
Volume 25, Number 5, September 2024


Volume 25, Number 5, September 2024
Behavioral Health
668 Methadone Initiation in the Emergency Department for Opioid Use Disorder
Daniel Wolfson, Roz King, Miles Lamberson, Jackson Lyttleton, Colin T. Waters, Samantha H. Schneider, Blake A. Porter, Kyle M. DeWitt, Peter Jackson, Martha W. Stevens, John Brooklyn, Richard Rawson, Elly Riser
Clinical Practice
675 Cross-Sectional Study of Thiamine Deficiency and Its Associated Risks in Emergency Care
Joseph Miller, Daniel Grahf, Hashem Nassereddine, Jimmy Nehme, Jo-Ann Rammal, Jacob Ross, Kaitlin Rose, Daniel Hrabec, Sam Tirgari, Christopher Lewandowski
680 Emergency Department Blood Pressure Treatment and Outcomes in Adults Presenting with Severe Hypertension
Farhan Chaudhry, Eliana Small, Steven J. Korzeniewski, Dana Benyas, Lydia Ross, Alex B. Hill, Amit Vahia, Candace McNaughton, Phillip Levy, Joseph Miller
Critical Care
690 Neutrophil-to-Lymphocyte Ratio Predicts Sepsis in Adult Patients Meeting Two or More Systemic Inflammatory Response Syndrome Criteria
Vamsi Balakrishnan, Anna Yang, Donald Jeanmonod, Harrison Courie, Spencer Thompson, Valerian Peterson, Rebecca Jeanmonod
697 The Nonlinear Relationship Between Temperature and Prognosis in Sepsis-induced Coagulopathy Patients: A Retrospective Cohort Study from MIMIC-IV Database
Guojun Chen, Tianen Zhou, Jingtao Xu, Qiaohua Hu, Jun Jiang, Weigan Xu
708 Scoping Review: Is Push-Dose Norepinephrine a Better Choice?
Michael Berkenbush, Lali Singh, Kelly Sessa, Raghad Saadi






Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Section Editors
Behavioral Emergencies
Leslie Zun, MD, MBA
Rosalind Franklin University of Medicine and Science
Marc L. Martel, MD
Hennepin County Medical Center
Cardiac Care
Fred A. Severyn, MD University of Colorado School of Medicine
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD
Carolinas Medical Center
Casey Clements, MD, PhD Mayo Clinic
Patrick Meloy, MD
Emory University
Nicholas Pettit, DO, PhD
Indiana University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD University of California, San Diego
Gabriel Wardi, MD University of California, San Diego
Joseph Shiber, MD University of Florida-College of Medicine
Matt Prekker MD, MPH Hennepin County Medical Center
David Page, MD University of Alabama
Erik Melnychuk, MD Geisinger Health
Quincy Tran, MD, PhD University of Maryland
Disaster Medicine
John Broach, MD, MPH, MBA, FACEP University of Massachusetts Medical School
UMass Memorial Medical Center
Christopher Kang, MD Madigan Army Medical Center
Education
Danya Khoujah, MBBS University of Maryland School of Medicine
University of Colorado
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of MedicineIrvine, California
University of California, Irvine School of MedicineIrvine, California
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Niels K. Rathlev, MD, Associate Editor Tufts University School of Medicine-Boston, Massachusetts
Rick A. McPheeters, DO, Associate Editor
R. Gentry Wilkerson, MD, Associate Editor University of Maryland
Michael Epter, DO
Maricopa Medical Center
ED Administration, Quality, Safety
Tehreem Rehman, MD, MPH, MBA Mount Sinai Hospital
David C. Lee, MD Northshore University Hospital
Gary Johnson, MD
Upstate Medical University
Brian J. Yun, MD, MBA, MPH Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH
Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine
University of California, Davis
Emergency Medical Services
Daniel Joseph, MD
Yale University
Joshua B. Gaither, MD University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD Yale School of Medicine
Stephen Meldon, MD Cleveland Clinic
Luna Ragsdale, MD, MPH
Duke University
Health Equity
Emily C. Manchanda, MD, MPH Boston University School of Medicine
Faith Quenzer
Temecula Valley Hospital
San Ysidro Health Center
Payal Modi, MD MScPH University of Massachusetts Medical
Infectious Disease
Elissa Schechter-Perkins, MD, MPH Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Stephen Liang, MD, MPHS
Shadi Lahham, MD, MS, Deputy Editor Kaiser Permanente- Irvine, California
Susan R. Wilcox, MD, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Elizabeth Burner, MD, MPH, Associate Editor University of Southern California- Los Angeles, California
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston Texas
Danya Khoujah, MBBS, Associate Editor University of Maryland School of Medicine- Baltimore, Maryland
Washington University School of Medicine
Victor Cisneros, MD, MPH Eisenhower Medical Center
Injury Prevention
Mark Faul, PhD, MA Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH Prisma Health Richland
Taylor Burkholder, MD, MPH Keck School of Medicine of USC
Christopher Greene, MD, MPH University of Alabama
Chris Mills, MD, MPH Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Indiana University School of Medicine
Statistics and Methodology
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH
Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS
Rick Lucarelli, MD Medical City Dallas Hospital
William D. Whetstone, MD University of California, San Francisco
Neurosciences
Antonio Siniscalchi, MD Annunziata Hospital, Cosenza, Italy
Pediatric Emergency Medicine
Paul Walsh, MD, MSc University of California, Davis
Muhammad Waseem, MD Lincoln Medical & Mental Health Center
M. Zeretzke-Bien, MD University of Florida
Henry Ford Hospital
John Ashurst, DO Lehigh Valley Health Network
Tony Zitek, MD Kendall Regional Medical Center
Trevor Mills, MD, MPH Northern California VA Health Care
Erik S. Anderson, MD Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD Henry Ford Hospital
Phillips Perera, MD Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS Virginia Commonwealth University
University of California, Irvine
Ultrasound J. Matthew Fields, MD
Shane Summers, MD Brooke Army Medical Center
Robert R. Ehrman Wayne State University
Ryan C. Gibbons, MD Temple Health
Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine


American Academy of Emergency Medicine


Integrating Emergency with Population Health
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
MAAEM
Amin A. Kazzi, MD, MAAEM
Amin A. Kazzi, MD, MAAEM
Gayle Galleta, MD
Gayle Galleta, MD
Beirut,
The American University of Beirut, Lebanon
The American University of Beirut, Beirut, Lebanon
Brent King, MD, MMM University Texas, Houston
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD
Ohio State University Wexner Medical Center
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Christopher E. San Miguel, Ohio State University Wexner Medical Center
Daniel J. Dire, MD
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
Daniel J. Dire, MD University Texas Health Sciences Center San Antonio
Douglas Ander, Emory University
Douglas Ander, MD Emory University
Emory University
Edward Michelson, MD Texas Tech University
Edward Michelson, Texas Tech University
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH South
Edward MD, MPH University South Alabama
Edward Panacek, MD, MPH University of South Alabama
Francesco
“Maggiore della Carità,” Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Novara, Italy
Francesco Della Corte, MD Azienda Ospedaliera Universitaria “Maggiore della Carità,” Novara, Italy
Elena Lopez-Gusman, JD
Elena Lopez-Gusman, JD
California ACEP
California ACEP
Elena Lopez-Gusman, JD California ACEP American College of Emergency
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog,
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Hjalti MD Icelandic Society of Emergency Medicine
Jaqueline Le, MD Desert Regional Medical Center
Jaqueline Le, MD Desert Medical Center
Regional
Jeffrey Love, MD
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jeffrey Love, The George Washington University School of Medicine and Health Sciences
Katsuhiro Kanemaru, MD University of Hospital, Miyazaki, Japan
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Leslie Zun, MD, MBA Chicago Medical School
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine
The George Washington University School of Medicine and Health Sciences Arizona, Chicago Medical School Librarian
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
Langdorf, MAAEM, FACEP
American of Emergency Physicians
American College of Emergency Physicians
Jennifer Kanapicki Comer, MD FAAEM
Jennifer Kanapicki Comer, MD FAAEM
California Chapter Division of AAEM Stanford University School of Medicine
California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE
DeAnna McNett, CAE
Kimberly Ang, MBA
Tufts University School of Medicine
Niels K. Rathlev, Tufts University School of Medicine
Niels K. Rathlev, MD Tufts University School of Medicine
Scott Zeller, MD
Scott Zeller, MD University of California, Riverside
Scott Zeller, MD University of California, Riverside
Pablo Fuenzalida, Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de
Bell,
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter A. Bell, DO, MBA Baptist Health University
Peter Sokolove, MD University of California, Francisco
Peter Sokolove, MD University of California, San Francisco
University of California, San Francisco
Rachel A. Lindor, MD, JD
Rachel A. Lindor, MD, JD Mayo Clinic
Rachel A. Lindor, MD, JD Mayo Clinic
Robert Suter, DO, MHA
Robert Suter, DO, UT Southwestern Medical Center
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
University of California, Davis
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Malaysia
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Scott Rudkin, MD, MBA
Scott Rudkin, MD, University of California, Irvine
Scott Rudkin, MD, MBA University of California, Irvine
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Steven H. Lim, Changi General Hospital, Simei, Singapore
Singapore
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP to the Netherlands Society of Emergency Physicians
Terry Mulligan, DO, MPH, FIFEM ACEP Ambassador to the Netherlands
Wirachin Hoonpongsimanont, MD, MSBATS
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Isabelle BS Executive Editorial Director
Isabelle Nepomuceno, BS Executive Editorial Director
UC Irvine Health School of Medicine
UC Irvine Health School of Medicine
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP
UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Robert Suter, DO, MHA American College of Osteopathic
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center
Visha Bajaria, BS WestJEM Editorial Director
Visha Bajaria, BS WestJEM Editorial Director
Cassandra Saucedo, MS Executive Publishing Director
Cassandra Saucedo, MS Executive Publishing Director
American College of Osteopathic Emergency Physicians
American College of Osteopathic Emergency Physicians
UC Irvine Health School of Medicine
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Kimberly Ang, MBA
Randall J. Young, MD, MMM, FACEP California ACEP
UC Irvine Health School of Medicine
American College of Emergency Physicians Kaiser Permanente
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians Kaiser Permanente
J. American College of Emergency Physicians Kaiser Permanente
Jorge Fernandez, MD, FACEP
Jorge Fernandez, MD, FACEP

UC San Diego Health School of Medicine
UC San Diego Health School of Medicine
Jorge Fernandez, MD, FACEP
UC San Diego Health School of Medicine

Emily Kane, MA WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Visha Bajaria, BS WestJEM Editorial Director WestJEM
Stephanie Burmeister, MLIS JEM Liaison

Nicole Valenzi, BA WestJEM Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
Cassandra Saucedo, MS WestJEM Publishing Director
June Casey, BA Copy Editor
June Casey, BA Copy Editor
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine

in Melvyl,
Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org
Editorial and Publishing Office: JEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
Education
715 Program Signaling in Emergency Medicine: The 2022–2023 Program Director Experience
Alexis E. Pelletier-Bui, Timothy Fallon, Liza Smith, Tania Strout, Michelle Fischer, Mark Olaf, Erin McDonough, Brian Barbas, Michael Cirone, Elizabeth Barrall Werley
725 Emergency Department Slit Lamp Interdisciplinary Training Via Longitudinal Assessment in Medical Practice
Samara Hamou, Shayan Ghiaee, Christine Chung, Maureen Lloyd, Kelly Khem, Xiao Chi Zhang
735 Emergency Medicine Milestones Final Ratings Are Often Subpar Diane L. Gorgas, Kevin B. Joldersma, Felix K. Ankel, Wallace A. Carter, Melissa A. Barton, Earl J. Reisdorff
739 Making A Difference: Launching a Multimodal, Resident-Run Social Emergency Medicine Program
Naomi P. Newton, Christopher Freeman, Patricia Panakos
Emergency Department Operations
748 Reduced Time to Admit Emergency Department Patients to Inpatient Beds Using Outflow Barrier Analysis and Process Improvement
Marjorie A. Erdmann, Ipe S. Paramel, Cari Marshall, Karissa LeHew, Abigail Kee, Sarah Soliman, Monica Vuong, Sydney Spillane, Joshua Baer, Shania Do, Tiffany Jones, Derek McGuire
758 Interfacility Patient Transfers During COVID-19 Pandemic: Mixed-Methods Study
Michael B. Henry, Emily Funsten, Marisa A. Michealson, Danielle Albright, Cameron S. Crandall, David P. Sklar, Naomi George, Margaret Greenwood-Ericksen
767 Impact of Medical Trainees on Efficiency and Productivity in the Emergency Department: Systematic Review and Narrative Synthesis
Jake Valentine, Jonathan Poulson, Jesus Tamayo, Amanda Valentine, Jacqueline Levesque, Shane Jenks
Emergency Medical Services
777 Telemedical Direction to Optimize Resource Utilization in a Rural Emergency Medical Services System
Ramesh Karra, Amber D. Rice, Aileen Hardcastle, Justin V. Lara, Adrienne Hollen, Melody Glenn, Rachel Munn, Philipp Hannan, Brittany Arcaris, Daniel Derksen, Daniel W. Spaite, Joshua B. Gaither
784 Impact of Prehospital Ultrasound Training on Simulated Paramedic Clinical Decision-Making
Andrea Roche, Evan Watkins, Andrew Pettit, Jacob Slagle, Isain Zapata, Andrew Seefeld, Nena Lundgreen Mason
793 Use of Long Spinal Board Post-Application of Protocol for Spinal Motion Restriction for Spinal Cord Injury
Amber D. Rice, Philipp L. Hannan, Memu-iye Kamara, Joshua B. Gaither, Robyn Blust, Vatsal Chikani, Franco Castro-Marin, Gail Bradley, Bentley J. Bobrow, Rachel Munn, Mary Knotts, Justin Lara
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
25, No. 5: September 2024
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
800 Association of Gender and Personal Choices with Salaries of New Emergency Medicine Graduates
Fiona E. Gallahue, Louis J. Ling, Leo Quigley, Dian Dowling Evans, Edward Salsberg, Robert E. Suter, Catherine A. Marco
Health Equity
809 Equity in the Early Pain Management of Long Bone Fractures in Black vs White Patients: We Have Closed the Gap
Dietrich Jehle, Krishna K. Paul, Stanley Troung, Jackson M. Rogers, Blake Mireles, John J. Straub, Georgiy Golovko, Matthew M. Talbott, Ronald W. Lindsey, Charles P. Mouton
817 A Cross-Sectional Review of HIV Screening in High-Acuity Emergency Department Patients: A Missed Opportunity
Jacqueline J. Mahal, Fernando Gonzalez, Deirdre Kokasko, Ahava Muskat
Health Policy Analysis
823 Preventive Health Services Offered in a Sampling of US Emergency Departments, 2022–2023
Christopher L. Bennett, M. Kit Delgado, Melissa Pasao, Janice A. Espinola, Krislyn M. Boggs, Carlos A. Camargo Jr.
