with Population Health Indexed in MEDLINE
Behavioral Health

823 Optimizing a Drone Network to Respond to Opioid Overdoses
Daniel J. Cox, Jinny J. Ye, Chixiang Zhang, Lee Van Vleet, João R. NickenigVissoci, Daniel M. Buckland
831 Does Housing Status Matter in Emergency Medical Services Administration of Naloxone? A Prehospital Cross-sectional Study

Tiffany M. Abramson, Corey M. Abramson, Elizabeth Burner, Marc Eckstein, Stephen Sanko, Suzanne Wenzel
Education
839 Application of a Low-cost, High-fidelity Proximal Phalangeal Dislocation Reduction Model for Clinician Training
Spencer Lord, Sean Geary, Garrett Lord
847 Gender and Inconsistent Evaluations: A Mixed-methods Analysis of Feedback for Emergency Medicine Residents
Alexandra E. Brewer, Laura Nelson, Anna S. Mueller, Rebecca Ewert, Daniel M. O’Connor, Arjun Dayal, Vineet M. Arora
855 COVID-lateral Damage: Impact of the Post-COVID-19 Era on Procedural Training in Emergency Medicine Residency



Daniel Frank, Thomas Perera, Moshe Weizberg
861 Improvement in Resident Scholarly Output with Implementation of a Scholarly Activity Guideline and Point System
Lauren Evans, Sarah Greenberger, Rachael Freeze-Ramsey, Amanda Young, Crystal Sparks, Rawle Seupaul, Travis Eastin, Carly Eastin
Contents continued on page iii
Volume 24, Number 5, September 2023 Open Access at WestJEM.com ISSN 1936-900X A Peer-Reviewed, International Professional Journal Western Journal of Emergency Medicine VOLUME 24, NUMBER 5, September 2023 PAGES 823-1004
Western Journal of Emergency Medicine: Integrating Emergency Care
West
Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Resident Editors
AAEM/RSA
John J. Campo, MD Harbor-University of California, Los Angeles Medical Center
ACOEP
Justina Truong, DO Kingman Regional Medical Center
Section Editors
Behavioral Emergencies
Leslie Zun, MD, MBA Chicago Medical School
Marc L. Martel, MD Hennepin County Medical Center
Cardiac Care
Fred A. Severyn, MD University of Colorado School of Medicine
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD
Carolinas Medical Center
Casey Clements, MD, PhD Mayo Clinic
Patrick Meloy, MD Emory University
Nicholas Pettit, DO, PhD
Indiana University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO
Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Gabriel Wardi, MD
University of California, San Diego
Joseph Shiber, MD
University of Florida-College of Medicine
Matt Prekker MD, MPH
Hennepin County Medical Center
David Page, MD
University of Alabama
Erik Melnychuk, MD
Geisinger Health
Quincy Tran, MD, PhD
University of Maryland
Disaster Medicine
John Broach, MD, MPH, MBA, FACEP
University of Massachusetts Medical School
UMass Memorial Medical Center
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of MedicineIrvine, California
Shahram Lotfipour, MD, MPH, Managing Editor University of California, Irvine School of MedicineIrvine, California
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Niels K. Rathlev, MD, Associate Editor Tufts University School of Medicine-Boston, Massachusetts
Rick A. McPheeters, DO, Associate Editor Kern Medical- Bakersfield, California
Gentry Wilkerson, MD, Associate Editor University of Maryland
Christopher Kang, MD Madigan Army Medical Center
Education
Danya Khoujah, MBBS University of Maryland School of Medicine
Jeffrey Druck, MD University of Colorado
John Burkhardt, MD, MA University of Michigan Medical School
Michael Epter, DO Maricopa Medical Center
ED Administration, Quality, Safety
Tehreem Rehman, MD, MPH, MBA Mount Sinai Hospital
David C. Lee, MD Northshore University Hospital
Gary Johnson, MD Upstate Medical University
Brian J. Yun, MD, MBA, MPH Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine


University of California, Davis
Emergency Medical Services
Daniel Joseph, MD Yale University
Joshua B. Gaither, MD
University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD Yale School of Medicine
Stephen Meldon, MD Cleveland Clinic
Luna Ragsdale, MD, MPH Duke University
Health Equity
Emily C. Manchanda, MD, MPH Boston University School of Medicine
Faith Quenzer
Temecula Valley Hospital
San Ysidro Health Center
Shadi Lahham, MD, MS, Deputy Editor Kaiser Permanente- Irvine, California
Susan R. Wilcox, MD, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Elizabeth Burner, MD, MPH, Associate Editor University of Southern California- Los Angeles, California
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston Texas

Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Mandy J. Hill, DrPH, MPH UT Health McGovern Medical School
Payal Modi, MD MScPH
University of Massachusetts Medical
Infectious Disease
Elissa Schechter-Perkins, MD, MPH
Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Kevin Lunney, MD, MHS, PhD University of Maryland School of Medicine
Stephen Liang, MD, MPHS Washington University School of Medicine
Victor Cisneros, MD, MPH Eisenhower Medical Center
Injury Prevention
Mark Faul, PhD, MA Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS
Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH
Prisma Health Richland
Taylor Burkholder, MD, MPH
Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Melanie S. Heniff, MD, JD Indiana University School of Medicine
Greg P. Moore, MD, JD Madigan Army Medical Center
Statistics and Methodology
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS
Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS Pacific Northwest University
Rick Lucarelli, MD Medical City Dallas Hospital
William D. Whetstone, MD
University of California, San Francisco
Neurosciences
Antonio Siniscalchi, MD
Annunziata Hospital, Cosenza, Italy
Pediatric Emergency Medicine
Paul Walsh, MD, MSc
University of California, Davis
Muhammad Waseem, MD
Lincoln Medical & Mental Health Center
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
Jacob Manteuffel, MD
Henry Ford Hospital
John Ashurst, DO
Lehigh Valley Health Network
Tony Zitek, MD
Kendall Regional Medical Center
Trevor Mills, MD, MPH
Northern California VA Health Care
Erik S. Anderson, MD
Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD Henry Ford Hospital
Phillips Perera, MD
Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS
Virginia Commonwealth University
Jeffrey R. Suchard, MD
University of California, Irvine

Ultrasound
J. Matthew Fields, MD
Thomas Jefferson University
Shane Summers, MD
Brooke Army Medical Center
Robert R. Ehrman
Wayne State University
Ryan C. Gibbons, MD Temple Health
Volume 24, No. 5: September 2023 i Western Journal of Emergency Medicine Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org Western Journal
Emergency Medicine
Integrating Emergency Care with Population Health Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
of
:
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine
Western
Amin A. Kazzi, MD, MAAEM The American University of Beirut, Beirut, Lebanon
Anwar Al-Awadhi, MD
Mubarak Al-Kabeer Hospital, Jabriya, Kuwait
Arif A. Cevik, MD United Arab Emirates University College of Medicine and Health Sciences, Al Ain, United Arab Emirates
Abhinandan A.Desai, MD University of Bombay Grant Medical College, Bombay, India
Bandr Mzahim, MD King Fahad Medical City, Riyadh, Saudi Arabia
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
David F.M. Brown, MD Massachusetts General Hospital/ Harvard Medical School
Douglas Ander, MD Emory University
Editorial Board
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Francesco Della Corte, MD
Azienda Ospedaliera Universitaria
“Maggiore della Carità,” Novara, Italy
Francis Counselman, MD Eastern Virginia Medical School
Gayle Galleta, MD
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Jacob (Kobi) Peleg, PhD, MPH Tel-Aviv University, Tel-Aviv, Israel
Jaqueline Le, MD Desert Regional Medical Center
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jonathan Olshaker, MD Boston University
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Khrongwong Musikatavorn, MD King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Nadeem Qureshi, MD St. Louis University, USA Emirates Society of Emergency Medicine, United Arab Emirates
Niels K. Rathlev, MD Tufts University School of Medicine
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Rachel A. Lindor, MD, JD Mayo Clinic
Robert M. Rodriguez, MD University of California, San Francisco
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Samuel J. Stratton, MD, MPH Orange County, CA, EMS Agency
Scott Rudkin, MD, MBA University of California, Irvine

Scott Zeller, MD University of California, Riverside
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Terry Mulligan, DO, MPH, FIFEM
ACEP Ambassador to the Netherlands Society of Emergency Physicians
Vijay Gautam, MBBS University of London, London, England
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Editorial Staff Advisory Board
Elena Lopez-Gusman, JD California ACEP American College of Emergency Physicians

Jennifer Kanapicki Comer, MD FAAEM California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE American College of Osteopathic Emergency Physicians

Kimberly Ang, MBA UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians Kaiser Permanente
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center

Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP UC San Diego Health School of Medicine
Isabelle Nepomuceno, BS Executive Editorial Director
Visha Bajaria, BS WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
June Casey, BA Copy Editor
Western Journal of Emergency Medicine ii Volume 24, No. 5: September 2023 Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine
Integrating Emergency Care with Population Health Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Journal of Emergency Medicine:
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
JOURNAL FOCUS
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
Table of Contents
Emergency Medical Services
868
Prehospital mSOFA Score for Quick Prediction of Life-Saving Interventions and Mortality in Trauma Patients: A Prospective, Multicenter, Ambulance-based, Cohort Study
Francisco Martin-Rodriguez, Ancor Sanz-Garcia, Ana Benito Justel, Almudena Morales Sánchez, Cristina Mazas Perez Oleaga, Irene Delgado Noya, Irene Sánchez Soberón, Carlos del Pozo Vegas, Juan F. Delgado Benito, Raúl López-Izquierdo
Health Equity
878 Social Determinants of Health in EMS Records: A Mixed-methods Analysis Using Natural Language Processing and Qualitative Content Analysis
Susan J. Burnett, Rachel Stemerman, Johanna C. Innes, Maria C. Kaisler, Remle P. Crowe, Brian M. Clemency
888 Racial Differences in Triage for Emergency Department Patients with Subjective Chief Complaints
Cassandra Peitzman, Jossie A. Carreras Tartak, Margaret Samuels-Kalow, Ali Raja, Wendy L. Macias-Konstantopoulos
894 Emergency Department Use Among Recently Homeless Adults in a Nationally Representative Sample
Caitlin R. Ryus, Elina Stefanovics, Jack Tsai, Taeho Greg Rhee, Robert A. Rosenheck
906 Race, Healthcare, and Health Disparities: A Critical Review and Recommendations for Advancing Health Equity
Wendy L. Macias-Konstantopoulos, Kimberly A. Collins, Rosemarie Diaz, Herbert C. Duber, Courtney D. Edwards, Anthony P. Hsu, Megan L. Ranney, Ralph J. Riviello, Zachary S. Wettstein, Carolyn J. Sachs
919 From the Editors – Future Directions to Strengthen the Emergency Department Safety Net Rama A. Salhi, Wendy L. Macias-Konstantopoulos, Caitlin R. Ryus
Musculoskeletal
921 Charcot Neuroarthropathy of the Foot and Ankle in the Acute Setting: An Illustrative Case Report and Targeted Review
Kian Bagheri, Albert T. Anastasio, Alexandra Krez, Lauren Siewny, Samuel B. Adams
Nueurology
931 A Shorter Door-In-Door-Out Time Is Associated with Improved Outcome in Large Vessel Occlusion Stroke
Adam Sigal, Derek L. Isenberg, Chadd K. Kraus, Daniel Ackerman, Joseph Herres, Ethan S. Brandler, Alexander Kuc, Jason T. Nomura, Derek R. Cooney, Michael T. Mullen, Huaquing Zhao, Nina T. Gentile
939 Treatment of Factor-Xa Inhibitor-associated Bleeding with Andexanet Alfa or 4 Factor PCC: A Multicenter Feasibility Retrospective Study
Adam J. Singer, Mauricio Concha, James Williams, Caitlin S. Brown, Rafael Fernandes, Henry C. Thode, Marylin Kirchman, Alejandro A. Rabinstein
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
Volume 24, No. 5: September 2023 iii Western Journal of
Medicine
Emergency
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Table of Contents continued
Pediatrics
950 Influence of Body Mass Index on the Evaluation and Management of Pediatric Abdominal Pain in the Emergency Department
Carly A. Theiler, Morgan Bobb Swanson, Ryan Squires, Karisa K. Harland
956 Comparison of Pediatric Acute Appendicitis Before and During the COVID-19 Pandemic in New York City
Priya Mallikarjuna, Saikat Goswami, Sandy Ma, Won Baik-Han, Kelly L. Cervellione, Gagan Gulati, Lily Quon Lew
Public Health
962 Expanding Diabetes Screening to Identify Undiagnosed Cases Among Emergency Department Patients
David C. Lee, Harita Reddy, Christian A. Koziatek, Noah Klein, Anup Chitnis, Kashif Creary, Gerard Francois, Olumide Akindutire, Robert Femia, Reed Caldwell
Trauma
967 Factors Associated with Overutilization of Computed Tomography of the Cervical Spine
Karl T. Chamberlin, Maureen M. Canellas, Martin A. Reznek, Kevin A. Kotkowski
Women’s Health
974 Sexual Assault Nurse Examiners Lead to Improved Uptake of Services: A Cross-Sectional Study
Meredith Hollender, Ellen Almirol, Makenna Meyer, Heather Bearden, Kimberly Stanford
983 Exploring Muslim Women’s Reproductive Health Needs and Preferences in the Emergency Department
Anum Naseem, Morgan Majed, Samantha Abdallah, Mayssa Saleh, Meghan Lirhoff, Ahmed Bazzi, Martina Caldwell
993 Mixed-methods Evaluation of an Expedited Partner Therapy Take-home Medication Program: Pilot Emergency Department Intervention to Improve Sexual Health Equity
Emily E. Ager, William Sturdavant, Zoe Curry, Fahmida Ahmed, Melissa DeJonckheere, Andrew A. Gutting, Roland C. Merchant, Keith E. Kocher, Rachel E. Solnick
Western Journal of Emergency Medicine iv Volume 24, No. 5: September 2023
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber
Albany Medical College
Albany, NY
Allegheny Health Network
Pittsburgh, PA
American University of Beirut
Beirut, Lebanon
AMITA Health Resurrection Medical Center
Chicago, IL
Arrowhead Regional Medical Center
Colton, CA
Baylor College of Medicine
Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center
Boston, MA
Boston Medical Center
Boston, MA
Brigham and Women’s Hospital
Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
California Chapter Division of American Academy of Emergency Medicine
Mediterranean Academy of Emergency Medicine
INTEGRIS Health
Oklahoma City, OK
Kaiser Permenante Medical Center
San Diego, CA
Kaweah Delta Health Care District
Visalia, CA
Kennedy University Hospitals
Turnersville, NJ
Kent Hospital
Warwick, RI
Kern Medical
Bakersfield, CA
Lakeland HealthCare
St. Joseph, MI
Lehigh Valley Hospital and Health Network
Allentown, PA
Loma Linda University Medical Center
Loma Linda, CA
Louisiana State University Health Sciences Center
New Orleans, LA
Louisiana State University Shreveport
Shereveport, LA
Madigan Army Medical Center
Tacoma, WA
Maimonides Medical Center
Brooklyn, NY
Maine Medical Center
Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical
Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine
Sociedad Argentina de Emergencias
Mayo Clinic
Jacksonville, FL
Mayo Clinic College of Medicine
Rochester, MN
Mercy Health - Hackley Campus
Muskegon, MI
Merit Health Wesley
Hattiesburg, MS
Midwestern University
Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health
New York, NY
North Shore University Hospital
Manhasset, NY
Northwestern Medical Group
Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center
Columbus, OH
Ohio Valley Medical Center
Wheeling, WV
Oregon Health and Science University
Portland, OR
Penn State Milton S. Hershey Medical Center
Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
Sociedad Chileno Medicina Urgencia
Thai Association for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Volume 24, No. 5: September 2023 v Western Journal of
Medicine
Emergency
Web
Citation Index Expanded
of Science, Science
Indexed
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber
Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program
St. Paul, MN
Rhode Island Hospital
Providence, RI
Robert Wood Johnson University Hospital
New Brunswick, NJ
Rush University Medical Center
Chicago, IL
St. Luke’s University Health Network
Bethlehem, PA
Spectrum Health Lakeland
St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University
Syracuse, NY
Temple University
Philadelphia, PA
Texas Tech University Health Sciences Center
El Paso, TX
The MetroHealth System/ Case Western Reserve University
Cleveland, OH
UMass Chan Medical School
Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham
Birmingham, AL
University of Arizona College of Medicine-Tucson
Tucson, AZ
University of California, Davis Medical Center
Sacramento, CA
University of California, Irvine
Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego
La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center
Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida
Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago
Chicago, IL
University of Iowa
Iowa City, IA
University of Louisville
Louisville, KY
University of Maryland
Baltimore, MD
University of Massachusetts
Amherst, MA
University of Michigan
Ann Arbor, MI
University of Missouri, Columbia
Columbia, MO
University of North Dakota School of Medicine and Health Sciences
Grand Forks, ND
University of Nebraska Medical Center
Omaha, NE
University of Nevada, Las Vegas
Las Vegas, NV
University of Southern Alabama
Mobile, AL
University of Southern California
Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington
Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine
Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center
Seattle, WA
University of Wisconsin Hospitals and Clinics
Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center
Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University
Winston-Salem, NC
Wake Technical Community College
Raleigh, NC
Wayne State
Detroit, MI
Wright State University
Dayton, OH
Yale School of Medicine
New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
Sociedad Chileno Medicina Urgencia
Thai Association for Emergency Medicine
Mediterranean Academy of Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Western Journal of Emergency Medicine vi Volume 24, No. 5: September 2023
in MEDLINE,
and Clarivate Web of Science, Science Citation Index Expanded
PubMed,



Save the Date Spring Seminar 2024 | April 27 - May 1 Signia Orlando Bonnet Creek • Orlando, Florida #ACOEP24
OptimizingaDroneNetworktoRespondtoOpioidOverdoses
DanielJ.Cox,MD,MEng*
JinnyJ.Ye,MD*
ChixiangZhang,MS†
LeeVanVleet,MHS,NREMT-P‡
JoãoR.NickenigVissoci,PhD*§
DanielM.Buckland,MD,PhD*∥
*DukeUniversity,DepartmentofEmergencyMedicine,Durham,NorthCarolina
† DukeUniversity,DepartmentofElectricalandComputerEngineering,Durham, NorthCarolina
‡ DurhamCountyEmergencyMedicalServices,Durham,NorthCarolina
§ GlobalHealthInstitute,DukeUniversity,Durham,NorthCarolina
∥ DukeUniversity,DepartmentofMechanicalEngineeringandMaterialsScience, Durham,NorthCarolina
SectionEditors: ShiraSchlesinger,MD,MPH,andGayleGalletta,MD
Submissionhistory:SubmittedDecember14,2022;RevisionreceivedMarch30,2023;AcceptedMay24,2023
ElectronicallypublishedAugust30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59609
Introduction: Effectiveout-of-hospitaladministrationofnaloxoneinopioidoverdosesisdependenton timelyarrivalofnaloxone.Delaysinemergencymedicalservices(EMS)responsetimecouldpotentially beovercomewithdronestodelivernaloxoneefficientlytothesceneforbystanderuse.Ourobjectivewas toevaluateamathematicaloptimizationsimulationforgeographicalplacementofdronebasesin reducingresponsetimetoopioidoverdose.
Methods: UsingretrospectivedatafromasingleEMSsystemfromJanuary2016
February2019,we createdageospatialdrone-networkmodelbasedoncurrenttechnologicalspecificationsandpotential baselocations.Geneticoptimizationwasthenusedtomaximizecountycoveragebydronesandthe numberofoverdosescoveredperdronebase.Fromthismodel,weidentifiedbaselocationsthat minimizeresponsetimeandthenumberofdronebasesrequired.
Results: Inadronenetworkmodelwith2,327opioidoverdoses,asthenumberofmodeleddronebases increasedthecalculatedresponsetimedecreased.Inageospatiallyoptimizeddronenetworkwithfour dronebases,responsetimecomparedtoambulancearrivalwasreducedby4minutes38secondsand covered64.2%ofthecounty.
Conclusion: Inouranalysiswefoundthatinamathematicalmodelforgeospatialoptimization, implementingfourdronebasescouldreduceresponsetimeof9–1–1callsforopioid overdoses.Therefore,dronescouldtheoreticallyimprovetimetonaloxonedelivery.[WestJEmergMed. 2023;24(5)823–830.]
INTRODUCTION
In2021over100,000peoplediedfromopioidoverdosesin theUnitedStates.1 Opioiddeathratesalsoincreased10-fold from2013to2019.2 Althoughdeathfromanopioidtypically occursoverafewhours,3 theremaybebystanderdelaysin calling9
1
1.4
6 Thereductionofdeathsfromopioid overdosesoftendependsonprompt9–1
1responseanduse ofthereversalmedicationnaloxone.
Naloxoneiscurrentlyavailablewithoutaprescriptionin intranasalandintramuscularformsthatlay-userscansafely
administerwithlittleskill.Becauseofthis,bystanderscan playavitalroleinpreventingdeathsfromopioidoverdoses throughtheadministrationofnaloxone.Despiteexpanded accessandeducationonnaloxone,peoplewhouseopioids maynotcarrythislife-savingmedication.7 Furthermore, timetoambulancearrival,whichcanimpedetheprovisionof naloxone,rangesfrom1.7
51minutes(median6.9 minutes).8 NationalFireProtectionAgencyStandard1710 establishestargetresponsetimesforEMSpersonnel.Itstates thatthegoalforresponsetimesis fiveminutesfor90%of
–
–
–
–
–
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 823 ORIGINAL RESEARCH
dispatchedincidents.9 Analysisfrom2017suggestedthat EMSresponsetimesaveraged7minutesintheUS,two minuteslongerthanNFPA1710.10
Unmannedaerialvehicles,ordrones,mayofferabridge forfasternaloxonedeliverywhileawaitingtrained first responders(firefighters,police,orparamedics).Droneshave previouslybeenusedformedicationdeliveryinruralareas,7 diseasesurveillanceandcollectionofbiosamples,11 andthey havebeeninvestigatedforuseinautomaticexternal defibrillatorsdeliveryincardiacarrest.12 Recently,astudyby Tukeletaldemonstratedthatdroneshavetheabilityto travelstraight-linedistancescarryinglife-savingopioid reversalmedicationsfasterthanambulances.13 Additionally, apre-printbyLejuneandMadescribesuseofastochastic methodtoimproveresponsetimesby78%in VirginiaBeach.14
Ourobjectiveinthisstudywastodeterminewhethera mathematicalmodelcouldbeusedtooptimizetheplacement ofdronebasestoreduceresponsetimetoopioidoverdoses. Giventhelocationsofopioidoverdoses,thismathematical modeldeterminesthenumberandlocationofdronebasesto meetanyspecifiedreductioninresponsetime.When comparedtoobservedambulanceresponsetimes,our optimizednetworkwasfoundtoreduceresponse timestoopioidreversalmedicationdeliverybyover fourminutes.
METHODS StudySetting
ThestudywasconductedinacountyinNorthCarolina withapopulationofover300,000peoplein2019on ≈750 squarekilometersoflandwithanaveragepopulationdensity of434persquarekilometer.15 AsingleEMSagencyresponds tomedicalemergenciesforthisarea.Inallsuspectedopioid overdosecalls, firefightersandsheriff’sdeputiesare dispatchedalongwithEMS.However,weonlyhadaccessto theEMSdataforthisstudy.Notethatthedatadoesnot includeresponsetimesforlawenforcement, firefighters,or otheremergencymedicalresponders.
Dispatchingambulancesuseahybridsystemstatus management(SSM).ThehybridSSMcoordinates respondingunitsbasedinstationsandautomaticvehicle location(AVL)toguidedispatch.TheAVLensuresthatthe unitclosesttothecallisassignedtotheresponsebasedon GPS.Theparamedicservicealsostrategicallypostsunits basedoncallvolume.Forexample,ifallrespondingunitsare busy,outlyingunitswillbesenttogeneralgeographicareas toprovidecoverageinuncoveredareasduringahigh-volume period.Generalstudysettinginformation(eg,county demographics,responsetimes)areshownin Table1.We defined “dispatchtime” asthetimebetweenwhenthecall cameinandwhenaunitordronewasassignedtothat particularincident.
StudyDesign
Usingaretrospectivecross-sectionaldesign,weuseddata inprospectivelycollectedelectronichealthrecordsaspartof routinecare.OuroveralldesignwasinspiredbyBoutilier etal,16 whichmathematicallyoptimizeddronenetworksfor automaticexternaldefibrillators(AED)forout-of-hospital cardiacarrestinToronto,Canada.Theirmethodoptimized byathresholdresponsetime,determininghowmany dronesateachprospectivebasewouldberequiredto reduceresponsetimesbyone,two,andthreeminutes.We furtheredthisanalysismethodbynotholdingthenumberof basesconstantandoptimizedthenumberofdronesand basesneededtoproducethegreatestcoveragearea andproducethegreatestdecreaseinresponsetime perdrone.
DATASOURCES OpioidOverdoseEpisodes
Weincludedinthisstudyalldispatchesforsuspected opioidoverdosesintheserviceareafromJanuary1, 2016–February17,2019(EmergencyMedicalDispatchcard number23ornaloxoneadministrationduringthecall) regardlessofcallpriority).Locationsofthesedispatches wereautomaticallygeocoded(convertingatext-based addresstogeographiccoordinates)basedonaddresses obtainedduringdispatchcalls.
CandidateBaseLocations
Forthedronenetwork,all fire,paramedic,andEMS administrativebuildingswereconsideredpotentialdrone bases.Theaddressesofeachstationwereobtainedfromthe localparamedicserviceandgeocodedintoUniversal TransverseMercator(GISGeography,Redlands,CA)
Characteristics Population(2017)311,640 Populationdensity(2017),km2 935.7 Averageannualnumberofopioidoverdoses743.1 Femalegenderinoverdoses43% Averagepatientage,years41 Numberofparamedicand firestations29 Dispatchtime,minutes/seconds Average03:01 90thpercentile05:00 Responsetime,minutes/seconds Average10:46 90thpercentile17:00 WesternJournal of EmergencyMedicineVolume24,No.5:September2023 824
Table1. SummarystatisticsforDurhamCounty,NorthCarolina. CountyDemographicandHistoricalResponseData
OptimizingaDroneNetworktoRespondtoOpioidOverdoses
Coxetal.
coordinates.Weused29suchcandidatestationsinour analysis.Dronebaseswereselectedamongthese candidatestations.
DroneSpecifications
Droneparametersforourmodelwerechosentoreflect current,cost-effectivedronecapabilities.Wesetthe maximumspeedas18kilometersperhourandamaximum distanceof7kilometersononebatterylife.Wechosemore conservativemetricsthanBoutilieretalbecausenaloxone willrequirelesspowertotransportcomparedtoanAED. However,Tukeletaluseddronesthatcouldreachspeedsof 94kilometersperhour,whichwouldlikelyfurtherimprove resultsfromthisstudy.Thesedroneshadtheabilitytocarry upto1.4kilogramsinpayload,whichshouldeasilyallowfor naloxonetobetransported.Becausethereisnopreviously standardizedlaunchtime,weassumeddroneliftoffand landingwouldeachtake60seconds.Wedidnotaccountfor timeforlay-userstoreachthedrone,removethemedication, andreturntothepatient’sside,asthesecalculationshavenot beenestablished.Ambulanceresponsetimealsodoesnot accountforthetimeintervalbetweenEMSarrivalonscene toarrivaltopatient.
Eachdrone’sgeographicalcatchmentareawassettoa 3.2kilometer-(twomile)radiusforthedrone’sabilityto flyto andfromthescene.Wealsoaccountedforwindspeedand rainonthedaysofoverdoseincidentsusinghourlyNorth Carolinaclimatedataintheservicearea.17 Assumingthe dronecouldwithstandalevel5wind(windspeedsof19–24 milesperhour),weset19milesperhourasthethreshold speedfordronestoworknormally.Formostdrones,itisnot recommendedtooperateinrainyconditions.Weassumed thatdroneservicewouldpauseduringthesetimes (precipitation >0).
ANALYSIS Measurements
Ourprimaryoutcomeswereambulanceanddrone responsetimesasdepictedin Figure1.Forourdataset,we definedambulanceresponsetimeasthedurationbetween EMSassignmentandarrivalatsceneasdocumentedinEMS records.Droneresponsetimewasconsideredtimebetween droneassignmentandarrivalatscene.Thesedefinitionswere equivalenttothoseusedbyBoutilieretal.Droneswouldbe collectedfromthescenewhenanambulancearrives.Time betweenarrivalonsceneandarrivaltothepatient wasnotcalculatedforeitherdroneorambulanceresponse times.Wecalculateddroneresponsetimesusingagenetic optimizationmodelandtechnologicalspecificationsof currentdronesasdescribedabove.Additionaltimewas addedtothecalculated flighttimetoaccountfordispatching thedroneandallowingittolandafterarrivingonthe field site.Thisadditionaltimeproducedaveryconservative estimateofthetotalresponsetimeforeachdrone flight.We excludedincidentswithmissingdataonscenelocationand responsetime.

GeneticOptimization
Geneticoptimizationisaniterativeprocessinspiredby naturalselectioninwhichthepropertiesofapotential solutiontoaproblemarechangedwitheachiteration.After eachiteration(generation),theperformance(fitness)is assessedforeachpotentialsolution.Thesubsequent generationofsolutionsisthendeterminedbasedonthe compositionofthecurrenthighestperformingsolutions. Inbiologicalterms,thebestsolutionsineachgeneration serveastheparentsforthenextsetofpotentialsolutions. Thisprocesscontinuesuntilasolutionmeetsasetof minimumcriteria.18,19
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 825 Coxetal. OptimizingaDroneNetworktoRespondtoOpioidOverdoses
Figure1. AmbulanceanddronetimelinesadaptedfromBoutilieretal2017.16 Theobjectiveofthedroneistogetnaloxonetothepatientas earlyaspossible.Iftheambulancearrives first,thedroneon-scenetimewillbezero.Ifthedronearrives first,naloxonecanbegivenwhilethe ambulanceisinroute.
Ourgoalwastodeterminetheoptimalnumberandspatial geographicdistributionofdronebasesthatwouldreduce naloxonedistributiontimestoopioidoverdoses.To accomplishthis,we firstusedlocationsofoverdoseincidents, numberofdronebases,andlocationsofdronebasestocreate dronebasenetworks.Thesenetworkseachhadaunique combinationofbaselocations,numberofbases,coverage rate(percentageofincidentscoveredbydronebases),and coveragedensity(numberofincidentscoveredbyadrone base).Giventheprespecifiednumberofbasesfrom0–29,the geneticoptimizationmodeldeterminesthegeographical locationsofdronesthatmaximizescoveragerateanddensity (inmathematicalterms,ifentropyconverged).Maximizing coveragerateanddensitydidnotaccountforruralandurban differencesinresponsetimes.Ouralgorithmsoughtto improvetheoveralldistributionofresponsetimes,regardless oflocation.Forexample,baselocationsforatwo-drone networkmaybecompletelydifferentthanathree-drone networkratherthansimplyaddinganotherdronelocation. Thegeneticoptimizerwasconsideredsuccessfulfordrone networkoptimizationifentropyconverged.Weconducted analyseswithPython3.6.8(PythonSoftwareFoundation, Wilmington,DE)onJupyterNotebookandArcGIS Desktop10.5.1(Esri).
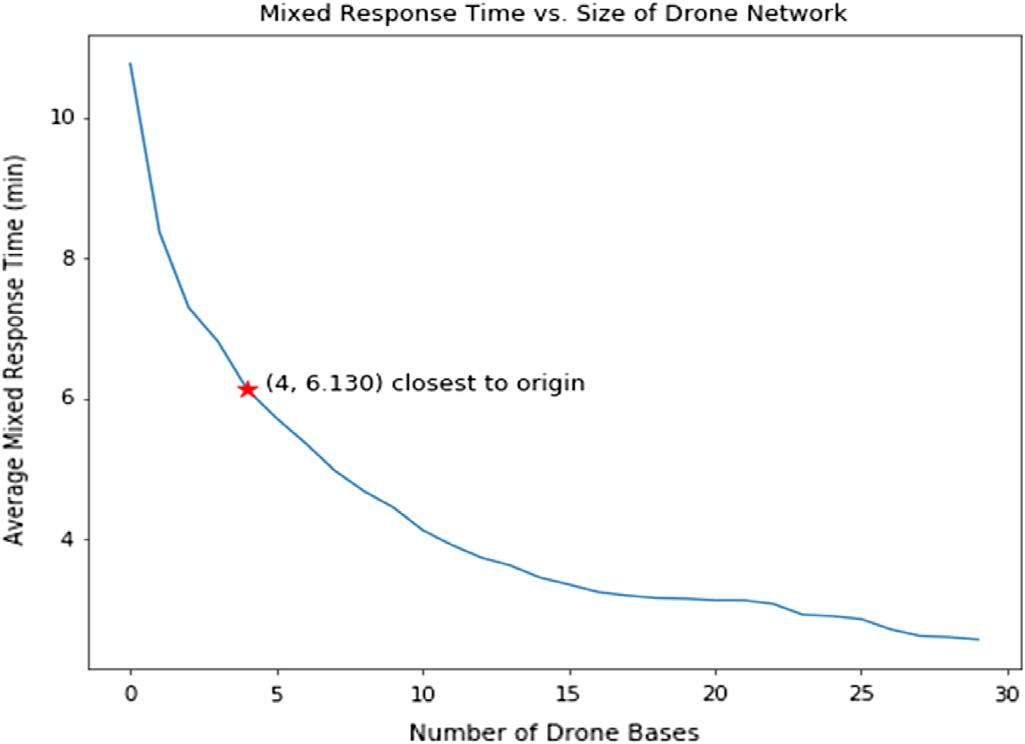
ObservedandEstimatedResponseTime
Wefoundthatthedronenetworksimprovedaverage responsetimeforeachaddeddronebase.Foreachreduction inresponsetime,weidentifiedthelocationsofthesedrone baseschosenfromcandidateEMS/firestations.We calculatedthedistributionsoftheobservedresponsetimes andestimateddroneresponsetimesforeachincident.A graphofresponsetimeandnumberofdronebaseswere plotted.Wechosetheoperatingpoint,orthepointclosestto thegraphorigin,astheoptimumnumberofdronebasesthat wouldminimizstheresponsetimeandnumberofbases.
WeperformedthetestofsignificancewithaStudent t -testbyproposingthenullhypothesis H 0:theaverage (orexpected)responsetimeofhistorical,optimized,andfully deployeddeliverynetworkisdifferentfromeachother.We calculatedthe P -valueforeachpairedcombinationof historical,optimizedandfullydeployeddeliverynetworks. P -valueslessthan0.05wereconsideredsignificant.
EthicsStatement
TheDukeUniversityInstitutionalReviewBoard determinedthisstudytobeexempt(Pro00101461).
RESULTS
CharacteristicsofStudySubjectsandClimate
From2016toearly2019,2,634callsweredispatchedfor suspectedopioidoverdose/poisoning.Aftereliminating duplicateincidentswithuniquerespondingunits,wefound 2,327distinctincidentsofsuspectedoverdose/poisoningor
dispatchcallsinwhichnaloxonewasused.Weexcluded303 casesinwhichresponsetimedataweremissing,threecasesin whichresponsetimesweregreaterthan40minutesand assumedtobeinaccuratedocumentation,andonecasethat wasgeocodedincorrectly,resultinginatotalof2020 final encounters.Summarycharacteristicsforopioidoverdoses areshownin Table1.Oftheincludedcasesofopioid overdoses43%involvedfemales,andtheaverageagewas 41yearsold.Dispatchtimetookanaverageof3minutes 1second,andresponsetimetookanaverageof10minutes 46seconds.Regardingclimate,nooverdosesoccurredwhen windsexceeded19milesperhour,while147incidents occurredduringrain.Wedidnotexcludeinthegenetic algorithmtheincidentsthatoccurredintherain.
MainResults
Theentropyofthegeneticoptimizationconvergedafter 60generations,meaningthedronebasenetworkwasableto beoptimized.Thechangeinresponsetimeandcoveragerate witheachaddeddronebaseisshownin Table2.Response timeandcoveragerateconsistentlyimprovedwithincreasing numberofdronebasesuptothe29availablelocations.For example,havingonlyonedronebasereducedresponsetime by2minutes24secondswitha36%coveragerate.Butatfull deploymentof29bases,responsetimewasreducedby8 minutes12secondsandcovered97.8%ofincidents.
Numberofdrone bases Improvementinresponse time,mm:ss Coverage rate% 000:000.0 102:2435.8 203:2850.5 303:5756.3 404:3864.2 505:0370.9 605:2473.0 705:4776.8 806:0579.9 906:1982.1 1006:3886.5 1106:5186.9 1207:0290.3 1307:0891.3 1407:1891.4 1507:2591.3 1607:3192.7 1707:3492.7 WesternJournal of EmergencyMedicineVolume24,No.5:September2023 826
Coxetal.
Table2. Dronenetworkcharacteristicsfortheresponsetime improvementinopioidoverdoses.
OptimizingaDroneNetworktoRespondtoOpioidOverdoses
Comparisonofresponsetimedistributions.Thetoprowdemonstratesthedistributionofhistoricalambulanceresponsetimes.The secondrowshowsthedistributionofestimatedresponsetimecorrespondingtothefour-basedronenetwork.Thethirdrowshowsthe distributionofestimatedresponsetimeifallcandidatebaseswerechosenasthepartofthedronenetwork.(Dronebasesarefullydeployed.) Solidverticallinesdemonstratethemeanresponsetime.Dashedverticallinesrepresentthe90thpercentileinresponsetime.
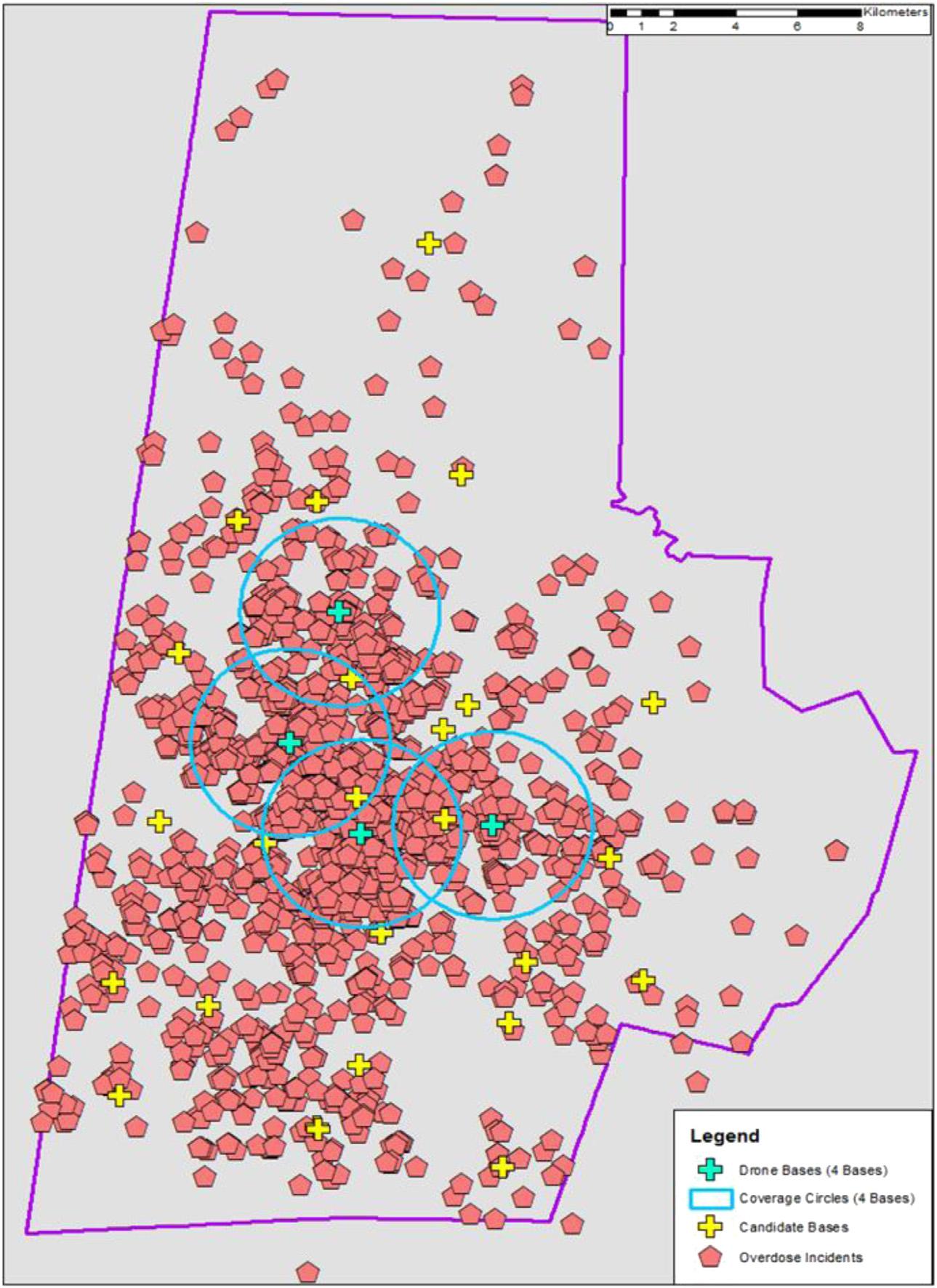
Thedistributionofresponsetimesalsonarrowedwithan increaseindronebases(Figure2).Asmoredronebaseswere introducedintothenetwork,theaverageandrangeof estimatedresponsetimesaremarkedlydecreasedcompared tohistoricalambulanceresponsetimes.Becauseresponse timecannotbeimprovedwithoutincreasingthenumberof dronebases,wechoseadronenetworkthatminimized responsetimeandnumberofbases,therebymaximizing resourceutilization.Thisidealnetwork,shownasthe pointclosesttoorigin(Figure3),wasfourdronebases. Theseoptimalcandidatebasesimprovedaverageresponse timeby4minutesand38secondswithacoveragerate of64.2%.Thesebasesareinareaswithmoreopioid overdoses(ie,urbanareas),leavingruralareaslargely uncoveredbydronesduetoconstraintson flighttimeand distance(Figure4).

DISCUSSION
Inthisstudyweevaluatedthepotentialbenefitofusing dronestoimprovetimetonaloxonedeliveryinsuspected opioidoverdoses.Ouranalysisfoundthatamathematical modelcanoptimizethelocationandnumberofbasesto reducenaloxonedeliverytimecomparedtohistorical ambulanceresponsetimes.Wefoundthatdronesnotonly improvetheaveragetimeofnaloxonedeliveryonscene (Table2),butalsoreducetheentireresponsetime distribution(Figure2).
Dronedeliveryofnaloxonehasthepotentialtoreducethe timetonaloxoneadministrationandtheoreticallyreduce
basesandresponsetime.Theredstarrepresentsthepointclosestto theorigin(x-axismustbeawholenumber).Thispointcorrespondsto themostefficientuseofdroneresources.
mortalityfromopioidoverdoses.Ourconservativemodel demonstratesthatdronescouldbeusedtodelivernaloxone aheadofambulances.Comparedtoambulances,dronesmay overcomechallengesanddelaysinreachingprivate locations.8 Insimulatedout-of-hospitalcardiacarrests, droneshavereducedresponsetimeby16minutescompared toEMS.12
Figure2.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 827 Coxetal.
Figure3. Averageresponsetimegivennumberofdronebases.This figuredemonstratestherelationshipbetweenthenumberofdrone
OptimizingaDroneNetworktoRespondtoOpioidOverdoses
Inouroptimizedmodel,thelocationsofourdronebases leavethemostrurallocationstobecoveredonlyby ambulances.Dronenetworkscancoverruralareas. However,thenumberofdronesneededtocoverruralareas wouldlikelynotbeeconomicalatthecurrentrangeof FederalAviationAdministration(FAA)-ratedcommercial dronesunlesstherewasaclusterofopioidoverdoseswhere dronescouldbestationednearby.Thegeneticalgorithmdid notdirectlyaccountforrural/urbandifferences.Instead,it focusedoncoveringthemaximumnumberofoverdoses,of whichthevastmajorityoccurinurbanareas.Thus,our dronenetworkmaximizesourchancesofreducingmortality inopioidoverdoses,especiallyduringtimesofincreased trafficandcallvolumewhichcanprolongambulance responsetimes.
Althoughallstatescurrentlyhavesomeformofnaloxone accesslaws,studiessuggestthatBlacksarelesslikelytohave accesstonaloxone.20–22 WithBlacksmakingup36.9%ofthe populationintheservicearea,adronenetworkhasthe potentialtoprovidethislifesavingtreatmenttothosewho maynothaveequitableaccess.
LIMITATIONS
Becausethemodeldependedontheestimatedincidenceof opioidoverdosesineachcatchmentarea,basesinhigh-call volumeareaswillhavemoredronebusytimeandrequire moredrones.However,theremainingparametersweremore conservative,likelyleadingtoanoverestimateindrone networksize.Weassumedonlyonedroneperbase,whereas inrealitymultipledronescouldbedeployedfromonebase,
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 828
Coxetal.
Figure4.Historicalopioidoverdoses,paramedicstationlocations,andoptimaldronenetwork. Thiscountymapdemonstrates locationsofhistoricalopioidoverdoses(redpentagons).Additionally,itshowsthelocationsofallcandidatedronebases(+ signs)andthe optimizeddronenetwork(blue + signs)anditscoveragearea(areainsidebluecircles).
OptimizingaDroneNetworktoRespondtoOpioidOverdoses
decreasingdronebusytime.Droneresourcesmayalsobe overestimatedbecauseweincludeddispatchesforopioid overdosesthatdidnotreceivenaloxone.Thissmallfraction ofcasesmayberuledoutforfuturedronedeployment. Additionally,dronetechnologyisprogressingrapidly. Withourconservativedronespecifications,response timesarelikelyanoverestimate.Furthermore,potential candidatebaseslocationssuchashospitalsandclinics werenotincludedinthemodel.Havingthese additionallocationscouldfurtherreducedrone responsetimes.
WeadditionallyusedEuclideandistancetosetour coverageareaanddidnotaccountforFAAregulationson drone flightpaths,whichmayrequireaslightlymore circuitouspathtobystandersthananticipatedbythismodel. Further,difficultweatherconditions(eg,windandrain)may limittheabilityto flydronesbasedontechnological capabilities.Reassuringly,thenumberofoverdoseincidents duringtheseconditionswereminimal.Thus,weexpectreallifeimplementationofdronestonotbemajorlyimpacted byweather.
Lastly,thedataweusedwasincompletebecausewedid nothaveaccesstodatafromlawenforcementor fire departments.Thismayhaveledtoanoverestimationof historicalambulanceresponsetimes.Inaddition,datawas basedonemergencymedicaldispatch(EMD)impressionof thechiefcomplaintasadrugoverdose.CallsinwhichEMS impressionwasopioidoverdose,butEMDimpressionwas not,mayhavebeenmissed.Weattemptedtoaccountforthis differencebyincludingallcallsinwhichnaloxonewas administered,regardlessofimpression.Otheropioid overdosecasesmayhavebeenunaccountedforduetodata exclusionbasedonincompleteorsuspectedinaccurate documentationonresponsetimes.However,becausewe excludedonly11.5%ofcasesbasedondocumentation,the impactofmissingdataislikelysmall.
CONCLUSION
Wehaveestablishedthatadronenetworkmathematically optimizedinlocationandnumberofdronebaseswould potentiallyreducetimetonaloxonedeliveryinopioid overdosescomparedtohistoricalambulanceresponsetimes. Ournextstepswillbetocloselyexaminethefeasibilityof implementingsuchadronenetworkbymeasuringGPS signals,confirming flightpaths,andcompletinglivedrone tests.Asdronetechnologyimprovesandcostdecreases, futureutilizationofdronenetworkscouldhelp temporizemanyemergencymedicalsituationsuntil EMSarrives.
AddressforCorrespondence:DanielBuckland,MD,PhD,Duke University,DepartmentofEmergencyMedicine,Departmentof MechanicalEngineeringandMaterialSciences,DukeUniversity
MedicalCenter3096,Durham,NC,USA27710.Email: dan. buckland@duke.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Coxetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.SpencerMR,MininoAM,WarnerM.DrugOverdoseDeathsinthe UnitedStates,2001–2021. NCHSdatabrief,2022(457):1–8.
2.MattsonCL,TanzLJ,QuinnK,etal.TrendsandGeographicPatternsin drugandsyntheticopioidoverdosedeaths-UnitedStates,2013-2019. MMWR,2021;70(6):202–7.
3.SporerKA.Acuteheroinoverdose. AnnInternMed,1999;(7):584–90.
4.ShermanSG,GannDS,ScottG,etal.Aqualitativestudyofoverdose responsesamongChicagoIDUs. HarmReductJ,2008;5(1):1–5.
5.TobinKE,DaveyMA,LatkinCA.Callingemergencymedicalservices duringdrugoverdose:anexaminationofindividual,socialandsetting correlates. Addiction,2005;100(3):397–404.
6.TracyM,PiperTM,OmpadD,etal.Circumstancesofwitnessed drugoverdoseinNewYorkCity:implicationsforintervention. DrugAlcoholDepend,2005;79(2):181–90.
7.HeaveySC,ChangY-P,VestBM,etal. ‘Ihaveitjustincase’ -Naloxone accessandchangesinopioidusebehaviours. IntJDrugPolicy, 2018;51:27–35.
8.Madah-AmiriD,ClauseT,MyrmelL,etal.Circumstancessurrounding non-fatalopioidoverdosesattendedbyambulanceservices. Drug AlcoholRev,2017;36(3):288–94.
9.SanchezTM,ChangestoNFPA1710andImpactstoBNA.2017, SandiaNationalLab.(SNL-NM),Albuquerque,NM.
10.MellH.K,MummaSN,HiestandB,etal.Emergencymedicalservices responsetimesinrural,suburban,andurbanareas. JAMASurgery, 2017;152(10):983–4.
11.RosserJC.Jr,VudathaV,TerwilligerBA.Surgicalandmedical applicationsofdrones:acomprehensivereview. JLeadershOrgan Stud,2018;22(3).
12.ClaessonA.,FredmanDM,SvenssonL,etal.Unmannedaerialvehicles (drones)inout-of-hospital-cardiac-arrest. ScandJTraumaResusc EmergMed,2016;24(1):124.
13.TukelCA,etal.Time-to-sceneforopioidoverdoses:areunmanned aerialdronesfasterthantraditional firstrespondersinanurban environment? BMJInnovations,2020:bmjinnov-2019-000357.
14.LejeuneM.,1074208andMaW.Drone-deliverynetworkforopioid overdose–nonlinearintegerqueueing-optimizationmodelsand methods.arXivpreprintarXiv:2206.14340,2022.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 829 Coxetal. OptimizingaDroneNetworktoRespondtoOpioidOverdoses
15.USCensusBureau.QuickFacts:DurhamCounty,NorthCarolina 2010–2019July1,2019[cited2021July15];Availableat: https://www.census.gov/quickfacts/durhamcountynorthcarolina AccessedAugust15,2021.
16.BoutilierJJ,BrooksSC,JanmohamadA,etal.Optimizingadrone networktodeliverautomatedexternaldefibrillators. Circulation, 2017;135(25):2454
65.
17.NorthCarolinaClimateOffice.WeatherAndClimateDatabase1/1/16 0:00-2/18/1923:00.[cited2021July15];Availableat: https://products. climate.ncsu.edu/cardinal/scout/?station=DURH&temporal=hourly AccessedAugust15,2021.
18.FuertesG.,VargasM,AlfaroM,etal.Chaoticgeneticalgorithm andtheeffectsofentropyinperformanceoptimization. Chaos, 2019;29(1):013132.
19.SmitS.K.,EibenA..Parametertuningofevolutionaryalgorithms: generalistvs.specialist.in EuropeanConferenceonthe ApplicationsofEvolutionaryComputation. 2010.NewYork, NY:Springer.
20.DaytonL,TobinK,OluwaseunNF,etal.Racialdisparitiesinoverdose preventionamongpeoplewhoinjectdrugs. JUrbanHealth-BulletinofY AcademyofMedicine,2020;97(6):823–30.
21.OngAR,LeeS,BonarEE.Understandingdisparitiesinaccessto naloxoneamongpeoplewhoinjectdrugsinSoutheastMichiganusing respondentdrivensampling DrugAlcoholDepend,2020;206:107743.
22.AbbasB,MarottaP,Goddard-EckrichD,etal.Socio-ecologicaland pharmacy-levelfactorsassociatedwithnaloxonestockingatstandingordernaloxonepharmaciesinNewYorkCity DrugAlcoholDepend, 2021;218:108388.
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 830 OptimizingaDroneNetworktoRespondtoOpioidOverdoses Coxetal.
DoesHousingStatusMatterinEmergencyMedicalServices
AdministrationofNaloxone?APrehospitalCross-sectionalStudy
TiffanyM.Abramson,MD*
CoreyM.Abramson,PhD†
ElizabethBurner,MD,MPH,MSc,PhD*
MarcEckstein,MD,MPH*
StephenSanko,MD*
SuzanneWenzel,PhD‡
*UniversityofSouthernCalifornia,KeckSchoolofMedicine,Department ofEmergencyMedicine,DivisionsofEmergencyMedicalServicesand Research,LosAngeles,California
† UniversityofArizona,SchoolofSociology,Tucson,Arizona
‡ UniversityofSouthernCalifornia,SuzanneDworak-PeckSchoolof SocialWork,LosAngeles,California
SectionEditors: MarcMartel,MD,andPatrickMaher,MD,MS
Submissionhistory:SubmittedFebruary19,2023;RevisionreceivedJuly10,2023;AcceptedJuly19,2023
ElectronicallypublishedAugust28,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.60237
Introduction: Personsexperiencinghomelessness(PEH)useemergencymedicalservices(EMS)at disproportionatelyhighratesrelativetohousedindividualsduetoseveralfactorsincludingdisparate accesstohealthcare.LimitedaccesstocareiscompoundedbyhigherratesofsubstanceuseinPEH. Despitegrowingattentiontotheopioidepidemicandhousingcrisis,differencesinEMSnaloxone administrationbyhousingstatushasnotbeensystematicallyexamined.Ourobjectiveinthisstudywas todescribeEMSadministrationofnaloxonebyhousingstatusintheCityofLosAngeles.
Methods: Thiswasa12-monthretrospective,cross-sectionalanalysisofelectronicpatientcarereports (ePCRs)forall9–1–1EMSincidentsattendedbytheLosAngelesFireDepartment(LAFD),thesole EMSagencyfortheCityofLosAngelesduringthestudyperiod,January-December2018.Duringthis time,theCityhadapopulationof3,949,776withanestimated31,825(0.8%)PEH.Weincludedinthe studyindividualstowhomLAFDrespondershadadministerednaloxone.Housingstatusisamandatory fieldonePCRs.TheprimarystudyoutcomewastheincidenceofEMSnaloxoneadministrationby housingstatus.Weuseddescriptivestatisticsandlogisticregressionmodelstoexaminepatterns bykeycovariates.
Results: Therewere345,190EMSincidentsduringthestudyperiod.Naloxonewasadministeredduring 2,428incidents.Ofthoseincidents608(25%)involvedPEH,and1,820(75%)involvedhoused individuals.Naloxoneadministrationoccurredatarateof19per1,000PEH,roughly44timestherateof housedindividuals.AlogisticregressionmodelshowedthatPEHremained2.38timesmorelikelyto receivenaloxonethantheirhousedcounterparts,afteradjustingforgender,age,andrespiratory depression(oddsratio2.38,95%confidenceinterval2.15–2.64).Themostcommonimpressions recordedbytheEMSresponderswhoadministerednaloxonewerethesameforbothgroups:overdose; alteredlevelofconsciousness;andcardiacarrest.Personsexperiencinghomelessnesswho receivednaloxoneweremorelikelytobemale(82%vs67%)andyounger(41.4vs46.2years) thanhousedindividuals.
Conclusion: IntheCityofLosAngeles,PEHaremorelikelytoreceiveEMS-administerednaloxone thantheirhousedpeersevenafteradjustingforotherfactors.Futureresearchisneededto understandoutcomesandimprovecarepathwaysforpatientsconfrontinghomelessnessandopioid use.[WestJEmergMed.2023;24(5)831–838.]
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 831
ORIGINAL RESEARCH
INTRODUCTION Background
Opioidoverdoseshavereachedepidemicproportionsin theUnitedStates(US),andoverdosedeathscontinueto increase.1,2 Opioidoverdoseisnowamongtheleadingcauses ofaccidentaldeaths.3 Theincidenceofoverdosedeathshas increasedwiththeintroductionoffentanylandother syntheticopioidsandtheaftermathoftheCOVID-19 pandemic.1,2,4–6 Althoughopioidusedisorders(OUD)and othersubstanceusedisorders(SUD)affectindividualsofall socioeconomicstatuses,personsexperiencinghomelessness (PEH)areatparticularrisk.7–9 In2021,9%ofallopioid overdose-relateddeathswereamongPEH.10
Thehousingcrisisisanotherpublichealthepidemicfacing theUS;ithascontributedtoarapidlygrowingpopulationof PEHwithmorethan1.5millionindividualsexperiencing homelessnesseachyear.11,12 LosAngelesCounty,whichhas oneofthehighesthousingcostsandthesecondlargest populationofPEHnationally,isnoexception.
Personsexperiencinghomelessnesshavehigherratesof chronicmedicalconditions,substanceabuse,andpsychiatric diagnoses,aswellasanoverallincreaseinmorbidityand mortality.13–16 Drugoverdoses,specificallythoseassociated withopioids,areacommoncauseofdeathinPEH.16
18 In oneBoston-basedstudy,drugoverdosewastheleadingcause ofdeathandwasresponsibleforoneinthreedeathsinadults experiencinghomelessnessundertheageof45.17 Further, PEHarelesslikelytohavearegularsourceofmedicalcare andhaveincreasedemergencydepartment(ED)utilization andengagementwithemergencymedicalservices(EMS).19
PersonsexperiencinghomelessnessuseEMSat disproportionallyhighratescomparedtotheirhoused counterparts.PriorresearchfoundthatPEHcallEMSata rate14timesthatoftheirhousedcounterparts.20 Atthesame time,EMScallsforopioidoverdoseappeartobeontherise withnaloxoneadministrationoccurringonalmosthalfa millionEMSrunsoveratwo-yearperiod.21 Asthehousing crisisandopioidepidemiccollide,itisimportanttodescribe howhousingstatusaffectsEMSutilizationandprehospital careforpresumedopioidoverdose.These findingsmaylead torecognitionofbiasincare,identificationofopportunities forinterventionsforthosewithOUDandlimitedaccessto care,andimprovementinEMSresponders’ education.
Importance
Despitegrowingattentiontotheopioidepidemicand housingcrisis,differencesinuseof9
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Personsexperiencinghomelessness(PEH) havehigherratesofchronicmedical conditionsandaredisproportionately representedamongopioidoverdosedeaths.
Whatwastheresearchquestion?
Doestheprevalenceofnaloxone administrationbyemergencymedicalservices (EMS)varybyhousingstatus?
Whatwasthemajor findingofthestudy?
Naloxonewasadministeredatahigherrateto PEH(19vs0.4/1000).TheadjustedORof naloxoneadministrationwas2.38timesthan thatofhousedpeers(95%CI2.15 – 2.64).
Howdoesthisimprovepopulationhealth?
These fi ndingscanhelpdriveEMSeducation and fi eldinterventionsandidentifyatarget forcommunityriskreductioninthis vulnerablepopulation.
implicationsforunderstandingandaddressingpublic healthdisparitiesattheintersectionofhousing,opioids, andpoverty.
METHODS
StudyDesign
Thiswasa12-monthretrospective,cross-sectional analysisofelectronichealthrecords(EHR)forall9
1 EMSincidentsattendedbytheLosAngelesFireDepartment (LAFD)fromJanuary1–December31,2018.Study designandreportingadheredtobestpracticesper StrengtheningtheReportingofObservationalStudiesin Epidemiology(STROBE)andReportingofStudies Conductedusingobservationalroutinelycollectedhealth data(RECORD)statements.22,23
StudySetting
1
1
1EMSresourcesfor treatmentofpresumedopioidoverdosebyPEHand subsequenttreatmentbyEMShasnotbeendescribed.
GoalsofthisInvestigation
Theprimaryoutcomeofinterestinthisstudywashowthe prevalenceofEMSadministrationofnaloxonevariesby housingstatusintheCityofLosAngeles.Thishasimportant
TheLAFDisthesoleentityproviding9–1–1EMS responsesfortheCityofLosAngeles,thesecondmost populouscityintheUS.TheLAFDreceivesmorethanone million9–1–1callsandrespondstoalmost400,000EMS incidentsannually.TheCityofLosAngelesspans480square milesandhas3,949,776inhabitants,withahomeless populationof31,285(0.8%).24,25
TheLAFDprovidesEMScareundertheguidanceofthe LACountyEMSAgencyanditstreatmentprotocols.Atthe
–
–
–
–
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 832
DoesHousingStatusMatterinEMSAdministrationofNaloxone? Abramsonetal.
timeofthestudy,thetreatmentprotocolfor “overdose/ poisoning/ingestion” includedintranasal,intramuscular orintravenousnaloxoneadministrationforsuspected opioidoverdosewithalteredmentalstatusand hypoventilation/apnea.26
SelectionCriteria
Weincludedall9–1–1EMScallsthatresultedinaunique incidentnumberandacompletedelectronicpatientcare report(ePCR)withdocumentationofEMS-administered naloxoneduringthestudyperiod.TheLAFDhasbeenusing thesameePCRandEHRsystem(HealthEMS,Stryker, Redmond,WA)since2011.TheEHRincludesinformation fromdispatch,theePCR,andbillinginformation. Responderimpressionsconsistof64standardizedoptions, whichremainedstableoverthestudyperiod.27 Housing statusisamandatory fieldonePCRs.PrehospitalEMS respondersaretrainedtoassessthequestion “Isthepatient homeless?” (yesvsno)oneveryLAFD-attended9
Wemodeledthesevariablesasbinary:housingstatus (currentlyunhousedyes/no,perEMSresponder),identified asfemale(yes/noperEMSresponder),respiratory depression(<12breathsperminutes:yes/no)andtransported (yes/no).TheEMSresponder’simpressionandpatient’ sage weremodeledascategorical.
TheprimaryoutcomewastheprevalenceofEMS administrationofnaloxonebyhousingstatus.Secondary outcomesincludedincidenceofnaloxonebypatient characteristics,EMSresponder’simpression,andtransport status.Wealsoexaminedwhetherdisparateratesof naloxoneadministrationremainedrobustaftercontrolling forpatientdemographicandclinicalcharacteristicsina regressionmodel.
Analysis
1
1EMS incidentbyaskingthepatientor,ifthepatientisunableor unwillingtorespond,byapplyingtheirbestjudgment.
DataExtraction
DatawasextractedelectronicallyfromHealthEMS.We mergedclinicaldataandEMSresponderdatausingcall numberandbookletnumber,whichareuniqueidentifiers. Casesinwhichboththeservicedateandcallnumberwere identicalweredroppedbeyondthe firstinstance.Asampleof thesecaseswerecheckedtoensuretheyweretrulyduplicates. Weincludedcasesinwhich “Narcan” or “Narcannasal spray ” werelistedasmedicationthatwasadministered duringtheincident.Westoredalldatawasstoredina password-protectedelectronicspreadsheet(MicrosoftExcel; MicrosoftCorporation,Redmond,WA).Theauthorsdid nothaveaccesstothestudypopulation.
VariableDefinitionandModeling
Toassesshousingstatus,EMSrespondersaskedeach patientwhethertheywerecurrentlyexperiencing homelessness.Ifthepatientwasunabletoanswer,theEMS responderwasinstructedtousetheirbestjudgmentbasedon theirtraining.
Wechosetodefinerespiratorydepression apriori as bradypneawitharespiratoryrateoflessthan12breathsper minute,basedontheLACountyEMSAgencyprotocoland priorworkevaluatingprehospitalnaloxone administration.28,29 Althoughrespiratorydepressionmay alsopresentashypopnea,itissubjectiveandnotreliably documentedintheprehospitalcarereport.
Weextractedtransportstatusfromthedisposition fieldon theePCR.Notransportwasdefinedasanentryof “ no transport/refusedcare,”“treated/notransport,” or “treated/ notransport(AMA).” Transportwasdefinedasanentry of “treated/transported.”
Ouranalysesusedstandardproceduresforcalculating descriptivestatisticsforthepopulationofincidents.Asour descriptiveanalysesweredrawnfromacomplete compilationofcallsratherthanasample,wefollowedthe standardpracticeofexcluding P -valuesforevaluating inferencesaboutwhetherthesamplestatistics(eg,sample means)providedareasonableestimateofthecorresponding populationparameters.
Tounderstandwhethertheobservedeffectwas explainablebycoreclinicalordemographicfactors,we performedalogisticregressionanalysis.Ourmodelincluded agecategories,gender,andclinicalindicationofrespiratory depressionbecausethesefactorswereshowntohaveaneffect inpriorliterature.20,29 Thelogisticregressionformalizedthis, allowingustotestwhetherobserveddifferencesbyPEH statuswere1)reducibletoclinicalneedor2)reducibleto otherdemographics.Thelogisticregressionsdonotprovide acompletemodelofallpossibleexplanationsorestablish causality,butratherhelpruleoutalternativeexplanations ofscientificandpolicysignificanceandtoquantify importanteffects.
Thedescriptivestatisticsusedthesetofdatafor caseswherenaloxonewasadministeredandforwhichwehad dataonhousingstatus.Regressionmodelsprovided informationonthemagnitudeanddirectionof demographicsandclinicaleffectsonnaloxone administrationforthefullpopulationofEMSincidents. Thesemodelswereusedtodescribeassociationsinourdata, notimplycausality.Missingvalueswereaccountedforby list-wisedeletion– acommonstrategyforlargedatasets withouthighlevelsofmissingdata.Alldatawereassembled, cleanedandmodeledinSTATA14(StataCorp,College Station,TX).Weproduced figuresusingtheggplot2package inR(TheRProjectforStatisticalComputing, Vienna,Austria).
Thestudywasreviewedandapprovedasexemptbythe InstitutionalReviewBoardoftheUniversityofSouthern California(HS-19-00472).
–
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 833
Abramsonetal.
DoesHousingStatusMatterinEMSAdministrationofNaloxone?
RESULTS
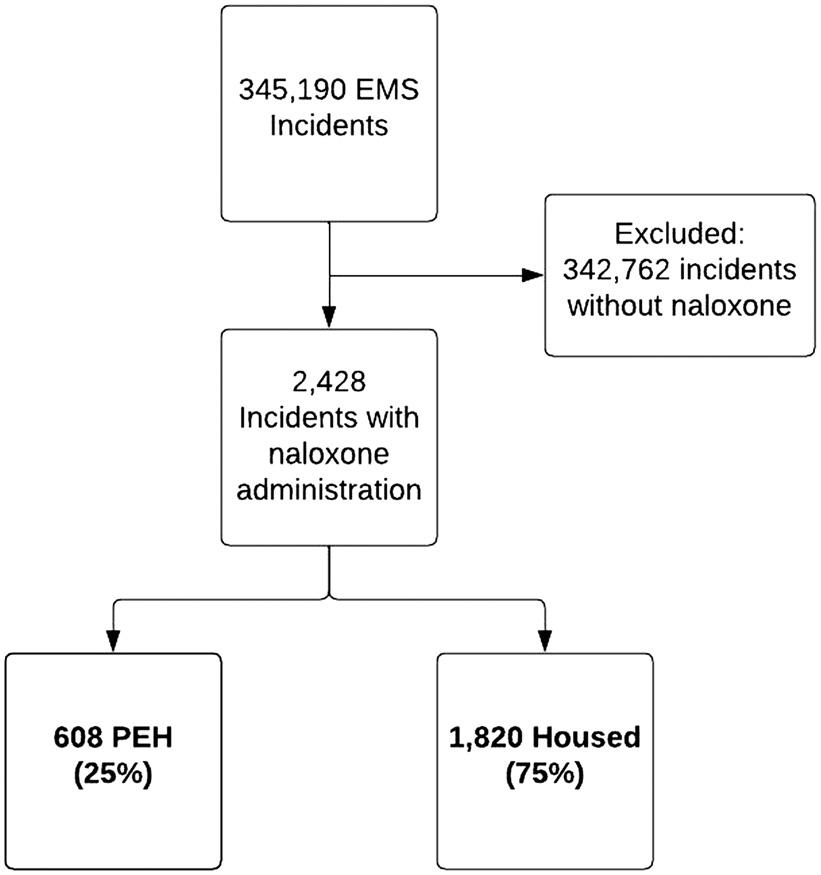
Ofthe345,190unique,recorded9
1
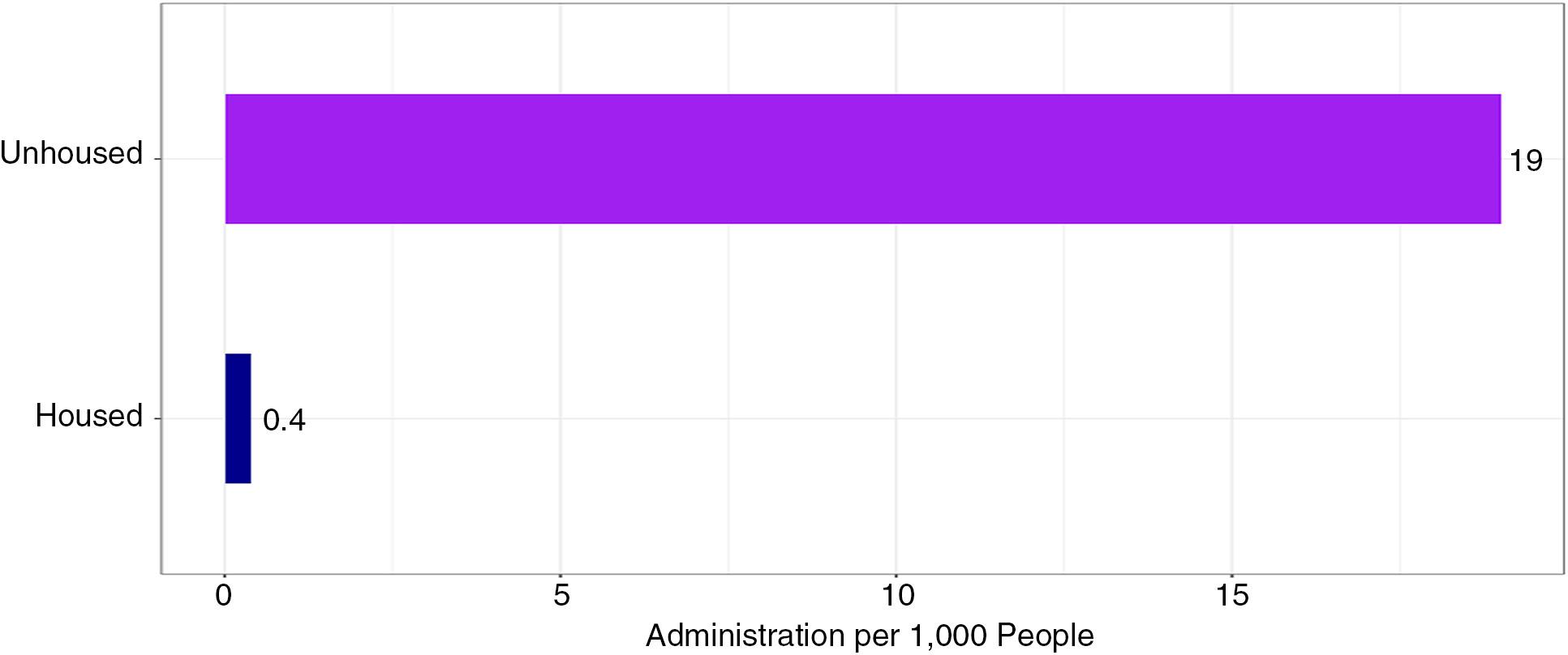
1EMSincidents duringthestudyperiod,2,428incidentsmetinclusioncriteria (Figure1).Inthe2,428incidentsinwhichEMSadministered naloxone,608(25%)incidentsinvolvedPEH,and1,830 (75%)involvedhousedindividuals.Incidentsthatresultedin naloxoneadministrationoccurredatarateof19per1,000 PEHcomparedto0.4per1,000housedindividuals,or roughly44timestherateofhousedindividuals(Figure2).
Thestudypopulationhadameanageof45years(SD 19.4)andwas70.7%male.Ofthepatientswhoreceived EMS-administerednaloxone,PEHwereyounger(mean 41.4years[SD14.1]vs46.2years[SD20.7])andmoreoften male(81.9vs66.9%).Theprevalenceofpatientswho declinedtransportwashigherforPEHthanforhoused individuals(17.3vs7.2%).ThetopthreemostcommonEMS
responderimpressionsforwhichnaloxonewasadministered werethesameinbothPEHandhousedgroups:overdose/ poisoning/ingestion,alteredlevelofconsciousnessand cardiacarrest(Table1).Amongthosepatientswhoreceived naloxone,aslightlygreaterproportionofthehoused individualswereincardiacarrestwhencomparedtothose experiencinghomelessness(6.9vs4.3%).Thisdoesnot changetheprimary findingoraccountforasubstantial portionoftheeffect.Introducingthecardiacarrestvariable inthemodeldecreasestheoddsratio[OR]from2.38to2.35.
Thelogisticregressionshownin Table2 demonstratesthat evenafteraccountingforkeycovariates(ie,age,respiratory depression,andgender),theoddsofPEHbeingadministered naloxonewas2.38thatofhousedpeers(95%confidence interval[CI]2.15
2.64).Thisisvisualizedin Figure3,which showsthepost-adjustmentoddsofnaloxoneadministration bygroup.
Thisdatashowsthatevenafteradjustingforgender,age, andrespiratorydepression,1)respiratorydepressionhadthe largesteffectonwhethernaloxonewasadministered(OR 49.32,95%CI45.17–53.873)and2)PEHhad2.38higher oddsofreceivingEMS-administerednaloxonerelativeto housedpeers.Thissuggeststhatwhileadministration mappedontoclinicalfactorsonaverage,EMSresponders administerednaloxoneathigherratestoPEHthantotheir housedcounterpartsirrespectiveofcondition.
DISCUSSION
Inthisstudy,PEHintheCityofLosAngelesreceived EMS-administerednaloxoneatsubstantiallyhigherrates thanthehousedpopulation.Whilesomeofthismayreflect need,PEHwerestillovertwotimesmorelikelytoreceivethe drugwhenallelsewasequal.
Secondarily,PEHwhoreceivednaloxonetendedtobe youngerandmoreoftenmalewhencomparedtotheirhoused counterparts,althoughthisdidnotexplaintheeffect.Thisis consistentwithpriorstudiesdocumentingEMSutilizationby PEHandthegeneraldifferencesindemographicsbetween
–
–
–
Figure1. Study flowdiagram. EMS,emergencymedicalservices; PEH,personsexperiencing homelessness.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 834 DoesHousingStatusMatterinEMSAdministrationofNaloxone? Abramsonetal.
Figure2. Naloxoneadministrationratebypopulation.
Abramsonetal. DoesHousingStatusMatterinEMSAdministrationofNaloxone?

= 1,820)
homelessandhousedcommunites.19,20,30,31 However,itis notablethatthemeanageofourstudypopulationwas youngerthantheaverageEMSuserintheCityofLosAngeles (45vs52years).Thisdifferenceismaintainedforboth thePEHandhousedgroups,46.2vs52.6yearsand 41.4vs46.1years,respectively,suggestingthatthosereceiving naloxonemaybeyoungerthanthegeneralpopulation.20
Personsexperiencinghomelessnessweremorethantwo timesaslikelytorefusetransportthantheirhoused counterpartwhoreceivedEMS-administerednaloxone. However,priorstudiesinLosAngeleshavedemonstrated thatoverall,PEHwerelesslikelytorefusetransportagainst medicaladvice.20 Further,independentofhousingstatus, refusaloftransportwashigherinpatientsreceivingEMSadministerednaloxonethanoverallrefusaloftreatmentand/
ortransportagainstmedicaladvicerateinLosAngeles duringthisstudyperiod.20 Thishighlightsthattheremaybe differencesinclinicalpresentation,EMScare,patient-EMS interaction,andsocialsituationsassociatedwiththe managementofpresumedopioidoverdoseandOUD.
Our findingsdescribedisproportionatelyhighratesof administrationofnaloxonetoPEHcomparedwiththeir housedcounterparts.Thelogisticregressionsuggeststhat experiencinghomelessnessisapredictorofnaloxone administrationnetofotherfactors.Thisdatahighlightsthe discrepancythatpersistsevenaftercontrollingforage, gender,andrespiratorystatus.However,thismodeldoesnot
VariableOR(95%CI) AdjustedOR (95%CI) Homeless2.61*(2.38,2.88)2.38*(2.15,2.64) Female0.65*(0.59,0.71) Respiratorydepression49.32*(15.16,53.87) Age 0–24 –25–491.11(0.98,1.27) 50–740.54*(0.47,0/62) >750.28*(0.23,0.33) *P < .01. OR,oddsratio; CI,confidenceinterval.
Table2. Oddsratiosforselectedassociationswithnaloxone administration.
All(N = 2,428)PEH(n = 608)Housed(n
Meanage(years)45(SD19.4)41.4(SD14.1)46.2(SD20.7) Medianage(years)53(IQR37)47(IQR23)54(IQR40) n%n%N% Gender Female71229.311018.160233.1 Male1,71670.749881.9121866.9 Respiratorydepression(RR < 12)1,13646.830249.7%83445.8 Nottransported2369.710517.3%1317.2% EMSprofessionalimpression1 Overdose/poisoning/ingestion1,37356.339966.2%97453.6% Alteredlevelofconsciousness69528.515325.4%54229.8% Cardiacarrest1546.3274.5%1277.0% 1ForEMSimpression,eightchartsweremissingvalues(n
Table1. Patientcharacteristicsbyhousingstatus.
= 2,420).Therewerenomissingvaluesforgender,respiratorydepression, nortransportstatus.
PEH, personsexperiencehomelessness; IQR,interquartilerange; RR,respiratoryrate.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 835
Figure3. Adjustedoddsofnaloxoneadministration. CI,confidenceinterval.
distinguishwhetherthisdifferenceisduetoavariationin clinicalpresentationsoranotherfactorthatisleadingEMS responderstoadministernaloxonewhenthepatient’ s medicalemergencyisrelatedtoanetiologyotherthanopioid overdose.Futurestudiesareneededtounderstandthe differencesincareprovidedbyEMStoPEHvshoused individualsandtoevaluatepatientoutcomedata.These findingscanhelpdrivefutureEMSeducationand field interventions,andpotentiallyhelpdevelopspecialized prehospitalprogramsthatfocusonopioidoverdoseandrisk reductioninthisvulnerablepopulation.
Althoughthisstudydoesnotaddresspatientoutcomes,we mustdiscussthepotentialclinicalimpactofhigherratesof naloxoneadministrationonpatientoutcomes.Naloxoneisa relativelysafedrug.However,therearerisksassociatedwith administeringhighdosesofnaloxonegiventhedosedependentrelationshipbetweennaloxoneandpulmonary edema.Arecentprehospitalstudydemonstratedhigherrates ofpulmonarycomplications,suchaspulmonaryedemaand needforventilatorysupport,incasesinwhichhigherdosesof out-of-hospitalnaloxonewereadministered.32 Further, administeringnaloxoneincaseswherepatientshaveOUD, butopioidoverdoseisnottheetiologyoftheirsymptoms, mayunnecessarilyprecipitateacuteopioidwithdrawal, vomiting,andaspiration.Finally,administeringexcessiveor unnecessarynaloxonedetractsfromEMSresponders’ ability tocriticallyassessthesituationandtreattheprimarymedical emergency.Thus,PEHareatpotentiallyhigherriskforpoor outcomesgiventhehigherratesofEMS-administered naloxone.Furtherstudiesareneededthatincorporate patientoutcomeaswellaspatientandEMSresponders’ experiencestoelucidatepotentialbiasesincare.
Further,thisstudyidentifiesapotentialtargetforpatientcenteredinterventions.Priorstudieshavesuggestedthatby increasingaccesstonaloxone,opioidoverdosemortalitycan bedecreased.33
35 However,inCaliforniaonly6%oflocal EMSagencieshadEMS-basedoutreachprogramsand9% oversawnaloxonedistribution.36 GiventhatEMSmaybe the first,oronly,medicalcarethatanindividualreceives,this interactionprovidesthepotentialforOUD-relatedcare, medication-assistedtherapy,naloxoneadministration, and/orlinkagetocare.TheEMSagencyisinaunique positionofhavingsituationalawarenessandregularcontact withPEH,whichcanbeleveragedtoaddresstheneedsofthis at-riskpopulation.Throughprehospitalinterventionsand novelcarepathways,theremaybeopportunitiestoimprove patientoutcomesinamorecost-effectiveandculturally acceptablemanner.
Finally,thisstudyisthe firststepindescribingthe disparitiesofEMS-administerednaloxonebyhousingstatus. Personsexperiencinghomelessnesswereadministered naloxoneatasubstantiallyhigherratethanthepopulationas awhole(19vs0.4per1,000membersofthepopulation). Muchofthisreflectsdifferencesinneed.However,our
analysesshowthatunhousedindividualsremainedmore thantwiceaslikelyashousedpeerstobeadministered naloxoneevenafteradjustingforclinicalanddemographic factors.Futureresearchwillbenecessarytodeterminethe causeandscopeofthesepatterns.
LIMITATIONS
Becausethiswasaretrospectiveobservationalstudyithas limitationsinherenttostudydesignandclinical documentation.Theavailabledataissubjecttoreporting errorsandmissingdatapoints.Norwereweabletoassess temporalityoftherespiratoryrateinrelationtothepatient receivingnaloxone,sincethetimingofvitalsand interventionsweredocumentedbytheEMSrespondersin retrospectand,therefore,werenotpreciseenough. Additionally,itispossiblethatadditionalclinical characteristicsotherthanbradypneaimpactanEMS responder’sdecisiontoadministernaloxone.Giventhe variabilityindocumentation,assessmentofneurologicstatus andairwaycompromisewerenotincludedinthisanalysisbut mayhaveimpactedwhetherapatientreceivednaloxone. Further,thisstudyreliesuponobservationdataandwasnot designedtoestablishcausality.Whiletheeffectof homelessnesswasnoteliminatedinmodelsadjustingforcore clinicalindicationsordemographics(age,gender),itis possiblethattheeffectisreducibletolatentvariablesor confoundersthatareabsentfromourdata.
Further,homelessnessisacomplexandsometimes transientissue.TheEMSresponderswereresponsiblefor documentingthepatients’ housingstatus.Giventhebinary optionintheePCRandthetrainingprovided,itispossible thatpatients’ housingstatuscouldpotentiallyhavebeen inaccuratelycodedineitherdirection.Thedecisionto documenthousingstatusashomelessmaybebiasedby appearance,environment,presenceofparaphernalia,and eventheuseofnaloxoneitself.
Additionally,thisstudyonlyaccountsfornaloxone administrationbyEMSanddoesnotincludenaloxone administeredbybystandersorother firstresponders,suchas lawenforcementorstreetmedicineteams.Further,although thisstudycapturesallpatientswhowereadministered naloxonebyEMS,itdoesnotcaptureallpatientswhomay havehadopioidorsubstanceusedisorders.Giventhe existingbodyofliteraturethatsuggestsahighincidenceof SUD,includingOUD,intheunhousedpopulation,itis likelythatanevenlargernumberofEMSpatientswhoare homelessmaybeexperiencinganemergencyrelatedto OUD/SUDevenwhennotexplicitlylabeledwithanEMS responder’simpressionrelatedtooverdoseorintoxicationor administerednaloxone.Whilethiscannotbefurther extrapolatedduetolimitationsintheePCRdata,this relationshiphaspreviouslybeendescribedintheemergency medicineliterature.30 Thus,anevenlargernumberof
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 836 DoesHousingStatusMatterinEMSAdministrationofNaloxone? Abramsonetal.
patientscouldpotentiallybenefitfromoutreachprogramsor otherinterventions.
Finally,thestudywasconductedinasinglecity.Asacity withoneofthelargestpopulationsofPEH,LosAngeleswas usedasalenstoevaluatetheevolvingsituationatthe intersectionoftheopioidepidemic,thehousingcrisis,and EMS.WhileLosAngelesmayhaveuniquecharacteristics, priorstudiessuggestthatthedemographicsofitshomeless populationaresimilartoothermajorUScities.31 Given nationaltrends,LosAngelesmayserveasabellwetherfor othermetropolitanareasintheUS.
CONCLUSION
PersonsexperiencinghomelessnessintheCityof LosAngelesreceivedEMS-administerednaloxoneathigher ratesthantheirhousedcounterparts,evenwhenaccounting fordifferencesinage,gender,andrespiratorydepression. Futureresearchisneededtovalidatethese findingsinother settingsandtounderstandthisdifferenceinadministration rates,characterizepatientoutcomes,andidentifypotential targetsforalternativecarepathwaysforpatientsconfronting homelessnessandopioidusedisorder.
AddressforCorrespondence:TiffanyM.Abramson,MD,University ofSouthernCalifornia,KeckSchoolofMedicine,1200N.State Street,Rm1011,LosAngeles,California90033.Email: tiffany. abramson@med.usc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Abramsonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.O’DonnellJ,TanzLJ,GladdenRM,etal.Trendsinandcharacteristicsof drugoverdosedeathsinvolvingillicitlymanufacturedfentanyls United States,2019–2020. MorbMortalWklyRep.2021;70(50):1740–6.
2.WilsonN,KariisaM,SethP,etal.Drugandopioid-involved overdosedeaths UnitedStates,2017–2018. MorbMortalWklyRep 2020;69(11):290–7.
3.AhmadFB,CisewskiJA,RossenLM,etal.Provisionaldrugoverdose deathcounts. NatlCentHealStat.2022.Availableat: https://www. cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
AccessedDecember7,2022.
4.GloberN,MohlerG,HuynhP,etal.ImpactofCOVID-19pandemicon drugoverdosesinIndianapolis. JUrbanHealth.2020;97(6):802–7.
5.GladdenRM,O’DonnellJ,MattsonCL,etal.Changesinopioidinvolvedoverdosedeathsbyopioidtypeandpresenceof benzodiazepines,cocaine,andmethamphetamine 25States, July–December2017toJanuary–June2018. MorbMortalWklyRep 2019;68(34):737–44.
6.CentersforDiseaseControlandPrevention.Deathratemaps&graphs. CentersforDiseaseControlandPrevention,National CenterforInjuryPreventionandControl.2022.Availableat: https:// www.cdc.gov/drugoverdose/deaths/index.html
AccessedDecember7,2022.
7.DoranKM,RahaiN,McCormackRP,etal.Substanceuseand homelessnessamongemergencydepartmentpatients. DrugAlcohol Depend.2018;188:328–33.
8.MarshallJR,GassnerSF,AndersonCL,etal.Socioeconomicand geographicaldisparitiesinprescriptionandillicitopioid-relatedoverdose deathsinOrangeCounty,California,from2010–2014. SubstAbus 2019;40(1):80–6.
9.YamamotoA,NeedlemanJ,GelbergL,etal.Associationbetween homelessnessandopioidoverdoseandopioid-relatedhospital admissions/emergencydepartmentvisits. SocSciMed 2019;242:112585.
10.CentersforDiseaseControlandPrevention.StateUnintentionalDrug OverdoseReportingSystem(SUDORS).Atlanta,GA:USDepartment ofHealthandHumanServices,CDC.Availableat: https://www.cdc.gov/ drugoverdose/fatal/dashboard.AccessedDecember8,2022.
11.HenryM,ShivjiA,deSousaT,etal.The2015AnnualHomeless AssessmentReport(AHAR)toCongressPart1:Point-in-Time EstimatesofHomelessness;2015.
12.HenryM,deSousaT,RoddeyC,etal.The2020AnnualHomeless AssessmentReport(AHAR)toCongress;2020.
13.KushelMB,PerryS,BangsbergD,etal.Emergencydepartmentuse amongthehomelessandmarginallyhoused:Resultsfroma community-basedstudy. AmJPublicHealth.2002;92(5):778–84.
14.HanB,WellsBL.Inappropriateemergencydepartmentvisitsanduseof thehealthcareforthehomeless. JPublicHealManagPract 2003;9(6):530–7.
15.BrownRT,KielyDK,BharelM,etal.Geriatricsyndromesinolder homelessadults. JGenInternMed.2012;27(1):16–22.
16.GambateseM,MarderD,BegierE,etal.Programmaticimpactof 5yearsofmortaliysurveillanceofNewYorkCityhomelesspopulations. AmJPublicHealth.2013;103(Suppl2):S193–8.
17.BaggettTP,HwangSW,O’ConnellJJ,etal.Mortalityamonghomeless adultsinBoston:shiftsincausesofdeathovera15-yearperiod. JAMA InternMed.2013;173(3):189–95.
18.BaggettTP,ChangY,SingerDE,etal.Tobacco-,alcohol-,anddrugattributabledeathsandtheircontributiontomortalitydisparitiesina cohortofhomelessadultsinBoston. AmJPublicHealth 2015;105(6):1189–97.
19.GallagherTC,AndersenRM,KoegelP,etal.Determinantsofregular sourceofcareamonghomelessadultsinLosAngeles. MedCare 1997;35(8):814–30.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 837 Abramsonetal. DoesHousingStatusMatterinEMSAdministrationofNaloxone?
20.AbramsonTM,SankoS,EcksteinM.Emergencymedical servicesutilizationbyhomelesspatients. PrehospEmergCare 2020;25(3):1–8.
21.GloberNK,GovindarajanaP.Population-basedestimatesof ambulanceutilizationandtreatmentpatternsforopioid-relatedoverdose inanationalsample. PrehospEmergCare.2018;21(10):97–152.
22.VonElmE,AltmanDG,EggerM,etal;STROBEInitiative. StrengtheningtheReportingofObservationalStudiesinEpidemiology (STROBE)statement:guidelinesforreportingobservationalstudies. BMJ.2007;335(7624):806–8.
23.BenchimolEI,SmeethL,GuttmannA,etal.Thereportingofstudies conductedusingobservationalroutinelycollectedhealthdata (RECORD)Statement. PLoSMed.2015;12(10):e1001885.
24.2003
2018GreaterLosAngelesHomelessCount-CityOfLos Angeles.Availableat: https://www.lahsa.org/documents?id=20032018-greater-los-angeles-homeless-count-city-of-los-angeles AccessedMarch4,2020.
25.AmericanCommunitySurvey.Availableat: https://data.census.gov/ table?q=DP05&g=160XX00US0644000&tid=ACSDP1Y2018.DP05 AccessedJuly10,2023.
26.PrehospitalCareManual.Reference1317.29.Availableat: https://dhs. lacounty.gov/emergency-medical-services-agency/home/ resources-ems/prehospital-care-manual/.AccessedDecember8,2022.
27.PrehospitalCareManual.Reference1200.3.Availableat: https://dhs. lacounty.gov/emergency-medical-services-agency/home/ resources-ems/prehospital-care-manual/.AccessedDecember8,2022.
28.PrehospitalCareManual.Reference1380.Availableat: https://dhs. lacounty.gov/emergency-medical-services-agency/home/ resources-ems/prehospital-care-manual/.AccessedDecember8,2022.
29.JenkinsC,LevineM,SankoS,etal.Useofnaloxonein9–1–1patients withoutrespiratorydepressioninLosAngelesCounty,California(USA). PrehospDisasterMed.2021;36(5):543–6.
30.SalhiBA,WhiteMH,PittsSR,etal.Homelessnessandemergency medicine:areviewoftheliterature. AcadEmergMed.2018;25(5):577–93.
31.RopersRH,BoyerR.Perceivedhealthstatusamongthenewurban homeless. SocSciMed.1987;24(8):669–78.
32.FarkasA,LynchMJ,WestoverR,etal.Pulmonarycomplications ofopioidoverdosetreatedwithnaloxone. AnnEmergMed 2020;75(1):39–48.
33.KeaneC,EganJE,HawkM.Effectsofnaloxonedistributionto likelybystanders:resultsofanagent-basedmodel. IntJDrugPolicy 2018;55:61–9.
34.WalleyAY,XuanZ,HackmanHH,etal.Opioidoverdoseratesand implementationofoverdoseeducationandnasalnaloxonedistribution inMassachusetts:interruptedtimeseriesanalysis. BMJ 2013;346(7894):1–13.
35.AboukR,PaculaRL,PowellD.Associationbetweenstatelaws facilitatingpharmacydistributionofnaloxoneandriskoffataloverdose. JAMAInternMed.2019;179(6):805–11.
36.GloberNK,HernG,McBrideO,etal.VariationsintheCalifornia emergencymedicalservicesresponsetoopioidusedisorder. WestJ EmergMed.2020;21(3):671–6.
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 838 DoesHousingStatusMatterinEMSAdministrationofNaloxone? Abramsonetal.
ApplicationofaLow-cost,High-fidelityProximalPhalangeal DislocationReductionModelforClinicianTraining
SpencerLord,MD*†
SeanGeary,MD*
GarrettLord,AIA‡
*AlbanyMedicalCenter,DepartmentofSurgeryandDepartmentofEmergencyMedicine, Albany,NewYork
† MassachusettsGeneralHospital,DepartmentofSurgery,Boston,Massachusetts ‡ DattnerAssociates,NewYork,NewYork
SectionEditor: JuanAcosta,DO,MS
Submissionhistory:SubmittedNovember20,2022;RevisionreceivedApril19,2023;AcceptedApril16,2023
ElectronicallypublishedAugust25,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59471
Introduction: Patientspresenttotheemergencydepartment(ED)relativelycommonlywithtraumatic closedproximalinterphalangealjoint(PIPJ)dislocations,anorthopedicemergency.Thereisapaucityof teachingmodelsandtrainingsimulationsforclinicianstolearneitherthecloseddislocateddorsalorvolar interphalangealjointreductiontechnique.Weimplementedateachingmodeltodemonstratetheutilityof anovelreductionmodeldesignedfromthree-dimensional(3D)printablecomponentsthatareeasyto connectanddonotrequirefurthermachiningorresinmodelstocomplete.
Methods: Studentswatchedatwo-minutevideoandamodeldemonstrationbytheauthors.Learners includingemergencymedicine(EM)residentsandphysicianassistantfellowsassessedmodel fidelity, convenience,perceivedcompetency,andobservedcompetency.
Results: Seventeenof21(81%)participantsagreedthemodelmimickeddorsalandvolarPIPJ dislocations.Nineteenof21(90%)agreedthemodelwaseasytouse,21/21(100%)agreedthedorsal PIPJmodeland20/21(95%)agreedthevolarPIPJmodelimprovedtheircompetency.
Conclusion: Our3D-printed,dorsalandvolardislocationreductionmodeliseasytouseandaffordable, anditimprovedperceivedcompetencyamongEMlearnersatanacademicED.[WestJEmergMed. 2023;24(5)839–846.]
INTRODUCTION
Traumaticdislocationsoftheproximalinterphalangeal joint(PIPJ)areamongthemostcommontypesof finger dislocation.Dorsaldislocationisduetoalateralloading forcewithhyperextensionleadingtodisruptionofthevolar plate,jointcapsule,andcompositeligamentsleadingtoa dorsaldislocation.1–3 Volardislocations,althoughmuch rarer,dooccurandareoftencausedbycompressionand rotationwithconcomitantPIPJ flexion.4 Despitethe prevalenceofthisinjurywithinthetraumapopulation,there arefewteachingmodelsavailablewithnopublishedpractice assessmentofthemodeltrainersforclinicians.5,6
Weprovideasimpletoprint,assemble,andreplacedorsal andvolarreductionmodelcreatedfromthree-dimensional (3D)printedcomponentswithoutrequiringmachining
(Figure1).7 Ourmodelfollowstheprincipleofsimpledorsal andvolardislocationthatrequiresmanagementusingthe exaggerationbydeformitydescribedbyRobertsandHedges etalin1998.8 Wedevelopedaworkshoptoassessthemodel byevaluatingmodel fidelity,modelconvenience,and cliniciancompetencyduringatrainingmodule.
METHODS ModelDesign
Wedevelopedaunique,interchangeablePIPJmodelto practicereducingnon-fracturedPIPJdorsalandvolar dislocations.Specificdetailsregardingmodelfunctionand jointarticulationarefullydescribedwithinLord2022etal.7 Wedevelopeda3D-printedhandmodelusingapalmbase fromtheopen-sourceFlexy-Handprosthetic(e-NABLE
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 839
RESEARCH
ORIGINAL
globalonlinecommunity).9 Wemodifiedthesecondand third fingerstofunctionasadislocatedPIPJinclosed complexdorsaldislocation(Figure2.1–3)withreduction achievedbytheexaggerationofdeformitymethod,andthe fourthand fifth fingerstofunctionasadislocatedPIPJ inclosedvolardislocation(Figure2.4–6).The fingersare alsodetachableforreconfigurationandeasy replacement(Figure3).
Supplies
FormodeldesignweusedRhinocerosV6software (McNeelandAssociates,Seattle,WA),UltimakerCura version4.9.0G-CODEsoftware(Ultimaker,Utrecht, Netherlands),aCrealityEnder33Dprinter(Creality, Schenzhen,China),and1.75mmPLA filament(Hatchbox, Pomona,CA).Specificallyforthejointapparatusweuseda single#6–32 × 1–1/2inmachinescrew,two#6 flatwashers, andfour5/32neoprenewashersfromahardwarestore, whichwecuttosizewitharazorblade(Figure4).The apparatuswashandtightenedforaddedstability. Table1 providesabreakdownofcosts.
PrintConfiguration
Theentireprinttakes33hoursand25minutesifeachpart isprintedseparately,witheach fingertaking3hoursand28 minutes(proximal,middle,distal,pin,andhinge).Anentire handrequirestheproductionoffourproximal,fourmiddle, andfourdistal fingercomponents,alongwitheightpinsand fourhingeconnectorsalongwithasinglepalmandsingle thumb.Thepropertiesofallprintedcomponentsare includedin Table2.The.stlprintisavailable,open source,at https://grabcad.com/library/proximalphalanx-traction-model-1.Weprovideastep-by-step assemblyofthedorsaldislocationandvolardislocation.
Supplemental file4 includeshowtouseCura
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Dorsaljointreductionsarecommon orthopedicemergencies,yettherearefew trainingmodelsforclinicians.
Whatwastheresearchquestion?
Doesanovellow-cost,high- fi delitymodel dorsaljointreductionmodelimprove competency?
Whatwasthemajor findingofthestudy?
100%ofparticipantsagreedthedorsal proximalinterphalangealjointmodel(PIPJ) and95%agreedthevolarPIPJmodel improvedcompetency.
Howdoesthisimprovepopulationhealth? Anaffordableeducationmodelenables medicaltraineestolearnthePIPJdislocation reductiontechniqueand,therefore,provide betterpatientcare.
Ultimakersoftwaretouploadyour.stl fileandassign yourprinter.
ModelAssembly
Thefollowing figuresshowthestepwiseassemblyofboth thedorsaldislocationandvolardislocation(Figure3).A step-by-stepvideoassemblyofthedorsalPIPJreductionis
Figure1. Proximalinterphalangealjoint(PIPJ)complexdorsaldislocationwith “exaggerationofdeformity” methodofthesecond finger(1A), hyperextensionofthePIPJ(1B),andreductionbacktotheneutralposition(1C).PIPJvolardislocationofthe fifth finger(1D), flexionreduction positionofthePIPJ(1E),andreductionbacktotheneutralposition(1F).
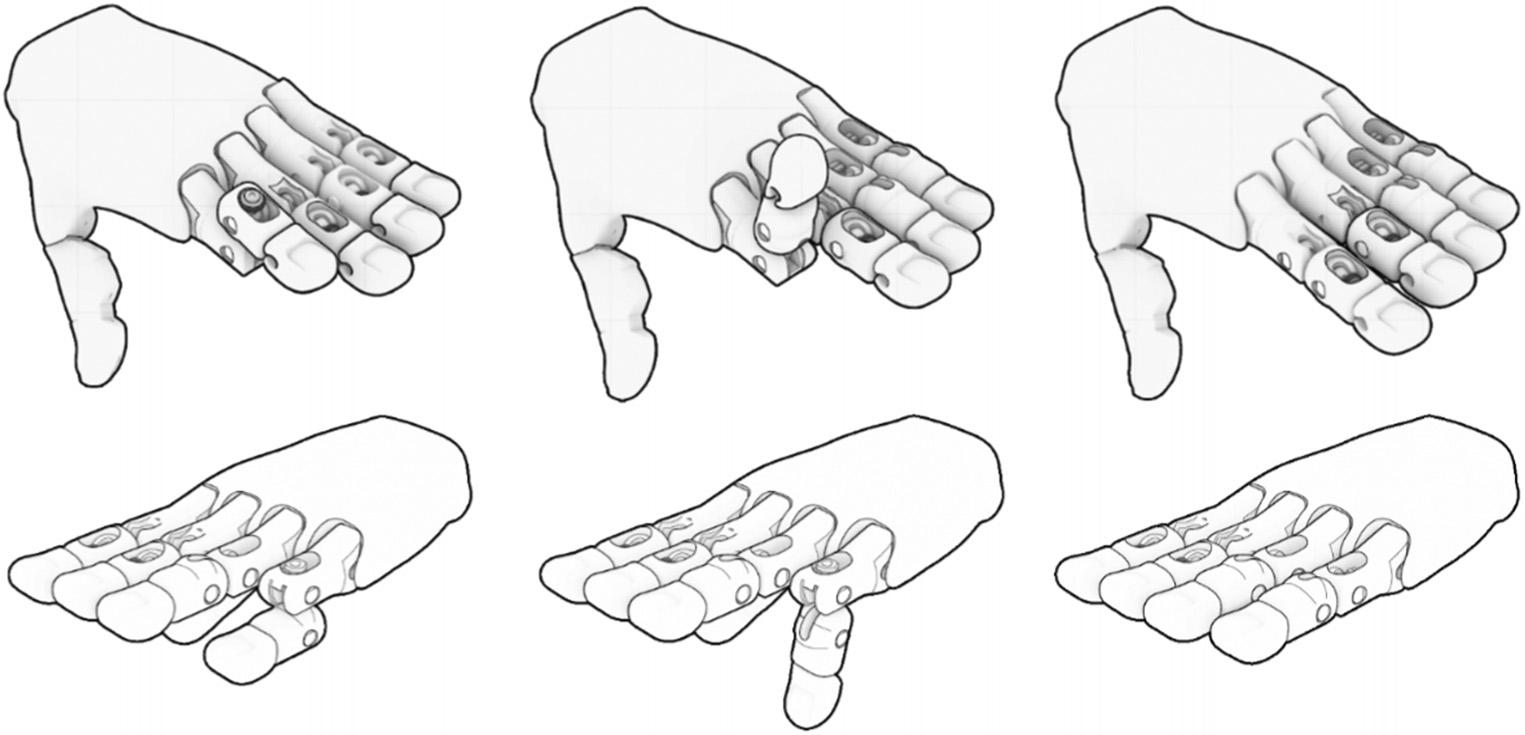
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 840 ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining Lordetal.
dislocationwithexaggerationofdeformitymethodofthesecond finger(2.1),hyperextensionofthePIPJ(2.2),andreductionbackto theneutralposition(2.3).PIPJvolardislocationofthefourth finger (2.4),hyperflexionreductionpositionofthePIPJ(2.5),andreduction backtotheneutralposition(2.6).

availableat(https://youtu.be/TkEyc3R2p9s)andvolarPIPJ reduction(https://youtu.be/_MCwHHbP-Sk).Anexploded assemblymodelisdescribedinLordetal2022.7
StudyDesign
Thiswasaprospectiveobservationalstudyperformed atasingle,LevelItraumacenteremergencymedicine (EM)residencyprogramduringthemonthsofNovember 2021andMarch2022.Allstudyparticipantswerecurrent EMresidentsandphysicianassistants,whoweregiven alivedemonstrationofhowtoperformavolarand dorsalreductionbytheexaggerationmethodonthe
providedteachingmodel[https://www.youtube.com/watch? v=i1XPiA3GYmQ].Participantswereassessedfor observedcompetencyusingastepwiseassessment,andthey inturnassessedthemodel’ s fidelityandconvenience,aswell astheirperceivedcompetency.(See supplemental1, supplemental2,and supplemental3.)10,11 Participantswere notassessedforpreviouscompetency.Institutionalreview boardapprovalwasgrantedforananonymoussurveyofan educationalexperiencewithdisseminationofsurveyresults forpublication.
Workshop
Followingthedemonstration,participantswereassessed forobservedcompetency.Thetotalteachingsectiontook placeduringa90-minutescheduledperiodwithinresidents’ protectededucationaltime.Participantsweregiventwo attemptstopracticeboththevolaranddorsaldislocation modelbeforeassessmentattempt.Proceduralstepswere scoredbasedonwhetherthetaskwascompletedortherewas hesitancyoromission/failure.Wedeterminedthathesitancy wouldbedefinedasapause >3seconds.Omissionwas definedasskippingastep,andwedefinedfailureas inappropriatelydeformingorbreakingthemodel.Following theworkshop,participantswereaskedtocompleteashort surveyusingasix-pointLikertscale(5stronglyagree, 4agree,3neutral,2disagree,1stronglydisagree, non-applicable)pertainingtoquestionsregardingmodel fidelity,convenience,andcompetency.11 Theworkshop directorwasavailableforquestionsaftertheparticipants attemptedthemodelandcompletedthequestionnaireand wasavailabletorebuildthemodelifparticipantscouldnot dosothemselves.
RESULTS
Duringthestudyperiodatotalof21participants comprising19residents(sixpostgraduateyear[PGY]1,
Figure2. Proximalinterphalangealjoint(PIPJ)complexdorsal
ItemBrandSizeUnitcost($)Totalcost MachinescrewEverbilt#6–32 × 1–1/2in0.424.98 FlatwasherEverbilt#60.364.36 MachinescrewnutEverbilt#6–320.111.28 NeoprenewasherEverbilt5/32in0.240.98 RazorbladeStanleyn/a1.971.97 1.75mm filament1kgHatchboxn/a22.9922.99 RhinocerosV6softwareMcNeelandAssociatesn/a195.00195.00 UltimakerCurasoftwareUltimakern/aFreeFree G-CODEsoftwareUltimakern/aFreeFree CrealityEnder33DprinterCrealityn/a179.99179.99 TotalCosts 411.55 Volume24,No.5:September2023WesternJournal of EmergencyMedicine 841 Lordetal. ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining
Table1. Itemizedlistofmodelcomponentsincludingcost.
Palm18hours42min(134g)45m0.8mm1.0mm50%/Cubic0.2mm
Proximal1hour23min8g2.81m0.8mm1.0mm50%/Cubic0.2mm
Middle1hour5min6g2.01m0.8mm1.0mm50%/Cubic0.2mm

Distal33min4g1.36m0.8mm1.0mm50%/Cubic0.2mm
Pin6min <1g0.13m0.8mm1.0mm50%/Cubic0.2mm
Hinge15min1g0.27m0.8mm1.0mm50%/Cubic0.2mm
Thumb1hour51min11g3.74m0.8mm1.0mm50%/Cubic0.2mm g,gram; m,meter; mm,millimeter.
sevenPGY2,andsixPGY3)andtwophysicianassistant fellowscompletedboththedorsalandvolarPIPJreduction model.Allparticipantsconsentedtoallowuseoftheirdata forresearchpurposes.Dataanalysiswasperformedwith Excel2006(MicrosoftCorp,Redmond,WA). Figure4 providesagraphicalrepresentationofmodelfeasibility, convenience,andperceivedcompetency.
ModelFeasibility
All21participantswereincludedinthefeasibility portion.Nineteenof21(95%)agreedthejointswere
palpableonexam;2/21(5%)didnotanswerthequestion. Seventeenof21(81%)participantseitheragreedorstrongly agreedthatthemodelmimickedadorsalproximal interphalangealjoint(dPIPJ)dislocation,and17/21(81%) agreedorstronglyagreeditmimickedavolarproximal interphalangealjoint(vPIPJ)dislocation.Also,13/21(62%) and12/21(57%)agreedorstronglyagreedthattension requiredforsuccessfuljointreductionofthedPIPJand vPIPJwasrealistic.Seventeenof21(81%)participants agreedthemodelmimickedadorsalandvolarPIPJ dislocation.Nineteenof21(90%)agreedthemodelwas
ItemPrinttime Filament weight(g) Filament length(m) Wallthickness (mm) Top/bottom thickness(mm)Infill%/type Layer height(mm)
Table2. Propertiesofallprintedcomponents.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 842 ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining Lordetal.
Figure3.3.1.Showsallcomponentpartsofthedorsallydislocated finger(lateralview). 3.2.Dorsalview. 3.3.Placepinandalignthecentral openingwithopeningsinthemiddleandproximal fingerportions. 3.4.Modifiedneoprenewashercut¼inx¼in. 3.5.Loadtwoneoprene washersandamachinescrewnut. 3.6. Loadthescrewdorsallythroughthepin. 3.7.passscrewthroughpininproximalphalangesasshown andattachscrewnutsinthisposition. 3.8.Placeinthereducedpositiontocheckresistance. 3.9.Showsallcomponentpartsofthevolar dislocated finger(lateralview). 3.10.Dorsalview. 3.11.Modifiedneoprenewashercut¼inx¼. 3.12.Loadtwoneoprenewashersand machinescrewnut. 3.13.Loadthescrewventrallythroughthepin. 3.14.Passscrewthroughpininproximalphalangesasshownand 3.15.attachscrewnutsinthisposition. 3.16.Placeinthereducedpositiontocheckresistance.
easytouse,and100%agreedthemodelimproved theircompetency.
Convenience
All21/21participantswereincludedintheconvenience portion.Nineteen(90%)agreedorstronglyagreedthatthe modelwaseasytouse.Oftheparticipantswhohadpracticed ona fingerreductionmodelbefore,6/10(60%)agreedor stronglyagreedthismodelwaseasiertouse,4/21(19%) thoughtthemodelwasneutralornodifferentinuse comparedtoothermodels,and11/21(52%)selected “non-applicable” astheyhadnomodeltocompare.Sixof the21participants(29%)didnothavetoreplacecomponents duringtheirtestingand,thus,theyresponded “ nonapplicable” tothequestion.
PerceivedCompetency
All21/21participantswereincludedintheperceived competencyportion.Twenty-one(100%)agreedthedPIPJ modelimprovedtheircompetencyindPIPJreduction technique.Nineteen(95%)agreedthevPIPJmodelimproved theircompetencyinvPIPJreductiontechnique.Nineteen (95%)agreedthemodelisadequatefortraining EMstaff.
ObservedCompetency
All21participantswereincludedintheobserved competencyportion(Figure5).Inboththevolaranddorsal reductiongroups,allparticipantsplacedthehandinaprone
position,palpatedthedeformityandstabilizedthejoint priortoreductionusingthecorrectpracticewithout hesitation.Fifteenof21(71%)performedcorrect hyperextensionandhyperflexionwithouthesitation,and 6/21(29%)performedhyperextensionandhyperflexionbut withhesitancy.InthedPIPJdislocation,17/21(81%) performedtraction/countertractioncorrectlyandwithout hesitation,2/21(10%)performedtraction/countertraction correctlybutwithhesitancy,and2/21(10%)performed traction/countertractionincorrectlyresultingin detachmentofthemetacarpal-phalangealjointfromthe handmodel.InthevPIPJdislocation,19/21(90%)performed traction/countertractioncorrectlywithouthesitancy.Twoof 21(10%)performedtraction/countertractioncorrectlybut withhesitation.
DISCUSSION
Thisisthe firstlow-cost,high-fidelityPIPJreduction modelpublishedinthemedicalliteraturedescribinga reproducible fidelitystudy.Themodelhasremovableand replaceablecomponentswithouttherequirementofresin moldproductionormachining.Thismodelalsoprovides appropriatecompetencytraininginalow-stress,teaching environmentforlearners.Themodelprovidesconvenience regardingassembly,replacement,anduse.Themodel mimicsreal-lifedPIPJandvPIPJsimpledislocationsand showsbothperceivedandobservedcompetencywith practice.Withfewmisapplications/omissionsnoted duringtheobservedperformance,ourmodelavoidsthe

