Volume 8, Number 2, May 2024



Volume 8, Number 2, May 2024
Clinicopathological Cases from the University of Maryland
83 54-year-old Woman with Chest Pain
Zachary R. Wynne, Kami M. Hu, Laura J. Bontempo, John David Gatz
Case Series
90 Using Point-of-care Ultrasonography to Diagnose Traumatic Arthrotomy of the Knee: A Case Series
Jordan Mullings, Henry Ashworth, Matthew Kongkatong, Daniel Mantuani
Case Report
95 A Critical Combination of Esophageal Rupture and Upside-down Stomach: A Case Report
Kay Nicole Tipton, Daniel Schroder
99 Acute Abdominal Pain and a Whirlpool Sign on Computed Tomography: A Case Report Christopher Libby, Evan Stern, Robyn Hoelle
102 Cardiac Arrest During a Ferric Derisomaltose Infusion Followed by Complete Heart Block: A Case Report
Michael Scott, Natalie Jansen, Leslie A. Bilello
107 Defibrillator Lead Perforation Leading to Concerning Electrocardiogram Findings: Case Report
Bryan Rosenberg, Max Hockstein, Cyrus Hadadi
111 Diabetic Ketoalkalosis: A Case Report
April Brill, Nirav Chheda, Daniel Strama, Ramesh Soundarajan
115 Emergency Department Doppler Assessment of a Central Retinal Artery Occlusion: Case Report Duncan McGuire, Robert Calleja, Eric Pai, Amit Bahl



Contents continued on page iii
















Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital, and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Penn State Health Lancaster Pediatric Center in Lancaster, Pa.; Penn State Health Lancaster Medical Center (opening fall 2022); and more than 3,000 physicians and direct care providers at more than 126 outpatient practices in 94 locations. Additionally, the system jointly operates various health care providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center, Hershey Endoscopy Center, Horizon Home Healthcare and the Pennsylvania Psychiatric Institute.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pa.


Indexed in PubMed and full text in PubMed Central
Rick A. McPheeters, DO, Editor-in-ChiefR. Gentry Wilkerson, MD, Deputy Editor University of Maryland School of Medicine
Mark I. Langdorf, MD, MHPE, Senior Associate Editor University of California, Irvine School of Medicine- Irvine, California
University of California, Irvine School of Medicine- Irvine, California
Shadi Lahham, MD, MS, Associate Editor Kaiser Permanente- Orange County, California
Manish Amin, DO, Associate Editor
John Ashurst, DO, Decision Editor/ ACOEP Guest Editor Kingman Regional Health Network, Arizona
Anna McFarlin, MD, Decision Editor
Louisiana State University Health Science Center- New Orleans, Louisiana
Lev Libet, MD, Decision Editor
Amin A. Kazzi, MD, MAAEM
The American University of Beirut, Beirut, Lebanon
BarryE. Brenner, MD, MPH Case Western Reserve University
Brent King, MD, MMM University of Texas, Houston
Daniel J. Dire, MD University of Texas Health Sciences Center SanAntonio
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Erik D. Barton, MD, MBA Icahn School of Medicine, Mount Sinai,
New York
Amal Khalil, MBA
Christopher Sampson, MD, Decision Editor University of Missouri- Columbia, Missouri
Joel Moll, MD, Decision Editor
Virginia Commonwealth University School of Medicine- Richmond, Virginia
Steven Walsh, MD, Decision Editor Einstein Medical Center Philadelphia-Philadelphia, Pennsylvania
University of Indiana School of Medicine- Indianapolis, Indiana
Austin Smith, MD, Decision Editor Vanderbilt University Medical Center-Nashville, Tennessee
Rachel A. Lindor, MD, JD, Decision Editor Mayo Clinic College of Medicine and Science
Jacqueline K. Le, MD, Decision Editor Desert Regional Medical Center
Christopher San Miguel, MD, Decision Editor Ohio State Univesity Wexner Medical Center
Francesco Dellacorte, MD
Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Gayle Galleta, MD
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Niels K. Rathlev, MD Tufts University School of Medicine
UC Irvine Health School of Medicine
Elena Lopez-Gusman, JD
California ACEP
American College of Emergency Physicians
DeAnna McNett, CAE
American College of Osteopathic Emergency Physicians
John B. Christensen, MD California Chapter Division of AAEM
Randy Young, MD
California ACEP
American College of Emergency Physicians
Mark I. Langdorf, MD, MHPE
UC Irvine Health School of Medicine

Jorge Fernandez, MD
California ACEP
American College of Emergency Physicians
University of California, San Diego
Peter A. Bell, DO, MBA
American College of Osteopathic Emergency Physicians
Baptist Health Science University
Robert Suter, DO, MHA
American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
UC Irvine Health School of Medicine
Brian Potts, MD, MBA
California Chapter Division of AAEM Alta Bates Summit-Berkeley Campus

PabloAguilera Fuenzalida, MD
Región Metropolitana, Chile
PeterA.Bell, DO,MBA Baptist Health Science University
Peter Sokolove, MD University ofCalifornia, San Francisco
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Scott Rudkin, MD, MBA University of California, Irvine
Scott Zeller, MD University of California, Riverside
Isabelle Nepomuceno, BS Executive Editorial Director
Visha Bajaria, BS CPC-EM Editorial Director
Emily Kane, MA CPC-EM Editorial Director
Stephanie Burmeister, MLIS
CPC-EM Staff Liaison
Clinical Forensic Medicine
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Vijay Gautam, MBBS University of London, London, England
Wirachin Hoonpongsimanont, MD, MSBATS Siriraj Hospital, Mahidol University, Bangkok, Thailand
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA CPC-EM Publishing Director
June Casey, BA Copy Editor

Available in MEDLINE, PubMed, PubMed Central, Google Scholar, eScholarship, DOAJ, and OASPA WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA the American Academy of Emergency Medicine

This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians California ACEP California Chapter Division of AmericanAcademy of Emergency Medicine
Academic Department of Emergency Medicine Subscribers
Albany Medical College Albany, NY
American University of Beirut Beirut, Lebanon
Arrowhead Regional Medical Center Colton, CA
Augusta University Augusta GA
Baystate Medical Center Springfield, MA
Beaumont Hospital
Royal Oak, MI
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Conemaugh Memorial Medical Center Johnstown, PA
Desert Regional Medical Center Palm Springs, CA
Doctors Hospital/Ohio Health Columbus, OH
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Emory University Atlanta, GA
Genesys Regional Medical Center Grand Blanc, Michigan
Hartford Hospital Hartford, CT
Hennepin County Medical Center Minneapolis, MN
Henry Ford Hospital Detroit, MI
Arizona
INTEGRIS Health
Oklahoma City, OK
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kern Medical Bakersfield, CA
Lakeland HealthCare
St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maricopa Medical Center Phoenix, AZ
Massachusetts General Hospital Boston, MA
Mayo Clinic College of Medicine Rochester, MN
Mt. Sinai Medical Center Miami Beach, FL
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Presence Resurrection Medical Center Chicago, IL
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
Southern Illinois University Carbondale, IL
St. Luke’s University Health Network Bethlehem, PA
Stanford/Kaiser Emergency Medicine Residency Program Stanford, CA
Staten Island University Hospital Staten Island, NY
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
University of Alabama, Birmingham Birmingham, AL
University of Arkansas for Medical Sciences Little Rock, AR
University of California, Davis Medical Center Sacramento, CA
University of California Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago, Chicago, IL
University of Colorado, Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
University of Illinois at Chicago Chicago, IL
University of Illinois College of Medicine Peoria, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of Nebraska Medical Center Omaha, NE
University of South Alabama Mobile, AL
University of Southern California/Keck School of Medicine Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Texas Health San Antonio, TX
University of Warwick Library Coventry, United Kingdom
University of Washington Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
Wake Forest University Winston-Salem, NC
Wright State University Dayton, OH
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
MediterraneanAcademyofEmergencyMedicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Sociedad Chileno Medicina Urgencia ThaiAssociationforEmergencyMedicine
To become a WestJEM departmental sponsor, waive article processing fee, receive print and copies for all faculty and electronic for faculty/residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Indexed in PubMed and full text in PubMed Central
Clinical Practice and Cases in Emergency Medicine (CPC-EM) is a MEDLINE-indexed internationally recognized journal affiliated with the Western Journal of Emergency Medicine (WestJEM). It offers the latest in patient care case reports, images in the field of emergency medicine and state of the art clinicopathological and medicolegal cases. CPC-EM is fully open-access, peer reviewed, well indexed and available anywhere with an internet connection. CPC-EM encourages submissions from junior authors, established faculty, and residents of established and developing emergency medicine programs throughout the world.
120 Face-off Droop: A Case Report of Pediatric Stroke
Duncan Robertson, Hayden F. Peirce, Marek D. Nicpon, Eric M. Otterson, Laurel O’Connor, Julia G. Rissmiller, Zachary W. Binder
125 Inferior Pancreaticoduodenal Artery Pseudoaneurysm Causing Biliary Obstruction: A Case Report
Patrick Meloy, Will S. Lindquester, Jeffrey Stebbins, Elaine Bromberek
129 Peritonsillar Abscess and Post-aspiration Bleed Identified with Point-of-care Ultrasound Using Endocavitary Probe: A Case Report
Jaclyn Floyd, Brandon Dahl, Matthew Whited, Ami Kurzweil
133 Permissive Hypotension in a Patient with Severe Hypernatremia: A Case Report
Andrea Hlady, David Kerner, Laura E. Walker
138 Profound Alkalosis and Prolonged QT Interval Due to Inappropriate Gastrostomy Tube Loss: A Case Report
Forrest Turner, Brandon Friedman, H. Pendell Meyers, Stephen W. Smith
143 Ruptured Ovarian Artery Aneurysm in a Postmenopausal Female: Case Report
Raj Patel, Amy Russell, Melanie M. Randall
147 Severely Painful and Pruritic Forearm Rash: A Case of Caterpillar Envenomation in South Florida
Cody M. Autrey, Stephanie A. Martinez, Michael Remaly, Eric Boccio
151 Silicone Embolism Syndrome Causing Altered Mental Status and Respiratory Failure After an Unlicensed Gluteal Silicone Injection: A Case Report
Christopher Lin, Jeremiah Robison
155 Transcatheter Arterial Embolization for Atraumatic Splenic Rupture in TEE-negative Endocarditis: A Case Report
Daniel P. High, Jose M. Acosta-Rullan, Danay Herrera, Mauricio Danckers, Daniel Heller, Daniel Zapata
159 Use of Point-of-care Ultrasound to Diagnose Rectus Abdominis Strain in the Acute Setting: A Case Report
Alejandro J. Sanoja, Michael Shalaby
163 When Educational Images Don’t Reflect the Population: Phlegmasia Cerulea Dolens, a Case Report
Kasha Bornstein, Elizabeth LaRosa, Kelsey Byrd, Dan Laney, Hector Ferral, Heather Murphy-Lavoie
Images in Emergency Medicine
168 Atraumatic Orbital Emphysema in a Young Woman
Eladio Albornoz, Janet Wildemuth, Josephine Valenzuela
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
No. 2: May 2024
Indexed in PubMed and full text in PubMed Central
Clinical Practice and Cases in Emergency Medicine (CPC-EM) is a MEDLINE-indexed internationally recognized journal affiliated with the Western Journal of Emergency Medicine (WestJEM). It offers the latest in patient care case reports, images in the field of emergency medicine and state of the art clinicopathological and medicolegal cases. CPC-EM is fully open-access, peer reviewed, well indexed and available anywhere with an internet connection. CPC-EM encourages submissions from junior authors, established faculty, and residents of established and developing emergency medicine programs throughout the world.
171 Child with Closed Head Injury and Persistent Vomiting Abdullah Khan
174 Clinical Images in Emergency Medicine: Cushing’s Disease
Jason D. Vadhan, Nathaniel Hansen, Fernando L. Benitez, Larissa I. Velez
176 One in a Million: A Woman Presenting with Unilateral Painful Ophthalmoplegia
Kevin Bennett, Eric Boccio
179 Rash and Fever in a Returned Traveler
Helena Kons, Elliott D. Herron, Zachary S. Pacheco, Erin F. Shufflebarger
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.


ZacharyR.Wynne,MD*†
KamiM.Hu,MD‡§
LauraJ.Bontempo,MD,MEd§ J.DavidGatz,MD§
*UniversityofMarylandMedicalCenter,DepartmentofEmergencyMedicine, Baltimore,Maryland
† UniversityofMarylandMedicalCenter,DepartmentofMedicine, Baltimore,Maryland
‡ UniversityofMarylandSchoolofMedicine,DepartmentofMedicine, Baltimore,Maryland
§ UniversityofMarylandSchoolofMedicine,DepartmentofEmergencyMedicine, Baltimore,Maryland
SectionEditor:JoelMoll,MD
Submissionhistory:SubmittedSeptember13,2023;RevisionreceivedNovember21,2023;AcceptedDecember1,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1666
Chestpainisacommonpresentationtotheemergencydepartment(ED)thatcanbecausedbya multitudeofetiologies.Itcanbechallengingtodifferentiatelife-threateningconditionsfrommorebenign causes.A54-year-oldwomanpresentedtotheEDcomplainingofchestpainwithdyspneainthesetting ofrecentblunttrauma.Thiscaseoffersathoroughyetpracticalapproachtothediagnosticworkupof chestpainwithdyspneaintheEDsetting.Thesurprising finaldiagnosisandcaseoutcomearethen revealed.[ClinPractCasesEmergMed.2024;8(2)83–89.]
A54-year-oldwomanwasbroughtintotheemergency department(ED)byemergencymedicalservices(EMS)for suspectedintoxication.TheEMSpersonnelfoundthepatient infrontofaconveniencestorewhostated, “afatladyfellon me. ” Shecomplainedofdiffusechestpain,whichwasworse withdeepbreaths,andshortnessofbreath.Prehospitalvital signswereunremarkable.Notreatmentswereinitiated,and thepatientwastransportedtotheED.Uponarrival,the patienttoldtheEDstaffthatearlierthatday,someonehad fallenontopofher.Shedeniedheadtraumaandhadnoloss ofconsciousness.Notlongafterward,shetriedtodrivehome butbegantofeellightheadedandpulledoveratthe conveniencestore.Thepatientcomplainedofongoing, continuouschestpainwithoutradiation.Therewasno associateddiaphoresis,paresthesias,orcough.Thepatient didcomplainofshortnessofbreathandagainstatedthather chestpainworsenedwithdeepbreathing.Shedeniedany feversorchills,abdominalpain,nausea,vomiting,diarrhea, urinarysymptoms,neckpain,orbackpain.
Hermedicalhistorywasnotableforchronicobstructive pulmonarydisease(COPD)forwhichsheusedhomeoxygen. Shealsohadaremotehistoryofbreastcancerpreviously treatedwithbilaterallumpectomies.Herhomemedications includedanasneededalbuterolinhaler, fluticasonenasal
spray,and fivemilligramtabletsofoxycodoneasneededfor chronicbackpain.Thepatientreportedahistoryoftobacco use,alcoholuse(lessthansevendrinksaweek),and occasionalmarijuana,cocaine,andecstasyuse.Shewas adamantshehadnotusedanysubstanceswithinthe prior24hours.
Oninitialpresentation,thepatient’svitalsignswere temperature36° Celsius,heartrate98beatsperminute, bloodpressure79/64millimetersofmercury(mmHg), respiratoryrate25breathsperminute,andoxygensaturation 99%onroomair.Herestimatedbodymassindexwas21 kilogramspersquaremeter.Onexamination,thepatientwas notdiaphoreticandnotinacutedistress.Herpupilswere equalandreactivewithoutmiosis.Herheadshowednosigns oftrauma.Herneckhadfullrangeofmotionwithnocervical spinetendernessandnojugularvenousdistention.Herheart hadregularrhythm,withborderlinetachycardia,andwith nomurmurs.Shehadsomeleftlateralchestwalltenderness withoutcrepitus,deformity,or flail.Herlungswereclearto auscultationandsymmetricbilaterally.Onabdominalexam, sheexhibitedrightupperandlowerquadranttenderness withoutreboundtendernessorguarding.Examinationofthe extremitiesshowednoedemaortenderness.Shewas neurologicallyintactwithaGlasgowComaScalescoreof15 andnofocaldeficits.
Table1. Initiallaboratoryresultsofa54-year-oldwomanwith chestpain.
TestPatientvalueNormalvalue
Completebloodcount
Whitebloodcellcount23.0 × 103/μL4.0–10.0 × 103/μL
Hemoglobin11.8g/dL12.0–14.7g/dL
Hematocrit37.9%36.0–45.0%
Platelets467 × 103/μL166–362 × 103/μL
Serumchemistries
Sodium139mmol/L136–145mmol/L
Potassium4.3mmol/L3.5–5.1mmol/L
Chloride100mmol/L98–107mmol/L
Bicarbonate22mmol/L21–30mmol/L
Bloodureanitrogen26mg/dL7–17mg/dL
Creatinine1.5mg/dL0.52–1.04mg/dL
Glucose295mg/dL70–99mg/dL
Aniongap17mmol/L
Calcium9.5mg/dL8.6–10.2mg/dL
Magnesium2.6mg/dL1.6–2.6mg/dL
Lactate-initial3.8mmol/L0.5–2.2mmol/L
Lactate-repeat3.1mmol/L0.5–2.2mmol/L
Hepaticstudies
Aspartate aminotransferase 55U/L14–36U/L
Alanine aminotransferase
13U/L0–34U/L
Alkalinephosphatase144U/L38–126U/L
Totalbilirubin0.4mg/dL0.3–1.2mg/dL
Cardiacstudies
Troponin0.9ng/mL <0.06ng/mL
NT-proBNP402pg/mL <300pg/mL
D-dimer5138ng/mLFEU <499ng/mLFEU
Urinalysisstudies
Whitebloodcellcount50perhpf0–5perhpf
Redbloodcellcount15–29perhpf0–2perhpf
Leukocyteesterase2+ Negative
NitriteNegativeNegative
BacteriaNegativeNegative
UrinepregnancytestNegativeNegative
K,thousand; mcL,microliter; g,gram; dL,deciliter; mmol,millimole; L,liter; mg,milligram; u,units; ng,nanogram; pg,picogram; FEU, fibrinogenequivalentunits; hpf,high-power field; NT-proBNP, N-TerminalPro-BrainNatriureticPeptide.
elevatedbloodureanitrogen(BUN)andcreatinine.Liver functiontestswerenotableforanelevatedaspartate aminotransferase(AST)withanormalalanine aminotransferase(ALT)levelalongwithanelevatedalkaline phosphatasewithnormaltotalbilirubin.Urinalysiswas notableforpyuria,hematuria,andleukocyteesterase.Initial lactatewas3.8millimolesperliter(mmol/L),whichtrended downto3.1mmol/Laftercrystalloidandvasopressor therapyinitiation.Troponinbiomarkerwaselevatedalong withNT-pro-B-natriureticpeptideandD-dimer.An electrocardiogram(ECG)andachestradiograph(CXR) wereobtainedaswell(Images1 and 2).
Thepatientreceivedintravenous(IV) fluidresuscitation withcrystalloid.Concurrently,shewasstartedona norepinephrineinfusiontomaintainameanarterialpressure (MAP)ofgreaterthan65mmHg.AsherMAPimproved, theinfusionwasthendiscontinued.Thepatientwasstarted onempiricantibioticswithpiperacillin/tazobactamdueto theconcernforsepsisofunknownetiologyasthecauseofher hypotension.Atestwassubsequentlyordered,anda diagnosiswasmade.
Presentedisa54-year-oldwomancomplainingofleftsided,pleuriticchestpain,lightheadedness,andshortnessof breathafterreportedblunttrauma.Thereisconcernfromthe accompanyingmedicthatillicitsubstanceusemaybe contributory,andthepatientfreelyadmitstosubstance use butover24hourspriortosymptomonset.Thereareno symptomsofrecentillnessorinfectionand,specifically pertinenttoatraumaevaluation,nootherpainsandno hematologicissues.
Thepatient’spastmedicalhistoryincludesadiagnosisof COPDonsupplementaloxygenatbaseline,whichmight predisposehertoaspontaneousortraumaticpneumothorax ifsheexperiencedablebrupture.Herhistoryofbreast cancer,presumablyinremission,doesgivemepause a recurrenceoflocalormetastaticdiseaseorsecondary pathologysuchasapulmonaryembolism(PE)relatedto malignancy-associatedhypercoagulabilitycouldpotentially berelatedtoherpresentationaswell.Hersurgicalhistory andmedicationlistdonotseemoutoftheordinaryforher providedhistory.Asnotedpreviously,sheadmitsto occasionalmarijuana,methylenedioxymethamphetamine (commonlyknownasMDMA, “ecstasy,” or “molly”),and cocaineuse,whichcancertainlycausecoronaryartery vasospasmandthesymptomsassociatedwithischemia.
Laboratorystudieswerecompleted(Table1).Complete bloodcountwasnotableforleukocytosis,mildanemia,and thrombocytosis.Basicmetabolicpanelwasnotableforan
Herphysicalexam findingsaremostremarkablefor hypotensionwithaquitenarrowpulsepressure,borderline tachycardia,andtachypneadespiteanotherwisenormal cardiopulmonaryauscultatoryexam,includinganormal saturationwithoutherhomeoxygen.Thisraisesconcernfor heartfailure,volumeloss,andcardiactamponade.Aortic stenosisasacauseofthenarrowpulsepressureisunlikely


giventhatnomurmurwasauscultatedonherexamination. Thepatientisnotonlytenderoverherleftchestwall,buton therightsideofherabdomenaswell,despitepreviously denyingabdominalpain.Thisraisesconcernfor intrabdominalpathologysuchastrauma-relatedliverinjury. Shehas,notably,noothersignsofinjury.
Themajorityofthepositivelab findingsarenon-specific, andtheirchronicityisunclear:theleukocytosisand thrombocytosiscouldbereactiveorinflammatory,andthe anemiaisborderline.HerBUNandcreatinineareelevated; however,evenifitwereacute,kidneyinjurydoesnotnarrow thedifferentialdiagnosis.Thetransaminitisismild,andan elevatedASTcouldmeaninjurytotheliver,skeletalmuscle, heart,kidney,orbrain.Ofnote,theALT,whichismore specifictotheliver,iswithinnormallimits,asisthetotal
bilirubinlevel,thusmakingprimaryliverpathologyless likely.Themostinterestinglababnormalitiesarethe elevatedtroponin,natriureticpeptide,andD-dimer levels,aswellasthelactatethatdoesnotclearwithIV fluidadministration.
HerCXRisgenerallyunremarkable,withouttheclassic (althoughuncommon) findingsassociatedwithPEsuchas Hamptonhump,Westermarksign,parenchymal consolidation,Fleischnersign,orpleuraleffusion.1 Theclear CXReliminatesalargehydro/pneumothoraxora flailchest astheetiologyofhersymptoms.HerECGdemonstratesa normalsinusrhythm,withnormalintervals,normalaxis, andanisolatedT-waveinversioninleadaVL,eliminating acutecoronarysyndromeasthecauseofher chestpain.
Primarilyneurologicdisordersareexcludedfromthe differentialdiagnosis,giventhelackofanycentralnervous systemrelatedphysicalexam findingsandthepresenceof hypotension.Pathologiescausingasecondaryincreasein intracranialpressurewouldbeaccompaniedbyanormalor elevatedbloodpressureandbradycardiaratherthan hypotension.Similarlyexcludedareisolatedpsychiatric disordersandmilderillnessessuchasgastritis,bronchitis, andmusclestrains,whichcouldbeconsistentwith hercomplaintsbutareinconsistentwithhervital signabnormalities.
Thepatienthasanelevatedglucoseandamildaniongap, butadiagnosisofdiabeticketoacidosisdoesnotexplainthe restofhercardiaclababnormalities.Sheisnotbradycardic andhasnoothercardinalsignsorcomplaintsassociatedwith hypothyroidismsuchasmyxedemaorhypothermia,nordoes shehavethehypertension,headaches,palpitations,or flushingusuallyassociatedwithpheochromocytoma.Her electrolytesandbloodpressureimprovementwith fluids makeadiagnosisofadrenalinsufficiencyunlikely,whilethe lab findingsofanelevatedplateletcountandnormaltotal bilirubinexcludethehematologicemergencythrombotic
Image1. Electrocardiogramofa54-year-oldwomanwithchestpain.thrombocytopenicpurpuraorotherhemolyticanemiasasa causeofhersymptoms.Aleukocytosiscanbeindicativeof hematologicmalignancy,butthewhitecountelevationistoo mildtobeacauseofleukostasisleadingtocardiacissues,and theleukemiasarenottypicallyassociatedwithhypotension withoutotherpathology.
Whilesometoxicologicentitiescancausehemodynamic instability,anelevatedlactate,andcardiovascularlab abnormalities,itisunlikelyforthispatient’spathologytobe attributabletococaineuseorsomethingsuchastricyclic antidepressanttoxicitywithoutnotable findingsonherECG (suchasT-waveandST-segmentchangesinthecaseofthe former,andPR-segmentprolongationorQRS-complex wideninginthelatter).Thelackofothersupportingevidence orhistoryforatoxiningestionorexposuremakesearly cyanidetoxicityandcarbonmonoxidepoisoningunlikely aswell.
Thepatient’svitalsignsdidimproveafterreceivinga broad-spectrumantibioticandIV fluids,whichcould supportadiagnosisofsepsisrelatedtoanunidentified infection.Infectiouspossibilitiesincludeaurinarytract infectionorotheretiologiesthatwouldcausechestpain,such asmediastinitis,septicarthritis,endocarditis,herpes zosterwithorwithoutbacterialcellulitis,andpneumonia withorwithoutempyema.Left-sidedchestwallpainisnot likelytoinvolveabonyjoint,andwithaclearCXRandno othersymptomsorphysical findingstosupportthese diagnoses,thepotentiallypositiveurinalysisisthe onlyindicationofinfection.Aurinarytractinfection isnotmuchofadiagnosticdilemma,andonewould expectadecreaseddiastolicpressureinsepsisfrom vasodilationratherthanisolatedsystolichypotension. Infectiousetiologiesare,therefore,removedfromthe differentialdiagnosis.
Gastrointestinal(GI)pathologiessuchasesophageal rupture,pepticulcerdiseasewithhemorrhage,and pancreatitiscancausesomeofthesymptomatology, includingchestpain,withwhichthepatientpresented, althoughagain,thereareno findingsonherradiographsto indicateanyofthese.Herlipaseisnotelevated,andshehas nohistoryofchronicpancreatitisoralcoholusethatmight indicateaburnt-outpancreasincapableofcausingan elevatedlipasedespitethepresenceofacutepancreatitisor pancreatictrauma.Althoughhersmokinghistorydoesput herathigherriskof Helicobacterpylori infection,sheisnot onanymedicationsthatwouldpredisposehertoulcer formation,andoverall,aprimaryGIetiologytoher presentationisunlikely.
Whatisleftthenaretheprimarilycardiovascularand traumaticdiagnosesthatcouldleadtoherpresentation.Even withinthesecategories,thedifferentialdiagnosisforchest painisvastandnotsignificantlynarrowedbytheadditional complaintofdyspnea.Incorporatingthe findingsof hypotensionandclearlungs,however,allowsrefinementof
thedifferentialtoamoremanageablelistthatpermits directedinterventionandstabilization.
Aspreviouslynoted,arelativelyblandECGandno mentionofpalpitationsorotherarrhythmiaswillstrikeacute coronarysyndromeandunstablearrhythmiasfromthe differentialdiagnosis.Althoughnot100%sensitive,aclear CXRwithoutshiftinthecardiacsilhouetteorsignofeffusion makesahemodynamicallysignificanthemothoraxor pneumothoraxunlikely;sothesewillcomeoffthedifferential diagnosisaswell.Lowerribfracturescouldcauseliveror spleniclacerations,buttocausehypotensiontheseentities shouldcauseamorepronouncedanemia,andtheydonot reallyaccountforthepronouncedcardiaclababnormalities andnormalALT.Whatremainsonmydifferentialdiagnosis thenarecardiomyopathy,PE,cardiactamponade,and aorticinjury.Despitetheelevatedcardiacmarkers,isolated cardiomyopathywithoutanincitingfactorisnotenoughofa diagnosis.Therearenosignsindicativeofasudden decompensatedheartfailureduetochronicillness,suchas pulmonaryedemaforleftheartfailure,orhypoxiadueto severepulmonaryhypertensionleadingtorightheart failurewithlowerextremityedemaor hepaticcongestion.
Aorticinjurycanbeassociatedwithsecondarycoronary ischemiaoreventamponade,buthertraumaticeventisnot consistentwiththehighshearstressthatcausesaortic trauma,whichtypicallyoccurswithhigh-speedmotor vehiclecollisionsorfallsfromgreatheight.BothPEand cardiactamponadecanbeassociatedwithanacute-onset obstructiveshock,withanelevatedD-dimer,troponin,and natriureticpeptide,withhepaticcongestionandelevated transaminases,withchestpainanddyspnea,andwithclear lungs.Lookingspecificallyatthetransaminases,the elevationofASTwithoutALTleansmoretowardinjuryofa non-hepatictissue,suchasthecardiacmuscle,ratherthan simplehepaticcongestion.ReturningtotheprovidedECG withthesetwodiagnosesinmind,electricalalternansisnoted tobepresent.Thus,consideringalltheabovefactorsandin thesettingofanadmittedlyunusualbutdefiniteblunt trauma,themostlikelydiagnosisiscardiactamponade,with apoint-of-careultrasoundbeingthediagnostictestofchoice.
Thepatientwassentforacomputedtomography,which showedmoderatehemopericardiumwithnoPEoraortic dissection.ShethenhadaformalechocardiogramintheED, whichshowedamoderatetolargepericardialeffusionwith impendingcardiactamponade.Thepatientwasultimately transferredtoatraumacenterandtakenimmediatelytothe operatingroomonarrival.Sternotomyandpericardial windowwereperformedatwhichtime300millilitersof bloodwasevacuated.Thesurgicalteamdiscovered thattheapexofthehearthadruptured,andthiswas repairedintraoperatively.

Image3. Postoperativeelectrocardiogramofa54-year-oldwomanwithchestpain.
Thefollowingday,thepatienthadanECG(Image3)that showedaninferiorST-segmentelevationmyocardial infarction.Repeattransthoracicechocardiogramshowed apicalhypokinesis.Coronaryangiographydonethesame dayshowedastumpedleftanteriordescendingartery,likely secondarytotherecentsurgicalrepair.Herpostoperative coursewascomplicatedbymultiplepneumothoraces,butshe wasultimatelydischargedfromthehospitalseveral weekslater.
Cardiactamponaderemainsarelativelyrarebutstriking presentationofobstructivecirculatoryshockcausedbyan accumulatingpericardialeffusion.Thepericardialeffusion canbearesultofmultipleetiologiesincludingblunttrauma (asinourpatient),penetratingtrauma,malignancy,infection (suchastuberculosis),autoimmuneconditions,uremia, andothers.2,3
Physiologically,cardiactamponadeismoreappropriately consideredasaspectrumofdiseaseratherthansimplyas beingpresentorabsent.4 Initially,thepatientwillhavea pericardialeffusionwithoutphysiologicsigns.With accumulationofthiseffusion,therewillbeanincreaseinthe pressureexertedbythepericardiumonthecardiacchambers. Patientsareoftenasymptomaticatthisstagebutare consideredatriskfortamponade.5 Therateofaccumulation ofthe fluiddeterminesthevolumethresholdatwhich symptomaticcardiactamponadeoccurs.3,5 Quickly accumulatingeffusions,suchasthoseseeninbluntor penetratingcardiacinjuries,willleadtotamponade physiologydevelopingatlowereffusionvolumes.Thisisdue totheinabilityofthe fibrouspericardialsactostretch rapidly.5 Inthecaseofsubacuteorchroniceffusions,the pericardialsaccancompensateovertime,leadingtoeffusion volumesashighasoneliterpriortothedevelopmentof cardiactamponade.5
Oncethepericardialpressureexceedstherightatrial pressure,venousinflowfromthevenacavaisimpaireddueto diastoliccollapseoftherightatrium.Thiscaninitiallybe
overcomewithincreasedcentralvenouspressurethrough fluidresuscitation.3 Eventually,increasingpericardial pressureleadstorightatrialcollapseinsystole(sensitivefor cardiactamponade)andventricularcollapseindiastole (specificforcardiactamponade).6,7 Next,thepericardial effusionbeginstoovercomediastolic fillingpressuresofall fourchambers.Thisleadstoincreasedinterventricular dependence,thestateinwhichallfourchambersmustsharea fixedintrapericardialvolume.8 Duringinspiration,decreased intrathoracicpressureandsubsequentdecreasedpulmonary vascularresistanceleadstoincreased fillingofright-sided chamberswithconsequentdecreased fillingofleftchambers inthis fixedvolume.Theoppositeoccursduringexpirationin whichleft-sidedchambersare filledmoresothantherightsidedchambersduetoincreasedresistanceencounteredby theright-sidedchambers.Thisphenomenonleadsto respiratoryvariationincardiacoutput,known aspulsusparadoxus(definedbyadeclineby10mmHg orgreaterinsystolicbloodpressure duringinspiration).8,9
Cardiacoutputisinitiallymaintainedbyincreasesinheart rateaswellasincreasedsystemicvascularresistanceby endogenouscatecholamines.Thesepatientsareoften hypertensiveearlyintheircourse;5 however,decreasedstroke volumesfromdecreasedchamber fillingeventuallyleadsto hypotension.Narrowpulsepressureremainsaphysiologic hallmarkofcardiactamponadeduetoworseningcardiac output.Eventually,pressuresofthefourcardiacchambers equalizeandpericardialpressuresbegintoincrease exponentially.Acriticalvolumeisreachedafter whichthesignificantlydecreasedcardiacoutputis unabletoperfusethecoronaryarteriessufficiently,knownas “lastdropphenomenon.” Patientsoftenthenhaveavagal responseanddevelopcardiacarrestduetocoronary arterialhypoperfusion.5
Typicalsymptomsofcardiactamponadeincludedyspnea, chestdiscomfortorpain,andtachypnea.5 Patientswithlatestagecardiactamponademayshowclinicalsignsof circulatoryshocksuchasalteredmentalstatusandcool
extremities.Patientswilloftenhaveclearlungsoundsifno otherpathologicprocessispresent.Subacuteformsof cardiactamponadewillshowsignsofrightheartfailure,such aslowerextremityedemaandjugularvenousdistension.3,5
Becktriad(jugularvenousdistension,muffledheartsounds, andhypotension)hasoftenbeentaughtinmedicalschoolsto clinicallydiagnosecardiactamponade,10 butrecentresearch suggeststhatthese findings,separateorincombination,may notsufficientlyexcludeorruleincardiactamponade.11,12
Electrocardiogram findingssuchaslowQRS-complex voltageandelectricalalternanscansuggestcardiac tamponadebutareneithersensitivenorspecificto thecondition.13
Asclinicaldiagnosiscanbeinaccurate,point-of-careor formalechocardiogramshouldbeobtainedinpatientswith undifferentiateddyspneawithconcernforpossiblecardiac tamponade.10,14 Thepresenceofapericardialeffusion shouldwarrantfurtherinvestigation.Thesizeoftheeffusion alonewillnotdeterminewhereapatientfallsonthespectrum ofillnessofcardiactamponade.Rightatrialcollapseduring systoleissensitiveforcardiactamponadewhileright ventriculardiastoliccollapseandleftatrialsystoliccollapse arespecific. 5–7 Aplethoricinferiorvenacavawithout respiratoryvariation,althoughnonspecific,furthersupports adiagnosisofcardiactamponade,whileitsabsencemakesit unlikely.Othersonographic findingsincludemitralinflow velocityrespiratoryvariation(alsoknownassonographic pulsusparadoxus),andhepatic flowreversal(measuredby pulsedwaveDoppler).6,7,15
Managementoftheobstructivecirculatoryshockcaused bycardiactamponadefocusesonremovalofthepericardial effusion.10,14 Priortoremovalof fluid,patientscanbe initiallystabilizedwith fluidresuscitationiftheyappear hypovolemic.3 Often,thesepatientshavemaximumintrinsic catecholaminestimulation,andfurtherinotropicsupport doesnotleadtoimprovedhemodynamics.5 Positivepressure ventilationshouldbeusedcautiouslyandonlyifabsolutely necessaryduetotheriskoffurtherdecreasesinvenousreturn fromincreasedintrathoracicpressure.3 Removalofthe pericardialeffusioncanbeaccomplishedinseveralways. Bedsidepericardiocentesiscanbeperformedinthesettingof impendingorongoingcardiacarrestorpersistent hypotensiondespite fluidresuscitationandvasopressor use.5,10,14 Patientswithpurulenteffusionsoreffusionsinthe settingoftraumacanhavepericardialdrainplacementdone intheoperatingroom,angiographysuiteorbyinterventional radiology.Inpatientswithtraumaticarrests,thoracotomy withpericardiotomycanbedonetorapidlydecompressthe pericardiumandassessforothertraumaticinjuries ofthethorax.16
Cardiactamponadefromventricularapexruptureinthe settingofbluntcardiactrauma
1.Patientswhopresentearlyinthecourseofcardiac tamponadewilloftenbetachycardicandhypertensive withnarrowpulsepressures.Hypotensionandsignsof end-organfailurearelate findings.
2.Thepressure,notthevolume,ofthepericardial effusionwilldeterminewhenapatientdevelopsclinical evidenceofcardiactamponade.Asloweraccumulationrateofpericardial fluidwillallowgreatereffusionvolumespriortosignsandsymptomsappearing.
3.Considerearlypoint-of-careechocardiographyin patientswithundifferentiateddyspneawhohaveno obviouspulmonaryetiology.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:J.DavidGatz,MD,Universityof Maryland,DepartmentofEmergencyMedicine,110SPacaStreet, 6thFloor,Suite200,Baltimore,MD21201.Email: jgatz@som. umaryland.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Dr.Gatzwassupportedbyagrantfrom theNationalFoundationofEmergencyMedicineduringthistime.
Copyright:©2024Wynneetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CocheE,VerschurenF,HainautP,etal.Pulmonaryembolism findings onchestradiographsandmultislicespiralCT. EurRadiol. 2004;14(7):1241–8.
2.AzarbalAandLeWinterMM.Pericardialeffusion. CardiolClin. 2017;35(4):515–24.
3.MekontsoDessapAandChewMS.Cardiactamponade. IntensiveCare Med. 2018;44(6):936–9.
4.ReddyPS,CurtissEI,UretskyBF.Spectrumofhemodynamicchanges incardiactamponade. AmJCardiol. 1990;66(20):1487–91.
5.SpodickDH.Acutecardiactamponade. NEnglJMed. 2003;349(7):684–90.
6.AlerhandSandCarterJM.Whatechocardiographic findingssuggesta pericardialeffusioniscausingtamponade? AmJEmergMed. 2019;37(2):321–6.
7.AlerhandS,AdrianRJ,LongB,etal.Pericardialtamponade: acomprehensiveemergencymedicineandechocardiographyreview. AmJEmergMed. 2022;58:159–74.
8.PetitMandVieillard-BaronA.Ventricularinterdependencein criticallyillpatients:fromphysiologytobedside. FrontPhysiol. 2023;14:1232340.
9.SwamiAandSpodickDH.Pulsusparadoxusincardiac tamponade:apathophysiologiccontinuum. ClinCardiol. 2003;26(5):215–7.
10.ChiabrandoJ,BonaventuraA,VecchiéA,etal.Managementofacute andrecurrentpericarditis. JAmCollCardiol. 2020;75(1):76–92.
11.StolzL,ValenzuelaJ,Situ-LaCasseE,etal.Clinicalandhistorical featuresofemergencydepartmentpatientswithpericardialeffusions. WorldJEmergMed. 2017;8(1):29–33.
12.RoyCL,MinorMA,BrookhartMA,etal.Doesthispatientwitha pericardialeffusionhavecardiactamponade? JAMA. 2007;297(16):1810–8.
13.GoyalM,WoodsKM,AtwoodJE.Electricalalternans:asign,nota diagnosis. SouthMedJ. 2013;106(8):485–9.
14.AdlerY,CharronP,ImazioM,etal.ESCScientificDocument Group.2015ESCguidelinesforthediagnosisandmanagementof pericardialdiseases:thetaskforceforthediagnosisandmanagement ofpericardialdiseasesoftheEuropeanSocietyofCardiology(ESC) endorsedby:TheEuropeanAssociationforCardio-ThoracicSurgery (EACTS). EurHeartJ. 2015;36(42):2921–64.
15.GinghinaC,BeladanCC,IancuM,etal.Respiratorymaneuversin echocardiography:areviewofclinicalapplications. Cardiovasc Ultrasound. 2009;7:42.
16.IshidaK,KinoshitaY,IwasaN,etal.Emergencyroomthoracotomyfor acutetraumaticcardiactamponadecausedbyabluntcardiacinjury: acasereport. IntJSurgCaseRep. 2017;35:21–4.
JordanMullings,MD*
HenryAshworth,MD,MPH*
MatthewKongkatong,MD†
DanielMantuani,MD*
SectionEditor:ShadiLahham,MD
*AlamedaHealthSystem,DepartmentofEmergencyMedicine,HighlandHospital, Oakland,California † UniversityofVirginiaHealthSystem,DepartmentofEmergencyMedicine, Charlottesville,Virginia
Submissionhistory:SubmittedOctober3,2023;RevisionreceivedOctober26,2023;AcceptedNovember16,2023
ElectronicallypublishedFebruary13,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1919
Introduction: Accuratediagnosisoftraumaticarthrotomyoftheknee(TAK)iscriticalforpatients presentingtotheemergencydepartment(ED)toensuretimelytreatment.Currentdiagnosticmodalities includingplainradiography,computedtomography(CT),andthesalineloadtest(SLT)haveadvantages anddisadvantages.Point-of-care-ultrasonography(POCUS)offersapossibletimely,low-cost,and efficientalternativemethodofdiagnosingTAK.InthiscaseserieswepresentthreecaseswherePOCUS wasusedtodiagnoseTAKintheED.
CaseSeries: Threepatientsintheirearly20spresentedtotheEDcomplainingofkneetraumawith woundsinproximitytothejoint.Mechanismsofinjuryincludedagunshotwoundinonecaseandblunt trauma(motorvehiclecollisionandbicyclecrash)intwocases.InallthreecasesTAKwassuggestedon POCUSexaminationsbythepresenceofintra-articularhyperechoicfociconsistentwithairartifact.All threecaseshadTAKconfirmedbyorthopedicevaluation.
Discussion: Ultrasoundmayhaveutilityintheevaluationofpatientspresentingwithkneetraumawhere TAKisaconcern.TheSLTisgenerallyconsideredthegoldstandardtestfordiagnosisofTAK,butitis invasiveandhasawiderangeofdiagnosticaccuracy.Intra-articularairhasbeenfoundtobeasensitive markerforTAKinCTstudies.Thus,additionalinvestigationsintothediagnosticaccuracyofPOCUSfor this findingshouldbeundertaken.[ClinPractCasesEmergMed.2024;8(2)90–94.]
Keywords: casereport;POCUS;traumaticarthrotomy;intra-articularair;musculoskeletalultrasound.
Traumaticarthrotomyoftheknee(TAK)involves damagetothecapsuleorsupportingstructures (eg,ligaments)thatresultsinviolationofthejointspace.1 Typically,traumaticarthrotomiesaretreatedbyoperative irrigationanddebridement,althoughthereisemerging evidencethatsmall,noncontaminateddefectscanbesafely treatedatthebedside.2 Delayindiagnosisandtreatmentcan resultinthedevelopmentofsepticarthritisresultingin significantincreasesinmorbidity(50%)and mortality(11–15%).3
Previousstudieshavedocumentedthediagnostic modalitiesthataremosteffectiveatdetectingTAKincases
whereitisnotobviousonphysicalexamination.4 These includeasalineloadtest(SLT)withorwithoutmethylene blueandcomputedtomography(CT).Radiographsare commonlyobtainedintheevaluationofjointinjuries.They havereasonablesensitivity(78%)andhighspecificity(90%) forTAKwhenintra-articularairisdetected.However,this findingmaybesubtleandoverlookedifthereaderis concentratingonevaluationforbonyinjury.1
TheSLTasadiagnostictoolcanbeunpredictable,with sensitivitiesreliantonmultiplefactors.5 Whileanincreased amountofinjectedsalineleadstoimprovedsensitivity(99% for175milliliters(mL),resultsvarybasedonjointlocation, patienttoleranceofinjection,andtimespentonprocedure.1,5
PassiverangingofthejointwhileperformingtheSLThas alsoshownsomeimprovementsinthesensitivityofthetest; however,combiningtheSLTwithmethyleneblueinjections hasshownlittletonobenefit.5 Therearealsosomestudies reportingthatoperatorproficiencycanleadtofalsenegative andfalsepositiveresults.5,6 TheSLTisalsopainful, particularlywhenlargevolumesareused,whichmaylimit theoperator’sabilitytoperformthetestthoroughly.
Computedtomographyhasbeeninvestigatedasan alternativetestfortraumaticarthrotomyinrecentyears.The modalityhasbeenshowntobebothhighlysensitive(100%) andspecificforTAKinacohortof62emergencydepartment (ED)patientspresentingwithwoundsaroundtheknee.7 In theseprotocolsintra-articularairisusedtomakethe diagnosisandCTissensitiveenoughtodetectaslittleas 0.1mLofair.8 Computedtomographyhasbeenshownto havesimilarperformanceintheevaluationoftraumatic arthrotomyofotherjointsaswell.1,9 Computedtomography canalsobettercharacterizefracturepatternsandinform treatmentdecisionscomparedtoradiograph.10 However, highutilizationofCTexposespatientstoincreasedamounts ofionizingradiation,incurssignificantcosttothehealthcare system,andrequiresthatthepatientleavethetreatmentarea.
Sinceintra-articularairappearstobeausefulimaging findingtodiagnoseTAK,point-of-care-ultrasonography (POCUS)maybeausefulbedsidetest,allowingforrapid diagnosiswhilesparingpatientsionizingradiationand painfuldiagnosticprocedures.Belowwedescribethe sonographicstepstodiagnoseTAK,followedbythreecases demonstratingtheutilityofultrasoundinidentifyingTAK.
Kneejointswerescannedusingahigh-frequencylinear probeinthesagittalplane,startingattheanteriorkneeinthe suprapatellarregion(Image1A).Initialorientationofthe probecollectedviewsofthefollowingstructuresinrelationto theprobemarker:patella(inferioraspectoftheview);joint
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Traumatickneearthrotomiescanleadto septicarthritisifnotidenti fi edand treatedappropriately.
Whatmakesthispresentationof diseasereportable?
Toourknowledge,thisisonlythesecondcase serieswherepoint-of-care-ultrasound (POCUS)wasusedtoaccuratelydiagnose traumaticarthrotomiesinlivingpatients.
Whatisthemajorlearningpoint?
Intra-articularairisreadilyseenonPOCUS ofkneejointsandhasprecedentofbeing agoodmarkerforarthrotomyin othermodalities.
Howmightthisimproveemergency medicinepractice?
Identi fi cationofintra-articularairon POCUSofjointsmayallowfortherapid, noninvasivediagnosisof traumaticarthrotomy.
capsule;anddistalfemur(superioraspectoftheview),as seenin Image1B (normalview).Imagescapturedinclude variousviewsinthedescribedorientationalonga

Image1. (A)Theorientationoftheprobeplacedinthesagittalplaneinthesuprapatellarregionwiththeprobemarkerorientedcranially; (B)ascanshowinganormalkneewiththetriangleindicatingthedistalfemurandthesquaremarkingthepatella.
medio-lateralpath.Abnormal findingswerecollectedand aredocumentedbelow.
A20-year-oldmalepresentedtotheEDwithagunshot woundtotheanterior,rightknee.Hereporteddifficulty walkingandlimitedrangeofmotionoftheknee.Onphysical examination,hehadtwomissilewoundsonthemedialaspect ofhisleg:onesuperiortothepatellaandoneinferiortothe tibialplateau.Theinitialradiographshowednooccult fracturebutdemonstratedbulletfragmentsneartheknee joint.APOCUSexaminationbytheemergencyphysician (EP)scanningthesuprapatellarrecessshowedinternal hyperechoiclinearstructuresconcerningforfreeair (Image2,Case1)withinhypoechoiceffusionwithanechoic bubblesconcerningforlipohemarthrosis.TheEPmadethe preliminarydiagnosisofTAK.ACTwasorderedtoconfirm TAK,butduetotheovernightburdenoftraumapatientsit wasnotperformeduntilsevenhoursafterpresentationwith interpretationtakinganadditionalhour.Orthopedicstook thepatienttotheoperatingroom(OR)thefollowingdayfor irrigationanddebridementwhereTAKwasconfirmed.The patientwasgivenaprophylacticseven-daycourseof cephalexin500milligrams(mg)everysixhoursand aone-weekfollow-upwithorthopedics.
A20-year-oldmalepresentedtotheEDwithadeep lacerationtotheleftkneeafterabicycleaccident fivehours prior.Onexamination,therewasadeep,15-centimeter(cm) longinfrapatellarlacerationwithexposedbutintacttendon. Thepatientwasambulatory,withoutneurologicdeficits,and hadfullrangeofmotionoftheleftknee.APOCUS examinationoftheleftkneewasperformedbytheEPand showedahypoechoicjointeffusioninthesuprapatellarspace
thatcontainednumerousmobile,hyperechoicstructures withposteriorshadowingalongthesuperioraspectofthe fluidcollection,suggestiveofTAK(Image2,Case2). Subsequentradiographsofthekneedemonstratednobony injurybutapossiblesmallfocusofgasinthesuprapatellar recess.Computedtomographyconfirmedthepresenceofgas withinthekneejointwiththeadditional findingofasmall, leftfemoralcondyleavulsionfracture.Thewoundwas irrigatedwithnormalsalineanddressed.Orthopedicswas consulted,andthepatientwasstartedonvancomycin intravenously.HewastakentotheORthenextdayfor irrigationandprimaryrepairofthejointcapsule.
A23-year-oldfemalepresentedtotheEDwitha lacerationneartherightkneeafteramoderate-speedmotor vehiclecollision.Onexaminationshehada4-cmlong lacerationmedialtothepatellathatextendedintothe subcutaneoustissueandsignificantpainwithpassiveranging oftheknee.Radiographsofthekneedidnotdemonstrate bonyinjury,butlucenciessuspiciousforairwerenotedbythe EPintheregionofthesuprapatellarrecess.
APOCUSexaminationofthekneejointwasperformed bytheEPshowingahypoechoicjointeffusioninthe suprapatellarrecesswithhyperechoicstructureswith posteriorshadowing(Image3).These findingswere interpretedasahemarthrosiswithintra-articularairbubbles suspiciousforTAK.Orthopedicswasconsulted,which confirmedthearthrotomywithapositiveSLT.Thepatient wastreatedwithonegramofcefazolinandtetanus vaccinationupdate.Orthopedicsperformedsalineirrigation ofthejointandprimaryrepairofthecapsulelacerationatthe bedside.Thepatientwasdischargedonaprophylacticcourse ofcephalexin500mgeverysixhoursfor fivedays.At two-weekfollow-upwithorthopedicsshehadnosignsof jointinfection.

