Volume 8, Number 3, August 2024



Volume 8, Number 3, August 2024
Clinicopathological Cases from the University of Maryland
182 A 77-Year-Old Male with a Rapid Change in Mental Status
Andrew Piner, Spencer S. Lovegrove, Laura J. Bontempo, T. Andrew Windsor
Case Reports
189 Pneumothorax Identified by a Remote Physician Using Paramedic-obtained Tele-ultrasound: Case Report
Shriman Balasubramanian, Michael DeFilippo, Michael Stone, Gabriela Galli, Matthew McCarty, Brock Daniels
194 Renal Artery Aneurysm Rupture as a Dangerous Mimic of Ovarian Cyst Rupture: A Case Report
Lauren Kaplan, Kaushal H. Shah, Christie Lech, Mary-Kate Gorlick
197 Capnocytophaga ochracea Septicemia After a Dog Bite: The Case of a Usual Suspect Transmitting an Unusual Organism
Clifford Chang, Vakula Atthota, Madison Lord, Michael P. Bonk, Muhammad Durrani
202 High-altitude Cerebral Edema and High-altitude Pulmonary Edema Diagnosed in the Desert: A Case Report
Bryn Walsh, Suneil Agrawal
206 Acute Confusional Migraines: A Case Report
Devin M. Howell, Garrett Lamouree
211 Spontaneous Osteomyelitis and Intraosseous Abscess: A Case Report
Meghan Chamberlain, Simon A. Sarkisian
215 A Case Report of Wünderlich Syndrome Causing Massive Hemorrhage During Hemodialysis
Karalee Bluhm, Ravali Kundeti, Nicole Maguire



Contents continued on page iii















Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital, and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Penn State Health Lancaster Pediatric Center in Lancaster, Pa.; Penn State Health Lancaster Medical Center (opening fall 2022); and more than 3,000 physicians and direct care providers at more than 126 outpatient practices in 94 locations. Additionally, the system jointly operates various health care providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center, Hershey Endoscopy Center, Horizon Home Healthcare and the Pennsylvania Psychiatric Institute.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pa.


Indexed in PubMed and full text in PubMed Central
Rick A. McPheeters, DO, Editor-in-Chief
R. Gentry Wilkerson, MD, Deputy Editor University of Maryland School of Medicine
Mark I. Langdorf, MD, MHPE, Senior Associate Editor University of California, Irvine School of Medicine- Irvine, California
University of California, Irvine School of Medicine- Irvine, California
Shadi Lahham, MD, MS, Associate Editor Kaiser Permanente- Orange County, California
John Ashurst, DO, Decision Editor/ ACOEP Guest Editor Kingman Regional Health Network, Arizona
Anna McFarlin, MD, Decision Editor Louisiana State University Health Science Center- New Orleans, Louisiana
Lev Libet, MD, Decision Editor
Amin A. Kazzi, MD, MAAEM
The American University of Beirut, Beirut, Lebanon
BarryE. Brenner, MD, MPH Case Western Reserve University
Brent King, MD, MMM University of Texas, Houston
Daniel J. Dire, MD University of Texas Health Sciences Center SanAntonio
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Erik D. Barton, MD, MBA Icahn School of Medicine, Mount Sinai,
New York
Amal Khalil, MBA
Christopher Sampson, MD, Decision Editor University of Missouri- Columbia, Missouri
Joel Moll, MD, Decision Editor
Virginia Commonwealth University School of Medicine- Richmond, Virginia
Steven Walsh, MD, Decision Editor Einstein Medical Center Philadelphia-Philadelphia, Pennsylvania
University of Indiana School of Medicine- Indianapolis, Indiana
Austin Smith, MD, Decision Editor Vanderbilt University Medical Center-Nashville, Tennessee
Rachel A. Lindor, MD, JD, Decision Editor Mayo Clinic College of Medicine and Science
Jacqueline K. Le, MD, Decision Editor Desert Regional Medical Center
Christopher San Miguel, MD, Decision Editor Ohio State Univesity Wexner Medical Center
Francesco Dellacorte, MD
Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Gayle Galleta, MD
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Niels K. Rathlev, MD Tufts University School of Medicine
UC Irvine Health School of Medicine
Elena Lopez-Gusman, JD
California ACEP
American College of Emergency Physicians
DeAnna McNett, CAE
American College of Osteopathic Emergency Physicians
John B. Christensen, MD
California Chapter Division of AAEM
Randy Young, MD
California ACEP
American College of Emergency Physicians
Mark I. Langdorf, MD, MHPE
UC Irvine Health School of Medicine

Jorge Fernandez, MD
California ACEP
American College of Emergency Physicians
University of California, San Diego
Peter A. Bell, DO, MBA
American College of Osteopathic Emergency Physicians
Baptist Health Science University
Robert Suter, DO, MHA
American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
UC Irvine Health School of Medicine
Brian Potts, MD, MBA
California Chapter Division of AAEM Alta Bates Summit-Berkeley Campus

PabloAguilera Fuenzalida, MD
Región Metropolitana, Chile
PeterA.Bell, DO,MBA Baptist Health Science University
Peter Sokolove, MD University ofCalifornia, San Francisco
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Scott Rudkin, MD, MBA University of California, Irvine
Scott Zeller, MD University of California, Riverside
Isabelle Nepomuceno, BS Executive Editorial Director
Visha Bajaria, BS CPC-EM Editorial Director
Emily Kane, MA CPC-EM Editorial Director
Stephanie Burmeister, MLIS
CPC-EM Staff Liaison
Clinical Forensic Medicine
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Vijay Gautam, MBBS University of London, London, England
Wirachin Hoonpongsimanont, MD, MSBATS Siriraj Hospital, Mahidol University, Bangkok, Thailand
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA CPC-EM Publishing Director
June Casey, BA Copy Editor

Available in MEDLINE, PubMed, PubMed Central, Google Scholar, eScholarship, DOAJ, and OASPA WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA the American Academy of Emergency Medicine

This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians California ACEP
Academic Department of Emergency Medicine Subscribers
Albany Medical College Albany, NY
American University of Beirut Beirut, Lebanon
Arrowhead Regional Medical Center Colton, CA
Augusta University Augusta GA
Baystate Medical Center Springfield, MA
Beaumont Hospital
Royal Oak, MI
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Conemaugh Memorial Medical Center Johnstown, PA
Desert Regional Medical Center Palm Springs, CA
Doctors Hospital/Ohio Health Columbus, OH
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Emory University Atlanta, GA
Genesys Regional Medical Center Grand Blanc, Michigan
Hartford Hospital Hartford, CT
Hennepin County Medical Center Minneapolis, MN
Henry Ford Hospital Detroit, MI
Arizona
INTEGRIS Health
Oklahoma City, OK
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kern Medical Bakersfield, CA
Lakeland HealthCare
St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maricopa Medical Center Phoenix, AZ
Massachusetts General Hospital Boston, MA
Mayo Clinic College of Medicine Rochester, MN
Mt. Sinai Medical Center Miami Beach, FL
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Presence Resurrection Medical Center Chicago, IL
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
Southern Illinois University Carbondale, IL
St. Luke’s University Health Network Bethlehem, PA
Stanford/Kaiser Emergency Medicine Residency Program Stanford, CA
Staten Island University Hospital Staten Island, NY
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
University of Alabama, Birmingham Birmingham, AL
University of Arkansas for Medical Sciences Little Rock, AR
University of California, Davis Medical Center Sacramento, CA
University of California Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago, Chicago, IL
University of Colorado, Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
University of Illinois at Chicago Chicago, IL
University of Illinois College of Medicine Peoria, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of Nebraska Medical Center Omaha, NE
University of South Alabama Mobile, AL
University of Southern California/Keck School of Medicine Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Texas Health San Antonio, TX
University of Warwick Library Coventry, United Kingdom
University of Washington Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
Wake Forest University Winston-Salem, NC
Wright State University Dayton, OH
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
MediterraneanAcademyofEmergencyMedicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Sociedad Chileno Medicina Urgencia ThaiAssociationforEmergencyMedicine
To become a WestJEM departmental sponsor, waive article processing fee, receive print and copies for all faculty and electronic for faculty/residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Indexed in PubMed and full text in PubMed Central
Clinical Practice and Cases in Emergency Medicine (CPC-EM) is a MEDLINE-indexed internationally recognized journal affiliated with the Western Journal of Emergency Medicine (WestJEM). It offers the latest in patient care case reports, images in the field of emergency medicine and state of the art clinicopathological and medicolegal cases. CPC-EM is fully open-access, peer reviewed, well indexed and available anywhere with an internet connection. CPC-EM encourages submissions from junior authors, established faculty, and residents of established and developing emergency medicine programs throughout the world.
219 A Case Report of Crotalidae Immune F(ab’)2-associated Coagulopathy Recurrence in a Preschool-age Child
Jean C.Y. Lo, E. Lea Walters, Brian Wolk
222 A Case Report of Delayed Opioid Toxidrome After Administration of Naloxone Maiya Cowan, Prasanna Kumar, Jenny McManus, Sean Bilodeau, Andrew Beck
226 Testicular Traction Technique with Intact Cremasteric Reflex, a Novel Approach for Manual Detorsion: Case Report
Garrett Trang, Taz Brinkerhoff
231 A Case Report of Hematogenous Osteomyelitis of the Manubrium Caused by Seeding from a Colovesicular Fistula Celina Wong, Tammy Phan, Emmelyn Samones, Sharmin Kalam
235 Ultrasound-guided Supraclavicular Brachial Plexus Block for Therapeutic Management of Postoperative Compressive Brachial Plexus Neuropathy: A Case Report
Daniela Usuga, Sofia Portuondo, David Farcy, Michael Shalaby
239 Neurogenic Pulmonary Edema Associated with Hyponatremia, Primary Polydipsia, and Cannabis Use: A Case Report
Christian Treat, Nicholas Ulloa, Alyssa Kettler, David Lawrence
243 Spontaneous Intracranial Hypotension Associated with Marfan Syndrome: A Case Report
Faiza Tariq, Wesley Eilbert
246 Atrial Fibrillation Occurring After Smoking Marijuana: A Case Report and Review of the Literature
Mary Unanyan, Christopher Colbert, Wesley Eilbert
250 ST-Elevation Myocardial Infarction Due to Coronary Vasospasm Associated with Eosinophilic Granulomatosis with Polyangiitis: A Case Report
Christopher Allen, Christopher Poyorena, Lauren B. Querin
254 Point-of-Care Ultrasound Findings in Occlusive Iliac Vein Thrombus During Pregnancy: A Case Report Donald Pettet III, John Forrester, Mathew Nelson, Tanya Bajaj
259 Rectus Sheath Blocks for Umbilical Hernia Reductions in the Emergency Department: A Case Series Katherine Vlasica, Amanda Hall
264 Angioedema Secondary to Tenecteplase Use in a Patient with Acute Ischemic Stroke: A Case Report Babette Newman, Matthew Poremba, R. Gentry Wilkerson
268 Tension Pyopneumothorax in an Immunocompetent Adolescent: A Case Report
Elizabeth May-Smith, Marc Olshan, Mark Supino
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
No. 3: August 2024
Indexed in PubMed and full text in PubMed Central
Clinical Practice and Cases in Emergency Medicine (CPC-EM) is a MEDLINE-indexed internationally recognized journal affiliated with the Western Journal of Emergency Medicine (WestJEM). It offers the latest in patient care case reports, images in the field of emergency medicine and state of the art clinicopathological and medicolegal cases. CPC-EM is fully open-access, peer reviewed, well indexed and available anywhere with an internet connection. CPC-EM encourages submissions from junior authors, established faculty, and residents of established and developing emergency medicine programs throughout the world.
273 Community-Acquired Candida albicans Empyema Leading to Tension Physiology: A Case Report
Jason Cinti, Paula Gomez, Suneil Agrawal
277 “K Cramps,” Recurrent Abdominal Pain in a Patient with Chronic Ketamine Use: A Case Report
Tucker Avra, Jesus Torres, Kumar Felipe Vasudevan, Elizabeth A. Samuels
282 Pupil Unleashed: Unraveling the Enigma of an Unusual Traumatic Head Injury: A Case Report
Akash Daswaney, Shuchi Abhishek, Sanjan Asanaru Kunju, Priya Pattath Sankaran, Ahlam Abdul Rahman
287 Spontaneous Hemothorax from Pulmonary Intralobar Sequestration: A Case Report
Clayton Korson, Jasmine Yu, John M. Pester
291 Median Nerve Measurement and Steroid Injection for Carpal Tunnel Syndrome: A Case Report
Gregory Oliva, Joseph McShannic, Yonghoon Lee, Michael Shalaby
Images in Emergency Medicine
295 Bezold Abscess in a Case of Eosinophilic Otitis Media
Satoshi Tsuruta, Takashi Fujiwara
298 Point-of-care Ultrasound Diagnosed Intraocular Breast Metastasis
Hamzah M. Yusuf, Timothy Batchelor, Nicholas Ashenburg
300 Spinal Arachnoid Web
Maiya Smith, Morgan Ketterling, Alexander Gallaer, Rowan Kelner, Christine Raps, Allison M. Beaulieu
302 A Woman with Right Shoulder Pain
Kitan Akinosho, William Weber
305 Point-of-Care Ultrasound for Earlier Detection of Pediatric Pneumonia
John H. Priester, Prasanna Kumar, Jesse Naumann, Katherine Dolbec, Peter Weimersheimer, Christian D. Pulcini
308 Painful Enlarging Cervical Mass in Young Male
Jacob Lawing, Jeremy Towns, Matthew A. Heimann
311 Atraumatic Infected Septal Hematoma in a Pediatric Patient
Osher Shefer, Jacqueline Le, Eshaan Daas, Eugene Hu
314 Brugada Syndrome and Sudden Cardiac Death: An Electrocardiographic History
Mark L. Moubarek, Gordon X. Wong, James S. Ford
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.



AndrewPiner,MD* SpencerS.Lovegrove,MD†
LauraJ.Bontempo,MD,MEd†
T.AndrewWindsor,MD†
SectionEditor:JoelMoll,MD
*UniversityofMarylandMedicalCenter,Baltimore,Maryland † UniversityofMarylandSchoolofMedicine,DepartmentofEmergencyMedicine, Baltimore,Maryland
Submissionhistory:SubmittedJanuary17,2024;RevisionreceivedMarch25,2024;AcceptedApril4,2024
ElectronicallypublishedJune14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7213
A77-year-oldmalewhopresentedtotheemergencydepartmentwithgeneralizedweaknessand worseningchronicdysphagiawasdiagnosedwithpneumonia.Shortlyafterreceivingvascularaccessfor histreatment,hehadarapidchangeinhismentalstatusandneurologicalexamination.[ClinPract CasesEmergMed.2024;8(3)182–188.]
Keywords: airembolism;stroke;CPC.
A77-year-oldmalepresentedtotheemergency department(ED)forgeneralizedweaknessaswellas worseningchronicdysphagia.Hewasaccompaniedbyhis wife,whoassistedinprovidingthehistory.Hispastmedical historyincludeddiabetes,hypothyroidism,athyroidgoiter, rightinternaljugular(IJ)thrombusforwhichhewastaking anticoagulation,andcirrhosis.Hissurgicalhistorywas significantforremotebilateralpercutaneousnephrostomy tubeplacement,yearsprior.Threeweeksprecedingthis hospitalvisit,hehadbeenadmittedanddischargedfromthe samehospitalafterreceivingathoracentesiswithdrainageof asimpletransudativepleuraleffusion.Thisincompletely relievedhishypoxia,andhewasdischargedonthreelitersper minute(L/min)ofoxygenvianasalcannula.
Sincereturninghome,thepatientthoughthisbreathing hadslightlyimproved,buthehaddifficultycompletinghis dailyactivities.Hehadapoorappetiteandwhenhedideat, heexperienceddysphagiafromhisgoiter,whichhefeltwas gettingworse.Hereportedgeneralmalaiseandchills.Hedid notfeelshortofbreathonexertion,ashehadduringhislast hospitalization,andhewasnotexperiencinganychest discomfort.Hedeniedanynausea,vomiting,constipation, diarrhea,dysuria,orurinarychanges.Hewasableto ambulatebuthaddifficultydoingsoduetohisweakness.
Thepatientwasrecoveringfromalcoholusedisorderand deniedhavinganyalcoholicdrinksinmultipleyears.Hehad aremote, fivepack-yeartobaccohistorybutdidnotsmoke anylonger.Hedeniedanyuseofillicitdrugs.Hiswife
oversawhismedications,whichhadnotchangedsincehis hospitaldischarge.Hetookmetoprolol,spironolactone, levothyroxine,andapixaban.Hehadnoknown drugallergies.
Thepatient’svitalsignsrevealedanoraltemperatureof 100.4° Fahrenheit(38° Celsius),heartrateof90beatsper minute,abloodpressureof90/40millimetersofmercury (mmHg),arespiratoryrateof15breathsperminute,andhis oxygensaturationwas94%on3L/minvianasalcannula.He weighed64kilograms(142pounds)andwas170centimeters tall(5feet7inches)withabodymassindexof22.1.
Onphysicalexamination,thepatientwasalertand orientedtoperson,place,time,andevents.Hewasableto speakinfullsentenceswithoutdyspnea.Hedidnotappearin acutedistress.Hehadevidenceofalargegoiteranddenied tendernessorthesensationofitexpandingorchanging.His breathsoundswerediminishedattherightlowerbasewith scatteredrhonchiandanoccasionalcough.Hisheartsounds wereregularwithoutmurmurs,rubs,orgallops.His abdomenwaslarge,protuberant,andhadasoft fluidwave thatcouldbeappreciated.Itwasnotincreasedinsizeperhis wife.Therewasnoguardingortenderness.Hehadtrace pedaledemawithoutlateralizingswelling.Hemovedall extremitieswithoutlocalizingweakness.Althoughhe reportedweakness,hisstrengthwas5/5symmetricallyinhis upperandlowerextremities.Hiscranialnerves(CN)II–XII wereintact.HisGlasgowComaScale(GCS)scorewas 15/15 – Eye4,Verbal5,Motor6.Hispupilswereequal, round,andreactivetolight.Hewasnotambulatedinthe
Table. Initiallaboratoryresultsofa77-year-oldmanwitharapid changeinmentalstatus.
Completemetabolicpanel
–99mg/dL
–17mg/dL
–1.04mg/dL
–10.2mg/dL
1.51.6–2.6mg/dL
2.92.5–4.5mg/dL
–8.2g/dL
10.3–1.2mg/dL
Aspartateaminotransferase4614–36units/L
Alanineaminotransferase210–34units/L
Alkalinephosphatase 8238–126units/L
Coagulation
–38seconds
–400mg/dL
–4mIU/L
6.60.8–1.8ng/dL
Additionaltests
Lactate 1.70.5–2.2mmol/L Ammonia 99–30 mcmol/L TroponinI0.02 <0.06ng/mL
dL, deciliter; g,grams; K,thousands; mcL,microliter; mcmol, micromole; mg,milligram; mIU,milli-internationalunits; mmol, millimole; ng,nanogram; L,liter.
Whatdowealreadyknowaboutthis clinicalentity?
Airembolismisararebutpotentiallylifethreateningcomplicationofvarious procedures,includingcentrallineplacement.
Whatmakesthispresentationof diseasereportable?
Thispatientexperiencedacerebralair embolismbutdidnothaveapatentforamen ovale,andtheairembolismremainedwithin thevenoussystem.
Whatisthemajorlearningpoint?
Althoughrare,cliniciansshouldconsiderair embolismforapatientwhohasanunexpected declineintheirconditionshortlyafteran intravascularprocedure.
Howmightthisimproveemergency medicinepractice?
Thiscasediscussestre atmentofthisserious condition,includingbedsidetreatmentand hyperbaricoxygentherapy.
roombuthadbeenseenearliermovingfromahospital wheelchairtothestretcherwithassistance.Therewasnoskin rashorjointswelling.
Initiallaboratoryresultsareshownin Table.An electrocardiogram(ECG)wasperformedandshowedasinus rhythmwithoutectopyorST-segmentchangesandwas unchangedfromhisprevioushospitalization.Chest radiography(CXR)wasobtained,shownin Image1.The radiologist’sinterpretationwas “[p]atchyopacityintheright lowerlobesuggestiveofpneumoniainthecorrectclinical setting.Goiterredemonstratedwhencomparedtoprevious. Normalcardiac findings.” Apoint-of-careultrasound (POCUS)oftheheartshowednopericardialeffusion,no suggestionofrightventriclestrain,novolumeoverload,and anormalleftventricle.
Beforetreatmentforpneumoniacouldbestarted,the nursealertedthephysiciantothelossofvascularaccess. Therewerenoreliableperipheralveinsseenviaultrasound; so,centralaccesswasobtainedintheleftIJveinvia ultrasoundguidancewhilethepatientwasinasemi-reclined position.Thewirewasconfirmedintheveinandremoved. Thephysicianinstilledabolusofagitatednormalsaline, confirmingthecentralaccesswasinthevenoussystemby PopulationHealthResearchCapsule
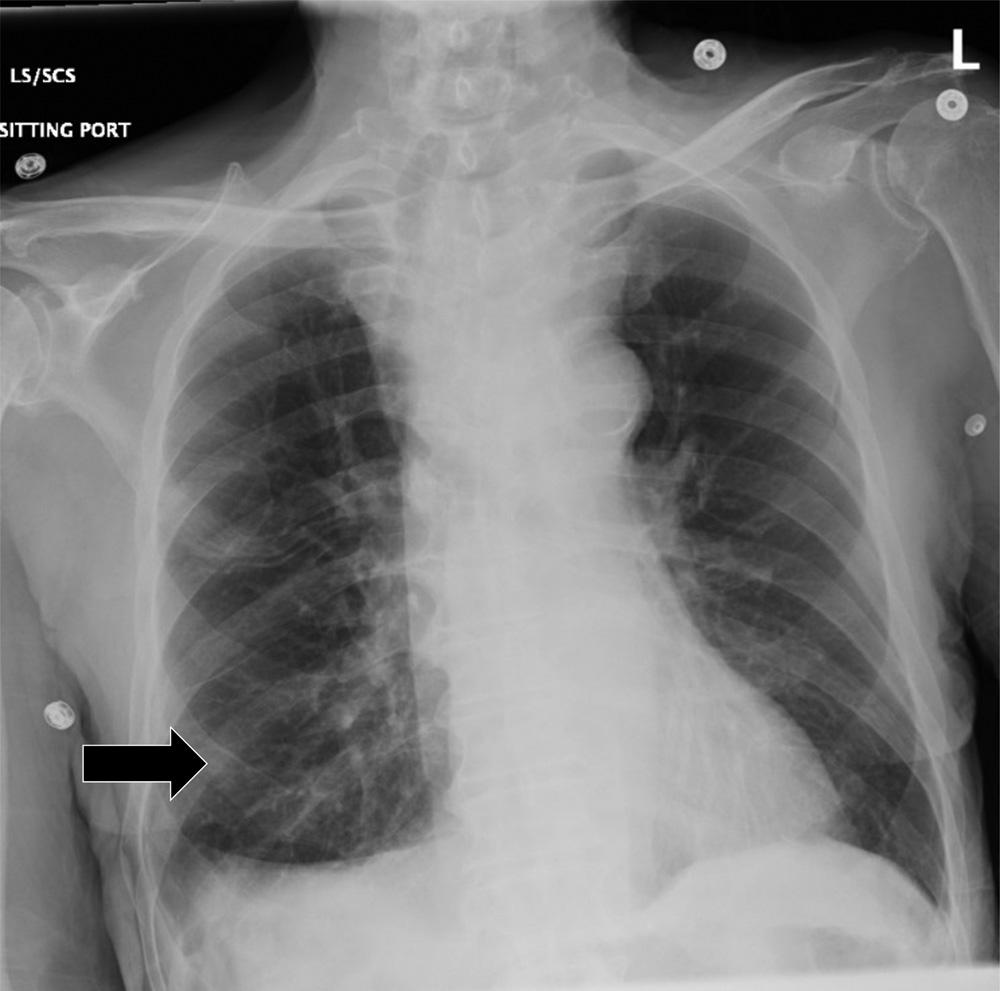
Image1. Initialchestradiographshowinganopacityintheright midlung(blackarrow)ina77-year-oldmanbeforeheexperienced arapidchangeinmentalstatus.
visualizingturbulent flowintherightatriumwithPOCUS. Thelinewassuturedanddressed.
Fifteenminuteslater,thephysicianwascalledtotheroom asthepatient’soxygenrequirementincreasedandhewasless responsive.Repeatphysicalexaminationrevealednew tachycardiawithameanarterialpressureof59mmHg.The patient’srespiratoryratewas20,andhisoxygensaturation remained94%on15L/minviaanon-rebreathermask. RepeatPOCUSshowedunchangedcardiacfunctionandno evidenceofpneumothorax.Thepatientwasunabletofollow commands,hiseyesopenedonlytopain,andhemuttered incomprehensiblewords.Hewasnotedtowithdrawtopain ontherightarmandleg,theleftarmwas flaccid,andtheleft legwas flexed.HisnewGCSwas8/15 – Eye2,Verbal2, Motor4.Hislefteyewasmidline,buthisrighteyewasnoted todeviatelaterallyandinferiorly.
Thepatientwasintubated,andaconfirmatoryCXR demonstratedintervalchangesofanewleftIJcentralline catheterandanendotrachealtubethatbothappeared adequatelypositionedasseenin Image2.
Atestwasperformed,andadiagnosiswasmade.
Thisisacaseofanelderlygentlemanwhoacutely decompensatedintheEDafterinitiallypresentingdueto worseningweaknessanddysphagia.Whenthereisapatient whoacutelydecompensatesintheED,asthispatientdid,itis importanttoconsiderwhetherthiswastheresultofthe
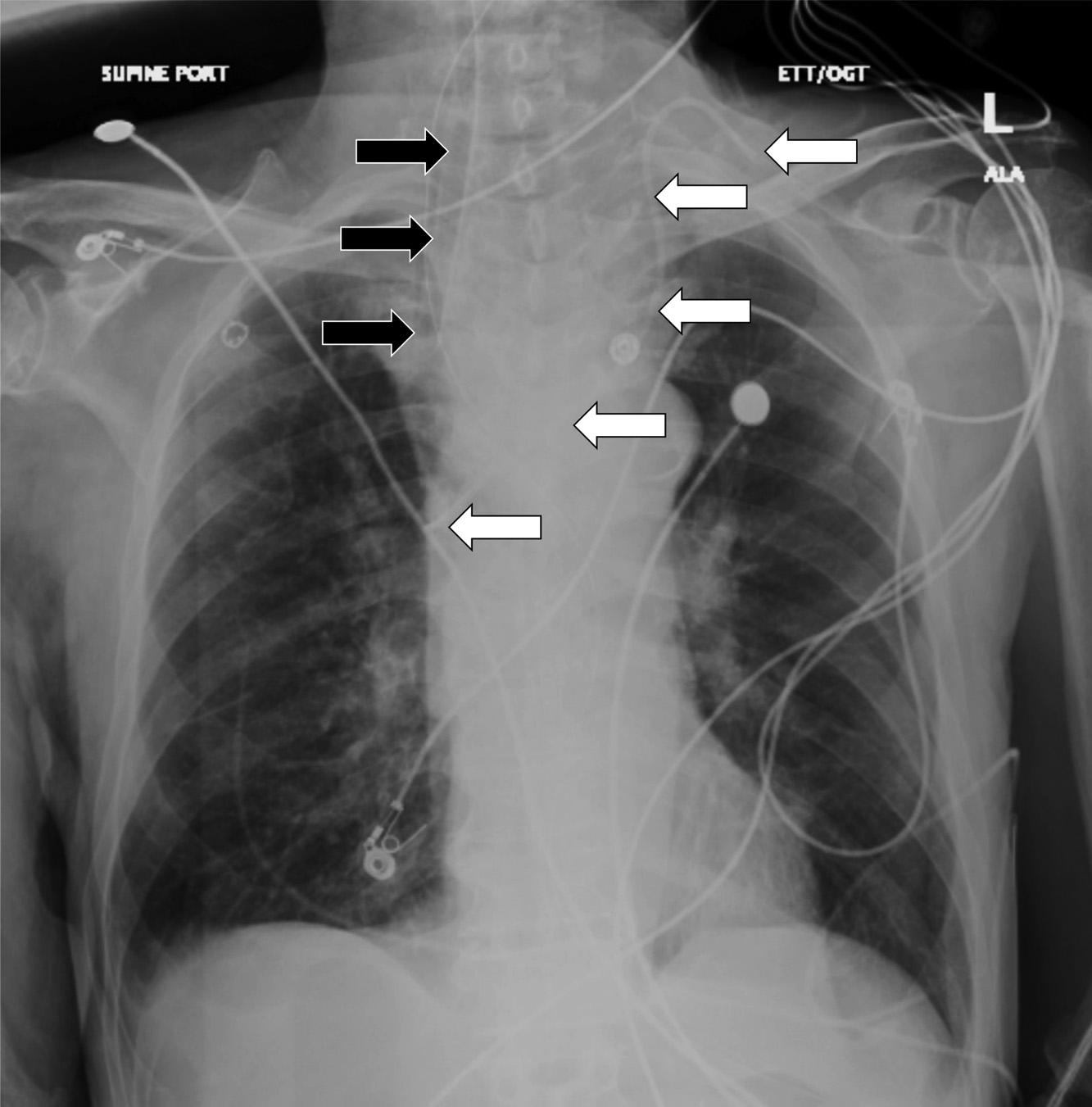
Repeatchestradiographofa77-year-oldmanaftera rapidchangeinmentalstatusshowingtheplacementofan endotrachealtube(blackarrows)andleftinternaljugularcentral line(whitearrows).
patient’snaturaldiseasecourse,somethingthathappenedin theED(iatrogenic),orevenalittlebitofboth.
Thepatient’sinitialcomplaintisworseningdysphagiaas wellasweakness.Hehasanextensivemedicalhistorythat includesdiabetes,hypothyroidism,goiter,rightIJthrombus, andanticoagulantuse.Hisphysicalexamisnotablefor multipleabnormalitiesincludingfever,hypotension, abnormalbreathsoundsinhisrightlung,andascites.Itis alsoimportanttopointoutthathisneurologicexamis normal,includingfullstrengthinallextremities.
Lookingoverthelabsandimaging,Idonotbelievethey provideasignificantamountofnewinformationbutcouldbe usedtoremovesomedifferentials.Thepatient’schemistry hadsomeslightabnormalitiesbutnothingunexpectedgiven hiscomorbidities.Hiscoagulationstudieswereconsistent withsomeonewithcirrhosis.Thereweresomeabnormalities inhisthyroidfunctionpanel,butIdonotthinktheyexplain hisacutechange.Wealsodonotknowthetimingofhis levothyroxinedose,andhisthyroidstimulatinghormone indicatesthathehaslikelybeentakingit.Theetiologyof hematuriaisunclear,buthisurineisotherwisewithoutany signofinfection.Hiscompletebloodcountdoesshow leukocytosisaswellasmildanemia.Lastly,hisCXRis subtle,butanopacityintherightmidlung,asinterpretedby radiology,wouldbeconsistentwithhisabnormal breathsounds.
Basedoffthehistory,physicalexam,anddiagnostic studies,thepatient’sinitialpresentationwasconcerningfor
sepsis,potentiallyfrompneumoniaassociatedwith aspirationorduetospontaneousbacterialperitonitis(SBP). However,Idonotbelievetheseissuesalonewould necessarilyprogresstocausesuchanabruptchangeinmental statusandneurologicfunction.Washisdysphagiabeing causedsimplybymasseffectofhisgoiter,orwasitsomething else?Couldtherebeanotherunderlyingetiologythatwas exacerbatedbythepatient’ssepticstate?
Oncehedecompensated,hisexamchanged,andthe differentialexpanded.HenowhadaGCSof8withgaze deviationofhisrighteye “downandout” totheright,buthis leftpupilismidline.Healsohada flaccidleftarmandhisleft legremained flexed.Hisrightarmandlegwithdrewtopain.I consideredthefollowingdifferentials,groupedbycategory, basedoffhisinitialpresentationandchiefcomplaintaswell astheeventsofhisEDvisit,asitisunclearwhetherthey arerelated.
Autoimmune: Forapotentialautoimmunecause,Idid considerpotentiallyundiagnosedmyastheniagravis(MG). Hehadaknownhistoryofgoiterandthyroiddisease,which doeshaveanassociationwithdevelopingMG.Patientswith MGcanpresentwithasymmetricmuscleweaknessthat commonlyinvolvestheextraocularmuscles.Asymmetric presentationscanmimicastroke.Perhapshisworsening dysphagiaandweaknesswerebeingcausedbyMG, andherapidlydeterioratedintheEDduetohissepsis. Hemayhavehadunrecognizedrespiratorymuscle compromiseandmayhavebecomehypercapnic,causinghis alteredmentalstatus.Thisisunlikelysincehehadno evidenceofanyweaknessonhisinitialexam,butitcould notreadilyberuledoutbytheresultsIwasgiven,soIkeptit onthedifferential.
Infectious: Aswediscussedearlier,itispossiblethathe haspneumoniaorSBP;however,Idonotthinktheywould causethesefocalneurologicabnormalities.Hisblood pressureisonthelowerend,potentiallyduetosepsis,butIdo notbelievehewouldhavesufferedawatershedinfarct causingthesespecificabnormalities.Similarly,Iconsidered meningitisorencephalitisduetohisfeverandalteredmental status,butagainIdonotthinktheyexplainhisrapid deteriorationandfocaldeficits.Healsodidnotcomplainof anyneckpainorheadachepriortohisdecompensation.
Cardiac: Arrythmiaisalwaysapotentialcauseofacute decompensation.Iwouldhavelovedtohaveseenarepeat ECGorrhythmstripatthetimeofdecompensation,but therewasnomentionofhimbeingparticularlytachycardic orbradycardicwithhisrepeatvitals,soIfeelthisisunlikely. Iconsideredthepossibilityofacuteheartfailureorcardiac tamponadecausinghypotensionandsubsequentpoor cerebralperfusionandalteredmentalstatus,butthepointof-careechocardiogramremainedessentiallynormal.
Pulmonary: Iconsideredpneumothoraxasa complicationofcentrallineplacementasacauseofthe acuterespiratorydecompensation;however,thiswasnot
seenonCXRafterplacement,anditshouldnotcausefocal neurologicdeficits.
Endocrine/metabolic: Hypoglycemiaandhyponatremia canbothcauseacutealteredmentalstatus;however,the patient’slabsshowednoevidenceofhyponatremiaor hypoglycemia,andthetreatmentshereceivedintheED shouldnothavecausedthem.Uremiaandhyperammonemia wereruledoutinhischemistrypanel.Iconsideredthyroid stormduetohisfeverandelevatedfreeT4;however,this patient’sT4ispresumablycomingfromhislevothyroxine. Withoutacutechangestohisregimenorsuspectedoverdose ofhismedications,Ifeltthiswasunlikely.
Toxicological: Thereisnohistoryofabnormalexposures. Hewasstartedonantibiotics,aswellasnorepinephrine. Someantibiotics,suchascefepime,canproduceneurologic abnormalitiessuchasseizures,butitwouldbeunlikelyto occurthisrapidlyafterinitialadministration.Healso presumablyreceivedlidocaineaspartofhiscentralline placement.Lidocainetoxicitycancausealteredmentalstatus andseizure.Often,whenadministeredaspartofcentralline placement,about5–10milliliters(mL)of1%lidocaineis used, andprecautionsaretakentoavoidvascular injection.Thisdosageshouldnotbehighenoughtocause acutelidocainetoxicity.
Hematologic: Ididconsiderthrombotic thrombocytopenicpurpura(TTP)asapotentialcause. InfectioncanpromptthedevelopmentofTTPandcould potentiallyexplainthepatient’sneurologicdeficits hematuriaandproteinuria.However,Ieliminatedthisfrom thedifferentialashehadonlymildanemiaandnosignificant thrombocytopeniaorevidenceofrenalfailure.
Neurologic: Thepatient’sacuteabnormalitiesthat developedintheEDwereprimarilyneurologic,whichmeans thisistheorgansystemIconsideredthemostheavily.The newphysicalexamisinterestingbecauseclassicallyina hemisphericstrokethereisconjugategazedeviation,with botheyeslookingtowardthelesion.Inseizure,theconjugate gazedeviationisclassicallyawayfromthelesion.The disconjugategaze,aswellastheleftarmweaknessinvolving theoppositesideasthegazedeviation,ledmeawayfroma largehemisphericischemicorhemorrhagicstroke.While consideringdiagnosesthatcouldcauseunilateralgaze deviation,Iagainconsideredmuscularweaknessbeing causedbyadisorderattheneuromuscularjunction,suchas MG;however,Ialsoconsideredischemicorcompressive lesionstoCNIII.Cavernoussinusthrombosishasbeen knowntocauseisolatedcranialnervepalsies,includingCN III,IV,V,andVI.Thispatientdidhaveahistoryof thrombosiswithapreviousIJthrombus,buthewascurrently takingananticoagulantandhadnotbeencomplaining ofheadache.
Thepatient’ssymptomswerefairlyconsistentwitha strokeinthemidbrainandWebersyndrome,whichis describedashavinganipsilateralCNIIIpalsywith
contralateralhemiplegia.However,thosepatientsgenerally havearelativelynormalmentalstatus,whereasourpatient hadaGCSof8.Itcouldbepossiblethathehadmultiple areasofinfarctordiseasethataremakingitdifficultto pinpointtheexactlocationofhislesionorlesions.
Afterconsideringthesedifferentialsandtheresultsthat wereavailable,Iultimatelynarrowedthedifferentialdown tothree finaldiagnoses.Anundiagnosedneuromuscular junctiondisorder,suchasMG,wouldpotentiallyexplainhis multipledeficitsandincorporatehisoriginalchiefcomplaint. Mylasttwodifferentialsaresimilarinthattheyareboth iatrogenicandrelatedtohiscentrallineplacementinvolving differenttypesofemboli.Hedecompensatedshortlyafterthe placementoftheline;so,apotentialiatrogeniccauseneeded heavyconsideration.
HehadaknownhistoryofpriorrightIJthrombus;so, perhapsacentrallinewasplacedthroughanew, undiagnosedleft-sidedIJthrombusandcausedashowerof embolicthrombi.However,forthistohavecausedastroke insteadofapulmonaryembolism,hewouldhavealsoneeded tohaveapatentforamenovaletoallowshuntingtothe arterialcirculation.Iftheclinicianusedultrasoundduring theplacementofthecentrallineandthepatienthasbeen takinghisanticoagulation,hopefullyplacementthrougha thrombuswouldhavebeenavoided.Thisright-to-left cardiacshuntingcouldalsohavebeendetectedduringthe bolusofagitatedsalinevisualizedforlineconfirmationon point-of-careechocardiogram,andtherewasnomention ofthis.
Formy finaldifferential,Iconsideredairembolism. Ashowerofairembolitothemidbrain,aswellasmultiple otherareasofthebrain,couldexplainhisfocalneurologic deficitsaswellashissuppressedmentalstatus.Thisisarare butpossiblecomplicationofcentrallineplacement,and retrogradevenous flowofairispossibleduetobuoyancyif thepatientisupright.Itwasnotedthatthepatientwassemireclinedduringplacement,ratherthaninthepreferable Trendelenburgposition,whichcanbeprotectiveagainstair embolus.Likeathrombus,airembolicouldalsobe transmittedtothearterialcirculationifthispatienthadan undiagnosedpatentforamenovale.
Ultimately,IdidnotchooseundiagnosedMGsincehis initialstrengthtestingwascompletelynormal.Withthe patientalreadytakinganticoagulation,anewthrombusis lesslikely;so,Ioptedtochooseairembolismasmy final diagnosisasitmakesthemostsensewiththetimingafter centrallineplacementandthemultipledifferentneurologic deficits.MytestofchoicefromtheEDwouldbecomputed tomography(CT)ofthehead.
ThepatientunderwentanemergentCTofthehead (Image3)duetothechangeinmentalstatus.Theradiology impressionoftheCTrevealed “extensivevenousgas,which
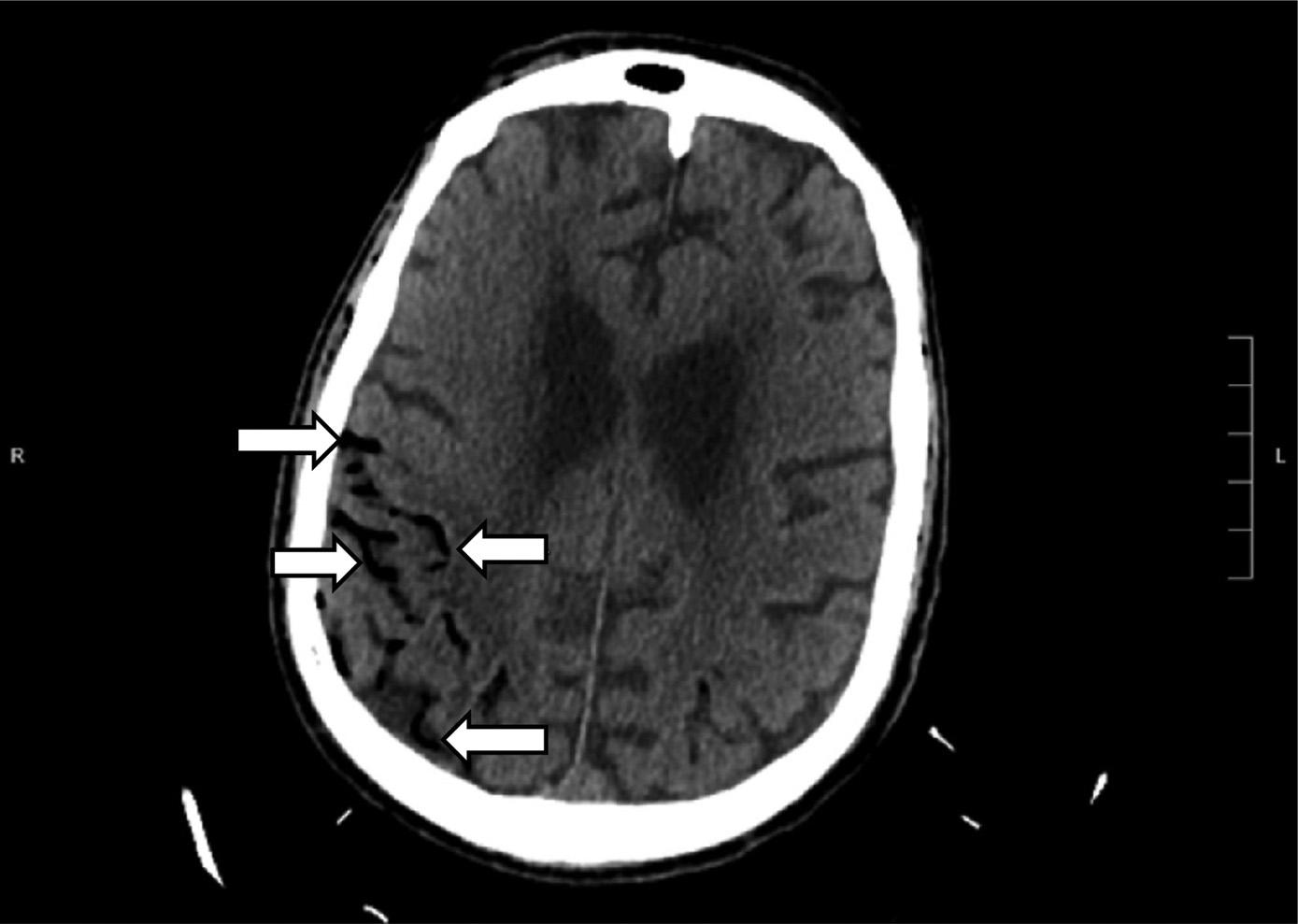
Computedtomographyofthebrainofa77-year-oldman afterarapidchangeinmentalstatusshowingextensivevenous gas(whitearrows)intherightparieto-occipitalregion.
mayindicategasemboluswithpossibleevolvinginfarctionin therightparietalregion.Nohemorrhageorshift.Further evaluationwithmagneticresonanceimaging[MRI]maybe useful.Largegoiter.” Immediatelytheteamassessedthe patient’scentralvenouscatheterandfoundanuncappedline. Aftertheairwaswithdrawnfromtheline,thelinewas capped.Thepatientwastransferredtotheintensivecareunit atourhospitalforfurthermanagementandahyperbaric medicineconsultation.Heunderwentahyperbaricoxygen therapytreatmentwithresolutionofthegasontherepeatCT head.Afollow-upMRIrevealedmultifocalinfarctsin multiplevascularterritories.
Inthefollowingdays,thepatient’smentalstatus unfortunatelyneverimproved.Palliativecarediscussions withthepatient’sfamilyindicatedthathewouldnotwantto haveanyfurtherartificialprolongationoflifewithoutany meaningfulneurologicfunctioning,andtheteam transitionedhiscaretocomfortmeasuresonly.Hewas transferredtohospicecareanddiedsurroundedby hisfamily.
Airembolismrepresentsararephenomenonwhenair enters eitherarterialorvenouscirculationwithsubsequent obstructionofthevasculature,preventingdistalblood flow. Theconditionrequiresthattherebeadirectconnection betweenthevasculatureandthegassource.Thiscanbedue tovasculartraumapromptinggasentryordirectentryfrom placementofanintravascularcatheter.Manyofthecasesof airembolisminvolveapreventableiatrogenicprocess, promptingtheCentersforMedicareandMedicaidServices atonepointtoclassifyitasa “neverevent” alongwithother preventableconditionssuchasfalls,retainedsurgicalobjects, andincompatiblebloodtransfusion.1
Therateofairembolismfollowingacentralline manipulation(insertion,drugdelivery,orremoval)is estimatedtobebetween0.3–2%.2 Consideringhow commonplacecentralaccessinsertionis,thiscouldinvolvea significantlevelofmorbidityandmortality.However,notall casesofairembolismareasdramaticorsymptomaticasin thiscase.Mostairemboliwillbeasymptomaticand unrecognized,astheirvolumeandrateofaccumulationmay beminiscule.Thelethaldosedependsonlocationofthe obstruction,volume,andrateofadministration,butlethal dosesrangebetween3–5milliliters(mL)perkilogramor about200–300mLinadults.3
Otheretiologiesofairembolismsinvolveblastinjuries, barotrauma,anddirectvasculartrauma.Surgeryhasbeen associatedwithairembolism,particularlyneurosurgery, wheretheincidenceofairembolismhasbeenreportedtobe higherwhenthepatientwasundergoinganopencraniotomy inaseatedorsemi-seatedposition.4
Thekeyforairembolismisprevention.Thisisparticularly importanttorememberwhenobtainingvascularaccess, manipulatingexistingcatheters,orotherhigh-risksurgical procedures.High-riskvascularaccessinvolveslarge-bore catheters,emergentplacement,accesssiteabovethelevelof theheart,andpressure-infused fluids(eg,arteriallineor rapidinfusionmachine).Carecanbetakentoproperly positionpatientswhenplacingcathetersandplacingthe vascularaccesspointatorabovetheleveloftheheart.Lines shouldbeimmediatelycappedorclampedtopreventdirect airentry.Althoughdebated,askingyourpatienttoexhale duringremovalmaypreventnegativeintrathoracicpressure, whichenhancesvenousreturnandcanpullairinifthereisan entryportal.Additionally,pressureshouldbeheldafterthe catheterisremovedinallcases.5
Promptrecognitioniscrucialfortreatment.Diagnosis shouldbemaderapidlyby firsthavingahighindexof suspicionandthenfollowedbytreatment.Thelocationinthe arterialorvenoussystem,amountofgas,andtheorgan affectedwilldictatethemanagement,aswellasthesignsand symptomsguidingtheworkup.
Iftheairembolismoccursinthepulmonarysystem,it couldbeexpectedtobehavelikeathromboticpulmonary embolism.However,ifthereisaconnectionbetweenthe venous/arterialside,asinthecontextofapatentforamen ovale,thenvenousgascouldtraverseandcausesymptomsof arterialischemia.Ourpatienthadcerebralvenousgas, likelyasaresultofretrograde flowwiththepatientinan uprightposition.
APOCUScanbeperformedtolookforagasbubbleinthe rightventricleaswellasalternativeexplanationsforthe changeinapatient’shemodynamics(forexample, pneumothoraxorpericardialtamponade).Transesophageal echocardiogram(TEE)ismoresensitivefordetection; however,thereislimitedaccesstothismethod,anditmaybe moreapplicableintheoperatingroom.Somehigh-risk
proceduresuseaTEEintraoperativelytoproactively monitorforsuchevents.Diagnosticmeasuresshouldbe orderedbasedonthesiteofthesuspectedembolism.These maycommonlyincludeatroponin,ECG,lactate,orrenal function.Imagingwillhelpconfirmthediagnosis;CT angiographyisthemostlikelydiagnosticmodality,although aircansometimesbeseenonplain films.
Ifanairembolismissuspected,thesiteofairentryshould becoveredifopen,pressureheld,andanyoffendingactions (lineinsertion,insufflation,pressureinfusion)shouldbe stopped.Thenextstepinvolvespositioningthepatientto trapgasinthevenoussystemandpreventitfromcausing completecardiovascularcollapseintheformofanairtrap. Thepatientshouldbeplacedintheleftlateraldecubitus positionintheTrendelenburgposition(headdown).Thisis calledtheDurantmaneuver.Thisallowsforbloodtostill passintothepulmonaryarterywhiledisplacingand hopefullytrappingtheairbubbleawayfromtheright ventricularoutflowtract.Italsopreventsright-to-left traversingofthegasbubble.5
Treatmentinvolvessupportivecareoftheorganaffected. Supplementaloxygenshouldbeappliedviaanon-rebreather mask.Ifanairembolismissuspectedandthereisacentral catheterinthesuperiorvenacava,thenonecanattemptto aspiratebloodfromthedistaltipinhopesofsuctioningthe airembolism.
Ifthesemeasuresfailtoalleviatethecardiovascular collapse,thenvenous-arterialextracorporealmembrane oxygenationcouldproviderescuetherapyasabridgeto definitivecare.Interestinglythough,thisprocedureitself hasahighriskofcausinganairembolismifthereisany airinthecatheterswhentheyarehookedtothecircuit. Thegoldstandardinvolveshyperbaricoxygenation therapywithearliertreatmentpreferred;however,cases havebeensuccessfullytreatedafter24hoursofsymptoms, astheavailabilityofdiveresourcesmayvarywidely amonginstitutionsandinvolveprolongedand carefultransport.6
Cerebralairembolismsecondarytocentral linecomplication.
• Rapidchangesinapatient’sclinicalstabilitymaybe relatedtoprogressionoftheknownpresentingdisease oranewprocessentirely.
• Centralvenouscatheterplacementisnotabenign procedure,andgivenitsfrequentuse,careshouldbe takentoavoidcomplications.
• Cerebralairembolismiscausedbyairentrydirectly intothevascularspace,whichmaypresentasachange inapatient’sneurologicalexamination.
• Preventioniskeyforairembolisms;however,if oneoccursthenoxygen,Durantmaneuver,and hyperbarictherapyarethecornerstonesoftherapy.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:T.AndrewWindsor,MD,Universityof MarylandSchoolofMedicine,DepartmentofEmergencyMedicine, 110SPacaSt.,6thFloor,Suite200,Baltimore,MD21201.Email: awindsor@som.umaryland.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Pineretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons
Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.MattieASandWebsterBL.CentersforMedicareandMedicaid Services’“neverevents”:ananalysisandrecommendationsto hospitals. HealthCareManag(Frederick). 2008;27(4):338–49.
2.ArcinasLA,LiuS,SchacterGI,etal.Cerebralairembolismfollowing centralvenouscatheterremoval. AmJMed. 2017;130(12):e549–50.
3.ToungTJ,RossbergMI,HutchinsGM.Volumeofairinalethalvenous airembolism. Anesthesiology. 2001;94(2):360–1.
4.GiraldoM,LoperaLM,ArangoM.Venousairembolisminneurosurgery. RevColAnest. 2015;43(Supp1):40–4.
5.McCarthyC,BehraveshS,NaiduS,etal.Airembolism:practicaltipsfor preventionandtreatment. JClinMed. 2016;5(11):93.
6.MurphyRandDonnellanJ.Ahigh-pressuresolutionforahigh-pressure situation:managementofcerebralairembolismwithhyperbaricoxygen therapy. Cureus. 2019;11(9):e5559.
ShrimanBalasubramanian,DO,MSc*
MichaelDeFilippo,DO*
MichaelStone,MD*
GabrielaGalli,MD*
MatthewMcCarty,MD†
BrockDaniels,MD,MAS,MPH†
SectionEditor:ChristopherSampson,MD
*NewYorkPresbyterianHospitalCornellandColumbia,Departmentof EmergencyMedicine,NewYork † WeillCornellMedicine,DepartmentofEmergencyMedicine,NewYork
Submissionhistory:SubmittedApril23,2023;RevisionreceivedSeptember20,2023;AcceptedOctober6,2023
ElectronicallypublishedJune3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1296
Introduction: Theuseoftelemedicineandultrasoundisemergingandnovelinthe fieldofcommunity paramedicine.However,thereisapaucityofdatasupportingitsuseandevenlessevidencethatshowsa morbidityandmortalitybenefit.Thiscasehighlightsauniquewaytodiagnoseacommonmedical emergency,whichcanleadtoagoodoutcome.
CaseReport: Wedescribetheuseoflungpoint-of-careultrasoundbyatrainedcommunityparamedic thatledtotheidentificationofapneumothoraxinan86-year-oldmaleatascheduledhomevisit.The imageswereinterpretedovertelehealthinreal-timebyanemergencyphysician,andthepatientwas transportedtotheemergencydepartmentwherethediagnosiswasconfirmedbychestradiography.He underwentchesttubeplacementandwasdischarged fivedayslaterafterreturningtohisbaseline.
Conclusion: Despiteminimaldatatosupportorrefutetheuseofparamedictele-ultrasound,thiscase highlightsauniqueopportunitytoexpandtheuseoftelemedicineandultrasoundincommunity paramedicinetoimprovepatientoutcomes.[ClinPractCasesEmergMed.2024;8(3)189–193.]
Keywords: telehealth;casereport;communityparamedicine;pneumothorax;point-of-careultrasound.
Withtheemergenceoftelemedicineandultrasounduse combinedwithcommunityparamedicine,healthsystemsare findingnovelwaystodiagnoseandtreatbothcommonand unusualdiseases.However,evidenceisstillsparseregarding theuseoftelehealthandultrasoundbyparamedics.Thiscase reporthighlightsanoveluseofultrasoundbyacommunity tele-paramedicprogram(CTP)todiagnoseapneumothorax intheprehospitalsettingandreferthepatienttoemergency care,leadingtoagoodoutcome.
Apneumothoraxoccurswhenairaccumulatesbetween theparietalandvisceralpleurainsidethechestwall,causing thelungparenchymatocollapse.1 Itcanbeeithertraumatic oratraumaticandisfurtherclassifiedassimple,tension,or open.Atraumaticpneumothoraxiseitherprimary,occurring
withoutanincitingevent,orsecondaryasinthesettingof pulmonarydisease.1,2 Traumaticpneumothoraxisseenin 20%ofbluntchesttrauma,andupto40%ofpenetrating trauma.2 Patientscanbeasymptomaticorpresentwith shortnessofbreath,chestpain,tachycardia,decreasedbreath sounds,jugularvenousdistention,hypotension,cyanosis, andcardiacarrest.1
Whilecomputedtomography(CT)remainsthegold standardofdiagnosis(despitesomedebate),thediagnosis canalsobemadewithultrasoundorwithchestradiography.3 Ultrasoundhasa94%sensitivityanduptoa100%specificity dependingontheoperator.2 Ultrasound findingsincludea lossoflungslidinginB-modeandthepresenceofa “barcode sign” onM-mode,signifyingthelossofpleuralmovement.2 ChestradiographyandCT findingsincludespacebetween
thepleuraandchestwall.3 Thedifferentialdiagnosisoften includescardiactamponade,aorticdissection,ribfracture, acutecoronarysyndrome,pulmonaryembolism,and pneumonia.1 Managementdependsontheseverityof pneumothoraxandcanincludethefollowing:needle decompression, fingerthoracostomy,pigtailthoracostomy, andlarge-boretubethoracostomy.
Theuniquenessofthiscaserevolvesaroundthemethodof diagnosis.ThecasepatientwasenrolledinaCTPprogram, whichispartofalarge,urbanacademicemergency department.Patientsarejointlyevaluatedbycommunity paramedics(CP)onsceneaswellasbyanemergency physician(EP)overvideoconference.Theseparamedics underwentaone-hourlongtrainingsessioninlungpoint-ofcare-ultrasound(POCUS)usingtheButterflyiQ(Butterfly Network,Burlington,MA)connectedtoamobiledevice. ImageswereobtainedbytheCPcrewusingthe “lung” preset ofthedevice,withtheprobemarkerpointingsuperiorly,and interpretedinreal-timebytheEPoverthetelehealth platform.Whilesomestudieshavereportedthefeasibilityof teachingemergencymedicalservices(EMS)professionals howtoobtainandreadPOCUSimages,thereisapaucityof dataregardingtheregularuseofPOCUSintheprehospital settingandevenfewerinvolvingliveimageinterpretationby anEP.7
Thiscasehighlightsan86-year-oldmalewhowasbeing followedcloselybytheCTPprogramofanurban,academic hospital-basedEMSsystem.Hismedicalhistoryincluded Parkinsondisease,stroke,peripheralneuropathy,atrial fibrillationstatus-postmultipleablations,direct-current cardioversion,andimplantationofaWatchmandevice, sicksinussyndromestatus-postautomaticimplantable cardioverterdefibrillatorplacement,congestiveheartfailure, chronicobstructivepulmonarydisease(COPD),and frequentfallsrequiringmultiplehospitalizations.He presentedataroutinehomevisitcomplainingofleftribpain andshortnessofbreathafterafalltwodaysprior.Ofnote, amonthbeforethisvisithehadbeenhospitalizedforafall anddeclinedtherecommendedsubacuterehabilitation placement.Theonlyhomecareserviceshereceived atthetimewereweeklyCTPvisits.
Duringhisinitialevaluationbyparamedicshedenied othercomplaints.Initialvitalswerepulse65beatsper minute,bloodpressure122/77millimetersofmercury,pulse oximetry100%onroomair,temperature36.6° Celsius,and respirations19breathsperminute.Hisphysicalexamwas significantforlethargy,althoughhewaseasilyarousableto voice;left-sidedchestwalltendernesstopalpation;bruising; crepitus;decreasedleftbreathsounds;andbilaterallower extremitypittingedema.Paramedicsobtainedbilateral anteriorviewsofthelung(Image1a),andimageswere interpretedinreal-timebythephysicianviaavideo
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Computedtomographyisgenerally consideredthegoldstandardfordiagnosis ofapneumothorax.
Whatmakesthispresentationof diseasereportable?
Usingreal-timevideo,anemergency physiciandiagnosedapneumothoraxby interpretingultrasoundimagesobtainedby theparamediconscene.
Whatisthemajorlearningpoint?
Theclinician ’ stelehealthconsultwiththe paramediconscenedemonstratesanovel solutiontodiagnosingconditionswheretime todiagnosisaffectsoutcomes.
Howmightthisimproveemergency medicinepractice?
Emergencyphysicianswillbeabletodiagnose andtreatpatientsearlier,potentiallyleading toimprovedpatientoutcomes.
telehealthplatform.TheEPnotedtheabsenceoflungsliding intheleftinferiorlung field(Image1b).
Thepatientwasplacedon100%oxygenvianonrebreathermaskandtransportedtoalocalemergency department(ED).UponarrivalattheEDhedeniednew complaints,andhisvitalsandphysicalexamwerenot significantlychanged.Hiselectrocardiogram(ECG)showed anatrialsensedpacedrhythmconsistentwithpriorECGs. Hehadachestradiograph(CXR)showingleft fifthandsixth ribfractureswithamoderatecircumferentialpneumothorax (Images2 and 3).
Headditionallyhadnon-contrastCTsoftheheadand cervicalspineshowingintervalresolutionofpriorsubdural andsubarachnoidhemorrhageswithoutanyacute findings. Serumcompletebloodcount,chemistrypanel,cardiac biomarkers,andcoagulationprofilewereunremarkable.He wascontinuedon100%oxygenviaanon-rebreathermask. TubethoracostomyplacementintheEDwasdeferreddueto thepatient’sclinicalstability,presenceofbilateralpleural effusions,andabsenceofasafewindowtoplaceachesttube onultrasound.Thepatientwasadmittedtothesurgical service.Onhospitaldayone,arepeatCXRshowedan unchangedpneumothorax.Heunderwentaninterventional radiologyCT-guidedpigtailthoracostomyplacement.

Image1. (A)Exampleofacommunitytele-paramedicvisitwithvideoconferenceandscreensharingusingmobileultrasound.Thepatientis seenatthetop,andtheemergencyphysicianisseenonthebottomscreen.(B)Thecasepatient’sb-modelungpoint-of-careultrasound, showingaccentuateda-lines,lossofb-lines,andinreal-timevideowithoutlungsliding(notpicturedhere).

Image2. Chestradiographwitharrowspointingtoleft-sidedmoderatecircumferentialpneumothorax.Thereisalossofsymmetry,avisible lungborder,andlossoflungmarkingsuperiortothelungborder.
Onhospitaldaythree,thechesttubewasclampedand subsequentlyremoved.Hewasrecommendedforsubacute rehabilitation;however,boththepatientandfamily declined.Hewasdischargedhomeonhospitalday fivewith
continuedweeklyfollowupwiththeCTPprogram,visiting nurses,andhomephysicaltherapy.
Thepatientwasseenwithfamilybyhisprimarycare physicianthreedaysafterhospitaldischarge.Homesafety
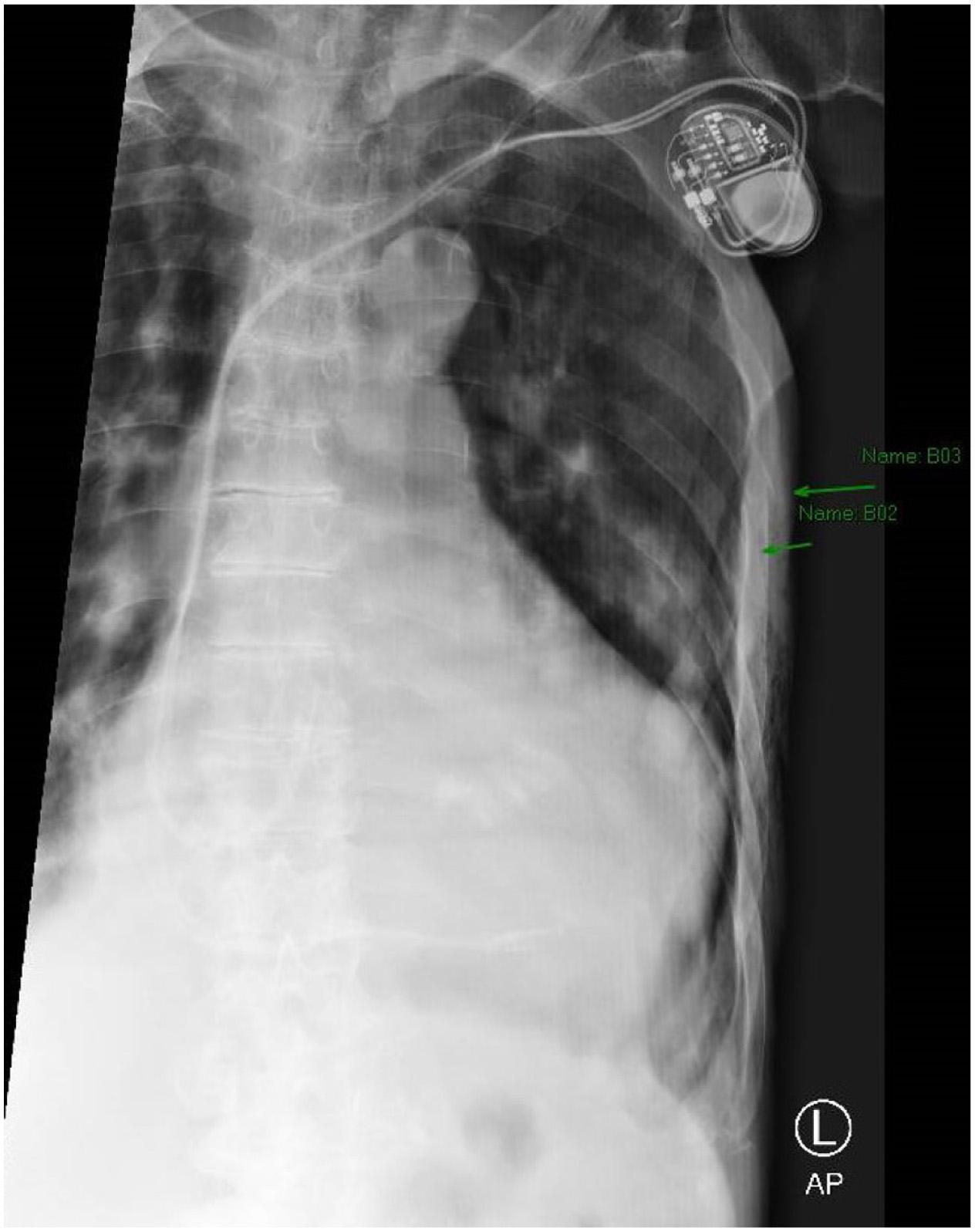
Image3. Magnifiedviewofthechestradiographdemonstrating fracturesofribs fiveandsix(arrows).
concernswereaddressed,fallpreventionteachingwasgiven, andthepatientchosea “donotresuscitate/donotintubate” status.HecontinuestobefollowedbytheCTPprogramona weeklybasis,andunfortunatelyhashadasubsequent admissionforcongestiveheartfailureexacerbationandtwo EDvisitsforfalls.
AlthoughpneumothoraxisnotarareconditionandEPs arequitefamiliarwiththediagnosisandtreatment,clinicians mustbeawareoftheincreasingpresenceofvirtualcare andmobileintegratedhealthcare(MIH).Thenovelty surroundingthiscaseliesinhowthediagnosiswasmade. TheparamedicsarepartofanEMSdivisionunderthe departmentofemergencymedicineatalarge,urban, academicmedicalcenter.TheyarespeciallytrainedasCPs providingscheduledhomevisitstopatientsprimarilywith heartfailure.Theirrolehasexpandedtoincludepost-EDor post-hospitaldischargefollow-upsforconditionssuchas COPDandfalls.
WhiletherearenationalEMSstandardsonCPtraining, therearefewtonostandardsregardingthetrainingofEMS professionalsintheuseofPOCUS.5 Ascopingreview regardingeducationalstandardsrevealedlessthan20 reviewarticles,withaconsensusshowinglittle-to-no
standardizationandnoconsiderationforleveloftraining. However,somestudieshaveshownthatafteratraining programparamedicscanaccuratelyacquireandinterpret lungPOCUSforpneumothoraxortensionpneumothorax withsimilaraccuracytoEPs.6,7 Itshouldbenotedthatmost ofthesestudieshadassessmentsofsimulatedpatientsor patientswithaknownpneumothoraxratherundifferentiated prehospitalpatients.Theresultsofsmallpilotstudieshave suggestedthatprehospitalPOCUSperformedbyparamedics andinterpretedviatelehealthplatformusingcellulardata has “good” to “verygood” qualityandthatremotelung POCUSisfeasible,althoughfurtherresearchonreliability andclinicaloutcomesisneeded.8,9
Thereisapaucityofqualitydatashowingthatimmediate interpretationoflungPOCUSleadstomorerapiddiagnosis, intervention,andbetterpatientoutcomesdespitethe potentialoflungPOCUStopositivelyimpactimmediate care.Inthiscasewedescribeauniquemethodofdiagnosis andrapidtreatmentleadingtoapositivepatientoutcome, whichmayhaveotherwisebeenmissedleadingtoclinical decline,significantmorbidityorevendeathifleftuntreated. ThiscasehighlightsanopportunityforbothEPsandEMS professionalstoexpandtheirscopeofpracticewithinthe prehospitalsetting.Theuseofreal-timeinterpretationbyan EPovertelemedicine(ascomparedtoparamedic-only interpretationorasynchronousstoreandforward)affords theopportunitytoguideimageacquisitionforlessexperiencedultrasonographersandincasesofdifficult patientwindows,whileprovidingadditionalclinicalcontext totheEPreadingtheimages.Overall,thishasthepotential toeffectivelytriagepatientstoappropriatedispositions startingfromveryearlyonintheircare.10
Onelimitationisthesmallbodyofliteratureevaluating whetherearlylungPOCUSreadbyanEPimprovesclinical outcomes.Thiscasereporthighlightstheneedforfurther implementationstudiestobetterunderstandtherisksand benefitsofPOCUSintheremotemanagementofpatient populationslivingwithchronicillnesssuchasheartfailure andCOPDwhererapidevaluationanddifferentiationofthe manycausesofdyspneaatthepatient’ssidecanbevaluable fordeterminingthemostappropriatetreatmentandlevel ofcare.
WiththecasereportwealsosoughttoincreaseEP awarenessofthepossibilityofprehospitaluseofPOCUS.A needsassessmentatourinstitutionsuggeststhatwhileEPs involvedintheremotemanagementofmedicallycomplex patientsthroughMIHprogramsbelieveremotelung ultrasoundisvaluable,mostwerenotawareitwasavailable, safe,oreffective.However,thedatareferredtoabove suggeststhatwiththerighttraining,paramedicsareableto obtainultrasoundimages.Asemergencymedicineexpands toinvolvemobileintegratedhealthcareandvirtualcare,we believeEPscanexpecttoseethatpatientassessmentsby paramedicsincludePOCUSimagestointerpret.
Thiscaseofcommunitytele-paramedicineuseoflung POCUSreadbyanEPasapneumothoraxshowsboththe diagnosticdiversityofpneumothoraxandthefeasibilityof EMSprofessionalsusingPOCUStoadvancepatientcare.It isimportanttorecognizeapneumothoraxandtreatitearly topreventprogressiontotensionphysiology.Bypartnering withEMS,wemaybeabletoidentifythisdiagnosisand initiateemergenttreatmentearlyon.Emergencyphysicians shouldbeawareofthegrowingprevalenceofprehospital ultrasoundanditsutilityinthediagnosisofcommon lungpathology.
WewouldliketoacknowledgeElisaAponteMD,Sophia Lin,MD,andRahulSharma,MD,fromtheDepartmentof EmergencyMedicineatNewYorkPresbyterianWeill CornellMedicinefortheirhardworkintheCommunity Tele-paramedicineProgram.Withtheirefforts,the departmentisabletoprovidevaluableservicestohigh-risk patientsandvaluableresearchtobetterhelpthecommunity.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ShrimanBalasubramanian,DO,MSc, NewYorkPresbyterianHospital,DepartmentofEmergyncy Medicine,525E.68th Street,NewYork,NY10065.Email: shb9291@nyp.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Balasubramanianetal.Thisisanopenaccess articledistributedinaccordancewiththetermsoftheCreative CommonsAttribution(CCBY4.0)License.See: http:// creativecommons.org/licenses/by/4.0/
1.McKnightCLandBurnsB.PneumothoraxIn StatPearls[Internet] TreasureIsland,Florida:StatPearlsPublishing;2023.
2.HusainLF,HagopianL,WaymanD,etal.Sonographicdiagnosisof pneumothorax. JEmergTraumaShock.2012;5(1):76–81.
3.WongA,GaliabovitchE,BhagwatK.Managementofprimary spontaneouspneumothorax:areview. ANZJSurg 2019;89(4):303–8.
4.DanielsB,GreenwaldP,HsuH,etal.284Usingcommunityteleparamedicinetoreduceunnecessaryemergencydepartmentvisitsand 30-dayreadmissionsamonghigh-riskpatientswithheartfailure, Ann EmergMed.2019;74(4):S112–3.
5.MeadleyB,OlaussenA,DelorenzoA,etal.Educationalstandardsfor trainingparamedicsinultrasound:ascopingreview. BMCEmergMed 2017;17:18.
6.BrookeM,WaltonJ,ScuttD,etal.Acquisitionandinterpretationof focuseddiagnosticultrasoundimagesbyultrasound-naiveadvanced paramedics:trialingaPHUSeducationprogramme. EmergMedJ 2012;29:322–6.
7.KhalilP,MerelmanA,RiccioJ,etal.Randomizedcontrolledtrialof point-of-careultrasoundeducationfortherecognitionoftension pneumothoraxbyparamedicsinprehospitalsimulation. PrehospDisasterMed.2021;36(1):74–8.
8.BerletM,VogelT,GharbaM,etal.Emergencytelemedicinemobile ultrasoundsusinga5G-enabledapplication:developmentandusability study. JMIRFormRes.2022;6(5):e36824.
9.PietersenPI,MikkelsenS,LassenAT,etal.Qualityoffocusedthoracic ultrasoundperformedbyemergencymedicaltechniciansand paramedicsinaprehospitalsetting:afeasibilitystudy. ScandJTrauma ResuscEmergMed.2021;29:40.
10.LangabeerJR2nd,GonzalezM,AlqusairiD,etal.Telehealth-enabled emergencymedicalservicesprogramreducesambulancetransport tourbanemergencydepartments. WestJEmergMed 2016;17(6):713–20.
LaurenKaplan,MD*
KaushalH.Shah,MD†
ChristieLech,MD,MHPE†
Mary-KateGorlick,MD*
SectionEditor:LevLibet,MD
*NewYork-PresbyterianHospital,NewYork,NewYork † NewYork-PresbyterianHospital;WeillCornellMedicalCenter,Departmentof EmergencyMedicine,NewYork,NewYork
Submissionhistory:SubmittedAugust2,2023;RevisionreceivedOctober8,2023;AcceptedNovember2,2023
ElectronicallypublishedMay14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1585
Introduction: Renalarteryaneurysmruptureisararebutmorbiddiagnosis,oftenrequiringemergency surgeryandnephrectomy.Clinicalpresentationcanmimicmorecommonpathologyinnon-pregnant womensuchasrupturedovariancyst.
CaseReport: Wepresentacaseofawomanwithapriorhistoryofovariancystpresentingwitha rupturedrenalarteryaneurysm.Promptcomputedtomography(CT)imagingrevealedaleftrenalartery aneurysmrupturewithhemoperitoneumandrenalinfarct.Sheunderwentemergencylaparotomyand nephrectomyandwasultimatelydischargedingoodcondition.
Conclusion: Whileovariancystruptureisthemostcommoncauseofspontaneoushemoperitoneumin non-pregnantwomenofchildbearingage,renalarteryaneurysmruptureshouldbeconsideredand promptCTimagingobtained,particularlyincasesofhemodynamicinstability,toensureprompt treatment.[ClinPractCasesEmergMed.2024;8(3)194–196.]
Keywords: casereport;aneurysm;renal;rupture.
Renalarteryaneurysm(RAA)isararediagnosis, estimatedtooccurin0.09%ofthegeneralpopulation.5
Ruptureisararebutmorbidcomplication,oftenrequiring emergentsurgeryandnephrectomy.Incontrast,ovariancyst ruptureisthemostcommoncauseofspontaneous hemoperitoneuminnon-pregnantwomenofreproductive ageandisusuallymanagedconservativelyintheabsenceof hemodynamiccompromiseorassociatedtorsion.1,2 We reportacaseofspontaneousrupturedRAAasadangerous mimicofovariancystrupture.
A52-year-oldwomanwithapastmedicalhistoryof ovariancystswasbroughtinbyemergencymedicalservices (EMS)toouremergencydepartment(ED)foracuteonsetof atraumaticleftlowerquadrantpain.Hersymptomsstarted abruptlywhileatwork,whichshestatedfeltlikesymptoms
oneyearpriorwhenshewasfoundtohaveovariancystsand likelyanovariancystrupture.Sheendorsedlightheadedness, butshedeniedanyshortnessofbreath,chestpain,cough, fevers,chills,orchangesinurination.
PerEMSreport,sheacutelybecamepaleandsomnolent, associatedwithbradycardiatothe40s.IntheEDshewas hypotensiveto84/48millimetersofmercury,withheartrate 84beatsperminute,oxygensaturation100%onroomair, andshewasafebrile.Physicalexaminationrevealedpallor, somnolence,coolextremities,andaperitonealabdomen. Focusedassessmentwithsonographyintraumaexamination waspositiveforfree fluidintheleftupperquadrant. Pregnancytestwasnegative.Initiallabswerenotablefor lactate4.59millimolesperliter(mmol/L)(referencerange 0.50–1.60mmol/L).Initialhemoglobinwas10gramsper deciliter(g/dL)(12.6–17.0g/dL);hematocrit30.5% (37.2–47.9%);platelets317,000permilliliter(mL) (156,000–325,000/mL);andwhitebloodcellcount
15,000/mL(3,120–8,440/mL).Coagulationfactors werenormal.Chemistrypanelwasnotableforsodium 130mmol/L(137–145mmol/L);potassium3.3mmol/L (3.5–5.1mmol/L);bicarbonate21mmol/L(19–27mmol/L); bloodureanitrogen18milligrams(mg)/dL(7–26mg/dL); andcreatinine1.0mg/dL(0.70–1.30mg/dL).Emergency physiciansactivatedamassivetransfusionprotocoland pagedtheobstetricsandgynecologyserviceduetoconcern forhemorrhagicrupturedovariancystvsovariantorsion.
Emergentcomputedtomographyoftheabdomenand pelvisrevealedalargeleftretroperitonealandperitoneal hematomasecondarytoleftRAArupture,aswellasconcern fordevelopingsplenicinfarctsintheleftlowerrenalpole (Image).Thepatientwastakenemergentlytotheoperating room(OR)forexploratorylaparotomywithintwohoursof EDarrival.Sheunderwentsuprarenalcross-clampingwith repairoftheleftrenalarteryandligationofrenalvessels.She returnedtotheORtwodayslaterforleftnephrectomyand abdominalclosure.Shewasextubatedandtransferredtothe floor.Shewasdischargedhometwodayslaterin goodcondition.
AlthoughtheincidenceofRAAisrare,rangingfrom 0.01–0.09%ofthepopulation,thiscasereportillustratesthe importanceoftimelydiagnosis.3,4 Contemporaryrupture ratesareestimatedatapproximately3%.5 Theyaremost commonlyfoundinwomen >60yearswithriskfactors includinghypertension, fibrodysplasia,andconnectivetissue disorderscausingarterialmedialwalldegeneration.Patients notablylacktraditionalcardiovascularriskfactorssuchas cigaretteuseanddiabetes.6,7 Aneurysmsareusually asymptomaticandfoundincidentallyonscreeningimaging, althoughpatientscanpresentwithsymptomssuchas hypertension, flankpain,hematuria,andabdominalpain.5

PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisclinical entity?
Renalarteryaneurysm(RAA)ruptureisa rarebutmorbiddiagnosisthatcanleadto emergencysurgeryandnephrectomy.
Whatmakesthispresentationofdisease reportable?
Wereportacaseofspontaneousruptured RAApresentingasadangerousmimicof ovariancystrupture,amorecommon pathologyinnon-pregnantwomen.
Whatisthemajorlearningpoint?
Emergencyphysiciansshouldmaintainanindex ofsuspicionforemergentvascularpathologyin non-pregnantwomenofchildbearingagewith spontaneoushemoperitoneum.
Howmightthisimproveemergencymedicine practice?
Maintaininganindexofsuspicionforrare diseaseprocessessuchasRAArupturewill ensurepromptrecognitionandtreatmentin theED.
AsthepresentationofarupturedRAAcanbeidenticalto themorecommonrupturedovariancyst,considerationof rareserioussurgicalpathologyshouldbemaintainedfor patientswithacuteabdominalpainandfree fluidonexam. Bradycardiainthesettingofhemoperitoneumisawell describedphenomenonparticularlyinrupturedectopic pregnancyandcanindicatehemorrhagicshock,bothof whichwereconsiderationsinthecasereportedhere.8,9 Other emergentcomplicationsofRAAincludethrombosis, embolism,andobstructiveuropathy.
Fornon-rupturedRAA,surgicalorendovascular interventionisrecommendedforaneurysmswithadiameter exceedingtwocentimeters,patientswithuncontrolled symptoms(ie.painorrefractoryhypertension),orinwomen ofchildbearingage(astherearehigherratesofruptureand mortalityinpregnancyandpuerperiumthaninthegeneral population).3,6 Theseguidelinesremainsomewhat controversialgiventheincreasedincidenceofaneurysms uncoveredbywidespreaduseofimagingcombinedwitha knowledgegapofthenaturalprogressionofdisease.2,4 Endovascularinterventionthroughstentingor angioembolizationisasafeandeffectivealternativetoopen repair,withstudiessuggestingatrendtowardshorter
hospitalstaysandfewercomplications.10 Incasesof hemodynamiccompromise,exploratorylaparotomyand nephrectomyareoftenindicated.2,3,4
Thisisacaseofspontaneousruptureofaleftrenalartery aneurysmasadangerousmimicofovariancystrupture. Whileovariancystruptureremainsthemostcommoncause ofspontaneoushemoperitoneuminnon-pregnantwomenof childbearingage,RAAshouldbeconsideredwith confirmationviacomputedtomography,particularlyin casesofhemodynamicinstabilitytoensureprompttreatment ofadiseasewithpotentiallyhighmorbidityandmortality.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:LaurenKaplan,MD,NewYorkPresbyterianHospital,525East68th Street,NewYork,NY10065. Email: Lek9048@nyp.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Kaplanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.LeeYR.CTimaging findingsofrupturedovarianendometrioticcysts: emphasisonthedifferentialdiagnosiswithrupturedovarianfunctional cysts. KoreanJRadiol.2011;12(1):59.
2.LimWH,WoodsN,LamaroVP.Trendsandoutcomesofruptured ovariancysts. PostgradMedJ.2021;98(1161):e9.
3.GonzalezJ,EstebanM,AndresG,etal.Renalarteryaneurysms. Curr UrolRep.2014;15(1):376.
4.VillianouNG,SikaraM,ZisisC.Ruptureofaleftrenalartery aneurysm:arareabdominalemergency. AmJEmergMed 2016;34(2):e347.e3–4.
5.KlausnerJQ,LawrencePF,Harlander-LockeMP,etal.The contemporarymanagementofrenalarteryaneurysms. JVascSurg 2015;61(4):978–84.
6.AugustinG,KulisT,KelloN,etal.Rupturedrenalarteryaneurysmin pregnancyandpuerperium:literaturereviewof53cases. ArchGynecol Obstet.2019;299(4):923–31.
7.ColemanDMandStanleyJC.Renalarteryaneurysms. JVascSurg 2015;62(3):779–85.
8.SnyderH.Lackofatachycardicresponsetohypotensionwithruptured ectopicpregnancy. AmJEmergMed.1990;8(1):23–6.
9.SomersMP,SpearsM,MaynardAS,etal.Rupturedheterotopic pregnancypresentingwithrelativebradycardiainawomannot receivingreproductiveassistance. AnnEmergMed 2004;43(3):382–5.
10.OrionKCandAbularrageCJ.Renalarteryaneurysms:movement towardendovascularrepair. SeminVascSurg.2013;26(4):226–32.
CliffordChang,MD*
VakulaAtthota,MD†‡
MadisonLord,DO‡
MichaelP.Bonk,MD§
MuhammadDurrani,DO*
SectionEditor:AustinSmith,MD
*InspiraHealthNetwork,DepartmentofEmergencyMedicine,Vineland,NewJersey † InspiraHealthNetwork,DepartmentofInfectiousDiseases,Vineland,NewJersey ‡ InspiraHealthNetwork,DepartmentofInternalMedicine,Vineland,NewJersey § RowanUniversity,CooperMedicalSchool,DivisionofCriticalCareMedicine, Camden,NewJersey
Submissionhistory:SubmittedNovember26,2023;RevisionreceivedJanuary17,2024;AcceptedJanuary23,2024
ElectronicallypublishedJuly11,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.5826
Introduction: Capnocytophagaochracea isfoundinthehumanoralmicrobiomeandisararecauseof antibiotic-resistant,opportunisticsepticemiainimmunocompromisedhosts.Thezoonotictransmission of Cochracea fromcaninestohumanshasnotyetbeenreportedintheliterature.Cohabitationwith peopleisassociatedwithoralcolonizationindogsandmaybeareservoirfor Capnocytophaga infections,whichhaveadecreasedsusceptibilityto first-lineantibioticscommonlyusedtotreat animalexposures.
CaseReport: Thisisthecaseofa70-year-oldmalewitharemotehistoryoflymphomastatuspost splenectomy,inremission,whopresentedwithstigmataof Capnocytophaga septicemiaafteradogbite, whichincludedpurpurafulminansonphysicalexamination.Initialbroad-spectrumcoveragewith cefepimefailedtoslowtheprogressionintomultiorganfailure.A Capnocytophaga strainwithextended resistancewassuspected.Antibioticsweretransitionedtomeropenem,andthepatienteventuallymade agoodrecovery.Bloodculturesisolated Cochracea.
Conclusion: Capnocytophaga infectionsshouldbesuspectedinpatientswithseveresepsisand purpurafulminansafteracanineexposure.Caninepetsmaybeareservoirfor Capnocytophaga species withincreasedantibioticresistances,suchas Cochracea,whichtracetheiroriginstothehumanoral microbiome.Athoroughmedicalhistoryisessentialtoidentifyriskfactorssuchasaspleniaandactive immunecompromisethatareassociatedwithinfectionsfromantibiotic-resistantstrainsandworse outcomes.For Capnocytophagainfectionsthatfailinitialtherapies,cephalosporinsshouldbe avoidedbecauseofhighresistancerates,andtheuseofcarbapenemsmaybefavoredover combinationbeta-lactam/beta-lactamaseinhibitorsinselectclinicalscenarios.[ClinPractCasesEmerg Med.2024;8(3)197–201.]
Keywords: capnocytophaga;antibioticresistance;dogbite;purpurafulminans;immunocompromise; extended-spectrum β-lactamases;ESBL.
Capnocytophag aisagenusofencapsulated,Gramnegativerodsthatresidesinthecommensalmammalian flora asfacultativeanaerobes.Nativetothecanineoral microbiome, Ccanimorsus iswellknowntocauseinfections inhumansthroughcanineexposuressuchasbites,licks,and
scratches.Otherspeciesof Capnocytophaga suchas Cochracea,Csputigena,andCgingivalis arenativetothe humanoralmicrobiomeandoftenfoundinassociationwith gingivitis.1 Bacteremiafromthesehumanoral Capnocytophaga (HOC)speciesdisproportionallyaffects severelyimmunocompromisedpatientsandisassociated
withpooroutcomes.Aretrospectivestudypublishedin2021 byChesdachaietalfoundthatthesix-monthmortalityof patientswithHOCbacteremiawashigherthanthosewith Ccanimorsus bacteremia,36.4%vs6.2%,respectively.2
Potentiatedbyacompromisedimmunesystem,the pathogenesisofHOCbacteremialikelyinvolvesself-seeding fromtheoralcavityintothesystemiccirculation.Whilethe majorityof Ccanimorsus infectionsareassociatedwith knownanimalexposures(upto77%),thezoonotic transmissionofHOCspeciessuchas Cochracea hasnotyet beenreportedintheliterature.2 Interestingly, Cochracea alongwithotherhumanoralmicrobesarefoundinthe mouthsofdogsthatcohabitatewithpeople.3,4 Suchpetsmay beareservoirofpotentiallypathogenicbacteriathatdonot yethaveatrackrecordforcausingzoonoticinfections.
Thepooroutcomesassociatedwith Cochracea andother HOCinfectionsaremultifactorialandincludethedegreeof hostimmunesuppression,thepresenceofunderlying diseasessuchashematologicmalignancy,andincreased antibioticresistance.Unlike Ccanimorsus ,whichisalmost universallysusceptibletonarrow-spectrumantibiotics(eg, penicillin), Cochracea andotherHOCspeciesareoften resistanttocommonlyusedbroad-spectrumantibioticsfor polymicrobialanimalexposures.Upto70%ofHOCisolates producebeta-lactamases,whichconferresistanceto firstgenerationcephalosporins(100%resistant),amoxicillin (86%),andthird-generationcephalosporins(63%).5–7
Although Capnocytophaga speciesaretypicallysensitive tocombinationbeta-lactam/beta-lactamaseinhibitorsin vitro,treatingcriticallyill,bacteremicpatientswith antibioticssuchasamoxicillin-clavulanateorpiperacillintazobactammayresultinpooroutcomes.Anoninferiority trialpublishedin2019randomized378patientswithGramnegativebacteremiademonstratingextendedspectrumbetalactamaseactivity(ESBL),definedasresistanceto ceftriaxone,toeithertreatmentwithpiperacillin-tazobactam ormeropenem.Despitehavingconfirmedinvitrosusceptibly tobothantibiotics,patientstreatedwithpiperacillintazobactam(12.3%)hadincreased30-daymortalitywhen comparedtomeropenem(3.7%).8
Hereinwedescribethe firstreportedcasetoour knowledgeofhumanoral-associated Capnocytophaga bacteremiatransmittedfromananimal.Thepatient describedinthiscasedevelopedsevere Cochracea septicemiawithpurpurafulminansafteradogbiteand eventuallyhadagoodoutcomeaftertreatment withmeropenem.
A70-year-oldmalewithahistoryofStageIIIdiffuselarge B-celllymphomastatuspostchemotherapyandsplenectomy 20yearsprior,currentlyinremission,presentedtoalarge communityemergencydepartmentwithgeneralized weaknessandalteredmentalstatusthreedaysafterhe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Humanoralbacteriaareoftenresistantto conventionalantibiotics.Cohabitationis associatedwiththeoralcolonizationofthese bacteriaindogs.
Whatmakesthispresentationof diseasereportable?
Thisisthe fi rstreportedcaseofahumanoral Capnocytophagaspeciescausingsepsisafter zoonotictransmissionviaadogbite.
Whatisthemajorlearningpoint?
Petbitesmaytransmitantibiotic-resistant bacteriathatoriginatefromthehumanoral microbiome.Theuseofcarbapenemsshould beconsideredwheninitialtherapiesfail.
Howmightthisimproveemergency medicinepractice?
Cliniciansshouldrecognizethechanging natureofinfectiousdiseasesandunderstand theroleofextendedspectrumantimicrobials.
sustainedabitetohisleftthumbfromapetdog.Thedogwas fullyvaccinatedandhadnotbeendemonstratingabnormal behaviorsleadinguptotheincident.Onarrivalthepatient appearedacutelyill.Vitalssignswerenotableforaheartrate of108beatsperminute,bloodpressureof78/43millimeters ofmercury,tachypneaatarateof38breathsperminute,and atemperatureof36.3° Celsius.Examinationoftheulnar aspectoftheleftthumbrevealedtwofaint,punctatebite marksthatlaterbecameduskyandlocallynecrotic (Image1).Darkpurple,non-blanchingmaculeswereseenin allextremitiesconsistentwithpurpurafulminansandhighly suggestiveof Capnocytophaga septicemia(Image2).
Theinitiallacticacidwas15.0millimolesperliter (mmol/L)(referencerange:0.5–1.5mmol/L),andthewhite bloodcellcountreachedapeakof90.0 × 109 cells/L(4.5 –11.0 × 109 cells/L).Giventheseverityofthepatient’sillness, vancomycinandcefepimewereinitiatedempirically.Despite broadspectrumantibioticsandtheresuscitationofseptic shockwithcrystalloid fluids,glucocorticoidtherapy,and escalatingvasoactivemedications,thepatientdeteriorated intomultiorganfailure.Withinthe firstdayofadmissionthe patientwasintubated,placedonmechanicalventilation, initiatedonrenalreplacementtherapy,developed coagulopathy,andrequiredintravenousinotropicsupport.

Image1. Lefthandwithpurpuraandlocalnecrosis(arrows)as wellaspetechiae(asterisk).

Image2. Pupurafulminans(arrows)oftheleftandrightlower extremities,respectively.
Echocardiogramdemonstratedsevereglobalhypokinesisof theleftventriclewithanewlydepressedejectionfractionof 20–25%consistentwithacutesepticcardiomyopathy.
Encapsulated Capnocytophaga infectionremained highestonthedifferentialgiventhepatient’shistoryof asplenia,recentcanineexposure,andpurpurafulminanson physicalexamination.However,thelackofresponseto cefepimeraisedconcernsforthepresenceofaresistant Capnocytophaga species,potentiallywithextended spectrumactivity.Thepatient’streatmentregimenwas transitionedtomeropenemonegrameveryeighthourson whichhebegantodemonstrateclinicalimprovement.
Capnocytophaga arefastidious,slow-growingbacteria, andoursuspicionforthisorganismwascommunicatedtothe microbiologylaboratorytoincreasecultureyields. Additionalgrowthmediawereused,andthespecimenswere
observedforalongerduration.Gram-negativebacilliwere foundintheaerobicbottlesafter fivedays,and Cochracea finallyspeciatedafter11days.Thespeciationwasconfirmed bybothbiochemicalmethods,usingRapIDANAII (ThermoFisherScientificInc,Waltham,MA)andmass spectrometrymatrix-assistedlaserdesorption/ionization (BrukerCorporation,Billerica,MA).Susceptibilitiesstudies wereunfortunatelynotperformedgivendifficultyof culturingtheorganism.
Afteragradualrecovery,thepatientwastransferredout oftheintensivecareunitninedaysafteradmissionand dischargedbackhomeonday18withvisitingrehabilitation servicesaswellastheremainderofafour-weektotalcourse ofmeropenem.Atdischarge,hewasambulatoryandhada recoveredleftventricularejectionfractionof50–55%.Other sequelaeincludedmultipletoeamputationsforvasopressor andcoagulopathy-associatedgangreneaswellaspostdebridementcontracturesofthelefthand.Despitehiscritical illnessandprolongedhospitalization,thepatientmadea remarkablerecovery.Hisgoalwastoeventuallyreturnto workfulltime.
Althoughmorecommonlythoughtofasacommensal organismintheoralmicrobiota,HOCspeciessuchas Cochracea areararecauseofsevere,opportunistic bacteremiainpatientswithriskfactorsforactiveimmune suppression.Acaseseriespublishedin2001reportedthatof 28cancerpatientswithneutropenicfeversrelatedtoHOC bacteremia,25(89%)hadanactivehematologicmalignancy andhalfhadmoderatetoseveremucositis.9 Identifiedin onethirdofcases, Cochracea wasthemostcommonly isolatedspecies.Amorerecentreviewpublishedin2021 foundthatall22patientswithHOCbacteremiahadatleast oneriskfactorforactiveimmunocompromise,most commonlyimmunosuppressivemedications(72%), hematopoieticstemcelltransplantation(54%),and hematologicmalignancy(40%).2
Thepatientdescribedinthiscaseunderwent chemotherapyandsplenectomyforalymphoma20years priorandhadbeeninremissionsince.Withoutsignsofan activemalignancy,hisprimaryriskfactorfor Capnocytophaga sepsiswaslikelyasplenia.Intermsof infectioussource,thepatientexhibitednosignsofmucositis andwasbittenonlythreedayspriortopresentation,whichis withintheonetosevendayincubationperiodof Capnocytophaga infections.10
Thespeciationof Cochracea insteadof Ccanimorsus fromthedogbitewasunanticipated.Inaretrospective reviewof Capnocytophaga bacteremia,animalexposurewas confirmedin68.8%of Ccanimorsus infectionswhileno patientswithinfectionsfromother Capnocytophaga species hadreportedexposures.2 Capnocytophagaochracea isnot thoughttobenativetothecanineoralmicrobiome;however,
severalHOCspecieshavebeenidentifiedintheoral microbiomesofpets.3 Cohabitationandclosecontactmay facilitatethetransmissionofmicroorganismsfromhumans topetanimals.Similartohowthehumanoralandgut microbiomeisoftentransmittedfrommotherstotheir children,theremaybetransmissionofhumanoralmicrobes topetdogsandcats.4,11,12 Thepotentialofpetsasreservoirs forHOCspecies,timingofsymptomsfollowinginoculation, andabsenceofstrongriskfactorsforspontaneous opportunisticbacteremiamakethecaseforzoonosisasthe sourceofourpatient’ s Cochracea sepsis.
Theantimicrobialsusceptibilityof Cochracea andother HOCinfectionsdiffersfromthatof Ccanimorsus. Capnocytophagacanimorsus strainsrarelyproducebetalactamasesandarelargelysusceptibletocommonantibiotics usedinthemanagementofpolymicrobialanimalexposures (ie,amoxicillin-clavulanate,clindamycin,third-generation cephalosporins).Upto70%ofHOCisolatesproducebetalactamases,andmorethan60%ofthoseareresistanttothirdgenerationcephalosporins.7 Additionally,therearereports ofmultidrugresistantstrainsof Cochracea,Csputigena , and Cgingivalis thatareresistanttofourth-generation cephalosporins(eg,cefepime).13,14 These findingsare concerningforextended-spectrum β-lactamases(ESBL) activityamongHOCspecies.
Combinationantibiotics(ie,amoxicillin-clavulanateor piperacillin-tazobactam)mayappeartobereasonable alternativesbasedoninvitrosusceptibilities;however,the treatmentofESBLGram-negativebacteremiawith piperacillin-tazobactamratherthanmeropenemis associatedwithdecreasedsurvival.8 Increasedbacterial densitywithininfectedtissuecanalterlocal pharmacokineticsthroughthewell-described “inoculum effect” wheresensitivitytopiperacillin-tazobactamcan decreasefrom95%atinvitrobacterialconcentrationsto58% atinvivoconcentrations.15 Thiseffectislimitedin carbapenemsandappearstobemediatedbythe downregulationoftargetproteins,synergisticenzymatic degradation,andbiofilmproduction.
Alimitationofourcaseisthelackofsusceptibilitydata; however,theprevalenceoflater-generationcephalosporin resistanceamong Cochracea strainsandthepatient’slackof clinicalimprovementwithcefepimeraisedoursuspicionfor thepresenceofextendedspectrumresistances.Inourcase, treatmentwithmeropenemultimatelyledtoa goodoutcome.
Capnocytophaga bacteremiashouldbesuspectedin patientswithseveresepsisandpurpurafulminansaftera canineexposure.Resistantinfectionsshouldbeconsideredin patientswhodonotrespondtoinitialtherapies.Patientswith aspleniaandactiveimmunocompromiseareathighestrisk. Insuchcases,cephalosporinsshouldbeavoidedbecauseof
highresistancerates,andtheuseofcarbapenemsmaybe favoredovercombinationbeta-lactam/beta-lactamase inhibitorsinselectclinicalscenarios.Caninepetsmaybea reservoirfor Capnocytophaga specieswithincreased resistances,suchas Cochracea ,whichtracetheiroriginsto thehumanoralmicrobiome.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:MuhammadDurrani,DO,Inspira VinelandMedicalCenter,DepartmentofEmergencyMedicine, 1505WestShermanAve.,Vineland,NJ08360.
Email: DurraniM1@ihn.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Changetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.IdateU,BhatK,KotrashettiV,etal.Molecularidentificationof Capnocytophaga speciesfromtheoralcavityofpatientswith chronicperiodontitisandhealthyindividuals. JOralMaxillofacPathol. 2020;24(2):397.
2.ChesdachaiS,TaiDBG,YetmarZA,etal.Thecharacteristicsof Capnocytophagainfection:10yearsofexperience. OpenForumInfect Dis. 2021;8(7):ofab175.
3.YamasakiY,NomuraR,NakanoK,etal.Distributionof periodontopathicbacterialspeciesindogsandtheirowners. ArchOral Biol. 2012;57(9):1183–8.
4.KatoY,ShiraiM,MurakamiM,etal.Moleculardetectionofhuman periodontalpathogensinoralswabspecimensfromdogsinJapan. JVet Dent. 2011;28(2):84–9.
5.Jolivet-GougeonA,Tamanai-ShacooriZ,DesbordesL,etal.Genetic analysisofanamblerclassAextended-spectrumbeta-lactamase fromCapnocytophagaochracea. JClinMicrobiol. 2004;42(2):888–90.
6.EhrmannE,HandalT,Tamanai-ShacooriZ,etal.Highprevalence of β-lactamandmacrolideresistancegenesinhumanoral Capnocytophaga species. JAntimicrobChemother. 2014;69(2):381–4.
7.Jolivet-GougeonA,Tamanai-ShacooriZ,DesbordesL,etal. Prevalenceoforopharyngealbeta-lactamase-producing Capnocytophaga spp.inpediatriconcologypatientsoveraten-year period. BMCInfectDis. 2005;5:32.
8.HarrisPNA,TambyahPA,LyeDC,etal.Effectofpiperacillintazobactamvsmeropenemon30-daymortalityforpatientswith
EcoliorKlebsiellapneumoniaebloodstreaminfectionandceftriaxone resistance:arandomizedclinicaltrial. JAMA. 2018;320(10):984–94.
9.MartinoR,RámilaE,CapdevilaJA,etal.Bacteremiacausedby Capnocytophaga speciesinpatientswithneutropeniaand cancer:resultsofamulticenterstudy. ClinInfectDis. 2001;33(4):E20–2.
10.OehlerRL,VelezAP,MizrachiM,etal.Bite-relatedandsepticsyndromes causedbycatsanddogs. LancetInfectDis. 2009;9(7):439–47.
11.TamuraK,NakanoK,HayashibaraT,etal.Distributionof10periodontal bacteriainsalivasamplesfromJapanesechildrenandtheirmothers. ArchOralBiol. 2006;51(5):371–7.
12.ArashimaY,KumasakaK,OkuyamaK,etal.Clinicobacteriological studyof Pasteurellamultocidaasazoonosisconditionofdogandcat
carriersof Pasteurella,andtheInfluenceforhumancarriersratebykiss withthepets. KansenshogakuZasshi. 1992;66(2):221–4.
13.WangHK,ChenYC,TengLJ,etal.Brainabscessassociatedwith multidrug-resistant Capnocytophagaochracea infection. JClin Microbiol. 2007;45(2):645–7.
14.MigiyamaY,AnaiM,KashiwabaraK,etal.Lungabscessfollowing bronchoscopyduetomultidrug-resistant Capnocytophagasputigena adjacenttolungcancerwithhighPD-L1expression. JInfectChemother. 2018;24(10):852–5.
15.ThomsonKSandMolandES.Cefepime,piperacillin-tazobactam,and theinoculumeffectintestswithextended-spectrumbeta-lactamaseproducingEnterobacteriaceae. AntimicrobAgentsChemother. 2001;45(12):3548–54.
BrynWalsh,DO SuneilAgrawal,MD
SectionEditor:JoelMoll,MD
Submissionhistory:SubmittedOctober20,2023;RevisionreceivedJanuary10,2023;AcceptedJanuary25,2024
ElectronicallypublishedMay28,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.3851
Introduction: Acutemountainsickness,high-altitudepulmonaryedema(HAPE),andhigh-altitude cerebraledema(HACE)areaspectrumofhigh-altitudeconditions,withHACEbeingthemostlifethreatening.Mostcasesdevelopataltitudesofgreaterthan4,000meters(~13,000feet)abovesealevel andafteroneto fivedays.
CaseReport: Apreviouslyhealthy46-year-oldfemalepresentedtotheemergencydepartmentwith ataxia,alteredmentalstatus,andvomitingthatdevelopedafterrapidlyascendingto~2,400meters (~7,800feet)abovesealevel.ShewastreatedforHACEandHAPEwithresolutionofhersymptoms within24hours.
Conclusion: High-altitudepulmonaryedemaandHACEcandeveloprapidlyandatmoderatealtitudes. Expeditiousrecognitionandtreatmentisimperativetoavoidlife-threateningcomplications.[ClinPract CasesEmergMed.2024;8(3)202–205.]
Keywords: acutemountainsickness;highaltitudepulmonaryedema;highaltitudecerebraledema; casereport;computedtomography.
High-altitudeconditionsinvolveaspectrumofdiseases includingacutemountainsickness(AMS),high-altitude pulmonaryedema(HAPE),andhigh-altitudecerebral edema(HACE).1–3 Acutemountainsicknessmanifestswith non-specificsymptoms,mostcommonlyheadache,nausea, andfatigue.Itusuallydevelops2–12hoursafterinitial arrivalathighelevation.1 High-altitudepulmonaryedema canpresentwithexertionaldyspnea,chesttightness,cough, anddecreasedexercisecapacity.4 High-altitudecerebral edemagenerallypresentswithvaryinglevelsofconfusion, ataxia,alteredmentalstatus,andvomiting,withataxia presentinupto60%ofreportedcases.1,4,5 EarlyHACEmay manifestassocialwithdrawalanddrowsiness.4 High-altitude cerebraledemarepresentstheleastcommonformofhighaltitudeillness;however,itisthemostimportanttodiagnose andtreatastheconditioncanrapidlyprogresstocoma secondarytobrainherniationanddeathinas fewas12hours.1,6
ThereportedprevalenceofHACEbetween4,200–5,000 meters(m)(~13,800to~16,400feet[ft])abovesealevelis 0.5–1%.3,4 WhenHACEdoespresent,itisthoughttooccur within1–5daysofanascentgreaterthan2,500–3,000m (8,200–9,800ft)abovesealevel,anditisrarelyseenat altitudeslowerthan2,500m(8,200ft)abovesealevelor withinthe first24hoursofarrival.4 Themostimportant factorsinthedevelopmentofsymptomsaretherateofascent andperiodofacclimatization.1 Thiscasehighlightsapatient whodevelopedsymptomsofHACEandHAPEwithinhours ofrapidlyascendingto~2,400m(~7,800ft)abovesealevel, whichonlyfewcaseshavepreviouslydemonstrated.
A46-year-oldfemalewithnopastmedicalhistoryand takingnomedicationspresentedtotheemergency department(ED)viaemergencymedicalservices(EMS)for acutealteredmentalstatusthatdevelopedwhilehikingon MountSanJacintoinSouthernCalifornia.Thepatienthad
traveledfromthecoastalregionofSouthernCalifornia (~20m[~60ft]abovesealevel)toPalmSprings,CA, (~150m[~490ft])abovesealevelwithawildernessgroup. AfterascendingviathePalmSpringsAerialTramwayovera 10–12minuteperiodandarrivingatthebasecampstation (~2,400m[~7,800ft]abovesealevel),thepatientbegan complainingofworseningmalaise,nausea,chesttightness, andheadache.Hersymptomsworsenedwhilehikingashort distancetoacampsite(~2,800m[~9,200ft]).Shortlyafter arriving,thepatientbeganvomiting,whichpromptedthe teamleadertodescendonthetramwiththepatientandcall EMS.Duringdescent,thepatientbecamemoreconfusedand ataxic,requiringassistancewithambulation.OnEMS arrivalatthebaseofthetram,thepatientwasmarkedly alteredandagitated.
IntheED,vitalswerebloodpressure132/86millimetersof mercury,heartrate84beatsperminute,respirations21 breathsperminute,andoxygensaturation100%on2liters nasalcannula.Onphysicalexam,thepatientwasnotedtobe tachypneic,mumblingincomprehensiblesounds,only openingeyestovoice,andwithdrawingtopain.Shewasnot answeringquestionsorfollowingcommands.Shewas intermittentlycombativeand fightingtogetoutofbed.Her GlasgowComaScorewas10(eyes-3,voice-2,motor-5). Therewasnoevidenceoftrauma.
WorkupintheEDincludedelectrocardiogram,complete bloodcount,metabolicpanel,urinalysis,drugscreen, ethanollevel,acetaminophenlevel,salicylatelevel, coagulationstudies,quantitativehumanchorionic gonadotropin,chestradiograph(CXR),andcomputed tomography(CT)ofthehead.Theonlylababnormalities wereinthemetabolicpanel,withasodiumof128 milliequivalentsperliter(mEq/L)(referencerange: 135–145mEq/L),potassiumof3.1mEq/L(3.5–5.0mEq/L), carbondioxideof18millimoles(mmol)/L(20–32mmol/L), andelevatedaniongapat22mEq/L(7–13mEq/L).Ethanol, acetaminophen,salicylate,andurinedrugscreenwere negative.TheCXR(Image)showeddiffusepulmonary vascularcongestion.SheremainedquiteagitatedintheED, requiring3milligrams(mg)oflorazepamintravenously(IV). TheheadCTinterpretationwaslimitedduetopatient motionbecauseofagitation,althoughnoacuteintracranial abnormalitywasseen.
Withoutanotherobviouscauseofherhypoxiaandaltered mentalstatus,HACE/HAPEtreatmentwasstartedinthe ED.Shewasgiven250mgacetazolamideIVand8mg dexamethasoneIV.Thepatientwasadmittedtothehospital forobservation,withneurologyandnephrologyspecialist consultationforalteredmentalstatusandminorelectrolyte abnormalities.Hersymptomscompletelyresolvedthe followingday,andherlabvaluesnormalized.Hermild hyponatremiaof128mmol/Lwasnotthoughttobethemain drivingfactorbehindhersymptoms.Atthetimeofdischarge shehadnomemoryofdescent,EMStransport,orhertimein
Whatdowealreadyknowaboutthis clinicalentity?
Mostcasesofhighaltitudecerebraledema (HACE)andhighaltitudepulmonaryedema (HAPE)occuratgreaterthan > 4000m (~13000ft)abovesealevel.
Whatmakesthispresentationof diseasereportable?
Thiscasehighlightsapatientwhodeveloped symptomsofHACEandHAPEwithinhours ofrapidlyascendingto~2400m(~7800ft) abovesealevel.
Whatisthemajorlearningpoint?
HAPEandHACEcanoccurmore rapidlyandatlowerelevationsthan previouslythought.
Howmightthisimproveemergency medicinepractice?
Giventhehighmortalityrateindelayed diagnosisofHAPEandHACE,itis imperativetokeepahighindexofsuspicion whensusceptibleindividualspresent.

Image. Oneviewanterior-posteriorchestradiographobtained duetopatient’scomplaintofchesttightnessduringascenttohigh altitudeandtachypneaonpresentation.Pulmonaryvascular congestionisseenthroughout.Thereisnoevidenceof pneumothorax,cardiomegaly,orconsolidation.
theED.Onceawake,shedeniedanypreviousdrugor alcoholuse.
Intheprogressionofhigh-altitudedisease,AMSgenerally develops first.5 Symptomsareusuallyseenafter2–12hours andreachmaximumintensityat18–24hoursataltitudes greaterthan2,500m(~8,200ft)abovesealevel.1,4,7 HighaltitudecerebraledemaandHAPEarerare,andusually occurathigheraltitudes(>4,000m[>13,000ft])aftera longerperiodoftime(1–5days).4 ProgressionofAMSto HACEisthoughttoresultfromdisruptionofthebloodbrain barrier,intracellularedemaand,possibly,venousoutflow obstruction.2,5 Hypoxialeadstocerebralvasodilationand increasedcapillarypressure,eventuallyleadingto fluidshifts intocellsandcerebraledema.2,5 Hypoxiaandcerebral vasodilationisthoughttocausetheinitialheadachesand lethargyseeninAMS,andalertpatientscanrapidly deterioratetocoma(within12hours),althoughthisisrare andusuallyoccursatextremealtitudes.2,5,8 InHAPE, pulmonaryarterypressuresincreasefromhypoxic pulmonaryvasoconstriction,causingcapillaryhypertension and fluidshifts.4,5 OfpatientswithHAPE,15%willalsohave HACE,andHACEhasbeenreportedataltitudesaslowas 2,500m(~8,200ft)abovesealevelinpatientswhohave concomitantHAPE.1,7,9
Riskfactorsforincreasedsusceptibilityforhigh-altitude illnessesincludefemalegender,youngerage,andahistoryof migraines.3 Inthecasedescribedabove,thepatientpresented withclassicsymptomsofbothHACE(ataxia,alteredmental status,vomiting)andHAPE(chesttightness,hypoxia, tachypnea).Itispossiblethatourpatient’sgenderpotentially contributedtoherrapidprogression.At46yearsofage,she wasonthecuspofthedefinedageriskofAMS,whichmay havealsoplayedapart.Thepatienthadnoreportedhistory ofmigraines.HistoryofAMShasalsobeencitedasarisk factorforrecurrentepisodes;however,shehadnoreported historyofAMS.3
Ourpatient’sinitialheadCT,althoughlimitedsecondary tomotionartifact,didnotrevealanyobviousedema.When findingsarepresent,CToftheheadcanshowdiffuselow densityintheentirecerebrum,whitemattersignal attenuationwith flatgyriandeffacedsulci,andsmall ventricles.5,8,10 Magneticresonanceimaging(MRI) findings canincludeedemainthegenuandspleniumofthecorpus callosumandthesubcorticalwhitematter.1,5 Microbleeds havealsobeenseeninthecerebralwhitemattertractsof HACEsurvivors,whichwerenotseeninpatientswithAMS orHAPEonly.1,7,11 Cerebralwhitemattercytotoxicedema onbrainMRIismoreconsistentlyseenafter22hoursof symptomonset.1 Hackettin1998detailedninepatientswith HACE,allofwhomrecoveredwithtreatment.Fourpatients whoweredefinedas “moderatelyill” hadnormalMRIs.11 In arecentstudyconductedbyLongetal,thebrainCTand
MRIfrom30patientsdiagnosedwithHACEwerereviewed fromJanuary2012–August2022.Findingsrevealeda100% sensitivityand100%specificityofMRIdiagnosis,anda 23.3%sensitivityand100%specificityofCTdiagnosis.12 Unfortunately,brainMRIwasnotdoneonourpatient duringhospitalization.Giventhebroadpotential findingson CTheadwithitspoorsensitivity,ifclinicalsuspicionishigh enoughtreatmentshouldnotbedelayedduetonegativeCT headimaging.
High-altitudepulmonaryedemacanmanifestaspatchy lunginfiltratesonCXR,whichareusuallyunevenly distributed.4,5,13 AsinHACE,CXR findingsresolveas clinicalfeaturesimprove.13 Whileourpatient’sCXRshowed pulmonaryedemaconsistentwithHAPE,thedistribution wasmoreeventhanwhatisclassicallyseen.Lower respiratorytractinfectionsbeforetravelareariskfactorthat mayaccountforHAPEatlowaltitudes.4 Virusescouldalter thepermeabilityofthealveolar-capillarybarrierandlower thepressurerequiredforformationofedema.4 Toour knowledge,thepatienthadnoknownviralsymptoms beforeascent.Thecasealsooccurredbeforethe2019 coronaviruspandemic.
Oncethereissuspicionforahigh-altitudeconditionofany degree,themostimportanttreatmentisdescent.Thisis especiallytrueinindividualswithHACEduetothecerebral edemaandriskofbrainherniation.2,12 WildernessMedical SocietyGuidelinesrecommendthatratherthantreating patientsbasedonaltitudeonly,treatmentshouldbebasedon symptoms.9 Symptomsusuallyresolveafterdescentof 300–1,000m(~980–3,200ft)abovesealevel.9 Interestingly,our patient’sconditionworsenedwithdescent.Oncedescendedor ifdescentisnotanoption,low-flowoxygencanbeappliedwith anoxygensaturationgoalofgreaterthan90%forpatientswith suspectedHAPE.Theuseofdexamethasoneinthetreatment ofAMSandHACEiswidelyaccepted,witharecommended doseof8mg(intramuscularly,IV,ororally),followedby4mg everysixhoursuntilsymptomsresolve.2,5,9 Dexamethasone mayhelpwithHAPE,althoughthisisunclear.9 Thereislimited dataontheuseofacetazolamideasatreatmentforAMSor HACE.However,currentliteraturerecommends considerationofitsuseinAMS.12 ForHAPE,acetazolamide maycausehypotension,especiallyifthereisconcomitant dehydration,whichcanworsendyspnea.9 Loopdiuretics shouldbeavoidedinHACEduetoassociateddehydration.5,9
Acutemountainsickness,HAPE,andHACEarea spectrumofconditionsundertheumbrellaofhigh-altitude illnesses.Whilerarelyseen,andgenerallyonlyatveryhigh elevations(>4,000m[>13,000ft]abovesealevel),HAPE andHACEcanoccurmorerapidlyandatlowerelevations thanpreviouslythought.Giventhehighmortalityratein delayeddiagnosisofHAPEandHACE,itisimperativethat physicianskeepahighindexofsuspicionwhenpotentially
susceptibleindividualspresent.Oncehigh-altitudesicknessis diagnosed,prompttreatmentiscrucialtoavoidlifethreateningcomplications.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:SuneilAgrawal,MD,DesertRegional MedicalCenter,1150N.IndianCanyonDr.,PalmSprings, CA92262.Email: Suneil.Agrawal@vituity.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Walshetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TurnerR,GattererH,FallaM,etal.High-altitudecerebraledema:its ownentityorend-stageacutemountainsickness? JApplPhysiol. 2021;131(1):313–25.
2.BasnyatBandMurdochDR.High-altitudeillness. Lancet. 2003;361(9373):1967–74.
3.BärtschPandSwensonER.Acutehigh-altitudeillnesses. NEnglJMed. 2013;368(24):2294–302.
4.LuksAM,SwensonER,BärtschP.Acutehigh-altitudesickness. Eur RespirRev. 2017;26(143):160096.
5.DavisCandHackettPH.Advancesinthepreventionand treatmentofhighaltitudeillness. EmergMedClinNorthAm. 2017;35(2):241–60.
6.JensenJandVincentAL.HighAltitudeCerebralEdema.In: StatPearls.TreasureIsland(FL):StatPearlsPublishing;2023. Availableat: https://www.ncbi.nlm.nih.gov/books/NBK430916/ AccessedAugust1,2023.
7.HackettPH,YarnellPR,WeilandD,etal.AcuteandevolvingMRIof high-altitudecerebraledema:microbleeds,edema,and pathophysiology. AJNRAmJNeuroradiol. 2019;40(3):464–9.
8.HackettPHandRoachRC.Highaltitudecerebraledema. HighAltMed Biol. 2004;5(2):136–46.
9.LuksAM,AuerbachPS,FreerL,etal.WildernessMedicalSociety ClinicalPracticeGuidelinesforthePreventionandTreatment ofAcuteAltitudeIllness:2019update. WildernessEnvironMed. 2019;30(4):S3–18.
10.KobayashiT,KoyamaS,KuboK,etal.Clinicalfeaturesofpatientswith high-altitudepulmonaryedemainJapan. Chest. 1987;92(5):814–21.
11.HackettPH,YarnellPR,HillRN,etal.High-altitudecerebraledema evaluatedwithmagneticresonanceimaging. JAMA. 1998;280(22):1920.
12.LongCandBaoH.Studyofhigh-altitudecerebraledemausing multimodalimaging. FrontNeurol. 2023;13:1041280.
13.KoyamaS,KobayashiT,KuboK,etal.Theincreasedsympathoadrenal activityinpatientswithhighaltitudepulmonaryedemaiscentrally mediated. JpnJMed. 1988;27(1):10–6.
DevinM.Howell,DO* GarrettLamouree†
*NorthwellHealth,DepartmentofEmergencyMedicine,Huntington,NewYork † BinghamtonUniversity,Binghamton,NewYork
SectionEditor:RachelLindor,MD,JD
Submissionhistory:SubmittedNovember4,2023;RevisionreceivedJanuary17,2024;AcceptedJanuary26,2024
ElectronicallypublishedMay14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.4918
Introduction: Acuteconfusionalmigraine(ACM)isararevariantofmigrainethatisbenignandselfresolvingbutdifficulttodiagnose.Withoutknowncausativepathophysiologyandalackofrecognitionin theInternationalClassificationofHeadacheDisorders(ICHD-3),ACMoffersapuzzlingclinical presentation.TherecurrentlyisnostandardizedtreatmentforACM,butwithagrowinganecdotal datasetthereistheopportunitytoformallyrecognizeandestablishprotocolstoimprovepatientcare andoutcomes.
CaseReport: A14-year-oldfemalepresentedtotheemergencydepartment(ED)withacuteonsetof confusion,visionchanges,right-sidedweakness,anddysarthriaonehourpriortoarrival.Astroke workupattheinitialEDofferednopertinent findings.Thepatientwastransferredtoapediatricspecialty EDwhereallsymptoms,asidefromnumbnessandamildheadache,resolvedduringtransfer.After administrationofamigrainecocktailatthepediatricspecialtyED,allremainingsymptomscompletely resolved.ThepatientwasdischargedhomefromtheEDthesameeveningwithoutpatientfollow-up.
Conclusion: ThiscasepresentsthedifficultyofdiagnosingandtreatingACMpriortoitsself-resolution.It highlightstheneedforformalrecognitionoftheconditionbytheICHD-3.Indoingso,greaterrecognition willpromotemoreresearch,awareness,andestablishmentofastandardizedtreatmentforACM.[Clin PractCasesEmergMed.2024;8(3)206–210.]
Keywords: pediatric;migraine;confusion;stroke;casereport.
Acuteconfusionalmigraine(ACM)afflictsallages,witha predominanceinchildren,andinvolvesasuiteofsymptoms, includingconfusion,aphasia,andhemiplegia.1 Withno knowncausativepathophysiologyandalackofrecognition intheInternationalClassificationofHeadacheDisorders (ICHD-3)asamigrainevariant,knowledgeofthis disorderislimitedamongclinicians,makingACMan exclusionarydiagnosis.1 TheclinicalpresentationofACM offersabroadrangeofdifferentialdiagnoses,makingit difficulttodiagnosepatientsintheabsenceofanindividual orfamilyhistoryofmigraines.2 Together,theseaspectshave likelyledtounderdiagnosisofACMandalackof standardizedtreatment.1,2
Wepresentthecaseofa14-year-oldfemalewhopresented totheemergencydepartment(ED)withanacuteonsetof confusion,visionchanges,right-sidedweakness,and
dysarthria,whichbeganonehourpriortoarrival.Her symptomswereprecededbyanincidentofminorhead traumathatoccurredthedayprior.BoththerarityofACM andthediscussionregardingACM-associatedheadtrauma makethiscaseauniqueaccountofthedisorder.
A14-year-oldfemalepresentedtotheEDwithacute alteredmentalstatus.Perthemother,anhourpriortoED arrival,thepatienthadanacuteonsetofconfusionwith visionchanges,followedbydysarthriaandright-sidedupper extremityweaknessandnumbness.Itwasdiscoveredthatthe patienthadsufferedaminorheadtraumafromabackward fallthedaypriorwithoutlossofconsciousnessorvomiting. Shewasnotevaluatedforherheadtraumapriortothe currentvisit.Thepatienthadahistoryofintermittent headaches(notformallydiagnosed)andafamilyhistoryof

oneepisodeoftransientglobalamnesiainhermother.There wasnootherreportedmedicalhistoryoranyprior psychiatrichistory.UponpresentationtotheED,thepatient wasnotorientedtoselfandcouldnotfollowcommands. Physicalexamination(PE)wascompletedwiththepatient responding “Idon’tknow” tomostquestionsandcommands asidefromhername,amildrightpronatordrift,andinability tofollowadditionalcommands,therebylimitingher examination.AllotherPE findingswereunremarkable, includinganysignsofexternaltrauma.
ANationalInstituteofHealthStrokeScale(NIHSS)was calculatedtobe6,andacodestrokewascalled.Deficits includedlevelofconsciousness,inthatsheonlyansweredone questioncorrectly(1)andperformedneithertaskforlevelof consciousnesscommandscorrectly(2).Hermotorfunction washinderedwithrightarmdrift,withthelimbholding90 (or45)degrees,butdriftingdownbeforethefull10seconds, butnothittingthebedorsupport(1).Her finaldeficitwas severeaphasia(2),withallcommunicationthrough fragmentedexpression,whichrequiredagreatneedfor inference,questioning,andguessingbythelistener. Therangeofinformationthatcouldbeexchangedwas limited;listenercarriedtheburdenofcommunication. Examinercouldnotidentifymaterialsprovidedfrom patientresponse.
Bothacomputedtomography(CT)(Image1)andCT angiogram(CTA)(Image2)ofthebrainwerecompleted.No pertinent findingswereyieldedfromtheCTA;however,the non-contrastCTwasreadbyneuroradiologyashavinga possiblepunctatefocusofhemorrhage,whichprompted furtheremergentimaging.Thispunctatefocuswasnot appreciatedbyourteam.Astatmagneticresonanceimaging (MRI)ofthebrainwasperformedwithoutsignificant findings(Image3).Laboratoryevaluation,includinga completebloodcount,comprehensivemetabolicpanel,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Acuteconfusionalmigraine(ACM)canbe treatedwithtraditionalmigrainemedications butmaypresentwithworryingsymptoms, includingsigni fi cantneurologicalde fi cits.
Whatmakesthispresentationof diseasereportable?
Acuteconfusionalmigraineisanunderreportedstrokemimicthatmaypresenttothe emergencydepartmentandshould,therefore, beconsidered.
Whatisthemajorlearningpoint?
CliniciansshouldbeawareofACM, particularlyinchildren,tohaveabroader differentialforthosepresentingwith stroke-likesymptoms.
Howmightthisimproveemergency medicinepractice?
ThroughincreasedawarenessofACM, emergencyphysiciansmaybeabletoavoid unnecessaryradiationandlabtesting.
pregnancytest,urinetoxicology,andserumdrugscreen, werecompletedwithnoremarkable findings.
DuringtheinitialEDvisit,thepatient’sclinicalstatus remainedunchangedasidefromanepisodewhereshe


becamesomnolent,desaturatingto75%withgoodwaveform andimprovingto99%uponarousal.Sheappearedtobe complainingofaheadacheandhadoneepisodeofvomiting; therefore,1000milligrams(mg)ofacetaminophenand4mg ofondansetronwereadministeredintravenously.
Thrombolytics,suchastissueplasminogenactivatoror tenecteplase,werenotadministeredthroughoutpatientcare, asneitherhavebeenstudiedinpediatricpatients.3
Interfacilitytransporttoaspecialtypediatrichospitalfor pediatricneurologyconsultationandmedicaladmissionwas arrangedatthattime.
Duringtransport,allsymptomsresolvedasidefroma headacheandmildnumbnessoftherightarm.Uponarrival atthepediatricED,thepatientwasabletospeakincomplete sentences,andherNIHSSimprovedto0.Thepatientwas givenamigrainecocktailof25mgketorolac,1000milliliters normalsaline,and7mgprochlorperazineintravenously. Followingadministration,thepatientstatedimprovementin headache,thusconcludinghersymptoms,whichintotal lastedapproximately6.5hours.Followingaformalpediatric neurologyconsult,theworkingdiagnosiswasACM.The patientwasconsideredstableandwassubsequently dischargedthateveningwithananticipatedoutpatient pediatricneurologyappointmentinonetotwoweeks.
Thediagnosticandtreatmentroutechosenforthispatient highlightsthedifficultyofclinicalpresentationto differentiatefromotherseriousdiagnoses,includingcerebral infarction,intracranialhemorrhage,nonconvulsivestatus epilepticus,andencephalitis,amongothers.1 Ischemic pediatricstrokeshaveanincidencerateof1.2–13/100,000, makingthemexceedinglyrare.4 However,witha10% mortalityrateandthecriticalconsequenceofneurological impairmentindevelopment,pediatricstrokesareaserious medicalemergency.4
Asidefromastutehistory-taking,oneofthefew promisingdiagnosticteststodiagnoseACMisan electroencephalogram(EEG).Inpreviousstudies,EEGhas shownslowingin49of50patientsduringtheonsetof symptomsthroughtheretrospectivestudyofpatientswith confusionalmigraines;therefore,werecommendtheuseof EEGinthesepatients,ifcapable.1 BeyondanEEG,noother diagnosticmodalityoffersanindicationforACMuntilthe benignresolutionofsymptoms,acharacteristicofACM knownsincethecases firstrecordedbyGasconandBarlow.5 Therefore,withoutanysignificantpatientorfamily historybeyondhermother’stransientglobalamnesia episode,orthecapabilityofperformingaspotEEG,aCT withoutcontrast,CTA,andMRIwerecompletedtoruleout seriousdisease.
Priortotheonsetofthepatient’sACM,thepatientnoted afallbackwardinwhichshehitherheadwithoutlossof consciousnessorvomiting.Althoughthepathophysiology hasnotbeenconfirmed,literaturereviewhasshownthatthe onsetofACMisprecededbymildheadtraumain37%of patients.1 SomeproposedmechanismsforACMviamild headtraumaincludeisolatedcerebraledemaandcortical spreadingdepression(CSD),inducingatemporarystateof brainstemdysfunction.6,7 Intheseinstancesofmild,traumainducedACM,thetypicaltimefromtraumaticinjuryto onsetofACMissecondstoapproximatelyfourhours, puttingourpatient’sfallwelloutsidethetypicaltimeframe ofonset.1
WhileconsideringtheCSDmechanism,inaretrospective studyof143migrainepatients72.2%ofthosesuffering migraineswithaurareporteddeficitsinhigherbrain function.7 Withresearchdemonstratinganassociationof migraineauraswithCSD,itisplausiblethatthehigher functiondeficitsseenincasesofACMarecausedby CSD,therebyallowingACMtobeseenasacomplexform ofaura.8 However,withformalrecognitionanda standardizedtreatmentforACMlackingwithinthe ICHD-3,thediscussionnowiswhetherACMshould haveitsowndistinction.
Throughretroactivestudiesithasbeenshownthatof 2,509diagnosedpatientswithinaneuropediatricward,2.7% ofthemigrainediagnosesqualifiedasACM.9 Withoutthe specificclassificationcriteriatodiagnosethesepatients, diagnosticuncertaintycanprevail,leadingtomisdiagnosis andunderdiagnosis,especiallyamongstadultswithanew diagnosisofmigraine.10 Similarly,withtheuseoftechniques suchasCT,pediatricpatientsareputatahigherriskof malignancyfollowingexposuretoionizingradiation.11 The useofCThighlightshowdiagnostictoolscanpotentiallybe hazardous,inadditiontodelayingdiagnosisandtreatment. ShouldapatienthaveapertinenthistoryforACM,excessive diagnosticsshouldbeavoided,aviewpointthathasbeenheld sinceACM’sidentificationinthe1970sandwellintothe 21st century.12,13
ShouldACMearnclassificationwithintheICHD-3, furtherformalresearchwouldlikelyoccurtoseekouta standardizedtreatmentforepisodes.Todate,duetoits rarity,knowledgeofACMisprimarilylimitedtocase reports,meaningstandardizedtreatmenthasyettobe determined.Although,consideringACMasamigraine variant,casestudieshaveshownsuccesswithtraditional migrainetreatmentwithsodiumvalproicacid.14 Inthiscase, mostsymptomsself-resolved;however,theadministrationof amigrainecocktailincludingketorolac,normalsaline,and prochlorperazinedidshowimprovementinthepatient’ s residualsymptoms,supportingthattraditionalmigraine treatmentsareeffectiveforACM.
Itshouldbenotedthatalthoughthereisnotenough researchonACMinparticular,migrainesareoften associatedwithavarietyofcomorbidities,rangingfrom psychiatricdisorderstoepilepsy,aswellasdifferentmeansof cardiovascularcompromise.Forthisreason,itisimportant torecognizeasitmaylimitpatientcareoptions,andwith futureresearchcouldoffergreaterinsightintothe mechanismbywhichACMarises.15
Withtheaforementionedinmind,itisimportantto considertheclinicalapproachforACM.Withapediatric patientpresentingwithalteredmentalstatus,onemustbegin toruleoutthebroadspectrumofdifferentialdiagnoses.A completesetofvitalsigns,includingrectaltemperature(as appropriate)andbloodglucoseshouldbeobtained. Thoroughhistory-takingshouldbeperformedfromthe patientand/oranybystanders,toincluderelevantmedical, surgical,psychiatric,andfamilialhistory.Caremustbe takentoalsoobtainpotentialingestions,includingthosethat areaccidental,suchasmedications,drugs(edibles), environmental(carbonmonoxide,chemical,cleaning products),etc.Athoroughphysicalexamshouldelicitany signsoftrauma,acompleteneurologicexam,evaluationof thecardiacandrespiratorysystems,andaskinexamination. Theapproachtolaboratorytestingshouldincludethe following,ifrelevant:completebloodcellcount;complete metabolicpanel;urinalysis;urineandserumtoxicology studies;thyroidfunctiontests;andcerebrospinal fluid testing.Ifconcernexistsforintracranialpathology, neuroimagingshouldnotbedelayedandaspotEEGcanbe performed,ifavailable.
Topursuearouteoftreatmentforapatientwithsuspected ACM,traditionalmigrainemedicationshaveshown promise.Treatmentoptionsmayincludethefollowing: sodiumvalproicacid,prochlorperazinewithorwithout diphenhydramine,metoclopramide,dihydroergotamine, triptans,ketorolac,steroids,ornormalsaline.Patientswith ACMwillclassicallyseefullresolutionofsymptomswithout anylastingconsequencesafterreceivingtreatment.Even withcompleteresolution,patientsmaybeadmittedfor formalEEGmonitoringordischargedwithcloseoutpatient neurologyfollow-up.
Acuteconfusionalmigrainesareararevariantof migrainethatprimarilyaf fl ictschildren.Lackofawareness ofthedisease,however,posesrisksfordelayeddiagnosis, delayedtreatment,andexcessivediagnostictestsin pediatricpatients.Thiscasecontributestothegrowing collectionofACMepisodesthatcontinuestovalidate theargumentforrecognitionofACMbytheICHD-3. Clinically,ACMposesachallengetodiagnose; therefore,withoutapertinentpatientorfamilyhistory, furtherdiagnosticsshouldbecarriedouttoruleoutserious disease.WithcasesofACM,althoughtheepisodic symptomsaresevere,physiciansshould fi ndsolacein knowingtheyarebenignandself-resolving,andthat traditionalmigrainetreatmentsshowpromiseinreducing orresolvingsymptoms.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:DevinM.Howell,DO,Northwell Health,270ParkAvenue,Huntington,NY11743.Email: Dhowell6@ northwell.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Howelletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SchipperS,RiedererF,SándorPS,etal.Acuteconfusionalmigraine: ourknowledgetodate. ExpertRevNeurother. 2012;12(3):307–14.
2.EhyaiAandFenichelGM.Thenaturalhistoryofacuteconfusional migraine. ArchNeurol. 1978;35(6):368–9.
3.CenterforDrugEvaluationandResearch.Aboutdrugs@fda. U.S.FoodandDrugAdministration.Availableat: https://www.fda.gov/ drugs/drug-approvals-and-databases/about-drugsfda AccessedNovember19,2023.
4.TszeDSandValenteJH.Pediatricstroke:areview. EmergMedInt. 2011;2011:734506.
5.GasconGandBarlowC.Juvenilemigraine,presentingasanacute confusionalstate. Pediatrics. 1970;45(4):628–35.
6.ShaabatA.Confusionalmigraineinchildhood. PediatrNeurol. 1996;15(1):23–5.
7.VincentMandHadjikhaniN.Migraineauraandrelatedphenomena: beyondscotomataandscintillations. Cephalalgia. 2007;27(12):1368–77.
8.HadjikhaniN,SanchezdelRioM,WuO,etal.Mechanismsofmigraine aurarevealedbyfunctionalMRIinhumanvisualcortex. ProcNatlAcad SciUSA. 2001;98(8):4687–92.
9.PachevaIandIvanovI.Acuteconfusionalmigraine:Isitadistinctformof migraine? IntJClinPrac. 2013;67(3):250–6.
10.FisherCM.Late-lifemigraineaccompanimentsasacauseof unexplainedtransientischemicattacks. CanJNeurolSci. 1980;7(1):9–17.
11.MeulepasJM,RonckersCM,SmetsAM,etal.Radiationexposurefrom pediatricCTscansandsubsequentcancerriskintheNetherlands. JNatlCancerInst. 2018;111(3):256–63.
12.EmeryES.Acuteconfusionalstateinchildrenwithmigraine. Pediatrics. 1977;60(1):110–4.
13.FarooqiA,PadillaJ,MonteithT.Acuteconfusionalmigraine: distinctclinicalentityorspectrumofmigrainebiology? BrainSci. 2018;8(2):29.
14.FujitaM,FujiwaraJ,MakiT,etal.Theefficacyofsodiumvalproate andaMRA findinginconfusionalmigraine. BrainDev. 2007;29(3):178–81.
15.ScherAI,BigalME,LiptonRB.Comorbidityofmigraine. CurrOpin Neurol. 2005;18(3):305–10.
MeghanChamberlain,MD SimonA.Sarkisian,DO
SectionEditor:ManishAmin,DO
CooperUniversityHospital,DepartmentofEmergencyMedicine,Camden,NewJersey
Submissionhistory:SubmittedNovember17,2023;RevisionreceivedJanuary26,2024;AcceptedJanuary29,2024
ElectronicallypublishedJune3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6568
Introduction: Acutehematogenousosteomyelitismayhavesignificantmorbidityandmortalityif undiagnosed.Becauseitisuncommonindevelopedcountriesandhasvariablepresentations,the patientmayundergoseveralhealthcarevisitspriortodiagnosis.
CaseReport: Wereportthecaseofa9-year-oldmalewhopresentedwithhipandkneepainwith associatedfeversandwasfoundtohaveosteomyelitisandintraosseousabscessinthediaphysisofthe rightfemur.Hehadmultipleemergencydepartmentandoutpatientvisitsbeforetheultimatediagnosis wasmade.Hewastreatedwithirrigationanddebridementinadditiontointravenousantibiotics.
Conclusion: Pediatricacutehematogenousosteomyelitiscanhavesubtlepresentations,andthiscase illustratessomeofthedifficultiesinmakingthediagnosis.Thisconditionshouldbeconsideredinthe workupofachildwithundifferentiatedfever,pain,ordecreaseinmobility.[ClinPractCasesEmergMed. 2024;8(3)211–214.]
Keywords: osteomyelitis;intraosseousabscess;pediatric;casereport.
Acutehematogenousosteomyelitisiscausedbybacteria proliferatingwithinthebone.Itoccursfromhematogenous spread,whereepisodesofbacteremiacombinewithturbulent flowatthemetaphysealarteriolar-venoussinusoidtransition toallowlocalinvasion.Theseepisodesoccurmore commonlyduringchildhood,astheimmatureboneisless capableofcontaininginfection.Mostcasesinvolvechildren youngerthan fiveyearsofage.1 Localtraumacontributesto riskofhematogenousinfection,presumedtobesecondaryto microvascularbleedingandstasis.Afterageone,male childrenaremuchmorelikelytosustainminortraumathan femalechildren,whichmayexplainwhyosteomyelitis disproportionatelyaffectsmales.2 Othercausesincludedirect inoculationfromaprocedureortraumasuchasintraosseous accessorspreadfromsurroundingtissues.
Inolderpatients,thebonesarethickerandtheperiostea isdenser;soosteomyelitisismorelikelytocauseformation ofanintraosseousabscess.Infectionsarepredominantly causedby Staphylococcusaureus ,withaboutonethird
beingmethicillinresistant.3 Patientswithsickle hemoglobinopathiesareatspecificriskforinfectionfrom salmonella.4 Patientscanhaveavarietyofpresentations includingfevers,irritability,decreasedextremityfunction, pointtenderness,swelling,andwarmth.Because Saureus hasvariablegrowthandtheinoculummaybesmall,the clinicalcoursemaybeindolentandpatientsmaypresent withoutfeverorwithonlylow-gradefever.Riskfactors includesicklecelldiseaseoranyimmunocompromisedstate, sepsis,minortrauma,andindwellingvascularcatheters.5
Anine-year-oldmalewithhistoryofHashimoto thyroiditisandRaynauddiseasepresentedtothe emergencydepartment(ED)forintermittentrighthipand kneepain,dailyfevers,anddifficultywithambulationfor16 days.Hehadnopriorhistoryofinjurytothelegorof intraosseousaccess.Hehadinitiallypresentedtoadifferent EDonday10ofillnesswherehehadanormalhip radiographandlabs.Thepatientwasevaluatedfor
autoimmuneandtick-borneillnesses.Hewasthenreferredto aninfectiousdiseasespecialistwhomhesawonday16.The patientwasultimatelysenttoourEDforfurtherevaluation andimaging.
Vitalsignswerenotableforatemperatureof37.9° Celsius orallyandheartrateof155beatsperminute.Onphysical exam,thepatienthadnotendernesstopalpationoftheright lowerextremity,normalrangeofmotionofalljoints,and wasabletoambulateandjumpwithoutpain.Noswellingof thehiporoverlyingskinchangeswerenoted.Thepatient’ s laboratorytestingwasnotableforC-reactiveprotein(CRP) elevatedat16.82milligramsperdeciliter(mg/dL)(reference range0.3–1.0mg/dL),erythrocytesedimentationrate(ESR) aboveassaylimitsatgreaterthan100millimetersperhour (mm/hr)(l0–15mm/hrinmales,0–20mm/hrinfemales),but noleukocytosis.Radiographsofhisrighthip,rightknee,and rightfemurwereunremarkable(Image1).
Thepatientwasadmittedforfurtherevaluationandfound tohavecontinuedintermittentfeversandrightlower extremitypain.OnDay17,hehadmagneticresonance imaging(MRI)oftherightlowerextremitywithandwithout contrast,whichrevealedrightfemoralosteomyelitiswith underlyingintraosseousabscess(Image2).Hewastakento theoperatingroomforarightfemurreamingandirrigation withdebridement.Bloodandtissueculturesgrewmethicillin susceptible Saureus ,andworkupwasnotableforan echocardiogramwithoutevidenceofvegetationand abdominalultrasoundwithoutevidenceofanintraabdominalsourceofinfection.Hereceivedintravenous

PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Acutehematogenousosteomyelitisiswell characterizedintheliteraturewithregardto thephysiology,epidemiology,presentation, andmanagement.
Whatmakesthispresentationof diseasereportable?
Asidefromthereportedhistory,thispediatric patienthadaclinicallybenignpresentationof thisuncommondiseaseprocess.
Whatisthemajorlearningpoint?
Considerdiagnosisofacutehematogenous osteomyelitisinpatientswithlocalizedpain andrecurrentfever,evenifthephysicalexam isunderwhelming.
Howmightthisimproveemergency medicinepractice?
Cliniciansshouldconsiderthisdiagnosis morefrequentlyandconsidermore intensiveevaluation.
cefazolinfor30daysandwasthentransitionedtotwoweeks oforalantibiotics,startingwithdoxycycline,whichwasthen changedtoorallevofloxacinduetosideeffects.His inflammatorymarkersweretrendedthroughouttherapy untiltheynormalized.Patienthadresolutionofhis symptomsandwasabletoambulatewithoutabnormality.
Acutehematogenousosteomyelitisisuncommon,withan estimatedincidenceofeightper100,000childrenperyear.3 Diagnosiscanbesubtle,andpatientsoftenpresentwithpain thatisnotwelllocalizedandwithoutsignsoflocalinfection. Patientstypicallypresentwithinoneweekofonset,but diagnosiscanrequiremultiplevisits,asoccurredwith ourcase. 6
AsystemicreviewoftheliteraturebyDarnelletalfound thatpresentingsymptomsweremostcommonlypain (81.1%),localizedsignsorsymptomsofinfection,suchas warmth,pointtenderness,orswelling(70%),fever(61.7%), reducedrangeofmotion(50.3%),andreducedweightbearing(49.3%).Themostcommonlaboratory abnormalitieswereelevatedinflammatorymarkers(ESR 91%,CRP80.5%),withorwithoutleukocytosis(35.9%). Theyalsofoundthatinitialimagingwaslimitedwith

Image2. Magneticresonanceimagingoftherightfemurwithcontrastdemonstratinglesionsintheproximal(left)andmid(right)femoral diaphysis(arrows).
sensitivityofradiograph16-20%,computedtomography (CT)67%,ultrasound55%,whileotherimagingmodalities hadsignificantlybettersensitivitywithbonescan53–100% andMRI80–100%.ThedecisiontoperformMRIwith contrastinchildreniscontroversialasthereisnoevidence thatcontrastimprovessensitivityorspecificityofdetection.7 BecauseMRIrequiresdeepsedationorgeneralanesthesiain youngchildren,childrenwithconcerningclinicalorlab findingsareusuallyhospitalizedforclosemonitoringand/or treatmentpendingMRIimaging.
Inasystematicreviewexaminingintraosseousabscess (termedBrodieabscess)byVanderNaaldetal,407 patientswereexamined.Ofthese,themediantimeto diagnosisfrominitialcomplaintwas12weekswithprimary presentingcomplaintsofpain(98%)andswelling(53%). Patientstypicallyhadfullresolutionofsymptoms;however, twooftheincludedpatients(0.5%)hadlastingsequelaefrom bonydestruction:limbshortening,andvertebralbody collapsecomplicatedbyneurologicdeficits.3
Thiscasedemonstratesthedifficultiesinevaluatingfor thiscondition.Whilethepatient’shistorywasconcerningfor possibleinfection,uponpresentationtotheEDhedidnot haveanylocalizingexam findingstosuggestunderlying infectionandhadnoidentifiableriskfactorsfordevelopment ofthiscondition.Thiscasewasuniquelydifficultaswell giventhattheabscesseswerelocalizedtothediaphysisofthe bone,whereaslesionsaretypicallylocatedinthemetaphysis orepiphysis.Furthercomplicatingthediagnosiswasthe patient’shistoryofautoimmuneconditions,namely HashimotothyroiditisandRaynaudsyndrome,which suggestedapossibleautoimmuneetiologyofhissymptoms. Thereisnoestablishedrelationshipbetweenthedevelopment
ofosteomyelitisandtheseconditions.Thedifferential forthispresentationisextensiveandincludestick-borne illnesses,autoimmuneconditions,musculoskeletalinjuries, andinfection.
Acutehematogenousosteomyelitiscanhaveserious consequencesifundiagnosed,includingsepsisandbony destruction.Notallpatientswillhaveidentifiableriskfactors andpresentationsmaybesubtle.Manypatientswilllack focaltendernessorswellingonexam,andthediagnosis shouldbeconsideredinpatientswhohaverecurrentfeversor complainoflocalizedpain.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:MeghanChamberlain,MD,Cooper UniversityHospital,DepartmentofEmergencyMedicine,401 HaddonAvenue,Camden,NewJersey08103.Email: Chamberlain-meghan@cooperhealth.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Chamberlainetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SonnenGMandHenryNK.Pediatricboneandjointinfections:diagnosis andantimicrobialmanagement. PediatClin.1996;43(4):933–47.
2.RivaraFP,BergmanAB,LoGerfoJP,etal.Epidemiologyofchildhood injuries:II.Sexdifferencesininjuryrates. AmJDisChild 1982;136(6):502–6.
3.VanderNaaldN,SmeeingDP,HouwertRM,etal.Brodie’sabscess: asystematicreviewofreportedcases. JBoneJointInfect 2019;4(1):33–9.
4.BurnettMW,BassJW,CookBA.Etiologyofosteomyelitiscomplicating sicklecelldisease. Pediatr.1998;101(2):296–7.
5.RiiseØR,KirkhusE,HandelandKS,etal.Childhoodosteomyelitisincidenceanddifferentiationfromotheracuteonsetmusculoskeletal featuresinapopulation-basedstudy. BMCPediatr.2008;8:45.
6.WoodsCR,BradleyJS,ChatterjeeA,etal.Clinicalpracticeguidelineby thePediatricInfectiousDiseasesSocietyandtheInfectiousDiseases SocietyofAmerica:2021guidelineondiagnosisandmanagementof acutehematogenousosteomyelitisinpediatrics. JPediatrInfectDis Soc.2021;10(8):801–44.
7.DartnellJ,RamachandranM,KatchburianM.Haematogenousacute andsubacutepaediatricosteomyelitis:asystematicreviewofthe literature. JBoneJointSurgBr.2012;94(5):584–95.
KaraleeBluhm,MD
RavaliKundeti,DO
NicoleMaguire,DO
Rutgers-RWJBH-CommunityMedicalCenter,DepartmentofEmergencyMedicine, TomsRiver,NewJersey
SectionEditor:R.GentryWilkerson,MD
Submissionhistory:SubmittedNovember26,2023;RevisionreceivedJanuary25,2024;AcceptedJanuary31,2024
ElectronicallypublishedMay14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1891
Introduction: Wünderlichsyndrome(WS)referstosubcapsular,perirenal,orpararenalhemorrhage duetonon-traumaticandiatrogenicconditions.Neoplasms,vasculardisease,renaletiology,and anticoagulantuseareunderlyingriskfactors.
CaseReport: WedescribeacaseofWSina79-year-oldmalewhowasundergoinghemodialysis, whichresultedinhemorrhagicshockrequiringmultipletransfusionsandembolizationby interventionalradiology.
Conclusion: Mostcommonly,patientspresentwith flankpain;acomputedtomographywithcontrastof theabdomenisessentialfordiagnosis.Surgicalinterventionisconsideredinhemodynamicallyunstable patients.Conservativetherapyandintravenousresuscitationswithbloodproductsareconsidereda priorityinhemodynamicallystablepatients.[ClinPractCasesEmergMed.2024;8(3)215–218.]
Keywords: Wünderlichsyndrome;hemorrhagicshock;renalemergency;casereport;dialysis.
Wünderlichsyndrome(WS)isararebutlife-threatening conditiondefinedasacute-onset,spontaneous,nontraumaticrenalhemorrhageintothesubcapsular,perirenal, orpararenalspaces.Fewerthan300documentedcaseshave beenreportedbetween1974–2016.Itischaracterizedbythe Lenktriad:acute flankpain, flankmass,andhypovolemic shock.1 However,theclinicalmanifestationscanbevaried andnonspecific.Presenceofallthreecomponentsofthetriad isuncommon,occurringinonly20%ofcases.Abdominal and flankpainarethemostfrequentsymptoms,occurringin 67%ofpatients,followedbyhematuria(40%)and hemorrhagicshock(26.5%).2
Approximately60–65%ofcasesarerelatedtorenal neoplasms,withangiomyolipomaleadingbenignneoplasm causesandrenalcellcarcinomathemaincauseofmalignant neoplasms.TheoverallprevalenceofWSasacomplication ofrenalcellcarcinomaoccursinonly0.3–1.4%ofcases, whereasitisestimatedtooccurin13–100%ofcasesofrenal angiomyolipoma.3 Othercausesincludetuberoussclerosis,
vascularlesions(eg,polyarteritisnodosa),arteriovenous malformations,renalarteryaneurysms,rupturedrenalcysts, renalcalculi,andcoagulopathy.4 Wünderlichsyndromeis oftenassociatedwithhypertension(33–50%)and atherosclerosis(80–87%).3 Wünderlichsyndromehasaslight malepreponderancewithanaverageageof46.8years,with mostcasesoccurringbetween30–60years.2
Traditionally,themanagementhasrangedfrom symptomaticcareandobservationtopartialorcomplete nephrectomy.Currently,thetreatmentofchoiceincludes stabilizationandtranscatheterarterialembolization(TAE), butthisdependsontheseverityofpresentationorunderlying causeofWS.Surgicaltreatmentorcurativenephrotomyis preferredinpatientswithdiagnosedrenalmalignancy,in casesofhemodynamicinstability,and/orfailedTAE.4,5
Wepresentthecaseofa79-year-oldmalewhopresented withaspontaneousleftrenalsubcapsularhematomaandan activeperinephrichemorrhagethatoccurredduring hemodialysis,leadingtohemorrhagicshockrequiring multiplebloodtransfusionsandarterialembolization.
A79-year-oldmalepresentedtotheemergency departmentwith30minutesofacuteandworsening abdominalpainthatoccurredsuddenlyduringthe firsthour ofhisscheduledhemodialysis.Hedescribedthepainas sharp,cramping,stabbing,constant,anddiffusebutworsein theleftupperquadrantand flankandassociatedwithacute abdominaldistention.Hedeniedanyrecenttrauma,chest pain,shortnessofbreath,paresthesias,nausea,vomiting,or urinarycomplaints.
Hispastmedicalhistoryincludedend-stagerenaldisease (onhemodialysis),type2diabetesmellitus,chronic obstructivepulmonarydisease,hypertension, hyperlipidemia,andhypothyroidism.Onchartreviewitwas notedthattherewasahistoryofleftrenalcyst,lastmeasuring 6.8centimeters(cm) × 5.5cm × 5.3cmfouryearspriorto presentationfoundincidentallyoncomputedtomography (CT).Follow-uprenalultrasoundwasorderedbutnever obtained.Thepatient’schronickidneydiseasewasrelatedto hisdiabetesandpoorlycontrolledhypertensionthatrequired treatmentwithfourantihypertensivemedications.His surgicalhistoryincludedtwounspecifiedherniarepairs, bilateralkneereplacements,looprecorderplacement, andsmallbowelresectionduetosmallbowelobstruction 15yearspreviously.Hissocialhistoryincludeddailyalcohol use,andhewasanon-smokerwholivedwithfamilyand wasretired.
Initialvitalsignsrevealedslighthypotensionwithblood pressureof98/42millimetersofmercury;otherwise,vitals werewithinnormallimits.Thepatienthadbeenawakeand alert,inobviousdistressduetopain,andhavingdifficulty sittingstill.Abdominalexamwasnotableforbeingobese withrigidity,distention,diffusetenderness,guarding,and withoutappreciablebowelsounds,reboundtenderness,or ecchymosis.Theremainderofhisexamwasunremarkable.
Apoint-of-careultrasound(POCUS)revealedagrossly positivefocusedassessmentwithsonographyfortrauma (FAST)inMorrison’spouchandsplenorenalrecess,with limitedsubxiphoidandsuprapubicviews.Hewastreated withfentanylintravenouslyandbolusedwithnormalsaline. TheCTangiogramoftheabdomenandpelviswasnotable foran18-cmleftrenalsubcapsularhematomaand hemorrhageintheleftperinephricspacewithactivecontrast blushcomingfromtheleftrenalsegmentalandinterlobar branches(Images1 and 2).Therewerealsomultiplesclerotic lesionsofthethoracicandlumbarspineindicatingpossible metastasis.Pertinentlabvaluesincludedwhiteblood cellcountof14.6 × 103/microliter(μL)(referencerange 4.3–12.0 × 103/μL),with83%neutrophils(5–13%), hemoglobin7.8gramsperdeciliter(g/dL)(13.4–17.4g/dL), hematocrit24.1%(40–54%),platelets271 × 103/μL (150–440 × 103/μL),internationalnormalizedratio1.09 (0.83–111),partialthromboplastintime29.3seconds (21.5–31.9seconds),prothrombintime12.7seconds
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Inpatientswithriskfactors,Wünderlich syndrome(WS)maypresentastheLenk triad:acute fl ankpain, fl ankmass,and hypovolemicshockduetorenalhemorrhage.
Whatmakesthispresentationof diseasereportable?
Fewerthan300reportedcasesofWShave beenreportedbetween1974 – 2016.Ithas neverbeenreportedinpatientsactively undergoinghemodialysis.
Whatisthemajorlearningpoint?
Presentationvariesfromvaguetolifethreatening.Promptcomputedtomography willaidindiagnosis;treatmentrangesfrom supportivetosurgicalmanagement.
Howmightthisimproveemergency medicinepractice?
ThisrarepresentationofWShighlightsthe importanceofawidedifferentialinthose presentingwiththeLenktriad.