Volume24,No.5:September2023WesternJournal of EmergencyMedicine 843 Lordetal. ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining
Figure4. Agraphicalrepresentationprovidinginterpretationofmodelconvenience,feasibility,andperceivedtrainingcompetency. vPIPJ,volarproximalinterphalangealjoint; dPIPJ,dorsalproximalinterphalangealjoint.
“fidelitytrap” (assumingparticipants “learninproportionto thelevelofrealism”)thatcanoccurwithhigh-fidelity teachingmodels.12,13
Ourdesignnotonlydepictsadislocation,butitalso requiresanatomicallycorrectmotionstosuccessfullyreduce thejointintothecorrectposition.Theuniquearticulation surfacesprevent “cheating,” enablelearnerstoexperiencethe significanttensionandpressureneededtosuccessfullyreduce thejointandallowforaneasyresettothedislocatedposition forthenextparticipant.Ourmodelprovidesimprovement overcurrentlyavailableproductsduetotestedrepeatability, relativeaffordability,andauniquejointapparatustoprevent incorrecttechnique.Itisthe firstmodelofitskindmadefrom reusable,replaceable3D-printedcomponentsfroma personal3Dprinterandeasilyavailablecomponentsfrom ahardwarestore.
Futurestudieswillfocusonaddressinglimitations, specificallycreatingamorerealistic fingercovertobetter replicatetheprocedureortrialingdifferentsilicone thicknesseswithoutaddingsignificantlymoreconstruction requirementsforthetrainee.Whilethesiliconecovering wechosewasanaffordableoption,itoftencaughtitself inthejointmakingthereductionattemptimpossible. Otheranticipatedmodelinnovationsincludetestingand refiningappropriateforcerequirementsduringreduction, ideallyusingaquantitativeforcetransducer.Further studiesareneededtoassessdifferentcliniciangroupswho performthisprocedureincludingprehospitalmedical services,militarypersonnel,moresenioremergency clinicians,andnon-emergencycliniciansincluding orthopedicandplasticsurgeons.
Three-dimensionalanatomicallearninghasbeenshownto beamoreeffectivestudyingtoolcomparedto2D technologies.14 Further,3Dteachingmodelsarenoninferior tocadavericteaching,areoftencheaper,andpotentially moreaccessible.15–17 Simpleandevencomplexjoint reductionscanbeperformedoutofhospital,andstudieshave showntherelativeeaseandsafetyofprehospitaljoint reductions.18–20
Proceduraltrainingusinghigh-fidelity teachingmodelsprovidestraineeswithnon-inferior proceduraltrainingintheabsenceofexpensivemannequins. Arecentmeta-analysisfoundthatoperativetimeand complicationratesimprovedwhenusing3Dmodelsfor surgicalplanning,andalargemultispecialtyreview highlightingtheroleof3Dprintingincomplexmedical proceduralplanningandtrainingshowedimproved competency.21,22 Thereisagrowing fieldinpreoperative planninginorthopediconcology,andorthopedic traumasurgery.23–25
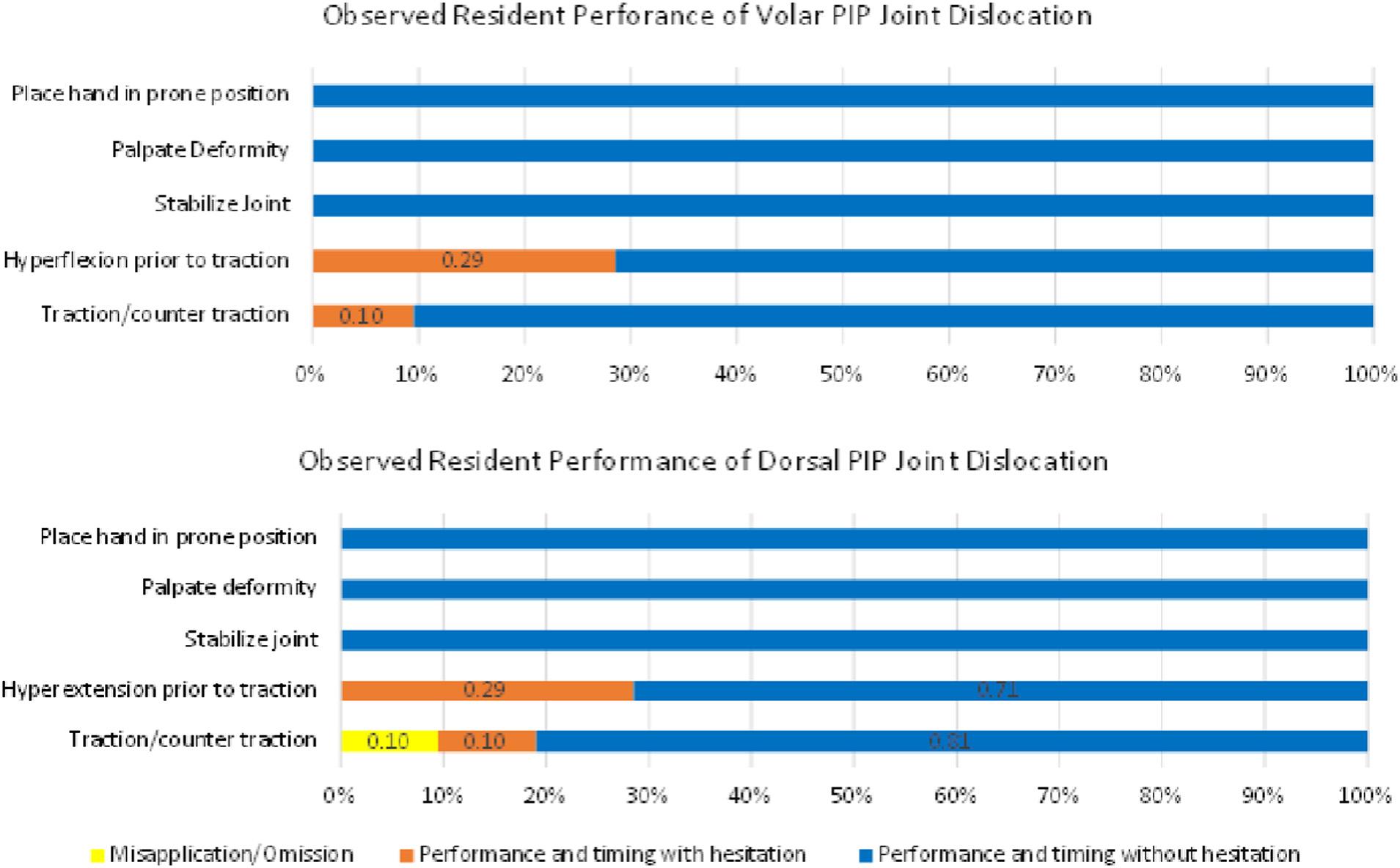
LIMITATIONS
Themodeldoeshavelimitations.Namely,thereareno modelsavailableforpurchasenoraretherepublished trainingmodelstocompare.5,6 Therefore,whileparticipants deemedthemodeleasytouse,wecouldnotobjectively comparefeasibility,competency,andconveniencetoother models.Themodelalsotakestimetoassembleduetothe intentionalmetacarpophalangealjointdislocation mechanismandassemblybynon-machinedparts.While mostparticipantsbelievedthemodelrepresentedarealistic PIPJdislocation,tomaintainstabilitywereducedthedegree ofrotationaldisplacementofthedislocatedjoint,therefore
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 844 ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining Lordetal.
Figure5. Observedcompetencyofthevolarproximalinterphalangealjoint(PIPJ)reductionmodelanddorsalPIPJreductionmodel.
reducingmodel fidelity.Furthermore,ourdorsal dislocationmodelismoreapplicablewhenthereisabayonet deformity(ie,whenthecondyleoftheproximalphalanx isnolongerincontactwiththebaseofthemiddlephalanx). Intheabsenceofbayonetting,thedegreeofhyperextension thatthemodelrequiresisnotalwaysneededinthe clinicalsetting.
Whilethejointapparatuswasfunctionalitwasdifficultto useandarticulatewiththepurchasedsiliconecoverings;half theparticipantsaskedtoremovethesilicone fingercoverprior toparticipatingintheevaluation;thus,learnerswereunableto practiceintheenvironmentofatrulycloseddislocation.While weattemptedtoassessobservedcompetency,wedidnot compareoutcomesbetweenthosewhohadreported performingadorsaldislocationreduction(7/21)(33%)or volardislocationreduction(2/21)(10%).Duetotherelatively smallsamplesizeofthisstudy,wedidnotaskabouttotal numberofattemptedlivereductionsorsuccessrateof attemptedliveprocedures.Further,withthesmallsample sizeandwithmostparticipantsbeingresidents,thisstudy lacksgeneralizability.
Whileprintingofthemodelwasreplicable,ageneral knowledgeofCuraUltimakersoftwareisneededtocomplete theprint,whichforthenon-engineersamongtheauthors, tooktwohoursofonlinetutorialinstructiontounderstand andbeself-sufficient.Thismaynotbeanaccuratelengthof timerequiredtolearnthesoftwareaswedidnotassessthisin ourstudy.
Oftheparticipantswhodidnotagreeorstronglyagree thatthetractionwasrealistic,40%attributedthistobelieving thetensionwastootight.Wedidnotconfirmwhetherthis wasthereasontwoparticipantsdidnotagreethemodel waseasytouse,norwhetherthereasonfourparticipants didnotagreeorstronglyagreethemodelmimickedvPIPJ anddPIPJdislocations.
Wedidnotuseaquantitativeforcetransduceraswecould not findasimplewaytoincorporateitintothestudymodel. Itwouldbeextremelybeneficialtofurtherrefinethedeviceto achievemoreaccuraterepresentationforforcesrequiredfor reduction.Also,itshouldbenotedthat8/21(38%) documented “non-applicable” fortheconvenience question “ThePIPJmodeliseasytoassemble” even thougheachparticipanthadtoattachthe fingerstothehand modelpriortouse.
CONCLUSION
Ouruniqueproximalinterphalangealjointdislocation modelprovidesareproducible,easy-to-printproductthat canbeusedwithinthelearningenvironmenttotrain practitioners.Themodeliseasytoassembleandprovidesa jointarticulationtotrainlearnersforbothdorsalandvolar PIPJdislocations.
AddressforCorrespondence:SpencerLord,MD,Massachusetts GeneralHospital,DepartmentofSurgery,55FruitSt.Boston Massachusetts,02114.Email: slord1@mgb.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Lordetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.VicarA.Proximalinterphalangealjointdislocationswithoutfractures. HandClin.1988;4(1):5–13.
2.GolanE,KangK,CulbertsonM,etal.Theepidemiologyof finger dislocationspresentingforemergencycarewiththeUnitedStates. Hand 2016;11(2):192–6.
3.PruczR,FriedrichJ.Fingerjointinjuries. Clin.SportsMed 2015;34(1):99–16.
4.JeromeT.Volardislocationoftheproximalinterphalangealjoint. J.OrthoplasticSurg 2021;5:6–8.
5.Luna(website).Availableat: https://lunainc.com/blog/athletic-trainingstudents-learn-technique-using-lunas-joint-reductiontrainer AccessedJune22,2021.
6.PolanksyRandKwonN.Reductionof fingerdislocation. Medscape Availableat: https://emedicine.medscape.com/article/ 109206-overview (embeddedinyoutube: https://youtu.be/tJjerc616rM) AccessedJune22,2021.
7.LordG,LordS,GearyS.PhalangealDislocationReductionModel.US PatentNo.63/396,914.USPatentandTrademarkOffice.
8.RobertsJ,HedgesJ,eds. ClinicalProceduresinEmergencyMedicine Philadelphia:ElsevierScience1998:838.
9.Adlughmin.2014.TheFLexy-Hand – TheMostInnovative,Useful, RealisticLooking3DPrintedProstheticHandYet.Availableat: https:// 3dprint.com/1500/the-flexy-hand-3d-printed-prosthetic AccessedJune22,2021.
10.SenurenC,YaylaciS,KayayurtK,etal.Developingcricothyroidotomy skillsusingabiomaterial-coveredmodel. WildernessEnvironMed 2020;31(3):291–7.
11.SullivanA,KhaitL,Favot.Anovellow-costultrasound-guided pericardiocentesissimulationmodel:demonstrationoffeasibility. JUltrasoundMed.2018;37(2):493–500.
12.CareyJandRosslerK.Thehowwhenwhyofhigh-fidelitysimulation. [Updated2022May8].In:StatPearls[Internet].TreasureIsland(FL): StatPearlsPublishing2022Jan-.Availableat: https://www. ncbi-nlm-nih-gov.elibrary.amc.edu/books/NBK559313/ AccessedJune21,2022.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 845 Lordetal. ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining
13.HelyerR,DickensP.Progressintheutilizationofhigh-fidelitysimulation inbasicscienceeducation. AdvPhysiolEduc.2016;40(2):143–4.
14.ZilverschoonM,CustersE,CateO,etal.Supportforusinga3D anatomyapplicationoveranatomicalatlasesinarandomized comparison. AnatSciEduc.2022;15(1):178–86.
15.LimK,LooZ,GoldieS,etal.Useof3Dprintedmodelsinmedication:a randomizedcontroltrialcomparing3Dprintsversuscadaveric materialsforlearningexternalcardiacanatomy. AnatSciEduc 2016;9:213–21.
16.YeZ,JiangH,NieC,etal.Theroleof3Dprintedmodelsintheteaching ofhumananatomy:asystematicreviewandmeta-analysis. BMCMed. Educ.2020;20(1):335.
17.CaiB,KanagasuntheramR,BayB,etal.Theeffectsofafunctional three-dimensional(3D)printedkneejointsimulatorin improvinganatomicalspatialknowledge. AnatSciEduc 2019;12(6):610–8.
18.WrightC,BrandonB,ReismanE.Closed-reductiontechniques forglenohumeral-,patellofemoral-,andinterphalangeal-joint dislocations. J.ofAthl.Train.2020;55(8):757–67.
19.LordS,BrodellJ,LenhardtH,etal.Implementationofaprehospital patelladislocationreductionprotocol. PrehospEmergCare 2020;24(6):800–3.
20.FennellyJ,GourbaultL,Neal-Smith,etal.Asystematicreviewofprehospitalshoulderreductiontechniquesforanteriorshoulderdislocation andtheeffectonpatientreturntofunction. Chin.J.ofTraumatol 2020;23(5):295–301.21.
21.YammineK,KarbalaJ,MaaloufA,DaherJ,AssiC.Clinicaloutcomesof theuseof3Dprintingmodelsinfracturemanagement:ametaanalysisofrandomizedstudies. EurJTraumaEmergSurg 2022;48(5):3479–91.
22.Meyer-SzaryJ,LuisM,MikulskiS,etal.Theroleof3Dprintingin planningcomplexmedicalproceduresandtrainingofmedical professionals cross-sectionalmultispecialtyreview. IJERPH 2022;19(6):3331.
23.PunyaratabandhuT,LiacourasP,PairojboriboonS.Using3Dmodelsin orthopediconcology:presentingpersonalizedadvantagesinsurgical planningandintraoperativeoutcomes. 3DPrintMed 2018;4(1):12.
24.ZhangM,GuoJ,LiH,etal.Comparingtheeffectivenessof3Dprinting technologyinthetreatmentofclavicularfracturebetweensurgeonswith differentexperiences. BMCMusculoskeletDisord.2022;23(1):1003.
25.WangJ,WangX,WangB,etal.Comparisonofthefeasibilityof3D printingtechnologyinthetreatmentofpelvicfractures:asystemic reviewandmetanalysisofrandomizedcontrolledtrialsandprospective comparativestudies. EurJTraumaEmergSurg 2021;47(6):1699–12.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 846 ApplicationofaLow-Cost,High-fidelityPPDReductionModelforClinicianTraining Lordetal.
GenderandInconsistentEvaluations:AMixed-methodsAnalysis ofFeedbackforEmergencyMedicineResidents
AlexandraBrewer,MA,PhD*
LauraNelson,MA,PhD†
AnnaS.Mueller,MA,PhD‡
RebeccaEwert,MA,PhD§
DanielM.O’Connor,MD∥
ArjunDayal,MD¶
VineetM.Arora,MD,MAPP#
*UniversityofSouthernCalifornia:LosAngeles,DepartmentofSociology, LosAngeles,California
† UniversityofBritishColumbia,DepartmentofSociology,Vancouver, BritishColumbia,Canada
‡ IndianaUniversity,DepartmentofSociology,Bloomington,Indiana
§ NorthwesternUniversity,Chicago,Illinois
∥ MassachusettsGeneralBrighamWentworth-DouglassHospital,Dermatologyand SkinHealth,Dover,NewHampshire
¶ RushCopleyMedicalGroup,Aurora,Illinois
# UniversityofChicago,PritzkerSchoolofMedicine,Chicago,Illinois
SectionEditors: JeffreyDruck,MD,andYaninaPurim-Shem-Tov,MD,MS
Submissionhistory:SubmittedJuly25,2023;RevisionreceivedApril23,2023;AcceptedMay25,2023
ElectronicallypublishedAugust22,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58153
Objectives: Priorresearchhasdemonstratedthatmenandwomenemergencymedicine(EM)residents receivesimilarnumericalevaluationsatthebeginningofresidency,butthatwomenreceivesignificantly lowerscoresthanmenintheir finalyear.Tobetterunderstandtheemergenceofthisgendergapin evaluationsweexamineddiscrepanciesbetweennumericalscoresandthesentimentofattached textualcomments.
Methods: Thismulticenter,longitudinal,retrospectivecohortstudytookplaceatfourgeographically diverseacademicEMtrainingprogramsacrosstheUnitedStatesfromJuly1,2013–July1,2015usinga real-time,mobile-based,direct-observationevaluationtool.Weusedcomplementaryquantitativeand qualitativemethodstoanalyze11,845combinednumericalandtextualevaluationsmadeby151 attendingphysicians(94menand57women)duringreal-time,directobservationsof202residents (135menand67women).
Results: Numericalscoresweremorestronglypositivelycorrelatedwithpositivesentimentofthetextual commentformen(r = 0.38, P < 0.001)comparedtowomen(r = 0.26, P < 0.04);morestrongly negativelycorrelatedwithmixed(r = 0.39, P < 0.001)andnegative(r = 0.46, P < 0.001)sentimentfor mencomparedtowomen(r = 0.13, P < 0.28)formixedsentiment(r = 0.22, P < 0.08)fornegative;and womenwerearound11%morelikelytoreceivepositivecommentsalongsidelowerscores,andnegative ormixedcommentsalongsidehigherscores.Additionally,onaverage,menreceivedslightlymore positivecommentsinpostgraduateyear(PGY)-3thaninPGY-1andfewermixedandnegative comments,whilewomenreceivedfewerpositiveandnegativecommentsinPGY-3thanPGY-1and almostthesamenumberofmixedcomments.
Conclusion: WomenEMresidentsreceivedmoreinconsistentevaluationsthanmenEMresidentsat twolevels:1)inconsistencybetweennumericalscoresandsentimentoftextualcomments;and 2)inconsistencyintheexpectedcareertrajectoryofimprovementovertime.These findingsreveal genderinequalityinhowattendingsevaluateresidentsandsuggestthatattendingsshouldbetrainedto provideallresidentswithfeedbackthatisclear,consistent,andhelpful,regardlessofresidentgender. [WestJEmergMed.2023;24(5)847–854.]
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 847 ORIGINAL RESEARCH
INTRODUCTION
Althoughwomennowgraduatefrommedicalschoolat thesamerateasmen,1 theyremainunderrepresentedin academicmedicine.2 Thegreatestattritionofwomenfrom academicmedicineoccursdirectlyafterresidency,1 pointing totheimportanceofgenderdynamicstakingplacewithin graduatemedicaleducationtotheproductionoflong-term inequalityinmen’sandwomen’smedicalcareers.Several recentstudieshaveexaminedhowgenderbiasinresidency mayhaveconsequencesforwomen’spursuitofacademic careersandpersistenceinacademicmedicine.3–6 Medicineis amale-typed field3,7:evenaswomenareincreasingly representedamongphysicians,therearestillstrong culturalassociationsbetweenmenandtheroleofdoctor, whichcanleadtoimplicitbiasagainstwomenphysicians.8 Associationsbetweenmenanddoctoringmaybe particularlystronginemergencymedicine(EM), whichisamongthemostmale-dominated medicalspecialties.9,10
Arecentstudyfromourgroupfoundthatagendergapin AccreditationCouncilforGraduateMedicalEducation (ACGME)milestoneattainmentappearstoemergeoverthe courseofEMresidency,withattendingsscoringmale residentshigherthanfemaleresidents.5 Thisattainmentgap wasnotdependentonthegenderoftheattendingphysician doingtheevaluation,orthegenderpairingbetweenthe attendingandresident.5 Researchbuildingonthisstudyhas usedthetextualcommentsattachedtonumericalscoresto unpackhowgenderbiasmayhaveinfluencedattendings’ numericalscores.Qualitativestudiesanalyzingthetextual commentsattachedtoattendings’ numericalscoresof residentperformancehavefoundthatEMfacultygive womenresidentslessconsistentfeedback,6 feedbackthatis morefocusedonpersonalitythanclinicalcompetence,6 harshercriticism,3 andlesshelpfulandreassuringfeedback3 thantomales.
Whileourpriorworkfocusedoneithernumericalor textualevaluations,withthisstudyourgoalwastoexamine concordancebetweennumericalscoresandtextual commentstobetterunderstandgendergapsinresident evaluationsintheemergencydepartment.Doesgenderbias influencehowattendingsphysiciansassignresidents numericalscores?Greaterdiscordancebetweentextual commentsandnumericalscoresforwomenthanmen suggestgenderbiasmayshapethewayfeedbackisprovided, whichinturnmaycontributetotheestablished gendergapinevaluationsandmayharm residenteducation.
METHODS
Weconductedamixedmethodsanalysisoftextualand numericalACGMEmilestone-basedevaluationsofEM residentsbyattendingphysicians.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
AgendergapinACGMEmilestone attainmentemergesoverthecourseof EmergencyMedicine(EM)residency,such thatwomenreceivesigni fi cantlylowerscores thanmenintheir fi nalyear.
Whatwastheresearchquestion?
Doesresidentgenderin fl uencehowattending physiciansscoreresidentsonACGME milestone-basedevaluations?
Whatwasthemajor findingofthestudy?
Maleresidentsreceivedmoreevaluations wherethenumericalscoreandsentimentof thetextualcommentmatchedthanfemale residents.
Howdoesthisimprovepopulationhealth?
Thisstudyidenti fi esbiasesandgender inequalitiesinEMworkforcetraining. Arepresentativeandwell-trainedEM workforcelikelyimprovespatientcare andoutcomes.
DataCollection
Wecollectedstudydatafromfourgeographicallydiverse, three-yearACGME-accredited,EMtrainingprogramsat universityhospitalsbetweenJuly1,2013–July1,2015. Trainingprogramswereincludedinthisstudyiftheyhad adoptedInstantEvalV2.0(MonteCarloSoftwareLLC, AnnandaleVA),adirect-observationmobileappfor collectingACGMEmilestoneevaluations,andiftheyenabled facultytoleavebothnumericalandtextualevaluations.
Weanalyzedatotalof11,845evaluationsby151 attendings(94menand57women)of202residents(135men and67women)acrossallthreeyearsofresidency.Each evaluationconsistedofanumericalACGMEEmergency MedicineMilestoneProject-basedperformancelevel (1,1.5,2,2.5,3,3.5,4,4.5,or5)on1of23possibleindividual EMsubcompetencies,11 alongwithanoptionaltext comment(limitedto1,000characters).Theapplication presentedfacultymemberswithdescriptorsofindividual milestonesandthemeaningofnumericalperformancelevels astheyperformedtheevaluation.Facultyweresupposedto assessonemilestoneperevaluation.Ascoreof1wastobe assignedincaseswheretheresidentperformedattheskill levelexpectedofanincomingresident;2whentheresident
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 848
GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents Breweretal.
wasimprovingbutnotyetperformingatmid-residencylevel; 3whentheresidenthadmasteredmostoftheskillsexpected ofagraduatingresident;4whentheresidentwasperforming attheskilllevelexpectedofagraduatingresident;and5when theresidentwasperformingbeyondthelevelexpectedofa graduatingresident.11 Mostprogramsencouraged1–3 evaluationspershift,butfacultycouldchoosewhento completeevaluations,whomtoevaluate,andhowmany evaluationstocomplete.
DataAnalysis
Ouranalyticstrategycombinedcomplementary quantitativeandqualitativemethods.12 Quantitative methodsallowedustoidentifybroadpatternsincomment typeandscoresacrossourdata,whileweusedqualitative methodstoconfirmthatthemechanismssuggestedbythe quantitativemethods(ie,inconsistentevaluations)were explicitlyapparentinthecommentsreceivedbytheactual residentsinourdata.
First,alltextualcommentsfromallfourhospitalswere qualitativelycodedinNVivo12(QSTInternational, Burlington,MA),aqualitativeanalysissoftwarepackage. Fourteammembersconductedfocusedcodingofcomments forpositive(containingonlypraise),negative(containing onlycriticism),mixed(bothpositiveandnegative),orneutral (containingneitherpraisenorcriticism)toneandcontent.
Seeexamplesin Table1.Toensureconsistency,atleasttwo offourteammemberscodedeverycomment,andany discrepanciesbetweencodeswerediscussedbyallfourteam membersuntilaconsensuswasreached.Informationabout residents’ andfacultymembers’ genderwashiddenduring qualitativecodingtopreventconfirmationbias.Thisprocess wasimperfectsincesomecommentsincludedgendered pronounsornamesofresidents.Whilewetriedusing sentimentanalysistechniquestoidentifyvalence,wefound thatthestandardtechniquesdidnotcapturethetruevalence ofthewordsinourdata.Forexample, patient isconsidereda positiveword(asintheadjectiverelatedtopatience)inmost sentimentdictionaries,butitisaneutralwordinourdata
(noun patients ).Wethusfoundhand-codingthemost reliableandaccuratemethodtoidentifycommentvalence.
Inoursecond,quantitativestep,wecalculatedthetotal numberofcommentsforeachvalencetypeandtheoverall averagescoreacrossallcommentsforeachresidentinallfour hospitals.Tomeasuretherelationshipbetweencomment valenceandnumericalscore,wecorrelatedthetotalnumber ofpositive,mixed,andnegativecommentswithaverage scorebyresidentgender,reportingthePearsoncorrelation coefficientanditsassociated P -valueasanindicationofthe magnitudeandsignificanceofthecorrelation.Tomeasure commenttypeoverthecourseofresidencytraining,we countedthenumberofpositive,mixed,andnegative commentsbyresidentgenderandbytheiryearinthe programandtabulatedtheaveragecountsbyresidentgender inallfourhospitals.
Third,weconducteda finalroundofdetailedqualitative codingtoassesswhetherpatternsinthequantitativeresults werelikelytobemeaningfultoresidents.Duringthisstage, wefocusedonasinglehospitalsitechosenbecauseitwasthe largest(intermsofnumberofattendings,residents,and evaluations)ofthefoursitesinourdataset.Allexamplesof commentsinthetextcomefromthissinglesite.Threeteam memberscodedall3,120textcommentsfromthissiteas eitherconsistentorinconsistentwithnumericalscore.
Consistencywasdefinedasa fitinsentimentbetweentextual commentsandnumericalscores,eg,apositivecommentwas attachedtoahigher-than-averagenumericalscore,and inconsistencyasamisfit.Threeanalystsconductedasingle roundofcodingonPGY-3datafromtheotherthree hospitalstoensurethisonehospitalwasnotidiosyncratic andfounditwasnot.
Allnamesusedinthetextarepseudonymstoprotect confidentiality.Sincenumericalscoreshavedifferent meaningsforresidentsatdifferentstagesoftraining,we presentqualitativeexamplesofPGY-1residentsintheresults forthesakeofsimplicity.Thisstudywasapprovedasexempt researchbytheUniversityofChicagoInstitutional ReviewBoard.
CodeDefinitionExample
PositiveCommentcontainspraiseof residentandnocriticism
NegativeCommentcontainscriticismof residentandnopraise
MixedCommentcontainsbothpraise andcriticism
NeutralCommentcontainsneitherpraise andcriticism
Residentistrulyabovehisleveloftraining.Heiscompleteandthoughtfulinhis treatmentofpatientsandunderstandstheoverallgoal.Performedverywellwitha difficultintubation.
Ihopethatthisisthe firstrotationintheED,otherwiseheisclearyruningbehindhis peers.Needsalotofprompting,lacksofinitiativeandinsight,looksscared,poorfollow uponhisownpatients.Performancebelowaverage.
Gooddatagathering,butneedstoworkondiffertialdiagnosis.Also,instaeadofasking questionsneedstotakesomeresponsabilityto figurethingsout,lookthingsup.
Workedtoplaceultrasoundguidedlinesthismonth.
Table1. DefinitionsofPositive,Negative,Mixed,andNeutralCodes.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 849 Breweretal.
GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents
Note:Ourunitisresident/year.Thesenumbersincludeduplicatecountsofresidentswhowereevaluatedovermultipleyears.Therewere64 residentswhowereevaluatedinboththeir firstandsecondyearsoftheprogram,and64whowereevaluatedinboththeirsecondandthird years,foratotalof330resident/yearunitsand202uniqueresidents.
PGY,postgraduateyear.
RESULTS
Wefoundthatattendings’ assessmentsoffemaleresidents werelessconsistentthanthoseofmaleresidents.
Inconsistencyoccurredattwolevels:1)inconsistency betweennumericalscoresandtextualcomments;and
2)inconsistencyintheexpectedcareertrajectory.
1.Inconsistencybetweennumericalscoreandtextual comment
Wefoundthatforbothmenandwomenresidents,there wasapositivecorrelationbetweenaverageevaluationscore andthenumberofpositivecommentstheresidentreceived, andanegativecorrelationbetweentheaveragescoreand numberofmixedandnegativecomments.However,this
relationshipwasstrongerforcommentsofallvalencesfor men,withaPearsoncorrelationcoefficientof0.26(anda P -value < 0.04)forpositivecommentsandscoreforwomen comparedto0.38formen(<0.001), 0.22(<0.08)for negativecommentsandscoreforwomenand 0.46(<0.001) formen,and 0.13(<0.28)formixedcommentsandscore forwomencomparedto 0.39(<0.001)formen.Forwomen, thecorrelationbetweenmixedandnegativecommentsand scorewasnotstatisticallysignificant(see Figure1).
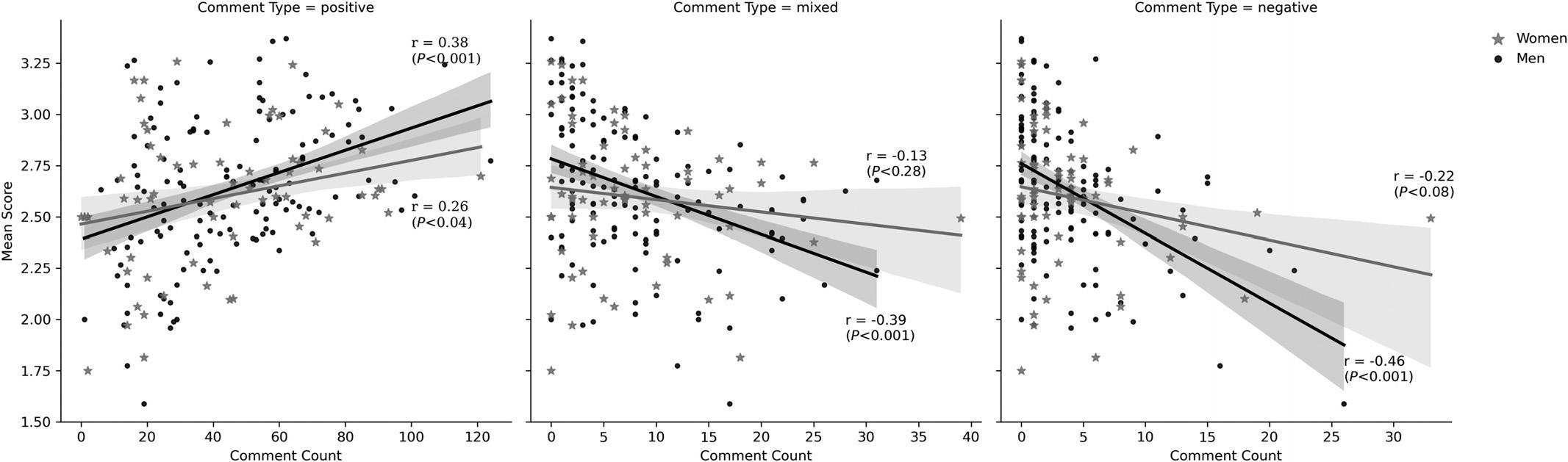
In-depthqualitativeanalysisfromonehospitalrevealed thattextualcommentsthatmatchednumericalscores providedclarityastowhatresidentsweredoingwelland wheretheyneededtoimprove.Considerthefollowing positivecommentwrittenbyattendingStevenforresident
Note: risPearsoncorrelationcoefficient(and P-value),byresidentgenderandcommenttype.Theshadedribbonsrepresentthe95% confidenceinterval.
Figure1. Scatterplotwithregressionline,correlationcoefficient(and P-value)fornumberofcommentsandmeanscore,byresidentgender andcommenttypeatfourhospitals.
PGY1PGY2PGY3 WomenMenWomenMenWomenMen 347143793370 Numberofresidents evaluatedMeanStd.Dev.MeanStd.Dev.MeanStd.Dev.MeanStd.Dev.MeanStd.Dev.MeanStd.Dev. Numberof Comments perResident 372236173521392132223419 PositiveComments perResident 291825142716311823182717 MixedCommments perResident 557555554534 NegativeComments perResident 353434231312 ScorebyResident2.30.22.30.22.70.22.70.22.90.33.00.3
Table2. Descriptivestatisticsbypostgraduateyearandresidentgenderinfourhospitals.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 850 GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents Breweretal.
Eugene: “Reallycontinuestocomealongnicely.Good followupandfollowthroughforresults,status,and disposition.” Thiscommentwasassociatedwithanumerical scoreof3.5outof5,indicatingthatSteventhoughtthat internEugenewasperformingatmid-residencylevel. Conversely,menreceivedloweraveragescoreswhenthey receivedmorenegativecommentscomparedtowomen acrossallfourhospitalsinoursample(Figure1),again indicativeofgreaterconsistencyintheirfeedbackfrom attendings.Inourqualitativeanalysisofasinglesite,the followingcommentsmadebyattendingsMichaelandGreg forresidentsZanderandSpencer,bothofwhichwere accompaniedbyanumericalscoreof1of5(thelowest possiblenumericalscore,indicatingthatresidentswerenot yetperformingatthelevelexpectedofanincomingintern), weretypicalofconsistentnegativefeedback.
• “Aswediscussedduringandaftershift,reviewingthe electronicmedicalrecordcanprovidesignificantuseful informationtoguideyourmanagement.Takeafew momentstolookfordischargesummariesorrecentED visits.” (MichaelforZander)
• “Continuetoworkonbuildingalistofdifferentialsfor eachpatient.Thiswillhelpyounotonly figureoutwhat studiesyouwanttoorderbutalsowhatquestionsyou needtoasktohelpnarrowitdown.” (GregforSpencer)
Ontheotherhand,attendingsweremoreinconsistentin howtheyassessedwomen’sperformances,assigningthema highernumberofnumericalscoresthatmismatchedtheir textualcomments.Ourqualitativeanalysisshowedthat whenitcametopositivecommentswithlowscores, attendingsoftensimultaneouslycommunicatedthatwomen weresucceedingandfailingatthesameskill.Forinstance, attendingHarrisonwroteaboutinternJosie, “Manageda patientwellwithcutsandabrasions,suturessmalllac, seemedtohavereasonableskillsforherlevel.” Whilethis commentcontainsmodestpraiseforJosie’sabilitytomanage wounds,HarrisonassignedJosieascoreof1of5forthis comment,aratingmeanttoindicatealower-than-intern skilllevel.
Thispatternwassimilarforpositivescoresassignedto negativecomments.Inonetypicalexample,attending MegangaveresidentKendallascoreof3of5,indicatingthat shewasperformingatmid-residencylevelininternyear,but criticizedherabilitytoformulateaplanforpatientcare, stating, “Seemstohesitatewithforming finalplan/dispofor patient,presentspatientknowingtheproblembutdoesn’t alwayshaveaclearplanofcareinmind.” Similarly, attendingAllisontoldresidentJade, “Needstostarttaking [the]nextstepforward. ‘I’mjustanintern’ willnotplayfor muchlonger.” Despitethiscriticism,Allisonassignedhera 3.5of5,indicatingthatherabilitieswerewellabove internlevel.
Ourdatasuggeststhat ≈11%morewomenthanmen (26of67women,and42of135men)receivedoverall “inconsistent” feedbackbetweentextualcommentsandscore, measuredbyresidentsreceivingahigher-than-average numberofcommentsbycommentvalenceandeitheralowerthan-averagescore(forpositivecomments)orahigher-thanaveragescore(formixedandnegativecomments).
2.Inconsistencyinexpectedcareertrajectory
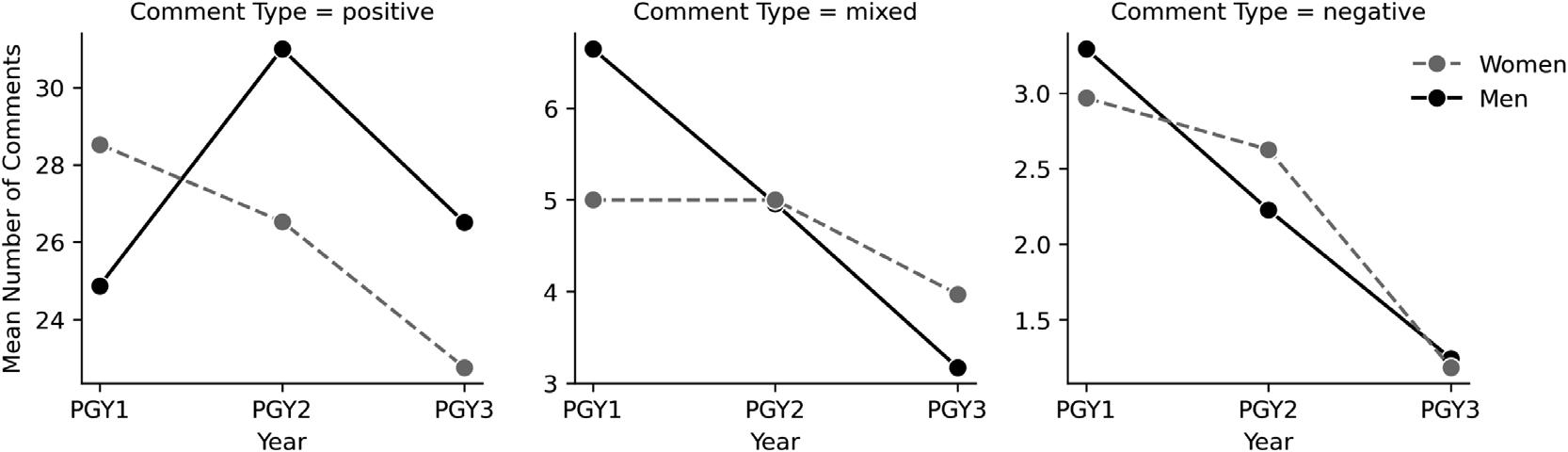
TheACGMEEMguidelinesoutlineacleartrajectory wherebyresidentsareexpectedtograduallyimproveoverthe courseofresidencythroughtheattainmentofskillsin23 subcompetencies.Theirrecommendationsforassigning numericalscorestoresidentprogressreflectthisideaoflinear progressovertime.
Ouranalysisshowsthatmenandwomenresidents’ numericalscoresareconsistentwiththisexpectedpattern. Attendingsgavebothmaleandfemaleresidentshigher numericalscoresfortheirperformanceinPGY-3(men receivedanaveragescoreof3.0andwomen2.9)thanin PGY-1(bothmenandwomenreceivedanaveragescoreof 2.3). Figure2 visualizesthedifferentpatternsintextual sentimentformenandwomenresidentsfromPGY-1to PGY-3.Maleresidentsreceivedmorenegativeandmixed commentsinPGY-1(anaverageofthreenegativecomments andsevenmixedcomments)thaninPGY-3(onenegative andthreemixed),whentheyreceivedalargerportionof positivecomments.(Menreceivedanaverageof25positive
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 851
Figure2. Meannumberofcommentsbyresidentgender,postgraduateyear,andcommenttypeatfourhospitals. PGY,postgraduateyear.
Breweretal. GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents
commentsinPGY-1and27inPGY-3.)Althoughmale residentsappeartobeassessedmoreharshlythantheir femalepeersinPGY-1inthattheyreceivemorenegativeand mixedcomments,theirtrajectoryovertimeisconsistentwith expectationsofimprovementasoneadvancesthrough residency.Femaleresidents,ontheotherhand,received morepositivecommentsinPGY-1andfewerinPGY-3(an averageof29positivecommentsinPGY-1and23inPGY-3) whiletheyreceivedalmostthesamenumberofmixed commentsonaverageinPGY-1andPGY-3(fivecompared tofour).Bothmenandwomenreceivedfewernegative commentsinPGY-3(onecomparedtothreeinPGY-1), althoughthenumberofnegativecommentsoverall islow.
DISCUSSION
Ourgoalforthisstudywastoexaminetherelationship betweennumericalandtextualperformanceevaluationsfor EMresidentstoshedlightonthe findingsofaprior quantitativestudy5 thatdemonstratedagendergapin milestoneattainmentduringEMresidency.Todothis,we usedcomplementaryquantitativeandqualitativemethodsto analyze11,845numericalandtextualevaluationsmadeby 151attendingphysiciansduringreal-timedirectobservations of202residents.Weidentifiedtwoformsofinconsistency betweennumericalscoresandtextualperformance evaluationsthatmayhaverelevancetowomen’slagging numericalscoresonACGMEmilestonesandtogender inequalityinresidency.
First,thedatarevealedthatwomen’snumericalscores werelessconsistentwiththesentimentoftheirtextual commentsthanthoseofmen.Womenresidentsinoursample weremorelikelytoreceivepositivecommentsalongside lowerscores,andnegativeormixedcommentsalongside higherscores.Second,thedatashowedthattextual commentsforwomen,butnotmen,wereinconsistentwith theexpectedEMcareertrajectoryofimprovementovertime. Onaverage,menreceivedslightlymorepositivecommentsin PGY-3thaninPGY-1andfewermixedandnegative comments,whilewomenreceivedfewerpositiveandnegative commentsinPGY-3thanPGY-1andalmostthesame numberofmixedcomments.
Inconsistentperformanceevaluationsareworthyof attentionforseveralreasons.First,inconsistentevaluations mayharmwomenresidents’ developmentasphysicians. Criticalfeedback,whenconstructive,canbeasourceof valuableadviceforimprovingone’sperformance.13,14 Our qualitative findingsdemonstratethatconsistencybetween numericalscoreandtextualcommentcanofferuseful informationtoresidentsbyprovidingaclearexplanationof whytheyearnedaparticularscoreand,onoccasion, actionablefeedbackabouthowtoimproveinthefuture. Inconsistentfeedbackcouldbeabarriertolearningfrom
errorsandtodevelopingskillsasaphysician,especiallyinthe earlierstagesofresidency,andcouldultimatelycontributeto thegendergapinACGMEmilestoneattainmentthat emergesoverthecourseofresidency.5
Additionally,inconsistentevaluationsmayharmwomen’ s confidenceintheirabilityasphysiciansand/ortheir commitmenttoacademicmedicine.Severalstudiessuggest thatwomeninmedicinesufferfromimpostersyndrome,the psychologicalphenomenonwherebypeopledoubttheir abilitieseveninthefaceofevidenceoftheirownsuccess.15,16 Inconsistentfeedbackcouldbeafactorthatcontributesto genderdisparitiesinfeelingsofimpostersyndromeduring residency:Ifwomenencountermorepraisethatiscombined withcriticism,thiscouldfosterdoubtintheirabilitiesas physicians.Further,priorresearchfromthesocialsciences showsthatconfidenceinone’sskillsiscriticalforthe persistenceofwomeninmale-typedprofessionslikeEM.17,18 Inconsistentfeedbackcouldbesomethingthatcontributes towomen’sattritionfromacademicEM,whichoccursata higherratethanthatofmen.19 Thefactthatwomeninour samplereceivedfewerpositivetextualcommentsasthey progressedfromPGY-1toPGY-3mayalsobe somethingthatharmstheirconfidenceandthatcould haveabroaderimpactontheircareers.Computational simulationshavesuggestedthatevenverysmallbiasesin everydayinteractions,suchasthosewe findhere,can compoundincomplexsystemstoproducemuchlarger patternsofinequalityinorganizations.20 Furtherstudyis warrantedtoexaminetheconnectionbetweeninconsistent evaluationsandattritionfrommedicalcareers,whether throughimpostersyndromeoranothermechanism.
Thisstudyprovidesfurthersupportfortheideathat genderbiascontributestothegendergapinevaluationsby showingthatattendingphysiciansevaluateresidents differentlybasedongender,withabiasinfavorofmen,even inthecontextofobjectivecriteriasuchastheACGME milestones.Basedonthese findings,wecautionagainstthe useofcompetency-basedgraduationfromresidency,even whenprogramsrelyonclearlyarticulatedstandardssuchas theACGMEmilestones.Movementtocompetency-based graduationwouldlikelydisadvantagewomenresidentsand deepeninequalitiesinthemedicalprofession.
LIMITATIONS
Therearelimitationstoourstudy.First,wedidnothave informationaboutthebroadercontextinwhichevaluations werewritten,includingconversationsthatmayhavetaken placebetweenattendingsandresidentsthatcouldhave providedadditionalinformationexplainingnumericalscores and/ortextualfeedback.Second,wedidnothavedataabout theraceorethnicityofthephysiciansinoursample,which maybeapertinentcovariategivenevidenceofbiasagainst peopleofcolorinthemedicalprofession.21
Third,sinceour datawascollectedin2013-15,itispossiblethatgender
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 852 GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents Breweretal.
GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents
dynamicsinresidencyprogramsmayhavechangedinthe interveningyears,especiallyasresidencyprogramshave investedinreducingbiasesintraining.Fourth,whilewetook severalstepstoguardagainstgenderbiasinourcoding procedures – includingusingmultiplecoders,requiring codingconsensus,andsuppressingattendingandresident gender
wedidnotsuppressallgenderedlanguageinthe textualcomments.Thismayhavebiasedouranalysis.Fifth, sinceweonlyanalyzedatafromfouruniversityhospitals,our findingsmaynotbenationallyrepresentativeofEMtraining programsintheUS.
Ourstudyalsohasseveralstrengths.First,facultydidnot knowthattheirevaluationswouldbeanalyzedforgenderbias, diminishingaHawthorneeffectorsocialdesirabilitybias,and givingusawindowintorealconditionsofgenderinequalityin medicaleducation.Second,drawingondatafromfour universityhospitalsacrosstheUSallowedustobemore confidentthattheinequalitieswefoundwerenotspecificto onehospitalenvironment,butrathermaybegeneralizable acrossdifferentorganizationalenvironments.
Futureresearchisneededtoexaminethefullscopeof inconsistentfeedbackingraduatemedicaleducation, includingcommentarygiventoresidentsinperson,aswellas theconsequencesofinconsistentfeedbackforphysicians’ careers,includingattritionfrommedicineandfeelingsof burnoutandimpostersyndrome.
CONCLUSION
Bypairingquantitativeandqualitativemethods,this studycontributestoresearchongenderinequalityin graduatemedicaleducationbyshowingmultiplelevelsat whichwomenreceiveinconsistentfeedbackinresidency. Initiativestoreducegenderinequalityinmedicineshould trainfacultytoofferallresidentsclear,consistent,and helpfulassessmentsoftheirperformance,regardlessof residentgender.
AddressforCorrespondence:AlexandraBrewer,MA,PhD, UniversityofSouthernCalifornia,DepartmentofSociology, 851DowneyWay,LosAngeles,California90089.
Email: breweral@usc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisprojectwassupportedbythe NationalCenterforAdvancingTranslationalSciencesoftheNational InstitutesofHealththroughGrantNumberUL1TR000430. AdditionalfundingwasprovidedbyaUniversityofChicagoDiversity SmallGrant(awardedtoVineetArora)andaUniversityofChicago GianinnoFacultyResearchAward(awardedtoAnnaS.Mueller).
Copyright:©2023Breweretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons
Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.LautenbergerDM,DandarVM,RaezerCL,etal.Thestateofwomenin academicmedicine:thepipelineandpathwaystoleadership, 2013–2014.Availableat: https://members.aamc.org/eweb/upload/The %20State%20of%20Women%20in%20Academic%20Medicine% 202013-2014%20FINAL.pdf.AccessedDecember7,2020.
2.FreundKM,RajA,KaplanSE,etal.Inequitiesinacademic compensationbygender:afollow-uptothenationalfacultysurvey cohortstudy. AcadMed.2016;91(8):1068–73.
3.BrewerAE,OsborneM,MuellerAS,etal.Whogetsthebenefitofthe doubt?Performanceevaluations,medicalerrors,andtheproductionof genderinequalityinemergencymedicaleducation. AmSocRev 2020;85(2):247–70.
4.EdmundsLD,OvseikoPV,ShepperdS,etal.Whydowomenchooseor rejectcareersinacademicmedicine?Anarrativereviewofempirical evidence. Lancet.2016;388(10062):2948–58.
5.DayalA,O’ConnorDM,QadriU,etal.Comparisonofmalevsfemale residentmilestoneevaluationsbyfacultyduringemergencymedicine residencytraining. JAMAInternMed.2017;177(5):651–7.
6.MuellerAS,JenkinsTM,OsborneM,etal.Genderdifferencesin attendingphysicians’ feedbacktoresidents:aqualitativeanalysis. JGradMedEduc.2017;9(5):577–85.
7.ReskinB.Sexsegregationintheworkplace. AnnRevSoc. 1993;19:241–70.
8.CookeM.Implicitbiasinacademicmedicine:#WhatADoctorLooksLike. JAMAInternMed.2017;177(5):657–8.
9.BennettCL,RajaAS,KapoormN,etal.Genderdifferencesinfaculty amongacademicemergencyphysiciansintheUnitedStates.2019. AcadEmergMed. 26(3):281–5.
10.DeFazioCR,CloudSD,VerniCM,etal.Womeninemergencymedicine residencyprograms:ananalysisofdatafromAccreditationCouncilfor GraduateMedicalEducation-approvedresidencyprograms. AEMEduc Train.2017;1(3):175–8.
11.AccreditationCouncilforGraduateMedicalEducationand AmericanBoardofEmergencyMedicine(ACGMEand ABEM).2015.Theemergencymedicinemilestoneproject.” Availableat: https://www.acgme.org/Portals/0/PDFs/Milestones/ EmergencyMedicineMilestonespdf.AccessedJanuary25,2018.
12.SmallMS,PamphileVD,McMahanP.Howstableisthecorediscussion network? SocNetworks 2015;40:90–102.
13.CorrellS,SimardC.Research:vaguefeedbackisholdingwomenback. HarvBusRev. April29,2016.Availableat: https://hbr.org/2016/04/ research-vague-feedback-is-holding-women-back AccessedDecember7,2020.
14.KingEB,BotsfordW,HeblMR,etal.Benevolentsexismatworkgender differencesinthedistributionofchallengingdevelopmental experiences. JManag.2012;38:1835–66.
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 853 Breweretal.
15.MullangiS,JagsiR.Impostersyndrome:treatthecause,notthe symptom. JAMA.2019;322(5):403–4.
16.ButkusR,SerchenJ,MoyerDV,etal.Achievinggenderequityin physiciancompensationandcareeradvancement:apositionpaperof theAmericanCollegeofPhysicians. AnnInternMed 2018;168(10):721–36.
16.HansenM,SchoonoverA.,SkaricaB,etal.Implicitgenderbiasamong USresidentphysicians. BMCMedEduc 2019;19(1):396.
17.CechE,RubineauB,SilbeyS,SeronC.Professionalroleconfidence andgenderedpersistenceinengineering. AmSocRev 2011;76(5):641–66.
18.CorrellS.Genderandthecareerchoiceprocess:theroleofbiasedselfassessment. AmJSoc.2001;106(6):1691–730.
19.LuDW,HartmanND,DruckJ,etal.Whyresidentsquit: nationalratesofandreasonsforattritionamongemergency medicinephysiciansintraining. WestJEmergMed 2022;20(2):351–6.
20.DuY,NordellJ,JosephK.Insidiousnonetheless:howsmalleffectsand hierarchicalnormscreateandmaintaingenderdisparitiesin organizations. Socius.2022;8.
21.FeaginJR,BennefieldZ.SystemicracismandU.S.healthcare. SocSci Med 2014;103(1):7–14.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 854 GenderandInconsistentEvaluations:AnAnalysisofFeedbackforEMResidents Breweretal.
COVID-lateralDamage:ImpactofthePost-COVID-19Era onProceduralTraininginEmergencyMedicineResidency
DanielFrank,MD* ThomasPerera,MD† MosheWeizberg,MD
*ZuckerHofstraSchoolofMedicine,NorthwellHealth,SouthShoreUniversityHospital, BayShore,NewYork
† ZuckerHofstraSchoolofMedicine,NorthwellHealth,NorthShore/LIJ, Manhasset,NewYork
‡ ZuckerHofstraSchoolofMedicine,NorthwellHealth,StatenIslandUniversityHospital, StatenIsland,NewYork
§ MaimonidesMedicalCenter/MaimonidesMidwoodCommunityHospital, Brooklyn,NewYork
SectionEditors: JeffreyDruck,MD,andWendyMacias-Konstantopoulos,MD,MPH,MBA
Submissionhistory:SubmittedDecember29,2022;RevisionreceivedMay19,2023;AcceptedJuly3,2023
ElectronicallypublishedSeptember1,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59771
Introduction: Hospitalizationsduringthecoronavirus2019(COVID-19)pandemicpeakedinNewYork inMarch–April2020.Inthemonthsfollowing,emergencydepartment(ED)volumesdeclined.Our objectiveinthisstudywastoexaminetheeffectofthisdeclineontheproceduralexperienceof emergencymedicine(EM)residentscomparedtothepre-pandemicperiod.
Methods: Weconductedthismulticenter,retrospectivecohortstudyofpatientsseenandkey proceduresperformedbyEMresidentsathospitalsspanningthreeAccreditationCommitteefor GraduateMedicalEducation-approvedEMresidenciesinNewYorkCityandNassauCounty,NY.We obtainednumbersofproceduresperformedduringMay–July2020andcomparedthemtothesametime periodfor2019and2018.Weaprioriclassifiedcriticalcareprocedures cardioversion,centrallines, chesttubes,proceduralsedation,andendotrachealintubation.Wealsostudied “fast-track” procedures fracture/jointreduction,incisionanddrainage(I&D),lacerationrepairs,andsplints.
Results: TotalnumberofcriticalcareproceduresinthemonthsfollowingtheCOVID-19peakdecreased from694to606( 12.7%,95%confidenceinterval[CI]10.3–15.4%),comparedtoanincreasefrom642 to694(+8.1%,95%CI6.1–10.5%)thepreviousyear(difference 9.3%).Totalnumberoffast-track proceduresdecreasedfrom5,253to3,369( 35.9%,95%CI34.6–37.2%),comparedtoadecreasefrom 5,333to5,253( 1.5%,95%CI1.2–1.9%)theyearbefore(difference 36.3%).Specificcriticalcare proceduresperformedin2020comparedtothemeanof2019and2018asfollows:cardioversion 33.3%;centrallines +19.0%;chesttubes 27.9%;proceduralsedation 30.8%;endotracheal intubation 13.8%.Specificfast-trackprocedures:reductions +33.3%;I&D 48.6%;lacerationrepair 17.3%;andsplintapplication 49.8%.
Conclusion: Emergencymedicineresidents’ criticalandfast-trackproceduralexperienceat five hospitalswasreducedduringthemonthsfollowingtheCOVID-19peakincomparisontoasimilarperiod inthetwoyearsprior.Trainingprogramsmayconsiderincreasingsimulation-labandcadaver-lab experiences,aswellasEDandcriticalcarerotationsfortheirresidentstooffsetthistrend.[WestJEmerg Med.2023;24(5)855–860.]
‡§
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 855 ORIGINAL RESEARCH
INTRODUCTION
Graduatemedicaleducation(GME)ofresidentsand fellowshasbeendramaticallyaffectedworldwidebecauseof thecoronavirus2019(COVID-19)pandemic.Similar influencesonGMEhavebeendescribedduringprevious epidemics,naturaldisasters,andeveninzonesofwarand conflict,althoughperhapsonadifferentscale.1–6 Duringthe severeacuterespiratorysyndrome(SARS)epidemicof2003, manyeducationalactivitiesweresacrificed,andoutside clinicalrotationsweredelayedduetofearofinter-site contaminationwhenresidentschangedservices.1,5 The ongoingconflictinIraqhasledtoasignificantimpairmentin qualityofeducation,andthemajorityoftraineesfelttheir safetytobeatrisk.3 Themajorityoftraineesalsoreported theirintenttoleaveIraqaftergraduation,furthercrippling thecriticalhealthcaresafetynetsomanycitizensrelyon.3
WhenHurricaneKatrinastruckLouisianaand Mississippiin2005,hundredsofresidentsandfellowshad theireducationdisrupted.TheAccreditationCouncilfor GraduateMedicalEducation(ACGME)respondedby quicklyassistinginplacingthesetrainees,eithertemporarily orpermanently,inotherprogramsthatcouldmeettheir educationalneeds.Theresultingpoliciesprovidedthe frameworkforinstitutionstorespondtotheneedsoftheir GMEprogramsduringHurricanesIkein2008andHarvey in2017.4,6
EarlyliteratureoneffectsonGMEoftheCOVID-19 pandemicfocusedonprocedure-basedspecialties,suchas surgery,urology,interventionalradiology,interventional cardiology,ophthalmology,andurology.7–11 Cancellationof electiveproceduresandredeploymentofresidentsand fellowscreatedadramaticreductionincasesneededfor adequatetraining.Surgicalprogramsespeciallyreported decreasedclinicalexperience,reducedcasevolume,and disruptededucationactivitiesasmajorconcerns.12 Additionally,theACGMEallowedinstitutionstoapplyfor “emergencystatus.” Thiseasedsomeofthemandatory trainingrequirementsthatwerenormallyinplace.To mitigatethisproblem,theAmericanBoardofSurgery announcedtheywouldaccepta10%reductioninoperative casesfromgraduatingresidents,whileotherspecialties suggestedtrainingmighthavetobeextendedtoensure adequatetraining,especiallyinaprolonged epidemicscenario.10,13,14
Emergencymedicine(EM)traineesweresimilarlyaffected bytheoveralldecreaseinpatientvolumesthatmany emergencydepartments(ED)experiencedthroughoutthe pandemic.Decreasedcasevariety,fewerprocedures,and fewerpatientswithseriousdiagnosesallnegativelyimpacted residenttrainingduringtheearlypandemicperiod.15,16
Throughouttheworld,GMEprogramsquickly respondedwithinnovationandutilizationofonline resourcesduringthepandemictominimizedisruptionsin residenteducation.Mostdidactics,journalclubs,andcase
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
TheCOVID-19pandemichaddramatic effectsongraduatemedicaleducationfor procedure-basedspecialtiessuchassurgery andinterventionalcardiology.
Whatwastheresearchquestion?
Whateffectdidthepost-COVID-19peak periodhaveontheproceduralexperiencein EMresidencytraining?
Whatwasthemajor findingofthestudy? Indexproceduresdecreased33.2%,critical careprocedures12.7%(10.3 – 15.4%); andfast-trackprocedures35.9% (34.6% – 37.2%).
Howdoesthisimprovepopulationhealth?
KnowingtheimpactofCOVID-19onEM proceduretrainingmayspurprograms toaugmentresidenteducationimpacted byinterruptions.
reviewsmovedonline,andlargeconferencesbecamevirtual. Manyoutpatientencountersweretakingplacevia telemedicineplatforms.Somesurgicalprogramsevenstarted workingwithsimulatorsbuiltinhouse,whileothers developedvirtualrealitytechnologyinanefforttomaintain technicalskills.8,9,11,14,17,18
Emergencymedicinetrainingprogramssimilarly confrontedchallengesinresidenteducationsincetheonset ofthepandemic.Allresidenttrainingdependsinlargepart onpatientencounterstogainexperienceanddevelop clinicalacumenandtechnicalskill.Traditionally, postgraduateyear(PGY)-1EMresidentswouldaverage0.7 patientencountersperhour,whilePGY-3residentscould see1.3patientsperhour.19 Thepandemic,however,caused adramaticreductioninEDpatientvolumes,especially amongpediatricpatients. 20 Duringtheearlypandemic period,EDvisitsintheUnitedStateswere42%lowerthan thesameperiodayearearlier,withthelargestproportional declineinpatients14yearsoryounger.21 Asaresultofthe pandemic,EMresidents’ criticalproceduralexperiences alsodecreased. 22 Moreovertherewasasigni ficantdeclinein allnon-COVID-19relatedpatientpresentations,with signi fi cantlylessresidentexposuretocardiac,psychiatric, surgical,andneurosurgicalcases. 23
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 856 ImpactofthePost-COVID-19EraonProceduralTraininginEMResidency Franketal.
HospitalizationsforCOVID-19peakedinNewYorkCity inMarchandApril2020.Inthemonthsfollowing,ED volumesdeclined.Ourobjectivewastostudytheeffectofthis declineontheproceduralexperienceofEMresidents comparedtothepre-pandemicperiod.Througha multicenterstudy,wesoughttodescribethevolume,types, andacuityofcasesseenbyEMresidentsduringthemonths followingtheCOVID-19peakwithinthreeseparateEM trainingprogramsinNewYorkCityandNassauCounty. Suchinformationcaninformdecisionsonhowbestto augmentresidenteducationandmaintainqualityoftraining duringprograminterruptionsandtimesofreducedpatient volume,clinicalexposure,andproceduralexperience.
METHODS
StudyDesign
Thiswasamulticenter,retrospectivecohortstudyofthe numberofpatientsseenandnumberofprocedures performedbyEMresidentsduringthemonthsfollowingthe COVID-19peak.Wecomparedthesenumberstothesame periodinthetwopreviousyears.Thestudywasreviewedby theinstitutionalreviewboardandwasdeemedtobenot humansubjectsresearch.
StudySettingandPopulation
Thiswasamulticenterstudyat fivehospitalsspanningtwo ACGME-approvedEMresidenciesandonecombined EM-IMresidencyinNewYorkCityandNassauCounty. Thehospitalsincludethreetertiarycarecenters,one communityhospital,andonechildren’shospital.Priorto COVID-19,thefouradultEDsrangedinpatientvolume from33,000to102,000patientsperyear,andthepediatric EDhadavolumeof60,000patientsperyear.Theresidency programsincludetwoEMprogramsinthePGY1–3format, aswellasonecombinedEM-internalmedicine(IM) program.Thenumberofresidentsateachprogramare30 and68fortheEMprogramsand10fortheEM-IMprogram.
OurstudytookplacefromMay–July2020.Thesedates werechosenbecausetheyrepresentedtheinitialperiod followingthemajor firstwaveofCOVID-19patientsin NewYork.Asacomparisongroup,wecollecteddatafrom thesamemonthsintheprecedingtwoyears.
StudyProtocol
Weperformedanelectronicdataquerytoextractdata fromourhealthsystem’selectronichealthrecord(EHR).We usedstandardrecordreviewpractices.24 Variablesobtained fromtheelectronicdataqueryincludedpatient demographics,disposition,authorshipofphysiciannote, diagnosis,andchiefcomplaint.Deidentifieddatawerestored inanExcelspreadsheet(MicrosoftCorp,Redmond,WA)on asecureserver.Wereviewedthetotalnumberofpatients seenbyEMresidentsduringthestudyperiod,aswellasthe admissionpercentage.Weidentifiedpatientsseenby
residentsbasedontheauthorshipofthephysiciannote.This wastoensureeachrecordwouldonlybecountedonce.We omittedpatientsseenbyphysicianassistants,nurse practitioners,orbyattendingsprimarily.
WereviewedourEHRbillingdataforthenumberof predeterminedproceduresperformedbyEMresidents duringthisperiod.Billingdatawascapturedfromprocedure noteswrittenbythephysicians.Westudiedcriticalcare procedures,specificallyelectricalcardioversion,centrallines, chesttubes,proceduralsedation,andendotracheal intubation.Thesearekeyproceduresrequiredbythe ResidencyReviewCommitteeinEmergencyMedicine (RRC-EM).Wealsostudied “fast-track” procedures, includingfracture/jointreduction,incisionanddrainage (I&D),lacerationrepairs,andsplints.Wecomparedthe numbersofprocedureperformedtothesameperiodinthe previoustwoyears.
MeasurementsorKeyOutcomeMeasures
Numbersofpatientsseenandproceduresperformedinthe monthsfollowingtheCOVID-19peakwerecomparedtothe numbersduringthesameperiodfor2019and2018.The primaryoutcomewasthechangeinthetotalnumberofindex proceduresduringthemonthsfollowingtheCOVID-19peak ascomparedtothemeanofthetwopreviousyears. Secondaryoutcomesincludedtotalnumberofpatients seen,andchangesinthenumberofcriticalcareand fast-trackprocedures.
DataAnalysis
WecalculatedstatisticsusingSASstatisticalsoftware (SASInstituteInc,CaryNC).Percentageofadmissionswas comparedusingchi-squaretests.
RESULTS
Totalnumberofpatientsseenbyresidentsduringthe monthsfollowingtheCOVID-19peakwas33,246, comparedto49,316in2019( 32.6%)and49,748in2018 ( 0.9%)(Table1).Admissionpercentagewas32.0%inthe monthsfollowingtheCOVID-19peakcomparedto28.5%in 2019and28.5%in2018.
Thetotalnumberofindexproceduresdecreasedfrom 5,947in2019to3,975in2020( 33.2%);comparedto virtuallynochangethepreviousyear(5,975to5,947). Totalcriticalcareproceduresinthemonthsfollowingthe
202020192018 P-value Total#ofpatientsseen byresidents 33,24649,31649,748 <0.001 Admissionpercentage32.0%28.5%28.5% <0.001 Volume24,No.5:September2023WesternJournal of EmergencyMedicine 857 Franketal. ImpactofthePost-COVID-19EraonProceduralTraininginEMResidency
Table1. ComparisonofpatientvolumefortheCOVID-19study periodandthecontrolperiod.
COVID-19peakdecreasedfrom694in2019to606in 2020( 12.7%,95%confidenceinterval[CI]10.3–15.4%), comparedtoanincreasefrom642to694(+8.1%,95%CI 6.1–10.5%)thepreviousyear(difference 9.3%).Totalfasttrackproceduresdecreasedfrom5,253in2019to3,369in 2020( 35.9%,95%CI34.6–37.2%),comparedtoadecrease from5,333to5,253( 1.5%,95%CI1.2–1.9%)theyear before(difference 36.3%)(Table2).
Thedatafortheindividualcriticalcareandfast-track proceduresarepresentedin Table3 and Table4.Duringthe studyperiod,therewasanotabledecreaseinthecriticalcare proceduresofcardioversion,chesttube,proceduralsedation, andendotrachealintubation.Theonlycriticalcare procedurethatdemonstratedanincreasewascentralline
placement.Therewasalsoadecreasenotedinfast-track proceduresofI&D,lacerationrepair,andsplintapplication. Theonlyfast-trackprocedurethatdemonstratedanincrease wasorthopedicreductions.
DISCUSSION
March–April2020representedthepeakofCOVID-19 casesinthe firstwaveintheNewYorkmetropolitanarea. DuringthistimeEDswere floodedwithextremelysick patients.ResidentsinEMwereoftenmanagingmultiple criticalpatientssimultaneously.Theywerealsoexposedto large-scaledeath,likelyforthe firsttimeintheircareers. Residentswereperforminglargenumbersofintubationsand medicalresuscitations.Thishadadramaticimpacton theirtraining.
Theimmediatepost-COVID-19era,however,sawa dramaticdeclineinEDvolume.Thiswaslikely multifactorial,withpatientsafraidtocometoEDsoutoffear ofcontractingCOVID-19,aswellastheiradherencetostayat-homeorders.ThisalsohadaneffectonEMresidency training.OurstudyfoundthatnumbersofEDpatientsseen byresidentsdecreasedby32.6%.Atthesametime,admission percentageincreasedby3.5%,suggestingthatloweracuity patientswerenotcomingtotheED.Thenumbersofboth criticalcareproceduresandfast-trackproceduresdecreased duringthisperiodascomparedtothepreviousyear.The mostdramaticchangeswerenotedinfast-trackprocedures, withnotabledecreasesinI&D,lacerationrepair,and splintapplication.
These findingscanhaveasignificantimpactonresident education.Ifthistrendcontinues,wemayseeresidents graduatingfromtrainingwithsignificantlylessprocedural experience,especiallyintherealmoffast-trackprocedures. Ourstudycaninformdecisionsonhowbesttoaugment residenteducationandmaintainqualityoftrainingduring programinterruptionsandtimesofreducedpatientvolume, clinicalexposure,andproceduralexperience.
Theseresultsarelikelymultifactorial.Intheimmediate post-COVID-19era,manypeoplewereafraidtocometothe hospitalduetoafearofcontractingthedisease.Alternative locationsforcarebecameavailableincludingtelemedicine andurgentcarecenters.Finally,patientsmayhavechosen nottoseekcareatall.
Residencyprogramsareencouragedtolookatthe numbersofproceduresthattheirresidentsareperforming, especiallyfast-tracktypeprocedures.Astheseprocedure numbersarenotrequiredtobereportedtotheACGME, thereisapossibilitythatresidencyprogramswillnotbe awareoftheindividualnumbersintheirownprogramsifnot specificallyexamined.Programsthat findtheirresidentshave adeficiencyinthenumberoffast-trackproceduresmaywish tosupplementtheirexperiencewithproceduraltrainingin thesimulationlaborcadaverlab.
202020192018 Difference2020from meanof2018/2019 Totalcritical careprocedures 606694642 9.3% Totalfast-track procedures 3,3695,2535,333 36.3% Total procedures 3,9755,9475,975 33.3%
Table2. Comparisonoftotalproceduresforthestudyperiodand thecontrolperiod.
Procedure202020192018 Difference2020from meanof2018/2019 Cardioversion71110 33.3% Centralline244212198 +19.0% Chesttube222734 27.9% Procedural sedation 126190174 30.8% Endotracheal intubation 207254226 13.8%
Table3. Comparisonofcriticalcareproceduresforthestudyperiod andthecontrolperiod.
Procedure202020192018 Difference2020from meanof2018/2019 Reductions363222 +33.3% Incisionand drainage 284551553 48.6% Laceration repair 1,7392,0902,115 17.3% Splint application 1,3102,5802,643 49.8% WesternJournal of EmergencyMedicineVolume24,No.5:September2023 858 ImpactofthePost-COVID-19EraonProceduralTraininginEMResidency Franketal.
Table4. Comparisonoffast-trackproceduresforthestudyperiod andthecontrolperiod.
LIMITATIONS
Thestudyhasseverallimitations,First,ittookplacein oneregionofthecountry,namelyNewYork.These findings maynotbegeneralizabletotherestoftheUS.However,we didstudythreedifferentprogramsat fivedifferenthospitals spanningfourdifferentcountiesinthearea.Second,thiswas aretrospectivecohortstudyand,therefore,ourdatais somewhatlimited.Itispossiblethatifthedatawouldhave beencollectedprospectively,wewouldhavehadamore completeandmoreaccuratedataset.
Ourresultswereobtainedfrombillingdata,whichis capturedfromprocedurenoteswrittenbythephysicians.Itis possiblethatsomeprocedureswereperformedwithouta procedurenotebeingwritten.Inthatscenario,theprocedure wouldnothavebeencapturedinourdataset.However,our billerscarefullyreviewallchartsandencouragephysiciansto completeallprocedurenotesiftheyhavenotbeen completed.Inaddition,thesamemethodsforcollecting proceduredatawereusedinboththestudypopulationand thecontrolpopulation.
Additionally,weonlylookedatdataforthreemonths.Itis possiblethatwhatweobservedwasatemporaryphenomenon andasvolumesinEDsbegantoreturn,proceduralavailability hasimprovedaswell.Finally,wedidnotlookatprocedure numbersduringtheactualCOVID-19peak.Itispossiblethat theincreaseincriticalcareproceduresduringthisperiodoffset thedecreasewesawinthestudyperiod.However,thiswould notaccountforthedecreaseinfast-trackprocedures,which essentiallywentawayduringtheCOVID-19peak.
CONCLUSION
Thepost-COVID-19eraresultedinlowerpatientvolume andlessavailabilityofcertainproceduresforEMresidentsin NewYorkCityandNassauCounty.Thisphenomenon shouldbewatchedcloselytodeterminewhethertrends appear.Ifso,interventionsmayneedtobeinstitutedto supplementresidenttraining.
AddressforCorrespondence:MosheWeizberg,MD,Maimonides MidwoodCommunityHospital,DepartmentofEmergencyMedicine, 2525KingsHighway,Brooklyn,NewYork11229.Email: mweizberg@maimonidesmed.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Franketal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.PepeD,MartinelloRA,Juthani-MehtaM.Involvingphysicians-intraininginthecareofpatientsduringepidemics. JGradMedEduc 2019;11(6):632–4.
2.MuyaI,GarsideJ,Van-derPlasM,etal.Emergencyhealtheducationin aconflictstrickenenvironment:asituationalanalysis. AfrJEmergMed 2018;8(4):129–33.
3.Barnett-VanesA,HassounahS,ShawkiM,etal.Impactofconflicton medicaleducation:across-sectionalsurveyofstudentsandinstitutions inIraq. BMJOpen.2016;6(2):e010460.
4.NewmanB,GallionC.HurricaneHarvey: firsthandperspectivesfor disasterpreparednessingraduatemedicaleducation. AcadMed 2019;94(9):1267–9.
5.SherbinoJ,AtzemaC. “SARS-Ed”:severeacuterespiratory syndromeandtheimpactonmedicaleducation. AnnEmergMed 2004;44(3):229–31.
6.Donini-LenhoffFG,RockeyPH,SurdykPM,etal.Emergency preparednessforresidency/fellowshipprograms:lessonslearned duringHurricaneKatrinaandappliedduringHurricaneIke. DisasterMed PublicHealthPrep.2010;4Suppl1:S71–4.
7.MishraD,NairAG,GandhiRA,etal.TheimpactofCOVID-19related lockdownonophthalmologytrainingprogramsinIndia outcomesofa survey. IndianJOphthalmol.2020;68(6):999–1004.
8.PorpigliaF,CheccucciE,AmparoreD,etal.Slowdownofurology residents’ learningcurveduringtheCOVID-19emergency. BJUInt 2020;125(6):E15–7.
9.GabrAM,LiN,SchenningRC,etal.Diagnosticandinterventional radiologycasevolumeandeducationintheageofpandemics: impactanalysisandpotentialfuturedirections. AcadRadiol 2020;27(10):1481–8.
10.GuptaT,NazifTM,VahlTP,etal.ImpactoftheCOVID-19pandemicon interventionalcardiologyfellowshiptrainingintheNewYork metropolitanarea:aperspectivefromtheUnitedStatesepicenter. CatheterCardiovascInterv.2021;97(2):201–5.
11.SchwarzkopfR,MaherNA,SloverJD,etal.theresponseofan orthopedicdepartmentandspecialtyhospitalattheepicenterofa pandemic:theNYULangonehealthexperience. JArthroplasty 2020;35(7S):S3–5.
12.ChenSY,LoHY,HungSK.WhatistheimpactoftheCOVID-19 pandemiconresidencytraining:asystematicreviewandanalysis. BMC MedEduc.2021;21(1):618.
13.FongZV,QadanM,McKinneyR,etal.Practicalimplicationsofnovel coronavirusCOVID-19onhospitaloperations,boardcertification, andmedicaleducationinsurgeryintheUSA. JGastrointestSurg. 2020;24(6):1232–6.
14.JamesHK,PattisonGTR.DisruptiontosurgicaltrainingduringCovid-19 intheUnitedStates,UnitedKingdom,Canada,andAustralasia:arapid reviewofimpactandmitigationefforts. JSurgEduc.2021;78(1):308–14.
15.StarkN,HayirliT,BhanjaA,etal.Unprecedentedtraining:experience ofresidentsduringtheCOVID-19pandemic. AnnEmergMed 2022;79(5):488–94.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 859 Franketal. ImpactofthePost-COVID-19EraonProceduralTraininginEMResidency
16.KimHS,CruzDS,ConrardyMJ,etal.Emergencydepartmentvisitsfor seriousdiagnosesduringtheCOVID-19pandemic. AcadEmergMed 2020;27(9):910–3.
17.ChielL,WinthropZ,WinnAS.TheCOVID-19pandemicandpediatric graduatemedicaleducation. Pediatrics.2020;146(2):e20201057.
18.DedeiliaA,SotiropoulosMG,HanrahanJG,etal.Medicalandsurgical educationchallengesandinnovationsintheCOVID-19era: asystematicreview. InVivo.2020;34(Suppl3):1603–11.
19.DouglassA,YipK,LumanauwD,etal.Residentclinicalexperiencein theemergencydepartment:patientencountersbypostgraduateyear. AEMEducTrain.2019;3(3):243–50.
20.LoHY,LinSC,ChaouCH,etal.WhatistheimpactoftheCOVID-19 pandemiconemergencymedicineresidencytraining:anobservational study. BMCMedEduc.2020;20(1):348.
21.HartnettKP,Kite-PowellA,DeViesJ,etal.ImpactoftheCOVID-19 pandemiconemergencydepartmentvisits UnitedStates, January1,2019-May30,2020. MorbMortalWklyRep 2020;69(23):699–704.
22.BrunoTW,JanwadkarR,ClaytonLM,etal.ImpactofCOVID-19on emergencymedicineresidentprocedureperformance. AEMEduc Train.2022;6(6):e10832.
23.BaughJJ,WhiteBA,McEvoyD,etal.Thecasesnotseen:patternsof emergencydepartmentvisitsandproceduresintheeraofCOVID-19. AmJEmergMed.2021;46:476–81.
24.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed.2005;45(4):448–51.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 860 ImpactofthePost-COVID-19EraonProceduralTraininginEMResidency Franketal.
ImprovementinResidentScholarlyOutputwithImplementationof aScholarlyActivityGuidelineandPointSystem
LaurenEvans,MD
SarahGreenberger,MD
RachaelFreeze-Ramsey,MD
AmandaYoung,MD
CrystalSparks,MSAM
RawleSeupaul,MD
TravisEastin,MD,MS
CarlyEastin,MD
UniversityofArkansasforMedicalSciences,CollegeofMedicine, DepartmentofEmergencyMedicine,LittleRock,Arkansas
SectionEditors: JeffreyDruck,MD,andYaninaPurim-Shem-Tov,MD,MS
Submissionhistory:SubmittedMarch5,2023;RevisionreceivedJune27,2023;AcceptedJuly19,2023
ElectronicallypublishedAugust15,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.60346
Introduction: Ensuringhigh-qualityscholarlyoutputbygraduatemedicaltraineescanbeachallenge. Withinmanyspecialties,includingemergencymedicine(EM),itisunclearwhatconstitutesappropriate residentscholarlyactivity.Wehypothesizedthatthequantityandqualityofscholarlyactivitywould improvewithaclearerguideline,includingapointsystemforeligiblescholarlyactivities.
Methods: AresidentScholarlyActivityGuidelinewasimplementedforEMresidentsinauniversity setting.Theguidelineconsistsofapointsysteminwhichpointvalues,rangingfrom1–10,areassigned tovarioustypesofscholarlyactivities.Residentsmustearnatleast10pointsandpresenttheirworkto meettheirscholarlygraduationrequirement.Wetrackedscholarlyactivitiesforgraduatesfromthe classesof2014–2020,withtheguidelinebeingimplementedfortheclassof2016.Inablindanalysis,we comparedmediantotalpointsperresident,meancountsoftheBoyermodelofscholarshipcomponents perresident,andmeancountsofsignificantscholarlyoutputperresidentbeforevsaftertheguideline wasimplemented.Significantscholarlyoutputwasdefinedasanimplementedprotocol, aresearchprojectwithdatacollectionandanalysis,aresearchabstractpresentation,oranoral abstractpresentation.
Results: Among64residentsanalyzed,48residentsusedtheguideline.Wefoundthatmedianpoints perresidentincreasedaftertheguidelinewasimplemented(median,interquartilerange:before7[7], after11[10,13], P = 0.002).Post-guidelinescholarlyactivitieswerefoundtorepresentmoreofBoyer’s componentsofscholarship[meanbefore0.81[SD0.40],meanafter1.52[SD0.71],meandifference 0.71,95%confidenceinterval[CI]0.332 ± 1.09, P < 0.001.Therewasnodifferenceinthemean significantscholarlyoutputperresident(meanbefore1.38[SD1.02],meanafter1.02[SD1.00],mean difference0.35,95%CI0.93 ± 0.23, P = 0.23).
Conclusion: ImplementationofaScholarlyActivityGuidelinepointsystemsignificantlyincreasedthe quantityand,byoneoftwomeasures,increasedthequalityofscholarlyoutputinourprogram.Ourpointbasedguidelinesuccessfullyincorporatedtraditionalandmodernformsofscholarshipthatcanbe tailoredtoresidentinterests.[WestJEmergMed.2023;24(5)861–867.]
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 861
EDUCATIONAL ADVANCES
INTRODUCTION
Scholarshiphasbeenafundamentalrequirementduring anyresidencytrainingsince1994,butexecutingthis requirementcanbechallengingduetoconfusionregarding whatconstitutesscholarship.1 Itisconsistentlythoughtthat alltraineesshouldbeexposedtothefourcomponentsofthe Boyermodelforscholarship:discovery;integration; application;andteaching.2,3 In2013,theCommonProgram Requirementsforresidencyprogramsaspublishedbythe AccreditationCouncilforGraduateMedicalEducation (ACGME)statedthat, “residentsmustparticipatein scholarship.”4 Whilethereweremorespecificfaculty scholarshipexpectations,theemergencymedicine(EM) requirementsdidnotdictatethetypeorextentofthis requirementforresidents.InJuly2022,theACGMEadded moredetailedlanguagetothesebroadrequirementsforEM (Table1),buttheycanstillbedifficultforprogramleadership toexecute.5
Notsurprisingly,therehasbeenbroadandsubjective applicationofthisrequirement.Forexample,in2015Geyer etalfoundthatwithinEM,39%ofprogramssurveyed requiredanoriginalresearchprojectupongraduationwhile 61%ofprogramsallowedcurriculardevelopmentprojectsor evidence-basedreviewsasanalternativetoatraditional researchprojectwithanassociatedpeer-reviewed manuscript.1 Inanattempttoaddressthisissue,in2018 representativesfromtwonationalEMgroupspublished
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Scholarlyactivitiesarearequiredpartof residencytraining,butde fi ningappropriate scholarshipremainsachallengefor residencyleadership.
Whatwastheresearchquestion?
Cananovelscholarlyactivityguidelineand pointsystemimprovethequalityandquantity ofresidentscholarship?
Whatwasthemajor findingofthestudy? Implementationofthepointsystemcorrelated withimprovedmedianscholarlypointsper resident(before7[IQR7],after11 [IQR10,13],P = 0.002).
Howdoesthisimprovepopulationhealth?
Aclear,concisescholar lyactivityguideline mayallowforimprovedresidentscholarly output,whichcontributestotheadvancement ofemergencycare.
2013Emergencymedicinerequirementsfor residentscholarlyactivities
Thecurriculummustadvanceresidents’ knowledgeofthebasicprinciplesofresearch, includinghowresearchisconducted,evaluated,explainedtopatients,andappliedto patientcare.
Residentsshouldparticipateinscholarlyactivity.
Thesponsoringinstitutionandprogramshouldallocateadequateeducational resourcestofacilitateresidentinvolvementinscholarlyactivities.
2022Emergencymedicinerequirementsfor residentscholarlyactivities
Residentsmustparticipateinscholarship.
Thecurriculummustadvancetheresidents’ knowledgeofthebasicprinciplesof research,includinghowresearchisconducted,evaluated,explainedtopatients,and appliedtopatientcare.
Atthetimeofgraduation,eachresidentshoulddemonstrate:
• activeparticipationinaresearchproject,orformulationandimplementationofan originalresearchproject,includingfundedandnon-fundedbasicscienceor clinicaloutcomesresearch,aswellasactiveparticipationinanEmergency Medicineemergencydepartmentqualityimprovementproject;or,
• presentationofgrandrounds,posters,workshops,qualityimprovement presentations,podiumpresentations,webinars;or,
• grantleadership,non-peer-reviewedprint/electronicresources,articlesor publications,bookchapters,textbooks,serviceonprofessionalcommittees,or servingasajournalreviewer,journaleditorialboardmember,oreditor;or
• peer-reviewedpublications.
Table1. EvolutionofemergencymedicineresidentscholarshiprequirementsasdesignatedbytheACGMEResidencyReviewCommittee foremergencymedicine.4,5
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 862 ImprovementinResidentScholarlyOutputwithaSAGandPointSystem Evansetal.
ACGME,AccreditationCouncilforGraduateMedicalEducation.
recommendationsbasedonsurveydata,suggesting appropriatetypesofscholarshipforEMresidentstoprovide morestructuretothescholarshiprequirement.6 However, theserecommendationshavebeencitedasbeingtoostrict andnottakingintoaccountmoremodernformsof scholarshipsuchassocialmedia,podcasts,oronline curricula,whicharenowrecognizedasfulfillingtheBoyer componentsofscholarship.7,8 Sinceacademicinstitutions areincreasinglyconsideringmorevariedtypesofscholarship inthefacultypromotionprocess,itisreasonabletosimilarly allowresidentstoparticipateintraditionaland nontraditionalactivitiesbasedontheirinterests.
Inadditiontothehistoricalvariationinprograms’ interpretationsofscholarshiprequirements,enforcinga singlestandardforthescholarlyactivityrequirementmay notbeappropriate,asmanytraineesdonotplantopursuea careerinacademicmedicine.Traineesoftenequateresearch orscholarlyactivitywithacademia,whichcanresultin diminishedengagementintheseprojectsiftheyintendto pursueadifferentcareerpath.Furthercomplicatingthe scholarlyprocess,manyresidentshavedifficultycompleting originalresearchprojectsduetolackofmentorshipor institutionalsupportfordatacollectionorstatistical analysis.1,9 Itis,therefore,notsurprisingthatinadequate scholarshiphasledtoahighrateofReviewCommittee(RC) citationssincethescholarshiprequirementwasintroduced in1994.1,9
In2018,ameta-analysisevaluatinggraduatemedical education(GME)scholarshipinitiativesfoundthat,whileno specificstrategywasmoreeffectiveatincreasingtrainee publications,therewasasignificantincreaseinpublications followingtheimplementationofanyinitiative.Theauthors concludedthata “cultureofemphasisonresident scholarship” wasthecriticalfactorinincreasingscholarly productionamongtrainees.10 Severalotherstrategieshave alsobeendescribedthatmayimproveresidentscholarly output,withthemosteffectivebeingprovidingdedicated timeforscholarship,havingaresearchcurriculum,adefined scholarshiprequirement,requiringapresentationata researchday,oracombinationofthese.11 However,the optimalapproachremainsunclear.
OBJECTIVE
Thepurposeofthisinnovationwastoimprovethe quantityandqualityofscholarshipbyprovidingawelldefinedscholarlyactivityframeworkforourtraineeswhile simultaneouslyincorporatingoptionsforavarietyof traditionalandmodernscholarlyactivities.
CURRICULARDESIGN DevelopmentoftheScholarlyActivityGuideline
Afteraliteraturereviewin2014,weusedexisting recommendationsforscholarlyoutputinanEMtraining programalongwithapreviouslypublishedunique
scholarshippointsystemtocreateaScholarlyActivity Guideline(SAG,SupplementalMaterial).3-5,12,13 Whilenot aprovenmethod,wechosethispointsystembasedonthe noveltyoftheideaandtheinclusionofawidevarietyof optionsforscholarship.Thepointsystemwastailoredtoour program ’sgoalsforfulfillingthescholarshiprequirement.It providesmultipleoptionsforscholarshipwithassociated pointvaluesrangingfrom1–10(Table2).
The firstversionofSAGrequiredthatresidentsobtaina minimumof10pointsonthescholarlypointsystem,attend onedepartmentresearchmeetingyearly,completeevidencebasedlearningmodules,andpresenttheirworkatourannual departmentalScholar’sDay.Themeetingandmodule requirementshavesincebeenremovedastheyareaddressed elsewhereintheresidencycurriculum.Theguidelineincludes asuggestedtimelineforcompletiontoassistinkeeping residentsonschedule.Finally,itincludesanideaformwhich servesasaguideforin-personprojectdiscussionswith
Table2. Theoriginalscholarlyactivitypointsystem,createdin2014, adaptedfromSeehusenetal.a
aTableadaptedfromSeehusenDA,AsplundCA,Friedman M.Apointsystemforresidentscholarlyactivity. FamMed 2009Jul–Aug;41(7):467–9.PMID:19582627.
IRB,institutionalreviewboard.
TypeofscholarlyactivityPoints IRB-approvedprojectcompletedwithmanuscript submittedtoapeer-reviewedjournal ≥10 Submissionofamanuscriptdescribingacaseseries, systematicreview,ormeta-analysis ≥10 Presentationofaposterororalpresentationata regional,national,orinternationalconference 5 Publicationofabookchapterorsection10 NonIRB-approvedquality-improvement(QI)project completedandresultssharedwithpeers 7 InitiationofIRB-approvedresearchorQIprojectbut projectstillongoingattimeofgraduation 8 – 10 Submissionofagrantforintramuralorextramural funding(withIRBapproval) 10 Creationandmaintenanceofanonlineteachingtool5 Publicationofalettertotheeditorinapeer-reviewed medicaljournal 3 – 5 Creationofsimulationcaseforsimulationcurriculum (notpublishedvspublished) 3 – 10 Submissiontopeer-reviewedjournalornational conferenceofaseriesofinterestingcases(ie,visual diagnosiscasesorphotocompetition) 3.5 Publicationsforthelaypublic,suchasnewspaper articles,onmedicaltopics 3 Participationonanationalcommittee5 Criticallyappraisedtopicwrite-upandsubmission tojournal 5
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 863 Evansetal. ImprovementinResidentScholarlyOutputwithaSAGandPointSystem
membersoftheresearchcommittee.Residentsarerequired toobtainapprovalfromtheResearchCommitteeforany scholarshipforwhichtheywishtoobtainpoints,but generallytheycanchooseanycombinationofactivitiesfrom theguidelinetoachievethegoalof10points.Ifthereisa projectthatdoesnot fitwellwithintheoptionslisted, residentscanpresenttheirideaforconsiderationtothe ResearchCommitteeand,ifapproved,thecommitteeassigns pointsbyconsensus.
TheSAGwasimplementedinAugust2014andwas first appliedtothegraduatingclassof2016aswellasall subsequentresidents.Thistimegapallowedtheinternclass of2014twoacademicyearstomeettheirrequirements.Asa matterofbackground,ourEMresidencyisalongstanding three-yearprogramlocatedataLevel1traumaandtertiary carehospitalintheSouthCentralUnitedStates.Priortothe introductionoftheSAG,therewasascholarship requirementforallresidentswithoutaspecificcurriculumor guidedefiningwhattypesofprojectswereappropriate.Over thesevenyearsofthisdataanalysis,ourresidency complementincreasedfromeightto10residentsperyear.We alsoaddedseveraladditionalfaculty,includingoneresearchfocusedfacultymember.
Forqualityimprovementpurposes,theguidelinehasbeen reviewedperiodicallyandadjustmentstoithavebeenmade whennecessary.Forexample,weremovedtherequirement toattendaresearchmeetingastheywerenotfoundtobehigh yield.Toavoiddiminishingeducationalvalue,restrictionson casereportswerealsoaddedtopreventresidentsfromonly completingcasereportsduringtheirtraining.Lastly,the categoryofabstractsforthe JournalofEmergencyMedicine wasadded,asoneoftheprogram’sfacultyisthesection editorfortheAbstractssectionofthejournalandallows residentstocontributeasauthors.
MethodsforAnalysisoftheScholarlyActivityGuideline
Aspartofroutineresidencydocumentation,scholarly activityoutputforallresidentsisrecordedinrealtime.In June2020weabstractedallrecordedscholarshipfor graduatesbetween2014-2020fromeachgraduate’sexitletter toassesstheimprovementinscholarlyoutputrelatedtothe introductionofthenewguideline.Whileallprojectsafter 2015hadpointsassignedtothematthetimetheywere completed,threeauthors(SG,RFR,AY)whowerenot membersoftheResearchCommitteeindependentlyassigned pointsforthepre-SAGcohortandre-measuredpointtotals foreachresidentinthepost-SAGgrouptoensure consistencyandreducebias.Tofurtherreducebias,two authors(TE,CE)removedthenameandgraduationyearof theresidentandreplacedtheprojecttitlewithaprojecttype. Thisblindedlistwasthenrandomizedandenteredinto RedCap,anelectronicdatacapturetoolhostedatUniversity ofArkansasforMedicalSciencesforrating.Thesame authors(SG,RFR,AY)alsoanalyzedthequalityofeach
resident’soutputbasedonhowmany,ifany,oftheBoyer componentsofscholarshipwererepresented.Therefore,our twoprimaryoutcomeswerethecomparisonofthemedian numberofpointsperresidentandthemeannumberofthe Boyercomponentsofscholarshippresentperresident,before andafterimplementationoftheSAG.
Althoughtheconsensusdocumentregardingappropriate scholarlyoutputforEMresidentsbyKaneetalwas publishedseveralyearsafterimplementationofour guideline,wewantedtoincorporatethesecriteriaintoour analysisaswell.6 Inadditiontorecommendingthat programsmaintainanarchiveinresidencyrecord files,Kane etalproposedfourotherprimaryelementsofresident scholarship:adevelopedandimplementedprotocol;a researchpaperwithahypothesis,collectedandanalyzed data,andaconclusion;aresearchabstractpresentation;or anoralresearchpresentation.Theconsensusauthorsstated thesewererecommendationsratherthanrequirements,and whilethoseoptionswereconsideredtobebestpractices,they stillbelievedthatprogramdirectorscouldacceptalternative typesofscholarship.6 Asapre-plannedsecondaryanalysis, ourthreeraters(SG,RFR,AY)alsoratedwhichprojects metatleastoneoftheconsensuscriteriaforscholarship, whichwedefinedas “significantscholarlyoutput.”
Theuniversity’sinstitutionalreviewboard(IRB)didnot considerthisreviewtobehumansubjectsresearchand, therefore,didnotrequireIRBoversight.Weuseddescriptive statisticswhereappropriate.Themedianvalueamongthe threeraterswasusedasthe finalcountforeachvariable.We treatedourscholarlyactivitypointvariable,asordinalas differentactivitiescouldachievedifferingpointvalues. CountsoftheBoyercomponentsandsignificantscholarly outputweretreatedascontinuous.Categoricalvariables werecomparedusingchi-squaredtests(ortheFisherexact testifcountswererare),ordinalvariableswerecompared usingtheMann-WhitneyUtest,andcontinuousvariables werecomparedusingindependent t -test.Wecalculatedinterraterreliability(FleissKappa)toassesstheagreement betweenthethreeraters.Analyseswereperformedusing SPSSStatisticsforMacintoshversion28.0(IBMCorp, Armonk,NY).
IMPACT AnalysisofScholarlyOutput
Sixty-fourresidentsgraduatedintheperiodstudied, producing676scholarlypoints.Beforetheguideline,onlyone of16(6.25%)residentswouldhavemettheminimumpoint requirement(Table3).SincetheSAGwasimplemented,40/48 (83.3%)residentsintheclassesof2016–2020mettheir scholarlypointrequirementsbasedontheblindedreview. Totalpointsperresidentincreasedsignificantlyafter implementationoftheguideline(median7pointsperresident [interquartilerange(IQR)7,7]beforevs11pointsperresident after[IQR10,13], P < 0.002).See Figure1 forgraphical
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 864 ImprovementinResidentScholarlyOutputwithaSAGandPointSystem Evansetal.
Guidelinegroup BeforeAfter
residentportfoliosaswellasatleastonesignificantscholarly achievementin71.8%(46/64).Whencomparingbeforeand aftertheSAG,wefoundasignificantincreaseinthemean numberofBoyercomponents(meanbefore0.81[SD0.40], meanafter1.52[SD0.71],meandifference0.71,95%CI 0.332–1.09, P < 0.001),althoughtheproportionof residentswithatleastonecomponentdidnotchange (81.25%vs95.3%,RR = 4.5,95%CI0.82–25.47, P = 0.10). Therewasnochangeintheaveragenumberofsignificant scholarlyoutputsperresident(meanbefore1.38[SD1.02], meanafter1.02[SD1.00],meandifference 0.35,95%CI 0.93 – 0.23, P = 0.23)orintheproportionofresidentswith atleastonesignificantscholarlyoutput(87.5%vs64.58%, RR0.35,95%CI0.09 = 1.36, P = 0.12).Overallinterrater agreementwasmeasuredasmoderate(Κ = 0.538,95%CI 0.499–0.577, P < 0.001).
AsanaturalconsequenceofseeingmoreoftheBoyer componentsofscholarshipwiththeSAG,wenoticedthatthe typesofscholarshipappearedtobemorevariedaswell.In thepre-guidelineperiod,mostscholarlyactivitieswerelocal qualityimprovementprojectsthatresultedindatacollection andanalysis,butmostwereonlypresentedlocally.Twoof theseresultedinresearchabstractspresentedatnational meetings,andtherewasoneresidentwhoparticipatedina multicenter,chartreviewstudy.Inthepost-guidelineperiod, residentsnotonlyhadregionalandnationalresearch abstractpresentations,peer-reviewedmanuscripts,andbook chapters,buttheyalsopublishedevidence-basedreviews, editedonlineresourcesformedicalstudents,wrotearticles forcommunitynewsletters,andrecordededucational, evidence-basedpodcasts.Inaddition,whileparticipationin nationalcommitteeswasinitiallyacontroversialadditionto ouracceptedformsofscholarship,residentswhohavechosen thisoptionhavebeenhighlyengagedandwereofteninvited tobeauthorsonsubsequentpublicationsorparticipatein nationalpresentations.
DISCUSSION
representationofalloutcomes.Ofnote,54.2%(26/48)of residentsinthepost-guidelineperiodendedtheirtrainingwith morepointsthantheminimumrequired,comparedwith 6.25%(1/16)before(relativerisk[RR]2.05,95%confidence interval[CI]1.47–2.85, P < 0.001).
Regardingthequalityofscholarship,wefoundatleastone oftheBoyercomponentsofscholarshipin92%(59/64)of
Weareexcitedabouttheimprovedresidentscholarship weachievedafterimplementationoftheSAG.Webelieve thathavingaclearerandmorediverselistofoptionshas allowedresidentstosuccessfullychooseprojectsinwhich theywouldfeelengagedwhilethepointrequirementhas ensuredaminimumstandardandaccountability.Although anecdotal,thefacultymembersoverseeingresident scholarshiphavenotedthattheclarityprovidedbytheSAG seemstohavereducedfrustrationonthepartofboth residentsandfaculty.WhiletheSAGconceptisnoveltoEM, thispointsystemwasadaptedfromasimilarsystemusedina familymedicineresidencybySeehusenetal.12 Our improvementsarecongruentwiththeincreasetheyfoundin theirscholarlyoutputwiththisapproach,describingmore presentations,bookchapters,andpeer-reviewed publications.Sinceimplementationofourguideline,
Table3. Scholarlyoutputresults,beforeandafter.
Count%Count% Successfullyachieved minimumpoints ≥10 points 16.3%4083.3% <10 points 1593.8%816.7% Boyercomponents present 0318.8%24.2% 11381.3%2347.9% 200.0%1939.6% 300.0%48.3% 400.0%00.0% AtleastoneBoyer componentpresent Yes1381.3%4695.8% No318.8%24.2% Signi ficantscholarly outputpresent 0212.5%1633.3% 1956.3%2245.8% 2318.8%36.3% 316.3%714.6% 416.3%00.0% Atleastonesignificant scholarlyoutput Yes1487.5%3164.6% No212.5%1735.4%
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 865 Evansetal. ImprovementinResidentScholarlyOutputwithaSAGandPointSystem
Figure1. Outcomesbeforevsafterscholarlyguideline. EM,emergencymedicine.
executionofasimilarpointsystemhasbeendescribedinthe radiologyliterature,butnoofficialquantitativeanalyses havebeenreported.14
Wefounditinterestingthatwhilethetotalpoints increasedandwefoundmoreoftheBoyercomponentsof scholarshippresentaftertheguideline,wedidnotseea differenceinsignificantscholarlyoutputasdefinedasoneof thefourcriteriadescribedbyKaneetalintheirconsensus statement.6 WhileKaneetal’srecommendationwasmade withinputandsupportfrommembersofseveralEM organizations,itwasprimarilycraftedbymembersofthe ResearchDirectorsInterestGroupandEvidence-based HealthcareImplementationinterestgroupsoftheSocietyfor AcademicEmergencyMedicine.Intheirstudy,theauthors identifiedthebestpracticesbasedonasurveyofpossible scholarlyoutputs,andonlythosewithhighconsensusamong respondentswereconsideredappropriatescholarship.While thesurveyrespondentswereaffiliatedwithmostofthe nationalEMgroups,representativesofseveralEMgroups, suchastheCouncilofResidencyDirectorsandvariousEM residentorganizations,respondedwithconcernthatthese recommendationsweretoostringentandthattheapproach usedtodeterminethecriteriawerenotconsistentwithwidely accepteddefinitionsofconsensus.7 Theyrecommendedusing alessstrictconsensusthreshold,whichwouldresultinamore variedlistofacceptablescholarshipopportunities.
Understandingthelimitationsoftheconsensus,itisnot surprisingthatgivenourinclusionofnon-traditionaland moremodernformsofscholarship(eg,onlineeducational resources,participationinnationalcommittees,or FOAMed),wedidnotseeasignificantincreaseinthosetypes ofscholarshipsonlynotedintheconsensusdocument.Itis certainlypossiblethatthelackofincreaseindicatesalackof impactofourscholarlyactivityguideline,butwefeelitmore reflectsthebiasoftheconsensusguidelinetowardmore traditionalresearchactivities.Forexample,inthepost-SAG group,wehadresidentspursuepodcasts,evidence-based reviews,andparticipateinnationalcommittees,alltypesof scholarshipwefeelarevaluablethatwouldnothave otherwisebeencountedintheconsensusguideline.
Thereareseveralotherpotentialexplanationsforthe smallchangeseeninouranalysis.Evenwiththeadditionof diversefacultyandincreasingthefocusonresident scholarship,ourresearchinfrastructurehasremained minimal,whichwefeelhasslowedtheadvancementofour researchmissionandpotentiallylimitedthepotentialofthe pointsystem.Themajorityofourresidentsalsobecome communityemergencyphysiciansandarenotnecessarily focusedonresearch,similartotraineesinmanyEM residencies.Whilewedidnotanalyzethepointsfrom residentswhopursuedcommunitypracticeagainstthose whopursuedfellowshipsoracademicmedicine,wesuspect thatthoseenteringcommunityemergencydepartmentslikely choselesstraditionalresearchandmayhavebeenmorelikely
to finishwiththeminimumpointsrequired.Iftrue,this wouldnotnecessarilybeanegativereflectionofthepoint system;rather,forusitwouldhighlightthe flexibilityofthis approachtoalltypesofresidents.Weneverexpectedthatall ourresidentswouldsuddenlyengageincomplexscholarship, butwedidhopeforanexplicitguideline,aclearminimum standardforcompletionand,overall,morehighquality output.Westillseeourimprovements,whilemodestfrom astatisticalstandpoint,asamajorcultureshiftfor ourprogram.
NextSteps
Webelievethatfuture,similarinvestigationswouldbe beneficialtoenhancegeneralizabilityofour findings.Ifother programswereto findsuccessinimplementingsimilar scholarlypointsystems,especiallyprogramswithavarietyof resources,wemaylearninwhichsettingsthepointsystem performsbest.Applyingthistoothergroupsmayalsobe useful.Forexample,ourprogramisconsideringcreatinga pointsystemforfacultytoimprovetheirscholarlyoutput andengagement.Whilestillintheplanningstage,this approachcouldhelplessresearch-focusedfaculty participateintheresearchmissionwithavarietyofoptions forcompliance.
BasedontheexperiencegainedbyimplementingtheSAG, wehaverealizedthatdocumentationisimperative,and suggesthavingclear,ongoingdocumentationfromthetime ofideagenerationthroughprojectcompletion.Thisprovides transparencyforprojectapprovalandprogression,how manypointswillbeawarded,andwhenthescholarlyworkis consideredcomplete.Wehavefounddocumentationof projectstatustobemostsuccessfulinasharedonlineformat withaccessfortheresident,theresearchcommittee,and programleadership.Additionally,onceapointsystemis implemented,periodicadjustmentsarenecessaryto incorporatenewareasofscholarship,ortoremoveorlimit itemsthatmaynotprovideincrementaleducationalbenefit tothelearner.
LIMITATIONS
Thisdatasetislimitedbyrecallbias,astherecouldbe projectsthatwerenotdocumentedandnotavailableto includeintheanalysis.Whiletheauthorsthatjudgedpoint valueswereblindedtoresidentnamesandgraduationyear, theymayhavebeenabletoidentifyresidents’ workbasedon theprojecttype.Additionally,whiletheratershad moderatelygoodagreement,theyhadnotpreviouslyjudged pointtotals,sothesenumbersmayhavebeenincongruent withthepointsawardedbytheresearchcommitteeinreal timebasedonknowingthespecificsoftheproject.Thisis particularlyevidentwhenconsideringthatatthetimeoftheir graduation,allresidentsinthepost-implementationgroup werefelttohavemetthe10-pointminimum,yetnotallwere judgedtohavemettherequirementinthisanalysis,
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 866 ImprovementinResidentScholarlyOutputwithaSAGandPointSystem Evansetal.
suggestingthatblindingledtounderestimationofpoints scored.However,wefeltthatcreatingablindedreview wouldallowforthemostunbiasedcomparison.
Itisalsopossiblethatretrospectiveapplicationofthe pointsystemmayhaveoverestimatedthedifference,butwe feelthisisunlikely.Anotherlimitationisthatadditional facultywerehiredatthetimeofandfollowingtheSAG implementation,andthesenewerfacultycouldhave improvedresidents’ abilitiestocompletehigh-quality scholarshipregardlessofguidelineimplementation.Lastly, whilewehavefoundtheSAGtobeeffectiveinourprogram, itispossiblethat,asWoodetalsuggest,anyinitiativethat providedenhancedemphasisonresidentscholarshipcould havebeenequallyeffective.10
CONCLUSION
Theimplementationofapoint-basedscholarlyactivity guidelineimprovesthequantity,breadthand,inouropinion, thequalityofscholarlyactivityamongemergencymedicine residents.Giventheinclusionofavarietyoftraditionaland non-traditionalformsofscholarshipanditssimplicity,this systemcouldbeeasilyadaptedforotherEMresidenciesor anyothersubspecialtytrainingprograms.
AddressforCorrespondence:CarlyEastin,MD,Universityof ArkansasforMedicalSciences,DepartmentofEmergency Medicine,DepartmentofPediatrics,4301WMarkhamSt,Slot584, LittleRock,Arkansas72211. Email:cdeastin@uams.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Evansetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.GeyerBC,KajiAH,KatzED,etal.Anationalevaluationofthescholarly activityrequirementinresidencyprograms:asurveyofemergency medicineprogramdirectors. AcadEmergMed.2015;22(11):1337–44.
2.PostonL,BoyerEL.Scholarshipreconsidered:prioritiesofthe professoriate. Academe.TheCarnegieFoundationforthe AdvancementofTeaching.1990.
3.GradyEC,RoiseA,BarrD,etal.Definingscholarlyactivityingraduate medicaleducation. JGradMedEduc.2012;4(4):558–61.
4.AccreditationCouncilforGraduateMedicalEducation.ACGME CommonProgramRequirements(Residency).Availableat: https:// www.acgme.org/globalassets/pfassets/programrequirements/ cprresidency_2022v3.pdf.AccessedJuly2020.
5.AccreditationCouncilforGraduateMedicalEducation.ACGME ProgramRequirementsforGraduateMedicalEducationinEmergency Medicine.Availableat: https://www.acgme.org/globalassets/pfassets/ programrequirements/110_emergencymedicine_2022_tcc.pdf AccessedNovember2022.
6.KaneBG,TottenVY,KrausCK,etal.Creatingconsensus:revisiting theemergencymedicineresidentscholarlyactivityrequirement. WestJEmergMed.2019;20(2):369–75.
7.PasichowSH,JarouZJ,NikollaDA,etal.Responseto “creating consensus:revisitingtheemergencymedicinescholarlyactivity requirement.” WestJEmergMed.2019;20(2):376–9.
8.QuinnA,ChanTM,SampsonC,etal.Curatedcollectionsfor educators: fivekeypapersonevaluatingdigitalscholarship. Cureus 2018;10(1):e2021.
9.LevineRB,HebertRS,WrightSM.Residentresearchandscholarly activityininternalmedicineresidencytrainingprograms. JGenIntern Med.2005;20(2):155–9.
10.WoodW,McCollumJ,KukrejaP,etal.Graduatemedicaleducation scholarlyactivitiesinitiatives:asystematicreviewandmeta-analysis. BMCMedEduc.2018;18(1):318.
11.StevensonMD,SmigielskiEM,NaifehMM,etal.Increasingscholarly activityproductivityduringresidency:asystematicreview. AcadMed 2017;92(2):250–66.
12.SeehusenDA,AsplundCA,FriedmanM.Apointsystemforresident scholarlyactivity. FamMed.2009;41(7):467–9.
13.SummersRL,FishS,BlandaM,etal.Assessmentofthe “scholarlyproject” requirementforemergencymedicineresidents: reportoftheSAEMResearchDirectors’ workshop.SAEM ResearchDirectors’ InterestGroup. AcadEmergMed 2008;6(11):1160–5.
14.BhattAA,GarnerHW,BowmanAW,etal.Residentscholarlyactivityfor diagnosticradiologyresidency:apointsystemapproach. CurrProbl DiagnRadiol.2022;51(3):301–3.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 867 Evansetal. ImprovementinResidentScholarlyOutputwithaSAGandPointSystem
PrehospitalmSOFAScoreforQuickPredictionofLife-Saving InterventionsandMortalityinTraumaPatients:AProspective, Multicenter,Ambulance-based,CohortStudy
FranciscoMartín-Rodríguez,PhD*†‡
AncorSanz-García,PhD‡§
AnaBenitoJustel,PhD†
AlmudenaMoralesSánchez,PhD†
CristinaMazasPerezOleaga,PhD#**
IreneDelgadoNoya,PhD#††
IreneSánchezSober´on,PhD†
CarlosdelPozoVegas,PhD*‡∥
JuanF.DelgadoBenito,MD†‡
RaúlL´opez-Izquierdo,PhD*‡¶
*UniversidaddeValladolid,FacultyofMedicine,Valladolid,Spain
† EmergencyMedicalServices(SACYL),AdvancedLifeSupport,Valladolid,Spain
‡ PrehospitalEarlyWarningScoring-SystemInvestigationGroup,Valladolid,Spain
§ UniversidaddeCastillalaMancha,FacultyofHealthSciences,Talaveradela Reina,Spain
∥ HospitalClínicoUniversitario,DepartmentofEmergencyMedicine, Valladolid,Spain
¶ HospitalUniversitarioRioHortega,DepartmentofEmergencyMedicine, Valladolid,Spain
# UniversidadEuropeadelAtlántico,DepartmentofEmergencyMedicine, Santader,Spain
**UniversidadInternacionalIberoamericana,DepartmentofEmergencyMedicine, Campeche,México
†† UniversidadeInternacionaldoCuanza,DepartmentofEmergencyMedicine, Cuito,Bié,Angola
SectionEditor: MarkLangdorf,MD,MHPE
Submissionhistory:SubmittedSeptember29,2022;RevisionreceivedMay17,2023;AcceptedMay19,2023
ElectronicallypublishedAugust8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59048
Background: Prehospitalemergencymedicalservices(EMS)arethemaingatewayfortraumapatients. Recentadvancesinpoint-of-caretestingandthedevelopmentofearlywarningscoreshaveallowedEMS toimprovepatientclassification.Weaimedtoidentifypatientspresentingwithmajortraumainvolvinglifesavinginterventions(LSI)usingthemodifiedSequentialOrganFailureAssessment(mSOFA)scoreinthe prehospitalscenario,andtocomparetheseresultswiththoseofothertraumascores.
Methods: Thiswasaprospective,ambulance-based,multicenter,training-validationstudyintrauma patientswhoweretreatedinaprehospitalsettingandsubsequentlytransportedtoahospital.Thestudy involvedsixAdvancedLifeSupportunits,38BasicLifeSupportunits,andfourhospitals.Theprimary outcomewasLSIperformedatthesceneorenrouteandintensivecareunit(ICU)admissionand all-causetwo-dayin-hospitalmortality.Wecollectedepidemiologicalvariables,creatinine,lactate,base excess,internationalnormalizedratio,andvitalsigns.Discriminativepower(areaunderthereceiver operatingcharacteristiccurve[AUC]),calibration(observedvspredictedoutcomeagreement),and decision-curveanalysis(DCA,clinicalutility)wereusedtoassessthereliabilityofthemSOFAin comparisontootherscores.
Results: BetweenJanuary1,2020–April30,2022,atotalof763patientswereselected.ThemSOFA score’sAUCwas0.927(95%confidenceinterval[CI]0.898–0.957)forLSI,0.845(95%CI0.808–0.882) forICUadmission,and0.979(95%CI0.966–0.991)fortwo-daymortality.
Conclusion: ThemSOFAscoreoutperformedtheotherscores,allowingaquickidentificationof high-riskpatients.TheroutineimplementationinEMSofmSOFAcouldprovidecriticalsupportinthe decision-makingprocessintime-dependenttraumainjuries.[WestJEmergMed.2023;24(5)868–877.]
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 868 ORIGINAL RESEARCH
BACKGROUND
Severalcomplexconsequencesfollowaseveretrauma (eg,hypoperfusion,coagulopathy,hypothermia,acidosis, andtissueinflammation).Theseresponsesincrease morbidityandmortalityintraumapatients.1 Discriminating majortraumathatrequirelife-savinginterventions(LSI)vs traumawithoutsystemicrepercussionsisaparticular challengeforemergencymedicalservices(EMS), particularlyinprehospitalcare.2,3 Theidentificationof patientsrequiringLSIonthesceneiscriticalindeciding whethertotransporttotheemergencydepartment(ED)ofa hospitalequippedtomanagecomplextraumacases(trauma center).Conversely,rapididentificationofpatientswhoare notathighriskallowsEMSpersonneltotransportthose patientstohospitalswithfewerresourcesand/orclinicians withlesstrainingintreatingcomplextrauma.Theabilityto quicklydifferentiatebetweenhigh-risktraumapatientsand thosenotatimmediateriskimprovesthetransferrateof high-complexitycasestotraumacenters,therebyoptimizing theuseofresources.Theuseoftraumascorestodetermine patientriskinnon-prehospitalscenarioshasbeen successfullyadoptedinclinicalpractice.4
Inprehospitalcare,theusefulnessofanearlywarning score(EWS)hasbeenbroadlydemonstratedandhasbecome standardpracticeacrossnumerousEMSagencies.5,6
However,fewspecificscoresareavailableforEMS applicationtotraumapatients(eg,therevisedtraumascore [RTS];7 newtraumascore[NTS];8 thecombinationof mechanism,GlasgowComaScale,age,andarterialpressure score[MGAP];9 ortheVittelcriteria).10 However, prehospitalpoint-of-caretesting(POCT)hasbeenwidely used.11 Measurementssuchashemoglobin,baseexcess,pH, lactate,creatinine,ortheinternationalnormalizedratio (INR)providerelevantfeedback,guidingtheresuscitationof polytraumapatientsfromthe firstmomentsofEMSarrival onthescene.12,13
ThemajoradvantageofusinganEWSorPOCT,either aloneorjointly,isthepotentialstandardizationofpatient assessment,enablingEMSpersonneltorecognizehigh-risk patientswithoutobviousclinicalsymptoms.On-sceneuseof diagnosticand/orprognosticstoolsstreamlinesthedecisionmakingprocess.Specifically,thesetoolsprovideEMS personneldetailedshort-termevolutiondatathatenables themtodecidewhethertotransportthepatienttoahigher resourcefacility.ApplyingEWSintraumapatientsalso makesitpossibletostandardizeatraumapatient’ s managementthroughouttheentirehealthcaresystem.This uniformterminologysimplifiespatienttransferbetween clinicians,ultimatelyloweringtheriskofadverseevents.14,15
Thecombinedapplicationofphysiologicalparameters andanalyticalmeasureshassignificantlyimprovedthe prognosticperformanceofbothEWSandPOCTinhelping toquicklyanddecisivelyidentifyhigh-riskpatients.A particularlystrikingexampleistheSequentialOrganFailure
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Prehospitalidenti fi cationofmajortrauma patientsrequiringlife-savinginterventions hasnotyetbeenelucidated.
Whatwastheresearchquestion?
DoesmSOFA(anearlywarningscore) allowquickidenti fi cationofhigh-risk traumapatients?
Whatwasthemajor findingofthestudy?
Majorcomparisonwithp-valueand confidenceinterval
ThemSOFAscorepresentsanareaunder thereceiveroperatingcharacteristic curveof0.927(95%CI0.898 – 0.957)for life-savinginterventions.
Howdoesthisimprovepopulationhealth?
UsingmSOFAtoquicklyidentifyhigh-risk traumapatientscouldimprovetreatmentand managementoftheserapidlyevolvingand complexcases.
Assessment(SOFA)score,whichcandiscriminate multiorgandamageandisroutinelyusedinintensivecare units(ICU).16 Morerecently,theTraumasis-SOFAscoring systemisusedspecificallyforpatientswhohavebeenina trafficcollision.17 Despitetechnologicaladvances,thereisno portablePOCTcapableofmeasuringbilirubinorplateletsin theprehospitalsetting;thus,prospectiveestimationofthe SOFAscoreisnotcurrentlyavailableatthesceneorwhileen routetotheED.TheSOFAscore,whichcombines physiologicalmeasurements(GlasgowComaScale[GCS], meanarterialpressure[MAP],andpulseoximetry saturation/fractionofinspiredoxygenratio[SaFi])with analyticaldeterminations(creatinineandlactate),was developedtobeusedatthesceneorenroute.18 Intheir2010 study,GrissometalproposedtheuseofamodifiedSOFA (mSOFA)score,19 whichwasspecificallydesignedand validatedforprehospitalcare,includingphysiologicaland analyticalparametersavailablebedside.
Inthisinvestigation,ourprimaryaimwastoevaluatethe effectivenessofprehospitalmSOFAscoresforpredictingthe needforLSI(invasivemechanicalventilation,and/or administrationoftranexamicacidand/ornoradrenaline)in traumapatients.Secondaryaimsweretoexplorethe performanceofmSOFAinpredictingICUadmissionsand two-dayin-hospitalmortality,andtocomparethemSOFA
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 869 Martín-Rodríguezetal. UseofPrehospitalmSOFAScoreinTraumaPatients
withfourtraumascores(RTS,NTS,MGAP,andtheBIG [basedeficit,INR,andGCS]score).
METHODS
StudyDesignandSettings
Thiswasaprospective,ambulance-based,multicenter, training-validationstudyoftraumapatientswhowere treatedintheprehospitalsettingandsubsequently transportedtoanED.ThestudyinvolvedsixAdvancedLife Support(ALS)units,38BasicLifeSupport(BLS)units,and fourEDs.Allthefacilities distributedoverthreeprovinces (coveringinnercityareas,suburbs,andruralareas) are partofthePublicHealthSystemofCastillayLe´on(Spain), withareferencepopulationof995,137inhabitants.TheBLS unitsarestaffedbytwoemergencymedicaltechnicians (EMT),andtheALSunitsarecomposedofanemergency registerednurse(ERN),aphysician,andtwoEMTs.
BetweenJanuary1,2020–April30,2022,patientdatawas collectedfromtwoback-to-backprospectivestudies conductedunderanidenticaloperativeguideline.The institutionalreviewboardofthePublicHealthService reviewedandapprovedtheinvestigation.Thestudywas registeredintheWHOInternationalClinicalTrialsRegistry Platform(ISRCTN48326533andISRCTN49321933);we followedtheTransparentReportingofaMultivariable PredictionModelforIndividualPrognosisorDiagnosis (TRIPOD)20 guidelines(Supplementarydatap3).
Participants
Weincludedinthisstudyadulttraumapatients (>18years)whowerescreenedbytheALSphysicianand evacuatedbyALSorBLSunitstotheED.Onlycaseswith venouslineandsubsequentbloodanalysisperformedatthe sceneorenroutewereincludedinthefollow-upcohort.
Exclusioncriteriaincludedthefollowing: cardiorespiratoryarrestnotrecoveredatthescene;pregnant women;potentialdangertostaff;dischargedinsitu(after evaluationbytheALSphysician);orinabilitytoobtain informedconsentatthesite,enroute,orattheED.
ScoreSelection
ThescorescomparedwiththemSOFAfulfilledthe followingconditions:theyhavebeenvalidated;theyare availableintheprehospitalscopeofcare;andtheyarebased onthedeterminationofstandardvitalsignsorclinical observationsand/orabasicbloodtest.Theexclusioncriteria includedthefollowing:scoreswithanalreadyknownmodest predictivecapacity(eg,shockindex21),complexanatomical scales(eg,InjurySeverityScore22);systemsrequiring laboratorytestsnotavailableatthescene(eg,Emergency TraumaScore23);orscoresrequiringimagingstudies (eg,Trauma-associatedSevereHemorrhageScore24).
Finally,theselectedscoresincludedtheRTS,7 NTS,8 MGAP,9 andBIG.25
OUTCOMES
PrimaryoutcomeofthecurrentstudywasLSIperformed atthesceneorenroute.ThefollowingLSIwereincludedin theanalysis:invasivemechanicalventilation(conventional orotrachealintubationandvideolaryngoscopeincasesof difficultairway);and/oradministrationoftranexamicacid and/ornoradrenaline(anydose).Wedidnotinclude additionalvasopressorsasLSI(eg,dopamine,dobutamine orvasopressin)forthecompositeoutcomebecause noradrenalineisthestandardpharmacologicagentinALS, inaccordancewiththeinternalprocedureguidelinesofour healthsystem,whichdescribenoradrenalineasthe vasopressorofchoiceforhypovolemicshockunresponsiveto volumewithhemodynamiccompromise.Neitherdidwe includebloodadministration,sincethisprocedureis conductedexclusivelyintheEDinourhealthsystem.Asa secondaryoutcomeweincludedunplannedICUadmission, andtwo-dayin-hospitalmortality(allcause).
Cases(ie,patientsshowingaconfirmedpositiveoutcome [LSIand/orICUadmissionand/ortwo-daymortality]),were allre-checkedbythestudycoordinator.Weexcludedfrom analysiscaseswithmissingdata(complete-casestudy).
PredictorsandDataAbstraction
Beforestartingtheproject,specifictrainingwasgivento allthestaffinthecorrectuseofthedatacollectionnotebook, howtotakebloodsamples,performtheanalysis,and maintainandcleanthedevicesusedforvariablescollection, whicharestatedbelow.Thestudycoordinatorregularly visitedalltheambulancestations.
Epidemiologicalvariables(gender,age,urbanorrural area,vectoroftransfer,andinterventiontimes)were collectedbyanEMT,andbaselinevitalsigns(respiratory rate,oxygensaturation,bloodpressure,heartrate, temperature,andGCS),werecollectedbytheERNduring the firstcontactoftheALSunitwiththetraumapatient. Pulseoxygensaturation,bloodpressure,andpulsewere determinedwiththeLifePAK15monitor-defibrillator (Physio-Control,Inc,Redmond,WA),andtemperaturewith theThermoScanPRO6000thermometer(WelchAllyn,Inc, SkaneatelesFalls,NY).
Subsequently,oncethevenouslinewascannulated,a bloodsamplewasextractedbytheERNforanalysisof parameters,includingcreatinine,lactate,baseexcess,and INR.BloodanalysiswasconductedusingtheepocBlood AnalysisSystem(SiemensHealthcareGmbH,Erlangen, Germany)andCoaguChekProIISystem(Roche DiagnosticsGmbH,Basel,Switzerland).
TheALSphysiciandocumentedtheapplicationofLSI (invasivemechanicalventilation,and/oradministrationof tranexamicacidand/ornoradrenaline),andthe final prehospitaldiagnosis.Twodaysaftertheindexevent,a researchassociatefromeachhospital,collectedthefollowing hospitaloutcomesviaelectronichealthrecords(EHR)
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 870 UseofPrehospitalmSOFAScoreinTraumaPatients Martín-Rodríguezetal.
review:hospital-inpatient,ICUadmission,andtwo-day mortality(anycause).
StatisticalAnalysis
Allpatientdatawasrecordedelectronicallyinadatabase createdspecificallyforthispurpose.Datawasprospectively collectedandregisteredinadatabasegeneratedwiththe IBMSPSSStatisticsforAppleversion20.0(IBMCorp, Armonk,NY).Thecaseloadentrysystemwastest-runto deleteunclearorambiguousitemsandtoverifytheadequacy ofthedata-gatheringsystem.TomakealinkbetweenEMS medicalrecordsandthehospital’sEHR,anexactmatchwas madewith fiveofthefollowingextractors:patientname; gender;age;day,arrivaltime,andincidentcode;and ambulancecodeand/orhealthcarecardnumber.
Datawasneverde-identifiedfortheteamresponsiblefor dataanalysis.Weassessedthedescriptiveresultsandthe associationbetweenpredictorsandtheoutcomeusingthe Mann-WhitneyUtestorthechi-squaredtest,asappropriate, andtheeffectsizewasprovidedasstandardizedmean difference.Weusedabsolutevaluesandpercentagesfor categoricalvariables,andmediansandinterquartileranges (IQR)forcontinuousvariables.Theaprioristatisticalplan wastousemediansandIQRsifcontinuousvariableswerenot normallydistributed.Sample-sizecalculationswere performedbyassessingthepowercalculationbasedona specificcomparisonusingpwrpackageinR(TheRProjectfor StatisticalComputing,Vienna,Austria),consideringa statisticalpower(from1
100)of97,asignificancelevelof P = .001,andamSOFAscoredifferencebetweencasesand non-casesof84%.Thesampleusedfortrainingand validation,derivedfromacrossvalidation(ie,n/10), wasn = 76.
Priortoscoredevelopmentandvalidationthesamplewas randomlysplit,preservingtheproportionoftheoutcome variable,byusinga10-foldcross-validation,whichhasbeen usedtoovercomeoverfitting.(Furtherdetailcanbefoundin supplementarydatap4.)ThemSOFAscorevalidationand calibrationrequireda firststepof fittingalogisticregression inwhichthescore(asacontinuousvariable)wasthe predictivevariableandtheLSI,two-daymortality,orICU admissiontheoutcome.Consideringthewholecohort,we plottedtheobserveddistributionoftheoutcomesandacurve ofthepredictedprobabilityoftheoutcomeaccordingtothe mSOFAscore,includingtheconfidenceinterval(CI).
ToassessthereliabilityofmSOFAanditscomparison againstotherwell-establishedscores,weevaluatedallthe scoresinthreedifferentways:withtheirdiscriminativepower (assessedbytheareaunderthereceiveroperating characteristic[ROC]curveandtheareaundertheROC curve[AUC]);theircalibration(observedvspredicted outcomeagreement;andwithdecisioncurveanalysis[DCA], clinicalutility).Inparticular,themSOFAdiscrimination capacitywasassessedbytheAUC.Thecalibrationwasalso
performedbycalculatingthecalibrationcurve,thatis, plottingpredictedvsobservedprobabilityoftheoutcome, anddeterminingseveralmetricsassociatedwithcalibration (explainedbelow).
WeassessedthediscriminativepowerofmSOFAbyROC curveanalysisandAUC,including95%CIs,a P -valueofthe hypothesistesting(H0:AUC = 0.5).All95%CIswere obtainedbybootstrapping(2,000iterations).Weassessed furtherparametersoftheROC:specificity;sensitivity; positivepredictivevalue;negativepredictivevalue;positive likelihoodratio;andnegativelikelihoodratio.Wealso reportedthemaximumpotentialeffectivenessachievedby thescores,withtheYoudenIndex(intermsofsensitivityand specificity)servingalsoasasummaryofthewholeROC curve.WecomparedAUCsusingtheDelongtest.
Weanalyzedthegoodnessof fitofthemodelagainstthe observedprobabilityusingdifferentadjustments:logisticand nonparametric fitusingLOWESS.Wecalculatedseveral additionalstatistics:Somers’ Drankcorrelation;ROCarea; Nagelkerke-Cox-Snell-Maddala-MageeR-squaredindex; discriminationindex;unreliabilityindex;thequalityindex; Brierscore(averagesquareddifferenceinpandy);intercept, slope,maximumabsolutedifferenceinpredictedandloesscalibratedprobabilities;theaverageofthepreviousparameter; the0.9ofthepreviousparameter;andtheSpiegelhalterZ-test forcalibrationaccuracyanditstwo-tailed P -value.
WeusedDCAtocomparemSOFAwiththosescores alreadyusedinclinicalpractice.
AllstatisticalanalyseswereperformedinRversion4.0.3 usingpackagesdescribedin supplementarydatap4
RoleoftheFundingSource
Thefunderofthestudyhadnoroleinstudydesign,data collection,dataanalysis,datainterpretation,orwritingof thereport.Thecorrespondingauthorshadfullaccesstoall thedatainthestudyandhad finalresponsibilityforthe decisiontosubmitforpublication.
RESULTS
PatientCharacteristics
Inthecurrentstudy,763patientsfrom44ambulance stations(sixALSand38BLS)fulfilledtheinclusioncriteria (supplementary figureS1).Theirmedianagewas52years (IQR:37–70years),and266(34.9%)werefemale.
Theprehospital-LSIratewas14.5%(111cases),while48 cases(6.3%)weretreatedwithtranexamicacid,28(3.7%) withnoradrenaline,and92cases(12.1%)withinvasive mechanicalventilation.In69oftheprehospital-LSIpatients (62.2%),onlyoneinterventionwasperformed;two prehospital-LSIwereperformedin27patients(24.3%),and in15patients(13.5%)allthreeprehospital-LSIwere required.TraumapatientssubjectedtoprehospitalLSIwere predominantlymale,18
49years,andpolytraumatized(lifethreateninginvolvementoftwoormoresystems),witha
–
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 871 Martín-Rodríguezetal. UseofPrehospitalmSOFAScoreinTraumaPatients
LSI,life-savinginterventions; NA,Notapplicable; ALS,AdvancedLifeSupport; RR,respiratoryrate; SpO2, oxygensaturation; FiO2, fraction ofinspiredoxygen; SaFi,pulseoximetrysaturation/fractionofinspiredoxygenratio; SBP,systolicbloodpressure; DBP,diastolicblood pressure; MBP,meanbloodpressure; HR,heartrate; GCS,Glasgowcomascale; BE,baseexcess; INR,Internationalnormalizedratio; mSOFA, modifiedSequentialOrganFailureAssessment; ICU,intensivecareunit. aValuesexpressedastotalnumber(fraction)andmedians[25th percentile-75th percentile],asappropriate. bTheCohend-testwasusedforestimatedeffectsize.
cTheMann-WhitneyUtest, t-test,orchi-squaredtestwasusedasappropriate.
Total Non-LSI LSI Standardizeddifference b P-valuec No.(%)withdataa 763(100) 652(85.5) 111(14.5) N.A. N.A. Age,years 52(37–70) 52(37–70) 50(34–65) 0.086 .402 Agegroups,years 0.101 .559 18–49 349(45.7) 295(45.2) 54(48.6) 50–74 269(35.3) 232(35.6) 37(33.3) >75 145(19) 125(19.2) 20(18) Gender,female 266(34.9) 234(35.9) 32(28.8) 0.151 .149 ALS 507(66.4) 401(61.5) 106(95.5) 0.909 <.001 Zone,urban 478(62.6) 422(64.7) 56(50.5) 0.292 .004 Isochronous,min Arrivaltime 11(8–16) 11(8–16) 12(10–23) 0.361 .001 Supporttime 31(23–40) 30(22–28) 34(26–48) 0.423 <.001 Evacuationtime 12(8–20) 12(8–19) 15(10–28) 0.44 <.001 Basalvitalsigns RR,breaths/min 18(14–21) 18(14–20) 18(12–27) 0.176 .147 SpO2,% 97(95–99) 97(95–99) 93(87–97) 0.894 <.001 FiO2,% 0.21(0.21–0.21)0.21(0.21–0.21)0.21(0.21–0.21) 0.608 .031 SaFi 462(448–471)462(452–471)429(310–462) 0.952 <.001 SBP,mmHg 133(117–146)134(120–147) 121(89–142) 0.523 <.001 DBP,mmHg 80(68–90) 80(70–90) 66(55–87) 0.508 <.001 MBP,mmHg 97(85–108) 98(88–108) 86(77–104) 0.543 <.001 HR,beats/min 84(71–100) 83(70–98) 92(77–118) 0.521 <.001 Temperature, °C 36(35.7–36.4)36(35.8–36.4)35.8(34.8–36.1) 0.474 <.001 GCS,points 15(15–15) 15815–15) 9(5–14) 1.634 <.001 Lactate,mmol/L 2.42(1.64–3.54)2.16(1.45–3.09)5.67(3.25–8.71) 1.158 <.001 Creatinine,mgr/dL 0.86(0.74–1.09)0.84(0.73–1.01)1.09(0.87–1.68) 0.616 <.001 BE,mEq/L 0.6( 2.6; 1.8)0.8( 1.6;1.9) 4.6( 10; 1.5) 1.143 <.001 INR 1(1–1.1) 1(1–1.1) 1(1–1.1) 0.228 .057 mSOFA,points 1(0–3) 1(0–2) 6(4–8) 1.994 <.001 Traumamechanism 0.419 <.001 Penetrating 39(5.1) 22(3.4) 17(15.3) Blunt 724(94.9) 630(96.6) 94(84.7) Traumatype 0.343 <.001 Polytraumatized 106(13.9) 53(8.1) 53(47.7) Polycontused 83(10.9) 83(12.7) 0 Headandneck 257(33.7) 221(33.9) 36(32.4) Thorax 52(6.8) 47(7.2) 5(4.5) Abdomen-pelvic 32(4.2) 25(3.8) 7(6.3) Spinal 46(6) 45(6.9) 1(0.9) Orthopedic 156(20.4) 153(23.5) 3(2.7) Burns 31(4.1) 25(3.8) 6(5.4) Hospitaloutcomes Hospital-inpatient 372(48.8) 265(40.6) 107(94.9) 1.501 <.001 ICUadmission 162(21.2) 58(8.9) 104(93.7) 3.204 <.001 2-daymortality 47(6.2) 8(1.2) 39(35.1) 0.979 <.001
Table1. Baselineclinicalandbiomarkercharacteristicsofthestudypopulation.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 872 UseofPrehospitalmSOFAScoreinTraumaPatients Martín-Rodríguezetal.
remarkablerateofpenetratingtrauma(15.3%).OftheLSI groupcases,93.7%presentedICUadmission(104cases),and thetwo-dayin-hospitalmortalityratewas35.1%(39cases).
ThemSOFA-associatedvariablesshowedstatistically significantdifferencesbetweencaseswithprehospital-LSI andnon-LSIcases(P < .001)(see Table1).
mSOFAValidation
ThevalidationofthemSOFAscorewasperformedby ROCanalysisassessingAUCvalues.TheAUCswereas follows:0.927(95%CI0.898–0.957)forLSI;0.845(95%CI
0.808–0.882)forICUadmission;and0.979(95%CI
0.966–0.991)fortwo-daymortality.Furtherdetailsonthe modelperformancecanbefoundin supplementarytableS2
Ascanbeobservedin Figure1,thepredictiveprobabilityfor eachoutcomeasafunctionofmSOFApresentedatypical

