantdifferenceofmatch locationamongallapplicantsapplyingtooneMidwestern EMresidencyprogramaftertheimplementationofvirtual interviews.Similarnumbersofapplicantsmatchedtothe sameERASregionastheirmedicalschoolregardlessofinpersonorvirtual-interviewformat.Applicantsfrom allopathicschoolsdidshowanincreasedproportion matchingattheirhomeorstateinstitutionsafterthe implementationofvirtualinterviews,andthis findingwas statisticallysignificant.Anincreasingnumberofosteopathic applicantsmatchedtoin-stateinstitutionsafterthe implementationofvirtualinterviews.Thistrenddidnot reachstatisticalsignificancebutdidapproachsignificance. Virtualinterviewsreducecosttoapplicantsandmayallow applicantstocompleteinterviewsatadditionalprograms. Correspondingly,thenumberofinterviewsconductedbythe programincreasedinthe firstyearofvirtualinterviewsprior tostabilizingatasomewhathighernumberthaninthe previoustimeframewithin-personinterviews.Increased numbersofinterviewsofferedmeantincreasedtimedemands fromfacultyparticipatinginthoseinterviewsandmayhave contributedtointerviewfatigue.Notably,oneobstetrics/ gynecologyprogramdidnot findanincreaseinnumbersof interviewsofferedtoorcompletedbyapplicants.6 Conversely,applicantshavingtheabilitytocompletemore interviewsmayallowforfewer financialdisparitiesto perpetuateamongstudents,assomestudentsmayhave previouslylimitedinterviewsduetocostconcerns.An AssociationofAmericanMedicalCollegessurveyshowed thatpreviousmonetarycostsforresidencyinterviewsranged from$1,000to$11,580(median$4,000).7 Usingavirtual processmayalsobenefit financiallychallengedstudentsby eliminatingthecostof flightsandhotels,andothertravel expensespreviouslynecessarytocompletetheinterview season.Thetransitiontovirtualinterviewsmayhave downstreameffectsonthediversityoftheEMworkforceif applicantsarelesslikelytomatchoutsidetheirhomeorinstateprograms.8
Table2. Allopathicandosteopathicapplicantmatchlocationbyyear.
Higherpercentagesofallopathicstudentsmatchingtoinhomeandin-stateprogramsmayindicatethatprogramsand applicantsalikepreferentiallyrankeachotherdueto familiarity,althoughgiventheuncertaintiesofthe COVID-19pandemicandrestrictionsonawayrotations from2021onward,itisdifficulttoattributethisincreaseto onefactor.Itiswellknownthatmoststudentshaveastrong geographicpreferencetomatchneartheirhomeandthat locationisasignificantdriverofresidencyprogramchoice.9
DOapplicants
MD, DoctorofMedicine; DO,DoctorofOsteopathicMedicine.
Thistrendhasalsobeenseeninorthopedicsurgeryprograms withtheirtransitiontoavirtualinterviewprocess10; however,thisdidnotholdtrueforneurologyandgeneral surgeryprograms.11,12 Students’ geographicpreferencesin EMseemtohavebeenamplifiedbythetransitiontovirtual interviews,particularlyamongallopathicapplicants.While virtualinterviewsarenottheonlychangethatoccurredinthe residentrecruitmentprocessduringthe2021andsubsequent interviewseasons,itisplausiblethatinterviewformatisone ofmanyfactorsinfluencingstudentinterviewbehavior, althoughwedidnot findevidenceofthisbehavioramongall applicantsinourstudy.
Itwasnotpossibletodeterminewhateffectotherfactors includingtravelrestrictions,societalunrest,andother changeshadonapplicantbehaviorandtheirprocessof selectingapplicationlocations,interviews,andultimately matchlocation.Further,itisdifficulttounderstandwhat effecttheadventofprogramsignalinghadonboth intervieweeandinterviewerbehaviorafteritsintroductionin 2022,andthisremainsanactiveareaofstudy. Understandingthestabilityofthein-regionmatchratesis difficulttointerpretbutsuggeststhatsimilarnumbersof studentsarelookingtoleavetheirmedicalschoolregionover time.TheERASregionswerealsodefinedduringthistime frame,whichmayhavealteredstudents’ perceptionsof region.Thesegeographicpreferencesareanareaforongoing studyasprogramsevaluateresidencymatchestoservetheir communitiesandensuremutuallybeneficialmatches betweenprogramsandapplicants.
Thisstudyhasmultiplelimitations.First,onlyonelarge, MidwesternEMresidencyprogramisrepresented.Thereare multipleotherfactorsincludingthenumeroussocialand societalchangesthattookplaceduringtheCOVID-19 pandemic,aswellastheintroductionofpreferencesignaling certainlyimpactedapplicants’ matchpreferencesand interviewbehaviorsinadditiontothetransitiontoavirtual interviewmodel.Wewereunabletocontrolforthesefactors orotherchangestoapplicantbehaviorsuchasthepotential desiretoremainclosertohomewhentravelwasmore constrainedduringtheglobalpandemicorasaresultof ongoingsocietalunrest.Ofnote,overallapplicantbehavior alsochangedacrossmatchyearswithadecreasein applicationsbeginningin2022andincreasedproportionsof osteopathicandinternationalmedicalgraduates.13 Additionally,EMapplicantscontinuetobeadvisedto completenomorethanoneawayrotationperinterview cycle,whichlimitsprogramandapplicantexposuretoeach other.Further,whileERASregionswereused,thisdoesnot accountforapplicantswhomayhavematchedjustacrossthe bordertoanotherregion,creatingafalseinflationof geographicdistance.
Virtualinterviewsarenowa fixtureoftheresidency applicationprocesswithEMprogramsrequiringthisprocess toparticipateinthematch.14 Wedidnot findstatistically significantdifferencesinhomeinstitutionorin-statematch ratesforallapplicants;however,allopathicapplicantsdid haveanincreaseinproportionofstudentsmatchingtotheir homeinstitution.Whileourdatadoesnotsuggestanoverall impactofvirtualinterviewsinmatchdecisionsmadeby applicantsorprograms,thesetrendswarrantadditional monitoringforongoingimpact,particularlyamong allopathicapplicantswhereanincreaseinhomeandin-state matcheswasstatisticallysignificant.Furtherlargerstudies wouldbehelpfultounderstandhowtransitioningtothis modelaffectsapplicantmatchbehavior.Additionalstudies wouldbebeneficialtohelpprogramsfurtherunderstandkey areasoffocusandensuresuccessfulinterviewplanningfor EMprograms.
AddressforCorrespondence:ChristineA.Motzkus,MD,PhD, IndianaUniversitySchoolofMedicine,DepartmentofEmergency Medicine,2651EDiscoveryPkwy.,RoomC3018,Bloomington, IN47408.Email: cmotzkus@iuhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Motzkusetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.JoshiA,BloomD,SpencerA,etal.Videointerviewing:areviewand recommendationsforimplementationintheeraofCOVID-19and beyond. AcadRadiol. 2020;27(9):1316–22.
2.PonterioJM,LevyL,LakhiNA.Evaluationofthevirtualinterview formatforresidentrecruitmentasaresultofCOVID-19 restrictions:residencyprogramdirectors’ perspectives. AcadMed. 2022;97(9):1360–7.
3.NewsomeK,SelvakumarS,McKennyM,etal.Shifting thesurgicalresidencymatchtoa100%virtualinterview formatduringtheCOVID-19pandemic:howhasitaffected placementintosurgicaltrainingprograms? AmerSurg. 2023;89(4):935–41.
4.BaghdassarianA,BaileyJA,CaglerD,etal.Virtualinterviewsandthe pediatricemergencymedicinematchgeography:anationalsurvey. WestJEmergMed. 2024;25(2):186–90.
5.PreacherK.J.2001.Calculationforthechi-squaretest:aninteractive calculationtoolforchi-squaretestsofgoodnessof fitandindependence [computersoftware].Availableat: http://quantpsy.org AccessedJanuary20,2024.
6.Santos-ParkerKS,HammoudMM,WinkelAF,etal.Distributionsof residencyinterviewswiththeimplementationofvirtualinterviews andstandardizationofinterviewofferdates. JSurgEduc. 2022;79(5):1105–12.
7.AssociationofAmericanMedicalColleges.2024.Thecostof interviewingforresidency.Availableat: https://students-residents. aamc.org/financial-aid-resources/cost-interviewing-residency AccessedMarch30,2024.
8.CapersQ,JohnsonA,BerlacherK,etal.Theurgentand ongoingneedfordiversity,equity,andinclusioninthe cardiologyworkforceintheUnitedStates. JAmHeartAssoc. 2021;10(6):e018893.
9.HasnieUA,HasnieAA,Preda-NaumescuA,etal.Exploringmatch space:howmedicalschoolandspecialtycharacteristicsaffect residencymatchgeographyintheUnitedStates. AcadMed. 2022;97(9):1368–73.
10.NestlerAJ,FeibelBM,BeasonAM,etal.Thestudentyouknow: orthopedicsurgeryhomeprogrammatchratesandgeographic relationshipsbeforeandafterCOVID-19. JSurgEduc. 2022;80(3):476–82.
11.BeinhoffP,AttlassyN,CarlsonC.Nogeographicdistributionchange amongresidencyapplicantsintheneurologymatchduringCOVID-19. Cureus. 2023;15(2):e34898.
12.BeesleyH,PernarL,KettoolaY,etal.Theassociationbetween virtualinterviewingandgeographicaldistributionofmatched residencyprogramsforgeneralsurgeryapplicants. JSurgEduc. 2022;80(2):194–9.
13.NationalResidencyMatchingProgram.2023.Resultsanddata:2023 mainresidencymatch.Availableat: https://www.nrmp.org/match-data/ 2023/06/results-and-data-2023-main-residency-match/ AccessedNovember6,2024.
14.AssociationofAmericanMedicalColleges.2024.AAMCinterview guidanceforthe2022–2023residencycycle.Availableat: https://www. aamc.org/about-us/mission-areas/medical-education/interviews-gmewhere-do-we-go-here.AccessedNovember6,2024.
CharlotteW.Croteau,MD
JoshuaN.Goldstein,MD,PhD
LaurenNentwich,MD
AliS.Raja,MD,DBA,MPH
MichaelVanRooyen,MD,MPH
JoshuaJ.Baugh,MD,MPP,MHCM
SectionEditor:LauraWalker,MD
HarvardMedicalSchool,MassachusettsGeneralHospital,Departmentof EmergencyMedicine,Boston,Massachusetts
Submissionhistory:SubmittedMarch4,2024;RevisionreceivedOctober23,2024;AcceptedOctober31,2024
ElectronicallypublishedDecember31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20303
Introduction: Emergencyphysicianshavethehighestratesofburnoutamongourphysicianpeers,with priorliteraturesuggestingclinicianschedulescanplayasignificantroleinburnout.Weassessedour transitionfromatenure-andage-basedparadigmtoanegalitarian,nightshiftbuy-outprogramthat allowsschedule flexibilityforphysiciansatallstagesoftheircareers.
Methods: Thenightshiftbuy-outprogramwasimplementedintheemergencydepartment(ED)ofan academic,quaternary-carecenterthattreatsapproximately100,000adultpatientsannuallywith56 facultyemergencyphysicians.Wesoughttocreateacost-neutralprogram,carefullybalancing incentivesbetweennocturnistsandthosewantingtoreduceallottednightshifts.Ultimately,theprogram wasdesignedtoallowallfacultytobuyoutofanynumberofnightsfor$500pernightshift,withthefunds generatedusedtoincreasenocturnistsalaries.Weanalyzedtwoyearsoftheprogram(July2022–June 2024)toassesstrendsinnightshiftbuy-outs,theprimaryoutcome.Wealsoconductedanall-faculty surveyaftertheprogram’s firstyeartogaugesentimentsabouttheprogram.
Results: Overtwoyears,22faculty(42%)fullyboughtoutofnights;anadditional10(15%)boughtoutof somenights.Byyeartwo,theprogramcouldgrantallfacultytheirpreferrednight-shiftallotment.Faculty whoboughtoutfullyhadworkedlongerinEMonaverage,workedfewerclinicalhoursperyear,were morelikelytobeassociate/fullprofessors,andwerelesslikelytobewomen.Nocturnistshadthehighest meanclinicalhoursofthefourgroups,hadthelowestaveragetenure,andwereleastlikelytobe associate/fullprofessors.Atotalof86%offacultyrespondedtothesurvey,towhichmorethan80%of thosebuyingoutreportedthatreducingthenight-shiftburdenwaseither “veryimportant” or “criticalfor continuinginthisjob.”
Conclusion: OuracademicEDtransitionedfromatenure-andage-based,overnightshiftparadigmto anegalitarianbuy-outprogramthatallowsphysicians flexibilityatallcareerstages.Thisapproachcould improvecareersatisfactionandreduceburnoutamongemergencyphysicians.[WestJEmergMed. 2025;26(2)290–294.]
Emergencyphysicians(EP)havethehighestratesof burnoutamongourphysicianpeers.1 Maslachdefines burnoutasthetriadofdepersonalization,emotional exhaustion,anddecreasedsenseofpersonal accomplishment.2 Whilemuchefforthasbeendirected toward findingmeaningfulsolutionstocounteractburnout inour field,theproblemonlyappearstobeworsening.Inthe
2022MedscapePhysicianBurnoutandDepression Report,therewasasignificantincreaseinburnout amongEPsbetween2021and2022,from43% to60%.3
Priorstudiessuggestthatonefactoraffectingburnoutin medicineisaphysician’sclinicalschedule.Nightshiftshave beenshowntonegativelyinfluencejobsatisfactionamong EPs.4 While “exhaustion” oftenrefersto “emotional exhaustion” intheburnoutliterature,sleepdeprivationhas beenidentifiedasacontributingfactortodecreasedpersonal well-being,lowerqualityofcare,andharmfulhealth outcomes.5–7 Sequentialnightshifts,inparticular,havebeen associatedwithreducedcognitiveperformanceinEPs,and shiftworkingeneralhasbeenassociatedwithadisruptionin circadianrhythms.8 Whileprovidingcarearoundtheclockis fundamentaltothedutyofemergencydepartments(ED),the 24/7shiftsalsolikelycontributetothehighburnoutrates amongEPs.
Despiteconcernsaboutnightshifts,somephysicianselect toworkonlyovernight.Reasonscitedforchoosinga nocturnistscheduleincludemoreindependence,moretime withfamily,highersalary,andscheduling flexibility.9 Hiring dedicatednocturnistsmayallowsomephysicianstoavoid undesirablenightshiftswhileenablingotherstooptintoa primarilynight-shiftschedule.AccordingtoMaslach’ s theoryofburnout,increasingemployees’ controlovertheir workcandecreaseburnout;allowingphysicianstooptinor outofnightsmaybeawin-winforeveryone’swell-being.2 In ouracademicED,wetransitionedfromatenure-andagebasednightsparadigmtoanegalitarian,nightshiftbuy-out programthatallowsphysicians flexibilityatallcareerstages. Goalsincludedbudgetneutrality,improvingequity(by givingallfaculty,irrespectiveofage,equaloptions),and increasingagency(bygivingallfacultyopportunitytoadjust theirscheduletomatchtheirownneeds).Thisstudyassessed patternsinnightshiftbuy-outsandEPs’ sentimentsabout theprogram.
StudyDesignandSetting
Thisretrospective,cohort,institutionalreviewboardexemptstudywasconductedinanEDwithinanacademic, quaternary-carecenterthatseesapproximately100,000adult patientsannually.Ourdepartmentincludesbothapediatric sectionandanadultsection;thisstudyfocusesonthestaffing oftheadultsection.Theadultattendinggroupinthestudy EDcomprises56facultyand7–9fellowsperyear.Only facultywereeligiblefortheovernightbuy-outprogram; fellowsdidnothavethisoption.Thereare13adultattending shiftsper24-hourperiod,threeofwhichareovernightshifts. Historicallyinourdepartment,attendingnightshiftswere allocatedbasedonacademicrank,withanadditionaloption tostopworkingnightsaltogetheratage60,regardlessof academicstatus.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencyphysicians(EP)havethehighest ratesofburnoutamongphysicians,withprior literaturesuggestingclinicianschedulescan playasigni fi cantrole.
Whatwastheresearchquestion?
Doesanightshiftbuy-outprogramimprove physiciancareersatisfactionandreduce burnoutamongemergencyphysicians?
Whatwasthemajor findingofthestudy?
Morethan80%ofphysiciansbuyingoutof nightshiftsreportedthiswaseither “ very important ” or “ criticalforcontinuingin thisjob. ”
Howdoesthisimprovepopulationhealth?
Wetransitionedfromatenure-andage-based overnightparadigmtoanegalitarianbuy-out program.Thiscouldimprovecareer satisfactionandreduceburnoutamongEPs.
Wesoughttocreateanewprogramwhereallfacultycould buyoutofnightshifts.Tofacilitatethis,werecognizedthe needtohiremorenocturnists.Ourgoalwasacost-neutral program,requiringcarefulbalancingofincentives. Therefore,severalruleswereestablishedfortheprogram.
Allfacultymemberswereeligibleafteroneyearofservice, regardlessofacademicrank;overtwoyearsourprogram evolvedintothesystemdescribedbelow.Todeterminehow manybaselinenightshiftsEPsinourdepartmentowed,we usedaproratedequationbasedontotalclinicaltime, adjustedeachyeardependingonthemakeupoftheattending rosterandschedulingneedsofthedepartment.Most physiciansinourdepartmentowedbetween12–24night shiftsperyear.Physicianswerethenofferedtheoptionof reducingtheirnumberofnightshiftsfortheyearinexchange forasalaryreductionofaspecificdollaramount($500)per nightshift.Thisnumberwaschosenbecauseitreflectsthe paydifferentialpershiftforanocturnistinourgroup. Physicianscouldbuyoutofanynumberofnightshifts;they coulddecreasetheirnightsbyasingleshift,buyoutofall nightshifts,oranythinginbetween.Totalannualclinical hoursowedbythesephysiciansdidnotchange:bought-out nightshiftswereinsteadconvertedtodaysandevenings.The fundsgeneratedbybought-outnightswereusedtoincrease thesalariesofnocturnistscomparedtonon-nocturnist
attendings,keepingtheprogramcost-neutral.Nocturnists couldalsopicktheexactdaystheywishedtowork,providing totalschedulecontrolasanaddedincentive.
Wedidmaintainanadditionaloptionforfacultyoverthe ageof60.Thesefacultyweregivenachoiceregardinghow theywouldliketodecreasetheirnights:theycouldbuyoutas above,workmoreweekendsinsteadofnightsina1:1 proportion,orincreasetheirtotalclinicalhoursinexchange fordecreasingnights.
TheEMnightshiftbuy-outprogramwasoriginally implementedonJuly1,2022.Allfacultyhadtocommitto theirbuy-outplanforonefullyear,withanoptiontomodify theirchoicesattheendofeachyear.Whilewearecurrentlyin yeartwoatthetimeofwriting,allbuy-outdecisionshave alreadybeenmadefortheprogram’sfullsecondyear.
Weanalyzedtwoyearsofprogramdatatoassesspatterns innightbuy-outsamongthefaculty,theprimaryoutcome measure.Wealsoevaluatedthedemographiccharacteristics ofparticipatingEPsseparatedintofourgroups:thosewho1) hadfullbuy-outfromnights;2)hadpartialbuyoutofnights; 3)hadnobuy-outofnights;and4)werenocturnists.
Demographicsassessedincludedthefollowing:yearsinEM, definedasyearssincemedicalschoolgraduation;academic rank,stratifiedasclinicalinstructororassistantprofessorvs associateorfullprofessor;clinicalhoursworked,expressed asapercentageofafull-timeclinicalrequirementinourED; andsex,definedasmale,female,orother.Thisdatawas assembledfromourfacultyhiringdatabaseaswellasour department’sschedulingsoftware,withanalysesperformed inExcel(MicrosoftCorporation,Redmond,WA).
Wealsoperformedasurveyduringtheprogram’ s first yearthatincludedallEMfaculty.Thisannualelectronic surveytypicallyassessesthewell-beingofourdepartment.In thewinterof2022,weaddedthefollowingquestionwith multiple-choice,Likertscaleanswerchoicesforfacultywho boughtoutofatleastsomenightshifts: “Howimportantisit foryoutobeabletodecreaseyournightshiftburden?”
Answerchoicesincludedthefollowing:notatallimportant; slightlyimportant;moderatelyimportant;veryimportant; andcriticalforcontinuinginthisjob.Giventhesmallsample size,onlydescriptivestatisticswereperformed.
Bytheendoftheprogram’ s firstyear,ourdepartment increaseditsnocturnistfacultyrosterfromthreetosix attendings.Inthe firstyear,wecouldnotallowattendings undertheageof60tofullybuyoutofnightsbecauseof clinicalcoverageneeds;thosedesiringfullbuy-outhadtheir nightsdecreasedby75%ratherthan100%.Withthree additionalnocturnistshired,wecouldfullyaccommodate buy-outrequestsforyeartwo.Overthetwoyears,22faculty
(42%)fullyboughtoutofnights,whileanadditional10 (15%)boughtoutofsomenightshifts.Sevenofthe10who choseapartialbuy-outdecreasedtheirnightsby50%, whiletheotherthreeboughtoutforfewerthan50%of theirnightshifts.
FacultywhoboughtoutfullyhadworkedinEMfor slightlylongeronaverage,hadlowertotalrequiredclinical hoursperyear,weremorelikelytobeassociateorfull professors,andwerelesslikelytobewomen(See Table for totalfacultygroupcharacteristics,aswellasdemographics bybuy-outcategory).Nocturnistshadthehighestmean clinicalhoursofthefourgroupsandthelowestaverage tenureandwereleastlikelytobeassociateorfullprofessors.
Overall,48of56faculty(86%)respondedtothesurveyat theendofyearone.Ofthe32facultywhoboughtoutatleast somenights,26(81%)respondedtothesurvey.Morethan 80%ofthosebuyingoutreportedthattheabilitytoreduce thenightshiftburdenwaseither “veryimportant” or “critical for continuinginthisjob” (Figure).
NightshiftscontributetoburnoutforsomeEPsandcan detractfromacademicproductivity.4 Forothers,working morenightshiftscanimprovejobsatisfaction,mainlyif doingsoprovidesadditionalschedulecontroland compensation.9 Manydepartmentscurrentlyreducenight shiftsforphysiciansoveracertainage,andtheAmerican CollegeofEmergencyPhysicianshasrecommended accommodationsforphysiciansintheirpre-retirement years. 10 Moreneedstobewrittenaboutoptionsfor physicianstocustomizetheirovernightshiftsatallstagesof theircareers.Ourdepartmentcreatedaprogramtoallowany facultymembertobuyoutofnightshifts,usingthefunds generatedfrombuy-outstoincentivizenocturnistpositions. Withintwoyearsofinitiatingtheprogram,weallowedevery facultymemberwithatleastoneyearofservicetobuyoutof theirdesirednumberofnightshiftswhilehiringthree additionalnocturnists.
AccordingtoanationalsurveyofacademicEMleaders regardingpoliciesaroundagingphysicians,overhalfofthe surveyedleadersreporteddecreasingoreliminating overnightshiftstoaccommodateagingphysicians.9 While thisisundoubtedlyanimportantoptionforsupporting longevityinEM,itdoesnotaddresstheimpactofnightshifts onyoungerphysicianswho,somestudiessuggest,experience thehighestratesofburnoutwithinmedicine.11 Duringyears whenphysiciansmayberaisingyoungchildrenwhileactively buildingtheircareers,increasedschedulecontrolmightbe beneficialformitigatingburnout.12 Inaddition,theremaybe non-agerelatedreasonsforsomeEPstobe
Table. Demographiccharacteristicsoffacultyineachbuy-outcategory.
Allfaculty(N=56)Fullbuy-out(n=22)Partialbuy-out(n=10)Nobuy-out(n=18)Nocturnist(n=6)
FTE, full-timeequivalent; EM,emergencymedicine.
Figure. Responsesfromfaculty(n=26)whousedthebuy-outprogramregardingtheimportanceofbuyingoutofnightshiftsasreportedon ourannualwell-beingsurvey.
disproportionatelyimpactedbynightshifts,including medicalissues,mentalhealthissues,orcaregiver responsibilities,whichcanbehardtoquantify.
Acriticalgoaloftheprogramwastopromoteequity acrossourfacultygroup.Programsthatreducenightshifts basedonage,academicrankortenuremayinadvertently propagateinequity,asphysicianswhoareolder,withlonger tenure,orofhigherrankmaybemorelikelytobemaleand Whitethanyoungerphysicians.13 Despiteofferingthesame buy-outoptionforallfaculty,wedidobservethatthosewho boughtoutofnightsentirelyweremorelikelytobemale, longer-tenured,andofhigheracademicrankthanourgroup average.Itshouldbenotedthatmalefacultydidhavehigher averageacademicrankthanfemalefaculty,butthisdidnot fullyexplainthegenderdifference;amongonlyhigh-ranking faculty,menwerealsomorelikelytobuyoutofnightsthan women.Thesetrendsmayberelatedtohistoricalpreferences inourdepartmentorto financialrealitiesforphysiciansat variouscareerstagesorwithdifferentfamilystructures, amongotherpotentialexplanations.Futureresearchmight explorereasonsfordifferencesinschedulepreferenceamong differentdemographicgroupsinEM.
Forthoseparticipatinginourprogram,mostfaculty reportedthattheabilitytoreducenightswasatleast “ very important,” with39%indicatingthiswascriticalfor
continuingintheirjobs.Priorresearchalsosuggeststhat simplygivingpeoplemorecontrolovertheirworkcanreduce burnout;theremaybebenefitsofincreasedschedulechoice forallfacultywithabuy-outprogram,notjustthosewho reducenightshifts.2 WithrecordburnoutinEMthreatening careerlongevityformany,providingincreasedschedule controlmaybeonestrategyforimprovingfacultyretention. Futureresearchshouldexaminewhetherself-reported answerstosurveyslikeoursultimatelypredictburnoutand careerdecisions.
Thisstudyassessedourexperiencewithapolicy implementedforasinglefacultygroupofphysiciansinone largeED.Thetrendsdiscussedheremay,therefore,be differentfromotherdepartments.Whilethisprogramcould beadoptedatotherinstitutions,theremaybeunique considerationsforimplementationinothersettings.Wealso observedtheeffectsofthepolicyoverarelativelyshort periodandwereonlyabletoassessimpactbasedonselfreport;futureworkmightexaminelongerintervalsalong withobjectivepatternsofhiringandretention.Wealsodid notspecificallystudythe financialimpactsoftheprogramon ourfaculty.Thepersonalimpactofthelossofsalaryfor attendingscouldbeworthinvestigatinginthefuture.
InourlargeacademicED,wesuccessfullytransitioned fromatenure-andage-basednightshiftparadigmtoan egalitariannightshiftbuy-outprogramthatallows flexibility forphysiciansatallstagesoftheircareers.Giventhe favorableresultsoftheprogram,wehavecontinuedtoallow thisoptionalovernightbuy-outforourfaculty.This approachhasthepotentialtoimprovecareersatisfaction, promoteequity,andreduceburnoutamong emergencyphysicians.
AddressforCorrespondence:CharlotteW.Croteau,MD,Harvard MedicalSchool,MassachusettsGeneralHospital,Departmentof EmergencyMedicine,55FruitSt.,Austen850,Boston,MA02114. Email: ccroteau1@mgb.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Croteauetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ShanafeltTD,BooneS,TanL,etal.BurnoutandsatisfactionwithworklifebalanceamongUSphysiciansrelativetothegeneralUSpopulation. ArchInternMed. 2012;172(18):1377–85.
2.MaslachC,JacksonSE,LeiterMP. MaslachBurnoutInventory Lanham,MD:ScarecrowEducation,1997.
3.KaneL.Physicianburnout&depressionreport2022: Stress,anxiety, andanger.Medscape.Availableat: https://www.medscape.com/
slideshow/2022-lifestyle-burnout-6014664?0=reg=1#2 AccessedJanuary2,2024.
4.Smith-CogginsR,BroderickK,MarcoC.Nightshiftsinemergency medicine:theAmericanBoardofEmergencyMedicine longitudinalstudyofemergencyphysicians. JEmergMed. 2014;47(3):372–8.
5.StewartNHandAroraVM.Theimpactofsleepandcircadiandisorders onphysicianburnout. Chest. 2019;156(5):1022–30.
6.HartenbaumNPandZeePC.Shiftworkandsleepoptimizing health,safety,andperformance. JOccupEnvironMed. 2011;53(5):S1–10.
7.MachiMS,StaumM,CallawayCW,etal.Therelationshipbetweenshift work,sleep,andcognitionincareeremergencyphysicians. AcadEmerg Med. 2012;19(1):85–91.
8.DulaDJ,DulaNL,HamrickC,etal.Theeffectofworkingserialnight shiftsonthecognitivefunctioningofemergencyphysicians. AnnEmerg Med. 2001;38(2):152–5.
9.TakakuwaKM,BirosMH,RuddyRM,etal.Anationalsurveyof academicemergencymedicineleadersonthephysicianworkforce andinstitutionalworkforceandagingpolicies. AcadMed. 2013;88(2):269–75.
10.ACEP.Considerationsforemergencyphysiciansinpre-retirement years.2021.Availableat: www.acep.org/patient-care/policystatements/considerations-for-emergency-physicians-in-preretirement-years.AccessedJan2,2024.
11.WestCP,DyrbyeLN,ShanafeltTD.Physicianburnout:contributors, consequencesandsolutions. JInternMed. 2018;283(6):516–29.
12.BaughJJ,TakayesuJK,WhiteBA,etal.BeyondtheMaslach burnoutinventory:addressingemergencymedicineburnout withMaslach’sfulltheory. JAmCollEmergPhysiciansOpen. 2020;1(5):1044–9.
13.MadsenTE,LindenJA,RoundsK,etal.Currentstatusofgenderand racial/ethnicdisparitiesamongacademicemergencymedicine physicians. AcadEmergMed. 2017;24(10):1182–92.
BryanA.Stenson,MD*
PeterS.Antkowiak,MD,MPH*
DavidT.Chiu,MD,MPH*
LeonD.Sanchez,MD,MPH†°
JoshuaW.Joseph,MD,MS,MBE‡°
SectionEditor:BrianYun,MD,MBA,MPH
*BethIsraelDeaconessMedicalCenter,DepartmentofEmergencyMedicine, Boston,Massachusetts
† BrighamandWomen’sFaulknerHospital,DepartmentofEmergency Medicine,Boston,Massachusetts
‡ BrighamandWomen’sHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts
° Contributedequallytothisworkintheroleofco-seniorauthor.
Submissionhistory:SubmittedJune7,2024;RevisionreceivedNovember21,2024;AcceptedNovember27,2024
ElectronicallypublishedJanuary31,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21298
Introduction: Advancepracticeclinicians(APC)playsignificantrolesinacademicandcommunity emergencydepartments(ED).Inattendingsandresidents,priorresearchdemonstratedthatproductivity isdynamicandchangesthroughoutashiftinapredictableway.However,thishasnotbeenstudiedin APCs.TheprimaryoutcomeofthisstudywastomodelproductivityforAPCsincommunityEDsto determinewhetheritchangesduringashiftsimilartothewayitdoesforattendingsandresidents.
Methods: Thiswasaretrospective,observationalanalysisof10-hourAPCshiftsattwosuburban hospitals,workedby14totalindividuals.Weexaminedthenumberofpatientsseenperhouroftheshift byexperiencedAPCswhoseeallacuityandstaffallpatientswithanattending.Weusedageneralized estimatingequationtoconstructthemodelofhour-by-hourproductivitychange.
Results: Weanalyzed862shiftsoveroneyearacrosstwosites,withthreeshiftstarttimes.Site1 10 AM–8 PM sawanaverageof13.31(95%confidenceinterval[CI]13.02–13.63)patientspershift;Site2 8 AM–6 PM sawanaverageof12.64(95%CI12.32–13.06)patientspershift;Site24 PM–2 AM sawan averageof12.53(95%CI12.04–12.82)patientspershift.Acrossallsitesandshifts,hour1sawthe highestnumberofpatients.Eachsubsequenthourwasassociatedwithasmall,statisticallysignificant decreaseovertheprevioushours.Thiswasmostpronouncedintheshift’slasttwohours.
Conclusion: TheproductivityofAPCsdemonstratesasimilarpatternofhourlydeclinesobservedin bothresidentandattendingphysicians.Thiscorroboratesprior findingsthatpatientsperhourisa dynamicvariable,decreasingthroughoutashift.Thisprovidesfurtherexternalvaliditytopriorresearchto includebothAPCsandcommunityEDs.Thesedepartmentsmusttakethisphenomenonintoaccount, asithasschedulingandoperationalconsequences.[WestJEmergMed.2025;26(2)295–300.]
Advancedpracticeclinicians(APC)playasignificantrole inthecareprovidedinmanyacademicandcommunity emergencydepartments(ED).APCsarenon-physician clinicians,suchasnursepractitioners(NP)andphysician assistants(PA),whoseeandevaluatepatientsunderthe supervisionof,andincollaborationwith,attending
physicians.TheuseofAPCshasincreasedinthepastfew decades,withthemostrecentNationalHospitalAmbulatory MedicalCareSurveyin2020estimatingthat10.1%ofED visitsinvolvedanNP,and13.4%ofvisitsinvolvedaPA.1
PreviousliteratureonAPCsintheEDislimitedbuthas rangedfromanalyzingresourceutilizationtodescribing overalltrendsinhowAPCsareusedandinwhichpractice
settings.2,3 OnegroupfoundthatAPCssawmorepatients perhourandgeneratedmorerelativevalueunits(RVU)per hour bothkeymarkersofproductivity thanaresident physicianinafasttracksetting,whilegeneratingfewer RVUsperpatient.4 Thistrendheldupinahigheracuity settinginthissamegroup.5 However,withsuchasignificant portionofEDvisitsinvolvinganAPC,thereisstilllimited dataonoverallproductivity.6
Amongthemetricscommonlyusedtomeasureclinical productivity,patientsseenperhourisoneofthemost essentialtoEDoperationsplanning.Itoftenleadsto importantstaffingdecisionsatalltypesofEDs,rangingfrom largeacademicEDstosmallcommunityones.7 While productivityisoftenthoughtofasastaticquantitymeasured acrossashift,inrealityitisdynamicandchangesthroughout thecourseofashiftinapredictableway.Thisphenomenon hasbeendemonstratedinemergencymedicine(EM) attendingsandresidents,anditmanifestsasastepwise decreaseinproductivityafterthe firstfewhoursofashift.8,9 Thisbehaviorwassimilarinbothofthesegroupsandis consistentwiththelivedexperienceofworkinginanED. Whenaphysicianshowsupfreshtoashift,theyhavemore bandwidthtoseenewpatients.Afterafewhours,aseachof thosepatientsstartstohaveresultsreturnandrequire additionaldecisions,thereislesstimetoseenewpatients.
Accountingforthisphenomenoncanhavesignificant operationalimpacts.Byunderstandingthetruehourly capacityoftheworkforce,administrativeleadershipcan ensurethisbestmatchesupwiththehourlypatient demand.10 Thishasthepotentialtoimprovekeyoperational metricssuchasdoor-to-cliniciantimeandtherateofpatients thatleavewithoutbeingseen,ametricthatisitselfnotstatic andisimpactedbyvariousdepartmentalfactors.11 Todate, however,thispatternhasnotbeenstudiedinAPCs practicingintheED.Ourprimaryoutcomeinthisstudywas todeterminewhetherthispatternwassimilarforAPCs workinginacommunityED,asthiswouldprovidefurther externalvalidationofthepreviousmodeltothecommunity settingandtoarelativelynewgroupoftheworkforce.
Weperformedaretrospective,observationalanalysisof APCshiftsattwosuburbanhospitalsintheNortheastern UnitedStatesfromJuly1,2020–June30,2021.Site1sawan averagedailyvolumeof54.46patientswithanEmergency SeverityIndex(ESI)scoremixof1.48%ESI1;30.00%ESI2; 50.65%ESI3;17.28%ESI4,and0.58%ESI5.Site2hadan averagedailyvolumeof79.71patientswithanESIscoremix of1.01%ESI1;26.7%ESI2;49.6%ESI3;20.4%ESI4;and 2.3%ESI5.
Fortheattendingshiftschedule,site1hadashiftschedule of7 AM–4 PM,2 PM–11 PM,and10 PM–7 AM forthe firstsix monthsofthestudy.Forthesecondsixmonthstheschedule changedto7 AM–2 PM,12 PM–7 PM,4 PM–11 PM,and11 PM–
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Patientsseenperhourisakeyproductivity metric.Forattendingsandresidents,ithas beenshowntobedynamicandchanges throughoutthecourseofashift.
Whatwastheresearchquestion?
Isthisproductivitypatternsimilarfor advancedpracticecliniciansworkingin communityEDs?
Whatwasthemajor findingofthestudy?
Meannumberofnewpatientsseendecreased ateachhouroftheshiftrelativetothe previoushour(P < 0.01).
Howdoesthisimprovepopulationhealth?
Understandinghowmanypatientsareseenat eachhouroftheday,basedoncliniciantype andhourofshift,couldinformstaf fi ngmodels andhelpthroughput.
7 AM toaddmoreattendingcoverage.Atsite2,theshiftswere 7 AM–3 PM,12 PM–9 PM,3 PM–11 PM,and10 PM–7 AM.The sign-outcultureatbothsitesisthatpatientswillhavean establishedplanfordispositionpriortotransitioningtothe newteam.
Atbothsites,APCshiftsare10hourslong.Atthe firstsite, thereisasingledailyAPCshiftfrom10 AM–8 PM.Atthe secondsite,thereweretwoAPCshiftsduringthestudy period,from8 AM–6 PM andfrom4 PM–2 AM.Therewere severaldaysduringwhichthe firstsitehadnoAPCcoverage, andthesecondsitehadonlyasingleshift.FiveAPCsworked theshiftsatsite1,includingamixofbothNPsandPAs,while 10APCsworkedtheshiftsatsite2,consistingsolelyofPAs. OneofthePAsworkedshiftsatbothsitesduringthestudy period.Intotaltherewere14APCs,2NPsand12PAs.The APCssawalllevelsofpatientacuity.Thesesitesemploya shared-visitmodel,andallpatientsseenbyanAPCare presentedto,andthenevaluatedby,anattendingphysician. TheAPCscontinuetopickupnewpatientsthroughoutthe shiftandarenotlimitedindoingsobyattendingavailability tostaff.Over70%oftheAPCsinthestudyhad >5yearsof clinicalexperienceatthestartofthestudyperiod.
Weusedade-identifiedqualityassurancedatabaseforthis study,whichisprimarilyusedforoperationsplanning.The databaseisautomaticallypopulatedbythesites’ electronic healthrecord(EHR).Timestampsofpatientarrivals,APC assignments,andpatientdispositionsareautomatically
recordedbytheEHR.Thetimestampdataiscompiledalong withadditionalaggregatedandde-identifiedpatient-level data,inaccordancewithHIPAA-SAFEHARBORcriteria, priortodataanalysis.OnlythepatientsseenbyanAPCwere includedforanalysis,andregistrationanomalieshadalready beenremoved.Thisstudywasgrantedanexemptionof informedconsent,aspartofalargerprojectusiingadeidentifiedadministrativedatasetofEDthroughputfor qualityassurancepurposes.Theexemptionwasgrantedby theinstitutionalreviewboardaffiliatedwiththeclinicalsites, whichincludesdirectinvolvementbypatientandcommunity representativesintheoversightandapprovalofall researchprotocols.
Theprimaryoutcomewasthenumberofnewpatients seenateachhourofastandard10-hourAPCshift.Weuseda generalizedestimatingequationtoconstructthemodelof APCproductivity,withtheindividualshiftasthegroupingin lightoftheuseofmultiplehourlymeasurementsfromthe sameshift.APoissondistributionwithaloglinkwasused,as theoutcomevariable(patientsseeninanhour)reflectsa positivecountvariableina fixedtimeinterval.Weevaluated themodelusinganautoregressivecovariancestructure,with alternatecovariancestructurestestedinsensitivityanalyses. Thehouroftheshiftandtheshifttimeandlocationwereused ascovariates.Wereport finalparsimoniousmodelsas determinedbyquasi-likelihoodscore.Atwo-sided P -value <.05wasconsideredstatisticallysignificant,withstrict correctionformultiplecomparisons.Forthepurposesof modelinterpretability,wereportthecalculatedmodel predictions,withtheraw(exponential)modelcovariatesina supplementalappendix.AnalysiswasconductedinPython 3.11usingtheStatsmodelsandSciPypackages(Python SoftwareFoundation,Wilmington,DE).
Duringthestudyperiod(July1,2020–June30,2021),we analyzed862shifts,ofwhich345wereatSite1(single coverage),and517wereatSite2(two-shiftcoverage).Allthe workedshiftsinthisperiodwereincludedinthestudy,andno aberranttimestampswerefoundinthedatabase,meaning thatthetimestampofAPCassignmentalwaysalignedwith
theshifthoursontheschedule.NoteveryAPCshiftwas staffedduringthestudyperiod,duetofactorsincluding quarantine,operationalreassignmentswithinthenetwork, andstaffingshortagesfromtheCOVID-19pandemic.
Sitecharacteristicsaresummarizedin Table1.AtSite1 withasingleAPCshiftfrom10 AM–8 PM,APCssawamean of13.31patientspershift(95%CI13.02–13.63).AtSite2, APCssaw12.64(95%CI12.32–13.06)patientsduring the8 AM–6 PM shift,and12.53(95%CI12.04–12.82) patientsduringthe4 PM–2 AM shift.Whilesmall,these differenceswerestatisticallysignificant(P < 0.01forall pairwisecomparisons).