Image1. Axialviewofcomputedtomographyangiogramofthe abdomenshowinglargeleftrenalhematomawithcontrastblush (arrow)suggestiveofactivebleeding. mm,millimeter.
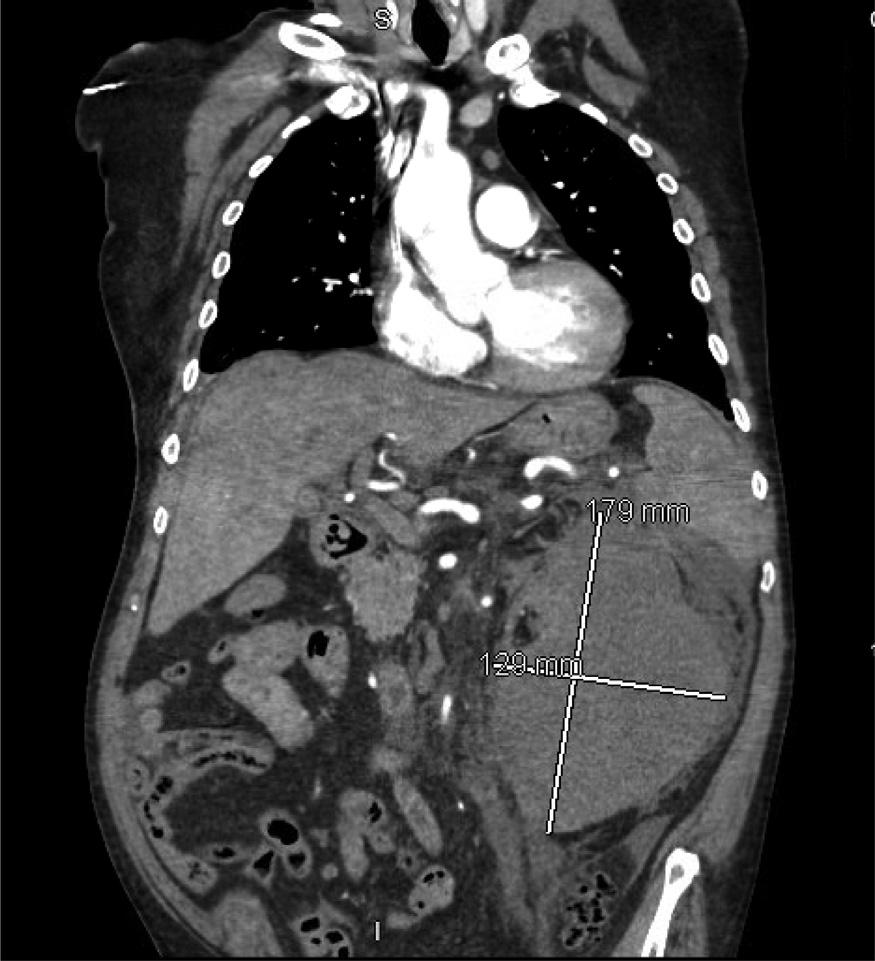
Wünderlichsyndromeisararecondition,butits occurrenceinadialyzedpatientisextremelyrarewithonlya handfulofotherreportsintheliterature.5,6 Wünderlich syndromeoccurringduringhemodialysishasnever previouslybeenreported.Ourcaseisanuncommonexample ofWSasitoccurredinapatientwithend-stagerenaldisease duringdialysiswithoutaknownhistoryofmalignancythat resultedinsignificanthemodynamicinstabilityrequiring emergenttransfusion,embolization,andintensivecare admission.ComputedtomographywithcontrastorCT angiogramarethediagnostictestsofchoice,7 butPOCUSis usefulinidentifyingintra-abdominal fluid,whichmay behemorrhage.
(10–13seconds),point-of-carelacticacid2.4millimolesper liter(mmol/L)(0.0–2.0mmol/L),glucose204milligramsper deciliter(mg/dL)(60–110mg/dL),bloodureanitrogen 47mg/dL(8–25mg/dL),andcreatinine7.13mg/dL (0.5–1.12mg/dL).
Whileawaitinginterventionalradiologyforrenal embolization,thepatientclinicallydeterioratedrequiring emergentcentrallineplacementandtwounitsofuncrossmatchedbloodadministeredbypressureinfuserandwarmer forhypotensionandactivebleeding.Duringembolization, multiplebranchesoftheleftkidneyincludingupperpole, mid-poleandlowerpolesubsegmentalarteries,aswellas interlobularandarcuatearteriesatallthreejunctures,were selectedandembolizedwithgoodangiographicresultandno evidenceofextravasationattheterminationofthe procedure.Thepatientwasthenadmittedtothesurgical intensivecareunitformonitoring.Hemaintainedstable bloodpressuresandwasdischargedhomeafterfournightsin thehospital.
Afterdischarge,hewassentforhematologyandoncology referralandpositronemissiontomographyduetoincidental findingsonhisCTduringthecurrentadmission.However, thepatientreturnedthreedaysafterdischargewith hypoglycemia,severeanemia,andactiveupper gastrointestinalbleed.Heunderwentan esophagogastroduodenoscopyandexploratorylaparotomy butultimatelydiedduetocomplicationsofthe gastrointestinalbleedwithinthreedaysofhissubsequent admission.Therewasnofurtheroncological workupperformed.
Althoughtheimagesinthisreportdonotdemonstrate fluidaroundtheliver,POCUSexamswiftlyrevealedamore diffuse,intra-abdominalhemorrhageasdemonstratedbythe positiveFASTexam,indicatingthatthebloodhadescaped theretroperitonealperinephricGerotafasciaintothe peritonealcavity.Unfortunately,wewerenotabletosavethe ultrasoundimages.Theuseofultrasound,whilenotnovel, didsubstantiallyreducethetimetakenfromcommencing caretodefinitivetreatment.Treatmentisbasedonthe patient’scondition,butstabilizationandtranscatheter arterialembolizationarestandardofcareforWScausing hemorrhagicshock.8,9
Ourpatienthadseveralriskfactorsthatmayhave contributedtothedevelopmentofWS.Hehadahistoryof hypertension,renalcysts,diabeticnephropathy,and atherosclerosis.Additionally,hehadadailyaspirinregimen, whichmighthaveexacerbatedhisoutcome.Apreviouscase ofbleedingintoasimplerenalcystcausinghemorrhagic shockwithoutotherriskfactorsknowntoWShasbeen reported.8 Hemorrhageinourpatientwaslocatedinthe kidney,whichhadthebackgroundofrenalcysts,suggesting non-malignantkidneymassesasanidusforhemorrhagethat isconsistentwithliteraturereview.
Furthermore,itispossiblethathehadanundiagnosed metastaticcancerasevidencedbylesionsnotedincidentally onCT.Furtherworkupwasunobtainableduetoclinical deterioration.Therelativeriskofrenalcellcarcinomain hemodialysispatientswasfoundtobe13.3to29-foldhigher thaninnormalsubjects,andhemodialysispatientshavea riskof2.3–3.3%ofdevelopingrenalcellcarcinoma.6 An autopsywasnotperformed;therefore,biopsyofthelesion wasnotobtained.
Thepatientwasondailyaspirinbutotherwisewasnot receivinganticoagulation.Hissubsequentadmissionalso revealedmassivebleeding;so,itispossibletherewassome underlyinghematologicalcomponentthatwascausingor contributingtohisbleedingdiathesis.Dailyalcoholusealso maybeariskfactorforWSortheseverityofpresentation. However,urologistshavedocumentedthaturemicpatients haveableedingtendencyassociatedwithplatelet
dysfunction10 becauseplateletsinuremicpatientshavea reducedaggregatingresponsetoadenosinediphosphate, epinephrine,andcollagen.11 Hemodialysispatients, therefore,aremorelikelytohavemoreseverebleeding,and treatmentshouldincludeconsiderationofoneora combinationofthefollowing:cryoprecipitate,desmopressin, andconjugatedestrogens.12
Duetoourpatient’ssuddenpresentationduring hemodialysis,weconsideredwhetherhemodialysismayhave beenariskfactorcausingenoughshiftsinpressuretoleadto spontaneousatraumaticrenalhemorrhage.Veryfewcasesof WSoccurinhemodialysispatients;therefore,thissubsetof patientswithWSriskfactorshasahigherlikelihoodof developingWS,particularlyiftheypresentwithelementsof theLenktriad.
Wünderlichsyndromeisararebutimportantdifferential toconsiderinatraumatic flankandabdominalpain.Mild presentationscaneasilybemisdiagnosedasbackpain, urolithiasis,orrenalinfections;so,keepingthisprocessin one ’sdifferential,especiallyinpatientswithriskfactors,is importantinobtainingthediagnosis.Point-of-care ultrasound,CT,andCTangiogramareparamountin identifyingintraperitonealfree fluidandactivehemorrhage. AlthoughseveralcasesofWShavebeeneffectivelymanaged conservatively,patientssuchasourscansufferfrom hemorrhagicshockresultingfromthesyndrome.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
AddressforCorrespondence:KaraleeBluhm,MD,RutgersRWJBH-CommunityMedicalCenter,DepartmentofEmergency Medicine,99Route37West,TomsRiver,NJ08755. Email: Karalee.Bluhm@rwjbh.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Bluhmetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ParmarN,LangdonJ,KaliannanK,etal.Wünderlichsyndrome:wonder whatitis. CurrProblDiagnRadiol. 2022;51(2):270–81.
2.GrubbSM,StuartJI,HarperHM.Suddenonset flankpain:spontaneous renalrupture. AmJEmerMed. 2017;35(11),1787.e1–.e3.
3.WangBH,PurezaV,WangH.AtaleofWünderlichsyndrome. JofSurg CaseRep. 2012;2012(11):rjs015.
4.KimJW,KimJY,AhnST,etal.Spontaneousperirenalhemorrhage (Wünderlichsyndrome):ananalysisof28cases. AmJEmerMed. 2019;37(1):45–7.
5.Tzu-ChengW,Kuo-HuaL,Pin-FangC,etal.Bilateralspontaneous massiverenalhemorrhageinaperitonealdialysispatient:acasereport. Medicine(Baltimore). 2021;100(44):e27549.
6.KawaharaT,KawaharaK,ItoH,etal.Spontaneousrenalhemorrhagein hemodialysispatients. CaseRepNephrolUrol. 2011;1(1):1–6.
7.ZagoriaRJ,DyerRB,AssimosDG,etal.Spontaneous perinephrichemorrhage:Imagingandmanagement. JofUrol. 1991;145(3):468–71.
8.BlakeleyCJandThiagalinghamN.Spontaneousretroperitoneal haemorrhagefromarenalcyst:anunusualcauseofhaemorrhagic shock. EmergMedJ. 2003;20(4):388.
9.AlbiG,DelCampoL,TagarroD.Wünderlich’ssyndrome: causes,diagnosisandradiologicalmanagement. ClinRadiol. 2002;57(9):840–5.
10.DiMinnoG,MartinezJ,McKeanML,etal.Plateletdysfunctionin uremia.Multifaceteddefectpartiallycorrectedbydialysis. AmJMed. 1985;79(5):552–9.
11.EvansEP,BranchRA,BloomAL.Aclinicalandexperimental studyofplateletfunctioninchronicrenalfailure. JClinPathol. 1972;25(9):745–53.
12.HedgesSJ,DehoneySB,HooperJS,etal.Evidence-basedtreatment recommendationsforuremicbleeding. NatClinPractNephrol. 2007;3(3):138–53.
JeanC.Y.Lo,MD
E.LeaWalters,MD
BrianWolk,MD
LomaLindaUniversityMedicalCenter,DepartmentofEmergencyMedicine, LomaLinda,California
SectionEditor:RachelLindor,MD,JD
Submissionhistory:SubmittedNovember26,2023;RevisionreceivedFebruary14,2024;AcceptedMarch7,2024
ElectronicallypublishedMay14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6583
Introduction: Pitviperenvenomationmaycausecoagulopathy.Thecoagulopathyhasbeentreated withcrotalidaepolyvalentimmunefragmentantigen-binding(Fab)ovineantivenomforthelastfew decadesintheUnitedStatesandusuallycorrectstheacutecoagulopathywithinhours.Daysafter receivingFab,coagulopathymayrecurinapproximatelyhalfofthepatients.Anotherdivalentantivenom, crotalidaeimmuneF(ab’)2 (equine)–F(ab’)2–wasapprovedbytheUSFoodandDrugAdministrationfor thetreatmentofpitviperenvenomation.F(ab’)2 iscomposedoftwolinkedantigen-bindingfragmentsof immunoglobulinG.SeveralstudieshavedemonstratedthatF(ab’)2 islesslikelytobeassociatedwith recurrence.ThereisnoreportedcaseofF(ab’)2-associatedlatecoagulopathyinveryyoungpatients.We reportthe firstcaseofrecurrenceassociatedwithF(ab’)2 useinapreschool-agechild.
CaseReport: Apreschool-agemaledevelopedlegswellingandhypofibrinogenemiaafterrattlesnake envenomation.F(ab’)2 wasadministeredtostabilizethelegedemaandtocorrectthe hypofibrinogenemia.Thepatientimprovedclinicallyandwasdischargedonhospitalday five.Seven daysaftertherattlesnakeenvenomation,hereturnedtotheemergencydepartmentasinstructed. Laboratorydatarevealedrecurrenthypofibrinogenemia.
Conclusion: TherearetwoantivenomsavailableintheUStotreatcrotalidenvenomation,Faband F(ab’)2.F(ab’)2 islesslikelytobeassociatedwithrecurrentcoagulopathyincomparisontoFab.We reportthe firstcaseofrecurrenceassociatedwithF(ab’)2 inapreschool-agechild.Itisimportantthatthe emergencyphysicianbeawareofpotentialF(ab’)2-associatedrecurrentcoagulopathy.Adultand pediatricpatientsmayneedtofollowuptobeevaluatedforhypofibrinogenemiaand/or thrombocytopeniaafterreceivingF(ab’)2.[ClinPractCasesEmergMed.2024;8(3)219–221.]
Keywords: pediatric;casereport;recurrence;F(ab’)2
Pitviper(Crotalinae )envenomationinNorthAmerica maycausecoagulopathy,whichmanifestsas hypofibrinogenemiaandthrombocytopenia.1 The coagulopathyhasbeentreatedwithcrotalidaepolyvalent immuneFab(ovine)(Fab)forthelastfewdecadesinthe UnitedStates.2 WhileFabcorrectstheinitialcoagulopathy withinhours,daysafterinitialFabadministration, coagulopathymayrecur.1,3,4,5 Recurrentcoagulopathymay beduetorapidclearanceofFab,whichhasaneffectivehalf
lifeoflessthan12hours.1 Approximatelyhalfofthepatients whoreceivedFabdeveloprecurrenthypofibrinogenemiaor thrombocytopenia.1 Theconcernwithrecurrence phenomenonisincreasedriskofbleeding.1,3,4
Anotherantivenom,crotalidaeimmuneF(ab’)2 (equine)–F(ab’)2–wasapprovedbytheUSFoodandDrug Administration(FDA)in2015forthetreatmentofNorth Americanpitviperenvenomation.6 F(ab’)2 iscomposedof twolinkedfragmentantigen-bindingregionswithalonger half-lifethanFab.7 Severalstudieshavedemonstratedthat
F(ab’)2 islesslikelytobeassociatedwithrecurrence.7,8,9 PreviousreportedcasesofF(ab’)2-associatedrecurrence werenotedinadultsandchildren >10yearsold.Wereport the firstcaseofrecurrentcoagulopathyassociatedwith F(ab’)2 inapreschool-agechild.
Apreschool-agemalepresentedtoanoutsideemergency department(ED)afterrattlesnakeenvenomationtohisleg. F(ab’)2 10vialsweregivenattheoutsidehospitalpriorto transfertoapediatricED.Vitalsignsrevealedtemperature 98.1o Fahrenheit,bloodpressure105/64millimetersof mercury,heartrate108beatsperminute,respiratoryrate18 breathsperminute,andoxygensaturation97%.Physical examdemonstratedleftlegedemawithecchymosis.The initial fibrinogenwas178milligramsperdeciliter(mg/dL) (referencerange200–393mg/dL).Thepatientdeveloped worseninglegswelling.HereceivedF(ab’)2 10vialsintheED andwasadmittedtothepediatricintensivecareunit(PICU). Anadditional28vialsofF(ab’)2 weregiveninthePICU (48vialsintotal).Hislegedemaandecchymosisstabilized. Noothersourceofbleedingwasnoted.His fibrinogenand plateletlevelremainedwithinnormalrangeduringthe admission.Thepatientwasdischargedonday five. HereturnedtotheEDsevendaysafterenvenomation. TheEDevaluationrevealed fibrinogenof147mg/dL. SubsequentEDvisitthreedayslaterrevealed fibrinogen improvedto162mg/dL.The Table includeshis fibrinogen trendafterrattlesnakeenvenomation.Hislegedemaand ecchymosisimproved.Nothrombocytopeniawasnoted duringadmissionorfollow-up.
Approximately5,000snakeenvenomationsarereportedto poisoncontrolcenterseachyearintheUS.10 Themajorityof thesesnakeenvenomationsaresecondarytorattlesnake envenomation.11 Crotalinae envenomationispredominately associatedwithlocaltissueeffectandhematologiceffects. Hematologiceffectsaretreatedwithantivenom.Overthelast fewdecades,Fabhasbeentheprimarytreatmentfor Crotalinae envenomationintheUS.2 Theplateletleveland fibrinogenlevel typicallyimprovewithinhoursofantivenomadministration.In approximatelyhalfofthepatientstheplateletand/or fibrinogen levelsdropagainafewdaysafterinitialFabadministration.1 Patientsareinstructedtofollowupwithaprimarycare physicianorreturntotheEDtorechecktheirplateletand fibrinogenlevelsafewdaysafterinitialFabadministration.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Recurrentcoagulopathyoccurscommonlyin patientswhoreceiveFab.Recurrenceisless commoninpatientswhoreceivedcrotalidae immuneF(ab ’ ) 2 (equine) – F(ab ’ ) 2 .
Whatmakesthispresentationof diseasereportable?
Untilnowtherehasbeennoreportedcase ofrecurrenceinveryyoungpatientswho receivedF(ab ’ ) 2 .Ourpatientdeveloped hypo fi brinogenemiaoneweekafter initialtreatment.
Whatisthemajorlearningpoint?
Recurrenceofhypo fi brinogenemiamayoccur inpatientsofallageswhoreceiveF(ab ’ ) 2 afterrattlesnakeenvenomation.
Howmightthisimproveemergency medicinepractice?
EmergencyphysicianswhoadministerF (ab ’ ) 2 topatientsafterrattlesnake envenomationshouldrecommendclose follow-upinaweek.
Patientswhodeveloprecurrencerequireclosefollow-up withfrequentmeasurementofplateletand fibrinogenlevels. Severethrombocytopeniaorhypofibrinogenemiahavebeen associatedwithincreasedriskofbleeding.4,5,6 Another antivenomF(ab’)2 wasapprovedbytheFDAin2015.6 F(ab’)2 islargerinsizeincomparisontotheFabfragment andisthoughttohaveaslowerrenalclearanceandlonger half-life.ThebenefitofF(ab’)2 overFabisthatF(ab’)2 isless likelytoresultinrecurrenceduetolongerhalf-life. Nowtherearetwocompetingantivenoms.F(ab’)2 appearstohavealowerriskofrecurrentcoagulopathyin multiplestudies.Arandomized-controlledtrialbyBushetal thatcomparedFabandF(ab’)2 revealedthatF(ab’)2 isless likelytobeassociatedwithrecurrencephenomenon.While 29.7%ofpatientsintheFabgroupdevelopedrecurrence, 10.3%patientsintheF(ab’)2 groupdevelopedrecurrence.
Table. Fibrinogentrendbetweendayoneandday10afterrattlesnakeenvenomation.
Dayafterrattlesnakeenvenomation 1234710
Fibrinogenlevelmilligramsperdeciliter(referencerange200–393)176396283297147162
Theplateletcountsand fibrinogenlevelswerelowerinthe FabgroupthanthoseintheF(ab’)2 group.Allsixpatients whodevelopedrecurrenceafterreceivingF(ab’)2 livedin inlandSouthernCalifornia.Onepossibilityisthat rattlesnakeenvenomationininlandSouthernCaliforniais morelikelytobeassociatedwithlatecoagulopathy. Furthermore,thestudybyBushincluded29.3%ofpatientsin theF(ab’)2 groupwhowereyoungerthan10yearsold.None ofthechildren <10yearsdevelopedrecurrence.7
AstudybyMascarenasetalalsoreportednolate coagulopathyassociatedwithF(ab’)2.Mascarenas compared37patients,11intheF(ab’)2 groupand26inthe Fabgroup.Therateofcoagulopathywas0%intheF(ab’)2 groupand29%intheFabgroup.8 AstudybyBoyeretal demonstratedthatmorepatientswhoreceivedFab developedthrombocytopeniaandhypofibrinogenemiain comparisontopatientswhoreceivedF(ab’)2.Ofthesix patientswhoreceivedF(ab’)2,onepatientdeveloped thrombocytopeniaandzeropatientshadalow fibrinogen level(<150mg/dL).9 Thesestudiesdemonstratedthat recurrenceislesslikelyinpatientswhoreceivedF(ab’)2 However,thereisstillanon-zeroriskforrecurrent coagulopathy,asillustratedbythiscase.Todate,therehas beennoreportedcaseofrecurrenceassociatedwithF(ab’)2 useinchildren <10.Wereportthe firstcaseofF(ab’)2associatedrecurrenceinapreschool-agechildwithout knownpre-existinghematopathologiccondition.
Limitationsofourreportincluderiskofextrapolation fromasinglecaseaswellasthefactthatthe fibrinogen concentrationdidnotreachalevelthatwouldsuggestahigh riskofbleeding.12 Alargerdatasetwouldberequiredto establishwhetherlaboratorysurveillanceismandatoryafter dischargeforchildrenreceivingF(ab’)2 antivenom.
TheantivenomcrotalidaeimmuneF(ab’)2 (equine)isless likelythanFabtoresultinrecurrenceorseverebleeding associatedwithlatecoagulopathy.ThebenefitofF(ab’)2 is lowerbleedingriskandpotentiallylessfrequentfollow-upfor laboratorytesting.WhileF(ab’)2-associatedlate coagulopathyisinfrequent,itdoesoccur.Adultandpediatric patientsmaystillrequirefollow-upfordetectionofrecurrent thrombocytopeniaandcoagulopathyafterreceivingF(ab’)2
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:JeanC.Y.Lo,MD,LomaLinda UniversityMedicalCenter,DepartmentofEmergencyMedicine, 11234AndersonSt.,LomaLinda,CA92354.Email: clo@llu.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Loetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
1.BoyerLV,SeifertSA,ClarkRF,etal.Recurrentandpersistent coagulopathyfollowingpitviperenvenomation. ArchInternMed. 1999;159(7):706–10.
2.GotoCandFengS.Crotalidaepolyvalentimmunefabforthetreatmentof pediatriccrotalineenvenomation. PedEmergCare. 2009;25(4):273–9.
3.BogdanGM,DartRC,FalboSC,etal.Recurrentcoagulopathyafter antivenomtreatmentofcrotalidsnakebite. SouthMedJ. 2000;93(6):562–6.
4.BaileyAM,JusticeS,DavisGA,etal.Delayedhematologictoxicity followingrattlesnakeenvenomationunresponsivetocrotalidae polyvalentantivenom. AmJEmergMed. 2017;35(7):1038.
5.KitchensCandEskinT.FatalityinacaseofenvenomationbyCrotalus adamanteusinitiallysuccessfullytreatedwithpolyvalentovine antivenomfollowedbyrecurrenceofdefibrinogenationsyndrome. J MedToxicol. 2008;4(3):180–3.
6.WilsonBZ,LarsenJ,SmelskiG,etal.UseofCrotalidaeequineimmune F(ab’)2 antivenomfortreatmentofanAgkistrodonenvenomation. Clin Toxicol(Phila). 2021;59(11):1023–6.
7.BushSP,RuhaAM,SeifertSA,etal.ComparisonofF(ab’)2 versusFab antivenomforpitviperenvenomation:aprospective,blinded, multicenter,randomizedclinicaltrial. ClinToxicol(Phila). 2015;53(1):37–45.
8.MascarenasDN,FullertonL,SmolinskeS,etal.ComparisonofF(ab’)2 andFabantivenomsinrattlesnakeenvenomation: firstyear’spostmarketingexperiencewithF(ab’)2 inNewMexico. Toxicon. 2020;186:42–45.
9.BoyerLV,ChasePB,DeganJA,etal.Subacutecoagulopathyina randomized,comparativetrialofFabandF(ab’)2 antivenoms. Toxicon. 2013;74:101–8.
10.GreenS,FoltJ,WyattK,etal.Epidemiologyoffatalsnakebitesinthe UnitedStates1989–2018. AmJEmergMed. 2021;45:309–16.
11.RuhaAM,KleinschimidtKC,GreeneS,etal.Theepidemiology,clinical course,andmanagementofsnakebitesintheNorthAmericansnakebite registry. JMedToxicol. 2017;13(4):309–20.
12.FaraoniD,WillemsA,SavanV,etal.Plasma fibrinogenconcentrationis correlatedwithpostoperativebloodlossinchildrenundergoing cardiacsurgery.aretrospectivereview. EurJAnaesthesiol. 2014;31(6):317–26.
MaiyaCowan,MD*†
PrasannaKumar,MD*†
JennyMcManus,MD,MPH*†
SeanBilodeau,DO*†
AndrewBeck,MD,MS†
SectionEditor:StevenWalsh,MD
*BrownUniversity,Providence,RhodeIsland † Lifespan/RhodeIslandHospital,DepartmentofEmergencyMedicine,Providence, RhodeIsland
Submissionhistory:SubmittedDecember13,2023;RevisionreceivedFebruary20,2024;AcceptedMarch8,2024
ElectronicallypublishedMay29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6622
Introduction: OpioiduseisanepidemicthatplaguestheUnitedStates.Patientsfrequentlypresentto theemergencydepartment(ED)afteropioidtoxicity,whichcanleadtorespiratoryfailure,apnea,and death.Althoughthereisaneffectiveantidote,naloxone,thecurrentguidelinessurroundingpostnaloxoneadministrationmonitoringarelooselydefined.
CaseReport: Wepresentacaseinwhichanindividualwasadministerednaloxoneafteranintentional opioidoverdoseandwasmonitoredforfourhours,asisstandardinourinstitution.HeremainedintheED foradditionalworkupfollowingthisobservationperiodandsubsequentlyexperiencedsignsofsevere respiratorydepression,requiringbag-valve-maskventilation,naloxone,andadmission.Hadhebeen discharged,asistypicalafterafour-hourobservationperiod,theconsequencescouldhavebeenfatal. Wepresentmultipletheoriesastowhyhisopioidtoxidromemayhavepresentedinadelayedmanner, includingingestionoffentanylanaloguesandvariabilityinmetabolizationofbothopioidsandnaloxone. WealsoexplorealternativeoverdoseantidoteproductsapprovedbytheUSFoodandDrug Administration,whichmayimpactpostoverdosecare.
Conclusion: Thiscasesuggeststhatthecorrectamountoftimetomonitorpatientsafternaloxone administrationmaybelongerthanoriginallythought.Ouraiminthisarticlewastofurtherthediscussion regardingthemostappropriateobservationperiodincasesofopioidtoxicity.[ClinPractCasesEmerg Med.2024;8(3)222–225.]
Keywords: naloxone;opioid;overdose;fentanyl;casereport.
Theopioidepidemicremainsaseriouspublichealthcrisis intheUnitedStates(US).Opioidoverdosesaccountfora largeproportionofemergencydepartment(ED)visits nationwideandarethenumberonecauseofdeathin individualsbetween25–64yearsofage.1,2 In2021,80,411 deathsinvolvingopioidoverdosewerereportedintheUS,an increasefrom68,630theyearprior.3 Naloxoneisa competitivemuopioidreceptorantagonistusedtoreverse thecentralandperipheraleffectsofopioidtoxicity.2
Currently,thereisnoconsensusregardingthedurationof observationafternaloxoneadministration.Variousstudies havecitedbetween1–4hoursassufficienttopreventadverse eventssuchasrecurrenceofrespiratorydepression, providingthepatienthasnormalvitalsignsand mentation.4,5 However,someauthorsrecommendeven longerobservationperiods.6 Thisreporthighlightsacaseof delayedopioidtoxidromeafternaloxoneadministration despiteanobservationperiodoffourhours,sheddinglight onpotentialpitfallswithcurrentpractice.
A30-year-oldmalewithpastmedicalhistoryof polysubstanceusedisorderandasthmapresentedtotheED followinganintentionalintranasalopioidoverdosewith illicitlypurchasedfentanyl.Hewasfoundunresponsive,and anambulancewascalled.Enroute,hereceivedatotalofsix milligrams(mg)ofintranasal(IN)naloxoneand0.4mg intravenous(IV)naloxonetoreversetheapneicstate.This washis firsttimeusingfentanyl,andhedeniedanyknown co-ingestion.Hedidnottakeanydailymedicationsorhave anyallergies.
Initialvitalsignswereasfollows:heartrate116beatsper minute;bloodpressure184/118millimetersofmercury; temperature97° Fahrenheit,andoxygensaturationof 94–100%ontwolitersofoxygen.Onexam,thepatientwas mildlysomnolentbutarousable,noddingoffduringthe interviewwithaGlasgowComaScale(GCS)of15.His pupilswerepinpoint.Thoughtcontentincludedactive suicidalideation(SI)withaplan.Hedemonstratednosigns oftrauma.Urinedrugscreen,animmunoassay,waspositive onlyforfentanyl,cannabinoids,andcocaine.Thiswaslater confirmedwithanextendeddrugpanel,whichwasalso negativeforthefollowing:methadone,benzodiazepines, buprenorphine,amphetamines,oxycodone,opiates,and phencyclidine.Acetaminophen,ethanol,toxicalcohol,and salicylatelevelswerenotdetected.Nootherlab abnormalitieswerepresent.
Thepatientwasgivenoneliterofnormalsalineandplaced ontelemetrywithconstantobservation.Afterfourhours,the patientwasmedicallystableashewasawake,alert,and cooperativewithaGCSof15.Atthispoint,hedemonstrated nosignsofrespiratorydepression,pupillaryabnormality,or mentalstatuschange.HeremainedintheEDforpsychiatric evaluationinthesettingofactiveSI.Duringthistime,hewas underconstantin-personobservationandhandcuffedtohis stretcher(arrestedonscene).Approximately5.5hoursafter initialnaloxoneadministration,thepatientbecameapneic andunresponsive.Hewasventilatedviabag-valve-maskand giventwomgofINnaloxonewithpromptclinicalresponse. HewasstartedonanIVnaloxoneinfusionat0.4mg/hour andadmittedtotheintensivecareunit.
Hewasontheinfusionforapproximatelytwohourswhen itwasdiscontinued.Approximatelythreehoursafter cessationoftheinfusion,hehadanotherepisodeofapnea. AnIVnaloxoneinfusionwasreinitiatedwitha0.2mgIV bolus,againwithappropriateclinicalresponse.Hewas successfullyweanedoffIVnaloxonelaterthatnight.Hewas dischargedtoacorrectionalfacilitywithpsychiatricfollowuptwodayslater.
Deathsfromopioidoverdosehavemorethantripledover thelastdecade.3 AsEDvisitsforopioid-relatedoverdoses continuetorise,itisparamounttohavestandardized
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Theopioidepidemicisasigni fi cantcause ofmorbidityandmortalityintheUnited States.Naloxoneisareadilyavailable antidotethatisclinicallyeffective.
Whatmakesthispresentationof diseasereportable?
Thepatientsufferedfromopioidtoxicitywell aftertheestablishedobservationperiodfor naloxoneuseatourinstitutionended.
Whatisthemajorlearningpoint?
Theremaynotbeauniversalobservation periodforopioidtoxicityintheemergency department,asindividualsmaymetabolize naloxoneandopioidsdifferently.
Howmightthisimproveemergency medicinepractice?
Thiscasemayencouragecliniciansto consideralongerobservationperiodor maintainahigherthresholdfordischarginga patientafteranopioidoverdose.
treatmentprotocolsinplace.Intranasalnaloxonehasgained momentumintheprehospitalandcommunitysettings,even becomingavailableoverthecounterin2023.Despiteits widespreaduse,therecontinuestobedisagreementover themostappropriateobservationperiodtoprevent adverseevents.
Theeliminationhalf-lifeofIVnaloxonerangesfrom 20–90minutes,whereasthatofmanyopioidscanbe substantiallylonger.5 Forexample,pharmaceuticalfentanyl hasahalf-lifeofapproximately3.6hours;andalthough humanstudiesarelacking,someanimalstudiessuggestthat carfentanilcanhaveahalf-lifeofupto7.7hours.7,8,9 Asa result,varioustimeperiodshavebeensuggestedasthemost appropriateforobservationaftertreatmentwithnaloxoneto preventrecurrenceoftoxicity.Therearestudiesthatciteone hourassafeandothersthatrecommendobservationperiods ofuptofourhours.4,5,10 Thepatientwasobservedforfour hoursinkeepingwithinstitutionalpolicyandsubsequently recrudesced,whichcouldhaveprovenfatal.
Therearemanyhypothesesastowhythispatient presentedatypicallyafteropioidintoxication:variabilityin naloxonemetabolism,ingestionoffentanylanalogues,and variabilityinopioidmetabolism.Theeliminationof
naloxonefollows firstorderkinetics.11 Consequently,after fourto fivehalf-lives,93.75–97%ofthedrugiseliminated, allowingfornegligibleremainingeffect.Basedonthewell documentedhalf-liferangeof20–90minutes,therateof eliminationamongtwopeopleoneitherendofthespectrum canbeapproximately4.5timesfasterorslower.5 Thisisa substantialdifference.Basedonthisrange,ifourpatient wereafastmetabolizerofnaloxone,helikelywouldhave requiredrepeatdoseswithintheobservationperiod. However,ifhewereaslowmetabolizer,hemayhavehad enoughnaloxonetopassafour-hourobservationperiodbut wouldexperiencereboundtoxicityonceitworeoff.Thereis scarcedatareviewingthisspecifictopic.
Onerecentstudysuggestsaprolongedobservationperiod between6–12hoursinchronicopioidusersorthosewho haveingestedmethadone,buprenorphine,orotherlongactingopioids.Additionally,once5mgormoreofIV naloxoneisadministered,admissionisrecommended.6 The rationaleisthatthisincreaseddosemayreflectthepotency andhalf-lifeoftheopioidingested.Ourcasemaybeanother datapointtosupportthenotionthattheremaybearolefor dose-dependentobservationperiodsafternaloxone administration.Thismaybehardtoquantifyasdosingis basedonclinicalresponseandmayoverestimatethe minimumamountofnaloxonerequiredforadequate reversal.Inaddition,thiswouldrequireamethodof standardizationwhencurrentobservationperiodsalready varygreatlyfromfacilitytofacility.5,10
Anotherexplanationisthatthepatientunintentionally ingestedalong-actingopioid,suchasafentanylanalogue. Fentanylanaloguesandnovelsyntheticopioidshave infiltratedtheunregulatedillicitdrugmarket.7 Data regardingpharmacokineticandpharmacodynamic propertiesoffentanylanalogues/novelsyntheticopioidsis scarce,andmuchofthedatacomefromanimalstudies.One example,carfentanil,haspermeatedthroughouttheillicit drugmarketandmaybeassociatedwithincreasing overdosesintheUS.7 Onesmallcohortstudyofhuman subjectsthatanalyzedpostoperativepainfoundthatfentanyl is50–100timesmorepotentthanmorphine,whilecarfentanil is10,000timesmorepotentthanmorphine.7 Thisis significantbecausepotency,affinityformuopioidreceptors, andeaseofdissociationcaninfluencehowmuchnaloxoneis neededtoreverseopioidtoxicity.8 Mostrelevanttothiscase, thehalf-livesofthesecompoundsvarygreatlyandwould havesignificantimplicationsforthedurationofmonitoring. Thehalf-lifeofpharmaceuticalfentanylis219minutes (~3.6hours),andanimaldatasuggeststhatthehalf-lifeof carfentanilis7.7hours.7,9,12 Giventhatthehalf-lifeof naloxoneis20–90minutes,thesecompoundscanbepresent formuchlongerthanthereversalagent,resultingin recurrenceoftoxicityandneedforlongermonitoringtimes. Toillustrate,onecaseserieshighlights18patientswho experiencedexaggeratedopioidtoxicityaftertestingpositive
forfentanylonalimiteddrugscreen.Seventeenofthese patientsrequirednaloxoneboluses,withfourrequiring prolongedinfusions(26–39hours).Furthermore,onepatient experiencedrecurrenttoxicityeighthoursafternaloxone discontinutation,10 similartothepatientpresentedinthis casereport.Thisshedslightontheneedformoredata regardingfentanylanditsanaloguesandpotentially increasingthetimeforobservationafterfentanyl ingestionsspecifically.
Considerationwasalsogiventothepossibilitythathehad self-administeredfentanylintheED.However,thiswas unlikelyashealwayshadastaffmemberpresentduetoSI andwasinhandcuffs.Anotherexplanationfordelayed opioidtoxidromecouldbevariablemetabolizationofthe drug.FentanylisprimarilymetabolizedbycytochromeP450 3A4(CYP4503A4)intheliverand,toalesserextent, duodenalmicrosomesandrenally.13 Fentanyliseliminated throughconversiontoinactive,nontoxicmetabolites.7 As withanyenzyme,metabolicfunctionmaybesubjectto variabilityamongindividualswithrespecttoexpressionand druginteractions.Forexample,patientswithhepatic impairmentwilllikelyhavedecreasedclearanceofthese medications.Additionally,drugsthatcompetewithfentanyl canresultinunforeseeninteractions.Toillustrate, benzodiazepinesarealsometabolizedbyCYP4503A4,and co-ingestioncouldresultindelayedconversionoffentanyl intoinactivemetabolites.13 Asaresult,ifmetabolismofthe opioidwasslowerthanthatofnaloxonethenthispatient couldhaveexperiencedreboundtoxicityoncenaloxone effectshaddiminishedorwaned.However,thispatient specificallydidnothaveanylaboratoryevidenceofhepatic impairmentorbenzodiazepineco-ingestion.
Whilenaloxoneisthestandardofcareforopioidoverdose reversal,otheremergingproductsinthepharmaceutical sectormayaddressbreakthroughpresentationssimilarto thiscase.Forinstance,in2023theUSFoodandDrug Administrationapprovednalmefeneasanintranasal alternativetonaloxone.Whilenalmefeneandnaloxoneare bothopioidantagonists,thebenefitofnalmefeneisthatits half-lifeisconsiderablylongerthannaloxoneat11.4hours.14 Morestudiesareneededtocompareitsefficacyandsideeffectprofiletonaloxone.However,itmayserveasa potentialalternativeforopioidoverdoses.
Thisdiscussionhighlightsacaseofdelayedopioid toxidromemorethanfourhoursafternaloxone administration.Themechanismofthese findingsisunclear butmayinvolveingestionoffentanylanaloguesorinterindividualvariabilityinmetabolizationofopioidsor naloxone.Whiledataislimitedonthisphenomenon, thiscasehighlightstheneedformorecontrolled studiesonappropriatedurationformonitoringafter naloxoneadministration.
Theauthorsattestthattheirinstitutionrequiresneither InstitutionalReviewBoardapproval,norpatientconsentfor publicationofthiscasereport.Documentationon file.
AddressforCorrespondence:MaiyaCowanMD,RhodeIsland Hospital,DepartmentofEmergencyMedicine,55ClaverickStreet, Providence,RI02903-4144.Email: Maiya_cowan@brown.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Cowanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SkolnickP.Treatmentofoverdoseinthesyntheticopioidera. PharmacolTher. 2022;233:108019.
2.BoyerEW.Managementofopioidanalgesicoverdose. NewEnglJMed. 2012;367(2):146–55.
3.NationalInstituteonDrugAbuse.DrugOverdoseDeathRates.2023. Availableat:~https://nida.nih.gov/research-topics/trends-statistics/ overdose-death-rates#:~:text=Opioid%2Dinvolved%20overdose% 20deaths%20rose,with%2080%2C411%20reported%20overdose% 20deaths.AccessedDecember10,2023.
4.ClemencyBM,EgglestonW,ShawEW,etal.Hospitalobservationupon reversal(HOUR)withnaloxone:aprospectiveclinicalpredictionrule validationstudy. AcadEmergMed. 2019;26(1):7–15.
5.HeatonJD,BhandariB,FaryarKA,etal.Retrospectivereviewof needfordelayednaloxoneoroxygeninemergencydepartment
patientsreceivingnaloxoneforheroinreversal. JEmergMed. 2019;56(6):642–51.
6.JordanMR,PatelP,MorrisonponceDNaloxone.In: StatPearls TreasureIsland(FL):StatPearlsPublishing;Availableat:~https://www. ncbi.nlm.nih.gov/books/NBK441910/#:~:text=The%20half%2Dlife% 20of%20naloxone,until%20obtaining%20a%20full%20recovery AccessedDecember10,2023.
7.ArmenianP,VoKT,Barr-WalkerJ,etal.Fentanyl,fentanylanalogsand novelsyntheticopioids:acomprehensivereview. Neuropharmacol. 2018;134(PtA):121–32.
8.LynnRRandGalinkinJL.Naloxonedosageforopioidreversal: currentevidenceandclinicalimplications. TherAdvDrugSaf. 2018;9(1):63–88.
9.ColeA,MutlowA,RamiroI,etal.Pharmacokineticsand pharmacodynamicsofcarfentanilandnaltrexoneinfemalecommon eland(Taurotragusoryx). JZooWildlMed. 2006;37(3):318–26.
10.WillmanMW,LissDB,SchwarzES,etal.Doheroinoverdose patientsrequireobservationafterreceivingnaloxone? ClinToxicol. 2017;55(2):81–7.
11.DowlingJ,IsbisterG,KirkpatrickC,etal.Populationpharmacokinetics ofintravenous,intramuscular,andintranasalnaloxoneinhuman volunteers. TherDrugMonit. 2008;30(4):490–6.
12.WolffK,Rostami-HodjeganA,ShiresS,etal.Thepharmacokineticsof methadoneinhealthysubjectsandopiateusers. BrJClinPharmacol. 1997;44(4):325–34.
13.LabrooRB,PaineMF,ThummelKE,etal.Fentanylmetabolismby humanhepaticintestinalcytochromeP4503A4:implicationsfor interindividualvariabilityindisposition,efficacy,anddruginteractions. DrugMetabandDisp. 1997;25(9):1072–80.
14.USFoodandDrugAdministration.HighlightsofPrescribingInformation. Availableat: https://www.accessdata.fda.gov/drugsatfda_docs/label/ 2023/217470Orig1s000.pdf.AccessedDecember10,2023.
GarrettTrang,BS TazBrinkerhoff,MD
TheUniversityofArizona,CollegeofMedicine-Phoenix,Phoenix,Arizona
SectionEditor:ChristopherSampson,MD
Submissionhistory:SubmittedAugust1,2023;RevisionreceivedFebruary19,2024;AcceptedMarch8,2024
ElectronicallypublishedMay29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1568
Introduction: Recognizingtesticulartorsionisextremelyimportantinpatientspresentingtothe emergencydepartment(ED)withacutescrotalpain.Traditionalmanualdetorsiontechniquesare frequentlyemployedbyemergencyphysiciansbutarenotalwayssuccessful.Delaysindetorsion increasetheriskoftesticularinfarctionandinfertility,andtheneedfororchiectomy.Noveltechniques suchasthetesticulartractiontechniquehavebeendescribedasapotentialsolutionfordifficult-todetorsetesticles.
CaseReport: Ourcasereportdescribesa20-year-oldmalewithnosignificantpastmedicalhistorywho presentedtoaruralEDwithacute,atraumatictesticularpainsecondarytotesticulartorsionwithanintact cremastericreflex.AfterconfirmingthediagnosisusingDopplerultrasound,manualdetorsionusingthe traditional “openbook” techniquewasattemptedandunsuccessful.Thepatientwassubsequently successfullydetorsedusingthenoveltesticulartractiontechnique.
Conclusion: Thetesticulartractiontechniqueisasafe,rapid,andeffectiveprimaryoradjunctive techniqueinmanualtesticulardetorsion.Giventhetime-sensitivenatureoftesticulartorsions,adjunctive techniquesplayacrucialroleinmanagingchallengingdetorsions,particularlyinresource-limitedrural settingswithlimitedaccesstourologicservices.Althoughitiscommonlythoughtthatthecremasteric reflexisabsentintesticulartorsions,itmaybepresentinrarecircumstances,anditspresenceshouldnot beanabsoluteinrulingouttorsion.[ClinPractCasesEmergMed.2024;8(3)226–230.]
Keywords: casereport;testiculartorsion;manualdetorsion;technique;cremastericreflex.
Scrotalcomplaintscompriseatleast0.5%ofallemergency department(ED)visits.1 Amongthedifferentialdiagnoses, testiculartorsionisoneofthemostseriousandisconsidered asurgicalemergency.Theannualincidenceoftesticular torsionisestimatedtobe3.8per100,000formales <18years ofage,andratesoforchiectomywerefoundtobeashighas 42%intheseboys.2,3 Giventhatthecomplicationsof testiculartorsionincludetesticularinfarctionandinfertility, quicklydiagnosingandtreatingitisimperative.3,4
IntheED,manualdetorsionisasafe,rapid,noninvasive treatmentthatshouldbeattemptedtoreverseischemiaand providerapidpainrelief.4 Sinceupto95%oftesticular torsionsareduetointernalrotation,thedetorsiontechnique
oftenrequiresexternalrotationofthetesticleasifonewas “openingabook.”5 Forasuspectedtorsionofthelefttesticle, thephysicianshouldplacehisorherrightthumbandindex fingeronthetesticleandrotate180degreesfrommedialto lateral(orclockwise).4 Theproceduremayberepeatedseveral timessincetorsioncaninvolverotationsof180–720degrees.4 Thesuccessrateofmanualdetorsionintheliteraturevaries;it canbeashighas76–95%whenperformedbyurologists,but otherstudiesfoundthesuccessratemorevariable.6–8 Given thevariablesuccessrateofthe “openbook” technique,itis importanttohaveanadjunctivetechniqueifitfailsorurologic interventionisnotimmediatelyavailable.
Thetesticulartractiontechniquewas firstdescribedin 2022byMellicketal9;itinvolvesgraspingthetesticlewith
oneorbothhandsandpullinginferiorlytostretchthe spermaticcordtoitsmaximumlength.Fromthere,manual detorsionofthetesticleisperformedbyexternallyrotating thetesticleusingthe “openbook” techniqueuntilthe spermaticcordfeelsnormal.Wedescribeasuccessful detorsionusingthetesticulartractiontechniqueafter conventionalmethodsfailed.
A20-year-oldWhitemalewithnoknownmedical conditionspresentedtoaruralEDwithcomplaintsof atraumaticandcontinuouspaintothelefttesticleand inguinalregionthatworsenedwithmovement.Thepain developedafteradayofworkinvolvingfrequentheavy lifting.Duringhisshowerathomeapproximately fivehours priortopresentation,henoticedthelefttesticularpainwas morepronouncedwithassociatedbulgingandtendernessin theleftscrotalregion.Hedeniedanyassociatedsymptoms suchasnauseaandvomiting.Hehadnohistoryoftorsion, undescendedtesticles,testicularmalignancy,orsurgeryto thetesticleorabdominalregion.
Onphysicalexam,thepatientappearedpale,nervous,and apprehensiveofmovement.Vitalsignswerewithinnormal limits.Genitourinaryexaminationrevealedahigh-riding andhardtesticlethatwasdiffuselytendertopalpation.There werenomassesintheinguinalregion,andnotesticular erythema,swelling,visiblemasses,orpeniledischarge.A hard,knot-likemasswaspalpatedonthesuperiorpoleofthe lefttesticlealongthespermaticcord,suspiciousforatorsed spermaticcord.Unexpectedly,thecremastericreflexwas present.Thesonographerwhoperformedtheultrasound approximatelysixhoursaftersymptomonsetnotedminimal blood flowtothelefttesticle(Image1).Theon-call radiologistquicklyconfirmedthediagnosisoftesticular
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Thetesticulartractiontechniquewas fi rst describedin2022asanadjunctivemanual detorsiontechniquefortesticulartorsions.
Whatmakesthispresentationof diseasereportable?
Apatientwithatesticulartorsionandan intactcremastericre fl exwasdetorsedusing thetesticulartractiontechnique.
Whatisthemajorlearningpoint?
Thisisasafe,noninvasivetreatmentthat providesrapidpainrelief.Absenceofthe cremastericre fl exmaynotalwaysbea reliablesignoftesticulartorsion.
Howmightthisimproveemergency medicinepractice?
Thetesticulartractiontechniqueisan effectiveprimaryoradjunctivetechnique fordif fi cult-to-detorsetesticles.
torsion.Theradiologyreportalsonotedatangled, heterogenousmasssuperiortothetesticlethatwasconsistent withthetorsedspermaticcordpalpableonphysicalexam (Image1).Therewasnonotableenlargementorchangesin echotexturethatwereconcerningforaninfarction ornecrosis.

Image1. Arterialandvenous flowinthelefttesticleandepididymisunderDopplerultrasound.Notethelackof flowinboththelefttesticle (yellowarrow)(A)andleftepididymis(orangearrow)(B).Therewasaheterogenousmass(orangearrow)superiortothelefttestiswithout blood flow,consistentwithtangledvasculature(B).Adiscussionwiththeradiologistdeterminedthatthespectralwaveformwasartifactand notvenous flow(A).
TRANS,transverseview; SAG,sagittalview.
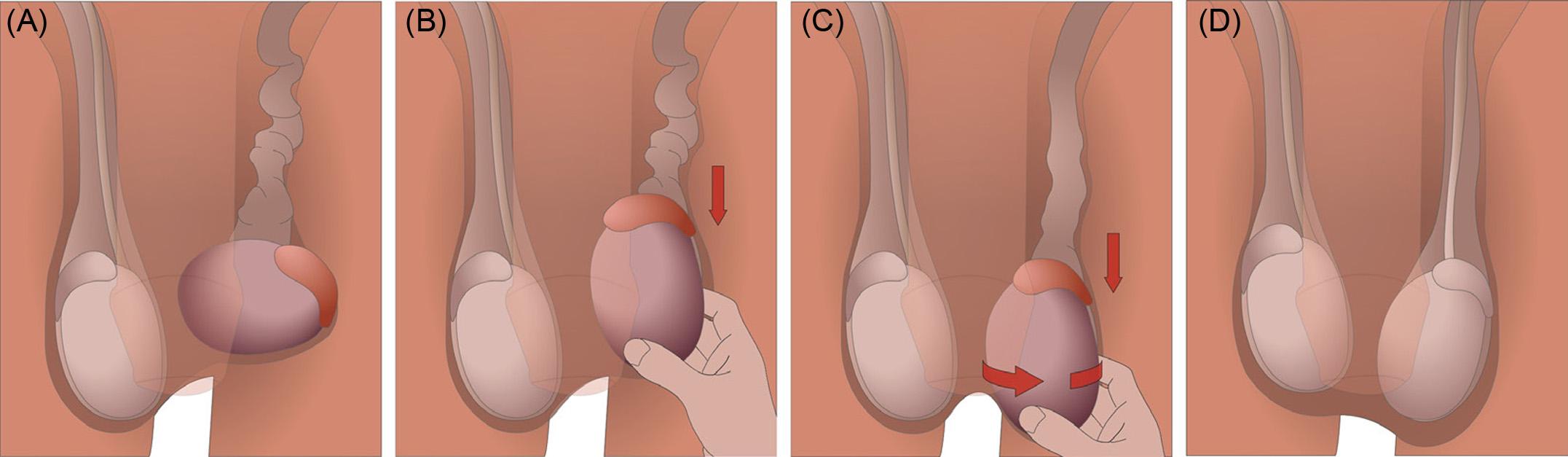
Figure. Thetesticulartractiontechnique.(A)Thetorsedlefttesticleisidentified.Typicalsymptomsincludeahigh-riding,hard,in flamed,and tendertesticleasdepictedhere.Atwistedspermaticcordmayalsobepalpatedsuperiortothetesticle.(B)Tractionisappliedtotheaffected testicleuntilthespermaticcordismaximallylengthened.Inourcase,theside-lyingangleofthetorsedtesticlewascorrectedtoamore natural,verticalangle.(C)Withthespermaticcordlengthened,thetesticleisrotatedexternallywhilemaintainingtraction.Mosttesticular torsionsaremediallytwisted;therefore,clockwiserotationshouldbeattemptedforthelefttesticleandcounterclockwiserotationfortheright testicle.Thephysicianshouldvisualizeandpalpateforany flippingorspinningofthetesticlethroughoutthemaneuver.(D)Successful detorsionisoftenrepresentedbyimmediateresolutionofpain.RepeatDopplerultrasoundshouldbeperformedtoconfirmrestorationof blood flowtotheaffectedtesticle.
Thepatientwaspreppedformanualdetorsionina standingpositionapproximatelysixhoursaftertheonsetof symptoms.Weattemptedthe “openbook” techniqueseveral timesinbothdirectionswithoutsuccessfuldetorsion.
Subsequently,thetesticulartractiontechnique(Figure)was performedby firstgraspingandapplyinginferiortractionto thelefttesticle,whilecorrectingtheside-lyingangletoamore naturalverticalangleofthetesticle.
Thetensionreducedthepalpablelumpofanticipated spermaticcordatthesuperiorpole.Whilemaintaining tractionandlengtheningthespermaticcord,thelefttesticle wasmanuallyrotatedclockwiseby~90°.Atthispoint,the testiclespontaneouslydetorsedbyatleast1–2turns.Itwas challengingtodeterminetheprecisenumberofrotations,as thetesticlerapidlyrotatedwithinthescrotum.However,the physiciancouldfeelthetesticularanatomyduringthis
movement.Resolutionwasapparentbybothvisibleand physicalexamsimmediatelyfollowingtheprocedure.The patientreportedinstantreliefofpain.ArepeatDoppler ultrasoundwasperformed,whichconfirmedthedetorsion andrestorationofnormalblood flowwithnoevidenceof infarctornecrosis(Image2).Basedonresolutionof symptomsandblood flow,theon-callurologistdetermined thatthepatientcouldfollowupinanoutpatientsetting urgentlyforelectiveorchiopexyprocedure.Follow-up informationwasnotavailable.
Thiscasereportsdescribesa20-year-oldmanwitha testiculartorsionandintactcremastericreflexthatwas successfullydetorsedwiththetesticulartractiontechnique. Thespermaticcordishighlymobileandstretchesand
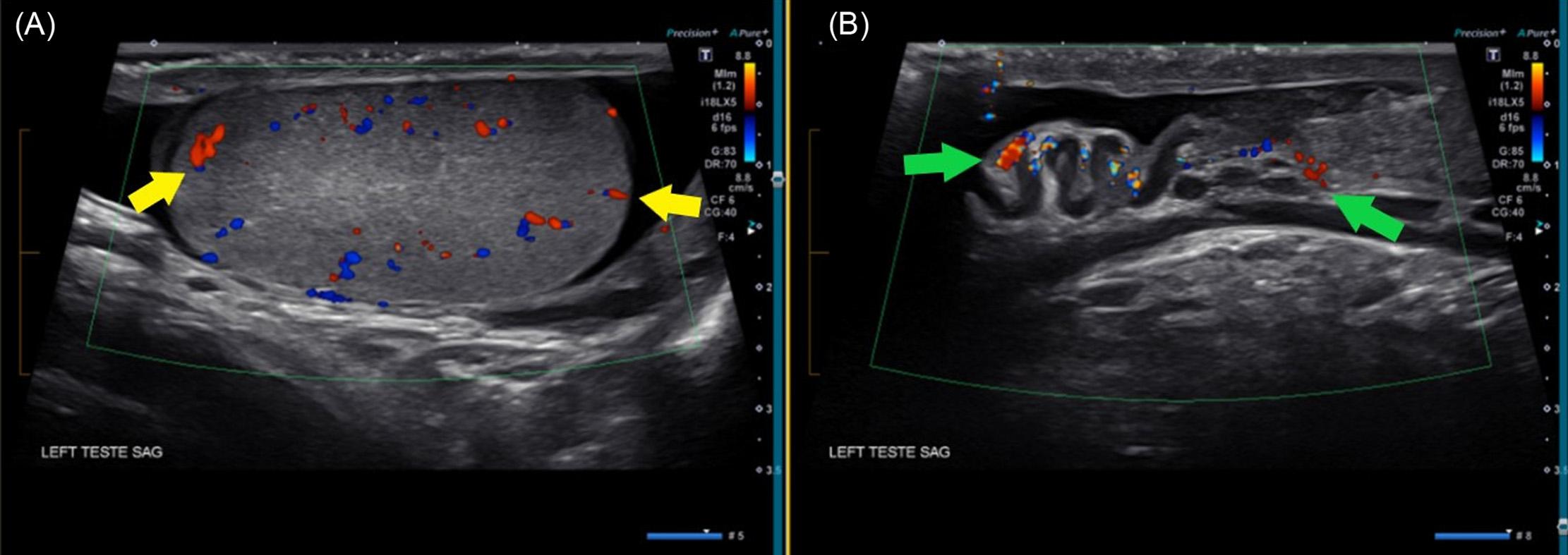
Image2. RepeatDopplerultrasoundofthelefttesticleaftermanualdetorsion.(A)Sagittalviewofthelefttesticleshowingrestoredarterialand venous flow(yellowarrows).(B)Sagittalviewofthespermaticcordandepididymiswithresolutionoftheheterogenousmassandrestoration ofblood flow(greenarrows),consistentwithsuccessfuldetorsion.
retractsundernormalphysiologicresponses.Asaresult,the tractionmaneuverinthetesticulartractiontechniqueshould bephysiologicallyandanatomicallytolerated.9 This techniqueisparticularlyusefulwhentorsionhasbeen prolongedandthespermaticcordbecomesedematous, increasedinvolume,andpartiallytrappedmakingextraction fromtheinguinalcanalnecessary.9 Theproposedmechanism ofthetechniqueisanalogoustostretchingatangledphone cordtoallowforpartialunravelingpriortoapplyinga rotationalforce.ScheierandLevyin2023describedasimilar phenomenonwhereeachtractionattemptreturnedtransient andpulsatileblood flowtothetesticledespitethemanual detorsionfailing.10
Ourcasewasconsistentwithwhatwasdescribedinthe firstcaseseriesreportinguseofthistechnique.9 Thetraction techniqueinourcasewasemployedasanadjunctmaneuver, whichremovedtheresistancefeltduringtheinitialdetorsion attemptusingstandardmethods.Whilethestretchingofthe spermaticcorddidnotdirectlyleadtounravelingofthe torsion,spontaneousunravelingdidoccuraftergentle externalrotationofthetesticle.Wehypothesizethatthe additionaldownwardforceofgravityinthestanding positionmayhavecontributedtothespontaneousdetorsion. However,thetechniquecouldbeperformedinasupine positionasdescribedinthepreviouscaseseries.
Themostimportantdeterminantsofanearlysalvagerate oftestesarethetimefromsymptomonsettodetorsionand thedegreeofspermaticcordtwisting.11 Thesensitivetime frameoftesticularsalvageintesticulartorsioncasesfurther emphasizestheimportanceoftimelydiagnosesandmanual detorsion.Inruralhospitalslikeours,subspecialityservices suchasurologyarenotimmediatelyavailable,andtransfer totertiarycarecentersmayprolongtesticularischemiaifnot successfullydetorsedintheED.Thecremastericreflexis oftenthoughttobeabsentin100%ofpatientswithtesticular torsion.Unexpectedly,thecremasterreflexwaspresentin ourcase,whichissimilartowhatwasreportedinothercase reports.12 Thecremastericreflexmaybeausefulsign,butits reliabilityindiagnosingorexcludingtesticulartorsionhas beenchallengedinrecentyears.13
Regardless,ascrotalultrasoundshouldbeimmediately performedonanypatientwhopresentswithacute atraumaticscrotalpain,andmanualdetorsionshouldbe attemptedinatimelyfashion.Theratesoforchiectomy followingtesticulartorsionvaryintheliterature; nonetheless,theyaresignificantlyhigherinpatientswho werenotsuccessfullymanuallydetorsed.14 Manualdetorsion intheEDcanbuyprecioustimethatisvitalforsuccessful surgicalsalvageandmaysometimesevenconvertan emergenturologicsurgeryintoanurgentbutelectiveone.6
Thetimewindowforsurvivalandsuccessfulsalvageofa torsedtesticlehadbeencommonlythoughttobe6–8hoursor less.15 Delayspastthistimewindowmayleadto orchiectomy,whichisassociatedwithreducedfertilityand
medico-legallitigation.Somephysiciansevenforgomanual detorsionbeyondthispoint.Inasystematicreviewby Mellicketalthatincluded2,116patientswithtesticular torsion,theyfoundthattesticularsurvivalwassignificantly beyondtheoriginal6–8hourtimeframe:90.4%survival whendetorsedwithinthe first12hours,54%from13–24 hours,and18.1%whenafter24hours.Successfuldetorsion maystillbeachievedpastthecommonlyacceptedwindow, butthedecisiontoattemptmanualdetorsionshouldbemade onacase-by-casebasis.
Theabsenceofthecremastericreflexmaynotalwaysbea telltalesigninidentifyingpatientswithanacutescrotum,and ultrasoundshouldbeperformedwhenevertesticulartorsionis suspected.Itiscommonlythoughtthattesticlesare unsalvageablepastthe6–8hourtimewindow;however,there isliteraturethatsupportslongersurvivability.Physicians shouldnotforgomanualdetorsionsolelybasedonthe durationoftorsion.Thetesticulartractiontechniqueisa rapid,easy-to-perform,andsafemaneuverthatcanbeusedas aprimaryoradjunctivetreatmentfordetorsioninanysetting. Despitelimitedpatientcases,thenoveltesticulartechnique showspromiseasasolutionfordifficult-to-reducetesticles.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:GarrettTrang,BS,TheUniversityof Arizona,CollegeofMedicine-Phoenix,475N5thSt.,HSEBBuilding C532,Phoenix,AZ85004.Email: gtrang@arizona.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Trangetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SchickMAandSternardBT.Testiculartorsion.In StatPearls[Internet] TreasureIsland,Florida:StatPearlsPublishing,2023.Availableat: https://www.ncbi.nlm.nih.gov/books/NBK448199/ AccessedMay22,2024.
2.ZhaoLC,LautzTB,MeeksJJ,etal.Pediatrictesticulartorsion epidemiologyusinganationaldatabase:incidence,riskoforchiectomy andpossiblemeasurestowardimprovingthequalityofcare. JUrol. 2011;186(5):2009–13.
3.SharpVJ,KieranK,ArlenAM.Testiculartorsion:diagnosis,evaluation, andmanagement. AmFamPhysician. 2013;88(12):835–40.
4.LaherA,RagavanS,MehtaP,etal.Testiculartorsionintheemergency room:areviewofdetectionandmanagementstrategies. OpenAccess EmergMed. 2020;12:237–46.
5.AggarwalD,ParmarK,SharmaAP,etal.Long-termimpactoftesticular torsionanditssalvageonsemenparametersandgonadalfunction. IndianJUrol. 2022;38(2):135–9.
6.DiasFilhoAC,OliveiraRodriguesR,RiccettoCLZ,etal.Improving organsalvageintesticulartorsion:comparativestudyofpatients undergoingvsnotundergoingpreoperativemanualdetorsion. JUrol. 2017;197(3):811–7.
7.HawtreyCE.Assessmentofacutescrotalsymptomsand findings.A clinician’sdilemma. UrolClinNorthAm. 1998;25(4):715–23.
8.DemirbasA,DemirDO,ErsoyE,etal.Shouldmanualdetorsionbea routinepartoftreatmentintesticulartorsion? BMCUrol. 2017;17(1):84.
9.MellickLBandWattersBC.Thetorsedtesticletractiontechniqueand 2casereports. PediatrEmergCare. 2023;39(5):364–7.
10.ScheierEandLevyES.Testiculartractiontechniqueinanadolescent withtorsion. PediatrEmergCare. 2023;39(11):75–6.
11.VisserAJandHeynsCF.Testicularfunctionaftertorsionofthe spermaticcord. BJUInt. 2003;92(3):200–3.
12.MurphyFL,FletcherL,PeaseP.Earlyscrotalexplorationinallcasesis theinvestigationandinterventionofchoiceintheacutepaediatric scrotum. PediatrSurgInt. 2006;22(5):413–6.
13.PaulEM,AlvayayC,PalmerL.Howusefulisthecremasteric reflexindiagnosingtesticulartorsion? JAmCollSurg. 2004;199(3):101.
14.Vuru ¸ skanE,ErçilH,KarkinK,etal.Theeffectofmanualdetorsionon testicularsalvageratesinadulttesticulartorsionpatients:singlecenter experience. DuzceMedJ. 2022;24(2):101–4.
15.MellickLB,SinexJE,GibsonRW,etal.Asystematicreviewoftesticle survivaltimeafteratorsionevent. PediatrEmergCare. 2019;35(12):821–5.
CelinaWong,MD
TammyPhan,BS
EmmelynSamones,BS
SharminKalam,MD
SectionEditor:JacquelineLe,MD
LomaLindaUniversityMedicalCenter,DepartmentofEmergencyMedicine, LomaLinda,California
Submissionhistory:SubmittedNovember28,2023;RevisionreceivedFebruary23,2024;AcceptedMarch11,2024
ElectronicallypublishedJune3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6591
Introduction: Osteomyelitiscanoccuratvariousosseouslocationsandcommonlypresentsinthe emergencydepartment(ED).Theincidenceofosteomyelitisis21.8casesper100,000persons annually.1 Hematogenousosteomyelitistypicallyoccursinthevertebrae;however,itmayseldomly occurinthemanubrium.Hematogenousosteomyelitiscanbeseeninpatientswithcomplicatedthoracic surgery,radiation,fracture,diabetes,immunosuppression,steroidtherapy,andmalnutrition.2 Because signsandsymptomsofosteomyelitismaybenonspecific,cliniciansmusthavehighsuspicionbasedon historyandphysical.Workupshouldincludeidentifyingthesource,imaging,andsurgicalcultures.
CaseReport: A60-year-oldmalewithhypertensionanddiabetespresentedwithatraumaticright shoulderandchestpain.ThepatientpresentedtwicetotheEDforclaviclepain fivedaysprior.Computed tomography(CT)ofthechestdetectedosseousinfectionofthemanubriumanduppersternum,right clavicle,andmediastinalphlegmon.ACToftheabdomenandpelvisrevealedosteomyelitisanddiscitis ofthe12th thoracicand firstlumbarvertebralbodywithgasatthepsoasmuscle,aswellassigmoid diverticulitiswithcolovesicular fistula.Thepatientwasstartedonbroadspectrumantibioticsand1,500 millilitersoflactatedRinger’sintheED.Afterevaluationbycardiothoracicsurgery,thepatientwastaken totheoperatingroomforneckexploration,incision/drainage,manubriectomy,andrightsternoclavicular jointresection.Surgical,blood,urine,andrespiratoryculturesgrew Klebsiellapneumoniae.Aftera 34-dayhospitalcourse,thepatientwasdischargedontwoweeksoforallevofloxacinandfollow-up appointmentswithcardiothoracicsurgeryandinfectiousdisease.Thepatienthadgoodprognosis andrecovery.
Conclusion: Hematogenousosteomyelitistothemanubriumisrareandmaypresentwithonlychest pain.Itisimportanttoconsiderothersourcesthatseedinthemanubriumandimagingtoevaluate multisiteinfection.Treatmentshouldincludeintravenousantibioticsand/orsurgicalinterventionfor debridementwithwashoutormanubriectomy.[ClinPractCasesEmergMed.2024;8(3)231–234.]
Keywords: hematogenousosteomyelitis;sternalosteomyelitis;discitis;colovesicular fistula; Klebsiellapneumoniae;casereport.
Osteomyelitisisdefinedasinfectionandinflammationof bonewithmultipletypesthatrequiredifferentinterventions andmanagement.Osteomyelitisdevelopsbythree mechanisms:bacteremialeadingtohematogenousspreadto thebone;contiguousspreadfromadjacentsofttissuetothe bone;ordirectinoculationintothebone.3 Theraresttypeof osteomyelitisisthatofhematogenousspread.4 Themost commonlocationofosteomyelitisisthevertebrae. Additionally,osteomyelitisofthemanubrium(outsideof
thoracicsurgery-relatedcomplications)isevenmore uncommonwithveryfewcasereportspublished;itcaneither leadtoorbearesultofhematogenousseeding.5 Typically, thesepatientswillhavemultipleriskfactorssuchasdiabetes orimmunodeficiencythatpredisposethemtoinfection. Treatmentsvaryfromintravenous(IV)antibioticsaloneto theadditionofsurgery.Thiscaseofmanubrium osteomyelitisisuniqueinthatitwastheresultof hematogenousspread;amanubriectomywasnecessaryin additiontolong-termIVandoralantibiotics.
A60-year-oldmalewithapastmedicalhistorysignificant forhypertensionanddiabetesmellituspresentedtothe emergencydepartment(ED)withright-sidedshoulderand chestpain.Thepatientinitiallypresented fivedayspriorwith complaintsofathree-dayhistoryofrightclaviclepain.There wasnoreporteddirecttrauma,butthepatientnoticedthe painstartedafterhewascatchingboxesatwork.Achest radiographanddedicatedrightclavicleradiographwas orderedatthetime,andbothimagingresultedasnormal. Thepatientwasthendischargedanddiagnosedwitha musculoskeletalstrain.Fivedayslater,thepatientpresented tothesameED,nowwithassociatedchestpain,fevers,and shortnessofbreath.Betweenthetwopresentations,the patientwasseenatanotherfacility,wherecomputed tomography(CT)revealedosteomyelitisofthe sternoclavicularjointandmanubrium.Accordingtothe patient,theCTalsomentionedcolonic fistulaandbecause thatfacilitydidnothaveacardiothoracicspecialistavailable, transferarrangementswereattemptedbutwereunsuccessful. Therefore,thepatientdecidedtoleaveagainstmedical adviceandpresenttotheEDdirectly.Thepatientdenied anyIVdruguse,tobaccouse,orhistoryof autoimmunedisorders.
Initialvitalsignswerethefollowing:temperature99.3° Fahrenheit,pulse120beatsperminute,bloodpressure 120/70millimetersofmercury,respiratoryrate24breathsper minute,andoxygensaturation97%onroomair.Onphysical exam,thepatientwasill-appearing.Therewasrightclavicle andright-sidedchestwalltendernessbutnoappreciationfor crepitusormass.Hiscardiopulmonaryexamrevealed tachycardia.Therewerenoheartmurmurs,andlungsounds wereclearbilaterally.Laboratoryvaluesrevealedawhite bloodcountof7.41109 perliter(referencerange4.8–11.4109 perliter),abloodsugarlevelof352milligramsperdeciliter (mg/dL)(70–140mg/dL),andanelevatedlactatelevelof3.5 millimolesperliter(mMol/L)(0.5–2.0mMol/L).
Additionally,therewasanelevatedsedimentationrateof84 millimetersperhour(mm/hr)(0–20mm/hr),anelevated C-reactiveproteinlevelof22.3mg/dL(0.0–0.8mg/dL),and anelevatedprocalcitoninlevelof12.90microgramsperliter (μg/L)(0.0–0.15 μg/L).ACTofthechestrevealedanosseous infectionofthemanubrium,uppersternum,andright
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Hematogenousosteomyelitisisarareformof osteomyelitisthatoccurswhenbacteria spreadstothebonethroughthebloodstream.
Whatmakesthispresentationof diseasereportable?
Wereportararelocationofthe hematogenousspreadtothemanubriumwith anevenmoreuncommontreatmentcourse.
Whatisthemajorlearningpoint?
Thiscaseteachestheimportanceofan extensiveworkuptoidentifytheprimary sourceofhematogenousosteomyelitiswhen foundinrarelocations.
Howmightthisimproveemergency medicinepractice?
Emergencyphysiciansshouldbeawareof hematogenousosteomyelitisandhow extensiveworkupwillaidinevaluatingthis diseaseprocess.
claviclewithanassociatedmediastinalphlegmonandsoft tissuegasextendingtotheneckandrightpectoralismajor muscle(Image1).ACToftheabdomenandpelvisrevealed osteomyelitisanddiscitisofthe12th thoracicand firstlumbar vertebralbodywithassociatedgasinthepsoasmusclebody atthatlevel(Image2).Additionally,sigmoiddiverticulitis withcolovesicular fistulawasnotedontheCTabdomenand pelvis(Image3),mentionedbythepatientasanotable findingattheoutsidehospital.
Differentialdiagnosisforthispatientincludedseptic shocksecondaryto Klebsiellapneumoniae bacteremia,with hematogenousspreadtothemanubriumand firstlumbar vertebralbody.Thesourcewassuspectedtobefromthe sigmoiddiverticulitiswithacolovesicular fistula.Alternative differentialdiagnosescouldincludenecrotizingfasciitisgiven thepresenceofgasinthenearbypsoasandpectoralmuscle, pulmonaryembolism,orendocarditisbasedonfeverand chestpain.
Thepatientwasstartedonbroadspectrumantibiotics (piperacillin-tazobactam,vancomycin,andclindamycin) andgivena1,500milliliter(mL)lactatedRinger’sbolus whileintheEDforpresumedsepsis.Thepatientthenbecame hypotensiveandwasstartedonanorepinephrinedripwith additionalcrystalloid fluidsgiven.Cardiothoracicsurgery
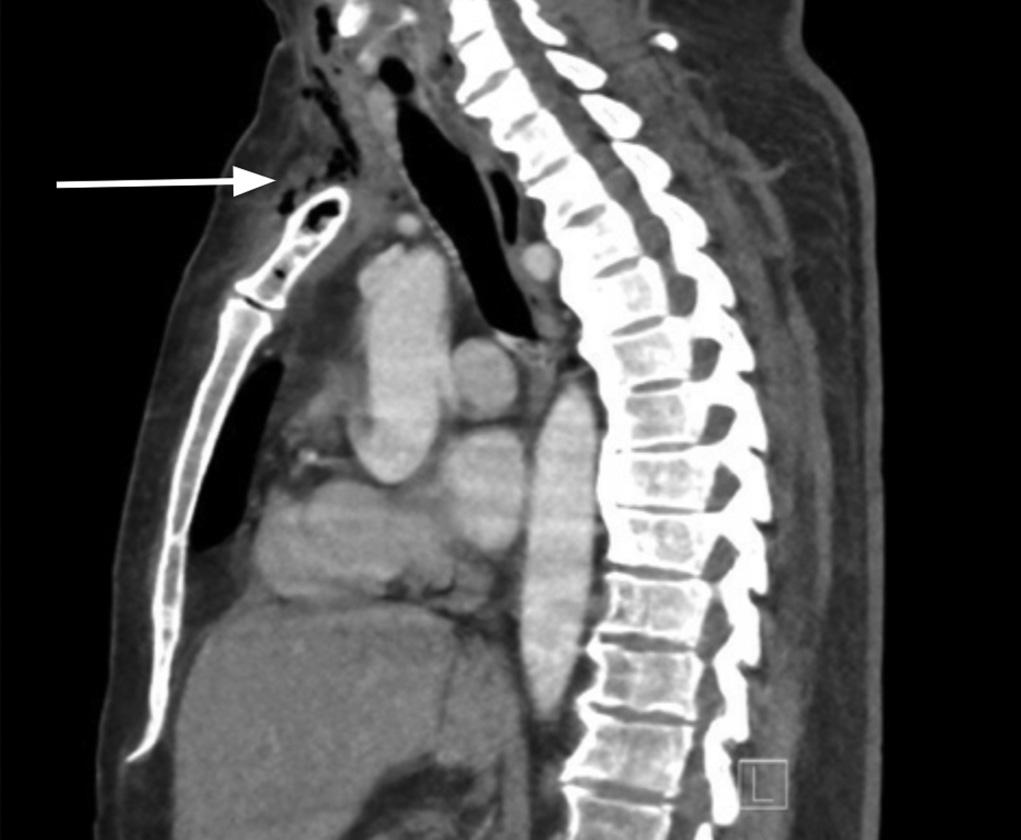
Image1. Asagittalviewofcomputedtomographyofthechest, revealingosseousinfectionofmanubriumwithsurroundinggas (arrow)extendingintotheneck.
wasconsultedforchest findings.Neurosurgerywasconsulted forthespine findings,andcolorectalsurgerywasconsultedto addressthe fistula.Afterbeingevaluatedbycardiothoracic surgery,thepatientwasimmediatelytakentotheoperating room(OR)fromtheEDforamanubriectomyandforsource