Image2. Case1)Asagittalviewofthesuprapatellarrecessshowingahyperechoicfocusofairwithposteriorshadowing(arrow)withinan effusion(star).Theeffusionhasmultiplecomponents,whichisindicativeoflipohemarthrosis.Case2)Asagittalviewofthesuprapatellar recessshowingahyperechoicfocusofairwithposteriorshadowingandreverberationartifact(arrow).Notehowthesignalfromthecortexof thefemur(triangle)isobscuredbytheshadowing.Asmalljointeffusionisalsovisualized(star).
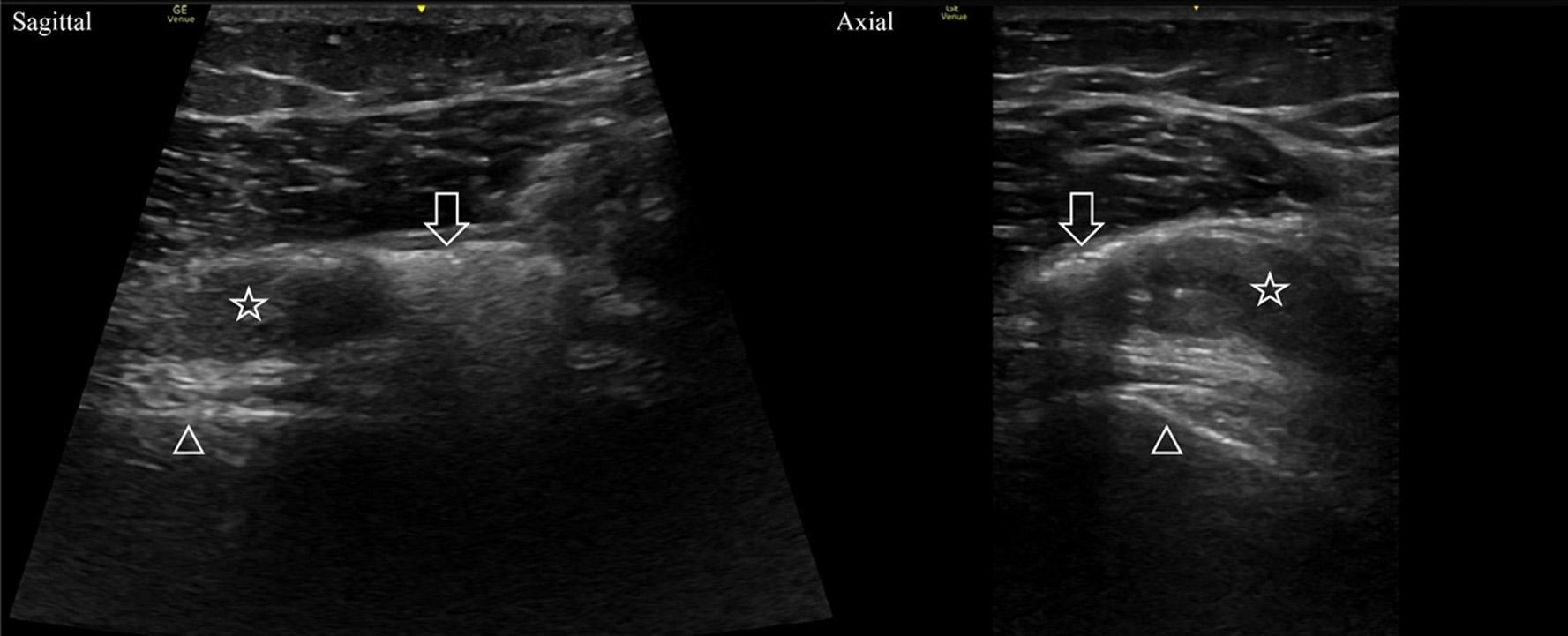
Image3. Sagittalandaxialviewsofthedistalfemurshowinghyperechoicfociwithposterioracousticshadowing(arrows)withinahypoechoic hemarthrosis(stars).Notetheshadowingobscuresthesignalfromthefemurcortex(triangles).
Traumaticarthrotomyshouldbeconsideredduringthe evaluationofapatientwithperiarticularwoundsduetothe riskofsepticarthritis.Currently,theSLTisrecommendedto diagnosetraumaticarthrotomyincaseswherearthrotomyis notobviousonphysicalexamination.Point-of-care ultrasonographyisanalternative,non-invasiveimaging modalitythathasbeendemonstratedtohaveutilityin evaluatingvariouskneepathologies.Onemeta-analysis foundthatultrasoundhadasensitivityof85%andspecificity of93%fortraumaticandatraumatickneeeffusions comparedtomagneticresonanceimaging.11 Another prospectivetrialofpatientswithacutekneetraumafound thatultrasonographywashighlyaccuratecomparedto radiographyindiagnosingintra-articularkneefractures whenlipohemarthrosiswaspresent.12 Point-of-care ultrasonographyhasthebenefitofbeingfreeofionizing radiationandlowercostthanCT,withthedrawbackof beingoperator-dependent.Computedtomographyisalsoa highlyusedresource,whichmayleadtodelaysindiagnosis suchasinCase1.
HerewedescribethreepatientswithprovenTAK first detectedbyPOCUSexaminations.Priortothiswriting,our literaturereviewresultedinonlyoneGerman-languagecase serieswherePOCUSexaminationsdiagnosedTAKin patientspresentingwithkneetraumaandperiarticular wounds.13 Asinourseries,the findingofintra-articularair ledtothecorrectdiagnosis.Theacousticimpedance mismatchbetweenairandsofttissuemakesairhighly echogenicwithresultantposteriorshadowing(Video). Reverberationartifactsmayalsobeseenwithlargerair bubbles.14 Literatureregardingthediagnosticperformance ofPOCUSfordiagnosingkneearthrotomyinlivepatientsis lacking.Onecadaverstudyfoundasensitivityof65%and specificityof75%for1mLofintra-articularair.15 The diagnosticperformanceofPOCUSforTAKshouldbe furtherinvestigated.
Point-of-care-ultrasonographyhasawidearrayof applicationsintheevaluationofEDpatients,includingbone andjointpathology.ThisseriessuggeststhatPOCUSmaybe effectiveindiagnosingtraumaticarthrotomyoftheknee, usingintra-articularairasthepositive finding.Sofar,the findingofintra-articularairinothermodalitieshasbeen showntobehighlysensitiveandspecificforTAK. Additionalstudiesshouldbeundertakento betterelucidatethediagnosticperformanceofPOCUS asamodalitytodiagnoseTAK.
Video. Intra-articularairisvisualizedasahyperechoiclinewith posteriorshadowing(whitearrow)thatobscurestheunderlying cortexsignal(blackarrow).
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
AddressforCorrespondence:MatthewKongkatongMD,University ofVirginiaHealthSystem,DepartmentofEmergencyMedicine, 1215LeeStreetCharlottesville,VA22908.
Email: mk3wk@uvahealth.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Mullingsetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ColmerHG4th,PirotteM,KoyfmanA,etal.Highriskandlowprevalence diseases:traumaticarthrotomy. AmJEmergMed.2022;54:41–5.
2.McKnightRR,RuffoloM,WallyMK,etal.Traumaticarthrotomies: Dotheyallneedtheoperatingroom? JOrthopTrauma 2021;35(11):612–8.
3.GoldenbergDL.Septicarthritis. Lancet.1998;351(9097):197–202.
4.BrubacherJW,GroteCW,TilleyMB.Traumaticarthrotomy. JAmAcad OrthopSurg.2020;28(3):102–11.
5.BrowningBB,VentimigliaAV,DixitA,etal.Doesthesalineloadteststill havearoleintheorthopaedicworld?Asystematicreviewofthe literature. ActaOrthopTraumatolTurc.2016;50(6):597–600.
6.KondaSR,HowardD,DavidovitchRI,etal.Thesalineloadtestofthe kneeredefined. JOrthopTrauma.2013;27(9):491–7.
7.KondaSR,DavidovitchRI,EgolKA.Computedtomographyscanto detecttraumaticarthrotomiesandidentifyperiarticularwoundsnot requiringsurgicalintervention:animprovementoverthesalineloadtest. JOrthopTrauma.2013;27(9):498–504.
8.KondaSR,HowardDO,GyftopoulosS,etal.Computedtomography scantodetectintra-articularairinthekneejoint:acadaverstudyto definealowradiationdoseimagingprotocol. JOrthopTrauma 2013;27(9):505–8.
9.PerloffE,PosnerA,MurtazaH,etal.CTscanversussalineloadtestfor detectionoftraumaticwristarthrotomy. JWristSurg 2021;11(2):154–60.
10.KondaSR,HowardD,DavidovitchRI,etal.Theroleofcomputed tomographyintheassessmentofopenperiarticularfractures associatedwithdeepkneewounds. JOrthopTrauma 2013;27(9):509–14.
11.MeyerR,LinC,YenokyanG,etal.Diagnosticutilityofultrasoundversus physicalexaminationinassessingkneeeffusions:asystematicreview andmeta-analysis. JUltrasoundMed.2022;41(1):17–31.
12.BonnefoyO,DirisB,MoinardM,etal.Acutekneetrauma:roleof ultrasound. ClinicalImaging.2007;31(2):147.
13.GrechenigW,ClementH,PeichaG,etal.SonographischerNachweis vonLuftimKniegelenk-eineexperimentelleStudieundklinischer Fallbericht. UltraschallMed.2002;23(01):47–51.
14.ButtarS,CooperDJr,OlivieriP,etal.Airanditssonographicappearance: understandingtheartifacts. JEmergMed.2017;53(2):241–7.
15.KongkatongM,ThomC,MoakJ.Canultrasoundidentifytraumaticknee arthrotomyinacadavericmodel? JEmergMed.2019;57(3):362–6.
KayNicoleTipton,DO,MS*†
DanielSchroder,DO*†
*UNCHealthSoutheastern,DepartmentofEmergencyMedicine, Lumberton,NorthCarolina
† CampbellUniversity,SchoolofMedicine,EmergencyMedicineResidency, Lumberton,NorthCarolina
SectionEditor:JoelMoll,MD
Submissionhistory:SubmittedJanuary15,2023;RevisionreceivedOctober5,2023;AcceptedOctober10,2023
ElectronicallypublishedApril17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.58206
Introduction: Spontaneousesophagealrupture,orBoerhaavesyndrome,andupside-downstomach arerarepathologiesassociatedwithgravesequelae.Boerhaavesyndromecanhaveamortalityrateas highas44%.Upside-downstomachaccountsforlessthan5%ofhiatalherniasandcanleadto incarcerationandvolvulus.
CaseReport: An80-year-oldwomanpresentedtotheemergencydepartmentwithsuddenonset,severe epigastricpain.Physicalexaminationrevealednormalvitalsignswithmildepigastrictenderness.Imaging obtainedrevealedalargehiatalherniaand findingsconcerningforesophagealperforation.Thepatient wasstartedon3.375gramsofintravenouspiperacillin/tazobactam,andtransfertoatertiarycarefacility wasinitiated.Aftertransfer,esophagographyconfirmedaperforationnearthegastroesophagealjunction and findingsconsistentwithanupside-downstomach.Thepatientunderwentsuccessfulrepairofthe esophagealperforationandgastropexyfollowedbyintensivecareunitadmissionandultimatelydischarge.
Conclusion: Boerhaavesyndromeandupside-downstomacharetwoconditionswithhighassociated morbidityandmortalityrequiringpromptintervention.Informationobtainedinthehistoryandphysical examinationincludingacuteonsetofchestpainaftervomiting,tachypnea,subcutaneousemphysema, andhypoxiacanassistinthediagnosisofthedescribedpathologies.Thesesignsandsymptomscanbe subtleonexaminationbutareimportantinraisingclinicalsuspicionforanotherwiserareetiologyfor acuteonsetchestpain.[ClinPractCasesEmergMed.2024;8(2)95–98.]
Keywords: esophagealrupture;Boerhaavesyndrome;upside-downstomach; hiatalhernia;casereport.
Spontaneousesophagealrupture,orBoerhaave syndrome,israrewithanincidenceaslowas3.1perone millionpeopleperyearandamortalityratethattripleswitha delayindiagnosisof48hoursfromsymptomonset.1,2 This conditionwas firstdescribedinapatientwhovomitedaftera largemealandsubsequentlydevelopedchestpainby HermannBoerhaave,aDutchprofessorofmedicine.1 Upside-downstomachoratypeIVhiatalherniaistherarest formofhiatalhernia,accountingforlessthan5%ofall hiatalhernias.3
Thiscombinationofpathology Boerhaavesyndromein thesettingofanupside-downstomach hasonlybeen describedoncepreviouslyinthesurgicalliterature.4 Each conditioncanindividuallyleadtosignificantmorbidityand mortality.Upside-downstomachhasahighdocumentedrisk ofincarceration,canleadtoesophagealoutletobstruction andperforation,andhaspreviouslybeensuggestedasa contributingfactortothedevelopmentofspontaneous esophagealrupture.4,5 Boerhaavesyndrome,ifnoturgently diagnosedandtreated,canrapidlyleadtomediastinitisand septicshockwithamortalityrateofupto44%.6
An80-year-oldwomanwithahistoryofgastroesophageal refluxandhypertensionpresentedtotheemergency department(ED)withsuddenonset,severe,sharpepigastric painwithradiationtoherback.Thepainbeganafteran episodeofemesisimmediatelyfollowingtheingestionof polyethyleneglycolapproximately11hourspriortoarrival. UponherpresentationtotheED,thepatientwasinapparent distresssecondarytopain;however,hervitalsignswere normalwithatemperatureof36.7° Celsius(C),blood pressureof142/65millimetersofmercury,heartrateof 80beatsperminute,andrespiratoryrateof18breathsper minute.Physicalexaminationrevealedonlymildepigastric tenderness.Nosubcutaneousemphysemawaspresentinthe tissueoverlyingtheneckorchest.Duetothepatient’sacute distressandcomorbidities,abroaddifferentialwas consideredforevaluationofcriticaletiologiesofherclinical presentationincludingaorticdissection,bowelperforation, esophagealrupture,acutecoronarysyndrome,mediastinitis, bowelobstruction,andpancreatitis.
Achestradiograph(CXR)(Image1)showedalargehiatal herniawithtracebilateralpleuraleffusionsanddisplacement ofthegastricbubbletotheright.Computedtomography (CT)withcontrastofthechest/abdomen/pelvis(Images2 and 3)demonstratedalargehiatalherniawithmostofthe stomachinthechest,associatedvolvulus,bilateralpleural effusions,rightgreaterthanleft,andacomplex,partially fluid-filledcollectionalongtheposterioraspectofthehiatal

Anterior-posteriorchestradiographdemonstratinglarge hiatalherniawithdisplacementofthegastricbubble(arrow)from lefttoright.

herniajustabovethediaphragm.Laboratorystudies revealedneutrophilicleukocytosiswith83.7%neutrophils andawhitecellcountof16.4 × 109 perliter(L)(4.8–10.8 × 109/L)andelevatedlacticacidof2.3millimolesperliter (mmol/L)(0.5–2.2mmol/L).Thepatientwasgiven3.375gof piperacillin/tazobactamintravenouslyforcoverageof gastrointestinal flora,andtransfertoatertiarycarefacility wasinitiated.WhileintheED,thepatientdevelopedroom airhypoxia,whichresolvedwiththreelitersofoxygen therapyvianasalcannula.
Aftertransfer,acontrastesophagramwasperformedand showedaperforationnearthegastroesophagealjunction.
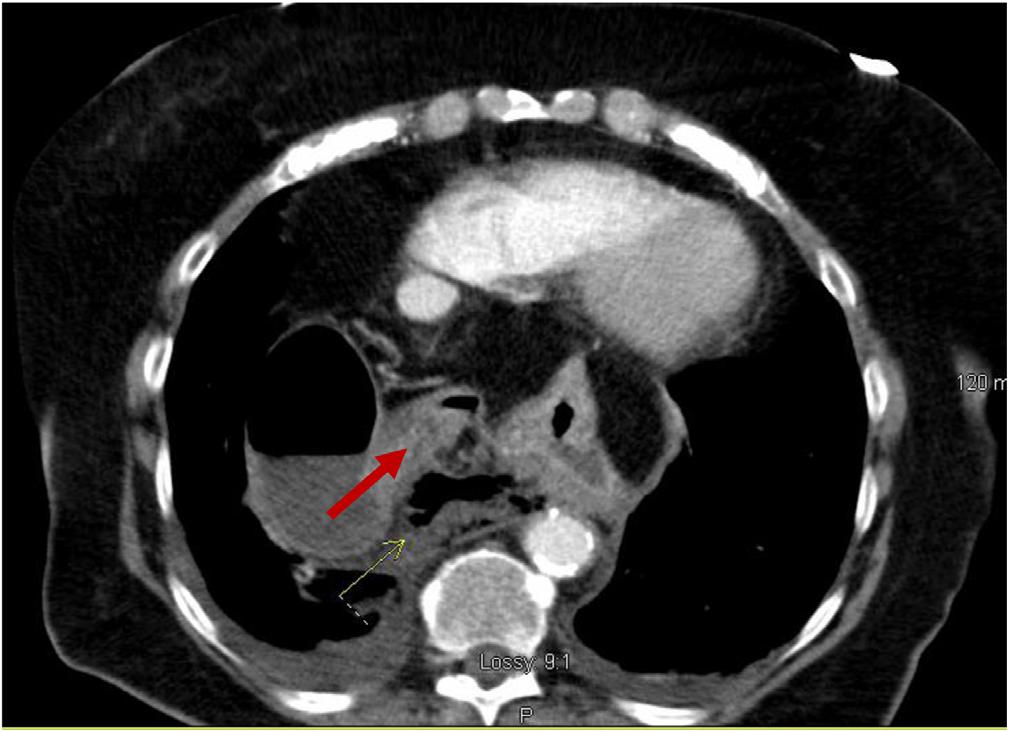
Image3. Transverseviewofcomputedtomographyofthechest/ abdomen/pelviswithanarrowindicatingpartially fluid-filled collectionposteriortoalargehiatalherniasuspiciousfor esophagealperforation.
Image1. Image2. Coronalviewofcomputedtomographyofthechest/ abdomen/pelvisshowinglargehiatalhernia(arrow).Thepatientunderwentanexploratorylaparotomy,which confirmedthepresenceofanesophagealrupturenearthe squamocolumnarjunctionandrevealedthepresenceofa gianthiatalherniawithanassociatedupside-downstomach. Surgicalrepairoftheesophagealperforationandgastropexy wasperformed.Thepatientwasadmittedtothesurgical intensivecareunitforatotalof fivedaysduringwhich shehadanepisodeofatrial fibrillationwithrapidventricular responsethatresolvedaftermetoprololanddiltiazem.
Onday fiveofherhospitalization,shewastransferredtoa cardiactelemetryunitafterbeingweanedoffsupplemental oxygen.Shewascontinuedonintravenous(IV) fluconazole 400milligrams(mg)daily,piperacillin/tazobactam3.375g everyeighthours,andvancomycindosedandmonitoredby pharmacyforatotalof14days.Multipleesophagramswere performed,whichrevealedapersistentleakfromthe esophagus;however;thisresolvedspontaneouslywith monitoringthroughouttheremainderofthehospitalcourse. Thepatientwasultimatelydischargedonhospitalday18 withcontinuedantibiotictherapyonamoxicillin-potassium clavulanate600–42.9mgtwicedailyforsevendays.After discharge,thepatientwasseenformultiplefollow-upvisits, withthelastfollow-upoccurringapproximately16months afterheroriginalpresentation.
Esophagealruptureisarareconditionwithhigh morbidityandmortalitythatisiatrogenicinnaturein approximately70%ofcases.2 Thespontaneousformofthis conditionisestimatedtoaccountforbetween15–30%of cases.1,7,8 Boerhaavesyndromeisthoughttobecausedbya suddenincreaseinintraesophagealpressureleadingtoa transmuraltearthroughtheesophagealtissue.4 Althoughit isimportanttomaintainacomprehensivedifferential diagnosis,physiciansmusthaveahighsuspicionforthis conditionasitisfrequentlymisdiagnosedasperforated ulcers,myocardialinfarction,orpulmonaryemboli.4
Thisconditionisanessentialdiagnosisforemergency physiciansduetoamortalityratereachingashighas44%. Riskfactorsfordevelopingspontaneousesophagealrupture includemalegenderandalcoholabuse.1 Asdescribedinthe caseabove,therehavebeendocumentedcasesassociated withpolyethyleneglycolingestionforcolonoscopy preparation.Thispreparationrequiresingestingalarge amountandcanleadtoforcefulvomiting.9 Inpatientswith Boerhaavesyndrome,themostcommonpresenting complaintispainthatisusuallyassociatedwiththesiteof perforationandcanoccurintheneck,chest,orabdomen.2 Thismaybeassociatedwithvomiting,painfulswallowing, andvoicechange,orfeverandphysicalexaminationmay revealthepresenceoftachycardia,tachypnea,and subcutaneousemphysema.1,2
ACXRmayshowevidenceofperforation;however,CTis preferredduetothelowersensitivityofplainradiography.If
suspicionremainshighforthecondition,acontrast esophagramisthepreferred diagnosticmodality.Barium shouldbeavoidedduetothepossibledevelopmentof mediastinitisifanesophagealleakispresent;instead,watersolublecontrastshouldbeused.1 Althoughnotcommonly includedinthestandarddiagnosisofBoerhaavesyndrome, bedsidepoint-of-careultrasoundhasbeenusedinspecific cases.Findingsonultrasoundincludethepresenceoffree fluid intheupperquadrantsoftheabdomenandairwithinthe pericardiumblockingthenormalvisualizationof cardiacwindows.10
Althoughthepatientinthiscasedidrequiresurgical intervention,thisisnottrueofallesophagealperforations. Fornon-operativemanagement,patientsmusthavesmall defectswithoutsignificantinvolvementofstructuresoutside theesophagus.ThesepatientsaretreatedwithIVantibiotics foratleast7–10daysandsupportivecaremeasuresincluding cardiacmonitoring,supplementaloxygen,ifnecessary,and adequateanalgesia.Accordingtoa2010articlebyKaman etal,therearenoclearrecommendationsforpatientswho shouldundergosurgicalinterventionalthoughitlikely includes, “earlypostemeticperforation,hemodynamic instability,intra-abdominalperforation,extravasationsof contrastintoadjacentbodycavitiesandpresenceof underlyingmalignancy,obstructionorstrictureintheregion oftheperforationandsurgically fitpatient.”2
Factorsthatincreasethemorbidityandmortalityofthis conditionincludetimetodiagnosis,sizeofthedefect,causeof thedefect,andassociationwithneutrophilicleukocytosis.6,8 Possiblythemostimportantfactoristhetimetodiagnosis. Adelayindiagnosisleadstoanincreasedpossibilityof developingmediastinitisandsepsissecondarytotheleakageof gastricenzymesandgastrointestinal flora.Aslittleasa 48-hourdelaycanleadtoathree-foldincreaseinmortality.2
Upside-downstomachisatypeIVhiatalhernia,most commonlycausedbytheweakeningofthediaphragmatic crura,whichaccountsforlessthan5%ofalldiagnosedhiatal hernias.3,5 Althoughsomepatientsmaybeasymptomatic, approximatelyone-thirdwilldeveloplife-threatening complicationsincludingvolvulus,incarceration,perforation, severegastricbleeding,andgastricischemia.3,4 Surgical repair,oftenlaparoscopic,isrecommendedurgently; however,emergentrepairisonlyrecommendedwhen complicationshaveoccurred,duetotheincreasedrisks associatedwithemergentsurgicalrepairs.3,5 Inapreviously describedcaseofcombinedupside-downstomachand esophagealrupture,itwasproposedthatthelargehiatal herniaresultedinblockageofthegastricoutletleadingto forcefulvomitingandultimaterupture.4
Emergencyphysiciansmustconsiderbroaddifferential diagnosesinallpatientstoensurethattime-sensitive diagnosesofconditionsaremadeeveninthosepatientswho
presentinitiallystable.Intheabovecase,thepatient presentationofabruptonsetepigastricpainimmediately afteranepisodeofemesisfollowingtheingestionof polyethyleneglycolledtorapiddiagnosisofthese rareconditions.Althoughthepatientdiddecompensatein theEDwiththedevelopmentoftachypneaandhypoxia, rapidmanagementofherconditionwithantibiotictherapy, oxygenadministration,prompttransfer,andsurgical interventionledtoafavorableoutcome.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:KayNicoleTipton,DO,MS,UNC HealthSoutheastern,300W27thSt.,Lumberton,NC28358. Email: Nictip616@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Tiptonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TurnerARandTurnerSD.Boerhaavesyndrome.In: StatPearls StatPearlsPublishing:TreasureIsland,FL,2022. Availableat: https://www.ncbi.nlm.nih.gov/books/NBK430808/
2.KamanL,IqbalJ,KundilB,etal.Managementofesophagealperforation inadults. GastroenterolRes;2010;3(6):235–44.
3.SchiergensTS,ThomasMN,HüttlTP,etal.Managementofacute upside-downstomach. BMCSurg.2013;13:55.
4.SaitoS,HosoyaY,KurashinaK,etal.Boerhaave’ssyndromeina patientwithanupsidedownstomach:acasereport, Int.J.Surg. CaseRep.2016;19:51–4.
5.MerzaN,LungJ,BazzazO,etal.Rarecaseofupside-downstomachin advancedhiatalhernia. SRCCC.2019;7(31):52–5.
6.ZimmermannM,HoffmannM,JungbluthT,etal.Predictorsofmorbidity andmortalityinesophagealperforation:retrospectivestudyof80 patients. ScandJSurg.2017;106(2):126–32.
7.SøreideJA,KonradssonA,SandvikOM,etal.Esophagealperforation: clinicalpatternsandoutcomesfromapatientcohortofWesternNorway. DigSurg.2012;29(6):494–502.
8.KimJD.Prognosticfactorsofesophagealperforationandrupture leadingtomortality:aretrospectivestudy. JCardiothoracSurg 2021;16(1):291.
9.YuJY,KimSK,JangEC,etal.Boerhaave’ssyndromeduringbowel preparationwithpolyethyleneglycolinapatientwithpostpolypectomy bleeding. WorldJGastrointestEndosc.2013;5(5):270–2.
10.DerrCandDrakeJM.Esophagealrupturediagnosedwithbedside ultrasound. AmJEmergMed.2012;30(9):2093.e1–3.
*CedarsSinaiHealthSystem,DepartmentofEmergencyMedicine, LosAngeles,California † HCAFloridaNorthFloridaHospital,DepartmentofGraduateMedicalEducation, Gainesville,Florida ‡ UniversityofCentralFlorida/HCAFloridaHealthcare,Gainesville,Florida
SectionEditor:ManishAmin,MD
Submissionhistory:SubmittedMay23,2023;RevisionreceivedOctober23,2023;AcceptedNovember6,2023
ElectronicallypublishedFebruary13,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1394
Introduction: Mesentericvolvulusisararecauseofabdominalpainandbowelobstructioninelderly patients.Whenamesentericvolvulusoccursinadultpatients,thesymptomsareoftennon-specific, whichcontributestodelaysindiagnosis.
CaseReport: Wepresentacaseofa75-year-oldfemalewhopresentedwithnon-specificabdominal pain.Therarewhirlpoolsignoncomputedtomographyidentifiedamesentericvolvulusasthecauseof smallbowelobstruction.Shewastakentotheoperatingroomand,aftersuccessfulresectionofthesmall bowel,sherecoveredandultimatelywasdischargedhome.
Conclusion: Earlyidentificationofawhirlpoolsignandearlysurgicalconsultationarekeytoproviding thebestchanceforsalvageofischemicsmallbowelduetomesentericvolvulusandtopreventafatal outcome.[ClinPractCasesEmergMed.2024;8(2)99–101.]
Keywords: mesentericvolvulus;malrotation;midgutvolvulus;whirlpoolsign;acuteabdominalpain.
Whileapproximately90%ofmidgutvolvuluscasesoccur beforetheageofoneyear,casesareidentifiedinpatientsof allages.1 Adult-onsetmidgutvolvulusisespeciallyrarewith anincidenceofonly0.2–0.5%.2,3 Whenadultspresentwith midgutvolvulus,theconditionpresentsasacuteonsetonly 10–15%ofthetime.4 Acuteonsetmidgutvolvuluspresents similarlytopatientswithacutebowelobstructions;however, subacutepresentationspresentmoreinsidiously.Patients withsubacutetochronicpresentationsmayhavenon-specific gastrointestinalsymptomssuchascramping,bloating, weightloss,nausea,andvomitingthatmaycomeandgofor weekstomonthsuntilanacutepresentationoradiagnosisis madeonadvancedimaging.Withoutahighdegreeof suspicion,patientswithsubacutemidgutvolvulusmaysuffer fromadelayindiagnosisintheemergencydepartment(ED) anddefinitivesurgicaltreatment.5 Inthepatientpresented here,initialsymptomsweresuggestiveofnumerous
abdominalpathologies.Diagnosiswasultimatelyrevealed oncomputedtomography(CT)byidentificationof thewhirlpoolsign,whichpromptedlife-saving surgicalintervention.
A75-year-oldwomanpresentedtotheEDforevaluation ofsuddenonsetofleftlowerquadrantabdominalpain.She reportedthatshebeganfeelingtheabdominalpain approximatelyfourhourspriortoarrivalbutdidnotcometo theEDuntilshebegantoexperiencenauseaanddryheaving withassociatedchills.Shereportedpassing flatusbuthadnot hadabowelmovementinthepreceding24hours.Shedenied anyrecenttraumatotheabdomenorpelvisanddidnot reportanyabdominalsurgicalhistory.Thepatientreporteda vaguehistoryof “abdominalinfections” withoutadiagnosis byherprimarycarephysicianorgastroenterology.She denieddrinkingwellwater,travelingrecently,orcamping.
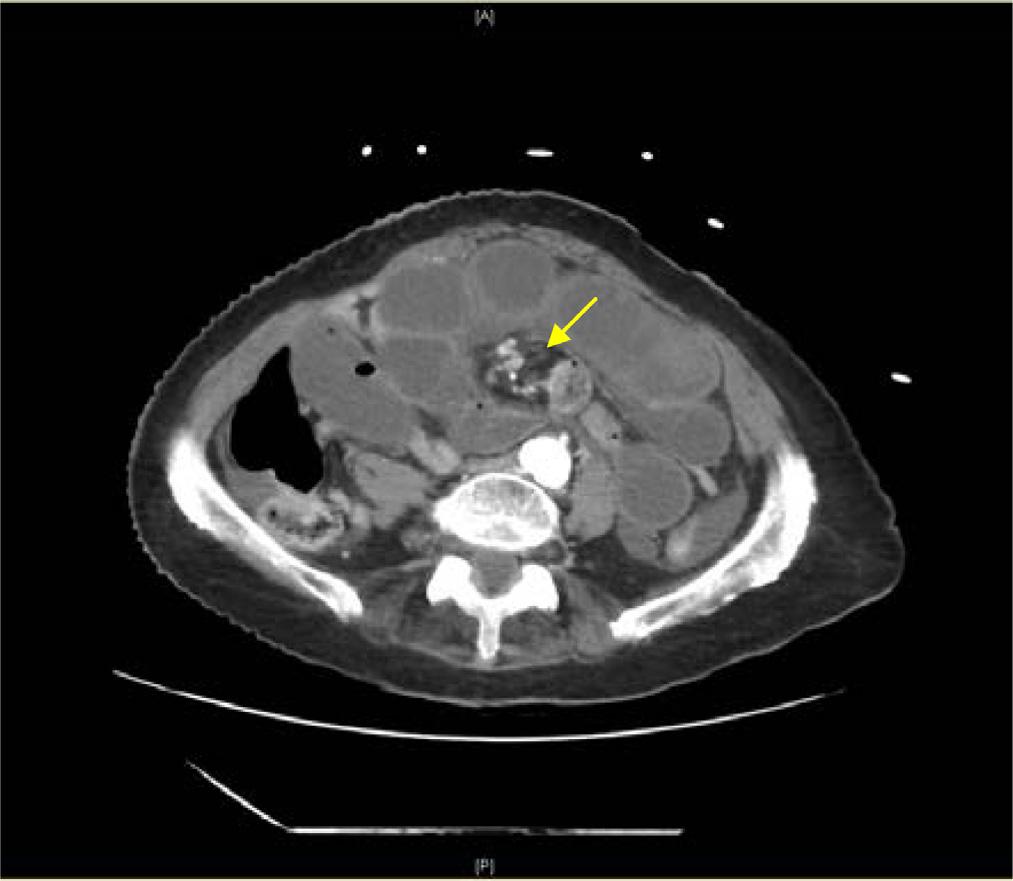
Image. Computedtomographyabdomenwithintravenouscontrast demonstratingdilated, fluid-filledloopsofsmallbowelandapattern ofswirlingmesentericvesselscalledthewhirlpoolsign(arrow).
Shereportedahistoryofpulmonaryemboli10yearsprior, butheldherwarfarindosethatmorningbecauseher internationalnormalizedratio(INR)was “high.”
Onpresentationthepatientwasinnoacutedistressbut wasclammyandtachycardicatarateof118beatsper minute.Onexam,herabdomenwasdiffuselytenderwithout distentionorperitonealsigns.Shehadanelevatedwhite bloodcellcountat17 × 103 permicroliter(K/μL)(reference range4.5–11.0K/μL),anINRof5.5,andalacticacidof 3.7millimolesperliter(mmol/L)(0.4–2.0mmol/L).An abdomenandpelvisCTwithintravenous(IV)contrast showed findingssuspiciousforclosedloop,smallbowel obstruction.TheCTalsodemonstratedevidenceofswirling ofthemesentericroot,knownasawhirlpoolsign(Image, Video).The findingsofthewhirlpoolsignonCTsuggested mesentericvolvulusasthecauseofherbowelobstructionand promptedemergentsurgicalconsultation.
ThepatientreceivedfreshfrozenplasmaandvitaminK forreversalofherINRinpreparationforemergentsurgery. Intraoperatively,hermesentericvolvuluswasreducedand eightfeet(~243cm)ofjejunumwasresectedduetoischemia. Sheremainednil-per-osforsevendayspost-surgerybefore beginningaclearliquiddiet,andsheremainedinthehospital foratotalofninedaysbeforebeingdischargedtoacute rehabilitation.Shecontinuedtorecoverandreturnedto baselineactivitiesoverthefollowingmonth.
Althoughhistory,physicalexam,andlaboratorytestsaid indiagnosingmidgutvolvulus,imagingisthemostuseful. Abdominalradiographsareveryquickandcanbedonein theEDatbedsidetoruleoutothercausesofabdominal
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Mesentericvolvulusisararecauseofsmall bowelobstruction.Itcanbedif fi cultto distinguishfromothercauseswithout appropriateimaging.
Whatmakesthispresentationof diseasereportable?
Thewhirlpoolsign swirlingofthe mesentericvesselsoncomputedtomography (CT)oftheabdomen isaclassic fi ndingfor amesentericvolvulus.
Whatisthemajorlearningpoint?
Amesentericvolvulusisasurgicalemergency, anddelaysindiagnosisinemergency departmentpatientsincreasemorbidity andmortality.
Howmightthisimproveemergency medicinepractice?
Whenidentifyingawhirlpoolsignon abdominalCT,emergencyphysiciansshould considermidgutvolvulusandobtain surgicalconsultation.
pathology.However,radiographsareofteninconclusivein midgutvolvulusbecauseevenapositive “doublebubble” signindicatingasmallbowelobstructiondoesnotruleouta concomitantmidgutvolvulus.7 Computedtomographywith IVcontrastgivesmuchgreaterdetailoftheabdomenandcan provideevidencesuggestiveofamidgutvolvulus.ClassicCT imaging findingsincludeawhirlpoolsignoftwisted mesentery,malrotatedbowelconfiguration,inverted superiormesentericarteryandsuperiormesentericvein relationship,bowelobstruction,andfree fluid/freegasin advancedcases.8 ThewhirlpoolsignseenonCTrepresents themesenteryandsuperiormesentericveinwrapping aroundthesuperiormesentericarteryina counterclockwisedirection.
Thediagnosisofamidgutvolvulusisconsideredasurgical emergency. 9 Surgicalconsultationshouldnotbedelayedfor additionaltestingoncethehistoryandimagingare suggestiveofavolvulus.Timetosurgicalcorrectionisthe mostimportantfactorinmortality,whichrangesfrom 0–25%inacuteonsetvolvuluslikeourpatientpresented.6 Whencorrectedbeforenecrosisofthebowelhasoccurred, mortalitycandecreasetoaslowas3–9%.1 Inadditionto
standardtreatmentforabowelobstruction,antibiotics coveringagainstanaerobesandgram-negativeorganismsof thegut florashouldbegiventopatientswithmidgutvolvulus duetothehighriskoftranslocationofbacteriasecondaryto bowelischemia.10
Abdominalpainintheelderlypopulationisacommon chiefcomplaintintheEDwithmanyetiologies.Smallbowel obstructionswithconcomitantmesentericvolvulusisa surgicalemergencythatrequiresearlyidentificationand surgicalconsultation,whichcanoftenbemissedinsubacute presentationswithnon-specificgastrointestinalcomplaints. DiagnosisbyCTabdomenandpelviswithcontrastremains theimagingmodalityofchoicetoidentifymidgutvolvulus. Emergencycliniciansshouldbefamiliarwiththecommon CT findingsforbothsmallbowelobstructionsandthe mesentericwhirlpoolsignsuggestiveofmidgutvolvulus,asit drasticallychangesthepatient’sprognosisandneedfor emergentsurgicalcare.
Video. Computedtomographyoftheabdomenandpelviswith intravenouscontrastshowsthesuperiormesentericarterybranching offfromtheaortaandultimatelyswirlingwiththemesenterytocreate thewhirlpoolsign,diagnosticofamidgutvolvulus.Additionally,the swirlservesasatransitionpointforthesmallbowelobstructionseen inthevideoasdilatedloopsof fluid-filledsmallbowel.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ChristopherLibby,MD,MPH,Cedars SinaiMedicalCenter,DepartmentofEmergencyMedicine,8700 BeverlyBoulevard,LosAngeles,CA90048.Email: Christopher. Libby@csmc.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisresearchwassupported(inwhole
orinpart)byHCAHealthcareand/oranHCAHealthcareaffiliated entity.Theviewsexpressedinthispublicationrepresentthoseofthe author(s)anddonotnecessarilyrepresenttheofficialviewsofHCA Healthcareoranyofitsaffiliatedentities.
Copyright:©2024Libbyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.FischerJEandBlandKI. MasteryofSurgery.6thed.Philadelphia,PA: LippincottWilliams&Wilkins;2012.
2.SinghS,DasA,ChawlaAS,etal.Ararepresentationofmidgut malrotationasanacuteintestinalobstructioninanadult:twocase reportsandliteraturereview. IntJSurgCaseRep.2013;4(1):72–5.
3.EmanuwaOF,AyantundeAA,DaviesTW.Midgutmalrotation first presentingasacutebowelobstructioninadults:acasereportand literaturereview. WorldJEmergSurg.2011;6(1):22.
4.DurkinET,LundD,ShaabanA,etal.Age-relateddifferencesin diagnosisandmorbidityofintestinalmalrotation. JAmCollSurg 2008;206(4):658–63.
5.ButterworthWAandButterworthJW.Anadultpresentationofmidgut volvulussecondarytointestinalmalrotation:acasereportandliterature review. IntJSurgCaseRep.2018;50:46–9.
6.DietzDW,WalshRM,Grundfest-BroniatowskiS,etal.Intestinal malrotation:ararebutimportantcauseofbowelobstructioninadults. DisColonRectum.2002;45(10):1381–6.
7.ReederMMandFelsonB. ReederandFelson’sGamutsinRradiology, ComprehensiveListsofRoentgenDifferentialDiagnosis,4thed. NewYork,NY:SpringerVerlag;2003.
8.PetersonCM,AndersonJ,HaraA,etal.Volvulusofthegastrointestinal tract:appearancesatmultimodalityimaging. Radiographics 2009;29(5):1281–93.
9.ValsdottirEandMarksJ.Volvulus:smallbowelandcolon. ClinColon RectalSurg.2008;21(2):91–3.
10.ZhengL,YuE,ZhangW,etal.Appropriatetreatmentofacutesigmoid volvulusintheemergencysetting. WorldJGastroenterol 2013;19(30):4979–83.
BethIsraelDeaconessMedicalCenter,DepartmentofEmergencyMedicine, Boston,Massachusetts
SectionEditor:MelanieHeniff,MD,JD
Submissionhistory:SubmittedSeptember5,2023;RevisionreceivedJanuary3,2024;AcceptedJanuary5,2024
ElectronicallypublishedApril17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1650
Introduction: Ferricderisomaltoseisthenewestavailableparenteralironformulation.Studieshave demonstratedagoodsafetyprofilewithimprovedtolerabilitycomparedtoalternativeparenteraliron formulations.Todatetherehavebeennoreportedacute,life-threateningcardiaceventsassociatedwith ferricderisomaltose.
CaseReport: An86-year-oldmalewhohadpreviouslytoleratedroutineironinfusionsreceiveda first doseofferricderisomaltoseatanoutpatientinfusionclinic.Sixminutesintotheinfusionthepatient becameunresponsivewithnopalpablepulse.Returnofspontaneouscirculationwasachievedaftertwo minutesofchestcompressions.Electrocardiogramshowedcompleteheartblockrequiring transcutaneouspacingandvasopressoradministration.Thepatientwastransferredtotheemergency departmentforstabilizationandthenadmittedtothecardiacintensivecareunit.Duringadmission, thepatientreceivedadual-chamber,permanentpacemakerwithoutcomplicationandwas ultimatelydischarged.
Conclusion: Itmaybereasonabletoconsiderparenteralironasatoxicologicaletiology forpatientspresentingwithcompleteheartblocktemporallyassociatedwithparenteral ironadministration,particularlyinpatientswithunderlyingconductionabnormalities.
[ClinPractCasesEmergMed.2024;8(2)102–106.]
Keywords: ferriccompounds;iron;heartblock;casereport.
Parenteralironisfrequentlyutilizedtotreatiron deficiencyanemia.Avarietyofparenteralironproductsare available;thenewestproductintheUnitedStatesisferric derisomaltose(FDI)followingUSFoodandDrug AdministrationapprovalinJanuary2020.Ferric derisomaltosewasintroducedinEuropein2010underthe nameironisomaltoside.Whileseriousadverseeventscaused byparenteralironinfusionsarerareandtypically characterizedasanaphylactic-typereactions,FDIallowsfor high-doserapidironinfusionwithimprovedtolerability comparedtoolderformulations.Ferricderisomaltosecan providefullironrepletionwithasingledose,thusreducing thenumberofinfusionsrequired.1,2 Herewedescribeacase
ofcardiacarrestsixminutesafterinitiationofFDI,withno obvioussignsofanaphylaxis,followedbypersistent completeheartblockuponachievingreturnofspontaneous circulation(ROSC).
An86-year-old,Farsi-speakingmalewithapastmedical historyoftype2diabetes,chronickidneydiseasestageIIIb (baselineserumcreatinine1.7–2.2milligramsperdeciliter (mg/dL),irondeficiencyanemia,gastroesophagealreflux disease,pepticulcerdisease,coloncancerstatuspost resection,coronaryarterydiseasestatuspostpercutaneous coronaryinterventionin2016,andParkinsondisease presentedtoanoutpatientinfusionclinicforaroutineiron
infusion.Hehadpreviouslyreceivedferumoxytolinfusions twicemonthlywithnodocumentedreactionsandwasbeing switchedtoFDItodecreaseinfusionrequirements.Home medicationsincludedatorvastatin,calcitriol,carbidopalevodopa,furosemide,lisinopril,tamsulosin,aspirin,and sodiumbicarbonate.Hehadnoknownallergies.
Ferricderisomaltosewasinitiatedat10:10 AM.At 10:16 AM thepatientbecameunresponsivewithagonal breathingandnopalpablepulse.Chestcompressionswere initiated,andROSCwasachievedafteronetwo-minuteround ofcompressions.Epinephrinewasnotadministered.PostROSCbloodpressure(BP)was60/30millimetersofmercury (mmHg),andpoint-of-carebloodglucosewas220mg/dL (referencerangeduringfastedstate:70–100mg/dL).Anormal saline1,000mLboluswasinitiated.Thepatientwasplacedon 100%oxygenvianonrebreathermask(NRB);intubationwas notrequired.Thepatientwastransferredtoanearby emergencydepartment(ED)andfoundtobeincomplete heartblockwithsignificantSTdepressionsintheprecordial leads(Image1).Transcutaneouspacingwasinitiated.Heart rateatthetimeoftranscutaneouspacinginitiationwasnot reported.Norepinephrineandvasopressinwereinitiated followingtheplacementofrighttibialintraosseousandright femoralcentrallines.Pacingwasdiscontinuedafteraheart rateabovethepacingthresholdwasachieved(60beatsper minute[bpm]).Vasopressinwasdiscontinued,andthe patientwastransferredtoourtertiary-careEDbyemergency medicalservices.
Uponarrival,thepatient’svitalsignsweredocumentedas heartrate92bpm,BP136/49mmHg,andoxygensaturation 92%onNRBwithrespiratoryraterange12–37breathsper minute.Norepinephrinewastheonlymedicationinfusingfor
CPC-EMPopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Ferricderisomaltoseisthemostrecently approvedparenteralironproductbytheUS FoodandDrugAdministration.
Whatmakesthispresentationof diseasereportable?
Wereportacaseofcompleteheartblockthat mayhavebeenprecipitatedbyparenteral irontherapy.
Whatisthemajorlearningpoint?
Althoughwell-tolerated,newerparenteral ironformulationsmayposerisksthathavenot yetbeenelucidated.
Howmightthisimproveemergency medicinepractice?
Itmaybereasonableforemergency physicianstoconsiderironchelationtherapy ifparenteralironisthesuspectedetiologic agentofcompleteheartblock.
hemodynamicsupportandwascontinuedat0.25 microgramsperkilogramperminute.Calciumgluconate 1gramintravenous(IV)andmagnesiumsulfate2gramsIV
 Image1. ElectrocardiogramshowingcompleteheartblockwithSTdepressionsinprecordialleadsuponinitialemergencydepartment presentationat11:14 AM
Image1. ElectrocardiogramshowingcompleteheartblockwithSTdepressionsinprecordialleadsuponinitialemergencydepartment presentationat11:14 AM