Acrossallsitesandshifts,the firsthouroftheshift demonstratedthehighestnumberofpatientsseen(Site1: 2.25[95%CI2.17–2.33],Site28 AM–6 PM:2.12[95%CI 1.98–2.26],andSite24 PM–2 AM:2.10[95%CI1.95–2.26]). Eachhourwasassociatedwithasmall,butstatistically significantdecreaseovertheprevioushours(Table2).This decreasewasmostpronouncedduringthelasttwohoursof theshift,leadingtoanaveragewellbelowasinglepatient seenperhourduringhours9(Site1:0.57[95%CI0.50–0.64], Site28 AM–6 PM:0.54[95%CI0.46–0.62],Site24 PM–2 AM: 0.53[95%CI0.45–0.62])and10(Site1:0.14[95%CI 0.11–0.17],Site28 AM–6 PM:0.13[95%CI0.10–0.17], Site24 PM–2 AM:0.13[95%CI0.10–0.17]).Thistrendcanbe visualizedin Figure. Asensitivityanalysisdidnotrevealany significantdifferenceinhourlyvolumeofpatientsseenby APCsbydayofweek.Priorresearchatthesehospitalshas shownadequatehourlypatientvolumessuggestingthereis notashortageofpatientstobeseen.9
Our findingsinthisstudysuggestthatAPCsmay demonstrateasimilarpatternofhourlydeclinesin productivitythathasbeenobservedinbothresidentand attendingphysicians.8,9 Thiscorroboratesprior findingsthat suggestthatpatientsseenperhourisadynamicvariable.An intuitiveexplanationofthis findingfollowsfromthefactthat patientevaluationstakeplaceovermultiplehoursofashift, andthatseeinganewpatientlaterintheshiftrequiresthe APCtobalancethedemandsofseeinganadditionalpatient
Table2. Modelsofnewpatientsseenperhour.
Site1:10 AM–8 PM shift
ShifthourMeannewpatients(95%CI) P-value
1 2.25(2.17–2.33) < 0.01
2 1.96(1.80–2.13) < 0.01 3 1.80(1.65–1.96) < 0.01
4 1.66(1.52–1.81) < 0.01
5 1.42(1.29–1.50) < 0.01
6 1.33(1.21–1.46) < 0.01
7 1.26(1.14–1.39) < 0.01
8 0.98(0.89–1.09) < 0.01
9 0.57(0.50–0.64) < 0.01 10 0.14(0.11–0.17) < 0.01
Site2:8 AM–6 PM shift
ShifthourMeannewpatients(95%CI) P-value
1 2.12(1.98–2.26) < 0.01
2 1.85(1.65–2.07) < 0.01
3 1.69(1.5–1.91) < 0.01
4 1.56(1.38–1.76) < 0.01
5 1.33(1.18–1.50) < 0.01
6 1.25(1.10–1.42) < 0.01
7 1.19(1.04–1.35) < 0.01
8 0.92(0.81–1.06) < 0.01
9 0.54(0.46–0.62) < 0.01 10 0.13(0.10–0.17) < 0.01
Site2:4 PM–2 AM shift
ShifthourMeannewpatients(95%CI) P-value
1 2.10(1.95–2.26) < 0.01
2 1.83(1.63–2.06) < 0.01
3 1.68(1.48–1.90) < 0.01
4 1.55(1.37–1.75) < 0.01
5 1.32(1.16–1.50) < 0.01
6 1.24(1.09–1.41) < 0.01
7 1.18(1.03–1.35) < 0.01
8 0.92(0.80–1.05) < 0.01
9 0.53(0.45–0.62) < 0.01
10 0.13(0.10–0.17) < 0.01
CI, confidenceinterval.
withconcurrentlycaringforexistingpatients.TheAPCsmay seemorepatientsearlierintheshiftpreciselybecausethey havethegreatestcognitivebandwidthatthestartofashift, withnoactivepatients.Asthosepatientsstarttogenerate resultsandrequirere-evaluation,interpretationofimaging

Figure. Meannumberofpatientsseenpershifthourbyadvanced practiceclinicians. APC,advancedpracticeclinician.
orlabs,orproceduresthataddtothecognitiveloadforan APC,theywillseefewernewprimarypatients.
However,therearesubstantialdifferencesinthepatternswe haveobservedinAPCsrelativetopatternsofphysician productivitypreviouslydescribedintheemergencymedicine operationsliterature.8,9 Notably,whileallofthesegroups demonstrateprogressivedeclinesinhourlyproductivityand seeahigherproportionofpatientsinthe firstfewhoursoftheir shifts,theAPCsinourstudydemonstratedbothasmaller “peak” atthebeginningoftheirshiftscomparedtothose reportedwithattendingphysicians,andamoregradual decreasefromhour-to-hourrelativetoresidentphysicians.The causeofthisislikelymultifactorial;however,intheprior studiesforbothattendingsandresidents,thosegroupswere incentivizedandgradedonproductivity;theAPCsinourstudy didnothavethesameexplicittietoproductivity.
Thishasimportantdownstreamconsequenceswhen creatingstaffingmodels.Whileshiftstypicallyspan10hours andthereisanadministrativeexpectationforequalcapacity duringallhoursofcoverage,the9th and10th hoursofashift donotprovidemuchinthewayofnewpatientevaluations. So,whenhiringandstaffingadepartmentandtryingtobest alignthenumberofhourlyarrivalswiththeavailablestaff (residents,attendingsorAPCs)theadministrationmusttake thispatternintoaccount.Understandinghowmanypatients areexpectedtobeseenataspecifichouroftheday,basedon whatstaffareavailableandthehourofeachperson’sshift, mayhelpthroughput.
Ourstudydoeshavemanylimitations.Itwasonlydoneat twocommunityhospitalsinasimilargeographicregion. Becausetherewereonlythreeshiftstarttimes,therewasless variabilitythanpriorstudiesperformedonresidentand attendingphysicians,whichalsohadagreatervarietyofshift startingandendingtimes,includingovernights.However,as longastherewereadequatepatientstobeseenateachhour oftheday asseeninpriorstudiesofattendingindependent productivityatthesesites thislimitationshouldbe mitigated.Therewerealsotwohoursofoverlapbetween shiftsatthesecondsite,whichmayhavecontributedtosome productivitydrop-offforthe8AM–6PMshiftatsite2. Additionally,withinthisnetworkAPCscaredforalllevelsof patientacuity,andeachvisitrequiredstaffingandevaluation byanattendingphysician.Thisdiffersfromothermodels whereAPCscandischargeloweracuitypatientswithoutan attendingevaluation.
Whilethedelayofwaitingforanattendingtoseethe patientmayprolongsometasksanddecisions,thisgroupof APCshadalotofexperienceandindependence(>70%with over fiveyearsofexperience)andcontinuedtopickupnew patientsintheinterim.Further,atthetwostudysitesAPCs wereusedtoseepatientsprimarily,andthismaynotbe applicabletootherwaystheyareusedindepartments,such
asmanagingobservationpatients.Lastly,asthisstudywas conductedattwosmallcommunitysitestherewereonlya fewtotalAPCs(14totalindividuals)whoprimarilywork onlyatasinglesite,andthisgroupmaynotberepresentative oflargergroupsofAPCsorthoseworkinginmultiple hospitalorurgentcaresettings.
Our findingssuggestthattheproductivityofadvanced practicecliniciansmayfollowapatternofdecreasingover successivehoursofashift,similartobothattendingsand residents.Thisstudyreinforcespriorliteraturethat demonstratesthatpatientsperhourisadynamicvariable, whichstartsatitshighestpointanddecreasessignificantly eachsubsequenthour.Byverifyingthatthispatternis consistentinAPCs,itbroadenstheproductivitymodelof priorresearch.CommunityEDs,whichareoftenstaffedwith APCsandhavenoresidentcoverage,mayneedtotakethis phenomenonintoaccountasithassignificantschedulingand operationalconsequences.
AddressforCorrespondence:BryanA.Stenson,MD,BethIsrael DeaconessMedicalCenter,DepartmentofEmergencyMedicine, OneDeaconessRd.,Boston,MA02215.Email: bstenson@bidmc. harvard.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Stensonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CairnsCandKangK.NationalHospitalAmbulatoryMedicalCare Survey:2020emergencydepartmentsummarytables.2022.Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2020-nhamcsed-web-tables-508.pdf.AccessedMay9,2023.
2.AledhaimA,WalkerA,VesselinovR,etal.Resourceutilizationinnonacademicemergencydepartmentswithadvancedpracticeproviders. WestJEmergMed. 2019;20(4):541–8.
3.HookerRS,KlockoDJ,LarkinGL.Physicianassistantsinemergency medicine:theimpactoftheirrole. AcadEmergMed. 2011;18(1):72–7.
4.JeanmonodR,DelcolloJ,JeanmonodD,etal.Comparisonofresident andmid-levelproviderproductivityandpatientsatisfactioninan emergencydepartmentfasttrack. EmergMedJ. 2013;30(1):e12.
5.HamdenK,JeanmonodD,GualtieriD,etal.Comparisonofresidentand mid-levelproviderproductivityinahigh-acuityemergencydepartment setting. EmergMedJ. 2014;31(3):216–9.
6.PinesJM,ZocchiMS,RitsemaT,etal.Theimpactofadvanced practiceproviderstaffingonemergencydepartmentcare: productivity, flow,safety,andexperience. AcadEmergMed. 2020;27(11):1089–99.
7.StensonBA,AndersonJS,DavisSR.Staffingandprovider productivityintheemergencydepartment. EmergMedClinNorthAm. 2020;38(3):589–605.
8.JosephJW,HenningDJ,StrouseCS,etal.Modelinghourly residentproductivityintheemergencydepartment. AnnEmergMed. 2017;70(2):185–90.e6.
9.JosephJW,DavisS,WilkerEH,etal.Modellingattendingphysician productivityintheemergencydepartment:amulticentrestudy. Emerg MedJ. 2018;35(5):317–22.
10.StensonBA,JosephJW,AntkowiakPS,etal.Understandingdemand andcapacitymismatchinanacademicemergencydepartmentusinga staircasemodelofprovidercapacityandstaggeredshiftstarttimes. J EmergMed. 2021;61(3):336–43.
11.ChiuDT,StensonBA,AlghamdiM,etal.Theassociationbetweenday ofarrival,timeofarrival,dailyvolumeandtherateofpatientsthat “left withoutbeingseen.” AmJEmergMed. 2023;67:24–8.
VincentKan,MD,MSc*
WilsonHuang,MD†
GrettaSteigauf-Regan,MD*
JillAnderson,MPH,MAT*
IvyDang,BS*
ChadDarling,MD,MSc*
SectionEditor:StephenW.Meldon,MD
*UMassChanMedicalSchool,DepartmentofEmergencyMedicine, Worcester,Massachusetts † UniversityofCaliforniaSanFrancisco,DepartmentofEmergencyMedicine, SanFrancisco,California
Submissionhistory:SubmittedSeptember5,2024;RevisionreceivedNovember20,2024;AcceptedNovember20,2024
ElectronicallypublishedJanuary30,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.35281
StudyObjective: Wesoughttodeterminetheoverallratesoftraumaticinjuriesandwhethertheratesof traumaticinjuriesandvariousclinicaloutcomesdifferedamongolderpatientspresentingtoatertiarycareemergencydepartment(ED)afteraground-levelfall(GLF)andwhounderwentwhole-body computedtomography.
Methods: Weconductedaretrospectivecohortstudyofpatients ≥65yearsofagewhopresentedtothe EDwithaGLFandreceivedawhole-bodyCTfromJanuary1–December31,2021.Agewasstratified intoagegroups:65–74;75–84;and85+.Wepresentedadescriptiveanalysisoftraumaticinjuries, intensivecareunit(ICU)admissions,andall-causemortalityrates.Weusedmultivariablelogistic regressiontodeterminetheassociationbetweenincreasingage,traumaticinjuries,and clinicaloutcomes.
Results: Of638patientsinthecohort,120(18.9%)sustainedthoracicinjuriesand80(12.5%)sustained intracranialhemorrhages.Only five(0.8%)patientssustainedanintra-abdominalinjury,while134 (21.0%)wereadmittedtotheICU,and31(4.8%)diedduringtheirindexhospitalization.Headinjuries (oddsratio[OR]6.21,95%CI3.65–10.6, P < 0.001)andthoracicinjuries(OR5.25,95%CI3.30–8.36, P < 0.001)wereassociatedwithincreasedoddsofICUadmission,whereasheadinjuries(OR3.21,95% CI1.41–7.31, P < 0.01)andcervicalinjuries(OR3.37,95%CI1.08–10.5, P < 0.05)wereassociatedwith increasedoddsofin-hospital,all-causemortality.Therewerenostatisticallysignificantdifferencesinthe ratesofinjuriessustainedbetweentherespectiveagegroups.Therewasnoassociationbetween increasingageandICUadmissionsorin-hospital,all-causemortalityrates.
Conclusion: Amongpatientsaged ≥65yearsofagewhopresentedtotheEDafteraground-levelfall andunderwentwhole-bodyCT,thoracicinjuriesandintracranialhemorrhageswereassociatedwith increasedoddsofICUadmissions.Wefoundnosignificantdifferencesininjuryratesoroutcomesacross agegroups,indicatingthatagealoneshouldnotguideICUadmissiondecisions.These findingssuggest thattheuseofwhole-bodyCTinthispopulationshouldbeselectiveandguidedbyclinicaljudgment ratherthanapplieduniversally.[WestJEmergMed.2025;26(2)301–306.]
Background
Fallsaretheleadingcauseoffatalandnon-fatalinjuries amongtheelderly.Upto40%ofmenandwomen ≥65years ofageinthecommunityfalleachyear.1 Injuriesrelatedto fallsamongtheelderlyaccountforthreemillionemergency department(ED)visitsand50billiondollarsofUS healthcarespendingannually.2 Ground-levelfalls(GLF), definedasfallsfromastandingheight,areparticularly commonamongolderpatients.Age-relatedphysiologic changescreatesignificantfall-relatedmorbidityand mortalityinthispatientcohort.3
PatientswhopresenttotheEDfortrauma-related complaintsareoftenevaluatedwithcomputedtomography (CT)fortheiraccuracyandreliabilityindetectinginjuries. Theroutineuseofnon-selective,whole-body(headtopelvis) CTisbecominganincreasinglycommondiagnosticmodality inthesepatients,particularlyinthoseinvolvedinhighenergymechanismssuchasmotorvehiclecollisions,dueto themorewidespreadavailabilityofCTimagingand changingclinicalpracticepatterns.4 Whilewhole-body CTisfrequentlyusedinhigh-energytrauma,itsapplication inlow-energymechanismslikeGLFsremainsless clearandmorevariable.Severalstudieshaveshown conflictingevidenceastowhetherwhole-bodyCTis warrantedintraumapatients.5,6 Giventhelowkinetic energyimpactfromGLFs,itisunclearwhetherthe indiscriminateuseofwhole-bodyCTinGLFscan improvepatients’ outcomesbydetectingclinically relevantinjuries.
Ourobjectivesofinthisstudyweretodeterminethe overallratesoftraumaticinjuriesandclinicaloutcomesand whethertheratesoftraumaticinjuriesandclinicaloutcomes wereassociatedwithincreasingageamongpatients ≥65yearsofagepresentingtoatertiary-careEDwithaGLF andwhounderwentwhole-bodyCT.Wehypothesizedthat duetodecreasedphysiologicalreservesandincreased fragility,theincidenceoftraumaticinjuriesandadverse outcomesafteraGLFamongthisselectivepopulationwould increasewithadvancingage.
ThisstudywasapprovedbytheHumanInstitutional ReviewBoard.Weconductedaretrospectivecohortstudyof patientstreatedatthistertiary-careLevelItraumaacademic medicalcenterwith90,000annualEDvisits.Weadheredto thepreviouslypublishedmethodologicalcriteriaforhealth recordreviewstudies.7
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Fallsaretheleadingcauseofinjuryinolder adults,yetoptimaluseofwhole-bodyCTin low-energymechanismssuchasground-level falls(GLF)isunclear.
Whatwastheresearchquestion?
Dotraumaticinjuryratesandclinical outcomesdifferwithageamongolder patientsundergoingwholebodyCTfor ground-levelfalls?
Whatwasthemajor findingofthestudy?
Thoracic(OR5.25,95%CI3.30 – 8.36)and headinjuries(OR6.21,95%CI3.65 – 10.6) afteraground-levelfallwereassociatedwith ICUadmissions.Only fi ve(0.8%)patients sustainedanintra-abdominalinjury.
Howdoesthisimprovepopulationhealth?
Selectivewhole-bodyCTuseinGLFpatients canimprovecareef fi ciencybyfocusingon clinicallysigni fi cantinjurieswhilereducing unnecessaryimaging.
Weidentifiedallpatients ≥65yearsofagewhopresented totheEDwithaGLFandreceivedawhole-bodyCT betweenJanuary1–December31,2021.Atourinstitution,a whole-bodyCTisdefinedasaCTofthehead,chest, abdomenandpelvis,cervicalspine,thoracicspine,and lumbarspine;itincludesintravenouscontrastadministration toevaluateforsofttissueinjuryofthethoraxandabdomen. AGLFisdefinedasfallingfromastandingheight,chair, wheelchair,oroutofbed.
Studyvariablescollectedincludedbasicdemographic characteristics(ageandsexasidentifiedbypatient), antiplateletoranticoagulantuse,medicalcomorbidities, initialGlasgowComaScale(GCS)score,initialheartrate andsystolicbloodpressure,andtraumaticinjuriesfoundon CT.Datawascollectedusingastandardizeddatacollection formthroughtheelectronichealthrecord(EpicSystems, Verona,WI)bytrainedresearchassistants(RA)anda residentphysician(WH).NoneofthetrainedRAsorthe residentphysicianknewthestudyobjectives.Datapoints collectedincludedallacutetraumaticinjuriesidentifiedon the finalCTimagingradiologyreports.Co-authorGS
performedaduplicatereviewof10%ofthehealthrecordsfor interobserverreliabilityassessment.WeusedtheCohen kappatodeterminetheinter-raterreliabilityof dataabstraction.
Ourprimarystudyoutcomemeasuresincludedtherateof variousacutetraumaticinjuries,admissiontotheintensive careunit(ICU),andall-cause,in-hospitalmortality. Traumaticinjuriesincludedintracranialhemorrhages(ICH), thoracicinjuries,intra-abdominalinjuries,cervicalspine fractures,thoracicspinefractures,andlumbarspinefractures. Intracranialhemorrhagesweredefinedasanyepidural, intraparenchymal,intraventricular,subarachnoid,orsubdural hematomasorhemorrhagethatwerebelievedtobetraumatic inetiology.Wedefinedthoracicinjuriesashemothoraces, pneumothoraces,pulmonarycontusions,orribfractures. Intra-abdominalinjuriesweredefinedasanysolidorganor hollowviscousinjuries.Weexcludedminorsofttissueinjuries orhematomas,subacuteorchronictraumaticinjury findings, andnon-traumatic findingsonCTimaging.Foroursecondary outcomemeasures,weanalyzedtheassociationbetweenage, traumaticinjuries,andclinicaloutcomes,includingICU admissionsandin-hospital,all-causemortality.Agewas stratifiedintoagegroups:65–74;75–84;and85+
Descriptivestatisticsarepresentedasmeans ± standard deviationsforcontinuousvariables,andcategorical variablesarereportedaspercentages.Incidencesof traumaticinjuries,ICUadmissions,andall-causemortality arereportedasproportionswithaccompanying95% confidenceintervals(CI).Differencesbetweenouragespecificcomparisongroups(65–74,75–84,85+)were examinedusingANOVAforcontinuousvariablesandchisquaredandFisherexacttestsforcategoricalvariables.Twotailedvaluesof P < 0.05wereconsideredstatistically significant.Weperformedbivariateanalysistoidentify variablesassociatedwithclinicaloutcomes.Usingthe65–74 cohortasthereferencegroup,weusedmultivariablelogistic regressiontodeterminetheassociationbetweenage, traumaticinjuries,andclinicaloutcomescontrollingfor medicalcomorbidities,antithromboticuse,andstatistically significanttraumaticinjuries.Dataanalysiswasperformed usingSTATA/MPVersion17(StataCorp,College Station,TX).
BaselinePatientCharacteristics
Atotalof638patientsmetourinclusioncriteriaduringthe one-yearperiodunderstudy.Theaverageageofthestudy populationwas82.1 ± 9.0years;60.0%werewomen,and 62.9%wereonatleastoneantithromboticagent,with33.7%
Antithrombotic,%
1Notstatisticallysignificant. CHF,congestiveheartfailure; COPD,chronicobstructivepulmonary disease; CVA/TIA,cerebrovascularaccident/transientischemic attack; GCS,GlasgowComaScale; MI,myocardialinfarction; HR, heartrate; SBP,systolicbloodpressure.
onanantiplateletand39.1%onananticoagulant.The averagenumberofcomorbiditieswas1.5 ± 1.3(Table1).
Amongthe638patientswhosustainedaGLF,120 patients(18.9%)sustainedthoracicinjuries,and80(12.5%) sustainedICH.Sixty(9.8%)patientssustainedthoracicspine injuries,51(8.0%)ssustainedlumbarspineinjuries,and34 (5.3%)patientssustainedcervicalspineinjuries.Only five Table1. Studypopulationcharacteristicsaccordingtoage.
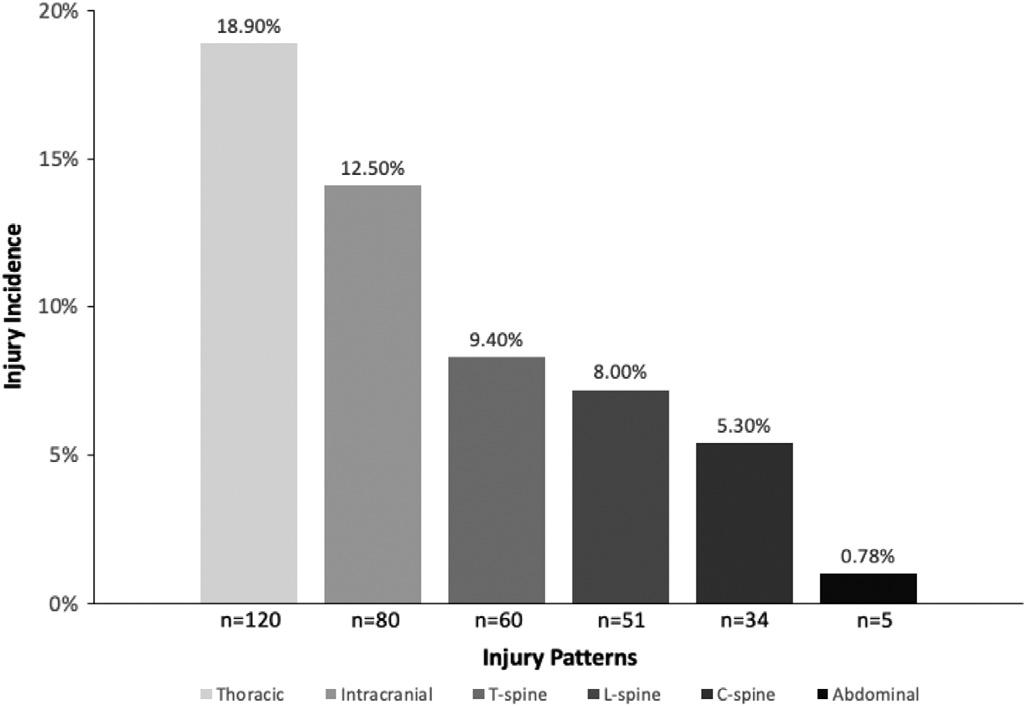
Figure. Incidenceproportionamongdifferentinjuries.
(0.8%)patientssustainedanintra-abdominalinjury(Figure). Ofthe fivepatientswithintra-abdominalinjuries,all five werefoundtohavepertinentphysicalexam findings,initial unstablevitalsigns(systolicbloodpressure <90orheartrate 100),orabnormalGCS(<15).Therewerenostatistically significantdifferencesintheratesofvariousinjuries sustainedbetweentherespectiveagegroups(Table2).
Atotalof134(21.0%)patientswereadmittedtotheICU, and31(4.8%)diedduringtheirindexhospitalization.There werenostatisticallysignificantdifferencesintheratesof clinicaloutcomesbetweentherespectiveagegroups.Using multivariablelogisticregressionmodels,wefoundno associationbetweenincreasingageandICUadmissionsor in-hospital,all-causemortalityrate(Table3).Incontrastto age,headinjuries(oddsratio[OR]6.15,95%CI3.62–10.5, P < 0.001)andthoracicinjuries(OR5.38,95%CI3.37–8.67, P < 0.001)wereassociatedwithincreasedoddsofICU
admission,whereasheadinjuries(OR3.21,95%CI 1.41–7.31, P < 0.01)andcervicalinjuries(OR3.37,95%CI 1.08–10.5, P < 0.05)wereassociatedwithincreasedoddsof in-hospitalmortality.
Amongthe10%ofthehealthrecordsreviewedbyacoauthor,wefoundthatourratersagreedon88%ofthe informationabstractedfromtherecords,resultingina Cohenkappacoefficientof0.8.
Inourstudypopulation,injuriessustainedafteraGLF werebroadlyconsistentamongallagegroups.Wefoundthat asubstantialminorityofolderpatientswhounderwent whole-bodyCTatthediscretionofthetreatingphysicians afteraGLFwerefoundtohaveclinicallysignificantinjuries
Table2. Traumaticinjuriesandemergencydepartmentdispositionsstratifiedbypatientage.
Traumaticinjuries,no.(%)
EDdisposition,no.(%)
Nostatisticalsignificance betweenallagegroups.
ED,emergencydepartment; ICU,intensivecareunit.
Table3. Associationbetweenincreasingageandclinicaloutcomes.
ICUadmissions
Mortality1
65–743(1.89%)1[Reference]1[Reference] 75–84
1In-hospital,all-causemortality.
ForICUadmissions:adjustedfortotalcomorbidities,headinjuries,thoracicinjuries. Formortality:adjustedfortotalcomorbidities,headinjuries,cervicalinjuries. OR,oddsratio; CI,confidenceinterval; ICU,intensivecareunit.
thatresultedinICUadmissions.Increasingagewasnot associatedwithanincreasedrateofICUadmissionordeath afteraGLF.ThoracicinjuriesandICHwereassociatedwith increasedoddsofICUadmission.Intracranialhemorrhages andcervicalfractureswereassociatedwithincreasedoddsof in-hospitalmortality.
Wefoundthatover30%oftheinjuriessustainedwere eitherICHorthoracicinjuries,bothofwhichwereassociated withincreasedoddsofICUadmissionsinourstudy population.Intracranialhemorrhagesandribfractures amongolderpatientsareinjuriesthatcanresultinhigh mortalityrates,8–10 thusrequiringfrequentmonitoringand necessitatingICUlevelofcare.Our findingsreinforcethe importanceofusingCTtoidentifytheseinjuriesinpatients presentingwithGLFs,particularlywhenthereisclinical suspicionofthoseinjuries.
Furthermore,ourstudydidnotshowanysignificant associationbetweenincreasingageandICUadmissionand mortality.Thiscontrastswiththeresultsofapreviousstudy, whichshowedastepwiseincrementintherateofcervical spineinjuriesandin-hospitalmortalityassociatedwith increasedageinGLFpatientsfromaninstitutionaltrauma registry.11 Patientsrecordedinatraumaregistrywilllikely havesustainedinjuriesrequiringtraumateamevaluation.In addition,wedidnot findanydifferenceintheratesofvarious injuriesafteraGLFbetweenthedifferentagegroups.Our studydiffersinthatitincludedallpatientswhosustained significantinjuriesandthosewhodidnot.Furthermore,we includedonlypatientswhounderwentwhole-bodyCTatthe discretionofthetreatingphysiciansafteraGLF.Basedon our findings,oneshouldbecautiousaboutusingincreased ageasariskfactoralonetodeterminewhetherapatient warrantswhole-bodyCTwithoutconsideringother clinicalfactors.
Overall,ourratesofdifferentinjuriesarehigherthan reportedintheliterature.Our findingsontherateofICH afteraGLFwas12.5%,whereastheratesofICHaftera GLFreportedintheliteraturehaverangedfrom 3.5–7%.12–15 Alarger,nationallyrepresentativeretrospective studyfoundtheratesofthoracicandlumbarspineinjuries were1.6%and2.5%,comparedto9.4%and8.0%inour study,respectively.16 Thediscrepancylikelyresultedfrom thefactthatweincludedonlypatientswhowereselectedby treatingphysicianstoundergowhole-bodyCTintheED. Thetreatingphysiciansprobablydeempatientsundergoing whole-bodyCTaftertraumatohavesustainedagreater numberofsignificantinjuriesduringtheinitialevaluation.
Wefoundthattherateofintra-abdominalinjurieswas low.Thisconclusionisbroadlyconsistentwiththe literature.11,17,18 Ofthe fivepatientsfoundtohaveintraabdominalinjuriesinourstudy,all fivewerefoundtohave eitherunstablevitalsigns,abnormalGCS,orabnormal physicalexamsoninitialevaluation.This findingis consistentwiththeliteraturewherehemodynamicallystable
patientswithnormalphysicalexamsareunlikelytohave intra-abdominalinjuriesafteraGLF.18–20 Performingfewer abdominalCTscansinthispopulationcouldhave substantialcostsavingswithoutreducingdiagnostic accuracy.Giventhesmallnumberofpatientswhosustained intra-abdominalinjuriesinourstudy,wewerenot adequatelypoweredtoidentifypotentialriskfactors associatedwithintra-abdominalinjuriesafteraGLF.Future prospectivestudiesareneededtoidentifyfactorsassociated withintra-abdominalinjuriesanddeterminethecosteffectivenessofaselectiveimagingalgorithminlow-risk GLFpatients.
Ourstudywasretrospectiveandsusceptibletobiases. Non-differentialmisclassificationcanoccurduringthe queryingofhealthrecords,whichwilllikelybiastheresults towardthenull.However,10%ofthehealthrecordswere reviewedbyco-authorGStolimitthisbias.Furthermore,we demonstratedexcellentinter-raterreliability.Thestudywas alsosusceptibletoselectionbias,andwaslimitedtopatients whoreceivedawhole-bodyCT.Atourinstitution,the decisiontoorderawhole-bodyCTonatraumapatient dependsonthetreatingphysician’spreference.Patientswho receivedawhole-bodyCTarelikelydeemedbythetreating physiciantohavesustainedsignificantinjuries.Therefore, ourstudylikelyoverestimatesinjuryincidenceduetothe selectivenatureofwhole-bodyCTuse.Moreover,wedidnot obtaininformationonolderpatientswhosustainedaGLF anddidnotreceiveawhole-bodyCT.Thosetwolimitations likelyresultedinourstudyoverestimatingtheincidence proportionofinjuriesreportedafteraGLF.Furthermore, thisstudywasbasedonasingleinstitutionatatertiary-care LevelItraumacenter;thus,itcannotbegeneralizedtoother institutions.Inaddition,thenatureofourquerydidnot allowustoobtainInjurySeverityScores.
Amongpatients ≥65yearsofagewhopresentedtotheED afteraground-levelfallandunderwentwhole-bodyCT, thoracicinjuriesandintracranialhemorrhages whilea minorityoftheinjuriessustained wereassociatedwith increasedoddsofICUadmissions.These findingshighlight theimportanceofcarefullyassessingtheseinjuriesinolder adults.Interestingly,wefoundnosignificantdifferencesin injuryratesorclinicaloutcomesacrossagegroups, suggestingthatagealoneshouldnotbethedetermining factorforICUadmissionormortalityriskinthispopulation. Givenour findings,weproposethattheremaybevaluein reassessingtraumascreeningprotocols,especiallyregarding theuseofwhole-bodyCTinpatientswhosustainalowenergyfall.Itsuseshouldbeselectiveratherthanapplied universally.Multicenterprospectivestudiesareneededto determinethebroaderutilityandcost-effectivenessofwhole-
bodyCTuseamongolderpatientswhopresenttotheED aftersustainingaground-levelfall.
AddressforCorrespondence:VincentKan,MD,UMassChan MedicalSchool,DepartmentofEmergencyMedicine,55NLake Ave.,Worcester,MA01655.Email: vincent.kan@umassmed.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Kanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TinettiME,SpeechleyM,GinterSF.Riskfactorsforfallsamongelderly personslivinginthecommunity. NEnglJMed. 1988;319(26):1701–7.
2.BergenG,StevensMR,BurnsER.Fallsandfallinjuriesamongadults aged ≥ 65years UnitedStates,2014. MMWRMorbMortalWklyRep. 2016;65(37):993–8.
3.SpaniolasK,ChengJD,GestringML,etal.Groundlevelfallsare associatedwithsignificantmortalityinelderlypatients. JTrauma. 2010;69(4):821–5.
4.BunnC,RinghouseB,PatelP,etal.Trendsinutilizationofwhole-body computedtomographyinblunttraumaafterMVC:analysisofthetrauma qualityimprovementprogram(TQIP)database. JTraumaAcuteCare Surg. 2021;90(6):951–8.
5.SalimA,SangthongB,MartinM,etal.Wholebodyimaginginblunt multisystemtraumapatientswithoutobvioussignsofinjury:Resultsofa prospectivestudy. ArchSurg. 2006;141(5):468–73;discussion473–5.
6.SierinkJC,TreskesK,EdwardsMJ,etal.Immediatetotal-bodyCT scanningversusconventionalimagingandselectiveCTscanningin patientswithseveretrauma(REACT-2):arandomisedcontrolledtrial. Lancet. 2016;388(10045):673–83.
7.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
8.BarneaY,KashtanH,SkornickY,etal.Isolatedribfracturesinelderly patients:mortalityandmorbidity. CanJSurg. 2002;45(1):43–6.
9.MaiHT,TranTS,Ho-LeTP,etal.Low-traumaribfractureinthe elderly:riskfactorsandmortalityconsequence. Bone. 2018;116:295–300.
10.StawickiSP,GrossmanMD,HoeyBA,etal.Ribfracturesintheelderly: amarkerofinjuryseverity. JAmGeriatrSoc. 2004;52(5):805–8.
11.BhattacharyaB,MaungA,SchusterK,DavisKA.Theoldertheyarethe hardertheyfall:Injurypatternsandoutcomesbyageaftergroundlevel falls. Injury. 2016;47(9):1955–9.
12.GanetskyM,LopezG,CoreanuT,etal.Riskofintracranialhemorrhage inground-levelfallwithantiplateletoranticoagulantagents. AcadEmerg Med. 2017;24(10):1258–66.
13.NishijimaDK,OffermanSR,BallardDW,etal.Riskoftraumatic intracranialhemorrhageinpatientswithheadinjuryandpreinjury warfarinorclopidogreluse. AcadEmergMed. 2013;20(2):140–5.
14.GrewalK,AtzemaCL,AustinPC,etal.Riskofintracranialhemorrhage betweendifferentdirectoralanticoagulantsinolderpatientsseeninthe emergencydepartmentwithaheadinjury:apopulation-basedcohort study. ThrombRes. 2022;214:47–52.
15.VardarZ,LoHS,MariyampillaiM,etal.Traumaticintracranial hemorrhageonCTafterground-levelfallinadultpatientsreceiving antithrombotictherapy:aretrospectivecase-controlstudy. AmJ Roentgenol. 2022;219(3):501–8.
16. GrabelZJ,LunatiMP,SegalDN,etal.Thoracolumbarspinalfractures associatedwithgroundlevelfallsintheelderly:ananalysisof254,486 emergencydepartmentvisits. JClinOrthopTrauma. 2020;11(5):916–20.
17.BahlAandSchaferS.Utilityofabdominalcomputedtomographyin geriatricpatientsonwarfarinwithafallfromstanding. JEmergTrauma Shock. 2018;11(2):88–91.
18.GartinCG,ReyesJ,HelmerSD,etal.Injurypatternsandincidenceof intra-abdominalinjuriesinelderlygroundlevelfallpatients:IsthePANSCANwarranted? AmJSurg. 2019;218(5):847–50.
19.HaganNE,BerdelHO,TefftA,etal.Torsoinjuriesafterfallfrom standing-empiricabdominalorthoracicCTimagingisnotindicated. Injury. 2020;51(1):20–5.
20.SiseMJ,KahlJE,CalvoRY,etal.Backtothefuture:Reducingreliance ontorsocomputedtomographyintheinitialevaluationofblunttrauma. J TraumaAcuteCareSurg. 2013;74(1):92–7;discussion97–9.
IraaGuleria,BS*
JenniferA.Campbell,PhD,MPH†
AbigailThorgerson,MPH* SanjayBhandari,MD‡
LeonardE.Egede,MD,MS†§
*MedicalCollegeofWisconsin,CenterforAdvancingPopulationScience, Milwaukee,Wisconsin
† UniversityatBuffalo,StateUniversityofNewYork,JacobsSchoolofMedicine andBiomedicalSciences,DepartmentofMedicine,DivisionofPopulation Health,Buffalo,NewYork
‡ MedicalCollegeofWisconsin,DepartmentofMedicine,DivisionofGeneral InternalMedicine,Milwaukee,Wisconsin
§ UniversityatBuffalo,StateUniversityofNewYork,JacobsSchoolofMedicine andBiomedicalSciences,UBMDInternalMedicine,BuffaloGeneralMedical Center,Buffalo,NewYork
SectionEditor:PayalModi,MD,MScPH
Submissionhistory:SubmittedDecember6,2023;RevisionreceivedOctober24,2024;AcceptedOctober25,2024
ElectronicallypublishedDecember31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18616
Background: Evidenceshowsthatsocialrisksarehighlyprevalentinthepatientpopulationthat presentstotheemergencydepartment(ED)forcare;however,understandingtherelationshipbetween socialriskfactorsandEDutilizationatthepopulationlevelremainsunknown.
Methods: WeusedtheNationalHealthInterviewSurveyfromthe2016–2018sampleadult files.The sampleincluded82,364individuals,representingapopulationsizeof238,888,238.Theprimary independentvariablesincludedsixsocialriskfactors:economicinstability;lackofcommunity; educationaldeficit;foodinsecurity;socialisolation;andinadequateaccesstocare.Theoutcome includedEDuseintheprioryear.Covariatesincludedage,race/ethnicity,insurancestatus,obesity, mentalhealth(depression/anxiety),andcomorbidities.Weranlogisticregressionmodelstotestthe relationshipbetweentheindependentanddependentvariablesadjustingforcovariates.
Results: Inthestudysample,20%hadatleastoneEDvisitintheprioryear.Inthefullyadjustedmodel, individualsreportingeconomicinstability(oddsratio[OR]1.33,95%confidenceinterval[CI]1.25-1.42), lackofcommunity(OR1.10,95%CI1.05-1.15),educationaldeficit(OR1.12,95%CI1.06-1.18),food insecurity(OR1.77,95%CI1.66-1.89),andsocialisolation(OR1.32,95%CI1.26-1.39)had significantlyhigheroddsofEDuse.Inadequateaccesstocarewassignificantlyrelatedtoloweroddsof EDuse(OR0.75,95%CI0.69-0.81).
Conclusions: SocialriskfactorsaresignificantlyassociatedwithhigheroddsofEDuseintheUnited Statesadultpopulation.Interventionsthatintegratesocialandmedicalneedsaregreatlyneeded,asis understandingtherolethatpreventivemedicinemayplayinreducingavoidableEDvisits.[WestJEmerg Med.2025;26(2)307–314.]
Emergencydepartment(ED)useintheUnitedStates remainshigh,withthemostrecentnationalestimates showing18%ofUSadultshadatleastonevisitintheprior12 months.1–3 CostofEDutilizationhasremainedover $76billionperyear,4 withanestimated$30billionspenton preventablehospitalizations.4 Althoughtheprimaryroleof anEDisprovidingmedicalservicestohigh-acuityor
life-threateningconditions,overuseandmisuseoftheEDin theUSremainsamajorconcernforpopulationhealth,with increasedattentionbeinggiventotheroleofunmetsocial needsunderlyingEDutilization.5,6
Ithasbeenwell-establishedthatanindividual’ssocialand physicalenvironmentplaysaroleinhealthoutcomesandis becomingincreasinglyimportantforunderstandingaccessto healthservices.7–11 Evidenceshowsthatsocialriskfactors, theadversesocialconditionssuchaseconomicinstability, foodandhousinginstability,andlimitedaccessto transportation,arehighlyprevalentamongpatientswho presenttotheED.6,12–19 Forexample,lowersocioeconomic statusandpovertyareassociatedwithincreasedEDand emergencyserviceutilizationrates,16–18 withevidence showingthatthosepresentingtotheEDaremorelikelytobe lowincome19 andinsuredthroughMedicaid.20 Atthe nationallevel,foodinsecurityisindependentlyassociated witha47%higherEDutilizationrate.14 Similarly, individualswithhousinginsecurityhaveatwo-foldincreased riskofEDuse,15 withahighriskforexperiencing homelessnessayearfollowinganEDvisit.21 Evidencealso showsthattransportationbarriersarehighamongthosewho presenttotheED.22
AsanyincreaseinEDutilizationrepresentsa correspondingincreaseinassociatedcosts,thereisanurgent needtounderstandtheunderlyingsocialdriversofED utilizationtoappropriatelydeveloptargetedinterventionsto accountforsocialriskburdenandtodecreaseEDutilization andimprovepopulationhealth.Whileexistingdatashows thatindividualsocialriskfactorsarelinkedtoincreasedED utilization,littlehasbeendonetounderstandtheprevalence ofmultiplesocialriskfactorsandtheirassociationwithED utilizationatanationallevel.Thepurposeofthisstudy, therefore,istoexaminetherelationshipbetweenmultiple socialriskfactors(economicinstability,lackofcommunity, limitededucationalattainment,foodinsecurity,social isolation,andlimitedaccesstocare)andEDutilizationina nationallyrepresentativesampleofUSadults.
DataSource
WeusedtheNationalHealthInterviewSurvey(NHIS), person,adult,andfamilyperson files.TheNHISgathers informationfrompeopleacrosstheUS.Information gatheredincludesdiseaseandconditionsinformationaswell ashealthcareinformation.23
Theprimaryindependentvariablesincludethesocialrisk factordomainsinitiallydescribedbyWrayetalin2022.24 Thesedomainsweretreatedasbinary:havingapositive responsetoanyiteminadomainwasconsidereda ‘1’ while havingnopositiveresponsesas ‘0.’ (Missingwasdefinedas missingallitemsinadomain.)Thepromptsandcriteriafor
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Socialriskfactorsplayaroleinaccessto healthcare.Prevalenceofmultiplesocialrisk factorsandtheirassociationwithEDuseata nationallevelremainsunclear.
Whatwastheresearchquestion?
Whatistherelationshipbetweenmultiple socialriskfactorsandEDuseinanationally representativesampleofUSadults?
Whatwasthemajor findingofthestudy?
Economicinstability,lackofcommunity, educationalde fi cit,foodinsecurity,and isolationincreased(P < 0.001)EDuse.
Howdoesthisimprovepopulationhealth?