Medical Education
828 Exploring Medical Student Experiences of Trauma in the Emergency Department: Opportunities for Trauma-informed Medical Education
Giselle Appel, Ahmed T. Shahzad, Kestrel Reopelle, Stephen DiDonato, Frances Rusnack, Dimitrios Papanagnou
Pediatrics
838 Drowning Among Children 1–4 Years of Age in California, 2017–2021
Phyllis F. Agran, Diane G. Winn, Soheil Saadat, Jaya R. Bhalla, Van Nguyen Greco, Nakia C. Best, Shahram Lotfipour
Technology
845 ChatGPT’s Role in Improving Education Among Patients Seeking Emergency Medical Treatment
Faris F. Halaseh, Justin S. Yang, Clifford N. Danza, Rami Halaseh, Lindsey Spiegelman
Letters to the Editor
856 Comments on “A Shorter Door-In-Door-Out Time Is Associated with Improved Outcome in Large Vessel Occlusion Stroke”
Gillian Cooper, Vainavi Gambhir, Zoe Gasparotti, Samantha Camp, William Gum, Robinson Okolo, Riya Raikar, Chad Schrier, Jessica Downing, Quincy K. Tran
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Albany Medical College Albany, NY
Allegheny Health Network Pittsburgh, PA
American University of Beirut Beirut, Lebanon
AMITA Health Resurrection Medical Center Chicago, IL
Arrowhead Regional Medical Center Colton, CA
Baylor College of Medicine Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center Boston, MA
Boston Medical Center Boston, MA
Brigham and Women’s Hospital Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
INTEGRIS Health Oklahoma City, OK
Kaiser Permenante Medical Center San Diego, CA
Kaweah Delta Health Care District Visalia, CA
Kennedy University Hospitals Turnersville, NJ
Kent Hospital Warwick, RI
Kern Medical Bakersfield, CA
Lakeland HealthCare St. Joseph, MI
Lehigh Valley Hospital and Health Network Allentown, PA
Loma Linda University Medical Center Loma Linda, CA
Louisiana State University Health Sciences Center New Orleans, LA
Louisiana State University Shreveport Shereveport, LA
Madigan Army Medical Center Tacoma, WA
Maimonides Medical Center Brooklyn, NY
Maine Medical Center Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
Mayo Clinic Jacksonville, FL
Mayo Clinic College of Medicine Rochester, MN
Mercy Health - Hackley Campus Muskegon, MI
Merit Health Wesley Hattiesburg, MS
Midwestern University Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health New York, NY
North Shore University Hospital Manhasset, NY
Northwestern Medical Group Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center Columbus, OH
Ohio Valley Medical Center Wheeling, WV
Oregon Health and Science University Portland, OR
Penn State Milton S. Hershey Medical Center Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
25, No. 5: September 2024
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program St. Paul, MN
Rhode Island Hospital Providence, RI
Robert Wood Johnson University Hospital New Brunswick, NJ
Rush University Medical Center Chicago, IL
St. Luke’s University Health Network Bethlehem, PA
Spectrum Health Lakeland St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University Syracuse, NY
Temple University Philadelphia, PA
Texas Tech University Health Sciences Center El Paso, TX
The MetroHealth System/ Case Western Reserve University Cleveland, OH
UMass Chan Medical School Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham Birmingham, AL
University of Arizona College of Medicine-Tucson Tucson, AZ
University of California, Davis Medical Center Sacramento, CA
University of California, Irvine Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
Emergency Medicine Association of Turkey Lebanese Academy of Emergency Medicine Mediterranean Academy of Emergency Medicine
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago Chicago, IL
University of Iowa Iowa City, IA
University of Louisville Louisville, KY
University of Maryland Baltimore, MD
University of Massachusetts Amherst, MA
University of Michigan Ann Arbor, MI
University of Missouri, Columbia Columbia, MO
University of North Dakota School of Medicine and Health Sciences Grand Forks, ND
University of Nebraska Medical Center Omaha, NE
University of Nevada, Las Vegas Las Vegas, NV
University of Southern Alabama Mobile, AL
University of Southern California Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center Seattle, WA
University of Wisconsin Hospitals and Clinics Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University Winston-Salem, NC
Wake Technical Community College Raleigh, NC
Wayne State Detroit, MI
Wright State University Dayton, OH
Yale School of Medicine New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
DanielWolfson,MD* RozKing,MSN*
MilesLamberson,BA* JacksonLyttleton,BS*
ColinT.Waters,MD,PhD* SamanthaH.Schneider,MS† BlakeA.Porter,PharmD‡ KyleM.DeWitt,PharmD‡ PeterJackson,MD§∥
MarthaW.Stevens,MD,MSCE* JohnBrooklyn,MD§¶ RichardRawson,PhD∥# EllyRiser,MD,MPH**
SectionEditor:MarcMartel,MD
*UniversityofVermontLarnerCollegeofMedicine,DepartmentofEmergencyMedicine, Burlington,Vermont
† RushUniversityMedicalCenter,CollegeofMedicine,Chicago,Illinois
‡ TheUniversityofVermontMedicalCenter,DepartmentofPharmacy,Burlington,Vermont
§ UniversityofVermontLarnerCollegeofMedicine,DepartmentofPsychiatry, Burlington,Vermont
∥ UniversityofVermont,VermontCenterforBehaviorandHealth,CenteronRural Addiction,Burlington,Vermont
¶ UniversityofVermontLarnerCollegeofMedicine,DepartmentofFamilyMedicine, Burlington,Vermont
# UniversityofCaliforniaLosAngelesSchoolofMedicine,LosAngeles,California **UniversityofVermontLarnerCollegeofMedicine,DepartmentofMedicine, Burlington,Vermont
Submissionhistory:SubmittedOctober26,2023;RevisionreceivedApril23,2024;AcceptedApril29,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18530
Introduction: Overdosedeathsfromhigh-potencysyntheticopioids,includingfentanylanditsanalogs, continuetorisealongwithemergencydepartment(ED)visitsforcomplicationsofopioidusedisorder (OUD).Fentanylaccumulatesinadiposetissue;althoughrare,thisincreasestheriskofprecipitated withdrawalinpatientsuponbuprenorphineinitiation.ManyEDshaveimplementedmedicationforopioid usedisorder(MOUD)programsusingbuprenorphine.However,fewoffermethadone,aproventherapy withouttheriskofprecipitatedwithdrawalassociatedwithbuprenorphineinitiation.Wedescribethe additionofanED-initiatedmethadonetreatmentpathwayandcomparedits72-hourfollow-upoutpatient treatmentengagementratestoourexistingED-initiatedbuprenorphineMOUDprogram.
Methods: WeexpandedourEDMOUDprogramwithamethadonetreatmentpathway.FromFebruary 20–September19,2023,wescreened20,504EDarrivals;5.1%hadsignsofOUD.Weenrolled61 patients:28inthemethadone;and33inthebuprenorphinepathways.Forpatientswhoscreened positiveforopioiduse,shareddecision-makingwasemployedtodeterminewhetherbuprenorphineor methadonetherapywasmoreappropriate.Patientsinthemethadonepathwayreceivedtheir firstdoseof upto30milligrams(mg)ofmethadoneintheED.Twoadditionalmethadonedosesofupto40mgwere dispensedatthetimeoftheEDvisitandheldinthedepartment,allowingpatientstoreturneachdayfor observeddosinguntilintakeatanopioidtreatmentprogram(OTP).Wecompared72-hourratesof outpatientfollow-uptreatmentengagementattheOTP(forthoseonmethadone)orattheaddiction treatmentcenter(ATC)(forthoseonbuprenorphine)forthetwotreatmentpathways.
Results: Ofthe28patientsenrolledinthemethadonepathway,12(43%)successfullyengagedin follow-uptreatmentattheOTP.Ofthe33patientsenrolledinthebuprenorphinepathway,15(45%) successfullyengagedinfollow-uptreatmentattheATC(relativerisk1.06;95%confidenceinterval 0.60–1.87).
Conclusion: MethadoneinitiationintheEDtotreatpatientswithOUDresultedinsimilar72-hourfollowupoutpatienttreatmentengagementratescomparedtoED-buprenorphineinitiation,providinganother viableoptionforMOUD.[WestJEmergMed.2024;25(5)668–674.]
TheopioidcrisisintheUnitedStatescontinuesunabated with106,699drug-involvedfatalitiesin2021,primarily involvingillicitlymanufacturedhigh-potencysynthetic opioids,andisfurthercomplicatedbyadulterantssuchas xylazineandgabapentin.1–6 Individualswithopioiduse disorder(OUD)facethehighestriskofdeathwithinthe first 48hoursfollowinganED(emergencydepartment)visitfora non-fataloverdose.7 TheEDidentificationofpatientswith OUDandinitiationofbuprenorphinetreatmenthasproven effectiveandissupportedbytheAmericanCollegeof EmergencyPhysiciansandtheCaliforniaBridgenetworkof hospitals.8–12 However,therisingprevalenceoffentanylin theillicitdrugsupplycomplicatestreatmentduetoits accumulationinadiposetissue,potentiallycausing precipitatedwithdrawaluponbuprenorphineinitiation.13–15 Additionally,abstainingfromfentanylfortherequiredpreinductionperiodmaybedifficultforsome,leadingthemto avoidfurtherbuprenorphineorfavormethadonefortheir medicationforOUD(MOUD).16–20 Methadone,asynthetic fullmu-opioidreceptoragonist,avoidsthesecomplications, asitdoesnotprecipitatewithdrawal.21,22 Inresponse,the UniversityofVermontMedicalCenter(UVM)enhancedits existingStartTreatmentandRecovery(STAR)program,an ED-basedinitiativetoinitiateMOUDinpatientswithOUD. Originallyfocusedonbuprenorphine,theprogramwas expandedtoincludemethadone,adaptingtotheshifting landscapeofopioiduseandpatientneeds.Wedescribethe implementationofanED-initiatedmethadonetreatment pathway,comparingits72-hourfollow-upoutpatient treatmentengagementratestoourexistingED-initiated buprenorphineMOUDprogram.
WeperformedanopentrialcomparingtwoMOUD treatmentpathwayswherepatientsintheEDwhometOUD criteriaandagreedtotreatmentchosebetweeninitiation ontobuprenorphineormethadone.FromFebruary 20–September19,2023wescreenedchartsof20,504ED arrivals,with1,051(5.1%)havingsignsofOUD.Ofthese, 903weredeterminedineligible,43patientsdeclined treatment,andsixpatientseloped.Patientsdeclining participationduetotimeconstraintsordeemedunsuitable forthestudyatcliniciandiscretionwereexcluded. EnrollmenttoinitiateMOUDintheSTARprogramwas completedfor61patientswith28initiatedonmethadoneand 33onbuprenorphine.Notincludedinthisanalysiswerean additional38patientswhowereenrolledinSTARbut admittedtothehospital(Figure1).TheSTARprogram coordinatorsscreenedpatientchartsfrom9 AM to9 PM daily andremainedoncallforenrollments24/7.Theyapproached identifiedpatientstoconfirmopioiduse,eligibility,and interestinstartingMOUD.
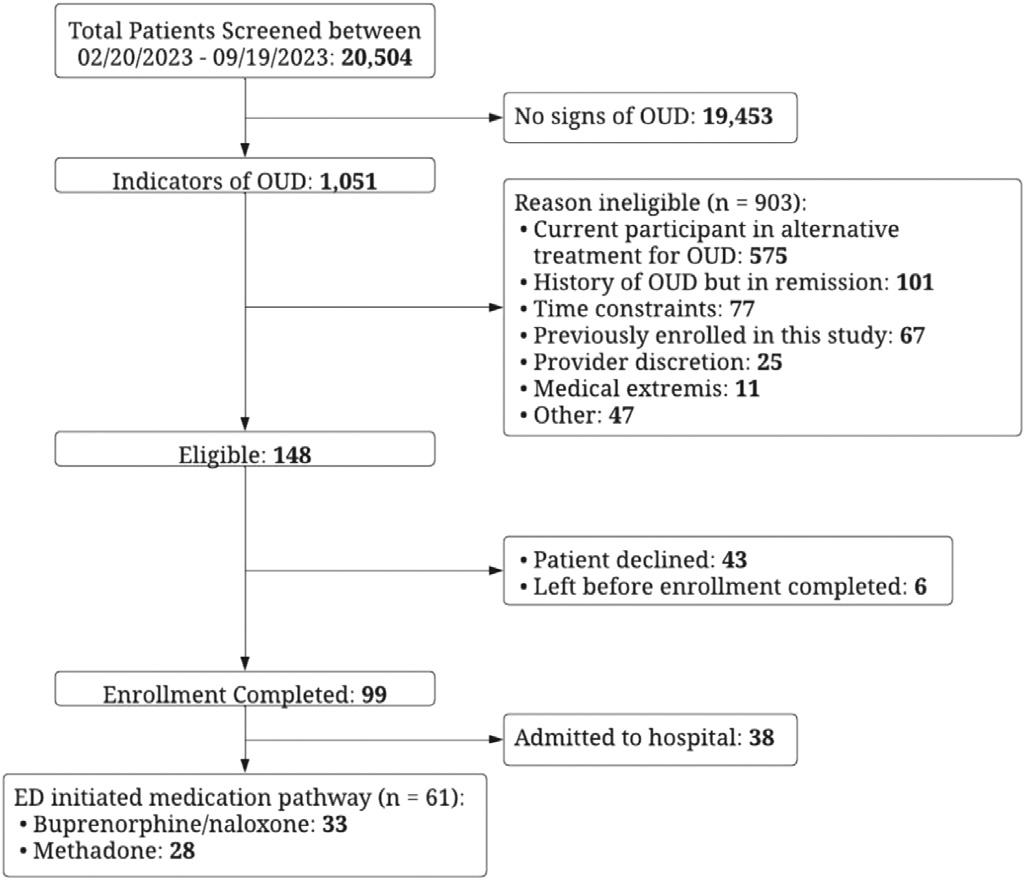
Figure1. Flowchartofscreeningofemergencydepartmentpatients andenrollmentinaSTAR(starttreatmentandrecovery)program. February20–September19,2023.
ED,emergencydepartment; OUD,opioidusedisorder.
Anemergencyclinicianthenusedthe Diagnosticand StatisticalManualofMentalDisorder s,5th Ed,criteriato confirmthediagnosisofOUDandassessreadinessfor treatment.Shareddecision-makingwasusedtodecideonthe mostappropriateMOUDtreatmentpathway:methadoneor buprenorphine/naloxone.Thisprocessinvolvedadiscussion betweentheclinicianandthepatientthatincludedareview oftherisksandbenefitsofeachmedication,theseverityof OUD,thepatient’spriorexperience/preference,andclinical factorssuchasdruginteractionsorQTprolongation.We comparedratesof72-hourfollow-uptreatmentengagement attheopioidtreatmentprogram(OTP)(forthoseon methadone)orattheUVMAddictionTreatmentCenter (ATC)(forthoseonbuprenorphine)forthetwotreatment pathwaysusingachi-squaretestStata/SE18.0(StataCorp, CollegeStation,TX).
Patientssignedadisclosureagreementallowingaccessto theirelectronichealthrecord,whichwassenttotheOTP/ATC viasecureemail.Patientsreceiveddetailsabouttheiroutpatient treatmentappointmentandwereprovidedwithtransportation vouchersandacellphone,whennecessary.Patientswerelinked toanEDpeerrecoverycoachwhoengagedwiththemduring theirEDvisitandcontinuedsupportthroughphonecallsforup to10daysfollowingdischarge.
MethadoneTreatmentPathway: Patientsreceiving methadoneweregiventhestandardUSFoodandDrug Administration-recommendedstartingdoseof30milligrams (mg)orallywithsubsequentdosingof40mgonthefollowing daysifbridgingdoseswererequireduntiltheOTP appointment.23 Theinitialdosewasreducedto20mgfor patientswithknownopioiduseinthepriorfourhours,ifthey
werecurrentlyusingothersedatives,orwithrelevantdrug interactions.Methadonewasnotofferedifthepatienthada respiratoryrate <10breaths/minute,anallergyto methadone,end-stageliverdisease,medicalextremis,ora knownQTc ≥ 500milliseconds.Electrocardiogramswere notroutinelyrequiredbutwereobtainedforriskfactorsin patienthistoryormedications.Basiclabsandurinedrug screenwereobtained.Patientswereinstructedtofollowupat theOTPthenextbusinessday.Ifapatientwasinitiatedon methadoneonaweekendorholiday,theappropriatenumber ofadditionalmethadonedosesweredispensedandheldina lockboxintheEDforobserveddosing.Thepatientwas
instructedtoreturntotheEDtoreceivefollow-updoses. Patientsreturningforre-dosingwerenotrequiredtocheckin asanEDpatientbutweregiventheirmethadonedose, observed,anddocumentedbyanurseusingascripted template(Figure2).24
Buprenorphine/naloxoneTreatmentPathway: Forpatients receivingbuprenorphine,theClinicalOpioidWithdrawal Scale(COWS)guideddosingstrategies.PatientswithaCOWS score <8underwenthomeinitiation.Forscoresof8–11, initiationintheEDwith8mgbuprenorphine/naloxonewas provided,andforscores >12,a16mgdosewasadministered. Allpatientsreceivedatake-homestarterpackwithathree-day

supplyofbuprenorphine/naloxoneandafollow-up appointmentattheATCwithin72hours(Figure3).25
InstitutionalReviewBoardReview: TheUniversityof VermontResearchProtectionsOfficedeemedthisprojectto meetcriteriaforresearchnotrequiringreview.
Patientsenrolledinthemethadoneorbuprenorphine pathwayshadsimilardemographicswithnosignificant differencesbetweengroupsbygender,race,ethnicity,age, modeofEDarrival,orEDdisposition.Ofthe28patientsin themethadonepathway,12(43%)attendedtheOTPfor
ongoingmethadonetreatment.Ofthe33patientsenrolledin thebuprenorphinepathway,15(45%)attendedthe ATCforongoingbuprenorphine/naloxonetreatment. The72-hourratesofsuccessfulfollow-upoutpatient treatmentengagementforpatientsenrolledinthe methadonevsbuprenorphinepathwayswerenot significantlydifferent(relativerisk1.06;95%confidence intervalCI,0.60–1.87).
WeenhancedourED ’ sexistingbuprenorphine-based MOUDprogrambyincorporatingatreatmentpathway

forinitiatingmethadone.Our fi ndingsshowthatEDinitiationofmethadoneforOUDispracticalandachieves 72-hourfollow-upoutpatienttreatmentengagementrates comparabletothoseofbuprenorphine.Whileprevious casestudieshavedocumentedsuccessfulinitiationof methadoneintheED,weareoneofthe fi rstto systematicallyreportontheimplementationofaclinical practicepathwayformethadoneinitiationintheED followedbylinkagetoongoingcare. 22 , 26 Traditionally, methadonehasnotbeenusedintheEDduetothepotential tocausefatalrespiratorydepressionifgivenindoses exceedinganindividual ’ stolerance;however,theEDisan ideallocationtosafelymonitorpatientsduringmethadone initiation. 27 Previousfederalregulationshadrestrictedthe useofmethadonetotreatOUDtolicensedOTPsinthe outpatientsetting. 28 TheEasyMedicationAccessand TreatmentforOpioidAddictionActimprovedthe fl exibilityofMOUDbyallowingpractitionersto dispenseuptoathree-daysupplyofnarcotics,including methadone,forthepurposeofinitiatingmaintenanceor detoxi fi cationtreatment. 29 – 33
Patientspreferselectingtheoptimaltreatmentpathway throughshareddecision-making,whichinvolvesa thoroughcomparisonoftheadvantagesanddisadvantages ofbuprenorphinevsmethadone.Thisapproachfosters informedandcollaborativehealthcarechoicesand potentiallyleadstoimprovedoutcomesandadherence. 22, 34 Wefoundmostpatientswilldirectlysaywhichtreatment pathwaytheypreferduetopastexperiencesoftreatment andprecipitatedwithdrawal.Buprenorphineis advantageousandpreferredasitislogisticallyeasierto take:thereislessriskofrespiratorydepression;thepatient canreceivetake-homemedicationsandprescriptions;and carecanultimatelybemanagedbythepatient ’ sprimary carephysicianwithoutdailytripstothemethadoneclinic fordosing. 19 However,patientswhohaveexperienced buprenorphine-precipitatedwithdrawalorwhocannot toleratecessationoffentanylfortherequiredprebuprenorphineinductiontime(often72hoursorlonger) maybene fi tfrommethadone. 35 Althoughsurveysfromotherinstitutionsindicate physicianshavemorecomfortinitiatingbuprenorphine overmethadone(88%vs45%),ourexperienceshows cliniciansreadilyadoptingthemethadonetreatment pathway. 36 TofosterclinicianacceptanceofEDMOUD, weimplementedseveralstrategies:sharingtestimonials fromourEDpeerrecoverycoaches;facilitatingone-on-one discussionsbetweenprojectchampionsandclinicians;and leveragingdirectclinicalexperience.Theseapproaches alignwithexistingresearch,whichdemonstratesincreased exposuretoimpactedpopulationseffectivelyreduces stigmatowardsthem. 37 Overcomingthesebarriers enhancedtreatmentoptionsthroughthesuccessful
implementationofamethadoneinitiationpathwayforED patientswithOUD.