Image2. Electrocardiogramuponarrivaltotertiary-careemergencydepartmentat1:26 PM
wereadministeredempirically.Onexam,thepatientwas alertandorientedandexhibitedbilaterallowerextremity edema.UponarrivaltoourED,electrocardiogram(ECG) wasrepeatedwithresolutionofpreviouslyappreciatedST depressions(Image2).Therefore,aposteriorECGto investigateforposterolateralmyocardialinfarctionwasnot performed.TroponinTwasslightlyelevatedat0.11 nanograms(ng)permL(referencerange0–0.01ng/mL)in thesettingofchronickidneydisease.Creatininekinase-MB isoenzymeresultedwithinnormallimits(Table),making acutecoronarysyndromelesslikely.Nofurtheracute interventionswererequiredintheED.
Thepatientwasadmittedtothecardiacintensivecareunit (ICU),andvitalsignsattimeoftransferfromtheEDtothe cardiacICUweredocumentedasheartrate75bpm,BP 134/64mmHg,andoxygensaturation99%on1liternasal cannula.ThepatientwasafebrilethroughouthisEDcourse. UponelectrophysiologyevaluationinthecardiacICU,the patientwasfoundtohavearightbundlebranchblockand leftanteriorfascicularblock.Duringadmissionadualchamber,permanentpacemakerwasplacedwithno complications,andthepatientwasdischarged shortlyafterward.
Whiletheexactsequenceofeventsprecedingthepatient’ s cardiacarrestisunknown,wesuspectanassociationbetween thearrestandFDI.Notably,itisunclearwhethertheiron infusionprecipitatedheartblockleadingtocardiacarrestor ifananaphylactic-typereactionprecipitatedthearrest. However,ananaphylactic-typereactionseemslesslikelyas therewerenoassociatedrespiratory,cutaneous,or
LaboratorytestResultReferencerange
Thyroidstimulatinghormone2.2 μIU/mL0.27–4.2 μIU/mL
LymeVsIE/PepC10PositiveNegative LymediseaseantibodyNegativeNegative Iron33 μg/dL45–160 μg/dL
Totalironbindingcapacity243 μg/dL260–470 μg/dL
Ferritin68ng/mL30–400ng/mL
Transferrin187mg/dL200–360mg/dL
Potassium4.5mEq/L3.5–5.4mEq/L
Calcium8.2mg/dL8.4–10.3mg/dL
Magnesium1.5mg/dL1.6–2.6mg/dL
Phosphorous3.1mg/dL2.7–4.5mg/dL
TroponinT0.11ng/mL < 0.10ng/mL
Creatinine1.9mg/dL0.5–1.2mg/dL
CK-MB6ng/mL0–10ng/mL
μIU,micro-internationalunit; mL,milliliter; VsIE/PepC10, Borrelia burgdorferi antigens; μg,microgram; dL,deciliter; ng,nanogram; mg,milligram; mEq,milliequivalent; L,liter; CK-MB,creatinine kinase-myoglobinbinding.
gastrointestinalsymptoms,andtheacuteeventresolved withoutepinephrineadministration.
Astootheretiologiesofthepatient’scardiacarrest,there wasnoreportedfamilyhistoryofprematurecoronaryartery disease,dysrhythmia,cardiomyopathy,orsuddencardiac death.HismostrecentlyavailableECGtakentwoyears priortothecardiacarrestshowedarightbundlebranch Table. Labresultsforelderlypatientwhosufferedcardiacarrest followingahigh-doserapidironinfusion.
blockandleftanteriorfascicularblock.Thepatient’sfamily reportedseveralepisodesofsyncopeovertheprevious month.AnECGwasnotrecordedsurroundingthese episodes.Oneepisodeoccurredafterusingthebathroom, andanotheroccurredwhilesittinginachair.Theseprior syncopaleventsandthearrestmayhavebeenprecipitatedby completeheartblockorvasovagalsyncope.However,vagal etiologyseemslesslikelyascompleteheartblockepisodes duringinpatientadmissionshowedasinusrateinthe90sand ventricularescapeinthe60s.
LaboratoryresultsindicatedthatLymecarditis, hyperkalemia,andhypothyroidismwerealsounlikely etiologies(Table),andthepatientwasnotprescribedany atrioventricularblockingmedications.Hypophosphatemia hasbeenassociatedwithparenteralironadministration, includingtheironisomaltoside/FDIformulation3 andmay resultinmyocardialcontractilityimpairmentandsudden cardiacdeath.However,labresultsshowedphosphorous levelswithinnormallimits.Ironoverloadmayexacerbate preexistingconductiondiseaseandleadtoheartblock,but ironstudieswerewithinnormallimitsduring admission,makingironoverloadanunlikely etiology4 (Table1).
Intheabsenceofotherobviouscauses,theironinfusion mayhaveexacerbatedanunderlyingconduction abnormalityandprecipitatedthearrest.However,one limitationofthisreportisthatthispatienthadmultiple comorbidities,includingpriorsyncopalevents.Whilethe FDIinfusionwastemporallyassociatedwiththispatient’ s cardiacarrest,wecannotconcludeforcertainthatthe infusionwasthesolecontributortotheeventasadditional factorsmayhaveplayedarole.
ThepathophysiologicbasisforFDIcausingcardiacarrest isnotentirelyclear.Animalmodelshavedemonstratedthat acuteirontoxicityleadstodecreasedmyocardial contractilityandcardiacoutput.5,6 Whiletheseeffectshave notbeenpreviouslydescribedfollowingparenteraliron administration,wehypothesizethatFDImayhave exacerbatedthispatient’sunderlyingcardiacabnormalities andprecipitatedthecardiacarrest.Roseandcolleagues demonstratedthatchronicironoverloadreducesvoltage dependentLtypealpha1Dsubunitcalciumchannel (CaV1.3)expressioninthesinoatrialnode,atria, atrioventricularnode,andproximalventricularconduction systemleadingtobradycardia,PR-intervalprolongation, heartblock,andconductiondeficits.4
Whileourpatientdidnothavechronicironoverload basedonlabresults,itisconceivablethatrapid administrationofIVironcouldacutelyprecipitatesimilar effectsinapatientwithunderlyingconduction abnormalities,despitetheadministeredironnotyethaving sufficienttimetodistributetothetissues.Anotherpossible pathophysiologicexplanationmaybeKounissyndrome,a syndromecharacterizedbyacutecoronaryeventsincluding
allergiccoronaryvasospasm,allergicmyocardialinfarction, orstentthrombosissecondarytoahypersensitivityreaction.7 Kounissyndromehasalsobeenimplicatedinmanifestingas fatalcompleteheartblock.8 Consideringparenteraliron’ s historyofinducingacutehypersensitivityreactions,itis plausiblethatparenteralironmayinduceKounis syndromeandprecipitatecompleteheartblock andcardiacarrestinapatientwithunderlying conductionabnormalities.
Seriousadverseeventscausedbyparenteralironinfusions arerareandtypicallycharacterizedasanaphylactic-type reactions,withonestudy findingonlytwodocumentedserious adverseeventsrequiringepinephrineadministrationoutof 35,737uniqueironinfusions.1 Ferricderisomaltosehasbeen demonstratedassafeandwelltoleratedcomparedtomore commonlyusedparenteralironproducts.9 Onestudy comparingFDItoironsucrose(IS)foundsinusnode dysfunctionin1/1,019patients(0.1%)and1/506(0.2%) patientsreceivingFDIandIS,respectively,and1/1,019(0.1%) patientsreceivingFDIhadcardiacarrestcomparedto2/506 (0.4%)intheISgroup.10 AnotherstudycomparingFDIto usualcare(noironororaliron)reportedbradycardiaratesof 2/559(0.4%)vs1/568(0.2%),completeatrioventricularblock ratesof1/559(0.2%)vs3/568(0.5%),andcardiacarrestrates of6/559(1.1%)vs15/568(2.6%),respectively.11 Itisunknown whetherdocumentedcardiaceffectsoccurredacutely followingparenteralironadministrationortheyoccurredat anothertimeduringthestudyperiodasbothstudiesanalyzed thelong-termsafetyofFDI.
Bradycardiaandheartblockarerarelyreportedinthe FDIliteratureandarenotreferencedasawarningor precautioninthepackageinsert.12 However,irondextran carriesawarningtousewithcautioninpatientswith preexistingcardiovasculardisease.13 Basedonthiscase,it maybeprudenttoconsiderthiswarningfornewerparenteral ironproductsaswell.
Bradycardiaandheartblockarerarelyreportedinthe parenteralironliterature.Althoughrare,itmaybe reasonabletoconsiderparenteralironasatoxicological etiologyforpatientspresentingwithcompleteheartblock temporallyassociatedwithaparenteralironinfusion, particularlyinpatientswithunderlyingconduction abnormalities.Inthecaseofongoingclinicalinstabilitywhen othercauseshavebeensufficientlyruledoutandacuteiron toxicityorchronicironoverloadissuspected,consultation withthelocalpoisoncontrolcenterforconsiderationof deferoxamineforironchelationmaybereasonable.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:MichaelScott,PharmD,BCPS, BCEMP,BethIsraelDeaconessMedicalCenter,Departmentof EmergencyMedicine,185PilgrimRd.,BakerBuilding,Suite BA-0101,Boston,MA02215-5412.Email: mscott10@bidmc. harvard.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Scottetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ArastuA,ElstrottB,MartensK,etal.Analysisofadverseeventsand intravenousironinfusionformulationsinadultswithandwithoutprior infusionreactions. JAMANetwOpen. 2022;5(3):e224488.
2.CancadoRandMunozM.Intravenousirontherapy:howfarhavewe come? RevBrasHematolHemoter. 2011;33(6):461–9.
3.SchaeferB,TobiaschM,ViveirosA,etal.Hypophosphatemiaafter treatmentofirondeficiencywithintravenousferriccarboxymaltoseor ironisomaltoside – asystematicreviewandmeta-analysis. BrJClin Pharmacol. 2021;87(5):2256–73.
4.RoseRA,SellanM,SimpsonJA,etal.IronoverloaddecreasesCaV1.3dependentL-TypeCa2+ currentsleadingtobradycardia,altered electricalconduction,andatrial fibrillation. CircArrhythmElectrophsiol. 2011;4(5):733–42.
5.ArtmanM,OlsonR,BoerthR.Depressionofmyocardialcontractilityin acuteirontoxicityinrabbits. ToxicolApplPharmacol. 1982;66(3):329–37.
6.VernonD,BannerW,DeanM.Hemodynamiceffectsofexperimental ironpoisoning. AnnEmergMed. 1989;18(8):863–6.
7.KounisNG.Coronaryhypersensitivitydisorder:theKounissyndrome. ClinTher. 2013;35(5):563–71.
8.KounisNG.Caspofungin-inducedfatalcompleteheartblock:another manifestationofKounissyndrome. JPharmacolPharmacother. 2013;4(2):161–2.
9.PollockRandBiggarP.Indirectmethodsofcomparisonofthesafetyof ferricderisomaltose,ironsucroseandferriccarboxymaltoseinthe treatmentofirondeficiencyanemia. ExpertRevHematol. 2020;13(2):187–95.
10.AmbrosyA,HaehlingS,KalraP,etal.Safetyandefficacyofintravenous ferricderisomaltosecomparedtoironsucroseforirondeficiencyanemia inpatientswithchronickidneydiseasewithandwithoutheartfailure. Am JCardiol. 2021;152:138–45.
11.KalraP,ClelandJ,PetrieM,etal.Intravenousferricderisomaltosein patientswithheartfailureandirondeficiencyintheUK(IRONMAN):an investigator-initiated,prospective,randomised,open-label,blindedendpointtrial. Lancet. 2022;400(10369):2199–209.
12.Monoferric.Packageinsert.PharmacosmosTherapeuticsInc.2020. Availableat: https://www.accessdata.fda.gov/drugsatfda_docs/label/ 2020/208171s000lbl.pdf. AccessedJuly14,2023.
13.INFeD.Packageinsert.AllerganUSA,Inc.2021.Availableat: https:// www.accessdata.fda.gov/drugsatfda_docs/label/2021/017441s179lbl. pdf.AccessedJuly14,2023.
BryanRosenberg,MD*
MaxHockstein,MD*
CyrusHadadi,MD†
SectionEditor:ManishAmin,DO
*MedstarWashingtonHospitalCenter;DepartmentofEmergencyMedicine;Washington, DistrictofColumbia
† MedstarWashingtonHospitalCenter;DepartmentofCardiology;Washington, DistrictofColumbia
Submissionhistory:SubmittedJune27,2023;RevisionreceivedOctober5,2023;AcceptedOctober9,2023
ElectronicallypublishedMarch25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1466
Introduction: Implantablecardioverter-defibrillator(ICD)leadperforationthroughthemyocardiummay resultinchestpainandelectrocardiogram(ECG)changesconcerningforST-segmentelevation myocardialinfarction.TheclinicalcontextoftheECGaidsinappropriatemanagement.
CaseReport: Wereportthecaseofa71-year-oldwomanexperiencingchestpainafteranICD placementtwoweeksearlier.Onpresentation,sheexhibitedST-segmentelevationonherECG. ComputedtomographyconfirmedICDleadmigration.Thepatient’shemodynamicswerenormal,and shewasdischargedhomeaftera five-dayhospitalstayfollowingaleadrevision.
Conclusion: Althoughrare,ICDleadperforationisapotentialcauseofchestpainandischemicECG changes.Emergencyphysiciansshouldconsiderleadperforationasapotentialdifferentialdiagnosis whenevaluatingchestpaininpatientswithICDs,takingintoaccountthepotentialcomplicationsof coronaryangiography.[ClinPractCasesEmergMed.2024;8(2)107–110.]
Keywords: casereport;ICD;leadperforation;currentofinjury;ECG.
Wepresentacaseofarightventricular(RV)implantable cardioverter-defibrillator(ICD)leadperforatingthe pericardium,resultinginapatientexperiencingchestpain withanelectrocardiogram(ECG)concerningforSTsegmentelevationmyocardialinfarction(STEMI).While rare,RVleadmigrationiscrucialforemergencymedicine physicianstoidentify.Ourcaseappearstobethe first presentationofchestpainandnewST-segmentelevation fromRVleadperforation.Theconsequenceofmisclassifying thispresentationmayhavegraveconsequences.
A71-year-oldfemalepresentedtotheemergency department(ED)withmildpleuriticchestpainanda twitchingfeltinherleftchest.Thepatienthadrecently incurredacardiacarrestduetoventricular fibrillationand hadundergoneICDplacementforsecondarypreventiontwo
weeksearlier.Shewasseenearlierinthedayat electrophysiologyclinicandwasnotedtohavechangesin RVleadimpedancesanddiaphragmaticstimulationduring thresholdtesting.Therefore,shewassenttotheEDfor furthermanagement.UponarrivaltotheED,anECGwas performed(Image1),whichshowedanormalsinusrhythm, leftaxisdeviation,andsignificantST-segmentelevation acrosstheprecordialandhighlateralleads.
Withahistoryofischemic-typechestpain,thisECGwas concerningforanacuteSTEMI.However,withthepatient’ s historyofrecentICDplacementinadditiontolargeand diffuseST-segmentelevations,itwasdeemedmorelikelyto beanICDcomplicationcausingacurrentofinjurythanan ischemicevent.Ahighsensitivitytroponinwasfoundtobe withinnormallimits,andpoint-of-careultrasoundshowed preservedleftventricularfunctionandnoevidenceof pericardialeffusion.Computedtomographychest demonstratedtheRVleadtipextendingthroughthe
myocardium,epicardialfat,andpericardium,withitstipin thepericardiacfat,againwithoutevidenceofpericardial effusionormediastinalcollection(Image2).
Thepatientexhibitednohemodynamicperturbations throughoutherEDstay,andshewasadmittedtothe electrophysiologyserviceforcontinuedcare.Duringher hospitalstay,serialtroponinsremainedlow,andthe perforatedRVleadwasrevised.TheECGfromaftertheRV leadrevisionshowedresolutionoftheST-segmentchanges (Image3).Herhospitalcoursewascomplicatedbyan episodeofventriculartachycardiawithaneffectiveICD shockinthesettingoflikelycoronaryvasospasm.The patientrecoveredwellandwasdischarged fivedaysafter initialpresentation.
AcombinationofchestpainwithconcerningECG findingsmaypromptimmediateinterventionalcardiology consultationforSTEMIinthecorrectclinicalcontext. Inthiscase,theaddedinformationfromthepatient’ s electrophysiologyvisitearlierthatdayprovidedthe necessarycontexttoguidecare.ChangesinRVlead impedanceanddiaphragmaticstimulationduringthreshold testingprovidedtheclinicianswithamorelikelyexplanation forthepatient’stwitchingsensationandECGchanges.
Implantablecardioverter-defibrillatorleadperforationis arare(0.14%)butpotentiallylife-threateningcomplication ofICDplacement.1 PredictorsforperforationofICD includeolderage,femalegender,leftbundlebranchblock, worsenedheartfailureclass,higherthannormalleft
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Leadperforationofanimplantable cardioverter-de fi brillator(ICD)isarare (0.14%)butpotentiallylife-threatening complicationofICDplacement.
Whatmakesthispresentationof diseassereportable?
Ourcaseappearstobethe fi rstpresentationof chestpainandnewST-segmentelevationson electrocardiogram(ECG)fromright ventricularleadperforation.
Whatisthemajorlearningpoint?
HistoryofrecentICDplacementwith ST-segmentelevationshouldpromptconcern forleadmigration.Anticoagulatingapatient withaperforatedICDcanleadtomortality.
Howmightthisimproveemergency medicinepractice?
Emergencyphysiciansshouldbeawareof thisrarebutimportantadditiontotheir differentialdiagnosiswhencontextualizing aworrisomeECGwithaclinicalhistory.
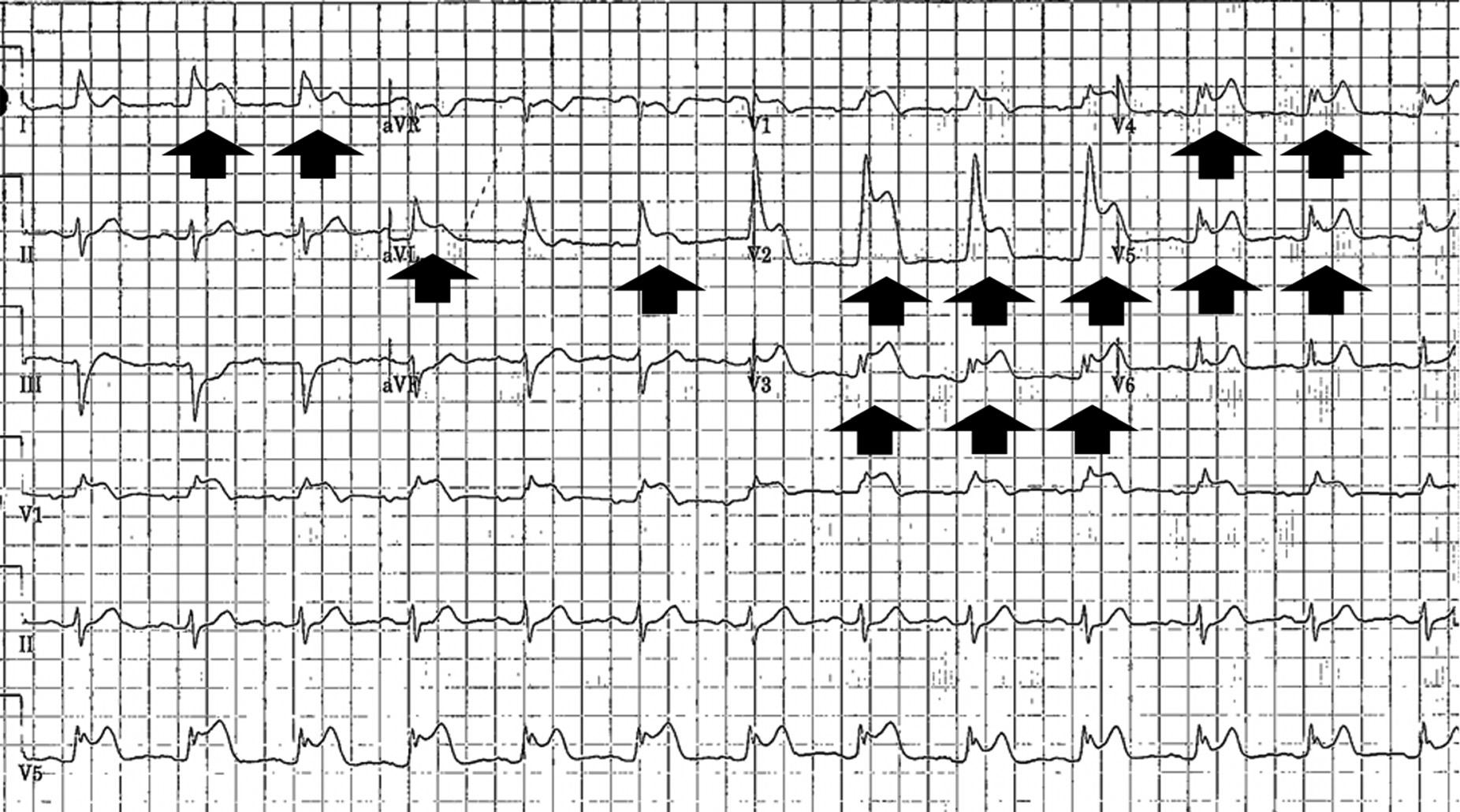
Image1. InitialelectrocardiogramonpresentationtotheemergencydepartmentshowingST-segmentelevations(arrows)acrossthe precordialandhighlateralleads.


ventricularejectionfraction,andnon–single-chamberICD implant.1 Themajorityofpacemakerordefibrillatorlead perforationsareeitheracuteorsub-acute,occurringwithin 30daysofimplantation.Delayedorchronicperforations occurringafter30daysofimplantationareuncommon. ThereareisolatedreportsofICDleadsperforatinganatomic structuresincludingribswithoutpleuralorpericardial
effusionorothercomplications,themediastinum complicatedbysepsis,andthecoronarysinusostium presentingwithoutsymptoms.2–5
Inthispresentation,therewasnoarrhythmia,pericardial effusion,hematoma,orotherdangerouspathologyfound.It appearstobeanovelpresentationofanECGconcerningfor STEMIleadingtoadiagnosisofRVleadmigration.The
Image3. ElectrocardiogramshowingresolutionofST-segmentelevationsafterperforatedpacerleadwassuccessfullyrevised.pathophysiologyofECGchangesfrompacerlead perforationrelatestocurrentofinjury,whichcanbe describedasthe flowofcurrentfromthedamagedareaofthe hearttotheundamagedportion.Thedamagedarearemains depolarized,andthecurrentofinjurypointstowardthe undamagedarea,leadingtotheST-segmentelevationsseen onourpatient’sECG.
AnypatientwithanICD,chestpain,andECGchanges requiresimmediateinterventionifhemodynamically unstable.Ifvitalsignsarenormal,workupshouldinclude serialtroponinsandECGs.Ifthereisconcernforlead perforation,advancedcardiacimagingwithorwithout electrophysiologyconsultationshouldbeconsidered.
Implantablecardioverter-defibrillatorleadperforationisa rarecomplicationofleadimplantationasevidencedbythe minimalavailableliteraturesurroundingitsepidemiologyand clinicalcourse.Theconstellationofchestpainandischemic ECGchangesinpatientswithICDsisevenmorerare.Not onlydoesthiscasebroadentherequireddifferentialofECGs demonstratingcurrentofinjurytoincludeICDlead perforation,butitalsoservesasguidancefortheemergency physiciantaskedwithworkingupchestpainandECG changesinapatientwithanICD.Cliniciansshouldlikewise appreciatethepotentialformisdiagnosis,leadingtopotential complicationssuchaspericardialeffusionassociatedwith anticoagulationinacatheterizationlaboratory.The appreciationofdeviceleadcomplicationsshouldprovidethe emergencyphysicianwithalesscommonbutimportant additiontotheirdifferentialdiagnosiswhencontextualizinga worrisomeECGwithaclinicalhistory.
Whilethereisnoclearguidancethatcanbeprovidedto physiciansgiventhelimitedexperience,therearethreetakehomepointswebelieveeveryemergencyphysicianshould keepinmindwhenevaluatingapatientwithanICDand chestpain:
1.HistoryofrecentICDplacementwithST-segment elevationshouldpromptconcernforleadmigration: withoutanelectrophysiologyvisitearlierthatday cluingtheauthorsintopotentialleadperforation, interventionalcardiologywouldhavelikelybeencalled forpossibleintervention.Imagingisrequiredtosecure thediagnosis.
2.AnticoagulatingapatientwithaperforatedICDcanlead tomortality:shouldthepatient’shistorybeunrecognized,
thepatientwouldbeatriskforreceivinganticoagulation duringcoronaryangiography,potentiallyleadingtolifethreateningpericardialtamponade.
3.PredictorsforperforationofICDincludeolderage, femalegender,leftbundlebranchblock,worsened heartfailureclass,higherleftventricularejection fraction,andnon-single-chamberICDimplant1:these factors,incombinationwiththeECGandfullclinical picture,mayhelpguidetheemergencyandcardiology teamswhenpresentedwithapatientwithICD placementandECGchanges,especiallywithin30days ofICDimplantation.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:BryanRosenberg,MD,Medstar WashingtonHospitalCenter;DepartmentofEmergencyMedicine, 110IrvingSt.NW,Washington,DC20010.Email: Bryan. Rosenberg@medstar.net
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Rosenbergetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.HsuJC,VarosyPD,BaoH,etal.Cardiacperforationfromimplantable cardioverter-defibrillatorleadplacement. CircCardiovascQual Outcomes.2013;6(5):582–90.
2.HerrMJ,CottrellJM,GarrettHEJr,etal.Erosionofarightventricular pacerleadintotheleftchestwall. SurgCaseRep.2020;6(1):262.
3.JainN,RavipatiV,KerutEK.Latepacemakerleadtipperforation documentedbychestCT. Echocardiography.2016;(9):1419–21.
4.HuangD,WilsonJ,GantiL.Isolatedshoulderpainsecondaryto pacerleadperforation. JAmCollEmergPhysiciansOpen 2022;3(2):e12615.
5.NakaoT,FujiuK,UeharaM,etal.Asymptomaticlong-termcardiac perforationbyapacemakerlead. InternMed.2019;58(16):2409–10.
AprilBrill,DO*
NiravChheda,DO*
DanielStrama,DO†
*FranciscanHealthOlympiaFields,EmergencyDepartment,OlympiaFields,Illinois † MidwesternUniversityChicagoCollegeofOsteopathicMedicine, DownersGrove,Illinois
RameshSoundararajan,MD*
SectionEditor:RachelLindor,MD,JD
Submissionhistory:SubmittedMay19,2023;RevisionreceivedNovember15,2023;AcceptedNovember17,2023
ElectronicallypublishedFebruary13,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1389
Introduction: Diabeticketoacidosis(DKA)isacommondiagnosisintheemergencydepartment(ED). However,onemustconsiderothercausesforacid-basedisturbanceswhenthepatternisnotconsistent withtypicalpresentation.
CaseReport: A52-year-oldfemalewithahistoryofinsulin-dependentdiabetesmellitustype2 presentedtotheEDwithabdominalpain,nausea,andvomitingforthreedays.Herdiagnosticworkup revealeddiabeticketoacidosisbutwithconcurrentmetabolicalkalosis.StandardtreatmentforDKAwas initiated,andtherewasimprovementofhermentationandresolutionofmetabolicderangements.
Conclusion: OverlookingadiagnosisofDKAbecauseofalkalosisonvenousbloodgastestingcould leadtoinappropriatetreatmentand,therefore,increasedriskofmorbidityandmortalityintheaffected patient.[ClinPractCasesEmergMed.2024;8(2)111–114.]
Keywords: DKA;diabeticketoalkalosis;bakingsodaingestion;casereport.
AccordingtoNationalDiabetesStatisticsReport2020, approximately34.2millionpeopleintheUnitedStatesalone hadbeendiagnosedwithdiabetes,whichaccountedfor about10%ofthetotalpopulation.1 Complicationsrelating tohyperglycemicepisodesaccountedfor224,000visitsto emergencydepartments(ED)in2016alone.1 Ithasbeen estimatedthatthetotalcostofcarerelatedtodiabeteshas increasedby49billiondollarsbetween2012–2017.Since diabeticcomplaintsandcomplicationsarecommon, emergencyphysiciansmustbefamiliarwiththedisease processandsequelae.1 Morbidityandmortalitydueto diabetesandrelateddisordersaccountedforgreaterthan 270,000deathsin2017andwastheseventhleadingcauseof deathintheUSin2017.1 Herewedescribeacaseofa52year-oldfemalepresentingwithauniquecauseofamixed acid-basedisorderforadiagnosisthatiscommonly encounteredintheED.Wediscussindepththeevaluationof mixedacid-basedisturbance.Thecasedemonstratesthe importanceofobtainingadetailedhistoryandphysicalexam wheneverpossible.
A52-year-oldfemalepresentedtotheEDbyambulance fromhomeforevaluationofhyperglycemia.Shereported complaintsofabdominalpain,nausea,andvomitingover thepriorthreedays.Shenotedthatsheadministeredherown medications,buttheremainderofthehistorywaslimiteddue toencephalopathy.Furtherhistorywasobtainedfromthe paramedicreportandelectronichealthrecordreview becausetherewasnofamilypresentatbedside.Onchart reviewitwasfoundthatshehadapastmedicalhistory ofinsulin-dependentdiabetestype2,gastroparesis, hypertension,seizuredisorder,hyperlipidemia,depression, substanceuse(tobacco,cocaine,andmarijuana), pancreatitis,andahiatalhernia.Briefreviewofsystemswas significantonlyfornauseaandvomiting,andshedenied suicidalityoruseofdrugsatthattime.Surgicalhistory wasnotableforpancreatectomywithpartialautologous transplantandappendectomy.Reportedhomemedications onthechartwereasfollows:amylase-lipase-protease 12,000–38,000–60,000unitsdelayedreleasecapsule;sodium phosphate;di/monoandpotassiumphosphatemonobasic
250milligram(mg)tablet,aspirin81mgtablet,atorvastatin 40mgtablet,calcium-vitaminD500mg-200unitpertablet, docusatesodium100mgcapsule,andinsulinglargineU-100 100unitspermilliliter(mL)vial.
Onphysicalexam,vitalsweretemperature36.4° Celsius, heartrate80beatsperminute,respiratoryrate18breathsper minute,bloodpressure135/72millimetersmercury(mmHg), oxygensaturation97%onroomair,andweightof36 kilograms.Shewasill-appearingandcachecticwithdry mucousmembranes,andherabdominalexamrevealedfocal epigastrictendernesswithoutguarding,rebound,orrigidity. Hercapillaryrefillandskinturgorwerenormal.She displayednofocalneurologicdeficitsandwasalertand orientedtoperson,place,andtime.However,herresponses weretangential,andshedisplayedpoorinsightintoher currentsituationandhealthproblems.
Initialabnormalchemistrylaboratory findingsweresodium 126milliequivalentsperliter(mEq/L)(referencerange133–144 mEq/L),potassium2.0mEq/L(3.5–5.1mEq/L),chloride 33mEq/L(98–107mEq/L),bicarbonategreaterthan45mEq/ L(21–31mEq/L),glucose448mg/deciliter(dL)(70–99mg/ dL),bloodureanitrogen(BUN)75mg/dL(7–25mg/dL), creatinine3.3mg/dL(0.6–1.2mg/dL),aniongap48mEq/L (6.2–14.7mEq/L),andmoderateacetone(negative).The mixedvenousbloodgaswasalsoabnormalwithapH7.64 (7.35–7.45);partialpressureofcarbondioxide65.1mmHg (35–45mmHg);hemoglobin11.9grams(g)/dL(14–18g/dL); andcalculatedbicarbonate71.1millimoles(mmol)/L(22–26 mmol/L).Serumalcoholwas <10mg/dL(<10mg/dL).Thefull labsarelistedinthe Table.Achestradiographrevealedno acutecardiopulmonary findings,andasingleviewabdomen radiographdemonstratedanon-obstructivebowelgaspattern. Electrocardiogramwasreadasnormalsinusrhythm,QTc490 milliseconds,andnoacuteST-Tchanges.
Giventhemarkedlyabnormalmetabolicderangements, initialtreatmentintheEDconsistedofthefollowing:two1-L fluidbolusesof0.9normalsalineintravenous(IV); ondansetron4mgIVpush,andpotassiumchloride(KCl) 60mEqIVoversixhoursfollowedbynormalsalinewith 20mEqKClat150mLperhour.Therewasconcernfor diabeticketoacidosis(DKA)giventhelaboratorystudies andavenousbloodgasthatdemonstratedamixedacid-base disorderwithanelevatedaniongap,moderateacetone,and elevatedglucose.Insulinwasinitiallyorderedbutcancelled whenthepotassiumhadnotcorrectedenoughpriortoher admissiontotheintensivecareunit(ICU).Duetothe complexityofexpectedmanagementofthemetabolic derangementsaswellasacutekidneyinjury,criticalcareand nephrologywereconsultedtodiscussfurthermanagement.
DuringherstayintheICU,shewaseventuallystartedona continuousinsulininfusionanddextrose5%inwaterwith 20mEqKCl.Heraniongapclosed,andhermetabolic derangementsresolved.Shewasswitchedbacktoherprior long-actingandsliding-scaleinsulinregimen.Ondaythreeof
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Diabeticketoacidosisisacommondiagnosis intheemergencydepartment(ED),andat least224,000visitsin2016weredueto complicationsofhyperglycemia.
Whatmakesthispresentationof diseasereportable?
Thiscasedemonstratesthesettingofan alteredpatientwhowasfoundtobe hyperglycemicbutalkaloticsecondaryto exogenousingestionofbakingsoda.
Whatisthemajorlearningpoint?
Thiscasediscussestheimportanceof reviewingalllabvaluesandtheimportanceof fl uidsandelectrolytereplacementasa standardofresuscitation.
Howmightthisimproveemergency medicinepractice?
Athoroughhistoryandphysicalexamincases ofmixedacid-basedisorderscanprovide pertinentinformationtohelpcounselpatients onappropriatehomemanagementofdiabetes andwhentoseekmedicalcare.
herstay,shewasmorecognizantandreportedthatshehad beenconsumingbakingsodaathomeforhersymptomsprior topresentation.Oncestabilized,shewasdowngradedtothe generalmedical flooranddischargedhomeonherprevious medicationregimenonhospitaldaysix.
Thecurrentliteraturereportsonseveralcasesofdiabetic ketoalkalosis,amixedmetabolicacidosisandalkalosis disorder,inthesettingofhypochloremia,althoughitremains ararediagnosis.2 Metabolicalkalosiswithhypochloremiacan besecondarytoexcessvomiting,metaboliccompensation, fastingorstarvationstate,oringestion.2–5 Wediscussthe specificingestionofbakingsodaasacauseforthepatient’ s metabolicderangements.Bakingsodamisusehasbeenshown tocausemetabolicderangementsresultinginhypokalemic metabolicalkalosis.2,6 Bakingsodafunctionsasanexcessbase withoneteaspoonproviding59mEqofbicarbonate comparedtothe7.7mEqfoundina650mgtabletofsodium bicarbonate.7 Therefore,thisingestionalsoledtomarkedly decreasedlevelsofchloride.8 Hypokalemicmetabolic
Table. Initiallaboratoryresultswithreferencerangesinparenthesis ofapatientwithdiabeticketoalkalosis.
CompletebloodcountCompletemetabolicprofile
WBC5.8(4.0–11.0 103/uL)Na126(133–144mEq/L)
Hg11.7(12.0–15.3g/dL)K2.0(3.5–5.1mEq/L)
Platelet561 (150–450103/uL)
Cl33(98–107mEq/L)
CO2 >45.0(21.0–31.0mEq/L)
Acetone:moderate(negative)Glucose448(70–99mg/dL)
Lacticacid:2.3 (0.5–2.0mmol/L)
BUN75(7–25mg/dL)
Cr3.3(0.6–1.2mg/dL)
Mixedvenousbloodgas:Calcium10.1(8.6–10.3mg/dL)
pH7.647(7.350–7.450)Totalprotein8.8(6.4–8.9g/dL)
PO2 91.1 (80.0–95.0mmHgb)
PCO2 65.1 (35.0–45.0mmHgb)
Albumin4.6(3.5–5.7g/dL)
Totalbilirubin0.8 (0.0–1.0mg/dL)
Hg11.9(14.0–18.0g/dL)Alkalinephosphatase169 (34–104U/L)
HCO3 71.1(22–26mmol/L)AST37(13–39U/L)
ALT15(7–52U/L)
Aniongap48(6.2–14.7mEq/L)
Mg2.5(1.6–2.6mg/dL)
Lipase88(11–82U/L)
Urinalysis:
Color:yellow(yellow)Bilirubin:negative(negative)
Appearance:hazy(clear)Protein100mg/dl(negative)
Ph7(5–8)Bloodurine:moderate(negative)
Specificgravity1.010 (1.005–1.030)
Urobilinogen:negative (negative)
Glucose >500mg/dl (negative) Nitrite:negative(negative)
Ketones20mg/dl(negative)Leukocyteesterase:negative (negative)
RBC0–2(0–2/hpf)Bacteria:noneseen(noneseen)
WBC0–5(0–5/hpf)Yeast:present(noneseen)
WBC, whitebloodcount; μL,microliter; Hg,hemoglobin; g,gram; dL, deciliter; mmol,millimole; L,liter; PO2,partialpressureofoxygen; mmHg,millimetersofmercury; PCO2,partialpressureofcarbon dioxide; HCO3,bicarbonate; mg,milligram; hpf,highpower field; RBC,redbloodcell; NA,sodium; mEq,milliequivalent; K, potassium; CI,chloride; CO2,carbondioxide; BUN,bloodurea nitrogen; Cr,creatinine; U,unit; AST,aspartateaminotransferase; ALT,alaninetransaminase; Mg,magnesium.
alkalosisduetoexcessbakingsodaconsumptioncanoccur eveninpatientswithnormalkidneyfunction.However,this patient’spoorrenalfunction,asindicatedbyherBUNand creatinine,furthercontributedtoherinabilitytoexpelexcess ingestedbicarbonate,leadingtoanelevatedlevel.8,9 This
elevatedlevelofbicarbonatealongwiththepatient’ s developingDKAresultedinadiabeticketoalkalosis.
Besidesthemetabolicderangements,excessbaseingestion canputpatientsatriskfordysrhythmias,seizures,and cardiopulmonaryarrest.9 Treatmentoftheexcessbakingsoda ingestionaswellastheconcomitantdiabeticketoalkalosis doesnotdifferfromthatofDKA.Afterdiscontinuinguseof theoffendingagentandinitiatingtherapywith fluids,insulin, andpotassium,allderangementsnormalized.2,10 Itis significanttoalsodiscussthatinsulintherapyisnot recommendeduntilhypokalemiaiscorrectedto >3.3mmol/L todecreaseriskofarrhythmiaandmuscleweakness.11
Thepatient’ssignificantlyelevatedaniongapof48mEq/L confirmsthemetabolicacidosis,whichwasfromDKA.Her severelyelevatedbicarbonatelevelinthechemistrypanelof greaterthan45mqE/L,aswellabloodgaswithacalculated bicarbonatelevelof71mmol/L,confirmsasignificant metabolicalkalosis.ThiscanalsobecorroboratedbyherpH of7.647.Withoutthecalculatedbicarbonatelevelavailable fromabloodgas,themodifieddeltagapcouldbeusedto screenforamixedmetabolicacid-basedisorder.Theformula isDeltagap=Na+-Cl- 36.12 Inthiscasethedeltagapwas +9andsignifiedpresenceofaconcomitantmetabolic alkalosissincetheriseintheaniongapwaslessthanthefall ofthebicarbonatelevel.12
Inthecaseofthispatient,attheonsetofhersymptomsshe mayhavehadsimplehyperglycemiathatresultedin gastroparesiswithnauseaandvomiting.Thehomeremedy ofbakingsodamayhavecausedhertoprogressintoDKAas wellasdelayherpresentationtohealthcarepersonnel. Patientsmustbecounseledonthepotentialrisksofhome remediesthatcanraisebicarbonatelevels.Thisisespecially trueofthoseconsideringanalkalinedietorconsuminga sodiumbicarbonateantacidasthiscanpredisposepatientsto hypokalemicmetabolicalkalosis.8,13
Thiscasehighlightstheneedforathoroughhistoryand physicalexamincasesofmixedacid-basedisorders,sincethe offendingagentwasnotidentifieduntilhospitaldaythree. Althoughhertreatmentalgorithmwouldnothavechanged withthisinformation,itwouldhaveprovidedpertinent informationtohelpcounselthepatientonappropriate homemanagementofherdiabetesandwhentoseek medicalattention.
TheInstitutionalReviewBoardapprovalhasbeendocumentedand filedforpublicationofthiscasereport.
AddressforCorrespondence:AprilBrill,DO,FranciscanHealth OlympiaFields,EmergencyDepartment,20201CrawfordAve, OlympiaFields,IL60461.Email: abrill@midwestern.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Brilletal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
1.CentersforDiseaseControlandPrevention.Nationaldiabetesstatistics report2020:estimatesofdiabetesanditsburdenintheUnitedStates. Availableat: https://www.cdc.gov/diabetes/pdfs/data/statistics/ national-diabetes-statistics-report.pdf.AccessedMay8,2023.
2.NanavatiS,KumarV,MelkiG,etal.Diabeticketoalkalosis:misnomeror undiagnosedvariantofdiabeticketoacidosis. BMJCaseReports 2018;2018:bcr2018226092.
3.YasudaK,HayashiM,MurayamaM,etal.Acidosis-induced hypochloremicalkalosisindiabeticketoacidosisconfirmedbythe modifiedbaseexcessmethod. JClinEndocrinolMetab 2016;101(6):2390–5.
4.FunkGC,ZaunerC,BauerE,etal.Compensatoryhypochloraemic alkalosisindiabeticketoacidosis. Diabetologia.2003;46(6):871–3.
5.BayatMandMøllerN.Diabetiskketoacidosemaskeretafmetabolisk alkalose[Diabeticketoacidosismaskedbymetabolicalkalosis]. Ugeskr Laeger.2013;175(46):2800–1.
6.Al-AbriSAandKearneyT.Bakingsodamisuseasahomeremedy:case experienceoftheCaliforniaPoisonControlSystem. JClinPharmTher 2014;39(1):73–7.
7.Al-AbriSAandOlsonKR.Bakingsodacansettlethestomach butupsettheheart:case filesoftheMedicalToxicologyFellowshipat theUniversityofCalifornia,SanFrancisco. JMedToxicol 2013;9(3):255–8.
8.CervantesCE,MenezS,JaarBG,etal.Anunusualcauseofmetabolic alkalosis:hidinginplainsight. BMCNephrol.2020;21(1):296.
9.SolakY,TurkmenK,AtalayH,etal.Bakingsodainducedsevere metabolicalkalosisinahaemodialysispatient. NDTPlus 2009;2(4):280–1.
10.SoiferJTandKimHT.Approachtometabolicalkalosis. EmergMedClin NorthAm.2014;32(2),453–63.
11.GosmanovAR,GosmanovaEO,KitabchiAE.Hyperglycemiccrises: diabeticketoacidosisandhyperglycemichyperosmolarstate. (2021).In:FeingoldKR,AnawaltB,BlackmanMR,etal.(Eds.), Endotext [Internet].SouthDartmouthMA:MDText.com,Inc. Availableat: https://www.ncbi.nlm.nih.gov/books/NBK279052/ AccessedOctober17,2023.
12.TsapenkoMV.Modifieddeltagapequationforquickevaluation ofmixedmetabolicacid-basedisorders. OmanMedJ 2013;28(1):73–4.
13.HoornEJ,BovéeDM,GeerseDA,etal.Diet-exercise-induced hypokalemicmetabolicalkalosis. AmJMed.2020;133(11):e667–9.
DuncanMcGuire,DO*
RobertCalleja,MD†
EricPai,MD†
AmitBahl,MD‡
SectionEditor:ShadiLahham,MD
*AscensionProvidenceHospital,DepartmentofEmergencyMedicine,Southfield,Michigan † BeaumontHealth,DepartmentofEmergencyMedicine,RoyalOak,Michigan ‡ CorewellHealth,DepartmentofEmergencyMedicine,RoyalOak,Michigan
Submissionhistory:SubmittedJuly13,2023;RevisionreceivedNovember2,2023;AcceptedNovember16,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1520
Introduction: Visionlossisasymptomfoundfrequentlyinpatientspresentingtotheemergency department(ED).Centralretinalarteryocclusion(CRAO)isanuncommonyettime-sensitiveandcritical causeofpainlessvisionlossinwhichdelayeddiagnosiscanleadtosignificantmorbidity.Emergency medicineliteraturedocumentstheabilitytodiagnoseaCRAOusingultrasoundbyidentifyingthe hyperechoicthrombus coinedtheretrobulbarspotsign.
CaseReport: Wepresentthecaseofapatientpresentingwithpainlessmonocularvisionlossforwhich CRAOwasdiagnosedintheEDusingpoint-of-careultrasoundenhancedbytheutilizationofserial Dopplerexaminationsaswellascalculationofthecentralretinalarteryresistiveindex.
Conclusion: Despitethepre-existingliteratureonpoint-of-careultrasoundinvestigationofcentralretinal arteryocclusion,therearenoemergencymedicinecasereportsdescribingserialexaminationofthe centralretinalarterybyspectralDopplerorcalculationofarterialresistiveindextoimprovethisevaluation andmonitorprogressionofthepathology.[ClinPractCasesEmergMed.2024;8(2)115–119.]
Keywords: centralretinalarteryocclusion;point-of-care-ultrasound;retrobulbarspotsign;resistive index;casereport.
Visionlossisafrequentlyencounteredsymptomresulting innumerousEDvisits.1 Whilesomeocularpathologiescan bereadilyidentifiedwithlimitedhistoryandevaluation, othersrequireexhaustiveapproachesincludingdilated fundoscopicexamination,specializedequipment, ophthalmologyconsultation,andevenadvancedimaging. Point-of-careultrasound(POCUS)oftheeyeisadiagnostic modalitythatcanbeappliedasaninitialscreeningtoolto helpidentifysomehigherriskdiagnosesefficientlyand accurately.2 Thisimagingmodalityallowsforhighresolutionevaluationofanteriorandposteriorchamber anatomy,aswellasretrobulbarstructuresincludingthe centralretinalarterywhichtravelswithintheoptic nervesheath.
Centralretinalarteryocclusion(CRAO)isthesudden blockageofthecentralretinalarterybyocclusivethrombus orembolusthatrequiresimmediateevaluationand treatmentatacomprehensivestrokecenter.3 AsCRAOisan uncommonyettime-sensitiveandcriticalcauseofpainless visionlossthatmaybedifficulttodistinguishfromother benigncauses,delayeddiagnosisofCRAOisanunfortunate reality.Theemergencymedicineliteraturedocumentsthe abilitytoidentifyCRAOusingPOCUSbyidentifyinga retrobulbarhyperechoicstructurewithinthedistaloptic nervesheath,representingcentralretinalarterythrombus (calledtheretrobulbarspotsign).4
Thereis,however,apaucityofliteraturedescribingthe EDapplicationofserialspectralDopplerexaminationas wellascalculationofthecentralretinalarteryresistiveindex
(RI)toimprovethisevaluationandmonitorpathology progression.WepresentthecaseofanEDusingPOCUS examination,enhancedbytheutilizationofserialDoppler examinationsaswellasRIcalculation,tomonitor diseaseprogression.
A60-year-oldfemalepresentedtoatertiary-careEDwith achiefcomplaintofpainless,right-sidedmonocularvision lossbeginning16hourspriortoarrivalwhileshewaseating dinner.Atthattime,sheexperiencedanacuteonsetrightsidedheadacheassociatedwithpainlessvisionlossinher righteye.Theheadachespontaneouslyresolvedafterthree minutes;however,thepersistenceofvisualdeficitsprompted herEDevaluation.UponarrivaltotheED,thepatient endorsedaworseningright-sidedsuperiorquadrantanopia. Shedeniedtrauma,otherneurologicdeficits,headache recurrence,systemicsymptoms,orahistoryof similaroccurrence.
Grossocularexaminationdemonstratedpupilsthatwere dilatedtofourmillimeters(mm)bilaterally.Therightpupil haddelayedconstrictionafterbothdirectandindirectlight exposurecomparedtotheleft,consistentwitharelative afferentpupillarydefect.Thepatient’srighteyecould perceivemovementonlyoutoftherightupperquadrant field.Visualacuitywas20/200oculusdexter(OD)and20/25 oculussinister(OS).Intraocularpressurewas16millimeters ofmercury(mmHg)ODand17mmHgOS.Anocular POCUSexaminationwasperformedbyemergency physiciansshortlyafterEDarrival.Thisdemonstratedright opticnervesheathdiameterof0.58centimeters(cm)andleft opticnervesheathdiameterof0.57cm(Image1).Therewas noevidenceofretinaldetachment,posteriorvitreous
Whatdowealreadyknowaboutthis clinicalentity?
Visionlossisafrequentlyencountered symptomintheED.
Whatmakesthispresentationof diseasereportable?
Point-of-careultrasound(POCUS)canbe rapidlyperformedintheEDtopreventdelays indiagnosisofcentralretinalartery occlusions(CRAO),apotentiallyvisionthreateningpathology.
Whatisthemajorlearningpoint?
SerialPOCUSexaminationintheEDcanbe usedtobothdiagnoseandmonitordisease progressioninCRAO.
Howmightthisimproveemergency medicinepractice?
Thiscaseemphasizestheimportanceof POCUSinevaluatingpatientswithpainless visionlosstoclinchthediagnosisandmonitor progressionofCRAO.
detachment,vitreoushemorrhage,retrobulbarhematoma, orlensdislocation.Uponcloserexaminationoftheoptic nervesheath,ahyperechoicsignalatthedistalaspectofthe

