Volume 25, Number 3, May 2024


Volume 25, Number 3, May 2024
Behavioral Health
303 Addressing System and Clinician Barriers to Emergency Department-initiated Buprenorphine: An Evaluation of Post-intervention Physician Outcomes
Jacqueline J. Mahal, Polly Bijur, Audrey Sloma, Joanna Starrels, Tiffany Lu
312 Factors Associated with Acute Telemental Health Consultations in Older Veterans
Erica C. Koch, Michael J. Ward, Alvin D. Jeffery, Thomas J. Reese, Chad Dorn, Shannon Pugh, Melissa Rubenstein, Jo Ellen Wilson, Corey Campbell, Jin H. Han
320 Implementation and Evaluation of a Bystander Naloxone Training Course
Scott G. Weiner, Scott A. Goldberg, Cheryl Lang, Molly Jarman, Cory J. Miller, Sarah Li, Ewelina W. Stanek, Eric Goralnick
Critical Care
325 Emergency Department SpO2/FiO2 Ratios Correlate with Mechanical Ventilation and Intensive Care Unit Requirements in COVID-19 Patients
Gary Zhang, Michael J. Burla, Benjamin B. Caesar, Carolyne R. Falank, Peter Kyros, Victoria C. Zucco, Aneta Strumilowska, Daniel C. Cullinane, Forest R. Sheppard
Education
332 Geographic Location and Corporate Ownership of Hospitals in Relation to Unfilled Positions in the 2023 Emergency Medicine Match
Zachary J. Jarou, Angela G. Cai, Leon Adelman, David J. Carlberg, Sara P. Dimeo, Jonathan Fisher, Todd Guth, Bruce M. Lo, Laura Oh, Rahul Puttagunta, Gillian R Schmitz
Emergency Department Operations
342 Imaging in a Pandemic: How Lack of Intravenous Contrast for Computed Tomography Affects Emergency Department Throughput
Wayne A. Martini, Clinton E. Jokerst, Nicole Hodsgon, Andrej Urumov




Integrating Emergency Care with Population Health Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Amin A. Kazzi, MD, MAAEM
The of MMM
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Douglas Ander, MD Emory University
Emory University
Edward Michelson, MD Texas Tech University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH
Edward Panacek, MD, MPH University of South Alabama
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
“Maggiore della Carità,” Novara, Italy
Gayle
Gayle Galleta, MD
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD
Icelandic Medicine
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Jaqueline MD
Desert
Jaqueline Le, MD Desert Regional Medical Center
Jeffrey Love, MD
The George Washington University School of Medicine and Health Sciences
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Katsuhiro University Miyazaki, Kenneth University
Leslie Chicago Medical School
Leslie Zun, MD, MBA Chicago Medical School
Linda University of
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Niels K. Rathlev, MD Tufts University School of Medicine
Tufts University School of Medicine
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Baptist University of California, San Francisco
Rachel A. Lindor, MD, JD Clinic
Rachel A. Lindor, MD, JD Mayo Clinic
Robert Suter, DO, MHA
Robert Suter, DO, MHA UT Southwestern Medical Center
Derlet, University of California, Davis
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD
Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Scott Rudkin, MD, MBA
Scott Rudkin, MD, MBA University of California, Irvine
Elena Lopez-Gusman, JD
Elena Lopez-Gusman, JD
California ACEP
California ACEP
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Isabelle Nepomuceno, BS Executive Editorial Director
Steven Changi
American College of Emergency Physicians
American College of Emergency
Jennifer Kanapicki Comer, MD FAAEM
AAEM School
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE
DeAnna McNett, CAE
Kimberly Ang, MBA
UC Irvine Health School of Medicine
UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
MPH FAAEM, FACEP
Shahram Lotfipour, MD, MPH FAAEM, FACEP
Visha Bajaria, BS WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Scott Zeller, MD University of California, Riverside
Scott Zeller, MD University
Singapore
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Wirachin MSBATS
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Mahidol Bangkok,
American College of Osteopathic Emergency Physicians
UC Irvine Health School of Medicine
American College of Osteopathic Emergency Physicians School
Randall J. Young, MD, MMM, FACEP
California ACEP
UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP
Jorge Fernandez, MD, FACEP
UC San Diego Health School of Medicine
UC San Diego Health School of Medicine
Visha Bajaria, BS WestJEM Editorial Director WestJEM
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Siriraj Hospital, Mahidol University, Bangkok, Thailand
American College of Emergency Physicians
Kaiser Permanente
American College of Emergency Physicians Kaiser Permanente
Physicians, :
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
Cassandra Saucedo, MS BA WestJEM Publishing Director Casey,
June Casey, BA Copy Editor
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine




PubMed, Central, CINAHL, Medscape, MDLinx Editorial and Publishing Office: JEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA
Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org
of Emergency
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
345 The Utility of Dot Phrases and SmartPhrases in Improving Physician Documentation of Interpreter Use
Katrin Jaradeh, Elaine Hsiang, Malini K. Singh, Christopher R. Peabody, Steven Straube
350 Best Practices for Treating Blind and Visually Impaired Patients in the Emergency Department: A Scoping Review
Kareem Hamadah, Mary Velagapudi, Juliana J. Navarro, Andrew Pirotte, Christopher Obersteadt
Endemic Infections
358 Association Between Sexually Transmitted Infections and the Urine Culture
Johnathan M. Sheele, Carolyn Mead-Harvey, Nicole R. Hodgson
368 Changing Incidence and Characteristics of Photokeratoconjunctivitis During the COVID-19 Pandemic
Yu-Shiuan Lin, Chih-Cheng Lai, Yu-Chang Liu, Shu-Chun Kuo, Shih-Bin Su
374 Operation CoVER Saint Louis (COVID-19 Vaccine in the Emergency Room): Impact of a Vaccination Program in the Emergency Department
Brian T. Wessman, Julianne Yeary, Helen Newland, Randy Jotte
382 Sexually Transmitted Infection Co-testing in a Large Urban Emergency Department
James S. Ford, Joseph C. Morrison, Jenny L. Wagner, Disha Nangia, Stephanie Voong, Cynthia G. Matsumoto, Tasleem Chechi, Nam Tran, Larissa May
International Emergency Medicine
389 Public Beliefs About Accessibility and Quality of Emergency Departments in Germany
Jens Klein, Sarah Koens, Martin Scherer, Annette Strauß, Martin Härter, Olaf von dem Knesebeck
Neurology
399 Support for Thrombolytic Therapy for Acute Stroke Patients on Direct Oral Anticoagulants: Mortality and Bleeding Complications
Paul Koscumb, Luke Murphy, Matthew Talbott, Shiva Nuti, George Golovko, Hashem Shaltoni, Dietrich Jehle
Pediatrics
407 Patient-related Factors Associated with Potentially Unnecessary Transfers for Pediatric Patients with Asthma: A Retrospective Cohort Study
Gregory A. Peters, Rebecca E. Cash, Scott A. Goldberg, Jingya Gao, Lily M. Kolb, Carlos A.Camargo
Public Health
415 Public Health Interventions in the Emergency Department: A Framework for Evaluation
Elisabeth Fassas, Kyle Fischer, Steven Schenkel, John David Gatz, Daniel B.Gingold
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Trauma
423 Trauma-informed Care Training in Trauma and Emergency Medicine: A Review of the Existing Curricula
Cecelia Morra, Kevin Nguyen, Rita Sieracki, Ashley Pavlic, Courtney Barry
Women’s Health
431 Relationship of Beta-Human Chorionic Gonadotropin to Ectopic Pregnancy Detection and Size
Duane M Eisaman, Nicole E. Brown, Sarah Geyer
436 Prevalence and Characteristics of Emergency Department Visits by Pregnant People: An Analysis of a National Emergency Department Sample (2010–2020)
Carl Preiksaitis, Monica Saxena, Jiaqi Zhang, Andrea Henkel
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Albany Medical College Albany, NY
Allegheny Health Network Pittsburgh, PA
American University of Beirut Beirut, Lebanon
AMITA Health Resurrection Medical Center Chicago, IL
Arrowhead Regional Medical Center Colton, CA
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
INTEGRIS Health Oklahoma City, OK
Kaiser Permenante Medical Center San Diego, CA
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Lakeland HealthCare St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Louisiana State University Shreveport Shereveport, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maine Medical Center Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Mayo Clinic Jacksonville, FL
Mayo Clinic College of Medicine Rochester, MN
Mercy Health - Hackley Campus Muskegon, MI
Merit Health Wesley Hattiesburg, MS
Midwestern University Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program St. Paul, MN
Rhode Island Hospital Providence, RI
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
St. Luke’s University Health Network Bethlehem, PA
Spectrum Health Lakeland St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
The MetroHealth System/ Case Western Reserve University Cleveland, OH
UMass Chan Medical School Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Tucson, AZ
University of California, Davis Medical Center Sacramento, CA
University of California, Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago Chicago, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Massachusetts Amherst, MA
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Nebraska Medical Center Omaha, NE
University of Nevada, Las Vegas Las Vegas, NV
University of Southern Alabama Mobile, AL
University of Southern California Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University Winston-Salem, NC
Wake Technical Community College Raleigh, NC
Wayne State Detroit, MI
Wright State University Dayton, OH
Yale School of Medicine New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
JacquelineJ.Mahal,MD,MBA*†
PollyBijur,PhD†
AudreySloma,MPH*
JoannaStarrels,MD,MS‡
TiffanyLu,MD,MS§
*JacobiMedicalCenter,DepartmentofEmergencyMedicine,Bronx,NewYork
† AlbertEinsteinCollegeofMedicine,DepartmentofEmergencyMedicine, Bronx,NewYork
‡ AlbertEinsteinCollegeofMedicine/Monte fi oreMedicalCenter,Departmentof Medicine,Bronx,NewYork
§ JacobiMedicalCenter,DepartmentofPsychiatry&BehavioralSciences, Bronx,NewYork
SectionEditor:MarcMartel,MD
Submissionhistory:SubmittedMay22,2023;RevisionreceivedJanuary3,2023;AcceptedJanuary4,2023
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18320
Introduction: Emergencydepartments(ED)areintheuniquepositiontoinitiatebuprenorphine,an evidence-basedtreatmentforopioidusedisorder(OUD).However,barriersatthesystemandclinician levellimititsuse.WedescribeaseriesofinterventionsthataddressthesebarrierstoED-initiated buprenorphineinoneurbanED.Wecomparepost-interventionphysicianoutcomesbetweenthestudy siteandtwoaffiliatedsiteswithouttheinterventions.
Methods: Thiswasacross-sectionalstudyconductedatthreeaffiliatedurbanEDswherethe interventionsiteimplementedOUD-relatedelectronicnotetemplates,clinicalprotocols,apeer navigationprogram,education,andreminders.Post-intervention,weadministeredananonymous, onlinesurveytophysiciansatallthreesites.Surveydomainsincludeddemographics,buprenorphine experienceandknowledge,comfortwithaddressingOUD,andattitudestowardOUDtreatment. Physicianoutcomeswerecomparedbetweentheinterventionsiteandthecontrolsiteswithbivariate tests.Weusedlogisticregressioncontrollingforsignificantdemographicdifferencestocompare physicians’ buprenorphineexperience.
Results: Of113(51%)eligiblephysicians,58completedthesurvey:27fromtheinterventionsite,and31 fromthecontrolsites.Physiciansattheinterventionsiteweremorelikelytospend <75%oftheirwork weekinclinicalpracticeandtobeinmedicalpracticefor <7years.Buprenorphineknowledge(including statusofbuprenorphineprescribingwaiver),comfortwithaddressingOUD,andattitudestowardOUD treatmentdidnotdiffersignificantlybetweenthesites.Physicianswere4.5timesmorelikelytohave administeredbuprenorphineattheinterventionsite(oddsratio[OR]4.5,95%confidenceinterval 1.4–14.4, P = 0.01),whichremainedsignificantafteradjustingforclinicaltimeandyearsinpractice, (OR3.5and4.6,respectively).
Conclusion: Physiciansexposedtointerventionsaddressingsystem-andclinician-level implementationbarrierswereatleastthreetimesaslikelytohaveadministeredbuprenorphineintheED. Physicians’ buprenorphineknowledge,comfortwithaddressingandattitudestowardOUDtreatmentdid notdiffersignificantlybetweensites.Our findingssuggestthatED-initiatedbuprenorphinecanbe facilitatedbyaddressingimplementationbarriers,whilephysicianknowledge,comfort,andattitudesmay behardertoimprove.[WestJEmergMed.2024;25(3)303–311.]
Opioid-relatedoverdosedeathsintheUShaveincreased sincethe1990s,andinthe12monthsendingJune2023 provisionaloverdosedeathsexceeded81,000.1 The emergencydepartment(ED)hasbeeninvolvedinaddressing theopioidcrisisbyimplementingopioid-sparingpain managementprotocolsandtreatingopioidoverdoses.Yet patientswithnon-fatalunintentionalopioidoverdosevisits totheEDarestill100timesmorelikelytodieofanoverdose withinayearoftheirindexvisitthanthosefroma demographicallymatchedpopulation.2 Emergency departmentsareintheuniquepositiontoinitiateandlinkto evidence-basedtreatmentforopioidusedisorder(OUD) whenapatientpresentsacutelywithopioidwithdrawalor non-fataloverdose.
Buprenorphine,apartialopioidagonist,isaneffective medicationtotreatOUDthathashistoricallynotbeen offeredinEDsettings.In2015,D’Onofrioetalpublisheda seminal,randomizedcontrolledstudydemonstratingthe efficacyofED-initiatedbuprenorphineandongoing engagementinOUDtreatmentat30-dayspostdischarge.3 Follow-upstudiesalsodemonstratedthatED-initiated buprenorphineisaneffectiveintervention,withongoing OUDtreatmentat30daysin50–86%ofthepatients.4,5 On theheelsofthese findings,theSubstanceAbuseandMental HealthServicesAdministrationpublishedaresourceguidein 2021acknowledgingtheEDasanimportantsitefor provisionofOUDtreatment.6 Inthesameyear,the AmericanCollegeofEmergencyPhysicianspublished consensusrecommendationsforOUDtreatmentincluding useofbuprenorphineintheED.7
WhilebuprenorphineuseintheEDhasincreasedinrecent years, 8 multiplebarriersatthesystemandclinicianlevellimit theimplementationofED-initiatedbuprenorphine.9–13 System-levelbarriersincludelackofstreamlinedordersets forOUDtreatment,difficultyreferringtoongoingtreatment servicesafterdischarge,limitedavailabilityofexpert physiciansandpharmacistsforconsultation,andlackof accesstodedicatedcarecoordinators,socialworkers,orpeer counselors.Clinician-levelbarriersincludelackof knowledge,comfortandexperiencewithbuprenorphineand OUDtreatment,ahistoricalneedforabuprenorphine prescribingwaiver,14 aswellasstigmatowardpatients withOUD.
Fewstudieshaveexaminedspecificinterventionsthat addressclinician-levelbarriersandpost-intervention clinicianoutcomes.Fosteretaldescribeda financial incentiveprogramforemergencyphysicianstocompletethe then-requiredbuprenorphinewaivertrainingandreporteda positivebutvariableincreaseinbuprenorphineprescribingin the fivemonthsaftertheincentive.14 Butleretalreportedona setofbehavioral-scienceinformedinterventionsthat increasedphysicianinitiationofOUD-relatedtreatments15
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
WhileED-initiatedbuprenorphineforthe treatmentofopioidusedisorderhas increased,system-andclinician-levelbarriers continuetolimititsuse.
Whatwastheresearchquestion?
Wesoughttocomparewhetherinterventions addressingbarrierstoED-initiated buprenorphinewouldimproveadministration ofbuprenorphine.
Whatwasthemajor findingofthestudy?
Physiciansattheinterventionsitewere 4.5timesmorelikelytohaveadministered buprenorphine(95%CI1.4 – 14.4,P = 0.01).
Howdoesthisimprovepopulationhealth?
ED-initiatedbuprenorphinecanbefacilitatedby addressingbothsystem-andclinician-level barriers,althoughphysicianknowledge, comfort,andattitudesmaybehardertoimprove.
atasingleacademicEDsitewitharobustaddictionclinic program.Khatrietalrandomizedphysicianstoaclinicianlevelinterventionofeitheradidactic-onlygrouporadidactic plusweeklymessaginganda financialincentivegroup.16 While33%ofallparticipantsprescribedbuprenorphinefor the firsttimeinthe90dayspost-intervention,buprenorphine administrationfrequencyorknowledgedidnotdiffer significantlybetweenthegroups.Inanongoing,multicenter effectivenessstudyofbuprenorphineinitiationintheED, D’Onofrioetaldescribedmultiplesystem-level implementationfacilitatorsthatincludeclinicalprotocols, learningcollaboratives,andreferralprograms.17,18 The implementationfacilitationperiodwasassociatedwitha highernumberofemergencyclinicianswhocompletedthe buprenorphineprescribingwaiver,aswellasEDvisitswhere cliniciansprescribedbuprenorphineandnaloxone.19
Wecontributetothegrowingbodyofliteratureby describingasetofinterventionsthataddressedmultiple system-andclinician-levelimplementationbarrierstoEDinitiatedbuprenorphineinasafety-netED.Weevaluated post-interventionphysicianoutcomesandcomparedthese betweentheEDsitewithtargetedinterventionsandtwo relatedsiteswithouttargetedinterventions.Ouraimwasto determinewhetheraddressingmultipleimplementation
barrierstoED-initiatedbuprenorphineisassociatedwith improvedbuprenorphineknowledge,comfortwith addressingOUD,andattitudestowardOUDtreatment amongphysiciansattheinterventionsite.Wehypothesize thatphysiciansattheinterventionsitehadimproved experiencewithadministeringbuprenorphineintheED.
Weconductedacross-sectionalstudyofattending physiciansatthreeEDsaffiliatedwithalarge,urban emergencymedicine(EM)residencyprogram.Physician knowledge,comfortwith,andattitudestowardOUD treatment,aswellasexperiencewithadministering buprenorphineintheED,werecomparedbetweenone interventionsite(whereamultifacetedsetofinterventions aimedataddressingclinician-andsystem-levelbarriersto ED-initiatedbuprenorphinewasimplemented)vstwo controlsites(whereinterventionsfocusedonED-initiated buprenorphinewerenotimplemented).Thestudywas approvedbytheaffiliatedinstitutionalreviewboards (IRB#2019-10920).
ThisstudytookplaceatthreeEDsaffiliatedwithalarge academicEMtrainingprogramwith84residentsperyear and100full-timeattendingphysiciansonfaculty.OneED siteispartoftheNewYorkCitymunicipalhospitalsystem, whiletheothertwoEDsitesarepartofalarge,private, academichealthsystem.AllthreeEDsseeahighvisitvolume around70,000perannumpersiteandprovidesafety-netcare toapayormixthatispredominantlypubliclyinsured.All threeEDsareintheboroughofTheBronx,NewYork, wheretheopioid-relatedoverdoseratewas73.6per100,000 in2022,representingthehighestofall fiveboroughsinNew YorkCity.20 ConsistentwithmostEMpracticesacrossthe country,thethreeEDtrainingsiteshavenothistorically offeredbuprenorphineforopioidwithdrawaland OUDtreatment.
BetweenNovember2018–June2020,themunicipal hospital-basedEDsite(hereinreferredtoas “intervention site”)implementedamultifacetedsetofinterventionsto addresssystem-andclinician-levelbarrierstoED-initiated buprenorphine.System-levelinterventionscustomizedforthe EDincludedthefollowing:1)anelectronichealthrecord (EHR)notetemplateforopioidwithdrawalandOUD assessment;2)aclinicalprotocolforadministering buprenorphineintheED;3)aclinicalworkflowtoprovide naloxonetrainingandtake-homekitsforoverdose prevention;and4)apeernavigationprogramtofacilitate referralandlinkagetooutpatientbuprenorphinetreatment, includinganin-housesubstanceusedisordertreatment
program.System-levelinterventionswerefundedand developedbyacentralizedleadershipteamfromthemunicipal publichospitalsystem.LocalEDimplementationwas facilitatedbyaclinicianchampion(JM)whoworkedclosely withaninterdisciplinaryteamofemergencymedicine, behavioralhealth,pharmacy,andsocialworkleadership. Initialsalarysupportforthisworkwasgrant-funded.
Clinician-levelinterventionsincludedthefollowing:1)a modest financialincentiveforvoluntarycompletionof buprenorphinewaivertrainingandobtainingtheprescribing waiver;2)regularupdatesandremindersaboutsystem-level interventionsatEMfacultymeetingseverytwoweeks;and 3)two,one-hourgrandroundslecturesthatreviewedthe evidenceforED-initiatedbuprenorphineandtheavailability ofclinicalprotocolstosupportbuprenorphinetreatment. Grandroundslecturesatthetimeofinterventionwere conductedinpersonandvoluntarilyattendedbyfacultyand residentsacrosstheEMresidencyprogram.Manyofthe interventionswereintroducedinanoverlappingmannerand refinediterativelyduringthetwo-yearimplementationperiod.
Duringthesameperiod,aclinicalprotocolandanorder settosupporthospital-initiatedbuprenorphinewerealso beingimplementedatthetwootherEDsitesbasedatthe private,academichealthsystem(referredtoas “thecontrol site”);however,theseinterventionsdidnotfocusontheED. PeernavigatorsbasedintheEDwereavailablebutwerenot dedicatedtosupportreferralandlinkagetooutpatient buprenorphinetreatment.Neitherwere financialincentives forcompletionofbuprenorphinewaivertrainingor physicianmeetingsdedicatedtoED-initiated buprenorphineoffered.
Werecruitedstudyparticipantsbasedonthefollowing criteria:1)licensedphysicianeligibletoobtainawaiverto prescribebuprenorphine;and2)attendingphysicians practicingateithertheinterventionorcontrolsite.Wedid notincluderesidentphysiciansinoursamplebecausethey rotateatboththeinterventionandcontrolsitesandwould haveexperiencedvariableexposuretotheinterventions aimedatED-initiatedbuprenorphine.Neitherdidweinclude physicianassistantswhoareanimportantpartoftheEM workforcebecausetheydidnotreceivethe financialincentive anddidnotattendfacultymeetingsorgrandroundswhere mostoftheclinician-facinginterventionsoccurred.
BetweenSeptember–December2020,weemailed113 eligibleemergencyphysiciansatthethreeEDsitesto introducetheopt-instudyandcontinuedtosendmonthly emailreminders.Wealsoannouncedthestudyinpersonat attendingphysicianmeetingsattwoofthethreesitesthat
couldallocatemeetingtimeduringtheCOVID-19public healthemergency.Individualizedemailremindersweresent toattendingphysiciansatallsitesinthelastmonthofstudy recruitment.Thesurveywasadministeredanonymouslyin EnglishusingtheonlineplatformQualtrics(Qualtrics, Provo,UT).Uponcompletionofthequestionnaire, participantswereeligibletoenteraraffletowinoneof five $50giftcards.
A22-itemsurveywasadaptedfrompreviouslypublished researchonclinicianbarrierstobuprenorphine prescribing.9,11 Thesurveyinstrumentwedeveloped consistedof fivedomains:demographics;buprenorphine experience;buprenorphineknowledge;comfortwith addressingOUD;andattitudestowardOUDtreatment.
Self-reporteddemographicsincludedage,gender,race, ethnicity,yearsinpractice,andamountoftimespent workingclinically(clinicaltime).Thenumberofyearsin practicewasmeasuredbythenumberofyearssince AmericanBoardofEmergencyMedicinecertificationdate, andrespondentswereconsideredjuniorattendingphysicians iftheyhadsevenorfeweryearsinpractice.Clinicaltimewas adichotomousmeasureoflessthanvs ≥ 75%,basedonthe rationalethatattendingphysicianswhospend <75%clinical timerepresentclinician-educators,researchers, oradministrators.
Forbuprenorphineexperience,participantswereaskedto answeryes/notoeveradministeringbuprenorphineinthe ED,completingthebuprenorphinewaivertraining,and receivingtheirbuprenorphineprescribingwaiver. Buprenorphineknowledgewasevaluatedwithseven questionsspecifictotheclinicaluseofbuprenorphineusinga three-pointLikertscale(“agree-neutral-disagree”),where agreeingordisagreeingcorrectlytotheknowledgequestions wasakeyoutcome.ComfortwithOUDtreatmentwasalso evaluatedwithathree-pointLikertscale(“comfortablesomewhatcomfortable-notcomfortable”)regarding managementofopioidwithdrawal,responsetoopioid overdose,counselingonandadministeringmedicationsfor OUD,andreferraltooutpatienttreatmentforsubstanceuse disorder.AttitudestowardOUDtreatmentweremeasured withlevelofagreement(“agree-neutral-disagree”)to stigmatizingstatementsdescribingpatientswithOUDas difficulttotreat,buprenorphineassubstitutingonedrugfor another,andprescribingbuprenorphineforOUDas increasingmedicolegalrisk.
Wecalculateddescriptivestatisticsfordemographic characteristics,buprenorphineexperience,and buprenorphineknowledgeforphysiciansattheintervention andcontrolsites.Fisherexacttestswereusedtoassess whetherphysicians’ demographiccharacteristicsand buprenorphineexperiencedifferedbysite.Weexamined buprenorphineknowledgebycalculatingacomposite
knowledgescorebasedonthenumberofcorrectanswersto thesevenknowledgequestionsandcomparedthembysite usingtheMann-WhitneyU-test.Physicians’ comfortwith addressingOUDandattitudestowardOUDtreatmentare describedwithproportionofresponseswith “comfortable” and “ agree, ” andcomparedbysitewithFisherexacttestsand Fisher-Freeman-Haldentests,forvariableswithmorethan twocategories.
Weconductedapost-hocmultivariableanalysisbecause ofastatisticallysignificantdifferencebetweenphysicians’ buprenorphineexperienceof “everadministered buprenorphine” bysite.Weexaminedpossibleconfounding ofthisassociationbythedemographiccharacteristicsthat aresignificantlyassociatedwiththesite.Weusedlogistic regressiontoassesstheassociationbetweenbuprenorphine administrationandsitewhilecontrollingforthesecovariates. Followingtherecommendationthatonevariableshouldbe usedforevery10participantswiththeoutcome,we ascertainedthatonlytwovariablescouldbeincludedina singleanalysisastherewere20participantswhohad “ ever administeredbuprenorphine.” Thus,werananalyseswith siteandeachofthepossibleconfoundersseparately.Alltests weretwo-sidedwithastatisticalsignificancecriterionof0.05. WeusedSPSSversion27(IBMCorp,Armonk,NY)forall statisticalanalyses.
Amongthe113eligibleattendingphysicians,58(51.3%) physiciansfullycompletedthesurvey,with27responses fromtheinterventionsiteand31responsesfromthecontrol site.Asshownin Table1,nosignificantdifferencesinthe demographiccharacteristicsofgender,race,andethnicity werefoundamongemergencyphysiciansbysite.Physicians weremorelikelytospend <75%oftimeinclinicalpracticeat theinterventionvscontrolsites,44.4%vs19.4%,respectively (P = 0.05).Nearlytwiceasmanyphysiciansatthe interventionsitewereinclinicalpracticeforsevenyearsor lesscomparedtothoseatthecontrolsite,70.4%vs38.7%, respectively(P = 0.02).Inotherwords,physiciansatthe interventionsiteweremorelikelytobeclinician-educators, researchersandadministrators,andjunior attendingphysicians.
Forbuprenorphineexperience,morephysiciansatthe interventionsitereported “everadministered buprenorphine” intheirclinicalpracticethanphysiciansat thecontrolsite,51.9%vs19.4%,respectively(P = 0.01).Over halfofthephysicianrespondentscompletedthewaiver trainingatboththeinterventionandcontrolsites,55.6%and 51.6%,respectively.Ofthosewhocompletedthewaiver training,mostphysiciansobtainedtheprescribingwaiver. Therewasnostatisticaldifferenceinwaivertraining completionandstatusbysite.Forbuprenorphine knowledge,themedianscoreofcorrectanswers(oftheseven knowledgequestions)wasthreeforphysiciansatthe
Table1. Demographic,experience,andknowledgeparticipantcharacteristics.
Demographiccharacteristics
Gender
Interventionsite N = 27n(%) Controlsites N = 31n(%) P-value
White 17(63.0%)22(75.9%)
Black 3(11.1%)3(10.3%)
Asian 2(3.7%)3(10.3%)
Other 2(7.4%)1(3.4%) Declinetoanswer4(14.8%)1(3.4%)
Obtainedprescribingwaiveramongthosewhocompletedwaivertraining0.74
Yes 12(80.0)12(75.0)
No 3(20.0)4(25.0)
Buprenorphineknowledge
Mean(SD)numberofcorrectresponses(7items)3.4(2.0)3.3(2.1)0.82 Median(range)3(0–7)4(06)0.88
*Statisticalsignificancewithp-valueforcomparison(p < .05).
interventionsite,whichwassimilartothemedianscoreof fouratthecontrolsite(Mann-WhitneyU = 428, P = 0.88). Asseenin Figures1 and 2,physicians’ comfortwith addressingOUDandtheirattitudestowardOUDtreatment didnotdiffersignificantlybetweentheinterventionand controlsites.
Thepost-hocanalysis(see Table2)oftheassociation betweenbuprenorphineadministrationandsiteindicates thatphysiciansattheinterventionsitewere4.5timesmore
likelytohaveadministeredbuprenorphinethanthoseatthe controlsite(OR4.5,95%CI1.4 – 14.4, P = 0.01).After adjustingforthetwodemographiccharacteristicsthat differedbysite(clinicaltimeandyearsinpractice),the likelihoodofbuprenorphineadministrationremainedhigh andstatisticallysignificantamongphysiciansatthe interventionsitecomparedtothecontrolsite(OR3.5 withclinicaltimecontrolled,4.6withyearsinpractice controlled,respectively).
Trea ng opioid withdrawal with buprenorphine will extend pa ent length of stay in the Emergency Department
Providing pa ents with buprenorphine for OUD will increase my medicolegal risk
Buprenorphine is subs tu ng one drug for another
Pa ents who have a history of OUD are difficult to treat
The Clinical Opiate Withdrawal Scale (COWS) is difficult to administer
PercentAgree(%)
Figure1. Physicianattitudestowardspatientslivingwithopioidusedisorder(OUD)1 anduseofbuprenorphinebysite(percentagree.)
Physicianagreementwiththestatementsalongtheverticalaxisbysite.Nostatisticaldifferencefound.
DISCUSSION
Inthisstudy,wefoundthatemergencyphysicianswho wereexposedtoamultifacetedsetofinterventionsthat addressedsystem-andclinician-levelbarrierstoED-initiated
Refertooutpa entsubstanceuse treatmentprograms
Counselpa entsaboutnaloxone take-homekits
Administermethadone
Administerbuprenorphine
Discussmedica onsforOUD
Respondtoopioidoverdose
TreatOpioidwithdrawal
buprenorphineattheirclinicalsitewereatleastthreetimesas likelytohaveadministeredbuprenorphineafteradjustingfor clinicaltimeandyearsinpractice.Yetphysicians’ buprenorphineknowledge,comfortwithaddressingOUD,
ControlSite Interven onSite
Percent(%)comfort
Figure2. Physicianpercentcomfortwithaddressingopioidusedisorderbysite. Physiciancomfortwiththeactivitieslistedalongtheverticalaxisbysite.*Statisticalsignificancewith P-valueforcomparison(P < .05).
*Statisticallysignificant P-value < 0.05. Ref,referencegroup; OR,oddsratio.
andattitudestowardOUDtreatmentdidnotdiffer significantlybetweentheinterventionandcontrolsites.Our findingssuggestthatED-initiatedbuprenorphinecanbe facilitatedbyaddressingsystem-levelimplementation barriers,whileclinicianknowledge,comfort,andattitudes maybehardertoimproveandmayrequirelong-termand/or differentinterventions.
Thesystem-levelinterventionsdescribedwereaseriesof toolsandservicesintroducedtotheEDbyinterdisciplinary stakeholderstoencouragetheuseofevidence-based,EDinitiatedbuprenorphinethathadnotpreviouslybeen consideredstandardtreatmentforpatientslivingwithOUD. IntegratedEHRtemplatesandclinicalprotocolsand workflowsweretoolstosupportclinicaldecision-making, whilethepeernavigationprogramprovidedharmreduction interventionsandsupportedpost-dischargeplanningand linkagetocare.Theimplementationofthesesystem-level interventionswasintendedtominimizetheburdenon cliniciansandtoreducevariationincare.21 Theimpactofeach interventionwasnotmeasuredindividuallybecausemany componentswereintroducedandrefinedinanoverlapping, iterativemannerduringtheimplementationperiod.(For example,announcementsandeducationregardingtheEHR ordersetsandclinicalprotocolsoccurredatasimilartimeand acrosssubsequentmeetings.)Thecross-sectionalstudy capturedonlyclinicianoutcomesafterreceivingthewholeset ofsystem-levelinterventions,whichisalimitationof measuringreal-worldimplementationfacilitation. Implementationofthesesystem-leveltoolsandservices requiredinterventionsattheclinicianleveltointroduce, familiarize,andremindcliniciansofavailabletoolsand supportservices.Frequentreminders,educational opportunities, financialincentivesforthethen-required buprenorphineprescribingwaivercourseworkwerean attempttoencourageknowledgeofandcomfortwithEDinitiatedbuprenorphinewiththegoaltosupportachangein clinicalpracticeto treat OUD,notjustrespondtoacute
overdoses,intheED.Ourclinician-levelinterventionseased theimplementationofsystem-levelinterventionsinasimilar manner,asthebehavioralscience-based “nudges” wereused toincreasethenumberofphysicianswhoobtainedawaiver atanotherurban,academicED.22 Thesamegroupalsoused clinician-levelnudgesintheformofbestpracticeadvisories intheEHRandmonthlyemailstoincreasetheuseof ambulatoryreferralstoaBridgeClinicandbuprenorphine administration.15 Animportantpartoftheprocessappears toincludeaclinicalchampionwhocanworkwith stakeholderstoovercomeinstitutionalbarriers18,19,23 to refineworkflowsandprotocols,andwhocanalsobea contentexpertresourcetocolleaguestointroduceevidencebasedpracticeupdatesandreminders.
Inourstudy,physicians’ clinicaltimeandyearsinpractice hadanimpactonthelikelihoodofpracticingED-initiated buprenorphine.Clinicaltimeinpracticeisavariableusedto differentiatebetweenphysicianswithorwithoutdedicated timeforclinicaleducation,research,andadministration, whichwashypothesizedtohaveanindependenteffecton adoptionofemergingclinicalpractices.Yearsinindependent clinicalpracticeisusedasameasuretoaccountforsecular trendsinEMtraining;attendingphysicianswithfewerthan sevenyearsinclinicalpracticemayhavebeenexposedto frequentpressontheopioidepidemicandchanging guidelinesforOUDtreatmentintheED.Imetalreportthat junioremergencyphysiciansaremorelikelytoviewOUDas achronicdiseaseandapproveofbuprenorphineinitiationin theED,24 evenifjunioremergencyphysiciansexpresseda similarsenseoffrustrationtreatingpatientswithOUDas seniorphysicians.Ourstudydidnotincluderesident physicianstominimizecross-contaminationofexposureto interventions.Otherstudieshavefoundthatemergency physiciansintheirresidencytrainingareeagertoimplement ED-initiatedbuprenorphine.15,22 Attitudesamong emergencyphysiciansaregenerallychangingtowardOUD, anditisincreasinglybeingviewedasachronicdiseasewith
acutemanifestationsthatshouldbetreatedinthe EDsetting.24,25
Theremovalofthebuprenorphine-prescribingwaiver requirementisanacknowledgmentthatthisclinician-level barrierimpededaccesstotreatmentforOUD.26,27 Whilethis studywascompletedatatimewhenthebuprenorphineprescribingwaiverrequirementwasstillineffect(and justified financialincentivesforemergencyclinicianswho voluntarilyobtainedaprescribingwaiver),weexpectthat futureinterventionstoaddressclinician-levelbarriersto buprenorphineinitiationintheEDwillstillrequireaclinical championwhocanregularlyprovideupdatesabout implementationandleadeducationefforts.
Limitationstoourstudyincludearelativelysmallsample sizewitha58%responserate,whichmayhavecontributedto asamplingbias.Ourclinicalsitesareinanurbanareawitha highprevalenceofopioidoverdoseandOUD,whichmay influencephysicianinterestinandknowledgeofOUDand, thus,participationinthesurvey.ImplementationofEDinitiatedbuprenorphineattheinterventionsitereceived financialsupportanddepartmentalresourcesinatertiarycaremunicipalhospitalaswellasinitialgrantfundingfor salarysupportoftheclinicalchampion,whichmaylimit generalizabilitytoEDsettingsinsmaller,ruraland/orunderresourcedhospitals.Withoutpre-/post-evaluationsforeach intervention,wewereunabletoassesswhetheraparticular interventioninfluencedthedifferenceinbuprenorphine administrationattheinterventionsite.Buprenorphine experienceisself-reported;responsesregarding buprenorphineadministrationintheEDarenotlinkedto pharmacydatafromtheinterventionalorcontrolsites. Lastly,cross-contaminationofattendingphysicians’ exposurestointerventionsmayhaveoccurredviaresidents whorotateamongtheinterventionandcontrolsites.Itmay havealsooccurredatthegrandroundslectureswhereall facultyfromtheresidencysitesareinvited;however,total facultyattendancetypicallyhoveredbelow10%forthethen in-personlectures.
OurstudycomparestheadministrationofED-initiated buprenorphineattwosimilarandrelatedEDsettingswhere physiciansatonesitewereexposedtoamultifacetedsetof interventionstoED-initiatedbuprenorphine.Physicians exposedtointerventionsdesignedtoaddresssystem-and clinician-levelbarriersweremorelikelytoinitiate buprenorphineforOUDtreatmentintheirclinicalpractice. Futureimplementationeffortsshouldexamineinterventions thataretailoredtoimplementationbarriersevenafterthe buprenorphine-prescribingwaiverrequirementhasbeen eliminated,includingresidencyeducationtoimprovethe
understandinganduptakeofED-initiatedbuprenorphine. Couplingpharmacy-levelbuprenorphineadministrationand prescribingdatawithphysician-reportedoutcomeswillalso helpparseoutimpactoffutureinterventions.
AddressforCorrespondence:JacquelineMahal,MD,MBA,Jacobi MedicalCenter,DepartmentofEmergencyMedicine,1400Pelham ParkwaySouth,Bronx,NY10461.Email: mahalj@nychhc.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Mahaletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AhmadFB,CisewskiJA,RossenLM,etal.Provisionaldrugoverdose deathcounts.NationalCenterforHealthStatistics.2023.Availableat: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm AccessedNovember20,2023.
2.Goldman-MellorS,OlfsonM,Lidon-MoyanoC,etal.Mortalityfollowing nonfatalopioidandsedative/hypnoticdrugoverdose. AmJPrevMed. 2020;59(1):59–67.
3.D’OnofrioG,O’ConnorPG,PantalonMV,etal.Emergencydepartmentinitiatedbuprenorphine/naloxonetreatmentforopioiddependence:A randomizedclinicaltrial. JAMA. 2015;313(16):1636–44.
4.KaucherKA,CarusoEH,SungarG,etal.Evaluationofan emergencydepartmentbuprenorphineinductionandmedicationassistedtreatmentreferralprogram. AmJEmergMed. 2020;38(2):300–4.
5.EdwardsFJ,WicelinskiR,GallagherN,etal.Treatingopioidwithdrawal withbuprenorphineinacommunityhospitalemergencydepartment:an outreachprogram. AnnEmergMed. 2020;75(1):49–56.
6.SubstanceAbuseandMentalHealthServicesAdministration (SAMHSA).UseofMedication-AssistedTreatmentinEmergency Departments.2021.Availableat: https://store.samhsa.gov/sites/ default/files/pep21-pl-guide-5.pdf.AccessedAugust16,2023.
7.HawkK,HoppeJ,KetchamE,etal.Consensusrecommendationson thetreatmentofopioidusedisorderintheemergencydepartment. Ann EmergMed. 2021;78(3):434–42.
8.RheeTG,D’OnofrioG,FiellinDA.Trendsintheuseofbuprenorphinein USemergencydepartments,2002–2017. JAMANetwOpen. 2020;3(10):e2021209.
9.HawkKF,D’OnofrioG,ChawarskiMC,etal.Barriersandfacilitatorsto clinicianreadinesstoprovideemergencydepartment-initiated buprenorphine. JAMANetwOpen. 2020;3(5):e204561.
10.MendiolaCK,GalettoG,FingerhoodM.Anexplorationofemergency physicians’ attitudestowardpatientswithsubstanceusedisorder, J AddictMed. March/April2018;12(2):132–5.
11.LowensteinM,KilaruA,PerroneJ,etal.Barriersandfacilitatorsfor emergencydepartmentinitiationofbuprenorphine:aphysiciansurvey. AmJEmergMed. 2019;37(9):1787–90.
12.SavageTandRossM.BarriersandattitudesreportedbyCanadian emergencyphysiciansregardingtheinitiationofbuprenorphine/ naloxoneintheemergencydepartmentforpatientswithopioiduse disorder. CJEM. 2022;24(1):44–9.
13.LoganG,MirajkarA,HouckJ,etal.Physician-perceivedbarriersto treatingopioidusedisorderintheemergencydepartment. Cureus. 2021;13(11):e19923.
14.FosterSD,LeeK,EdwardsC,etal.Providingincentiveforemergency physicianX-waivertraining:anevaluationofprogramsuccessand postinterventionbuprenorphineprescribing. AnnEmergMed. 2020;76(2):206–214.
15.ButlerK,ChavezT,WakemanS,etal.Nudgingemergencydepartmentinitiatedaddictiontreatment. JAddictMed. 2022;16(4):e234–9.
16.KhatriU,LeeK,LinT,etal.Abriefeducationalinterventiontoincrease EDinitiationofbuprenorphineforopioidusedisorder(OUD). JMed Toxicol. 2022;18(3):205–13.
17.D’OnofrioG,EdelmanEJ,HawkKF,etal.Implementationfacilitationto promoteemergencydepartment-initiatedbuprenorphineforopioiduse disorder:protocolforahybridtypeIIIeffectiveness-implementation study(ProjectEDHEALTH). ImplementSci. 2019;14(1):48.
18.WhitesideLK,D’OnofrioG,FiellinDA,etal.Modelsforimplementing emergencydepartment-initiatedbuprenorphinewithreferralforongoing medicationtreatmentatemergencydepartmentdischargeindiverse academiccenters. AnnEmergMed. 2022;80(5):410–9.
19.D’OnofrioG,EdelmanEJ,HawkKF,etal.Implementationfacilitationto promoteemergencydepartment–initiatedbuprenorphineforopioiduse disorder. JAMANetwOpen.2023;6(4):e235439.
20.TuazonE,BaumanM,SunT,etal.UnintentionalDrugPoisoning (Overdose)DeathsinNewYorkCityin2022.NewYorkCityDepartment
ofHealthandMentalHygiene:EpiDataBrief(137);September2023. Availableat: https://www.nyc.gov/assets/doh/downloads/pdf/epi/ databrief137.pdf.AccessedFebruary13,2024.
21.CentersforMedicareandMedicaidServices.QualityMeasurementand QualityImprovement.2023.Availableat: https://www.cms.gov/ Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/ Quality-Measure-and-Quality-ImprovementAccessedNovember23,2023.
22.MartinA,KunzlerN,NakagawaJ,etal.Getwaivered:aresident-driven campaigntoaddresstheopioidoverdosecrisis. AnnEmergMed. 2019;74(5):691–6.
23.WoodK,GiannopoulosV,LouieE,etal.Theroleofclinicalchampionsin facilitatingtheuseofevidence-basedpracticeindrugandalcoholand mentalhealthsettings:asystematicreview. ImplementResandPract. 2020;1:2633489520959072.
24.ImDD,CharyA,CondellaAL,etal.Emergencydepartmentclinicians’ attitudestowardopioidusedisorderandemergencydepartmentinitiatedbuprenorphinetreatment:amixed-methodsstudy. WestJ EmergMed. 2020;21(2):261–71.
25.SokolR,TammaroE,KimJY,etal.LinkingMATTERS:barriersand facilitatorstoimplementingemergencydepartment-initiated buprenorphine-naloxoneinpatientswithopioidusedisorder andlinkagetolong-termcare. SubstUseMisuse. 2021;56(7):1045–53.
26.OfficeofNationalDrugControlPolicy(ONDCP).Dr.Guptaapplauds removalofX-waiverinomnibus,urgeshealthcareproviderstotreat addiction.2022.Availableat: https://www.whitehouse.gov/ondcp/ briefing-room/2022/12/30/dr-gupta-applauds-removal-of-xwaiver-in-omnibus-urges-healthcare-providers-to-treat-addiction AccessedFebruary23,2023.
27.USDepartmentofJustice,DrugEnforcementAdministration,Diversion ControlDivision.EliminationoftheDATAwaiverprogram.Availableat: https://www.deadiversion.usdoj.gov/pubs/docs/dear_registrant_ AM_01122023.html.AccessedNovember20,2023.
EricaC.Koch,MD*†**
MichaelJ.Ward,MD,PhD,MBA*†§
AlvinD.Jeffery,PhD‡§∥
ThomasJ.Reese,PharmD§
ChadDorn,PSM§ ShannonPugh,RN* MelissaRubenstein,MPH*
JoEllenWilson,MD,MPH†¶ CoreyCampbell,DO#
JinH.Han,MD,MSc*†
*VanderbiltUniversityMedicalCenter,DepartmentofEmergencyMedicine, Nashville,Tennessee
† TennesseeValleyHealthcareSystem,GeriatricResearch,Education,andClinical Center,Nashville,Tennessee
‡ VanderbiltUniversitySchoolofNursing,Nashville,Tennessee
§ VanderbiltUniversityMedicalCenter,DepartmentofBiomedicalInformatics, Nashville,Tennessee
∥ TennesseeValleyHealthcareSystem,NursingServices,Nashville,Tennessee
¶ VanderbiltUniversityMedicalCenter,DepartmentofPsychiatry, Nashville,Tennessee
# TennesseeValleyHealthcareSystem,PsychiatricServices,Nashville,Tennessee
**VeteransAffairsQualityScholarsProgram,Nashville,Tennessee
SectionEditor:PhilipsPerera,MD
Submissionhistory:SubmittedMarch23,2023;RevisionreceivedNovember17,2023;AcceptedJanuary10,2024
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.17996
Introduction: TheUnitedStatesVeteransHealthAdministrationisaleaderintheuseoftelementalhealth (TMH)toenhanceaccesstomentalhealthcareamidstanationwideshortageofmentalhealth professionals.TheTennesseeValleyVeteransAffairs(VA)HealthSystempilotedTMHinitsemergency department(ED)andurgentcareclinic(UCC)in2019, withfull24/7availabilitybeginningMarch1,2020. Followingimplementation,preliminarydatademonstratedthatveterans ≥65yearsoldwerelesslikelyto receiveTMHthanyoungerpatients.Wesoughttoexaminefactorsassociatedwitholderveteransreceiving TMHconsultationsinacute,unscheduled,outpatientsettingstoidentifylimitationsinthecurrentprocess.
Methods: ThiswasaretrospectivecohortstudyconductedwithintheTennesseeValleyVAHealth System.Weincludedveterans ≥55yearswhoreceivedamentalhealthconsultationintheEDorUCC fromApril1,2020–September30,2022.Telementalhealthwasadministeredbyamentalhealthclinician (attendingphysician,residentphysician,nursepractitioner,orphysicianassistant)viaiPad,whereasinpersonevaluationswereperformedintheED.Weexaminedtheinfluenceofpatientdemographics,visit timing,chiefcomplaint,andpsychiatrichistoryonTMH,usingmultivariablelogisticregression.
Results: Ofthe254patientsincludedinthisanalysis,177(69.7%)receivedTMH.Veteranswithhighriskchiefcomplaints(suicidalideation,homicidalideation,oragitation)werelesslikelytoreceiveTMH consultation(adjustedoddsratio[AOR]:0.47,95%confidenceinterval[CI]0.24–0.95).Comparedto attendingphysicians,nursepractitionersandphysicianassistantswereassociatedwithincreasedTMH use(AOR4.81,95%CI2.04–11.36),whereasconsultationbyresidentphysicianswasassociatedwith decreasedTMHuse(AOR0.04,95%CI0.00–0.59).TheUCCusedTMHforallbutoneencounter. Patientcharacteristicsincludingtheirvisittiming,gender,additionalmedicalcomplaints,comorbidity burden,andnumberofpsychoactivemedicationsdidnotinfluenceuseofTMH.
Conclusion: High-riskchiefcomplaints,location,andtypeofmentalhealthclinicianmaybekey determinantsoftelementalhealthuseinolderadults.Thismayhelpexpandmentalhealthcareaccessto areaswithashortageofmentalhealthprofessionalsandpreventpotentiallyavoidabletransfersinlowacuitysituations.FurtherstudiesandinterventionsmayoptimizeTMHforolderpatientstoensuresafe, equitablementalhealthcare.[WestJEmergMed.2024;25(3)312–319.]
In2020,52.9millionpeopleintheUnitedStates(US) sufferedfromamentalhealthorsubstanceusedisorder.1,2 Emergencydepartment(ED)visitsandadmissionsfor psychiatricconcernscontinuetoincrease.3–7 Despitethe increaseddemand,thereisawidespreadmentalhealth professionalsshortageintheUS,whichnegativelyaffects accesstotimely,efficientmentalhealthcareforsociety’smost vulnerablepopulations.Anestimated7,632cliniciansare neededtobridgethegapinlow-resourcedareas.8 Approximately66%ofruralorpartiallyruralcountiesare designatedbythefederalgovernmentasmentalhealth professionalshortageareas.8 Patientsintheseareashave beenfoundtohaveworsehealthoutcomes,includingshorter lifeexpectancyandhigherrateofsuicide.9–11 Innovative solutionsareneededtoaddressthesekeygapstoexpand accesstoequitablementalhealthservices,particularlyinthe settingofacutecrises.
Telehealthwas firstdescribedinclinicalpracticeinthelate 1950s.12 Overthepasttwodecades,usehasexpandedina varietyofclinicalsettings.13 TheVeteransHealth Administrationhasadoptedtelehealthacrossavarietyof settings,includingmentalhealthcomplaints.14 By2016, nearlyhalfofEDsintheUSreportedtheuseoftelehealth, with20%usingitformentalhealthpurposes(telemental health[TMH]).15,16 TheuseofTMHinroutineEDclinical practicegrewdramaticallyduringtheCOVID-19 pandemic.5 FormanyEDs,itistheonlyavenueto emergencypsychiatriccare.15
OnMarch1,2020,theTennesseeValleyVeteransAffairs HealthSystemimplementedfull-timeTMHforveteranswho presentedtotheEDformentalhealthcomplaints.Both TMHandin-personconsultationsperformedbyamental healthclinicianwereavailable7daysaweek,24hoursaday, includingholidays,attheEDandduringalloperatinghours attheUCC(daily8 AM – 8 PM).Consultationmodalitywas lefttothechoiceofthementalhealthclinician.In-person cliniciancoveragewasalwaysavailablebyanattending physician,residentphysician,nursepractitioner,or physicianassistantduringfacilityoperatinghours. Capabilitiesdidnotchangedependingontheroleofthe clinician.Amoredetaileddescriptionoftheprogramis providedelsewhere.17 Despitetheimplementationofthis TMHprogram,preliminarydatashowed20%ofmental healthconsultationsstilloccurredinperson.17 Veteranswho receivedin-personmentalhealthevaluationswerenotably oldercomparedtothosereceivingTMH,with31%in-person consultsoccurringinveteransages ≥65vs18%of TMHconsults.17
Olderpatientswithmentalhealthcomplaintsfaceunique challengesintheemergencysetting.Attentiontothese patientsduringtheimplementationofnewprocessesofcare isvitaltoensuretheyreceivehigh-qualitymentalhealth evaluation.Withtheexponentialgrowthprojectedforthe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Thereisawidespreadshortageofmental healthprofessionalsintheUS,which decreasesaccesstotimelyemergency mentalhealthcare.
Whatwastheresearchquestion?
Whatfactorsareassociatedwitholder veteransreceivingacute,unscheduled telementalhealth(TMH)vsinpersonconsults?
Whatwasthemajor findingofthestudy?
High-riskchiefcomplaints(suicidalor homicidalideation,oragitation)were associatedwithdecreasedTMHuse (OR0.39,95%CI0.18 – 0.81).Typeof clinicianandlocationofcarewerealso associatedwithTMHuse.
Howdoesthisimprovepopulationhealth?
TMHrepresentsanopportunitytoexpand accesstomentalhealthcare,therebyreducing potentiallyunnecessarypatienttransfersand shorteningboardingtimes .
olderpopulationintheUS,understandingfactorsassociated withvariabilityofTMHusewillinformfuture implementationandsustainabilityinacutecaresettings.18 In thisstudywesoughttoexaminefactorsassociatedwitholder veteransreceivingTMHconsultationsinacute,unscheduled, outpatientsettingstoidentifypotentialbarriersto widespreaduseofTMHintheED.Encountersinvolving patientsolderthan75,urbanlocation,residentphysicians, andhigheracuitywerehypothesizedtobemorelikelyto occurinperson.
StudyDesign,Setting,andPatientPopulation
Thiswasanexploratory,retrospective,cohortstudy conductedattheTennesseeValleyVAHealthSystemED andurgentcareclinic(UCC).20 Describedinmoredetail elsewhere,thisTMHprogramwasinitiallypilotedduring limitedhoursin2019andthenwentlivewith24/7coveragein March2020withtheonsetoftheCOVID-19pandemic.17 PatientswereinitiallyevaluatedbyanEDorUCCclinician (attendingphysician,residentphysician,nursepractitioner, orphysicianassistant)anddeterminedtoneedmentalhealth consultation.Aconsultorderwasthenrequestedthroughthe
electronichealthrecord(EHR)withdirectcommunication betweentheemergencyphysicianandon-callmentalhealth clinician(nursepractitioner,physicianassistant,orattending psychiatrist).Consultmodalitywaslefttothedecisionofthe on-callmentalhealthclinician.TheTMHvisitwasprovided viaAppleiPad(AppleInc,Cupertino,CA)withaudioand visualcapabilities,whereasin-personevaluationswere performedbythesamementalhealthclinicianintheEDor UCC.Bothin-personandTMHconsultationswereavailable 24/7intheEDandduringoperatinghours oftheUCC.
Weincludedveteranswhowere ≥55yearsandreceiveda mentalhealthconsultationintheEDbetweenApril1, 2020–September30,2022.Sincethereisnouniversally acceptedagethatdefines “olderage,” wechose55yearsold asthecut-offtomaximizeoursamplesizewhilemaintaining amedianageof65yearsold,atraditionalcut-point.Nonveteranswithoutservicebenefits,directadmissionswhodid notpresentthroughtheED,andpatientswithamissing modalityofconsultationwereexcluded.Forveteranswith multipleEDmentalhealthencounters,onlythe first consultationencounterwasincluded.Of1,478initialvisits withinthestudyperiod,weselected510chartstoreview;497 hadcompletementalhealthconsultationsinthechart.A substantialproportionofpatientsreceivedTMHduringthe studyperiod.Therefore,2–3TMHconsultationswere includedforeachin-personconsultation.Webalancedthe numberofchartsselectedforeachmonthofthestudyto reducetemporalbias.Wethenexcludedallpatients <55yearsfromthisanalysis.Thisstudywasapprovedbythe localinstitutionalreviewboardasexempt.
Wedesignedthechartreviewmethodologytofollow acceptedguidelines.21 Datawasmanuallyextractedfromthe VAEHRandClinicalDataWarehouse.Thefollowing patientfactorswereincludedinthisanalysis:age;race; gender;maritalstatus;rurality;EDtriagechiefcomplaint; mentalhealthhistory;totalactivenumberofpsychoactive medications;andpresenceofadditionalnon-psychiatric medicalcomplaint(eg,chestpain).Ruralitywasdetermined bytheRural-UrbanCommutingAreaCodesbasedonthe patient’sZIPcode.22 Weconsideredthefollowingsystemlevelfactors:location(EDvsUCC);timingofpresentation (9 AM – 5 PM ornights/weekends)andmentalhealthclinician type(nursepractitioner,physicianassistant,resident physician,orattendingphysician).
Patientdemographics,visitdate,homelessness, psychiatrichistory,andmedicationsweremanually abstractedbyaphysician(ECK)andnurse(SP).Senior authorstrainedabstractorspriortodatacollection.Each reviewerunderwentmentoredtrainingonhowtorevieweach chartwithatrialperiodofmanualdouble-checkingbythe seniorauthortoensurecompetency.Eachchartwas
reviewedbyeitherthephysicianornursereviewerandthen wascarefullydouble-checkedbythesamereviewerfor inaccuracies.Eachchartwasreviewedbyoneperson.Data abstractionformswereused,andthedatawascompiled usingREDCapelectronicdatacapturetoolshostedatUS DepartmentofVeteransAffairs.
Weusedthetotalnumberofpsychiatricconditions documentedintheEHRpriortotheindexEDvisitto determinepsychiatriccomorbidityburden.Anymentionof suicidalideation,homicidalideation,andagitationqualified ashigh-riskmentalhealthchiefcomplaints,regardlessof whetherthiswasthepatient’sprimaryreasonforED evaluation.Additionalmedicalreasonsforthe EDvisitwerecollectedbyreviewingtriageand physiciandocumentation.
Theprimarydependentvariableofinterestwasreceiptof TMHvsin-personmentalhealthconsultationbyamental healthclinicianwhowasanattendingphysician,resident physician,ornursepractitioner.
Wereportedcentraltendencyanddispersionasmedians andinterquartilerangesforcontinuousvariables. Categoricalvariableswerereportedasfrequenciesand percentages.Amultivariablelogisticregressionanalysiswas performedtodeterminefactorsassociatedwithuseofTMH. Wecreatedamoderatelysaturatedmodelwith7–8 covariatestominimizeoverfitting.23 Giventhesmallsample size,independentvariableswererankedaprioribasedon expertopinionfrompsychiatrists(EJW,CC)andemergency physicians(MJW,JHH)whoroutinelycareformental healthpatients.ThetopsevenrankedfactorsforTMHvsinpersonmentalhealthevaluationincludedage,race,high-risk chiefcomplaint,presenceofdementia,urbanlocation, timingofpresentation,andhistoryofsubstanceabuse.To exploreadditionalfactorsassociatedwithTMHvsin-person mentalhealthconsultation,weperformedahighlysaturated modelincorporatingallfactorsintothemultivariablelogistic regressionmodel.Becausesite(EDvsUCC)ofpatient presentationmayhavestronglyinfluencedTMHvsinpersonmentalhealth,thisfactorwasincorporatedintothe models.Adjustedoddsratios(aOR)with95%confidence intervals(CI)arereported.Weconductedallstatistical analyseswithRstatisticalsoftware,v3.6.2(TheRProjectfor StatisticalComputing,Vienna,Austria).
Ofthe510healthrecordsreviewed,254patientsmetage inclusioncriteria(≥55yearsofage)andwereincludedinthe study.Characteristicsofthisoldercohortvstheentirecohort ofchartsreviewedisincludedasasupplementaltable. Ofthoseeligible,177(69.7%)veteransreceivedTMH
Table1. Baselinedemographicdataofpatientspresenting totheemergencydepartmentorurgentcarecenterreceiving psychiatricconsultation.
Variable In-person (n = 77) Telemental health(n = 177)
Age,(years)65[61,71]65[61,70]
Gender,n(%)
Female3(3.9)14(7.9)
Male74(96.1)163(92.1)
Race,n(%)
Black30(39.0)72(40.7)
Non-Black47(61.0)105(59.3)
Maritalstatus,n(%)
Married26(33.8)44(24.9)
Unmarried/unknown51(66.2)133(75.1)
Chiefcomplaintrisk,n(%)
Low49(63.6)130(73.4)
High28(36.4)47(26.6)
Historyofdementia,n(%)
Yes10(13.0)18(10.2)
No67(87.0)159(89.8)
Location,n(%)
ED76(98.7)151(85.3)
UCC1(1.3)26(14.7)
Rural,n(%)
Rural24(31.2)45(25.4)
Urban53(68.8)132(74.6)
ESIscore ≥ 2,n(%)77(100.0)177(100.0)
ESIscore,n(%)
<322(28.6)61(34.5)
≥355(71.4)116(65.5)
Timingofpresentation, n(%)
Offhours28(36.4)64(36.2)
Businesshours49(63.6)113(63.8)
Historyofsubstance abuse,n(%)
No36(46.8)74(41.8)
Yes41(53.2)103(58.2)
Mentalhealthclinician type,n(%)
Attendingphysician62(80.5)123(69.5)
Residentphysician7(9.1)1(0.6)
Nursepractitioneror physicianassistant 8(10.4)53(29.9)
Totalpsychoactive medications, median[IQR]
(Continuedonnextcolumn)
Table1. Continued. Variable In-person (n = 77)
Telemental health(n = 177)
Totalpsychiatric comorbidities,median [IQR] 1.00[1.00,2.00]2.00[1.00,2.00]
Additionaltriagemedical complaint,n(%)
No48(62.3)118(66.7)
Yes29(37.7)59(33.3)
Homelessness,n(%)
No64(83.1)144(81.4)
Yes13(16.9)33(18.6)
CCIscore,median[IQR]2.00[1.00,4.00]2.00[1.00,5.00]
ESI,EmergencySeverityIndex; IQR,interquartilerange; CCI, CharlsonComorbidityIndex; UCC,urgentcareclinic; ED, emergencydepartment.
consultations,and77(30.3%)veteransreceivedanin-person evaluation.Therewerenomissingdatapointsonchart review.Intheunadjustedresults,UCClocationand consultationperformedbynursepractitionersandphysician assistantswasassociatedwithastatisticallysignificanttrend towardsTMHuse(Table1).Consultationsperformedby residentmentalhealthphysiciansweremorelikelytooccurin personbutrepresentedfewconsultsoverall(Table1). Age,race,presenceofdementiaorsubstanceusedisorder inmedicalhistory,totalpsychoactivemedications, psychiatriccomorbidityburden,homelessness,andmarital statuswerenotassociatedwithsignificantdifferencesin consultmodality.
Wethenperformedmultivariablelogisticregression analysis.Modelswereadjustedforlocationtoaccountfor sitepracticedifferencesattheEDandUCC,astheUCC performednearlyallconsultsviaTMH. Table2 demonstratesamoderatelysaturatedriskmodel.Nofactors weresignificantlyassociatedwithTMHusebeyondurgent carelocation(AOR15.15,95%CI1.98–116.04).Inahighly saturatedmodel,patientsevaluatedbyresidentphysicians werelesslikelytoreceiveTMH(AOR0.04,95%CI: 0.00–0.58),whilethoseevaluatedbynursepractitionersand physicianassistantsreceiveditmorefrequently(A5.07,95% CI:2.13–12.03),comparedtoattendingphysicians(Table3). Patientswithhigh-riskchiefcomplaints(suicidalideation, homicidalideation,oragitation)werelesslikelytoreceive TMH(AOR:0.39,95%CI:0.18–0.81)inthehighlysaturated riskmodel(Table3).Gender,age,race,comorbidityburden, timingofpresentation,historyofsubstanceusedisorder, historyofdementia,andhomelessnesswerenotassociated significantdifferencesinconsultmodality.
Table3. Multivariableregressionanalysis – highlysaturatedmodel.
modality.Specifically,weobservedthatpatientswithhighriskpsychiatricchiefcomplaints(suicidalideation, homicidalideation,andagitation)weremorelikelytoreceive in-personconsultations.Residentphysiciansperforming consultswerelesslikelytouseTMH,whilenurse practitionersandphysicianassistantsweremorelikelyto chooseTMH.TheUCCusedTMHnearuniversally.
Themoderatelysaturatedriskmodelofmosthighly rankedapriorifactorsshowedAORsgreaterthan1inurban location,timingofpresentationduringoffhours,andhistory ofsubstanceusedisorder.However,the95%CIweretoo widetobesignificant.These findingsweresimilarinthe highlysaturatedmodel.Whilenotstatisticallysignificant, thesefactorsmayholdclinicalrelevance.Further studieswithahighersamplesizeareneededtoclarify anysignificance.
–2.26
–12.03
–0.58
–1.32
–1.54
–1.40 Homelessness1.130.47–2.71
–1.23
UCC,urgentcareclinic; CCI,CharlsonComorbidityIndex.
DISCUSSION
InanoldercohortofveteranspresentingtotheEDor UCCwithacutepsychiatriccomplaints,wefoundthathighriskpsychiatricchiefcomplaints,cliniciantype,andlocation ofthementalhealthconsultwerekeydriversofconsultation
Onepotentialexplanationforreduceduseamonghigher severitycomplaintsisthatmentalhealthcliniciansmayfeel morecompelledtoconductin-personconsultationinhigher acuitysituationsbecausethisiswhattheyaremostfamiliar with.PracticechangessuchastheuseofTMHmaycreatea disruptionasphysiciansstruggleto “unlearn” whattheyare mostfamiliarwithpriortoestablishinganewpractice pattern.24 Alternatively,asrecognizedbytheSocietyfor AcademicEmergencyMedicineConsensusConferenceon EmergencyTelehealth,littleresearchhasbeendoneonthe qualityandsafetyoftelehealth.25 Recentworkhassoughtto addressthis.Evidencesuggestspatientspresentingwithacute psychosismaytoleratetelehealthwell.26,27 Telementalhealth hasbeenfoundtohavenodifferenceinlong-termoutcomes ofrehospitalizationanddeathinpatientswithsuicidal ideationandsuicideattemptscomparedtoin-person consultation.26,28 Additionally,recentworkhassuggested thatTMHisnotassociatedwithincreased30-dayreturn visits,readmissions,ordeathcomparedtoin-person evaluationsinacutecaresettings.26 Therefore,EDand mentalhealthcliniciansshouldbeeducatedonthesafetyof TMHinolderEDpatientswithhigh-riskmentalhealth chiefcomplaints.
Priorresearchdemonstratedthatclinicianscontribute substantialvariabilitytothedecisiontousetelehealthand maypartiallyexplainwhytherearesuchdifferencesinthe useofTMHbycliniciantype(ie,residentphysiciansvsnurse practitionersandphysicianassistants).29 Therewereno differencesinclinicianschedulingthatcouldaccountforthe findingsinourstudy.Allmentalhealthclinicians,including residents,wereavailabletoperformin-personorTMH evaluations.Therefore,locationdidnotmakeresidentsmore orlesslikelytoevaluatepatientsinperson.Thepandemic demonstratedvariabilityintelehealthusewithclinician factorshavingagreaterinfluenceontheuseofvideo telehealthwhencomparedwithpatientfactors.29 Moreover, priorstudiesindicatetherearevariabilitiesinpatientswho areofferedtelehealthdespitebeingvideo-capable.30 Prior
qualitativestudiessuggestthatincreasedexposureto telehealthimprovedclinicianattitudes,whileperceptionsof complexitywithintheprocessledtoreducedutilization.31 Furtherresearchisneededtobetterunderstandwhether inequitiesandanycontributingfactorsexist.
Systemswithunanimousleadershipbuy-inandpolicies usetelehealthmorefrequently.31 Despitetheavailabilityof anin-personmentalhealthclinician,theUCCusedTMHfor nearlyeveryencounter.Itisplausiblethatsimilarsystemic factorsmaybecontributingtothisphenomenon. Investigatingthepoliciesanddecision-makingprocesses throughqualitativestudiescouldshedlightontheunderlying reasonsforthenear-universaluseofTMHattheUCC,as factorsnotcapturedinthisstudyarelikelyinvolved.
ReluctancetoadoptTMHmaycontributetopotentially avoidabletransfersinEDswithlimitedmentalhealth resources.Priorresearchfoundthatmentalhealthpatients werethemostlikelytobetransferredfromVAEDsand representthelargestgroupofpotentiallyavoidabletransfers, definedasthosetransfersrapidlydischargedfromtheEDor within24hoursfromhospitaladmission(withouta procedure).32 Our findingssuggestthatmentalhealth cliniciansfeltcomfortableevaluatingpatientsviaTMHin low-acuitysituations.Inplaceswithoutaccesstoin-person mentalhealthconsultation,patientswithloweracuity complaintsmaybeevaluatedandsafelydischargedvia TMH,reducingtheriskofunnecessarytransfer.33
WeidentifiedonlyoneresidentTMHencounter throughouttheentirestudyperiod.Asresidentsgenerally rotatebetweenmultipleVAandnon-VAclinicalservices, this findingmaybeduetolackoffamiliaritywiththeprocess inthissystem.Duetothelowoverallnumberof consultationsperformedbyresidents,itisdifficulttodraw conclusionsregardingthisdata.Educationalinitiatives targetingtelehealthuseamongresidentphysiciansmay increasefamiliaritywithTMH.34,35 Astelehealth expandedacrossmultiplespecialtiesduringthepandemic, medicaltrainingcurriculacouldbeadaptedtoinclude telehealthinitiatives.34,35
Limitationsofthisstudyincludedasmallsamplesize.Our samplesizemayhavebeentoosmalltoidentifyriskfactors forTMHuse.Additionally,becausethisstudywas conductedinasinglecenteritmaynotbegeneralizableto othersettings.Riskfactorsidentifiedinourexploratory analysisandthesignificantassociationsobservedmayhave beensecondarytooverfittingasstatisticalsignificancewas onlynotedinthehighlysaturatedmodel.Asaresult,these findingsshouldbeconfirmedinalargersamplesize. Additionally,theVAhasalowproportionofwomen veterans(estimated11.5%),potentiallylimitingthe generalizabilityofourstudyoutsidetheVApopulation.36 FurtherstudiesoutsidetheVApopulationareneededto
assessforanygender-specificdifferencesthatmayimpact consultmodalitychoice.
TheED/UCCclinicianandmentalhealthclinician generallyhadaverbalconversationoncallpriortomental healthconsultation.Theseconversationsmayhave influencedmodalitychoicebythementalhealthclinician. Ourquantitativedatawouldnothavebeenabletocapture theseconversations.Furtherqualitativeworkmaybridge thisgaptounderstandaclinician’smodalitychoice.
Therearepotentialconfounderstothisstudythatwerenot accountedfor.Severityofillnesslikelyaffectsboththe likelihoodofacutecarepresentationandtheconsult modalitychoice.Whileweadjustedforhigh-riskpsychiatric complaintstoaccountforseverityofillness,residual confoundinglikelystillexists.Encountersthatoccurred duringtheCOVID-19pandemicalsolikelyinfluencedboth thelikelihoodofacutecarepresentationandtheconsult modalitychoice.Morementalhealthcliniciansmayhave optedforTMHtoreducetheriskofvirustransmission, especiallyduringperiodsofwidespreadCOVID-19 transmission.Patientsmayhavealsobeenmorefearfulof presentingtotheEDforcareduringthesetimes.Ongoing post-pandemicdataanalysisbothatthisfacilityand externallyshouldbeperformedtoevaluatetheeffectsofthe COVID-19pandemiconTMHuse.
Inthisexploratoryretrospectiveanalysis,illnessseverity, location,andcliniciancharacteristicsappearedtoinfluence useoftelementalhealthinpatientsoverage55.Loweracuity, olderpatientsrepresentapatientpopulationwithwhom moreclinicianswouldbecomfortableusingTMH.For resource-poorsettings,TMHmayrepresentanopportunity toexpandaccesstomentalhealthcareinshortageareasand reducepotentiallyunnecessarypatienttransfersthatcould otherwisebepreventedviaremoteconsultation.Further researchisneededtoexaminehesitancytoadoptTMHin moreacutelyillpopulationsandthegeneralizabilityofthe findingspresentedinthiswork.
AddressforCorrespondence:JinH.Han,MD,MSc,Vanderbilt UniversityMedicalCenter,DepartmentofEmergencyMedicine, 2215GarlandAvenue,LightHallSuite203,Nashville,TN37232. Email: jin.h.han@vumc.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thismaterialisbaseduponwork supported(orsupportedinpart)bytheDepartmentofVeterans Affairs,VeteransHealthAdministration,OfficeofRuralHealth, VeteransRuralHealthResourceCenter–IowaCity(Award#ORH10808).AlvinD.Jefferyreceivedsupportforthisworkfromthe AgencyforHealthcareResearchandQuality(AHRQ)andthe
Patient-CenteredOutcomesResearchInstitute(PCORI)under AwardNumberK12HS026395.Thecontentissolelythe responsibilityoftheauthorsanddoesnotnecessarilyrepresentthe officialviewsofAHRQ,PCORI,ortheUnitedStatesgovernment. Therearenootherconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2024Kochetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SubstanceAbuseandMentalHealthServicesAdministration.Key substanceuseandmentalhealthindicatorsintheUnitedStates:Results fromthe2020NationalSurveyonDrugUseandHealth.2021.Available at: https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/ NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121. pdf.AccessedMarch22,2023.
2.OwensP,FingarK,McDermottK,etal.InpatientStaysInvolvingMental andSubstanceUseDisorders,2016.HealthcareCostandUtilization Project(HCUP)StatisticalBriefs.2019.Availableat: https://hcup-us. ahrq.gov/reports/statbriefs/sb249-Mental-Substance-Use-DisorderHospital-Stays-2016.jsp.AccessedMarch22,2023.
3.BallouS,MitsuhashiS,SankinLS,etal.Emergencydepartmentvisits fordepressionintheUnitedStatesfrom2006to2014. GenHosp Psychiatry. 2019;59:14–9.
4.TheriaultKM,RosenheckRA,RheeTG.Increasingemergency departmentvisitsformentalhealthconditionsintheUnitedStates. JClin Psychiatry. 2020;81(5):20m13241.
5.ZhuD,PaigeSR,SloneH,etal.Exploringtelementalhealthpractice before,during,andaftertheCOVID-19pandemic. JTelemedTelecare. 2024:30(1):72–8.
6.AgencyforHealthcareResearchandQuality(AHRQ).Trendsin emergencydepartmentvisits,2006–2014.HCUPStatisticalBrief#227. 2017.Availableat:~https://hcup-us.ahrq.gov/reports/statbriefs/ sb227-Emergency-Department-Visit-Trends.jsp#:~:text=Overall%2C% 20the%20number%20of%20ED,U.S.%20population%20grew%206. 9%20percent.AccessedMarch22,2023.
7.FairchildR,Ferng-KuoS-F,RahmouniH,etal.Anobservationalstudy oftelementalcaredeliveryandthecontextforinvoluntarycommitment formentalhealthpatientsinagroupofruralemergencydepartments. TelemedRep. 2020;1(1):22–35.
8.DesignatedHealthProfessionalShortageAreasStatistics:Third QuarterofFiscalYear2022DesignatedHPSAQuarterlySummary (BureauofHealthWorkforce:HealthResourcesandServices Administration(HRSA):U.S.DepartmentofHealth&HumanServices). 2022.Availableat: https://data.hrsa.gov/Default/ GenerateHPSAQuarterlyReport.AccessedMarch22,2023.
9.KuBS,LiJ,CathyLally,ComptonMT,etal.Associationsbetween mentalhealthshortageareasandcounty-levelsuicideratesamong adultsaged25andolderintheUSA,2010to2018. GenHosp Psychiatry. 2021;70:44–50.
10.Ivey-StephensonAZ,CrosbyAE,JackSPD,etal.Suicidetrendsamong andwithinurbanizationlevelsbysex,race/ethnicity,agegroup,and mechanismofdeath-UnitedStates,2001–2015. MMWRSurveill Summ. 2017;66(18):1–16.
11.SinghGKandSiahpushM.Wideningrural-urbandisparitiesinlife expectancy,U.S.,1969–2009. AmJPrevMed. 2014;46(2):e19–29.
12.BrownFW.Ruraltelepsychiatry. PsychiatrServ. 1998;49(7):963–4.
13.ShoreJH.Telepsychiatry:videoconferencinginthedeliveryof psychiatriccare. AMJPsychiatry. 2013;170(3):256–62.
14.BeechEH,YoungS,AndersonJK,etal.Evidencebrief:safetyand effectivenessoftelehealth-deliveredmentalhealthcare.2022. Availableat: https://www.hsrd.research.va.gov/publications/esp/ telehealth-mh-brief.cfm.AccessedMarch22,2023.
15.ZhongC,FreemanRE,BoggsKM,etal.Receiptoftelepsychiatryand emergencydepartmentvisitoutcomesinNewYorkState. PsychiatrQ. 2021;92(3):1109–27.
16.ZachrisonKS,BoggsKM,HaydenME,etal.Anationalsurveyof telemedicineusebyUSemergencydepartments. JTelemedTelecare. 2020;26(5):278–84.
17.WardMJ,ShusterJlJr,MohrNM,etal.Implementationoftelehealthfor psychiatricareinVAemergencydepartmentsandurgentcareclinics. TelemedJEHealth. 2022;28(7):985–93.
18.VincentGK,VelkoffVA,SensusBereauUS.(2010).Thenextfour decades:theolderpopulationintheUnitedStates:2010to2050.City, State/Country:U.S.DepartmentofCommerce,Economicsand StatisticsAdministration,U.S.CensusBureau.
19.Populationestimatesandprojections.U.S.Dept.ofCommerce, EconomicsandStatisticsAdministration,U.S.CensusBureau; 2010:14.
20.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. Lancet. 2007;370(9596):1453–7.
21.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. AnnEmergMed. 2005;45(4):448–51.
22.OnegaT,WeissJE,Alford-TeasterJ,etal.Concordanceofrural-urban self-identityandZIPcode-derivedRural-UrbanCommutingArea (RUCA)designation. JRuralHealth. 2020;36(2):274–80.
23.HarrellFE.RegressionModelingStrategiesWithApplicationstoLinear Models,LogisticandOrdinalRegression,andSurvival Analysis. 2nded. Cham,Switzerland:Springer;2015.
24.GuptaDM,BolandRJ,Jr,AronDC.Thephysician’sexperienceof changingclinicalpractice:astruggletounlearn. ImplementSci. 2017;12(1):28.
25.HaydenEM,DavisC,ClarkS,etal.Telehealthinemergencymedicine: aconsensusconferencetomaptheintersectionoftelehealthand emergencymedicine. AcadEmergMed. 2021;28(12):1452–74.
26.HanJH,KochE,JefferyAD,etal.Theeffectoftelementalversusinpersonmentalhealthconsultsintheemergencydepartmenton30-day utilizationandprocessesofcare. AcadEmergMed. 2023;30(4):262–9.