sigmoidcurve,meaningthatthenumberofcases(forallthe outcomes)increasedwithincreasingmSOFAvalues.Curves weresteeperforLSIandICU,indicatingthatthemSOFA valueatwhichthecasesincreasedforthisoutcomewaslower thanthatformortality.
Finally,thecalibrationresultsshowedthatthebest performanceofmSOFAwasformortalityaccordingto Brier,resultingin0.06(95%CI0.063–0.067)forLSI;0.11 (95%CI0.110–0.115)forICU;and0.03(95%CI 0.019–0.049)formortality.However,whenconsideringthe slopeorthecalibration-in-the-large(orintercept),thebest performancewasforICU,followedbyLSIandmortality(in thatorder).Resultsofslopewere0.98(95%CI0.73–1.23)for LSI;1.00(95%CI0.86–1.15)forICU;and0.89(95%CI 0.48–1.30)formortality,whilethoseofcalibrationin-the-largewere0.02(95%CI 0.39–0.45)forLSI;
mSOFA,modifiedSequentialOrganFailureAssessment; ICU,intensivecareunit.
Figure1. ProbabilityofdifferentoutcomesbasedonthevalueofmSOFAinprehospitalcare:a)life-savinginterventions;b)ICUadmission; andc)two-daymortality.Thesolidlineshowsthepredictedprobabilityoftheoutcome;gray-shadowedareashowsthe95% confidenceinterval.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 873 Martín-Rodríguezetal. UseofPrehospitalmSOFAScoreinTraumaPatients
0.004(95%CI 0.24–0.25)forICU;and 0.50(95%CI 1.82–0.82)formortality.
mSOFAvsOtherScoringSystems
ThecomparisonbetweenmSOFAandtheotherscores wasassessedbythreedifferentprocedures.First,the discriminationpowerusingtheAUCcomparisonshowed thatmSOFAoutperformedtheotherscoresforallthe outcomesevaluated(Figure2);thiswascorroboratedbythe resultsfromtheDelongtest(SupplementarytableS3)in whichmSOFApresentedstatisticallysignificantdifferences vsallthescoresforalloutcomes(P -valuerangedbetween P < .01and P < .001,exceptforLSIinwhich P = .078vsRTS,and P = .061vsMGAP).Secondly,
similarlytodiscriminationanalysis,DCA(Figure3)showed ahighernetbenefitformSOFAthanotherscoresthroughout allthethresholdprobabilityandforalloutcomes,withthe exceptionofthehigherthreshold,inwhichthenetbenefitwas similarforLSIorlowerforICUadmissioncompared toRTS.
Thirdly,thecalibration-derivedmetricsshowedthat mSOFApresentedthebestperformanceforLSI.For instance,theBrierscoreofmSOFAwasthelowestcompared totheotherscoresforalltheevaluatedoutcomes. Interestingly,whenconsideringthe fittedcalibrationcurves, eitherlogisticornonparametric(LOWESS),mSOFA presentedthebest fit.Furtherdetailsonthecalibration resultscanbefoundin supplementaryFigureS4
Figure2. Discriminationanalysisresultsofeachmodel.Discriminationcapacityofthescoreswasassessedbytheareaunderthereceiver operatingcharacteristic(ROC)curve(AUC)fora)life-savinginterventions;b)intensivecareunit(ICU)admission;andc)two-daymortality. Redline = modifiedSequentialOrganFailureAssessment(mSOFA);greenline = revisedtraumascore(RTS);blueline = combinationof mechanism,GlasgowComaScale,age,andarterialpressurescore(MGAP);blackline = BIGscore;yellowline = newtraumascore(NTS).
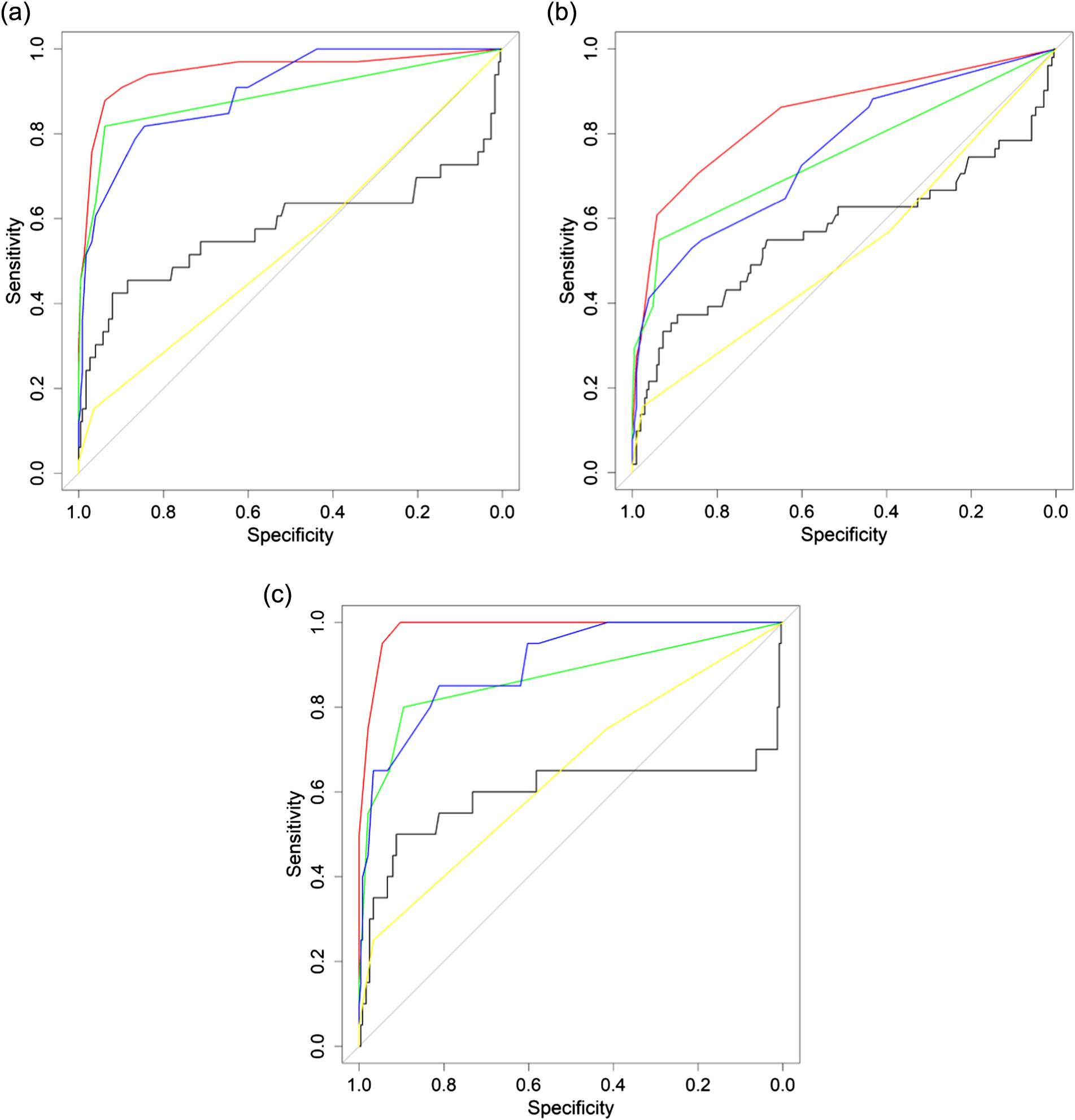
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 874 UseofPrehospitalmSOFAScoreinTraumaPatients Martín-Rodríguezetal.
DISCUSSION
Toourknowledge,thisisthe firststudytoanalyzethe predictiveabilityofprehospitalmSOFAscorestodetect high-risktraumapatientsatthesceneorenroute.The mSOFAscorepresentedanexcellentAUCforpredictionof prehospitalLSI,unplannedICUadmissions,andtwo-day in-hospitalmortality,outperformingallthescoresanalyzed.
TheX-A-B-C-D-Eresuscitationguidelinesclearlyoutline theprioritiesinprimaryassessmentandinitialcareofmajor trauma.26 Uponidentificationandcontrolofexternal bleedinghemorrhage,thenextlife-threateningpriorityisto ensureairwaypatencyand/orineffectiveventilation,coupled withquickrecognitionofsubtlesignsofshockatearlyonset thatallowrapidtreatmentstart.Consideringtheabove,in
the firstmomentspost-injury,EMSpersonnelshould prioritizetherapididentificationandresponseto hypovolemicshockofhemorrhagicoriginasatoppriority, togetherwithinitialairwaymanagementonscene.27,28
Severalscoreshavebeendevelopedtoforecasttheseverity ofatraumapatient’scondition;however,studiesevaluating thepredictiveabilityofdifferentscorestodetermine prehospitalLSIrequirementarescarce.Galvagnoetal11 analyzedtheperformanceofvenouslactatetopredict prehospitalLSI,showinganAUCof0.71.Radowskyetal29 examinedtheabilityoftheprehospital,handheld,tissue oximetertoidentifyoccultshock,withpoorresults (AUC = 0.51).Liuetal30 studiedthecapabilityofdifferent standardvitalsigns(heartrate,lowersystolicbloodpressure,
Figure3. Decisioncurveanalysisresultsofeachmodel:a)life-savinginterventions;b)intensivecareunitadmission;andc)two-day mortality.Redline = modifiedSequentialOrganFailureAssessment;greenline = revisedtraumascore);blueline = combinationof mechanism,GlasgowComaScale,age,andarterialpressurescore;blackline = BIGscore;yellowline = NewTraumaScore. BIGscore,admissionbasedeficit + internationalnormalizedratio + GlasgowComaScale.
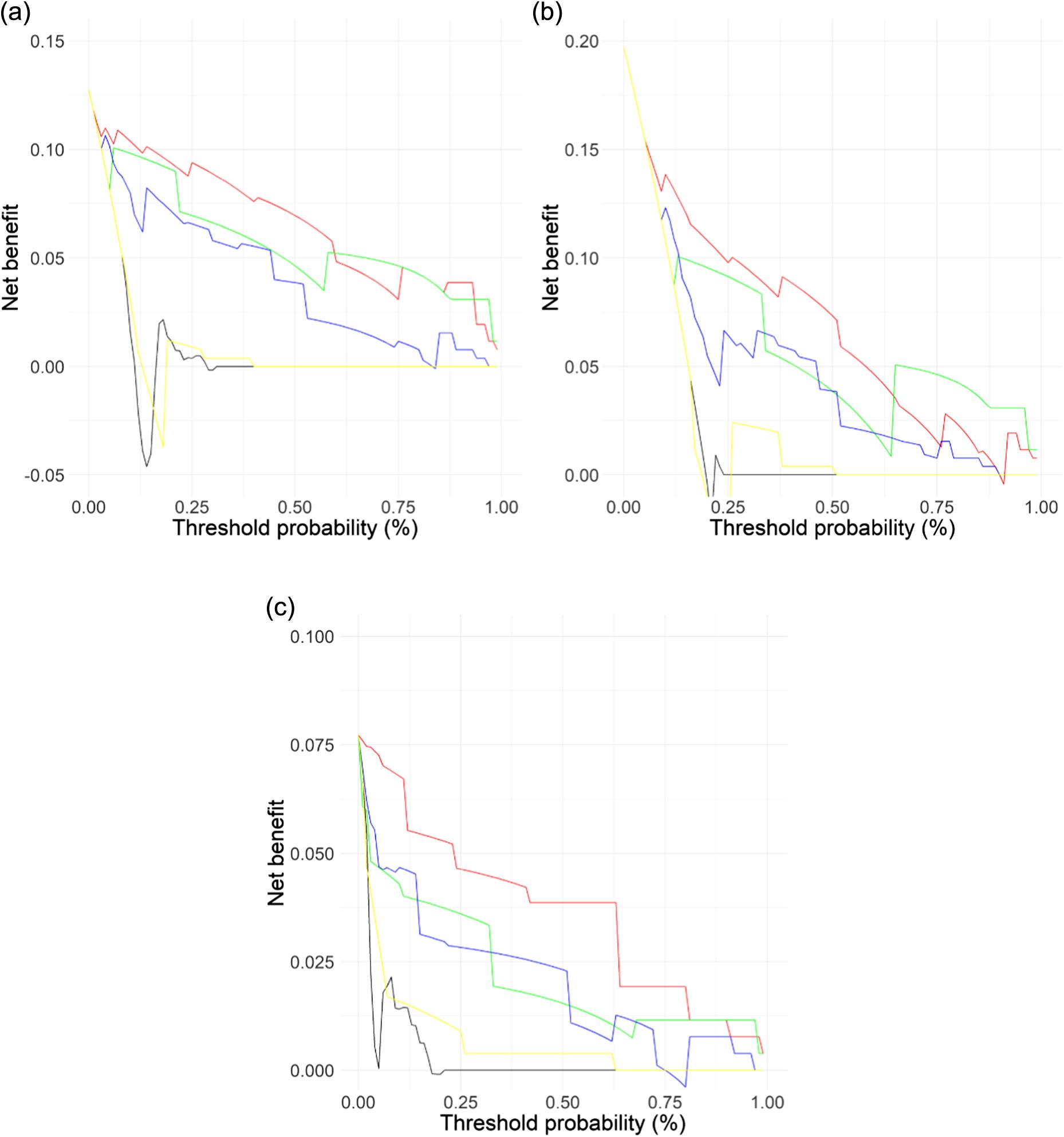
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 875
Martín-Rodríguezetal.
UseofPrehospitalmSOFAScoreinTraumaPatients
shockindex,pulsepressure,andGCScomponents),while Kumaretal31 analyzedthefeasibilitytopredictLSIofa modelbasedonheartratevariability.Inbothcasesoverall resultsweremodest(AUC = 0.72and0.75,respectively).In summary,isolatedstudieshaveanalyzedstandardvitalsigns and/ortraumascores,reportingAUCslowerthanthatofthe mSOFAscore.
ThemSOFAisa five-parametersystemassessablein prehospitalcarefromthe firstcontactwithpatients,18 which allowstheidentificationofpotentialhigh-risktrauma patients.Thisscoringsystemincludesrespiratory(SaFi), hemodynamic(MAP),neurological(GCS),andoxidative metabolism(creatinineandlactate)endpoints,providinga globaloverviewofthetraumapatient’sstatus.
LIMITATIONS
Whilethestrengthsofthepresentstudyarethelarge numberofEMSrecordsweexaminedoveralongperiodof timeandtheuseofstandardizedproceduresforthe managementoftraumapatients,aswellasthehomogeneous trainingofallEMSpersonnelinvolved,thestudydoeshave severallimitations.First,thedatawasnotblinded.To minimizebias,datawascollectedcontinuously24hoursa daythroughouttheyear,andambulancesservedbothurban andruralareas,involvingdifferentEDs.Inaddition,EMS personneldidnotknowthescoresanalyzedortheir interpretationorcalculatedrisks,andtheoutcomeswerenot knowntohospitalinvestigatorassociates.Asadouble-check setup,thestudycoordinatorauditedallnotifiedpatientswith aprimarypositiveoutcome.Second,someofthescores testedrequiredtheuseofprehospitalPOCT,whichrequiresa certaintrainingandisnotwidelyimplementedinEMS. Third,eventhoughthoracicdecompressiontechniquesare consideredtobeLSI,theywerenotincludedinthestudynor wasthereexactdataonthecrystalloidvolumeadministered. (Infuturestudiestheseinputswillberecordedtoimprove predictivecapacityandtoimprovetheidentificationofhighriskpatients.)
Fourth,theongoingstudystartedbeforethecurrent COVID-19pandemicandwasinprogress,continuously addingcasesintothedatabase.Thepotentiallong-term consequencesofCOVID-19areyettobedetermined;thus,it remainsunclearwhattheeffectofthisnewpathologyhason patientswhohavealreadysufferedthediseaseoritslongtermsequelae.Largerstudiesarerequiredtounderstandthe impactofthepandemiconmedicalemergencycare,and specificallyontraumapatients.Fifth,theinterpretationof theDCAandcalibrationresultsshouldbeinterpreted fromaqualitativepointofview,ratherthanfroma quantitative/statisticalpointofview.Theyareintendedto supporttheAUC findingsratherthanbeinterpretedalone. Finally,thecurrentstudywasdevelopedinasinglecountry, withparticularconditionsoftheSpanishhealthsystem,such asPOCTavailabilityintheEMS.Thegeneralizability
ofthisstudywillrequirefurtherstudiesindifferent healthsystems.
CONCLUSION
ThemSOFAscorecanhelpEMSpersonnelrecognize high-riskpatients.Theidentificationofthreekey outcomes life-savinginterventionsonscene,unplanned ICUadmission,andtwo-daymortality canplayacritical roleinbettermanagementoftheserapidlyevolvingand complexcases.
AddressforCorrespondence:AncorSanz-García,PhD,Universidad deCastillalaMancha,FacultyofHealthSciences,Avda.Real FábricadeSeda,s/n45600,TalaveradelaReina,Toledo. Email: ancor.sanz@uclm.es, ancor.sanz@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financialrelationshipswithanycompaniesthatarerelevanttothis study.Therearenoconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2023Martín-Rodríguezetal.Thisisanopenaccess articledistributedinaccordancewiththetermsoftheCreative CommonsAttribution(CCBY4.0)License.
See: http://creativecommons.org/licenses/by/4.0/
REFERENCES
1.PapeHC,MooreEE,McKinleyT,etal.Pathophysiologyinpatientswith polytrauma. Injury.2022;53(7):2400–12.
2.MitraB,Bade-BoonJ,FitzgeraldMC,etal.Timelycompletionofmultiple life-savinginterventionsfortraumatichaemorrhagicshock: aretrospectivecohortstudy. BurnsTrauma.2019;7:22.
3.MeizosoJP,ValleEJ,AllenCJ,etal.Decreasedmortalityafter prehospitalinterventionsinseverelyinjuredtraumapatients. JTrauma AcuteCareSurg.2015;79(2):227–31.
4.ServiáL,BadiaM,MontserratN,etal.Severityscoresintraumapatients admittedtoICU.Physiologicalandanatomicmodels. MedIntensiva (EnglEd).2019;43(1):26–34.
5.Martín-RodríguezF,Sanz-GarcíaA,Medina-LozanoE,etal.Thevalue ofprehospitalearlywarningscorestopredictin-hospitalclinical deterioration:amulticenter,observationalbase-ambulancestudy. PrehospEmergCare.2021;21(5):597–606.
6.WilliamsTA,TohiraH,FinnJ,etal.Theabilityofearlywarningscores (EWS)todetectcriticalillnessintheprehospitalsetting:asystematic review. Resuscitation.2016;102:35–43.
7.FilipescuR,PowersC,YuH,etal.Improvingtheperformanceofthe RevisedTraumaScoreusingShockIndex,PeripheralOxygen Saturation,andTemperature:aNationalTraumaDatabasestudy2011 to2015. Surgery.2020;167(5):821
8.
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 876 UseofPrehospitalmSOFAScoreinTraumaPatients Martín-Rodríguezetal.
8.JeongJH,ParkYJ,KimDH,etal.Thenewtraumascore(NTS):a modificationoftherevisedtraumascoreforbettertraumamortality prediction. BMCSurg.2017;17(1):77.
9.CassignolA,MarkarianT,CotteJ,etal.Evaluationandcomparisonof differentprehospitaltriagescoresoftraumapatientsonin-hospital mortality. PrehospEmergCare.2019;23(4):543–50.
10.CotteJ,CourjonF,BeaumeS,etal.Vittelcriteriaforseveretrauma triage:characteristicsofover-triage. AnaesthCritCarePainMed 2016;35(2):87–92.
11.GalvagnoSM,SikorskiRA,FloccareDJ,etal.Prehospitalpointofcare testingfortheearlydetectionofshockandpredictionoflifesaving interventions. Shock.2020;54(6):710–6.
12.Martín-RodríguezF,L´opez-IzquierdoR,Medina-LozanoE,etal. Accuracyofprehospitalpoint-of-carelactateinearlyin-hospital mortality. EurJClinInvest.2020;50(12):e13341.
13.SchöttU.Prehospitalcoagulationmonitoringofresuscitationwithpointof-caredevices. Shock.2014;41(Suppl1):26–9.
14.Martín-RodríguezF,L´opez-IzquierdoR,DelPozoVegasC,etal. Amulticenterobservationalprospectivecohortstudyofassociationof theprehospitalnationalearlywarningscore2andhospitaltriagewith earlymortality. EmergMedInt.2019;51478008.
15.Durantez-FernándezC,Martín-ContyJL,Medina-LozanoE,etal.Early detectionofintensivecareneedsandmortalityriskbyuseof fiveearly warningscoresinpatientswithtraumaticinjuries:anobservational study. IntensiveCritCareNurs.2021;67:103095.
16.McCarthySL,StewartL,ShaikhF,etal.PrognosticvalueofSequential OrganFailureAssessment(SOFA)scoreincriticallyillcombat-injured patients. JIntensiveCareMed.2022;37(11):1426–34.
17.JoS,JeongT,ParkB.Evaluationofthesequentialorganfailure assessmentscoreandnewlyintroducedcriteria-Traumasis-intraffic collisionpatients. AmJEmergMed.2022;51:98–102.
18.Martín-RodríguezF,Sanz-GarcíaA,DelPozoVegasC,etal.Timefora prehospital-modifiedSequentialOrganFailureAssessmentscore:an ambulance-basedcohortstudy. AmJEmergMed.2021;49:331–7.
19.GrissomCK,BrownSM,KuttlerKG,etal.AmodifiedSequentialOrgan FailureAssessmentscoreforcriticalcaretriage. DisasterMedPublic HealthPrep.2010;4(4):277–84.
20.CollinsGS,ReitsmaJB,AltmanDG,etal.TransparentReporting ofaMultivariablePredictionModelforIndividualPrognosisor Diagnosis(TRIPOD):theTRIPODstatement. AnnInternMed 2015;162(1):55–63.
21.HaradaM,TakahashiT,HagaY,etal.Comparativestudyonquick SequentialOrganFailureAssessment,systemicinflammatoryresponse syndromeandtheshockindexinprehospitalemergencypatients: single-site retrospectivestudy. AcuteMedSurg.2019;6(2):131–7.
22.GalvagnoSM,MasseyM,BouzatP,etal.Correlationbetweenthe RevisedTraumaScoreandInjurySeverityScore:implications forprehospitaltraumatriage. PrehospEmergCare 2019;23(2):263–70.
23.ParkHO,KimJW,KimSH,etal.UsabilityverificationoftheEmergency TraumaScore(EMTRAS)andRapidEmergencyMedicineScore (REMS)inpatientswithtrauma:aretrospectivecohortstudy. Medicine (Baltimore).2017;96(44):e8449.
24.SperryJL,GuyetteFX,BrownJB,etal.Prehospitalplasmaduringair medicaltransportintraumapatientsatriskforhemorrhagicshock. NEnglJMed.2018;379(4):315–26.
25.YoonTJ,KoY,LeeJ,etal.PerformanceoftheBIGscoreinpredicting mortalityinnormotensivechildrenwithtrauma. PediatrEmergCare 2021;37(12):e1582–88.
26.KondoY,FukudaT,UchimidoR,etal.AdvancedLifeSupportvs. BasicLifeSupportforpatientswithtraumainprehospitalsettings: asystematicreviewandmeta-analysis. FrontMed(Lausanne) 2021;8:660367.
27.FecherA,StimpsonA,FerrignoL,etal.Thepathophysiologyand managementofhemorrhagicshockinthepolytraumapatient. JClin Med.2021;10(20):4793.
28.TranA,YatesJ,LauA,etal.Permissivehypotensionversus conventionalresuscitationstrategiesinadulttraumapatientswith hemorrhagicshock:asystematicreviewandmeta-analysisof randomizedcontrolledtrials. JTraumaAcuteCareSurg 2018;84(5):802–8.
29.RadowskyJS,DuBoseJJ,ScaleaTM,etal.Handheldtissueoximetry fortheprehospitaldetectionofshockandneedforlifesaving interventions:technologyinsearchofanindication? AirMedJ 2019;38(4):276–80.
30.LiuNT,HolcombJB,WadeCE,etal.Inefficacyofstandardvital signsforpredictingmortalityandtheneedforprehospitallife-saving interventionsinblunttraumapatientstransportedviahelicopter: arepeatedcallfornewmeasures. JTraumaAcuteCareSurg 2017;83(Suppl1):S98–S9S103.
31.KumarA,LiuN,KohZX,etal.Developmentofaheartratevariabilityand complexitymodelinpredictingtheneedforlife-savinginterventions amongsttraumapatients. BurnsTrauma.2019;7:12.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 877 Martín-Rodríguezetal. UseofPrehospitalmSOFAScoreinTraumaPatients
SOCIAL EMERGENCY MEDICINEAND POPULATION HEALTH
SocialDeterminantsofHealthinEMSRecords: AMixed-methodsAnalysisUsingNaturalLanguage ProcessingandQualitativeContentAnalysis
SusanJ.Burnett,MS,EMT-P*
RachelStemerman,PhD†
JohannaC.Innes,MD*
MariaC.Kaisler,MD*
RemleP.Crowe,PhD,NREMT†
BrianM.Clemency,DO,MBA*
SectionEditor: DanielJoseph,MD
*JacobsSchoolofMedicineandBiomedicalSciences,UniversityatBuffalo, TheStateUniversityofNewYork,DepartmentofEmergencyMedicine, Buffalo,NewYork
† ESO,Austin,Texas
Submissionhistory:SubmittedSeptember30,2022;RevisionreceivedApril17,2023;AcceptedApril10,2023
ElectronicallypublishedAugust8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59070
Introduction: Socialdeterminantsofhealth(SDoH)areknowntoimpactthehealthandwell-beingof patients.However,informationregardingthemisnotalwayscollectedinhealthcareinteractions,and healthcareprofessionalsarenotalwayswell-trainedorequippedtoaddressthem.Emergencymedical services(EMS)professionalsareuniquelypositionedtoobserveandattendtoSDoHbecauseoftheir presenceinpatients’ environments;however,thetransmissionofthatinformationmaybelostduring transitionsofcare.DocumentationofSDoHinEMSrecordsmaybehelpfulinidentifyingandaddressing patients’ insecuritiesandimprovingtheirhealthoutcomes.Ourobjectiveinthisstudywastodetermine thepresenceofSDoHinformationinadultEMSrecordsandunderstandhowsuchinformationis referenced,appraised,andlinkedtootherdeterminantsbyEMSpersonnel.
Methods: UsingEMSrecordsforadultpatientsinthe2019ESODataCollaborativepublic-useresearch datasetusinganaturallanguageprocessing(NLP)algorithm,weidentifiedfree-textnarratives containingdocumentationofatleastoneSDoHfromcategoriesassociatedwithfood,housing, employment,insurance, financial,andsocialsupportinsecurities.FromtheNLPcorpus,werandomly selected100recordsfromeachoftheSDoHcategoriesforqualitativecontentanalysisusing groundedtheory.
Results: Ofthe5,665,229recordsanalyzedbytheNLPalgorithm,175,378(3.1%)wereidentifiedas containingatleastonereferencetoSDoH.ReferencestothoseSDoHwerecenteredaroundthesocial topicsofaccessibility,mentalhealth,physicalhealth,andsubstanceuse.Therewereinfrequentexplicit referencestootherSDoHintheEMSrecords,butsomerelationshipsbetweencategoriescouldbe inferredfromcontexts.Appraisalsofpatients’ employment,food,andhousinginsecuritieswere mostlynegative.Narrativesincludingsocialsupportand financialinsecuritieswerelessnegatively appraised,whilethoseregardinginsuranceinsecuritiesweremostlyneutralandrelatedtoEMS operationsandprocedures.
Conclusion: ThesocialdeterminantsofhealthareinfrequentlydocumentedinEMSrecords.Whenthey areincluded,theyareinfrequentlyexplicitlylinkedtootherSDoHcategoriesandareoftennegatively appraisedbyEMSprofessionals.Giventheiruniquepositiontoobserveandsharepatients’ SDoH information,EMSprofessionalsshouldbetrainedtounderstand,document,andaddressSDoHintheir practice.[WestJEmergMed.2023;24(5)878–887.]
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 878
INTRODUCTION
Socialdeterminantsofhealth(SDoH),includinghousing, employment,education,income,neighborhoods,accessto healthcare,andeducationareknowntoimpactthehealth andwell-beingofpatients,yetthesevariablesarenotalways accountedforduringinteractionswiththehealthcare system.1,2 Whileunmetbasicsocialneedshavemeasurable impactsonindividuals,communities,andthepublichealth system,1,3,4 littleguidanceexistsforhealthcarecliniciansto addresspatients’ SDoH,andcurrentstrategiesfocusonthe populationandpolicylevels.5 Greaterattentionisneededto individual-levelsocialissues,asleavingthemunaddressed leadstopoorclinicaloutcomes,healthdisparities,and increasedhealthcarecosts.3 Patientswithunmetsocialneeds frequentlyaccesshealthcarethroughhospitalsand, particularly,emergencydepartments(ED)only,warranting anincreasedfocusonSDoHinemergencymedicine(EM).6
8 Emergencymedicalservices(EMS)professionals operatingattheintersectionofpublicsafety,publichealth, andhealthcareareuniquelypositionedtoobserveandattend toSDoHinproductiveandinfluentialways.9 Theyusetheir perceptionsofpatients’ socialandphysicalenvironmentsto aidinmedicaldecision-making,suchasdeterminingwhether totransportthepatienttothehospitalornot.10 Additionally, conveyinginformationtoEDstaffaboutfactorssuchas unsafehousing,lackofaccesstomedications,orinabilityof patientstosafelycareforthemselvescanultimatelyaffect whetherornotthatpatientcanbesafelydischargedfromthe ED.Nevertheless,informationexchangethroughverbal hand-offsfromEMSprofessionalstoEDnursingstaffand subsequentreportingtoadditionalhospitalpersonneloften resultsinlostinformationandmiscommunication.11–19
ElectronichealthrecorddocumentationbyEMSisa reliablechannelthroughwhichinformationaboutapatient’ s SDoHcanbesharedwithallhealthcarepersonnelassociated withthepatient’shospitalization.20 Thereisapaucityof SDoHinformationinEMSrecordsforpediatricpatients,21 butthepresence,appraisal,andconnectionsofSDoH informationinEMSrecordsforadultpatientsisunknown. Ourobjectiveinthisstudywastodeterminethepresenceand frequencyofSDoHdocumentationinadultEMSrecords andunderstandthewaysinwhichthoseinsertionsare referenced,appraised,andlinkedtootherdeterminants.
METHODS
StudyDesignandSetting
Weretrospectivelyanalyzed9-1-1recordsforadult patients(≥18years)inthe2019ESODataCollaborative public-useresearchdataset.TheESODataCollaborative consistsofde-identifiedprehospitalelectronicpatientcare recordscreatedbyEMSpersonnelduringthecourseof patientcare.AllEMSagenciesthatcontributetothedataset agreetosharetheirde-identifieddataforresearchand benchmarking.Annualresearchdatasetsaremadeavailable
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Theabilityofemergencymedicalservices (EMS)personneltoassesspatients ’ social determinantsofhealth(SDoH)canhavea greatimpactonpatientcare.
Whatwastheresearchquestion?
Wesoughttoevaluatethepresence,appraisal, andrelationshipsofSDoHdocumentationin EMSrecords.
Whatwasthemajor findingofthestudy?
Of5,665,229adultpatientEMSrecordswe analyzed,3.1%wereidenti fi edascontaining atleastonereferencetoSDoH.
Howdoesthisimprovepopulationhealth?
UnderstandinghowEMSpersonnelrecognize anddocumentpatients ’ SDoHiskeyto identifyingtheirdiverseneedsandexpanding out-of-hospitalcareoptions.
freeofchargefollowingaproposalprocessandreviewbyan institutionalreviewboard(IRB).Weselectedthisdatabase forthediversityofincludedpracticesettingsandtheability torequestfree-textnarratives.In2019,thisdatabase containedmorethaneightmillionrecordsfrom1,322EMS agencieswithencountersacrossallfourUSCensusregions (South:58%;Midwest:22%;West:16%;andNortheast:5%) and6%ofencountersoccurringinruralsettings.Atotalof 31%ofencountersoccurredincommunitiesclassifiedwithin themostvulnerablequartileofsocioeconomicstatusbased ontheUSCentersforDiseaseControlandPrevention’ s socialvulnerabilityindex.22 Thisstudywasdesignatednot humansubjectsresearchbytheStateUniversityofNew YorkatBuffaloIRB.
SelectionofCases
Allcases,regardlessofcomplaintordisposition,were screened.Weusedamultilabelclassificationmachinelearningmodelwhich,whenidentifyingSDoHtopics,has areaunderthecurvereceiveroperatingcharacteristicsof 93.9.23 Thisnaturallanguageprocessing(NLP)algorithm hasaframeworkofapplicationstoEMandEMS records.21,23 Byapplyingthisalgorithm,weidentified free-textnarrativescontainingdocumentationofat leastoneSDoHfromcategoriesassociatedwithfood, housing,employment,insurance, financial,andsocial supportinsecurities.
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 879 Burnettetal. EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing
MeasuresandAnalysis
Weperformeddescriptivestatisticalanalysisand randomizationofrecordsforqualitativeanalysisusingStata MPversion17.0(StataCorpLLC,CollegeStation,TX). FromthecorpusproducedbytheNLPalgorithm,arandom sampleof100narrativeswaschosenfromeachdeterminant categoryforqualitativecontentanalysis.Usingan interpretiveparadigm,24 thethreestudyteammembersread eachnarrativetounderstandthe first-personperspectivesof theEMSprofessionalswhodocumentedtheirinteractions withpatientsintherecordstheykept.Thisapproachwas necessarytofacilitateahermeneuticalapproachand understandthesocialconstructionofthoseEMS professionals’ experiencesonthecallsaboutwhichthey documented.Teammembersusedagroundedtheory framework24–26 todescribethecontentfoundinthe EMSrecords.
Threeresearchers(JCI,anEDattending,EMSphysician, andparamedic;MCK,anEDattendingandEMSfellow; andSJB,aparamedicandEMSeducator)reviewed narratives,performedprimarycodingtounderstandthe contentoftheEMSrecords,andfurtherimmersed themselvesinthedatabydiscussingtheir findingsforeach categorywiththeotherqualitative-analysisstudyteam members.24,27 Duringthisdataimmersionphase,codeswere developed.Forexample,patientswhoweredocumentedas nothavingeateninseveraldayswerecodedasfoodinsecure (iftheircaseswerenototherwisecategorizedinthefood insecuritydeterminantcategorybytheNLPcorpus),or patientswhoreportedtheycouldnotaffordmedications werecodedas financiallyconstrained.Then,usingthe constantcomparativemethod,24,28 researchersorganizedthe primarycodesintosecondarycodestosynthesizesocial topicsillustratedbythedatathroughoutthedeterminant categories.Forexample,patientswhoreported financial constraintswerecategorizedashavingaccessibility problems.Researchersfurthercollaboratedtoassurethatthe contentoftheEMSrecordswasrepresentedbythesocial topicsandeachconceptwasrobustlysupportedbydata.29
Inaseparateroundofpurposivecoding,researchers lookedfordocumentationofotherinsecuritiesineach determinantcategorytodeterminetherelationship, frequency,anddirectionalityoftheirreference.Forexample, ifanarrativewasdeterminedbytheNLPcorpustocontain informationaboutsocialsupportinsecurities,butthepatient wasdocumentedasnothavingeateninseveraldays,they werecodedasfoodinsecure,asreferredtointhesocial supportcategory.Additionally,theteammembers qualitativelyappraisedeachnarrativetoidentifythevalence ofthenarrativesasameansoffurtherunderstandingthe EMSprofessionals’ perspectives.Tolimitpotential perceptionsofbias,thequalitativeresearchersfrequently checkedinwiththemselvesandtheothersasameansof reflexivity.24,28 Theyverifiedthattheirinterpretationsand
modelswererepresentativeofthedataandthattheirownand theothers’ experiencesandbiasesdidnotresultin misinterpretation.Theyalsocollaborativelybuiltmodels andinterrogatedtheirdatatoassuretheir findings werestronglysupportedbythedatafromtheEMS recordnarratives.
RESULTS
Of5,665,229recordsanalyzedbytheNLPalgorithm, 175,378(3.1%)wereidentifiedascontainingatleastone referencetoaSDoH.Oftherecordsinthiscorpus,171,740 (97.93%)containedonlyoneidentifiablereferencetoSDoH, while3,580records(2.04%)containedtwoidentifiable references;57(0.03%)containedthreeidentifiablereferences; andoneoftherecords(<0.01%)containedfouridentifiable referencestoSDoH.Recordscontainingappearancesof SDoHinthecorpuswereasfollows:housing(52.28%); employment(33.06%);general financial(8.04%);insurance (4.73%);socialsupport(3.86%);andfood(0.14%).
SocialTopicsIllustratedinEmergencyMedicalServices Records
SimilarSDoHtopicswereidentifiedthroughoutthe varioussocialdeterminantcategories.TheseSDoHtopics wereaccessibility,mentalhealthconcerns,physicalhealth concerns,andsubstanceuse.Examplesofthesocialtopics’ appearancesineachdeterminantcategorycanbefoundin theTable.
Accessibility
Alldeterminantcategoriesincludeddocumentationof concernsaboutpatients’ lackofaccesstoservicesorgoods, oftenbecauseofaninabilitytoaffordorphysicallygetto theirneededinterventions.Patientswithemployment/ incomeinsecuritiesweredocumentedasunabletoaffordsafe housing,medications,ormedicalcare.AttendingEMS professionalslinkedthese financialconstraintstothecallsfor help,particularlywhenambulanceswereusedasameansof transportationorfacilitatorsforadditional,non-urgentcare, suchasaccesstomedications,treatments,orsocialservices. Itwasalsonotedthat financialbarrierstoaccess compoundedexistinghealthconditionsbecausepatients couldnotaffordnecessarymedicationsorfollow-upcare. Whenotherpatientswithdocumented financialinsecurities encounteredEMSfornon-chronicconditions(eg,motor vehiclecollisionsorfalls),theyrefusedtreatmentand transportbyEMSbecauseofreportedinabilitiestoafford ambulanceorhospitalbills.
Whendocumentingfoodinsecurities,EMSpersonnel wrotethatpatientscouldnotreadilyaffordoraccess nutritiousfoodstuffs.Insomecases,patientswerereportedas selling,skipping,ormisusingmedicationstodivertfundsto theirfoodbudgets.Housinginsecurityinformationwas documentedbecauseofpatients’ lackofsafeorpermanent
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 880 EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing Burnettetal.
SocialTopics
Table1. Representativequotesforeachsocialtopicwithineachdeterminantcategory.
AccessibilityMentalhealthPhysicalhealthSubstanceuse
“ Herelayshewasonameth bingeovertheweekendandfeels tiredbutneedstobeheretoget hisfoodstampsfortheweek. ”
“ < Thepatient > statesshe vomitedyesterdayandherchest hurtstoday ::: shewenttoWIC todaytogetfoodatthefood bank. ”
“ < Thepatient > advisedthathe wassuicidalbecausehis roommateshadbeenbullying himbytakinghisbelongings, includinghisphone,foodstamps, etc. < He > alsoadvisedthathe wasfeelinghomicidal,butthat thosefeelingshadpassed. ”
“ She hadbeenstandinginline outside < thefoodbank > for approx.30min,feltlightheaded < sic > ,andpassedout ::: states shehasn ’ teatensince yesterday. ”
Dispatchedtoamotelfora stroke: “ < thepatient > is homelessbutcametostaywith hersister
< thepatient > admittedtosmokingmarijuana thismorning
Sheadvised < of medicalhistoryincluding > drug useandshehasn ’ tdrank < sic > alcoholinseveraldays ::: or eateninafewdays. ”
“ < Thepatient > stateshefelt dizzyandwenttogroundfrom seatedposition. < Thepatient > stateshefeels fi neandis refusingalltreatmentor transport
< he > statesheisa diabeticbut < cannot > afford medicalbill < s > < His mother > statesshewilltakehimto theED. ”
Afterreceivingnaloxone, “ she begantocomearound.She admittedtoalcoholusebutno otherdrugs ::: shewantedto signoutofthehospitalbeforeshe accumulatedanybillsbecause shefelttheycouldnotafford them. ”
“ Thepatientstatedshehasa historyofCOPDandhad complications < with > breathing forthepast12hours ::: The patientstatedsheisnormallyon homeoxygenbuthasbeen unabletoaffordhermedications thismonth. ”
ThepatientleftanEDforaheroin overdose
“ patientbecame belligerentandaggressivewhen askedaboutdrugusesince leaving < hospital > patientstated theblood < onhisface > wasfrom himvomitingbloodandthe abrasionswerefor < an > allergic reactiontothe < heroin > ::: patientdoesnothaveinsurance. ”
( Continued onnextpage )
Food
SDoH categories
Patientlivinginacommunity facility “ startedhaving hallucinations
< Thepatient > wastalkingaboutbabygeese thatstaffdidnotsee. ”
Maleatdaylaborstaf fi ngbuilding “ wasstandingnexttothecounter andbeganhavingaseizure < thepatient > stateshedoes haveahxofseizuresandhas beenoffhisKeppraforquite sometimenow, ‘ stateshecan ’ t affordit. ’”
Employment/ income
Arepresentativefromthe patient ’ sbankcalledbecausethe patient “ hadmadesuicidal commentstothemduringa phoneconversationinvolvinga bill ::: < thepatient > statesthat sheisdepressedaboutthe passingofherhusbandandhas beenhaving fi nancialissuesas well. ”
FinancialThepatientpresentedas “ hyperglycemic,hypertensive, < withalteredmentalstatus > ::: Hehasahistoryofhypertension anddiabetes,butitisnot controlledwithmedications,ashe hasbeenunabletoaffordthem forseveralmonths. ”
AfteranMVC,apatient complainedof “ lowerback pain
Patientstatedshe wantedtobecheckoutbyEMS butrefusetobetransportbyEMS duetonoinsurance. ”
Callforpsychiatriccomplaints andcrewfoundthepatient requestingassistance “ gettingher Medicaid
ptwasbeing uncooperativeandyelling angrily : ptrefused < transport > , becomingangryagainand statingshedidn ’ twanttogoto theEDandthatshejustwanted herMedicaidagain. ”
InsurancePatient “ reportingaheadache thatstartedlastnightat1900 hoursduetowithdrawalsfrom Depakoteandamitriptyline.She reportsshehasbeenoutapprox. oneweekduetothecost becauseshelostherMedicaid. ”
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 881 Burnettetal. EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing
Table1. Continued.
SocialTopics
AccessibilityMentalhealthPhysicalhealthSubstanceuse
Anelderlyfemalewholivedalone wascheckedonbyafriendwho found herstatingshehad “ progressivelybeenfeeling weakeroverthepastweek ::: pt isnormallyabletowalkandtake careofherselfwithno assistance.
” Thepatient ’ sfriend alsorevealedthepatient “ isan alcoholicandwasdrinkingheavily upuntiloneweekago. ”
Thepatientcalled911forchest painandreportedinability “ to sleep ::: nauseaandfeltlikeshe mightfaint.Shewaitedtoseeif shewouldimprove.astimewent by,shestatesshebecamemore worriedand fi nallydecidedtocall 911. ” Sherefusedtransportand “ admitsheranxietywasa signi fi cantfactorinhercalling 911.Ptfrequentlycalls911.Pt livesalone. ” Hervisitingnurse wasduesoonandthe “ patient doesnotbelievehernursewill makehergoassheisfeeling better. ”
“ Patientadvisedheisaddictedto methandwantstogethelpwith detox. ” Uponarrivingthe homelessshelter, “ hedidabout½ gramofmethabouttwohours ago ::: heattemptedtospray ‘ bleachbathroomcleaner ’ inhis mouthtoassisthiminpassinga drugtest. ”
“ Founda < femalepatient > at localwomen ’ sshelterwithc/cof contractions,abdominalpain. < Thepatient > statessheis34w pregnantwithtwins. ”
’ sfriendreported, “ she startedhidingindifferentplaces inthehouse ::: < thenwent > into aneighbor ’ sgarage < to > hide fromherfriend ::: ” Whena policeof fi cerarrived,thepatient “ statedshedidnotwanttobe shotandputherhandsoverher headasifshewastoldtoraise herhands. ” Afterspeakingwitha mentalhealthprofessionalon scene, “ afamilyfriendcameand statedthatshewouldtake hertothehospitalandpickup hermedication. ”
Thepatient
Patient ataphysician ’ sof fi cewas foundhypertensive. “ Thepatient ’ s niecerelatedthattherehasbeen aproblemwiththepatient ’ s pharmacyand < themedications havenotbeeninstock > . ” The niecealsoreportedthepatient livesaloneand,whileshechecks onhim, “ shefeelsthatheisnot takingthembecausehedoesn ’ t rememberto < takehis medications > ”
Social support
Homelessshelterstaffcalled becausethepatient “ waswalking aroundwithbrokenglassbottles andwasparanoid. ” Thepatient was “ hyperparanoid.Andstated, ‘ theyaretryingtokillme. ’ < The patient > advisedthat ‘ someputa hit ’ outonherandthatsomeone hasbeenfollowingher. ”
HousingCallforpatientatfacilitywho seized: “ staffstates < thepatient waswithout > hismedicationsx1 week. < Thepatient > statesthey werestolenfromhimwhileheas atthehomelesscenter.
”
Approx., approximately; min,minute; WIC, Women,InfantsandChildren; hx, history; ED, emergencydepartment; pt, patient; MVC, motorvehiclecollision; EMS, emergency medicalservices; w ,weeks.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 882 EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing Burnettetal.
housing,whichmayhavepresentedproblemsupon discharge.Insuranceinsecuritiesweredocumentedbecause ofalackofaccesstohealthinsurance,sometimessecondary tolackofemployment;however,moreoften,EMSpersonnel wroteaboutpatients’ usingthe9-1-1systemtoexpresstheir desirestoobtaininsuranceorcarecoveredbyinsurance. Thesepatientsexplicitlyrequestedhelpinsigningupfor insuranceorreferralstoothersectorsofthehealthcare system,andinonecaseapersoncalled9-1-1fortransportto afacilitytohaveanalreadyprescribedmedicalprocedure becausetheirinsurancewouldnototherwisecoveritasan outpatienttreatment.Inthedocumentationofsocialsupport insecurities,patientslackedfamilymembers,friends,or healthcarepersonneltoaidinsafelycaringfortheir conditions,accessingfood,or findingsafeliving environments.Whenstrongsocialsupportwasavailable, accesstoresourcesandassistancewasclearlydocumented inthisdeterminantcategory.
MentalHealthConcerns
Whenmentalhealthconcernsweredocumented, regardlessofdeterminantcategory,EMSprofessionals conveyedtheywereprecipitatedbytheinsecurities.Patients withemploymentandfoodinsecuritiesexpresseddepression orsuicidalitywhilepatientswithhousinginsecurities primarilydescribedanxiety.Thosewithdocumented financialandinsuranceinsecuritiesalsoreportedsuicidality, buttheEMSprofessionalsexplicitlylinkedthecauseof financialconstraintsasongoingexpensesofchronichealth
conditions.Additionally,therewerecasesofdocumented elderor financialabuseperpetratedonorbypatientswho interactedwithEMS.Thosewithsocialsupportinsecurities wereprimarilyanxiousornervousaboutlivingalone,but theseissuesoftenwerenotthereasonsforwhythecallswere madeforemergencyservices.
PhysicalHealthConcerns
Patientswithemploymentandhousinginsecuritieswere oftenfoundoutside,exposedtotheelements,andwith complaintsrelatedtothoseconditions.Forexample,many complainedofpainintheirlegsorbacksthatcouldhavebeen attributedtotheirfrequentwalkingorhot-orcold-related issues.Someofthesecaseswereresultsofcallsforother conditions,butEMScrewsoftenfoundthesepatientswere moreinterestedinshelterthanmedicalcareatthehospital. Thosewithfoodinsecuritiescomplainedofweakness, hypoglycemia,ornearorcompletedsyncope,particularly whilestandinginline,awaitingaccesstoafoodbank.Some reportedbeingwithoutfoodbecauseof financialproblems, butothersreportedtheyhadnootherwayofaccessinggoods withoutcommunityresources.Insomecases,patients reportedprioritizingaccessingmedicationsoverfood.Those with financialandinsuranceinsecuritiesmostoften complainedofmanifestationsoftheirchronicconditionsand inabilitytotreatthem.Insomecases,patientswithboth determinanttypeshadacutehealthconcernsandmanyhad diagnoses,buttheycouldnotaffordorotherwiseaccessthe prescribedtreatments.Patientswithsocialsupport
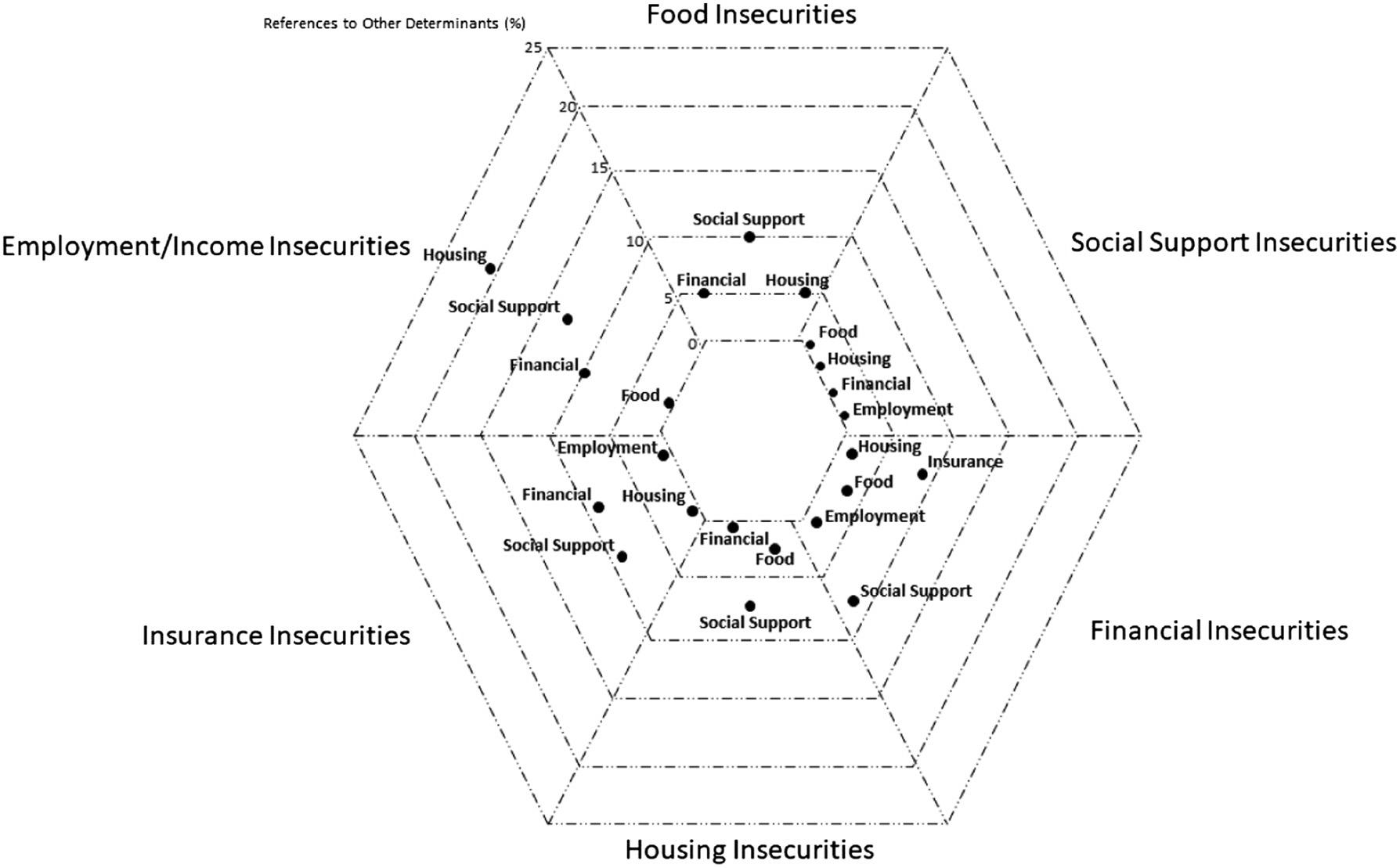
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 883 Burnettetal. EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing
Figure1. Explicitreferencestootherdeterminantcategoriesincharts(%).
insecuritiesmostoftencomplainedofacutemedical-or trauma-relatedissuesandaninabilitytoproperlyaddress them.Thesepatientsweremostoftenelderlypatientswho complainedofweaknessandfalls.
SubstanceUse
Patientswithdocumentedemploymentandhousing insecuritiesweremoreoftendescribedtobeusingor withdrawingfromvarioussubstances.Thosewithfood insecuritieswerealsodescribedasengaginginheavyuseof substanceswhiletheirabilitytoaccessornotaccessfoodwas documented.Documentationofalcoholusewithfood, financial,housing,insurance,andsocialsupportinsecurities wererarelyassociatedwithpatients’ complaintsor conditions,buttheywerefrequentlywrittenaboutaspart ofthescene-settingdescriptions.
RelationshipsBetweenDeterminantCategories
Withinthesocialdeterminantscategories,EMSpersonnel sometimesdocumentedlinkstootherdeterminant categories.Forexample,whenachartwas flaggedbecauseof adocumentedfoodinsecurity,EMSpersonnelincluded informationaboutconcurrenthousing, financial,orsocial supportinsecurities.(SeeFigureforarticulatedrelationships betweendeterminantcategories.)Someoftheserelationships wereunidirectional(eg,insuranceinsecuritieswerelinkedto socialsupportinsecurities,butsocialsupportinsecurities werenotlinkedtoinsuranceinsecurities),althoughthere werefrequentbidirectionalreferralsbetweendeterminants butforvaryingreasons.Forexample,patientswith financial insecuritiesrefusedEMStreatmentandtransportbecause theyweredocumentedasreportingalackofinsurance,but patientswithinsuranceinsecuritiesrequestedEMS transportationbecausetheycouldnotaffordalternative treatmentortransport.
Mostoften,however,theotherdeterminantswerenot explicitlyreferencedinthedocumentation,butplausible explanationscouldbeinferredfromcontext.Forexample,in thecaseofapatientwithhousinginsecurity,theEMS professionaldocumentedthepatienthadnoteatenortaken theirmedicationsinseveraldays.Theseelementscouldbe indicativeoffood,insurance,or financialinsecurities,but theywerenotexplicitlycited.
AppraisalofEMSProfessionals’ Perspectives
WhenEMSprofessionalswroteaboutemployment,food, andhousinginsecurities,mostoftheappraisalswerenegative andappearedtodiscursivelypositionthepatientsasatfault fortheir9-1-1complaintsandlifeconditions.Someofthe contentinthesenarrativeswasunnecessaryandunrelatedto thepatients’ needswithinthecontextoftheEMScall.For example,inthecaseofapatientwithhousinginsecuritywho complainedoflowerextremitypain,thewriterincluded severalinsertionsabouthowthepatientdidnotappearto
havediscomfortorunsteadygaitandhypothesizedthe patienthadulteriormotivesforthecallto9-1-1.Forthose withinsuranceinsecurity,mostofthedocumentationinthe EMSnarrativesincludedinabilityforpatientsorcrew memberstoobtainthebillinginformationforanotherpartof thechart.Narrativesforpatientswith financialorsocial supportinsecuritiescontainedlessperceivablenegativityin thedescriptionsofthosepatients’ conditions.
Withinthesocialsupportcategory,specifically,the narrativesweregenerallymuchlongerthanintheother categoriesandthescenesweredescribedwithgreaterdetail. Althoughsomeofthepatientsweredocumentedasrepeat customers,theovertonewaspositive,andtheEMS professionalsdescribedtheirfamiliarityinassociationwith thehelptheyprovidedforthepatientsinthecurrentand previousinteractions.Onlythesocialsupportinsecurities categorycontaineddescriptionsoftheadvocacywork providedbytheEMScrewsonthescene,includingreferrals tomobileintegratedhealthorothercommunityresources, assistinginpatients’ errands,callingapatient’sprimary healthcarephysicianforthem,ordeliveringfoodfromtheir ownstationsothepatientcouldeatameal.Thiscategory alsocontainedricherdescriptionsofsafetyconcernsfor patientswholivedinhomes,generallyalone,yetthe reflectionofsafetyconcernsdidnotcomeupforpatientswho didnothavehomes,food,medications,ormoney.
DISCUSSION
UnderstandinghowEMSprofessionalsdocumentSDoH withinelectronichealthrecordsisvitalforimproving emergencycare,subsequenttreatment,andoutcomesfor patientswithinsecurities.Mostoften,SDoHinformation wasnotincludedinEMSrecordsand,whenpresent,was neitherholisticnorinterconnectedtootherinsecuritiesthat mayimpactapatient’ s healthandwell-being.Additionally, EMSpersonneloften likelyunintentionally wroteabout patients’ insecuritieswithanegativevalenceortone.Such negativityinhealthrecordshasdemonstrateddownstream impressionsofthepatientsthemselves.30
BecauseEDsarevenuesthatperformassafetynetsfor myriadhealthandsocialproblems,thereareproposalsfor employingsocialemergencycaretoscreenandconnect patientswiththeresourcestheyneedtoaddresstheir insecurities.6,31 Asmembersofthepatients’ careteams,EMS professionalsshouldbeincludedinanyeffortstocollectand applyinformationaboutpatients’ SDoH.Patientnavigators andotherhospitalpersonnelcollectdataandaddSDoH informationtopatients’ medicalrecords,31,32 buthospital personnelshouldbeawareoftheEMSrecords’ contentand thereducedlikelihoodofsocialdesirabilitybiasorinfluence bytheEMSprofessionals.
SocialEMisaburgeoningsub-fieldofEM6 andcanbe seenasawayfortheEMSprofessiontoexpanditsscope,as well.Callstoexpandtrainingandcurriculaforemergency
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 884 EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing Burnettetal.
practitioners33,34 canbeextendedtoEMSprofessionalsto improvethequantityandqualityofSDoH-relatedcontentin EMSrecords.WhileaddressingSDoHinallmedicalrecords, terminologyshouldbeconsistenttoavoid miscommunication.8 Systematicandprescribedformatting forverbalhand-offsfromEMStoEDpersonnelhave improvedefficacyandinformationtransmission,11,16,18,35 andtheNationalEmergencyMedicalServicesInformation System(NEMSIS)36 hasstandardizedandimprovedthe collectionofEMSdata.Thecreationofaspecificdata collectiontoolcanincreaseandimproveinformation acquisitionandneutralreportingofpatients’ SDoH. Additionally,recentinitiativestoaddresspatients’ needs andavoidunnecessarytransportstooverwhelmedEDs suchastheEmergencyTriage,Treat,andTransport(ET3) Model37 byaddressingSDoHthroughcommunity engagementhaveresultedinfewerunnecessarycallsto9-1-1, fewerunnecessaryvisitstoEDs,lessout-of-servicetimefor firstresponderunits,anddecreasedincidenceofpatient falls.38,39 AllEMSpersonnelshouldlearnaboutthe resourcesavailableintheirowncommunitiesforaddressing SDoH(eg,emergencyshelters,foodbanks,orhome healthcareandoutreachorganizations).IfEMS professionalsareawareofsupportservicesintheir communities,theymaybemorelikelytohelptheirpatients makenecessaryconnections.Emergencymedicalservices personnelofalllevelsandinallorganizationtypes shouldundergospecifictrainingtorecognizeandaddress patients’ insecurities.FutureresearchaboutEMS personnel’sknowledgeaboutSDoH,theirrolesinthis typeofdatacollection,andperceptionsofeducationabout thetopicmaybeinformativetoEMSandother fields’ implementationofinterventionstoimprovelongitudinal patientcare.
Overthepastseveralyears,increasedrecognitionand researchlinkingemergencycareandSDoHhave significantlyimpactedthevolumeofliteratureinthissalient area.ThesestudieshaveexaminedSDoHand training,33,34,40,41 documentationandscreening,8,23,42–44 interventions,6,45,46 homelessness,47 mentalhealth,48,49 insurancetypes,50 andlinkstochronicoracuteillnessand injuries.7,51–54 NearlyallofthesestudiesfocusedonEDs, whicharenottheonlypointsofcontactforallpatients seekingemergencycareandlacktheperspectiveofseeing fromwhereapatienthails.Emergencymedicalservices personnelhavethebenefitofsharinginpatients’ lived experiencesandinteractingwithpatientswhomaynot subsequentlypresenttoEDs.Thisstudyprovidesaview fromthisnovelvantagepoint.
LIMITATIONS
ThenarrativesanalyzedinthisstudywerefromEMS recordsfromvarioussourcesthroughouttheUS,including firstresponseagencies,transportingambulanceagencies,
and flightEMSorganizations.Thecertificationlevelsofthe EMSpersonnelwereunknownduringanalysis.Theremay bedifferencesindocumentationofSDoHbasedon geographiclocation,organizationtypes,orlevelsoftraining. Sincethiswasaretrospectiveanalysisoffree-textnarratives, wedidnotassessothersectionsoftherecordsforinformation aboutpatients’ SDoH.Giventhede-identifiednatureofthis dataset,itwasalsounclearwhetherindividualagencies providedguidancetotheirpersonnelaboutSDoHortheir documentation.Additionally,thisanalysisleveragedrecords fromalargeconveniencesampleofEMSagenciesthatusea single,privatelyownedelectronichealthrecordsystem; thus,thegeneralizabilityofthese findingstocommunities servedbyEMSagenciesusingotherdocumentationsystems isunknown.
Theuseofthreequalitativeresearchersandjointanalysis sessionsmayhaveincreasedthepotentialforgroupthink, whichcouldhavenarrowedthefocusonthemesandconcepts forthebenefitofconsensus-building.Futurestudiesshould evaluatewhetherthesevariablesareassociatedwithSDoH documentationandvalenceofEMSpersonnel’ s perspectives.Useoftheinterpretiveparadigmand hermeneuticalapproachcouldaccountforanypotential differencesinmessagereceptionandintention duringdocumentation.
CONCLUSION
Addressingsocialdeterminantsofhealthcanleadto improvedhealthoutcomes,reducedstrainonhealthcare systems,anddecreasedhealthspending.Emergency medicalservicesprofessionalsareuniquelypositionedto collectandshareinformationonpatients’ SDoHthrough theirdocumentation,buttheoverwhelmingmajorityof EMSrecordslacksuchcontent.EducationaboutSDoH andtheirrelationshipstooneanother,alongwithtraining onhowtoneutrallyincludesuchcontentintheir documentationcanbebene fi cialforEMSprofessionalsand theirpatients.Thecreationofstandardizededucational contentanddocumentationtoolstocollectSDoH informationandcollectionsoforganizations’ community resourcesforaddressinginsecuritiesmayimproveEMS professionals’ awareness,documentation,andtreatment ofSDoH.
AddressforCorrespondence:SusanJ.Burnett,MS,EMT-P,Jacobs SchoolofMedicineandBiomedicalSciencesUniversityatBuffalo, TheStateUniversityofNewYork,DepartmentofEmergency Medicine,77GoodellSt.,Buffalo,NY14203.Email: burnett8@ buffalo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 885 Burnettetal. EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing
relationshipswithanycompaniesthatarerelevanttothisstudy. Dr.Clemencyisaspeaker/consultantforStryker.Theotherauthors havenofundingorconflictsofinteresttodisclose.
Copyright:©2023Burnettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.CentersforDiseaseControlandPrevention.AboutSocial DeterminantsofHealth(SDOH).PublishedMarch10,2021.
Availableat: https://www.cdc.gov/socialdeterminants/about.html
AccessedSeptember24,2022.
2.ThorntonRLJ,GloverCM,CenéCW,etal.Evaluatingstrategiesfor reducinghealthdisparitiesbyaddressingthesocialdeterminantsof health. HealthAff(Millwood).2016;35(8):1416–23.
3.HammondG,JohnstonK,HuangK,etal.Socialdeterminantsofhealth improvepredictiveaccuracyofclinicalriskmodelsforcardiovascular hospitalization,annualcost,anddeath. CircCardiovascQual Outcomes.2020;13(6):e006752.
4.OfficeofDiseasePreventionandHealthPromotionUSDofHandHS. SocialDeterminantsofHealth-HealthyPeople2030| health.gov
Availableat: https://health.gov/healthypeople/priority-areas/ social-determinants-health.AccessedMarch7,2022.
5.GottliebL,SandelM,AdlerNE.Collectingandapplyingdataonsocial determinantsofhealthinhealthcaresettings. JAMAInternMed 2013;173(11):1017–20.
6.AndersonES,LippertS,NewberryJ,etal.Addressingsocial determinantsofhealthfromtheemergencydepartmentthroughsocial emergencymedicine. WestJEmergMed.2016;17(4):487–9.
7.FosterCC,SimonTD,QuP,etal.Socialdeterminantsofhealth andemergencyandhospitalusebychildrenwithchronicdisease. HospPediatr.2020;10(6):471–80.
8.Samuels-KalowME,CiccoloGE,LinMP,etal.Theterminologyofsocial emergencymedicine:measuringsocialdeterminantsofhealth,social risk,andsocialneed. JAmCollEmergPhysiciansOpen 2020;1(5):852–6.
9.NationalHighwayTrafficSafetyAdministrationOfficeofEMS. EMS.gov|WhatisEMS?WhatisEMS?Availableat: https://www.ems. gov/whatisems.html.AccessedSeptember24,2022.
10.HalterM,VernonS,SnooksH,etal.Complexityofthedecision-making processofambulancestaffforassessmentandreferralofolder peoplewhohavefallen:aqualitativestudy. EmergMedJ 2011;28(1):44–50.
11.BostN,CrillyJ,PattersonE,ChaboyerW.Clinicalhandoverofpatients arrivingbyambulancetoahospitalemergencydepartment:aqualitative study. IntEmergNurs.2012;20(3):133–41.
12.MeiselZF,SheaJA,PeacockNJ,etal.Optimizingthepatienthandoff betweenemergencymedicalservicesandtheemergencydepartment. AnnEmergMed.2015;65(3):310–7.e1.
13.HorskyJ,SuhEH,SayanO,etal.Uncertainty,casecomplexityandthe contentofverbalhandoffsattheemergencydepartment. AMIAAnnu SympProc.2015;2015:630–9.
14.GoldbergSA,PoratA,StrotherCG,etal.Quantitativeanalysisofthe ontentofEMShandoffofcriticallyillandinjuredpatientstothe emergencydepartment. PrehospEmergCare.2017;21(1):14–7.
15.HorwitzLI,MoinT,KrumholzHM,etal.Consequencesofinadequate sign-outforpatientcare. ArchInternMed.2008;168(16):1755–1760.
16.MaddryJK,AranaAA,ClemonsMA,etal.ImpactofastandardizedEMS handoff tooloninpatientmedicalrecorddocumentationataLevelI traumacenter. PrehospEmergCare.2021;25(5):656–63.
17.OngMS,CoieraE.Asystematicreviewoffailuresinhandoff communicationduringintrahospitaltransfers. JtCommJQualPatient Saf.2011;37(6):274–84.
18.ReayG,NorrisJM,NowellL,etal.TransitionincarefromEMSproviders toemergencydepartmentnurses:asystematicreview. PrehospEmerg Care.2020;24(3):421–33.
19.TroyerL,BradyW.BarrierstoeffectiveEMStoemergencydepartment informationtransferatpatienthandover:asystematicreview. AmJ EmergMed.2020;38(7):1494–503.
20.AmericanCollegeofEmergencyPhysicians.TransferofPatientCare BetweenEMSProvidersandReceivingFacilities.Availableat: https:// www.acep.org/patient-care/policy-statements/transfer-of-patientcare-between-ems-providers-and-receiving-facilities/ AccessedMarch7,2022.
21.LoweryB,D’AcuntoS,CroweRP,etal.Usingnaturallanguage processingtoexaminesocialdeterminantsofhealthinprehospital pediatricencountersandassociationswithEMStransportdecisions. PrehospEmergCare.2022;0(0):1–6.
22.DataandResearch-ESO.Published2023.Availableat: https://www. eso.com/data-and-research/.AccessedMarch21,2023.
23.StemermanR,ArguelloJ,BriceJ,etal.Identificationofsocial determinantsofhealthusingmulti-labelclassificationofelectronic healthrecordclinicalnotes. JAMIAOpen.2021;4(3):ooaa069.
24.TracyS. QualitativeResearchMethods:CollectingEvidence,Crafting Analysis,CommunicatingImpact.Hoboken,NJ:Wiley-Blackwell,2013.
25.GlaserBG,StraussAL. TheDiscoveryofGroundedTheory:Strategies forQualitativeResearch.Manchester,UK:JohnRylandsLibrary:Aldine Publishing;1967.
26.StraussAL,CorbinJM. BasicsofQualitativeResearch:Techniquesand ProceduresforDevelopingGroundedTheory.ThousandOaks, CA:Sage;1998.
27.SaldanaJ. TheCodingManualforQualitativeResearchers.3rded. ThousandOaks,CA:Sage;2016.
28.CharmazK. ConstructingGroundedTheory.2nded.ThousandOaks, CA:Sage;2014.
29.LowJ.APragmaticdefinitionoftheconceptoftheoreticalsaturation. SociolFocus.2019;52(2):131–9.
30.ParkJ,SahaS,CheeB,etal.Physicianuseofstigmatizinglanguagein patientmedicalrecords. JAMANetwOpen.2021;4(7):e2117052.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 886 EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing Burnettetal.
31.FriedmanNL,BanegasMP.Towardaddressingsocialdeterminantsof health:ahealthcaresystemstrategy. PermJ.2018;22:18–95.
32.Thomas-HenkelC,SchulmanM.Screeningforsocialdeterminantsof healthinpopulationswithcomplexneeds:implementation considerations.2017.Availableat: https://www.chcs.org/media/ SDOH-Complex-Care-Screening-Brief-102617.pdf AccessedSeptember25,2022.
33.AxelsonDJ,StullMJ,CoatesWC.Socialdeterminantsofhealth: amissinglinkinemergencymedicinetraining. AEMEducTrain 2017;2(1):66–8.
34.MoffettSE,ShahidiH,SuleH,etal.Socialdeterminantsofhealth curriculumintegratedintoacoreemergencymedicineclerkship. MedEdPORTAL.2019:10789.
35.SmithCJ,BuzalkoRJ,AndersonN,etal.Evaluationofanovelhandoff communicationstrategyforpatientsadmittedfromtheemergency department. WestJEmergMed.2018;19(2):372–9.
36.NationalHighwayTrafficSafetyAdministrationOfficeofEMS.Whatis NEMSIS.NEMSIS.Availableat: https://nemsis.org/what-is-nemsis/ AccessedSeptember25,2022.
37.CentersforMedicare&MedicaidServices.EmergencyTriage,Treat, andTransport(ET3)Model.PublishedJuly28,2022.Availableat: https://cmmicoordinator.survey.fm/was-this-helpful?iframe=https%3A %2F%2Finnovation.cms.gov%2Finnovation-models%2Fet3&ft=1 AccessedSeptember25,2022.
38.BronskyES,McGrawC,JohnsonR,etal.CARES:acommunity-wide collaborationidentifiessuper-utilizersandreducestheir9-1-1call, emergencydepartment,andhospitalvisitrates. PrehospEmergCare
2017;21(6):693–9.
39.YoderCM,PeschMS.Anacademic-firedepartmentpartnership toaddresssocialdeterminantsofhealth. JNursEduc
2020;59(1):34–8.
40.BalharaKS,IrvinN.Acommunitymuraltour:facilitatingexperiential learningaboutsocialdeterminantsofhealth. WestJEmergMed
2021;22(1):60–2.
41.GrossmanLG,MechanicOJ,OrrZ,etal.Ananalysisofsocial determinantsofhealthandstructuralcompetencytraininginglobal emergencymedicinefellowshipprogramsintheUnitedStates.
AEMEducTrain.2021;5(S1):S28–32.
42.GottliebL,HesslerD,LongD,etal.Arandomizedtrialonscreeningfor socialdeterminantsofhealth:theISCREENstudy. Pediatrics
2014;134(6):e1611–8.
43.HsiehD.Achievingthequadrupleaim:treatingpatientsaspeopleby screeningforandaddressingthesocialdeterminantsofhealth. AnnEmergMed.2019;74(5):S19–24.
44.WallaceAS,LutherBL,SislerSM,etal.Integratingsocialdeterminants ofhealthscreeningandreferralduringroutineemergencydepartment care:evaluationofreachandimplementationchallenges. ImplementSci Commun.2021;2(1):114.
45.WalterLA,SchoenfeldEM,SmithCH,etal.Emergency department
basedinterventionsaffectingsocialdeterminantsof healthintheUnitedStates:Ascopingreview. AcadEmergMed 2021;28(6):666–74.
46.OrdonezE,DowdellK,NavejarNM,etal.Anassessmentofthesocial determinantsofhealthinanurbanemergencydepartment. WestJ EmergMed.2021;22(4):890–7.
47.DoranKM,KunzlerNM,MijanovichT,etal.Homelessnessandother socialdeterminantsofhealthamongemergencydepartmentpatients. JSocDistressHomelessness.2016;25(2):71–7.
48.BarkerLC,BronskillSE,BrownHK,etal.Hospitaladmissionatthetime ofapostpartumpsychiatricemergencydepartmentvisit:theinfluenceof thesocialdeterminantsofhealth. EpidemiolPsychiatrSci.2021;30:e33.
49.ShymanL,SukhorukovR,BarbicD,etal.Socialdeterminants ofhealthanddepressioninadultspresentingtotheemergency department:Implicationsforfamilymedicine. CanFamPhysician 2021;67(12):e337–47.
50.McCarthyML,ZhengZ,WilderME,etal.Theinfluenceofsocial determinantsofhealthonemergencydepartmentsvisitsinamedicaid sample. AnnEmergMed.2021;77(5):511–22.
51.BalharaKS,FisherL,ElHageN,etal.Socialdeterminantsofhealth associatedwithhemodialysisnon-adherenceandemergency departmentutilization:apilotobservationalstudy. BMCNephrol 2020;21(1):4.
52.BaptisteDL,Turkson-OcranRA,HanHR,etal.Socialdeterminantsof emergencydepartmentvisitsamongpersonsdiagnosedwithcoronary heartdiseaseandstroke. EthnDis.31(1):41–6.
53.CortrightL,BuckmanC,TuminD,etal.Socialdeterminantsofhealth andemergencydepartmentuseamongchildrenwithsicklecelldisease. JPediatrHematolOncol.2020;42(1):e42–5.
54.SinguS,AcharyaA,ChallagundlaK,etal.Impactofsocialdeterminants ofhealthontheemergingCOVID-19pandemicintheUnitedStates. FrontPublicHealth.2020.Availableat: https://www.frontiersin.org/ articles/10.3389/fpubh.2020.00406.AccessedMarch3,2023.
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 887 Burnettetal. EMSDocumentationofSocialDeterminantsofHealthwithNaturalLanguageProcessing
SOCIAL EMERGENCY MEDICINEAND POPULATION HEALTH
RacialDifferencesinTriageforEmergencyDepartment PatientswithSubjectiveChiefComplaints
CassandraPeitzman,MD,PhD,MPH
JossieA.CarrerasTartak,MD,MBA
MargaretSamuels-Kalow,MD,MSHP,MPhil
AliRaja,MD,MBA,MPH
WendyL.Macias-Konstantopoulos,MD,MPH,MBA
SectionEditor: RamaSalhi,MD
MassachusettsGeneralHospital,HarvardMedicalSchool, DepartmentofEmergencyMedicine,Boston,Massachusetts
Submissionhistory:SubmittedSeptember29,2022;RevisionreceivedMarch30,2022;AcceptedApril10,2023
ElectronicallypublishedAugust30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59044
Introduction: BlackandHispanicpatientsarefrequentlyassignedloweracuitytriagescoresthanWhite patients.Thiscanleadtolongerwaittimes,lessaggressivecare,andworseoutcomes.Inthisstudywe aimedtodeterminewhethertheseeffectsaremorepronouncedforpatientswithsubjectivecomplaints.
Methods: Weperformedaretrospectiveanalysisforalladultvisitsbetween2016-2019atanurban academicemergencydepartment(ED)withacuity-basedpods.Wedeterminedratesofinitialhigh-acuity triagebothacrossallpatientsandamongthesubsetlocatedinthehigh-acuitypodattimeofdisposition (eitherthroughinitialassignmentorsubsequentup-triage).Analysiswasperformedforcommonchief complaintscategorizedassubjective(chestpain,dyspnea,anypain);observed(alteredmentalstatus); numeric(fever,hypotension);orprotocolized(stroke,ST-elevationmyocardialinfarction). Weconstructedlogisticregressionmodelstocontrolforage,race,gender,methodofarrival, and finaldisposition.
Results: Weanalyzed297,355adultEDvisits.BlackandHispanicpatientswerelesslikelytobetriaged tohigh-acuitybeds(adjustedoddsratio[aOR]0.76,95%confidenceinterval[CI]0.73-0.79forBlack,and aOR0.87,95%CI0.84-0.90forHispanicpatients).Thiseffectwasmorepronouncedforthosewith subjectivechiefcomplaints,includingchestpain(aOR0.76,95%CI0.73-0.79forBlackand0.88,95%CI 0.78-0.99forHispanicpatients),dyspnea(aOR0.79,95%CI0.68-0.92and0.8,95%CI0.72-0.99),and anypain(aOR0.83,95%CI0.75-0.92and0.89,95%CI0.82-0.97,respectively).Amongpatientsinthe high-acuitypodattimeofdisposition,BlackandHispanicpatientsweredisproportionatelytriagedto loweracuitypodsonarrival(aOR1.47,95%CI1.33-1.63forBlackandaOR1.27,95%CI1.15-1.40for Hispanicadults),withsignificantdifferencesobservedonlyforsubjectivechiefcomplaints.No differenceswereobservedforobserved,objective,orprotocolizedcomplaintsineitheranalysis.
Conclusion: BlackandHispanicadults,includingthosewhoultimatelyrequiredhigh-acuityresources, weredisproportionatelytriagedtoloweracuitypods.Thiseffectwasmorepronouncedforpatients withsubjectivechiefcomplaints.Additionalworkisneededtoidentifyandovercomepotential biasintheassessmentofpatientswithsubjectivechiefcomplaintsinEDtriage.[WestJEmergMed. 2023;24(5)888–893.]
INTRODUCTION
Overthepastseveraldecades,arobustliteraturehas developeddemonstratingracial-,gender-,andlanguage-
baseddisparitiesinthequalityandintensityofmedicalcare intheUnitedStates.1–5 BlackandHispanicpatientsare consistentlyofferedlessintensivecare,6–8 subjectedtolonger
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 888
waittimes,9 andseenaslessacutelyillthentheirWhite counterparts,evenwhencontrollingforotherpossible explanatoryfactors.10,11 Insomecases,thesedifferencescan leadtodelaysincare,inadequateintensityofinterventionor monitoring,12–16 andgreaterriskofadverseoutcomes.17
Triageprovidesanaturalcontextinwhichtoassess encounter-leveldriversofsuchdisparitiesbecauseofbothits well-defined,episodicnatureandbecauseitinitiatesa treatmentpaththatmayinfluenceapatient’ scare throughouttheirclinicalcourse.Inthisstudywesoughtto 1)determinewhetherracialdifferencesarepresentineither initialratesofhigh-acuitytriageorneedforlaterreassignmenttoahigh-acuitypodand2)whetherthese differencesvarybypatientchiefcomplaint.Wehypothesized thatBlackandHispanicpatientsexperiencehigherratesof under-triage,andthesedifferencesaremorepronouncedfor patientspresentingwithsubjectiveorsymptom-basedchief complaints.Thishypothesisisinkeepingwithpriorliterature suggestingthatsubjectiveassessmentswithincomplete informationmayleadtogreaterintroductionofbias,18 whereaschiefcomplaintsthattriggerclearprotocols(suchas ST-elevationmyocardialinfarction[STEMI]orstrokealerts) maytendtowardmoreprescriptiveand,therefore,lessbiased triageprocesses.Wehopethatbyidentifyingthe circumstancesunderwhichracialdisparitiesintriageappear, wemaybetterunderstandandtherebyinterveneandact uponthephenomenathatdrivethem.
METHODS
Weconductedaretrospectiveanalysisofalladultpatient visitsbetween2016–2019toanurbanacademicEDwith nursing-ledtriagetoacuity-basedpods(includinglowacuity/fast-track,mid-acuity,andcritical-care/high-acuity pods)basedonhospital-specific,resource-basedguidelines. Ouranalysisconsideredboththefullsetofvisitsandselected chiefcomplaints,whichwerechosentorepresentfourtypes ofcomplaint: “subjective” complaintswerethoserelatingto patients’ reportsoftheirownsymptoms; “objective” complaintsweredefinedbynumericcutoffsinprehospitalor homeassessments; “observed” complaintsweresubjectively definedbutreportedbasedonassessmentsbyathirdparty; and finally, “protocolized” chiefcomplaintsweredefinedas thoseforwhichtriageisassignedbyprotocol.
Forthis,weincludedthethreemostcommonchief complaintswithatleasta20%rateofhigh-acuitytriage(chest painandshortnessofbreathas “subjective” complaintsand alteredmentalstatusas “observed”). “Objective” complaints includedboththemostcommonandhighestacuity complaintswithnumericaldefinitions(feverand hypotension).Twocommon “protocolized” chiefcomplaints (STEMIandstroke)werealsoincluded.Tobetterassessa broadgroupofsubjectivecomplaints,weassessedan additionalcategoryofanychiefcomplaintincluding “pain,” (approximately10%ofwhichwasinitiallytriagedashigh
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Racialdisparitiesintriagecanleadtoless aggressivecareandworseoutcomes.
Whatwastheresearchquestion?
Israce-basedtriagemorepronouncedfor patientswithsubjectivechiefcomplaints,such aspainanddyspnea?
Whatwasthemajor findingofthestudy?
BlackandHispanicpatientswerelesslikelythan similarWhitepatientstobetriagedtohighacuitybayswhenpresentingwithchestpain (aOR0.76forBlackand0.88forHispanic patients),dyspnea(aOR0.79and0.80),orany pain(aOR0.83and0.89).However,patients whosecomplaintsactivatedprotocolized pathways(e.g., “CodeStroke”)weretriaged identicallyacrossracialgroups.
Howdoesthisimprovepopulationhealth? Furtherintegrationofobjectivedata(eg,vital signsandECGs)andprotocolsforspeci fi c complaintsmayhelpreducedisparities intriage.
acuity).Chiefcomplaintswereidentifiedviasearchand manualreviewoffree-textchiefcomplaintsenteredattriage. Racialcategoriesweretakenfromdataenteredattimeof registration,withpooledcategoriesincludingBlack,White, Asian,multiracial,other,andunknown.Recordswithmissing variables(316total)wereexcludedfromtheanalysis. Weevaluatedtwooutcomesofinterest:relativeprobability ofinitialtriagetothehigh-acuitypod(Table2a)andrelative probabilityofhavingrequiredup-triage(reassignmenttothe
Meanage (years) Percentage male Percentage high-acuity triageNumber White50.752.9%19%210,596 Black 42.452.7%11.7%32,645 Hispanic34.049.9%10.6%49,973 Asian41.547.1%14.3%14,875 Multiracial41.4851.5%14.6%8,216 Other37.751.4%11%10,833 Unknown39.453.7%20.1%7,154 Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 889 Peitzmanetal. RacialDifferencesinTriageforEDPatientswithSubjectiveChiefComplaints
Table1. Summarizedracial,gender,andagedistributionoffulladult emergencydepartmentsample2016–2019.
Table2. (A)Adjustedoddsofinitialtriagetohigh-acuitypodand(B)adjustedoddsofinitiallower-acuitytriageamongpatientscompleting emergencydepartment(ED)courseinhigh-acuitypodamongadultEDpatients2016–2019,stratifiedbychiefcomplaint.Controlsincluded forage,agesquared,agecategories(18
44years,45–64years,65+ years),EDdeathandadmission. “Other” and “Unknown” racial categoriesomittedforclarity.STEMIandstroke-alertpatientswereuniformlytriagedtoahigh-acuitysettingand,therefore,regression analysiswasnotpossible.Resultsreportedasadjustedoddsratioswith95%confidenceintervals.
2A.Adjustedoddsoftriagetohigh-acuitypodbyrace
2B.Adjustedoddsofinitiallower-acuitytriageforpatientsrequiringhigh-acuityresourcespriortodispositionbyrace
high-acuitypod)forpatientsultimatelyrequiringhigh-acuity care(Table2b).Logisticregressionwasperformedtoassess therelationshipbetweentheseoutcomevariablesandselfreportedrace,acrossboththefullsampleandbychief complaint.Controlswereincludedforgender,age(including squaredandbinterms),methodofarrival(ambulancevs walk-in),and finaldisposition(admission,observation, discharge,ordeath).Weperformedanalysiswasperformedin R4.1.0(RFoundationforStatisticalComputing,Vienna, Austria),19,20 withresultsreportedasoddsratiosforeaseof
interpretation.Althoughmoderatecollinearitywasidentified amongourcontrolvariables,varianceinflationfactorswere <2inallcases,andmaineffectswererobusttomultiplemodel specifications.(SeeAppendix1forrepresentativesensitivity analyses.)Thestudywasreviewedandapprovedbythe hospitalInstitutionalEthicsReviewBoard.
RESULTS
Of297,355adultEDvisitsanalyzed,66%(196,040)were ofpatientswhoidentifiedasWhite,approximately10%
–
ChiefcomplaintAllpatientsChestpainDyspneaPainFeverHypotensionAMS Black 0.76***0.77***0.79**0.83***1.08 0.99 1.06 (0.73, 0.79)(0.67,0.88)(0.68,0.92)(0.75,0.92)(0.85,1.37)(0.70,1.41)(0.44,2.54) Hispanic 0.87***0.88*0.84*0.89** 1 0.99 1.07 (0.84,0.90)(0.78,0.99)(0.72,0.99)(0.82,0.97)(0.77,1.30)(0.76,1.29)(0.46,2.51) Asian 1.06*1.071.151.131.24 1.33* 2.63 (1.01,1.12)(0.88,1.30)(0.92,1.44)(0.99,1.30)(0.84,1.82)(1.01,1.75)(0.74,9.30) Multiracial 0.91*1.15 0.9 1.050.69 1.05 2.32 (0.85,0.98)(0.88,1.50)(0.68,1.20)(0.88,1.26)(0.44,1.06)(0.62,1.78)(0.27,20.20) Gender(male)1.26***1.55***1.27***1.58***1.03 1.21* 1.23 (1.23,1.28)(1.43,1.68)(1.18,1.38)(1.50,1.67)(0.91,1.18)(1.04,1.40)(0.82,1.84) BIBAª 3.01***2.66***1.78***2.59***2.16***2.39***1.80** (2.95,3.07)(2.45,2.88)(1.64,1.93)(2.45,2.73)(1.88,2.48)(2.04,2.81)(1.20,2.69) Observations297,03416,17113,15073,4864,1086,331 638
Chief complaintAllpatientsChestpainDyspneaPainFeverHypotensionAMS Black 1.47***1.68***1.31.47***1.15 0 1.28 (1.33, 1.63)(1.25,2.26)(0.90,1.89)(1.18,1.83)(0.49,2.70)(0.00,Inf)(0.64,2.55) Hispanic 1.27***1.081.54*1.111.34 1.28 1.17 (1.15,1.40)(0.79,1.47)(1.06,2.24)(0.90,1.37)(0.72,2.48)(0.12,13.10)(0.52,2.63) Asian 1.09 1.091.011.151.23 2.3 1.52 (0.94,1.26)(0.70,1.72)(0.57,1.79)(0.85,1.56)(0.65,2.35)(0.26,20.40)(0.53,4.37) Multiracial 1.11 1.64 1 1.59*1.68 0 2.06 (0.91,1.36)(0.98,2.77)(0.45,2.19)(1.08,2.35)(0.53,5.26)(0.00,Inf)(0.70,6.05) Gender(male)0.91**1.030.77*0.910.94 0.35 1.34 (0.86,0.96)(0.85,1.25)(0.63,0.95)(0.80,1.03)(0.66,1.35)(0.08,1.48)(0.90,2.02) BIBAª 0.65***0.52***0.870.65***0.84 0.62 0.61* (0.61,0.69)(0.43,0.63)(0.71,1.07)(0.57,0.74)(0.57,1.23)(0.15,2.52)(0.40,0.94) Observations51,9025,5354,5647,845932 419 1,895 *P < 0.05; **P < 0.01;***P < 0.001. AMS,alteredmentalstatus; BIBA,broughtinbyambulance. WesternJournal of EmergencyMedicine Volume24,No.5:September2023 890 RacialDifferencesinTriageforEDPatientswithSubjectiveChiefComplaints Peitzmanetal.
(29,214)whoidentifiedasBlack,and13%(38,396)who identifiedasHispanic.Patientswere48%(143,079)female, 52%(154,268)male,andhadameanageof51years.
Overall,theadjustedoddsoftriagetothehighacuitypod werelowerforBlack(adjustedoddsratio[aOR]0.76,95% confidenceinterval[CI]0.73-0.79andHispanicpatientsaOR 0.87,95%CI0.84-0.90).Amongouridentifiedchief complaints,thiseffectwasonlydemonstratedforpatients withsubjectivechiefcomplaints,includingchestpain(aOR 0.76,95%CI0.73,0.79forBlack,andaOR0.88,95%CI 0.78,0.99forHispanicpatients),dyspnea(aOR0.79,95%CI 0.68-0.92forBlack,andaOR0.84,95%CI0.72-0.99for Hispanicpatients),andanypain(aOR0.83,95%CI 0.75-0.92forBlack,andaOR0.89,95%CI0.82-0.97for Hispanicpatients).Nodifferencesweredetectedacross observed,numeric,orprotocolizedcomplaints.
Weperformedanalysisofneedforup-triageonthesubset ofpatientslocatedinthehigh-acuitypodattimeofED disposition(death,hospitaladmission,ordischarge), constitutingapproximately16%ofadultvisits(51,959). Patientswereconsideredtohaverequiredup-triageifthey wereinitiallyassignedtoaloweracuitypodandrequired reassignmenttothehigh-acuitypodduringtheirEDcourse. Racialdifferenceswerealsoidentifiedinthismeasure,with BlackandHispanicadultsexperiencinghigherratesofuptriage.Thiswasdemonstratedacrossthefullall-complaint studysample(aORof1.47,95%CI1.3-1.63forBlack, andaORof1.27,95%CI1.15-1.40forHispanicadults),as wellasforBlackpatientspresentingwithchestpain(aOR 1.68,95%CI1.25-2.26),oranypain(aOR1.47, 95%CI1.1-1.83)andHispanicpatientspresentingwith dyspnea/shortnessofbreath(aOR1.54,95%CI1.06-2.24). Nodifferenceswereobservedforobserved,objective,or protocolizedcomplaints.
DISCUSSION
InouranalysiswefoundthatBlackandHispanicadultsin ourpopulationweredisproportionatelytriagedtolower acuityareas,andthatthisphenomenonwasmore pronouncedforpatientspresentingwithsubjectivechief complaints.Furtheranalysesdemonstratedthatofpatients requiringcriticalcare/high-acuityresourcesatthetimeofED discharge,BlackandHispanicpatientstendedtohavebeen disproportionatelytriagedtoloweracuitypodsduringinitial assessment.These findingssuggestthatthepatternoflower acuitytriagecannotbeexplainedbytruedifferencesin resourcerequirementsovertheEDcourse(ie,accurate predictionoflowerresourcerequirementsrelatedtoless severeclinicalpresentations),butratheratendencyto consistentlyunderestimatetheneedsofBlackandHispanic adults.Thispatternisalsomorepronouncedfor patientspresentingwithsubjectivechiefcomplaints, suggestingthattriageclinicians’ assessmentsoftheseverity
ofpatient-reportedsymptomsforBlackandHispanic patientsmayhaveplayedaroleinthisunderestimation.
Manypotentialmechanismsmayunderliethispattern, possiblyincludingraciallycorrelateddifferencesinpatients’ descriptionsoftheirsymptoms,21,22 differencesinaffective communicationandstoicism,23 differencesinsymptom presentationfrom “canonical” caseshistoricallyusedin medicaleducation,24,25 differencesinstyleorcontentof reportorinactionstakenbyprehospitalpersonnel,26 differentialimpactofclinicians’ cognitive “heuristics” regardingdiseasepresentation,27–29 anddifferencesin patient-clinicianinteractionstyleorotherformsofbias.30
32 Thesephenomenamayalsohavebeenexacerbatedby structuralfactors(suchaseaseofaccesstointerpreter serviceswhenneeded,crowding,clinicianfatigueor cognitiveburden,timeofday,etc),whicharebeyondthe scopeofouranalysis.Reassuringly,wedidnotobserve raciallycorrelatedtriagedifferencesinprotocolized chiefcomplaints.
LIMITATIONS
Thiswasasingle-centerstudythatusedanacuity-based triagesystemtoidentifyrace-relateddifferencesintriage assignment,potentiallylimitinggeneralizabilityofthis finding.ThisanalysisalsofocusedonasubsetofEDchief complaintsthatrepresentapproximately32%oftotalED presentationsandweredevelopedbasedonfrequency, acuity,andeaseofidentificationinourdata.Itispossible thatthesepatternswouldnotemergeinadatasetwhereother chiefcomplaintsweremorecommon,morefrequently representedhigh-acuitypresentations,orweremorereadily identifiable.Thisanalysiswasalsoperformedondata collectedunderhospital-developedtriageguidelinesbut priortothe2021-2022implementationofaformalized EmergencySeverityIndex(ESI)assignmentprotocolwithin oursystem,whichmayalterthesepatterns.
Inadditiontothepotentialstructuralfactorslistedabove, wedidnotcontrolforotherinterpersonalorindividual factorsthatmaycontributetopodselectionwithinthis system(includingcurrentstaffing,hourlythroughputtime, relativecrowding,recenttriagetothesamepod,etc).Neither didweassessnursingfactors(includingrace,age,seniority, languagesspoken,etc.).Thus,furtherworkwillbeneededto bothassesstheseadditionalfactorsandtoidentifypotential mechanismsunderlyingour findings.
CONCLUSION
Overall,ouranalysisidentifiesapatternofsignificant racialdifferencesintriageaccuracy,whichtendsto underestimatethecritical-careneedsofBlackandHispanic adults,especiallythosewithsymptom-basedcomplaints, potentiallycompromisingboththetimelinessand appropriatenessoftheircare.These findingssuggestthat furtherworktobetterunderstandandimprovetriage
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 891 Peitzmanetal.
RacialDifferencesinTriageforEDPatientswithSubjectiveChiefComplaints
encountersandthenatureoftheinteractionswithin themmaybeimportantinhelpingtoreducedisparitiesin EDcare.
ACKNOWLEDGMENTS
TheauthorswouldliketothankCassieKrausandthe MGHEDQualityandAnalyticsprogramfortheirsupport indataidentificationandstewardship.
AddressforCorrespondence:CassandraPeitzman,MD,PhD,MPH, MassachusettsGeneralHospital,DepartmentofEmergency Medicine,55FruitSt.,Boston,Massachusetts02114. Email: cpeitzman@partners.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financialrelationshipswithanycompaniesthatarerelevanttothis study.Therearenoconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2023Peitzmanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.SmedleyBD,StithAY,NelsonAR. UnequalTreatment:Confronting RacialandEthnicDisparitiesinHealthCare(FullPrintedVersion) Editors,CommitteeonUnderstandingandEliminatingRacialandEthnic DisparitiesinHealthCare.2003;782.
2.KelleyE,MoyE,StryerD,etal.TheNationalHealthcare QualityandDisparitiesReportsanOverview. MedCare 2005;43(3Suppl):18–8.
3.CooperLA,PoweNR.Disparitiesinpatientexperiences,health careprocesses,andoutcomes:theroleofpatient – provider racial,ethnic,andlanguageconcordance. CommonwFund. Publishedonline2004.
4.ZhangX,CarabelloM,HillT,etal.Racialandethnicdisparitiesin emergencydepartmentcareandhealthoutcomesamongchildreninthe UnitedStates. FrontPediatr.2019;7:525.
5.WilliamsRA.EliminatingHealthcareDisparitiesinAmerica:Beyondthe IOMReport.Totawa,NJ:HumanaPress;2007.
6.GroeneveldPW,KruseGB,ChenZ,etal.Variationincardiacprocedure useandracialdisparityamongVeteransAffairshospitals. AmHeartJ 2007;153(2):320–7.
7.SotoGJ,MartinGS,GongMN.Healthcaredisparitiesincriticalillness. CritCareMed.2013;41(12):2784–93.
8.L´opezL,WilperAP,CervantesMC,etal.Racialandsexdifferencesin emergencydepartmenttriageassessmentandtestorderingforchest pain,1997-2006. AcadEmergMed.2010;17(8):801–8.
9.LuFQ,HanchateAD,Paasche-OrlowMK.Racial/ethnicdisparitiesin emergencydepartmentwaittimesintheUnitedStates,2013–2017. AmJEmergMed.2021;47:138–44.
10.SchraderCD,LewisLM.Racialdisparityinemergencydepartment triage. JEmergMed.2013;44(2):511–8.
11.VigilJM,AlcockJ,CoulombeP,etal.Ethnicdisparities inEmergencySeverityIndexscoresamongU.S.Veteran’s Affairsemergencydepartmentpatients. PLoSOne 2015;10(5):1–10.
12.NataleJE,JosephJG,RogersAJ,etal.Relationshipofphysicianidentifiedpatientraceandethnicitytouseofcomputed tomographyinpediatricblunttorsotrauma. AcadEmergMed 2016;23(5):584–90.
13.WelchLC,TenoJM,MorV.End-of-lifecareinblackandwhite:race mattersformedicalcareofdyingpatientsandtheirfamilies. JAmGeriatr Soc.2005;53(7):1145–53.
14.ElTurabiA,AbelGA,RolandM,etal.Variationinreportedexperience ofinvolvementincancertreatmentdecisionmaking:evidencefrom theNationalCancerPatientExperienceSurvey. BrJCancer 2013;109(3):780–7.
15.BurgessDJ,Crowley-MatokaM,PhelanS,etal.Patientraceand physicians’ decisionstoprescribeopioidsforchroniclowbackpain. Soc SciMed.2008;67(11):1852–60.
16. HendersonJ,GaoH,RedshawM.Experiencingmaternitycare:thecare receivedandperceptionsofwomenfromdifferentethnicgroups. BMC PregnancyChildbirth.2013;13:196.
17.ChapmanEN,KaatzA,CarnesM.Physiciansandimplicitbias:how doctorsmayunwittinglyperpetuatehealthcaredisparities. JGenIntern Med.2013;28(11):1504–10.
18.BurgessDJ.Areprovidersmorelikelytocontributetohealthcare disparitiesunderhighlevelsofcognitiveload?Howfeaturesofthe healthcaresettingmayleadtobiasesinmedicaldecisionmaking. Med DecisMak.2010;30(2):246–57.
19.RCoreTeam.(2021)R:Alanguageandenvironmentforstatistical computing.RFoundationforStatisticalComputing,Vienna, Austria.Availableat: https://www.R-project.org/ AccessedMarch16,2023.
20.RStudioTeam.(2020)RStudio:IntegratedDevelopmentforR.RStudio, PBC,Boston,MA.Availableat: http://www.rstudio.com/ AccessedMarch16,2023.
21.PayneJS.Influenceofraceandsymptomexpressiononclinicians’ depressivedisorderidentificationinAfricanAmericanmen. JSocSocial WorkRes.2012;3(3):162
77.
22.Carpenter-SongE,ChuE,DrakeRE,etal.Ethno-culturalvariations intheexperienceandmeaningofmentalillnessandtreatment: implicationsforaccessandutilization. TranscultPsychiatry 2010;47(2):224–51.
23.MeintsSM,CortesA,MoraisCA,etal.Racialandethnicdifferencesin theexperienceandtreatmentofnoncancerpain. PainManag 2019;9(3):317
34.
–
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 892 RacialDifferencesinTriageforEDPatientswithSubjectiveChiefComplaints Peitzmanetal.
24.AmutahC,GreenidgeK,ManteA,etal.Misrepresentingrace therole ofmedicalschoolsinpropagatingphysicianbias. NEnglJMed 2021;384(9):872–8.
25.McSweeneyJC,O’SullivanP,ClevesMA,etal.Racialdifferencesin women’sprodromalandacutesymptomsofmyocardialinfarction. AmJCritCare.2010;19(1):63–73.
26.KennelJ,WithersE,ParsonsN,etal.Racial/ethnicdisparitiesinpain treatment:evidencefromOregonemergencymedicalservices agencies. MedCare.2019;57(12):924–9.
27.O’SullivanED,SchofieldSJ.Cognitivebiasclinicalmedicine. JRColl PhysiciansEdinb.2018;48(3):225–32.
28.CroskerryP.Achievingqualityinclinicaldecisionmaking: cognitivestrategiesanddetectionofbias. AcadEmergMed 2002;9(11):1184
204.
29.TverskyA,KahnemanD.Judgmentunderuncertainty:heuristicsand biases.Biasesinjudgmentsrevealsomeheuristicsofthinkingunder uncertainty. Science.1974;185(4157):1124–31.
30.ElliottAM,AlexanderSC,MescherCA,etal.Differencesin physicians’ verbalandnonverbalcommunicationwithblack andwhitepatientsattheendoflife. JPainSymptomManage 2016;51(1):1–8.
31.Mende-SiedleckiP,Qu-LeeJ,BackerR,etal.Perceptualcontributions toracialbiasinpainrecognition. JExpPsycholGen 2019;148(5):863–89.
32.RLSJr,GordonH,HaidetP.Physicians’ communicationand perceptionsofpatients:Isithowtheylook,howtheytalk,orisitjust thedoctor? SocSci.2010;65(3):586–98.
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 893 Peitzmanetal. RacialDifferencesinTriageforEDPatientswithSubjectiveChiefComplaints
SOCIAL EMERGENCY MEDICINEAND POPULATION HEALTH
EmergencyDepartmentUseAmongRecentlyHomeless AdultsinaNationallyRepresentativeSample
CaitlinRyus,MD,MPH*
ElinaStefanovics,PhD†‡
JackTsai,PhD‡§∥
TaehoGregRhee,PhD†‡ ¶ RobertA.Rosenheck,MD†‡
*DepartmentofEmergencyMedicine,YaleUniversitySchoolofMedicine, NewHaven,Connecticut
† U.S.DepartmentofVeteransAffairsNewEnglandMentalIllnessResearch, Education,andClinicalCenter,WestHaven,Connecticut
‡ DepartmentofPsychiatry,YaleUniversitySchoolofMedicine,NewHaven, Connecticut
§ VANationalCenteronHomelessnessamongVeterans,Washington,DC
∥ SchoolofPublicHealth,UniversityofTexasHealthScienceCenteratHouston, Houston,Texas
¶ DepartmentofPublicHealthSciences,UniversityofConnecticutSchoolofMedicine, Farmington,Connecticut
SectionEditor: TonyZitek,MD
Submissionhistory:SubmittedSeptember29,2022;RevisionreceivedMay11,2023;AcceptedMay24,2023
ElectronicallypublishedAugust11,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59054
Introduction: Inthisstudyweexaminedtheassociationofhomelessnessandemergencydepartment (ED)use,consideringsocial,medical,andmentalhealthfactorsassociatedwithbothhomelessnessand EDuse.Wehypothesizedthatsocialdisadvantagealonecouldaccountformostoftheassociation betweenEDuseandhomelessness.
Methods: WeusednationallyrepresentativedatafromtheNationalEpidemiologicSurveyonAlcohol andRelatedConditions(NESARC-III).Emergencydepartmentusewithintheprioryearwascategorized intonouse(27,674;76.61%);moderateuse(1–4visits:7,972;22.1%);andhighuse(5ormore visits:475;1.32%).Weusedbivariateanalysesfollowedbymultivariable-adjustedlogisticregression analysestoidentifydemographic,social,medical,andmentalhealthcharacteristicsassociatedwith EDuse.
Results: Among36,121respondents,unadjustedlogisticregressionshowedprior-year homelessnesswasstronglyassociatedwithmoderateandhighprior-yearEDuse(oddsratio [OR]2.31and7.34,respectively, P < 0.001).Afteradjustingforsociodemographicfactors,the associationsofhomelessnesswithmoderate/highEDusediminished(adjustedOR[AOR]1.27 and1.62,respectively,both P < 0.05).Adjustingformedical/mentalhealthvariables,alone,similarly diminishedtheassociationbetweenhomelessnessandmoderate/highEDuse(AOR1.26, P < .05 and2.07, P < 0.001,respectively).Ina fi nalstepwisemodelincludingsocialandhealth variables,homelessnesswasnolongersigni fi cantlyassociatedwithmoderateorhighEDuse intheprioryear.
Conclusion: Afteradjustmentforsocialdisadvantage andhealthproblems,wefoundnostatistically significantassociationbetweenhomelessnessandEDuse.Theimplicationsofour findings suggestthatEDservicedeliverymustaddressbothhealthissuesandsocialfactors.[WestJEmergMed. 2023;24(5)894–905.]
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 894
INTRODUCTION
Emergencydepartments(EDs)havelongservedasa healthcaresafetynetforthemedicalneedsofmarginalized populationsintheUS,suchaspeopleexperiencing homelessness.1 Overthepastseveralyears,therehasbeen increasingrecognitionthatinprovidingthisservice,EDs playadistinctroleindelivering “socialemergencymedicine” toaddressthestructuraldeterminantsofpoorhealthsuchas poverty,racism,inadequatehousing,andfoodinsecurity.2–4 “Emergencydepartmentuseiscostly,5 andsomequestionthe appropriatenessandefficiencyofaddressingsocialproblems withintheEDandhealthcaresystem,especiallyintheUS wheresocialservicesarelimited.5,6
PreviousstudieshaveshownthatEDpatientsarefarmore likelytobehomelessthanotheradults.7,8 Amultisitestudy conductedinNortheasternPennsylvaniaestimatedthatthe prevalenceofhomelessnessinEDsrangedfrom7–18%.7 At oneEDinNewYorkCity,14%ofpatientswerehomeless and25%hadbeenconcernedaboutbecominghomeless duringthepriortwomonths.8 Homelessnessisspecifically associatedwithhighlevelsofEDuse.9–14 Nationaldatafrom theVeteransHealthAdministrationfoundthatpatients experiencinghomelessnesswere6.6timesmorelikelythan otherstohavemorethan25EDvisitsannually.15
Furthermore,patientsexperiencinghomelessnessarefour timesmorelikelythanotherstore-presenttotheEDwithin threedaysofapriorevaluation.16 Althoughhomelessnessis stronglyassociatedwithhighEDuse,itmaynotbe independentlyassociatedwithsuchusesincemanysocialand medicalfactorsmaydrivethisassociation;however,this needstobeempiricallyexamined.
PreviousresearchonEDutilizationamongpatients experiencinghomelessnesshasbeenalmostexclusivelybased ondatafrompatientpopulationssampledinclinicalsettings, potentiallybiasingourunderstandingofhowhomelessness relatestoEDuseinthegeneralpopulation.7–11,13–16 Few studieshaveexaminedEDuseinnationallyrepresentative samplesthatincludednon-healthserviceusers.Thefew availablereportsfromcommunity-basedstudiesamong homelessindividualssuggestthatonlyasmallminority (8–12%)usetheEDmorethanthreetimesperyear.17,18 Thus,thereisaneedtoexaminethisissueinanationally representativesample.
Inthisstudy,weusedanationallyrepresentativesurvey, theNationalEpidemiologicSurveyonAlcoholandRelated Conditions(NESARC-III),toexaminetheassociationof recenthomelessnessandfactorsthatmaybeassociatedwith EDuse.19 Wehypothesizedthatsocialdisadvantage (eg,poverty,racism,educationalattainment,and neighborhoodenvironment)mightaccountformuchofthe extensiveEDusebyhomelessadults,althoughwesuspected thathealth-relatedfactorswouldalsoplayarole.Wethus soughttoexamineevidencetoclarifyhowsocial,medical, andmentalhealthfactorsplayintotheassociationbetween
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Previousresearchamongpatientpopulations inclinicalsettingsdemonstratedastrong associationbetweenhomelessnessandhigh frequencyEDuse
Whatwastheresearchquestion?
Dosocialdisadvantageandhealth-related factorsaccountformuchoftheextensiveED usebyhomelessadults?
Whatwasthemajor findingofthestudy?
Adjustedforsocialandhealthfactors, homelessnessandEDusewerenot signi fi cantlyassociated(AOR1.27,95%CI 0.79 – 2.03) .
Howdoesthisimprovepopulationhealth?
Thecomplexinterplaybetweensocialand medicalissuesshouldencouragethe developmentofservicedeliverymodels linkingtheseintersectingdimensionsofneed
homelessnessandEDuseamongthemostsocially disadvantagedsectorsoftheUSpopulation.
METHODS DataSourceandStudySample
Weperformedacross-sectionalanalysistoassessthe associationbetweenhomelessnessandEDuseusingdata fromNESARC-III.TheNESARC-IIIisanationally representativesurveyof36,906adults,whichincludes informationonexperiencesofprior-yearhomelessnessand emergencycareutilizationaswellasdemographicandrecent social,medical,andmentalhealthcharacteristics.19 This dataallowsexaminationoftheassociationofbothrecent homelessnessandotherfactorsthatarelikelytobe associatedwithEDuse,thusofferinganexaminationofthe independentassociationofhomelessnessandEDusewhen social,medical,andmentalhealthfactorsaretakeninto consideration.ThesurveywassponsoredbytheNational InstituteonAlcoholAbuseandAlcoholism(NIAAA)and conductedbetweenApril2012–June2013amongthenoninstitutionalizedUScivilianpopulation ≥18yearsold.19 Multistageprobabilitysamplingwasusedtorandomlyselect personsfromthispopulation.Primarysamplingunitswere individualcountiesorgroupsofcontiguouscounties. Secondarysamplingunitsconsistedofareasegmentsof census-definedblocks.Householdswithinthesampled
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 895 Ryusetal. NationalSampleofEDUseAmongRecentlyHomelessAdults
secondarysamplingunitswerethenselected.Finally,eligible adultswithinthesampledhouseholdswererandomly selected.19 Aninitial43,364eligiblesamplepersonswere identified,and36,309participatedintheNESARC-III,while 7,055wereclassifiedasnonresponders,foraperson-level responserateof84.0%.19
Atotalof36,309respondentscompletedtheAlcoholUse DisorderandAssociatedDisabilitiesInterviewSchedule, DSM-5version(AUDADIS-5),afullystructured, computer-assisteddiagnosticinterviewconductedbytrained NIAAAinterviewers.20 Institutionalizedindividuals(eg,in nursinghomes,prisons,hospitals,orshelters)wereexcluded alongwithactivedutymilitarypersonnel.Racial/ethnic minoritieswereoversampledtoassurerepresentative analysis.Datawasadjustedforoversamplingand nonresponseandthenweightedtorepresenttheUScivilian populationbasedonthe2012AmericanCommunity Survey.21 Informedconsentwaselectronicallyrecorded,and respondentsreceived$90forparticipation.Institutional reviewboards(IRB)attheUSNationalInstitutesofHealth andWestat,Inc.(Rockville,MD)approvedthestudy protocol.ThisstudywasapprovedbytheIRBsofthe DepartmentofVeteransAffairsConnecticutHealthcare SystemandYaleSchoolofMedicine.
MEASURES EDUtilization
Wemeasuredtheprimaryoutcomevariable,ED utilization,basedonself-reportbyrespondentsand categorizedintoathree-levelvariablerepresentingnouse (0visits),moderateuse(1–4visits),andhighuse(5ormore visits)intheprioryear.
Sociodemographics
Sociodemographiccharacteristicsincludedage,gender, race,maritalstatus,annualhouseholdincome,levelof education,employmentstatus,militaryservice,ruralvs urbanresidence,andhealthinsurancecoverage.
SocialHistory
Socialhistoryvariablesaddressedhomelessness, incarceration,interactionwithlawenforcement,parental socialhistory,adversechildhoodexperiencessuchassexual abuseorneglect,experiencesofracialdiscrimination,social contacts,andsocialsupport.Wecreatedtwodichotomous homelessnessvariablesthatidentifiedadultswith homelessnessinthepastyearandhomelessnesspriortothe mostrecentpastyear.Lifetimehomelessnesswasassessed withthisquestion: “Sinceyouwere15,didyouhaveatime thatlastedatleastonemonthwhenyouhadnoregularplace tolive likelivingonthestreetorinacar?” Aseparate question “Inthelast12months,haveyouatanytimebeen homeless?” wastheindependentvariableofcentralinterest inthisstudy.ApreviousstudyusingNESARC-IIIdata
reportedthelifetimeandone-yearprevalenceofhomelessto be4.2%and1.5%,respectively.22
Othersocialhistoryvariablesincludedquestionssuchas “Duringthelast12months,didyouhaveserioustroublewith thepoliceorlaw?” whichwascodedintoadichotomous variableforpoliceinvolvement.Experiencingracial discriminationwasacontinuousvariableassessedfromsix questionswithinAUDADIS-5thathavebeenshowntohave goodvalidityandreliabilityformeasuringexperiencesof racialdiscrimination.22 Thesixdiscriminationquestionsask aboutexperiencedracialdiscriminationinsixcontexts: obtaininghealthcare/healthinsurance;receivingcare; inpublic;obtainingajob;beingcalledracistnames;being hit/threatenedwithharm.WeusedaLikertscaletoassessthe frequencyofexperiencesofdiscriminationinthepastyear: 0 = never;1 = almostnever;2 = sometimes;3 = fairlyoften; or4 = veryoften.
Parentalhistoryincludedexperiencesofincarceration, psychiatrichospitalization,suicideattemptorcompletion, andsubstanceuse.Theextentofsocialsupportwasassessed usingtheInterpersonalSupportEvaluationList23,24: perceivedavailabilityofotherstoshareactivities,talkabout one ’sproblemsandfromwhomtopotentiallyreceive materialsupport.Socialcontactswereassessedthrougha seriesofquestionsregardinghowmanypeoplethe respondentshadcontactwithintheprevioustwoweeks, whichweresummedtocreateanindexofsocialcontacts. Veteranswereidentifiedasthosewhorespondedtothe question “HaveyoueverservedonactivedutyintheU.S. ArmedForces,MilitaryReserves,orNationalGuard?” with “Yes,inthepast,butnotnow.”
Medical,MentalHealth,andServiceUseHistory
Medicalhistoryvariablesincludednumberofmedical comorbidities,upto18;presenceofmoderatetoseverepain; numberofinjuriesinthepastyear;cancerhistory;bodymass index(BMI) > 40;andmental-andphysicalhealth-related qualityoflife.Respondentswereaskedwhetherornotthey hadeachof18medicalconditions(eg,arthritis,diabetes,and insomnia)inthepast12months.Thosewhoresponded positivelywerefurtherasked, ‘‘Didadoctororhealth professionaltellyouthatyouhad[amedicalcondition]?’’
Usingthesetwoquestionnaireitemsforeachmedical condition,wecreatedameasureofchronicconditions experiencedinthepastyear.Qualityoflifewasmeasured usingtheShortForm-12,version2(SF-12),areliableand validmeasureofhealthstatuscommonlyusedinpopulation surveys.25,26 The12questionscanbescoredintosubscalesto yieldamentalcomponentsummary(MCS)scoreanda physicalcomponentsummary(PCS)scoreaswellasoverall subjectivehealthstatus.Thenumberofinjuriesreportedby respondentswasassessedbythequestion, “Duringthelast 12months,howmanyinjurieshaveyouhadthatcausedyou toseekmedicalhelportocutdownyourusualactivitiesfor
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 896 NationalSampleofEDUseAmongRecentlyHomelessAdults Ryusetal.
morethanhalfaday?” Thisvariablewasmeasuredasa continuousvariable.
WeassessedlifetimeorpastyearpresenceofDSM-5 mentalhealthdiagnoseswiththeAUDADIS-5andincluded thefollowing:mooddisorders(majordepressivedisorder, bipolarIdisorder,dysthymia);anxietydisorders(generalized anxietydisorder,specificphobia,panicdisorder);posttraumaticstressdisorder(PTSD),andeatingdisorder.We usedAUDADIS-5scoringforalldisordersexcept schizophrenia/psychosis,whichwasaddressedwiththe followingquestion, “Didadoctororotherhealth professionaltellyouthatyouhadschizophreniaora psychoticillnessorepisode?” Personalitydisordersincluded antisocial,borderline,andschizotypal.Lifetimeandpast yearsubstanceusedisorders(SUD)includedalcoholuse disorder,aswellascannabis,cocaine,opiate,heroin, stimulant,andsedativeusedisorders(consideredtogetheras non-alcoholdrugusedisorders),andtobaccousedisorder.
Multimorbiditywasaddressedwithdichotomous variablesindicatingthefollowing:thepresenceofonlyone psychiatricdiagnosisandanotherindicatingtwoormore suchdiagnoses;thepresenceofonlyoneSUDdiagnosisand anotherindicatingtwoormoresuchdiagnoses.An additionalmeasurecapturedthepresenceofbothpsychiatric disorderandSUD(dualdiagnosis).
DataAnalysis
Weusedaseriesofbivariateanalysestoevaluatethe associationofeachdemographic,social,ormedicaland mentalhealthcharacteristicwitheachlevelofEDusage. Becausetherewasinflatedstatisticalpowergiventhelarge samplesize,weselectedvariablesforinclusioninsubsequent multivariableanalysesbasedoneffectsizesratherthan P -values.Weidentifiedriskratios > 1.5or < 0.7as representingsubstantialandmeaningfuleffectsfor dichotomousvariables.27 Forcontinuousvariablesweused Cohendasanindicatorofeffectsize,withd > 0.20or < 0.20 indicatingatleastasmalleffectsize.28
Wethenconductedaseriesoffourlogisticregression analysesconductedseparatelywithdifferentsetsof independentvariables,allincludingpastyearhomelessness. The firstlogisticregressionwasunadjustedandincludedonly pastyearhomelessnessastheindependentvariable.The secondmodelwasadjustedonlyfordemographicandsocial variablesmeetingcriteriaforsubstantialbivariateeffectsand thusevaluatedtheconcurrentroleofsocialdeterminantsof health.Athirdlogisticmodelexaminedonlyco-occurring medicalandmentalhealthvariablesshowingsubstantial associationwithEDuseinbivariateanalyses.Weincluded variablesregardingparentalsuicide,druguse,and psychiatrichospitalizationinthethird(health)model, whereasparentalprisonhistorywasincludedinthesecond modelofnon-medicalsocialriskfactors.Finally,weentered allvariableswithmeaningfuleffectsizespertheabove
criteriaintoastepwisemultinomiallogisticregression analysiswithforwardselectiontoidentifyaparsimoniousset ofstatisticallysignificantfactorsthatwereindependently associatedwithmoderateandhighEDuse.Sinceallthese variableshadpassedtheeffectsizescreensonbivariate analysis,weappliedaconventional P < 0.05levelof statisticalsignificancetothesemodels.
Wecomputedstandardizedregressioncoefficientsto allowidentificationofvariablesmoststronglyassociated withEDuse.Comparisonof 2loglikelihoodindicators wereusedtoassessgoodnessof fitwithlargervalues indicatingsuperior fit.WeperformedallanalysesusingSAS version9.4(SASInstituteInc,Cary,NC).
RESULTS Sample
Ofthetotal36,121respondentswithcompletedata, 27,674(76.61%)reportednoEDuseinthepastyear,7,972 (22.07%)reportedmoderateEDuse,and475(1.32%) reportedhighuse.Havingexperiencedhomelessnesswithin thepastyearwasreportedby559(1.55%)respondents,and 1,541(4.27%)respondedthattheyhadexperienced homelessnesswithintheirlifetime.
BivariateCorrelatesofEDUse
Bivariateanalysesshowedpastyearhomelessness (relativerisk[RR] = 6.83)tobeamongthethreevariables moststronglyassociatedwithhighEDuse,exceededonlyby pastyearsuicideattempt(RR = 11.51)andreceiptofa diagnosisofschizophreniaorpsychosisinthepastyear (RR = 8.61)(Tables1–3).Demographicvariables substantiallyassociatedwithmoderateandhighEDuse includedreceivingdisabilitybenefits(RR = 2.71and RR = 7.68,respectively).Havingacollegeeducationwas protective(Table1).
Amongthesocialvariables(Table2)associatedwith moderateandhighEDuse,homelessnessinthepastyear (RR = 2.27andRR = 6.83)andhomelessnesswithinone’ s lifetime(RR = 1.97andRR = 4.38)wereassociatedwiththe highest relativerisk.Experiencingtroublewiththepolice (RR = 4.17)andhistoryofincarcerationbeforeandafterage 18(RR = 3.74andRR = 2.64)werealsoassociatedhighED use,aswereadversechildhoodeventssuchasneglect,sexual abuse,parentalsuicideattempts,parentalsuicide completion,parentalimprisonment,parentaldruguse,and parentalpsychiatrichospitalization.AsBlackracewas associatedwithhighEDuse,itshouldbenotedthat experiencingracialdiscriminationinthepastyearwasalso significantlyassociatedwithhighEDuse.
Healthstatusvariables(Table3)associatedwithmoderate andhighEDuseincludedworsegeneralhealth(Cohen d = 1.11and1.12),experiencingmoderateorseverepain,and aBMI > 40.HigherscoresonboththePCSandMCS wereprotective.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 897 Ryusetal. NationalSampleofEDUseAmongRecentlyHomelessAdults
Table1. Bivariateassociationsofdemographicvariableswithemergencydepartmentuse.
BivariateanalysescomparemoderateandhighEDuserstonon-users.
*Denotes continuousvariablewithCohendformeasureofassociation. ED,emergencydepartment;
,relativerisk;
,VeteransAdministration.
EDuse Group1 N = 27,674 EDuse Group2 n = 7,972 EDuse Group3 n = 475Bivariateanalysis 0visits1–4visits ≥5visits2vs13vs1 Variablemean(SD)/%mean(SD)/%mean(SD)/%RR/Cohend* RR/Cohend* Gender Male 49.15% 44.91% 36.57% 0.91 0.74 Age* 46.25(17.48)47.61(18.76)44.82(17.59) 0.08 0.08 Annualincome <$20,000 20.80% 28.20% 51.05% 1.36 2.45 $20,000–40,000 23.47% 26.46% 25.81% 1.13 1.1 $40,000–60,000 22.51% 20.87% 11.77% 0.93 0.52 >$60,000 33.22% 24.47% 11.39% 0.74 0.34 Race Black 10.74% 15.01% 20.90% 1.4 1.95 White 66.26% 66.37% 61.79% 1 0.93 Hispanic 15.25% 13.17% 10.09% 0.86 0.66 Other 7.75% 5.45% 7.24% 0.7 0.93 Maritalstatus Separatedordivorced 12.81% 16.89% 25.09% 1.32 1.96 Widowed 5.27% 7.48% 8.54% 1.42 1.62 Nevermarried 22.58% 21.82% 29.68% 0.97 1.31 Marriedorcohabitating59.34% 53.81% 36.69% 0.91 0.62 Employment Receivesdisability 3.61% 9.77% 27.70% 2.71 7.68 Lookingforwork 6.98% 8.65% 13.99% 1.24 2 Otheremployment 16.92% 17.60% 18.89% 1.04 1.12 Retired 16.68% 20.76% 14.11% 1.24 0.85 Employed 72.36% 63.01% 49.85% 0.87 0.69 Militaryservice Anymilitaryservice 9.08% 11.94% 10.54% 1.32 1.16 Rurality Urban 78.96% 78.21% 75.06% 0.99 0.95 Highestlevelofeducation Pre-highschool 12.17% 15.27% 23.65% 1.26 1.94 Highschool 25.01% 28.31% 31.24% 1.13 1.25 Pre-college 32.41% 35.29% 36.49% 1.09 1.13 College 30.42% 21.14% 8.62% 0.69 0.28 Healthinsurancecoverage Medicaid 8.22% 16.58% 32.40% 2.02 3.94 VATricare 4.18% 6.42% 8.20% 1.53 1.96 Medicare 19.43% 27.71% 32.85% 1.43 1.69 Anyinsurance 79.43% 83.49% 85.30% 1.05 1.07 Privateinsurance 59.83% 51.99% 35.23% 0.87 0.59
RR
VA
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 898
Ryusetal.
NationalSampleofEDUseAmongRecentlyHomelessAdults
BivariateanalysescomparemoderateandhighEDuserstonon-users. *Denotes
AmongthementalhealthvariablesassociatedwithED use(Table3),suicideattemptinthepastyearwasthemost stronglyassociatedwithbothmoderate(RR = 5.01)andhigh EDuse(RR = 11.51).ModerateandhighEDusewereboth associatedstronglywithpersonalitydisordersanddiagnosis ofschizophreniaorpsychosiswithinone’slifetime. Havingmorethanonesubstanceusedisorder,more thanonepsychiatricdisorder,ordualdiagnosiswithin thepastyearwerealsoallassociatedwithmoderateandhigh use(Table3).
MultivariateMultinomialLogisticRegressionAnalyses
Unadjustedlogisticregressionanalysisdemonstratedthat peoplewithexperienceofhomelessnesswithinthepastyear wereapproximatelytwiceaslikelytoreportmoderateED use(oddsratio[OR]2.31;95%confidenceinterval[CI]
1.93–2.76; P < 0.001)andseventimesmorelikelytoreport highEDuse(OR7.34;95%CI5.04–10.68; P < 0.001) comparedtothosewithoutpastyearexperience(Figure1).