Image2. Asagittalboneviewofcomputedtomographyofthe abdomenandpelvisrevealinggaswithinthetwelfththoracicand firstlumbarvertebralbody(circle)suspiciousforosteomyelitis.

andpelvisdemonstratingsigmoiddiverticulitiswitha colovesicular fistula(circle,arrows).
control.IntheOR,thesurgeonsperformedaneck exploration,anincisionanddrainage,amanubriectomy,and aresectionoftherightsternoclavicularjoint.Thepatientwas thenadmittedtothesurgicalintensivecareunitafterbeing intubated,andhecontinuedtorequirevasopressors. Surgical,blood,urineandrespiratoryculturesgrew Kpneumoniae ,whichwaspresumedtobethesourceof infection.Ondaysix,thepatientwasfoundtohave additionalsepticembolionCThead.Alumbarpuncturewas performedondayeight;however,cerebrospinal fluid culturesgrewnobacteria.Thepatientwaseventually extubated,weanedoffvasopressors,andmanagedonthe medical/surgical flooronday11.
Duringhishospitalstayonthesurgical floor,thepatient completedasix-weekcourseofintravenous(IV)antibiotics andwasswitchedtooralantibiotics.Onhospitalday30, thepatientunderwentadditionalsurgeryforaright sternocleidomastoidmuscle flap,debridementofthe sternoclavicularjoint,andclosureoftheneckwound. Aftera34-dayhospitalcourse,thepatientwasdischarged onorallevofloxacinforanadditionaltwoweekswith follow-upwithcardiothoracicsurgeryandinfectious diseasespecialists.
Fewcasereportshavebeenpublishedregardingprimary sternalosteomyelitis,withthethoughtthatmoststemfrom hematogenousspread.4,5 Thisagainissupportedbyour patient’spresentation,wherethereweremultiplesitesof infectionincludingvertebralosteomyelitis,extensiveneck andpsoasmuscleabscesses,andsepticemboliinfarcts.
Inhematogenousosteomyelitis,bacteriaintheblood flowing throughthevasculatureinthebonecanadheretoit.Bacteria maycauseinflammatorychanges,breakingdownthebony cortexandperiosteum,whichcancausefurtherinvasionof thebacteriaandnecrosisofthebone.6 Typically,riskfactors forhematogenousosteomyelitisincludeendocarditis,IV druguse,sicklecelldisease,hemodialysis,orthopedic hardware,andintravasculardevices.7 However,thispatient didnotpresentwithanyknownriskfactors.Thepatient’ s historyofdiabetesmellitusmayhavebeenariskfactorfor contiguousspreadfromdiabeticulcersintotheadjacent bone.Additionally,thepatientpresentedwithonlychest painwithnochestmassasseeninothercasereportsof sternumosteomyelitis.5,8,9,10
Furthermore,whentakingacloserlookatthepathogen isolatedinthiscase, Kpneumoniae wasfoundbothinthe vertebraeandthemanubriumsurgicalcultures. Kpneumoniae isatypicalanaerobicorganismofthe gastrointestinal(GI)tract.Onestudyshowedittocause severebacterialinfectionswheretherewasacorrelationwith increasedmorbidityseeninpatientswithGI fistulas.11 Similarly,withthiscaseitisassumedthatthe fistulamay havecausedhematogenousspreadoftheinfection,thus causingthemultiplesitesofosteomyelitis.Treatmentfor hematogenousosteomyelitisisnormallyIVantibiotics alone.4 However,forthiscaseamanubriectomywas performedforsourcecontrolduetothepatient’sseptic shock.Typically,surgicaltreatmentforsternum osteomyelitishasincludedsurgicaldebridement,surgical washout,andevenhyperbaricoxygentherapy.5,12 In additiontosurgery,thispatientdidreceiveaprolonged courseofIVandoralantibiotics.
Hematogenousosteomyelitistothemanubriumisrare andmaypresentwithonlychestpain.Workupincludes obtaininginflammatorymarkers,aswellasCTimagingof thechest.Additionally,itisimportanttoconsiderother sourcesthatmayhaveseededthemanubrium,suchas inthispatientwithcolovesicular fistula,andtoobtain additionalimaging/workuptoevaluateformultiplesitesof infection.Oncethediagnosisismade,treatmentatminimum shouldincludeIVantibioticsbutmayrequiresurgical interventionsuchasdebridementwithwashoutor evenamanubriectomy.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:SharminKalam,MD,LomaLinda UniversityMedicalCenter,DepartmentofEmergencyMedicine, 11234AndersonSt.,RoomA890A,LomaLinda,California92354. Email: Skalam@llu.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Wongetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KremersHM,NwojoME,RansomJE,etal.Trendsintheepidemiology ofosteomyelitis:apopulation-basedstudy,1969to2009. JBoneJoint SurgAm. 2015;97(10):837–45.
2.GillGSandPulciniM.Maxillaryosteomyelitisinapatientwith pansinusitisandrecentlydiagnosedfocalsegmental glomerulosclerosis. Cureus. 2019;11(8):e5347.
3.KolinskyDCandLiangSY.Musculoskeletalinfectionsintheemergency department. EmergMedClinNorthAm. 2018;36(4):751–66.
4.LewDPandWaldvogelFA.Osteomyelitis. Lancet. 2004;364(9431):369–79.
5.PlattMAandZieglerK.Primarysternalosteomyelitiswithbacteremia anddistalseeding. JEmergMed. 2012;43(2):e93–5.
6.SchmittSK.Osteomyelitis. InfectDisClinNorthAm. 2017;31(2):325–38.
7.RenzN,HaupenthalJ,SchuetzMA,etal.Hematogenousvertebral osteomyelitisassociatedwithintravasculardevice-associated infections-aretrospectivecohortstudy. DiagnMicrobiolInfectDis. 2017;88(1):75–81.
8.CarnevaleA,RighiR,ManiscalcoP,etal.Primarysepticarthritisofthe manubriosternaljointinanimmunocompetentyoungpatient:acase report. RadiolCaseRep. 2017;12(4):682–5.
9.DiNardoAR,SchmidtD,MitchellA,etal.Firstdescriptionoforal Cryptococcusneoformans causingosteomyelitisofthemandible, manubriumandthirdribwithassociatedsofttissueabscessesinan immunocompetenthost. ClinMicrobiolCaseRep. 2015;1(3):017.
10.RodríguezLorenzoP,FernándezMartínezB,PérezAlbaM,etal. Primarysternalosteomyelitis. ArchArgentPediatr. 2023;121(5):e202201449.
11.LiJ,RenJ,WangW,etal.Riskfactorsandclinicaloutcomesof hypervirulent Klebsiellapneumoniae inducedbloodstreaminfections. EurJClinMicrobiolInfectDis. 2018;37(4):679–89.
12.deNadaiTR,DanielRF,deNadaiMN,etal.Hyperbaricoxygentherapy forprimarysternalosteomyelitis:acasereport. JMedCaseRep. 2013;7:167.
DanielaUsuga,MS*
SofiaPortuondo,MD†
DavidFarcy,MD‡
MichaelShalaby,MD‡
SectionEditor:ShadiLahham,MD
*FloridaInternationalUniversity,HerbertWertheimCollegeofMedicine,Miami,Florida † MountSinaiMedicalCenterMiamiBeach,DepartmentofEmergencyMedicine, MiamiBeach,Florida ‡ FloridaInternationalUniversity,HerbertWertheimCollegeofMedicine, DepartmentofEmergencyMedicineandCriticalCare,Miami,Florida
Submissionhistory:SubmittedNovember30,2023;RevisionreceivedFebruary27,2024;AcceptedMarch11,2024
ElectronicallypublishedJune14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6600
Introduction: Compressiveneuropathyofthebrachialplexusisacommonissuefollowinglaparoscopic androboticsurgeries.
CaseReport: A71-year-oldmale,post-lumbarspinalsurgery,presentedwithexcruciatingrightupper extremitypainandparesthesias.Asupraclavicularbrachialplexus(SBP)blockwithbupivacaine providedsignificantpainrelief,lasting36hours.Subsequentphysicaltherapyledtogradualpainand weaknessimprovementincompressiveneuropathy.
Discussion: TheSBPblock,facilitatedbyultrasoundguidance,isasafeprocedurewithfewserious complications.Itprovesbeneficialformanagingpostoperativecompressiveneuropathy,allowing patientstobreakpaincyclesandparticipateinrehabilitation.
Conclusion: TheSBPblockisaneffectiveadditiontothemanagementofpostoperativecompressive neuropathy,givenitsease,safety,andpotency.Althoughregionalanesthesiaprovidesonlytemporary relief,patientscanexperienceabreakindebilitatingpaincyclesassociatedwithcompressive neuropathy.[ClinPractCasesEmergMed.2024;8(3)235–238.]
Keywords: SupraclavicularBrachialBlock;ultrasound;compressiveneuropathy;brachialplexus.
Thebrachialplexusarisesfromthespinalnerverootsof fifthcervicalto firstthoracicandsuppliessensoryandmotor innervationtotheupperlimbandshouldergirdle. Compressiveneuropathy,alsoknownasentrapment neuropathy,occursfromthecompressionofanerveandcan resultintemporaryorpermanentweaknessandpain,which canbedebilitating.1 Thebrachialplexusislocatedinthe posteriortriangleintheneckandpassesproximallybetween thescalenemuscleanddistallybetweenthe firstriband clavicle.2 Withincreasedutilizationoflaparoscopicand roboticsurgery,therehasbeenanincreasedincidenceof
brachialplexusneuropathy,3 especiallygiventheprolonged timethatthepatientspendsintheTrendelenbergposition.2–4 Previouslypublishedcasereportsandcaseserieshave reportedbrachialplexusneuropathyfollowingprolonged spinalsurgery.5–7 Spinalsurgeriesinwhichthepatientisin thepronepositionwiththeirarmsabductedatanangle greaterthan90° havebeendemonstratedtohave significantlyincreasedincidenceofpostoperativebrachial plexusinjury.6 Suchcaseshavealsobeenreplicatedinanimal studies,inwhichinterruptedblood flowtoorprolonged stretchingofthebrachialplexusresultsinintraneural capillaryruptureandhematomaformation.4
Parsonage-Turnersyndrome,alsoknownasidiopathic brachialplexopathyorneuralgicamyotrophy,isarare conditioncharacterizedbyadiverserangeofsymptoms.8 It typicallymanifestswithsuddenonsetshoulderpainonone side,followedbyprogressiveneurologicalissuessuchas motorweakness,dysesthesias,andnumbness.Whilethe exactcauseofthesyndromeisnotwellunderstood,ithas beenobservedinvariousclinicalscenarios,including postoperativecompressive,postinfectious,post-traumatic, andpost-vaccinationsettings.8
Ourpatientwasa71-year-oldmanwhohadafourth lumbarto fifthlumbarposteriorlumbarinterbodyfusion withthirdlumberto fifthlumbarposterolateral decompressionandfusiononemonthbeforepresentation. Hepresentedtoouremergencydepartment(ED)withachief complaintofpainfulparesthesiasoftheentirerightupper extremity.Afterremainingonhisrightlateraldecubitusfor anextendedperiodintraoperatively,thepatient subsequentlydevelopedpainfulparesthesiasintheright shoulderandrightarm.Hehadseenaneurologistinthe clinic,whoprescribedgabapentin300milligrams(mg)three timesdailyandmethocarbamol750mgthreetimesdailyfor compressiveneuropathy.However,thepatienthadachieved minimalanalgesiawiththisregimen,andheratedhispainas a10/10uponpresentationtotheED.Thepatient’sphysical examshowedintactstrengthandreflexesinupperextremities bilaterally.However,hehaddecreasedsensationtosharp touchovertheentireupperextremitycomparedtotheleft.
Thepatientconsentedtoasupraclavicularbrachialplexus (SBP)block,whichwasperformedwith15milliliters(mL) bupivacaine0.5%withepinephrine.Hetoleratedthe procedurewellandwaspain-freewhendischarged.At follow-upviaphonecalloneweeklaterhestatedthathe’d had36hoursofpainrelieffromthebrachialplexusblock. Sincetheprocedure,thepatienthasbeeninphysicaltherapy andhispainfromhiscompressiveneuropathyhasbeen slowlyimproving.
Anultrasound(US)-guidedSBPblockinvolvesinstilling anestheticwithinthenervesheathtoanesthetizetheupper, middle,andlowertrunksofthebrachialplexus.TheSBPcan typicallybevisualizedbyplacingashortlinearUSprobe withinthesupraclavicularfossa,thespaceimmediately posteriortothemiddletomedialclavicle(Image).Inthis view,thesubclavianarteryisviewedmedialtotheSBP,the firstribcaudal,andthepleuradeeptothe firstrib(Figure). Withanin-planeneedletechnique,thephysicianusesa shallowneedleapproachfromlateraltomedialtoguidethe needletowardtheSBP.Oncetheneedleisclearlyvisualized withintheSBPsheath,thephysicianslowlyinjectsaliquotsof 5mLofanestheticatatime,makingsuretoaspiratepriorto
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Brachialplexuscompressionisacommon post-operativecomplication,exacerbatedby prolongedproceduressuchasrobotic surgeriesintheTrendelenbergposition.
Whatmakesthispresentationof diseasereportable?
Wereportsuccessfultreatmentofpostoperativebrachialplexusneuropathywith ultrasound-guidedsupraclavicularbrachial plexus(SBP)block.
Whatisthemajorlearningpoint?
Ultrasound-guidedSBPblockoffers signi fi cantpainreliefforpost-operative compressiveneuropathy,breakingpaincycles untiloutpatientmanagementisfeasible.
Howmightthisimproveemergency medicinepractice?
Ultrasound-guidedSBPblockisasafe, effectiveoptiontobreakpaincycles,enabling therapyandenhancingpost-operative compressiveneuropathymanagement.
anyinjection.Furthermore,injectingatthe “cornerpocket” (Figure)closesttothesubclavianarteryhelpstoguarantee completeanesthesiaoftheinferiortrunkofthebrachial plexus.9 TheSBPisverysuperficial,typically1–2centimeters deepintheskin;thus,a22-gauge,non-spinalneedlecan usuallybeusedforthisprocedure.TheMillerweight-based localanestheticdosingshouldbeusedtocalculatetheideal anestheticdosagebasedonidealbodyweight.10 However, 15–20mLoflocalanestheticisusuallyadequatefor anesthesiaoftheupperlimb.The firstribservesasa backstop,shouldthephysicianaccidentallyovershootthe SBP,toavoidcausingapneumothorax.10 Besides pneumothorax,othercomplicationsoftheSBPinclude axonaldamage,hemidiaphragmaticparalysis,and subclavianarterypuncture.10
TheuseofUStoperformaSBPblock,asopposedtothe landmark-basedtechnique,significantlyreducesthe likelihoodofpneumothoraxandneuronalinjury,asreported inpreviousstudies.11,12 Additionally,shouldtheperforming physicianmaintainproperneedlecontrolthroughoutthe procedure,thepleuraandsubclavianarteryremain comfortablyoutsidetheneedle’strajectorytotheSBP.9 Byanesthetizingalltrunksofthebrachialplexus,the

Image. Ultrasoundprobeplacementinthesupraclavicular fossatoidentifyandanesthetizethesupraclavicularbrachial plexus.Theneedleisshownbeforeintroductionfromalateralto medialapproach(shownhereonamodelpatient).
Figure. Graphicdemonstratingthesupraclavicularbrachialplexus (yellow),subclavianarterymedial(red), firstribdeep(beige),and pleura(pink).Theneedleshaftmakesashallowangletowardsthe brachialplexus.Theblueasteriskrepresentsthe “cornerpocket.”
SBPblockprovidesreliableanesthesiaofmostoftheupper extremity,includingtheshoulder,butsparingtheupper medialarm(whichisinnervatedbythesecondthoracic spinalnerve).13,14,15
Thebrachialplexushasincreasedvulnerabilitytoinjury duetoitssuperficiallocationintheneckandtopatient positioningduringcertainprolongedsurgicalprocedures. Whileourpatienthadnotyetreceivedaformaldiagnosisof Parsonage-TurnerSyndromebyhisneurologist,his symptomswereconsistentwiththedisease.Althoughchronic painresultingfromcompressiveneuropathyoften fluctuates inintensity,ourpatientexperiencedexcruciatingpain,which causedhimtopresenttotheEDthatday.Whileregional anesthesiadoesnotprovideapermanentsolution,itcan affordasubstantialamountofreliefintheshorttermand breakpaincycles.
Subsequently,ourpatientwasabletoresumehisphysical therapywithoutrevisitingtheEDduetopain.Forpatients grapplingwithsimilardebilitatingpaincausedby compressiveneuropathy,regionalanesthesiacanbeasafe andeffectiveoption.Furthermore,pertheAmericanSociety ofRegionalAnesthesia,post-surgicalcompressive neuropathyisnotacontraindicationtotreatmentwith regionalanesthesia.16 TheSBPblockisfeasiblefor emergencyphysicianstoperformatthebedside,andtheuse ofUSsignificantlyreducescomplications.6,16–19
Consideringtheease,safety,andpotencyoftheSBP block,emergencyphysiciansshouldincludetheSBPblockin themultimodalapproachtothemanagementof postoperativecompressiveneuropathy.Whilepainfrom compressiveneuropathyischronic,italsowaxesandwanes andattimescanbecomedebilitating.Thus,regional anesthesiaingeneralcanprovidesignificantrelieffor patientsexperiencingsimilarpain.
Video. Performanceofanultrasound-guidedsupraclavicular brachialplexusblock.
SA,subclavianartery; BP,brachialplexus; NS,needleshaft.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
AddressforCorrespondence:DanielaUsuga,MS,Florida InternationalUniversity, Herbert WertheimCollegeofMedicine, 11200SW8thSt.,AHC2,Miami,FL33199.Email: 15danielausuga@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Usugaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ThatteMRandMansukhaniKA.Compressiveneuropathyintheupper limb. IndianJPlastSurg. 2011;44(2):283–97.
2.KwannJHandRappaportI.Postoperativebrachialplexuspalsy.astudy onthemechanism. ArchSurg. 1970;101(5):612–5.
3.ThomasJ.Post-operativebrachialplexusneuropraxia:aless recognisedcomplicationofcombinedplasticandlaparoscopic surgeries. IndianJPlastSurg. 2014;47(3):460–4.
4.ChinPandPooleG.Bilateralbrachialplexusinjuryduringlaparoscopic sigmoidcolectomy. ANZJSurg. 2003;73(1–2):86–8.
5.SchwartzDM,SestokasAK,HilibrandAS,etal.Neurophysiological identificationofposition-inducedneurologicinjuryduringanterior cervicalspinesurgery. JClinMonitComput. 2006;20(6):437–44.
6.ThanKD,MummaneniPV,SmithZA,etal.Brachialplexopathyafter cervicalspinesurgery. GlobalSpineJ. 2017;7(1Suppl):17S–20S.
7.UribeJS,KollaJ,OmarH,etal.Brachialplexusinjuryfollowingspinal surgery. JNeurosurgSpine. 2010;13(4):552–8.
8.FeinbergJHandRadeckiJ.Parsonage-turnersyndrome. HSSJ. 2010;6(2):199–205.
9.SoaresLG,BrullR,LaiJ,etal.Eightball,cornerpocket:theoptimal needlepositionforultrasound-guidedsupraclavicularblock. RegAnesth PainMed. 2007;32(1):94–5.
10.ShalabyM,SmithM,TranL,etal.Utilityofsupraclavicularbrachial plexusblockforanteriorshoulderdislocation:coulditbeuseful? WestJ EmergMed. 2023;24(4):793–7.
11.BendtsenTF,LopezAM,VandepitteC.Ultrasound-guided supraclavicularbrachialplexusnerveblock.2018.Availableat: https:// www.nysora.com/topics/regional-anesthesia-for-specific-surgical-
procedures/upper-extremity-regional-anesthesia-for-specific-surgicalprocedures/anesthesia-and-analgesia-for-elbow-and-forearmprocedures/ultrasound-guided-supraclavicular-brachial-plexus-block/ AccessedOctober1,2023.
12.KapralS,KrafftP,EibenbergerK,etal.Ultrasound-guided supraclavicularapproachforregionalanesthesiaofthebrachialplexus. AnesthAnalg. 1994;78(3):507–13.
13.ShalabyMandSahniR.Supraclavicularbrachialplexusblock:the unsungheroofemergencydepartmentregionalanesthesia. ClinExp EmergMed. 2023;10(3):342–4.
14.BrownDL,CahillDR,BridenbaughLD.Supraclavicularnerveblock: anatomicanalysisofamethodtopreventpneumothorax. AnesthAnalg. 1993;76(3):530–4.
15.D’SouzaRSandJohnsonRL.SupraclavicularBlock.In: StatPearls TreasureIsland(FL):StatPearlsPublishing;2023.
16.PerlasA,LoboG,LoN,etal.Ultrasound-guidedsupraclavicular block:outcomeof510consecutivecases. RegAnesthPainMed. 2009;34(2):171–6.
17.TogiokaBMandWuCL.Supraclavicularblock.2019.Availableat: https://www.asra.com/news-publications/asra-updates/blog-landing/ legacy-b-blog-posts/2019/08/07/supraclavicular-block AccessedSeptember20,2023.
18.WilliamsSR,ChouinardP,ArcandG,etal.Ultrasoundguidancespeeds executionandimprovesthequalityofsupraclavicularblock. Anesth Analg. 2003;97(5):1518–23.
19.FrancoCD,GlossFJ,VoronovG,etal.Supraclavicularblock intheobesepopulation:ananalysisof2020blocks. AnesthAnalg. 2006;102(4):1252–4.
ChristianTreat,MD,MSPH
NicholasUlloa,MD
AlyssaKettler,MD
DavidLawrence,DO
SectionEditor:JoelMoll,MD
StonyBrookUniversity,DepartmentofEmergencyMedicine,StonyBrook,NewYork
Submissionhistory:SubmittedNovember15,2023;RevisionreceivedFebruary27,2024;AcceptedMarch12,2024
ElectronicallypublishedJune3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6562
Introduction: Neurogenicpulmonaryedemaisarareandpotentiallylife-threateningconditionthatcan presentasseverepulmonaryedemaaftersignificantneurologicinsults.Thisisthe firstdocumented instancethatshowsaplausiblecausallinkbetweencannabisconsumption,psychogenicpolydipsia,and thesubsequentdevelopmentofneurogenicpulmonaryedemaassociatedwithstatusepilepticus secondarytoacutehyponatremia.
CaseReport: Wereportacaseofa34-year-oldfemalewhopresentedtotheemergencydepartment alteredandpostictalafterawitnessednew-onsetseizure.Shedevelopedsignificantrespiratorydistress thatrequiredintubation.Hersodiumwas121millimolesperliter(mmol/L),from137mmol/L36hours prioronroutineoutpatientlabs.Furtherhistoryrevealedexcessivewateringestionaftereatinga cannabisediblepriortotheseizure.
Conclusion: Thiscasehighlightstheimportanceofrecognizingneurogenicpulmonaryedemain connectionwithpsychogenicpolydipsia,severehyponatremia,andstatusepilepticussubsequentto cannabisconsumption.[ClinPractCasesEmergMed.2024;8(3)239–242.]
Keywords: neurogenicpulmonaryedema;hyponatremia;primarypolydipsia;cannabisintoxication; casereport.
Neurogenicpulmonaryedema(NPE)isarareand potentiallylife-threateningconditionthatcanoccurasa complicationofneurologicinsultssuchasseizures,traumatic braininjury,andintracranialhemorrhage.1 Itisbelievedto resultfromasuddenincreaseinsympathetictoneleadingto increasedpulmonarycapillaryhydrostaticpressureand increasedpulmonaryvascularpermeability.2,3 Neurogenic pulmonaryedemaisoftenassociatedwithsignificant morbidityandmortality,andearlyrecognitionand managementarecrucialforfavorableoutcomes.Inthiscase report,weillustrateaplausiblecausallinkbetweencannabis consumption,psychogenicpolydipsia,andthesubsequent developmentofNPEassociatedwithstatusepilepticus secondarytoacutehyponatremia.
A34-year-oldfemalewithamedicalhistoryofwellcontrolledHIV,depression,andanxietypresentedtothe emergencydepartment(ED)withnew-onsetseizures. Accordingtoherpartner,shehadconsumedanedible cannabiscookieearlierinthedayandthendrank approximatelyeight16.9-ouncebottlesofwateroverthe courseofonehourinresponsetoherseverethirst. Emergencymedicalserviceswerecalledbecauseshehada witnessed,generalizedtonic-clonicseizurethatlasted approximately fiveminutes.Prehospitalvitalsigns werenotableforperipheraloxygensaturation(SpO2) of69%onroomairanda fingerstickglucoseof 254milligramsperdeciliter(mg/dL)(normalrange 70–99mg/dL).
OnarrivaltotheED,thepatient’sheartratewas104beats perminute,bloodpressure117/71millimetersofmercury (mmHg),respiratoryrateof39breathsperminute,andSpO2 69%onroomair.Anon-rebreathermaskwasplacedwith improvementofSpO2 to90%.Shewascombativeand altered,unabletofollowcommandstonotremovethenonrebreathermask,anddemandingwaterfromEDstaff.Due toexcessiveagitation,50mgofintravenous(IV)ketamine wasgiventothepatienttoallowustoobtainanemergent computedtomography(CT)headwithoutcontrast,CT angiogramheadandneck,andCTchestwithoutcontrast. FollowingCTimaging,shehadanotherseizureandher SpO2 inthelow80%rangedespitenon-rebreathermask. Inthesettingofherrefractoryhypoxia,alteredmentalstatus, andseizures,thedecisionwasmadetointubate.Weuseda delayedsequenceintubationtopreoxygenatethepatientby firstadministering100mgofIVketamine.Thisimproved SpO2 to96%.Thenweproceededwithparalysiswith100mg ofrocuroniumandintubatedsuccessfullywithoutepisodes ofhypoxia.Post-intubation,weadministeredpropofolata rateof20micrograms(mcg)/kg/minute.
Laboratoryevaluationofthepatientrevealedmarked hyponatremiaof121millimolesperliter(mmol/L), comparedtoherbaselinelevelof137mmol/Lobtained 36hourspriorduringaroutineoutpatientvisit(normalrange 135–146mmol/L).Twoampules(100mL)of8.4%sodium bicarbonatewereadministeredtothepatientforacute symptomatichyponatremia.Acetaminophen,salicylate,and ethanollevelswereallnegative.Aurinetoxicologyscreen waspositiveforcannabis,andanexpandedurinetoxicology panelwassenttoanexternallaboratory.EmergentCT imagingshowednormal findingsonnon-contrastheadand angiographyoftheheadandneck,andaCTperfusionstudy demonstratednosignsofacuteinfarction.Thenon-contrast CTchestrevealedmultifocalairspaceanddiffusebilateral ground-glassopacities,withnoevidenceofeffusion orpneumothorax.
Arterialbloodgasanalysisrevealedthefollowingresults afterintubation:pH7.20(normalrange7.35–7.45),partial pressureofcarbondioxide(PaCO2)59mmHg(35to45mm Hg),partialpressureofoxygen(PaO2)83mmHg(normal range80–100mmHg),andbicarbonate23mmol/L(22–26 mmol/L).Thepatient’sventilationstatusnecessitatedhigh levelsofpositiveend-expiratorypressure(PEEP)and fractionofinspiredoxygen(FiO2),16centimetersH2Oand 100%,respectively.Shewasadmittedtotheintensivecare unitforacutehyponatremiaandhypoxemicrespiratory failure.Afterreceivingtwoampulesofsodiumbicarbonate intheED,hersodiumlevelsincreasedfromaninitiallevelof 121mmol/Lto123mmol/Lafterfourhours.Subsequently, shewasadministeredtwodosesof100mLof3%saline, resultinginarepeatsodiumlevelof131mmol/Lafter 13hoursfrominitialsodiumlevel.Finally,hersodium reached135mmol/Lafter29hoursfrominitiallevel.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Neurogenicpulmonaryedema(NPE)isa rare,life-threateningcomplicationarising fromneurologicalinsultssuchasseizuresand intracranialhemorrhage.
Whatmakesthispresentationof diseasereportable?
Thisreporthighlightsanovelcaseof psychogenicpolydipsiafromcannabisuse leadingtoNPEwithstatusepilepticusdue tohyponatremia.
Whatisthemajorlearningpoint?
Cannabisusemayleadtopsychogenic polydipsia,symptomatichyponatremia,and potentiallyinduceneurologicsequelae includingseizuresandNPE.
Howmightthisimproveemergency medicinepractice?
Patternsofincreasingcannabisuseinthe UnitedStatesshowtheneedtoconsiderlesser knowncomplicationsinpatientswith cannabis-relatedEDvisits.
Herexpandeddrugtoxicologypanelthatwassenttoan outsidelaboratoryreportedthatherurinewaspositivefor >500mcg/mL11-nor-9-carboxy-tetrahydrocannabinol(the psychoactivecompoundfoundincannabis)andnegativefor 3,4-methylenedioxymethamphetamine(MDMA), amphetamines,barbiturates,benzodiazepine,cocaine, methadone,opiates,phencyclidine,andpropoxyphene.
Thepatient’sventilatoryrequirementswereweanedto FiO2 40%,PEEP10cmH2O,withpH7.35,PaCO2 37mm Hg,andPaO2 155mmHg,andshewasextubatedtofour litersnasalcannula14hoursafterintubationandtransferred tothegeneralmedical floorsonhospitaldaythree.
Anechocardiogramperformedshowednormalcardiac parameterswithanejectionfractionof71%andnormal valvularstructures.Anelectrocardiogramshowedsinus rhythm,shortPRinterval,narrowQRS,andnormalQTc. Telemetrywaswithoutevidenceofanyventricular arrhythmias.Follow-upchestradiographs(CXR)showed resolvingpulmonaryedema.
Intravenousceftriaxoneandazithromycinwere continuedforherhospitalcourse.Thepatientwasafebrile, hadnoleukocytosis,andreportednorespiratoryissues
post-extubation.Theinfectiousworkupalsoincludeda sputumculturewithnormal flora,negativeurinarylegionella andpneumococcalantigens,negativebloodcultures,and negativeurinecultures.Additionally,aCD4leveldrawntwo dayspriortoadmissionwas752cellspermicroliter,HIV viralloadwasundetectable,andarespiratorypathogen panel,includingtestingforrespiratorysyncytialvirus, influenzavirus,andSARS-CoV-2,wasnegative.The patientunderwent24-hourvideoelectroencephalogram monitoring,whichrevealednoseizureactivityandshe returnedtonormalneurologicalstatusbyhospitaldayone aftersodiumcorrection.
Onsocialworkevaluation,shewasadherenttohermental healthcaretreatmentregimen,regularlyattendedtherapy, andusedescitalopramfordepressionandanxiety.Shehad nodocumentedpsychiatrichospitalizations,suicidalor homicidalideation,orhallucinationsintheprioryear. Shewasdischargedtohomeonhospitaldaysix.She reportednoacuteconcernsathersubsequentprimary careandnephrologyfollow-upvisits,sevenand 22dayslater,respectively.
ThiscaseshowsthedevelopmentofNPEfromsevere acutehyponatremiacausedbypsychogenicpolydipsia relatedtocannabisuse.Toourknowledge,thisspecificacute complicationofcannabishasnotbeenextensivelyreported. Preliminarydatahasshowntheassociationbetweenchronic cannabisuseandhyponatremia.Inratmodels,chronic marijuanaadministrationreducedserumsodiuminratsover a12-weekperiod,likelyviainhibitoreffectsonsodium channels.4 Anotherstudyusedspectrophotometryto estimateserumsodiumlevelsinasampleofregular marijuanasmokersandnon-marijuanasmokingcontrols andfoundsignificantlydecreasedmeansodiumlevelsof 119 ± 26mmol/Lcomparedtomeansodiumlevelsof 140 ± 6mmol/L.5 Takentogether,thisevidenceindicates marijuanacandisruptsodiumbalance,whichemergency physiciansshouldrecognizeasanimportantpossible complicationofcannabisuse.
Anyacutecentralnervoussystemeventthatabruptly triggersasympatheticdischargecanpotentiallytriggerNPE. Multiplereferenceslinkstatusepilepticustononcardiogenic pulmonaryedema,emphasizingtherelevanceofconsidering NPEinthecontextofseizure-relatedcomplications.For instance,onereportdescribedastrongerassociationbetween seizureslastinggreaterthan200secondsandthe developmentofpulmonaryedemaonCXR.6
ProposedcriteriaforthediagnosisofNPEincludethe following:bilateralopacities,PaO2/FiO2 ratio <200;no evidenceofleftarterialhypertension,presenceofneurologic injury,andabsenceofothercausesofacuterespiratorydistress syndrome.7 Ourpatient,whopresentedwith first-timeseizures, hadbilateralopacitiesandmetcriteriaforsevereacute
respiratorydistresssyndrome(ARDS)withaPaO2/FiO2 of83. Theechocardiogram findings,includingnormalleftventricular size,wallthickness,globalsystolicfunction,absenceof hypertrophy,andnosignsofimpaireddiastolicfunctionorleft atrialenlargement,collectivelysuggestednoevidenceofleft arterialhypertensioninthepatient.
Intriguingly,Ayus-Arieffsyndromeisacondition characterizedbyhyponatremia-inducedcerebraledema leadingtothedevelopmentofpulmonaryedemaandhas beendocumentedincasereports,particularlyincontexts involvingMDMAuseandinmarathonrunners.8,9 No reportscurrentlylinkittocannabisconsumption.The syndromebecameasignificantconsiderationforourpatient, whoexperiencednew-onsetseizuresinthecontextofacute hyponatremia,attributabletopolydipsiasecondaryto cannabisintoxication.Subsequently,sherequiredintubation duetoacutehypoxemicrespiratoryfailureassociatedwith ARDS.Notably,athoroughworkuprevealednormal cardiologicalandinfectiousparameterswitharapidreturn toclinicalbaselinefollowingcorrectionofsodium.
Effectivemanagementofhyponatremiarequiresa tailoredapproachbasedonunderlyingcausesandseverity. Hyponatremiastemsfromdiversecauses,includingsevere renalfailure,excessivewaterintake,hypovolemicfactors suchasgastrointestinallossesordiuretics,euvolemic conditionssuchasadrenalinsufficiencyandsyndromeof inappropriateantidiuretichormone(SIADH),and edematousstatessuchasheartfailureorcirrhosis.Patients withacutehyponatremiaexhibitserumsodiumlevelsbelow 135mmol/Lwithin48hours,whilechronichyponatremia developsovermorethan48hoursorisassumedinthe absenceofaknownbaseline.Themanagementof hyponatremiaiscriticallyinfluencedbyitschronicityand severity.Immediateconcernsinsymptomatichyponatremia involveseizures,cerebraledema,andbrainherniation.In chroniccases,theriskliesinthepotentialforrapid correction.Althoughosmoticdemyelinationisrareifthe initialsodiumlevelexceeds120mmol/L,itbecomesa concernwithahighrateofsodiumrise,typicallysurpassing 8mmol/Lina24-hourperiod.10
Thepatient’sacutehyponatremiaappearedtobelinkedto psychogenicpolydipsiagiventhehistoricalcontext,likely duetoexcessivewaterintakeinthesettingofcannabis intoxication.Givenherhistoryofdepressionandanxiety,an alternativediagnosiscouldbeSIADH,whichisknowntobe associatedwithantidepressants.11 Thissyndrometendsto haveamoreinsidiousonset,makingthisdiagnosislesslikely ashersodiumwaswithinnormalrangethedayprior tohospitalization.
Intermsofmanagement,patientswhodevelopsevere symptomssuchasseizuresorcoma,shouldbetreated promptlyandaggressivelywithhypertonic3%saline.Of note,multiplestudiesconfirmthat3%salineissafeto administerthroughaperipheralline.12–14 Therefore,
attemptingcentralaccessisunnecessaryandshouldnotdelay treatment.DependingontheED,3%salinemayrequirethe pharmacytoprepare,whichwillfurtherdelaytreatment.In thosecircumstances,ampulesofsodiumbicarbonatearea resourcefulalternativeforthetreatmentofsevere hyponatremia.Forexample,oneampuleofsodium bicarbonatehasthesameosmolarityof5.8%saline, essentiallytwicetheosmolarityof3%saline.15 Therefore, 50mLofsodiumbicarbonate,oroneampule,isroughly equivalentto100mLof3%saline.Forourpatient,we administered100mL,ortwoampules,ofsodium bicarbonatebecauseitwasthemostrapidmethodtotreather severehyponatremia.Thisincreasedhersodiumto123 mmol/L,whichwaswithinourgoal.
Thiscaseunderscorestherareoccurrenceofneurogenic pulmonaryedemalinkedtopsychogenicpolydipsia,severe hyponatremia,andstatusepilepticusfollowingcannabis consumption.Thesignificanceofthispotentialassociation withcannabisisheightenedagainstthebackdropofthe escalatingconsumption,decriminalization,andlegalization trendsobservedintheUnitedStates.Thisnotonly underscorestheclinicalcomplexityofthecasebutalso emphasizestheurgentneedforthoroughinvestigationand awarenessascannabisusagepatternsevolve.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ChristianTreat,MD,MSPH, RenaissanceSchoolofMedicineatStonyBrookUniversity, DepartmentofEmergencyMedicine,101NicollsRoad,StonyBrook, NY11794.Email: Christian.Treat@stonybrookmedicine.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Treatetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.RogersFB,ShackfordSR,TrevisaniGT,etal.Neurogenicpulmonary edemainfatalandnonfatalheadinjuries. JTrauma. 1995;39(5):860–6.
2.HallSRR,WangL,MilneB,etal.Intrathecallidocaineprevents cardiovascularcollapseandneurogenicpulmonaryedemain aratmodelofacuteintracranialhypertension. AnesthAnalg. 2002;94(4):948–53.
3. ŠedýJ,Kuneš J,ZichaJ.Pathogeneticmechanismsofneurogenic pulmonaryedema. JNeurotrauma. 2015;32(15):1135–45.
4.TaiwoOA,DosumuOA,UgbajaRN,etal.Oraladministrationof marijuanaproducesalterationsinserotonin5-hydroxytryptamine receptor3Agene(HTR3A)andelectrolyteimbalancesinbrainofmale Wistarrats. MolBiolResCommun. 2021;10(1):5–11.
5.OsadolorHBandEmokpaeAM.Effectsofmarijuanaonsodium andpotassium(Na+&K+)ionshomeostasisamongsmokersin BeninCity-ametropolitancityinNigeria. IntJPharmBioSci. 2010;3(1):1–3.
6.KennedyJD,HardinKA,ParikhP,etal.Pulmonaryedemafollowing generalizedtonicclonicseizuresisdirectlyassociatedwithseizure duration. Seizure. 2015;27:19–24.
7.DavisonDL,TerekM,ChawlaLS.Neurogenicpulmonaryedema. Crit Care. 2012;16(2):212.
8.AyusJC,VaronJ,ArieffAI.Hyponatremia,cerebraledema,and noncardiogenicpulmonaryedemainmarathonrunners. AnnInternMed. 2000;132(9):711–4.
9.ThakkarA,ParekhK,ElHachemK,etal.AcaseofMDMA-associated cerebralandpulmonaryedemarequiringECMO. CaseRepCritCare. 2017;2017:6417012.
10.Rondon-BerriosH.Therapeuticreloweringofplasmasodiumafter overlyrapidcorrectionofhyponatremia:whatistheevidence? ClinJAm SocNephrol. 2020;15(2):282–4.
11.PinkhasovA,XiongG,BourgeoisJA,etal.ManagementofSIADHrelatedhyponatremiaduetopsychotropicmedications:anexpert consensusfromtheAssociationofMedicineandPsychiatry. J PsychosomRes. 2021;151:110654.
12.MoussaviK.Safetyofperipherallineadministrationof3%hypertonic salineandmannitolintheemergencydepartment. JEmergMed. 2019;56(4):431–6.
13.MengL,NguyenCM,PatelS,etal.Associationbetweencontinuous peripheralIVinfusionof3%sodiumchlorideinjectionandphlebitisin adults. AmJHealthSystPharm. 2018;75(5):284–91.
14.DillonRC,MerchanC,AltshulerD,etal.Incidenceofadverseevents duringperipheraladministrationofsodiumchloride3%. JIntensiveCare Med. 2018;33(1):48–53.
15.FarkasJ.EmergenttreatmentofhyponatremiaorelevatedICPwith bicarbampules.2015.Availableat: https://emcrit.org/pulmcrit/ emergent-treatment-of-hyponatremia-or-elevated-icp-with-bicarbampules/. AccessedJune7,2023.
FaizaTariq,MBBS WesleyEilbert,MD
UniversityofIllinois,CollegeofMedicine,DepartmentofEmergencyMedicine,Chicago,Illinois
SectionEditor:JacquelineLe,MD
Submissionhistory:SubmittedJanuary23,2024;RevisionreceivedMarch6,2024;AcceptedMarch12,2024
ElectronicallypublishedMay29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7223
Introduction: Spontaneousintracranialhypotension(SIH)isanuncommonandfrequently misdiagnosedconditioncharacterizedbyalower-than-normalvolumeofcerebrospinal fluid(CSF) causedbyleakageofCSFthroughtheduralmembrane.TheprimarymanifestationofSIHisan orthostaticheadache,whichisfrequentlyaccompaniedbynauseaandvomiting.Patientswith connectivetissuedisordersareatincreasedriskforspontaneousCSFleaksduetothestructural weaknessoftheirduralmembranes.
CaseReport: An18-year-oldwomanwithnoreportedpastmedicalhistorypresentedtotheemergency departmentwith10daysofabifrontalheadachethatwasorthostaticinnaturewithassociatednausea andvomiting.Shewasnotedtohaveseveralmarfanoidfeaturesonphysicalexamination.Spontaneous intracranialhypotensionwasultimatelydiagnosedandtreatedsuccessfullywithanepiduralbloodpatch. SubsequentgenetictestingrevealedadiagnosisofMarfansyndrome.
Conclusion: Spontaneousintracranialhypotensionisanuncommoncauseofheadache.Individuals withconnectivetissuedisorderssuchasMarfansyndromeareatincreasedriskforSIH.Knowledgeof therelationshipbetweenthesetwoconditionsallowsforamorerapiddiagnosisofSIH.[ClinPractCases EmergMed.2024;8(3)243–245.]
Keywords: spontaneousintracranialhypotension;Marfansyndrome;meningealdiverticulum;spinal cerebrospinal fluidleak;casereport.
Firstdescribedin1938,spontaneousintracranial hypotension(SIH)isaconditioncharacterizedbyalowerthan-normalvolumeofcerebrospinal fluid(CSF)causedby leakageofCSFthroughtheduralmembrane.1,2 Patientswith connectivetissuedisordersareatincreasedriskfor spontaneousCSFleaksduetothestructuralweaknessof theirduralmembranes.3 TheprimarymanifestationofSIHis anorthostaticheadachethatmaybeaccompaniedbynausea, tinnitus,andphotophobia.4 Wereportthecaseofayoung womanwithpreviouslyundiagnosedMarfansyndromewho presentedwithSIH.
An18-year-oldwomanpresentedtothe emergencydepartment(ED)complainingofabifrontal headachepresentfor10days.Theheadachewas ofinsidiousonsetandwassignificantlyworseintheupright position,betterwhensupine.Shereportednausea withtheheadacheandoneepisodeofvomitingtwodays earlier.Onphysicalexamination,shehadseveral marfanoidfeaturesincludingatall,slenderbuildwith disproportionatelylongarms,legs,and fingers. Shewasafebrileandhadanormal neurologicexamination.
Computedtomographyofherbrainshowednosignificant abnormalitiesandmagneticresonanceimaging(MRI)ofthe brainwithvenogramwasorderedbecauseofconcernfor possibleduralvenoussinusthrombosis.TheMRIshowed duralthickeningandincreasedduralenhancement suggestiveofintracranialhypotension.Thepatientwas admittedtothehospital,andMRIofthecervical,thoracic, andlumbarspineperformedthenextdayshowedno extradural fluidcollectionstosuggestaCSFleak.Shehad modestimprovementofherheadacheafteranepiduralblood patchandwasdischargedonhospitaldaythree.
ThepatientreturnedtotheED fivedayslatercomplaining ofareturnoftheheadache.AsecondMRIofthespinewas performedthatshowedameningealdiverticulumarising fromtheleft firstandsecondthoraciclevelwithanadjacent pleuraleffusionconcerningforapossiblerupturednerveroot sleevediverticulum(Image).Shereceivedasecondepidural bloodpatchwithcomplete,longstandingreliefofthe headache.Subsequentoutpatientgenetictestingrevealeda pathogenicvariantoftheFBN1geneconsistentwitha diagnosisofMarfansyndrome.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Spontaneousintracranialhypotension(SIH) iscausedbyleakageofcerebrospinal fl uid throughtheduralmembrane,whichcanbe weakenedbyconnectivetissuedisorders.
Whatmakesthispresentationof diseasereportable?
Awomanwhopresentedwithanorthostatic headachewasultimatelydiagnosedwithSIH. Genetictestinglaterrevealedadiagnosisof Marfansyndrome.
Whatisthemajorlearningpoint?
Individualswithconnectivetissuedisorders suchasMarfansyndromeareatincreased riskforspontaneouscerebrospinal fl uidleaks resultinginSIH.
Howmightthisimproveemergency medicinepractice?
Spontaneousintracranialhypotensionisdistinguished fromothercausesofCSFleaksofknowncausesuchas spinalsurgery,craniospinaltrauma,and,mostcommonly, lumbarpunctureorspinalanesthesia.Spontaneous intracranialhypotensionisanuncommoncauseof headacheintheED,withanestimatedannualincidenceof 5/100,000individuals halftheincidenceofsubarachnoid hemorrhage. 5 WomenarediagnosedwithSIHmore frequentlythanmen,withafemale-maleratioof approximately2:1. 6 Spontaneousintracranialhypotension isofteninitiallymisdiagnosed,with94%ofpatients receivinganincorrectinitialdiagnosisinonestudy.7 The headachecausedbySIHisbelievedtobetheresultof downwarddisplacementofthebrainduetolossofCSF buoyancy,resultingintractiononpain-sensitive fi bersin theduramater. 3, 6 TheorthostaticheadachecausedbySIH istypicallydescribedasdiffuse,occipital,orfrontal. 4 Other associatedsymptomsareoftenpresent(Table1).4
Knowledgeofthepredilectionofpatientswith connectivetissuedisordersforSIHmayassist cliniciansinthediagnosisofsimilarcases.
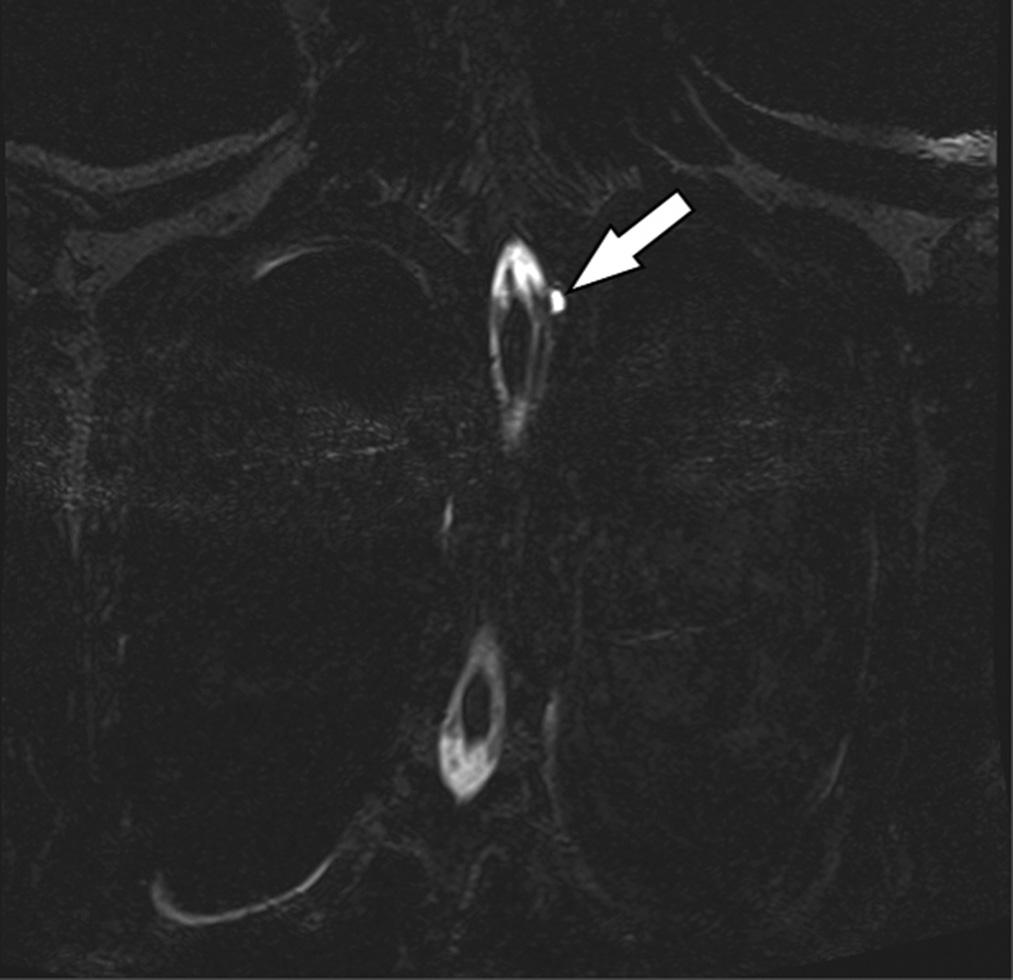
Table2. Diagnosticcriteriaforspontaneous intracranialhypotension.
1.AnyheadacheattributedtolowCSFpressureorCSF leakage thatmeetscriterion3below.
2.Eitherorbothofthefollowing:
a.LowCSFpressure(<60mmH2OCSF)
b.EvidenceofCSFleakageonimaging
3.HeadachethatdevelopedintemporalrelationtothelowCSF pressureorCSFleakage,orthatleadstoitsdiscovery.
4.Absenceofaprocedureortraumaknowntobeabletocause CSFleakage.
5.Headachenotbetteraccountedforbyanotherdiagnosis.
CSF, cerebrospinal fluid; mmH2O,millimetersofwater.
ThelocationoftheCSFleakwithSIHisoftennot determinedsincespinalCSFleaksgenerallydonotcause localsymptoms.6 ExtraduralspinalCSFcollectionsare foundinapproximatelyhalfofallpatientswithSIH.2 The majorityofidentifiedspinalCSFleaksoccuratthethoracic orcervicothoracicspinelevel.8 SpinalCSFleaksoccurvia threemainmechanisms:meningealdiverticula;ventraldural tears;andCSF-venous fistulas,withdiverticulabeingmost common. 9 Patientswithgeneticconnectivetissuedisorders suchasMarfansyndrome,Ehlers-DanlossyndromeTypeII, andautosomaldominantpolycystickidneydiseaseareat higherriskforspontaneousCSFleaksduetothestructural weaknessoftheirduralmembranes.3,10 Oneprospective studyfoundthatuptotwo-thirdsofpatientswith spontaneousspinalCSFleakshadsomeevidenceofa connectivetissuedisorder.10
DiagnosticcriteriaforSIHhavebeenproposed (Table2).2,11 BrainMRIwithcontrastisthemostsensitive imagingstudyfordiagnosingSIH.4,9 Smooth,generalized duralenhancementisthefeaturemostcommonlyseen, presentin73%ofpatientswithSIH.2,4 ManycasesofSIH resolvespontaneouslywithnospecifictreatmentrequired.12 Initialconservativetreatmentsofbedrest,oralhydration, andcaffeineareeffectiveinapproximately25%ofpatients.4 Epiduralbloodpatchingisthemostcommonlyperformed interventionforspinalCSFleaks,withestimatesofefficacy rangingfrom36–90%.9
Spontaneousintracranialhypotensionisanuncommon causeofheadacheandisfrequentlymisdiagnosed. IndividualswithMarfansyndromeandotherconnective tissuedisordersareatincreasedriskforSIHduetothe structuralweaknessoftheirduralmembranespredisposing tospontaneousCSFleaks.Knowledgeoftherelationship betweentheseassociatedconditionsallowsformorerapid diagnosisofSIH.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:WesleyEilbert,MD,Universityof Illinois,CollegeofMedicine,DepartmentofEmergencyMedicine, 1819W.PolkSt.,Room469,Chicago,IL60612.
Email: weilbert@uic.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Tariqetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SchaltenbrandG,Neureanschauungenzurpathophysiologieder liquorzirkulation(RecentviewsonthepathophysiologyofCSF circulation). ZentralblNeurochir. 1938;3:290–300.
2.SchievinkWI.Spontaneousintracranialhypotension. NEnglJMed. 2021;385(23):2173–8.
3.DobrockyT,NicholsonP,HaniL,etal.Spontaneousintracranial hypotension:searchingfortheCSFleak. LancetNeurol. 2022;21(4):369–80.
4.D’AntonaL,JaimeMerchanMA,VassiliouA,etal.Clinicalpresentation, investigation findings,andtreatmentoutcomesofspontaneous intracranialhypotensionsyndrome:asystematicreviewandmetaanalysis. JAMANeurol. 2021;78(3):329–37.
5.SchievinkWI,MayaMM,MoserF,etal.Frequencyofspontaneous intracranialhypotensionintheemergencydepartment. JHeadache Pain. 2007;8(6):325–8.
6.SchievinkWI.Spontaneousspinalcerebrospinal fluidleaksand intracranialhypotension. JAMA. 2006;295(19):2286–96.
7.SchievinkWI.Misdiagnosisofspontaneousintracranialhypotension. ArchNeurol. 2003;60(12):1713–8.
8.MokriB,MaherCO,SencakovaD.SpontaneousCSFleaks:underlying disorderofconnectivetissue. Neurology. 2002;58(5):814–6.
9.KranzPG,GrayL,MalinzakMD,etal.Spontaneousintracranial hypotension:pathogenesis,diagnosisandtreatment. Neuroimaging ClinNAm. 2019;29(4):581–94.
10.SchievinkWI,GordonOK,TourjeJ.Connectivetissuedisorderswith spontaneousspinalcerebrospinal fluidleaksandintracranial hypotension:aprospectivestudy. Neurosurgery. 2004;54(1):65–70.
11.HeadacheClassificationCommitteeoftheInternationalHeadache Society(IHS).TheInternationalClassificationofHeadacheDisorders, 3rded. Cephalgia. 2018;38(1):1–211.
12.DavenportRJ,ChatawaySJ,WarlowCP.Spontaneousintracranial hypotensionfromaCSFleakinapatientwithMarfan’ssyndrome. J NeurolNeurosurgPsychiatry. 1995;59(5):516–9.
MaryUnanyan,DO
ChristopherColbert,DO WesleyEilbert,MD
SectionEditor:StevenWalsh,MD
UniversityofIllinoisatChicago,CollegeofMedicine,DepartmentofEmergencyMedicine, Chicago,Illinois
Submissionhistory:SubmittedJanuary23,2024;RevisionreceivedMarch2,2024;AcceptedMarch2,2024
ElectronicallypublishedJuly11,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7227
Introduction: Atrial fibrillation(AF)isthemostcommoncardiacarrhythmia,occurringprimarilyin individualswithknownriskfactorssuchasadvancedage,heartfailure,andcoronaryarterydisease. Cannabisuseproducesseveralcardiovascularchangesresultinginproarrhythmiceffectsontheheart.
CaseReport: A38-year-oldwomanwithnosignificantpastmedicalhistorypresentedtotheemergency department(ED)complainingofpalpitationswithassociatedshortnessofbreathoccurringaftersmoking marijuana.ShewasfoundtobeinAF.EvaluationintheEDandduringhospitalizationfoundnocardiac ormetabolicconditionsthatpredisposedtoAF.TheAFresolvedwithinthreehoursofonset withoutintervention.
Conclusion: Cannabisuseshouldbeconsideredasapossibleetiologyofnew-onsetAF, especiallyinrelativelyyoungpatientswithnootherpredisposingriskfactors.[ClinPractCasesEmerg Med.2024;8(3)246–249.]
Keywords: atrial fibrillation;marijuana-inducedatrial fibrillation;marijuana-inducedarrhythmia; cannabis-inducedarrhythmia;casereport.
Atrial fibrillation(AF)isthemostcommoncardiac arrhythmia,occurringin1–3%ofthegeneralpopulationand inupto17%ofindividuals >80yearsinage.1 Themajorityof AFcasesoccurinpatientswithknownriskfactorssuchas advancedage,heartfailure,andcoronaryarterydisease.1 We reportacaseofparoxysmalAFina38-year-oldwomanwith noassociatedriskfactorsaftersmokingmarijuana.
A38-year-oldwomanwithahistoryofobesitypresented totheemergencydepartment(ED)complainingof palpitationswithassociatedshortnessofbreath,dizziness, andchestdiscomfort.Thesymptomshadbegunabruptly approximatelyonehourearlierwhileshewasapatientina nearbydentalclinic.Sheadmittedtorecreationalmarijuana useandreportedshehadsmokedmarijuanajustpriortoher dentalappointmenttoalleviateherrelatedanxiety.
Onphysicalexamination,shehadapulseof93beatsper minutewithanirregularrhythm,andherbloodpressurewas 123/90millimetersofmercury.Herlungswereclearto auscultation.Anelectrocardiogramrevealedanirregular rhythmwithanarrowQRScomplexandanabsenceofP waves,consistentwithAF(Image).Noischemicchanges werepresent.
LaboratorytestingintheEDwasremarkablefora minimallyelevatedserumhigh-sensitivitytroponinIlevelof 15nanogramsperliter(ng/L)(referencerange:0–15ng/L) andaserumthyroidstimulatinghormonelevelinthenormal range.Approximately90minutesafterEDarrival,the patientspontaneouslyconvertedtoanormalsinusrhythm. ShewasadmittedtothehospitalforevaluationofnewonsetAF.
Thepatientremainedinasinusrhythmwhileinthe hospital.Serialserumhigh-sensitivitytroponinIlevelswere notindicativeofmyocardialdamage.Herserummagnesium
levelwasfoundtobejustbelowthenormalrangeat1.7 milligramsperdeciliter(mg/dL)(1.8–2.4mg/dL).Herurine toxicologicalscreeningwaspositiveonlyforcannabinoids. Hertransthoracicechorevealednostructuralabnormalities oftheheartandnormalleftventricularfunction.Thepatient wasdischargedhomeonhospitaldaytwoonnonew medicationsasherAFwasfelttobeparoxysmalinnature.
CannabisisthemostwidelyusedillicitdrugintheUnited States(US).2 ThepercentageofUSadultsthatusemarijuana hasmorethandoubledsince2001,andcannabisinvarious formsforrecreationalormedicinaluseisnowlegalin46 states.3,4 Thepotencyofcannabishasalsoincreased significantlyinthepast20yearsintheUS.5 Asof2021, approximately75%ofUSadultsbelievedcannabisusewas assafeorsaferthantobaccouse.6
ParoxysmalAFfollowingmarijuanausewas first reportedin2000.7 Sincethen,severalsimilarcaseshavebeen described,ofteninyoungpeoplewithstructurallynormal heartsandnootherriskfactorsforAF.8 ItispossiblethatAF aftermarijuanauseisunder-reportedbecausepatientsare reluctanttoseekmedicalcarewhileundertheinfluenceofthe drugduetolegalconcerns.Also,palpitationssuggestiveof AFexperiencedbyusersmaybeinterpretedassimplyan expectedcardiovasculareffectofcannabisuse.Atrial fibrillationfollowinguseofsyntheticcannabinoidshasalso beendescribed.9
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Atrial fi brillation(AF)occursprimarilyin individualswithknownriskfactors. Marijuanausehasseveralproarrhythmic effectsontheheart.
Whatisthemajorimpactoftheimage(s)?
ApatientwithnoriskfactorsforAFpresented totheEDwithparoxysmalAFaftersmoking marijuana.NoothercauseofherAFwas identi fi edafterhospitaladmission.
Howmightthisimproveemergency medicinepractice?
Useofcannabisshouldbeconsideredasa possibleetiologyofnew-onsetAF,especially inpatientswithnootherpredisposingfactors.
Variouscardiacarrhythmiashavebeenreportedwith marijuanause,withAFandventricular fibrillationthemost common(Table).10–12 Themechanismsbywhichmarijuana inducescardiacarrhythmiasisunknown,althoughseveral