27.SharpIR,KobakKA,OsmanDA.Theuseofvideoconferencingwith patientswithpsychosis:areviewoftheliterature. AnnGenPsychiatry. 2011;10(1):14.
28.VakkalankaJP,HarlandKK,WittrockA,etal.Telemedicineisassociated withrapidtransferandfewerinvoluntaryholdsamongpatientspresenting withsuicidalideationinruralhospitals:apropensitymatchedcohort study. JEpidemiolCommunityHealth. 2019;73(11):1033–9.
29.RodriguezJA,BetancourtJR,SequistTD,etal.Differencesintheuseof telephoneandvideotelemedicinevisitsduringtheCOVID-19pandemic. AmJManagCare. 2021;27(1):21–6.
30.BenjenkI,FranziniL,RobyD,etal.Disparitiesinaudio-only telemedicineuseamongMedicarebeneficiariesduringthecoronavirus disease2019pandemic. MedCare. 2021;59(11):1014–22.
31.ConnollySL,SullivanJL,LindsayJA,etal.Factorsinfluencinguptakeof telementalhealthviavideoconferencingathighandlowadoptionsites withintheDepartmentofVeteransAffairsduringCOVID-19:aqualitative study. ImplementSciCommun. 2022;3(1):66.
32.MohrNM,WuC,WardMJ,etal.Potentiallyavoidableinter-facility transferfromVeteransHealthAdministrationemergencydepartments: acohortstudy. BMCHealthServRes. 2020;20(1):110.
33.JumreornvongO,YangE,RaceJ,etal.Telemedicineand medicaleducationintheageofCOVID-19. AcadMed. 2020;95(12):1838–43.
34.KirklandEB,DuBose-MorrisR,DuckettA.Telehealthfortheinternal medicineresident:a3-yearlongitudinalcurriculum. JTelemedTelecare. 2021;27(9):599–605.
35.ZhangJ,BodenM,TraftonJ.Mentalhealthtreatmentandthe roleoftele-mentalhealthattheVeteransHealthaAdministration duringtheCOVID-19pandemic. PsycholServ. 2022;19(2):375–85.
36.AffairsUSDoV.VeteranPopulation:Age/Gender.2020.Availableat: https://www.va.gov/vetData/veteran_population.asp AccessedMarch22,2023.
ScottG.Weiner,MD,MPH*
ScottA.Goldberg,MD,MPH*
CherylLang,MPH†
MollyJarman,PhD,MPH†
CoryJ.Miller,BS*
SarahLi,BA*
EwelinaW.Stanek,PA-C*
EricGoralnick,MD,MS*
SectionEditor:MarcMartel,MD
*BrighamandWomen’sHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts † BrighamandWomen’sHospital,DepartmentofSurgery,Boston,Massachusetts
Submissionhistory:SubmittedMarch13,2023;RevisionreceivedSeptember26,2023;AcceptedJanuary12,2024
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.60409
Introduction: Bystanderprovisionofnaloxoneisakeymodalitytoreduceopioidoverdose-related death.Naloxonetrainingcoursesareavailable,butnostandardizedprogramexists.Aspartofa bystanderempowermentcourse,wecreatedandevaluatedabriefnaloxonetrainingmodule.
Methods: Thiswasaretrospectiveevaluationofanaloxonetrainingcourse,whichwaspairedwithStop theBleedtrainingforhemorrhagecontrolandwasofferedtoadministrativestaffinanofficebuilding. Participantsworkedinanorganizationrelatedtohealthcare,butnonewereclinicians.Thecurriculum includedthefollowingtopics:1)backgroundabouttheopioidepidemic;2)howtorecognizethesignsof anopioidoverdose;3)actionsnottotakewhenencounteringanoverdosevictim;4)thecorrectstepsto takewhenencounteringanoverdosevictim;5)anoverviewofnaloxoneproducts;and6)Good Samaritanprotectionlaws.The20-minutedidacticsectionwasfollowedbyahands-onsessionwith nasalnaloxonekitsandasimulationmannequin.ThecoursewasevaluatedwiththeOpioidOverdose Knowledge(OOKS)andOpioidOverdoseAttitudes(OOAS)scalesfortake-homenaloxonetraining evaluation.WeusedthepairedWilcoxonsigned-ranktesttocomparescorespre-andpost-course.
Results: Twenty-eightparticipantscompletedthecourse.TheOOKS,measuringobjectiveknowledge aboutopioidoverdoseandnaloxone,hadimprovedscoresfromamedianof73.2%(interquartilerange [IQR]68.3%–79.9%)to91.5%(IQR85.4%–95.1%), P < 0.001.ThethreedomainsontheOOASscore alsoshowedstatisticallysignificantresults.Competencytomanageanoverdoseimprovedona fivepointscalefromamedianof2.5(IQR2.4–2.9)toamedianof3.7(IQR3.5–4.1), P < 0.001.Concerns aboutmanaginganoverdosedecreased(improved)fromamedianof2.3(IQR1.9–2.6)tomedian1.8 (IQR1.5–2.1), P < 0.001.Readinesstointerveneinanopioidoverdoseimprovedfromamedianof4 (IQR3.8–4.2)toamedianof4.2(IQR4–4.2), P < 0.001.
Conclusion: Abriefcoursedesignedtoteachbystandersaboutopioidoverdoseandnaloxonewas feasibleandeffective.Weencouragehospitalsandotherorganizationstouseandpromulgatethis model.Furthermore,wesuggesttheconveningofanationalconsortiumtoachieveconsensuson programcontentanddelivery.[WestJEmergMed.2024;25(3)320–324.]
Timeisacriticalcontributingfactorinpatientoutcomes inmanyemergencies.IntheUnitedStates,theaverage responsetimebyemergencymedicalservicestoa9-1-1callis sevenminutes.1 Tobridgethisgap,manyeffortshavebeen launchedtoempowerlaypersons,whoaretypically firston thescene,tointerveneandemployskillsrangingfrom cardiopulmonaryresuscitation(CPR)andautomated externaldefibrillator(AED)usetobleedingcontrol interventions.2 BasicLifeSupport(BLS)coursecontentis baseduponrigorousandfrequentlyupdatedconsensus(ie, AmericanHeartAssociation[AHA]GuidelinesUpdatefor CPRandEmergencyCardiovascularCare).3,4 Thesecourses aretaughtinastandardizedfashionbytheAHAandthe AmericanRedCross.Likewise,theStoptheBleed(STB) program,anationalinitiativelaunchedin2015focusedon empoweringthepublicandpublicsafetyprofessionalsto recognizeandcontrollife-threateningbleeding,hasseveral typesofcourses,themostprominentbeingtheAmerican CollegeofSurgeons’ (ACS)BasicHemorrhageControl Course(BCon).5,6
WhileCPR,AEDandSTBtrainingfocusonpreventable deaths,anothersignificantsourceofpreventabledeathsisthe opioidoverdoseepidemic,whichremainsoneofthemost pressingpublichealthissuesofourtime,havingclaimed about1,000,000livesintheUSsince1999.7 Thenumberof overdosedeathshasincreasedgreatlyinrecentyears,with yetanotherrecordnumberin2021,predominantlydueto fentanyl.8 Bystandernaloxoneadministration,whichcanbe usedtoreverseanopioidoverdose,hasbeenintroducedas onepotentialmitigatingfactor.In2018,theUSSurgeon Generalissuedanadvisoryonnaloxoneandopioidoverdose thatencouragescommunitymemberswhocomeintocontact withpeopleatriskforopioidoverdosetoknowhowtouse naloxoneandkeepitwithinreach.9 Likewise,theUS DepartmentofHealthandHumanServices’ overdose preventionstrategyincludesharmreduction,withagoalto widenaccesstoopioidoverdosereversaltreatments.10
UnlikeCPR,thereisnoonestandardizedcoursefor bystandernaloxonetraining.Onlinecoursesareofferedby agenciessuchastheCentersforDiseaseControland Prevention(CDC),11 theAmericanRedCross,12 individual states(eg,Massachusetts13 andNewYork14),andothernonprofits(eg,GetNaloxoneNow15).Thecourseslacka standardizedcorecontent,measuresofeffectiveness,oragreedupondeliverymethods(inperson,hybrid,remote,simulation, didactic,etc).Althoughanecdotesexistoflaypersonuse,we havealimitedunderstandingofaneffective,layperson naloxone-empowermentcurriculum,andgapsremainin knowledgeabouttrainingparametersandstrategies.16
Inthisstudy,weevaluatedanoverdose-responsenaloxone trainingprogramadministeredtolaypersons.We emphasizedthestructureandcurriculumofthecourseand evaluatedefficacywithavalidatedscreeningtool.
Thenaloxonecoursewasdesignedtobeabrief interventionwith20minutesofdidacticsand20minutesof practicalexperiencewithamannequin.Thecoursewas bundledwiththeACSBConcourseaspartofabystander empowermentprogram.Courseinstructorswerethree board-certifiedemergencyphysicians.Thesessiontookplace ataprofessionalofficebuilding.Althoughtheparticipants workedinanorganizationrelatedtohealthcare,allworked asofficestaffandnonewereclinicians.Twoidenticalsessions wereoffered,andbothtookplaceinJune2018during normalbusinesshours.Participantswerenotcompensated specificallyforparticipatingbutattendedinlieuoftheir normalduties.Weadministeredanonymouspre-andpostcourseevaluations.Theprojectwasdeterminedtonotmeet thecriteriaforhumansubjectresearchbytheMassGeneral BrighamHumanResearchOffice.
Createdbythecourseinstructors,thecurriculumincluded thefollowingtopics:1)backgroundabouttheopioid epidemic;2)howtorecognizethesignsofanopioid overdose;3)actionsnottotakewhenencounteringan overdosevictim;4)thecorrectstepstotakewhen encounteringanoverdosevictim;5)anoverviewofnaloxone products;and6)GoodSamaritanprotectionlaws.Content wascreatedby firstsearchingforexistingtrainingresources online,includingtrainingmanualsfromthestatesofNew York(https://www.dhses.ny.gov/naloxone-informationfirst-responders)andTexas(https://txoti.org),andCanadian provinceManitoba(https://www.gov.mb.ca/health/ publichealth/docs/training_manual_overdose.pdf).This informationwasintegratedwithadditionalcontentfrom courseinstructorexpertiseintoadidacticmodulecontaining 30slides(Appendix1),andparticipantswereprovidedwitha hardcopyoftheslides.Thepracticalmoduleentailedsmall groupsaroundasimulationmannequinwithacourse instructor.Participantswereabletopracticewithtwotypes ofnaloxonekits(pre-packagednasalnaloxonesprayandan autoinjector)onthemannequin.Discussionwasencouraged untilallparticipants’ questionsandconcernswereaddressed.
Toevaluatetheefficacyofthecourse,weusedtheOpioid OverdoseKnowledge(OOKS)andOpioidOverdose Attitudes(OOAS)scalesfortake-homenaloxonetraining evaluation.17 The firsthalfofthisvalidatedtool(OOKS)asks objectivequestionsaboutopioidoverdosetoevaluatetrainee knowledge,includingindicatorsofopioidoverdose,howto manageanoverdose,themechanismofactionofnaloxone, anditsdurationofaction.Thesecondpart(OOAS)asks questionspertainingtoperceptionsofcompetenciesto manageanopioidoverdose,concernsaboutmanagingan overdose,andreadinesstointerveneinanopioidoverdose.
Allparticipantscompletedpre-andpost-evaluationson paperforms.Subjectswereaskedtowritethesamerandom four-digitnumberoneachofthetwoevaluationsforpaired analysispurposes.Responsesweretransferredtoa spreadsheet,andasecondinvestigatorconfirmedthe accuracyofthetranscription.TheOOKSscaleisaseriesof true/falsestatements,andthecorrectanswersweresummed, withatotalpossible41points.Wemodifiedtheoriginal 45-pointversionslightly,asmultiplepointswerepossiblefor severalindividualquestions(eg, “Whatisnaloxoneused for?” and “Howcannaloxonebeadministered?”)andwe countedthemonlyasonepointeach.Therewasalsoachoice of “don’tknow” forseveralquestions,andthatwas consideredanincorrectanswerasindicatedinthescoring instructions.TheOOASscaleis28questionsdividedinto threedomainsandmeasuredona five-pointLikertscale (5 = completelyagreeand1 = completelydisagree). Althoughthepost-testOOKSresultsandoneofthedomains ontheOOASwerenormallydistributedasdeterminedbythe Shapiro-Wilktest,theremainderofresultswerenon-normal. Thus,allresults,includingthescalesoneachdomainofthe OOASandtheoverallscoreontheOOKS,aredescribed withmediansandinterquartilerange(IQR)andcompared withthepairedWilcoxonsigned-ranktest.Weanalyzeddata withJMPv16(JMPStatisticalDiscoveryLLC,Cary.NC).
Twenty-eightparticipantstookthecourse.Allcompleted thepre-testandthepost-test,althoughthreeparticipantsdid notanswerallquestionsonthepre-testOOASscale. Therefore,thecorrespondinganswersinthedomainsfor thesethreeindividualsonthepost-testwerenotincludedin theanalysis.TheOOKS,measuringobjectiveknowledge aboutopioidoverdoseandnaloxone,hadimprovedscores fromamedianof73.2%(IQR68.3%–79.9%)to91.5%(IQR 85.4%–95.1%), P < 0.001.ThethreedomainsontheOOAS scorealsoshowedstatisticallysignificantresults. Competencytomanageanoverdoseimprovedfroma medianof2.5(IQR2.4–2.9)toamedianof3.7(IQR 3.5–4.1), P < 0.001.Concernsaboutmanaginganoverdose decreased(improved)fromamedianof2.3(IQR1.9–2.6)to median1.8(IQR1.5–2.1), P < 0.001.Readinesstointervene inanopioidoverdoseimprovedfromamedianof4(IQR 3.8–4.2)toamedianof4.2(IQR4–4.2), P < 0.001.
Increatingandevaluatinganaloxonetrainingprogram forbystanders,wefoundimprovementinbothsubjective attitudesandobjectiveknowledgeaboutopioidoverdose andnaloxone.Thetrainingisrelativelybrief(lastingunder anhour)andeffective.Wehavesubsequentlytaughtthis curriculumseveraltimestolocalcommunityorganizations, includingthosewhoworkwithpeoplewhousedrugs.
Althoughwedidnotmeasureobjectiveoutcomes subsequently,theconceptofbystanderempowerment, teachingbothnaloxoneandSTBskills,hasbeenwell receivedandrepresentsimportantoutreachfromour hospitaltothelocalcommunity.
Onekeyquestionthatremainsiswhetherthistrainingis necessaryforbystanders.Inourpreviousresearch,wefound that49of50bystanderswereabletocorrectlyadminister naloxoneinasimulatedexperienceonapublicsidewalkwith guidancebyasimulated911dispatcher.18 However,not everyonewillhavetheguidanceofadispatcherwhenusing naloxone,andtheremaybeconfusionabouthowtousethe kitandthetimingofaseconddose(ifneeded)withoutthat assistance.Bystandertrainingmayalsobevaluableasaway tofosterself-efficacy,increasingthelikelihoodthata laypersonwillrecognizeandrespondtoanoverdose.Inour course,wealsocoverwhenbystandersshouldadminister naloxoneanddispelmythsaboutanyharmthatcanbe causedbygivingit,aswellashowtoaccessnaloxone.
Naloxoneforbystandersiscurrentlyavailablevia standingorderinseveralstates,meaningthatindividualscan obtainitfrompharmacieswithoutaprescription.19–22 Standingordersareassociatedwithreductionsinfatal overdosesinthecommunity.23 Thecurrentpackagingof prescriptionnasalnaloxonehasa flapthatopensgivingjustin-time(JIT)instructionstothebystander,butthatmaynot besufficient.TheUSFoodandDrugAdministration(FDA) recentlyapprovedmakingnasalnaloxoneanover-thecountermedication,eventhoughitsbriefingdocument describedseveralcasesofincorrectlyadministerednaloxone, includinganindividualwhodidnotplacethetipofthe dispenserfullyinthenostril,someonewhosqueezedthe devicebutdidnotpushtheplunger,anotherwhoplacedthe deviceupsidedownsothattheplungerwasinthenostril,and severalindividualswhodidnotwait2-3minutesbefore administeringaseconddose.24 WhiletheFDAadvisors votedunanimouslytomakenaloxoneavailablewithouta prescription,25 theseerrorsinadministrationindicate theneedforabystandercoursethatcouldfurther improveoutcomes.
Anotherreasontoteachsuchacourseistoaddressstigma, whichispervasivewhenconsideringopioidusedisorder (OUD).26 Arecentstudyofindividualswhodidnotuseillicit opioidsthemselvesbutknewotherswhodidreportedstigma aboutOUDandmisinformationaboutopioid-related risks.27 Naloxone-basedinterventionscanintroducethe conceptofharmreduction,empowerbystanders,and encourageindividualstocarrynaloxoneincasethey encounteranoverdosevictim.28
Althoughnotapartofourstudy,despitethepositive resultsonourobjectiveandsubjectivetesting,wedo encouragethecreationofstandardizedtraining.TheSTB BConportionofourcoursewascreatedandendorsedby theACS,usingstandardizedcontentandcertifiedtrainers.
Asimilarprocesscouldbeusedfornaloxone,eitheraspartof aBLStraining,suchasfromtheAHAorAmericanRed Cross,fromaspecialtysociety,suchastheAmerican AcademyofEmergencyMedicine,theAmericanCollegeof EmergencyPhysicians,ortheAmericanSocietyofAddiction Medicine,orfromanationaladvocacygroupsuchas Shatterproof.Suchbrandingandpromotionmayempower morebystanderstobecometrainedandfurtherreduce stigmaandmisconceptionsaboutOUDamongthe generalpopulation.
WhileCPRtrainingforlaypersonsisthegoldstandard, manygapsinimplementingbystandertrainingremain,and aninvestmentinthestudyoftheeffectivenessoftherelatively simplestepsofnaloxoneadministrationmayhelpuslearn andimprovetechniquesofCPRandSTBtrainingaswell. Forexample,despiteeducationalinitiativesthatbeganinthe 20thcentury,onlyone-thirdofout-of-hospitalcardiacarrest patientsreceivebystanderCPR.Time,location,and durationhaveallbeenperceivedbythepublicasbarriersto CPRclasses.29 BlacksandHispanicsarelesslikelythan WhitestoreceiveCPRathomeorinpublic.30 Inthelast decade,therehavebeenmanyinitiativeswithvariable efficacy,inmostcasesnotmeasured,touseJITtoolslike flashcards,videoortalkingkitstoprovideuserswithrealtimeinstructionsfortheuseofautomatedexternal defibrillatorsorSTBequipment.Whiletheagreementof coursecontentandidentifyingefficacyisa firststep,future workshouldalsofocusondeveloping,trialing,andscaling effectiveJITnaloxone-administrationtools.
Therearelimitationstoourstudy.Wetaughtthiscourse toasmallsampleofadministrativeprofessionalsinasuburb ofMassachusetts,astatewithahighburdenofopioidrelatedoverdose.Itispossiblethatbystandersfromdifferent backgroundsandgeographiclocationswouldhaveanswered thequestionsdifferently.Wealsodidnotcollectany demographicdataaboutourstudyparticipantstoprotect confidentiality.However,thisinformationmighthave determinedthecharacteristicsofindividualswhomaybenefit mostfromthetraining.Thecontentofthepracticalsessionof thecoursewasnotstandardized.Finally,wedidnot measureknowledgeretentionoruseofnaloxonefollowing thecourse.
Abriefcoursedesignedtoteachbystandersaboutopioid overdoseandnaloxonewasfeasibleandeffective.We encouragehospitalsandotherorganizationstouseand promulgatethismodel.Furthermore,wesuggestconvening ofanationalconsortiumtoachieveconsensusonprogram content,delivery,andopportunitiesfordevelopmentofjustin-timetoolstoadministernaloxone.
AddressforCorrespondence:ScottG.Weiner,MD,MPH,Brigham andWomen’sHospital,DepartmentofEmergencyMedicine,75 FrancisStreet,NH-226,Boston,MA02115.Email: sweiner@bwh. harvard.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Outsideofthisresearch,ScottG. WeinerissupportedbyNationalInstitutesofHealthgrant5-R01DA044167,theFoundationforOpioidResponseEfforts,andthe ElevanceFoundation.ScottG.Weinerisanadvisorycommittee memberofVertexPharmaceuticals,Inc.andCessation Therapeutics,Inc.Therearenootherconflictsofinterestorsources offundingtodeclare.
Copyright:©2024Weineretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.MellHK,MummaSN,HiestandB,etal.Emergencymedicalservices responsetimesinrural,suburban,andurbanareas. JAMASurg. 2017;152(10):983–4.
2.FederalEmergencyManagementAgency.Youarethehelpuntil helparrives.Availableat: https://community.fema.gov/ PreparednessCommunity/s/until-help-arrives?language=en_US AccessedAugust20,2023.
3.AmericanHeartAssociation.2020AmericanHeartAssociation GuidelinesforCPRandECC.Availableat: https://cpr.heart.org/en/ resuscitation-science/cpr-and-ecc-guidelines AccessedAugust20,2023.
4.SoarJ,DonninoMW,MaconochieI,etal.2018InternationalConsensus onCardiopulmonaryResuscitationandEmergencyCardiovascular CareSciencewithTreatmentRecommendationssummary. Circulation. 2018;138(23):e714–30.
5.GoralnickE,ChaudharyMA,McCartyJC,etal.Effectivenessof InstructionalInterventionsforHemorrhageControlReadinessfor LaypersonsinthePublicAccessandTourniquetTrainingstudy (PATTS):arandomizedclinicaltrial. JAMASurg. 2018;153(9):791–9.
6.GoolsbyC,JacobsL,HuntRC,etal.StoptheBleedEducation Consortium:educationprogramcontentanddeliveryrecommendations. JTraumaAcuteCareSurg. 2018;84(1):205–10.
7.CentersforDiseaseControlandPrevention.DrugOverdoseDeaths. Availableat: https://www.cdc.gov/drugoverdose/deaths/index.html AccessedAugust20,2023.
8.NationalCenterforHealthStatistics.ProvisionalDrugOverdoseDeath Counts.Availableat: https://www.cdc.gov/nchs/nvss/vsrr/ drug-overdose-data.htm.AccessedAugust20,2023.
9.UnitedStatesHealthandHumanServices.U.S.SurgeonGeneral’s AdvisoryonNaloxoneandOpioidOverdose.Availableat: https://www. hhs.gov/surgeongeneral/reports-and-publications/addiction-
and-substance-misuse/advisory-on-naloxone/index.html AccessedAugust20,2023.
10.UnitedStatesHealthandHumanServices.HarmReduction.Available at: https://www.hhs.gov/overdose-prevention/harm-reduction AccessedAugust20,2023.
11.CentersforDiseaseControlandPrevention.NaloxoneTraining. Availableat: https://www.cdc.gov/opioids/naloxone/training/index.html AccessedAugust20,2023.
12.AmericanRedCross.FirstAidforOpioidOverdosesOnlineCourse. Availableat: https://www.redcross.org/take-a-class/opioidoverdose AccessedAugust20,2023.
13.CommonwealthofMassachusetts.Overdose&NaloxoneTraining Resources.Availableat: https://www.mass.gov/service-details/ training-resources.AccessedAugust20,2023.
14.NewYorkState.CommunityCalendarofOpioidOverdoseTrainings. Availableat: https://www.health.ny.gov/diseases/aids/general/ opioid_overdose_prevention/training_calendar.htm AccessedAugust20,2023.
15.GetNaloxoneNow.Availableat: https://www.getnaloxonenow.org/ #home.AccessedAugust20,2023.
16.Moustaqim-BarretteA,DhillonD,NgJ,etal.Take-homenaloxone programsforsuspectedopioidoverdoseincommunitysettings:a scopingumbrellareview. BMCPublicHealth. 2021;21(1):597.
17.WilliamsAV,StrangJ,MarsdenJ.DevelopmentofOpioidOverdose Knowledge(OOKS)andAttitudes(OOAS)scalesfortake-home naloxonetrainingevaluation. DrugAlcoholDepend. 2013;132(1-2):383–6.
18.GoldbergSA,DworkisDA,LiaoVT,etal.Feasibilityofbystander administrationofpublic-accessnaloxoneforopioidoverdose. Prehosp EmergCare. 2018;22(6):788–94.
19.IjiomaSC,FernándezEV,GatewoodSB,etal.Communitypharmacists inVirginiadispensingnaloxoneunderastandingorder:aqualitative study. JAmPharmAssoc(2003). 2021;61(6):753–60.e1.
20.SugarmanOK,BreithauptJ,WangX,etal.Characteristicsandhealth serviceuseofMedicaid-insuredindividuals fillingnaloxoneundera
standingorderinLouisiana. JAmPharmAssoc(2003). 2023;63(3):904–8.e1.
21.AbbasB,MarottaPL,Goddard-EckrichD,etal.Socio-ecologicaland pharmacy-levelfactorsassociatedwithnaloxonestockingatstandingordernaloxonepharmaciesinNewYorkCity. DrugAlcoholDepend. 2021;218:108388.
22.ChatterjeeA,YanS,XuanZ,etal.Broadeningaccesstonaloxone: communitypredictorsofstandingordernaloxonedistributionin Massachusetts. DrugAlcoholDepend. 2022;230:109190.
23.TaylorM,PradhanA,OgandoYM,etal.Impactofthenaloxonestanding orderontrendsinopioidfataloverdose:anecologicalanalysis. AmJ DrugAlcoholAbuse. 2022;48(3):338–46.
24.UnitedStatesFederalDrugAdministration.JointNonprescriptionDrug AdvisoryCommitteeandAnestheticandAnalgesicDrugProducts AdvisoryCommitteeMeeting.2023.Availableat: https://www.fda.gov/ media/165338/download.AccessedAugust20,2023.
25.AntrimA.FDAAdvisoryCommitteesRecommendNaloxoneBe AvailableOTC.2023.Availableat: https://www.pharmacytimes.com/ view/fda-advisory-committees-recommend-naloxone-be-available-otc AccessedAugust20,2023.
26.FomiattiR,FarrugiaA,FraserS,etal.Addictionstigmaandthe productionofimpedimentstotake-homenaloxoneuptake. Health (London). 2022;26(2):139–61.
27.SlocumS,OzgaJE,JoyceR,etal.Ifwebuildit,willtheycome? Perspectivesonpharmacy-basednaloxoneamongfamilyandfriendsof peoplewhouseopioids:amixedmethodsstudy. BMCPublicHealth. 2022;22(1):735.
28.MillerNM,Waterhouse-BradleyB,CampbellC,etal.Howdonaloxonebasedinterventionsworktoreduceoverdosedeaths:arealistreview. HarmReductJ. 2022;19(1):18.
29.McGovernSK,BlewerAL,MurrayA,etal.Characterizingbarriersto CPRtrainingattainmentusingTwitter. Resuscitation. 2018;127:164–7.
30.GarciaRA,SpertusJA,GirotraS,etal.Racialandethnicdifferencesin bystanderCPRforwitnessedcardiacarrest. NEnglJMed. 2022;387(17):1569–78.
GaryZhang,MD*
MichaelJ.Burla,DO*†§
BenjaminB.Caesar,MD*
CarolyneR.Falank,PhD* PeterKyros,MD*
VictoriaC.Zucco,BS* AnetaStrumilowska,BS‡
DanielC.Cullinane,MD* ForestR.Sheppard,MD*
SectionEditor:ChristopherTainter,MD
*MaineMedicalCenter,DepartmentofSurgery,Portland,Maine † SouthernMaineHealthcare,DepartmentofEmergencyMedicine,Biddeford,Maine ‡ UniversityofNewEnglandCollegeofOsteopathicMedicine,Biddeford,Maine § TuftsSchoolofMedicine,Boston,Massachusetts
Submissionhistory:SubmittedMarch31,2023;RevisionreceivedJanuary8,2024;AcceptedJanuary10,2024
ElectronicallypublishedApril18,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.17975
Background: Patientswithcoronavirus2019(COVID-19)areathighriskforrespiratorydysfunction. Thepulseoximetry/fractionofinspiredoxygen(SpO2/FiO2)ratioisanon-invasiveassessmentof respiratorydysfunctionsubstitutedforthePaO2:FiO2 ratioinSequentialOrganFailureAssessment scoring.Wehypothesizedthatemergencydepartment(ED)SpO2/FiO2 ratioscorrelatewithrequirement formechanicalventilationinCOVID-19patients.OurobjectivewastoidentifyCOVID-19patientsat greatestriskofrequiringmechanicalventilation,usingSpO2/FiO2 ratios.
Methods: WeperformedaretrospectivereviewofpatientsadmittedwithCOVID-19attwohospitals. HighestandlowestSpO2/FiO2 ratios(percentsaturation/fractionofinspiredO2)werecalculatedon admission.Weperformedchi-square,univariate,andmultipleregressionanalysistoevaluatethe relationshipofadmissionSpO2/FiO2 ratioswithrequirementformechanicalventilationandintensive careunit(ICU)care.
Results: Atotalof539patients(46%female;84%White),withameanage67.6 ± 18.6years,met inclusioncriteria.Patientswhorequiredmechanicalventilationduringtheirhospitalstaywerestatistically youngerinage(P = 0.001),hadahigherbodymassindex(P < .001),andtherewasahigherpercentage ofpatientswhowereobese(P = 0.03)andmorbidlyobese(P < .001).Shortnessofbreath,cough,and feverwerethemostcommonpresentingsymptomswithamediantemperatureof99°F.Averagewhite bloodcountwashigherinpatientswhorequiredventilation(P =<0.001).AhighestobtainedEDSpO2/ FiO2 ratioof ≤300wasassociatedwitharequirementformechanicalventilation.AlowestobtainedED SpO2/FiO2 ratioof ≤300wasassociatedwitharequirementforintensivecareunitcare.Therewasno statisticallysignificantcorrelationbetweenEDSpO2/FiO2 ratios >300andmechanicalventilationor intensivecareunit(ICU)requirement.
Conclusion: TheEDSpO2/FiO2 ratioscorrelatedwithmechanicalventilationandICUrequirements duringhospitalizationforCOVID-19.TheseresultssupportEDSpO2/FiO2 asapossibletriagetooland predictorofhospitalresourcerequirementsforpatientsadmittedwithCOVID-19.Furtherinvestigationis warranted.[WestJEmergMed.2024;25(3)325–331.]
Thecoronavirus2019(COVID-19)pandemicprofoundly impactedhospitalsystemsworldwide.Identifyingpatients presentingwithCOVID-19intheemergencydepartment (ED)atgreatestriskforrequiringmechanicalventilationor intensivecareunit(ICU)careisofparamountimportance sincethiswouldfacilitatemoreefficientallocationoflimited medicalresources.SevereCOVID-19infectioncanbelifethreateningandisassociatedwithsignificanthypoxemiaand thedevelopmentofacuterespiratorydistresssyndrome (ARDS).1,2 Identifyingearlypredictorsofrespiratoryfailure andICUneedisvitalbothforpatientcareandlogisticsinthe settingofaglobalpandemicwithlimitedICUresources.
Thepulseoximetry/fractionofinspiredoxygen(SpO2/ FiO2 ratio)haspreviouslybeenusedasapredictorofhighflownasalcannulafailure,needforintubation,and mechanicalventilation.3 TheSpO2 valuehasbeen demonstratedtobeareliablesurrogateforpartialpressureof oxygeninthearterialblood(PaO2),4,5 andtheSpO2/FiO2 ratiodoesnotrequireanybloodtests.TheSpO2/FiO2 ratiois anon-invasiveassessmentofrespiratorydysfunctionthat canbequicklyobtainedatthebedside.Measuredatthetime ofpresentation,theSpO2/FiO2 ratiohasbeendemonstrated tobeanindependentindicationofARDSdevelopment.6 The abilitytoquicklydeterminerequiredlevelofcarefor vulnerablepatientsisessentialtopreventpooroutcomes, particularlyinresource-limitedenvironments.TheCOVID19pandemicledtoEDcrowdingandadecreaseinventilator andICUavailability.7 Avalidatedprognosticindicatortool akintothesystematicinflammatoryresponsesyndromeor SequentialOrganFailureAssessmentcriteriaforsepsis8 is vitalforEDusetoidentifyCOVID-19patientsathighestrisk ofventilatorandICUneed.TheSpO2/FIO2 ratiopredictive valuehaspreviouslybeenvalidatedinARDS,6 andearly measurementmayserveasanindicatorandtriagetoolin COVID-19withregardtorespiratoryfailure/ventilationrisk andICUneed.
OurobjectiveinthisstudywastoevaluateEDSpO2/FIO2 ratiosinCOVID-19patientsandcorrelatethemwith subsequentrespiratoryfailure,necessitatingtheneedfor ICUlevelofcareand/ormechanicalventilationduring hospitalization.Useofthisratiomayhelphospitalsystems moreefficientlyuseresourcesandeffectivelypreparefora patient’sneedforICUcareormechanicalventilation.
StudyDesignandParticipantSelection
Thiswasaretrospectivestudythatevaluatedadmission encountersfrombothMaineMedicalCenter(MMC)and SouthernMaineHealthCare(SMHC).Theseinstitutions workcloselytogether,withMMCbeingtheregion’stertiary carecenterwithover70,000annualEDvisitsandatotalof 45multipurposeICUbeds.TheSMHCisacommunity hospitalwithincloseproximitytoMMC,averaging ≈55,000
totalEDvisitsandnineICUbeds.COVID-19patientswho were ≥18yearsoldandrequiredadmissiontoeitherhospital metinclusioncriteria.Encounterswerecollectedbetween March–December28,2020;thus,nopatientshadbeen vaccinatedagainstCOVID-19.Patientswereexcludedifthey didnotrequireadmission.Thisstudywasperformedunder approvaloftheinstitutions’ reviewboards.
Weperformedretrospectivechartreviewtoidentify patientdemographics,diagnoses,levelofhospitalcare,and hospitaloutcomesdatafromelectronichealthrecords.The FiO2 valueswerecalculatedusingnasalcannula flowrate.9 Werecordedthepatient’slowestandhighestSpO2 andFiO2 valuesintheEDandcalculatedSpO2/FiO2 ratios.
Theprimaryoutcomewastheneedformechanical ventilation.SecondaryoutcomesincludedICUlevelofcare, ventilatordays,in-hospitalcomplications,escalationofcare followinginitialtriage,ICUlengthofstay(LOS),hospital LOS,andin-hospitalmortality.
WeanalyzeddatausingRStudio2020(RStudioInc, Boston,MA).Descriptivestatisticswerepresentedas frequencyandpercentage.Normallydistributedcontinuous datawerereportedasmeanwithSDs,andordinalnonnormallydistributedcontinuousdataweredescribedwith medianswithinterquartileranges.Weusedmultivariable logisticregressiontoassesstheassociationbetweeneither loworhighSpO2/FiO2 ratioswithintheED,anticoagulation use,asthma,coronaryarterydisease(CAD),congestive healthfailure(CHF),chronicobstructivepulmonarydisease (COPD),diabetes,hyperlipidemia,hypertension,and gastroesophagealrefluxdisease(GERD),ortheneedfor mechanicalventilation,adjustedforageandbodymass index(BMI).Bivariableanalysisofcategoricalvariableswas doneusingthe χ2test,andnonparametricvariablesbythe Kruskal-Wallistest.Regressionmodelscontrolledforboth ageandBMI.
Atotalof539patients,withameanage67.6 ± 18.6years, metinclusioncriteria.Patientswerestratifiedintotwo cohortsbasedontheneedformechanicalventilation (Table1).Asshowninthetable,patientswhorequired mechanicalventilationduringtheirhospitalstaywere statisticallyyoungerinage(P = 0.001),hadahigherBMI (P < .001),andtherewasahigherpercentageofpatientswho wereobese(P = 0.03)andmorbidlyobese(P < .001). Shortnessofbreath,cough,andfeverwerethemostcommon presentingsymptoms,withamediantemperatureof99°F. Theaveragewhitebloodcountwashigherinpatientswho
Table1. Baselinecharacteristicsofpatientswithcoronavirus2019.
Demographicdata
Mean ± SD,median,rangeorn(%)
Notmechanically ventilatedn = 451 Mechanically ventilatedn = 88 P-value
Age(median,IQR)72,2666,19.750.001
BMI(median,IQR)28.9,9.432.3,10.9 <.001
Gender
Female217(48%)31(35%)0.03
Male234(52%)57(65%)0.03
Race
Asian11(2%)5(6%)0.03
Black31(7%)5(6%)0.73
NativeHawaiianorotherPacificIslander1(0.2%)0(0%)0
Unknown/notreported2(0.4%)2(2%)0.003
Morethanonerace3(0.6%)0(0%)0.47
White397(88%)73(83%)0.20
Other6(1%)3(3%)0.13
Ethnicity
HispanicorLatino9(2%)3(3%)0.56 NotHispanicorLatino440(98%)84(95%)0.10
Unknown/notreported2(0.4%)1(1%)0.46
Origin
Home282(63%)54(61%)0.72
Nursinghome61(14%)9(10%)0.31
Skillednursinghome31(7%)0(0%)0.01
Rehab1(0.2%)2(2%)0.03
Other*76(17%)23(26%)0.05
Comorbidconditions
Alcoholuse23(5%)8(9%)0.14
Anticoagulationtherapy52(12%)13(15%)0.44
Asthma66(15%)14(16%)0.81
Cerebrovascularaccident41(9%)4(5%)0.22
COPD71(16%)16(18%)0.64
Chronicheartfailure67(15%)13(15%)1
Chronickidneydisease73(16%)12(14%)0.64
Cancer57(13%)9(10%)0.44
Coronaryheartdisease/heartfailure105(23%)19(22%)0.84
Currentsmoker30(7%)2(2%)0.08
Dementia75(17%)5(6%)0.01
Diabetesmellitus156(35%)38(43%)0.15
GERD132(29%)26(30%)0.85
Myocardialinfraction39(9%)5(6%)0.36
Hypertension282(63%)57(65%)0.72
Hyperlipidemia222(49%)49(56%)0.23
Morbidlyobese14(3%)11(13%) <.001
Obese81(18%)25(28%)0.03
(Continuedonnextpage)
Table1. Continued.
Demographicdata
Presentingsymptoms
Mean ± SD,median,rangeorn(%)
Notmechanically ventilatedn = 451
Mechanically ventilatedn = 88 P-value
Fever176(39%)34(39%)1
Myalgia72(16%)15(17%)0.82
Arthralgias21(5%)2(2%)0.22
Headache50(11%)4(5%)0.09
GIsymptoms140(31%)17(19%)0.02
Cough229(51%)54(61%)0.09
Shortnessofbreath253(56%)57(65%)0.12
Other233(52%)43(49%)0.61
AveragetemperatureintheED ± SD(Fahrenheit)97.1 ± 12.4,99.1,7.3–104.598.1 ± 10,99,37–1030.48
WBCcountintheED(median,IQR)6.2,4.78,7.4 <.001
Diagnoses
Neurologicaldiagnoses128(28%)40(45%)0.002
Renaldiagnoses129(29%)55(63%) <.001
Liverdiagnoses44(10%)23(26%)
Heartdiagnoses168(37%)56(64%) <.001
Pulmonarydiagnoses280(62%)69(78%)0.004
Shock10(2%)46(52%) <.001
Respiratoryfailure153(34%)75(85%) <.001
Renalfailure29(6%)22(25%) <.001
ICU
PatientswhorequiredICUcareatanypoint75(17%)84(95%) <.001
RequiredmorethanoneICUadmissions2(0.4%)6(7%) <.001
ICULOS(median,IQR)2,313,16 <.001
Intubated
Patientswhowereintubated0(0%)84(95%) <.001
Daysintubatedn/a2,4
Non-procedurebasedintubation0(0%)51(58%) <.001
Mechanicalventilators
Ventilatordays(median,IQR)n/a9,13
Requiredreintubationn/a7(8%)
Escalationofcarefrominitialtriage60(13%)56(64%) <.001
HospitalLOS(median,IQR)6,617.5,19 <.001
Dischargedisposition
Homeorself-care193(43%)8(9%) <.001
Homewithservices97(22%)17(19%)0.53
Hospice/palliativecareunit11(2%)1(1%)0.52
Mentalhealth/psychiatrichospital8(2%)0(0%)0.18
Nursinghome17(4%)1(1%)0.16 (Continuedonnextpage)
Table1. Continued.
Demographicdata
Mean ± SD,median,rangeorn(%)
Notmechanically ventilatedn = 451 Mechanically ventilatedn = 88 P-value
Other62(14%)34(39%) <.001
Rehab15(3%)24(27%) <.001
Skillednursingfacility48(11%)3(3%)0.02
In-hospitalmortality36(8%)28(32%) <.001
*Otherincludeshomeless,transfersin,grouphome,Primarycarephysicianfollowup,mentalhealthfacility.
BMI,bodymassindex; IQR,interquartilerange; COPD,chronicobstructivepulmonarydisease; GERD,gastroesophagealrefluxdisease; WBC,whitebloodcount; ED,emergencydepartment; ARDS,acuterespiratorydiseasesyndrome; GI,gastrointestinal; ICU,intensivecare unit; LOS,lengthofstay.
requiredventilation(P =<0.001)(Table1).Patients requiringmechanicalventilationhadhigherdiagnoses ofARDS(P < .001),pneumonia(P < .001),shock (P < .001),respiratoryandrenalfailure(P < .001), andworsehospitaloutcomeswithanin-hospitalmortality of32%vs8%(P < .001)andamedianhospitalLOSof 17.5vs6days(P < .001).
TheSpO2/FiO2 ratiosintheEDandtheirassociations withmechanicalventilationorneedforICUcareare presentedin Table2.AhighestobtainedEDSpO2/FiO2 ratioof300orbelowwasstatisticallyassociatedwitha requirementformechanicalventilationduring hospitalization.AlowestobtainedEDSpO2/FiO2 ratioof 300orbelowwasstatisticallyassociatedwitharequirement forICUcareduringhospitalization.Therewasno statisticallysignificantrelationshipbetweenEDSpO2/FiO2 ratiosabove >300andmechanicalventilationorICUlevel ofcare.
Chronicobstructivepulmonarydiseasewasa confoundingfactorforCOVID-19patientswhorequired mechanicalventilation(adjustedR2 value = 0.1132; P < .001).Nostatisticallysignificantassociationswere identifiedbetweenthefollowingco-morbidities: anticoagulationuse;asthma(adjustedR2 = 0.096, P = 0.75); CAD(adjustedR2 = 0.102; P = 0.07);CHF(adjustedR2 = 0.096; P = 0.95);diabetes(adjustedR2 = 0.10; P = 0.07); hyperlipidemia(adjustedR2 = 0.11; P = 0.08);hypertension (adjustedR2 = 0.096; P = 0.58);andGERD(adjustedR2 = 010; P = 0.28)fortherequirementofmechanicalventilation.
ThisstudydemonstratedthatthehighestobtainedED SpO2/FiO2 ratioof300orbelowcorrelatedwiththeneedfor mechanicalventilationduringhospitalization.Additionally, alowestobtainedEDSpO2/FiO2 ratioof300orbelowwas associatedwitharequirementforICU-levelcare.Although COPDwasaconfoundingfactorforpatientsrequiring mechanicalventilation,otherco-morbiditieswerenot independentlyassociatedwithhigherratesofmechanical
ventilationandtheEDSpO2/FiO2.Thissuggeststhatthe SpO2/FiO2 ratiocanbeusedasaprognosticindicatorto stratifyseverityofillnessinpatientswithCOVID-19during theirinitialevaluationintheED.SincetheSpO2/FiO2 ratiois non-invasiveandcanbequicklyobtainedandtrendedduring apatient’sevaluation,thisratiocouldbeanimportantfactor inpatienttriageanddisposition.
Multipleprognosticindicatorshavebeenproposedinthe previousliteraturetohelpstratifyARDSseverityandpredict outcomes.10–13 ThePaO2:FiO2 (P:F)ratioisawidelyused measureofARDSseverity;however,multiplestudieshave shownthattheP:Fratioisnotanindependentpredictorof mortality.10–13 Anotherprognostictool,theoxygenation index,(OI[FIO2/PaO2 × meanairwaypressure × 100])has beendemonstratedtobeanindependentriskfactorfor mortalityinadultswithARDS,11,12 butitrequires mechanicalventilationandarterialbloodgasanalysisfor calculation.Oxygensaturationindex(OSI[FIO2 × mean airwaypressure × 100)/SaO2])isameasurethatcorrelatesto OIandisanindependentpredictorofclinicaloutcomes.12 AlthoughOSIcalculationdoesnotrequirebloodanalysis,it stillrequiresmechanicalventilation.Anotherprognostic tool,theLungInjuryPredictionScore(LIPS),has applicabilityintheED.13 However,theLIPStoolrequiresa detailedpastmedicalhistory(e.g,alcoholusedisorder)and thepatient’spH,requiringabloodgas.Althoughallthese toolsprovidesomeprognosticvalue,eachhaslimitations, resultinginbarrierstodeploymentfortriagingpatientsin theED.
Incontrast,theSpO2/FiO2 ratiorequiresnobloodtests andisquicklyandeasilyobtainedatthebedside.Measured atthetimeofpresentation,ithasbeenshowntobean independentindicationofARDSdevelopment.6 Thisstudy suggeststhattheSpO2/FIO2 ratiomayofferanestimateof diseaseseverityinpatientswithCOVID-19before progressiontoovertrespiratoryfailure,servingasatriage tooltoidentifythoseatgreatestriskforneedingmechanical ventilationandcriticalcare.TheSpO2/FiO2 ratiocanbeused asatoolorpartofaprotocoltoassesswhetherapatient
Table2. SpO2/FiO2 ratiosandtheirassociationwithintensivecareunitormechanicalventilationneeds. VariableSpO2/FiO2 ratios*
LowestEDSpO2/FiO2
*ForpatientswhohadEDSpO2/FiO2 values. CI,confidenceinterval; OR,oddsratio; ED,emergencydepartment; ICU,intensivecareunit.
meetstransfercriteriawithinahospitalsystem.Many regionalhealthsystemsoperateundera “hubandspoke” modelwherealargecentralinstitutionsupportsanetworkof smallerhospitals.Rapididentificationofpatientsatriskfor decompensationandwithneedforhigherlevelcarewould facilitateaccesstolimitedcriticalcareresourceswhilealso decreasingtheincidenceofover-triagetothehubhospital.
Thestudyisretrospectivewithinherentlimitationsin controllingconfoundingvariables.Thecohortwaslimitedto onehospitalsystem,andthuscannotaccountforpractice variationsinotherhealthcaresystems.Thehospitals evaluatedinthisstudymayhavehaddifferentcriteriafor ICUadmission.Additionally,FiO2 valueswerebasedlargely
onnasalcannula flowrates;limitingtohigh flownasal cannulawouldpermitmoreaccurateFiO2 butwould alsolimitapplicability.Atthetimeofdatacollection, nopatientswerevaccinated,thuslimitingtheapplicability of findingstopopulationswithsomeformof COVID-19vaccination.
Insummary,EDSpO2/FiO2 ratioscorrelatewith mechanicalventilationandICUrequirementsduring hospitalizationforCOVID-19infection.Theseresults supportEDSpO2/FiO2 asatriagetoolandpredictorof hospitalresourcerequirementsforpatientsadmittedwith COVID-19.Furtherstudyisrequiredwithaprospective analysisassessingaccuracyoftheSpO2/FiO2 ratioin
predictingmechanicalventilationandneedforICUlevelcare.
AddressforCorrespondence:MichaelJ.Burla,DO,SouthernMaine HealthCare,DepartmentofEmergencyMedicine,SouthernMaine HealthCare,1MedicalCenterDr,Biddeford,ME04005. Email: Michael.burla@Mainehealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisworkwassupportedinpartbythe NorthernNewEnglandClinicalandTranslationalResearchgrant U54GM115516.Therearenoconflictsofinterestorothersourcesof fundingtodeclare.
Copyright:©2024Zhangetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ArentzM,YimE,KlaffL,etal.Characteristicsandoutcomesof21 criticallyillpatientswithCOVID-19inWashingtonState. JAMA. 2020;323(16):1612–4.
2.BellaniG,LaffeyJG,PhamT,etal.Epidemiology,patternsofcare,and mortalityforpatientswithacuterespiratorydistresssyndromein intensivecareunitsin50countries. JAMA. 2016;315(8):788–800.
3.RocaO,CaraltB,MessikaJ,etal.Anindexcombiningrespiratoryrate andoxygenationtopredictoutcomeofnasalhigh-flowtherapy. AmJRespirCritCareMed. 2019;199(11):1368–76.
4.BilanN,DastranjiA,GhalehgolabBehbahaniA.Comparisonofthe SpO2/FiO2 ratioandthePaO2/FiO2 ratioinpatientswithacutelunginjury
oracuterespiratorydistresssyndrome. JCardiovascThoracRes. 2015;7(1):28–31.
5.RiceTW,WheelerAP,BernardGR,etal.ComparisonoftheSpO2/FIO2 ratioandthePaO2/FIO2 ratioinpatientswithacutelunginjuryorARDS. Chest. 2007;132(2):410–7.
6.FesticE,BansalV,KorDJ,etal.SpO2/FiO2 ratioonhospital admissionisanindicatorofearlyacuterespiratorydistress syndromedevelopmentamongpatientsatrisk. JIntensiveCareMed. 2015;30(4):209–16.
7.SandhuP,ShahAB,AhmadFB,etal.Emergencydepartmentand intensivecareunitovercrowdingandventilatorshortagesinushospitals duringtheCOVID-19pandemic,2020–2021. PublicHealthRep. 2022;137(4):796–802.
8.ZhaoC,XinMY,LiJ,etal.ComparingtheprecisionofthepSOFAand SIRSscoresinpredictingsepsis-relateddeathsamonghospitalized children:amulti-centerretrospectivecohortstudy. WorldJEmergMed. 2022;13(4):259–65.
9.MarkovitzGH,ColthurstJ,StorerTW,etal.Effectiveinspiredoxygen concentrationmeasuredviatranstrachealandoralgasanalysis. Respir Care. 2010;55(4):453–9.
10.WareLB.PrognosticDeterminantsofacuterespiratorydistress syndromeinadults:impactonclinicaltrialdesign. CritCareMed. 2005;33(3Suppl):S217–22.
11.GajicO,AfessaB,ThompsonBT,etal.Predictionofdeathand prolongedmechanicalventilationinacutelunginjury. CritCare. 2007;11(3):R53.
12.DesPrezK,McNeilB,WangC,etal.Oxygenationsaturationindex predictsclinicaloutcomesinARDS. Chest. 2017;152(6):1151–8.
13.Elie-TurenneMC,HouPC,MitaniA,etal.Lunginjurypredictionscore fortheemergencydepartment: firststeptowardspreventioninpatients atrisk. IntJEmergMed. 2012;5(1):33.
ZacharyJ.Jarou,MD,MBA*†
AngelaG.Cai,MD,MBA‡
LeonAdelman,MD,MBA§
DavidJ.Carlberg,MD∥
SaraP.Dimeo,MD,MEHP¶
JonathanFisher,MD,MPH# ToddGuth,MD,MHPE**
BruceM.Lo,MD,MBA††‡‡ LauraOh,MD§§
RahulPuttagunta,MD*†
GillianR.Schmitz,MD∥∥
*AscensionProvidenceHospital,DepartmentofEmergencyMedicine, South field,Michigan
† MichiganStateUniversity,EastLansing,Michigan
‡ UniversityofPennsylvania,DepartmentofEmergencyMedicine, Philadelphia,Pennsylvania
§ IvyClinicians,Raleigh,NorthCarolina
∥ GeorgetownUniversity,DepartmentofEmergencyMedicine,WashingtonDC
¶ DignityHealthEastValleyRehabilitationHospital,ChandlerRegionalMedical Center,Chandler,Arizona
# TexasChristianUniversity,BurnettSchoolofMedicine,FortWorth,Texas
**UniversityofColoradoSchoolofMedicine,DepartmentofEmergencyMedicine, Denver,Colorado
†† SentaraNorfolkGeneralHospital,Virginia
‡‡ EasternVirginiaMedicalSchool,Virginia
§§ EmoryUniversity,DepartmentofEmergencyMedicine,Atlanta,Georgia
∥∥ UniformedServicesUniversityofHealthSciences,DepartmentofMilitaryand EmergencyMedicine,Bethesda,Maryland
SectionEditor:GaryJohnson,MD
Submissionhistory:SubmittedAugust18,2023;RevisionreceivedDecember8,2023;AcceptedDecember14,2023
ElectronicallypublishedMarch29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18436
Introduction: Inthe2023NationalResidentMatchingProgram(NRMP)match,therewere554unfilled emergencymedicine(EM)positionsbeforetheSupplementalOfferandAcceptanceProgram(SOAP). WesoughttodescribefeaturesofEMprogramsthatparticipatedinthematchandtheassociation betweenselectprogramcharacteristicsandunfilledpositions.
Methods: Theprimaryoutcomemeasuresincludedtheproportionofpositions filledinrelationtostate andpopulationdensity,hospitalownershiptype,andphysicianemploymentmodel.Secondaryoutcome measuresincludedcomparingprogram-specificattributesbetween filledandunfilledprograms, includingoriginalaccreditationtype,yearoforiginalaccreditation,thetotalnumberofapprovedtraining positions,lengthoftraining,urban-ruraldesignation,hospitalsizebynumberofbeds,resident-to-bed ratio,andthepercentageofdisproportionatesharepatientsseen.
Results: TheNRMPMatchhad276uniqueparticipatingEMprogramswith554unfilledpositions.Six statesoffered52%ofthetotalNRMPpositionsavailable.Fivestateswereassociatedwithtwo-thirdsofthe unfilledpositions.Publichospitalshadastatisticallysignificanthighermatchrate(88%)whencomparedto non-profitandfor-profithospitals,whichhadmatchratesof80%and75%,respectively(P < 0.001). Programswithfacultyemployedbyahealthsystemhadthehighestmatchrateof87%,followedbyclinician partnershipsat79%andprivateequitygroupsat68%(P < 0.001overallandbetweenallsubgroups).
Conclusion: The2023matchinEMsawincreasedratesinthenumberofresidencypositionsand programsthatdidnot fillbeforetheSOAP.Publichospitalshadhighermatchratesthanfor-profitornonprofithospitals.Residencyprogramsthatemployedacademicfacultythroughthehospitalorhealth systemwereassociatedwithhighermatchrates.[WestJEmergMed.2024;25(3)332–341.]
Emergencymedicine(EM)hashistoricallybeenahighly competitivespecialty, fillingallornearlyalltheavailable residencypositionsaspartoftheMainResidencyMatch (match)organizedbytheNationalResidencyMatching Program(NRMP).Afterarecordnumberofapplicantsin 2021,thepasttwoyearshaveseenadeclineinthenumberof studentapplicantswhilethenumberofavailableEM residencypositionshascontinuedtoincrease,ultimately resultinginariseinunfilledprogramsandpositions.Inthe 2022NRMPmatch,therewere219unfilledEMpositions among69programsbeforetheSupplementalOfferand AcceptanceProgram(SOAP),andin2023that figure approximatelydoubledto554unfilledpositionsamong 131programs.Manyareconcernedthatthedramatic increaseinpre-SOAPunfilledpositionsrepresentsa declineinthedesirabilityandcompetitivenessof thespecialty.1
ThisisanobservationalstudydescribingfeaturesofEM residencyprogramsthatparticipatedinthe2023NRMP matchandtheassociationbetweenselectprogram characteristicsandunfilledpositions.Itisunclearwhether certaincharacteristicsincludingstate-basedgeographic locationandpopulationdensity,hospital financingmodels, facultyphysicianemploymentmodels,orspecific programcharacteristicssuchasthesizeofprogramorlength oftrainingareassociatedwithhigherratesofunfilled positions.Transparencyoffactorsassociatedwithunfilled positionswillguidethespecialty’sresponsetothematchand programaccreditationrequirementswithobjectivedata. Priorstudieshaveexaminedsimilarfactorsbutprovided limiteddetailandnuanceonthetopicofcorporate ownership,whichweexpounduponin ourstudy.2,3
StudyDesignandSetting
Inthisobservationalstudyweusedpubliclyavailable datasetstoanalyzethematchresultsforEMresidency programsparticipatinginthe2023NRMPMatchbasedon STROBEguidelines.4 Theinstitutionalreviewboard determinedthisstudytobeexempt.AllEMresidency programsandthepositionstheyofferedthatparticipatedin the2023NRMPMatchwereincludedin thestudy.
VariablesandMeasurements
WeobtainedalistofEMresidencyprogramsandtheir numberofofferedand filledpositionsfromtheNRMP.Each NRMPIDwaslinkedtotheprogram’sAccreditation CouncilforGraduateMedicalEducation(ACGME) ProgramID,whichprovidedinformationabouttheyearof accreditation,programlength,numberofapproved
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Priorstudiesexaminedprogramfeaturesand ownershippredictorsofun fi lledpositionsbut withoutdeeperanalysisofcorporate ownershiptrendsandassociations.
Whatwastheresearchquestion?
Whatprogramfeaturesandhospitalor facultyownershipareassociatedwiththe un fi lled2023match?
Whatwasthemajor findingofthestudy?
Public,for-pro fi t,andnon-pro fi tmatched 88%,80%,and75%(P < 0.001).Program facultyemployed,clinicianpartnership,and privateequitymatched87%,79%,and 68%(P < 0.001).
Howdoesthisimprovepopulationhealth?
Understandingfactorsformatchsuccesshelp ensurestableinputstotheemergency medicineworkforce.
positions,andtrainingsites.Wealsoobtainedalistof ACGMEprogramsthatwereformallyaccreditedbythe AmericanOsteopathicAssociation(AOA)andtheyearof earliestAOAaccreditationtype.TheACGMESiteIDfor eachprimarysitewaslinkedtothehospital’sCentersfor MedicareandMedicaidServices(CMS)Certification Numberandthe2023CMSInpatientProspectivePayment SystemFinalRuleData,whichincludesinformationabout hospitalownershiptype,urban-rurallocation,numberof hospitalbeds,resident-to-bedratio,andpercentageof disproportionatesharehospital(DSH)patients.Hospitals werelinkedtothehealthsystemsthatoperatethem. Informationaboutthephysiciangroupstaffingeach hospital’semergencydepartmentandtheownershiptypeof thosegroupsasofMarch2023wasobtainedfromIvy Clinicians.5 Wedefinedphysiciangroupsas “privateequity” iftherewasamajority-ownershipinterestbyaprivateequity firm. “Clinicianpartnerships” weredefinedasbeingmajority ownedbyphysicians.Thisincludedindependentfaculty physiciangroupsaffiliatedwithahealthsystem,equalpartnershipdemocraticgroups,groupswherecertain cliniciansmayownalargerpercentageofshares,andgroups withminority-interestownershipbyaprivateequity firm.We definedphysiciangroupsas “healthsystem” iftheywere
employeddirectlybythephysicianorganizationofthe hospital,healthsystem,medicalschool,oracademic medicalcenter.
Theprimaryoutcomemeasuresincludedtheproportion ofpositions filledbystateandpopulationdensity,hospital ownershiptype,andphysicianemploymentmodel. Secondaryoutcomemeasurescomparedotherprogramspecificattributesbetween filledandunfilledprograms, includingoriginalaccreditationtype,yearoforiginal accreditation,yearofACGMEaccreditation,thetotal numberofACGME-approvedtrainingpositions,lengthof training,urban-ruraldesignation,hospitalsizebynumberof beds,resident-to-bedratio,andthepercentageofDSH patientsseen.Aprogramwasclassifiedasunfilledifthere wereoneormoreunmatchedpositionsacrossanyofits NRMPIDs;programswithzerounfilledpositionsacrossany ofitsNRMPIDswereclassifiedas filled.
Weperformedalldataextraction,transformation,and analysisusingRStudioversion2023.03.0 + 386runningR version4.2.3(RStudio,PBC,Boston,MA).Wedescribed continuousvariablesusingmediansandinterquartileranges. Categoricalvariablesweredescribedusingfrequencyand percentages.Wecomparedcontinuousvariablesusingthe Wilcoxonrank-sumtest.Wecomparedcategoricalvariables usingPearsonchi-squaredtestingwithBonferroni post-hocanalysiswheremorethantwogroupswere compared. P -valueslessthan0.05wereconsideredtobe statisticallysignificant.
CharacteristicsofStudySubjects
AsofMarch2023,therewere283ACGME-accredited EMresidencies;however, fiveoftheseweremilitary programsthatdonothistoricallyparticipateintheNRMP match,andthereweretwoadditionalprogramsthatdidnot participateinthe2023match.Therewere11EMprograms withdualNRMPIDs,whereoneoftheIDsmaybeusedto offerasinglepositiontoaspecialtypeofapplicant,suchas international/private-fundedpositions,researchpositions,or forthree-yearMDpathresidents.6 Atotalof276EM programsparticipatedinthematch,offering3,010positions in43statesplustheDistrictofColumbiaandPuertoRico. Therewere131programs(48%)with554positions(18%) thatwereunfilledbeforetheSOAP.
Sixstatesoffered52%ofthetotalNRMPEMpositions available:NewYork(338),California(285),Michigan(236), Florida(234),Pennsylvania(234),andTexas(184).There
wassignificantvariationinthenumberofresidencypositions availableperstatepopulation.Amongthesixstatesthat offeredthelargestnumberofresidencypositions,Michigan hadthemostNRMPpositionsperpopulationat23.5 residentspermillioncitizensinthe2020census,while Texashadonly6.1residentspermillioncitizens.Fivestates wereassociatedwithtwo-thirdsoftheunfilledpositions: Michigan(92);NewYork(83);Pennsylvania(78); Ohio(56);andFlorida(49).Therewasalsosignificant variationinthepercentageofunmatchedpositionsby state(Table1).
Themajority(63%)ofresidencyEMpositionswere offeredby177programsatnon-profithospitals(1,880/ 3,010),while68publichospitalprogramsoffered28%of positions(831/3,010),and31for-profithospitalprograms offered10%ofpositions(299/3,010).Therewasastatistically significantdifferenceinthepercentageofunmatched positionsbyhospitalownershiptype(P < 0.001)(Table2). Publichospitalshadastatisticallysignificanthighermatch rate(88%),comparedtonon-profitandfor-profithospitals, whichhadmatchratesof80%and75%,respectively (P < 0.001).Therewasnodifferenceinmatchratesbetween non-profitandfor-profithospitals.Seventeenhealthsystems operatedthreeormoreresidencyprograms,ofwhich11were non-profit,threewerefor-profit,andtwowerepublic.The healthsystemofferingthelargestnumberofresidency programswasHCAHealthcare(19programs,189positions, 70%matchrate).
AmongEMfacultygroupownershipandemployment models,halfofEMresidencypositions(52%)hadprogram facultythatwereemployedbyhealthsystems(1,574/3,010, 134programs),with31%havingclinicianpartnershipfaculty (941/3,010,87programs),and16%ofpositionshaving privateequity-employedfaculty(495/3,010,55programs). Fiveemployergroupsmetthedefinitionofmajorityprivate equityownership.ThesegroupsincludedAmerican PhysicianPartners,EnvisionPhysicianServices,SCP Health,SoundPhysicians,andTeamHealth.
Therewasastatisticallysignificantdifferenceinthe percentageofunmatchedpositionsbytheemployment modeloffacultyphysicians(P < 0.001)(Table3).Programs withfacultyemployedbyahealthsystemhadthehighest matchrateof87%,followedbyclinicianpartnershipsat79% andprivateequitygroupsat68%(Table3).Thirteen physiciangroupsoperatedthreeormoreresidencyprograms. Thephysiciangroupsstaffingthelargestnumberofresidency programswereEnvisionPhysiciansServices(24programs, 230positions,71%matchrate)andTeamHealth (21programs,197positions,75%matchrate).
Table1. Residencymatchresultsbystateandemergencymedicinepositionsperstatepopulation.
Alabama218194%6%5.13.5
Arizona551590%10%7.46.9
Arkansas216944%56%35.3
California242852292%8%397.3
Colorado1170100%0%5.82.9
Connecticut2370100%0%3.610.2
Delaware218667%33%117.7
DistrictofColumbia2220100%0%0.732.7
Florida222344979%21%22.210.5
Georgia558690%10%10.95.3
Illinois12144994%6%12.611.4
Indiana1210100%0%6.83.1
Iowa1100100%0%3.23.1
Kansas110460%40%2.93.4
Kentucky2250100%0%4.55.5
Louisiana4420100%0%4.69.1
Maine1100100%0%1.47.2
Maryland2230100%0%6.23.7
Massachusetts572297%3%710.3
Michigan252369261%39%1023.5
Minnesota3320100%0%5.75.6
Mississippi328968%32%2.99.5
Missouri5511178%22%6.28.3
Nebraska1120100%0%26.1
Nevada3251156%44%3.27.9
NewHampshire160100%0%1.44.3
NewJersey121222778%22%9.313.2
NewMexico1120100%0%2.15.7
NewYork313888379%21%19.719.7
NorthCarolina7852274%26%10.77.9
Ohio171585665%35%11.813.4
Oklahoma533876%24%48.2
Oregon1110100%0%4.22.6
Pennsylvania232347867%33%1318
PuertoRico216194%6%3.25
RhodeIsland222386%14%1.120.1
SouthCarolina555493%7%5.310.4
Tennessee548590%10%7.16.8
Texas151841592%8%306.1
Utah1120100%0%3.43.5
Vermont160100%0%0.69.3
(Continuedonnextpage)
Table1. Continued.
NRMP,NationalResidentMatchingProgram.
ProgramandHospital-specificAttributes
Whencomparing filledandunfilledprogramsby accreditationhistoryandhospital-levelcharacteristics, unfilledprogramsweremorelikelytobesmallerinsizebased
onthenumberofpositionsoffered(P < 0.001),previously accreditedbytheAOA(P < 0.001),andstartedinmore recentyears(P < 0.001).Therewasnodifferencein filledvs unfilledprogramsbyprogramlength(P = 0.78).Unfilled
Table2. Associationofhospitalownershiptypeonunfilledemergencymedicinepositions. Healthsystem
Byhospitalownershiptype(P < 0.001,Pearsonchi-squaredtest)
Overall,theproportionsof filled/unfilledpositionsdidvarybyhospitalownershiptype(X2 = 34.126,df = 2, P < 0.001).Post-hocBonferroni comparisonsbetweenhospitaltypesshowedthatpublichospitalshadalowerproportionofunfilledpositionscomparedtobothfor-profitand non-profithospitals(rawandadjusted P-values <0.001),whiletherewasnodifferenceintheproportionofpositions filledbetweenfor-pro fit andnon-profithospitals(raw P = 0.05,adjusted P = 0.16).
NRMP = NationalResidentMatchingProgram. UPMC,UniversityofPittsburghMedicalCenter.
Table3. 2023emergencymedicinematchratesbyfacultyphysiciangroup/type.
Physiciangroup Group type
Numberofresidency programs NRMPpositions available NRMPpositions matched Unmatched positions(%)
Byresidencyfacultyphysiciangrouptype(P < 0.001,Pearsonchi-squaredtest)
Healthsystem(HS)1341574137513%
Clinicianpartnership(CP)8794174421%
Privateequity(PE)5549533732% Total2763010245618.4%
Byresidencyfacultygroup(operating3+ EMresidencies) AmericanPhysicianPartnersPE426677% ApolloMDCP4362336% EnvisionPhysicianServicesPE2423016329%
IntegrativeEmergency Services
NorthwellHealthHS3393413%
PhysicianAffi
Overall,theproportionsof filled/unfilledpositionsdidvarybyresidencyfacultyphysiciangrouptype(X2 = 99.007,df = 2, P < 0.001).PosthocBonferronicomparisonsbetweengrouptypesshowedthatprogramswithhealthsystememployedfacultyhadthelowestproportionof unfilledpositions,followedbyclinicianpartnershipfaculty,whileresidencieswithprivateequityemployedfacultyhadthehighestproportionof unfilledpositions(rawandadjustedp-valuesforallpairwisecomparisons <0.001).
NRMP,NationalResidentMatchingProgram; UPMC,UniversityofPittsburghMedicalCenter.
programstendedtobeinlessurbanareas(P = 0.03),at hospitalswithasmallernumberofbeds(P < 0.001),lower resident-to-bedratios(P < 0.001),andfewer disproportionatesharepatients(P < 0.001)(Table4).
Weexaminethefactorsandprogramcharacteristics associatedwithunfilledpositionsintheEMmatch.Five stateswereassociatedwithtwo-thirdsoftheunfilled positions.Publichospitalshadastatisticallysignificant highermatchrate(88%)whencomparedtonon-profitand for-profithospitals,whichhadmatchratesof80%and75%, respectively(P < 0.001).Publichospitalsincludethose ownedbygovernmententities(local,state,federal government)ortheVeteransHealthAdministration.Nonprofitandfor-profithospitalsareprivatelyownedand differentiatedbytheirtaxstatus(discussedfurtherbelow). Programswithfacultyemployedbyahealthsystemhadthe
highestmatchrateof87%,followedbyclinicianpartnerships at79%andprivateequitygroupsat68%(P < 0.001overall andbetweenallsubgroups).Ouranalysisconfirmsand expands findingsfromrecentstudies.Onestudyidentifiedsix characteristicsofunfilledprograms(indescendingorderof predictivestrength):unfilledpositionsinthe2022match; smallerprogramsize;Mid-Atlanticlocation;priorAOA accreditation;EastNorthCentrallocation;andprivate equitymajorityownershipofphysicianfacultygroup.3 Anotherstudyofcombined2022and2023matchdatafound programsatriskofnot fillinghadaccreditationwithinthe prior fiveyears,hadafor-profitprimaryclinicalsite, andwereingeographicareaswithhighnumbersof positionsoffered.2
ThenumberofunmatchedpositionsintheEMmatchwas drivenbyadramaticincreaseinthenumberofEMprograms
Table4. Comparingattributesof filled/unfilledprogramsin2023emergencymedicinematch. Filled(n = 145)Unfilled(n = 131)Total
Originalaccreditationtype
ACGME141(97%)84(64%)225(82%)
AOA4(3%)47(36%)51(19%)
Yearoforiginalaccreditation
Median199520102003
Q1,Q31982,20091993,20181988,2016
YearofACGMEaccreditation
Median199520172008
Q1,Q31982,20112006,20191990,2017
TotalapprovedACGMEpositions
Median393036
Q1,Q330,5422,3624,44
Lengthoftraining
3years116(80%)103(79%)219(80%) 4years29(20%)28(21%)57(21%)
Largeurbanarea89(61%)64(49%)153(55%)
Otherurbanarea55(38%)61(47%)116(42%)
Ruralarea1(1%)6(5%)7(3%)
Numberofhospitalbeds <0.001b
Median571359450
Q1,Q3382,730260,534318,680
Resident-to-bedratio(per100beds)
Median472938
Q1,Q330,7016,4521,63
Disproportionatesharehospitalpatients[%]
Median393336
Q1,Q331,5228,4330,47
aPearsonchi-squaredtest. bWilcoxonrank-sumtest.
ACGME,AccreditationCouncilforGraduateMedicalEducation; AOA,AmericanOsteopathicAssociation; Q,quartertile.
andpositionsofferedoverthepastdecade,aswellasamore recentdecreaseinapplicantsoverthepriortwoyears.
Between2014–2023,therewasa29%increaseinthenumber ofEMprogramsanda46%increaseinthenumberof postgraduateyear(PGY)-1positionsofferedinthematch, suggestingthatthegrowthofpositionsisnotonlyrelatedto thecreationofnewprogramsbutalsotheexpansionof existingprograms.Inrecentyears,EMhasexperiencedthe largestgrowthrateofPGY-1positionsacrossallmedical specialties.7 Thematchrateisalsoimpactedbyadecreasein thenumberofapplicantsovertime.ApplicantsinEM peakedin2021at4,391applicants.Itisunclearwhetherthis recordhigh,representinga16%increaseovertheyearbefore, wasanoutlier.Theoverall five-yeartrendisan8%decrease
inapplicantscontrastedwiththe23%increaseinpositions.8 Thisunprecedentedgrowthhasoutstrippedthenumber studentsapplyingtotraininEMandplayedalargerolein thenumberofunfilledspotsin2023.
Between2013–2020,therewassignificantgrowthofEM residenciesinstatesthatalreadyhadmultipleEMtraining programs.Anumberofstatesnearlydoubledthenumberof trainingprogramsinthattimeframe:NewYork(21to31), Pennsylvania(12to21),andCalifornia(14to22),while othersgrewevenmoreOhio(9to18),Michigan(11to25), andFlorida(5to19).9,10 Newprogramsare disproportionatelygrowinginurbanareas,whereassome ruralstatesdonothaveanyEMtrainingprograms.10 Only sevenEMresidencyprogramsarelocatedinruralareas,six
ofwhichdidnot fill.11 Ourdatademonstratesthatmanyof theunfilledspotsin2023occurredinstatesthathadthe highestabsolutenumberofresidentpositionsaswellas numberofresidentspercapitapopulation.Nostate-level regulationsexisttolimitthenumberofresidencytraining programs.WhilesomehavecalledontheACGMEtorestrict thenumberofEMtrainingpositions,itiscurrentlyagainst ACGMEpolicyandaviolationofstateandfederalantitrust lawfortheACGMEtoimplementanationalworkforce policytoestablishthenumberofpracticingphysicians.12 The ACGMEcancreateandadjuststandardsforaccreditationto optimizethelearningenvironment.Somehaveexpressed concernregardingtheacademicqualityofsomeofthenewer programs.Onestudyfoundthatnearly25%ofprograms weregiven “withwarning” accreditationoninitial accreditationcomparedtolessthan3%ofprogramson continuedaccreditation.7,13
Debateexistsoverwhoisresponsiblefortheincreased growthofresidencyprograms.Anewresidencyprogram requiresasponsoringinstitution,whichtheACGMEdefines asan “organizationorentitythatassumesultimate financial andacademicresponsibilityforaprogram.” Sponsoring institutionsmayincludeuniversities,medicalschools, hospitals,healthcaredeliverysystems,orphysiciangroup practices.14 Currently,areviewoftheACGMElistings revealsthatallEMresidencyprogramsaresponsoredby hospitalsandhealthsystems,withnonebeingsponsoredby physicianstaffinggroups. 13 Theroleandmotivationofthe physiciangroupswhoserveasfacultyfornewresidency programsthataresponsoredbyhospitalsandhealthsystems mayvary.Graduatemedicaltrainingprogramsoffer financialbenefitstohospitalsandrecruitmentbenefitsto hostinginstitutionsandstaffinggroups. 15 Newprogram growthcouldbedrivenatthephysiciangroup,hospitalor healthsystemlevel,orboth.Forexample,HCAHealthcare hasatransparentobjectivetoexpandGMEpositionsstating, “With270+ residencyandfellowshipprograms,HCA HealthcareplanstocontinuetogrowthelargestGME communityintheUnitedStates.”16 Itisreasonableto surmisethatfacultygroupsfeelpressuretostartandstaffnew programstoalignwiththehealthsystem’sintenttomaintain contracts.HospitalsthatcreatedGMEprogramsafter2015, knownas “GME-naive,” haveastrongincentivetoincrease thenumberofresidentsattheirsitewithin fiveyearsof startingbecauseCMScalculatestheirtrainingcapafterthe fifthyear.17
Unfilledspotsmayrepresentmarketforcesrightsizingthe numberandgeographicdistributionofresidencyslots, althoughthecomplexitiesofGMEfundingandtrainingcaps createregulatorybarrierstomarketcorrections.9 Unfilled positionsdonotreceiveGMEfunding,whichcouldleadto residencyclosureswithoutalternatesourcesoffunding.18 Whenanesthesiaexperiencedasimilarplightofdecreasing fillratesinthe1990s,acumulativedropof77%ofapplicants
overasix-yearperiodresultedin16%ofallanesthesia residenciesinthecountryclosingtheirdoors.11 However, marketcorrectionswillnotoccurifunfilledspotsintheinitial matcharesubsequently filledintheSOAP,whichoccursa fewdayslater.MostoftheunfilledEMpositionsinthe2022 Matchsubsequently filledintheSOAP.19 Discussion continuesonhowbesttomaintainthequalityandstabilityof theEMworkforce.1
Weobservedsignificantdifferencesinmatchratesby hospitalownershiptypewithpublichospitalshavingthe fewestunmatchedpositions.Non-profithospitalscontinueto makeupthemajorityofEMtrainingsites,andtherewasno statisticaldifferenceinmatchratesbetweennon-profitand for-profithospitals.Overthepast20years,therehasbeen increasedconsolidationandcorporatizationinhealthcare includingEMpracticeandtraining.20–22 Manyfearthat increasedfor-profitandinvestorsponsorshipofresidency programsmayresultinlowerqualitytrainingorthe commoditizationofGME.23,24 Whiletherehasbeen increasedscrutinyoncorporateinvestmentinhealthcareand medicaleducation,andsomestudiesonhealthorworkforce outcomesinotherspecialties,nosuchstudiesexistin EM.20,25,26 TheproportionofEMresidenciescreatedatforprofithospitalshasincreasedconsiderably.7 Priorto2016, only5%ofEMresidencyprogramshadprimarysitesatforprofithospitals(10total),comparedto30%(21/71)ofnew programsbeingbasedatfor-profithospitals.Whilehospitals arefrequentlydifferentiatedbynon-profitorfor-profit status,thisdifferentiationbasedontaxstatushaslimitations incapturingthebusinessincentivesoftheinstitution.27
Ourdatashowsthatpublichospitalswereassociatedwith thehighestmatchrates.Therewasnodifferencebetweenforprofitandnon-profithospitalswithregardtomatchrates.A priorstudysimilarlydidnot findastatisticallysignificant differentgreaterriskofnot fillingatfor-profitsites (comparedtonon-profitorgovernmentsites)butdid finda 50%greaterriskofnot fillingwhenexamining2022and2023 matchdata.2 Wedid findsignificantvariationbetween groupswithinthesametaxdesignation.Forexample,ofthe 17healthsystemsthatoperatethreeormoreprograms, TrinityHealth,anon-profithealthsystem,hadthehighest percentageofunmatchedpositionsat56%(sixprograms total,23/41unmatched)andtheUniversityofCalifornia,a publichealthsystem,had0unfilledpositions(fiveprograms total,67positions).Thehealthsystemoperatingthelargest numberofEMresidenciesisHCAHealth,afor-profithealth system,whichoffered189positionsat19programs,ofwhich 30%wereunmatched.TenetHealthcare,anotherfor-profit healthsystem,whichoffered44positionsatfourprograms, hadamatchrateabovethenationalaverage, filling91%ofits positions.Hence,althoughpublichospitalshadahigher matchrateoverall,thereissignificantvariability.