Limitationsofthisstudyincludeasmallsamplesizethat restrictsthegeneralizabilityofresultsandimpactsstatistical significance.Additionally,theabsenceoflong-termoutcome data,suchassix-monthfollow-upmetrics,limitsinsightsinto theintervention’seffectiveness.Theexclusionofpatients concurrentlyenrolledinothertreatmentprograms introducedselectionbias,potentiallyaffectingthestudy’ s applicabilitytothewiderOUDpopulation.Finally, individualclinicianbiasesmayhaveinfluencedboth participantselectionandtreatmentchoice,potentially affectingstudyoutcomes.
EDinitiationofmethadoneforpatientswithopioiduse disorderispractical,achieves72-hourfollow-uptreatment engagementratescomparabletothoseofbuprenorphine treatment,andprovidesanotheroptionforMOUDthat benefitssomepatients.
AddressforCorrespondence:DanielWolfson,MD,Universityof VermontLarnerCollegeofMedicine,DepartmentofEmergency Medicine,111ColchesterAve.,Burlington,VT05401.Email: Daniel. Wolfson@uvmhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ThisstudywasfundedbytheSubstance AbuseandMentalHealthServicesAdministration(SAMHSA) 1H79TI085330andthe2019UniversityofVermontHealthNetwork InnovationGrant.Therearenootherconflictsofinterestorsources offundingtodeclare.
Copyright:©2024Wolfsonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SpencerMR,MininoAM,WarnerM.DrugoverdosedeathsintheUnited States,2001–2021.2022.Availableat: https://www.cdc.gov/nchs/ products/databriefs/db457.htm.AccessedMarch23,2023.
2.NationalInstituteonDrugAbuse.Drugoverdosedeathrates.2023. Availableat: https://nida.nih.gov/research-topics/trends-statistics/ overdose-death-rates.AccessedMarch23,2023.
3.O’DonnellJ,TanzLJ,GladdenRM,etal.Trendsinandcharacteristicsof drugoverdosedeathsinvolvingillicitlymanufacturedfentanyls-United States,2019–2020. MMWRMorbMortalWklyRep. 2021;70(50):1740–6.
4.MattsonCL.Notesfromthe field:trendsingabapentindetection andinvolvementindrugoverdosedeaths 23statesandthe DistrictofColumbia,2019–2020. MorbMortalWklyRep. 2022;71(19):664–6.
5.KariisaM,PatelP,SmithH,etal.Notesfromthe field:xylazinedetection andinvolvementindrugoverdosedeaths-UnitedStates,2019. MorbMortalWklyRep. 2021;70(37):1300–2.
6.FriedmanJ,MonteroF,BourgoisP,etal.Xylazinespreadsacross theUS:agrowingcomponentoftheincreasinglysyntheticand polysubstanceoverdosecrisis. DrugAlcoholDepend. 2022;233:109380.
7.WeinerSG,BakerO,BernsonD,etal.One-yearmortalityofpatients afteremergencydepartmenttreatmentfornonfatalopioidoverdose. AnnEmergMed. 2020;75(1):13–7.
8.HawkK,HoppeJ,KetchamE,etal.Consensusrecommendationson thetreatmentofopioidusedisorderintheemergencydepartment. Ann EmergMed. 2021;78(3):434–42.
9.HerringAA.Postoverdoseinitiationofbuprenorphineafternaloxoneprecipitatedwithdrawalisencouragedasastandardpracticein theCaliforniaBridgenetworkofhospitals. AnnEmergMed. 2020;75(4):552–3.
10.SnyderH,KalminMM,MoulinA,etal.Rapidadoptionoflow-threshold buprenorphinetreatmentatCaliforniaemergencydepartments participatingintheCABridgeprogram. AnnEmergMed. 2021;78(6):759–72.
11.D’OnofrioG,O’ConnorPG,PantalonMV,etal.Emergencydepartmentinitiatedbuprenorphine/naloxonetreatmentforopioiddependence:a randomizedclinicaltrial. JAMA. 2015;313(16):1636–44.
12.BoganC,JenningsL,HaynesL,etal.Implementationofemergency department-initiatedbuprenorphineforopioidusedisorderinarural southernstate. JSubstAbuseTreat. 2020;112S:73–8.
13.HuhnAS,HobelmannJG,OylerGA,etal.Protractedrenalclearanceof fentanylinpersonswithopioidusedisorder. DrugAlcoholDepend. 2020;214:108147.
14.ComerSDandCahillCM.Fentanyl:receptorpharmacology,abuse potential,andimplicationsfortreatment. NeurosciBiobehavRev. 2019;106:49–57.
15.D’OnofrioG,HawkKF,PerroneJ,etal.Incidenceofprecipitated withdrawalduringamultisiteemergencydepartment-initiated buprenorphineclinicaltrialintheeraoffentanyl. JAMANetwOpen. 2023;6(3):e236108.
16.ShearerD,YoungS,FairbairnN,etal.Challengeswithbuprenorphine inductionsinthecontextofthefentanyloverdosecrisis:acaseseries. DrugAlcoholRev. 2022;41(2):444–8.
17.SpadaroA,FaudeS,PerroneJ,etal.Precipitatedopioidwithdrawal afterbuprenorphineadministrationinpatientspresentingtothe emergencydepartment:acaseseries. JAmCollEmergPhysicians Open. 2023;4(1):e12880.
18.SueKL,CohenS,TilleyJ,etal.Apleafrompeoplewhousedrugsto clinicians:newwaystoinitiatebuprenorphineareurgentlyneededinthe fentanylera. JAddictMed. 2022;16(4):389–91.
19.SchoenfeldEM,WestaferLM,BeckSA,etal. “Justgivethemachoice”: patients’ perspectivesonstartingmedicationsforopioidusedisorder intheED. AcadEmergMed. 2022;29(8):928–43.
20.VarshneyaNB,ThakrarAP,HobelmannJG,etal.Evidenceof buprenorphine-precipitatedwithdrawalinpersonswhousefentanyl. JAddictMed. 2022;16(4):e265–8.
21.BartG.Maintenancemedicationforopiateaddiction:thefoundationof recovery. JAddictDis. 2012;31(3):207–25.
22.ChurchB,ClarkR,MohnW,etal.Methadoneinductionforapatientwith precipitatedwithdrawalintheemergencydepartment:acasereport. JAddictMed. 2023;17(3):367–70.
23.SubstanceAbuseandMentalHealthServicesAdministration (SAMHSA).Tip63:medicationsforopioidusedisorder.2021.Available at: https://store.samhsa.gov/product/tip-63-medications-opioid-usedisorder/pep21-02-01-002.AccessedFebruary21,2024.
24.CABridge.Methadonehospitalquickstart.2023.Availableat: https:// cabridge.org/resource/methadone-hospital-quick-start/ AccessedMay11,2023.
25.CABridge.Buprenorphineemergencydepartmentquickstart.2023. Availableat: https://bridgetotreatment.org/resource/buprenorphinebup-hospital-quick-start/.AccessedApril8,2024.
26.HuoS,HeilJ,SalzmanMS,etal.Methadoneinitiationintheemergency departmentforopioidusedisorder:acaseseries. JEmergMed. 2023;64(3):391–6.
27.BartG.Maintenancemedicationforopiateaddiction:thefoundationof recovery. JAddictDis. 2012;31(3):207–25.
28.SubpartC Certificationandtreatmentstandardsforopioidtreatment programs.Availableat: https://www.govregs.com/regulations/ expand/title42_chapterI_part8_subpartC_section8.12 AccessedMay12,2023.
29.DrugEnforcementAdministration.Dispensingofnarcoticdrugsto relieveacutewithdrawalsymptomsofopioidusedisorder.2023. Availableat: https://www.federalregister.gov/documents/2023/08/08/ 2023-16892/dispensing-of-narcotic-drugs-to-relieve-acute-withdrawalsymptoms-of-opioid-use-disorder.AccessedSeptember21,2023.
30.LaksJ,KehoeJ,FarrellNM,etal.Methadoneinitiationinabridge clinicforopioidwithdrawalandopioidtreatmentprogramlinkage: acasereportapplyingthe72-hourrule. AddictSciClinPract. 2021;16(1):73.
31.21CFR1306.07 Administeringordispensingofnarcoticdrugs.2024. Availableat: https://www.ecfr.gov/current/title-21/chapter-II/part-1306/ subject-group-ECFR1eb5bb3a23fddd0/section-1306.07 AccessedApril3,2023.
32.DrugEnforcementAdministration.DEA’scommitmenttoexpanding accesstomedication-assistedtreatment.2022.Availableat: https:// www.dea.gov/press-releases/2022/03/23/deas-commitmentexpanding-access-medication-assisted-treatment AccessedApril3,2023.
33.BILLS-116hr2281rfs.pdf.2020.Availableat: https://www.govinfo.gov/ content/pkg/BILLS-116hr2281rfs/pdf/BILLS-116hr2281rfs.pdf AccessedApril3,2023.
34.YarboroughBJH,StumboSP,McCartyD,etal.Methadone, buprenorphineandpreferencesforopioidagonisttreatment:a qualitativeanalysis. DrugAlcoholDepend. 2016;160:112–8.
35.SilversteinSM,DaniulaityteR,MartinsSS,etal. “Everythingisnotright anymore”:buprenorphineexperiencesinaneraofillicitfentanyl. IntJ DrugPolicy. 2019;74:76–83.
36.HeilJ,GanetskyVS,SalzmanMS,etal.Attitudesonmethadone utilizationintheemergencydepartment:aphysiciancross-sectional study. WestJEmergMed. 2022;23(3):386–95.
37.CorriganPWandNieweglowskiK.Stigmaandthepublichealth agendafortheopioidcrisisinAmerica. IntJDrugPolicy. 2018;59:44–9.
JosephMiller,MD,MS*
DanielGrahf,MD†
HashemNassereddine,MD‡
JimmyNehme,MD§
Jo-AnnRammal,BS*
JacobRoss,DO§
KaitlinRose,MD∥
DanielHrabec,MD*
SamTirgari,MD*
ChristopherLewandowski,MD*
SectionEditor:PatrickMeloy,MD
*HenryFordHealthandMichiganStateHealthServices,Departmentof EmergencyMedicine,Detroit,Michigan
† AdvocateHealth,DivisionofCriticalCareMedicine,Chicago,Illinois ‡ CorewellHealthUniversityHospital,DepartmentofEmergencyMedicine, RoyalOak,Michigan
§ HenryFordHealthandMichiganStateHealthSciences,DepartmentofInternal Medicine,Detroit,Michigan
∥ UniversityofMichigan,DepartmentofEmergencyMedicine, AnnArbor,Michigan
Submissionhistory:SubmittedSeptember18,2023;RevisionreceivedJanuary30,2024;AcceptedApril4,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18472
Background: Growingdataindicatesthatthiaminedeficiencyoccursduringacuteillnessintheabsence ofalcoholusedisorder.Ourprimaryobjectivewastomeasureclinicalfactorsassociatedwiththiamine deficiencyinpatientswithsepsis,diabeticketoacidosis,andoncologicemergencies.
Methods: Thiswasananalysisofpooleddatafromcross-sectionalstudiesthatenrolledadult emergencydepartment(ED)patientsatasingleacademiccenterwithsuspectedsepsis,diabetic ketoacidosis,andoncologicemergencies.Weexcludedpatientswhohadknownalcoholusedisorderor whohadreceivedEDthiaminetreatmentpriortoenrollment.Investigatorscollectedwholeblood thiaminelevelsinadditiontodemographics,clinicalcharacteristics,andavailablebiomarkers.We definedthiaminedeficiencyasawholebloodthiaminelevelbelowthenormalreferencerangeand modeledtheadjustedassociationbetweenthisoutcomeandage.
Results: Therewere269patients,ofwhomtheaverageagewas57years;46%werefemale,and80% wereBlack.Fifty-five(20.5%)patientshadthiaminedeficiency.Inunivariateanalysis,age >60years (oddsratio[OR]2.5,95%confidenceinterval[CI],1.3–4.5),femalegender(OR1.9,95%CI1.0–3.4), leukopenia(OR4.9,95%CI2.3–10.3),moderateanemia(OR2.8,95%CI1.5–5.3),and hypoalbuminemia(OR2.2,95%CI1.2–4.1)wereassociatedwiththiaminedeficiency.Inadjusted analysis,thiaminedeficiencywassignificantlyhigherinfemales(OR2.1,95%CI1.1–4.1),patients >60years(OR2.0,95%CI1.0–3.8),andpatientswithleukopenia(OR5.1,95%CI2.3–11.3).
Conclusion: Inthisanalysis,thiaminedeficiencywascommonandwasassociatedwithadvancedage, femalegender,andleukopenia.[WestJEmergMed.2024;25(5)675–679.]
Thiamine(vitaminB1)isacrucialcofactorfornumerous metabolicprocesses,especiallycarbohydratemetabolism.1 Itsdeficiencyisassociatedwithdiseaseswithsignificant morbidity,includingWernicke-Korsakoffsyndromeand beriberi.2 Dataincriticalillnessalsoshowsanassociation withincreasedmorbidityandmortalityindependentofthese specificsyndromes.3,4
Thiaminestoresareentirelydependentonregulardietary intakeorartificialsupplementation,andbodystorescan
becomedepletedwithinthreeweekswithoutadequate intake.5–7 Studiesindicatethatconditionsroutinelyseenin theemergencydepartment(ED)thatincreasemetabolic strainareassociatedwiththiaminedeficiency,including diabeticketoacidosis(DKA),sepsis,andcancer.3,4,8–13 In studiesofseveresepsisandsepticshock,upto35%ofpatients showthiaminedeficiency,withevidencethatlevelsimprove withrecoveryinchildren.3,8,9,14 CasereportsofWernicke’ s encephalopathyinpatientswithcancerarenumerous.15–19 In recentobservationalstudiesofgastrointestinaland hematologicalcancerpatients,thiaminedeficiencywas commonandassociatedwithneurologicalsymptoms.20 Studieshavealsodemonstratedthiaminedeficiencyinupto 35%ofchildrenandadultswithDKA.10,11
Althoughtheexistingliteraturedemonstratesan associationbetweensuchdiagnosesandthiaminedeficiency, furtherassessmentofclinicalriskfactorsfordeficiencycould definewhomaybenefitmostfromthiaminetreatment.Inthis study,wesoughttoexploretheassociationofclinicalrisk factorswiththiaminedeficiencyinEDpatients.Such informationcouldguidefuturetherapeuticandpreventative approachesinthemanagementofat-riskpatients.
DesignandSetting
Thisisananalysisofpooleddatafromtwocross-sectional studiesperformedatasingle-center,urbanacademicmedical center.Enrollmentoccurredinthecenter’sED,whichhas approximately92,000patientencounterseachyearand servesaprimarilyBlackpopulation.Thisresearchwas approvedbytheinstitutionalreviewboard,whichgranted waiverofinformedconsentforthestudy.
Thisanalysiswasinclusiveofadultpatients(age ≥18years)intheEDfromtwostudies.The firststudy enrolledpatientswithdiabeticorinfectiousemergencies fromApril2015–February2018.Thesecondstudyenrolled patientswithactivemalignancybetweenMarch 2017–October2018.Forbothstudies,weexcludedpatients whohadknownalcoholusedisorderorreceivedthiamine treatmentintheEDorthroughhomesupplementationprior toenrollment.
Eligiblepatientsprovidedawholebloodsampleinthe ED,whichmeasuresthiamine-diphosphate.Thesamples wereprotectedfromlight,frozen,andsenttoanoffsite laboratory(WardeMedicalLaboratory,AnnArbor,MI)for thiamine-leveltestingusinggaschromatography–mass spectrometry.Wecollecteddemographics,clinical characteristics,andin-hospitalmortalitydataonallpatients. Wealsorecordedlaboratoryinformationobtainedduring routinecareintheED,includingchemistriesandblood
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencypatientswithhighmetabolic strain,suchasoccursincriticalillness,have signi fi cantratesofthiaminede fi ciencyinthe absenceofalcoholusedisorder.
Whatwastheresearchquestion?
Canclinicalfactorspredictpatientsmost likelytohavethiaminede fi ciencyinthe absenceofalcoholusedisorder?
Whatwasthemajor findingofthestudy?
Factorssuchasage > 60years(OR2.0,95% CI1.0 – 3.8)andleukopenia(OR5.1,95%CI 2.3 – 11.3)areassociatedwithde fi ciency.
Howdoesthisimprovepopulationhealth?