Image. Thepatient’selectrocardiogramshowingatrial fibrillation.
Table. Cardiacarrhythmiasreportedwithmarijuanause.
SupraventriculararrhythmiasVentriculararrhythmias
Atrial fibrillation
Ventriculartachycardia
Atrial flutter Ventricular fibrillation
Ectopicatrialtachycardia Asystole
Supraventriculartachycardia
Junctionalrhythm
Sinusbradycardia
Sinusarrest
FirstdegreeAVblock
SeconddegreeAVblock
ThirddegreeAVblock
AV, atrioventricular.
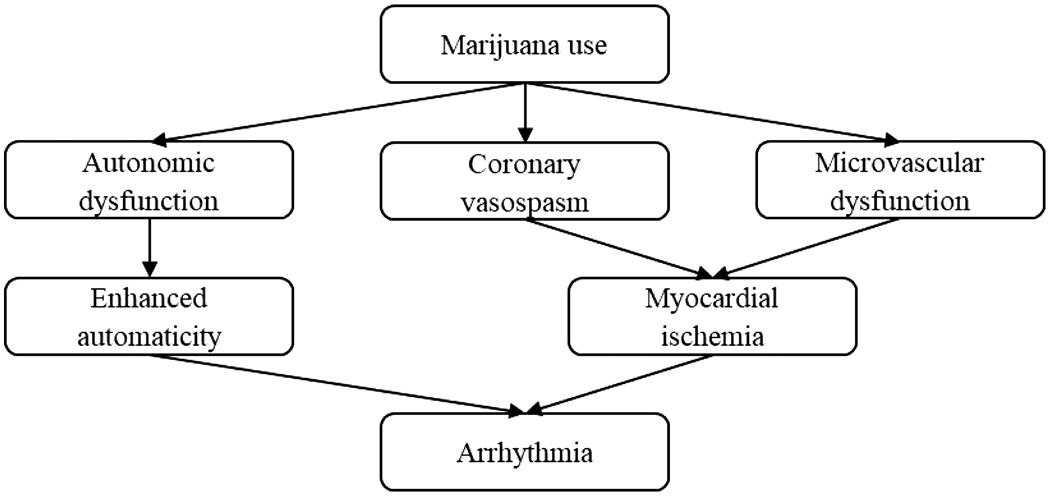
Figure. Proposedmechanismsofmarijuana-induced cardiacarrhythmias.
mechanismshavebeenproposed(Figure).8–10 Autonomic dysfunctionbeginswithinminutesaftersmokingmarijuana, causingabiphasicanddose-dependenteffect.Sympathetic stimulationispredominantatlowerdoses,leadingto tachycardiaandenhancedcardiacautomaticity.Athigher doses,parasympatheticactivationleadstobradycardiaand hypotension.8,13 Cannabismayalsoinducecoronary vasospasmandhaveadetrimentaleffectonthecoronary microcirculation,leadingtomyocardialischemia.8,10 Allof thesecardiovascularchangesresultinproarrhythmiceffects ontheheart.
TheincidenceofAFrelatedtomarijuanauseisdifficultto estimate,althoughtheprevalenceofcannabisusedisorder amongpatientsadmittedforAFisincreasing,withthe greatestincreaseinpercentageprevalenceamongyounger patients.14 Atrial fibrillationrelatedtomarijuanauseatthis pointseemstobeatransientandrelativelybenign phenomena,leadingsomeauthorstocompareitto “holiday heart” occurringwithethanoluse.15 Screeningforcannabis usebyhistoryorlaboratorytestingshouldbeconsideredin patientswithnew-onsetAF,especiallyinthoseotherwise youngandhealthy.
Atrial fibrillationassociatedwithmarijuanausehasbeen increasinglydescribedinthepast20years.Theexact mechanismbywhichmarijuanainducesAFisunknown. Thisphenomenonistypicallytransientandrelativelybenign inpatientsthatareotherwiseyoungandhealthy.Cannabis useshouldbeconsideredasapossibleetiologyofnewonset AF,especiallyinyoungpatientswithnootherpredisposing riskfactors.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:MaryUnanyan,DO,Universityof IllinoisatChicago,CollegeofMedicine,DepartmentofEmergency Medicine,Room469CME1819WPolkSt.,ChicagoIL,60612. Email: munany2@uic.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Unanyanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.FreedmanB,HindricksG,BanerjeeA,etal.WorldFederationRoadmap onAtrialFibrillation-a2020update. GlobHeart. 2021;16(1):41.
2.CentersforDiseaseControlandPrevention.MarijuanaandPublic Health.2021.Availableat: https://www.cdc.gov/marijuana/datastatistics.htm.AccessedDecember28,2023.
3.HasinDS,SahaTD,KerridgeBT,etal.Prevalenceofmarijuanause disordersintheUnitedStatesbetween2001–2002and2012–2013. JAMAPsychiatry. 2015;72(12):1235–42.
4.DISAGlobalSolutions.Marijuanalegalitybystate.2023.Availableat: https//www.disa.com/marijuana-legality-by-state AccessedDecember29,2023.
5.ChenM,LuYL,ChenXF,etal.Associationofcannabisusedisorder withcardiovasculardiseases:atwo-sampleMendelianrandomization study. FrontCardiovascMed. 2022;9:966707.
6.ChambersJ,KehaniS,LingPM,etal.Perceptionsofdailycannabisvs tobaccosmokingandsecondhandsmokeexposure,2017–2021. JAMANetwOpen. 2023;6(8):e2328691.
7.KosiorDA,FilipiakKJ,SolarzP,etal.Paroxysmalatrial fibrillationina younghealthyfemalepatientfollowingmarijuanaintoxication-acase reportapossibleassociation. MedSciMonit. 2000;6(2):386–9.
8.KorantzopoulosP,LiuT,PapaioannidesD,etal.Atrial fibrillationand marijuanasmoking. IntJClinPrac. 2008;62(2):308–13.
9.EfeTH,FelekogluMA,CimenT,etal.Atrial fibrillationfollowing syntheticcannabinoiduse. TurkKardiolDernArs. 2017;45(4):362–4.
10.KariyannaPT,WengrofskyP,JayarangaiahA,etal.Marijuana andcardiacarrhythmias:ascopingreview. IntJClinResTrials. 2009:4;132.
11.DesaiR,PatelU,DeshmukhA,etal.Burdenofarrhythmiainrecreational marijuanausers. IntJCardiol. 2018;264:91–2.
12.RichardsJR,BlohmE,TolesKA,etal.Theassociationofcannabisuse andcardiacdysrhythmias:asystematicreview. ClinToxicol(Phila). 2020;58(9):861–9.
13.YahudE,PaulG,RahkovichM,etal.Cannabisinduced cardiacarrhythmias:acaseseries. EurHeartJCaseRep. 2020;4(6):1–9.
14.ChouairiF,MillerPE,GuhaA,etal.Cannabisusedisorderamongatrial fibrillationadmissions,2008–2018. PacingClinElectrophysiol. 2021;44(11):1934–8.
15.CharbonneyE,SztajzelJM,PolletiPA,etal.Paroxysmalatrial fibrillationafterrecreationalmarijuanasmoking:another “holidayheart”? SwissMedWkly.2005;135(27–28):412–4.
AssociatedwithEosinophilicGranulomatosiswithPolyangiitis:
ChristopherAllen,BS*
ChristopherPoyorena,BS*
LaurenB.Querin,MD,MEd,MSc*†
SectionEditor:R.GentryWilkerson,MD
*MayoClinicAlixSchoolofMedicine,Scottsdale,Arizona † MayoClinicHospitalPhoenix,DepartmentofEmergencyMedicine, Phoenix,Arizona
Submissionhistory:SubmittedFebruary7,2024;RevisionreceivedMarch12,2024;AcceptedApril1,2024
ElectronicallypublishedJune14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.19412
Introduction: ST-elevationmyocardialinfarction(STEMI)canbecausedbyunderlyingcoronaryartery vasospasm(CAV)withorwithoutassociatedatheroscleroticdisease.Coronaryarteryvasospasmisa rarebutpotentiallydevastatingmanifestationofeosinophilicgranulomatosiswithpolyangiitis(EGPA).
CaseReport: Wedescribea54-year-oldmalewithaknownhistoryofEGPAandcoronaryartery diseasepresentingtotheemergencydepartmentwithchestpainandaninferiorSTEMIon electrocardiogram.Hewasultimatelytakenforcoronaryangiographyandfoundtohaveadiscrete vasospasticlesionintherightcoronaryarterythatwastreatedwithintra-coronarynitroglycerinand calciumchannelblockers.Hewascontinuedonimmunosuppressantagents(prednisoneand mepolizumab)formanagementofEGPAandfollowedupwithoutpatientcardiologyandrheumatology forvasospasticangina.
Conclusion: ThiscasehighlightsararecauseofSTEMI,discussesthenuancesintreatmentofSTEMI duetoCAV,andprovidesbackgroundonpathophysiologyandtreatmentofEGPA.[ClinPractCases EmergMed.2024;8(3)250–253.]
Keywords: casereport;STEMI;coronaryarteryvasospasm;eosinophilicgranulomatosis withpolyangiitis.
ThemostcommoncauseofST-elevationmyocardial infarction(STEMI)isacuteplaqueruptureassociatedwith atheroscleroticdisease.However,about5–25%ofcasesare causedbyanon-atheroscleroticevent,suchascoronary arteryvasospasm(CAV).1 DifferentiatingSTEMIdueto atherosclerosisvsCAVischallengingandoftenrequires coronaryangiographyfordefinitivediagnosis.1 Although rare,CAVhasbeenassociatedwithvasculitisseenin rheumatologicandsystemicinflammatoryconditions.2,3 Eosinophilicgranulomatosiswithpolyangiitis(EGPA) (formerlyChurg-Strausssyndrome)isarare,small-and medium-vesselvasculitis.4 Coronaryarteryvasospasmisa potentiallydevastatingcomplicationofEGPA.Wereporta
uniquecaseofaninferiorSTEMIsecondarytoCAV associatedwithunderlyingEGPA.
A54-year-oldmalepresentedtotheemergency department(ED)withacute-onset,severeleft-sidedchest painanddiaphoresis.Hehadtaken81milligramsaspirinand sublingualnitroglycerinpriortopresentation,whichdidnot alleviatehissymptoms.Pastmedicalhistorywasnotablefor hypertension,hyperlipidemia,coronaryarterydisease (CAD),andEGPA.Hehadfourpriorrightcoronaryartery (RCA)stents,withthemostrecentatanoutsidehospitalone monthprior.Healsoreportedseveralmonthsofanginal chestpainthoughttobesecondarytocoronaryvasospasm.
Initialvitalsignsincludedbloodpressure148/99 millimetersofmercury(mmHg),heartrate69beatsper minute(bpm),respiratoryrate26breathsperminute, temperature36.7° Celsius,andpulseoximetry98%onroom air.Onexamhewasdiaphoreticanduncomfortable appearingwithmildtachypnea,buthiscardiopulmonary examwasotherwisenormal.Initialelectrocardiogram (ECG)(Image1)showedanormalsinusrhythmwithSTsegmentchangesconcerningforinferiorSTEMI.Thepatient wastreatedwithaspirin,morphine,andsublingual nitroglycerin,andacodeSTEMIwasactivated. IntervalECGobtained15minuteslaterdemonstratedno significantchange.
Thepatientwastakenforcoronaryangiography,which revealedahigh-gradestenosisofthedistalRCAduetoa discrete99%vasospasticlesion(Figure).Intracoronary nitroglycerinwasadministered,ultimatelyresultingin resolutionofthestenosis.Hispreviousstentswerepatent withoutrestenosis,andtherewasnosignificant atheroscleroticdisease.Followingcatheterization,the patientwasstartedonanitroglycerindripanddiltiazem.A post-catheterizationECG(Image2)showedevidenceof recentinferiorinfarct.Hewasdischargedtwodayslateron dualantiplatelettherapy,diltiazem,isosorbidemononitrate, L-arginine,prednisone,andmepolizumabtherapy.
AnginalchestpainsecondarytoCAVoccurswhenoneor morecoronaryarteriesconstrict,leadingtoocclusionofthe affectedvessel(s).Thiscanevolveintoacutemyocardial
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicentity?
ST-elevationmyocardialinfarction (STEMI)iscausedbyacuteplaquerupture withatheroscleroticdisease.Asmallsubsetis causedbynon-atheroscleroticevents, includingcoronaryarteryvasospasm.
Whatmakesthispresentationof diseasereportable?
Thisisarareunderlyingcauseofarelatively commonand “ can ’ tmiss ” diagnosisof STEMIintheED.
Whatisthemajorlearningpoint?
Coronaryarteryvasospasm(CAV)is associatedwithunderlyingvasculitisandcan causeSTEMI.Managementshould includevasodilators.
Howmightthisimproveemergency medicinepractice?
RarecausesofSTEMI,includingCAVand itsriskfactors(eg,vasculitis),shouldbekept ondifferentialssothatearlyinterventioncan beimplemented.

Image1. InitialelectrocardiogramdemonstratinganormalsinusrhythmwithSTelevationsinleadsII,III,andaVFaswellasreciprocalmild STdepressionsinleadsIandaVLraisingconcernforinferiorST-elevationmyocardialinfarction.
Volume8,No.3:August2024ClinicalPracticeandCasesinEmergencyMedicine
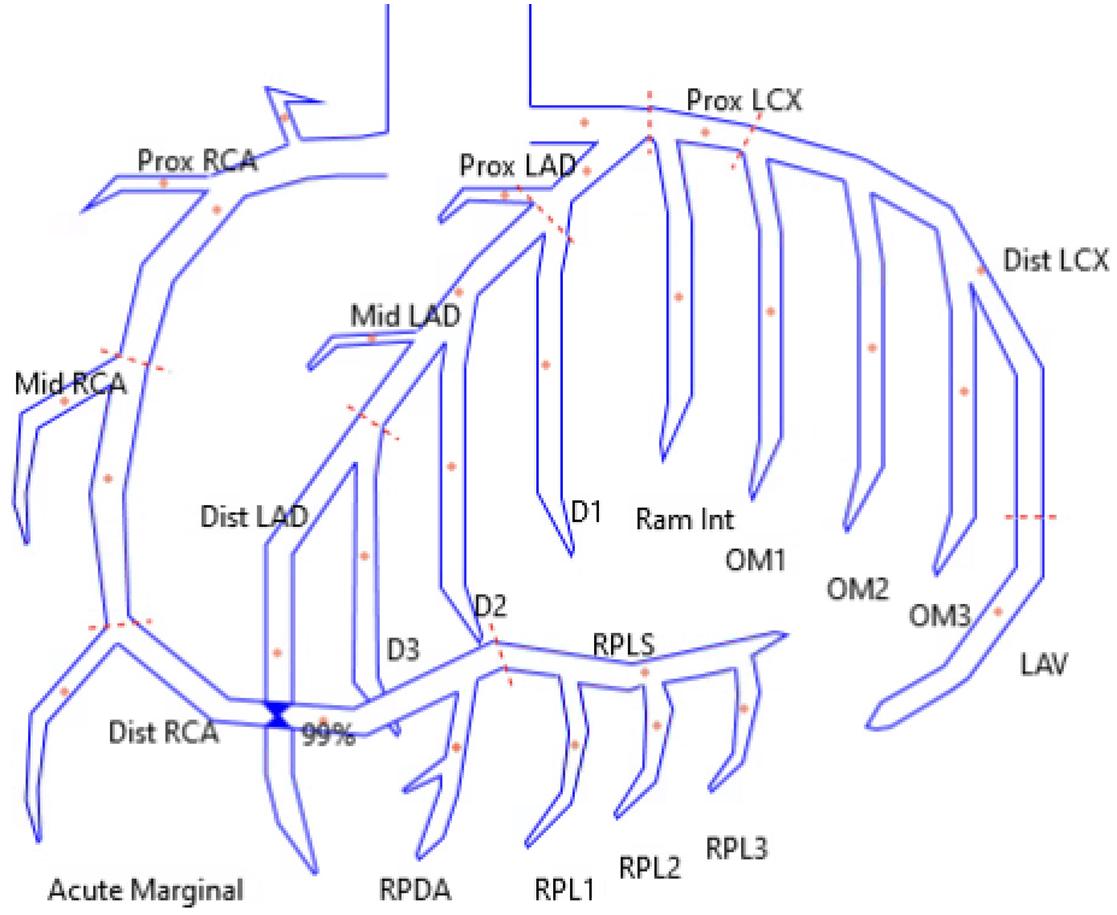
Figure. Reconstructeddrawingofcoronaryarteryanatomy demonstratingthelocationofthedistalrightcoronaryartery 99%stenosis.
RCA,rightcoronaryartery.
infarction(MI),asseeninthiscase.1,5 RiskfactorsforCAV includefemalegender,JapaneseorKoreanlineage, emotionalstress,tobaccouse,sympathomimeticdrugs,and systemicinflammatoryconditions(vasculitis).6,7
Eosinophilicgranulomatosiswithpolyangiitisisarare vasculitisthoughttobecausedbyanti-neutrophilcytoplasmic antibody-inducedendothelialdamageandmultisystem eosinophilicinfiltration.8,9 Typicalpresentingfeaturesinclude adult-onsetasthma,rhinosinusitis,andconstitutional
symptoms.However,involvementofendorgansmaybeseen, leadingtorenaldysfunction,gastrointestinalsymptoms,skin, and/orcardiacmanifestations.4,10 Cardiacinvolvementin EGPAtypicallymanifestsascardiomyopathy, myopericarditis,and/ordysrhythmia.11 Coronaryartery vasospasmandMIarerarelyreported.Although pathogenesisisnotfullyunderstood,itispostulatedthat eosinophilicinflammationinduceshypercontractionof coronarysmoothmusclethroughactivationofmastcellsand releaseofvasoactivesubstances.12,13
Thepresentationandinitialtreatmentofacutevasospastic anginaisthesameirrespectiveoftheunderlyingcauseofthe vasospasm.DuringtheacutepresentationofCAV, symptomsarenearlyidenticaltoatheroscleroticetiologiesof acutecoronarysyndromes,includingchestpain,diaphoresis, anddyspnea.Subtledifferencesexist,includingthatCAV oftenpresentsatrest,especiallyduringrapideye movement(REM)sleepandintheearlymorning.5,14
Electrocardiogram findingsarevariableandcanrangefrom normaltoST-elevationsmeeting STEMIcriteria.1
Differentiatingbetweenatheroscleroticplaqueruptureand CAVasetiologyofSTEMIcanbechallenging.However, definitivetreatmentdiffersand,therefore,physiciansshould beattentiveinconsideringCAV,particularlyinpatientswith underlyingriskfactors.1 Coronaryarteryvasospasmmaybe suggestedifonrepeatECGthereisresolutionorimprovement ofSTchangesfollowingadministrationoffast-actingnitrate. However,definitivediagnosisrequirescoronaryangiography, especiallyifthediagnosisisunclear,orifsymptomspersist.5 Emergencyphysiciansshouldinitiaterapidinvolvementof
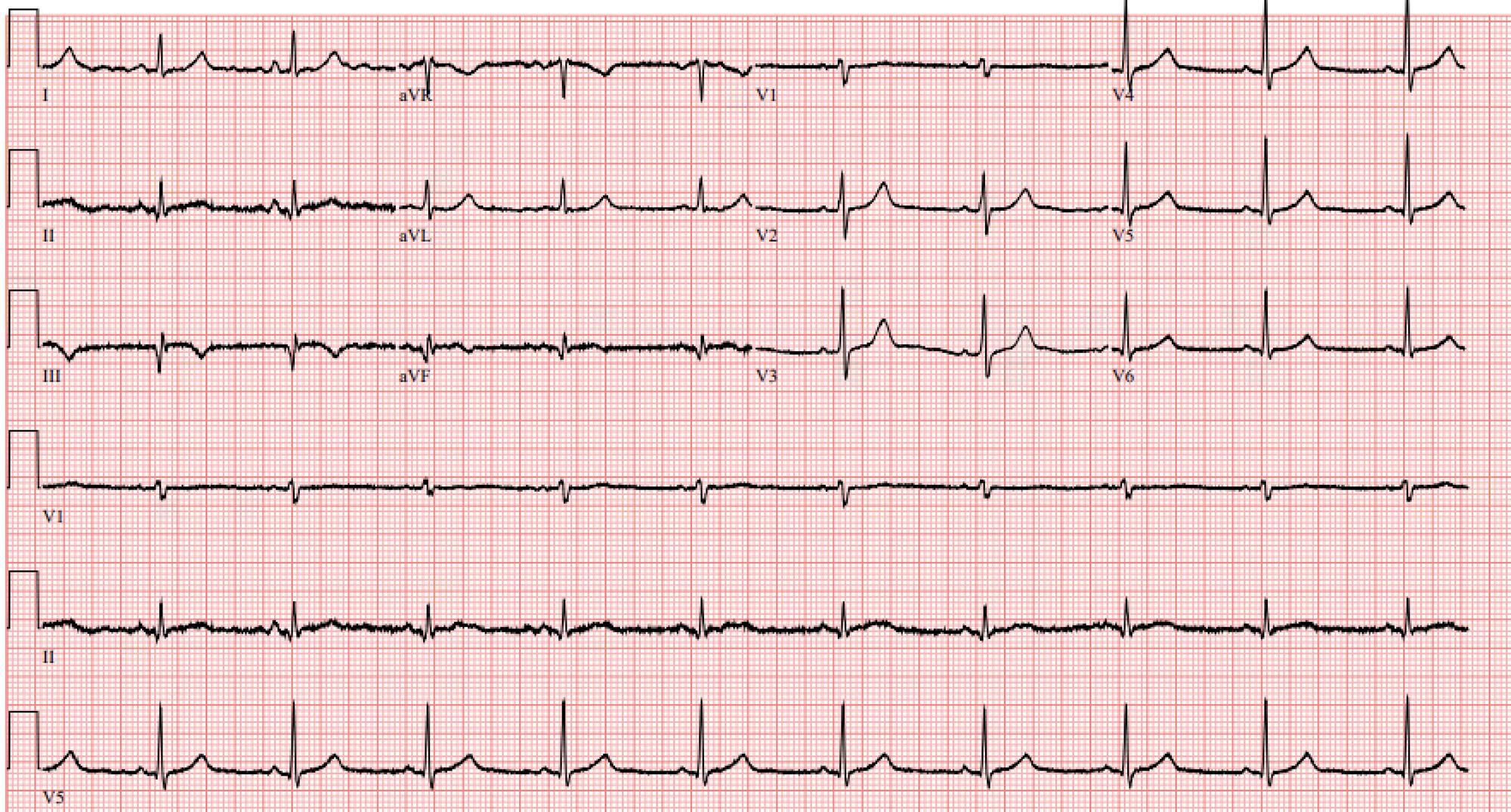
Image2. Electrocardiogramondayofdischarge(post-catheterization)demonstratinganormalsinusrhythmwithevidenceofinferiorinfarct withQwavesinleadsII,III,aVFandnewT-waveinversionsinleadsIIIandaVF.ThereisresolutionofpreviouslyseenSTelevations anddepressions.
interventionalcardiologycolleagues,whilesimultaneously startingvasodilatorytreatmentinpatientswithSTEMIand suspectedCAV.
MainstaytherapyofCAViscenteredaroundvasodilation ofthecoronaryvasculature.Non-dihydropyridinecalcium channelblockers(CCB)andnitratesarethe pharmacotherapiesofchoice.1,14 Additionally,lifestyle changes,treatmentofunderlyingconditions,and optimizationofcardiovascularrisk,areindicated.
PrimarytreatmentofEGPAiscorticosteroids,alongwith otherimmunosuppressiveagents.15 Treatmentofvasospastic anginainEGPAislessestablishedanddependentonacuityof presentation.Casereportsincardiologyliteraturehighlight treatmentwithsystemicandintracoronarynitroglycerinand calciumchannelblockers,asutilizedinthiscase.2,3
ThispatienthadknownEGPAwitharecenthistoryof anginalchestpainthatraisedsuspicionforvasospastic angina.However,healsohadriskfactorsfor,andpreviously diagnosed,CADwitharecentstentplacement,whichraised concernforplaqueruptureorstentthrombosis.Therefore, thepatientunderwentcoronaryangiography,whichallowed fordefinitivediagnosisandtreatment.Upondischarge,the patientwascontinuedonnitroglycerin,CCB,anddualantiplatelettherapy.Additionally,treatmentwith prednisoneandmepolizumab(interleukin-5inhibitor)were continuedtoaddresstheunderlyingEGPAinhopesof preventingrecurrentvasospasticangina.
Coronaryarteryvasospasmisararebutpotentially devastatingmanifestationofEGPA.AcuteSTEMIcanbe causedbyCAV,whichisprimarilytreatedmedicallywith nitratesandcalciumchannelblockers,asopposedto coronarystentplacementfrequentlyusedtotreatSTEMI duetounderlyingatheroscleroticdisease.Emergency physiciansshouldmaintainsuspicionforCAVinpatients withunderlyingriskfactors,includinginthosewithEGPA, intheappropriateclinicalcontext.Initiationandreferralfor treatmentofEGPAisalsokeyforpreventionofrecurrent vasospasticangina.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:LaurenB.Querin,MD,MEd,MSc, MayoClinicHospitalPhoenix,DepartmentofEmergencyMedicine, 5777E.MayoBlvd.,Phoenix,AZ85054.Email: querin.lauren@ mayo.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Allenetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.BeijkMA,VlastraWV,DelewiR,etal.Myocardialinfarctionwithnonobstructivecoronaryarteries:afocusonvasospasticangina. NethHeart J. 2019;27(5):237–45.
2.BitarAY,ThompsonCD,TanCW,etal.Coronaryartery vasospasmandcardiogenicshockastheinitialpresentationfor eosinophilicgranulomatosiswithpolyangiitis. JCardiolCases. 2015;13(4):105–8.
3.WatanabeK,YamochiW,OshitaniT,etal.Low-dosecorticosteroid therapyimprovesrefractorycoronaryvasospasmaccompaniedby eosinophilicgranulomatosiswithpolyangiitis. JCardiolCases. 2020;23(2):69–72.
4.ChakrabortyRKandAeddulaNR.EosinophilicGranulomatosisWith Polyangiitis(Churg-StraussSyndrome).In: StatPearls.TreasureIsland (FL):StatPearlsPublishing;2023.
5.SwarupS,PatibandlaS,GrossmanSA.CoronaryArteryVasospasm. In: StatPearls.TreasureIsland(FL):StatPearlsPublishing;2023.
6.FernandezD,RosenthalJE,CohenLS,etal.Alcohol-induced Prinzmetalvariantangina. AmJCardiol. 1973;32(2):238–9.
7.RanzaniOT,ZampieriFG,ForteDN,etal.C-reactiveprotein/albumin ratiopredicts90-daymortalityofsepticpatients. PLoSOne. 2013;8(3):e59321.
8.LieJT.Illustratedhistopathologicclassificationcriteriaforselected vasculitissyndromes.AmericanCollegeofRheumatology SubcommitteeonClassificationofVasculitis. ArthritisRheum. 1990;33(8):1074–87.
9.MohammadAJ.AnupdateontheepidemiologyofANCA-associated vasculitis. Rheumatology(Oxford). 2020;59(Suppl3):iii42–50.
10.GuillevinL,CohenP,GayraudM,etal.Churg-Strausssyndrome. Clinicalstudyandlong-termfollow-upof96patients. Medicine (Baltimore). 1999;78(1):26–37.
11.DennertRM,vanPaassenP,SchallaS,etal.Cardiacinvolvementin Churg-Strausssyndrome. ArthritisRheum. 2010;62(2):627–34.
12.ChapmanFA,DhaunN,DweckM,etal.Coronaryvasospasmin eosinophilicgranulomatosiswithpolyangiitis. Rheumatology(Oxford). 2020;59(12):e144–6.
13.PetrakopoulouP,FranzWM,BoekstegersP,etal.Vasospasticangina pectorisassociatedwithChurg-Strausssyndrome. NatClinPract CardiovascMed. 2005;2(9):484–90.
14.HanSH,LeeKY,HerSH,etal.Impactofmulti-vesselvasospastic anginaoncardiovascularoutcome. Atherosclerosis. 2019;281:107–13.
15.ChungSA,LangfordCA,MazM,etal.2021AmericanCollegeof Rheumatology/VasculitisFoundationguidelineforthemanagementof antineutrophilcytoplasmicantibody-associatedvasculitis. Arthritis Rheumatol. 2021;73(8):1366–83.
DonaldPettetIII,DO
JohnForrester,DO
MathewNelson,DO
TanyaBajaj,MD
NorthShoreUniversityHospital,DepartmentofEmergencyMedicine,Manhasset,NewYork
SectionEditor:ShadiLahham,MD
Submissionhistory:SubmittedJanuary5,2024;RevisionreceivedMarch11,2023;AcceptedMarch13,2024
ElectronicallypublishedJune14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.6658
Introduction: Diagnosingdeepvenousthrombosesandvenousthromboemboli(DVT/VTE)inpregnant patientspresentsauniquechallengeforemergencyphysicians.TheriskofDVT/VTEincreasesduring pregnancy,andthepotentialconsequencesofmisdiagnosesaresevere.Point-of-careultrasonography (POCUS)isfrequentlya first-linediagnosticimagingmodality.However,recentstudieshaveshowna highincidenceofthrombosesproximaltothecommonfemoralveinduringpregnancy,andthesewould notbevisualizedusingcompressiveultrasonography,whichtraditionallycanonlyvisualizethromboses distaltothefemoralvein.
CaseReport: A38-year-oldfemale,25-weeksprimiparous,presentedtotheemergencydepartment withathree-dayhistoryofleftlowerextremityswelling.Point-of-carethree-pointcompressiontesting wasusedtoevaluateforaDVT;however,nothrombuswasvisualized.Givenhighclinicalsuspicion, colorandspectralDopplertestingwereperformedanddemonstratedturbulent flowandreduced respiratoryvariationinthecommonfemoralvein.Thispromptedfurtheradditionaltestingforaproximal DVTusingmagneticresonancevenography,whichrevealedanocclusiveleftexternaliliacthrombus. Thepatientwassubsequentlystartedondailysubcutaneousenoxaparinanddischargedhomewith closefollow-up.
Conclusion: EmergencyphysiciansplayacriticalroleinevaluationsforthepresenceofDVT/VTE, particularlyinpregnantpatients.WeendorsetheuseofPOCUSwiththree-pointcompressiontesting,as wellascolorandspectralDopplerimaging,tohelpidentifyproximalDVTsinthispatientpopulation.This casereportcanaidphysiciansinthediagnosisofthispathologicalconditionthatifleftuntreatedcanhave severeconsequences.[ClinPractCasesEmergMed.2024;8(3)254–258.]
Keywords: deepveinthrombosis;DVT;pregnancy;point-of-careultrasound;casereport.
Diagnosingdeepvenousthromboses(DVT)andvenous thromboemboli(VTE)inpregnantpatientspresentsaunique challengeforemergencyphysicians.Pregnancyincreasesthe riskofDVT/VTE.Thepotentialconsequencesof misdiagnosesaresevereandincludeDVT/VTErecurrence, post-thromboticsyndrome,pulmonaryembolism,andeven death.1 Venousultrasonographyisa first-linediagnostic imagingmodalityintheemergencydepartment(ED)for
patientswithamoderatetohighpretestprobabilityforDVT/ VTE.2 However,recentstudieshaveshownahigherincidence ofthrombosesproximaltothecommonfemoralveinduring pregnancy. 3 Forthisreason,incaseswhereclinicalsuspicion remainshighdespitenegativethree-pointcompressiontesting, adjunctiveultrasoundimagingmodalitiesandmore comprehensiveimagingmayberequired.
Inthisreport,wepresentacaseofapreviouslyhealthy pregnantwomaninhersecondtrimesterwithaDVTwithin
theleftexternaliliacvein,whichwasnotinitiallydetected withpoint-of-careultrasonography(POCUS)andthreepointcompressiontesting.Withlimitationsregardingtheuse ofultrasonographytodetectthrombosesproximaltothe commonfemoralvein,thiscaseunderscorestheimportance ofconsideringthisentityinpregnantpatientswith suspectedDVT/VTE.4
A38-year-oldfemalepresentedtotheEDwithathree-day historyofprogressivelyworseningswellinginherleftlower extremity.Atthetimeofpresentation,shewas25weeks pregnantandhadnosignificantmedical,surgical,orfamily history.Physicalexaminationrevealedcircumferential swellinginherleftlowerextremityextendingfromtheknee tothedistalforefoot.Additionally,sheexhibitedleftcalf tendernessuponpalpation.
ToevaluateforthepresenceofaDVTinherleftlower extremity,weusedPOCUSwiththree-pointcompression testing.Thefemoralandpoplitealregionsdemonstrated normalmanualcompressibility,andnothrombuswas visualized.Despitethese findings,thepatient’sexamand clinicalhistoryraisedsuspicionforthrombosis.Asaresult, colorandspectralDopplertestingwereperformed,which revealedturbulent flowandreducedrespiratoryvariationin thecommonfemoralvein.These findingsprompted additionaltestingforaproximalDVTusingmagnetic resonancevenography(MRV),whichultimatelyrevealedan occlusiveDVTintheleftexternaliliacvein.Thepatientwas subsequentlyevaluatedbyhematology,startedondaily subcutaneousenoxaparinsodiuminjections,anddischarged homewithclosefollow-up.
ADVTisconsidered “proximal” whenitisidentified withinthepopliteal,femoral,oriliacveinsofthelower extremityonradiographicimaging.Theinitialpresentation forpatientswithproximalDVTscanvarysignificantly,but commonsymptomsincludeswelling,discoloration,and crampingsensationswithinthecalfandthighoftheeffected limb.IntheED,theinitialdiagnosticapproachinvolvesan assessmentofpretestprobabilitywithconsiderationforthe patient’shistory,geneticandacquiredriskfactors,andsigns andsymptoms.Oneriskfactorofparticularimportanceto theemergencyphysicianistheassociationofDVT/VTE withpregnancy.
Observationalstudiesandmeta-analyseshaveestablished pregnancyasariskfactorforDVT/VTE,withasmanyas 1.0–1.8%ofpregnantpatientsdevelopingthiscondition.4 Thisthromboembolicriskincreasesthroughoutpregnancy tonine-foldduringthethirdtrimester,andpeakstwotosix weekspostpartumwhentheriskis80timeshigherthanin non-pregnantpatients.5 Itisimportanttonotethatunlikein menandnon-pregnantwomen,pregnantpatientsaremore
Whatdowealreadyknowaboutthis clinicalentity?
Pregnantpatientsareatincreasedriskfor deepveinthromboses(DVT)proximaltothe femoralvein.
Whatmakesthispresentationof diseasereportable?
Whilethree-pointcompressiontestingis frequentlyappliedintheemergency department,thiscasehighlightsfalsenegativeresultsduetoaproximalDVT.
Whatisthemajorlearningpoint?
Three-pointcompressiontestingmayleadto false-negativeresultsinpregnantpatientsdue toincreasedratesofthrombosesproximalto thefemoralvein.
Howmightthisimproveemergency medicinepractice?
ConsiderationforproximalDVTinpregnant patientsmayhelpavoidadverseoutcomes relatedtofalse-negative,three-point compressiontesting.
likelytodevelopproximalratherthandistalthromboses. Previousstudiesinvestigatingtheanatomicdistributionof DVTsinpregnantpatientsfoundthrombosestomore commonlybeleft-sided(84%)andrestrictedtothe iliofemoral(64%)andiliac(12%)veins.6 Giventhat9.3%of pregnancy-relateddeathsareduetopulmonaryemboli,the importanceofidentifyingsuchthrombosesinthispatient populationcannotbeoverstated.7
Inpregnantpatients,theformationofDVT/VTEis heavilyinfluencedbyphysiologichypercoagulabilityand intra-abdominalanatomicalchanges.Pregnancyis characterizedbyahypercoagulablestatecausedbyan increaseinclottingfactors,adecreaseinnatural anticoagulants,andalterationsin fibrinolyticactivity.8 These changesarethoughttobeprotectiveagainsthemorrhage duringdelivery,buttheyalsopredisposepatientsto thromboses.Theapproximationofthegraviduteruswiththe vertebralbodiesduetoincreasedlordosisalsopredisposes pregnantpatientstothrombosesthroughvenous compression.9 Theinfluenceoftheseanatomicalchangesis highlightedincasesofaortocavalcompressionwhen pregnantpatientsarelyingsupine.
Otheranatomicalinfluencesmayalsoplayarole.For example,May-Thurnersyndromeisaconditioninwhich compressionoftheleftcommoniliacveinbytheoverlying rightcommoniliacarterymayleadtoinflammation, sclerosis,venousstasis,andthromboses.May-Thurner syndromehasbeenidentifiedinover30%ofall-comers previouslydiagnosedwithleftlowerextremityDVTandis oftenoverlooked.10 OtherriskfactorsforDVT/VTEin pregnancyincludeimmobility,advancedmaternalage, obesity,smoking,multiplegestations,andapersonalor familyhistoryofthromboembolicdisease.Itisimportantfor emergencyphysicianstobeawareoftheseriskfactorsand maintainahighlevelofsuspicionforDVT/VTEinpregnant patientspresentingwithlowerextremityswellingorpain.
Theinitialimagingtestofchoicewhenevaluatinga pregnantpatientforaDVTisvenousultrasonography. Traditionally,theinitialdiagnosticimagingmodalityof choicehasbeenthecompleteduplexultrasound.However, withtheemergenceofPOCUS,three-pointcompression testinghasbeenemployedintheEDtoevaluatepatientsfor DVTs,withadvocateshighlightingimprovedtimestostudy completion,decreasedcosts,andtheavoidanceof unnecessarytransfersandtreatments.11–13 Thismethod involvesevaluationsofthecommonfemoralveinonetotwo centimetersabovethebifurcationwiththesaphenousvein, thecommonfemoralveinatthebifurcationwiththe saphenousvein,thefemoralveinatthebifurcationwiththe deepfemoralvein,andthepoplitealvein.
Lossofcompressibilityisconsideredthemostreliable indicatorofaDVT,andcolorDopplerimagingmaybeused todifferentiatebetweencompleteandincompleteocclusions. Multiplestudieshavevalidatedthisapproachand
demonstratedfalsenegativeresultsinaslittleas1.4%.14,15 A recentsystematicreviewandmeta-analysisbyHerczetal additionallyfoundapooledsensitivityof90%andspecificity of95%usingemergencyphysician-performedultrasound evaluationsforDVTs.16 Unfortunately,studiesevaluating theuseofthree-pointcompressiontestingduringpregnancy arenotavailable.Importantly,theAmericanCollegeof ObstetricsandGynecologyguidelinesrecommendclose follow-upwithrepeatimagingatthreeandsevendaysif ultrasoundevaluationsarenegativeandaniliocaval thrombosisisnotsuspected.7 Thiscasehighlightsthe diagnosticchallengethatemergencyphysiciansmay encounter,asthree-pointcompressiontestingcanyield negativeresultseveninthepresenceofanocclusive iliocavalthrombus.
Giventhepossibilityoffalse-negativeresultswiththreepointcompressiontestinginpregnantpatients,POCUS evaluationsshouldincorporatecolorandspectralDoppler studiesofthecommonfemoralveins.ColorDopplerenables clinicianstovisualizeturbulent flowpatterns,alsoknownas “rouleaux,” whilespectralDopplercanidentifychangesin respiratoryphasicity,suggestingavenousocclusion proximaltotheareaofinsonation.17 Undernormal conditions,spectralDopplertestingshoulddemonstrate phasicvariationsinwaveformthroughoutthecardiac cycleduetorespiration.AnabnormalspectralDoppler waveformthatis flatandcontinuousindicatesdecreased respiratoryvariationandshouldraiseconcernfora venousobstructionproximally.18 Importantly,toobtain accurateresultsphysiciansshouldensurethattheangleof incidenceisbelow60degreesandcompareresultstothe contralateralextremity.
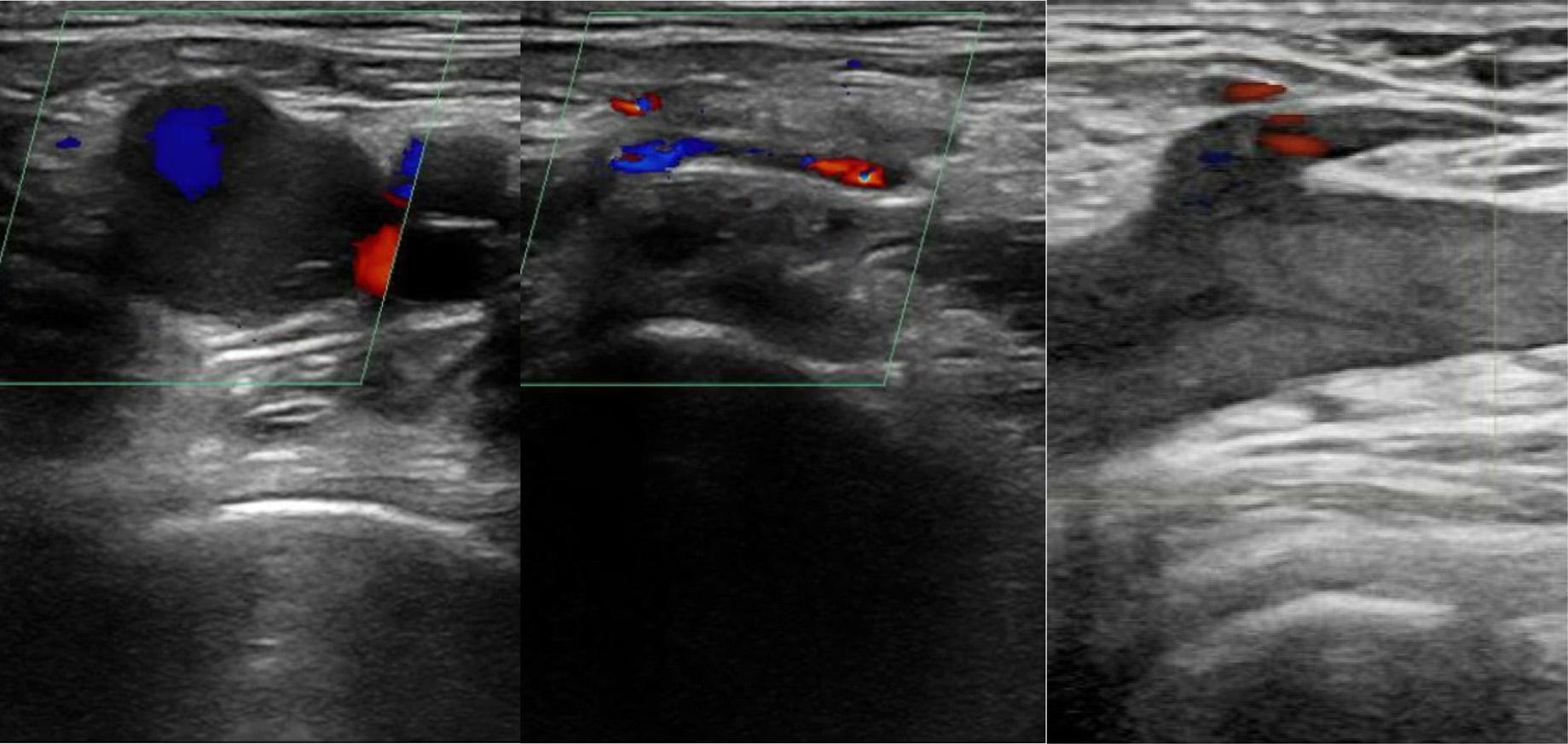
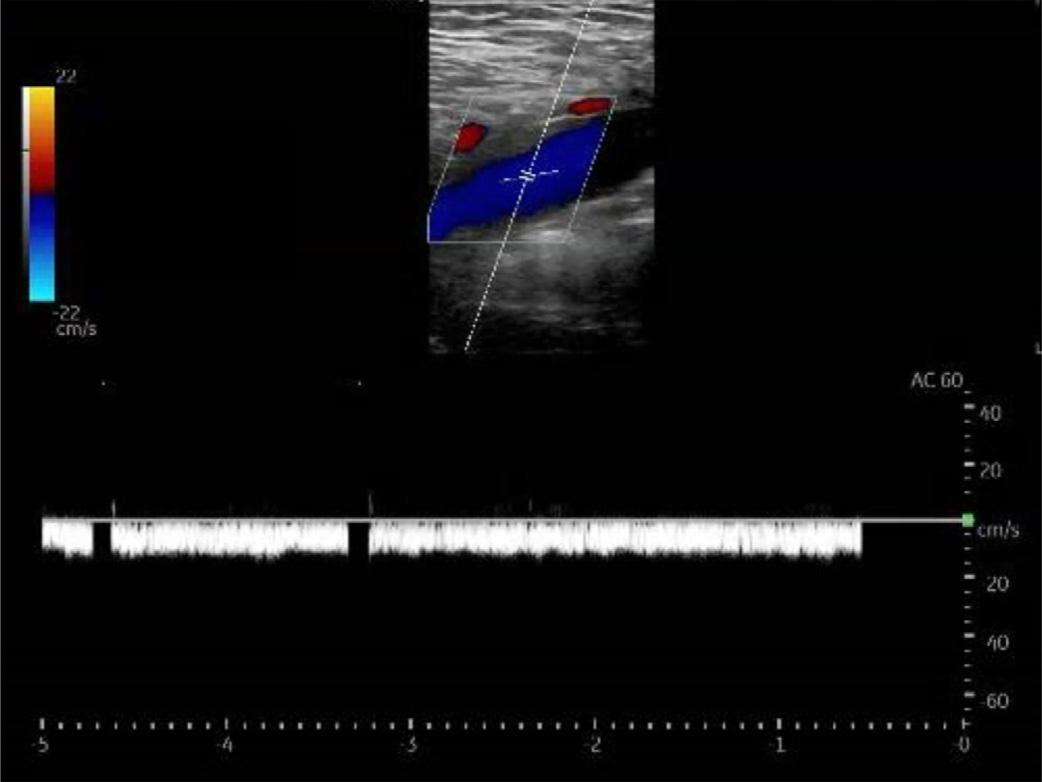
Image2. Point-of-careultrasoundimageoftheleftcommon femoralveininlongitudinalviewdemonstratinglackofnormal respiratoryphasicitywithspectralDoppler.

Image3. Magneticresonancevenogramimageoftheleftexternal iliacveindemonstratingadeepveinthrombosis(whitearrow).
Despitenegativeresultswiththree-pointcompression testing,circumferentiallegswellinginthispatient’ scase promptedcolorandspectralDopplerassessmentsfora proximal,iliocavalthrombus.Thesestudiesultimately demonstratedturbulent flowpatternsanddecreased respiratoryphasicity(Images1 and 2).Ifthereisevidenceof aproximalvenousobstructiononultrasoundimaging, computedtomographyandMRVhavebeenestablishedas theimagingmodalitiesofchoiceduetolimitationsofduplex ultrasonographyabovetheinguinalplane.19,20 Inthis patient’scase,magneticresonanceimagingwasobtainedand identifiedaDVTwithintheleftexternaliliacvein(Image3). Overall,thiscasehighlightstheimportanceofinvestigations
forthrombosesproximaltothecommonfemoralveinin pregnantpatientswhensuspicionishigh,evenwhenthreepointcompressiontestingisnegative.
Emergencyphysiciansplayacriticalroleintheevaluation ofhigh-riskpatientsforthepresenceofDVT/VTE, particularlyinpregnantpatientswhomayhavefamilial, genetic,oranatomicfactorsthatincreasetheirriskfor thromboses.Cliniciansevaluatingpregnantpatientsshould maintainahighdegreeofclinicalsuspicionandhavealow thresholdtoobtaincomprehensiveultrasoundstudiesand magneticresonancevenographywhennecessary.The informationprovidedinthiscaseunderscorestheimportance ofconsideringDVTsproximaltothecommonfemoralvein inpregnantpatientsandmayaidcliniciansinthediagnosisof thispathologicalcondition,whichifleftuntreatedcanresult inseriousconsequences,includingDVT/VTErecurrence, post-thromboticsyndrome,pulmonaryembolism,and evendeath.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:JohnForrester,DO,NorthShore UniversityHospital,DepartmentofEmergencyMedicine, 300CommunityDrive,Manhasset,NY11030.Email: jforrest@ northwell.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Pettetetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.LeizoroviczA.Long-termconsequencesofdeepveinthrombosis. Haemost. 1998;28(Suppl.3):1–7.
2.BatesSM,JaeschkeR,StevensSM,etal. DiagnosisofDVT: AntithromboticTherapyandPreventionofThrombosis,9thed: AmericanCollegeofChestPhysiciansEvidence-BasedClinical PracticeGuidelines. CHEST. 2012;141(2):e351S–418S.
3.ChanWS,SpencerFA,LeeAYY,etal.Safetyofwithholding anticoagulationinpregnantwomenwithsuspecteddeepvein thrombosisfollowingnegativeserialcompressionultrasoundandiliac veinimaging. CanMedAssocJ. 2013;185(4):E194–200.
4.JainAK,SoultMC,ResnickSA,etal.Detectingiliacveinthrombosis withcurrentprotocolsoflowerextremityvenousduplexultrasound. JVascSurgVenousLymphatDisord. 2018;6(6):724–29.
5.JamesAH,JamisonMG,BrancazioLR,etal.Venousthromboembolism duringpregnancyandthepostpartumperiod:Incidence,riskfactors, andmortality. AmJObstetGynecol. 2006;194(5):1311–15.
6.ChanWS,SpencerFA,GinsbergJS.Anatomicdistributionof deepveinthrombosisinpregnancy. CanMedAssocJ. 2010;182(7):657–60.
7.AmericanCollegeofObstetriciansandGynecologists’ Committeeon PracticeBulletins Obstetrics.ACOGpracticebulletinno.196: thromboembolisminpregnancy[publishedcorrectionappearsinObstet Gynecol.2018Oct;132(4):1068]. ObstetGynecol. 2018;132(1):e1–17.
8.JacobsenAF,SkjeldestadFE,SandsetPM.Incidenceandrisk patternsofvenousthromboembolisminpregnancyandpuerperium a register-basedcase-controlstudy. AmJObstetGynecol. 2008;198(2):233.e1–233.7.
9.Schrufer-PolandTL,FlorioK,GrodzinskyA,etal.Managementof May-Thurnersyndromeinpregnantpatients. JCardiovascDevDis. 2022;9(12):410.
10.DixC,ClementsW,GibbsH,etal.Venousanomaliesand thromboembolism. ThrombJ. 2023;21(1):45.
11.PedrazaGarcíaJ,ValleAlonsoJ,CeballosGarcíaP,etal.Comparison oftheaccuracyofemergencydepartment-performedpoint-of-careultrasound(POCUS)inthediagnosisoflower-extremitydeepvein thrombosis. JEmergMed. 2018;54(5):656–64.
12.VarriasD,PalaiodimosL,BalasubramanianP,etal.Theuseofpoint-ofcareultrasound(POCUS)inthediagnosisofdeepveinthrombosis. JClinMed. 2021;10(17):3903.
13.BlaivasM,LambertMJ,HarwoodRA,etal.Lower-extremitydopplerfor deepvenousthrombosis:canemergencyphysiciansbeaccurateand fast? AcadEmergMed. 2000;7(2):120–6.
14.FrazeeBW,SnoeyER,LevittA.Emergencydepartmentcompression ultrasoundtodiagnoseproximaldeepveinthrombosis. JEmergMed. 2001;20(2):107–12.
15.LeeJH,LeeSH,YunSJ.Comparisonof2-pointand3-point point-of-careultrasoundtechniquesfordeepveinthrombosis attheemergencydepartment:ameta-analysis. Medicine. 2019;98:e15791.
16.HerczD,MechanicOJ,VarellaM,etal.UltrasoundPerformedby EmergencyPhysiciansforDeepVeinThrombosis:ASystematic Review. WestJEmergMed.2024;25(2):282–90.
17.BlancoPandVolpicelliG.Commonpitfallsinpoint-of-careultrasound: apracticalguideforemergencyandcriticalcarephysicians. CritUltrasoundJ. 2016;8(1):15.
18.NeedlemanL,CronanJJ,LillyMP,etal.Ultrasoundfor lowerextremitydeepvenousthrombosis. Circulation. 2018;137(14):1505–15.
19.LiuD,PetersonE,DoonerJ,etal.Diagnosisandmanagementof iliofemoraldeepveinthrombosis:clinicalpracticeguideline. CanMed AssocJ. 2015;187(17):1288–96.
20.DronkersCE,SrámekA,HuismanMV,etal.Accuratediagnosis ofiliacveinthrombosisinpregnancywithmagneticresonance directthrombusimaging(MRDTI). BMJCaseRep. 2016;2016:bcr2016218091.
KatherineVlasica,DO AmandaHall,DO
SectionEditor:AustinSmith,MD
St.Joseph’sHealth,Paterson,NewJersey
Submissionhistory:SubmittedJanuary26,2024;RevisionreceivedMarch20,2024;AcceptedApril4,2024
ElectronicallypublishedJuly31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7233
Introduction: Rectussheathblockshavebeenusedfordecadesintheoperatingroomforanalgesia followingumbilicalsurgicalprocedures.Wepresentthe firstreportedcaseseriesofarectussheathblock usedintheemergencydepartment(ED)forthereductionofanumbilicalhernia.
CaseSeries: FourpatientspresentedtotheEDforpainful,non-reducibleumbilicalhernias.An ultrasound-guidedbilateralrectussheathblockwasusedinallfourpatientswithcompletepainreliefand aneasyherniareduction.
Conclusion: Rectussheathblocksareanexcellentadditiontoamultimodalanalgesicregimenin periumbilicalpainandpainfulprocedures.Thisblockiseasytoperformandimplementforpaincontrolin umbilicalherniasinanEDsetting.[ClinPractCasesEmergMed.2024;8(3)259–263.]
Keywords: rectussheathblock;umbilicalhernia.
Umbilicalherniasareacommonentitypresentingtothe emergencydepartment(ED)andfrequentlypresentapain managementchallengefortheemergencyphysician. Umbilicalherniasaccountfor6–14%ofalladultabdominal wallherniasandaremorecommoninwomenand individualswithincreasedintraabdominalpressureasin pregnancy,obesity,orascites.1 Patientswithincreased abdominalpressuretypicallyhaveunderlyingpathology, makinganysurgicalinterventionahighriskfor complications.Ofnote,20%ofallcirrhoticpatientswill developanumbilicalhernia,whichmakesasurgical interventionorproceduralsedationdeemedhighriskfor complications.1 Thiscaseseriesexamineshowwecanusea bilateralrectussheathblock(BRSB)forsafeandefficientED umbilicalherniareduction.
TheBRSBwas firstdescribedintheliteraturein1899. ThroughoutitslifespantheBRSBwasprimarilyusedinthe operatingroom(OR)asatargetedanalgesicintervention reducingpostoperativenausea,vomiting,constipation,and opioidconsumption.2,3,4 ABRSBprovidesmidlineanalgesia totherectusmuscleandoverlyingskinfromthexiphoid
processtothesymphysispubis.Therectusabdominismuscle isamedialoval-shapedmusclethatliesinsideitsrectus sheathformedbythesplitaponeurosisoftheexternal oblique,transversusabdominus,andinternaloblique, borderedbythelineaalbamediallyandthelineasemilunaris laterally.Theninththrougheleventhintercoastalnerves, epigastricarteryandveinsareinthespacebetweentherectus abdominismuscleanditsposteriorrectussheath. Deeptotherectussheathisthetransversalisfasciaand abdominalcavitycontainingperitoneumandabdominal viscera.Intherectussheathblock0.1milliliters(mL)per kilogram(kg)toamaximumof10mLpersideisdeposited bilaterally,resultinginatotalvolumeof20mLoflocal anesthetic.Thelocalanestheticisdepositedbetweenthe posteriorrectussheathandrectusabdominusmuscletoallow forasuccessfulblock(Image1).Theblocktypicallyworks unilaterallyfromapproximatelythesevenththrough elevenththoraciclevel.4
Allfourpatientsunderwentthesametechniquefora BRSB.Consentwasobtainedpriortotheprocedure,andthe
patientwasplacedonacardiacmonitor.Withtheskin disinfected,atransducerwasplacedinatransverseaxis abovetheumbilicusslightlylateraltothemidline.Color Dopplerwasusedtoidentifyandavoidtheepigastric arteries.Ablunt-tippedhyperechoicblockneedlewas insertedinplanethroughthesubcutaneoustissue,anterior rectussheath,andrectusmuscleuntilresistancewasfeltas theblunt-tippedneedlecontactedtheposteriorrectussheath (Image1).Initially,1–2mLofsalinewereusedtoconfirm placementafteraheme-negativeaspiration.Wetheninstilled 10mLof0.5%ropivacaineundertheposterioraspectofthe rectusmuscle,effectivelyliftingitfromtheposteriorrectus sheath(Video).Theprocesswasrepeatedonthe contralateralside.Eachpatientreceivedatotalof20mLof 0.5%ropivacaine,totaling100milligrams(mg)of ropivacaine.Maximumdoseofropivacaineis3mg/kg. Allthepatientswerewellwithinthesafetymarginof maximumdosing.
ThevideoisaSonoClip(SonoClipShare.com) demonstratingtherelevantanatomyandrectussheathblock performance.Anechogenicblockneedleenterstherectus sheathfromalateraltomedialdirection.Thetargetareaof injectionisbetweentheundersideoftherectusabdominus andposteriorrectussheath.Ananechoiclocalanestheticis seenliftingtherectusabdominusmusclefromtheposterior rectussheath.
A60-year-oldmalewithapastmedicalhistoryofchronic umbilicalherniaandalcoholusedisorderpresentedtothe EDfollowingafallresultinginanon-reducibleumbilical herniaandleftanklepain.Thepatientwasgiven400mgof ibuprofenorallyand15mgofketorolacintravenously(IV) forhisanklepaincausedbyadistal fibularfracture.His anklepainwascontrolled,buthestillhadpainwithbedside
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Bilateralrectussheathblockshavebeenused fordecadesintheoperatingroomfor periumbilicalsurgicalanesthesia.
Whatmakesthispresentationof diseasereportable?
Thisisthe fi rstreportedcaseseriesofa bilateralrectussheathblockusedintheED forbedsidereductionofanincarcerated umbilicalhernia.
Whatisthemajorlearningpoint?
Thebilateralrectussheathblockcanbesafely performedintheEDandshouldbeadded totheproceduralarmamentariumof emergencyphysicians.
Howmightthisimproveemergency medicinepractice?
Bilateralrectussheathblockperformedinthe EDinlieuofproceduralsedationprovides targetedanalgesiainapatientwithan incarceratedumbilicalhernia.
reductionattempts.AftertheBRSBtheumbilicalherniawas easilyreduced.Thepatientwasdischargedhomeformedical optimizationandanelectiveumbilicalherniarepairatthe patient’sconvenience.
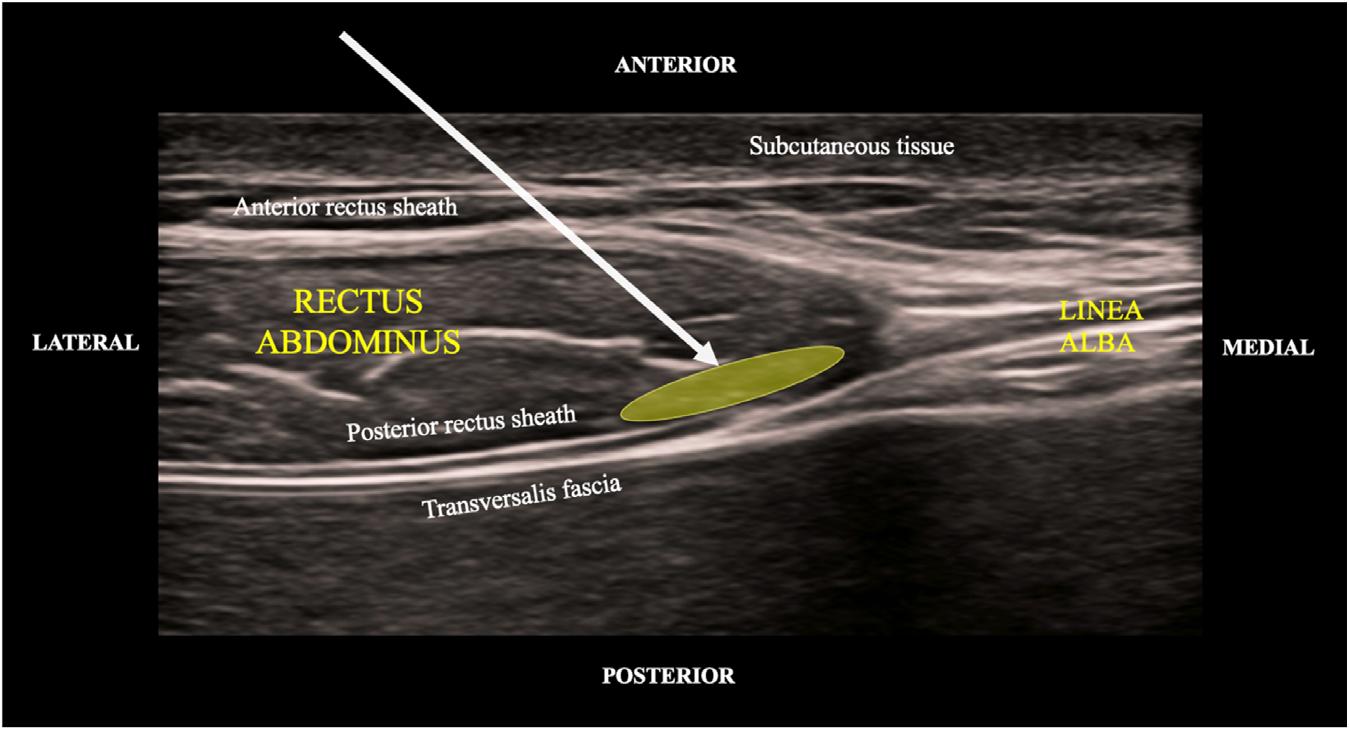
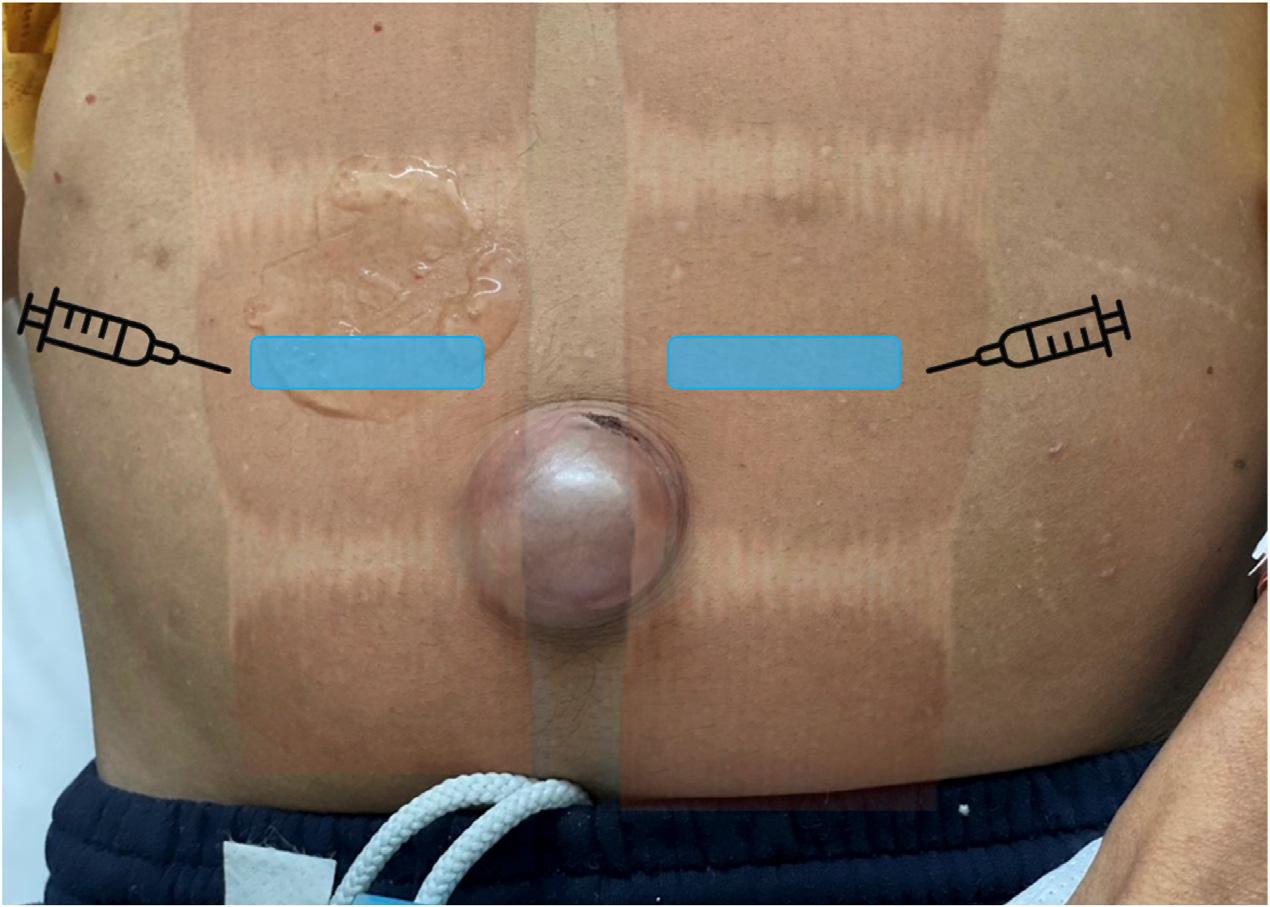
Patientwithanincarceratedumbilicalherniapriortothebilateralrectussheathblockperformedforpaincontrol.Blueboxesindicate footprintsoflinearprobeforabilateralrectussheathblock.Theneedleisinsertedinthelateraltomedialdirection,inplanewiththelinear transducerprobe.
A60-year-oldmalewithpastmedicalhistoryofopioid abuse,ascitessecondarytoalcoholiccirrhosis,inguinal hernia,andumbilicalherniapresentedtotheEDwith complaintsofgraduallyworseningsevereabdominalpain withaworseningumbilicalbulge(Image2).Thepatientwas initiallygivenfentanyl100microgramsIVandhaloperidol 5mgIVforpainandnausea.Therewasanobviousumbilical herniaidentifiedwithskinchangesandabdominal tenderness.Computedtomography(CT)oftheabdomen andpelvisshowedanumbilicalherniacontainingasmallbowelloopresultinginasmall-bowelobstruction. IncarcerationwasunabletobeexcludedonCT.Surgerywas consulted,andthepatientwasscheduledtoundergoan emergentoperativerepair.Duetocontinuedseverepaina BRSBwasperformed.Shortlyaftertheblockthepatient reportedsignificantimprovementofpainandwas transferredtothepreoperativearea.Threehourslaterthe patientwasre-evaluatedinthepreoperativeareabythe surgicalteam;thepatient’sherniahadspontaneously reduced,andhewaspainfreeandrestingcomfortably.Given thepatient’snumerouscomorbidities,thedecisionwasmade topostponethesurgeryformedicaloptimization.The patientwasmonitoredinthehospitalforafewdays,normal bowelpatternsreturned,paindidnotresume,andhewas dischargedhomefourdaysafterinitialpresentation. AftertheBRSBthepatientdidnotrequireany additionalanalgesia.
A49-year-oldfemalewithapastmedicalhistoryof obesity,hypercholesterolemia,non-insulin-dependent
diabetes,andhypertensionpresentedtotheEDfor abdominalpainatthesiteofapreviousumbilicalhernia repair.Thepatientstatedshehadbeenadmittedmultiple timesforpaincontrolanddischargedwithinstructionsto scheduleanelectiveoperativerepairasoutpatient.Physical examshowedanobesefemalewithmildtendernessto palpationoftheumbilicus.Thepatienttookacetaminophen 975mgathomepriortoarrivalandreceivedketorolac 15mgIVintheEDwithimprovementofpainbuthad persistenttendernesstopalpationofhernia.ABRSBwas performedintheED.Thepatient’sherniaspontaneously reduced,andshehadcompleteresolutionofherpain.She wasdischargedforoutpatientfollow-upwithher generalsurgeon.
Thelastcasewasa42-year-oldmalewithnopastmedical historywhopresentedtotheEDforeightmonthsof intermittentumbilicalpain,thathadworsenedovertheprior threedays.Hehadnotsoughtmedicalcarepriortoarrivalin theED.Onexamhehadatenderumbilical,non-reducible hernia,approximately4centimeters(cm)insize. Computerizedtomographyrevealeda3 × 3.7 × 3.4cm,fatcontainingumbilicalherniawithanarrowneckmeasuring 15millimeters.Initialbedsidereductionwasunsuccessful afteradministrationofketorolac15mgIV,placementin Trendelenburgposition,andapplicationoficetothe umbilicus.Surgicalconsultwascalled,andafterdiscussion withthesurgicalteamthepatientunderwentaBRSB. Approximately20minutesaftertheblocktheherniawas reducedatbedsidewithoutdifficulty,andthepatientwas dischargedhomewithoutpatientsurgicalfollow-up.
TheBRSBhasbeenusedintheORfordecadestoprovide sensoryanalgesiatotheanteriorabdominalwall.Inthepast therectussheathblockwasperformedwithoutvisualization, usingaloss-of-resistanceapproachastheblunt-tippedblock needlepassedthroughfascialandmuscleplanesoftherectus sheathtoanesthetizetheanteriordivisionsoftheseventh thoracicto firstlumbarspinalnerves.Thisprocedurewas typicallynotperformedintheEDduetofearofepigastric vesselpunctureorbowelperforationduetoinaccurateneedle placement.However,theriseofultrasounduseinED proceduresoverthelastdecadehasledtotheadaptationof manyultrasound-guidedregionalanesthesia(UGRA) techniquesfromtheirORprovenance.Theabilityto visualizethedistributionofanalgesicmedicationsaround andnearnerveshasincreasedaccuracyoftheseblocksand limitedaccidentalinjectionintovasculatureor damagetosurroundinganatomy.Tothebestofour knowledge,thesefourcasesrepresentthe firstreporteduseof BRSBforthemanagementofanumbilicalhernia intheED.
Giventherisingratesofsubstanceusedisordersinthe US,thespotlighthasbeenplacedonopioidusageand prescribing.Physiciansareconstantlyevaluatingnovel methodsoftargetedanalgesiaforpainfulEDconditionsasa partofamultimodalpainregimen.Asdemonstratedinthis caseseries,webelieveBRSBisavaluabletoolforcontrolof umbilicalherniapainintheED.Allfourpatientshad completeresolutionoftheirpainwithminimaluseofopioids, allowingforaneitherspontaneousormanualreductionof umbilicalherniaswithsignificantlylessprocedural discomforttothepatient.
Therectussheathblockcanbeperformedquicklyand safelyatthebedside,providingrapidpainreliefwithout parenteralopioidsorthelargemobilizationofresources requiredforproceduralsedation.Alltheprocedureswere performedbyanemergencymedicineresidentandan UGRA-credentialedemergencyattendingphysician, provingthesafety,easeofperformanceandgeneralizability ofthiscaseseries.
Ultrasound-guidedregionalanesthesiahasproventohave numerousadvantagesoverparenteralanalgesictherapiesfor patientspresentingwithpainfulinjuriestotheED:decreased incidenceofcentralsensitizationleadingtochronicpain5; decreasedadverseeffectssuchashypoxia,nauseaand vomiting6,7;reducedopioidrequirements8,9;anddecreased lengthofstay.10,11 Inmultiple,publishedanesthesia literaturecasesithasbeendemonstratedthatBRSBswere performedastheprimaryanestheticinhigh-riskpatientsin casesofbothinguinalandumbilicalherniarepairwith success. 4 InthisEDcaseseries,aBRSBprovidedan expeditiousandsaferesolutionofthepatient’spainwithno complications,minimalopioidutilization,andnoneedfora fullproceduralsedation.Whilethereareriskstoboth
proceduralsedationandUGRA,therisksofprocedural sedationandparenteralopioidmedicationsaremore complexandpotentiallysevereinthepatientpopulation typicallypronetoumbilicalhernias.Allpatientsavoided emergentoperativerepairsubsequenttosuccessful reductionoftheirumbilicalhernias,enablingthem tobedischargedwithoutpatientschedulingfor medicaloptimization.
Ultrasound-guidedregionalanesthesiaallowsphysicians totreatnumerousacutelypainfulconditionsandpainful proceduresinatimely,expeditious,andsafemanner.The abovecasesdescribetheuseofUGRAforthereductionof umbilicalherniaswithouttheneedforproceduralsedationor emergentsurgicalintervention.Inallfourcasesthepainwas controlledwithminimalEDuseofopioids,andthehernia wasreducedwithoutproceduralsedation.Withoutthis interventionthepatientsmayhaverequiredemergent operativerepairratherthananelectiveoutpatientrepair.
Asemergencyphysiciansexpandtheirknowledgebase andskillset,UGRAincludingtherectussheathblockisa techniquewecanusewithherniareduction,abdominalwall abscess,andanyotherpainfulperiumbilicalconditions. Thesefourcasesdemonstratedtheutilityofabilateral rectussheathblockinavertingtheneedforprocedural sedationandemergentoperativerepairsfromtheED,also resultingindecreasedresourceutilization,opioid consumption,andlengthofstay.Overall,theBRSBisagreat additiontothearmamentariumoftheemergency physicianasanexpeditiouspaincontroloptionfor periumbilicalconditions.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:KatherineVlasica,DO, St.Joseph’sHealth,703MainSt.,PatersonNJ07043. Email: Vlasicak@sjhmc.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Vlasicaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CosteAH,BamarniS,LeslieSW.Umbilicalhernia.[Updated2024Feb 27].In: StatPearls [Internet].TreasureIsland(FL):StatPearls
Publishing.2024.Availableat: https://www.ncbi.nlm.nih.gov/books/ NBK459312/.AccessedMarch20,2024.
2.ManasseroA,BossolascoM,MeineriM,etal.Spread patternsandeffectivenessforsurgeryafterultrasound-guidedrectus sheathblockinadultday-casepatientsscheduledfor umbilicalherniarepair. JAnaesthesiolClinPharmacol. 2015;31(3):349–53.
3.PhuaDS,PhooJW,KoayCK.Theultrasound-guidedrectussheath blockasananaestheticinadultparaumbilicalherniarepair. Anaesth IntensiveCare. 2009;37(3):499–500.
4.KaraarslanE,TopalA,Avcı O,etal.Researchontheefficacyofthe rectussheathblockmethod. Agri. 2018;30(4):183–8.
5.QuekKHandPhuaDS.Bilateralrectussheathblocksasthesingle anaesthetictechniqueforanopeninfraumbilicalherniarepair. SingaporeMedJ. 2014;55(3):e39–41.
6.LevinM.Nerveblocksinthetreatmentofheadache. Neurotherapeutics. 2010;7(2):197–203.
7.WathenJE,GaoD,MerrittG,etal.Arandomizedcontrolled trialcomparingafasciailiacacompartmentnerveblockto atraditionalsystemicanalgesicforfemurfracturesina
pediatricemergencydepartment. AnnEmergMed. 2007;50(2):162–71.
8.TezelO,KaldirimU,BilgicS,etal.Acomparisonofsuprascapularnerve blockandproceduralsedationanalgesiainshoulderdislocation reduction. AmJEmergMed. 2014;32(6):549–52.
9.BeaudoinFL,HaranJP,LiebmannO.Acomparisonofultrasoundguidedthree-in-onefemoralnerveblockversusparenteralopioidsalone foranalgesiainemergencydepartmentpatientswithhipfractures:a randomizedcontrolledtrial. AcadEmergMed. 2013;20(6):584–91.
10.NeubrandTL,RoswellK,DeakyneS,etal.Fasciailiaca compartmentnerveblockversussystemicpaincontrolforacutefemur fracturesinthepediatricemergencydepartment. PediatrEmergCare. 2014;30(7):469–73.
11.BlaivasM,AdhikariS,LanderL.Aprospectivecomparisonofprocedural sedationandultrasound-guidedinterscalenenerveblockfor shoulderreductionintheemergencydepartment. AcadEmergMed. 2011;18(9):922–7.
12.StoneMB,WangR,PriceDD.Ultrasound-guidedsupraclavicular brachialplexusnerveblockvsproceduralsedationforthetreatmentof upperextremityemergencies. AmJEmergMed. 2008;26(6):706–10.
BabetteNewman,DO*
MatthewPoremba,PharmD†
*
R.GentryWilkerson,MD
SectionEditor:StevenWalsh,MD
*UniversityofMarylandMedicalCenter,DepartmentofEmergencyMedicine, Baltimore,Maryland
† UniversityofMarylandMedicalCenter,DepartmentofPharmacy, Baltimore,Maryland
Submissionhistory:SubmittedJanuary9,2024;RevisionreceivedApril9,2024;AcceptedApril16,2024
ElectronicallypublishedJuly11,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7190
Introduction: Angioedema,aswellingofthesubcutaneousorsubmucosallayersoftheskinor gastrointestinaltract,isapotentialcomplicationtothrombolytictherapyinthetreatmentofacute ischemicstrokes.Inthesecases,angioedemadevelopsduetoincreasedlevelsofbradykininasaresult oftheactivationofthe fibrinolyticpathwayandcontactactivationsystem.Angioedemacaninvolvethe tongue,larynx,andvocalcords,leadingtoocclusionoftheairwayanddeathduetoasphyxiation.Itis vitalfortheemergencyphysiciantoknowthatthiscomplicationcanoccurtoensureappropriate monitoringfordevelopmentofangioedema.
CaseReport: Wereportthecaseofa65-year-oldBlackmanwhopresentedwithsignsofanacute ischemicstrokeandwastreatedwithtenecteplase.Thepatient’sstrokesymptomsmostlyresolved within90minutes;however,hedevelopedswellingofhisrightupperlipconsistentwithangioedema.The patientwastreatedwithsteroidsandantihistamines.Hewascloselymonitoredanddidnotrequire airwayintervention.Theangioedemawasalmostfullyresolvedbythefollowingday.
Conclusion: Angioedemaisaknowncomplicationofthrombolytictherapyforacuteischemicstroke. Riskfactorsforalteplase-associatedangioedemaincludeuseofangiotensin-convertingenzyme inhibitors,femalegender,diabetes,andinfarctsoftheinsulaandfrontalcortex.Ashospitalsystems switchfromalteplasetotenecteplaseforthetreatmentofacuteischemicstrokesforreasonsofcostand easeofadministration,itisimportanttorecognizethatangioedemaisalsoapotentialcomplicationof tenecteplase.[ClinPractCasesEmergMed.2024;8(3)264–267.]
Keywords: angioedema;tenecteplase;stroke;airway.
Angioedemadescribesthedevelopmentofswellingofthe subcutaneousorsubmucosallayersofthecutaneousand gastrointestinaltracts.Numerousmechanismscanresultin thedevelopmentofangioedema,andtheseareusually classifiedbasedontheunderlyingsubstancecausingthe swelling.Histaminergicangioedemaisduetothereleaseof histamineandisseenincasesofallergyandanaphylaxisas wellasotherimmunologicprocesses.Bradykinin-mediated angioedemaincludeshereditaryangioedema(HAE),which isusuallycausedbydeficientquantityorfunctionof
C1-esteraseinhibitor(C1-INH),acquiredangioedemawhere thelevelsofC1-INHarelowduetoincreasedconsumption, andmedication-associatedincreasesinbradykininincluding angiotensin-convertingenzyme(ACE)inhibitors.1 InACE inhibitor-inducedangioedema,theACEenzyme,whichalso actsastheprimaryenzymetobreakdownbradykinin,is inhibitedleadingtoincreasedlevelsofbradykinin.2
Numerouscasereportshavedescribedthedevelopmentof angioedemafollowingadministrationofalteplaseforthe treatmentofacuteischemicstroke.Inmanyofthesecasesthe swellingiscontralateraltotheinfarctedhemisphere.3 When
plasminogenisactivatedtoplasmin,theplasminactivates FactorXIItoFactorXIIa,whichinturnconverts prekallikreintokallikrein,theenzymeresponsibleforthe cleavageofbradykininfromhighmolecularweight kininogen.1 Hereinwedescribeacaseofangioedemathat developedafteradministrationoftenecteplase(TNK). Individualreportsofangioedemasecondarytotenecteplase haverarelybeendescribed,4 andtodatenonehavebeenina patientnottakinganACEinhibitor.
A65-year-oldmanpresentedtotheemergencydepartment (ED)viaemergencymedicalservicesasastrokealertforacute onsetright-sidedfacialdroop,dysarthria,andaphasia.The patientwasreportedlyfoundoutsidebyaneighborwho noticedthathewashavingtroublespeaking.Onarrival,the patient’sneighborandfamilymemberscouldnotbereached foradditionalinformation,buthislastknownwelltimewas estimatedtobeapproximatelyonehourpriortoarrivalinthe ED.Thepatientdeniedanyprecedingheadtraumaaswellas associatedheadache,dizziness,visionchanges,chestpain, shortnessofbreath,nausea,orvomiting.Hispastmedical historyincludedhypertension,well-controlledHIV,and previoussuccessfultreatmentforhepatitisC.Hehadno historyofpriorstrokesandwasnottakinganticoagulants.He haddocumentedallergiestolisinoprilandshellfish.The patient’sinitialvitalsignswerenotableforhypertensionto 156/84millimetersofmercury(mmHg),butotherwisewere withinnormallimitswithheartrate96beatsperminute, respiratoryrate18respirationsperminute,pulseoximetry 96%onroomair,andtemperature98.4° Fahrenheit. Onphysicalexam,thepatientwasalertandinteractive. Hisspeechwasmoderatelydysarthricandaphasicbut intelligiblewitheffort.Hehadfacialparalysisontheright. Hewasabletoansweronequestioncorrectlyandfollowtwo commandscorrectly.Therewasnogazedeviation,visual fieldloss,extremitydrift,sensoryloss,limbataxia,or extinction.HisinitialNationalInstitutesofHealthStroke Scalescorewas five.Thebrainattackteamwascalled,and thepatientwasquicklytakenforcomputedtomography (CT)oftheheadaswellasCTangiographyoftheheadand neckwithperfusion.Imagingrevealednointracranial hemorrhageorlargevesselocclusion.Sincethepatient presentedwithin4.5hoursofsymptomonsetandtherewere noobviouscontraindications,thedecisionwasmadeto administerTNKwithemergencyconsent.
Thepatientreceivedanintravenous(IV)0.25milligrams perkilogram(mg/kg)bolusofTNK,16mgtotal.Shortly afterTNKadministration,hisbloodpressureincreasedto 188mmHg,sohewasstartedonaclevidipineinfusionat 1mg/hour.Approximately90minutesafterTNK administration,thepatient’sneurologicdeficitshad improved,buthewasfoundtohavedevelopedprofound swellingofhisrightupperlip,consistentwithangioedema
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Bradykinin-mediatedangioedemaoccursdue toC1-esteraseinhibitorde fi ciency, angiotensin-convertingenzyme(ACE) inhibitors,andthrombolytics.
Whatmakesthispresentationof diseasereportable?
Therearefewreportsofangioedemadueto tenecteplase.Thisisthe fi rstdescription involvingapatientnotonanACEinhibitor.
Whatisthemajorlearningpoint?
Cliniciansshouldbeawareofangioedemaasa potentialcomplicationoftenecteplaseuse. Itoccursinabout1.1%ofpatients receivingtenecteplase.
Howmightthisimproveemergency medicinepractice?
Thisreportunderscorestheneedforclose patientmonitoringaftergivingtenecteplase, asthepatient ’ sairwaymaybecome compromisedduetoangioedema.
(Image).Therewasnoassociatedtongueswelling,drooling, orstridor.Hehadnoincreasedworkofbreathingand continuedtosaturatewellat95%onroomair.Thepatient wastreatedwithIVmethylprednisolone125mg,famotidine 20mg,anddiphenhydramine50mg,andclosemonitoring wascontinuedintheED.Hewasultimatelyadmittedtothe neurologicintensivecareunitwheretheangioedemawas notedtobealmostfullyresolvedbythefollowingday. Magneticresonanceimagingwasperformedthefollowing daydemonstratingadistalleftmiddlecerebralarteryinfarct.
Alteplaseisthecurrentstandardofcaretreatmentfor acuteischemicstrokeandistheonlyUSFoodandDrug Administration-approvedagentforthisindication. Tenecteplaseisconsideredanalternativetoalteplaseinthe 2019AmericanHeartAssociation/AmericanStroke Associationguidelines.5 Itisageneticallymodifiedalteplase variantwithincreased fibrinspecificityandalongerhalf-life. ThesemodificationsallowTNKtobegivenintravenouslyas asingle,rapidbolusdose,whereasalteplaserequiresabolus dosefollowedbyaone-hourinfusion.6 Recently,multiple trialscomparingTNKwithalteplasefortreatmentofstroke