Theseresultsprovidetargetsforintervention developmentandclinicalscreening programstoreduceunnecessaryEDuse andhealthcarecosts.
eachdomainarelistedin Table2.Theoutcomewasbinary anddefinedashavinganyvisitstotheEDintheprioryear (0visitsvs ≥1visits).Wealsoincludedthefollowing covariates:age;race/ethnicity;insurancestatus;obesity; mentalhealth(depression/anxiety);andcomorbidities (hypertension,coronaryheartdisease,heartattack,stroke, asthma,ulcer,cancer,emphysema/chronicobstructive pulmonarydisease,kidneydisease,diabetes,liverdisease, arthritis,migraine,andchronicpain).
Wecomparedsampledemographics,reportedas percentagesandmeans,usingchi-squareandanalysisof variancestatistics.Logisticregressionmodelswereusedto assesstheunadjustedindependentassociationbetweenED useasabinaryvariableandeachofthesixsocialrisk domains,followedbydomain-adjustedmodels(ie, simultaneouslycontrollingforallsixsocialrisks).Then,we usedthefullyadjustedlogisticregressionmodelstoevaluate theindependentassociationbetweenEDuseasabinary variableandeachofthesixsocialriskdomains,adjustingfor covariates,includingage,race/ethnicity,insurancestatus, obesity,mentalhealth,andcomorbidities.Covariateswere selectedforinclusioninthemodelbasedonpriorevidenceon therelevanceofthesevariablesaswellasbasedon P =<0.25 inbivariateanalyses.Weperformedstatisticalanalysiswith Rv4.0.3(RFoundationforStatisticalComputing,Vienna,
Austria).Toaccountforthecomplexsurveydesignand producepopulationlevelestimates,weightingwasdone usingthesvydesignfunctioninR.Statisticalsignificancewas setat P =< 0.05.
Thestudysamplewascomprisedof82,364individualsin the2016–2018period,whichrepresents238,888,238adultsin theUSpopulation.Thistimeframewasselectedforits robustsetofsocialriskfactorsavailableinthedataset. Table1 showsdemographiccharacteristicsofourstudy population.Almost20%reportedusingtheEDoneormore times.Middle-agedadults(ages40-64)accountedforabout 42%ofthissample,withyoungadults(ages18-39) representing38%.Olderadults(65+)accountfor approximately20%ofthestudysample.Themajority (64.8%)identifiedasnon-HispanicWhite,withHispanic accountingforthesecond-highestgroup(16.1%),followed bynon-HispanicBlacksat12%,andnon-Hispanicotherat 7.2%.About9%oftheadultswereuninsured. Approximately42%had1-2comorbiditiesand23.2%had threeormore,withchronicpain(34%)andhypertension (31%)representingthetwomostcommoncomorbidities.
Table2 showscharacteristicsofsocialriskdomainsinour studypopulation.Atotalof73.5%reportedeconomic instability,40.5%reportedlackofcommunity,23.5% reportedfoodinsecurity,27.2%reportedsocialisolation,and 13.1%reportedinadequateaccesstocare.
Table3 displaysunadjusted,domain-adjusted (controllingforonlysocialrisks),andfullyadjustedmodels (controllingofsocialrisks,comorbidities,andallother covariatesoutlinedinthetable).Allsocialriskfactors (economicinstability,lackofcommunity,educational deficit,foodinsecurity,socialisolation,andinadequate accesstocare)weresignificantlyassociatedwithhigherodds ofEDvisitsintheunadjustedmodels,withfoodinsecurity, economicinstability,andsocialisolationamongthosewith higheroddsratios(OR)(OR2.46,95%confidenceinterval [CI]2.32-2.59;OR2.10,95%CI1.99-2.22;andOR2.02,95% CI1.94-2.11,respectively).Inthefullyadjustedmodels, economicinstability(OR1.33,95%CI1.25-1.42),lackof community(OR1.10,95%CI1.05-1.15),educationaldeficit (OR1.12,95%CI1.06-1.18),foodinsecurity(OR1.77,95% CI1.66-1.89),andsocialisolation(OR1.32,95%CI1.261.39)wereassociatedwithhigheroddsofEDutilization. However,inadequateaccesstocarewasnegatively associatedwithEDuseinbothadjustedmodels(fully adjusted:OR0.75,95%CI0.69-0.81).
Overall,~20%ofUSadultshadatleastoneEDvisit,and socialriskfactorswerehighlyprevalentinthestudysample with74%havingeconomicinstability,41%reportinglackof community,37%reportingeducationaldeficits,27%
Table1. Characteristicsofadults,NationalHealthInterviewSurvey, 2016–2018.
COPD, chronicobstructivepulmonarydisease; ED,emergencydepartment.
Table2. Characteristicsofsocialdeterminantsofhealthdomainsin adults,NationalHealthInterviewSurvey,2016–2018.
Table2. Continued.
(Continued onnextcolumn)
SNAP, SupplementalNutritionAssistanceProgram; WIC,Women, InfantsandChildrenProgram.
reportingsocialisolation,24%reportingfoodinsecurity,and 13%reportinginadequateaccesstocare.Inaddition,fully adjustedmodelsshowedthateconomicinstability,lackof community,educationaldeficits,foodinsecurity,andsocial isolationwereindependentlyassociatedwithincreasedodds ofEDvisits,whileinadequateaccesstocarewassignificantly associatedwithloweroddsofEDvisits.Thisisoneofthe firststudiestoourknowledgethathasassessedthe relationshipbetweenmultipledomainsofsocialrisk factorsandEDutilizationinanationallyrepresentative USadultpopulation.
Our findingsareconsistentwithexistingliteratureonthe associationofsocialriskswithEDutilization.Forexample, studiesbyEstrella25 andDean26 showfoodinsecurityis significantlyassociatedwithincreasedEDuseandED expenditureevenafteradjustmentforpotential confounders.25,26 Seim16 hasshownthateconomicinstability andcommunityfactors,throughneighborhoodpoverty,are positivelyassociatedwith9-1-1ambulanceutilization,a surrogateforEDutilization.16 Inanotherstudy,Ku27 providesevidencethatfrequentusersoftheEDmaybe disproportionatelyhomeless.27 Similarly,availableliterature highlightstherelationshipbetweensocialisolationandED use.Inanobservationalstudyofolderpatients,Mosen26 foundthatthosewhoexperiencesocialisolationweremore likelytohaveatleastoneEDvisitthanthosewhorarelyor neverexperiencedsocialisolation.28
Thecurrent findingsshowlackofaccesstocareis negativelyassociatedwithEDuse.Availableevidenceonthe associationbetweenaccesstohealthandEDuseismixed.29 Evidencesuggeststhatgreateraccesstocarecantranslateinto greaterreceiptofpreventativecareandbeingmorecognizant ofdiseasesandhealth,resultinginincreaseduseacrossED andprimarycarevisits.30 Conversely,lackofaccesscanresult inloweruseoftheED,asthecurrent findingsshow.Onthe
Table3. Logisticregressionforbinaryemergencydepartmentvisits.
UnadjustedDomainadjustedFullyadjusted
Lack ofcommunity
Age
50–64
*P =< 0.05, **P =< 0.01,***P =< 0.001. COPD,chronicobstructivepulmonarydisease; ED,emergencydepartment.
contrary,someevidenceshowsthatanincreaseinaccessto outpatientcareisassociatedwithadecreaseinEDuse.29 Giventhemixed findings,thereremainsanurgentneedfor furtherevidenceonhowthepresenceorlackofaccessimpacts EDutilizationacrosspopulations.
Overall,thisstudyprovidesnewevidencefor understandingtherelationshipbetweensocialriskfactors andEDuseforadultsatthenationallevelwithimplications acrossresearch,practice,andpolicy.Specifically,available evidenceshowsEDvisitratesarehigherforpatientsinlower-
incomeandsociallyvulnerablecommunities,highlighting theneedforspecificinitiativesaimedatunderstandingthe driversoftheirincreasedEDuse,andtheneedtopayclose attentiontosocialrisksandeffectivewaystoaddressthem.10 FederaleffortstoreduceEDoverusecurrentlyfocuson improvingprimarycare;10 however,initiativesthathave lookedtoincreasetheavailabilityoflow-costoptionsforthe patientsseekingtheseservices,typicallyoflowacuity,have yieldedlittleintermsofreducingcosts.31,32 Whileourstudy underscoresthelinkageofindividualsocialriskswithED utilization,italsohighlightsagreateropportunitytoreduce costsbyaddressingsocialrisks.Furtherresearchcan elucidatewhetheraddressingeachofthesesocialriskswill translateintodecreasedEDuseandcost.
Althoughvariousprofessionalorganizationsrecommend thathealthsystemsandcliniciansincorporatesocial determinantsofhealthandsocialriskscreeningintocare models,10,11 avastmajorityofhealthcaresystemsand hospitals(ie,70%)donothavededicatedfundstoaddress socialneeds,withmanyhealthsystemslackingcommunitylevelsocialneedsdatatoinforminvestment.33,34 Evenwhen asocialriskisidentified,emergencycliniciansmaynotbe awareoflocalresourcesor findithardtobestaddressit.25 DoranandcolleaguesdevelopedascreeningtoolforED patientstoidentifytheriskofbecominghomelesstoreferfor servicesandsupportforhomelessnessprevention9;toolssuch asthese,usingmodelsforreferralservices,35 aregreatly neededtoassessacrossthespectrumofsocialriskfactors knowntoimpacthealthandleadtoadditionalED utilization.9 Whileourstudyaddstotheevidenceontherole ofsocialrisksonEDutilization,thereisneedforresearch investigatinghoweachriskisdrivingEDuse,whatinitiatives canbetakenbycommunitiesandpolicymakerstoreduce suchrisks,andhowEDscanbetteraccommodatethe patientswhoareexperiencingtheserisks,bothtoreduce costsandEDburden,andalsotoimprovetheir healthoutcomes.
Physicianscanlooktosocialemergencymedicine(EM), anemerging fieldwithinEM,asapathforwardtoaccount fortheintersectionbetweenemergencycareandsocial determinantsofhealth.36 SocialEMemphasizesamore holisticcaremodelintheEDtobetterservethepopulations whofrequentlyvisittheEDandreceivecarewithout adequateunderstandingbycliniciansofthesocialforcesat play.Our findingssupporttheimportanceofthisevolving fieldasapromisingplatforminmitigatingthesocialrisk burdenonabroaderscaleandreducingEDutilization, especiallyamongsociallyvulnerablepopulations.37
Therearesomelimitationsthatmustbeconsideredwhile interpretatingourstudy findings.Althoughourstudyis basedonanationallyrepresentativesample,itexcluded institutionalizedindividuals;therefore,the findingmaynot
generalizetothatsegmentoftheUSpopulation.Secondly,to maintainarobustsetofsocialriskfactors,thedataset includedNHISdatapriortothe2019revision.Forthis reason,thisstudydoesnotcaptureadditionalsocialrisk factorsthatmayhavedevelopedasaresultoftheCOVID-19 pandemic.Inaddition,whileourmodelscontrolledfor relevantconfoundingvariables,wedidnothavedataonall possibleconfounders,whichmayhavebiasedourestimates. Also,sincetheresponsestoallsurveyquestionsarebasedon self-report,theyaresubjecttorecallbias.Finally,giventhat thestudyiscross-sectional,wecannotspeaktocausality.
Thisstudyofanationallyrepresentativesampleofadults indicatesthatsocialriskfactorsaresignificantlyassociated withEDutilization.Specifically,economicinstability,lack ofcommunity,educationaldeficit,foodinsecurity,andsocial isolationareassociatedwithhigheroddsofEDuse,whereas inadequateaccesstocareisassociatedwithlowerEDusein fullyadjustedmodels.Furtherresearchisneededtobetter understandpotentialpathwaysandmechanismsthat underlietheseassociations.Interventionsthatcaneffectively addresssocialriskshaveapotentialtoreduceunnecessary EDutilizationandreducehealthcarecosts.Emphasisshould beplacedonbuildinginfrastructureforscreeningand preventionprogramsforhandoffsandreferrals.
AddressforCorrespondence:LeonardE.Egede,MD,MS,UBMD InternalMedicineUniversityatBuffalo,JacobsSchoolofMedicine andBiomedicalSciencesBuffaloGeneralMedicalCenter, DepartmentofMedicine,100HighSt.,D2-76,Buffalo,NY14203. Email: legede@buffalo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Guleriaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CentersforDiseaseControlandPrevention.Emergencydepartment visits.2024.Availableat: https://www.cdc.gov/nchs/fastats/emergencydepartment.htm.AccessedSeptember12,2024.
2.CairnsCandKangK.NationalHospitalAmbulatoryMedicalCare Survey:2020emergencydepartmentsummarytables.Availableat: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2020-nhamcs-edweb-tables-508.pdf.AccessedApril1,2023.
3.NationalCenterforHealthStatistics.Emergencydepartmentvisitsinthe UnitedStates,2016–2021.Availableat: https://www.cdc.gov/nchs/ dhcs/ed-visits/index.htm. AccessedMay24,2023.
4.MooreBJandLiangL.StatisticalBrief#268:Costsofemergency departmentvisitsintheUnitedStates,2017.2020.Availableat: www. hcup-us.ahrq.gov/reports/statbriefs/sb268-ED-Costs-2017.pdf AccessedApril1,2023.
5.OfficeoftheAssistantSecretaryforPlanningandEvaluation,U.S. DepartmentofHealthandHumanServices.Trendsintheutilizationof emergencydepartmentservices,2009–2018.2021.Availableat: https://aspe.hhs.gov/pdf-report/utilization-emergency-departmentservices.AccessedApril1,2023.
6.LooS,AndersonE,LinJG,etal.Evaluatingasocialriskscreeningand referralprograminanurbansafety-nethospitalemergencydepartment. JAmCollEmergPhysiciansOpen. 2023;4(1):e12883.
7.MayhewM,DentonA,KenneyA,etal.Socialdeprivation, theareadeprivationindex,andemergencydepartmentutilization withinacommunity-basedprimaryandpreventivecareprogram ataFloridamedicalschool. JournalofPublicHealth. 2024;32(5):827–35.
8.DoranKM,KunzlerNM,MijanovichT,etal.Homelessnessandother socialdeterminantsofhealthamongemergencydepartmentpatients. JSocDistressHomeless. 2016;25(2):71–7.
9.DoranKM,JohnsE,ZuiderveenS,etal.Developmentofa homelessnessriskscreeningtoolforemergencydepartmentpatients. HealthServRes. 2022;57(2):285–93.
10.U.S.DepartmentofHealthandHumanServices,OfficeofDisease PreventionandHealthPromotion.Healthypeople2023.Availableat: https://health.gov/healthypeople/objectives-and-data/socialdeterminants-health. AccessedApril1,2023.
11.NationalAcademiesofSciences,Engineering,andMedicine. AFrameworkforEducatingHealthProfessionalstoAddresstheSocial DeterminantsofHealth.Washington,DC:TheNationalAcademies Press;2016.
12.RouthierG,MijanovichT,SchretzmanM,etal.Associationsbetween differenttypesofhousinginsecurityandfutureemergencydepartment useamongacohortofemergencydepartmentpatients. JHealthCare PoorUnderserved. 2023;34(3):910–30.
13.WangR,LukoseK,EnszOS,etal.Emergencydepartmentvisit frequencyandhealthcarecostsfollowingimplementationofan integratedpracticeunitforfrequentutilizers. AcadEmergMed. 2024;31(11):1112–20.
14.BerkowitzSA,SeligmanHK,MeigsJB,etal.Foodinsecurity,healthcare utilization,andhighcost:alongitudinalcohortstudy. AmJManagCare. 2018;24(9):399–404.
15.Clemenzi-AllenA,NeuhausJ,GengE,etal.Housinginstabilityresults inincreasedacutecareutilizationinanurbanHIVcliniccohort. Open ForumInfectDis. 2019;6(5):ofz148.
16.SeimJ,EnglishJ,SporerK.Neighborhoodpovertyand9-1-1 ambulancecontacts. PrehospEmergCare. 2017;21(6):722–8.
17.KangoviS,BargFK,CarterT,etal.Understandingwhypatientsoflow socioeconomicstatuspreferhospitalsoverambulatorycare. HealthAff. 2013;32(7):1196–203.
18.KeetCA,MatsuiEC,McCormackMC,etal.Urbanresidence, neighborhoodpoverty,race/ethnicity,andasthmamorbidityamong childrenonMedicaid. JAllergyClinImmunol. 2017;140(3):822–7.
19.KriegC,HudonC,ChouinardMC,etal.Individualpredictorsoffrequent emergencydepartmentuse:ascopingreview. BMCHealthServRes. 2016;16(1):594.
20.NationalCenterforHealthStatistics.Estimatesofemergency departmentvisitsintheUnitedStates,2016–2022.Availableat: https://www.cdc.gov/nchs/dhcs/ed-visits/index.htm Accessed:September17,2024.
21.DoranKM,JohnsE,SchretzmanM,etal.Homelessshelterentryinthe yearafteranemergencydepartmentvisit:resultsfromalinkeddata analysis. AnnEmergMed. 2020;76(4):462–7.
22.WolfeMK,McDonaldNC,HolmesGM.Transportationbarrierstohealth careintheUnitedStates: findingsfromtheNationalHealthInterview Survey,1997–2017. AmJPublicHealth. 2020;110(6):815–22.
23.NationalCenterforHealthStatistics.AbouttheNationalHealth InterviewSurvey.2022.Availableat: https://www.cdc.gov/nchs/nhis/ about_nhis.htm.AccessedApril1,2023.
24.WrayCM,TangJ,L´opezL,etal.Associationofsocialdeterminantsof healthandtheircumulativeimpactonhospitalizationamonganational sampleofcommunity-dwellingUSadults. JGenInternMed. 2022;37(8):1935–42.
25.EstrellaA,ScheidellJ,KhanM,etal.Cross-sectionalanalysisoffood insecurityandfrequentemergencydepartmentuse. WestJEmergMed. 2021;22(4):911–8.
26.DeanEB,FrenchMT,MortensenK.Foodinsecurity,healthcare utilization,andhealthcareexpenditures. HealthServRes. 2020;55Suppl2(Suppl2):883–93.
27.KuBS,FieldsJM,SantanaA,etal.Theurbanhomeless:super-usersof theemergencydepartment. PopulHealthManag. 2014;17(6):366–71.
28.MosenDM,BanegasMP,Tucker-SeeleyRD,etal.Socialisolation associatedwithfuturehealthcareutilization. PopulHealthManag. 2021;24(3):333–7.
29.SommersBD,BlendonRJ,OravEJ,etal.Changesinutilization andhealthamonglow-incomeadultsafterMedicaidexpansion orexpandedprivateinsurance. JAMAInternMed. 2016;176(10):1501–9.
30.FinkelsteinAN,TaubmanSL,AllenHL,etal.EffectofMedicaid coverageonEDuse furtherevidencefromOregon’sexperiment. NEnglJMed. 2016;375(16):1505–7.
31.MacKinneyT,VisotckyAM,TarimaS,etal.Doesprovidingcarefor uninsuredpatientsdecreaseemergencyroomvisitsand hospitalizations? JPrimCareCommunityHealth. 2013;4(2):135–42.
32.SmulowitzPB,HonigmanL,LandonBE.Anovelapproachtoidentifying targetsforcostreductionintheemergencydepartment. AnnEmerg Med. 2013;61(3):293–300.
33.GargA,Boynton-JarrettR,DworkinPH.Avoidingtheunintended consequencesofscreeningforsocialdeterminantsofhealth. JAMA. 2016;316(8):813–4.
34.KreuterMW,ThompsonT,McQueenA,etal.Addressingsocialneedsin healthcaresettings:evidence,challenges,andopportunitiesforpublic health. AnnuRevPublicHealth. 2021;42:329–44.
35.MakarounLK,HalaszynskiJJ,RosenT,etal.LeveragingVAgeriatric emergencydepartmentaccreditationtoimproveelderabusedetection
inolderveteransusingastandardizedtool. AcadEmergMed. 2023;30(4):428–36.
36.ShahR,DellaPortaA,LeungS,etal.Ascopingreviewofcurrentsocial emergencymedicineresearch. WestJEmergMed. 2021;22(6):1360–8.
37.KraynovL,QuarlesA,KerriganA,etal.Proceedingsfromthe2021 SAEMConsensusConference:researchprioritiesforinterventionsto addresssocialrisksandneedsidentifiedinemergencydepartment patients. WestJEmergMed. 2023;24(2):295–301.
MargaretE.Samuels-Kalow,MD,MPhil,MSHP* RebeccaE.Cash,PhD,MPH,NRP*
KoriS.Zachrison,MD,MSc* AurioleCorelRodneyFassinou,BS† NormanHarrisII,BS‡
CarlosA.CamargoJr.,MD,DrPH*
SectionEditor:IoannisKoutroulis,MD,MBA,PhD
*HarvardMedicalSchool,MassachusettsGeneralHospital, DepartmentofEmergencyMedicine,Boston,Massachusetts † CornellUniversity,Ithaca,NewYork ‡ TempleUniversity,LewisKatzSchoolofMedicine, Philadelphia,Pennsylvania
Submissionhistory:SubmittedOctober26,2023;RevisionreceivedNovember5,2024;AcceptedNovember6,2024
ElectronicallypublishedJanuary15,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18526
Introduction: Thedisproportionateimpactofcoronavirus2019(COVID-19)onBlackandHispanic communitieshasbeenwidelyreported.Manystudieshaveusedneighborhoodracial/ethniccomposition tostudysuchdisparities,butlessisknownabouttheinterplaybetweenindividualrace/ethnicityand neighborhoodracialcomposition.Therefore,ourgoalinthisstudywastoassesstherelative contributionsofindividualandneighborhoodrisktodisparitiesinCOVID-19incidenceandoutcomes.
Methods: Weperformedacross-sectionalstudyofpatientswithemergencydepartment(ED)and inpatientvisitstoanacademichealthsystem(12hospitals;February1–July15,2020).Theprimary independentvariablewasrace/ethnicity;covariatesincludedindividualage,sex,comorbidity,insurance andneighborhooddensity,poverty,racial/ethniccomposition,educationandoccupation.Theprimary outcomewassevereacuterespiratorysyndromecoronavirus2(SARS-CoV-2)positivity;secondary outcomesincludedadmissionanddeathafterCOVID-19.Weusedgeneralizedestimatingequationsto assesswhetherrace/ethnicityremainedsignificantlyassociatedwithCOVID-19afteradjustmentfor individualandneighborhoodfactors.
Results: Therewere144,982patients;5,633(4%)wereSARS-CoV-2positive.Ofthose,2,961(53%) wereadmittedand601(11%)died.DiagnosisofCOVID-19,admission,anddeathweremorecommon amongnon-HispanicBlack,Hispanic,Spanish-speakingpatients,andthosewithpublicinsurance.Inthe basemodel(adjustingforrace/ethnicity,age,sex,andcomorbidities),race/ethnicitywasstrongly associatedwithCOVID-19(non-HispanicBlackoddsratio[OR]4.64[95%confidenceinterval(CI) 4.18–5.14],andHispanicOR6.99[CI6.21–7.86]),whichwasslightlyattenuatedbutremainedsignificant afteradjustmentforneighborhoodfactors.AmongpatientswithCOVID-19,therewasnosignificant associationbetweenrace/ethnicityandhospitaladmission,otherthanforpatientswithunknownrace.
Conclusion: Thisdatademonstratesapersistentassociationbetweenrace/ethnicityandCOVID-19 incidence,withBlackandHispanicpatientsatsignificantlyhigherrisk,whichwasnotexplainedby measuredindividualorneighborhoodfactors.Thissuggeststhatusingexistingneighborhood factorsinstudiesexamininghealthequitymaybeinsufficient,andmoreworkisneededtoquantifyand addressstructuralfactorsandsocialdeterminantsofhealthtoimproveequity.[WestJEmergMed. 2025;26(2)315–325.]
Thedisproportionateimpactofcoronavirus2019 (COVID-19)onBlackandHispaniccommunitieshasbeen extensive.1–9 Alongwiththeassociationwithindividualrace andethnicity,multiplestudieshaveshownassociations betweenneighborhooddemographicsandCOVID-19 incidenceandoutcomes.Areaswithhigherproportionsof BlackandHispanicresidentshavehigherCOVID-19 incidenceandfatalityrates.10–13 Althoughanumberofother neighborhoodvariableshavebeenassociatedwithincreased ratesofCOVID-19,includingpoverty,insurancecoverage,13 unemployment,essentialserviceemployment,14 and neighborhoodeducationlevels,11 theassociationwith neighborhooddemographiccompositionmaybestronger thanthatwithneighborhoodsocioeconomicstatus(SES).15 Importantly,theassociationbetweencommunity-levelsocial determinantsofhealth,suchasneighborhoodpovertyand COVID-19rates,doesnotseemtobeexplainedby differentialtestingrates.14
Theconnectionbetweensocialdeterminantsofhealth, unequalexposuretosevereacuterespiratorysyndrome coronavirus2(SARS-CoV-2),andrace/ethnicityisa reflectionofstructuralracism16 the “discriminatory policies,practices,andsystemsthatreinforceanunequal distributionofpowerandresourcesinsocialinstitutions.”17 Non-Whitepatientshaveincreasedrepresentationinserviceindustryorlow-incomejobs,increased financialinsecurity, morefrequentresidenceinsharedorcongregatehousing,18 andaresultingincreasedriskofexposuretoCOVID-19.In addition,structuralracismalsoaffectspatients’ lived experienceinthecommunityandhealthcaresettings,and specificallytheirabilitytoaccesscare.19 Ourpreviouswork usingdatafromalargeacademichealthsystemhas demonstratedco-location(overlap)ofneighborhoodfactors, suchaspercentageofthepopulationthatwasHispanic,nonHispanicBlack,withouthealthinsuranceorlivingin poverty,andCOVID-19cases.13 However,recentresearch hasdemonstratedthatrelyingonneighborhood-levelsocial riskfactorsalonemayover-attribute findingstothe neighborhood-levelfactor.20 Therefore,ourgoalinthisstudy wastoassesstherelativecontributionsofindividualand neighborhoodrisktothosedisparitiesinadatasetwherewe couldassessindividualdemographics,insurancestatus(asa proxyforindividualSES),andcomorbidities.
Weperformedacross-sectionalstudyofallemergency department(ED)andinpatientvisitsfromFebruary1–July 15,2020withinalargeacademichealthsystemof12hospitals, includingtwoacademicmedicalcenters,inNewEngland. Datawereabstractedfromtheelectronichealthrecord (EHR).Visitswereeligibleforinclusioniftheywereeither(1) the firstencounter(EDvisitoradmission)toanyhealthsystem
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
ThedisproportionateimpactofCOVID-19on BlackandHispaniccommunitieshasbeen widelyreported.
Whatwastheresearchquestion?
Wesoughttoassesstherelativecontributions ofindividualandneighborhoodriskto disparitiesinCOVID-19incidence andoutcomes.
Whatwasthemajor findingofthestudy?
Race/ethnicitywasassociatedwithCOVID19andremainedsigni fi cantafteradjustment forneighborhoodfactors.
Howdoesthisimprovepopulationhealth?
Thisdatasuggeststhatusingexisting neighborhoodfactorsinstudiesexamining healthequitymaybeinsuf fi cient.
facilityduringthestudyperiodwherethepatientwasSARSCoV-2positiveor(2)the firstvisitifthepatientwasnever SARS-CoV-2positive.Patientswereeligibleiftheywerea Massachusettsstateresidentbasedonrecordedaddress.We excludedpatientsiftheiraddresswasaPOboxoriftheywere undomiciledornotabletobegeocodedviaEpicorArcGIS (EnvironmentalSystemsResearchInstitute,Inc,Redlands, CA)(foratotalof2,233or2%ofparticipants;seeeFigure1). Eachpatientwasincludedonlyonce.
Allmethodswerecarriedoutinaccordancewith institutionalguidelines;inparticular,thestudywasdeemed exemptfrominformedconsentrequirementsbytheMass GeneralBrighamInstitutionalReviewBoard.Becauseof this,thedatasetsgeneratedandanalyzedduringthecurrent studyarenotpubliclyavailableduetopatientprivacy concernsanddataconfidentialityrules.
Theprimarypredictorvariablewasrace/ethnicity.Fora subsetof2,494patientsinthehealthsystem,Hispanic/Latino wasincludedasarace.Patientswereconsideredtobe HispaniciftheirracewasHispanic/Latino,iftheirethnicity wasHispanic/Latinoregardlessofrace,oriftheirethnicity was “Brazilian,”“Dominican,”“Honduran,”“Puerto Rican,”“Salvadoran,”“Guatemalan,”“Columbian,” or “Mexican,MexicanAmerican,Chicano,” regardlessofrace.
Patientswereotherwisecategorizedbasedonreportedrace andcategorizedasnon-HispanicWhite,non-Hispanic Black,Asian,other,missing,orunknown.
Sexwasdefinedasmaleorfemale;dataoneightpatients whosesexassignmentatbirthwasnotknownwascodedas “missing.” Similarly,dataon22patientswhosereportedage was >107yearswasalsorecordedas “missing” asitwas presumedtorepresentanerrorintheEHR.Giventhelimited dataonindividualsocialdeterminantsofhealthintheEHR, wechosetouseinsurancestatusandlanguageasfactorsthat areassociatedwithaccessandutilizationofcare generally21,22 and,specifically,forCOVID-19.13,23 Insurance statuswasdefinedaspublic,privateorother(seeAppendix), andpreferredlanguageabstractedfromtheEHRwas English,Spanish,Portuguese,Creole-Haitian,Arabic,other, ormissing/unknown(null,declined,unavailable).
WeascertainedcomorbiditiesbycalculationoftheCharlson ComorbidityIndex(CCI)calculatedfromInternational ClassificationofDiseases,10th Rev,ClinicalModification codesintheproblemlist,24,25 andbydirectidentificationof obesity,pulmonarydisease,chronickidneydisease,diabetes mellitus,andhypertensionintheproblemlist(seeAppendix). Comorbiditieswerechosenbasedonpreviouslypublished associations2,26,27 andinstitutionalguidanceregardingrisk factorsforpooroutcomesfromCOVID-19.
Neighborhoodfactorstoassesssocialdeterminantsof healthweredrawnfromthe2015–2019American CommunitySurvey five-yearestimates28 andincluded neighborhoodpoverty,13 educationalattainment,service occupation,29 andpopulationdensity30 aswellasproportion Hispanic/Latino,non-HispanicBlack,non-HispanicAsian, bachelor’sdegreeorhigher,andworkinginservice occupationanalyzedatthecensustractlevel.Wederived quintilesforneighborhoodfactorsforanalysisusingall censustractsinthestateofMassachusettsratherthanthose includedinthesample.
TheprimaryoutcomewasSARS-CoV-2positivity (COVID-19positivity),definedaspolymerasechainreaction testresultofpositiveoradmission/dischargestatus documentedas “COVID-19Positive” or “PatientExpired (COVID-19).” Secondaryoutcomeswerehospitaladmission afterSARS-CoV-2positivity(admissionafterCOVID-19), definedasadmissionduring firstencounterwhereSARSCoV-2positiveorwithin14daysofthe firstencounter;or deathafterSARS-CoV-2positivity(deathafterCOVID-19), definedasdeathatanytimeduringthestudyperiodafterthe firstencounterwheretheSARS-CoV-2testresultwas positive.OutcomeswereascertainedfromtheEHR.
WeperformedallstatisticalanalyseswithStataSE15.1 (StataCorp,CollegeStation,TX),with P < 0.05considered
statisticallysignificant.Continuousvariablesaredisplayed asmean(SD).Categoricalvariablesaredisplayedas numbers(percentage)ofparticipantswithineachgroup. Participantswithmissingdatawereexcludedfrommodels. Wecalculateddescriptivestatisticsforpatientsand neighborhoodcharacteristicsinthesampleoverallandby COVID-19outcomes.
Associationbetweenrace/ethnicityandindividual-level riskfactors
Weusedmultivariablelogisticregressionmodelstoassess theassociationbetweencomorbiditiesandindividualrisk factorsandrace/ethnicity.Giventhatwehypothesizedthat comorbiditieswerelikelyonthecausalpathwaybetween race/ethnicityandincreasedCOVID-19burdenofdisease, wealsoassessedtheindividualcomorbiditiesasmediatorsof theassociationbetweenrace/ethnicityandCOVID-19 incidenceandoutcomes.WeusedtheBaronandKenny methodologytoassessformediation.31 First,weconfirmeda significantassociationbetweenrace/ethnicityandeach outcome(COVID-19positivity,admission,anddeath)and betweenrace/ethnicityandeachmediator.Next,weincluded eachmediatorinamodelwithrace/ethnicityandthe outcome.Weassessedforanymajorchangeinestimates,in particularachangeinmagnitude,direction,orstatistical significance.Completemediationwouldbeindicatedbythe associationbetweenrace/ethnicityandtheoutcome becomingnon-significantoncethemediatorwasincluded.
Oncewehaddeterminedthattherewerenosignificant mediationeffects,weassessedneighborhoodfactorsfor multicollinearityusingvarianceinflationfactors(VIF)ina linearregressionmodel.AVIFgreaterthan10was consideredindicationofpotentialmulticollinearity.Weused generalizedestimatingequationstoassesswhetherrace/ ethnicityremainedsignificantlyassociatedwithCOVID-19 positivityafteradjustmentforneighborhoodfactorsand insurancestatus.Weusedalogitlink,binomialdistribution, andworkingindependencecorrelationstructuretoestimate oddsratiosseparatelyforeachoutcome(COVID-19 positivity,admission,anddeath)withrobuststandarderrors andclusteringattheneighborhoodlevel.Foreachoutcome, abasemodelwascreatedthatincludedage,sex,andCCI.We chosetousetheCCIasasummarymeasureofoverall comorbiditystatus.Wethengeneratedmodelsincluding eachneighborhoodfactorindividuallyandafully adjustedmodel.
Weconductedsensitivityanalysesstratifiedby comorbidityandincludinginsurancestatusinthebase model.Theanalysisstratifiedbycomorbiditieswasdesigned toaddresstheconcernthatthedistributionofcomorbidities
inourpopulationwouldbeunequalbyrace32,33 and, therefore,adjustingforcomorbiditiesmightdiminishthe overallimpactofstructuralracismanddisadvantage.The inclusionofinsurancewasdesignedtoassesstheimpactof includingaproxymeasureofindividualSESinthemodel.
Therewere144,982patientswithEDvisitsorhospital admissionsduringthestudyperiodofwhom5,633(4%)were COVID-19positive(Table1).Ofthose,2,961(53%)were admittedand601(11%)died.Althoughnon-HispanicBlack
Table1. PatientcharacteristicsoverallandbyCOVID-19outcomes. AmongCOVID-19positive PatientcharacteristicOverallCOVID-19positiveAdmittedDied
Race/ethnicity, n(%)
Comorbidities,n(%)
, coronavirus2019.
patientswere9%oftheoverallcohort,theyrepresented16% oftheCOVID-19positivepatients,17%oftheadmitted patients,and15%ofthepatientswhodiedaftertesting positiveforCOVID-19.
Similarly,Hispanicpatientswere13%oftheoverall cohort,30%oftheCOVID-19positivepatients,23%ofthe admittedpatientsand10%ofthepatientswhodiedwith COVID-19.Patientswhowerelistedashavingalanguage preferenceofSpanishwere9%oftheoverallcohortbut30% oftheCOVID-19positivepatients,25%oftheadmitted patients,and12%ofthosewhodiedwithCOVID-19. Although36,384patients(25%)intheoverallpopulationhad onlypublicinsurance,39%oftheCOVID-19positive,40% ofthepatientsadmittedafterCOVID-19,and37%ofthe patientswhodiedafterCOVID-19hadonlypublic insurance.Wheninsurancewasexaminedasthosewhohad anypublicinsurance(60,515,42%),therewerehigher percentagesofpatientswithpublicinsurancewhowere COVID-19positive(55%),admittedafterCOVID-19(61%), ordiedafterCOVID-19(70%)thanintheoverallcohort.
Regardingneighborhoodcharacteristics(Table2),there wasagreaterrepresentationofpatientsfromneighborhoods inthehighestquintileofpoverty,percentageHispanic population,percentagenon-HispanicBlackpopulationand percentageserviceoccupation,andlowestquintileofnonHispanicWhitepopulationandeducationalattainment withintheCOVID-19outcomegroups(testedpositive, admitted,died).
FortheoutcomeofCOVID-19positivity,wedetected multicollinearitywhenincludingpatientrace/ethnicityand allneighborhoodrace/ethnicityvariables;excludingvariable forquintilesofnon-HispanicWhitepopulationresolvedthe collinearityissues.Fortheoutcomesofadmissionwithin14 daysof firstCOVID-19positivepresentationanddeathany timeafter firstCOVID-19positivepresentation(among COVID-19positivepatients),multicollinearitywasdetected betweenrace/ethnicityvariablesandserviceoccupation. Removingthevariablesforquintilesofnon-HispanicWhite populationandserviceoccupationresolvedthecollinearity.
IndividualComorbidityandRiskFactors:Association andMediation
Thereweresignificantassociationsbetweenrace/ethnicity andeachcomorbidity,withtheexceptionofnon-Hispanic Blackandhypertension(HTN)(eTable1).Intheunadjusted modelforCOVID-19positivity(Table3),race/ethnicitywas asignificantpredictorofCOVID-19positivity(nonHispanicBlackoddsratio[OR]3.36[3.09–3.64]and HispanicOR4.28[4.00–4.58]).Theassociationwithrace/ ethnicityremainedsignificantevenafteradjustmentforeach individualcomorbidityandriskfactor(Table3).Therewas potentialpartialmediationbylanguagepreference(Table3),
astheORwassubstantiallydecreasedbutstillstatistically significantafteradjustmentforlanguagepreference. Intheunadjustedmodelforadmissionamongthepatients withCOVID-19,non-HispanicBlackandHispanicpatients hadloweroddsofbeingadmitted(OR0.62[0.52–0.72]and 0.36[0.32–0.41],respectively),andthedirectionalityand significanceoftheassociationwasnotalteredbyadjustment foranyoftheindividualcomorbiditiesorriskfactors (eTables2and3);asimilarpatternwasseenfordeathsafter COVID-19(eTables4and5).Together,thisdatasuggests thattheindividualcomorbiditiesandsocialriskfactorsare notsignificantmediatorsoftheassociationbetweenrace/ ethnicityandCOVID-19incidenceandoutcomes.
Oncetherewaslessconcernforcomorbiditiesservingasa mediatoroftheassociation,wecreatedabasemodelthat includedage,sex,andtheCCItoexaminehowthe associationsbetweenrace/ethnicityandCOVID-19 outcomes wouldchangewiththeinclusionofneighborhood factors.Inthebasemodel(Table4),race/ethnicitywas stronglyassociatedwithCOVID-19positivity(non-Hispanic Black,OR4.64[4.18–5.14],Hispanic,OR6.99[6.21–7.86], whichwasslightlyattenuatedbutremainedsignificantafter adjustmentforneighborhoodfactors(non-HispanicBlack, OR3.27[2.90–3.69],Hispanic,OR4.10[3.66–4.60]]).Trends forotherracial/ethnicgroupsaredisplayedin Table4 AmongpatientswithCOVID-19,therewasnosignificant associationbetweenrace/ethnicityandhospitaladmission, otherthanthatpatientswithmissingorunknownracewere lesslikelytobeadmitted,andthatassociationremained consistentafteradjustmentforneighborhoodfactors.For theoutcomeofdeathafterCOVID-19,Hispanic(OR0.62 [0.46–0.83])andAsian(0.46[0.25–0.86])patientshadlower oddsofdyingascomparedtonon-HispanicWhitepatientsin thebasemodel,andthatassociationpersistedafter adjustmentforneighborhoodfactors(HispanicOR0.61 [0.44–0.85],AsianOR0.47[0.25–0.91])(Table4).
Wefurtherexaminedtheassociationbetweenrace/ ethnicityandCOVID-19outcomesinmodelsstratifiedby comorbidity(eTables6–10).Forpatientswithandwithout obesity,race/ethnicityremainedsignificantlyassociatedwith COVID-19positivityinboththebaseandfullyadjusted models,althoughtheassociationwassmallerintheobese patientsforthosewhowereBlackorHispanicandlargerfor thosewhowereAsian.Similartrendswereseenfor pulmonarydisease,althoughwithsmallerchanges.For patientswithchronickidneydisease,diabetesandHTN,the associationwithrace/ethnicitywasweakerinpatientswith theconditionthanthosewithout,althoughitremained significantinallmodels.
Asasensitivityanalysis,wemodeledtheassociation betweenrace/ethnicityandCOVID-19includingnotonly
Table2. NeighborhoodcharacteristicsoverallandbyCOVID-19outcomes.
AmongCOVID-19positive NeighborhoodcharacteristicOverallCOVID-19positiveAdmittedDied Density,mean(SD),populationpersquaremile10,032(11984)16,121(13,592)15,062(13529)12,402(11711)
Families livingbelowpoverty,n(%)
Lowestquintile(0–1.5%)
2(1.6–3.4%)
3(3.5–6.3%)
4(6.4–13.5%)
28,375(20) 634(11) 382(13) 83(14)
29,941(21) 655(12) 391(13) 95(16)
26,173(18) 712(13) 400(14) 80(13)
32,572(22)1,736(31) 902(31)191(32)
Highestquintile(13.6–65.2%) 27,849(19)1,890(34) 882(30)152(25)
Missing 72 6 4 0
Hispanic/Latinopopulation,n(%)
Lowestquintile(0–2.2%) 21,932(15) 363(6) 211(7) 63(10)
2(2.3–4.5%) 27,409(19) 584(10) 379(13) 99(16)
3(4.6–8.3%) 28,998(20) 698(12) 430(15) 82(14)
4(8.4–19.1%) 27,399(19) 962(17) 498(17)110(18)
Highestquintile(19.2–100%) 39,202(27)3,024(54)1,443(49)247(41)
Non-HispanicBlackpopulation,n(%)
Lowestquintile(0–0.6%)
474(8) 292(10) 62(10)
2(0.7–2.0%) 24,281(17) 506(9) 282(10) 73(12)
3(2.1–4.2%)
4(4.3–9.2%) 27,814(19) 970(17) 511(17) 98(16)
Highestquintile(9.3–82.9%)
Non-HispanicAsianpopulation,n(%)
Lowestquintile(0–0.7%) 20,830(14) 556(10) 296(10) 71(12)
2(0.8–2.2%) 22,773(16) 786(14) 422(14)106(18)
3(2.3–4.9%)
4(5.0–10.9%)
Highestquintile(11.0–59.2%)
Non-HispanicWhitepopulation,n(%)
Lowestquintile(0–50.2%)
2(50.3–72.3%)
30,938(21)1,194(21) 602(20)110(18)
37,281(26)1,869(33) 972(33)171(28)
33,118(23)1,226(22) 669(23)143(24)
38,229(26)2,977(53)1,384(47)227(38)
28,958(20)1,098(20) 606(20)129(21)
3(72.4–83.7%) 31,217(22) 742(13) 464(16)105(17)
4(83.8–91.4%)
28,150(19) 574(10) 366(12) 98(16)
Highestquintile(91.5–100%) 18,386(13) 240(4) 141(5) 42(7)
Bachelor’sdegreeorhigherlevelofeducation,n(%)
Lowestquintile(0–22.3%) 24,773(17)1,926(34) 878(30)136(23)
2(22.4–34.4%)
3(34.5–46.5%)
4(46.6–63.9%)
Highestquintile(64.0–95.6%)
Personsinserviceoccupations,n(%)
Lowestquintile(0–10.8%)
21,154(15)1,097(19) 578(20)106(18)
27,471(19) 756(13) 406(14)101(17)
34,611(24) 949(17) 525(18)125(21)
36,930(25) 903(16) 574(19)133(22)
33,289(23) 817(15) 509(17)112(19)
2(10.9–14.8%) 31,728(22) 723(13) 430(15)111(18)
(Continued onnextpage)
Table2. Continued.