Muchscrutinyhasfocusedoncorporate,specifically privateequity(PE),ownershipandinvestmentinEM. Amongthedifferenttypesofnon-physiciancorporate investors,PEhasundergoneparticularcriticismdueto significantexpansionwithinEM,evidenceofpooroutcomes inotherareasofhealthcare,andshort-termprofit incentives.28 Privateequityandpubliclytradedcompany controloftheemergencyphysicianstaffingmarketincreased from8.6%to22%from2009to2019.26 Privateequityacquiredhospitalsnowaccountfor8%ofall nongovernmentalhospitals.29 Ourdatashowsthat503/3,010 (17%)ofEMresidencypositionsinthe2023matchwere staffedbyphysiciangroupsthataremajorityownedbyPE. Toourknowledge,therehasneverbeenanoutcomes comparisonstudybetweenemploymentmodelswithin residencytrainingprogramstopredictsuccessinpractice aftergraduation.Employmentmodelsofphysiciansare changingwithincreasedconsolidationinhealthcare. Emergencymedicine-boundstudentshaveexpressedconcern aboutcorporateinfluenceinEM,butitisuncleartherelative contributionofthisonstudentrecruitmentespeciallyinlight ofotherfactors.30 Academicfacultycanbeemployedin multipleemploymentmodelssuchasbyamedicalschool,a healthsystem,alargenationalgroup,aregionalgroup,ora singleownershipgroup.Emergencymedicineprogramswith thehighest fillratesinthematchwereassociatedwith employmentmodelsinwhichfacultyweredirectlyemployed bythehospital,healthsystem,ormedicalschool.Therewas significantvariability,however,betweenemployersand employmenttypes.
Thisanalysishasseveralimportantlimitations.Thereare manyreasonsamedicalstudentmayrankandmatriculateat aresidencyprogram.Uniquecharacteristicsofaprogram thatmayinfluenceaparticularapplicant’sinterestandrank listwerenotcapturedforanalysis.Thenumberofapplicants interviewedandrankedbyprogramsareadditionalfactors thatimpactmatchrates,whichwerenotmeasured.Thepast twoyearsdidnotincludein-personapplicantinterviews, whichmayhavealsoimpactedmatchrates.
Additionally,therelationshipsbetweenhospitals,health systems,physicianfacultygroups,andindividualresidency programsarecomplexandevolving,andthismustbe consideredwheninterpretingresults.Forexample,one healthsystemmayemployphysiciansundermultiplemodels suchasdirectemploymentorathird-partystaffinggroup. Thecurrenthealthsystemorstaffinggroupattheprogramin thisanalysismaynothavebeenthesameonepresentwhen theresidencystartedduetomergersandacquisitions.Since thisanalysistherehavebeenmajorchangesintheemergency physicianstaffinglandscapeincludingtheclosureof AmericanPhysiciansPartnersandChapter11Bankruptcyof
Envision,whichoperatedfourand24residenciesinthe2023 EMmatch,respectively.31
Therearenocurrentlyagreedupondefinitionsfor classifyingphysician-groupownershipstructures.Thevaried spectrumofcorporateinvestor(eg,PE)ownershipstakesin EMgroupsfromminoritytowholecomplicatesthecreation ofdiscretecategories.Ourclassificationofhealthsystems wasnotabletodifferentiatebetweenthevariouscomplex relationshipsthatcomprisehealthsystems,suchasas whetherthehealthsystemphysiciangroupiswhollyowned bythehealthsystemandortheyareownedbyamedical school,academicmedicalcenter,orhospital.Most fundamentally,ownershiponlyservesasaproxyforother importantfeaturessuchasphysicianautonomyand educationalquality.
The2023matchinEMsawincreasedratesinthenumber oftrainingslotsandprogramsthatdidnot fillbeforethe SOAP.Publichospitalshadhighermatchratesthanforprofitornon-profithospitalsoverall,buttherewas significantvariabilitywithinhospitalsandhealthsystems. Residencyprogramsthatemployedacademicfacultydirectly throughthehospitalorhealthsystemwereassociatedwith highermatchrates.
AddressforCorrespondence:AngelaG.Cai,Universityof Pennsylvania,DepartmentofEmergencyMedicine,GroundFloor Ravdin,3400SpruceSt.,Philadelphia,PA19104.Email: angela. cai@pennmedicine.upenn.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Jarouetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SchmitzGRandJarouZJ.Theemergencymedicinematch:Isthesky fallingoristhisjustgrowingpains? AnnEmergMed. 2023;82(5):608–10.
2.GettelCJ,BennettCL,RothenbergC,etal.Unfilledinemergency medicine:ananalysisofthe2022and2023matchbyprogram accreditation,ownership,andgeography. AEMEducationandTraining. 2023;7(4):e10902.
3.PreiksaitisC,KrzyzaniakS,BowersK,etal.Characteristicsof emergencymedicineresidencyprogramswithunfilledpositionsinthe 2023match. AnnEmergMed. 2023;82(5):598–607.
4.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. IntJSurg. 2014;12(12):1495–9.
5.AdelmanL.IvyClinicians2023StateoftheEmergencyMedicine EmployerMarket(February2023).;2023.
6.TheMatch-NationalResidentMatchingProgram.MainResidency MatchDataandReports.2023.Availableat: https://www.nrmp.org/ match-data-analytics/residency-data-reports/ AccessedAugust17,2023.
7.CarlbergDJ.Theemergencymedicineeducationalcommunityandthe supplysideoftheworkforce. WestJEmergMed. 2022;24(1):64–7.
8.AAMC.ERAS® statistics.Availableat: https://www.aamc.org/ data-reports/data/eras-statistics-data.AccessedAugust17,2023.
9.CommitteeontheGovernanceandFinancingofGraduateMedical Education,BoardonHealthCareServices,InstituteofMedicine,etal. 2014. Graduatemedicaleducationthatmeetsthenation’shealthneeds WashingtonDC:NationalAcademiesPress.
10.BennettCL,ClayCE,EspinolaJA,etal.UnitedStates2020emergency medicineresidentworkforceanalysis. AnnEmergMed. 2022;80(1):3–11.
11.HaasMRC,HopsonLR,ZinkBJ.Toobigtoofast?PotentialImplications oftherapidincreaseinemergencymedicineresidencypositions. AEM EducTrain. 2020;4(Suppl1):S13–21.
12.NascaTJandCarlsonD.Graduatemedicaleducationspecialtymixand geographicresidencyprogrammaldistribution:IsThereaRoleforthe ACGME? AMAJEthics. 2016;18(3):258–63.
13.ACGME-accreditationdatasystem(ADS).AcademicYear2022–2023. Availableat: https://apps.acgme.org/ads/Public/Reports/Report/1 AccessedJuly22,2022.
14.AccreditationCouncilforGraduateMedicalEducation. Common ProgramRequirements(Residency).2022.Availableat: https://www. acgme.org/programs-and-institutions/programs/common-programrequirements/.AccessedAugust17,2023.
15.KimKandOrnelas-DorianC.Educationasthenewbattleground.In: SchlicherNandHaddockA,eds. EmergencyMedicineAdvocacy Handbook.Irving,Texas:EmergencyMedicineResidents’ Association;2023.
16.HCAHealthcare.GraduateMedicalEducation.Availableat: https:// hcahealthcaregme.com/.AccessedAugust17,2023.
17.CaliforniaHealthCareFoundation.Expandinggraduatemedical educationinCalifornia:theroleofGME-naivehospitals.2021. Availableat: https://www.chcf.org/publication/expandinggraduate-medical-education-gme-naive-hospitals/ AccessedAugust18,2023.
18.U.S.GovernmentAccountabilityOffice.PhysicianWorkforce:Capson Medicare-FundedGraduateMedicalEducationatTeachingHospitals. Availableat: https://www.gao.gov/products/gao-21-391 AccessedAugust17,2023.
19.GutmanA.1in4emergencymedicineresidencyspotsatJefferson Health,EinsteinunfilledaheadofMatchDay,following “unprecedented”
nationaltrend.2023.Availableat: https://www.inquirer.com/health/ match-day-residency-emergency-medicine-spots-jefferson-einsteinnazareth-20230317.html.AccessedAugust17,2023.
20.CouncilonMedicalEducation. GraduateMedicalEducationandthe CorporatePracticeofMedicine.AmericanMedicalAssociation.2020. Availableat: https://councilreports.ama-assn.org/councilreports/ downloadreport?uri=/councilreports/CME_02_I_20_annotated.pdf AccessedAugust17,2023.
21.June2022ReporttotheCongress:MedicareandtheHealthCare DeliverySystem.Availableat: https://www.medpac.gov/document/ june-2022-report-to-the-congress-medicare-and-the-health-caredelivery-system/.AccessedAugust17,2023.
22.AmericanCollegeofEmergencyPhysicians.RequestforInformationon MergerEnforcement.2022.Availableat: https://www.acep.org/ globalassets/acep-response-to-ftc-and-doj-rfi-on-mergerguidelines-04.20.22.pdf.AccessedAugust17,2023.
23.KadakiaKT,ZhengJ,BruchJD,etal.Comparisonofthe financialand operationalcharacteristicsoffor-profitandnonprofithospitalsreceiving federalgraduatemedicaleducationpayments,2011-2020. JAMA. 2023;329(2):173–5.
24.CouncilonMedicalEducation. TheImpactofPrivateEquityonMedical Training.AmericaMedicalAssociation.2022.Availableat: https:// councilreports.ama-assn.org/councilreports/downloadreport?uri=/ councilreports/CME_01_I_22_final_annotated.pdf AccessedAugust17,2023.
25.MedPac.June2022ReporttotheCongress:Medicareand theHealthCareDeliverySystem.Availableat: https://www. medpac.gov/document/june-2022-report-to-the-congressmedicare-and-the-health-care-delivery-system/ AccessedAugust17,2023.
26.AdlerL,MilhauptC,ValdezS.Measuringprivateequitypenetrationand consolidationinemergencymedicineandanesthesiology. Health AffairsScholar. 2023;1(1):qxad008.
27.HerringB,GaskinD,ZareH,etal.Comparingthevalueofnonprofit hospitals’ taxexemptiontotheircommunitybenefits. Inquiry. 2018;55:46958017751970.
28.LevinsH.Theeffectofprivateequityinvestmentinhealthcare.Penn LDI.2023.Availableat: https://ldi.upenn.edu/our-work/researchupdates/the-effect-of-private-equity-investment-in-health-care/ AccessedAugust17,2023.
29.OffodileACII,CerulloM,BindalM,etal.Privateequityinvestmentsin healthcare:anoverviewofhospitalandhealthsystemleveraged buyouts,2003-17. HealthAff. 2021;40(5):719–26.
30.MurphyJA.EMresidencyapplicationsaredown.Whatdoesthismean forourfuture?Availableat: https://www.emra.org/emresident/article/ presidents-message-january-february-march-2023 AccessedAugust17,2023.
31.AdelmanL.APP’sCauseofDeath-ThePEBusinessModel.2023. Availableat: https://emworkforce.substack.com/p/apps-causeof-death-the-pe-business.AccessedNovember5,2023.
WayneA.Martini,MD*
ClintonE.Jokerst,MD†
NicoleHodsgon,MD* AndrejUrumov,MD*
*MayoClinicArizona,DepartmentofEmergencyMedicine,Phoenix,Arizona † MayoClinicArizona,DepartmentofRadiology,Phoenix,Arizona
SectionEditor:LeonSanchez,MD,MPH
Submissionhistory:SubmittedOctober20,2023;RevisionreceivedDecember18,2023;AcceptedDecember22,2023
ElectronicallypublishedMarch29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18515
Introduction: Duringthecoronavirus2019pandemic,hospitalsintheUnitedStatesexperienceda shortageofcontrastagent,muchofwhichismanufacturedinChina.Asaresult,therewasasignificantly decreasedamountofintravenous(IV)contrastavailable.Wesoughttodeterminetheeffectofrestricting theuseofIVcontrastonemergencydepartment(ED)lengthofstay(LOS).
Methods: Weconductedasingle-institution,retrospectivecohortstudyonadultpatientspresentingwith abdominalpaintotheEDfromMarch7–July5,2022.Of26,122patientencountersreviewed,3,028 (11.6%)includedabdominopelvicCTwithacomplaintincluding “abdominalpain.” Weexcludedpatients withoutsideimagingandnon-EDscans.RoutineIVcontrastagentwasadministeredtoapproximately 74.6%ofpatientsbetweenMarch7–May6,2022,whenwealteredusageguidelinesduetoanationwide shortage.BetweenMay6–July5,2022,32.8%ofpatientsreceivedIVcontrastafterinstitutional recommendationsweremadetolimitcontrastuse.Wecomparedpatientdemographicsandclinical characteristicsbetweengroupswithchi-squaretestforfrequencydata.WeanalyzedEDLOSwith nonparametricWilcoxonrank-sumtestforcontinuousmeasureswithfocusbeforeandafternewED protocols.Wealsousedstatisticalprocesscontrolchartsandplottedthe1,2and3sigmacontrollimitsto visualizethevariationinEDLOSovertime.Thechartsincludetheaverage(mean)ofthedataandupper andlowercontrollimits,correspondingtothenumberofstandarddeviationsawayfromthemean.
Results: AfteruseofroutineIVcontrastwasdiscontinued,EDLOS(229.0vs212.5minutes, P =<0.001)declinedby16.5minutes(95%confidenceinterval 10, 22).
Conclusion: IntravenouscontrastaddssignificantlytoEDLOS.DecreaseduseofroutineIVcontrastin theEDacceleratestimetoCTcompletion.ApolicychangetolimitIVcontrastduringanationalshortage significantlydecreasedEDLOS.[WestJEmergMed.2024;25(3)342–344.]
Abdominopelviccomputedtomography(CT)isroutinely orderedfromtheemergencydepartment(ED)toevaluatefor abdominalpain.1 Historically,IVcontrasthasbeenusedto highlightdifferencesbetweensofttissuesthatwould otherwiselookthesame.Intravenous(IV)contrastforCTis oftensourcedfromoverseas,andcurrentestimatesarethat
abouthalfofhospitalsintheUnitedStatesgetmostoftheir IVcontrastagentfromGEHealthcare.Muchofthecontrast dyeismanufacturedatGE’splantinShanghai.Duringthe COVID-19relatedlockdownsinChinatheplantwasclosed oroperatingatreducedcapacityforweeks.Asaresult,many hospitalshadasignificantlydecreasedsupplyofIVcontrast, whichforcedthemtodecreaseutilizationbyupto80%.
AnticipatingcontinueddeficienciesinthesupplyofIV contrast,MayoClinicArizonainMay2022initiatedcritical protocolstolimitcontrastusetopotentiallylife-threatening conditions.ThisdecreasedutilizationwithintheEDcreated auniquecircumstanceinwhichwehadtheopportunityto explorethetheoreticalbenefitofomittingIVcontrast materialfromroutineEDabdominopelvicCTtodetermine whetheritwouldsignificantlydecreaseEDlengthofstay (LOS),whichinourinstitutionwemeasureasthepatient’ s totaltimeinthedepartment.Lengthofstayisabenchmark usedbytheCentersforMedicareandMedicaidServicesasa hospitalqualitymetric.2 Additionally,shorteneddurationof LOShasbeenshowntodecreasetheratethatpatientsleave againstmedicaladvice,whileincreasingpatientsatisfaction, andpotentiallyimprovingtreatmentoutcomes.3
Priortothecontrastshortagealert,theIVcontrastagent iohexolwasroutinelyadministeredtoEDpatientsin conjunctionwithCTexaminationsoftheabdomenand pelvis.StartingMay6,2022,ourEDincollaborationwith theradiologydepartmentagreedtodiscontinueIVcontrast materialforroutineCTexceptintwospecificscenarios: patientsrequiringabdominalimagingwhohadabodymass index(BMI) <25;andpatientswithaBMI >25inwhom therewasanacute,time-dependentconcernthatrequiredIV contrasttofurtherdiagnose.
Wedesignatedthe “beforeinterventionperiod” asthe 60dayspriortoMay6,andthe “afterinterventionperiod” as the60daysafterMay6.Sincethestudywasfocusedon processratherthanpatients,thenormalrequirementfor institutionalreviewboardoversightwaswaived.Weincluded inthestudypatientswhopresentedtotheEDwithabdominal painandunderwentabdominopelvicCTatthediscretionof thetreatingattendingemergencyphysician.Theprimary outcomewasEDLOS,whichwasdefinedasthelengthoftime betweenwhenthepatientregisteredforcareintheEDandthe timeofEDdisposition(admitordischargetime).
Medianandinterquartilerange(IQR)valueswere expressedforallcontinuousmeasuresbetweengroups (beforevsafterperiods).Wecomparedpatientdemographics andclinicalcharacteristicsbetweengroupswithchi-square testforfrequencydataandnonparametricWilcoxonranksumtestforcontinuousmeasures.Theprimaryoutcomewas EDLOS.Weanalyzeddatausingstatisticalprocesscontrol charts(with1,2and3sigmacontrollimits),andweadjusted confidencelimitsusinganXmRchart,whichhelpsto determinehowaprocesschangesovertime.TheXmR controlchartisrecommendedforLOSandreal-worldED operationaldata.4 Controlchartswererunforallscansand separatedoutbycontrastadministrationforbothtime periods. P -values <0.05wereconsideredstatistically significant.WeusedRversion4.1.2ggQCpackage (RStudio,Boston,MA)forstatisticalanalysis.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Intravenouscontrastisusedtohighlight differencesbetweensofttissuesthatwould otherwiselookthesame.
Whatwastheresearchquestion?
Doesdecreaseduseofcontrastforcomputed tomography(CT)improveEDlengthof stay(LOS)?
Whatwasthemajor findingofthestudy?
IfthereisashortageofIVcontrastforCT, usingcontrastonfewerpatientsmayimprove patientthroughputduetoshortenedLOS.
Howdoesthisimprovepopulationhealth?
IfthereisashortageofIVcontrastforCT, usinglesscontrastmayimprovepatient throughputduetoshortenedLOS.
Therewere26,122patientencounterswithinthestudy period,ofwhich3,028(11.6%)metthestudycriteria: complaintattriageofabdominalpain;age >18;and indicationsforCTexclusiveofureterolithiasis.Medianage was60years(IQR40–72).Followingprotocolchange,there wasa41.8%absolutedecreaseinabdominopelvicCTstudies thatusedIVcontrast:74.6%(1,120/1,502)beforevs32.8% (500/11,526)after; P < 0.001).Therewasalsoa16.5-minute decreaseinLOS(95%confidenceinterval 10, 22)from 229.0vs212.5minutes(Table).
Webelievethatradiologycansignificantlyimpactpatient throughput.5 Our findingssuggestthatdecreaseduseofIV contrastinnon-essentialimagingoftheabdomenandpelvis isassociatedwithadecreaseinEDLOS,therebyimproving EDthroughput.While16.5minutesmayseemlikeabrief lengthoftime,inthispatientsamplingitreducedLOSby about7.2%(229vs212.5minutes)andreducedaggregate LOSbyacombinedtotalof420hoursoverthecourseofnine weeks.Thistimesavingsmultipliedbythemillionsof patientswhopresenttotheEDannuallyforabdominalpain cantranslateintoalargemagnitudeoftimesaved,further decreasingthestrainontheEDandpotentiallyimproving patientsatisfaction.6 Asourstudywasperformedatan institutionwithhighnursingstafflevels(2–3patientsper nurse)andtechratios(sixpatientspertech),thereby optimizingtimetoIVaccessandkidneyfunctiontestresults,
Table. Beforevsafterrestrictionsonuseofintravenouscontrastforabdominal/pelviccomputedtomography,demonstratingtheimpacton lengthofstayintheemergencydepartment.
Before(n = 1,502)After(n = 1,526)Total(N = 3,028) P-value
TotalLOS(minutes) <0.001
Mean(SD)239.6(89.2)226.3(96.3)232.9(93.1) Median229.0212.5220.0 Q1,Q3176.0,293.0156.3,281.0167.0,287.0
Contrastreceived <0.001
No382(25.4%)1026(67.2%)1408(46.5%)
Yes1120(74.6%)500(32.8%)1620(53.5%)
LOS,lengthofstay; Q,quartile; SD,standarddeviation.
wehypothesizetherewouldbeevenmorepronounced improvementinLOSatfacilitiesthatareshortstaffed. Additionally,discontinuationofcontrastcanhelpto reduceincidenceofneedforIV-lineplacement,andtheriskfor allergy/anaphylaxis.Inconversationswiththeradioloy department,theradiologistsemphasizedthattheyfeltmore confidenceintheaccuracyoftheirdiagnoseswiththeuseof contrastandthatnon-urgent findingssuchascarcinoma wouldmorelikelybemissedwithoutcontrast.Theysuggested thatreduceduseofIVcontrastwouldbeappropriatein settingswhereartificialintelligencehasimprovedpathology recognitionorintheeventofanothershortageofcontrast agent.Moreresearchwillbeneededtoinvestigatetheclinical effectofdiscontinuingIVcontrastinthissetting.
Thereareseverallimitationstoourstudy.Afterreviewing thedataatothersites(MayoClinicRochester,MayoClinic Florida,andMayoClinicHealthSystem)wedecidedtomake thisasingle-centerstudyasothersiteswerenotaffectedinthe samewaybytheshortage,andtheyhadamoregradual rolloutofIVcontrastrestrictions.Whilewenotedareduction inLOS,wewereunabletoclearlyparseoutwhetheritresulted fromdecreasedneedforIVaccessandlabresults,ordecreased timeinradiologydepartment.Additionally,ourstudy encompassedalimitedtimeframeofonlyabout60days,after whichIVcontrastagentbecamemoreavailable.Lastly,more researchisneededtofurtheranalyzethepotentialneedfor repeatimagingorpossiblereturnvisitstotheEDasaresultof notusingIVcontrast.
Inthissingle-centerstudy,wefoundthataninstitutional policychangereducingtheuseofcontrastinabdominalpelvicCTduringtheCOVID-19pandemicwassignificantly associatedwithshorterlengthofstayintheED.
AddressforCorrespondence:WayneA.Martini,MD,MayoClinic ArizonaDepartmentofEmergencyMedicine,5777E.MayoBlvd., Phoenix,AZ85054.Email: Martini.Wayne@Mayo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbe perceivedaspotentialsourcesofbias.Noauthorhasprofessional or financialrelationshipswithanycompaniesthatarerelevantto thisstudy.Therearenoconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2024Martinietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.FishmanEK.SpiralCT:applicationsintheemergencypatient. Radiographics. 1996;16(4):943–8.
2.ChangAM,LinA,FuR,etal.Associationsofemergencydepartment lengthofstaywithpubliclyreportedquality-of-caremeasures. Acad EmergMed. 2017;24(2):246–50.
3.GarnderRM,FriedmanNA,CarlsonM,etal.Impactofrevisedtriageto improvethroughputinanEDwithlimitedtraditionalfasttrackpopulation. AmJEmergMed. 2018;36(1):124–7.
4.PimentelLandBarruetoF.Statisticalprocesscontrol:separatingsignal fromnoiseinemergencydepartmentoperations. JEmergMed. 2015;48(5):628–38.
5.SweenyA,KeijzersG,O’DwyerJ,etal.Predictorsofalonglengthof stayintheemergencydepartmentforolderpeople. InternMedJ. 2020;50(5):572–81.
6.DeSteenwinkelM,HaagsmaJA,vanBerkelECM,etal.Patient satisfaction,needs,andpreferencesconcerning informationdispensationattheemergencydepartment:a cross-sectionalobservationalstudy. IntJEmergMed. 2022;15(1):5.
KatrinJaradeh,MD*†
ElaineHsiang,MD*†
MaliniK.Singh,MD,MPH,MBA*†
ChristopherR.Peabody,MD,MPH*†
StevenStraube,MD,MBA*†
SectionEditor:MatthewTews,MD
*DepartmentofEmergencyMedicine,UniversityofCalifornia, SanFrancisco,California
† SanFranciscoGeneralHospital,SanFrancisco,California
Submissionhistory:SubmittedJune6,2023;RevisionreceivedDecember8,2023;AcceptedDecember14,2023
ElectronicallypublishedApril2,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18352
Background: PatientswithlimitedEnglishproficiency(LEP)experiencesignificanthealthcare disparities.Cliniciansareresponsibleforusinganddocumentingtheiruseofcertifiedinterpretersfor patientencounterswhenappropriate.However,thedataoninterpreterusedocumentationinthe emergencydepartment(ED)islimitedandvariable.Wesoughttoassesstheeffectsofdotphraseand SmartPhraseimplementationinanadultEDontheratesofdocumentationofinterpreteruse.
Methods: Weconductedananonymoussurveyaskingemergencyclinicianstoself-report documentationofinterpreteruse.WealsoretrospectivelyrevieweddocumentationofinterpreterservicesuseinEDchartsatthreetimepoints:1)pre-interventionbaseline;2)post-implementationofa clinician-drivendotphraseshortcut;and3)post-implementationofaSmartPhrase.
Results: Mostemergencycliniciansreportedusinganinterpreter “almostalways” or “often.” Ourmanual auditrevealedthatatbaseline,interpreterusewasdocumentedin35%oftheinitialcliniciannote,4%of reassessments,and0%ofprocedurenotes;52%ofdischargeinstructionswerewritteninthepatients’ preferredlanguages.AfterimplementationofthedotphraseandSmartPhrase,respectively,ratesof interpreter-usedocumentationimprovedto43%and97%ofinitialcliniciannotes,9%and6%of reassessments,and5%and35%ofprocedurenotes,with62%and64%ofdischargeinstructions writteninthepatients’ preferredlanguages.
Conclusion: Therewasadiscrepancybetweenreportedratesofinterpreteruseandinterpreter-use documentationrates.Thelatterincreasedwiththeimplementationofaclinician-drivendotphraseand thenaSmartPhrasebuiltintothenotes.Ensuringaccuratedocumentationofinterpreteruseisan impactfulstepinlanguageequityforLEPpatients.[WestJEmergMed.2024;25(3)345–349.]
Asof2019,over65millionpeopleintheUnitedStates (US)speakalanguageotherthanEnglish,with approximately20%ofhouseholdsreportingspeaking Englishlessthan “verywell,” alsoknownaslimited-English proficiency(LEP).1 IntheUS,presidentialExecutiveOrder 13166,enactedin2000,ensuresthatLEPpatientsareoffered interpretationservicesathealthcarefacilitiesreceiving federalassistance.2,3 Thelackofaccesstolanguage-
concordantcarecontributestohealthcaredisparitiesamong LEPpatients.4
Intheemergencydepartment(ED),LEPpatientswere morelikelytohaveunplannedrevisitswithin72hours5 with limitedevidencesuggestingdifferencesintriageoradmission decisionsdependingoninterpreteruse.6 Recentdata demonstratesincreasedunnecessarytestingandhospital admissionwithlongerlengthsofstayamongLEPpatients whodidnotreceiveprofessionalinterpretingservices.7,8
Documentationofinterpreteruseisoftenusedasa proxyforinterpreteruse.Severalgroupsofresearchers studiedtherateofinterpreter-usedocumentationinthe hospital.Onefoundthat41%(30/74)ofpatientshada consentformintheirnativelanguageorthataninterpreter hadsignedit.8
Interventionshavebeenimplementedtoimprove documentationofinterpreteruse.Benderetalfoundthat whentheyplaced flyersintheEDandmadepre-work shiftannouncements,documentationofinterpreteruse increasedfromabaselinerateof5%to25%.9 In2021,astudy amongpatientsadmittedtoapediatricservicefoundthat usingadotphraseincreasedinterpreterusefrom64%to81%, andinterpreter-usedocumentationincreasedfrom69%to 98%.10 Toourknowledge,therehavebeennostudies investigatingtheuseofadotphrase(textinsertedwith keyboardshortcuts)oraSmartPhrase(abbreviationsor wordsusedtopulllongphrasesintoaphysician’snote)inan adultEDtoimprovedocumentationofinterpreteruse.We assessedtheeffectsofadotphraseandaSmartPhraseinan adultEDontheratesofdocumentationofinterpreteruse. Wehypothesizedtheseinterventionswouldincrease documentationrates.
WeconductedthisstudyataLevelIacademictrauma centerinanadultED,whereinterpretersareavailableover thephone24/7andinpersonduringdesignatedhours.First, wegatheredpatients’ medicalrecordnumbers(MRN)from interpreterservicesthatdocumentedaninterpreterhadbeen used.Apre-interventionretrospectivechartreviewwas conductedtoassessthebaselinerateofinterpreter-use documentationintheelectronichealthrecord(EHR). Second,wesurveyedemergencyclinicianstoassesstheir perspectiveoninterpreteruseanddocumentation.Third,we implementedadotphraseandthenaSmartPhraseand retrospectivelyreviewedchartsfordocumentationof interpreteruse.Bothinstrumentswerebeingdevelopedatthe sametime,butthedotphrasewascompletedmorequickly andimplemented first.Documentationofinterpreterusewas capturedwithinthehistoryandphysical(H&P), reassessments,procedurenotes,anddischargeinstructions (DCI),whichincludesaverbaldiscussion,written instructions,andattachments.Weexcludedchartsfromthe studyifthepatientonlyspokeorpreferredtospeakin English,leftwithoutbeingseen,MRNswerenotfound,orif ititwasaduplicaterecord.Therewasnopriortrainingon documentationofinterpreteruse.Weanalyzeddatausing descriptivestatistics.Thisstudywasdeemedexemptbyour institutionalreviewboard.
WeverifiedMRNsfromtheinterpreterservicedata intheEHR.Anumbergeneratorwasusedtorandomize
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
PatientswithlimitedEnglishpro fi ciency experiencehealthcaredisparities.Using interpretersreducesunnecessarytestingand hospitalizationsforthispopulation.
Whatwastheresearchquestion?
Doesimplementingadotphraseand SmartPhraseincreasedocumentationof interpreteruse?
Whatwasthemajor findingofthestudy?
Documentationofinterpreteruseinthe historyandphysicalrosefrom35%to 43%(dotphrase)andthento 97%(SmartPhrase).
Howdoesthisimprovepopulationhealth?
Aninterventiontoimprovedocumentationof interpreterusehelpsensurelanguageequity forlimitedEnglishpro fi ciencypatients.
andidentifypatientsforchartreview.Tominimize clinician-specificpracticepatterns,weauditedone chartperdayfromJuly–September2021fromvarious shifttimestoestimatethepre-interventionrateofinterpreter usedocumentation.
Weemailedananonymoussurveyto128EDattendings, fellows,residents,andnursepractitionersregarding interpreter-usedocumentationafterthepre-intervention datawascollected.Onefollow-upemailwassent.Wecreated asurveyof14multiple-choicequestionshostedonQualtrics (Qualtrics,Provo,UT).Thesurveyincludeddemographics, questionsaboutinterpreteruse,documentation,andwaysto improvedocumentation.
Adotphraseisablockoftextinsertedusingakeyboard shortcutproceededbyadotthatfacilitatesclinician’ s documentation.Clinicianscaninputthephrase “.EDinterpreter” forthestatement “A[phone,in-person] [languageoptions]interpreterwasusedon[dateandtime], [INTERPRETERID#]” tobeaddedintheEHR.Thedot phrasewasavailableonJuly1,2022.Allchartsfrom interpreterservicesdatawereauditedbetween July1–October14,2022.
WeembeddedaSmartPhraseintotheH&Pandprocedure notescreatinga “hardstop” whereclinicianscouldnotsign theirnotesuntiltheSmartPhrasewascompleted.Thiscould bebypassedbydeletingtheSmartPhrase.Ifanon-English languagewasselected,theSmartPhrasewouldpromptto choosethepatient’spreferredlanguage.TheSmartPhrase wasavailableonNovember1,2022.Allchartsfrom interpreterservicesdatawereauditedbetween November1–February1,2023.
Of91auditedcharts,Spanish(61%)wasthemost preferredlanguage,followedbyCantonese/Mandarin/ Taishanese(37%),andRussian(2%).Useofaninterpreter wasdocumentedin35%ofH&Ps,4%ofreassessments,and in0%ofprocedurenotes.Withinthedischargeinstructions, 6%ofchartsindicateddiscussinginstructionsusingan interpreter;52%ofwrittenDCIsand89%ofattachments wereprovidedinthepatient’snativelanguage(Figure1).
Of128emergencyclinicianswhoreceivedthesurvey,67 (52%)initiatedand65(51%)completedit.Ofthe respondents,46%wereresidents,37%attendings,9%NPs, and8%fellows.Cliniciansreporteduseofaninterpreter “almostalways” or “often” 66%and25%ofthetimewhen interactingwithLEPpatients.Additionally,23%and8%of cliniciansreported “almostalways” or “often” documenting useofaninterpreterintheH&P(Figure2a).Clinicians reported “almostalways” documentinguseofaninterpreter
inthereassessment(3%),procedure(15%),andDCI(8%) portionsofthenote(Figure2b, 2c, 2d).Whenaskedwhatcan makedocumentationeasier,41%suggestedadditionstothe EDnotetemplatewith29%recommendingadotphrase.
Of866auditedcharts,weanalyzed809(93%).Spanish (67%)wasthemostpreferredlanguage,followedby Cantonese/Mandarin/Taishanese(32%),andRussian(1%). Forty-threepercentofH&Ps,9%ofreassessments,and5%of procedurenoteshaddocumentationofinterpreteruse. Documentationofinterpreteruseduringdischargeremained at6%.ThewrittenportionandattachmentsoftheDCIwere inthepatient’snativelanguagein62%and94%ofcharts.
Of779auditedcharts,weanalyzed646(83%).Spanish (64%)wasthemostpreferredlanguage,followedby Cantonese/Mandarin/Taishanese(35%),andRussian (0.62%).Ninety-sevenpercentofH&P,6%ofthe reassessments,and35%ofprocedurenoteshad documentationofinterpreteruse.RegardingtheverbalDCI, 4%documentedinterpreteruse.Thewrittenportionand attachmentswereinthepatient’snativelanguagein64%and 94%ofcharts(Figure1).
Documentationratesofinterpreteruseincreasedafter implementationofadotphraseandaSmartPhrase.After implementingtheSmartPhrase,almost100%oftheH&Ps and35%ofprocedurenotesdocumentedinterpreteruse. BecausetheSmartPhrasewasembeddedonlyinH&Psand
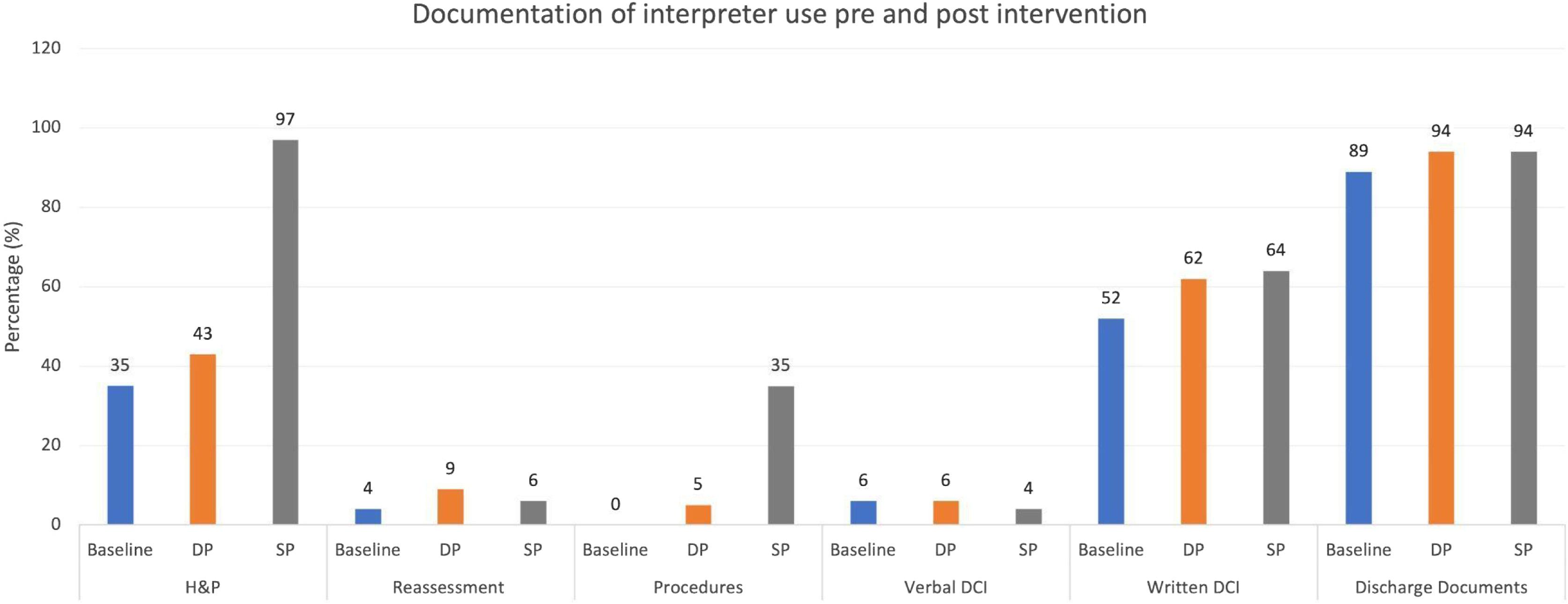
Figure1. Percentageofpatientchartswithdocumentationofinterpreteruseatbaseline(blue),afterthecreationofthedotphrase(orange), andafterthecreationoftheSmartPhrase(gray).
H&P,historyandphysical; DCI,dischargeinstructions; DP,dotphrase; SP,SmartPhraseandprocedurenoteimplementation.
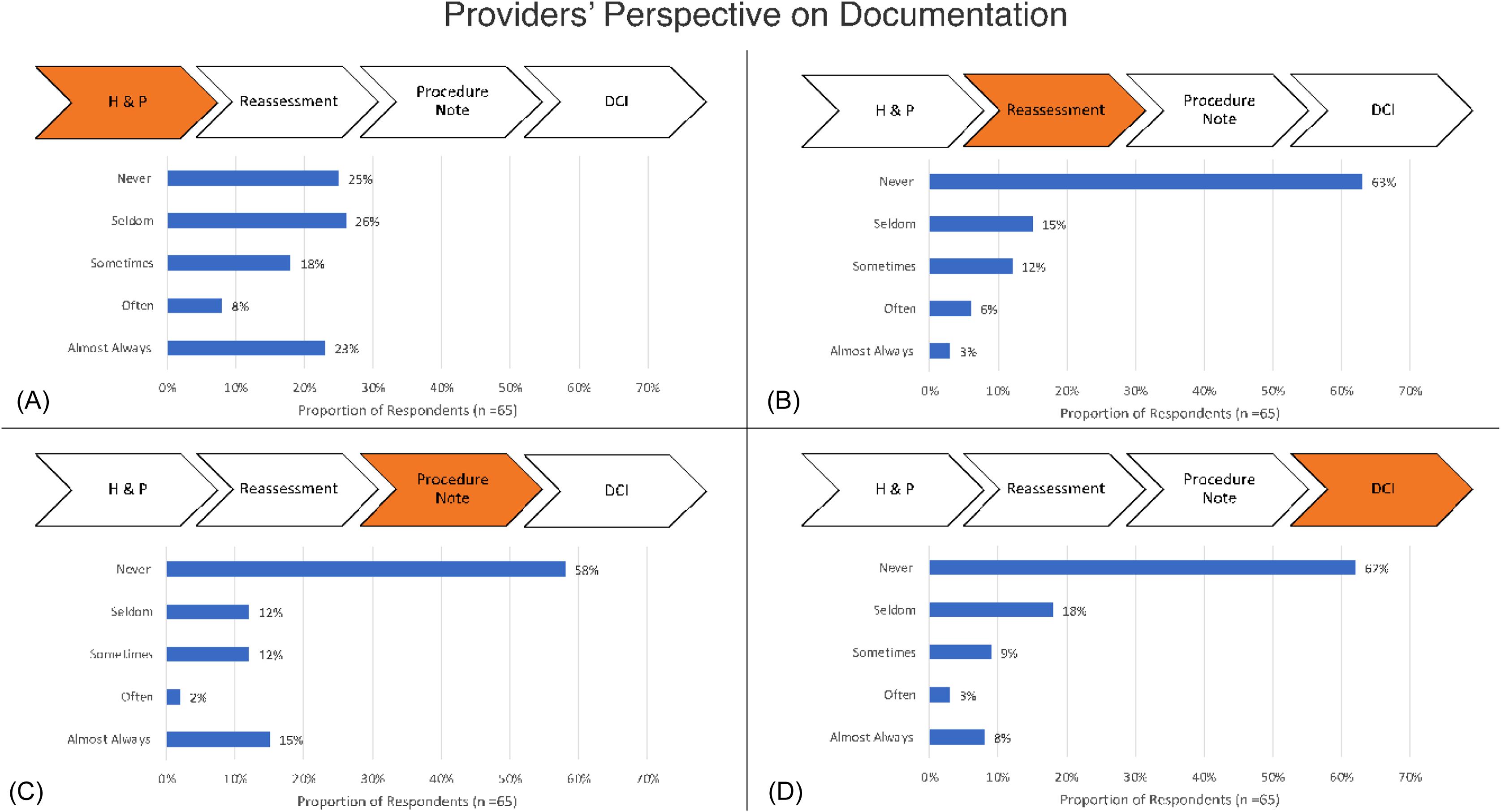
Figure2. (a)Emergencyclinicians’ perspectiveondocumentationofinterpreteruseinthehistoryandphysical.(b)Emergencyclinicians’ perspectiveondocumentationofinterpreteruseinthereassessment.(c)Emergencyclinicians’ perspectiveondocumentationofinterpreter useintheprocedurenote.(d)Emergencyclinicians’ perspectiveondocumentationofinterpreteruseintheDCI. H&P,historyandphysical; DCI,dischargeinstructions.
procedurenotes,wedidnotexpectincreasesintheDCIand reassessments.Thegeneralratesofinterpreter-use documentationinthisstudyandpreviousstudiesvary. Behairyetalfoundthatattheirchildren’shospital documentationofinterpreterusewas0%,11 whereasTaira etalfounddocumentationofinterpreteruseintheirpublic EDtobe4.6%.12 Toourknowledge,thisisoneofthe firststudiesontheimpactofadotphraseandaSmartPhrase ondocumentationofinterpreteruseinan adultED.
Therewasadiscrepancybetweenreportedratesof interpreteruseanddocumentationofinterpreteruse.Despite 66%ofcliniciansreporting “almostalways” usingan interpreter,only23%reported “almostalways” documentingtheiruseintheH&P.Thesamediscrepancy wasseenamongreassessments(3%),procedurenotes(35%), andDCIs(8%)wherecliniciansreportedthey “almost always” documentedtheiruse.Whilewedidnotspecifically askclinicianswhentheyuseaninterpreter(whilegathering theH&P,etc,settingdocumentationasaproxyfor interpreteruse,manycliniciansspeakingtotheirpatients withaninterpreterwouldnothavethedocumentationto supporttheirclaim.Lastly,cliniciansmayhaveusedanad hocinterpreter(familymemberoramemberofthe healthcareteam),asthesurveydidnotspecifyuseof professionalinterpretation.Thismayaccountforsome
ofthediscrepancybetweenthereportedandactualratesof interpreteruseperinterpreterservicesdata.
Next,wehopetoassesstheimpactofimproved documentationonpatientcare.
Thiswasasingle-institutionstudyandresultsmaynotbe generalizable.Variabilityindocumentationamong emergencyclinicians,andintimeanddayofshiftwerenot captured.Sinceonlyonechartperdaywasreviewedforpreinterventiondata,documentationratesmayhavebeenmore influencedbytimeofdaythanpost-interventionrates, affectingthedifferencesinpre-/post-interventionchanges. WedidnottrackthedataofdotphraseandSmartPhraseuse. Further,despitetheSmartPhraseleadingtoa “hardstop,” clinicianscoulddeletetheSmartPhrase.However,we includedboththedotphraseandSmartPhraseas interventionssinceclinicianscouldaddthedotphrase intootherelementsoftheEHRwhentheyusedan interpreter(eg,reassessments).
Documentationofinterpreteruseisvaried.Therewasa discrepancybetweenreportedratesofinterpreteruseand interpreter-usedocumentation.Implementationofadot phraseandaSmartPhraseimproveddocumentationof
interpreteruse,suggestingitsfeasibilitytoimprove cliniciandocumentation.
AddressforCorrespondence:KatrinJaradeh,MD,Universityof CaliforniaSanFrancisco,DepartmentofEmergencyMedicine,533 ParnassusAve.,SanFrancisco,CA94143.Email: katrin.jaradeh@ ucsf.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ChristopherPeabodyworksasa consultantinunrelatedcapacitiesforFujiFilmandSonoSite.There arenootherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Jaradehetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.UnitedStatesCensusBureau.2022.WhatLanguagesDoestheUnited StatesSpeak?AGeographicAnalysisoftheLanguagesSpokenat HomeintheUnitedStates,2015–2019.Availableat: https://www. census.gov/library/visualizations/2022/demo/lang-geogr-distrob.html AccessedOctober27,2022.
2.U.S.DepartmentofJusticeCivilRightsDivision.2015.ExecutiveOrder 13166.Availableat: https://www.justice.gov/crt/executive-order-13166 AccessedApril21,2023.
3.U.S.DepartmentofJusticeCivilRightsDivision.2015.TitleVIofthe CivilRightsActof196442U.S.C.§2000dEtSeq.Availableat: https:// www.justice.gov/crt/fcs/titlevi-overview.AccessedApril21,2023.
4.Eneriz-WiemerM,SandersLM,BarrDA,etal.ParentallimitedEnglish proficiencyandhealthoutcomesforchildrenwithspecial healthcareneeds:asystematicreview. AcadPediatr 2014;14(2):128–36.
5.NgaiKM,GrudzenCR,LeeR,etal.Theassociationbetweenlimited Englishproficiencyandunplannedemergencydepartmentrevisitwithin 72hours. AnnEmergMed.2016;68(2):213–21.
6.MarteD,BairdJ,BristerJ,etal.240Evaluatingtheimpactoflimited Englishproficiencyoncaredeliveryinapediatricemergency department. AnnEmergMed.2019;74(4):S94.
7.LindholmM,HargravesJL,FergusonWJ,etal.Professionallanguage interpretationandinpatientlengthofstayandreadmissionrates. JGenInternMed.2012;27(10):1294–9.
8.SchenkerY,WangF,SeligSJ,etal.Theimpactoflanguage barriersondocumentationofinformedconsentatahospital withon-siteinterpreterservices. JGenInternMed 2007;22(2):294–9.
9.BenderD.(2021) ImprovingInterpreterDocumentationinthe EmergencyDepartment.RutgersUniversity-Schoolof Nursing – RBHS.
10.RajbhandariP,KeithMF,BraidyR,etal.Interpreteruseforlimited Englishproficiencypatients/families:aQIstudy. HospPediatr 2021;11(7):718–26.
11.BehairyM,AlencheryA,Cuesta-FerrinoC,etal.Increasing languageinterpreterservicesuseanddocumentation: aqualityimprovementproject. JHealthcQualJHQ 2023;45(1):19.
12.TairaBRandOrueA.LanguageassistanceforlimitedEnglish proficiencypatientsinapublicED:determiningtheunmetneed. BMCHealthServRes.2019;19(1):56.
KareemHamadah,BS*‡
MaryVelagapudi,DO,BSN†‡
JulianaJ.Navarro,MD,MPH†‡
AndrewPirotte,MD†‡§¶
ChrisObersteadt,EMT†‡#
*UniversityofKansasSchoolofMedicine,KansasCity,Kansas
† UniversityofKansasHealthSystem,KansasCity,Kansas
‡ UniversityofKansasMedicalCenter,KansasCity,Kansas
§ UniversityofKansasMedicalCenter,DepartmentofEmergencyMedicine, KansasCity,Kansas
¶ UniversityofKansasMedicalCenter,OfficeofStudentAffairs, KansasCity,Kansas
# RockhurstUniversity,KansasCity,Kansas
SectionEditor:MuhammadWaseem,MD
Submissionhistory:SubmittedAugust8,2023;RevisionreceivedNovember21,2023;AcceptedJanuary19,2024
ElectronicallypublishedMay3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.61686
Introduction: Blindandvisuallyimpairedindividuals,anunder-representedpopulationofthe emergencydepartment(ED),possesscomorbiditiesandhaveahigherchanceofin-hospitalsequelae, includingfalls.Thispotentiallyvulnerablepopulation,ifnottreatedmindfully,canbesubjecttodecreased qualityofcare,recurrentand/orlongerhospitalizations,persistenceofhealthissues,increased incidenceoffalls,andhigherhealthcarecosts.Forthesereasons,itiscrucialtoimplementholistic practicesandtrainclinicianstotreatblindandvisuallyimpairedpatientsintheEDsetting.
Methods: Weidentifiedandusedacomprehensivearticledescribingbestpracticesforthecareofblind andvisuallyimpairedpatientstoestablishtheED-specificrecommendationspresentedinthispaper. AscopingreviewoftheliteraturewasthenperformedusingPubMedtoidentifyadditionalarticlesto supporteachrecommendation.Toensurethatrecommendationscouldbeimplementedina representative,scalable,andsustainablemanner,weconsultedanadvocatefortheblindtohelprefine andprovideadditionalsuggestions.
Results: Weidentified14recommendationsthatfocusoncommunicationstrategies,EDresource access,andcontinuityofcare.Themainrecommendationisforthecliniciantosupporttheunique healthcareneedsofthevisuallyimpairedindividualandmaintainthepatient’sautonomy.Another recommendationistheconsistentuseofassistivedevices(eg,canes,guidedogs)toaidpatientsto safelyambulateintheED.Alsoidentifiedasbestpracticesweredischargeeducationwiththeuseofa screenreaderandtimelyfollow-upwithaprimarycarephysician.
Conclusion: Whilewesummarizeavarietyofrecommendationsinthisarticle,itisimportantto implementonlythestrategiesthatworkbestforthepatients,personnel,andenvironmentspecifictoyour ED.Afterimplementation,itisvitaltorefine(asfrequentlyasneeded)theinterventionstooptimizethe strategies.Thiswillenabletheprovisionofexceptionalandequalcaretoblindandvisuallyimpaired patientsintheED.[WestJEmergMed.2024;25(3)350–357.]
Theblindandvisuallyimpaired(VI)areasmallbuthighly marginalizedpopulationintheUnitedStatesandaroundthe world.1,2 ThereareapproximatelyninemillionVIpeoplein theUS,withblindpeoplemakingupslightlylessthan1%of thepopulation.Globally,about2%ofchildrenare consideredVI.3 EstimatesintheUSareexpectedtodouble by2050,withtheVIpopulationprojectedtobemore prevalentinracialminoritiesandinthesouthernUS.The reasonforthisincreaseismultifactorialbutmaybeduetoan ever-increasingagingpopulationanddifferentialaccessto preventativeservicesamongminoritygroups.4,5 Datais limitedontheexactnumberofVIpatientswhoareseeninthe emergencydepartment(ED).However,approximately0.2% ofpatientsadmittedtoUShospitalsareconsideredVI.6 StatesthathavenotexpandedMedicaidcoverageseehigher ratesofVIpatientsintheirEDs.7 Patientswithother disabilities,suchasthoseinthedeafandhard-of-hearing (DHH)community,arealsomorelikelytoseekEDcare comparedtothosenotintheDHHcommunity.8–12
AlthoughVIpatientsrepresentarelativelysmall proportionofpatientsseenintheEDandadmittedtothe hospital,theyhavesignificantlyworseoutcomes:Theyare admittedandreadmittedmoreoften,incurhigherhealthcare costs,andmayhaveahigherin-hospitalmortalityrate.6,13,14 Visuallyimpairedpatientsaremorelikelytoexperience multiplemorbidities,thusfurtherincreasingtheirriskof needingEDcare.15 Fallsandtheirsequelae,suchaship fractures,areamongthemostcommonreasonsforblind patientstobeseenintheED.16–18 PediatricVIpatientsare particularlylikelytoincurorthopedicinjuriesandarealso morelikelytohavefracturesuponpresentation.19 HospitalizedpatientswhoareVIarealsomorelikelyto experiencedelirium,20 awell-knownriskfactorformorbidity andmortality.21 TheseinjuriesandconditionsamongtheVI occurinothercountries22 andtootherdisabledgroups.12,23 IntheUS,theseissuesarefurthercompoundedbythe intersectionsofraceandage.2 Blackpatientsandpatients insuredbyMedicare(ie,those ≥65yearsold)arethemost likelytohaveextendedhospitalstays.13
OptimalcareforallpatientsintheEDremainsanongoing challenge;careofVIpatientspresentsuniquechallengesthat offeranumberofopportunities.Amindfulapproachtocare ofVIpatientsrequiresthatEDsandclinicianspursuebest practices,supportstaff,impactfuleducation,andspecialized considerations.Aswithmanypopulations,theneedsofVI patientsimpacttheirexperienceduringEDcare.Inthis article,wepresentbestpracticeconsiderations.Thisscoping reviewisintendedtopromptimprovedpracticeandto furtherdiscussiontooptimizeEDcareforVIpatients.
WeperformedascopingreviewtoidentifyPubMed articlesrelatedtoblindnessandVIintheED,withparticular
emphasisonassessingtheexperiencesofVIpatientsinthe ED.Articleswereincludediftheymetoneormoreofthe followingcriteria:centeredontheexperiencesofdisabled people,particularlyVIpeople,inhealthcare;discussedthe experiencesorepidemiologyofdisabledpatientsinEDsor hospitalsregardlessofgeographicregion;providedbest practicerecommendationsforthecareofVIpatients regardlessofspecialty;anddiscussedoutcomesofdisabled patientsintheEDorhospital.Weexcludedarticles discussingthecareofacuteblindnessorVI,asthefocusof thisreviewwasonpatientswithpre-existingvisual impairment.Duetotheoveralllackofdataonthistopic, guidelinesfromotherspecialties(eg,ophthalmology)were includedandadaptedtotheEDsetting.
WeusedtheAmericanswithDisabilitiesAct(ADA) ChecklistbyMarshallandJoffee(2006)asthebasisofour recommendations,asitprovidesacomprehensivelistofbest practicesforallhealthcareclinicians.Fromthispaper,we selected15recommendationsmostrelevantandapplicableto theEDsetting(Table).Recommendationswere supplementedusingfocusgroupandsurveydatafoundon PubMed.Thesearchphrase “(visuallyimpaired)AND (accessibility))AND(emergencydepartment)” resultedin28 results.WefoundonerelevantstudybyCarmichaeletal (2023),inwhich12disabledindividualswereinterviewed(six ofwhomwereVI).DuetoalackofdataspecifictoVI patients,thesearchwasexpandedtoincludetheexperiences ofpatientswithotherphysicalandcognitivedisabilities, whichyieldedanadditionalstudybyMorrisetal(2021).
WeevaluatedtrendsinEDuseamongdisabledpatientsto contextualizetherecommendationsprovided.Finally,we usedarticlesbytheNationalFederationoftheBlind(NFB) toensurethatthevoicesofVIauthorsandacademicswere wellrepresentedandtoinformseveralrecommendations (eg,language).Mostofthedatawereobservationaland retrospective.Wealsoconsultedasubjectmatterexpertwho wasbornblindanddedicatedhercareertoadvocatingfor otherVIpeopletoensurethatwewerebestrepresentingthe needsofVIpatients.Usingthisdata,weidentifiedactionable recommendationsandbestpractices.
WeperformedPubMedsearchestoidentifysupporting articlesforall14recommendations(see Table).Articleswere selectedusingthepreviouslydescribedinclusionand exclusioncriteria.ExcludingtheADAChecklistby MarshallandJoffee,whichwasusedtodevelop eachrecommendation,wefoundfourarticlessupporting recommendationone.Threearticleswerefoundsupporting recommendationtwo.Fivearticleswerefound supportingrecommendationthree,andonearticlewas foundsupportingrecommendationfour.Wefoundthree articlessupportingrecommendation five,sixarticles supportingrecommendationsix,andfourarticlessupporting
Table. Summaryofrecommendationsforinteractingwithvisuallyimpairedpatientsintheemergencydepartment. RecommendationsRationaleReferences
Useoptimallanguage:disability- firstoftenpreferred.Betterrepresentsthepatient’slivedexperiences24
Introduceyourselfeverytimeyouentertheroom(consider placingsignagetoalertstaff).
Ensurespatientisawareofwhoisintheroomatall timesandmayhelppreventdelirium
Tellthepatientwhatyou’regoingtodobeforedoingit, includingbeforeleavingtheroom.
Listentothepatient’scaregiver(s),ifapplicable,butonly aftergatheringasmuchinformationfromthepatientas youcan.
Ifavailableatyourfacility,askwhetherthepatientwould likeanadvocate.
Accommodatetheneedsofthepatient,butdonot over-focusonvisualimpairmentduringtheHPI.
PlacethepatientinquietestpartoftheED.Mayhelppreventdelirium32,35,41
Ensurethepatienthasaccesstomobilityequipment (eg,cane,guidedog)atalltimes.
Ensurethepatienthasaccesstopersonaltechnology (eg,phone,smartwatch,etc).
Ensurethepatientknowswherethecalllightisand howtouseit.
Ensuresmaximalpatientautonomyandmayhelp preventdelirium
preventdelirium
Usethecorrectstrategieswhenguidingapatient.Helpsensurepatientsafety31,32 Clearlynotethepatient’svisualimpairmentinthemedical record(ICD-9:369;ICD-10:H54).
Helpsensureallhealthcareworkersareawareofthe patient’sVIandcanproviderelevant accommodations
AdvocateforMedicaidexpansionatthestateandmedical society(eg,AAEM)level,andencouragepatientstoapply. MayhelpdecreasefrequencyofEDvisits7,32
HelpthepatientestablishcarewithaPCP.HelpstopreventrecurrentEDvisits32,44,45
HPI,historyofpresentillness; ED,emergencydepartment; VI,visuallyimpaired; ICD,InternationalClassificationofDiseases,Rev9or10; AAEM,AmericanAcademyofEmergencyMedicine;PCP,primarycarephysician.
recommendationseven.Threearticleswerefound supportingrecommendationeight.Onearticlewasfound supportingrecommendation9–13.Finally,wefoundtwo articlessupportingrecommendation14.Allsupporting articlesandwhichrecommendationstheyinformedcanbe foundin Table
CommunicationStrategies
OptimalLanguage
Theuseofperson-first(eg,personwhoisblind)and disability-first(eg,blindperson)languageisacontentious issue.Academicsconsiderperson-firstlanguagetobemore dignifyingasitplacesfocuslessonthedisabilityandmoreon theindividual.24,25 However,manyblindpeopleandblind advocatesstronglydisagreewithperson-firstlanguageasit mayinadvertentlystigmatizedisability.Blindadvocatesalso arguethatdisability-firstlanguagemoreaccurately representsdisabledexperiences.25–27 Thiscontentionfurther emphasizestheimportanceoflisteningtodisabledpatients andusingtheterminologytheyprefer.Ifablindpatient
preferstobecalleda “blindpatient” ora “patientwhois blind,” thatpreferenceshouldbeaccommodatedlikeany other.Disability-firstlanguagewillbeusedinthispaperfor brevityand,moreimportantly,becauseitisgenerally preferredbytheVIcommunity.
Consentisanintegralcomponentofpatientcare,andall effortsshouldbemadebyemergencycliniciansandpatient carestafftoobtaininformedconsentatalltimes.28 However, thewaythatconsentisobtainedcannotbeuniformlyapplied toallpatients.Forexample,blindpatientscannotseewhois enteringtheirroom,sotheymaynotimmediatelybeableto tellwhetherthepersonwhojustwalkedinisadoctor,nurse, familymember,etc.Thus,itisimperativeforeachperson enteringablindpatient’sroomtoverballyinformthepatient oftheirnameandroleeverytimetheyentertheroom.29 This isespeciallyimportantintheED,anoftenhecticand disorientingplaceforallpatients,andparticularlyforthose withdisabilities.30 Justasimportantasannouncingwhenyou walkintoapatient’sroomisannouncingwhenyouor
othersinvolvedinpatientcareleavetheroom.29 Ifthis isnotdone,thepatientmayattempttospeaktosomeone whotheylogicallyassumeisstillintheroomonlytobe metwithsilence.Thisisnotonlypotentiallyembarrassing butdisorienting.31,32
InformedconsentdiscussionsalsomustbetailoredforVI patients.Inadditiontothetypicaldiscussionstogain consent,VIpatientsbenefitfromtheclinicianmaintainingan ongoingdialogueduringaprocedure,explainingwhatwillbe donenextandprovidingclear,actionableinstructionswhen necessary.29,33 Addingthisextralayerofcommunicationcan beinstrumentalinensuringpatientsafetyandadherence,and theoverallefficacyofthemedicalinterventionforblind patients.Furthermore,itservestomaintainrespectfortheir autonomy,helpsfosteracooperativeenvironment,and minimizessurpriseordiscomfortduringtheprocedure, aparticularlyimportantconsiderationinanEDsetting wherethepaceofcareisoftenrapidandpotentially anxiety-inducing.34,35
Ifacaregiverisnotpresent,youmayaskthepatientor checkthepatient’schartforapotentialcaregiver’scontact information.However,donotassumeapatienthasor requiresacaregiverbecausetheyareVI.Duringthecourseof treatmentofaVIpatient,thecaregiver(ifapplicable)maybe abletoprovidehelpfulinformationorcontextregardingthe patient.36 Forexample,thecaregivermayprovide informationaboutthepatient’sbaselineindependenceand ActivitiesofDailyLiving theskillsneededto independentlycareforoneself.Thisinformationcanbe helpfulduringthecourseoftreatmentintheED,aswellas upondischargetocustomizeinstructionstothepatient. However,itisimportanttorememberthatcaregivers areanadjuncttopatientcareandnotthepatientsthemselves. Thus,besuretogatherasmuchinformationfromthe patientaspossibleaswellasfromtheircaregiver.29,32 This helpsmaintainarespectfulandautonomouspatientclinicianrelationship.
Patientadvocatescanplayasignificantroleintheholistic careofapatient.37,38 DuringthecourseoftreatmentforaVI patient,itisimportanttoaskthepatientwhethertheyhave anadvocate,whichcanbedoneasearlyasthetriageprocess. Ifthepatientdoesnotalreadyhaveanadvocateorcannot thinkofsomeone,itisimportanttoworkcollaboratively withthepatienttoidentifyanadvocate,iftheywouldlike one.Thereareseveralpotentialpeoplewhocanbeadvocates includingfamilyandfriendsofthepatient,workcolleagues,
caregivers,socialworkers,andhospitalvolunteers (eg,premedicalstudentsandnavigators).32,33
Theroleofanadvocatemayvary;therefore,itiscriticalto establishclearrolesandresponsibilitiesfortheadvocate.One oftheirkeyresponsibilitiescanbetoaccompanythepatientin thewaitingroom.Iftheadvocateisanemployeeofthe hospitalorfamiliarwiththeED,itcanbehelpfulforthe advocatetodiscusstheoverallEDprocess.Thiswillprovide predictabilityofwhattoexpectandclarifytheEDprocessfor thepatient.37 Afterthewaitingroom,theadvocatecanalso providesupportduringtransporttotheroomandinmeeting healthcarepersonnelandexplainingtheworkupand proceduresforlabsorimaging.Finally,duringdisposition,the advocatecanappropriatelyadvocateonbehalfofthepatient forresourcesrequiredfollowingdischargeorduringthe admissionprocess.Theoverallrolesandresponsibilitiescan varybypatientandEDsetting,butitisimportantforthe patientandtheadvocatetoestablishamutualunderstanding.
Whengatheringthehistoryofpresentillness(HPI)onaVI patient,emergencycliniciansshouldstrivetotreatthepatient assimilarlytootherpatientsaspossible.Forexample, lookingatthepatientdirectlywhenyouarespeaking,asyou wouldforotherpatients,isconsiderateand thoughtful.29,31–33 ItisalsoimportanttorecognizethatVI existsonaspectrumfromslightlydecreasedvisualacuitytoa completelackofvision,andmostpeopletypicallyconsidered blindhavesomelevelofvisualfunction.39 Acknowledging thisspectrum,cliniciansshouldattempttodiscernthe patient’suniqueneedstoprovideoptimalcare.Itisalso important not topresumelowercognitiveabilityorother disabilitiesduetovisualimpairment.36 Ininteractionswith thepatient,beconsiderateoftheirvisualimpairment,butdo notoverlyfocusonit.Remember,EDvisitsforblindnessand lowvisionareexceedinglyrare40;thus,ablindpatientis unlikelytobeseekingemergencycarefortheirblindness. Treattheblindpatientasyouwouldyourotherpatientsas muchaspossible,anddonotoverlyplacatethepatient.For example,iftheblindpatientneedstosignaconsentform,you canmakethenecessaryaccommodationssuchasreadingthe formoutloud.29,32,33
OptimalLocationforPatientsintheED
ItiscommonforpeoplewhoareVItohaveheightened sensorysensitivity,particularlytosound.41,42 Thisis especiallytrueforpeoplewithearlyvisionloss.43 Therefore, makingconsiderationsforadaptingthecareenvironment cancontributetoamorecomfortablepatientexperience.For example,placingthepatientinthequietestpartoftheED canhelp.32,35 Thismayalsohelppreventdelirium, particularlyifapatientneedstostayintheEDfora prolongedperiodoftime.
EnsureAccesstoAssistiveDevices
Accessibilitytopersonalassistivedevices,suchasmobility equipment,shouldbeconsidered.32 Thesedevices,likecanes orguidedogs,areconsideredanextensionofthepersonand arelegallyrecognizedasmedicalequipmentundertheADA. Forpatientswithaguidedog,cliniciansandotherhealthcare staffshouldunderstandthatthedoghasaspecificjoband, thus,shouldnotbebotheredorinhibited.Healthcarestaff arenotrequiredtodirectlycareforaguidedogbutmayassist withcaretasksifthepatientrequestsandtimepermits.By ensuringthatVIpatientshavecontinualaccesstotheseaids, wecanhelpfacilitateindependentnavigationandmobility, whichservestopreservetheirautonomyandreduces potentialdistressduringtheirstay.29,33,35
Phonesorsmartwatchescanalsohelpbridgegapsin healthcareequitybyservingseveralfunctions.Forexample, VIpatientsoftenusespeech-to-textsoftwareornavigational aids,whichtheymayaccessthroughtheirpersonaldevices.30 Manyhospitalsofferappsoronlinetoolstotrack appointments,viewlabresults,orcommunicatewith clinicians.Ensuringaccesscan,therefore,facilitate communicationwithmedicalstaffandcontributetoamore comprehensiveunderstandingoftheircare.Finally,personal devicesenablepatientstomaintaincontactwiththeirsocial networks,friends,orfamily,whichcanhelppromote emotionalwell-beingduringapotentiallystressfulhospital stay.30 Somepatientsmayrelyontheirdevicesfor entertainmentordistraction,whichcanmakethestressful EDenvironmenteasiertocopewith.Inall,maintaining accesstopersonaltechnologyisnotmerelyaconveniencefor VIpatients;itplaysacrucialroleinensuringequityand inclusivitybyfosteringamorepatient-centeredapproachto careandempoweringtheminthemanagementoftheir healthcare.30,32 Finally,ensuringthatpatientsareawareof thelocationandoperationofthecalllightcanfurther empowerthemandfacilitateimmediatecommunication, especiallyinemergencysituations.30,32 Thesesimple strategiesmayalsohelppreventdeliriuminVIpatientswho arealreadyathigherrisk.
IfaVIpatientneedstomovesomewhere(eg,tousethe bathroom),andisstableenoughtoambulate,itisimportant toknowhowtobestassistthepatient.Allowingambulatory patientstowalkalsoprovidesthemwithautonomy.Guiding canbeadauntingtaskforthosewhohaveneverdoneit,but thistaskisrelativelysimple.First,thehealthcarestaffshould askthepatientwhethertheywouldlikeaguideandwhether theywouldliketobringtheirassistivedevice(ie,caneor guidedog).Iftheysayyes,allowthemtostand;then,the healthcareworkershouldstandnexttothepatientandtap thepatient’sarm.Thepatientwillthentaketheperson’ sarm orelbowandwillbereadytobeguided.Thehealthcare workershouldwalkatanormalpace.Iftheworkerispassing
throughatightarea,theyshouldsimplymovetheirelbow behindtheirbackandholditthere.Thiswillsignalthe patienttowalkbehindthestaffmember.Whenit’ssafefor thepatienttoreturntotheclinicianorhealthcareworker’ s, theworkershouldmovetheirelbowbacktotheirside;this willsignalitissafetoreturntowalkingbytheworker’sside. AlthoughunlikelyintheED,ifthehealthcareworker encountersaledgeorstairs,theyshouldinformthepatient andpausewhentheygettothearea.Thiswillgivethepatient enoughtimetogainstablefooting.After,walkupordown thestairsatanormalpace.IftheEDstaffmember encountersadoor,openthedoorandensurethepatienthasa handonthedoor.Thiswillensuretheyareabletocontrol whenthedoorcloses.Ifthepatientisusingthebathroom, assistthemin findingthetoiletandsink;thenleavethe bathroomandgivethepatientprivacy.When finished,the patientwillletthestaffmemberknow,andtheycanbe guidedbacktotheirroom.31,32
Whentreatingablindpatient,itisimportanttonote visualimpairmentasearlyaspossibleandasclearlyas possibleinthechartand/oronthewristbandthatthe personiswearing,forexample.30,32 Theidealtimetonote visualimpairmentwouldbeduringtheintakeortriage process.TheInternationalClassificationofDiseases,Rev9 and10codesforBlindnessandLowVisionare369andH54, respectively.Thiswouldenablethedownstreamhealthcare workerstoappropriatelyadjusttheircaretoapatientwith visualimpairment.
Uponrecognizingthatthepatientisblind,thepatient’ s chartshouldbeupdatedtoclearlyreflectthevisual impairment,asperhospitalorEDprotocol.Ifyour healthcaresettingdoesnothaveaprotocol,youcanseekto establishastandardizedprotocol.Beforeimplementing, considerthattheprotocolshouldbeimplementableacross bothelectronicandpaperhealthrecords.Oneexamplecould bean “ eye ” iconinanelectronichealthrecord(EHR)ora coloredstickerforpapercharts.Additionally,thesamecoloredstickercanalsobeappliedasapatientwristband. Finally,ensurethattheprotocoldoesnotoverlaporconflict withanotherexistingdepartment/hospitalprotocol.For example,ifyourhospitalusesayellowwristbandtosignifya fall-riskpatient,itisbesttouseanalternatecolortosignifya patientwithvisualimpairment.Similarsignageusedfor “fall-risk” orinfectionprecautionscanbeusedonthe patient’sdoor,ifadmitted.32
Duringdischarge,patientsareoftengivenpapercopiesof theirdischargeinstructions.However,thisisnotaccessible forVIpatients.Thus,itisimportantto findalternativemeans ofprovidingthisinformation.29,32,33 ManyEHRsystems
havewebsitesorappspatientscanusetoaccesstheirhealth information.Forexample,Epic(EpicSystemsCorporation, Verona,WI)usestheMyChartsystem,whichisscreenreaderaccessible.Screenreadersaresoftwarenatively installedordownloadedontodevicesthatusethedevice’ s microphonetoreadoutloudwhatisonscreen.TheMyChart appcanbeusedwithIOSandAndroidscreenreaders, VoiceoverandTalkback,respectively,andthewebsitecanbe accessedwithJAWSandNVDA,thetwomostcommonly usedWindowsscreenreaders.Althoughit’simpossibleto testeveryEHR,youcanreachouttoyourinformation technologydepartmenttodeterminewhetheryoursystemis screen-readeraccessible,andifnot,toadvocateforupdates tobemadesoallpatientscanaccesstheirhealthrecordsand dischargeinstructions.
StatesthathaveexpandedMedicaidcoverageseea decreasedrateofEDvisitsamongdisabledpatients.Thisis likelybecauseitdecreasesthe financialburdenfordisabled patientstoseekpreventativecare.7 Importantly,thismay alsodecreaseclinicianburden.Werecommendadvocating forMedicaidexpansioninyourstate.Thiscanbedonein manyways,suchascontactingyourmemberofcongressor representativesatyourmedicalsociety(eg,American AcademyofEmergencyMedicine).Additionally,hospital financialservicesorsocialworkersmaybeabletoassist patientsinapplyingtoMedicaid.32
Itisknownthataccesstoaprimarycarephysician(PCP) isassociatedwithsignificantlyreducedEDvisits.44 ForVI patientswhohaveamyriadofuniqueneeds,itisespecially importanttoconnectthemwithaPCPbeforetheyare discharged.32 Thishasalsobeenfoundtodecreaserecurrent EDvisitsamongdisabledpatients.45
ThisreviewislimitedbythelackofdataonVIpatientsin theED.Itisalsoimportanttonotethatdisabledindividuals’ experiencesarevariedandhighlypersonal,sothe recommendationsprovidedinthispaperaregeneral.Alldata usedinthisreviewareretrospectiveandobservationaland, thus,subjecttothelimitationsinherenttothosestudytypes. Moreresearchisneededtodeterminetheshortcomingsof EDcareofVIpatients.
Thereareavarietyofimpactfulinterventionsthatcan improveEDcareforvisuallyimpairedpatients.These interventionsarereproducible,notresource-intensive,and profoundlyhelpfulforVIpatientsintheED.LikemanyED interventions,theserecommendationsarenotstaticor comprehensivebutratherservethepurposeoffurtheringa
much-neededconversation.Theserecommendationsshould alsobefurtherstudiedtodeterminetheirpatient-centered impact,ideallyinpartnershipwithnationalandstate organizationsrepresentingVIpeople.Optimalcareinthe EDforvisuallyimpairedpatientsisoptimalcareforall patients.Pleaseconsiderimplementingsomeorallofthese interventionsandapproachingthecareofVIEDpatients mindfullyandintentionally.
TheauthorswouldliketothankSheilaStyronforher feedbackonthispaperfromtheperspectiveofaVIperson andadvocateatTheWholePerson.
AddressforCorrespondence:KareemHamadah,Universityof KansasSchoolofMedicine,4000CambridgeSt,KansasCity, KS66103.Email: khamadah@kumc.edu
ConflictsofInterest: Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Hamadahetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.UlldemolinsAR,LansinghVC,ValenciaLG,etal.Socialinequalitiesin blindnessandvisualimpairment:areviewofsocialdeterminants. Indian JOphthalmol. 2012;60(5):368–75.
2.BesagarS,YonekawaY,SridharJ,etal.Associationofsocioeconomic, demographic,andhealthcareaccessdisparitieswithseverevisual impairmentintheUS. JAMAOphthalmol. 2022;140(12):1219–26.
3.YektaA,HooshmandE,SaatchiM,etal.Globalprevalenceandcauses ofvisualimpairmentandblindnessinchildren:asystematicreviewand meta-analysis. JCurrOphthalmol. 2022;34(1):1–15.
4.ChanT,FriedmanDS,BradleyC,etal.Estimatesofincidenceand prevalenceofvisualimpairment,lowvision,andblindnessintheUnited States. JAMAOphthalmol. 2018;136(1):12–9.
5.VarmaR,VajaranantTS,BurkemperB,etal.Visualimpairment andblindnessinadultsintheUnitedStates:demographicand geographicvariationsfrom2015to2050. JAMAOphthalmol. 2016;134(7):802–9.
6.HarrisCMandWrightSM.Severevisionimpairmentandblindnessin hospitalizedpatients:aretrospectivenationwidestudy. BMC Ophthalmol. 2021;21(1):263.
7.Horner-JohnsonW,LindnerS,LevyA,etal.Timetrendsinemergency departmentuseamongadultswithintellectualanddevelopmental disabilities. DisabilHealthJ. 2022;15(2):101225.
8.RaschEK,GulleySP,ChanL.Useofemergencydepartmentsamong workingageadultswithdisabilities:aproblemofaccessandservice needs. HealthServRes. 2013;48(4):1334–58.
9.KuehnBM.Disabilitiesandemergencycare. JAMA. 2013;309(8):759.
10.JamesTG,CoadyKA,StacciariniJMR,etal. “They’renotwillingto accommodatedeafpatients”:communicationexperiencesofdeaf AmericanSignLanguageusersintheemergencydepartment. Qual HealthRes. 2022;32(1):48–63.
11.JamesTG,McKeeMM,MillerMD,etal.Emergencydepartment utilizationamongdeafandhard-of-hearingpatients:aretrospective chartreview. DisabilHealthJ. 2022;15(3):101327.
12.McKeeMM,WintersPC,SenA,etal.Emergencydepartmentutilization amongdeafAmericanSignLanguageusers. DisabilHealthJ. 2015;8(4):573–8.
13.MorseAR,YatzkanE,BerberichB,etal.Acutecarehospital utilizationbypatientswithvisualimpairment. ArchOphthalmol. 1999;117(7):943–9.
14.CreweJM,SpilsburyK,MorletN,etal.Healthserviceuseandmortality oftheelderlyblind. Ophthalmology. 2015;122(11):2344–50.
15.ZhengDD,ChristSL,LamBL,etal.Patternsofchronicconditions andtheirassociationwithvisualimpairmentandhealthcareuse. JAMAOphthalmol. 2020;138(4):387–94.
16.SinghRRandMauryaP.Visualimpairmentandfallsamongolder adultsandelderly:evidencefromlongitudinalstudyofageinginIndia. BMCPublicHealth. 2022;22(1):2324.
17.LoriautP,LoriautP,BoyerP,etal.Visualimpairmentandhipfractures: acase-controlstudyinelderlypatients. OphthalmicRes. 2014;52(4):212–6.
18.PatinoCM,McKean-CowdinR,AzenSP,etal.Centralandperipheral visualimpairmentandtheriskoffallsandfallswithinjury. Ophthalmology. 2010;117(2):199–206.e1.
19.S¸ahinAA,Keles¸S¸ahinA,UzunA,etal.Therelationship betweenextremityfracturesandvisualimpairmentinchildhood: acase-controlstudy. UlusTravmaVeAcilCerrahiDerg. 2022;28(5):662–667.