Image. Angioedemaoftherightupperlipinapatientfollowing administrationoftenecteplase(arrow).
haveshownTNKtobenotinferiorinbothefficacyand safety.7,8 Datafromthesetrials,incombinationwiththeease ofadministrationandimprovedcosteffectiveness,has promptedmanyhealthsystemstoswitchfromalteplaseto TNKforstroketreatment.2,9
PublishedstudiescomparingTNKandalteplasefor treatmentofstrokemostcommonlyreportsymptomatic intracranialhemorrhageoranyintracranialhemorrhageas theirprimarysafetyendpoints,whileratesofangioedemaare reportedinconsistently.Thelargestpublishedtrial comparingalteplasetoTNKreportedthat9/800patients (1.1%)receivingTNKand9/763patients(1.2%)receiving alteplaseexperiencedangioedema.3 Inasingle-center retrospectiveanalysisofpatientstreatedwithalteplase,the rateofangioedemawasreportedtobe7.9%.10 Roseetal performedasystematicreviewandmeta-analysisof complicationsofTNKandalteplaseforstrokeandfound cumulativeangioedemaratesof0.56%inpatientswithTNK comparedto0.63%inpatientsreceivingalteplase.11
Overallratesofangioedemaappeartobesimilarbetween alteplaseandTNK,butspecificcharacteristicsofpatientswho experienceangioedemaareseldomreported.A2022metaanalysisfromMasSerranoetal foundpriortreatmentwith ACEinhibitors,diabetes,dyslipidemia,femalegender,and hypertensiontobeassociatedwithdevelopmentof angioedemaafteralteplaseadministration.12 Strokesinvolving thefrontalcortexandinsulahavealsobeendescribedashaving increasedriskofangioedema.3 Potentialriskfactorsfor experiencingangioedemaafterTNKadministrationarenot
welldescribedincurrentliterature,althoughtheyareexpected tobesimilartothoseseenwithalteplasegivenbothagents sharetheirmechanismofaction.Theonlypublishedcase reportsofangioedemaafterTNKadministrationoccurredina patientswhowerecurrentlyusinganACEinhibitor,whichisa knownriskfactorfordevelopmentofangioedema.4,13 Our patientwasnotcurrentlytakinganACEinhibitoratthetime hereceivedTNK,althoughhehaddocumentedhistoryofan allergicreactiontotheACEinhibitorlisinopril.
Therehavebeennostudiestodeterminethebesttreatment ofangioedemafollowingTNKadministration.Theprimary goalistoensureairwaypatency.Despitehistaminenotbeing thesubstratecausingangioedemafollowingTNK administration,somehavesuggestedthatitshouldbetreated similarlytoallergicreactionsbyadministering antihistamines,steroids,andinsomecasesepinephrine.The useofmedicationsthatareapprovedforHAEhavenotbeen studiedandarecurrentlynotrecommendedforthis indication.Thelysineanalog,tranexamicacid(TXA),could haveapotentialbenefitasitbindstoplasmin,preventingthe activationofFactorXIIleadingtodecreasedproductionof bradykinin.Tranexamicacidisanantifibrinolyticinthatit preventsplasmindegradationof fibrin-to-fibrindegradation products.UseofTXAmayleadtoworseoutcomesin patientswithacuteischemicstrokes.
Thiscasereportprovidesdetailsregardingthe developmentofangioedemainapatientbeingtreatedwith tenecteplaseforanacuteischemicstroke.Whileitisknown thatangioedemaisapotentialcomplicationofTNK administration,thedetailsofindividualcasesarerarely reported.Itisimportantfortheemergencyphysiciantobe awareofthispotentialcomplicationofTNKsothatpatients donotexperiencefurthermorbidityandmortality.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:R.GentryWilkerson,MD,Universityof MarylandMedicalCenter,DepartmentofEmergencyMedicine, 110SPacaSt.,6thFloor,Suite200,Baltimore,MD21201. Email: gwilkerson@som.umaryland.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Newmanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.WilkersonRGandMoellmanJJ.Hereditaryangioedema. EmergMed ClinNAm. 2021;40(1):99–118.
2.WilkersonRGandWintersME.Angiotensin-convertingenzyme inhibitor-inducedangioedema. EmergMedClinNAm. 2021;40(1):79–98.
3.HillMD,LyeT,MossH,etal.Hemi-orolingualangioedemaandACE inhibitionafteralteplasetreatmentofstroke. Neurology. 2003;60(9):1525–7.
4.ShiG,LvJ,WuW,etal.Ipsilateralorolingualangioedemafollowing rhTNK-tPAadministrationforacuteischemicstroke. AmJEmergMed. 2024;77:231.e1–3.
5.PowersWJ,RabinsteinAA,AckersonT,etal.Guidelinesfortheearly managementofpatientswithacuteischemicstroke:2019update tothe2018guidelinesfortheearlymanagementofacuteischemic stroke:aguidelineforhealthcareprofessionalsfromtheAmerican HeartAssociation/AmericanStrokeAssociation. Stroke. 2019;50(12):e344–418.
6.NohL,PhamF,HaddadL,etal.Apracticegamechanger: impactoftenecteplaseforacuteischemicstrokeinamulticenter qualityimprovementproject. AmJHealthSystPharm. 2022;79(9):e149–53.
7.MenonBK,BuckBH,SinghN,etal.Intravenoustenecteplase comparedwithalteplaseforacuteischaemicstrokeinCanada(AcT):
apragmatic,multicentre,open-label,registry-linked,randomised, controlled,non-inferioritytrial. Lancet. 2022;400(10347):161–9.
8.BurgosAMandSaverJL.Evidencethattenecteplaseisnoninferiorto alteplaseforacuteischemicstroke:meta-analysisof5randomized trials. Stroke. 2019;50(8):2156–62.
9.DittmarE,WolfelT,MenendezL,etal.Conversionfromintravenous alteplasetotenecteplasefortreatmentofacuteischemicstrokeacross alargecommunityhospitalhealthsystem. AnnPharmacother. 2023;57(10):1147–53.
10.HurfordR,RezvaniS,KreimeiM,etal.Incidence,predictorsandclinical characteristicsoforolingualangio-oedemacomplicatingthrombolysis withtissueplasminogenactivatorforischaemicstroke. JNeurol NeurosurgPsychiatry. 2015;86(5):520–3.
11.RoseD,CavalierA,KamW,etal.Complicationsofintravenous tenecteplaseversusalteplaseforthetreatmentofacuteischemic stroke:Asystematicreviewandmeta-analysis. Stroke. 2023;54(5):1192–204.
12.Mas-SerranoM,García-PastorA,Iglesias-MohedanoAM,etal.Related factorswithorolingualangioedemaafterintravenousalteplaseinacute ischemicstroke:resultsfromasingle-centercohortandmeta-analysis. NeurolSci. 2022;43(1):441–52.
13.LapostolleA,Weisenburger-LileD,YgerM,etal.Bradykinin-mediated angioedemafollowingtenecteplaseadministrationinanacuteischemic stroke. Stroke. 2022Oct;53(10):e446–7.
ElizabethMay-Smith,MD
MarcOlshan,MD
MarkSupino,MD
SectionEditor:AnnaMcFarlin,MD
JacksonMemorialHospital,DepartmentofEmergencyMedicine,Miami,Florida
Submissionhistory:SubmittedNovember28,2024;RevisionreceivedApril12,2024;AcceptedApril16,2024
ElectronicallypublishedJuly18,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6590
Introduction: Tensionpyopneumothoraxisarare,life-threateningconditionthatoccursasa complicationofintrathoracicinfectionorbronchopleural fistula.Inthefewcasesreportedintheliterature, thepatientstypicallyhavemultiplecomorbidities,underlyinglungdisease,and/oran immunocompromisedstate.
CaseReport: Thiscasedescribestensionpyopneumothoraxinapreviouslyhealthyadolescentmale withnoexistingriskfactorsforthisdisease.Afteremergentstabilizationandadmission,surgical explorationofthechestrevealedno fistulasorpleuraldefects.Extensiveworkupdidnotshowany underlyingriskfactorsfordevelopmentofthiscondition.
Conclusion: Thiscaseofpyopneumothoraxwithprogressiontotensionphysiologyisexceedinglyrare. Uniquely,thepatienthadnounderlyingmedicaloranatomicalpredispositiontodevelopingthis condition.Thecasealsoemphasizespediatricpatients’ capacitytocompensateinthesettingofcritical illness.[ClinPractCasesEmergMed.2024;8(3)268–272.]
Keywords: tensionpyopneumothorax;thoracostomy;empyema;casereport;pediatrics.
Tensionpneumothoraxisastandardemergency department(ED)diagnosis,typicallyseeninthesettingof trauma,andrequiresimmediateclinicalrecognition andintervention.Tensionphysiologycanlesscommonly occurwithotherpathologyinsidethechest,suchas infection.Tensionpyopneumothoraxisarare, life-threateningconditionthatcandevelopinthesettingof intrathoracicinfection.Therearefewcasesdescribed intheliterature.Thediagnosistendstooccurinpatients withmultiplecomorbiditiesandunderlyinglung pathology. 1, 2 Wedescribeacaseoftension pyopneumothoraxinapreviouslyhealthyadolescentwith slowdevelopmentoverseveralweeks.Management includespromptthoracostomy,respiratorysupport, antibioticsand,often,surgicalmanagementfor adequatesourcecontrol. 3 , 4
Thepatientwasa12-year-oldHispanicmalewho presentedtotheEDaccompaniedbyhisfatherforshortness ofbreath.Onarrival,thepatientwasdiaphoretic, profoundlytachypneic,andappearedfrightenedintriage. Thefatherreportedthatthepatienthadcomplainedofsevere chestpainanddifficultybreathingforseveraldays.The patientwaspromptlymovedtotheresuscitationroom, whereinitialvitalsignswereasfollows:temperature 37.1° Celsius,heartrate150beatsperminute,respiratory rate60breathsperminute,oxygensaturation91%onroom air,andbloodpressure120/90millimetersofmercury. Heweighed69kilogramswithabodymassindexof28. Uponauscultation,absentbreathsoundswerenotedover theleftchest.Therewasinitialconcernforspontaneous pneumothorax.Asthepatientwasbeingconnectedtothe monitorandastatportablechestradiograph(CXR)was
ordered,apoint-of-careultrasounddemonstratedabsentlung slidingovertheleftchest.No fluidwasnotedatthattimeon ultrasound.Onfurtherphysicalexam,thepatientwasalert withappropriatementationbutappearedtobeinsignificant distress.Inthewheelchairbeforetransferringtothestretcher hewasinatripodpositionandprofoundlytachypneic.Hewas tachycardicwithintactperipheralpulse,capillaryrefillof2–3 seconds,andnojugularvenousdistensionwasnoted.The patient’sfatherelaboratedthatthepatienthadcomplainedof shortnessofbreathandmalaiseformorethanoneweek leadinguptohispresentationbutdeniedanycoughorfevers. Hereportedthatthepatienthadnopastmedicalhistory,no knownallergies,andnopriorsurgeries.Thepatientwasupto dateonallvaccinationssinceimmigratingtotheUnitedStates fiveyearspriorfromCentralAmerica.
ArapidportableCXRdemonstratedaleft-sidedapical pneumothoraxwitheffusionatthebaseandevidenceof tensionphysiology(Image1A).Needledecompressionwas deferredasthepatientwasnormotensivewithoutsignsof imminentcirculatorycollapse,andtheteamquicklysetup fortubethoracostomy.Theteamwasworriedthat intubationwouldexacerbateunderlyingtensionphysiology andcirculatorystatus;sothepatientwasmaintainedonnonrebreatheroxygenationandsedatedwithketamineforthe procedure.Apigtailcatheterplacementwasattemptedwith lateralapproach;however,asyringeofbloody,purulent malodorous fluidwasaspirated;thus,theteamswitchedtoa traditionallarge-borethoracostomywitha28Frenchtube. Uponaccessingthechest,alargevolumeoffoul-smelling purulent fluidwasextruded.Apost-procedureradiograph showedthechesttubeinproperpositionandimproved positionofmediastinalstructures,withsomepersistentleft pneumothoraxandeffusion(Image1B).Thepatient’sheart rateimprovedto130beatsperminute,respiratoryrate decreasedto30breathsperminute,oxygensaturationof 100%on15litersoxygennon-rebreather,andhisblood pressureremainedthesame.
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Tensionpyopneumothoraxisarareclinical presentationintheemergencydepartment thatrequiresswiftrecognitionand intervention.
Whatmakesthispresentationof diseasereportable?
Thisisthe fi rstdescribedcaseinan immunocompetentpediatricpatientdue totheorganism StreptococcusConstellatus.
Whatisthemajorlearningpoint?
Clinicianswithsuspicionforthispresentation shouldconsiderlarge-boretubethoracostomy andtransfertoafacilitywithpediatric surgicalcapability.
Howmightthisimproveemergency medicinepractice?
Timelyinterventioniskeytopreventing morbidityandmortality.Point-of-care ultrasoundandpromptthoracostomywillaid indiagnosisandmanagement.
Bloodworkwassignificantforawhitebloodcellcountof 26,000permicroliter(μL)(normalrange4,500–13,000/μL), lactateof3.1millimolesperliter(mmol/L)(0.7–2.1mmol/L), albuminof2.8gramsperdeciliter(g/dL)(3.9–5.0g/dL),mild transaminitis,normalrenalfunction,andnormalpHon venousbloodgas.Onfurtherchartreview,wefoundthatthe patienthadbeenseenintheEDtwoweekspriorforback

Image1. Emergencydepartmentchestradiograph(CXR):A) firstsemi-upright,oneviewradiographofthechestdemonstratingleft-sided hydropneumothorax(whitearrow)withshiftingofthemediastinalstructurestowardtheright(arrow);B)oneviewCXRpost-procedure demonstratingintervalchesttubeplacementontheleftsidewithexpansionofleftlung(arrow),improvedhydropneumothorax,andresolved tensionphysiology(blackarrow).
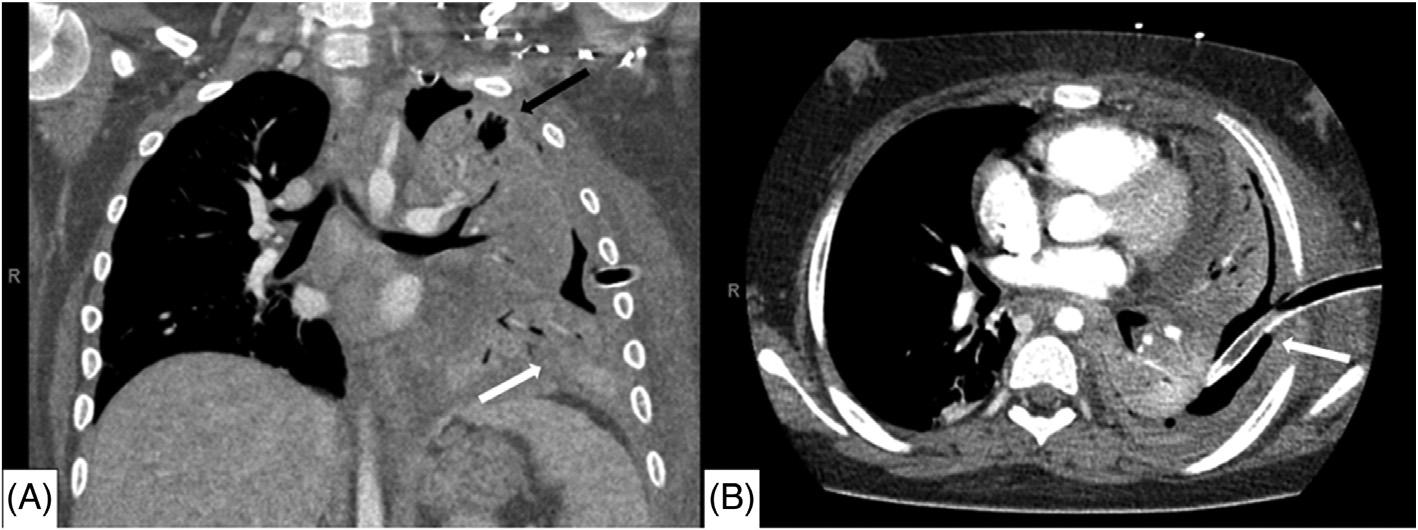
Image2. Computedtomographyimagingofthechestduringearlyhospitalcourse:A)coronalviewandB)axialviewdemonstratingresidual moderatelefthydropneumothoraxwithdiffuseopacificationofleftlungrepresentingextensivepneumonia(whitearrow),andperipheralair lucenciesontheleftsuggestiveofloculations(blackarrow).Chesttubenotedtobeingoodpositionwith fluidanddebrisobstructingthelumen oftube(whitearrow).
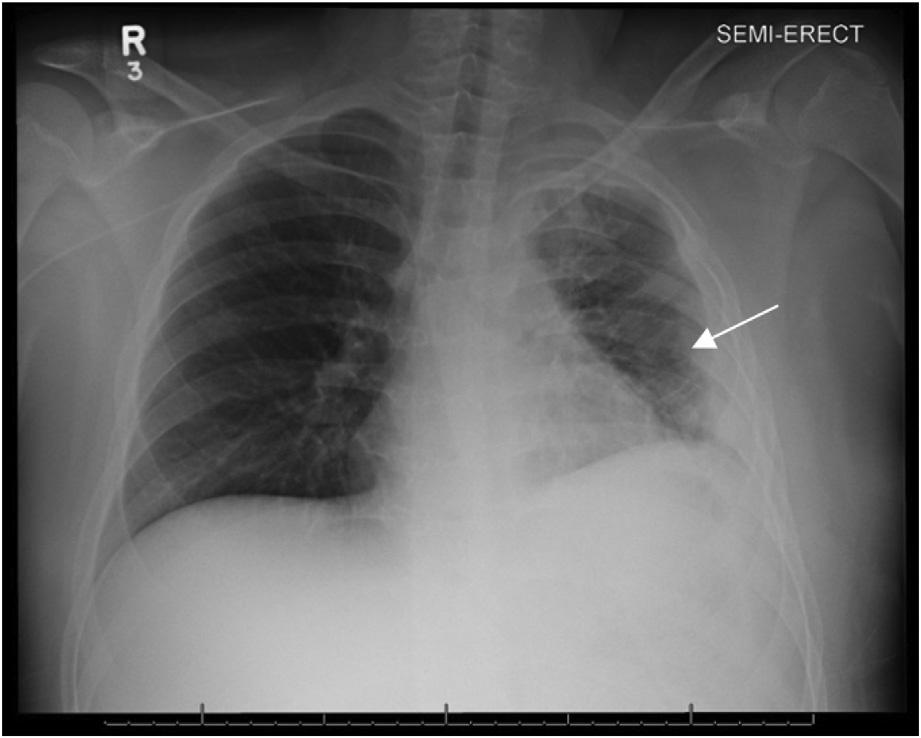
Image3. Chestradiographoneviewthatshowsre-expansionof thelungwithimprovedopacificationandsomeresidualdiffuse interstitialprominenceoftheleftlung(arrow).Intervalremovalof chesttube.
painandhadanormalCXRatthattime.Broadspectrum antibioticswereadministeredintheED,thepatientwas placedonhigh-flownasalcannula,andhewasadmittedto thepediatricintensivecareunit(PICU).Bythetimehe transferredoutoftheED,greaterthan1.5litersofpurulent outputfromthechesttubehademptiedintotheclosedchest drainagesystem.Oncethepatientwasstabilizedinthe PICU,computedtomographyofthechestwasobtainedthe followingdaythatshowedamoderateleft hydropneumothorax,diffuseopacificationoftheleftlungin thesettingofextensivepneumonia,andperipheralair lucenciesontheleft,likelyrepresentingloculations (Image2).
ThepatientremainedinthePICUforthreeweeks.He continuedparenteralantibioticsandrequiredmultipledoses ofintrapleuralalteplasetocleardebrisfromthechesttube. Onhospitalday five,heunderwentavideo-assisted
thorascopic(VATS)procedureforwashoutofthechestand replacementoftheoriginalchesttube.Operativereportfrom theVATSproceduredescribed fibrinousdebrisonthe surfaceofthelunguponentryintothechestcavity,aswellas denseadhesionsbetweenthelungandpleuralsurfaceofthe chestwall.Grossexaminationandrecruitmentmaneuvers didnotrevealanyotherfocalabnormalitiesofthelungitself, andnobronchopleural fistulaswereobserved.
Cultureofthechesttubeoutputgrew Streptococcus constellatus forwhichantibioticswerenarrowedto ampicillin-sulbactam.Thepatientrequiredintermittent bilevelpositiveairwaypressureforthe firsttwoweeksof admissionbutwaseventuallyweanedfromallsupplemental oxygen.Furtherworkupfortuberculosis,underlying immunodeficiency,andmalignancywerenegative. Ultimatelythe finalCXRdemonstratedimprovedaeration oftheleftlung(Image3).Thepatientwasdischarged homeafteratotalofonemonthinthehospital.Heattended onefollow-upappointmentonemonthafterhospital dischargeandreportednoresidualrespiratorysymptoms atthattime.Unfortunately,hewaslosttofollow-upafter thatappointment.
Tensionpyopneumothoraxisarare,life-threatening conditioninwhichairandpuscompressthelungandother intrathoracicstructures,anditoccursasacomplicationof pneumonia,trauma,aspiration,lungabscess,orpreexisting bronchopulmonaryorpleural fistula.3 Intheabsenceofa pleuraldefect,itisalsotheorizedthatapyopneumothorax canarisefromanabscess,empyema,orpyogenicinfection withagas-formingorganisminsidethechest.5 Thetension physiologyinthiscasewascharacterizedbysevere respiratorydistressandsignsofshockincludingtachycardia andmildhypoxiawithvisibleshiftingofmediastinal structuresonradiograph.Althoughthepatientwas normotensiveoninitialassessment,hebecamehypertensive throughouthospitalizationandrequiredantihypertensive
medicationsupondischarge.Thissuggeststhathispresenting bloodpressurewaslikelybelowhisbaselineandasignof earlycirculatorycompromise.
Therearefewcasereportsdescribingthiscondition,and onlyahandfulofcasesaredescribedinthepediatric population.Mostdocumentedcasesoftension pyopneumothoraxhavearapidlyprogressiveclinicalcourse andoccurredinpatientswithunderlyingdiseaseor immunocompromise,suchasmalignancy,Parkinson disease,cerebralpalsy,substanceuse,recurrentpneumonias, and/oraspirationevents.Thereisonesimilarcasethat describesdevelopmentofsymptomsandprogressionto tensionphysiologyoverseveralweeksinapediatricpatient.3
Ourpatient’scaseisquiteuniqueinthatthepatienthada gradualdevelopmentofapyogenicpneumoniathatledto tensionphysiologywithoutanyidentifiableunderlying diseaseorimmunocompromise.
Anaerobicbacteriaareimplicatedin30%ofpyothorax, althoughacombined floracanbeseenincasesofpyothorax withaspirationetiology.6,7 Sconstellatus wastheculprit organisminourpatient’spyopneumothorax.Sconstellatus ispartofthe Sanginosu sgroup;theseanaerobesarenativeto differentsystemsinthebodyincludingtheupperrespiratory tract,oralcavity,gastrointestinaltract,andreproductive tract.2 SincetheseGram-positivebacteriaarenativetothe respiratorytract,itcanbedifficulttodistinguishthem fromcontaminantorcausativeorganismonculture;rarely, thesebacteriacanleadtoaggressivepyogenicinfections.8 Sconstellatus hasbeenassociatedwithabscessformation andempyema.Duetoitsanaerobicmetabolism, Sconstellatus producesgas,whichcouldleadto developmentoftensioninpyogenicintrathoracicinfections.5
Patientswithsevereinfectionstypicallyhaveriskfactors suchasextensivesmokinghistory,malignancy,chroniclung disease,periodontaldisease,andinfectiousdiseasessuchas HIVandhepatitis.2 Onecasereportdescribesa57-year-old malepatientwithhistoryofhepatitisC,tobaccouse,and chronicobstructivepulmonarydiseasewhowasfoundto haveanaggressive Sconstellatus cavitarylesionasasequela ofarecentsubsegmentalpulmonaryemboli.9 Despiteearly initiationofbroad-spectrumantibioticcoverage,thelesion rapidlyexpanded,necessitatingextensivesurgical managementincludingpartialpleurectomyandlocalized resectioninadditiontoantibiotics.Ourcaseisthe firstto describe Sconstellatus asthecausativeorganismin pyopneumothoraxwithtensionphysiology.
Themainstayoftreatmentfortensionpyopneumothorax ispleuraldrainageandparenteralantibiotics,althoughfor somepatientswithunderlying fistulaorotherstructural abnormalitiesofthelung,resectionorlobectomymaybe required.4,10 Needledecompressionisindicatedintension physiologyduetoimpendingcirculatorycollapse;however, thisstepwasnotperformedinourpatientdueto normotensionandrapidcapabilitytoperformtube
thoracostomy.Initialpleuraldrainageinthesecasescanbe donewithsmall-orlarge-boretubethoracostomy.Smallboreorpigtailcathetersaregenerallybettersuitedfor pneumothoracesandtransudativeeffusionsduetotheir smalldiameterandpotentialforocclusion.11 Inthiscase, small-borethoracostomywasattemptedbutaborteddueto aspirationofbloodandpurulenceintothesyringe.Even whenthepatienthadsuccessfulinitialdrainagewithalargeborethoracostomy,heeventuallyrequiredmultipledaysof intrapleuralalteplaseduetotubeocclusionanddefinitive VATSproceduretoachievesourcecontrol.Similarcases presentingtosmallercommunityhospitalswouldrequire transfertoalargercenterwherepediatricthoracicsurgery consultandmanagementisavailable.
Ourpatientpresentedwithaprogressive Sconstellatus pneumoniaandempyemathatledtoformationofatension pyopneumothorax,arare,life-threateningcondition.Thiscase isuniqueinthatthepatientdidnothaveanyriskfactorsfor developmentofthetensionpyothoraxorseverepyogenic infectionfrom Sconstellatus, andheexhibitedasubacute courseleadingtoEDpresentation.Additionally,ourcase highlightstheresilienceofpediatricpatientsandtheirabilityto compensateduringactivediseaseprocesses.Ourpatient presentedcriticallyillfromaseverepneumoniathathadbeen developingforatleastoneweek.Despitethetension physiologyhedevelopedfromtheunderlyingpneumonia,his mentalstatusandbloodpressurewereintact.Thepatientdid wellafterinitialmanagement withtubethoracostomyand furtherparenteralantibiotics,supplementaloxygen,anda VATSprocedure.Thepatientmighthavebenefitedfrom earliersurgery,whichwouldhaveresultedinmorerapidsource controlofsuchanaggressiveinfection,buthewasultimately liberatedfromallrespiratorysupportandcompletedseveral weeksofparenteralantibioticstomakeafullrecovery.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:ElizabethMay-Smith,MD,Jackson MemorialHospital,DepartmentofEmergencyMedicine,1611NW 12th Ave.,Miami,FL,33136.Email: elizabeth.smith@jhsmiami.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024May-Smithetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KanaiO,FujitaK,OkamuraM,etal.Afebriletensionpyopneumothorax duetoanaerobicbacteria: fistulaorgasproduction? RespirMedCase Rep. 2021;32:101372.
2.NoguchiS,YateraK,KawanamiT,etal.Theclinicalfeaturesof respiratoryinfectionscausedbythe Streptococcusanginosus group. BMCPulmMed. 2015;15:133.
3.WhitemanPJ,WilsonMT,BarcayD,etal.Tensionpyopneumothoraxin achild:acasereport. JEmergMed. 2003;24(4):429–31.
4.MitsuiSandTauchiS.Tensionpyopneumothorax. BMJCaseRep. 2021;14(3):e242197.
5.HsiehC-F,LinH-J,FooN-P,etal.Tensionpyopneumothorax. Resuscitation. 2007;73(1):6–7.
6.TsangKY,LeungWS,ChanVL,etal.Complicated parapneumoniceffusionandempyemathoracis:microbiology
andpredictorsofadverseoutcomes. HongKongMedJ. 2007;13(3):178–86.
7.JerngJ-S,HsuehP-R,TengL-J,etal.Empyemathoracisandlung abscesscausedbyviridansstreptococci. AmJRespirCritCareMed. 1997;156(5):1508–14.
8.PortaG,Rodriguez-CarballeiraM,GomezL,etal.Thoracic infectioncausedby Streptococcusmilleri EurRespirJ. 1998;12(2):357–62.
9.VulishaAK,SamR,NurH,etal.Aggressivepresentationof Streptococcusconstellatus Cureus. 2021;13(4):e14534.
10.ReidJM,BarclayRS,StevensonJG,etal.Themanagementof spontaneouspyopneumothoraxandempyemainyoungchildren. Dis Chest. 1966;49(2):175–8.
11.AndersonD,ChenS,GodoyL,etal.Comprehensivereviewofchest tubemanagement. JAMASurg. 2022;157(3):269–74.
JasonCinti,DO
PaulaGomez,DO
SuneilAgrawal,MD
DesertRegionalMedicalCenter,DepartmentofEmergencyMedicine,PalmSprings,California
SectionEditor:ChristopherSanMiguel,MD
Submissionhistory:SubmittedFebruary10,2024;RevisionreceivedApril19,2024;AcceptedApril19,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.19426
Introduction: Atensionempyema,inwhichpurulentmaterialaccumulatesinthechestcavityandleads tocardiopulmonarydysfunction,isararecomplicationofempyemas.Moreover,fungalempyemasthat grow Candidaalbicans andcausetensionphysiologyhavenotyetbeenpreviouslydescribed.
CaseReport: Inthisreport,wepresentanimmunocompetent30-year-oldmalewhopresentedtothe emergencydepartmentwithworseningshortnessofbreathandwasfoundtohavealeft-sidedfungal empyemacausingtensionphysiology.Leftchestthoracostomyyieldedapproximately4litersofpurulent fluid.Pleuralcultureseventuallygrew Calbicans,andafterantifungaltherapy,surgicaldecorticationof thelung,andaprolongedintensivecareunitstay,thepatientwasdischargedhomeinstablecondition.
Conclusion: Whilemortalityfrom Calbicans empyemasthatcauserespiratorycompromiseis exceedinglyhigh,ourcasehighlightsthataggressivemanagementwithrapidchestthoracostomyand antifungaltherapycanleadtoafavorableoutcome.[ClinPractCasesEmergMed.2024;8(3)273–276.]
Keywords: casereport;empyemathoracis;tensionempyema;Candidaalbicans;severehyponatremia.
Tensionempyemadescribesalargeaccumulationof purulentmaterialinthechestcavity,whichthenentrapsthe lungandcompressesmediastinalstructures.Thiscauses cardiopulmonarydysfunctionbypreventingadequate ventilationandcanleadtoseverelyreducedcardiacoutput viaincreasedintrathoracicpressuresanddecreasedvenous return,resultinginlife-threateningcardiacarrest.1
Empyemasareoftenpolymicrobial,composedofboth aerobicandanaerobicbacteria,andaremostcommonly causedbypneumoniaandparapneumoniceffusion.2,3 Those thatgrowfungiareparticularlyrare. Candidaalbicans empyemahaspreviouslybeendescribedasapotential complicationofcommunity-acquiredpneumonia.4 However,mostcandidalempyemashavebeendiagnosedin patientswithprecedingabdominalandintrathoracic surgeriesorpatientswithesophagealrupture.5 Toour knowledge,therehavebeennocasesintheliteraturethat describecandidaempyemathatdemonstratetension
physiology.Inthiscasewepresentanimmunocompetent patientwithnoreportedpastmedicalhistorywhopresented totheemergencydepartment(ED)withachiefcomplaintof shortnessofbreath.Hewasfoundtohaveatension empyemathatgrew Calbicans .
A30-year-oldmalewithnoreportedpastmedicalhistory presentedtotheEDbyambulancewiththechiefcomplaint ofshortnessofbreath.Hereportedprogressivelyworsening dyspneaandaproductivecoughfortheprior6–8weeks.He wasgivenanalbuterolbreathingtreatmentbyemergency medicalservices(EMS)withnoreliefofhissymptoms,and hewasplacedonanon-rebreathermaskat15litersper minute(L/min)byEMSduetoaninitialoxygensaturationof 80%.Thepatientdeniedrecentfevers,chills,chestpain, nausea,vomiting,abdominalpain,urinarycomplaints,leg swelling,recentsickcontacts,orrecenttravel.Hedenieda historyofintravenousdruguse;however,hedidendorse
dailytobaccosmokingandheavyalcoholuse,particularly beer.Hismotherprovidedadditionalhistory,statingthatthe patienthadbeendrinkingover10beersperdayfortheprior severalweekswithminimalfoodintake.
InitialvitalsintheEDwerenotablefortachycardiaat115 beatsperminute,tachypneaat30breathsperminute,and hypoxiaat82%ona15L/minnon-rebreathermask.Hewas afebrile,andhisbloodpressurewas135/85millimetersof mercury(mmHg).Physicalexamrevealedatoxicappearing,uncomfortablemaleinmoderaterespiratory distress.Hewasdiaphoretic.Hehaddecreasedbreath soundsovertheleftlowerlobeandclearbreathsoundsonthe right.Hischestwallwasasymmetrical,withtheleftchest appearinglargerandmoreprotrudingthantherightchest. Laboratorybloodworktakenonarrivalrevealeda leukocytosisof20 × 103 whitebloodcellspermicroliter (109/L)(referencerange4.2–10.8 × 109/L),severe hyponatremiaat104milliequivalents(mEq)/L (137–145mEq/L),alacticacidosisat3.22millimoles (mmol)/L(mmol/L)(0.8–2.0mmol/L),andanegativeblood alcohollevel.Therestofthebasicmetabolicpanelrevealeda potassiumof5.3mEq/L(3.4–5.0mEq/L),chlorideof69 mEq/L(98–107mEq/L),bicarbonateof21mEq/L(21–30 mEq/L),glucose138mg/dL(70–110mg/dL),calciumof7.0 milligramsperdeciliter(mg/dL(7.8–9.8mg/dL)),bloodurea nitrogenof8.0mg/dL(9.0–20mg/dL),creatinineof0.3mg/dl (0.7–1.3mg/dL),andanalbuminof2.7grams(g)/dL (3.5–5.0g/dL).Theurinedrugscreenwaspositiveonly fortetrahydrocannabinol.
Thepatientwasstartedonbroadspectrumantibiotics withvancomycinandcefepimeintheED.Duetodelaysin radiographs,thepatienthadacomputedtomography(CT) ofthechestwithintravenouscontrasttofurtherinvestigate thecauseofhisdifficultybreathing.TheCTwasimmediately reviewedbytheemergencyphysician,andthepatientwas foundtohavealargecollectionof fluidandgasintheleft chest,withadeviatedtracheaandextensiverightward deviationoftheheart(Image1).Whilenottruetension physiologygiventhepatient’sindolentonsetofsymptoms (6–8weeks)andinitialhemodynamicstability,astension
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Tensionempyemasarelargeaccumulations ofpurulentmaterialinthechestcavity thatentrapthelung,leadingto cardiopulmonarydysfunction.
Whatmakesthispresentationof diseasereportable?
Fungalempyemasthatgrow Candidaalbicans andcausetensionphysiologyhavenotbeen previouslydescribed.
Whatisthemajorlearningpoint?
Tensionphysiologyandcardiovascular collapsearerarebutpossiblecomplicationsof empyemas;thus,itiscriticalthatphysicians quicklyidentifyandtreatit.
Howmightthisimproveemergency medicinepractice?
physiologytypicallydescribesamoreacutecondition involvinghemodynamiccollapse,such findingsonCTwere certainlyconcerningforimpendingtensionphysiology.
Basedonthe findingsonCTandhisincreasingworkof breathing,hewasintubatedemergently.Hisoxygen saturationpriortointubationwas84%ona15L/minnonrebreathermask.Hebecamehypotensivepost-intubation aftersedationandwasstartedonnorepinephrineinfusion. Giventhelargeamountof fluidandairseenonCT,itwas
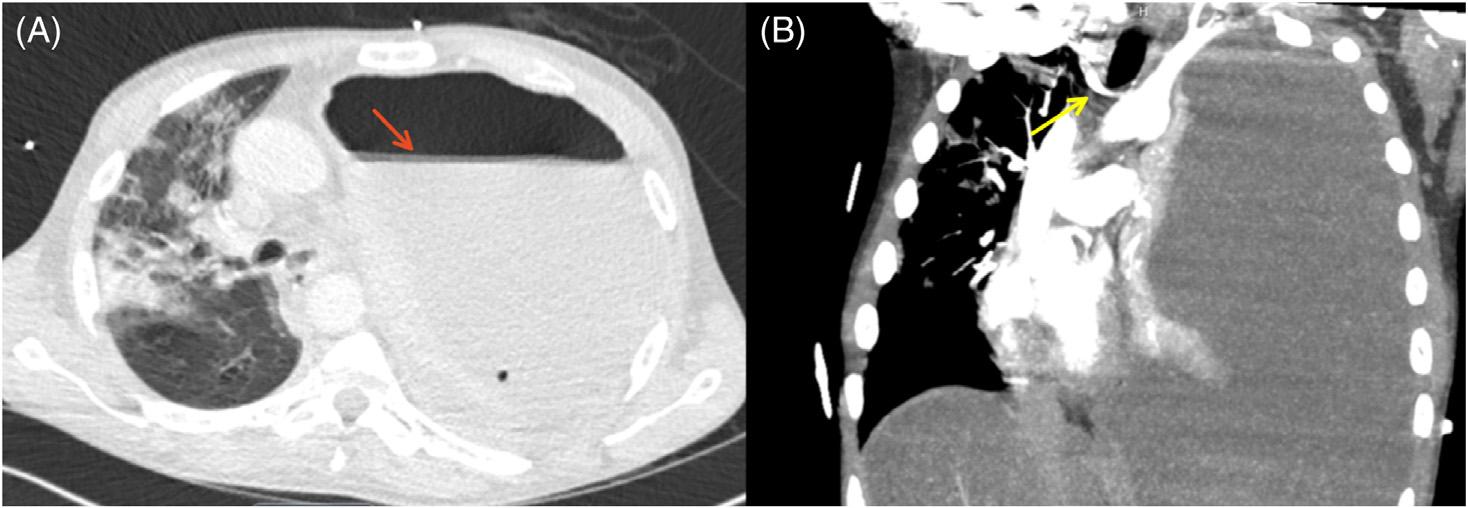
Aggressivemanagementwithchest thoracostomyandantifungaltherapycanlead toafavorableoutcomedespitethehigh mortalityassociatedwiththisdiseaseprocess. Image1. A.Axialviewofinitialcomputedtomographychestshowinglargelefthydropneumothoraxwithcompleteleftlungcollapse(red arrow).B.Coronalviewofsignificantrightwardshiftofthetracheaandmediastinum(yellowarrow).
initiallythoughtthatthepatientmayhavehada diaphragmaticherniawithextrusionofthestomachintothe leftthorax.Forthisreason,generalsurgerywasconsulted.A subsequentCToftheabdomenandpelvisshowedno diaphragmaticruptureorabdominalinvolvement.The surgeryresidentperformedaleft-sidedthoracostomy,with immediateoutputoffourlitersofthick,purulent,andhighly malodorousmaterial.Hemodynamicsimprovedafterchest tubeinsertion,withimprovementinhisbloodpressurefrom 88/55mmHgto113/64mmHg.Thepatientwasadmittedto theintensivistcareunit(ICU)onmechanicalventilationand remainedon15micrograms/minofnorepinephrine.
Duringhisinpatientstay,pleural fluidanaerobiccultures grew Prevotellaoris ,suggestingoralmicrobesand aspirationpneumoniawithparapneumoniceffusionand empyema.Pleural fluidandsputumculturesaswellasblood culturesalsogrew Calbicans .OnrepeatCTchestoneday later,thepatienthadapersistentempyema.Toevacuatethe empyema,cardiothoracicsurgerywasconsultedand performedaleftthoracoscopywithtotaldecortication,lysis ofadhesions,andtotalparietalpleurectomy.Postoperative CTchestshowedpersistentbutreducedempyemaand improvedmediastinalshift(Image2).
Thepatientwassuccessfullyextubatedsixdaysafterthe cardiothoracicprocedure,thechesttubeswereremoved,and hewasdowngradedfromtheICUtothetelemetryunit15 daysafteradmission.Hishyponatremiaresolvedondaynine afteradmissionwithcareful fluidrestrictionand maintenance fluids.Owingtorapidinitialovercorrection, desmopressinanddextrose5%inwaterwereusedtoprevent centralpontinemyelinolysis.
RepeatCTchestpriortodischargeshowedresidual airspacedensitiesinthelungswithimprovedaeration comparedtothepriorstudy,persistentatelectasisattheleft

Image2. Repeataxialcomputedtomographychestwithcontrast ondaysixofintensivecareunitadmissionshowingpersistent largeempyemareducedinsize(redarrow)withresolutionof mediastinalshift.Chesttubestillinplace(yellowarrow),and bilateralground-glassopacitiespresent.
lowerlobewithintervalre-expansionoftheleftupperlobe, anddiffusepleuralthickeninginthelefthemithoraxwith loculatedlefthydropneumothorax,significantlysmaller comparedtothepriorstudy.Hewasdischargedhomewitha walker24daysafteradmissionwithfollow-upwith cardiothoracicsurgeryintwoweeks.
Inthisreportwedescribeacaseof Calbicans empyema causingimpendingtensionphysiologyina30-year-oldmale withahistoryofalcoholism,withover4litersofpurulent, malodorousoutputafterinitialtubethoracostomy.Thereare onlyafewcasereportsintheliteraturethatdescribetension empyemas,andnonethatweareawareofthatdescribe tensionphysiologyfromafungalempyema.Ookoetal discussatensionempyemacausingcardiacarrestinayoung, immunocompromisedpatientwithHIVandtuberculosis, with~2900milliliters(mL)ofpusoutputafter thoracostomy.6 Ahernetaldescribea28-year-oldfemale withHIVwithpost-intubationcardiacarrestandoutputof ~1500–2000mLofpurulentexudate.7 Bramleyetaldiscussa 42-year-oldmalewithdiabetesmellitustype1andtrisomy21 whopresentedinpulselesselectricalactivityandahypoinflatedlefthemithoraxwithabsentbreathsounds,with ~900mLofmalodorouspusoutput.8 Noneofthesecases wereoffungaletiology.Untilourcase,thelargestfungal empyemadescribedintheliteraturewasbySrinivasnakshatri etalin2014,with~2500mLof fluidthatgrew Ckrusei and Ctropicalis drainedover48hours.9 Theimmediatedrainage of4litersofpusgrowing Calbicans inourcaseis thusunprecedented.
Thecaseisalsounusualinthatempyemasthatgrow Calbicans areoftenaresultofesophagealperforation, fistulaformation,orprecedingabdominalandintrathoracic surgeries.4 Inthe firstretrospectiveanalysisof67patients withfungalempyemainTaiwanbyKoetal,themost commonunderlyingcause(30%)wasabdominaldisease, especiallypriorabdominalsurgeryorgastrointestinal perforation.5 Ourpatientdidnothaveaprecedingsurgeryor gastrointestinalperforation.Itislikelythathehadan aspirationeventowingtohisexcessivealcoholusethat ultimatelyledtopneumoniawithsubsequent parapneumoniceffusion,whichisfurtherreflectedbythefact thatthepleural fluidalsogrew Prevotella ,predominantlyan oralmicrobe.Thisisacommonmechanism:inone retrospectivestudyof63patientswith Candida empyema thoracis,55.6%ofthesewerefromcontiguousinfection.10
Inanotherretrospectiveanalysisof81patients, Candida empyemawasfromanintrathoracicsourcein51%of patients.4 Thesecondmostcommonunderlyingcauseof fungalempyemaintheanalysisbyKoetalwas bronchopulmonaryinfectionsat22%.5 However,giventhat ourpatientwasfoundtohavecandidemia,itisalsopossible thatanexistingtriggerinthepleuralspace,suchasa
hemothorax,chylothorax,orhydrothorax,becameinfected dueasystemicinfectionviahematogenousspread.Thisisless commonlyreportedintheliterature,with2%ofpatients havingconcurrentcandidemiainSengeretaland27% havingconcurrentfungemiainKoetal.4,5
Furthermore,mortalityfrom Calbicans empyemasis extremelyhighandismorelikelytooccurinolderpatients andthoseinanimmunocompromisedstate.Inthe retrospectiveanalysispreviouslydiscussedbyKoetal, mortalityinpatientswithfungalempyemawas73%.5 Lin etal’sretrospectivestudyofpatientswith Candida empyema thoracisfoundmortalitytobe61.9%.10 Calbicans empyema wasmostcommon.Patientswhopresentedwithrespiratory failure,asourpatientdid,wereassociatedwithhigher mortality.Inconjunction,thesetwostudiesshowthatfungal empyemaofanykindisassociatedwithveryhighmortality.
Animmunocompromisedstateappearstoplayarolein Candida empyemasaswell.Wesawthisassociation previouslyinpatientswithtensionempyemaswithoutfungal etiologieswhowereimmunocompromisedsecondaryto HIV,tuberculosis,andtype1diabetesmellitus.6,8 Twoother casereportsdescribepatientswith Calbicans empyemaswho wereimmunocompromisedsecondarytocarcinoma, specifically,esophagealcarcinoma,andoneofwhichdidnot involvegastrointestinalperforation.11,12 Fortunately,our youngpatientwithnosignificantmedicalhistoryotherthan alcoholusesurvivedthetensionempyemaandwas eventuallydischargedfromthehospital.Inourcase, however,itislikelythatthepatientdevelopedan immunocompromisedstatenotfromHIVbutfromchronic alcoholismandmalnutrition.
Tensionphysiologyandcardiovascularcollapsearerare complicationsofempyemathoracis.Thiscasereportis uniqueinthatthiswasacommunity-acquired Calbicans infection,notassociatedwithgastrointestinalperforation, HIV,orrecentsurgery,anddemonstratedimpendingtension physiologyonphysicalexamandimaging.Duetothehigh riskofmortalityassociatedwithpulmonaryfungal infections,itiscriticalthatphysiciansquicklyidentify tensionphysiologyandkeepabroaddifferentialwhen choosingappropriateantibiotictreatment.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:SuneilAgrawal,MD,Desert RegionalMedicalCenter,DepartmentofEmergencyMedicine, 1150NIndianCanyonDr.,PalmSprings,CA92262. Email: suneil.agrawal@vituity.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Cintietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.WhitemanPJ,WilsonMT,BarcayD,etal.Tensionpyopneumothoraxin achild:acasereport. JEmergMed. 2023;24(4):429–31.
2.McCauleyLandDeanN.Pneumoniaandempyema:causal,casualor unknown. JThoracDis. 2015;7(6):992–8.
3.IshiguruT,TakayanagiN,IkeyaT,etal.Isolationof Candida speciesis animportantclueforsuspectinggastrointestinaltractperforationasa causeofempyema. InternMed. 2010;49(18):1957–64.
4.SengerSS,ThompsonGR,SamantaP,etal. Candida empyema thoracisattwoacademicmedicalcenters:newinsightsintotreatment andoutcome. OpenForumInfectDis. 2021;8(4):ofaa656.
5.KoSC,ChenKY,HsuehPR,etal.Fungalempyemathoracis. Chest. 2000;117(6):1672–8.
6.OokoPB,OngondiM,WhiteRE.Tensionempyemathoracis. AnnAfr Surg. 2015;12(2):109–10.
7.AhernTLandMillerGA.Tensionpyothoraxcausingcardiacarrest. West JEmergMed. 2009;10(1):61.
8.BramleyD,DowdH,MuwangaC.Tensionempyemaasareversible causeofcardiacarrest. EmergMedJ. 2005;22(12):919–20.
9.SrinivasnakshatriVK,SubramaniP,VenkateshwaraprasadKN,etal.A fatalcaseoffungalempyemadueto Candidakrusei and Candida tropicalis:arareoccurrencewithanatypicalpresentation. JClinDiagn Res. 2014;8(11):DD01–2.
10.LinK-H,LiuY-M,LinP-C,etal.Reportofa63-caseseriesof Candida empyemathoracis:9-yearexperienceoftwomedicalcentersincentral Taiwan. JMicrobiolImmunoInfect. 2014;47(1):36–41.
11.HullJH,KendallA,LoftsF.Fungalempyemathoraciscomplicating treatmentofesophagealcarcinoma. PostgradMedJ. 2004;80(941):154.
12.BaradkarVP,MathurM,KulkarniSD,etal.Thoracicempyemadueto Candidaalbicans IndianJPatholMicrobiol. 2008;(512):286–8.
TuckerAvra,DVM* JesusTorres,MD,MPH,MSc†
KumarFelipeVasudevan,MD‡ ElizabethA.Samuels,MD,MPH,MHS†
SectionEditor:StevenWalsh,MD
*UCLADavidGeffenSchoolofMedicine,LosAngeles,California † UCLADavidGeffenSchoolofMedicine,DepartmentofEmergency Medicine,LosAngeles,California ‡ UCLADavidGeffenSchoolofMedicine,DepartmentofInternal Medicine,LosAngeles,California
Submissionhistory:SubmittedFebruary16,2024;RevisionreceivedApril19,2024;AcceptedApril22,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.19431
Introduction: MedicalandnonmedicalketamineuseisincreasingintheUnitedStates.Thiswilllikelylead toanincreaseinemergencydepartment(ED)visitsinindividualsexperiencingassociatedsideeffects. Physicianswillneedtobeabletoeffectivelyrecognizeandmanageketamine-relatedcomplications.
CaseReport: A31-year-oldmalewithathree-yearhistoryofinhalational,intramuscular,and intravenousnonmedicalketamineusepresentedtotheEDtwicewithinaweekwithsymptomsofsevere atraumaticbackpain,abdominalpain,anddyspepsia.Acomprehensiveworkup,includingadvanced imaging,wasunrevealingforidentifiablecauses,andthepatientwasdischargedwithinstructionsfor primarycarefollow-upforfurtherevaluation.ThepatientusedinformationsharedonReddit,anonline forumandsocialnetwork,toidentifythatthecauseofhispainwasrelatedtochronicketamineuse. Subsequently,upondiscontinuationofketamine,thepainimprovedin24hours.Thepatientselfnavigatedtoaddictiontreatment.
Conclusion: Emergencyphysiciansshouldconsidersequelaeofchronicketamineuseasapossible causeforgastrointestinalandurologicsymptomsintheED.Inadditiontothoroughexaminationand assessmentforotheracutemedicalproblems,patientsshouldbeofferededucation,symptomatic treatment,andlinkagetoharmreductionandsubstanceusedisordertreatmentservices.[ClinPract CasesEmergMed.2024;8(3)277–281.]
Keywords: ketamine;casereport;harmreduction;substanceusedisorder;ketamineusedisorder.
KetamineisbecomingincreasinglyusedintheUnited States(US)foravarietyofmentalhealthconditions,most notablytreatment-resistantdepression.1 Intranasal esketamine(S-enantiomerofketamine)wasapprovedin 2019bytheUSFoodandDrugAdministration(FDA)for treatment-resistantdepression.Thereisalsowidespreadofflabelmedicaluseofintravenous(IV)ketamineforother mentalhealthconditions,includingpost-traumaticstress disorder,anxiety,eatingdisorders,andmooddisorders. Ketamineisalsousedrecreationallyforitsdissociative andpsychedeliceffects.Overthelasttwodecades,
self-reported,nonmedicalketamineuseandexposuresinthe UShavebeengraduallyincreasing,andseizuresofillicit ketamineincreased349%from2017to2022.2 Asratesof recreationalandmedicaluseofketaminerise,physicians needtoknowhowtorecognizeandtreatsideeffectsand complicationsofketamineuse.However,thereisapaucityof USliteraturediscussinghowtoidentifyandmanageside effectsofchronicketamineuse.StudiesintheUnited Kingdom,HongKong,andItalydescribeavarietyofclinical presentationsinpeoplewithchronicketamineuse,including urological,neurological,andgastrointestinal(GI) symptoms.3,4 Commonpresentationsofthesesymptoms
includedysuriaforurologicalsymptoms,intoxicationor hallucinationsforneurologicalsymptoms,andabdominal painforGIsymptoms.Inthiscasereport,wedescribe clinicalpresentationandmanagementofrecurrentsevere abdominalpain knowninformallyas “Kcramps” in thecommunityofpeoplewhouseketamine associated withlong-termuse.
A31-year-oldmalewithahistoryofchronicketamineuse, majordepressivedisorder,andchronicbackpainpresented totheemergencydepartment(ED)withtwodaysof increasinglyseverebackpainandchesttightness.Hehada similarepisodeofbackpainandchesttightnesseightweeks priorthatlastedfor10days,withnoothersymptoms.Hedid notseekmedicaltreatmentforthatepisode,andthepain slowlyresolvedonitsown.Thepatienttookintramuscular andIVketaminedailyforeightmonths,witheachday’ s dosesrangingfrom1–3grams.BeforeintramuscularandIV use,hehadbeeninsufflating0.5–1grameverydayfor threeyears.
AtpresentationtotheED,hewasafebrile,heartrateof 77beatsperminute,bloodpressureof131/86millimetersof mercury,andanoxygensaturationof100%onroomair. Hewasawakeandalertandinmilddistress.Physical examinationrevealedmildtendernessonthoracicparaspinal musclepalpation,mildtendernesstopalpationintheleft upperquadrant,andwasotherwiseunremarkable.Complete bloodcount,completemetabolicpanel,urinalysis, electrocardiogram,troponin,andD-dimerwerewithin normallimits.Chestradiographswerenegativefor pneumonia,pneumothorax,pneumomediastinum,or subcutaneousair.Givenbackpainandinjectionuse,a thoracicspinemagneticresonanceimaging(MRI)was performedtoruleoutanepiduralabscess.TheMRIrevealed noinfection, fluidcollection,discdisease,fractures,orother acuteabnormalitythatcouldaccountforhissymptoms. Twosetsofbloodculturewerenegative.Thepatientwas treatedwithacetaminophenanddischargedwithinstructions tocontinueacetaminophenandibuprofenathomefor painmanagement.
Thefollowingday,thepainmigratedtohisupper abdomenandhedevelopeddyspepsia.Hereportedtaking famotidine,calciumcarbonate,acetaminophen,and ibuprofendaily,withnoimprovementinsymptoms.He continueddailyketamineuseforrecreationalpurposes andtocontrolthepain.Everynight,thepainwokehimup at4 AM.Thepain,whichthepatientdescribedasadeep aching/crampingsensation,wasworseaftereatingand improvedwithfasting.Theintensityremainedsevere,andhe returnedtotheED fivedayslaterforreevaluation. OnthesecondEDvisit,thepatientreported9/10 abdominalpainonarrival.Again,vitalsignsshowedno abnormalities.Hewasawakeandalertandinmoderate
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Abdominalpainisacommoncomplication fromchronicketamineuse,butunderlying mechanismsarepoorlyunderstood.
Whatmakesthispresentationof diseasereportable?
Thisisthe fi rstreportedcaseofabdominal painassociatedwithketamineuseinthe UnitedStatespeer-reviewedliterature.
Whatisthemajorlearningpoint?
Gastrointestinalsideeffectsshouldbeonthe differentialwhenassessingabdominalpainin individualswhouseketamine.
Howmightthisimproveemergency medicinepractice?
Withincreasesinket amineuse,emergency physicianswillneedtobeabletorecognize andcareforpatientswithnon-neurologic complicationsofchronicketamineuse.
distress.Physicalexaminationrevealedrightlower quadranttendernesstopalpationandmildrightupper quadranttenderness.
Hewastreatedwith4milligramsIVmorphineand1liter lactatedRinger’sIV fluid.Thepainimprovedtoan8/10and themorphinewasrepeatedtwohourslater,resultingin6/10 abdominalpain.Computedtomographyoftheabdomen andpelviswithcontrastwasperformedandrevealedno evidenceofanacuteintra-abdominalprocess. Acompleteabdominalultrasoundwasperformed,revealing a2–3mmadherentgallstoneanda3mmgallbladder polyp.Thepatientwasdischargedwithinstructionsto continueibuprofenandacetaminophen,followupwith primarycare,andreturntotheEDintwodaysiftherewas noimprovement.
Afterdischarge,thepatientsearchedforhissymptomson Reddit,wherehediscoveredseveraldiscussionforumsabout “KCramps/KPains,” Redditusersdescribethepainas feelinglikesomeonewassqueezingtheirorgansashardas theycould,painthatreachesdownintotheupperabdomen andcreepsthoughthechest,andfeelinglikeahotknifewas runningthroughthebacktothefrontofthestomach.He followedpeerrecommendationstotakehotbathsand discontinueketamine.Afterdiscontinuingketamine,the painimprovedwithin24hours.Herestartedrecreational
ketamine72hourslater,withinitialrecurrenceofdyspepsia fourhoursafteruse.Thefollowingdayhedevelopedthe severeabdominalpainagain,whichlastedfortwodaysuntil hediscontinuedketamineagainandadmittedhimselftoa residentialsubstanceusedisorder(SUD)treatmentprogram. Thepainimproved30hoursafterstartingSUDtreatment. ThepatientcommunicatedthisinformationtohisED treatmentteamduringhisresidentialtreatmentstay.
Wereportacaseofrecurrentabdominalpainassociated withchronichighdosesofketamine,colloquiallyknownas “Kcramps.” Thepatientinitiallypresentedwithreported backpainandchesttightnesswithabdominaltendernesson physicalexamthatprogressedtosevereupperabdominal pain.Diagnosticsruledoutinfectionorotherlife-threatening causesofhissymptoms,andthepatientwasdischargedwith instructionstocontinueacetaminophenandibuprofenand returnintwodaysifthepainhadnotimproved.Thepatient wasopenabouthisketamineusetotheemergency physicians.However,outsideofpossibleepiduralabscessor infectionduetoat-homeIVandintramuscularketamineuse, therewasnoconsiderationofthepossibleassociationof symptomsasasideeffectorcomplicationofketamineuse. Inaddition,therewasnorecommendationorcounselingto reduceuse,harmreductioncounseling,motivational interviewing,orscreening,briefintervention,andreferral totreatment.
Cross-sectionalstudieshavedescribedthemostcommon toxicitypatternsassociatedwithketamine,primarily presentingwithneurological,urological,andgastrointestinal symptoms.3 Areviewof233EDvisitsamongpeoplewhouse ketamineinHongKongshowedthatthemostcommon
presentingsymptomswerealteredconsciousness(45%), abdominalpain(21%),urinarysymptoms(12%),and dizziness(12%)(Table).6 Inaddition,manyforumsonthe internetdescribeandverifyabdominalpainasacommon symptommanifestationforpatients.
“KCramps” ismentionedonlyonetimeinpeer-reviewed literature,describedas “severeabdominalpains” that “ can feellikeseveregaspainsbutmuchworse.”5 Inonecrosssectionalstudyofpatientsseekingtreatmentforketamine uropathy,27.5%reportedupperGIsymptoms,including epigastricpainandrecurrentvomiting.4 Somecasereports indicatethepainisbiliaryorgastricinetiology.Biliary causesincludecholestasis,chronicacalculousbiliarycolic, andcommonbileductdilation.7,8 Abnormalliverfunction testshavealsobeenassociatedwiththerapeuticketamine use,andthemechanismisunknown.9,10 Poonetalevaluated GIproblemsamongindividualswithinhalationalketamine use.Among28patientswithGIsymptoms,14patientshad endoscopies,with Helicobacterpylori -negativegastritisas themostcommonhistopathological finding,followedby gastroduodenitis.9 Theonlyreportedtreatmentfor ketamine-associatedabdominalpaininthepeer-reviewed literatureisabstinence,althoughRedditthreadsreveal numeroussupportivemeasures,includinghotshowersand baths,hotbeverages,andsmallmeals,tosupportpatientsin managingtheirpain.
Inadditiontoabdominalpain,emergencyphysicians shouldbefamiliarwiththesevereneurologicandurologic complicationsofchronicketamineuse.Patientsmay experiencealteredmentalstatus,agitation,musclerigidity, anddissociativeemergencereactionsthatmayinclude hallucinations,fear,and “outofbody” experiences.3 Benzodiazepinesaretheprimarytreatmentfordissociative
Table. Clinicalpresentations,mechanismsofaction,andtreatmentofsideeffectsassociatedwithketamineuse.
SystemaffectedSymptom(s)FindingsMechanismofactionTreatment
NeurologicIntoxication
Alteredmentalstatus
Agitation
Musclerigidity
Hallucinations
Dissociativeemergentreactions
UrologicDysuria
Urinaryurgency
Hematuria
NMDA,N-methyl-D-aspartate.
Acalculousbiliarycolic
Commonbileductdilation
Abnormalliverfunctiontests
Gastritis
Gastroduodenitis UnknownHotbaths
Sterileurine
Ulcerativecystitis
Obstructivenephropathy
Directdamagetourothelial liningbyketamineand ketaminemetabolites
Hotbeverages
Cessationof ketamineuse
Cessationof ketamineuse
emergencereactions,musclerigidity,andagitationdueto ketamineuse.11 Theurologicalsideeffectsofketamineuse arewelldescribedandreportedlyaffectapproximatelyonethirdofchronicketamineusers.12 Clinicalsymptomsof urologicaltoxicityaredysuria,urinaryurgency,andpossible progressiontopainfulhematuria.Thesesymptomsare associatedwithulcerativecystitissecondarytoketamineand itsmetabolitesthatmayprogresstoobstructivenephropathy andbladder fibrosis.13,14 Abstinenceofketamineuseis describedastheonlytreatment,withnoreportsofresolution ofurologicalsymptomswithpersistentketamine use(Table).12
TherearelimitedcasereportsintheUSofclinical presentationsassociatedwithketaminetoxicity.Ketamine sideeffectsshouldbeonthedifferentialwhenassessing abdominalpainanddysuriainindividualswhoadmitto ketamineuse.However,itisadiagnosisofexclusionafter otheremergentorinfectiouscausesareappropriatelyruled out.Whilenopharmacotherapyhasbeenapprovedbythe FDAforketamineusedisorder,primarycounselingto addresssymptomsshouldfocusonreductionorcessationof ketamineuse,includingmotivationalinterviewingand referralandlinkagetoaddictiontreatment.Forallpatients whoinjectdrugs,emergencyphysiciansshouldbefamiliar withandprovideresourcesonsterileconsumption equipmentandsaferinjectiontechniqueforinfection prevention.Furthermore,giventhefrequentpresenceof fentanyladulterantsinthedrugsupply,allpatientswhouse drugsshouldbeofferedtake-homenaloxone(ornaloxone prescription)andfentanylteststripsforoverdose prevention.15
Inthiscase,lackofclinicianknowledgeabout “Kcramps” contributedtodelayedaddictiontreatmentengagementand resolutionofsymptoms.Thepatientreliedonadviceand inputfromanonlineforumofpeoplewhouseorhaveused ketaminetoself-guidehistreatment.Giventhatthepatient reportedusing1–3gramsofketaminedailyheshouldhave beenreferredforaddictiontreatment.Peoplewhousedrugs havehistorically,andcurrently,developed and subsequentlytested strategiestoreducemorbidityand mortalityamongthemselvesandtheirpeers.Thishas includedharmreductionstrategiessuchassyringeservices programs,naloxonedistribution,drugcheckinginitiatives, andpeersupportandinformationsharing.Asnonmedical ketamineuseincreasesintheUS,emergencyphysiciansmay seemorepatientswithsymptomsandcomplicationsrelated tochronicuse.Furtherworkisneededtounderstandthe etiologyandtreatmentofGIsymptomsrelatedtoketamine use,whichshouldincludebeingawareoftheknowledgeand perspectivesofpeoplewhohaveusedketamineandtesting thestrategiestheyhavedevelopedtotreatGIsymptoms.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:TuckerAvra,DVM,UCLADavid GeffenSchoolofMedicine,10833LeConteAve.,LosAngeles, CA90095.Email: TAvra@mednet.ucla.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Dr.Samuelsispartiallysupportedbythe CentersforDiseaseControlandPrevention(R01CE003516).The opinionsexpressedheredonotreflectthoseoftheCentersfor DiseaseControlorPrevention.
Copyright:©2024Avraetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.WalshZ,MollaahmetogluO,RootmanJ,etal.Ketamineforthe treatmentofmentalhealthandsubstanceusedisorders: comprehensivesystematicreview. BJPsychOpen. 2021;8(1):e19.
2.PalamarJJ,WilkinsonST,CarrTH,etal.Trendsinillicitketamine seizuresintheUSfrom2017to2022. JAMAPsychiatry. 2023;80(7):750–1.
3.PavarinRM,MaraniS,TurinoE.Ketamineabusersreferringto emergencydepartmentsinnorthernItaly:across-sectionalstudy. AnnIstSuperSanita. 2019;55(4):338–44.
4.LiuSYW,NgS,TamY,etal.Clinicalpatternandprevalenceofupper gastrointestinaltoxicityinpatientsabusingketamine. JDigDis. 2017;18(9):504–10.
5.JansenKLR.Areviewofthenonmedicaluseofketamine: use,usersandconsequences. JPsychoactiveDrugs. 2000;32(4):419–33.
6.NgSH,TseML,NgHW,etal.Emergencydepartmentpresentationof ketamineabusersinHongKong:areviewof233cases. HongKongMed J. 2010;16(1):6–11.
7.NyirendaTJ,Shirazi-NejadA,SolimanAS.Persistentketamineinducedcholangiopathy:anapproachtomanagement. Cureus. 2020;12(11):e11611.
8.LoRSC,KrishnamoorthyR,FreemanJG,etal.Cholestasisandbiliary dilatationassociatedwithchronicketamineabuse:acaseseries. SingaporeMedJ. 2011;52(3):e52–5.
9.PoonTL,WongK,ChanM,etal.Uppergastrointestinalproblemsin inhalationalketamineabusers. JDigDis. 2010;11(2):106–10.
10.NoppersIM,NiestersM,AartsL,etal.Drug-inducedliverinjury followingarepeatedcourseofketaminetreatmentforchronic paininCRPStype1patients:areportof3cases. Pain. 2011;152(9):2173–8.
11.ZhouJY,HamiltonP,MacresS,etal.Updateonketamine. AdvAnesth. 2020;38:97–113.
12.KalsiSS,WoodDM,DarganPI.Theepidemiologyandpatternsof acuteandchronictoxicityassociatedwithrecreationalketamineuse. EmergHealthThreatsJ. 2011;4(1):7107.
13.ShahaniR,StreutkerC,DicksonB,etal.Ketamine-associated ulcerativecystitis:anewclinicalentity. Urology. 2007;69(5):810–2.
14.SelbyNM,AndersonJ,BungayP,etal.Obstructivenephropathyand kidneyinjuryassociatedwithketamineabuse. NDTPlus. 2008;1(5):310–2.
15.Macias-KonstantopoulosW,HeinsA,SachsC,etal.Between emergencydepartmentvisits:theroleofharmreductionprogramsin mitigatingtheharmsassociatedwithinjectiondruguse. AnnEmerg Med. 2021;77(5):479–92.
AkashDaswaney,MBBS*
ShuchiAbhishek,MBBS†
SanjanAsanaruKunju,MD,DNB‡ PriyaPattathSankaran,MD§ AhlamAbdulRahman,MD∥
*DepartmentofEmergencyMedicine,KasturbaMedicalCollege,Manipal, ManipalAcademyofHigherEducation,Manipal,Karnataka,India
† KasturbaMedicalCollege,Manipal,ManipalAcademyofHigherEducation, Manipal,Karnataka,India
‡ DepartmentofEmergencyMedicine,KasturbaMedicalCollege,Mangalore, ManipalAcademyofHigherEducation,Manipal,Karnataka,India
§ DepartmentofRadiodiagnosisandImaging,KasturbaMedicalCollege, Manipal,ManipalAcademyofHigherEducation,Manipal, Karnataka,India
∥ DepartmentofAnaesthesiology,KasturbaMedicalCollege,Mangalore, ManipalAcademyofHigherEducation,Manipal,Karnataka,India
SectionEditor:R.GentryWilkerson,MD
Submissionhistory:SubmittedMarch5,2024;RevisionreceivedApril19,2024;AcceptedApril22,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem
DOI: 10.5811/cpcem.20308
Introduction: Isolatedoculomotornervepalsyaftermildtraumaticbraininjuryisunusualand prognosticallysignificantduetounclearmechanismsandrecoverychallenges.Wepresentacaseof isolatedoculomotornervepalsyfollowingminorheadtrauma,sheddinglightonthisunusualoccurrence.
CaseReport: A24-year-oldmaleexperiencedseverevisionlossandright-sidedoculomotornerve palsyafteramotorvehiclecollision.Initialimagingshowedahemorrhagicfocusintheleftposteriorfossa andacontusioninthecorpuscallosum,yetnodirectcauseforthenervepalsywasfound.Partial recoverywasobservedafter12months.
Conclusion: Thiscaseunderscorestheimportanceofmaintainingaheightenedsuspicionforoccult intracranial findings,especiallywhentheinitialnon-contrastcomputedtomographywasinconclusive. Timelyclinicalassessmentandappropriateradiologicalinvestigationsbyemergencyphysiciansare crucialforimprovingtheprognosis.[ClinPractCasesEmergMed.2024;8(3)282–286.]
Keywords: oculomotornervepalsy;minorheadtrauma;emergencydepartment;casereport.
Isolatedoculomotornervepalsyfollowingmildheadinjury isarareoccurrence.Themechanismrequiredtodamagethe nerveisusuallysevereandisoftenassociatedwithbasilarskull fracture,orbitalinjury,subarachnoidhemorrhage,or neurologicaldeficitssuchaslossofconsciousness.1 Injuryto thenervecouldbedirectduetoshearingforcebetweenthe brainstemandsupratentorialstructurescausingrootlet avulsionanddistalfasciculardamageorindirect,causedby compression,displacement,ordeformityofthenerveduetoa space-occupyinglesionlikeanexpandinghematoma.2 Itis
oftendescribedtooccurfollowinganexpandingintracranial masslesion,causinguncalherniation.3 Therecoveryrate,in termsofsympatheticandparasympatheticoculomotor function,followingcompleteoculomotornervepalsyis prolonged,oftenresultinginincompleteresolution.Inthis case,wedescribeapatientwhodevelopedisolatedright oculomotornervepalsyfollowingminorclosedheadtrauma (GlasgowComaScale[GCS]15).Apeculiarfeaturewasthe lackofassociationbetweenthemagneticresonanceimaging (MRI) findingsandclinicalmanifestationsthatgaveusinsight intotheinjurymechanismtothenerve.
Apreviouslyhealthy24-year-oldhelmetedmale, motorbikeriderpresentedtotheemergencydepartment (ED)ofatertiarycarecenterafteraroadtrafficaccident. Unabletocontrolthespeedofhismotorcycle,heskiddedand fellwhiletakingasharpturn.Onadmission,hehadsevere painoverhisrightshoulderandhip,diminutionofvisionon therightside,inabilitytoopenhisrighteye,right-sided diplopia,andinabilitytorecollectanyeventssurrounding theincident.Hedeniedlossofconsciousness,nosebleeding, vomiting,orseizures.
Atpresentation,hewasconsciouswithaGCSscoreof15. Thevitalsrecordedwereheartrate90beatsperminute, bloodpressure140/90millimetersofmercury(mmHg), respiratoryrate16breathsperminute,100%oxygen saturationonroomair,andafebrile.Initialneurological examinationshowedthathewascooperative,alert,andwell orientedtoperson,place,andtime.Therewasptosis,lateral deviationoftheeyeball,anda fixed,dilated,andnonreactivepupilmeasuring7millimeters(mm)onexamining therighteye.Hewasunabletoadduct,elevate,ordepressthe righteyeball(Image1).Orbitalmarginswereintact.The conjunctivaappearednormal,thecorneawasclear,the anteriorchamberlookednormal,andthelenswas transparent.Thelefteyeappearednormalwithnolimitation inextraocularmovements,andthepupilwas2mmand reactive.Allotherophthalmicexaminations,including measurementofintraocularpressure,revealednormal findings.Examinationofothercranialnervesandsystemic examinationwasunremarkable.