These fi ndingspointtotheneedforfurther investigationintomicronutrientde fi ciencyin populationsthatemergencyclinicians commonlyserve.
counts.Toaccountformissinglaboratorydataforserum albuminandhematologyresults,weperformedmultiple imputationpriorto finalanalysis.Becausepreclinicaldata suggeststhatmetforminmayinterferewithintestinal thiaminetransporters,dataspecifictometforminusewas alsocollected.21 Finally,werecordedanyclinical documentationofabnormalgaitordiagnosisofdelirium throughoutapatient’sEDorhospitalstay.Wedidnot performstandardizedassessmentofgait,delirium,or nutritionalstatus.
Weevaluatedclinicalcharacteristicsandoverall prevalenceofthiaminedeficiencyusingdescriptivestatistics. Discretedatawasreportedasfrequenciesandpercentages. Wereportedcontinuousdataasmeansormedianswhere appropriate.Analysisconsistedofunivariatecomparisons andmultivariablelogisticregressiontoassessriskfactorsfor theprimaryoutcomeofthiaminedeficiency,definedasa wholebloodlevelbelowthecentrallab’sreferencerange (38–122microgramsperliter).Basedoncommonclinically meaningfulcutoffs,wecreatedcategoricalvariablesforage >60years(primarycovariateofinterest)andlaboratory findingsofleukopenia(whitebloodcellcount <4 × 109/L), moderateanemia(hemoglobin <10gramsperdeciliter [g/dL]),andhypoalbuminemia(serumalbumin <3.4g/dL). Withstatisticallysignificantcategoricalvariables,we
performedstepwiselogisticregression(significancelevelfor entry0.2andtostay0.1)toconstructa finalmodelthatwas inclusiveofage >60years,gender,presenceofleukopenia, andhypoalbuminemia.Analysisalsoincludedtestingforan interactionofgenderandage >60years.
Resultsarereportedasoddsratios(OR)witha95% confidenceinterval(CI).A P -value <0.05(two-tailed)was consideredstatisticallysignificantforalltests.Duetothe exploratorynatureofthisanalysis,wedidnotperforma poweranalysisandusedthesamplesizeavailable. WeusedSAS9.4(SASInstitute,Inc,Cary,NC)for allanalyses.
Therewere269patientsenrolledfromMarch 2015–October2018.Theirmeanagewas57years,and46% werefemale.MostpatientsidentifiedasBlack(80%).There were55(20.5%)patientswhohadthiaminedeficiency.When comparedtopatientswithnormalthiaminelevels,thiaminedeficientpatientswereolder(P = 0.001)andmorecommonly female(P = 0.04).Wereportdemographicandclinical characteristicswithcomparisonsbythiaminestatus in Table1.
Significantlaboratory findingsassociatedwiththiamine deficiencyinthecohortincludedleukopenia,anemia,and hypoalbuminemia.Intheadjustedanalysis,femalegender, leukopenia,andage >60yearsweresignificantlyassociated withthiaminedeficiency. Table2 demonstratesthese unadjustedandadjustedassociations.Finally,unadjusted ratesofin-hospitalmortality,60-daymortality, findingsof abnormalgait,anddeliriuminpatientswithorwithout thiaminedeficiencyareshownin Table3.
Itiswellestablishedthatthiaminedeficiencycanresult fromalcoholusedisorderorseverenutritionaldeficiencies. However,thiaminedeficiencyisalsoprecipitatedbyacute illnesswithhighmetabolicdemand,anddataindicatesitmay becommoninconditionssuchasDKA,sepsis,andcancer. Determiningadditionalclinicalfactorsassociated withthiaminedeficiencyinsuchpopulationscould aidintailoringthiamineadministrationto appropriatepatients.
WithinthisanalysisofEDpatientswithsepsis,DKA,and cancer,wefoundthat20.5%ofpatientswerethiamine deficientbasedonEDbloodlevels.Weidentifiedadvanced age,femalegender,andleukopeniaashavinggreater adjustedoddsofthiaminedeficiency.Theseresultsongender andleukopeniaareunique.Priordataindicatesan associationbetweenadvancedageandthiaminedeficiency.22 Genderorthepresenceofleukopeniaarenotwell-described riskfactors.PriorresearchindicatesthatB12deficiencyis morecommoninmen,23 butwearenotawareofdata indicatingahigherriskofthiaminedeficiencybasedon
Table1. Demographicsandclinicalcharacteristicsofpatientsbased onpresenceorabsenceofthiaminedeficiency.
Normal thiamine N = 214 Thiamine deficiency N = 55 P-value
Demographics
Female,no.(%)91(42.5)32(58.2)0.04
Age,years,mean(SD)54.8(18.0)63.6(17.6)0.001
Age >60years, no.(%) 89(41.6)35(63.6)0.003
Blackrace,no.(%)169(79.0)47(85.5)0.28
Medicalhistory,no.(%)
Diabetesmellitus*123(57.5)22(40.0)0.02
Metforminuse33(15.4)11(20.0)0.41
Myocardialinfarction20(9.4)2(3.6)0.17
Chronickidneydisease57(26.6)16(29.1)0.72
Hypertension131(61.2)35(63.6)0.74
Stroke26(12.2)6(10.9)0.80
Cancer74(34.6)29(52.7)0.01
Congestiveheartfailure19(8.9)6(10.9)0.64
Laboratoryvalues
Whitebloodcell × 109/L, mean(SD)
Creatinine,mg/dL,mean (SD)
Serumalbumin,g/dL3.43(0.83)2.86(0.89) <0.001
Bodymassindex, kg/m2,mean(SD)
*Diabetesmellitusincludedanypatientwiththisclinical diagnosis(type1or2).Regardlessofbeingpartofthediabetic ketoacidosiscohort. g/dL,gramsperdeciliter; mg,milligrams; kg/m2,kilogramsper squaremeter.
femalegender.The findingthathypoalbuminemiamaybe associatedwiththiaminedeficiencyisalsonovel,although this findingdidnotreachstatisticalsignificanceinan adjustedanalysis.Itisalsonoteworthythatthisanalysis includedmostlyBlackpatients.Muchoftheexisting literatureonthiaminedeficiencyincriticalillnessisinclusive ofamainlyWhitepopulation.3,10,20,22 Nonetheless,wefound
Table2. Unadjustedandadjustedanalysisofpatientcharacteristicsandlaboratoryvaluesassociatedwiththiaminedeficiency. Unadjustedanalysis* Adjustedanalysis
Oddsratio(95%CI) P-valueOddsratio(95%CI) P-value
Femalegender1.88(1.03–3.43)0.0392.13(1.11–4.07)0.02
Age >60years2.46(1.33–4.54)0.0041.98(1.03–3.81)0.04
Cancer2.11(1.16–3.84)0.015
Diabetesmellitus2.03(1.11–3.71)0.022 WBC <4*109/L4.87(2.31–10.30) <0.0015.12(2.31–11.30) <0.001
Albumin <3.4g/dL2.20(1.19–4.08)0.0121.82(0.94–3.54)0.08
Hemoglobin <10g/dL2.81(1.49–5.32)0.002
*Categoricalvariablesincludedinstepwiselogisticregressionmodel.Adjustedanalysisdisplaysonlyresultsforretainedvariables. CI,confidenceinterval; WBC,whitebloodcellcount.
Table3. Unadjustedclinicaloutcomesbasedonpresenceor absenceofthiaminedeficiency.
60-daymortality,no.(%)34(15.9)15(27.3)0.05
Abnormalgait,no.(%)58(27.1)25(45.5)0.009
Delirium,no.(%)64(30.1)22(40.0)0.16
overallcomparableratesofthiaminedeficiencywithina Blackcohort.
Nutritionaldeficiencymaybecontributorytoour findings.Whilewedidnotperformnutritionalsurveysin thesecohorts,otherresearchindicatesthatEDpatientshave significantratesofmalnutrition,approachingashighas60% intheelderly.24 Futureresearchinthisareacouldbenefit fromspecificmeasuresoffoodinsecurityandnutritional statusindiversepopulations.Whilewecouldpresumethat lowalbuminlevelsarereflectiveofpoornutritionalstatus,it ischallengingtodeterminewhetherhypoalbuminemiaisdue topoorproteinintakevsinflammatoryconditions orhighmetabolicdemandsthatsuppress albuminsynthesis.23
Thecurrentstudyhasseveralnotablelimitations.First,we includedanarrowsubsetofdiagnoses,whichlimitsthe generalizabilityofthese findingstootherconditions.Overall patientenrollmentwaslowduetolimitedcoordinator coverage,whichmayhaveintroducedbiasinpatient selection.Asnoted,wedidnotperformstandardized nutritionalassessmentsorneurologicalassessmentsthat mighthaveteasedouttheclinicalimpactofthiamine deficiency.Ofnote,ourresultshighlighteddetectionofacute
deficiencyanddidnotmeasureglobalthiaminestores.We performedthisinanurbansettingwithsignificantratesof foodinsecurity.Such findingsmaynottranslateto suburbansettings.
Thestudywasalsounderpoweredtoassesscertaindrugs associatedwiththiaminedeficiencysuchasfurosemide.25 Nonetheless,theseresultsaddtoagrowingbodyofevidence onthiaminedeficiencyinEDpatientswithconditionssuchas DKA,sepsis,andcancerwhodonothavealcoholuse disorder.3,10,11,20 Furthertestinginbroaderpopulationsis neededtomeasurehowage,gender,nutritionalstatus,and otherclinicalfactorsinterrelatewiththiaminedeficiency.
InouruniquestudypopulationofEDpatientswithouta historyofalcoholusedisorderwhohadsepsis,canceror diabeticketoacidosis,independentriskfactorsforthiamine deficiencywereadvancedage,femalegender,and leukopenia.Furtherresearchisindicatedtodefinethe epidemiologyofthiaminedeficiencyinabroadcohortof adultswithacuteillness.
AddressforCorrespondence:JosephMiller,MD,MS,2799WGrand Blvd.,Detroit,MI48202.Email: jmiller6@hfhs.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Fundingfortheworkwasthrougha unrestrictedphysicianscientistawardgiventoJosephMillerby HenryFordHealth(grantnumberA20300).Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Milleretal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.LonsdaleD.Areviewofthebiochemistry,metabolismandclinical benefitsofthiamin(e)anditsderivatives. EvidBasedComplement AlternatMed. 2006;3(1):49–59.
2.DonninoMW,VegaJ,MillerJ,etal.Mythsandmisconceptionsof Wernicke’sencephalopathy:Whateveryemergencyphysicianshould know. AnnEmergMed. 2007;50(6):715–21.
3.DonninoMW,CarneyE,CocchiMN,etal.Thiaminedeficiencyin criticallyillpatientswithsepsis. JCritCare. 2010;25(4):576–81.
4.HolmbergMJ,MoskowitzA,PatelPV,etal.Thiamineinsepticshock patientswithalcoholusedisorders:anobservationalpilotstudy. JCrit Care. 2018;43:61–4.
5.WhitfieldKC,BourassaMW,AdamolekunB,etal.Thiaminedeficiency disorders:diagnosis,prevalence,andaroadmapforglobalcontrol programs. AnnNYAcadSci. 2018;1430:3–43.
6.SicaDA.Loopdiuretictherapy,thiaminebalance,andheartfailure. CongestHeartFail. 2007;13(4):244–7.
7.VelezRJ,MyersB,GuberMS.Severeacutemetabolicacidosis(acute beriberi):anavoidablecomplicationoftotalparenteralnutrition. J ParenterEnteralNutr. 1985;9(2):216–9.
8.AttaluriP,CastilloA,EdrissH,etal.Thiaminedeficiency:an importantconsiderationincriticallyillpatients. AmJMedSci. 2018;356(4):382–90.
9.RajKM,BaranwalAK,AttriSV,etal.Thiaminestatusinchildrenwith septicshockfromadevelopingcountry:aprospectivecase-control study. JTropPediatr. 2021;67(1):fmaa107.
10.MoskowitzA,GraverA,GibersonT,etal.Therelationshipbetween lactateandthiaminelevelsinpatientswithdiabeticketoacidosis. JCrit Care. 2014;29(1):182.e5–8.
11.RosnerEA,StrezleckiKD,ClarkJA,etal.Lowthiaminelevelsinchildren withtype1diabetesanddiabeticketoacidosis:apilotstudy. PediatrCrit CareMed. 2015;16(2):114–8.
12.AndersenLW,HolmbergMJ,BergKM,etal.Thiamineasanadjunctive therapyincardiacsurgery:arandomized,double-blind,placebocontrolled,phaseIItrial. CritCare. 2016;20:92.
13.DonninoMW,CocchiMN,SmithlineH,etal.Coronaryartery bypassgraftsurgerydepletesplasmathiaminelevels. Nutrition. 2010;26(1):133–6.
14.EqueyL,AgyemanPKA,VeraguthR,etal.Serumascorbicacidand thiamineconcentrationsinsepsis:secondaryanalysisoftheSwiss pediatricsepsisstudy. PediatrCritCareMed. 2022;23(5):390–4.
15.BrownSandHutt-WilliamsS.Wernicke’sencephalopathyinadvanced cancer. BMJSupportPalliatCare. 2022;12(4):460–2.
16.KocaO,DemirB,DerinS,etal.AcasereportofWernickeKorsakoff syndromeinapatientwithcholangiocellularcarcinoma:an underestimatedcauseofencephalopathyincancerpatients. Medicine. 2022;101(48):e31904.
17.NikjooA,RashidH,ChungR,etal.ArarecaseofWernicke encephalopathyinstageIVgastriccancer. Neurocase. 2022;28(1):123–5.
18.SlimS,AyedK,TrikiW,etal.Gayet-Wernicke’sencephalopathy complicatingprolongedparenteralnutritioninpatienttreatedforcolonic cancer-acasereport. BMCNutr. 2022;8(1):83.
19.ZhangY,WangL,JiangJ,etal.Non-alcoholicWernicke encephalopathyinanesophagealcancerpatientreceiving radiotherapy:acasereport. WorldJClinCases. 2022;10(17):5810–5.
20.IimuraY,AndohS,KawamataT,etal.Thiaminedeficiencyand neurologicalsymptomsinpatientswithhematologicalcancerreceiving chemotherapy:aretrospectiveanalysis. JNeurosciRuralPract. 2021;12(4):726–32.
21.LiangX,ChienHC,YeeSW,etal.Metforminisasubstrateandinhibitor ofthehumanthiaminetransporter,THTR-2(SLC19A3). MolPharm. 2015;12(12):4301–10.
22.LeeDC,ChuJ,SatzW,etal.Lowplasmathiaminelevelsinelder patientsadmittedthroughtheemergencydepartment. AcadEmerg Med. 2000;7(10):1156–9.
23.MargalitI,CohenE,GoldbergE,etal.VitaminB12deficiencyandthe roleofgender:across-sectionalstudyofalargecohort. AnnNutrMetab. 2018;72(4):265–71.
24.PereiraGF,BulikCM,WeaverMA,etal.Malnutritionamongcognitively intact,noncriticallyillolderadultsintheemergencydepartment. Ann EmergMed. 2015;65(1):85–91.
25.KattaN,BallaS,AlpertMA.Doeslong-termfurosemidetherapycause thiaminedeficiencyinpatientswithheartfailure?Afocusedreview. AmJ Med. 2016;129(7):753.e7–11.
FarhanChaudhry,MD,MS*†
ElianaSmall,DO‡
StevenJ.Korzeniewski,PhD†
DanaBenyas,MD*
LydiaRoss,MD§
AlexB.Hill,BS†
AmitVahia,MD,MPH∥
CandaceMcNaughton,MD,PhD¶
PhillipLevy,MD,MPH#
JosephMiller,MD,MS‡
SectionEditor:KennethScottWhitlow,DO
*DepartmentofSurgery,DetroitMedicalCenter/WayneStateUniversitySchool ofMedicine,Detroit,Michigan
† DepartmentofFamilyMedicineandPopulationHealthSciences,WayneState UniversitySchoolofMedicine,Detroit,Michigan
‡ DepartmentofEmergencyMedicine,HenryFordHealthandMichiganState UniversityHealthSciences,Detroit,Michigan
§ DepartmentofEmergencyMedicine,BaylorCollegeofMedicine, Houston,Texas
∥ AscensionSt.JohnHospital,Detroit,Michigan
¶ DepartmentofEmergencyMedicine,UniversityofToronto,Toronto,Canada
# DepartmentofEmergencyMedicine,WayneStateuniversity,Detroit,Michigan
Submissionhistory:SubmittedMay14,2023;RevisionreceivedApril13,2024;AcceptedApril16,2024
ElectronicallypublishedJuly17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18126
Background: Patientswhopresenttotheemergencydepartment(ED)withseverehypertension definedasasystolicbloodpressure(SBP) ≥180millimetersofmercury(mmHg)ordiastolic(DBP) ≥120 (mmHg)withoutevidenceofacuteend-organdamageareoftendeemedhighriskandtreatedacutelyin theED.However,thereisadearthofevidencefromlargestudieswithlong-termfollow-upforthe assessmentofmajoradversecardiovascularevents(MACE).Weconductedthelargeststudytodateof patientspresentingwithseverehypertensiontoidentifypredictorsofMACEandexaminewhetherblood pressureatdischargeisassociatedwithheightenedrisk.
Methods: WeenrolledEDpatientswithaSBPof180–220mmHgbutwithoutsignsofend-organ damageandfollowedthemforoneyear.TheprimaryoutcomewasMACEwithinoneyearofdischarge. Secondarily,weperformedapropensity-matchedanalysistotestwhetherSBP ≤160mmHgat dischargewasassociatedwithreducedMACEat30days.