20.MorandiA,InzitariM,UdinaC,etal.Visualandhearingimpairment areassociatedwithdeliriuminhospitalizedpatients:resultsof amultisiteprevalencestudy. JAmMedDirAssoc. 2021;22(6):1162–7.e3.
21.AungTheinMZ,PereiraJV,NitchinghamA,etal.Acalltoactionfor deliriumresearch:meta-analysisandregressionofdeliriumassociated mortality. BMCGeriatr. 2020;20(1):325.
22.KimAM,LeeJY,KimJ.Emergencydepartmentutilizationamong peoplewithdisabilitiesinKorea. DisabilHealthJ. 2018;11(4):598–605.
23.MerrifieldJ.Meetingtheneedsofpeoplewithalearningdisabilityinthe emergencydepartment. IntEmergNurs. 2011;19(3):146–51.
24.ForgeJ.Preferredlanguagepracticeinprofessionalrehabilitation journals. JRehabil. 1991;57:49.
25.GernsbacherMA.EditorialPerspective:Theuseofperson-first languageinscholarlywritingmayaccentuatestigma. JChildPsychol Psychiatry. 2017;58(7):859–61.
26.VaughanCE.People-firstlanguage:anunholycrusade. Braille Monitor.2009.Availableat: https://nfb.org/sites/default/files/images/ nfb/publications/bm/bm09/bm0903/bm090309.htm AccessedApril9,2023.
27.StreeterL.Thecontinuingsagaofpeople-firstlanguage. Braille Monitor.2010.Availableat: https://nfb.org/sites/default/files/images/ nfb/publications/bm/bm10/bm1005/bm100509.htm AccessedApril9,2023.
28.HallDE,ProchazkaAV,FinkAS.Informedconsentforclinicaltreatment. CMAJ 2012;184(5):533–40.
29.SchneiderK.Caringbetterforpatientswhoareblindorvisually impaired. AmFamPhysician. 2013;88(11):774.
30.MorrisMA,WongAA,DorseyHollimanB,etal.Perspectivesofpatients withdiversedisabilitiesregardinghealthcareaccommodationsto promotehealthcareequity:aqualitativestudy. JGenInternMed. 2021;36(8):2370–7.
31.StevensS.Assistingtheblindandvisuallyimpaired:guidelines foreyehealthworkersandotherhelpers. CommunityEyeHealth. 2003;16(45):7–9.
32.MarshallSandJoffeeE.ADAChecklist:HealthCareFacilitiesand ServiceProviders–EnsuringAccesstoServicesandFacilitiesby PatientsWhoAreBlind,Deaf-Blind,orVisuallyImpaired.TheAmerican FoundationfortheBlind.2006.Availableat: https://www.afb.org/ blindness-and-low-vision/your-rights/advocacy-resources/ ada-checklist-health-care-facilities-and.AccessedMay2,2023.
33.CarmichaelJH,KalagherKM,ReznekMA,etal.Improvingaccessibility intheemergencydepartmentforpatientswithdisabilities:aqualitative study. WestJEmergMed. 2023;24(3):377–83.
34.RotoliJ,BacksterA,SappRW,etal.Emergencymedicineresident educationoncaringforpatientswithdisabilities:acalltoaction. AEMEducTrain. 2020;4(4):450–62.
35.PoffenbergerCM,CoatesWC,BacksterA,etal.Makingemergency medicineaccessibleforall:thewhat,why,andhowofproviding accommodationsforlearnersandphysicianswithdisabilities. AEMEducTrain. 2022;6(S1):S71–6.
36.HeydarianNM,HughesAS,MoreraOF,etal.Perspectivesof interactionswithhealthcareprovidersamongpatientswhoareblind. 2021.Availableat: https://nfb.org/images/nfb/publications/jbir/jbir21/ jbir110203.html.AccessedApril3,2023.
37.AmericanCollegeofEmergencyPhysicians(ACEP).Emergency departmentpatientadvocateroleandtraining.Policystatement. AnnEmergMed. 2015;65(1):130–1.
38.ChoiPP.Patientadvocacy:theroleofthenurse. NursStand. 2015;29(41):52–8.
39.LeeSYandMesfinFB.(2023)Blindness.In: StatPearls Availableat: http://www.ncbi.nlm.nih.gov/books/NBK448182/ AccessedJuly30,2023.
40.VaziriK,SchwartzSG,FlynnHW,etal.Eye-relatedemergency departmentvisitsIntheUnitedStates,2010. Ophthalmology. 2016;123(4):917–9.
41.NilssonMEandSchenkmanBN.Blindpeoplearemoresensitivethan sightedpeopletobinauralsound-locationcues,particularlyinter-aural leveldifferences. HearRes. 2016;332:223–32.
42.KolarikAJ,RamanR,MooreBCJ,etal.Theaccuracyofauditoryspatial judgmentsinthevisuallyimpairedisdependentonsoundsource distance. SciRep. 2020;10(1):7169.
43.BauerCM,HirschGV,ZajacL,etal.MultimodalMR-imagingreveals large-scalestructuralandfunctionalconnectivitychangesinprofound earlyblindness. PLoSONE. 2017;12(3):e0173064.
44.TsaiMH,XirasagarS,CarrollS,etal.Reducinghigh-users’ visitstothe emergencydepartmentbyaprimarycareinterventionfortheuninsured: aretrospectivestudy. InqJMedCareOrganProvisFinanc. 2018;55:0046958018763917.
45.ChuL,SoodN,TuM,etal.Reductionofemergencydepartment useinpeoplewithdisabilities. AmJManagCare. 2017;23(12):e409–15.
JohnathanM.Sheele,MD,MHS,MPH*
CarolynMead-Harvey,MS†
NicoleR.Hodgson,MD‡
SectionEditor:IoannisKoutroulis,MD,MBA,PhD
*MayoClinic,DepartmentofEmergencyMedicine,Jacksonville,Florida † MayoClinic,DivisionofClinicalTrialsandBiostatistics, Scottsdale,Arizona ‡ MayoClinicHospital,DepartmentofEmergencyMedicine, Phoenix,Arizona
Submissionhistory:SubmittedFebruary1,2023;RevisionreceivedDecember13,2023;AcceptedJanuary16,2014
ElectronicallypublishedMay3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.60033
Introduction: Bacterialurinarytractinfections(UTI)andsomesexuallytransmittedinfections(STI)can haveoverlappingsignsandsymptomsornonspecific findings,suchaspyuriaonurinalysis. Furthermore,resultsfromtheurinecultureandthenucleicacidamplificationtestforanSTImaynotbe availableduringtheclinicalencounter.Wesoughttodeterminewhethergonorrhea,chlamydia,and trichomoniasisareassociatedwithbacteriuria,informationthatmightaidinthedifferentiationofSTIs andUTIs.
Methods: Weusedmultinomiallogisticregressiontoanalyze9,650encountersoffemalepatientswho wereaged ≥18yearsandwhounderwenttestingforSTIs.TheEDencounterstookplacefromApril18, 2014–March7,2017.Weusedamultivariableregressionanalysistoaccountforpatientdemographics, urinalysis findings,vaginalwet-mountresults,andpositiveornegative(orno) findingsfromtheurine cultureandtestingfor Neisseriagonorrhoeae,Chlamydiatrachomatis, or Trichomonasvaginalis.
Results: Inmultivariableanalysis,infectionwith Tvaginalis, Ngonorrhoeae, or Ctrachomatis wasnot associatedwithhavingaurinecultureyielding10,000ormorecolony-formingunitspermililiter(CFU/mL) ofbacteriacomparedwithaurinecultureyieldinglessthan10,000CFU/mLornourinecultureobtained. ThediagnosisofaUTIintheEDwasnotassociatedwithhavingaurinecultureyielding10,000ormore CFU/mLcomparedwithaurinecultureyieldinglessthan10,000CFU/mL.
Conclusion: Afteradjustingforcovariates,noassociationwasobservedbetweenurinecultureresults andtestingpositivefortrichomoniasis,gonorrhea,orchlamydia.Ourresultssuggestthathavinga concurrentSTIandbacterialUTIisunlikely.[WestJEmergMed.2024;25(3)358–367.]
Keywords: chlamydia;emergencydepartment;emergencymedicine;gonorrhea;Trichomonas; urinarytractinfection.
Urinarytractinfection(UTI)isoneofthemostcommon bacterialinfectionsdiagnosedintheemergency department(ED). 1 , 2 SymptomsofUTIarethereasonfor approximately1%ofallambulatoryvisitsandresultin2 – 3 millionEDvisitsintheUSeachyear. 2 Urinecultureresults cantakemorethanaday,andtheurinalysis fi ndingscan
causediagnosticuncertaintyabouttheexistenceofa bacterialUTI.Addingtotheproblemisthattheincidence ofsomesexuallytransmittedinfections(STI)suchas gonorrhea,chlamydia,andtrichomoniasisisincreasingin theUS, 3 , 4 andclinicalmanifestationsofUTIsandSTIs mayoverlap.Theseoverlappingsignsandsymptomsmay leadtounderdiagnosingSTIsinpatientswithurinary
concernsandovertreatingforSTIsinpatientswithgenital concerns. 5 – 9 Previousstudy fi ndingshaveshownthatSTIs areassociatedwithsterilepyuriaandothernon-speci fi c fi ndingsonurinalysis. 5 , 9 , 10 Diagnosticconfusionmaybe mostcommonwhentrichomoniasisisidenti fi edintheED byurinalysisorwetmountandtheclinicianmustconsider whethertheurinein fl ammatorychangesarecausedby Trichomonasvaginalis onlyorbyaconcurrent bacterialUTI.
Inthisanalysis,wesoughttodeterminewhether infectionwithgonorrhea,chlamydia,andtrichomoniasis wasassociatedwithspeci fi curinecultureresults. Speci fi cally,weattemptedtodeterminethefrequencyof STIsandhavingaurinecultureyield10,000ormore colony-formingunitspermilliliter(CFU)/mL)ofbacteria. Theresearchquestionwesoughttoanswerwasasfollows: Forawomansuspectedofhavingorfoundtohave gonorrhea,chlamydia,ortrichomoniasisduringtheED encounterwhohasgenitourinaryconcerns,arethe in fl ammatorychangesobservedonurinalysismostlikely causedonlybytheSTI,orisconcurrentbacteriuria (eg,UTI)contributing?
Dataset
Weusedanexistingdatasetof75,000EDencountersof patients ≥18yearsinagefromasinglehealthsystem.11–22 All patientsinthedatasetreceivedtestingforgonorrhea, chlamydia,ortrichomoniasisorunderwentbothurinalysis andurineculture.Patientsundergoingonlyurinalysis, regardlessofSTItesting,werenotincludedinthedataset.All EDencounterstookplaceApril18,2014–March7,2017. Thedatasetwascreatedbytheinstitution’sinformation technologyteamwhoextractedretrospectivedatafromthe electronichealthrecords(EHR).Forouranalysis,we includedwomenwhowerenotadmittedtothehospitaland whohadanucleicacidamplificationtest(NAAT)for gonorrhea,chlamydia,ortrichomoniasisorhadavaginal wetmount.DataontheNAATswabsitewerenotavailable. IndividualpatientscouldhavemorethanoneEDencounter. Ourprojectwasapprovedbytheinstitutionalreviewboard withanexemptionfromfullreview,andinformedconsent waswaived.Articleshavebeenpublishedusingthe originaldataset.11–22
Patientsinthedatasetwereidentifiedashaving trichomoniasisiftheparasitewasseenwithurinemicroscopy (amethodhavingverylowsensitivitybuthighspecificity), vaginalwetmount(moderatesensitivityandhigh specificity),orNAAT(highsensitivityandspecificity).22–24 Toavoidmulticollinearityinthemultivariableanalysis,we consolidated findingsfromvaginalwetmountandurine microscopyfor Tvaginalis intoasinglevariablelabeled T vaginalis infectionstatusknownduringtheEDencounter. The Tvaginalis NAAT(Aptima,Hologic,Inc,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Thereisanoverlapinthesigns,symptoms, and fi ndingsonurinalysisforwomenwith urinarytractinfections(UTIs)andsexually transmittedinfections(STIs).
Whatwastheresearchquestion?
Forawomansuspectedofhavingorfoundto haveanSTI,arethein fl ammatorychanges observedonurinalysismostlikelycausedonly bytheSTI,orcouldshehave concurrentbacteriuria?
Whatwasthemajor findingofthestudy?
Afteradjustingforcovariates,noassociation wasobservedbetweenurinecultureresults andtestingpositiveforanSTI,suggesting concurrentSTIandbacterialUTI areunlikely.
Howdoesthisimprovepopulationhealth?
ConcurrentSTIsandbacterialUTIs areunlikely.
Marlborough,MA)result,orthe Neisseriagonorrhoeae or Chlamydiatrachomatis NAAT(Aptima),wasconsidered separatelybecausetheresultwasnotobtaineduntilafterthe EDvisit.Womenmayhavetestedpositivefor Tvaginalis by morethanonetestduringtheirencounter,andanypatient withapositive Tvaginalis testwasconsideredtobeinfected with Tvaginalis. AllSTItestingwasperformedatthe discretionofthetreatingclinician.
Wereportedthevaginalwetmountasnotperformedifthe patienthadnoresultsfromthevaginalwetmountforwhite bloodcells(WBC),yeast, Tvaginalis ,orcluecells.The vaginalwetmountWBCswereanalyzedas0–10/11ormore cellsperhigh-power field(HPF).16 Forthevaginalwet mount,yeast,cluecells,and Tvaginalis werereportedbythe clinicallaboratoryaspresentorabsent.
Weconsideredaurinalysistohavebeenperformedifany componenttestfromtheurinalysiswasreported.Theurine samplewasreportedtohavebeencollectedbythefollowing methods:cleancatch/voided;missingornotdocumentedby nursing;or “other” (eg,bladdercatheter,straightcatheter, ileostomy,nephrostomy,suprapubic,orurostomy).From theurinalysis,weconsideredthefollowingvariables:bacteria (0–4+);blood(0–3+);glucose(positiveornegative);ketones
(positiveornegative);leukocyteesteraselevel(0–3+);mucus (0–4+);nitrites(positiveornegative);protein(positiveor negative);redbloodcells(RBC)(0–101cells/HPF); Trichomonas (positiveornegative);WBCclumps(positive vsnegative);WBCs(0–101cells/HPF);andyeast(presentor absent).IfarangeofurineRBCsandWBCswasreported, weusedthemedianoftherangeintheanalysis,andifmore than100cells/HPFwerereported,weusedtheresult “101 cells/HPF” foranalysis.Allurinetestswereorderedatthe discretionofthetreatingclinician.
Weincludedthefollowingdemographicandtriage informationifitwasavailableduringtheEDencounter: methodofEDarrival;maritalstatus;age;race;andthetriage EmergencySeverityIndex.Ageinyearswasconvertedtoa categoricalvariabletoaccountforthenonlinearrelationship withSTIs.25
WomenwereconsideredtohaveaUTIdiagnosisifthey hadaspecificEDcodeonthe InternationalClassi fi cationof Diseases,9 th or10 th Rev(ICD-9/ICD-10) (Supplement1). Womenwereconsideredpregnantiftheyhadadocumented positivepregnancytestoraspecific ICD-9 or ICD-10 code(Supplement1).
Wesummarizedcontinuousvariablesasmedianand interquartilerange,withanalysisofvariance F testsusedto testassociations.Wereportedcategoricalvariablesascounts andpercentages,witha χ 2 testusedtotestassociations.We perfomedmultinomiallogisticregressionanalysis accountingformultipledemographic,clinical,and diagnostictestingvariables,withtheWaldtestusedto determine P values.Multivariableanalyseswereperformed forpatientswhohadcompletedataforallmodelcovariates. Oddsratiosand95%confidenceintervalswerecalculated fromthemultivariablemodel.A P valuelessthan.05was consideredsignificant.Weconductedstatisticalanalyses withstatisticalsoftwareJMPPro14(JMPStatistical Discovery,LLC,Cary,NC)andSASversion9.4(SAS Institute,Inc,Cary,NC).
Amongthe75,000EDencountersintheoriginaldataset, 16,755womenmetourinclusioncriteria.Asummaryofthe clinicalencountersisshownin Table1.Amongthe1,631 patientencounterswithapositivetestresultforgonorrhea, chlamydia,orboth,1,443(88.5%)hadurinalysis,443 (27.2%)hadurineculture,and438(26.9%)hadboth urinalysisandurineculture.Amongthe1,354womenwith Tvaginalis identifiedonvaginalwetmountand418women withapositiveNAATresultfor Tvaginalis ,1,203(88.8%) and374(89.5%)patients,respectively,hadurinalysis.
Table2 showsencounterswithapositiveSTItestresultand theresultsoftheurineculture.Amongthe443patientswith gonorrhea,chlamydia,orbothwhohadaurineculture
result,341(77.0%)hadlessthan10,000CFU/mLofbacteria, and102(23.0%)had10,000ormoreCFU/mLofbacteriain theurineculture.
Intotal,1,804patientencountershadapositivetestresult for Trichomonas byurinemicroscopy,vaginalwetmount,or NAAT.Ofthese,1,612(89.4%)hadaurinalysistestresult, 548(30.4%)hadaurinecultureperformed,and538(29.8%) hadbothaurinalysisandurinecultureresult.Atotalof9,650 clinicalencountershadcompleteobservationsforallmodel covariatesandwereincludedinthemultivariableanalysis (Table3).Thisnumberincluded2,414patientencounters withlessthan10,000CFU/mLofbacteria,722patientswith 10,000ormoreCFU/mLofbacteria,and6,514patientswith nourinecultureperformed.
Thefollowingvariablesweresignificantlymorelikelyto beassociatedwithaurineculturewith10,000ormore CFU/mLcomparedwithlessthan10,000CFU/mL:higher bacteriuriaonurinalysis;higheramountofbloodintheurine nitrite-positiveurinepresenceofurinaryWBCclumps; higherurinaryWBCcount;andfewerWBCsonthevaginal wetmount(all P ≤ 0.01; Table3).Thesevariableshada significantlylowerlikelihoodofbeingassociatedwithaurine culturewith ≥10,000CFU/mL:no Tvaginalis NAATresult (comparedwithanegative Tvaginalis NAAT)andprotein intheurine(both P ≤ 0.01; Table3).Thefollowingvariables weresignificantlymorelikelytobeassociatedwith ≥10,000 CFU/mLofbacteriaintheurineculture(comparedwithno urinecultureperformed):married/lifepartner(vssingle); higherbacteriuriaonurinalysis;higherurineleukocyte esteraselevel;nitrite-positiveurine,proteinintheurine, presenceofurinaryWBCclumps,UTIdiagnosedintheED, andhigherurinaryWBCcount(all P ≤ 0.02; Table3).These variableshadasignificantlylowerlikelihoodofbeing associatedwithaurineculturewith ≥10,000CFU/mL (comparedwithnourinecultureperformed):no Tvaginalis NAATresult(comparedwithanegative Tvaginalis NAAT),proteinintheurine,andnovaginalwetmountclue cells(comparedwithpresent)(all P ≤ 0.01; Table3). Neisseriagonorrhoeae or CtrachomatisdetectedbyNAAT, orknown Tvaginalis infectionintheED,wasnot associatedwithaurinecultureyielding10,000ormore CFU/mL.Additionally,UTIdiagnosedintheED wasnotassociatedwithaurinecultureyielding 10,000ormoreCFU/mLcomparedwithlessthan 10,000CFU/mL.
BothUTIsandSTIscanhaveoverlappingsignsand symptomsandcancauseinflammatorychangesintheurine. DistinguishingbetweenUTIandSTIcanbechallengingin theED.5,6,26 Wesoughttoassesstherelationshipbetween bacteriuriaandSTIs.Ourresearchquestionwasasfollows: Forawomansuspectedofhavingorfoundtohave gonorrhea,chlamydia,ortrichomoniasisduringtheED
Table1. Demographicsandclinicalcharacteristicsbyurinecultureresult.
Characteristic
(N = 16,755)
(n = 12,372)
Urineculture, <10,000 CFU/mL(n = 3,534)
Urineculture, ≥10,000 CFU/mL(n = 849) P
Age,y,no.(%) .002a
18–2810,524(62.8)7,769(62.8)2,201(62.3)554(65.3)
29–394,328(25.8)3,252(26.3)894(25.3)182(21.4)
≥401,903(11.4)1,351(10.9)439(12.4)113(13.3)
Race,no.(%)(n = 16,683)(n = 12,311)(n = 3,523) <.001a
Black14,855(89.0)11,090(90.1)3,017(85.6)748(88.1)
NotBlack1,828(11.0)1,221(9.9)506(14.4)101(11.9)
Maritalstatus,no.(%)(n = 16,708)(n = 12,336)(n = 3,526)(n = 846) <.001a
Marriedorlifepartner1,488(8.9)1,050(8.5)359(10.2)79(9.3)
Separated,divorced, orwidowed
670(4.0)460(3.7)168(4.8)42(5.0)
Single14,550(87.1)10,826(87.8)2,999(85.1)725(85.7)
Pregnant,no.(%) <.001a
No13,105(78.2)9,725(78.6)2,681(75.9)699(82.3)
Yes3,650(21.8)2,647(21.4)853(24.1)150(17.7)
ESI,no.(%)(n = 15,793)(n = 11,810)(n = 3,365)(n = 798)0.06a 1and2353(2.2)255(2.2)77(2.3)21(2.6)
311,937(74.7)8,777(74.3)2,574(76.5)586(73.4) 4and53,683(23.1)2,778(23.5)714(21.2)191(23.9)
MechanismofEDarrival, no.(%) (n = 16,663)(n = 12,309)(n = 3,507)(n = 847)0.46a
EMSorpolice1,122(6.7)815(6.6)244(7.0)63(7.4)
Publictransportationor onfoot 852(5.1)630(5.1)170(4.8)52(6.1)
Privatevehicle14,689(88.2)10,864(88.3)3,093(88.2)732(86.4)
Urinespecimensource,no.(%)
Cleancatheter/voidedurine3,309(19.7)0(0.0)2,703(76.5)606(71.4)
Other71(0.4)0(0.0)51(1.4)20(2.4)
Notdocumentedormissing13,375(79.8)12,372(100.0)780(22.1)223(26.3)
NAATfor Chlamydia trachomatis, no.(%)
Negative14,985(89.4)11,123(89.9)3,127(88.5)735(86.6)
Positive1,303(7.8)958(7.7)266(7.5)79(9.3)
Notestresult467(2.8)291(2.4)141(4.0)35(4.1)
NAATfor Neisseria gonorrhoeae,no.(%) <.001a
Negative15,819(94.4)11,745(94.9)3,292(93.2)782(92.1)
Positive477(2.8)342(2.8)104(2.9)31(3.7)
Notestresult459(2.7)285(2.3)138(3.9)36(4.2)
NAATfor Trichomonas vaginalis, no.(%)
Negative4,505(26.9)3,409(27.6)854(24.2)242(28.5)
Positive418(2.5)293(2.4)94(2.7)31(3.7)
Notestresult11,832(70.6)8,670(70.1)2,586(73.2)576(67.8)
(Continuedonnextpage)
Characteristic
DiagnosedwithUTIintheED, no.(%)
<10,000 CFU/mL(n = 3,534)
≥10,000 CFU/mL(n = 849)
No14,849(88.6)11,456(92.6)2,900(82.1)493(58.1)
Yes1,906(11.4)916(7.4)634(17.9)356(41.9)
Treatmentofgonorrheaand chlamydia,no.(%)
No13,593(81.1)10,051(81.2)2,855(80.8)687(80.9)
Yes3,162(18.9)2,321(18.8)679(19.2)162(19.1)
Vaginalwetmount, WBCs/HPF,no.(%)
11–1005,296(31.6)3,716(30.0)1,287(36.4)293(34.5) ≤1010,868(64.9)8,233(66.5)2,119(60.0)516(60.8)
Notperformed591(3.5)423(3.4)128(3.6)40(4.7)
Vaginalwetmount, yeast,no.(%)
Present1,027(6.1)762(6.2)217(6.1)48(5.7)
None14,538(86.8)10,765(87.0)3,036(85.9)737(86.8)
Notperformed1,190(7.1)845(6.8)281(8.0)64(7.5)
Vaginalwetmount,cluecells, no.(%)
None8,826(52.7)6,449(52.1)1,908(54.0)469(55.2)
Present6,941(41.4)5,232(42.3)1,386(39.2)323(38.0)
Notperformed988(5.9)691(5.6)240(6.8)57(6.7)
.001a
Leukocyteesterase(urine) <.001b
No.(missing)14,616(2,139)10,381(1,991)3,403(131)832(17)
Median(IQR)0.0(0.0–1.0)0.0(0.0–1.0)1.0(0.0–2.0)2.0(1.0–3.0)
Range0.0–3.00.0–3.00.0–3.00.0–3.0
Nitrite(urine),no.(%)(n = 14,818)(n = 10,505)(n = 3,480)(n = 843) <.001a
Negative14,257(96.2)10,236(97.4)3,417(98.5)604(71.6)
Positive561(3.8)269(2.6)53(1.5)239(28.4)
WBCs(urine) <.001b
No.(missing)10,692(6,063)7,199(5,173)2,699(835)794(55)
Median(IQR)5.0(2.5–13.0)3.0(2.5–12.5)8.0(2.5–16.0)31.5(10.0–101.0)
Range0.0–101.00.0–101.00.0–101.00.0–101.0
Bacteria(urine) <.001b
No.(missing)10,688(6,067)7,194(5,178)2,700(834)794(55)
Median(IQR)1.0(0.0–1.0)1.0(0.0–1.0)1.0(0.0–1.0)1.0(1.0–2.0)
Range0.0–4.00.0–4.00.0–4.00.0–4.0
Blood(urine) <.001b
No.(missing)14,604(2,151)10,361(2,011)3,411(123)832(17)
Median(IQR)0.0(0.0–1.0)0.0(0.0–1.0)0.0(0.0–1.0)1.0(0.0–2.0)
Range0.0–3.00.0–3.00.0–3.00.0–3.0 (Continuedonnextpage)
Table1. Continued.
Characteristic
Total (N = 16,755)
Nourineculture (n = 12,372)
Urineculture, <10,000 CFU/mL(n = 3,534)
Urineculture, ≥10,000 CFU/mL(n = 849) P value
Glucose(urine),no.(%)(n = 14,809)(n = 10,500)(n = 3,467)(n = 842)0.39a
Negative14,216(96.0)10,092(96.1)3,322(95.8)802(95.2)
Positive593(4.0)408(3.9)145(4.2)40(4.8)
Ketones(urine),no.(%)(n = 14,786)(n = 10,477)(n = 3,467)(n = 842) <.001a
Negative12,220(82.6)8,740(83.4)2,808(81.0)672(79.8)
Positive2,566(17.4)1,737(16.6)659(19.0)170(20.2)
Mucus(urine) 0.88b
No.(missing)10,692(6,063)7,202(5,170)2,696(838)794(55)
Median(IQR)1.0(0.0–2.0)1.0(0.0–2.0)1.0(0.0–2.0)1.0(0.0–2.0)
Range0.0–4.00.0–4.00.0–4.00.0–4.0
Protein(urine),no.(%)(n = 14,800)(n = 10,494)(n = 3,464)(n = 842) <.001a
Negative10,553(71.3)7,716(73.5)2,366(68.3)471(55.9)
Positive4,247(28.7)2,778(26.5)1,098(31.7)371(44.1)
RBCs(urine) <.001b
No.(missing)10,693(6,062)7,196(5,176)2,701(833)796(53)
Median(IQR)2.5(2.0–12.5)2.5(1.0–12.5)2.5(2.0–12.5)5.0(2.3–22.8)
Range0.0–101.00.0–101.00.0–101.00.0–101.0
WBCclumps(urine),no.(%)(n = 10,578)(n = 7,116)(n = 2,672)(n = 790) <.001a
None10,118(95.7)6,915(97.2)2,549(95.4)654(82.8)
Present460(4.3)201(2.8)123(4.6)136(17.2)
Yeast(urine),no.(%)(n = 10,628)(n = 7,154)(n = 2,684)(n = 790)0.04a
Present280(2.6)171(2.4)80(3.0)29(3.7)
None10,348(97.4)6,983(97.6)2,604(97.0)761(96.3)
Tvaginalis statusduringED encounter,no.(%) (n = 16,308)(n = 11,987)(n = 3,478)(n = 843) <.001a
Nowetmountperformed720(4.4)451(3.8)216(6.2)53(6.3)
Negativec 14,176(86.9)10,554(88.0)2,922(84.0)700(83.0)
Positive1,412(8.7)982(8.2)340(9.8)90(10.7)
a χ 2 test.
bAnalysisofvariance F test.
cNegativevaginalwetmountandurinemicroscopy(ifperformed).
CFU,colony-formingunits; ED,emergencydepartment; EMS,emergencymedicalservices; ESI,EmergencySeverityIndex; HPF,highpower field; NAAT,nucleicacidamplificationtest; RBCs,redbloodcells; UTI,urinarytractinfection; WBCs,whitebloodcells.
encounterwhohasgenitourinaryconcerns,arethe inflammatorychangesobservedonurinalysismostlikely causedonlybytheSTI,orisconcurrentbacteriuria(eg,UTI) contributing?Ourresultsshowthatinfectionwith gonorrhea,chlamydia,ortrichomoniasiswasnotassociated withalsohavingaurinecultureyielding ≥10,000CFU/mLof bacteriacomparedwith <10,000CFU/mLornourine cultureperformed.Animportant findingwasthatwhen Tvaginalis wasidentifiedduringtheEDencounteronurine microscopyorvaginalwetmount,therewasnosignificant associationwithbacteriaintheurineculture.Whenan emergencyclinicianisevaluatingawomanwith
genitourinaryconcernsandanSTIissuspectedoractually identified,asisthecaseonurinemicroscopyorvaginalwet mountfor Tvaginalis, bacteriuriaisnotmorelikelyto coexist.Our findingssupportrecommendationsforscreening forbothUTIsandSTIsinappropriatepatients.7,8 For instance,womenundergoingpelvicexamination whowerealsodiagnosedwithaUTIintheEDwere subsequentlyfoundtohavehighratesofSTIs.7 However, emergencycliniciansfrequentlydonotscreenforSTIsin womenwithdysuriawhoarediagnosedwithaUTI.8 Furthermore,our findingssupportthoseof smallerstudies.6,27
Table2. PositiveSTItestresultsbyurineculture.a
Urinecultureresult, CFU/mL
Positiveforgonorrhea,chlamydia,orboth onNAAT(n = 1,631)
Positivefor Trichomonasvaginalis bytestmethod
Urinemicroscopy (n = 275)
Vaginalwetmount (n = 1,354) NAAT (n = 418)
Nourineculture1,188(72.8)186(67.6)943(69.6)293(70.1)
0 <10,000341(20.9)71(25.8)326(24.1)94(22.5)
10,000 <100,00015(0.9)5(1.8)16(1.2)6(1.4) >100,00087(5.3)13(4.7)69(5.1)25(6.0)
aDataispresentedasNo.(%).Womenmayhavetestedpositivefor Tvaginalis bymorethan1test. CFU,colony-formingunits; NAAT,nucleicacidamplificationtest; STI,sexuallytransmittedinfection.
Table3. Multinomiallogisticregressionusingurinecultureresultastheoutcomevariable(N = 9,650).
NAATfor Chlamydia trachomatis
NAATfor Neisseria gonorrhoeae
Separated,divorced, orwidowed Single1.04(0.66–
4and51and21.42(0.72–
NotestresultNegative0.87(0.17–
NotestresultNegative1.20(0.23–
NAATfor Trichomonas vaginalis PositiveNegative0.90(0.53–1.52)0.690.95(0.58
MechanismofEDarrivalEMS/policePrivate vehicle
Publictransportation/ onfoot Private vehicle
DiagnosedwithUTIintheEDYesNo1.17(0.94–
Treatmentofgonorrheaand chlamydia YesNo0.79(0.62–
Tvaginalis statusduringED encounter Nowetmount performed Negativec
Bacteria(urine)1-UnitincreaseNone1.13(1.05–1.23) <.0011.19(1.10–1.28) <.001 (Continuedonnextpage)
Glucose(urine)PositiveNegative0.91(0.59–1.42)0.680.98(0.65–1.49)0.93
Ketones(urine)PositiveNegative1.03(0.80–1.31)0.831.13(0.90–1.42)0.31
Leukocyteesterase(urine)1-UnitincreaseNone0.98(0.88–1.09)0.661.16(1.05–1.29) <.001
Mucus(urine)1-UnitincreaseNone0.99(0.92–1.06)0.810.98(0.92–1.05)0.62
Nitrite(urine)PositiveNegative15.7(10.8–22.76) <.0015.72(4.45–7.34) <.001
Protein(urine)PositiveNegative0.71(0.57–0.88).0020.76(0.62–0.93) <.001
WBCclumps(urine)PresentNone1.54(1.10–2.15)0.011.89(1.39–2.56) <.001
Yeast(urine)PresentNone1.18(0.70–1.98)0.531.33(0.82–2.18)0.25
WBCs(urine)1-UnitincreaseNone1.02(1.02–1.02) <.0011.02(1.02–1.02) <.001
Vaginalwetmount,cluecellsPresentNone0.91(0.75–1.11)0.350.78(0.65–0.94) <.001
NotperformedNone0.33(0.06–1.70)0.190.53(0.12–2.43)0.42
Vaginalwetmount,WBCs/HPF11–100 ≤100.68(0.55–0.84) <.0010.84(0.69–1.02)0.09 Notperformed ≤101.01(0.36–2.88)0.980.96(0.35–2.64)0.94
Vaginalwetmount,yeastPresentNone0.96(0.64–1.42)0.820.77(0.53–1.12)0.17 NotperformedNone2.68(0.50–14.45)0.253.50(0.74–16.59)0.11
aCovariateWaldtestfromthemultinomiallogisticregressionmodel.
bAgewasgroupedas18–28,29–39,and ≥40years.
cNegativetestresultbyvaginalwetmountandurinemicroscopy(ifperformed).
CFU,colony-formingunits; ED,emergencydepartment; EMS,emergencymedicalservices; ESI,EmergencySeverityIndex; HPF,highpower field; NAAT,nucleicacidamplificationtest; OR,oddsratio; RBCs,redbloodcells; UTI,urinarytractinfection; WBC,whitebloodcell.
AstudybyPrentissetalshowedthatamongadolescent girlswithurinarytractsymptomsintheED,9%hadanSTI, 57%hadaUTI,and6%hadbothanSTIandaUTI.6
Clinicianaccuracywas83%forSTIsand71%forUTIs, whereasonly23%correctlydiagnosedpatientswithboth UTIandSTI.6 Shapiroetal27 foundthatamong92women withurinarytractsymptoms,STIrateswerenotdifferent betweenwomenwithapositivevsanegativeurineculture (102 CFU/mL).Additionally,aretrospectivestudyofED patientsfoundthatpatientswhoweretreatedforaUTI, testedpositiveforgonorrhea,chlamydia,ortrichomoniasis, andhadpyuriaweresignificantlymorelikelytohavea negativeurineculturethanapositiveurineculture.9
Relianceonpositiveurinenitriteandpyuriatotreatfor UTIinpatientswithconfirmedorsuspectedSTImay resultinovertreatmentwithantibiotics.However,patients withanSTIandapositiveurineculturehadsignificantly higherurineleukocytesthanthosewithnegative cultureresults.9
Wealsofoundthatclinicalencountersinwhichpatients werediagnosedwithaUTIintheEDwerenotmorelikelyto haveaurinecultureof ≥10,000CFU/mLofbacteria comparedwith <10,000CFU/mLPossibly,patientswho werediagnosedwithaUTIbutwhohad <10,000CFU/mL
weremorelikelytohaveanSTI,butthisassociationwasnot examinedinthecurrentstudy.Becausethediagnosisofa UTIwasnotpartofourinclusioncriteria,notallwomen withaUTIdiagnosisarerepresentedinourcohort.Wewere abletostudyonlywomenwhohadbothaurinalysisand urineculture,notjustaurinalysis.Therefore,theassociation betweenaUTIdiagnosisandbacteriuriadeserves furtherinvestigation.
Althoughourstudyusedalargedataset,ithassome limitations.First,notallwomenfromourdatasetunderwent urinalysis,urineculture,vaginalwetmount,andNAATfor STIs.Furthermore,notallwomendiagnosedwithaUTI underwentSTItestingoravaginalwetmount.Second, modeling Tvaginalis intheEDhasinherentlimitations becausetheurinalysisandvaginalwet-mountresultsare availabletotheclinicianduringtheencounter,buttheylack highsensitivity,whereasNAATishighlysensitiveand specificbuttypicallydoesnotyieldresultsduringthepatient encounter.Third,womenundergoingSTItestingwhoalso hadaurineculturemayhavebeenmorelikelytobe concernedabouturinarysymptoms,whichcouldhavebiased ouranalysistothosewomenwithgenitourinaryconcerns. Table3. Continued.
Becausewewereunabletoincludehistoryandphysical examination findingsinouranalysis,wecouldnot differentiatebetweenpatientswithmoregenital concernsandthosehavingmoreurinarysymptoms. Alternatively,somewomenincludedintheanalysismay havehadasymptomaticbacteriuriaoranasymptomaticSTI, althoughthispossibilityisthoughttobelesslikely. Wedidnotattempttodifferentiatebetween contaminatedurineculturesandthoseyielding classicuropathogens.5
Fourth,ourdatasetrepresentedalimitedgeographical areaintheUS,andthepatientswerepredominantlyBlack; therefore,ourresultsmaynotbegeneralizabletoother locationsandraces.Fifth,thedatadidnotincludepediatric patientsormen;soourresultscannotbeextrapolatedto thosegroups.Sixth,patientswhoweretreatedpresumptively forSTIswithoutspecifictestingwereexcludedfrom analysis,andthiscouldhaveresultedinselection bias.Finally,inherentlimitationsexisttousinga datasetextractedfromtheinstitution’sEHRand ICD codes.
Inourregressionanalysis,positivegonorrhea,chlamydia, andtrichomoniasistestresultswerenotassociatedwith bacteriuriayielding ≥10,000CFU/mLcomparedwith <10,000CFU/mLornourinecultureobtained.
AddressforCorrespondence:JohnathanM.Sheele,MD,MHS, MPH,MayoClinic,DepartmentofEmergencyMedicine, 4500SanPabloRd.,Jacksonville,FL32224. Email: sheele.johnathan@mayo.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Sheeleetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.LongBandKoyfmanA.Theemergencydepartmentdiagnosisand managementofurinarytractinfection. EmergMedClinNorthAm. 2018;36(4):685–710.
2.Flores-MirelesAL,WalkerJN,CaparonM,etal.Urinarytractinfections: epidemiology,mechanismsofinfectionandtreatmentoptions. NatRev Microbiol. 2015;13(5):269–84.
3.BarrowRY,AhmedF,BolanGA,etal.Recommendationsforproviding qualitysexuallytransmitteddiseasesclinicalservices,2020. MMWR RecommRep. 2020;68(5):1–20.
4.CrowleyJS,GellerAB,VermundSH. SexuallyTransmittedInfections: AdoptingaSexualHealthParadigm.Washington,DC:National AcademiesPress;2021.
5.TomasME,GetmanD,DonskeyCJ,etal.Overdiagnosisofurinarytract infectionandunderdiagnosisofsexuallytransmittedinfectioninadult womenpresentingtoanemergencydepartment. JClinMicrobiol. 2015;53(8):2686–92.
6.PrentissKA,NewbyPK,VinciRJ.Adolescentfemalewithurinary symptoms:adiagnosticchallengeforthepediatrician. PediatrEmerg Care. 2011;27(9):789–94.
7.BergE,BensonDM,HaraszkiewiczP,etal.Highprevalenceofsexually transmitteddiseasesinwomenwithurinaryinfections. AcadEmerg Med. 1996;3(11):1030–4.
8.WilbanksMD,GalbraithJW,GeislerWM.Dysuriaintheemergency department:misseddiagnosisof Chlamydiatrachomatis WestJEmerg Med. 2014;15(2):227–30.
9.ShipmanSB,RisingerCR,EvansCM,etal.Highprevalenceofsterile pyuriainthesettingofsexuallytransmittedinfectioninwomen presentingtoanemergencydepartment. WestJEmergMed. 2018;19(2):282–6.
10.HuppertJS,BiroFM,MehrabiJ,etal.Urinarytractinfectionand chlamydiainfectioninadolescentfemales. JPediatrAdolescGynecol. 2003;16(3):133–7.
11.BonnerM,SheeleJM,Cantillo-CamposS,etal.Adescriptiveanalysisof mendiagnosedwithepididymitis,orchitis,orbothintheemergency department. Cureus. 2021;13(6):e15800.
12.CamposSC,ElkinsJM,SheeleJM.Descriptiveanalysisofprostatitisin theemergencydepartment. AmJEmergMed. 2021;44:143–7.
13.ElkinsJM,HamidOS,SimonLV,etal.AssociationofBartholincystsand abscessesandsexuallytransmittedinfections. AmJEmergMed. 2021;44:323–7.
14.ElkinsJM,Cantillo-CamposS,SheeleJM.Frequencyofcoinfectionon thevaginalwetpreparationintheemergencydepartment. Cureus 2020;12(11):e11566.
15.ElkinsJM,Cantillo-CamposS,ThompsonC,etal.Descriptive evaluationofmaleemergencydepartmentpatientsintheUnitedStates withgonorrheaandchlamydia. Cureus. 2020;12(10):e11244.
16.SheeleJM,ElkinsJM,MohseniMM,etal.Vaginalleukocytecountsfor predictingsexuallytransmittedinfectionsintheemergencydepartment. AmJEmergMed. 2021;49:373–7.
17.MohseniM,SimonLV,SheeleJM.Epidemiologicandclinical characteristicsoftubo-ovarianabscess,hydrosalpinx,pyosalpinx, andoophoritisinemergencydepartmentpatients. Cureus. 2020;12(11):e11647.
18.MohseniMM,BenardRB,Mead-HarveyC,etal.Sexuallytransmitted infectionsintheemergencydepartmentarenotassociatedwithholidays orschoolbreaks. AmJEmergMed. 2021;45:642–4.
19.SheeleJM,LibertinCR,FinkI,etal.Alkalineurineintheemergency departmentpredictsnitrofurantoinresistance. JEmergMed. 2022;62(3):368–77.
20.SheeleJM,NiforatosJD,ElkinsJM,etal.Predictionmodelfor gonorrhea,chlamydia,andtrichomoniasisintheemergency department. AmJEmergMed. 2022;51:313–9.
21.FoxHTandSheeleJM.Associationofmaritalstatusinthetestingand treatmentofsexuallytransmittedinfectionsintheemergency department. Cureus. 2021;13(8):e17489.
22.LawingLF,HedgesSR,SchwebkeJR.Detectionoftrichomonosisin vaginalandurinespecimensfromwomenbycultureandPCR. JClin Microbiol. 2000;38(10):3585–8.
23.BlakeDR,DugganA,JoffeA.Useofspunurinetoenhancedetectionof Trichomonasvaginalis inadolescentwomen. ArchPediatrAdolesc Med. 1999;153(12):1222–5.
24.ChapinKandAndreaS.APTIMA® Trichomonasvaginalis,a transcription-mediatedamplificationassayfordetectionof Trichomonas vaginalis inurogenitalspecimens. ExpertRevMolDiagn 2011;11(7):679–88.
25.WorkowskiKA,BachmannLH,ChanPA,etal.Sexuallytransmitted infectionstreatmentguidelines,2021. MMWRRecommRep. 2021;70(4):1–187.
26.SheeleJM,SmithJ,NiforatosJD,etal.History,physicalexamination, andlaboratory findingsassociatedwithinfectionandtheempiric treatmentofgonorrheaandchlamydiaofwomenintheemergency department. Cureus. 2019;11(12):e6482.
27.ShapiroT,DaltonM,HammockJ,etal.Theprevalenceofurinarytract infectionsandsexuallytransmitteddiseaseinwomenwithsymptomsof asimpleurinarytractinfectionstratifiedbylowcolonycountcriteria. AcadEmergMed. 2005;12(1):38–44.
Yu-ShiuanLin,MD*
Chih-ChengLai,MD†
Yu-ChangLiu,MD‡§
Shu-ChunKuo,MD*∥
Shih-BinSu,MD,PhD¶#
*ChiMeiMedicalCenter,DepartmentofOphthalmology,Tainan,Taiwan
† ChiMeiMedicalCenter,DivisionofHospitalMedicine,DepartmentofInternalMedicine, Tainan,Taiwan
‡ ChiMeiMedicalCenter,DepartmentofEmergencyMedicine,Tainan,Taiwan
§ NationalChengKungUniversity,CollegeofMedicine,DepartmentofEnvironmentaland OccupationalHealth,Tainan,Taiwan
∥ ChungHwaUniversityofMedicalTechnology,DepartmentofOptometry,Jen-Teh, Tainan,Taiwan
¶ ChiMeiMedicalCenter,DepartmentofOccupationalMedicine,Tainan,Taiwan
# ChiMeiMedicalCenter,DepartmentofFamilyMedicine,Tainan,Taiwan
SectionEditor:WirachinHoonpongsimanont,MD,MSBATS
Submissionhistory:SubmittedFebruary12,2023;RevisionreceivedJanuary11,2024;AcceptedJanuary17,2024
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.17882
Introduction: Photokeratoconjunctivitis(PKC)isprimarilycausedbywelding.However,inappropriate useofgermicidallamps,whichhavebeenwidelyusedfollowingtheCOVID-19outbreak,canalsocause PKC.OurgoalinthisstudywastoinvestigatetheincidenceofandchangesinthecausesofPKCduring thecoronavirus2019(COVID-19)pandemic.
Methods: Weconductedasingle-center,retrospectiveobservationalstudy.Thehealthrecordsof patientswhovisitedtheemergencydepartmentinatertiarycarehospitalfromJanuary1, 2018–December31,2021andwerediagnosedwithPKC,werereviewed.Wethenconductedan analysistocomparethecharacteristicsofPKCbeforeandafterCOVID-19beganandthefeaturesof PKCcausedbyweldingandgermicidallamps.
Results: Therewere160PKCcaseswithaclearetiologybeforetheCOVID-19pandemicand147cases duringtheCOVID-19pandemic.Nosignificantdifferencesinageandgenderweredetectedbetweenthe twogroups.TheincidenceofPKCinducedbytheuseofgermicidallampsduringtheCOVID-19 pandemicwassignificantlyhigher(10.2%)thantheincidencebeforethepandemic(3.1%).Theratioof femalestomalesinthegermicidallampsubgroupwassignificantlyhigherthantheratiointhewelding subgroup.Limitationsincludedincompleteinformationduetotheretrospectivenatureofthestudy, underestimationofincidence,andpossiblerecallbias.
Conclusion: IntheeraofCOVID-19,cliniciansshouldbeawareofthehazardsofgermicidallamps. AlthoughtheCOVID-19pandemicseemstoshowsignsofeasing,newinfectiousdiseasesthatrequire protectivemeasurescouldstillemergeinthefuture.Therefore,injuriesrelatedtogermicidallamps deservemorepublichealthattention.[WestJEmergMed.2024;25(3)368–373.]
Keywords: COVID-19;SARS-CoV-2;ultravioletlight;photokeratoconjunctivitis;germicidallamp; welding.
Photokeratoconjunctivitis(PKC),orphotophthalmia,is relatedtoultravioletradiation(UVR)exposure.Exposureto ultravioletB(UV-B)andultravioletC(UV-C)candamage theocularsurface,includingthecornealorconjunctival epithelialcells.1 Theclinicalmanifestationsincludeocular painorforeignbodysensation,tearing,photophobia,and evenblurredvisioninseverecases.Thephotochemical reactiontypicallytakes6–12hourstocausesymptoms.2 Therefore,patientsoftenexperiencesymptomsatnightafter daytimeexposure,leadingtoemergencydepartment(ED) visitsatnight.3 ExposuretoUVRcanbeclassifiedinto naturalandartificialsources.Naturalsourcesincludedirect orreflectedsunlightduringskiingortimespentatthebeach.4 Artificialsourcesincludeworkplacewelding flashes,which arethemostcommoncauseofPKC,andcuringlights, printingmachines,high-techindustrialprocesses,laser engravers,andgermicidallamps.3
Thecoronavirusdisease2019(COVID-19)iscausedby thesevereacuterespiratorysyndromecoronavirus2(SARSCoV-2).TheCOVID-19outbreakbeganinDecember2019 andwasdeclaredapandemicbytheWorldHealth Organizationin2020.5,6 Tocontrolthespreadofthishighly contagiousvirus,severalpreventativeandcontrolmeasures wereimplemented,includingwearingmasks,social distancing,handhygiene,anduseofpersonalprotective equipmentanddisinfectants,suchasdilutedbleachsolutions or70%ethanol.6,7 Ultraviolentradiationwasinvestigated forirradiationofthecoronavirus8;UVRdisinfectsby damagingDNAstructures,includingviralDNA.Different wavelengthshavedifferentdisinfectingeffects.9 The potentialhazardofgermicidallampstotheeyeswas recognizedbeforetheCOVID-19pandemic.10,11 However, germicidallampuseincreasedsignificantlyduringthe COVID-19pandemic,andtheincreasedusagemayleadto morecasesofPKC.
ChangesinophthalmicEDvisitsaftertheCOVID-19 pandemicbeganwererecentlydiscussed.Adecreased numberofoveralleyeinjurieswasnotedinseveral studies.12,13 Additionally,severalstudiesreportedcasesof PKCduetogermicidallampsaftertheCOVID-19pandemic began,andaneight-weekcomparisonstudysuggestedan upwardtrend.14–16 However,long-termdataaboutthe causesofPKCaftertheCOVID-19pandemicislimited.In thisstudyweaimedtoinvestigatetheincidenceofand changesinthecausesofPKCbeforeandafterthe COVID-19pandemic.
Wedividedpatientsintotwogroups:patientswithPKC beforetheCOVID-19pandemic(betweenJanuary1, 2018–December31,2019)andpatientswithPKCafterthe COVID-19pandemicbegan(betweenJanuary1,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Photokeratoconjunctivitis(PKC)ismainly causedbywelding.Germicidallamps,which alsocausePKCifimproperlyused,were widelyusedaftertheCOVID-19outbreak.
Whatwastheresearchquestion?
Whataretheincidenceofandchangesinthe causesofPKCduringtheCOVID-19 pandemic(overatwo-yearperiod)?
Whatwasthemajor findingofthestudy?
TheincidenceofPKCinducedbyuseof germicidallampsincreasedsigni fi cantlyafter COVID-19began(10.2%vs3.1%).
Howdoesthisimprovepopulationhealth?
Thepotentialinjuriesfromgermicidallamps deservemorepublichealthattentionboth duringtheCOVID-19eraandfornew infectiousdiseasesinthefuture.
2020–December31,2021).Demographicdata,including gender,age,month,time,etiology,occupation,andexposure time,werecollected.
Patientswhovisitedthetertiary-carecenterEDin TaiwanbetweenJanuary1,2018 –December31,2021and werediagnosedwithPKCwereenrolledinthestudy. Photokeratoconjunctivitiswasdiagnosedaccordingtothe followingcriteria:UVexposurehistorywithinoneday; typicalsymptoms,includingocularforeignbodysensation, pain,photophobia,andtearing;andophthalmicclinical fi ndings,suchasconjunctivalhyperemiaandcorneal super fi cialpunctatelesions.Weexcludedpediatricpatients, giventhepossibilityofuncooperativephysicalandocular examination.BasedonthecausesofPKCmentionedinthe medicalrecords,patientsweredividedintothreegroups basedontheetiology:germicidallamps;welding;andother. Patientswhosemedicalrecordsspeci ficallymentionedthe useofgermicidallampswereassignedtothegermicidal lampgroup,patientswhosemedicalrecordsmentioned exposuretoweldingwereassignedtotheweldinggroup, andthosewhosecauseswereunknownorrelatedtodirector re fl ectivesunlightwereassignedtotheothersgroup. ThisstudywasapprovedbytheInstitutionalReviewBoard
ofChiMeiMedicalCenter,Tainan,Taiwan(Applicant’ s No:11108-010).
Theprimaryoutcomeofthestudywastheincidenceand causesofPKCbeforeandafterCOVID-19began.The secondaryoutcomewasthecharacteristicsofthegermicidal lampandweldinggroups.
WeanalyzeddatausingSPSSStatisticsforWindows, version22(IBMCorp,Armonk,NY).ThePearsonchisquaredtestandFisherexacttestwereusedtocompare categoricalvariables.Continuousvariableswerecompared usingtheStudent t -test.Thethresholdforstatistical significancewasdefinedasa P -valuelessthan0.05.
PatientCharacteristics
Duringthestudyperiod,307PKCpatientswererecruited. FewercasesofPKCoccurredafterCOVID-19began(147vs 160)comparedwiththenumberofPKCcasesbeforethe COVID-19period.Themeanpatientageswere41.85 ± 0.97years(range,20–71years)beforeCOVID-19and 40.07 ± 1.09years(range,20–78years)afterCOVID-19.No significantdifferencesinageorgenderweredetectedbetween thegroupsbeforeandafterCOVID-19began.Amajorityof patientswenttotheEDatnight;90%wenttotheED between8 PM–07:59 AM,andthemostprevalentperiodwas 12 AM–03:59 PM.ThecharacteristicsofthepatientswithPKC aresummarizedin Table1.
IncidenceandDemographicDataofGermicidalLamprelatedPKC
ThetotalnumberofPKCcasesslightlydecreasedafterthe COVID-19pandemicbegan.TheetiologiesofPKCwere differentbeforeandafterCOVID-19began.Thepercentage ofpatientsinthegermicidallampgroupbeforeCOVID-19 (5,3.1%)waslowerthanthepercentageofpatientsinthe germicidallampgroupafterCOVID-19began(15,10.2%); thus,theincidenceofPKCinthegermicidallampgroup increasedsignificantlyafterCOVID-19began(P = 0.03). Withinthegermicidallamp-relatedPKCsubgroup,themean ageswere39.20 ± 3.69years(range,31–51years)and42.73 ± 3.88years(range,21–78years)beforeandafterCOVID-19 began,respectively,andnosignificantdifferencesinageor genderweredetectedbetweenthegroups(Table2).All patientsinthegermicidallampgroupwenttotheED between8 PM–07:59 AM
ComparisonBetweentheWeldingandGermicidal LampGroups
MostpatientswithPKCweremales(morethan90% beforeandafterCOVID-19began),andmostpatientsinthe
Table1. Characteristicsofpatientswithphotokeratoconjunctivitis.
Before COVID-19 (N = 160)
After COVID-19 (N = 147) P value
Age:mean ± SD41.85 ± 0.9740.07 ± 1.090.22
Gender(%)0.88
Male154(96.3)141(95.9)
EtiologyofPKC(%) P = 0.03
Welding144(90.0)118(80.3)
Germicidallamp5(3.1)15(10.2)
Othercauses11(6.9)14(9.5)
TimeofEDvisit(%)0.89
00:00–03:59100(62.5)93(63.3)
04:00–07:5918(11.3)16(10.9)
08:00–11:592(1.3)2(1.4)
12:00–15:591(0.6)2(1.4)
16:00–19:592(1.2)3(2.0)
20:00–23:5937(23.1)31(21.1)
COVID-19,coronavirusdisease2019; ED,emergencydepartment; PKC,photokeratoconjunctivitis.
Table2. Demographicdataofpatientswithgermicidallamp-induced photokeratoconjunctivitisbeforeandafterCOVID-19began. Before COVID-19 (n = 5) After COVID-19 (n = 15)
Male2(40.0)10(66.7)
TimeofEDvisit(%)0.51
00:00–03:592(40)10(66.67)
04:00–07:591(20)1(6.67)
08:00–11:590(0)0(0)
12:00–15:590(0)0(0)
16:00–19:590(0)0(0)
20:00–23:592(40)4(26.67)
*Fisherexacttest.
COVID-19,coronavirusdisease19; ED,emergencydepartment; PKC,photokeratoconjunctivitis.
weldingsubgroupweremales(Tables1 and 3).However,the percentageoffemalesinthegermicidallampsubgroupwas higherthanthepercentageoffemalesintheweldinggroup (P < 0.001).ThetimespatientswenttoEDwerenot significantlydifferentbetweenthegermicidallampgroup andtheweldinggroup.
Table3. Thecomparisonbetweenthephotokeratoconjunctivitis subgroupsofgermicidallampandwelding.
InformationAboutIndividualsintheGermicidal LampGroup
Informationaboutpatientsinthegermicidallampgroup ispresentedin SupplementalTables1and2).Theexposure durationrangedfromafewsecondstotwohours.The domesticcomponentaccountedfor60%(3/5)ofthePKC casesbeforeCOVID-19and40%(6/15)ofthecasesafter COVID-19began.BeforeCOVID-19,theoccupational componentincludedmedicalpersonnel/staff(2/5).After COVID-19began,theoccupationalcomponentexpandedto medicalstaff(3/15),workersintherestaurantandhotel industry(3/15),acleaner(1/15),aschoolemployee(1/15), andaconstructionindustryworker(1/15).
Inthisstudywecomparedtheincidenceandcausesof PKCbeforeandafterCOVID-19began.Weselected January1,2020,asthestartingpointfortheobservation periodfortwoprimaryreasons.The firstreasonwasthe
geographicalproximitybetweenTaiwanandMainland Chinaandthefrequentbusinesstripsbetweenthetwo nations.Secondly,basedonthepreviouspainfulexperience oftheSARSoutbreakinTaiwanin2003,ourgovernment andpeopletreatedthisincidentwithgreatcautionatavery earlystage.AtapressconferenceonDecember31,2019,the TaiwanMinistryofHealthandWelfare,announced epidemicinformationandinitiationofaborderquarantine inaccordancewithstandardprocedure.
Theproportionofgermicidallamp-relatedPKCcases significantlyincreasedafterCOVID-19began.Theincrease inPKCcasesisattributedtotheincreasednumberof germicidallamp-relatedPKCcasesandthedecreased numberoftotalPKCcases.ThenumberofgermicidallamprelatedPKCcaseslikelyincreasedafterCOVID-19began duetotheincreaseduseoftheselampsfordisinfection. Previousstudiesconcerninggermicidallamp-relatedPKC casesafterCOVID-19beganareshownin Table4.Leung reportedthreecases(sixeyes)inHongKongandSengillo reportedsevencases(14eyes)intheUnitedStates.Wangetal comparedgermicidallamp-relatedPKCcaseseightweeks beforeandeightweeksafterCOVID-19beganandreported thepercentageofPKCduetodisinfectionincreased significantlyfrom9.1%to56.9%afterCOVID-19began.14 Wangetalalsomentionedthatthecasenumberdecreased substantiallyaftergoodpublichealtheducation.InTaiwan, germicidallampshadproductinstructionsandwarnings aboutimproperuse.Thenewsmediaalsoemphasizedthe hazardsofgermicidallamps.Despitethespreadofpublic educationontheuseofgermicidallamps,somepatientswere
Table4. Summaryofrecentstudiesaboutgermicidallamp-inducedphotokeratitisafterCOVID-19pandemicbegan.
Reference
Wang 202114 109cases inChina
Sengillo 202115 7cases (14eyes) inUSA
Leung 202116 3cases (6eyes)in HongKong
Lin202215cases inTaiwan
Retrospective32.1(range, 21–54) M:F = 55:54NorecordAverage:16.7 minutes
Caseseries40(range, 24–59)
CasereportOneis17;no recordabout othertwo patients
Retrospective42.7(range, 21–78)
M:F = 5:2P3:38W UV-C germicidal lamp(AURA)
± 0.02 logMAR
P6:38W UV-C germicidal lamp(Uvlizer) 10minute-4 hoursin5 cases,2 without documentation 20/30or betterin 13/14eyes (93%) Norecord
M:F = 1:2UV-C Effective illumination area:40m2 15,20,60 minutes
All3were 6/12 bilaterally
All3were6/6 bilaterally
M:F = 10:5Norecordfewseconds to2hours,5 caseswithout documentation NorecordNorecord
UV,ultraviolet; VA,visualacuity; M:F,maletofemale; logMAR;logarithmoftheminimumangleofresolution.
unawareofthedangers.However,publiceducationmay havepreventedupwardspikesintheincidenceofPKC.
OurstudyalsoshowedthatthenumberoftotalPKC(160 before;147after)patientsandthenumberofpatientsinthe weldingsubgroup(144before;118after)slightlydecreased afterCOVID-19began.Thereareseveralexplanationsfor thisdecrease.First,patientsdidnotgototheEDdueto concernsaboutSARS-CoV-2.17,18 Second,theoutbreak forcedmanycompaniesandfactoriestohaltproduction (lockdown),whichpredominantlyinfluencedshort-termor part-timeworkers.AccordingtoastudybyYenetal,3 longtermworkerscompliedwithsafetyregulationsbetterthan short-termworkersandworeprotectiveequipmentmore. Therefore,theweldingcasesdecreased,andgermicidallamprelatedPKCcasesincreased,leadingtothesignificantly increasedproportionofgermicidallamp-relatedPKCcases afterCOVID-19began.
Thedomesticcomponentinthegermicidallampsubgroup declinedfrom60%(3/5)beforeCOVID-19to40%(6/15) afterCOVID-19began.Incontrast,workplacecases increasedfrom40%(2/5)beforeCOVID-19to60%after COVID-19(9/15)began.This findingimpliesthathospitals/ clinics/nursinghomes,restaurants,andhotelsrequiredmore germicidallampuse.InTaiwan,manyhotelsservedas quarantinehotels,wheregermicidallampswerefrequently usedfordisinfection.InLeung’sreport,thethreecases belongedtoclusteringathome.16 InthestudyofWang etal,14 clusteringplayedanimportantrole.Ourcasesof germicidallamp-relatedPKCwereallsporadicratherthan clusteringepisodes,whichmayindicategoodpublicpolicies andstaffsafetyeducationinmostcompanies andworkplaces.
Therearesomedifferencesbetweenwelding-associated andgermicidallamp-relatedPKC.Thewavelength emanatingfromgermicidallampsismostlyUV-C (254nanometers),andthecornea,whichabsorbsmostofthe UV-C,ispredominantlydamaged.9,19,20 Thewavelength emanatingfromweldingequipmentisintheUV-Bspectrum. Theoretically,theenergyofUV-Cisgreaterthantheenergy fromUV-Band,therefore,causesmoredamagetothe corneaatthesamedistanceandexposuretime.However, mostpreviousstudiesreportedvisualacuityasagood prognosisingermicidallamp-relatedPKCcases(Table4) Becauseitisprimarilymenwhoworkinthewelding industry,theproportionoffemalesinthegermicidal-lamp groupwassignificantlyhigherthanthefemalesinthewelding groupinourstudyandpreviousstudies.14
Thereweresomelimitationstoourstudy.Duetoits retrospectivenature,somedata(suchasexposuretime, visualacuity,brand,andwavelengthofthemachine)was incomplete.However,thismissingdatadidnotaffectour results.Second,wemayhaveunderestimatedtheincidenceof
germicidallamp-relatedPKC.Ourstudyfocusedonthe adultpopulation;sopediatricpatientsshouldbetakeninto accountinfutureresearch.Inaddition,wedidnotanalyze patientswithoutaclearPKCcausetomaintaintherigorof ourstudy.Thus,theremightberecallbias.Inourclinical experience,patientsdeniedUVRoranyotherstronglight exposureuntiltheywerespecificallyaskedaboutexposureto germicidallampsorUV-enableddishdryers.Ifthemedical staffdidnotdirectlyaskpatientsabouttheirexposureto certainmachines,theexactcauseofthePKCwasdifficultto determine.Third,theresultsmaynotbegeneralizedtoother nationsbecauseofdifferencesinrace,culture,education status,pandemicseverity,andaccessibilitytoUVR machines.Despitetheselimitations,wehopeourstudy focusesmorepublicattentionontherelatedissuesand potentialhazards.Theeffectsofnewsmediaandpublic safetyeducationonthetrendofgermicidallamp-related PKCafter2022mayrequirefurtherstudiestoevaluate.
Germicidallamp-relatedPKCincreasedduringthe COVID-19era.Wefoundthattheincidenceincreased significantlyoveratwo-yearperiodfrom3.1%before COVID-19to10.2%afterCOVID-19began.Whileit appearsthattheCOVID-19pandemicisgraduallysubsiding, itisimportanttorecognizethatnewinfectiousdiseasesmay emergeinthefuture,necessitatingprotectivemeasures. Therefore,cliniciansshouldpayattentiontothispotential causeofPKCandtakemoreaccuratehistories.Thepotential hazardofgermicidallampsisanimportantpublichealth issuethatshouldbeemphasizedtopreventfurtherinjury fromthissourceofultravioletradiation.
WewouldliketothankEnagofortheEnglishrevision.
AddressforCorrespondence:Shih-BinSu,MD,PhD,ChiMei MedicalCenter,DepartmentofOccupationalMedicine,901 ZhonghuaRoad,YongkangDistrict,TainanCity710,Taiwan. Email: shihbin1029@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Linetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
1.YamJCandKwokAK.Ultravioletlightandoculardiseases. Int Ophthalmol. 2014;34(2):383–400.
2.CullenAP.Photokeratitisandotherphototoxiceffectsonthecorneaand conjunctiva. IntJToxicol. 2002;21(6):455–64.
3.YenYL,LinHL,LinHJ,etal.Photokeratoconjunctivitiscausedby differentlightsources. AmJEmergMed. 2004;22(7):511–5.
4.IzadiM,Jonaidi-JafariN,PouraziziM,etal.Photokeratitisinducedby ultravioletradiationintravelers:amajorhealthproblem. JPostgradMed. 2018;64(1):40–6.
5.MarfakA,AchakD,AziziA,etal.ThehiddenMarkovchainmodellingof theCOVID-19spreadingusingMoroccandataset. DataBrief. 2020;32:106067.
6.SharmaA,AhmadFaroukI,LalSK.COVID-19:areviewonthenovel coronavirusdiseaseevolution,transmission,detection,controland prevention. Viruses. 2021;13(2):202.
7.GunerR,HasanogluI,AktasF.COVID-19:Preventionandcontrol measuresincommunity. TurkJMedSci. 2020;50(SI-1):571–7.
8.KumarA,RajA,GuptaA,etal.PollutionfreeUV-Cradiationtomitigate COVID-19transmission. GondwanaRes. 2023;114:78–86.
9.ChangCP,LiuHH,PengCY,etal.UVRmeasurementofaUV germicidallamp. HealthPhys. 2007;92(3):242–50.
10.ZaffinaS,CamisaV,LemboM,etal.AccidentalexposuretoUV radiationproducedbygermicidallamp:casereportandrisk assessment. PhotochemPhotobiol. 2012;88(4):1001–4.
11.StrippMP,DulaneyAR,BeuhlerMC,etal.Photokeratitisamong restaurantworkers:acaseseries. AmJIndMed. 2018.Inpress.
12.YanM,XiangyuS,JingM,etal.Analysisofdiseasespectrumand epidemiologicalcharacteristicsofemergencyoculartraumaduring
outbreakofnovelcoronaviruspneumonia. OphthalmologyinChina. 2020;29(3):224.
13.LiangH,ZhangM,ChenM,etal.OculartraumaduringCOVID-19 pandemic:asystematicreviewandmeta-analysis. AsiaPacJ Ophthalmol(Phila). 2022;11(5):481–7.
14.WangY,LouJ,JiY,etal.Increasedphotokeratitisduringthe coronavirusdisease2019pandemic:clinicalandepidemiological featuresandpreventivemeasures. Medicine(Baltimore). 2021;100(24):e26343.
15.SengilloJD,KunklerAL,MedertC,etal.UV-photokeratitisassociated withgermicidallampspurchasedduringtheCOVID-19pandemic. Ocul ImmunolInflamm. 2021;29(1):76–80.
16.LeungKCPandKoTCS.Improperuseofthegermicidalrange ultravioletlampforhouseholddisinfectionleadingtophototoxicityin COVID-19suspects. Cornea. 2021;40(1):121–2.
17.TankelJ,KeinanA,BlichO,etal.Thedecreasingincidenceofacute appendicitisduringCOVID-19:aretrospectivemulti-centrestudy. World JSurg. 2020;44(8):2458–63.
18.AlenaziTH,AlArbashH,El-SaedA,etal.Identifiedtransmission dynamicsofMiddleEastrespiratorysyndromecoronavirusinfection duringanoutbreak:implicationsofanovercrowdedemergency department. ClinInfectDis. 2017;65(4):675–9.
19.WorldHealthOrganization,WorldMeteorogicalOrganization,United NationsEnvironmentProgramme,etal. GlobalSolarUVIndex: APracticalGuide.Geneva,Switzerland:WorldHealth Organization;2002.
20.McCartyCAandTaylorHR.Areviewoftheepidemiologicevidence linkingultravioletradiationandcataracts. DevelopOphthalmol 2002;35:21–31.
BrianT.Wessman,MD*†
JulianneYeary,PharmD‡
HelenNewland,PharmD‡
RandyJotte,MD*
*WashingtonUniversityinSaintLouis,DepartmentofEmergencyMedicine, St.Louis,Missouri
† WashingtonUniversityinSaintLouis,DepartmentofAnesthesiology, DivisionofCriticalCareMedicine,St.Louis,Missouri
‡ BJCHealthCare,DepartmentofPharmacyServices,St.Louis,Missouri
SectionEditor:AsitMisra,MD,MSDEd,CHSE
Submissionhistory:SubmittedMay22,2023;RevisionreceivedJanuary4,2024;AcceptedJanuary9,2024
ElectronicallypublishedApril30,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18325
Introduction: Coronavirus2019(COVID-19)inequitablyimpactedminoritypopulationsandregionswith limitedaccesstohealthcareresources.TheBarnes-JewishEmergencyDepartmentinSt.Louis,MO, servessuchapopulation.TheCOVID-19vaccineisanavailabledefensetohelpachievecommunity immunity.Theemergencydepartment(ED)isapotentialsocietalresourcetoprovideaccesstoa vaccinationintervention.OurobjectiveinthisstudywastodescribeandevaluateanovelEDCOVID-19 vaccineprogram,includingitsimpactonthelocalsurroundingunderservedcommunity.
Methods: Thiswasaretrospective,post-protocolimplementationreviewofanEDCOVID-19 vaccinationprogram.Overtheinitialsix-monthperiod,wecompileddataonallvaccinatedpatientsoutof theEDtoevaluatedemographicdataandtheimpactonunderservedregionalareas.
Results: WereportasuccessfulED-basedCOVID-19vaccineprogram(withover1,000vaccines administered).Thisprogramhelpedraiseregionalandstatevaccinationrates.Over50%ofthe populationthatreceivedtheCOVID-19vaccinefromtheEDwerefromdefinedsociallyvulnerable patientpopulations.Noadverseeffectsweredocumented.
Conclusion: OperationCoVER(COVID-19VaccineintheEmergencyRoom)SaintLouiswasableto successfullyvaccinateasociallyvulnerablepatientpopulation.Thisfree,COVID-19ED-basedvaccine programwithdedicatedpharmacysupport,wasnovelinemergencymedicinepractice.SimilarED-based vaccineprogramscouldhelpwithfuturevaccinedistribution.[WestJEmergMed.2024;25(3)374–381.]
Coronavirus2019(COVID-19) firstimpactedtheUnited Statesinearly2020.ByFebruary2021,morethen500,000 individualshaddiedintheUSafterbecominginfected.1–4 Variousstrategieswereemployedtolimitthespreadofthe virusincludingcommunitylockdowns,socialdistancing, contacttracing,andmasking,withvariedsuccessand waningadherenceovertime.5 TheCOVID-19pandemic inequitablyimpactedminoritypopulationsandregionswith limitedaccesstohealthcareresources.6–8 TheBarnes-Jewish
HospitalEmergencyDepartment(BJHED)inSaintLouis, MO,staffedbyWashingtonUniversitySchoolofMedicine inSt.Louisemergencyphysicianswithdedicatedpharmacy supportservessuchapopulationforthebi-stateregionof MissouriandIllinois.
Oneofthestrongestdefensesagainstthisnovelvirusis vaccines.Developmentandmorewidespreaddistributionof vaccinesbeganinSpring2021.BySeptember2021,COVID19vaccinationwasestimatedtoprevent56%ofexpected hospitalizationsand58%ofexpecteddeaths.9 Toachieve
community or “herd” immunityandtherebyreducing theriskofcommunityspread,approximately67–90%ofthe populationmustachieveimmunity,eitherbyvaccinationor infection.However,vaccinehesitancy,miseducation,and lackofaccesstovaccinesaremajorbarrierstoachievingthis herdimmunitygoal.10–16 Asthesafetynetformany communities,theemergencydepartment(ED)providesa multitudeofhealthcare,educational,andsocialservices.17,18 WehypothesizedthattheEDcouldalsoplayapivotalrole withvaccineeducation,distribution,andaccessforan underservedpopulation.Priorstudieshaveevaluatedthe theoreticalbenefitofusingtheEDasapotentialvaccination resourcesite.19–25 Atthetimeofprojectinitiation,thestateof Missourirankednationallyinthebottom10ofstatesfor populationvaccinationrates,presentingopportunityfor improvement.4
WestartedofferingCOVID-19vaccinestopatients presentingtoBJHEDonJuly21,2021,initiallyboththe PfizerandJohnson&Johnson(J&J)vaccines.Ofnote,this initiationdatewaswellintothedeltavariantsurgeofthe pandemic.Additionally,vaccinationwasapprovedand availableforthepublicthroughotherpublichealthsources. Toourknowledge,thisfreeCOVID-19vaccineprogramby emergencyphysicianswithpharmacysupport,basedoutof anED,wasnovelinemergencymedicinepractice.Wenamed ourproject:OperationCoVER(COVID-19Vaccineinthe EmergencyRoom)STL(SaintLouis).
CollaborationontheEDvaccinationimplementation projectbetweenBJHEDhospitaladministration,Washington Universityemergencyphysicians,andthepharmacy departmentbeganinSpring2021.Ona24/7basis,theEDteam offersat-the-momenthealthcarewithconfidentiality,patientcenterededucation,andaccesstofollow-upresources (includingcompletionoftheinitialvaccinationseries,if indicated).Suchavailabilitydifferedfromothercommunity resources.Barriersthroughouttheprocesswereidentifiedand resolved.TheseincludedPfizervaccinestoragerequirements (ultra-lowtemperaturefreezer[ 80°Cto 60°C]);avoidanceof vaccinewastage(asonceavialwasdiluted,contentshadtobe usedwithinsixhours);handdeliveryfrominpatientpharmacy totheED;administrationofthevaccinewithintwohoursfrom vialextraction;record-keepingofappropriateviallotnumber; expirationdateandinjectionsite;andclinician/nursetraining. Vaccineeducationwasprovidedtoourphysicians,nurse practitioners,physicianassistants,andnurses.Allwere encouragedtooffereverypatienttheCOVID-19 vaccination.Signage,educationalmaterials,andadvertising weredevelopedanddistributedtoraiseawarenessoffree vaccinationaccessintheED.Schedulingsubsequentdosesto completetheinitialvaccineserieswasfacilitatedbyour dischargenursecoordinators.Weeklyemailreminders trackingvaccinesadministeredwerecirculatedtothe
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
TheCOVID-19vaccineisanavailable defensetohelpachievecommunityimmunity. TheEDisapotentialsocietalresourceto provideaccesstoavaccinationintervention.
Whatwastheresearchquestion?
Ourgoalwastodescribeandevaluateanovel EDCOVID-19vaccineprogram,including itsimpactonthelocalsurrounding underservedcommunity.
Whatwasthemajor findingofthestudy?
ThisED-basedCOVID-19vaccineprogram resultedinover1,000vaccinesadministered.
Howdoesthisimprovepopulationhealth?
Theprogramhelpedraiseregional/state vaccinationrates.Over50%ofthose whoreceivedthevaccinefromtheED werefromde fi nedsociallyvulnerable patientpopulations.
WashingtonUniversityemergencyphysician/nurse practitionerandphysicianassistant/residentgroup.
Basedonregionalvaccinationratesandthehealthcare accessofourpatientpopulation,anassumptionwasmade thatapproximatelyone-thirdofpatientswouldarrive vaccinated.Alsoconsideringcriticalillness/trauma presentation,acuteillness,vaccinehesitancy,andclinician forgetfulness,weanticipatedanotherone-thirdofpatients wouldnotbeavailabletoconsentforvaccination.Ofthe remainingpatients,avaccinationgoalrateof5–10% (approximately5–15patientsaday)wasencouraged.This wasdiscussedatlengthwithpharmacytosupportthe componentofvaccinestorage,preparation,and administrationinatimelyfashionfortheED patientpopulation.
Allpatientswererequiredtoconsenttoreceivingthe vaccine,whichwasdocumentedelectronicallyuponorder entrybytheclinician.Patientsnoteligibletoreceivethe vaccineincludedthosewithacontraindicationtothevaccine, anactiveCOVID-19infection,orthosewithadocumented COVID-19infectionwithintherecentpast(current recommendationofpriorseven-dayperiod).Allvaccines werekeptinacentralizedpharmacylocationtomeetstorage requirementsofboththePfizerandJ&Jvaccines.Pharmacy staffwithdrewdosesfortherequestedvaccineandhand deliveredittotheEDbedsidenursealongwithvaccinevial
information(manufacturer,expirationdate,lotnumber,and timeofdosewithdrawal)andablankstandardizedCOVID19vaccinecard(issuedbytheUSCentersforDisease ControlandPrevention[CDC]).
Thebedsidenursewouldadministerthevaccinedoseas soonaspossibleinviewofthetwo-hourlimitbetweenvial withdrawalandadministration.Nursesalsoprovidedpatient educationregardingpotentialsideeffectsandadverseevents afterreceivingthevaccine.Finally,nursesprovidedeach vaccinatedpatientwitheducationregardingfollow-up requirements.UponBJHEDdischarge,patientswould receivevaccineinformationsheetsandscheduling informationforthesecondvaccinedeadline,ifapplicable. Dischargenursecoordinatorswouldreceiveareportofall patientswhoreceivedtheir firstvaccineintheseriesand wouldcallpatientstoconfirmtheyhadasecondvaccine completedorscheduled,asapplicable.