Image1. Photographofthepatientthatshowedfeaturesof oculomotornervepalsyonrightside:a)ptosis(whitearrow), indicativeofinvolvementofthelevatorpalpebraesuperioris (sympatheticinvolvement);b)absentpupillarylightreflex ‘“fully blownoutdilatedpupil’”(whitearrowhead)indicativeofinvolvement ofthesphincterpupillae(parasympatheticinvolvement);c)intact left-sidedpupillarylightreflex(blackarrow).
Whatdowealreadyknowaboutthis clinicalentity?
Isolatedoculomotornervepalsyfollowing mildtraumaticbraininjury(TBI)israre,and indirectinjuriespredominate.
Whatmakesthispresentationof diseasereportable?
Thiscaseunderscoresisolatedoculomotor nervepalsypost-mildTBI,prompting re-evaluationduetoabsenceoffocalde fi cits andcorrelatingradiological fi ndings.
Whatisthemajorlearningpoint?
Preciseimagingenhancesoculomotornerve palsymanagement.Thoroughassessmentand tailoredtreatmentarevitalinmildTBIcases.
Howmightthisimproveemergency medicinepractice?
Thoroughclinicalassessmentandimaging, precisestrategies,andadvocating standardizedevaluationacrossinjury severitieselevateemergencymedicine standards.
Inthiscase,owingtotheintricatenatureofthepatient’ s presentationcharacterizedbyisolatedoculomotornerve palsyaftermildheadtrauma,amultidisciplinaryteam comprisingexpertsfromemergencymedicine,neurology, ophthalmology,andradiologycollaboratedtodeliver meticulousandcomprehensivecare.Laboratory examinationswerenormalexceptforanelevatedwhiteblood cellcount.Radiographsoftheshoulderandhipontheright siderevealedaclaviclefractureandanintertrochanteric fractureofthefemur,respectively.Non-contrastcomputed tomography(CT)ofthebrainandorbitsrevealedawelldefinedhemorrhagicfocusmeasuring~0.9 × 2.2centimeters intheleftposteriorfossathatdidnotcorrelatetothe observedclinical findings(Image2).Thepatientwas transferredtotheintensivecareunitforfurthermonitoring, andamultitudeofadditionaldiagnosticscanswere performed.Magneticresonanceimagingofthebrain revealedasmallhemorrhagiccontusionoverthebodyofthe corpuscallosumontherightsideandminimal intraventricularhemorrhageintheposteriorhornoftheright lateralventricle(Image2).
Anophthalmologistrecommendedtoinstillantibiotic(to preventasuperimposedbacterialinfection)andlubricanteye
Volume8,No.3:August2024
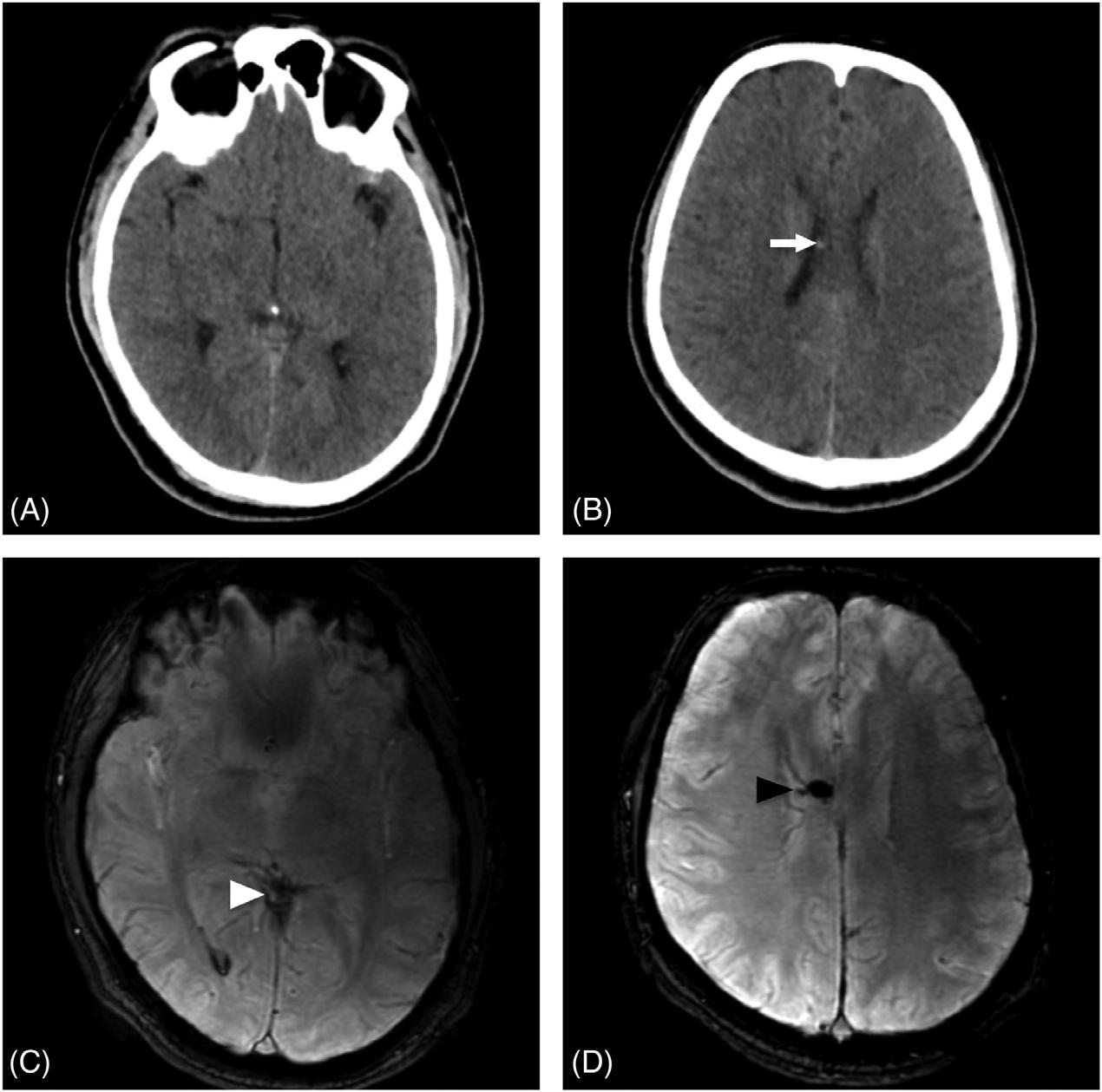
Image2. Non-contrastcomputedtomographybrainofa24-year-oldmale(axialview):a)withoutanyevidenceofIntraparenchymalinjury; b)showingtinyhemorrhagicfoci(whitearrow).Magneticresonanceimagingofthebrain(axial3-Dsusceptibility-weightedangiography)at thecorrespondingsectionshowed;c)bloomingfociintheposteriorhornoftherightlateralventricle(whitearrowhead)suggestiveofminimal intraventricularhemorrhage;d)bloomingfociinthebodyofcorpuscallosumontherightside(blackarrowhead),measuring6.0 × 8.0mm likelyminorhemorrhagiccontusion.
dropsintherighteyeandtodocoldcompressesovertheright eyethreetimesadayforoneweek.Arepeatevaluationtwo dayslatershowedthepupilsizetobe5mm, fixed,and dilated.Thiswasanimprovementcomparedtothe7mm notedintheED.Inaddition,thefundusexaminationofthe

Image3. Photographofthesamepatienttaken10monthsafterthe injury:a)persistenceofmildptosis(whitearrow)intherightupperlid atrest;b)improvementofptosis(whitearrowhead)onraising theeyebrows.
righteyewasnormal.Hewasadvisedtocontinuethesame treatmentandwasdischargedafterninedays.Overthenext 12months,heexperiencedpartialimprovementinsome aspectsofhisrightoculomotorfunction(Image3).
Apatientwhopresentswithblurringofvision,headache, diplopia,ptosis,evidenceoftrauma,andfocalneurological deficitspointsanemergencyphysiciantoapotentially alarmingsituation.Duetothisdiversepresentationand thevastdifferential,anoculomotornervepalsyencounter shouldbeginwithathoroughhistory,physicalexamination, andradiologicalinvestigation.
Traumaticinsults(eg,traumaticbraininjury[TBI], subduralhematoma,basilarskullfracture,brainherniation syndromes),autoimmuneexacerbations(eg,multiple sclerosis,myastheniagravis),vascularanomalies (eg,cerebrovascularaccidents,posteriorcommunicating arteryaneurysm,basilararteryaneurysm,subarachnoid hemorrhage),neoplasms(eg,pituitaryapoplexy,skull-based tumors),andinfections(eg,orbitalcellulitispredisposing acavernoussinusthrombosis)representtheemergent spectrumofthirdcranialnervepalsies.4
Previousstudieshaveemployed “theruleofthepupil” to determinehowradiologicalinvestigationsareexpeditedin suchcases.5 Thesubarachnoidlocationofthepupillary constrictor fibersmakesthemeasilycompressibleby posteriorcommunicatingorbasilararteryaneurysms. Therefore,thelackofpupilinvolvementwouldoftenpointto alessemergentconditionsuchasischemiasecondaryto diabetesmellitus.Similarly,frequentphysicalexaminations andliberalconsultationsleadtoclinicalclues(unilateralvs bilateralinvolvement,immediatevsdelayedpresentation, completevspartialextraoculardysfunction,signsofbasilar skullfracture,focalneurologicaldeficits,Cushingtriad)that helpruleoutemergentconditions.6
Inourcase,thepatientpresentedwithanisolatedrightsidedoculomotornervepalsyfollowingamildTBI.The absenceofaccompanyingred flags,signs,orsymptomsand thelackofexplanatoryradiological findingsmakethiscase unique.Contrastingly,inboththeSolomonsetaland Memonetalstudies,noisolatedthirdnervepalsycaseswere causedbymildheadinjury.3,7 Only0.04%oftraumatic oculomotornervepalsyhadbeenreportedbyastudydonein 19,800mildheadinjurycases.Inourcase,theimpactwasa directright-sidedfrontalblowwiththeradiographic finding thatdoesnotcorrelatewiththeclinicalpresentationof theTBI.8
However,theexactmechanismofisolatedoculomotor nervepalsycausedbymildTBIisnotprecise.Theinjuryto theoculomotornervecanoccuranywherealongitscourse fromthemidbraintoorbit.4 Threecriticalpartswhereitcan bedamagedareatthesitewherethenerveemergesfrom cerebralpeduncles,uponenteringthecavernoussinus,and withinthecavernoussinus.Whileindirectinjuries(resulting fromadisturbanceinbloodsupplyordetrimental biomechanicaleffectsfollowingaheadinjury)havebeen reportedtohaveahigherincidencethandirectinjuries (mechanicaldamage),informationisscarceon inconsequentialthirdnervepalsymanagementinsuch settings.Furthermore,suchpatientswouldhavedelayed presentation,whichwasnotthecaseinthisscenario.2
AccordingtoKaidoetal,arostrocaudallineofforceis generatedfollowingafrontalblow.Thedirectionisparallel tothethirdnerveandcancausetractionat fixationpoints, causingstretchingandintraneuralhemorrhage.9 The “ open Vformation” ofbothoculomotornerveslikelyprevents bilateraldirectthirdnerveinjury,andthatiswhyitisrarely observedclinically.7 Ashockwavegeneratedatthetimeof impactcanalsocausedamagetothethirdnerve.10 Diffusion tensorimagingand fibertractographyarerecentimaging techniquesthatcouldassesswhite fiberdamageandmayhelp usindiagnosing,predicting,andprognosticating oculomotornervepalsy.11
Itisuncommonto findatraumaticcauseofisolated oculomotornervepalsywithoutcorrelatingradiological findings.Multipositional,high-resolutionMRIwithT1-and
T2-weightedimagesinmostpatientswithsuspectedthird nervepalsymayshowabnormalenhancementofthe oculomotornervebecauseofischemia,inflammation,or demyelinatingconditions.1 Afewstudiesreported radiologicalevidenceofinjurytothenerveasitpassesover thetoughpetroclinoidligament.9,12 Incontrasttothe radiologicalfeaturespresentinthesestudies,our findingson MRIincludedaminorhemorrhagiccontusionoverthebody ofthecorpuscallosumontherightsideandminimal intraventricularhemorrhageintheposteriorhornoftheright lateralventriclethatneitherrevealedthecausenorlocation oftheinjury.Thelackofrelationbetweenimaging abnormalitiesandobservedclinical findingsgaveusan insightintotheotherprobablemechanismsofthirdnerve injuryinmildTBI.
Basedoncurrentevidence,theappropriatemanagement ofisolatedoculomotornervepalsycausedbymildTBIisstill unclear.Ourrecommendationwouldbe,tobeginwith,a non-contrastCTheadtodeterminetheneedforimmediate surgicalintervention(evacuationviaacraniotomyorburr holeorresectionofatumor)withorwithoutsteroids.1 If inconclusive,athree-dimensionalMRIofbrainandblood vessels(includingT1-andT2-weightedimages,magnetic resonanceangiography,anddiffusion-weightedimages) shouldbeconsidered.Inadditiontothis,Felixetalsuggested anisotropic,high-resolution,T2-weightedconstructive interferencesteadystate(CISS)sequenceandcontrastenhanced,axialandcoronalT1sequencestodetectdirect andindirectmechanismsofinjury.13
Similartothetreatmentrationaleinpatientswithdelayed facialnervepalsy,somestudieshavesuggestedusingsteroids asitreducesendoneurialedematopreventsecondary neuronaldamage.1,14 Asopposedtoothercases,therewasno indicationforsurgicaltreatmentinourpatient.Observation andfollow-uparethecornerstonesofmanagementin patientswithnodefiniteintracranial findings.Asimilar strategywasadoptedinourcase:instillingantibioticand lubricanteyedrops fivetimesadayandcoldcompressevery eighthours.Thepupilsizehadreducedfrom7mmto5mm onthefourthday,indicatingslightimprovement.Afew reportsintroducereading-relatedneurorehabilitationlike facialmassageandeye-trackingexercisesandinjecting botulinumtoxinintothelateralrectusmuscletoprevent contractureandmayreducethemorbidity.1,2
Theprognosisofthirdnervepalsyisgenerallypoor,with fullrecoverybeinguncommon,resultinginhighmorbidity.15 Ptosishasbeenreportedtoresolveearlierthanimpaired extraocularmusclemovement,whilethepupillarysizeand lightreflexshowtheleastdegreeofrecoveryfollowingthe courseofevents.Althoughthetimeintervaltoresolution varied,ourreviewrevealedthatpatientswhohadmildTBI withinitialGCSscoresof13ormoreexperiencedatleast partialresolution.Ourpatientexperiencedatleastpartial improvementinsomeaspectswithin12months(Image3).
Thepresenceof fixedanddilatedpupilsfollowingTBIin theemergencydepartmenthasbeenassociatedwithhigh mortality.However,wehighlighttheoccurrenceofisolated thirdnervepalsyinmildTBIwithnootherfocalneurological deficitsthroughthiscase.Althoughtheappropriate managementofisolatedoculomotornervepalsycausedby mildTBIisstillunclearbasedoncurrentevidence,areview ofmanagementandoutcomeshelpsestablishgoal-oriented treatmentplansandrehabilitation.Moreover,westressthe importanceofacomprehensiveclinicalassessment.Also,we recommendradiologicalimagingtestsregardlessofinjury severitytoassessthecauseofdamagetoplanfortreatment andimproveprognosticoutcomes.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
AddressforCorrespondence:SanjanAsanaruKunju,MD,DNB, DepartmentofEmergencyMedicine,KasturbaMedicalCollege, Mangalore,ManipalAcademyofHigherEducation,Manipal, Karnataka,India-576104,India.Email: sanjan.a@manipal.edu; sanjan.asanar@gmail.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Daswaneyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KimEandChangH.Isolatedoculomotornervepalsyfollowingminor headtrauma:caseillustrationandliteraturereview. JKoreanNeurosurg Soc. 2013;54(5):434.
2.MuthuPandPrittyP.Mildheadinjurywithisolatedthirdnervepalsy. EmergMedJ. 2001;18(4):310–1.
3.MemonMYandPaineK.Directinjuryoftheoculomotornervein craniocerebraltrauma. JNeurosurg. 1971;35(4):461–4.
4.UbertiM,HasanS,HolmesD,etal.Clinicalsignificanceofisolated thirdcranialnervepalsyintraumaticbraininjury:adetaileddescriptionof fourdifferentmechanismsofinjurythroughtheanalysisofour caseseriesandreviewoftheliterature. EmergMedInt. 2021;2021:5550371.
5.WoodruffMMandEdlowJA.Evaluationofthirdnervepalsyinthe emergencydepartment. JEmergMed. 2008;35(3):239–46.
6.BalcerLJ,GalettaSL,BagleyLJ,etal.Localizationoftraumatic oculomotornervepalsytothemidbrainexitsitebymagneticresonance imaging. AmJOphthalmol. 1996;122(3):437–9.
7.SolomonsNB,SolomonDJ,deVilliersJC.Directtraumaticthirdnerve palsy. SAfrMedJ. 1980;58(3):109–11.
8.CoelloAF,CanalsAG,GonzalezJM,etal.Cranialnerveinjuryafter minorheadtrauma. JNeurosurg. 2010;113(3):547–55.
9.KaidoT,TanakaY,KanemotoY,etal.Traumaticoculomotornerve palsy. JClinNeurosci. 2006;13(8):852–5.
10.DhaliwalA,WestAL,TrobeJD,etal.Third,fourth,andsixthcranial nervepalsiesfollowingclosedheadinjury. JNeuroophthalmol. 2006;26(1):4–10.
11.JacquessonT,FrindelC,KocevarG,etal.Overcomingchallengesof cranialnervetractography:atargetedreview. Neurosurgery. 2019;84(2):313–25.
12.TakeuchiS,TakasatoY,MasaokaH,etal.Isolatedtraumatic oculomotornervepalsycausedbyminorheadtrauma. BrainNerve ShinkeiKenkyuNoShinpo. 2008;60(5):555–8.
13.EisenhutF,GernerST,GoelitzP,etal.High-resolutionmagnetic resonanceimaginginisolated,traumaticoculomotornervepalsy:acase report. RadiolCaseRep. 2021;16(2):384–8.
14.NakagawaY,TodaM,ShibaoS,etal.Delayedandisolatedoculomotor nervepalsyfollowingminorheadtrauma. SurgNeurolInt. 2017;8:20.
15.ChenC,PaiY,WangR,etal.Isolatedoculomotornervepalsyfrom minorheadtrauma. BrJSportsMed. 2005;39(8):e34.
ClaytonKorson,MD*
JasmineYu,BS†
JohnM.Pester,DO*
SectionEditor:LevLibet,MD
*St.Luke’sUniversityHealthNetworkEmergencyDepartment,Bethlehem,Pennsylvania † RockyVistaUniversityCollegeofOsteopathicMedicine,Parker,Colorado
Submissionhistory:SubmittedOctober19,2023;RevisionreceivedApril18,2024;AcceptedMay3,2024
ElectronicallypublishedJuly31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.3259
Introduction: Pulmonarysequestrationisararelyreportedphenomenonwhereaberrantlungtissue existsindependentlyfromtherestofthetracheobronchialnetwork.Complicationsmayinclude hemothorax;however,thereisapaucityofdescriptionsofthisconditionintheliterature.
CaseReport: Wedescribeacaseofapulmonaryintralobarsequestrationresultinginatraumatic tensionhemothorax.A73-year-oldwomanpresentedtoourfacilityinextremisandwithcomplaintsof acute-onset flankpain.Herevaluationwasnotableforalargepulmonarysequestrationwithapresumed, moderate-sizedeffusion;however,initialreviewdidnotrevealanobviousunderlyingcauseforher symptoms.Shortlyafterherarrivaltotheemergencydepartment(ED)sheexperiencedacardiacarrest. Onsecondaryreviewofhercomputedtomographicangiography,itwasdeterminedthatwhatwas previouslythoughttobeapleuraleffusionwasalargehemothorax.Followingthis finding,a finger thoracostomywasperformed,whichresultedintheimmediateevacuationofhemothorax.The thoracostomywasthenconvertedintoanEDthoracotomytoassessforactivehemorrhagewithbrief returnofspontaneouscirculation.Priortoproceedingwithemergentoperativeintervention,thepatient’s spouserequestedthatallfurtherresuscitativeeffortscease,andthepatientwasallowedtoexpire.Ina reviewofthecase,itwasdeterminedthatthepatientsufferedfromcardiacarrestduetoaspontaneous hemothoraxsecondarytoalargeintralobarpulmonarysequestration.
Conclusion: Pulmonaryintralobarsequestrationcanresultinspontaneoushemorrhagewithfatal results.EarlyandcorrectinterpretationofimagingandsurgicalinterventionarecrucialinED management.[ClinPractCasesEmergMed.2024;8(3)287–290.]
Keywords: hemothorax;tension;thoracotomy;intralobar;sequestration.
Pulmonarysequestrationisarareabnormalityinwhich non-functionallungtissueexistsinisolationfromtherestofthe tracheobronchialtreeandreceivesananomalousbloodsupply fromthesystemiccirculation.1 Coughisthemostcommonly describedpresentingsignwithhemoptysisnotedinsevere cases;however,mostpatientsareasymptomatic.1,2 Intralobar pulmonarysequestration(IPS)asacauseofhemothoraxisa rarelyreportedentity.3–6 Wepresentanuncommoncase ofIPScomplicatedbyatraumatichemothoraxrequiring emergencythoracotomyforstabilization.
A73-year-oldwomanpresentedtoourfacilitywith complaintsofsuddenonset,left-sided flankpain.Thepain beganshortlypriortoarrival.Itwassharpinnatureand locatedintheleft flankregionwithinitialradiationofpain fromherleftcollarbonedowntoherpelvis.Later,she describedthepainasradiatingtothemidthoracicspine.Of note,shehadacomplexpastmedicalhistorythatincluded transcatheteraorticvalvereplacement,chronicheartfailure withareducedejectionfraction,leftintralobarpulmonary sequestration,coronaryarterydisease,hypertension,and
biventricularpacemaker.Shealsohadchronicosteomyelitis ofhersternumstatuspostwashoutwithanantibioticcourse.
Onarrival,thepatientappearedcriticallyill,diaphoretic, andclammy.Herinitialvitalsignsincludedabloodpressure of93/57millimetersofmercury,oxygensaturationof90%on roomair,respiratoryrateof26breathsperminute,heartrate of60beatsperminute,andatemperatureof36.7° Celsius. Onphysicalexam,thepatientwasill-appearing,diaphoretic, anduncomfortable.Shewasalertandorientedandexhibited noneurologicaldeficits.Heartsoundswereregularwithout evidenceofrubsormurmurs.Herlungswereclearto auscultationbilaterally.Shehad2+ pulsesinallfour extremitieswithoutevidenceofbruits,thrills,mottling,or cyanosis.Hercapillaryrefillwaslessthantwoseconds.She hadnoevidenceofecchymoses,deformities,orrashes.
Immediatelyaftertheinitialevaluation,abroad evaluationwasobtained,whichincludedanemergent computedtomographyangiography(CTA)toevaluatefor aorticdissection,anelectrocardiogram(ECG),troponin, completebloodcount,metabolicpanel,lipase,and hydromorphoneforpaincontrol.HerECGwasnotablefora biventricularlypacedrhythm,atarateof103,withfrequent prematureventricularcomplexesandwithoutevidenceof acuteischemia.TheCTAwasreviewedinrealtime(Image1) andshowednoevidenceofacuteaorticpathology.
Shedidhavealarge,complex,heterogeneousleft intralobarmass,consistentwithherknownpulmonary sequestration,aswellaswhatwaspresumedtobea moderate,left-sidedpleuraleffusion.Uponreviewingreports fromanoutsidehospital(withouttheabilitytoviewthe

Whatdowealreadyknowaboutthis clinicalentity?
Intralobarpulmonarysequestration(IPS) occurswhenlungtissueisperfusedby systemiccirculationratherthanfrom pulmonarycirculation.
Whatmakesthispresentationof diseasereportable?
Althoughrare,fatalhemorrhageduetoIPS canoccur.Themostcommonpresentationsof IPSarecoughandrecurrentpneumonia.
Whatisthemajorlearningpoint?
IPSmaycauserapidhemorrhageresulting incardiovascularcollapseduetotension hemothora,orexsanguination.Earlysurgical interventionmaybenecessary.
Howmightthisimproveemergency medicinepractice?
Cliniciansshouldbeawarethatfatal hemorrhagecanresultfromIPS. Resuscitativethoracotomycanaidin decompressionoftensionhemothoraxand hemorrhagecontrol.
actualimages),itwasdeemedthatthese findingswere chronicinnatureandunchanged.AdelayedsequenceCTA wasobtainedshortlyafter,whichdidnotshowevidenceof blushoninitialreview(Image2).
Herlaboratoryworkupwasnotableforawhitebloodcell countof12.54 × 103 cellspermicroliter(μL)(referencerange 4.5–11 × 103 cells/μL).hemoglobinof13.5gramsperdeciliter (g/dL)(12.1–15.1g/dL),bloodsugarof161milligrams (mg)/dL(70–100mg/dL),andahighsensitivitytroponin of9nanogramsperliter(ng/L)(0–4ng/L).
Thepatientcontinuedtodeteriorate,becoming progressivelymorediaphoretic.RepeatECGshoweda biventricularlypacedrhythm,rateof121,withoutevidence ofacuteischemia.Givenherworseningstatus,cardiology wasconsultedforpossibleacutecoronarysyndrome(ACS) thatmayhavebeenmaskedbyherventricularlypaced rhythm.Whilecardiologywasintheprocessofobtaininga transthoracicechocardiogramtoassessforregional wallmovementabnormalities,thepatientwentinto cardiacarrest.Cardiopulmonaryresuscitationwasstarted usingstandardAdvancedCardiacLifeSupport(ACLS) protocol.Duetoalargevolumeofemesis,esophageal

diversionintubationwasperformed,followedby endotrachealintubation.
TheACLSwascontinuedforapproximately20minutes withoutreturnofspontaneouscirculation.Systemic thrombolyticswereconsideredforpresumedACS.Priorto

Image3. Computedtomographyangiographyaxialimage. Delayedsequenceimagingdemonstratingswirling contrastwithinthehemothorax,consistentwithactive hemorrhage(arrows).
administrationofthrombolytic,however,herCTAwas reviewedagain,andablushwasnoted.Whatwaspreviously thoughttobeapleuraleffusionwasactuallyalarge hemothoraxwithactivehemorrhage(Image3).Giventhis finding,a fingerthoracostomywasperformedontheleftside, whichresultedintheimmediateexpulsionofalargevolume ofblood.Thisprocedurewasthenconvertedintoan emergentthoracotomytoassessforsourceofhemorrhage andresultedintheevacuationofapproximately500 millilitersofadditionalblood.Amassivetransfusion protocolwascommenced,acutecaresurgeryarrivedatthe bedside,andreturnofspontaneouscirculationwasachieved.
Priortoproceedingwithfurthersurgicalintervention, goalsofcarewerediscussedwiththepatient’shusbandwho wishedtoceaseallfurtheraggressivemanagement.The patientexpiredthereafter.
Inreview,itwasdeterminedthatthepatientsufferedfrom cardiacarrestduetoaspontaneous,atraumatichemothorax secondarytoalarge,hemorrhagicIPS.
Pulmonarysequestrationisarareconditioninwhicha segmentofabnormallungtissueexistswithnoidentifiable tracheobronchialcommunicationandreceivesitsarterial bloodsupplyfromthesystemiccirculation.Pulmonary sequestrationisfurtherdividedintoextralobularand intralobularsequestration.Inextralobarpulmonary sequestration,thelungmassisenclosedinitsownpleuralsac, whereasinIPSthemasslieswithinthevisceralpleura.1
LiteraturereviewofIPScasereportsdescribecoughand recurrentrespiratoryinfectionasthemostcommon presentingsymptoms.2 Inonlyafewpublishedcaseshas hemothoraxbeenreportedasacomplicationofIPS,likely causedbyspontaneousruptureofanarteryfeedingthe anomalouspulmonarytissue.3–6 Theliteraturesupportsthe useofcomputedtomographicangiographyforthediagnosis ofpulmonarysequestrationanddemonstrationofthe arterialsupply.Perpriorreports,themostcommonsiteof intrapulmonarytypesequestrationistheleftlowerlobeofthe lung,whichisconsistentwithourpatient’ s findings.7 Ofthe reportedcasesthatdescribehemothoraxasarare presentationofIPS,twodescribetheuseofemergency thoracotomyto findtheoriginofbleedingandtoachieve hemostasisinemergentcaseswithpatientspresentingwith massiveintrapulmonaryhemorrhageandinshock.3,4 Followinginitialstabilizationmeasures,allstudies describingIPScomplicationsadvocateforresection ofthesequesteredtissueforpreventionoffuturemajor medicalcomplications.
Thiscasereportdescribesararepresentationofintralobar pulmonarysequestrationwithspontaneoushemothorax resultingincardiacarrest.Earlydiagnosisandresectionof
theabnormallungtissueshouldbeconsideredinallpatients with findingsofpulmonarysequestration.Ourcasealsoadds totheliteraturearareinstancewhereemergencydepartment thoracotomyshouldbeconsideredtoaidinthestabilization ofamedicalpatient.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:JohnPester,DO,St.Luke’sUniversity HealthNetwork,EmergencyMedicineResidency,801Ostrum Street,Bethlehem,PA18015.Email: Jonathan.pester@sluhn.org
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Korsonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ChakrabortyRK,ModiP,SharmaS.Pulmonarysequestration. [Updated2023Jul24].In StatPearls [Internet].TreasureIsland(FL): StatPearlsPublishing.2024.Availableat: https://www.ncbi.nlm.nih.gov/ books/NBK532314/.AccessedJuly2,2024.
2.YoshitakeS,HayashiH,OsadaH,etal.Emergencylaparotomyhelped theresectionofanintralobarpulmonarysequestrationwith haemorrhagicshock. EurJCardiothoracSurg. 2013;43(1):190–2.
3.HofmanFN,PaskerHG,SpeekenbrinkRG.Hemoptysisandmassive hemothoraxaspresentationofintralobarsequestration. AnnThorac Surg. 2005;80(6):2343–4.
4.IliásL,PálffyG,Sz´onyiP,etal.Massivehaemothoraxcausedby intralobarpulmonarysequestration. OrvHetil. 1996;137(23):1263–5.
5.ZapateroJ,BaamondeC,BellánJM,etal.Hemothoraxasrare presentationofintralobarpulmonarysequestration. ScandJThorac CardiovascSurg. 1983;17(2):177–9.
6.ArsalaneA,ParrotA,AssouadJ,etal.Spontaneoushemothorax:arare butseriouscomplicationofintralobularpulmonarysequestration. RevPneumolClin. 2006;62(1):30–3.
7.SavicB,BirtelFJ,TholenW,etal.Lungsequestration:report ofsevencasesandreviewof540publishedcases. Thorax. 1979;34(1):96–101.
GregoryOliva,DO*
JosephMcShannic,MD*
YonghoonLee,MD* MichaelShalaby,MD†
*MountSinaiMedicalCenterMiamiBeach,DepartmentofEmergencyMedicine, MiamiBeach,Florida † HerbertWertheimCollegeofMedicineatFloridaInternationalUniversity, DepartmentofEmergencyMedicineandCriticalCare,MiamiBeach,Florida
SectionEditor:R.GentryWilkerson,MD
Submissionhistory:SubmittedJanuary11,2024;RevisionreceivedMay6,2024;AcceptedMay6,2024
ElectronicallypublishedJuly11,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7194
Introduction: Carpaltunnelsyndromeisanentrapmentneuropathythataffects3%ofadultsinthe UnitedStates.Thecurrenttechniquesusedfordiagnosishavelimitedspecificity/sensitivity,andthe techniquesusedfortreatmenthavelimitedefficacy.
CaseReport: A34-year-oldfemalepresentedtotheemergencydepartmentwithtwomonthsof worseningpainfulparesthesiasinherrightthenareminence.Ultrasoundwasperformedshowinga mediannerveareaof20.4squaremillimeterswithinthecarpaltunnel.Mediannerveblockwas performedwithinthecarpaltunnelcausingcompleteresolutionofherpain.
Conclusion: Emergencyphysiciansskilledinpoint-of-careultrasoundandneedle-guidedprocedures candiagnoseandtreatcarpeltunnelsyndrome.[ClinPractCasesEmergMed.2024;8(3)291–294.]
Keywords: carpaltunnelsyndrome;mediannerve;ultrasound;steroidinjection;casereport.
Carpaltunnelsyndrome(CTS)isacommonentrapment neuropathycausedbycompressionofthemediannerveasit travelsthroughthewristwithinthecarpaltunnel.Carpal tunnelsyndromeaccountsfor90%ofallentrapment neuropathiesandaffects3%ofadultsintheUnitedStates.1 Carpaltunnelsyndromeinducespain,numbness,and paresthesiasalongthepalmaraspectsofthe first,second, third,andlateralportionofthefourthdigit,aswellasthe thenareminence.Inadvanceddisease,symptomsprogressto weaknessofthumbabduction,decreasedgripstrength,and thenaratrophy.1 Whilethediagnosisisclinicalandis supportedby findingssuchasTinelsign(percussionof proximalwristcausingparesthesias)andPhalensign (holdingwristsin60degreesof flexionelicitingsymptoms), physicalexammaneuvershavealowsensitivityand specificity.2 Thegoldstandardforconfirmationofthe diagnosisisanerveconductionstudy.3
Ultrasound(US)measurementsofthemediannervecan beusedtoassesssymptomaticpatients,revealinganenlarged
nerveareainindividualswithCTS.4 Numerousstrategies havebeenemployedtoalleviatethesymptomsofCTS.These includediuretics,pyridoxine,non-steroidalantiinflammatorydrugs,yoga,steroidinjections,UStherapy, andacupuncture.5 Thesetechniquescandecrease inflammationandprovidesomereliefbutdonotalways causecompleteresolutionofpain.Herein,wedescribea patientwithnew-onsetCTSwhosetreatmentinthe emergencydepartment(ED)withcombinedlocalanesthetic andcorticosteroidinjectionprovidedcompletereliefof symptoms.Thisisthe firstcasereportdetailingtheutilization ofultrasound-guidedmediannerveblockintheEDsetting.
A34-year-oldfemalepresentedtotheEDwithtwo monthsofworseningpainfulparesthesiasinherrightthenar eminence.Onphysicalexam,positiveTinelandPhalensigns werenoted,alongwithreducedsensationofthepalmar aspectofher firstthreedigits.Muscularstrengthwas5/5in bilateralupperextremities.Thedifferentialdiagnoses
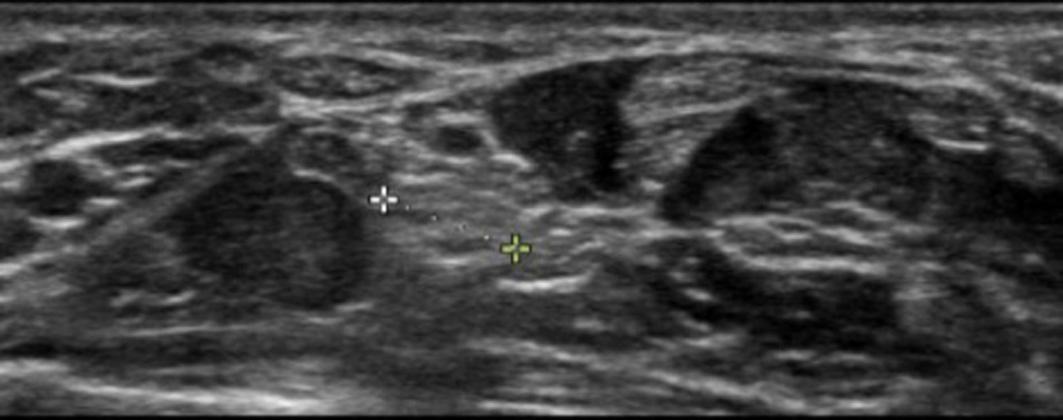
Image1. Enlargeddiameterofthemediannervewithinthecarpal tunnel,measuring5.1millimeters,whichcorrespondstoanareaof 20.4squaremillimeters.
encompassedcervicalradiculopathy,thoracicoutlet syndrome,pronatorteressyndrome,andanterior interosseousneuropathy.Consideringthesymptomlocation andabsenceofsensoryalterations,weakness,ortenderness proximaltothewrist,theleadingexplanationwas compressionofthemediannervewithinthecarpaltunnel. Ultrasoundwasperformedshowingamediannerveareaof 20.4squaremillimeters(mm2)(referencerange8.5–10mm2) withinthecarpaltunnel(Image1).
Thepatientconsentedtoamediannerveblock,whichwas performedwithinthecarpaltunnelwith10milliliters(mL)of 0.25%bupivacaineand1mLof40milligrams(mg)/mL triamcinolone.Aftertheprocedure,thepatientdeveloped completeresolutionofherpain.Shewasplacedinawrist splintanddischargedhomewithinformationforhand surgeryfollow-up.Despitenumerousphonecalls,thepatient wasunfortunatelylosttofollowup.
Themediannervearisesfromtheanterolateraland anteromedialcordsofthebrachialplexusandcomprisesthe sixthcervicalto firstthoracicnerveroots.6 Distally,thenerve coursesdeeptothe flexorretinaculumandentersthecarpal tunnel,travelinginananteriorandlateraldirection alongsidethetendonsofthe flexordigitorumsuperficialis.6 It isatthispointthatentrapmentismostcommon.Beyondthe carpaltunnel,itdividesintoamotorbranchthatservesthe thenarcompartment,aswellasthe firstandsecond lumbricals,andasensorybranchthatdividesintofour palmarbranchesforthe fingers. 6 Toperformamediannerve blockwithinthecarpaltunnel,thenerveis firstidentified betweenthe flexordigitorumsuperficialisand flexor digitorumprofundus,andthentraceddistallytoitsposition withinthecarpaltunnel.7 Onceatthisposition,thenervecan beidentifiedmedialtothe flexorcarpiradialisandlateralto thepalmarislongus(Image2).
Anin-planeapproachisusedtoadvancetheneedlebefore instillinglocalanestheticaroundthenerve.Usually, ≤5mL localanestheticsufficesformediannerveblockade.Local anestheticssuchasbupivacaineandropivacaineprovide longerpainreliefandare,therefore,preferredover
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Carpaltunnelsyndrome(CTS)isprevalent, affecting3%ofadultsintheUnitedStates, butdiagnosisandtreatmentmethodsare limitedinef fi cacy.
Whatmakesthispresentationof diseasereportable?
Mediannerveblockintheemergency department(ED)ef fi cientlyaidsindiagnosis andrelievesnewlydiagnosedCTS.
Whatisthemajorlearningpoint?
Emergencyphysiciansskilledinpoint-of-care ultrasoundandneedle-guidedprocedurescan diagnoseandtreatCTSeffectively.
Howmightthisimproveemergency medicinepractice?
EarlyEDdiagnosisallowsforprompt intervention,potentiallyimproving patientoutcomes.
lidocaine.7 Whilephysiciansinotherspecialtieshave previouslyemployedthisprocedure,thiscasereport representsthe firstdocumentationofultrasound-guided

Image2. Theexternalanatomyofthewristforoptimalultrasoundguidedneedleplacementisillustratedasfollows:thebluecircle denotestheneedleinsertionsite,whilethepinkboxrepresents theplacementoftheultrasoundprobe.Additionally,thered, yellow,andorangeboxesindicatethepositionsofthe flexorcarpi radialis,mediannerve,andpalmarislongus,respectively.
mediannerveblockbeingusedinanEDsetting.Ingeneral, mediannerveareaofgreaterthan8.5–10mm2 atthe midchannelisassociatedwithCTS.4 Inourcase,we calculatedthemediannerveareatobe20.4mm2.Withthese findings,wededucedthatthenervewasexhibitingsigns ofinflammation.
Carpaltunnelsyndromeisapainfulconditionaffecting >8millionpeopleyearly.8 Carpaltunnelreleaseisthesecond mostcommontypeofmusculoskeletalsurgerywithover 230,000casesannually.8 Whiletheprocedurecanbeeffective atrelievingpain,itisinvasiveandcostly,andresultsare poorerforpatientswithlongstandingdisease.9 Patientswith operativeinterventionearlierinthecourseofthediseasehave beenshowntohavebetteroutcomes.9 Toreferpatientsfor treatmentinatimelyfashion,thediagnosismustbetimely. Whilediagnosisisusuallymadeclinically,calculationofthe mediannervecross-sectionalareaandnerveblockadecan provideadefinitivediagnosisandtimelyanalgesia. Furthermore,instillingcorticosteroidwithinthesheathcan provideprolongedanalgesia.Theintroductionof dexamethasonehasbeenobservedtoresultinprolonged nerveblockdurations,reducedopioidrequirements,andan extendedtimeuntilthenextanalgesicdoseisneeded.10–12 Whendecidingwhethercorticosteroidsshouldaccompany localanestheticsfornerveblocks,thechoiceshould hingeonthedesireddurationoftheblockadeand considerationsofcontraindications.Accordingtothe AmericanSocietyofRegionalAnesthesiaandPain Medicine,dexamethasoneisamongthefrequentlyused agentsforextendinganalgesia.However,official recommendationsareimpededbythelowqualityand clinicaldiversityofpublishedtrials.13
Ultrasoundguidancefacilitatesmediannerveblockadeby allowingemergencyphysicianstofeasiblyandprecisely targetthemediannervewithinthecarpaltunnel.Therefore, insteadofperformingamediannerveblockintheusualmidforearmlocation,weoptedtoinstillanestheticaroundthe nervewithinthecarpaltunneltoincludeacorticosteroidat thesiteofcompression.Moreover,injectionofanesthetic directlyintothecarpaltunnelhasbeenshowntoprovide improvedsymptomseverityandfunction.14
Nerveblocksmayentailvariouscomplications,suchas neuronaldamage,bleeding,andlocalanestheticsystemic toxicity(LAST)syndrome.15 Peripheralnerveinjuryisan infrequentoutcome,withanestimatedincidenceranging from0.5 –1.0%. 15 Althoughnerveinjuryencompassesa spectrumofissues,permanentnervedamageoccursin approximately1.5casesper10,000. 15 Inadvertentvascular punctureposesrisksofbleedingwithhematomaformation or,iftheanestheticentersthevessel,triggeringLAST syndrome.15 SymptomsofLASTsyndromecanrangefrom mild,suchascircumoralnumbness,metallictaste,and auditorychanges,tosevere,includingseizures,coma, respiratoryarrest,hypotension,ventriculararrhythmias,
andcardiacarrest. 15 Recentstudiessuggestthat usingUSguidancereducesthelikelihoodof inadvertentvascularpuncture,therebymitigating thesecomplications.15
Whiledexamethasoneiscommonlyemployedtoextend analgesia’sdurationinperipheralnerveblocks,itsusageis cautionedagainstindiabeticpatientsduetotheassociated hyperglycemicresponse.16 Absolutecontraindicationsfor corticosteroidinjectionincludelocalinfection,sepsis,and bacteremia,astheyposerisksofinfectiondissemination. Relativecontraindicationsincludejuxta-articular osteoporosisduetoconcernsaboutexacerbatingbone densityloss,coagulopathy,andinjectionsthreetimes annuallyorwithinasix-weekperiod.17
Mediannerveblockisaneffectiveandefficientwayto bothdiagnoseandprovidereliefofnewlydiagnosedcarpal tunnelsyndromethatpresentstotheED,andemergency physiciansshouldconsiderusingitwithintheirpractice forsuch.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:GregoryOliva,DO,MountSinai MedicalCenterMiamiBeach,DepartmentofEmergencyMedicine, 4300AltonRd.,MiamiBeach,FL33140.Email: gregory.oliva@ msmc.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Olivaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SevyJO,SinaRE,VaracalloM.CarpalTunnelSyndrome.[Updated 2023Oct29].In: StatPearls [Internet].TreasureIsland(FL):StatPearls Publishing;2024.Availableat: https://www.ncbi.nlm.nih.gov/books/ NBK448179/.AccessedApril14,2024.
2.ArabAA,ElmaghrabiMM,EltantawyMH.Carpaltunnelsyndrome: evaluationofitsprovocativeclinicaltests. EgyptJNeurosurg. 2018;33(14):14.
3.RosarioNBandDeJesusO.ElectrodiagnosticEvaluationofCarpal TunnelSyndrome.[Updated2023Aug23].In: StatPearls [Internet]. TreasureIsland(FL):StatPearlsPublishing;2024.Availableat: https:// www.ncbi.nlm.nih.gov/books/NBK562235/.AccessedApril14,2024.
4.CartwrightMS,Hobson-WebbLD,BoonAJ,etal.Evidence-based guideline:neuromuscularultrasoundforthediagnosisofcarpaltunnel syndrome. MuscleNerve. 2012;46(2):287–93.
5.EbenbichlerGR,ReschKL,NicolakisP,etal.Ultrasoundtreatmentfor treatingthecarpaltunnelsyndrome:randomised “sham” controlledtrial. BrMedJ. 1998;316(7133):731–5.
6.MeyerP,LintingrePF,PesquerL,etal.Themediannerveatthecarpal tunnel andelsewhere. JBelgSocRadiol. 2018;102(1):17.
7.PesterJM,BechmannS,VaracalloM.MedianNerveBlockTechniques. [Updated2023Aug4].In: StatPearls [Internet].TreasureIsland(FL): StatPearlsPublishing;2024.Availableat: https://www.ncbi.nlm.nih.gov/ books/NBK459141/.AccessedApril14,2024.
8.AmericanAcademyofOrthopedicSurgeons.11astoundingcarpal tunnelstatistics.2019.Availableat: https://www.orthoarlington.com/ contents/patient-info/conditions-procedures/11-astoundingcarpal-tunnel-statistics.AccessedNovember16,2023.
9.MasudM,RashidM,MalikSA,etal.Doesthedurationand severityofsymptomshaveanimpactonreliefofsymptoms aftercarpaltunnelrelease? JBrachialPlexPeripherNerveInj. 2019;14(1):e1–8.
10.BrusichKT.Corticosteroidsasadjuvantsforperipheralnerveblocks:a minireview. IntJAnaesthRes. 2018;1(1):14–7.
11.RasmussenSB,SaiedNN,BowensC,etal.Durationofupperandlower extremityperipheralnerveblockadeisprolongedwithdexamethasone
whenaddedtoropivacaine:aretrospectivedatabaseanalysis. PainMed. 2013;14(8):1239–47.
12.GianniniF,PasseroS,CioniR,etal.Electrophysiologicevaluationof localsteroidinjectionincarpaltunnelsyndrome. ArchPhysMed Rehabil. 1991;72(10):738–42.
13.RanganathYS,SeeringMS,MarianAA.Curbyourenthusiasm:local anestheticadjuvantsforperipheralnerveblocks.2020.Availableat: https://www.asra.com/news-publications/asra-newsletter/curb-yourenthusiasm/asra-news/2020/11/01/curb-your-enthusiasm-localanesthetic-adjuvants-for-peripheral-nerve-blocks AccessedApril14,2024.
14.KarimzadehA,EsmailyH,RaeissadatSA,etal.Comparisonofthe effectofintracarpalinjectionofketorolacwithtriamcinoloneincarpal tunnelsyndrome:Arandomizedcontrolledtrial. AnnPharmacother. 2024;58(3):205–13.
15.JengCL,TorrilloTM,RosenblattMA.Complicationsofperipheralnerve blocks. BrJAnaesth. 2010;105(1):i97–107.
16.WilliamsBA,MurinsonBB,GrableBR,etal.Futureconsiderations forpharmacologicadjuvantsinsingle-injectionperipheralnerve blocksforpatientswithdiabetesmellitus. RegAnesthPainMed. 2009;34(5):445–57.
17.SimurinaT,MraovicB,ZupcicM.Localanestheticsandsteroids: contraindicationsandcomplications – Clinicalupdate. ActaClinica Croatica. 2019;58(1):53–61.
SatoshiTsuruta,MD
TakashiFujiwara,MD,PhD
SectionEditor:ManishAmin,MD
KurashikiCentralHospital,DepartmentofOtolaryngology,Kurashikicity, Okayama,Japan
Submissionhistory:SubmittedSeptember29,2023;RevisionreceivedMay14,2023;AcceptedMay16,2023
ElectronicallypublishedJune6,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.21313
CasePresentation: A57-year-oldmanwithahistoryofbronchialasthmaandeosinophilic sinusitispresentedtotheemergencydepartmentwithanexacerbationofotitismedia.Hisprimary complaintswereotopyorrhea,headache,andneckpainwithredness.Contrast-enhancedcomputed tomographyrevealedaposteriorneckabscesscontiguouswiththemastoidprocess.Thepatient underwentmastoidectomyandreceivedantimicrobialtherapy.Eosinophilicgranulationtissueinthe middleearobstructedthemiddleearaditusanddirectedtheinflammatoryprocesstowardthe mastoidtip.
Discussion: Bezoldabscessisarareextracranialcomplicationofacutemastoiditis.Therefore, cliniciansshouldconsiderneckpainwithrednessasanimportantphysicalsignthatsuggestsBezold abscessinpatientswithotitismedia.[ClinPractCasesEmergMed.2024;8(3)295–297.]
Keywords: Mastoiditis;otitismedia;abscess;eosinophilicotitismedia.
A57-year-oldmanwithahistoryofbronchialasthma andeosinophilicsinusitispresentedtotheemergency departmentwithanexacerbationofotitismedia.Hehad previouslyreceivedtreatmentwithtympanostomyand antimicrobialtherapyforacuteotitismediaofhisrightear, buthisconditiondidnotimprove.Heexperienced otopyorrhea( Image1),worseningpaininhisrightearand neckwithredness,headache,andimpairedconsciousness. Contrast-enhancedcomputedtomographyrevealed bilateralotitismedia,thrombosisfromtherightinternal jugularveintothesigmoidsinus,andaposteriorneck abscesscontiguouswiththemastoidprocessontheright side( Image2).
Thepatientunderwentmastoidectomyandwastreated withantimicrobialandantithrombotictherapies.During surgery,itwasfoundthattherightmiddleearwas filledwith eosinophilicgranulationtissue,withtheformationofapath betweenthemastoidpartofthetemporalboneandthe posteriorneck(Image3).Intraoperativeintratympanic steroidadministrationeliminatedthegranulationtissuea fewdaysafterthesurgery.Thepatientwastreatedwith antimicrobialtherapyforsixweeks.Hewasdischargedwith higherfunctionalimpairmentandgaitdisturbance.

Image1. Otoscopicviewofthemiddleeardemonstrating anerythematous,bulgingtympanicmembranewith purulenteffusion.
However,hecontinuedhisrehabilitationandcoulddrive twomonthsafterdischarge.Furthermore,thepatient successfullyreintegratedintosocietyandwasfoundto beingoodhealthoneyearlater.
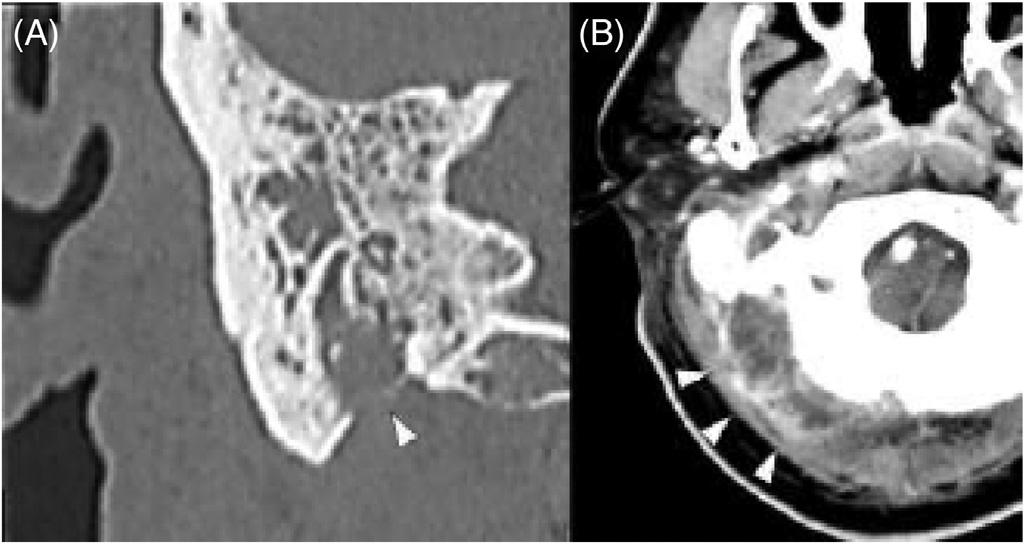
Image2. (A)Computedtomography(CT)ofthemastoidwith intravenous(IV)contrastshowingmastoidprocessperforation (arrowhead);(B)CToftheneckwithIVcontrastdemonstratinga posteriorneckabscess(arrowheads).