Afteradjustingonlyfordemographic,socialvariables,the associationofhomelessnessanditsstatisticalsignificance weregreatlydiminishedaspeoplewithpastyearexperience ofhomelessnesswereonly27%morelikelytoreport moderateEDusethanothers(adjustedOR[AOR]1.27;95% CI1.05–1.54; P = 0.014)and62%morelikelytoreporthigh EDuse(AOR1.62;95%CI,1.05–2.50; P = 0.030)(Figure1).
Thethirdmodel,whichadjustedonlyformedicaland mentalhealthvariables,alsoshowedmarkeddeclineinORs comparedtotheunadjustedmodelasparticipants experiencingpastyearhomelessnesswere26%morelikelyto reportmoderateuse(AOR1.26;95%CI1.03–1.55; P = 0.025)andabouttwiceaslikelyastohavehighEDuse (AOR2.07;95%CI,1.33–3.24; P = 0.001).
Inthe finalstepwisemodelwithforwardselectionat P < 0.05,includingallsubstantiallyimportantvariables(social, medical,andmentalhealth),homelessnesswasnolonger significantlyassociatedwitheithermoderateorhighEDuse at P < 0.05.Afurtheranalysisinwhichpastyear
EDuseGroup1 n = 27,674 EDuseGroup2 n = 7,972 EDuseGroup3 n = 475Bivariateanalysis 0visits1–4visits ≥5visits2vs13vs1 Variablemean(SD)/%mean(SD)/%mean(SD)/%RR/Cohend* RR/Cohend* Homelessness Past year 1.14% 2.59% 7.81% 2.27 6.83 Lifetime 3.39% 6.68% 14.84% 1.97 4.38 Incarcerationhistory Policetroubleinpastyear 1.30% 2.50% 5.41% 1.92 4.17 Incarceratedbeforeage18 3.33% 5.86% 12.47% 1.76 3.74 Incarceratedafterage18 9.56% 14.91% 24.47% 1.61 2.64 Socialhistoryandsocialsupport Historyofchildneglect* 12.22(5.02)13.49(6.21)15.62(8.35) 0.19 0.52 Historyofchildsexualabuse*4.37(1.54)4.76(2.40) 5.49(3.18) 0.17 0.47 Racialdiscriminationinthe pastyear* 1.21(.43)1.29(.52) 1.47(.70) 0.14 0.48 Socialsupport* 3.02(.464)2.96(.51) 2.83(.61) 0.12 0.37 Numberofcontactsinthe pasttwoweeks* 16.36(15.08)15.91(15.08)14.28(14.28) 0.02 0.11 Parentalhistory Parentwithsuicideattempt 2.81% 4.20% 10.46% 1.49 3.72 Parentwithprisonhistory 6.48% 11.49% 19.07% 1.77 2.94 Parentwithsuicidecompletion0.86% 0.98% 2.42% 1.14 2.82 Parentwithdrugusehistory 4.99% 8.15% 11.26% 1.63 2.38 Parentpsychiatrichospitalization history 4.74% 7.47% 11.26% 1.58 2.38
Table2. Bivariateassociationsofsocialvariableswithemergencydepartmentuse.
continuousvariablewithCohen’sdformeasureofassociation. ED,emergencydepartment; RR,relativerisk. Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 899 Ryusetal. NationalSampleofEDUseAmongRecentlyHomelessAdults
Bivariateanalysescomparemoderateandhighuserstonon-users.
*Denotes continuousvariablewithCohen’sdformeasureofassociation. ED,emergencydepartment; RR,relativerisk; BMI,bodymassindex.
homelessnesswasforcedintothemodeltoassessthepoint estimateoftheeffectsizeassociationofrecenthomelessness withEDuseshowedanAORformoderateEDuseof1.13 (95%CI0.91–1.40,notsignificant)andAOR1.27(95%CI 0.79–2.03,notsignificant)forhighEDuse(Figure1).
Closerexaminationofthe finalmodel(Table4)showeda notablecommonalityinvariablesassociatedwithboth moderateandhighEDuse(Table4).Variableswiththe highestassociationswith moderate useincludednumberof
injuries(AOR1.79,95%CI1.73–1.86,standardized regressioncoefficient[SRC] = 0.8),numberormedical conditions(AOR1.33,95%CI1.30–1.37,SRC = 0.18),and Medicaidinsurance(AOR1.49,95%CI1.37–1.62, SRC = 0.07).
Variableswiththestrongestindependentassociationswith high EDusealsoincludednumberofinjuriesinthepastyear (AOR = 1.82,95%CI1.75–1.89,SRC = 0.82),numberof
= 1.53,95%CI1.43–1.64,
medicalconditions(AOR
EDuseGroup 1n = 27,674 EDuseGroup 2n = 7,972 EDuseGroup 3n = 475Bivariateanalysis 0visits1–4visits ≥5visits2vs13vs1 Variablemean(SD)/%mean(SD)/%mean(SD)/%RR/Cohend* RR/Cohend* Psychiatricandsubstanceusedisorders Past yearsuicideattempt 0.10% 0.50% 1.16% 5.01 11.51 Schizotypaldisorder 5.04% 10.10%22.14% 2.01 4.4 Antisocialdisorder 3.58% 6.48% 15.61% 1.81 4.37 Lifetimediagnosisofschizophreniaor psychosis 1.73% 3.57% 7.41% 2.07 4.29 Pastyeargreaterthanonesubstance usedisorderdiagnosis 1.79% 3.54% 6.84% 1.98 3.82 Pastyearsingledrugusedisorder diagnosis 3.15% 5.93% 11.30% 1.88 3.58 Pastyeargreaterthanonepsychiatric diagnosis 6.72% 13.51%23.34% 2.01 3.47 Borderlinepersonalitydisorder 7.96% 16.87%29.72% 2.01 3.47 Pastyeardualdiagnosis:psychiatric/ substanceusedisorder 4.00% 7.16% 9.48% 1.79 2.37 Pastyearsinglepsychiatricdiagnosis12.57%16.91%24.93% 1.35 1.98 Multiplerecurringtraumas 12.86%16.00%22.00% 1.24 1.71 Lifetimealcoholusedisorderdiagnosis27.97%32.56%38.13% 1.16 1.36 Pastyearsinglesubstanceusedisorder diagnosis 12.85%15.03%17.01% 1.17 1.32 Pastyearalcoholusedisorder diagnosis 13.16%16.05%17.01% 1.22 1.29 Medicalhistory Medicalconditions(range1–18)* 0.62(0.97)1.28(1.48)2.26(1.97) 0.45 1.12 Numberofinjuries* 0.20(2.11)0.96(4.50)2.44(8.00) 0.16 0.46 Generalhealth(scaleof1to5)* 2.33(1.04)2.84(1.15)3.64(1.14) 1.11 0.46 ShortForm-12mentalcomponent*51.62(9.18)48.63(11.42)43.37(12.56) 0.27 0.75 ShortForm-12physicalcomponent*50.91(9.49)45.51(12.37)36.68(12.85) 0.47 1.23 Moderateorseverepain 15.80%32.77%63.90% 2.07 4.04 Anyhistoryofcancer 3.65% 6.20% 12.94% 1.70 3.55 BMI >40 3.76% 6.76% 10.78% 1.8 2.86
Table3. Bivariateassociationsofmedicalandmentalhealthvariableswithemergencydepartmentuse.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 900 NationalSampleofEDUseAmongRecentlyHomelessAdults Ryusetal.
SRC = 0.27),andMedicaidinsurance(AOR = 1.97,95%CI 1.55–2.51,SRC = 0.11),alongwithparentaldrugusehistory (AOR1.95,95%CI1.40–2.71;SRC = 0.09).Thestrongest protectivevariablesforbothmoderateandhighEDuse includedhighSF-12componentscores,collegeeducation, andbeingmarriedorcohabitating.
Comparisonof 2loglikelihoodindicatorsofmodel fit showedthemodelofhomelessnessalone( 2LL = 41495, degreesoffreedom[df] = 2)hadapoorergoodnessof fitthan boththemodelofsocial( 2LL = 38,777,df = 40)andthe modelofmedicalandmentalhealthfactorsalone( 2LL = 36,076,df = 52),andallthreehadapoorermodel fitthanthe finalcombinedstepwisemodel( 2LL = 35,188,df = 42)with eachmodel fitsignificantlysuperiortothatoftheprevious modelat P < 0.005.
DISCUSSION
Thisstudyshowedthathomelessnesswasstrongly associatedwithEDuseinanunadjustedmodel,ashasbeen foundinmanyotherstudies.9–14 However,estimatesofthe independent associationofhomelessnessandEDuse, adjusting firstformeasuresofdemographiccharacteristics andsocialdisadvantageandthenseparatelyformedicaland mentalhealth,showedthatbothsetsoffactorslargely accountedforthisassociation.Thissuggestsanimportant potentialmediatingroleofthesefactors.Theassociationof homelessnesswithEDusewasfurtherreducedtononsignificancewhenbothtypesoffactorswereincluded ascovariates.
Thestrongestriskfactorsinthe finalmodelwereinjuries, medicalconditions,Medicaidcoverage,andparentaldrug usewhilethestrongestprotectivevariableswerehigh
physical-andmentalhealth-relatedqualityoflife,college education,andbeingmarriedorcohabitating.These findings areconsistentwithexistingliteraturethathasdemonstrated lowersocioeconomicstatus,lowereducationalattainment, publicinsurance,andpoorerperceivedhealthwere predictorsoffrequentEDuse.29 Physicalinjurieshavealso beenshowntobeassociatedwithfrequentEDvisits, includingreturnvisits.30
Thestrongunadjustedassociationbetweenhomelessness andEDuseisconsistentwithpriorliterature.15,31 However, inthisstudywefurtherconsideredmedicalandsocialfactors asseparateblockstoexploretheassociationofhomelessness andEDuseadjustingforthesefactors.Additionally,our studywasbasedonanationallyrepresentativesample extendingitsgeneralizabilitytopopulationsthatincluded peopleoutsideclinicalsettings.17,18 TheNESARC-III datasetwasalsoexceptionalinthericharrayofsocial variablesunavailableinmedicalrecords(eg,education, parentalhistories,adversechildhoodevents,socialisolation, andcriminaljusticeinteraction.)
Implications
Ithasbeensuggestedthatthehighcostofhealthcareinthe UScomparedtootherwealthycountriesreflectslimited provisionofsocialservices.5 Healthpolicyexperts increasinglyrecognizethesocialdeterminantsofhealth,and federalandlocalinitiativesareemergingtoaddresssocial needsandreducehealthcareserviceuseandcosts,including EDcosts.32,33 WhilefrequentEDusersrepresentonly4
8% ofEDpatients,theyaccountfor21–28%ofallEDvisitsand generatesignificantcosts.34 Recentstudiesshowthat individualizedcasemanagementinterventionscanmodestly
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 901 Ryusetal. NationalSampleofEDUseAmongRecentlyHomelessAdults
Figure1. AssociationofpastyearhomelessnesswithmoderateandhighEDuse:UnadjustedandAdjustedOddsratiosfrommultinomial logisticregressionmodels. OR,oddsratio.
reduceEDuse.35–37 Otherstudiesthatfocusonprimarycare accessarelesspromisingsincemostfrequentEDusers alreadyusehighlevelsofprimarycare.15 Housing-focused
initiativessignificantlyreducehomelessnessbuthavehad limitedeffectonthephysicalormentalhealthofclients,on decreasingEDuse,oronreducinghealthservicecosts.
38–42
Variable ModerateEDusevsNon-use* Variable HighEDusevsNon-use* OR(95%CI) Standardized regression coefficientOR(95%CI) Standardized regression coefficient Numberofinjuries 1.79 (1.73–1.86) 0.8 Numberofinjuries 1.82 (1.75–1.89) 0.82 Medicalconditions 1.33 (1.30–1.37) 0.18ShortForm-12physical component 0.95 (0.94–0.96) 0.32 ShortForm-12physical component 0.98 (0.977–0.983) 0.12MedicalConditions 1.53 (1.43–1.64) 0.27 Medicaidinsurance 1.49 (1.37–1.62) 0.07Collegeeducation 0.47 (0.32–0.68) 0.19 ShortForm-12mental component 0.99 (0.987–0.993) 0.06Marriedorcohabitating 0.56 (0.45–0.69) 0.16 Black 1.34 (1.23–1.46) 0.05ShortForm-12mental component 0.98 (0.966–0.984) 0.14 Anytraumaticexperience 1.2 (1.13–1.27) 0.05Medicaidinsurance 1.97 (1.55–2.51) 0.11 Collegeeducation 0.81 (0.76–.87) 0.05Parentwithdrugusehistory1.95 (1.40–2.71) 0.09 Pastyearsuicideattempt3.03 (1.74–5.27) 0.03Black 1.56 (1.19–2.05) 0.08 VATricare 1.29 (1.14–1.46) 0.03Racialdiscriminationinthe pastyear 1.35 (1.14–1.59) 0.07 Parent withprisonhistory1.23 (1.11–1.37) 0.03Policetroubleinpastyear2.06 (1.25–3.38) 0.05 Borderlinepersonality disorder 1.20 (1.09–1.21) 0.03Pastyearhomelessness ** ** Socialsupport 1.14 (1.07–1.21) 0.03Pastyearsuicideattempt ** ** Historyofchildsexualabuse1.03 (1.01–1.04) 0.03VATricare ** ** Pastyeargreaterthanone substanceusedisorder diagnosis 1.28 (1.08–1.52) 0.02Pastyeargreaterthanone substanceusedisorder diagnosis ** ** Marriedorcohabitating 0.91 (0.86–0.97) 0.02Parentwithprisonhistory ** ** Pastyearhomelessness ** **Anytraumaticexperience ** ** Policetroubleinpastyear ** **Borderlinepersonality disorder ** ** Parentwithdrugusehistory** **Socialsupport ** ** Racialdiscriminationinthe pastyear ** **Historyofchildsexualabuse** ** *Allvariableswitha P-value forWaldchi-square <.01. **Variablenotincludedinthe finalstepwiseregression. ED,emergencydepartment; OR,oddsratio; CI,confidenceinterval; VA,VeteransAdministration. WesternJournal of EmergencyMedicine Volume24,No.5:September2023 902 NationalSampleofEDUseAmongRecentlyHomelessAdults Ryusetal.
Table4. StepwisemultinomiallogisticregressionmodelsoftheassociationofEDuseandsocial,medical,psychiatric,andsubstanceuse disorders.
Thesemixed findingssuggestthereisalargercontext beyondserviceintegrationandsupportedhousingthat requiresattention.
Theconcurrenceofhomelessness,socialdisadvantage, andchronicmedicalandmentalillnesspointstoa vulnerabilitydeeperthanmerelyhavingmultiple,chronic illnessesandmaybebestunderstoodthroughtheevolving conceptofallostaticburden.43 Allostasisisthegeneral adaptivecapacityofapersontorespondeffectivelyto physicalorsocialdemands.Allostaticburdenreferstothe magnitudeofthedemandforandpotentialfailureof adaptivecapabilities.Inindividualswithhighallostatic burden,thecumulativeeffectofchronicstressandlifeevents overwhelmsadaptivecapacitiesinabroadsense.Allostatic burdenhasbeenshowntobeassociatedwithpoorerhealth outcomesincardiovasculardisease,diabetes,preeclampsia, geriatricfrailty,periodontaldisease,PTSD,psychotic disorders,andalcoholdependence,43 andtoarisefrom conditionsofpoverty,segregation,discrimination,sexual trauma,andloweducationalattainmentandthusexceeds anyconceptionofchronicdiseasethatmerelyreflects illnessescontinuingoveralong-termcourse.43 Many indicatorsofallostaticburdenweresignificantinourmodel ofhighEDuseandaredisproportionatelyrepresentedinthe homelesspopulation.Whilenostudiestodatehave examinedtheassociationofallostaticloadandfrequentED use,theallostaticburdenmodelmayfacilitateunderstanding offrequentEDuse,andspecificallyhighuseamongpeople experiencinghomelessness.
Inrecognitionofwhatiscurrentlyknown,social emergencymedicine(EM)shouldbeaddedtotheEM researchagendaandincludedinthecorecurriculumforED residentsviabothdidacticsandcommunity-based learning.44 Ausefulframeworkcoulddifferentiatethree distinctlevelsofcare:acutecareforimmediateproblems (eg,appendicitis,traumaticinjuries);acute-on-chronic careforurgenttreatmentofexacerbatedheartfailure; diabeticketoacidosis,etc;andcareforlong-term overwhelmingallostaticburden,thecomplexoflifelong socialandmedicalproblemsthatchallengestheability ofanindividualtomaintainthemselvesinthesociety inwhichtheylive,andaboutwhichmuchremainsto belearned.2,44
LIMITATIONS
Severallimitationswarrantconsideration.First,specific dataontheimmediatereasonsforindividualEDvisitswere notavailableinNESARC-III.Whilemedicalandmental healthproblemsaccountformuchoftheassociation betweenEDuseandhomelessness,itisunclearwhetherED visitsweredirectlyrelatedtotreatmentofthesehealthissues. Previousstudiesfoundthatthemajorityofvisitsamong patientswithmentalillnesswereforphysicalhealth conditionsratherthanreasonsrelatedtomental
health.45–48 Weheuristicallyseparatedmedicaland mentalhealthproblemsbutrecognizethattheyare tightlyintertwined.49–51
Second,ourstudywascross-sectionalandcannotsupport conclusionsaboutcausality.Thevariablerepresenting homelessnessreferredtoprioryearhomelessnesswithout dataontherecencyorchronicityofthehomelessness episode.Additionally,ourcross-sectionaldataisfrom 2012–2013andassociationsmayhavechangedinthe interveningtime.Our findingssuggesttrendstobeexplored inlongitudinalstudiesofhowEDuseamonghomeless adults,aswellasothers,relatestooverwhelminglong-term allostaticburden.
Third,thesampleexcludedinstitutionalizedadults, omittingpertinentpopulationsathighriskforhomelessness suchasincarceratedindividualsandthoseinhomeless shelters.Thislimitationisnotuniquetoourstudy,although itismorecomprehensivethaninpreviousliterature.Finally, someNESARC-IIIvariablesthemselvesareimpreciseandof uncertainvalidity.HomelessnessandEDusewerebasedon self-reportandthussubjecttorecallbias.TheEDuseitem waslimitedtoamaximumof10ormorevisitsperyear, limitingtheprecisionwithwhichwecouldanalyzethe constructof “high” EDuse.Itispossiblethatattheextremes ofEDuse,theremayhavebeenanevenstrongerassociation withhomelessnessandotherevidenceofextreme allostaticburden.15
CONCLUSION
HomelessindividualsusetheEDathigherratesthanother individuals,butwhenadjustingforothersocialandmedical factors,wedidnot findanindependentassociationbetween homelessnessandhigherEDusage.Thishighlightsthe complexinterplaybetweensocialandmedicalissuesand shouldencouragethedevelopmentandevaluationofmore fullyintegratedtrainingandservicedeliverymodelslinking theseintersectingdimensionsofneed.
AddressforCorrespondence:CaitlinRyus,MD,MPH, YaleSchoolofMedicine.DepartmentofEmergencyMedicine 464CongressAve.,Suite260,NewHaven,CT06519. Email: caitlin.ryus@yale.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Ryusetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 903 Ryusetal. NationalSampleofEDUseAmongRecentlyHomelessAdults
REFERENCES
1.SelbyS,WangD,MurrayE,etal.Emergencydepartmentsasthehealth safetynetsofsociety:adescriptiveandmulticenteranalysisofsocial workersupportintheemergencyroom. Cureus.2018;10(9).
2.AlterHJ,FahimiJ,WangNE.Socialemergencymedicine:historyand principles.In: SocialEmergencyMedicine. NewYori,NY:Springer; 2021:3–12.
3.FahimiJ,GoldfrankL.Principlesofsocialemergencymedicine. Ann EmergMed.2019;74(5):S6
S10.
4.TheriaultKM,RosenheckRA,RheeTG.Increasingemergency departmentvisitsformentalhealthconditionsintheUnitedStates. JClinPsychiatry.2020;81(5).
5.BradleyE,TaylorL. TheAmericanHealthCareParadox:WhySpending MoreIsGettingUsLess.NewYork,NY:PublicAffairs,PerseusBooks Group;2013.
6.MooreBJ,LiangL.CostsofEmergencyDepartmentVisitsintheUnited States,2017.In: HealthcareCostandUtilizationProject(HCUP) StatisticalBriefs[Internet].AgencyforHealthcareResearchandQuality (US);2020.
7.FeldmanBJ,CalogeroCG,ElsayedKS,etal.Prevalenceof homelessnessintheemergencydepartmentsetting. WestJEmerg Med.2017;18(3):366.
8.DoranKM,JohnsE,SchretzmanM,etal.Homelessshelterentryinthe yearafteranemergencydepartmentvisit:resultsfromalinkeddata analysis. AnnEmergMed.2020;76(4):462–7.
9.KuBS,FieldsJM,SantanaA,etal.Theurbanhomeless:super-usersof theemergencydepartment. PopulHealthManag.2014;17(6):366–71.
10.LaCalleEJ,RabinEJ,GenesNG.High-frequencyusersofemergency departmentcare. JEmergMed.2013;44(6):1167–73.
11.CawleyC,RavenMC,MartinezMX,etal.UnderstandingThe100 HighestUsersofHealthandSocialServicesinSanFrancisco. AcadEmergMed. 2021.
12.KanzariaHK,NiedzwieckiM,CawleyCL,etal.Frequentemergency departmentusers:focusingsolelyonmedicalutilizationmissesthe wholeperson. HealthAffairs.2019;38(11):1866–75.
13.TsaiJ,DoranKM,RosenheckRA.Whenhealthinsuranceisnotafactor: nationalcomparisonofhomelessandnonhomelessUSveteranswho useVeteransAffairsemergencydepartments. AmJPublicHealth 2013;103(S2):S225–31.
14.TsaiJ,RosenheckRA.RiskfactorsforEDuseamonghomeless veterans. AmJEmergMed.2013;31(5):855–8.
15.DoranKM,RavenMC,RosenheckRA.Whatdrivesfrequentemergency departmentuseinanintegratedhealthsystem?Nationaldatafromthe VeteransHealthAdministration. AnnEmergMed.2013;62(2):151–9.
16.KuBS,ScottKC,KerteszSG,etal.Factorsassociatedwithuseofurban emergencydepartmentsbytheUShomelesspopulation. PublicHealth Reports.2010;125(3):398–405.
17.MooreDT,RosenheckRA.Factorsaffectingemergencydepartment usebyachronicallyhomelesspopulation. PsychiatricServices 2016;67(12):1340–7.
18.KushelMB,PerryS,BangsbergD,etal.Emergencydepartmentuse amongthehomelessandmarginallyhoused:resultsfromacommunitybasedstudy. AmJPublicHealth.2002;92(5):778–84.
19. GrantB,ChuA,SigmanR,etal.NationalInstituteonAlcoholAbuseand AlcoholismNationalEpidemiologicSurveyonAlcoholandRelated Conditions-III(NESARC-III)sourceandaccuracystatement.Bethesda, MD:NIAAA.2015.
20.HasinDS,GreensteinE,AivadyanC,etal.TheAlcoholUseDisorder andAssociatedDisabilitiesInterviewSchedule-5(AUDADIS-5): proceduralvalidityofsubstanceusedisordersmodulesthroughclinical re-appraisalinageneralpopulationsample. DrugAlcoholDepend 2015;148:40–6.
21.U.S.CensusBureau.AmericanCommunitySurvey,2012.In: CommerceUSDo,ed.Suitland,MD:U.S.CensusBureau2013.
22.TsaiJ.Lifetimeand1-yearprevalenceofhomelessnessintheUS population:resultsfromtheNationalEpidemiologicSurveyonAlcohol andRelatedConditions-III. JPublicHealth. 2018;40(1):65–74.
23.BommersbachTJ,RheeTG,StefanovicsEA,etal.ComparisonofBlack andWhiteindividualswhoreportdiagnosesofschizophreniaina nationalsampleofUSadults:discriminationandserviceuse. Schizophr Res. 2021.
24.CohenS,MermelsteinR,KamarckT,etal.Measuringthefunctional componentsofsocialsupport.In: SocialSupport:Theory,Researchand Applications.NewYork,NY:Springer;1985:73
94.
25.WareJ,KosinskiMJr,Turner-BowkerD,etal. Howtoscoreversion2of theSF-12HealthSurvey(withasupplementdocumentingversion1) Lincoln,RI:QualityMetricInc.2002.
26.HasinDS,StinsonFS,OgburnE,etal.Prevalence,correlates, disability,andcomorbidityofDSM-IValcoholabuseanddependence intheUnitedStates:resultsfromtheNationalEpidemiologic SurveyonAlcoholandRelatedConditions. ArchGenPsych 2007;64(7):830–42.
27.FergusonCJ.Aneffectsizeprimer:aguideforcliniciansand researchers. ProfessionalPsychology:ResearchandPractice, 40(5):532–538. https://doi.org/10.1037/a0015808
28.CohenJ.Statisticalpoweranalysisforthebehavioralsciences [Internet]. StatisticalPowerAnalysisfortheBehavioralSciences. 1988:567.
29.GiannouchosTV,KumHC,FosterMJ,etal.Characteristicsand predictorsofadultfrequentemergencydepartmentusersintheUnited States:asystematicliteraturereview. JEvalClinicalPrac 2019;25(3):420–33.
30.LafertéC,DépelteauA,HudonC.Injuriesandfrequentuseof emergencydepartmentservices:asystematicreview. BMJOpen 2020;10(12):e040272.
31.DavisCI,MontgomeryAE,DichterME,etal.Socialdeterminantsand emergencydepartmentutilization: findingsfromtheVeteransHealth Administration. AmJEmergMed.2020;38(9):1904–9.
32.WilenskyG.AddressingsocialissuesaffectinghealthtoimproveUS healthoutcomes. JAMA.2016;315(15):1552–3.
–
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 904 NationalSampleofEDUseAmongRecentlyHomelessAdults Ryusetal.
33.CMS.AccountableHealthCommunitiesModel.CentersforMedicaid andMedicareServices.Availableat: https://innovation.cms.gov/ innovation-models/ahcm.Published2021. AccessedNovember27,2021.
34.LaCalleE,RabinE.Frequentusersofemergencydepartments:the myths,thedata,andthepolicyimplications. AnnEmerMed 2010;56(1):42–8.
35.SorilLJ,LeggettLE,LorenzettiDL,etal.Reducingfrequentvisitstothe emergencydepartment:asystematicreviewofinterventions. PLoS ONE.2015;10(4):e0123660.
36.RavenMC,KushelM,KoMJ,etal.Theeffectivenessofemergency departmentvisitreductionprograms:asystematicreview. AnnEmerg Med.2016;68(4):467–483.e415.
37.SandbergSF,EriksonC,OwenR,etal.HennepinHealth:asafety-net accountablecareorganizationfortheexpandedMedicaidpopulation. HealthAffairs.2014;33(11):1975–84.
38.NationalAcademiesofSciencesE,Medicine.Permanentsupportive housing:evaluatingtheevidenceforimprovinghealthoutcomesamong peopleexperiencingchronichomelessness.2018.
39.GoeringPN,StreinerDL,AdairC,etal.TheAtHome/ChezSoitrial protocol:apragmatic,multi-site,randomisedcontrolledtrialofaHousing Firstinterventionforhomelessindividualswithmentalillnessin five Canadiancities. BMJOpen.2011;1(2):e000323.
40.RosenheckRA,LamJ,MorrisseyJP,etal.Servicesystemsintegration andoutcomesformentallyillhomelesspersonsintheACCESS program. PsychiatSer.2002;53(8):958–66.
41.SadowskiLS,KeeRA,VanderWeeleTJ,etal.EffectofaHousingand CaseManagementProgramonEmergencyDepartmentVisitsand HospitalizationsAmongChronicallyIllHomelessAdults:arandomized trial. JAMA.2009;301(17):1771–8.
42.TinlandA,LoubièreS,BoucekineM,etal.Effectivenessofahousing supportteaminterventionwitharecovery-orientedapproachonhospital
andemergencydepartmentusebyhomelesspeoplewithsevere mentalillness:arandomisedcontrolledtrial. EpidemiolPsychiatrSci 2020;29.
43.GuidiJ,LucenteM,SoninoN,etal.Allostaticloadanditsimpacton health:asystematicreview. PsychothePsychosom.2021;90(1):11–27.
44.RyusCR,YangD,TsaiJ,etal.Usingcommunity-basedparticipatory researchmethodstoinformcareforpatientsexperiencing homelessness:anopportunityforresidenteducationonhealthcare disparities. AEMEducTrain.2021;5:S121–5.
45.MerrickEL,PerloffJ,TompkinsCP.Emergencydepartmentutilization patternsforMedicarebeneficiarieswithseriousmentaldisorders. PsychiatServ.2010;61(6):628–31.
46.Mehl-MadronaLE.Prevalenceofpsychiatricdiagnosesamongfrequent usersofruralemergencymedicalservices. CanadianJRuralMed 2008;13(1):22.
47.TsaiJ,SzymkowiakD,KerteszSG.Top10presentingdiagnosesof homelessveteransseekingcareatemergencydepartments. AmJ EmergMed.2021;45:17–22.
48.PaudyalV,GhaniA,Shafi T,etal.Clinicalcharacteristics,attendance outcomesanddeathsofhomelesspersonsintheemergency department:implicationsforprimaryhealthcareandcommunity preventionprogrammes. PublicHealth 2021;196:117–23.
49.BrewerLC,CooperLA,PattenCA.Diabetesself-management educationforspecialpopulations:thesocialdeterminantsofhealth matter. PublicHealthRep.2019;134(3):313–4.
50.HardmanR,BeggS,SpeltenE.Whatimpactdochronicdiseaseselfmanagementsupportinterventionshaveonhealthinequitygapsrelated tosocioeconomicstatus:asystematicreview. BMCHealthServRes 2020;20(1):1–15.
51.MuenchbergerH,KendallE.Predictorsofpreventablehospitalizationin chronicdisease:prioritiesforchange. JPublicHealthPolicy 2010;31(2):150–63
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 905 Ryusetal. NationalSampleofEDUseAmongRecentlyHomelessAdults
SOCIAL EMERGENCY MEDICINEAND POPULATION HEALTH
Race,Healthcare,andHealthDisparities:ACriticalReviewand RecommendationsforAdvancingHealthEquity
WendyL.Macias-Konstantopoulos, MD,MPH,MBA*†
KimberlyA.Collins,MD,MPH‡
RosemarieDiaz,MD§
HerbertC.Duber,MD,MPH∥¶
CourtneyD.Edwards, DNP,RN,CLN#
AntonyP.Hsu,MD**
MeganL.Ranney,MD,MPH††
RalphJ.Riviello,MD,MS‡‡
ZacharyS.Wettstein,MD§§
CarolynJ.Sachs,MD,MPH∥∥
*CenterforSocialJusticeandHealthEquity,DepartmentofEmergencyMedicine, Boston,Massachusetts
† HarvardMedicalSchool,DepartmentofEmergencyMedicine,Boston,Massachusetts
‡ TampaGeneralHospital,Tampa,Florida
§ UniversityofCalifornia-LosAngeles,DepartmentofEmergencyMedicine, LosAngeles,California
∥ UniversityofWashingtonSchoolofMedicine,DepartmentofEmergencyMedicine, Seattle,Washington
¶ WashingtonStateDepartmentofHealth,Tumwater,Washington
# SamfordUniversity,Moffett&SandersSchoolofNursing,Birmingham,Alabama
**TrinityHealthAnnArborHospital,DepartmentofEmergencyMedicine, Ypsilanti,Michigan
†† YaleUniversity,YaleSchoolofPublicHealth,NewHaven,Connecticut
‡‡ UniversityofTexasHealthSanAntonio,DepartmentofEmergencyMedicine, SanAntonio,Texas
§§ UniversityofWashingtonSchoolofMedicine,DepartmentofEmergencyMedicine, Seattle,Washington
∥∥ RonaldReagan-UCLAMedicalCenterandDavidGeffenSchoolofMedicineat UniversityofCalifornia-LosAngeles,DepartmentofEmergencyMedicine, LosAngeles,California
SectionEditors: DavidThompson,MDandShahramLotfipour,MD,MPH
Submissionhistory:SubmittedAugust15,2022;RevisionreceivedApril17,2023;AcceptedMay24,2023
ElectronicallypublishedAugust8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58408
Anoverwhelmingbodyofevidencepointstoaninextricablelinkbetweenraceandhealthdisparitiesin theUnitedStates.Althoughraceisbestunderstoodasasocialconstruct,itsroleinhealthoutcomeshas historicallybeenattributedtoincreasinglydebunkedtheoriesofunderlyingbiologicalandgenetic differencesacrossraces.Recently,growingcallsforhealthequityandsocialjusticehaveraised awarenessoftheimpactofimplicitbiasandstructuralracismonsocialdeterminantsofhealth,healthcare quality,andultimately,healthoutcomes.Thismorenuancedrecognitionoftheroleofraceinhealth disparitieshas,inturn,facilitatedintrospectiveracialdisparitiesresearch,rootcauseanalyses,and changesinpracticewithinthemedicalcommunity.Examiningthecomplexinterplaybetweenrace,social determinantsofhealth,andhealthoutcomesallowssystemsofhealthtocreatemechanismsforchecks andbalancesthatmitigateunfairandavoidablehealthinequalities.
Asoneofthespecialtiesmostintertwinedwithsocialmedicine,emergencymedicine(EM)isideally positionedtoaddressracisminmedicine,develophealthequitymetrics,monitordisparitiesinclinical performancedata,identifyresearchgaps,implementprocessesandpoliciestoeliminateracialhealth inequities,andpromoteanti-racistidealsasadvocatesforstructuralchange.Inthiscriticalreviewouraim wasto(a)provideasynopsisofracialdisparitiesacrossabroadscopeofclinicalpathologyinterests addressedinemergencydepartments communicablediseases,non-communicableconditions,and injuries and(b)througharace-consciousanalysis,developEMpracticerecommendationsfor advancingacultureofequitywiththepotentialformeasurableimpactonhealthcarequalityandhealth outcomes.[WestJEmergMed.2023;24(5)906–918.]
Keywords: healthdisparities;socialdeterminantsofhealth;structuralracism;implicitbias.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 906
INTRODUCTION
Socialdeterminantsofhealth(SDoH)asdefinedbythe USCentersforDiseaseControlandPrevention(CDC)are theconditionsinwhichpeoplelive,learn,work,andplaythat aredeterminedbythedistributionofmoney,power,and resourcesandthataffectawiderangeofhealthandqualityof-liferisksandoutcomes.1 Influencedbythesocialconstruct ofrace,SDoHexertdisparateimpactsonthehealthof subpopulations.Economicdisparitiesdisproportionately placeBlack,indigenous,andpeopleofcolor(BIPOC)within zonesmarkedbysubstandardhealthpromotionand excessivehealthrisks.Thecompoundingnatureofadverse SDoH,suchashousinginstability,foodinsecurity,poor healthcareaccess,andhazardousexposures,hasserious healthimplications.Healthdisparitiesarethe profounddownstreameffectofthesocioeconomic disadvantagesthatBIPOCendureunderthemoniker structuralracism .
Inadditiontostructuralracism, implicitbias definedas unconsciousattitudes,positiveornegative,towardaperson, group,oridea oftenleadstodifferentialtreatmentbasedon perceivedrace.2,3 Implicitbiasfurtherrestrictsquality healthcareasaseparatefactoraboveandbeyondinequities ofstructuralracism.Emergencydepartment(ED)data indicatesthatBlack(vsWhite)patientshavelonger treatmentwaittimes,4 longerlengthsofstay,5 andlower triageacuitylevels.6 Additionally,BlackEDpatientshavea 10%lowerlikelihoodofadmissionand1.26timeshigher oddsofEDorhospitaldeaththanWhitepatients.7 Researchalsosuggeststhatphysicians’ ownimplicitracial biasesmaycontributetodisparitiesinhealthcarequality anddelivery.8–10
Inthiscriticalreviewweexplorethecomplexeffectsof race,implicitbias,andstructuralracismonSDoH, healthcarequalityand,ultimately,healthoutcomes. Althoughnotintendedasacomprehensiveliteraturereview onhealthdisparities,thisexerciseinformsaconceptual frameworkthroughwhichactionablestepsandpractice recommendationsforemergencymedicine(EM)are proposedasonepartofalargersystemwideeffortthat requiresthoughtfulactionandtransformativepolicyto dismantlethehard-wiredinequitiesofstructuralracismand advancehealthequity.
METHODS CriticalReviewMethodology
Weconductedabroad-scopecriticalreviewoftheextant healthdisparitiesliteratureacrossthreeareasofclinical pathologyinterest:communicablediseases;noncommunicableconditions;andinjuries.Thereviewwas conductedthrougharace-consciouslenstoexaminethe impactofraceonhealthoutcomesandinformaconceptual frameworkforthedevelopmentofactionablestepsand practicerecommendations.
Criticalreviewsinclude “adegreeofanalysisand conceptualinnovation” resultinginaproductcapableof launchinganewphaseofevaluation.11 AccordingtoGrant andBooth,thecriticalreviewdoesnotcallforasystematic evaluationofalltheliteraturerelatedtoatopic,butrather theemphasisisonthecontributionofeachpieceofevidence includedtothereview’sconceptualproduct.11 Asdescribed bytheSearch,Appraisal,Synthesis,andAnalysis framework,criticalreviewsaredesignedtoidentifykey findingsinthe fieldofinterest(healthdisparitiesliterature), evaluatetheevidenceinaccordancewithitscontribution (racialhealthdisparitiesattributabletoSDoH),synthesize theevidenceinorganizedfashion(clinicalpathology interestsrelevanttoEM),andprovideaconceptualoutputof analysisthatcontributestotheliterature(actionablesteps andpracticerecommendations).11
Inthisreviewweaimedtoexamineracialhealth disparitiesthroughtheSDoHmodelandapply socioenvironmentaltheory12 andresourcedeprivation theory13 asrace-conscious filtersthroughwhichracial disparitiesdataisanalyzedandsynthesized(Table1). Theanalysisinformedtheconceptualframeworkthrough whichwedevelopedandproposeactionablestepsand practicerecommendations.
RESULTS CommunicableDiseases HIV/AIDS
Racialandethnicdisparitiesintheincidenceand prevalenceofHIVinfectionandAIDShavebeen documentedintheUSsincethe1980s.14 Despiteprevention, identification,andtreatmentadvances,Black-Whiteand Hispanic-Whitediseaseincidencedisparitieshaveincreased since1984.In2013,BlacksandHispanicsaccountedfor46% and21%ofnewHIVinfectionsand49%and20%ofnew AIDSdiagnosesdespiterepresenting12%and16%ofthe totalUSpopulation,respectively.14 AlthoughHIVincidence rateshaveimprovedinrecentdecades,BlacksandHispanics havebenefittedlessfromantiretroviraltherapy advancements.15 Incidencerates(IR)havedeclinedwiththe adventofpre-exposureprophylaxis(PrEP);however,PrEP usageremainsdisparatelylowamongBlack(5.9%)and Hispanic(10.9%)adultswithanindicationascomparedto Whites(42.1%).16,17
EDActionableSteps: IncreaseaccesstoHIVtestingand referralstoPrEPandpost-exposureprophylaxis.
ViralHepatitis
HepatitisCvirus(HCV)istheleadingcauseofliver disease-relateddeathintheUS.18 Racialdisparitiesindisease prevalenceexistatarategreaterthantwicethatofWhites; BlacksintheUShavethehighestprevalenceratio(PR)of disease(PR2.29,95%confidenceinterval[CI]1.94
2.70).18
RatesoftreatmentforchronichepatitisCarealsohigher
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 907 Macias-Konstantopoulosetal. Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations
12
Socioenvironmentaltheory
Socioenvironmentaltheory holdsthatracialresidential segregationiscentraltoracialandethnichealthdisparities. Accordingtothistheory,racial/ethnicminoritygroupshave considerablydifferentlevelsofhealthriskduetothemultiple socialandenvironmentalfactorsthatdetrimentallyimpacttheir healthwithinthecontextoflongstandingresidentialsegregation anditsdeeplyrootedsocioeconomicdisadvantages.
amongWhitesascomparedtoBlack,Hispanic,andAsian individuals.19 Direct-actingantivirals(DAA)became availablein2014andareachievinggreaterthan90%cure rates.20 EarlyresearchfoundthatBlackandHispanic patientswerelesslikelythanWhitestobenefitfromDAA initiation(adjustedrateratio[aRR]0.7,95%CI0.7–0.8and 0.8,95%CI0.7–0.9,respectively).21 Follow-updatafroma nationalcohortfoundthattheseracial-ethnicgapshad closedby2016;however,morerecentdataisneededto determinewhetherequitableaccesshaspersistedbeyond initialevidence-drivenefforts.20
EDActionableSteps: IncreaseaccesstoHCVtestingand referralstoDAAtreatment.
SexuallyTransmittedInfections
Disparitiesinsexuallytransmittedinfections(STI)have beendescribedextensivelyintheliterature.Ratesof primaryandsecondarysyphilis,HIV/AIDS,chlamydia, andgonorrheaamongBlacksrangefrom5.4to17.8times theratesamongWhitesintheUS.22 TheSDoHassociated withincreasedSTIprevalencehavebeendiscussed extensively,rangingfrominequitiesinhealthcare,income, incarceration,residentialsegregation,andsubstanceuse, amongothers. 23 ,24 Importantly,prevalencemustbe interpretedwithinthecontextofSTIscreening,the oddsofwhicharehigheramongBlackandHispanic womenthantheirWhitecounterparts(adjustedodds ratio[aOR]2.56,95%CI2.60 –3.10and1.42,95%CI 1.39 –1.46,respectively). 25
EDActionableSteps: IncreaseaccesstoSTItestingand ED-basedtreatment.
DiarrhealDisease
Anestimated500,000casesofshigellosisoccurannuallyin theUS.26 Incidenceratesofinfectionper100,000aregreatest amongBlack(7.2)andHispanic(5.6)individualsas comparedtoWhites(2.6).26 Despitethepreventablenature ofshigellosis,ananalysisofover25,000laboratoryconfirmedcasesreportedtotheCDCfoundastrong
Resourcedeprivationtheory13
Resourcedeprivationtheory holdsthatthelongstanding deprivationofresourcesexperiencedbyracial/ethnicminority groupsiscentraltoracialandethnicdisparities.Duetochronic deprivation,racial/ethnicminoritygroupslackthenecessary infrastructuretosupporthealth.Resourcesarenotrestrictedto materialpossessions;theyincludeeducation,employment, housing,neighborhoodsafety,andpsychologicalwellbeing. Accordingtoevidence-basedinterpretationsofthistheory,gap closurecannotbeachievedthroughequaldistributionof resources,butrathertargeteddifferentialdistributionofresources thatlevelstheplaying fieldforracial/ethnicminoritygroups.
associationbetweenitsincidenceandresidenceinareas markedbyUSCensusTract-levelpovertyandhousehold crowding.RacialandethnicIRdisparities,however, persistedevenaftercontrollingforthesesocioeconomic indicators,26 andtheratesofsevereinfectionamongadults arehighestamongBlackpersons.27 Similarly,Black(vsnonBlack)infants <6monthsinagehadhigherratesofdiarrheaassociatedhospitalizationsthatpersistedevenafterthe introductionoftherotavirusvaccinesin2006.28
EDActionableSteps: Educatepatientsandparentsabout transmissionmechanismsandmitigationstrategies(eg,hand hygiene,low-costwatertreatmentoptions,vaccination), andconsiderofferingvaccinationintheEDwhennecessary andreasonable.
PandemicRespiratoryViralInfection
Disparitiesexistamongpandemicrespiratoryviral infections,includinginfluenzaH1N1andsevereacute respiratorysyndromecoronavirus2(SARS-CoV-2),resulting inhigherdiseaseincidenceandmortalityamongminority groups. 29–31 Coronavirusdisease2019(COVID-19)casesand hospitalizationrateswere2.5-4.5timeshigheramongBlack, Hispanic,andNativeAmericanpopulationsthanWhites. ThroughMay2021,COVID-19deathsamongHispanicand Blackpopulationswere17%and10%greater,respectively, thanexpectedbyUSpopulationrepresentationafter controllingforage.32 ElevatedCOVID-19infectionanddeath rateshavealsobeenobservedinsociallydisadvantaged countieswithlargerproportionsofBIPOC.32,33 Among residentsofapredominantlyBlackandHispanicCOVID-19 hotspot,veryhighanddisparatepositivityrateswereobserved amongBlack(68.5%)andHispanic(65.3%)patientsas comparedtoWhites(53%).34 Higherhospitalizationratesfor Blacks(60.2%)andHispanics(62.3%)ascomparedtoWhites (47.7%)werealsoobserved,althoughtherewereno differencesinadmissionratestotheintensivecareunit.34 MortalityratesamongCOVID-19inpatientsalsoshow BIPOCdisparities.35,36 RecentCDCdatashowshigher mortalityriskratiosforNativeAmericans(2.4),Hispanics
Table1. Race-consciousanalysistoolsemployedincriticalreview.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 908 Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations Macias-Konstantopoulosetal.
(2.3),andBlacks(1.9)comparedtoWhites.37 Thereare severalreasonscitedtoexplainthehigherout-of-hospital mortalityrates,diseaseburden,andseverityofillness amongBIPOC.36,38–40 Severalauthorshaveconcludedthat population-baseddisparitiesinCOVID-19hospital mortalityarebestexplainedbydifferentialdisease incidence,prevalenceofcomorbidconditions,and socioeconomicmarginalizationamongBlackand Hispanicindividuals.34,39,40
OverallracialandethnicdisparitiesinCOVID-19risk, severity,morbidity,andmortalityarisefromacombination ofsocial,economic,andhealthdeterminants.36,38 Dueto economicstrain,BIPOCaremorelikelytoliveincrowded housing(multigenerationalorcommunalhouseholds)and denselypopulatedneighborhoods.Theyarealsomorelikely toworkinconsumer-facingpublicserviceindustriesandrely onpublictransportation,increasingtheirexposurerisk. Additionally,higherratesofcomorbidities(eg,heartdisease, diabetes,hypertension,andobesity)increaseBIPOC’srisk forsevereCOVID-19disease.Barrierstohealthinsurance andhealthserviceslimitaccesstotreatmentsandtoaccurate knowledgeregardingSARS-CoV-2transmission,prevention strategies,diseasesymptoms,andreasonsforseeking care. 41
43 Interestingly,despitethepositiveimpactof Medicaidexpansiononhealthcareaccess,mortality,and disparities,onestudyfailedto findanassociationbetween COVID-19mortalityandexpansionvsnon-expansion,44,45 likelyreflectingabenefitnegatedbytheheightenedsocialrisk ofstructuralracism.
Disparitiesinvaccinationcoveragewereevidentbythe endofApril2021.Whenalladultagegroupswereeligible, vaccinationratesamongBlack(46.3%)andHispanic (47.3%)adultswerelowerthanamongWhites(59%)and Asians(69.6%).46
Despitepoliciestoensureequitable COVID-19vaccineaccess,vaccinationhesitancy originatingfromdistrustinthemedicalestablishmentand resultingfromlongstandingsystemicracisminhealthcare andresearch requiredcommunitypartnerships andconcertedeffortsbytrustedsourcesofinformation toovercometheslowerratesofvaccination amongBIPOC.46
EDActionableSteps: Increaseaccesstoviraltesting, educatepatientsandparentsabouttransmissionmechanisms andmitigationstrategies(eg,masks,isolation,vaccination), andconsiderofferingvaccinationintheEDwhennecessary andreasonable.
Non-CommunicableConditions AcuteCoronarySyndromeandAcuteMyocardial Infarction
Disparitiesinacutecoronarysyndrome(ACS)carehave beenwell-documented.ComparedtoWhitepatientswith door-to-balloon(DTB)timesof103.4minutes,Blackand HispanicpatientsexperiencesignificantlylongerDTBtimes
(122.3and114.8minutes,respectively).47 Overthelast decade,DTBtimeshaveimprovedsignificantlyacrossall groups;however,BlackAmericanshavealowerlikelihood ofexperiencingDTBtimes <90minutes48 andhave experiencedonlyamodestdeclineinrecurrent hospitalizationforacutemyocardialinfarction(AMI) comparedtoWhites.49 BlackpatientsexperienceworseAMI outcomeswitha five-yearmortalityrateof29%comparedto 18%amongWhites.50
EDActionableSteps: ConsiderprotocolizedEDtriage andearlymanagementofpotentialACS/AMI-related complaintsbeyondchestpain.
Type2DiabetesMellitus
Type2diabetesprevalenceratesamongBlack(13.2%) andHispanic(12.8%)Americansaresimilarandhigherthan ratesamongWhites(7.6%).51 Well-controlledglycemiaand hospitalizationrates,qualityindicators,arebothworse amongBlackpatients(37.6%and26.5%,respectively) comparedtoWhites(44%and16.1%,respectively).51 The markerofglycemiccontrol,hemoglobinA1c (HgbA1c),is statisticallyworseamongBlackvsWhitepatients(HgbA1c 9.1 ± 2.9%vs.8.5 ± 2.2%, P = 0.001).52 BlackandHispanic patientshavehigheroddsofdiabetes-relatedEDvisits (oddsratio[OR]1.84,95%confidenceinterval[CI]
1.7–2.0and1.60,95%CI1.4–1.8,respectively) thanWhites.53
EDActionableSteps: Educatepatientsaboutthe complicationsofpoorglycemiccontrolandconsider navigationpartnershipswithprimarycareforexpedited post-EDvisit,outpatientfollow-upofpatientswithdiabetesrelatedchiefcomplaintsandcomplications.
Hypertension
Racialandethnicdisparitiesinhypertensionarelikely multifactorialrelatedtoupstreamSDoH,includingaccessto healthcare,affordablemedications,low-sodiumfoods,and safegreenspacesforphysicalactivity.54 UniquetoBlack patients,race-consciousnesssignificantlyincreasesdiastolic bloodpressure(BP),andtheself-perceptionofhavinga lowersocialstandingasafunctionofraceisassociatedwith medicationnon-adherenceandhighersystolicBP.54
ResearchhasalsodemonstratedthatBlackandAsian patientshavehigheroddsofahighBPreadingattheirlast clinicvisit(OR0.36,95%CI0.21–0.60and0.40,95%CI 0.16–0.97,respectively)andBlackandAmericanIndian/ AlaskaNativepatientshavehigheroddsofanEDvisitor hospitalization(OR3.61,95%CI1.88–6.91and5.31, 95%CI2.13–13.20,respectively).55
EDActionableSteps: Educatepatientsaboutthe complicationsofpoorBPcontrolandconsidernavigation partnershipswithprimarycareforexpeditedpost-EDvisit, outpatientfollow-upofpatientswithhypertension-related chiefcomplaintsandcomplications.
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 909 Macias-Konstantopoulosetal. Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations
End-stageRenalDisease
Racialandethnicdisparitiesareprofoundinrenaldisease. BlackpatientsexperiencehigherIRsofend-stagerenal disease(ESRD)inadolescence,greaterprobabilityof progressiontoadvanceddiseasestagesbeforeinitiationof dialysis,lowerlikelihoodofperitonealvshemodialysis treatment,lowerlikelihoodoftransplantwaitlistplacement, andlongerwaitingtimesfortransplantation.56 Pediatric nephrologyregistrydatafoundthatamongchildrenwho progressedtoESRD,41.8%ofWhitechildrenreceived transplantscomparedto16.3%and27%ofBlackand Hispanicchildren,respectively,and70%ofWhitechildren weretransplantedwithintwoyearsofwaitlistplacement comparedto44%ofBlackpediatricpatients.57 Subsequent analysesconfirmthepersistenceofthesedisparitieswith BlackandHispaniclesslikelythanWhitechildrentoreceive preemptivetransplants(8.7%and14.2%vs27.4%, respectively),andBlackpediatrictransplantrecipientswere lesslikelythanWhitetoexperienceallograftsurvivalat five years(63%vs80.8%,respectively).58
Similardisparitiesamongnon-WhiteadultESRD patientsincludelowerratesoftransplantreferrals,delayed timestotransplantwaitlistplacement,andlongerwaittimes fortransplant.56 NationalmortalitystatisticsindicateBlacks experiencesignificantlyhigherdeathratesfromESRDthan HispanicandWhiteAmericans(24.6vs11.1and12.1 age-adjusteddeathrateper100,000,respectively).59
EDActionableSteps: Advocateforincreasedaccessto dialysis,particularlyfortheuninsured,andconsider navigationpartnershipswithnephrologyandlocal dialysiscentersforexpeditedpost-EDvisit,outpatient follow-upofpatientswithESRD-relatedchiefcomplaints andcomplications.
Obesity
Asariskfactorforheartdisease,type2diabetes, hypertension,andotherchronicconditions,obesityposesa realchallengetopopulationhealthmanagementefforts. Nationaldatademonstratesthatthehighestprevalenceof adultobesityoccursamongBlackAmericans(38.4%) followedbyHispanics(32.6%)andWhites(28.6%).60 Much likehypertension,racialandethnicdisparitiesinobesityare multifactorialandrequireamultifacetedinterventionto targetsocial(fooddeserts),biological(hormone dysregulationsecondaryadversechildhoodevents),and behavioral(physicalactivity)determinants.61 Researchhas revealedahighburdenoffast-foodestablishmentswithin predominantlyBlackcommunities.62–64 Treatment disparitiesarealsopresentwithBIPOCdemonstrating decreasedresponsivenesstoweight-losspharmacotherapy, decreasedlikelihoodweight-losscenterreferral,and decreasedlikelihoodofbariatricsurgery.65
EDActionableSteps: Considerpartnershipswith communityprogramsfocusedonhealthylifestylechangeand
prescribevoucherstopatientswhosehealthwouldbene
fromweightloss.
MentalHealth
Racialdisparitiesinthemanagementofpsychiatricillness havealsocometotheforefrontinrecentyears.Ratesof depressiontreatmentareloweramongBlackandHispanic patientsascomparedtoWhitepatients,whoarehalfaslikely andathirdaslikely,respectively,toreceivecarethanWhite patients.66 AccordingtotheCDC,Blackadultshadthe highestratesofmentalhealth-relatedEDvisitsin2018-2020, hadlongerEDwaittimes,andwerelesslikelytobeadmitted ortransferredtoanotherhospital.67 Ananalysisofnational datafoundthatBlackpatientspresentingtotheEDwitha psychiatricemergencyhaveagreaterprobabilityofchemical sedationthanWhitepatients.68,69 Additionally,single-and multisitestudieshavefoundthatBlack69
71 andHispanic patients71 aremorelikelytobephysicallyrestrainedinthe EDthanWhitepatients.
EDActionableSteps: Useanequitylenstoconducta thoroughreviewofpoliciesrelatedtorestraintuse,consider protocolizedscreeningandmanagementofagitation inclusiveofearlyoralmedicationandwithdrawaltreatment, andconsidernavigationpartnershipswithhospital-based andcommunity-basedcounselingservices.
Injuries
EnvironmentalHazard-RelatedInjuries
Ambient fine-particulatematterexposure(PM2.5)isa riskfactorforahostofconditionsincludingreactiveairway disease,coronaryarterydisease,andcerebrovascular disease.72 Theinequitabledistributionofhazardoussites, namelyindustrialfacilities,utilities,andlandfills,isoneof thegreatestconcernsinthe fieldofenvironmentaljustice. Extensiveliteraturehasdemonstratedthatnon-Whitesare morelikelytoresidenearstationarysourcesofPM,with BlackAmericansexperiencingahigherburdenofPM exposurethanWhitesandthegeneralpopulation.73
Racialdisparitiesinhazardousexposureburdenarenota recentphenomenon.The1987groundbreakingstudythat firstexposedthedisproportionateco-locationoftoxicwaste sitesandminoritycommunitiesfoundthatthreeofevery five BlackandHispanicAmericanslivedinsuchconditions.74 TheNationalResearchCouncilconductedastudythat observedgreaterprevalenceofhealthproblems spontaneousabortions,birthdefects,heartdisease,gastric cancer,leukemia,andHodgkin’slymphoma amongthose livinginproximitytohighlytoxicchemicalsandcarcinogens (eg,benzene,polychlorinatedbiphenyls,mercury,arsenic, andlead).75 Geo-mappingofhazardoussitesfoundthata disproportionatenumberoftownsoverburdenedbytoxic sourceswerealsohometohighproportionsofBIPOC,a robustpositivepredictorofhazardouswastesitelocations.76
fit
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 910 Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations Macias-Konstantopoulosetal.
EDActionableSteps: Increasesyndromicsurveillance collaborationswithpublichealthdepartmentsfor earlydetectionandcommunitynotificationof hazardousconditions,andadvocatefortargetedpolicy interventionsbyhighlightingtheharmfulhealthimpacts onlocalcommunities.
Long-boneFractures
BlackandHispanicpatientsarelesslikelytoreceive opioidanalgesiaforacutepainintheEDandopioid prescriptionsatdischargecomparedtoWhite counterparts.77–79 Researchshowsthatalthoughaverage painscoresdonotdifferbetweenWhiteandnon-White patientswithlong-bonefractures(LBF),Whitepatientsare morelikelytoreceiveopiates(70%vs50%, P < 0.001).78 AmongchildrenpresentingforEDmanagementofLBF,the dataissimilar:BlackandHispanicchildrenwerelesslikelyto receiveopioidanalgesics(aOR0.86,95%CI077–0.95and 0.86,95%CI0.76
0.96,respectively)andlesslikelyto achieveoptimalpainreduction(aOR0.78,95%CI0.67–0.90 and0.80,95%CI0.67–0.95,respectively).80
EDActionableSteps: ConsiderprotocolizedEDtriage andearlymanagementofLBF,includingadequateanalgesia dosingschedules.
FirearmInjuries
FirearmviolenceisapublichealthepidemicintheUS.In 2018, firearmsweretheleadingmethodofhomicideand suicide,majorcausesofprematuredeath.PertheCDC, 39,707Americansdiedfrom firearmviolencein2019, averaging109deathsperdayandcomprising60%suicides, 35%homicides,and1.4%lawenforcementinterventions.81
Whilemost firearmsuicidedeathsimpactWhites andAmericanIndian/AlaskaNatives,homicides disproportionatelyplagueBlackAmericans.In2018, firearm homicideswerehighestamongBlacks.Blackmalesand femalesaged20
34yearsdiedby firearmhomicideatnearly 17timeshigherandnearlysixtimeshigherratesthantheir Whitecounterparts,respectively.Amongyouthaged0–19, Blackmaleshadthehighest firearmhomiciderateat14times higherthantheirWhitepeers.AmericanIndian/Alaska Nativemaleyouthhadthesecondhighestyouthhomicide rate.Blackmalesaredisproportionatelykilledbylaw enforcementinterventionwith firearmsatarate1.71times thatofnon-HispanicWhitemales.82
EDActionableSteps: Remaininformedoflocal firearm injurystatisticsandadvocateforadequatepolicyresponses byhighlightingtheharmfulhealthimpactsonlocal communities.
DISCUSSION
Acrossclinicalpathologyinterestsandinalmostevery areastudied,BIPOCcommunitiesexperienceworsepatient careandhealthoutcomes.Contrarytohistoricalmedical
teachings,thereisnobiologicalevidencefortheconceptof raceasagenomichumansubspeciestoexplainhealth disparities.83,84 Rather,itisthesocialinterpretationof peopleinarace-conscioussocietythatdisparatelyimpacts health.85 Thesystemofstructuringopportunityand assigningvalue,basedonassumptionsaboutgroupsof peoplewithcertainphysicalattributes,systematically privilegessomewhiledisadvantagingothersandundergirds thedeadlyproblemofstructuralracism.Compoundingthe well-recognizedtheoryofresourcedeprivationamong racially/ethnicallysegregatedcommunities(eg,quality primaryeducation,adequatehousing,greenspace)is socioenvironmentaltheory,whichpointstoactsof commissionthatinequitablyposehealthrisks(eg,air pollution,72,73 toxicwaste,74–76 andfast-food,62–64 alcohol,86 andtobaccooutlets87).
Physiciansmustacknowledgetheinsidioushealththreat thatimplicitbiasesandstructuralracismpose. Disproportionatelevelsofsocioeconomicdisadvantage, socialvulnerability,andpoorhealthoutcomesare manifestationsoflong-establishedanddeeplyentrenched racialsegregationandracialdeprivation.Onecouldargue thattheadversehealtheffectsofstructuralracismoverthe centurieshavecreatedafargreaterpublichealthcrisisthan theCOVID-19pandemic,andyetbeyondtheir identification,theyhavenotreceivedtheattentionthey demand.Perhaps,infutureyears,ourcollectiveresponseto thevolatilesociopoliticaleventsofthelast fiveyearswillbe viewedastheforcethatchangedthenarrative.Many academicmedicalcentershavecreatedexecutivepositions focusedonequity,diversity,andinclusionandhaveworked toimplementeducationalcurriculaaimedatdismantling structuralracism.88
Thequestionthatremainstoday howdoweas individualsandcollectivelyasaninstitutionandspecialty bestadvancesocialjusticeandhealthequity? demands thoughtfulactionsandtransformativepolicies.Arecent scopingreviewfound37publishedinterventionpaperswith onlyathirdincludingempiricalresearch.89 Clearly,the implementationsciencebehindthismassivemulti-pronged processwilltaketimetodevelop,90 butthereappearstobe sufficientdirectiontoproposepotentialactionablesteps (Table2)andpracticerecommendations.
LIMITATIONS
Ascriticalreviewsfocusonadvancingthoughtthrough conceptualinnovationfollowingananalysisoftheliterature, themethodology,bydesign,doesnotnecessitatean exhaustivecomprehensivereviewoftheliteraturenorthe samesystematicityandqualityassessmentasinothermore structuredreviewapproaches.11 Additionally,theobjective oftheconceptualproductofacriticalreviewistoproposea newphaseofresearchwithinthe fieldinquestion,11 andasa result,theactionablestepsandpracticerecommendations
–
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 911 Macias-Konstantopoulosetal. Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations
Table2. Potentialactionablestepsforemergencyphysicians.
Communicable diseases
1. DPH-funded,communitypartnershipsforpop-upscreeningclinicsinthecommunitydesignedtoprovide rapidtestingandcounselingregardingtreatmentinitiationforHIV,hepatitisC,andSTIs.
2.DPH-funded,communitypartnershipsforpop-upvaccinationclinicsinthecommunitydesignedtoprovide testing, vaccination,andtransmission-mitigationeducationinthecommunity.
3.Self-guidededucationandpeereducationabouttheincreasedriskforsevereCOVID-19andother respiratoryanddiarrhealmorbidityandmortalityamongethnicandraciallydiversepopulations.
4.Empowerpatientswithathoroughunderstandingofcommunicablediseases,includingnaturalcourseof illness,methodsoftransmission,transmissionprevention,andreasonsforreturning;discharge counselingtechniquesmayincludedischargenursingteach-backorread-backofinstructions.
5.DPH-medical-communitypartnershipsdesignedtofocuseffortsinareasofhightransmissionriskwhen planningresourcedistributionoftesting,treatment,andvaccinationsuppliesrelatedtoCOVID-19and otherpandemic-relatedillnesses.
Non-communicable conditions
1. EducateEPsaboutlong-standingracialandethnicgapsinED-basedcareandhealthoutcomes;and promoteopportunitiesforimplicitbiastraining.
2.Developequitymetrics,monitorclinicalperformancedataonqualitymeasures,identifyinequitiesinclinical and research,andimplementprocessandpolicychangestoclosedisparitygaps.
3.Supporthealthequityinitiativesattheindividual,departmental,andorganizationallevelsthataimtoeducate patientsaboutcertainmedicalconditions(eg,hypertension,diabetes),earlywarningsignsofserious complications(eg,acutecoronarysyndrome,renalfailure),andavailabletreatmentoptions;educational strategiesmayinvolvesmartdocumentsandwaitingroomvideoeducationalmodules.
4.Supportandpartnerwithexistingpatientcarenavigatorandcommunityhealthworkerprogramstoengage patientsbeyondtheindexEDvisitandensuremedicationandtreatmentplanadherence,outpatientfollowupscheduling,andregularassessmentsofanybarrierstodiseasecontrol.
5.Partnerwithlocalcommunityorganizationsdesignedtopromotehealthylifestyle(eg,smokingcessation, nutritionalfoodplanning,localfarmfoodcollaborative,reduced-feegymmemberships,etc).
Injuries
1. Considerthepotentialenvironmentaldeterminantsoflungin flammationandinjuryinBIPOCpatients withdifficult-to-controlasthmasymptoms;educatepatientsaboutPManditsrelationshiptoasthmaand counselthemonpreventativemeasuresandimportanceofmaintenancemedicationadherence.
2.Supportandadvocateforstateandfederallegislationandpolicyaimedatpreventionoftoxicwaste dumping, containmentefforts,periodictestingofsoilandwatersupplies,increasedtestingfor environmentalexposuresamongcommunitieslivinginhigh-riskexposureareas,andinvestmentin industrialwastedecontamination,saferhousing,andqualitymedicalcareforaffectedcommunities.
3.Self-guidededucationandpeereducationaboutthesignsandsymptomsoftoxicityduetocommon hazardouswastecontaminants,andtheavailabletreatments.
4.ProvideopioidanalgesiaforacuteseverepainintheEDbasedonlikelydiagnosis,objectivemeasuresof pain,andoptimalpainreduction(atleasta2-levelreductioninpainscoreforinitialtreatment).
5.Supportepidemiologicandnarrativeresearchof firearmviolence,bothnonfatalinjuriesanddeaths,to betterunderstandriskandprotectivefactorsasthebasisforintervention.
6.Usetheresultsofepidemiologicandnarrativeresearchtopartnerwithcommunitiestodevelopand implementeffectiveinterventionsespeciallytargetedathigh-riskyouthandyoungadultsofcolor.
7.Partnerwithexistingprogramsandpersonnelthathaveoperatedtraumacenterresourcesforcommunity and firearmviolencetoextendtheirinpatientworktoreachagreaterproportionofthoseinneedby developingandimplementingEDprotocolstoidentify,counsel,andreferat-riskpopulations.
8.EducateEPsontheeffectivecounselingofpopulationsatdisproportionateriskforcommunityand firearm violenceandincorporatesmartdischargephrasesintotheelectronichealthrecordsystem.
9.DevelopstrongcollaborationswithcommunitygroupsandsocialservicestowhomtheEDcouldtransition primaryandsecondaryprevention;incorporatethesereferralsintodischargematerials.
10.Encouragestateandfederallegislationandpolicyaimedatdecreasing firearmhomicidesandnonfatal injuries(eg,decreaseaccesstoillegal firearms,increasefederalfundingforresearchon firearm violence,decreasetheproductionofviolentvideogamesandmediaandreplacethemwithgamesinwhich theprotagonistmustsavelivesratherthankilltowin).
BIPOC,Black,indigenousandpeopleofcolor; DPH,DepartmentofPublicHealth; ED,emergencydepartment; EP,emergencyphysician; PM,particulatematter; STIs,sexuallytransmittedinfections.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 912 Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations Macias-Konstantopoulosetal.
madehaveyettobeproveneffectivebutinsteadserveasa startingpointforanewphaseofimplementationscience.
CONCLUSION
Thesuggestedactionablestepsandfollowingpractice recommendationsconstitutetheconceptualproductofthis criticalreview,demandinganewphaseofimplementation andevaluationresearchthatidentifieseffectivestrategies andbestpracticesformitigatingracialhealth inequities.Emergencyphysicians,asindividualsand organizationalleaders,canactfromseveralpositionsinthe socialstructure:
A.Societalmembers
1.Participateinlocal,state,andfederalgovernment forumsadvocatingforhealththroughresources andadvantageshistoricallyinaccessibletoBIPOC:
a.Affordable,safehousing
b.Foodsecurity(ie,sufficient,safe,andnutritious sustenance)
c.Firearmsafety,neighborhoodsafety,and supportforsurvivorsofviolence
d.Health-promotinglifestyle(eg,greenspaceand densityrestrictionsonfast-food,tobacco,and alcoholoutlets)
e.Comprehensivecommunityhealthcenterswith expandedhoursofoperations
2.Developmeaningfulindividualandorganizational partnershipswithantiraciststakeholdersand communities (ie,BlackLivesMatter,WhiteCoatsforBlack Lives,etc).
3.Engageleadershipandrepresentativesof first responderagenciesinupholdingthevalueof everyhumanlife.
B.Stewardsofmedicine
1.Engagemedicalleadershipinchanging organizationalculturetoonethatconsistently prioritizesequity,addressesinequitiesinclinical andprofessionalspaces,andrecognizesthe systematicadvantageofprivilege.
2.Createpermanentpositionsaccountabletoequity, diversity,andinclusioninitiatives91 andensure coreleadershiparticulatesdiversityasan institutionalpriorityanddialoguesconstructively withallrelevantstakeholders.92
3.IncreaseBIPOCrepresentationwithinthepipeline andacrossallorganizationalstrata.93
4.Identifyracialdisparitiesandtheirsourceswithin thesystem,conductrootcauseanalyses,and implementstrategiestoremedyinequities.94
Describe,document,andproactivelyworkto mitigatethehealthimpactofracism.95
5.Draftpoliciesandenforceprotocolsfordealing withrace-basedaggressionbypatientsandother staff.
6.Educatemedicalpersonnelthroughmultimodal continuousmedicaleducationontraumainformedcare,anti-racismpractice,andcultural humility.96
7.Offermedicaleducationcurriculaandperiodic trainingsforstudents,residents,community physicians,andfacultythatincludethe following:93,97
a.SDoH:Althoughtheprospective,patientorientedoutcomeissparse,manymedical schoolsandresidencyprogramshaveadopted SDoHcurriculum,whichmayleadto measurablechangesinthefuture98 andisa statedpriorityoftheInstituteofMedicine.99 Comprehensivetrainingmaterialsarefree andavailableontheweb.100
b.Culturalhumilitytrainingtoaddressimplicit bias,stereotypes,andprejudice.101
c.Anti-racismandtrauma-informedcaretraining toimprovepatientcarecommunicationand bedsideskills.
8.Evaluatetheimpactofeducationalprogramson patientcareandhealthoutcomestocurate efforts.102 Disseminateevidence-basedbest practices.
9.Endeavorasaninstitutionandspecialtyto eliminateracializedconceptionsofdisease susceptibility(eg,castingBlacksasinnately diseasedanddehumanizingtheirsuffering).103
C.EDstaff
1.Developequitymetrics,monitorclinical performancedata,identifyclinicalandresearch gaps,andimplementprocessandpolicychanges toeliminatehealthdisparities.
2.Abandonthepracticeofstatingthepatient’ srace inthenarrativeofthehistoryandphysicalasithas minimalbenefit,risksintroducingbias,andis offensivetominorityphysicians.104
3.Ceasetheuseofcorrectionformulasthatuserace asaproxyforpathologywhentheirusefurthers healthinequities.105
4.Makedeliberateeffortstotreatracialgroups similarlyonindividualandpopulationlevelsasa concrete firststepinamelioratingracialhealth disparities.Althoughphysiciansundoubtedly carryimplicitracialbiasesequaltothegeneral population,thereissomeevidencethat emergencyphysiciansshowlessimplicitracial biasthanthegeneralpopulation.106
5.Addressracistpatientattitudesprofessionallyeven whenthesecausemoraldistress.107 Addressing
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 913 Macias-Konstantopoulosetal. Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations
racismandattemptingtorebuildtherapeutic alliancesispartoftheleadershipand professionalismthatemergencyphysiciansmust emulate.
D.Hospitalexecutives
InstitutionalleadersmustassureappropriateED ancillarystaffingandaddresshospitalpolicies(eg, inpatientcensuslevels,directandtransferadmissions) thatresultinEDcrowding,medicalerror,morbidity andmortality,andstaffdemoralization.108
Emergencyphysiciansareexpertsinrapidcognition orthin-slicing,butwiththatpracticecomesthe expressionoflatentstereotypesandbiasesthat requireadeliberate “bias-check” pausetobetter understandthepatientand,thus,achievebetter outcomes.109 Researchhasdemonstratedthat overstressingphysiciansbeyondreasonablelevelsis associatedwithincreasesinimplicitbias.110
E.Clinicalcaregivers
1.Employatrauma-informedcareapproachwith individualpatientinteractions.111 TheBIPOC communitiessufferunderthepervasivenessof historicalandpersonaltraumaaswellasthe psychologicaltraumainflictedbylaw enforcementkillingsofunarmedBlacks.112
Moreover,BIPOCminoritiesareexposeddaily tostressfulandtraumaticeventsatmuchgreat ratesthanthegeneralpopulation.113 Toadopt thetrauma-informedcareframework:
a.Abandonpowerimbalancescommonin traditional,paternalisticdoctor-patient dynamics.
b.Empowerpatientstobepartnersintreatment decisions.
c.Offerpatientsvalidation,explanation,and choice.
d.Practiceculturalhumility,anorientationto carethatisbasedonself-reflexivity, appreciationofpatients'layexpertise, opennesstosharingpowerandknowledge withpatients,anddesiretolearnfrom patients.114
2.Recognizeandcounterpotentiallyracistclinical decisionsbydoingthefollowing:
a.Followevidence-basedrace-blindadmission andsurgicalcriteria.
b.Provideprofessionalpeer-to-peerfeedback withcoachingondeliveryofdifficult conversations.115
c.Buildrace-blindanalgesiaprotocols.116
d.Createpoliciestoaddressinterprofessional microaggressionsandpatient-to-clinician racism.Micro-andmacroaggressions
contributetoburnoutandmustbecombated toensureinclusionandcareerlongevity.117,118
Inconclusion,fromamedicalstandpoint,thereisonlyone race thehumanrace andwemustrecognizeandcounter ourimplicitbiases.Asfellowhumans,wemustacknowledge thatstructuralracismdriveshealthinequities,andas emergencyphysicianswecanchoosetoaddressitby employinganyoralltheactionsandrecommendations proposedherein.
AddressforCorrespondence:WendyLMacias-Konstantopoulos, MD,CenterforSocialJusticeandHealthEquity,Departmentof EmergencyMedicine,MassachusettsGeneralHospitalandHarvard MedicalSchool,55FruitStreetZeroEmerson,Suite3B,Boston, Massachusetts02114.Email: wmacias@mgh.harvard.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Macias-Konstantopoulosetal.Thisisanopen accessarticledistributedinaccordancewiththetermsofthe CreativeCommonsAttribution(CCBY4.0)License.See: http:// creativecommons.org/licenses/by/4.0/
REFERENCES
1.CenterforDiseaseControlandPrevention. SocialDeterminantsof HealthatCDC.2022.Availableat: https://www.cdc.gov/about/sdoh/ index.html.AccessedJuly9,2023.
2.GreenwaldAG,BanajiMR.Implicitsocialcognition:attitudes, self-esteem,andstereotypes. PsycholRev. 1995;102(1):4–27.
3.FitzGeraldC,HurstS.Implicitbiasinhealthcareprofessionals: asystematicreview. BMCMedEthics.2017;18:19.
4.QiaoWP,PowellES,WitteMP,etal.Relationshipbetweenracial disparitiesinEDwaittimesandillnessseverity. AmJEmergMed. 2016;34(1):10–5.
5.PinesJM,LocalioAR,HollanderJE.Racialdisparitiesinemergency departmentlengthofstayforadmittedpatientsintheUnitedStates. AcadEmergMed. 2009;16(5):403–10.
6.SchraderCD,LewisLM.Racialdisparityinemergencydepartment triage. JEmergMed. 2013;44(2):511–8.
7.ZhangX,CarabelloM,HillT,etal.Trendsofracial/ethnicdifferencesin emergencydepartmentcareoutcomesamongadultsintheUnited Statesfrom2005to2016. FrontMed. 2020;7:300.
8.GreenAR,CarneyDR,PallinDJ,etal.Implicitbiasamongphysician anditspredictionofthrombolysisdecisionsforBlackandWhitepatients. JGenInternMed. 2007;22(9):1231–8.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 914 Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations Macias-Konstantopoulosetal.
9.JohnsonTJ,HickeyRW,SwitzerGE,etal.Theimpactofcognitive stressorsintheemergencydepartmentonphysicianimplicitracialbias. AcadEmergMed. 2016;23(3):297–305.
10.DehonE,WeissN,JonesJ,etal.Asystematicreviewoftheimpactof physicianimplicitracialbiasonclinicaldecisionmaking. AcadEmerg Med. 2017;24(8):895–904.
11.GrantMJ,BoothA.Atypologyofreviews:ananalysisof14reviewtypes andassociatedmethodologies. HealthInfoLibrJ. 2009;26(2):91–108.
12.WilliamsDR,CollinsC.Racialresidentialsegregation:afundamental causeofracialdisparitiesinhealth. PublicHealthRep. 2001;116(5):404–16.
13.AssariS.Unequalgainofequalresourcesacrossracialgroups. IntJHealthPolicyManag. 2018;7(1):1–9.
14.Chapin-BardalesJ,RosenbergES,SullivanPS.Trendsinracial/ethnic disparitiesofnewAIDSdiagnosesintheUnitedStates,1984–2013. AnnEpidemiol. 2017;27(5):329–34.e2.
15.NosykB,KrebsE,ZangX,etal. “Endingtheepidemic” willnothappen withoutaddressingracial/ethnicdisparitiesintheUnitedStates humanimmunodeficiencyvirusepidemic. ClinInfectDis. 2020;71(11):2968–71.
16.HarrisNS,JohnsonAS,HuangY-LA,etal.Vitalsigns:statusofhuman immunodeficiencyvirustesting,viralsuppression,andHIVpreexposure prophylaxis UnitedStates,2013–2018. MMWRMorbMortalWkly. 2019;68(48):1117–23.
17.BeerL,BradleyH,MattsonCL,etal.Trendsinracialandethnic disparitiesinantiretroviraltherapyprescriptionandviralsuppressionin theUnitedStates,2009–2013. JAcquirImmuneDeficSyndr. 2016;73(4):446–53.
18.BradleyH,WallEW,RosenthalEM,etal.HepatitisCvirusprevalencein 50U.S.statesandD.C.bysex,birthcohort,andrace:2013-2016. HepatolCommun. 2020;4(3):355–70.
19.VutienP,HoangJ,BrooksL,etal.Racialdisparitiesintreatmentrates forchronichepatitisC. Medicine. 2016;95(22):e3719.
20.JungJ,DuP,FeldmanR,etal.Racial/ethnicandsocioeconomic disparitiesinuseofdirect-actingantiviralsamongMedicare beneficiarieswithchronichepatitisC,2014-2016. JManagCareSpec Pharm. 2019;25(11):1236–42.
21.MarcusJL,HurleyLB,ChamberlandS,etal.Disparitiesininitiationof direct-actingantiviralagentsforhepatitisCvirusinfectioninaninsured population. PublicHealthRep. 2018;133(4):452–60.
22.HogbenM,LeichliterJS.Socialdeterminantsandsexuallytransmitted diseasedisparities. J SexTransmDis. 2008;35:S13–8.
23.AdimoraAA,SchoenbachVJ.Socialcontext,sexualnetworks,and racialdisparitiesinratesofsexuallytransmittedinfections. JInfecDis. 2005;191(s1):S115–22.
24.Owusu-EduseiK,ChessonHW,LeichliterJS,etal.Theassociation betweenracialdisparityinincomeandreportedsexuallytransmitted infections. AmJPublicHealth. 2013;103(5):910–6.
25.ParekhN,DonohueJM,CorbelliJ,etal.Screeningforsexually transmittedinfectionsaftercervicalcancerscreeningguidelineand
Medicaidpolicychanges:apopulation-basedanalysis. MedCare. 2018;56(7):561–8.
26.LibbyT,ClogherP,WilsonE,etal.Disparitiesinshigellosisincidenceby censustractpoverty,crowding,andrace/ethnicityintheUnitedStates, FoodNet,2004–2014. OpenForumInfectDis. 2020;7(2):ofaa030.
27.McCrickardLS,CrimSM,KimS,etal.Disparitiesinsevereshigellosis amongadults FoodborneDiseasesActiveSurveillanceNetwork, 2002-2014. BMCPublicHealth. 2018;18(1):221.
28.YenC,SteinerCA,BarrettM,etal.Racialdisparitiesindiarrheaassociatedhospitalizationsamongchildrenin fiveUSStates,before andafterintroductionofrotavirusvaccines. Vaccine. 2010;28(46):7423–6.
29.YayaS,YeboahH,CharlesCH,etal.Ethnicandracialdisparitiesin COVID-19-relateddeaths:countingthetrees,hidingtheforest. BMJ GlobalHealth. 2020;5(6):e002913.
30.SmithAR.EmergencydepartmentvisitsforCOVID-19byraceand ethnicity 13States,October–December2020. MMWRMorbMortal WklyRep. 2021;70(15):566–9.
31.QuinnSC,KumarS,FreimuthVS,etal.Racialdisparitiesinexposure, susceptibility,andaccesstohealthcareintheUSH1N1influenza pandemic. AmJPublicHealth. 2011;101(2):285–93.
32.KhazanchiR,BeiterER,GondiS,etal.County-levelassociationof socialvulnerabilitywithCOVID-19casesanddeathsintheUSA. JGenInternMed. 2020;35(9):2784–7.
33.MilletGA,JonesAT,BenkeserD,etal.Assessingdifferentialimpactsof COVID-19onBlackcommunities. AnnEpidemiol. 2020;47:37–44.
34.KabarritiR,BrodinNP,MaronMI,etal.Associationofraceandethnicity withcomorbiditiesandsurvivalamongpatientswithCOVID-19atan urbanmedicalcenterinNewYork. JAMANetwOpen. 2020;3(9):e2019795.
35.CentersforDiseaseControlandPrevention. ExcessDeathsAssociated withCOVID-19.2023.Availableat: https://www.cdc.gov/nchs/nvss/vsrr/ covid19/excess_deaths.htm.AccessedJuly9,2023.
36.ChenJT,KriegerN.RevealingtheunequalburdenofCOVID-19by income,race/ethnicity,andhouseholdcrowding. JPublicHealthManag andPract. 2021;27(Suppl1),COVID-19andPublicHealth:Looking Back,MovingForward:S43–56.
37.NationalCenterforHealthStatistics(NCHS)provisionaldeath counts. CentersforDiseaseControlandPrevention.Published2021. Availableat: https://data.cdc.gov/NCHS/
Provisional-Death-Counts-for-Coronavirus-Disease-C/pj7m-y5uh AccessedJune10,2021.
38.COVID-19RacialandEthnichealthdisparities.CentersforDisease ControlandPrevention.Published2020.Availableat: https://www.cdc. gov/coronavirus/2019-ncov/community/health-equity/ racial-ethnic-disparities/increased-risk-exposure.html#ref1 AccessedJune10,2021.
39.Munoz-PriceLS,NattingerAB,RiveraF,etal.Racialdisparitiesin incidenceandoutcomesamongpatientswithCOVID-19. JAMANetw Open. 2020;3(9):e2021892.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 915 Macias-Konstantopoulosetal. Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations
40.YehiaBR,WinegarA,FogelR,etal.Associationofracewithmortality amongpatientshospitalizedwithcoronavirusdisease2019(COVID-19) at92USHospitals. JAMANetwOpen. 2020;3(8):e2018039.
41.AlobuiaWM,Dalva-BairdNP,ForresterJD,etal.Racialdisparitiesin knowledge,attitudesandpracticesrelatedtoCOVID-19intheUSA. JPublicHealth. 2020;42(3):470–8.
42.AlsanM,StantchevaS,YangD,etal.Disparitiesincoronavirus2019 reportedincidence,knowledge,andbehavioramongUSadults. JAMA NetwOpen. 2020;3(6):e2012403.
43.JonesJ,SullivanPS,SanchezTH,etal.Similaritiesanddifferencesin COVID-19awareness,concern,andsymptomsbyraceandethnicityin theUnitedStates:cross-sectionalsurvey. JMedInternetRes. 2020;22(7):e20001.
44.GuthM,AmmulaM.Buildingontheevidencebase:studiesonthe effectsofMedicaidexpansion,February2020toMarch2021.
KaiserFamilyFoundation.Published2021.Availableat: https://files.kff. org/attachment/Report-Building-on-the-Evidence-Base-Studieson-the-Effects-of-Medicaid-Expansion.pdf AccessedAugust23,2021.
45.LiaoTF,DeMaioF.Associationofsocialandeconomicinequalitywith coronavirusdisease2019incidenceandmortalityacrossUScounties. JAMANetwOpen. 2021;4(1):e2034578.
46.KrissJL,HungMC,SrivastavA,etal.COVID-19vaccinationcoverage, byraceandethnicity NationalImmunizationSurveyAdultCOVID Module,UnitedStates,December2020-November2021. MMWRMorb MortalWklyRep. 2022;71(23):757
63.
47.BradleyEH,HerrinJ,WangY.Racialandethnicdifferencesintimeto acutereperfusiontherapyforpatientshospitalizedwithmyocardial infarction. ACCCurrJRev. 2004;13(12):8.
48.CavenderMA,RassiAN,FonarowGC,etal.Relationshipofrace/ ethnicitywithdoor-to-balloontimeandmortalityinpatientsundergoing primarypercutaneouscoronaryinterventionforST-elevationmyocardial infarction: findingsfromGetwiththeGuidelines-CoronaryArtery Disease. ClinCardiol. 2013;36(12):749–56.
49.ChaudhrySI,KhanRF,ChenJ,etal.Nationaltrendsinrecurrent AMIhospitalizations1yearafteracutemyocardialinfarctionin Medicarebeneficiaries:1999–2010. JAmHeartAssoc. 2014;3(5):e001197.
50.GrahamGN,JonesPG,ChanPS,etal.Racialdisparitiesinpatient characteristicsandsurvivalafteracutemyocardialinfarction. JAMA NetwOpen. 2018;1(7):e184240.
51.FerdinandKC,NasserSA.Racial/ethnicdisparitiesinprevalenceand careofpatientswithtype2diabetesmellitus. CurrMedResOpin.
2015;31(5):913
23.
52.GaryTL,McguireM,McCauleyJ,etal.Racialcomparisonsofhealth careandglycemiccontrolforAfricanAmericanandWhitediabetic adultsinanurbanmanagedcareorganization. DisManag.
2004:7(1):25
34.
53.MenchineMD,WiechmannW,PeterAL,etal.TrendsindiabetesrelatedvisitstoUSEDsfrom1997to2007. AmJEmergMed.
2012;30(5):754
8.
54.DoyleSK,ChangAM,LevyP,etal.Achievinghealthequityin hypertensionmanagementthroughaddressingthesocialdeterminants ofhealth. CurrHypertensRep. 2019;21(8):58.
55.SripipatanaA,PouratN,ChenZ,etal.Exploringracial/ethnicdisparities inhypertensioncareamongpatientsservedbyhealthcentersinthe UnitedStates. JClinHypertens. 2019;21(4):489–98.
56.MinnickML,BoyntonS,NdiranguJ,etal.Sex,race,andsocioeconomic disparitiesinkidneydiseaseinchildren. SeminNephrol. 2010;30(1):26–32.
57.NAPRTCS.2007. NorthAmericanPediatricRenalTransplant CooperativeStudy(NAPRTICS)2007AnnualReport.Rockville,MD: TheEMMESCorporation.
58.PatzerRE,MohanS,KutnerN,etal.Racialandethnicdisparitiesin pediatricrenalallograftsurvivalintheUnitedStates. KidneyInt. 2015;87(3):584–92.
59.NationalCenterforHealthStatistics. Health,UnitedStates,2015:With SpecialFeatureonRacialandEthnicHealthDisparities.DHHS PublicationNo.2016-1232.Hyattsville,MD:CentersforDiseaseControl andPrevention,U.S.DepartmentofHealthandHumanServices; 2016.Availableat: https://stacks.cdc.gov/view/cdc/39108 AccessedAugust15,2022.
60.PetersenR,PanL,BlanckHM.Racialandethnicdisparitiesinadult obesityintheUnitedStates:CDC’strackingtoinformstateandlocal action. PrevChronicDis. 2019;16:E46.
61.KruegerPM,ReitherEN.Mindthegap:race\ethnicandsocioeconomic disparitiesinobesity. CurrDiabRep. 2015;15(11):95.
62.HilmersA,HilmersDC,DaveJ.Neighborhooddisparitiesinaccessto healthyfoodsandtheireffectsonenvironmentaljustice. AmJPublic Health. 2012;102(9):1644–54.
63.KwateNO,YauCY,LohJM,etal.Inequalityinobesigenicenvironments: fastfooddensityinNewYorkCity. HealthPlace. 2009;15(1):364–73.
64.LewisLB,SloaneDC,NascimentoLM,etal.AfricanAmericans’ access tohealthfoodoptionsinSouthLosAngelesrestaurants. AmJPublic Health. 2005;95(4):668–73.
65.ByrdAS,TothAT,StanfordFC.Racialdisparitiesinobesitytreatment. CurrObesRep. 2018;7(2):130–8.
66.McGregorB,LiC,BaltrusP,etal.Racialandethnicdisparitiesin treatmentandtreatmenttypefordepressioninanationalsampleof Medicaidrecipients. PsychiatrServ. 2020;71(7):663–9.
67.PetersZJ,SantoL,DavisD,etal.Emergencydepartmentvisitsrelated tomentalhealthdisordersamongadults,byraceandHispanicethnicity: UnitedStates,2018-2020. NatlHealthStatReport. 2023;(181):1–9.
68.KhatriUG,DelgadoMK,SouthE,etal.Racialdisparitiesinthe managementofemergencydepartmentpatientspresentingwith psychiatricdisorders. AnnEpidemiol. 2022;69:9–16.
69.SmithCM,TurnerNA,ThielmanNM,etal.AssociationofBlackracewith physicalandchemicalrestraintuseamongpatientsundergoing emergencypsychiatricevaluation. PsychiatrServ. 2022;73(7):730–6.
70.SchnitzerK,MeridethF,Macias-KonstantopoulosW,etal.Disparitiesin care:theroleofraceontheutilizationofphysicalrestraintsinthe emergencysetting. AcadEmergMed. 2020;27(10):943–50.
–
–
–
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 916 Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations Macias-Konstantopoulosetal.
71.CarrerasTartakJ,BrisbonN,WilkieS,etal.Racialandethnicdisparities inemergencydepartmentrestraintuse:amulticenterretrospective analysis. AcadEmergMed. 2021;28(9):957–65.
72.MikatiI,BensonAF,LubenTJ,etal.Disparitiesindistributionof particulatematteremissionsourcesbyraceandpovertystatus. AmJPublicHealth. 2018;108(4):480–5.
73.TessumCW,PaolellaDA,ChamblissSE,etal.PM2.5polluters disproportionatelyandstructurallyaffectpeopleofcolorintheUnited States. SciAdv. 2021;7(18):eabf4491.
74.CommissionforRacialJustice. ToxicWastesandRaceintheUnited States:ANationalReportontheRacialandSocio-Economic CharacteristicsofCommunitieswithHazardousWasteSites.NewYork, NY:UnitedChurchofChristCommissionforRacialJustice;1987.
Availableat: https://www.nrc.gov/docs/ML1310/ML13109A339.pdf AccessedAugust15,2022.
75.NationalResearchCouncil.1991. EnvironmentalEpidemiology: VolumeI:PublicHealthandHazardousWastes.NationalResearch CouncilCommitteeonEnvironmentalEpidemiology.Washington,DC: NationalAcademiesPress.
76.FaberDR,KriefEJ.Unequalexposuretoecologicalhazards: environmentalinjusticesintheCommonwealthofMassachusetts. EnvironHealthPerspect. 2002;110(Suppl2):277–88.
77.LeeP,LeSauxM,SiegelR,etal.Racialandethnicdisparitiesinthe managementofacutepaininUSemergencydepartments:Metaanalysisandsystematicreview. AmJEmergMed. 2019;37(9):1770–7.
78.BenzingAC,BellC,DerazinM,etal.Disparitiesinopioidpain managementforlongbonefractures. JRacialEthnHealthDisparities. 2020;7(4):740–5.
79.SinghalA,TienYY,HsiaRY.Racial-ethnicdisparitiesinopioid prescriptionsatemergencydepartmentvisitsforconditions commonlyassociatedwithprescriptiondrugabuse. PLoSOne. 2016;11(8):e0159224.
80.GoyalMK,JohnsonTJ,ChamberlainJM,etal.Racialandethnic differencesinemergencydepartmentpainmanagementofchildrenwith fractures. Pediatrics. 2020;145(5):e20193370.
81.EducationalFundtoStopGunViolence.NewCDCDataReveals PersistentlyHighRatesofU.S.GunDeaths.2019.Availableat: https:// efsgv.org/press/new-2019-cdc-data/.AccessedJanuary7,2021.
82.EducationalFundtoStopGunViolence.GunViolenceinAmerica:An Analysisof2018CDCData.2020.Availableat: https://efsgv.org/report/ gun-violence-in-america-an-analysis-of-2018-cdc-datafebruary-2020/.AccessedJanuary7,2021.
83.SmedleyA,SmedleyBD.Raceasbiologyis fiction,racismasasocial problemisreal:anthropologicalandhistoricalperspectivesonthesocial constructionofrace. AmPsychol. 2005;60(1):16–26.
84.Nieblas-BedollaE,ChristophersB,NkinsiNT,etal.Changinghowrace isportrayedinmedicaleducation:recommendationsfrommedical students. AcadMed. 2020Dec;95(12):1802–6.
85.CooperRS.Raceinbiologicalandbiomedicalresearch. ColdSpring HarbPerspectMed. 2013;3(11):a008573.
86.AlanizML.Alcoholavailabilityandtargetedadvertisingin racial/ethnicminoritycommunities. AlcoholHealthResWorld. 1998;22(4):286–9.
87.LeeJGL,SunDL,SchleicherNM,etal.Inequalitiesintobaccooutlet densitybyrace,ethnicity,andsocioeconomicstatus,2012,USA:results fromtheASPiREstudy. JEpidemiolCommunityHealth. 2017;71(5):487–92.
88.Esquierdo-LealJL,HoumanfarRA.CreatingInclusiveandequitable culturalpracticesbylinkingleadershiptosystemicchange. BehavAnal Prac. 2021;14(2):499–512.
89.HassenN,LoftersA,MichaelS,etal.Implementinganti-racism interventionsinhealthcaresettings:ascopingreview. IntJEnvironRes PublicHealth. 2021;18(6):2993.
90.BrownsonRC,KumanyikaSK,KreuterMW,etal.Implementation scienceshouldgivehigherprioritytohealthequity. ImplementSci. 2021;16(1):18.
91.ParkerRB,StackSJ,SchneiderSM,etal.Whydiversityandinclusion arecriticaltotheAmericanCollegeofEmergencyPhysicians’ future success. AnnEmergMed. 2017;69(6):714–7.
92.CampbellKM,TuminD.Missionmatters:associationbetweena medicalschool’smissionandminoritystudentrepresentation. ZweigenthalVEM,ed. PLoSOne. 2021;16(2):e0247154.
93.LewisJH,LageOG,GrantBK,etal.Addressingthesocialdeterminants ofhealthinundergraduatemedicaleducationcurricula:asurveyreport. AdvMed. 2020;11:369–77.
94.Eslava-SchmalbachJ,Garz´on-OrjuelaN,EliasV,etal.Conceptual frameworkofequity-focusedimplementationresearchforhealth programs(EquIR). IntJEquityHealth. 2019;18(1):80.
95.BaileyZD,FeldmanJM,BassettMT.Howstructuralracismworks racistpoliciesasarootcauseofUSracialhealthinequalities. NEnglJ Med. 2020;384(8):768–73.
96.CurtisE,JonesR,Tipene-LeachD,etal.Whyculturalsafetyratherthan culturalcompetencyisrequiredtoachievehealthequity:aliterature reviewandrecommendeddefinition. IntJEquityHealth.
2019;18(1):1–17.
97.HeronSL,LovellEO,WangE,etal.Promotingdiversityinemergency medicine:summaryrecommendationsfromthe2008Councilof EmergencyMedicineResidencyDirectors(CORD)Academic AssemblyDiversityWorkgroup. AcadEmergMed.
2009;16(5):450–3.
98.LewisNM,FriedrichsM,WagstaffS,etal.DisparitiesinCOVID-19 incidence,hospitalizations,andtesting,byarea-leveldeprivation–Utah, March3–July9,2020. MMWRMorbMortalWklyRep.
2020;69(38):1369–73.
99.InstituteOfMedicine(U.S.).CommitteeonEducatingHealth ProfessionalstoAddresstheSocialDeterminantsofHealth;Boardon GlobalHealth;InstituteofMedicine;NationalAcademiesofSciences, Engineering,andMedicine.2016. AFrameworkforEducatingHealth ProfessionalstoAddresstheSocialDeterminantsofHealth Washington,DC:NationalAcademiesPress(US).
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 917 Macias-Konstantopoulosetal. Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations
100.NeffJ,HolmesSM,KnightKR,etal.Structuralcompetency:curriculum formedicalstudents,residents,andinterprofessionalteamsonthe structuralfactorsthatproducehealthdisparities. MedEdPORTAL. 2020;16:10888.
101.OgunyemiD.Defeatingunconsciousbias:theroleofastructured, reflective,andinteractiveworkshop. JGradMedEduc. 2021;13(2):189
94.
102.HorvatL,HoreyD,RomiosP,etal.Culturalcompetenceeducation forhealthprofessionals. CochraneDatabaseSystemRev. 2014;(5):CD009405.
103.BaileyRK,SaldanaAM,SaldanaAM.RichardAllenWilliams,MD: acareer fightingdisparitiesandfosteringequity. JRacialEthnHealth Disparities. 2021;8(3):566–9.
104.OlufadejiA,DuboshNM,LandryA.Guidelinesontheuseofraceas patientidentifiersinclinicalpresentations. JNatlMedAssoc. 2021;113(4):428–30.
105.DiaoJA,WuGJ,TaylorHA,etal.Clinicalimplicationsof removingracefromestimatesofkidneyfunction. JAMA. 2021;325(2):184
6.
106.ClevelandManchandaEC,Macias-KonstantopoulosWL.Tackling genderandracialbiasinacademicemergencymedicine:the perceivedroleofimplicitbiasinfacultydevelopment. Cureus. 2020;12(11):e11325.
107.HuffmanA.Whenracebecomesanissueinemergencydepartment treatment. AnnEmergMed. 2018;71(1):A16–8.
108.KelenGD,WolfeR,D’OnofrioG,etal.Emergencydepartment crowding:thecanaryinthehealthcaresystem. NEJMCatalyst,2021.
Availableat: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0217
AccessedAugust14,2022.
109.GladwellM.2013. Blink:ThePowerofThinkingWithoutThinking NewYork,NY:BackBayBooks.
110.JohnsonTJ,HickeyRW,SwitzerGE,etal.theimpactofcognitive stressorsintheemergencydepartmentonphysicianimplicitracialbias. GersonL,ed. AcadEmergMed. 2016;23(3):297–305.
111.AgboolaIK,CoupetEJr,WongAH. “Thecoatsthatwecantakeoffand theoneswecan’t”:theroleoftrauma-informedcareonraceandbias duringagitationintheemergencydepartment. AnnEmergMed. 2021;77(5):493–8.
112.BorJ,VenkataramaniAS,WilliamsDR,etal.Policekillingsand theirspillovereffectsonthementalhealthofBlackAmericans: apopulation-based,quasi-experimentalstudy. Lancet. 2018;392(10144):302–10.
113.GillespieCF,BradleyB,MercerK,etal.Traumaexposureand stress-relateddisordersininnercityprimarycarepatients. Gen HospPsychiatry. 2009;31(6):505–14.
114.LekasHM,PahlK,FullerLewisC.Rethinkingcultural competence:shiftingtoculturalhumility. HealthServInsights. 2020;13:117863292097058.
115. StoneD,HeenS.2015. ThanksfortheFeedback:TheScienceandArt ofReceivingFeedbackWell(evenwhenitisoffbase,unfair,poorly delivered,andfrankly,you’renotinthemood).NewYork,NY: PortfolioPenguin.
116.Tamayo-SarverJH,HinzeSW,CydulkaRK,etal.Racial andethnicdisparitiesinemergencydepartmentanalgesicprescription. AmJPublicHealth. 2003;93(12):2067–73.
117.SudolNT,GuaderramaNM,HonsbergerP,etal.Prevalenceandnature ofsexistandracial/ethnicmicroaggressionsagainstsurgeonsand anesthesiologists. JAMASurg. 2021;156(5):e210265.
118.MolinaMF,LandryAI,CharyAN,etal.Addressingtheelephantinthe room:microaggressionsinmedicine. AnnEmergMed. 2020;76(4):387–91.
–
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 918 Race,Healthcare,andHealthDisparities:ACriticalReviewandRecommendations Macias-Konstantopoulosetal.
FromtheEditors – FutureDirectionstoStrengthen theEmergencyDepartmentSafetyNet
RamaA.Salhi,MD,MHS,MSc*
WendyL.Macias-Konstantopoulos,MD,MPH,MBA*
CaitlinR.Ryus,MD,MPH**
SectionEditor: MarkLangdorf,MD,MHPE
Submissionhistory:SubmittedApril17,2023;RevisionreceivedMay31,2023;AcceptedJune1,2023
ElectronicallypublishedAugust8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.60719
Emergencymedicineasaspecialtypridesitselfonbeing thesafetynetforthecommunitiesweserve.Alwaysopen,we providecaretoallcomers,regardlessofinsurancestatusor abilitytopay,oftenontheworstdaysoftheirlives.Over time,wehavecometoappreciatethatthiscanmean fracturedlimbs,cardiacarrest,oracancerdiagnosis;butjust asfrequentlywecareforindividualswhoaresufferingthe ramificationsoftheinnumerablewaysinwhichoursystem hasfailedthem.Thisincludespoverty,structuralracism,lack ofhousing,foodinsecurity,communityviolence,andwidely disparateincarcerationrates.1–3
Weacknowledgeseveralfundamentaltruths:
1.Discriminationbyage,race,genderidentity,sexual orientation,housingstatus,psychiatricillness(andthe listgoeson)exists.
2.Ourpatients,colleagues,andcommunitiesgrapplewith discriminationanditshealthramificationseveryday.
3.Implicitbiasesanddiscriminatorypracticesarenot static.Wecontinuetoseetheimpactofpastpractices, andourcurrentdecisionswillimpactmanydecades tocome.
4.Emergencycliniciansareuniquelypositionedand privilegedtocontributetoadvancingequity.
Aswestrivetounderstandmorefullythehealthimpactof thesesocialinequitiesandinjustices,ourclinicalspecialtyhas seentherapidexpansionofsocialemergencymedicine. Increasinglyrecognizedasasubspecialty,socialemergency medicinehasestablishedagrowingfoundationofknowledge repletewithpeer-reviewedliterature,academicjournal specialissues,textbooks,researchandeducational conferences,fellowships,andrepresentationwithinour professionalsocieties.4–6 Theburgeoningmultidisciplinary workofsocialemergencymedicineisatestamenttothe nuancewithwhichwemustunderstandsocialandstructural determinantsofhealth.Thislevelofnuanceisrequiredto evenbegintounderstandourroleasemergencyphysicians,
administrators,educators,researchers,andultimately advocatesintheirsolutions.
Despitetheseadvances,thebodyofliteraturethat constitutesthefoundationofsocialemergencymedicineisstill beingbuilt.Manyofthesocialdeterminantsofhealththatwe seektoaddresscanbedifficulttoquantitativelystudydueto smallorinaccessiblepopulations,discriminationand mistrust,orfailuretoscreenandidentify.Hereiswherewe find thevalueofcasestudies,qualitativestudies,hypothesisgeneratingstudies,andnarrativereviews.Showcasedinthis WesternJournalofEmergencyMedicine specialissueare studiesbyauthorswhoendeavoredtocontributetoour growingfoundationofknowledgeandcoverabroadrange oftopics.
Asemergencyphysicians,webearwitnessdailytothe healthimpactsofsocialinequitiesandinjusticesonthe individualsandcommunitiesweserve.Althoughthe structuralsolutionsneededtoaddressourmostvexing socialproblemsmaynotliesquarelywithinourcontrol asaspecialty,wehaveboththeresponsibilityandthe opportunitytocreate,inform,andparticipateinchange. Systematicallyinvestigatingthecompoundinghealtheffects ofcomplexandinterrelatedsocialproblemsallowsusto fulfillourpromisetoourcommunities:Nomatterwhoyou are,nomatteryourproblem,wearehere24hoursaday, 365daysayear.
AddressforCorrespondence:RamaA.Salhi,MDMHSMSc, MassachusettsGeneralHospital,DepartmentofEmergency Medicine,125NashuaSt.,Suite920,Boston,Massachusetts 02114.Email: rsalhi@mgh.harvard.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
*MassachusettsGeneralHospital,Departmentof EmergencyMedicine,Boston,Massachusetts **YaleSchoolofMedicine,DepartmentofEmergency Medicine,NewHaven,Connecticut
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 919
EXPERT COMMENTARY
Copyright:©2023Salhietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.DarbyA,ClevelandManchandaEC,JanewayH,etal.Race,racism, andantiracisminemergencymedicine:Ascopingreviewofthe literatureandresearchagendaforthefuture. AcadEmergMed 2022;29(11):1383–98.
2.SalhiBA,WhiteMH,PittsSR,etal.Homelessnessandemergency medicine:areviewoftheliterature. AcadEmergMed 2018;25(5):577–93.
3.WulzA.Emergencydepartmentvisitsbyincarceratedadultsfor nonfatalinjuries UnitedStates,2010–2019. MorbMortalWklyRep. 2023;72.
4.AlterHJ.Forewordtoconferenceproceedings,inventingsocial emergencymedicine. AnnEmergMed. 2019;74(5):S1–S2.
5.AlterHJ,DalawariP,DoranKM,etal. SocialEmergency Medicine:PrinciplesandPractice.London,UK:Springer Nature;2021.
6.GoldbergL,UrquhartS,DesCampR,etal.Trainingfuture leaders:socialemergencymedicinefellowships. AAEM-Common Sense.2021.Availableat: https://www.aaem.org/UserFiles/ SocialPopulationJulyAugust2021.pdf.AccessedApril14,2023.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 920 FromtheEditors – FutureDirectionstoStrengthentheEDSafetyNet Salhietal.
CharcotNeuroarthropathyoftheFootandAnkleintheAcute Setting:AnIllustrativeCaseReportandTargetedReview
KianBagheri,BA*
AlbertT.Anastasio,MD†
AlexandraKrez,BA‡
LaurenSiewny,MD§
SamuelB.Adams,MD†
*CampbellUniversity,SchoolofOsteopathicMedicine,Lillington,NorthCarolina
† DukeUniversityHospital,DepartmentofOrthopedicSurgery,Durham,NorthCarolina
‡ DukeUniversity,SchoolofMedicine,Durham,NorthCarolina
§ DukeUniversityHospital,DepartmentofEmergencyMedicine,Durham,NorthCarolina
SectionEditors:JuanAcosta,DO,MS,andEdwardMichelson,MD
Submissionhistory:SubmittedJanuary9,2023;RevisionreceivedJuly14,2023;AcceptedJuly18,2023
ElectronicallypublishedAugust30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59833
Charcotneuroarthropathy(CN)isararebutserioussequelaofdiabetesandotherdiseasesthatcause peripheralneuropathy.Itismostcommonlycharacterizedbydegenerationofthefootand/oranklejoints leadingtoprogressivedeformityandalteredweight-bearing.Ifleftuntreated,thedeformitiesofCNlead toulceration,infection,amputation,andevendeath.Becauseoftheassociatedperipheralneuropathy andproprioceptiondeficitsthataccompanyCN,patientstypicallydonotperceivetheonsetofjoint destruction.Moreover,inthehandsoftheuntrainedclinician,theinitialpresentationofCNcaneasilybe mistakenforinfection,osteoarthritis,gout,orinflammatoryarthropathy.Misdiagnosiscanleadtothe aforementionedserioussequelaeofCN.Thus,anearlyaccuratediagnosisandoff-loadingofthe involvedextremity,followedbypromptreferraltoaspecialisttrainedinthecareofCNarecrucialto preventthelate-termsequelaeofthedisease.Thepurposeofthisarticlewastocreateanopportunityfor enhancedunderstandingbetweenorthopedicsurgeonsandemergencyphysicians,toimprove patientcarethroughtheoptimizationofdiagnosisandearlymanagementofCNintheemergentsetting.
[WestJEmergMed.2023;24(5)921–930.]
Keywords: Charcotneuroarthropathy;Charcotfoot;diabetesmellitus;midfootcollapse;emergency.
INTRODUCTION
Duetotheprogressivelossofprotectivesensationin advancedcasesofdiabetesmellitus(DM),identifying DM-relatedfootandanklepathologyintheearlystagesisa challengeforbothpatientsandclinicians.Oneincreasingly commoncomplicationofadvancedDMisCharcot neuroarthropathy(CN),aprogressive,destructivepathology oftheboneandjointsofthefoot.Safavietalestimatedthat CNhasaprevalenceofupto13%inpoorlycontrolled diabeticpatients.1 Oncethoughttobeararecomplication, thisdiagnosishasbecomeincreasinglycommonastheglobal incidenceofDMcontinuestorise.
DiagnosingdiabeticCNischallenging,andeventhemost experiencedclinicianscanstruggletodifferentiatethedisease frompathologiesthatmasqueradeasCN.Limitedspecificity withregardtophysicalexamination,imaging,andlabwork findingsinCNcancloudthediagnosis.Moreover,whenCN
presentsasanacutelyinflamedfoot,itoftenpresents similarlytomuchmorecommonpathologiesofthefootand ankle,suchascellulitis,osteomyelitis,orgout.Delayed treatmentresultsinthedevelopmentoffootandankle deformities,whichincreasestheriskofulceration,infection, andamputation.2–5
Thiscaseillustrationandreview,authoredbyorthopedic surgeonsandemergencyphysicians,focusesontheearly clinicalpresentation,diagnosis,andmanagementofCN, particularlyintheemergentandoutpatientsetting.While manyauthorshaveprovidedreviewarticlesonCN,2–5 none todatehaveprovidedamanuscriptspecificallygeared towardthefacilitationofcross-talkbetweentheinvolved specialtiestoaidindifferentiatingthischallengingdiagnosis fromothersimilarpathologies.Astheincidenceofpoorly controlledDMgrows,theabilitytodistinguishthesubtle presentationofCNfromothermorecommonfoot
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 921 REVIEW
pathologiestakesonunprecedentedimportance.We advocateforenhancedcollaborationbetweenorthopedic surgeonsandemergencyphysicianstobetterunderstandour respectiverolesintheearlydiagnosisandtreatmentofCN, andtoultimatelyimprovethecareofpatientswith thiscondition.
ETIOLOGYANDPATHOPHYSIOLOGYOF CHARCOTNEUROARTHROPATHY
EarlyrecognitionofthecomplicationsofDMsuchasCN iscriticalinpreventingdamaging,long-termoutcomes.In patientswithpoorlycontrolledDM,lackofprotective sensationfacilitatesrepetitivemicrotrauma,perpetuatinga damagingfeedbackloopthatisthoughttocontributetothe CNpathologicprocess.SomedegreeofCNexistsingreater than80%ofpatientswhohavepoorlycontrolledDMfor morethan10years.2 However,itisessentialtoemphasize thatdiabetesaloneisnotthesolepredisposingfactorforthe developmentofCN.Anyconditionthatcausessensoryor autonomicneuropathycanleadtoCN.Examplesinclude syphilis,inwhichdegenerationanddemyelinationofthe dorsalcolumnsandrootscanleadtoprogressivesensory ataxia,chronicalcoholism,inwhichnutritionaldeficiency (especiallythiamine)andoxidativestresscanleadtofree radicaldamagetonerves,6 andspinalcordinjuryinwhich thesomatosensorysystemisdamaged.7
TheexactpathogenesisofCNisnotentirelyunderstood, buttherearetwotheoriesofwhatisbelievedtocontributeto thepathogenesisofthedisease.2 Theneurovasculartheory postulatesthatincreasedblood flowtothebones,whichisa resultofdamagetothe “trophicnerves,” leadstobone resorptionandweakening.Thesepathophysiologicchanges predisposepatientstoincreasedsusceptibilitytofractures anddeformities.Alternatively,theneuro-traumatictheory statesthatrepetitivetraumacancausefracturesand deformationduringhealing.
PATIENTCASEREPORT
A75-year-oldwomanwithlongstanding,poorly controlledtype2DMwithperipheralneuropathytothemidcalfregionpresentedtotheemergencydepartment(ED)with complaintsofrightfootdeformityandpainforninedays. Whilethepatientdidnotrecallanyspecificinjury,she attributedtheappearanceandsymptomstoananklesprain. Shewasinitiallyevaluatedbyherprimarycarephysician, wherethediagnosisofcellulitiswasmadeandshewastoldto gototheEDforfurtherevaluation.Atthetimeof presentation,hererythrocytesedimentationrate(ESR)was 103,herwhitebloodcellcount(WBC)waswithinnormal limits,andhervitalsignswerewithinnormallimits.Physical examrevealedaswollen,diffuselyerythematousfootwith diminishedsensationto finetouch.Nostandardfootand ankleradiographswereobtained,butsheunderwent magneticresonanceimaging(MRI)thatshoweda fluid
collectionposteriortotheanklejoint,whichwasdrainedand yieldedaclear,serous fluidthatdidnotgrowanyorganisms ofculture.Adiagnosisofcellulitiswasmade,andthepatient wasplacedonintravenousclindamycinandadmittedtothe hospital.Shewasdischargedonoralantibiotics five dayslater.Therewerenolimitationsplacedonher weight-bearingstatus.
Shortlyafterdischarge,thepatienttraveledacrossthe country,bearingweightontheinvolvedfoot.Afteraweek, herfootswellingandrednessprogressedinseverity.SherepresentedtoadifferentED.ArepeatMRIatthattimewas concerningforosteomyelitis,andshewasstartedon cefepimeandvancomycin.Duringthispresentation,herlab valueswerewithinnormallimitsandshewasagainafebrile. Shewasadmittedtothehospitalandlaterdischargedon vancomycinviaaperipherallyinsertedcentralcatheter.No standardfootandankleradiographswereobtainedduring thisadmission.Threeweeksafterthatadmission,her creatinineincreasedto4.41andhervancomycintroughwas foundtobe16.8microgramspermicroliter(mcg/mL) (referencerange:5–15mcg/mL).Subsequently,thepatient wasadmittedtothehospital,thistimeforacuterenalfailure secondarytovancomycintherapy.
Physicalexamatthetimerevealeda fixedabduction deformityofthefootwithasevereequinuscontractureofthe Achillestendon.Shedidnothaveprotectivesensationto Semmes-Weinsteinmonofilamenttestingwith5.07.Finally, radiographicimagingwasobtained,whichdemonstrated severemidfootandhindfootcollapsewithhindfootvalgus alignmentandforefootabduction(Figure1).Hertaluswas nearlyinaverticalplantar flexedposition.Advanced imagingintheformofcomputedtomography(CT)further demonstratedthese findings,withadvancedstageCN, withdegenerativechangeatthetalonavicularjointand midfoot(Figure2).
ShewaseventuallydiagnosedwithCNaswellasendstagerenaldisease,requiringchronichemodialysis.Afterthe correctdiagnosisofCNhadbeenmade,thepatientfollowed upintheorthopedicsurgeryclinicatourinstitution,where shereceivedfurthercare,includingosteotomywithmedial andlateralcolumn fixation(Figure3).
CaseSummation
Thiscasehighlightstheimportanceofearlyrecognitionof CNinanacutelyinflamedfootinpatientswithDM, especiallyinthepresenceofadvancedneuropathy.Despite carefulattentionfromvariousclinicians,nostandard radiographswereobtainedandthediagnosisofCNwas missed,contributingtokidneyinjuryinadditiontoincreased destructivechangesofthefootfromCNthatmayhavebeen avoidedwithpromptdiagnosis.Inthecaseofourpatient,no individualclinicianonthecareteamwasatfault;CNcanbe achallengingdiagnosistomakeduetothenumberof pathologieswithwhichitcanbeeasilyconfused.Orthopedic
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 922 CNofFootandAnkleinAcuteSetting:CaseReportandReview Bagherietal.