Thiswasaretrospectivepost-protocolimplementation reviewofallBJHEDpatientsreceivingtheCOVID-19 vaccinethroughOperationCoVERSTLbetweenJuly1, 2021–January20,2022.Wereportimpactonvaccineefforts forvariousdemographicsofourregion.Datawascollected fromtheelectronichealthrecord.Weanalyzedadditional CDCdatatocomparevaccineregionaluptake.Specifically, theSocialVulnerabilityIndex(SVI)wascollectedfromCDC data,specifictoourpatientpopulation’saffectedarea. Sociallyvulnerablepopulationsareespeciallyatriskduringa publichealthemergencyduetofactorssuchas socioeconomicstatus,householdcomposition,minority status,accesstotransportation,housingtype,andlackof resources. 5–7 TheCDCusesthisindextohelpdetermine wheretoleveragehealthcareresourcestohelpalleviate humansufferingandeconomicloss(estimatesupplies,need foremergencyshelters,evacuationplanning,required emergencypersonnel).TheSVIdatabasewasimportant duringtheCOVID-19outbreaktodeterminewhich communitieswouldbeaffectedmoreandrequireadditional support(ie,vaccineimplementation).26 Thedataisfurther dividedintoquartilesinwhichquartile “A” representsthe lowest/leastlevelofvulnerabilityandquartile “D” represents thehighest/most.Weobtainedappropriateinstitutional reviewboardapproval(classifiedas “exempt”)toconduct thisretrospectivestudyatourinstitution.
Atotalof874COVID-19vaccinedoseswereadministered betweenJuly21,2021–January20,2022(averageof4.78 vaccinedosesperday).Thetotalnumberofimpacted patientswas824individuals.(Aminorityofpatientsusedthe EDfortheirsecondvaccinedoseadministration.)Themean patientagewas44.4yearsold(±15.6years).Thedistribution inraceincluded76%(626/824)Black,27.2%(224/824) White,and2.91%(24/824)AmericanIndian,Asian,or “other” ethnicitypatients(Table1, Figure1).
Table1. Demographicdataonpatientswhoreceivedthe COVID-19vaccine.
N = 874vaccinesadministered;N = 824patient
Meanage(years)44.4 ± 15.6
MeanEDduration(hours)7.49 ± 5.05
Admitted(yes%[n])21.6[189] DischargedfromED(Yes%[n])78.4[685] Deceased(yes%[n])0.11[1] MeannumberofEDvisitsinprior5years11 Gender(female%[n])45.3[396] Race(%[n])
Black76.0[626/824] White27.2[224/824] AmericanIndian0.73[6/824] Asian0.24[2/824]
Unabletoanswer1.94[16/824]
Meanweight(kg)82.38 ± 24.1
Meanheight(cm)170.6 ± 10.64
Insurancestatus
Self-pay%[n]29.5[258] Insurance%[n]70.5[616] MOMedicaid%[n]22.3[195] MOmanagedcare%[n]10.1[88]
Primarycareprovider
Yes%[n]51.4[449] No%[n]48.6[425]
COVID-19vaccinegiven Pfizer%[n]81.1[709] Johnson&Johnson%[n]18.9[165]
Historyof +COVID-19priortovaccination (Yes%[n])
8.7[76]
COVID-19+ aftervaccination(Yes%[n])4.9[43]
Timeofvaccinegivenpershift
1st shift(0700–1500)%[n]42.4[371] 2nd shift(1501–2300)%[n]30.8[269]
3rd shift(2301–0659)%[n]26.0[227]
Medicationsgiven
EpiPen%[n]0.23[2]
Diphenhydramine%[n]1.03[9]
Steroids%[n] (Methylprednisolone,prednisolone, prednisone,ordexamethasone)
Patientaddress/homestates
0.80[7]
Missouri89.7[784] Illinois9.61[84] Indiana0.11[1]
(Continuedonnextpage)
Texas0.11[1]
Unknown0.11[1]
CDCData
Missouridata
AveragepercentageoftheMOpopulationthat received1doseofanyCOVID-19vaccine by7/21/21
AveragepercentageoftheMOpopulationthat completedthevaccineseriesby7/21/21
AveragepercentageoftheMOpopulationthat received1doseofanyCOVID-19vaccine by1/20/22
AveragepercentageoftheMOpopulationthat completedtheseriesby1/20/22
Countydata
AveragepercentageoftheSt.LouisCity Countypopulationthatreceived1doseofany COVID-19vaccineby7/21/21
AveragepercentageoftheSt.LouisCity Countypopulationthatcompletedtheseries by7/21/21
AveragepercentageoftheSt.LouisCity Countypopulationthatreceived1doseofany COVID-19vaccineby1/20/22
AveragepercentageoftheSt.LouisCity Countypopulationthatcompletedtheseriesby 1/20/22
AveragepercentageoftheSt.LouisCounty populationthatreceived1doseofany COVID-19vaccineby7/21/21
AveragepercentageoftheSt.LouisCounty populationthatcompletedtheseries by7/21/21
AveragepercentageoftheSt.LouisCounty populationthatreceived1doseofany COVID-19vaccineby1/20/22
AveragepercentageoftheSt.LouisCounty populationthatcompletedtheseries by1/20/22
SocialVulnerabilityIndex (timeframe:7/21/21 – 1/20/22) A(0–
C(0.5001–0.75)36%
D(0.7501–1.0)16%
ED,emergencydepartment; MO,Missouri; COVID-19,coronavirus 2019; CDC,USCentersforDiseaseControlandPrevention.
NumberofBarnes-JewishHospitalEmergency Departmentpatientsvaccinatedbyrace.
Thegeographicdistribution(basedonlistedhomeZIPcode) included89.7%(784/874)ofMissouripatientsand9.61%(84/ 874)ofIllinoispatients(Figure2).Otherrepresentedstates includedIndiana,Kentucky,Mississippi,Tennessee,and Texas.Approximately22%ofvaccinatedpatientswere admitted,and78%weredischargedfromtheED.Themean numberofEDvisitsintheprior fiveyearsperpatientinthe vaccinatedcohortwas11totalEDvisits.
AtthetimeoftheirBJHEDvisitandvaccination,29.5% (258/874)ofpatientslackedhealthinsurance.Ofthe70.5% (616/874)ofpatientswithinsurance,22.3%(195/874)had MissouriMedicaidand10.1%(88/874)hadMissouri ManagedCare,bothofwhichprovidemedicalinsuranceto lowerincomehouseholds.AtthetimeoftheirBJHEDvisit, 51.4%(449/874)ofpatientshadaknownprimary carephysician.
Duringthestudiedtimeframe,16%ofthepatients vaccinatedbytheBJHEDvaccineprogramlivedinareasof highsocialvulnerability(quartileDoftheSVI),withan additional37%residinginareasofmedium-highsocial vulnerability(quartileC).Altogether,greaterthan50% (51.3%)ofthepatientsimpactedbytheBJHEDvaccine administrationprogramwerefromareasofmedium-high andhighsocialvulnerability(Figure3).Seeincludedmaps (Figure2)demonstratinggeographicimpactonourregion (MissouriandIllinois).
DatafromSaintLouisCityandSaintLouisCounty(the twolargestsurroundingregions)showeda21.1%increasefor St.LouisCityandan18.2%increaseforSt.LouisCountyfor patientsreceivingatleastonedoseoftheCOVID-19vaccine overthetemporalperiodofOperationCoVERSTL.Wealso revieweddataonadverseoutcomes,specificallyreviewingall medicationsprovidedduringeachpatientencounter.Useof agentsforanaphylacticreactions(epinephrine, corticosteroids,antihistamines)werelimitedinthepatient cohort.Twopatientsreceivedepinephrine0.3milligrams intramuscularinjectionsduringtheirEDstay;however,both wereunrelatedtothevaccineadministration(onepresented totheEDafteraninsectstingandanotherwithangioedema asthepresentingchiefcomplaint,priortoreceivingtheir COVID-19vaccineatdischarge).Wewereunabletoassess

Figure2. GeographicdistributionofvaccinatedBarnes-JewishemergencydepartmentpatientsbylistedZIPcode(forstatesofMissouri andIllinois).
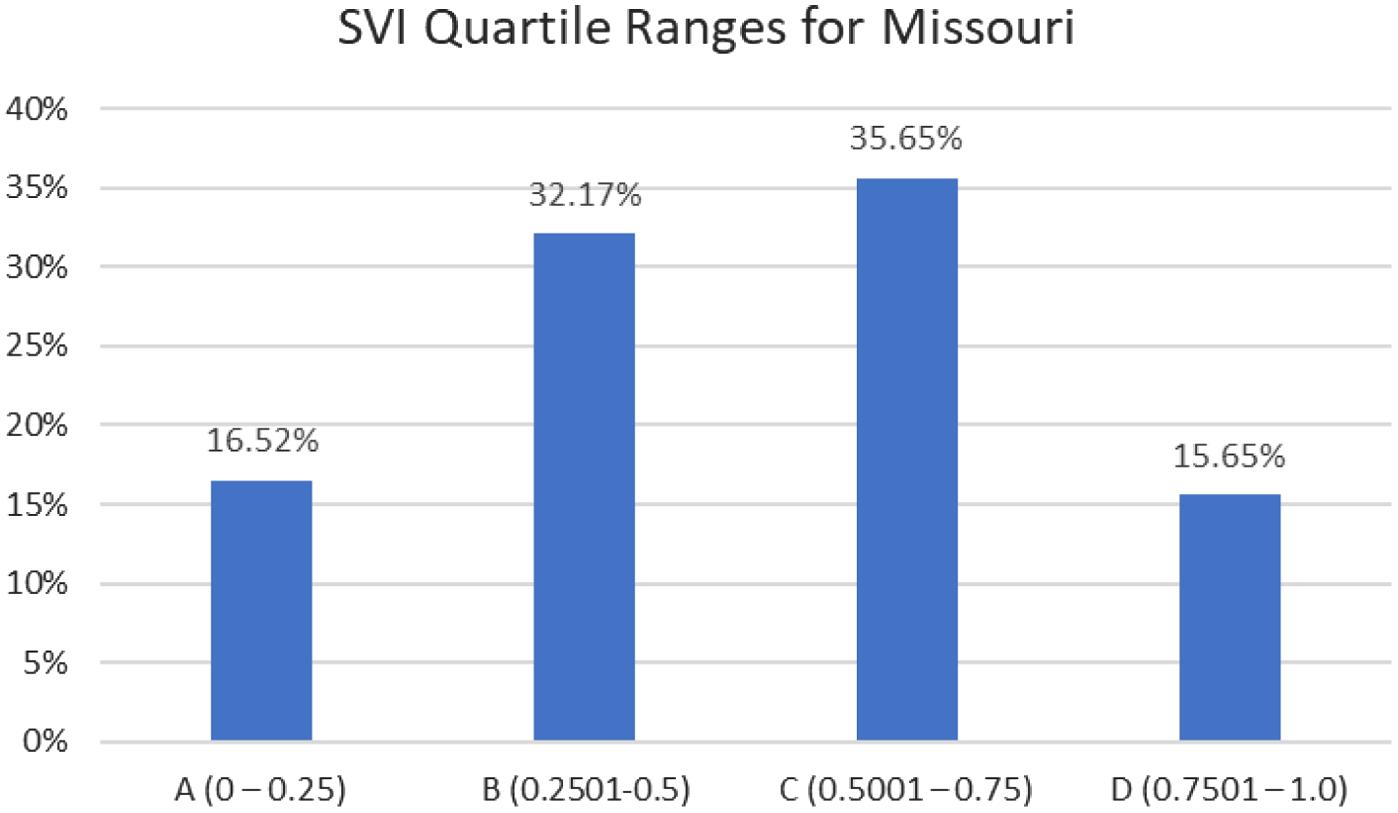
Figure3. Socialvulnerabilityindexforimpactedpostalcodesfor vaccinatedBarnes-Jewishemergencydepartmentpatients(Ais low/leastvulnerableandDishigh/mostvulnerable).
forotherpotentialadverseeventssuchaspericarditisorlocal siteirritation;however,wedidnotrecordanyrepeatvisitsin thispatientcohortforthesepresentingdiagnoses.
OperationCoVERSTLisanovel,ED-basedvaccination programthatmeetstheneedsofanunderservedcommunity withahighsocialvulnerabilityrisk.TheWashington UniversityDepartmentofEmergencyMedicineservesasthe locusofprimarycareformanyofourregionalpatients.The BJHEDcensusaverages185–240patientsdaily,with upwardof80,000adultpatientvisitsperyear.Emergency cliniciansareadeptatordering,administering,and documentingvaccines;themostcommonexampleisthe tetanus,diphtheria,andpertussisvaccine,whichis administeredalmostdailyintheEDforopen-wound prophylaxisintraumapatients.Wehavepreviouslybeen
involvedwithotherpublicvaccinationeffortsincluding offeringtheinfluenzavaccineinprior “fluseasons, ” although withvariablesuccess.
TheaveragenumberofEDvisitsperpatientsinthis vaccinatedcohortwas11(overtheprior fiveyears), demonstratingtheuniqueroletheBJHEDservesfor healthcareinourregionalcommunity.Populationswithinour communityaredependentontheBJHEDtoreceivemuchof theirhealthcare,reflectingwhyOperationCoVERSTLwas impactful.Thispracticeissimilaramongotherlargeurban areas,withanEDfulfillingtheroleofcentralandessential “healthcare” deliveryforanunderservedpatientpopulation.
WeevaluatedCDCdataonvaccinationratesforCOVID19vaccineuptakeinMissouriduringourED-based initiative.Onday0ofOperationCoVERSTL,32.9%ofthe statepopulationhadreceivedonedoseofanyCOVID-19 vaccineand28.6%ofthestatepopulationhadcompletedthe COVID-19vaccineseries(two-doseregimenformRNA vaccines).OnJanuary20,2022(enddatacohortdate),this ratehadincreasedto45.2%ofthestatepopulationhaving receivedonedoseofanyCOVID-19vaccineand39.0%ofthe populationhavingcompletedtheCOVID-19vaccineseries (Figure4).ProgramssuchasOperationCoVERSTLhelped alongwithotherinitiativesandprogramstoachievethis 12.3%increaseininitialvaccinationratesfortheMissouri population(16.6%increaseincompletedvaccinationseries).
WewereabletoaccessdatafromtheCDCtoanalyzeand understandourimpactontheregion.TheSVIdatawas assessedbytheimpactedZIPcodesassociatedtotheED visit.TheZIPcodesofourpatientcohortwereinhigh-risk sociallyvulnerableregions,indicatingapproximately52%of ourvaccinationrecipientswerefromsociallyvulnerable populations.TheSVIrateshelpdemonstratethatmany patientsservedbyBJHEDandWashingtonUniversity emergencyphysiciansarethosewithahigherimpactfrom publichealthemergenciesandresideinareasinneedof additionalsupport.
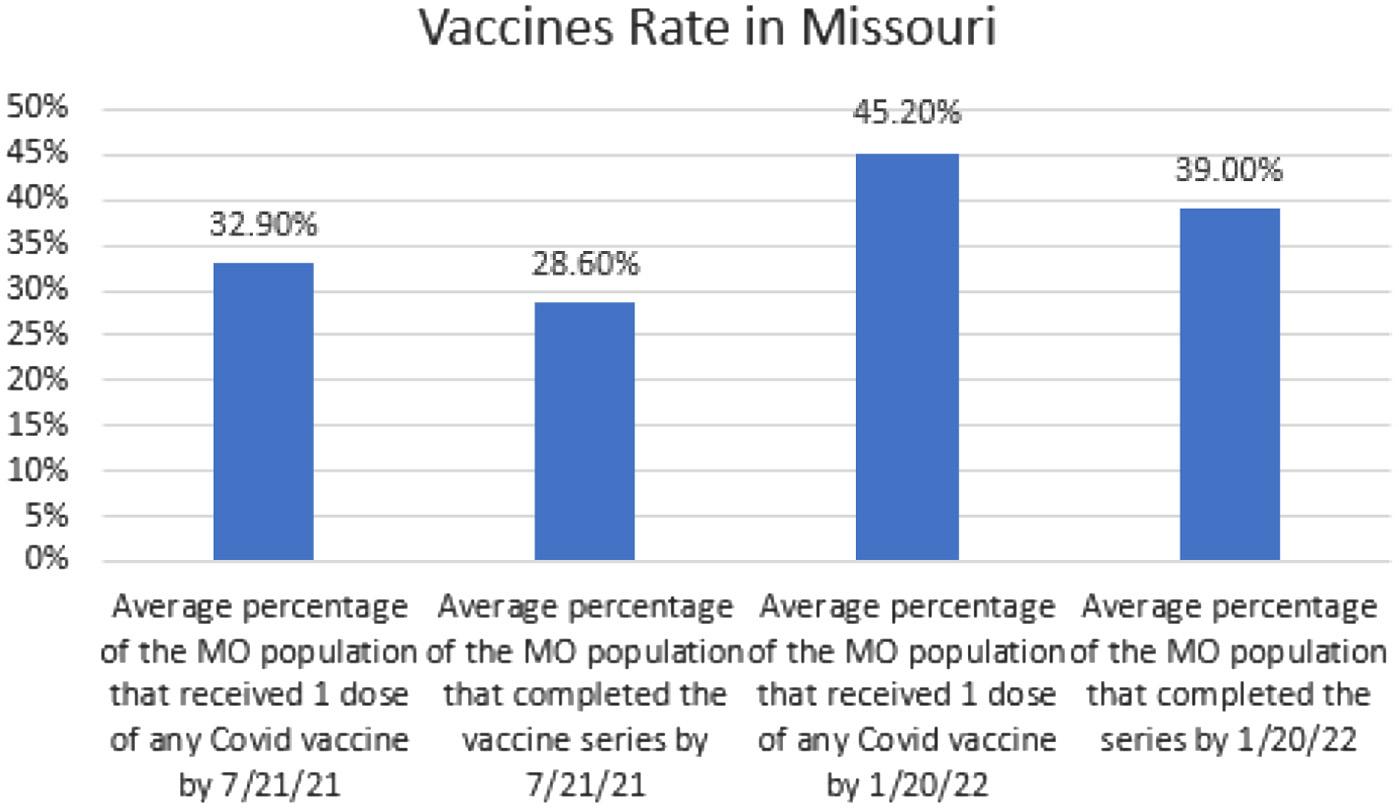
WealsolookedattheracialdistributionofOperation CoVERSTLefforts.Thedistributionofvaccinesprovidedin ourcohortincluded76%Black(626/824patients)and27.2% White(224/824patients).Thiscorrespondstotheracial distributionofthegeographicareaservedbytheBJHED, whichincludesSt.Louiscityandthesurroundingbistate regionsofMissouriandIllinois.Asof2022,thecensusofSt. Louiscitydemonstratedthat “BlackorAfricanAmerican alone” madeup44.8%ofthecitypopulationand “White alone” madeup46.3%ofthecitypopulation.27 However,our hospitalcensusnumberstypicallyreflectahigherpercentageof “BlackorAfricanAmerican” patientsusingtheBJHEDto accesshealthcare.Duringthesix-monthperiodofthiscohort, theBJHEDprovidedcarefor39,570patients.Theracial distributionoftheEDpopulationincluded61.29% “Black” and33.92% “White” (Table2).Thismayagainreflecttherole theBJHEDservesforspecificpopulationsinourcity(higher SVIZIPcodes)whoaresociallyvulnerableandwhyOperation CoVERSTLdidprovideauniquepublichealthresource.
Wehavealsobeguntolookatclinicianattitudesand supportofthisprogramthroughsurveystobetterunderstand
allparametersofthispilot.WehopeourED-based vaccinationprogramcanserveasamodelforotherEDswith similarsociallyvulnerablepopulations.
WehavecontinuedtoofferOperationCoVERSTL throughourBJHED.WenowofferthePfizervaccineand booster(s),ifeligible.Ofnote,wedidremoveaccesstothe J&JvaccineunderCDCpublicguidance.Wehaveexpanded ourvaccinationeffortstoincludeboosterimmunizationsfor eligiblepatients.Asweapproachedtheone-yearanniversary ofthestartofthisinitiative,wehadvaccinatedover1,236 patientsasofJanuary20,2023).
Thisretrospectiveanalysisisnotwithoutlimitations includingitsobservationalnatureandoursingle-center analysis.Vaccinationsweregivenonaclinician-preference basis,andwereliedheavilyuponcliniciansinitiatingthe conversationofvaccineswithpatients.Ofnote,thepublic visualannouncementsofvaccineaccessintheEDwaiting room,individualpatientcareareas,andrestroomsdidlead somepatienttoinitiatethe vaccineconversationwith WashingtonUniversiyemergphysicians.Vaccinehesitancy wasnotscreenedfororassessedinthisstudy,butanecdotally wasacommonthemelimitingvaccineuptake.Withthe retrospective,blindeddesignofourdatacohort,wewere unabletoinvestigateindividualfactorsimpactingpatient vaccinationdecisions.OnJanuary20,2022(enddatacohort date),only39%oftheMissouripopulationhadcompleteda COVID-19vaccineseries(Figure4),demonstratingthatless thanhalfofourstatepopulationhadgoneforwardwitha decisiontovaccinate.Weare awareofmultipleemergency cliniciansatourinstitutionreportingpatientsrefusingtoreceive thevaccinewhenofferedasanadditionalbenefitoftheirED visit.Ouroriginalvaccinationgoalwassetat5–15vaccinesper day.Weendedupadministering4.78vaccinedoseseachday; thus,vaccinehesitancycouldhaveimpactedourdailyrates.
Duetocrowdingissues,theBJHEDhasaprolongedwait timeandlengthofstay.Itisnotuncommonformiddle-to low-acuitypatientstowait4-6hoursinthetriageareaprior tohavingaccesstoaclinicianinanEDroom.Itispossible thattheseprolongedEDtimescouldhaveimpacted vaccinationrates.Typically,anEDpatientarriveswithan acute “ emergency ” chiefcomplaint.SomeEDsmayhave fasterevaluationanddispositiontimes,duringwhichtime additionalrequirements(vaccinedefrosting,administration) maynegativelyimpactpatient flow.However,withalonger EDlengthofstay,theEDstaffmayhavemoreopportunities toengagewiththepatienttodiscussspecificconcernsabout vaccineadministration.Furthermore,thepatientmaywant togetasmanypotentialavailableservicestomaximizecare duringtheirprolongedwait.Ourlarge,academicEDhas directaccesstopharmacywithadedicatedEDclinical pharmacist.SmallerEDswithoutdirectpharmacistaccess maybelimitedwithasimilarvaccineprotocoldesign
requiringpharmacysupport.Finally,thepatientpopulation inourareaisprimarilyurban,potentiallylimiting applicabilitytoruralareas.
Herewereportonthedevelopmentandimplementation ofasuccessfulED-basedCOVID-19vaccinationprogram. Ourprogramwasabletovaccinateanunderservedpatient populationbymeetingthepatientswheretheyreceivedtheir standardhealthcare.Thisprogramcanserveasamodelfor otheremergencydepartmentslookingtoimpacttheirregions throughvaccinationefforts.Futurestudiesshouldevaluate longevityofsuchprograms,aswellaspublicperceptionand clinicianattitudes.
AddressforCorrespondence:BrianT.WessmanMD,Washington UniversityinSaintLouis,DepartmentofEmergencyMedicine, 660S.EuclidAve.,CB8054,St.Louis,MO,63110.Email: brianwessman@wustl.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Wessmanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.YesudhasD,SrivastavaA,GromihaMM.COVID-19outbreak:history, mechanism,transmission,structuralstudiesandtherapeutics. Infection. 2021;49(2):199–213.
2.ShahriarS,RanaMS,HossainMS,etal.COVID-19:epidemiology, pathology,diagnosis,treatment,andimpact. CurrPharmDes. 2021;27(33):3502–25.
3.QuL,LiJ,RenH.COVID-19:theepidemiologyandtreatment. BrJHospMed(Lond). 2020;81(10):1–9.
4.CentersforDiseaseControlandPrevention(CDC).UnitedStates COVID-19Cases,Deaths,andLaboratoryTesting(NAATs)byState, Territory,andJurisdiction:caseslast7daysrateper100,000.2021. Availableat: https://stacks.cdc.gov/view/cdc/107545 AccessedMay12,2023.
5.CraneMA,ShermockKM,OmerSB,etal.Changeinreported adherencetononpharmaceuticalinterventionsduringtheCOVID-19 pandemic,April-November2020. JAMA. 2021;325(9):883–5.
6.KhanijahaniA,IezadiS,GholipourK,etal.Asystematicreviewofracial/ ethnicandsocioeconomicdisparitiesinCOVID-19. IntJEquityHealth. 2021;20(1):248.
7.MackeyK,AyersCK,KondoKK,etal.Racialandethnicdisparitiesin COVID-19-relatedinfections,hospitalizations,anddeaths:asystematic review. AnnInternMed. 2021;174(3):362–73.
8.WebbHooperM,NápolesAM,Pérez-StableEJ.COVID-19andracial/ ethnicdisparities. JAMA. 2020;323(24):2466–7.
9.SteeleMK,CoutreA,ReedC,etal.EstimatedmumberofCOVID-19 infections,hospitalizations,anddeathspreventedamongvaccinated personsintheUS,December2020toSeptember2021. JAMANetw Open. 2022;5(7):e2220385.
10.JoshiA,KaurM,KaurR,etal.PredictorsofCOVID-19vaccine acceptance,intention,andhesitancy:ascopingreview. FrontPublic Health. 2021;9:698111.
11.GhasemiyehP,Mohammadi-SamaniS,FirouzabadiN,etal.Afocused reviewontechnologies,mechanisms,safety,andefficacyofavailable COVID-19vaccines. IntImmunopharmacol. 2021;100:108162.
12.ShenSCandDubeyV.Addressingvaccinehesitancy:clinicalguidance forprimarycarephysiciansworkingwithparents. CanFamPhysician. 2019;65(3):175–81.
13.SevinAM,RomeoC,GagneB,etal.Factorsinfluencingadults’ immunizationpractices:apilotsurveystudyofadiverse,urban communityincentralOhio.2016.Availableat: https://doi.org/10.1186/ s12889-016-3107-9.AccessedMay12,2023.
14.AttwellK,NavinMC,LopalcoPL,etal.Recentvaccinemandatesinthe UnitedStates,EuropeandAustralia:acomparativestudy. Vaccine. 2018;36(48):7377–84.
15.SmithMJ.Promotingvaccineconfidence. InfectDisClinNorthAm. 2015;29(4):759–69.
16.PaltielAD,SchwartzJL,ZhengA,etal.ClinicaloutcomesofaCOVID19vaccine:implementationoverefficacy. HealthAff(Millwood). 2021;40(1):42–52.
17.LaneBH,MallowPJ,HookerMB,etal.TrendsinUnitedStates emergencydepartmentvisitsandassociatedchargesfrom2010to 2016. AmJEmergMed. 2020;38(8):1576–81.
18.WallsCA,RhodesKV,KennedyJJ.Theemergencydepartmentas usualsourceofmedicalcare:estimatesfromthe1998NationalHealth InterviewSurvey. AcadEmergMed. 2002;9(11):1140–5.
19.RodriguezRM,TorresJR,ChangAM,etal.Therapid evaluationofCOVID-19vaccinationinemergencydepartments forunderservedpatientsstudy. AnnEmergMed. 2021;78(4):502–10.
20.ChenG,KazmiM,ChenD,etal.Identifyingassociationsbetween influenzavaccinationstatusandaccess,beliefs,andsociodemographic factorsamongtheuninsuredpopulationinSuffolkCounty,NY. J CommunityHealth. 2020;45(6):1236–41.
21.GuM,TaylorB,PollackHA,etal.ApilotstudyonCOVID-19vaccine hesitancyamonghealthcareworkersintheUS. PLoSOne. 2022;17(6):e0269320.
22.KhubchandaniJ,SharmaS,PriceJH,etal.COVID-19vaccination hesitancyintheUnitedStates:arapidnationalassessment. JCommunityHealth. 2021;46(2):270–7.
23.ReiterPL,PennellML,KatzML.AcceptabilityofaCOVID-19vaccine amongadultsintheUnitedStates:Howmanypeoplewouldget vaccinated? Vaccine. 2020;38(42):6500–7.
24.KaighC,BlomeA,SchreyerKE,etal.Emergencydepartment-based hepatitisAvaccinationprograminresponsetoanoutbreak. WestJEmergMed. 2020;21(4):906–8.
25.KapurAKandTenenbeinM.Vaccinationofemergency departmentpatientsathighriskforinfluenza. AcadEmergMed. 2000;7(4):354–8.
26.DasguptaS,BowenVB,LeidnerA,etal.Associationbetweensocial vulnerabilityandacounty’sriskforbecomingaCOVID-19hotspot UnitedStates,June1–July25,2020. MorbMortalWklyRep. 2020;69(42):1535–41.
27.UnitedStatesCensusBureau.QuickFacts:St.Louis,Missouri. Availableat: https://www.census.gov/quickfacts/fact/table/ stlouiscitymissouri/PST045222.AccessedSept25,2023.
JamesS.Ford,MD*
JosephC.Morrison†
JennyL.Wagner,PhD,MPH‡ DishaNangia§
StephanieVoong,MPH∥
CynthiaG.Matsumoto,PhD¶ TasleemChechi,MPH∥
NamTran,PhD# LarissaMay,MD,MSPH∥
*UniversityofCaliforniaSanFrancisco,DepartmentofEmergencyMedicine, SanFrancisco,California
† UniversityofCaliforniaDavis,Davis,California
‡ CaliforniaStateUniversity,DepartmentofPublicHealth,Sacramento,California
§ UniversityofCaliforniaDavis,SchoolofMedicine,Sacramento,California
∥ UniversityofCaliforniaDavisHealth,DepartmentofEmergencyMedicine, Sacramento,California
¶ UniversityofCaliforniaDavisHealth,LearningHealthSystem,Departmentof PopulationHealthandAccountableCare,Sacramento,California
# UniversityofCaliforniaDavisHealth,DepartmentofPathologyandLaboratory Medicine,Sacramento,California
SectionEditor:JuanAcosta,DO,MS
Submissionhistory:SubmittedJuly19,2023;RevisionreceivedNovember17,2023;AcceptedDecember22,2023
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18404
Introduction: Theincidenceofsexuallytransmittedinfections(STI)increasedintheUnitedStates between2017–2021.ThereislimiteddatadescribingSTIco-testingpracticesandtheprevalenceofSTI co-infectionsinemergencydepartments(ED).Inthisstudy,weaimedtodescribetheprevalenceof co-testingandco-infectionofHIV,hepatitisCvirus(HCV),syphilis,gonorrhea,andchlamydia,inalarge, academicED.
Methods: Thiswasasingle-center,retrospectivecross-sectionalstudyofEDpatientstestedforHIV, HCV,syphilis,gonorrheaorchlamydiabetweenNovember27,2018–May26,2019.In2018,thestudy institutionimplementedanED-basedinfectiousdiseasesscreeningprograminwhichanypatientbeing testedforgonorrhea/chlamydiawaseligibleforopt-outsyphilisscreening,andanypatient18–64years whowashavingblooddrawnforanyclinicalpurposewaseligibleforopt-outHIVandHCVscreening.We analyzeddatafromallEDpatients ≥13yearswhohadundergoneSTItesting.Theoutcomesofinterest includedprevalenceofSTItesting/co-testingandtheprevalenceofSTIinfection/co-infection.We describedatawithsimpledescriptivestatistics.
Results: Duringthestudyperiodtherewere30,767EDencountersforpatients ≥13years(meanage: 43 ± 14years,52%female),and7,866(26%)weretestedforatleastoneofHIV,HCV,syphilis, gonorrhea,orchlamydia.Weobservedthefollowingtestingfrequencies(andprevalenceofinfection): HCV,7,539(5.0%);HIV,7,359(0.9%);gonorrhea,574(6.1%);chlamydia,574(9.8%);andsyphilis,420 (10.5%).Infectiousetiologieswithuniversaltestingprotocols(HIVandHCV)madeupthemajorityofSTI testing.Inpatientswithsyphilis,co-infectionwithchlamydia(21%,9/44)andHIV(9%,4/44)washigh.In patientswithgonorrhea,co-infectionwithchlamydia(23%,8/35)andsyphilis(9%,3/35)washigh,andin patientswithchlamydia,co-infectionwithsyphilis(16%,9/56)andgonorrhea(14%,8/56)washigh. PatientswithHCVhadlowco-infectionproportions(<2%).
Conclusion: PrevalenceofSTIco-testingwaslowamongpatientswithclinicalsuspicionforSTIs; however,co-infectionprevalencewashighinseveralco-infectionpairings.Futureeffortsareneededto improveSTIco-testingratesamonghigh-riskindividuals.[WestJEmergMed.2024;25(3)382–388.]
Keywords: emergencydepartment;sexuallytransmittedinfection;sexuallytransmitteddisease;public health;humanimmunodeficiencyvirus;HIV;hepatitisCvirus;syphilis;gonorrhea;chlamydia.
Anestimatedonein fiveindividualsintheUnitedStates (US)areinfectedwithasexuallytransmittedinfection (STI).1,2 Between2017–2021,theincidenceofsyphilisand gonorrheaincreasedandtheincidenceofchlamydia infectionsremainedhigh.2 Withwidespreaduseof antiretroviraltreatment,theoverallincidenceofHIVhas declinedoverthesameperiod,butincidencehasplateauedin certainhigh-riskgroups,suchaspeoplewhoinjectdrugs.3 WhilecurativetreatmentforHCVbecameavailableinthe USin2011,theincidenceofHCVdoubledbetween 2013–2020.4,5 Moreover,just33%ofthosewithchronic HCVhavebeencured,andlessthan17%ofyoung (<40years),uninsuredpatientshaveachievedsustainedviral clearance.6 Lowtestingfrequencies,patientunawarenessof infection,pooraccesstotraditionaltreatmentsettings(ie, primarycareclinics)andre-infectionfollowingcureall contributetothesesub-optimaldata.6,7
Theemergencydepartment(ED)isanimportantsafety netforunderserved,high-riskpopulations,makingitavital settingtodeliverhealthcareservicestopatientswithout accesstoprimarycare.8,9 Emergencydepartment-based infectiousdiseasesscreeningprogramshavedemonstrated successinidentifyingSTIsandlinkingpatientsto treatment.10–12 ItiswellknownthatcontractionofoneSTI increasesapatient’sriskofco-infectionwithotherSTIs.13,14 OneED-basedstudyshowedthatamongpatientswho receivedtestingforSTI,co-testingforasecondSTIwasas lowas8%;however,thisstudydidnotreportprevalenceof infection/co-infection.15 OtherED-basedstudiesreport prevalenceofco-infectionbutonlysingleSTI pairings.10,15–17 UnderstandingEDSTIco-testing frequenciesandprevalenceofco-infectionsisimperativefor optimizingpublichealthinfectiousdiseasesurveillanceand treatment,particularlyamongpatientswithoutaccessto traditionalprimarycareservices.Inthisstudy,weaimedto describeco-testingandco-infectionprevalenceofHIV, hepatitisCvirus(HCV),syphilis,gonorrhea,andchlamydia, inalarge,academicED.
Overview
In2018,thestudyinstitutionimplementedanopt-out, ED-basedinfectiousdiseasesscreeningprogramthat employedelectronichealthrecord(EHR)bestpracticealerts (BPA).Anypatientbeingtestedforgonorrhea/chlamydia waseligibleforopt-outsyphilisscreening.Additionally,any
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Dataonsexuallytransmittedinfection(STI) testingandprevalencearelimitedinthe emergencydepartment(ED)setting.
Whatwastheresearchquestion?
WhatistheprevalenceofSTItesting,cotestingandco-infectionamongEDpatients .
Whatwasthemajorquantitative finding ofthestudy?
Co-testingforSTIswasinfrequent,butcoinfectionwithchlamydiawashighamong patientswithsyphilis(21%)and gonorrhea(23%).
Howdoesthisimprovepopulationhealth?
ThisstudyhighlightstheneedtoimproveSTI co-testingratesamonghigh-riskindividuals.
EDpatient18–64yearsofagewhowashavingblooddrawn foranyclinicalpurpose,waseligibleforopt-outHIVand HCVscreening.Fundingforlabtestswasobtainedby chargingthepatient’sinsurance,abillingstrategyemployed bysimilarscreeningprogramsandstudies.18 Ifapatient requestedthattheirinsurancenotbecharged,ortheydidnot haveinsurance,testingwaspaidforbytheprogramgrant. Physicians(includingallresidents),nursepractitionersand physicianassistantscouldordertesting.Thefulldetails ofthesescreeningprogramshavebeenpreviously described.10–12 AnexampleBPAisavailablein Figure1.In thisstudyweexaminedSTItesting/co-testingfrequencies andinfectionprevalenceintheED.Asdatawasinitially collectedforqualityassurancepurposes,thestudywas deemednottobehumansubjectsresearchbythe InstitutionalReviewBoardQualityImprovementSelfCertificationTool.
Thiswasaretrospective,cross-sectionalstudyofED patientstestedforHIV,HCV,syphilis,gonorrhea,or
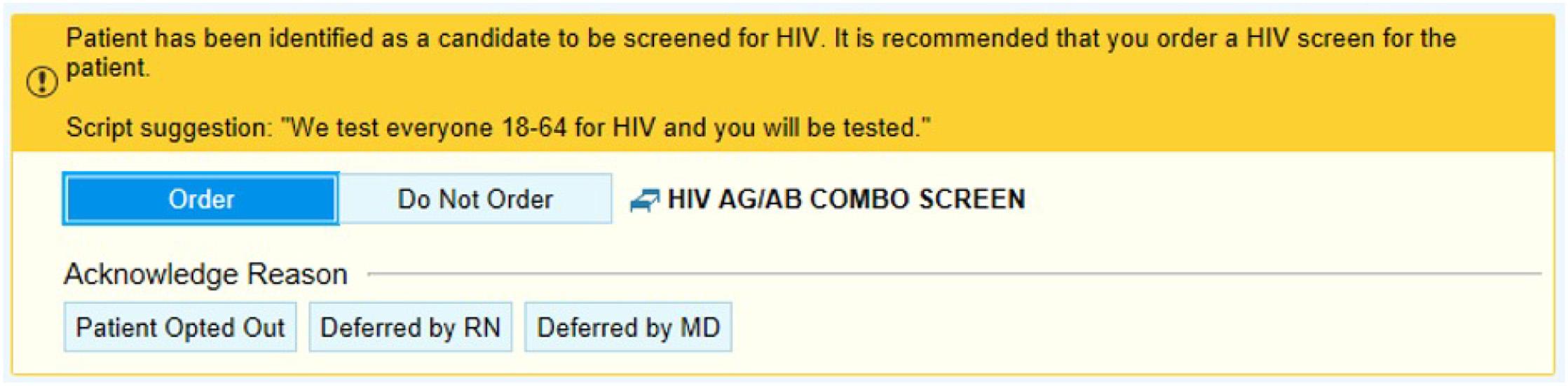
Figure1. Exampleofabestpracticealertinsidetheelectronichealthrecord.
chlamydiaduringthesix-monthperiodfollowing implementationoftheED-basedinfectiousdiseases screeningprogram.Thestudyinstitutionwasaquaternary care,academic,LevelItraumacenterinNorthernCalifornia thatseesmorethan80,000patientvisitsannually.
Weincludeddatafromallpatients ≥13yearswhohad undergonetestingforoneormoreofHIV,HCV,syphilis, gonorrhea,orchlamydiaintheEDbetweenNovember27, 2018–May26,2019.
WeabtracteddatafromtheEHR(EpicSystemsCorp, Verona,WI)usingcomputer-generatedreportsbyquerying patientswhohadreceivedEDSTItestsduringthestudy period.Weincludeddemographicfactors(age,gender,race, ethnicity)andresultsofSTItesting.Thedataanalyst responsibleforprocuringthesereportswasblindedtothe hypothesisofthestudy.WedefinedSTIco-testingastesting fortwoormoreofthefollowingSTIs:gonorrhea,chlamydia, syphilis,HIV,andHCV.Topreventduplicatedata,we includedonlyapatient’ s firstEDvisitwheretheyreceived HCVtestingwhencalculatingco-testing/co-infection prevalence.Weexaminedsubsequenttestingthatoccurredin futureEDvisitstoidentifyinstanceswherebroaderSTI testingcouldhaveidentifiedinfectionsearlier.Datawas storedinde-identifieddatasets,andpatientsweregiven uniqueidentifierstomaintainpatientconfidentiality. HIVscreeningwasperformedusingaHIVP24antigen (Ag)andHIV-1/HIV-2antibody(Ab)combinationtestwith theARCHITECTi1000SRimmunoanalyzer(Abbott Laboratories,AbbottPark,IL),anddiagnoseswere confirmedusingBio-RadRapidTestMultispotHIV-1/HIV2Abreflextesting(Bio-RadLaboratories,Inc,Hercules, CA).ScreeningforHCVintheEDwasperformedusinga chemiluminescentanti-HCVARCHITECTi1000SR immunoassay,anddiagnoseswereconfirmedbyHCV ribonucleicacidviralload(VL)withCobasHCV4800assay (RocheMolecularSystems,Pleasanton,CA).Patientswere consideredpositiveforHCVonlyiftheyhadadetectable
VL.Multiplexgonorrheaandchlamydiaurinepolymerase chainreactiontestingwasalsoperformedviatheCobas4800 assay.Patientsweretestedfor Treponemapallidum IgM/IgG antibody(TPA)usingBio-Rad’smultiplex flow immunoassay(MFI),Bioplex2200.19 Specimenswith reactiveTPAMFIresultsunderwentreflexiveconfirmatory quantitativenon-treponemalassaytesting,usingrapid plasmareagin.Iftestresultswerediscordant,thespecimen wastestedreflexivelyusingthe Tpallidum particle agglutinationtestasanadditionalconfirmatory treponemaltest.
Theoutcomesofinterestincludedtheprevalence ofSTItesting/co-testingandprevalenceofSTI infection/co-infection.
Wedescribeddatausingdescriptivestatistics.Categorical variableswereexpressedaspercentagesandproportions,and continuousvariableswereexpressedasmeans ± standard deviations.WeperformedallstatisticalanalysesusingStata 15.1(StataCorpLLC,CollegeStation,TX).
Therewere30,767EDpatientencountersforpatients aged ≥13yearsduringthestudyperiod.Ofthese,7,866(26%) weretestedforatleastoneofHIV,HCV,syphilis, gonorrhea,orchlamydia.Themeanageofpatientswas 43 ± 14years,and4,077(52%)werefemale.Themost commonracewasWhite(39%),andmostpatientswerenonHispanic(76%).MostpatientstestedhadMedicaid insurance(56%).See Table1 forfullpatientcharacteristics.
ThemostcommonlytestedSTIswerethosewithuniversal screeningindications:HCV(24.5%,7,539/30,767);andHIV (23.9%,7,359/30,767).Gonorrhea/chlamydia(1.9%,74) testingwasmorecommonthansyphilistesting(1.4%,
Table1. Characteristicsof7,866emergencydepartmentpatients whounderwenttestingforatleastonesexuallytransmittedinfection.
Meanage(years)1
Genderr
43 ± 14
Male48%(3,789)
Female52%(4,077)
Race/ethnicity2
White39%(3,034)
Black22%(1,698)
Asian7%(517)
Mixed/other32%(2,517)
Ethnicity3
Hispanic24%(1,845)
Non-Hispanic76%(5,933)
Sexuality(self-identified)4
Heterosexual93%(1,386)
LGBTQ7%(105)
Housingstatus5
Domiciled91%(5,982)
Undomiciled9%(614)
Insurancetype
Private27%(2,162)
Medicare13%(1,025)
Medicaid56%(4,399)
Self/uninsured4%(280)
1Reportedasmean ± standarddeviation.
2Datamissingfor100patients.
3Datamissingfor88patients.
4Datamissingfor6,375patients.
5Datamissingfor1,270patients.
LGBTQ,Lesbian,Gay,Bisexual,Transgender,Queer.
420/30,767).OfthosewhoreceivedtestingforSTIs,6.5% (508/7,866)weretestedforasingleSTI.Patientsweretested fortwoormoreSTIsin95.6%(7,521/7,866)ofcasesand threeormoreSTIsin5.6%(437/7,866)ofcases.Patientswere testedforHIV,HCV,syphilis,andgonorrhea/chlamydiain 3.6%(286/7,866)ofcases.See Table2 foroverallco-testing.
Table2. Overalltesting/co-testingproportionsamongemergency department(ED)patientstestedforsexuallytransmittedinfections duringtheir firstEDvisit.
OneSTItestedTestingproportion
HCVonly24.5%(7,539/30,767)
HIVonly23.9%(7,354/30,767)
Syphilisonly1.4%(420/30,767)
Gonorrhea1.9%(574/30,676)
Chlamydia1.9%(574/30,676)
TwoSTIsco-testedCo-testingproportion
Gonorrhea + Chlamydia1 100%(574/574)
HCV + HIV95%(7,240/7,650)
HCV + syphilis4.4%(333/7,626)
HCV + Gonorrhea4.4%(344/7,769)
HCV + Chlamydia4.4%(344/7,769)
HIV + syphilis4.5%(357/7,417)
HIV + Gonorrhea4.6%(346/7,582)
HIV + Chlamydia4.6%(346/7,582)
Syphilis + Gonorrhea57%(361/633)
Syphilis + Chlamydia57%(361/633)
ThreeSTIsco-testedCo-testingproportion
HCV + HIV + syphilis2.1%(314/14,680)
HCV + HIV + Gonorrhea2.2%(319/14,829)
HCV + HIV + Chlamydia2.2%(319/14,829)
HCV + syphilis + Gonorrhea2.0%(303/14,861)
HCV + syphilis + Chlamydia2.0%(303/14,861)
HIV + syphilis + Gonorrhea4.0%(306/7,736)
HIV + syphilis + Chlamydia4.0%(306/7,736)
FourSTIsco-testedCo-testingproportion
HCV + HIV + Syphilis + Gonorrhea286(3.6%)
HCV + HIV + Syphilis + Chlamydia286(3.6%)
All fiveSTIsco-testedCo-testingproportion
HCV + HIV + syphilis + Gonorrhea + Chlamydia 286(3.6%)
1Gonorrheaandchlamydiawerealwaystestedtogether. STI,sexuallytransmittedinfection; HCV,hepatitisCvirus.
Theseroprevalenceofinfectionwashighestforsyphilis (44/420,10.5%[95%CI7.7–13.8]),followedbychlamydia (56/574,9.8%[95%CI7.4–12.5]),gonorrhea(35/574,6.1% [95%CI4.3–8.4]),HCV(373/7,470,5.0%[95%CI4.5–5.5]), andHIV(67/7,354,0.9%[95%CI0.7–1.2]).Among67 patientswhotestedpositiveforHIV,HCVwasthemost commonco-infection(sevenpatients,10.4%).Among373 patientswhotestedpositiveforHCV,HIVwasthemost commonco-infection(seven,0.9%).Among44patientswho testedpositiveforsyphilis,chlamydiawasthemostcommon co-infection(nine,20.5%).Among35patientswhotested positiveforgonorrhea,chlamydiawasthemostcommoncoinfection(eight,22.9%).Amongpatientswhotestedpositive forchlamydia,syphiliswasthemostcommonco-infection (nine,16.1%).OnepatientwasinfectedwiththreeSTIs (HCV,HIV,andsyphilis).Nopatientswereinfectedwith morethanthreeconcurrentSTIs.Overallco-infectiondatais availablein Table3.
Table3. Infectionandco-infectionproportionsforsexually transmittedinfections.
Infectiontype%(Proportion)
Syphilisinfection10.5%(44/420)
Chlamydiaco-infection20.5%(9/44)
HIVco-infection9.1%(4/44)
Gonorrheaco-infection6.8%(3/44)
HCVco-infection2.3%(1/44)
Gonorrheainfection6.1%(35/574)
Chlamydiaco-infection22.9%(8/35)
Syphilisco-infection8.6%(3/35)
HIVco-infection2.9%(1/35)
HCVco-infection2.9%(1/35)
Chlamydiainfection9.8%(56/574)
Syphilisco-infection16.1%(9/56)
Gonorrheaco-infection14.3%(8/56)
HCVco-infection1.8%(1/56)
HIVco-infection0%
HIVinfection0.9%(67/7,354)
HCVco-infection10.4%(7/67)
Syphilisco-infection5.9%(4/67)
Gonorrheaco-infection1.5(1/67)
Chlamydiaco-infection0%
HCVinfection5.0%(373/7,470)
HIVco-infection1.9%(7/373)
Chlamydiaco-infection0.3%(1/373)
Gonorrheaco-infection0.3%(1/373)
Syphilisco-infection0.3%(1/373)
Gonorrheaandchlamydiawerealwaystestedtogether. HCV,hepatitisCvirus.
Atotalof633patientsreceivedtargetedSTItestingdueto clinicalconcernduringtheir firstEDvisit(testedforcombo gonorrhea/chlamydiaand/orsyphilis).However,co-testing betweensyphilisandgonorrhea/chlamydiaoccurredinonly 57%(361/633)ofthesetestingencounters.Only63% (397/633)ofthesepatientsreceivedHIVco-testing,andonly 59%receivedHCVco-testing.SomepatientsreceivedSTI testingforoneormoreSTIs,butnotall fiveSTIs(gonorrhea, chlamydia,syphilis,HIV,HCV),duringtheir firstEDvisit. InthisgroupwithincompleteSTItesting,weassessed whetherpatientsreceivedfurtherSTItestinginanyoftheir nextfourdocumentedEDvisitswithinthestudyperiodand foundthefollowingtestingcountsandpositiveresults:HCV, 81(9positive[11.1%]);HIV,61(1positive[1.6%]);syphilis, 49(3positive[6.1%]);andgonorrhea/chlamydia, 55(1gonorrheapositive[1.8%]).
InourstudyweexaminedSTItesting/co-testingand infection/co-infectionprevalenceinEDpatientswhowere testedforatleastoneofHIV,HCV,syphilis,gonorrhea,or chlamydia.Toourknowledge,thisisthe firstED-based studytoreportEDSTIco-testingandco-infection frequenciesforeverycombinationofgonorrhea,chlamydia, syphilis,HIV,andHCV.Overall,STIco-testingwas infrequent,butco-infectionprevalencewashighamong severalSTIco-testpairings.
TheHIV/HCVtestingco-testingoccurredfrequently, likelyrelatedtothepresenceoftheuniversalscreeningBPA. AccordingtotheUSCentersforDiseaseControland Prevention,approximately21%ofindividualswithHIVin high-riskpopulations(ie,menwhohavesexwithmen,people whousedrugs)areco-infectedwithHCV.20 Whilepublished dataislimited,previousED-basedstudiesfoundthat8–33% patientswithHIVwereco-infectedwithHCV.21–24 Inour study,10.5%ofpatientswithHIVwereco-infectedwith HCV,butonly1.9%ofpatientswithHCVwereco-infected withHIV.PreviousstudiesinthisEDpopulationfoundthat patientssharedsome(malegender,unhousedstatus,history ofillicitdruguse,andMedicareinsurancestatus)butnotall riskfactorsforinfection.25,26 Itispossiblethatco-infection proportionsmaydifferamongpatientswithHCVandHIV duetosomeotherunmeasuredriskfactor.Alternatively, giventheimmunosuppressivepropertiesofHIV,patients whoareexposedtoHCVmaybemorelikelytoprogresstoa chronicinfection.27
Amongpatientswithgonorrhea,23%wereco-infected withchlamydia.Conversely,only14%ofthoseinfectedwith chlamydiawereco-infectedwithgonorrhea.Thisdifferential co-infectionpatternhasbeenpreviouslyreportedinatleast oneotherED-basedstudy(gonorrhea+,chlamydia+:44%; chlamydia+,gonorrhea+:17%).28 Amongpatientswith syphilis,wealsoobservedahighprevalenceofchlamydiacoinfection(21%).Inourstudy,therewasaBPAthatprompted clinicianstotestpatientsforsyphiliswhowereundergoing gonorrhea/chlamydiatesting,andco-testingoccurredinjust 57%ofpatients.Previousstudiesreporttheprevalenceof syphilisandgonorrhea/chlamydiaco-testing(9–39%); however,wecouldnot findanyED-basedstudiesthat reportedproportionsofco-infection.29 Similarly,wefound thatpatientswhoweretestedforsyphilisand/orgonorrhea/ chlamydia,co-testingforHIVandHCVoccurred infrequently.Giventhatpatientswithsyphilis,gonorrhea, andchlamydiahadthehighestprevalenceofco-infection withotherSTIs.Theseinstancesrepresentpotentialmissed opportunitiesfordiagnosisandlinkagetocare.
Inourstudy,therewereseveralpatientswhotested positiveforspecificSTIsinsubsequentEDvisitsandwere nottestedfortheseSTIsintheirinitialvisit.Itispossiblethat patientscontractedtheSTIexposureaftertheindexEDvisit, andhadtheybeentestedattheindexvisittheymayhavebeen
negative.However,itisalsopossiblethatthesediagnoses werepresentattheindexvisitandweremissed,suggesting thatincreasedco-testingcanleadtoincreaseddiagnosisof clinicallysignificantco-infectionswiththepotentialtoreduce transmissioninthecommunity.
Thiswasaretrospectivestudywithdataobtainedfromthe EHRatasingleinstitution;thus,our findingsmaynotbe generalizabletoallsettings.OurstudyhadmultipleBPAsin placethatlikelyinfluencedclinicianco-testingbehavior.We didnotreportchiefcomplaints,makingitdifficultto differentiatepatientswithtrueclinicalindicationfortesting, andpatientswhowerebeingscreenedaspartofascreening protocol.Sincetestingforsyphilisandgonorrhea/chlamydia wasnotuniversal,thereportedproportionsareunlikelyto representtheprevalenceforthewholeED,butratherthe prevalenceofinfectionamongpatientswithclinical suspicionforSTI.WhileHIVandHCVscreeningwas universallyorderedformostpatientsundergoingbloodwork, patientscouldstilloptout,whichmayhavebiasedthe prevalenceestimatesfortheseinfections.
Prevalenceofco-testingforsexuallytransmittedinfection waslowamongpatientswithclinicalsuspicionforSTI; however,co-infectionprevalencewashighinseveralcoinfectionpairings.EncounterswithsingleSTItesting representamissedopportunitytoscreenforco-infections. FutureeffortsareneededtoimproveSTIco-testingrates amonghigh-riskindividuals.Withtheincidenceofmany STIsincreasing,theEDcanserveasanimportantscreening settingforSTIs,especiallyinpatientswithoutaccessto traditionaloutpatientservices.
AddressforCorrespondence:LarissaMay,MD,MSPH,Universityof CaliforniaDavisHealth,DepartmentofEmergencyMedicine, 4150V.St.,PSSB2100,Sacramento,CA95817.Email: lsmay@ ucdavis.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ThisworkwassupportedbyGileadfundedFrontlinesofCommunitiesintheUnitedStates(FOCUS). TheFOCUSProgramisapublichealthinitiativethatenables partnerstodevelopandsharebestpracticesinroutineblood-borne virus(HIV,HCV,HBV)screening,diagnosis,andlinkagetocarein accordancewithscreeningguidelinespromulgatedbytheUS CentersforDiseaseControlandPrevention,theUSPreventive ServicesTaskForce(USPSTF),andstateandlocalpublichealth departments.FOCUSfundingsupportsHIV,HCV,andHBV screeningandlinkagetothe firstmedicalappointmentafter diagnosis.FOCUSpartnersdonotuseFOCUSawardsforactivities
beyondlinkagetothe firstmedicalappointment.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Fordetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CentersforDiseaseControlandPrevention(CDC).PressRelease: CDCestimates1in5peopleintheU.S.haveasexuallytransmitted infection.2021.Availableat: https://www.cdc.gov/nchhstp/newsroom/ 2021/2018-STI-incidence-prevalence-estimates-press-release.html AccessedMay20,2022.
2.CentersforDiseaseControlandPrevention(CDC),U.S.Departmentof HealthandHumanServices,NationalCenterforHIV,ViralHepatitis, STD,andTBPrevention,etal.SexuallyTransmittedDisease Surveillance2019.2021.Availableat: https://www.cdc.gov/std/ statistics/2019/std-surveillance-2019.pdf.AccessedMay20,2022.
3.CentersforDiseaseControlandPrevention(CDC).HIVIncidence. Availableat: https://www.cdc.gov/hiv/statistics/overview/in-us/ incidence.html.AccessedJuly18,2023.
4.MannsMPandMaasoumyB.BreakthroughsinhepatitisCresearch: fromdiscoverytocure. NatRevGastroenterolHepatol. 2022;19(8):533–50.
5.CentersforDiseaseControlandPrevention(CDC).HepatitisC Surveillance2020.2020.Availableat: https://www.cdc.gov/hepatitis/ statistics/2020surveillance/hepatitis-c.htm.AccessedJuly18,2023.
6.WesterC,OsinubiA,KaufmanHW,etal.HepatitisCvirusclearance cascade-UnitedStates,2013–2022. MorbMortalWklyRep. 2023;72(26):716–20.
7.RyersonAB,SchillieS,BarkerLK,etal.VitalSigns:newlyreported acuteandchronichepatitisCcases-UnitedStates,2009–2018. MMWR MorbMortalWklyRep. 2020;69(14):399–404.
8.StanfordKA,HazraA,SchneiderJ.Routineopt-outsyphilisscreeningin theemergencydepartment:apublichealthimperative. AcadEmerg Med. 2020;27(5):437–8.
9.FordJS,MarianelliLG,FrassoneN,etal.HepatitisBscreeninginan ArgentineED:increasingvaccinationinaresource-limitedsetting. AmJ EmergMed. 2020;38(2):296–9.
10.FordJS,ChechiT,OtmarM,etal.EDsyphilisandgonorrhea/chlamydia cotestingpracticesbeforeandaftertheimplementationofanelectronic healthrecord-basedalert. EmergMedJ. 2021.21:emermed-2020210331.
11.FordJS,ChechiT,ToosiK,etal.UniversalscreeningforhepatitisC virusintheEDusingabestpracticeadvisory. WestJEmergMed. 2021;22(3):719–25.
12.FordJ,RouleauS,VoongS,etal.UniversalHIVscreeninginthe emergencydepartment:aninterruptedtimeseriesanalysis. AIDS. 2022.Inpress.
13.ChoudhryS,RamachandranVG,DasS,etal.Characterizationof patientswithmultiplesexuallytransmittedinfections:Ahospital-based survey. IndianJSexTransmDisAIDS. 2010;31(2):87–91.
14.PakianathanMR,RossJD,McMillanA.Characterizingpatientswith multiplesexuallyacquiredinfections:amultivariateanalysis. IntJSTD AIDS. 1996;7(5):359–61.
15.BarnesA,JetelinaKK,BettsAC,etal.Emergencydepartmenttesting patternsforsexuallytransmitteddiseasesinNorthTexas. SexTransm Dis. 2019;46(7):434–9.
16.SeballosSS,LopezR,HusteyFM,etal.Co-testingforhuman immunodeficiencyvirusandsexuallytransmittedinfectionsinthe emergencydepartment. SexTransmDis. 2022;49(8):549–50.
17.WhiteDA,AlterHJ,IrvinNA,etal.Lowrateofsyphilisscreeningamong high-riskemergencydepartmentpatientstestedforgonorrheaand chlamydiainfections. SexTransmDis. 2012;39(4):286–90.
18.Schechter-PerkinsEM,MillerNS,HallJ,etal.Implementationand preliminaryresultsofanemergencydepartmentnontargeted,opt-out hepatitisCvirusscreeningprogram. AcadEmergMed. 2018;25(11):1216–26.
19.MarangoniA,NardiniP,FoschiC,etal.EvaluationoftheBioPlex2200 syphilissystemasa first-linemethodofreverse-sequencescreeningfor syphilisdiagnosis. ClinVaccineImmunol. 2013;20(7):1084–8.
20.CentersforDiseaseControlandPrevention(CDC).Peoplecoinfected withHIVandviralhepatitis.Availableat: https://www.cdc.gov/hepatitis/ populations/hiv.htm#ref07.AccessedFebruary14,2023.
21.BurrellCN,SharonMJ,DavisS,etal.Usingtheelectronic medicalrecordtoincreasetestingforHIVandhepatitisCvirusinan
Appalachianemergencydepartment. BMCHealthServRes. 2021;21(1):524.
22.Martel-LaferriereV,BarilJG,AlarieI,etal.Opt-outuniversalHCVand HIVscreeninginaCanadianemergencyroom:across-sectionalstudy. BMJOpen. 2022;12(1):e048748.
23.CieplyL,SimmonsR,IjazS,etal.SeroprevalenceofHCV,HBVandHIV intwoinner-cityLondonemergencydepartments. EpidemiolInfect. 2019;147:e145.
24.TorianLV,FelsenUR,XiaQ,etal.UndiagnosedHIVandHCVinfection inaNewYorkCityemergencydepartment,2015. AmJPublicHealth. 2018;108(5):652–8.
25.FordJS,HollywoodE,SteubleB,etal.RiskfactorsforhepatitisCvirus infectionatalargeurbanemergencydepartment. JViralHepat. 2022;29(10):930–7.
26.FordJS,MousaMA,VoongS,etal.RiskfactorsforHIVinfectionata largeurbanemergencydepartment:across-sectionalstudy. Sex TransmInfect. 2023;99(6):404–8.
27.ThomasDL,LeoutsakasD,ZabranskyT,etal.HepatitisCin HIV-infectedindividuals:cureandcontrol,rightnow. JIntAIDSSoc. 2011;14:22.
28.WilsonSP,VohraT,KnychM,etal.Gonorrheaandchlamydiainthe emergencydepartment:continuedneedformorefocusedtreatmentfor men,womenandpregnantwomen. AmJEmergMed. 2017;35(5):701–3.
29.EricksonJL,WuJ,FertelBS,etal.Multidisciplinaryapproachtoimprove humanimmunodeficiencyvirusandsyphilistestingratesinemergency departments. OpenForumInfectDis. 2022;9(12):ofac601.
JensKlein,PhD* SarahKoens,PhD*
MartinScherer,MD†
AnnetteStrauß,MD†
MartinHärter,PhD,MD‡
OlafvondemKnesebeck,PhD*
SectionEditor:GayleGalletta,MD
*UniversityMedicalCenterHamburg-Eppendorf,InstituteofMedicalSociology, Hamburg,Germany
† UniversityMedicalCenterHamburg-Eppendorf,DepartmentofGeneralPractice andPrimaryCareHamburg,Germany
‡ UniversityMedicalCenterHamburg-Eppendorf,DepartmentofMedical Psychology,Hamburg,Germany
Submissionhistory:SubmittedMay16,2023;RevisionreceivedDecember20,2023;AcceptedJanuary22,2024
ElectronicallypublishedMay3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18224
Background: Itiswellestablishedthatemergencydepartment(ED)crowdingleadstoworsehealth outcomes.AlthoughvariouspatientsurveysprovideinformationaboutreasonstovisitEDs,lessis knownintermsofbeliefsaboutEDsamongthegeneralpopulation.Thisstudyexaminespublicbeliefs regardingaccessibilityandqualityofEDsandtheirassociationswithsocialcharacteristics(gender,age, education,immigrationbackground)aswellasknowledgeaboutemergencycareservicesand healthliteracy.
Methods: Weconductedacross-sectionalstudybasedonarandomsampleof2,404adultslivingin Hamburg,Germany,inwinter2021/2022.Wedevelopedeightstatementsregardingaccessibilityand qualityofEDsleadingtotwoscales(Cronbach’s α accessibility = 0.76andqualityofcare = 0.75). Descriptivestatisticsoftheeightitemsareshownandlinearregressionwereconductedtodetermine associationsofthetwoscaleswithsocialcharacteristicsaswellasknowledgeaboutemergencycare servicesandhealthliteracy(HLS-EU-Q6).
Results: Nearly44%oftherespondentsagreedthat “youcanalwaysgotoanED,ifyoudonotgeta short-termappointmentwithageneralpractitionerorspecialist.” And38%agreedwiththestatement, “If youdonothavethetimeduringnormalpracticehoursduetoyourwork,youcanalwaysgotoanED.” In termsofquality,38%believedthatdoctorsinEDsaremorecompetentthandoctorsingeneralpractice, and25%believedthatdoctorsinEDsaremorecompetentthandoctorsinspecializedpractices.Inthe fullyadjustedmodel,publicbeliefsaboutemergencycareaccessibilityandqualityofEDswere significantlyassociatedwithallsocialcharacteristicsandknowledgeofemergencycareoptionswiththe strongestassociationsbetweenknowledgeandaccessibility(β = 0.17; P < 0.001)andbetween educationandquality(β = 0.23; P < 0.001).
Conclusion: WefoundendorsementofpublicbeliefsaboutaccessibilityandqualityofEDsthatcan leadtoinappropriateutilization.Ourresultsalsosuggestthatknowledgeofdifferentemergencyservices playsanimportantrole.Therefore,aftersystem-relatedreorganizationsofemergencycare,information campaignsaboutsuchservicestailoredtosociallydeprivedpopulationsmayhelpalleviatetheissueof crowding.[WestJEmergMed.2024;25(3)389–398.]
Crowdingofemergencydepartments(EDs)hasbecome animportantissueinmanycountries.1–3 Twocontributing causesofcrowdingareboardingofadmittedpatients (primary)andinappropriateutilizationoftheEDfornonurgentconditions(secondary).3–5 Intermsofthe firstcause, accessblock(ie,accesstohospitalbedsisblockedandno admissiontoaninpatientwardispossible)andhospital admissionsforambulatorycare-sensitiveconditions(ACSC) havebeenextensivelydiscussed.6,7 Inthisstudyweaimedto addressthesecondcause.AmongOrganizationfor EconomicCooperationandDevelopmentcountries,the increaseofEDuseinGermanyiscomparativelyhigh.8
Emergencydepartmentcrowdinghasbeenshownto negativelyaffectpatientsafety.3–5 Variousstudieshave examinedassociationsbetweencrowdedEDsandworse healthcareoutcomes(eg,delaysincriticaltreatments, medicationerrors,returnvisits,complicationrates,and mortality).9–11 Forinstance,recentresearchintheUnited KingdomfoundthatEDcrowdingisassociatedwith treatmentdelayandanincreaseinall-cause,30-day mortality.12 ToreducepatientnumbersinEDs,researchis focusedonavoidableEDvisitsofpatientswithnon-urgent conditions.StudieshaveshownthatthepercentageofallED visitsjudgedtobenon-urgentisabout30–40%,eventhough studydesignswereveryheterogeneous.13 Moreover,astudy fromGermanyfoundthatmorethanhalfofthepatients visitinganEDdidnotthinkthattheirconditionrequired urgenttreatmentandthusdidnotmeetthedefinitionofa medicalemergency.14
Innumerouspatientsurveys,differentreasonsforvisiting EDswithnon-urgentconditionswerereported.Access barrierstooutpatientcare,assumptionsofhigherqualityof careandmorehealthcareoptionsatEDs(aswellasnegative perceptionsaboutprimarycarephysicians),perceivedneed andanxiety,convenience(eg,24/7availability,no appointments,transport),andreferralfromhealthcare professionalsweremostfrequentlymentionedinvarious internationalsurveys.13,15–17 Patientsurveysconductedin GermanyfoundfourmainmotivationsforpatientswhoselfreferredtotheED:distress/perceivedurgency;access;quality ofcare;andconvenience.14,18,19
Alowersocioeconomicstatus(SES) mostlyassessedby educationallevel,income,occupationonindividualor regionallevel,andimmigrationstatus predictmore frequentEDutilizationandahigheruseforlow-acuity presentations,20–23 eventhoughsomecurrent findingsdidnot completelyconfirmtheseinequalitiesforGermany.19 Inthis context,theconceptofhealthliteracyplaysanimportant role.24 Lowhealthliteracywasshowntobeassociatedwith preventableEDvisitsduetominorornon-urgentproblems andwithmorefrequentutilizationofEDsandemergency services,25–27 althoughsomeotherstudiesdidnotshow thisassociation.28
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
CrowdedEDsareassociatedwithpoorhealth outcomes.Patientsurveyshaveshown problematicassumptionsaboutED accessibilityandquality.
Whatwastheresearchquestion?
WesoughttoexaminebeliefsabouttheED andtheirassociationswithvarious characteristicsinapopulationsurvey.
Whatwasthemajor findingofthestudy?
44%ofrespondentsagreed, “ youcanalways gotoanED,ifyoucan ’ tgetanappointment withanof fi cedoctororspecialist, ” and38% saidyoucouldusetheEDforcareduring non-businesshours.
Howdoesthisimprovepopulationhealth?
ByunderstandinginappropriateEDuse, wecandevelopeducationprogramsfor vulnerablegroupstoinformthemabout alternativevenuestoobtaincare.
Whilecurrentevidenceprovidesinformationabout reasonsandpredictorsoffrequentorinappropriateEDuse, nearlyall findingsarederivedfrompatientsurveysthatwere conductedatEDsorwerebasedonEDrecords.These surveysexaminetherecordedhealthcareutilizationofactual patientsratherthanthebeliefsaboutEDsamongthegeneral population.Thisresearchgapconcerningpublicbeliefs aboutEDsandtheiraccessibilityandqualitywasour rationaleforconductingthisstudy.Publicbeliefsabout emergencycarearehighlyrelevantastheymaycontributeto abetterunderstandingofinappropriateEDuseandtothe developmentofcampaignstoimprovehealthliteracy.29 Againstthisbackground,weexploredtworesearch questions:1)Whatarethepublic’sbeliefsaboutEDsinterms ofaccessibilityorconvenienceandqualityofcare;and2)Are therevariationsinthesebeliefsaboutEDsaccordingtosocial characteristics(age,gender,educationlevel,and immigrationstatus)andhealthliteracy(generalhealth literacyandknowledgeofemergencycareoptions)?
Across-sectionaltelephonesurveywasconductedin Hamburg,Germanyinwinter2021/2022viacomputerassistedtelephoneinterviews.Weobtainedarandomsample
ofGerman-speakingpeopleaged ≥18yearsusingallpossible telephonenumbersinHamburg,includingnon-registered numbers,viarandomdigitaldialing.Onlylandlinenumbers couldbeincludedasmobiletelephonenumbersarenot providedonaregionallevel.About83%ofallhouseholdsin Germanyhavealandlinetelephone.30 Thus,alargemajority ofthepopulationcanbereachedvialandlinenumbers. Repeatedcallsweremadebytrainedinterviewersofa professionalsurveyresearchinstitute(USUMA,Berlin, Germany)ondifferentweekdays.WeappliedtheKish selectiongridtorandomlyselectthetargetpersoninthe contactedhouseholds.31 Priortothis,thesamesurvey researchinstituteconductedapilotstudyamong30 individualsinthegeneralpopulation.
Wechoseatelephonesurveyasthemethodfordata collectionduetothevignettedesignofthestudy.Atthe beginningofthesurvey,recordedaudio filesdescribing differentsymptomsweredirectlyplayedtotherespondents. Toguaranteeastandardizedstimulusandimmediate response,telephonesurveysareusuallyfavoredandan establishedmethod.32 Subsequently,astandardized questionnairewasapplied.Samplesizewascalculatedbased onavignettedesign(48vignettesintotal)appliedinthe study.Accordingtopowercalculations,asamplesizeof50 respondentspervignettewascalculatedtoidentifymedium sizedifferencesresultinginabout2,400requiredparticipants (statisticalpower0.8,andtype-Ierror0.05).Thesevignettes werenotusedinthepresentanalyses.Thesampleconsisted of2,404respondents.
Duetodifferentapproachesforthedefinitionofeligibility intelephonesurveys,differentresponserates(RR)canbe calculated.33 Thus,aRRinthissurveyvariedbetween 10.9–46.0%(AmericanAssociationofPublicOpinion ResearchRR334 17.3%).Togainarepresentativesample,we weighteddataforhouseholdsize,gender,age,educational level,andplaceofresidence(districtinHamburg)usingthe officialstatisticsregardingtheadultpopulationlivingin Hamburg.35–37 InaccordancewithHalbeslebenand Whitman,38 weconductedasample/populationcomparison toassessnonresponsebias. Table1 showsthattheweighted sampleadequatelyrepresentsthegeneraladultpopulationof Hamburgregardingthedistributionofgender,age,and educationallevel.35,36 ThesurveywasapprovedbytheLocal PsychologicalEthicsCommitteeattheCenterfor PsychosocialMedicine,UniversityMedicalCenter Hamburg(No.LPEK-0200).Respondentsgavetheir informedconsentfortheparticipationandtheuseof theirdata.Consentsandrefusalsweredocumentedby theinterviewers.
Measures
Toassessthepublic’sbeliefsaboutEDs,wedevelopedeight items(statementsaboutEDs)basedonareviewofthe literature.13–16,18,19,39 Asdescribedabove,themain
Table1. Samplecharacteristicsofsurveyrespondentscompared withofficialstatisticsforthepopulationinHamburgbypercentage.
Samplea (N = 2,404)
Adultpopulationof Hamburg2020b Pc
Gender (0)d
Male48.548.40.95
Female51.551.6
Age(years) (0)
18–249.69.40.83 25–3419.719.6
35–4417.217.5
45–5417.516.6
55–6414.115.1 65–7410.110.0 ≥7511.811.8
Educationlevel (71)
Migration background (46) Nomigration background
2nd generation11.2 –g 1st generation10.9 –g
aWeighted; b34,35; cPearson’schi2; dNumberofmissingcasesinbracketsinitalics; eDataforeducationonlyavailableforpeople ≥15yearsold. fNoexactdataavailable. gAstherewasnodiscreteweightingforimmigrationbackground,test statisticswerenotconducted.
motivationsforpreferringEDsin patientsurveyswererelated tobarrierstoaccessofoutpatientcare,convenience, assumptionsofhigherqualityofcare,anddistressorsubjective need.Wedevelopedfourstatementsregardingaccessbarriers andconvenience,aswellasfourstatementsrelatedtothe qualityofcareprovidedinEDs(Figure1).Asthesurveywas conductedamongthegeneralpopulationandnotacute patientsinEDs,wedidnotincludestatementsregarding distressandsubjectiveneed.Responsecategorieswere “fully agree, ”“ratheragree,”“ratherdisagree,”“fullydisagree” and, additionally, “don’tknow,” withhighervaluesindicating strongeragreement.Validitywastestedinaccordancewith someaspectsofMessick'sunifiedframework.40
Wecollectedcontentvalidityevidencethroughan extensiveliteraturescreeningofpatientsurveysidentifying themainmotivationsforpreferringEDs.Additionally,
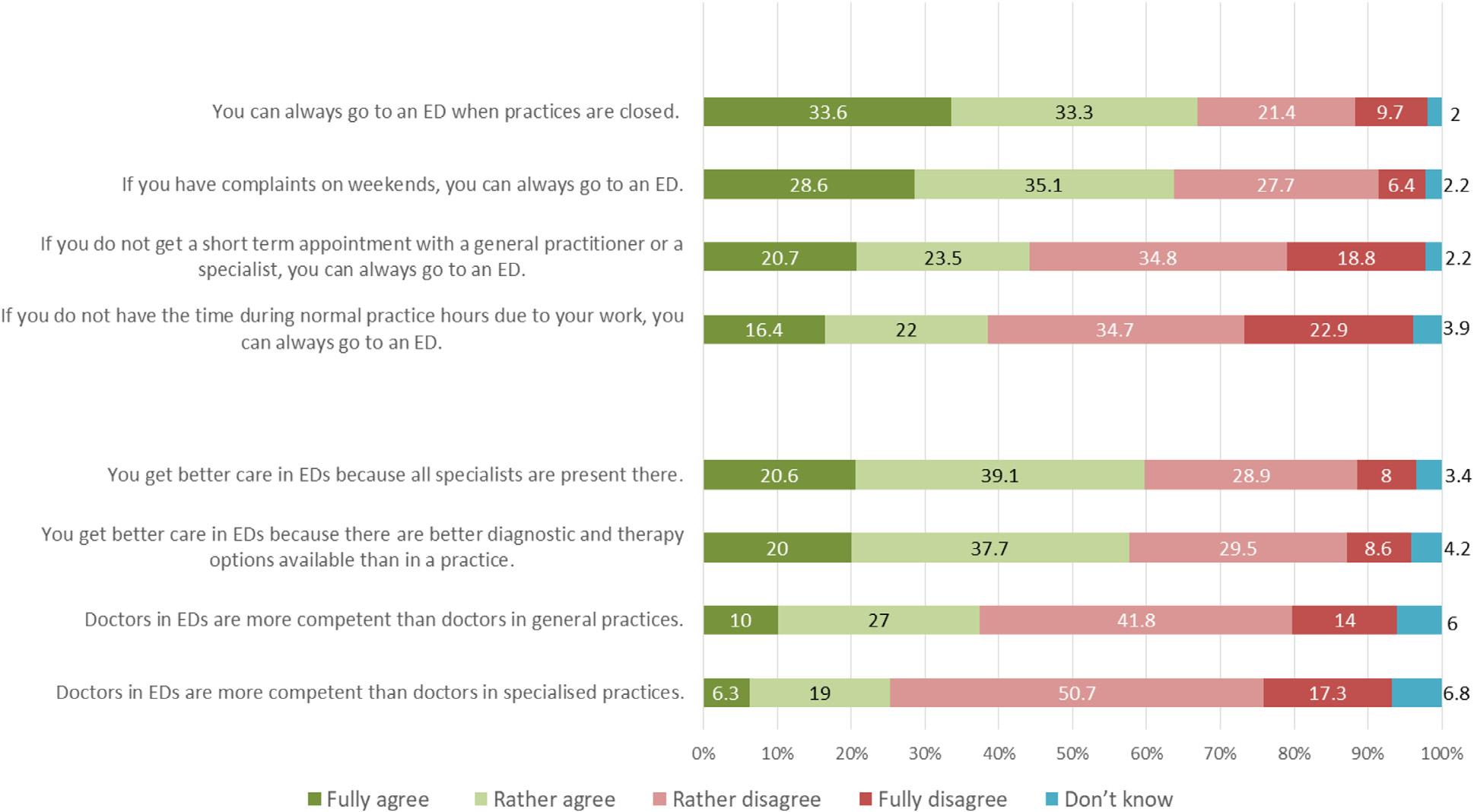
Figure1. Publicbeliefsaboutaccessibilityandqualityofemergencydepartments(N = 2,404). ED, emergencydepartment.
expertsinemergencycarewereinvolvedintheitem development.Usingapilotstudy,wepretesteditemsand responseconsistencies.Furthermore,internalstructure validitywastestedthroughCronbach’ s α andthefactorial structureoftheinstrumentviaprincipalcomponentanalysis. Theweightingofdemographicsinourstudywasaimedto meetexternalvalidity.