C:Retrobulbarspotsignnotedwithinthe opticsheathoftherighteyeasindicatedby arrow
Image1. Point-of-care-ultrasound findingsdemonstratingnormalright-(A)andleft-sided(B)opticnervesheathdiameters,aswellasan acutethrombusinthecentralretinalarterycalledtheretrobulbarspotsign(C). cm,centimeter.
sheath,knownasaretrobulbarspotsign,was appreciated(Image1).
ColorDopplerwasappliedtoassessforcentralretinal arterial flow,andapplicationofpulsedwaveDoppler revealedanarterial flowpatternwithanRI([peaksystolic velocity – enddiastolicvelocity]/peaksystolicvelocity]) calculatedtobe0.71(Image2).AfterPOCUSexamination, thepatientunderwentadditionalimaging,ophthalmology, andlaboratoryevaluation.Anon-contrastheadcomputed tomography(CT)didnotdemonstrateacuteintracranial pathology.Fundoscopicexamperformedbyophthalmology demonstratedretinalwhiteningwithsuperiormacular sparingintherighteyewithsupero-nasalchorioretinal hyperpigmentation.Thecuptodiscratiowas 0.2∶1bilaterally.
UponrepeatPOCUSexaminationonehourlater,there wasnoevidentcentralretinalarterial flowindicating completeCRAO(Image2).Duetothisdevascularization,a centralretinalarteryRIwasunabletoberecalculated. BecauseofthedelayedEDpresentationaftersymptom onset,thepatientwasnotacandidatefortissueplasminogen activator(tPA);therefore,ocularmassagetherapywas initiated,andshewasgivenadropofbrimonidine 0.1%ocularsolutionintheaffectedeye.Anteriorchamber decompressionwasrecommended;however,thepatient declined.Giventheatypicalheadacheassociatedwiththe patient’svisionloss,erythrocytesedimentationrate(ESR) andC-reactiveprotein(CRP)wereorderedintheED andwereelevated(ESR = 40mm/hr[referencerange = 0–20mm/hr]andCRP23.4milligramsperliter[mg/L] [referencerange =<3mg/L]).Incasethevisionlossoccurred
secondarytotemporalarteritis,thepatientwasstartedon high-dosesolumedrol(250mgeverysixhoursfor12doses followedbyprednisone80mgdaily.
NeurologywasalsoconsultedintheED,andthepatient wasadmittedtothehospitalforfurthermanagement.Her hospitalstayincludedacompleteevaluationforstrokeand inflammatorypathologies.Shewasdischargedfourdays lateronsteroid,brimonidine,andaspirintherapy.The patientwasprovidedwithinstructionstofollowupwith neurology,ophthalmology,cardiology,andrheumatology forcontinuedevaluationandmanagement.Onsubsequent reevaluationonemonthfollowingherCRAO,thepatient’ s visionhadimprovedto20/70-3ODwithextremeenhanced cornealcompensationand20/30+2OS.Ophthalmology advisedhertocontinuebrimonidineeyedropsandmaintain strictbloodglucose,bloodpressure,andlipidcontrol.
Centralretinalarteryocclusionshouldbeaconsideration inpatientsexperiencingpainlessvisionloss,anddilated fundoscopicexaminationisthegoldstandarddiagnostic approach.5 Giventhenuancesoftheprocedureincluding availabilityofspecializedequipment,timeneededfor dilation,andenvironmentalfactors,emergencyphysicians arelimitedintheirabilitytoaccuratelyandefficiently performfundoscopicevaluations.Asophthalmology consultationisnotalwaysreadilyavailableinmanyEDs, identifyingCRAOcanbeadiagnosticconundrumwith inevitabledelays.Centralretinalarteryocclusionisatimesensitivediagnosisandresultsindamagetoretinalcellsinas littleas12–15minutes,underscoringtheimportanceofearly

Image2. Centralretinalarterywithacutethrombusandcolor flowoncolorDopplerevaluation(A),centralretinalarterywithincreased resistanceto flowandanelevatedresistiveindex(B),andabsenceofcentralretinalarterycolorDoppler flowuponrepeatevaluation(C).
detection.5 Fortunately,emergencyphysicianexposureto ocularPOCUSisrapidlyincreasing,withtheAmerican CollegeofEmergencyPhysiciansrecognizingocular ultrasoundasoneof12coreemergency ultrasoundapplications.6
Whilebothglobeandretrobulbarstructurescanbereadily identifiedusingocularPOCUS,evaluationforCRAOisonly sparselydescribedinemergencymedicinecasereportsor series.7 Additionally,therearenoemergencymedicine accountsofserialcolorDopplerexamsperformedonpatients withthediagnosisofCRAOenhancedbythecalculationofan RI.Thereareseveralultrasound findingsthatmaybepresent intheocularPOCUSexaminationofapatientsufferingfrom aCRAO,includingthefollowing:anabsenceofpulsatile centralretinalarteryblood flowusingcolorandpulsedwave Doppler,anincreasedRImeasuredusingpulsedwave Doppler,andtheretrobulbarspotsign.3 Theretrobulbarspot signisahyperechoicstructurefoundposteriortotheeye withintheopticnervesheath.Itispostulatedthatthis structurehasahyperechoicsonographicappearancebecause itisacalcifiedcholesterolandthrombinemboluslodged withinthecentralretinalartery.4
AcolorDopplergaitcanbeappliedtotheopticnerve sheath,revealingpulsatile flowwithinthecentralretinal artery.8 Oncethisisidentified,apulsedwavegaitcanbelaid overthisarterialcolorpattern.Thisallowsforthecalculation ofthecentralretinalartery’sRI,theamountofresistanceto blood flowwithinavessel.Itiscalculatedbydetectingthe variationinpeaksystolicandenddiastolicvelocities.A normalcentralretinalarteryRIislessthan0.7.9 Presumably, theRIwouldbeelevatedinCRAO,althoughadditional researchiswarrantedtoevaluatefortheefficacyofthis modalityinpredictingaccuratecentralretinalartery vascularresistance.10 Additionally,theremaybeanabsence ofcentralretinalarteryDoppler flowifthereiscomplete occlusionofthevessel.
Currently,orbitalCTangiographyor fluorescein angiographyaretheimagingmodalitiesrecommendedwhen attemptingtodiagnoseCRAO.5 Diffusion-weighted magneticresonanceimagingcanalsobeperformedto evaluateforthispathologyandretinalanatomy.11 However, thesetestsarenotwithouttheir flawsastheytaketimeto perform,exposethepatienttoradiationandintravenous contrast,areexpensive,andaresusceptibletomotion artifact.ByusingPOCUSasanadjunctdiagnosticmodality inpatientssuspectedtohavethisdiagnosis,emergency physicianscanclinchthisvision-threateningdiagnosis, therebyavoidingfurtherdelaysinthediagnosticand therapeuticpathways.
WithintheED,ocularpoint-of-careultrasoundinpatients experiencingacuteonsetpainlessvisionlosscanenable
physicianstorapidlydiagnoseandacceleratetreatmentof centralretinalarteryocclusion.Ourcasehighlightsanovel useofPOCUSindiagnosingandmonitoringprogressionof thiscriticalentitybyusingserialexaminationsaidedby theapplicationofspectralDoppleraswellasresistive indexcalculation.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:DuncanMcGuire,DO,FAWM, AscensionProvidenceHospital,DepartmentofEmergency Medicine,3601W13MileRd,RoyalOak,MI48073. Email: mcguire.duncan@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024McGuireetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ChannaR,ZafarSN,CannerJK,etal.Epidemiologyof eye-relatedemergencydepartmentvisits. JAMAOphthalmol 2016;134(3):312.
2.PropstSL,KirschnerJM,StrachanCC,etal.Ocularpoint-of-care ultrasonographytodiagnoseposteriorchamberabnormalities. JAMA NetwOpen.2020;3(2):e1921460.
3.Rojas-BartoloméL,Ayo-MartínÓ,García-GarcíaJ,etal.Contributionof orbitalultrasoundtothediagnosisofcentralretinalarteryocclusion. J ClinMed.2022;11(6):1615.
4.NedelmannM,GraefM,WeinandF,etal.Retrobulbarspotsignpredicts thrombolytictreatmenteffectsandetiologyincentralretinalartery occlusion. Stroke.2015;46(8):2322–2324.
5.MacGroryB,SchragM,BiousseV,etal.ManagementofCentralRetinal ArteryOcclusion:AScientificStatementFromtheAmericanHeart Association. Stroke.2021;52(6):e282–94.
6.AmericaCollegeofEmergencyPhysicians.UltrasoundGuidelines: Emergency,Point-of-Care,andClinicalUltrasoundGuidelinesin Medicine.2023.Availableat: https://www.acep.org/patient-care/ policy-statements/ultrasound-guidelines-emergency-point-of–care-and-clinical-ultrasound-guidelines-in-medicine AccessedJune10,2023.
7.GalustH,BanksS,RiscintiM.Point-of-careultrasoundinthe detectionofcentralretinalarteryocclusioninapatientwithrecent COVID-19. JAmCollEmergPhysiciansOpen 2022;3(6):e12842.
8.WilliamsonTH,BaxterGM,DuttonGN.ColourDopplervelocimetryof thearterialvasculatureoftheopticnerveheadandorbit. Eye 1993;7(1):74–9.
9.KhatriM,SaxenaS,KumarM,etal.Resistiveindexofcentralretinal arteryisabioimagingbiomarkerforseverityofdiabeticretinopathy. IntJ RetinaVitreous.2019;5(1):38.
10.PolskaE,KircherK,EhrlichP,etal.RIincentralretinalarteryas assessedbyCDIdoesnotcorrespondtoretinalvascularresistance. Am JPhysiolHeartCircPhysiol.2001;280(4):H1442–7.
11.SiebertE,Rossel-ZemkouoM,VillringerK,etal.Detectabilityofretinal diffusionrestrictionincentralretinalarteryocclusionislinkedtoinner retinallayerthickness. ClinNeuroradiol.2022;32(4):1037–44.
DuncanRobertson,MD*
HaydenF.Peirce,MD†
MarekD.Nicpon,MD‡
EricM.Otterson,PA-C*
LaurelO’Connor,MD*
JuliaG.Rissmiller,MD‡
ZacharyW.Binder,MD†
SectionEditor:JoelMoll,MD
*UniversityofMassachusetts,ChanMedicalSchool,DepartmentofEmergencyMedicine, Worcester,Massachusetts
† UniversityofMassachusetts,ChanMedicalSchool,DepartmentofPediatrics, Worcester,Massachusetts
‡ UniversityofMassachusetts,ChanMedicalSchool,DepartmentofRadiology, Worcester,Massachusetts
Submissionhistory:SubmittedNovember27,2023;RevisionreceivedJanuary26,2024;AcceptedJanuary29,2024
ElectronicallypublishedApril24,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.6586
Introduction: Cerebrovascularaccidentsrarelyoccurinchildren;theincidenceofischemicstrokein patients <16yearsofageisbetween0.6–7.9/100,000.However,theyarethefourthmostcommon causeofacuteneurologicaldeficitsinthepediatricpopulation,andpossiblecasesshouldbeevaluated withahighindexofsuspiciontoensuretimelyintervention.
CaseReport: Wedescribeapreviouslyhealthy17-year-oldmalewhopresentedtothepediatric emergencydepartmentwithaleftfacialdroopandhemiparesisconsistentwithastroke.Thepatient’s ageandlackofcomorbiditiesmadethisanextremelyuncommonpresentation.Ourpatient’sneurologic symptomswerebelievedtohavebeencausedbyarecenttraumaticclavicularinjurysustainedtwo weeksprior,whichsubsequentlyledtovascularinsult.
Conclusion: Cerebrovascularaccidentsareanimportantcauseofmorbidityandmortalityinpediatric patients.Cerebrovascularaccidentsinchildrenaremostoftensecondarytocongenitalcauses; however,careshouldbetakentoassessforacquiredcauses,suchastraumatomajorbloodvessels. Whilerarelyimplicatedintraumaticinjuries,arterialstructuresposteriortothemedialclaviclecanresultin severecomplications.[ClinPractCasesEmergMed.2024;8(2)120–124.]
Keywords: stroke;claviclefracture;pseudoaneurysm.
Whilemorecommoninolderadults,strokes,or cerebrovascularaccidents(CVA),rarelyoccurinchildren. Theincidenceofischemicstrokeinchildren <16yearsofage isbetween0.6–7.9/100,000,andinyoungadults <45years oldisbetween8–100/100,000peryear.1,2 Thetraditionalrisk factorsforstroke hypertension,smoking,diabetes,and hypercholesterolemia arelessprevalentinpediatric patients.Inchildren,CVAsaremorecommonlyassociated withcardiacconditions,hematologicconditions, vasculopathies,andmetabolicdisorders.1 Pregnancy, exogenoushormoneuse,smoking,illicitdruguse,and prematureatherosclerosiscanincreasetheriskofCVAin youngadults.1 Wepresentthecaseofahealthyadolescent
malewhopresentedtothepediatricemergencydepartment (PED)withastrokedespitehavingnoidentifiablerisk factors.Writtenpermissionfromthepatient’sguardiansand assentfromthepatientwereobtainedtopresentthiscase.
Emergencymedicalservices(EMS)respondedtoahockey rinkforachiefcomplaintof “neckinjury.” Paramedics encountereda17-year-oldmalelyingsupineonthelocker room floor.Thepatient’strainerreportedthatthepatient hadcollapsedontheiceandcouldnotstand.Thepatient complainedoflight-headednessandwasnotedtohaveleftsidedfacialdroopandparalysisofhisleftupperextremity. Hedeniedheadacheorneckpain.Therewasnoreported
traumaticinjuryonthedayofpresentation.Thepatient deniedmedicalorsurgicalhistory,druguse,oralcoholuse.A videooftheincidentwasobtained(Video1).
TheexamperformedbyEMSwasnotablefor tachycardia,left-sidedfacialdroop,andabsentstrengthof theleftshoulder,elbow,forearm,hand,and fingers.Spinal precautionswereapplied,andEMSbypassedacommunity hospitalinfavoroftheregionalpediatrictraumacenter. UponarrivaltothePED,thepatientwasactivatedasa trauma.Onassessmentintheresuscitationbay,apersistent leftlowerfacialdroop,aGlasgowComaScaleof15,anda negativeextendedfocusedassessmentwithsonographyin traumawaspresent.Noexternalsignsoftraumawerenoted ontheexam.
Atthattimethepatientwasidentifiedasasuspected strokewithaNationalInstituteofHealthStrokeScalescore ofthree.Pediatricneurologywasconsulted,andthepatient wasemergentlytakenforcomputedtomography(CT)head, CTcervicalspine,andCTangiogram(CTA)oftheheadand neck.Computedtomographydidnotdemonstrateany acuteintracranialabnormalityorfractureofthecervical spine.TheCTAoftheheadandneckshowed “a1.8cm amorphoushyperdensityabuttingtheanterioraspectofthe junctionofthebrachiocephalicandrightcommoncarotid arterieswithanapparentneckextendingfromthe brachiocephalicartery,suggestingpseudoaneurysmor containedrupture” (Image1).

Image1. Sagittalmultiplanarreconstructionofthecomputed tomographyangiogramoftheheadandneckdemonstratesa 1.8cmamorphous,hyperdense,ovalstructureabuttingthe anterioraspectofthejunctionofthebrachiocephalicandright commoncarotidarteries,withanapparentconnectingneck extendingfromthebrachiocephalicartery(arrows),suggestinga pseudoaneurysmorcontainedrupture.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Cerebrovascularaccident(CVA)isamajor causeofmorbidityandmortalityforpatients ofallagesandcanarisefrommany differentetiologies.
Whatmakesthispresentationof diseasereportable?
Ouryoungpatienthadnoriskfactorsfor strokeexceptforanoccultinjurythatarose frompriortrauma.Thisinitiallyconfounded thecauseduringinitialpresentation.
Whatisthemajorlearningpoint?
AlthoughCVAisrelativelyrareinthe pediatricpopulation,itmustremainonthe differentialasremotetraumaticinjurymay createanidusforthromboembolism.
Howmightthisimproveemergency medicinepractice?
ExpedientcareofCVAintheEDisdependent onquickrecognitionandmustbeconsidered eveninthosewithfewperceivedriskfactors.
Anon-occlusive fillingdefectintheproximalright subclavianarterywassuggestiveofthrombusandraised concernforanembolicprocess.Decreased flowintheright distalsecondsegmentandthirdsegmentsoftherightvertebral arterysupportedaconcernforathrombus.Therewereno largevesselocclusionsorsignificantstenosesofthemajor intracranialarteries.Finally,aSalter-HarrisIfractureofthe rightclavicularheadwithsurroundingcontusion/hematoma wasnoted,alongwithdislocationofthesternoclavicularjoint. Theposteriorlydisplacedclaviclewasnotedtoabutthe pseudoaneurysm/containedrupture(Image2).
Afterthese findingsweremaderadiographically,the patientwasaskedspecificallyaboutinjurytohisrightupper chest.Hereportedthattwoweeksearlierhehadsustaineda bluntinjurytotheareaduringhockeypractice.Hehadbeen evaluatedbyhisschooltrainer,andradiographshadbeen obtainedthatwereinterpretedasnegative.Hehadcontinued toplayhockeyoverthesubsequenttwoweekswithmoderate butimprovingpain.Aspartofthepatient’strauma evaluation,achestradiographwasperformed,which demonstratedlefttrachealdeviation,likelyduetotheclavicle fracture.Laboratorydatarevealednormalcoagulation studiesandlipidprofile.

Image2. Three-dimensionalreconstructionofthethoracicinlet usingthecomputedtomographyangiogramoftheheadandneck demonstratesfractureoftherightclavicularheadwithananterior fracturefragmentposteriordisplacementoftheclaviclewith abutmentofthepseudoaneurysm/containedrupture(arrows). Theconnectingneckextendingfromthebrachiocephalicarteryis alsodepicted.
Oncethesubclavianarterywasidentifiedasanapparent thromboticsource,consultationswereplacedtovascular surgeryandcardiothoracicsurgery.Thepatientwastaken emergentlytotheoperatingroomforrepairoftheright innominatearterypseudoaneurysmviasternotomy. Additionally,anembolectomyoftherightsubclavianartery wasperformed.Thepatientawokepost-operativelywitha strongrightradialpulseandneurologicallyintact.
Magneticresonanceimaging(MRI)performedthe followingdayrevealedseveralsmallacuteinfarctstothe rightfrontallobe,theposteriormarginoftherightinsular cortex(Image3),andtherightparietallobe.These findings supportthehypothesisthatanembolicprocesscausedour patient’spresentingneurologicsymptoms.Hewasplacedon aspirin(81milligramsdailyforthreemonths)andwas
dischargedneurologicallyintactonpostoperativedaythree withplansforvascularsurgeryfollow-upandintervalrepair oftheclaviculardislocationbyorthopedicsurgery.
Thiscasedescribesa17-year-oldmalewhopresentedto thePEDwithweaknessofhisleftfaceandarm.Imaging revealedapseudoaneurysmofthebrachiocephalicartery likelyduetoarightclavicularfracture.Thepseudoaneurysm wasrepaired,andthepatientwasdischargedfromthe hospitalwithoutneurologicaldeficits.Thereareseveral noteworthyconsiderationsinthiscase.First,CVAisrarein children,especiallyinthosewithoutmedical comorbidities.1,2 OlderpatientsexperiencingaCVAtendto presentwithsignsofaphasia,visualdisturbance,and hemiparesis.Incontrast,pediatricpatientsmaypresentwith alteredmentalstatus,lethargy,andseizures.3,4
Pediatricstrokesecondarytocardiacdiseaseisassociated withbilateraldeficits,anteriorandposteriorcirculation involvement,andseizures.4 Conversely,strokesecondaryto traumaorembolicphenomenonisassociatedwithposterior circulationinvolvement,andismorelikelytopresentwith dysarthria,hemiparesis,visual fielddefect,orataxia. 5 While rare,strokeisthefourthmostcommoncauseofacutefocal neurologicaldeficitinchildrenafterhemiplegicmigraine, seizure,andBell’spalsy.6 Paramounttotheevaluationof strokeisimaging.Diffusion-weightedMRIcoupledwith vascularMRangiographyisthegoldstandardinthe evaluationofischemicstroke.7,8 Ifunavailablewithinthe firsthourofpresentation,guidelinesrecommendnoncontrastCTandCTAoftheheadandneck.8 Whileradiation isafactortoconsiderintheevaluationofpediatricpatients, thebenefitsofCTimaginginthiscircumstanceoutweigh potentialharm.
Themanagementofpediatricstrokerequiresa multidisciplinaryapproachinvolvingtheED,neurology, pharmacy,thepatient,andthepatient’sfamily.

Image3. Non-contrastbrainmagneticresonanceimagingdemonstratesahyperintenselesionontheaxialT2-weightedimageinthe posteriorrightinsularcortex(A)withrestricteddiffusionasdemonstratedbyfocusofhyperintensesignalonthediffusionweightedimage(B), andafocusofhypointensesignalontheapparentdiffusioncoefficientmap(C),consistentwithanacuteinfarct.Similarlesionswerealso identifiedintheanteriorrightfrontallobeandanterioraspectoftherightparietallobe.
Antiepilepticsshouldbeinitiatedifseizuresarepresent.7–10 Treatmentofacuteischemicstrokewithtissueplasminogen activator(tPA)orendovascularinterventionhaveshown benefitsinadults;however,thesetherapiesremain controversialinchildren.AjointstatementbytheAmerican HeartAssociation/AmericanStrokeAssociation recommendsthattPAorendovascularinterventionbe consideredinpediatricpatientswhohaveradiographically confirmedlargearteryocclusionandpersistentdisabling neurologicaldeficits,inconsultationwithneurologyand endovascularsurgery.10
Itissuspectedthatthepseudoaneurysmandsubsequent emboliformationinourpatient’ssubclavianarterywerethe mostlikelycauseofhisCVA.Twopotentialmechanismshave beensuggested:1)directembolizationfromthesubclavian arteryclotintothecarotidartery;or2)migrationofthe brachiocephalicarteryclotintothesubclavianartery withsmallerembolithentransitingthroughthe carotidartery.
Anotherremarkableaspectofthiscasewastheprofound sequelaofthepatient’sclavicularinjury.Hisneurologic symptomsultimatelyarosefromaclaviclefracturethathad occurredtwoweeksprior.Wesuspectthatthefracture causedtheinitialinsulttothebrachiocephalicartery,which thenledtotheformationofthepseudoaneurysm.Clavicle fracturesaremanagedbasedontheirlocation,angulation, andthedegreeofcompromisetosurroundingtissue.Distal andmidshaftclavicularfracturesaretypicallymanaged conservativelywithaslingandorthopedicsurgeryfollowup. 11 Fracturesofthemedialclavicle,suchastheone sustainedbyourpatient,arerare,representing2–6%ofall claviclefractures.12,13
Themedialclavicularphysisclosesbetween22–25yearsof age.Asaresult,fracturesofthemedialclaviclemostoften occurinpatients <25yearsold.14 Thesefracturesare associatedwithinjuriestovascularstructureswithinthe mediastinumsuchasthebrachiocephalicartery,aorta,and subclavianartery.14 Attentionmustbetakentoensurethat thesevascularstructuresarenotinjuredwhenevaluating medialclavicularfractures.15 Areviewoftheliterature yieldedasinglereportofasimilarincidentwhereatraumatic clavicularinjurycausedasecondaryCVAinayoungadult; however,thereislittleavailabledataontheincidenceof CVAcausedbyblunttraumaticinjuryinpediatricor adultpatients.16
Finally,earlyandeffectivecommunicationbetweenteams canminimizedelaysintheassessmentandmanagementof patientswithtime-sensitiveand/oruncommonED presentations.Inthiscase,EMSdivertedtoapediatric traumacenterandthemultidisciplinaryteamwaspresenton arrival.Onceacutetraumawasdeemedlesslikely,thepatient wasidentifiedasasuspectedstrokevictim,whichresultedin expeditedneurologicalevaluation.Thisidentificationofa strokemaynothavehappenedasrapidlywithouta
conscientiousassessmentbyEMSandfrontlineparamedics. Anydelaycouldhaveresultedinpermanentneurologic injury.Ourpatientlikelybenefittedfrombeingtransported directlytoamedicalcenterwiththeappropriateresourcesto treathisrarepresentation.
Whilerarerthaninadults,CVAsareanimportantcause ofmorbidityandmortalityinpediatricpatients. Cerebrovascularaccidentsinchildrenaremostoften secondarytocongenitalcauses;however,careshouldbe takentoassessforacquiredcauses,asoccurredinour patient.Theregionposteriortothemedialclavicle,while rarelyimplicatedintraumaticinjury,holdsmanyimportant arterialstructures.Asaresult,injuriestothisareashouldbe evaluatedwithahighindexofsuspicion.Finally,when pediatricstrokeisbeingconsidereditisimportantto useallavailableresourcestoobtainpromptimaging andexpediteevaluationtoincreasethechancesofa favorableoutcome.
Video1. Thepatient(#22)canbeseeninitiallyattherightofthe video.Asthecamerapanstowardtheright,thepatientisseenatthe center.Asheskatesbackwardhefalls.Onmultipleattemptstoget backup,itappearshisleftlegandarmhavedecreasedcoordination andweakness.Heisescortedofftheicetobeevaluatedby medicalpersonnel.
TheInstitutionalReviewBoardapprovalandPatientConsenthave beendocumentedand filedforpublicationofthiscasereport.
AddressforCorrespondence:DuncanRobertson,MD,Universityof Massachusetts,ChanMedicalSchool,DepartmentofEmergency Medicine,55LakeAve.North,Worcester,MA01655.Email: duncan. robertson@umassmemorial.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theprojectdescribedwassupportedby theNationalCenterforAdvancingTranslationalSciences,National InstitutesofHealth,throughGrantKL2TR001454.TheNIHhadno roleinthedesignandconductofthestudy.Thecontentissolelythe responsibilityoftheauthorsanddoesnotnecessarilyrepresentthe officialviewsoftheNIH.
Copyright:©2024Robertsonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PutaalaJ,MetsoAJ,MetsoTM,etal.Analysisof1008consecutive patientsaged15to49with first-everischemicstroke. Stroke. 2009;40(4):1195–203.
2.GiroudM,LemesleM,GouyonJB,etal.Cerebrovasculardiseasein childrenunder16yearsofageinthecityofDijon,France:astudyof incidenceandclinicalfeaturesfrom1985to1993. JClinEpidemiol. 1995;48(11):1343–8.
3.MallickAA,GanesanV,KirkhamFJ,etal.Childhoodarterialischaemic strokeincidence,presentingfeatures,andriskfactors:aprospective population-basedstudy. LancetNeurol. 2014;13(1):35–43.
4.AbendNS,BeslowLA,SmithSE,etal.Seizuresasapresenting symptomofacutearterialischemicstrokeinchildhood. JPediatr. 2011;159(3):479–83.
5.AsakaiH,CardamoneM,HutchinsonD,etal.Arterialischemicstrokein childrenwithcardiacdisease. Neurology. 2015;85(23):2053–9.
6.ShellhaasRA,SmithSE,O’ToolE,etal.Mimicsofchildhoodstroke: characteristicsofaprospectivecohort. Pediatrics. 2006;118(2):704–9.
7.FerrieroDM,FullertonHJ,BernardTJ,etal.ManagementofStrokein NeonatesandChildren:ascientificstatementfromtheAmericanHeart Association/AmericanStrokeAssociation. Stroke. 2019;50(3):e51–96.
8.BernardTJ,FriedmanNR,StenceNV,etal.Preparingfora “pediatric strokealert.” Pediatricneurology. 2016;56:18–24.
9.RoyalCollegeofPaediatricsandChildHealth.StrokeInChildhoodClinicalGuidelineforDiagnosis,ManagementandRehabilitation.2017. Availableat: http://www.rcpch.ac.uk/stroke-guideline
Accessed:March8,2023
10.FerrieroDM,FullertonHJ,BernardTJ,etal.Managementofstrokein neonatesandchildren:ascientificstatementfromtheAmericanHeart Association/AmericanStrokeAssociation. Stroke. 2019;50(3):e51–96.
11.CanadianOrthopaedicTraumaSociety.Nonoperativetreatment comparedwithplate fixationofdisplacedmidshaftclavicularfractures. Amulticenter,randomizedclinicaltrial. JBoneJointSurgAm. 2007;89(1):1–10.
12.GoldfarbCA,BassettGS,SullivanS,etal.Retrosternaldisplacement afterphysealfractureofthemedialclavicleinchildrentreatment byopenreductionandinternal fixation. JBoneJointSurgBr. 2001;83(8):1168–72.
13.KihlströmC,MöllerM,LönnK,etal.Claviclefractures:epidemiology, classificationandtreatmentof2,422fracturesintheSwedish FractureRegister;anobservationalstudy. BMCMusculoskeletDisord. 2017;18(1):82.
14.KhanLA,BradnockTJ,ScottC,etal.Fracturesoftheclavicle. JBone JointSurgAm. 2009;91(2):447–60.
15.HoogervorstP,vanSchieP,vandenBekeromMP.Midshaftclavicle fractures:currentconcepts. EFORTOpenRev. 2018;3(6):374–80.
16.GhazalehD,SalariA,MohlL,etal.Acuteischemicstrokewith devastatingconsequencescanoccurduetoposteriorsternoclavicular jointdislocation. Life(Basel). 2022;12(11):1836.
PatrickMeloy,MD*
WillS.Lindquester,MD†
JeffreyStebbins,PA-C*
ElaineBromberek,MD*
*EmoryUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Atlanta,Georgia
† EmoryUniversitySchoolofMedicine,DivisionofInterventionalRadiologyand Image-guidedMedicine,Atlanta,Georgia
SectionEditor:ChristopherSanMiguel,MD
Submissionhistory:SubmittedAugust8,2023;RevisionreceivedNovember24,2023;AcceptedDecember1,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.1598
Introduction: Visceralarterialaneurysmsandpseudoaneurysmsarerarebutdangerouspathologies, withreportedincidenceof0.01–0.2%oftheworldwidepopulation,asfoundonautopsy. Pancreaticoduodenalarterypathologyaccountsforapproximately2%ofallvisceralaneurysms;itis commonlycausedbychronicinflammatoryprocesses,suchaspancreatitisoradjacentpseudocysts. Morbidityandmortalitycommonlyresultfromruptureoftheaneurysmitself,leadingtolife-threatening hemorrhageintotheperitoneumorgastrointestinaltract.
CaseReport: Herewepresentthecaseofa64-year-oldmalepatientwithprevioushistoryofalcoholuse disorderleadingtochronicpancreatitisandpriorembolizationofaninferiorpancreaticoduodenal pseudoaneurysm,whopresentedtotheemergencydepartment(ED)withabdominalpain,nausea,and vomiting,andwasfoundtohavealargerecurrentinferiorpancreaticoduodenalpseudoaneurysmwith associatedobstructivecholangitisandpancreatitisviacontrast-enhancedcomputedtomography(CT)of theabdomenandpelvis.Thepatientwasmanagedemergentlybyinterventionalradiologyangiography withemboliccoilingandpercutaneousbiliarycatheterplacement,andhesubsequentlyunderwentbiliary ductstentingwithgastroenterology.Thepatientwassuccessfullydischargedafterabriefhospitalization afterresolutionofhispancreatitisandassociatedhyperbilirubinemia.
Conclusion: Pancreaticoduodenalarteryaneurysmsandpseudoaneurysmsarerareanddangerous visceralpathologies.PatientscanbediagnosedrapidlyintheEDwithCTimagingandneed urgentendovascularmanagementtopreventmorbidityandmortality.[ClinPractCasesEmergMed. 2024;8(2)125–128.]
Keywords: casereport;visceralpseudoaneurysm;pancreaticoduodenalpseudoaneurysm;obstructive jaundice;alcoholusedisorder.
Visceralarteryaneurysmsareclinicallyrareentitiesand aretypicallyfoundincidentallyonabdominalimagingorvia autopsy.1,2 Patientswhopresentwithsymptoms,suchas abdominalpain,vomiting,orgastrointestinalbleeding,are morelikelytobeexperiencingatrueemergency,with8.5%of allcasesresultingindeath.2 Aneurysmsofthe pancreaticoduodenalarteriesrepresent2%ofallvisceral aneurysmsandarethemostlife-threatening.2 Comparedto
trueaneurysms,patientswithpseudoaneurysmshave profoundlyhigherrupturerates,upto76%comparedto3%, andrequireemergenttreatmentforstabilization.3
Inthiscase,thepatientpresentedwithsymptomatic abdominalpainandtendernessandwasfoundtohaveavery largerecurrentpseudoaneurysmoftheinferior pancreaticoduodenalartery,thesizeofwhichledto obstructivebiliarydiseaseandcholangitis.Thepatient underwentemergentembolizationofhispseudoaneurysm
andpercutaneousbiliarycatheterplacementwith interventionalradiology(IR)tomanagehissevere diseaseprocess.
A64-year-oldmalepatientwithapastmedicalhistoryof pancreatitis,alcoholusedisorder,glaucoma,andprior gastrointestinalbleed,presentedtotheemergency department(ED)complainingoftwoweeksofabdominal pain,nausea,andvomiting.Hereportedthathehadchronic abdominalpainthathadworsenedinthepriortwoweeks.He washospitalizedatanoutsidefacilityonemonthpriorfora gastrointestinalbleed,butasourceofbleedingwasnever identified.Hissurgicalhistorywassignificantforcoil embolizationofaninferiorpancreaticoduodenalartery (IPDA)pseudoaneurysmsac,measuring2.2centimeters (cm)atthetimeofembolization,withadditionalcoilingof thegastroduodenalartery(GDA)topreventcollateral filling ofthepseudoaneurysm.Hehadalsoundergonetotal kneereplacement.
Onarrival,hisvitalsignsweretemperature 36.8° Celsius(C)(oral),heartrate85beatsperminute, respiratoryrate16breathsperminute,bloodpressure139/67 millimetersofmercury,andoxygensaturation99%onroom air.Hisphysicalexamwasnotableforscleralicterusand moderateabdominaltenderness,worseovertheepigastrium, butwithoutreboundtendernessorguarding.Intravenous (IV)accesswasestablished,labsweredrawn,andthepatient wasgivenoneliterlactatedRinger’s,4milligrams(mg)IV morphine,and4mgIVondansetron.
Thepatient’slaboratorystudiesweresignificantforan initialwhitebloodcellcount(WBC)of14.0permicroliter (109/liter)(referencerange4.5–11.0 × 109/liter),hemoglobin 8.6gramsperdeciliter(g/dL)(14–18g/dL),hematocrit 26.6%(41–50%),andplateletsof486 × 109/liter(150–400 × 109/liter).Lipasewaselevatedat225unitsperliter(U/L) (0–160U/L).Liverfunctiontestswerealsoobtainedand wereconcerningfortotalbilirubin6.0mg/dL (0.1–1.2mg/dL),aspartatetransaminase102U/L (8–33U/L),andalaninetransaminase127U/L(7–56U/L). Thepatienthadevidenceofcoagulopathywithprothrombin timeof21seconds(10–13seconds)andinternational normalizedratio1.86(referencerangelessthan1.1),despite lackofanysystemicanticoagulation.
Initialcomputedtomography(CT)withIVcontrastofthe abdomenandpelvisrevealeda6.6-cmenhancinglesioninthe regionofthepancreaticheadandcommonbileduct, consistentwithalargevisceralpseudoaneurysmwithout arterialextravasation(Images1 and 2).Coilsfromtheprior embolizationwerepresentwithinthepseudoaneurysmsac, indicatingthatthiswasarecurrencewithsignificant enlargementofthepreviouslytreatedpseudoaneurysm. Severeintrahepaticbiliaryductaldilationanddiffuse dilationofthegallbladderwasalsoseen,withthepresumed
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Visceralarteryaneurysmsarerarebut dangerous.Pancreatitisisacauseof pancreaticoduodenalarteryaneurysm,and rupturecanleadtohemorrhageinto theperitoneum.
Whatwastheresearchquestion?
Thiscasedetailsananeurysmpresentinupto 0.2%oftheworldwidepopulation.Itssizeand locationledtobiliaryobstruction,which aidedinrapiddiagnosis.
Whatwasthemajor findingofthestudy?
Visceralarteryaneurysmsarediagnosedwith CTangiography;considerationshouldbe giventourgentinterventionalradiology coilingorembolizationforstability.
Howdoesthisimprovepopulationhealth?
Cliniciansshouldconsidervisceralartery aneurysmsinpatientswithunexplained obstructivebiliarypathologyandobtainCT angiographyfordiagnosis.

Image1. Axialcontrast-enhancedcomputedtomographyinthe arterialphase,pre-procedure,demonstratingalargevisceral pseudoaneurysmintherightupperquadrant(bracketswith measurements);andanartifactfromtheendovascularcoilswithin thelesionfrompriorembolization(arrow).

Image2. Coronalcontrast-enhancedcomputedtomographyin thearterialphase,pre-procedure,demonstratingalargevisceral pseudoaneurysmintherightupperquadrant(bracketswith measurements);andanartifactfromtheendovascularcoilswithin thelesionfrompriorembolization(arrow).
GDApseudoaneurysmcausingmasseffectonthecommon bileduct(Image3).
TheimagingresultswerediscussedimmediatelywithIR, andthepatientwaspreppedforemergentembolization. Additionally,IRplannedurgentpercutaneousbiliarycatheter placementgivenconcernforcholangitisinthesettingofan elevatedWBCcountandobstructivecholangiopathy. AngiographydemonstratedalargeIPDApseudoaneurysm arisingfromthebranchesofthesuperiormesentericartery. Coilembolizationofthearterialinflowandoutflowwas successfulwithnopersistent fillingofthepseudoaneurysm