AmongCOVID-19positive NeighborhoodcharacteristicOverallCOVID-19positiveAdmittedDied
3(14.9–18.9%)
4(19.0–25.2%)
23,812(16) 565(10) 316(11) 80(13)
23,950(17)1,028(18) 508(17)116(19) Highestquintile(25.3–69.2%)
COVID-19, coronavirus2019.
age,sex,andtheCCI,butalsoinsurancestatusasamarkerof individualSES.Again,raceremainedstronglyassociated withCOVID-19positivity;onlymissingracewasassociated withadmissionforCOVID-19,andHispanicandAsianrace/ ethnicitywereassociatedwithloweroddsofdeathafter COVID-19(Table5).
Inthiscross-sectionalstudyofhealthsystemdatafromthe initialstagesoftheCOVID-19pandemic,non-HispanicBlack,
Hispanic,andAsianrace/ethnicityweresignificantly associatedwithincreasedCOVID-19positivity,andthe associationremainedsignificantafteradjustmentforboth individualriskfactors(age,sex,comorbidity,insurance)and neighborhoodriskfactors(density,poverty,racial/ethnic composition,educationalattainment,occupation).These resultsdemonstrateapersistentassociationwithrace/ethnicity afteradjustmentforpotentialexplanatoryfactors(eg, comorbidities).Importantly,wedidnot findthatcomorbidities orindividualinsurancestatus(asamarkerofSES)were
Table3. Associationofrace/ethnicityandCOVID-19positivitya,unadjustedandadjustedforeachcomorbidityandindividualriskfactor.
Race/ethnicity(primaryexposure),OR(95%CI)b
riskfactor
foreachcomorbidity
aCOVID-19positivitywasde finedasPCRtestresultofpositiveoradmission/dischargestatusdocumentedas “COVID-19Positive” or “PatientExpired(COVID-19).” bPresentedareoddsratios(95%CI)fortheoutcome(COVID-19positivity)foreachrace/ethnicitygroupcomparedtonon-HispanicWhites (referent, firstcolumn),withtheunadjustedvaluesinthe firstrowandafteradjustmentforthevariablesseparatelyinfollowingrows. CCI,CharlsonComorbidityIndex; COVID-19,coronavirus2019.
Table4. Oddsratiosa fortheassociationbetweenrace/ethnicityandCOVID-19outcomes. COVID-19positivity (N = 117,589;clustern = 1,447)
Race/ethnicity
AdmissionafterCOVID-19 (n = 4,895;clustern = 848)
DeathafterCOVID-19 (n = 4,895;clustern = 848) BasemodelFullyadjustedb BasemodelFullyadjustedc BasemodelFullyadjustedc
(referent)
aEstimatedusinggeneralizedestimatingequations(binomialdistribution,logitlink,workingindependencecorrelationstructure)withrobust standarderrorsandclusteringattheneighborhoodlevel.Allmodels(baseandfullyadjusted)includerace/ethnicity,age,sex,andthe CharlsonComorbidityIndex.
bIncludesallneighborhoodfactors(density,poverty,Hispanic/Latino,Non-HispanicBlack,Non-HispanicAsian,Bachelor’sdegreeorhigher levelofeducationandserviceoccupation).Non-HispanicWhitepopulationwithinthecensustract(neighborhoodlevelvariable)was excludedduetomulticollinearity.
cIncludesallneighborhoodfactors(density,poverty,Hispanic/Latino,Non-HispanicBlack,Non-HispanicAsian,Bachelor’sdegreeorhigher educationlevel).Non-HispanicWhitepopulationwithinthecensustract(neighborhoodlevelvariable)andserviceoccupationexcludeddue tomulticollinearity.
COVID-19,coronavirus2019.
meaningfulmediatorsoftheassociationbetweenrace/ethnicity andCOVID-19incidenceoroutcomes,meaningthatwedid notseeevidencethattheywereonthecausalpathwayforthis association.Additionally,theassociationwasnotfully explainedbymeasuredneighborhoodrisk.
Fromtheseresultswedrawtwomajorconclusions. Firstly,recognizingthattheresidualassociationwith measuredrace/ethnicityrepresentsstructuralracismrather thanbiologicalvariationandthatthereisnostandard measurementforstructuralracisminadministrative datasets,thisdataemphasizestheneedforimproved measurementofindividual-levelsocialdeterminantsof healthandtheimpactofstructuralracism.Similartoprior reports,wefoundstrongerassociationsbetweenrace/ ethnicityandCOVID-19positivity,againsuggestingthat higherratesinBlackandHispanicpopulationsaredrivenby exposure, 4 andthatthemortalitytrendsaremorecomplex.6,7 Thisdatabuildsuponpriorreportsthatshowaconsistent impactofraceandethnicitythatappearstobemodifiedor mediatedbysocialdeterminantsofhealth.26,30,34,35 Similarly,arecentstudydemonstratedlimitedabilityof insurancetocorrectlyclassifySES,asdefinedbyeducation andincome.36 Additionalworkisneededtodefineand reliablymeasureindividualsociodemographicfactors
associatedwithdiseasevulnerabilityandusethemtodefine areasforpotentialintervention.
Thesecondmajorconclusionofourstudyurgescaution intheuseofneighborhoodsocioeconomicfactorsaloneto examinedisparities.Neighborhoodfactorsrepresentthe ecologicalexposureandnottheindividualexperience,and thisstudydemonstratesthecomplexinterplaybetween theseindividualandneighborhoodfactors.Forexample,a studyexamininghospitalizedpatientswithCOVID-19in Michiganfoundthatthosefromsociallyvulnerable neighborhoodsweremorelikelytopresentwithsevere disease,evenafteradjustmentforage,sex,and comorbidities,butthatneighborhoodvulnerabilitywasnot associatedwithmortality. 37 Overall,thisdataemphasizes theimportanceofmeasuringthefactors(eg,individual housinginsecurity,crowding,andessentialoccupations thatcouldnotbecompletedremotely)thatre fl ectstructural racism,andmayserveaspotentialmediatorsinthe associationbetweenrace/ethnicityandCOVID-19,rather thanrelyingonneighborhood-levelmeasurementsalone. Futuredirectionsforthisresearchcouldincludeusing improvedmeasurementsofindividual-levelsocial determinantsofhealthinfutureinvestigationsinother conditionsandinterventionstoreducethedisproportionate burdenofdisease.
Table5. Oddsratiosa fortheassociationbetweenrace/ethnicityandCOVID-19outcomes,includingadjustmentforinsurancestatus. COVID-19positivity (N = 116,631;clustern = 1,447)
AdmissionafterCOVID-19 (n = 4,895;clustern = 848)
DeathafterCOVID-19 (n = 4,895;clustern = 848) BasemodelFullyadjustedb BasemodelFullyadjustedc BasemodelFullyadjustedc
Race/ethnicity
aEstimatedusinggeneralizedestimatingequations(binomialdistribution,logitlink,workingindependencecorrelationstructure)withrobust standarderrorsandclusteringattheneighborhoodlevel.Allmodels(baseandfullyadjusted)includerace/ethnicity,age,sex,theCharlson ComorbidityIndex,andinsurancestatus.
bIncludesallneighborhoodfactors(density,poverty,Hispanic/Latino,Non-HispanicBlack,Non-HispanicAsian,Bachelor’sdegreeorhigher educationlevelandserviceoccupation).Non-HispanicWhitepopulationwithinthecensustract(neighborhoodlevelvariable)wasexcluded duetomulticollinearity.
cIncludesallneighborhoodfactors(density,poverty,Hispanic/Latino,Non-HispanicBlack,Non-HispanicAsian,Bachelor’sdegreeorhigher educationlevel).Non-HispanicWhitepopulationwithinthecensustract(neighborhoodlevelvariable)andserviceoccupationexcludeddue tomulticollinearity.
COVID-19,coronavirus2019.
Limitationsofthisstudyincludethatthedatawasdrawn fromasinglehealthsystemand,therefore,mayminimize hospital-leveldifferencesanddisparitiesincare38 andmay notfullycapturetheunderlyingpopulation.Thisis particularlyimportantbecausedatafromourcityhasshown differencesintheracial/ethnicmakeupofpatientpopulations byhospital.39,40 However,thehealthsystemincludesthe hospitalthathascaredforthehighestnumberofadmitted COVID-19patientsinthearea,41,42 andourpriorwork showedthatourhealthsystemdataidentifiedsimilarclusters tothestatedatawithinourcatchmentarea.13 Earlyinthe pandemicthereweredisparitiesintestingaccess,43,44 althoughotherstudiesinMassachusettshavefound disparitiesthatwerenotfullyexplainedbytestingaccess differences.14 Additionally,notallcomorbiditiesmay havebeencodedintheproblemlist,particularlyfor patientswhowerenewtoourhealthsystem,potentially limitingourabilitytoascertainthem.Weusedinsurance statusasaproxyforindividualSESbecausewedonothave fulldataonsocialdeterminantsofhealthforallpatients inthecohort.
Itischallengingtodeterminewhetherthemeasured differencesinadmissionanddeathwereduetounmeasured
differencesinillnessseverityorcomorbidities,represented ascertainmentbiasduetouseofEHRdata,orwerea manifestationofimplicitbias.Increasedmortalityhasbeen reportedinHispanicpopulations,8,9 whichwasnot demonstratedinourdata,potentiallyreflectingunmeasured confoundingfromdifferencesintheHispanicpopulationin ourcohort(eg,healthyimmigranteffect).45 Becausewewere interestedinneighborhoodeffects,wewerenotableto includepatientswithoutanaddress,andtheremaybea differentrelationshipbetweensocialriskandCOVID-19 incidenceandoutcomesinanundomiciledpopulationthat wewereunabletoexamine.Finally,withtheabilityof patientstoaccessvaccination,andtheevolutionofnew COVID-19variants,thedisparitiesinCOVID-19continue toevolve.
ThedatashowsapersistentassociationbetweennonHispanicBlack,Hispanic,andAsianrace/ethnicityand higherCOVID-19incidencethatisnotexplainedbyincluded individualorneighborhoodfactors.Theresultsemphasize theimportanceofimprovingthemeasurementofstructural factorsandsocialdeterminantsofhealthandcareful attentiontotheuseofindividual-levelandneighborhood-
levelriskfactorsinstudiestoenableinterventionstoimprove theequityofpandemicresponse.
AddressforCorrespondence:MargaretE.Samuels-Kalow,MD, MPhil,MSHP,HarvardMedicalSchool,MassachusettsGeneral Hospital,DepartmentofEmergencyMedicine,125NashuaSt.,Suite 920,BostonMA,02114.Email: Msamuels-kalow@partners.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisprojectwassupportedbyagrant fromtheMGHExecutiveCommitteeonResearch.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Samuels-Kalowetal.Thisisanopenaccess articledistributedinaccordancewiththetermsoftheCreative CommonsAttribution(CCBY4.0)License.See: http:// creativecommons.org/licenses/by/4.0/
1.BoserupB,McKenneyM,ElkbuliA.Disproportionateimpactof COVID-19pandemiconracialandethnicminorities. AmSurg. 2020;86(12):1615–22.
2.KalyanaramanMarcelloR,DolleJ,GramiS,etal.Characteristicsand outcomesofCOVID-19patientsinNewYorkCity’spublichospital system. PLoSOne. 2020;15(12):e0243027.
3.BassettMT,ChenJT,KriegerN.Variationinracial/ethnicdisparitiesin COVID-19mortalitybyageintheUnitedStates:across-sectionalstudy. PLoSMed. 2020;17(10):e1003402.
4.ZelnerJ,TrangucciR,NaraharisettiR,etal.Racialdisparitiesin coronavirusdisease2019(COVID-19)mortalityaredrivenbyunequal infectionrisks. ClinInfectDis. 2021;72(5):e88–95.
5.GoyalMK,SimpsonJN,BoyleMD,etal.Racialand/orethnicand socioeconomicdisparitiesofSARS-CoV-2infectionamongchildren. Pediatrics. 2020;146(4):e2020009951.
6.RentschCT,Kidwai-KhanF,TateJP,etal.PatternsofCOVID-19 testingandmortalitybyraceandethnicityamongUnitedStates veterans:anationwidecohortstudy. PLoSMed. 2020;17(9):e1003379.
7.WangZ,ZheutlinA,KaoYH,etal.HospitalisedCOVID-19patientsof theMountSinaiHealthSystem:aretrospectiveobservationalstudy usingtheelectronicmedicalrecords. BMJOpen. 2020;10(10):e040441.
8.DaiCL,KornilovSA,RoperRT,etal.Characteristicsandfactors associatedwithCOVID-19infection,hospitalization,andmortality acrossraceandethnicity. ClinInfectDis. 2021;73(12):2193–204.
9.FeldmanJMandBassettMT.VariationinCOVID-19mortalityintheUS byraceandethnicityandeducationalattainment. JAMANetworkOpen. 2021;4(11):e2135967.
10.BaltrusPT,DouglasM,LiC,etal.PercentageofBlackpopulationand primarycareshortageareasassociatedwithhigherCOVID-19caseand deathratesinGeorgiacounties. SouthMedJ. 2021;114(2):57–62.
11.HawkinsRB,CharlesEJ,MehaffeyJH.Socio-economicstatusand COVID-19-relatedcasesandfatalities. PublicHealth. 2020;189:129–34.
12.HansonAE,HainsDS,SchwadererAL,etal.VariationinCOVID-19 diagnosisbyZIPCodeandraceandethnicityinIndiana. FrontPublic Health. 2020;8:593861.
13.Samuels-KalowME,DornerS,CashRE,etal.Neighborhood disadvantagemeasuresandCOVID-19casesinBoston,2020. Public HealthRep. 2021;136(3):368–74.
14.HawkinsD.SocialdeterminantsofCOVID-19inMassachusetts, UnitedStates:anecologicalstudy. JPrevMedPublicHealth. 2020;53(4):220–7.
15.GagliotiAH,LiC,DouglasMD,etal.Population-leveldisparitiesin COVID-19:measuringtheindependentassociationoftheproportionof BlackpopulationonCOVID-19casesanddeathsinUScounties. JPublicHealthManagPract. 2021;27(3):268–77.
16.ClevelandManchandaE,CouillardC,SivashankerK.Inequityincrisis standardsofcare. NEnglJMed. 2020;383(4):e16.
17.FairMAandJohnsonSB.Addressingracialinequitiesinmedicine. Science. 2021;372(6540):348–9.
18.EssienURandVenkataramaniA.Dataandpolicysolutionstoaddress racialandethnicdisparitiesintheCOVID-19pandemic.Availableat: https://jamanetwork.com/channels/health-forum/fullarticle/2765498 AccessedMay19,2020.
19.BaileyZD,FeldmanJM,BassettMT.Howstructuralracismworks racistpoliciesasarootcauseofU.S.racialhealthinequities. NEngJ Med. 2020;384(8):768–73.
20.BeckettMK,MartinoSC,AgnielD,etal.Distinguishingneighborhood andindividualsocialriskfactorsinhealthcare. Health ServRes. 2022;57(3):457–71.
21.JohnsonWGandRimszaME.Theeffectsofaccesstopediatriccare andinsurancecoverageonemergencydepartmentutilization. Pediatrics. 2004;113(3Pt1):483–7.
22.LoweJT,MonteiroKA,ZonfrilloMR.Disparitiesinpediatricemergency departmentlengthofstayandutilizationassociatedwithprimary language. PediatrEmergCare. 2022;38(4):e1192–7.
23.KimHN,LanKF,NkyekyerE,etal.AssessmentofdisparitiesinCOVID19testingandinfectionacrosslanguagegroupsinSeattle,Washington. JAMANetwOpen. 2020;3(9):e2021213.
24.CharlsonME,PompeiP,AlesKL,etal.Anewmethodofclassifying prognosticcomorbidityinlongitudinalstudies:developmentand validation. JChronicDis. 1987;40(5):373–83.
25.QuanH,SundararajanV,HalfonP,etal.Codingalgorithmsfordefining comorbiditiesinICD-9-CMandICD-10administrativedata. MedCare. 2005;43(11):1130–9.
26.Munoz-PriceLS,NattingerAB,RiveraF,etal.Racialdisparitiesin incidenceandoutcomesamongpatientswithCOVID-19. JAMANetw Open. 2020;3(9):e2021892.
27.ExpertonB,TettehHA,LurieN,etal.Apredictivemodelforsevere COVID-19intheMedicarepopulation:atoolforprioritizing primaryandboosterCOVID-19vaccination. Biology(Basel). 2021;10(11):1185.
28.UnitedStatesCensusBureau.Americancommunitysurvey(ACS). Availableat: https://www.census.gov/programs-surveys/acs AccessedMay21,2020.
29.WasfyJH,HidrueMK,RockettH,etal.Socioeconomicand demographiccharacteristicsofbothinpatientsandoutpatientswith positivetestingforSARS-CoV-2. JGenInternMed. 2021;36(8):2522–4.
30.VahidyFS,NicolasJC,MeeksJR,etal.Racialandethnicdisparitiesin SARS-CoV-2pandemic:analysisofaCOVID-19observationalregistry foradiverseUSmetropolitanpopulation. BMJOpen. 2020;10(8):e039849.
31.BaronRMandKennyDA.Themoderator-mediatorvariabledistinction insocialpsychologicalresearch:conceptual,strategic,andstatistical considerations. JPersSocPsychol. 1986;51(6):1173–82.
32.ThorntonPL,KumanyikaSK,GreggEW,etal.Newresearchdirections ondisparitiesinobesityandtype2diabetes. AnnNYAcadSci. 2020;1461(1):5–24.
33.NicholasSB,Kalantar-ZadehK,NorrisKC.Socioeconomicdisparitiesin chronickidneydisease. AdvChronicKidneyDis.2015;22(1):6–15.
34.RozenfeldY,BeamJ,MaierH,etal.Amodelofdisparities:riskfactors associatedwithCOVID-19infection. IntJEquityHealth. 2020;19(1):126.
35.TungEL,PeekME,RivasMA,etal.Associationofneighborhood disadvantagewithracialdisparitiesinCOVID-19positivityinChicago. HealthAff(Millwood). 2021;40(11):1784–91.
36.MonuteauxMC,DuM,NeumanMI.Evaluationofinsurancetypeasa proxyforsocioeconomicstatusinthepediatricemergencydepartment: apilotstudy. AnnEmergMed. 2024;83(6):562–7.
37.TipirneniR,KarmakarM,O’MalleyM,etal.Contributionofindividualandneighborhood-levelsocial,demographic,andhealthfactorsto
COVID-19hospitalizationoutcomes. AnnInternMed. 2022;175(4):505–12.
38.AschDA,IslamMN,SheilsNE,etal.Patientandhospitalfactors associatedwithdifferencesinmortalityratesamongBlackandWhiteUS MedicarebeneficiarieshospitalizedwithCOVID-19infection. JAMA NetwOpen. 2021;4(6):e2112842.
39.KowalczykL,WallackT,DungcaN,etal.Colorlinepersists,in sicknessandinhealth.Availableat: https://apps.bostonglobe.com/ spotlight/boston-racism-image-reality/series/hospitals/ AccessedMay30,2020.
40.TikkanenRS,WoolhandlerS,HimmelsteinDU,etal.Hospitalpayer andracial/ethnicmixatprivateacademicmedicalcentersinBostonand NewYorkCity. IntJHealthServ. 2017;47(3):460–76.
41.CommonwealthofMassachusetts.COVID-19responsereporting. Availableat: https://www.mass.gov/info-details/covid-19response-reporting#covid-19-weekly-public-health-reportAccessedJune8,2020.
42.WenP.Here’salistofcoronaviruscasesinMassachusettsbyhospital. Availableat: https://www.bostonglobe.com/2020/04/13/nation/ coronavirus-cases-by-hospital/.AccessedJuly27,2020.
43.DoddsCandFakoyaI.Covid-19:Ensuringequalityofaccesstotesting forethnicminorities. BMJ. 2020;369:m2122.
44.RaderB,AstleyCM,SyKTL,etal.GeographicaccesstoUnitedStates SARS-CoV-2testingsiteshighlightshealthcaredisparitiesandmaybias transmissionestimates. JTravelMed. 2020;27(7):taaa076.
45.NgE,QuinlanJ,GiovinazzoG,etal.All-causeacutecarehospitalization ratesofimmigrantsandtheCanadian-bornpopulation:alinkagestudy. HealthRep. 2021;32(9):3–13.
RaymenR.Assaf,MD,MPH,MA*†
ChloeKnudsen-Robbins,MD‡ TheodoreHeyming,MD*§ KellieBacon,MPH*
ShelbyK.Shelton,MPH* BharathChakravarthy,MD,MPH§ SoheilSaadat,MD,MPH,PhD§ JasonA.Douglas,PhD∥ VictorCisneros,MD,MPH,CPH,FAAEM§¶
*Children’sHospitalofOrangeCounty,Orange,California
† UniversityofCaliforniaIrvine,SchoolofMedicine,Departmentof Pediatrics,Irvine,California
‡ UniversityofCincinnatiCollegeofMedicine,Departmentof EmergencyMedicine,Cincinnati,Ohio
§ UniversityofCaliforniaatIrvine,DepartmentofEmergency Medicine,Orange,California
∥ UniversityofCaliforniaIrvine,DepartmentofHealth,Society, &Behavior,Irvine,California
¶ EisenhowerHealth,DepartmentofEmergencyMedicine, RanchoMirage,California
# UniversityofCaliforniaRiverside,SchoolofMedicine,Departmentof EmergencyMedicine,Riverside,California
SectionEditor: RonnieDellWaldrop,MD
Submissionhistory:SubmittedFebruary12,2024;RevisionreceivedNovember5,2024;AcceptedNovember6,2024
ElectronicallypublishedJanuary15,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.19435
Introduction: Foodandhousinginsecurityinchildhoodistroublinglywidespread.Emergency departments(ED)arewellpositionedtoidentifyandsupportfood-andhousing-insecurechildrenand theirfamilies.However,thereisnoconsensusregardingthemostefficientscreeningtoolsormost effectiveinterventionsforEDuse.
Objective: Inthiscross-sectionalstudyweaimedtoinvestigatetheimplementationofafood/housing insecurityscreeningtoolandresourcereferraluptakeinapediatricED.
Methods: Duringthestudyperiod(March1–December9,2021),therewere67,297EDvisitsatthestudy institution,whichisafreestandingchildren’shospital.CaregiversofpatientspresentingtotheEDwere approachedforparticipationinthestudy;1,908familiesparticipated(2.8%ofallEDvisitsduringthe studyperiod)andwerescreenedforfoodandhousinginsecurity.Caregiversurveysincluded demographic,foodandhousinginsecurity,caregiver/patienthealthstatus,andhealthcareutilization questions.Caregiverswhoscreenedpositiveforfoodand/orhousinginsecurityreceivedprinted materialswithfoodand/orhousingresources.Weanalyzeddatausingdescriptivestatistics,one-way analysisofvariance,andthePearsonchi-squaredtest.
Results: Atotalof1,908caregiversweresurveyed:416(21.8%)screenedpositiveforfoodand/or housinginsecurity.Ofthosewhoscreenedpositive,147/416completedfollow-upsurveys.Onfollow-up, 44(30.0%)nolongerscreenedpositiveforfoodand/orhousinginsecurity,while15(10.2%)reported usingatleastoneresourcereferral.Themostfrequentlyreportedreferralutilizationbarrierwaslossor reportednon-receiptofthereferral.
Conclusion: Thisstudydemonstrateshighfood-andhousing-insecurityratesamongfamilies presentingtoapediatricED,emphasizingtheurgencyandnecessityofscreeningandinterveninginthis environment.Thefoodandhousinginsecuritychangebetweenbaselineandfollow-upreportedhereand theoveralllowresourceuptakehighlightschallengeswithED-basedscreeningandinterventionef ficacy. [WestJEmergMed.2025;26(2)326–337.]
OneinsixofallchildrenintheUnitedStates(US)arefood insecure,whileonein18undertheageofsixareunhoused.1 In2017,over1.5millionchildrenenrolledinpublicschools wereunhoused.2,3 Beyondastatisticalrepresentationof societalshortcomingsofmeetingthebasicneedsofchildren, these figuresaredistressingasfoodandhousinginsecurity hasrepeatedlybeenshowntobeassociatedwithadverse mental,physical,anddevelopmentalhealthoutcomes.1,4–12 Foodandhousinginsecuritydisproportionatelyburdens underservedcommunitiesofcolor,particularlythosein whichmorethan20%ofresidentsliveinpoverty,and downstreamhealthdisparitiesarecommon.13
Since2015theAmericanAcademyofPediatricshas advocatedforthescreeningoffoodinsecurityduringwellchildvisits,andthisapproachhasnowexpandedtoavariety ofhealthcaresettings.14 Theemergencydepartment(ED)is particularlywellpositionedtoassessforhealth-relatedsocial needs(HRSN)andtopotentiallyintervene.Over15%ofall USchildrenvisittheEDeachyear,manywithbarriersto routinepreventivecare,andfood/housinginsecurityhasbeen showntobeassociatedwithincreasedEDuse.15–18 Several studieshavedemonstratedthefeasibilityofvariousscreening methodsandresourcereferralforfoodandhousing insecurityintheED.19–25 However,thereisnocurrent consensusregardingthemosteffectivetechniquesfor reliable,widespreadscreeningintheEDor recommendationsforoptimizingcaregiverresource utilization.Inthisstudyweaimedtoinvestigatethe implementationofafoodandhousinginsecurityscreening toolandresourcereferraluptakeinapediatricED.
Thiscross-sectionalstudyincludedpatientspresentingto theEDofafreestandingchildren’shospitalwithaLevelII traumacenterbetweenMarch1–December9,2021.This institution,locatedinasuburbancommunityinthe SouthwesternUS,hasanannualEDcensusof approximately100,000visitsperyear;67,297visitsoccurred duringthestudyperiod.Inthestudycounty,approximately 24%ofhouseholdsreportahouseholdincomeofunder $50,000/year,25%report$50,000–100,000,31%report $100,000–$200,000,and19%reportover$200,000.An estimated11%ofchildrenlivebelowthepovertyline.26 This studywasapprovedbythestudyinstitution’sinstitutional reviewboard(IRB#200326).
Usingaconveniencesampleofadultcaregiversofpatients <18,trainedresearchassistants(RA)approached prospectiveparticipantsduringtriage,describedthestudy, invitedthemtoparticipate,andobtainedverbalconsent fromthosewhoagreed.TheRAsapproachedeligiblepatient caregiversduringthehoursof8 AM – 5 PM Mondaythrough Fridayduringthestudyperiod.TheRAsadministered surveysviaREDCap(ResearchElectronicDataCapture
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Foodandhousinginsecurityinterventionsare increasinginthepediatricemergency department(ED)yetlackastandard approachtooptimizingresourceutilization.
Whatwastheresearchquestion?
Whatarebarrierstouptakeoffoodand housinginsecuritycommunity-resource referralsinapediatricED?
Whatwasthemajor findingofthestudy?
Onfollow-up,only10%ofparticipating familiesreportedusingatleastone resourcereferral.
Howdoesthisimprovepopulationhealth?
Thisstudyidenti fi esmultiplebarriersto communityresourceuseandfollow-upamong familiesparticipatinginapassivereferral approachinapediatricED.
hostedatUCIrvineEmergencyDepartment)onelectronic tablets,inwhichparticipantsdirectlyenteredtheirresponses. SurveyswereavailableinEnglishandSpanish.Thebaseline surveyincludedanexpandeddemographicssectionfollowed by16questionsregardingfoodinsecurity,accesstofood, housinginsecurity,neighborhoodsafety,caregiverselfreportedhealth,caregiver-reportedpatienthealth,and healthcareutilization(SupplementaryMaterialsAppendix A).Wealsogarneredcaregiverself-reportedrace/ethnicityas wellasinsurancestatusfrompatientregistrationdata. SurveysweredevelopedbyRA,VC,andJD,authorswith expertiseinpublichealth.
Weassessedanddefinedfoodinsecuritybasedontwo previouslyvalidatedscreeningquestions: “Withinthepast12 months,IworriedwhethermyfoodwouldrunoutbeforeI gotmoneytobuymore”;and “Withinthepast12months, thefoodIboughtjustdidn’tlastandIdidn’thavemoneyto getmore.”27 Affirmativeresponsestoeitherorboth questionswasconsideredapositivescreen.Weassessed housinginstabilityonanaffirmativeresponseeitherto1) “In thepast12months,haveyouhadtroublepayingyourrent/ mortgage/utilitybills,” or2)aresponseof “Stayatafriend’ s home” or “Idonotliveinstablehousing” tothesurvey question “Inthepast12months,haveyoubeenlivingin stablehousingthatyou ” Thisdefinitionisconsistentwith priorstudies,althoughhistoricallyhousinginstabilityhas beendefinedbyvariouscriteriainfederalbodiesand
scientificliterature,renderingitmoredifficulttoconsistently measurethanfoodinsecurity.4
Allcaregiverswhocompletedthesurveyreceivedcurated printedmaterialswithcurrentlocalfoodand/orhousing resources.TheRAsprovidedtheseresourcesimmediately aftertheparticipantscompletedthesurvey.Direct communicationbetweenresearchpersonnelandcommunity resourcesaboutindividual-levelneed(eg,warmhand-offs) werenotpartofthestudymethods.Thestudyinstitution’ s socialworkteamworkedwithauthorsRAandVCto developdocumentscontaininganextensivelistofvetted localcommunityresources.Additionally,thosewho screenedpositiveforfoodorhousinginsecuritywere contactedbyRAsthreeweeksandsixweeksaftertheindex EDvisittoconductfollow-upsurveys.TheRAsconducted follow-upsurveysviatelephoneandattemptedtocontact familiesuptothreetimes.Follow-upsurveysincluded questionsregardinguseofprovidedresources,barriersto use,andfood/housinginsecurityinthepriorthreeweeks (SupplementaryMaterialsAppendixB).Follow-upstatus (foodinsecure,housinginsecure,orbothfoodandhousing insecure)wasrecordedbasedon finalresponses(ie,atthree weeksifcaregiversdidn’trespondtothesix-weeksurveyor sixweeksiftheyrespondedtobothsurveys).
DatawasscreenedandcleanedpriortoanalysesbyPKP. Descriptivestatisticswereusedtoanalyzedemographic, healthcareutilization,andclinicalcharacteristics.We analyzedpatientageandEDlengthofstay(bothcontinuous variables)usingtheFisher t -testorWelchone-wayanalysis ofvariance.Allothervariables(categorical)wereanalyzed usingthePearsonchi-squaredtestwithMonteCarlo simulationandstandardizedresiduals(z)tointerpret significantassociations.
Atotalof2,144adultcaregiversparticipatedinthesurvey. Initialfood/housinginsecuritystatuswasindeterminatefor 236patientsastheircaregiversdidnotrespondtothefood/ housingquestionsdescribedaboveand,thus,thisgroupwas excludedfromdataanalysis.Oftheremaining1,908 respondents(2.8%oftotalEDvisitsduringthestudyperiod), atotalof416(21.8%)screenedpositiveforfoodand/or housinginsecurity.Additionally,164caregivers(8.6%) screenedpositiveforfoodandhousinginsecurity,95(4.98%) forsolelyfoodinsecurity,and157(8.2%)forsolely housinginsecurity.
Demographics
Themeanageforallpatientswhosecaregivercompleteda surveywas6.68 ± 5.26years.Onaverage,patientswithfood orhousinginsecurity(7.42 ± 5.40years),foodandhousing
insecurity(7.95 ± 5.44years)wereolderthanthosewithout (6.41 ± 5.18years; P < 0.001).Slightlymorethanhalfofall patientsweremale(52.8%);therewasnosignificant differencewithrespecttosexamongpatientswithand withoutfoodand/orhousinginsecurity; P = 0.43.Among thosesurveyed,64.1%wereHispanic,20.4%WhitenonHispanic,7.3%Asian,and2.5%Black.Justover75%of caregiverswhoscreenedpositiveforfoodorhousingsecurity wereHispanic,11.5%wereWhitenon-Hispanic,4.4%were Asian,and2.0%wereBlack.Caregiverswhowerebothfood andhousingsecureweremorelikelytoreportWhitenonHispanicraceandethnicity(z = 2.9, P < 0.001).Overtwothirds,67.5%,ofpatientshadpublichealthinsurance; caregiverswhowerefoodand/orhousinginsecureweremore likelytohavepublichealthinsurancethanprivatehealth insurance(z = 4.22, z = 4.41, P < 0.001).Complete demographicsstratifiedbytotalpopulation,andthose withandwithoutfoodand/orhousinginsecurityareincluded in Table 1
Ofallcaregiverssurveyed,72.9%reportedalwaysfeeling safeintheirneighborhoodand76.2%reportedneverbeing concernedaboutthepatient’ssafetyintheirneighborhood. Caregiversscreeningpositiveforbothfoodandhousing insecuritywerelesslikelytoreportalwaysfeelingsafeintheir neighborhood(z = 4.5)andmorelikelytoreportsometimes beingconcernedaboutthepatient’ssafetyintheir neighborhood(z = 4.5, z = 7.1, P < 0.001).
Only35.3%ofcaregiversratedthepatient’shealthas excellent,whileevenfewer,25.1%,ratedtheirownhealthas excellent.Thosescreeningpositiveforhousingand/orfood insecuritywerelesslikelytoratethepatient’shealthas excellent(z = 3.1, z = 3.2, P < 0.001)aswellastheirown healthasexcellentorverygood(z = 2.8, z = 3.4, P < 0.001).Caregiverswhoscreenedpositiveforboth housingandfoodinsecurityweremorelikelytoreportthat atsometimeaphysiciantoldthemthepatientwasobese (z = 3.22),hadanxiety(z = 3.82),orhademotional challenges(z = 3.80, P < 0.001).
Inourstudy,68.3%ofcaregiversreportedthepatienthad notvisitedtheEDinthepreviousyear,19.6%reporteda singlevisit,and12.1%reportedtwoormorevisitsduringthe sametimeframe.Caregiversscreeningpositiveforbothfood andhousinginsecurityweremorelikelytoreportvisitingthe EDatleastonce(z = 3.0, P < 0.001).
Themajority(65.1%)ofpatientsweretriagedto EmergencySeverityIndex(ESI)level3anddischargedhome fromtheindexEDvisit(80.9%),whilethemeanlengthof stayintheEDwas4.5 ± 3.19hours.Therewasnosignificant
Table1. Initialsurvey:demographicsandclinicalcharacteristicsasstratifiedbyfoodandhousinginsecuritystatus.
Baselinestatus(N = 1,908)
Characteristics
Demographic
$20,000,n(%)
$60,000 – $79,999,n(%)
Missingorprefernottoanswer, n(%)
Respondent’shighesteducationlevel <0.001
Lessthanhighschool,n(%)
HighschooldiplomaorGED,n(%)499(26.3%)71(28.2%)54(32.9%)374(25.1%)
Somecollege,n(%)
Collegedegree,n(%) 542(28.4%)37(14.7%)21(12.8%)484(32.4%)
Missingorprefernottoanswer, n(%)
Numberoftimesmovedduringpast 12months
0,n(%) 1,294(67.8%)141(56%)88(53.6%)1,065(71.4%) 1,n(%) 274(14.4%)55(21.8%)39(23.8%)180(12.1%)
(Continued onnextpage)
Table1. Continued.
Characteristics Totalpopulation (N = 1,908)
Respondent’sperceptionof neighborhoodsafety: “Doyoufeelsafeinyour neighborhood?”
Respondent’sconcernforpatient’s safetyinneighborhood: “Areyou concernedaboutyourchild’ssafety inyourneighborhood?”
Baselinestatus(N = 1,908)
Respondent’sperceptionof patienthealth
Excellent,n(%)
674(35.3%)60(23.8%)34(20.7%)580(38.9%)
Verygood,n(%) 654(34.3%)97(38.5%)50(30.5%)507(34.0%)
Good,n(%) 442(23.2%)68(27.0%)55(33.5%)319(21.4%)
110(5.8%)24(9.5%)22(13.4%) 64(4.3%)
Respondent’sperceptionof ownhealth <0.001
Excellent,n(%) 479(25.1%)41(16.3%)26(15.9%)412(27.6%)
Verygood,n(%) 676(35.4%)79(31.3%)32(19.5%)565(37.9%) Good,n(%) 594(31.1%)91(36.1%)64(39.0%)439(29.4%) Fair,n(%) 148(7.8%)39(15.5%)37(22.6%) 72(4.8%)
Level3,n(%) 1,243(65.1%)172(68.3%)109(66.5%)962(64.5%) (Continued onnextpage)
Table1. Continued.
Baselinestatus(N = 1,908)
Characteristics
Discharged,n(%) 1,544(80.9%)206(81.7%)138(84.1%)1,200(80.4%)
Admitted,n(%)
Leftagainstmedicaladvice,n(%)1(0.1%)
EDlengthofstay,meanhours(SD)4.52(3.19)4.92(2.80)4.82(2.87) 4.85(3.45)0.95
NumberofEDvisitsduringpast 12months
2ormore,n(%) 230(12.1%)43(17.1%)21(12.8%)166(11.1%)
Adoctorhasstatedthatpatient has(checkallthatapply):
Noneofthoselisted
*Note: Despite thissignificant P-value,noneofthe z’swere ≥2.58;Type1errorpossible. ED,emergencydepartment; GED,GeneralEducationalDevelopment.
differenceinEDdispositionorlengthofstayamong caregiversreportingfoodand/orhousinginsecurity comparedtothosewhowerefoodandhousingsecure.
Movesintheprecedingyear
Baselinesurveyresultsindicatedthat20caregivers(1.0% ofthesample)reportedmovingthreeormoretimesinthe previous12months.Ofthose,nonescreenedpositivefor solelyfoodinsecurity,35%screenedpositiveforsolely housinginsecurity,40%screenedpositiveforbothfoodand housinginsecurity,and25%didnotscreenpositiveforfood orhousinginsecurity.
Ofthe416familiesscreeningpositiveforfoodorhousing insecurity,contactwassuccessfullymadewith147(35.3%) caregiversatthreeweeks,andofthose,70(47.6%)responded tosurveysatsixweekspost-EDvisit.
Food/housinginsecuritystatus
Ofthe147caregiverswhoparticipatedinfollow-up,25 weresolelyfoodinsecureattheindexEDvisit.Ofthose, seven(28%)continuedtoreportfoodinsecurityatthetimeof follow-up,two(8%)reportedsolelyhousinginstability withoutfoodinsecurity,three(12%)reportedbothfoodand
housinginsecurity,and12(48%)nolongerscreenedpositive foreitherfoodorhousinginsecurity.Ofthe60caregivers whoscreenedpositiveforsolelyhousinginsecurityatthe indexEDvisitandparticipatedinfollow-up,19(31.7%) continuedtoreporthousinginsecurityatthetimeoffollowup,three(5%)reportednewfoodinsecurityonly,11(18.3%) reportedbothfoodandhousinginsecurity,and26(43%)no longerscreenedpositiveforeitherfoodorhousinginsecurity.
Ofthe62caregiverswhoscreenedpositiveforbothfood andhousinginsecurityattheindexEDvisitandparticipated infollow-up,31(50%)continuedtoreportbothfoodand housinginsecurity,15(24.2%)reportedfoodinsecurityonly, 10(16.1%)reportedhousinginsecurityonly,andsix(9.7%) nolongerscreenedpositiveforfoodorhousinginsecurity. Follow-upstatuswasunknownduetomissingdatafortwo families.(Onereportedfoodinsecurity,andtheother reportedhousinginstabilityattheindexEDvisit.)
Transitionsfrompositivefoodand/orhousinginsecurity screeningtonegativescreening
Ofthe147caregiverswhoreportedfoodand/orhousing insecurityattheindexEDvisitandparticipatedinfollow-up, 44(29.9%)nolongerscreenedpositiveforeitherfoodor housinginsecurityatfollow-up.Familiesofthoseinitially screeningpositivewhosubsequentlydidnotscreenpositive appearedgenerallysimilarwithrespecttodemographics, neighborhoodsafety,healthstatus/healthcareutilization, andEDvisitcharacteristics(Table2).Youngerpatientage wasassociatedwithatransitionfromapositivetonegative screen(P = 0.02). Table2 includescomparisonsofall collectedvariablesforthesetwogroups.Giventherelatively lownumberoffamiliesthatfollowedupandreported resourceuse,itwasnotpossibletodeterminewhetherthere wasanyassociationbetweenreferraluseandtransitionfrom positivetonegativescreens.
Ofthe147caregiverswhoparticipatedinfollow-up,only 15(10.2%)reportedusingatleastoneoftheresource referrals.Themostfrequentlyreportedbarrierforthose reportingabarriertoresourceusewaslosingornotreceiving thereferral(41.7%).Othercommonreasonsincludednot havingtime(15.2%)andresourcesnot fittingtheirneeds (10.6%).The Figure demonstratescaregiver-reported barrierstoreferraluse.
Demographicsofthosewithandwithoutfollow-up
Patientswhosecaregiversparticipatedinfollow-uphad largelysimilardemographicstothosewhodidnot,exceptfor languagespokenathome.Spanish-speakingcaregiverswere lesswellrepresentedamongthosewithfollow-up(z = 3.06, P < 0.001).Supplementary Table1 demonstrates demographics,neighborhoodsafety,healthstatus,
healthcareutilization,andEDvisitcharacteristicsofthose withandwithoutfollow-up.