Gender,age,educationallevel,andimmigration background(noimmigrationbackground, firstgeneration, secondgeneration)wereintroducedassocialcharacteristics oftherespondents.Educationlevelwasbasedonyearsof schooling(9years = low;10years = middle; ≥12 = high).A personwasconsideredtohaveanimmigrationbackgroundif heorsheoratleastoneparentwasbornabroad. Respondentswithanimmigrationbackgroundwhowere borninGermanyareconsideredsecond-generation immigrants,whilethosewithimmigrationexperienceare subsequentlytermed first-generationimmigrants.We assessedgeneralhealthliteracyusingaEuropeanhealth literacysurveyquestionnaire,theHLS-EU-Q6,ashortform oftheestablishedHLS-EU-Q47.41 Onafour-point Likertscale,theanswercategorieswere “verydifficult,” “fairlydifficult,”“fairlyeasy,” and “ veryeasy, ” including “don’tknow.” TheCronbach’ s α = 0.60ofthescaleis acceptableforaninstrumentthatisshortandfeatures discreteelementsofliteracy.42 Wecomputedasumscaleby averagingtheresponsestothesixitemsresultinginarange between1–4,withhigherscoresindicatinganincreased healthliteracy.
Tospecificallyassessknowledgeaboutavailable emergencycareservices,weaskedtherespondentstoname alloptionsofemergencycaretheyknewof(open-ended question).IntheGermanhealthcaresystem,patients basicallyhavefouroptionsofemergencycare.43 Theycan1) calltherescueservice(telephonenumber112);2)gotoan ED;3)gotoanemergencypractice(practicesthatareusually openfrom6 PM tomidnightforurgentconditions); or4)contactthemedicalon-callservice(alsoknownas “116117,” referringtothetelephonenumber)inurgentor emergencycases.Inthesurvey,thisquestionwaslocated beforetheitemaboutarespondent’sbeliefsconcerningEDs. Basedontheresponses(respectiveemergencycareservice mentioned = 1,notmentioned = 0),wecalculatedasum scalewithapossiblerangefrom0–4withhigherscores indicatingmoreknowledge.
Wepresentpercentagesofagreementoftheeightsingle itemstoassessbeliefsaboutEDsasdescriptiveresults. Furthermore,weconductedaprincipalcomponentanalysis includingtheeightitemsassessingpublicbeliefs.Theanalysis revealedtwocomponentswitheigenvalues ≥1reflecting accessibility(eigenvalue:3.22,explainedvariance:40.3%) andqualityofcare(eigenvalue:1.41,explainedvariance: 17.6%),whichaccountedfor57.9%ofthetotalvariance (rotatedloadingsbetween0.66–0.78).Eigenvaluesareused todeterminetherelativeimportanceandtheexplained varianceofeachprincipalcomponent.Usually,onlyfactors
witheigenvalues ≥1areconsidered.44 Accordingly,forthe multivariateanalyses,twoscalesrepresentingaccessbarriers andconvenience(subsequentlylabelledas “accessibility,” fouritems)andqualityofcare(“quality,” fouritems)were calculatedrangingfrom1–4.Higherscoresindicatestronger agreementwitheasyaccessibilityandsuperiorcarequality withregardtoEDs.Intermsofreliability,internal consistencyofthetwoscalesrevealedsatisfactoryresults (Cronbach’ s α = 0.76[accessibility]and0.75[quality]).
Wecalculatedlinearregressionmodelstoanalyze associationsbetweensocialcharacteristics,healthliteracy, andpublicbeliefsaboutaccessibilityandqualityofEDs. Dependentvariableswerethetwoscalesregarding accessibilityandqualityofEDs.Aspredictorvariables, gender,age,educationlevel,immigrationbackground, generalhealthliteracy,andknowledgeofemergencyservices wereintroduced.Ina firststep,wecalculatedsimple unadjustedmodelsshowingthesingleestimatesand significancesofeachpredictorvariable.Thereafter,inthefull model,thepredictorvariableswereenteredsimultaneously adjustingallvariablesforeachother.Wedocumented regressionestimates(B),standardizedB(β),significances(P ), andexplainedvariance(R2).Resultswith P < 0.05were consideredstatisticallysignificant.Asmanyparticipants chosetheoption “don’tknow” whencompletingtheHLSEU-Q6,whichhadtobeconsideredasmissingvalue,the multivariateanalyseswereconductedwithasamplesizeof 1,751(quality)or1,826(accessibility),respectively. Moreover,variouskeyassumptionsforlinearregression models(linearrelationship,normaldistributionofresiduals, auto-correlation,homoscedasticity,andmulticollinearity) weresuccessfullytested.Allanalyseswerecalculatedwith
weighteddataandcarriedoutusingtheStatisticalPackage fortheSocialSciencesV27(SPSS,Inc,ChicagoIL).45
Meanageoftherespondentswas48.8years(SD19.0); 51.5%werefemale.Almosthalfofthesample(48.5%)hada higheducationallevel(middlelevel:24.1%;lowlevel: 27.4%).About11%eachbelongedtothegroupof first-or second-generationimmigrants,whileabout78%ofthe samplehadnoimmigrationbackground(Table1).Themean (SD)was2.56(0.49)forhealthliteracy(HLS-EU-Q6)score (range1–4).Regardingknowledgeofavailableemergency services,onaveragetherespondentsknewtwooffour options. Figure1 showsthedistributionoftheeightitems measuringbeliefsaboutaccessibilityandqualityofEDs. Agreement(percentageofrespondentswho “fully” and “rather” agreedsummedup)totheitemsrelatedtoaneasy accessofEDsrangedbetween38.4%(“Ifyoudonothavethe timeduringnormalpracticehoursduetoyourwork,youcan alwaysgotoanED”)and66.9%(“Youcanalwaysgotoan EDwhenpracticesareclosed”).Intermsofqualityofcare providedinEDs,25.3%oftherespondents “fully” or “rather” agreedwiththeitem “DoctorsinEDsaremore competentthandoctorsinspecializedpractices,” while68% “rather” or “fully” disagreed.Regardingtheitem “Youget bettercareinEDsbecauseallspecialistsarepresentthere,” 59.7%expressedagreement.
Table2 showstheresultsoflinearregressionanalyseswith thesumscaleindicatingaccessibilityofEDsasthedependent variable.Ascanbeseenintheunadjustedmodels,all predictorvariablesindicatedsignificantassociationswith beliefsaboutaccessibility.Strongestassociationswereshown
B = regressionestimate, β = standardizedB, P = significance(significantassociations[P < 0.05]arebold). aHighervaluesindicatestrongeragreement(range1to4). bAllanalysesbasedonthesamplesizeofthefullyadjustedmodel.
cGender = reference:male,age = range18–96years,education = range1–3;migrationbackground = reference:nomigrationbackground; healthliteracy = range1–4;knowledgeofemergencycareservices = range0–4. dEmergencydepartment/emergencypractice/rescueservice/medicalon-callservice.
Table3. Beliefsaboutemergencydepartments:sumscalequalitya (N = 1,751b)(linearregressions) UnadjustedmodelsFullyadjustedmodel
B = regressionestimate, β = standardizedB,p = significance(significantassociations[P < 0.05]arebold). aHighervaluesindicatestrongeragreement(range1to4).
bAllanalysesbasedonthesamplesizeofthefullyadjustedmodel.
cGender = reference:male,age = range18–96years,education = range1–3;migrationbackground = reference:nomigrationbackground; healthliteracy = range1–4;knowledgeofemergencycareservices = range0–4. dEmergencydepartment/emergencypractice/rescueservice/medicalon-callservice.
foreducationlevelandknowledgeofemergencycareservice. Inthefullyadjustedmodel,femalerespondentslessoften agreedthatEDsarecharacterizedbyeasyaccessibility. Moreover,agreementincreasedwithage,whileit decreasedwitheducationlevelandknowledgeof emergencycareserviceoptions.Comparedtorespondents withoutanimmigrationbackground, first-andsecondgenerationimmigrantsmorestronglybelievedinthe easyaccessibilityofEDs.Highest β-valuesinthefully adjustedmodelwereshownforeducation(β = 0.13, P < 0.001),knowledge(β = 0.17, <0.001)andage (β = 0.13, P < 0.001).
IntermsofbeliefsaboutsuperiorcarequalityinEDs, significantassociationswereshownforallpredictorsexcept immigrationbackground(secondgeneration)inthe unadjustedmodels(Table3).Again,educationleveland knowledgeofemergencycareserviceindicatedhighest βvalues.Regardingthefullyadjustedmodel,significant negativeassociationswitheducationlevel,emergencycare knowledge,andhealthliteracyemerged.Furthermore,these beliefsincreasedwithageandweremorepronouncedamong first-generationimmigrantsandmales.Educationlevel showedthestrongestassociation(β = 0.23, P < 0.001)in thefullyadjustedmodel.
BasedonapopulationsurveyinaGermanmetropolis,we assessedthepublic’sbeliefsaboutaccessibilityandqualityof careofEDs.Nearly44%oftherespondentsagreedthat “ you canalwaysgotoanED,ifyoudonotgetashort-term appointmentwithageneralpractitioneroraspecialist.” Still, 38%agreedtothestatement “Ifyoudonothavethetime
duringnormalpracticehoursduetoyourwork,youcan alwaysgotoanED.” Intermsofsuperiorquality,38% believedthatdoctorsinEDsaremorecompetentthan doctorsingeneralpracticeand25%regardeddoctorstobe morecompetentinspecializedpractices.Inaddition,nearly 60%agreedthat “yougetbettercareinEDsbecauseall specialistsarepresentthere.” Furthermore,thepublic’ s perceptionsofemergencycarearesignificantlyassociated withsocialcharacteristics(gender,age,educationlevel, immigrationbackground)andknowledgeofemergencycare options.Regardingaccessibility,knowledgeshowedthe strongestassociation:Themoreoptionsofemergencycare respondentsnamed,thelessrespondentsagreedthatEDsare alwaysaccessible.Intermsofbeliefsaboutqualityofcare, educationlevelturnedouttobethestrongestpredictor:The lesseducatedtherespondentswerethemoretheyagreedthat thequalityofcareissuperiorinEDs.
Astherearemanypatientsurveysbutveryfew population-basedstudies,comparabilityofourresultswith previousresearchislimited.Someresearchersalsoaimedto assesspublicperceptionsaboutEDs,buttheirmethodsvary considerably.27,46 Regardingattitudestowardaccessibility andquality,males,olderpeople,ethnicminorities,and peoplewithlowerSESshowedatendencytouseemergency services,evenforminorproblems,morefrequently.An Australianstudyamongthegeneralpopulationshowedthat perceivedurgency,goodaccessibility,andbetterhealthcare provisionwerestatedasreasonstovisitanED.46 However, nofurtheranalysisaboutpredictingfactorswasconducted. InaBritishsurveyusingcasevignettes,thetendencytocall foranambulanceortovisitanEDinlessurgentcaseswas significantlyincreasedformales,olderage,andthosewho
wereofethnicminoritiesandhadalowerpaidoccupation andalowerlevelofhealthliteracy.27
Whendevelopingthestatementsconcerningaccessibility, wedeliberatelychosestrictwording(“always”),sothatthe itemswerenottooleading.Toagreetothefourstatements wasnotcompletelywrong,butitwasinappropriateinterms offavorednavigationwithintheGermanhealthcaresystem. ServicesintheEDaregenerallyprovidedforlife-threatening conditionsorseriousacuteproblemsthatcannotwaitand needtobetreatedbyadoctorimmediately.Inlessurgent cases,otheralternativesshouldbepreferred.Forthesecases, mainlytwoservicesareprovidedwhenpracticesareclosed: emergencypracticesandthemedicalon-callservice(also knownas “116117” referringtothetelephonenumber).In fact,thesetwoserviceswereimplementedtounburdenEDs. Thiswastakenintoaccountwhenwedevelopedthefour statementsconcerningbeliefsaboutaccessibility.Itissimilar inthecaseofthestatementsregardingbetterqualityofcare inEDs.Thereisconcentratedexpertiseinhospitals,butthe ratingofworseexpertiseofoutpatientdoctorsandthe assumptionthatallspecialistsareavailableintheemergency wardaredoubtfulandcouldleadtounrealisticexpectations regardingtheuseofEDs.Inthisregard,thepresentstudy couldhelpustounderstandthepublic’sbeliefsonwhich inappropriateutilizationofEDsarebased.However,it cannotberuledoutthatsomeparticipantsdidnotcorrectly understandtheitems.
The findingsprovidedataaboutthelackofhealth educationamongthegeneralpopulation.Particularly, males,olderandlesseducatedpeople,andthosewithlimited knowledgeofemergencycareoptionsshowedapotentially inappropriateutilizationoftheED.Intermsofimmigration status,especially first-generation,immigrantsshowedalack ofinformationthatcouldbeduetolessexperiencewiththe healthcaresystem,languagebarriers,differentexpectations andpreferences,aswellasformalaccessbarriers(eg,waiting timesortraveldistances).47 Regardinggender-specific differences,previousresearchshowedahigherED attendancefornon-urgentproblemsandahigheruseofoutof-hourshelp-seekingamongmen.27,48 Potentially,this preferencecouldbeduetolongerworkinghoursamongmen andlesswillingnesstobeabsentfromworkbecauseof healthcare.Thus,socialinequalitiesshouldbeconsidered whenimplementinginterventions(eg,information campaigns).Tomodifypublicbeliefsabouthealthcarein generaloremergencycareinparticular, “ emergency literacy” campaignsareawaytoaddresstheproblemofED crowding.Inthisregard,knowledgeabouttheavailabilityof differentemergencycareservices,navigationwithinthe healthcaresystem,andtheassessmentofsymptomscould beaddressed.
PeopleshouldbeeducatedthattheEDisforlifethreateningandseriousconditionssuchasheavybleeding, brokenbones,chestpainorstroke,andthatmanysymptoms
canbetreatedmoreappropriatelyelsewhere.AnAustralian behaviorchangecampaignthatfocusedonattitudes, awareness,andknowledgewassuccessfulinreducingthe numberofinappropriateornon-urgentcallstoambulance servicesormedicalemergencyphonenumbers.29 Currently, aqualitativestudyfromGermanypositivelyevaluatedan educationalinterventiontailoredforEDpatientswithlowacuityconditions.49 Anotherstudyexaminedphysiciandirectedstrategiesforimprovingpatienthealthliteracyin EDs.50 Furthermore,lowerhealthliteracywasfoundamong peoplewhowereofolderageandhadlowereducationlevels, lessaffluence,andwithimmigrationbackgrounds,51,52 which arefactorsthatwerealsoshowntobeassociatedwithhigher andinappropriateEDuseinsomestudies.25–27 Asourdata ofpublicbeliefssupportsthe findingsofsocialinequalitiesin inappropriateEDuse,tailoredhealtheducationhastotake placeinmoredeprivedareaswherevulnerablegroupsare livingandtheavailabilityofhealthcareservicesispotentially limited.Informationindifferentlanguagesandindigitaland non-digitalversionscouldhelptoreachthepopulationina betterway.
Inthisstudy,wefocusedonbeliefsthatmayfosteran inappropriateutilizationoftheEDfornon-urgent conditionsasonecauseofcrowding.Anotherandmore importantreasonisrelatedtoboardingofadmittedpatients.3 Inthiscontext,accessblockandhospitaladmissionsfor ambulatorycare-sensitiveconditions(ACSC)are discussed.6,7 Accessblockisthesituationinwhichaccessto hospitalbedsisblockedandnoadmissiontoaninpatient wardispossible.6 HospitaladmissionsforACSCaredefined asadmissionsinhospitalwardsincludingEDsformedical conditionsthatarepotentiallyavoidableiftheyaremanaged intheoutpatientcare.7 ThroughACSC,theavailability, accessandqualityofoutpatientcarecanbeevaluated,and socialinequalitiescanberevealed.7 Somereviewssummed uppossibleimplicationsandinterventionsintermsof reorganizationofEDwardsandavailabilityofoutpatient care. 53–55 Recently,reformsofemergencycarehavebeen discussedinGermanyintermsofallocatingandtriaging patients(ie,implementationofacoordinationcenterfor first telephonecontactandfurtherallocation,andageneral counterforinitialassessmentandtriagingatEDs).
Thisstudyhassomelimitationsthatneedtobediscussed. Eventhoughthedatawasweightedforgender,age,and educationlevel,andthecomparisonofsampleand populationshowedreasonableresults,apotentialselection biasduetonon-responseandtheexclusiveuseoflandline numberscannotberuledout.Inthisregard,aresponserate ofbetween10.9–46%(dependingondefinitionofeligibility) canbeconsideredacceptablecomparedtoothertelephone surveys. 56 Moreover,83%ofhouseholdscanbereachedvia landlinenumbersinGermany.30 Ourdatareferstothe
situationofhealthcareprovisioninaGermanmetropolis. Theconditionsinothercountriesandinmoreruralregions couldbedifferent.
Astherewasnovalidatedmeasureforpublicbeliefsabout availabilityofEDs,wedevelopedeightitemsbasedona reviewoftheliteratureofpatientsurveys.Although psychometricpropertiesofthetwoscalesseemadequate (Cronbach’ s α = 0.76[accessibility]and0.75[quality]),42 thesescalesneedtobefurtherdevelopedandtested.Interms ofmissingvalues,someitemsoftheaccessibilityandquality scale(n = 185andn = 320),andnotablyitemsoftheHLSEU-Q6scaleyieldedahighnumberofmissingvaluesdueto “don’tknow” answers(434).Althoughthisprocedurewasin accordancewiththeoriginalHLS-EUinstrument,theoption of “don’tknow” inquestionnairesshouldnotbe automaticallytreatedasmissingvalues.Therefore,amissing analysiswasconducted.Theresultsrevealedonlya consistentpatternforage(significantlyincreasedmissing valuesamongpeoplewitholderage).Thus,therelevanceof agecouldbeunderestimatedintheregressionanalyses,and duetosubjectivedataacommonmethodbiascouldnotbe ruledout.Finally,theevaluationofgeneralhealthliteracy wasconductedwithanestablishedinstrumentoftheHLSEUconsortium,butwiththeshortestversionavailable (HLS-EU-Q6).41 So,amorecomprehensiveinstrument wouldpossiblyleadtoanimprovedassessment.
Thisstudysuggeststhatthepublic’ sperceptionsabout EDqualityandaccessibilitycontributetoinappropriate EDutilizationandcrowdinginGermany.Particularly,this holdstrueforpeopleofolderage,malegender,lower educationlevel,andthosewhoare fi rst-generation immigrantsandwhohavelessknowledgeaboutavailable emergencycareservices.The fi ndingshelpinunderstanding inappropriateutilizationofemergencycareservicesand developinghealtheducationprogramstailoredtosocially deprivedpopulations.
AddressforCorrespondence:JensKlein,PhD,UniversityMedical CenterHamburg-Eppendorf,InstituteofMedicalSociology, Martinistr.52,Hamburg,Germany20146.Email: j.klein@uke.de
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Kleinetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.MorleyC,UnwinM,PetersonGM,etal.Emergencydepartment crowding:asystematicreviewofcauses,consequencesandsolutions. PLoSOne. 2018;13(8):e0203316.
2.VashiAA,UrechT,CarrB,etal.Identificationofemergencycaresensitiveconditionsandcharacteristicsofemergencydepartment utilization. JAMANetwOpen. 2019;2(8):e198642.
3.HigginsonI.Emergencydepartmentcrowding. EmergMedJ. 2012;29(6):437–43.
4.PinesJM,HiltonJA,WeberEJ,etal.Internationalperspectives onemergencydepartmentcrowding. AcadEmergMed. 2011;18(12):1358–70.
5.TrzeciakSandRiversEP.Emergencydepartmentovercrowdinginthe UnitedStates:anemergingthreattopatientsafetyandpublichealth. EmergMedJ. 2003;20(5):402–05.
6.AffleckA,ParksP,DrummondA,etal.Emergencydepartment overcrowdingandaccessblock. CJEM. 2013;15(6):359–84.
7.JohnsonPJ,GhildayalN,WardAC,etal.Disparitiesinpotentially avoidableemergencydepartment(ED)care:EDvisitsforambulatory caresensitiveconditions. MedCare. 2012;50(12):1020–28.
8.BerchetC.Emergencycareservices:trends,driversandinterventions tomanagethedemand.2015.Availableat: https://www.oecd-ilibrary. org/social-issues-migration-health/emergency-care-services_ 5jrts344crns-en.AccessedDecember11,2023.
9.SunBC,HsiaRY,WeissRE,etal.Effectofemergencydepartment crowdingonoutcomesofadmittedpatients. AnnEmergMed. 2013;61(6):605–11.e6.
10.KimD-U,ParkYS,ParkJM,etal.Influenceofovercrowdinginthe emergencydepartmentonreturnvisitwithin72hours. JClinMed. 2020;9(5):E1406.
11.KimJ-S,BaeH-J,SohnCH,etal.Maximumemergencydepartment overcrowdingiscorrelatedwithoccurrenceofunexpectedcardiac arrest. CritCare. 2020;24(1):305.
12.JonesS,MoultonC,SwiftS,etal.Associationbetweendelaystopatient admissionfromtheemergencydepartmentandall-cause30-day mortality. EmergMedJ. 2022;39(3):168–73.
13.Uscher-PinesL,PinesJ,KellermannA,etal.Emergencydepartment visitsfornonurgentconditions:systematicliteraturereview. AmJManag Care. 2013;19(1):47–59.
14.SchererM,LühmannD,KazekA,etal.Patientsattendingemergency departments. DtschArzteblInt. 2017;114(39):645–52.
15.CosterJE,TurnerJK,BradburyD,etal.Whydopeoplechoose emergencyandurgentcareservices?Arapidreviewutilizinga systematicliteraturesearchandnarrativesynthesis. AcadEmergMed. 2017;24(9):1137–49.
16.PearsonC,KimDS,MikaVH,etal.Emergencydepartmentvisitsin patientswithlowacuityconditions:factorsassociatedwithresource utilization. AmJEmergMed. 2018;36(8):1327–31.
17.AbarB,HolubA,HongS,etal.Latentclassanalysisofbarriersto careamongemergencydepartmentpatients. WestJEmergMed. 2019;20(2):256–61.
18.SchmiedhoferM,MöckelM,SlagmanA,etal.Patientmotivesbehind low-acuityvisitstotheemergencydepartmentinGermany:aqualitative studycomparingurbanandruralsites. BMJOpen. 2016;6(11):e013323.
19.HolzingerF,OslisloS,MöckelM,etal.Self-referredwalk-inpatientsin theemergencydepartment – whoandwhy?Consultationdeterminants inamulticenterstudyofrespiratorypatientsinBerlin,Germany. BMC HealthServicesResearch. 2020;20(1):848.
20.KriegC,HudonC,ChouinardM-C,etal.Individualpredictorsoffrequent emergencydepartmentuse:ascopingreview. BMCHealthServRes. 2016;16(1):594.
21.CredéSH,SuchE,MasonS.Internationalmigrants’ useofemergency departmentsinEuropecomparedwithnon-migrants’ use:asystematic review. EurJPublicHealth. 2018;28(1):61–73.
22.LynchB,FitzgeraldAP,CorcoranP,etal.Driversofpotentially avoidableemergencyadmissionsinIreland:anecologicalanalysis. BMJQualSaf. 2019;28(6):438–48.
23.CarlsonLC,ZachrisonKS,YunBJ,etal.Theassociationof demographic,socioeconomic,andgeographicfactorswithpotentially preventableemergencydepartmentutilization. WestJEmergMed. 2021;22(6):1283–90.
24.QuaglioG,SørensenK,RübigP,etal.Acceleratingthehealthliteracy agendainEurope. HealthPromotInt. 2017;32(6):1074–80.
25.BalakrishnanMP,HerndonJB,ZhangJ,etal.Theassociationofhealth literacywithpreventableemergencydepartmentvisits:acrosssectionalstudy. AcadEmergMed. 2017;24(9):1042–50.
26.SchumacherJR,HallAG,DavisTC,etal.Potentiallypreventableuseof emergencyservices:theroleoflowhealthliteracy. MedCare. 2013;51(8):654–8.
27.O’CathainA,SimpsonR,PhillipsM,etal.Tendencytocallan ambulanceorattendanemergencydepartmentforminorornon-urgent problems:avignette-basedpopulationsurveyinBritain. EmergMedJ. 2022;39(6):436–42.
28.VandenboschJ,VandenBrouckeS,VancorenlandS,etal.Health literacyandtheuseofhealthcareservicesinBelgium. JEpidemiol CommunityHealth. 2016;70(10):1032–38.
29.BorgK,WrightB,SannenL,etal.Ambulancesareforemergencies: shiftingattitudesthrougharesearch-informedbehaviourchange campaign. HealthResPolicySyst. 2019;17(1):31.
30.FederalStatisticalOfficeofGermany.Equipmentofhouseholdswith informationandcommunicationtechnology.Availableat: https://www. destatis.de/EN/Themes/Society-Environment/Income-ConsumptionLiving-Conditions/Equipment-Consumer-Durables/Tables/ liste-equipment-households-information-communicationtechnology-germany.html#55714.AccessedDecember11,2023.
31.KishL.AProcedureforobjectiverespondentselectionwithinthe household. JAMA. 1949;44(247):380–7.
32.HäderM.(2012).Dataqualityintelephonesurveysviamobileand landlinephone.InHäderS,HäderM,KühneM,(Eds), Telephone SurveysinEurope:ResearchandPractice(247-62).Heidelberg, Germany:SpringerBerlin.
33.MartsolfGR,SchofieldRE,JohnsonDR,etal.Editorsandresearchers beware:calculatingresponseratesinrandomdigitdialhealthsurveys. HealthServRes. 2013;48(2Pt1):665–76.
34.AmericanAssociationforPublicOpinionResearch.Standarddefinitions - finaldispositionsofcasecodesandoutcomeratesforsurveys. 2016.Availableat: https://aapor.org/wp-content/uploads/2022 /11/Standard-Definitions20169theditionfinal.pdf
AccessedDecember11,2023.
35.StatisticalOfficeforHamburgandSchleswig-Holstein.(2020). Hamburg StatisticalYearbook2019/2020.Hamburg,Germany:StatisticalOffice forHamburgandSchleswig-Holstein.
36.FederalStatisticalOffice.Educationlevelofthepopulationresultsofthemicrocensus2019;2020.Availableat: https://www. destatis.de/EN/Themes/Society-Environment/EducationResearch-Culture/Educational-Level/Tables/educationalattainment-population-germany.html
AccessedDecember11,2023.
37.KolenikovS.Calibratingsurveydatausingiterativeproportional fitting (raking). StataJ 2014;14(1):22–59.
38.HalbeslebenJRBandWhitmanMV.Evaluatingsurveyqualityinhealth servicesresearch:adecisionframeworkforassessingnonresponse bias. HealthServRes. 2013;48(3):913–30.
39.UnwinM,KinsmanL,RigbyS.Whyarewewaiting?Patients’ perspectivesforaccessingemergencydepartmentserviceswithnonurgentcomplaints. IntEmergNurs. 2016;29:3–8.
40.MessickS.Validityofpsychologicalassessment:validationof inferencesfrompersons’ responsesandperformancesasscientific inquiryintoscoremeaning. AmPsychol. 1995;50:741–49.
41.PelikanJ,GanahlK,VandenBrouckeS,etal.(2013).Measuringhealth literacyinEurope:introducingtheEuropeanhealthliteracysurvey questionnaire(HLS-EU-Q).In:OkanO,BauerU,Levin-ZamirD, PinheiroP,SørensenK(Eds), InternationalHandbookofHealth Literacy(115-38).Bristol,England:PolicyPress.
42.TaberKS.TheUseofCronbach’salphawhendevelopingandreporting researchinstrumentsinscienceeducation. ResSciEduc. 2018;48(6):1273–96.
43.vondemKnesebeckO,KoensS,SchäferI,etal.Publicknowledge aboutemergencycare – resultsofapopulationsurveyfromGermany. FrontPublicHealth. 2022;9:2204.
44.KaiserHF.Theapplicationofelectroniccomputerstofactoranalysis. EducPsycholMeas. 1960;20(1):141–51.
45.IBMCorp.IBMSPSSStatisticsforWindows,Version27.0.2019. Availableat: https://www.ibm.com/products/spss-statistics AccessedDecember11,2023.
46.FitzGeraldG,TolooGS,AitkenP,etal.Publicuseandperceptionsof emergencydepartments:apopulationsurvey. EmergMedAustralas. 2015;27(4):336–42.
47.KleinJ,vondemKnesebeckO.Inequalitiesinhealthcareutilization amongmigrantsandnon-migrantsinGermany:asystematicreview. Int JEquityHealth. 2018;17(1):160.
48.KeizerE,ChristensenMB,CarlsenAH,etal.Factorsrelatedtoout-ofhourshelp-seekingforacutehealthproblems:asurveystudyusingcase scenarios. BMCPublicHealth. 2019;19(1):33.
49.KümpelL,OslisloS,CantuRR,etal.Exploringtheviews oflow-acuityemergencydepartmentconsultersonaneducational interventionandgeneralpractitionerappointmentservice: aqualitativestudyinBerlin,Germany. BMJOpen. 2023;13(4):e070054.
50.Nwanaji-EnweremJC,Smith-WilkersonM,GordonB,etal.Universal precautionsplus:physician-directedstrategiesforimprovingpatient healthliteracyintheemergencydepartment. WestJEmergMed. 2023;24(1):110–3.
51.SørensenK,PelikanJM,RöthlinF,etal.HealthliteracyinEurope: comparativeresultsoftheEuropeanhealthliteracysurvey(HLS-EU). EurJPublicHealth. 2015;25(6):1053–8.
52.NutbeamDandLloydJE.Understandingandrespondingtohealth literacyasasocialdeterminantofhealth. AnnuRevPublicHealth. 2021;42:159–73.
53.BaierN,GeisslerA,BechM,etal.Emergencyandurgentcaresystems inAustralia,Denmark,England,France,GermanyandtheNetherlands – analyzingorganization,paymentandreforms. HealthPolicy. 2019;123(1):1–10.
54.VandenHeedeKandVandeVoordeC.Interventionstoreduce emergencydepartmentutilisation:areviewofreviews. HealthPolicy. 2016;120(12):1337–49.
55.CowlingTEandGunningEJ.AccesstogeneralpracticeinEngland: political,theoretical,andempiricalconsiderations. BrJGenPract. 2016;66(650):e680–e682.
56.DutwinDandLavrakasP.Trendsintelephoneoutcomes,2008-2015. SurveyPractice. 2016;9(3).
PaulKoscumb,MD*
LukeMurphy,MD*
MatthewTalbott,DO*
ShivaNuti,BS*
GeorgeGolovko,PhD†
HashemShaltoni,MD‡
DietrichJehle,MD*
SectionEditor:RichardLucarelli,MD
*UniversityofTexasMedicalBranch,DepartmentofEmergencyMedicine, Galveston,Texas
† UniversityofTexasMedicalBranch,DepartmentofPharmacologyandToxicology, Galveston,Texas
‡ UniversityofTexasMedicalBranch,DepartmentofNeurology,Galveston,Texas
Submissionhistory:SubmittedApril10,2023;RevisionreceivedOctober25,2023;AcceptedDecember11,2023
ElectronicallypublishedApril8,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18063
Background: Alteplase(tPA)istheinitialtreatmentforacuteischemicstroke.CurrenttPAguidelines excludepatientswhotookdirectoralanticoagulants(DOAC)withintheprior48hours.InthispropensitymatchedretrospectivestudywecomparedacuteischemicstrokepatientstreatedwithtPAwhohad receivedDOACswithin48hoursofthrombolysistothosenotpreviouslytreatedwithDOACs,regarding threeoutcomes:mortality;intracranialhemorrhage(ICH);andneedforacutebloodtransfusions(asa markerofsignificantbloodloss).
Methods: UsingtheUnitedStatescohortof54healthcareorganizationsintheTriNetxdatabase,we identified8,582strokepatientstreatedwithtPAonDOACswithin48hoursofthrombolysisand46,703 strokepatientstreatedwithtPAnotonDOACssinceJanuary1,2012.Weperformedpropensityscore matchingondemographicinformationandsevenpriorclinicaldiagnosticgroups,resultinginatotalof 17,164acutestrokepatientsevenlymatchedbetweengroups.Werecordedmortalityrates,frequencyof ICH,andneedforbloodtransfusionsforeachgroupovertheensuing7-and30-dayperiods.
Results: PatientstreatedwithtPAonDOACshadreducedmortality(3.3%vs7.3%;riskratio[RR]0.456; P < 0.001),fewerICHs(6.8%vs10.1%;RR0.678; P < 0.001),andlessriskofmajorbleedingas measuredbyfrequencyofbloodtransfusions(0.5%vs1.5%;RR0.317; p < 0.001)at7dayspost thrombolytic,thanthetPApatientsnotonDOACS.Findingsfor30dayspost-thrombolyticsweresimilar/ statisticallysignificantwithlowermortalityrate(7.2%vs13.1%;RR0.550; P < 0.001),fewerICHs(7.6% vs10.8%;RR0.705; P < 0.001),andfewerbloodtransfusions(0.9%vs2.0%;RR0.448; P < 0.001).
Conclusion: AcuteischemicstrokepatientstreatedwithtPAwhoreceivedDOACswithin48hoursof thrombolysishadlowermortalityrates,reducedincidenceofICH,andlessbloodlossthanthosenoton DOACs.OurstudysuggeststhatprioruseofDOACsshouldnotbeacontraindicationtothrombolysisfor ischemicstroke.[WestJEmergMed.2024;25(3)399–406.]
IntheUnitedStates,strokeremainscommon,withthe estimatedriskofstrokeoveranindividual’slifetime
approachingoneinfour.Ischemicstrokerepresents87%of acuteinsultswithintracerebralhemorrhageand subarachnoidhemorrhagemakinguptheremaining
balance.1,2 Forpatientswhoareeligible,themainstayof treatmentofischemicstrokeisrestorationofblood flowvia thrombolyticsand/orthrombectomy.Alteplase(tPA)is currentlytheonlythrombolyticapprovedforuseinacute ischemicstrokebytheUSFoodandDrugAdministration.3
Thromboembolismfromatrial fibrillationisafrequent causeofischemicstrokeandbecomesparticularlyprevalent withaging.IntheFraminghamstudy,atrial fibrillation representeda1.5%riskofstrokeinthe50–59agegroupand rosetoa23.5%riskinthe80–89agegroup.4 Asa preventativemeasure,mostpatientswithatrial fibrillation aretreatedwithanticoagulation,whichcaneffectively reducetheriskofstrokebyapproximatelytwo-thirdswhen comparedtoplacebo.5–9 Patientswithvalvularatrial fibrillationshouldbetreatedwithoralvitaminKantagonists (VKA).10,11 However,directoralanticoagulants(DOAC), whichincludedirectthrombininhibitorsandfactorXa inhibitors,havedemonstratednon-inferioritytoVKAsinthe preventionofacuteischemicstrokeinpatientswithnonvalvularatrial fibrillation.12–15
Themostrecent2019updatetothe2018AmericanHeart Association(AHA)guidelinesontPAexcludespatientswith concomitantusageofDOACswithin48hoursofthelast doseintake,unlesscoagulationparametersareobtainedand normal.Coagulationparametersincludetestssuchas activatedpartialthromboplastintime(aPTT),prothrombin time(PT),plateletcount,thrombintime(TT),ordirect factorXaactivityassay.16 Recentdatahassuggestedthatthe useofDOACsmaynotincreasetheriskofsymptomatic intracerebralhemorrhageevenintheabsenceofreversal agents,17–20 butthishasnotyetledtoachangeinguidelines. Promptadministrationofthrombolyticstopatientswith acuteischemicstrokehasthepotentialtoleadtoclot breakdownand,ideally,restoredcerebralperfusion.Patients withacuteischemicstrokewhoaretreatedwith thrombolyticshaveimprovedneurologicaloutcomeatthree months21,22 andhavealowerriskoflong-termmortality23; therefore,itiscriticaltoidentifythemaximumnumberof patientsthatcansafelyreceivethisintervention.Theuseof DOACshasrapidlyincreasedinthepastdecadebothfor primarystrokepreventioninpatientswithatrial fibrillation, andinthetreatmentofvenousthromboembolism.24,25 Therefore,thisrepresentsalargecohortofpatientswhomay bedeprivedofthepotentialbenefitsofreperfusiontherapy. WesoughttoassesswhetherpatientsreceivingDOACs whoalsoreceivedtPAwouldhaveanincreasedriskof adverseevents.Weevaluatedmortalityandrateof hemorrhagicconversionacrossalarge,retrospectivedataset. Duetothenatureofthehealthcaredataset,wewerenotable toassessforseverityofallotherbleedingdirectly.Thus,we evaluatedforwhetherpatientsrequiredbloodtransfusionas asurrogatemarkerforclinicallysignificantbleeding. Weanalyzedthesethreeoutcomesat7and30days postthrombolytic.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
WhiletPAistheinitialtreatmentforischemic stroke,guidelinesexcludepatientstaking directoralanticoagulants(DOAC)dueto theoreticalriskofbleeding.
Whatwastheresearchquestion?
DopatientstakingDOACswhoreceive tPAhaveworseoutcomesthanthosenot takinganticoagulants?
Whatwasthemajor findingofthestudy?
WithDOACtherewasreducedmortality (3.3%vs7.3%;RR0.456;P < 0.001)and intracerebralhemorrhage(6.8%vs10.1%; RR0.678;P < 0.001)
Howdoesthisimprovepopulationhealth?
UseofDOACsisincreasing;thisshouldnot preventpatientstakingDOACsfrom receivingthebene fi tsofreperfusiontherapy forischemicstroke.
TriNetXisaglobalfederatedhealthresearchnetwork providingde-identifiedaccesstoretrospectiveelectronic healthrecords(diagnoses,procedures,medications,lab values,genomicinformation)fromapproximately91million patientsin54largehealthcareorganizations(HCO)within theUnitedStates.26 InthisstudyweusedtheUS CollaborativeNetworktoidentifypatientswhoweretreated withtPAforacutestroke.Twocohortswereidentifiedfor thisstudywithinthegroupofpatientstreatedwithtPAon thedayoforwithinonedayofthediagnosisofacutestroke: Cohort1consistedofacutestrokepatientstreatedwithtPA whohadreceivedaDOAConthedayoforonedaypriorto theirpresentationwithacutestroke;andCohort2consisted ofactuestrokepatientstreatedwithtPAwhohadnot receivedaDOACwithinsevendaysofthediagnosis ofstroke.
Weidentifiedstrokepatientsofallethnicities,races,and gendersusingInternationalClassificationofDiseases,10th modification(ICD-10)codeI63(CerebralInfarction,1.49 millioncases).Inthedatabasetherewere565,835patients whoweretreatedwithtPAusingRxNORM:8410.The datasetwaslimitedtothosepatientswhoseindexevent occurredonorafterJanuary1,2012,andwhohadthe diagnosisofcerebralinfarctionsoastoexcludepatients
treatedwithtPAforacutecoronarysyndrome,pulmonary embolism,etc.Wethengeneratedtwocohorts.InCohort1, patientshadreceivedaDOAC(edoxaban,dabigatran, apixaban,orrivaroxaban)onthedayoforonedaypriorto theirstrokeandthrombolyticusingRxNORM1599538, 1037042,1364430,or1114195,resultingin8,582patients. Cohort2wasdefinedasstrokepatientstreatedwithtPAwho weredocumentedtonotbeonDOACsintheprior7days, resultingin46,703patients.
Tocontrolforpotentiallyconfoundingriskfactorsforthe measuredoutcomes,weperformedpropensityscore matchingbasedontheageatstrokediagnosis,race, ethnicity,gender,presenceofhypertensivediseases(ICD-10 codesI10-I16),diabetesmellitus(E08-E13),acutekidney failureandchronickidneydisease(N17-N19),overweight status/obesity(E66),heartfailure(I50),cardiacarrest(I46), andischemicheartdiseases(I20-I25).Weusedthebalanced cohorttoolinTriNetXformatching.26
Weperformedtheoutcomeanalysisbetweenthetwo cohortsforthreeevents:death(vitalstatus:deceased); nontraumaticintracranialhemorrhage(ICH)andblood transfusions(CurrentProceduralTerminologycode36430). NontraumaticICHwasdefinedasnontraumatic subarachnoid – ICD-10codeI60;nontraumatic intracerebralhemorrhage – ICD-10:I61,ornontraumatic acutesubduralhemorrhage – ICD-10:I62.01.Ratesofblood transfusionwereusedasamarkerofsignificantbloodloss postthrombolyticadministration.Alltestedoutcomes occurredonorafterthedayofdiagnosisofstroke.We measuredoutcomesoveraperiodof7and30dayspost thrombolytics.Patientswhohadtheoutcomeatthetimeof orpriortothedesignatedtimewindowweresubsequently excludedfromtheanalysis.26
Weperformedunivariateanalysisusingthemeasure-ofassociationtoolinTriNetX,whichcomparesoutcomes withinthedesignatedtimeframesforeachcohortreported bothasriskratios(RR),oddsratios,95%confidence intervals(CI)oftheseratiosandriskdifferenceasa P -value. Weobtainedde-identifiedpatientdatafromtheTriNetXUS CollaborativeNetworkdatabaseonNovember4,2022,and weperformedthedataanalysesonthesamedate.We reportedouroutcomesasRRswith95%CIsandrisk differences.TheTriNetXplatformprovidesaccessto aggregatedcountsandstatisticalsummariesofde-identified patientrecords.Noprotectedhealthinformationor personaldataisavailabletotheplatformusers;therefore, thisprojectwasexemptfrominstitutionalreview boardreview(www.trinetx.com).26 Ourmanuscript followsSTROBEguidelinesforobservational cohortstudies.27
Weidentified91,1707,410patientsintheTriNetXUnited StatesCollaborativeNetworkfrom54academicmedical
centers/healthcareorganizations.InCohort1ofpatients treatedwithtPAonDOACswithin48hoursofthrombolysis forstrokeweidentified8,582patients.InCohort2ofpatients treatedwithtPAforstrokedocumentedtonotbeonDOACs inthepriorsevendays,therewere46,703patients.After propensityscorematchingonbasicdemographic informationandsevenpriorclinicaldiagnosticgroups associatedwithmortalitytherewereatotalof17,164acute strokepatientsevenlymatchedbetweentheDOACandnoDOACgroups.
Mostofthedemographicgroupsexceptforgender(male/ female)werestatisticallydifferentbetweenthetwocohorts beforematching.Allpre-existingmedicalconditions associatedwithmortalitywerestatisticallydifferentbetween cohorts.Afterpropensitymatchingmostofthedemographic groupsorpre-existingmedicalconditionswerestatistically differentbetweenthecohorts. Tables1 and 2 presentthe demographiccharacteristicsandpre-existingconditionsin Cohorts1and2beforeandafterpropensitymatching. TriNetXreportsinfrequenteventswithoutcomesthatare ≤10as10;sothedifferencebetweenthetwocohortsmay havebeenslightlygreaterfortheNativeAmericanand Hawaiiandemographicgroupswherethenumberinthe DOACgroupislistedas10.
Weexcludedpatientsiftheyhadanoutcomeatthetimeof orpriortothedesignatedindexeventbasedonwhatis recordedinthehealthrecords.Theriskanalysisforthe mortalityoutcomehad193patientsexcludedfromCohort1 (DOAC)and171patientsfromCohort2(no-DOAC).These exclusionsarenecessarywhenthetimingofanoutcome diagnosisisuncertainoroccursbeforethetimewindow. Theseexclusionsarealsoinpartnecessarywhentheoutcome andindexeventoccurswithinhoursofeachother,asthe TriNetXdatabasedoesnotalwayshavethedegreeof granularitytodistinguishwhicheventoccurred first.The DOACsweremuchlessfrequentlyusedmorethan10years ago(introducedapproximately13yearsago);thus,we eliminatedthisperiodfromthetreatmentandcontrolgroups toavoidconfounding.
PatientstreatedwithtPAonDOACswerefoundtohave reducedmortality(3.3%vs7.3%;RR0.456; P < 0.001), lowerincidenceofICH(6.8%vs10.1%;RR0.678; P < 0.001),andlessriskofmajorbleedingasmeasured byfrequencyofbloodtransfusions(0.5%vs1.5%;RR0.317; P < 0.001)atsevendayspostthrombolytic,thanthetPA patientswhohadnotbeenonDOACS.Wefoundsimilar statisticallysignificant findingswithlowermortalityrate (7.2%vs13.1%;RR0.550; P < 0.001),lowerincidenceof ICH(7.6%vs10.8%;RR0.705; P < 0.001),andfewerblood transfusions(0.9%vs2.0%;RR0.448; P < 0.001)at30days aftertheadministrationofthethrombolyticagentinthe 10-yeardataset.Thisinformationregardingthepatient outcomesatsevendays(Table3)and30days(Table4)post thrombolyticisbelow.The95%CIsfortheRRofdeath,
Table1. Cohort1(N = 8,582)andCohort2(N = 46,703)characteristicsbeforepropensityscorematching. Demographics CohortMean
ICH,andsignificantotherbleedingarealsopresentedin thesetables.
Inthislarge,multicenter,propensity-matched, retrospectivestudy,patientswithischemicstrokewho receivedtPAandhadreceivedDOACswithintwodaysof
thrombolyticswerefoundtohavesignificantlylowerriskof death,ICH,andbleedingwhencomparedtopatientswho receivedtPAwithoutpriorDOACs.These findings werestatisticallysignificantatboth7and30days post-thrombolytic.Thisissignificantbecausecurrentstroke guidelinesrecommendagainstadministrationof thrombolysisinpatientswhohavetakenaDOACwithin
Table2. Cohort1(N = 8,582)andCohort2(N = 8,582)characteristicsafterpropensityscorematching.
48hoursofpresentationduetoatheoreticalincreasedriskof bleeding.AlthoughpriorstudieshaveindicatedthatDOAC usemaynotincreasetheriskofintracerebralhemorrhage,to ourknowledgeourstudyisthe firsttosuggestadecreased riskofbleedingaswellasadecreasedriskofdeath.
Recommendationsforwithholdingthrombolyticsfrom patientsusingDOACsintheabsenceoflabtestingsuchas
activatedpartialthromboplastintime(aPTT),prothrombin time(PT),plateletcount,thrombintime(TT_,ordirect factorXaactivityassaywere firstinstitutedin2013basedon consensusopinionwithlimited-to-nodata(ClassIIIC recommendation).28 Theserecommendationsmayhavebeen prudentatthetimeasDOACswerearelativelynovelclassof medication,anddatasurroundingtheirusewasonly
Table3. Outcomesat7Daysafterpropensityscorematching.
OutcometPA + DOAC* (n = 8,582)tPA-DOAC(n = 8,582)RiskRatio(95%CI‡)Probability(p)
*DirectOralAnticoagulant.
‡ConfidenceInterval. †IntracranialHemorrhage.
Table4. Outcomesat30Daysafterpropensityscorematching.
OutcometPA + DOAC*(n = 8,582)tPA-DOAC(n = 8,582)RiskRatio(95%CI‡)Probability(p)
Mortality7.2%13.1%0.550(.500,0.604) <
BloodTransfusion0.9%2.0%0.448(0.341,0.590)
beginningtoemerge.However,theclinicalutilityofmany commoncoagulationparametersinpatientsonDOACsis limited.TheAPTT,PT,andTTarereadilyavailablebut poorlysensitiveandspecificformonitoringofDOACsand shouldnotbeusedquantitativelytoevaluatethedegreeof anticoagulationeffect.Bycontrast,plasmadrug concentrationandanti-factorXaassaysmayquantifythe degreeofanticoagulationbutarenotalwaysavailableand mayrequirespecializedlaboratorysend-outtesting.29 Atour institution,diluteTTisonlyperformedtwiceweekly,and anti-factorXaforDOACsisnotperformedbyour hematologylabdespiteourinstitutionbeinga comprehensivestrokecenter.Wesuspectthatthisissimilar tomanycomprehensivestrokecentersnationwide.Awaiting theaboveresultsisproblematicsincetPAadministrationis timesensitive;therefore,patientsarefunctionallyexcluded fromreceivingtPAduetothetimerequiredtoobtain thesestudies.
IthasbeenknownfornearlyadecadenowthatDOACuse isnon-inferiortowarfarininthepreventionofacuteischemic strokeinpatientswithnonvalvularatrial fibrillation.12–15 However,whileadequateanticoagulationdecreasestherisk ofstroke,itdoesnotcompletelynegatetherisk,withthe estimatedannualriskofischemicstrokedespiteoral anticoagulationbeingapproximately1–2%.30 Weconjecture thatperhapsthiscohortofpatients,whilestillexperiencing ischemicstroke,hasrelativelymilderstrokeswithsmaller thrombusburden,whichputsthesepatientsatlowerriskof deathregardlessoftPAadministration.Furthermore,these patientsmayhavesmallerareasofinfarction,whichmayput thematadiminishedriskofhemorrhagicconversiondueto lessvolumeoffragiletissue.
OurresultsfavoringDOACsareinlinewithotherdata thatalsosuggestthatDOACsareassociatedwithlowerrisk
offatalordisablingstrokewhencomparedtocoumadin.31 Furtherstudyinthisareacouldseektostratifypatientsby initialNationalInstitutesofHealthStrokeScalescoreor volumeofinfarctiononimagingtoconfirmthesehypotheses. Thesehypothesesdonotfullyexplainthethirdoutcome demonstratingalowerrateofbloodtransfusionasa surrogateforextracranialbleeding.Itispossiblethatless debilitatingstrokesamongpatientsonDOACscouldplace lessmetabolicstressonthebodyandresultinalessglobally criticalconditionofthepatient.Itisknown,forexample, thatlengthofintensivecareunitstayincreasestheriskof gastrointestinalbleeding.32 IfpatientsreceivingDOACs havesmallerstrokesandlessseverediseaseresultingin decreasedmultisystemorganfailure,thenthismayaccount forthedifferencesseeninourdataset.Itisalsopossiblethat thelimitedhalf-lifeofDOACmedicationsallowsfora reductionintheirbleedingeffectevenwithatimeof abstinencelessthan48hours.Themaximalhalf-lifeof rivaroxabanisapproximately12hours,andthatofapixaban issimilar.Warfarin’smeanhalf-lifeontheotherhandis40 hours,andthiscanvarywidely.
TherateofICHseeninthisstudyisslightlyhigherthan wasseeninpriorstudies,forexample,intheNINDStrial wherethesymptomaticICHratewasfoundtobe6.4%in patientstreatedwiththrombolytics.Thiswasdefinedas “ any CT[computedtomography]-documentedhemorrhagethat wastemporallyrelatedtodeteriorationinthepatient’ s clinicalconditioninthejudgmentoftheclinicalinvestigator” within36hoursoftreatment.21 Ourstudyevaluatedfor outcomesat7and30daysfollowingtreatment,andthemore expansivetimeframemaypartiallyexplaintheincreased hemorrhagerateseeninourstudy.Additionally,ourstudy includedallICH,notonlysymptomaticICH.Institutional strokeprotocolsmaymandateforaroutineCTbrainforall
patientstreatedwiththrombolyticsregardlessofwhether theyweresymptomatic,andthismayhavecapturedpatients includedinourstudywhowouldhavebeenexcluded fromothers.
Theretrospectivecohortdesignofthisstudymakes establishingcausalitydifficult.However,toourknowledge ourstudyismuchlargerthananyotherintheliterature evaluatingoutcomesaftertPAinpatientstakingDOACsvs thosenottakingDOACs.Thesizeofourstudy,combined withthepropensitymatchingthatweperformedonour sample,givesitmorepowertoevaluatefordifferencesin outcomes.Furthermore,thegeneralizabilityofourstudyis increasedbythenumberofinstitutionsqueriedbyTriNetX.
Weperformed1:1propensitymatchingforage,gender, race,hypertensivediseases,ischemicheartdisease,diabetes mellitus,acuteandchronickidneyfailure,heartfailure, overweightstatus/obesity,andpriorcardiacarrest,asthese areknownriskfactorsformortality.Itisimportanttonote thatalthoughweselectedmultiplepotentiallyconfounding variablesformatching,avariablethatwedidnotinclude couldhaveconfoundedtherelationshipbetweendrug treatmentandmortality.Authorsthathavebeencriticalof propensitymatchingtechniquesacknowledgethatmost potentialdeficienciesofthistechniqueareminimizedin largerdatasetssuchasthisone.
Additionally,weusedbloodtransfusionasasurrogate markerofsignificanthemorrhage,althoughthiscannotbe determinedtobesecondarytothethrombotic administration.Thisoutcomewasinvestigatedoveraperiod of7and30dayspost-thrombotictreatment,whichshould limitconfoundingduetoothercausesofbleeding.
Wedidnotexcludewarfarinusefromourtwopatient populations.Itispossible,butunlikely,thatthepresenceof warfarinuseinsomenon-DOACpatientcohortmayhave skewedtowardhigherratesofICH.However,2019AHA guidelinesspecificallyrecommendagainsttreatmentof ischemicstrokeswiththrombolyticsinpatientswithan internationalnormalizedratio >1.7,whichwouldexclude mostpatientstherapeuticonwarfarin.Inaddition,patients takingwarfarinareunlikelytobeconcurrentlytreatedwith aDOAC.
Weareunsurewhythepatientsincludedinthisstudywere treatedwiththrombolytics,contrarytocurrentstroke guidelines.Itispossiblethatthesewerepatientswho, throughcoagulationassayssuchasdirectfactorXa,were foundnottobeanticoagulated.However,duetothetimeconsumingnatureofthesestudiesandtheneedtoadminister thrombolyticsinatime-sensitivemannerandtheirlimited availabilityevenatcomprehensivestrokecenterssuchasour own,webelieveitisunlikelythatthesepatientswereincluded inasystemicmannerorinlargenumbers.Wewereunableto evaluatewhethertherewasaclusteringofpatientson
DOACswhoreceivedthrombolyticsatcertaincenters,asthe TriNetXprivacypolicydoesnotallowustoviewthis informationduetothede-identifiednatureofthedataset. Thede-identifiednatureofthedatasetalsorequiredustobe dependentonaccurateinputoftheelectronichealthrecordto evaluatewhetherornotthepatientwastakingaDOAC.
Inthislarge,retrospective,multicenterstudy,patients takingDOACswhoreceivedtPAforacuteischemicstroke hadareducedriskofdeath,lowerincidenceofICH,and decreasedbloodlossincomparisontothosewhoreceived tPAandwerenottakingDOACs.Ourstudyaddstothe increasingevidencethatDOACuseshouldnotbea contraindicationtothrombolyticsintheinitialtreatmentof acuteischemicstroke.Thestrokeguidelinesshouldbe updatedtoreflectthese findings.
AddressforCorrespondence:PaulKoscumb,MD,Universityof TexasMedicalBranch,DepartmentofEmergencyMedicine, 301UniversityBlvd.,Galveston,TX77555-1173.Email: pakoscum@utmb.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisresearchwassupportedbythe InstituteforTranslationalSciencesattheUniversityofTexas MedicalBranch,supportedinpartbyaClinicalandTranslational ScienceAward(UL1TR001439)fromtheNationalCenterfor AdvancingTranslationalSciencesattheNationalInstitutesofHealth (NIH).Thecontentissolelytheresponsibilityoftheauthorsanddoes notnecessarilyrepresenttheofficialviewsoftheNIH.Thereareno conflictsofinteresttodeclare.
Copyright:©2024Koscumbetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GBD2016LifetimeRiskofStrokeCollaboratorsFeiginVL,NguyenG, etal.Global,Regional,andCountry-SpecificLifetimeRisksofStroke, 1990and2016. NEnglJMed.2018;379(25):2429–37.
2.TsaoCW,AdayAW,AlmarzooqZI,etal.HeartDiseaseandStroke Statistics-2022Update:AReportFromtheAmericanHeartAssociation [publishedcorrectionappearsin Circulation.2022;146(10):e141]. Circulation.2022;145(8):e153–639.
3.PotlaNandGantiL.Tenecteplasevs.alteplaseforacuteischemic stroke:asystematicreview. IntJEmergMed.2022;15(1):1.
4.WolfPA,AbbottRD,KannelWB.Atrial fibrillationasanindependentrisk factorforstroke:theFraminghamStudy. Stroke.1991;22(8):983–8.
5.PetersenP,BoysenG,GodtfredsenJ,etal.Placebo-controlled, randomisedtrialofwarfarinandaspirinforpreventionof
thromboemboliccomplicationsinchronicatrial fibrillation.The CopenhagenAFASAKstudy. Lancet.1989;1(8631):175–9.
6.StrokePreventioninAtrialFibrillationStudy.Finalresults. Circulation 1991;84(2):527–39.
7.BostonAreaAnticoagulationTrialforAtrialFibrillation InvestigatorsSingerDE,HughesRA,etal.Theeffectoflow-dose warfarinontheriskofstrokeinpatientswithnonrheumaticatrial fibrillation. NEnglJMed.1990;323(22):1505–11.
8.ConnollySJ,LaupacisA,GentM,etal.CanadianAtrialFibrillation Anticoagulation(CAFA)Study. JAmCollCardiol.1991;18(2):349–55.
9.EzekowitzMD,BridgersSL,JamesKE,etal.Warfarinintheprevention ofstrokeassociatedwithnonrheumaticatrial fibrillation.VeteransAffairs StrokePreventioninNonrheumaticAtrialFibrillationInvestigators [publishedcorrectionappearsin NEnglJMed.1993;328(2):148]. NEnglJMed.1992;327(20):1406–12.
10.ConnollySJ,KarthikeyanG,NtsekheM,etal.Rivaroxabaninrheumatic heartdisease-associatedatrial fibrillation. NEnglJMed 2022;387(11):978–88.
11.EikelboomJW,ConnollySJ,BrueckmannM,etal.Dabigatranversus warfarininpatientswithmechanicalheartvalves. NEnglJMed 2013;369(13):1206–14.
12.ConnollySJ,EzekowitzMD,YusufS,etal.Dabigatranversuswarfarin inpatientswithatrial fibrillation[publishedcorrectionappearsin NEnglJ Med.2010;363(19):1877]. NEnglJMed.2009;361(12):1139–51.
13.PatelMR,MahaffeyKW,GargJ,etal.Rivaroxabanversuswarfarinin nonvalvularatrial fibrillation. NEnglJMed.2011;365(10):883–91.
14.GrangerCB,AlexanderJH,McMurrayJJ,etal.Apixabanversus warfarininpatientswithatrial fibrillation. NEnglJMed 2011;365(11):981–92.
15.GiuglianoRP,RuffCT,BraunwaldE,etal.Edoxabanversuswarfarinin patientswithatrial fibrillation. NEnglJMed.2013;369(22):2093–104.
16.PowersWJ,RabinsteinAA,AckersonT,etal.GuidelinesfortheEarly ManagementofPatientswithAcuteIschemicStroke:2019Updateto the2018GuidelinesfortheEarlyManagementofAcuteIschemic Stroke:AGuidelineforHealthcareProfessionalsfromtheAmerican HeartAssociation/AmericanStrokeAssociation[published correctionappearsin Stroke.2019;50(12):e440-1]. Stroke 2019;50(12):e344–418.
17.ShahjoueiS,TsivgoulisG,GoyalN,etal.Safetyofintravenous thrombolysisamongpatientstakingdirectoralanticoagulants:a systematicreviewandmeta-analysis[publishedcorrectionappearsin Stroke.2020;51(3):e59]. Stroke.2020;51(2):533–41.
18.XianY,FederspielJJ,HernandezAF,etal.Useofintravenous recombinanttissueplasminogenactivatorinpatientswithacute ischemicstrokewhotakenon-vitaminKantagonistoralanticoagulants beforestroke. Circulation.2017;135(11):1024–35.
19.SeiffgeDJ,HooffRJ,NolteCH,etal.Recanalizationtherapiesinacute ischemicstrokepatients:impactofpriortreatmentwithnoveloral anticoagulantsonbleedingcomplicationsandoutcome. Circulation 2015;132(13):1261–9.
20.SuzukiK,AokiJ,SakamotoY,etal.LowriskofICHafterreperfusion therapyinacutestrokepatientstreatedwithdirectoralanti-coagulant. JNeurolSci.2017;379:207–11.
21.NationalInstituteofNeurologicalDisordersandStrokert-PAStroke StudyGroup.Tissueplasminogenactivatorforacuteischemicstroke. NEnglJMed.1995;333(24):1581–7.
22.HackeW,KasteM,BluhmkiE,etal.Thrombolysiswithalteplase 3to4.5hoursafteracuteischemicstroke. NEnglJMed 2008;359(13):1317–29.
23.SchmitzML,SimonsenCZ,HundborgH,etal.Acuteischemicstroke andlong-termoutcomeafterthrombolysis:nationwidepropensityscorematchedfollow-upstudy. Stroke.2014;45(10):3070–2.
24.Sindet-PedersenC,PallisgaardJL,StaerkL,etal.Temporaltrendsin initiationofVKA,rivaroxaban,apixabananddabigatranforthetreatment ofvenousthromboembolism. SciRep.2017;7(1):3347.
25.YuAYX,MaloS,SvensonLW,etal.Temporaltrendsintheuseand comparativeeffectivenessofdirectoralanticoagulantagentsversus warfarinfornonvalvularatrial fibrillation. JAmHeartAssoc 2017;6(11):e007129.
26.MurphyL,HillTP,PaulK,etal.Tenecteplaseversusalteplaseforacute stroke:mortalityandbleedingcomplications. AnnEmergMed 2023;82(6):720–8.
27.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. JClinEpidemiol 2008;61(4):344–9.
28.JauchEC,SaverJL,AdamsHPJr,etal.GuidelinesfortheEarly ManagementofPatientswithAcuteIschemicStroke:aguidelinefor healthcareprofessionalsfromtheAmericanHeartAssociation/ AmericanStrokeAssociation. Stroke.2013;44(3):870–947.
29.ConwaySE,HwangAY,PonteCD,etal.Laboratoryandclinical monitoringofdirectactingoralanticoagulants:whatcliniciansneedto know. Pharmacotherapy.2017;37(2):236–48.
30.StaerkL,GerdsTA,LipGYH,etal.Standardandreduceddosesof dabigatran,rivaroxabanandapixabanforstrokeprevention inatrial fibrillation:anationwidecohortstudy. JInternMed 2018;283(1):45–55.
31.CostelloM,MurphyR,JudgeC,etal.Effectofnon-vitamin-Koral anticoagulantsonstrokeseveritycomparedtowarfarin:ameta-analysis ofrandomizedcontrolledtrials. EurJNeurol.2020;27(3):413–8.
32.KumarS,RamosC,Garcia-CarrasquilloRJ,etal.Incidenceandrisk factorsforgastrointestinalbleedingamongpatientsadmittedtomedical intensivecareunits. FrontlineGastroenterol.2017;8(3):167–73.
GregoryA.Peters,MD*†‡
RebeccaE.Cash,PhD,MPH*†
ScottA.Goldberg,MD,MPH*‡
JingyaGao,MS†
LilyM.Kolb,MPH§
CarlosA.CamargoJr.,MD,DrPH*†∥
*HarvardMedicalSchool,Boston,Massachusetts
† MassachusettsGeneralHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts
‡ BrighamandWomen’sHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts
§ TheDonaldandBarbaraZuckerSchoolofMedicineatHofstra/Northwell, Hempstead,NewYork
∥
HarvardT.H.ChanSchoolofPublicHealth,DepartmentofEpidemiology, Boston,Massachusetts
SectionEditor: DavidThompson,MD
Submissionhistory:SubmittedJuly12,2023;RevisionreceivedDecember8,2023;AcceptedDecember28,2023
ElectronicallypublishedApril9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18399
Background/Objective: Asthmaisacommonchronicmedicalconditionamongchildrenandthemost commondiagnosisassociatedwithinterfacilitytransportsforpediatricpatients.Asmanyas40%of pediatrictransfersmaybeunnecessary,resultinginpotentialdelaysincareandunnecessarycosts.Our objectivewastoidentifythepatient-relatedfactorsassociatedwithpotentiallyunnecessarytransfersfor pediatricpatientswithasthma.
Methods: WeusedpatientcaredatafromtheCaliforniaDepartmentofHealthCareAccessand Informationpatientdischargeandemergencydepartment(ED)datasetstocaptureEDvisitswherea pediatricpatient(age2–17years)presentedwithasthmaandwastransferredtoanotherEDoracute carehospital.Theoutcomeofinterestwasapotentiallyunnecessarytransfer,definedasavisitwhere lengthofstayaftertransferwas <24hoursandnoadvancedserviceswereused,suchasrespiratory therapyorcriticalcare.Patient-relatedcharacteristicswereextracted,includingage,gender,race/ ethnicity,primarylanguage,insurancestatus,andclinicalcharacteristics.First,weuseddescriptive statisticstocomparenecessaryvsunnecessarytransfers.Second,weusedgeneralizedestimating equationsaccountingforclusteringbyEDtoestimateoddsratios(OR)andidentifyfactorsassociated withpotentiallyunnecessarytransfers.
Results: Atotalof4,233pediatricEDpatientsweretransferredwithadiagnosisofasthma,including461 (11%)transfersthatmetcriteriaaspotentiallyunnecessary.Medianagewas12years(interquartile range7–15),and46%werefemale.Factorsassociatedwithincreasedoddsofpotentiallyunnecessary transferwhilecontrollingforkeyfactorsincludedyoungerage(eg,2–5years,OR2.0,95%confidence interval[CI]1.4–2.9),malegender(OR1.4,95%CI1.1–1.7),andHispanicethnicity(OR1.6,95%CI 1.2–2.1),whilemultiplehospitalizationsforasthmaperyearwasassociatedwithdecreasedodds(OR 0.2,95%CI0.1–0.4).
Conclusion: Severalpatient-relatedfactorswereassociatedwithincreasedordecreasedoddsof potentiallyunnecessarytransfersamongpediatricpatientspresentingtotheEDwithasthma.These factorscanbeconsideredinfutureworktobetterunderstand,predict,andreduceunnecessarytransfers andtheirnegativeconsequences.[WestJEmergMed.2024;25(3)407–414.]
Asthmaisacommonchronicmedicalconditionamong children,1 affecting7.5%oftheoverallpediatricpopulation2 withpeakprevalenceinyoungteenagers(12–14years)at nearly11%.3 Childrenwithasthmaexacerbationsaccount forapproximately650,000emergencydepartment(ED) visitsintheUSannually,andmanyofthesevisitsresultin hospitaladmission,includingviainterfacilitytransferby emergencymedicalservices(EMS)toanotherhospital.4 Indeed,asthmaisthemostcommonprimarymedical diagnosisassociatedwithinterfacilitytransportforpediatric patients.5 Interfacilitytransfersaretypicallyinitiatedby emergencyphysicians,citinganeedforahigherlevelofcare (ie,criticalcare),recommendationofspecialtyservices(eg, pediatricpulmonology),orcapacity-relatedlimitations(ie, currentavailabilityofbedsorotherresources).Despitethe commonplacenatureofpediatrictransfersforasthmainthe ED,thereisnopriorliteraturetosupportpolicymakersand otherstakeholdersthatincludeemergencyphysicians andadministratorswhennavigatingthisroutine decision-makingprocess.
Priorworkhasshownthatmorethan40%of undifferentiatedpediatrictransferswereeitherdischarged directlyfromthereceivingEDorwithin24hoursofdirect admissionupontransfer,6 andthatonlyone-quarterofall pediatrictransfersarecompletedtoprovideahigherormore specializedlevelofcaretothepatient.7 Theseoutcomesare importantbecauseinterfacilitytransfersareassociatedwith misseddosesofmedication,prolongedtimetoinitiationof inpatientcare,andasubstantial financialburdenonfamilies andtaxpayers.7,8 Withtheserisksandcostsinmind,arecent studyof1.7millionpediatrictransfersintheUSreportedthat only12.3%ofallpediatrictransfersmetcriteriafora medicallynecessarytransfer,demonstratingthelimited directbenefittopatientcareinmanycasesretrospectively.9 Moreover,socioeconomicallyvulnerablepopulationsare disproportionallyaffectedbyasthma,10–14 andthe disproportionate financialburdenofinterfacilitytransferson underservedruralpatientshasbeenpreviouslydescribed,8 indicatingtheimportantlikelyhealthequityimplicationsof thistopic.Theseconsiderationsunderscoretheneedfor improvedguidanceforpolicymakerswhencontemplating theroutinepracticeofinterfacilitytransferofpediatric patientswhopresenttotheEDwithasthma.
Weaimedtodescribethepatient-relatedfactors associatedwithpotentiallyunnecessaryinterfacilitytransfer ofpediatricpatientspresentingtotheEDwithasthma.Our ultimategoalinthisworkistostimulatediscussionand futureresearchregardingthecharacteristicsofpatientsmost
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Asthmaisthemostcommondiagnosis associatedwithinterfacilitytransferof pediatricpatients.Transfersentailcosts, delaysincare,andresourcestrain.
Whatwastheresearchquestion?
Whichpatient-relatedfactorsareassociated withunnecessarytransferforpediatric asthmaexacerbations?
Whatwasthemajor findingofthestudy?
Youngerage(OR2.0,95%CI1.4-2.9)and Hispanicethnicity(OR1.6,95%CI1.2 – 2.1) wereassociatedwithunnecessarytransfer.
Howdoesthisimprovepopulationhealth?
Severalpatient-relatedfactorswere associatedwithincreasedoddsofunnecessary transfer,whichcancausepreventablestrain onfamiliesandhealthcaresystems.
likelytoexperiencetheconsequencesofunnecessarytransfer andtodevelopinterventionstoreduceunnecessarystrainon patientsandtheirfamilies,EMS,andhospitalresources.
Weusedaretrospectivecohortstudytoanalyzepatient careandhealthcareadministrativedatafromasampleof pediatricpatientswhopresentedtotheEDwithasthma.The primarysourceofdataforthisstudywastheCalifornia DepartmentofHealthCareAccessandInformation (HCAI),fromwhichwereceivedanon-publicversionofthe EmergencyDepartmentandAmbulatorySurgery(EDAS) DataandPatientDischargeData(PDD)datasets.The HCAIcompilesitsdataviamandatorystandardized collectionfromalllicensedhospitalsthroughoutthestateof California.TheHCAIorganizesdataasuniqueencounters betweenapatientandhealthcarefacility,suchthateach recordcorrespondstoonepatientencounteratagiven facility(eg,aninterfacilitytransferwouldgeneratetwo recordsforthatpatient).VisitstotheEDthatresultinsamehospitaladmissionareincludedinthePDD,whereasall otherEDvisits,includingthosethatresultininterfacility transfer,areincludedintheEDAS.CombiningEDASand PDDforagivenyearprovidesafulldatasetofallunique, unduplicatedEDvisitsinCaliforniawithinthatyear.The HCAIdatasetsaresubjecttostandardizedqualityassurance
procedures.MoredetailedinformationaboutHCAIcanbe foundonitswebsite.15
ThisstudyfollowedtheStrengtheningtheReportingof ObservationalStudiesinEpidemiology(STROBE) reportingguidelineforcross-sectionalstudies16 andwas approvedbytheMassGeneralBrighamHumanResearch CommitteeandtheCaliforniaCommitteefortheProtection ofHumanSubjects.
WeextractedallEDvisitsfromtheEDASandPDD datasetsfromHCAIduring2016–2019.Weincludedall patientsaged2–17yearstospecificallystudypediatric patients,andweexcludedpatientsyoungerthantwoyearsof agebecausewheezingatthisyoungageismorelikely attributabletoatransientconditionsuchasbronchiolitis ratherthanachroniconesuchasasthma.17,18 Weincluded pediatricpatientswhopresentedtotheEDandhada diagnosisofasthma(ie,InternationalClassificationof Diseases,Rev10,codesJ45,J98.01,andR06.2)forany documenteddischargediagnosis.Finally,weincluded pediatricasthmaEDvisitsthatresultedinaninterfacility transferfromtheED,regardlessoftheinitialcaresettingat thereceivingfacility(eg,EDtoED,EDtoinpatient floor, EDtointensivecareunit,etc).Insummary,the finalstudy sampleincludedpatientsaged2–17yearswhopresentedto anEDinCaliforniaduring2016–2019,werediagnosedwith asthma,andweretransferredviaEMStoanotherfacility.
Theprimaryoutcomemeasureusedforthisstudywas potentiallyunnecessaryinterfacilitytransfer.Thismeasure wasdesignedtocapturepatienttransfersthat withinthe limitationsofthisdatasource werenotassociatedwith clearretrospectiveindicationsthatthepatientreceived clinicallynecessaryservicesthatrequiredtransfer.We definedpotentiallyunnecessarypediatrictransferbasedon recentliterature(includingallchiefcomplaintcategories),9 wherethetransferdidnotresultinadispositionofdeathor admission >24hours,involvesedationoradvancedimaging (definedasanyimagingstudyapartfromplainradiographs), orincuroperatingroomorcriticalcarecharges.Weadded respiratorytherapyasanadditionalmarkerofnecessary transferinthecaseofasthma,inadditiontoservicescaptured undercriticalcaresuchaspositive-pressureventilation.All remainingtransferswereconsiderednecessary.
Moregenerally,weidentifiedinterfacilitytransfersby findingtwoencountersassociatedwithasingleunique patientidentifierwithinonedayofeachotherperencounter date,wheretheencountersoccurredattwoseparate hospitals,andwheredispositionatthesendingfacilitywas designatedasatransfer.Additionalvariablesofinterest includedsociodemographiccharacteristicsanddetailsto describepatients’ medicalhistoryandhealthcareutilization
relatedtoasthma.Demographicdataincludedpatientage, gender,race,ethnicity,primarylanguage,residence urbanicity,andinsurancestatus.Wealsoincludedthe numberofEDvisitsandhospitaladmissionseachpatient hadperyearwhereasthmawaslistedasthedischarge diagnosis.Finally,wecalculatedthenumberofcomplex chronicconditionsfromeachpatient’spastmedical historyperthePediatricComplexChronicCondition version2system(includingtechnologydependenceand organtransplantation).19,20
First,weuseddescriptivestatisticstocomparepediatric transfersforasthmathatmetvsdidnotmeetcriteriafor potentiallyunnecessarytransfer.Comparisonsbetween groupsweremadeusing t -tests,Wilcoxonrank-sumtests,or chi-squaretestsasappropriate.Weusedgeneralized estimatingequations(GEE)accountingforclusteringby facilitytocalculateadjustedoddsofunnecessarytransfer, estimatedwithbinominaldistribution,logitlinkfunction, workingindependencecorrelation,androbuststandard errors.Covariatesincludedthepatient-relatedfactors describedabovethatwereincludedaprioribasedonprior literatureandsubstantivereasoning.Weperformedall statisticalanalysesusingStataversion15.0(StataCorp, CollegeStation,TX).
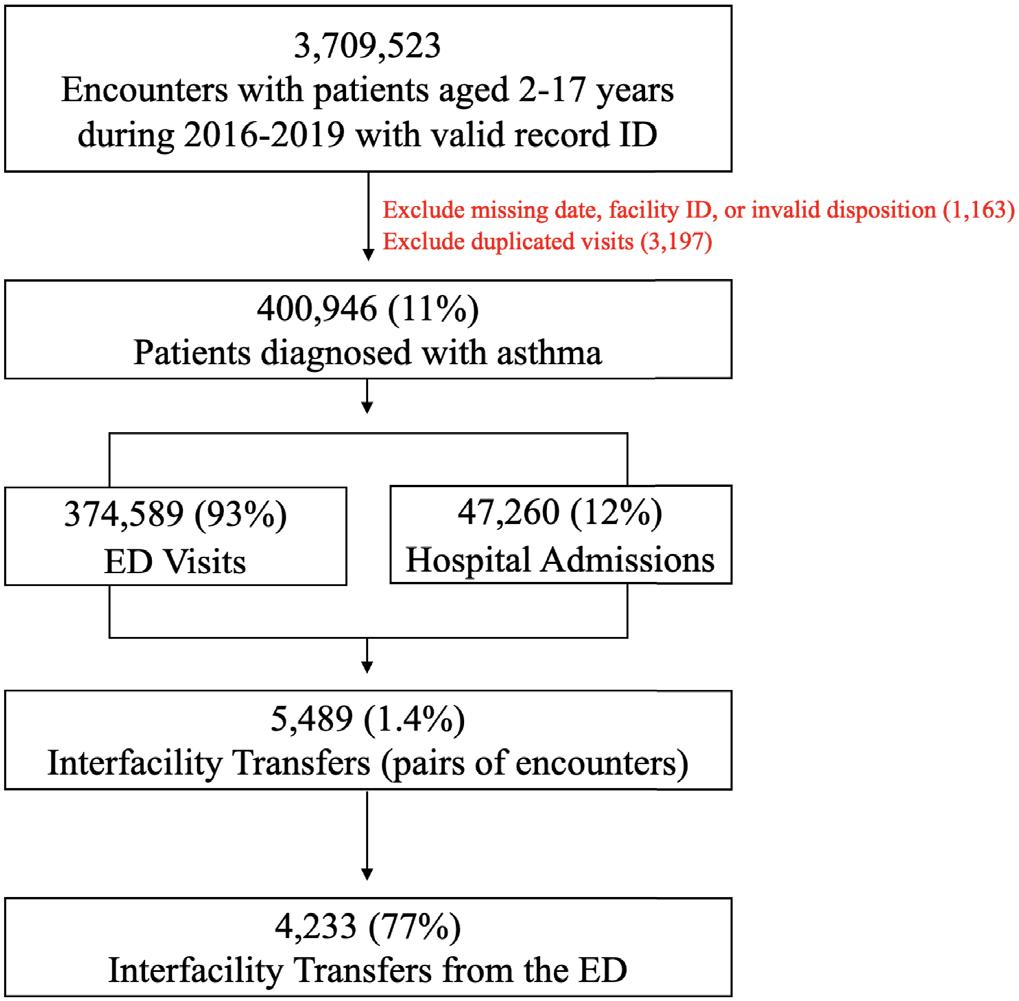
Figure1. Inclusionandexclusioncriteriausedtodevelopthe final studysample.Statisticsregardingemergencydepartmentvisitsand hospitaladmissionsdonotrepresentpatientsbeingincludedor excluded;insteadtheyprovidecontexttoaidinunderstandingthe relativerateofpatienttransferswithinthesample. ED,emergencydepartment.