Image3. Intraoperativeimagesduringmastoidectomy.(A)Before mastoidectomy:Drainageofpusfromthemastoidprocesswas observed(arrowheads).(B)Aftermastoidectomy:Thedashed whitelinerepresentstheposteriorwalloftheearcanal,whereas thedashedyellowlineindicatesthemastoidtip.Apathbetween themastoidantrumandneckisvisible(arrowhead),through whichsurgicalinstrumentscouldbeinsertedfromthenecktothe mastoidantrum.
Bezoldabscess,arareextracranialcomplicationofacute mastoiditis,occurswhenaninfectionerodesthroughthelateral mastoidcortexmediallytowardtheneck.Althoughthe incidenceofBezoldabscesshasdecreasedwiththe developmentofantimicrobialagentsandimprovednutrition,
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Patientswithmiddleeardisease,particularly cholesteatoma,areathighriskofdeveloping Bezoldabscess.
Whatisthemajorimpactoftheimage(s)?
Thisisthe fi rstreportedcaseofBezold abscessduetoeosinophilicotitismedia.
Howmightthisimproveemergency medicinepractice?
Emergencyphysiciansshouldrecognizethat eosinophilicotitismediacancausethecondition.
individualswithmiddleeardisease,particularlycholesteatoma, remainatahigherriskofdevelopingthiscondition.The presenceofmiddleeardisease(eg,cholesteatoma)canobstruct themiddleearaditusanddirecttheinflammatoryprocess towardthemastoidtip.Inthepresentcase,Bezoldabscess occurreddespitetheadministrationofappropriate antimicrobialagentsandtympanostomy.
Thepatienthadahistoryofbronchialasthmaand eosinophilicsinusitis,leadingtothediagnosisofeosinophilic otitismedia.Acuteotitismediaexacerbatesthedevelopment ofeosinophilicgranulationtissueinthemiddleear,which canobstructthemiddleearaditus,leadingtoneckabscess formation.Toourknowledge,thisisthe firstcaseofBezold abscessduetoeosinophilicotitismedia.Thus,emergency physiciansshouldrecognizethateosinophilicotitismedia cancauseBezoldabscess.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval.Patientconsenthasbeenobtainedfor publicationofthiscasereport.Documentationon file.
AddressforCorrespondence: TakashiFujiwara,MD,Kurashiki CentralHospital,DepartmentofOtolaryngology,Miwa1-1-1, Kurashikicity,Okayamaprefecture,710-8602,Japan. Email: t.fujiwarabi@gmail.com
ConflictsofInterest:BytheCPC-EMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Tsurutaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AlkhaldiAS,AlwabiliM,AlbilasiT,etal.Bezold’sabscess: acasereportandreviewofcasesover20years. Cureus 2022;14(1):e21533.
2.UchidaY,UedaH,NakashimaT.Bezold’sabscessarisingwith recurrentcholesteatoma20yearsafterthe firstsurgery:withareviewof the18casespublishedinJapansince1960. AurisNasusLarynx. 2002;29(4):375–8.
HamzahM.Yusuf,MD
TimothyBatchelor,MD
NicholasAshenburg,MD
SectionEditor:ShadiLahham,MD
StanfordUniversity,DepartmentofEmergencyMedicine,PaloAlto,California
Submissionhistory:SubmittedSeptember25,2023;RevisionreceivedJanuary22,2024;AcceptedJanuary29,2024
ElectronicallypublishedMay14,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.1686
CasePresentation: A60-year-oldfemalepresentedtotheemergencydepartmentwithunilateraleye painandvisionloss.Point-of-careultrasound(POCUS)wasperformed,whichdemonstratedocular metastaticlesionsofbreastcancer.
Discussion: Ocularmetastasisisrare,clinicallychallenging,andmaypresentwithawiderangeof ophthalmicsymptoms.However,POCUSmaysafelyandrapidlyidentifymetastaticlesionstodirect furthercare.[ClinPractCasesEmergMed.2024;8(3)298–299.]
Keywords: POCUS;ocularultrasound;emergencymedicine;breastcancer;metastasis.
A60-year-oldfemalewithahistoryofrecentlydiagnosed breastcancerwithliver,lung,andbonemetastasespending biopsyresultspresentedtotheemergencydepartmentwith onedayofprogressivelefteyepain,blurryvision,andcentral scotoma.Shedeniedmyodesopsia,photopsia,orrecenteye trauma.Fluoresceinstainingwasunremarkable.Hervisual acuitywas20/30bilaterally.Shehadintraocularpressuresof 19millimetersofmercury(mmHg)bilaterally(reference range10–20mmHg),andequallyroundandreactivepupils. Shehadfullextraocularmovement.Herslitlampexamwas notableformild,lefteyeconjunctivalinjection.
Usingalinearultrasoundprobe,weperformedpoint-of-care ultrasound(POCUS)toobtainsagittalandtransverseviews evaluatingtheanteriorchamber,posteriorchamber,retina, lenslocation,andoverallstructureofthelefteye.Twoposterior masseswereidentifiedovertheopticnerve(Image). Ophthalmologywasconsultedand,ondilatedfundusexam, identifiedtwo,paleyellowchoroidallesionsincloseproximity totheopticnerveandopticnervetilting,withstrongconcern forleptomeningealinvolvement.Thepatientwasthenadmitted tothehospitalforenhancedimagingandfacilitationofcare.
Aninpatientmagneticresonanceimagingstudyofthe brainwithandwithoutcontrastdemonstratedhypointense nodularityinseveralareaswithintheglobe,withseveral,
scattered,smallenhancingcerebrallesions.Shewasstarted oncorticosteroidsandofferedwholebrainvsstereotactic bodyradiationtherapy,aswellasexternalbeamtherapyfor intraoculartumors.Shewassubsequentlydischargedfor outpatientradiology-oncologycare.
Ocularmetastasisrepresentsarareandclinically challengingmanifestationofadvancedcancer.Breastcancer remainsamoreprevalentsourceofocularmetastasisdueto itshighincidence,aggressivenature,andpropensityfor systemicdissemination.Theocularstructures,includingthe choroid,retina,iris,andopticnerve,serveaspotentialsites forsecondarytumorgrowth,leadingtovisualimpairment andsignificantmorbidity.1 APOCUSexammayshowa hypoechoicdomeorplateau-shapedlesiontypicallyoverthe choroidwithminimalinternalvascularization.2
Clinically,ocularmetastasiscanmanifestasawiderange ofophthalmicsymptoms,includingblurredvision,pain, photophobia,metamorphopsia,oritcanbe asymptomatic.1,3 Estimatingtheincidenceofophthalmic metastasishasprovenchallengingasasymptomatic manifestationsmaygounnoticed,buttheprevalenceof ocularmetastasisinmetastaticbreastcancerhasbeen estimatedbetween9.7–30%.4 Differentialdiagnosesmay
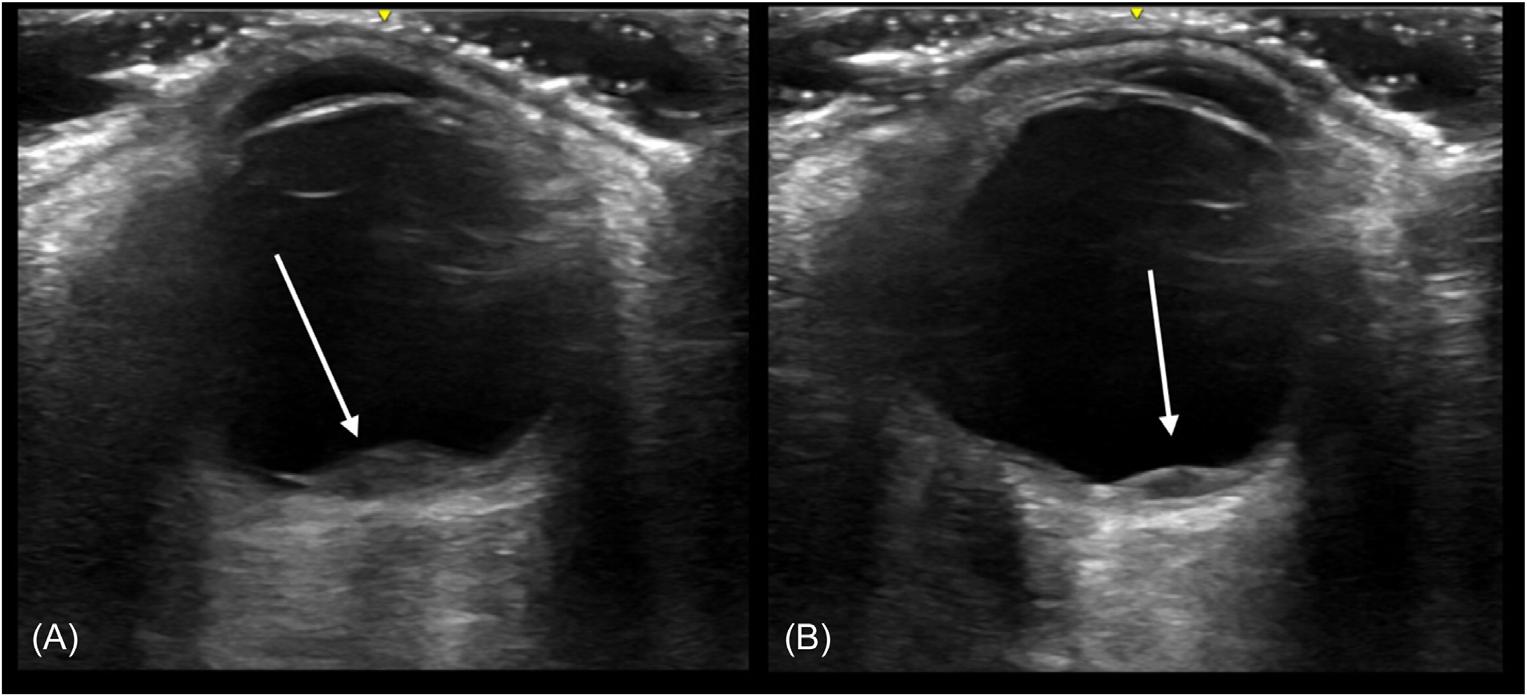
Image. Point-of-careultrasoundusingliner8-megahertztransducerintransverseviewdemonstrating,(A)hypoechoiclenticular-shaped opticmetastasis(3.2millimeters[mm]by1.5mm)overtheopticnerve,and(B)asmallerlenticular-shapedmetastasis(1.7mmby1.0mm) withthepatientinleftwardgaze.
includeprimaryocularmalignancies,hemangioma, sclerochoroidalcalcification,granuloma,andinfection, underscoringtheimportanceofaccuratediagnosistoguide appropriatemanagementstrategies.
Subclinicalmetastasismaynotindicatetargeted treatment.Atinitialdiagnosis,patientsmayreceivesystemic adjuvanttreatmenttoeliminatemicrometastaticdiseaseand preventfurthermetastasis.5 Systemictreatmentmayinclude endocrinetreatment,cytotoxicchemotherapy, corticosteroids,orimmunotherapy.Targetedtreatmentto ocularmetastasesincludesexternalbeamradiation,which canbeusefulinpatientswithfovealinvolvementbutmay resultincataractsorradiationretinopathy.
Theauthorsattestthattheirinstitutionrequiresneither InstitutionalReviewBoardapproval,norpatientconsentfor publicationofthiscasereport.Documentationon file.
AddressforCorrespondence:HamzahM.Yusuf,MD,Stanford University,DepartmentofEmergencyMedicine,900WelchRd., Suite350.PaloAlto,CA94304.Email: hyusuf@stanford.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Yusufetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.WickremasingheS,DansinganiKK,TranosP,etal.Ocular presentationsofbreastcancer. ActaOphthalmolScand 2007;85(2):133–42.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Ocularmetastasisrepresentsarare, clinicallychallengingmanifestationof advancedcancer.
Whatisthemajorimpactoftheimage(s)?
Wedescribeanexampleofbreastcancer metastasisonpoint-of-careultrasound (POCUS),itsclinicalmanifestations,and potentialtreatments.
Howmightthisimproveemergency medicinepractice?
Emergencyphysiciansmaybeableto diagnoseocularmalignancyusingPOCUS, afastandeasy-to-usebedsidetool.
2.BlasiMA,MaceroniM,CaputoCG,etal.Clinicalandultrasonographic featuresofchoroidalmetastasesbasedonprimarycancersite: long-termexperienceinasinglecenter. PLoSONE 2021;16(3):e0249210.
3.MaheshwariAandFingerPT.Cancersoftheeye. CancerMetastasis Rev.2018;37(4):677–90.
4.BarakA,NeudorferM,HeilweilG,etal.Decreasedprevalenceof asymptomaticchoroidalmetastasisindisseminatedbreastandlung cancer:argumentagainstscreening. BrJOphthalmol.2007;91(1):74–5.
5.CuiY,YinS,QinX,etal.Advancesinthetreatmentofintraocular malignancies:aliteraturereview. FrontMed(Lausanne) 2022;9:975565.
MaiyaSmith,MD
MorganKetterling,DO
AlexanderGallaer,MD
RowanKelner,MD
ChristineRaps,MD
AllisonM.Beaulieu,MD,MAEd
SectionEditor:RachelLindor,MD,JD
UniversityofUtah,DepartmentofEmergencyMedicine,SaltLakeCity,Utah
Submissionhistory:SubmittedJanuary10,2024;RevisionreceivedMarch7,2024;AcceptedMarch8,2024
ElectronicallypublishedJune3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7189
CasePresentation: Wedescribeacaseofa57-year-oldmalewithmultiplemedicalcomorbiditieswho presentedtotheemergencydepartmentwithatwo-weekhistoryofupperbackpainwithassociated numbness.Physicalexamdemonstratedsensorylossinabilateralthirdandfourththoracicdermatome distribution.Thediagnosisofspinalarachnoidwebwasmadebasedonneurologicalexamand imaging findings.
Discussion: Spinalarachnoidwebisararediagnosis,butconsiderationisimportant,asearly recognitionandsurgicalinterventioncanresolvesymptomsandpreventworseningneurological sequelae.[ClinPractCasesEmergMed.2024;8(3)300–301.]
Keywords: spinalarachnoidweb;neurology.
A57-year-oldmalewithhistoryoftypeIIdiabetes mellitus,renaltransplant,coronaryarterydisease,and hypertensionpresentedtotheemergencydepartment(ED) fornumbnessinhischestfortwoweeks,withassociated upperbackpainradiatingtohischestbilaterally,and shortnessofbreath.Hepresentedtoanoutpatient clinicforsimilarcomplaintsonedaypriorandwas startedonafour-daycourseofprednisonefor presumedpleurisy.
OnexaminationintheED,thepatientwasfoundtohave decreasedsensationinhisthirdandfourththoracic dermatomeinaband-likedistributionwithoutadditional neurologicdeficitsorskin findings.Magneticresonance imaging(MRI)ofthecervicalandthoracicspinewere obtained,showingadorsalspinalarachnoidweb(SAW) withslightcompressionofthespinalcordlocatedatthethird andfourththoraciclevels(Image, Video).
Neurosurgerywasconsulted,evaluatedthepatientand reviewedimaging.Nosurgicalinterventionwasofferedat thattimeduetothepatient’ssignificantcomorbiditiesand
moderatesymptoms.HewasdischargedhomefromtheED withrecommendedcloseoutpatientfollow-up.
Spinalarachnoidwebisararediagnosis.Withinthe meninges,therearethreelayers:thedura,arachnoid,and pia.Thearachnoidisathinmembranebetweentheduraand piathatadherestothebrainandspinalcord.1 ASAW specificallyreferstoafocalthickeningofthearachnoid, typicallyinthethoracicspine,whichcausescompressionof thespinalcordandinterfereswiththefree flowofspinal fluid withinthedorsalsubarachnoidspace.ItisthoughtthatSAW representsavariantofarachnoidcystformation.Whilethis patientdidnothaveradiographicevidenceofsyringomyelia, SAWistypicallyassociatedwithsyringomyeliaand doesnotseemtobeassociatedwithtrauma, hemorrhage,orinflammation.2 Presentingsymptoms includebackpain,upper/lowerextremityweakness, andnumbness.3
ImagingincludesMRIorcomputedtomography myelographyandoftendemonstratesa “scalpelsign”

Image. Magneticresonanceimagingwithandwithoutcontrast showingfocalanteriordisplacementofthethoracicspinalcordat thethirdandfourththoraciclevels(arrow).Inthesettingofa prominentdorsalsubarachnoidspacewithalteredcerebrospinal fluid flowdynamics,the findingsdemonstrateadorsal arachnoidweb.
deformityatthesiteoftheSAW,representingthefocal dorsalindentationcausedbytheweb,reminiscentofthe pointededgeofascalpel.3 However,theonlydefinitive diagnosisforSAWisthroughsurgicalconfirmation.
Spinalarachnoidwebislikelyunder-recognizedandunderdiagnosedgivenitsrarity.Diagnosisusuallytakesyears,and treatmentinvolvessurgicallysisofthearachnoidband.2–4 Surgicalinterventioncancompletelyresolvesymptoms.2
FailuretodiagnoseSAWmayresultinworseningspinalcord functionandneurologicfunction.Patientswhohave progressivelyworseningpain,paresthesia,orweaknessina dermatomaldistributionwithouttraumaorprior neurosurgicalinterventionshouldpromptconsideration ofthisdiagnosis.Emergencyphysiciansneedtobe awareofthisrarediagnosisgivenitspossiblyirreversible neurologicalsequelaeincludingpain,numbness,weakness, andparalysis.2–4
Video. Magneticresonanceimagingwithandwithoutcontrast demonstratingthe “scalpelsign” seenatthethirdandfourththoracic levels(arrow)duetothespinalarachnoidweb.
TheInstitutionalReviewBoardapprovalhasbeendocumentedand filedforpublicationofthiscasereport.
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
Whatdowealreadyknowaboutthis clinicalentity?
Spinalarachnoidwebisararediagnosisthat presentswithnumbnessandotherneurologic sequelaesecondarytothickeningofthe arachnoidandcompressionofspinalcord.
Whatisthemajorimpactoftheimage(s)?
Thickeningofthearachnoidcanbeseenon magneticresonanceimagingasa “scalpelsign,” aidinginthisultimatelysurgicaldiagnosis.
Howmightthisimproveemergency medicinepractice?
Thisrarediseaseisreversiblewhentreated early.Physicianawarenessanduseof imagingwillaidindiagnosisandpreventionof neurologicmorbidity.
AddressforCorrespondence:MaiyaSmith,MD,Departmentof EmergencyMedicine,HelixBuilding,5050,30NMarioCapecchi Drive,Level2South,SaltLakeCity,UT84112.Email: maiya.smith@ hsc.utah.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Smithetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GhannamJYandAlKharaziKA.Neuroanatomy,cranialmeninges. In:StatPearls.TreasureIsland,FL:StatPearlsPublishing;2024. Availableat: http://www.ncbi.nlm.nih.gov/books/NBK539882/ AccessedFebruary18,2024.
2.ParamoreCG.Dorsalarachnoidwebwithspinalcordcompression: variantofanarachnoidcyst?Reportoftwocases. JNeurosurgSpine. 2000;93(2):287–90.
3.ReardonMA,RaghavanP,Carpenter-BaileyK,etal.Dorsalthoracic arachnoidwebandthe “scalpelsign”:adistinctclinical-radiologicentity. AmJNeuroradiol. 2013;34(5):1104–10.
4.BrodbeltARandStoodleyMA.Syringomyeliaandthearachnoidweb. ActaNeurochir(Wien). 2003;145(8):707–11;discussion711.
KitanAkinosho,MD* WilliamWeber,MD,MPH†
*BethIsraelDeaconessMedicalCenter,DepartmentofEmergencyMedicine, Boston,Massachusetts † RushUniversityMedicalCenter,DepartmentofEmergencyMedicine,Chicago,Illinois
SectionEditor:JacquelineLe,MD
Submissionhistory:SubmittedJanuary18,2024;RevisionreceivedMarch20,2024;AcceptedApril2,2024
ElectronicallypublishedJune3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7200
CasePresentation: Wereportacaseofan89-year-oldfemalewhopresentedwithpaininherright shoulderfollowingafallontoheroutstretchedhand.Uponpresentation,herrighthandwasheldbehind herheadandelbowheldaboveherheadin flexion.Therewasobviousdeformityseenandfeltinher axilla.Radiographoftheshouldershowedaninferiorshoulderdislocationandimpactedhumeralneck fracture.Givenherageandcomorbidosteoporosis,abedsidereductionwasperformedbyorthopedics wherethehumeralheadwasintentionallydislocatedfromthehumeralshaft.Thirteendaysaftertheinitial shoulderdislocation,thepatient’sshoulderwassuccessfullyrepairedbyopenreduction.
Discussion: Luxatioerecta,whichmeans “erectdislocation” inLatin,referstoaninferiorshoulder dislocation.Itaccountsforlessthan1%ofshoulderdislocations.Ourcasereporthighlightsaninferior shoulderdislocationwitharare,concomitanthumeralneckfracture,managedviastagedreductionby orthopedicswithintentionaldislocationofthehumeralheadgivenconcernoverpatient’sageand osteoporosis.Thepatientwaseventuallysuccessfullyrepairedviaarthroplastywithintwoweeks.[Clin PractCasesEmergMed.2024;8(3)302–304.]
Keywords: inferiorshoulderdislocation;luxatioerecta;shoulderpain.
An89-year-oldfemalewithahistoryofosteoporosis presentedafteramechanicalfallwithrightshoulderpain. Shetrippedandfellwithherarmraisedaboveherheadand infrontofher.Shereporteddifficultymovingherrightarm fromitspositionaboveherhead.Onphysicalexam,herright armwasneurovascularlyintact,butheldaboveherhead withpalpableinferiordisplacementofthehumeralhead intheaxilla.Radiographwasperformedandisshown below(Image1).
Thisradiographshowsaninferiorshoulderdislocation, alsoknownasluxatioerecta,anuncommonshoulderinjury thataccountsforlessthan1%ofshoulderdislocations.1 Luxatioerectatypicallyresultsfromsuddenhyperabduction, whichforcesthehumeralheadinferiorly,oftentearingthe inferiorcapsule.Patientsgenerallypresentwiththearmfully abductedandtheirhandneartheirheadforcomfort.2 Patientsmostcommonlyfracturethegreatertuberosity,but
thispatientwithosteoporosisexperiencedahumeral neckfracture.
Twoimportantapproachconsiderationsdifferentiate inferiorshoulderdislocationsfromtypicalanterioror posteriordislocations:rateofconcomitantinjuryandvector ofreduction.Physiciansshouldpaycloseattentionfor neurovascularcompromise,withtheaxillarynerveand axillaryarteryverysusceptibletoinjury.Studieshavefound highratesofbonyinjury(60%),neurologicinjury(29%),and vascularinjury(10%)associatedwiththeinjury.1,3 Reductionsforinferiorshoulderdislocationstypically employsuperiorandexternaltraction.4 Alternatively, anteriortractioncanconvertaninferiordislocationtoan anteriordislocation,whichcanthenbereducedwithavariety ofmethods.
Inthiscase,orthopedicswasconsultedduetothemultiple concomitantfractures.Typically,theremainderofthe humeruscanbeusedtodistractthehumeralheadandallow reduction,butinthiscasethehumeralheadwasseparated.In thiscase,orthopedicschosetousetraction-countertraction
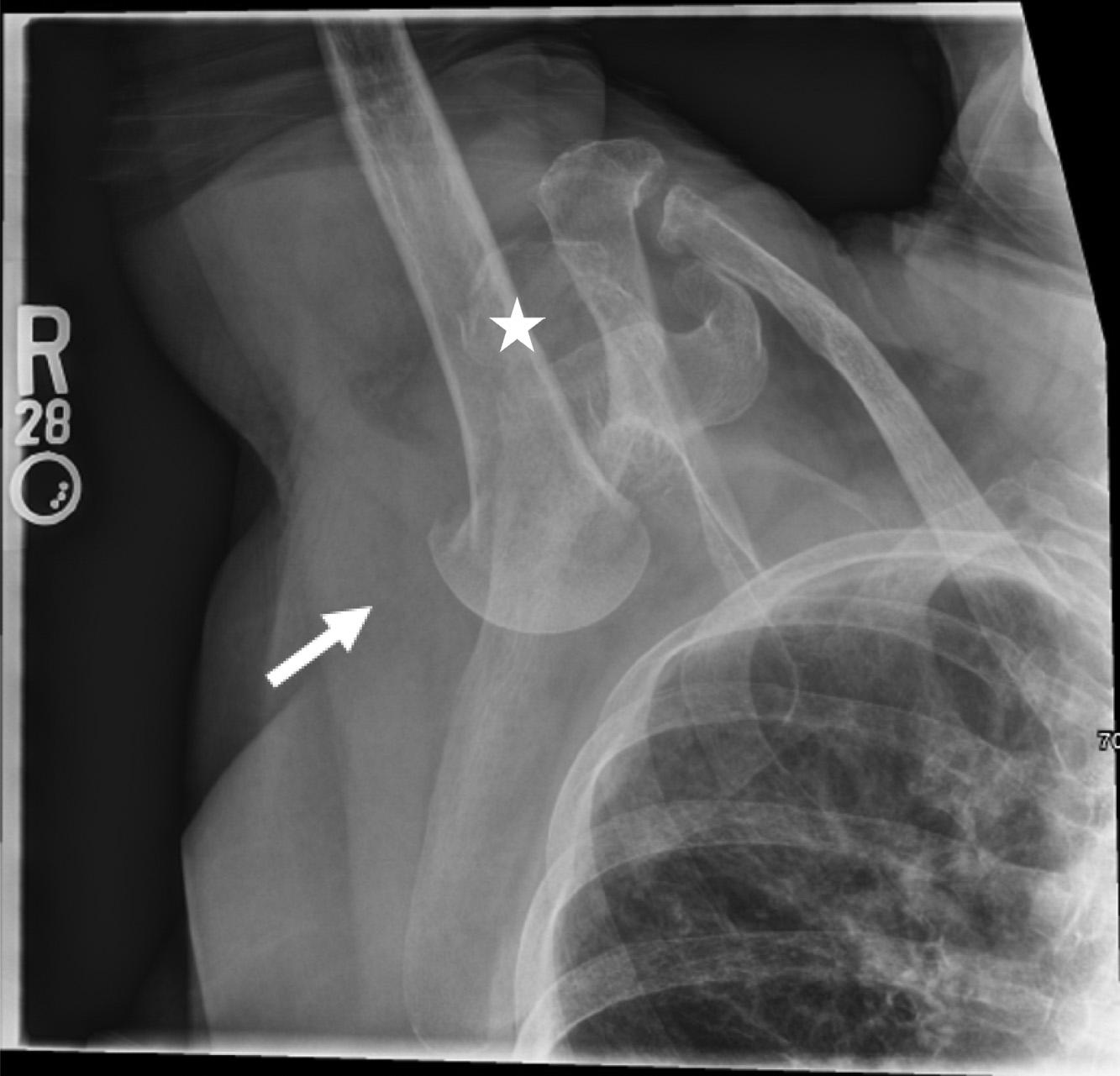
Initialradiographofrightshouldershowsarightinferior dislocation[luxatioerecta]withaconcomitantimpactedhumeral neckfracture(arrow).Amildlydisplacedrightglenoidfractureis alsonoted(star).
withasuperiorandexternalvectorawayfromthepatientto reducetheremainderofthehumerusforcomfortand neurovascularsafetywhileleavingthehumeralhead dislocatedforopenrepair(Image2).Thepatientwas providedashoulderslingintheinterimuntilcardiacrisk

PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Luxatioerecta(inferiorshoulder dislocation)isarareoccurrence( < 1%)that carriesahighrateofconcomitantvascular, neurologic,andbonyinjury.
Whatisthemajorimpactoftheimage(s)?
Wehighlightaluxatioerectawitha superimposedhumeralfracture,managedvia bedsidereductionwithintentionaldislocation ofthehumeralheadpriortosurgery.
Howmightthisimproveemergency medicinepractice?
Theapproachtoreducingluxatioerecta differsfromothershoulderdislocations. Maintainhighsuspicionforotherinjuriesand considerorthopedicconsult.
evaluationclearedherforoperativerepair(Image3).The patientexperiencednolong-termneurologiccompromise fromherinjury.

TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:KitanAkinosho,MD,BethIsrael DeaconessMedicalCenter,OneDeaconessRoad,Rosenberg2, Boston,MA02215.Email: kakinosh@bidmc.harvard.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Akinoshoetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.NambiarM,OwenD,MooreP,etal.Traumaticinferiorshoulder dislocation:areviewofmanagementandoutcome. EurJTraumaEmerg Surg. 2018;44(1):45–51.
2.VasiliadisAV,KalitsisC,KantasT,etal.Inferiordislocationofshoulder complicatedwithundisplacedgreatertuberosityfracture,ruptureofthe supraspinatustendon,andbrachialplexusinjuryintheelderly:case reportandliteraturereview. CaseRepOrthop. 2020;2020:9420184.
3.OstermannRC,JoestlJ,HofbauerM,etal.Associatedpathologies followingluxatioerectahumeri:aretrospectiveanalysisof38cases. J ClinMedRes. 2022;11(2):453.
4.NhoSJ,DodsonCC,BardzikKF,etal.Thetwo-stepmaneuver forclosedreductionofinferiorglenohumeraldislocation(luxatio erectatoanteriordislocationtoreduction). JOrthopTrauma. 2006;20(5):354–7.
JohnH.Priester,MD*
PrasannaKumar,MD†
JesseNaumann,BS,EMT*
KatherineDolbec,MD*
PeterWeimersheimer,MD*
ChristianD.Pulcini,MD,MEd,MPH*‡
SectionEditor:ShadiLahham,MD
*UniversityofVermont,LarnerCollegeofMedicine,Departmentof EmergencyMedicine,Burlington,Vermont
† BrownUniversity/RhodeIslandHospital,DepartmentofEmergency Medicine,Providence,RhodeIsland
‡ UniversityofVermont,LarnerCollegeofMedicine,Departmentof Pediatrics,Burlington,Vermont
Submissionhistory:SubmittedJanuary25,2024;RevisionreceivedApril19,2024;AcceptedApril19,2024
ElectronicallypublishedJuly18,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.7216
CasePresentation: An8-month-oldinfantpresentedtoageneralemergencydepartmentwithchief complaintsofrhinorrhea,decreasedactivity,andfever.Apoint-of-carelungultrasound(LUS)was performedatbedsidewithpotentialearly findingsofpneumonia.Basedonthese findingsonLUS,a chestradiograph(CXR)wasorderedandperformedwithnoacute findings.Hewasdischargedwithout antibioticsbasedonthese findings;unfortunately,hereturnedtwodayslaterwithworseningsymptoms requiringchesttubeplacement,mechanicalventilation,andprolongedhospitalizationforcomplicated bacterialpneumonia.
Discussion: Pneumoniaisamajorcauseofpediatricmorbidityandmortalityworldwide.Despite evidencesupportingtheutilizationofLUSforthediagnosisofpediatricpneumonia,CXRremainsthe defaultimagingforclinicaldecision-makinginmostsettings.Inthiscase,earlierantibioticsandhigher relianceonLUSforclinicaldecision-makingmayhavepreventedthemorbidityassociatedwiththis hospitalization.[ClinPractCasesEmergMed.2024;8(3)305–307.]
Keywords: point-of-careultrasound;pneumonia;lungultrasound;chestradiograph;pediatrics.
An8-month-oldinfantpresentedtotheemergency department(ED)withoneweekofrhinorrhea,decreased activity,andfever.Reportedsymptomsovertheprior24 hoursincludedincreasedworkofbreathing,decreasedoral intake,andfewerwetdiapers.Onarrival,physicalexam findingsincludedgrunting,retractions,tachycardia, tachypnea,andfeverof39.3° Celsius.Withantipyreticshis respiratorysymptomsimproved.Achestradiograph (Image1)wasperformedtofollowuponaneducationalpointof-carelungultrasound(LUS)(Image2),whichwas suggestiveofearlypneumonia.Hewasdischargedhome withoutantibioticsgivenhisnegativechestradiograph (CXR)(Image1).
Heunfortunatelyreturnedtwodayslaterwithcontinuing fever,decreasedoralintake,andemesis.Repeatradiography
demonstratedrightlungopacity,andhewasdiagnosedwith methicillin-sensitive Staphylococcusaureus communityacquiredpneumoniawithempyema(Image3).Hewas admittedandtreatedforpneumonia,andhiscoursewas complicatedbyacutehypoxicrespiratoryfailureand empyema,necessitatingmechanicalventilationandchest tubeplacement.Hewasdischargedonhospitalday21.
Community-acquiredpneumoniaisamajorcauseof pediatricmorbidityandmortality.1 Ourcaseaddstothe currentliteraturesupportingLUSassuperiorinidentifying pediatricpneumoniacomparedtoCXR,yetCXRremains themostcommonmodalityusedforclinicaldecision-making inthispopulationintheED.2 Previousresearchhas comparedLUStoCXRinthediagnosisofpneumoniain

Image1. Chestradiographfrominitialevaluationinthe emergencydepartment,withoutevidenceofpneumonia.
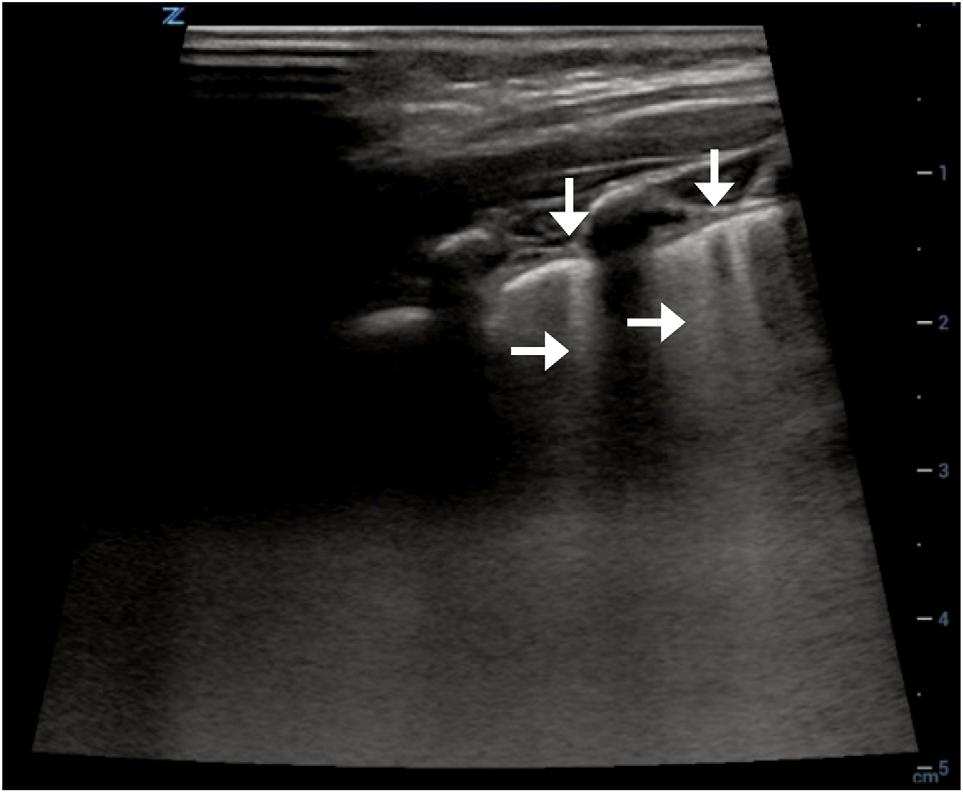
Image2. Focalpleuralirregularities(verticalarrows)andB-lines (horizontalarrows)suggestiveofpneumoniafromrightlung ultrasoundperformedoninitialvisittotheemergencydepartment.
childrenwithsensitivityandspecificityofLUSashighas 96%and93%,respectively.2 Further,upto28%oflesionsin pediatricpneumoniaidentifiedwithLUSwerenotvisible withradiograph.3 Inthecasepresentedhere,significant morbiditymayhavebeenavoidedhadantibiotictherapy beeninitiatedfollowingtheinitialevaluationwithLUS.
TheadvantagesofLUSwhencomparedtoCXRextend beyondeffectivenessandaccuracy.Earlierdetectionof disease,reducedradiationexposure,andefficientbedside assessmentarealsoclearadvantages.1,3–5 Inaddition,LUS canberepeatedatbedsidetomonitordiseaseprogressionor regression,allowingforinformedongoingtreatment decisions.Aspoint-of-careultrasonographybecomesan integralpartofemergencymedicineresidencyprogramsand standardofcare,wehopetoseemorephysicianstrainedto effectivelyperform,interpret,andclinicallyapplyLUS, notablyinthepediatricpopulation.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Chestradiographyistheconventional imagingmodalityofdiagnosingpediatric pneumonia.However,lungultrasoundoffers similar,ifnotbetter,sensitivity andspeci fi city.
Whatisthemajorimpactoftheimage(s)?
Thiscasedemonstrateshowlungultrasound candiagnosepediatricpneumoniaearlierthan chestradiographyandshouldbethebasisfor clinicaldecisionmaking.
Howmightthisimproveemergency medicinepractice?
Inthepresenceofabnormallungultrasound fi ndingsandnormalchestradiography, emergencymedicinephysiciansshould stronglyconsiderinitiatingtreatment.
Thiscasepresentationdemonstratestheadvantagesof usingLUSforclinicaldecision-makinginthepediatric population.EarlyinitiationofantibioticsbasedonLUSmay helptoavoidmorbidityandmortalityfromtreatmentdelay, andourcaselendscredencetothelingeringquestionamong emergencycliniciansofwhethertotreatwithantibiotics basedonultrasound findingsthatarediscrepantwithaCXR. Emergencycliniciansshouldstronglyconsiderprioritizing

Image3. Chestradiographonday3,followingreturntothe emergencydepartment.Rightlungconsolidationsuggestiveof pneumoniaisvisible.
the findingsofLUSindiagnosingandtreatingpediatric pneumonia,aswellassupportthetraininganddissemination ofLUSasthesuperiormodalitytooptimizecareofthis potentiallyvulnerablepopulation.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:PrasannaKumar,MD,Brown University,AlpertMedicalSchool,DepartmentofEmergency Medicine,55ClaverickSt.,Suite100,Providence,RI02903. Email: Prasanna_kumar@brown.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Priesteretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.JonesBP,TayET,ElikashviliI,etal.Feasibilityandsafetyof substitutinglungultrasonographyforchestradiographywhen diagnosingpneumoniainchildren:arandomizedcontrolledtrial. Chest. 2016;150(1):131–8.
2.NajgrodzkaP,BudaN,ZamojskaA,etal.Lungultrasound inthediagnosisofpneumoniainchildren:ameta-analysis andareviewofpediatriclungimaging. UltrasoundQ. 2019;35(2):157–63.
3.IorioG,CapassoM,PriscoS,etal.Lungultrasound findings undetectablebychestradiographyinchildrenwithcommunity-acquired pneumonia. UltrasoundMedBiol. 2018;44(8):1687–93.
4.IannielloS,PiccoloCL,BuquicchioGL,etal.First-linediagnosisof paediatricpneumoniainemergency:lungultrasound(LUS)in additiontochest-X-ray(CXR)anditsroleinfollow-up. BrJRadiol. 2016;89(1061):20150998.
5.MartínezRedondoJ,ComasRodríguezC,PujolSaludJ,etal.Higher accuracyoflungultrasoundoverchestx-rayforearlydiagnosis ofCOVID-19pneumonia. IntJEnvironResPublicHealth. 2021;18(7):3481.
JacobLawing,MD
JeremyTowns,MD
MatthewA.Heimann,MD
SectionEditor:MelanieHeniff,MD
UniversityofAlabamaatBirmingham,DepartmentofEmergencyMedicine, Birmingham,Alabama
Submissionhistory:SubmittedJanuary7,2024;RevisionreceivedApril15,2024;AcceptedApril24,2024
ElectronicallypublishedJuly31,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.6664
CasePresentation: A32-year-oldmalewhorecentlyimmigratedfromKenyapresentedtothe emergencydepartment(ED)withapainful,enlarging,right-sidedneckmassforeightweeksduration. Point-of-careultrasoundwasusedtorevealalargecysticmasswithinternalseptationsandnumerous hypoechoicroundlesions.InitialtuberculosisbloodtestorderedintheEDwaspositivewithcultures ultimatelygrowing Mycobaceteriumtuberculosis
Discussion: Scrofulashouldbeconsideredinthedifferentialinpatientspresentingwithenlarging neckmasseswhohaveepidemiologicalriskfactorsfortuberculosis.[ClinPractCasesEmergMed. 2024;8(3)308–310.]
Keywords: scrofula;neckmass;tuberculosis;lymphadenitis.
A32-year-oldmalepresentedtotheemergency department(ED)duetoapainful,enlarging,right-sidedneck massforeightweeks.Notably,hehadimmigratedfrom Kenyaapproximatelyoneyearprior.Hereportedsubjective feversbutdeniedweightloss,nightsweats,orpulmonary symptoms.Physicalexamrevealedamoderate-sizedareaof focalswellingnotedtorightlateralneckassociatedwith cervicallymphadenopathy(Image1).
AT-SPOT.TBtest(aninterferon-gammareleaseassay) wasorderedfromtheEDandreturnedpositive.Empiric treatmentwithcefepimewasstarted,andthepatientwas admittedtothehospitalforultrasound-guidedlymphnode biopsy.Limitedpoint-of-careultrasound(Image2)and computedtomographyoftheneckwithcontrast(Image3) wereperformed.
Thisdiagnosisofscrofulawasultimatelymadethrough acid-fastbacillusculture,whichgrew Mycobacterium tuberculosis. Scrofula,ormycobacteriallymphadenitis,isa typeofextrapulmonarytuberculosis(TB)causedby hematogenousorlymphaticdisseminationofpulmonary TBorreactivationoflatentTB.Commonpresentations includeanenlargingmasswithorwithouttendernessand
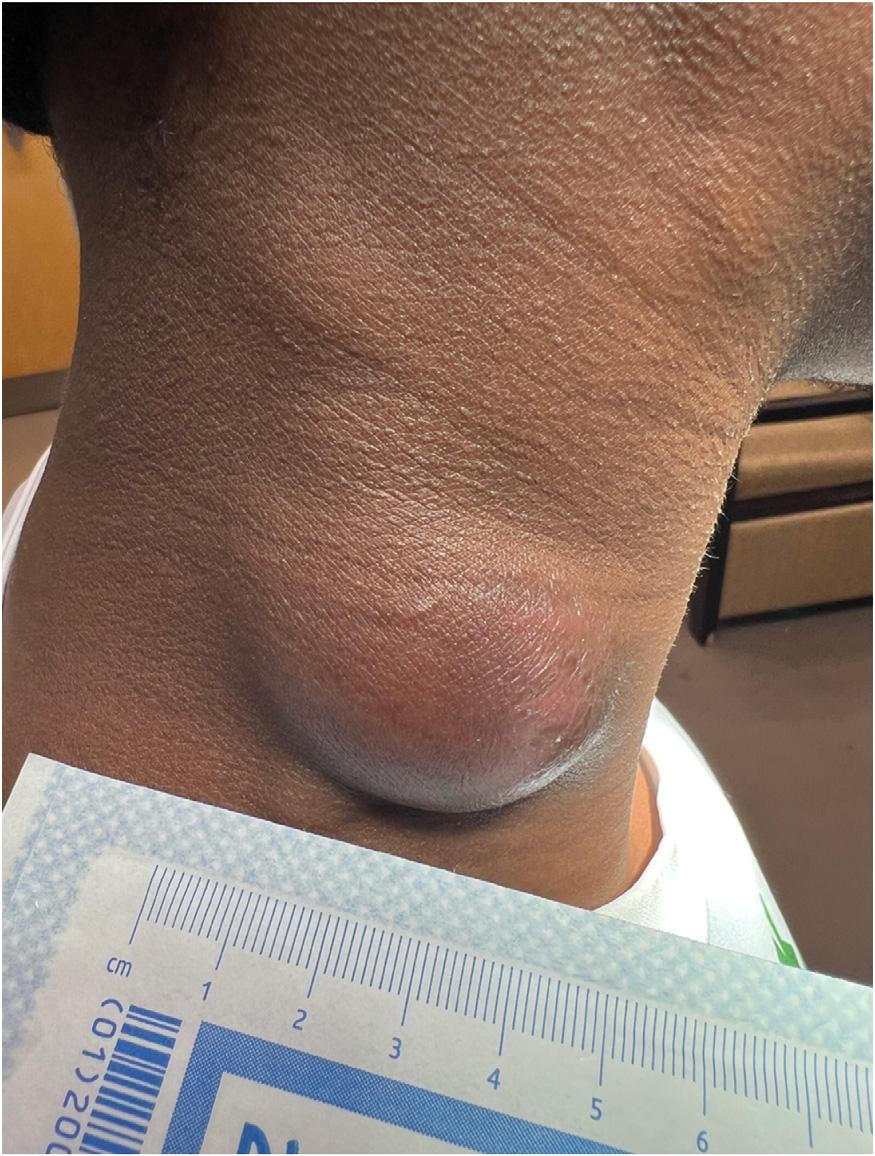

Image2. Point-of-careultrasoundrevealinglargecysticmasswith internalseptations(whitearrow)andcervicaladenopathy (blackarrow).
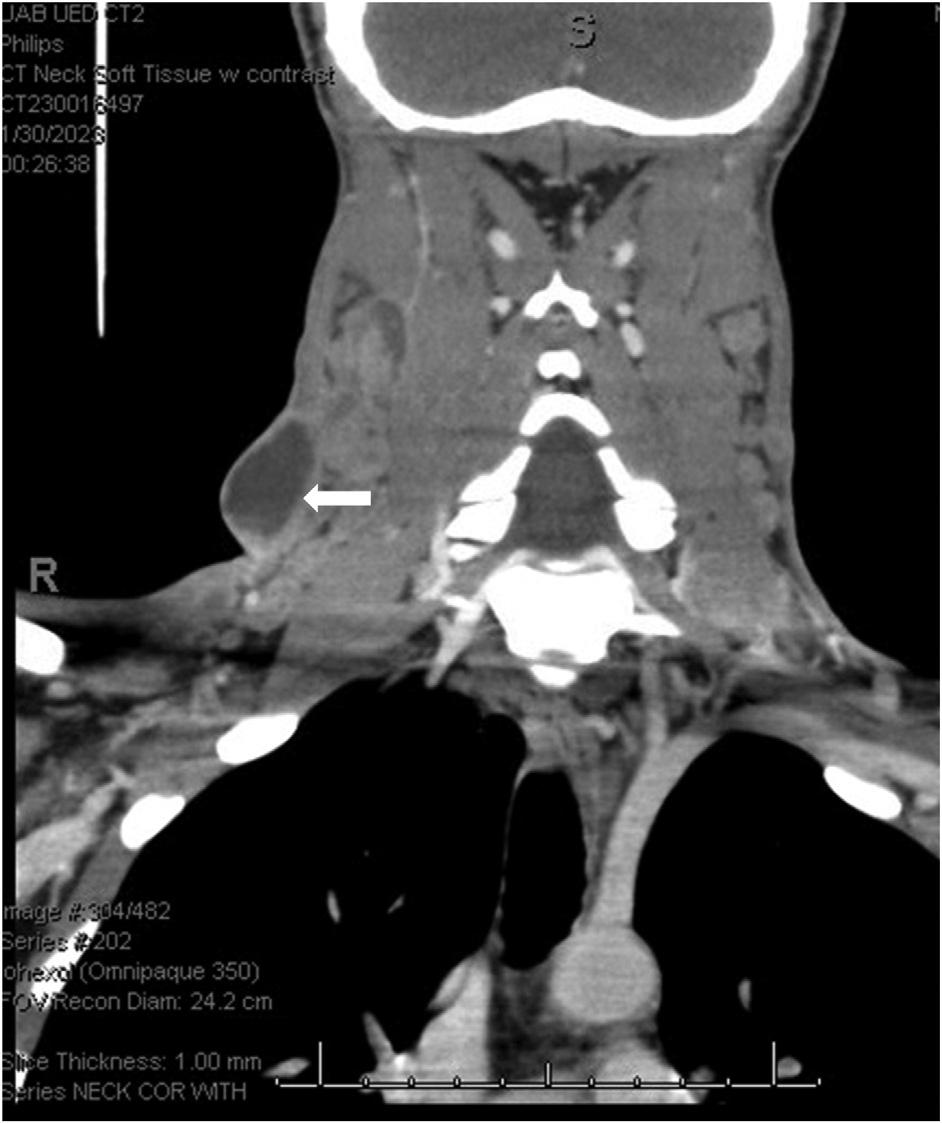
Image3. Computedtomographyoftheneckwithintravenous contrastrevealedmultiplenecroticandcystic-appearinglymph nodes(arrow).
erythemalocatedwithinthe cervicalorsupraclavicular lymphnodes.1 Associatedsymptomsincludefever,rigors, andnightsweats.2 Point-of-careultrasoundoftuberculous nodeswillbehypoechoicandround,withintranodalcystic necrosisandadjacentsoft-tissueedema.Diagnosisismade
Whatdowealreadyknowaboutthis clinicalentity?
Scrofula,ormycobacteriallymphadenitis, isatypeofextrapulmonarytuberculosisthat commonlypresentsasanenlargingmass withinthecervicalorsupraclavicular lymphnodes.
Whatisthemajorimpactoftheimages?
Identi fi cationofacysticmasswith internalseptationsonpoint-of-care ultrasound(POCUS)canhelpdistinguish thisentityfromothercausesof cervicalmasses.
Howmightthisimproveemergency medicinepractice?
TheuseofPOCUSoncervicalmassesin patientswithendemicriskfactorscangreatly aidinthediagnosisofscrofula.
byhistopathologyalongwithasmearofacid-fastbacilli andcultureoflymphnodes.Treatmentincludesrifampicin, isoniazid,pyrazinamide,andethambutol.Itisimperative toobtainappropriateimagingsuchasultrasoundor computedtomographyinen largingneckmasseswith epidemiologicriskfactorsofTBandensureclose follow-up.
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:JacobLawing,MD,Universityof AlabamaatBirmingham,DepartmentofEmergencyMedicine, 52119thSt.South,Suite203,Birmingham,AL35233. Email: jglawing@uabmc.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Lawingetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/ ImagesinEMCapsule
1.BhandariJandThadaPK.Scrofula.In: StatPearls[Internet] TreasureIsland,FL:StatPearls,2023.Availableat: https://www.ncbi.nlm.nih.gov/books/NBK557700/ AccessedDecember20,2023.
2.PoleskyA,GroveW,BhatiaG.Peripheraltuberculouslymphadenitis: epidemiology,diagnosis,treatment,andoutcome. Medicine (Baltimore). 2005;84(6):350–62.
3.AhujaATandYingM.Sonographicevaluationofcervicallymphnodes. AmJRoentgenol. 2005;184(5):1691–9.
OsherShefer,MD
JacquelineLe,MD
EshaanDaas,MD
EugeneHu,MD
SectionEditor:LevLibet,MD
DesertRegionalMedicalCenter,DepartmentofEmergencyMedicine,PalmSprings,California
Submissionhistory:SubmittedFebruary22,2024;RevisionreceivedMay2,2024;AcceptedMay6,2024
ElectronicallypublishedJune26,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.19476
CasePresentation: Wepresentacaseofa10-year-oldmalewhodevelopedanatraumatic,nasal septalhematomawithabscessfollowingseveraldaysofrhinorrheaandcough.Hischiefcomplainttothe emergencydepartmentwasatwo-dayhistoryofnasalswellinganddiscomfort,associatedwithdifficulty breathingthroughhisnose.Thepatientwaswell-appearingwithswellingandtendernessalongthe externalnasalridgeandnasalseptalswellingthatoccludedbothnares.Contrast-enhancedmaxillofacial computedtomographyrevealedarim-enhancing, fluid-filledcollectiontotheanteriornasalseptum.The patientunderwentsuccessfulincisionanddrainagebyotolaryngology.
Discussion: Infectedseptalhematomasarerarebutimportanttorecognizeastheycanresultinseptal deformityandpotentiallylife-threateningsequelae,suchasintracranialinfections.Mostaresecondary tonasaltraumainadultpatients.Thiscasehighlightsauniquepresentationofatraumaticseptal hematomawithabscessformationinanimmunocompetentpediatricpatient.[ClinPractCasesEmerg Med.2024;8(3)311–313.]
Keywords: nasalseptalabscess;nasalseptalhematoma;pediatric;atraumatic;ear-nose-throat(ENT).
A10-year-oldmalewithnopastmedicalorsurgical historypresentedtoourhigh-volumecommunityemergency departmentwithatwo-dayhistoryofnasalswellingand discomfortassociatedwithcoughandrhinorrheathatbegan afewdaysprior.Hehaddifficultyinhalingthroughhisnose butdeniedanytrauma,dentalpain,fevers,orvomiting.No seasonalallergiesorallergiestomedicationswerereported bythepatient’sfamily.
Thepatientwaswell-appearing,withanelevatedbodymass indexof32(referencerange18.5–24.9forhealthyweight). Vitalsignswerewithinnormallimits,withtemperatureof 37.2° Celsius,heartrateof95beatsperminute,respiratoryrate of18breathsperminute,andoxygensaturationof98%on roomair.Physicalexaminationrevealedswellingand tendernessoftheexternalaspectofthenosewithoutevidence ofskinlesionsortrauma.Theseptumwasedematous extendingintoandobstructingbothnares,andclearnasal dischargewaspresent(Image1).Hehadnorespiratory distress,andoropharynxwasclearwithnormaldentition.
Theotolaryngology(ENT)servicewasconsulted,and theyrecommendedmaxillofacialcomputedtomography (CT)withcontrast.Computedtomographyimagingwas significantfora3.7 × 2.8 × 2.1centimetermidlinerimenhancing, fluidcollectionattheanteriornasalseptumwith obstructionofthebilateralnasalcavity(Image2).Therewas mildparanasalmucosalthickeningwithoutbony destruction.Whitebloodcellcountrevealedaleukocytosisof 20.1 × 109/liter(referencerange5.0–14.5 × 109/liter)withleft shiftof85.8%neutrophils(42–77%)and10%lymphocytes (20–40%).Analgesiawithacetaminophenandempiric intravenousantibioticsofvancomycinandpiperacillin/ tazobactamwereinitiatedforsuspectednasalseptalabscess. Thepatientwastransferredtoatertiarycarefacilitywith pediatricENTservices.
Thefollowingday,pediatricENTperformedanincision anddrainageofthenasalseptalcollectionwithreported bloodyoutputandscantpurulence.Culturesubsequently revealedlightgrowthof Staphylococcusaureus, Corynebacteriumamycolatum, and Sepidermidis. The
patientwasdischargedthedayaftersurgeryinstable conditionwithoutoutpatientantibiotics.
Nasalseptalhematomasandabscessesarecollectionsof bloodorpurulentmaterial,respectively,withinthenasal septumandarerareclinicaloccurrences.Nasalseptal abscessesarealmostexclusivelydescribedaftertraumaand arethoughttoarisesecondarytoseptalhematoma formation.1–4 Inonecaseseries,all20pediatricpatientswho presentedwithseptalhematomaand/orabscesshada reportedhistoryofnasaltrauma.1 Lesscommoncausesof septalabscessincludedentalinfection,rhinosinusitis,and postoperativesequelae.2,3 Typicalpathogensinclude Saureus,Streptococcuspneumoniae,Haemophilus in fl uenzae, andanaerobicbacteria.2 Atraumaticnasalseptal abscesseshavebeenmorecommonlyreportedin immunocompromisedadults,andaspontaneousnasalseptal hematomawithabscesshasbeenreportedinanadult.5 Our caseisnovelinthatwepresentanatraumatic,infectedseptal hematomainanimmunocompetentpediatricpatient.
Aclinicalpresentationofpainandswellingwith examination findingsseenin Images1 and 2 shouldprompt considerationofseptalhematomaorabscess.InourcaseENT
CPC-EMCapsule
Whatdowealreadyknowaboutthis clinicalentity?
Nasalseptalabscessisacomplicationof traumaticseptalhematomawithpotential sequelaesuchascartilagenecrosis,cavernous sinusthrombosis,andmeningitis.
Whatisthemajorimpactoftheimages?
Theimagesshowatraumatic,infectedseptal hematomainanimmunocompetentpediatric patient,representingarareclinical presentationinanuncommondemographic.
Howmightthisimproveemergency medicinepractice?
Infectedseptalhematomasarerareand requiretimelydiagnosis,whichcanbe achievedwithclinicalsuspicionguidedby visualrecognitionofcardinalfeatures.
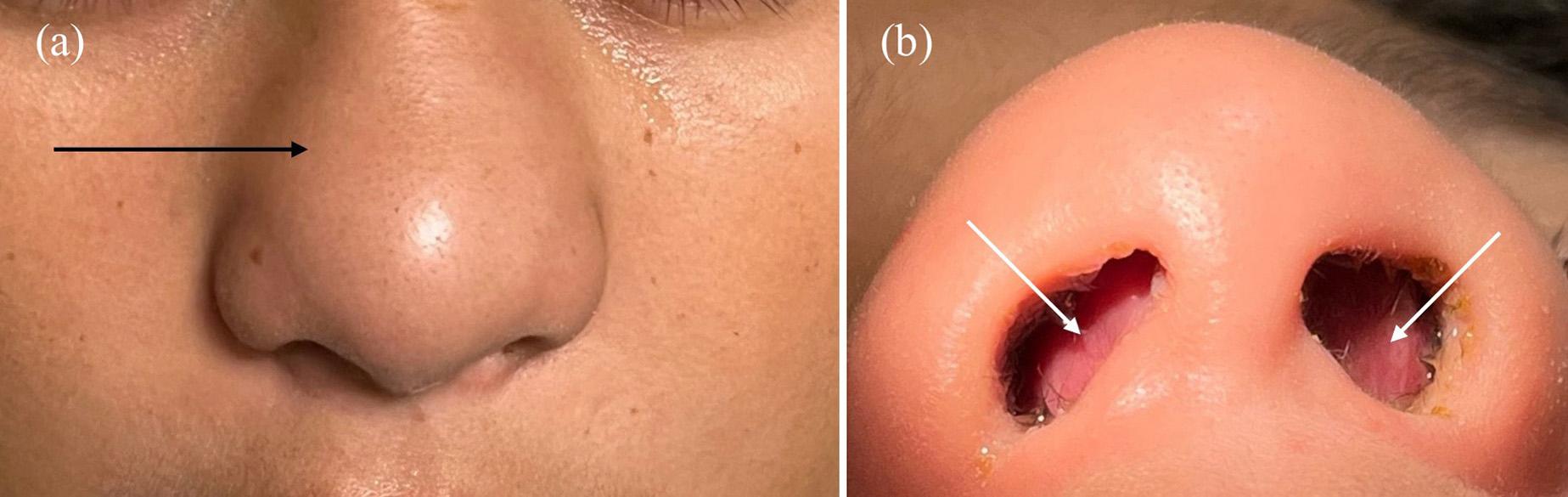
Image1. Externalnasalexamination(a)ofthepatientdemonstrateddiffuseedemasuperiortobothala(blackarrow).Internalnasalexamination (b)revealedamarkedlyedematousnasalseptumthatextendedandoccludedbothnares(whitearrows).Clearrhinorrheawasnoted.
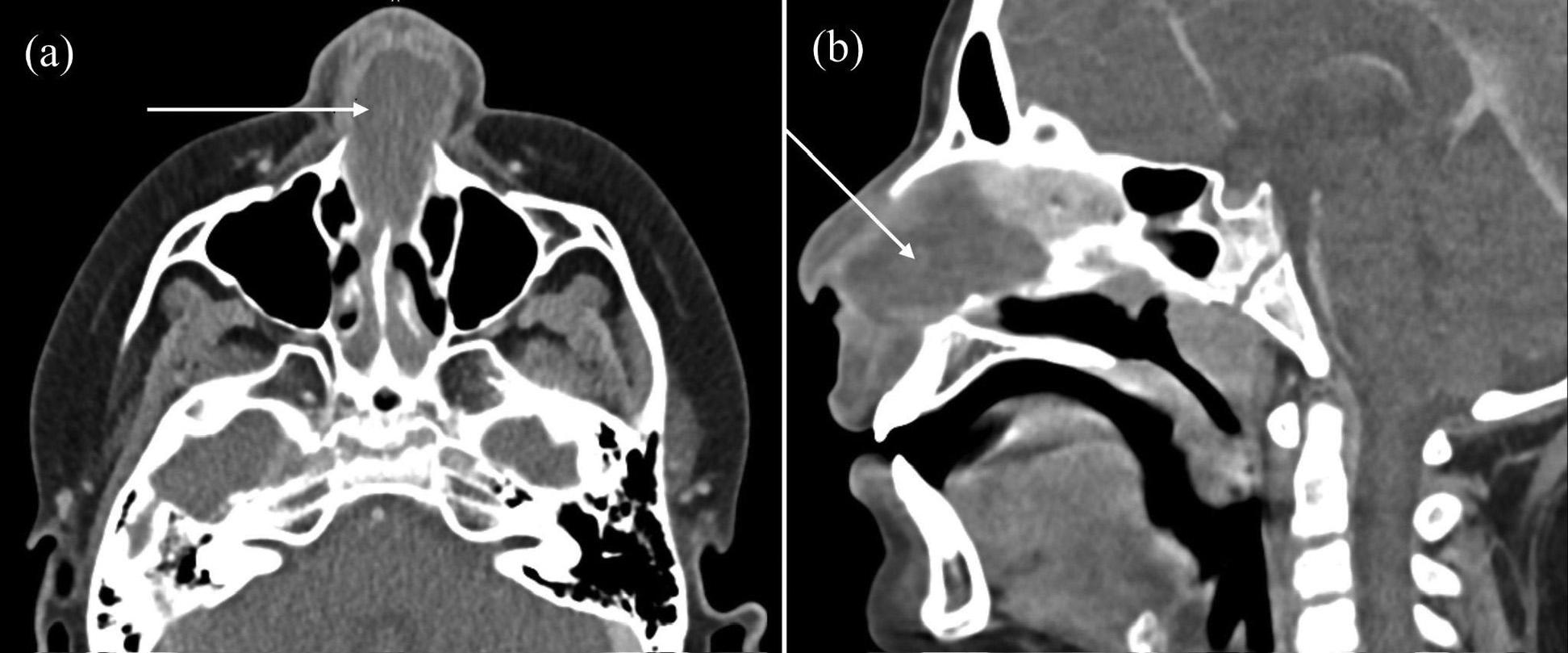
Image2. Axial(a)andsagittal(b)imagesofcontrast-enhancedmaxillofacialcomputedtomographydemonstratingalargemidlinerimenhancing, fluid-filledmassattheanteriornasalseptum(arrows)withobstructionofbothnasalcavities.
recommendedadvancedimagingandtransfertoasitewith pediatricENTavailability.Timelyrecognitionanddiagnosis ispivotaltooptimalpatientoutcomesandminimizing potentialcomplicationsincludingnasaldeformity,septal perforation,andintracranialinfection.2
Patientconsenthasbeenobtainedand filedforthepublicationofthis casereport.
TheauthorsattestthattheirinstitutiondoesnotrequireInstitutional ReviewBoardapprovalforpublicationofthiscasereport. Documentationon file.
AddressforCorrespondence:JacquelineLe,MD,Desert RegionalMedicalCenter,DepartmentofEmergencyMedicine, 1150N.IndianCanyonDr.,PalmSprings,CA92262. Email: Jacqueline.Le@vituity.com
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Sheferetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CantyPAandBerkowitzRG.Hematomaandabscessofthe nasalseptuminchildren. ArchOtolaryngolHeadNeckSurg. 1996;122(12):1373–6.
2.HuangYC,HungPL,LinHC.Nasalseptalabscessinan immunocompetentchild. PediatrNeonatol. 2012;53(3):213–5.
3.TienDA,KrakovitzP,AnneS.Nasalseptalabscessinassociation withpediatricacuterhinosinusitis. IntJPediatrOtorhinolaryngol. 2016;91:27–9.
4.AlshaikhNandLoS.Nasalseptalabscessinchildren:fromdiagnosis tomanagementandprevention. IntJPediatrOtorhinolaryngol. 2011;75(6):737–44.
5.MooneyCPandRimmerJ.Spontaneousnasalseptalhaematoma andabscess:acasereportandliteraturereview. RhinolOnline. 2018;1(1):122–6.
MarkL.Moubarek,MD*
GordonX.Wong,MD†
JamesS.Ford,MD,MAS‡
*UniversityofCalifornia,DavisHealth,DepartmentofEmergencyMedicine, Sacramento,California
† UniversityofCalifornia,DavisHealth,DepartmentofInternalMedicine, DivisionofCardiovascularMedicine,Sacramento,California
‡ UniversityofCalifornia,SanFrancisco,DepartmentofEmergencyMedicine, SanFrancisco,California
SectionEditor:R.GentryWilkerson,MD
Submissionhistory:SubmittedFebruary21,2024;RevisionreceivedMay3,2024;AcceptedMay5,2024
ElectronicallypublishedAugust2,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.19477
CasePresentation: A22-year-oldmalewithahistoryofanti-neutrophilcytoplasmicantibodyvasculitis, renaltransplant,hypertension,andnoknownfamilyhistoryofsuddencardiacdeathsuffereda witnessedcardiacarrest.Aninitialrhythmstriprecordedbyemergencymedicalservicesrevealed ventricular fibrillation.Returnofspontaneouscirculationwasachievedafterthreeroundsof cardiopulmonaryresuscitation,defibrillation,andintravenousepinephrine.Thepatientwasbroughtto theemergencydepartmentandadmittedtotheintensivecareunit.HewasdiagnosedwithBrugada syndrome,andanautomaticimplantablecardioverter-defibrillator(AICD)wasplacedafterdischarge.
Discussion: Brugadasyndromeischaracterizedelectrocardiographicallyby ≥2millimeters(mm) ST-segmentelevationinleadsV1–V2 witheither “covedtype” (type1)or “saddleback” (type2) ST-segmentmorphology,or ≤2mmST-segmentelevationinV1–V2 witheither “coved” or “saddleback” morphology(type3).Theabsenceofthesepatternsonisolatedelectrocardiograms(ECG)doesnot excludethediagnosis,asdynamic fluctuationsinECGpatternsarewell-documentedandcanbe inducedbyvariousphysiologicstressors.Thiscaseprovidesanuncommon,complete electrocardiographichistoryofBrugadasyndrome,fromout-of-hospitalcardiacarresttoAICD placementanddepictsdynamic fluctuationsbetweenBrugadapatternsandnormalECGs.This highlightstheimportanceofserialECGsindiagnosis,assuddencardiacdeathisoftenthe firstoronly presentationofBrugadasyndrome.[ClinPractCasesEmergMed.2024;8(3)314–317.]
Keywords: Brugadasyndrome;suddencardiacdeath;cardiacarrest;covedST-segmentelevation; saddlebackST-segmentelevation.
A22-year-oldmale,withahistoryofanti-neutrophil cytoplasmicantibodyvasculitis,renaltransplant, hypertension,andnoknownfamilyhistoryofsuddencardiac death,sufferedawitnessedout-of-hospitalcardiacarrest, receivingbystandercardiopulmonaryresuscitation(CPR). Aninitialelectrocardiogram(ECG)rhythmstripinthe field revealedventricular fibrillation(VF)(Image1).Thepatient achievedreturnofspontaneouscirculation(ROSC)after threemilligrams(mg)ofintravenous(IV)epinephrine,
450mgIVamiodarone,andthreeroundsofCPRand defibrillation.Hewasintubatedinthe field.Apost-ROSC ECGdemonstratedBrugadatype1ST-segmentelevationin V1–V2 (Image2A).1 Intheemergencydepartment(ED)an ECGshoweddynamicresolutionoftheBrugada pattern(Image2B).
Thepatientwasgivencalciumgluconateempiricallyfor thetreatmentofpresumptivehyperkalemia,givenhishistory ofrenaltransplant.IntheED,labswerenotableforapHof 6.90(referencerange7.35–7.40);partialpressureofcarbon
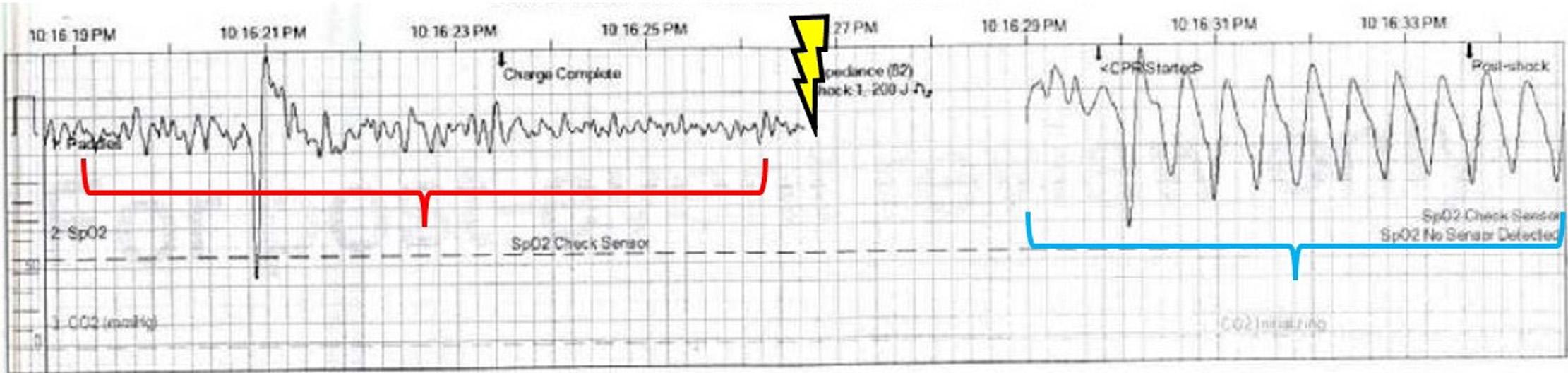
Image1. Rhythmstripperformedbyemergencymedicalservicesshowingventricular fibrillation(redbracket)followedbydefibrillation (lightningsymbol),withconversiontoawide-complextachycardiaconsistentwithventriculartachycardia(bluebracket).
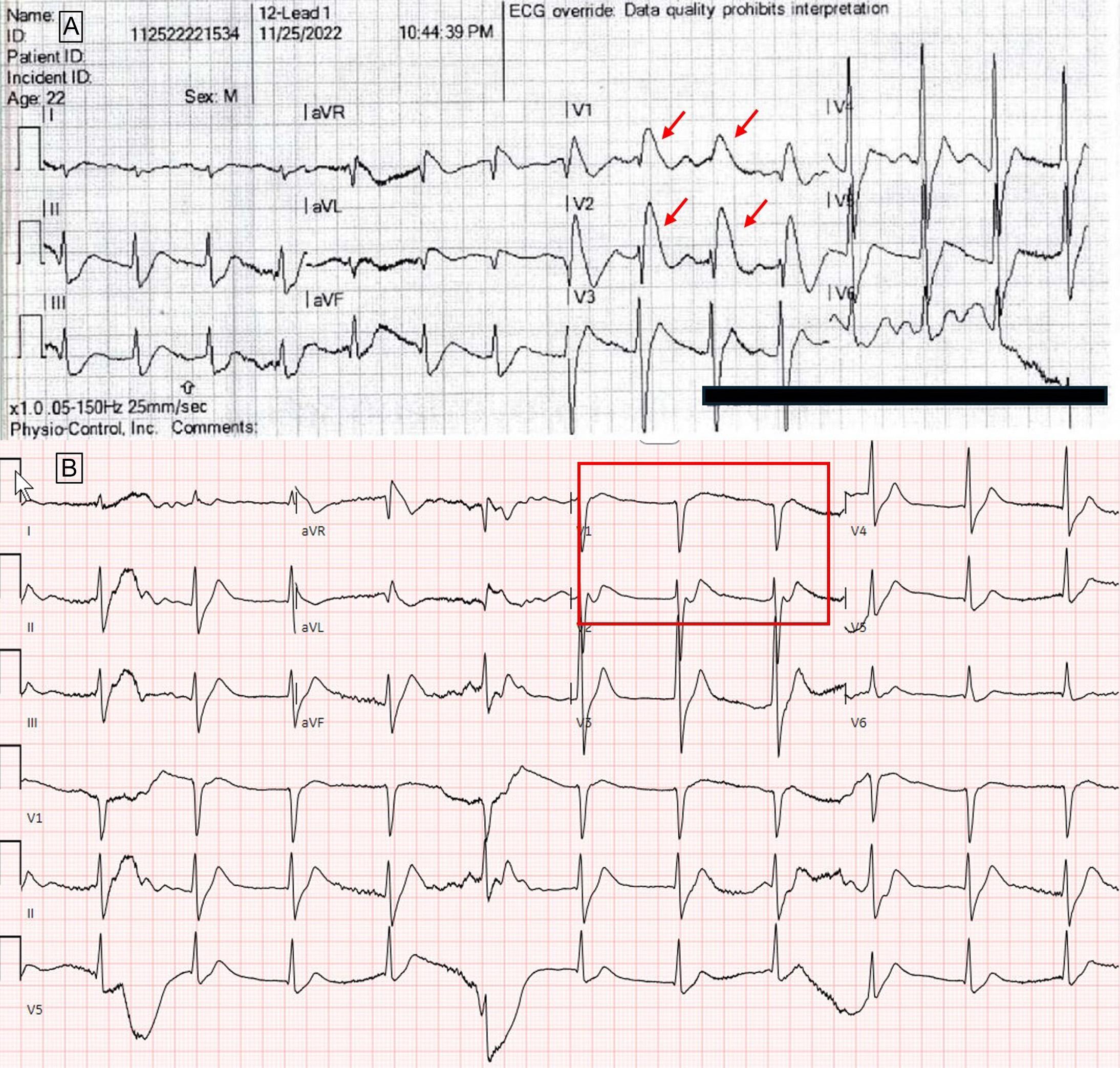
Image2. A.Electrocardiogramperformedbyemergencymedicalservicespriortoarrivaltotheemergencydepartment,showingBrugada pattern(type1)ST-segmentelevationinleadsV1–V2 (redarrows).B.InitialECGperformedintheED,withresolutionofBrugadapattern ST-segmentelevations(redbox).
dioxide67millimetersofmercury(mmHg)(35–45mmHg), bicarbonate13milliequivalentsperliter(mEq/L)(22–28 mEq/L),andpotassium2.4mEq/L(3.5–5.2mEq/L).Four
hourslater,pHandpotassiumnormalizedwithoutfurther intervention.Thepatientbrieflyrequiredanorepinephrine infusionforlowbloodpressureandwasgivenempiricbroad
spectrumantibioticstocoverforpossiblesepsis.Antibiotics werediscontinuedafteranegativeinfectiousworkup. Anechocardiogramandcomputedtomographyofthe head,chest,abdomen,andpelviswereunremarkable.The patientwasadmittedtotheintensivecareunitandunderwent targetedtemperaturemanagement.AnECGfromhospital day fivere-demonstratedatype1Brugadapattern (Image3A),andanECGfromhospitalday10showedatype 3Brugadapattern(Image3B).2 Giventhere-demonstration ofBrugadapatternsdespitenormalizationoflaboratory derangementsandnootheridentifiedcauseofcardiacarrest, hewasdiagnosedwithBrugadasyndrome.Noformal
electrophysiologictestingwasperformed.Hewasdischarged onhospitalday28withaLifeVest(ZollMedical Corporation,Pittsburgh,PA)afteranear-completephysical andneurologicrecovery,andheunderwentoutpatient automatic-implantable-cardioverter-defibrillator(AICD) placement.Genetictestingperformedlaterasanoutpatient wasinconclusive.
Brugadasyndromeischaracterized electrocardiographicallyby ≥2mmST-segmentelevationin leadsV1–V2 witheither “covedtype” (type1)or
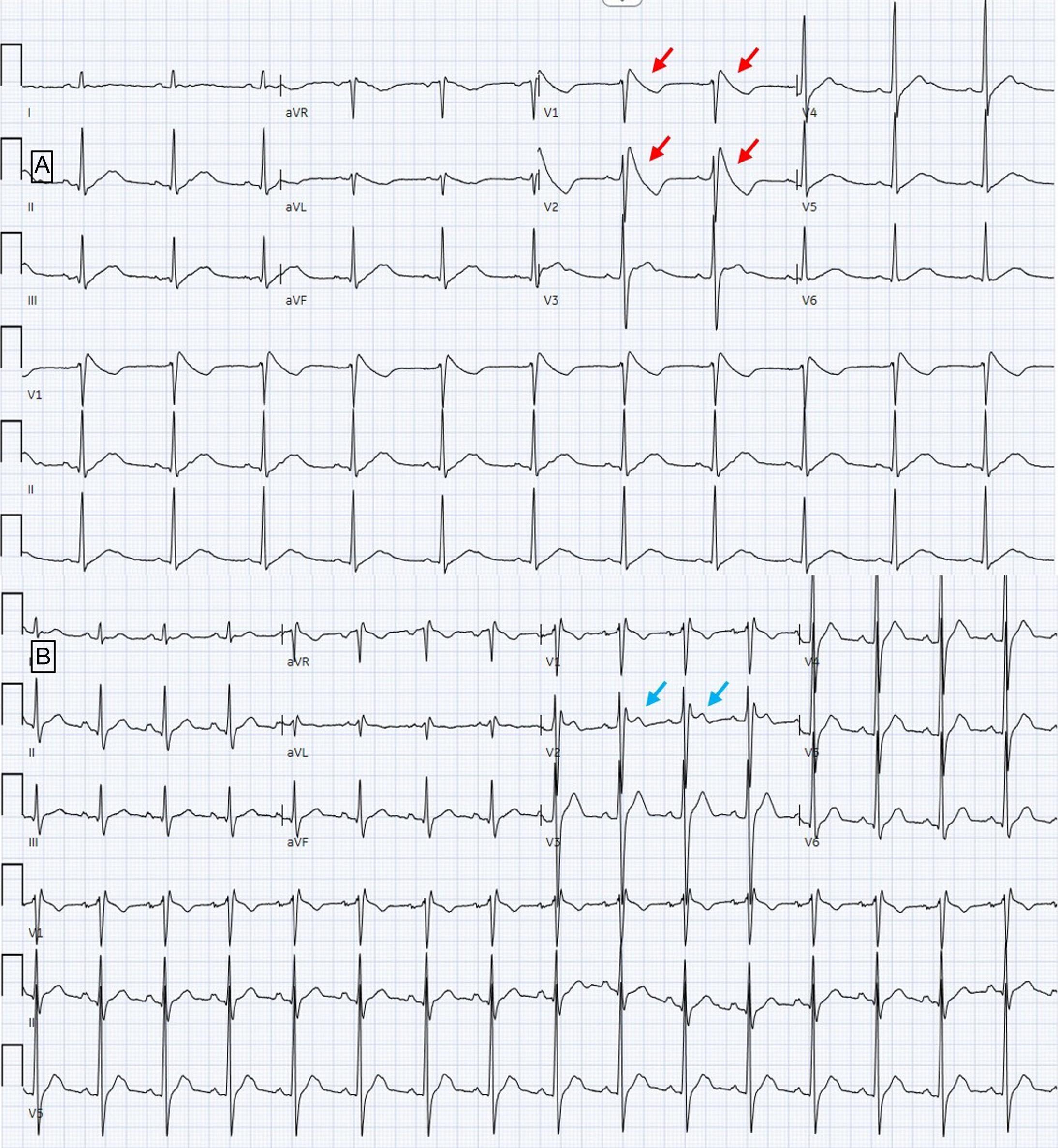
Image3. A.Electrocardiogram(ECG)performedapproximately60hourspostinitialcardiacarrest,againwithdown-slopingST-segment (Type1)elevationsinleadsV1–V2 (redarrows).B.ECGperformed10daysafterinitialcardiacarrestshowingsaddlebackST-segment elevation <2mm(type3)inleadV2 (bluearrows).
Whatdowealreadyknowaboutthis clinicalentity?
TheabsenceofclassicBrugadapatterns ( “ coved ” or “ saddleback ” ST-segment elevations)onisolatedelectrocardiograms (ECG)doesnotexcludethediagnosis.
Whatisthemajorimpactoftheimages?
Imagesdepictdynamicchangesbetween BrugadapatternsandnormalECGs,from cardiacarresttoautomaticimplantable cardioverter-de fi brillatorplacement.
Howmightthisimproveemergency medicinepractice?
SerialECGsareimportantindiagnosis,as suddencardiacdeathisoftenthe fi rstoronly presentationofBrugadasyndrome.
“saddleback” (type2)ST-segmentmorphology,or ≤2mm ST-segmentelevationinV1–V2 witheither “coved” or “saddleback” morphology(type3).1,2 Theabsenceofthese patternsonisolatedECGsdoesnotexcludethediagnosis,as dynamic fluctuationsinECGpatternsarewell-documented andcanoccurinresponsetomedications,fever,exerciseor otherstressors 1,3 Whilethispatientdidnotundergoformal electrophysiologictesting,establisheddiagnosticcriteriado notnecessitatethis,anditsutilityisquestionableinVFsurvivors.2 Similarly,thispatient’sgenetictestingwas inconclusive;only10–30%ofpatientshavebeensuccessfully genotyped,owingtothebroadheterogeneityandcomplexity ofunderlyinggeneticriskfactorsthatcanpredisposean individualtoBrugadasyndrome.2
Thiscaseprovidesanuncommon,complete electrocardiographichistoryofBrugadasyndrome,from out-of-hospitalcardiacarresttoAICDplacementand depictsclassicdynamic fluctuationsbetweenBrugada
patternsandnormalrhythmsonECG.Thishighlights theimportanceofserialECGsindiagnosis,assudden cardiacdeathisoftenthe firstoronlypresentationof Brugadasyndrome.4
TheauthorsattestthattheirinstitutionrequiresneitherInstitutional ReviewBoardapproval,norpatientconsentforpublicationofthis casereport.Documentationon file.
AddressforCorrespondence:MarkL.Moubarek,MD,Universityof California,Davis,DepartmentofEmergencyMedicine,450VStreet, PatientSupportServicesBuilding,Suite2100,Sacramento, CA95817.Email: mlmoubarek@ucdavis.edu
ConflictsofInterest:Bythe CPC-EM articlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsdisclosednone.
Copyright:©2024Moubareketal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PrioriSG,WildeAA,HorieM,etal.HRS/EHRA/APHRSexpert consensusstatementonthediagnosisandmanagementof patientswithinheritedprimaryarrhythmiasyndromes:document endorsedbyHRS,EHRA,andAPHRSinMay2013andby ACCF,AHA,PACES,andAEPCinJune2013. HeartRhythm. 2013;10(12):1932–63.
2.WildeAA,AntzelevitchC,BorggrefeM,etal.Proposeddiagnostic criteriafortheBrugadasyndrome:consensusreport. Circulation. 2002;106(19):2514–9.
3.VeltmannC,SchimpfR,EchternachC,etal.Aprospectivestudyon spontaneous fluctuationsbetweendiagnosticandnon-diagnosticECGs inBrugadasyndrome:implicationsforcorrectphenotypingandrisk stratification. EurHeartJ. 2006;27(21):2544–52.
4.ProbstV,VeltmannC,EckardtL,etal.Long-termprognosisofpatients diagnosedwithBrugadasyndrome:resultsfromtheFINGERBrugada syndromeregistry. Circulation. 2010;121(5):635–43.