Thisstudydemonstratedhighlevelsofsocialneedin patientspresentingtoapediatricED.Overonein five patientsscreenedpositiveforfoodand/orhousinginsecurity. Thereportedrateoffoodinsecurityfoundinthisstudydoes appearsomewhatlowerthanthenationalaverageaswellas comparedtopreviousstudiesinvestigatingfoodinsecurityin thepediatricED,althoughoverallnumbersvarywidely basedondatasource.1,22,23,25,27 Wedid findhigherfood insecurityratesthanthatofthesurroundingcountyinthe studyyear.28 Still,ourstudydesignwaslimitedby conveniencesamplinganda2.8%responserateof participantsintheED,limitingthegeneralizabilityofour findings.OtherpediatricED-basedstudiesdemonstrate similarchallenges,withlowresponserate(3.6%)29 and health-relatedsocialneed-positivescreeningrate(16%).30 It isimportanttonotethateveniffamiliesscreenpositivefor socialrisk,asubstantialproportionmaystilldecline assistance.31 Similarly,socialneedsnavigationfollow-uphas beenshowntobechallengingintheEDsetting,withlow participationrate(7%)32 andpersistenceofsocialneed(56%) despiteparticipationinnavigationservices.19
Inourstudy,follow-upsurveydatarevealedanoverall reductioninthereportedratesoffoodandhousing insecurity,yetcommunityresourcereferraluptakewaslow. Thislikelyreflectsthecomplexityandburdenofpatient socialcircumstancesandamultitudeofenvironmental factors.Amongthosewhowerefoodinsecureatbaseline, almosthalfnolongerscreenedpositiveforfoodorhousing insecurity,andamongthosewhowerehousingunstableat baseline,over40%nolongerscreenedpositiveforfoodor housinginsecurity.Thosewithfoodandhousinginsecurity atbaselinedemonstratedtheleastreductioninsocialneed, withjustunder10%nolongerscreeningpositiveforeither foodorhousinginsecurityatfollow-up.However,despite theseapparentpositiveshifts,itisdifficulttoascertain whetherthesedevelopmentswereassociatedwithED interventions.Indeed,itseemsunlikelygiventhatthe majorityofcaregiverswithwhomwefollowedupdidnot endorseresourceuse.
Itisbeyondthescopeofthisstudytodiscerntheetiology ofthistrend.Itispossiblethatcaregiversunder-reported resourceuse,thatcompletionofthesurveyitselfmayhave precipitatedachange,randomchance,orarangeofother explanationsincludinganinterplayofsocialdeterminantsof health.Interestingly,Kanaketaldemonstratedsomewhat similar findingsusinganinterventionavailableontabletand personalsmartphone(theHelpStepsapp),reportingthat only23%ofcaregiversdescribedusingthetool.19 Only14% contactedatleastonereferralagency,yet44%reportedtheir primaryneedeithercompletelyorsomewhatresolved.19 As
Table2. Follow-upsurvey:demographicsandclinicalcharacteristicsasstratifiedbyfood/housinginsecuritystatus. Follow-upstatus* Characteristics
– $39,999,n(%)
– $79,999,n(%)
$80,000 – $99,999,n(%)
Numberoftimesmovedduringpast12months
Respondent’sperceptionofneighborhoodsafety,n(%)
(Continued onnextpage)
Table2. Continued. Follow-upstatus
Adoctorhasstatedthatpatienthas: noneofthoselisted,n(%)
(Continued onnextpage)
*Follow-upstatusunknownduetomissingdatafortwofamilies(onefoodinsecureandonehousinginsecureatbaseline).
**Despite thissignificant P-value,noneofthe z’swere ≥2.58;Type1errorpossible. ED,emergencydepartment; GED,GeneralEducationalDevelopment.

inthecurrentstudy,Kanaketalfoundhousingneedstobe morepersistentthanfoodinsecurityaswell.19 Libermanetal alsoexaminedsocialneedsinterventionsinthepediatricED withtrainednavigatorsandnotedmuchgreateruseof resources(45.6%ofthosewhofollowedupreported contactingatleastoneresource);however,itwasdifficultto determinewhetherthesewerehousing-andfood-related resourcesastheserepresentedonly21%and20%, respectively,ofreferralresourcesprovided.21
Inthecurrentstudy,themostcommonbarriertoresource usereportedbycaregiverswasthattheyeitherlostordidnot receivethereferral.Whilethisinitiallyappearssomewhat discouragingitalsomaypotentiallyprovethesimplest obstacletoaddressinfuturework.Itmaybehelpfulto provideelectronicformsofresourcesinadditiontowritten copies,assuggestedbycaregiversinotherpediatricEDbasedstudies.21,29 Itisremarkablethatamongcaregiversina studybyCullenetalwhoscreenedpositiveforfood insecurityandoptedtoreceiveadirectphonecallfromafood resourceagency,only35.9%wereabletobereached,andof those,31%werenolongerinterestedinfood-resource referrals.23 Itispossiblethatfutureresearchmayalsoelicit appropriatemethodsofneedsreassessmentandtimingfor suchreassessment.Increasedengagementandcollaboration
Theassociationofageandsocialneedislikely multifactorialandmayincludevariablessuchasreduced Table2. Continued.
withthecommunity,bothwiththoseinneedandwiththose providingresources(ie,foodbanks),maypavethewayfor improvedscreeningdesignandresourceinformation deployment,aswellasmoresuccessfulandincreased useofinterventions.
Thecurrentstudyreinforcesassociationsdemonstrated throughouttheliteraturebetweenfood/housinginsecurityand caregiver/patientphysicalandmentalhealth.1,4–12 Thisserves tounderscoretheimportanceofattemptingtoaddressfood andhousinginsecurityateveryopportunity.Theassociation ofneighborhoodsafetyandfoodandhousinginsecurity,while notunexpected,likelyadditionallycompoundsthechronic illnessessuchasanxiety,obesity,andasthmaalsofoundinthe currentstudytobeassociatedwithfoodandhousing insecurity.Notabledemographicassociationswithfoodand/ orhousinginsecurityincludedolderage;agealsoappearedto beassociatedwiththetransitionfrompositivetonegative screensforfoodand/orhousing.Gonzalezetalalsofound increasingageandpublichealthinsurancetobeassociated withfoodinsecurity;however,unlikeinthecurrentstudythey didnot findassociationsbetweenfoodinsecurityandchronic healthconditions.25
resourcesavailableforfamilieswitholderchildren,and increasedmonetaryrequirementsofolderchildrenpossibly representmoredeeplyentrenchedsocialneed.Interestingly, despitepreviousliteraturedemonstratinganassociation betweenfoodinsecurityandincreasedhealthcareutilization suchasEDvisits,thecurrentstudyfoundsomewhat equivocaldata.15,17 OneEDvisitwithinthepastyearwas morelikelytobeassociatedwithfoodandhousing insecurity;however,twoormorewasnot.Additionally,the transitionfrompositivetonegativescreenswasalso associatedwithaslightlyincreasedmeannumberofED visitswithintheprioryear.Itisdifficulttohypothesizewhat maybedrivingtheseseeminglydiscordantresults;however, itispossiblethatitistheunequalinterplayofmultiple variables;forexample,youngerchildrenwhoarealsomore likelytotransitionfrompositivetonegativescreensaremore likelytovisittheEDoverall.
Therewereseverallimitationsinherenttothedesignof thisstudy,includingtheuseofconveniencesamplingwith datacollectorspresentonlyduringthedayandearlyevening. Thissamplingtechniquemaynothavecapturedthosewith particularlychallengingsocialcircumstances, underestimatingthetrueratesoffoodandhousing insecurity,whileincreasingthelikelihoodofsamplebias andpresenceofconfoundingfactors.Additionally, thisstudyrelieduponself-reportforidentificationoffood/ housinginsecurityaswellasresourceuse;therefore, reportingbiasmayhaveimpactedourresults.Althoughwe attemptedtodesignthestudyinsuchawaytoreduce potentialdiscomfortasmuchaspossible, financialmeans andsocialneedingeneralremainsensitivetopics,and concernsregardingprivacyandstigmamayhavecontributed furthertoreporterbias.Thisisespeciallypertinentasfollowupsurveyswereconductedoverthephonewhileinitial surveyswerecompletedonelectronictablets,possibly contributingto fluctuationsinthereportingoffoodand/or housinginsecurity.
Familieswerecontactedbystudyresearchpersonnel,and thismechanismmaybelesseffectivethanestablishedclosedloopreferralmechanismsinwhichthecommunity-based socialserviceitselfislinkeddirectlywiththehealthcare institution.Thefollow-upperiodofthreetosixweeksmay alsobesomewhatlimited,anditispossiblethatresourceuse, especiallyformorecomplexneedssuchashousing,maynot effectchangewithinthisshortperiod.Itisalsoworth considering,forexample,thatwhilefoodbanksareessential socialresourcestoaddresshunger,theyareatemporary solution,anddonotincreasetheabilityofacaregiverto purchaseadequatefood.Difficultiesincontactingfamilies forfollow-upalsopresentedasignificantlimitationand restrictedourabilitytoevaluatestudyinterventions.During thestudyperiod,researchersatthesameinstitutionwerealso
conductingastudyexaminingadversechildhood experiences;aspartofthisconcurrentstudy,socialworkers mayhavebeenconsultedforsomeofthesefamilies, potentiallyalteringresourcereferraldistributionforthose families.Lastly,becausethisstudytookplaceduringthe COVID-19pandemictheresultantincreasedsocialneeds andrapidlychangingeconomiclandscapelikelyaffectedour results,possiblyreducingthegeneralizabilityofthiswork.
Thisstudysuggeststhatscreeningandinterventionamong twocommonsocialdeterminantsofhealth foodand housinginsecurity maybefeasibleinapediatricEDsetting. Atthesametime,itillustratesthatachievingwidespread participationamongfamiliesmaybeasignificantchallenge. Althoughasignificantproportionofcaregiversreporteda changeinfoodandhousinginsecurityonfollow-up,itis difficulttoascertainwhatmayhavecontributedtothis finding, especiallygiventhelimitedresponserateandreportedresource use.Furthersocialneeds-interventionresearchinthepediatric EDsettingshouldbedesignedtocapturelargerresponserates (includinganassessmentofsocialneeddisclosureindayand overnightperiods),whileassessingtheperformanceofclosedloopreferralandfollow-upmechanismsforthosefamilieswho indicateadesireforassistance.
TheauthorswouldliketothankPhungK.Pham,PhD,for heressentialstatisticalcontributionstothispaper.This researchwaspartiallysupportedthroughthestudy institution’sChiefScientificOfficerSeedGrant.Thisfunding sourcewasnotinvolvedinstudydesign,datacollection,data analysis, interpretationofdata,manuscriptdrafting,or decisiontosubmitforpublication.
AddressforCorrespondence:VictorCisneros,MD,MPH, EisenhowerHealth,DepartmentofEmergencyMedicine,39000Bob HopeDr.,RanchoMirage,CA92270.Email: vcisneros2@ eisenhowerhealth
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsourcesand financialormanagementrelationshipsthatcouldbeperceivedas potentialsourcesofbias.Thisresearchwassupportedthrougha Children’sHospitalofOrangeCountyChiefScientificOfficer(CSO) SeedGrant(Grant#16962002).Thisfundingsourcewasnotinvolved instudydesign,datacollection,dataanalysis,interpretationofdata, manuscriptdrafting,ordecisiontosubmitforpublication.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Assafetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BrochierA,GargA,PeltzA.Clinicalandpublicpolicyinterventionsto addressfoodinsecurityamongchildren. CurrOpinPediatr. 2022;34(1):2–7.
2.NationalCenterforHomelessEducation.Federaldatasummaryschool years2015–16to2017–18:educationforhomelesschildrenandyouth. 2020.Availableat: https://nche.ed.gov/wp-content/uploads/2020/01/ Federal-Data-Summary-SY-15.16-to-17.18-Published-1.30.2020.pdf AccessedNovember9,2023.
3.YamashiroAandMcLaughlinJ.Earlychildhoodhomelessnessstate profiles:2018–19.2019.Availableat: https://www2.ed.gov/about/ offices/list/opepd/ppss/reports.html.AccessedNovember9,2023.
4.BessKD,MillerAL,MehdipanahR.Theeffectsofhousinginsecurityon children’shealth:ascopingreview. HealthPromotInt. 2023;38(3):daac006.
5.CainKS,MeyerSC,CummerE,etal.Associationoffoodinsecuritywith mentalhealthoutcomesinparentsandchildren. AcadPediatr. 2022;22(7):1105–14.
6.StPierreC,VerPloegM,DietzWH,etal.Foodinsecurityandchildhood obesity:asystematicreview. Pediatrics. 2022;150(1):e2021055571.
7.PantellMS,KaiserSV,TorresJM,etal.Associationsbetweensocial factordocumentationandhospitallengthofstayandreadmission amongchildren. HospPediatr. 2020;10(1):12–9.
8.LeeAM,ScharfRJ,FilippSL,etal.Foodinsecurityisassociated withprediabetesriskamongU.S.adolescents,NHANES2003-2014. MetabSyndrRelatDisord. 2019;17(7):347–54.
9.ThomasMMC,MillerDP,MorrisseyTW.Foodinsecurityandchild health. Pediatrics. 2019;144(4):e20190397.
10.DrennenCR,ColemanSM,EttingerdeCubaS,etal.Foodinsecurity, health,anddevelopmentinchildrenunderagefouryears. Pediatrics. 2019;144(4):e20190824.
11.SandelM,ShewardR,EttingerdeCubaS,etal.Unstablehousingand caregiverandchildhealthinrenterfamilies. Pediatrics. 2018;141(2):e20172199.
12.CuttsDB,MeyersAF,BlackMM,etal.UShousinginsecurity andthehealthofveryyoungchildren. AmJPublicHealth. 2011;101(8):1508–14.
13.AmegbletorDY,GoldbergD,PopeDA,etal.Foodandnutritionsecurity associaldeterminantsofhealth:fosteringcollectiveimpacttobuild equity. PrimCare. 2023;50(4):633–44.
14.GittermanBA,ChiltonLA,CottonWH,etal.CouncilonCommunity Pediatrics;CommitteeonNutrition.Promotingfoodsecurityforall children. Pediatrics. 2015;136(5):e1431–8.
15.RigdonJ,MontezK,PalakshappaD,etal.Socialriskfactorsinfluence pediatricemergencydepartmentutilizationandhospitalizations. JPediatr. 2022;249:35–42.e4.
16.FosterCC,SimonTD,QuP,etal.Socialdeterminantsofhealthand emergencyandhospitalusebychildrenwithchronicdisease. Hosp Pediatr. 2020;10(6):471–80.
17. PeltzAandGargA.Foodinsecurityandhealthcareuse. Pediatrics. 2019;144(4):e20190347.
18.McDermottKW,StocksC,FreemanWJ.(2018). HealthcareCostand UtilizationProject(HCUP)StatisticalBriefsno.242:Overviewof PediatricEmergencyDepartmentVisits,2015.Rockville,MD:Agency forHealthcareResearchandQuality(US).
19.KanakMM,FleeglerEW,ChangL,etal.Mobilesocialscreeningand referralinterventioninapediatricemergencydepartment. AcadPediatr. 2023;23(1):93–101.
20.MurrayE,RooseveltGE,VogelJA.Screeningforhealth-relatedsocial needsintheemergencydepartment:adaptabilityand fidelityduringthe COVID-19pandemic. AmJEmergMed. 2022;54:323.e1–4.
21.LibermanDB,PhamPK,Semple-HessJE.Socialemergencymedicine: capitalizingonthepediatricemergencydepartmentvisittoscreenand connectpatientsandfamiliestocommunityresources. AcadPediatr. 2022;22(6):1049–56.
22.CullenD,WoodfordA,FeinJ.Foodforthought:arandomizedtrialof foodinsecurityscreeningintheemergencydepartment. AcadPediatr. 2019;19(6):646–51.
23.CullenD,AbelD,AttridgeM,etal.Exploringthegap:foodinsecurityand resourceengagement. AcadPediatr. 2021;21(3):440–5.
24.DeMarchisEH,HesslerD,FichtenbergC,etal.Assessmentofsocial riskfactorsandinterestinreceivinghealthcare-basedsocialassistance amongadultpatientsandadultcaregiversofpediatricpatients. JAMA NetwOpen. 2020;3(10):e2021201.
25.GonzalezJV,HartfordEA,MooreJ,etal.Foodinsecurityinapediatric emergencydepartmentandthefeasibilityofuniversalscreening. WestJ EmergMed. 2021;22(6):1295–300.
26.U.S.CensusBureau.Censusreporter.Availableat: https:// censusreporter.org.AccessedNovember9,2023.
27.HagerER,QuiggAM,BlackMM,etal.Developmentandvalidityofa 2-itemscreentoidentifyfamiliesatriskforfoodinsecurity. Pediatrics. 2010;126(1):e26–32.
28.FeedingAmerica.Foodinsecurityamongoverall(allages)populationin California:2021foodinsecurityinCalifornia.Availableat: https://map.feedingamerica.org/county/2021/overall/california AccessedNovember9,2023.
29.AssafRR,AssafRD,PadlipskyPS,etal.Afamily-centeredapproachto socialneedsawarenessinthepediatricemergencydepartment. PEC Innov. 2024;4:100283.
30.TedfordNJ,KeatingEM,OuZ,etal.Socialneedsscreeningduring pediatricemergencydepartmentvisits:disparitiesinunmetsocial needs. AcadPediatr. 2022;22(8):1318–27.
31.KanakMM,StewartAM,ChangL,etal.Health-relatedsocialrisks versusneedsinapediatricemergencydepartment. AmJPrevMed. 2024;67(2):291–5.
32.WallaceAS,LutherBL,SislerSM,etal.Integratingsocialdeterminants ofhealthscreeningandreferralduringroutineemergencydepartment care:Evaluationofreachandimplementationchallenges. Implement SciCommun. 2021;114(2):1–12.
SumanThakur,MD* VivekChauhan,MD†
SagarGalwankar,MD‡ FatimahLateef,MBBS,FRCS§ PiaDaniel,MD∥
ZeynepCakir,MD¶ KatiaM.Lugo,MD#
SamjhanaBasnet,MD** BusraBildik,MD††
Authorscontinuedatendofpaper
SectionEditor: ElisabethCalhoun,MD,MPH
*IndiraGandhiMedicalCollege&Hospital,DepartmentofEmergency Medicine,Shimla,India
† IndiraGandhiMedicalCollege&Hospital,DepartmentofMedicine, Shimla,India
‡ SarasotaMemorialHospital,FloridaStateUniversityCollegeofMedicine EmergencyMedicineResidencyProgram,DepartmentofEmergency Medicine,Sarasota,Florida
§ SingaporeGeneralHospital,DepartmentofEmergencyMedicine,Singapore
∥ DownstateHealthSciencesUniversity,DepartmentofEmergencyMedicine, Brooklyn,NewYork
Af
filiationscontinuedatendofpaper
Submissionhistory:SubmittedJuly16,2024;RevisionreceivedOctober24,2024;AcceptedOctober28,2024
ElectronicallypublishedDecember31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.29331
Background: TheFemaleLeadershipAcademyforMedicalExcellence,membersoftheWorld AcademicCouncilofEmergencyMedicine,conductedthissystematicreview,whichexploresgender disparitiesinburnoutamongemergencyphysicians(EP)usingtheMaslachBurnoutInventory-Human ServicesSurvey(MBI-HSS).Burnoutisacriticalissueinhealthcare,particularlyinemergencymedicine wherehighstressanddemandingworkenvironmentsprevail.
Methods: FollowingPRISMAguidelines,wesearchedPubMedandEpistemonikosforstudiesusing MBI-HSStomeasureburnoutinEPs.Inclusioncriteriaencompassedpeer-reviewed,English-language articlesreportingburnoutbysex.Dataextractionfocusedonproportionsofburnoutandits subcomponents,meanscores,andoddsratios,withqualityassessedusingJoannaBriggs Institutecriteria.
Results: Weincluded18studiesspanning26,939EPsfrom10countries.Whileoverallburnoutratesdid notsignificantlydifferbetweenthesexes,theproportionoffemaleEPswithhighemotionalexhaustion (EE)(69%)andlowsenseofpersonalaccomplishment(PA)(45%)weresignificantlyhighercomparedto maleswithhighEEin57%andlowPAin29%,respectively(P < 0.001forboth).Proportionwithhigh depersonalization(DP)scorewas44%inbothmaleandfemaleEPs.Meanscoresrevealedfemales experiencinghighermeanEE(26.8 ± 15.7)scoresvsmales(25.4 ± 15.9) P < 0.001.Maleshadmean DPscores(8.6 ± 8.0)andmeanPAscores(26.6 ± 12.7)comparedtofemaleswithlowermeanDP scores(7.4 ± 7.2)andhigherPAscores(27.7 ± 11.9),respectively P < 0.001forboth.Oddsratios indicatedvaryingrisks,predominantlyhigherEEoddsamongfemales,varyingfrom0.72to2.3.
Conclusion: Thisreviewunderscoresgender-specificmanifestationsofburnoutamongemergency physicians,withfemalesmoresusceptibletoemotionalexhaustionandlowersenseofpersonal accomplishment.Standardizedreportingmethodsarecrucialforfuturemeta-analysestorefinegenderspecificinterventionscombatingburnoutinemergencymedicine.Targetedstrategiesaddressing distinctmanifestationsofburnoutareimperativetosupportthewell-beingandretentionofEPs,fostering sustainablehealthcaredelivery.[WestJEmergMed.2025;26(2)338–346.]
Theterm “burnout,” introducedbyFreudenbergerin 1974,referstojob-relateddissatisfactionprimarilycausedby work-relatedstress.1 Themostwidelyvalidatedtoolfor measuringburnoutamongphysiciansistheMaslach BurnoutInventory-HumanServicesSurvey(MBI-HSS) 22-itemtool.2 TheMBI-HSSmeasuresburnoutinthree subcomponents:emotionalexhaustion(EE); depersonalization(DP);andpersonalaccomplishment (PA).2 BurnoutissuggestedbyahighscoreinEEandDP, andalowscoreonPA.2
Thereisapalpablegendergapinacademicemergency medicine(EM)wherefemaleemergencyphysicians(EP)are lesslikelytoholdmajorleadershippositions,morelikelyto spendagreaterpercentageoftimeinclinicalandteaching activities,publishlessinpeer-reviewedjournals,andareless likelytoachievesenioracademicranksintheirmedical schools. 3 Evenafteradjustingforfactorssuchasrace, region,rank,yearsofexperience,clinicalhours,corefaculty status,administrativeroles,boardcerti fi cation,and fellowshiptraining,themean(±SD)salaryofwomenwas foundtobe$19,418( ±$3,736)lessthanthatofmen ( P < 0.001). 4 Thisgenderdisparitycannegativelyimpact theretentionoffemaleEPsandpredisposethemto higherburnout.
Althoughtherearesystematicreviewsthathavedescribed burnoutamongEPs,nonehavefocusedonthegendergapin burnoutamongEPs.5–7 Therefore,theFemaleLeadership AcademyforMedicalExcellence(FLAME)membersofthe WorldAcademicCouncilofEmergencyMedicine performedasystematicreviewtodescribethegender disparityinburnoutamongEPsatagloballevel.Tothebest ofourknowledge,thisisthe firstsystematicreviewfocusing ongenderdisparityinburnoutamongEPsasmeasuredby thevalidatedMBItool.
METHODS
Weperformedasystematicreviewfollowingthe PRISMAmethods8 usingtheprotocolpublishedin PROSPERO(CRD42024558794).
SearchStrategy
Wesearchedtwoopenaccessdatabases,PubMedand EpistemonikosonJune30,2024,forpeer-reviewedarticles onburnoutandemergencyphysicians.Weoperationalized differentpermutationsofeachkeywordasfollows:
Burnout: “Maslachburnoutinventory” ORMBIOR burnoutORburn-outOR “burnedout” OR depersonalizationOR “emotionalexhaustion” OR “compassionfatigue”
EmergencyPhysician: “emergencyphysician*” OR “emergencydoctor*” OR “EMphysician*” OR “EM doctor*” OR “emergencyresident*” OR “EMresident*” OR “emergencyconsultant*” OR “EMconsultant*” OR
“emergencyfaculty*” OR “EMfaculty*” OR “ emergency professor*” OR “EMprofessor*” OR “ emergency attending*” OR “EMattending*”
Weappliedthe field “All fields” forsearchingonPubMed and “TitleandAbstracts” forsearchingthesame combinationofkeywordsinEpistemonikos.
Weappliedaseriesofinclusionandexclusioncriteria. Articleswereincludediftheywere1)writteninEnglish, 2) publishedinapeer-reviewedjournal,3)originalarticles, and4)appliedanyversionoftheMBI-HSStomeasure burnout.Theywereexcludedifthey1)didnotdescribethe resultsseparatelybysex,2)didnotincludeEPsintheirstudy, or3)wereasystematicreview.
Extractionwasperformedbytwoinvestigators independently.Thefollowinginformationwasextracted: studycharacteristics(firstauthor,yearofpublication, country,numberofparticipantsthatresponded); characteristicsofparticipants(meanage,proportionof malesandfemales);andoutcomedata(proportionofhigh burnoutinmalesandfemales,proportionofmalesand femaleswithhighEE,highDPandlowPA,meanscoresin malesandfemalesforEE,DPorPAandoddsofburnoutor itssubcomponents EE,EP,orPA infemaleEPs.
WeusedtheJoannaBriggsInstitute’scriticalappraisal checklistforevaluationofthequalityoftheprevalence studies.9 Thetoolassessedqualityusingninequestions.A scoreof1wasassignedfora “Yes” asananswer,andascore of0wasassignedforananswerthatwas “No,”“Unclear,” or “NotApplicable.” Thescoresweregradedaslow,moderate orhighifthetotalscorewas ≤ 4,5–7,and ≥ 8,respectively. Thequalityassessmentwasperformedindependently bytwoinvestigators,andanydisagreementwassettled bydiscussion.
Ourinitialsearchresultedin331articlesinPubMedand 13inEpistemonikos,whichwereimportedintoEndNote referencemanagementsoftware(ClarivateAnalytics, Philadelphia,PA).Ofthese344articles,ninewerefoundto beduplicates,leavingatotalof335articlesforthescreening andeligibilitystages(Figure).Ofthe335articlesscreened,we excluded226thatdidnotmeettheinclusioncriteria,leaving uswith109articlesforretrieval.Wereviewedthese109full textsforeligibility,resultingintheexclusionofthefollowing:
• 3articlesthatweresystematicreviews
• 7articlesthatwerenotpeer-reviewedoriginalarticles
• 5articlesthatdidnotincludeemergencyphysicians
• 41articlesthatdidnotusetheMaslachBurnout Inventoryformeasuringburnout
• 35articlesthatdidnotreporttheirdatabysex,
Thisleftatotalof18articlesforthe finalreview.The processofscreeningandselectingstudiesisshowninthe PRISMA flowdiagram(Figure).
Weincluded18studiesfrom10differentcountriesinthe finalanalysis(Table1).ThetotalnumberofEPsstudiedin these18studieswas26,939,including8,864(33%)female EPs,resultinginamale-to-femaleratioof2:1.Fifteenof thesestudiesusedthe22-itemMBI-HSStoolformeasuring burnout,whiletwostudiesusedthetwo-itemtoolbasedon theMBI-HSS,andoneincludedthenine-itemMBItool (Table1).Allweremulticentricstudiesexceptforone,which wasasingle-centerstudy.IncludedwereEPsofbothsexesin allstudiesexceptforone,whichincludedonlyfemaleEPs.
Allincludedstudieswereconductedinthelast10years(2014 topresent),exceptforonestudyconductedin1996.Six studieswerescoredashighquality,whiletheremaining12 weremoderatequalitystudies.Theresponseratesvaried from30–94.1%.
BurnoutcalculatedbyMaslachBurnoutInventory
Sevenstudiesreportedtheburnoutproportionsseparately inmaleandfemaleEPs(Table2).Thestudiesthatincludedthe 22-itemMBI-HSStoolhadatotalof1,181maleand542 femaleEPs,withanaveragepooledproportionofhigh burnoutat58.7%and58.3%,respectively(P = 0.8).Two studiesusedthetwo-itemMBI,includingatotalof4,868male and2,736femaleEPs,withanaveragepooledproportionof highburnoutat27%and34%,respectively(P < 0.001).
SevenstudiesreportedindividualcomponentsoftheMBIHSS,specificallytheproportionofparticipantswithhigh
Identification of studiesvia databases and registers
Recordsidentified from PubMed (n=331) Epistemonikos (n=13)
Recordsscreened (N=335)
Reportssought for retrieval (n=109)
Reportsassessed for eligibility (n=109)
Recordsremoved before screening:
Duplicate records removed (n=9)
Recordsexcluded by screening Titles and abstracts (n=226)
Reportsnot retrieved (n=0)
Reportsexcluded: Maslach Burnout Inventory not used (n=41)
Data not given by Gender (n=35)
Not original articles (n=7)
Did not study emergency physicians (n=5)
Systematic reviews (n=3)
Studies included in review (n=18)
Table1. Characteristicsoftheincludedstudies.
, MaslachBurnoutInventory.
Table2. Proportionofmaleandfemaleemergencyphysicianswithhighlevelsofburnout.
2-itemMBItool (n=4,868)n=1,502(31.4%)(n=2,736)n=903(33%)
2item4,768 1,478(31%) 2,698 890(33%) 0.05
2item100 24(24%) 38 13(35%)
MBI, Maslach BurnoutInventory.
EE,highDP,andlowPAseparatelyformaleandfemaleEPs (Tables3 and 4).Fourofthesestudiesreportedthe proportionofparticipantswithsubcomponentssuggestiveof burnout(Table3),andthreeofthesestudiesreportedthe meanandstandarddeviationsoftheMBIsubcomponents (Table4).FemaleEPshadproportionatelyhigherEEand lowerPAthanmaleEPs(P < 0.001).TheDPlevelswere similaramongmaleandfemaleEPs(Table3).Thecombined
meanEEscorewashigherinfemaleEPs(P < 0.001),while thecombinedPAscorewashigherandtheDPscorewas lowerinfemaleEPscomparedtomaleEPs(P < 0.001) (Table4).Fourstudiespresentedtheirresultsintheformof oddsorrelativerisk(Table5),andthreeoftheseshowed higheroddsamongfemalesofburnoutwhileonehadlower odds.Threeofthesestudiesreportedonlyonesubcomponent ofMBI-HSS(ie,EE)(Table5).
Table3. Proportionofparticipantswithhighlevelsofemotionalexhaustion,highdepersonalization,andlowsenseofpersonal accomplishment,theindividualcomponentsoftheMaslachBurnoutInventory,amongmaleandfemaleemergencyphysicians.
Author Male (n=371)HighEELowPAHighDP
Female (n=399)HighEELowPAHighDP BaturA18 223135(61%)69(31%)- 166119(72%)83(50%)ElhadiM20 8251(62%)21(25%)39(47%)7253(74%)13(18%)35(49%) SarwarS33 6626(39%)18(27%)27(41%)8440(48%)22(26%)31(37%) SoltanifarA34 0 - - - 7765(85%)62(81%)37(48%)
Total 371212(57%)108(29%)66(44%)399277(69%)180(45%)103(44%) P-value(Fisherexacttest) <0.001 <0.0010.77
EE, emotionalexhaustion; PA,personalaccomplishment; DP,depersonalization.
Table4. Mean(standarddeviation)valuesofsubcomponentsoftheMaslachBurnoutInventoryamongmaleandfemale emergencyphysicians.
Author Male (n=10,837)HighEELowPALowDP
Female (n=4,691)HighEELowPAHighDP
LovellLP28 4929.4(11.7)45.5(8)11.8(5.7)6232.5(12.1)43.4(6.8)13(6.7)
YanS35 10,65025.4(16.1)26.5(12.8)8.5(8.1)4,59326.8(15.7)27.6(11.9)7.4(7.2) ErdurB21
Unpaired t-test P-value <0.001 <0.001 <0.001 EE, emotionalexhaustion; PA,personalaccomplishment; DP,depersonalization.
Table5. Oddsorrelativeriskofburnoutoritssubcomponentsbygenderamongemergencyphysicians.
AuthorsMalesFemalesReportedparameterValue
ThestressfulenvironmentofEMisaknowncontributor tothenegativeimpactsofburnout.10 Burnoutcanbethe resultofgood-intentionedphysicianswhostrivefor perfectionatwork.10 Emergencyphysiciansbecome frustratedwhentheirworkenvironmentfallsshortof supportingwell-meaninggoals,leadingtoEPburnout.10
Moralinjuryisnowrecognizedasasignificantfactor contributingtoburnoutamongEPs.Theyoftenface challengingdecisionssuchasprioritizingcareinlife-or-death situations,dealingwithresourcelimitations,andfrequently witnessingsufferinganddeath.Theemotionaltollofmoral injurycanleadtosymptomsofdepression,anxietyandstress disorders,whicharecloselylinkedtoburnout.FemaleEPs, inaddition,facesex-baseddiscrimination,bias,unequal treatment,andfeweropportunitiesforcareeradvancement.3 Theyaremoreburdenedwithbalancingprofessionaland
familyresponsibilities.Femalesareexpectedtodisplaymore empathyandprovideemotionalsupporttopatientsand colleagues,whichcanincreaseemotionallaborandmoral injuryiftheyareunabletomeettheseexpectations.
TheMBIassessestheseverityofthethreeprimary symptomsofburnout:exhaustion;depersonalization;andlack ofpersonalaccomplishment.Developedinthe1970s,ithas becomethegoldstandardformeasuringburnoutacross variousprofessionsandindustries.TheMBI-HSSisspecifically designedforuseinhumanservicesprofessionssuchassocial work,counseling,andhealthcare.2 Aburnoutsurveyof7,288 USphysiciansfromallspecialties,usingtheMBI-HSStool, showedthathighburnoutwasreportedby38%ofUS physiciansandthatburnoutismorecommonamong physiciansthanotherUSworkers.11 Amongallspecialties,EM hadthehighestburnoutrates,withover60%ofEPsreporting highburnoutlevels.11 Emergencymedicineisafrontline
specialty,andseveralfactorscontributetohighburnoutinEPs, includingnightshifts,sleepdisorders,job-relatedstrain,fearof makingmistakes,andworkplaceviolence.12
Inrecentyears,morefemalephysicianshaveenteredthe workforce,leadingtoincreaseddataavailabilityforstudying sexdifferencesinburnoutsymptoms.Insomecultures,female patientspreferentiallyaskforfemaleEPstoattendtothemin theED.13 ArecentlyconductedsystematicreviewofUS physiciansfoundthatwomenphysicianshaveahigher likelihoodofexperiencingburnoutcomparedtomale physicians,particularlywithrespecttotheEEdimensionof burnout.14 StudiesfocusingonEPscorroboratethis finding, indicatingthatfemaleEPsareathigherriskofburnout comparedtomaleEPs.Additionally,femaleshavehigher attritionratescomparedtotheirmalecounterparts.3,4,15 Factors citedascontributingtothediscrepancyinburnoutinclude greaterlevelsofwork-familyconflict,greatertendenciesto emotionallyinvestinpatients/work,andgreaterdiscrimination insalariesandpromotionsbyfemalephysicians.14
Incontrasttotheabovestudies, findingsfromasystematic reviewof16,016physiciansfromtheEasternMediterranean regionindicatednosignificantdifferenceinburnoutrates betweenmaleandfemalephysicians.16 However,noneofthe studiesinDoraiswamy’ssystematicreviewweredesignedto comparedifferencesbysex,limitingtheinterpretationsofthe findings.15 Anothersystematicreviewthatincluded109,628 physiciansconcludedthatinconsistenciesindefinitionsand assessmentmethodsforburnoutacrossstudiespreventeda reliabledeterminationoftheassociationbetweenburnout andthesexofthephysician.17
Thesereviewshighlightvariabilityin findingsacross differentregionsandcontexts,suggestingthatthe relationshipbetweenburnoutandsexmayvarydepending onfactorssuchasculturalnorms,healthcaresystem characteristics,andstudymethodologies.Therefore,while somestudiesmayindicateagenderdisparityinburnout, othersmaynot findsuchdifferences,emphasizingtheneed fornuancedinterpretationandcontext-specific understandingofburnoutinhealthcareprofessions.
Weconductedthissystematicreviewtoaddress inconsistentdataonthegendergapinburnoutamongEPs. Rotensteinetalhavehighlightedintheirreviewthe inconsistenciesinthedefinitionsandassessmentmethodsof burnout;therefore,wefocusedspecificallyonstudiesthat usedtheMBI-HSStoolforassessingburnout.17 Despite usingacommonassessmenttool,theincludedstudies employedvariousmethodsforreportingburnoutscores.Of the18studiesincludedinourreview,18–35 sevenreported burnoutasthepercentageofparticipantswithhighburnout; fourreportedthepercentageofparticipantswithhigh individualcomponentsofburnout(EE,DP,PA)butnot overallburnout;threereportedthemeanscoresforEE,DP, andPA;andfourreportedoddsratiosandrelativerisksfor EE(Tables2–5).Thisapproachallowedusto
comprehensivelyexamineandcomparethegender disparitiesinburnoutamongEPsacrossdifferentstudies.
Wecollateddatafromstudiesreportingburnoutasa percentageofthepopulationhavinghighburnoutandfound thatof1,181maleEPsand542femaleEPs,highburnoutwas reportedin58.8%and58.4%,respectively,whichindicates nearlyequalratesofburnoutbetweenmaleandfemale EPs22–24,26,27 (Table2).Thetwo-itemtool,knownforits brevityandeaseofadministration,caneffectivelyidentifyatriskEMresidentsshowingearlysignsofburnout.36 Thistool usestwoquestionsfromtheMBI-HSSandenables consistent,widespread,andlongitudinalmonitoringof burnoutamongEMresidentsatlocal,regional,andnational levels.36 Inoursystematicreview,weincludedtwostudies thatusedthetwo-itemtooltomeasureburnoutamong4,778 maleand1,502femaleEPs.Thereportedburnoutrateswere 31%amongmaleEPsand33%amongfemaleEPs (P = 0.05).29,32 Thisslightdifferencesuggestsatrendtoward higherburnoutamongfemaleEPs,asindicatedbythese specificstudiesusingtheabbreviatedMBItool.
Fouradditionalstudiesincludedinoursystematicreview, totalling317maleand399femaleEPs,reportedindividual componentsofburnout(EE,DP,PA)aspercentagesof participantswithhighorlowscores(Table3).18,20,33,34 These studiesfoundthattheproportionoffemaleEPswithhighEE andlowPAwassignificantlyhighercomparedtomaleEPs (P < 0.001).However,levelsofDPwerecomparable betweenbothgenders(P = 0.77).Thisindicatesthatfemale EPsmayexperiencegreaterEEandlowerPA,highlighting potentialareasofconcernforgender-specificburnout interventionsinemergencymedicine.
Lastly,amongtheremainingstudiesthatreportedodds ratiosorrelativerisksforburnout,3of4studiesindicateda higherriskofburnoutamongfemaleEPs,whileonestudy showedahigherriskamongmaleEPs(Table5).19,25,30,31 Specifically,femaleEPswerefoundtohaveahigherriskfor theEEcomponentofburnoutcomparedtomaleEPs,as suggestedbythese findings.Thisunderscoresthegender disparityinburnoutriskwithintheEMprofession, emphasizingtheneedfortargetedinterventionstomitigate thesedisparitiesandsupportthewell-beingofallEPs.
Inoursystematicreview,weencounteredchallengesin performingameta-analysisduetothevariabilityinhow authorsreportedtheir findingsusingtheMBItooltomeasure burnoutamongEPs.Specifically,therewerelimitations stemmingfromthelimitednumberofstudiesthatreported resultsseparatelyformaleandfemaleEPs,aswellasthe diversityinhowparametersofburnoutwerereportedacross thesestudies.Thevariationinreportingincludeddifferences inthefollowing:
• Whetherburnoutwasreportedasoverallscoresor individualcomponents(EE,DP,PA)
• Thespecificmetricsusedtodefinehighburnout
• Themethodsusedtoanalyzeandpresentdata (percentages,means,oddsratios,etc).
Thisvariabilitymakesitchallengingtoaggregatedata acrossstudiesforameta-analysis,whichtypicallyrequiresa consistentapproachtodatareportingandstatistical measures.Asaresult,whileourreviewprovidesvaluable insightsintothegenderdisparitiesinburnoutamongEPs,the heterogeneityinreportingpreventsaquantitativesynthesis ofthe findings.
Movingforward,standardizingthereportingofMBIHSSresultsandburnoutparametersinfuturestudieswould facilitatemorerobustmeta-analyticalapproachestofurther elucidatethegendergapinburnoutamongEPsandinform targetedinterventionstomitigateburnoutinthiscritical healthcarespecialty.
AspertheoriginatorsoftheMBI-HSSthepre-2016 versionsofthetoolusedarbitraryclassificationsofhigh burnout,dividingthenormativepopulationintotertiles labelledashigh,moderate,andlowburnout.Thisapproach waslateracknowledgedasamistake,leadingtotheremoval ofthesecutoffclassificationsfromallversionsoftheMBIHSSstartingwiththefourtheditionin2016.Thischange allowedresearcherstoviewburnoutasacontinuumwithin thecontextofspecificpopulations.37
Inoursystematicreview,despiteincluding14studies conductedafter2016,onlythreestudiesreportedthemean (±SD)scoresofindividualcomponentsofburnoutseparately formaleandfemaleEPs.21,28,35 Notably,thesestudies highlightedsignificantdifferences:femalesexhibited significantlyhigherEEscores,whilemalesshowed significantlyhigherDPandlowerPAscores(P < 0.001).21,28,35 ItisimportanttonotethatthestudybyYanetalinChina includedalargecohortof15,243participants,whichmayskew theoverall findingstowardthisstudy’sresults.35
Inmostotherstudiesincludedinourreview,researchers derivedcutoffsbycombiningresultsfromindividual components(EE,DP,PA),whichcouldexplainwhyoverall burnoutscoresappearedequivocalacrossthesestudies (Table2).Thisvariabilityinreportingunderscoresthe ongoingchallengeofharmonizingburnoutmeasurements acrossdifferentstudiesandemphasizestheneedfor standardizedreportingpracticestofacilitateclearer comparisonsandmeta-analysesinfutureresearch.