Fromaninitialsampleof3,709,523pediatricencounters, atotalof4,233patientswithasthmaweretransferredfrom
anED(eachincludingapairoftwoencounters,oneatthe sendingfacilityandasecondatthereceivingfacility; Figure1).Amongthissample,461(11%)metcriteriaas
Table1. Descriptivecharacteristicsandcomparisonofnecessaryandpotentiallyunnecessaryinterfacilitytransfers.
FactorOverallNecessaryUnnecessary
Totaln4,2333,772(89)461(11)
Ageinyears
Mean(SD)10.8(4.8)11.0(4.8)9(4.6) <
Agecategory,n(%) <0.001
Child(2–5years)843(20)718(19)125(27)
Schoolage(6–12years)1,451(34)1,249(33)202(44)
Teen(13–17years)1,939(46)1,805(48)134(29)
Gender,n(%)
Female1,952(46)1,789(47)163(35)
Male2,281(54)1,983(53)298(65)
Race/ethnicity,n(%)
Non-HispanicWhite1,041(25)961(26)80(17)
Non-HispanicBlack918(22)835(22)83(18)
Hispanic1,724(41)1,491(40)233(51)
Non-Hispanicother518(12)455(12)63(14)
English3,874(92)3,467(92)407(88)
Spanish322(8)275(7)47(10)
Otherormissing37(1)30(1)NR
EDvisitswithouttransferforasthmaperyear
Mean(SD)2.1(1.9)2.1(2.0)1.6(1.6) <0.001 >2EDvisitperyear,n(%)1,068(25)983(26)85(18)
Admissionsforasthmaperyear
Mean(SD)1.2(0.8)1.2(0.8)0.6(0.7) <
>1admissionperyear,n(%)688(16)669(18)19(4) <0.001
Anycomplexchroniccondition†,n(%)463(11)425(11)38(8)0.050 Patientresidenceurbanicity,n(%)
Rural83(2)78(2)NR
Urban4,131(98)3,679(98)452(99) Missing 1915NR
Insurancestatus,n(%)
Public2,514(59)2,235(59)279(61) Private1,548(37)1,385(37)163(35) Self-pay/other/missing171(4)152(4)19(4)
Columnpercentagesshown.Percentagesmaynotsumto100duetorounding.
*T-testorchi-squaretestasappropriate.
†Complexchronicconditionsdefinedusingversion2definitionfromFeudtneretal,2014,(https://bmcpediatr.biomedcentral.com/articles/10. 1186/1471-2431-14-199),adaptedfromKurowskietal,2014.(https://pubmed.ncbi.nlm.nih.gov/25039935/).Notably,theversion2definition includestechnologydependenceandtransplantbutdoesnotaddthesetothetotal.Inthisanalysis,technologydependenceandtransplant areincludedintotalcomplexchroniccondition.
ED,emergencydepartment; NR,notreported(duetodatareportingrestrictions).
potentiallyunnecessary.Themeanageofallpediatric patientswithatransferforasthmawas10.8years(SD4.8), 47%werefemale,and41%wereHispanic(Table1).Patients withapotentiallyunnecessarytransferwereyounger(9vs 11years, P < 0.001),moreoftenmale(65%vs53%, P < 0.001),andmoreoftenhadHispanicethnicity (51%vs40%, P < 0.001).Intermsofclinicalcharacteristics,
Table2. Oddsofunnecessarytransferusinggeneralizedestimating equationstoaccountforclusteringbyhospital.
Agecategory
Child(2–5years)2.011.39,2.91
Schoolage(6–12years)2.031.50,2.73
Teen(13–17years)1.00(referent)
Gender
Female1.00(referent)
Male1.391.15,1.70
Race/ethnicity
Hispanic1.00(referent)
Non-HispanicBlack0.630.45,0.86
Non-HispanicWhite0.630.48,0.83
Non-Hispanicother0.880.65,1.20
Primarylanguage
English1.00(referent)
Spanish1.180.82,1.70
Otherormissing1.690.74,3.87
EDvisitsforasthmaperyear
0–21.00(referent)
≥30.940.68,1.28
Admissionsforasthmaperyear
0–11.00(referent)
≥20.220.13,0.36
Complexchroniccondition*
None1.00(referent)
≥10.790.55,1.15
Patientresidenceurbanicity
Rural0.720.35,1.58
Urban1.00(referent)
Insurancestatus
Public0.980.75,1.28
Private1.00(referent)
Self-pay/other/missing1.020.55,1.89
*Complexchronicconditionsdefinedusingversion2de finition.In thisanalysis,technologydependenceandtransplantareincluded intotalcomplexchroniccondition.
AOR,adjustedoddsratio; CI,confidenceinterval; ED,emergencydepartment.
patientswhometcriteriaforpotentiallyunnecessarytransfer lessoftenhadacomplexchroniccondition(8%vs11%, P = 0.05)andovertheprioryearexperiencedfewerED visits(1.6vs2.1, P < 0.001)andhospitaladmissions (0.6vs1.2, P < 0.001)forasthma.
UsingtheGEEmodeltoaccountforclusteringbyhospital (Table2),wefoundthatyoungeragegroupswereassociated withincreasedadjustedoddsofpotentiallyunnecessary transfer(ie,age2–5years,oddsratio[OR]2.01,95% confidenceinterval[CI]1.39–2.91,comparedtoage 13–17years).Malegender(OR1.39,95%CI1.15–1.70)was alsoassociatedwithincreasedoddsofpotentially unnecessarytransfer.Noassociationswerefoundwith insurancestatus,residenceurbanicity,orprimarylanguage. PatientsofHispanicethnicity,comparedtonon-Hispanic Whitepatients,hadincreasedoddsofpotentially unnecessarytransfer(OR1.59,95%CI1.21–2.10).(Note thatHispanicethnicitywasusedasthereferentin Table2 giventhatthiswasthelargestracial/ethnicgroupinthis sample.)Twoormorehospitaladmissionsforasthmaper yearwasassociatedwithdecreasedoddsofpotentially unnecessarytransfer(OR0.22,95%CI0.13–0.36),whereas noassociationswerefoundwithEDvisitsforasthmaor absenceofanycomplexchronicconditions.
Usingacomprehensive,statewidedatasetofEDvisitsand admissions,wefoundseveralpatientcharacteristics associatedwithpotentiallyunnecessarytransferofpediatric patientswhopresenttotheEDwithasthma.These findings describethepatient-levelcharacteristicsassociatedwith elevated(orreduced)oddsofpotentiallyunnecessary transfer,whichcaninformpolicymakersandED administratorstoconsidersubpopulationswithelevatedrisk ofunnecessarytransferwhendevelopingfuturestudiesand policiesrelatedtothetransferofpediatricpatientswith asthma.Potentiallyunnecessarytransfersmarkcaseswhere patientsdonotshowevidenceofthebenefitsoftransfer,such asahigherlevelofcareoraccesstoaspecialistbutdo experiencetherisksandcostsassociatedwithtransfer.
Therateofpotentialunnecessarytransferamongthis cohortwas11%,whichismuchlowerthanreported previouslyinstudiesofundifferentiatedpediatricpatients, includingratesofone-in-twotonearlynine-tenths.9,21,22 However,inpriorliteraturethediagnosticcategoryof respiratoryemergencieshadthegreatestnumberof transferredpediatricpatientsandwastheonlydiagnostic categoryassociatedwithdecreasedoddsofdirectdischarge homefromtheED,whichmayatleastpartiallyexplainwhy weobservedalowerrateofpotentiallyunnecessary transfer.21 Perhapsrespiratoryemergenciesarerelativelyless likelytobequicklydischargedfromthereceivingfacility comparedtootherdiagnosesbecausetheyaremorelikelyto involveanobservationperiod(eg,continuousoxygen
saturationmonitoring,gradualreductioninfrequencyof respiratorytreatments),orperhapsbecauseemergency physicianshavemorecomfortwithdecision-makingfor thesetransfersduetotheirmorecommonplacenature. Similarly,theincreasedprevalenceofobservationunitsmay havecontributedtothis findingcomparedtoearlierstudies whenthisoptionwaslessavailable.
Demographicfactorsassociatedwithincreasedoddsof unnecessarytransfersincludedyoungerage,malegender, andHispanicethnicity.Youngerpatientswereassociated withincreasedoddsofpotentiallyunnecessarytransfer, whichwasconsistentwithpriorreportsthatfound particularlyhighriskamongpreschool-agepatients.9,22 One possibleexplanationforthis findingcouldsimplybe relativelyinferiorcomfortamongclinicianscaringfor youngerpatients.Increasedoddsofpotentiallyunnecessary transferamongmalepatientswasnotexpectedaprioriand wasnotfoundintheliteratureamongundifferentiated pediatricpatients,wherefemalepatientsaremoreoften foundtobeathigherriskwhengender-baseddifferencesare found.9 Priorresearchhassuggestedthatmalepediatric patientstendtohavegreaterprevalenceandillnessseverityof asthmabeforepuberty,incontrasttogreaterprevalenceand severityamongfemalesafterpuberty,withsomeindication thatsexhormonesmayplayarole.23,24 Furtherresearch focusedonthetransferofpediatricpatientswithasthmawill beneededtodeterminewhethergender-relateddifferences arewidespread,andifso,whatmayaccountfor thisdisparity.
Hispanicethnicitywasalsofoundtobeassociatedwith increasedoddsofpotentiallyunnecessarytransfer.One possiblecontributingfactortothis findingmighthavebeen languagebarriers;however,evenaftercontrollingfor primarylanguagespoken,wefoundanindependent associationwithHispanicethnicity.Hispanicethnicityhas previouslybeenreportedtobeassociatedwithincreasedodds ofunnecessarytransfer,butthereasonsforthisremain unclear.9,25 Giventheknown financialcostsandmedical risksthatcanbeassociatedwithinterfacilitytransfer7,8 and prior findingsthatHispanicpatientsincurgreatercosts associatedwiththeirasthma-relatedcareingeneral,26 we encouragefurtherworktoevaluatethistrendtogainabetter understandingofhowtominimizedisparitiesintheburden ofundueriskassociatedwithpotentiallyunnecessary interfacilitytransfer.
Wefoundnoassociationwithpatientresidenceurbanicity orwithinsurancestatus,incontrasttopriorresearchthat foundincreasedriskofpotentiallyunnecessarytransfer amongurbanpatientsandthosewithpublichealth insurance.9 Incontrasttoour findings,importantpriorwork hashighlightedthatruralpatientsaremorelikelyto experiencepotentiallyunnecessarytransferbecausetheir nearesthospitalstendtobelessresourced,especiallyfor pediatriccare,comparedtourbanpatientswhoaremore
likelytoresideingeographicproximitytomoreresourced centersthatarelesslikelytotransferpediatricpatients.8 CharacteristicsspecifictothestateofCaliforniamayaccount forthesedifferences,althoughratesofpublicinsuranceand urbanresidencewerequitesimilarinthiscohortcomparedto priorwork.Alternatively,ourfocusonasthmacouldbethe explanatoryfactor,giventhatasthmaismorecommonin urbansettings(particularlyinthepresenceofotherfactors thattendtoaffectsuchareas,suchasenvironmentaland housing-relatedinsults)andisconsideredanambulatory care-sensitiveconditionshowntobemodulatedbychanges ininsurancestatusamongpopulations.14,27 Takentogether, asolid,generalizableconclusionregardingthepotential associationbetweenpotentiallyunnecessarytransferand urbanicityorinsurancestatusremainsdifficulttoreach.
Finally,regardingclinicalpatient-levelfactors,wefound thatmultiplehospitaladmissionsforasthmaperyearwere associatedwithdecreasedoddsofpotentiallyunnecessary transfer,whereasnoassociationwasfoundwith ≥3EDvisits orthepresenceofacomplexchroniccondition.The finding thatmultiplehospitaladmissionsforasthmawasassociated withdecreasedriskisnotunexpected.Theincreasedriskof mortalityassociatedwithrecenthospitalizationforasthma notonlysuggestsgreaterlikelihoodofincreasedclinical severityamongthiscohortbutisalsoawelldocumentedand widelytaughtpieceofevidencethatdirectlyfactorsinto clinicaldecision-making,whichmakesitlesslikelyforsuch patientstomeetcriteriaforpotentiallyunnecessary transfer.28,29 However,thesamelineofworkthattendsto indicatetheassociationbetweenhospitalizationsand mortalityoftenhighlightssimilarassociationswithEDuse, albeitanintuitivelyweakerassociationgiventhatchildren whovisittheEDandareadmittedpresumablyhavemore severeasthmathanthosewhoareinsteaddischarged.
Priorresearchhasshownthatcomplexchronicconditions tendtobeassociatedwithlongerlengthofstayandgreater resourceutilizationwhentransferredcomparedtonot transferredforadmission,suggestingthatcomplexpediatric patientstendtobeappropriatelytransferred.However,we didnot finddecreasedriskamongthiscohort,perhapsdueto over-triageinsomecaseswhereanasthmaexacerbationwas relativelymild,buttransferwasneverthelesspursuedoutof concernforpoorreserveandlikelyclinicaldeteriorationorto provideahigherlevelofspecializedcare,perhapsinsome caseswithteamstowhomthepatientisknown.
Therearelimitationsassociatedwiththisstudy.First,the HCAIdataincludesamixofadministrativeandclinicaldata sourcedfrompatienthealthrecords.Thus,definitionsofkey variables,suchasrace/ethnicityandevenincludingthe diagnosisofasthma,aresubjecttoinformationbiasand misclassification.Mostnotably,theprimaryoutcome measureusesacompositedefinitionpreviouslyestablishedin
theliteraturebutslightlyadaptedforthepurposesofastudy focusedonasthma.Thisdefinitionofpotentiallyunnecessary transferisausefultoolforretrospectiveresearchbutisfar fromperfectandlikelyincludessomedegreeoferror associatedwithmisjudgmentintheabsenceofmore detailedcase-by-caseinformation.Moreover, appropriatenessofdischargewithin24hourswasnot assessed,suchasthoroughdocumentationofreturnvisits. Similarly,definingtheinclusioncriteriaforthisstudyrelied uponassumptionsandtrade-offs,suchasincludingpatients withanyactivediagnosisofasthmaexacerbation,rather thanprimarydiagnosis,toovercomethelimitationsofthis datasetdespitetheriskofincludingpatientswithother primarydiagnoses.
Second,theHCAIdatasetisrestrictedtothestateof California.Californiaisalarge,heavilypopulated,and diversestate,whichmakes findingsfromsamplesofits residentsmorenationallyrelevantthanthosefrommost states.However,thegeneralizabilityofthese findingsto otherstatesandnationallyisunclear.Third,themodelsused inthisanalysisfocusonpatient-levelcharacteristics, thereforeneglectingthemanyotherfactorsthathavebeen reportedtoplayintothedecisionforinterfacilitytransfer, includingpatientvolumesandhospitalcapacities,hospitalrelatedfactorssuchasresourcesavailable,andcommunityrelatedfactorssuchastheavailabilityofoutpatient physicians.Fourth,weusedaretrospectivecohort design,whichlimitstheinterpretationof these findings.
Fifth,datawasfrom2016–2019,priortotheCOVID-19 pandemic.TheCOVID-19pandemichadwidespreadand complexeffectsontheUShealthcaresystem,includingthe managementofrespiratoryconditionsandthereallocation ofpediatricandcriticalcareresourcesthroughoutsystems; thus,useofdatapriortothepandemicmightmoreclosely relatetocurrentconditionsastheUShealthcaresystem continuestoadaptandfurthernormalize.Ongoingresearch intotheeffectsoftheCOVID-19pandemiconthe interfacilitytransferofpediatricpatientswithrespiratory complaintswillprovideadditionalinformationtobetter evaluatethisassessment.
UsingastatewidedatasetofEDvisitsandadmission,we foundthatyounger,Hispanic,andmalechildrenwho presentedtotheEDwithasthmahadhigheroddsof experiencingpotentiallyunnecessaryinterfacilitytransfer. Patientswithmultiplehospitaladmissionsforasthmawithin theprioryearwerefoundtohavedecreasedoddsof potentiallyunnecessarytransfer.Importantnextstepsinthis lineofinvestigationincludestudiestargetedatdiscrepancies betweenthese findingsandpriorresearch,investigationof the financialcostsassociatedwithunnecessarytransferof pediatricpatientswithasthma,andanalysisofthehealthcare
systems-relatedfactorsassociatedwithpotentially unnecessaryinterfacilitytransfers.Theseinsightscanbe consideredbypolicymakersandEDadministratorsto identifysubpopulationsofpatientsthataremorelikelytobe impactedbynewinterventionsortoinformfuturestudies concernedwithdisparitiesindelaysincareor financialcosts associatedwithunnecessarytransfer.Findingsfromthis studywillneedvalidationthroughamorerigorous prospectivestudytoconfirmthepatientcharacteristicsthat mightbeassociatedwithincreasedriskofpossiblyavoidable transfersandthepotentialconsequencesassociated withthem.
AddressforCorrespondence:CarlosACamargo,MDDrPH, MassachusettsGeneralHospital,DepartmentofEmergency Medicine,125NashuaSt.,Suite920,Boston,MA02114. Email: ccamargo@partners.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ThisresearchwasfundedbytheSociety forAcademicEmergencyMedicineFoundation.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Petersetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.HealthResources&ServicesAdministration.NationalSurveyof Children’sHealth:NSCHDataBrief.2020.Availableat: https://mchb. hrsa.gov/sites/default/files/mchb/about-us/nsch-data-brief.pdf AccessedJune12,2021.
2.CDC.Table4–1CurrentAsthmaPrevalencePercentsbyAge,United States:NationalHealthInterviewSurvey,2018.2019.Availableat: https://www.cdc.gov/asthma/nhis/2018/table4-1.htm AccessedDecember25,2020.
3.CDC.MostRecentNationalAsthmaData.2023.Availableat: https:// www.cdc.gov/asthma/most_recent_national_asthma_data.htm AccessedFebruary2,2021.
4.CDC.Asthmaemergencydepartment(ED)visits2010–2018.2021. Availableat: https://www.cdc.gov/asthma/asthma_stats/ asthma-ed-visits_2010-2018.html.AccessedJuly6,2021.
5.RosenthalJL,HiltonJF,TeufelRJ,etal.Profilinginterfacilitytransfers forhospitalizedpediatricpatients. HospPediatr. 2016;6(6):345–53.
6.LiJ,MonuteauxMC,BachurRG.Interfacilitytransfersofnoncriticallyill childrentoacademicpediatricemergencydepartments. Pediatrics. 2012;130(1):83–92.
7.StolteE,IwanowR,HallC.Capacity-relatedinterfacilitypatient transports:patientsaffected,waittimesinvolvedandassociated morbidity. CJEM. 2006;8(4):262–8.
8.MohrNM,HarlandKK,ShaneDM,etal.Potentiallyavoidablepediatric interfacilitytransferisacostlyburdenforruralfamilies:acohortstudy. AcadEmergMed. 2016;23(8):885–94.
9.RichardKR,GlissonKL,ShahN,etal.Predictorsofpotentially unnecessarytransferstopediatricemergencydepartments. Hosp Pediatr. 2020;10(5):424–9.
10.WrightRJandSubramanianSV.Advancingamultilevelframework forepidemiologicresearchonasthmadisparities. Chest. 2007;132(5Suppl):757S–769S.
11.FornoEandCeled´onJC.Healthdisparitiesinasthma. AmJRespirCrit CareMed. 2012;185(10):1033–5.
12.GoldDRandWrightR.Populationdisparitiesinasthma. AnnuRev PublicHealth. 2005;26(1):89–113.
13.Bryant-StephensT.Asthmadisparitiesinurbanenvironments. JAllergy ClinImmunolGlob. 2009;123(6):1199–206.
14.PetersGA,OrdoobadiAJ,CashRE,etal.AssociationofAffordable CareActimplementationwithambulanceutilizationforasthma emergenciesinNewYorkCity,2008–2018. JAMANetwOpen. 2020;3(11):e2025586.
15.HCAI.DataResources.Availableat: https://hcai.ca.gov/data/ data-resources/.AccessedMay1,2023.
16.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. AnnInternMed. 2007;147(8):573–7.
17.MartinezFD,WrightAL,TaussigLM,etal.Asthmaandwheezinginthe firstsixyearsoflife. NEngJMed 1995;332(3):133–8.
18.NASEMSO.NationalModelEMSClinicalGuidelinesVersion3.0.2022. Availableat: https://nasemso.org/wp-content/uploads/National-ModelEMS-Clinical-Guidelines_2022.pdf.AccessedApril9,2022.
19.MurtaghKurowskiE,ByczkowskiT,Grupp-PhelanJM. Comparisonofemergencycaredeliveredtochildrenandyoungadults
withcomplexchronicconditionsbetweenpediatricand generalemergencydepartments. AcadEmergMed. 2014;21(7):778–84.
20.FeudtnerC,FeinsteinJA,ZhongW,etal.Pediatriccomplexchronic conditionsclassificationsystemversion2:updatedforICD-10and complexmedicaltechnologydependenceandtransplantation. BMC Pediatr. 2014;14(1):199.
21.PeeblesER,MillerMR,LynchTP,etal.Factorsassociatedwith dischargehomeaftertransfertoapediatricemergencydepartment. PediatrEmergCare. 2018;34(9):650.
22.GattuRK,TeshomeG,CaiL,etal.Interhospitalpediatricpatient transfers factorsinfluencingrapiddispositionaftertransfer. Pediatr EmergCare. 2014;30(1):26.
23.ChowdhuryNU,GunturVP,NewcombDC,etal.Sexandgenderin asthma. EurRespirRev. 2021;30(162):210067.
24.FuseiniHandNewcombDC.Mechanismsdrivinggenderdifferencesin asthma. CurrAllergyAsthmaRep. 2017;17(3):19.
25.OsenHB,BassRR,AbdullahF,etal.Rapiddischargeaftertransfer:risk factors,incidence,andimplicationsfortraumasystems. JTraumaAcute CareSurg. 2010;69(3):602.
26.GlickAF,TomopoulosS,FiermanAH,etal.Disparitiesinmortalityand morbidityinpediatricasthmahospitalizations,2007to2011. Acad Pediatr. 2016;16(5):430–7.
27.GrantTLandWoodRA.Theinfluenceofurbanexposuresand residenceonchildhoodasthma. PediatrAllergyImmunol. 2022;33(5):e13784.
28.ChangY-L,KoH-K,LuM-S,etal.Independentriskfactorsfordeathin patientsadmittedforasthmaexacerbationinTaiwan. NPJPrimCare RespirMed. 2020;30(1):1–8.
29.D’AmatoG,VitaleC,MolinoA,etal.Asthma-relateddeaths. Multidiscip RespirMed. 2016;11:37.
ElisabethFassas,MD,MSc
KyleFischer,MD,MPH
StephenSchenkel,MD,MPP
JohnDavidGatz,MD
DanielB.Gingold,MD,MPH
SectionEditor:TonyZitek,MD
UniversityofMarylandSchoolofMedicine,Baltimore,Maryland
Submissionhistory:SubmittedMay21,2023;RevisionreceivedDecember14,2023;AcceptedDecember15,2023
ElectronicallypublishedMarch29,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18316
Emergencydepartments(ED)intheUnitedStatesserveadualroleinpublichealth:aportalofentryto thehealthsystemandasafetynetforthecommunityatlarge.PublichealthofficialsoftentargettheED forpublichealthinterventionsduetotheperceptionthatitisuniquelyabletoreachunderserved populations.However,undertimeandresourceconstraints,emergencyphysiciansandpublichealth officialsmustmakecalculateddecisionsinchoosingwhichinterventionsintheirlocalcontextcould providemaximalimpacttoachievepublichealthbenefit.Weidentifyhowdecisionsregardingpublic healthinterventionsareaffectedbyconsiderationsofcost,time,andavailablepersonnel,andfurther considertheroleoflocalcommunityneeds,healthdepartmentgoals,andpoliticalenvironment.We describeasampleofED-basedpublichealthinterventionsanddemonstratehowtouseaproposed frameworktoassessinterventions.Wepositaseriesofquestionsandvariablestoconsider:local diseaseprevalence;abilityoftheEDtoperformtheintervention;relativeefficacyoftheEDvscommunity partnershipsastheprimaryinterventionlocation;andexpectedoutcomes.Inusingthisframework, cliniciansshouldbeempoweredtoimprovethepublichealthintheircommunities.[WestJEmergMed. 2024;25(3)415–422.]
Emergencydepartments(EDs)intheUnitedStatesservea dualroleinpublichealth:aportalofentrytothehealth system,andasafetynetforthecommunityatlarge. Clinically,itspositionisclear;theEDprovidesunscheduled acutecare,regardlessofapatient’sabilitytopay.Givenits functionasasafetynetforpeoplelackingconsistentaccessto care,however,theEDisoftenidentifiedforpotentialpublic healthinterventionsduetoaperceptionthatithasaunique abilitytoreachunderservedpopulations.Unsurprisingly,the fieldofemergencymedicine(EM)hastakenonthischallenge andpioneeredanumberofeffectivepublichealth interventions,rangingfromcommunityviolenceprevention1 totreatmentofopioidusedisorder.2
Onestudy3 identified43conditionsproposedinthepeerreviewedliteratureforED-basedpublichealthscreening and/orintervention.Giventhelogisticalimprobabilityofany departmentemployingallproposedinterventions,clinicians
mustmakecalculateddecisionsabout which interventionsto deployand how toimplementthemsuccessfully. Unfortunately,thereisalackofevidence-basedguidancein theEMliteratureonhowEDsshouldprioritizeand implementsuchinterventionssoastomaximallybenefitthe publichealthoftheirlocalcommunity.Thesedecisionsare increasinglyimportantgiventhegrowingstressanddemands alreadyplacedonEDsaroundthecountry.Annualpatient volumeshaveincreasedsubstantially.Patientacuityis gettingmorecomplex.Emergencydepartmentboardinghas becomeanationalcrisis.4 Giventhesignificantresource limitationsoftheEDfromthesetypesoffactors,anypublic healthinterventionbeyondcoreclinicalcaremusthavea clearroleintheEDsetting.
Inthispaper,weproposeaframeworkgroundedin implementationscienceprinciplesforEDstoprioritize interventionsthatmaximizepublichealthbenefitsandreview thekeyelementsofsuccessfulimplementation.Wepresent
thisfromtheperspectiveofourownexpertise:EDmedical directorswhohaveimplementednumerousED-basedpublic healthinterventions;anemergencymedicalservicesmedical directorworkingonpopulationhealthprojects;publichealth researchersandadvocates;publicpolicyexperts;and emergencyphysicians.Werecognizethattheconversation regardingED-basedpublichealthinterventionsis challengingandaffectedbymanyconsiderationsboth internalandexternaltotheED,butwebelievesuccessis possiblewiththerightapproach.
Thevolumeofpotentialpublichealthproposals necessitatesaframeworkfordeterminingwhicharemost meaningfullydeployedasinterventionsinaspecificED.As eachadditionalpublichealthscreeningorinterventiontakes timewithinthecontextofanEDvisit,thereisatangiblecost totheindividualpatientassociatedwithparticipationin publichealth-focusedinterventions.Prioritizationis challengingforEDadministrators,asproposedinitiatives rarelyarisebya fixedprocessbutratherfromaconstellation offactors:acutepublichealthemergencies;issuesoflongstandingconcernwithindividualinterestorexpertisefroma frequentlychangingphysicianandnursingstaff;strategic initiativesfromhospitalsystems;andoftenchanging prioritiesfromlocalpublichealthdepartmentsorpolitical
leaders.Considerationsoffunding,time,andcapacityto providetheinterventionwith fidelityareoftenincomplete. Moreover,interventionsmaybeimplementedwithoutaplan forrigorousevaluationtojustifytheircontinuedpresence. Giventhesechallenges,asystematicapproachtodecisionmakingmaymaximizehealthoutcomes.
Inthiscontext,weprovideaframeworkforconsidering themeritsofconductingaparticularinterventionwithinan EDvisit.Asnoidealframeworkyetexists,wehaveadapted constructsfromtheConsolidatedFrameworkfor ImplementationResearch(CFIR).Thisimplementation frameworkwasoriginallypublishedin2009,7 representing thecumulativeknowledgeofimplementationscienceatthe time.Itisa “pragmaticstructure” foreffective implementationofprogramsandsystemschange precisely whatisneededforenactingeffectivepublichealthprograms intheED.Wedidnot findallconstructsofCFIRpertinentto determiningtheappropriatenessofanew,ED-basedpublic healthintervention.Thoseconstructsdeemedmostrelevant, byauthorconsensus,areoutlinedin Table1 asamodified frameworkforconsideringthemeritsofapotential intervention.Theframeworkwepresentisthusa commentary,basedonourexperienceinEMandpublic healthadministration.
TheCFIRgroupsimplementationscienceconstructs across fivedomains(intervention,process,individuals,inner
Table1. Recommendedconsiderationsforimplementingnewemergencydepartment-basedpublichealthinterventions(Consolidated FrameworkforImplementationResearchmodel).
CFIRmajor domains RelevantCFIR constructsQuestionstoconsider
Intervention characteristics
1.Evidencestrength andquality
• Hastheproposedinterventionshowneffectivenessinpatient-centered outcomesintheEDsetting?
• Ifnot,hastheinterventionshownbenefitthatislikelytotranslatetotheED setting?
• Howstrongistheevidencebase?
2.Relativeadvantage
3.Adaptability
4.Trialability
5.Complexity
• AretherelocationsotherthananED,eitherinthehospitalorinthecommunity thatmaybeamorepatient-centricinterventionsite?
• Cananyoftheselocationsperformthisinterventionmoreeasily,efficiently, cheaply,oreffectively?
• Willthelocalcontextrequireanydeviationsfromtheestablishedprogram model?Ifso,howcouldthesedifferencesimpactefficacy?
• Doestheproposedinterventionhavethe flexibilitytoevolve,asnecessary,after initialimplementation?
• Whatisthetimelineoftheintervention?Isthereaclearendpoint?
• Willitbepossibletoendtheinterventionifnoteffective?
• Whatchallengesmightarisetomaintaining fidelitytotheestablishedprogram model?
• Whatarepossibleunintendedadverseeffectsoftheinterventionfornonparticipants?Arecostsshared,orarespecificpopulationsdisproportionately harmed?
• Aretherehealthequityconsiderations?
(Continuedonnextpage)
Table1. Continued.
CFIRmajor domains RelevantCFIR constructsQuestionstoconsider
Externalcontext*1.Patientneedsand resources
• Whatisthelocalprevalenceofthetargetedconditioninthegeneralpopulation? TheEDpopulation?
• IsthetargetedpopulationmostreadilyaccessiblewithintheED?Arethere alternativeandpotentiallymorepatient-centeredlocations?
• HowdoestheconditionaffectlocalEDutilization,includingreturnvisitsand hospitalization?
Organizational characteristics**
2.Externalnetworking
3.Peerpressure
4.Externalpolicyand incentives
1.Culture
2.Compatibility
3.Relativepriority
4.Leadership engagement
5.Availableresources
6.Accesstoknowledge andinformation
Characteristicsof individualsinvolved
1.Knowledge&beliefs abouttheintervention
2.Individualstageof change
3.Otherpersonal attributes
Processof Implementation
1.Planning
2.Opinionleaders
3.Champions
4.Executing
5.Reflectingand evaluating
• ArethereeffectivesystemsinplacetocontinuecareafterEDdischarge?
• Howmighttheabsence,change,orlossofexternalpartnersaffectthe intervention?
• Howdoestheengagementofothersintheareaaffecttheneedforthe interventionandthepotentialforefficacy?
• Whatstakeholdersorpolicymakersareencouragingimplementation?
• Forprogramsrelyingonexternalfunding,whatisthelong-termstabilityofthis funding?
• Doestheintervention fitwithintheorganizationalmissionoftheED?
• Doestheintervention fitwithintheorganizationalmissionofthehospital?
• Howdoesthisintervention fitwithintheexistingworkflowoftheED?
• HowwouldtheinterventionalterEDperformancemetrics?
• WhatessentialEDprocessesmightbeimpactedbytheintervention?For example,willthroughputbereduced,waittimesincreased,ortriageburdened?
• Whatotherprogramsmayneedtobesacrificedforimplementation?
• Doexpectedbenefitsoutweighpotentialdisruption?
• Istherebuy-infrombothEDandhospitalleadership?
• IstherebandwidthwithintheEDleadershipfortheintervention?
• WilladditionalresourcesberequiredtoaccomplishtheinterventionintheED? Howmightthoseresourcesbemadeavailable?
• Arethereadditionaloutsideresourcesthatthatcouldbebroughttobear?
• Isthisaconditioninwhichemergencyclinicianshavespecificexpertise?
• Whatsourcesofpublichealthexpertisecanbetappedwithinthedepartment?
• Whatadditionaltrainingortechnicalexpertisemightbeaccessed?
• AretheassumptionssupportingimplementationintheEDvalid?
• Arefront-linestaffmotivatedtoparticipateintheintervention?
• Whatcultural,religious,orpoliticalconcernsmaystaffhaveaboutthe intervention?
• Howwilltheplanbedevelopedanddisseminated?
• Howmuchtimeisneededtodevelopanimplementationplanandformulate alliances?
• Whatsupportoroppositionwillimplementationhavefromopinionleaders?
• Howisaprojectchampiongoingtobeidentified?
• Wouldthatchampionhavethebandwidth,expertise,andinfluencetoovercome obstaclestotheintervention?
• Whatistheprocessforcontinuedmonitoringandimprovement?
• Whatwillbetheprocessforevaluationofinterventioneffectiveness?
*TheoriginalCFIRmodelwordingcalledexternalsetting “outersetting.” Thelanguagewaschangedforclaritywhenweadaptedtheframework.
**TheoriginalCFIRmodelcalledorganizationalcharacteristics “innersetting.” Thelanguagewaschangedforclaritywhenweadapted theframework.
CFIR,ConsolidatedFrameworkforImplementationResearch; ED,emergencydepartment.
setting,outersetting)thatcanassistsystematicassessmentof opportunitiesandbarrierstosuccessfulimplementation. Manyofthesearewellsuitedtobeconsideredevenearlierin theimplementationprocess,asaninitialassessmentofvalue andappropriateness.Theseareposedaspriorityquestionsin Table1.Wefurtherexplorethisproposedframeworkby discussingitsapplicationtoseveralestablishedand experimental,ED-basedinterventions.Theseexamplesare meanttoberepresentativeofbenefitsandchallengesthat mayaccompanytheimplementationofcertaininterventions. Theyarenotmeanttobecomprehensive.
Table2 listsmany(butnotall)proposedpublichealth interventionsintheEDaccordingtolevelofacceptanceand penetrance.Someinterventionshavebecomesoengrainedin theEDworkflowthattheynolongerareperceivedas “public health” interventions.Tetanusvaccines,aswellasscreening forsexuallytransmittedinfections,fallunderthiscategory. Below,weexploretheproposedframeworkusingindividual interventionsascasestudiesasaguidefromwhichtoexplore theproposedquestions.Eachexamplewasselectedto
highlightmajorconsiderationsrequiredtodeployand maximizepublichealthbenefits,andeachvariesintheextent towhichtheinterventionisacceptedandimplementedin EDsthroughoutthecountry.Weconsidertheoveralldisease prevalenceandimpactoftheinterventionsasitrelatesto futureEDutilization.Weexplorewhethertheinterventionis typicallyintegratedwith,runsparallelto,orisseparatefrom theworkflowofanEDvisit.Similarly,weexaminetheability andappropriatenessofperformingtheinterventionsby consideringboth financialcostsandrequisiteresources.
TheUSCentersforDiseaseControlandPrevention endorsedED-basedscreeningforundiagnosedHIVin2001,8 buttheserecommendationshavenotrisentothelevelof officialguidelinesorqualitymetrics.Suchprogramshavethe potentialtotestlargepopulationsandmay findindividuals whodonothaveaccesstotraditionaltestingprograms.
Multiplestudieshaveexaminedhowtobest fitHIV screeningintoexistingEDworkflowordevelopparallel workflows. 9 Frequentquestionsincludewhichpatientsto test(universalvssymptomsvsrisk-basedscreening);who
Table2. Selectiveoverviewofthecurrentstateofemergencydepartment‒basedpublichealthinterventions.
Levelof acceptanceConceptSelectexamplesNotes
EstablishedAcceptedinterventionsthatare well-integratedintheEDsetting
SupportedInterventionsforwhichimplementation iscontextdependentbasedon,for example,localepidemiology,local resources,andcommunitypriorities.
• Sexuallytransmitteddiseasetesting
• Tetanusvaccination
• Bloodpressurescreening
• Smokingandtobaccoscreening
• Intimatepartnerviolencescreening
• Substanceusescreening, intervention,andreferraltotreatment
• HIVscreeningandreferralfor treatment
• HepatitisAandCscreeningand referralfortreatment
• Naloxoneprovisionforsubstance useandoverdose
• BuprenorphineinitiationintheEDfor opioidusedisorder
• Communityviolenceintervention programs
• Depressionscreeningandreferral
Typicallycodifiedbycurrentfederal guidelinesorrecommendations,such asTheJointCommission,The CentersforMedicareandMedicaid Servicesrequirementsor reimbursement,USPreventive ServicesTaskforcerecommendations.
Potentiallywidelydiscussedinthe emergencymedicineliterature,these aretypicallynon-regulated interventionsthatmaybethetopicsof grantsorregionalimplementation. Nationalguidelinesmaybesupportive butnotnecessarilywithinthe EDsetting.
ExperimentalInterventionsarediscussedor implementedatasmallnumberof selectdepartments,often experimentalorotherwiseresearch oriented.
• HepatitisAvaccination
• Earlypregnancylinkagetocare
• Dementiascreening
• Naloxoneprovisionforallopioid prescriptions
• COVID-19vaccination
• Screeningforhousinginsecurityand otherhealth-relatedsocialneeds
ED,emergencydepartment; COVID-19,coronavirusdisease2019.
Potentiallygrantfunded,thesemay alsobeindividualdepartmental projectsorthesubjectsoftrials.Well establishedguidancewithinoroutside theEDisrare.
shouldinitiatescreening(counselororclinician);andthe operationalneedsofsuchprograms.9 Arecentlarge, randomizedtrialcomparinguniversalscreeningagainsttwo typesoftargetedscreeningshowedsimilareffectivenessin identifyingnewcases,butwithlowerresourceexpenditureof targetedscreeningprograms.9 Researchdemonstratingthat clinician-basedtestingresultsinlowerscreeningrates suggeststhepotentialbenefitofdedicatingadditionalstaffing andfundstosuchinitiativestomaximizeeffectiveness. Operationalchallengesmayfurthercomplicateeffortsto establishED-basedHIVscreenings,includingpoorlinkage tocare,10,11 lowwillingnesstotestamongmarginalized populations,12,13 andlackofculturalcompetency surroundingtestinginitiatives.14,15 Factorssuchaslower HIVincidence,improvedcommunityawarenessandriskmitigation,increasedtestingduringroutinemedicalcare, fewerregulatorybarrierstoHIVscreeninginotherlocations, moreeffectiveanti-retroviralmedication,anddecreased stigmaofthediseasemayalsohavechangedthebenefitof ED-basedprogramssincetheywere firstdevelopedmore than20yearsago.
Intimatepartnerviolence(IPV)refersto “physical violence,sexualviolence,stalkingandpsychological aggressionbyacurrentorformerpartner” andaffectsan estimatedoneinfourwomenandonein10men nationwide.16 ScreeningforIPVinwomenofreproductive agemayhelpamelioratephysicalandpsychologic sequelae.17,18 TheUSPreventiveServicesTaskForce (USPSTF)providesaGradeBrecommendationthat “cliniciansscreenforIPVinwomenofreproductiveageand provideorreferwomenwhoscreenpositivetoongoing supportservices.”
Screeningforphysicalinjurycouldbereadilyintegrated intoanED’sexistingassessmentofacuteinjuries.However, forcomplaintswithlessobviousconnectionstoIPV,suchas mentalhealthconditionsexacerbatedbyIPVexposure, integrationofscreeningmaybehardertodefineor standardizeintheabsenceofuniversalscreeningprotocols. Inpractice,universalscreeningisoftendeployedwhile collectingpatientinformationonamyriadofothervariables (eg,pastmedicalhistory,medicationhistory,suicide screening),andmaybeproneto “clickfatigue,” whereinthe screener,taskedwithcompilingalargeamountofdataina shortamountoftime,isunabletoperformthescreening questionswiththeintended fidelity.19 Patientsalsocanbe fatiguedbytimespentscreeningforconditionsnotrelatedto theirchiefcomplaintandmaybereluctanttodivulge sensitiveinformationinthissetting.However,focused screeningofhigh-riskpopulationsmaymisspatientsandis pronetobias.
TheexistingevidencebasecitedbytheUSPSTFincludes 30studies,includingthreerandomcontrolledtrials(RCT),
whichyieldednuancedresultshighlightingthenecessityof bothcomponentsofscreeningandrobustintervention.As Feltneretalreportintheirconclusion: “Althoughavailable screeningtoolsmayreasonablyidentifywomenexperiencing IPV,trialsofIPVscreeninginadultwomendidnotshowa reductioninIPVorimprovementinqualityoflifeover3to 18months.”20 Thishighlightsthechallengeoftranslating positivescreensintopositivehealthoutcomes.Practicing clinicianswillrecognizethatinterveningtoprotectvictimsof IPVischallengingwhenpatientspresentexplicitlywiththis complaint,letalonewhenpatientsmaybeunwillingor unabletodivulgesymptomsofabuse.Closerelationships withcommunityresourcesequippedtoassistvictimsofIPV arenecessarytoensureeffectiveness,whichrequires substantialandsustainedadministrativesupport.
GunviolenceintheUnitedStatesremainsanintractable publichealthproblem,with2020recording19,384 homicides.21 Inresponse,hospitalshaveimplemented hospitalviolenceinterventionprograms(HVIP)inEDsand wards.22 Theseprogramsusewhatisdescribedasa “golden moment” ofopportunitywhenpatientsareinthehospitalto fosterclose,long-termcarerelationshipsbetweenculturally competentviolencepreventionprofessionalsandpatients. Thisincludesthecreationofcomprehensiveneeds assessments,deliveryofcasemanagementservices,longtermpeersupport,mentalhealthservices,andaddressing socialdeterminantsofhealthasrootcausesofviolence.
InitialstudiesofHVIPshavedemonstratedpromising resultswithdecreasedinjuryrecidivismandimproved intermediateoutcomessuchasdeliveryofmentalhealth services.23 However,toachievetheseoutcomes,significant commitmentisrequiredbyEDs,includingbuy-infrom multiplehospitaldepartments,communitypartners,and internalprogramchampions.Thecostsofhiringspecially trainedstaffaresignificant,astimeandexpertisetoperform thisinterventionisoftenoutsidethetypicalworkloadof emergencyclinicians.Manyprogramsrequireanannual budgetofgreaterthan$300,000.Thisfundinghas historicallybeenchallenging,althoughrecentdevelopments allowforreimbursementthroughtheMedicaidprogramina minorityofstates.24
HepatitisAvirus(HAV)isavaccine-preventable transmissibleinfectionwiththepotentialforlong-term,fatal liverdisease.Asinglevaccinedosageisupto98%effectiveat preventingtransmission.25 Consequently,ED-basedHAV vaccinationhasthepotentialtolimitlong-termsequelaein thoseathighestriskofcontractingtheillness.Still,the processofidentifyingtheseat-riskindividualsrelieson simplescreeningquestionsthatareoftenincorporatedinto standardhistory-takinginstrumentsandpracticesinthe
emergencycontext.Storageandprovisionofvaccinescan leverageexistinghospitalpharmacyandnursingprotocols. Whileat-riskgroups,includingindividualsexperiencing homelessnessorusingintravenousdrugs,menwhohavesex withmen,andthosewhohavebeenincarcerated26 frequently receivehealthcareintheemergencysetting,therearealso outpatientclinicsandother,non-healthcareentities(eg, homelessshelters,nightclubs,jails,substanceusetreatment facilities)tailoredtoservethispopulation.Targetingthese communitysitesmayachievebetterpenetranceofthe interventionforunderservedpopulationmorequickly atlowercost,givenmodestenrollmentof ED-basedprograms.27
VaccinationeffortsbasedintheEDwerealsobolsteredby thepresumptiveviewthattheEDpatientpopulationmight nothavereadyaccesstovaccinationoutsidetheED,28 aswell asbyadesireonthepartofmanystaffmemberstotakepart inanationaleffortofclearimport.29 AnED-based vaccinationseemedtobeanobviousextensionofhospitalbasedvaccinationprograms.TheEDvaccinationcould leverageresourcessuchasreadyaccesstopharmacyand freezers,arelativelysmallpoolofstaffwhocouldbetrained toadministervaccines,andculturalcompetencyinoffering vaccinations.Absenttheseconsiderationswasanassessment ofresourceandvaccineavailabilityinthesettingofCOVID19-relatedstaffingshortages.Themultipledosingregimen forCOVID-19addedcomplexityandrequiredaseparate workflowwithintheEDcontextandrequiredfollow-upthat wassometimesnotpossiblewithintheEDsetting. Additionally,muchwasunknownaboutwhethertheED offeredvaccinationtoanewordifferentpopulationorwas redundanttootherhospital,state,orlocalcommunity efforts.Withvaryingdiseaseincidenceandincreasing vaccinationrates,therewaslikelyashortwindowtorealizea modestbenefitfortheintervention.
Emergencyphysiciansarecommittedtoimprovingpublic healthoutcomes,asevidencedbythe2009and2021Society forAcademicEmergencyMedicineconsensus conferences30,31 andthedevelopmentofseveralpost-EM fellowshipsinrecentyearscommittedtopublichealthand publicpolicy.32 Emergencydepartmentshaveembraced manypublichealthtaskssuchasscreening,surveillance,and interventionsoutsidethetraditionalscopeofemergencycare. Withlimitedtimeandresources,notallpublichealthprojects canbeundertaken.Tomaximizepublicbenefit,caremustbe takentoselectinterventionsthathavethelargestimpact whilemaintainingintegritytotheED’scoreclinicalmission. Whileemergencyphysicianstakeprideinthemantra, “anyone,anything,anytime,” wemustrecognizethatsome resourcesmaybebetterspentoutsidethewallsoftheED.
Thisdoesnotmeanabandoningcertainpatientpopulations, butratherbringingtheskillsofemergencyphysiciansbeyond thewallsoftheEDthroughavarietyofcreativeways,such ascollaborationswithpublichealthornonprofit organizations,leveragingemergencymedicalservices experienceandconnectionstodevelopmobileintegrated healthprograms,33 ordeployingthetacticsof “streetmedicine.”
Additionally,emergencyphysiciansshouldconsidernot justhowtheprogramdesignaffectsthatsingleconditionbut howadaptabletheinterventionisforaspecificdepartment andavailableresources.Considerahypothetical interventionthatmayhave90%sensitivityforuniversal screening,butonly70%fortargetedscreening.Depending onthedifferenceinstafftimebetweenthetwo,implementing thelowersensitivitytargetedapproachmayinfactallowthe sameEDtodeployaninterventionforanadditionalpublic healthconcernwiththemarginalresourcesneededfor universalscreening,thusmaximizingoverallbenefit.
Screeningprogramsthatcollectdatabutdonotprovide aninterventioninresponsetopositivescreensareunlikelyto beimpactful.Wepositthatthehighestvaluescreening programshaveappropriatesensitivityandspecificityfor theirtargetcondition,arecosteffective,andareactionable. Thevalueofascreeningprogramshouldbeassessedbased onthepatientpopulationmostinneedofthisscreening,the effectivenessofapossibleintervention,andtheproposed rationaleorrelativeadvantagefordoingitintheED. Additionally,buy-inforaninterventionisnecessaryfrom stakeholdersacrossmultiplelevelsoftheorganization: hospitalandEDleadership,physicians,nursing,andstaff. Failuretoobtainsupportfromleadershipallocating resourcesorstaffcarryingouttheinterventioncandamage moraleandlimitprogramefficacy.
Interventionsforpositivescreeningresults,whetherfor chronicinfectiousdiseaseorhealth-relatedsocialneeds,may needtobeprovidedoutsidetheED.Therefore,robust externalnetworksbetweentheEDandoutpatientclinicsand socialservicesarethemostimportantpartofascreeningand referralprogram.MostEDsenthusiasticallyembrace additionalresourcestocoordinatecarefortheirmost vulnerablepatients,withorwithoutformalizedscreening programs.Thus,intheplanningprocessEDsshouldensure thereissignificantbuy-infrompotentialexternalpartners,so thatanyscreeningimplementedhastangibledownstream effects.Manymaybepublicclinicsornonprofit organizationsthatmaythemselvesbeunderfundedand understaffed,necessitatingexternalfundingthatshouldbe equitablydistributedbetweenstakeholders.External partnersoftenbenefitfromachampionpointofcontactin theEDtoadvertise,monitor,andcoordinate referralpathways.
PatientopennesstoacceptinganinterventionintheEDis alsoanimportantfactorinanED-basedintervention.What
expectationsdopatientsbringintotheED?Forexample,a patientsufferinganankleinjurymaynotwanttoanswer questionsabouttheirmaritalsexualpracticesorsmoking habitswhileawaitingtheresultsofaradiograph.Such questionsmaybeperceivedasirrelevanttothestatedreason forthevisit,andthepatientmay findtheminvasive oralienating.
Identifyingaliteraturebaseforproposedinterventions thatshowsbenefittopatient-centeredoutcomes(eg, improvedbloodpressure,reducedmortality),orpopulationbasedoutcomes(e.g.,fewercommunityoverdosesor shootings),isanoptimalstandardforconsidering implementationofpublichealthinterventionintheED. Observationalstudieswithoutwell-matchedcontrolsare oftensubjecttoselectionbiasandregressiontothemean. Rigorousevaluationmethodologythatisolatestheeffectof theinterventiononmeaningfuloutcomes,suchasRCTs,is preferredtoidentifythemostimpactfulinterventions. Ideally,implementedinterventionswillcontinuemonitoring andevaluationofkeymetricstoensurelocalefficacy.When thatevidenceisabsent,wehopethatthisframeworkcan informthedecision-makingprocessanalogoustothewaywe makeclinicaldecisionsintheabsenceofrobustevidence.
Emergencydepartmentsareintimatelyfamiliarwiththe waysinwhichsocialneedsdrivehealthcareutilizationand outcomes.However,disparitiesinpopulation-basedhealth outcomesarenotdrivenprimarilybylackofquality emergencycare,butbydisparitiesinbroadersocial determinantsofhealth.Thesedisparitiesareunlikelytobe amelioratedbyaone-timeinterventionwithintheED context.Thus,emergencyphysiciansmustconsider implementingpublichealthprogramsnotasaone-time isolatedinterventionbutratherasthebeginningprocessof long-term,transformative,structuralchangeofthe healthcareandsocialservicessystemsasawhole.34
Emergencycliniciansandstaffcaredeeplyaboutthe publichealthofthecommunitiestheyserve.Tomaximize publichealthbenefit,emergencyphysiciansfacechallenging decisionsregardingwhichpublichealthinterventionshold themostpotentialforimpact,aswellasthewaytheyare deployed.Localdynamicswillinformdecision-making the balanceofbenefitsandharmsmaydifferonaccountof context-specificcircumstances.Manyproposed interventionscouldalsobeimplementedeffectivelyinsome settingsbutnotinothers.Giventhatthereisno “onesize fits all” approach,wehaveproposedaframeworkgroundedin implementationsciencetoassesspotentialinterventionsina systematicmannertomaximizepublichealthintervention withoutdetractingfromtheED’scorefunction.Itiscritical touseaguidingframeworktoproperlyevaluateefficiency, feasibility,localcontext,andcostbeforedeploymentofany ED-basedpublichealthintervention.
AddressforCorrespondence:JohnDavidGatz,MD,Universityof MarylandSchoolofMedicine,DepartmentofEmergencyMedicine, 110SouthPacaSt.,6thFloor,Suite200,Baltimore,MD21201. Email: jgatz@som.umaryland.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Dr.Gatzwassupportedbyaresearch grantfromtheNationalFoundationofEmergencyMedicineduring thistime.Therearenootherconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2024Fassasetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ZunLS,DowneyL,RosenJ.TheeffectivenessofanED-basedviolence preventionprogram. AmJEmergMed. 2006;24(1):8–13.
2.D’OnofrioG,O’ConnorPG,PantalonMV,etal.Emergencydepartmentinitiatedbuprenorphine/naloxonetreatmentforopioiddependence:a randomizedclinicaltrial. JAMA. 2015;313(16):1636–44.
3.KelenGD.Publichealthinitiativesintheemergencydepartment:notso goodforthepublichealth? AcadEmergMed. 2008;15(2):194–7.
4.MareinissDP.Theimpendingstorm:COVID-19,pandemicsandour overwhelmedemergencydepartments. AmJEmergMed. 2020;38(6):1293–4.
5.BabcockIrvinC,WyerPC,GersonLW.Preventivecareinthe emergencydepartment,PartII:Clinicalpreventiveservices–an emergencymedicineevidence-basedreview.SocietyforAcademic EmergencyMedicinePublicHealthandEducationTaskForce PreventiveServicesWorkGroup. AcadEmergMed. 2000;7(9):1042–54.
6.RhodesKV,GordonJA,LoweRA.Preventivecareintheemergency department,PartI:Clinicalpreventiveservices–Aretheyrelevantto emergencymedicine?SocietyforAcademicEmergencyMedicine PublicHealthandEducationTaskForcePreventiveServicesWork Group. AcadEmergMed. 2000;7(9):1036–41.
7.DamschroderLJ,AronDC,KeithRE,etal.Fosteringimplementationof healthservicesresearch findingsintopractice:aconsolidated frameworkforadvancingimplementationscience. ImplementSci. 2009;4:50.
8.BransonBM,HandsfieldHH,LampeMA,etal.Revised recommendationsforHIVtestingofadults,adolescents,andpregnant womeninhealth-caresettings. MMWRRecommRep. 2006;55(RR-14):1–CE4.
9.EscuderoDJ,BahamonM,PanakosP,etal.Howtobestconduct universalHIVscreeninginemergencydepartmentsisfarfromsettled. J AmCollEmergPhysiciansOpen. 2021;2(1):e12352.
10.MenonAA,Nganga-GoodC,MartisM,etal.Linkage-to-caremethods andratesinU.S.emergencydepartment-basedHIVtestingprograms:a
systematicliteraturereviewbriefreport. AcadEmergMed. 2016;23(7):835–42.
11.EhrenkranzPD,AhnCJ,MetlayJP,etal.Availabilityofrapidhuman immunodeficiencyvirustestinginacademicemergencydepartments. AcadEmergMed. 2008;15(2):144–50.
12.MerchantRC,SeageGR,MayerKH,etal.Emergencydepartment patientacceptanceofopt-in,universal,rapidHIVscreening. Public HealthRep. 2008;123Suppl3(Suppl3):27–40.
13.HaukoosJS,HopkinsE,ByynyRL,etal.Patientacceptanceofrapid HIVtestingpracticesinanurbanemergencydepartment:assessmentof the2006CDCrecommendationsforHIVscreeninginhealthcare settings. AnnEmergMed. 2008;51(3):303–9,309.e1.
14.MerchantRC,LiuT,ClarkMA,etal.FacilitatingHIV/AIDSandHIV testingliteracyforemergencydepartmentpatients:arandomized, controlled,trial. BMCEmergMed. 2018;18(1):21.
15.TorresM.RapidHIVscreeningintheemergencydepartment. Emerg MedClinNorthAm. 2010;28(2):369–80.
16.CentersforDiseaseControlandPrevention.Intimatepartnerviolence. 2021.Availableat: https://www.cdc.gov/violenceprevention/ intimatepartnerviolence/index.html.AccessedAugust30,2022.
17.CDC.Preventingintimatepartnerviolence.CentersforDiseaseControl andPrevention.UpdatedOctober11,2022. https://www.cdc.gov/ violenceprevention/intimatepartnerviolence/fastfact.html AccessedSeptember2,2022.
18.USPreventativeServicesTaskForce.FinalRecommendation Statement – IntimatePartnerViolence,Elderabuse,andAbuseof VulnerableAdults:Screening.2018.Availableat: https://www. uspreventiveservicestaskforce.org/uspstf/recommendation/ intimate-partner-violence-and-abuse-of-elderly-and-vulnerableadults-screening.AccessedSeptember2,2022.
19.CollierR.RethinkingEHRinterfacestoreduceclickfatigueand physicianburnout. CMAJ. 2018;190(33):E994–5.
20.FeltnerC,WallaceI,BerkmanN,etal.Screeningforintimatepartner violence,elderabuse,andabuseofvulnerableadults:evidencereport andsystematicreviewfortheUSPreventiveServicesTaskForce. JAMA. 2018;320(16):1688–1701.
21.GramlichJ.WhatthedatasaysaboutgundeathsintheU.S.Originally published2019.LastupdatedApril26,2023.Availableat:~https://www. pewresearch.org/fact-tank/2022/02/03/what-the-data-says-aboutgun-deaths-in-the-u-s/#:~:text=The%2019%2C384%20gun% 20murders%20that,75%25%20increase%20over%2010%20years AccessedOctober10,2022.
22.BonneS,HinkA,ViolanoP,etal.Understandingthemakeupofa growing field:aCommitteeonTraumasurveyofthenationalnetworkof hospital-basedviolenceinterventionprograms. AmJSurg. 2022;223(1):137–45.
23.StrongBL,ShipperAG,DowntonKD,etal.Theeffectsofhealthcarebasedviolenceinterventionprogramsoninjuryrecidivismandcosts:a systematicreview. JTraumaAcuteCareSurg. 2016;81(5):961–70.
24.ZavalaC,BuggsSA,FischerKR.StatesshoulduseMedicaidtosupport violenceinterventionefforts. JTraumaAcuteCareSurg. 2022;92(2):e25–7.
25.CentersforDiseaseControlandPrevention. ViralHepatitis:HepatitisA 2020.Availableat: https://www-cdc-gov.proxy-hs.researchport.umd. edu/hepatitis/hav/index.htm.AccessedSeptember20,2022.
26.KaighC,BlomeA,SchreyerKE,etal.Emergencydepartment-based hepatitisAvaccinationprograminresponsetoanoutbreak. WestJ EmergMed. 2020;21(4):906–8.
27.JamesTL,AschkenasyM,EliseoLJ,etal.ResponsetohepatitisA epidemic:emergencydepartmentcollaborationwithpublichealth commission. JEmergMed. 2009;36(4):412–6.
28.RodriguezRM,TorresJR,ChangAM,etal.TheRapidEvaluationof COVID-19VaccinationinEmergencyDepartmentsforUnderserved PatientsStudy. AnnEmergMed. 2021;78(4):502–10.
29.WaxmanMJ,MoschellaP,DuberHC,etal.EmergencydepartmentbasedCOVID-19vaccination:Wheredowestand?. AcadEmergMed. 2021;28(6):707–9.
30.BernsteinSLandD’OnofrioG.Publichealthintheemergency department:AcademicEmergencyMedicineConsensusConference executivesummary. AcadEmergMed. 2009;16(11):1037–9.
31.SchoenfeldEM,LinMP,Samuels-KalowME.Executivesummaryofthe 2021SAEMConsensusConference:Frombedsidetopolicy:advancing socialemergencymedicineandpopulationhealththroughresearch, collaboration,andeducation. AcadEmergMed. 2022;29(3):354–63.
32.SocietyforAcademicEmergencyMedicine.FellowshipsDirectory. Availableat: https://member.saem.org/SAEMIMIS/SAEM_Directories/ Fellowship_Directory/SAEM_Directories/P/FellowshipMap.aspx AccessedMay7,2022.
33.GingoldDB,LiangY,StryckmanB,etal.Theeffectofamobile integratedhealthprogramonhealthcarecostandutilization. Health ServRes. 2021;56(6):1146–55.
34.Samuels-KalowME,BoggsKM,CashRE,etal.Screeningforhealthrelatedsocialneedsofemergencydepartmentpatients. AnnEmerg Med. 2021;77(1):62–8.
CeceliaMorra,BA*
KevinNguyen,BS*
RitaSieracki,MLS*
AshleyPavlic,MD,MA†
CourtneyBarry,PsyD,MS‡
SectionEditor:MuhammadWaseem,MD
*MedicalCollegeofWisconsin,Milwaukee,Wisconsin
† MedicalCollegeofWisconsin,DepartmentofEmergencyMedicine, Milwaukee,Wisconsin
‡ MedicalCollegeofWisconsin,DepartmentofPsychiatryandBehavioralMedicine, Milwaukee,Wisconsin
Submissionhistory:SubmittedJuly7,2023;RevisionreceivedDecember29,2023;AcceptedJanuary4,2023
ElectronicallypublishedApril8,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18394
BackgroundandObjectives: Greaterlifetimeexposuretopsychologicaltraumacorrelateswitha highernumberofhealthcomorbiditiesandnegativehealthoutcomes.However,physiciansoftenarenot specificallytrainedinhowtocareforpatientswithtrauma,especiallyinacutecaresettings.Ourobjective wastoidentifyimplementedtrauma-informedcare(TIC)trainingprotocolsforemergencyand/ortrauma servicephysiciansthathavebothsufficientdetailthattheycanbeadaptedandoutcomedataindicating positiveimpact.
Methods: WeconductedacomprehensiveliteraturesearchinMEDLINE(Ovid),Scopus,PsycInfo,Web ofScience,CochraneLibrary,Ebsco’sAcademicSearchPremier,andMedEdPORTAL.Inclusion criteriawereEMandtraumaserviceclinicians(medicaldoctors,physicianassistantsandnurse practitioners,residents),adultand/orpediatricpatients,andtrainingevaluation.Evaluationwasbased ontheKirkpatrickModel.
Results: Wescreened2,280uniquearticlesandidentifiedtwodifferenttrainingprotocols.Results demonstratedthetrainingincludedpatient-centeredcommunicationandinterprofessionalcollaboration. Onecurriculumdemonstratedthattargetedoutcomeswereduetothetraining(Level4).Bothcurricula receivedoverallpositivereactions(Level1)andillustratedbehavioralchange(Level3).Neitherwere foundtospecificallyillustratelearningduetothetraining(Level2).
Conclusion: Study findingsfromourreviewshowapaucityofpublishedTICtrainingprotocolsthat demonstratepositiveimpactandaredescribedsufficientlytobeadoptedbroadly.Currenttraining protocolsdemonstratedanincreasingcomfortlevelwiththeTICapproach,integrationintocurrent practices,andreferralstotraumainterventionspecialists.[WestJEmergMed.2024;25(3)423–430.]
Greaterpsychologicaltraumaexposurewithinone’ s lifetimecorrelateswithanincreasednumberofhealth comorbiditiesandnegativehealthoutcomes.1 Childhood exposurestotraumaarelinkedtoincreasedhealthrisksin adulthoodforsubstanceusedisorder,depression,obesity, heartdisease,cancer,andmore.Experiencingtraumais oftenthoughtofasarareoccurrence,butthefoundational adversechildhoodexperiences(ACE)studyhasshownhow
commonandpervasivetraumaticeventsarewithintheUS. Thestudyinvestigateddifferentcategoriesofchildhood traumathatincludedphysical/sexual/emotionalabuse, parentalincarceration,andparentaldruguse.Morethan halfoftheparticipantsreportedatleastoneACE,and25% reportedmorethantwocategoriesofACEs.From 2011–2015,thestateofWisconsinrantheBehavioralRisk FactorSurvey,whichfoundthat57%ofthe25,518adult participantsreportedoneormoreACEs.2
ManystudiesrecommendscreeningforACEsinthe emergencydepartment(ED),butthishasnotbecome commonpractice.3 TheACEquestionnaireremainsthemost commontoolusedforsuchscreening1;however,morerecent researchhassuggestedthattrauma-informedcare(TIC) shouldbeappliedinallpatientinteractionsbecausepatients withahistoryoftraumainfrequentlyclassifythemselvesas such.4 Practicingwiththeassumptionthateachpatienthas experiencedsomeformoftraumaallowsthehealthcareteam toavoidre-traumatization,orthere-experiencingofaprior traumawhenexposedtoanewtraumaticevent,andto delivercompassionateandpatient-centeredcare,whichisa criticalpieceinTIC.5–7
Becauseapatient’ s firstcontactwiththehealthcaresystem isoftenintheacutecaresetting,itiscrucialthatthese cliniciansareequippedwiththeappropriateresourcesand knowledgetoprovideTIC.5,8,9 Thisencouragesthemtousea moremindfulapproachtoassessingpatients.Studieshave indicatedthat11–61%ofEDpatientspresentwithatrauma historyand20%ofpatientsatadmissionreportsuffering fromacuteemotionaldistress.10,11 Intheseacutecare settings,therearemultiplescenariosinwhichretraumatizationcanoccur.Forexample,althoughitisnot surprisingto findthatrestraintuseonapatientcanbe harmful,studiessuggestthatevenaroutinephysicalexam withoutverbalcuescanunintentionallyre-traumatizea patient.12,13 Sucheventscancausepatientstowithdrawfrom thehealthcareinteractionanddecision-making,whichleads toaportrayalofpatientnon-adherence.Furthermore, patientswithtraumahistoryarelesslikelytoseekouta primarycarephysician,insteadrelyingontheEDfor treatment.14,15 Thus,ifTICisnotpracticedinthesesettings, long-termhealthoutcomesareimpairedandmorbidityis increased.Itisessentialthatmedicalstaffbetrainedin trauma-informedpracticestoprovidehigh-qualitycareand promotehealing.
TheTICpyramidoutlines fiveoverarchingprinciples: 1)patient-centeredcommunicationandcare; 2)understandingthehealtheffectsoftrauma; 3)interprofessionalcollaboration;4)understandingyour ownhistoryandreactions;and5)screening,including universaltraumaprecautionsandtrauma-specificstrategies (Figure1).16 The firsttwoprinciplesareuniversal precautionsthatfostertrustandrapportandcanbeused withoutestablishingapatient’straumahistory.The remainingthreeprinciplesarespecificforwhentheclinician knowsthepatienthasexperiencedtrauma.
ThepositiveimpactofTICinbothacutecareandprimary caresettingshasbeenwelldocumentedinthe literature.9,17–23 TheuseofTIChasbeenassociatedwith improvedchildhoodandfamilyadjustmentduringperiodsof increasedadversity,enhancedhealthoutcomes,increased satisfactionwithcare,andbettermentalhealthoutcomes,
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Manypatientswhoaccessemergencycare haveahistoryofpsychologicaltrauma.Best practicesrecommendatrauma-informedcare (TIC)approach.
Whatwastheresearchquestion?
WhatTICtrainingprotocolshaveshown apositiveimpactforemergencyand traumaclinicians?
Whatwasthemajorquantitative findingofthe study?Majorcomparisonwithp-valueand confidenceinterval.
OnlytwoTICcurriculaintheliteratureshow positiveimpactandarereproducible.
Howdoesthisimprovepopulationhealth?
Thelimitedexistingcurriculashowthat targetedTICtrainingincreasesclinicianuse ofTICpracticesandimprovespatient outcomesandsatisfaction.
withdecreasedsubstanceabuseratesandreducedposttraumaticstressdisordersymptoms.22
PracticingTICcanalsodecreasethepsychologicaland emotionalburdenonthehealthcareteam.10,23 Frequent occupationalexposuretothetraumaexperiencesofothersis consideredsecondarytraumaandisthoughttohavea cumulativeeffectonclinicianwell-being,resultingingreater distressovertime.24 Theimpactoftheseexperienceshasbeen describedasclinicianburnout,compassionfatigue,and
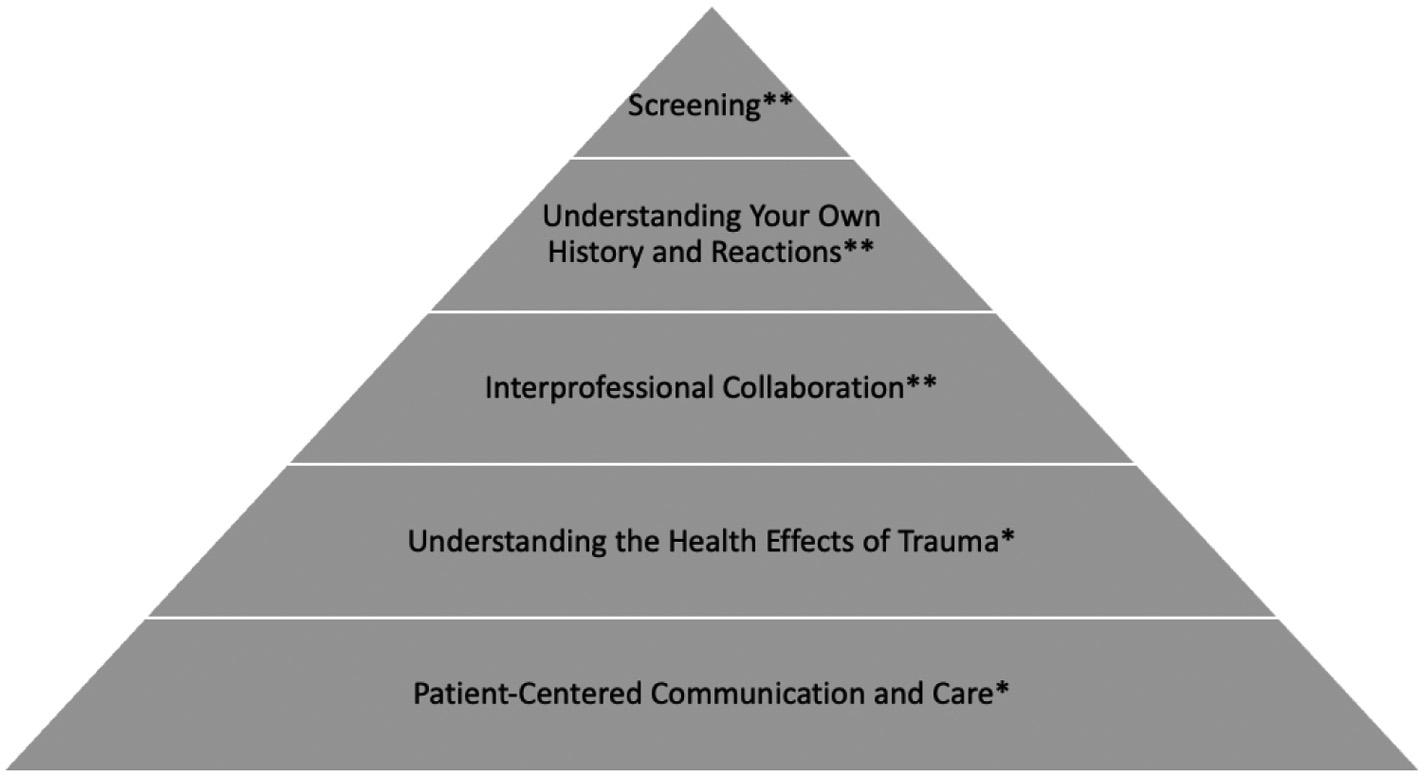
Figure1. Trauma-informedcarepyramidadaptedfrom Rajaetal(2015). Universaltraumaprecautions*;trauma-specificcare.**16
secondarytraumaticstress.Clinicianburnouthasbeen showntoleadtopoorsleep,distraction,anddefensiveness, amongotherphysicalandpsychologicalramifications.23 Thesereactionsimpairaclinician’sabilitytodelivercare, increasingthelikelihoodofmedicalerrorsandmaking patientsfeellesssafe.23 PracticingTICallowsthehealthcare teamtonotonlyidentifyandattendtoapatient’sprior trauma,mitigatenewtraumaduetocurrentmedicalcare, andbetterunderstandthereactionsandbehaviorsofpatients andtheirfamilies,butalsoencouragesthemedicalteamto recognizetheirownhistorywithtrauma.
OuraiminthisscopingreviewwastoidentifyTICtraining protocolsdesignedforUSEDsandtraumaservicesthathave demonstratedpositiveimpactinordertodevelopanew trainingprotocoltobeusedinthesesettings.Identifying implementedtrainingwillassistclinicians,healthcare practices,andteachingprogramsinterestedinimproving knowledgeandclinicalpracticetoaddresstrauma. Reviewingexistingtrainingprotocolswillfacilitate adaptationanddevelopmentoffuturetrainingtofurther improvepatientcare.
LiteratureSearch
WeusedthePRISMAExtensionforScopingReviews (PRISMA-ScR)checklistasareportingguideforthis review.25 Furthermore,wemodeledthispaperfroma previouspublishedpaperonascopingreviewonTICwithin theprimarycaresetting.21 Acomprehensiveliteraturesearch wasdevelopedbyamedicallibrarianandpeerreviewedusing thePRESSguideline.26 Searcheswereconductedin MEDLINE(Ovid),Scopus,PsycInfo,WebofScience, CochraneLibrary,Ebsco’sAcademicSearchPremier,and MedEdPORTAL,andthesearcheswereconductedtwice. SearcheswerelimitedtoEnglishlanguagearticles.Therewas norestrictiononyearorstatusofpublication;weincluded articlesthroughNovember24,2021,inthesearch.Search strategieswerecreatedusingmedicalsubjectheadings (MeSH)andkeywordscombinedwithdatabase-specific advancedsearchtechniques.MeSHtermsandkeywords wereidentifiedtorepresenttrauma-informedapproach trainingforemergencyandtraumacareclinicians.Thefull searchstrategyfromOvidMedlineisfurtherdetailedin Table1.Wedownloadedatotalof6,786resultsfromthe literaturesearchesintoEndNote,andduplicatearticleswere removed;2,280uniquepublicationswereuploaded intoRayyan(RayyanSystemsInc,Boston,MA; https://www.rayyan.ai/)forscreening(Figure2).
Alltheresultswerescreenedbythreeindependent reviewerstodetermineeligibilityforthisreview.The first phaseofscreeningwasablindedtitle/abstractreview conductedinRayyan,andpotentiallyrelevantarticleswere
movedtothesecondphaseofscreeningforthefulltextofthe publications.Conflictswereresolvedwithgroupdiscussion andconsensus.Finalanalysisincludedidentificationof specifictrainingprotocolsfromeachofthearticles.
AlthoughmanypapersreferenceTICtraining,we specificallysoughttrainingprotocolsthatweredescribedto thelevelthattheycouldbeduplicatedandthathadbeen evaluatedwithaminimaldegreeofrigor.Studieswere selectediftheymetthefollowingcriteria:thepopulation includedemergencyortraumaserviceclinicians(medical doctors,nurses,residents,nursepractitionersandphysician assistants);studydesigninvolvedTICtrainingforemergency ortraumacliniciansandincludedevaluationofthetraining, andthesettingwasaUSEDortraumahospital environment.OnlyarticleswritteninEnglishwereincluded. Weevaluatedtrainingprotocolsbasedonwho participated,modeandlengthoftraining,evaluation methods,results,andKirkpatricklevels(Table2).The KirkpatrickModel,developedin1959,remainsthemost commonmethodforevaluatingtheimpactoftraining programsandisprimarilyusedtoassessmedicaltraining.As awell-establishedtoolforevaluation,theKirkpatrickModel iswidelyconsideredtobeavalidandreliabletoolthatcanbe implementedwitheasetomeasuretheeffectivenessof trainingonaparticulartargetgoal.Themodelusesfour levelsoftrainingevaluation:Level1:Reaction how favorable,engaging,andrelevanttrainingistothe participants’ jobs;Level2:Learning didparticipants acquiretheintendedknowledge,skills,attitude,confidence, andcommitmentthroughparticipation;Level3:Behavior willparticipantsapplywhattheylearnedinpractice;and Level4:Results aretargetedoutcomes(changesinclinician behaviorsandimprovedpatientoutcomes)duetotraining.27
Afterreviewing2,280uniquearticles,weincluded16 articlesforfull-textreview.Ofthe16articles,onlytwowere includedinthe finalanalysis.Fourteenarticleswereexcluded fortargetingtheincorrectpopulation,23,28 havingatraining centerlocationoutsidetheUS,29,30 notdescribingtheTIC trainingcurriculum,31–39 orlackingevaluationofthe curriculum.40 Theincludedarticleshighlightdifferent trainingprotocols,oneaddressingthetreatmentofagitation andoneencouragingclinicianreferrals.6,7 Botharticlescover subjectmatterrelatedtopatient-centeredcommunication, usein-personlearningmethodologies,includingdidactic sessionsorroleplays,andaddressinterprofessional collaborationaspartofthetraining.6,7 Thesetwoarticles detailthedevelopmentofTICcurriculaforemergencyand traumacliniciansfromtheirdesigntotheirimpact,providing comprehensiveinsightthatwillbeabletoinformthe developmentoffuturetrainingprotocols.
Table1. OvidMEDLINEsearchstrategy(throughNovember24,2021).
1(traumainformedor(acesoradversechild*event*oradversechild*experience*)).mp.
2trauma.ti.ortrauma.ab.ortraumatiz*.mp.ortraumatis*.mp.orretraumatis*.mp.orretraumatiz*.mp.
3expstress,psychological/orpsychologicalstress*.mp.orstressfulevent*.mp.orstressfulexperience*.mp.orexplifechange events/orlifechang*event*.mp.
4expRESILIENCE,PSYCHOLOGICAL/orresilien*.mp.orcoping.mp.orcope.mp.orcoped.mp.
5expAdaptation,Psychological/or(psychological*adj5adapt*).mp.or(emotional*adj5adjust*).mp.orexpemotionaladjustment/ 6expStressDisorders,Post-Traumatic/orposttraumaticstressdisorder*.mp.orposttraumaticstressdisorder*.mp.orptsd.mp.or posttraumaticneuros*.mp.orposttraumaticneuros*.mp.or(moral*adj5injur*).mp. 7expsocialsupport/orsocialsupport*.mp.orsocialnetwork*.mp.
8expselfcare/orselfcare.mp.
9wellbeing.mp.orexp “QualityofLife”/orqol.mp.orqualityoflife.mp.orlifequality.mp.
102or3or4or5or6or7or8or9
11patientcentered*.mp.orexpPatient-CenteredCare/orpatientfocused*.mp.ormedicalhome*.mp.orclientcentered*.mp.