Image3. Axialcontrast-enhancedcomputedtomographyinthe arterialphase,pre-procedure,demonstratingsevereintra-hepatic biliaryductaldilation(arrow).
postembolization,withassociatedpreservationofthe surroundingjejunalarteriesviacollaterals.
Giventhatthepatientwasalsofoundtohavebiliary ductaldilationwithobstructionandconcernforcholangitis, aleft-sidedbiliarydrainwasplacedfordecompression.The patienttoleratedtheinitialprocedureandwasadmittedto thesurgicalintensivecareunitforongoingmonitoring.Over thefollowingfourdays,hehadimprovementofhisliver functiontestsandleukocytosisandwassubsequently dischargedhome.Fiveweeksafterdischarge,thepatienthad repeatimagingoftheabdomenandpelvis,whichdidnot showanypatentpseudoaneurysmpresent.Hesubsequently underwentbiliarystentplacementwithgastroenterologyand removalofhisbiliarycatheter.
Apseudoaneurysmisdefinedasanencapsulatedhematoma incommunicationwiththelumenoftherupturedvessel,where theexternalwallconsistsofadventitia,perivasculartissue, fibrosis,orclot.2 Pseudoaneurysmsusuallyoccurinthe proximityofpseudocysts,whicherodeintoandcommunicate withavesseltocreateapseudoaneurysm.2,3 Pseudoaneurysms usuallydonotoccurimmediatelyafteranepisodeofacute pancreatitisbutaremorecommonlyfound3–5weeksafterthe initialepisode.Bleedingandhemorrhagehavebeenseen anywherefromtwomonthstoeightyearsafterasingleepisode ofpancreatitis.5,6 Gastroduodenalarterypseudoaneurysms areseeninupto20%ofarterialpseudoaneurysmscomplicated bypancreatitis,whilepancreaticoduodenalarteriesare involvedinupto10%ofcases.2,5
Althoughpancreaticpseudoaneurysmsareuncommon,itis importanttorecognizethisconditionearly,asitcanresultin life-threateningcomplications.Patientswilltypicallypresent withgastrointestinalbleedingorabdominalpain.2 Pseudoaneurysmsmaycausegastrointestinalbleedingby erosionintotheadjacentbowelortheymaydirectlyrupture, causingbleedingintotheretroperitoneum.1 Computed tomographyusuallyprovidesappropriatediagnosticimages; however,angiographyhasbeendemonstratedtobethemost informativeinvestigationfordiagnosisaswellastreatment. Computedtomographyangiographyhasahighrateof sensitivityandspecificitybutdoesnotfacilitateintervention concurrently.Angiographydefinesthecharacterandlocation ofthelesions,aswellasprovidesanopportunitytogaincontrol overthebleedingbytranscatheterembolizationorpossible stenting.1 Aseriesof35patientsfrom1993–2003indicated95% ofpseudoaneurysmsweredetectedwithangiographywhile only90%weredetectedwithCTangiography.1 AlthoughCT angiographyisanimportanttoolintheEDtodiagnosethese cases,managementpertheIRteamisparamountforsuccess. Endovascularuseofmetalliccoilsisfrequentlyusedasthe definitivetreatmentofthesepseudoaneurysms.Othertools includingcoveredstents,detachableballoons,gelfoam,or particleshavealsobeenusedwithsuccessratesofupto85%.1
Surgicaltreatmenthasbeenshowntobechallengingand associatedwithhighmorbidityrates,thusreservingsurgical interventionincasesoffailedembolizationor hemodynamicallyunstablepatients.1 Thereportedincidence ofrecurrenthemorrhageafterthrombosisisashighas30%, withembolizationofpancreaticpseudoaneurysmsrequiring long-termfollow-upinthesepatients.13 Inthecaseofour patient,IRwasabletosuccessfullyembolizethelargeIPDA pseudoaneurysmwithfollow-upimagingdemonstrating ongoingresolution.
Pancreaticoduodenalandgastroduodenalartery pseudoaneurysmsarerareanddangerousvisceralpathologies. Pseudoaneurysmsusuallyoccurintheproximityof pseudocystsorchronicinflammatoryconditionsandarea knowncomplicationofchronicpancreatitis.Patientscanbe diagnosedintheEDwithCTangiographyandneedurgent endovascularmanagementwithinterventionalradiologyto preventmorbidityandmortality.Duetohighratesof recurrenthemorrhageafterthrombosis,patientsshouldhave closefollow-upandserialimagingtoassessfor pseudoaneurysmoraneurysmrecurrence.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:PatrickMeloy,MD,EmoryUniversity SchoolofMedicine,DepartmentofEmergencyMedicine, 531AsburyCircle,AnnexBuilding,SuiteN340,Atlanta,GA30322. Email: patrickmeloy@emory.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Meloyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PittonMB,DappaE,JungmannF,etal.Visceralarteryaneurysms: incidence,management,andoutcomeanalysisinatertiarycarecenter overonedecade. EurRadiol.2015;25(7):2004–14.
2.KumarV,AbbasAK,AsterJC. RobbinsBasicPathology.10thed. (KumarV,AbbasAK,AsterJC,eds.).Elsevier-HealthSciences Division;2021.
3.MendelsonRM,AndersonJ,MarshallM,etal.Vascularcomplicationsof pancreatitis. ANZJSurg.2005;75(12):1073–9.
4.YamaguchiK,FutagawaS,OchiM,etal.Pancreaticpseudoaneurysm convertedfrompseudocyst:transcatheterembolizationandserialCT assessment. RadiatMed.2000;18(2):147–50.
5.DorffelY,WruckU,RuckertRI,etal.Vascularcomplicationsinacute pancreatitisassessedbycolorduplexultrasonography. Pancreas 2000;21(2):126–33.
6.BalthazarEJ.AcutePancreatitis:Assessmentofseveritywithclinical andCTevaluation. Radiology.2002;223(3):603–13.
7.BoudghèneF,L’HerminéC,BigotJM.Arterialcomplicationsof pancreatitis:diagnosticandtherapeuticaspectsin104cases. JVasc IntervRadiol.1993;4(4):551–8.
8.AgrawalG,JohnsonPT,FishmanEK.Splenicarteryaneurysmsand pseudoaneurysms:clinicaldistinctionsandCTappearances. AJRAmJ Roentgenol.2007;188(4):992–9.
9.BradleyEL.Complicationsofchronicpancreatitis. SurgClinNorthAm 1989;69(3):481–97.
10.Vázquez-RuizJ,L´opez-FlorV,Aguado-PérezM,etal.Pancreatic pseudoaneurysms:formsofpresentationandtherapeuticoptions. Cir Cir(EnglishEdition).2015;83(5):454–5.
11.BergertH,DobrowolskiF,CaffierS,etal.Prevalenceandtreatmentof bleedingcomplicationsinchronicpancreatitis. Langenbeck’sArchSurg 2004;389(6):504–510.
12.GuillonR,GarcierJM,AbergelA,etal.Managementof splenicarteryaneurysmsandfalseaneurysmswithendovascular treatmentin12patients. CardiovascInterventRadiol 2003;26(3):256–260.
13.dePerrotM,BerneyT,BuhlerLH,etal.Managementofbleeding pseudoaneurysmsinpatientswithpancreatitis. BrJSurg 1999;86(1):29–32.
PeritonsillarAbscessandPost-aspirationBleedIdentifiedwith Point-of-careUltrasoundUsingEndocavitaryProbe: ACaseReport
JaclynFloyd,MDBrandonDahl,DO
MatthewWhited,MD
AmiKurzweil,MD
SectionEditor:JoelMoll,MD
EisenhowerMedicalCenter,DepartmentofEmergencyMedicine,RanchoMirage,California
Submissionhistory:SubmittedAugust30,2023;RevisionreceivedNovember15,2023;AcceptedNovember17,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1645
Introduction: Peritonsillarabscessesformbetweenthetonsillarcapsule,thesuperiorconstrictor,and palatopharyngeusmuscles.Physicianstraditionallymakethisdiagnosisclinically;however,ultrasound allowsclinicianstofurtheridentifyanddifferentiatebetweenperitonsillitis,peritonsillarabscess,and phlegmonformation.Byincreasingboththesensitivityandspecificity,ultrasoundimprovesthe diagnosticaccuracyforpatientswithperitonsillarabscesses.Thiscasedemonstratestheutilizationof ultrasoundinperitonsillarabscessesandtheapplicationofpoint-of-careultrasound(POCUS)in identifyingcomplicationsofproceduresusedfortreatmentintheemergencydepartment(ED).
CaseReport: A19-year-oldmalepresentedtotheEDwithcomplaintsofseveresorethroatandfeverfor theprior fivedays.APOCUSusinganendocavitaryprobewithsterilecoverdemonstratedhypoechoic debriswitha “swirlsign.” Ultrasoundwasusedtosuccessfullyguideneedleaspirationbyusingin-plane needleguidance.Thepatienthadsignificantbleedingafterneedleaspiration,andrepeatPOCUSclearly identifiedanewpocketofbloodthathadformedandwascontainedinthesofttissue.Wemonitoredthe sizeofthehematomainrealtimewithultrasoundtoensurethehematomahadnorapidexpansionand wasstable.
Conclusion: Amongthedifferentialdiagnosesforsorethroat,thediagnosisofperitonsillarabscessis particularlyconcerningasitisbothcommonandgenerallyrequiresswiftintervention.Presentationscan rangefromamildinfectiontoalife-threateningemergencywithpotentialairwaycompromise.Thetwo primaryavenuesfortreatmentincludeeitherneedleaspirationorincisionanddrainage.Ultrasoundcan successfullyidentifytheabscessandotherlandmarksforsafeandsuccessfuldrainage,aswellasearly identificationofcomplications.[ClinPractCasesEmergMed.2024;8(2)129–132.]
Keywords: peritonsillarabscess;endocavitaryultrasoundprobe;ultrasound;otolaryngology; casereport.
Peritonsillarabscessisthemostcommondeep-space infectionoftheheadandneck.Casesarecommonly polymicrobialbutmostcommonlycausedbystreptococcus. Patientsmaypresentwithfever,odynophagia,dysphagia, trismusandpossiblyamuffledvoicecolloquiallyknownas
“hotpotatovoice.” Diagnosisofperitonsillarabscessusing historyandphysicalalonehasasensitivityandspecificityof 75%and50%,respectively.Diagnosisusingultrasound,in additiontohistoryandphysical,usinganendocavitaryprobe placedintraorallyshowedasensitivityandspecificityof91% and75%,respectively,whiletranscervicalshoweda
sensitivityandspecificityof80%and81%,respectively.7 This casehighlightsaninterestingcomplicationofacutebleed demonstratedbypoint-of-careultrasound(POCUS)during peritonsillardrainage.Ultrasoundidentificationof peritonsillarabscessisontheconsensuslistforcompetencies inemergencymedicineresidency3;proficiencyinultrasound isincreasinglyexpectedintrainees,andthisparticular scenarioexemplifiesitsutility.
A19-year-oldmalewithnopast medicalhistorypresented totheemergencydepartment(ED)withthecomplaintofsix daysofsorethroat,primarilyontherightside.Healsohad feverandchills,otalgia,andodynophagia.Onphysicalexam thepatient’svoicehadamuffledtone,hefeltwarmtotouch, andtherewasswellingnexttotherighttonsilwithuvular deviation.Hewasnothavinganydifficultybreathing,andno stridorwasnoted.Computedtomography(CT)hadbeen ordered,whichreturnedshowinga rightperitonsillarabscess measuring23 × 32 × 45millimeters,enlargementof Waldeyer’sring,andright-sidedlevelIIandIII lymphadenopathy.APOCUSusingtheendocavitaryprobe withsterilecoverdemonstratedencapsulated,swirling echogenicdebrisapproximately3centimeters(cm)deep.This wasusedtoclearlymarkthelocationforneedleaspiration.
Needleaspirationwasperformedwithremovalof 10milliliters(mL)ofpurulence,andthepatientstartedtohave significantbleeding,approximately200millilitersofboth bloodandsalivainthesuctioncannisterwithinafewminutes. Asolutionof4%cocainewassoakedontolongcottontips,and pressurewasheldfor10minutes.Repeatultrasoundwas performedeverytwominutes,whichshowedahyperechoic pocket,likelyrepresentingfreshhematoma,notexpanding. Twophysicianswereintheroom,withonephysician continuingtoholdpressure,althoughmovingslightlylaterally ateachtwo-minuteintervaltoallowspaceforthesecond physiciantoperformarepeatultrasound.Eachrepeat ultrasounddemonstratedstabilityofthehematoma,andat10 minutesthehematomawasconsideredcontrolled.Clinicallyat thispoint,thepatienthadnofurtheroropharyngealbleeding.
Otolaryngologywasconsultedregardingthe findingsand recommendedadditionalincisionanddrainage(I&D)given theinitialsizeoftheabscessfoundonCT.Inaddition,they recommendedintravenous(IV)antibiotics,IVdexamethasone, softdiet,andadmission.TheI&Dwasperformedinthe operatingroom,andthepatientwasdischargedthefollowing dayonclindamycin,orallyandamedroldosepack.
Peritonsillarabscessisafrequentlymadediagnosisbothin urgentcareandintheED.Itaffectsanestimated 45,000peopleperyear,withoverhalfbeingadmittedfor furthertreatment.10 Physicalexamwillrevealaunilateral (rarelybilateral)swellingaboveandlateraltothetonsilswith
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Peritonsillarabscessisthemostcommon deep-spaceinfectionoftheheadandneck.
Whatmakesthispresentationof diseasereportable?
Thiscasehighlightstherapidonsetofa hematomafollowingneedleaspirationandthe useofultrasoundtomonitoritsprogression.
Whatisthemajorlearningpoint?
Hematomadevelopmentmaybeonecause ofbleedingafterneedleaspirationof peritonsillarabscessandthiscanbeseenwith apoint-of-careultrasound.
Howmightthisimproveemergency medicinepractice?
Clinicianscanutilizeultrasoundguidanceto helpmanagecomplicationsofneedle aspirationsforperitonsillarabscess,withan imageandvideoforreference.
contralateraldeviationoftheuvula.Peritonsillarabscessisa medicalemergencyduetothepossibilityofupperairway obstructionandthepatient’sinabilitytoprotecttheirown airway.Diagnosisisclinical;however,ultrasoundcanbe usedtodifferentiatebetweenperitonsillitisandperitonsillar abscess.TreatmentincludesI&Dorneedleaspiration andantibiotics.
UltrasoundcanbeusedtoperformI&Dorneedle aspirationandhasbeenshownhelpfulinidentifyingthe locationoftheabscessandincreasingthesafetyofthe procedurebyaidinginidentifyingarterialvasculaturesuch astheunderlyingcarotidarteryanditsdistancefromthe abscesspocket(Image).Whileultrasoundcanhelpminimize complications,theycanstilloccur.Themostfrequent complicationsofperitonsillarabscessincludemediastinitis, necrotizingfasciitis,Lemierresyndrome,and retropharyngealabscess.2 Antibiotictreatmentshouldcover staphylococcusandstreptococcus,anaerobes, Eikenella corrodens, and Haemophilusin fl uenzae .Intravenous antibioticoptionsincludeampicillin/sulbactam, piperacillin/tazobactam,clindamycinorceftriaxone. Outpatientantibioticoptionsincludeclindamycinor amoxicillin/clavulanate.
Ultrasoundcanbehelpfulinidentifyingcrucialaspectsof eachofthesecomplications.Forexample,innecrotizing

Image. Point-of-careultrasoundwithendocavitaryprobedemonstratingswirlingechogenicdebrisencapsulatedapproximately3 centimetersdeep,representinginitialabscess(arrow).Colorboxrepresentsvasculature,includingcarotidartery.
fasciitisultrasoundhasahighsensitivityinidentifyingfree air.9 Forretropharyngealabscess,ultrasoundcanidentify thepocketof fluid,autilizationthathasmostlybeen describedinpediatrics.11 Thiscaseshowsanunexpected complicationofneedleaspiration.Thehematomashownin Video wasmonitoredusingtheendocavitaryprobetoensure itwasnotrapidlyexpandingaspressurewasheldonthe cavityexteriorly.Pressurewasheldcontinuouslyfor10 minutes,whiletheendocavitaryprobewasusedeverytwo minutestomonitorthehematoma.Thiscaseexemplifieshow theendocavitaryprobeapproachcanbeextremelyusefulin helpingtomanageaperitonsillarabscessaswellas complicationsthatmayarise.
Theskillofusingultrasoundtodetectperitonsillarabscess isacknowledgedasakeycompetencyforemergency medicineresidents.3 Thiscasestudydemonstratestheutility ofpoint-of-careultrasoundinbothidentifyingperitonsillar abscessesandprovidingguidanceduringtheaspiration procedure.Gainingavisualdiagnosiswhencomplications arisecanprovetobeexceptionallyvaluable.
Video. Point-of-careultrasounddemonstratinghyperechoicpocket, representingfreshhematoma(arrow).
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:JaclynFloyd,MD,Eisenhower MedicalCenter,DepartmentofEmergencyMedicine,39000Bob HopeDr,RanchoMirage,CA92270.Email: jfloyd@ eisenhowerhealth.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Floydetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ChangBA,ThambooA,BurtonMJ,etal.Needleaspirationversus incisionanddrainageforthetreatmentofperitonsillarabscess. Syst Rev. 2016;12(12):CD006287.
2.KlugTE,GreveT,HentzeM.Complicationsofperitonsillarabscess. AnnClinMicrobiolAntimicrob.2020;19(1):32.
3.HaidarD,PetersonW,MingesP,etal.Aconsensuslistofultrasound competenciesforgraduatingemergencymedicineresidents. AEMEduc Train.2022;6(6):e10817.
4.BryczkowskiC,HaussnerW,RomettiM,etal.Impactofbedside ultrasoundonemergencydepartmentlengthofstayandadmissionin patientswithasuspectedperitonsillarabscess. Cureus 2022;14(12):e32207.
5.MillsLD,MayK,MihlonF.Peritonsillarabscesswithuvularhydrops. WestJEmergMed.2010;11(1):83–5.
6.KimDJ,BurtonJE,HammadA,etal.Testcharacteristicsofultrasound forthediagnosisofperitonsillarabscess:asystematicreviewandmetaanalysis. AcadEmergMed.2023;30(8):859–69.
7.DonaldsonR,SwartzJ,LuK,etal.Peritonsillarabscess.WikEM.2021. Availableat: https://wikem.org/wiki/Peritonsillar_abscess AccessedFebruary26,2023.
8.BallewJD.UnlockingCommonEDprocedures-peritonsillarabscess drainage.EmDOCs.net-EmergencyMedicineEducation,EmDOCs. 2019.Availableat: https://www.emdocs.net/unlocking-common-ed-
procedures-peritonsillar-abscess-drainage/ AccessedFebruary26,2023.
9.YenZS,WangHP,MaHM,etal.Ultrasonographicscreening ofclinicallysuspectednecrotizingfasciitis. AcadEmergMed 2009;9(12):1448–51.
10.GlasierCM,StarkJE,JacobsRF,etal.CTandultrasoundimagingof retropharyngealabscessesinchildren. AJNRAmJNeuroradiol 1992;13(4):1191–5.
11.OrtegaBK,ShortS,KaneBG,etal.Managementof peritonsillarabscesswithinalocalemergencydepartment: aqualityanalysisstudy. Cureus.2021;13(8):e17545.
AndreaHlady,MD*
†
DavidKerner,MD LauraE.Walker,MD,MBA†SectionEditor:AnnaMcFarlin,MD
*MayoClinicHealthSystem,DepartmentofEmergencyMedicine, AlbertaLea,Minnesota † MayoClinic,DepartmentofEmergencyMedicine,Rochester,Minnesota
Submissionhistory:SubmittedMay31,2023;RevisionreceivedOctober18,2023;AcceptedNovember1,2023
ElectronicallypublishedMarch25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1422
Introduction: Severehypernatremiaisacriticalsituation,andwhencoupledwithintravasculardepletion andhypotensioncancreateatreatmentdilemma.
CaseReport: Wepresentthecaseofamedicallycomplexpatientwhohadgraduallyworsening alterationofmentalstatusandmeanarterialpressuresinthe50sonpresentationtothe emergencydepartment.
Conclusion: Finaldiagnosesincludedseverehypernatremiaandhypovolemicshocksecondarytopoor oralintake.Weusedjudicious fluidrepletionwithgradualimprovementinsodiumlevelsandpermissive hypotensiontoavoidrapidosmoticshifts.Balancingreperfusionandtheriskforosmoticeffects ofaggressive fluidresuscitationcanbeachallengingsituationforthemultidisciplinary team.[ClinPractCasesEmergMed.2024;8(2)133–137.]
Keywords: metabolicdisturbance;hypernatremia;permissivehypotension;casereport.
Mentalstatuschangeinolderadultsisacommon presentingcomplaintandoftenduetosystemicprocesses suchasinfection,trauma,centralnervoussystem(CNS) impairment,medications,metabolicderangements, cardiopulmonarydysfunction,oriatrogeniceffects.1 Taken asamultifactorialprocess,riskofdeliriumisincreasedby nursinghomeresidents’ cognitiveimpairment,hearing impairment,andhistoryofstroke,withpotentialstrong associationswithfrailtyandmalnutrition.2 Duetothebroad differential,evaluationsfordeliriumandmentalstatus changesoftenincludescreeningforunderlyinginfections, metabolicderangements,dehydration,primaryCNScauses, trauma,andothercausesofendorgandamage.
Hypernatremia,serumsodiumgreaterthan145 milliequivalentsperliter(mEq/L),iscommoninolderadults, andnursinghomeresidentsareparticularlyatriskasoral rehydrationcanbechallenging.3 Mostcasesarefoundatthe extremesofage,whenindividualsarelessabletoactonor detectthirst.Additionalcausesincludeinsensiblelosses,
gastrointestinallosses,centralornephrogeniccauses,and diuresis.Increasedoralintakeofsodiumwithout concomitantfreewatercanalsoresultinhypernatremia. Treatingboththeunderlyingconditionandrestoringnormal physiologyunderliestheapproachtocareintheemergency department(ED).Acutevschroniconsetofhypernatremia determinestherateatwhichsodiumiscorrectedtoavoid iatrogeniccerebraledema.4 Wedescribeacaseinwhich hemodynamicinstabilityandseverehypernatremia presentedtogether,creatingacomplexscenariofor EDresuscitation.
WeadheredtotheCAREguidelinesforreporting casestudies.5
A64-year-oldwomanwastransportedtotheEDvia emergencymedicalservices(EMS)withalteredmentalstatus andgeneralizedweakness.Hermedicalhistorywas significantforcontracturesofunknownetiology, osteoporosis,psoriaticarthritis,bullouspemphigoid,
paroxysmalsupraventriculartachycardia,hypertension,and mildcognitiveimpairment.Sherequiredongoingnursing careduetoherlimitedmobilitycausedbyhercontractures.
UponEDarrivalshewasunabletocontributetothe historysecondarytohermentalstatuschanges.Family informedtheEDteamthatshehadbeenunwellfortheprior threedayswithdecreasedoralintakeandincreased confusion.Theyhadnoticedthatshewasnoteatingather recentbirthdaycelebrationandthatherspeechseemed “off” whenspeakingviatelephone.Onthedayofpresentationshe hadnotcalledherfamilyand,therefore,afamilymember requestedthatanursecheckinonher.Theyalsovisitedthe patientlaterthatday findingherconfused,prompting activationofEMS.
OnarrivaltotheEDherbloodpressurewasinitially measuredat101/64millimetersofmercury(mmHg)but within30minuteswas75/63mmHg,heartrate137beatsper minute,respiratoryrate34breathsperminutewithnormal saturationsof97%,andatemperatureof36.6° Celsius(C). Herweightwas35.3kilograms.Shewasconfusedandunable toanswerquestionsorfollowcommands.Sheappeared cachectic,withbitemporalwasting.Hereyesweresunken, andtherewaspurulentdrainagefromtherighteye.Mucous membranesweredry.Hereyeswereopen,shewasmoaning withincomprehensiblespeech,andshewithdrewfrompain. Shehadweakperipheralpulses.Cardiopulmonaryexam revealedtachycardiaandclearlungsbilaterally.Her abdomenwassoft,althoughshedidappeartohave voluntaryguarding.Shehadseverecontractionsoftheupper andlowerextremities.Herskinwaswarmanddry.
Withherhemodynamicabnormalitiesthepriorityafter primarysurveywastoobtainintravenous(IV)access.This wasimpairedbythediffusecontracturesaswellas hypovolemia.Ultrasound-guidedperipheralIVandcentral venouscatheteraccesswereattempted,butveinsappearedto benon-compressibleandconcerningfordiffuseclotburden precludingadditionalattempts.Intraosseousaccesswas obtained,andthepatientwasgivenabolusofoneliter normalsalineandstartedonlactatedRinger’satarateof 200millilitersperhour(mL/hr).Atimelineof patientcareispresentedinthe Table1
Labstudiesincludedelectrolytes,completebloodcount, lactate,coagulationprofile,bloodcultures,andCOVID-19 andinfluenzaswabs,aswellasurinalysis.Significant findings areshowninthe Table2.Upondiscoverythathersodium was176mEq/L, fluidresuscitationwaspausedtodetermine appropriaterateofadministrationforsafecorrection.
Table1. Atimelineofthepatientepisodeofcare.
Elapsed TimeEvent
00:00Patientarrival
00:12 Initialphysicianevaluation
00:18Attemptsatperipheralaccessunsuccessful HR:137;BP:101/64
00:291liter0.9%normalsalinebolusinitiated
00:44Point-of-careglucose87mg/dL Labsdrawn
00:48HR:136;BP:75/63
00:53Completebloodcountresulted 01:07Lactateresulted
01:16Basicmetabolicpanelresulted 01:18HR:136;BP:75/65
01:48HR:140;BP:75/58
01:51Urinalysisresulted
Familypresenttoprovideadditionalhistory
1:58
Intraosseousneedleplaced 02:00HR:140;BP:114/98
02:29Bedsideechocardiogram:hyperdynamic myocardium,collapsedIVCnoted
02:48HR:116
02:50Urineosmolalityresulted
03:03HR:131;BP:73/55
03:24PeripheralIVaccessobtained
04:31Point-of-carevenousbloodgasobtained,repeat lactateimproving
04:33Pipercillin/sulbactamadministered,lactated Ringer’sinitiatedat200mL/hour HR:122;BP:73/46
04:47Arteriallineplaced 04:48HR118;BP:73/47
05:03HR114;BP:76/48
05:18Heparindripinitiatedduetoconcernforclot HR:119;BP:71/43
05:21Imagingresultsreassuring,decisiontoadmitto medicalintensivecareunit
05:48HR:122;BP:83/51
06:03HR:122;NP:81/49
Patienttransportedtointensivecareunit
8:00–30:00D5Wadministeredatvaryingrates BP(MAP)rangesfrom55-69 86:00Sodiumlevel145mEql/L
HR, heartrate; BP,bloodpressure; IVC,inferiorvenacava; IV, intravenous;mL,milliliters; D5W,dextrose5%inwater; MAP, meanarterialpressure; mg/dL,milligramsperdeciliter; mEq/L, milliequivalentsperliter.
Table2. Notablelabstudies.
WBC 27.4 × 109/L
Neutrophilcount21.89cells/L
Hematocrit47.6%
Sodium176mEq/L
Chloride131mEq/L
Creatinine2.85mg/dL(baseline0.7)
BUN85mg/dL
INR1.8
Lactate3.7mEql/L
UrineRedappearance,cloudy; + RBCs, + WBCs, + ketones, + nitrites, + leukocyteesterase
WBC, whitebloodcells; BUN,bloodureanitrogen; INR,international normalizedratio; RBC,redbloodcells;mEq/L,milliequivalentsper liter; mg/dL,milligramsperdeciliter.
Herhypotension,apparentabdominaldiscomfort,and concernfordiffuseclottingpromptedseveralimaging studies.Theseweredelayedsecondarytodifficultyobtaining IVaccessandconcernforpotentialsignificantclotburden. Ultimatelywhentheywereobtainedcomputedtomography (CT)oftheabdomenandpelvisdemonstratednoacute findings,CTofthebrainshowednoapparentabnormalities, andlowerextremityultrasounddidnotrevealacutedeep veinthrombosis.
Thepatientcontinuedtohavetachycardiaand hypotensionfollowingtheinitialliterofcrystalloidprovided. Thediscoveryofprofoundhypernatremiaprompteda treatmentdilemma,inwhichslowcorrectionofsodiumwas pursuedratherthanrapidcorrectionofhemodynamics.Our assessment,basedonthehistoryprovidedbythefamily,was thatthiswaslikelyachronicdevelopmentofhypernatremia. Clinically,sheappeareddehydratedandinneedof additional fluids.Inadditiontodehydrationandresulting hypernatremia,weconsideredthepossibilityofsepsiswitha possibleurinarysource.Herelevatedlactate,creatinine,and urinaryketones,aswellasherhemodynamics,wereevidence ofaneedforadditional fluids.Thedegreeofsodium elevationshehadisassociatedwithariskofmortalityof 75%6;additionally,herelevatedlactateinthesettingof infectioncontributedadditionalriskofmortalitywithin 28days.7
Aftertheinitialoneliterofnormalsalinewasgiven andwediscoveredherhypernatremia,weadjusted fluid administrationtoachieveagoalrateofsodiumcorrection between10–12mEq/Lperday,startingwithlactated Ringer’sat200cc/hr.AnEDpharmacistassistedtoensure appropriatetherapy.Shewastreatedempiricallyforpossible
urosepsiswithpiperacillin-sulbactam(2.25g)pending cultureresults.
DuringherEDstayourteamstruggledwiththe conflictingdesirestotreatherhypotensionandtachycardia andprovideresuscitationforhersepsis/hypovolemiawhile managingherhypernatremia.Aggressiverehydrationwould havelikelyresultedincerebraledemaandaverypoor outcome.Weoptedtopursuepermissivehypotensioninthe ED,andthiscourseofcarewascontinuedintotheintensive careunit(ICU).UponICUadmission,shewasstartedon dextrose5%inwateratarateof100millilitersperhour (mL/hr)withadditionalfreewateradministeredvia nasogastrictubeat50mL/hr.
Duringhospitalization,nutritionalstudiesrevealedsevere malnutrition.Additionalhistoryatthattimeuncoveredshe hadover20%weightlossoverthecourseoftheprioryear. Shewastransferredtotheregularmedical floorwhenher sodiumreached152mEq/mL,twodaysafteradmission.Her hospitalcoursewascharacterizedbydifficultywithoral intake.Apalliativecareconsultwasperformed,andafamily decisionwasmadetopursuefeedingvianasogastrictube followedbypercutaneousendogastrictube.Anemia developedfollowingrehydration,thoughttoalsobe associatedwithfrequentlabdraws,andshewastransfused withoneunitofpackedredbloodcells.Shehadepisodesof aspirationwithresultingtachycardiaandtachypnea. Imagingstudiesrevealedanexudativepleuraleffusionwith negativecultures.Hersymptomsimprovedwithout antibiotics.Sheremainedstablefortheremainderofher hospitalizationandwasdischargedonhospitalday24toa skillednursingfacilitywithparenteralfeeding. Figure1 demonstratestherateofsodiumcorrectionalongwith representativemeanarterialpressure(MAP)during thisperiod.
Managementofhypernatremiaisa “breadandbutter” topicinemergencymedicine.However,theroleofpermissive hypotensioninresuscitationismostoftencitedinreference topatientswithtraumaandseverehemorrhage,8 ruptured abdominalaorticaneurysm,9 andvasodilatoryshock.10 Neitheratthetimecarewasprovided,norsubsequently,did weidentifyliteraturediscussingthetenuousresuscitationof patientswithseverehypovolemiaandhypotensioninthe settingofprofoundhypernatremia.
Theimmediatecareforthispatientpresentedasituation thatwasstressfulfortheEDteam.Persistenthypotension andtachycardiaintheEDwerenotedbyteammembers includingnursing,physiciantrainees,andpharmacists. Thiswasremediatedbygoodteamcommunicationand collaboration.Asharedunderstandingoftheorderof operationswewouldundertakeandthereasoningbehind
Figure. Hourlytrendsofsodiumlevelandmeanarterialpressure. MAP,meanarterialpressure;mEq/dL,milliequivalentsperdeciliter.
permissivehypotensionwascrucialtoprovidingappropriate careforthepatient.Whenwearepushedoutofourtypical algorithmof “airway,breathing,circulation” andinstead needtotendtolong-termsurvivabilityduetopotential metabolic/neurologiccompromise,thesmoothcarewe typicallyaimtoprovideisdisrupted.Knowingwhenand howtogo “offprotocol” fromthebasicapproachto resuscitationisakeyskillinemergencymedicine.
Thegoaloftreatinghypotensionistoreduceendorgan injury.Thisisprimarilyachievedthrough fluidresuscitation andvasopressors.However,therearetimeswheneither fluidsorvasopressorsmaybedetrimental.Consider aggressive fluidresuscitationinpulmonaryembolismor hypernatremia,crystalloidresuscitationinhemorrhagic shock,orhighvasopressoruseandtissuehypoxiaaswellas increasedmortalityinvasodilatoryandhemorrhagic shock.8,11–15 Intheseinstances,permissivehypotensionmay beinthebestinterestofthepatient,butwhataretheeffectsof long-termcontrolledpermissivehypotensionandwhat degreeofhypotensionshouldweallow?
Thereareveryfewstudiesdiscussingthisissueandeven fewerthatcandirectourpractice.Moststudiesarefocused ontheeffectsofhemorrhagicshock.Aretrospectivecohort studyofICUpatientssuggeststhattheMAPatwhich terminalcardiovascularcollapseoccursissomewhere between30–46mmHg15;andwearetaughtthat65mmHgis theoptimalMAPgoal,andinsomeinstanceshigher (eg,post-operativespinalcordperfusion).Inarandomized controltrialevaluatingICUpatients ≥65yearscomparing
permissivehypotensiontousualcare,theydidnot finda statisticallysignificantdifferencein90-daymortalityandno differenceinseriousadverseevents.Mostadverseevents relatedtoacuterenalfailureandsupraventricularcardiac arrythmias.Cognitivedeclineandhealth-relatedqualityof lifeat90daysandatoneyearweresimilarbetweenthetwo groups. 10 Allowingpermissivehypotensionanddeferringto otherprioritiesinresuscitationmayofferanadvantagewith minimaldownsideincasessuchasseverehypernatremiaand volumedepletion.
Theprimarytake-awaysfromthiscaseincludethe importanceofrapidreassessmentandpivotingfrom aggressivecrystalloidresuscitationwhenhypernatremiawas identified;andtheuseofpermissivehypotensionin hypovolemichypernatremiatoprioritizecentralnervous systemstabilityandestablishasharedunderstandingofthe treatmentprioritiesforEDteammembers.Webelievethat EDandsubsequentICUcarewereessentialtothepatient’ s survivaltodischarge.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:LauraE.Walker,MD,MBA,Mayo Clinic,DepartmentofEmergencyMedicine,200FirstSt.SW, Rochester,MN55902.Email: Walker.laura@Mayo.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Hladyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.HanJHandWilberST.Alteredmentalstatusinolderpatientsinthe emergencydepartment. ClinGeriatrMed.2013;29(1):101–36.
2.OliveiraJESL,BerningMJ,StanichJA,etal.Riskfactorsfor deliriuminolderadultsintheemergencydepartment:a systematicreviewandmeta-analysis. AnnEmergMed 2021;78(4):549–65.
3.MorleyJE.Dehydration,hypernatremia,andhyponatremia. ClinGeriatr Med.2015;31(3):389–99.
4.MuhsinSAandMountDB.Diagnosisandtreatmentof hypernatremia. BestPractResClinEndocrinolMetab 2016;30(2):189–203.
5.RileyDS,BarberMS,KienleGS,etal.CAREguidelinesforcasereports: explanationandelaborationdocument. JClinEpidemiol 2017;89:218–35.
6.KimSW.Hypernatemia:successfultreatment. ElectrolyteBloodPress 2006;4(2):66–71.
7.ShapiroNI,HowellMD,TalmorD,etal.Serumlactateasapredictorof mortalityinemergencydepartmentpatientswithinfection. AnnEmerg Med.2005;45(5):524–8.
8.WoodwardLandAlsabriM.Permissivehypotensionvs.conventional resuscitationinpatientswithtraumaorhemorrhagicshock:areview. Cureus.2021;13(7):e16487.
9.MorenoDH,CacioneDG,Baptista-SilvaJC.Controlledhypotension versusnormotensiveresuscitationstrategyforpeoplewith rupturedabdominalaorticaneurysm. CochraneDatabaseSystRev 2018;6(6):CD011664.
10.MounceyPR,Richards-BelleA,ThomasK,etal.Reducedexposureto vasopressorsthroughpermissivehypotensiontoreducemortalityin criticallyillpeopleaged65andover:the65RCT. HealthTechnol Assess.2021;25(14):1–90.
11.BelenkieI,DaniR,SmithER,etal.Effectsofvolumeloadingduring experimentalacutepulmonary-embolism(InEnglish). Circulation 1989;80(1):178–88.
12.FrancisSandKabrhelC.Currentcontroversiesincaringforthecritically iiipulmonaryembolismpatient(InEnglish). EmergMedClinNAm 2020;38(4):931–44.
13.HarjolaVP,MebazaaA,CelutkieneJ,etal.Contemporarymanagement ofacuterightventricularfailure:astatementfromtheHeartFailure AssociationandtheWorkingGrouponPulmonaryCirculationandRight VentricularFunctionoftheEuropeanSocietyofCardiology(InEnglish). EurJHeartFail.2016;18(3):226–41.
14.LamontagneF,DayAG,MeadeMO,etal.Pooledanalysis ofhigherversuslowerbloodpressuretargetsforvasopressor therapysepticandvasodilatoryshock. JIntensiveCareMed 2018;44(1):12–21.
15.BrunauerA,KokoferA,BataarO,etal.Thearterialbloodpressure associatedwithterminalcardiovascularcollapseincriticallyillpatients: aretrospectivecohortstudy. CritCare.2014;18(6):719.
ForrestTurner,MD*
BrandonFriedman,MD*
H.PendellMeyers,MD*
StephenW.Smith,MD†
SectionEditor:JoelMoll,MD
*CarolinasMedicalCenter,DepartmentofEmergencyMedicine,Charlotte,NorthCarolina † HennepinHealthcareandUniversityofMinnesotaSchoolofMedicine,Departmentof EmergencyMedicine,Minneapolis,Minnesota
Submissionhistory:SubmittedJuly14,2023;RevisionreceivedJanuary17,2024;AcceptedJanuary25,2024
ElectronicallypublishedApril30,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1519
Introduction: Severemetabolicalkalosesarerelativelyrarebutcancarryahighmortalityrate. Treatmentinvolvessupportivecareandtreatmentofunderlyingcauses.
CaseReport: A55-year-oldmaledependentonagastrojejunostomytubepresentedtotheemergency departmentforalteredmentalstatus.Thepatienthadmetabolicalkalosis,electrolyteabnormalities,and prolongedQTintervalonelectrocardiogram.Examinationandhistoryrevealedthatchronicdrainageof gastric fluidviamalfunctioningagastrojejunostomytuberesultedinprofoundalkalosis.Thepatient recoveredwithsupportivecare,electrolyterepletion,andgastrojejunostomytubereplacement.
Conclusion: Thiscasehighlightstheimportanceofgastr ointestinalacid-basepathophysiology. [ClinPractCasesEmergMed.2024;8(2)138 – 142.]
Keywords: metabolicalkalosis;prolongedQTinterval;casereport.
Metabolicalkalosisaccountsforapproximatelyhalfof acid-basederangementsinhospitalizedpatients.However, casesofseverealkalosis(pH > 7.55)arelesscommonand carryasurprisinglyhighmortality.1–4 Andersonetal reportedamortalityof27.9%inpatientswithpH > 7.48, risingto48.5%inpatientswithpH > 7.60.5 Metabolic alkalosis,whichischaracterizedbyelevatedplasmapHand serumbicarbonateanddecreasedserumchloride,canresult inelevatedpartialpressureofcarbondioxide(pCO2)via respiratorycompensation.Itisoftenassociated withhypokalemia.
Metabolicalkalosesrelatedtodiureticuseor gastrointestinallossesarereferredtoaschlorideresponsive, astheyareassociatedwiththedepletionofsodiumchloride andvolume.Thisresultsinasecondaryhyperaldosteronism, therebyexacerbatingpotassiumwastingandretentionof bicarbonatewithinthenephron.Therapyisfocusedon repletingvolumeandelectrolytes.Non-chlorideresponsive metabolicalkalosishasmanycausesincluding
hyperaldosteronismofanyetiology(eg,primary,secondary, exogenousmineralocorticoid),hypomagnesemia, hypokalemia,orexogenousalkaliinthesettingofrenal insufficiency.Clinicalmanifestationsofmetabolicalkalosis canbenon-specificandwilloftenoverlapwithother associatedelectrolytederangements;theseincludeconfusion, musclecramping,tetany,seizure,cardiacdysrhythmia, andhypoventilation.6
A55-year-oldmalewithpastmedicalhistoryofcerebral palsy,spasticquadriplegia,seizuredisorder,anddysphagia, anddependentonagastrojejunostomytubepresentedfroma skillednursingfacilitywithalteredmentalstatus.Thepatient wasmorelethargicandlessinteractiveascomparedtohis baseline,accordingtostaffatthefacility.Otherwise,hehad nocommunicablecomplaintsandalimitedreviewofsystems duetolethargy.Hecouldstatehisnameandfollowsimple commandsbutwasunabletoarticulatehissymptoms.The patienthadnotbeenprescribeddiureticmedicationsandhad
nohistoryofrecentvomitingordiarrhea.Initialvitalsigns includedheartrateof57beatsperminute(BPM),blood pressure103/65millimetersofmercury(mmHg),respiratory rateof12breathsperminute,andanoxygensaturationof 93%ontwolitersofoxygenbynasalcannula.(Thepatient hadnobaselineoxygenrequirement.)
Initiallaboratorystudieswerenotableforhyponatremia, hypochloremia,hypokalemia,hypocalcemia,acutekidney injury,andaserumbicarbonateabovemeasurablerangefor thelab.Thesestudiesaresummarizedinthe Table.The initialvenousbloodgasmeasuredapHof7.61(reference range:7.31–7.41);pCO2 77mmHg(35–45mmHg); bicarbonate77millimolesperliter(mmol/L)(24–28mmol/L) andbaseexcess47( 2 – +2).Theinitialelectrocardiogram (Image1)wasnotableforsinusbradycardiaatarateof 56BPMandmarkedlyprolongedQTorQUintervalof approximately690milliseconds(ms),withdiffuseT-wave flatteningandbiphasicmorphology,likelyfollowedby prominentUwaves.
Oncloserinspectionthegastricportofthepatient’ s feedingtubewasnotedtobedrainingbygravityintoaFoley collectionbag.Thestaffatthenursingfacilityreportedthat thepatient’sgastric fluidwasallowedtodraintogravityinto aFoleybagforunclearreasons,yieldingapproximately 200millilitersperdaythatwasthendiscardedforanunclear numberofweeks.Thegastricportwasdisconnectedfromthe collectionbagandsealed.Thepatientwasadministered intravenous(IV)normalsalineandelectrolyteinfusions.
Thepatientwasadmittedtotheintensivecareunitand maintainedoncontinuouscardiactelemetryforhighriskof ventriculardysrhythmias.Hiselectrolytederangements begantoimprove,andhisQTintervalnormalizedto approximately450mswithin24hours,asshownin Image2 Hedidnotexperienceanysignificantdysrhythmias,buthe didhaveoneuncomplicatedbreakthroughseizure.By hospitalday2,physiciansnoticedintermittentdysfunction
Table. Initiallabvaluesofpatientinseveremetabolicalkalosis.
SerumPatientresultReferencerange
Sodium(mEq/L)120136–145
Chloride(mEq/L)5098–106
Potassium(mEq/L)2.03.5–5.0
Bicarbonate(45mmol/L) >45a 20–29
Bloodureanitrogen(mg/dL)308–20
Creatinine(mg/dL)0.54b 0.7–1.3(male)
Calcium(mg/dL)4.28.6–10.2
Magnesium(mEq/L)2.21.6–2.6
aBicarbonatelevelwasabovethelab’smeasurablerange. bPatient’spriorbaselinecreatininenotedtobe0.25mg/dL. mEq/L,milliequivalentsperliter;mmol/L,millimolesperliter;mg/dL, milligramsperdeciliter.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Metabolicalkalosisisfrequentlyencountered intheemergencydepartment.The managementofseverealkalosisiswell documentedintheliterature.
Whatmakesthispresentationof diseasereportable?
Severemetabolicalkalosisislesscommonly encounteredbyemergencyphysicians.We describethe fi rstreportedcasedueto inappropriategastrostomytubelosses.
Whatisthemajorlearningpoint?
Thiscasehighlightsthepresentationand recognitionofseveremetabolicalkalosisand underlyingpathophysiologyanddescribes managementstrategies.
Howmightthisimproveemergency medicinepractice?
Severemetabolicalkalosiscarriesahigh mortality.Byhighlightingitsrecognitionand management,wecouldimprovethe resuscitationofthesepatients.
andcloggingofthejejunostomylumenofhis gastrojejunostomytube,requiringreplacementby interventionalradiology.Physicianssurmisedthatfeeding tubedysfunctionandinabilitytotolerategastricsecretions likelyledtosymptomsthat,unfortunately,inspirednursing facilitystafftoventhisgastricporttogravity,andthe underlyingcausewasnotaddresseduntilhospitaladmission. Hisencephalopathy,alkalosis,hypokalemia,andother electrolytederangementshadresolvedbydischargeon hospitalday7.
Thiscaseillustratesacriticallyillpatientwithcomplex metabolicderangements.Thepatienthadongoinggastric secretionlossesoveraperiodofweeks,resultinginaslowbut steadylossofvolume,aswellaslossofhydrogen,chloride, sodium,andpotassiumions.7 Theinitialinsultwas maintainednotonlybycontinuouslossesinthepatientover timebutbyhypovolemiaandtheincreasingactivityof aldosterone.Thisresultedinfurtherlossofpotassiumand impairedthekidney’sabilitytoexcretebicarbonate.6
Forapatientwithseveremetabolicalkalosisand bradycardia,themostimminentlylife-threatening

Image1. Thepatient’selectrocardiogramonarrivaltotheemergencydepartment,withadditionalannotationsshowingsinusrhythmwithout obviousischemiaandextremelyprolongedQTorQUinterval.SeveralexamplemeasurementsfortheQUintervalareshowninblue.Inthe precordialleads,greenverticallinesmarktheapproximatepositionoftheTwave,whichappears flatinmanyleads.Redlinesmarkthe positionoftheterminalcomponentofrepolarization,whicharebestdescribedasUwaves. ms,milliseconds; BPM,beatsperminute.