Twelveofthearticlesincludedinourstudywerepublished in2020orlater,and fivestudieswereconductedduringthe peakoftheCOVID-19pandemicin2020–2021.Itislikely thatthepandemiccausedunusualfatigueandburnout, resultingindifferentburnoutlevelsamongmalesandfemales acrossdifferentregions.
Thissystematicreviewencounteredseverallimitations. Onemajorchallengewasthevariabilityinhowstudies
reportedburnout,evenwhenusingtheMBI-HSStool.Some studiesfocusedonoverallburnout,whileothersreported individualcomponentssuchasEE,DPandPA. Additionally,studiesemployeddifferentmetrics (percentages,means,oroddsratios),makingitdifficultto aggregate findingsforameta-analysis.Thelimited numberofstudiesreportinggender-specificdatafurther constrainedourabilitytomakedefinitiveconclusionsabout thegendergapinburnoutamongEPs.Moreover,some studiesusedoutdatedversionsoftheMBI-HSS,whichrelied onarbitrarycutoffsforhighburnout,affectingtheaccuracy ofburnoutclassification.Finally,severalstudieswere conductedduringtheCOVID-19pandemic,aperiod markedbyincreasedfatigueandburnout,potentially skewingthe findingsandlimitingtheirgeneralizability beyondthattimeframe.
Thisreviewhighlightsthatthescienceofexamining physicianburnoutiscomplexandinfluencedbyawide rangeoffactors.Notwostudiesareperfectlycomparable, evenwhenusingsimilarassessmenttools,suchasthe MaslachBurnoutInventory-HumanServicesSurvey. Variableslikethetypeofwork,workload,acuityoftasks,job satisfaction,hoursworked,frequencyofrapiddecisionmaking,criticalthinkingdemands,work-lifebalance, competinginterests,culturalbeliefs,andsocietal norms suchaspowerdistanceandhierarchy all impactburnoutdifferently.
Despitethe findingsthatfemaleemergencyphysicians reporthigheremotionalexhaustionandlowersenseof personalaccomplishmentthantheirmalecounterparts, itisessentialforsocietiesandcountriestodelvedeeperinto thisissue,tailoringstudiestotheirspecificcontexts andcultures.Thisreviewunderscorestheneedfor gender-specificstrategiestocombatburnoutamongEPs. Whilebothmenandwomenexperiencesignificantburnout, thenatureoftheirburnoutdiffers,necessitatingtargeted interventionstosupportthewell-beingofallEPs.
1. UniformReportingofResults: Futurestudieson burnoutamongEPsshoulduniformlyreportresults, includingthemean(±SD)fortheindividual componentsoftheMBI-HSStool EE,DPandPA forbothmaleandfemaleEPs.Thisstandardized approachwillfacilitateaclearerunderstandingof thegendergapinburnoutacrossdifferentsettings and populations.
2. FurtherResearchFocus: Thereisacriticalneedfor furtherresearchtodelveintotheunderlyingreasons behindthedisparitiesinEE,DP,andPAbetween maleandfemaleEPs.Understandingthesefactorsis essentialfordevelopingtargetedinterventionsthat
addressthespecificneedsofeachgender,thereby effectivelymitigatingburnout.
3. MoveAwayfromArbitraryCutoffScores: Thepractice ofusingarbitrarycutoffscores(high,moderate,low burnout)tocategorizeburnoutlevelsshouldbe abandoned.Thisapproach,discouragedbythe originatorsoftheMBI-HSStool,doesnotaccurately capturethenuancedexperiencesofburnoutandmay leadtomisleadingconclusions.
4. HolisticAssessmentofBurnout: Ratherthanfocusing solelyonoverallburnoutscores,futurestudiesshould emphasizethedetailedassessmentofEE,DP,andPA. Thisholisticapproachprovidesamorecomprehensive understandingofburnoutdynamicsamongEPsand allowsfortargetedinterventionsbasedonspecific componentsofburnout.
Basedontheobservationsregardingburnoutamong womeninEMandfemaleEPs,weareproposingthe followingmeasures:
1. IncreasedAwarenessandEducation:
○ Enhanceawarenessandrecognitionofburnout withintheEMcommunity.
○ Incorporateburnout-relatedsessionsintoEM residencytrainingandcorecurriculum.
2. ProactiveFacultyandLeadership:
○ FacultyandEMleadershipshouldcloselymonitor allstaff,includingbothfemaleandmaleEPs,for signsofwork-relatedstress,cognitiveoverload, andotherrelevantcommitments.
○ Emphasizeaddressingburnoutasawork-related issueratherthanagender-relatedone,especially whenthereisnoconfirmedevidenceofgenderspecificcauses.
3. OpenDiscussionsonBurnout:
○ Fosteranopen,non-judgmentaldialogueabout burnoutduringdepartmentalpeer-reviewsessions.
○ Ensurethatstaffatalllevelscansharetheir experienceswhilemaintainingpsychologicalsafety.
○ Addressburnoutopenlytopreventitfrombecoming a “silentcrisis.”
4. PsychologicalWellnessInitiatives:
○ Leadershipandmanagementshouldimplement psychologicalwellnessinitiatives,suchas “Joy@ Work,” iTHRIVEinitiatives,andwellnessgrants.
5. Peer-SupportCommittees:
○ Establishinterprofessionalpeer-supportcommittees orteams.
○ Encouragestafftodiscussburnoutwithpeers,who maybemoreapproachable,andsharebestpractices formanagingburnout.
AUTHORSANDAFFILIATIONSCONTINUED
SihamAzahaf,MD‡‡ SevilayVural,MD§§ BusraH.Difyeli,MD∥∥ LisaMoreno-Walton,MD¶¶
¶ AtaturkUniversity,DepartmentofEmergencyMedicine, Erzurum,Türkiye
# HCA/USFMorsaniCOM:GMEOakHillHospital, DepartmentofEmergencyMedicine,Brooksville,Florida **DhulikhelHospitalKathmanduUniversityHospital, DepartmentofGeneralPracticeandEmergencyMedicine, Kavre,Nepal
†† KarabukUniversity,FacultyofMedicine,Departmentof EmergencyMedicine,Karabuk,Türkiye
‡‡ AmsterdamUniversityMedicalCenters,Departmentof InternalMedicine,Amsterdam,Netherlands
§§ YozgatBozokUniversity,DepartmentofEmergency Medicine,Azizli,Türkiye
∥∥ AlmusStateHospital,DepartmentofEmergencyMedicine, Almus/Tokat,Türkiye
¶¶ LouisianaStateUniversityHealthSciencesCenter, SectionofEmergencyMedicine,NewOrleans,Louisiana
AddressforCorrespondence:SumanThakur,MD,IndiraGandhi MedicalCollege&Hospital,DepartmentofEmergencyMedicine, Shimla,India,171001.Email: Suman_thakur13@yahoo.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Thakuretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.FreudenbergerHJ.Staffburn-out. JSocIssues. 1974;3091:159–65.
2.MaslachC,JacksonSE,LeiterMP.(1997).Maslachburnoutinventory: 3rded.In EvaluatingStress:ABookofResources (191–218).Lanham, MD:ScarecrowEducation,1997.
3.CydulkaRK,D’OnofrioG,SchneiderS,etal.Womeninacademic emergencymedicine. AcadEmergMed. 2000;7(9):999–1007.
4.MadsenTE,LindenJA,RoundsK,etal.Currentstatusofgenderand racial/ethnicdisparitiesamongacademicemergencymedicine physicians. AcadEmergMed. 2017;24(10):1182–92.
5.SomvilleF,VanBogaertP,WellensB,etal.Workstressandburnout amongemergencyphysicians:asystematicreviewoflast10yearsof research. ActaClinBelg. 2024;79(1):52–61.
6.VerougstraeteDandHachimiIdrissiS.Theimpactofburn-outon emergencyphysiciansandemergencymedicineresidents:asystematic review. ActaClinBelg. 2020;75(1):57–79.
7.ZhangQ,MuMC,HeY,etal.Burnoutinemergencymedicine physicians:ameta-analysisandsystematicreview. Medicine (Baltimore). 2020;99(32):e21462.
8.ThePRISMAstatementforreportingsystematicreviewsandmetaanalysesofstudiesthatevaluatehealthcareinterventions:explanation andelaboration. BMJ. 2009;339:b2700.
9.MunnZ,MoolaS,LisyK,etal.Chapter5:systematicreviewsof prevalenceandincidence.In:AromatarisEandMunnZ.(Eds.). JBIManualforEvidenceSynthesi. 2020.
10.BragardI,DupuisG,FleetR.Qualityofworklife,burnout,andstressin emergencydepartmentphysicians:aqualitativereview. EurJEmerg Med. 2015;22(4):227–34.
11.ShanafeltTD,BooneS,TanL,etal.BurnoutandsatisfactionwithworklifebalanceamongUSphysiciansrelativetothegeneralUSpopulation. ArchInternMed. 2012;172(18):1377–85.
12.MoukarzelA,MicheletP,DurandAC,etal.Burnoutsyndromeamong emergencydepartmentstaff:prevalenceandassociatedfactors. BiomedResInt. 2019;2019:6462472.
13.AlomarM,AlkandariF,AsfoorMA,etal.Howemergencyphysicians’ gendershapedbypatientsattendingemergencydepartmentsin culturallyconservativesociety. TraumaEmergCare. 2018;3(2):1–5.
14.HoffTandLeeDR.Burnoutandphysiciangender:whatdoweknow? MedCare. 2021;59(8):711–20.
15.GettelCJ,CourtneyDM,AgrawalP,etal.Emergencymedicine physicianworkforceattritiondifferencesbyageandgender. Acad EmergMed. 2023;30(11):1092–100.
16.DoraiswamyS,ChaabnaK,JitheshA,etal.Physicianburnoutin theEasternMediterraneanregion:influenceofgenderandrelated factors-systematicreviewandmeta-analysis. JGlobHealth. 2021;11:04043.
17.RotensteinLS,TorreM,RamosMA,etal.Prevalenceofburnoutamong physicians:asystematicreview. JAMA. 2018;320(11):1131–50.
18.BaturA,AksanA,MeneksedagY,etal.Impostorphenomenonand burnoutsyndromeamongemergencyphysicians:across-sectional study. ArchEnvironOccupHealth. 2023;78(7–8):379–88.
19.deWitK,MercuriM,WallnerC,ClaytonN,ArchambaultP, RitchieK,etal.Canadianemergencyphysicianpsychologicaldistress andburnoutduringthe first10weeksofCOVID-19:amixed-methods study. JAmCollEmergPhysiciansOpen. 2020;1(5):1030–8.
20.ElhadiM,MsherghiA,ElgzairiM,etal.Thementalwell-beingoffrontline physiciansworkingincivilwarsundercoronavirusdisease2019 pandemicconditions. FrontPsychiatry. 2020;11:598720.
21.ErdurB,ErginA,YükselA,etal.Assessmentoftherelationofviolence andburnoutamongphysiciansworkingintheemergencydepartments inTurkey. UlusTravmaAcilCerrahiDerg. 2015;21(3):175–81.
22.FeeksC,ChaoJ,SinertR.Prevalenceandriskfactorsforburnoutin pediatricemergencymedicinefellows. Pediatr EmergCare. 2020;36(5):236–9.
23.GoldbergR,BossRW,ChanL,etal.Burnoutanditscorrelatesin emergencyphysicians:fouryears’ experiencewithawellnessbooth. AcadEmergMed. 1996;3(12):1156–64.
24.IyerS,SulemanS,QiuY,etal.Riskfactorsforphysicianburnout:a perspectivefromTanzania. PanAfrMedJ. 2022;41:298.
25.JaliliM,SadeghipourRoodsariG,BassirNiaA.Burnoutandassociated factorsamongiranianemergencymedicinepractitioners. IranJPublic Health. 2013;42(9):1034–42.
26.TakayesuJK,RamoskaEA,ClarkTR,etal.Factorsassociatedwith burnoutduringemergencymedicineresidency. AcadEmergMed. 2014;21(9):1031–5.
27.LiuR,VanAarsenK,SedranR,etal.Anationalsurveyofburnout amongstCanadianRoyalCollegeofPhysiciansandSurgeonsof Canadaemergencymedicineresidents. CanMedEducJ. 2020;11(5):e56–61.
28.LovellLP,AtherleyAEN,WatsonHR,etal.Anexplorationofburnout andresilienceamongemergencyphysiciansatthreeteachinghospitals intheEnglish-speakingCaribbean:across-sectionalsurvey. Lancet RegHealthAm. 2022;15:100357.
29.LuDW,ZhanT,BilimoriaKY,etal.Workplacemistreatment, careerchoiceregret,andburnoutinemergencymedicine residencytrainingintheUnitedStates. AnnEmergMed. 2023;81(6):706–14.
30.MercuriM,ClaytonN,ArchambaultP,etal.Canadianemergency medicinephysicianburnout:asurveyofCanadianemergency physiciansduringthesecondwaveoftheCOVID-19pandemic. CJEM. 2022;24(3):288–92.
31.MorikawaM,UechiT,HanakiN,etal.BurnoutamongJapanese emergencymedicinephysicians:amulticentricquestionnairestudy. AcuteMedSurg. 2023;10(1):e848.
32.Salmoirago-BlotcherE,FitchettG,LeungK,etal.Anexplorationofthe roleofreligion/spiritualityinthepromotionofphysicians’ wellbeingin emergencymedicine. PrevMedRep. 2016;3:189–95.
33.SarwarS,MahmoodA,RajaMF,etal.Burnoutandhealthrelated qualityoflifeamongemergencyphysiciansworkingatemergency attertiarycarehospitalinLahore,Pakistan. PakJMedSci. 2023;39(5):1372–7.
34.SoltanifarA,PishbinE,AttaranMashhadiN,etal.Burnoutamong femaleemergencymedicinephysicians:anationwidestudy. Emerg MedAustralas. 2018;30(4):517–22.
35.YanS,ShenX,WangR,etal.Challengesfacedbyemergency physiciansinChina:anobservationfromtheperspectiveofburnout. FrontPsychiatry. 2021;12:766111.
36.Li-SauerwineS,RebillotK,MelamedM,etal.A2-questionsummative scorecorrelateswiththemaslachburnoutinventory. WestJEmerg Med. 2020;21(3):610–7.
37.MaslachC,JacksonSE,LeiterMP,etal.MaslachBurnoutToolkit™ formedicalpersonnel:2024MindGarden,Inc.2024.Availableat: https://www.mindgarden.com/329-maslach-burnout-toolkit-formedical-personnel#horizon.AccessedJuly14,2024.
StephenD.Hallisey,MD*†
ChristianaK.Prucnal,MD,ScM†‡§
AnnetteM.Ilg,MD*†
RaghuR.Seethala,MD,MSc*†
PaulS.Jansson,MD,MS*†
SectionEditor:ChristopherR.Tainter,MD
*BrighamandWomen’sHospital,DepartmentofEmergencyMedicine, DivisionofEmergencyCriticalCareMedicine,Boston,Massachusetts
† HarvardMedicalSchool,DepartmentofEmergencyMedicine, Boston,Massachusetts
‡ BrighamandWomen’sHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts
§ MassachusettsGeneralHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts
Submissionhistory:SubmittedJuly12,2024;RevisionreceivedNovember20,2024;AcceptedNovember26,2024
ElectronicallypublishedJanuary30,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.29328
Introduction: Non-depolarizingagentssuchasrocuroniumandvecuroniumarefrequentlyusedinthe emergencydepartment(ED)tofacilitateintubationbutmayleadtodelayinneurologicexaminationand intervention.Sugammadexisusedforreversalofneuromuscularblockadebynon-depolarizingagents butitsroleinthereversalofneuromuscularblockadeforneurologicexaminationintheEDis poorlydefined.
Methods: Thiswasamulticentercohortstudyusingretrospectivechartreview.WereviewedallED encountersfromJune21,2016–February9,2024oftheelectronichealthrecordofMassGeneral Brigham,alargemultistatehealthsystem,andabstractedallEDadministrationsofsugammadexto facilitateneurologicexamination.Wecalculateddescriptivestatisticsandassessedoutcomes.
Results: In3,080,338EDvisitsduringthestudyperiod,48patientsreceivedsugammadextofacilitate neurologicexamination.Ofthosepatients,23(47.9%)underwentaprocedurewithin24hours.Three (6.3%)hadbradycardia,andone(2.1%)hadhypotensionfollowingsugammadexadministration.Atotal of23patients(47.9%)ultimatelydiedduringtheiradmission,and24(50%)diedwithin30days.
Conclusion: PatientswhoreceivedsugammadexintheEDtofacilitateneurologicexaminationduring thestudyperiodhadrareassociatedadverseeffects,highratesofprocedureswithin24hoursof administration,andsignificantin-hospitalmortality.Prospectivedataisneededtoassesstheimpactof sugammadexondecision-making.[WestJEmergMed.2025;26(2)347–352.]
Neuromuscularblockade(NMB)isfrequently administeredaspartofrapidsequenceinductioninthe emergencydepartment(ED)andprehospitalsettings.Nondepolarizingaminosteroidneuromuscularblockingagents (NMBA)suchasrocuroniumandvecuroniumare commonlyadministeredtofacilitateintubationintheED,1 butadministrationmayleadtoprolongedparalysis anddelayinneurologicexaminationandsurgical
decision-makinginpatientspresentingwithneurological injury.Sugammadexisamodifiedgamma-cyclodextrinused forthereversalofNMBfromaminosteroidNMBAs.2 When comparedtoacetylcholinesteraseinhibitorssuchas neostigmine,sugammadexisassociatedwithfastertimeto reversal,longerdurationofaction,andlowerratesof cholinergicsideeffectssuchasbradycardia,nausea,and vomiting.3 Asaresult,itdoesnotrequirethe co-administrationofatropineorglycopyrrolate.Itis
currentlyrecommendedoverneostigmineasa first-lineagent forthereversalofrocuroniumintheoperatingroom.4 Despitethisrecommendation,littleisknownabouttheuseof sugammadexintheED.
Tworecentstudieshavehighlightedthepotentialforits useintheEDsetting.5,6 Ourrecentreviewoftheuseof sugammadexintheEDfoundthatthemostcommon indicationwasforneurologicexamination,with93.7%of patientsreceivingsugammadexforthisindication.7 Inthat series,wefoundthattheuseofsugammadexforother indicationswasrare:onepatientreceivedsugammadexafter inadvertentNMBadministration;onereceivedsugammadex tofacilitateterminalextubation;andonereceived sugammadexfollowingincompletereversalofNMBatan ambulatorysurgerycenter.Nopatientsreceived sugammadexforacannot-intubate-cannot-ventilate scenario.Onlytwosmallstudieshavedescribedtheuseof sugammadextofacilitateneurologicalexamination.A retrospectivestudyof11patientsreceivingsugammadexin theEDforneurologicalexaminationfoundthatthe majorityofpatientswhoreceivedsugammadexhad achangeintheirexaminationandconcludedits administrationtobeuseful.8 Asecondretrospectivestudy thatevaluateditsusein24patientsfoundthatdosingof2 milligramsperkilogram(mg/kg)and4mg/kgwereequally effectiveinachievingatrainoffour(TOF)offour.9 We soughttofurtherdefinethesafety,efficacy,andoutcomesof sugammadexusetofacilitateneurologicexaminationin theED.
Thiswasamulticentercohortstudyusingretrospective chartreview.Weadheredtoallelementsofoptimal retrospectivechartreviewinemergencymedicineresearchas previouslydefinedbyWorsteretalwiththeexceptionof interobserverreliabilityuseandtesting,aschartabstraction wasperformedbyoneauthor.10 Weperformedastructured chartabstractionofallEDencountersbetweenJune21,2016 (thedateofsugammadexadditiontotheformulary)and February9,2024,intheelectronichealthrecord(EHR)(Epic Systems,Verona,WI)ofMassGeneralBrigham,alarge multistateregionalhealthsystemwithtwoaffiliated academicmedicalcentersandsevenaffiliatedcommunity, acutecarehospitals.
Weusedchartabstractiontoidentifyalladministrations ofsugammadexduringanEDencounter.Chartswere manuallyreviewedbytheseniorauthor(PSJ)toverifyusage ofsugammadextofacilitateneurologicalexamination. Patientdemographics,dosingweight,andlaboratoryvalues wereautomaticallyabstractedfromtheEHRforthelinked EDencounter.ForNMBAsadministeredwithinthe healthsystem,dosingweight,doseadministered, andtimeofadministrationwereautomatically abstractedfromthelinkedrecordoftimeofmedication
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Littleisknownabouttheuseofsugammadex intheED.Priordatahasshownitismost commonlyusedtofacilitateneurologicexam.
Whatwastheresearchquestion?
Whataretheoutcomesofpatientswhoreceive sugammadexforneurologicexamintheED?
Whatwasthemajor findingofthestudy?
47.9%ofpatientswhoreceivedsugammadex intheEDultimatelyunderwentaprocedure within24hours,and50%diedwithin30days.
Howdoesthisimprovepopulationhealth?
Thisstudyprovidesinputontheoutcomesof patientsreceivingsugammadexintheEDfor neurologicexam,whichisdonerarelyandin high-acuityandtime-sensitive clinicalsituations.
administrationintheEHR.ForNMBAsadministered outsideofthehealthsystem,linkedEHRs, triagenotes,andambulancerunreportsweremanually reviewedtodeterminedoseandtimingof NMBadministration.
Manualchartreviewandabstractionwasthenperformed bythe firstauthor(SDH)todeterminetheneurological injurytype,proceduretypeandtiming,majoradverseevents, mortality,andin-hospitalchangestoacomfort-oriented codestatus.
Wherepossible,GlasgowComaScale(GCS)was abstractedfromnursingandphysiciannotes.Wecalculateda modifiedRankinScale(mRS)basedonthephysical examinationandphysicaltherapynotesincludedinthe dischargesummary.Descriptivestatisticswerecalculated. ThisresearchwasapprovedbytheMassGeneralBrigham institutionalreviewboard.
FromJune21,2016–February9,2024,therewere 3,080,338EDvisitsatMassGeneralBrigham-affiliated acute-carehospitals.Forty-eightpatientsreceived sugammadextofacilitateneurologicalexamination.The mean(±SD)ageatadministrationwas59.9(±20.9) yearsofage(range21–94years).Sixteenpatients (33.3%)werefemale,and32patientsweremale (66.7%)(Table).
Table. Patientcharacteristics.
Age,mean(SD),years
Sex, n(%)
59.9(20.89)
Male 32(66.7%)
Female
Weight,mean(SD)kg
Sugammadexdose,mean(SD),mg 345.63(200)
Sugammadexdose,mean(SD),mg/kg 4(2.8)
Neurologicinjury,n(%)
Subduralhematoma 6(12.5%)
Subarachnoidhemorrhage 7(14.6%)
Multicompartmentalhemorrhage 15(31.3%)
Intraparenchymalhemorrhage 11(22.9%)
Ischemicstroke 3(6.3%)
Cervicalspineinjury
Other 3(6.3%)
Trauma,n(%) 25(52%)
Mortality,n(%)
Within72hoursofsugammadex
Within30daysofsugammadex
Changetocomfortmeasuresonly,n(%)
Within72hoursofsugammadex 16(33.3%)
Duringhospitalization 22(45.8%)
Locationofparalytic,n(%)
Outsidehospital
GCS,median,whenrecorded
Pre-sugammadex
Post-sugammadex
Changepre-/post-sugammadex
Procedureperformed,n(%)*
Craniotomy
Externalventriculardrain 7(14.6%)
Angiogram/embolization/thrombectomy 4(8.3%)
Spinalfusion/decompression 3(6.3%)
Other 5(10.4%)
*Somepatientshadmorethanoneprocedure.
GCS, GlasgowComaScore; kg,kilogram; mg,milligram.
Dosing,Timing,andLocation
Themeandosingweight(±SD)was77.3kgs(±18.9kg). RocuroniumwasthemostcommonNMBAtobereversed, usedin46ofthe48patients(95.8%).Wewereabletoabstract accuratedosingofrocuroniumfor35patients,andthemean
(±SD)dosewas104.7mg(±18.3mg)orameanof 1.37mg/kg(±0.30mg/kg).Accuratedosingofvecuronium wasobtainedfromonepatient,whoreceived 10mg(0.13mg/kg).
Sugammadexwasgivenatameandoseof346mg(range 100–2,000mg,interquartilerange[IQR]200–377.5mg).The mostcommondosewas4mg/kg(25patients)withamean doseof4mg/kg(range2–18mg/kg,IQR2.8–4mg/kg).The NMBandsugammadexwereadministeredinthesameED encounterfor15patients.ForNMBgiveninalternate contexts,themostcommonlocationwasprehospital (18patients),atareferringhospital(13patients),andduring interfacilitytransport(twopatients).Alldosesof sugammadexwereadministeredinthetwoacademicmedical centerEDs.Wewereabletoobtainaccuratetimeof administrationforbothNMBandsugammadex for22patients.Themean(range, ±SD)timefrom NMBtosugammadexadministrationwas109.9 (31–283, ±66.8)minutes.
Withregardtohepaticandrenalclearance,allpatients hadacreatininelevelobtainedduringtheEDvisit,and46of 48(96%)hadtransaminaselevelsobtained.Thirty-three patientshadnormaltransaminaselevels(definedasboth aspartateaminotransferaseandalanineaminotransferase < 50unitsperliter)and35patientshadnormalcreatinine levels(definedas < 1.2mg/deciliter).
Theprimaryneurologicalinjuryvaried,butthemajority (40,83.3%)ofpatientspresentedwithintracranial hemorrhage.Three(6.3%)presentedwithacuteischemic strokes;twopatients(4.2%)hadextracranialvascularinjury; onewithaTypeAaorticdissectioncausingcommoncarotid arteryocclusionandonewithavertebralarterydissection andpseudoaneurysm.Two(4.2%)patientshadprimary spinalcordtrauma,andonepatient(2.1%)presentedwitha brainmass.Twenty-five(52.1%)ofthepatientspresented followingtrauma.
AnaccurateGCSwasobtainedbeforeadministrationof sugammadexin43(89.6%)patientsandwas3tinallbutone (whowas4t).AnaccurateGCSwasobtainedafter administrationofsugammadexin35(72.9%)patientswitha mean(±SD)of6.4(±2.4).Thirty-four(70.8%)hadareliable GCSobtainedbeforeandafteradministrationof sugammadex;themean(range, ±SD)increaseinGCSwas 3.38( 1to +8, ±2.5)points.
Twenty-threepatients(47.9%)underwentaninvasive procedurewithin24hoursofsugammadexadministration, andanotherthree(totalof26or54.2%)underwenta procedurewithin72hours(Table1).Twelvepatients(25.0%) died within72hoursofsugammadexadministration,while 24patients(50%)diedwithin30days.Thecodestatuswas
changedto “comfortmeasuresonly” for16patients(33.3%) within72hoursofsugammadexadministration,andfor22 patients(45.8%)duringthehospitalization.Adverseevents wererare,withtwo(4.1%)patientsexperiencinghypotension aftersugammadexadministration,four(8.2%)patients experiencingbradycardia,andnopatientsexperiencing cardiacarrest.
ThemRSforneurologicdisability11,12 atdischarge (rangingfrom0–6,withhigherscoresindicatingmoresevere disability),excludingallpatientswithadischargemRSof6 (deceased),wasanaverageof3.9(SD ±1.36),whereascore of4indicatesmoderatelyseveredisability.
Non-depolarizingNMBAsarefrequentlyusedinboththe EDandprehospitalsettingduringairwaymanagementof neurologicallyinjuredpatients.Theuseofnon-depolarizing NMBAsleadstoprolongedparalysis,whichimpairs accurateneurologicexaminationessentialtoguideemergent andtime-sensitivetherapyforneurologicinjury.Beyond neurologicexaminationbeingacriticalpartofdecisionmakingregardingtherapy,prognosisrelatedtoinitial neurologicexaminationmaybevaluabletofamiliesasthey considerearlygoalsofcare.Thisisreflectedinourdatasetas 33.3%ofpatientsreceivingsugammadexwhosestatuswas changedto “comfortmeasuresonly” within72hoursof receivingsugammadex.
Rocuronium,themostcommonlyusedNMBAinour cohort,hasanexpecteddurationofactionof30–60 minutes.13 However,longerdurationofactionhasbeenwell described.14–17 Thetimetoadministrationofsugammadexin ourstudyreflectsthis,aspatientsreceivedsugammadexas longas283minutesfollowingrocuroniumadministration withchangeinneurologicexamination.Additionally,we wereunabletoobtainaccuratetimesforsomeprehospital andreferringhospitaladministrationsofneuromuscular blockade,whichmayhavebiasedtheresultstowardthose administeredinthesameEDencounter.Thispotentially extendeddurationofactionforNMBwasunlikelydueto impairmentsofrenalorhepaticmetabolismasthesewas predominantlynormalinourcohort;instead,itmayhave beenduetohigherNMBdosesused,greaterpatientage,or touncharacterizedhypothermiaorhypovolemia,thelatter ofwhichwasnotcapturedinourstudy.18–20 Alldosesof sugammadexoccurredatthetwoacademicmedicalcenters. Weattributedthistobothhospitalsbeingreferralcentersfor neurosurgicaltraumaandforpost-strokecare.Becauseof this,weareunabletodrawanyconclusionsaboutitsusein communityhospitals.
Ourstudyreplicatedprevious findingsseenintherelevant literatureincludingthatsugammadexuseintheEDfor neurologicexamisoverallrareandappearsmostprevalentat academicmedicalcenters.Thislikelyreflectsthecapacityfor advancedtherapeuticsandneurosurgicalinterventionfor
whichrapidNMBreversalforneurologicexamisindicated atthesecentersandthatadverseeffectsassociatedwithitsuse arerare.5,7
AlimitationofourstudywaslackofrecordedTOF monitoring.WithoutTOFmonitoring,itisdifficultto commentonwhetherthesugammadexdosesadministered wereadequateatfullyreversingNMB.Becauseofthe retrospectivenatureofthestudy,wewereunableto determinetheexacttimeofneurologicalexamination. Additionally,itispossiblethatdocumentedchangeinGCS wasduetootherfactorssuchaschangesinsedationor underlyingneurologicstatus.Anadditionallimitationofour studywasthatrecordedGCSwasbasedonexamsperformed bymanydifferentindividualswithvariabletraining backgroundsincludingnursing,emergencymedicine residentsandattendings,neurologyandneurosurgery residents,andneurosurgeryattendings.Further,thepre-and post-GCSwasoftenbasedonexaminationsperformedby separateindividuals,andvariationinexambetween clinicianscouldhavecontributedtochangeinGCS,rather thantrueclinicalchange.TimeofGCSexaminationswas alsonotrecorded,whichalsomayhaveaffectedtheresultsof theexamaftersugammadexadministration.Althoughour cohortdescribessugammadexuseamongpatientswitha rangeofneurologicalpathology,wedidnotcaptureany patientswithstatusepilepticusastheunderlyinginjury,one potentiallyrelevantdiseasecategoryforwhichNMBreversal hasbeenpreviouslydescribed.5
Anadditionallimitationwaslackofbispectralindex monitoringordataregardingawarenessduringparalysis. AwarenessduringparalysisisknowntooccurinEDpatients receivingmechanicalventilation,withrocuroniumbeing associatedwithincreasedfrequencyofawarenessduring paralysis.21 Furthermore,theimpactoftheuseof sugammadexonclinicaldecision-makingwasdifficultto determinegiventheretrospectivenatureofthestudy. Accurateneurologicalexaminationisanessential aspectofclinicaldecision-makingduringneurologic emergenciesandlikelyplayedanimportantroleinclinical courseregardlessofwhetherinterventionwasperformed followingrepeatexam.Prospectiveresearchisneededto determinetheimpactofsugammadexonclinical decision-making.
Despitetheselimitations,sugammadexadministration waswelltolerated,withrareadverseeffects.Althoughthere weretwoepisodesofhypotensionandfourepisodesof bradycardia,itwasdifficulttodeterminewhetherthesewere attributabletosugammadexgivenpossibleconfounderssuch assedationadministrationandunderlyingcriticalillness. Overall,thecohortwasassociatedwithhighacuityreflective ofthecriticalnatureofneurologicemergenciesrequiring intubation.Mortalitywashighinthiscohort,andmRSat
dischargewasreflectiveofmanypatientshavingsevere disabilityatdischarge.Despitehighmortalityandsevere disabilityinsurvivors,itisdifficulttoconsidersugammadex administrationandsubsequentproceduresasfutileassome patientsmaygoontorecoverconsiderablywith aggressiverehabilitation.
Administrationofsugammadextofacilitateneurologic examinationisarareoccurrenceintheED.Inthis multicenter,retrospectivestudy,wefoundthatpatientswho receivedsugammadexintheEDduringthestudyperiodhad infrequentassociatedadverseeffects,highratesof procedureswithin24hoursofadministration,andsignificant in-hospitalmortality.ChangeinGlasgowComaScalewas observeddespitemostpatientsinthiscohortreceiving sugammadexgreaterthanonehourafterNMB administrationwithamaximalobservedintervalofgreater thanfourhoursafterNMBadministration.Codestatus ultimatelychangedto “comfortmeasuresonly” fornearly halfofthesepatientsand,onaverage,patientsdischarged fromahospitalizationwheresugammadexhadbeen administeredintheEDhadmoderatelysevereneurologic disability.Prospectivedataisneededtoassesstheimpactof sugammadexondecision-making.
AddressforCorrespondence:StephenD.Hallisey,MD,Brigham andWomen’sHospital,DepartmentofEmergencyMedicine, DivisionofEmergencyCriticalCareMedicine,75FrancisSt., Boston,MA02115.Email: shallisey@mgb.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Halliseyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BrownCA,BairAE,PallinDJ,etal.Techniques,success,andadverse eventsofemergencydepartmentadultintubations. AnnEmergMed. 2015;65(4):363–70.e1.
2.NicholsonWT,SprungJ,JankowskiCJ.Sugammadex:anovelagent forthereversalofneuromuscularblockade. Pharmacotherapy. 2007;27(8):1181–8.
3.IwasakiH,RenewJR,KunisawaT,etal.Preparingforthe unexpected:specialconsiderationsandcomplicationsafter sugammadexadministration. BMCAnesthesiol. 2017;17(1):140.
4.ThilenSR,WeigelWA,ToddMM,etal.2023AmericanSocietyof Anesthesiologistspracticeguidelinesformonitoringandantagonismof neuromuscularblockade:areportbytheAmericanSocietyof AnesthesiologistsTaskForceonNeuromuscularBlockade. Anesthesiology. 2023;138(1):13–41.
5.ChenB.Sugammadex:alimitedbutimportantrole inemergencymedicine. PediatrEmergCare. 2020;36(6):296–301.
6.LentzS,MorrissetteKM,PorterBA,etal.Whatistheroleof sugammadexintheemergencydepartment? JEmergMed. 2021;60(1):44–53.
7.JanssonPS,PimentelMPT,SeethalaRR.Emergencydepartment usageofsugammadexinalargeregionalhealthsystem. AcadEmerg Med. 2024;31(7):713–5.
8.FalksenJAandSchomerKJ.Neurologicexaminationfacilitatedby reversalofrocuroniumwithsugammadex. JPharmPract. 2024;37(4):880–4.
9.HileGB,OstinowskyME,SanduskyNP,etal.Evaluationof sugammadexdosingforneurologicalexaminationintheemergency department. JPharmPract. 2024;37(4):838–44.
10.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
11.BanksJLandMarottaCA.Outcomesvalidityand reliabilityofthemodifiedRankinscale:implicationsforstroke clinicaltrials:aliteraturereviewandsynthesis. Stroke. 2007;38(3):1091–6.
12.vanSwietenJC,KoudstaalPJ,VisserMC,etal.Interobserver agreementfortheassessmentofhandicapinstrokepatients. Stroke. 1988;19(5):604–7.
13.TevaParentalMedicines.(2008). Rocuronium[packageinsert].Irvine, CA:TevaParentalMedicines,Inc.
14.MoralesMartínAC,VaqueroRonceroLM,MurielVilloriaC.Extremely prolongedneuromuscularblockadeafterrocuronium:Acasereport. ActaAnaesthesiolScand. 2009;53(7):957–9.
15.OlivieriLandPlourdeG.Prolonged(morethantenhours) neuromuscularblockadeaftercardiacsurgery:reportoftwocases. Can JAnaesth. 2005;52(1):88–93.
16.CooperRA,MaddineniVR,MirakhurRK,etal.Timecourseof neuromusculareffectsandpharmacokineticsofrocuronium bromide(Org9426)duringisofluraneanaesthesiainpatients withandwithoutrenalfailure. BrJAnaesth. 1993;71(2):222–6.
17.RobertsonEN,DriessenJJ,BooijLHDJ.Pharmacokineticsand pharmacodynamicsofrocuroniuminpatientswithandwithoutrenal failure. EurJAnaesthesiol. 2005;22(1):4–10.
18.JainA,WermuthHR,DuaA,etal.Rocuronium.In: StatPearls[Internet] TreasureIsland,FL:StatPearlsPublishing,2024.
19.BaykaraN,SolakM,TokerK.Predictingrecoveryfromdeep neuromuscularblockbyrocuroniumintheelderly. JClinAnesth. 2003;15(5):328–33.
20.VestedM,PapeP,KristensenCM,etal.Rocuronium0.3or0.9mg/kg comparingonsettime,durationofaction,andintubatingconditionsin patients80yearsandolder:arandomizedstudy. ActaAnaesthesiol Scand. 2022;66(7):811–7.
21.PappalRD,RobertsBW,MohrNM,etal.TheED-AWARENESSstudy: aprospective,observationalcohortstudyofawarenesswithparalysisin mechanicallyventilatedpatientsadmittedfromtheemergency department. AnnEmergMed. 2021;77(5):532–44.
Ba ¸ sakBayram,MD*
MuratCetin,MD†
ÖnderLimon,MD‡
BritLong,MD§
MichaelGottlieb,MD∥
* IzmirMetropolitanMunicipalityE ¸ srefpa ¸ saHospital,Izmir,Türkiye
† Dr.BehçetUzChildren’sEducationandResearchHospital,DepartmentofEmergency Medicine,Konak,Izmir,Türkiye
‡ IzmirUniversityofEconomics,FacultyofMedicine,MedicalpointHospital,Departmentof EmergencyMedicine,Kar ¸ sıyaka,Izmir,Türkiye
§ SanAntonioUniformedServicesHealthEducationConsortium,DepartmentofEmergency Medicine,FortSamHouston,Texas
∥ RushUniversityMedicalCenter,DepartmentofEmergencyMedicine,Chicago,Illinois
SectionEditor:SoheilSaadat,MD,MPH,PhD
Submissionhistory:SubmittedMay15,2024;RevisionreceivedDecember6,2024;AcceptedDecember13,2024
ElectronicallypublishedFebruary14,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.21201
Introduction: Alternativemetrics(altmetrics)haveemergedasinvaluabletoolsforassessingthe influenceofscholarlyarticles.InthisstudyweaimedtoevaluatecorrelationsbetweenAltmetricAttention Scores(AAS),andsourcesandactualcitationsinarticlesdisplayingthehighestAASwithinemergency medicine(EM)journals.
Methods: WeconductedananalysisofEMjournalslistedintheScienceCitationIndexExpanded (SCIE)usingtheAltmetricExplorertool.Weanalyzedthejournalsthatreceivedthehighestnumberof mentions,thesourcesofAAS,theregionsmostfrequentlymentioned,andthegeographicaldistribution ofmentions.Inthesubsequentstageofouranalysis,weconductedanexaminationofthe200toprankedarticlesthathadreceivedhighAASandwerepublishedinSCIEEMjournalsfromJanuary1, 2013–January1,2023.WesoughttodeterminethecorrelationsbetweentheAASandthecitationcounts ofarticlesonGoogleScholarandtheWebofScience(WOS).
Results: Of40,840researchoutputsevaluated,therewere510,047sharesacrossmultipleplatforms. TheAASwerepresentfor36,719articles(89.9%),while10.1%hadnoscore.Inthereviewofthetop200 articleswiththehighestAAS,themedianscorewas382.5(interquartilerange301.3–510.8).Ofthe researchoutputevaluated,38%wereobservationalstudies,13%casereports,and13%reviews/metaanalyses.Themostcommonresearchtopicswereemergencydepartment(ED)managementand COVID-19.TherewasnocorrelationbetweenAASandWOScitationnumbers(rs = 0.041, P = 0.563, 95%confidenceinterval[CI] 0.175–0.087).TherewasaweakcorrelationidentifiedbetweenWOS citationsandmentionsonX,andamoderatecorrelationobservedforWOScitationsandblogmentions (rs = 0.330, P < .001,95%CI0.174to0.458;rs2 = 0.109,andrs = 0.452, P < .001,95%CI0.320–0.566; andrs2 = 0.204,respectively).However,wefoundastrongpositivecorrelationbetweenWOScitations andthenumberofMendeleyreaders(rs = 0.873, P < .001,95%CI0.82–0.911,rs2 = 0.762).
Conclusion: WhilemostarticlesinEMjournalsreceivedanAAS,wefoundnocorrelationwithtraditional citationmetrics.However,Mendeleyreadershipnumbersshowedastrongpositivecorrelationwith citationcounts,suggestingthatacademicplatformengagementmaybetterpredictscholarlyimpact. [WestJEmergMed.2025;26(2)353–363.]