Results: Atotalof12,044patientswereenrolled.TheprevalenceofMACEwithinoneyearwas1,865 (15.5%).Olderage,malegender,historyofcardiovasculardisease,cerebrovasculardisease,diabetes, smoking,presentationwithchestpain,alteredmentalstatus,dyspnea,treatmentwithintravenousand oralhydralazine,andoralmetoprololwereindependentpredictorsforone-yearMACE.Additionally, dischargewithanSBP ≤160mmHgwasnotassociatedwith30-dayMACE-freesurvivalafterpropensity matching(hazardratio0.99,95%confidenceinterval0.78–1.25, P = 0.92).
Conclusion: One-yearMACEwasrelativelycommoninourcohortofEDpatientswithsevere hypertensionwithoutacuteend-organdamage.However,dischargebloodpressurewasnotassociated with30-dayorone-yearMACE,suggestingthatBPreductioninandofitselfisnotbeneficialinsuch patients.[WestJEmergMed.2024;25(5)680–689.]
Background
Hypertensiveemergenciesareasignificantconcernwhen patientspresenttotheemergencydepartment(ED)with severelyelevatedbloodpressure(BP),definedas ≥180 millimetersofmercury(mmHg)systolicor ≥120mmHg diastolicpressure.1 Nevertheless,veryfewofthesepatients haveevidenceofacuteend-organdamage.(EOD)andoften haveonlyseverelyuncontrolledchronichypertension (HTN).2,3 SeverelyelevatedBP,butwithoutEOD,isoften called “hypertensiveurgency.” Thereissignificantlong-term evidenceregardingcharacteristicsassociatedwithincreased majoradversecardiovascularevents(MACE)forpatients withchronicallyelevatedBP,butthereisalackoflong-term evidenceregardingcharacteristicsassociatedwithincreased MACEinthosepresentingwithhypertensiveurgencyinthe ED.2 Evenwithoutthislong-termevidence,thereis temptationandexpectationtoacutelylowerBP.Recent retrospectiveEDstudiessuggestthattheremaybeno immediatebenefitfromacutelyreducingBPinthesettingof severehypertensionwithoutEOD.4,5 Thiscouldbebecause thereisevidencetosuggestagreaterriskforsevereadverse effectswithantihypertensivesinthesettingofseverely elevatedBPwithoutEOD.5,6 However,largeroutcomedata forreachingalowertargetBPforthispopulationpriorto dischargeislacking.
Rationale
Giventhattherearesignificantlymorepatientspresenting totheEDwithsevereHTNwithoutEOD,identifying characteristicsassociatedwithMACEinthiscohorthas becomeincreasinglymoreimportant.1,3,7 Likewise,thereis uncertaintyregardingthevalueofreachingasignificantly lowertargetpressurepriortodischargefromtheEDforthis cohort.AssessingtheimpactofreachingatargetBPon MACEwouldalsoprovideclinicalutilityfor emergencyphysicians.
Toaddresstheseuncertainties,weconductedthelargest observationalcohortstudytodatetoidentifyriskfactorsfor MACEatoneyearamongpatientsdischargedhomefromthe EDwhopresentedwithseverelyelevatedBPwithoutEOD. Wealsotestedwhethertargetingalowersystolicblood pressure(SBP)priortodischargewasassociatedwithreduced MACEat30daysinthiscohort.Ourhypothesisforour primaryanalysiswasthatpatientswithSBPbetween 180–220mmHgwithoutdocumentedEODandtreatedwith anti-hypertensiveswouldhavelessMACEatoneyear.We usedanSBPgreaterthan180mmHgasthisisthecutofffor hypertensivecrisisaccordingtotheAmericanHeart Association(AHA).8 Oursecondaryhypothesiswasthat propensity-matchedpatientswithaninitialSBPbetween 180–220mmHgwithoutdocumentedevidenceofEOD,but
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Patientswithworseninglevelsofuncontrolled bloodpressurehaveincreasingriskoflongtermcardiovascularevents.
Whatwastheresearchquestion?
Howcommonaremajoradverse cardiovascularevents(MACE)withinone yearforpatientsdischargedfromtheEDwith severehypertension?
Whatwasthemajor findingofthestudy?
While15.5%hadacardiovascularevent withinayear,wefoundnoassociationwith initialEDencounterforso-called “ hypertensiveurgency. ”
Howdoesthisimprovepopulationhealth?
Severehypertensionintheabsenceof hypertensiveemergencyidenti fi espatientsat signi fi cantriskofMACE,butacuteBP reductionintheEDmaynotbe immediatelybene fi cial.
whoweredischargedwithalowertargetSBP(≤160mmHg), wouldhavelessMACEat30days.WeusedaSBP ≤160mm Hg,as >160mmHgisthecutoffforGrade2hypertensionand hasbeenshowntobeassociatedwithahighriskofEOD.8
Subjectsincludedpatientsbetween18–90yearsofagewho presentedtooneofeightEDsinanintegratedhealthsystem (HenryFordHealthSystem,Detroit,MI)fortreatmentof anymedicalconditionbetweenJanuary2014–July2015. TheseEDsconsistedofonetertiary-careacademicteaching hospital,threecommunityteachinghospitals,andfour freestandingEDs.TheEDlocationsservedurban communitieswithlowsocioeconomicstatusaswellas suburban,moreaffluentcommunities.WeincludedED encountersthatresultedindischargefromtheEDanddid notresultinadmissionorbeingplacedinobservation.Adult patientencounterswereabstractedfromtheelectronichealth record(EHR)sharedbyallEDsincludedinthestudy(Epic SystemsCorporation,Verona,WI).WeincorporatedallED encountersforadultsforinitialabstraction.Ofthese encounters,weexcludedpatientencounterswithSBP >220mmHgorbelow <180mmHgandencounterswith missingorincorrectlycodedpatientvariables.Forthisstudy
wedefinedacuteEODasanenteredclinicaldiagnosisat presentationofacutecoronarysyndrome,stroke,heart failureexacerbation,oracutekidneyinjuryintheEHR.
Thestudywasapprovedbytheinternationalreviewboard (IRB)atHenryFordHospitalSystem.Datacollection includedthepatient’ s firstEDBPanddischargeBP, demographicinformation,comorbidities,insurancestatus, tobaccouse,andclinicalpresentation.Weusedchief complaintastheprimarysymptomfortheirvisit.Wealso recordedwhethertheywerereferredtotheEDprimarilyfor hypertension(HTN).Comorbiditiesincludedhistoryof cardiovasculardisease,stroke,diabetes,andchronickidney disease.Weclassifiedinsurancestatusintoinsured (Medicare,Medicaid,commercial)ornotinsured.Wealso collectedthemedianincomefortheZIPcodewhereeach patientresided.ThemedianincomesforeachZIPcodewere groupedintoquartilesforsubsequentanalysis.Thepatient’ s antihypertensivetherapiesduringthevisitwererecorded. WeusedamethodcriteriondescribedbyWorsteretal.9 1)Twodataabstractorsweretrainedwiththestudycriteria describedabove;.2)Theinclusionandexclusioncriteriaused wereasstatedabove.3)Variablesweredefinedpriorto analysis.4)Weusedastandardabstractionform.
5)Abstractorperformancewasbasedonthenumberof recordsscreenedandverifiedbasedonaccuracyof incorporatingthecriteriainrecordselection.6)Abstractors duringabstractionofrecordswereblindedtothehypothesis. 7)Interobserverreliabilitywasdiscussed,8)butitwaswas notmeasuredduetolownumberofobserverstoperforma statisticaltest.9)Thehealthrecorddatabasewasidentified. 10)Methodofsamplingwasdescribedpreviously.11)Any missingvariabledataofpreidentifiedvariablesofinterest resultedinremovaloftheentirepatientrecordfromthe study.12)TheIRBdidreviewthestudy.
Eachpatientwastrackedinthehealthsystem’sEHRupto oneyearfollowingthedateofthepatient’ s firstED encounter.Weconsideredpatientstohavetheprimary outcome,MACE,iftheyhadadocumenteddiagnosisof acuteheartfailure,acutestroke(hemorrhagicorischemic), acutecoronarysyndrome,ordeathwithinoneyearfollowing theirEDvisit.Weselectedaone-yearfollow-upperiodto increasethenumberofeventsandtherebyimprovestatistical powergiventhesamplesize.
Ifapatienthadmorethanonecardiovasculareventinthe 12-monthperiod,weonlycountedtheir firsteventforthe purposeoftheprimarystudyoutcome.DocumentedMACE fromEpic’sCareEverywherenetworkwasalsoincluded,so thatwewouldnotmissanyMACEifthepatientpresentedto anoutsidehealthcaresystemwithinthestateofMichigan usingthesameEHR.Thisincorporatesdeathsidentifiedby
thestateofMichigan;however,ifaneventoccurredoutside thestate,thenthiscouldnotbeincorporated.TheCare EverywherenetworkincorporatestheEHRsofmultiplecare systemsinthestateofMichigan,andrecordscreatedwithin thesecaresystemsareautomaticallyuploadedandvalidated inCareEverywhere.However,outsiderecordsmayhave beenmissedand,thus,maybealimitationtothestudy.
Thesecondaryoutcomewastime-to-MACEwithin 30daysfromdischarge:a)becauseeventsthatoccurnear dischargearemoreplausiblycausallyrelatedthanareevents thatoccurlongafterdischarge;andb)totestfordifferences ininstantaneousriskvelocity(ie,hazardratio[HR]) conditionalonsurvival(ie,toidentifyfactorsthatare associatedwithshorterintervals-to-MACEat30days).
Weuseddescriptivestatisticstoassessbaseline demographicandclinicalcharacteristicsofthecohort. Continuousvariableswereexpressedasmedianinterquartile range(IQR),whilecategoricaldatawereexpressedas frequenciesandproportions(ie,%).TheMann-Whitney U-testandthechi-squaretestwereusedtoexamine differencesindistributionsandproportions,respectively.In theprimaryregressionanalysis,weusedlogisticregressionto estimatemagnitudesofassociationbetweenpatient characteristicsandMACEatoneyear.Wechoselogistic regressionbecausethesymmetricnatureoftheoddsratio (OR)enablesinferencesaboutassociationsbetween antecedentsandoutcomesorviceversa,unlikerelative risk.10 Symmetryisidealgiventhepotentialforconfounding byindicationinnon-randomizedclinicalstudies;thatis,only ORsallowinferencesabouttreatmentgivenoutcomeand viceversa.10,11 Potentialconfoundersweredefinedapriorias factorsthatareassociatedwithbothanexposureand outcomewhoseadjustmentalterstheestimatedmagnitudeof associationby >10%.Weemployedatwo-stagemodel selectionstrategy.Firstly,weselectedallfactorsthatwere associatedwithdischargeSBPandMACEbothinourstudy andbasedonpriorknowledge(ie,fullmodel).Next,to reducethenumberofcovariablesandpotentialimpactof multicollinearity,weusedanagnosticstrategythat optimizedmodelaccuracymeasuredbypartialareaunder thecurveata10% fixed-false-positiverateacross1,000 bootstrapreplicatesoftraining(70%)andtestingdatasets (30%).WhenconsideringZIPcodecharacteristics,we includedarandomintercepttoaccountforsimilarities amongpatientsnestedinthesamegeographicarea.
Inthesecondaryregressionanalysis,weusedtheCox proportionalhazardsmodeltoestimatethemagnitudeof associationbetweenpatientfactorsatEDdischargeand time-to-MACEat30days.Giventhepotentialfor confoundingbyindication,andbecausewewantedto examinetheclinicalrelevanceofdischargeSBP,we performedapropensity-matchedanalysistobalancethe
distributionofpotentialconfoundersbetweenstudygroups thathadSBP ≤160mmHgor >160mmHg.12 Weusedthe MatchItR-packageto findpairsofobservationswithsimilar propensityscoresbutthatdifferintreatmentstatus.13 That is,theprimarylogisticregressionmodelwasusedtoderive propensity-matchedgroups;factorsthatnevertheless differedbetweenpropensity-matchedgroupswereincluded inthe finalmultivariableCoxmodelaspotential confounders.Inboththeprimaryandsecondaryanalyses, magnitudesofassociation(ie,ORandHR)with95% confidenceintervals(CI)thatdonotincludethenullestimate (ie, ‘1.0’)arestatisticallysignificant.Allanalysiswas performedusingRversion4.0.3(RFoundationfor StatisticalComputing,Vienna,Austria).
DemographicsandClinicalCharacteristics
Of222,028EDencountersreviewedduringthestudy period,13,042(5.8%)patientsmetinclusioncriteria.There were12,044(92.4%)whohadcompleterecordsandwere usedforsubsequentanalysis.Theoverallnumberofpatients thathadMACEwithinoneyearwas1,865(15.5%),inclusive of176deaths(9.5%).
Table1 demonstratestheoveralldemographicand clinicalcharacteristicsofthecohort.Univariateanalysis foundthatpatientswithMACEwithinoneyearfollowing EDdischargeweresignificantlymorelikelytobeolder(ages 65–90,OR6.66[95%CI5.44–8.24] P < 0.001),andmale (779/1,865[41.8%]vs3,719/10,179[36.5%];OR1.25 [1.13–1.38], P < 0.001),butlesslikelytobeBlack(646/1.865 [34.6%]vs3,814/10,179[37.5%];OR0.89[0.80–0.98], P < 0.05).AlsosignificantlyassociatedwithMACEwithin oneyearwerehistoryofcardiovasculardisease(495/1,865 [26.5%]vs251/10,179[2.47%],OR14.3[13.2–16.8], P < 0.001);cerebrovasculardisease(202/1,865[10.8%]vs 136/10,179[1.33%],OR8.97[7.18–11.2], P < 0.001); diabetesmellitus(607/1,865[32.5%]vs1,092/10,179[10.7%], OR4.02[3.58–4.51], P < 0.001);andchronickidneydisease (352/1,865[18.9%]vs337/10,179[3.31%],OR6.80 [5.80–7.97], P < 0.001).Patientswhousedtobacco,had insurance,andthosewholivedinaZIPcodewithamedian annualincomeof$54,973–$70,439US(75%quartile)were morelikelytohaveMACEwithinoneyearincomparisonto thosewithlessthan$44,583(25%quartile)(OR2.59 [2.24–2.87], P < 0.001,3.81[2.78–5.39], P < 0.001,and1.17 [1.02–1.34], P < 0.05, respectively).
Table1. Patientcharacteristicsandunivariatelogisticregressioncomparisonsforoutcomes.
Demographic
Age rangeinyears,n(%)
18–45
46–65
65–90
Male,n(%)
2,243/12,044(18.6%)2,139/10,179(21.0%)104/1,865(5.58%)
4,995/12,044(41.5%)4,409/10,179(43.3%)586/1,865(31.4%)2.74(2.22–3.41) P < 0.001
4,806/12,044(39.9%)3,631/10,179(35.7%)1,175/1,865(63.0%)6.66(5.44–8.24) P < 0.001
4,498/12,044(37.3%)3,719/10,179(36.5%)779/1,865(41.8%)1.25(1.13–1.38) P < 0.001
Black,n(%) 4,460/12,044(37.0%)3,814/10,179(37.5%)646/1,865(34.6%)0.89(0.80–0.98) P < 0.05
Medicalhistory
Cardiovasculardisease,n(%)746/12,044(6.19%)251/10,179(2.47%)495/1,865(26.5%)14.3(12.2-16.8) P < 0.001
Cerebrovasculardisease, n(%) 338/12,044(2.81%)136/10,179(1.33%)202/1,865(10.8%)8.97(7.18–11.2) P < 0.001
Diabetesmellitus,n(%)1,699/12,044(14.1%)1,092/10,179(10.7%)607/1,865(32.5%)4.02(3.58–4.51) P < 0.001
Chronickidneydisease,n(%)689/12,044(5.72%)337/10,179(3.31%)352/1,865(18.9%)6.80(5.80–7.97) P < 0.001
Socialhistory
Tobaccosmoker,n(%)3,176/12,044(26.3%)2,358/10,179(23.1%)818/1,865(43.8%)2.59(2.24–2.87) P < 0.001
Hasinsurance,n(%) 11,258/12,044(93.5%)9,431/10,179(92.7%)1,827/1,865(98.0%)3.81(2.78–5.39) P < 0.001
ZIPcodemedianannualincomerangein$US
Lessthan44,583,n(%)4,663/12,044(38.7%)3,979/10,179(39.1%)684/1,865(36.7%) 44,584–54,972,n(%)1,857/12,044(15.4%)1,549/10,179(15.2%)308/1,865(16.5%)1.16(1.00–1.34)0.05 54,973–70,439,n(%)2,634/12,044(21.9%)2,192/10,179(21.5%)442/1,865(23.7%)1.17(1.02–1.34) P < 0.05 (Continued onnextpage)
Table1. Continued.