Image2. Thepatient’selectrocardiogramfollowingrepletionofelectrolytesdemonstratingimprovementinQTinterval.
complicationisventriculardysrhythmiasincluding ventricular fibrillationandpolymorphicventricular tachycardia.ProlongedQTintervalisconsideredarisk factorfortorsadesdepointes(TdP),whichisaformof polymorphicventriculartachycardiaprecededbylongQT interval.AQTinterval(orcorrectedQTintervalwhenthe heartrateisgreaterthan60BPM)greaterthan485–500ms bytheBazettformulaisconsideredariskfactorforthe developmentofTdP.Whilethepatientinthiscasedidhavea profoundlyprolongedQTinterval,hedidnotsufferany acutedysrhythmias.
Mostcasesofmetabolicalkalosiscanbeadequately treatedwithcorrectionoftheprecipitatingcauseandsimple repletionofvolumeandelectrolytes.Inmoresevereor complicatedcases,additionaltreatmentswiththegoalof directlyimprovingthealkalosismaybeindicated. Acetazolamideinhibitscarbonicanhydrase,preventing conversionofhydrogenandbicarbonateionstocarbon dioxideandwater,resultinginrenallossofsodiumand bicarbonate,resultingindiminutionofthealkalosis. Intravenous(IV)administrationofacetazolamide 500milligrams(mg)every12hourshasshownasmallbut
statisticallysignificanteffectinreducingbicarbonatelevels andisequivalenttomorefrequentdosingschedules.8 In patientswithgastricacidlossasthecauseofthealkalosis, histamine-2receptorantagonistsorprotonpumpinhibitors havebeenusedasanadjunctivetherapywhileaddressingthe underlyingcause.9 Inrenallyimpairedpatients,dialysisby variousmethodscanbeusedtodirectlylowerserum bicarbonatequicklyandeffectivelyusingeithernormalor low-bicarbonatedialysate.10,11
Intravenousacidsolutions,mostcommonlyhydrochloric acid,havealsobeenusedinthemanagementofmetabolic alkalosis.Itisindicatedwhenmetabolicalkalosisisnot correctingornotanticipatedtocorrectwithlessaggressive management.Multiplecasereportsandcaseseries demonstratethesafetyofhydrochloricacidinfusions.12–14 Twocasereportscitechestwallnecrosisresultingfrom hydrochloricacidinfusions,highlightingtheimportanceof administeringinfusionsviacentrallinesconfirmedtobein goodpositionandviathemostdistalport.15,16 Hydrochloric acidinfusiondosingcanbeestimatedbycalculatingthe amountofhydrogenionrequiredviacalculatingthe bicarbonateexcess.
Bicarbonateexcesscanberoughlycalculatedby multiplyingthedesireddecreaseinplasmabicarbonate(in milliequivalentsperliter[mEq/L])bythetotalbodywater contentinliters,whichisroughly60%ofleanbodymassin kilograms(kg)formalesand50%ofleanbodymassin females.17 Hydrochloricacidsolutionswithconcentrations of0.1to0.2mmol/kg/hour otherwiseknownas0.1to0.2 normal(N)solutions aresafeformulations,withhigher concentrationsassociatedwithworsenedrenaloutcomes. Aliterof0.1Nhydrochloricacidcontains100mEqeachof hydrogenandchlorideions.Suggestedmaximuminfusion ratesinclude125mL/houror0.2mEq/kg/hour.Infusionscan berepeated,guidedbyserialelectrolytetesting,andIV tubingshouldbechangedevery12hoursduetotheoretical concernsaboutbreakdownofplastic.
Alternativestohydrochloricacidinfusionsinclude ammoniumchlorideandargininemonohydrochloride, althoughthesearebothdependentonhepaticmetabolism.18 Finally,controlledhypoventilationhasbeenproposedasan optionforcriticallyillintubatedpatientswithsevere alkalosis.Whilenodataexiststosuggestspecifictargetsof minuteventilationorpCO2 inseveremetabolicalkalosis,a fewcasereportsmentionusingcontrolledhypoventilationto exaggeratethephysiologicrespiratorycompensationof alkalemiainmechanicallyventilatedpatients.14
Althoughlossofgastrointestinalsecretionsisoneofthe mostcommoncausesofmetabolicalkalosis,priorcase reportsofseveremetabolicalkalosiscausedbymistakenly intentionalprolongedgastrostomytubedrainagearenotin theliterature.Drainageorventingofagastrostomytube canbeatemporarytherapytotreatsymptomssuchas
fullnessorbloatingorincasesofobstruction 19;however, prolongeddrainageofgastrointestinalsecretionswithout addressingtheunderlyingproblemcanbedetrimentalto thepatient.
Thiscase,whichhighlightsfundamentalunderstandingof gastrointestinalandacid-basephysiology,demonstratesthe dangersofongoinglossofgastricsecretionsandmetabolic alkalosis.Itservesasanexampleofidentifyingthe underlyingcauseofalkalosisandsubsequent treatmentoptions.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ForrestTurner,MD,CarolinasMedical Center,DepartmentofEmergencyMedicine,1000BlytheBlvd., Charlotte,NC28203.Email: forrestturnermd@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Turneretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SoiferJTandKimHT.Approachtometabolicalkalosis. EmergMedClin NorthAm. 2014;32(2):453–63.
2.PatelKB,EspinosaJ,WileyJ,etal.Severealkalemia(pH7.85): compatiblewithlife?Atripleacid-baseconundrum. MathewsJCase Rep. 2016;1(2):10.
3.MennenMandSlovidCM.Severemetabolicalkalosisintheemergency department. AnnEmergMed. 1988;17(4):354–7.
4.TripathyS.Extrememetabolicalkalosisinintensivecare. IndianJCrit CareMed. 2009;13(4):217–20.
5.AndersonLEandHenrichWL.Alkalemia-associatedmorbidityand mortalityinmedicalandsurgicalpatients. SouthMedJ. 1987;80(6):729–33.
6.DuBoseTJr.Acidosisandalkalosis.In: Harrison’sPrinciplesofInternal Medicine,20th ed.NewYork,NY:McGrawHill;2018.
7.LyuHGandSminkD.Stomach&duodenum.In: CurrentDiagnosis& Treatment:Surgery,15th ed.NewYork,NY:McGrawHill;2020.
8.FaisyC,MezianiF,PlanquetteB,etal.Effectofacetazolamidevs placeboondurationofinvasivemechanicalventilationamongpatients withchronicobstructivepulmonarydisease:arandomizedclinicaltrial. JAMA. 2016;315(5):480–8.
9.KirschBM,Sunder-PlassmannG,SchwarzC.Metabolicalkalosisina hemodialysispatient-successfultreatmentwithaprotonpumpinhibitor. ClinNephrol. 2006;66(5):391–4.
10.HsuSC,WangMC,LiuHL,etal.Extrememetabolicalkalosis treatedwithnormalbicarbonatehemodialysis. AmJKidneyDis. 2001;37(4):E31.
11.AyusJC,OliveroJJ,AdroguéHJ.Alkalemiaassociatedwithrenal failure.Correctionbyhemodialysiswithlow-bicarbonatedialysate. Arch InternMed. 1980;140(4):513–5.
12.BrimioulleS,VincentJL,DufayeP,etal.Hydrochloricacidinfusionfor treatmentofmetabolicalkalosis:effectsonacid-basebalanceand oxygenation. CritCareMed. 1985;13(9):738–42.
13.GuffeyJD,HaasCE,CrowleyA,etal.Hydrochloricacidinfusionforthe treatmentofmetabolicalkalosisinsurgicalintensivecareunitpatients. AnnPharmacother. 2018;52(6):522–6.
14.JonesMWandWilliamsM.Acid-basecorrection:acasereportand reviewoftheliterature. JIntensiveCareSoc. 2010;11(2):126–9.
15.JankauskasSJ,GurselE,AntonenkoDR.Chestwallnecrosis secondarytohydrochloricaciduseinthetreatmentofmetabolic alkalosis. CritCareMed. 1989;17(9):963–4.
16.BuchananIB,CampbellBT,PeckMD,etal.Chestwallnecrosisand deathsecondarytohydrochloricacidinfusionformetabolicalkalosis. SouthMedJ. 2005;98(8):822–4.
17.MehtaAandEmmettM.Treatmentofmetabolicalkalosis.In: UpToDate AlphenaandenRijn,Netherlands;WoltersKluwer:2022.Availableat: https://www.uptodate.com/contents/treatment-of-metabolic-alkalosis? search=metabolic+alkalosis&source=search_result&selectedTitle= 2~150&usage_type=default&display_rank=2.AccessedJune15,2023.
18.MartinWJandMatzkeGR.Treatingseveremetabolicalkalosis. Clin Pharm. 1982;1(1):42–8.
19.GleesonNC,HoffmanMS,FioricaJV,etal.Gastrostomy tubesaftergynecologiconcologicsurgery. GynecolOncol. 1994;54(1):19–22.
RajPatel,DO
AmyRussell,MD MelanieM.Randall,MDSectionEditor:AustinSmith,MD
RiversideUniversityHealthSystem,DepartmentofEmergencyMedicine, MorenoValley,California
Submissionhistory:SubmittedAugust28,2023;RevisionreceivedOctober27,2023;AcceptedNovember2,2023
ElectronicallypublishedMarch25,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1643
Introduction: Ovarianarteryaneurysmisararediagnosis,primarilyassociatedwithlatepregnancyand thepostpartumperiod.Itcancauselife-threateninghemorrhagewhenruptured.Evenmorerareare ovarianarteryaneurysmsinpostmenopausalwomen.
CaseReport: Wepresentacaseofapostmenopausalfemalepresentingtotheemergencydepartment with flankpain.Point-of-careultrasoundshowedfree fluidintheabdomen.Shewasdiagnosedwith anovarianarteryaneurysmoncomputedtomographyangiographyandtreatedsuccessfully withembolization.
Conclusion: Rupturedovarianarteryaneurysmisanuncommoncauseofintra-abdominalhemorrhage inwomen.[ClinPractCasesEmergMed.2024;8(2)143–146.]
Keywords: intra-abdominalhemorrhage;ovarianartery;aneurysm;casereport.
Ovarianarteryaneurysms(OAA)andpseudoaneurysms areprimarilydiagnosedduringthelatepregnancyandearly postpartumperiods.Hemodynamicandendocrinechanges duringpregnancycanleadtoaneurysmformation.1 Other lesscommonriskfactorsincludetraumaandchronic inflammatoryconditions.Themostcommonpresenting symptomissignificantabdominaland flankpain.Ruptureof theaneurysmresultsinintraperitonealand/or retroperitonealhemorrhageoftenrequiringemergent intervention.Incidenceofthisdiagnosisislow.2 Wepresent anuncommoncaseofapostmenopausalfemalefoundto havearupturedleftOAA.
A51-year-old,postmenopausal,gravidathree,parathree femalepresentedtoouremergencydepartment(ED)with worseningleft flankpainandnewleft-sidedabdominalpain. Shehadbeendischargedfromourhospitaltwodaysprior. Duringthatadmission,sheunderwentaleftrenalbiopsythat wascomplicatedbyaperirenalandintraabdominal
hematoma.Hermedicalhistoryincludedsystemiclupus erythematosus,chronickidneydisease,antiphospholipid syndrome,andhypertension.Hergynecologichistorywas significantforapriorcesareansectionandatuballigation. Shewasonwarfarinduetoherhypercoagulablestate.
UponpresentationtotheED,hervitalsignswere temperature36.6° Celsius,heartrate69beatsperminute, bloodpressure116/75millimeters(mm)ofmercury, respiratoryrate16perminute,andoxygenlevel96%on roomair.Physicalexamrevealedatired-lookingfemalein milddistress.Sheexhibitedleft flanktendernessnearher renalbiopsysitewithnoexternalsignsofbleedingor infection.Additionally,shehadabdominaltendernessinthe leftupperquadrant(LUQ).Therewasnoabdominalrigidity orsignsofperitonitis.Apoint-of-careultrasoundwas positiveforfree fluidintheLUQ(Image1).
Herlaboratoryvalueswerehemoglobin6.6gramsper deciliter(g/dL)(referencerange12.1–15.1g/dL),platelet count374 × 109 perliter(×109/L)(150–450 × 109/L),blood ureanitrogen63milligramsperdL(mg/dL)(7–30mg/dL), creatinine3.7mg/dL(0.7–1.2mg/dL),prothrombintime
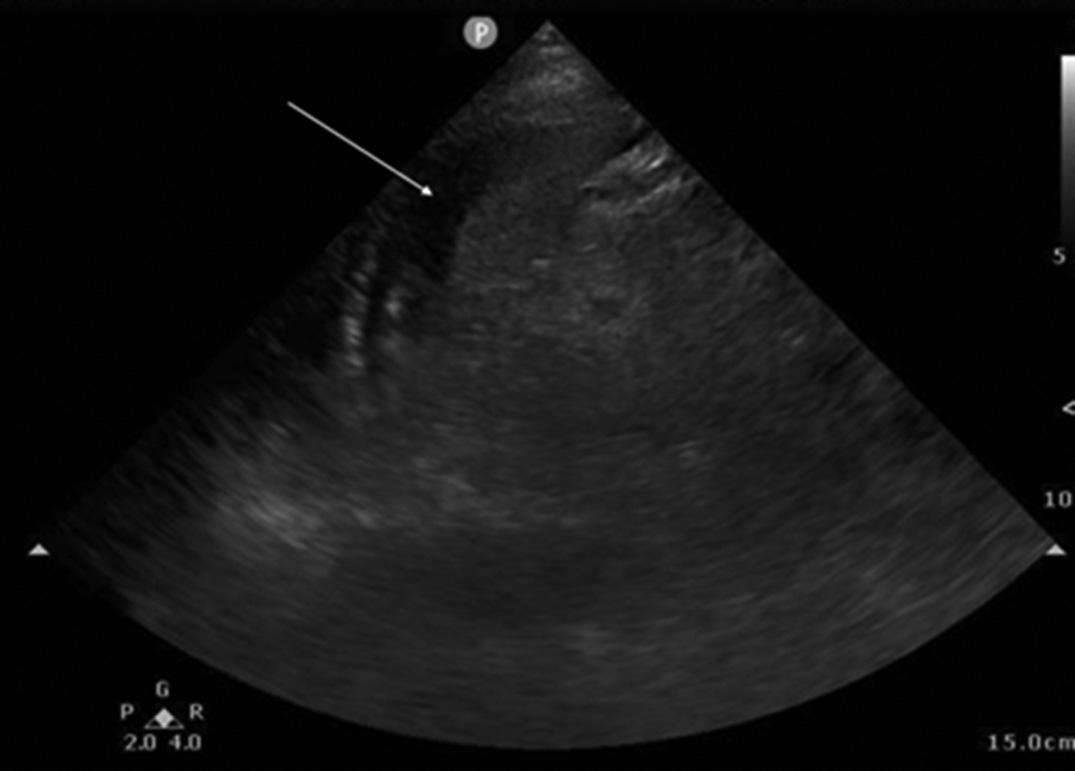
15.8seconds(10–13seconds),andinternationalnormalized ratio1.3(0.89–1.16).Thepatient’shemoglobinlevelthree dayspriorwas9g/dL.
Interventionalradiology(IR)wasconsultedduetothe patient’srecentcomplicatedbiopsy,newlaboratory derangements,andfree fluidonultrasound.Computed tomography(CT)angiographywasrecommendedtoassess forbleedinglocationandruleoutabscess,perforation,or ischemia.Computedtomographyoftheabdomenandpelvis revealedanew10mmenhancementwithintheintraabdominalhemorrhage.Thisabnormalitywasidentifiedasa ruptured,bleedingdistalOAA(Image2).Thepatientwas givenoneunitofpackedredbloodcellsandtakentoIRfor definitivemanagement.Sheunderwentgelfoamandcoil embolizationoftheleftgonadalartery,resultingincessation ofbleeding(Image3).Afteranuncomplicatedhospital course,shewasdischarged.
Ovarianarteryaneurysmruptureisararebutlifethreateningdiagnosis.Theclinicalpresentationis
Whatdowealreadyknowaboutthis clinicalentity?
Ovarianarteryaneurysmsarerareandmost oftenrelatedtopregnancy.Rupturecanlead tolife-threateninghemorrhage.
Whatmakesthispresentationof diseasereportable?
Fewovarianarteryaneurysmshavebeen describedinpostmenopausalwomenor presentingtotheemergencydepartment.
Whatisthemajorlearningpoint?
Ovarianarteryaneurysmisararebutserious diagnosisthatcanpresentwithsigni fi cant intra-abdominalhemorrhage.
Howmightthisimproveemergency medicinepractice?
Thiscaseaddstotheexistingdifferential diagnosesforintra-abdominalhemorrhageof unknownorigin.
non-specificbutcaninclude flankpain,abdominalpain,and hemodynamicinstability.Imagingwillshowintraperitoneal and/orretroperitoneal fluid.Point-of-careultrasoundmay assistindiagnosisifadequateintraperitoneal fluidvolumeis present.DefinitivediagnosisrequiresCTangiography, traditionalangiography,ordirectoperativevisualization. ManagementrequiresIRembolizationina hemodynamicallystablepatientorlaparotomywithligation inanunstablepatient.2,3
Althoughsymptomatologyandphysicalexaminationare non-specific,medicalhistorymaybehelpfulinthe
 Image1. Point-of-careultrasoundshowingfree fluidintheleftupper quadrantabdomenbetweenthespleenandkidney(arrow).
Image2. Computedtomographyangiographydemonstratingextravasationfromleftovarianarteryaneurysm(arrows).
Image1. Point-of-careultrasoundshowingfree fluidintheleftupper quadrantabdomenbetweenthespleenandkidney(arrow).
Image2. Computedtomographyangiographydemonstratingextravasationfromleftovarianarteryaneurysm(arrows).
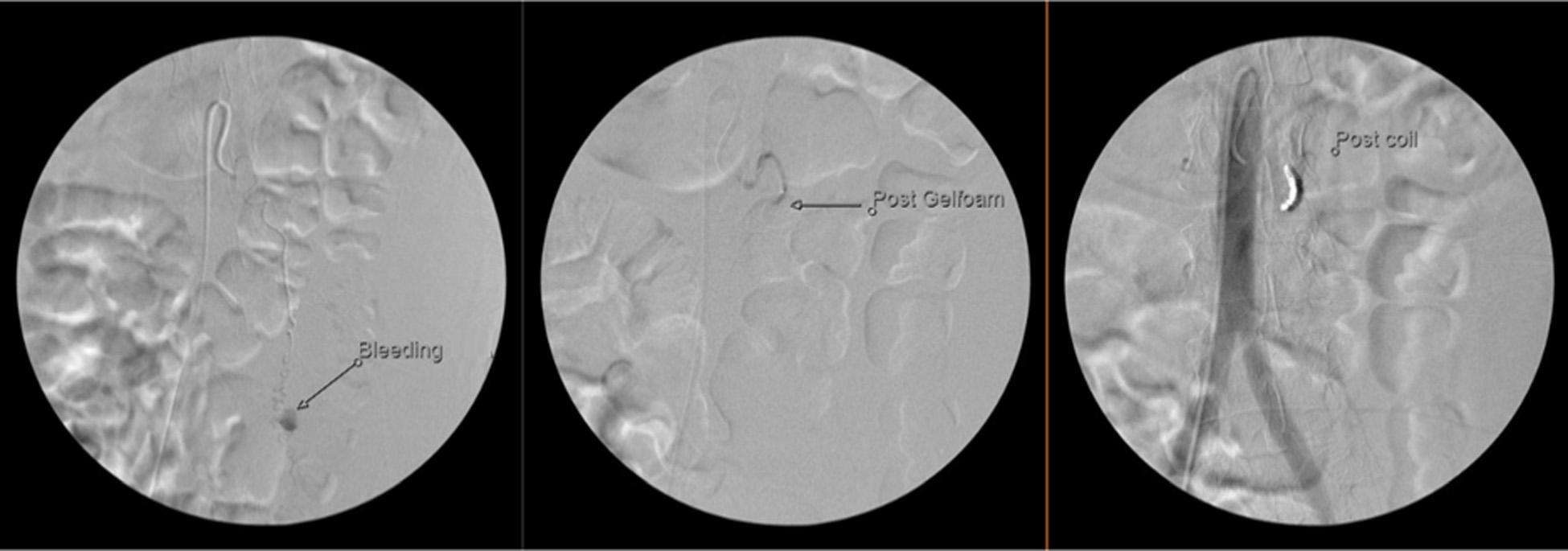
Image3. Angiographyillustratingfromlefttorighttheovarianarteryaneurysmwithactivebleeding;aftergelfoamembolization;and aftercoiling.
considerationofthediagnosisandthechoiceofimaging. Whilemostcommonlyassociatedwithpregnancy,OAAhas alsobeendescribedinpatientswith fibroids,chronic hypertension,trauma,vasculopathy,andinthe postoperativephase.2–11 Increasedplasmavolume,increased cardiacoutput,andhormonalchangesduringpregnancy havebeenproposedasfactorspredisposingpatientstoOAA. Mostdocumentedcasesoccurredinmultiparouswomen, suggestingthatrepeatpregnancymaybeariskfactordueto thecompoundingeffectofthesephysiologicchanges.2,4
Finally,thereareindependentcasesofOAApatientswith chronicinflammatoryconditionsincludingchronic lymphocyticleukemia,rheumatoidarthritis,HIV,and lupus.6,7,9 Theexactinfluenceofchronicinflammationon aneurysmformationorgrowthisunclear.
Ovarianarteryaneurysmisarareandseriousdiseasemost commonlyassociatedwithpregnancy.Wepresentarare presentationinapostmenopausalfemaleintheED.Dueto itsemergentnature,OAAcanbeconsideredinthe differentialdiagnosisofafemalepatientpresentingwith nontraumaticabdominalor flankpainwithcertain appropriateriskfactors.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:MelanieRandall,MD,Riverside UniversityHealthSystem,DepartmentofEmergencyMedicine, 26520CactusAvenue,MorenoValley,CA92555. Email: m.randall@ruhealth.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived
aspotentialsourcesofbias.MelanieRandallreceivesamonthly administrativestipendfromVituityEmergencyPhysicians PartnershipastheResearchDirectorfortheRiversideUniversity HealthSystememergencydepartment.
Copyright:©2024Pateletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.EnakpeneCA,SternT,BarzalloSalazarMJ,etal.Spontaneousrupture ofanovarianarteryaneurysm:ararepostpartumcomplication. Case RepObstetGynecol.2016;2016:1029561.
2.WadaK,AoyagiS,MatsuuraY,etal.Pregnancy-unrelated spontaneousruptureofarightovarianarteryaneurysm. RadiolCase Rep.2021;16(11):3270–4.
3.AlmuhannaAF,AlkhalifaMA,AltaweelFY,etal.Traumaticovarian arterypseudoaneurysmpost-ovumpickup:ararecomplication. Cureus 2021;13(12):e20825.
4.HuYH,OuhYT,KimC,etal.Spontaneousruptureofovarianartery aneurysminapostmenopausalwoman:acasereportandliterature review. JMenopausalMed.2021;27(2):102–5.
5.ChaoLWandChenCH.Spontaneousruptureofanovarianartery aneurysm:casereportandreviewoftheliterature. GynecolObstet Invest.2009;68(2):104–7.
6.ZorrillaAM,FeinLA,JamesK,etal.Retroperitonealhematoma secondarytospontaneousruptureofovarianarterypseudoaneurysms: casereportandreviewofliterature. JObstetGynaecol 2019;39(3):422–4.
7.KirkJS,DeitchJS,RobinsonHR,etal.Stagedendovasculartreatment ofbilateralrupturedandintactovarianarteryaneurysmsina postmenopausalwoman. JVascSurg.2009;49(1):208–10.
8.NakajoM,OhkuboK,FukukuraY,etal.Embolizationofspontaneous ruptureofananeurysmoftheovarianarterysupplyingtheuteruswith fibroids. ActaRadiol.2005;46(8):887–90.
9.HerskowitzMM,WongCM,LeonardoRF.Rupturedovarianartery pseudoaneurysminapostmenopausalpatienttreatedwith transcatheterembolization. CaseRepRadiol.2020;2020:6728318.
10.ErdoesLSandEntzianD.Rupturedtraumaticovarianartery pseudoaneurysminapregnantpatient. JVascSurgCases 2015;1(1):36–8.
11.TaoY,MatsubaraS,YagiK,etal.Intra-abdominalhemorrhage duetosegmentalarterialmediolysisofanovarianartery pseudoaneurysmandconcomitantaneurysmalsubarachnoid hemorrhage:illustrativecase. JNeurosurgCaseLessons 2022;4(5):CASE22233.
CodyM.Autrey,BS*
StephanieA.Martinez,MPH* MichaelRemaly,DO† EricBoccio,MD,MPH†
SectionEditor:ShadiLahham,MD
*FloridaInternationalUniversity,HerbertWertheimCollegeofMedicine, Miami,Florida
† MemorialHealthcareSystem,DepartmentofEmergencyMedicine, Hollywood,Florida
Submissionhistory:SubmittedSeptember20,2023;RevisionreceivedNovember22,2023;AcceptedDecember1,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1697
Introduction: Theaspcaterpillar(Megalopygeopercularis)isendemictothesoutheasternUnited States,withmostsightingsinFlorida,Texas,andLouisiana.Afewhundredcaterpillarenvenomations arereportedannuallywithmostcasesoccurringinJuly–November.Aspcaterpillarshavehollowspines alongtheirbacksthatcontainvenom.Contactwiththesespinesiswhatproducesthecharacteristic “sting” resultingincontactdermatitisandalocalizedhypersensitivityreactioncollectivelyreferredtoas lepidopterism.Symptomsoflepidopterismmayincludesevereburningpain,pruritis,edema,nausea, vomiting,abdominalpain,andheadache.Symptomsareoftenselflimited,andtreatmentshouldfocuson expeditedremovalofimplantedspinesandaggressivesymptommanagement.
CaseReport: Wepresentthecaseofapatientpresentingtotheemergencydepartment(ED)withacuteonsetsevereleftforearmpainwithassociatedpruriticrashincurredwhileworkinginaretailstore.Initial therapeuticmanagementincludedadministrationofanalgesics,antihistamines,andsteroids.After obtainingacomprehensivehistoryandconsultingwiththePoisonControlCenter,wesuspectedanasp caterpillarenvenomation.Followingextractionofthecaterpillarspineswithsilktape,thepatient’s symptomsimproved.AfteraperiodofobservationintheED,thepatientwasdischargedhomewithout anyknownsequelae.
Conclusion: Althoughaspcaterpillarstypicallyinhabittreesandfoliage,humanexposuretothecaterpillar mayoccurindevelopedenvironments.Effectivehistory-taking,promptcommunicationwithtoxicologic experts,andcompleteremovalofintactspinesareessentialforearlyidentificationandeffectiveclinical managementofaspcaterpillarenvenomation.[ClinPractCasesEmergMed.2024;8(2)147–150.]
Keywords: Megalopygeopercularis;aspcaterpillar;caterpillarenvenomation;lepidopterism; casereport.
Theaspcaterpillar(Megalopygeopercularis ),alsoknown asthewoollyslugcaterpillarorpusscaterpillar,isthelarva formofthesouthern flannelmoth.Ithasawidegeographic distributionstretchingfromMarylandtoMexicoandis endemictothesoutheasternUnitedStateswithmost sightingsinFlorida,Texas,andLouisiana.1 Peakmonthsof
aspcaterpillarreportsoccurbetweenJuly–November.2 The aspcaterpillaristypically2.5–4centimeters(cm)inlength, anditshairsrangeincolorfromgraytoyellow-browngiving ititscharacteristicwoollyappearance.Withinthedensehair coatarehiddenspinescalledsetae,whicharehollowand containapoisongland.Contactmaycausethesetaeto fractureandinjectvenom,resultinginbothtoxiceffectsand
typeIVhypersensitivity/immunoglobulinE-mediated reactions.Theaspcaterpillarstingisreportedtobethemost potentofallcaterpillarstingsintheUnitedStates.3
Whilemostcaterpillarenvenomationsarebenignanddo notnecessitatemedicalevaluation,variousclinicalsequelae havebeendescribed.Theaspcaterpillarstingcausesa characteristicgrid-like,hemorrhagiceruption,andtherashis associatedwithexcruciatingpainandirritation,puncture wounds,pruritis,andedema.4 Stingreactionsinclude erucism(localizedurticarialdermatitis),lepidopterism(skin andsystemicreactions),ophthalmianodosa(ocular inflammatoryreaction),andlonomism(apotentiallylifethreateningbleedingdiathesis).5 Systemictoxicitymay manifestaslymphadenopathy,headache,nausea,vomiting, abdominalpain,andpseudoappendicitis.6–8 Thereactionis oftenself-limiting;managementshouldfocusonexpeditious removalofanyremainingimplantedsetaeandaggressive symptommanagement.Albeitrare,therehavebeen severalreportsofanaphylacticshockresultingfrom caterpillarenvenomation.9
Wereportanunusualcauseofacute,suddenonset,severe leftforearmpainandpruritisinanadultmalewhowasat workinaretailstoreinSouthFlorida.Althoughthese caterpillarstypicallyinhabittreesandfoliage,thiscase highlightsthathumanexposuretoaspcaterpillarsmayoccur indevelopedenvironments.Effectivehistory-taking, heightenedclinicalsuspicion,promptcommunicationwith toxicologicexperts,andcompleteremovalofintactspines areessentialforearlyidentificationandeffectiveclinical managementofaspcaterpillarenvenomation.
A20-year-oldmalewithnoknownpastmedicalhistoryor allergiespresentedtotheemergencydepartment(ED) complainingofacute,suddenonset,leftforearmpainand rash.Thepatientwasworkingataneyeglassesandcontacts storeandstatedthatthepainstartedwhenheknelttolift somethingupfromgroundlevel.Indoingso,heplacedhis leftelbowonhisleftthigh.Heimmediatelyfeltastinging sensationinhisleftelbowwithsevere10/10painradiating downtheextremitytotheleftforearmandhand.Shortly afterwardhenoticedtheaffectedareahadbecome erythematous,thushepresentedtotheEDforanemergent medicalevaluation.Pertinentnegativesincludedabsenceof fever,chills,cough,shortnessofbreath,chestpain,nausea, vomiting,diarrhea,urinarycomplaints,backpain, andheadache.
Thepatientarrivedhypertensivewithinitialblood pressuremeasuring130/91millimetersofmercury.Triage vitalsignswereotherwisenormal.Onphysicalexamination, thepatientappearedanxious.Theprimarysurveyofairway, breathing,andcirculationwasunremarkable.Focused examinationoftheaffectedregiondemonstratedan approximately1 × 2-cmareaoferythemaandedemaover
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Aspcaterpillar( Megalopygeopercularis) envenomationisanunusualcauseofa severelypainfulrashaffectingpatientsinthe southeasternUnitedStates.
Whatmakesthispresentationof diseasereportable?
Whileexposurerisksaregreatestoutdoors neartreesandfoliage,caterpillarstingsmay alsooccurincommercialbuildingsand residentialsettings.
Whatisthemajorlearningpoint?
Comprehensivehistory-taking,heightened clinicalsuspicion,interdisciplinary collaboration,andeffectivetherapeutic managementarenecessaryto treatenvenomation.
Howmightthisimproveemergency medicinepractice?
Awarenessofexposurerisksandsymptomsof erucismandrecognitionofthecharacteristic erythematousrashwillfacilitatetimely diagnosisandpropertreatment.
theproximalposteriorforearmwithanassociatedgrid-like patternofraisedurticaria.Therashwaslocalizedanddidnot exhibitdesquamation(Image1).
Theleftupperextremitywasotherwiseneurovascularly intactwithapalpableradialpulseandcapillaryrefillless thanthreeseconds.Assessmentofmotorfunctionandactive andpassiverangeofmotionattheelbowwasnormal. Laboratoryassessmentandimagingweredeterminedtobe ofnoutilityandwerenotordered.Uponfurtherinquiry,the patientmentionedthathisarmmayhavecontacteda caterpillar,whichwasfoundonthegroundatthesitewhere hispain firstbegan.Aphotoofthecaterpillarwas eventuallyobtainedandprovidedonthepatient’ s smartphone(Image2).
TheemergencyphysiciancalledthePoisonControl Center(PCC)hotline,whichconfirmedthatthesymptoms werelikelytheresultofanaspcaterpillarenvenomation.Of note,theexpertatthePCCmentionedthatthepresentation wasparticularlyunusualgiventhatitoccurredina commercialbuildingdevoidoftreesandfoliage.Other diagnosesconsideredwereallergicreaction,insectbite/sting, contactdermatitis,cellulitis,andtraumaticinjury.

Image1. Erythematousspotsappearingatthesiteofasp caterpillarenvenomationontheposteriorproximal forearm(arrow).
Therapeuticmanagementfocusedonaggressivesymptom management.Duetoconcernforadeveloping hypersensitivityreaction,dexamethasone8milligrams(mg) intravenous(IV),acetaminophen-codeine300-30mgperos (PO),famotidine20mgIV,ketorolac30mgIV,and diphenhydramine25mgIVwereadministered.Uponfurther inspectionoftheaffectedarea,severalspineswerevisualized penetratingthepatient’sskin.Silktapewasappliedtothe affectedareaandcarefullyremoved,thusstrippingawaythe

Image2. Photofromsmartphoneofanaspcaterpillar (Megalopygeopercularis)onthecarpeted floorofaneyeglass andcontactlensstore.
offendingspines.Thepatient’spainrapidlyimproved.The patientreceivedanadditional25microgramsoffentanylIV afterreassessmentanhourlater.Heunderwentaperiodof observationintheEDandwasdischargedwithprescriptions formethylprednisolone4mgPOandoxycodoneacetaminophen5–325mgPO.Attemptstocontacthimafter dischargetoarrangefollow-upandawoundcheckwere unsuccessful.Therewerenosubsequentpatientencounters documentedintheelectronichealthrecord.
Wedescribeacasereportofa20-year-oldmalewithno knownpastmedicalhistoryorallergieswhopresentedtothe EDwithseverelocalizedpain,erythema,andswellingofthe leftforearm.Afocusedassessmentrevealedan erythematous,swollen,andtenderareacontainingseveral raisederythematouslesionsinagrid-likepattern.Upon closerinspection,severalspineswerevisualizedremainingin theskin.Effectivehistory-taking,recognitionofthe characteristicrash,timelyinvolvementofan interdisciplinaryteamthatincludedtoxicologicexpertsatthe PCCandspeciesidentificationusingavailabletechnologies facilitatedtimelydiagnosisandappropriate clinicalmanagement.
Typically,aspcaterpillarstingsoccurinoutdoorsettings whenanindividualunknowinglybrushesagainstthe caterpillarorthecaterpillarfallsfromatreewhereit normallyresides.Thiscasechallengestheconventional exposureriskstoaspcaterpillars,describinganencounter thatoccurredindoorsinanareadevoidofanysurrounding treesorfoliage.Itispossiblethatthecaterpillarwascarried intothestorewhileattachedtothepatient’sclothing,within infestedgoods,oronadeliverypackage.Theabsenceof detailedentomologicalinvestigationslimitedourabilityto definitivelyascertainhowtheaspcaterpillarmayhave enteredthestore.
Interdisciplinaryteamcollaborationplayedanessential roleinthiscase.Effectivecommunicationbetween healthcareprofessionalsandlocaltoxicologicexpertsatthe PCCwasinstrumentalinestablishingthediagnosisand guidingtherapeuticmanagement.Thecontentknowledge regardingregionalinsectpatternsandvenomousspecies possessedbytoxicologicexpertsaidedinspecies identificationandreliableprognostication.
Duetothepaucityofreportsintheliteratureand presumedunderreportingintheclinicalenvironment, theprevalenceofatypicalandseverepresentationsofasp caterpillarenvenomationisunknown.Thetherapeutic managementofaspcaterpillarenvenomationisvariable. Usuallybenignandself-limiting,managementshouldfocus onremovingtheoffendingagentandsymptommanagement. Administrationofanalgesicscanbesupplementedwith topicalandinjectedlocalanesthetics.10,11 Ananalysisofasp caterpillarstingsreportedtoTexasPoisonCentersfound
thatnumeroustreatmentssuchasdilution,irrigationand washing,antihistamines,steroids,andantibioticshavebeen effectivelyused.4 Whileanalgesics,antihistamines,and steroidsarethestaplesofcaterpillarenvenomation,no consensusguidelinesexistforitsmanagementinthe EDsetting.
Althoughaspcaterpillarstypicallyinhabittreesand foliage,humanexposuremayoccurindeveloped environments.Caterpillarenvenomationismostlikely underreportedandmistreatedduetothelackofpatientand clinicianknowledge,lackofdetailinthehistoryofpresent illness,andcommonmimicsoferucism.Effectivehistorytaking,heightenedclinicalsuspicion,prompt communicationwithtoxicologicexperts,andcomplete removalofintactspinesareessentialforearlyidentification andeffectiveclinicalmanagementofaspcaterpillar envenomation.Therelativelyhighprevalenceofasp caterpillarenvenomationjustifiesfuturestudyofitsvenom, developmentofapotentialantivenom,andguidelinesfor clinicalmanagement.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
AddressforCorrespondence:EricBoccio,MD,MPH,Memorial HealthcareSystem,DepartmentofEmergencyMedicine,3501 JohnsonStreet,Hollywood,FL33021.Email: eboccio@mhs.net
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Autreyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.EaglemanDM.Envenomationbytheaspcaterpillar(Megalopyge opercularis). ClinToxicol(Phila). 2008;46(3):201–5.
2.GoldmanBSandBraggBN.Caterpillarandmothbites.In: StatPearls [Internet].2023.Availableat: https://www.ncbi.nlm.nih.gov/books/ NBK539851/?report=reader.AccessedNovember9,2023.
3.McGovernJP,BarkinGD,McElhenneyTR,etal. Megalopyge opercularis:observationsofitslifehistory,naturalhistoryofitsstingin man,andreportofanepidemic. JAMA. 1961;175(13):1155–8.
4.ForresterMB. Megalopygeopercularis caterpillarstings reportedtoTexaspoisoncenters. WildernessEnvironMed. 2018;29(2):215–20.
5.HosslerEW.Caterpillarsandmoths. DermatolTher. 2009;22(4):353–66.
6.KoehlerAWandZaveriKG.Lepidopterismcausedbythepuss caterpillar. JAmAssocNursePract. 2021;34(1):169–71.
7.Konstat-KorzennyE,YudovichA,Morgenstern-KaplanD. Lepidopterism:casereportandreviewoftheliterature. Cureus. 2020;12(1):e6567.
8.GreeneSCandCareyJM.Pusscaterpillarenvenomation:erucism mimickingappendicitisinayoungchild. PediatrEmergCare. 2020;36(12):e732–4.
9.Morales-CabezaC,Prieto-GarcíaA,AceroS,etal.Systemic mastocytosispresentingasoccupationalIgE-mediatedanaphylaxisto pineprocessionarycaterpillar. AnnAllergyAsthmaImmunol. 2016;117(3):333–4.e1.
10.BrancoMMP,Borrasca-FernandesCF,PradoCC,etal.Managementof severepainafterdermalcontactwithcaterpillars(erucism):a prospectivecaseseries. ClinToxicol(Phila). 2019;57(5):338–42.
11.TorrentsR,SimonN,SchmittC,etal.Envenomationbycaterpillarsof thegenus Megalopyge inFrenchGuianawithanatypicalclinical presentation,basedonthreeobservations. ClinToxicol(Phila). 2015;53(8):844–5.
SectionEditor:JoelMoll,MD
Submissionhistory:SubmittedJuly19,2023;RevisionreceivedDecember22,2023;AcceptedDecember28,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1441
Introduction: Unlicensedcosmeticprocedures,whichcomeatincreasedriskofinfectionandpotential surgicalcomplications,haveintroducednewchallengesinhealthcare.Physiciansshouldbeawareof presentationsthatmayarisesecondarytotheseprocedures.
CaseReport: Wedescribeacaseinwhichapreviouslyhealthy,28-year-oldfemalepresentedwith new-onsetseizuresandacuterespiratorydistresssyndrome(ARDS)inthesettingofarecentcosmetic procedurewithsiliconeinjectionstotheglutealregion.Thepatient’shospitalcoursewascomplicatedby alteredmentalstatus,respiratoryfailure,rapidhemodynamiccompromise,andeventualdeath.
Conclusion: Inrarecases,onepossiblecomplicationofcosmeticproceduresissiliconeembolism syndrome,whichischaracterizedbypneumonitis,alveolarhemorrhage,andARDS.Thepatient describedinthisreportalsoexperiencedneurologicsymptomsincludingseizureandalteredmental status.Thisisaclinicaldiagnosisthatreliesuponthoroughhistory-takinganddetailedphysicalexam. Documentationonthisphenomenonislimited,andmedicalmanagementhasnotyetbeenstandardized forthiscondition.Morbidityandmortalityremainhigh.[ClinPractCasesEmergMed.2024;8(2)151–154.]
Keywords: casereport;siliconeembolizationsyndrome;ARDS;cosmeticsurgery.
Unlicensedcosmeticprocedureshaveresultedin complicationsincludin ginfectionandcosmetic deformities.Treatmentofthesecomplicationsmayrequire antibiotictherapy,hospit aladmission,andattimes surgicalintervention. 1 – 3 Limiteddocumentationincases ofunlicensedcosmeticsurgerybringsadditional challengestouncoveringhistoryandpatient management. 4 – 7 Siliconeinjectionsarenotapprovedby theUSFoodandDrugAdministrationduetotheir associationwithinfection,permanentdis fi gurement, embolism,anddeath.Theserestrictionshaveprompted individualstoseekcertain cosmeticproceduresby unlicensedpractitionerswithintheUnitedStatesor abroad.Inthesecases,practitionersmaybeunquali fi edfor thecosmeticinterventionsperformed.Additionally,the
cosmetic fi llersusedmaybepronetoimpuritiesduetothe absenceofregulations. 2
Theincreasedprevalenceofmedicaltourismforcosmetic procedureshascontributedtocomplicationssecondaryto unlicensedmedicalpractice.WithintheUS,themajorityof patientswhoundergomedicaltourismareHispanic females;traveldestinationsareprimarilywithinLatin America,withtheDominicanRepublicthemostfrequented destination.1 Whiledataislimited,itissuspectedthat individualspursuecosmeticoptionsinforeigncountriesdue tolower financialcosts;onestudyfoundthatthemajorityof patientsaffectedareMedicaidrecipientsandoflower socioeconomicbackgrounds.2
Liquidsilicone(polydimethylsiloxane)isacommonly usedsubstanceforcosmeticinjections,primarilyasasoft tissueexpander.Inrarecases,siliconeembolismsyndrome
(SES),acomplicationassociatedwithillicitcosmetic modificationsinvolvingsiliconeinjections,canoccur.This conditionisassociatedwithpneumonitis,alveolar hemorrhage,andacuterespiratorydistresssyndrome (ARDS).4–7 Currentliteraturesuggeststhatthepulmonary findingsarecausedbyasiliconeembolismfromdirect intravenousinjection.Alternatively,theymaybecaused afterlocaltissuedestruction.Afterreachinglungtissue,the siliconetriggersacascadeofinflammatoryresponses includingproteolysisandrecruitmentofneutrophils.4 The embolusitselfcanresultinocclusionofmicrovasculature, furtheraffectingpulmonaryfunction.Pulmonary hemorrhageandedemacanoccurrapidly.
Symptomshavebeenreportedasearlyaswithin72hours ofcosmeticsurgery.However,delayedpresentationsupto 18yearsafterinitialsurgeryhavebeendocumented.4,8 Due tothelimitednumberofcasereportsregardingthis condition,theaveragetimecoursefromsurgerytosymptom onsetisunclear.Presentationsvary,althoughmostreports indicatesymptomonsetwithinhourstodays.Imaging reportsarelargelyconsistentbetweencases,withcomputed tomography(CT)revealingdiffusealveolarinfiltratesor ground-glassopacities.4–8
Anotherwisehealthy,28-year-oldHispanicfemalewith noknownpastmedicalhistorywasbroughttotheemergency departmentbyemergencymedicalservices.Accordingtothe historyprovided,thepatienthadbeenwalkingwithafriend beforeexperiencingsuddenonsetabdominalpainfollowed byseizureactivity.Afteranepisodeofemesisand repeatseizureduringinitialtriageevaluation,thepatientwas takentotheresuscitationbayforfurtherevaluation. Furtherhistory-takingfromfamilyrevealedthatthe patienthadattendeda “cosmeticparty” earlierthat day(withintheprior24hours)andreceivedgluteal soft-tissueinjections.
Initialvitalswerenotablefortachycardiawithaheartrate of116beatsperminute(bpm),andtachypneawitha respiratoryrateof34breathsperminute.Thepatientwas alsofoundtobehypoxicat70%saturationonpulse oximetry.Temperatureandbloodpressurewere98.3° Fahrenheitand137/82millimetersofmercury(mmHg), respectively.Seizureactivitywascontrolledwith 4milligrams(mg)oflorazepam.Thepatientremained unabletoprovidehistoryorfollowcommands,with continuedhypoxiaandsignsofrespiratorydistressdespite supplementaloxygenwithanonrebreathermask.Dueto respiratoryfailure,rapidsequenceintubationwas performed.Thephysicalexamwasnotablefor findings suggestiveofrecentglutealinjections,withsurgicalpen markings,injectionsites,andoozingofclearliquid.After intubation,bloody fluidfromtheendotrachealtubewas suggestiveofalveolarhemorrhage.
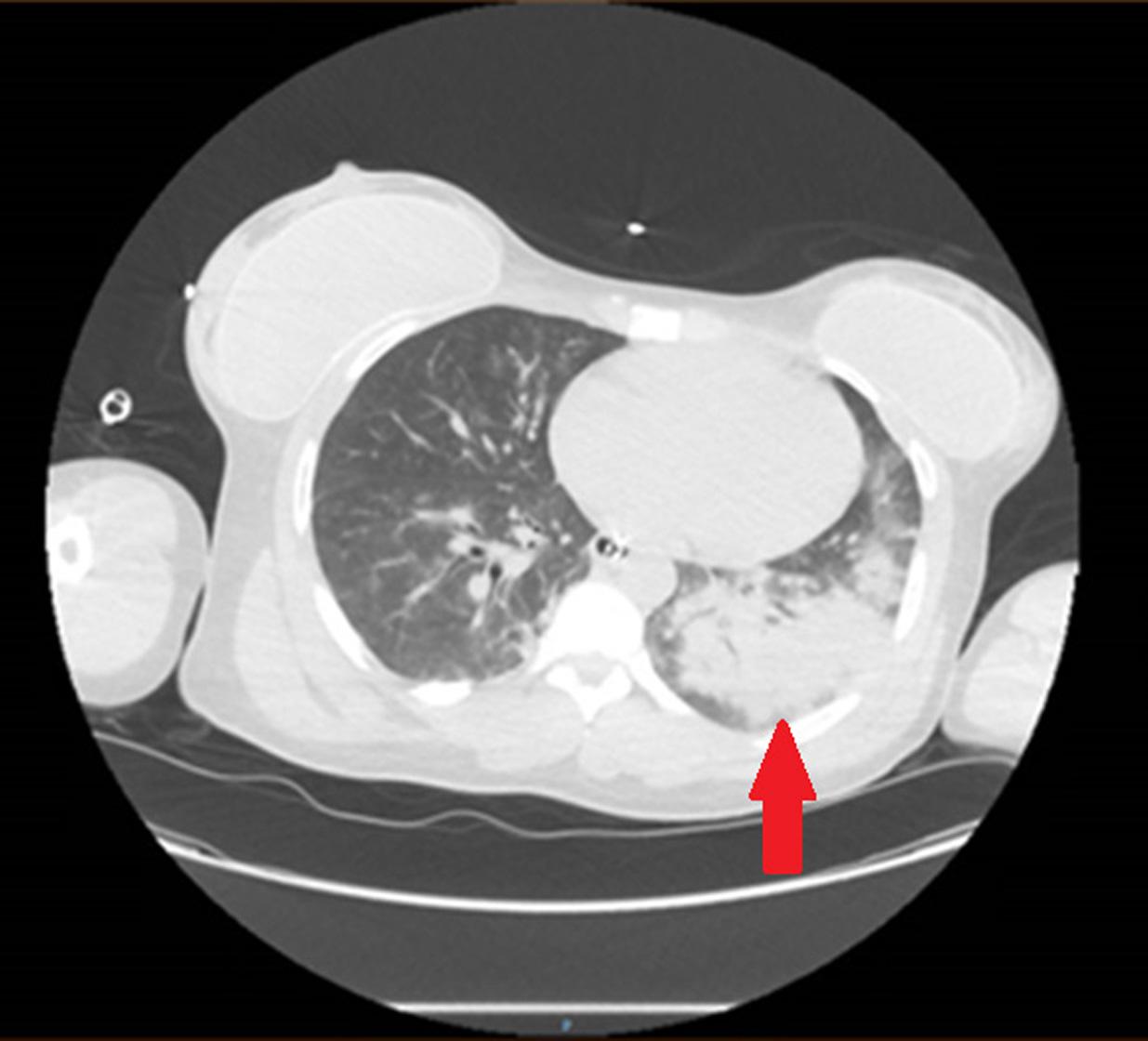
Image1. Computedtomographyofthechestwithcontrast demonstratingbilateralpulmonaryairspacedisease,more pronouncedintheleftlung(arrow).
Chestradiographobtainedimmediatelyafterintubation demonstratedleft-sided,ground-glassopacities.Computed tomographydemonstratedextensivebilateralpulmonary airspacediseaseaswellasopacitiesintheglutealarea suggestiveofcosmeticinjections,consistentwiththephysical exam(Images1 and 2).Asubsegmentalpulmonary embolismwasalsopresent.Broadspectrumantibioticswere initiatedduetoconcernforasurgicalsiteinfection,given subcutaneousemphysemaalsopresentonCT(Image3). BloodgasresultswerenotableforalacticacidosiswithapH of7.24(referencerange7.35–7.45).Adecreasedratioof arterialoxygenpartialpressuretofractionalinspiredoxygen
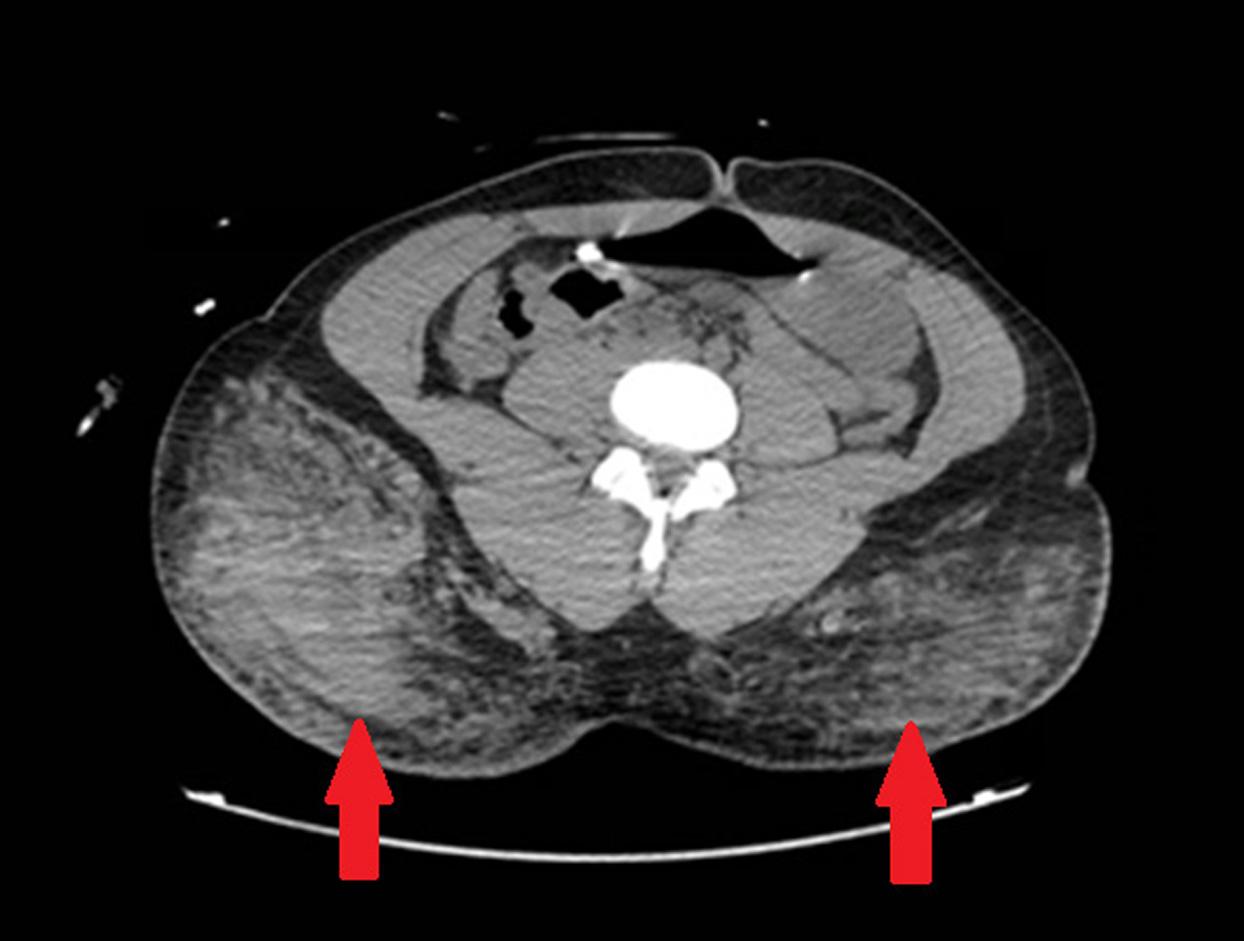
Image2. Computedtomographyoftheabdomenandpelviswith contrastdemonstratingopacitiesinglutealsubcutaneousfat, suggestiveofinflammationfromsiliconeinjections(arrows).