Alternativemetrics(altmetrics)emergedintheearly2010s inresponsetothelimitationsoftraditionalcitation-based metrics.1 Altmetricsuseabroadersetofindicatorssuchas pageviews,downloads,socialmediamentions,newsmedia coverage,andexpertrecommendationstoprovideamore comprehensiveunderstandingofanarticle’sinfluence. 2 PlatformslikeAltmetric.comandPlumAnalyticsprovide toolsforevaluatingthereachandimpactofscholarly articles,helpingtotracktheironlinedisseminationinreal time.Anincreasingamountofevidenceindicatesthat maintaininganactiveonlinepresencecandirectlyinfluencea researcher’scredentialsasevaluatedbyconventional measures. 3 Byconsideringvariousaspectsbeyondcitations alone,altmetricsprovidesresearchersandinstitutionswitha moreholisticassessmentoftheirwork’ssocietalimpact. Whilethepurposeofthesemetricsistomeasuresocial impact,earlysocialmediavisibilityafterpublicationcanalso increaseandpredictcitations.4 Assessingtheseactivities couldprovidefasterevaluationsofanarticle’simpactand predictcitations,servingasanearlyidentifierforemerging areasofresearchgrowth.5
Withinthemedical fieldspecifically,thesemetricsoffer insightsintobothscholarlyrecognitionandpublicreception ofresearch findings.Moreover,therelationshipbetween thesemetricsunderscoresthechanginglandscapeof scholarlycommunication,asresearchers,clinicians,andthe publicalikeengagewithandcontributetothedissemination ofresearch findingsthroughonlineplatforms.Withthe growthofdigitalcommunicationandsocialmedia,thespeed andthescaleofinformation-sharinghaveaccelerated, makingaltmetricsaninvaluabletoolforassessingreal-time impactofarticles.6 Emergingtrendscanbekeytoamore efficientlyfunctioning fieldofmedicine.7 Emergencymedicine(EM)thrivesonthetimely disseminationofresearchandinformationthatdirectly impactspatientcare.8 The firstaltmetricsanalysisinEM conductedbyBarbicetalfoundthatthemost-citedarticles onsocialmediainEMfrom2011wereoftenpublishedin non-EMbiomedicaljournals.9 Althoughthismaysuggest thatauthorsinthe fieldofEMselecthigh-impactjournalsto increasetheeffectivenessoftheirpublications,altmetric scoresandjournalimpactfactorsarenotcorrelated.10 The socialimpactofanarticlemaybebetterassessedbyfocusing onindividualaltmetricscoresourcesratherthantheoverall score. 11 Thiswassupportedbyarecentstudythatfounda directcorrelationbetweenX(formerlyTwitter)mentions andarticlecitationsamongEMresearch.12 Ouraiminthis studywastoinvestigatethecorrelationsbetweenthe altmetricscores,theirsources,andcitations.
Inthe firststageofthestudy,weusedtheAltmetric ExplorertoolfromAltmetric.com(AltmetricLLP,London,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Altmetricsemergedinthe2010stoaddress thelimitationsoftraditionalcitation-based metricsinevaluatingresearchimpact.
Whatwastheresearchquestion?
Weexploredthecorrelationsbetween AltmetricAttentionScores,theirsources,and citationcountsforarticlespublishedin EMjournals.
Whatwasthemajor findingofthestudy?
NocorrelationwasfoundbetweenAASand WebofScience;itwasweakforXmentions, moderateforblogs,butstrongforMendeley readership(r s = 0.873,95%CI0.822 – 0.911).
Howdoesthisimprovepopulationhealth?
Focusingonarticledisseminationthrough individualaltmetricsources,ratherthantotal scores,canhelpresearchersmoreeffectively reachtheirtargetaudiences.
UK)toassesstheAltmetricAttentionScores(AAS)of scholarlyarticlespublishedinEMjournalsindexedinthe ScienceCitationIndexExpanded(SCIE).TheAASisa metricthatevaluatestheattentionaresearchoutputreceives usingaweightedsystemthatassignsdistinctvaluestovarious sources,suchasnewsoutlets,blogs,andsocialmedia platforms.Sourceswithgreaterimpact,suchasnewsarticles, areattributedhigherweightscomparedtosocialmedia mentions.Thescoreiscalculatedbyasophisticated algorithmthatfactorsinnotonlythenumberofmentionsbut alsovariablessuchasduplicatepostsandthecredibilityof thenewssources.13
AllAltmetricExplorerassessmentswereconductedand downloadedasaCSV fileonSeptember2,2023.Theinitial analysisfocusedonexaminingthedistributionofaltmetric databycountryandjournal,aswellasevaluatingthesources ofAASscoresovertime.The2022JournalCitation Indicator(JCI)scoresforthejournalswereobtainedfromthe WebofScience(WOS)MasterJournalList.TheseJCIscores representtheaveragecitationimpactofarticlespublished between2019–2021.
Inthesecondstageweidentifiedthetop200articleswith thehighestAASpublishedinSCIEEMjournalsbetween January1,2013–January1,2023.WeassessedtheAASof thesearticlesalongwiththesourcesoftheirmentions. Citationcountsforthesearticleswereevaluatedusingboth
WOSandGoogleScholar.Tocalculatetheannualcitation number,wedividedthetotalcitationcountsobtainedfrom thesearchenginesbythenumberofyearssincethearticles’ publication.Weobtainedfull-textaccessforthearticlesto determinethearticle’ssubject(eg,emergencydepartment management,trauma,toxicology,resuscitation,criticalcare, COVID-19)andtype(randomizedcontrolledtrial, observationalstudy,casereports,reviews(systematicreview andmeta-analysis).Additionally,wedeterminedthecountry ofthe first-namedauthorofeacharticle.
WeassessedthecorrelationbetweentheAASandcitation countsofthearticles.Furthermore,twoEMspecialistsfrom theresearchteamindependentlyreviewedtheAASandall screeningprocessesofthestudy.Incaseswherethetwo evaluatorsdidnotreachaconsensus,athirdEMspecialist conductedtheevaluation.Thestudywasapprovedbythe LocalEthicsCommitteeof ˙ IzmirProvincialHealth DirectorateDr.BehcetUzPediatricDiseasesandSurgery TrainingandResearchHospital.
WeperformedstatisticalanalysisusingSPSS29.0for Windows(SPSSStatistics,IBMCorp,Armonk,NY). CategoricalvariableswereevaluatedusingtheKolmogorovSmirnovtest.Amongthevariables,thosethat fitthenormal distributionwerepresentedasthemean ± standard deviation,andthosethatdidnot fitthenormaldistribution werepresentedasmedian(interval)ormedian(interquartile range[IQR]).WeusedMann-WhitneyUandKruskalWallisteststocomparenumericalvariables.Spearman correlationanalysiswasusedtoassesstherelationship betweenAAS,theirsources(mentions),andWOSand GoogleScholarcitationnumbers.Spearmancorrelation analysiswasusedtoanalyzedistributionsofAAS,thesource ofthescores(mentions),andWOSandGoogleScholar
citationnumbers.Weinterpretedthecorrelationsasweak, moderate,strong,andverystrongbasedontheresulting coefficients.14 Statisticalsignificancewasrecognized whenP < 0.05.
Ofthe40,840researchoutputsevaluated,510,047were sharedacrossmultipleplatforms.AltmetricAttentionScores werepresentfor36,719articles(89.9%),while10.1%hadno score.Theonlineengagementforthiscontentincluded 459,391tweetsfrom114,708uniquetweetersin206 countries,14,355Facebookpostson2,141uniquepagesin 60countries,19,571newsstoriesby1,988uniqueoutletsin86 countries,and2,791policydocumentsfrom79unique sourcesin18countries.Thetop10journalshadnomentions onPinterest,Syllabi,orLinkedIn.Onlytwojournals receivedmentionsontheChinesemicrobloggingplatform Weibo,eachmentionedonce. Figure illustratesthe frequencyofmentionscorrespondingtothe publicationyears.
TheAltmetrics–Xdemographicsdatarevealedthetop five countriescontributingtomentionsfortheanalyzedcontent. Thecountrywasnotspecifiedin193,148posts(42.0%)and 54,517profiles(47.5%).Thelargestnumberofpostswere fromtheUnitedStates(Table1).
Overall,90%ofthe36,780articleshadanAAS ≥ 1.The median(IQR)valuesforthesearticleswereasfollows:AAS3 (1–9),Xmentions3(1–9);Mendeleyreadership24(9–50); Dimensionscitations5(1–15);andblogmentions0(0–24). WefoundastrongcorrelationbetweenAASandXmentions (rs = 0.712,95%CI0.707–0.717, P < .001)andaweak correlationbetweenAASandthenumberofMendeley readers(rs = 0.338to356, P < .001).
WefoundtwojournalsthatlackedAAS.Themediantotal mentionsforEMjournalswere14,154(rangingfrom
Table1. Countrydistributionofaltmetrics-Xdemographics.
Spain 13,538(2.9%) 3,863(3.4%)
*Apostreferstoanindividualmentionorengagementonasocialmediaplatform(suchasanXmention,Facebookpost,blogentry,etc) where aspecificresearchoutputissharedordiscussed.
**Aprofilereferstotheuniquesocialmediaaccountoruser(eg,anXorFacebookaccount)thatmadethepostormention.
57–77,460).MentionsonXhadamedianof12,284(ranging from56–68,078),Facebookmentionshadamedianof234 (rangingfrom0–2,180),blogmentionshadamedianof126.5 (rangingfrom0–1,866),andnewsmentionshadamedianof 288(rangingfrom0–5,040).
TheEMjournalswiththehighesttotalnumberof mentionswere AnnalsofEmergencyMedicine, Resuscitation,andtheAmericanJournalofEmergency Medicine .Conversely,theAASperarticlewashighestfor AcademicEmergencyMedicine,AnnalsofEmergency Medicine,andtheEmergencyMedicineJournal , respectively(Table2).Wefoundamoderatecorrelation (rs = 0.518, P = 0.07,95%CI0.152–759)betweenthe2022 JCIandthetotalnumberofmentions.
Inthereviewofthetop200articleswiththehighestAAS, themedianscoreofthearticleswas382.5(IQR301.3–510.8). TheAASwithsourcesandnumberofcitationsofthetop50 articlesareprovidedin Table3.ThemedianWOScitations forthearticleswas16(IQR5–39),withanannualcitation countof4.7(IQR1.8–8.9).ThemedianGoogleScholar citationswas29(IQR11–65),withanannualcitationcount of7.5(IQR3.2–15.1).Amongthesearticles,38%were observationalstudies,whilecasereportsandreviews/metaanalysesconstituted13%.Themostcommonresearchtopics wereEDmanagementandCOVID-19(Table4).
TheAASofreviewsandguidelineswerelower,while observationalstudiesandcasepresentationswerehigher (P = 0.02).TheAASwashigherfortopicsrelatedto toxicology,COVID-19,andcriticalcare(P = 0.02).While therewasanincreaseinAASandWOScitationsin COVID-19-relatedpapers,thesevariationswerenot significant(P = 0.09and P = 0.08,respectively).
TherewasnosignificantcorrelationbetweenAASand WOScitationnumbers(rs = 0.041, P = 0.56,95%CI 0.175–0.087,rs2 = 0.0017)orGoogleScholarcitations (rs = 0.038, P = 0.59,95%CI 0.174–0.101,rs2 = 0.0014). However,therewasaverystrongpositivecorrelation betweenWOSandGoogleScholarcitationnumbers(rs = 0.973, P < .001,95%CI0.955–0.984,rs2 = 0.947).Despite theweakcorrelationidentifiedbetweenWOScitationsandX
mentions,andthemoderatecorrelationobservedforblog mentions(rs = 0.330, P < .001,95%CI0.174to0.458, rs 2 = 0.109,andrs = 0.452, P < .001,95%CI0.320to0.566, rs 2 = 0.204,respectively),therewasaverystrongpositive correlationobservedinthenumberofMendeleyreaders. (rs = 0.873, P < .001,95%CI0.822–0.911,rs2 = 0.762). Nocorrelationwasobservedbetweennewsmentions (rs = 0.107, P = 0.10,95%CI 0.246–0.046,rs2 = 0.0012), andvideomentions(rs = 0.037, P = 0.60,95%CI 0.078to 0.145,rs2 = 0.0013).
ThisstudyexaminedaltmetricsofEMjournalarticles fromthe2013–2023.TenpercentofEMjournalarticleswere nevermentionedonsocialmedia.ComparedtoBarbicetal’ s investigationsfrom2011,AASforthemostcited publicationshaveincreasedsignificantlyinthesubsequent decade.9 SocialmediafollowersforEMjournalarticleshave increasedsignificantlyinrecentyears.Interestingly,threequartersofthe200most-citedarticleswerepublishedafter thisstudy,with45%publishedaftertheCOVID-19 pandemic.SocialmediafollowersforEMjournalarticles haveincreasedsignificantlyinrecentyears.
Kolahietalidentifiedaweakbutpositivecorrelation betweenAASandcitationsintheirmeta-analysis;the authorsemphasizedtheimportanceofcontinuingtoexamine thetemporaldynamicsofthisrelationship.15 Inourstudy, althoughnocorrelationwasfoundbetweenAASand traditionalcitationcounts,weobservedaweakcorrelation betweenAASandXmentions,andamoderatecorrelation betweenAASandblogmentions.Notably,therewasavery strongcorrelationobservedbetweenAASandtheMendeley readershipnumbers.
TheAASiscalculatedbasedonthesourceandfrequency ofsharing.Inthiscalculation,news,blogmentions,Wiki pages,policydocuments,andpatentshavethemostweight, whileXhaslessweight.Mendeleyreadershipandcitations arenotconsidered.16 Itshouldbenotedthattheprimary purposeofaltmetricsistomeasuresocialinterestinagiven topic,ratherthantopredictthepotentialcitationcountofan
Table2. Journalswiththehighesttotalnumberofmentions.
1.56 46,94523.972,3321,1091995841,615101,17899258225061
2.377,46020.855,0401,8662215868,078191,8301361074016051
1.246,19616.921,0251,0941591642,30321,37480114182010
Journaltitle
AcademicEmergency Medicine
AnnalsofEmergency Medicine
Resuscitation1.8764,94115.081,53284540015159,34112,1801492183229361
1.0620,34514.917933901062818,29835201018123021
TheWesternJournal ofEmergency Medicine
0.7525,41414.882653901771523,7911620107375107
CanadianJournalof EmergencyMedicine
1.3216,90114.81224145481816,02132864975193010
ScandinavianJournal ofTrauma, Resuscitationand EmergencyMedicine
1.235,63412.661,2987981473332,356363118894285251
JournalofEmergency Medicine
1.4750,0289.632,1561,1903355544,442161,502172681710164
AmericanJournalof EmergencyMedicine
0.7716,9215.5230843097614,43441,534431204050
PediatricEmergency Care
Δ JCI:JournalCitationIndicator. δ Thejournalsarerankedbasedonthetotalmentionsperarticle.
Med
Med
Med
Med
Med
Med
Table3. Top50articleswithhighestaltmetricscores.
1N95respiratorcleaningandreusemethodsproposed by theinventoroftheN95maskmaterial
2Associationbetweendelaystopatientadmissionfrom theemergencydepartmentandall-cause30-day mortality
4Vaccine-inducedmyocarditisintwointerndoctorsin thesamenightshift
5 Loperamideabuseassociatedwithcardiac dysrhythmiaanddeath
6Alayperspectiveandcommentaryontheassociation betweendelaystopatientadmissionfromthe emergencydepartmentandall-cause30-daymortality
7Characteristicsofpaediatricout-of-hospitalcardiac arrestintheUnitedStates
8Acoronavirusdisease2019(COVID-19)patientwith bilateralorchitis
9Theassociationoftreatmentwithhydroxychloroquine andhospitalmortalityinCOVID-19patients
10Priapisminapatientwithcoronavirusdisease2019 (COVID-19)
11Esophagealruptureafterghostpepperingestion
12Accidentaloccupationalexposuretoalargevolumeof liquidfentanylonacompromisedskinbarrierwithno resultanteffect
13VitaminDde fi ciencyisassociatedwithhigherrisksfor SARS-CoV-2infectionandCOVID-19severity: aretrospectivecase –controlstudy
14Characterizationofinfl ightmedicaleventsinvolving childrenoncommercialairline fl ights
15Interrogationofpatientsmartphoneactivitytracker toassistarrhythmiamanagement
16 AWARE AWArenessduringREsuscitation A prospectivestudy
17AlarmingtrendsinUSdomesticviolenceduringthe COVID-19pandemic
18Useofantibioticcoatedintramedullarynailsinopen tibiafractures:aEuropeanmedicalresourceuseand cost-effectivenessanalysis
19Bilateralretinaldetachmentsinahealthy22-year-old womanafterModernaSARS-COV-2vaccination
20 Stoppinghaemorrhagebyapplicationofrope tourniquetoringuinalcompression(SHARCstudy)
Theuseoftheword “ quiet ” in theemergency departmentisnotassociatedwithpatientvolume: arandomizedcontrolledtrial
Med
22Aromatherapyversusoralondansetronforantiemetic therapyamongadultEmergencydepartmentpatients: arandomizedcontrolledtrial
23Cyclicvomitingpresentationsfollowingmarijuana liberalizationinColorado
24Removalofiliosacralscrews:thewasherproblem
25Persistenthiccupsasanatypicalpresentingcomplaint ofCOVID-19
26Itisn ’ tlikethisonTV:revisitingCPRsurvivalrates depictedonpopularTVshows
27In-hospitalcardiacarrestoutcomesamongpatients withCOVID-19pneumoniainWuhan,China
28 Identifyingsafecorridorsforanteriorpelvic percutaneousinstrumentationusingcomputed tomography-basedanatomicalrelationships
29Riskofacutekidneyinjuryafterintravenouscontrast mediaadministration
30 Acutekidneyinjuryaftercomputedtomography: ameta-analysis
31Trendsininequitiesinthetreatmentofandoutcomes forwomenandminoritieswithmyocardialinfarction
32Singleversusdualincisionapproachesfordualplating ofbicondylartibialplateaufractureshavecomparable ratesofdeepinfectionandrevisionsurgery
33Comparisonoforalibuprofenatthreesingle-dose regimensfortreatingacutepainintheemergency department:arandomizedcontrolledtrial
34 Youngwomanwithparaplegiafollowingamotor vehiclecrash
Med
35Associationbetweentheopeningofretailclinicsand low-acuityemergencydepartmentvisits
36STEMImimic:focalmyocarditisinanadolescent patientaftermRNACOVID-19vaccine
Med
Med
37 One-yearmortalityofpatientsafteremergency departmenttreatmentfornonfatalopioidoverdose
38Academicemergencymedicinephysicians ’ anxiety levels,stressors,andpotentialstressmitigation measuresduringtheaccelerationphaseofthe COVID-19pandemic
39 BystanderCPRisassociatedwithimproved neurologicallyfavourablesurvivalincardiacarrest followingdrowning
withmorequestionsthananswers
waittimesintheemergencydepartment
externalde fi brillatorsinEngland?
workforceanalysis
inhospitalsthatprovideemergencycare
LongitudinaltrendsinU.S.drugshortagesfor medicationsusedinemergencydepartments (2001 –2014)
ofurinarycatheterusein18emergencydepartments
Rapidadoptionoflow-thresholdbuprenorphine treatmentatCaliforniaemergencydepartments participatingintheCABridgeProgram
fi rstaiddecreasesskingrafting requirementsinpediatricburns:acohortstudyoftwo thousandfourhundredninetyfi vechildren
Table4. Thecitationsarecategorizedbasedonthetopicsandtypesofthetop200articleswiththehighestAltmetricAttentionScores.
Articletype
Topics EDmanagement39(19.5)369.0(295.0–
–
AnalysisofCOVID-19articles
ED, emegencydepartment; IQR,interquartilerange; WOS,WebofScience.
article.Traditionalcitationsremainthegoldstandardfor academicrecognition.However,therelationshipbetween socialmediaandcitationssupportsthepositiveimpactof researchersandscientificjournalsusingsocialmediato enhancethevisibilityandinfluenceoftheirarticles. Incorporatingtheimpactofsocialmediaintothegold standardofcitationcountscouldbeawaytoacknowledge thisevolvinglandscape.
Theresultsofastudyexaminingtheimpactofpromoting Cochranesystematicreviewsinthe fieldofpediatricEM usingXandblogpostsrevealedasignificantincreaseof 10timesintheAASofthereviews.17 Thedistribution patternofarticlesonsocialmediamightvarybasedonthe natureofthesharing.Infographicsarevisualrepresentations ofdatameanttoenhanceengagementandstreamlinethekey elementsofagivenstudy.18 Somedatasuggeststhat presentingresearch findingsvisuallyonsocialmediamay leadtoa5–7timeshighernumberofinteractionscompared tostudieswithoutvisualcontent.19,20 Althoughusingvisual presentationstoshareresultscanreachalargeraudience,this effectmayonlyapplytospecificareasofexpertise.
Theextenttowhichsharinginfluencesthenumberof downloadsandcitationsofapaperremainsuncertain.21
However,altmetricstodayplayacrucialroleasmarkersfor assessingthespreadofcontentviasocialmediatoreachthe intendedaudience.Temporalpatternsinarticlealtmetrics
exhibitvariationacrossdifferentdatasources.Astudy investigatingaltmetricstemporaltrendsreportedthatX engagementstartedandendedquickly,whileMendeley readershipincreasedsteadilyoverthenextfewyears.22 An excellentwaytomaintaininterestinpublishedarticlesistouse altmetricsdatasourcesincombinationwithmethodsthat engagethetargetaudienceandregularlyupdatethecontent.
DuringtheCOVID-19pandemic,therewasanotable increaseinthedisseminationofinformationonsocialmedia platforms,withhealthcareprofessionalsusingthese platformsmorefrequently.Ouranalysisshowsthatnearly halfofthetop200publicationsinEMjournalswere publishedaftertheonsetofthepandemic.Additionally, whenevaluatingthecomprehensivealtmetricsofarticlesin EMjournals,wefoundtherewasaclearriseinmentions during2020–2021.Theevaluationundertakeninthisstudy encompassesreferencesmadeuntilthestartof2023.While futurestudieswilldeterminewhetherthisupwardtrendwill persist,itisforeseeablethatthesurgeinresearchersusing socialmediatomonitorscientificinformationwillcontinue asaresultoftheCOVID-19pandemic.Thisrisecanbe linkedtothesurgeinsharingactivitiesassociatedwith COVID-19.Nevertheless,ourinvestigationfoundno discernibledistinctionbetweenAASandWOScitations whencomparingpaperslinkedtoCOVID-19andthose unrelatedtoit.
Thisstudyhasseverallimitations,particularlyits emphasisonquantitativedataanalysisandtheuseofasingle datasource.ThecurrentAltmetricdatabasemainly emphasizesthenumberofmentions,andouranalysis exclusivelycomparedthesemetrics.Inapproximately50%of thementionsonXwewereunabletodeterminethecountry associatedwiththeaccount.Inadditiontotheincreased interactionoftheattributesofsocialmediashares,itismore importanttoevaluatetherelationshipoftheinformationto thetargetaudience,reference,anddownload.20 Intheearly partofthestudy,weanalyzedallarticlespublishedinEM journals,butwemadecomparisonswithtraditional referencesforonly200articles.Incontrasttoprevious studies,weevaluatedarticleswiththehighestAASinsteadof thealtmetricsofthemostcitedarticlesintraditional referenceindices.Anotherlimitationofthisstudyisthe inabilitytofullydifferentiatetheimpactofincreasedsocial mediausageduringtheCOVID-19pandemiconAAS.The surgeinonlinecontentandinteractionsduringthepandemic mayhaveartificiallyinflatedAASvalues,particularlyfor articlespublishedduringthisperiod,potentiallyaffectingthe relationshipbetweenAASandtraditionalcitationcounts.
TherehasbeenanotableriseinAltmetricsAttention Scoresinrecentyears,drivenbyincreaseduseofsocialmedia forfollowingscientificresearch,particularlyduringthe COVID-19pandemic.Articlesfocusingontoxicology, COVID-19,andresuscitation/criticalcaretendtoreceivethe highestAAS.Whilenocorrelationwasfoundbetweentotal AASandcitationcountsfromWOSandGoogleScholar, thereisastrongpositivecorrelationbetweenWOScitations andthenumberofMendeleyreaders.Additionally,weak andmoderatecorrelationswereobservedformentionson Xandblogs,respectively.Furtherresearchisneededto exploretherelationshipbetweenaltmetricsandtraditional citationmetrics,aswellastheimpactofsocialmediaon academicresearchvisibilityinEM.
TheauthorswishtoacknowledgeAltmetric.comfor generouslyprovidingno-costaccesstoessentialdatathrough theAltmetricResearcherDataAccessProgram.Altmetric hadnoinvolvementinthedesignofthestudy,thedata analysis,orthewritingofthemanuscript.Additionally,they didnotparticipateinreviewingorapprovinganyversionof themanuscript.
AddressforCorrespondence:MuratÇetin,MD,Dr.BehçetUz Children'sEducationandResearchHospital,Departmentof EmergencyMedicine,Konak,35210,Izmir,Türkiye.Email: muratcetinn@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Bayrametal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PriemJ,TaraborelliD,GrothP,etal.Altmetrics:amanifesto.2010. https://zenodo.org/records/12684249.AccessedSeptember15,2024.
2.PriemJ,GrothP,TaraborelliD.Thealtmetricscollection. PLoSOne. 2012;7(11):e48753.
3.BikHMandGoldsteinMC.Anintroductiontosocialmediaforscientists. PLoSBiol. 2013;11(4):e1001535.
4.PriemJ,PiwowarHA,HemmingerBM.Altmetricsinthewild:using socialmediatoexplorescholarlyimpact. arXiv:1203.4745.
5.EysenbachG.Cantweetspredictcitations?Metricsofsocialimpact basedonTwitterandcorrelationwithtraditionalmetricsofscientific impact. JMedInternetRes. 2011;13(4):e123.
6.MaloneTandBurkeS.Academiclibrarians’ knowledgeofbibliometrics andaltmetrics. EvidBasedLibrInfPract. 2016;11(3):34–49.
7.WuDandZhangQ.Analtmetricsstudyofartificial ıntelligencein medicine.In: Proceedingsofthe2021InternationalConferenceon ComputationalScienceandComputationalIntelligence (p196-8). LasVegas,NV(2021).
8.HueckerMR,ShrefflerJ,PlattM,etal.Emergencymedicinehistoryand expansionintothefuture:anarrativereview. WestJEmergMed. 2022;23(3):418–23.
9.BarbicD,TubmanM,LamH,etal.Ananalysisofaltmetricsin emergencymedicine. AcadEmergMed. 2016;23(3):251–68.
10.FassoulakiA,VassiA,KardasisA,etal.Altmetricsshouldnotbeused forrankingofanaesthesiajournals. BrJAnaesth. 2018;121(2):514–6.
11.ThelwallM,HausteinS,LarivièreV,etal.Doaltmetricswork?Twitter andtenothersocialwebservices. PLoSOne. 2013;8(5):e64841.
12.DemirHAandDoganS.Correlationbetweenacademiccitationsin emergencymedicinejournalsandTwittermentions. AmJEmergMed. 2022;58:33–8.
13.Altmetric.com.Howisthealtmetricattentionscorecalculated?2024. Availableat: https://help.altmetric.com/support/solutions/articles/ 6000233311-how-is-the-altmetric-attention-score-calculated-T AccessedSeptember13,2024.
14.SchoberP,BoerC,SchwarteLA.Correlationcoefficients:appropriate useand ınterpretation. AnesthAnalg. 2018;126(5):1763–8.
15.KolahiJ,KhazaeiS,IranmaneshP,etal.Meta-analysisofcorrelations betweenaltmetricsattentionscoreandcitationsinhealthsciences. BiomedResInt. 2021;2021:6680764.
16.Garcia-VillarC.Acriticalreviewonaltmetrics:canwemeasurethe socialimpactfactor? InsightsImaging. 2021;12(1):92.
17.GatesA,FeatherstoneR,ShaveK,etal.Disseminationof evidenceinpaediatricemergencymedicine:aquantitativedescriptive evaluationofa16-weeksocialmediapromotion. BMJOpen. 2018;8(6):e022298.
18.GottliebM,IbrahimAM,MartinLJ,etal.Educator’sblueprint:a how-toguideforcreatingahigh-qualityinfographic. AEMEducTrain. 2022;6(4):e10793.
19.IbrahimAM,LillemoeKD,KlingensmithME,etal.Visualabstractsto disseminateresearchonsocialmedia:aprospective,case-control crossoverstudy. AnnSurg. 2017;266(6):e46–8.
20.OskaS,LermaE,TopfJ.Apictureisworthathousandviews:atriple crossovertrialofvisualabstractstoexaminetheir ımpact onresearchdissemination. JMedInternetRes. 2020;22(12):e22327.
21.SoreideK.Numbersneededtotweet:socialmediaandimpacton surgery. EurJSurgOncol. 2019;45(2):292–5.
22.SlowTaylorM.Slow,quick,quick,slow: fivealtmetricssources observedoveradecadeshowevolvingtrends,byresearchage, attentionsourcematurityandopenaccessstatus. Scientometrics. 2023;128(4):2175–200.
SamuelJ.Stellpflug,MD*
WilliamH.Menton,PhD†
BjornC.Westgard,MD*
RyanD.Johnsen,MD*
AlexanderM.Coomes,MD*
RobertC.LeFevere,MD*
MichaelD.Zwank,MD*
SectionEditor:JeffreyR.Suchard,MD
*RegionsHospital,DepartmentofEmergencyMedicine,SaintPaul,Minnesota † VAHealthcareSystem,Minneapolis,Minnesota
Submissionhistory:SubmittedJune28,2024;RevisionreceivedSeptember2,2024;AcceptedNovember27,2024
ElectronicallypublishedFebruary6,2025
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.24998
Introduction: Thegoldstandardforquantifyingethanolintoxicationinpatientsisserumtesting. However,breathtestingisfaster,lessexpensive,andlessinvasive.Itisunknownwhetherperceived effortduringabreathethanoltestimpactstheaccuracyofthetestandthecorrelationwithserum concentration.Inthisstudyweanalyzedwhetherperceived “poor” effortduringbreathethanoltesting wouldresultinworsecorrelationthanperceived “normal” breath-testingeffortwithrespecttoserum ethanolconcentration.
Methods: Subjectswereidentifiedretrospectivelyovera49-monthperiodiftheyhadbothabreath ethanoltestandaserumethanoltestobtainedduringthesameEDvisitwithin60minutesofeachother,if theyhadtheireffortduringthebreathtestrecordedas “normal” or “poor” bythepersonadministeringthe test,andhadnon-zerobreathandserumethanolconcentrations.Wecompleteddescriptiveand correlationanalyses.
Results: Atotalof480patientswereenrolled,245withnormaland235withpooreffort.Thepatientswith normalbreath-testefforthadmeanbreathandserumconcentrationsof0.19gramsperdeciliter(g/dL) and0.23g/dL,respectively.Thepatientswithpoorbreath-testefforthadmeanbreathandserum concentrationsof0.19and0.29g/dL,respectively.Thecorrelationcoefficientbetweenbreathandserum ethanolvalueswas0.92(95%confidenceinterval(CI)0.84–0.96)forgoodeffortand0.63(95%CI 0.53–0.74)forpooreffort.
Conclusion: Theassessmentofbreathexhalationeffortismeaningfulindetermininghowwella patient’sbreathethanollevelcorrelateswiththeserumethanolconcentration.Poorbreatheffort,when comparedtonormalbreatheffort,wasassociatedwithhigherethanollevelsaswellasalargerdifference andagreatervariabilitybetweenbreathandserumvalues.Ifanaccurateethanollevelisimportantfor clinicaldecision-making,aphysicianshouldnotrelyonapoor-effortbreathalyzervalue.[WestJEmerg Med.2025;26(2)364–366.]
Breathtestingforethanolhasbeendiscussedinmedical literaturefornearly150years.1 Ethanoltestingisoftenused inemergencydepartments(ED)andhashistoricallyincluded bloodtesting,breathtesting,orboth.Breathtestinghasbeen usedasasurrogateforthegoldstandardserumtestingand hasdistinctadvantagesoverblood:itisfaster,lessinvasive, andlessexpensive.2 Despitelongstandingstudyofthetopic
andwideacceptanceofitsuse,ithasnotbeenwellestablished whetherapoorexpiratoryeffort,asjudgedbythetester, affectstheaccuracyofthetest.
Whenadministeringabreathethanoltest,theoperatorsof thedevicewilloftencommentontheexpiratoryeffortofthe patient.Theinferenceisthataneffortdeemed “ poor ” bythe testerwillnotbeasaccurateasa “normal”-appearing expiratoryeffort.Theimpactofapparentexhalationeffort onthecorrelationbetweenbreathandserumlevelshasnot beenclearlyestablished.Clarifyingthiscouldimpactpatient careandcouldprovideutilityinforensicevaluation.Our primaryobjectiveinthisstudywastodeterminewhethera patient’sexpiratoryeffort,asperceivedbythetester,affected thebreathethanoltestresultswhencomparedtoserum. Secondaryobjectivesincludeddeterminingoverall correlationsbetweenbreathandbloodtestingwithinasingle hospitalencounter.
ThisstudywasapprovedbytheHealthPartners institutionalreviewboard.Aretrospectiveelectronichealth record(EHR)inquirywasperformedtoincludeallpatients overa49-monthperiodwhohadbreathethanoltestingwith documentedperceivedexhalationeffort(“normal” or “ poor ”)andserumethanoltestingcompletedduringasingle EDvisitatalarge,tertiary-carehospital.Atthishospital,the individualperformingthebreathtest,typicallyanemergency medicinetechnicianorregisterednurse,choosesoneofthese twoeffortcategoriesasanelectroniccheckboxwhenentering theethanolvalueintotheEHR.Theassessmentofeffortis doneusingtheirownclinicaljudgment.Allbreathethanol testswereperformedusingtheAlco-SensorFST(AlcoPro Inc,Knoxville,TN).Allserumethanoltestsweredoneusing theARCHITECTc8000(AbbottLaboratories,Abbott Park,IL).
Datacollectedforthisstudyincludedthefollowing:time ofbreathethanoltest;thepatient’sperceivedbreathtesting effort;theresultofthebreathethanoltest;thetimeofthe blooddrawforserumethanoltesting;andtheresultofthe serumethanoltest.Subjectswereincludediftheyhadbotha bloodandbreathethanoltestdonewithina60-minutetime
interval.Subjectswereexcludedifeitherthebreathorserum concentrationwas0gramsperdeciliter(g/dL).Thiswasdone becausesomeoftheblooddrawandbreathtestshadenough timebetweentheminthesamesubjectsuchthata0g/dL valuemayhaveinaccuratelyimpactedthecorrelation calculations,asthepatientmayhavenaturallyreacheda levelof0g/dLwellbeforethesecondtestoccurred.
Theassociationsbetweenbreathandserumethanollevels, controllingforbreatheffort,appearedhighlylinearoninitial graphicalvisualizationofthedata.Therefore,the relationshipsbetweenthesevariableswereexploredfurther usingacombinationofzero-orderPearsoncorrelationsand linearregression.Weexaminedthepropertiesofbreath ethanolconcentrations,serumethanolconcentrations,and theassociationsbetweenthem.
Atotalof480subjectswereincludedinthestudy.Ofthese subjects,245showednormaleffortand235were documentedaspooreffort.Additionally,237patientshada timeintervaloflessthan15minutesbetweenbreathand serumvalues,112hadatimeintervalof16–30minutes,and 131hadatimeintervalof31–60minutes.Therewere184 patientswhohadblooddrawnbeforethebreathalyzerand 288whohadblooddrawnafterthebreathalyzer;eight patientsweretestedconcurrently.Amongallpatients,the meanbreathethanolwas0.19g/dL,whilethemeanserum ethanolwas0.26g/dL.Thepatientswithnormalbreathtest efforthadmeanbreathandserumconcentrationsof 0.19g/dLand0.23g/dL,respectively.Thepatientswithpoor breathtestefforthadmeanbreathandserumconcentrations of0.19and0.29g/dL,respectively.Thecorrelation coefficientbetweenbreathandserumwas0.92(95% confidenceinterval[CI]0.84-0.96)withnormaleffortand 0.63(95%CI0.53-0.74)withpooreffort.Descriptiveresults andcorrelationanalysisbetweenthetestsarepresentedinthe Table. Aplotdisplayingindividualbreathandserumvalues, aswellaslinesofbest fitbyeffortgroup,ispresentedin the Figure
Patientethanollevels(breathandserum;gramsperdeciliter)andcorrelationcoefficients.
Correlationcoefficientbetweenbreathandserum[95%CI]0.75[0.7,0.82]0.92[0.84,0.96]0.63[0.53,0.74] EtOH, ethanol; CI,confidenceinterval.
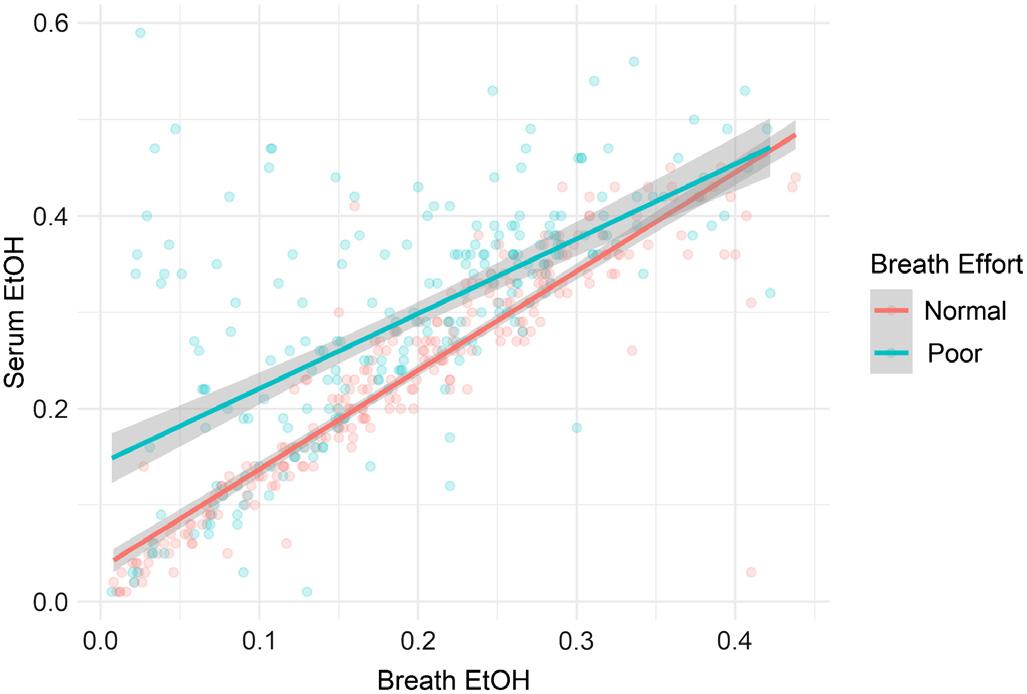
Figure. Plotofbreathandserumethanolvaluesandlinesofbest fit for “normal”-and “poor” effortgroups.
Ourprimaryobjectiveinthisstudywastodetermine whethertheperceivedlevelofexpiratoryeffortduringa breathethanoltestimpactstheaccuracyofthebreathtest whencomparedtoaserumethanoltest.Wedocumentedthe subject’seffortasperceivedbythetesterbecauseitreflectsa commonassessmentintheclinicalsetting.Cliniciansare oftengiventheresultofthebreathtestalongwiththe assessor ’ssubjectivedescriptionofthebreatheffort.
Theresultsofthisstudyindicatethattheassessmentof breathexhalationeffortismeaningfulindetermininghowwell apatient’sbreathethanollevelcorrelateswiththeirserum ethanolconcentration.Whilebreathethanolvalueswere generallylowerthanserumethanolvalues(regardlessof effort),thisdifferencewasbothgreaterandmorevariable amongpatientswithpooreffort.Thisisshownbyagreater differenceinvaluesforthosepatientswithpooreffort(Table), byahigherstandarddeviationindifferencevalues,andbya lowercorrelationcoefficientinthisgroup(Table and Figure). Thisisconsistentwithprior findingsinastudybyGibbetal whoexaminedwhether “cooperativeness” withthe breathalyzerwasassociatedwithdifferencesinbreathvs serumvalues.2 Cooperationwasdefinedaswhetherapatient “understoodandfollowedthroughwiththeinstructionsto performasmooth,forcedexpirationintotheanalyzer.” While thiswasaninformativestudy,inpractice,documentationis relatedtoeffortandnottocooperation.Thus,ourstudyisa morepracticalassessmentofreal-worldexperience.
The “pooreffort” groupalsodemonstratedsubstantially higherserumalcoholconcentrationsthanthe “normaleffort” group(0.29g/dLvs0.23g/dL).Thisisperhapsunsurprising andsuggestspossiblyreducedabilitytocoordinateagood expiratoryeffortorlessmotivationtoparticipateintesting. Wedidnotextendtheanalysispasta60-minuteinterval betweenbreathandserumtestsbecauseanyconclusions
beyondthistimeframewerenotfelttobeclinicallyapplicable. Analysisofsubjectswithanarrowtimedifferencebetween breathandserumtestingisimportanttominimizeanypossible impactofongoingethanolmetabolismbetweenexecutionof thedifferenttestingmodalities.
Assessmentofpatientexpiratoryeffortinbreathethanol testingisasubjectivemeasure.However,itisthesame subjectivemeasureassessedduringrealpatientcare.More formalmeasurementofexpiratorycapacitycouldadd perspectiveandpotentiallyaccuracyaswell.Inaddition, giventheretrospectiveobservationalnatureofourdata, breathtestingandbloodsamplesforserumtestingwereoften notperformedsimultaneously.Wediduseanarrowtime frameforanalysis,thusnegatingmuchmetabolism.A prospectivestudyobtainingbloodsamplesforserumethanol testingatthetimeofbreathethanoltestingwouldbe necessarytoeliminatethispotentialconfounder.Finally, whilethebreathalyzerusedatourhospitalisacommonly useddevice,otherdevicesmaybeusedelsewhere,andtheir measurementpropertiesmayvary.
Breathethanolconcentrationsweregenerallylowerthan serumethanolconcentrations.Poorexhalationefforton breathethanoltestingcorrelatedwithalargerdifference betweenbreathandserumethanolconcentrationsandwith greatervariabilityinthedifferencebetweenthetwo.Thiscan berelevantinclinicalandforensicsettings.
AddressforCorrespondence:SamuelJ.Stellpflug,MD,Regions Hospital,DepartmentofEmergencyMedicine,640JacksonSt.,Saint Paul,MN55101.Email: samuel.j.stellpflug@healthpartners.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Stellpflugetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AnstieFE.Finalexperimentsontheeliminationofalcoholfromthebody. Practitioner. 1874;13:15–28.
2.GibbKA,YeeAS,JohnstonCC,etal.Accuracyandusefulnessofa breathalcoholanalyzer. AnnEmergMed. 1984;13(7):516–20.