VariableTotalNo1-yearMACE1-yearMACEOR(95%CI)
Over70,440,n(%) 2,889/12,044(24.0%)2,459/10,179(24.2%)431/1,865(23.1%)1.02(0.89–1.16) 0.77
Presentation
Headache,n(%) 398/12,044(3.31%)346/10,179(3.41%)52/1,865(2.79%)0.81(0.60–1.08)0.70
Chestpain(%) 990/12,044(8.22%)799/10,179(7.86%)191/1,865(10.2%)1.34(1.13–1.58) P < 0.001
Alteredmentalstatus(%)92/12,044(0.772%)53/10,179(0.530%)39/1,865(2.09%)4.01(2.63–6.05) P < 0.001
Dyspnea(%) 465/12,044(3.86%)329/10,179(3.23%)136/1,865(7.29%)2.36(1.91–2.89) P <
Referralforhypertension(%)781/12,044(6.48%)675/10,179(6.63%)106/1,865(6.02%)0.85(0.68–1.04)0.13
Systolicbloodpressurerange inmmHg(%)
180–200 9,572/12,044(79.5%)8,158/10,179(80.1%)1,414/1,865(75.8%)
201–220
Diastolicbloodpressurerange inmmHg(%)
Lessthan80
80–100
2,472/12,044(20.5%)2,021/10,179(19.9%)451/1,865(24.2%)1.288 (1.15–1.45)
1,530/12,044(12.7%)1,182/10,179(11.6%)348/1,865(18.6%)
6,600/12,044(54.8%)5,577/10,179(54.8%)1,023/1,865(54.9%)0.62(0.54
Greaterthan101 3,914/12,044(32.5%)3,420/10,179(33.6%)494/1,865(26.5%)0.49(0.42–0.57)
Treatment 3,528/12,044(29.3%)2,345/10,179(23.0%)1,183/1,865(63.3%)5.80(5.22–6.44) P < 0.001
Clonidineoral(%) 1,220/12,044(10.1%)897/10,179(8.81%)323/1,865(17.3%)2.17(1.89–2.49)
EnalaprilatIV(%) 114/12,044(0.946%)74/10,179(0.727%)40/1,865(2.14%)2.99(2.01–
Labetaloloral(%) 241/12,044(2.00%)159/10,179(1.56%)82/1,865(4.40%)2.90(2.20–3.79)
827/12,044(6.87%)559/10,179(5.49%)268/1,865(14.4%)2.89(2.47–3.37)
Metoprololoral(%) 1,603/12,044(13.3%)809/10,179(7.95%)794/1,865(42.6%)8.59(7.64–9.65)
316/12,044(2.62%)174/10,179(1.71%)142/1,865(7.61%)4.74(3.77
655/12,044(5.44%)319/10,179(3.13%)336/1,865(18.0%)6.79(5.78–7.99)
Hydralazine IV(%) 1,086/12,044(9.01%)656/10,179(6.4%)430/1,865(23.1%)4.35(3.81
Outcome
DischargesystolicbloodpressurerangesinmmHg(%)
90–160 4,356/12,044(36.2%)3,641/10,179(35.8%)715/1,865(38.3%)
160–220 7,688/12,044(63.8%)6,538/10,179(64.2%)1,150/1,865(61.6%)0.90(0.81–0.99) P < 0.05
Acutecoronarysyndrome(%)1,190/12,044(9.88%)
1,190/1,865(63.8%)
Heartfailureadmission(%)705/12,044(5.85%) 705/1,865(37.8%)
Stroke(%) 488/12,044(4.05%) 488/1,865(26.2%)
Death(%) 176/12,044(1.46%) 176/1,865(9.47%)
MACE, majoradversecardiacevent; OR,oddsratio; CI,confidenceinterval; mmHG,millimetersofmercury; IV,intravenous.
SymptomsandPresentingBP
Patientspresentingwithchestpain,alteredmentalstatus, dyspneaandaSBPof201–220insteadof180–200mmHg weresignificantlymorelikelytosufferMACE(OR1.34 [1.13–1.58], P < 0.001,4.01[2.63–6.05], P < 0.001,2.36 [1.91–2.89], P < 0.001,and1.29[1.15–1.45], P < 0.001), respectively.Achiefcomplaintofheadacheorreferralfor HTNwasnotsignificantlyassociatedwithMACE(OR0.81 [0.60–1.08], P = 0.17andOR0.85[0.68–1.04], P = 0.13).
Patientswithapresentingdiastolicbloodpressureranging
from80–100mmHgor101mmHgandgreaterwereless likelytosufferMACE(OR0.62[0.54–0.72], P < 0.001;0.49 [0.42–0.57], P < 0.001).
Therewere3,528/12,044(29.3%)patientswhohadany antihypertensivetreatmentduringtheirEDvisit,andthis treatmentwassignificantlyassociatedwithahigherrateof MACEwithinoneyearcomparedtothosewhodidnot receiveantihypertensivetreatment(OR5.80,95%CI
5.22–6.44).Univariateanalysisforeachtypeof antihypertensivemedicationdemonstratedthateachwas associatedwithMACEatoneyear.Furthermore,patients whoweredischargedwithaSBPabove160–220mmHgwere lesslikelytosufferMACEatoneyear(OR0.90,95%CI 0.81–0.99, Table1).
Tocreateaparsimoniousmultivariablelogisticregression model,thebootstrapreceiveroperatingcurvemodelretained age,gender,historyofcardiovasculardisease, cerebrovasculardisease,diabetesmellitus,chronickidney, smokingstatus,presentationwithchestpain,alteredmental status,dyspnea,treatmentwithhydralazine(oralandIV), oralmetoprolol,anddischargeSBPasvariables(Supplement S1).Thebefore-variableselectionAUCwas0.842,andthe after-variableselectionAUC0.839.Giventhattheestimated variancefromtherandomeffectofpatientZIPcodeswaslow (0.0759,SD0.275),thisrandomeffectwasnotincludedin our finalanalysis.Intheadjustedmodel,olderagerange, malegender,historyofcardiovasculardisease, cerebrovasculardisease,diabetesmellitus,smoking,
Table2. Multivariablelogisticregressionofpatientcharacteristics withamajoradversecardiacevent(MACE)atone-yearvsthose withoutaMACE. OR(95%CI) P-value
Agerangeinyears
18–45
46–65
1.90(1.53–2.39) P < 0.001
65–90 4.04(3.27–5.04) P < 0.001
Male 1.35(1.19–1.52) P < 0.001
Historyofcardiovasculardisease4.62(3.78–5.66) P < 0.001
Historyofcerebrovasculardisease4.62(3.48–6.15) P < 0.001
Historyofdiabetesmellitus1.64(1.41–1.91) P < 0.001
Historyofchronickidneydisease1.19(0.96–1.48)0.11
Tobaccosmoker 1.35(1.19–1.54) P < 0.001
Chestpain 1.38(1.13–1.68) P < 0.01
Alteredmentalstatus 3.27(1.92–5.49) P < 0.001
Dyspnea 1.47(1.11–1.93) P < 0.001
TreatedwithhydralazineIV1.98(1.67–2.35) P < 0.001
Treatedwithhydralazineoral2.15(1.74–2.65) P < 0.001
Treatedwithmetoprololoral4.88(4.26–5.59) P < 0.001
DischargesystolicbloodrangesinmmHg
90–160
161–220 0.94(0.83–1.06)0.295
Multivariatelogisticregressionresultsafterachievingparsimonywith ROC-bootstrap method.
CI,confidenceinterval; IV,intravenous; mmHg,millimeters ofmercury.
presentationwithchestpain,alteredmentalstatus,treatment withIVandoralhydralazine,andoralmetoprololwere significantindependentpredictorsforMACEatoneyear (Table2).Themodelhadapseudo-R2 of0.260. RetrospectivepoweranalysisperformedwithGPower3 (https://www.psychologie.hhu.de/arbeitsgruppen/ allgemeine-psychologie-und-arbeitspsychologie/gpower. html)showedastatisticalpowerofthisstudyover90%.14
Wecomparedshort-termoutcome(30-dayMACE-free survival)forpatientswhoweredischargedwithaSBP ≤160mmHgvsthosewithSBP >160mmHg.Therewere significantgroupdifferencesforage,gender,historyof cerebrovasculardisease,smoking,presentationofheadache, chestpain,presentingSBP,andreceptionofantihypertensive treatmentsbetweenthosewhoweredischargedwithaSBP ≤160mmHgcomparedtothosewithaSBP >160mm Hg(Table3).
Afterpropensity-scorematching,4,356controlswithSBP >160mmHgand4,356patientswithSBP ≤160mmHgwere matched.Chestpainwastheonlyvariablethatremained significantlydifferentbetweenpatientswithSBP >160mm HgvsthosewithSBP <160mmHg.Thiswasincludedasa variableforadjustmentforthefollowingCoxregression analysisfor30-dayMACE(Table4).Inthepropensity-score matchedanalysisachiefcomplaintofchestpainwas independentlyassociatedwithanincreasedriskof30-day MACE(HR1.76,95%CI1.30–2.37, P < 0.001, Table4). However,dischargewithanSBP ≤160mmHgwasnot associatedwith30-dayMACE-freesurvivalafteradjusting forcovariates(HR0.99,95%CI0.78–1.25, P = 0.92). Survivalcurveshowsnosignificantsurvivalbenefitfor patientswhoweredischargedwithaSBP ≤160mmHgvs thosedischargedwithSBP >160mmHg(Figure1).
ThisstudyrepresentsalargecohortofEDpatientswith severelyelevatedBPwithoutEOD.TherewerehighMACE ratesatoneyear(15.5%)inourcohort.Independentrisk factorsforMACEatoneyearafteranEDvisitwhere severelyelevatedBPwasnotedincludedadvancedage,male gender,historyofcardiovasculardisease,cerebrovascular disease,diabetesmellitus,andsmoking.Presentingsignsof chestpainandalteredmentalstatus,butnotheadache,were alsofoundtobeindependentriskfactorsforMACE. Treatmentwithhydralazineormetoprololwasassociated withhigherratesofMACEatoneyearaswell.Similarto findingsbyPateletal,wefoundthatreferraltotheEDforBP managementbyaclinicwasnotassociatedwithanincreased riskofMACEatoneyear.4
Weusedpropensity-matchedanalysistomeasurethe associationbetweenreducingSBPintheEDandmore immediate,30-dayMACE-freesurvival.Inthisanalysis,
Table3. Pre-vspost-propensityscorematchingpatientcharacteristicsbetweenpatientsdischargedwithasystolicblood pressure ≤160vs >160.
Historyofcardiovascular disease(%)
477/7,688(6.2%)269/4,356(6.18%)0.949277/4,356(6.29%)269/4,356(6.18%)0.72
Historyofcerebrovascular disease(%) 198/7,688(2.58%)140/4,356(3.21%)
Historyofdiabetes mellitus(%) 1,086/7,688 (14.1%) 614/4,356(14.1%)0.979597/4,356(13.4%)614/4,356(14.1%)0.60
Historyofchronickidney disease(%)
458/7,688(5.97%)231/4,356(5.30%)0.132209/4,356(5.07%)231/4,356(5.30%)0.28 Tobaccosmoker(%)1,972/7,688 (25.7%) 1,204/4,356 (27.6%)
Headache(%) 223/7,688(2.90%)176/4,356(4.03%) P < 0.01212/4,356(4.82%)176/4,356(4.04%)0.06
Chestpain(%) 422/7,688(5.48%)569/4,356(13.0%) P < 0.001421/4,356(9.69%)569/4,356(13.1%) P < 0.001
Alteredmentalstatus(%)56/7,688(0.73%)37/4,356(0.85%)0.47645/4,356(0.90%)37/4,356(0.85%)0.38
Dyspnea(%) 229/7,688(2.98%)236/4,356(5.41%) P < 0.001228/4,356(5.23%)236/4,356(5.42%)0.70
PresentingmedianSBP inmmHg(IQR) 190(184–199)190(184–198)
antihypertensive treatment(%)
0.001189(184–198)190(184–198)0.45
Pre-vspost-propensitydemographics,presentationcharacteristicsandoutcomes. T-test comparisonsareshown. SBP,systolicbloodpressure; mmHg,millimetersofmercury; IQR,interquartilerange,
therewasnosignificantassociationbetweenareductionin SBP ≤160mmHguponEDdischargeand30-dayMACE. Thiswasfoundevenafterpropensitymatchingforreception ofantihypertensiveagents.Thisdataaddstoprior observationalstudiesshowingnoassociatedbenefitwitha targetBPpriortodischargefromtheED.5
Table4. Coxregressionanalysisfor30-dayMACE*-freesurvival afterpropensitymatching.
Variable30day-MACEHR(95%CI) P-value
Chestpain 1.76(1.30–2.37) P < 0.001
Discharge SBP ≤1600.99(0.78–1.25)0.92
Coxregressionanalysisfor30-dayMACE-freesurvival;discharge SBP≤160 variableisadjustedforchestpainaspresentingclinical symptomafterpropensityscorematching.
*MACE,majoradversecardiacevent; HR,hazardratio; CI, confidenceinterval; SBP,systolicbloodpressure.
Therewasanassociationwithcertainantihypertensive treatmentsintheEDandhigherone-yearMACE.Whileitis unlikelythatthisantihypertensivetreatmentledtohigher ratesofMACEuptooneyearfollowingtreatment,itis plausiblethatcliniciansperceiveaclinicalneedtotreatBPor heartrateimmediatelyinpatientswithhigherriskfor MACE.This findingcoincideswithourpreviouswork illustratingthatseverelyhypertensivepatientswhowereat higherriskforMACEweremorelikelytobegiven medicationsthatquicklylowerBPintheED,suchas nitrates,clonidine,hydralazine,metoprolol,labetalol, enalapril,andnicardipine,inadditiontocontinuingtheir chronicHTNmedications.5 Asrecentdatashowsan associationwithinpatientantihypertensivetreatmentand higherratesofacutekidneyinjuryat30days,futurework mayconsiderthisoutcomeinassessingthepracticeofacute BPloweringintheED.15
Ofnote,wefoundnoassociationbetweenBlackraceand one-yearMACEinpatientswithsevereHTNonadjusted
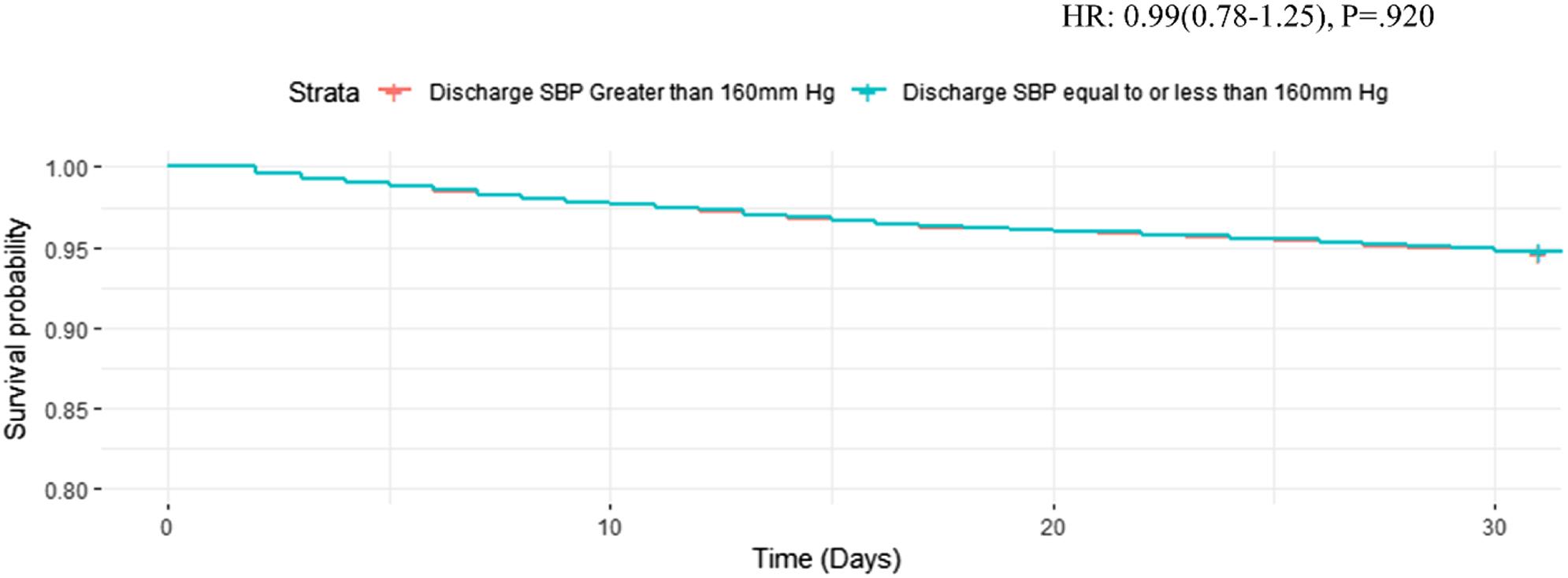
Figure1. 30-dayMACE*-freesurvivalcurvefordischargingpatientwithanSBP ≤160afterpropensityscorematchingandadjustingforchest painaspresentingclinicalsymptom.
*MACE, majoradversecardiacevent; HR,hazardratio; SBP, systolicbloodpressure; mmHg,millimetersofmercury.
analyses.Studieshavepreviouslydemonstratedsignificant associationbetweenBlackraceandincreasedincidenceof MACE,attributingcausationtohigherprevalenceof cardiovascularcomorbidities,genetics,lowersocioeconomic status,anddifferenttreatmentreceivedduring hospitalization.16,17 SevereHTNismorecommoninBlacks andispresentatayoungerageincomparisontootherraces; therefore,theremaybeaprotectivebiasamongthis population.Itisimportanttonote,however,thatchronic HTNisdifferentfromanacutepresentationofsevereHTN, inwhichitiswellestablishedthatBlackshavesignificantly worseoutcomes.18
Inourcohort,chestpain,alteredmentalstatus,and dyspneawerethreechiefcomplaintsindependently associatedwithone-yearMACE.Priordatahasindicated thatpatientswhopresenttotheEDwithchestpain,withor withoutelevatedBP,haveabouta5%chanceofdeveloping MACEatoneyear.19 Ofthe990patientsinthisstudywho presentedwithachiefcomplaintofchestpainandhad severelyelevatedBP,191(19.3%)developedMACEatone year.Ofthe92patientswhopresentedwithalteredmental status,39(42.4%)developedMACE.Additionally,ofthe 465patientswhopresentedwithdyspnea,136(29.2%) developedMACE.Thecombinationofseverelyelevated BPandthesecomplaintsmayindicatepoorcontrolof comorbidconditions,whichcontributestovascular endothelialdysfunctionandacuteend-organinjury.While headacheinthesettingofseverelyelevatedBPisconsidered bysometobeindicativeofahypertensiveemergency,itis notablethatwefoundnoassociationbetweenthisand MACEinourstudy.