ARDS,andalveolarhemorrhage.4–8 Here,wedescribeacase ofSESresultinginrespiratoryfailure,althoughthiswasalso associatedwithrapidhemodynamicinstabilityanddeath. Forthispatientcase,clinical findingsinadditiontoautopsy resultsconfirmedthatrecentcosmeticsurgerybyan unlicensedpractitionerresultedinsiliconeembolismto multipleorgansystems.Seizureactivityasnotedduringthe initialpatientpresentationwaslikelyattributedto siliconeembolismtothebrain.These findingssuggestthat siliconeembolicandirectlyaffectmultipleorgansystems;we suspectthatinvolvementofthecentralnervoussystem, characterizedbyemboliandischemicchangeswithinthe brain,isassociatedwithincreasedmortalityandrapid clinicaldeterioration.
of73wasalsopresent,suggestiveofsevereARDS.Altered mentalstatusandrespiratoryfailurearesuspectedtobe secondarytoeffectsofsiliconeemboli.
Thepatientwasadmittedtotheintensivecareunitfor furthermanagement.Thehospitalcoursewascomplicated byfurtherhemodynamicinstabilityandworseningacidemia. Thepatientexperiencedrapidlyworseningtachycardiaand hypotension,withtheheartrateincreasingto144bpmand meanarterialpressuredecreasingto60mmHgwithinaonehourtimespan.Increasingtroponinlevelsfrom0.49 nanogramspermilliliter(ng/mL)to1.64ng/mL(reference range0–0.5ng/mL)werealsonoted.Sevenhoursafter arrivalatthehospital,thepatientexperiencedacardiac arrest.Despiteaggressiveinterventioninvolvingonehourof cardiopulmonaryresuscitationandtheadministrationof alteplaseforsuspectedembolism,thepatientwas pronounceddead.
Reviewbythemedicalexaminerlaterconfirmedinitial clinicalimpressions.Examwasremarkableformultiple puncturemarksattheglutealregion.Multiplecysts filled withviscousmaterialandgranulationtissuewerepresent. Thepatientwasnotedtohavemultipleembolisystemically, presentinthelungs,kidneys,heart,andbrain.Alveolar hemorrhageofthelungswasnoted;histologicalanalysis demonstratedlipoidmaterialinthevasculatureaswellas withinmacrophages.Microscopicanalysisofembolic materialwasconsistentwithsilicone.Theautopsyreport identifiedevidenceofsiliconeembolismtomicrovascular structuresofthebrain,withischemicchangesnoted.
Isolatedcasereportshavedocumentedpulmonary complicationssecondarytoliquidsiliconeinjections. Siliconeembolismsyndromeresultsinmultiplesystemic findings,includingmentalstatuschanges,seizureactivity,
AlthoughmedicalmanagementofSEShasnotyetbeen standardized,ofthecasereportsthatdetailthis phenomenon,resolutionofARDSandoverallrecoveryhave beenassociatedwithcorticosteroiduseandlung-protective mechanicalventilation.4–8 Intravenousmethylprednisolone hasmostcommonlybeenusedinthetreatmentofrespiratory distressinthesettingofSES.Improvedoutcomesare believedtobesecondarytodecreasedairway inflammation.4–7 Othercasestudiesnotedimprovementafter theuseofextracorporealmembraneoxygenation(ECMO)in thesettingofrespiratoryfailureandpersistent hypotension.9,10 Neurologicmanifestations,including alteredmentalstatusandcoma,mayoccurandare associatedwithpooreroutcomes.6,9,11 Seizureonset,as documentedinthiscasestudy,isanatypicalpresentation thathasnotbeenextensivelydocumentedinotherreports. Casesofsurvivalhavebeenreported;prognosismaydepend onvolumeofsiliconeandpressureofinjection.4–7
One2019casereportdescribesacaseofSESthat respondedtoaregimenofmethylprednisolone125mgevery sixhours.Thepatientinthatcase,whoalsoreceivedECMO, recovered.Presentationwasacuteandwithintwodaysofa siliconeinjection.11 Another2013studyalsoreported administrationofmethylprednisoloneatthesamedosing withpatientsurvival.Onsetwasalsowithintwodaysofa glutealinjection.7 Thesepatientcases,inadditiontotheone describedinourcasereport,describearelativelyquickonset ofsymptomsaftercosmeticsurgery.
Withregardtoclinicalpractice,siliconeinjectionscreatea challengeinwhichtheunderlyingetiologyofacriticallyill, otherwisehealthypatient,maynotbereadilyapparent.The locationofpotentialcosmeticsurgerymayberevealedbya thoroughphysicalexamorCT.Withunlicensedprocedures, afullhistorymaynotbeavailablefromhealthrecordsalone. Patientsmaynotbeforthcomingwithsensitivehistory regardingcosmeticsurgery,especiallyifappearingnottobe directlyrelatedtonew-onsetpulmonarychanges.Incritically illpatients,verbalhistorymaynotbeavailable.Physicians shouldconsiderthediagnosisofsiliconeembolisminyoung patientswithacutehemodynamicormentalstatuschanges,
whenhistoryorexam findingsaresuggestiveofrecent cosmeticsurgery.
Unlicensedcosmeticprocedureshaveresultedin complicationsthatintroducenewmedicalchallengesfor emergencyphysicians.Inrarecases,embolizationofsilicone mayresultinacuterespiratoryfailureandmayprogressto systemic findingsthatincludeneurologicchangesand cardiopulmonarycompromise.Volumeofsiliconeinjection, inadditiontotheextentofembolization,maybefactorsthat affectmortality.Inthecasewereportherethesudden hemodynamicchangesandmentalstatuschangeswerelikely secondarytowidespreadsiliconeemboli,whichwere identifiedinmultipleorgansystems.Earlyidentificationof potentialsiliconeembolismsyndromeandaggressive supportivecareappeartobebeneficial.Furtherstudies documentinginterventionsandoutcomeswillhelpguide futuremanagement.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ChristopherLin,MD,SaintBarnabas Hospital,DepartmentofEmergencyMedicine,BrakerBuilding Floor4,44223rdAve.,Bronx,NY10457. Email: clin7@mail.einstein.yu.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Linetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.McAuliffePB,MussTEL,DesaiAA,etal.Complicationsofaesthetic surgicaltourismtreatedintheUSA:asystematicreview. AestheticPlast Surg. 2023;47(1):455–64.
2.ZhengC,QuentzelJ,BrustJCM.Complicationsofsiliconecosmetic proceduresamongmedicaltouristsfromtheBronx, NewYork:aretrospectivenalysis. JClinAesthetDermatol. 2019;12(10):24–8.
3.MayerJEandGoldbergDJ.Injuriesattributabletocosmeticprocedures performedbyunlicensedindividualsintheUnitedStates. JClinAesthet Dermatol. 2015;8(10):35–7.
4.NgBH,MatWRW,AbeedNNN,etal.Siliconepneumonitisaftergluteal filler:acasereportandliteraturereview. RespirolCaseRep. 2020;8(3):e00538.
5.EckleVS,LambirisN,GrundD,etal.Akutesrespiratorischesversagen durchsilikon-injektion[Acuterespiratoryfailureaftersiliconeinjection]. Pneumologie. 2019;73(10):582–5.
6.ClelandDA,TsaiCHH,VoJ,etal.COVID-19infectionor buttockinjections?Thedangersofaestheticsandsocializing duringapandemic. JCritCareMed(TarguMures). 2022;8(1):49–54.
7.EssenmacherACandAstaniSA.Respiratorydiseasefollowing illicitinjectionofsilicone:acasereport. CaseRepMed. 2013;2013:743842.
8.AroraA,InatyH,MukhopadhyayS,etal.Chronicpulmonarysilicone embolismrelatedtosalinebreastimplants. AnnAmThoracSoc. 2016;13(1):139–41.
9.MadanN,KhanU,MartinsA,etal.Recurrentsiliconeembolism syndromerequiringVAECMO. RespirMedCaseRep. 2022;36:101576.
10.MolinaCFandRetalisZP.Pulmonaryembolismsecondarytosilicone injection. IntJMedStud, 2019;7(2):41–4.
11.SingarajahA,WangA,SayeghJ,etal. “Botched”:acasereportof siliconeembolismsyndromeafterpenileandscrotalinjection. ClinPract CasesEmergMed. 2020;4(4):595–8.
DanielP.High,MD*
JoseM.Acosta-Rullan,MD†
DanayHerrera,DO†
MauricioDanckers,MD*
DanielHeller,MD,FCCP*
DanielZapata,MD‡
SectionEditor:LevLibet,MD
*HCAFloridaAventuraHospital,DepartmentofPulmonaryandCriticalCare Medicine,Aventura,Florida
† HCAFloridaAventuraHospital,DepartmentofInternalMedicine,Aventura,Florida ‡ HCAFloridaKendallHospital,DepartmentofPulmonaryandCriticalCareMedicine, Miami,Florida
Submissionhistory:SubmittedMay24,2023;RevisionreceivedNovember2,2023;AcceptedNovember16,2023
ElectronicallypublishedFebruary13,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1399
Introduction: Spontaneoussplenicruptureisanextremelyrarecomplicationofinfectiveendocarditis.
CaseReport: Wepresentacaseofa56-year-oldimmunocompetentfemalewithporcinebioprosthetic mitralvalvereplacement,automatedimplantedcardioverter-defibrillator,andatrial fibrillationon apixabanwhowasfoundtohavein-hospitalatraumaticsplenicrupturecomplicatinginfective endocarditiswith Haemophilusparainfluenza. Therupturewastreatedsuccessfullybyendovascular embolization.Usualtreatmentwithsixweeksofantibioticsprovideddurablecurewithoutfurther complication,andnosurgicalinterventionwasneededforeitherthevalveorspleen.
Conclusion: Transcatheterarterialembolizationshouldbeconsideredearlyinatraumaticsplenic rupture.Relevantabdominalandcerebralimagingshouldbeconsideredinallcasesofsuspectedor confirmedinfectiveendocarditiswhereunexplainedsymptomsarepresent.[ClinPractCasesEmerg Med.2024;8(2)155–158.]
Keywords: atraumaticsplenicrupture;splenicarteryembolization;endocarditis;casereport.
Thespleen,anencapsulatedhematopoieticorgan,isthe mostfrequentlyinjuredvisceralorganduringabdominal blunttrauma.1 Patientswhosufferfromasplenicrupture oftenpresentwithnon-specificandsubtlesymptomsthat mayincludesuddenonsetleftupperquadrantabdominal pain(LUQ),abdominaldistention,arapiddecreasein bloodpressureand,ifsevereenough,alterationsin mentalstatus.Whileblunttraumaistheleadingcauseof splenicrupture,atraumaticsplenicrupture(ASR)isa life-threateningconditionthatcanoccurspontaneouslyand intheabsenceofanyapparentinjury.Liuetalreport ASRasarareconditionwithanestimatedincidencerateof 3.2%ofallsplenicruptures,andAkouryetalpoints outthatitisoftenmisdiagnosedforother,more commoncausesofLUQabdominalpainsuch aspancreatitis.2,3
Atraumaticsplenicrupturecarriesahighmortalityrate estimatedat12.2%becausedelaysindiagnosismayleadto persistentinternalbleeding,hemodynamicinstabilityand, subsequently,death.Herewereportourteam’semergent managementofararecaseof Haemophilusparain fl uenzae endocarditis-associatedatraumaticsplenicrupture.This subsetofatraumaticsplenicruptureisquiterare,andtheuse ofendovascularratherthansurgicaltreatmentisalso relativelynovel.Inareviewoftheliteraturewefoundno othersimilarcasestreatedthisway.
A56-year-oldimmunocompetentwomanwith nonischemiccardiomyopathywithautomatedimplanted cardioverterdefibrillator(AICD),bioprostheticmitralvalve replacementsecondarytorheumaticheartdisease, paroxysmalatrial fibrillationonanticoagulation,andhistory
ofnephrolithiasispresentedtotheemergencydepartment (ED)withLUQpain.Shedeniedanyrecenthistoryof trauma.Laboratorydataandcomputedtomography(CT)of theabdomenandpelviswithintravenous(IV)contrastwere unremarkable.Secondaryreviewofimagingdonebyan independentradiologistforpublicationconfirmedalackof splenicpathology.Thepatientwasnotedtohavehematuria anddischargedfromtheEDwithsuspicionfor nephrolithiasis-associatedrenalcolicfromastonethathad alreadybeenpassedoutoftheurethra.Fivedayslater,she wasaskedtoreturntothehospitalduetopositiveblood culturesgrowing Haemophilusparain fl uenzae .On admission,shemetmodifiedDukecriteriaforpossible infectiveendocarditis(IE).ShewasstartedonIVceftriaxone andcontinuedonapixabanhomeregimen.A transesophagealechocardiogram(TEE)wasperformed withoutevidenceofAICDleadorvalvularvegetations, althoughmildmitralvalveregurgitationwasnoted.
PersistentLUQpainbyhospitaldaythreeprompteda follow-upCTwithoralandIVcontrastoftheabdomenand pelvisthatrevealedalargehemoperitoneumwithasplenic hematomameasuring15 × 9 × 15centimeters.(Image)There wasnodefinitivecontrastblush,butactivesplenic hemorrhagewasstronglyfavoredbythereadingradiologist. Herhemoglobinhaddroppedfrom11.9gramsperdeciliter (g/dL)to7.1g/dL(referencerange:11.2–15.7g/dL).
Emergentangiogramconfirmedactiveextravasationatthe inferiorpoleofthespleenduringselectiveangiographyofthe

Image. Contrast-enhancedcoronalcomputedtomographyofthe abdomendemonstratingalarge(15 × 9 × 15centimeter)perisplenic hematoma(arrow)withconcomitanthemoperitoneumdueto atraumaticrupture.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Atraumaticsplenicrupturerarely complicatesinfection,malignancy,and in fl ammatorydisease.Treatmentfollows pathwaysformorecommontraumatic splenicinjuries.
Whatmakesthispresentationof diseasereportable?
Wedescribede fi nitivemanagementoflate, atraumaticsplenicrupturecomplicating transesophagealechocardiogram-negative endocarditisusingsplenicembolization andantibiotics.
Whatisthemajorlearningpoint?
Rareclinicalentitiescancoexistandwillnot alwaysbereadilyidenti fi ableduringaninitial emergencydepartmentvisit.
Howmightthisimproveemergency medicinepractice?
Transcathetersplenicarteryembolization shouldbeconsideredearlyasasafe alternativetosurgicalmanagementof atraumaticsplenicrupture.
splenicartery,andthesplenicarterywasembolizedwith sevencoilsandgelfoam.Thepatientreceivedthreeunitsof packedredbloodcells.Apixabanhadbeenheldformore than12hours,andnoreversalagentwasindicated.Further intensivecareunitandhospitalcoursewereuncomplicated, andthepatientwasdischargedondayeighttocompletea six-weekcourseofIVceftriaxoneonhome anticoagulationregimen.
Shereturnedtoanearbyhospitalthenextdayfor continuedabdominalpain.Noevidenceofbleedingwasseen atthattime,butanticoagulationwasheldforatotaloffour months.Noneurovascularcomplicationswereevidenced duringthisperiodnorrecurrenceofbleedingwhen anticoagulationwasrestarted.Surveillanceculturesafter antibioticregimencompletionwerenegative,andfollow-up TEEdidnotshownew findings.
Atraumaticsplenicrupturecanbefurtherdividedintotwo categories:pathological(93%)andidiopathic(7%).The pathologicaletiologiesincludemalignancies(30%), infectious(30%)inflammatorydiseases(15%),medical
treatments(10%),ormechanicalcauses(7%).3 Less commonly,ASRhasalsobeenreportedasafatal complicationofIE(firstreportedcasebyLakeandKevinin 1919).4 Here,wepresentararecaseofnon-traumatic, spontaneoussplenicruptureinthesettingof Hparain fl uenzae endocarditis.
Spontaneoussplenicruptureisanextremelyrare complicationofIE.Whilerare,missingthediagnosismaybe catastrophic;therefore,ahighindexofsuspicionisneeded. Incaseseriestheconditioncarriesamortalityrateof 15–58%.6 Themortalityrateisvariabledependingonthe etiology:neoplastic(21.4%),infectious(8.7%),inflammatory (9.5%),medicaltreatment(13%),mechanical(17%),and idiopathic(2%).7 Riskstratificationandchoiceof interventionshouldbeundertakenwiththesebaseline mortalityrisksinmind.7
Itiscrucialtoinquireregardingrecentinfections,surgical history,bleedingdisorders,anduseofanticoagulants, antiplatelets,ornonsteroidalanti-inflammatorydrugs. Therearethreepathophysiologicalmechanismsofsplenic ruptureinendocarditis:1)ruptureofsplenicabscess; 2)ruptureofamycoticaneurysm;and3)ruptureofa hematomasecondarytosuppuratingintrasplenicvessel, subcapsulardissection,anddelayedcapsulartear.8 Computedtomographyisthecurrentimagingmodalityof choicetodiagnosesplenicinjury,butincorporatingmagnetic resonanceimagingoftheabdomenandbrainmayalsobe consideredwithconcurrentIEasithasbeenshownto upgradecertaintyofIEdiagnosisorchangetreatmentin28% ofIEcases.10
Surgicalsplenectomyisthemostcommoninterventionfor ASR,althoughorgan-preservingsplenorrhaphycanalsobe donelesscommonlywhenappropriate;pediatriccases,for example,aremorecommonlymanagedconservativelyor withorgan-preservingtreatment.7 Transcatheterarterial embolization(TAE)isbecomingamorefrequenttreatment modality,particularlyincasesinvolvinganticoagulants, viralorprotozoanetiology,orwithactivebleedingasthis methodmayallowmorerapidandsaferhemostasisthan surgeryalone.12
ThediagnosisofIEwasmadeusing fiveminorDuke endocarditiscriteriaforfever,mitralvalvereplacement, presumedsplenicemboli,glomerulonephritispresumed basedonhematuriawithoutbiopsyproof,andbloodcultures notmeetingmajorcriteria.Circumstancesprecludedtimely repeatbloodculturestoobtainbloodculturemajorcriteria, andrepeatculturesweretakenafter fivedaysofantibiotics. Therewasunnecessaryrisktothepatientthatprecluded kidneybiopsytoprovehematuriawasrelatedto glomerulonephritisgivenitwouldnothavechanged management.Assplenectomywasnotperformed,no histopathologywasperformedonthespleentoprove embolismvsintrinsicsplenicpathology.NorepeatTEEwas performedduringthehospitalcourseorthatwereavailable
afterdischarge.Inthesettingofdelayedsplenicrupture,risk ofongoinginfectionwastoohightojustifyashorter antibiotictreatmentcourse.
WhenpatientswithpossibleordefinitiveIEhave unexplainedsymptoms,thereshouldbealowthresholdof clinicalsuspicionforadvancedimagingofthebrainand abdomentoassessforembolicphenomenaincludingsplenic lesions.Suchclinicalinformationcanprovecrucialfor identifyingmajorcomplicationsincasesofTEE-negative endocarditissuchastheonepresentedhere.Inaddition,TAE canbeastabilizingandtemporizingmeasureusedin combinationwithcriticalcaremonitoringandintervention evenifdefinitivesurgicalmanagementmaysometimesbe neededlater.CliniciansshouldconsiderTAEearlyinASR andconsideritaprimaryoptionduringinterdisciplinary decision-makingtoachievefavorablepatientoutcomesinthis time-sensitiveandhigh-riskclinicalentity.Wedemonstrate herefavorableanduncomplicatedsurvivalusingTAEas definitivemanagementinadjuncttousualantibiotictreatment ofASRcomplicating Hparain fl uenzae IE.
Thisresearchwassupported(inwholeorinpart)by HCAFloridaAventuraHospital.Theviewsexpressed inthispublicationrepresentthoseoftheauthor(s)and donotnecessarilyrepresenttheofficialviewsofHCA FloridaAventuraHospitaloranyofitsaffiliatedentities. WewishtothankKevinJaszewski,MD,forimageprocessingassistance.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
AddressforCorrespondence:DanielP.High,MD,HCAFlorida AventuraHospital,DepartmentofPulmonaryandCriticalCare Medicine,20900BiscayneBlvd.,Aventura,FL33180.Email: danphigh@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudywasfundedinwholebythe authorsandHCAFloridaAventuraHospital.
Copyright:©2024Highetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.IsenhourJLandMarxJ.Advancesinabdominaltrauma. EmergMed ClinNorthAm,2007;25(3):713–33.
2.LiuJ,FengY,LiA,etal.Diagnosisandtreatmentofatraumaticsplenic rupture:experienceof8cases. GastroenterolResPract 2019;2019:5827694.
3.AkouryTandWhetstoneDR.Splenicrupture. StatPearls. 2022. Availableat: https://www.ncbi.nlm.nih.gov/books/NBK525951/ AccessedOct25,2023.
4.LakeNCandKevinHK.Threeuncommonabdominalcasesillustrating somepitfalls. TheLancet.1919;194(5001):13.
5.DimitrakakisG,VonOppellU,ZilidisG,etal.Splenicrupture complicatingaorticvalvereplacementforbacterialendocarditis. Interact CardiovascThoracSurg.2008;7(1):138–40.
6.Hershman-SarafovM,PazA,PotasmanI.Echo-negativeendocarditis: analysisof538consecutivetransesophagealechocardiographies. OpenForumInfectDis.2016;3(suppl1):1105.
7.RenzulliP,HostettlerA,SchoepferAM,etal.Systematicreviewof atraumaticsplenicrupture. BrJSurg.2009;96(10):1114–21.
8.VergneR.Ruptureofthespleenininfectiveendocarditis. ArchIntern Med.1975;135(9):1265–7.
9.WalkerAandFoleyE.Surgicalmanagementofatraumaticsplenic rupture. IntSurgJ.2016;3(4):2280–8.
10.LungB,KleinI,MourvillierB,etal.Respectiveeffectsofearlycerebral andabdominalmagneticresonanceimagingonclinicaldecisionsin infectiveendocarditis. EurHeartJCardiovascImaging 2012;13(8):703–10.
11.MurdochDR.Clinicalpresentation,etiology,andoutcomeofinfective endocarditisinthe21stcentury. ArchInternMed.2009;169(5):463.
12.TonoliniM,IerardiAM,CarrafielloG.Atraumaticsplenicrupture:an underratedcauseofacuteabdomen. InsightsImaging 2016;7(4):641–6.
13.GedikE,GirginS,AldemirM,etal.Non-traumaticsplenicrupture:report ofsevencasesandreviewoftheliterature. WorldJGastroenterol 2008;14(43):6711.
SectionEditor:ShadiLahham,MD
Submissionhistory:SubmittedSeptember14,2023;RevisionreceivedDecember6,2023;AcceptedDecember7,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1670
Introduction: Rectusabdominismusclestrainsarecommonandcanbedebilitatinginbothprofessional andamateurathleteswhoengageinstrenuousactivity.
CaseReport: Wereportararecaseofrectusabdominismuscletearinanamateurbodybuilder diagnosedbypoint-of-careultrasound(POCUS)intheemergencydepartment(ED).Thepatienthad presentedtotheEDthreeseparatetimesafterstrenuousexercise,receivedcostlydiagnosticworkups, andultimatelywasdiagnosedonthethirdvisitwithgrade2bilateralrectusabdoministear.Thepatient wasgivenappropriateeducationandsportsmedicinefollow-up.Heunderwentrehabilitationfocusedon trunkandcorestability.Ateight-weekfollow-up,thepatienthadmadeafullrecovery.
Conclusion: Toourknowledge,acaseofbilateralrectusabdoministeardiagnosedbyultrasoundinthe emergencysettinghasnotbeenpreviouslypublished.OurcasereporthighlightstheutilityofPOCUSin diagnosingmusculoskeletalpathologyandpreventingcostlybounce-backvisits.[ClinPractCases EmergMed.2024;8(2)159–162.]
Keywords: rectusabdominis;ultrasound;muscletear;emergencydepartment;casereport.
Rectusabdominismusclestrainsarecommonand debilitatinginbothprofessionalandamateurathletesbut canbeeasilymisdiagnosedinanemergencysettingorby physicianswhodonottreatathletesregularly.1–10 Point-ofcareultrasound(POCUS)isahelpfultooltoaidinexpedient diagnosisandgradethedegreeofseverityofrectus abdominisstrain.7 Herewedescribeacase ofrectusabdominismusclestrainthathighlights theutilityofPOCUS,theimportanceofdiscriminating betweenintra-abdominalandabdominalwall pathology,andthepreventionofpoor functionaloutcomes.
Thepatientwasa40-year-oldmalerecreational bodybuilderwithnosignificantpriormedicalhistorywho presentedtotheemergencydepartment(ED)withlower abdominalpain.Hetrained fivedaysaweekwithafocuson
weightliftingandincludedavarietyofenduranceexercisesin hisregimen.Ofnote,hehadrecentlyincreasedhisendurance trainingandcoreisolationexercises.
Atthepatient’ s firstEDvisit,hecomplainedof debilitatingabdominalpainthatwaslocatedbelowthe umbilicus,constantandprogressivelyworsening.Hispain wasaggravatedbyrunning,abdominalisolationexercises, anddeadlifting.Thepatienthadnottriedanymedicationsto alleviatethepain.Hedeniedanyconstitutionalsymptoms, dysuria,hematuria,vomiting,ordiarrhea.Physicalexam wassignificantforseveresuprapubictendernesstopalpation. Labworkwaswithinnormallimits,andcomputed tomography(CT)oftheabdomenandpelviswithoraland intravenouscontrastrevealednoabnormalities.Thepatient wasgivenondansetron,normalsaline,viscouslidocaine, andfamotidineandwasdischargedhomewithprimary carefollow-up.
Thepatientreturnedthreemonthslaterwithpersistent lowerabdominalpain.Hereportedthathisaggravatingand
alleviatingfactorshadnotchanged,butthathisabdominal painhadprogressed.Hehadnotfollowedupwithaprimary carephysicianoranyotherspecialistsincehis firstvisit.He onceagainhadlabsdrawnandCTabdomenandpelvis imaging,whichwereagainwithinnormallimits.The patientwasagaingivenpainmedicinesandwasdischarged homewithadiagnosisof “unspecifiedlowerabdominal pain,” andgivenfollow-upwithgastroenterology andurology.
Thepatientpresentedagainafteranotherthreemonths withcontinuedabdominalpain,whichhenotedstilloccurred afterthesameexacerbatingexercisesfromprior.Physical examinationwassignificantforpainelicitedwith flexionof theabdominalmusclesandpalpation.Additionally,the patientwasevaluatedbysofttissueultrasoundoverthemost painfulareaoftheabdomen.Point-of-careultrasound (POCUS)oftheabdominalrectusmuscledemonstrated disruptedabdominalmuscle fibersbilaterallywithanechoic fluidbetweenabdominismusclelayers(Image1)andstreaks ofedemaintramuscularly(Image2).Theemergency physiciandiagnosedthepatientwithrectusabdominisstrain andinstructedhimtorestandfollowupwithasports medicinephysician.
Thepatientwascontactedtwomonthsafterdischarge fromtheED.Hehadstoppedperformingtheculprit exercisesuntilhisabdomennolongerhurt.Hemodified aggravatingisolationabdominalexercisesandprogressively overthecourseoftwomonthsreturnedtohisprevious normalactivitywithoutpain.
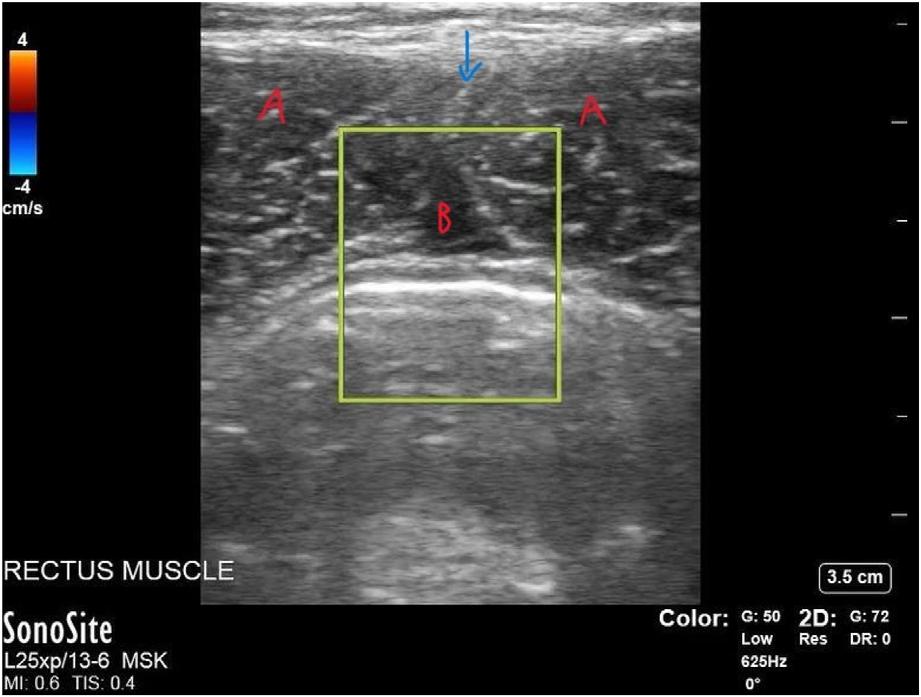
Image1. Point-of-careultrasoundoftherectusabdominusin short-axisviewdemonstratingasmall,1 × 2-centimetercollection of fluid.Inthenear fieldisskinandsubcutaneoustissue.The hyperechoicmidlinestripebetweenthetwotriangularrectus abdominismusclebellies(“A”)oneithersideisthelineaalba(blue arrow).Thehypoechoicarea(labeled “B”)betweentherectus abdominismusclesandbelowthelineaalbaislikelyedema.The yellowrectangleisacolor flowapplication,whichindicatesarterial (red)orvenous(blue)blood flow.Inthiscase,thereisno flow, whichisexpectedinthecaseofedema.
PopulationHealthResearchCapsule
Whatdoweknowaboutthisclinicalentity?
Rectusabdominismusclestrainsareeasily misdiagnosedintheemergencysetting.point ofcareultrasound(POCUS)hasbeenshown toaideindiagnosisinthesports medicineliterature.
Whatmakesthispresentationof diseasereportable?
Therehasneverbeenareportedcaseofrectus abdominisstrainthatwasdiagnosedby POCUSintheemergencymedicineliterature.
Whatisthemajorlearningpoint?
ThiscasereportemphasizeshowPOCUSis animportant,sensitive,andcost-effective aideinevaluatingabdominalwallpathology.
Howmightthisimproveemergency medicinepractice?
Thismayencourageemergencymedicine physicianstoroutinelyusePOCUSwhen suspectingmusculoskeletalpathology.
Abdominalrectusinjuriesareoverallarareentityinthe generalpopulation;however,theyoccurinphysicallyactive individualswhoengageinfrequentstrenuousexercise.1 The literaturedescribestheseinjuriesinadiversityofprofessional andrecreationalathletes,includingrecreational
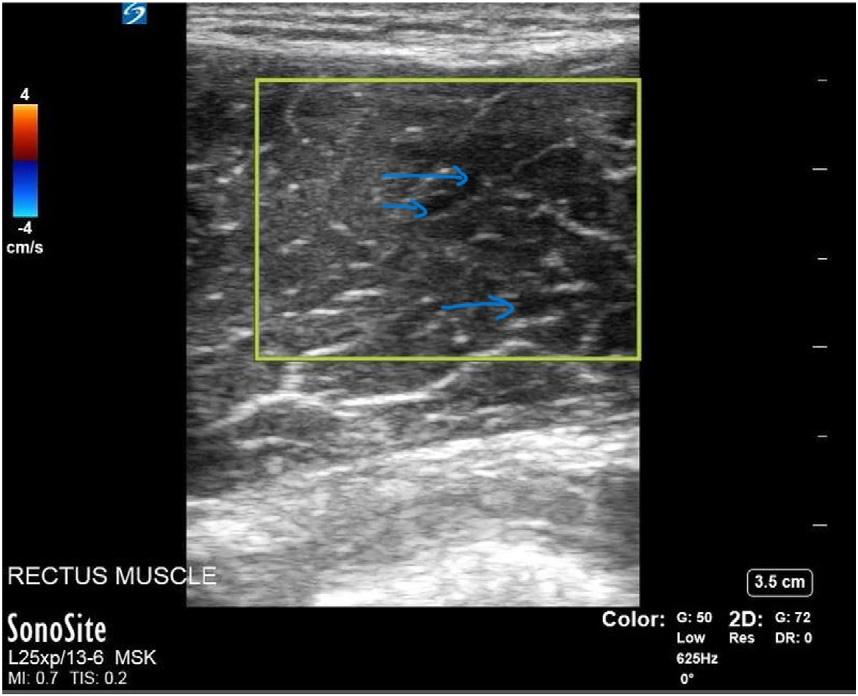
Image2. Point-of-careultrasoundoftherightrectusabdominus muscleintheshort-axisviewdemonstratingmuscle fiber elongationwithintramuscularedemaindicatedbytheblue arrows.Again,theyellowrectangledemonstratesnoevidenceof smallvascularstructures.
weightlifters.1–9 Clinically,therearenotablehistoricaland examination findingsthatarehelpfultodistinguish abdominalwallfromvisceralpathology.Abdominalwall injuriestendtobemorelocalized,elicitedbymovement,and aretendertopalpationregardlessofmusclecontractility. TheCarnettsigniselicitedwhenthepointofmaximal abdominaltendernesspersistswhenthepatient’sabdomenis palpatedwhiletensed.IftheCarnettsignispositive,thenthe painislikelytoarisefromtheabdominalwall.1 Visceralpain canbemorediffuse,referred,constant,andiselicitedwhen themusclesarerelaxed.Additionally,thereisanotable absenceofnausea,vomiting,diarrhea,constitutional symptoms,orothersymptomscommoninintra-abdominal pathologies.1 Asinthiscase,thepresentationcanbe ambiguous,andPOCUSisapowerfultoolthatcanbeused toaidindiagnosis.
Inthiscase,bothimprovedphysicalexamandultrasound wereinvaluableinreliablydiagnosingthepatientwithrectus abdominismuscletearandpreventingfurtherdelayin treatment.Afewcasereportshighlightultrasoundasatool tobothdiagnoseandtreatabdominalmuscletears.1–7,9 Ruff etalandMaquirriainetalrecommendusingultrasoundto estimatediseaseseverity.Thegoalofultrasonographyinthe settingofsuspectedmuscularpathologyistoidentifyatear, asthisprognosticatestimetorecoveryandtosport.7 Tears arecharacterizedbydisturbedmuscle fibers,intramuscular edema,and fluidcollections.Aswithourpatient,rectus abdominisstraincanbeeasilyoverlookedwhenapatientisin acutedistressduetopain.Thepatientpresentedthreetimes totheEDbeforeacorrectdiagnosiswasmade.Thiscanlead tounnecessarytestingandinappropriatetreatment. RevisionofCTimagingbyanattendingemergency physicianafterultrasounddiagnosisshowednosignificant acuteabnormality.Revisionbyaradiologistwasnot performed,butthesecondCTreportincludedarevisionof the firstscanforcomparison.BothCTstudies,readbytwo differentradiologists,showednoacuteabdominalwall pathology.Ultrasoundandmagneticresonanceimagingare preferredteststoevaluateformuscularpathologydueto increasedsensitivityandspecificity.1,2,10 Computed tomographyhaslimitedutilityformuscularlesional evaluationbutwillassessforfractureandintrabdominal pathology.Asdiscussedabove,ultrasoundisbothspecific andsensitiveindetectingmuscletears.10 Magneticresonance imagingcanprovideadditionalinformationandistypically orderedfortheprofessionalathlete.However,numerous studieshaveshownPOCUStobebothsensitiveandspecific indetectingmuscularpathologyandhastheaddedbenefitof beingcost-effectiveandrapidlyavailableinmostEDs.4,7,10 Treatmentformostrectusabdominaltearsis conservative.Thecornerstoneoftreatmentintheacute periodisrest,ice,analgesia,andavoidanceoftheoffending action.1,5 Earlyrehabilitationisconsideredkeytoreducing timetoplay.5 Rehabilitationfocusesonfunctional
restorationexercises.1,5–8 Severalcasereportssupporttheuse ofplateletrichtherapiesandcorticosteroidinjectionin professionalathletesinadditiontorehabilitation.3,4 The patientdiscussedhereimprovedwithconservative managementandaprogressivereturntoweightlifting.
Identificationofabdominalwallinjuryiseasily overlookedbyacutecarephysicians,butitiscrucialto preventdelayedtreatment,poorfunctionaloutcomes,and costlymedicalworkup.Thiscasedemonstrateshow ultrasonographycanbeusedtodiagnoseabdominalmuscle tearsinboththeEDandoutpatientclinic.Ultrasoundis reliable,quick,andcost-effective.Toourknowledge,there arefewerthan12casereportsonthistopic,withnone occurringintheEDthatresultedinreal-timediagnosis.We supporttheroutineuseofPOCUStoevaluate musculoskeletalpathologyintheEDandinthe outpatientsetting.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:AlejandroSanoja,MD,MountSinai MedicalCenter,DepartmentofEmergencyMedicine, 4300AltonRoad,MiamiBeach,FL33140.
Email: alejandro.sanoja@msmc.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Sanojaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.JohnsonR.Abdominalwallinjuries:rectusabdominisstrains,oblique strains,rectussheathhematoma. CurrSportsMedRep. 2006;5(2):99–103.
2.MaquirriainJ,GhisiJP,KokaljAM.Rectusabdominismusclestrainsin tennisplayers. BrJSportsMed. 2007;41(11):842–8.
3.DautyM,MenuP,DuboisC.Uncommonexternalabdominaloblique musclestraininaprofessionalsoccerplayer:acasereport. BMCRes Notes. 2014;7:684.
4.StevensKJ,CrainJM,AkizukiKH,etal.Imagingandultrasound-guided steroidinjectionofinternalobliquemusclestrainsinbaseballpitchers. AmJSportsMed. 2010;38(3):581–5.
5.BayerML,Hoegberget-KaliszM,SvenssonRB,etal.Chronicsequelae aftermusclestraininjuries:influenceofheavyresistancetrainingon
functionalandstructuralcharacteristicsinarandomizedcontrolledtrial. AmJSportsMed. 2021;49(10):2783–94.
6.GozubuyukOB,KoksalC,TasdemirEN.Rehabilitationofapatientwith bilateralrectusabdominisfullthicknesstearsustainedinrecreational strengthtraining:acasereport. PhysiotherTheoryPract. 2022;38(13):3216–25.
7.RuffAN,CornelsonSM,PanterAS,etal.Rectusabdominismuscletear diagnosedwithsonographyanditsconservativemanagement. J Ultrasound. 2020;23(3):401–6.
8.KawamaR,IkeA,SomaA,etal.Side-to-sidedifferencein electromyographicactivityofabdominalmusclesduringasymmetric exercises. JSportsSciMed. 2022;21(4):493–503.
9.GuermaziA,RoemerFW,RobinsonP,etal.Imagingofmuscle injuriesinsportsmedicine:sportsimagingseries. Radiology. 2017;285(3):1063.Erratumfor: Radiology 2017;282(3):646–63.
10.DraghiF,CoccoG,RichelmiFM,etal.Abdominalwallsonography:a pictorialreview. JUltrasound. 2020;23(3):265–78.
KashaBornstein,MD,MPH*
ElizabethLaRosa,MD,MPH†
KelseyByrd,DO†
DanLaney,MD‡
HectorFerral,MD‡
HeatherMurphy-Lavoie,MD†
SectionEditor:RachelLindor,MD,JD
*LouisianaStateUniversityHealthSciencesCenter,DepartmentofInternaland EmergencyMedicine,NewOrleans,Louisiana
† LouisianaStateUniversityHealthSciencesCenter,DepartmentofEmergency Medicine,NewOrleans,Louisiana
‡ LouisianaStateUniversityHealthSciencesCenter,DepartmentofInterventional Radiology,NewOrleans,Louisiana
Submissionhistory:SubmittedOctober4,2023;RevisionreceivedJanuary4,2024;AcceptedJanuary8,2024
ElectronicallypublishedApril17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1905
Introduction: Phlegmasiaceruleadolens(PCD)isanuncommon,potentiallylife-threatening complicationofacutedeepvenousthrombosesthatrequiresatimelydiagnosis.Thenameofthe condition,thevisualdiagnosticcriteria,andthepreponderanceofcasesintheliteraturereferencing findingsexclusivelyinpatientswithlighterskincomplexionsmeansthatPCDmaynotbeonthe differentialdiagnosisforthepatientwithmoremelanatedskinwhoisexperiencingthistime-sensitive vascularemergency.
CaseReport: WedescribeonecaseofPCDinapatientwithdarkerskincomplexionandtheimportance ofidentifyingclinical findings,regardlessofskincolor,giventhepaucityofreferenceimagesforPCDin darkercomplectedpatients.Ourliteraturereviewyielded60casereportsforPCD.Onlytwopapers includedimagesreferencingpatientsofcolor.
Conclusion: Accuratediagnosisrequiresrecognitionofdiagnostic findings,whichmayvary significantlybetweenphenotypicallydistinctpopulations.Manypathognomonicphysicalexam findings relyondescriptorsbasedonpresentationinphenotypicallywhitepatients.[ClinPractCasesEmergMed. 2024;8(2)163–167.]
Keywords: casereport;healthdisparities;deepvenousthrombosis.
Phlegmasiaceruleadolens(PCD)isarareandpotentially life-threateningcomplicationofacutedeepvenous thrombosis(DVT),especiallyifdelayedindiagnosis.Itis characterizedbymarkedextremityswelling,pain,andskin colorchange.Additional findingsincludenon-palpable distalpulsesandparesthesias.1 Phlegmasiaceruleadolens resultsfromcriticalthrombosisofboththedeepand superficialvenoussystemsofthelimb,leadingtoarterial ischemia,gangrene,andlimbloss.Themortalityratefor PCDrangesbetween20–40%;lethalcomplicationsinclude pulmonaryemboli(PE),rhabdomyolysis, fluid sequestration,hyperkalemia,andshock.2 Evenwith
aggressiveintervention,amputationratesarebetween 12–50%.3 Theexistingliteraturehasapaucityofreference imagesforPCDinpatientswithdarkerskintones.We describeonecaseofPCDinapatientwithadarkerskin complexion,highlightingdistinctionsinexam findingsin patientsofcolor.
A68-year-oldmanwithahistoryofpulmonary adenocarcinomapresentedtotheemergencydepartment (ED)reportingprogressivegeneralizedweaknessandright lowerextremitypainfor10days.Onemonthprior,hehad beenhospitalizedforshortnessofbreathanddiagnosedwith
amalignantpleuraleffusion.Thiswasmanagedwitha tunneledpleuralcatheterforcontinuousdrainage.During thathospitalization,hewasfoundtohavebilateralDVTsof theposteriortibialveinsandsegmentalembolitotheleft pulmonaryartery.Hewasstartedonanticoagulationatthat timebutsubsequentlydevelopedhemorrhagicpleural drainage.Anticoagulationwasheld,andinterventional radiology(IR)placedaninferiorvenacava(IVC) filter.He wasdischargedhometocontinueoncologictreatment.
UponhissecondEDpresentation,hisexamwas significantforsinustachycardia,normoxemictachypnea, andhypotension.Theskinaroundtherightpleuralcatheter wasclean,dry,andnon-erythematous.Pleuralcatheter drainagewasscantandclear.Pulmonaryexamwas otherwiseunremarkablewithoutadventitiouslungsounds. Hisrightlowerextremityhadcircumferential,non-pitting edemafromthefoottothegroin,withareasoferythema, mottling,andpurplingaboutthedigits,shin,andknee.His rightfootwasdarkenedandcooltotouch(Image1).
Popliteal,posteriortibial,anddorsalispedispulseswere palpable.Heendorsedpainonpassivemotion,paresthesias, anddecreasedsensationdistaltotheknee.Hewasableto flex andextendatthehipjointbuthadcompleteparalysisbelow theknee.Hisleftlowerextremitywaswarmandwellperfused,withnoedemaorneurologicabnormalities.The remainderofhisphysicalexamwasunrevealing.Laboratory analyseswerenotablefornormocyticanemiawith hemoglobinof7.7gramsperdeciliter(g/dL)(referencerange 13.2–16.6g/dL),consistentwithhisprioradmission,

Image1. Patient’srightlegwithevidenceofenlargement(red bracket),darkeningofskinaroundjoints(blackarrows),subtle reddeningandpurplingoftissues(whitearrow).
Whatdowealreadyknowaboutthis clinicalentity?
Phlegmasiaceruleadolens(PCD)isa potentiallylife-threateningsequelaofdeep veinthrombosischaracterizedbyextremity swelling,pain,andskincolorchange.
Whatmakesthispresentationofthe diseasereportable?
WedescribeacaseofPCDinapatientwith darkercomplexion,emphasizingdistinctions inexam fi ndings.
Whatisthemajorlearningpoint?
Physiciansarenotprimedtovisuallydiagnose conditionsinpatientswithdarker-complected skin,astheliteraturealmostuniformly references fi ndingsinWhitepatients.
Howmightthisimproveemergency medicinepractice?
Phenotypicdifferencesconfersigni fi cant variationuponexam fi ndings.Diagnosis requiresrecognitionofpathologybetween distinctpopulations.
leukocytosisof12.8 × 103 permicroliter(μL) (4.5–11 × 103/μL),potassiumof5.5millimolesperliter (mmol/L)(3.5–5mmol/L),creatinineof1.76milligrams (mg)/dL(0.74–1.35mg/dL),upfrom1.22mg/dLonprior discharge.Lactatewaselevatedto2.7mmol/L(reference range <2).COVID-19polymerasechainreactionwas negative.Lowerextremityduplexultrasonographywas performed,demonstratingcompletethrombosisoftheright commonfemoral,greatersaphenous,popliteal,andcalf veins(Image2A, 2B).
Additionalthrombiwereidentifiedintheleftfemoral, popliteal,anduppercalfveins.Thisclotburdenwasgreater thanhadbeenseenduringtheprioradmission;ultrasoundat thattimerevealedthrombiintherightperonealandtheleft poplitealveins.Computedtomography(CT)ofthechest revealednoevidenceofPE.Computedtomographyofthe abdomenandpelvisdemonstratedextensivebilateraliliofemoralDVTextendingtotheIVC filter(Image2C).
Thepatientwas fluidresuscitatedandstartedonaheparin infusion.Interventionalradiologywasconsultedand performedpercutaneousvenousthromboaspirationfromthe poplitealveinstotheIVC.Flowwassuccessfullyrestored throughouttherightlowervenousvasculature,and70%of