ChristineE.Ren,MD*†
AnastasiaTernovskaia,BS‡
FatimaMikdashi,BS‡
HassanSyed,MD§
IshaVashee,BS‡
VainaviGambhir‡
NatalieChao,BA§
JessicaV.Downing,MD∥*
DavidDreizin,MD¶
QuincyK.Tran,MD,PhD‡∥#
*R.AdamsCowleyShockTraumaCenter,UniversityofMarylandMedicalCenter, DepartmentofEmergencyMedicine-SurgicalCriticalCare,Baltimore,Maryland † OregonHealthandScienceUniversity,DepartmentofEmergencyMedicineand CriticalCareMedicine,Portland,Oregon
‡ UniversityofMarylandSchoolofMedicine,DepartmentofEmergencyMedicine, ResearchAssociateProgram,Baltimore,Maryland
§ UniversityofMarylandSchoolofMedicine,Baltimore,Maryland
∥ UniversityofMarylandSchoolofMedicine,DepartmentofEmergencyMedicine, Baltimore,Maryland
¶ UniversityofMarylandSchoolofMedicine,DepartmentofDiagnosticRadiologyand NuclearImaging,DivisionofEmergencyandTraumaImaging,Baltimore,Maryland
# R.AdamsCowleyShockTraumaCenter,UniversityofMarylandMedicalCenter, PrograminTrauma,Baltimore,Maryland
SectionEditor: PierreBorczuk,MD
Submissionhistory:SubmittedApril20,2024;RevisionreceivedOctober29,2024;AcceptedOctober30,2024
ElectronicallypublishedDecember31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20346
Background: Diffuseaxonalinjury(DAI),afeatureseeninseveretraumaticbraininjury(TBI),is associatedwithsubstantialmorbidityandmortality.Althoughbloodpressurevariability(BPV)hasbeen showntoimpactTBIoutcomesoverall,itsrelevanceinDAIcasesremainsuncertain.Weinvestigated whether24-hourpost-injuryBPVandotherclinicalfactorswerelinkedtopatientoutcomes.
Methods: WeconductedaretrospectiveanalysisofLevelItraumacenter-admittedTBIpatientswith radiographicDAIdiagnosis(computedtomography/magneticresonanceimaging).Hospitaldisposition (home,nursingfacility,hospice/death)andGlasgowComaScale(GCS)onhospitalday5(HD5GCS) wereoutcomesofinterest.Weassessedassociationswithclinicalfactorsusingordinallogisticregression.
Results: Among153patients(meanage49 ± 20years,74%male),medianadmissionGCSwas5.0 (3.0-12.5),HD5GCSwas8.0(6.0-11),andmedianhospitalstaywas25(15.5-34.5)days.TheBPV, measuredassuccessivevariationinsystolicbloodpressure(SBPSV)andstandarddeviationinsystolic bloodpressure(SBPSD),wasnotsignificantlyassociatedwithhospitaldisposition.SBPSV andSBPSD werealsonotassociatedwithoursecondaryoutcomeofHD5GCS.Initialinternationalnormalizedratio (INR)(Coefficient-3.67,oddsratio[OR]0.03,95%confidenceinterval[CI]0.00-0.70),cerebralcontusion (Coeff-2.39,OR0.09,95%CI0.01-0.75),andHD5GCS(Coeff0.59,OR1.80,95%CI1.30-2.49)were associatedwithincreasedoddsofdischargetohospiceordeath.Administrationofbloodproducts(Coeff 1.06,OR2.89,95%CI1.10-7.60),vasopressors(Coeff1.40,OR4.05,95%CI1.37-11.96),and hyperosmolartherapy(Coeff1.23,OR3.41,95%CI1.36-8.54),andconcurrentintraventricular hemorrhage(Coeff0.99,OR2.70,95%CI0.86-6.49)werelinkedtopoorerHD5GCS.
Conclusion: Bloodpressurevariabilitywasnotcorrelatedwithoutcomesinpatientswithdiffuseaxonal injury.LowGlasgowComaScoreonhospitalday5,highinitialINR,andconcomitantcerebralcontusion wereassociatedwithpooreroutcomes.[WestJEmergMed.2025;26(2)367–377.]
Diffuseaxonalinjury(DAI),alsoreferredtoastraumatic axonalinjury,isanincreasinglyrecognizedcomponentof traumaticbraininjury(TBI),nowestimatedtooccurinover 40%ofpatientshospitalizedwithotherformsofTBI.1,2 DAI iscausedbyrotationalacceleration-decelerationinertial forcesthatshearthewhitemattertractsinthebrain.This mechanismdisruptsaxonaltransport,leadingtoaxonal swelling,secondaryaxonaldisconnection,andsubsequent degeneration.3 Thisinjuryismostoftenassociatedwith high-velocityevents,suchasmotorvehiclecollisions orlongfallsfromheight.Clinicalmanifestationscanvary widely,rangingfromminimalsignificanceto profoundneurologicalimpairment,dependingon injuryseverity.
SeverecasesofDAIoftenleadtopersistentcomasor substantialdeficitsinneurologicalrecoveryandare associatedwithsignificantmortality.4 Lesionsassociated withDAImaynotinitiallybeapparentordetectableon computedtomography(CT);patientswithsuspectedDAI oftenduetopersistenceofpoormentalstatusintheabsence ofsignificantedemaonCTorfollowingneurosurgical evacuationofextra-axialhematoma areoftenevaluated withmagneticresonanceimaging(MRI)fordiagnosis.4,5 TheseverityofDAIappreciatedonMRIischaracterized accordingtothedegreeandlocationofidentifiedwhite matterlesions;Grade1isprimarilyassociatedwithlesionsin thecortex,Grade2inthecorpuscallosum,andGrade3in thebrainstem.6
Giventhevariabilityinclinicalmanifestationsand potentiallyhighratesofcognitivemorbidityandmortality associatedwithDAI,numerousstudieshavesoughtto identifyfeaturesassociatedwithimprovedorpoorpatient outcomes,suchasradiographic findings,initialGlasgow ComaScale(GCS)scores,andhypertension(definedas systolicbloodpressure[SBP] ≥160millimetersofmercury (mmHg),amongothers.4,7–9 Theroleofbloodpressure variability(BPV)hasnotyetbeeninvestigatedinpatients withDAI;BPVdescribesoscillationsinbloodpressure betweenconsecutivemeasurementsorwithinadefined timeframe.Variationsinbloodpressurearecommonafter TBI,possiblyduetoimpairedcerebrovascular autoregulationordecreased “baroreflexsensitivity” asa resultoftheinjury,andpriorresearchsuggestsalinkto pooroutcomes.10
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Bloodpressurevariability(BPV)hasbeen associatedwithpooreroutcomesinpatients withtraumaticbraininjury(TBI).
Whatwastheresearchquestion?
IsBPVassociatedwithworsedisposition outcomesinTBIpatientswithdiffuseaxonal injury(DAI)?
Whatwasthemajor findingofthestudy?
ForTBIpatientswithDAI,blood pressurevariabilitydidnotimpact dischargedestination.
Howdoesthisimprovepopulationhealth?
WhileBPVwasnotassociatedwithpoorer outcomesinourstudy,furtherstudiesare neededtodeterminewhetherother interventionscanimpactoutcomesin thesepatients.
Bloodpressurevariabilityhasbeenassociatedwith deviationsfromoptimalcerebralperfusionpressures (CPPopt),whichareinturnlinkedtounfavorableoutcomes inTBIpatients.11 Wehavepreviouslyinvestigatedthe connectionbetweenBPVandoutcomesinpatientswith traumaticintraparenchymalhemorrhageandfoundan associationwithlowerratesofdischargetohome,indicating worsefunctionaloutcomesupondischarge.12 Inadditionto TBI,BPVhasbeenpreviouslyassociatedwithadverse outcomesinischemiccerebrovascularaccidentsand spontaneousintracranialhemorrhage(ICH).13–17
InthisstudyweinvestigatedtheimpactofBPVinthe initial24hoursfollowinghospitalarrivalonoutcomesin patientswithDAIandevaluatedclinicalfeaturesthatmay correlatewithpatientoutcomes,withthegoalofimproving theaccuracyofprognosticassessmentsandproviding importantinformationtoguidefuturestrategiesinmanaging post-injuryTBIandpatientsdiagnosedwithorsuspectedof havingDAI.
ThisstudywasperformedatR.AdamsCowleyShock TraumaCenter,aregional,quaternarytraumacenterand neurotraumaspecialtycenterthatadmitstraumapatients directlyfromthe fieldandactsasareferralcenterforother hospitalswithinthestate.Uponarrivalatourinstitution, patientsare firstevaluatedbythetraumateamandundergo appropriatescreeningimagingstudies,includingCT,as clinicallyindicated.PatientswithidentifiedICHorcontusion areevaluatedemergentlybytheneurosurgeryteam.Patients withCTorclinicalcharacteristicssuggestiveofDAI subsequentlyundergoabrainMRIforconfirmationand furthercharacterizationofdiseaseseveritywhentheyare clinicallystableenoughtotolerateMRI.Previousstudies haveidentifiedthatradiographicpresenceofDAIonMRIis
itselfindependentlyassociatedwithpooroutcomes7,18;thus, wechosepatientswhoalsohadanMRIperformedduring theiracutehospitalizationwithin30daysfromtheir admissionevenifDAIwassuspectedontheirinitialCT images.Thisapproachallowedustobetterevaluatespecific radiographicfeaturessuchashemorrhagicvolumeofburden andlesionlocation.
Weconductedaretrospectivecohortstudyofalladult traumapatients(≥18yearsold)admittedtoourhospital betweenJanuary1,2016–December31,2019withthe diagnosisofTBI.Patientswithradiographicevidenceof DAIwhounderwentbothCTandMRIwithin30daysof admissionwereeligible.Weexcludedpatientswhodidnot havecompleteclinicalinformationorimagingstudies.
PatientswitharadiographicdiagnosisofDAIwereidentified fromourinstitution’sRadiologyInformationSystem,a databaseusedforthemanagementofradiographicimages; furtherdatawascollectedfromthepatient’selectronichealth record(EHR).
Dataabstractionfollowedpreviouslypublished methodologicalguidelinesonretrospectivechartreview.19 Priortodatacollection,investigatorsevaluatedsetsof five patientchartsanddirectlycomparedtheir findingstothoseof theseniorinvestigatorandprincipalinvestigator(Q.T.)until accuracyreached90%.Datacollectorswerenotblindedto thehypothesis.Radiographicinformationwasinterpreted andprovidedbyanattendingradiologist.AnExcel spreadsheet(MicrosoftCorporation,Redmond,WA)with standardizedcategorieswasusedtorecordclinicaldatafrom de-identifiedpatients.
Demographicsandclinicaldataofinterest,selecteda prioriaccordingtoapreviousstudy,18 includedthe following:patient’sage;sex;pastmedicalhistory;serum lactatelevel;internationalnormalizedratio(INR); mechanismofinjury;initialGCSatadmissionandhighest recordedGCSathospitalday5(HD5GCS);administration ofbloodproducts(packedredbloodcells,freshfrozen plasma,platelets,cryoprecipitate);vasopressors (norepinephrine,vasopressin,orepinephrinearethemost commonlyusedvasopressorsforthispatientpopulationat ourinstitution);hyperosmolartherapy(hypertonicsalineor mannitol);intravenous(IV)antihypertensives,antiepileptic medications,locationandvolumeofDAIburden; concurrentpresentationwithseizures,intracranial contusion,intracerebralhemorrhage,intraventricular hemorrhage(IVH),orsubarachnoidhemorrhage(SAH); andallrecordedSBPmeasurementswithinthe first24hours ofadmission.Forpatientswholeftthehospitalorexpired beforehospitalday5,theirHD5GCSlevelswereinputas3 (forexpiredpatients)orthelastrecordedGCSpriorto hospitaldischarge.
Allbloodpressuremeasurementswerecollectedasthey wererecordedinpatients’ chartsbynursingstaff.Our institution’sclinicalstandarddictatesthatpatientsadmitted tointensivecareunitshaveatleastonesetofvitalsigns documentedperhour.Wecollectedallbloodpressure measurements,asdocumentedbyournursingstaff,evenif theyexceededmorethanonesetofvitalsignsperhour. Methodologyofobtainingbloodpressure,eitherbymanual bloodpressurecuff,automaticbloodpressurecuff,orby arterialbloodpressuremonitoring(radialorfemoralaccess) wasdecidedbythebedsideclinicians.Atourinstitution, invasivemonitoringwitharterialbloodpressuremonitoring isstronglyencouragedforallpatientswhoreceive antihypertensivesorvasopressorinfusions.Forpatientswho haddocumentationofbotharterialbloodpressureandcuff pressure,wecollectedthearterialbloodpressurevalues.
Bloodpressurevariabilityquantifiesbloodpressure fluctuationsoveraspecifiedtimeinterval.TheBPVcanbe studiedwithrespecttoSBP,diastolicbloodpressure,and meanarterialpressure(MAP).Here,weexaminedvariability inSBP,asspecificSBPgoalsaretraditionallyusedfor managementofpatientswithICHorTBI.20 Weevaluated threedifferentmodalitiesofmeasuringandreportingsystolic BPV:successivevariationofsystolicbloodpressure(SBPSV); standarddeviationinsystolicbloodpressure(SBPSD);and coefficientofvariationinsystolicbloodpressure(SBPCV).21 WealsocollectedSBPmax andSBPmin fromthe first24hours ofadmission.TheSBPSV isthesquarerootoftheaveraged squareddifferencebetweenanytwosuccessiveSBP measurementsanddemonstratestherateofchangebetween consecutivemeasurements.TheSBPSD representstheextent ofvariationordispersionofindividualSBPmeasurements aroundtheaverageSBPwithinagiventimeframe,indicating thelevelof fluctuationorstabilityinbloodpressurevalues. TheSBPCV iscalculatedastheratioofthestandarddeviation ofSBPtothemeanSBPandoffersastandardizedmeasureof SBPvariabilityrelativetotheaverageSBP.
ThepresenceofDAIwasestablishedbasedonMRI findings,whichwereinterpretedanddocumentedbyan attendingradiologist.Theimaginginformationprovided includedthelocationofDAIwithinsevenregions:thecorpus callosum;basalganglia;thalami;parahippocampalregion; cerebellum;brainstem;andgray-whitejunction.Thevolume ofDAIhemorrhageburdennotedonsusceptibilityweighted imageswasmeasuredineachlocationusingthe3Dslicer version4.102(https://www.slicer.org)spherebrushpaint toolandquantificationmodule.Additionally,presenceor absenceofconcomitantinjuries,specificallycontusion,SAH, IVH,andintraparenchymalhemorrhage,weredocumented usingradiologyreports.
Ourprimaryoutcomewashospitaldischargedisposition, usedasasurrogatemarkerforneurocognitivedisabilityat dischargeamongpatientswithTBI.Dischargedestinations includedhome,rehabilitationfacilities,andhospice/death. Beingdischargedhomedirectlyfromthehospitalsignifiesa favorableoutcomewithahigherlikelihoodoffunctional recoveryandpreservationofindependentliving.Onthe otherhand,beingdischargedtoarehabilitationfacility suggeststheneedforongoingsupportandtherapydue tosignificantneurologicdeficits.22 Hospice/death representsthepoorestoutcome.Thesecondaryoutcomeof HD5GCShasbeenshowntohaveprognosticvaluein predictinglong-termoutcomesandisconsideredan importantindicatorofneurologicalrecoveryinpatients withspontaneousICH.23,24
Weuseddescriptivestatisticstopresentcontinuousdata asmean(standarddeviation)ormedian(interquartilerange), dependingonthedistributionofthedataafterthedata’ s histogramswereinspected.The t -testorMann-WhitneyU testwasemployedforcontinuousdatacomparisons,while categoricaldatacomparisonswereconductedusingthechisquaretestorFisherexacttest,asappropriate.Weused ordinallogisticregressionsfortheoutcomesofbothhospital dispositionandHD5GCS.Hospitaldispositionwasranked inthreeordersfromlowesttohighestseverity:0(home); 1(rehabilitation);and2(hospice/death).Patients’ HD5GCS scoreswererankedinorderfrom0(GCS3-8),1(GCS9-12), 2(GCS13-14),or3(GCS15).Fortheordinallogistic regressions,thecoefficientsrepresenttheassociationofthe independentvariablesandtheoutcomes.Apositive coefficientindicatedincreasedoddsofassociationwiththe lowestnumberrank(rank0),whileanegativecoefficientwas associatedwiththehighestrankoftheoutcomes.
Weperformedalldescriptiveanalysesandordinal regressionswithMinitabversion19(MinitabLLC,State College,PA).Allanalyseswith2-tail P =< 0.05were consideredstatisticallysignificant.
PatientCharacteristics
Fromtheinitial174patientsidentifiedintheEHR fitting ourinclusioncriteria,weincluded153inthe finalanalysis. Theremaining23patientswereexcludedduetoinadequate recordingofbloodpressure,laboratory,orotherclinicaldata (Figure).Themeanageofincludedpatientswas49years (SD20),and113(74%)weremale(Table1).Motorvehicle collisionswerethemostcommonmechanismofinjury, accountingfor66%ofthepatients’ causeofinjuries.Median GCSatadmissionwas5(3-13).Amongthestudypopulation, 141patients(92%)requiredmechanicalventilationduring theirstay,and94patients(61%)underwentatracheostomy
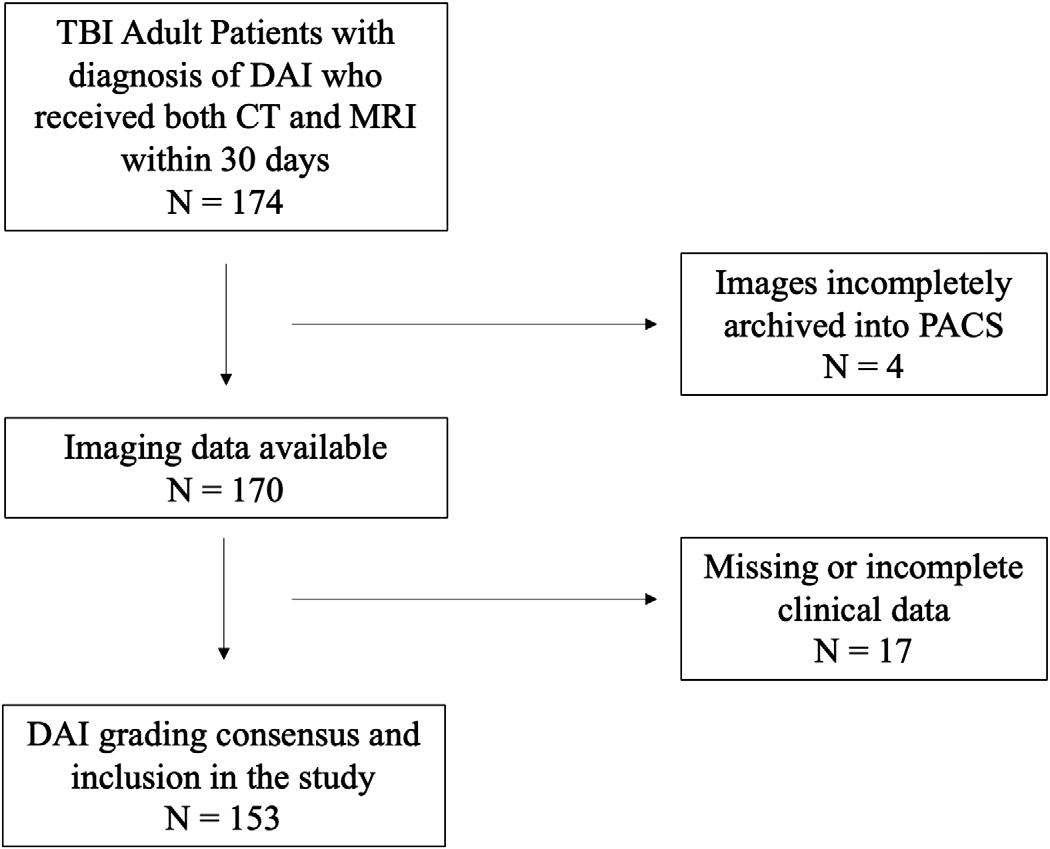
Figure. Flowdiagramforpatientselection.
TBI,traumaticbraininjury; CT,computedtomography; MRI, magneticresonanceimaging; PACS,picturearchivingand communicationsystem.
procedure.ThemostcommonlocationofDAIburdenwas thecorpuscallosum(58%)followedbytheparahippocampus (35%),basalganglia(27%)andthalami(25%)(Table1). Withinthe first24hours,allpatientshadreceivedsomeform ofopioidmedication,98%ofthepatientsreceivedIV fluids (IVF),95%receivedasedativemedication,87%receivedan anti-epilepticmedication,and82%requiredvasopressor support(Table2).
Ouranalysisidentifiednosignificantassociationbetween twoseparatemeasurementsofBPV– SBPSV (Coefficient0.02,OR0.98,95%CI0.87-1.10, P = 0.74)andSBPSD (Coeff 0.03,OR0.97,95%CI0.81-1.16, P = 0.74)–andhospital dispositionamongpatientsadmittedforTBIanddiagnosed withDAI.Wefoundthat11.8%ofpatientswithDAIeither diedinthehospitalorweredischargedtohospicecare.This groupofpatientshadahighermeanageof63(19)andlower GCSscoresat24hoursand5days(5[4-6.3]forboth)than survivors(Table1).Allthesepatientsrequiredintubation,all werediagnosedwithaconcurrentbraincontusion,and94% hadaconcurrentIVH.Thecorpuscallosumwasidentifiedas thepredominantlocationofDAIamongpatientswhodied, andahighervolumeofhematomawasobservedinthe corpuscallosumofthisgroupwhencomparedtosurvivors (Table1).Nosignificantdifferenceswerefoundintermsof sex,pastmedicalhistoryofhypertensionanddiabetes,or mechanismofinjury.
Weusedordinallogisticregressionanalysistoinvestigate therelationshipbetweendemographicandclinicalfactors andthelikelihoodofasignificantdiscrepancyintheprimary
Table1. Demographicsandclinicalfeaturesofpatientswithdiffuseaxonalinjuriesfortheoutcomeofmortality.
Sex, N(%)
Pastmedicalhistory,N(%)
Clinicalvariables
Volumeofburdenbylocationofinjury,(mm3)median[IQR]
Continued onnextpage
Table1. Continued.
Boldedvaluesindicatestatisticalsignificance.
CI, confidenceinterval; IQR,interquartilerange; GCS,GlasgowComaScore; mg,milligram; dL,deciliter; INR,internationalnormalizedratio; EVD,externalventriculardrain; IPH,intraparenchymalhemorrhage; IVH,intraventricularhemorrhage; SAH,subarachnoidhemorrhage; ARDS,acuterespiratorydistresssyndrome; MVC,motorvehiclecollision; mm,millimeter.
Table2. Clinicalfeatureswithin24hoursforpatientswithdiffuseaxonalinjuries.
Bloodpressurevariability
Hospitaldisposition,N(%)
DAI, diffuseaxonalinjury; IVF,intravenous fluid; PRBC,packedredbloodcells; FFP,freshfrozenplasma; SBP,systolicbloodpressure; max, maximum; min,minimum; SBPSV,systolicbloodpressuresuccessivevariation; SBPSD,systolicbloodpressurestandarddeviation; SBPCV, systolicbloodpressurecoefficientofvariation.
Table3. Resultsfromordinallogisticregressionassessingassociationbetweenpatients’ demographicandclinicalfactorsandpatients’ disposition,whereorderofhospitaldispositionwasrankedfrom0 = home,1 = acuterehab,to2 = hospice/death.Allindependentvariables reportedinthistablewereaddedinthemodel.
Pastmedicalhistory
Bolded P-values indicatestatisticalsignificance.
OR,oddsratio; CI,confidenceinterval; GCS,GlasgowComaScore; INR,internationalnormalizedratio; AED,antiepilepticdrugs; IPH,intraparenchymalhemorrhage; IVH,intraventricularhemorrhage; SAH,subarachnoidhemorrhage.
Table4. Resultsfromordinallogisticregressionassessingassociationbetweenbloodpressurevariabilityandpatients’ disposition,where orderofhospitaldispositionwasrankedfrom0 = home,1 = acuterehab,to2 = hospice/death.
OR, oddsratio; CI,confidenceinterval; SBP,systolicbloodpressure; SBPSV,systolicbloodpressuresuccessivevariation; SBPSD,systolic bloodpressurestandarddeviation; SBPCV,systolicbloodpressurecoefficientofvariation.
outcomeofdisposition(Table3).TheSBPvariation measurementsdidnotdemonstrateanassociationwiththe dispositionoutcome(Table4).Otherclinicalfactorssuchas age,contusions,GCSscores,basalgangliainvolvement,and thepresenceofSAHwerefoundtobeassociatedwith dischargedestination.
Amongthedemographicfactors,agedemonstrateda marginalassociationwiththeoutcome(OR0.97,95%CI 0.93-1.00, P = 0.05,Coeff-0.03),suggestingthatyounger patientsmaybemorelikelytoachievefavorableoutcomesin termsofdisposition.Thepresenceofanycerebralcontusion (OR0.09,95%CI0.01-0.75, P = 0.03,Coeff-2.39)and higherinitialINR(OR0.03,95%CI0.00-0.70, P = 0.03, Coeff-3.67)correlatedwithpoordispositionoutcomes. Thesenegativecoefficientsindicatethatifthereis contusionpresentorthevalueoftheinitialINR increases,theassociationwithhigheroutcomenumbers strengthens;inthiscasethehighestoutcomenumber ishospice/death.
Additionally,weidentifiedGCSat fivedaysasa significantfactoraffectingtheoutcomesofdisposition(OR 95%CI1.30-2.49, P =< 0.001,Coeff0.59).HigherGCS scoresat fivedayswerestronglyassociatedwithanincreased probabilityofachievingmorefavorableoutcomes,suchas dischargetohomeorrehabilitation.Regardingthelocation ofburden,patientswithinvolvementofthebasalgangliahad poorerprognosis(OR5.02,95%CI1.02-24.62, P = 0.05, Coeff1.61).ThepresenceofSAHwasunexpectedly identifiedwithbetterdispositionoutcomes(OR7.26,95%CI 1.14-46.42, P = 0.04,Coeff1.98).
TheSBPSV (Coeff0.02,OR1.02,95%CI0.95-1.1, P = 0.51)andSBPSD (Coeff0.02,OR1.02,95%CI0.91-1.13, P = 0.75)werenotassociatedwithoursecondaryoutcomeof HD5GCS(Table5).Receivinganybloodproducts(OR2.89, 95%CI1.10-7.60, P = 0.03,Coeff1.06),aswellastreatment withvasopressors(OR4.05,95%CI1.37-11.96, P = 0.01, Coeff1.40),hyperosmolartherapy(OR3.41,95%CI1.368.54, P = 0.01,Coeff1.23),andthepresenceofconcurrent IVH(OR2.70,95%CI0.86-6.49, P = 0.03,Coeff0.99)were allassociatedwithanincreasedlikelihoodofalower
HD5GCS(Table6).Ontheotherhand,theuseof antiepilepticdrugs(OR0.27,95%CI0.07-0.99, P = 0.05, Coeff-1.31)wasassociatedwithanincreasedlikelihood ofahigherHD5GCS.
Inthisstudyweinvestigatedtheimpactof24-hoursystolic BPVonoutcomesinpatientsdiagnosedwithDAIand soughttoidentifyrelevantclinicalfeaturesthatmaycorrelate withpatientoutcomestoimproveprognosticassessments. Wedidnot findasignificantassociationbetweenBPVand outcomesinpatientswithDAI.Thisstandsincontrastto priorstudies,suchasthatbySvedungWetterviketal,who linkedBPVtodeviationsfromoptimalCPPoptand unfavorableoutcomesinpatientswithTBI.25 Ithasbeen proposedthatthenegativeimpactofBPVonpatient outcomesmaybeattributedtothedevelopmentof compromisedcerebralblood flowregulationinTBIandthe potentialforsecondaryinjuriessuchascerebral hypoperfusionorhyperemia;however,theexactpathways andunderlyingprocessesarenotfullyunderstood.26,27 There arealsoseveralnuances,suchasthedurationandfrequency ofBPVmonitoring,thetimingofBPVinrelationtotheonset ofinjury,andthesensitivityofdifferentBPVparameters, suchasdiastolicbloodpressureorMAPvariability,that requireadditionalinvestigationandmayalsoplayarolein predictingoutcomes.28,29
Itisalsounknownwhatrolebloodpressuremanagement mightplayinmitigatingtheimpactsofBPV.Itisstandard practiceatourinstitutiontomanagehypertension(definedat thetimeofthisstudyasSBP >160mmHgforpatientswith TBI)andhypotension(MAP <65mmHg)inpatientswith TBIusingtitratableinfusionsofantihypertensivesand vasopressors.Strictmanagementofbloodpressuremayhave dampenedBPVandlimitedourabilitytodetectaneffecton patientoutcomes.Lastly,BPVmayhavenoimpacton improvingthedamagecausedbyaxonalshearinginDAI,or inpreventingsecondaryaxotomy.Additionalstudiesare neededtoclarifytheinterplaybetweenBPV,cerebral hemodynamics,andDAIpathology,aswellastodetermine themostrelevantandsensitiveBPVparametersfor predictingoutcomes.
Table5. Resultsfromordinallogisticregressionassessingassociationbetweenbloodpressurevariabilityandpatients’ hospitalday five GlasgowComaScore(GCS),whichwasrankedinorderfrom0(GCS3-8),1(GCS9-12),2(GCS13-14),3(GCS15).
GCS, GlasgowComaScore; OR,oddsratio; CI,confidenceinterval; SBP,systolicbloodpressure; SBPSV,systolicbloodpressure successivevariation; SBPSD,systolicbloodpressurestandarddeviation; SBPCV,systolicbloodpressurecoefficientofvariation.
Table6. Resultsfromordinallogisticregressionassessingassociationbetweenpatients’ demographicandclinicalfactorsandpatients’ hospitalday fiveGlasgowComaScore(GCS),whichwasrankedinorderfrom0(GCS3-8),1(GCS9-12),2(GCS13-14),3(GCS15).All independentvariablesreportedinthistablewereaddedinthemodel.
Pastmedicalhistory
Bolded P-values indicatestatisticalsignificance. GCS,GlasgowComaScore; OR,oddsratio; CI,confidenceinterval;INR,internationalnormalizedratio; AED,antiepilepticdrugs; IPH,intraparenchymalhemorrhage; IVH,intraventricularhemorrhage; SAH,subarachnoidhemorrhage.
Ourstudyrevealedseveralclinicalfactorscorrelatingwith patientoutcomes,specificallyincreasedinitialINR, concurrentcerebralcontusion,andlowGCSathospital day5.OuridentificationofinitialINRasapoorprognostic factorwithrespecttohospitaldispositioncontributestothe growingbodyofevidenceontheassociationbetween coagulopathyandpoorclinicaloutcomesinpatientswith TBI,specificallythosewithDAI.30,31 Thedisturbancein coagulationstatusatadmissionmayexacerbatebleedingand contributetoapoorerprognosis.Coagulopathyinducedby TBIfollowsadistinctpathogenicpathway,separatefrom coagulopathyinducedbyextracranialtraumaand hemorrhagicshock.Itcaninvolvedisruptionsinthe
blood-brainbarrier,whichallowleakageof fluidandrelease procoagulantsubstances.Thesesubstancesmayalso accelerateandenhance fibrinolysis.Earlymonitoringand managementofcoagulationabnormalitieshold thepotentialtoimprovepatientsurvivalandreducerates ofmortality.30
Concurrentcerebralcontusions,whichcontributeto secondarybraininjury,andlowGCSscoresatday5of hospitalization,whilenotalwaysintervenable,playcrucial rolesinidentifyingpatientsathigherriskofpoorneurologic outcomes.Althoughour findingsshowthatconcurrentIVH inpatientswithDAIwasnotassociatedwithincreased mortality,itwasassociatedwithlowerHD5GCS,whichisa
predictorofpooroutcomes.Theseresultsalignwithprior researchthatsuggeststhatthepresenceofIVHisassociated withsevereDAI.32
Thisstudyalsohighlightedthatpatientswhoreceived bloodproducts,vasopressors,orhyperosmolartherapyin the first24hoursofadmissionhadahigherlikelihoodofa lowGCSscoreathospitalday5.Thisfollowsclinical reasoninginsuggestingthatthesetherapiesandinterventions aremorecommonamongpatientswithmoresevere impairmentinneurologicalfunctionwhoareathigherrisk forpooreroutcomes,althoughbasedonour findingswe cannotconcludewhetherthesetherapiesthemselvesmaybea driverofpooroutcomes.ThepresenceofIVHwasalso associatedwithahigherlikelihoodofalowerGCSscore, furtheremphasizingtheimpactofconcurrentIVHon neurologicalimpairment.Incontrast,theuseofantiepileptic drugs(AED)wasassociatedwithahigherlikelihoodof achievingahigherGCSscoreonhospitalday5,suggestinga potentialbeneficialeffectofAEDsinpreservingneurological function.Withinthiscontext,itisinterestingtonotethat therewasnosignificantassociationbetweenseizureduring admissionandHD5GCS.Furtherstudiesareneededto establishaconclusiveassociationbetweenAEDuseand improvedGCSscoresinDAIpatients,andtoinvestigate whetherthisassociationvariesacrossdifferentAEDs.(Our institutiontypicallyusesaprophylacticregimenof levetiracetam1.5grams[g]followedby1gBIDforseven days.)ThepotentialneuroprotectiveeffectsofAEDs warrantadditionalinvestigation.
Theretrospectivedesignofourstudyandtherelianceon EHRfordatacollectionintroducedinherentbiasesand constraintstoaccuracyofdatacollectionthatwewere unabletoaudit,suchasthepossibilityofmanualinputerrors orinaccuratetimemeasurements.Itisimportantto acknowledgethatthecollectionofbloodpressurevaluesin ourstudylackedstandardization.Variationsinthetypeof equipmentused,whetherinvasiveornon-invasive readingswereemployed,andthetimingofdatacollection couldhaveintroducedvariabilityintothemeasured BPvalues.
AspatientswithDAIareassociatedwithsevereTBI,our populationwasalsolikelytohavebeenmorecriticallyill. Thisisalsoevidencedbythepercentageofourstudy populationrequiringmechanicalventilation(92%)and eventualtracheostomy(61%).Thismayhaveintroducedan indicationbias,inwhichtherewasclosermonitoringand tightercontrolofbloodpressureparameters.Another limitationisthatouranalysiswasconductedatasingle center,whichisaregional,quaternarytraumaand neurotraumaspecialtycenter.Thissettingpotentiallylimits thegeneralizabilityofour findingstopatientswithDAI presentinginotherhealthcaresettings.Variationsinpatient
characteristics,treatmentprotocols,andaccesstoresources acrossdifferentcentersmayin fluencetheobserved associations.Additionally,therelativelysmallsamplesizeof ourstudymayhavelimitedthestatisticalpowertodetect smallerassociationsbetweenBPVandDAIoutcomes.
Patientswithradiographicallydiagnoseddiffuseaxonal injuriesfacehighratesofmorbidityandmortality;only8% ofpatientswithinourstudypopulationweredischarged homedirectlyfromthehospital.Bloodpressurevariability wasnotidentifiedasapredictorofdischargedisposition.We identifiedthatGlasgowComaScoreathospitalday5,initial INR,andconcurrentcerebralcontusionaspotentialdrivers ofpooroutcomes.Itisunclearfromourstudywhether interventionsaimedatthesevariables(eg,correctingan elevatedINR)wouldhaveaffectedpatients’ outcomes,or whethertightcontrolofpatients’ bloodpressureswith titratableinfusions(bothantihypertensivesand vasopressors)mayhavemaskedtheimpactofBPV onoutcomes.
AddressforCorrespondence:ChristineE.Ren,MD,OregonHealth andScienceUniversity,DepartmentofEmergencyMedicineand CriticalCareMedicine,3181SWSamJacksonParkRd.,Portland, OR97239.Email: rench@ohsu.edu
ConflictsofInterest: Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2025Renetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AngelovaP,KehayovI,DavarskiA,etal.Contemporaryinsightinto diffuseaxonalinjury. FoliaMed(Plovdiv). 2021;63(2):163–70.
2.MeythalerJM,PeduzziJD,EleftheriouE,etal.Currentconcepts:diffuse axonalinjury-associatedtraumaticbraininjury. ArchPhysMedRehabil. 2001;82(10):1461–71.
3.GrahamNSN,JollyA,ZimmermanK,etal.Diffuseaxonalinjurypredicts neurodegenerationaftermoderate-severetraumaticbraininjury. Brain. 2020;143(12):3685–98.
4.VieiraRC,PaivaWS,deOliveiraDV,etal.Diffuseaxonalinjury: epidemiology,outcomeandassociatedriskfactors. FrontNeurol. 2016;7:178.
5.LiXYandFengDF.Diffuseaxonalinjury:novelinsightsintodetection andtreatment. JClinNeurosci. 2009;16(5):614–9.
6.AdamsJH,DoyleD,FordI,etal.Diffuseaxonalinjuryinhead injury:definition,diagnosisandgrading. Histopathology. 1989;15(1):49–59.
7.HumbleSS,WilsonLD,WangL,etal.Prognosisofdiffuseaxonal injurywithtraumaticbraininjury. JTraumaAcuteCareSurg. 2018;85(1):155–9.
8.PalmieriM,FratiA,SantoroA,etal.Diffuseaxonalinjury:clinical prognosticfactors,molecularexperimentalmodelsandtheimpactofthe traumarelatedoxidativestress.Anextensivereviewconcerning milestonesandadvances. IntJMolSci. 2021;22(19):10865.
9.LohaniS,BhandariS,RanabhatK,etal.DoesdiffuseaxonalinjuryMRI gradereallycorrelatewithfunctionaloutcome? WorldNeurosurg. 2020;135:e424–6.
10.MalecJF,MandrekarJN,BrownAW,etal.Injuryseverityanddisability intheselectionofnextlevelofcarefollowingacutemedicaltreatmentfor traumaticbraininjury. BrainInj. 2009;23(1):22–9.
11.SvedungWettervikT,HowellsT,EnbladP,etal.Temporal neurophysiologicaldynamicsintraumaticbraininjury:roleofpressure reactivityandoptimalcerebralperfusionpressureforpredicting outcome. JNeurotrauma. 2019;36(11):1818–27.
12.TranQK,FrederickH,TranC,etal.Bloodpressurevariabilityand outcomeintraumaticbraininjury:apropensityscorematchingstudy. WestJEmergMed. 2022;23(5):769–80.
13.ZhaoJ,YuanF,FuF,etal.Bloodpressurevariabilityandoutcomein acuteseverestroke:aposthocanalysisofCHASE-arandomized controlledtrial. JClinHypertens(Greenwich). 2021;23(1):96–102.
14.PreiksaitisA,KrakauskaiteS,PetkusV,etal.Associationofsevere traumaticbraininjurypatientoutcomeswithdurationofcerebrovascular autoregulationimpairmentevents. Neurosurgery. 2016;79(1):75–82.
15.DivaniAA,LiuX,DiNapoliM,etal.Bloodpressurevariabilitypredicts poorin-hospitaloutcomeinspontaneousintracerebralhemorrhage. Stroke. 2019;50(8):2023–9.
16.AndalibS,LattanziS,DiNapoliM,etal.Bloodpressurevariability:anew predictingfactorforclinicaloutcomesofintracerebralhemorrhage. J StrokeCerebrovascDis. 2020;29(12):105340.
17.TranC,FrederickH,BaqaiH,etal.Traumaticbraininjuryand intraparenchymalhemorrhageprogression:bloodpressurevariability matters. AmJEmergMed. 2022;52:119–27.
18.vanEijckMM,SchoonmanGG,vanderNaaltJ,etal.Diffuseaxonal injuryaftertraumaticbraininjuryisaprognosticfactorforfunctional outcome:asystematicreviewandmeta-analysis. BrainInj. 2018;32(4):395–402.
19.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
20.ArimaH.Threerulesforbloodpressuremanagementinacute intracerebralhemorrhage:fast,intenseandstable. HypertensRes. 2023;46(1):264–5.
21.deHavenonA,FinoNF,JohnsonB,etal.Bloodpressurevariabilityand cardiovascularoutcomesinpatientswithpriorstroke:asecondary analysisofPRoFESS. Stroke. 2019;50(11):3170–6.
22.CuthbertJP,CorriganJD,Harrison-FelixC,etal.Factorsthatpredict acutehospitalizationdischargedispositionforadultswithmoderateto severetraumaticbraininjury. ArchPhysMedRehabil. 2011;92(5):721–30.e3.
23.MaasMB,FrancisBA,SanghaRS,etal.Refiningprognosisfor intracerebralhemorrhagebyearlyreassessment. CerebrovascDis. 2017;43(3-4):110–6.
24.TardifPA,MooreL,BoutinA,etal.Hospitallengthofstayfollowing admissionfortraumaticbraininjuryinaCanadianintegrated traumasystem:aretrospectivemulticentercohortstudy. Injury. 2017;48(1):94–100.
25.SvedungWettervikT,HowellsT,LewénA,etal.Bloodpressure variabilityandoptimalcerebralperfusionpressure-newtherapeutic targetsintraumaticbraininjury. Neurosurgery. 2020;86(3):E300–9.
26.AleksandrovaEV,OshorovAV,SychevAA,etal.Autoreguliatsiia mozgovogokrovotokapritiazhelomdiffuznomaksonal’nom povrezhdeniigolovnogomozga:rol’ neı ˘roanatomicheskikhfaktorov [Autoregulationofcerebralblood flowinseverediffuseaxonalbrain injury:theroleofneuroanatomicalfactors]. ZhVoprNeirokhirImNN Burdenko. 2018;82(3):5–14.
27.CarneyN,TottenAM,O’ReillyC,etal.Guidelinesforthemanagement ofseveretraumaticbraininjury,4th ed. Neurosurgery. 2017;80(1):6–15.
28.TullyPJ,YanoY,LaunerLJ,etal.Associationbetweenbloodpressure variabilityandcerebralsmall-vesseldisease:asystematicreviewand meta-analysis. JAmHeartAssoc. 2020;9(1):e013841.
29.ChungPW,KimJT,SanossianN,etal.Associationbetween hyperacutestagebloodpressurevariabilityandoutcomeinpatientswith spontaneousintracerebralhemorrhage. Stroke. 2018;49(2):348–54.
30.ZhangJ,ZhangF,DongJF.Coagulopathyinducedbytraumatic braininjury:systemicmanifestationofalocalizedinjury. Blood. 2018;131(18):2001–6.
31.ShammassianBH,RonaldA,SmithA,etal.Viscoelastichemostatic assaysandoutcomesintraumaticbraininjury:asystematicliterature review. WorldNeurosurg. 2022;159:221–36.e4.
32.Mata-MbembaD,MugikuraS,NakagawaA,etal.Intraventricular hemorrhageoninitialcomputedtomographyasmarkerofdiffuse axonalinjuryaftertraumaticbraininjury. JNeurotrauma. 2015;32(5):359–65.