12exp “DeliveryofHealthCare,Integrated”/or(behavioraladj5healthadj5integrat*).mp.or(behaviouraladj5healthadj5integrat*). mp.or(integratedadj5care).mp.
1311or12
1410and13
151or14
16expeducation/orexpcurriculum/orexpeducation,professional/orexpeducation,medical/orcurricul*.mp.ored.fs. 17(educat*ortrain*ororientat*orlectur*orteach*orworkshop*orpre-postorimplement*orassessment*).mp. 18expsimulation/orsimulat*.mp.orscreen*.mp.
19expTEACHING/orexpTEACHINGMATERIALS/orexplectures/
20expEducation,Medical,Continuing/orcontinuingmedicaleducat*.mp.orcme.mp.
21expHealthPersonnel/edorinterprofessionaleducat*.mp.
22expprogramdevelopment/or(program*adj5develop*).mp.
23expqualityimprovement/or(qualityadj5improv*).mp.
24expEvaluationStudiesasTopic/or(researchadj5evaluat*).mp.or(program*adj5evaluat*).mp.
2516or17or18or19or20or21or22or23or24
26AdvancedTraumaLifeSupportCare/orexpemergencymedicine/oremergencynursing/orexpEmergencyService,Hospital/
27(emergencyoremergicenter*oremergencycenter*ortraumaservice*ortraumaunit*ortraumacenter*oradvance*trauma*).mp.
28(emergencydepartment*oremergencyhospitalservice*oremergencyoutpatientunit*oremergencyroom*oremergencyunit*or emergencyward*orhospitalemergencyservice*oremergencyservice*oremergencynurs*oremergencyphysician*or emergencymedicine).mp.
2926or27or28
3015and25and29
31limit30toEnglishlanguage
FivePointsofTrauma-InformedCare
OneoftheTICtrainingprotocols,entitledtheFivePoints ofTIC,wasimplementedforLevelItraumacenter clinicians.7 CliniciansandstafffromthedepartmentsofEM, pediatrics,surgery,andsocialwork,aswellasmedical studentsandnurses,amongothers,participatedintraining thatconsistedofa90-minuteworkshop,facilitatedbya pediatricianandformerpatients.Thismodeloutlined five pillarstoguidecliniciansandaidfamiliesaffectedbytrauma
orviolentinjury:safety;screening;understandingcontext; avoidingre-traumatization;anddischargeplanning. Additionally,thetrainingfocusedonpromotingapatient’ s senseofsafety,whichcanhelpimprovetheirhealingand establishtrustbetweenclinicianandpatient.7 Thisincludes factorssuchasprivacy,aconsistentanddependable clinician,andasoothingenvironment.
Withinthisworkshop,participantsdiscussedcorrelating clinicalcases,complextrauma,andahospital-basedviolence
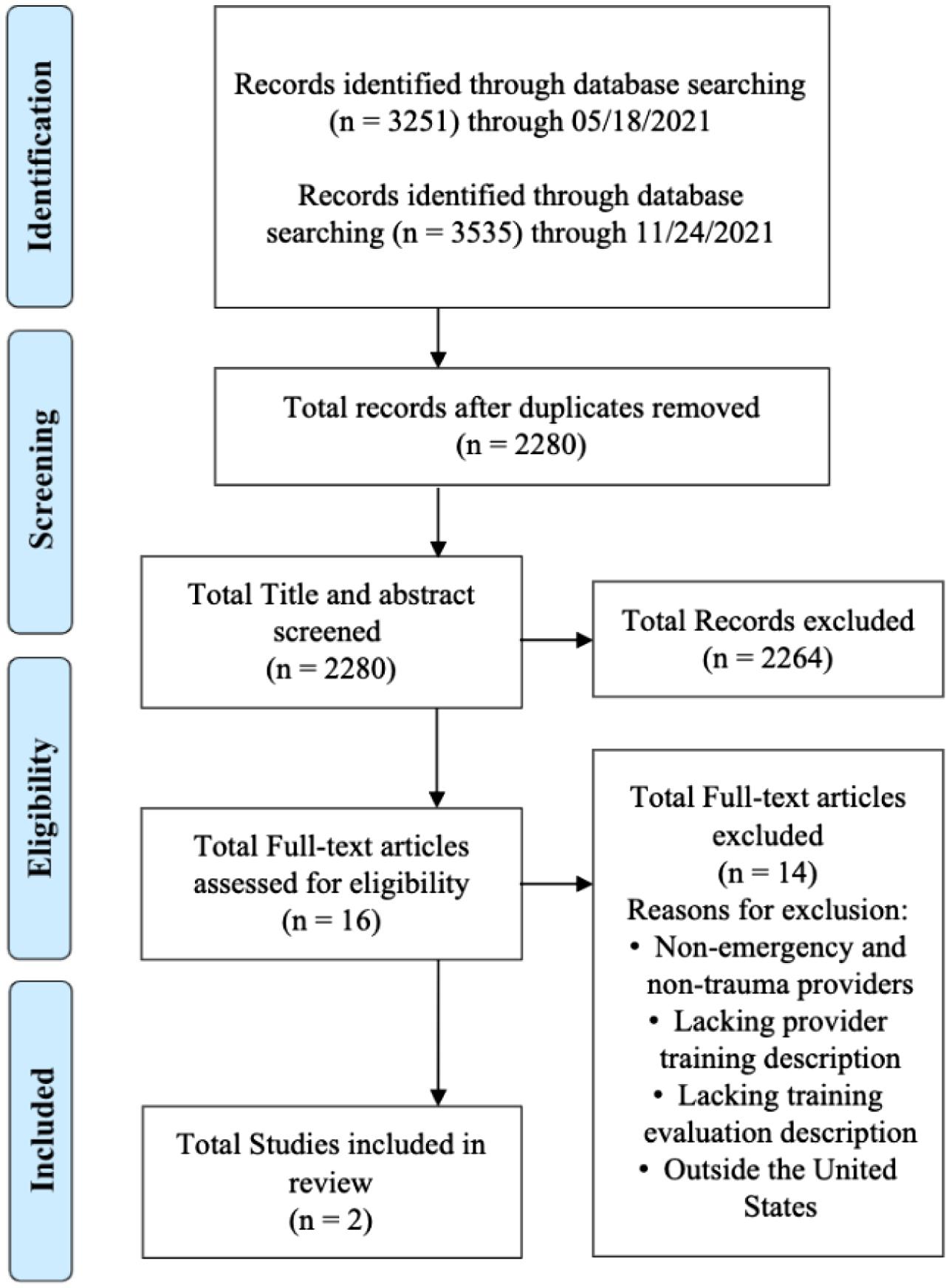
interventionprogram(VIP).TheVIPincludedtrauma interventionspecialistswhocouldprovidecrisisintervention, support,andpsychoeducationontrauma.Next,participants reviewedtheFivePointsofTICanddiscussedpatientcases. Followingthecases,theyheldapatientpanelandVIPpanel, wherepatientswereabletosharetheirexperienceswith trauma-sensitivecommunicationskillsandhealing.
TheKirkpatricklevelshighlightedforthisprotocolinclude Levels1and3.Participantscompletedpre-andpostworkshopsurveysassessingcomfortwiththeFivePointsof TIC.Resultsdemonstratedanincreaseincomfortlevelswith TIC(P < .001)forattendings,residents,fellows,andmedical students,withmedicalstudentshavingthehighestincreasein comfortlevels(Level1).Additionally,behavioralchangewas directlyassessed,withVIPreferralsfromphysicians significantlyincreasingfrom7.3%in2014to47.8%ofpatients referredin2018followingthecourse(P < .001)(Level3). Theseresultsdemonstratethatasaresultoftraining,therecan beanimprovementinTICcomfortandfamiliaritywithTIC approaches,leadingtosubstantivechangeinpractice.
AnotherTICtrainingprotocolwascompletedbynurses, andlaterallstaff,intheED.6 Participantscompleted
ManagementoftheAgitatedPatientintheEmergency Departmenttraining,partoftheBestPracticesinEvaluation andTreatmentofAgitation(BETA)project,whichfocuses onevidence-basedguidelinesandnon-pharmacological interventionstominimizeuseofrestraintsandseclusion whencaringforagitatedpatients.De-escalationtechniques, environmentalmodifications,andsensoryapproachesare thefoundationofthisapproach.
Thefour-hourtrainingconsistedofdidacticsimulations androleplay.Beyondstaffeducation,theprotocolalso calledforthedevelopmentofnewclinicalprocessesand ongoingmonitoringandfeedback.BasedontheKirkpatrick Modeloftrainingevaluation,learningassociatedwiththis protocolincludedLevels1,3,and4.Followingcompletion ofthetraining,resultsindicatedthatthenursesfoundit valuableandabletobeeasilyintegratedintotheirpractice (Level1).Participantsreportedimprovedconfidenceand satisfactionwithmanagingaggressivepatients(Level1). Therewasalsoasignificantreductioninrestraintuseinthe ED,demonstratingthatabehavioralchangeandimproved outcomescanoccurthroughprovidingstaffwithTIC knowledgeandtheskillstoaddressunderlyingcausesof patientbehaviors(Level3and4).
Thisreviewhighlightstheneedforcontinueddevelopment andevaluationofoutcomesofTICtrainingsforemergency andtraumaservicephysicians.Althoughonlytwocurricula wereidentifiedthatmettheinclusionandexclusioncriteria establishedforthisreview,severalstudieshighlightedthe importanceofTICtraining(Hawkins,Fisher).9,34 These studiesdonot,however,includespecificcurriculathatwere usedtotrainemergencyandtraumaservicephysicians.To promotetheliteratureonthistopicandaidinstitutions strivingtobringTICtotheirEMortraumaservices,itis importanttonotonlyidentifythetrainingcurriculaavailable foremergencyandtraumaserviceclinicians,buttoevaluate the effectiveness oftheTICtraining.
Priortodesigningandimplementingatrainingprotocol,a needsassessmentcanbeconductedtodeterminethespecific deficitswithinaninstitutionorpractice.21,41 Thisisastep thatwasnotindicatedinthecurrentincludedresultsandmay beanimportantpiecepriortocreatingacurriculum.6,7 To createthemostimpactfulcurriculum,theneedsofthe clinicians,patients,andcommunitiesmustbeunderstood. First,thisinvolvessurveyingclinicianattitudesandbeliefs aboutTIC,aswellasspecificknowledgeofwhatTIC encompassesanditsroleinbuildingtrustwithinthemedical system.8 Second,thisinvolvesaskingclinicianswhattheyfeel theymayneedinTICtrainingandtheoutcomestheyare hopingfor.
Theneedsasperceivedbyphysiciansonatraumaservice maydifferdramaticallyfromthoseasperceivedby outpatientprimarycarephysicians.21 Furthermore,aneeds
Table2. Summaryoftwoapproachestotrauma-informedcaretrainingforemergencyandtraumaphysicians.
Kirkpatrick Modellevel oflearning ColeR (2014) Twonewnursesand fourrecentgraduate nurses(pilotgroup) atanacute-care, LevelIItrauma center.Expandedto includeallEDstaff
SourcePopulation Training methodologyEvaluationResults
Four-hourpilot trainingcourse:read 2BETAProject articlesandcomplete homeworkbefore workshop;didactic sessionsand roleplay
• Post-test
• Classevaluation bypilotgroup
McNamara M,etal (2020)
318cliniciansand hospitalstaff membersattwo LevelIpediatric traumacenters
90-minuteworkshops from2015–2018plus patientexpertadvice andapanel discussion,followed byimplementationof “FivePointsofTIC” curriculum
• Pre-/post-workshop surveys
• Trackedreferralsto theViolence Intervention Program(VIP)from 2014–2018
1.Mostparticipantsfoundthe trainingvaluableandintegrable intotheirexistingpractice.
2.Initially,15–20episodesof restraintorseclusionpermonth decreasedto0episodes.
3.Overallbehavioralhealth seclusion/restrainthoursreduced from38.5h/mo.(August2011)to 0h/mo.(September2013)with overallshorterepisodeduration andimproveddocumentation compliance.
1.Increasedreferralsto VIPfromphysicians (P < 0.001;7.3%to47.8%).
2.Decreasedprobabilityofpatients beingidentifiedonlybyVIPstaff (P < 0.001;62.1%to23.4%).
3.Self-reportedcomfortwithTIC afterworkshopsimprovedby21% (P < 0.001).
ED,emergencydepartment; BETA,BestPracticesinEvaluationandTreatmentofAgitation; h/mo,hours/months; TIC,trauma-informedcare.
assessmentwouldpromoteunderstandingofanyTIC approachesthatarealreadybeingimplemented(whetheror nottheyareexplicitlyrecognizedasTIC)withintheEDor traumaservicesetting.Finally,thisneedsassessmentwould focusonaddressingconcernsoftheuniquepatient populationsthattheclinicianscarefor.EvenacrossEDsand traumaservices,theremaybemarkeddifferencesinpatient populationsandcommunityresourcesalreadyavailable, whichmayimpactwhatisemphasizedinahospital-based TICtraining.
Whendevelopingatrainingprotocol,outcomeshave indicatedthatevenmoderatetrainingimprovestheabilityof thehealthcareteamtoprovideTIC;however,moreintensive protocolsarecorrelatedwithimprovedresults.35 Protocols suchastheFivePillarsofTICandtheBETAProject,which usein-personworkshopswithcase-baseddiscussions,roleplay,andsimulationsversusdidacticsalone,showgreater clinicianproficiencyassociatedwithimprovedpatientreportedoutcomesandphysiciancomfortlevels.6,7,35
Althoughtheliteratureregardingtheoutcomesof implementingTICtrainingforemergencyandtrauma servicephysiciansislimited,researchonthedevelopmentof suchtrainingprogramssuggeststhattrainingand simulationsshouldencourageamultidisciplinaryapproach, mirroringtherealityoftheenvironment.41 Thismethodhelps bothtoidentifysystem-levelconditionsthatmightimpact
• Reaction – Level1
• Behavior – Level3
• Results – Level4
• Reaction – Level1
• Behavior – Level3
thedeliveryofTIC,suchasorganizationalissues,andto highlightanysocialdynamicsorauthorityhierarchiesthat coulddiscourageteammembersfromvoicingconcerns.
AsnotedintheincludedarticlesbyCole(2014)and McNamaraetal(2020),thesuccessofaTICprotocolcanbe evaluatedthroughpre-andpost-trainingsurveysor evaluationstogaugetheimpactofthecourseonhealthcare cliniciansandtheirpractice.6,7,35 Metricsthatincludereferral tooutsideresources,involvementofsocialworkers,and patientsatisfactioncanbeusedtotracksuccessful implementationofTICmethodsasillustratedthroughthe BETAProject.7 Thesecanbemonitoredbymonthlyor quarterlychartauditsandpatientsurveys.6 Additionally, long-termevaluationofbehavioralchanges,knowledgeand beliefs,andcomfortwithprovidingTICshouldbetrackedto monitortheimpactofthetrainingprogram.
Finally,futureresearchshouldemphasizethewaysin whichTICcanimprovehealthcarecosts,clinician satisfactionandwell-being,andlong-termhealthoutcomes forpatientsaffectedbytraumaticexperiences,including reducedre-traumatization,decreasedhealthcareutilization, improvedmentalandphysicalhealthoutcomes,and decreasedsubstanceuse.19 Existingevidencesuggeststhat recognizingtrauma’simpactonpatientbehaviorandhealth allowsclinicianstoavoidunnecessaryinterventions, decreasereadmissions,andimprovehealthoutcomes.5
Additionally,evaluatingTICpracticestoreduceclinician burnoutcouldlimitstaffturnoverandassociatedrecruitment andtrainingcosts.10,23,24 Thisdata,alongwithmorerobust datafromemergencyandtraumaservicesthathave implementedTICprotocols,iscriticalinultimately providingthemostconsiderateandappropriatecare forpatients.
Thisreviewislimitedinthatonlytwoarticleswerefound tomeetinclusioncriteria.Whiletherewasmoreavailable researchonTICtrainingevaluationswithinmentalhealth andprimarycaresettings,theuniquenatureofEDsand traumaserviceswarrantedstrictinclusioncriteria,which resultedinanarrowselectionofliterature.Inthesesettings, patientsarefacedwithunfamiliarphysiciansandfast-paced interactions,andthereisevidenceindicatingthatalarge proportionofpatientsinthesesettingsreportahistoryof traumaandoftenrelyonacutecareforallhealthcare needs.11,12,15,16 Anenvironmentemphasizingempathyand safetyisparamountinTIC,especiallyinthese departments.7,10 Theprimaryintentionofincluding evaluationsofTICtrainingonlyinUShealthcarefacilities wastoaccountfordifferencesinhealthcaresystemresources andinvestmentintrainingcomparedtoothercountries. ExcludedwerearticlesdiscussingthepotentialofcertainTIC trainingandpracticeswithoutevaluationofeffectiveness thatwouldinformfuturecurriculadevelopment.Withthe necessarycriteriathatwereestablishedforarobustreview, the finalresultsyieldedlimiteddatafordeterminingthemost optimalfeaturesofaTICtrainingprotocol.
Ourreviewdemonstratesaconsiderablepaucityinthe literatureregardingimplementedandevaluatedtraumainformedcarecurriculaforemergencyandtraumaservice clinicians.However,theexistingtrainingprotocols demonstratethat,withtargetedtraining,cliniciansbecome morecomfortablewithTICandcanintegrateaspectsofTIC intocurrentpractices.
AddressforCorrespondence:CeceliaMorra,BA,MedicalCollegeof Wisconsin,8701W.WatertownPlankRd.,Milwaukee,WI53226. Email: cmorra@mcw.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Morraetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons
Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.FelittiVJ,AndaRF,NordenbergD,etal.Relationshipofchildhood abuseandhouseholddysfunctiontomanyoftheleadingcausesof deathinadults.TheAdverseChildhoodExperiences(ACE)Study. AmJ PrevMed. 1998;14(4):245–58.
2.ChildAbuseandNeglectPreventionBoard.AdverseChildhood ExperiencesinWisconsin:2011–2015BehavioralRiskFactorSurvey Findings.2018.Availableat: https://preventionboard.wi.gov/ Documents/ACE-Brief_2018FINAL.pdf.AccessedFebruary23,2022.
3.BinnieV,LeBrocqueR,JessupM,etal.Adultfrequentpresentationto emergencydepartmentsandadversechildhoodexperiences:ascoping review. AustralasEmergCare. 2021;24(4):264–79.
4.GuestH.Aconceptanalysisoftrauma-informedcare. NursForum. 2021;56(4):1000–7.
5.CochranCB.Infusingtheprinciplesoftrauma-informedcareinto emergencynursing:acomprehensiveapproachtochangepractice. JForensicNurs. 2019;15(4):206–13.
6.ColeR.Reducingrestraintuseinatraumacenteremergencyroom. NursClinNorthAm. 2014;49(3):371–81.
7.McNamaraM,CaneR,HoffmanY,etal.Traininghospitalpersonnelin trauma-informedcare:assessinganinterprofessionalworkshopwith patientsasteachers. AcadPediatr. 2021;21(1):158–64.
8.HawkinsBE,CoupetEJr,Saint-HilaireS,etal.Trauma-informedacute careofpatientswithviolence-relatedinjury. JInterpersViolence. 2022;37(19–20):NP18376–93.
9.FischerKR,BakesKM,CorbinTJ,etal.Trauma-informedcarefor violentlyinjuredpatientsintheemergencydepartment. AnnEmergMed. 2019;73(2):193–202.
10.BodyR,KaideE,KendalS,etal.Notallsufferingispain: Sourcesofpatients’ sufferingintheemergencydepartmentcallfor improvementsincommunicationfrompractitioners. EmergMedJ. 2015;32(1):15–20.
11.OphuisRH,OlijBF,PolinderS,etal.Prevalenceofpost-traumatic stressdisorder,acutestressdisorderanddepressionfollowingviolence relatedinjurytreatedattheemergencydepartment:asystematicreview. BMCPsychiatry. 2018;18(1):311.
12.BonnerG,LoweT,RawcliffeD,etal.Traumaforall:apilotstudyofthe subjectiveexperienceofphysicalrestraintformentalhealthinpatients andstaffintheUK. JPsychiatrMentHealthNurs. 2002;9(4):465–73.
13.U.S.DepartmentofHealthandHumanServices,SubstanceAbuseand MentalHealthServicesAdministration.SAMHSA’sConceptofTrauma andGuidanceforaTrauma-InformedApproach.2014.Availableat: https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4884.pdf AccessedFebruary28,2022.
14.HargreavesMK,MoutonCP,LiuJ,etal.Adversechildhoodexperiences andhealthcareutilizationinalow-incomepopulation. JHealthCare PoorUnderserved. 2019;30(2):749–67.
15.KoballAM,RasmussenC,Olson-DorffD,etal.Therelationship betweenadversechildhoodexperiences,healthcareutilization,costof careandmedicalcomorbidities. ChildAbuseNegl. 2019;90:120–6.
16.RajaS,HasnainM,HoerschM,etal.Trauma-informedcareinmedicine: currentknowledgeandfutureresearchdirections. FamCommunity Health. 2015;38(3):216–26.
17.BruceMM,Kassam-AdamsN,RogersM,etal.Traumaproviders’ knowledge,views,andpracticeoftrauma-informedcare. JTrauma Nurs. 2018;25(2):131–8.
18.CorbinTJ,PurtleJ,RichLJ,etal.Theprevalenceoftraumaand childhoodadversityinanurban,hospital-basedviolenceintervention program. JHealthCarePoorUnderserved. 2013;24(3):1021–30.
19.CorbinTJ,RichJA,BloomSL,etal.Developingatrauma-informed, emergencydepartment-basedinterventionforvictimsofurbanviolence. JTraumaDissociation. 2011;12(5):510–25.
20.CunradiCB,CaetanoR,AlterHJ,etal.Adversechildhoodexperiences areassociatedwithat-riskdrinking,cannabisandillicitdrugusein femalesbutnotmales:anemergencydepartmentstudy. AmJDrug AlcoholAbuse. 2020;46(6):739–48.
21.GundackerC,BarryC,LaurentE,etal.Ascopingreviewoftraumainformedcurriculaforprimarycareproviders. FamMed. 2021;53(10):843–56.
22.MeléndezGuevaraAM,LindstromJohnsonS,ElamK,etal.Culturally responsivetrauma-informedservices:amultilevelperspectivefrom practitionersservingLatinxchildrenandfamilies. CommunityMent HealthJ. 2021;57(2):325–39.
23.WeissD,Kassam-AdamsN,MurrayC,etal.Applicationofaframework toimplementtrauma-informedcarethroughoutapediatrichealthcare network. JContinEducHealthProf. 2017;37(1):55–60.
24.RobinsPM,MeltzerL,ZelikovskyN.Theexperienceofsecondary traumaticstressuponcareprovidersworkingwithinachildren’s hospital. JPediatrNurs. 2009;24(4):270–9.
25.TriccoAC,LillieE,ZarinW,etal.PRISMAextensionforscopingreviews (PRISMA-ScR):checklistandexplanation. AnnInternMed. 2018;169(7):467–73.
26.McGowanJ,SampsonM,SalzwedelDM,etal.PRESSpeerreviewof electronicsearchstrategies:2015guidelinestatement. JClinEpidemiol. 2016;75:40–6.
27.AlsalamahAandCallinanC.TheKirkpatrickModelfortraining evaluation:bibliometricanalysisafter60years(1959–2020). Industrial andCommercialTraining. 2021;54(1):36–63.
28.NandiM,PuranamS,Paccione-DyszlewskiM,etal.Makinguniversal trauma-informedhealthcareareality:apilotinitiativetotrainfuture
providers. TheBrownUniversityChildandAdolescentBehaviorLetter. 2018;34(12):1–6.
29.DearieV,CharlestonR,HallA,etal.Evaluationofemergency departmentstafftrainingtousetrauma-informedcareformentalhealth consumers. IntJMentHealthNurs. 2015;24(0):14–5.
30.HallA,McKennaB,DearieV,etalT.Educatingemergencydepartment nursesabouttraumainformedcareforpeoplepresentingwithmental healthcrisis:apilotstudy. BMCNurs. 2016;15:21.
31.AgboolaIK,CoupetEJr,WongAH. “Thecoatsthatwecantakeoffand theoneswecan’t”:theroleoftrauma-informedcareonraceandbias duringagitationintheemergencydepartment. AnnEmergMed. 2021;77(5):493–8.
32.GargA,PandaP,MalayS,etal.Ahumantraffickingeducational programandpoint-of-carereferencetoolforpediatricresidents. MedEdPORTAL. 2021;17:11179.
33.GoldstonDBandAsarnowJR.Qualityimprovementforacutetraumainformedsuicidepreventioncare:introductiontospecialissue. Evid BasedPractChildAdolescMentHealth,2021;6(3):303–6.
34.HawkinsBE,CoupetEJr,Saint-HilaireS,etal.Trauma-informedacute careofpatientswithviolence-relatedinjury. JInterpersViolence. 2022;37(19-20):NP18376–93.
35.DarnellD,ParkerL,EngstromA,etal.EvaluationofaLevelItrauma centerprovidertraininginpatient-centeredalcoholbriefinterventions usingtheBehaviorChangeCounselingIndexratedbystandardized patients. TraumaSurgAcuteCareOpen. 2019;4(1):e000370.
36.Traumacaresystemsdevelopment,evaluation,andfunding.American CollegeofEmergencyPhysicians. AnnEmergMed. 1999;34(2):308.
37.AlpertEJ.Ajustoutcome,or ‘just’ anoutcome?Towardstraumainformedandsurvivor-focusedemergencyresponsestosexualassault. EmergMedJ. 2018;35(12):753–4.
38.IrvinN.Commentary:Usingatrauma-informedcareframeworkto addresstheupstreamanddownstreamcorrelatesofyouthviolence. AnnEmergMed. 2019;74(5S):S55–8.
39.DennisBM,NolanTL,BrownCE,etal.Usingachecklisttoimprove familycommunicationintraumacare. AmSurg. 2016;82(1):59–64.
40.AuerbachM,ButlerL,MyersSR,etal.Implementingfamilypresence duringpediatricresuscitationsintheemergencydepartment:familycenteredcareandtrauma-informedcarebestpractices. JEmergNurs. 2021;47(5):689–92.
41.ArmeniaS,ThangamathesvaranL,CaineAD,etal.Theroleofhighfidelityteam-basedsimulationinacutecaresettings:asystematic review. SurgJ(NY). 2018;4(3):e136–51.
SectionEditor:PatrickMeloy,MD
*UniversityofPittsburgh † ChathamUniversity ‡ UniversityofPittsburghMedicalCenter
Submissionhistory:SubmittedJuly18,2023;RevisionreceivedJanuary10,2024;AcceptedJanuary19,2024
ElectronicallypublishedMay3,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18396
Introduction: Ectopicpregnanciesareasignificantcauseofmorbidityandmortalityinthe firsttrimester ofpregnancy.Hospitalprotocolsrequiringaspecificbeta-humanchorionicgonadotropin(β-hCG)levelto qualifyfordiagnostictesting(pelvicultrasound)candelaydiagnosisandtreatment.Inthisstudywe soughttodeterminetherelationshipbetween β-hCGlevelandthesizeofectopicpregnancywith associatedoutcomes.
Methods: Weperformedaretrospectivecasereviewofpatientsdiagnosedwithectopicpregnancyinan urban,academicemergencydepartmentspecializinginobstetricalcare,fromJanuary1, 2015–December31,2017.Variablesextractedincludedpresentation,treatment,adverseoutcomes, andratesofrupture.
Results: Weidentified519uniqueectopicpregnancies.Ofthoseectopicpregnancies,22.9%presented withevidenceofruptureonultrasound,and14.4%showedevidenceofhemodynamicinstability(pulse >100beatsperminute;systolicbloodpressure <90millimetersofmercury;orevidenceofsignificant bloodloss)onpresentation.Medicalmanagementoutcomeswereasfollows:of177patientswho receivedsingle-dosemethotrexate,14.7%failedmedicalmanagementandrequiredsurgical intervention;of46whoreceivedmulti-dosemethotrexate,36.9%failedmedicalmanagementand requiredsurgicalintervention.Ultimately,55.7%ofpatientsrequiredoperativemanagementoftheir ectopicpregnancy.Mean β-hCGlevelatinitialpresentationwas7,096milli-internationalunitsper milliliter(mIU/mL)(SD88,872mIU/mL)withamedianof1,289mIU/mL;50.4%ofectopicpregnancies presentedwith β-hCGlevelslessthanthestandarddiscriminatoryzoneof1,500mIU/mL.Additionally, 44%ofthepatientswhopresentedwithevidenceofrupturehad β-hCGlevelslessthan1,500mIU/mL. Comparisonofsizeofectopicpregnancy(basedonmaximumdimensioninmillimeters)to β-hCGlevels revealedaveryweakcorrelation(r = 0.144, P < .001),anddetectionofectopicpregnanciesby ultrasoundwasindependentof β-hCGlevels.
Conclusion: Levelsof β-hCGdonotcorrelatewiththepresenceorsizeofanectopicpregnancy, indicatingneedfordiagnosticimagingregardlessof β-hCGlevelinpatientswithclinicalsuspicionfor ectopicpregnancy.Almostone-sixthofpatientspresentedwithevidenceofhemodynamicinstability, andapproximatelyonequarterofpatientspresentedwithevidenceofrupturerequiringemergent operativemanagement.Ultimately,morethanhalfofpatientsrequiredanoperativeprocedureto definitivelymanagetheirectopicpregnancy.[WestJEmergMed.2024;25(3)431–435.]
Ectopicpregnanciesarenotarareoccurrence,affecting approximately2%ofallpregnancies.1–3 Thereisno centralizedsystemtomonitorratesofectopicpregnancy; thus,thetrueincidenceislikelyhigherthanthisestimate.2 Ectopicpregnancyisaleadingcauseofmorbidityand mortalityinthe firsttrimesterofpregnancy.Medical managementrequiresmorefromapatientintermsoffollowup(multipleblooddraws,ultrasounds,andappointments) whencomparedtosurgicalmanagement;between12–24%of patientswillfailmedicalmanagementandultimatelyrequire surgicalmanagement.4
Theclassicpresentationofanectopicpregnancyis unilateralpelvicpainwithvaginalbleedinginthepresenceof apositivepregnancytest.Riskfactors(presentin50%of thosewithectopicpregnancy)includepriorectopic pregnancy;historyofpelvicinflammatorydiseaseorpelvic surgery;assistedreproductivetechnologyforconception;age >35years;tobaccouse;intrauterinediethylstilbestrol exposure;andpresenceofanintrauterinedeviceatthetime ofconception.1,2 About96%ofectopicpregnancieswill occurwithintheadnexa;rarerlocationsincludethecervix, cesareansectionscars,ovaries,andabdominalcavity.1,3,5
Diagnosticworkupforsuspectedectopicpregnancy includesbloodworktocheckforbeta-humanchorionic gonadotropin(β-hCG)levels,Rhtype,hemoglobinlevel,and transvaginalultrasoundtovisualizelocationofthepregnancy (intra-vsextrauterine).Thepublisheddiscriminatoryzonefor β-hCGlevels(1,500–4,000milli-internationalunitsper milliliter[mIU/mL])canbeusedtoaidforcorrelationto expectedultrasound findings.Patientswitha β-hCG >3,500 mIU/mLshouldhave findingsonultrasoundthatdemonstrate thelocationofthepregnancy(intrauterine[gestationalsac plusyolksacwithintheendometrialcavity]vsectopic[lackof intrauterinepregnancywithanextrauterinemasswith sonographiccharacteristicsconsistentwithectopic pregnancy]).1 Whilethediscriminatoryzoneishelpfulto determinewhenanintrauterinegestationshouldbeseenon ultrasound,signsofanectopicpregnancymaybevisibleat significantlylower β-hCGlevels.6 Inthisstudywesoughtto determinewhether β-hCGlevelscorrelatewiththesizeofan ectopicpregnancyaswellastherateoftreatmentfailureof ectopicpregnancy.
Weperformedaretrospectivecasereviewofpatientsseen inanurban,academicEDhousedinatertiary-carefacility specializinginobstetricalcare.Casesoccurredbetween January1,2015–December31,2017,forpatientswhowere diagnosedwithanectopicpregnancy.Thisstudywas approvedbytheinstitutionalreviewboard;participant consentwasnotrequired.Thecriterionforinclusionwasa diagnosedectopicpregnancyinthechartand/oron ultrasound,identifiedbysearchingbillingcodesfor “Ectopic
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Beta-humanchorionicgonadotropin ( β -hCG)levelsandthediscriminatory zonecutoffsareusedtodetermine ultrasound-orderingalgorithmsat manyhospitals.
Whatwastheresearchquestion?
Do β -hCGlevelscorrelatewithsize ofanectopicpregnancyand/orrateof treatmentfailure?
Whatwasthemajor findingofthestudy?
50.4%ofectopicpregnancies,and44%who hadrupture,had β -hCGlevelslessthan1,500 mIU/mL.Theectopicpregnancy β -hCGlevels onlyveryweaklycorrelated(r = 0.144, P < .001)withectopicsize.
Howdoesthisimprovepopulationhealth?
β -hCGlevelsshouldnotbeafactorinordering transvaginalultrasoundinapatientwith suspectedectopicpregnancy.
Pregnancy,”“EctopicPregnancy,Other,”“Abdominal Pregnancy,”“TubalPregnancy,”“EctopicPregnancy, Nonspecific, ” and “OvarianPregnancy.” Thissearchyielded 1,265visitsduringtheresearchperiodwith519uniquecases ofectopicpregnancy(whereeachcasecouldhavemultiple associatedvisits).Patientsofallageswereincludedinthe studyiftheymettheinclusioncriterion.Exclusioncriteria waslossofpatienttofollow-upafterinitialpresentation(thus makingitimpossibletoconfirm finaldiagnosisofectopic pregnancyand/oroutcomesrelatedtotreatment)orifthe patientwasultimatelyfoundtohaveadiagnosisotherthan ectopicpregnancy(ie,intrauterinepregnancy).Forthe519 casesofectopicpregnancy,dataextractedfromeachchart includedthefollowingvariables:presentation(including initial β-hCGlevelsandultrasound findings[sizeofectopic pregnancy,evidenceofrupture,and/orfetalheartbeat]); treatment(expectant,medical,and/orsurgical);and treatmentoutcomes(successful,failure,orrupture).Data wasextractedbytwoindividuals;theprincipalinvestigator (xx)reviewedtheextracteddataevery fivecasestoensure consistencyofdataextraction.Wecompareddatausing standardmeans,thePearsoncorrelationcoefficient,and Student t -testingusingExcel(MicrosoftCorp,Redmond, WA).Forchartswheredatawasincomplete(forexample, missingultrasoundevidenceofectopicpregnancy),we
includedthechartintheanalyseswheredatacouldbe extractedandweexcludeddatafromtheanalyseswhereit wasmissing.
Thedatasetcontained519uniqueectopicpregnancies presentingtotheEDduringathree-yearperiod(Table).The averageageofthesubjectsatpresentationwas29.39years withnearequalracialdistributionbetweenself-reported BlackandWhite.Evidenceofectopicrupturewaspresentin 22.9%ofcasesonpresentation,and14.4%hadevidenceof hemodynamicinstability.Aheartbeatwasdetected9.1%of thetime,whichpercurrentAmericanCollegeof ObstetriciansandGynecologists(ACOG)recommendation
Table. Ageofpatientinyears,reportedrace,rateofectopicrupture atpresentation,unstableatpresentation(heartrate >100bpm, systolicbloodpressure <90mmHg,ordocumentationofinstability), rateofmethotrexatefailureaftertreatment,rateofliveectopicat presentation, β-hCGlevelsforvisualizedectopic, β-hCGlevelsfor rupturedvsnon-rupturedectopic,andgreatestdiameterof visualizedectopic.
VariableassessedFindings
Age(Years)29.39(SD4.42)
Race(Mayincludemorethanone)
Rupturedatpresentation22.9%
Unstableatpresentation14.4%
Methotrexatefailurerate
Liveectopicatpresentation9.1%
β-hCGlevels(mIU/mL)
Ruptured7,005(SD8,949)
Non-ruptured7,609(SD8,773)
T-test P = 0.51
β-hCGforvisualizedectopicpregnancy(mIU/mL;n = 456)
Mean4,964(SD12,217)
Median1,209
Greatestdiameterofvisualizedectopicpregnancy (mm;n = 456)
Mean24(SD14.3)
Median21
β-hCG,beta-humanchorionicgonadotropin; mlU/ML,milliinternationalunitspermilliliter; mm,millimeter.
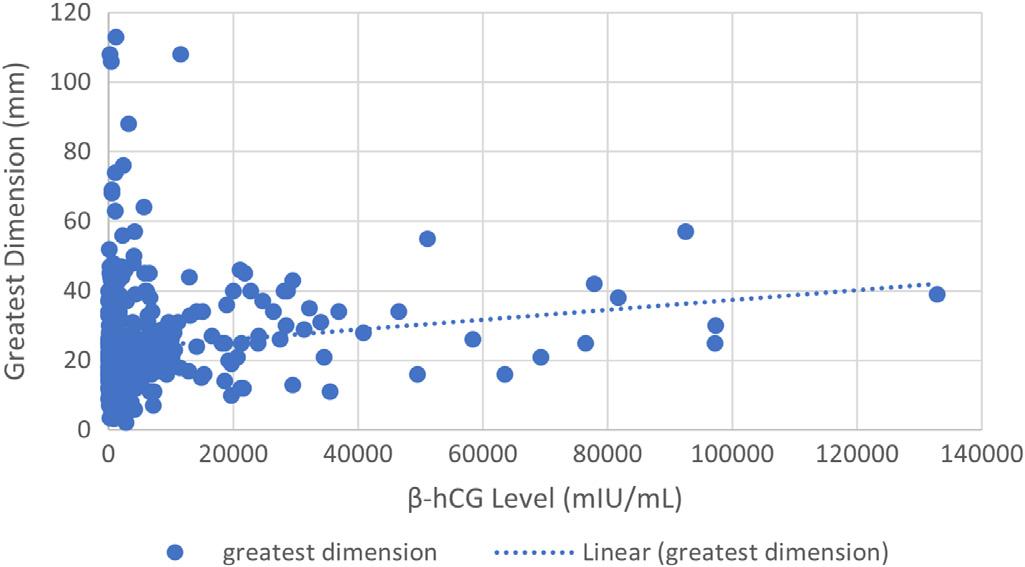
Figure. β-hCGlevelinrelationtothegreatestdimensionofectopic pregnancy(n = 456).Pearsoncorrelationbetween β-hCGleveland greatestdimensionwasr = 0.144(P < .001),demonstratingavery weakcorrelation.
β-hCG,beta-humanchorionicgonadotropin; mm,millimeters; mIU/mL, milli-internationalunitspermilliliter.
isarelativecontraindicationfortreatmentwith methotrexate.1 Subjectsreceivingsingle-dosemethotrexate treatmenthadafailurerateof14.7%.Subjectswhoreceived multi-dosemethotrexate(generallybecausetheydidnot meetACOGrequirementsforsingle-dosemethotrexate treatment)hadafailurerateof36.9%.The β-hCGlevels forbothrupturedandnon-rupturedectopicpregnancies weresimilar.
Greatestdimensionofectopicpregnancy(diameterin millimeters[mm])wascorrelatedwith β-hCGlevel(milliinternationalunitspermilliliter[mIU/mL])foreachpatient (Figure).Weexcludedfromthisanalysispatientswhodidnot haveanextrauterinemassvisualizedonultrasoundas dimensionsofectopicsizewereunknown.Mean β-hCGfor thisgroupof456subjectswas4,964mIU/mL(SD12,217; 95%confidenceinterval[CI]3,793–6.135),andmedian β-hCGwas1,209mIU/mL;meangreatestdiameterwas 24mm(SD14.3;95%CI22.69–25.31)andmedianwas 21mm.ThePearsoncorrelationcoefficient(r-value)ofthis groupwasr = 0.144(P < .001),indicatingaveryweak correlationbetween β-hCGlevelandgreatestdimensionof ectopicpregnancy.WealsocalculatedthePearson correlationfor β-hCGcomparedtoectopicvolume(inmm3); theresultswerenotstatisticallysignificant.
Nearly25%ofpatientswithanectopicpregnancyinthis studypresentedwithevidenceofrupture,andabout15%of patientspresentedwithevidenceofhemodynamicinstability, bothscenariosrequiringemergentsurgicaltreatment.The ectopicrupturerateseeninthisstudywasgreaterthanprior reportedratesof15%,although,interestingly,lessthan10% ofrupturedectopicpregnanciesinthestudyrequiredablood transfusion(datanotshown),whichissimilartoprevious publisheddataof8.7%.7,8
Themajorityofvisualizedectopicpregnanciesinthe currentstudyhad β-hCGlevelsbelowthetraditional1,500 mIU/mLdiscriminatoryzone,withthelowest β-hCGlevelin thestudybeing9mIU/mL(whichhadsonographicevidence ofanectopicpregnancy).The β-hCGlevelsweresimilar betweenrupturedandnon-rupturedectopicpregnancies. Priorstudieshavealsodemonstratedlow β-hCGlevelsin ectopicpregnancies,withlevelsaslowas <10mIU/mL documented.9 Whileectopicpregnanciestypicallyhave lower β-hCGlevelscomparedtointrauterinepregnancies, thepresenceofverylow β-hCGlevelsindocumentedectopic pregnancycasesisstriking.9 Onestudyfoundthat41%of ectopicpregnancieshada β-hCGlevel <2,000mIU/mLat thetimeofdiagnosis,andapproximately9%(18of204cases) hada β-hCGlevelunder100mIU/mL.9 These findings combinedwithourresults(50.4%ofcaseshada β-hCG <1,500mIU/mL,and8.5%hadalevel <100mIU/mL) emphasizetheneedtoconsiderandworkupsuspected ectopicpregnanciesfullyatthetimeofpresentation, regardlessofserum β-hCGlevel,toavoidmissingthe diagnosisofectopicpregnancy.Thus,discriminatorycutoffs of β-hCGlevelsshouldnotbeadeterminingfactorwhen orderingtransvaginalultrasonographytoevaluatefor ectopicpregnancy.10
Wefoundaveryweakcorrelationbetween β-hCGandsize ofectopicpregnancy,whenlookingatgreatestdimension, andnocorrelationof β-hCGtovolumeofectopicpregnancy. These findingsareinstarkcontrasttopriorstudies,where β-hCGlevelsandectopicpregnancyvolumewerefoundtobe stronglycorrelated.9 Therefore,thisstudyindicatesthat β-hCGlevelsmayhavelesspredictivevalueforestimating thesizeorvolumeofanectopicpregnancythanpreviously thought,furtherstrengtheningtheneedfortransvaginal ultrasoundattainmentregardlessof β-hCGlevel.
Post-methotrexatefailureorruptureisnotuncommon; about20%ofpatientsinthecurrentstudyultimately requiredsurgicalmanagement(higherthanthe10.2% reportedinpreviousstudies).11 Thisincreasedrateofpostmethotrexatefailuremightberelatedtostudylocation (tertiary-carecenterforobstetricalcare),patientdelayin seekingcare,orhigherrateofcasesnecessitatingmultipledosemethotrexatetreatment(duetotreatmentatatertiarycarecenter),althoughanyconclusionregardingthese variablesisdifficult.Patientsreceivingmethotrexatefor ectopicpregnancywithcomplaintsofneworworsening abdominalpainorincreasedvaginalbleedingshouldbe evaluatedforpotentialectopicpregnancyrupture.
Thestudytookplaceatasingle-siteacademiccenter, wherethepopulationoftheEDcouldhavebeenskeweddue tolocation(urban),referralcenterstatus(tertiarycarefor obstetricalcare),andhigheracuitylevelofcarecomparedto manyhospitals.Inaddition,patientencounterstookplace
between2015–2017usingACOGguidelinespublishedin 2008;however,currentACOGguidelines(releasedin2018) aresimilartothoseusedduringthetimeframeofpatientcare; thus,anypotentialeffectonthedatawasnegligible.1,12
Inthesettingofapositivepregnancytest,pelvicpainand/ orvaginalbleedingshouldpromptacompleteworkupfor ectopicpregnancytoincludeRhstatus,hemoglobin, β-hCG level,andtransvaginalpelvicultrasound(regardlessof β-hCGlevel).Cliniciansmustconsidertheongoingriskof ectopicpregnancyruptureaftermethotrexatetreatment. Finally,patientsmaybelosttofollow-upandhavean untreatedectopicpregnancy,whichcanleadtosignificant morbidityand/ormortality.
AddressforCorrespondence:NicoleE.Brown,MSChatham University,ChathamEastside166,WoodlandRoad,Pittsburgh, PA15232.Email: nbrown1@chatham.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Eisamanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AmericanCollegeofObstetriciansandGynecologists.ACOG PracticeBulletin:TubalEctopicPregnancy. ObstetGynecol. 2018;131(3):e91–103.
2.MannLM,KreiselK,LlataE,etal.Trendsinectopicpregnancy diagnosesinUnitedStatesemergencydepartments,2006–2013. MaternChildHealthJ. 2020;24(2):213–21.
3.NaveedAK,AnjumMU,HassanA,etal.Methotrexateversusexpectant managementinectopicpregnancy:ameta-analysis. ArchGynecol Obstet. 2022;305(3):547–53.
4.AiobA,YousefH,AbuShqaraR,etal.Riskfactorsandpredictionof ectopicpregnancyrupturefollowingmethotrexatetreatment:a retrospectivecohortstudy. EurJObstetGynecolReprodBiol. 2023;285:181–5.
5.EbnerF,VargaD,SorgF,etal.Treatmentcostevaluationof extrauterinegravidity:aliteraturereviewofmedicalandsurgical treatmentcosts. ArchGynecolObstet. 2015;291(3):493–8.
6.Sobecki-RauschJ,MadrigalJM,CavensA,etal.Evaluationof adherenceratesfollowingectopicpregnancytoinformmanagement decisionsinapublichospitalsystem. JGynecolObstetHumReprod. 2021;50(9):102180.
7.CulliferRM,HuynhTQ,PacisMM,etal.Riskfactorsforblood transfusioninwomenrequiringsurgicalmanagementofectopic pregnancy. JMinInvasiveGynecol. 2020;27(7):S134.
8.MullanyK,MinneciM,MonjazebR,etal.Overviewofectopicpregnancy diagnosis,management,andinnovation. JWomen’sHealth(Lond). 2023;19:17455057231160349.
9.SaeedUandMuzharN.CorrelatingserumbetahCGlevelswith transvaginalsonographicfeaturesofectopicpregnancy. JRawalpindi MedColl. 2017;21(1):64–7.
10.HirschlerLEandSotiV.Theutilityofmonitoringbeta-human chorionicgonadotropinlevelsinanectopicpregnancy. Cureus. 2023;15(1):e34063.
11.SendyF,AlShehriE,AlAjmiA,etal.Failurerateofsingledose methotrexateinmanagementofectopicpregnancy. ObstetGynecolInt. 2015;2015:902426.
12.AmericanCollegeofObstetriciansandGynecologists.ACOG PracticeBulletin:TubalEctopicPregnancy. ObstetGynecol. 2008;131(3):613–5.
CarlPreiksaitis,MD*
MonicaSaxena,MD,JD*
JiaqiZhang,MS†
AndreaHenkel,MD,MS†
SectionEditor:StephenMeldon,MD
*StanfordUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Stanford,California † StanfordUniversitySchoolofMedicine,DepartmentofObstetricsandGynecology, Stanford,California
Submissionhistory:SubmittedMarch18,2023;RevisionreceivedOctober5,2023;AcceptedJanuary9,2024
ElectronicallypublishedApril2,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.60461
Introduction: Thenumberandcharacteristicsofpregnantpatientspresentingtotheemergency department(ED)hasnotbeenwelldescribed.Ourobjectiveinthisstudywastodeterminethe prevalenceandcharacteristicsofpregnantpatientspresentingtoEDsintheUSbetween2010–2020.
Methods: Wecompletedaretrospective,cross-sectionalstudyofpatientencountersathospital-based EDsintheUSfrom2010–2020.UsingtheEDsubsampleoftheNationalHospitalAmbulatoryMedical CareSurvey(NHAMCS)weidentifiedEDvisitsforfemalepatientsaged15–44years.Wedefineda subsampleoftheseasvisitsforpregnantpatientsusingdischargediagnosiscodesspecificto pregnancy.Wecomparedthispopulationofpregnantpatientvisitstothosefornon-pregnantpatients andcomputedpointestimatesfornationallyweightedvalues.Multivariablelinearregressionwasusedto determinefactorsindependentlyassociatedwithpregnantpatientvisits.
Results: The2010–2020NHAMCSdatasetincluded255,963EDvisits.Ofthesevisits59,080werefor femalepatients15–44yearsold,and6,068ofthosevisitswereforpregnantpatients.Pregnantpatients accountedfor3%(95%confidenceinterval[CI]2.7–3.2)ofallEDvisitsand8.6%(95%CI8–9.3)ofall visitsamongfemalepatients15–44years.Weightingtoanationalsample,thisequatesto2.77million pregnantpatientspresentingforEDvisitsannually.PregnantpatientsweremorelikelytobeBlack, Hispanic,ortousepublicinsurance.
Conclusion: PregnantpatientsmakeupasignificantnumberofEDvisitsannuallyandaremorelikelyto bepeopleofcolororpubliclyinsured.Interventionstoaddresstheeffectsofchangingabortionlegislation onemergencymedicinepracticemaybenefitfromconsiderationthatcertainpopulationsofpregnant peoplearemorelikelytopresenttotheEDforcare.[WestJEmergMed.2024;25(3)436–443.]
Background
InJune2022,theUSSupremeCourtruledon Dobbsv JacksonWomen ’ sHealthOrganization anddeterminedthat thereisnoconstitutionalrighttoabortion,allowing individualstatestolegislateabortionrestrictions.1 This decisionhasmultipleanticipatedimplicationsforemergency clinicians,includinganincreaseinpregnantpatients
presentingtotheemergencydepartment(ED)asaresultof barrierstocare,complicationsofself-managedabortions,or delayedpresentationofemergentdiagnosisduetofearof legalrepercussions.2
UseoftheEDishighamongpregnantpatients,with studiesshowingthatapproximately35%ofthesepatients
willvisittheEDatleastonceduringtheirpregnancy.3,4 Thesepatientsaremorelikelytobeofracialandethnic minorities,publiclyinsured,andhavebarrierstoprenatal careaccess.3,5,6 Lessisknown,however,aboutthetotal populationofpregnantpatientswhopresenttotheED.A secondaryanalysisofthe2006–2016NationalHospital AmbulatoryMedicalCareSurvey(NHAMCS)identified thattherewereapproximately900,000visitstotheEDfor earlypregnancyloss,butthetotalpopulationofpregnant patientswasnotdescribed.5
Oldercohortstudiesdisagreeonthepregnancyrate amongreproductive-capablefemalepatients,reporting valuesrangingfrom2.3–33%.7–9 Thesestudiesreportthat manypregnanciesare firstidentifiedintheED,buttherateof incidentalpregnancyinmorerecentyearsandhowoften thesepatientsareprovidedwithcounselinghasnotbeen described.10 Infact,beforetherepealof RoevWade there wasanidentifiedneedforfurtheremergencyphysician traininginpatient-centeredreproductivehealthcare.5,10 Withincreasedlegalrestrictions,theneedforemergency medicinepolicyandphysicianeducationhasneverbeen greater.2,11 Todothissuccessfully,wemusthaveabetter understandingofthepopulationthatwillbeaffectedbythese changes:pregnantpeople.Thishasnotbeenrecently reportedintheliterature,whichledustoundertake thisstudy.
GoalsofthisInvestigation
Theprimaryobjectiveofourstudywastoidentifythe prevalenceofandcharacterizepregnantpatientspresenting toUSEDsbetween2010–2020.
StudyDesignandDataSource
Wecompletedaretrospective,cross-sectionalstudyof patientencountersathospital-basedEDsintheUSfrom 2010–2020.Thisperiodwasselectedas2010sawthepassage oftheAffordableCareAct,whichhadmanyeffectsfor expandinghealthcareandcontraceptivecoveragefor women. 12 DatawasfromthepubliclyavailableED subsampleoftheNHAMCS.13 TheNHAMCSisasurvey conductedannuallybytheNationalCenterforHealth Statistics(NCHS),apartoftheUSCentersforDisease ControlandPrevention(CDC).14
TheNHAMCSusesathree-stageprobabilitysampling designinanefforttoprovidearepresentativesampleofall EDsinthecountry.14 First,112geographicprobability samplingunits,determinedbyvariouscounties,towns,and citiesarechosen.Theseareselectedtoberepresentativeof differentgeographicalregionsandurbanandruralareas. Withinthesesamplingunits,450–500short-stayhospitals (averagelengthofstayfewerthan30days)aresampledto ensureadiversityofhospitalsizeandtype.Finally,EDsthat provideunscheduledcare24hoursaday/7daysaweekat
thesesampledhospitalsareselectedforinclusion.Each includedEDhasvisitdatarecordedoverarandomly assigned4-weekperiod.Duringthisperiod,datafrom selectedvisitsisabstractedfromthechartandenteredintoan electronicformbytrainedcensustakers.
FurtherdescriptionoftheNHAMCSsurveyisavailable ontheNCHSwebsite.14 TheNHAMCSproducesadataset thatreflectsabroadspectrumofEDvisits.Usingthesurvey’ s samplingdesign,eachdataentryisassignedaweightto accountfortherelativecontributionofthatentrytothe largersample.Asaresult,eachdatapointinthedataset representsavaryingnumberofactualvisits,dependingonits assignedweight.
Todetermineourstudypopulation,weidentifiedthetotal EDvisitsforNHAMCSbetween2010–2020forallpatients. Visitswereselectedforwomenofreproductiveage,defined bytheCDCasbeingbetweenages15–44years.15 We acknowledgethatresearchsurroundingpregnancyoften assumescisgenderidentities,whichmaynotdescribepeople whoaretransgenderornon-binary.Weattemptedtouse languagethatisasinclusive;however,thedataanalyzedin thisstudyusesgenderlabelsthatcannotbechangedwhile remainingaccuratetothesourcematerial.
Wedefinedvisitsforpregnantpatientswithinourcohort asthosevisitsthathadanInternationalClassificationof DiseasesRevisions9or10(ICD-9and-10)diagnosiscode specifictopregnancyasoneofthedischargediagnoses(eg, ectopicpregnancy;excessivevomitinginpregnancy; pregnantstate,incidental).Specificdiagnosiscodesusedfor patientidentificationarelistedin Appendix1.Thesewere initially filteredbySPSSStatisticsv27(IBMCorporation, Armonk,NY)andwerethenhand-verifiedbyonestudy author(CP).WeexcludedencounterswithoutICDdiagnosis codesorcodedonlyas “elopement” or “leftwithout beingseen.”
Asthishasimportantimplicationsforemergency clinicians,asecondarygoalofouranalysiswastoidentifyan estimateoftheincidenceofnewpregnancydiagnosisinthe ED thatis,visitswherepatientswere firstidentifiedas pregnantduringtheirEDvisit.Wedefinedasubsetof pregnantpatientvisitsas “incidentalpregnancy” through EDreason-for-visit(RFV)codesandwhetherpregnancywas testedforintheED.TheRFVcodesincludethechief complaint,aswellasothersymptomsormedicalproblems relatedtotheEDvisit.16 WeexaminedRFVcodesand excludedpatientvisitswithcodesthatsuggestedaprevious diagnosisofpregnancy(eg,1790.0Problemsandother conditionsrelatedtopregnancy;2735.0Diagnosed
complicationsofpregnancyandpuerperium).Withthegoal ofobtainingaconservativeestimate,wealsoexcluded patientvisitswithRFVcodesforvaginalbleeding.Patient visitsfromthisgroupthathadapregnancytestsentintheED madeupour “incidentalpregnancy” population.Toobtain evidenceofconstructvalidity,weexaminedtheICD-9and ICD-10dischargecodesforthe “incidentalpregnancy” populationtoensuretheywereconsistentwithanew pregnancydiagnosis.
Availabledemographicsincludedpatientage;race/ ethnicity(non-HispanicBlack,non-HispanicWhite, Hispanic,andother);payment/insurancestatus(private insurance,publicinsurance[Medicare,Medicaidorother state-basedprogram],self-pay,andotherorunknown insurance);andresidence(private,unhoused,orother).
Visitcharacteristicsincludeddayoftheweekthevisittook place(weekendorweekday),season(Fall,Winter,Spring,or Summer),andyearofvisit.Visitcharacteristicsalsoincluded hospitaladmission,whetherapregnancytestwassent,useof ultrasound,consultation,lengthofvisit,waittimetoseea clinician,andreturnvisitwithin72hours.Pregnancytest, ultrasounduse,hospitaladmission,consultation,andreturn visitwithin72hoursweredichotomousvariables,andreturn visitreferredtowhetherthepatientwasseeninthesameED intheprior72hoursforanyreason.Wedefinedwaittimeas thetimefromarrivalto firstcliniciancontact,andlengthof visitwasdefinedasthetimefromarrivaltodischarge.We analyzedbothvaluesascontinuousvariables.
Hospital-levelcharacteristicsincludedgeographicregion (Midwest,Northeast,South,andWest)andmetropolitan statisticalarea,reflectinganurbanvsrurallocationas definedbytheUSOfficeofManagementandBudget.
WefollowedtheStrengtheningtheReportingof ObservationalStudiesinEpidemiology(STROBE) reportingguidelines.17 WedescriptivelyanalyzedEDvisits forpregnantpatientsanddeterminedtheproportionofED visitsforpregnantpatientsamongallEDvisits(forwomen andmen)aswellasamongwomen15–44yearsold. Demographic,visit,andhospitalcharacteristicsof presentationsofpregnantpatientsamongwomenof reproductiveageweresimilarlyanalyzed.Wecomparedthe characteristicsofvisitsforpregnantreproductive-aged womentothosefornon-pregnantreproductive-agedwomen usingchi-squaredtestsforcategoricalfactorsandtwosample t -testforcontinuousvariables.Statistical significancewassetat P < 0.01asrecommendedby NHAMCSdocumentation.13
Wecomparedcharacteristicsofvisitsforpregnant patientstonon-pregnantpatientsusingmultivariablelogistic regression.Weexaminedunadjustedassociationsandthen
usedmultivariablelogisticregressionmodelstodetermine factorsindependentlyassociatedwithvisitsforpregnant patients.Modelsgeneratedoddsratios(OR)and95% confidenceintervals(CI).Statisticalcalculationswere completedwithSASOnDemandforAcademics(SAS,Inc, Cary,NC).
WeightedresultsrepresentativeofallEDvisitsroundedto thenearestthousandintheUSwerepresentedforanalysis unlessotherwisestated,asrecommendedbyNHAMCS.13,18 BasedonbestpracticesfortheuseofNHAMCSdatain research,weensuredthatallreportedestimateswerebased on >30unweightedrecords,hadarelativestandarderrorof <30%,anddidnotincludeanyitemswithanon-response rate >30%inouranalysis.14,18 TheNHAMCSimputesdata formissingvaluesinage,gender,race,andethnicityusinga model-basedsingle,sequentialregressionmethod.13 Race andethnicityhadthehighestaverageproportionofmissing valuesinourdataset(17%and21%,respectively); therefore,weperformedasensitivityanalysistoensure resultdurability.
DatafromtheNHAMCSarede-identifiedandpublicly available.Useofthisdataforresearchpurposeshasbeen reviewedandapprovedbytheNationalCenterforHealth StatisticsEthicsReviewBoard(Protocol#2021-03).
The2010–2020NHAMCSdatasetincluded255,963visits (weightedn = 1,502,215,000,95%CI 1,342,435,000–1,661,995,000),including59,080visitsamong womenages15–44(weightedn = 353,012,000,95%CI 310,947,000–395,078,000).Atotalof6,068ofthesevisits wereforpregnantpatients(weightedn = 30,489,000,95%CI 26,117,000–34,861,000).Pregnantpatientvisitsaccounted for3.0%(95%CI2.7–3.2)ofallEDvisits.Thisequatesto 2.77millionpregnantpatientspresentingforEDvisits annually.Limitingthepopulationtowomenages 15–44years,pregnantpatientvisitsaccountedfor8.6%(95% CI8–9.3)ofallEDvisits.
Incidentalpregnancywasidentifiedin672patientvisits (weightedn = 4,056,000,95%CI3,323,000–4,789,000). Incidentalpregnancyvisitsaccountedfor13.3%(95%CI 12.7–13.7)ofallpregnantEDvisits.Annually,thisequates to368,000(95%CI352,000–379,000)visitswherepregnancy isdiagnosedintheED.Themajority(52%)oftheICD-9and 10codesforthesevisitswereforpregnancy-related complaints(eg,hyperemesisgravidarum,infectionofthe genitaltractinpregnancy),andtheremainderwere diagnosesofpregnancy(eg,encounterforsupervisionof normal firstpregnancy,pregnantstate,incidental),aligning withourassumptionthatthesevisitsrepresentednew pregnancydiagnoses.
Themedianageofwomenpresentingwithpregnancywas 25years(interquartilerange21–30years),withoverhalf (57.9%)betweentheagesof20–29years(Table1).Visitsfor pregnantpatientsweremorelikelytobeforBlack(31.6%vs 26.3%fornon-pregnantwomen)andHispanic(22.0%vs 15.5%)women.Pregnantpatientvisitsweremorelikelyto usepublicinsurancethannon-pregnantvisits.
Therewerenosignificantdifferencesinpresentationof pregnantpatientsbetweenweekdaysandweekendsoracross seasons.Thenumberofpregnantpatientspresentingtothe EDdidnotsignificantlyvaryacrossyears,evenwhen normalizedtototalpatientsinourpopulation.Regional
distributionofpregnantpatientvisitsdidnotdiffer.Pregnant patientsweremorelikelytopresenttoahospitalinanurban area(89%vs84.7%, P < 0.001).Only44.8%ofpatientvisits includedapregnancytest,and44%includedanultrasound; 17.5%ofpregnantpatientvisitsincludedapelvicexam. Sevenpercentofpregnantpatientvisitsresultedin hospitalizationvs4.7%ofnon-pregnantpatientvisits (P < 0.001);and11.5%ofpregnantpatientvisitsincluded evaluationbyaconsultingphysician.
Therewasnosignificantdifferenceinwaittimebetween pregnantvsnon-pregnantpatientvisits.TheEDvisits generallylastedlongerforpregnantpatients(33.6%over fourhoursvs24.5%, P < 0.001).Most(84.4%)patientswere seenbyanattendingphysician,withoutmeaningful differencesbetweengroupsthatwereseenbyotherclinicians.
Table1. Characteristicsoffemalepatientsaged15–44yearsoldpresentingtotheemergencydepartmentforcare,2010–2020,weighted andstratifiedbypregnancystatus.
Age25(21–30)28(22–36)
15–19years4,185,000(13.7)47,282,000(14.7)
20–29years17,640,000(57.9)124,098,000(38.5)
30–39years7,802,000(25.6)103,558,000(32.1)
40–44years862,000(2.8)47,586,000(14.8)
Race/ethnicity
Non-HispanicWhite13,199,000(43.3)178,581,000(55.4)
Non-HispanicBlack9,642,000(31.6)84,808,000(26.3)
Hispanic6,695,000(22.0)49,863,000(15.5)
Non-HispanicOther952,000(3.1)9,271,000(2.9)
Paymentsource
Privateinsurance8,039,000(26.4)96,150,000(29.8)
Publicinsurance15,197,000(49.8)133,820,000(41.5)
Self-pay3,289,000(10.8)46,446,000(14.4)
Other1,164,000(3.8)13,203,000(4.1)
Unknown2,800,000(9.2)32,905,000(10.2)
Residence 0.21
Privateresidence29,464,000(96.6)309,823,000(96.1)
Homeless76,000(0.2)1,556,000(0.5)
Other226,000(0.7)3,517,000(1.1)
Unknown723,000(2.4)7,628,000(2.4)
Visitcharacteristics
EDvisitday
Weekend8,087,000(26.5)86,105,000(26.7)
Weekday22,403,000(73.5)236,419,000(73.3) (Continuedonnextpage)
Table1. Continued.
Fall7,503,000(24.6)85,173,000(26.4)
Winter7,735,000(25.4)77,058,000(23.9)
Spring7,536,000(24.7)81,156,000(25.2)
Summer7,715,000(25.3)79,136,000(24.5)
Year
20102,453,000(8.0)17,134,000(5.3)
20112,716,000(8.9)32,089,000(9.9)
20122,363,000(7.8)30,316,000(9.4)
20132,362,000(7.7)30,350,000(9.4)
20142,570,000(8.4)32,656,000(10.1)
20153,028,000(9.9)31,333,000(9.7)
20163,073,000(10.1)31,538,000(9.8)
20172,902,000(9.5)30,809,000(9.6)
20182,710,000(8.9)27,058,000(8.4)
20193,558,000(11.7)31,182,000(9.7)
20202,743,000(9.0)28,059,000(8.7)
Hospitaladmittance2,147,000(7.0)15,048,000(4.7) <0.001
Pregnancytest13,665,000(44.8)87,455,000(27.1) <
Ultrasound13,423,000(44.0)18,889,000(5.9) <
72-hourrevisit1,293,000(4.2)12,776,000(4.0)0.03
Seenbyconsultant3,498,000(11.5)19,499,000(6.0) <
Lengthofvisit <
<1hr1,769,000(7.6)29,062,000(11.8)
1–2hr3,221,000(13.9)64,011,000(26)
2–4hr10,413,000(44.9)93,180,000(37.8)
>4hr7,789,000(33.6)60,415,0000(24.5)
Waittime
<30min15,538,000(59.5)172,983,000(61.6)
30min-1hr4,830,000(18.5)50,720,000(18.1)
1–2hr3,475,000(13.3)35,543,000(12.7)
>2hr2,280,000(8.7)21,565,000(7.7)
Hospitalcharacteristics
Geographicregion
Northeast4,241,000(13.9)51,007,000(15.8)
Midwest7,302,000(23.9)73,129,000(22.7)
South12,631,000(41.4)130,591,000(40.5)
West6,315,000(20.7)67,797,000(21.0)
Metropolitanstatisticalarea(MSA) <0.001
MSA25,040,000(89.0)247,480,000(84.7)
Non-MSA3,085,000(11.0)44,727,000(15.3)
Dataaren(%),median(interquartilerange). ED,emergencydepartment.
MultivariableAnalysis
UnadjustedandadjustedORsforassociationsofpatient demographicsandhospitalcharacteristicswithpresentation ofpregnantpatientscomparedtonon-pregnantpatientsto theEDarepresentedin Table2.Inthegeneratedmodel,age 20–29years,Hispanicethnicity,publicinsurancestatus,and metropolitanlocationweresignificantlyassociatedwith visitsforpregnantpatients.Theseresultsheldthrough sensitivityanalysestoensurethatimputationinthedataset didnotaffectour findings.
Table2. Bivariableandmultivariablelogisticregressionmodels.
Age
15–19yearsReferenceReference
Race/ethnicity
Non-HispanicWhiteReferenceReference
Residence
PrivateresidenceReferenceReference
EDvisitday Weekend0.99(0.90–
WeekdayReferenceReference
EDvisitseason
Geographicregion
West1.12(0.95–1.32)0.981.03(0.86–1.22)0.09
Metropolitanstatisticalarea(MSA) MSA1.47(1.22–1.76) <0.0011.41(1.18–1.67) <0.001
Non-MSAReferenceReference
OR,oddsratio; ED,emergencydepartment.
Inthisstudy,usingdataavailablefromNHAMCS,we estimatedthatthereare2.77millionEDvisitsforpregnant patientsannuallyintheUnitedStates.Mostcommonly, womenpresentingtotheEDwithpregnancyarebetweenthe agesof20–29years,publiclyinsured,andidentifyasBlackor Hispanic.Ofthesepregnantpatientvisits,weestimatethat 13.3%oftheseresultedinanewdiagnosisofpregnancyinthe ED,equivalenttoapproximately370,000pregnancies first identifiedintheEDannually.
Wefoundthat8.6%ofvisitsamongwomenbetweenages 15–44yearswereforpregnantpatients,whichgenerally alignswithpreviouslyreportedvalues;however,therewasa largeamountofvariabilityinreported figures. 7–9 Benson etalperformingasimilarevaluationforpatientspresenting forearlypregnancylossreportedapproximately900,000 visitsannually,whichwouldrepresent32%ofthe2.77 millionpregnantpatientvisitswedescribe.5 Thisishigher thantheoftenreportedrateof20%earlypregnancyloss, whichwesuspectisduetoearlypregnancylossbeinga commonreasonforEDpresentation.19
Ourdatashowsthatpregnantpatientsseekingcareinthe EDaremorelikelytobeBlack,Hispanic.orpublicly insured.Thesepopulationsarelesslikelytoreceiveroutine prenatalcareandhaveahigherratesofpregnancy-related morbidityandmortalitywhencomparedtoWhitepatients.20 Furthermore,unintendedpregnancyratesarehigherandthe rateofreferralfordesiredfamilyplanningservicesislowerin thesepatientgroups.21–23 Currentlymorethanonehalfof abortionsareamongwomenofcolordespitethesepatients experiencinggreaterbarrierstoaccessingfamilyplanning services.24 PatientsonMedicaidsimilarlyhavechallenges accessingabortioncareduetolimitedcoverageforthese services.24 The Dobbs decisionislikelytoexacerbatethese disparitiesandmaydisproportionatelyaffectpregnant patientspresentingtotheED.24 Futurestudiesshould investigatetheseimpactsaslegislationchangesandexamine howEDpresentationsandcaredifferbetweenstatesthat enactrestrictiveabortionlegislationcomparetostates withoutrestriction.
Ourresultssuggestthatalargeproportion(13.3%)of pregnantpatientswhoseekcareintheEDare firstdiagnosed duringtheirEDencounter.Basedonhistoricaldata,halfof thesepregnanciesareunplanned,andhalfwouldendin abortioninthepre-Dobbs era. 21 Discoveryofthese pregnanciesintheEDoffersanopportunityforcounseling andreferraltoavailableabortionservicesifdesired.Thisis especiallyimportantinstateswherestrictrestrictionson gestationalageforlegalabortionexist.Thesepatientsmay facebarrierstocareanddelaysincarefollowingED discharge,suggestingacriticalneedforcounselingand linkagetocareduringtheEDencounter.
Nationwideaccesstothesereproductivehealthcare servicesissupportedbytheAmericanCollegeofEmergency
Physicians.AlthoughtheEDistakingalargerrolein offeringthiscare,furtherresearchisrequiredtoidentifythe needsofthispopulation.25,26 Specifically,futurestudies coulddirectlymeasuretherateofnewpregnancydiagnosisin theED,determinecounselingpracticesamongemergency clinicians,andexaminehowthesepatientsarelinkedtocare ifapregnancyisundesired.Thisdata,alongwith comparisonsbetweenstateswithvaryingdegreesof legislationchange,couldhelpinformpolicychanges.
ResultsarebasedondatafromtheNHAMCS,whichhas several,well-reportedlimitations.18 AlthoughtheNHAMCS makesgreateffortstoincludearepresentativesample,itis possiblethattheincludedvisitsarenotcompletely representativeofEDvisitsnationwide.Nevertheless,the NHAMCSisthelargestdatasettodatewithpopulationbasedestimatesofEDvisitsintheUS.Non-responseratefor itemsintheNHAMCSmayalsobiasresults;however,all ourvariablesofinteresthadnon-responseratesthatfell withinacceptablemargins,andthosewithhighernonresponserates(raceandethnicity)wereevaluatedwith sensitivitytestingtoensureimputedvaluesdidnot compromiseresults.
Wedefinedvisitswithpregnantpatientsinourpopulation bypregnancy-relatedICD-9and-10diagnoses,whichmay havebeenenteredinerrorfornon-pregnantpatients.Visits withanincidentalpregnancydiagnosiswerebasedontriage dataandpregnancytesting,whichmayhavemisclassified pregnanciesasincidentalorfailedtoidentifyotherincidental pregnanciesnotcaptured.Toobtainaconservativeestimate, weexcludedpatientpresentationsforvaginalbleeding, whichmayhaveraisedclinicianorpatientsuspicionof pregnancy.Duetothenatureofthedatasetweanalyzed,we werenotabletoprovidedefinitiveinformationabout completionofapreviouspregnancytestorultrasound,nor aboutthepatient’ssuspicionforpregnancy,whichwouldbe preferredmarkersforidentifyingnewpregnancydiagnoses.
Finally,wewereunabletoprovideinformationabout whetherthesepregnanciesweredesired,whetherpatientshad establishedcarewithanobstetrician,ortheoutcomesof thesepregnancies.
Ourstudyrevealsthatpregnantpatientsmakeup3%of EDvisitsannually.Givenrecentlegislativechanges concerningreproductivehealthcare,thesepatientscouldbe significantlyimpacted.TheED,oftenseenasthehealthcare system’ssafetynet,providescrucialcarethatmightnotbe availableelsewhere.Withthepossibilityofpregnantpatients turningmoreoftentotheEDforcare,thereisanurgentneed todevelopandimplementeducationalandpolicystrategies thatsupportthesepatientsinnavigatingtheincreasingly complexrealmoffamilyplanningservices.
AddressforCorrespondence:CarlPreiksaitis,MD,Stanford UniversitySchoolofMedicine,DepartmentofEmergencyMedicine, 900WelchRoad,Suite350,PaloAlto,CA94304.Email: cpreiksaitis@stanford.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Preiksaitisetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1. Dobbsv.JacksonWomen’sHealthOrg.597U.S.2022.
2.Samuels-KalowME,AgrawalP,RodriguezG,etal.Post-Roe emergencymedicine:policy,clinical,training,andindividual implicationsforemergencyclinicians. AcadEmergMed. 2022;29(12):1414–21.
3.MalikS,KothariC,MacCallumC,etal.Emergencydepartmentusein theperinatalperiod:anopportunityforearlyintervention. AnnEmerg Med. 2017;70(6):835–9.
4.MatenchukBA,RosychukRJ,RoweBH,etal.Emergencydepartment visitsduringpregnancy. AnnEmergMed. 2023;81(2):197–208.
5.BensonLS,MagnussonSL,GrayKE,etal.Earlypregnancylossinthe emergencydepartment,2006–2016. JAmCollEmergPhysicians Open. 2021;2(6):e12549.
6.KilfoyleKA,VreesR,RakerCA,etal.Non-urgentandurgentemergency departmentuseduringpregnancy:anobservationalstudy. AmJObstet Gynecol. 2017;216(2):181.e1–7.
7.StengelCL,SeabergDC,MacLeodBA.Pregnancyintheemergency department:riskfactorsandprevalenceamongallwomen. AnnEmerg Med. 1994;24(4):697–700.
8.RamoskaEA,SacchettiAD,NeppM.Reliabilityofpatienthistoryin determiningthepossibilityofpregnancy. AnnEmergMed. 1989;18(1):48–50.
9.StroteJandChenG.Patientselfassessmentofpregnancystatusinthe emergencydepartment. EmergMedJ. 2006;23(7):554–7.
10.RobertsSCM,WingoE,KimportK.Aqualitativeexplorationofwomen’s experiencesdiscoveringpregnanciesintheemergencydepartment. ContraceptX. 2020;2:100024.
11.ACEPNow.Taskforceformedtoexamineemergencydept. reproductivehealth.2022.Availableat: https://www.acepnow.com/ article/task-force-formed-to-examine-emergency-dept-reproductivehealth/.AccessedNovember8,2022.
12.LeeLK,ChienA,StewartA,etal.Women’scoverage,utilization, affordability,andhealthaftertheACA:areviewoftheliterature. Health Aff(Millwood). 2020;39(3):387–94.
13.2020NHAMCSMicro-data filedocumentation.2020.Availableat: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/ Dataset_Documentation/NHAMCS/doc20-ed-508.pdf AccessedNovember1,2022.
14.NAMCS/NHAMCS-AmbulatoryHealthCareDataHomepage.2022. https://www.cdc.gov/nchs/ahcd/index.htm AccessedNovember8,2022.
15.ZambranoLD,EllingtonS,StridP,etal.Update:characteristicsof symptomaticwomenofreproductiveagewithlaboratory-confirmed SARS-CoV-2infectionbypregnancystatus UnitedStates,January 22–October3,2020. MorbMortalWklyRep. 2020;69(44):1641–47.
16.SchneiderD,AppletonL,McLemoreT.Areasonforvisitclassification forambulatorycare. VitalHealthStat2. 1979;(78):1–63.
17.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. AnnInternMed. 2007;147(8):573–7.
18.McCaigLFandBurtCW.UnderstandingandinterpretingtheNational HospitalAmbulatoryMedicalCareSurvey:keyquestionsandanswers. AnnEmergMed. 2012;60(6):716–21.e1.
19.ACOGPracticeBulletinNo.200:Earlypregnancyloss. ObstetGynecol. 2018;132(5):e197.
20.HillL,ArtigaS,RanjiU.Racialdisparitiesinmaternalandinfanthealth: currentstatusandeffortstoaddressthem.2022.Availableat: https:// www.kff.org/racial-equity-and-health-policy/issue-brief/racialdisparities-in-maternal-and-infant-health-current-status-andefforts-to-address-them/.AccessedNovember7,2022.
21.FinerLBandZolnaMR.DeclinesinunintendedpregnancyintheUnited States,2008–2011. NEnglJMed. 2016;374(9):843–52.
22.DehlendorfC,HarrisLH,WeitzTA.Disparitiesinabortionrates:apublic healthapproach. AmJPublicHealth. 2013;103(10):1772–9.
23.NobelK,LukeAA,RiceWS.Racialdisparitiesinpregnancyoptions counselingandreferralintheUSSouth. HealthServRes. 2023;58(1):9–18.
24.ArtigaS,HillL,RanjiU,etal.Whataretheimplicationsoftheoverturning ofRoev.Wadeforracialdisparities?Availableat: https://www.kff. org/racial-equity-and-health-policy/issue-brief/what-are-theimplications-of-the-overturning-of-roe-v-wade-for-racial-disparities/ AccessedNovember18,2022.
25.ACEPCouncilResolution24.Availableat: https://www.acep.org/ what-we-believe/actions-on-council-resolutions/councilresolution/ AccessedDecember3,2022.
26.PreiksaitisCandHenkelA.Theevolvingroleofemergencymedicinein familyplanningservices. CurrOpinObstetGynecol. 2023;35(6):484–9.