Image2. Top:Ultrasoundoftherightcommonfemoralvein demonstratingclot(A)withincompressibilityofthevein(B).
Bottom:Computedtomographyoftheabdomenandpelvis demonstratingthrombosisoftheinferiorvenacavatothelevelof implantedinferiorvenacava filter(C).
thethromboticburdenwasaspiratedfromtheIVC (Image3).Followingintervention,thepatientwasadmitted totheintensivecareunitforcontinuedmanagementof hypotensionandanticoagulation.Rightlowerextremity discoloration,edema,andparesthesiasresolvedwithin24 hoursfollowingintervention.Hishemodynamicsimproved, andhewastransferredtoInternalMedicine.Hewas dischargedtoaskillednursingfacilityonhospitalday15.
Phlegmasiaceruleadolensisanuncommon,lifethreateningmanifestationofDVT,resultingfromcritical thrombosisofthedeepandsuperficialvenoussystems leadingtoarterialcompromiseanddecreasedperfusion. RiskfactorsforPCDaresimilartootherDVTandinclude malignancy,hereditarycoagulopathies,surgery,trauma, IVC filterplacement,pregnancy,smoking,anduseof hormonalcontraception.4,5 UnlikesimpleDVT,PCDalso carriesriskofcompartmentsyndrome,rhabdomyolysis, electrolytedisturbances,tissueischemia,gangreneandlimb loss, fluidsequestrationleadingtohemodynamic compromise,andconsequentmultiorganfailure.3
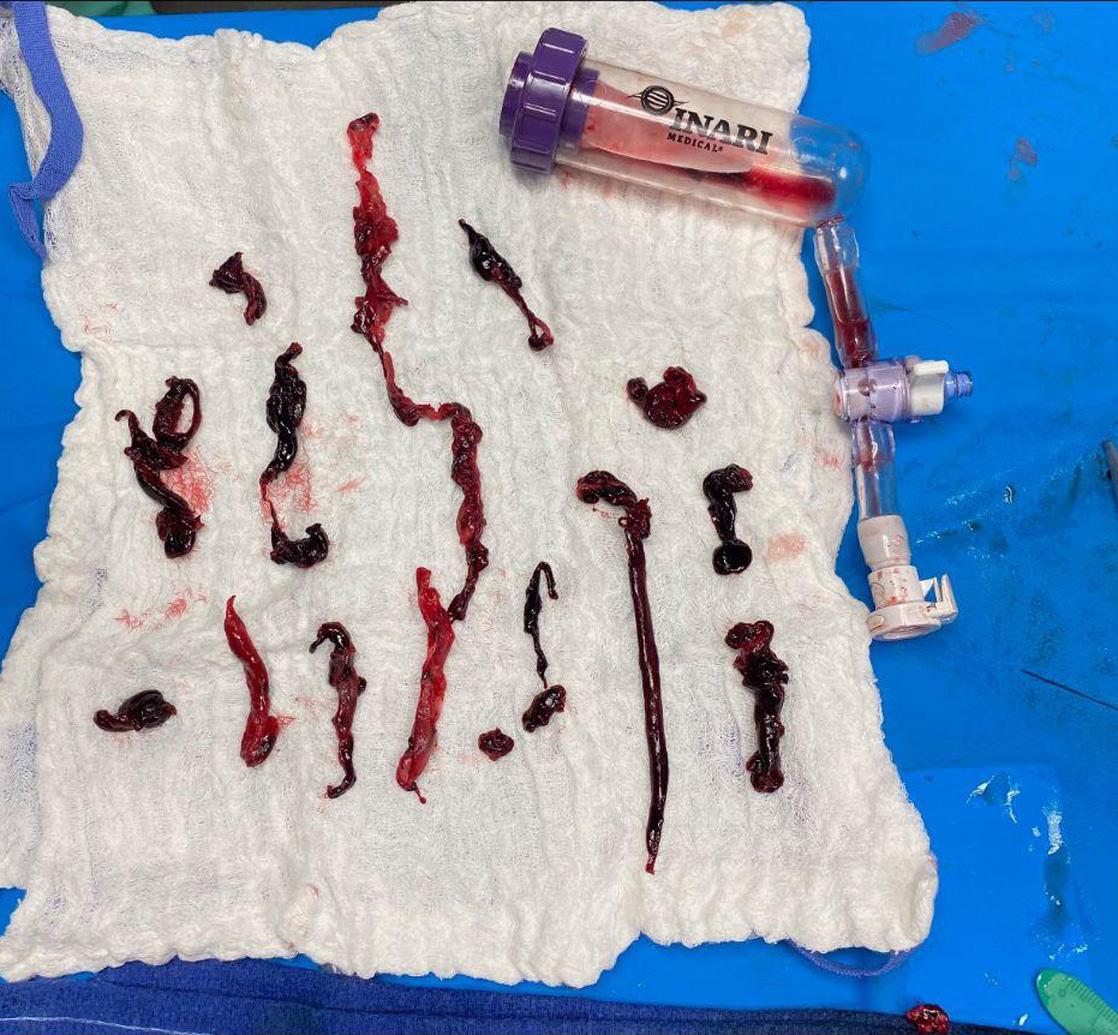
Demonstrationofclotburdenfollowing thromboaspirationbyInterventionalradiologyserviceusingclot retrieverdevice.
Recognizingthisseriousconditionisessential.Exam findingssuggestiveofPCDincludedarkeningofthelimb(s), extremityedema,decreasedskinsensation,paresis,and muscularorsuperficialtenderness.Crucialphysicalexam componentsincludeinspectionandpalpationoftheentire extremitytoevaluatearterialpulses,temperature,and capillaryrefill.Adetailedneurologicalexamshouldassess sensoryandmotorfunctionofthelimb.Earlyduplex ultrasoundiscriticalforassessingnon-compressibleveins fromthedistaltoproximalvasculatureoftheaffected extremity.Asatime-sensitivecondition,angiographyand othervascularimagingisunnecessaryunlesssuspicionis raisedforconcomitantPE.Managementincludes hemodynamicstabilization,treatmentofelectrolyte derangements,initiationofanticoagulation,andvascular surgeryorIRconsultationforthrombectomy.2
Accuratediagnosisandmanagementoflife-orlimbthreateningconditionsisanessentialroleofemergency physicians.Webelievethiscaseillustratesthatthisobjective wasachievedinthecareofthispatient.However,ouraim wasnotsimplytoillustrateacaseofPCD.Wepresentthis casetoemphasizethepotentialconsequencesofmedical educationresourcesthatinsufficientlydepictPCDinnonwhitepatients.Althoughthispatienthadmanyoftherisk factorsandclassicphysicalexam findingsofPCD,(active malignancy,presenceofanIVC filter,extremitypain,and paresis)thediagnosiswasbrieflydelayedbydifficulty recognizingthesefeaturesinapatientwhoseleg physiologicallycouldnotbeblue.Byvirtueofthecondition’ s name painfulblueinflammation physiciansare notprimedtovisuallydiagnosethisconditionin
Image3.darker-complectedskin,aseducationalresourcesalmost uniformlyreferenceexam findingsinwhitepatients.
Casereportsonpatientswithlight-complectedskin predominatethemedicalliteratureonPCD,implicitlymaking palerskinthedefault.Casesinpatientswithdarkerskinmaybe missedormisdiagnosedsimplybecauseofunfamiliaritywith skinthatappearsmoreashen,purple,orhyperpigmented ratherthanblue.6 Thispatientdidnotpresentwiththe ostensiblypathognomonic “brightblueleg” frequently encounteredinbotheducationalresourcesandclinicalimaging seriespublishedinacademicjournals.7,8 Manyotherclinical exam findingsincludingcyanosis,livedoreticularis,jaundice, andpurpuraaredistinctbetweenpatientpopulationsof differentskincomplexionbutarebasedonareferenceframeof patientswithlightlycomplectedskin.Expectingtoseeblue, ratherthanhyperpigmented,purpuric,orashenskincan undergirdascertainmentbiasanddiagnosticerrors,with delayeddispositionandtreatmentinthisandothercritical illnesses.Inacasereportaboutapatientwithtoxicepidermal necrolysis,Lester,Taylor,andChren(2021)describeapatient whospentmanyhoursinthehospitalwaitingroom decompensating,theircaredelayedbecause “thecharacteristic redness” facilitatingdiagnosis “canbesubtlein skinofcolor.9
Thesesubtletiesareunder-representedinthemedical literature.Ourliteraturereviewyielded60casereportson PCD.Onlytwoincludedimagesinvolvingpatientsofcolor.In astudyassessingrepresentationofskincolorindermatologyrelatedGooglesearches,Kurrti,AustinandJagdeoetalfound that91.7%displayedlightskin.10 AlthoughBlackpeople comprise13.5%oftheUnitedStatespopulation,Black physiciansaccountforonly5%ofthephysicianworkforcein theUSasof2019.Peopleofcolormoregenerallyaccountfor fewerthanone-thirdofphysicians.11,12 Physician demographicdisparitiesderivefrommultipleinterconnected causesincludingstructuralandinstitutionalracism,historical segregationinmedicaleducation,andmarginalizationof historicallyBlackmedicalschools.7
The1910FlexnerReport,whichinstigatedmajorreformsin medicaleducationintheUS,alsopromptedtheclosureofall buttwohistoricallyBlackmedicalschoolsinaneraduring whichmodernbiomedicaldiagnosticswereestablished.13 Flexner’sviewoftheroleforBlackphysicianswasproviding “hygiene” forBlackcommunitiestopreventhookwormand tuberculosisfromaffectingWhitepopulations.13 Itisno historicalaccidentthatmanycontemporarydescriptorsfor clinicalexam findingsreflecttheirpresentationinWhite patients;theprivilegeofelaboratinganatomopathological nomenclaturetodescribefeaturesofdiseasewasdeliberately restrictedtoWhitephysicianswhosepracticewascarriedoutin raciallysegregatedenvironments.Consequentially,medical practicetodayinvolvesunexamineduseofterminology thatmayunintentionallybiastheuserawayfrom correctdiagnosis.
Accuratediagnosisrequiresrecognitionofpathologyand variousdiagnosticcriteria,whichmayvisuallyvary significantlybetweenphenotypicallydistinctpopulations. Manypathognomonicphysicalexam findingsinvolve descriptorsbasedontheirpresentationinWhitepatients. Whileraceisnotabiologicalphenomenon,phenotypic differencesconfersignificantdistinctionsinmanifestationof pathologic findings.Historicalracismsituatingwhitenessas defaultinfluencedthedevelopmentofclinicalnomenclature, potentiallylimitingtheappropriatenessandfulldiagnostic scopeoftermsformanyclinicalexam findings.Asatimesensitivecondition,thenamingofphlegmasiaceruleadolens canbeadisservicetocliniciansandpatientsalike. Emergencycliniciansshouldbeconsciousofthecorefeatures seeninthisclinicalentity;significantdiscolorationtoan entireextremitywithassociatedpain,swelling,and paresthesia,particularlyinapatientwithanunderlying acquiredorinheritedthrombophilia.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:KashaBornsteinMD,MPH,Louisiana StateUniversityHealthSciencesCenter,DepartmentofInternaland EmergencyMedicine,2021PerdidoSt.,Room5141,NewOrleans, LA70112.Email: borns@lsuhsc.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Bornsteinetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GardellaLandFaulkJB.Phlegmasiaalbaandceruleadolens.In: StatPearls.TreasureIsland(FL)2023.Availableat: https://www.ncbi. nlm.nih.gov/books/NBK563137/.AccessedJuly8,2022.
2.ChaochankitWandAkaraborwornO.Phlegmasiaceruleadolenswith compartmentsyndrome. AnnVascDis. 2018;11(3):355–7.
3.ChinsakchaiK,TenDuisK,MollFL,etal.Trendsinmanagementof phlegmasiaceruleadolens. VascEndovascularSurg. 2010;45(1):5–14.
4.ChiWK,TanGM,YanBP.May-Thurnersyndromeresultsinlifethreateningcondition:phlegmasiaceruleadolensandrhabdomyolysis. JInvasiveCardiol. 2020;32(7):E190.
5.NicklerM,HaubitzS,MendezA,etal.Phlegmasiaceruleadolens-an uncommonbutalarmingmanifestationofdeepveinthrombosis. Vasa. 2020;49(5):422–6.
6.PenedoAlonsoJR,Aranda-GarciaY,Ly-PenD,etal.Incidenceand characteristicsofphlegmasiaceruleadolens.A17-year,descriptive studyinathird-levelhospitalinMadrid. IntJContempMedRes. 2019;6(11):K7–9.
7.BakerWandKimS.Riskinglifeandlimb:managementofphlegmasia albaandceruleadolens.2015.Availableat: https://www.emra.org/ emresident/article/risking-life-and-limb-management-of-phlegmasia–alba-and-cerulea-dolens.AccessedJuly8,2022.
8.ThurmanRJandStackL.Blueleg.2015.Availableat: https://www. emra.org/emresident/article/blue-leg.AccessedJuly8,2022.
9.LesterJC,TaylorSC,ChrenM-M.Under-representationofskinofcolour indermatologyimages:notjustaneducationalissue. BrJDermatol. 2019;180(6):1521–2.
10.KurttiA,AustinE,JagdeoJ.Representationofskincolorin dermatology-relatedGoogleimagesearches. JAmAcadDermatol. 2022;86(3):705–8.
11.GuevaraJP,WadeR,AysolaJ.Racialandethnicdiversityat medicalschools Whyaren’twethereyet? NEnglJMed. 2021;385(19):1732–4.
12.DiversityinMedicine:FactsandFigures2019.2019. Availableat: https://www.aamc.org/data-reports/workforce/report/ diversity-medicine-facts-and-figures-2019 AccessedJuly8,2022.
13.LawsT.Howshouldwerespondtoracistlegaciesinhealthprofessions educationoriginatingintheFlexnerReport? AMAJEthics. 2021;23(3):E271–5.
EladioAlbornoz,BS*
JanetWildemuth,MSPAS†
JosephineValenzuela,MD‡§
*ArizonaStateUniversity,DepartmentofMedicalStudies,Phoenix,Arizona
† ValleywiseHealth,DepartmentsofEmergencyMedicineandInternalMedicine, Phoenix,Arizona
‡ CreightonUniversityofPhoenix,Phoenix,Arizona
§ UniversityofArizonaPhoenix,Phoenix,Arizona
SectionEditor:StevenWalsh,MD
Submissionhistory:SubmittedSeptember28,2023;RevisionreceivedJanuary3,2024;AcceptedJanuary5,2024
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1897
CasePresentation: Wedescribethepresentation,evaluation,andmanagementofayoungfemale patientpresentingtotheemergencydepartmentwithatraumaticorbitalemphysema,ararecondition. Thispatientwasdiagnosedusingpoint-of-careultrasoundandcomputedtomographyandwas managedexpectantly.
Discussion: Atraumaticorbitalemphysemaisarareclinicalconditionmorecommoninearly middle-agedfemalepatientswithcertainhistoricalfeaturessuchaschronicsinusitis,facial surgeryortrauma,tobaccosmoking,orcurrentupperrespiratorysymptoms.Whilemostcaseswill resolvespontaneously,rarelythisconditioncanleadtovision-threateningorbitalcompartment syndrome,requiringlateralcanthotomyorneedledecompression.[ClinPractCasesEmergMed. 2024;8(2)168 –170.]
Keywords: atraumaticorbitalemphysema;point-of-careultrasound;casereport.
A36-year-oldwomanpresentedtotheemergency departmentwithpainandswellingaroundherrighteyeafter blowinghernosetheeveningprior(Image1).Shedenied headache,fever,eyedischarge,andvisualchanges.She deniedanyhistoryoftrauma,recentsurgery,orupper respiratorysymptoms.Physicalexaminationwasnotablefor periorbitalswelling.Therewascrepitustopalpationofthe area.Pupilswereequal,round,andreactivetolight.Visual acuitywas20/30inbotheyes,withanelevatedintraocular pressureintheaffectedeyeof32millimetersofmercury (mmHg)(referencerange10–20mmHg),butwithout proptosis.Eyemovementswerenormalandpainless.There wasnoconjunctivalinjection,hemorrhage,tearing,or dischargefromtheeye.
Thepatientwaslaidsupine,andapoint-of-care ultrasoundwasperformedwithalineartransducer (Image2).Notable findingsincluded “dirtyshadowing” andring-downartifactconsistentwithairintheperiorbital softtissue.Computedtomography(CT)confirmed adefectinthelaminapapyraceaoftheethmoid
sinus(themedialorbitalwall),withairtrappedinthe orbit(Image3).
Orbitalemphysemaisanuncommonconditionthat resultsfromtrappingofairintheorbitandperiorbital tissue.1 Typicalsignsandsymptomsincludeperiorbital swelling,crepitus,pain,proptosis,chemosis,visionchanges, andrelativeafferentpupillarydefect.1 Itisnormally associatedwithtrauma,althoughdozensofotheretiologies havebeenreported,includingsneezing,nose-blowing, coughing,postoperativecomplication,anduseofa continuouspositiveairwaypressuredevice.1–3 Nontraumaticetiologiesaremorecommoninpatientswhoare earlymiddle-aged,female,andhaveahistoryoffacial trauma,surgery,sinusitis,ortobaccosmoking,orhave currentupperrespiratorysymptoms.4 Itistheorizedthat chronicinflammationand/orremotetraumacanweakenthe laminapapyraceaoftheethmoidsinus,sothatpositive pressurethencausesafractureandairentryintotheorbit.2 Thedifferentialdiagnosisofatraumaticorbitalemphysema

shouldincludeorbitalcellulitis,malignancy,orbitalforeign body,andhematoma.1 Apartfromageandgender,this patienthadnoadditionalriskfactors.
Whensuspectedonhistoryandphysicalexamination,a diagnosisismadeonCToftheface.Point-of-care ultrasound fi ndingsdemonstratingairinthesubcutaneous tissuecanincreasetheindexofsuspicionforthisentitybut cannotde fi nitivelyestablishthediagnosis.Regarding management,mostcasesresolvein7–10days spontaneously.Inrarecases,orbitalcompartment syndromecandevelop,withtrappedaircompressingeither theopticnerveitselfortheophthalmicartery,causing ischemia.Thisisavision-threateningcomplication requiringemergentlateralcanthotomyandcantholysisor needledecompression. 5 Orbitalcompartmentsyndromeis detectedbyincreasedintraocularpressureandabnormal visualacuityonphysicalexamination. 5
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Orbitalemphysemaisanuncommonclinical conditionusuallycausedbytrauma,though atraumaticetiologieshavebeenreported aswell.
Whatisthemajorimpactoftheimages?
Whileexamplesoforbitalemphysemaare common,thisisthe fi rstpublishedexample ofapoint-of-careultrasoundof thiscondition.
Howmightthisimproveemergency medicinepractice?
Familiaritywiththisconditionmayprompt thecliniciantoselectsuitableimaging,screen fororbitalcompartmentsyndrome,and consultaspecialist.
Inthiscase,thepatient’sintraocularpressurewasonly mildlyelevated,withnormalvisualacuity;thus,ouron-call ophthalmologistandplasticsurgeonrecommended expectantmanagement.Thepatientfollowedupinplastic surgeryclinicthreedayslaterwithsignificantlyreducedpain andswelling.Shewasaskedtocontinuetofollowsinus precautions,includingnonose-blowing,sneezingwith mouthclosed,strawusage,diving, flyingonairplanes,or smoking,forseveralmoreweeks.
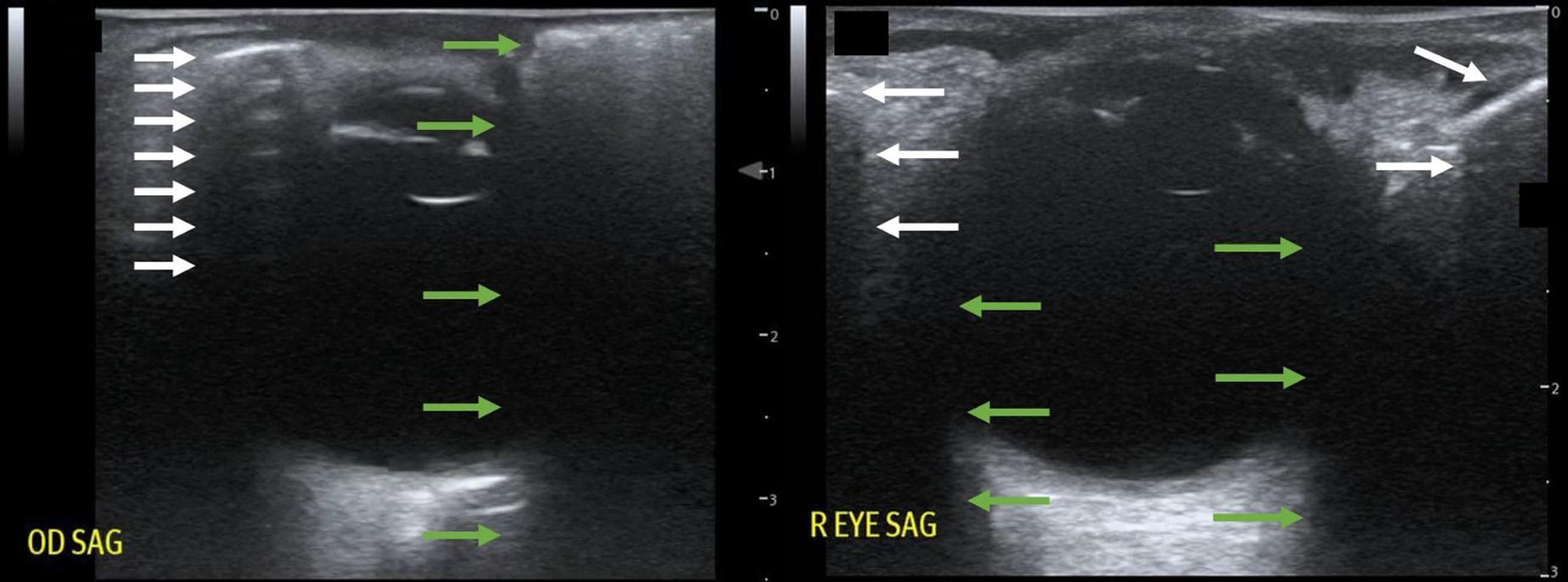
Image2. Point-of-careultrasoundofthepatient’seye(left)comparedwithanormaleyeultrasound(right).Inthepatient’sultrasoundonthe left,ahyperechoiclineisseenjustbelowtheskinsurface(topwhitearrow),whichrepresentstheair-tissueinterfaceofsubcutaneous emphysema.Belowareequallyspaced,repeatinglinesofreverberationartifact(additionalwhitelines),typicalofhighlyreflectiveair-tissue interfaces,analogousto “A-lines” onnormallungultrasound.Comparatively,intherightimage,theshadowofthebonyorbitinanormaleye ultrasound(whitearrows)originatesdeeperbelowtheskinsurface,issharplydemarcatedattheedges,andlacksreverberationartifact.Also showninthepatient’sultrasoundontheleftisthe “dirtyshadowing” associatedwithsubcutaneousair(greenarrows.).Comparedtothe shadowsofedgeartifactindicatedbythegreenarrowsinthenormalultrasoundontheright,these “dirtyshadows” originatefromanirregular surface,appearmore “smeared,” andarenotwell-demarcatedattheedges.
Image1. Periorbitalswellingoftherighteyeinafemalepatient.
Image3. Computedtomographyofthefacialbones,axialviewontheleftandcoronalviewontheright,demonstratingsubcutaneous periorbitalemphysema(whitearrows),intraconalorbitalspaceemphysema(blackarrows),withadefectinthelaminapapyraceaofthe ethmoidsinus(greenarrows).
Theauthorsattestthattheirinstitutionexemptedthiscasereport fromInstitutionalReviewBoardapproval.Thepatientprovided informedconsentforpublicationofthiscasereport. Documentationon file.
AddressforCorrespondence:JosephineValenzuela,MD, DepartmentofEmergencyMedicine,2601E.RooseveltSt., Phoenix,AZ85008.Email: Josephine_Valenzuela@dmgaz.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Albornozetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.RoelofsKA,StarksV,YoonMK.Orbitalemphysema:acasereportand comprehensivereviewoftheliterature. OphthalmicPlastReconstrSurg. 2019;35(1):1–6.
2.GonzalezF,CalV,ElhendiW.Orbitalemphysemaaftersneezing. OphthalmicPlastReconstrSurg. 2005;21(4):309–11.
3.RoshAJandSharmaR.Orbitalemphysemaafternoseblowing. JEmergMed. 2008;34(3):327–9.
4.KomroJJ,WilliamsPJ,LinDJ.Orbitaldefectandemphysema afternoseblowing:acasereportandliteraturereview. Cureus. 2022;14(12):E32958.
5.McCallumE,KerenS,LapiraM,etal.Orbitalcompartment syndrome:anupdatewithreviewoftheliterature. ClinOpthalmol. 2019;12(6):2189–94.
SectionEditor:MelanieHeniff,MD,JD
Submissionhistory:SubmittedOctober28,2023;RevisionreceivedJanuary17,2024;AcceptedJanuary26,2024
ElectronicallypublishedApril17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.4814
CasePresentation: Wepresentthecaseofasix-year-oldchildwithautismwhopresentedwith persistentvomitinginthesettingofaclosedheadinjury(CHI).Computedtomographyoftheheadwas normal,butduetopersistentvomitingaradiographoftheabdomenwasdone,whichshowedmultiple, rare-earthmagnetsintheabdomen.Therewasnohistoryofwitnessedingestion.Thesemagnetshad causedenteroenteric fistulaformationleadingtopersistentvomiting.
Discussion: InthesettingofCHI,vomitingcanbeasignofconcussionorintracranialhemorrhage.In casesofCHIwhereintracranialpathologyisruledoutandvomitingstillpersists,itisimportanttoexplore intra-abdominalcausesofvomiting,especiallyindevelopmentallychallengedchildrenastheyhavehigher incidenceofunwitnessedforeignbodyingestions.[ClinPractCasesEmergMed.2024;8(2)171 –173.]
Keywords: closedheadinjury;rare-earthmagnets;vomiting.
Asix-year-oldautisticchildpresentedtotheemergency departmentwithmultipleepisodesofnon-bloody,nonbiliousvomitingaftersustainingaclosedheadinjury(CHI). Thepatienthadfallenfaceforwardonthegroundfroma heightof fivetosixstairsteps.Noassociatedlossof consciousness,seizures,abdominalpain,difficultybreathing, ear,eye,ornasaldischargeswerereported.Thephysical examinationrevealedatwo-centimetercontusiononthe forehead.Therestoftheocular,auditory,abdominal, respiratoryexaminationsincludingGlasgowComascale werenormal.Initiallythepatientreceivedondansetron,but vomitingcontinuedafterthemedication.Duetopersistent vomiting,completebloodcount,bloodelectrolytes,liver functiontests,lipaselevel,andurinalysiswereobtainedfrom thelaboratory,andCToftheheadwithoutcontrastwas performed.AlllabtestsandCTwerenormal.Aradiograph oftheabdomenincidentallyshowedaclusterofsmallround ballsofrare-earthmagnetswithnosignsofobstructionor pneumoperitoneum(Image1).
Therewasnohistoryofwitnessedingestion.General surgerywasconsulted,andthepatientwasadmittedtothe hospital.Initially,thepatientwasmanagedconservatively withantiemeticsandlaxatives;butduetopersistentvomiting andlackofmovementofthemagnets,thepatientwastaken
totheoperatingroom.Duringthelaparotomy,itwasnoticed thatthemagnetshadcausedformationofanenteroenteric fistula(Image2).The fistulawasdivided,themagnetswere extracted,andtheedgesofthe fistulawereclosed.(Image3). Thepatientrecoveredwithoutanycomplicationsandwas dischargedfromthehospital.
Rare-earthmagnets(neodymiummagnets)are commerciallysoldas3–6millimetersroundrecreational objects;theyare fiveto10timesmorepowerfulthannormal magnets.Whenmorethanoneofthesemagnetsareingested, thebowelcangetcompressedbetweenthem,whichleadsto obstruction,necrosis,perforation,and fistulaformation.1 Duetothesmallsizeofthesemagnets,patientscandevelop localizedintestinalperforationsand fistulaswithout significantsymptomsandradiologic findings.Therefore,in patientswithingestionofmultiplerare-earthmagnets, surgicalorendoscopicremovalofthemagnetsshouldbe performedeveninasymptomaticpatients.2 Theincidenceof foreignbodyingestionishigherintoddlersandpreschool children,whereasahigherincidenceofingestionisnoticedat olderageinchildrenwithneurologicaldisabilities.3 Because foreignbodyingestionsinthesechildrenareoften unwitnessed,itpresentsachallengeindiagnosis.1,3 In


PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Rare-earthmagnetsaremorepowerfulthan regularmagnets,andwheningested inmultiplenumberscancause intestinalcomplications.
Whatisthemajorimpactoftheimage(s)?
Inanautisticchildpresentingwithclosed headinjury,abdominalimagingincidentally showedingestedrare-earthmagnets.
Howmightthisimproveemergency medicinepractice?
Foreignbodyingestionsshouldbeconsidered inthedifferentialdiagnosisofvomiting. especiallywhenevaluatingchildrenwith neurodevelopmentaldisabilities.

summary,foreignbodyingestionsshouldbeinthe differentialdiagnosisinchildrenwithneurologicaldisability presentingwithunexplainedvomiting.Additionally,incases withingestionofmultiplerare-earthmagnets,conservative managementmay not betheappropriatechoice.
TheauthorattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:AbdullahKhan,MD,FAAD,FACEP, SidraMedicineDepartmentofEmergencyMedicine,AlGharrafa Street,Ar-Rayyan,Doha,Qatar,POBOX3050. Email: abdullahkhan120@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Image1. Supineradiographoftheabdomenshowingmultiplerareearthmagnets(bluearrow). Image2. Viewofbowelduringlaparotomyshowingenteroenteric fistula(blackarrow).Copyright:©2024KhanThisisanopenaccessarticledistributedin accordancewiththetermsoftheCreativeCommonsAttribution(CC BY4.0)License.See: http://creativecommons.org/licenses/by/4.0/
1.KhanA,EldosY,AlansariK.Clinicalpresentationandoutcomeof multiplerareearthmagnetingestionsinchildrenofQatar.asinglecenterexperience. QatarMedJ. 2023;2023(1):9.
2.ZhengY,ZhangZ,YanK,etal.Retrospectiveanalysis ofpediatricpatientswithmultiplerare-earthmagnetsingestion: asingle-centerexperiencefromChina. BMCPediatr. 2021;21(1):179.
3.DestroF,CarusoAM,MantegazzaC,etal.Foreignbody ingestioninneurologicallyimpairedchildren:achallenging diagnosisandmanagementinpediatricsurgery. Children. 2021;8(11):956.
NathanielHansen,MD
FernandoL.Benitez,MD
LarissaI.Velez,MD
SectionEditor: MelanieHeniff,MD
UTSouthwesternMedicalCenter,DepartmentofEmergencyMedicine,Dallas,Texas
Submissionhistory:SubmittedOctober29,2023;RevisionreceivedJuly12,2023;AcceptedJuly13,2023
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.59302
CasePresentation: A22-year-oldfemalepresentedtotheemergencydepartmentwithatwo-month historyofworseningfatigue,unintentionalweightgain,andprogressivefacialswelling.Physical examination findingsincludedhirsutism,moonfacies,andabdominalstriae.Subsequentbrainmagnetic resonanceimagingrevealedthepresenceofa2.4-centimeterpituitarymacroadenoma,confirmingthe diagnosisofCushing’sdisease.Thepatientwasthenadmittedforneurosurgicaltumorresection.
Discussion: Cushing’sdiseaseisexceedinglyrareandoftenpresentswithsymptomsresemblingmore prevalentdisorders,contributingtodelaysindiagnosis.Therefore,maintainingahighindexofsuspicion forthisdiseaseiscrucialforemergencyphysicians.[ClinPractCasesEmergMed.2024;8(2)174–175.]
Keywords: Cushing’sdisease;Cushingsyndrome;pituitaryadenoma;casereport.
A22-year-oldfemalewithapastmedicalhistoryof hypertensionanddiabetespresentedtotheemergency departmentwithtwomonthsofabdominalstriae,persistent fatigue,unintentionalweightgainexceeding30pounds,and progressivefacialswelling.Physicalexamrevealedthe presenceofabdominalstriae(Image1),facialandtrapezius adiposity(Image2),andhirsutism(Image3).Sincethe patientwasnotreceivingsteroidtherapyatthetime,her

symptomsraisedsuspicionforCushing’sdisease. Subsequently,abrainmagneticresonanceimaging (MRI)withintravenouscontrastwasperformed,revealinga 2.4-centimeterpituitarymacroadenomacausing severeupwarddisplacementoftheopticchiasm (SupplementaryImage).Neurosurgerywassought,andthe patientwasadmittedforoperativemanagement.
 Image1. Lowerabdominalstriaeduetohypercortisolism.
Image1. Lowerabdominalstriaeduetohypercortisolism.

Image3. Hirsutismofthefaceduetoincreasedadrenocorticotrophic hormoneproduction,resultinginhyperandrogenism.
Cushing ’ sdiseaseisararedisordercharacterizedby excessivecortisolproductionfromtheadrenalglands, whichcaneitherbefromtheadrenalsdirectlyorfrom corticotropin-releasingtumorsinthelungsorpituitary gland. 1 Theterm “ Cushing ’ sdisease ” refersexplicitlytothe presentationofCushing ’ ssyndromecausedbyapituitary tumor.Cushing ’ sdiseaseismorecommonlyobserved amongwomen,typicallyappearingbetween20 – 40yearsof age. 1 Clinicalmanifestationsar eattributedtoincreased cortisolproduction,whichca usesweightgain,fatigue, poorconcentration,hypertension,hyperglycemia, excesshairgrowth,abdominalstriae,adiposedeposition, andmenstrualirregularity. 2 Unfortunately,these symptomsarenonspeci fi candoverlapwithcommon medicalconditionssuchasdiab etes,hypertension,and polycysticovariansyndrome.Consequently,the diagnosisofCushing ’ sdiseaseisoftendelayed,withan averagetimetodiagnosisexceedingthreeyearsfrom symptomonset. 3
TheevaluationforCushing’sdiseaseistypicallyinitiated inanoutpatientsettingandinvolvesvarioustests,including midnightsalivarycortisolmeasurement,low-dose dexamethasonesuppressiontest,or24-hoururine-free cortisollevelassessment.2 However,intheemergency department,obtainingabrainMRImaybewarrantedto detectavisiblepituitarytumor,whichcanbeseen approximately50%ofthetime,asinthiscase.2 When pituitarytumorsarediscovered,neurosurgicalconsultation andoperativeresectionareoftennecessary.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
Whatdowealreadyknowaboutthis clinicalentity?
Cushing ’ sdisease,causedbypituitary adenomas,oftenleadstodelayeddiagnosis duetononspeci fi csymptoms.
Whatmakesthispresentationof diseasereportable?
Thisreporthighlightstheclassicclinical presentationofCushing ’ sdiseaseincluding distinctivephysicalexam fi ndings.
Whatisthemajorlearningpoint?
Maintainingahighindexofsuspicionforrare diseaseslikeCushing ’ sintheemergency departmentisessentialfortimelydiagnosis.
Howmightthisimproveemergency medicinepractice?
PromptrecognitionofCushing ’ sdisease symptomscanleadtoatimelydiagnosisand appropriatede fi nitivecare,ultimately improvingpatientoutcomes.
AddressforCorrespondence:JasonD.Vadhan,UTSouthwestern MedicalCenter,DepartmentofEmergencyMedicine,5200Harry HinesBlvd,Dallas,TX53235.Email: jason.vadhan@phhs.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Vadhanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GardnerDG,ShobackDM. Greenspan’sBasicandClinical Endocrinology.NewYork,NY:McGraw-HillEducation;2017.
2.NiemanL,SwearingenB.Cushing’ssyndromeandCushing’sdisease. CMMGlobal.2013:1–12.
3.RubinsteinG,OsswaldA,HosterE,etal.TimetodiagnosisinCushing’s syndrome:ameta-analysisbasedon5367patients. JClinEndocrinol Metab.2019;105(3):e12–22.
SectionEditor:JacquelineLe,MD
MemorialHealthcareSystem,DepartmentofEmergencyMedicine,Hollywood,Florida
Submissionhistory:SubmittedOctober9,2023;RevisionreceivedNovember22,2023;AcceptedJanuary8,2023
ElectronicallypublishedApril17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.2582
CasePresentation: A52-year-oldfemalepresentedtotheemergencydepartmentwithfourdaysofright periorbitalpain,ipsilateraltemporalheadache,diplopia,andphotophobia.Physicalexaminationoftherighteye revealedpainfulophthalmoplegia,cranialnervesIIIandVIparesis,increasedintraocularpressure,andmild proptosis.Magneticresonancevenogramandmagneticresonanceimagingorbitswithcontrastdemonstrated anabnormalsignalsurroundingtherightcavernoussinus/petrousapex.Tolosa-Huntsyndrome(THS)was diagnosed.Perneurologyrecommendations,thepatient wasplacedonasteroidregimenoverthecourseof threeweeks.Shewasdischargedonhospitaldayninefollowingresolutionofsymptoms.Shehadno recurrenceofsymptomsorresidualdeficitsnotedathertwo-weekfollow-upappointment.
Discussion: Withanestimatedannualincidenceofonecasepermillion,THSisasinisteretiologyof unilateralheadache,painfulophthalmoplegia,andoculomotorpalsy.Tolosa-Huntsyndromeiscaused bygranulomatousinflammationinthecavernoussinusandishighlyresponsivetocorticosteroids. MagneticresonanceimagingstudiesofthecavernoussinusandorbitalapexarehighlysensitiveforTHS andcharacteristicallyshowenlargementandfocal-enhancingmasseswithintheaffectedcavernous sinus.[ClinPractCasesEmergMed.2024;8(2)176–178.]
Keywords: Tolosa-Huntsyndrome;ophthalmoplegia;cavernoussinus.
A52-year-oldBlackfemalewithhistoryofirondeficiency anemiapresentedtotheemergencydepartmentwithfourdays ofrightperiorbitalpain,ipsilateraltemporalheadache, diplopia,andphotophobia.Incidentally,thepatientreported sinuscongestiononemonthpriorthathadrespondedto fluticasonepropionateintranasal.Triagevitalsignswere withinnormallimits.Physical examinationoftherighteye demonstratedblurryvisionwithpositivelightperception,pupil equal,round,andreactivetolight,anincreasedocularpressure of39millimetersofmercury(mmHg)(referencerange: 10–21mmHg),andmildproptosis.CranialnervesIIIandVI paresiswasobservedresultinginptosisandimpaired abduction,adduction,andupwardanddownwardgaze.The patientdidnottolerateafundoscopicexaminationand voluntarilykeptherrighteyelidclosedduetophotophobia. Laboratorytests,includingacompletebloodcount,basic metabolicpanel,andurinepregnancy,wereunremarkable.
Theelectrocardiogramdemonstratedanormalsinusrhythm. Computedtomography(CT)brainandCTangiogrambrain andcarotidsrevealedacavernoussinus fillingdefect concerningforsinusvenousthrombosis,andaheparin infusionwasinitiated.Magneticresonancevenogramand magneticresonanceimagingorbitswithcontrast demonstratedanabnormalsignalsurroundingtheright cavernoussinusandpetrousapex(Image1).
Tolosa-Huntsyndrome(THS)wasdiagnosed,andthe heparininfusionwasdiscontinued.Neurologywasconsulted; 250milligrams(mg)solumedrolintravenous(IV)was administered,andthepatientwasadmittedtotheintermediate medicalcareunit.Sheunderwentalumbarpuncture,which demonstratedanormalopeningpressureandnegative cerebrospinal fluidanalysis.Perneurologyrecommendations, shewasplacedonasteroidregimenconsistingofthreedaysof 250mgsolumedrolIVdailyfollowedbyoneweekof80mg prednisoneperosdailyfollowedbyataperof20mgperweek

Image1. Coronal(A)andaxial(B)slicesofmagneticresonanceimagingorbitswithcontrastdemonstratinganabnormalsignalsurrounding therightcavernoussinusandpetrousapexsuspiciousforTolosa-Huntsyndrome(arrows).
Whatdowealreadyknowaboutthis clinicalentity?
Tolosa-Huntsyndrome(THS)isararecause ofheadache,painfulophthalmoplegia,and oculomotorpalsywithcharacteristic fi ndings onMRI.
Whatisthemajorimpactoftheimage?
Magneticresonanceimagingoftheorbits demonstratingfocalenhancementofthe affectedcavernoussinusandpetrousapexis characteristicofTHS.
Howmightthisimproveemergency medicinepractice?
Recognizingtheappropriateradiographic modalityand fi ndingsofTHSwill leadtoearlierdiagnosisandtherapeutic managementwhileavoiding unnecessarytests.
overthecourseofthreeweeks.Thepatientwasdischargedon hospitalday9followingresolutionofsymptoms.Shehadno recurrenceofsymptomsnorresidualdeficitsnotedathertwoweekfollow-upappointment.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:EricBoccio,MD,MPH,Departmentof EmergencyMedicine,MemorialHealthcareSystem,703NFlamingo Road,PembrokePines,FL33028.Email: eboccio@mhs.net
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Bennettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BugemeM,CisséO,MukukuO,etal.Tolosa-Huntsyndrome:apainful ophthalmoplegia. CaseRepNeurolMed. 2020;2020:8883983.
Withanestimatedannualincidenceofonecasepermillion, THSisasinisteretiologyofunilateralheadache,painful ophthalmoplegia,andoculomotorpalsy.1,2 Thereported averageageofonsetis41yearsold.(Pediatriccaseshaveonly rarelybeendescribed).3 Granulomatousinflammation involvinglymphocytesandplasmacellsincreasesthepressure withinthecavernoussinusandmayresultincompressionof cranialnervesIII,IV,andVIaswellasthesympatheticplexus surroundingtheinternalcarotidartery.4,5 Whiletheetiologyis presumedtobeidiopathic,thereisastrongassociationwith autoimmunedisorderssuchassystemiclupuserythematosus andsarcoidosis.6,7 Magneticresonanceimagingstudiesofthe cavernoussinusandpetrousapexarehighlysensitiveforTHS andcharacteristicallyshowenlargementandfocal-enhancing masseswithintheaffectedcavernoussinus.8,9 Whilethereisno consensusnorarethereguidelinesformanagingsymptoms attributedtoTHS,high-dosesteroidsareconsidered first line.10 Rapidresponsetosteroidtherapyisthehallmarkof THS,andpatientstypicallyrecoverwithnoresidualdeficits.11
2.AmrutkarCandBurtonEV.Tolosa-Huntsyndrome.In: StatPearls [Internet].2023.Availableat: https://www.ncbi.nlm.nih.gov/books/ NBK459225/.AccessedOctober9,2023.
3.TsirigotakiM,NtouliosG,LioumpasM,etal.Tolosa-Huntsyndrome: clinicalmanifestationsinchildren. PediatrNeurol. 2019;99:60–3.
4.GladstoneJPandDodickDW.Painfulophthalmoplegia:overviewwitha focusonTolosa-Huntsyndrome. CurrPainHeadacheRep. 2004;8(4):321–9.
5.KahlNandPelucioM.Casereportofamanwithrighteyepainand doublevision. JEducTeachEmergMed. 2022;7(1):V22–5.
6.CalistriV,MostardiniC,PantanoP,etal.Tolosa-Huntsyndromeina patientwithsystemiclupuserythematosus. EurRadiol. 2002;12(2):341–4.
7.Brandy-GarcíaA,Suárez-CuervoC,Caminal-MonteroL.Tolosa-Hunt syndromeasaninitialpresentationofsarcoidosis. ReumatolClin(Engl Ed). 2021;17(3):178–9.
8.CakirerS.MRI findingsinTolosa-Huntsyndromebefore andaftersystemiccorticosteroidtherapy. EurJRadiol. 2003;45(2):83–90.
9.JainR,SawhneyS,KoulRL,etal.Tolosa-Huntsyndrome:MRI appearances. JMedImagingRadiatOncol. 2008;52(5):447–51.
10.KoseA,BozkurtS,UmayST,etal.Acaseofheadache,doublevision andptosisinemergencydepartment:Tolosa-Huntsyndrome. TurkJ EmergMed. 2017;18(3):134–6.
11.BeckhamS,KimH,TruongA.Painfulophthalmoplegiaoftherighteyein a20-year-oldman. JEmergMed. 2013;44(2):e231–4.
HelenaKons,MD
ElliottD.Herron,BS
UniversityofAlabamaatBirminghamHeersinkSchoolofMedicine, DepartmentofEmergencyMedicine,Birmingham,Alabama
ZacharyS.Pacheco,MD
ErinF.Shufflebarger,MD,MSPH
SectionEditor:StevenWalsh,MD
Submissionhistory:SubmittedSeptember30,2023;RevisionreceivedDecember8,2023;AcceptedDecember11,2023
ElectronicallypublishedMarch26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1911
CasePresentation: A21-year-old,otherwisehealthyfemalepresentedtotheemergencydepartment withfeveramongothernonspecificsymptomsafterrecentlyreturningfromGhana.Onphysicalexam, shehadacharacteristicupperextremityrash,andatourniquettestrevealednumerouspetechiae.The diagnosisofdenguewassuspectedandsubsequentlyconfirmed.
Discussion: Dengueisoneofmanyviralillnessesthatshouldbeconsideredinreturningtravelers presentingwithfeverandothernonspecificsymptoms.Emergencyphysiciansmustkeepabroad differentialwhenevaluatingfeverinreturnedtravelersandprioritizehistoryandphysicalexam findingsto helpnarrowthediagnosisandprovideappropriatemanagementandsupportivecarewhileawaiting furtherconfirmatorytesting.[ClinPractCasesEmergMed.2024;8(2)179–181.]
Keywords: feverinreturnedtraveler;tropicalmedicine;dengue.
A21-year-old,otherwisehealthyfemalepresentedtothe emergencydepartment(ED)withfeverafterrecently returningfromGhana.Shereportedintermittentfever, headachewithphotophobia,diarrhea,jointpains,and generalizedweakness.Shealsonoticedadiffuse, intermittentlypruriticrash.WhileinGhana,shevolunteered atarefugeehospital,atelocalstreetfood,andhadexposure tolocalanimalsincludingdogs,sheep,andamonkey.
OnarrivaltotheED,shehadatemperatureof39.4° Celsiusandwastachycardicat126beatsperminute.Her othervitalsignswerewithinnormallimits.Physicalexam revealedanuncomfortable-appearingfemalewitha maculopapularrashtotheextremitiesandchest,confluent erythemanotedinsomeareas(Image1),andscattered papuleswithsomesurroundingexcoriationaroundthe ankles,whichthepatientstatedweremosquitobites.Initial labresultsrevealedmildlyelevatedtransaminaseswith alaninetransaminase58unitsperliter(U/L)(referencerange 7–52U/L),aspartateaminotransferase42U/L(12–39U/L), thrombocytopeniawithplatelets125.3 × 103 percubic millimeter(mm3)(150–400 × 103/mm3),andleukopeniawith whitebloodcells2.78 × 103/cmm(4–11 × 103/mm3).
Abedsidetourniquettest1 wasperformed(Image2)toassess forcapillaryfragility.
Thepatientreceivedintravenous fluidsand acetaminophenforfeverandwasstartedonempiricoral doxycyclinetocoverfortick-relatedillnesspriorto admissionforobservation.Herlabsremainedstable,andher symptoms,includingfever,improvedduringher36-hour hospitalstay.Approximatelyoneweekafterdischargefrom thehospital,boththedenguefevervirusantibodies immunoglobulinGandMresultedpositive.
Dengueisanacuteviralfebrileillnesstransmittedbythe Aedesaegypti mosquito.2 ItisendemictoSoutheastAsia, LatinAmerica,andAfrica.2 WithintheUnitedStates,it remainsanuncommondiagnosis,with814documented casesreportedin2021.3 Denguecommonlypresentswith nonspecificsymptomsincludingfever,headache,vomiting, transientmacularrash,myalgiasandarthralgias.2 This nonspecificpresentationmimicsotherviral,bacterial,and parasiticillnesses,makingitdifficulttodiagnosein theacutesetting.Forexample,chikungunyasymptomscan mirrorthoseofdenguewithfever,rash,andmyalgias.4

Image1. Rashonupperextremitywithcharacteristicconfluent erythemaandsmallareasofsparedskin(arrow).
Malariaisalsomosquito-borneandcanpresentwithfever andthrombocytopenia.4
Focusingonspecificdetailsincludingregion(s)visited, timingoffeverrelativetoincubationperiod,exposures encountered,symptomsexperienced,physicalexam findings, andlabresultscannarrowdownthepathogen.4 Detectionof denguevirusantigensremainsthediagnosticgoldstandard; however,thisrequirestimeandspecializedequipment.5 Therefore,emergencyphysiciansmustkeepabroad differentialwhenevaluatingfeverinreturnedtravelersand prioritizehistoryandphysicalexam findingstohelpnarrow

Image2. Appreciablepetechiaevisibleintheantecubitalfossa afterinflatingabloodpressurecuffaroundtheupperarmfor five minutesatapressurehalfwaybetweenthepatient’ssystolicand diastolicbloodpressure.This “tourniquettest” isdeemedpositive ifmorethan10petechiaearepresentwithinasquareinchofskin, suggestingcapillaryfragility.1
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Anacuteviralfebrileillnesstransmittedby mosquito,dengueisendemictoSoutheast Asia,LatinAmerica,andAfrica.
Whatmakesthispresentationof diseasereportable?
Thisnonspeci fi cpresentationoffeverandrash illustratesthechallengeofdiagnosing mosquito-borneviruses.
Whatisthemajorimpactoftheimage?
A “ tourniquettest ” revealingpetechiae helpednarrowthediagnosis.
Howmightthisimproveemergency medicinepractice?
Itisnecessarytokeepabroaddifferential whenevaluatingfeverinreturnedtravelers andtoprioritizehistoryandphysical exam fi ndings.
thediagnosisandprovideappropriatemanagementwhile awaitingconfirmatorytesting.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ErinF.Shufflebarger,MD,University ofAlabamaBirminghamHeersinkSchoolofMedicine,Department ofEmergencyMedicine,GSBSuite203,52119th StreetSouth, Birmingham,AL35233.Email: erinshufflebarger@uabmc.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Konsetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GrandeAJ,ReidH,ThomasE,etal.Tourniquettestfor denguediagnosis:systematicreviewandmeta-analysis ofdiagnostictestaccuracy. PLoSNeglTropDis. 2016;10(8):e0004888.
2.WorldHealthOrganization.Dengueandseveredengue.2023. Availableat: https://www.who.int/en/news-room/fact-sheets/detail/ dengue-and-severe-dengue.AccessedSeptember29,2023.
3.CentersforDiseaseControlandPrevention.Dengue:historicdata (2010–2022).2022.Availableat: https://www.cdc.gov/dengue/ statistics-maps/2020.html.AccessedAugust1,2023.
4.ThwaitesGEandDayN.Approachtofeverinthereturningtraveler. NEnglJMed. 2017;376(6):548–60.
5.YowKS,AikJ,TanEY,etal.Rapiddiagnostictestsforthedetectionof recentdengueinfections:anevaluationofsixkitsonclinicalspecimens. PLoSOne. 2021;16(4):e0249602.