Whilehypertensiveemergenciesrequireemergent treatment,bestpracticesremaincontroversialwhenpatients
haveseverelyelevatedBPandlackacuteEOD.1 Often termed “hypertensiveurgency,” amisnomerthatimplies sometypeofurgentinterventionisneeded,currentguidance formanagementofsuchpatientsislargelybasedonexpert opinionandvariessignificantly.20 Observationaldatashows noassociatedbenefitforoutpatientclinicreferraltotheED forasymptomaticsevereHTN.4,21 Guidancefromthe AmericanCollegeofEmergencyPhysiciansrecommends againstantihypertensivetherapyintheEDforpatientswith asymptomaticsevereBPelevation.22 Whilesomehave advocatedthatthepotentialfordevelopingEODis concerningenoughwithseverelyelevatedBPtojustify urgentmanagementintheED,particularlyinpopulations withpoorEDfollow-upcare,thereisnodefinitiveevidence thatinterveninginsuchamannerimprovesshort-orlongtermoutcomes.20 Infact,ourstudyprovidesnewevidence suggestingthattheincreaseinlong-termriskofMACEin thiscohortismostlyduetoestablishedcardiovascularrisk factors.ReachingalowertargetSBPdoesnotappeartobe beneficial.Whileobservationalstudiessupportthis conclusion,arandomizedclinicalstudyiswarrantedtohelp confirmthisstatement.ManagementofseverelyelevatedBP shouldbereservedfortheoutpatientsetting.Weidentified keypredictorsformortalityinthispopulation,andefforts shouldconcentrateonbetteroutpatientmanagementof patientswiththesecharacteristics.
Animportantlimitationtothisstudyisthepotentialfor unmeasuredconfoundersthatmayhaveaffectedoutcomes. Neitherdidweaccountforpriormedicationadherenceor newlydiagnosedHTN,factorsthatmayimpactaclinician’ s approachtotreatmentintheED.5,21 Anotherlimitationis thelackoflongitudinalfollow-upBPandantihypertensive medicationuseoveroneyearfollowingtheEDvisit.While
otherpublishedreportsindicatethatEDpatientswith severelyelevatedBPoftencontinuetohaveuncontrolledBP, wedidnotcollectsuchlongitudinaldata.4 Furthermore,we failedtocollectpotentiallyrelevantbiomarkerssuchas troponinandB-typenatriureticpeptidetomoreaccurately definepatientswithEOD.Thus,itispossiblethatclinicians mayhavemisseddiagnosingpatientswhomayhavebeen sufferingfromEOD.Eventsthatoccurredoutsidethishealth system,whichwerenotdocumentedintheCareEverywhere network,werenotcaptured,andpatientsmayhavesuffered subclinicalorunreportedevents.Itisunknownhowmany hospitalsareregisteredintheCareEverywherenetwork. Together,theseconsiderationsmayhaveledtoan underestimationofthetotalnumberofevents.
Ourstudyshowsthattheriskofsubsequentmajoradverse cardiovasculareventsinEDpatientswithseverelyelevated bloodpressurewithoutend-organdamageishigh.Patientsat higherriskofMACEoftensufferfromwell-established cardiovascularriskfactors.Whilethesepatientsstandto benefitfromcarefullycoordinatedfollow-upfor cardiovascularriskreduction,reachingatargetBPin theEDisnotassociatedwithimprovedoutcomes.This dataaddstomountingevidenceagainsttheutilityof havingatargetBPpriortodischargefromtheEDand suggestthattheterm “hypertensiveurgency” beavoided todescribesuchindividuals,asthereisnoneedfor urgentintervention.
AddressforCorrespondence:JosephMiller,MD,MS,HenryFord Hospital,DepartmentofEmergencyMedicine,2799WGrandBlvd., Detroit,MI48202.Email: jmiller6@hfhs.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Rossetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PeixotoAJ.Acuteseverehypertension. NEnglJMed. 2019;381(19):1843–52.
2.WheltonPK,CareyRM,AronowWS,etal.ACC/AHA/AAPA/ABC/ ACPM/AGS/APhA/ASH/ASPC/NMA/PCNAguidelineforthe prevention,detection,evaluation,andmanagementofhighblood pressureinadults:areportoftheAmericanCollegeofCardiology/
AmericanHeartAssociationTaskForceonClinicalPracticeGuidelines. Hypertension. 2017;71(6):e13–115.
3.McNaughtonCD,SelfWH,ZhuY,etal.IncidenceofhypertensionrelatedemergencydepartmentvisitsintheUnitedStates,2006to2012. AmJCardiol. 2015;116(11):1717–23.
4.PatelKK,YoungL,HowellEH,etal.Characteristicsandoutcomesof patientspresentingwithhypertensiveurgencyintheofficesetting. JAMAInternMed. 2016;176(7):981–8.
5.LevyPD,MahnJJ,MillerJ,etal.Bloodpressuretreatmentand outcomesinhypertensivepatientswithoutacutetargetorgandamage:a retrospectivecohort. AmJEmergMed. 2015;33(9):1219–24.
6.GrossmanE,MesserliFH,GrodzickiT,etal.Shouldamoratorium beplacedonsublingualnifedipinecapsulesgivenfor hypertensiveemergenciesandpseudoemergencies? JAMA. 1996;276(16):1328–31.
7.JankeAT,McNaughtonCD,BrodyAM,etal.Trendsintheincidenceof hypertensiveemergenciesinUSemergencydepartmentsfrom2006to 2013. JAmHeartAssoc. 2016;5(12):e004511.
8.UngerT,BorghiC,CharcharF,etal.2020InternationalSocietyof Hypertensionglobalhypertensionpracticeguidelines. Hypertension. 2020;75(6):1334–57.
9.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed. 2005;45(4):448–51.
10.GeorgeA,SteadTS,GantiL.What’stherisk:differentiatingriskratios, oddsratios,andhazardratios? Cureus. 2020;12(8):e10047.
11.BoscoJL,SillimanRA,ThwinSS,etal.Amoststubbornbias:No adjustmentmethodfullyresolvesconfoundingbyindicationin observationalstudies. JClinEpidemiol. 2010;63(1):64–74.
12.MiaoB,HernandezAV,AlbertsMJ,etal.Incidenceandpredictorsof majoradversecardiovasculareventsinpatientswithestablished atheroscleroticdiseaseormultipleriskfactors. JAmHeartAssoc. 2020;9(2):e014402.
13.HoD,ImaiK,KingG,etal.MatchIt:Nonparametricpreprocessingfor parametriccausalinference. JStatSoftw. 2011;42(8):1–28.
14.FaulF,ErdfelderE,LangA-G,etal.G*Power3:A flexiblestatistical poweranalysisprogramforthesocial,behavioral,andbiomedical sciences. BehavResMethods. 2007;39(2):175–91.
15.RastogiR,SheehanMM,HuB,etal.Treatmentandoutcomesof inpatienthypertensionamongadultswithnoncardiacadmissions. JAMA InternMed. 2021;181(3):345–52.
16.FraneyEG,Kritz-SilversteinD,RichardEL,etal.Associationofraceand majoradversecardiacevents(MACE):theAtherosclerosisRiskin Communities(ARIC)cohort. JAgingRes. 2020;2020:7417242.
17.CaiA,DillonC,HillegassWB,etal.Riskofmajoradverse cardiovasculareventsandmajorhemorrhageamongWhiteandBlack patientsundergoingpercutaneouscoronaryintervention. JAmHeart Assoc. 2019;8(22):e012874.
18.LacklandDT.Racialdifferencesinhypertension:Implicationsforhigh blood pressuremanagement. AmJMedSci. 2014;348(2):135–8.
19.MolKA,SmoczynskaA,RahelBM,etal.Non-cardiacchestpain: prognosisandsecondaryhealthcareutilization. OpenHeart. 2018;5(2):e000859.
20.KatzJN,GoreJM,AminA,etal.Practicepatterns,outcomes,andendorgandysfunctionforpatientswithacuteseverehypertension:the StudyingtheTreatmentofAcuteHypertension(STAT)registry. Am HeartJ. 2009;158(4):599–606.e591.
21.BrodyA,TwinerM,KumarA,etal.Surveyofemergencyphysician approachestomanagementofasymptomatichypertension. JClin Hypertens. 2017;19(3):265–9.
22.WolfSJ,LoB,ShihRD,etal.Clinicalpolicy:criticalissuesinthe evaluationandmanagementofadultpatientsintheemergency departmentwithasymptomaticelevatedbloodpressure. AnnEmerg Med. 2013;62(1):59–68.
Neutrophil-to-LymphocyteRatioPredictsSepsisinAdultPatients
VamsiBalakrishnan,MD*
AnnaYang,MD†
DonaldJeanmonod,MD*
HarrisonCourie,MD*
SpencerThompson,MD‡
ValerianPeterson,MD§
RebeccaJeanmonod,MD*
SectionEditor:PatrickMeloy,MD
*St.Luke’sUniversityHealthNetwork,Bethlehem,Pennsylvania † RegionalOneHealth,Memphis,Tennessee ‡ LinnCountyEmergencyMedicinePC,CedarRapids,Iowa § MedicalCollegeofWisconsin,DepartmentofEmergencyMedicine, GrandRapids,Michigan
Submissionhistory:SubmittedSeptember14,2023;RevisionreceivedMarch28,2024;AcceptedApril4,2024
ElectronicallypublishedJune28,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18466
Introduction: Determiningwhichpatientswhomeetsystemicinflammatoryresponsesyndrome(SIRS) criteriahavebacterialsepsisisadifficultchallengeforemergencyphysicians.Wesoughttodetermine whethertheneutrophil-to-lymphocyteratio(NLR)couldbeusedtoexcludebacterialsepsisinadult patientswhomeet ≥2SIRScriteriaandarebeingevaluatedforsepsis.
Methods: Consentingadultpatientsmeeting ≥2SIRScriteriaandundergoingevaluationforsepsiswere enrolled.Werecordedpatientage,gender,vitalsigns,andlaboratoryresults.Wethenlaterreviewed healthrecordsforcultureresults,endorgandysfunction,survivaltodischarge,and finaldiagnoses. Patientswereclassifiedashavingsepsisiftheymet ≥2SIRScriteriaandwereultimatelydiagnosed withabacterialsource.Weanalyzeddatausingdescriptivestatisticsandsensitivityand specificityanalyses.Areceiveroperatingcharacteristiccurve(ROC)wascreatedtodetermine testcharacteristics.
Results: Atotalof231patientshadcompletedatasets.Patients’ medianagewas69(interquartilerange [IQR]54–81),and49.6%weremale.Therewere154patients(66.7%)ultimatelydiagnosedwithsepsis withanidentifiedbacterialsource,while77patientswith ≥2SIRScriteriahadnon-infectiousreasonsfor theirpresentations(33.3%).SepticpatientshadamedianNLR12.36(IQR[interquartilerange] 7.29–21.69),comparedtothosewithoutsepsis(medianNLR5.62,IQR3.89–9.11, P < 0.001).TheNLR valueof3appliedasacutoffforsepsishadasensitivityof96.8(95%confidenceinterval[CI]92.2–98.8), andaspecificityof18.2(95%CI10.6–29.0).TheROCforNLRhadanareaunderthe curveof0.74.
Conclusion: Theneutrophil-to-lymphocyteratioisasensitivetooltohelpdeterminewhichpatientswith abnormalSIRSscreenshavebacterialsepsis.[WestJEmergMed.2024;25(5)690–696.]
Theclinicalprogressionofsystemicinflammatory responsesyndrome(SIRS)fromaseriousinfectiontosepsis tosepticshockisamajorcauseofpatientmorbidityand
mortality.Sepsisaffects1.7millionadultsintheUnited Stateseachyear,resultinginatleast350,000deaths.1 Worldwide,sepsisistheleadingcauseofdeath,passing cardiovasculardiseaseandcancer.2
Thehealthcarecostsassociatedwithsepsisarealsohigh, withanestimatedannualeconomicburdenof$57billionin theUSin2019.3 Notsurprisingly,thecostincurredfromany individualcaseofsepsisincreaseswithincreasingdisease severity,anddiseaseseverityincreasesovertime.4,5 Therefore,rapididentificationandtreatmentofsepsishas beenahighprioritywithinthehospitalsettingfordecades, andperformanceimprovementprogramswith standardizationandprotocolizationofsepsismanagement havedemonstratedimprovementinoutcomes.6–8 Since87% ofcasesofsepsisarepresentuponarrivaltothehospital(as opposedtobeinghospitalacquired),emergencyphysicians playacrucialroleinpromptlyrecognizingandintervening withthesehigh-riskpatients.1,9 Emergencyphysiciansare alsotaskedwithlimitingunnecessaryuseofbroad-spectrum antibioticsaspartoftheantibioticstewardshipgoals outlinedbytheInfectiousDiseaseSocietyofAmerica,the SocietyforHealthcareEpidemiologyofAmerica,andthe PediatricInfectiousDiseaseSociety.10
Identificationofsepsiscontinuestobeachallenge. Screeningtoolsbasedonclinicaland/orlaboratorycriteria, suchasQuickSequentialOrganFailureAssessment (q-SOFA)andSIRS,arecommonlyusedtoidentifypatients withsepsis,but15–60%ofpatientswhomeetthosecriteria donotgoontohaveanactualdiagnosisofsepsis.11–13
Cardiacdysrhythmias,primarylungdisease,viralillness, trauma,endocrinedisease,andnumerousotherprocesses canresultinapositiveSIRSorq-SOFAscreen;more importantly,forrisk-stratificationtools,highsensitivityis criticallyimportanttoavoidmissingcasesofsepsis.In multipletrials,SIRSwithsuspicionforinfectionoutperforms qSOFAintermsofsensitivitybutisinferiorfor specificity.14–18 Lactateisanothertoolcommonlyused primarilyforprognosticationandassessmentofresponseto treatmentinpatientswithdiagnosesofsepsis.19,20 Althoughspecificlactatevaluesareusedasdefiningcriteria inthediagnosesofseveresepsisandsepticshock, lactateisneithersensitivenorspecificduring earlysepsis.
Theneutrophil-to-lymphocyteratio(NLR)hasbeen demonstratedtobeareliableandeasy-to-obtainmeasureof patientimmuneresponsetoavarietyofdifferentinfectious andnon-infectiousconditions.21 AnormalNLRisgenerally considered <3,althoughneonatalliteratureusesmore conservativecutoffs.21 TheNLRhasbeenassociatedwith thepresenceofbacteremiaandappearstoberelevantto prognosisandprogressioninsepsis.22–25 Inneonates, researchdemonstratesthattheNLRcanbepredictiveof bothearlyandlatesepsis.26–28 Inthisstudy,wesoughtto determinewhethertheNLRcouldbeusedtoexcludesepsis inadultpatientswhomettwoormoreSIRScriteria orhadapositiveq-SOFAscreenwhowerebeingevaluated forsepsis.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Currentscreeningforbacterialsourcesof sepsisisneithersensitivenorspeci fi c.
Whatwastheresearchquestion?
Cantheneutrophillymphocyteratio(NLR) beusedtoexcludebacterialsepsisinpatients meeting ≥ 2SIRScriteriaforsystemic in fl ammatoryresponsesyndrome?
Whatwasthemajor findingofthestudy?
AnNLRvalueof3hadasensitivityof96.8% (CI92.2 – 98.8),andaspeci fi cityof18.2% (10.6 – 29.0).TheROCforNLRhadanarea underthecurveof0.74.
Howdoesthisimprovepopulationhealth?
Bacterialsepsisisamajorcauseofmorbidity andmortality.TheNLRisasensitiveand inexpensivetoolthatcanhelpdetermine whichpatientshavebacterialsepsis.
Thiswasaprospectivecohortstudyofadult(≥18years) emergencydepartment(ED)patientswhowerebeing evaluatedforsepsis.Allpatientscompletedwritteninformed consentorhadsurrogateinformedconsent.Thestudywas reviewedandapprovedbytheinstitutionalreviewboard.
ThestudytookplaceatasingleacademicEDwithan annualcensusof50,000patients.Patientswereenrolledfrom April2019–March2020.Adultpatientswereeligiblefor enrollmentiftheywerepositiveonSIRSscreening(≥2values present)oronq-SOFAscreeningonarrivaltotheEDand wereundergoingevaluationforsepsis.TheSIRScriteriaare temperature >100.4°Fortemperature <96.8°F;heartrate >90beatsperminute;respiratoryrate(RR) >20orpCO2 < 32millimetersofmercury(mmHg);andwhitebloodcell count >12,000or <4,000,orbandcount >10%.AqSOFA scoreiscalculatedbygivingthepatientapointforaltered mentalstatus,systolicbloodpressurelessthan100mmHg, orRR ≥22,with ≥2pointsconsideredindicativeofhighrisk. Patientswereidentifiedthroughtheelectronichealthrecord (EHR)(EpicSystemsCorporation,Verona,WA),which generatesanautomaticcomputeralertforpatientswith positiveqSOFAandSIRSscreens.Afteridentificationof
potentialpatientsthroughthecomputeralert,eligibility formswerecompletedbyclinicians.