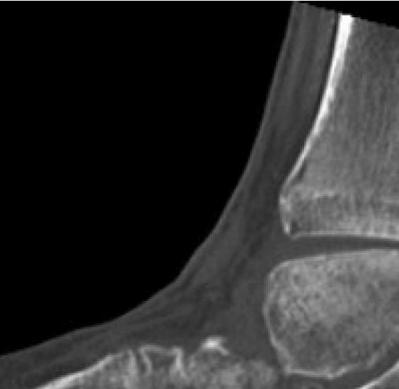
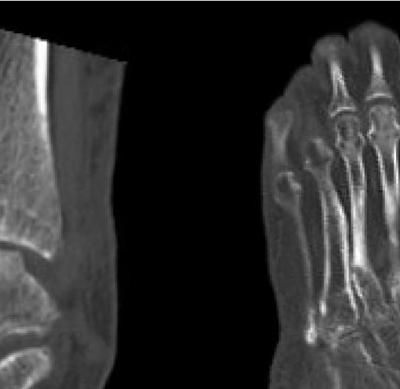


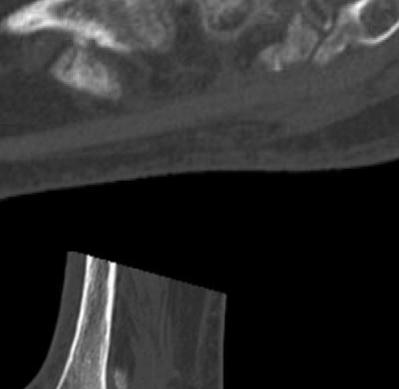
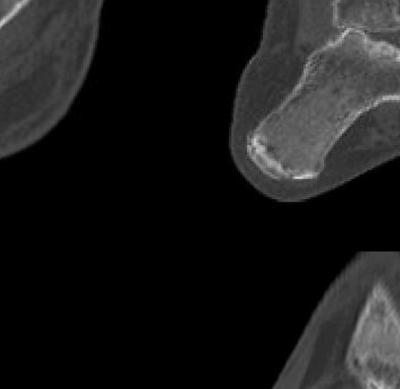


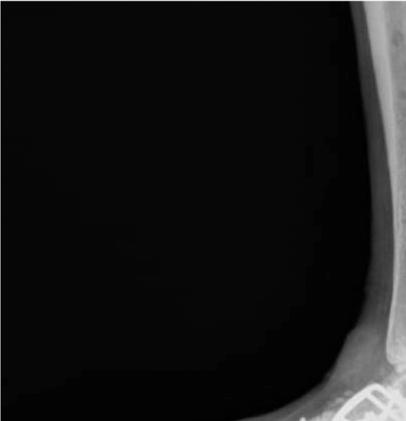









 (A)
(B)
(C)
(D)
Figure2. Computedtomographywith(A,C,D)multiplesagittalcuts,and(B)acoronalcutafterfollow-upinorthopedicclinicdemonstrating findingsconsistentwithadvancedstageCharcotjointwithmarkedpesplanus,mid-footcollapse,andhindfootvalgus.
(A)
(B)
Figure3. Mostrecentradiographsat finalfollow-up.(A)Lateralradiograph.(B)Bilateralanterior-posteriorradiograph,revealingrestorationof thearchofthefoot,throughtheuseofmultipleosteotomysitesandinternal fixationwithavarietyofplate,screw,andbeamconstructs.
(A) (B)
(A)
(B)
(C)
(D)
Figure2. Computedtomographywith(A,C,D)multiplesagittalcuts,and(B)acoronalcutafterfollow-upinorthopedicclinicdemonstrating findingsconsistentwithadvancedstageCharcotjointwithmarkedpesplanus,mid-footcollapse,andhindfootvalgus.
(A)
(B)
Figure3. Mostrecentradiographsat finalfollow-up.(A)Lateralradiograph.(B)Bilateralanterior-posteriorradiograph,revealingrestorationof thearchofthefoot,throughtheuseofmultipleosteotomysitesandinternal fixationwithavarietyofplate,screw,andbeamconstructs.
(A) (B)
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 923 Bagherietal. CNofFootandAnkleinAcuteSetting:CaseReportandReview
Figure1. Weight-bearingradiographs:(A)Bilateralanterior-posterior.(B)Lateralradiographs1.5yearsafterthepatient’sinitialpresentation totheemergencydepartment.Thereisevidenceofdegenerativechangesatthetalonavicularjoint(A – redcircle)inadditiontomidfoot collapse(B – redarrow).
surgeonsreceivespecifictrainingondifferentiatingCNfrom otherconditionsduringfootandanklesubspecialtytraining, butthebreadthofknowledgerequiredforotherspecialties mayprecludeextensiveawarenessofCN.Thus,ourgoal withthisreviewwastodiscussthedifferentialdiagnosisofa patientwithperipheralneuropathyandswellingtothefoot andankleandtoexpandupontheinitialdiagnosisandearly treatmentoptionsofCN.Ourultimateaimistofacilitate understandingbetweenorthopedicsurgeons,emergency physicians,andprimarycarephysicianstooptimizethecare ofthediabeticpatientwithCN.
ClinicalPresentationintheEmergentSetting
ThetypicalpatientpresentingtotheEDwithCNisan individualwithpoorlycontrolleddiabetes,usually50years ofageorolder,withsignsofadvanceddiseasesuchas peripheralneuropathy,retinopathy,orchronickidney disease.Aclinicianmayencounterthefrequentscenarioofa patientwithprevioustraumatothefoot,suchasafall,that re-presentsweeksormonthslaterwithpersistentswelling andpain.However,patientsoftendonotrecallanyspecific trauma,whichmakespromptdiagnosischallenging.
IntheearlyphaseofCN,painisanuncommon finding. However,ifpresent,painisusuallyinsidiousinonset, progressingoverdaysorweeks.Between25–50%ofpatients recallnotraumaorincitingevent.3 Aclinicalexamwill revealunilateralwarmthandanerythematousfootwithsoft tissueswelling.Itisoftendifficultforthepatientto fitthe affectedfootintonormalshoes.Alowthresholdshouldbe maintainedforreferraltoorthopedicsurgery.
Withouttreatment,earlyCNcanprogresstoachronic stage,whereunfortunatelymostcasesofCNarediagnosed. Latediagnosisincreasesthelikelihoodofbonydestruction andresorption,whicheventuallyleadstofootdeformities, ulceration,andsubsequentinfection,oftenwarranting amputation.5,8
InasystematicreviewbySafavietalin2021, theaveragetimefromsymptomonsettoa finaldiagnosisof CNwas84.8days,and48%ofpatientsexperienceda misdiagnosis.1 AsystematicreviewbyKorstetalin2022 foundsimilarresults;thedurationfromsymptomonsetto correctdiagnosiswas86.9days,and53.2%ofcasesofCN wereinitiallymisdiagnosed.9 Thesealarmingstatistics highlightthechallengeinmakingthediagnosisofCN,which callsattentiontotheimportanceofaccuratediagnosisand prompttreatment.
DifferentialDiagnosis
Charcotneuroarthropathysharesmanyoverlapping featureswithothercommonpathologiesofthefootand ankle,whichcancomplicatepromptandaccuratediagnosis. Thus,wediscusscommonpathologiesofthefootandankle thatcanmisleadclinicianstooverlookthediagnosisofCN andofferclinical “pearls” thatcanhelpdifferentiateone fromtheother(Table1).
Infection:Cellulitis,SepticArthritis,andOsteomyelitis
ThediagnosisthatisthemostcommonlymadeoverCNis footandankleinfection,includingcellulitis,septicarthritis, andosteomyelitis.ThisisbecauseacuteCNcausesfoot swellinganderythema.Ingeneral,anacutelyinfectedfootis oftenpainfulandaccompaniedbyafever,whereasCNmay presentwithminimalpainandanafebrilestatus.However, varyingpresentationsofmoreindolentinfectiousetiologies inafebrilepatientswhomaylackperipheralsensationand painsymptomscanmisleadthediagnosis.Thesepatientsalso tendtohavepoorlycontrolledbloodglucoselevelsdueto elevatedcortisol,whichantagonizestheactionofinsulin,10 furthercausingthepotentialformisdiagnosis.
Charcotneuroarthropathyshouldalwaysbeconsideredin patientswithrecurrentcellulitiswithoutsystemicsigns, symptoms,or findingsthatsuggestinfectiononlaboratory analysis.3 Specifically,cellulitiscanbeaccompaniedbysigns ofsystemictoxicitysuchasleukocytosisandelevated inflammatorymarkers.Thelackofthese findingsinthe presenceoferythemamayindicateanearlystageofCN. Acommonorthopaedicteachingpointregardingthe differentiationofCNfrominfectiousetiologiesinvolves assessingthelimbforimprovementinerythemawith elevation.Aftertheinvolvedfoothasbeenelevatedfor30 minutes,erythemashoulddecreaseinCNbutwillremainin thesettingofinfection.3 Anotherdistinguishingfactoris laboratorymarkers.InCN,WBCcount,C-reactiveprotein (CRP),andESRmaybenormal,butthesemarkersare almostalwayselevatedtosomeextentinthesetting ofinfection.2,11
Regardingspecificinfectiousetiologies,osteomyelitis sharesmanyoverlappingfeaturesandcanbeconcomitantly presentwithCN.Osteomyelitisshouldbesuspectedinthe presenceofulcersandshouldbeassumedinthesettingofan ulcerthatprobestobone.12 TheESRmaybeelevatedinboth osteomyelitisandCN,butadownwardtrendwith appropriateantibiotictherapyfavorsthediagnosisof osteomyelitis.13 Asafurtherdifferentiatingfactor, osteomyelitisofteninvolvesasingleboneregion,whereas CNinvolvesmultiplebonesandjoints.14
ImagingcanfurtherhelpdelineatebetweenCNand infectiousetiologiesofthefootandankle.Plainradiography canbeusedtodiagnoseCN,but findingsmaynotappear untiltwotothreeweeksaftersymptomonset.Moreover,it hasbeendemonstratedthata40–50%lossinbonemassina patientwithCNisrequiredtonoteadifferencefrompatients withoutCN.12 Thus,MRIisareasonablealternativetoplain radiography.Unfortunately,severallimitationstoMRIfor thediagnosisofCNexist,suchasinthesettingofrecent surgery,retainedhardware,orrenalinsufficiencythatmay precludepatientsfromreceivingcontrast.Abonebiopsy, whichhaslongbeenconsideredthegoldstandardfor diagnosingosteomyelitis,canbedoneaftera14-day antibiotic-freeperiodifthediagnosisofosteomyelitisismore
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 924 CNofFootandAnkleinAcuteSetting:CaseReportandReview Bagherietal.
Table.1 Asummaryofriskfactors,physicalexam,laboratory,andimaging findings,andtreatmentforCharcotneuroarthropathy(CN)and diseasesthatpresentsimilarlytoCN.
DifferentialRiskfactors
Charcot neuropathy
• Chronicalcoholuse
• Diabeticneuropathy
• Heavymetalpoisoning
• Myelomeningocele
• Leprosy
• Syphilis
• Syringomyelia
• VitaminB12deficiency
Physicalexam findings
• Commonlypainless
• Decreasedrangeof motion
• Edema
• Erythemathatmay decreasewith elevation
• Peripheral neuropathy
• Structuraldeformity
• Warmth
Abnormallab findings frominitialevaluationImaging findingsTreatment
• ElevatedHbA1cor randomserum glucose
• Plainradiograph: Delayedimagingwith evidenceofjointspace narrowing,fragmentation ofarticularsurfaces, coalescenceof fragments,bone resorption,softtissue calcification,deformity andremodelingofthe fracturefragments
• MRI:Maydetectsubtle changesaboveinthe earlierstagesaswellas periarticularedema
Gout
• Chemotherapy
• Chronickidneydisease
• Excessiveintakeof ethanol,dietarypurineor fructose
• Hemolyticdisorders
• Inheritedenzymedefects leadingtopurine overproduction
• Lymphoproliferative disorders
• Malesex
• Myeloproliferative disorders
• Obesity
• Olderage
• Psoriasis
• Useofmedications associatedwith hyperuricemia
Deepvein thrombosis
• Chronicinflammatory states
• Heartfailure
• Obesity
• Olderage
• Malegender
• Malignancy
• May-Thurnersyndrome
• Myeloproliferative disorders
• Pregnancyorpostpartum status
• Previousdeepvein thrombosis
• Prolongedimmobilization
• Recenttraumaorsurgery
• Tobaccouse
• Useoforal contraceptivesor hormonereplacement therapy
• Decreasedrangeof motion
• Edema
• Erythema
• Fever
• Jointpain
• Jointtenderness
• Subcutaneous nodules
• Suddenonsetof symptoms
• Warmth
• Elevatedserumuric acid
• Jointaspirationwith negativebirefringent monosodiumurate crystals
• Plainradiograph: Periarticularerosionwith scleroticborders,joint spacenarrowing,soft tissuecrystaldeposition
• Contactcasting
• Orthotics
• Optimize underlyingrisk factors
• Surgical management
• Edema
• Erythema
• Increasedvisible skinveins
• Pratt’ssign
• Sigg’ssign
• Unilateralpainand edemamost commonlyincalf
• Warmth
• ElevatedD-dimer
• Ultrasound: Noncompressiblevein positiveforthrombus
• Nonsteroidalantiinflammatory drugs
• Colchicine
• Corticosteroids
• Allopurinol
• Optimize underlyingrisk factors
• Anticoagulants
• Optimize underlyingrisk factors
(Continuedonnextpage) Volume24,No.5:September2023WesternJournal of EmergencyMedicine 925 Bagherietal. CNofFootandAnkleinAcuteSetting:CaseReportandReview
DifferentialRiskfactors
Osteoarthritis
• Femalegender
• Historyofjointtraumaor overuse
• Obesity
• Olderage
• Muscleweakness
Physicalexam findings
• Boneovergrowthor deformity
• Decreasedrangeof motion
• Gradualonsetof symptoms
• Jointinstability
• Jointtenderness
• Maybepolyarticular
• Morningstiffness
≤30minutes
• Painwithmovement andrelievedwith rest
Osteomyelitis
• Diabetes
• Injectiondruguse
• Immunocompromised
• Indwellingcatheter
• Olderage
• Orthopedichardware
• Peripheralneuropathy
• Poorvascularsupply
• Recenttrauma
• Sicklecell
Cellulitis
• Diabetes
• Injectiondruguse
• Lymphaticdrainage disruption
• Obesity
• Peripheralarterydisease
• Recentsurgery
• Saphenousveinharvest
• Skinbarrierdisruption
• Skininflammation
• Venousinsufficiency
Septic arthritis
Abnormallab findings frominitialevaluationImaging findingsTreatment
• Plainradiographs:Joint spacenarrowing, presenceofosteophytes, andsubchondral sclerosis
• Nonsteroidalantiinflammatory drugs
• Physicaltherapy
• Optimize underlyingrisk factors
• Surgical management
• Decreasedrangeof motion
• Drainingsinustract
• Gradualonsetof symptoms
• Fever
• Erythema
• Edema
• Tenderness
• Pain
• Presenceofulcers
• Warmth
• Breachinskin barrier
• Edema
• Erythemawithout dissipationupon elevationofaffected extremity
• Fever
• Tenderness
• Warmth
• Elevatederythrocyte sedimentationrate andC-reactiveprotein Positiveboneculture
• Leukocytosis
• Plainradiograph:After2 weeksmayobserve bonelossandperiosteal reaction
• MRI:Inadditionto
findingonplain radiograph,T2boneand softtissueedemaanda penumbrasignmaybe present
• Antibiotics
• Irrigationand debridement
• Optimize underlyingrisk factors
• Amputation
• Elevatederythrocyte sedimentationrate andC-reactiveprotein
• Leukocytosis
-
• Antibiotics
• Diabetes
• End-stagerenaldisease
• Acuteonsetof symptoms
• Immunocompromised
• Indwellingcatheters
• Injectiondruguse
• Olderage
• Recentsurgery
• Recenttrauma
• Skinorsofttissue infection
• Elevatederythrocyte sedimentationrate andC-reactiveprotein
• Antibiotics
• Decreasedrangeof motion
• Edema
• Erythemawithout dissipationupon elevationofaffected extremity
• Fever
• Jointpain
• Tenderness
• Warmth
• Leukocytosis
• Positivesynovial fluid gramstainandculture
• Plainradiographs:Joint spacenarrowing,joint effusion,periarticular osteopenia,destruction ofsubchondralbone
• Surgicaldrainage MRI,magneticresonanceimaging.
Table.1 Continued.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 926 CNofFootandAnkleinAcuteSetting:CaseReportandReview Bagherietal.
heavilyfavoredthanCN.15 Insummation,differentiating CNfrominfectiousetiologiesofthefootandankleisa clinicalchallengethatinvolvescarefulconsiderationofa varietyofclinical,laboratory,andimaging-based findings.
Gout
Goutmostcommonlymanifestssymptomaticallyinthe footandankle,makingthisdiagnosiseasytoconfusewith CN.RiskfactorsforgoutandCNoverlap,suchasDMand obesity,butafewspecialconsiderationsmeritfurther discussion.Forexample,certainmedicationscanprecipitate gout,themostcommonofwhicharethiazidediuretics.Thus, werecommendathoroughmedicationreconciliationupon presentationincasesofsuspectedgoutvsCN.Heavyalcohol useisanotherriskfactoroftenassociatedwithgout. However,chronicalcoholismhasbeenshowntobearisk factorfortheprogressionofCN,16,17 andsothepresenceof heavyalcoholusedoesnotnecessarilyfavoronediagnosis overtheother.Anadditionaldiagnosticclueisthepresence orabsenceofperipheralneuropathy.Thepresence ofperipheralneuropathycoupledwithextensive alcoholconsumptionpointsmoretowardCNovergout, especiallyifthepatientdoesnothaveaprevioushistoryof gouty flares. 18
Tofurtherdifferentiateagout flarefromCN,painand tendernessthatdissipateoverashortdurationfavorthe diagnosisofgoutoverthemorelong-term,subacutepain seenwithCN.Laboratoryanalysismayrevealnonspecific changesconsistentwithinflammationduringagout flare, andtheseelevationsmayalsobepresentinCN.Uricacid levelsarenotconsistentlyelevatedingout19 andshouldnot beusedasamarkertodistinguishgoutfromCN.Ifgoutis suspected,synovial fluidtestingwithcellcountsand differentialwhitecount,Gramstainandculture,andcrystal examinationunderpolarizinglightmicroscopyis recommended.20
22 Thepresenceofmonosodiumurate crystalsconfirmsthediagnosisofgout.
DeepVeinThrombosis
Deepveinthrombosis(DVT),whilemorecommonly relegatedtothecalf,mayalsopresentsimilarlytoCN.Oneof themostreliableclinicalsignsofDVTisunilateralleg swellingthatinvolvesthecalf.23 RiskfactorsforDVT includerecentsurgery,pregnancy,smoking,cancer,and prolongedimmobility,whicharedistinctfromCN.24
Furthermore,aD-dimerlevelhasahighsensitivityforruling outDVT.IftheD-dimeriselevated,venousduplex ultrasonographybecomestheimagingstudyofchoicein patientswithsuspectedDVT.25,26 Theresultofthisstudywill benormalinpatientswithCN.
Osteoarthritis
Osteoarthritisisachronicconditionthatprogressively worsensoverthecourseofapatient’slife.27 Painisthe
cardinalsymptomofosteoarthritis,whichmayormaynot alwaysbepresentinCN,givenlossofprotectivesensation. However,thepaininosteoarthritisisclassicallyexacerbated byactivityandimprovedbyrest.28 Osteoarthritisalsohas characteristic findingsonradiographs,suchasjointspace narrowing,thepresenceofosteophytes,andsubchondral sclerosis.29,30 Inaddition,bonyfragmentationandcallus formationarenotseeninosteoarthritisbutcanbeseen inCN.
Diagnosis
DiagnosticdelaysindiabeticCNarecommonbut avoidableifcliniciansmaintainahighindexofsuspicionin patientswithriskfactorsforCN.Weencouragecliniciansto alwaysconsiderCNintheirdifferentialdiagnosiswhena diabeticpatientwithperipheralneuropathypresents withfootedema,redness,andwarmth,especiallyin theabsenceofpain.DiagnosisofCNincludesa thoroughhistoryandphysicalexam,imaging,and laboratoryevaluation.
PhysicalExam
DiagnosisofCNbeginswithacompletephysicalexam. Vitalsignsshouldbeassessedforevidenceofsystemicillness, suchasthepresenceoffever,tachycardia,orhypotension.In addition,thepatient’sfeetshouldbeinspectedforthe presenceofulcersorbreaksintheskin.Althoughgross sensationtestinginpatientsatriskofneuropathyissimple andrapidintheemergentsetting,itisunreliableforassessing diabeticpatientsatriskofCN.31 Semmes-Weinstein monofilamenttestinghaslongbeenconsideredthegold standardfordetectingclinicallyrelevantneuropathyin diabeticpatients.31 Thisnon-invasive,low-cost,andrapid testisthemostsensitiveindicatorofCN.32 Inadditionto sensationtesting,skintexture,bonydeformities,signsof vascularorneurologiccompromise,anddetailsoffootwear shouldberecorded.2 Finally,elevatingtheaffectedfootfor 30minutesisasimpleyeteffectivewayofnarrowingthe differentialdiagnosisintheemergentsetting.Rednesswill decreaseinCNbutnotinthesettingofinfection.3
LaboratoryTesting
LaboratorytestinginpatientssuspectedofCNshould includeacompletebloodcount(CBC),WBCwith differential,andtestingofrenalfunction(viabloodurea nitrogenandcreatinine).Patientsshouldalsobescreenedfor diabetes,eveniftheydonothaveahistoryofthediseaseorits presentingriskfactors.Dependingontheclinicalsetting,this canbeachievedbyassessingfastingglucose,hemoglobin A1c(HbA1c),orrandombloodglucoselevels.TheESRand CRPcanalsobehelpful,aselevationsinthesevaluesareseen morecommonlyinotherconditions,suchasosteomyelitis orinfection.
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 927 Bagherietal. CNofFootandAnkleinAcuteSetting:CaseReportandReview
Imaging
Imagingisalsohelpfultohelpestablishthediagnosisof CN;however,itisimperativetoemphasizethatnormal radiographsdonotruleoutCN.Radiographsareoften unremarkableintheearlystagesofthediseaseandarenota reliableindicatorofdiseaseprogression.Nonetheless,plain filmradiographsmustbeobtainedbecausetheyserveasa baselineandallowforthedetectionofsubtlechangesthat mayportendinstability.3
Ininstanceswheretheradiographisnegative,butthere remainsahighindexofsuspicionforCN,MRIcanbeused forfurtherevaluation.Magneticresonanceimagingismore sensitiveindetectingsubtlechangesintheearlyphaseofthe diseaseandcanhelpruleoutotheroverlappingpathologies suchasosteomyelitis.32 IninstanceswhenMRIis contraindicatedorcannoteffectivelydistinguishCNfrom otherpathologies,nuclearmedicinestudiessuchas leukocyte-labeledbonescansarehighlyspecificfor distinguishingbetweenCNandinfection.33 Inthisprocess, WBCsareremovedfromthepatient,taggedwitha radioisotopesuchasindium-111,andinjectedintravenously backintothepatient.Thetaggedleukocytesthenlocalizeto areasofrelativelynewinfection.
Treatment
Immobilization
Charcotneuroarthropathyisamedicalemergencythat canleadtoirreversibleskeletaldestructionandpermanent deformitiesifnotpromptlyaddressed.33 Inpatientswith concomitantriskfactorsforCN,immobilizationandnonweightbearingoftheinvolvedfootisrecommendeduntilthe correctdiagnosisisconfirmed.OncethediagnosisofCNis established,itisvitaltocontinueimmobilizationandnonweightbearingoftheaffectedextremity.32 Ataminimum, thepatientshouldbeplacedinacontrolledanklemotion (CAM)boot.Wecautionagainstsplintingorcastinginthe EDincasethepatientgetslosttofollow-up.Along-term splintorcastcouldleadtoulcerationinthesettingof decreasedsensation.Ifanulcerispresent,thepreferred methodofimmobilizationisatotalcontactcast.3,33 Full methodologyfortheapplicationoftotalcontactcastingis outsidethescopeofthismanuscriptbutgenerallyincludesa thinlayerofcastpaddingtoallowforweightdistributionto offloadpointsofulcerationandbonychange.Totalcontact castingshouldcontinueuntillowerextremityedemaand warmthresolveandserialradiographyshowsevidenceof osseousconsolidation.3 Thisprocesstypicallyoccursafter threetofourmonthsbutcantakeaslongas12months.ACT orMRIcanalsobeusedtomonitortheresolutionofCN.
DISCUSSION
Charcotneuroarthropathycontinuestoemergeasa significantcontributortopatientmorbidityworldwide.In recognitionoftheimportanceofearlydiagnosisofthis
condition,anumberofauthorshavereportedonvarious interventionsaimedtoimprovethedetectionofCN.Astudy byFoltzetallookedatthevascularandneurologic findings thatwerethemosthelpfulindifferentiatingfactorsbetween patientswithandwithoutCN.34 Theyfoundthatsimple neurologictestingcombinedwithacomprehensivepatient historywerethemostbeneficialtoolstodeterminepatientsat highriskofdevelopingCN.Theyfoundstatistically significantassociationsforhistoryofretinopathy, nephropathy,andpreviousfootulcerinadditiontothe neurologicphysicalexam findingsofvibratorysensation, deeptendonreflexes,andSemmes-Weinsteinmonofilament testingwithCN.Notably,vascularexaminationswerenot predictiveofCN.These findingshaveimportantimplications foremergencyphysicianswhoareconsideringadiagnosis ofCN.
AnotherstudybyChantelauetalassessedtheclinical courseofacuteCNin24patientswithoutevidenceofdefinite fracturesontheinitialradiographaftertheonsetof symptoms.35 Alarmingly,19ofthe24patientsinthisstudy hadbeenmisdiagnosedpriortoreferral,highlightingthe difficultyinachievinganaccuratediagnosisofCN.Themost commonmisdiagnosisamongthesepatientswasanankle sprain,followedbycellulitis.Fourteenofthepatients progressedtodefinitefracturesofeitheralltarsometatarsal jointsorofthetalonavicularjoint.Thisstudyemphasizesthe importanceofearlydiagnosis,treatment,andreferralofCN topreventtheprogressionofthedisease.
IfCNispromptlydiagnosed,earlytreatmenthasshown excellentsuccessatmitigatingitspossiblelong-term ramifications.AstudybyParisietalin2013lookedatthe radiographicandfunctionalresultsinthetreatmentofthe earlystagesofCNwithaCAMbootandimmediateweightbearing.36 Thestudyincluded22patientswithtype2 diabetes.AmericanOrthopedicFootandAnkleSociety scoresshowedstatisticallysignificantimprovementatthe terminationofthestudy.Theseauthorsconcludethatthe utilizationofaCAMbootinconjunctionwithimmediate weight-bearingforCNshowedgoodfunctionaloutcomes andhaltedtheprogressionofdeformityonradiographic assessment.Incontrast,whenthediagnosisofCNisdelayed andpatientspresenttotheEDwiththepresenceofa Charcot-relatedfootwound,outcomescanbemuchworse. AstudybyWukichetalfoundthatthepresenceofa Charcot-relatedfootwoundatpresentationincreasedthe likelihoodofamajorlowerextremityamputationbyafactor ofsix.37
CONCLUSION
Charcotneuroarthropathyisahighlycomplexdisorder, anditspathophysiologyisnotfullyunderstood.Whileoncea rarediagnosis,asobesityanddiabetesratesrise,CNis becomingmorecommon.Evenexperiencedcliniciansmay struggletodiagnoseCN,giventhelargenumberofother
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 928 CNofFootandAnkleinAcuteSetting:CaseReportandReview Bagherietal.
conditionsthatcanpresentsimilarly.Itshouldalwaysbeon thedifferentialinadiabeticpatientwithperipheral neuropathyandsignsoffootedema,redness,andwarmth, especiallyintheabsenceofpain.IfCNissuspected, immediateimmobilizationandnon-weightbearingare recommendeduntilorthopedicfollow-up.Amultidisciplinary approachshouldbeemphasizedinthecareofpatientswith CN,withenhancedcollaborationbetweenemergency physiciansandorthopedicsurgeonstoensurethebest outcomeforpatientswiththiscomplexcondition.
AddressforCorrespondence:KianBagheri,BA,DukeUniversity Hospital,200TrentDrive,Durham,NorthCarolina27710.Email: k_bagheri1204@email.campbell.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Bagherietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.ShazadehSafaviK,JanneyC,ShazadehSafaviP,etal.Inappropriate antibioticadministrationinthesettingofCharcotarthropathy: acaseseriesandliteraturereview. PrimCareDiabetes 2022;16(1):202
06.
2.TriebK.TheCharcotfoot:pathophysiology,diagnosisand classification. BoneJointJ 2016;98-B(9):1155–9.
3.MarmolejoVS,ArnoldJF,PonticelloM,etal.Charcotfoot:clinicalclues, diagnosticstrategies,andtreatmentprinciples. AmFamPhysician 2018;97(9):594
99.
4.Al-BusaidiIS,MasonR,LuntH.DiabeticCharcotneuroarthropathy:The diagnosismustbeconsideredinalldiabeticneuropathicpatients presentingwithahot,swollenfoot. NZMedJ 2015;128(1423):77–80. [publishedOnlineFirst:20151016]
5.GoldsmithL,BarlowM,EvansPJ,etal.Acutehotfoot:Charcot neuroarthropathyorosteomyelitis?Untanglingadiagnosticweb. BMJ CaseRep 2019;12(5).[publishedOnlineFirst:20190513]
6.ChopraK,TiwariV.Alcoholicneuropathy:possiblemechanisms andfuturetreatmentpossibilities. BrJClinPharmacol 2012;73(3):348–62.
7.ChambelSS,TavaresI,CruzCD.Chronicpainafterspinalcordinjury:Is therearoleforneuron-immunedysregulation? FrontPhysiol 2020;11:748.[publishedOnlineFirst:20200707]
8.FauziAA,ChungTY,LatifLA.RiskfactorsofdiabeticfootCharcot arthropathy:acase-controlstudyataMalaysiantertiarycarecentre. SingaporeMedJ 2016;57(4):198–203.
9.KorstGS,RatliffHT,TorianJ,etal.DelayeddiagnosisofCharcotfoot:a systematicreview. JFootAnkleSurg 2022;61(5):1109–13. [publishedOnlineFirst:20220223]
10.ButlerSO,BtaicheIF,AlanizC.Relationshipbetweenhyperglycemia andinfectionincriticallyillpatients. Pharmacotherapy 2005;25(7):963–76.
11.CarroGV,RicciA,TorterolaI,etal.DifferentialdiagnosisofCharcot neuroarthropathyinsubacuteandchronicphases:unusualdiseases. Int JLowExtremWounds 2021:15347346211054326.[publishedOnline First:20211115]
12.WomackJ.Charcotarthropathyversusosteomyelitis:evaluationand management. OrthopClinNorthAm 2017;48(2):241–7.[published OnlineFirst:20170201]
13.BuryDC,RogersTS,DickmanMM.Osteomyelitis:diagnosisand treatment. AmFamPhysician 2021;104(4):395–402.
14.MarcusCD,Ladam-MarcusVJ,LeoneJ,etal.MRimagingof osteomyelitisandneuropathicosteoarthropathyinthefeetofdiabetics. Radiographics 1996;16(6):1337–48.
15.DoneganR,SumpioB,BlumePA.Charcotfootandanklewith osteomyelitis. DiabetFootAnkle 2013;4[publishedOnlineFirst: 20131001]
16.ArapostathiC,TentolourisN,JudeEB.Charcotfootassociatedwith chronicalcoholabuse. BMJCaseRep 2013;2013[publishedOnline First:20130405]
17.ShibuyaN,LaFontaineJ,FraniaSJ.Alcohol-inducedneuroarthropathy inthefoot:acaseseriesandreviewofliterature. JFootAnkleSurg 2008;47(2):118–24.
18.LioteF.[Diagnosisofcrystal-inducedarthritis]. PresseMed 2011;40(9Pt1):869–76.[publishedOnlineFirst:20110803]
19.PittmanJR,BrossMH.Diagnosisandmanagementofgout. AmFam Physician 1999;59(7):1799–806,810.
20.HainerBL,MathesonE,WilkesRT.Diagnosis,treatment,and preventionofgout. AmFamPhysician 2014;90(12):831–6.
21.SiveraF,AndresM,QuilisN.Gout:Diagnosisandtreatment. MedClin (Barc) 2017;148(6):271–76.[publishedOnlineFirst:20161205]
22.DalbethN,MerrimanTR,StampLK.Gout. Lancet 2016;388 (10055):2039–52.[publishedOnlineFirst:20160421]
23.HansraniV,KhanbhaiM,McCollumC.Thediagnosisand managementofearlydeepveinthrombosis. AdvExpMedBiol 2017;906:23–31.
24.GoldhaberSZ.Riskfactorsforvenousthromboembolism. JAmColl Cardiol 2010;56(1):1–7.
25.Barrosse-AntleME,PatelKH,KramerJA,etal.Point-of-careultrasound forbedsidediagnosisoflowerextremityDVT. Chest 2021;160(5):1853–63.[publishedOnlineFirst:20210713]
26.KatzDS,HonM.CurrentDVTimaging. TechVascIntervRadiol 2004;7(2):55–62.
27.BeckerJA,DailyJP,PohlgeersKM.Acutemonoarthritis:diagnosisin adults. AmFamPhysician 2016;94(10):810–6.
28.Taruc-UyRL,LynchSA.Diagnosisandtreatmentofosteoarthritis. Prim Care 2013;40(4):821–36,vii.[publishedOnlineFirst:20130926]
–
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 929 Bagherietal. CNofFootandAnkleinAcuteSetting:CaseReportandReview
29.RoemerFW,DemehriS,OmoumiP,etal.Stateoftheart:imagingof osteoarthritis-revisited2020. Radiology 2020;296(1):5–21.[published OnlineFirst:20200519]
30.BraunHJ,GoldGE.Diagnosisofosteoarthritis:imaging. Bone 2012;51(2):278–88.[publishedOnlineFirst:20111203]
31.ObolenskyL,TrimbleK.ImportanceofclosesurveillanceforCharcot arthropathyindiabeticpatientspresentingtotheemergencydepartment withlow-energyfootinjuries. EmergMedJ 2010;27(6):484–5.
32.VopatML,NentwigMJ,ChongACM,etal.Initialdiagnosisand managementforacuteCharcotneuroarthropathy. KansJMed 2018;11(4):114–9.[publishedOnlineFirst:20181129]
33.MascarenhasJV,JudeEB.TheCharcotfootasacomplicationof diabeticneuropathy. CurrDiabRep 2014;14(12):561.
34.FoltzKD,FallatLM,SchwartzS.Usefulnessofabriefassessment batteryforearlydetectionofCharcotfootdeformityinpatientswith diabetes. JFootAnkleSurg 2004;43(2):87–92.
35.ChantelauEA,RichterA.TheacutediabeticCharcotfootmanagedon thebasisofmagneticresonanceimaging–areviewof71cases. Swiss MedWkly 2013;143:w13831.[publishedOnlineFirst:20130729]
36.ParisiMC,Godoy-SantosAL,OrtizRT,etal.Radiographicand functionalresultsinthetreatmentofearlystagesofCharcot neuroarthropathywithawalkerbootandimmediateweightbearing. DiabetFootAnkle 2013;4.[publishedOnlineFirst:20131029]
37.WukichDK,SadoskasD,VaudreuilNJ,etal.Comparisonofdiabetic charcotpatientswithandwithoutfootwounds. FootAnkleInt 2017;38(2):140–8.[publishedOnlineFirst:20161024]
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 930 CNofFootandAnkleinAcuteSetting:CaseReportandReview Bagherietal.
AShorterDoor-In-Door-OutTimeIsAssociatedwithImproved OutcomeinLargeVesselOcclusionStroke
AdamSigal,MD*
DerekL.Isenberg,MD†
ChaddK.Kraus, DO,DrPH‡
DanielAckerman,MD§
JosephHerres,DO∥
EthanS.Brandler,MD¶
AlexanderKuc,MD#
JasonT.Nomura,MD**
DerekR.Cooney,MD††
MichaelT.Mullen,MD‡‡
HuaqingZhao,PhD§§
NinaT.Gentile,MD†
SectionEditor: ShadiLahham,MD
*ReadingHospital,DepartmentofEmergencyMedicine,WestReading,Pennsylvania
† LewisKatzSchoolofMedicineatTempleUniversity,DepartmentofEmergencyMedicine, Philadelphia,Pennsylvania
‡ GeisingerHealth,DepartmentofEmergencyMedicine,Danville,Pennsylvania
§ St.Luke’sHealthSystem,DepartmentofNeurology,Bethlehem,Pennsylvania
∥ EinsteinHealthSystem,DepartmentofEmergencyMedicine,Philadelphia,Pennsylvania
¶ StateUniversityofNewYork-StonyBrook,DepartmentofEmergencyMedicine, StonyBrook,NewYork
# CooperUniversityHealthcare,DepartmentofEmergencyMedicine,Camden,NewJersey
**ChristianaCare,DepartmentofEmergency,Newark,Delaware
†† StateUniversityofNewYork-Upstate,DepartmentofEmergencyMedicine, Syracuse,NewYork
‡‡ LewisKatzSchoolofMedicineatTempleUniversity,DepartmentofNeurology, Philadelphia,Pennsylvania
§§ LewisKatzSchoolofMedicineatTempleUniversity,CenterforBiostatisticsand Epidemiology,Philadelphia,Pennsylvania
Submissionhistory:SubmittedSeptember27,2022;RevisionreceivedApril21,2023;AcceptedApril18,2023
ElectronicallypublishedAugust30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58946
Introduction: Endovascularthrombectomy(EVT)significantlyimprovesoutcomesinlargevesselocclusion stroke(LVOS).WhenapatientwithaLVOSarrivesatahospitalthatdoesnotperformEVT,emergent transfertoanendovascularstrokecenter(ESC)isrequired.Ourobjectivewastodeterminetheassociation betweendoor-in-door-outtime(DIDO)and90-dayoutcomesinpatientsundergoingEVT.
Methods: WeconductedananalysisoftheOptimizingPrehospitalStrokeSystemsofCare-Reactingto ChangingParadigms(OPUS-REACH)registryof2,400LVOSpatientstreatedatnineESCsintheUnited States.WeexaminedtheassociationbetweenDIDOtimesand90-dayoutcomesasmeasuredbythe modifiedRankinscale.
Results: Atotalof435patientswereincludedinthe finalanalysis.ThemeanDIDOtimeforpatientswith goodoutcomeswas17minuteshorterthanpatientswithpooroutcomes(122minutes[min]vs139min, P = 0.04).AbsoluteDIDOcutofftimesof ≤60min, ≤90min,or ≤120minwerenotassociatedwith improvedfunctionaloutcomes(46.4vs32.3%, P = 0.12;38.6vs30.6%, P = 0.10;and36.4vs28.9%, P = 0.10,respectively).Thisheldtrueforpatientswithhyperacutestrokesoflessthanfour-houronset. LowerbaselineNationalInstitutesofHealthStrokeScale(NIHSS)score(11.9vs18.2, P =<.001)and youngerage(62.5vs74.9years(P < .001)wereassociatedwithimprovedoutcomes.Onmultiple regressionanalysis,age(oddsratio[OR]1.71,95%confidenceinterval[CI]1.45–2.02)andbaseline NIHSSscore(OR1.67,95%CI1.42–1.98)wereassociatedwithimprovedoutcomeswhileDIDOtime wasnotassociatedwithbetteroutcome(OR1.13,95%CI0.99–1.30).
Conclusion: AlthoughtheDIDOtimewasshorterforpatientswithagoodoutcome,thiswasnonsignificantinmultipleregressionanalysis.ReceiptofintravenousthrombolysisandtimetoEVTwerenot associatedwithbetteroutcomes,whilemalegender,lowerage,arrivalbyprivatevehicle,andlower NIHSSscoreportendedbetteroutcomes.NoabsoluteDIDO-timecutofformodifiablefactorwas associatedwithimprovedoutcomesforLVOS.ThisstudyunderscorestheneedtostreamlineDIDO timesbutnottosetanartificialDIDOtimebenchmarktomeet.[WestJEmergMed.2023;24(5)931–938.]
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 931
ORIGINAL RESEARCH
INTRODUCTION
Endovascularthrombectomy(EVT)significantly improvesoutcomesinpatientswithlargevesselocclusion stroke(LVOS).1 Timetothrombectomyisamajor determinantofneurologicoutcomewithshortertimes associatedwithbetterfunctionaloutcomesat90days.2,3 Key componentsinmanagingLVOSincludeidentifyingthe LVOS,determiningeligibilityforthrombolyticsandEVT, andoptimizingmanagementuntilreperfusionoccurs.4 Many hospitalsintheUnitedStatesdonothaveEVTcapabilities andmusttransferLVOSpatientstoendovascularstroke centers(ESC)forEVT.5
Itisnotclearhowthelengthoftimespentatthe transferringnon-ESCimpactspatientoutcomes.Timespent atnon-ESChospitalspriortotransferisdefinedasthedoorin-door-outtime(DIDO).LongerDIDOtimesatthenonESCmayworsenoutcomesbydelayingrecanalizationand reperfusion.6 However,thereisapaucityofevidenceonthe relationshipbetweenDIDOandfunctionaloutcomes.Inthis study,weexaminedtherelationshipbetweenDIDOtimes and90-dayfunctionaloutcomesinamulticenterregistry.We hypothesizedthatlongerDIDOtimeswouldbeassociated withworsefunctionaloutcomesat90days.
METHODS
ThisstudywasconductedbytheOptimizingPrehospital StrokeSystemsofCare-ReactingtoChangingParadigms (OPUS-REACH)consortium.TheOPUS-REACHisa consortiumofninehealthsystemsintheNortheastUS.The structureoftheOPUS-REACHconsortiumhasbeen previouslydescribed.7 TheOPUS-REACHregistryincludes allpatientswhounderwentEVTatoneofthenineESCs betweenJanuary1,2015
December31,2020.AnESCwas definedasathrombectomy-capablestrokecenteror comprehensivestrokecentercapableofperformingEVT 24hoursadayonanemergencybasis.Weincludedall patientswhoinitiallypresentedtoanon-ESCandwerelater transferredtoanESCforEVT.Weexcludedpatientsfrom analysisiftheirstrokeoccurredafterarrivalatthehospital, their90-dayfunctionaloutcomewasunknown,orifDIDO timeatthenon-ESCwasnotavailable.
Weextractedallinformationfromtheelectronichealth records(EHR)attheindividualhospitalsandsubmittedto TempleUniversitythatservesasthecentralrepositoryfor OPUS-REACHdata.Trainedresearchassociatesornurses ateachoftheninesitesusedastandardizedcasereportform toabstractdatafromtheEHR.Theprincipalinvestigatorat eachoftheninesitesverifiedthedatapriortosubmissionto University.Thedataabstractedwereexplicitvariables withoutneedforinterpretation.Missingdatawasnot imputedexceptformissing90-daymodifiedRankinScale (mRS)scores.
ThemRSscorewasobtainedfromdocumentationinthe EHRorbyestimationbythesiteinvestigatorusingtheEHR.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Door-in-door-out(DIDO)time(thetime spentintheEDatatransferringhospital)is usedasabenchmarkinstrokepatients transferredtoahigherlevelofcare.
Whatwastheresearchquestion?
WhatistheassociationbetweenDIDOtime andoutcomesinpatientsundergoing endovasculartherapy?
Whatwasthemajor findingofthestudy?
Themeantimeforpatientswithgood outcomeswas122minutesvs139minutesfor patientswithpooroutcomes(P = 0.04).
Howdoesthisimprovepopulationhealth?
Thisstudyunderscorestheneedtostreamline DIDOtimesbutnottosetanarti fi cialDIDOtimebenchmarkfortransferringhospitals tomeet.
Ifno90-daymRSscorewasdocumentedintheEHRorinthe hospital’sstrokeregistry,thesiteinvestigatorateachESC reviewedtheEHRtoidentifyacliniciannotefromthe90-day timeframe.Thiscouldhavebeenanotefromneurology, emergencymedicine,primarycare,physicaltherapy,orany otherlicensedclinician.Usingthisnote,thesiteinvestigator estimatedwhetherthepatienthadagood(mRS0–2)orpoor (mRS3–6)functionaloutcome.Forexample,iftheEHR reflectedthatthepatientneededcareinaskillednursing facultythiswouldbecodedasapooroutcomewhileifthe notereflectedthepatienthadminimalneurologicaldeficits andwalkedwithoutassistance,thepatientwouldbeassigned agoodoutcome.ThisestimationofthemRSscorehasbeen previouslyshowntohavegoodcorrelationwithin-person derivedmRSvalues.8 Wecollectedandmanagedstudydata usingREDCapelectronicdatacapturetoolshostedat TempleUniversity.1,2 REDCap(ResearchElectronicData Capture)isasecure,web-basedsoftwareplatformdesigned tosupportdatacaptureforresearchstudies.
Theprimaryoutcomewas90-dayfunctionaloutcomeas assessedbythemRS.10–13 AmRSscoreof0–2was consideredagoodoutcomewhileamRSscoreof3–6was consideredapooroutcome.
Descriptivesummarystatisticsarepresentedasmeans (SD)forcontinuousvariablesandasfrequencieswith percentagesforcategoricalvariables.Weusedthe
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 932 AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke Sigaletal.
two-sample t -testtocomparecontinuousvariablesandchisquaretesttocomparecategoricalvariablesbetweengood andpooroutcomes.Univariatelogisticregressionwas performedtoestablishpotentialfactorsthatmaycontribute togoodoutcomes.Apriori,wedefineda P -valueof <0.05as significantintheunivariateanalysis.Multiplevariable logisticregressionwasconductedtodeterminethe associationofvariablestoestimateanoddsratioofagood outcome.WeperformedstatisticalanalyseswithSAS StatisticsSoftware,SAS9.4(SASInstituteInc,Cary,NC). Univariateanalysiswasperformedusing t -teststoobtaina P -value.Apriori,wedefined aP-value of <0.05as significant.Weconductedmultiplelogisticregressionto determinetheassociationofvariablestoestimateanodds ratio.Theinstitutionalreviewboardsofallnineparticipating institutionsapprovedthisstudy.
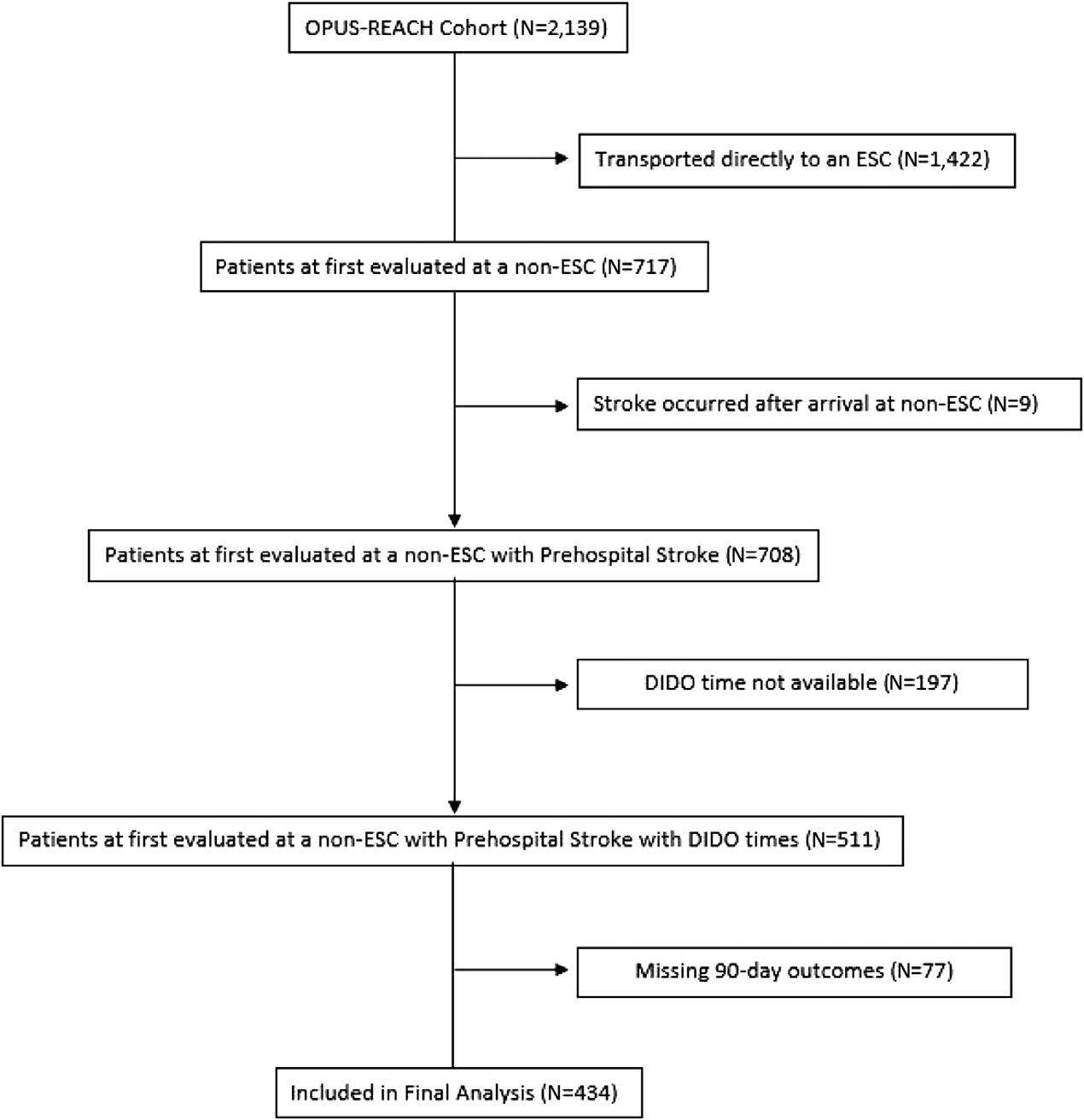
RESULTS
Ofthe2,139patientsintheOPUS-REACHregistry,we included434inthe finalanalysis(Figure1).Patientswere predominantlyWhitewithanevendistributionbygender. Themedianagewas71years(Table1).Ofthe378patients forwhomthetimeofvascularimagingwasknown,56%
ofpatientshadvascularimagingperformedatthe transferringhospital.
Wefoundthat33%ofpatientshadagoodoutcome (mRS0–2).Patientswhohadfavorable90-dayoutcomeshad alowerbaselineNIHSSscorethanthosewithpooroutcomes (NIHSS11.9vs18.2, P < 0001).Patientswithbetter outcomesweremorelikelytoarrivebyprivatetransportthan byemergencymedicalservices(EMS)(56.5vs30.6%, P = 0.004).Overall,patientswithgoodoutcomeshada 17-minutefasterDIDOtimethanpatientswithpoor outcomes(122.6minutes[min]vs139.8min, P = 0.037).This trend,however,didnotmeetstatisticalsignificance whenanalyzedwithDIDOcutofftimesof ≤60, ≤90, or ≤120min(Table2).
Weperformedasubgroupanalysisforpatientswho arrivedatthenon-ESCwithinfourhoursoftheonsetoftheir strokes(hyperacutestroke).Here,wesawnodifferenceinthe meanDIDOtimesbetweenthegroupwithgoodoutcomes andthegroupwithpooroutcomes(Table3).Again,lower ageandlowerinitialNIHSSscoreportendedbetter outcomes.Onmultiplevariableanalysis,wefoundthatage andlowerbaselineNIHSSscoreweretheonlyvariables associatedwithimprovedoutcomesinLVOSpatients.There
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 933 Sigaletal. AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke
Figure1. Enrollmentdiagram.Oftheinitialcohortof2,129patients,434wereincludedinthe finalanalysisbasedoncompleteDIDOtimes andneurologicoutcomes. ESC,endovascularstrokecenter.
werenomodifiablefactorsassociatedwithimproved outcomes.(Table4).
DISCUSSION
Althoughpatientswithgoodoutcomehadslightlyfaster DIDOtimesoverall,wecould findnospecificDIDO thresholdupto120minthatwasassociatedwithimproved outcomesat90dayswhetherearlyorlateinthestroke process.TheinitialNIHSSscoreandthepatient’ sagewere morepredictivethanDIDOtimeforfavorableoutcome.We foundsomesurprisingfactorsthatwerenotassociatedwith outcomesamongourpatients.ArrivalbyEMSwas significantlyassociatedwithimprovedoutcomesinour cohort.ArrivalbyEMSwascloselylinkedtoahigher NIHSSscore.Therefore,EMSarrivalwasnotsignificanton multiplevariableanalysis.Receiptofintravenous thrombolysis(IVT)wasborderlinesignificantonunivariate analysis.Thismayberelatedtoasmallsamplesizeor tothefactthatthemeanarrivaltimetothenon-ESCwas greaterthan4.5hours,makingmanypatientsineligible forIVT.
Mostinteresting,timetoEVTwasnotassociatedwith betteroutcomes,despitepriorresearchshowingdelaysto EVTwereassociatedwithworseoutcomes.Forexample, Jahanetalfoundthateach15-mindelaytoEVTwas associatedwithworseoutcomes.14 However,thiseffectonly persistedupto270min.Therefore,thelongertimetoEVTin ourcohortmayhavedilutedeffectsoftimetoEVT.
AlthoughDIDOtimeislinkedtoEVTtime,therearemany moretimeintervalsinvolvedinstrokeonsettoEVT.Itmay bethattimefromhospitalarrivaltoEVTortimefrom imagingtoEVTaremoreimportantfactorsinoutcomes afterLVOS.
Themodelfortransferringpatientstohigherlevelsofcare andconcernthatdelaysmayimpactlong-termfunctionisan adaptationofthemodelsdevelopedformanagingacuteSTelevationmyocardialinfarction(STEMI).AmongSTEMI transferpatients,thosewithprolongedDIDOtimeshad increasedmortalityat30days.15 Transferredpatientswith DIDOtimes <30minhadbothshorterperfusiontimesand lowerin-hospitalmortality,withtheoddsratioof1.56for thosewithtimes >30min.16
Inonemetanalysisofnearly16,000patients,theauthors foundthatthosewithDIDOtimeof <30minhada2.8% 30-daymortalitycomparedto6.0%forpatientswithDIDO timesof >30min.17 However,DIDOtimesfortransferred patientsundergoingprimarypercutaneousintervention rarelymeettherecommended30-mingoal.18,19 Common delaysintransferincludetransportdelays,diagnostic uncertainty,andclinicalinstabilitypriortotransfer.20
Asregionalstrokesystemsofcaredevelop,DIDOhas beenproposedasametricfortransferringhospitalstofollow. Choietaldemonstratedthataprimarystrokecentercan achievemedianDIDOtimesof <60min.21 However, comparedtotheSTEMItransferprocess,thediagnosisof LVOSismorecomplex.WhereasaSTEMIdiagnosiscanbe madebasedona12-leadelectrocardiogramandan abbreviatedhistory,thediagnosisofanLVOSrequiresa thoroughneurologicexam,advancedcomputed tomography,radiologicinterpretation,andconsultation withaneurologist.CurrentlytheAmericanHeart Association(AHA)makesnorecommendationsastoan optimalDIDOtimeforLVOS.1 WhilethebenefitofEVTis timedependentearlyoninLVOS,andsystemsofcareshould prioritizerapidtransferofLVOSpatientstoanESC,more researchisneededtoidentifyaclinicallymeaningfulDIDO threshold,priortoadoptingnationalbenchmarks.Fromour data,wecannotrecommendaspecificDIDOtimeforLVOS patientsinananalogousmannertoSTEMIpatients.
LIMITATIONS
Ourstudyhasseverallimitations.Asitwasaretrospective study,wedidnothavecompletedataonallthepatients transferredtothrombectomycentersforEVT.Wewere missingDIDOtimesfor197patientslargelybecauseof
Table1. Demographics. DemographicN = 434(%) Race American Indian/AlaskaNative 1(0.2) BlackorAfricanAmerican 62(15.0) White 347(83.8) Asian/NativeHawaiian/PacificIslander 2(0.5) Other 2(0.5) Unknown 22(5.0) Hispanicethnicity Yes 16(3.7) No 416(96.3) Unknown 4(0.9) Age Mean(SD) 70.7(16.2) Range 25–103 Gender Male 211(48.4) Female 225(51.6) BaselinePatientCharacteristics MeaninitialNIHSS(SD) 16.1(8.1) Meantimefromlastknownwelltoarrivalat non-ESCinminutes(SD) 276(325) MeantimefromlastknownwelltoEVTin minutes(SD) 505(344)
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 934 AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke Sigaletal.
NIHSS, NationalInstitutesofHealthStrokeScale; EVT, endovascularthrombectomy.
Table2. Univariateanalysisofentirecohort.
DIDO, door-in-door-out; ESC,endovascularstrokecenter; EMS,emergencymedicalservices; IVT,intravenousthrombolysis; PSC,primary strokecenter; LKW,lastknownwell; EVT,endovascularthrombectomy; NIHSS NationalInstitutesofHealthStrokeScale.
VariableOverall(N = 434)Good(N = 144)Poor(N = 290) P-value 434 144 290 Mean DIDOtimeatnon-ESC(SD) 134.1(86.7) 122.6(74.0)139.8(91.9)0.04 Meansofarrivaltonon-ESC(n = 415) <.001 EMS 369(88.9) 113(30.6) 256(69.4) PrivateVehicle 46(11.1) 26(56.5) 20(43.5) ReceivedIVT 0.08 No 263(60.6) 79(30.0) 184(70.0) Yes 171(39.4) 79(38.0) 106(62.0) Vascularimagingperformedatnon-ESC(n = 324) 0.73 No 141(43.5) 46(32.6) 95(67.4) Yes 183(56.5) 63(34.4) 120(65.6) Levelofnon-ESC(n = 434) 0.90 Notcertified 59(13.6) 20(33.9) 39(66.1) PSC 375(86.4) 124(33.1) 251(66.9) Race(n = 412) 0.55 AmericanIndian 1(0.2) 0 1(100.0) Asian/PacificIslander 2(0.5) 0 1(100.0) Black 62(15.1) 23(37.1) 39(62.9) White 345(83.7) 111(32.2) 234(67.8) Other 2(0.5) 0 2(100.0) Hispanicethnicity(n = 430) 0.57 No 415(96.5) 137(33.0) 278(67.0) Yes 15(3.5) 6(40.0) 9(60.0) Meanage(SD) 70.8(15.1) 62.5(15.0) 74.9(13.5) <.001 Gender 0.02 Female 224(51.5) 63(28.1) 161(71.9) Male 211(48.5) 81(38.4) 130(61.6) DIDOtimeatnon-ESC ≤60minutes(min) 28(6.5) 13(46.4) 15(53.6) 0.12 >60min 406(93.6) 131(32.3) 275(67.7) ≤90min 140(32.3) 54(38.6) 86(61.4) 0.10 >90min 294(67.7) 90(30.6) 204(69.4) ≤120min 247(56.9) 90(36.4) 157(63.6)0.10 >120min 187(43.1) 54(28.9) 133(71.1) LKWtoarrivalatnon-ESC(n = 401) 0.31 Meantimeinminutes(SD) 278.83(330.1)254.63(300.1)290.57(343.6) LKWtoarrivalatnon-ESCin <4hours(n = 266) 88(33.1) 178(66.9)0.80 LKWtoEVT(n = 394) 0.28 Meantimeinminutes(SD) 497.4(334.8)471.4(307.5)510.4(347.5) InitialNIHSSscore(n = 430)[SD] 16.1(8.1) 11.9(7.3) 18.2(7.7) <.001
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 935 Sigaletal. AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke
Table3. Univariateanalysisofpatientswithhyperacutestrokepresentation(onsettoarrivalofnon-endovascularstrokecenterof <240minutes).
VariableTotalGoodoutcomePooroutcome P-value 265 87 178 Mean DIDOtime(SD) 126.3(71.2)116.6(62.4)131.1(74.9)0.12 MeansofarrivaltoNnon-ESC(n = 254) EMS 227(89.4) 67(29.5) 160(70.5) <.001 Privatevehicle 27(10.6 15(55.6) 12(44.4) ReceivedIVT No 106(40.0) 28(26.4) 78(73.6) 0.07 Yes 159(60.0) 59(37.1) 100(62.9) Vascularimagingperformedatnon-ESC(n = 200) No 88(44.0) 28(31.8) 60(68.2) 0.82 Yes 112(56.0) 34(30.4) 78(69.6) Levelofnon-ESC 265 Notcertified 41(15.5) 13(31.7) 28(68.3) 0.87 PSC 224(84.5) 74(33.0) 150(67.0) Race(n = 249) 249 AmericanIndian 1(0.4) 0 1(100) 0.83 AsianorPacificIslander 1(0.4) 0 1(100) Black 32(12.9) 11(34.4) 21(65.6) White 214(85.9) 68(31.8) 146(68.2) Other 1(0.4) 0 2(100) Hispanicethnicity(n = 263) No 252(95.8) 84(33.3) 168(66.7) 0.68 Yes 11(4.2) 3(27.3) 8(72.7) Meanage <.001 Mean(SD) 70.87(15.14)62.86(14.83)74.78(13.71) Gender(n = 245) 0.04 Female 146(55.1) 40(27.4) 106(72.6) Male 119(44.9) 47(39.5) 72(60.5) DIDOtimeatnon-ESC ≤60minutes(min) 16(6.0) 6(37.5) 10(62.5) 0.68 >60min 406(93.6) 131(32.3) 275(67.7) ≤90min 91(34.3) 34(37.4) 57(62.6) 0.26 >90min 294(67.7) 90(30.6) 204(69.4) ≤120min 158(59.6) 57(36.1) 101(63.9) 0.17 >120min 187(43.1) 54(28.9) 133(71.1) LKWtoarrivalatnon-ESC 0.35 Mean(SD) 79.31(53.2)74.95(53.4)81.43(53.1) LKWtoEVT(n = 260) 0.97 Mean(SD) 301.13(114.2)300.69(114.9)301.35(114.1) InitialmeanNIHSSscore(SD)[n = 263] 263 DIDO, door-in-door-out; ESC,endovascularstrokecenter; IVT,intravenousthrombolysis; EMS,emergencymedicalservices; PSC,primarystrokecenter; LKW,lastknownwell; EVT,endovascularthrombectomy. WesternJournal of EmergencyMedicine Volume24,No.5:September2023 936 AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke Sigaletal.
Table4.
HyperacuteStrokePresentation(onsettoarrivalof non-ESC of <240minutes)
Non-endovascularstrokecentersshouldfocusonfollowing AHA/AmericanStrokeAssociationguidelinesforinitial strokecare,includingintravenousthrombolysis administration,andappropriatetransfertoanESC.
AddressforCorrespondence:DerekIsenberg,MD,LewisKatz SchoolofMedicineatTempleUniversity,DepartmentofEmergency Medicine,1316WestOntarioStreet,10th Floor,Philadelphia, Pennsylvania19140.Email: derek.isenberg@tuhs.temple.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Dr.DerekIsenbergandDr.JasonT. NomurareceivedagrantfromtheAmericanHeartAssociationto supportOPUS-REACH.Theauthorsdisclosednoconflicts ofinterest.
DIDO, door-in-door-out; NIHSS,NationalInstitutesofHealthStroke Scale.
missingdatafromthetransferringhospitals.Asdatawas collectedretrospectively,recordsfromthetransferring hospitalweresometimesmissingfromtheEHRoftheESC. Inaddition,thethree-monthoutcomewasbasedonamRS scorethatattimeswasestimate-based.Priorstudieshave validatedthismethodology,however.8
Inaddition,weincludedpatientscaredforbyninehealth systemsandover100non-ESCs.Althoughmostfollowed standardAHA/AmericanCollegeofCardiologystroke guidelinesforcareandaredesignatedasESCs,thereare variationsinprehospitalEMScommunications,transfer processes,initialimaging,andthrombolysisprocessatthe initialhospitalsfromwhichtheyreceivepatients.However, theinclusionofmanyhealthsystemsinawidecontiguous geographicregionimprovesgeneralizabilityandprovides informationaboutoutcomesinroutineclinicalpractice, ratherthanclinicaltrials.Allpatientsinourstudywere knowntohaveLVOSandunderwentEVT.Wedonotknow theDIDOtimesforpatientswhoweretransferredbutdidnot undergoEVT.
CONCLUSION
Althoughthemeandoor-in-door-outtimeisshorterfor patientswithgoodfunctionaloutcomesafterlargevessel occlusionstrokethereisnoabsoluteDIDOcutofftimeupto 120minutesthatimproved90-dayfunctionaloutcomefor patientswithanLVOSundergoingendovascular thrombectomy.BeforeestablishingDIDOmetricsfor referringhospitals,moreresearchisneededonfactorsthat improveclinicaloutcomes.Themostimportantpredictorof 90-dayoutcomesisthepatient’sageandinitialNIHSSscore.
Copyright:©2023Sigaletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.AdeoyeO,NystrümKV,YavagalDR,etal.Recommendationsforthe establishmentofstrokesystemsofcare:a2019update. Stroke. 2019;50(7):e187–210.
2.JahanR,SaverJL,SchwammLH,etal.Associationbetweentimeto treatmentewithendovascularreperfusiontherapyandoutcomesin patientswithacuteischemicstroketreatedinclinicalpractice. JAMA. 2019;322(3):252–63.
3.SaverJL,GoyalM,vanderLugtA,etal.Timetotreatmentwith endovascularthrombectomyandoutcomesfromischemicstroke:a meta-analysis. JAMA. 2016;316(12):1279.
4.McTaggartRA,AnsariSA,GoyalM,etal.Initialhospitalmanagementof paitentswithemergentlargevesselocclusion(ELVO):reportofthe standardsandguidelinescommitteeoftheSocietyof NeuroInternventionalSurgery. JNeuroIntervSurg. 2017;9:316–23.
5.JauchEC,SchwammLH,PanagosPD,etal.Recommendationsfor RegionalStrokeDestinationPlansinRural,SuburbanandUrban CommunitiesFromthePrehospitalStrokeSystemofCareConsensus Conference:AConsensusStatementFromtheAmericanAcademyof Neurology,AmericanheartAssociation/AmericanStrokeAssociation, AmericanSocietyofNeuroradiology,NationalAssociationofEMS Physicians,NationalAssociationofStateEMSOfficials,Societyof NeuroInterventionalSurgeryandSocietyofVascularandInterventional Neurology:EndorsedbytheNeurocriticalCareSociety. Stroke. 2021;52(5):e133–52.
6.McTaggartRA,ModovanK,OliverLA,etal.Door-in-door-outtimeat primarystrokecentersmaypredictoutcomeforemergentlargevessel occlusionpatients. Stroke. 2018;49(12):2969–74.
7.IsenbergDL,HenryKA,SigalA,etal.OptimizingPrehospitalStroke SystemsofCare-ReactingtoChangingParadigms(OPUS-REACH):a
Oddsratio 95%Confidence limits DIDO 1.13 0.991.30 Not insame hospitalsystem 1.98 1.183.31 NIHSS 1.67 1.421.98 Age 1.71 1.452.02
Multipleregressionanalysisforentirecohort.
Oddsratio 95%Confidence limits DIDO 1.22 0.991.50 Not insame hospitalsystem 3.02 1.496.11 NIHSSscore 1.76 1.412.20 Age 1.80 1.432.25
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 937 Sigaletal. AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke
pragmaticregistryoflargevesselocclusionstrokepatientsto createevidence-basedstrokesystemsofcareandeliminate disparitiesinaccesstostrokecare. BMCNeurology. 2022;22(1):132.
8.IsenbergD,PrusN,RamseyF,NTG.TheModifiedRankinScalecan accuratelybederivedfromtheelectronicmedicalrecord. TransformativeMedicine. 2022;1(2):31–5.
9.HarrisPA,TaylorR,ThielkeR,etal.Researchelectronicdatacapture (REDCap)-ametadata-drivenmethodologyandworkflowprocessfor providingtranslationalresearchinformaticssupport JBiomedInform. 2009;42(2):377–81.
10.RankinJ.Cerebralvascularaccidentsinpatientsovertheageof60.I. Generalconsiderations. ScottMedJ. 1957;2(4):127–36.
11.RankinJ.Cerebralvascularaccidentsinpatientsovertheageof60.II. Prognosis. ScottMedJ. 1957;2(5):200–15.
12.RankinJ.Cerebralvascularaccidentsinpatientsovertheageof60.III. Diagnosisandtreatment. ScottMedJ. 1957;2(6):254–68.
13.vanSwietenJC,KoudstaalPJ,VisserMC,etal.Interobserver agreementfortheassessmentofhandicapinstrokepatients. Stroke. 1988;19(5):604–7.
14.JahanR,SaverJL,SchwammLH,etal.Associationbetweentimeto treatmentwithendovascularreperfusiontherapyandoutcomesin patientswithacuteischemicstroketreatedinclinicalpractice. JAMA. 2019;322(3):252–63.
15.ShiO,KhanAM,RezaiMR,etal.Factorsassociatedwithdoor-into door-outdelaysamongST-segmentelevationmyocardialinfarction (STEMI)patientstransferredtoprimarypercutaneouscoronary intervention:apopulation-basedcohortstudyinOntario,Canada. BMC CardiovascularDisorders. 2018;18(1):1–9.
16.WangTY,NallamothuBK,KrumholzHM,etal.Associationofdoor-into door-outtimewithreperfusiondelaysinoutcomesamongpatients transferredforprimarypercutaneouscoronaryintervention. JAMA. 2011;305(24):2540–7.
17.YamaguchiJ,MatobaT,KikuchiM,etal.Effectsofdoor-intodoor-out timeonmortalityamongST-segmentelevationmyocardialinfarction patientstransferredforprimarypercutaneouscoronaryinterventionsystemicreviewandmeta-analysis. CircRep. 2022;4(3):109–15.
18.HerrinJ,MillerLE,TurkmaniDF,etal.Nationalperformanceondoor-in todoor-outtimeamongpatientstransferredforprimarypercutaneous coronaryintervention. ArchInternMed. 2011;171(21):1879
86.
19.LambertLJ,BrownKA,BoothroydLJ,etal.Transferofpatientswith ST-elevationmyocardialinfarctionforprimarypercutaneouscoronary intervention. Circulation. 2014;129(25):2653–60.
20.MiedemaMD,NewellMC,DuvalS,etal.Causesofdelayand associatedmortalityinpatientstransferredwithST-segment-elevation myocardialinfarction. Circulation. 2011;124:1636–44.
21.ChoiPMC,TsoiAH,PopeAL,etal.Door-in-door-outtimeof60minutes forstrokewithemergentlargevesselocclusionataprimarystroke center. Stroke. 2019;50:2829–34.
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 938 AShorterDIDOTimeIsAssociatedwithImprovedOutcomeinLVOStroke Sigaletal.
TreatmentofFactor-XaInhibitor-associatedBleedingwith AndexanetAlfaor4FactorPCC:AMulticenter FeasibilityRetrospectiveStudy
AdamJ.Singer,MD*
MauricioConcha,MD,MHS†
JamesWilliams,DO‡
CaitlinS.Brown,PharmD§
RafaelFernandes,MS*
HenryC.ThodeJr.,PhD*
MarylinKirchman,MSN,RN,SCRN†
AlejandroA.Rabinstein,MD∥
SectionEditor:MarkLangdorf,MD,MHPE
*RenaissanceSchoolofMedicineatStonyBrookUniversity,Departmentof EmergencyMedicine,StonyBrook,NewYork
† SarasotaMemorialHospital,DepartmentofNeuroscience, Sarasota,Florida
‡ MeritusHealth,DepartmentofEmergencyMedicine,Hagerstown,Maryland
§ MayoClinic-Rochester,DepartmentofPharmacy,Rochester,Minnesota
∥ MayoClinic-Rochester,DepartmentofNeurosurgery, Rochester,Minnesota
Submissionhistory:SubmittedMarch31,2023;RevisionreceivedJuly6,2023;AcceptedJuly20,2023
ElectronicallypublishedAugust22,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.60587
Background: Therearenorandomizedtrialscomparingandexanetalfaand4factorprothrombin complexconcentrate(4F-PCC)forthetreatmentoffactorXainhibitor(FXa-I)-associatedbleeds,and observationalstudieslackimportantpatientcharacteristics.Wepursuedthisstudytodemonstratethe feasibilityofacquiringrelevantpatientcharacteristicsfromelectronichealthrecords.Secondarily,we exploredoutcomesinpatientswithlife-threateningFXa-Iassociatedbleedsafteradjustingfor thesevariables.
Methods: Weconductedamulticenter,chartreviewof100consecutiveadultpatientswithFXa-I associatedintracerebralhemorrhage(50)orgastrointestinalbleeding(50)treatedwithandexanetalfaor 4F-PCC.Wecollecteddemographic,clinical,laboratory,andimagingdataincludingtimefromlastfactor FXa-Idoseandbleedonset.
Results: Mean(SD)agewas75(12)years;34%werefemale.EstimatedtimefromlastFXa-Idoseto bleedonsetwaspresentinmostcases(76%),andpatientstreatedwithandexanetalfaand4F-PCC weresimilarinbaselinecharacteristics.Hemostaticefficacywasexcellent/goodin88%and76%of patientstreatedwithandexanetalfaand4F-PCC,respectively(P = 0.29).Ratesofthromboticevents within90dayswere14%and16%inandexanetalfaand4F-PCCpatients,respectively(P = 0.80). Survivaltohospitaldischargewas92%and76%inandexanetalfaand4F-PCCpatients,respectively (P = 0.25).Inclusionofanexploratorypropensityscoreandtreatmentinalogisticregressionmodel resultedinanoddsratioinfavorofandexanetalfaof2.01(95%confidenceinterval0.67–6.06)for excellent/goodhemostaticef ficacy,althoughthedifferencewasnotstatisticallysignificant.
Conclusion: Importantpatientcharacteristicsareoftendocumentedsupportingthefeasibilityofalarge observationalstudycomparingreal-lifeoutcomesinpatientswithFXa-I-associatedbleedstreated withandexanetalfaor4F-PCC.Thesmallsamplesizeinthecurrentstudyprecludeddefinitive conclusionsregardingthesafetyandefficacyofandexanetalfaor4F-PCCinFXa-I-associatedbleeds. [WestJEmergMed.2023;24(5)939–949.]
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 939
ORIGINAL RESEARCH
INTRODUCTION
TheuseoffactorXainhibitors(FXa-I)hasrapidly increasedoverthelastdecadeduetotheirimproved pharmacokineticproperties,efficacy,andsafetycompared withoralvitaminKantagonists.1–4 Asaresult,thenumberof patientsrequiringtreatmentforlife-threateningbleeding associatedwithFXa-Iusehasalsoincreased.5 Priortothe availabilityofaspecificreversalagentforbleedingsecondary totheFXa-I,thesebleedsweretreatedwith4-factor prothrombincomplexconcentrates(4F-PCC)containing coagulationfactorsII,VII,IXandX,6,7 butbecausepatients treatedwiththeFXa-Iarenotdeficientinthesecoagulation factors,themechanisticrationalefortheirusehasbeen questioned.8 Andexanetalfa(morerecentlyknownas coagulationfactorXa[recombinant],inactivated-zhzo) isaspecificallydesignedrecombinantfactorXadecoy molecule.9 DuetoitshighaffinitytotheFXa-I,andexanet alfabindswithapixabanandrivaroxabanreleasingnative FXaandresultinginthrombingeneration,clotformation, andhemostasis.
Theefficacyandsafetyofandexanetalfainpatients treatedwithFXa-Ipresentingwithlife-threateningbleedsis supportedbytheANNEXA-4clinicaltrial.10 However, ANNEXA-4wasasinglearmtrial.Anongoingrandomized clinicaltrial(RCT),ANNEXA-I,iscomparingandexanet alfaheadtoheadwithcoagulationfactorreplacement strategy(anticipatedtomostlybe4F-PCC)forfactorFXa-Irelatedintracerebralhemorrhage(ICH)(ClinicalTrials.gov NCT03661528).Yettheresultsofthistrialarenot anticipatedforatleast1
2years,anditwillonlyprovide resultsforintracerebralbleeds.
Whileanumberofstudieshavedescribedtheuseof4FPCCfortreatmentoflife-threateningbleedsinpatients treatedwithaFXa-I,6,7 relativelyfewstudieshavecompared 4F-PCCtoandexanetalfaandnonehavebeenRCTs.11–16 Directcomparisonofpatientstreatedwith4F-PCCand andexanetalfaischallengingduetodifferencesinpatient populationsandendpoints.Aretrospectivereviewof electronichealthrecords(EHR)from45hospitalscompared outcomesof3,030patientshospitalizedwithmajorbleeding relatedtoFXa-Iandtreatedwithandexanetalfaor4F-PCC. Inthisstudy,treatmentwithandexanetalfawasassociated withthelowesthospitalmortalityacrossdifferentbleed types.14 However,thisstudydidnotcollectcriticalbaseline informationsuchastimefromlastFXa-Idoseanddidnot controlforconfoundingvariables,limitingitsconclusions. Furthermore,thisstudywaslimitedtohospitaloutcomes onlywithnolongertermoutcomes.
Anotherretrospectivestudyof322patientstreatedwith andexanetalfafromtheANNEXA-4study10 thatwere propensityscorematched(PSM)with88patientsfromthe ORANGEstudy15 foundlower30-dayadjustedmortality ratesinpatientstreatedwithandexanetalfa.13 Thisstudyis alsolimitedsincepatientsincludedintheANNEXA-4study
weregenerallylessseverelyillthanthoseincludedinthe ORANGEstudy.Incontrast,otherretrospective comparisonsofpatientstreatedwithandexanetalfaor4FPCChavenotshowncleardifferencesinoutcomes.11,12,16,17 Importantly,thesestudiesoftenfailedtocontroltheir analysesforrelevantpatientcharacteristicsthatarepotential confoundingvariables,suchastimingfromlast FXa-Idose,timingfromonsetofbleedingepisode,initial ICHvolume,timefromICHonsetto firstheadCT,or severityofillness.18
Ourobjectiveinthiscurrentfeasibilitystudywasto conductamulticenterretrospectivechartreviewto determinewhetherdataregardingimportantpatient characteristicswasgenerallydocumentedintheEHRandto exploretheassociationbetween4F-PCCorandexanet alfaandoutcomesinpatientswithprimaryICHand gastrointestinalbleeds(GIB)associatedwithuseof apixabanorrivaroxaban.
METHODS StudyDesign
Weperformedastructured,retrospectivechartreview, consistentwiththerecommendedmethodologyofKaji etal.19 OurstudyalsofollowedtheStrengtheningof ReportingofObservationalStudiesinEpidemiology (STROBE)reportingguidelinesforcross-sectionalstudies.20 Becauseoftheretrospectivedesign,wereceivedinstitutional reviewboard(IRB)approvalwithwaiverofinformed consent.Duetothenatureofthisstudyasafeasibilityand exploratorypilot,nosamplesizecalculationsweremade.
PatientsandSettings
WeincludedalladultpatientspresentingwithanICH(50) orGIB(50)eventwhoreceivedreversalwithandexanetalfa (50)orreplacementwith4F-PCC(50).Wechosetoinclude 50patientsineachtreatmentgroupandbleedingtypeapriori sincewefeltthatthisnumberwouldbeadequateto determinethefeasibilityofalargerstudy.Weexcluded patientswhoweretreatedwithbothagentsaswellaspatients treatedwithandexanetalfaplusothercoagulationfactor concentrates.Wealsoexcludedpatientstransferredtooneof thestudysitesfromanotherhospital.Thestudyperiod wasfromMay2018(whentheUSFoodandDrug Administration[FDA]approvedandexanetalfa)until December2021.Consecutivepatientswereenrolledin reversechronologicalorderstartingwiththemostrecentdate (basedoneachinstitution’sIRBapproval)untiltherequired numberofpatientswereidentified.Thestudysitesincluded twolargeacademicmedicalcentersandtwolarge communitysettings.Initially,eachhospitalwasrequestedto contributecasesequally.However,duetoimbalancesin numberofpatientstreated,the finalnumberofstudypatients fromeachsitewasnotequal.Onesitedidnothaveandexanet alfaonformularyandonlycontributedcasestreatedwith
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 940 TreatmentofFXa-IBleedingwithAndexanet
α or4F-PCC Singeretal.
4F-PCC.Attheotherthreesitesandexanetalfawasaddedto theformularyinJune2018.
Decisiononhighorlowdosefollowedthestandard recommendations.Nopatientinthestudyhadrepeated doses.Andexanetalfawasusedinpatientswhoreported lastdoseofapixabanorrivaroxabanwithin18hoursand metthefollowingindications:i)acute,overtmajororlifethreateningbleedingepisode;ii)acutebleedingina criticalareaororgan,suchaspericardial,intracranial, orintraspinal;iii)signsorsymptomsofsignificant hemodynamiccompromisedespiteaggressive fluidand bloodproductresuscitation;iv)patientswithICHmusthave hadaGlasgowComaScore(GCS) ≥7andanestimated intracerebralhematomavolumeof60millilitersasassessed bycomputedtomography(CT)ormagneticresonance imaging.Duringthestudyperiod,prescriptionofandexanet alfawasrestrictedtoneurology,neurosurgery,hematology, emergencymedicine,andtraumasurgery.The4F-PCC prescriptionwasnotrestrictedbyspecialty,anddosewas weight-based.Thedecisiontotreatpatientsandtheselection ofthereversalagentwasatthediscretionofthe treatingphysician.
DataCollection
Structureddatacollectionwasperformedbyphysicians, pharmacistsortrainedresearchassistantsusingaHIPPAcompliantencrypteddatabase(REDCap,hostedat VanderbiltUniversity,Nashville,TN).Wedevelopeda libraryofthedefinitionsofdatacollected(Supplement1). Datacollectedincludeddemographic,clinical,laboratory, andimagingdataonpatientpresentationandthroughout theirentirehospitaladmissionandextendingto90daysafter discharge.Thepresenceofcomorbiditieswasdeterminedby chartreview.Amongthevariablescollectedwespecifically searchedallEHRsfortimeofbleedingonset,timefromlast doseoforalFXa-I,timefrompresentationtoimaging, clinicalriskscores(GCSforICHandalbuminlevel <3.0 gramsperdeciliter,internationalnormalizedratio[INR] >1.5,alteredmentalstatus,systolicbloodpressurelessthan 90millimetersofmercury,andage >65years[AIMS65] forGIB)21,22 andconcomitanttreatmentsincluding bloodproducts,reversalagents,andprocedures.(See Supplements2
4fordatacollectiontools.)Thrombotic eventswerecollectedduringindexhospitalizationandat30 and90daysafterdischarge.Wedefinedthromboticeventsas deepveinthrombosis(DVT),pulmonaryembolism(PE), ischemicstroke,myocardialinfarction,orotherarterialor venousthromboembolicevents.Doortoneedletimewas definedastimefromhospitalpresentationtoreceiptof reversalagent.OnsettoCTtimewascalculatedusingthe differencebetweeninitialCTandtimeofbleedingonset, wheretheybothexisted;onsettoCTtimefortheremainder ofcaseswasdeterminedbycombiningcategoricalonsetto presentationtime(<6,6–12,12–24,24–48,and >48hours),
usingthemediantimeforeachcategory,withdoortoCT time.Wedefinedallstudydataandvariablespriorto initiatingthestudyandtrainedourdataabstractorsusinga libraryofdefinitions(see Supplement1).Weperiodically monitoreddatacollectionandprovidedfeedbacktothedata abstractorsduringandafterdatacollectionandentry regardingmissing,conflicting,orobviouslyerroneousdata. Thenumberofdataabstractorsateachinstitutionvaried from1–3.Thedataabstracterswerenotblindedtotherapy.
Outcomes
Wedevelopedallstudyoutcomesapriori.Theprimary outcomeswerepresenceofestimatedtimesfromlastdoseof FXa-Iandtimefrombleedingonsettoadministrationof 4F-PCCorandexanetalfa.Secondaryoutcomeswere hemostaticefficacyasdefinedbytheANEXXA-4criteria,23 survivaltohospitaldischarge,thromboticeventsduringthe indexhospitalizationandat30and90days,andrebleeding eventssuchasICH,rectalbleeding,melena,orhematemesis.
DataAnalysis
Weuseddescriptivestatisticstosummarizethedata. Categoricaldataarepresentedasnumbersorpercentages andcomparedbetweengroupsusingchi-squareorFisher exacttestsasappropriate.Continuousvariablesare presentedwithmeansandstandarddeviationsormedians andinterquartileranges(IQR)basedontheirdistribution andcomparedwith t -testsortheMann-WhitneyUtests,as appropriate.Becausethiswasapilotstudy,noformalsample sizecalculationwasperformed.Wechosetoinclude25 patientsineachofthefourstudysubgroups:ICHtreated withandexanetalfa;ICHtreatedwith4F-PCC;GIBtreated withandexanetalfa,andGIBtreatedwith4F-PCC.An exploratoryPSMmodelwasconstructedtoestimatetheodds ofexcellent/goodhemostaticefficacyinpatientstreatedwith andexanetalfaor4F-PCCadjustingforage,gender, comorbidities,timefromlastdoseofFXa-I,time frombleedonsettotreatment,andindication foranticoagulation.
RESULTS
GeneralCharacteristicsandFeasibility
Intotal,thestudyenrolled100patientswhoweretreated witheitherandexanetalfaor4F-PCCforreversaloflifethreateningbleedsaftertakingapixabanorrivaroxaban (Table1).Asintentionallydesigned,halfofthepatientshad anICHandhalfhadaGIB.Withinthetwogroupsof patients,halfweretreatedwithandexanetalfawhilethe otherhalfweretreatedwith4F-PCC.Mean(SD)ageofall patientswas75(12)years,and34%werefemale.Most patientswereonapixaban(72%),andtherestwereon rivaroxaban.Commoncomorbiditiesincludedhypertension (78%)anddiabetes(25%).Antiplateletagentswereusedin abouthalfofthepatients,mostlyaspirin(40%)followedby
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 941 Singeretal. TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC
Table1. Comparisonofpatientswithintracerebralhemorrhageand gastrointestinalbleeding.Resultsarepresentedasnumbers(%) unlessotherwisespecified.
Number(%)unlessotherwise specified
Allcases (N = 100) ICH (n = 50) GIB (n = 50)
Mean(SD)age,years75(12)75(15)75(10)
Gender
Female34(34)15(30)19(38)
Male66(66)35(70)31(62)
Ethnicity
Non-Hispanic95(95)48(96)47(94)
Hispanic3(3)1(2)2(4)
Unknown2(2)1(2)1(2)
Race
White91(91)47(94)44(88)
Black2(2)1(2)1(2)
Asian2(2)02(4)
NativeHawaiian/Pacific Islander 1(1)01(2)
Unknown4(4)2(4)2(4)
Meanheight(SD),cm*170(13)173(10)167(15)
Meanweight(SD),kg84(24)84(20)85(27)
MeanBMI*30(15)28(6)31(21)
Codestatusat presentation
Fullcode62(62)31(62)31(62)
DNR/DNI10(10)5(10)5(10)
DNR2(2)2(4)0
Unspecified26(26)12(24)14(28)
Comorbidities
None3(3)03(6)
Hypertension78(78)44(88)34(68)
Diabetesmellitus25(25)11(22)14(28)
Liver4(4)2(4)2(4)
Chronickidneydisease13(13)2(4)11(22)
Alcoholabuse8(8)3(6)5(10)
Priorbleed16(16)3(6)13(26)
Priorstroke18(18)9(18)9(18)
FactorXainhibitor
Apixaban72(72)36(72)36(72)
Rivaroxaban28(28)14(28)14(28)
Bleedtype
Traumatic5(5)4(8)1(2)
Spontaneous94(94)46(92)48(96)
Unspecified1(1)01(2)
(Continuedonnextcolumn)
Table1. Continued. Number(%)unlessotherwise specified
Indicationsfor anticoagulation
Atrial fibrillation68(68)33(66)35(70)
Deepveinthrombosis28(28)15(30)13(26)
Pulmonaryembolism15(15)6(12)9(18)
ProphylaxisofVTE000
Other6(6)4(8)2(4)
Antiplateletagents
None52(52)24(48)28(56)
*9casesmissingheightandbodymassindex. ICH,intracerebral; GIB,gastrointestinalbleed; BMI,bodymass index; VTE,venousthromboembolism; DNR,donotresuscitate.
Allcases (N = 100) ICH (n = 50) GIB (n = 50)
Aspirin40(40)23(46)17(34) Clopidogrel9(9)4(8)5(10) Ticagrelor2(2)1(2)1(2) Treatments Andexanetalfa50(5)25(50)25(50) 4F-PCC50(50)25(50)25(50) Numberof4F-PCC doses 143(86)19(76)24(96) 27(14)6(24)1(4) VitaminK12(12)9(18)3(6) Freshfrozenplasma8(8)08(16) Packedredbloodcells38(38)038(76) Platelets22(22)11(22)11(22) FactorIX5(5)2(4)3(6) Desmopressin7(7)6(12)1(2) Cryoprecipitatepooled 5-packstatus 1(1)01(2) Intravenous fluids59(59)31(62)28(56) Other7(7)3(6)4(8) Outcomes Thromboticevents in-hospital 11(11)5(10)6(12) Hemostaticef
Excellent62(62)35(71)27(55) Good16(16)5(10)11(22) Poor20(20)9(18)11(22) Unknown2(2)1(2)1(2) Rebleedin-hospital7(7)1(2)6(12) Survival(todischarge)83(83)42(84)41(82)
ficacy
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 942 TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC Singeretal.
clopidogrel(9%)andticagrelor(2%).Overallhemostatic efficacywasexcellentin62%andgoodinanadditional16%. Mortalityathospitaldischargewas16%,andthe overallratesofthrombosisandrebleedingwere15% and7%,respectively.
WhiletheexacttimingoflastdoseofFXa-Iandbleed onsetwasrarelyavailable,estimatedrangesoftime(in6–12hourintervals)fromlastdoseandbleedonsetwereavailable intheEHRinmostcases.OfthosewithICH,96%ofpatients whoreceivedandexanetalfaand80%ofthosewhoreceived 4F-PCChaddocumentationofanestimatedtimefromlast FXa-I.InpatientswithGIB,thedocumentationoflast FXa-Iwaspresentin92%ofthosereceiving4F-PCCand in68%ofthosereceivingandexanetalfa.
IntracerebralHemorrhage
Acomparisonofbaselinecharacteristicsofpatientswith ICHbasedonreversalagentispresentedin Table2.Overall, thetwostudygroupswerefairlywellbalancedforthe variablesmeasured.Morepatientsinthe4F-PCCgrouphad apriorstrokeandintraventricularextension.Themost commonsitesofbleedingwerelobarandthedeepwhite matter.Median(IQR)initialGCSinpatientstreated withandexanetalfaand4F-PCCwere14(12–15)and 14(13
15),respectively.
Inbothgroups,overtwothirdsofpatientspresented withinsixhoursoftheonsetofbleeding.Theproportionof patientspresentingwithinsixandwithin12hoursoftheirlast doseoforalFxa-Iamongthosetreatedwithandexanetalfa were28%and52%,respectively,ascomparedwith4%and 44%amongthosetreatedwith4F-PCC(P = 0.06).Initial hematomavolumesinpatientstreatedwithandexanetalfa and4F-PCCwere15 +/ 23mland28+/ 37ml,respectively, P = 0.07.Timetoimagingandtimetoadministrationofthe reversalagentwererelativelyshortandcomparable.
Hemostaticefficacywasexcellentin80%ofthosetreated withandexanetalfaand60%amongpatientstreatedwith 4F-PCC.Survivaltohospitaldischargeamongthosetreated withandexanetalfaand4FPCCwere92%and76%, respectively(P = 0.25).Ofthe fivethromboticeventsthat occurredin-hospital,threewereinpatientstreatedwith andexanetalfa(oneischemicstroke,oneDVT,andonePE), andtwowereinpatientstreatedwith4F-PCC(twoDVTs).
Therateofadditionalthromboticeventsbeyondtheindex hospitalizationamongpatientstreatedwithandexanetalfa and4F-PCCwere0%and5%at30daysand0%and5% at90days,respectively.
GastrointestinalBleeding
Of50patientswithGIB,25(50%)hadanuppersourceof GIB,16(32%)hadalowersourceofGIBandinnine(18%) patients,thesourcewasunknown.Acomparisonofbaseline characteristicsofpatientswithGIBbasedontreatment strategyispresentedin Table3.Overall,thetwostudygroups
Table2. Andexanetalfavs4F-PCCinpatientswithintracerebral hemorrhage.Resultsarepresentedasnumbers(%)unless otherwisespecified.
–
Andexanet alfa (n = 25) 4F-PCC (n = 25) Pvalue Gender0.54 Female9(36)6(24) Male16(64)19(76) Mean(SD)age,years77(12)73(17)0.38 Ethnicity0.35 Non-Hispanic23(92)25(100) Hispanic1(4)0 Unknown1(4)0 Race0.22 White23(92)24(96) Black01(4) Asian00 NativeHawaiian/Pacific Islander 00 Unknown2(8)0 Comorbidities None00Hypertension23(92)21(84)0.67 Diabetesmellitus8(32)3(12)0.17 Liverdisease02(8)0.49 Chronickidneydisease1(4)1(4)1.00 Alcoholabuse1(4)2(8)1.00 Priorbleed03(12)0.24 Priorstroke1(4)8(32)0.02 Indicationsforanticoagulation Atrial fibrillation17(68)16(64)1.00 Deepveinthrombosis8(32)7(28)1.00 Pulmonaryembolism4(16)2(8)0.67 Other1(4)3(12)0.61 ICHlocation Deepwhitematter9(36)8(32)1.00 Lobar11(44)13(52)0.78 Brainstem2(8)00.49 Cerebellum3(12)3(12)1.00 Intraventricularextension1(4)7(28)0.049 Hematomavolume,mean (SD),ml 15(23)28(37)0.07 Estimatedtimefromlastdose ofapixaban/rivaroxabanto presentation 0.06 <6hrs.7(28)1(4) 7–12hrs.13(52)11(44) (Continuedonnextpage) Volume24,No.5:September2023WesternJournal of EmergencyMedicine 943 Singeretal. TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC
Diagnosticangiography1(4)0
Angiographicrepair01(4)
*EstimatedtimefrombleedonsettoCTimagingwascalculatedby addingthemedianoftheestimatedtimeintervalfrombleedonsetto presentationtothetimefromdoortoCTimaging.
ICH,intracerebral; IQR,interquartilerange; CT,computed tomography.
Table3. Andexanetalfav.4F-PCCinpatientswithgastrointestinal bleeding.Resultsarepresentedasnumbers(%)unlessotherwise specified.
Andexanet alfa(n = 25) 4F-PCC (n = 25) Pvalue
Gender1.00
Female9(36)10(40)
Male16(64)15(60)
Mean(SD)age,years72(11)78(9)0.049
Ethnicity0.22
Non-Hispanic23(92)24(96)
Hispanic2(8)0
Table2. Continued. Andexanet alfa (n = 25) 4F-PCC (n = 25) Pvalue 8–18hrs.4(16)5(20) 19–24hrs.01(4) >24hrs.02(8) Unknown1(4)5(20) Estimatedtimefrombleed onsettopresentation 0.26 <6hrs.18(72)17(68) 7–12hrs.1(4)4(16) 8–18hrs.2(12)0 19–24hrs.1(4)2(8) >24hrs.1(4)2(8) Unknown1(4)0 Median(IQR)GCS14(12–15)14(13–15)0.40 DoortoCTtime(median ([IQR]),hrs. 0.45 (0.22–1.22) 0.53 (0.26–1.16) 0.89 Estimatedtimefrom bleedonsettoCT*,(median [IQR]),hrs. 4.5 (3.2–6.9) 2.5 (1.1–7.2) 0.25 Doortoneedletime,median (IQR),hrs. 1.8 (1.4–3.0) 1.7 (1.5–2.6) 0.99 Outcomes Thromboticeventinpatient3(12)2(8)1.00 Hemostaticefficacy0.50 Excellent20(80)15(60) Good2(8)3(12) Poor3(12)6(24) Unknown01(4) Groupedhemostatic efficiency 0.29 Excellent/Good22(88)18(76) Fair/Poor3(12)6(24) Rebleed01(4)1.00 Survival(tohospital discharge) 23(92)19(76)0.25 Interventions Endotrachealintubation2(8)11(44)0.10
Craniotomy08(32)0.11 Externalventriculardrain03(12)0.24
Unknown01(4) Race0.39 White21(84)23(92) Black01(4) Asian2(8)0 NativeHawaiian/Pacific Islander 1(4)0 Unknown1(4)1(4) AIM65criteria Albumin < 3g/dL10(48)10(42)0.77 INR > 1.510(43)9(39)1.00 Alteredmentalstatus6(24)4(17)0.73 SBP < 90mmHg9(36)7(29)0.76 Age > 65years19(76)23(92)0.25 Median(IQR)AIMS65score2(1–2)2(2–2)0.90 Comorbidities None2(8)1(4)1.00 Hypertension16(64)18(72)0.76 Diabetesmellitus7(28)7(28)1.00 Liverdisease02(8)0.49 Chronickidneydisease6(24)5(20)1.00 Alcoholabuse2(8)3(12)1.00 Priorbleed5(20)8(32)0.52 Priorstroke4(16)5(20)1.00 Indicationsforanticoagulation Atrial fibrillation15(60)20(80)0.22 Deepveinthrombosis6(24)7(28)1.00 Pulmonaryembolism5(20)4(16)1.00 Other2(8)00.49 Estimatedtimefromlastdose ofapixaban/rivaroxabanto treatment <0.001 <6hrs.4(16)9(36) 7–12hrs.1(4)6(24) 8–18hrs.3(12)7(28) (Continuedonnextpage) WesternJournal of EmergencyMedicineVolume24,No.5:September2023 944 TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC Singeretal.
Excellent16(64)11(44)
Good4(16)7(28)
Poor5(20)6(24)
24hoursorunknownin16%and32%inpatientstreatedwith andexanetalfaand12%and8%inpatientstreatedwith 4F-PCC,respectively.ThetimeofthelastdoseofFxa-Iwas 12hoursorlessin20%and60%inpatientstreatedwith andexanetalfaand4F-PCC,respectively.Median[IQR] timesfromarrivaltoEDtoadministrationofthetreatment drugwerealsorelativelyshortandcomparableinpatients treatedwithandexanetalfaand4F-PCC(3.6[2.2–16.0]vs3.3 [1.3–7.0],respectively).
Hemostaticefficacywasexcellentin64%and44%ofthose treatedwithandexanetalfaand4F-PCC,respectively(P = 0.40).Survivaltohospitaldischargeamongthosetreated withandexanetalfaand4F-PCCwere76%and88%, respectively(P = 0.46).Therateofthromboticeventsamong patientstreatedwithandexanetalfaand4F-PCCwere8%in eachgroup.Ofthesixthromboticeventsthatoccurredinhospital,fourwereinpatientstreatedwithandexanetalfa (twoDVTs,andtwoother)andtwowereinpatientstreated with4F-PCC(twoischemicstrokes).
ThromboticEvents
Therewere15caseswithrecordedthromboticevents (Tables4 and 5).Ofthese,11caseshadin-hospital thromboticevents,threehadthromboticeventsat30days, andoneeventoccurredbetween30-90daysofindexbleed.Of allthromboticevents,sevenoccurredinpatientstreatedwith andexanetalfaandeightoccurredinpatientstreatedwith 4F-PCC.Ofthe15patientswhohadathromboticevent10 patientswererestartedonanticoagulationpriortothe
INR,Internationalnormalizedratio; SBP,systolicbloodpressure; IQR,interquartilerange; PRBC,packedredbloodcells.
werefairlywellbalancedforthevariablesthatwere measured.Median(IQR)initialAIMS65scoresinpatients treatedwithandexanetalfaand4F-PCCwere2(1–2)and 2(2–2),respectively.Mostpatientinbothgroupshad hypertensionordiabetes.
Thepercentagesofpatientspresentingwithin6or12 hoursofbleedingonsetamongthosetreatedwithandexanet alfawere40%and0%,whilethepercentagesofpatients presentingwithin6or12hoursofbleedingwere52%and8%, respectively,amongpatientstreatedwith4F-PCC.Thetime frombleedingonsettopresentationwasgreaterthan
Table3.
Andexanet alfa(n = 25) 4F-PCC (n = 25) Pvalue 19–24hrs.1(4)1(4) Unknown16(64)2(8) Estimatedtimefrombleed onsettopresentation 0.10 <6hrs.10(40)13(52) 7–
8
19–24hrs.3(12)2(8) >24hrs.4(16)3(12) Unknown6(32)2(8) Doortoneedletime,median (IQR) 3.6 (2.2–16.0) 3.3 (1.3–7.0) 0.22 Outcomes Thromboticevent in-hospital 4(16)2(8)0.67 Hemostaticeffi
Continued.
12hrs.02(8)
–18hrs.03(12)
cacy0.40
Rebleedin-hospital5(20)1(4)0.09 Survival(tohospital discharge) 19(76)22(88)0.46 Interventions Mean(SD)unitsPRBC over24hours 1.6(1.8)2.2(1.6)0.26 Endoscopy14(56)21(84)0.06 Interventionalradiology1(4)2(8)1.00 Surgery2(8)1(4)1.00
Unknown01(4) Groupedhemostaticefficiency0.74 Excellent/Good20(80)18(76) Fair/Poor5(20)6(24)
Andexanetalfa (n = 50) 4F-PCC (n = 50) P-value Hemostaticefficacy0.26 Excellent36(72)26(52) Good6(12)10(20) Poor8(16)12(24) Groupedhemostatic efficiency 0.32 Excellent/good42(84)36(72) Fair/poor8(16)12(24) Rebleedingeventsin hospital 5(10)2(4)0.26 Survivaltohospital discharge 42(84)41(82)1.00 In-hospitalthrombotic events 7(14)4(8)0.53 Totalthromboticevents throughday90 7(14)8(16)0.80 Volume24,No.5:September2023WesternJournal of EmergencyMedicine 945 Singeretal. TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC
Table4. Outcomesbytreatmentwhenbleedingtypesarecombined. Numbers(percent).
4F-PCCICH2(2DVT)1(DVT)1(DVT)
GIB2(2strokes)2(2DVT)
*Acuteleftlowerextremityarterialthrombosiswithischemia(n = 1); bowelinfarctionandsplenicinfarcts(n = 1).
ICH,intracerebralhemorrhage; DVT,deepveinthrombosis; PE, pulmonaryembolism; GIB,gastrointestinalbleeding.
thromboticevent.Abreakdownofthromboticeventsbysite ofbleedingandtherapyispresentedin Table5.
PropensityScoreMatchedModel
Outcomesinpatientstreatedwithandexanetalfaand4FPCCwhenallstudypatientswerecomparedregardlessofsite ofbleedingaresummarizedin Table4.Therewereno statisticallysignificantdifferencesinanyofthestudy outcomesbetweenthetwotreatmentgroups.Usingallcases combined(98,excludestwomissinghemostaticefficacy)and fortheendpointofhemostaticefficacy,categorizedinto excellent/goodandpoor,apropensityscorewasdetermined usingage,gender,comorbidities,timefromlastdose,time frombleedingonset,andindicationforanticoagulation. Inclusionofthepropensityscoreandtreatmentinalogistic regressionmodelresultedinanoddsratio(OR)infavorof andexanetalfaof2.01(95%confidenceintervalCI, 0.67
6.06)fortheendpointofexcellent/good hemostaticefficacy.
AdditionalExploratoryAnalysesforHemostaticEfficacy
Forthe49ICHcases(onewithmissingdataexcluded)and fortheoutcomeofhemostaticefficacy,categorizedinto excellent/goodandpoor,apropensityscorewasdetermined usingage,hematomavolumecategorizedinto <30vs ≥30 milliliters,GCSscorecategorizedinto <13vs ≥13,timefrom lastdoseofFXa-I,andonsettoCTtime.Twocaseswere excluded(both4F-PCC)becauseonedidnothaveaninitial CTtimeandonehadinitialCTtimepriortohospital presentation.Inclusionofthepropensityscoreandtreatment inalogisticregressionmodelresultedinanORofandexanet alfato4F-PCCof3.30(95%CI0.59–18.52)inpredicting excellent/goodhemostaticefficacy.
For49GIBcases(onewithmissingdataexcluded)and fortheoutcomeofhemostaticefficacy,categorizedinto excellent/goodandpoor,apropensityscorewasdetermined usingage,timefromlastFXa-Idose,timeofbleedonset,
andAIMS65categorizedinto <2vs ≥2.Inclusionofthe propensityscoreandtreatmentinalogisticregressionmodel resultedinanORofandexanetalfato4F-PCCof 1.67(95%CI0.29–9.71)inpredictingexcellent/good hemostaticefficacy.
DISCUSSION
Ourmulticenterstudydemonstratesthatacomparative studyofpatientswithICHandGIBtreatedwithandexanet alfaor4F-PCCcanbeadequatelyconductedbycollecting andanalyzingdataroutinelyavailableintheEHR retrospectively.Wewereabletoacquireinformationon manyimportantfactorsaffectingoutcomes,including severalthathadbeenconsistentlymissingfromprevious studies.18 Forexample,documentationofestimatedranges oftimefromlastFXa-Idoeswerepresentin80
96%of patientswithICHandin68%–92%ofpatientswithGIB. Theseresultssuggestthatareliablestudyevaluatingreal-life practiceinpatientsundergoingFXa-Ireversalwith andexanetalfaor4F-PCCafterICHorGIBshouldbe feasibleinamuchlargercohortofpatientsincenterslike thoseincludedinthestudy.
CurrentliteratureonreversalstrategiesforFXa-Ihas majorlimitations.Therehavebeenonlynon-randomized cohortstudiesevaluatingandexanetalfaand4F-PCC.24–26 Mostofthesestudieshavebeensingle-arm,single-center, orboth.6,7,11,12,16,27–35
Someusehistoricalratherthan contemporarycontrols,oratbestindirectlycomparedtwo independentdatasetstryingtoaccountformajorbaseline differencesbyusingasuboptimalPSM.13 Otherstudiesused propensityscoretreatmentweightingratherthanPSMand wereabletoaccountforbleedsize/volume,whichwasnot capturedintheORANGEindirectcomparison.36,37 None hasincludedallpertinentvariablestosufficientlyreducethe riskofconfoundingbias.18
EvenANNEXA-4,10,23 a prospectivestudythatservedtosupporttheFDAapproval ofandexanetalfaforreversalofanticoagulationwithFXa-I inpatientswithlife-threateningbleeding,hadasinglearm andfailedtocontrolforcrucialfactors,suchastimefrom ICHonsetto firstheadCT akeyvariablebecausetherisk ofhematomaexpansionismuchgreaterinpatients presentingearlyafterICHonset.38 Otherpertinentvariables oftenmissedinmostpreviousstudiesincludetimebetween ICHonsetandhospitalpresentation,timebetweenlastdose ofFXa-Iandhospitalpresentation,precisehematoma volumeandlocation,measuresofseverityofGIB, concomitantadministrationofantiplateletagents,detailed accountingofcomorbidities,restrictionsinthelevelof medicalcare,andfunctionaloutcomes.18 Up-to-dateassays tomeasurelevelofanticoagulationinpatientstreatedwith FXa-Iarenotcommerciallyavailable.Intheabsenceof informationontheintensityofanticoagulation,time variables(eg,timefromlastdoseofanticoagulant)become keysurrogatesinacontrolledanalysisofhemostaticefficacy.
–
–
Bleed site In-hospital event30days90days Andexanet alfa ICH3(1DVT, 1stroke,1PE) 00 GIB4(2DVT, 2other*) 00
Table5. Summaryofthromboticevents.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 946 TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC Singeretal.
OneofthemajoradvantagesofRCTsisthattheactof randomizationreducesthechanceofbetween-groupbiasdue toimbalancesinmeasuredandunmeasuredconfounding variables.Thus,anyclaimsregardingtherelativeefficacy andsafetyofandexanetalfavs4F-PCCinpatientswith FXa-Ibleedswillonlyberesolvedwiththecompletionofa RCTcomparingthesetreatmentsheadtohead.Thatsaid,in themeantimereal-worlddatacanbeusefulifthe studiesadjustasmuchaspossibleforpotential confoundingvariables.
Ourfour-centerstudywasdesignedtodeterminethe feasibilityofcollectingallrelevantinformationfromthe EHRofmultiplecenters.Duetothesmallsamplesize, adjustmentofcovariatesinamultivariateanalysiswas limited,andnodefinitiveconclusionscanbemaderegarding therelativeefficacyandsafetyofandexanetalfaand 4F-PCC.OurexploratoryanalysisincludingPSMmodels suggestedbetterhemostaticefficacywithandexanetalfafor bothindications,ICHandGIB.However,theseresultswere veryimprecise(asindicatedbythewide95%CIs)andshould thereforebeinterpretedwithgreatcaution.
Thestrengthofourstudyresidesinthegranularityofthe datacollection.AmongpatientswithICH,wewereableto obtaininformationontimebetweenlastdoseofFXa-Iand symptomonsetandtheintervalsbetweensymptomonsetand hospitalpresentationand firstheadCT.Whileexacttimes werenotconsistentlydocumented(infact,thisinformationis oftennotknownwithprecisionindailypractice),estimated timerangeswereavailableinnearlyallpatients.Clinical severityassessedbytheGCSscoreandtheuseof concomitantantiplateletagentswereroutinelyavailable. Intracerebralhematomavolumeswerealsoavailablesince allpatientswithICHhadinitialheadCTsaswellasrepeat CTswithin6
24hours,allowingprecisecalculationof hematomavolumeandhematomaexpansion.Forpatients withGIB,wewereabletoadjustforillnessseverityusingthe AIMS65riskassessmentscore.Thehemostaticefficacyin patientswithGIBistypicallydeterminedbytheneedfor bloodtransfusionsandtheireffectonhemoglobinand hematocritoverthecourseofthe first12hours.However, bleedingcessationoftenrequiresadvancedinterventions, suchasendoscopichemostasisorembolizationby interventionalradiology.Dataontheseadvanced interventionsarealsoimportanttoreport;however,many priorstudiesdidnotreportontheseinterventions.
Ofnote,themortalityinthesubgroupofpatientswith GIBinthisstudywasconsiderablyhigherthanpreviously reported,39 suggestingthatpatientswithGIBwhiletaking FXa-Iareaparticularlyhigh-riskgroupandrequire immediateandaggressivetherapy.Existingriskprediction scores,suchastheAIMS65,40 donotaccountforongoing useofFXa-I,yetthisfactormustbeconsideredinthe managementpatientswithGIB.DuetothelackofRCTsand thesmallnumberofreportedstudiesevaluatinguseof
andexanetalfaforacuteGIBtheAmericanCollege ofGastroenterologyandtheCanadianAssociationof Gastroenterologyrecommendagainsttheuseofandexanet alfaforreversinglife-threateninggastrointestinalbleeds.35 Moredataisneededtoidentifytheidealpatientandreversal agentforFXa-I-associatedGIB.
LIMITATIONS
Thisstudyhasvariouslimitationsinadditiontothesmall sizeofthefourgroupsexamined.Selectionbiasmayhave affectedour findings,andthedirectionofthisbiasisdifficult toinferfromourdata.Ininstitutionswherebothandexanet alfaand4-PCCareavailable,thetreatedgroupsbecome selectivelydifferentandsoistheirprognosis.Forexample, becauseofstrictercriteriafortheuseofandexanetalfathe useof4-PCCmayberelegatedtopatientswithworsebleeds andlessfavorablechancesofrecovery.Ontheotherhand, andexanetalfacouldhavebeenpreferentiallyusedin patientsdeemedtobeathigherriskofhematoma expansion.Thus,confoundingbyindicationcannotbe excluded.Studyingamuchlargercohortwithadequate adjustmentforcovariatesmightbeabletoaccountfor theseissues.
Also,functionaloutcomesafterdischargewereavailable inonlysomeoftheparticipatingcenters.Informationon thromboticeventswasconsistentlyavailableinthehospital butnotafterdischarge.Oneoftheparticipatingcentersdid nothaveavailabilityofandexanetalfaandconsequentlythe otherthreecentershadtocontributemorecasestreatedwith thisagent.Thismayhaveintroducedadditionalbiastoour study.Identificationofthromboticeventsanddeathsthat occurredafterhospitaldischargemayhavebeen underestimatedsincesomepatientsmayhavefollowedupat hospitalsitesotherthantheindexhospital.
Duetothenatureofthestudybeingafeasibilitypilot,data abstractionwasperformedbyinvestigatorswhowerenot blindedtotherapy.Thismayhaveintroducedobserverbias thatmayhaveaffectedtheexploratoryresults.Whileoverall documentationofimportantconfoundingvariablesatthe fourstudysiteswasgoodtoexcellent,itispossiblethatother sitesmayhavehadless(ormore)documentationofthese variables.InthisstudywechosetheAIMS65scoretocontrol forgastrointestinalbleedingseverity.Weacknowledgethat theAIMS65hasnotbeenvalidatedinlowerGIBandmay notbethebestindexofseverityeveninupperGIB.In addition,sincethemedianAIMS65scorewasrelativelylow inbothstudygroups,ourresultsmaynotbegeneralizableto moreseveregastrointestinalbleeds.
Anotherlimitationofourstudyisthatitincludedmostly Whitepatientsandmaynotbeasrepresentativeofother racialminoritygroups.Whilenoneofthepatientsreceived morethanonedoseofandexanetalfa,someofthepatients receivedaseconddoseof4F-PCC.However,itisunclear whyaseconddosewasgiven.Finally,wehaveno
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 947 Singeretal. TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC
informationregardingcompliancewithFXa-Iafter dischargefromthehospital,whichmaycontributetoahigh rateofthromboticevents.
CONCLUSION
Thisfeasibilitystudyindicatesthatcarefulcollectionof informationroutinelyavailableintheelectronichealth recordsofacademicandcommunityhospitalspermitsthe developmentofadjustmentmodelsincorporatingmostofthe factorsthatcaninfluencetheprognosisofpatientswith intracranialhemorrhageandgastrointestinalbleedsand confoundtheinterpretationofthetherapeuticeffectsof anticoagulationreversalwithandexanetalfaorreplacement with4F-PCC.Untilmoredefinitivedatafromrandomized controlledtrialsbecomesavailable,amuchlargerstudywith moreparticipatingcentersmayproducecomparativereallifeexperiencethatcanhelpdeterminewhetherthetreatment selectedforreversalofFXa-I(ie,andexanetalfavs4F-PCC) hasanimpactonpatient-centeredoutcomesindailypractice. Furthermore,ourdatahasadditionalbenefitsinceitreflects clinicalpracticewherepatientsarenotnecessarilytreatedas inwellcontrolledtrials.
AddressforCorrespondence:AdamJ.Singer,MD,StonyBrook University,RenaissanceSchoolofMedicine,Departmentof EmergencyMedicine,HSC-L4-050,101NicollsRoadStonyBrook, NewYork11794.Email:adam.singer@stonybrook.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.AdamJ.SingerandJamesWilliams haveservedonanadvisoryboardforAlexionandAstraZenecaand areonthespeaker’sbureauofAlexionandAstraZeneca.Research fundinghasbeengivenbyAlexiontotheinstitutionsof AdamJ.Singer,MauricioConcha,JamesWilliams,and AlejandroA.Rabinstein.
Copyright:©2023Singeretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.BarnesGD,LucasE,AlexanderGC,etal.Nationaltrendsinambulatory oralanticoagulantuse. AmJMed.2015;128:1300–5e1302.
2.LutseyPL,WalkerRF,MacLehoseRF,etal.Directoralanticoagulants andwarfarinforvenousthromboembolismtreatment:trendsfrom2012 to2017. ResPractThrombHaemost.2019;3:668–73.
3.ZiakasPD,KourbetiIS,PoulouLS,etal.MedicarepartDprescribingfor directoralanticoagulantsintheUnitedStates:cost,useandthe “rubber effect.” PLoSONE.2018;13:e0198674.
4.YaoX,AbrahamNS,SangaralinghamLR,etal.Effectiveness andsafetyofdabigatran,rivaroxaban,andapixabanversus
warfarininnonvalvularatrial fibrillation. JAmHeartAssoc 2016;5.
5.GellerAI,ShehabN,LovegroveMC,etal.Emergencyvisitsfororal anticoagulantbleeding. JGenInternMed.2020;35:371–3.
6.MajeedA,AgrenA,HolmstromM,etal.Managementofrivaroxaban-or apixaban-associatedmajorbleedingwithprothrombincomplex concentrates:acohortstudy. Blood.2017;130:1706–12.
7.SchulmanS,GrossPL,RitchieB,etal.Prothrombincomplex concentrateformajorbleedingonfactorXainhibitors:aprospective cohortstudy. ThrombHaemost.2018;118:842–51.
8.LuG,LinJ,BuiK,etal.Andexanetversusprothrombincomplex concentrates:differencesinreversaloffactorXainhibitorsininvitro thrombingeneration. ResPractThrombHaemost.2020;4:1282–94.
9.YehCH,FredenburghJC,WeitzJI.Therealdecoy:anantidoteforfactor Xa-directedanticoagulants. CircRes.2013;113:954–7.
10.ConnollySJ,CrowtherM,EikelboomJW,etal.Fullstudyreportof andexanetalfaforbleedingassociatedwithfactorXainhibitors. NEnglJ Med.2019;380:1326–35.
11.AmmarAA,AmmarMA,OwusuKA,etal.Andexanetalfaversus4-factor prothrombincomplexconcentrateforreversaloffactorXainhibitorsin intracranialhemorrhage. NeurocritCare.2021;35:255–61.
12.BarraME,DasAS,HayesBD,etal.Evaluationofandexanetalfaand four-factorprothrombincomplexconcentrate(4F-PCC)forreversalof rivaroxaban-andapixaban-associatedintracranialhemorrhages. JThrombHaemost.2020;18:1637–47.
13.CohenAT,LewisM,ConnorA,etal.Thirty-daymortalitywithandexanet alfacomparedwithprothrombincomplexconcentratetherapyforlifethreateningdirectoralanticoagulant-relatedbleeding. JAmCollEmerg PhysiciansOpen.2022;3:e12655.
14.ColemanCI,DobeshPP,DaneseS,etal.Real-worldmanagementof oralfactorXainhibitor-relatedbleedswithreversalorreplacement agentsincludingandexanetalfaandfour-factorprothrombincomplex concentrate:amulticenterstudy. FutureCardiol.2021;17:127–35.
15.GreenL,TanJ,MorrisJK,etal.Athree-yearprospectivestudyofthe presentationandclinicaloutcomesofmajorbleedingepisodes associatedwithoralanticoagulantuseintheUK(ORANGEstudy). Haematologica.2018;103:738–45.
16.PhamH,MedfordWG,HorstS,etal.Andexanetalfaversusfour-factor prothrombincomplexconcentrateforthereversalofapixaban-or rivaroxaban-associatedintracranialhemorrhages. AmJEmergMed. 2022;55:38–44.
17.TroyerC,NguyenW,XieA,etal.Retrospectivereviewofandexanet alfaversus4-factorprothrombincomplexconcentrateforreversalof DOAC-associatedintracranialhemorrhage. JThrombThrombolysis. 2023;55(1):149–55.
18.ConchaM,CohenAT.Recommendationsforresearchassessing outcomesforpatientswithanticoagulant-relatedintracerebralbleeds. Stroke.2021;52:1520–6.
19.KajiAH,SchrigerD,GreenS.Lookingthroughtheretrospectoscope: reducingbiasinemergencymedicinechartreviewstudies. AnnEmerg Med.2014;64:292–8.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 948 TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC Singeretal.
20.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. AnnInternMed 2007;147:573–7.
21.SaltzmanJR,TabakYP,HyettBH,etal.Asimpleriskscoreaccurately predictsin-hospitalmortality,lengthofstay,andcostinacuteupperGI bleeding. GastrointestEndosc.2011;74:1215–24.
22.ThandasseryRB,SharmaM,JohnAK,etal.Clinicalapplicationof AIMS65scorestopredictoutcomesinpatientswithupper gastrointestinalhemorrhage. ClinEndosc.2015;48:380–4.
23.ConnollySJ,MillingTJJr,EikelboomJW,etal.Andexanetalfaforacute majorbleedingassociatedwithfactorXaInhibitors. NEnglJMed 2016;375:1131–41.
24.NederpeltCJ,NaarL,KrijnenP,etal.Andexanetalfaorprothrombin complexconcentrateforfactorXainhibitorreversalinacutemajor bleeding:asystematicreviewandmeta-analysis. CritCareMed 2021;49:e1025–36.
25.ShresthaDB,BudhathokiP,AdhikariA,etal.Efficacyandsafetyof andexanetalfaforbleedingcausedbyfactorXaInhibitors:ASystematic ReviewandMeta-Analysis. Cureus.2021;13:e20632.
26.Gomez-OutesA,AlcubillaP,Calvo-RojasG,etal.Meta-analysisof reversalagentsforseverebleedingassociatedwithdirectoral anticoagulants. JAmCollCardiol.2021;77:2987–3001.
27.BrownCS,ScottRA,SridharanM,etal.Real-worldutilizationof andexanetalfa. AmJEmergMed.2020;38:810–4.
28.CastilloR,ChanA,AtallahS,etal.Treatmentofadultswithintracranial hemorrhageonapixabanorrivaroxabanwithprothrombincomplex concentrateproducts. JThrombThrombolysis.2021;51:151–8.
29.GiovinoA,ShomoE,BuseyKV,etal.An18-monthsingle-center observationalstudyofreal-worlduseofandexanetalfainpatientswith factorXainhibitorassociatedintracranialhemorrhage. ClinNeurol Neurosurg.2020;195:106070.
30.RauchS,MullerHP,DreyhauptJ,etal.Andexanetalfaforreversalof factorXainhibitorsinintracranialhemorrhage:ObservationalCohort Study. JClinMed.2022;11.
31.VestalML,HodulikK,Mando-VandrickJ,etal.Andexanetalfaandfourfactorprothrombincomplexconcentrateforreversalofapixabanand
rivaroxabaninpatientsdiagnosedwithintracranialhemorrhage. JThrombThrombolysis.2022;53:167–75.
32.ParselsKA,SeaburyRW,ZyckS,etal.Andexanetalfaeffectiveness andsafetyversusfour-factorprothrombincomplexconcentrate (4F-PCC)inintracranialhemorrhagewhileonapixabanorrivaroxaban: Asingle-center,retrospective,matchedcohortanalysis. AmJEmerg Med.2022;55:16–9.
33.PanosNG,CookAM,JohnS,etal,NeurocriticalCareSociety PharmacyStudyG.FactorXainhibitor-relatedintracranialhemorrhage: resultsfromamulticenter,observationalcohortreceivingprothrombin complexconcentrates. Circulation.2020;141:1681–9.
34.BradshawPG,KeeganS,FoertschM,etal.Andexanetalfaafter 4-factorPCCadministrationforintracranialhemorrhage:acaseseries. JThrombThrombolysis.2022;54:295–300.
35.AbrahamNS,BarkunAN,SauerBG,etal.AmericanCollegeof Gastroenterology-CanadianAssociationofGastroenterologyClinical PracticeGuideline:ManagementofAnticoagulantsandAntiplatelets DuringAcuteGastrointestinalBleedingandthePeriendoscopicPeriod. AmJGastroenterol.2022;117:542–58.
36.CostaOS,ConnollySJ,SharmaM,etal.Andexanetalfaversus four-factorprothrombincomplexconcentrateforthereversalof apixaban-orrivaroxaban-associatedintracranialhemorrhage: apropensityscore-overlapweightedanalysis. CritCare 2022;26:180.
37.HuttnerHB,GernerST,KuramatsuJB,etal.Hematomaexpansion andclinicaloutcomesinpatientswithfactor-Xainhibitor-related atraumaticintracerebralhemorrhagetreatedwithintheANNEXA-4trial versusreal-worldusualcare. Stroke.2022;53:532
43.
38.BrouwersHB,GreenbergSM.Hematomaexpansionfollowingacute intracerebralhemorrhage. CerebrovascDis.2013;35:195–201.
39.StanleyAJ,LaineL.Managementofacuteuppergastrointestinal bleeding. BMJ.2019;364:l536.
40.KimMS,ChoiJ,ShinWC.AIMS65scoringsystemiscomparableto Glasgow-BlatchfordscoreorRockallscoreforpredictionofclinical outcomesfornon-varicealuppergastrointestinalbleeding. BMC Gastroenterol.2019;19:136.
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 949 Singeretal. TreatmentofFXa-IBleedingwithAndexanet α or4F-PCC
uenceofBodyMassIndexontheEvaluationandManagement ofPediatricAbdominalPainintheEmergencyDepartment
CarlyA.Theiler,MD*
MorganBobbSwanson* RyanSquires,MD†
KarisaK.Harland,MPH,PhD*
SectionEditor: WestJEMPublishingOffice
*UniversityofIowa,DepartmentofEmergencyMedicine,IowaCity,Iowa † IndianaUniversity,DepartmentofEmergencyMedicine,Bloomington,Indiana
Submissionhistory:SubmittedOctober28,2022;RevisionreceivedMarch14,2023;AcceptedApril28,2023
ElectronicallypublishedAugust8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59287
Introduction: ChildhoodobesityisaseriousconcernintheUnitedStates,withoveronethirdofthe pediatricpopulationclassifiedasobese.Abdominalpainisoneofthemostcommonchiefcomplaints amongpediatricemergencydepartment(ED)visits.Wehypothesizedthatoverweightandobese childrenbeingevaluatedintheEDforabdominalpainwouldhavehigherresourceutilizationthantheir normalandunderweightpeers.
Methods: Thiswasaretrospectivereviewofpediatricpatients <18yearswhopresentedwithabdominal paintotheEDofatertiarycarecenterfromJanuary1,2014–September3,2020.Patientswereexcluded iftheydidnothavebothaheightandweightrecorded.Wecategorizedpatientsasunderweight(body massindex[BMI] <5th percentile);normalweight(BMI5th to <85th percentile),overweight(BMI85th to <95th percentile);orobese(BMI ≥95th percentile).Descriptivestatisticswereusedtoexaminethestudy population.Weusedchi-squareteststoexaminethedifferencesinpatientcharacteristicsbetween normal/underweightpatientsandoverweight/obesepatients.TheKruskal-Wallistestwascompletedfor examiningdifferencesinthemedians.Weusedmultivariablelogisticregressiontoexaminevisit characteristicsassociatedwithoverweight/obesepatients,includingEDinterventions,testing,and lengthofstay(LOS).
Results: Ofthe184subjectsincludedintheanalysis,nine(4.9%)wereunderweight,108(58.7%)were normalweight,21(11.4%)wereoverweight,and46(25.0%)wereobese.PatientswithaBMIof ≥85th percentilewereolder(median15vs13years, P = 0.01).Theywereotherwisesimilarindemographics. Therewasnosignificantdifferencebetweennormal/underweightandoverweight/obesesubjectsin disposition(37%vs43%discharge, P = 0.38),72-hourreturn(7%vs6%, P = 0.82),EDLOS(median 4.42vs3.95hours, P = 0.195),orinpatientLOS(median42.0vs34.2hours, P = 0.06).Therewereno statisticallysignificantdifferencesintotalnumberofEDtestsorinterventionsreceivedbyoverweight/ obesepatientscomparedtonormal/underweightpatients,andeachsubjectreceivedamedianofsix tests(interquartilerange[IQR]4–7)andtwointerventions(IQR1–3).
Conclusion: AmongpediatricpatientspresentingtotheEDwithabdominalpain,wefoundthatpatient characteristicsandEDresourceutilization(includingtesting,intervention,disposition,andLOS)didnot differsignificantlyacrossBMIcategories.[WestJEmergMed.2023;24(5)950–955.]
INTRODUCTION
ChildhoodobesityisaseriousconcernintheUnited States,withoveronethirdofthepediatricpopulation
classifiedasoverweight/obese.1,2 Abodymassindex (BMI)elevatedabovenormalhasbeenassociatedwith numerousillnessesinchildhoodandhigherhealthcare
Infl
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 950 BRIEF RESEARCH REPORT
utilization/expenditures,includingincreasedoutpatient visits,prescriptiondruguse,andemergencydepartment (ED)visits,aswellasahigherlikelihoodofhospital admission.3,4 Inaddition,overweightandobesechildren aremorelikelythantheirnormal-weightpeerstoreceive theirroutinemedicalcareinanEDratherthanaprimary caresetting.5
Abdominalpainisacommonchiefcomplaintamong pediatricEDvisits.6 PatientswithanelevatedBMIhavebeen foundtohavehigherratesoffunctionalgastrointestinal(GI) disordersincludingconstipation,gastroesophagealreflux disease,irritablebowelsyndrome,encopresis,andfunctional pain.7,8 Obesepediatricpatientsalsohavehigherratesof persistentpainwithfunctionalGIdisorders,andhigherrates ofoverallpainreportingintheoutpatientsetting.9,10 Obesity mayalsolimittheaccuracyofaphysicalexamandisa comorbiditythatmaycontributetomissedordelayed diagnosis.11,12 Inaddition,inchildrenwhopresenttothe EDwithappendicitis,thereisincreasedlikelihoodof non-diagnosticultrasoundandneedforfurtherimaging inobesechildren.13,14
Wehypothesizedthatoverweightandobesechildren beingevaluatedintheEDforabdominalpainwouldhave higherresourceutilizationthantheirnormaland underweightpeers.Todate,nostudytoourknowledge hasexaminedthesefactorsinthepediatricabdominal painpopulation.
METHODS
Thiswasaretrospectivereviewofpediatricpatientsseen intheEDatamidwesternacademiccenterwitha freestandingtertiarychildren’shospital,withanannual pediatricEDcensusofapproximately15,000patients.This wasaninstitutionalreviewboard-approvedstudy.We abstracteddatafromtheelectronichealthrecord(EHR)for EDvisitsbetweenSeptember1,2014–September3,2020. Patientswereincludedwhowere <18yearsofageand presentedtotheEDwithachiefcomplaintofabdominal pain.Becausebothheightandweightarerequiredto calculateBMI,weexcludedpatientsiftheydidnothavea recentheightrecordedintheEHR.Oncepatientswere identifiedusingthissimplecriterion,asinglephysician completedtemplatedchartabstractionandrecorded objectivedemographicandvisit-leveldatadirectlyintoa secureRedCapdatabasehostedatUniversityofIowa.1,2 REDCap(ResearchElectronicDataCapture)isasecure, web-basedsoftwareplatformdesignedtosupportdata captureforresearchstudies.Asecondblindedabstractor randomlyreviewed10%ofchartstoensureinterrater reliability;therewerenodiscrepancies.
PediatricBMIcutoffsaredefinedusingaBMI-for-age percentile;therefore,wecalculatedBMIasapercentileusing theUSCentersforDiseaseControlandPreventionagebasedcalculator.15 Patientswerecategorizedasunderweight
(BMI <5th percentile);normalweight(BMI5th to <85th percentile);overweight(BMI85th to <95th percentile),or obese(BMI ≥95th percentile).WedefinedEDinterventions aspediatricgastroenterologyconsult,pediatricsurgery consult,oradministrationofantiemetic,intravenous fluids, orpainmedications,andwedefinedEDtestingasbloodwork (basicmetabolicpanel,liverfunctiontest,lipase,complete bloodcount,C-reactiveprotein,erythrocytesedimentation rate),entericpanel,urinalysisorurineculture,abdominal radiograph,abdominalultrasound,orotheradvanced imaging(computedtomographyabdomenormagnetic resonanceimagingabdomen).
Descriptivestatisticswereusedtoexaminethestudy population,andweusedchi-squareteststoexaminethe differencesinpatientcharacteristicsbetweennormal/ underweightpatients(BMI <85th percentile)andoverweight/ obesepatients(BMI ≥85th percentile),with P < 0.05 consideredstatisticallysignificant.TheKruskal-Wallistest wascompletedforexaminingdifferencesinthemedians.We usedmultivariablelogisticregressiontoexaminevisit characteristicsassociatedwithoverweight/obesepatients, controllingforage.Allstatisticalanalyseswereperformed usingStatisticalAnalysisSoftwareversion9.3(SASInstitute Inc,Cary,NC).
RESULTS
Weincludedatotalof184patientencountersinthe analysis.Ofthe184subjects,nine(4.9%)wereunderweight (BMI <5th percentile),108(58.7%)werenormalweight(BMI 5th to <85th percentile);21(11.4%)wereoverweight(BMI 85th to <95th percentile);and46(25.0%)wereobese(BMI ≥95th percentile).Demographiccharacteristicsofthestudy populationareshownin Table1.PatientswithaBMIof ≥85th percentilewereolder(median15yearsvs13years, P = 0.01)butwereotherwisesimilarindemographics includinggender,race,andtriagelevel.
Table2 showsvisitcharacteristicsincludingED interventionsandtesting,withadjustedoddsoftheseafter controllingforage.Overall,112patients(61%)were admittedtoinpatientfromtheED,and12patients(7%) returnedtotheEDwithin72hours.Therewasnosignificant differencebetweennormal/underweightandoverweight/ obesesubjectsindisposition(37vs43%dischargefromthe ED, P = 0.38)or72-hourreturnrates(7vs6%, P = 0.82). TheoverallmedianEDLOSwas4.09hours(IQR 3.08–5.53),withnosignificantdifferencebetweennormal/ underweightandoverweight/obesesubjects(median4.42vs 3.95hrs, P = 0.20).Amongthe112patientswhowere admitted,themedianinpatientLOSwas37.7hrs(20.9
76.7 hrs),withnosignificantdifferencebetweennormal/ underweightandoverweight/obesesubjects(median42.0vs 34.2hrs, P = 0.06).
Therewasnostatisticallysignificantdifferenceintotal numbersofEDtestsorinterventionsreceivedbyoverweight/
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 951 Theileretal. InfluenceofBMIonPediatricAbdominalPain
obesepatientscomparedtonormal/underweightpatients. EachsubjectreceivedamedianofsixEDtests(IQR4–7)and twoEDinterventions(IQR1–3).Therewasnodifferencein thenumberofEDinterventions(P = 0.20)orEDtests (P = 0.618)byBMIgroup.Onbivariateanalysis, overweight/obesesubjectswerelesslikelythannormal/ underweightsubjectstohaveanabdominalradiograph (22vs38%, P = 0.03)andlesslikelytohaveapediatric surgeryconsult(33vs49%, P = 0.04);however,after controllingforage,this findingwasnotfoundtobe statisticallysignificantforeitherabdominalradiograph (aOR0.51,95%confidenceinterval[CI]0.26–1.03)or pediatricsurgeryconsult(aOR0.58,95%CI0.31–1.11). Therewerenosignificantdifferencesintherateofother individualtestsorinterventionsbetweenthetwogroups.
DISCUSSION
OurresultsdidnotshowasignificantdifferenceinED resourceuse(testingorintervention)orLOSforoverweight/ obesepediatricpatientspresentingtotheEDwithabdominal paincomparedtonormal/underweightpatients.We analyzed184pediatricpatientspresentingtotheEDwitha chiefcomplaintofabdominalpain.Ofthese,4.9%were underweight,58.7%normalweight,11.4%overweight,and 25.0%wereobese.PatientswithaBMIof ≥85th percentile wereolder(median15yearsvs13years, P = 0.01)but otherwisesimilarindemographics.
Therewasnosignificantdifferencebetweennormal/ underweightandoverweight/obesesubjectsindisposition (37vs43%dischargefromtheED, P = 0.38); 72-hourreturn(7vs6%, P = 0.82),EDLOS(median
VariableLevelN Overall N = 184 BMI <85% percentilen = 117 BMI ≥85% percentilen = 67 P-ValueMetrics Age(years)18413.64 (9.63,16.44) 13.02 (8.5,15.87) 15.08 (11.67,16.7) 0.01Median (Q1,Q3) 13–18184103(55.98%)59(50.43%)44(65.67%)0.13N(%) 2–627(14.67%)19(16.24%)8(11.94%)N(%) 7–1254(29.35%)39(33.33%)15(22.39%)N(%) BMI18473(39,94.5)47(26,72)96(94,99) <.001Median (Q1,Q3) Height(cm)184157.5(134,167.6)152.4(130,165.1)161.3(149.9, 167.6) 0.02Median (Q1,Q3) Weight(kg)18452.55(30.1, 70.25) 46.7(25,56.4)75.3(59.5,93.2) <.001Median (Q1,Q3) GenderFemale184109(59.24%)68(58.12%)41(61.19%)0.68N(%) Male75(40.76%)49(41.88%)26(38.81%)N(%) RaceAsian1844(2.17%)3(2.56%)1(1.49%)0.31N(%) BlackorAfricanAm16(8.70%)7(5.98%)9(13.43%)N(%) Missing22(11.96%)13(11.11%)9(13.43%)N(%) White142(77.17%)94(80.34%)48(71.64%)N(%) ModeoftransferAirambulance632(3.17%)1(2.44%)1(4.55%)0.89N(%) Groundambulance50(79.37%)33(80.49%)17(77.27%)N(%) Privatevehicle11(17.46%)7(17.07%)4(18.18%)N(%) ModeofarrivalAmbulance1836(3.28%)3(2.59%)3(4.48%)0.76N(%) Privatevehicle/Public transportation 114(62.30%)72(62.07%)42(62.69%)N(%) Transferfromanother facility 63(34.43%)41(35.34%)22(32.84%)N(%) TriagelevelEmergent18428(15.22%)20(17.09%)8(11.94%)0.35N(%) Non-urgent2(1.09%)2(1.71%)0(0.00%)N(%) Urgent154(83.70%)95(81.20%)59(88.06%)N(%) BMI,bodymassindex; cm,centimeter; kg,kilogram; Am,American. WesternJournal of EmergencyMedicineVolume24,No.5:September2023 952 InfluenceofBMIonPediatricAbdominalPain Theileretal.
Table1. Characteristicsofstudypopulation.
1Adjustedforageofpatientasacontinuousvariable.
2ThemediandifferenceforthosewithaBMIinthe ≥85%percentilevsthe <85%percentile.
BMI,bodymassindex; aOR,adjustedoddsratio; DC, discharge; ED,emergencydepartment; LOS,lengthofstay; Inpt,inpatient; hrs,hours; Ped,pediatric; GI,gastroenterology; IV,intravenous.
4.42vs3.95hrs, P = 0.20),orinpatientLOS(median42.0vs 34.2hrs, P = 0.06).Therewasnostatisticallysignificant differenceintotalnumberofEDtestsorinterventions receivedbyoverweight/obesepatientscomparedtonormal/ underweightpatients.
ThelackofstatisticaldifferencesinEDresourceuseand LOSacrossBMIgroupsinourpopulationwassurprising,as ourhypothesis pediatricpatientswithelevatedBMIwho presenttotheEDwithabdominalpainwouldhavehigher resourceutilization wasbasedonpriorstudies
VariableLevel Overall N = 184 BMI <85% percentile n = 117 BMI ≥85% percentile n = 67P-ValueaOR(95%CI)1 DispositionAdmit112(60.87%)74(63.25%)38(56.72%)0.381.02(0.52,1.97) DCtohome72(39.13%)43(36.75%)29(43.28%)1.00(ref) 72-hourreturnN172(93.48%)109(93.16%)63(94.03%)0.821.00(ref) Y12(6.52%)8(6.84%)4(5.97%)0.91(0.26,3.21) EDLOS(hrs)4.09(3.08,5.53)4.42(3.33,5.57)3.95(2.58,5.2)0.20 0.45( 1.17,0.28)2 InptLOS(hrs)37.7(20.9,76.7)42.0(26.7,88.2)34.2(18.9,44.1)0.06 7.2( 23.6,9.2)2 Intervention – AntiemeticsY88(47.83%)59(50.43%)29(43.28%)0.350.77(0.42,1.42) N96(52.17%)58(49.57%)38(56.72%)1.00(ref) Intervention – PedGIY12(6.52%)7(5.98%)5(7.46%)0.701.39(0.41,4.70) N172(93.48%)110(94.02%)62(92.54%)1.00(ref) Intervention – PedsurgeryY79(42.93%)57(48.72%)22(32.84%)0.040.58(0.31–1.11) N105(57.07%)60(51.28%)45(67.16%)1.00(ref) Intervention – IV fluidsY128(69.57%)84(71.79%)44(65.67%)0.390.90(0.46,1.75) N56(30.43%)33(28.21%)23(34.33%)1.00(ref) Intervention – PainmedsY59(32.07%)37(31.62%)22(32.84%)0.871.04(0.54,2.01) N125(67.93%)80(68.38%)45(67.16%)1.00(ref) AnybloodworkN18(9.78%)15(12.82%)3(4.48%)0.071.00(ref) Y166(90.22%)102(87.18%)64(95.52%)3.48(0.95,12.7) EntericpanelY16(8.70%)8(6.84%)8(11.94%)0.242.17(0.75,6.27) N168(91.30%)109(93.16%)59(88.06%)1.00(ref) Urinalysis/UrinecultureY143(77.72%)90(76.92%)53(79.10%)0.730.95(0.45,2.02) N41(22.28%)27(23.08%)14(20.90%)1.00(ref) AbdominalradiographY60(32.61%)45(38.46%)15(22.39%)0.030.51(0.26,1.03) N124(67.39%)72(61.54%)52(77.61%)1.00(ref) AnyabdominalultrasoundN96(52.17%)64(54.70%)32(47.76%)0.371.00(ref) Y88(47.83%)53(45.30%)35(52.24%)1.44(0.78,2.66) AnyadvancedimagingN131(71.20%)82(70.09%)49(73.13%)0.661.00(ref) Y53(28.80%)35(29.91%)18(26.87%)0.95(0.48,1.88) AnylabN6(3.26%)5(4.27%)1(1.49%)0.311.00(ref) Y178(96.74%)112(95.73%)66(98.51%)2.27(0.25,20.5) AnyimagingN46(25.00%)24(20.51%)22(32.84%)0.061.00(ref) Y138(75.00%)93(79.49%)45(67.16%)0.53(0.26,1.05) NumberofEDinterventions2(1,3)2(1,3)2(1,3)0.200.00( 0.54,0.54)2 NumberofEDtests6(4,7)6(4,7)6(5,7)0.620.00( 0.45,0.45)2
Table2. Visitcharacteristics.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 953 Theileretal. InfluenceofBMIonPediatricAbdominalPain
5,7
9
demonstratinghigherEDutilizationandhigherratesof functionalabdominalpaininoverweightandobesepediatric patients.3
Thislackofstatisticaldifferencebetween BMIgroupsinregardtoEDresourceuseforabdominalpain couldpotentiallybeexplainedbythegeneraltendencyto verycloselyevaluateandobserveallpediatricabdominal painintheED,particularlywhenconsideringthehigher ratesofatypicalpresentationsofacuteappendicitisor misseddiagnosesintheyoungerpopulation.16 Interestingly, our findingsdemonstratinglackofdifferenceinED resourceutilizationacrossBMIgroupsinthepediatric abdominalpainpopulationparallelthe findingsofsimilar adultstudies.11,17
LIMITATIONS
WewereabletoanalyzeonlysubjectswhoseBMIcouldbe calculated(bothheightandweightrecordedintheEHR). Unfortunately,heightisnotroutinelyobtainedintheED, andinthisretrospectivereviewwelikelymissedalarge numberofpatientsduetonoheightbeingrecorded,resulting inalimitedsamplesize.Notably,wedid findthatthe majorityofpatientswithheightandweightrecordedalsohad aprimarycarephysician(PCP)atthesametertiarycare institutionwherethestudytookplace.Itcouldbe hypothesizedthatthe “missedpopulation” (patientswhodid nothaveaheightrecordedintheEHR)mayhave representedalargerproportionofpatientswhoeitherresided inamoreruralareawithaPCPoutsidethetertiarysystem’ s EHR,orwhodidnothaveaPCPatall.Inasub-sampleof pediatricpatientswithabdominalpainidentifiedduringthe studytime,thosewithheightandweightrecordedinthe EHRwereolderthanthosewhodidnothaveheightand weightrecordedintheEHR,suggestingthatthe “missed population” mayhavehadadditionalcharacteristicsthat differedfromthestudypopulation.Futureprospective studiescouldbeaimedatobtainingaheightandweightonall patientstoeliminatethisselectionbias.
CONCLUSION
WefoundthattheEDevaluationofpediatricpatients withachiefcomplaintofabdominalpaindidnotdiffer significantlybasedonbodymassindexinregardtoresource utilization,includingtesting,intervention,andlengthofstay. Furtherresearchiswarrantedtoassesswhetherthis findingis replicatedoutsideapediatrictertiarycarecenter,inthe generalpediatricpopulation.
AddressforCorrespondence:CarlyTheiler,MD,FAAP,Universityof IowaDepartmentofEmergencyMedicine200HawkinsDrive,1008RCP,IowaCity,Iowa,52242.Email: carly-theiler@uiowa.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources
and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Theileretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.FryarCD,CarrollMD,AffulMS.Prevalenceofoverweight,obesity,and severeobesityamongchildrenandadolescentsaged2–19years: UnitedStates,1963–1965through2017–2018. NCHSReports December2020.
2.HalesCM,CarrollMD,FryarCD,etal.Prevalenceofobesityamong adultsandyouth:UnitedStates,2015-2016. NCHSDataBrief 2017;(288):1–8.
3.TrasandeL,ChatterjeeS.Theimpactofobesityonhealthservice utilizationandcostsinchildhood. Obesity(SilverSpring) 2009;17(9):1749–54.
4.KovalerchikO,PowersE,HollandML,etal.Differencesinfrequencyof visitstopediatricprimarycarepracticesandemergencydepartmentsby bodymassindex. AcadPediatr.2020;20(4):532–9.
5.Bianchi-HayesJ,CalixteR,HuangJ,etal.Healthcareutilizationby obeseandoverweightchildren. JPediatr.2015;166(3):626–31e2.
6.McDermottKW,StocksC,FreemanWJ.OverviewofPediatric EmergencyDepartmentVisits,2015: StatisticalBrief#242.Healthcare CostandUtilizationProject(HCUP)StatisticalBriefs.Agencyfor HealthcareResearchandQuality (US);2006.
7.TeitelbaumJE,SinhaP,MicaleM,etal.Obesityisrelatedtomultiple functionalabdominaldiseases. JPediatr.2009;154(3):444–6.
8.PhatakUP,PashankarDS.Prevalenceoffunctionalgastrointestinal disordersinobeseandoverweightchildren. IntJObes(Lond) 2014;38(10):1324–7.
9.BonillaS,WangD,SapsM.Obesitypredictspersistenceofpainin childrenwithfunctionalgastrointestinaldisorders. IntJObes(Lond) 2011;35(4):517–21.
10.GroutRW,Thompson-FlemingR,CarrollAE,etal.Prevalenceofpain reportsinpediatricprimarycareandassociationwithdemographics, bodymassindex,andexam findings:across-sectionalstudy. BMC Pediatr.2018;18(1):363.
11.ChenEH,ShoferFS,HollanderJE,etal.Emergencyphysiciansdonot usemoreresourcestoevaluateobesepatientswithacuteabdominal pain. AmJEmergMed.2007;25(8):925–30.
12.MahajanP,BasuT,PaiCW,etal.Factorsassociatedwithpotentially misseddiagnosisofappendicitisintheemergencydepartment. JAMA NetwOpen.2020;3(3):e200612.
13.TantisookT,AravapalliS,ChotaiPN,etal.Determiningtheimpact ofbodymassindexonultrasoundaccuracyfordiagnosing appendicitis:Isitlessusefulinobesechildren? JPediatrSurg 2021;56(11):2010
15.
–
–
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 954 InfluenceofBMIonPediatricAbdominalPain Theileretal.
14.SchuhS,ManC,ChengA,etal.Predictorsofnon-diagnostic ultrasoundscanninginchildrenwithsuspectedappendicitis. JPediatr 2011;158(1):112–8.
15.BMIPercentileCalculatorforChildandTeen.CentersforDisease ControlandPrevention.Availableat: https://www.cdc.gov/ healthyweight/bmi/calculator.html.AccessedFebruary22,2020.
16.BeckerT,KharbandaA,BachurR.Atypicalclinicalfeaturesofpediatric appendicitis. AcadEmergMed.2007;14(2):124–9.
17.Platts-MillsTF,BurgMD,SnowdenB.Obesepatientswithabdominal painpresentingtotheemergencydepartmentdonotrequiremoretime orresourcesforevaluationthannonobesepatients. AcadEmergMed 2005;12(8):778–81.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 955 Theileretal. InfluenceofBMIonPediatricAbdominalPain
ComparisonofPediatricAcuteAppendicitisBeforeand DuringtheCOVID-19PandemicinNewYorkCity
PriyaMallikarjuna,MD*
SaikatGoswami,MBBS*
SandyMa,MD*
WonBaik-Han,MD*
KellyL.Cervellione,MPhil†
GaganGulati,MD*
LilyQ.Lew,MD*
*FlushingHospitalMedicalCenter,DepartmentofPediatrics,Flushing,NewYork † MedisysHealthNetwork,DepartmentofClinicalResearch,Jamaica,NewYork
SectionEditors:CristinaZeretzke,MD,andMarkLangdorf,MD,MHPE
Submissionhistory:SubmittedNovember10,2022;RevisionreceivedMarch27,2023;AcceptedMay25,2023
ElectronicallypublishedAugust22,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59393
Background: Acuteappendicitis(AA)isthemostcommonabdominalsurgicalemergencyinchildren andadolescents.Intheyearimmediatelyfollowingthedeclarationofthecoronavirusdisease2019 (COVID-19)pandemicbytheWorldHealthOrganization(WHO),therewasaprecipitousdeclinein emergencydepartment(ED)visitsespeciallyforsurgicalconditionsandinfectiousdiseases.Fearof exposuretosevereacuterespiratorycoronavirus2infectionresultedindelayinpresentationandtimeto surgery,andashifttowardmoreconservativemanagement.
Objective: OurgoalwastocomparetheincidenceandseverityofAAbeforeandduringthe COVID-19pandemic.
Methods: Patientsaged2–18yearsadmittedwiththediagnosisofAAtoFlushingHospitalMedical CenterorJamaicaHospitalMedicalCenterinQueens,NewYork,wereselectedforchartreview.Data extractedfromelectronichealthrecordsincludeddemographics,clinical findings,imagingstudies,and operativeandpathological findings.WecalculatedtheAlvaradoscore(AS)forincidenceandthe AmericanAssociationfortheSurgeryofTrauma(AAST)gradeforseverity.Wecomparedpatients admittedbetweenMarch1,2018–February29,2020(pre-pandemic)topatientsadmittedbetween March1,2020–February28,2021(pandemic).Wethencomparedpre-pandemicandpandemicgroups todeterminedifferencesinpediatricAAincidenceandseverity.
Results: Of239patientsdiagnosedwithAA,184(77%)wereinthepre-pandemicgroupand55(23%)in thepandemicgroup.Incidence(numberperyear)ofAAdeclinedby40%.Thepandemicgrouphad significantlygreateroverallASof ≥7,indicatingincreasedlikelihoodtorequiresurgery,(P = 0.04)and higherAASTgradedemonstratingincreasedseverity(P = 0.02).
Conclusion: TherewasadeclineinthenumberofAAcasesseeninourpediatricEDsandadmitted duringthe firstyearofthepandemic.CliniciansneedtobeawareofincreasedseverityofAAattimeof presentationduringpublichealthemergenciessuchasapandemic,possiblyduetomodifiedpatient behavior.[WestJEmergMed.2023;24(5)956–961.]
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 956 BRIEF RESEARCH REPORT
INTRODUCTION
InMarch2020the firstcaseofcoronavirusdisease2019 (COVID-19)wasidentifiedinNewYorkCity(NYC),and theboroughofQueensbecametheepicenterwithindays. FollowingtheWorldHealthOrganization(WHO) declarationofaglobalpandemic,practicestoreducethe spreadofsevereacuterespiratorysyndromecoronavirus2 (SARS-CoV-2)includedclosingallnonessentialbusinesses andschools,useofpersonalprotectiveequipment,social distancing,anddensityreduction.1 Routinepediatricand emergencydepartment(ED)visitsduringthepandemic declinedprecipitously.2 Acuteappendicitis(AA),themost commonabdominalsurgicalemergencyinpediatrics,was impacted.ThereisapaucityofdataonpediatricEDvisitsin urbanteachingcommunityhospitalsandonwhetherthe trendsaffectedpresentationorprogressionofAAinthistype ofsetting.WecomparedtheAlvaradoscore(AS)for incidenceandtheAmericanAssociationforthe SurgeryofTrauma(AAST)gradeforseverityinpatients withAAbeforeandduringthe firstyearofthe COVID-19pandemic.
METHODS
TheinstitutionalreviewboardsofFlushingHospital MedicalCenter(FHMC)and JamaicaHospitalMedical Center(JHMC)approvedthestudy.Weanalyzedchartsof patientsmeetinginclusioncriteriawhowereseenand admittedwithAAtoeitherFHMCorJHMC.Data extractedfromelectronichealthrecordsincluded
demographics,clinicalprese ntation,imagingstudies,and operativeandpathologicalcriteriatodeterminetheASand AASTgrade.Demographicsincludedage,gender,and ethnicity.TheASusesa10-pointclinicalscoringsystemto identifyAAbasedoncriteriasuchasmigrationofpain, anorexia,nausea,tendernessinrightlowerquadrant, rebound,fever,leukocytosisandleftshiftofleukocytosis. Rightlowerquadrantpainandleukocytosisareassigned twopointsandtheremainingsixcriteriaassignedonepoint each.Apatientwithascoreof1
6isleastlikelytorequire surgerywhileapatientwithascoreof7 – 10ismorelikelyto requiresurgery.3 TheAASTgradeincludeswhetherthe appendixisin fl amed,gangrenous,orperforated.Thegrade rangesfromItoV,withgradeItheleastsevereandgradeV themostsevere.4 PatientsdiagnosedwithAAweregrouped accordingtotimeper iod,betweenMarch1, 2018 – February29,2020asthepre-pandemicgroupand betweenMarch1,2020 – February28,2021asthe pandemicgroup.
Weincludedpatientsaged2–18yearswhowerediagnosed withAAbetweenMarch1,2018–February28,2021 (Figure1).Datawerecollectedinadherencetothe methodologicalstandardsproposedformedicalrecord reviewstudiesbyWorsteretal.5 WeusedAStodetermine incidence3 andAASTtodetermineseverity.4 Weanalyzed thedatausingSPSSversion22software(SPSSInc,Chicago, IL).Independentsample t -tests,chi-squaretestsandFisher exacttestswereusedforbetween-groupanalyses; P < 0.05 wasconsideredsignificant.
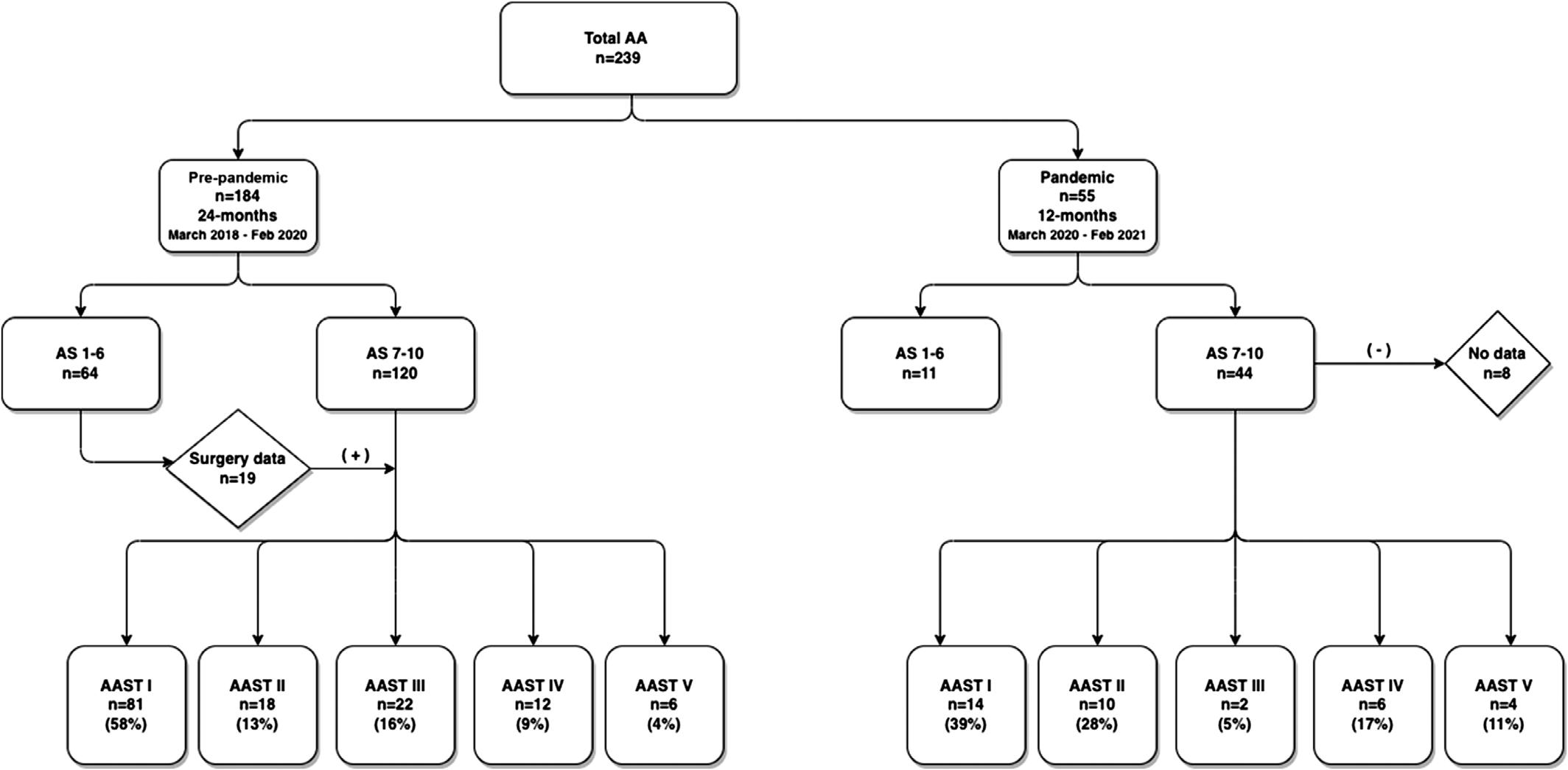
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 957 Mallikarjunaetal. ComparisonofPediatricAABeforeandDuringCOVID-19inNYC
Figure1. FlowchartofpatientsreviewedbeforeandduringCOVID-19pandemic. AA,acuteappendicitis; AS,Alvaradoscore; AAST,AmericanAssociationfortheSurgeryofTraumagrade.
RESULTS
Demographics
Wereviewed239patientcharts.Therewere184(77%) patientsinthepre-pandemicgroupand55(23%)inthe pandemicgroup.Theaveragenumberofpatientsperyearin thetwoyearsprecedingthepandemicwas92(38%peryear) comparedto55(23%)inthe firstpandemicyear,adeclineof 40%.Themeanageofpatientsinourstudygroupwas10.2 ± 3.9years.Malegenderwaspredominant(60%).Themajority ofourpatientswereofHispanicorAsianethnicity,reflective
ofourQueenscommunity.Meanage,gender,andethnicity weresimilarforpre-pandemicandpandemicgroups.
AlvaradoScore
Inboththepre-pandemicandpandemicgroups,tenderness intherightlowerquadrantwastheprimaryclinical finding, andleukocytosiswithleftshiftwasthemostfrequent laboratory finding.AnASof7–10wasmorelikelyinpatientsin thepandemicgroup.Pre-pandemicAScomparedtopandemic ASwassignificant(OR2.13,95%CI1.03–4.41; P = 0.04).
Variables Pre-pandemic n = 184 (24-months) n(%) Pandemic n = 55 (12-months) n(%) P-value Demographics Age(years)mean(SD)10.21(3.9)10.2(3.9)0.85 Gender 0.84 Male111(60.3)34(61.8) Female73(39.7)21(38.2) Ethnicity Caucasian6(3.3)1(1.8)0.58 Hispanic134(72.8)45(81.8)0.18 AfricanAmerican6(3.3)3(5.5)0.45 Asian36(19.6)6(10.9)0.14 Other2(1.1)0(0)0.67 Alvaradoscore Migrationofpain84(48.3)34(64.2)0.04* Anorexia72(52.9)32(69.6)0.05* Nausea142(78.9)42(80.8)0.77 Tendernessinrightlowerquadrant179(97.8)55(100)0.27 Reboundpain44(27.7)17(38.6)0.16 Leftshift178(96.7)54(98.2)0.58 Fever77(41.8)29(52.7)0.15 Leukocytosis159(86.4)51(92.7)0.41 TotalAlvaradoscore 0.04* 1–664(34.8)11(20.0) 7–10120(65.2)44(80.0) AmericanAssociationfortheSurgeryofTrauma(AAST)grade I:Acuteinflamedappendixintact81(58.3)14(38.9)0.37 II:Gangrenousappendicitisintact18(12.9)10(27.8)0.31 III:Perforatedappendixwithlocalcontamination22(15.8)2(5.6)1.00 IV:Perforatedappendixwithphlegmonorabscess12(8.6)6(16.7)1.00 V:Perforatedappendixwithgeneralizedperitonitis6(4.3)4(11.1)1.00 TotalAASTgrade 0.02*
< 0.05wassignificant. WesternJournal of EmergencyMedicineVolume24,No.5:September2023 958 ComparisonofPediatricAABeforeandDuringCOVID-19inNYC Mallikarjunaetal.
Table1. AlvaradoscoreandAmericanAssociationfortheSurgeryofTraumagradebeforeandduringtheCOVID-19pandemic.
*P
UltrasoundoftheAppendix
Weobtainedanimagingstudyin53%ofpatientsinthe pre-pandemicgroupandin47%ofpatientsinthepandemic group, P = 0.39.
AmericanAssociationfortheSurgeryofTraumaGrade
TheAASTwasappliedtothosewithAS7 –10andtoan additional19patientswithAS <7andsurgicaldata(totalof 139inthepre-pandemicgroup,36inthepandemicgroup). Inthepandemicgroup,eightpatients(15%)were transferredtoatertiarycarecenter.Themajorityofpatients inthepre-pandemicgrouphadgradeI,andtheleast numberofpatientswerecategorizedwithgradeV.Mostof thepatientsinthepandemicgrouphadgradeIandgradeII severityandtheleasthadgradeIIIandgradeIVseverity. Chi-squareanalysisrevealedasigni fi cantdifferenceinthe AASTseveritygradedistributionsbetweenpre-pandemic andpandemicgroups(OR0.36,95%CI0.1–1.35, P = 0.02)(Table1).Onlythreepatientstestedpositive forSARS-CoV-2.
DISCUSSION
Acuteappendicitisisthemostcommonabdominal surgicalemergencyinpediatricsandgenerallyoccurs frequentlyinmales10
19yearsinage.6,7 Thetypical presentationincludesperiumbilicalpainthatmigratestothe rightlowerquadrantoftheabdomenassociatedwithfever between37.2
38.0° Celsius,nausea,lossofappetite,and diarrhea.Sincethesesymptomsmimicotherconditions, diagnosisofAAcanbechallenging.TheASassistsinthe diagnosisofAA,andvisualizationoftheappendixon ultrasoundisconfirmatory.Delayindiagnosiscanresultin ruptureoftheappendix.6 Earlysurgicalinterventionis associatedwithlowerriskofperforation.However,thereare ongoingstudiesinvestigatingwhetherappendectomycanbe delayedby12-24hoursandtheroleofnon-operative managementwiththeuseofantibioticsasaneffective treatmentalternative.7 AnASof ≥7ismorelikelytorequire surgery. 3 TheAASTanatomicgradingsystemfor appendicitisisavalidatedtooltoassessseverity.Ahigher AASTgradeisassociatedwithmostseverecasesandhigher complicationrates.4 WeusedtheAStodetermineincidence andtheAASTgradetodetermineseverity.Eachpatientwas assignedtothehighestgroupforanalysis.
TheWHOdeclaredtheCOVID-19pandemicinMarch 2020asthevirusspreadworldwide.8 Measurestomitigate thespreadofthevirusmodifiedthebehaviorofpatientsand thedeliveryofhealthcare.9 Thefearofexposureresultedin declineinpediatricroutineandEDvisits.1,2,10 Emergency departmentswereoverwhelmedwithCOVID-19cases,while theremainderofthehospitalandmedicalstaffwas reorganizedtocareforthosewhowereadmitted.Elective surgerieswerecanceled,andnon-urgentsurgerieswere delayed.11 Studieshavereportedthepossibleeffectofthe
COVID-19pandemiconpresentation,management,and outcomesonappendicitis.12–16 Asmallpercentage(5%)of ourpatientswithAAtestedpositiveforSARS-CoV-2, despiteareportedpossibilityofAAasapost-inflammatory complicationofSARS-CoV-2infection.17,18
Inourstudy,themedianageandgenderofourpatients wereconcordantwithknownepidemiologyofAA.The numberofpatientsineachethnicgroupisreflectiveofour community.ThemeannumberofpatientswithAAperyear pre-pandemiccomparedtopandemicdeclinedby40%, similarto findingsbytheUSCentersforDiseasesControl andPrevention.19 ForeachclinicalcriterionontheAS,prepandemicandpandemicgroupswerenotsignificantly different.Thepercentageofultrasoundoftheappendix performedwaslowerinthepandemicgroupandwasalsonot significantlydifferent.However,thehighernumberof patientswithAS ≥7inthepandemicgroupwassignificant. AllourpatientswithAS1–6weremanagedwithantibiotics. Inbothgroups,only66%ofpatientshadcompletesurgical andpathologicaldata.ThepercentageofgradesIand IIwashigherinthepre-pandemicgroup,andthe percentageofgradesIVandVwashigherinthepandemic group.ThehigherAASTgradewassignificantinthe pandemicgroup.
OtherstudiesregardingincidenceandseverityofAA duringtheCOVID-19pandemicwerevariable.Inonestudy, alowerincidenceandahighercomplicationrateinadults withAAwereobservedinamulticenterstudyinthe Netherlandsduringthesameperiodstudiedbyus.20 Lucero etalreportedareductioninEDvisitsinbothchildrenand adultsacrossourcountry.2 WeconcurwithadeclineinED visitsforAA.StudiesrelatedtoseverityofAAinchildren wereallretrospectiveandbasedonpatientswithdelayed presentationandincreasedincidenceof complications.13,15,21,22 Wedidnotcorrelatedelayed presentationwithseverity.Incidenceofcomplicationswas assessedusingASSTgrade.Geralletalreportedinasmall sampleof48patientsinthepandemicgroupwithdelayed presentationandincreasedseveritybasedonclinical presentationandradiologicalimagingofperforationand intra-abdominalabscess.23 Wedidseeanincreasein perforationwithabscess(gradeIV)inourpandemicgroup comparedtothestudyfromItalybyLaPergolaetalinwhich thepandemicgrouphadoveralldecreasedhospital admissionandunchangednumberofcomplicated appendectomiesasanindicationofseverity,24 andtothe studyfromLithuaniabyVansevičienė etalwhenasurgical delayoffourhourswasnotassociatedwithincreased complications.25 Notallstudiesconfirmeddelayin presentationordemonstratedincreasedseverityofAA duringthepandemic.13,26 Theremaybeunmeasurable factorscontributingtothechangesseenduringthepeakof thepandemicaffectingthebehaviorandrelationshipofour patientsandhealthcaresystems.
–
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 959 Mallikarjunaetal. ComparisonofPediatricAABeforeandDuringCOVID-19inNYC
LIMITATIONS
Thiswasaretrospectivestudyconductedintwo community,non-profit,teachinghospitals.Wefocusedon the firstyearofthepandemicinNYCwhentheCOVID-19 vaccinewaslimitedfortheagegroupstudiedandafter worldwidespread.Changeinmedicalcoverageandparental healthliteracywerenottakenintoconsiderationwhen evaluatingpatientbehavior.Wedidnotincludedataontime fromEDtooperatingroom,outcomes,orfollow-upafter hospitaldischarge.
CONCLUSION
Inoursamplefromtwourbancommunityhospitals,there wasadeclineinthenumberofAAvisitsinourpediatricEDs. Theseverityofacuteappendicitisinchildrenandadolescents whopresentedtotheEDwasheightenedduringtheCOVID19pandemic.Cliniciansneedtobeawareofincreased severitywhenevaluatingAAandpossibleincreasedriskof complicationsduringapublichealthemergency.The increasinguseoftelemedicinetoscreenpatientsandofsocial mediatoobtainhealthinformationbypatientsfueledbythe COVID-19pandemicmaycontributetothechanging presentationofmanyconditions,includingAA.
AddressforCorrespondence:LilyQ.Lew,MD,FlushingHospital MedicalCenter,DepartmentofPediatrics,4500ParsonsBlvd, Flushing,NewYork11355.Email: llew2.flushing@jhmc.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Mallikarjunaetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.PinesJM,ZocchiMS,BlackBS,etal.Characterizingpediatric emergencydepartmentvisitsduringtheCOVID-19pandemic. AmJ EmergMed. 2021;41:201–4.
2.LuceroAD,LeeA,HyunJ,etal.Underutilizationoftheemergency departmentduringtheCOVID-19pandemic. WestJEmergMed. 2020;21(6):15–23.
3.OhleR,O’ReillyF,O’BrienKK,etal.TheAlvaradoscoreforpredicting acuteappendicitis:asystematicreview. BMCMed. 2011;9:139.
4.FinnesgardEJ,HernandezMC,AhoJM,etal.TheAmerican AssociationfortheSurgeryofTraumaemergencygeneralsurgery anatomicseverityscoringsystemasapredictorofcostinappendicitis. SurgEndosc. 2018;32(12):4798–804.
5.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
6.AddisDG,ShafferN,FowlerBS,etal.Theepidemiologyofappendicitis andappendectomyintheUnitesStates. AmJEpidemiol. 1990;132(5):910–25.
7.KrzyzakM,MulrooneySM.Acuteappendicitisreview:background, epidemiology,diagnosis,andtreatment. Cureus. 2020;12(6):e8562.
8.CucinottaD,VanelliM.WHOdeclaresCOVID-19apandemic. Acta Biomed. 2020;91(1):157–60.
9.NewYorkStateCOVID-19data.Availableat: https://coronavirus.health. ny.gov/home.AccessedMarch17,2021.
10.Delgado-MiguelC,GarciaUrbánJ,DelMonteFerrerC,etal.Impactof theCOVID-19pandemiconacuteappendicitisinchildren. JHealthc QualRes. 2022;37(4):225–30.
11.KvasnovskyCL,ShiY,RichBS,etal.Limitinghospitalresourcesfor acuteappendicitisinchildren:lessonslearnedfromtheU.S.epicenterof theCOVID-19pandemic. JPediatrSurg. 2021;56(5):900–4.
12.LiC,SalehA.EffectofCOVID-19onpediatricappendicitis presentationsandcomplications. JPediatrSurg. 2022;57(5):861–5.
13.TristánJG,RomeroHS,PelliteroSE,etal.Acuteappendicitisinchildren duringtheCOVID-19pandemic:neitherdelayeddiagnosisnorworse outcomes. PediatrEmergCare. 2021;37(3):185–90.
14.LotfallahA,AameryA,MoussaG,etal.Surgicalversusconservative managementofacuteappendicitisduringtheCOVID-19pandemic:a single-centreretrospectivestudy. Cureus. 2021;13(3):e14095.
15.PawelczykA,KowalskaM,TylickaM,etal.ImpactoftheSARS-CoV-2 pandemiconthecourseandtreatmentofappendicitisinthepediatric population. SciRep. 2021;11(1):23999.
16.PlaceR,LeeJ,HowellJ.Rateofpediatricappendicealperforationata children’shospitalduringtheCOVID-19pandemiccomparedwiththe previousyear. JAMANetwOpen. 2020;3(12):e2027948.
17.MalhotraA,SturgillM,Whitley-WilliamsP,etal.PediatricCOVID-19and appendicitis:agutreactiontoSARS-CoV-2? PediatrInfectDisJ. 2021;40(2):e49–55.
18.MalbulK,KatwalS,MaharjanS,etal.Appendicitisasapresentationof COVID-19:acasereport. AnnMedSurg. 2021;69:102719.
19.HartnettKP,Kite-PowellA,DeViesJ,etal.Impactofthe COVID19pandemiconemergencydepartmentvisits – UnitedStates January1,2019–May30,2020. MorbMortalWklyRep. 2020;69(23):699–704.
20.ScheijmanJGC,BursteinABJ,PuylaertCAJ,etal.Impactofthe COVID-19pandemiconincidenceandseverityofacuteappendicitis:a comparisonbetween2019and2020. BMCEmergMed. 2021;21(1):61.
21.RaffaeleA,CervoneA,RuffoliM,etal.Criticalfactorsconditioningthe managementofappendicitisinchildrenduringCOVID-19pandemic: experiencefromtheoutbreakareaofLombardy,Italy. BrJSurg. 2020;107(11):e529–30.
22.SnapiriO,RosenbergDanzigerC,KrauseI,etal.Delayeddiagnosisof paediatricappendicitisduringtheCOVID-19pandemic. ActaPaediatr. 2020;109(8):1672–6.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 960 ComparisonofPediatricAABeforeandDuringCOVID-19inNYC Mallikarjunaetal.
23.GerallCD,DeFazioJR,KahanAM,etal.Delayedpresentationandsuboptimaloutcomesofpediatricpatientswithacuteappendicitisduringthe COVID-19pandemic. JPediatrSurg. 2021;56(5):905–10.
24.LaPergolaE,SgroA,RebosioF,etal.Appendicitisinchildren inalargeItalianCOVID-19pandemicarea. FrontPediatr. 2020;8:600320.
25.Vansevičienė I,Bučinskaitė D,MalciusD,etal.DidtheCOVID-19 pandemicprolongthetimetilldiagnosisandworsenoutcomesfor childrenwithacuteappendicitis? Medicina. 2021;57(11):1234.
26.NassiriAM,PrudenRD,HolanCA,etal.Pediatricappendicitisinthe timeoftheCOVID-19pandemic:aretrospectivechartreview. JAmer CollEmergPhysiciansOpen. 2022;3(2):e12722.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 961 Mallikarjunaetal. ComparisonofPediatricAABeforeandDuringCOVID-19inNYC
ExpandingDiabetesScreeningtoIdentifyUndiagnosedCases AmongEmergencyDepartmentPatients
DavidC.Lee,MD,MS*†‡
HaritaReddy,MPH*
ChristianA.Koziatek,MD*‡
NoahKlein*
AnupChitnis,MD*
KashifCreary*
GerardFrancois*
OlumideAkindutire,MD*
RobertFemia,MD,MBA*‡
ReedCaldwell,MD*
*NewYorkUniversity,NYUGrossmanSchoolofMedicine,RonaldO.Perelman DepartmentofEmergencyMedicine,NewYork,NewYork
† NewYorkUniversity,NYUGrossmanSchoolofMedicine,DepartmentofPopulation Health,NewYork,NewYork
‡ BellevueHospitalCenter,DepartmentofEmergencyMedicine,NewYork,NewYork
SectionEditors: ErikAnderson,MD,andGayleGalletta,MD
Submissionhistory:SubmittedJanuary21,2023;RevisionreceivedMay30,2023;AcceptedJuly8,2023
ElectronicallypublishedAugust8,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.59957
Introduction: Diabetesscreeningtraditionallyoccursinprimarycaresettings,butmanywhoareathigh riskfacebarrierstoaccessingcareandthereforedelaysindiagnosisandtreatment.Thesesamehighriskpatientsdofrequentlyvisitemergencydepartments(ED)and,therefore,mightbenefitfromscreening atthattime.Ourobjectiveinthisstudywastoanalyzeoneyearofresultsfromamultisite,ED-based diabetesscreeningprogram.
Methods: Weassessedthedemographicsofpatientsscreened,identifieddifferencesinratesofnewly diagnoseddiabetesbyclinicalsite,andthegeographicdistributionofhighandlowhemoglobinA1c (HbA1c)results.
Results: Weperformeddiabetesscreening(HbA1c)among4,211EDpatients40–70yearsold,witha bodymassindex ≥25,andnopriorhistoryofdiabetes.Ofthesepatientsscreenedfordiabetes,9%hada HbA1cresultconsistentwithundiagnoseddiabetes,andnearlyhalfofthesepatientshadaHbA1c ≥9.0%.RatesofnewlydiagnoseddiabeteswerenotablyhigheratEDslocatedinneighborhoodsoflower socioeconomicstatus.
Conclusion: Emergencydepartment-baseddiabetesscreeningmaybeapracticalandscalablesolution toscreenhigh-riskpatientsandreducehealthdisparitiesexperiencedinspecificneighborhoodsand demographicgroups.[WestJEmergMed.2023;24(5)962–966.]
INTRODUCTION
Amongthe35millionAmericanswithdiabetes,nearly oneinfourareunawareoftheircondition.1 Diabetes screeningtraditionallyoccursinprimarycaresettings,but manypeopleathighriskofdiabetesfacesubstantialbarriers whenaccessinghealthcare.2,3 Therefore,diagnosisisdelayed amongthosemostlikelytodevelopdiabetesatanearlyage, andthereisgreaterriskofdiabetes-relatedmorbidityand
mortalitythatwouldotherwisehavebeenpreventable.4,5 Manyhigh-riskpatients,however,dohavefrequent interactionswiththehealthcaresystem.Patientswith socioeconomicburdensandtimeconstraintsaremorelikely tovisitemergencydepartments(ED)forcare.6–8
InJune2019,webegananEDinitiativetotest hemoglobinA1c(HbA1c)forpatientswithoutahistoryof diabeteswhometUSPreventiveServicesTaskForce
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 962 BRIEF RESEARCH REPORT
(USPSTF)guidelinesforscreening.Ourgoalinthisstudy wastoevaluateoneyearofresultsfromthisscreening programtoassessprogramefficacyandthedemographicsof EDpatientswithnewlydiagnoseddiabetes.Weaimedto examinewhetherED-baseddiabetesscreeningcanbe scalableandeffectiveinhelpingaddressdisparitiesinthe diagnosisofnewdiabetesandidentifyingpatientswhoneed linkagetooutpatientcareformanagement.
METHODS
StudyDesign
Weperformedaretrospectivechartreviewofpatients screenedfordiabetesfromFebruary2021–January2022 withaHbA1ctestatfourEDsinNewYorkCity.The primaryoutcomeofinterestwasthepercentageofpatients withanelevatedHbA1c.Weanalyzedthedemographic characteristicsofscreenedpatients,differencesbyclinical site,andthegeographicdistributionofresultsamong patientsscreened.
StudyPopulation
Patientsscreenedincludedanyonealreadyreceivingblood workfortheirclinicalcarewhometUSPSTFguidelinesfor diabetesscreening.Atthetimeofthestudy,thoseguidelines recommendedscreeningforadults40–70yearsoldwitha bodymassindex(BMI) ≥25.Eligiblepatientswere automaticallyidentifiedthroughtheelectronichealthrecord (EHR)asnothavingahistoryofdiabetes(basedonproblem list,auto-populatedviathesharedhealthrecordsystemCare Everywhere[CareEverywhereLLC,Natick,MA]orby patient-providedpastmedicalhistoryatEDtriage),andas nothavingaHbA1ctestintheprevioussixmonths.The HbA1ctestswereofferedatnocharge,andpatientswere giventheopportunitytodeclinethetest,althoughdataon thosedeclinedwasnottracked.
StatisticalAnalysis
Weperformedadescriptiveanalysisofscreenedpatients duringthestudyperiod,forboththeoverallstudypopulation andbyclinicalsite.WeanalyzedBMIcategorically: overweight(BMI25.0–29.9);obese(30.0–39.9);and morbidlyobese(≥ 40).TheHbA1cresultwascategorizedas normal(<5.7%),prediabetes(5.7%–6.4%),diabetes (6.5%–8.9%),andpoorlycontrolleddiabetes(≥9.0%).To identifystatisticallysignificantdifferencesinpatient characteristicsamonghospitals,weusedANOVA forcontinuousvariablesandchi-squaredtestsfor categoricalvariables.
Weconductedageospatialanalysistodeterminewhether highandlowHbA1cvalueswereconcentratedinspecific geographicareas.Todothis,weperformedaGetis-OrdGi* hotspotanalysisonHbA1cvalues,acommonlyused approachtoidentifysignificantspatialclusteringofhighand
lowvaluesforagivenvariable.9,10 WeusedtheK-nearest neighborstomodelspatialproximity.
StatisticalanalyseswereperformedusingStata16.1(Stata Corp,CollegeStation,TX).Geographicanalysiswas performedusingArcGISPro2.8.3(ESRI;Redlands,CA). Thisstudywasapprovedbytheinstitutionalreviewboardat NewYorkUniversitySchoolofMedicine.
RESULTS
StudyPopulation
Wescreened4,211EDpatients40–70yearsold,withBMI ≥25andnopriorhistoryofdiabetes(Table1).Ofthepatients screened,58%wereminorities;theproportionofeachrace/ ethnicitydifferedamongthefoursites.Demographic differencesateachsitegenerallyreflectedthelocal populationslivingnearthoseEDs.Ofthepatientsscreened, 16%reportedthatEnglishwasnottheirprimarylanguage. Byinsurancetype,55%ofpatientsscreenedhadprivate/ commercialinsurance,15%wereinsuredbyMedicare,25% byMedicaid,and5%wereself-payoruninsured.Thirty-four percentofpatientsscreenedatNYUBrooklynwereinsured byMedicaid,muchhigherthantheproportionattheother EDs.IntermsofBMI,43%wereobese,10%weremorbidly obese,andtheremainderwereoverweight,giventheBMI screeningcutoffof25.
PrimaryOutcome
EighteenpercentofscreenedEDpatientshadaHbA1c resultconsistentwithprediabetes,and9%hadHbA1cresults consistentwithundiagnoseddiabetes.Notably,almosthalf ofEDpatientswithanewdiagnosisofdiabeteshadaHbA1c ≥9.0%,consistentwithpoorlycontrolleddiabetes. Comparingtheproportionofpatientsnewlydiagnosedwith diabetesateachofthefourEDs,rateswerenotablyhigherat NYUBrooklyn(16%)andNYUCobbleHill(9%)compared toNYU-TischHospitalinManhattan(6%)andNYULong Island(6%)(P -value < 0.01).
GeospatialAnalysisofHbA1cResults
Inageospatialanalysis,weidentifiedstatistically significantclusteringofhighandlowHbA1cvaluesinthe NewYorkCityarea(Figure1).Sensitivityanalysesforthe numberofnearestneighborsdemonstratedagenerally similargeographiclocationofthesehotandcoldspots, whichsuggeststhatthese findingswererobust(notaffected bychangingthenumberofnearestneighborsspecified).11
DISCUSSION
OurstudyreviewedoneyearofdatafromanED-based diabetesscreeningprogramandfoundahighrateof previouslyundiagnoseddiabetesamongEDpatients meetingUSPSTFcriteriatobescreened.Manyofthese patientshadpoorlycontrolleddiabetes(HbA1cof >9.0%). WhileEDsarenotdesignedtoprovidelong-term
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 963 Leeetal. DiabetesScreeningforUndiagnosedEDPatients
Asian129(3%)33(3%)32(3%)12(2%)47(3%)
Other345(8%)120(11%)108(10%)47(8%)62(4%)
Other172(4%)44(4%)86(8%)6(1%)62(2%)
Insurance
Medicare733(17%)229(21%)183(17%)88(15%)248(16%)
Medicaid1,035(24%)240(22%)367(34%)141(24%)295(19%)
Self-pay172(4%)22(2%)97(9%)18(3%)31(2%)
BMI
Overweight2,026(47%)557(51%)529(49%)253(43%)698(45%) < 0.01
Obese1,854(43%)437(40%)453(42%)253(43%713(46%)
Morbidlyobese431(10%)98(9%)97(9%)82(14%)140(9%)
HbA1cresult
≥ 9.0%172(4%)22(2%)97(9%)24(4%)31(2%) < 0.01
6.5%to8.9%216(5%)44(4%)76(7%)29(5%)62(4%)
5.7%to6.4%776(18%)164(15%)183(17%)88(15%)326(21%) < 5.7%3,147(73%)863(79%)723(67%)448(76%)1,132(73%)
BMI,bodymassindex; HbA1c,hemoglobinA1c.
managementofchronicdiseases,ratesofundiagnosed diabetesareknowntobetwotimeshigheramongpatients withpooraccesstoprimarycare.12 Patientsdiagnosedwith diabetesthroughpreventivescreeningarediagnosedmuch earlier,andhavelowermortality,whencomparedtopatients diagnosedwithdiabetesduetoclinicalsymptoms.13,14 The EDprovidesasettingfordiabetesscreeningwherenewcases couldbediagnosedthatmightotherwisegoundetected, especiallyamonghigh-riskpatientswithpooraccessto primarycare.PreviouslypublishedeffortstoscreenED patientsfordiabeteshavedemonstratedevenhigherrates ofundiagnoseddiabetes,whichmaybeduetothe screeningcriteriausedorthepatientpopulationsinthose healthsystems.15–19
Ourstudyalsofoundhigherratesofundiagnoseddiabetes inourEDsthatarelocatedprimarilyinneighborhoodsof lowersocioeconomicstatus,includingthosewithahigh proportionofpatientsforwhomEnglishisnottheprimary language.LeveragingtheEDtopromotediabetesscreening hasthepotentialtoreduceracialandethnicdisparitiesin diabetesburden,especiallyamongpatientswhomayface languagebarriers.Limitingpreventivescreeningtothe primarycaresettingriskstheperpetuationofpoorhealth outcomesforthosepatientswhofacebarrierstohealthcare access.Iftheprimaryconcernisthatthesenewlydiagnosed EDpatientsmaynotfollowupforappropriateoutpatient care,theneffortsshouldfocusonhowtoimprovecare coordinationfromtheEDtotheprimarycaresetting.
Population characteristicsAllhospitals NYU-TischHospital Manhattan NYU Brooklyn NYUCobble Hill NYULong Island P-valuefor differences Patients4,3111,0921,0795891,551 Age(median)5455535155 < 0.01 Gender Female2,155(50%)513(47%)496(46%)330(56%)807(52%) < 0.01 Male2,156(50%)579(53%)583(54%)259(44%)744(48%)
White1,811(42%)491(45%)345(32%)194(33%)776(50%) < 0.01 Black905(21%)229(21%)129(12%)224(38%)310(20%)
Table1. CharacteristicsofemergencydepartmentpatientsscreenedfordiabetesandhemoglobinA1cresults.
Race/ethnicity
Hispanic1,121(26%)218(20%)464(43%)112(19%)357(23%)
English3,621(84%)1,005(92%)712(66%)565(96%)1,334(86%) < 0.01
Language
Spanish517(12%)44(4%)281(26%)18(3%)186(12%)
Private2,371(55%)612(56%)432(40%)342(58%)977(63%) < 0.01
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 964 DiabetesScreeningforUndiagnosedEDPatients Leeetal.
Ourstudydemonstratesthatthehighestyieldofthis diabetesscreeningwasinEDsseeingahighproportionof patientsoflowersocioeconomicstatus.Inamultivariable analysiscontrollingforage,gender,race/ethnicity,language, andinsurancetype,wefoundmalegender,allnon-White race/ethnicities,otherlanguage,andself-payinsurancestatus werestatisticallysignificantpredictorsofpreviously undiagnoseddiabetes.Inaddition,thelocationofhotand coldspotsofHbA1cvaluescorrelatedwellwithpriorstudies ofthegeographicdistributionofpoorglycemiccontrol amongdiabetespatientsinNewYorkCity.20 Promoting diabetesscreeninginEDsthatservehigh-riskpatient populationscanhelpidentifyundiagnosedcasesofdiabetes intheseneighborhoods,whichmaybeacriticalstepin addressingpoorhealthoutcomesexperiencedinthese geographicareas.
LIMITATIONS
Ourstudyhasseverallimitations.First,EDpatients receivingbloodworkarelikelytohavesomedifferencesfrom patientsnotreceivingbloodwork;these findingsmaynotbe generalizabletoeveryEDpatient.Additionally,ourstudy wasinonemetroarea,andwhileour findingsdo fitwellwith existingdiabetesliteraturefortheNewYorkCityarea,itis possiblethatothergeographicareaswillhavedifferent patienttypesvisitingtheEDand,therefore,mayhave differentamountsofundiagnoseddiabetesthanfoundinour study.Itisalsopossiblethatpatientsidentifiedasnewly diagnosedinourstudydidhaveapreviousdiagnosis
elsewhere,whichtheydidnotdiscloseduringtheirEDvisit andwasnotavailableinourEHRdata.Finally,theremay havebeenotherconfounders(eg,dietarybehaviors)thatare highlycorrelatedwiththefactorsanalyzedinourstudy, whichmaybeanunmeasuredpredictorofundiagnosed diabetesandmaybealimitationofrelyingonlyon EHRdata.
CONCLUSION
WefoundahighpercentageofscreenedpatientsintheED withundiagnoseddiabetes.Wefurtherfoundthattheburden ofundiagnoseddiabetesintheEDisconcentratedincertain geographicareas,corroboratingknownsocioeconomic elementstoundiagnoseddiabetes.Thissuggeststhat ED-baseddiabetesscreeningcanbeascalablesolutionfor addressingdisparitiesintheburdenofdiabetesand identifyingpatientswhoneedlinkagetooutpatientcare. Furtherworkcanfocusonimprovedscreeningcriteria specifictotheEDpopulationtoimproveyieldand follow-onsystemsdevelopmentforfurthercareofnewly diagnosedpatients.
AddressforCorrespondence:ReedCaldwell,MD,NewYork University,NYUGrossmanSchoolofMedicine,RonaldO.Perelman DepartmentofEmergencyMedicine,5501stAvenue,NewYork, NewYork10016.Email: reed.caldwell@nyulangone.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Leeetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
REFERENCES
1.MenkeA,CasagrandeS,GeissL,etal.Prevalenceofandtrendsin diabetesamongadultsintheUnitedStates,1988–2012. JAMA 2015;314(10):1021–9.
2.LiaoY,BangD,CosgroveS.Surveillanceofhealthstatusinminority communities-RacialandEthnicApproachestoCommunityHealth AcrosstheU.S.(REACHU.S.)RiskFactorSurvey,UnitedStates,2009 -PubMed. MorbMortalWklyRep.2011;60(6):1–44.

3.GaryTL,VenkatNarayanKM,GreggEW,etal.Racial/ethnic differencesinthehealthcareexperience(coverage,utilization,and satisfaction)ofUSadultswithdiabetes. EthnDis.2003;13(1):47–54.
4.LeeDC,YoungT,KoziatekCA,etal.Agedisparitiesamongpatients withtype2diabetesandassociatedratesofhospitaluseanddiabetic complications. PrevChronicDis.2019;16:E101.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 965 Leeetal. DiabetesScreeningforUndiagnosedEDPatients
Figure1. Geographicdistributionofemergencydepartmentpatients screenedfordiabetesintheNewYorkCityareaandmarked locationsoftheemergencydepartments.
5.GopalanA,MishraP,AlexeeffSE,etal.Prevalenceandpredictorsof delayedclinicaldiagnosisoftype2diabetes:alongitudinalcohortstudy. DiabetMed.2018;35(12):1655–62.
6.CappR,KelleyL,EllisP,etal.Reasonsforfrequentemergency departmentusebyMedicaidenrollees:aqualitativestudy. AcadEmerg Med.2016;23(4):476–81.
7.MalechaPW,WilliamsJH,KunzlerNM,etal.Materialneedsof emergencydepartmentpatients:asystematicreview. AcadEmergMed 2018;25(3):330
59.
8.KangoviS,BargFK,CarterT,etal.Understandingwhypatientsoflow socioeconomicstatuspreferhospitalsoverambulatorycare. HealthAff (Millwood).2013;32(7):1196–203.
9.SoltaniA,AskariS.Exploringspatialautocorrelationoftrafficcrashes basedonseverity. Injury.2017;48(3):637
47.
10.BesserLM,MeyerOL,JonesMR,etal.Neighborhoodsegregationand cognitivechange:multi-ethnicstudyofatherosclerosis. Alzheimers Dement.2023;19(4):1143–51.
11.Vizuete-JaramilloE,Meza-FigueroaD,Reyes-CastroPA,etal.Usinga sensitivityanalysisandspatialclusteringtodeterminevulnerabilityto potentiallytoxicelementsinasemiaridcityinNorthwestMexico. Sustain.2022;14(17):10461.
12.ZhangX,GeissLS,ChengYJ,etal.Themissedpatientwithdiabetes: howaccesstohealthcareaffectsthedetectionofdiabetes. Diabetes Care.2008;31(9):1748–53.
13.FeldmanAL,GriffinSJ,FhärmE,etal.Screeningfortype2diabetes:do screen-detectedcasesfarebetter? Diabetologia.2017;60(11):2200–9.
14.UmpierrezGE,IsaacsSD,BazarganN,etal.Hyperglycemia: anindependentmarkerofin-hospitalmortalityinpatientswith undiagnoseddiabetes. JClinEndocrinolMetab 2002;87(3):978–82.
15.DanielsonKK,RydzonB,NicosiaM,etal.Prevalenceofundiagnosed diabetesidentifiedbyanovelelectronicmedicalrecorddiabetes screeningprograminanurbanemergencydepartmentintheUS. JAMA NetwOpen.2023;6(1):e2253275.
16.MenchineMD,AroraS,CamargoCA,etal.Prevalenceofundiagnosed andsuboptimallycontrolleddiabetesbypoint-of-careHbA1Cin unselectedemergencydepartmentpatients. AcadEmergMed 2011;18(3):326–9.
17.CharfenMA,IppE,KajiAH,etal.Detectionofundiagnoseddiabetes andprediabeticstatesinhigh-riskemergencydepartmentpatients. AcadEmergMed.2009;16(5):394–402.
18.GeorgePM,ValabhjiJ,DawoodM,etal.Screeningfortype2 diabetesintheaccidentandemergencydepartment. DiabetMed 2005;22(12):1766–9.
19.AndersonES,DworkisDA,DeFriesT,etal.Nontargeteddiabetes screeninginaNavajoNationemergencydepartment. AmJPublic Health.2019;109(2):270–2.
20.LeeDC,JiangQ,TabaeiBP,etal.Usingindirectmeasuresto identifygeographichotspotsofpoorglycemiccontrol:cross-sectional comparisonswithanA1Cregistry. DiabetesCare 2018;41(7):1438–47.
–
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 966 DiabetesScreeningforUndiagnosedEDPatients Leeetal.
FactorsAssociatedwithOverutilizationofComputedTomography oftheCervicalSpine
KarlT.Chamberlin,MD
MaureenM.Canellas,MD,MBA
MartinA.Reznek,MD,MBA
KevinA.Kotkowski,MD,MBA
UniversityofMassachusettsChanMedicalSchool,DepartmentofEmergency Medicine,Worcester,Massachusetts
SectionEditors: DavidThompson,MD,andPatrickMaher,MD,MS
Submissionhistory:SubmittedSeptember19,2022;RevisionreceivedJune23,2023;AcceptedJuly3,2023
ElectronicallypublishedAugust28,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58948
Introduction: Despitethewideavailabilityofclinicaldecisionrulesforimagingofthecervicalspineafter atraumaticinjury(eg,NEXUSC-spineruleandCanadianC-spinerule),thereissignificantoverutilization ofcomputedtomography(CT)imaginginpatientswhoaredeemedtobeatlowriskforaclinically significantcervicalspineinjurybytheseclinicaldecisionrules.Thepurposeofthisstudywastoidentify themajorfactorsassociatedwiththeoveruseofCTcervicalspineimagingusingalogistic regressionmodel.
Methods: ThiswasaretrospectivereviewofalladultpatientswhounderwentCTcervicalspineimaging forevaluationofatraumaticinjuryatatertiaryacademicemergencydepartment(ED)andthreeaffiliate communityEDsinJanuaryandFebruary2019.Weperformedmultivariablelogisticregressiontoidentify factorsassociatedwithobtainingCTcervicalspineimagingdespitelow-riskclassificationbytheNEXUS C-spineRule.
Results: Atotalof1,051patientsunderwentCTcervicalspineimagingfortraumaticindicationsduring thestudyperiod,and889patientswereincludedintheanalysis.Ofthesepatients,376(42.3%)were negativebytheNEXUSC-spinerule.Variablesthatwereassociatedwithincreasedlikelihoodof unnecessaryimagingincludedageover65,EmergencySeverityIndex(ESI)score2and3,arrivalasa walk-in,andanticoagulationstatus.PatientswhopresentedtothetertiaryacademicEDhada significantlylowerlikelihoodofunnecessaryimaging.Twenty-onepatients(2.4%)werefoundtohave cervicalspinefracturesonimaging,twoofwhomwerenegativebytheNEXUSC-spinerule,butneither hadaclinicallysignificantfracture.
Conclusion: CervicalspineimagingisvastlyoverusedinpatientspresentingtotheEDwithtraumatic injuries,asadjudicatedusingtheNEXUSC-spineruleasareferencestandard.Olderage,ESIlevel, arrivalasawalk-in,andtakinganticoagulationdrugswereassociatedwithoverutilizationofCTimaging. Conversely,presentingtothetertiaryacademicEDwasassociatedwithalowerlikelihoodofundergoing unnecessaryimaging.ThismodelcanguidefutureinterventionstooptimizeEDCTutilizationand minimizeunnecessarytesting.[WestJEmergMed.2023;24(5)967–973.]
INTRODUCTION
Evaluationofpotentialcervicalspineinjuryisacommon reasonforpresentationtotheemergencydepartment(ED). Annually,morethan2.5millionpatientsintheUnitedStates seekcareatanEDforevaluationofapotentialinjurytothe
cervicalspine.1 Ithasbeenpreviouslyestimatedthat3–10% ofthesepatientsmayhaveclinicallysignificantcervicalspine injuries.2–5 Inrecentdecades,thevolumeofradiographic imagingperformedinEDshasincreasedexponentially, particularlycomputedtomography(CT).6,7
Thisdramatic
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 967
RESEARCH
ORIGINAL
increaseinimagingstudiespresentsnumerouspotential negativeimplications,includingincreasedhealthcarecosts, risksofradiation,longerlengthsofstay,moreincidental findings,andinefficienciesinEDthroughput.8–10 Therefore, itisavaluableobjectivetomoderatetheuseofimaginginthe EDtoavoidunnecessaryimaging.
Clinicaldecisionruleshavegainedtractioninemergency medicinetoassistwithdecision-making,andseveralclinical decisionruleshavebeenwell-studiedandvalidatedto determinetheneedforimagingofthecervicalspineaftera traumaticinjury.Themostuseddecisionrulesarethe NEXUSC-spineruleandtheCanadianC-spinerule.11,12
TheNEXUSC-spineruleestablishescriteriathatcanbeused torisk-stratifypatientsandtherebyidentifypatientswhoare atlowriskforaclinicallysignificantcervicalspineinjuryand forwhomcervicalspineimagingisthusunnecessary.
Althoughtheseclinicaldecisionrulesarewidelyavailable, utilizationoftheserulesisvariable.Priorliteraturehas demonstratedthatapproximately25%ofCTC-spinestudies wereperformedonpatientswhodidnotmeetNEXUS criteriaforimaging.13–16 Todateitisnotwellunderstood whythehighrateofCTC-spineoverutilizationpersists despitevalidateddecisionruleshavingbeeninplaceand broadlycommunicatedforthelasttwodecades. UnderstandingfactorscontributingtotheoveruseofCT C-spinemayinformtargetedstrategiestoincreasedecisionruleadherenceandtherebyreduceunnecessaryimaging studies.Ourobjectiveinthisstudywastoidentifythemajor factorsassociatedwiththeoverutilizationofCTcervical spineimaging,asadjudicatedbytheNEXUSC-spineruleas areferencestandard,usingalogisticregressionmodel.
METHODS
Thiswasamulticenter,retrospectivereviewofalladult patientswhounderwentCTcervicalspineimagingfor evaluationofblunttraumaticspinalinjury.Weobtained dataonpatientswhopresentedtoanurban,tertiary academicED(approximately77,000annualpatient encounters)andthreeaffiliatecommunityEDs(ranging fromapproximately13,000–43,000annualpatient encounters)inJanuaryandFebruary2019.Exclusion criteriaincludedpatients <18yearsofage,andCT indicationsthatwerenontraumatic,penetratingtrauma,or unspecified.Thisstudywasgrantedaninstitutionalreview boardexemption.
Weextracteddatafromtheelectronichealthrecordonall patientswhounderwentCTofthecervicalspineintheED duringthepre-specifiedperiod.Inadditiontothe demographicdataobtained,eachchartwasmanually reviewedbyasinglereviewerforthepresenceofeachofthe fiveNEXUScriteria:focalneurologicaldeficit;midline cervicalspinetenderness;distractinginjury;intoxication;or alteredmentalstatus.Duringinitialchartreview,wealso collecteddataontheCanadiancriteria.However,therewas
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
CTofthecervicalspineisfrequently performedonpatientswhoarelowriskfora clinicallysigni fi cantinjurybywell-validated criterialiketheNEXUSC-spinerule.
Whatwastheresearchquestion?
Wesoughttoidentifyfactorsthatare associatedwithoverutilizationofCT cervicalspine.
Whatwasthemajor findingofthestudy?
Variablesassociatedwithoveruseincludeage > 65,lowerEmergencySeverityIndexscore, arrivalnotbyEMS,anticoagulation,and non-universityacademicsite.
Howdoesthisimprovepopulationhealth?
Thesevariablesmayguidefuture interventionstoreduceoveruseofCTcervical spine,resultinginimprovedEDef fi ciency, reductioninradiationexposure,andlower healthcarecosts.
inadequatedatatoproceedwithanalysisoftheCanadian C-spinerulebecauseofinsufficientclinicaldocumentationof low-riskfactorsandrangeofmotionoftheneck.Duetothe demandsofchartreviewandthenumberofcases,weselected atwo-monthstudyperiodforfeasibility.
WedefinedtheNEXUScriteriaasfollows:1)focal neurologicaldeficit anyacuteabnormalityofthemotoror sensoryexamthatwasnotattributedtopain;2)midline tenderness bonyormidlinetendernessoftheneckor cervicalspine;3)distractinginjuries fracturesofthe humerus,radius,ulna,femur,tibia, fibula,orsternum, multipleribfractures,oranyotherinjurythatwas documentedas “distracting”;4)intoxication clinical signsofintoxicationonexam,historyofrecentalcohol intake,oradetectableserumethanollevel;and5)altered mentalstatus GlasgowComaScorebetween3–14as documentedbythephysicianornurse,ordocumentation thatthepatientwasdisoriented,confused,nonverbal,or unresponsive.Eachofthesecriteriahashighclinical relevancethatwarrantsdocumentationinthehealthrecord; therefore,NEXUScriteriathatwerenotdocumented werepresumedtobeabsent.Patientswhowerenegativefor all fivecriteriaweredeemedatlowriskforaclinically significantcervicalspineinjurybyNEXUScriteria.We classifiedtheCTcervicalspinestudiesas “overutilization” if
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 968
FactorsAssociatedwithOverutilizationofComputedTomographyoftheC-Spine
Chamberlinetal.
theywereorderedonpatientswhowereatlowriskby NEXUScriteria.
Weperformedmultivariablelogisticregressiontoidentify factorsassociatedwithobtainingCTcervicalspineimaging despitelow-riskclassificationbytheNEXUSC-spinerule. Thefollowingvariableswereincludedintheregression analysis:age;gender,mechanismofinjury;EDsite; EmergencySeverityIndex(ESI)score;arrivaltimeofday; arrivaldayofweek;meansofarrival;anticoagulationstatus; concurrentheadCT;traumaactivationlevel(ie,1,2,3,or none);physicianleveloftraining(ie,residentorattending); andorderingattending.Therewerenomissingorimputed values.Traumaactivationlevel,ESI1,physicianlevelof training,andorderingattendingwereremoveddueto significantmulticollinearity(over70%)withEDsite. Variablestatisticalsignificancewasdenotedbya P -value oflessthan0.05.WeperformedallanalysesusingR version4.0.2(RFoundationforStatisticalComputing, Vienna,Austria).
RESULTS
Duringthetwo-monthstudyperiod,1,051CTsofthe cervicalspinewereperformedacrossallsites,and889metthe inclusioncriteria.Baselinecharacteristicsofthestudy populationareshownin Table1.Ofthescansthatmet inclusioncriteria,376(42.3%)didnotmeetanyofthe NEXUScriteria.Notably,ofthe376CTsthatwere performedonNEXUS-negativepatients,373(99.2%)were negativeforanyacutefracture.Twoimageswerepositivefor
(Continuedonnextcolumn)
clinicallyinsignificanttransverseprocessfracturesthatdid notrequireintervention.Onewasnondiagnosticdueto motionartifact,andthispatientdidnotsubsequentlyrequire furtherimaging,intervention,ormanagement.Noneofthe patientsintheNEXUS-negativegroupwereidentifiedto haveaclinicallysignificantcervicalspinefracture.Inthe NEXUS-positivegroup,19/513CTs(3.7%)werepositivefor fracture,and fivewereindeterminateforfracture.All five patientswithindeterminateinitialimagingunderwent follow-upimagingwithMRIorrepeatCT.Fourhadno injuryonfollow-upimaging,andonewasfoundtohave aclinicallysignificantfracture.Theseresultsareshown in Figure1
Variablen% Age 18–4417519.7 45–6420723.3 65–8430033.7 ≥8520723.3 Gender Male43849.3 Female45150.7 Mechanismofinjury Fall66074.2 MVC15417.3 Assault202.2 Seizure171.9 Pedestrianstruck101.1 Other283.1
Table1. Populationbaselinecharacteristicsforadultpatientswho presentedtofouremergencydepartmentsforevaluationofpotential cervicalspinetraumaticinjury.
Variablen% Siteofarrival AcademicED58565.8 CommunityED#19510.7 CommunityED#217219.3 CommunityED#3364.0 EmergencySeverityIndexscore 1525.8 229422.1 343148.5 410511.8 510.1 Traumaactivationlevel 1242.7 216919.0 3171.9 None67976.4 Meansofarrival Emergencymedicalservices72881.9 Walk-in16118.1 Anticoagulation Yes13515.2 No74884.1 ConcurrentCThead Yes77587.2 No11412.8 Roleoforderingclinician Resident48054.0 Attending40445.4 Advancedpracticepractitioner40.4
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 969 Chamberlinetal. FactorsAssociatedwithOverutilizationofComputedTomographyoftheC-Spine
Table1. Continued.
MVC, motorvehiclecollision; ED, emergencydepartment; CT
, computedtomography.
Theregressionanalysisoutputisshownin Table2. Variablesassociatedwithincreasedlikelihoodof unnecessaryimagingincludeage65–84(P < 0.001);age ≥85years(P < 0.001);arrivalbywalk-in(P < 0.001);ESI2 (P < 0.01);ESI3(P < 0.001);andanticoagulationuse (P < 0.05).Patientswhopresentedtothetertiaryacademic EDhadasignificantlylowerlikelihoodofunnecessary imaging(P < 0.01).
DISCUSSION
Ourinvestigationidentifiedmultiplefactorsassociated withoverutilizationofCTC-spineimaging.Inaddition,our studyconfirmedpriorreportsrelatedtoC-spineevaluation, redemonstratingthesensitivityoftheNEXUSC-spinerule andthesignificantoverutilizationofcervicalspineimaging. Thisstudyexpandstheverylimitedpublishedliteratureon CToverutilizationintheEDsetting.Itisthe firstmulticenter investigationtoevaluateCTC-spineoverutilizationandthe
firsttostudythetopicincommunityEDs.Thesenovel findingshavepotentialimplicationsforfutureeffortsto reduceunnecessaryCTimagingofthecervicalspine.
TheoutcomesforNEXUS-negativepatientsinthisstudy alignwithpriordatavalidatingthesensitivityoftheNEXUS C-spineruleforidentifyingcervicalspinefractures.Noneof thepatientsintheNEXUS-negativecohortwerefoundto haveaclinicallysignificantcervicalspineinjury.Despitethis sensitivitywithinourownpatientpopulation,nearlyhalfof allcervicalspineCTswereordereddespitethepatient’ s statusasNEXUSnegative.
Ourregressionanalysisdemonstratedthatpatientagewas stronglyassociatedwithoverutilization,withgeriatric patientsmorelikelytoundergoCTimagingdespitebeing NEXUS-negative.Thereareseveralfactorsthatmaybe drivingthisassociation.Somephysiciansmaybeinfluenced intheirpracticebytheCanadianC-spinerule,which recommendsimagingforpatients >65yearsinage.Some

VariableOddsratio P-valueCI2.5%CI97.5% AcademicED0.56 <0.050.390.79 Age65–843.40 <0.0011.936.09 Age85+ 3.63 <0.0011.986.78 Walk-inarrival2.61 <0.0011.694.06 ESI24.08 <0.011.7011.46 ESI35.35 <0.0012.2315.09 Onanticoagulation1.55 <0.051.012.40 ED
Table2. Theoutputofthelogisticregressionanalysisshowsthatthevariablessignificantlyassociatedwithoverutilizationofcomputed tomographyC-spineincludeEDsite,age,meansofarrival,ESIscore,andanticoagulationstatus.
,emergencydepartment; ESI,EmergencySeverityIndex; CI,confidenceinterval.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 970 FactorsAssociatedwithOverutilizationofComputedTomographyoftheC-Spine Chamberlinetal.
Figure1. Ofthe1,051computedtomographyC-spinestudiesperformedinthestudyperiod,889metinclusioncriteria.Forty-twopercentof thestudieswereperformedonNEXUS-negativepatients,andnoneoftheNEXUS-negativepatientswerefoundtohaveaclinically significantcervicalspineinjury.
cliniciansmayalsobelessjudiciouswithimagingingeriatric patients,particularlybecauseofaperceivedhigher likelihoodofinjuryandlowerlong-termriskofradiation amongolderadults.Nonetheless,ourresultsreinforcethat ageshouldnotinfluenceCTdecision-making;noneofthe NEXUS-negativepatientsinourstudypopulation,including thepatientswhowereover65,werefoundtohaveaclinically significantfracture.FutureeffortstoreduceCT overutilizationshouldemphasizethatalthoughradiation maybelessofaconcernintheelderlypopulation,wedidnot findanyadditionalriskbasedonagealone,andthereare othersignificantnegativeramificationsofoverutilization includingcost,EDthroughput,andincidental findings.
Incontrasttoage,concurrentCTheadwassurprisingly notassociatedwithoverutilizationofCTC-spine.We hypothesizethatsomephysiciansmayorderaCTofthe cervicalspineonaNEXUS-negativepatientifthepatientis alreadygoingtobeundergoingaCThead,andtheclinician maynotperceivemuchadditionalrisktoorderinga concurrentCTC-spine.However,inthispopulation,this variablewasnotsignificant,likelyduetocollinearity(though underthe70%threshold)betweenorderingofCTheadand CTC-spine.Thevastmajorityofthepatientsinthisstudy underwentaconcurrentCThead,andtherewasnota statisticallysignificantdifferencebetweentheNEXUSpositiveandNEXUS-negativecohorts.
Meansofarrivalwasalsonotedtobeasignificantvariable inthismodel,withanincreasedlikelihoodofoverutilization inpatientswhoarrivedaswalk-ins.Thisislikelyrelatedto patientself-sortingofarrivalmodality.Wehypothesizedthat patientswhowalkintotheEDarecategoricallylesslikelyto haveasignificantinjury.Furthermore,walk-inpatientsare lesslikelytomeetcertainNEXUScriteria,suchashavinga distractinginjuryoraneurologicaldeficit,whichtypically warrantEMStransport.Thus,itislikelythatfewerCTs areorderedonwalk-inpatients,whichmaybedriving thisphenomenon,althoughadefinitiveexplanation remainsunclear.
Patientswhowereonanticoagulantsweremorelikelyto receiveunnecessaryCTimagingofthecervicalspine.Our studywasnotdesignedtoexploretheunderlyingdriversof thisbehaviorortoinfercausality.Itispossiblethatpatients onanticoagulationweremorelikelytoundergoCThead, evenwithrelativelyminormechanismsofinjury,and cliniciansreflexivelyorderedaconcurrentCTC-spine,asit hasbeenestablishedthatacommonpracticepatterninour studypopulationinvolvesconcurrentorderingofCThead andCTC-spine.However,furtherresearchwouldbeneeded toexplorethishypothesis.
Additionally,ESIscoresof2and3werealsoassociated withoverutilization.This findingwasofunclearsignificance, butitmayofferpotentialtargetsforfutureinterventionsto reduceCToverutilization.TheEDsiteofpresentationwas significantlyassociatedwithoverutilizationinthisstudy.At
theacademictertiarycareED,therewassignificantlyless overutilizationcomparedtothecommunityEDs.Itis hypothesizedthatacademicfacultyandresidentsmaybe morelikelytofollowevidence-basedguidelinesthan physicianspracticingatcommunitysites;however,thereis notablysignificantoverlapintheclinicianswhopracticeat eachofthesitesinthisstudy.Thiscouldalsobearesultof patientself-selectionsimilartomodeofarrivaldiscussed above.Furtherinvestigationiswarrantedwithregardtoour observationsofoverutilizationintheacademiccentervs communitysitesbecauseifthisisageneralizedphenomenon, itmaybetterinformstrategiestoreduceCToverutilization onanationallevel.Furthermore,todate, findingsrelatedto resourceutilizationonteachingvsnon-teachingsettingshave showneitherequivalenceoroveruseintheacademic setting.17–20 Ourresultsappeartorefutethistrend,atleast forCTC-spineutilization,forreasonsthatremainunclear.
Theassociationsidentifiedinthisstudycanbeusedto informstrategiestoimprovedisseminationandadoptionof theNEXUSC-spineruleand,thus,reduceunnecessaryCT imaging.AreductioninoverutilizationofCTimagingmay reducehealthcarecosts,minimizeunnecessaryradiationto patients,andimproveEDthroughput.Ataminimum, emphasisonclinicianeducationregardingsensitivityof NEXUSinelderlypatientsmaybeneeded.Itmayalsobe prudenttofocuseducationalstrategiesatcommunity practicesites,whichdemonstratedhigherratesof overutilizationinourstudy.Additionally,thisinformation couldbeusedinauditandfeedbackstrategiestoincludenot justutilizationratesbutagerangesandratesofidentifying significantinjuries.
LIMITATIONS
Foremost,ourinvestigationwasnotdesignedto determinecausalitybutratheronlyassociation.Therefore, whilemanyofthevariablesusedinthisregressionwere correlatedwithoverutilizationofCTimaging,wewere unabletoproveacausativerelationshipforthesefactors. Furthermore,whileourinvestigationdidincludefourEDs thatdifferedinsizeandpatientpopulations,theywere staffedbymembersofasingleacademicdepartmentof emergencymedicine,limitinggeneralizability.
Thisstudywasalsolimitedbythedocumentationthatwas availableuponchartreview.ItispossiblethatNEXUS criteriacouldhavebeenpresentbutwerenotdocumentedby theclinician,causingtherateofoverutilizationtobe overestimated.However,giventheclinicalimportanceof eachoftheNEXUScriteriaintheevaluationofpatientswith potentialcervicalspineinjury,itislikelythatpositivecriteria wouldhavebeenincludedintheclinician’sdocumentation. Inadditiontoreviewingcliniciandocumentation,chart reviewersalsoreviewedlabstudies,imaging,and nursingnotestoidentifyanyinformationregardingthe NEXUScriteria.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 971 Chamberlinetal. FactorsAssociatedwithOverutilizationofComputedTomographyoftheC-Spine
Tosupportfeasibility,ourstudywaslimitedtoatwomonthperiod.Theseoccurredduringwintermonths,and someofthepatientshadseason-specificmechanismsof injury.Forexample,mechanismsofinjuryincludedskiing/ snowboardingaccidentsandsnowmobilecollisions. Althoughnoneofthemechanismsofinjuryinthisstudywere significantlyassociatedwithoverutilizationofCTimaging, theremaybesignificantmechanismsofinjurywithseasonal variationthatwerenotidentifiedinthispopulationduetothe timingofthestudy.
Overall,therateofoverutilizationatthesitesinthisstudy washigherthantheratesidentifiedpreviouslyinthe literature.Inthiscohort,nearlyone-halfofthepatientswho underwentCTofthecervicalspinewerenegativebyNEXUS criteria.Althoughthisishigherthanpreviouslyreported rates,itshouldbenotedthatthereisverylimitedpublished dataonthistopic,andpriorresearchhasbeenlimitedto academicmedicalcenters.12–14 Itisunclearwhetherorhow thismayhaveaffectedourobservedresults.
Lastly,theremaybesignificantvariabilityinindividual physicianpracticepatterns,whichmaybeafactorassociated withoverutilizationofCTimaging.However,duetothe limitednumberofstudiesthatwereorderedbyeach physicianduringthestudyperiod,wewereunabletoassess theassociationbetweenindividualphysicianpractice patternsandoverutilization.Futureinvestigationwith alargerstudypopulationwouldbeneededtoanswer thisquestion.
CONCLUSION
ComputedtomographyC-spineimagingcontinuestobe overutilizedintheEDsetting.Factorsthatwereassociated withoveruseofCTimaginginclude >65yearsold,ESIscores 2and3,arrivalbywalk-in,anticoagulation,andpresenting toacommunityED.These findingsmayassistinguiding futureinterventionstooptimizeresourceutilizationand promotesaferandmoreefficientemergencycare.
AddressforCorrespondence:KarlT.Chamberlin,MD,Universityof MassachusettsChanMedicalSchool,DepartmentofEmergency Medicine,55LakeAvenueNorth,Worcester,Massachusetts01615. Email: karl.chamberlin@umassmemorial.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Chamberlinetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.CairnsC,KangK. NationalHospitalAmbulatoryMedicalCareSurvey: 2019EmergencyDepartmentSummaryTables.Hyattsville,Maryland: NationalCenterforHealthStatistics;2022.
2.InabaK,ByerlyS,BushLD,etal.Cervicalspinalclearance:a prospectiveWesternTraumaAssociationmulti-institutionaltrial. JTraumaAcuteCareSurg.2016;81(6):1122–30.
3.HaslerRM,ExadaktylosAK,BouamraO,etal.Epidemiologyand predictorsofcervicalspineinjuryinadultmajortraumapatients:a multicentercohortstudy. JTraumaAcuteCareSurg
2012;72(4):975
81.
4.MilbyAH,HalpernCH,GuoW,etal.Prevalenceofcervicalspinalinjury intrauma. NeurosurgFocus.2008;25(5):E10.
5.YoungAJ,WolfeL,TinkoffG,etal.Assessingincidenceandriskfactors ofcervicalspineinjuryinblunttraumapatientsusingtheNational TraumaDataBank. AmSurg.2015;81(9):879–83.
6.LarsonDB,JohnsonLW,SchnellBM,etal.NationaltrendsinCTusein theemergencydepartment:1995–2007. Radiology
2011;258(1):164–73.
7.BerdahlCT,VermeulenMJ,LarsonDB,etal.Emergencydepartment computedtomographyutilizationintheUnitedStatesandCanada. Ann EmergMed.2013;62(5):486–94.e3.
8.MillsAM,RajaAS,MarinJR.Optimizingdiagnosticimaginginthe emergencydepartment. AcadEmergMed.2015;22(5):625
31.
9.BellolioMF,HeienHC,SangaralinghamLR,etal.Increased computedtomographyutilizationintheemergencydepartmentandits associationwithhospitaladmission. WestJEmergMed 2017;18(5):835–45.
10.EvansCS,ArthurR,KaneM,etal.Incidentalradiology findingson computedtomographystudiesinemergencydepartmentpatients: asystematicreviewandmeta-analysis. AnnEmergMed 2022;80(3):243–56.
11.HoffmanJR,MowerWR,WolfsonAB,etal.Validityofasetofclinical criteriatoruleoutinjurytothecervicalspineinpatientswithblunttrauma. NationalEmergencyX-RadiographyUtilizationStudyGroup. NEnglJ Med.2000;343(2):94–9.
12.StiellIG,ClementCM,McKnightRD,etal.TheCanadianC-spinerule versustheNEXUSlow-riskcriteriainpatientswithtrauma. NEnglJ Med.2003;349(26):2510–8.
13.GriffithB,BoltonC,GoyalN,etal.ScreeningcervicalspineCTinalevel Itraumacenter:overutilization?. AJRAmJRoentgenol 2011;197(2):463–7.
14.GriffithB,KellyM,ValleeP,etal.ScreeningcervicalspineCTinthe emergencydepartment,phase2:aprospectiveassessmentofuse. AJNRAmJNeuroradiol.2013;34(4):899–903.
15.GriffithB,ValleeP,KruppS,etal.ScreeningcervicalspineCTinthe emergencydepartment,phase3:increasingeffectivenessofimaging. JAmCollRadiol.2014;11(2):139–44.
16.UriellML,AllenJW,LovasikBP,etal.Yieldofcomputedtomography ofthecervicalspineincasesofsimpleassault. Injury 2017;48(1):133–6.
–
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 972 FactorsAssociatedwithOverutilizationofComputedTomographyoftheC-Spine Chamberlinetal.
17.ReznekMA,MichaelSS,HarbertsonCA,etal.Clinicaloperationsof academicversusnon-academicemergencydepartments:adescriptive comparisonoftwolargeemergencydepartmentoperationssurveys.
BMCEmergMed.2019;19(1):72.
18.SalazarA,CorbellaX,OnagaH,etal.Impactofaresidentstrikeon emergencydepartmentqualityindicatorsatanurbanteachinghospital.
AcadEmergMed.2001;8(8):804–8.
19.FrenchD,ZwemerFLJr,SchneiderS.Theeffectsoftheabsenceof emergencymedicineresidentsinanacademicemergencydepartment. AcadEmergMed.2002;9(11):1205–10.
20.KhaliqAA,HuangCY,GantiAK,etal.Comparisonofresourceutilization andclinicaloutcomesbetweenteachingandnonteachingmedical services. JHospMed.2007;2(3):150–7.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 973 Chamberlinetal. FactorsAssociatedwithOverutilizationofComputedTomographyoftheC-Spine
SOCIAL EMERGENCY MEDICINEAND POPULATION HEALTH
SexualAssaultNurseExaminersLeadtoImproved UptakeofServices:ACross-SectionalStudy
MeredithHollender,MPP*
EllenAlmirol,MPH,MAMS†
MakennaMeyer,BS†
HeatherBearden,RN,SANE-A‡
KimberlyA.Stanford,MD,MPH†‡
SectionEditor: TehreemRehman,MD,MPH
*UniversityofChicago,PritzkerSchoolofMedicine,Chicago,Illinois
† ChicagoCenterforHIVElimination,Chicago,Illinois
‡ UniversityofChicago,SectionofEmergencyMedicine,Chicago,Illinois
Submissionhistory:SubmittedNovember29,2022;RevisionreceivedApril13,2023;AcceptedMay24,2023
ElectronicallypublishedAugust11,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59514
Introduction: SexualAssaultNurseExaminers(SANE),whoaretrainedtoprovidecomprehensiveand compassionatespecialtycaretosexualassaultsurvivors,areincreasinglyusedintheemergency department(ED),butthereislittlepublishedliteraturetosupporttheirbenefit.Inthisstudyweaimedto compareservicesofferedandreceivedbysexualassaultsurvivorsintheEDwhencarewasprovidedby aSANEvsthosewithtraditionalcareteams,hypothesizingthatSANEutilizationwillbeassociatedwith improveduptakeofrecommendedservices.
Methods: Thiswasaretrospectivereviewexaminingallpatientencountersinwhichasexualassault wasdisclosedinalarge,urban,adultEDbetweenJune1,2019–June30,2022.Weextractedtimeline informationfromtheEDencounter,demographicinformation,resourcesofferedtoandacceptedbythe patient,clinicalcaredata,andcontinuityofcaredatafromthemedicalrecord.Weusedunadjustedand adjustedanalysestocomparepatientdemographicsandservicesofferedandacceptedbetweenSANE andnon-SANEencounters.
Results: Weincludedatotalof182encountersintheanalysis,ofwhich130(71.4%)involvedSANEs. Demographicsweresimilarbetweengroups,excepttherewasalargerproportionofcisgendermenin thenon-SANEgroup(14.0%vs5.5%),andthetimingofvisitsdiffered,withnon-SANEvisitsmore commonduringtheovernightshift.Allrecommendedtesting,prophylaxis,andresourceswereoffered morefrequentlyduringSANEvisits,andallbutoneweremorefrequentlyacceptedbypatientsduring SANEvisits,althoughnotallcomparisonsreachedstatisticalsignificance.
Conclusion: PatientswhoreceivedcarefromaSANEweremoreoftenofferedrecommendedservices andresourcesandmorefrequentlyacceptedthem.MakingSANEcareavailableatalltimestothese vulnerablepatientswouldbothimprovepatientoutcomesandallowhospitalstomeetrequiredquality metrics.StatesshouldconsiderexpandinglegislationtoencourageandfundSANEcoverageforall hospitalstosupportaccesstovitalresourcesintheEDforsurvivorsofsexualassault.[WestJEmerg Med.2023;24(5)974–982.]
INTRODUCTION
Sexualassault(SA)isamajorpublichealthissue thataffectspeopleofallsocioeconomicandcultural backgrounds.EachyearintheUnitedStates,morethan 100,000survivorsofSAseekcareintheemergency
department(ED).1 UnderstandingthatsurvivorsofSA areavulnerablegroupwithuniqueacuteandchroniccare needs,therehavebeenrecentmovestowardimplementing legislationthatwillhelpsupportcomprehensiveand compassionatehospitalcareforsurvivors,includingthe
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 974
federalSurvivors’ BillofRightsActof2016,theIllinois SexualAssaultSurvivorsEmergencyTreatmentAct (SASETA)amendedin2019,andtheNoSurprisesfor SurvivorsAct,introducedin2022.2–4 Theselawsaimto protectSAsurvivorsfrom financialruinaftertheirhospital visit,ensuremedicalforensickitsareprocessedinan efficientandtimelymanner,establishcareguidelines andreportingsystemsforhospitalsthattreatSA survivors,andpromotetheprovisionofcomprehensive, trauma-informedcare.
Thegoaloftheseinitiativesistoaddressinequitiesin accesstocarefacedbysurvivorsofSA,amongwhom themostvulnerablemembersofsociety particularly young,socioeconomicallydisadvantagedwomen are disproportionatelyrepresented.5–7 Survivorsfacemany barrierstoreceivingoptimalcare,withfewerthanonein five UShospitalsprovidingall10metricsofwhatisconsidered “comprehensivemedicalcaremanagement” forSAsurvivors intheED.6 Oneproposedmechanismtoaddressthisgapisto usespeciallytrainedSexualAssaultNurse Examiners(SANE).
SexualAssaultNurseExaminerprogramsweredeveloped in1976toaugmenttraining,addressconcernsofphysicians aboutcaringforsurvivorsofsexualassault,decreaselong EDwaittimes,andsupportsensitiveandsociallycompetent care. 8 Manyemergencyphysiciansandnursesfeel unpreparedanduncomfortableprovidingsomeorall necessarypatientcareincasesofSA.9 Theymayalsoface significantchallengesduetotheuniqueEDenvironment, includingcrowding,caringformultiplepatients simultaneously,orneedingtocareforpatientswhorequire immediateattention.Earlierstudieshaveshownthatwhen SANEsprovidecare,theydosoinacompassionate, respectful,andsafemannerthatisassociatedwithfeelingsof confidenceandreliefinsurvivors.10,11 TheSANEsareableto buildaunique,trustingrelationshipwiththeirpatientsthatis focusedonprovidingSAsurvivorswithcontrolandchoices surroundingtheircaredecisions.12
SexualAssaultNurseExaminerprogramsareincreasingly common,andthereisrisingawarenessoftheimportance ofspecializedSANEtraining;however,thereisstilla nationwideshortageofSANEs.13 Ruralareashavefew SANEsandarelesslikelythanurbanareastohave24-hour continuousSANEcoverage.14 Eveninurbanareas,85.5%of nursesindicatethattheyarenotSANE-trained,yettheyhave caredforSAsurvivorsintheirhealthcareinstitution.13 While somestudieshaveexaminedtheimpactofSANEsonthe patientexperience,fewhaveevaluatedtheeffectsofSANE careonqualitymetricsintermsoftheactualdeliveryof recommendedservicesandresources.
Weconductedthisstudyatalarge,urban,tertiarycare hospitalwithaLevelItraumacenter.Approximately60 – 80 adultsurvivorsofSAvisitourEDannually.InthisED, aSANEisunavailableintheadultEDapproximately
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Fewstudieshaveexaminedtheimpactof SexualAssaultNurseExaminers(SANE)on thepatientexperience,orevaluatedtheir effectsondeliveryofrecommendedservices.
Whatwastheresearchquestion?
Weresexualassaultsurvivorsmorelikelyto receiverecommendedhealthcareservicesin theEDiftheywerecaredforbyaSANE?
Whatwasthemajor findingofthestudy?
PatientscaredforbyaSANEweremore likelytobeofferedadvocateservices (P < 0.05),medicalforensicexamkits (P < 0.05),andresourcepackets(P < 0.05).
Howdoesthisimprovepopulationhealth?
SexualassaultsurvivorscaredforbyaSANE aremorelikelytoreceiverecommended treatmentintheED,whichmayhavemajor impactsonlong-termoutcomesforthem.
20-30%ofthetime,mostlyovernight.CareforaSAsurvivoris alwaysprovidedbyaSANE,ifavailable;ifnot,thencareis providedbyaphysicianornon-physiciancliniciananda registerednurse,whichisthestandardofcare.Duringavisit forSA,patientsareofferedamedicalforensicexamination kit,ifappropriate,whichcanbeusedasevidenceshoulda casegototrial,testingandprophylaxisforHIVandother sexuallytransmittedinfections(STI),apregnancytest, andemergencycontraception.Theyshouldalsohavethe opportunitytospeakwithpolice,aSAadvocate,andsocial services,andaccessotherhospitalresourcesasneeded,such asbehavioralhealthsupportorsafehousingoptions,and theyaregivenapacketofpost-visitresourcesbefore discharge.BothSANEsandregisterednurseshaveaccessto achecklistoftheseitemsthatshouldbecompletedduring theEDvisit.Thisstudycomparedtherateatwhichthese serviceswereofferedoracceptedbetweenencountersin whichcarewasprovidedbyaSANEvsthosewith traditionalcareteams,hypothesizingthatSANEswouldbe morelikelytoofferservices,andthattheirpatientswouldbe morelikelytoacceptthem.Increaseduptakeof recommendedserviceswithSANEcarewouldsupport theadoptionandexpansionofSANEprograms,which wouldultimatelyaddressdisparitiesincarefacedby SAsurvivors.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 975 Hollenderetal. SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices
METHODS StudyDesign
Thiswasaretrospectivereviewofalladultpatient encountersinwhichaSAwasdisclosed(definedasatriage chiefcomplaintorEDdiagnosiscodeforSA)intheED betweenJune1,2019–June30,2022.Encounterswere includedevenifthepatientleftbeforethevisitwas consideredcomplete,providedanyserviceshadbeenoffered. Forpatientswhowereincludedmorethanonce(i.e.,hadtwo instancesofSAduringthestudyperiod),eachencounterwas consideredanindependentevent,asthedetailsoftheassault andtheEDencounterwereunique.Thisstudywasapproved byourinstitutionalreviewboard.
Measures
Dataextractedfromtheelectronichealthrecord(EHR) includedthefollowing:demographics(e.g.,age,gender,race/ ethnicity);thetimethepatientwasadmittedtotheED;days sinceincidentreported;clinicalcaredata(e.g.,STItesting andprophylaxis,forensickitcollection,pregnancytesting andprovisionofemergencycontraceptives);andcontinuity ofcaredata(e.g.,linkagetoprimarycareormentalhealth resources).Encountertimewasdividedaccordingtoshift timesintheED,with6:30 AM
2:30 PM consideredthe morning,2:30 PM
10:30 PM consideredtheafternoon, and10:30 PM–6:30 AM consideredovernight.
Theprimaryoutcomesofthisstudyweretheproportions ofpatientsofferedandacceptingserviceswhencaredforbya SANEornon-SANEteam.Incertaincases,forwhicha servicewasnotapplicableduringtheEDvisit(e.g.,already completedelsewhere,toomuchtimepassedsincethe incident,orpregnancytestingforindividualswithouta uterus),thesewereremovedfromthedenominatorof servicesoffered.Ifanapplicableservicewasnotexplicitly documentedtohavebeenofferedoracceptedintheEHR, itwasconsiderednotofferedornotacceptedforthe purposesoftheanalysis.Ifaservicewaspartiallyaccepted (e.g.,prophylaxisforgonorrheaandchlamydiabutnot hepatitis),theoutcome(e.g.,STIprophylaxis)was consideredacceptedintheanalysis.
StatisticalAnalyses
Wecomparedpatientdemographicsandtheproportionof patientsofferedandacceptingservicestoidentifydifferences betweenSANEandnon-SANEevaluatedpatients,using a t -testforcontinuousvariablesandchi-square(χ2)testor theFisherexacttestforcategoricalvariables.Weused logisticregressiontocalculateoddsratiosbetweengroups, adjustingforpatientarrivaltimeasapotentialconfounderin themodel.Offeringthemedicalforensickit,accepting thedischargeresourcepacket,andacceptingthesocial workconsultwereexcludedfromthelogisticregression analysisduetothepresenceofzeroresponses.Differences wereconsideredsignificantat P ≤ 0.05.Weperformed
allstatisticalanalysesusingRversion4.2.1.(RCore Team,RFoundationforStatisticalComputing, Vienna,Austria).
RESULTS
ParticipantCharacteristics
Overthethree-yearstudyperiod,weidentified182adult EDencountersforSA,including177uniqueindividuals, five ofwhompresentedontwoseparateoccasionsforSA.Ofall encounters,130(71.4%)receivedcarefromaSANE,while52 (28.6%)receivedthestandardofcarewithaphysician/nurse team(Table1).Cisgenderwomen(90.4%)andnon-Hispanic Blackindividuals(82.7%)representedthemajorityof encounters,withameanageof30years(range18–79). Demographicsweresimilarbetweenthetwogroups; however,thenon-SANEgrouphadmorecisgendermen thantheSANEgroup(14.0%vs5.5%)andnotransgender individuals.Thegroupsdifferedbytimeofpatientarrival, withalargerproportionofSANEencounters(48.5%)inthe afternoon,andthelargestproportionofnon-SANE encounters(50.0%)duringtheovernightshift(P < 0.01). BothSANEandnon-SANEgroupspresentedtotheED withinsimilartimeframesaftertheassault(mean1.16days, SD1.44,non-SANEvsmean1.28days,SD1.72,SANE; P = 0.65).Additionally,therewasasignificantdifference inthenumberofpatientswholeftbeforetreatmentwas complete(15.4%non-SANEvs2.3%SANE, P < 0.01).
Resources,MedicalCare,andServicesOffered andAccepted
Whilenotalldifferenceswerestatisticallysignificant, everytypeofrecommendedresourceorcarestudiedwas offeredinahigherproportionofSANEencountersthannonSANEencounters(Table2).Significantdifferencesobserved inservicesofferedbetweenSANEandnon-SANEgroups includedSAadvocate(97.7%SANEvs89.4%non-SANE; oddsratio[OR]5.04,95%confidenceinterval[CI]1.1621.99, P = 0.03),medicalforensickit(100%vs93.6%, P = 0.02); pregnancytesting(96.2%vs86.1%;OR4.11,95% CI1.09-15.54, P = 0.05);anddischargeresourcepacket (69.0%vs48.9%;OR2.33,95%CI1.16-4.65, P = 0.03). AhigherpercentageoftheSANEgroupwasoffered emergencycontraception(94.3%vs82.4%, P = 0.07), althoughnotsignificant.Theproportionofencounters offeredsafedispositionplanning(28.7%vs21.7%) orasocialworkconsult(33.3%vs27.7%)wasmarkedly lowinbothgroups,althoughitisunknownwhether thiswasrelatedsimplytolackofdocumentationaround theseservices.
Forthoseservicesdocumentedtohavebeenapplicable andoffered,theproportionofrecommendedresourcesand careacceptedinSANEencounterswasalsohigherfor everyservicecategoryexceptthedischargeresourcepacket, whichwascomparablebetweengroups(98.9%SANEvs
–
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 976 SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices Hollenderetal.
SANE, SexualAssaultNurseExaminer.
*Indicatesa P-value ≤ 0.05;Fishertestswereconductedduetothesmallcellcounts.
+Gender(n = 177)andrace/ethnicity(n = 177),giventhat fiveindividualshadtwoencounters.
^Patientarrivaltimeswerecategorizedintothefollowing:morning6:30 AM–
Missingvaluesforrace/ethnicity(n = 15,8%)anddayssinceincident(n = 7,4%).
100.0%non-SANE, P = 1.00).Amuchlargerproportionof encountersintheSANEgroupacceptedSAadvocate services(78.7%vs61.9%;OR2.28,95%CI1.07-4.84, P = 0.05)andamedicalforensickit(88.4%vs68.2%;OR 3.55,95%CI1.54-8.15, P < 0.01).Largedifferencesthatdid notreachstatisticalsignificancewerefoundforseveral servicetypes,includingmakingapolicereport(82.4%vs 67.5%),HIVprophylaxis(76.3%vs64.1%),HIVtesting (93.4%vs85.7%)andSTItesting(93.5%vs86.0%), emergencycontraception(66.3%vs57.1%),andsocial workerconsultation(100%vs84.6%).
BecauseSANEencountersoccurredmoreoftenduring theafternoonandnon-SANEencountersmoreoften overnight,additionalmodelswerecreatedtoadjustforthe effectsofpatientarrivaltimeonservicesofferedandaccepted (Tables3 and 4).Intheadjustedanalysis,SANEencounters werestillmorelikelytoofferrecommendedservicessuchas SAadvocates(adjusted[aOR]5.51,95%CI1.26-24.05, P = 0.03)andtoacceptboththeadvocateservices (aOR2.60,95%CI1.22-5.52, P = 0.02)andthemedical forensickit(aOR2.90,95%CI1.26-6.66, P = 0.02).Ofnote, afteradjustingforarrivaltime,thehigherproportionof SANEencounterscompletingapolicereportwassignificant (aOR2.63,95%CI1.17-5.93, P = 0.03).Whilethe
non-SANEgrouphadahigherproportionofcisgendermen thantheSANEgroup(Table1),themodelwasnotadjusted forpatientgender,asthisobserveddifferencedidnotreach statisticalsignificance.
DISCUSSION
WefoundthatsurvivorscaredforbyaSANEweremore oftenofferedtherecommendedcareandresourcesinevery categoryexamined,andtheyacceptedthisoffermoreoften forallbutonecategory.TheSANEsweresignificantlymore likelytoofferapregnancytestandemergencycontraception, andsurvivorscaredforbyaSANEweresignificantlymore likelybothtobeofferedandtoacceptSAadvocateservices andamedicalforensicexaminationkit.Whileonlyafew categoriesreachedstatisticalsignificance,thisislikelydueto thesmallsamplesizeinherentinstudyingarelatively uncommonevent,andtheresultsofthisstudysuggestmajor potentialbenefitsfromSANEcare.
17
Providing
RecentdatashowsaconcerningtrendinUSEDvisitsfor SA,whichhaveincreasedmorethan1,533.0%from2006to 2019.5 Young,low-incomewomenaredisproportionately representedamongsurvivorsofSA.5 Survivorsmayhave increasedriskforavarietyofmentalhealthcomplications, substanceuse,andchronichealthconditions.15
–
Allencounters (n = 182) SANE (n = 130) Non-SANE (n = 52) P-value n(%)n(%)n(%) Age(mean,SD) 30.2(13.1)30.1(13.5)30.6(12.3)0.81 Gender+ 0.11 Female160(90.4%)117(92.1%)43(86.0%) Male14(7.9%)7(5.5%)7(14.0%) Transgender/Non-binary3(1.7%)3(2.4%)0(0.0%) Race/Ethnicity+ 0.83 Non-HispanicWhite14(8.4%)10(8.1%)4(9.3%) Non-HispanicBlack138(82.7%)101(81.5%)37(86.0%) Hispanic9(5.4%)8(6.5%)1(2.3%) Other6(3.6%)5(4.0%)1(2.3%) Patientarrivaltime^ <0.01* Morning48(26.4%)32(24.6%)16(32.0%) Afternoon73(40.1%)63(48.5%)10(18.0%) Overnight61(33.5%)35(26.9%)26(50.0%) Dayssinceincident(mean,SD)1.191.511.161.441.281.720.65
Table1. DemographicsofemergencydepartmentpatientencountersforsexualassaultfromJune1,2019–June30,2022, bytypeofcareteam.
2:30
PM–10:30 PM;andovernight10:30 PM–6:30 AM
PM;afternoon2:30
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 977 Hollenderetal. SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices
Table2. BivariateanalysisofservicesofferedandacceptedbyemergencydepartmentpatientsevaluatedaftersexualassaultfromJune1, 2019–June30,2022,bytypeofcareteam.
Safedischargeplanning
SANE, SexualAssaultNurseExaminer; STI,sexuallytransmittedinfections.
*Indicatesa P-value ≤ 0.05; +Fishertestswereperformedduetosmallcellcounts.
SANE(n = 130)Non-SANE(n = 52) P-value n/N(%)n/N(%) Testingandprophylaxis HIV testing Offered+ 122/128 (95.3%) 42/46 (91.3%) 0.46 Accepted+ 113/121 (93.4%) 36/42 (85.7%) 0.20 STItesting Offered+ 124/129 (96.1%) 43/47 (91.5%) 0.25 Accepted+ 115/123 (93.5%) 37/43 (86.0%) 0.20 Pregnancytesting Offered+ 102/106 (96.2%) 31/36 (86.1%) 0.05* Accepted+ 94/101 (93.1%) 28/31 (90.3%) 0.70 HIVprophylaxis Offered+ 115/126 (91.3%) 39/44 (88.6%) 0.56 Accepted 87/114 (76.3%) 25/39 (64.1%) 0.20 STIprophylaxis Offered+ 122/129 (94.6%) 41/46 (89.1%) 0.31 Accepted 103/121 (85.1%) 33/41 (80.5%) 0.65 Emergencycontraception Offered+ 99/105 (94.3%) 28/34 (82.4%) 0.07 Accepted 65/98 (66.3%) 16/28 (57.1%) 0.50 Servicesandresources Medicalforensickit Offered+ 129/129 (100.0%) 44/47 (93.6%) 0.02* Accepted 114/129 (88.4%) 30/44 (68.2%) <0.01* Sexualassaultadvocate Offered+ 127/130 (97.7%) 42/47 (89.4%) 0.03* Accepted 100/127 (78.7%) 26/42 (61.9%) <0.05* Policereport Offeredtocall+ 119/125 (95.2%) 40/44 (90.9%) 0.29 Reportcomplete 98/119 (82.4%) 27/40 (67.5%) 0.08 Resourcepacket Offered 89/129 (69.0%) 22/45 (48.9%) 0.03* Accepted+ 88/89 (98.9%) 22/22 (100.0%) 1.00 Socialworkerconsult Offered 43/129 (33.3%) 13/47 (27.7%) 0.60 Accepted+ 43/43 (100.0%) 11/13 (84.6%) 0.05
Offered 37/129 (28.7%) 10/46 (21.7%) 0.47 Accepted+ 36/37 (97.3%) 9/10 (90.0%) 0.38 Leftbeforetreatmentcomplete 3/130 (2.3%) 8/52 (15.4%) <0.01
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 978 SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices Hollenderetal.
STI, sexuallytransmittedinfections.
*Indicatesa P-value ≤ 0.05;referencegroup = non-SexualAssaultNurseExaminers.Analysesareadjustedforpatientarrivaltime.Odds ratioanalysiscouldnotbecalculatedforN/Aentriesdueto0responsesinasinglegroup.
Table4. OddsratiosofservicesacceptedbyemergencydepartmentpatientsevaluatedaftersexualassaultfromJune1,2019,throughJune 30,2022,bytypeofcareteam.
*Indicatesa P-value ≤ 0.05;Referencegroup = non-SexualAssaultNurseExaminers.Analysesareadjustedforpatientarrivaltime.Odds ratioanalysiscouldnotbecalculatedforN/Aentriesdueto0responsesinasinglegroup.
comprehensiveandtrauma-informedcaretosurvivorsof SAintheEDisvitaltothelong-termoutcomesforthese vulnerablepatients.However,timeconstraints,crowding,
lackofawarenessortrainingintrauma-informedcare,and manyotherchallengesoftheEDenvironmentcanpresent majorobstacles.
Unadjusted oddsratio 95%Confidence interval P-value Adjusted oddsratio 95%Confidence interval P-value Testingandprophylaxis HIV testing 2.35 (0.77,7.24)0.131.93(0.63,5.95)0.27 STItesting 2.33 (0.76,7.16)0.142.40(0.78,7.36)0.15 Pregnancytesting 1.44 (1.00,16.96)0.621.41(0.87,14.79)0.64 HIVprophylaxis 1.80 (0.82,3.95)0.141.87(0.86,4.10)0.14 STIprophylaxis 1.39 (0.55,3.48)0.492.11(0.48,3.04)0.70 Emergencycontraception 1.43 (0.61,3.38)0.411.61(0.68,3.80)0.29 Servicesandresources Medicalforensickit 3.55 (1.54,8.15) <0.01*2.90(1.26,6.66)0.02* Sexualassaultadvocate 2.28 (1.07,4.84)0.03*2.60(1.22,5.52)0.02* Policereport 2.25 (1.00,5.06)0.052.63(1.17,5.93)0.03* Resourcepacket N/A N/A Socialworkerconsult N/A N/A Safedischargeplanning 4.00 (0.23,70.30)0.343.64(0.21,63.91)0.40
Table3. OddsratiosofservicesofferedtoemergencydepartmentpatientsevaluatedaftersexualassaultfromJune1,2019–June30,2022, bytypeofcareteam.
Unadjusted oddsratio 95%Confidence interval P-value Adjusted oddsratio 95%Confidence interval P-value Testingandprophylaxis HIV testing 1.94 (0.52,720)0.322.04(0.55,7.58) 0.32 STItesting 2.31 (0.59,8.99)0.232.04(0.52,7.94) 0.33 Pregnancytesting 4.11 (1.09,15.54)0.04*3.59(0.95,13.55)0.08 HIVprophylaxis 1.34 (0.44,4.10)0.611.07(0.35,3.26) 0.92 STIprophylaxis 2.13 (0.64,7.06)0.221.59(0.48,5.29) 0.47 Emergencycontraception 3.54 (1.05,11.78)0.04*3.00(0.90,9.97) 0.08 Servicesandresources Medicalforensickit N/A N/A Sexualassaultadvocate 5.04 (1.16,21.99)0.03*5.51(1.26,24.05)0.03* Policereport 1.98 (0.53,7.39)0.311.87(0.50,6.96) 0.37 Resourcepacket 2.33 (1.16,4.65)0.02*1.96(0.98,3.93) 0.07 Socialworkerconsult 1.21 (0.58,2.54)0.591.05(0.50,2.19) 0.91 Safedischargeplanning 1.45 (0.65,3.23)0.361.34(0.60,2.98) 0.49 STI, sexuallytransmittedinfections.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 979 Hollenderetal.
SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices
Recentfederalandstatelawshavebeenpassedor proposedtotrytoaddressthisproblem,requiringcertain standardsforallvisitsforSA.Forexample,theIllinois SASETAactcreateduniversalcareandreportingguidelines andrequiresEDstohavecontinuouscoveragebyaSANEor aclinicianwithequivalenttraining.4 Guidelinesfromthe AmericanCollegeofEmergencyPhysiciansonmanagement ofpatientspresentingafterSAemphasizetheimportanceof “speciallytrained,non-physicianmedicalpersonnel,” which mayincludeSANEs,and “accesstoappropriatemedical, technical,andpsychologicalsupport” forpatients.18 In addition,withtherecentincreasingpopularityofthevaluebasedreimbursementmodel,therewillbe financialincentives forhospitalstoprovideservicestoSAsurvivorsbeyondbasic medicalcare.19 Similarly,theremaybe financialpenaltiesor legalramificationsforhospitalsthatdonotmeetthese qualitymetricsinstatesthathaveimplementedlaws likeSASETA.
TheSANEprogramshavebeenproposedto fillthese gaps,usingdedicatedcarepersonnelwithspecializedtraining incaringforsurvivorsofSA.Theseprogramshavebeen showntoreducepatientwaittimes,increasequalityof examinationandevidencecollection,andprovideoverall comprehensiveandcompassionatecareinatimelymanner.20 DespitegrowingevidenceandguidelinessupportingSANE services,SANEutilizationandavailabilityarehighly variable.Onestudyfoundthat35.5%ofhospitalshadno accesstoSANEservicesatall.13 Hiringandretaininga speciallytrainedgroupofnursestobeavailableatalltimes,if needed,isexpensiveandchallenging.Forhospitalswithout themeanstoexpandSANEcoverage,communityefforts havelaidthegroundworkfortelehealthSANEcoveragein ruralareas.21
Whilethereisagrowingbodyofevidencedemonstrating thebenefitsofSANEcare,thusfarlittlehasbeenpublished ontheeffectofSANEcareonqualitymetrics,whichare importantbothforindividualpatientoutcomesand regulatoryand financialreasons.Evidenceofanassociation betweenSANEcareandimprovedservicedeliverycould encourageexpandedsupportforthedevelopmentand adoptionofSANEprograms.Priorstudiessuggestthat specializedtrainingmayhelpnursesapproachpatientsabout receivingmedicalservicesforaSAinamannerthat encouragesengagementincare.11,22 Whencareisprovided byaSANE,patientsreportpositivepsychologicaloutcomes, suchasfeelingsofempowermentandcompassion.11,22
OnestudyfoundthatSANEsgobeyond “collecting evidence,” andthat “themannerinwhichitwasbeingdone” madeapositiveimpactonpatients.10 Patientsinterviewedin thatstudyfoundthatSANEsprovideda “clearandthorough explanationoftheexamprocessand findings.”10 Inthe presentstudy,moresurvivorscompletedtreatmentintheED whencarewasprovidedbyaSANE.Thismayreflectthe additionaltrainingintrauma-informedcareorthelackof
concurrentclinicaldutiesduringSANEcare,bothofwhich mayleadpatientstoengagemoreintheircare.Additionally, whenserviceswereofferedtosurvivors,theywereacceptedat muchhigherrateswhenofferedbyaSANE.Thislikely reflectsthewayinwhichtheresourcewaspresentedor describedtothesurvivor,whichcertainlycouldbeaffected bytrainingandawareness.
InvolvementofSANESincareisassociatedwithmore medicalservicesprovided,moreforensickitscollected,and morepolicereports filed.23 Thesametrendwasidentifiedfor SANEcareincasesofpediatricSA.24 Inthecurrentstudy, afteradjustingforpatientarrivaltime,policereportswere completedduringSANEencountersatasignificantlyhigher rate.Thepolicereportingoptionsforpatientsarecomplex, therecanbesignificantdelayswaitingforpolicetoarriveto fileareport,andnon-SANEnursesmaynotbefamiliarwith alltheoptions,whichmayleadtomissedopportunitiesto file apolicereport.
Non-SANEnursescaringforSAsurvivorshavea checklistofservicestoofferand,therefore,theoretically shouldoffertheseservicesatthesamerate.However,SANEs receivesubstantialadditionaltrainingthatmayaffordthem abetterunderstandingoftheimportanceoftheseresources andtheskillstodiscussthemsensitivelywithatraumatized patient.ASANE-trainednursemayhaveamorepositive attitudetowardSAsurvivorsingeneral.13 Theymayalso havemoretimetotalkwiththepatients,astheyarenot responsibleforanyotherpatientcaredutiesatthesametime; orthehigherresourceacceptanceratesamongSANE patientsmaysimplyreflectthefactthatSANEnurseshave self-selectedforadditionaltrainingduetoaninterestin helpingSAsurvivors,whichmayallowthemtoprovidemore sensitivecare.Regardlessofthereason,givenmounting evidencetosupportthebenefitsofSANEcaretopatientand qualityoutcomes,SANEprogramsshouldbeexpandedand supportedwheneverpossible.
LIMITATIONS
Themajorlimitationofthisstudywastherelianceon retrospective,routinecaredatacollectedfromtheEHR.Itis possiblethatsomeservicesorresourceswereofferedand/or acceptedbypatientsandsimplynotdocumented,anditis unknownwhetheronegroupwasmorelikelytodocument thantheother.Anyservicenotdocumentedwasconsidered tonothavebeenofferedorreceivedforthepurposesofthe analysis,whichmayhaveaffectedtheoutcomesifalarge proportionofthoseservicesnotdocumentedwereeithernot applicableorwereactuallyprovided.Additionally,there were fiveindividualswhopresentedforSAtwiceduringthe studyperiod.Eachencounterwasanalyzedindependently, butitispossiblethatthe firstEDexperienceimpactedtheir choicesduringthesecondencounter.However,giventhat theseindividualsrepresentedsuchasmallproportionofthe sample,itisunlikelythattheirinclusionsignificantlyaffected
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 980 SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices Hollenderetal.
SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices
theresultsofthestudy.Duetothesmallsamplesize,the effectsofsurvivorgendercouldnotbefullyexplored,as genderdifferencesbetweengroupswerenotstatistically significant.Itispossiblethatthelargerproportionof cisgendermeninthenon-SANEcohortaffectedoutcomes, orthattheirgenderaffectedeitherthelikelihoodofSANE careortheirlikelihoodofacceptingservices,asmenmaybe lesstrustingoftheircareteamduetosignificantstigma.24,25 Furthermore,muchofthestudyperiodincludedthe COVID-19pandemic,whichmayhaveimpactedclinical documentation,availabilityofEDservices,orwillingnessof patientstoremainintheEDwhilewaitingforresultsor referrals,althoughtheseshouldhaveimpactedbothSANE andnon-SANEgroupssimilarly.Lastly,thiswasasingle-site study.Whileitislikelythattheresultsaregeneralizableto otherlarge,urban,adultEDs,furtherstudiesareneededto validatetheseresultsinotherEDsettings.
CONCLUSION
Thisstudyrevealedthatsexualassaultsurvivorsinthe EDwhoreceivedcarefromaSexualAssaultNurse Examinerweremorelikelytobeofferedandtoaccept standard-of-careSAservicesandresources.Thismayrefl ect theincreasedsensitivityandexpandedskillsetaffordedby SANEtraining,ortheabilityofadedicatedSANEtowork outsidethetime,space,andworkfl owconstraintsofabusy ED.WhilearrangingforcontinuousSANEcoverageinthe EDcanbelogisticallyand fi nanciallychallenging,itmay notonlybene fi tpatientoutcomesbutallowhospitalsto meetrecommendedqualitymetrics,whichmayberequired bygoverningbodiesoreventiedtoreimbursementinthe value-basedcaremodel.LegislativesupportforSANE coverageshouldbeexpandednationally,withparallel increasesinfundingtohelphospitalsimplementcontinuous SANEcoverage.Thiswillpositivelyimpactthequalityof careforsurvivorsofSA,whomaythenbemorelikelyto receivetheservicesandtreatmentthattheyneedaftera traumaticevent.
AddressforCorrespondence:MeredithHollender,MPP,University ofChicago,PritzkerSchoolofMedicine,924E57thStreet,Chicago, IL60637.Email: mhollender@uchicagomedicine.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Hollenderetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.ShortNA,LechnerM,McLeanBS,etal.Healthcareutilizationby womensexualassaultsurvivorsafteremergencycare:resultsofa multisiteprospectivestudy. DepressAnxiety.2021;38(1):67–78.
2. Survivors’ BillofRightsActof2016.114thCongress.Availableat: https://www.congress.gov/bill/114th-congress/house-bill/5578 AccessedMarch28,2023.
3. NoSurprisesforSurvivorsActof2022.117thCongress.Availableat: https://www.congress.gov/bill/117th-congress/house-bill/8891/. AccessedMarch28,2023.
4. SexualAssaultSurvivorsEmergencyTreatmentAct(SASETA).Illinois GeneralAssembly.Availableat: https://www.ilga.gov/legislation/ilcs/ ilcs3.asp?ActID=1531&ChapterID=35.AccessedMarch28,2023.
5.VogtEL,JiangC,JenkinsQ,etal.TrendsinUSemergencydepartment useaftersexualassault,2006-2019. JAMANetwOpen 2022;5(10):e2236273–e2236273.
6.PatelA,PanchalH,PiotrowskiZH,etal.Comprehensivemedicalcare forvictimsofsexualassault:asurveyofIllinoishospitalemergency departments. Contraception.2008;77(6):426–30.
7.PatelA,RostonA,TilmonS,etal.Assessingtheextentofprovisionof comprehensivemedicalcaremanagementforfemalesexualassault patientsinUShospitalemergencydepartments. IntJGynaecolObstet 2013;123(1):24–8.
8.AhrensCE,CampbellR,WascoSM,etal.SexualAssaultNurse Examiner(SANE)programs:alternativesystemsforservicedeliveryfor sexualassaultvictims. JInterpersViolence.2000;15(9):921–43.
9.ChandramaniA,DussaultN,ParameswaranR,etal.Aneeds assessmentandeducationalinterventionaddressingthecareofsexual assaultpatientsintheemergencydepartment. JForensicNurs 2020;16(2):73–82.
10.Fehler-CabralG,CampbellR,PattersonD.Adultsexualassault survivors’ experienceswithSexualAssaultNurseExaminers(SANEs). JInterpersViolence.2011;26(18):3618–39.
11.CampbellR,PattersonD,AdamsAE,etal.Aparticipatoryevaluation projecttomeasureSANEnursingpracticeandadultsexualassault patients’ psychologicalwell-being. JForensicNurs.2008;4(1):19–28.
12.PoldonS,DuhnL,CamargoPlazasP,etal.Exploringhowsexual assaultnurseexaminerspractisetrauma-informedcare. JForensic Nurs.2021;17(4):235–43.
13.NielsonM,StrongL,StewartJ.Doessexualassaultnurseexaminer (SANE)trainingaffectattitudesofemergencydepartmentnursestoward sexualassaultsurvivors? JForensicNurs.2015;11(3):137–43.
14.ThiedeE,MiyamotoS.RuralavailabilityofSexualAssaultNurse Examiners(SANEs). JRuralHealth.2021;37(1):81–91.
15. DworkinER,DeCouCR,FitzpatrickS.Associationsbetweensexual assaultandsuicidalthoughtsandbehavior:ameta-analysis. Psychol Trauma.2022;14(7):1208–11.
16.Young-WolffKC,SarovarV,KlebanerD,etal.Changesinpsychiatric andmedicalconditionsandhealthcareutilizationfollowingadiagnosis ofsexualassault:aretrospectivecohortstudy. MedCare 2018;56(8):649
57.
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 981
–
Hollenderetal.
17.SantaulariaJ,JohnsonM,HartL,etal.Relationshipsbetweensexual violenceandchronicdisease:across-sectionalstudy. BMCPublic Health.2014;14(1):1286.
18.AmericanCollegeofEmergencyPhysicians.Managementofthe PatientwiththeComplaintofSexualAssault.Availableat: https://www. acep.org/patient-care/policy-statements/management-of-thepatient-with-the-complaint-of-sexual-assault/ AccessedMarch28,2023.
19.CrookHL,ZhengJ,BleserWK,etal.Howarepaymentreforms addressingsocialdeterminantsofhealth?Policyimplicationsandnext stepsissuebrief.Availableat: https://www.milbank.org/wp-content/ uploads/2021/02/Duke-SDOH-and-VBP-Issue-Brief_v3.pdf AccessedMarch28,2023.
20.LittelK.SexualAssaultNurseExaminer(SANE)programs:improving thecommunityresponsetosexualassaultvictims.U.S.Departmentof Justice,OfficeofJusticePrograms,OfficeforVictimsofCrime.
Availableat: http://www.vawnet.org/sites/default/files/assets/files/ 2016-09/OVC_SANE0401-186366.pdf.AccessedMarch28,2023.
21.MiyamotoS,ThiedeE,DornL,etal.TheSexualAssaultForensic ExaminationTelehealth(SAFE-T)Center:acomprehensive,nurse-led telehealthmodeltoaddressdisparitiesinsexualassaultcare. JRural Health.2021;37(1):92–102.
22.CampbellR,PattersonD,LichtyL.Theeffectivenessofsexualassault nurseexaminerprograms:areviewofpsychological,medical,legal,and communityoutcomes. TraumaViolenceAbuse.2005;6(4):313–29.
23.CrandallC,HelitzerD.ImpactevaluationofaSexualAssaultNurse Examiner(SANE)program.Availableat: https://www.ojp.gov/pdffiles1/ nij/grants/203276.pdf.AccessedMarch28,2023.
24.BechtelK,RyanE,GallagherD.Impactofsexualassaultnurse examinersontheevaluationofsexualassaultinapediatricemergency department. PediatrEmergCare.2008;24(7):442–7.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 982 SexualAssaultNurseExaminersLeadtoImprovedUptakeofServices Hollenderetal.
SOCIAL EMERGENCY MEDICINEAND POPULATION HEALTH
ExploringMuslimWomen’sReproductiveHealthNeeds andPreferencesintheEmergencyDepartment
AnumNaseem,MD*
MorganMajed,MSPH*
SamanthaAbdallah,MD*
MayssaSaleh,BSN†
MeghanLirhoff,MD†
AhmadBazzi,MD†
MartinaT.Caldwell,MD,MS†
SectionEditor: MarkI.Langdorf,MD,MHPE
*WayneStateUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Detroit,Michigan
† HenryFordHospitalDepartmentofEmergencyMedicine,Detroit,Michigan
Submissionhistory:SubmittedSeptember19,2022;RevisionreceivedApril27,2023;AcceptedMay1,2023
ElectronicallypublishedAugust22,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58942
Objective: WeexploredindividualMuslimwomen’sreproductivehealthcareexperiences,preferences, beliefs,andbehaviorsintheemergencydepartment(ED)andingeneral.
Methods: ThiswasaqualitativestudyconductedatacommunityEDusingsemi-structuredinterviews withapilotedinterviewguide.WeinterviewedparticipantsawaitingcareintheEDwiththefollowing criteria:femalegender;EnglishorArabicspeaking;aged ≥18years;andself-identifiedasMuslim.We conductedinterviewsinbothEnglishandArabicuntilthematicsaturationwasreached.Transcriptswere codedusinganiterativelydevelopedcodebook,maintainingintercoderagreementgreaterthan80%.We usedaninductivethematicanalysistoidentifythemes,andresultswereinterpretedinthecontextof interviewlanguageandpatient’sage.
Results: Weinterviewed26Muslim-identifiedfemaleEDpatients.Wefoundthatculturalrepresentation andsensitivityamongEDstaffmitigateddiscriminationandpromotedinclusionforMuslimEDpatients. However,assumptionsaboutMuslimidentityalsoimpactedtheparticipants’ healthcare.Most participantsendorsedapreferenceforafemaleclinicianfortheirreproductivehealthcareingeneral,but notnecessarilyforotherareasofmedicine.Clinicianculturalconcordancewasnotalwayspreferredfor participantsintheEDduetofearsaboutthelossofconfidentiality.Maritalstatusimpactedbeliefsabout reproductiveandsexualhealthinthecontextofMuslimidentity.Overall,familyplanningwasacceptable andencouragedinthispatientpopulation.
Conclusion: Thethemeselucidatedinthisstudymayguidecliniciansindevelopingculturally sensitivepracticeswhenprovidingreproductivehealthcaretotheMuslimpopulation.[WestJEmerg Med.2023;24(5)983–992.]
INTRODUCTION
Racialandethnicminoritiescontinuetohaveinequitable healthcareaccessandoutcomes,frompreventivemeasuresto thetreatmentofacuteillness.1–4 Withanincreasinglydiverse patientpopulation,muchfocushasbeenonimproving patient-cliniciancross-culturalinteractionstoprevent stereotyping,biases,andlackoftrustthatimpedethe
deliveryofqualitycare.2 Modelsofculturalcompetence emphasizeapatient-centeredapproachtoenhance healthcaredeliverytominoritygroupswithculturaland linguisticdifferences.5 Thisisespeciallyimportantinthe emergencydepartment(ED),asafety-netcaresettingin whichcliniciansdonottypicallyhaveestablished relationshipswithpatients.6,7
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 983
HealthoutcomesandculturalpreferencesoftheMuslim populationarenotwellestablishedinthehealthcare literatureorpracticeguidelines.8 Anestimated3.3million MuslimsliveintheUnitedStatestoday,makingIslamthe thirdmostprominentreligioninthecountry.9 TheMuslim populationisgrowingandprojectedtoreach8.1millionby 2050,largelyduetoincreasedimmigration.10 Considering theprevalenceofMuslimsnationally,itisimportant thatcliniciansarewelltrainedindeliveringcarethatis sensitivetotheuniqueperspectivesandbeliefsof thesepatients.
EnsuringthatcliniciansareknowledgeableaboutMuslim patients’ preferencesregardingreproductivehealthis especiallyimportantintheEDwherepatientsoftenpresent forobstetricorgynecologicalcomplaintsandthereisno establishedpatient-clinicianrelationship.11 Althoughbest practicesforcareofMuslimpatientsintheEDhavebeen published,thereisalackofliteraturethatisderivedfrom patientpreferencesthatspecificallyfocusesonreproductive healthcareforfemaleMuslimsintheED.11–14 Moreover,the Muslimpopulationconstitutesaveryheterogenous populationthatincludesmanydifferentethnicgroups,andin whichreligiousidentityisoftenconfoundedbyspecific culturalvalues.Understandingperspectivesofindividual patientscanhelpelucidatehowtobestaddressthediversity ofidentitywithinthispopulation.15 Therefore,weaimedto exploreMuslimwomen’sreproductivehealthcare experiences,preferences,beliefs,andbehaviorsintheED andingeneral.
METHODS StudyDesignandSetting
Weconductedsemi-structured,face-to-faceinterviews usingapilotedinterviewguidewithfemaleMuslimpatients ofreproductiveagepresentingtoacommunityEDlocatedin amidwesternsuburbwithalargeMuslimpopulation.The studywasapprovedbytheinstitutionalreviewboardatthe institutionwheredatacollectionoccurred.Toensureour interviewguidewasculturallysensitive,weperformed cognitiveinterviewsinEnglishwhilepilotingthe interviewguide.
Twoteammembers(ANandMS)conductedallstudy activitiesinEnglishorArabicaccordingtotheparticipant’ s preference.AN,athird-yearmedicalstudent,conductedall oftheEnglishinterviews,andMSworkedasaregistered nurseatthestudysiteandconductedalloftheArabic interviews.BothANandMSarereproductive-aged, cisgenderfemaleswhoidentifyasMuslim,butneitherwear thehijab.ANisSouthAsianandisfamiliarwiththe communitythroughhermedicaleducationactivitiesand volunteerism.MSisLebaneseandalife-longmemberofthe localMuslimcommunity.Bothwerenewtoqualitative researchandweretrainedbyMC,whohasextensivetraining andexperienceinqualitativemethodsandcommunity-based
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
BestpracticecaremodelsforMuslimpatients thathavebeenpublishedtoimprovecultural competencyamongclinic iansarenotderived frompatientpreferences.
Whatwastheresearchquestion?
WeaimedtoexploreMuslimwomen ’ s reproductivehealthcareexperiencesand preferencesintheEDandingeneral.
Whatwasthemajor findingofthestudy?
Mostwomenpreferredafemaleclinicianfor theirreproductivehealthcare,butcultural concordancewasnotalwaysdesireddueto fearsaboutcon fi dentiality.Familyplanning wasacceptable,anddesiredinthispatient population.
Howdoesthisimprovepopulationhealth?
Thethemeselucidatedheremayguide cliniciansindevelopingculturallysensitive practiceswhenprovidingreproductive healthcaretothispopulation.
participatoryresearch.NotethatallArabicresearch documentswereprofessionallytranscribedandcertified bythehealthsystem’sapprovedcompany,aswellas reviewedbymultipleArabic-speakingmembersofthe studyteam.
SelectionofParticipants
WhilepatientsawaitedmedicaltreatmentintheED,a studyteammemberscreenedtheelectronichealthrecord (EHR)trackboardforinclusioninthisstudyandapproached potentiallyeligibleparticipants.Participantswhometthe followingcriteriawereincluded:1)femalegenderperthe EHR;2)age ≥18yearspertheEHR;and(3)self-identifiedas Muslim.AnyindividualwhowasidentifiedbytheEHRto meetthe firsttwoinclusioncriteriawereapproachedand askedwhethertheyself-identifiedasMuslimtoavoid profiling.Individualswhometthefollowingcriteriawere excluded:1)inphysical,mental,oremotionaldistress, includingEmergencySeverityIndex1(thehighestacuity); 2)prisoners;3)cognitivelydelayed;or4)couldnotunderstand andconverseaboutreproductivehealthinEnglishorArabic. InterviewswereconductedintheEDpatientrooms withoutthepresenceoffamilymembersinthe majorityofcases.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 984 ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED Naseemetal.
Measurements
Participantscompletedabriefscreeningquestionnaireto obtaindemographicinformation.Writteninformedconsent wasobtainedfromallparticipantsintheirpreferred language.Participantsreceiveda$20cashcompensationfor participatinginthe30-to40-minuteinterviews.Interviews wereaudiorecorded,transcribed,andde-identifiedbya professionaltranscriptioncompany.Arabictranscriptswere subsequentlytranslatedintoEnglishandverifiedbyMHand AB,whoareArabic-speaking,Muslimresidentphysicians. Interviewersdocumented fieldnotesoftheirobservations andexperiencesforeachinterview,whichwereusedto contextualizeinterviewdataduringanalysis.
Analysis
Interviewswerecollecteduntilthematicsaturationwas reachedorwhenrecurringthemeswereidenti fi edinthe manuscripts,whichwasfoundtobeat26interviews.No repeatinterviewsneededtobeconducted.Thestudyteam developedacodebookusingaxialandopencoding, resolvingdisagreementsusingaconsensusprocess.The codebookwasiterativelyrevisedthroughoutcodingto includeemergingcontent.Priortocoding,andevery fi ve transcriptsthereafter,codersperformedanintercoder agreementtrialandmaintainedintercoderagreementator above80%.Usingqualitativedataanalysissoftware Dedooseversion7.0.23(SocioCulturalResearch Consultants,LLC,LosAngeles,CA),twotrainedcoders (MM,aMuslimgraduatestudentandSA,aMuslim medicalstudent)employedcodesfromthecodebooktothe transcribedandde-identi fi edinterviews.ANusedan inductivethematicprocesstoanalyzethetextdata. Findingswerevalidatedbytheentireresearchteam,which iscomprisedofmostlyMuslimmembersandtwononMuslims.Thematicresultswereconvergedwith demographicdataobtainedinthequestionnaire.
RESULTS
CharacteristicsofStudySubjects
Weinterviewed26participants,ofwhom14wereEnglishspeakingand12wereArabic-speaking(Table1).The majorityofparticipants(16)wereofreproductiveage, definedas18
50yearsold;19wereUScitizens;23had publiclyfundedhealthinsurance;and14identifiedashaving moretraditionalIslamicreligiousviews.TheArabicspeakinggroupwasolderthantheEnglish-speaking interviewees(39vs33yearsold).AlltheArabic-speaking participantswerebornoutsidetheUS,andthisgrouphad lowereducationallevelswith41.6%reportinganeighthgradeeducationorless.TheEnglish-speakingpopulation mostlyidentifiedasLebanese(11),whereastheethnicity mostoftenrepresentedamongtheArabic-speakinggroup wasYemeni(sixparticipants).
MainResults
Wegroupedthemesintotwomaincategories:1)impactof Muslimidentityonreproductivehealthexperiencesin general;and2)impactofMuslimidentityonreproductive healthpreferences,beliefs,andbehaviors(Table2).The supportingquotesareformattedasfollows:interview language(E = English,A = Arabic);participantnumber; andparticipantageinyears(y).
ImpactofMuslimIdentityonReproductiveHealth ExperiencesinGeneral
I.Culturalrepresentationandculturalsensitivity mitigateexperiencesofdisc riminationandpromotefeelings ofinclusion. Themostprevalentthemeintheinterviews addresseddiscrimination,culturalrepresentation,and culturalsensitivityinhealthcareingeneral.When interviewersaskedparticipantswhethertheyhadeverfelt discriminatedagainstwhilereceivingreproductivehealth servicesbecauseoftheirreligion,themajorityofparticipants deniedsuchexperiencesintheEDandinhealthcareatlarge. Forexample,manyparticipantsseemedtoagreethat “Idon’tseeanydifference[inreceivingreproductive healthcare]whetherIwearahijabornot.Theytreatus thesameway” (A2,34y).Putmoreexplicitly, “I’mtreated thesamebyeverydoctorandnursethatIencounter,soI think[discrimination]isnotaproblem” (E15,24y).
Manyparticipantsalludedtotheuniquecultural representationinthelocalcommunityasbeingamajor protectivefactoragainstdiscriminationandbias.One participantsaid, “comingin[totheED]andseeingMuslim people itjustmakesmemorecomfortable ” (E15,24y). Anotherparticipantdescribedhow “[inthishospital],since theyknowthere’ salotofArabsandstuff,andtheyalways haveArabnurses,theycancommunicate,sohereit ’ s better” (E7,35y)indicatingthatculturalrepresentationis animportantpartofbuildingcomfortwithclinicians. Additionally,someparticipantsalsosuggestedthat, “alotoftheAmericandoctors[inthiscommunity] know ourculture ::: butifyougooutsidelikeFloridaand stuff ::: Iheardthattheywouldtreat[Muslims]differently” (E7,35y).
Notableexceptionstothisthemeseemedrelatedto languageandreligiousclothing,suchasthehijab.One participantstated, “I’veheard[alotofstoriesof discrimination]anditusually[involved]womenwhodidn’t speakEnglish” (E8,27y).Anotherparticipantconcurred that “probablybecause[anotherMuslimwoman]hadan accentand[she]couldn’tspeakEnglishwell,[theclinicians] werekindofrudeto[her]” (E7,35y).Oneparticipantshared astoryofhersupportofanotherMuslimwomanwhoworea hijab,describing, “alittlescarflady shecouldn’tdefend herself,soIhadtodefendherbecause[theclinicianswere] talkinglikeshe’sstupid” (E6,27y).OneoftheEnglishspeakingparticipantsexplainedthatshehadnever
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 985 Naseemetal. ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED
ED, emergencydepartment; GED,GeneralEducationalDevelopment. *Notalldataaddupto100%becauseofmissingdataorrounding.
encountereddiscriminationduetoherMuslimreligion, “maybebecauseIdon’twearaheadscarf,it’sdifferent.And IcomeoutspeakingEnglish-youwouldn’tmistakemefora Muslim.” Despiteherownexperiences,shehadheardstories
ofotherMuslimsbeingtreated “rudeanddisrespectful” (E4,30y).
TheArabic-speakingparticipantsdidnotshare experiencesoflanguagebiasandhadoverwhelmingly
English (n = 14) Arabic (n = 12) Total (N = 26) Averageage,years 33 39 38 ED visitsinthelast12months,mean 1.6 2.9 2.7 Placeofbirth(%) IntheUnitedStates 42.8(6) 0(0) 23.0(6) OutsidetheUnitedStates 57.2(8) 83.3(10) 69.2(18) Citizenship(%) UScitizen,bybirth 50(7) 0(0) 26.9(7) UScitizen,bynaturalization 28.5(4) 50(6) 38.4(10) UScitizen,bornabroadbyparentswhoareUScitizen 14.2(2) 0(0) 7.6(2) NotaU.S.citizen 7.1(1) 41.6(5) 23(6) Healthinsurance(%) Publicinsurance 92.8(13) 83.3(10) 88.4(23) Privateinsurance 7.1(1) 16.6(2) 11.5(3) Ethnicity(%) Iraqi 14.2(2) 25(3) 19.2(5) Lebanese 78.5(11) 16.6(2) 50(13) Palestinian 0(0) 8.3(1) 3.8(1) Yemeni 7.1(1) 50(7) 26.9(8) Maritalstatus(%) Nevermarried 28.6(4) 8.3(1) 19.2(5) Married 50(7) 66.7(8) 57.6(15) Divorced 14.3(2) 8.3(1) 11.5(3) Separated 0(0) 8.3(1) 3.8(1) Widowed 7.1(1) 0(0) 3.8(1) Religiosity(%) Traditional 64.3(9) 41.6(5) 53.8(14) Neithertraditionalnornon-traditional 21.4(3) 25(3) 23(6) Non-traditional 7.1(1) 16.6(2) 11.5(3) Highestgrade/degreecompleted(%) 8th gradeorless 7.1(1) 41.6(5) 23(6) Highschoolgraduate/GED 50(7) 8.3(1) 30.8(8) Somecollegeorassociate’sdegree 28.6(4) 33.3(4) 30.8(8) Bachelor’sdegreeorhigher 14.3(2) 8.3(1) 11.5(3) Difficultyforyouoryourhouseholdtopaybillsinlast12months,(%) Hard 50(7) 33.3(4) 42.3(11) Neitherhardnoreasy 35.7(5) 0(0) 19.2(5) Easy 7.1(1) 50(6) 26.9(7)
Table1. ParticipantdemographicsofEnglish-andArabic-speakinginterviewsconductedintheemergencydepartment.*
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 986 ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED Naseemetal.
Table2. Supportingquotesfromstudyparticipants.
ThemesIllustrativequotes
I.Culturalrepresentationandcultural sensitivity mitigateexperiencesof discriminationandpromotefeelingsof inclusion
• “They’reveryunderstanding,especiallyaroundhereinthecommunity” (E13,34y).
• “I feellikeifIweretogooutofstateoranywhere,everybodywouldlookatmedifferently,just becauseI’maMuslim” (E9,20y).
• “Wherewegoweseeracismsowedon’tfeelcomfortable.Everywhere,notonlyinthehospital. ThankGod,Iwasn’ttreatedwithracisminthehospital.Theytreateveryoneequally” (A1,29y).
• “Ihavebeenhereforaverylongtime,[doctors]neverdifferentiate[betweenanon-Muslimanda Muslim]” (A12,49y).
• “[Thedoctors]areniceandtheyhavemercy,itdoesn’tmakeadifferenceforthemifweare Muslimsornot theyhavemoremercythanwedo” (A4,60y).
• “Ifeelthat[thedoctors]aregood theydealinaniceway,theydon’tdiscriminatewhetheryou areSunni,Shia,AmericanorArab” (A7,27y).
• “Weallgettreatedthesame[intheED]” (E3,33y).
• “WhenIcame[totheED],theytreatedmeinaveryniceway,ingynecology,theyrespectthatI wearaHijabandtheytakecareofme” (A12,49y).
• “They’reveryunderstanding[ofmyHijab]especiallyaroundhereinthecommunity.Mostofthe doctorsknowandthey’reawareofallthat,sotheydowhatevertheycantoaccommodateit (E13,34y).
II.AssumptionsaboutMuslimidentity
• “Whenyouwalkinandyou’recovered amaledoctorwillwalkin,theydogetalittle ‘Are youokaywith[mebeinghere]?’ or ‘Doyouwantusto,youknow–?’ butnotifitwasn’ta coveredwomanoraMuslimwoman” (E2,31y).
• “Just becausetheyseeyoucoveredupdoesn’tmeanyoudon’tspeaktheirlanguage.Ithinkthey havethatmentality,butit’sfarfromthetruth” (E8,27y).
• “IftheyseeIdon’thaveaweddingringonandI’mMuslim,they’relike ‘Oh,soyou’renotpregnant forsure she’savirgin.Shedoesn’tdrink.I’mgoingtoquicklygooverthisquestion’ whereas peoplecanbevaryinglevelsofreligiositydependingonwhethertheyweartheheadscarfornot” (E15,24y).
III.Preferenceforafemalecliniciantendsto
• “Someproblemsshouldonlybediscussedwithafemaledoctor womantowomanthere’s nothingtohide” (A5,37y).
• “If theyhavetodothevaginaltest,yes[wouldpreferawoman] becauseweareMuslims” (E11,31y).
• “Becauseheisastranger,youknowthatinourreligionthat’snotacceptable,itisHaramunlessif itisanemergencyandherlifeisindanger,thenitisacceptable .Iamonlytalkingaboutgenital organs,butitis fineinotherspecialties.” (A8,47y).
• “Ithink[cliniciangender]doesn’tmatterexceptifIamgoingtohaveagynecologicalexam” (A8,47y).
• “Ifitisafemaledoctor,Ifeelmorecomfortablebecausewearethesame” (A2,34y).
• “WhenIgavebirthtomyeldestson,thefemaledoctorwasn’tthere,andIhadtodealwithamale doctor,itwasembarrassingbutIaccepteditbecauseitwasanemergencycase” (A1,29y).
• “Iknowthatmostofmyrace,subconsciouslytheywilljudgeyouregardlessofiftheytellyou theydon’t Idon’tliketobecriticizedorjudgedorlookedatinacertainwayjustbecauseof howIlookorwhatI’mherefor whatmybloodresultswillcomeoutto” (E2,31y).
• “They prefertogotoaCaucasianoranyotherraceofpsychologiststhanonejustlikethem,infear orworrythatIwillgossipinthecommunity anditworksbothways.LikeIwouldbescaredtoo” (E15,24y).
• “Ithinktherearealotofgirlsthatareyounger.Theygetabortions.Buttheydon’thavenobodyto talkto especiallybeingArab,youcan’t.Youhavetogosomewherenobodyknows about Theproblemisn’twiththedoctor.Theproblemiswiththe wholeenvironment.You reallycan’tsaymuchinDearborn” (E3,33y).
• “IfIhaddonesomethingorwantedtotalkaboutit,I’llbeworried ifthere’speoplelisteninginthe hallway,orifsomeonerecognizesme” (E15,24y).
V.Maritalstatusimpactsideasabout intercourse
• “InthepastmaybelikebeforeIgotmarried[preferredfemaledoctor],beforeIhadkids.But afterallthatit’slike,they’veseeneverything.You’rejustopenaboutit.Youdon’tcare anymore” (E13,34y).
• “[Intercourse]is[notpermissible]inourreligion onlywithherhusband” (A8,47y).
• “Muslimgirlsdon’tweartamponsifthey’renotmarriedyet” (E15,24y).
• “You’renotsupposedtodo[pelvicexams]untilbasicallyyou’remarried” (E9,20y).
VI.Religiouspermissibilityforcontraception
• “Ididn’tknowthat[birthcontrol]hadanythingtodowithreligion” (E2,31y).
• “I wouldnevertakebirthcontrolnorwouldIwantmydaughtersto it’snotthat[Islamis]against it.It’snotnaturalbutthenagain,itistheirchoicebutIwouldadvisethemdon’ttakeit” (E10,54y).
• “[Birthcontrol]isnotsomethingpeopletalkaboutthatmuch,butpeopleourage,Ithinkit’snota bigdealforus” (E15,24y).
bespecifictoreproductivehealth
IV.Preferencefornon-Muslim/non-Arab clinician
(Continuedonnextpage) Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 987 Naseemetal. ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED
ThemesIllustrativequotes
• “Itisnormaltotakebirthcontrolpills,ifIdon’twanttogetpregnant,itistotally finetotakebirth controlpills” (A7,27y).
• “Ifthewomanisweakandcan’tsupportanewpregnancybecauseofseveralprevious miscarriages,sheshouldusebirthcontrolpillstoprotectherhealthorifthewomanhas enoughchildren,sheshouldusethemaswell” (A8,47y).
• “I’veusedcontraceptivepillsandthat’sokay[inmyreligion]” (A11,67y).
• “Idon’tknowwhatIslamicreligionsaysaboutbirthcontrolpillsbutpersonallyIusedtotakethem whenIwasinLebanon.Ididn’tthinkaboutreligionatthattime,butitisabadthingtobringababy tothisworldifyoucan’ttakecareofhim” (A12,49y).
• “Religionisnotagainstbirthcontrolpills infactit’squitetheopposite.It’sforthesethings, becauseyoucan’triskgettingpregnanteveryday” (A9,57y).
positiveexperiencestosharewhenaskedaboutfeelingsof discrimination.Oneparticipantexplained, “Idon’tfeelthat [non-Muslimsaretreatedbetter]no tobehonestIwould liketothanktheAmericansinthisregard theyrespect you ” (A6,47y).Anotherparticipantagreedsaying, “Ihave beenhere17yearsandIhaveneverfelt[discriminated againstinhealthcare]” (A2,34y).Allofthesesentiments appliedtotheirreproductivehealthcare,aswellastheir healthcareexperiencesingeneral.
II.AssumptionsaboutMuslimidentity. Althoughmost participantsdidnotfeelreligiouslydiscriminatedagainst, somesharedfeelingstereotypedbyclinicians.Participants explainedhowvisiblereligiousexpressions,suchaswearing thehijab,ledtocliniciansmakingassumptionsabouttheir preferences. “Whenyouwalkinandyou’recovered ::: a maledoctorwillwalkin,theydogetalittle ‘Areyouokay with[mebeinghere]?’ butnotifitwasn’tacovered womanoraMuslimwoman” (E2,31y).Anotherparticipant shared “justbecausetheyseeyoucoveredupdoesn’tmean youdon’tspeaktheirlanguage.Ithinktheyhavethat mentalitybutit’sfarfromthetruth” (E8,27y).These assumptionsmayaffectthecareMuslimpatientsreceive,as oneparticipantmentioned “iftheyseeIdon’thaveawedding ringonandI’mMuslim,they’relike ‘Oh,soyou’renot pregnantforsure she’savirgin.Shedoesn’tdrink. I’mgoingtoquicklygooverthisquestion’ ::: whereas, peoplecanbeofvaryinglevelsofreligiositydepending onwhethertheyweartheheadscarfornot” (E15,24y).
ImpactofMuslimIdentityonReproductiveHealth Preferences,BeliefsandBehaviors
I.Preferenceforafemalecliniciantendstobespeci fi cto reproductivehealth .Mostparticipantspreferredafemale clinicianfordiscussionsaboutreproductivehealthand reproductivephysicalexaminations.Participantsexplained that “itisdifficult forArabwomenandespeciallythosewho wearhijabtodiscuss[reproductivehealth]withmale doctors” (A1,29y).Anotherparticipantagreed: “Ialways
preferifit’sawomaniftheyaregoingtocheckprivateparts andstuff” (E5,50y).
TheArabic-speakingparticipantsweremore fi xedthan theEnglish-speakingparticipantsabouttheirpreferences forreproductivehealthcliniciangender.Asoneparticipant said, “ Ican ’ texposemygenitalareatoamaledoctor. That ’simpossible ::: thatisnotacceptable” (A8,47y). Anotherparticipantindicatedthatinthepastbecauseofa maleclinician “[I]did[refuseagynecologicalexam]one time ” (A5,37y).AnotherArabic-speakingparticipant explainedhowthepreferencewasin fl uencedbytraditions morethanjustpersonalchoiceas, “ somewomendon’ t acceptifthedoctorismalebecauseoftheirtraditions.In Iraq,ifwehaveanemergency,weaccepttobeexaminedby amaledoctorbutwhenitcomestolabororgynecological emergencies,somewomencan ’ tacceptbecausetheir husbanddon’ tacceptorbecausetheirreligionorfamilies ” (A1,29y).However,participantsoverwhelminglyagreed thatinanemergency “ ifthereisonlyamaledoctor,Iwould acceptthat.Ihavenochoice ” (A2,34y).Otherexceptionsto thepreferenceforafemaleclinicianonlyappearedinthe Englishinterviews,astwoparticipantsmentionedthatthey actuallypreferredmalecliniciansbecause “they ’ revery gentle” (E4,30y)and “ womenhaveatendencyto overthink” (E10,54y).Theydidnotprovidefurthercontext intothesebeliefs.
Whenparticipantswereaskedtodescribethebestperson tocarefortheirreproductivehealth,almostallparticipants discussedcharactertraitsratherthangender.Theseincluded traitslike “listen[ing]andunderstand[ing]” (E12,47y)and “aslongasthey’requalifiedandhaveaheartandcan understandwhatI’mgoingthrough” (E10,54y).Gender preferenceseemedtoberelatedonlytoreproductivehealth, asmostparticipantsreportedthat “ifIamhavinga gynecologicalexam,itshouldbeafemaledoctor.Butforany otherproblems,thereisnodifferencebetweenmaleorfemale doctors” (A3, 57y).Anotherparticipantconcurredthat “outsideoftheemergency[sic],ifitissomethingrelatedto OBGYN,Iwouldpreferafemaledoctoronly.Butforany
Table2. Continued.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 988 ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED Naseemetal.
A,Arabic-speakingparticipant; E,English-speakingparticipant; ED,emergencydepartment; y,ageinyears.
otherhealthproblems,itdoesn’tmatterifitisamaledoctor” (A7,27y).
II.Preferenceforanon-Muslim/non-Arabclinician. Multipleparticipantsdiscussedadesireforanon-Muslim/ non-Arabclinicianwhilereceivingreproductivehealthcare, citingconcernsaboutprivacy.Oneparticipantexplainedthat discussingherreproductivehealthwithaMuslimorArab clinicianwouldcause “fearorworry[about]gossipinthe community” (E15,24y).Anotherparticipantagreedthat “subconsciously [MuslimorArabclinicians]willjudge youregardlessofiftheytellyoutheywon’t” (E2,31y).
Someparticipantssharedbeliefsthatclinicianswhodid notcomefromtheircommunitywerebetter.Forexample, oneparticipantsuggestedthat “peoplearesojudgmental, andI’mArabic,sotrustmeIknowhowtheyare Ilovemy race butI’dratherhavea[clinicianbea]nicewhiteladyor aniceblackguy,Chinese,whatever ::: they’regood” (E6,47y).Anotherparticipantconcurred, “Ithinkthat AmericanshavemoremercythanArabs” (A8,47y).
III.Maritalstatusimpacts ideasaboutreproductive health. Formanyparticipants,maritalstatuswasvitally importanttoreproductivehealth,becauseitprovidesan importantcontextfortheroleintercourseplaysintheir religion,health,andhealthcare.Manyinterviewees emphasizedthat “[intercourse]is[generallynotpermissible] inourreligion ::: onlywithherhusband” (A8,47y).For someparticipants,womenwho “hadsexand[weren’t] married there’snowayinhell[they]couldtellthatto anybody” (E3,33y),indicatingthatthesubjectofsexual activityistabooandmaynotbediscussedreadily,ifatall,by someMuslimwomen.Anotherparticipantexplainedthis further,describing, “IbrokemyvirginityandIwasn’t married.ButIwouldstillgotalktomygynecologist[who was]anoldwhiteguy AndImadesurethatIdidn’tknow nobodythatworkedatthatoffice ” (E3,33y).Similarly, maritalstatusalsoinfluencedideasaboutgeneral reproductivehealthtopicslikemenstruationsince “Muslim girls don’tweartamponsifthey’renotmarriedyet” (E15,24y).Anotherparticipantagreed, “ you ’renot supposedtodo[pelvicexams]untilbasicallyyou’ re married” (E9,20y).
IV.Religiouspermissibilityforcontraception. When participantswerespecificallyaskedhowtheirreligiousbeliefs impactedtheirchoicesaroundcontraception,theresponses wereoverwhelminglypositiveandemphasizedreligious permissibility.Asoneparticipantexplained, “No,[birth control]won’tbeconsideredagainstGodorreligionbecause Godknowshowmyhealthis.HeknowsthatIcannolonger tolerateanotherpregnancy ::: Weallknowourselves,maybe wearen ’tabletoraisethechildrenandtoberesponsible aboutthem.Thesepillsaren’tagainstIslamatall” (A2,34). Anotherparticipantemphasizedhowthesechoicesare personalsince, “Irathernot[usebirthcontrol]becauseI think[ifapregnancyis]meanttobe,thenit’smeanttobe :::
[Thesefeelingsare]justpersonal.Ifbirthcontrolworksfor youthenuseit” (E6,27).Notonlydidparticipantsexpress religiouspermissibility,butoneparticipantarticulated religiousnecessityforthenon-contraceptiveeffectsof contraception. “WhenIwaslike14,wewenttotheIslamic pilgrimage,Hajj.Andtodothat,Ihadtogetonbirthcontrol sothatIdon’tgetmyperiodthereandmisstheopportunity topraythere” (E15,24).
DISCUSSION
Inthisstudy,weaimedtoexploreMuslimwomen’ s reproductivehealthcareexperiences,preferences,beliefs,and behaviors.Wewereabletoelucidatekeythemesfrom participantsthatcaninformculturallysensitivecareforthis population.Morespecifically,thisexplorationhighlighted thehighproportionofMuslimrepresentationinhealthcare inthecommunitywesampled,whichhelpedmitigate discriminationandpromotedinclusion.Previousstudiesin minoritypopulationshavehighlightedtheneedforcultural representationandsensitivityastoolstobetterservea community.16 Yetthereweredrawbackstotheinsularnature ofthiscommunity,suchasthepotentialforlossof confidentialitythatmayleadtostigmaaroundreproductive healthbehaviors.ThisinfluencedpreferencesfornonMuslimcliniciansforsomeparticipants.Otherstudieshave shownthatminoritycommunitiesreceivebettercarefrom membersoftheirowncommunity,butthatcultural concordanceisnotalwayspossible.16–19 Whennotpossible, environmentsshouldbeintentionalinhiringadiverse workforcetohelpincreasetheculturalknowledgeof cliniciansoutsidetheminoritypopulation.Allclinicians, includingthosewhoarereligiouslyandculturally concordant,shouldexploreandbesensitivetotheirpatients’ concernsaboutprivacy,especiallyfortaboosubjectslike reproductiveandsexualhealth.
Interestingly,thereweremajordifferencesthat dichotomizedtheresultsbetweenEnglish-andArabicspeakingparticipants,emphasizingthediversityofthe Muslimpopulation.Theconcernsaboutprivacyand judgmentwerealmostexclusivelyconveyedbytheEnglishspeakingparticipants.TheEnglish-speakinggroupwas younger,moreeducated,andmorelikelytobenativetothe UScomparedtotheArabic-speakinggroup.Inthisway,the English-speakingparticipantsmayexhibitlesstraditional beliefsandbehaviorsthanothersubgroupsintheir community,suchasolderorimmigrantwomen.Thefactthat membersoftheArabic-speakinggroupweremore fixedin theirpreferenceforafemalecliniciansupportstheideathat thisgroupmaybemoretraditional.Althoughreligiositywas explicitlyexploredinourdemographicsurvey,thisisa termthatisbothsubjectiveandrelative,makingitdifficultto measure.Thispotentiallyexplainsthediscrepancy betweenourhypothesisandtheresults findingthatthe
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 989 Naseemetal. ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED
English-speakinggroupreportedmoretraditional religiousbeliefs.
Additionally,theArabic-speakingparticipantsoveralldid notendorsefeelingsofdiscriminationwhilereceiving reproductivehealthcare,despitetheEnglish-speaking participantsreportingthatlanguagebarriersplayedarolein theirobservationofdiscriminationagainstArabic-speaking Muslimwomen.TheArabic-speakinggroupwasexclusively bornoutsidetheUSandlikelyhadmoreexperiences receivingreproductivehealthcareoverseas.Theirpositive reproductivehealthcareexperiences,contextualizedinthis US-basedstudysetting,maybeattributedtosocial desirabilitybiasorideasaboutsuperiorhealthcareinthe US.20 Furthermore,sincetheEnglish-speakinggroup predominantlyidentifiedasLebanese,whereastheArabicspeakinggroupwerelargelyYemeni,itisdifficultto elucidatewhetherthesedifferencesweretrulyrelatedto Muslimidentityandreligiosityorratherinherentethnic dissimilarities.Althoughthisstudywasfocusedonexploring theexperiencesofMuslimwomen,itisimportanttoconsider thechallengesincapturingdatathatcanbepurelyattributed toreligiousidentitywithoutbeingconfoundedbyethnicor culturalnuances.
Themajorityofparticipantsdesiredafemaleclinicianfor reproductivehealthcareintheEDunlessitwasanemergency situation,consistentwithpreviousstudiesthathave demonstratedthispreferenceinalmostallgroups,regardless ofraceorreligion.21 Yetmanyoftheparticipantsdiscussed certainpersonalitytraits,suchasempathyandgoodlistening skills,asthemostimportantattributeswhendescribingthe bestclinicianforreproductivehealthcareintheED.Thisis anideathathasbeenestablishedinpreviousstudies, suggestingthatitisnotuniquetoMuslimpatientsto prioritizeclinicianqualitiesovergenderforreproductive healthcare.22,23 Additionally,mostparticipantsagreed thattheydidnothaveagenderpreferencewhenreceiving non-reproductivehealthcare.Therefore,cliniciansshould avoidassumptionsaboutgenderpreferenceinthe Muslimpatientpopulation.Thisalsoemphasizestheneed forgenderdiversityinhealthcarewhenpossibleand creatingpoliciestosupportpatientclinicianpreferences forreproductivehealthwhenitcanbefeasibly accommodated.
Maritalstatuswasalsofoundtodictatewhatwas permissibleregardingreproductivehealth.Participants discussedhowsexualactivityoutsideofmarriagewaslargely consideredtaboowithmajorpotentialconsequenceswithin theMuslimcommunity.Thisalsoinfluencedconcerns aboutmenstruationandpelvicexamscompromising virginity.Thisisimportantknowledgeforcliniciansbecause theymaybeapatient’sonlyconfidantonthesesubjects. Itisalsoanareawhereclinicianscanprovidesexualhealth educationandaddressmisinformationwithsensitivityto deeplyheldbeliefs.
Lastly,thisstudyhelpedelucidateMuslimwomen’ s attitudestowardfamilyplanning,anareawellknowntobe influencedbyreligiousandculturalnorms.24–26 Participants conveyedbeliefsaboutthereligiouspermissibilityof contraception,aswellasinsomecases,religiousnecessity. Thisisinlinewitharecentself-reportedsurveythat examinedAmericanMuslim’scontraceptionutilization patterns,whichdemonstratedthatMuslimrespondents reportedhighercontraceptionusethanthenational proportion.27 Participantsalsoemphasizedthatchoices aboutcontraceptionwerepersonalandshouldnotbe influencedbyothers’ beliefs.Theseareimportanttakeaways becausetheydemonstratethatfamilyplanningcounseling shouldbetailoredtoanindividual’smotivationsand goals,ratherthanbasedonassumptionsaboutculturalor religiousbelief.28
Previousliteraturethathasfocusedoncultural competencyinprovidingmedicalcaretotheMuslim populationhaslargelyincludedgeneralizationsaboutthe Muslimpopulation,suchaspreferenceforafemaleclinician orassumptionsaboutsexualactivitybeforemarriage.29
31 Thisstudyfocusedonindividualexperiencesthatattimes contradictedthesegeneralizations.Our findingalignswith theculturalempowermentmodelofculturalcompetencethat emphasizesthedynamicnatureofculturalcompetency.15 Morespecifically, “becauseofthespecificnatureofeach patient-clinicianinteractionwithinitsparticularsocialand politicalenvironment,culturallycompetentbehaviorinone contextmaybeculturallyincompetentinanother.”15 This providesaframeworkforprovidingcaretotheMuslim populationwhoexhibitalargerangeofdiversity suchas race,ethnicity,andlanguage thatmayheavilyinfluencethe wayonepracticestheirreligion.
LIMITATIONS
Thisstudyhadseverallimitations.WeenrolledEnglishandArabic-speakingpatientsfromasingleEDwithina predominantlyMiddleEasterncommunity;therefore,the resultsmaynotbegeneralizedtoallMuslims.However,the qualitativeapproachwasdesignedtobeexploratoryand generatehypothesesandfutureresearchquestionsthatmay beevaluatedforgeneralizabilityinthefuture.The demographicsurveyandinterviewsinArabicmayhavebeen affectedbyparticipantcomprehensionandliteracyor translationnuancesthatchangedthemeaningofconcepts, whichisalimitationofthestudy.Additionally,the demographicsoftheinterviewersmayhaveaffectedthe sentimentsourstudyparticipantsfeltcomfortablesharing duetosocialdesirabilitybias.Morespecifically,ANwas youngerandnotvisiblyMuslim,soparticipantsmayhave spokenmorefreelyaboutstigmatizingtopicswithherthan withMS,alifelongmemberofthelocalMuslimcommunity whoisanurseatthestudysite.
–
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 990 ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED Naseemetal.
CONCLUSION
Our findingscontributetothegrowingbodyofliterature focusingonculturalsensitivityintreatingtheMuslim population.Wefoundthatculturalrepresentationand sensitivityamongEDstaffmitigateddiscriminationand promotedinclusionforMuslimEDpatients.However, assumptionsaboutMuslimidentityalsoimpactedthe participants’ healthcare.Mostparticipantsendorseda preferenceforafemaleclinicianfortheirreproductive healthcareingeneral,butnotnecessarilyforotherareasof medicine.Clinicianculturalconcordancewasnotalways preferredbyparticipantsinthisEDstudyduetofears aboutthelossofconfidentiality.Maritalstatusimpacted beliefsaboutreproductiveandsexualhealthinthecontext ofMuslimidentity.Overall,familyplanningwasacceptable andencouragedinthispatientpopulation.
Thisstudyisuniquebecauseitemphasizespatient preferencesandfocusesonfemaleMuslims’ reproductive healthpreferences,anareaofclinicalimportancethathasnot beenthoroughlyexplored.Ultimately,our findings underscoretheneedforfutureworktocaptureamorediverse perspectiveofMuslimwomenandbetterelucidatethe reproductivehealthpreferencesandneedsthatareuniqueto thispopulation.
AddressforCorrespondence:AnumNaseem,MD,WayneState UniversitySchoolofMedicine,DepartmentofEmergencyMedicine, 540E.CanfieldAve,Detroit,Michigan,48201.Email: mmajed2@ hfhs.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Naseemetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.WheelerSM.Racialandethnicdisparitiesinhealthandhealthcare.
ObstetGynecolClinNorthAm.2017;44:1–11.
2.OwenCM,GoldsteinEH,ClaytonJA,etal.Racialandethnichealth disparitiesinreproductivemedicine:anevidence-basedoverview.
SeminReprodMed.2013;31:317
24.
3.AssociationofAmericanMedicalColleges.Whatyoudon’tknow:the scienceofunconsciousbiasandwhattodoaboutitinthesearchand recruitmentprocess.Availableat: https://www.aamc.org/initiatives/ leadership/recruitment/178420/unconscious_bias.html
AccessedApril12,2020.
4.CommitteeonHealthCareforUnderservedWomen.ACOGCommittee OpinionNo.649:Racialandethnicdisparitiesinobstetricsand gynecology. ObstetGynecol.2015;126:e130–34.
5.ButlerM,McCreedyE,SchwerN,etal.ImprovingCulturalCompetence toReduceHealthDisparities[Internet].Rockville(MD):Agencyfor HealthcareResearchandQuality(US);2016Mar.(Comparative EffectivenessReviews,No.170.)Table21,Culturalcompetence models.
6.AmericanCollegeofEmergencyPhysicians.Culturalawarenessand emergencycare. AnnEmergMed.2008;52:189.
7.SoaresWEIII,KnowlesKJII,FriedmannPD.Athousandcuts: racialandethnicdisparitiesinemergencymedicine. MedCare 2019;57:921–3.
8.PadelaAI,GunterK,KillawiA,etal.Religiousvaluesandhealthcare accommodations:voicesfromtheAmericanMuslimcommunity. JGen InternMed.2012;27:708–15.
9.MohamedB.AnewestimateoftheU.S.Muslimpopulation.Availableat: http://www.pewresearch.org/fact-tank/2016/01/06/a-new-estimateof-the-u-s-muslim-population/.AccessedMarch1,2017.
10.delaCruzGP,BrittinghamA.TheArabpopulation:2000.Availableat: https://www.census.gov/prod/2003pubs/c2kbr-23.pdf AccessedJanuary25,2021.
11.EzenkweleUA,RoodsariGS.Culturalcompetenciesinemergency medicine:caringforMuslim-AmericanpatientsfromtheMiddleEast. JEmergMed.2013;45:168–74.
12.PadelaAI,CurlinFA.Religionanddisparities:consideringthe influencesofIslamonthehealthofAmericanMuslims. JReligHealth 2013;52:1333–45.
13.YosefARO.Healthbeliefs,practice,andprioritiesforhealthcare ofArabMuslimsintheUnitedStates. JTranscultNurs 2008;19:284–91.
14.PadelaAI,delPozoPR.Muslimpatientsandcross-genderinteractions inmedicine:anIslamicbioethicalperspective. JMedEthics 2011;37:40–44.
15.GarrettPW,DicksonHG,WhelanAK,etal.Whatdonon-Englishspeakingpatientsvalueinacutecare?Culturalcompetencyfromthe patient’sperspective:aqualitativestudy. EthnHealth 2008Nov1;13(5):479–96.doi: 10.1080/13557850802035236 PMID:18850371.
16.CooperLA,RoterDL,JohnsonRL,etal.Patient-centered communication,ratingsofcare,andconcordanceofpatientand physicianrace. AnnInternMed.2003;139:907–15.
17.SwartzTH,PalermoAS,MasurSK,etal.Thescienceandvalueof diversity:closingthegapsinourunderstandingofinclusionand diversity. J InfectDis.2019;220:S33–S41.
18.LaVeistTA,Nuru-JeterA,JonesKE.Theassociationofdoctor-patient raceconcordancewithhealthservicesutilization. JPublicHealthPolicy 2003;24:312–23.
19.StrumpfEC.Racial/ethnicdisparitiesinprimarycare:theroleof physician-patientconcordance. MedCare.2011;49:496–503.
–
Volume24,No.5:September2023 WesternJournal of EmergencyMedicine 991 Naseemetal. ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED
20.BergenN,LabontéR. “Everythingisperfect,andwehavenoproblems”: detectingandlimitingsocialdesirabilitybiasinqualitativeresearch. Qual HealthRes.2020;30:783–92.
21.DeroseKP,HaysRD,McCaffreyDF,etal.Doesphysiciangenderaffect satisfactionofmenandwomenvisitingtheemergencydepartment?
JGenInternMed.2001;16:218–26.
22.TurrentineM,RamirezM,StarkL,etal.Roleofphysiciangenderinthe modernpracticeofobstetricsandgynecology:doobstetriciangynecologistsperceivediscriminationfromtheirsex? SouthMedJ 2019;112:566–70.
23.TamTY,HillAM,Shatkin-MargolisA,etal.Femalepatientpreferences regardingphysiciangender:anationalsurvey. MinervaGinecol 2020;72:25–9.
24.PinterB,HakimM,SeidmanDS,etal.Religionandfamilyplanning. EurJContraceptReprodHealthCare.2016;21:486–95.
25.JacksonAV,KarasekD,DehlendorfC,etal.Racialandethnic differencesinwomen’spreferencesforfeaturesofcontraceptive methods. Contraception.2016;93:406–11.
26.HillNJ,SiwatuM,RobinsonAK. “Myreligionpickedmybirthcontrol”:the influenceofreligiononcontraceptiveuse. JReligHealth 2014;53:825–33.
27.BudhwaniH,AndersonJ,HearldKR.Muslimwomen’suseof contraceptionintheUnitedStates. ReprodHealth.2018;15:1.
28.DehlendorfC,GrumbachK,SchmittdielJA,etal.Shareddecision makingincontraceptivecounseling. Contraception.2017;95:452–455. Erratumin:Contraception.2017;96:380.
29.HasnainM,ConnellKJ,MenonU,etal.Patient-centeredcareforMuslim women:providerandpatientperspectives. JWomensHealth(Larchmt) 2011;20:73–83.
30.HammoudMM,WhiteCB,FettersMD.Openingculturaldoors:providing culturallysensitivehealthcaretoArabAmericanandAmericanMuslim patients. AmJObstetGynecol 2005;193:1307–11.
31.AttumB,HafizS,MalikA,etal.CulturalCompetenceintheCare ofMuslimPatientsandTheirFamilies.[Updated2021Jul7].In: StatPearls[Internet].TreasureIsland (FL):StatPearlsPublishing; 2021Jan.
WesternJournal of EmergencyMedicine Volume24,No.5:September2023 992 ExploringMuslimWomen’sReproductiveHealthNeedsandPreferencesintheED Naseemetal.
Mixed-methodsEvaluationofanExpeditedPartnerTherapy
Take-homeMedicationProgram:PilotEmergencyDepartment InterventiontoImproveSexualHealthEquity
EmilyE.Ager,MD,MPH*
WilliamSturdavant,MD*
ZoeCurry,MD†
FahmidaAhmed,MD*
MelissaDeJonckheere,PhD*
AndrewA.Gutting,BS‡
RolandC.Merchant,MD,MPH,ScD§
KeithE.Kocher,MD,MPH*∥
RachelE.Solnick,MD,MSc,MS§
*UniversityofMichigan,SchoolofMedicine,DepartmentofEmergency Medicine,AnnArbor,Michigan
† VanderbiltUniversityMedicalCenter,SchoolofMedicine,Departmentof EmergencyMedicine,Nashville,Tennessee
‡ UniversityofMichigan,MichiganMedicine,DepartmentofClinicalQuality, AnnArbor,Michigan
§ IcahnSchoolofMedicineatMountSinai,NewYork,NewYork
∥ UniversityofMichigan,InstituteforHealthcarePolicyandInnovation, AnnArbor,Michigan
SectionEditors:ErikAnderson,MD,andMarkLangdorf,MD,MHPE
Submissionhistory:SubmittedNovember28,2023;RevisionreceivedMay31,2023;AcceptedJune1,2023
ElectronicallypublishedAugust25,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59506
Background: Treatmentforpartnersofpatientsdiagnosedwithsexuallytransmittedinfections(STI), referredtoasexpeditedpartnertherapy(EPT),isinfrequentlyusedintheemergencydepartment(ED). ThiswasapilotprogramtoinitiateandevaluateEPTthroughmedication-in-hand(“take-home”)kitsor paperprescriptions.InthisstudyweaimedtoassessthefrequencyofEPTprescribing,theefficacyofa randomizedbestpracticeadvisory(BPA)ontheuptake,perceptionsofemergencycliniciansregarding theEPTpilot,andfactorsassociatedwithEPTprescribing.
Methods: WeconductedthispilotstudyatanacademicEDinthemidwesternUSbetween August–October2021.TheprimaryoutcomeofEPTprescriptionuptakeandtheBPAimpactwas measuredviachartabstractionandanalyzedthroughsummarystatisticsandtheFisherexacttest.We analyzedthesecondaryoutcomeofbarriersandfacilitatorstoprogramimplementationthroughEDstaff interviews(physicians,physicianassistants,andnurses).Weusedarapidqualitativeassessment methodfortheanalysisoftheinterviews.
Results: Duringthestudyperiod,52EDpatientsweretreatedforchlamydia/gonorrhea,andEPTwas offeredto25%(95%CI15%–39%)ofthem.Expeditedpartnertherapywasprescribedsignificantlymore often(42%vs8%; P < 0.01)whentheinterruptivepop-upalertBPAwasshowncomparedtonotshown. BarriersidentifiedintheinterviewsincludedworkflowconstraintsandknowledgeofEPTavailability.The BPAwasviewedpositivelybythemajorityofparticipants.
Conclusion: InthispilotEPTprogram,expeditedpartnertherapywasprovidedto25%ofEDpatients whoappearedeligibletoreceiveit.Theinterruptivepop-upalertBPAsignificantlyincreasedEPT prescribing.BarriersidentifiedtoEPTprescribingshouldbethesubjectoffutureinterventionstoimprove provisionofEPTfromtheemergencydepartment.[WestJEmergMed.2023;24(5)993–1004.]
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 993 ORIGINAL RESEARCH
INTRODUCTION
In2020,therewere677,769casesofgonorrheainthe UnitedStates,anincreaseof111%since2009,1 and1.58 millioncasesofchlamydia.Emergencydepartment(ED) visitsforbacterialsexuallytransmittedinfections(STI)inthe USarealsoincreasinginfrequency.2 TheEDisacritical accesspointforSTIcare.PatientspresentingtotheEDfora possibleSTIaremorelikelytobepositiveforaSTI thanthosevisitinganoutpatientclinic.3 Treatmentofa patient’spartnerisalsocrucial,particularlyforfemale reproductivehealth,asthereisanestimated14%rate ofchlamydiareinfection,4 whichcanleadto severecomplications.5
Expeditedpartnertherapy(EPT)isonemethodtoreduce STIre-infection.Itisasafeandeffectiveharm-reduction practiceoftreatingthesexpartner(s)ofpatientswithSTIs withoutaclinicalexamination.6 Large,multisite, randomizedtrialshaveshownthatEPTissuperiorin preventingreinfectioncomparedtostandardpartner referral,7,8 andmeta-analyses9,10 havefoundthatpatients offeredEPThadareductioninpersistentorrecurrent gonorrheaorchlamydiainfections;notably,twoofthese studiesinvolvedEDpatients.7,8 Additionally,EPTmay decreasepopulationincreasesinchlamydiaatthe statelevel.11
Expeditedpartnertherapyissupportedbyhealth organizations5 includingtheAmericanCollegeof EmergencyPhysicians.12 Therehavebeennoadversedrug eventsreportedinpriorstudiesofEPT9 orinoveradecadeof monitoringbytheCaliforniaDepartmentofHealth.13 While usedinmostpubliclyfundedfamilyplanningclinicsinthe US,14 EPTisinfrequentlyprovidedintheinpatient setting15
17 orinEDs.18 Medicaldirectorshavereported poorknowledgeofhowtoprescribeEPT,18 andemergency clinicians’ abilitytoprescribeEPTmedicationscanvary greatly.18 ManystateregulationsprohibitEPTmedication costsfrombeingchargedtoanindexpatient’shealth insurancepolicy.Toaddressthebarrierofapartner’ saccess toSTItreatment,twopromisingapproachesforEDsinclude eithertodistributemedication-in-hand(“take-home”)kitsor paperprescriptionsforthepatienttogivetotheirsex partner(s).However,researchevaluatingtheseapproachesin theEDislacking.
ToinvestigatepossiblesolutionstoEPTimplementation inEDsweimplementedapilotprogramatasingleEDto dispensebothtake-homekitsandpaperprescriptions. Emergencyclinicianswereinterviewedabouttheir perceptionsofthepilotandassessedthefrequencyofEPT prescribing.Inaddition,weexaminedtheefficacyofabest practiceadvisory(BPA)toencourageprescribing.Lastly,we exploredvariationsinEPTprescribingbypatient demographicfactors,healthinsurancestatus,cliniciantype, andSTItestingresults.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Despiterisingratesofsexuallytransmitted infections(STI),EDsrarelyuseexpedited partnertherapy(EPT),whichcandecrease recurrentSTIs.
Whatwastheresearchquestion?
WhatarethebarriersandfacilitatorsoftakehomeEPTandtheeffectofabestpractice advisory(BPA)onEPTuse?
Whatwasthemajor findingofthestudy?
In25%ofeligiblepatientsEPTwasused morewhenBPAwasshownvswhennot, 42%vs8%,P < 0.01.
Howdoesthisimprovepopulationhealth?
Partneringwithalocalhealthdepartmentto offertake-homeEPTtopatientsempirically treatedforSTIswouldexpandtreatmentto high-riskpopulations.
METHODS
SettingandParticipants
ThepilotstudywasconductedbetweenAugust
October 2021atanacademicEDinthemidwesternUSwithapatient volumeofover100,000visitsperyear.InMichigan,EPTis legalandencouragedbytheMichiganDepartmentofHealth andHumanServices(MDHHS)forchlamydia,gonorrhea, andtrichomoniasis.19 Beforetheonsetofthispilotstudy,the MDHHSbeganaUSCentersforDiseaseControland Prevention(CDC)grant-fundedinitiativetoincrease statewideuseofEPT,whichincludeddonatingEPT medicationstoseveralEDsinthestateforindexpatientsto delivertotheirpartner(s)viatake-homekits.TheEPT medicationswerebasedonCDCguidelinesonthe presumptivetreatmentofgonorrheaandchlamydiausingan oral-onlyregimen.6
TheMDHHSobtainedthesemedicationsfroma pharmacydistributorandrepackagedthemintopre-labeled kitswithinformationandinstructionsforEPT.Toabideby drugsafetyregulationsregardingthetransferofmedications, aT3documentinwhichadrugmanufacturerdetailsall productinformationtoanewrecipient,wasobtainedand approvedbytheEDpharmacy.Thetake-homekitswere thendeliveredtotheEDinpackagesforeitherpotentially pregnant(containingcefiximeandazithromycin)ornot
–
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 994 Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram Ageretal.
Ageretal.
Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram
pregnant(containingcefiximeanddoxycycline)patients. PregnancystatuswasbasedonEDserumorurine testing.Thisstudywasapprovedbythestudysite’ s institutionalreviewboard(HUM00199376) and(HUM00196451).
PilotExpeditedPartnerTherapyProgram
ThemechanismoftheEPTpilotisdetailedviaaswimlaneprocessmap(Figure1).Aspartofalargerquality improvementinitiative,asexualhealthEHRordersetwas createdtoassistemergencyclinicianswithorderinglabtests andtreatmentforpatientsbeingevaluatedforSTIs (Appendix3).TheordersetprovidedalinktoanEPT protocolandthefollowing:1)standardizedEPT prescriptionsforprintingonplainpaper;2)progressnoteto indicatetheprovisionofEPT;and3)EPTdischarge instructionsandresourcesto findlocalloworno-costsexual healthclinics.
WithassistancefromEDpharmacyleadership,an ED-specificprotocolwasdesignedtodispenseEPTkits.For the “take-home” medicationkits,theclinicianprintedthe EPTprescriptions,broughttheprescriptionstotheED
pharmacylocatedadjacenttotheclinician’sworkspace,and thenthepharmacisttookthekittothepatientandprovided medicationcounseling.Emergencyclinicianscouldoffer patientsEPTpaperprescriptionsasanalternativetothekits. Atthetimeofthepilot,Michiganlawstillallowedplain paperprescriptionsfornon-controlledsubstances.20 Clinicianscouldchooseeitherapproachpertheprotocol.
Abestpracticeadvisory(BPA)wasalsocreatedasan interruptivealertdesignedtoappearwhenclinicians empiricallytreatedpatientsforgonorrheaandchlamydia (Appendix4a).TheinterruptiveBPAappearedwiththe followingtriggercriteria:1)patientwas ≥18yearsinage; 2)gonorrheaorchlamydiatestwasordered;and 3)ceftriaxoneandazithromycinorceftriaxoneand doxycyclinewereordered.Metronidazoleorderingwas initiallyincludedasaBPAtriggercriterionbutwaslater removedasittoofrequentlytriggeredtheBPAforpatients treatedforbacterialvaginosis.Additionally,anoninterruptivealertappearedintheEHRDischargeNavigator foralltriggercriteriapatientsifEPThadnotbeenorderedto notifycliniciansthatthepatientwaseligibleforEPT (Appendix4b).PrescribingcliniciansreceivedtheBPA;
Thisswim-laneprocessmapdepictstheEPTprogramresponsibilitiesrepresentedbyhorizontalswimlanesorganizedbytheroleofthe stakeholder:emergencydepartment(ED)patient,clinician,EDpharmacy,DepartmentofHealth,andpartner.Basedontheinterviewsand additionaldiscussionwiththeMichiganDepartmentofHealthandHumanServicesMDHHSandEDpharmacyoverthecourseoftheproject, fourphasesforpilotimplementationaredisplayedacrossthetopoftheprocessmapbymajoractivitydomains:1)supplyandpreparation, 2)patientselection,3)clinicianadoptionandpatientcounseling,4)patientdeliverytopartner.Captionsunderneaththemapsummarizekey pointsofthecorrespondingsection.
 Figure1. Swim-laneprocessmapoftheexpeditedpartnertherapy(EPT)pilotprogram.
Figure1. Swim-laneprocessmapoftheexpeditedpartnertherapy(EPT)pilotprogram.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 995
STI,sexuallytransmittedinfection; EPT,expeditedpartnertherapy; ED,emergencydepartment; Rx,prescription.
nursesdidnotreceivetheBPA.Toevaluatetheefficacyofthe interruptiveBPA,itwasprogrammedtoappearrandomly forapproximatelyhalfofEDvisitsthatmettrigger criteria(1:1randomizationofvisits,BPAalert,ornoBPA alertappearance).
BeforetheBPAintroduction,thepilotEPTprogram elementswerepresentedatEDfaculty,nursing,and physicianassistant(PA)meetingsandEMresidency didactics,followedbyemailsofpresentedmaterials.In addition,EDpharmacystaffpostedtheprotocoland educationalmaterialsonabulletinboardinahigh-trafficked areaoftheED.
EDStaffInterviewsAboutthePilotEPTProgram
Structuredinterviewswereconductedwithemergency clinicianscaringforEPT-eligiblepatientstoexplorebarriers andreasonsforEPTuptake.Weusedpurposivesamplingto interviewtheattendings,residents,PAs,andnurseswho caredforEPT-eligiblepatients.Eachclinicianwasinvitedvia emailtoatelephoneinterviewwithin72hoursofthe patient’svisit.Participantscouldparticipateinonlyone interview,eveniftheyhadprovidedcaretomultiple EPT-eligiblepatients.
Anindependentlygenerated,semi-structuredinterview guidewaspreparedusingelementsfromtheConsolidated FrameworkforImplementationResearch(CFIR)21 and publishedmanuscriptsonEPTimplementation.22–24 Thereis currentlynovalidatedinterviewguiderelatedtoEPT.The interviewguidewaspilot-testedanditerativelyrevisedwith threecliniciansunaffiliatedwiththisprojectbyconducting cognitive-basedassessmentsusingthe “think-aloud”25 approachtoensurecomprehensionand fidelitytothe questionintent(Appendix1).Eachtelephoneinterview beganwithquestionsontheparticipant’sbackground,as wellastheirEPTknowledgeandbeliefs.Participantswere thenaskedabouttheirrecentEPT-eligiblepatientencounter, includingreasonsforprescribingornotprescribingEPTand anybarriersorfacilitatingfactorstheyencounteredwiththe EPTprocess.The finalportionoftheinterviewincluded questionsregardingtheBPA.Threemultiple-choice questionswerealsoincorporatedtointroduceeachinterview topic.InterviewswererecordedusingaHealthInsurance PortabilityandAccountabilityAct(HIPAA)-compliant audiocall(ZoomVideoCommunications,Inc,SanJose, CA),auto-transcribedviaZoomclosedcaptioning,and savedtoapassword-protectedwebsitefor150days. Participantswereawareofthesubjectoftheinterviewbefore agreeingtoparticipate.Theywerenotcompensated.Each interviewwas10
15minutesinduration.
TheleadresearcherRSisanemergencyphysicianwith formaltraininginqualitativemethodsandhealthservices research.Theinterviewteamwascomposedofnine individuals:oneexpertinqualitativemethodologywho guidedtheanalyticalapproach(MD);threeresident
physicians(AK,EA,WS);andfourmedicalstudents(AR, JL,LD,ZC).Allinterviewteammembersreceivedtraining intherapidassessmentqualitativemethodologyfromthe leadresearcher.RSdidnotconductanyoftheinterviewers. Noneoftheinterviewershadasupervisoryrolerelatedto participants.Interviewerswerenotcompensated.
Outcomes
TheprimaryoutcomewasEPTprovisionandtheimpact oftheBPAonEPTuse.WeexaminedvariationsinEPT orderingbypatientdemographicfactors,insurancestatus, cliniciantype,andSTItestingresultsasanexploratory outcome.Thesecondaryoutcomeswerebarriersand facilitatorstoEPTprogramimplementation,whichwere assessedthroughEDclinicianinterviews.Thesemethodsare describedinfurtherdetailbelow.
AnalysisofExpeditedPartnerTherapyProvision
Anelectronichealthreport(EHR)prompt(EPICSystems Corporation,Verona,WI)wascreatedtoautomaticallysend same-day,dailyemailstotheresearchteamaboutEDvisits thatmetthepreviouslydescribedcriteriafortheinterruptive pop-upalertBPA.EachoftheseEDvisits’ EHRAssessment andPlansectionwerereviewedbyaresearchassistantto confirmthatthepatientwasbeingtreatedforapresumedSTI ratherthanforanotherbacterialinfection.ForEDvisitsthat metthesestudycriteria,researchassistantsextractedthe followingdataelements:patientdemographics(age,gender, race/ethnicity,insurancepayer,STItestingresults);clinician demographics(resident,attendingorPA);andwhetherthe clinicianhadbeenexposedtotheinterruptiveBPAforEPT. Summarystatisticsarereportedwiththefrequencyofeach categorybyEPTordering.Weconductedunivariable analysiswiththeFisherexacttestcomparingdistributionsby receiptofEPT.Proportionsarecalculatedwithalogit transformed95%confidenceinterval(CI).Weperformed statisticalanalysesusingStataversion16(StataCorpLLC, CollegeStation,TX).
AnalysisofInterviewswithEmergencyDepartmentStaff Weanalyzeddatausingarapidassessmentmethod.26
Duringtheinterviews,researchersparaphrasedresponsesin real-timeortranscribedselectquotesverbatimimmediately followingtheinterview,withassistancefromtheautotranscriptionandZoomrecording.Interviewersalsocoded thedataimmediatelyfollowingeachinterview.Interviewees wereemailedalistoftheirreportedverbatimquotesand askedtocommentontheaccuracyoftheirquotesand provideanyneededcorrections.Codeswerecreated accordingtoaCFIR-basedcodingschemeandpriorrelevant EPTliterature.22,23,27,28
Interviewersiterativelyaddedcodes toreflectnewideasnotincludedintheaprioricodingscheme untildatasaturationwasachieved.Themeswerederived deductivelyandorganizedbyCFIRdomains,with
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 996 Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram Ageretal.
Ageretal.
Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram
additionalthemesaddedbasedonpatternsinthecoding elements.Tworeviewers(EA,WS)independentlyevaluated thecodeddatatoidentifypatterns,whileathird(RS) reconciledanydiscrepancies.WeusedtheStandardsfor QualityImprovementReportingExcellence(SQUIRE2.0) andConsolidatedCriteriaforReportingQualitative Research(COREQ)reportingguidelinesasaframeworkfor reportingdata(Appendix2).29,30
RESULTS
ExpeditedPartnerTherapyProvision
Duringthestudyperiod,52EDpatientsweretestedand empiricallytreatedforSTIsatthestudyinstitution.Their demographiccharacteristicsareprovidedin Table1.Only
physicianresidentsorPAsweretheprescribingclinician type,whichistypicalatthisacademicinstitution.Ofthe52 patients,14patients(27%;95%CI16–41%)hadalabconfirmedtestforeithergonorrhea,chlamydia,or trichomoniasis,and13patients(25%;95%CI15–39%)were providedwithEPT.Ofthe14patientswithalab-confirmed testforeithergonorrhea,chlamydia,ortrichomoniasis,three (21%;95%CI6–53%)receivedEPT.TheEPTprescribing didnotdifferbydemographics,thetypeofemergency clinicianinvolvedinthepatient’sEDvisit,orwhetherthe patienthadalab-confirmedtestforeithergonorrhea, chlamydia,ortrichomoniasis.However,EPTwasprescribed significantlymorefrequentlywhentheprescribingclinician hadbeenrandomlyshowntheinterruptivepop-upalertBPA
) P-value N = 5275%(39)25%(13)
Private48%(25)51%(20)38%(5)
Medicaid31%(16)31%(12)31%(4)
Medicare4%(2)3%(1)8%(1)
Self-Pay4%(2)3%(1)8%(1)
Missing13%(7)13%(5)15%(2)
HasPCP54%(27)53%(20)58%(7)1.00
Lab-confirmedSTI27%(14)28%(11)25%(3)1.00
Chlamydia10%(5)8%(3)15%(2)0.59
Gonorrhea12%(6)13%(5)8%(1)1.00
Trichomoniasis8%(4)10%(4)0%(0)0.56
Clinicianfactors
EDPrescribingcliniciantype
Physicianresident44%(23)36%(14)69%(9)0.054
PA46%(24)51%(20)31%(4)0.34
ExposuretoBPA
ShownBPA50%(26)38%(15)85%(11)0.009
NotshownBPA50%(26)62%(24)15%(2)
P-valueiscalculatedfromtheFisherexacttest.
EPT,expeditedpartnertherapy; PCP,primarycarephysician; PA,physicianassistant, BPA,bestpracticeadvisory; STI,sexually transmittedinfection.
Total%(n)EPTnotordered%(n)EPTordered%(n
Patientfactors Age30(9)30(10)29(5)0.66 Female56%(29)54%(21)62%(8)0.75 Race 0.090 White48%(25)56%(22)23%(3) Black40%(21)33%(13)62%(8) Asian6%(3)5%(2)8%(1) Other4%(2)3%(1)8%(1) Missing2%(1)3%(1)0%(0) Insurance 0.37
Table1. ExpeditedpartnertherapyutilizationandcharacteristicsofEDpatientspresumptivelytreatedforsexuallytransmittedinfections.
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 997
(11/26;42%)comparedtowhentherewasnoBPAshown(2/ 26;8%)(P < 0.01).
InterviewswithEmergencyDepartmentStaffAbout ExpeditedPartnerTherapy
Ofthe106emergencycliniciansinvitedtobeinterviewed, 20participated(Table2).Ofthe20interviewees,11were attendingphysicians, fivewereemergencymedicine residents,twowerePAs,andtwowerenurses.Thirteenwere female.Additionalrepresentativequotesaredisplayedin Table3,andkeyconsiderationsaresummarizedbytheir respectiverolesontheprocessmap(Figure1).
OuterSetting(PatientNeedsandResources,External PolicyandIncentives) ImprovingSTITreatment
ManyparticipantsnotedthepublichealthbenefitofEPT andtheuniqueroletheEDhasincaringforunderserved patients.MostremarkedthatitwasimportantforEDs,in general,topreventSTIreinfectionandthatEPTiseffective inpreventingSTIreinfectioninEDpatients.
IthinkthiscouldbereallyhelpfultolotsofEDs;wesee limitedencountersforthisindication,butforthosewe doseeithasthepotentialtobeveryvaluable especiallyifwebringthistopatientsinanonjudgmentalway.[EPTis]veryimportant-weseelots offolksthatdon ’ thaveaprimarycaredoctoror gynecologist.Wehavetheopportunitytoeducate, treat,[and]preventthelong-termsequelaeofthese typesofinfections.(Participant9)
InnerSetting(Culture,StructuralCharacteristics,Accessto KnowledgeandInformation,ImplementationClimate)
Unfamiliarity,IncreasedWorkload
Frequentlymentionedinner-settingcharacteristics includedknowledgeofthebasicconceptofEPTandtime constraintsinusingit.Almostallparticipantswereableto accuratelyoratleastpartiallydefineEPT.Althoughmost participantswerefamiliarwiththeconcept,onlyabouthalf knewhowtoorderEPTatthestudysite.
Ididn’tknowtheprogramexistedanddidnotknowhow tousetheordersetorthatitwasavailable.(Participant8)
WhilethemajorityweresupportiveofhavingEPT availableasanoption,theextraworkinvolvedineducation wascitedbyseveralparticipantsasabarrier.Theystatedthat somepatientsmaynotunderstandSTIsandthusneedextra counseling.EspeciallyinabusyED,theextratimeinvolved inbridgingtheseknowledgegapswasundesirable.
[Abarrieris]explainingtothepatienthowtoexplain topartner,whichcanbechallenging not insurmountable.(Participant19)
Cultureatthestudysitewasalsofrequentlycitedasa barrier.ThesecliniciansstatedthatEPTisnotacommon practiceanditwaschallengingtoremembertouseit. Further,severalparticipantsviewedEPTaslessimpactfulin EDswithalowervolumeofSTIvisits.
Itfeelsstrangetowriteaprescriptionwithoutanameonit. Givingittosomeoneyou’venevermetorinteractedwith feelsstrange;it’sachangeinpractice.(Participant1)
Participantsalsomentionedwaystochangethisculture. TwocliniciansstatedthatincorporatingEPTintothe standardofpracticeisthebestlong-termsolutionfor clinicianstoorderEPTconsistently.
Ithinkeveryonejustneedstodoitonce,andthenitwillbe apartofourpractice.Thevolumeofusseeinganexposure needstogrowandthenjustknowingtodoitfromnowon. (Participant6)
ParticipantcharacteristicNumber(%) Self-identi fiedgender Male13(65) Female7(35) Age(years),median(range;IQR)35 (27–61;32–43) 20–293(15) 30–3911(55) 40–492(10) 50–592(10) 60–692(10) 70+ 0(0) RoleinED MD/MBBS16(80) Physician(attending)11(69) Physician(resident)5(31) Physicianassistant2(10) Registerednurse2(10) Yearsinpracticepost-residency(years), median(range;IQR) 3.5(0–37;0–13) 05(25) 1–99(45) 10–193(15) 20+ 3(15) ED,emergencydepartment; MBBS,BachelorofMedicine,Bachelor ofSurgery; IQR,interquartilerange. WesternJournal of EmergencyMedicineVolume24,No.5:September2023 998 Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram Ageretal.
Table2. Characteristicsofphysicians,physicianassistants,and nurseswhoparticipatedinclinicianinterviews.
Table3. RepresentativeclinicianquotesregardingexpeditedpartnertherapyorganizedbyCFIR*domainandconstructs.
CFIRdomainCFIRconstructsTopicRepresentativequote
OutersettingPatientneedsandresources,external policyandincentives ImprovingSTI treatment
Itissuperimportant[topreventSTIreinfection]to publichealthandtothehealthofourpatients,andto loweringthebarrierstheyhavetomedicalcare. (Participant5)
[We]seepatientswhodon’tinteractwiththemedical systemfrequently – weareapointofcontactforthem andhavetheopportunitytogivethemthisintervention thatimprovespublichealth.(Participant20)
Ithinkit’scapturingagroupofpatientswedon’talways seeintheED.(Participant18)
Ithinkitwouldbehelpfulfromacommunityhealth perspective,and[it]wouldhelplimitthespreadof disease.(Participant10)
InnersettingCulture,structuralcharacteristics,access toknowledgeandinformation, implementationclimate
Unfamiliarity, increased workload
[Abarrieris]thinkingaboutdoingit.(Participant5) Unfortunately,[abarrieris]justtheextraworkinvolved. (Participant16)
Istillthinkit’sweirdtowriteaprescriptionforsomeone Ihaven’tseenasapatientbutIamnotopposedto doingit.(Participant1)
It’snotentirelyuptotheEDbutweshouldplayarole andtakeadvantageofthetoolsavailabletous, includingEPT.(Participant16)
Thelong-termansweristhatitbecomes[the]standard ofcare.(Participant4)
Characteristics
Intervention characteristics Complexity,costTake-home program, distribution
I’mconcernedmostlyforsafety – iftheyareallergic, [havea]drugreaction,orsometypeofkidneydisease that’sundiagnosed.(Participant15)
Ithinkiftheyleavewithmedicationsinhandthat’s betterbecausethere’slesssteps.(Participant17)
Moreoptionsarebetter.Iliketheideaofgiving medicationmoreasgettingmedicationsseemseasier. (Participant5)
Itwouldbegreatifitmakesittotheintended individual.Dotheyactuallygetthemedication? (Participant12)
Whatwouldhappenifyougaveascripttosomeone whoseallergiesyoucannotcheck?(Participant19)
ThisBPAshouldexistbecauseitisfor[an]intervention that,withoutahard-stopreminder,itwouldnotbe prescribedotherwise.(Participant20)
[The]take-homemedkitispreferable;[it]reducesextra stepfor[the]patienttogive[the]partneraprescription [and]to fillthatprescription.(Participant20)
Thepatientwasdischargedandwasinahallwayspot waitingfor30–40minuteswaitingforthemedications; thepatientalmostleftwithoutmedicationsbecausehe wasreadytogo.(Participant15)
(Continuedonnextpage)
ofindividuals Knowledgeandbeliefsaboutthe intervention Unseen partner, uncertain delivery
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 999 Ageretal. Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram
CFIRdomainCFIRconstructsTopicRepresentativequote
DesignqualityandpackagingOrderset,best practice advisory
AsIrecalltheordersetwasprettystraightforward. (Participant12)
BPAswouldbethebestreminder;ifyouwantpeople topayattentionanddosomethingyouneedaBPA. (Participant8)
I’msureit’shelpfulbutmoreBPAsarepainful.The moretimesI’minterruptedthemoreI’mlikelytomake amistakeonthethingIwantedtodo.(Participant4)
CharacteristicsofIndividuals(KnowledgeandBeliefsAbout theIntervention)
Unseenpartner,uncertaindelivery
Oneclinicianexpressedreluctancerelatedtotreatinga patient’spartnerwhentheindexpatienthadanunconfirmed STIstatus.
Alimitationisthatwedon’thaveconfirmedtestresults andsowithoutresults,Imayattimesfeelreluctantto sendapartnerhomewithakit.(Participant5)
Medicationcostwhen fillingpaperprescriptionswasalso listedasareasonforareluctancetoorderEPT.
Ihaveconcernsthatthemedicationscostalotofmoney andwemaybeaddingaburdentothepatient.
(Participant8)
Aminorityofclinicianswereconcernedaboutprescribing forsomeonetheyhadn’tevaluatedasapatientandadverse medicationeffectsorallergies.WhenaskedabouttheEPT take-homekit,aparticipantstated,
Some[doctors]maybereluctanttodothatbecausethey haven’tbeenabletoexaminethepatient’spartner.
(Participant10)
InterventionCharacteristics(Complexity,Cost)
Take-homeProgram,Distribution
Participantspreferredthetake-homeEPTkitsoverpaper prescriptionsduetothefewerstepsfortreatmentofsex partnersbutrecognizeditwaslikelyashareddecision betweenpatientandclinician.
Itdependsonthepatient’ssituation.Youneedtodiscuss withthepatientiftheyarewillingorwanttodispense medicationtoapartnerorifaprescriptionwillbe effective.(Participant16)
Aprocessbarrierobservedbysomeparticipantswasa delayintheEDpharmacist fillingthetake-homeEPTkit, withonecliniciannotingthatthepatienthadtowait30 minutesafterdischargeforthekit.
Factorsoutsidethecontrolofemergencyclinicians, includingthepatient’sactions,werefrequentlycitedas barrierstotheimplementationofEPT.Halfofthe participantswereconcernedthatthesuccessofEPT dependedonpatientfactors,suchasdeliveringthetakehomekittotheirsexpartneror fillingthepaperprescription. Theyworriedthatthepatientwouldnolongerhavecontact withtheirsexpartnerorwouldnotdeliverthetake-homekit orprescriptiontotheirsexpartner.
Thebiggest[barrier]isiftheycan’tgetintouchwiththeir partneragain-Idon’tevenknowthispartnersoI’mnot goingtogivethemtheprescription.(Participant6)
InterventionCharacteristics(DesignQualityand Packaging)
Orderset,BestPracticeAdvisory Participantsnotedthesimplicityof findingandnavigating theEPTEHRorderset.Whenasked “whatwentwellwith theEPTprocessintheED,” aquarterindicateditwas “ easy touse.” Participantsstatedthattheordersetwas straightforward,well-designed,andeasyto findintheEHR. TheEPT-specificdischargeinstructionswerealsoconsidered efficientandhelpedwithpatienteducation.
PerspectivesonBPAsweremixedbutgenerallypositive. AlmosthalfoftheparticipantssuggestedusingaBPAwhen askedhowtoimplementED-basedEPT.Whenasked, “howdoyoufeelaboutareminderBPAforEPTthatpops upwhenyouorderempirictherapy, ” therewere13 responsesfor “appreciateitasareminder,” sevenresponses for “like, ” andfourresponsesfor “don’ tlike. ” Participants alsostatedthattheysupportBPAsthataremore “ patientcentered” ratherthanintendedfor fi nancialormedicolegal purposes.
Table3. Continued.
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 1000 Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram Ageretal.
*CFIR, ConsolidatedFrameworkforImplementationResearch; STI, sexuallytransmittedinfection; MBBS, BachelorofMedicine,Bachelorof Surgery; IQR, interquartilerange; BPA, bestpracticeadvisory.
IthinktheBPAisthemoststreamlinedwaytodoit;if therewasn’tahardstopImaynothavewrittenthe prescriptioninthiscircumstance;Iknowsomepeople areagainstBPAsingeneralbutIlikedit.Ithinkif we ’rereallytryingtoimplementthis,ahard-stopBPA isthebestwaytonotmisstheseprescriptions.Itis probablythemosteffectiveway.(Participant18)
Severalparticipantshadconflictedfeelingstowarda “hard-stop” BPA,statingthatcliniciansalreadyencounter numerousBPAs,whichcanbedisruptivetoclinician workflow.Conversely,severalstatedtheywouldsupport a “hard-stop” BPAsincetheinterventionmaybe otherwiseforgotten.
I’ mconflictedaboutit.IdislikeBPAsprobablybecauseof howmanywehave.So,addinganotheronemakesme cringe.Butifthere’sawaytodoitatthetimeof dischargeratherthanduringtheencounterthenI wouldn’thateit.(Participant17)
Additionalnon-BPA-basedsuggestionsforearly adoptionincludedencouragingattendingstoremind residentstouseEPT,involvingtheEDpharmacistmore extensivelyintheEPTprocess,andhavinga “standing nursingorder” toorderEPTmedications.
DISCUSSION
Thispilotstudydemonstratesthefeasibilityof anovelED-based,EPTtake-homemedicationpilotprogram andtheeffectivenessofEHRinterventionstofacilitate adoption.WeexaminedEPTuseamongallpatients beingpresumptivelytreatedforgonorrheaorchlamydia,as wellastheefficacyofaninterruptiveBPAforEPT. WhiletheBPAgreatlyincreasedEPTprescribing,EPTwas onlyofferedto25%ofEPT-eligibleEDpatients. ThislowlevelofEPTprescribingwassurprising,especially giventhatmostintervieweesaccuratelyconveyed theconceptofEPTandsupporteditsprovisionfrom theED.
ThelowlevelofEPTorderingmaybeduetoseveral factors.First,therewasaneducationalgapinhowtoorder EPT;halfoftheparticipantsstatedthattheydidnotknow howtoorderEPT.Second,patientsofferedEPTmayhave declined,whichthisstudycouldnotmeasure.Inasurveyof pediatricEDpatients,participantsuninterestedinEPTcited thattheywereconcernedforpartnersafety,wantedthe partnertogetadiagnosis,orfeltEPTwoulddetractfromthe partner’saccountability.31 Third,lowusemayhavebeen relatedtologisticaldifficultiesinvolvedinprovidingtakehomemedications.Althoughclinicianspreferredtake-home kitsoverpaperprescriptions,theyalsorecalledthelong processofkitdistribution,possiblyduetopharmacists’ unfamiliaritywiththeprocess.
Inthefuture,thiswillbeanessentialconsideration,as delaysinprovidingthemedicationinhandareapotential back-endissue.Addressingthisconcernmaynotonly increaseorderratesamongcliniciansbutincreaseefficiency andpreventdelaysincare.Fourth,emergencyclinicians couldhaveforgottentoprescribeEPT,asevidencedby intervieweeswhoreportedthatrememberingtoprescribe EPTwaschallenging.TheinterruptiveBPAlikelyreduced thisissue.Thenon-interruptiveBPAintheDischarge Navigatorusedinthisprojectwasprobablyoverlooked,as nonementionedseeingit.
DespitemixedfeelingsamongclinicianstowardBPAsin general,themajoritysupportedanEPT-specificBPA,with nearlyhalfsuggestingusingaBPAtoincreaseEPTordering. Further,theovertwo-foldincreaseinEPTorderingduring BPA-exposedvisitssupportsitsefficacyforEPT implementation.Thisstudyaddstothegrowingresearchon clinicianacceptability32 ofusingBPAstoimprovepatient care. 33–38 AstudyfromanurbanEDincluding75,901 patientsdemonstratedthatatargetedBPAincreasedsyphilis screeningby124%comparedtoclinician-initiatedtesting.39 However,BPAsareknowntocontributetoalarmfatigue40 andmustbedesignedtominimizeinappropriate interruptions.41 FutureworkonEPTprescribing mayinvestigatewhentodiscontinueaBPAasclinician familiarityincreases.
Onlythreepatientsoutofthe13providedEPThadalabconfirmedSTI,suggestingpresumptiveEPTmayleadto overprescribing.Apotentialsolutiontoimprovethe accuracyofED-basedEPTprovisionisrapidtestingfor chlamydiaandgonorrhea.42–45 Ontheotherhand,EPT couldstillbeappropriateevenwhenlabtestingisnegativeif thepatientwastestedbeforethetestcouldaccuratelydetect theinfection(ie,a “windowperiod” afterexposure).Without rapidtesting,manyEDshavedevelopeddedicatedfollow-up teamstoaddresspositivetestresultsafterEDdischarge. OfferingEPTduringsuchfollow-upinteractionscouldhelp targetEPTtopatientswithlab-confirmedinfections.
AninnovativeaspectofthisEPTprogramwastheability toprovide “take-home” EPTkits.WhileEPThasbeen demonstratedtoincreasefollow-uprateswiththeindex patient’spartnerandreducereinfectionratesamongthe indexpatient,46 priorstudieshavefoundthatthetotalrateof treatmentofthepatient’spartnerisstillrelativelylow,owing inpartduetolowprescription fillingrates,sometimesfound tobelessthan50%.47,48 Thisstudydemonstratesonemethod foraddressingthisback-endissue:providingtake-home medicationsratherthanawrittenprescription.Thiswould reducetheimpactofonemajorlimitingfactorinthe completionoftreatment.Forthisreason,theCDC recommendationsonEPTstateapreferencefortake-home medications.6 Otherstudieshaveshownthebenefitof “med tobed” or “take-home” programstofacilitatemedication compliancewhenthereisconcernaboutapatient’ s
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 1001 Ageretal. Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram
access,suchasinanticoagulantsandmedicationsfor opioidusedisorder.49–51
AlthoughotherED “take-home” medicationsmaybe chargedtoapatient’shealthcareinsuranceplan,this mechanismisnotcurrentlypossibleforEPT,asmosthealth insurerswillnotpayformedicationforanyoneotherthanthe coveredindividual.OneknownexceptionisCalifornia, where,sinceFebruary2020,thestateMedicaidprovider –includingMedi-CalandFamilyPACTinsurance – must coverpartnerEPTmedicationsforlow-incomepatients.52,53 Additionally,certainfamilyplanningclinics,health departmentSTIclinics,andFederallyQualifiedHealth CenterspayforEPTmedicationsviagovernmentalgrants.54 Givendisparitiesinhealthcareaccessamongpatientswho receiveSTIcareinEDs,55,56 expandingED-EPTmedication fundingmechanisms(suchastheMichiganDepartmentof Health’sprovisionofmedicationsinthiscurrentstudy),and insuranceregulatorychanges(suchasCalifornia’sMedicaid regulations)tootherstateswouldincreaseEPTprovision.
LIMITATIONS
Limitationsofthisstudyincludethesmallsamplesize, whichreducedtheabilitytoidentifydifferencesbetween groupsiftheyexisted.Externalvalidityislimitedbecausethe studywasconductedatoneEDwhosepopulation,setting, andresourcesmaybedifferentfromothersettings. Additionally,theoveralllowresponseratetotheinterview invitationintroducedthepotentialforselectionbias.Dueto limitationsindatacollectionbasedondailyEHRreports, datawascollectedonlyonhowmanypatientsreceivedEPT ratherthanhowmanypatientsmayhavebeenofferedbut thendeclinedEPT.Inaddition,theabilityofthisEPT programtoprovidepaperprescriptionscouldbeunique. ElectronicmedicationprescriptionisthenormintheUS,57 althoughsomestatesallowpaperprescriptionsforEPT.58 In addition,theBPAdidnottriggerforpatientsbeingtreated fortrichomonas,asthisinfectionwastooinfrequently diagnosedinthisEDandkeepingmetronidazoleasatrigger criterionsignificantlydecreasedthesensitivityofthe screeningforeligiblepatients.
Giventhelimitsofthispilotstudymethodology,patients’ compliancetoprovidethe “take-home” kitsorpaper prescriptionstotheirpartners,ifthepaperprescriptionswere filled,orifthemedicationsweretakenisunknown.Thelack offollow-uplimitedourabilitytoconfirmmedication adherenceandcompletionoftreatmentinthispatient population.Priorrandomizedcontroltrialswithfollow-up thatalsotrackedsubsequentSTIinfectionshavefounda rangeinthenumberneededtotreat(NNT)toprevent recurrentorpersistentchlamydiaorgonorrheaintheindex patient,from fiveinastudyofheterosexualmen46 to33ina studyofwomenandheterosexualmen.7 Ourcurrentstudy lacksthefollow-uptomakeanyconclusionsonNNTor completionoftreatmentonceprovided.
CONCLUSION
Inthispilot,expeditedpartnertreatmentprogram,EPT wasprovidedto25%ofEDpatientswhoappearedeligibleto receiveit.Theinterruptivebestpracticesadvisoryincreased EPTprescribingmorethantwo-fold.Multiplebarriersto EPTprescribingfromthisEDwereidentified,whichcanbe thesubjectoffutureinterventionstoimproveprovisionof EPTtopatientsintheED.
ACKNOWLEDGEMENTS
WethankBiancaClarkeMPHfromtheMichigan DepartmentofHealth,aswellasAaronKrumheuerMD, AsavariRajpurkarMD,JefferineLiMD,LauraDurecka PA-C,RichMedlinMD,MSIS,andJoyceLeeMD,MPH fortheircontributionstothisproject.
AddressforCorrespondence:RachelE.Solnick,MD,MSc,The MountSinaiHospital/IcahnSchoolofMedicine,Departmentof EmergencyMedicine – ResearchDivision,555West57thStreet5th FloorSuite5-25,NewYork,NewYork10019.Email: Rachel. Solnick@mountsinai.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Dr.SolnickwassupportedbytheInstituteforHealthcarePolicyand InnovationattheUniversityofMichiganNationalClinicianScholars Programduringaportionofthisstudy.Therearenoconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2023Ageretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.CentersforDiseaseControlandPrevention.SexuallyTransmitted DiseaseSurveillance2020.Atlanta:USDepartmentofHealthand HumanServices;2022.Availableat: https://www.cdc.gov/std/statistics/ 2020/2020-SR-4-10-2023.pdf.AccessedOctober27,2022.
2.PearsonWS,PetermanTA,GiftTL.Anincreaseinsexuallytransmitted infectionsseeninUSemergencydepartments. PrevMed 2017;100:143–4.
3.JamisonCD,Greenwood-EricksenM,RichardsonCR,etal. Associationbetweenchlamydiaandroutineplaceforhealthcare intheUnitedStates:NHANES1999-2016. PLoSONE. 2021;16(5):e0251113.
4.HosenfeldCB,WorkowskiKA,BermanS,etal.Repeatinfectionwith chlamydiaandgonorrheaamongfemales:asystematicreviewofthe literature. SexTransmDis.2009;36(8):478–89.
5.HillisSD,OwensLM,MarchbanksPA,etal.Recurrentchlamydial infectionsincreasetherisksofhospitalizationforectopicpregnancy
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 1002 Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram Ageretal.
andpelvicinflammatorydisease. AmJObstetGynecol. 1997;176(1Pt1):103–7.
6.WalenskyR,HouryD,JerniganD,etal.Sexuallytransmittedinfections treatmentguidelines,2021. MMWRRecommRep. 2021;70(4):1–187.
7.GoldenMR,WhittingtonWLH,HandsfieldHH,etal.Effectofexpedited treatmentofsexpartnersonrecurrentorpersistentgonorrheaor chlamydialinfection. NEnglJMed.2005;352(7):676–85.
8.SchillingerJA,KissingerP,CalvetH,etal.Patient-deliveredpartner treatmentwithazithromycintopreventrepeatedchlamydiatrachomatis infectionamongwomen:arandomized,controlledtrial. SexTransmDis 2003;30(1):49–56.
9.TrelleS,ShangA,NarteyL,etal.Improvedeffectivenessofpartner notificationforpatientswithsexuallytransmittedinfections:systematic review. BMJ.2007;334(7589):354.
10.FerreiraA,YoungT,MathewsC,etal.Strategiesforpartnernotification forsexuallytransmittedinfections,includingHIV. CochraneDatabase SystRev. 2013;(10):CD002843.
11.MmejeO,WallettS,KolenicG,etal.Impactofexpeditedpartnertherapy (EPT)implementationonchlamydiaincidenceintheUSA. SexTransm Infect.2018;94(7):545–7.
12.AmericanCollegeofEmergencyPhysicians(ACEP).ExpeditedPartner TherapyforSelectedSexuallyTransmittedInfections.Policy
Statements.Availableat: https://www.acep.org/patient-care/ policy-statements/expedited-partner-therapy-for-selected-sexuallytransmitted-infections.AccessedOctober27,2022.
13.CaliforniaDepartmentofPublicHealth.Patient-deliveredpartner therapy(PDPT)forchlamydia,gonorrhea,andtrichomeniasis:guidance formedicalprovidersinCalifornia.2016.Availableat: https://www.cdph. ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/ ClinicalGuidelines_CA-STD-PDPT-Guidelines.pdf
AccessedOctober27,2022.
14.ZolnaMR,FrostJJ.Publiclyfundedfamilyplanningclinicsin2015: patternsandtrendsinservicedeliverypracticesandprotocols. GuttmacherInstitute.2016.Availableat: https://www.guttmacher.org/ report/publicly-funded-family-planning-clinic-survey-2015
AccessedOctober27,2022.
15.CramerR,MartinezN,RobertsC,etal.Useofexpeditedpartner therapyforsexuallytransmitteddiseasesincollegeanduniversity healthcentersintheUnitedStates,2011-2012. SexTransmDis 2015;42(10):580
4.
16.IsolaM,FrancisJ.UseofExpeditedpartnertherapyfortreatment ofchlamydiainadolescents. JPediatrAdolescGynecol 2018;31(2):178.
17.TaylorMM,ReilleyB,YellowmanM,etal.Useofexpeditedpartner therapyamongchlamydiacasesdiagnosedatanurbanIndianhealth centre,Arizona. IntJSTDAIDS.2013;24(5):371–4.
18.SolnickRE,CortesR,ChangE,etal.Anationalstudyofexpedited partnertherapyuseinemergencydepartments:asurveyofmedical directorknowledge,attitudesandpractices. medRxiv.2023.Available at: https://www.medrxiv.org/content/10.1101/2023.04.01.23287999v1. article-info.AccessedOctober27,2022.
19.DivisionofHIVandSTIPrograms,FieldServicesandSTIPrevention Section. GuidanceforHealthCareProviders:ExpeditedPartner Therapy(EPT)forChlamydia,Gonorrhea,andTrichomoniasis [MichiganDepartmentofHealthandHumanServices];2021.
20.MichiganLicensingandRegulatoryAffairsBureauofProfessional Licensing.ElectronicPrescribingFAQ.2022.Availableat: https://www. michigan.gov/lara/-/media/Project/Websites/lara/bpl/HealthProfessional-Licensing-page/Electronic-Prescribing-FrequentlyAsked-Questions.pdf?rev=308cccd61a7748099a0f30199b9edc9f AccessedOctober27,2022.
21.DamschroderLJ,AronDC,KeithRE,etal.Fosteringimplementationof healthservicesresearch findingsintopractice:aconsolidated frameworkforadvancingimplementationscience. ImplementSci 2009;4:50.
22.McCool-MyersM,SmithADY,KottkeMJ.Expertinterviewsonmultilevel barriersinimplementingexpeditedpartnertherapyforchlamydia. JPublicHealthManagPract. 2020;26(6):585–9.
23.FahertyE,BoraasC,SmithK,etal.Expeditedpartnertherapyfor sexuallytransmittedinfectionsinMinnesota:amixed-methodsreviewof currentpracticesandbarrierstoimplementation. ValueHealth 2021;24:S103.
24.WongJ,ZakherB,ConsolacionT,etal.Facilitatorsandbarriersto expeditedpartnertherapy:resultsfromasurveyoffamilyphysicians. SexTransmDis.2020;47(8):525–9.
25.ArtinoARJr,LaRochelleJS,DezeeKJ,etal.Developingquestionnaires foreducationalresearch:AMEEGuideNo.87. MedTeach 2014;36(6):463–74.
26.SoboEJ,SimmesDR,LandsverkJA,etal.Rapidassessmentwith qualitativetelephoneinterviews:lessonsfromanevaluationof California’sHealthyFamiliesProgram&Medi-CalforChildren. AmJ Eval.2003;24(3):399–408.
27.SolnickR,CortesR,ChangE,etal.175Anationalstudyofbarriersand facilitatorsofexpeditedpartnertherapyuseinemergencydepartments: aqualitativestudy. AnnEmergMed.2021;78(4):S70.
28.NiccolaiLM,WinstonDM.Physicians’ opinionsonpartnermanagement fornonviralsexuallytransmittedinfections. AmJPrevMed 2005;28(2):229–33.
29.OgrincG,DaviesL,GoodmanD,etal.SQUIRE2.0(Standardsfor QualityImprovementReportingExcellence):revisedpublication guidelinesfromadetailedconsensusprocess. BMJQualSaf 2016;25(12):986–92.
30.TongA,SainsburyP,CraigJ.Consolidatedcriteriaforreporting qualitativeresearch(COREQ):a32-itemchecklistforinterviewsand focusgroups. IntJQualHealthCare.2007;19(6):349–57.
31.ShamashZ,CatallozziM,DayanPS,etal.Preferencesforexpedited partnertherapyamongadolescentsinanurbanpediatricemergency department:amixed-methodsstudy. PediatrEmergCare 2019;37(3):e91–6.
32.TrinkleyKE,BlakesleeWWMDD.Clinicianpreferencesfor computerisedclinicaldecisionsupportformedicationsinprimarycare:a focusgroupstudy. BMJHealthCareInform. 2019;26(1).
–
Volume24,No.5:September2023WesternJournal of EmergencyMedicine 1003 Ageretal. Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram
33.CohenS,BostwickJR,MarshallVD,etal.Theeffectofacomputerized bestpracticealertsysteminanoutpatientsettingonmetabolic monitoringinpatientsonsecond-generationantipsychotics. JClin PharmTher.2020;45(6):1398–404.
34.BejjankiH,MrambaLK,BealSG,etal.Theroleofabestpracticealertin theelectronicmedicalrecordinreducingrepetitivelabtests. Clinicoecon OutcomesRes.2018;10:611
8.
35.PalatnikA,TillisB,TsaihSW,etal.674Effectofabest-practicealerton theratesofsmokingcessationduringpregnancy. AmJObstetGynecol 2021;224(2):S423–4.
36.Najafi N,CucinaR,PierreB,etal.Assessmentofatargetedelectronic healthrecordinterventiontoreducetelemetryduration:aclusterrandomizedclinicaltrial. JAMAInternMed.2019;179(1):11–5.
37.DeSilvaMB,KodetA,WalkerPF.Abestpracticealertforidentifying hepatitisB-infectedpatients. AmJTropMedHyg.2020;103(2):884–6.
38.FunkeM,KaplanMC,GloverH,etal.Increasingnaloxoneprescribing intheemergencydepartmentthrougheducationandelectronic medicalrecordwork-aids. JtCommJQualPatientSaf 2021;47(6):364
75.
39.FordJ,ChechiT,OtmarM,etal.Emergencydepartmentsyphilis screeningpracticesbeforeandaftertheimplementationofanelectronic healthrecord-basedbest-practicealert. SupplAnnEmergMed:ACEP ResearchForum.2020;76:s54.
40.EmbiPJ,LeonardAC.EvaluatingalertfatigueovertimetoEHR-based clinicaltrialalerts: findingsfromarandomizedcontrolledstudy. JAm MedInformAssoc.2012;19(e1):e145–8.
41.FryC.Developmentandevaluationofbestpracticealerts:methodsto optimizecarequalityandcliniciancommunication. AACNAdvCritCare 2021;32(4):468–72.
42.LehtoE,AndersonB,ReedJ,etal.Impactofrapidtestingforgonorrhea andchlamydiainanurbanpediatricemergencydepartment. JAdolesc Health.2022;70(6):910–4.
43.GaydosCA,AkoMC,LewisM,etal.Useofarapiddiagnostic forchlamydiatrachomatisandNeisseriagonorrhoeaeforwomen intheemergencydepartmentcanimproveclinicalmanagement: reportofarandomizedclinicaltrial. AnnEmergMed 2019;74(1):36–44.
44.RothmanR,DugasA,LewisM.RapidTestingforchlamydiaand gonorrheainemergencydepartments.AmericanSexualHealth Association.Availableat: http://chlamydiacoalition.org/rapidtesting-for-chlamydia-and-gonorrhea-in-emergency-departments/ AccessedOctober27,2022.
45.MayL,WareCE,JordanJA,etal.Arandomizedcontrolledtrial comparingthetreatmentofpatientstestedforchlamydiaandgonorrhea afterarapidpolymerasechainreactiontestversusstandardofcare testing. SexTransmDis.2016;43(5):290.
46.KissingerP,MohammedH,Richardson-AlstonG,etal.Patientdeliveredpartnertreatmentformaleurethritis:arandomized,controlled trial. ClinInfectDis.2005;41(5):623–9.
47.SlutskerJS,TsangLYB,SchillingerJA.Doprescriptionsforexpedited partnertherapyforchlamydiaget filled?Findingsfromamultijurisdictionalevaluation,UnitedStates,2017–2019. SexTransmDis 2020;47(6):376–82.
48.SchillingerJ,SlutskerJ,TsangLY,etal.P076Doprescriptionsfor expeditedpartnertherapyget filled?Findingsfromamulti-jurisdictional evaluation,US,2017–2018. SexTransmInfect.2019;95(Suppl1):A107.
49.HayesBD,ZaharnaL,WintersME,etal.To-gomedicationsfor decreasingEDreturnvisits. AmJEmergMed.2012;30(9):2011–4.
50.BlomeA,KaighC,ShafferC,etal.Emergencydepartmentmedication dispensingreducesreturnvisitsandadmissions. AmJEmergMed 2020;38(11):2387–90.
51.KabrhelC,VinsonDR,MitchellAM,etal.Aclinicaldecisionframework toguidetheoutpatienttreatmentofemergencydepartmentpatients diagnosedwithacutepulmonaryembolismordeepveinthrombosis: Resultsfromamultidisciplinaryconsensuspanel. JAmCollEmerg PhysiciansOpen.2021;2(6):e12588.
52.EssentialAccessHealth:CaliforniaStatePolicy.EssentialAccess Health.Availableat: https://www.essentialaccess.org/advocacy/ policy-priorities.AccessedOctober27,2022.
53.AnthemBlueCross.ExpeditedpartnertherapyforthepreventionofSTI reinfections.2021.Availableat: https://providers.anthem.com/docs/ gpp/CA_CAID_PU_partnertherapySTIreinfections.pdf? v=202106011845.AccessedOctober27,2022.
54.AboutTitleX.EssentialAccessHealth.Availableat: https://www. essentialaccess.org/programs-and-services/about-title-x AccessedOctober27,2022.
55.PearsonWS,TrombleE,JenkinsWD,etal.Choosingthe emergencydepartmentasanalternativeforSTDcare:potential D=disparitiesinaccess. JHealthCarePoorUnderserved 2022;33(3):1163–8.
56.WareCE,AjabnoorY,MullinsPM,etal.Aretrospectivecross-sectional studyofpatientstreatedinUSEDsandambulatorycareclinicswith sexuallytransmittedinfectionsfrom2001to2010. AmJEmergMed 2016;34(9):1808–11.
57.E-PrescribingStateLaws.Availableat: https://mdtoolbox.com/ eprescribe-map.aspx?AspxAutoDetectCookieSupport=1 AccessedOctober27,2022.
58.ExceptionstoElectronicPrescribing.Availableat: https://www.health. ny.gov/professionals/narcotic/electronic_prescribing/ exceptions_to_ep.htm.AccessedOctober27,2022.
–
–
WesternJournal of EmergencyMedicineVolume24,No.5:September2023 1004 Mixed-MethodsEvaluationofaPilotED-basedExpeditedPartnerTherapyProgram Ageretal.
EMERGENCY MEDICINE IS THE ONLY SPECIALTY WITH ITS OWN BUDGET ALLOCATION. CALIFORNIAACEPSECURED $200MANNUALLYTO INCREASEMEDI-CAL REIMBURSEMENTFOR EMERGENCYPHYSICIANS! @CALIFORNIAACEP www.californiaacep.org Medi-cal Medi-cal rrateincrease ateincrease















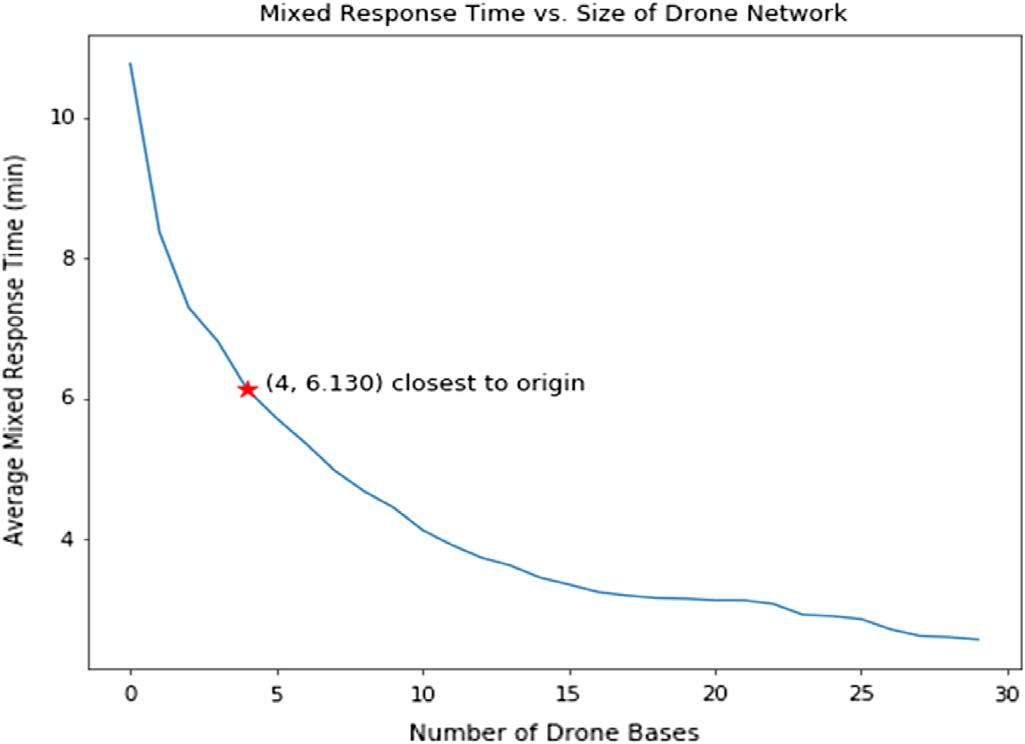

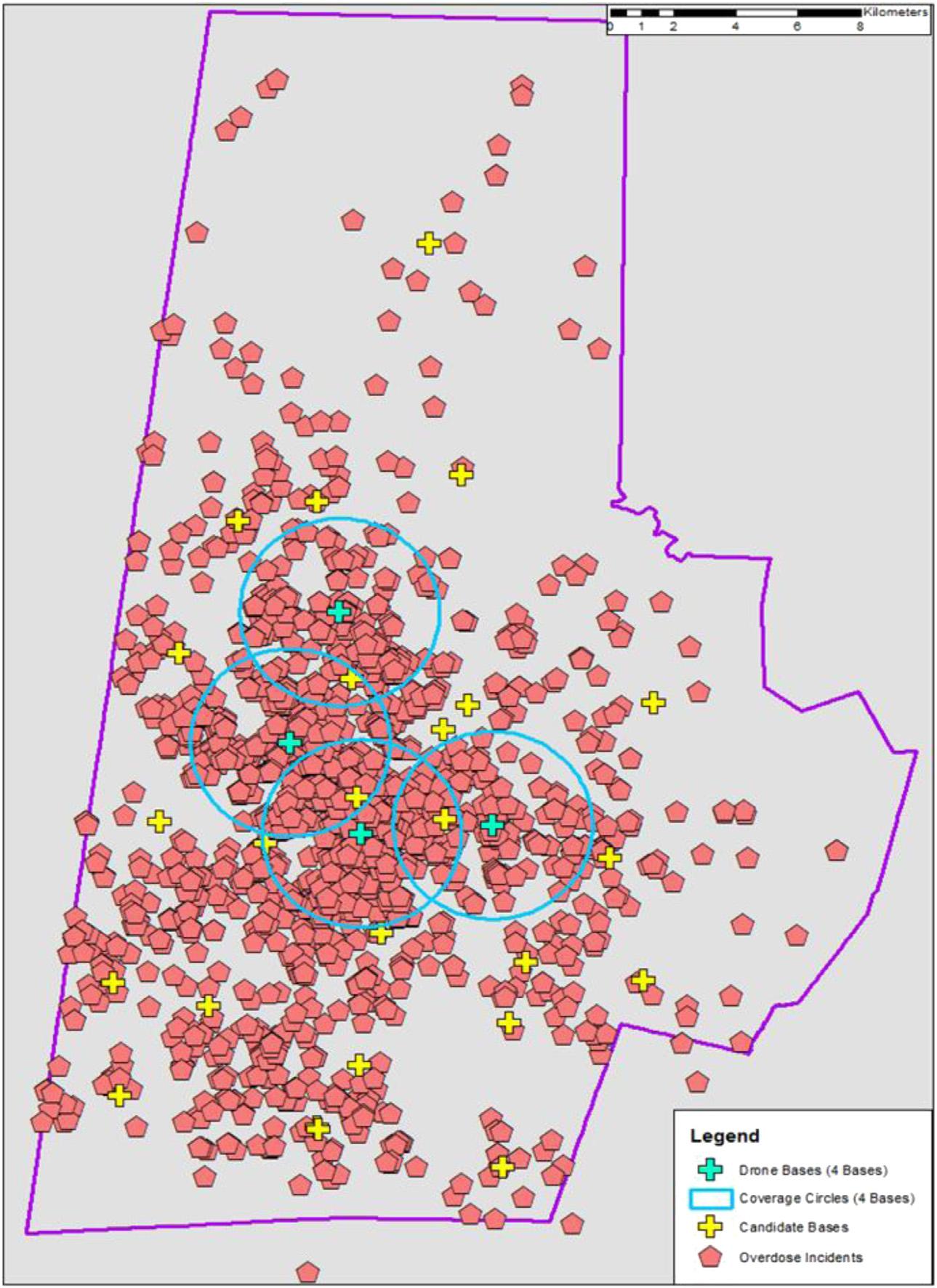
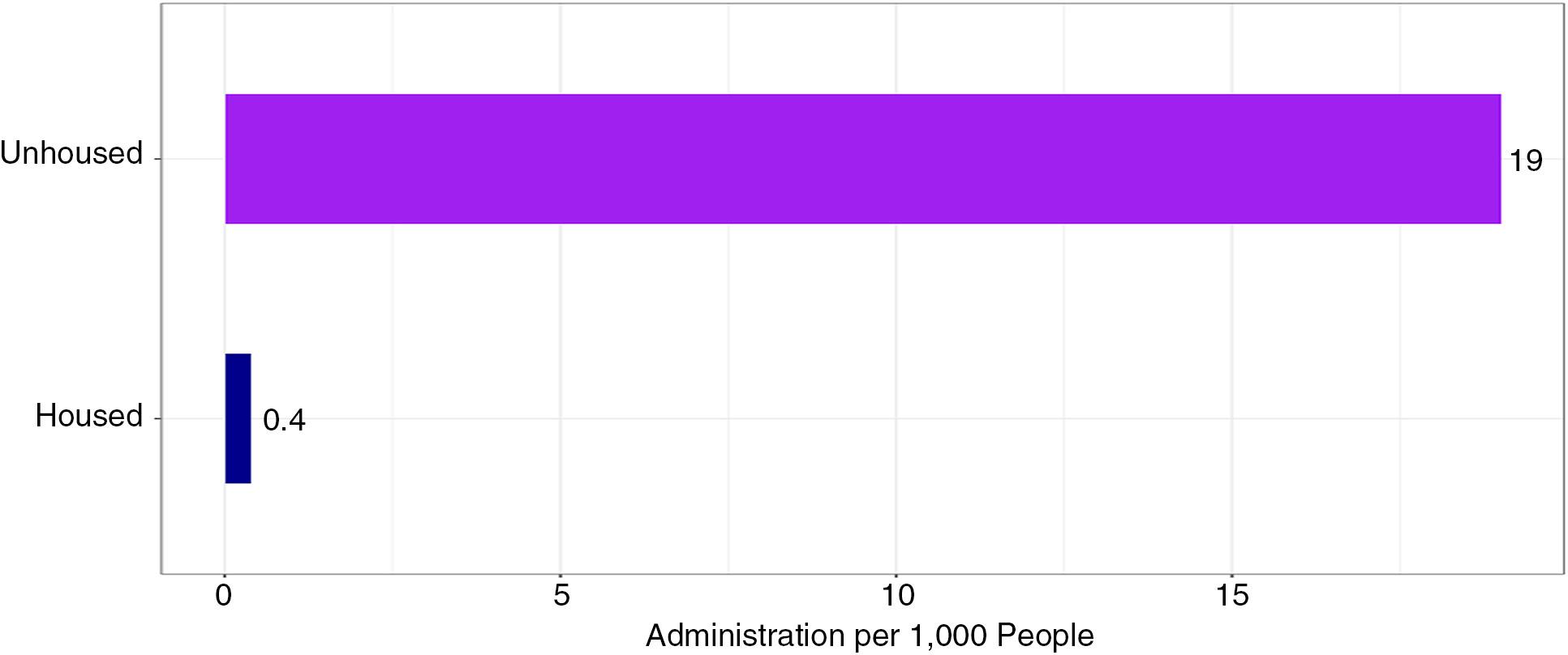
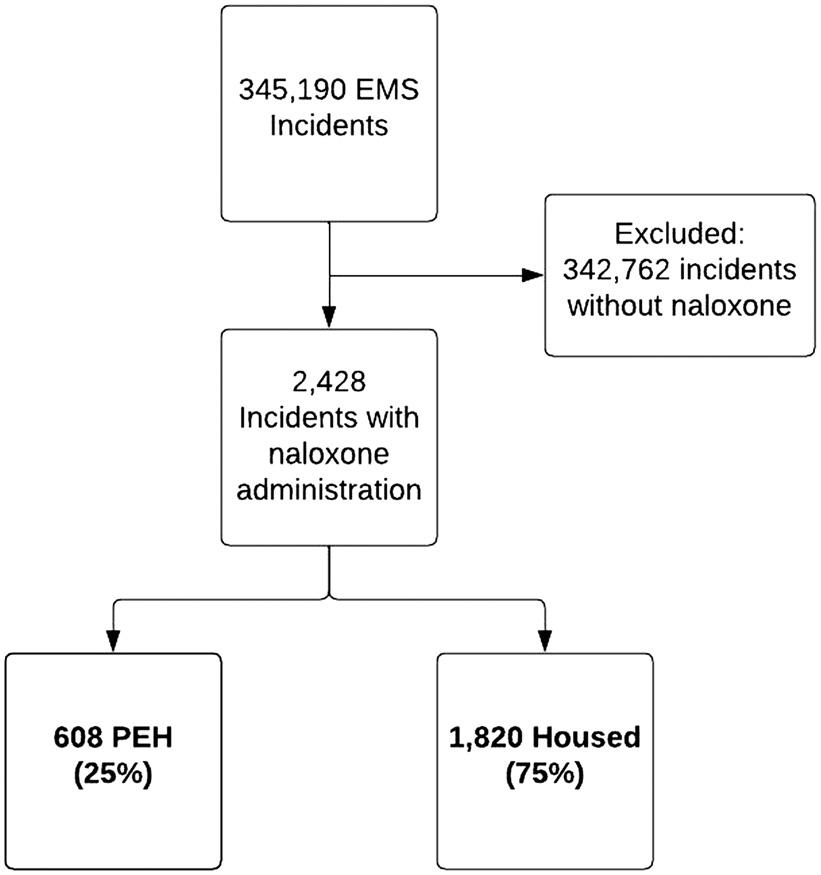

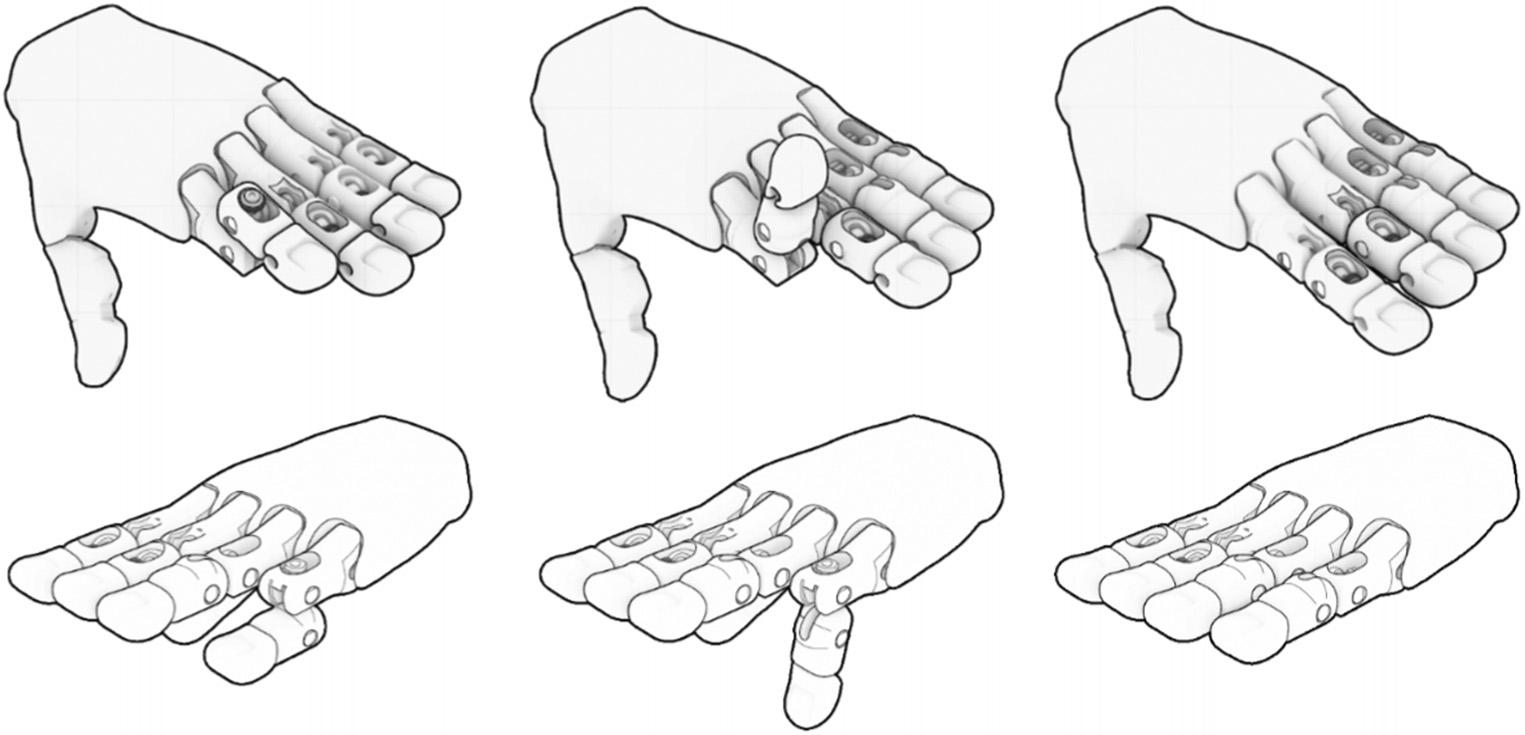



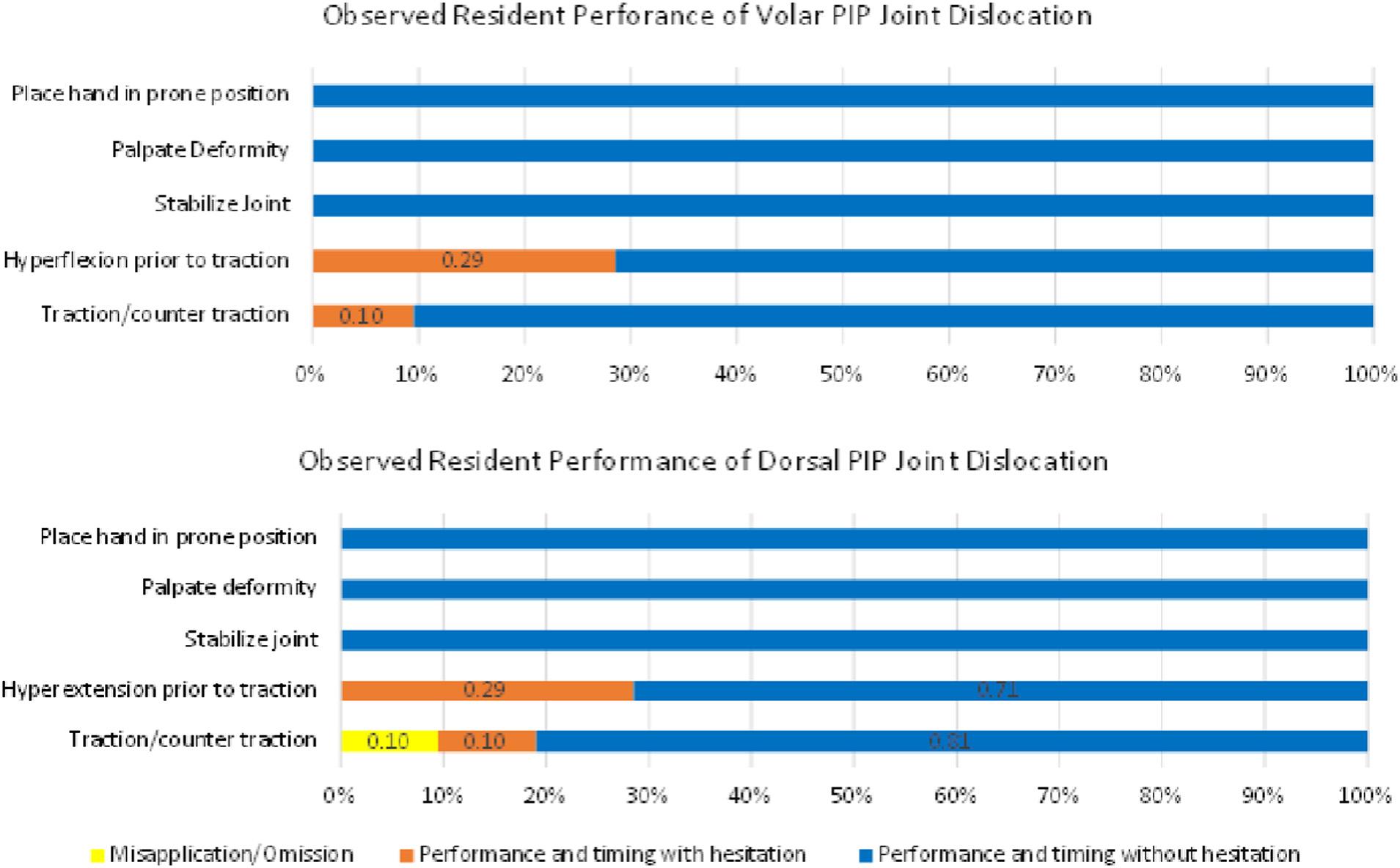
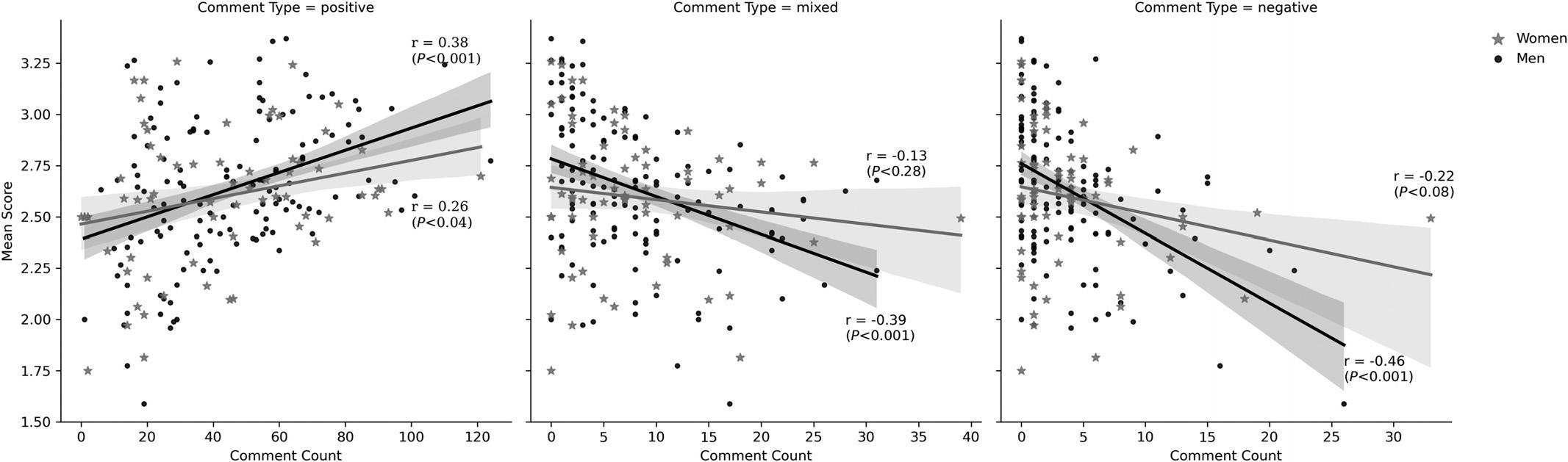
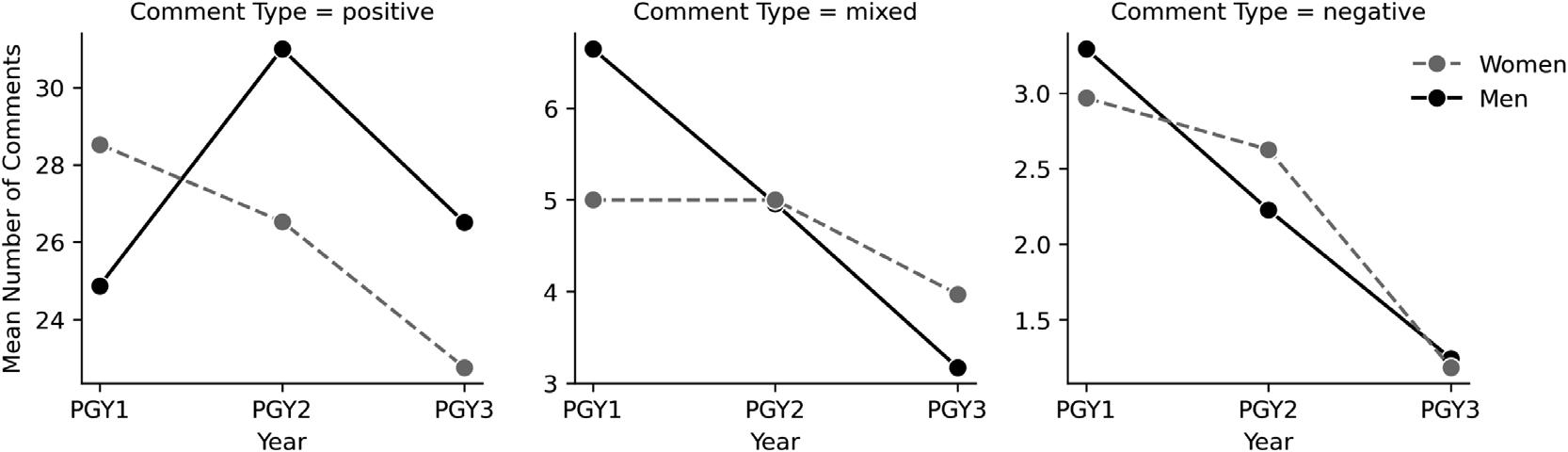

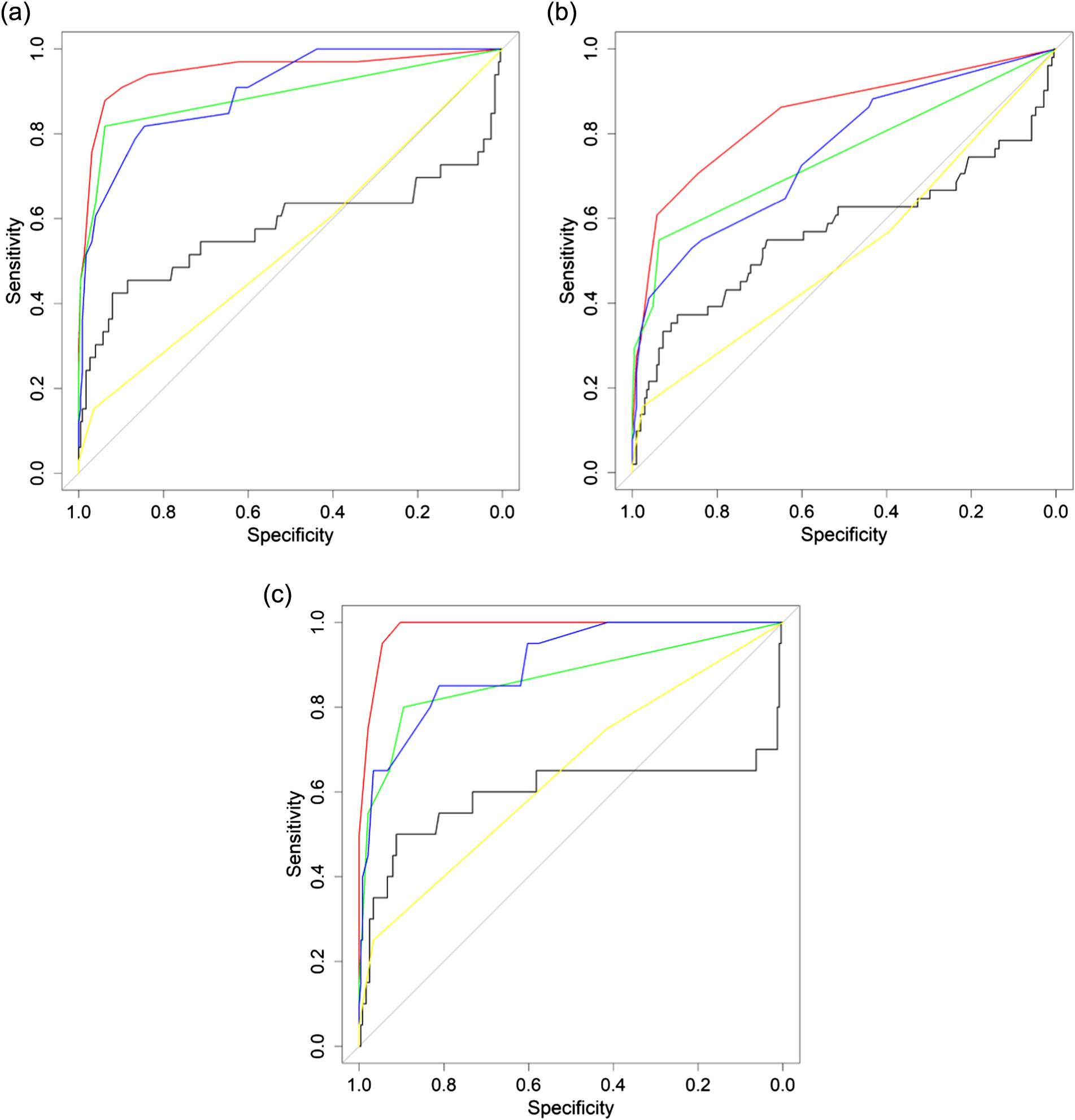
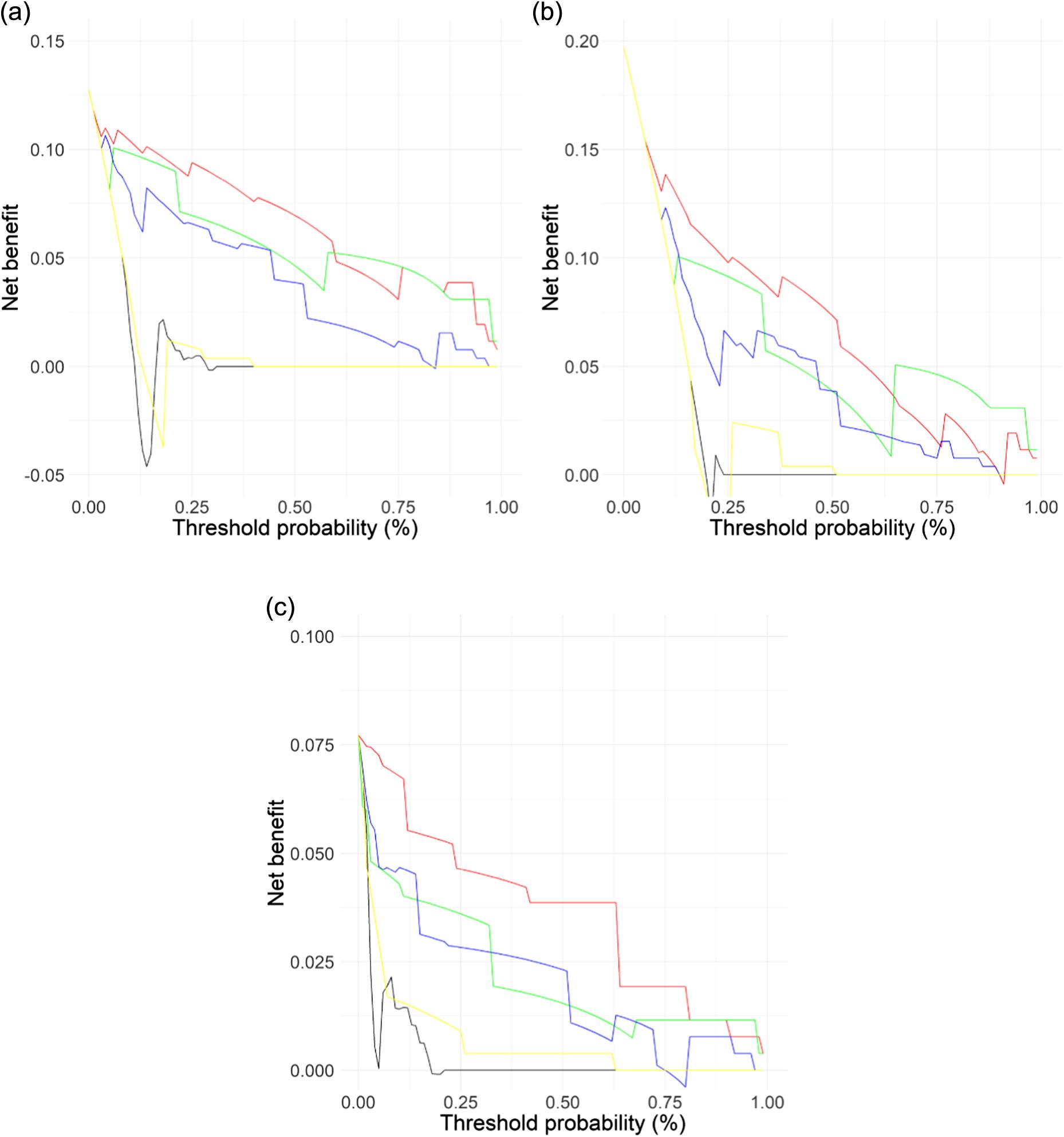
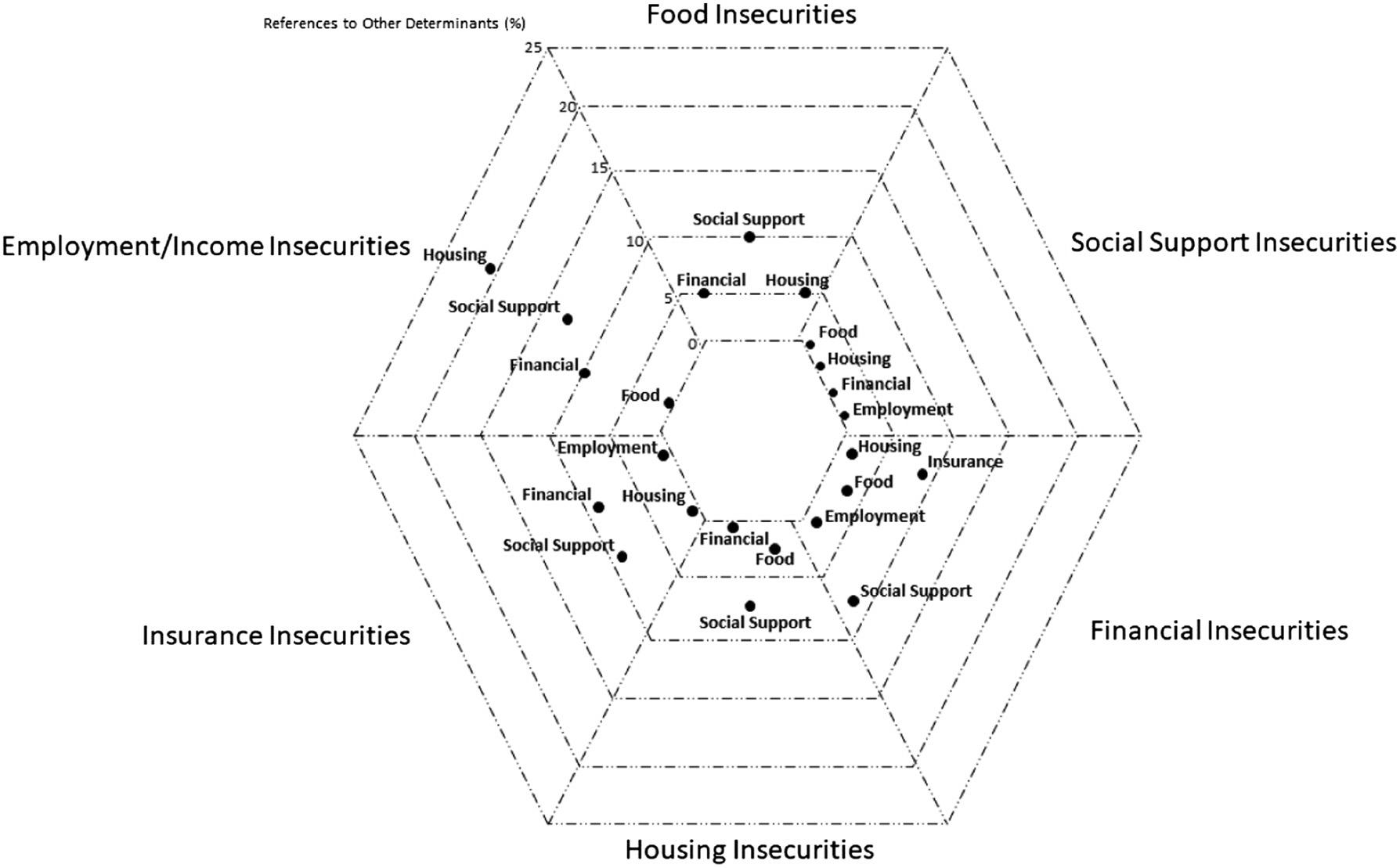

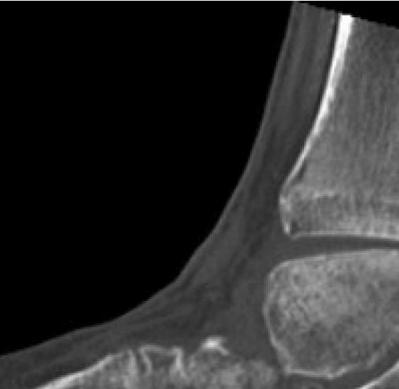
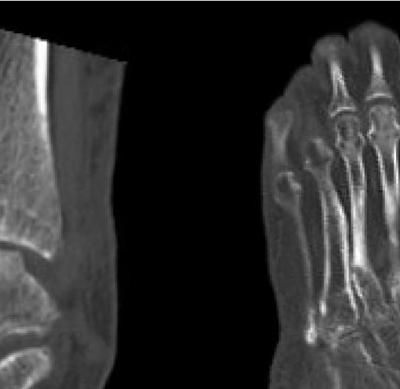


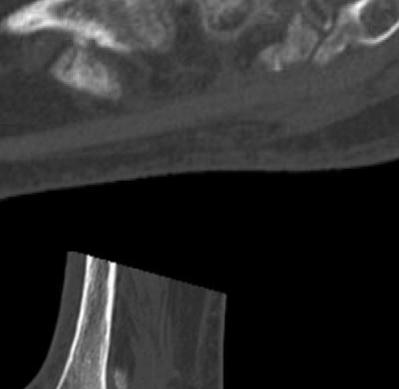











 (A)
(B)
(C)
(D)
Figure2. Computedtomographywith(A,C,D)multiplesagittalcuts,and(B)acoronalcutafterfollow-upinorthopedicclinicdemonstrating findingsconsistentwithadvancedstageCharcotjointwithmarkedpesplanus,mid-footcollapse,andhindfootvalgus.
(A)
(B)
Figure3. Mostrecentradiographsat finalfollow-up.(A)Lateralradiograph.(B)Bilateralanterior-posteriorradiograph,revealingrestorationof thearchofthefoot,throughtheuseofmultipleosteotomysitesandinternal fixationwithavarietyofplate,screw,andbeamconstructs.
(A) (B)
(A)
(B)
(C)
(D)
Figure2. Computedtomographywith(A,C,D)multiplesagittalcuts,and(B)acoronalcutafterfollow-upinorthopedicclinicdemonstrating findingsconsistentwithadvancedstageCharcotjointwithmarkedpesplanus,mid-footcollapse,andhindfootvalgus.
(A)
(B)
Figure3. Mostrecentradiographsat finalfollow-up.(A)Lateralradiograph.(B)Bilateralanterior-posteriorradiograph,revealingrestorationof thearchofthefoot,throughtheuseofmultipleosteotomysitesandinternal fixationwithavarietyofplate,screw,andbeamconstructs.
(A) (B)
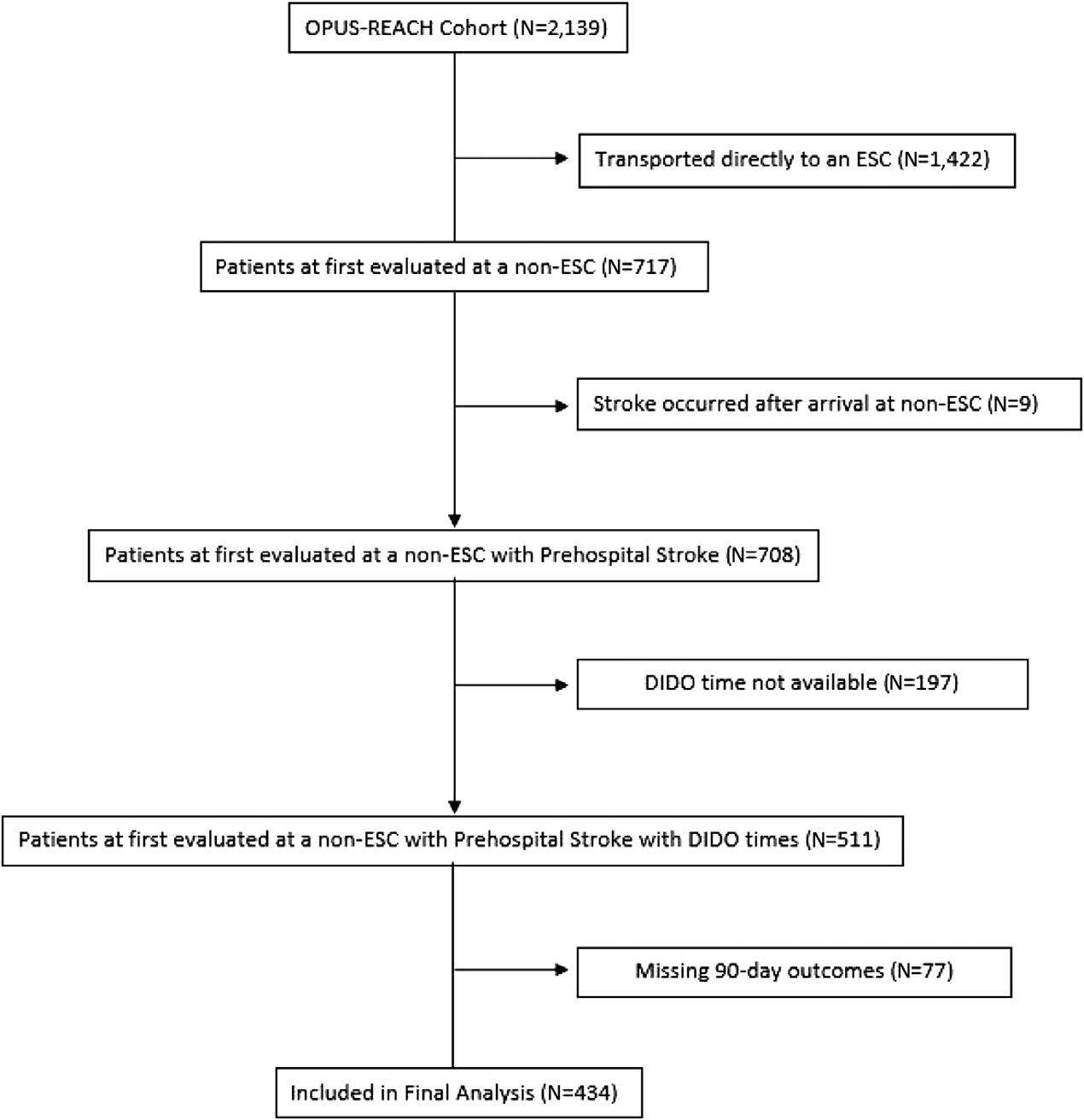
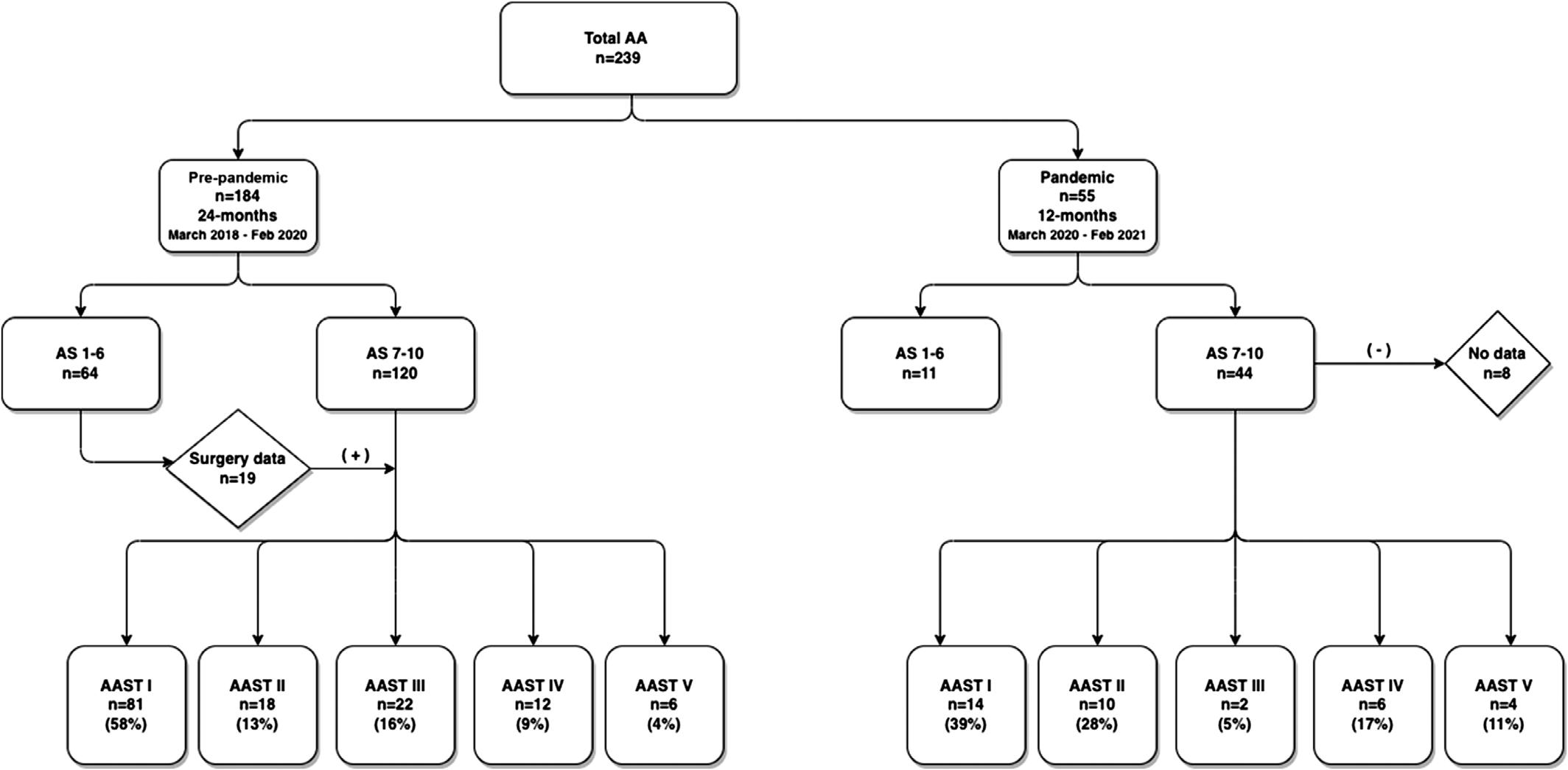


 Figure1. Swim-laneprocessmapoftheexpeditedpartnertherapy(EPT)pilotprogram.
Figure1. Swim-laneprocessmapoftheexpeditedpartnertherapy(EPT)pilotprogram.