Patientswererequiredtoprovidewritteninformed consent.Incaseswherepatientsweretooill,cognitively impaired,orintubatedandcouldnotconsent,consentwas soughtfromtheirhealthcareproxy,ifavailable.Weexcluded non-English-speakingpatientsandpatientsforwhomtheir evaluationscouldnotbedelayedtoaccommodatethe consentprocess.Pregnantpatientsandpatientstriagedtothe traumabaywerealsoexcluded.Traumabaytriagecriteria arelistedin Appendix1
Aftereligibilityformswerecompletedbyclinicians involvedinthepatients’ care,theformswerescreenedby studyinvestigatorswhothenapproachedthepatientsto obtainconsent.Onceconsentwascompleted,werecorded clinicaldataforeachSIRS-positiveandqSOFApatient enrolled,includingage,gender,vitalsigns,completeblood count(CBC)andlactatelevels.Welaterreviewedhealth recordsoutto90daysforcultureresults;endorgan dysfunction(includingrenalfailure,shockliver,pulmonary failure,cardiacfailure,delirium);survivaltodischarge; disposition(home,rehab,nursingfacility,ordeathwithin 90days);and finaldiagnoses.Wecollecteddataina standardizedExcelspreadsheet(MicrosoftCorp,Redmond, WA)onapassword-protectedcomputerbelongingtoastudy investigator.Alldatawasenteredfromaprepopulatedpulldownmenutoreducedataentryerrors.Onceallclinicaldata collectionwascomplete,thedatabasewaspurgedofpatient identifierspriortoanalysis.
Patientswereclassifiedashavingsepsisiftheymet ≥2 SIRScriteriaor2+ qSOFAcriteriaandwereultimately diagnosedwithabacterialsource.Patientswereclassifiedas nothavingsepsisiftheymetSIRS/qSOFAcriteriabut werediagnosedwithanalternativesourceforthose abnormalitiesandhadnobacterialsourceidentified. Bacterialsourcesofsepsiswereclassifiedasurinary, pulmonary,centralnervoussystem,intra-abdominal,skin andsofttissue,hematogenous,orother.Cutoffvaluesfor analysisofNLRwere3,whichisacommonlyreported numberintheliteratureasbeingabnormallyhigh, and10,whichisavaluereportedtohavenegative prognosticimplications.
OnlyphysicianswhohadcompletedmandatoryCITI trainingandgoodclinicalpracticetrainingconsentedand enrolledpatientsinthisstudy.Althoughallclinicians workingintheEDwereinformedandremindedofthestudy duringweeklyeducationaltimeandwerepermittedto completeeligibilityforms,onlytrainedinvestigatorswere permittedtoenrollpatients.Inadditiontomandatory researchtraining,investigatorsmetwiththeprincipal
investigator(AY)whodesignedthedatacollectiontooland weretrainedinitsuse.
Weanalyzeddatausingdescriptivestatistics.Sensitivity andspecificitycalculationswereperformedusingMedCalc (MedCalcSoftwareLtd,Ostend,Belgium)andVassarStats (RichardLowry1998–2023).Wecreatedreceiveroperating characteristic(ROC)curvestodeterminetestcharacteristics.
Weenrolled233patients.Twohadincompletedatasets, leaving231patientsfordataanalysis.Thepatients’ median agewas69,withaninterquartilerangeof54–81;49.6%were male.Twenty-fivepatients(10.7%)wereadmittedtothe intensivecareunit,18patients(7.7%)diedinthehospital duringtheindexvisitorweredischargedtohospice,and32 (13.7%)diedwithin90daysoffollow-up.Fivepatientswere enrolleddespitenotmeetingSIRSorqSOFAcriteriaon initialpresentation.Theywereincludedinthisanalysisonan intent-to-treatbasis.Furtherpatientcharacteristicsare showninthe Table.
Ofthe231eligiblepatients,154patients(66.7%)were ultimatelydiagnosedwithsepsiswithanidentifiedbacterial source(Figure1).Seventy-sevenhadnon-infectioussources identified(33.3%).Themostcommonlyidentifiedsources werepulmonaryandurinarytract,followedbybacteremia andsofttissueinfections(Figure2).Somepatientshadmore thanoneidentifiedsource.Themostcommonlyidentified reasonsforpatientsmeetingSIRScriteriawithoutbacterial sourceofsepsiswereviralsyndromes(28patients); congestiveheartfailure(10);asthma/chronicobstructive pulmonarydiseaseexacerbations(5);medication/drugs(5); malignancyrelated(5);pneumonitis(5);andcomplications ofendocrinedisease(3).Patientswithsepsiswithan identifiedbacterialsourcehadamedianNLRof12.36 (interquartilerange[IQR]7.29–21.69),comparedtoa medianNLRof5.62(IQR3.89–9.11)inthosethatdidnot haveabacterialsource(P < 0.001)(Figure3).
TheNLRvalueof3appliedasacutoffforsepsishada sensitivityof96.8(95%confidenceinterval[CI]92.2–98.8), andaspecificityof18.2(CI10.6–29.0).Inthispopulation withahighprevalenceofdisease,thepositivepredictive valueofNLRwas70.3(CI63.6–76.2),withanegative predictivevalueof73.7(CI48.6–89.9),withaperformance oddsratioof6.86(CI2.37–19.89)forhavingdisease.When anNLRcutoffof10wasused,thespecificityincreased significantlyto73%,althoughwithamarkedsacrificeof sensitivitydownto60.5%.TheROCforNLRyieldedan areaunderthecurveof0.74(Figure4).
Mosthospitalsusesomevariationofscreeningforsepsis asrequiredtomeetcoresepsismetricsimplementedbythe
Table. Characteristicsofpatientsundergoingevaluationfor bacterialsourceofsepsis.
Total(N = 231)
Medianage(IQR)69(54–81)
Gender(%)
Male114(49.4)
Female117(50.6)
Dispositionfromindexvisit(%)
Home156(67.5)
Assistedlivingandnursinghome55(23.8)
Hospice14(6.1)
Death5(2.2)
Unknown1(0.4)
NumberofSIRScriteria(%) 00(0) 16(2.6) 2102(44.2) 393(40.3) 426(11.3) 54(1.7)
NumberofqSOFAcriteria(%)
094(40.7) 1113(48.9) 223(10)
31(0.4)
IQR,interquartilerange; SIRS,systemicinflammatoryresponse syndrome; qSOFA,quickSequentialOrganFailureAssessment.
CentersforMedicareandMedicaidServices.Theseare typicallybasedonSIRSand/orqSOFAcriteriawith suspicionforinfection.Manyhospitalshavebestpractice advisorywarningsautomaticallyimplementedintotheEHR basedonthesestratificationtoolstohelpcliniciansearlier identifypotentiallyillpatientswhomaybenefitfrom escalationofcare.Thisinitialrecognitionofahigherrisk cohortofpatientsisanimportant firststep.Becausethese initialscreensarehistoricallyinsensitive(bothwith sensitivitiesofabout50%)butalsonotadequatelyspecific,a secondaryscreenwouldbeusefultohelpdeterminewhich patientsmighthavesepsisasthereasonfortheir presentation.13,29 ANLRisasimplecalculation requiringonlyacompletebloodcount(CBC)with differentialtoberesultedandcouldbeusedasa secondaryscreen.
Althoughvirtuallyeverypatientwithsuspectedsepsishas theirCBCanalyzed,thegoalofthisbloodtestistraditionally todetermineabsolutewhitebloodcellcountandpercentage ofbands,astheseareexistingcriteriawithinSIRS.TheNLR hasnotbeenpositedasbeingusefulinthedeterminationto initiateantibioticsorasapotentialscreenforsepsis.Fora computer-generatedalert,usingaNLRiseasytoimplement andcouldprovideusefulguidanceinprescreened high-riskpatients.
Inourstudy,patients allofwhomwereprospectively beingevaluatedforsepsis aNLR >3gaveanoddsratioof 6.9ofsepsis,withasensitivityof96.8%.Thissuggeststhatit maybereasonabletoinitiatebroad-spectrumantibioticsin high-riskpatientswithanelevatedNLR.SinceaCBChasa rapidlabturnaroundtime,thismayhastentreatmentin
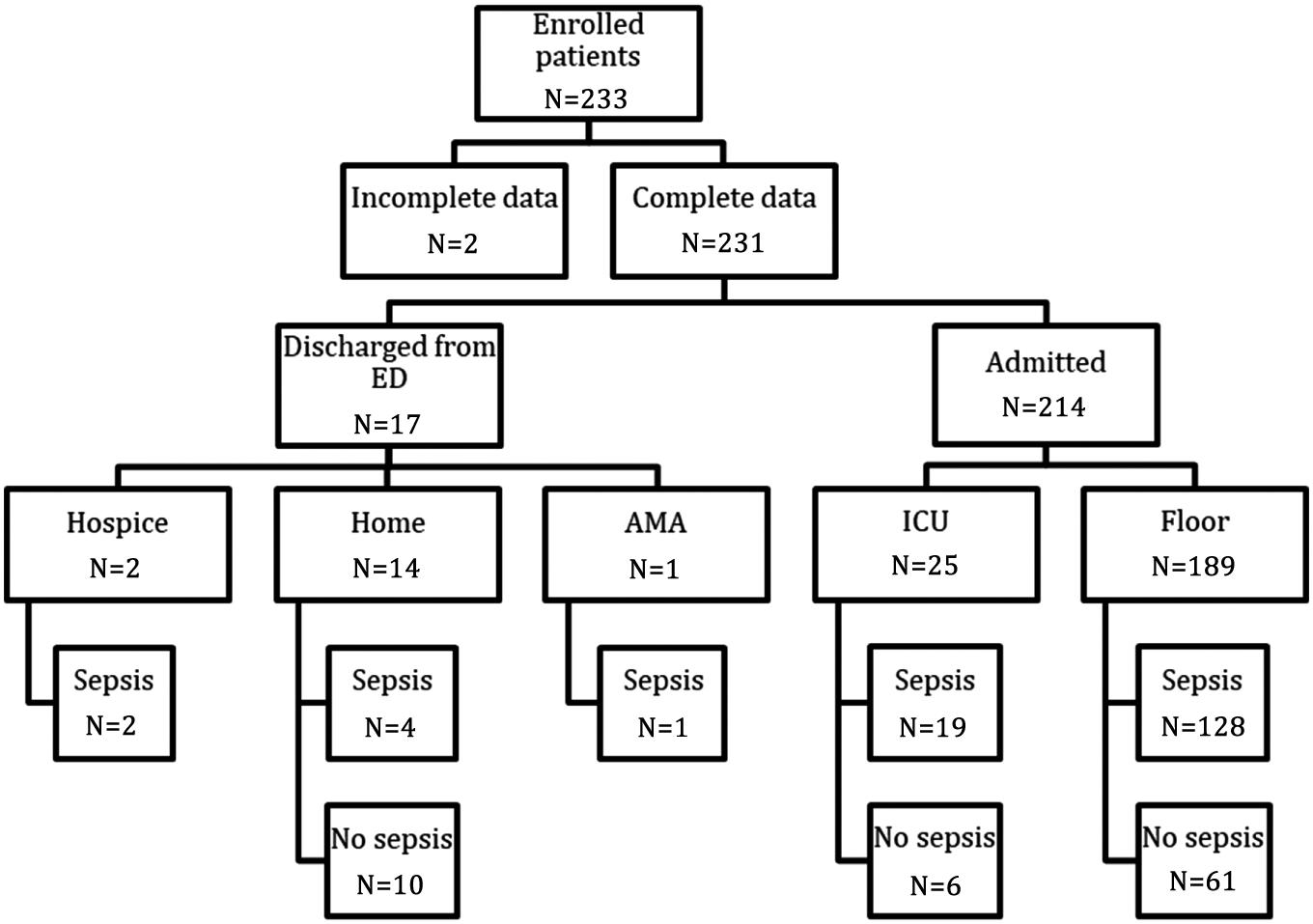
,againstmedicaladvice; ICU,intensivecareunit.
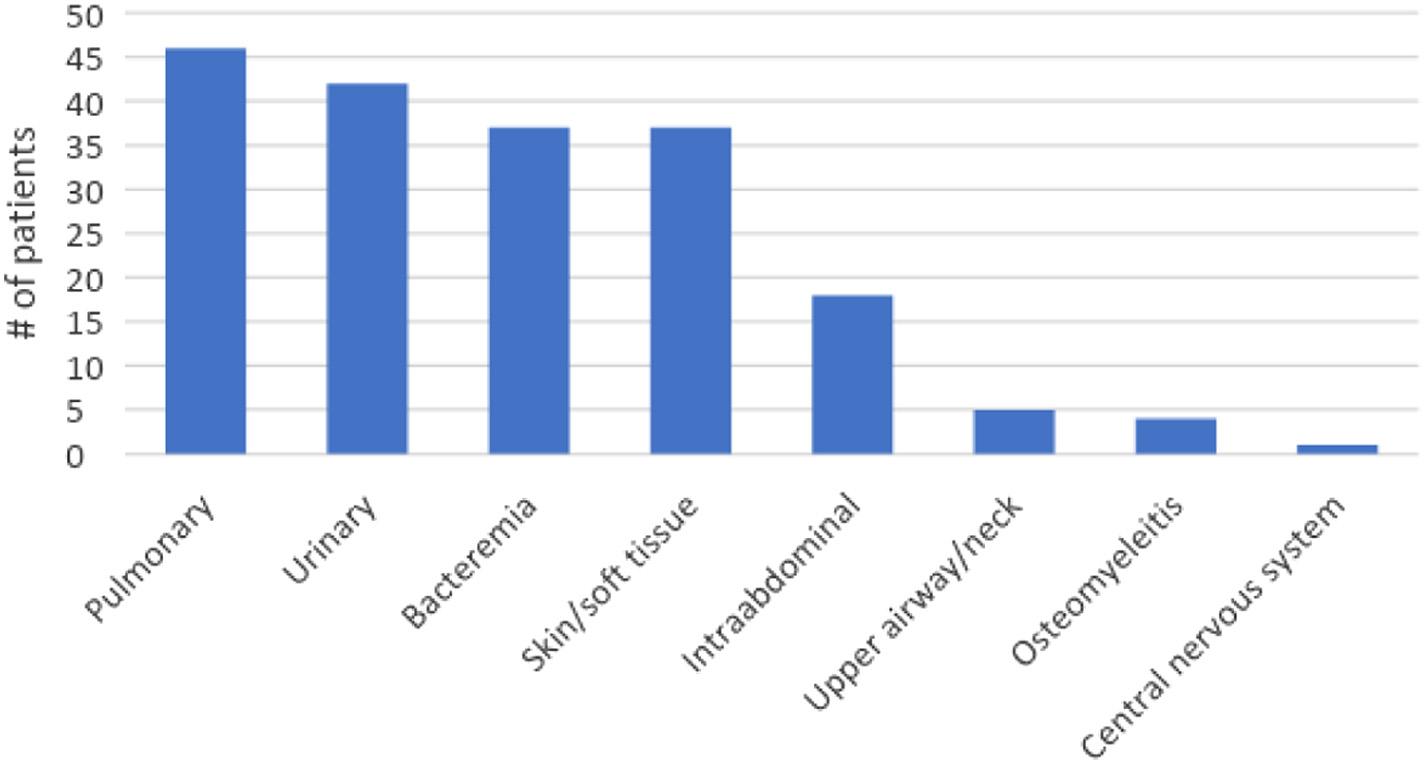
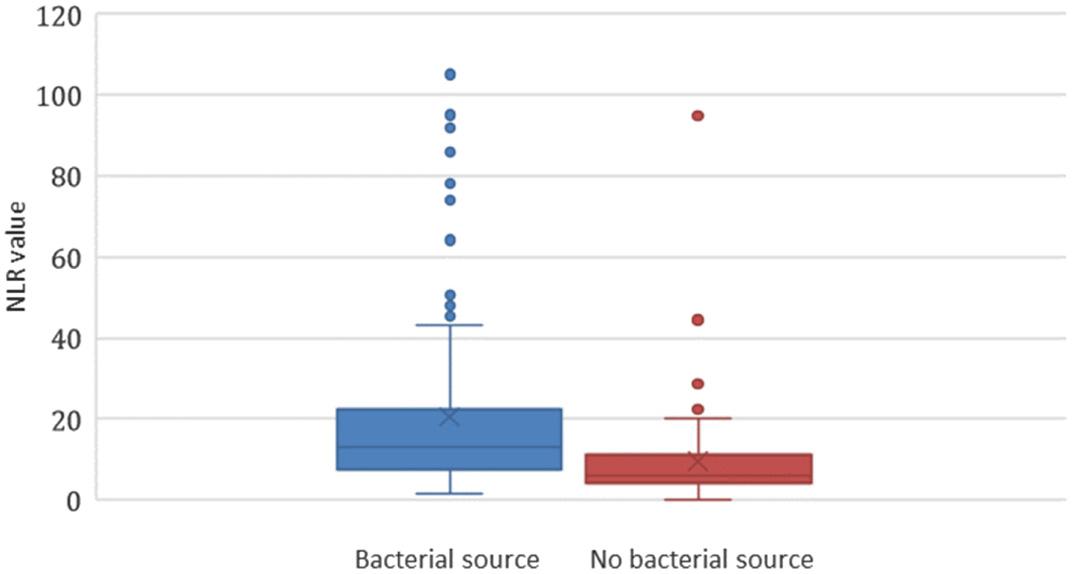
Figure3. Neutrophil-to-lymphocyteratioinpatientswith ≥2 SIRS*criteria.
*SIRS,systemicinflammatoryresponsesyndrome; NLR,neutrophilto-lymphocyteratio.
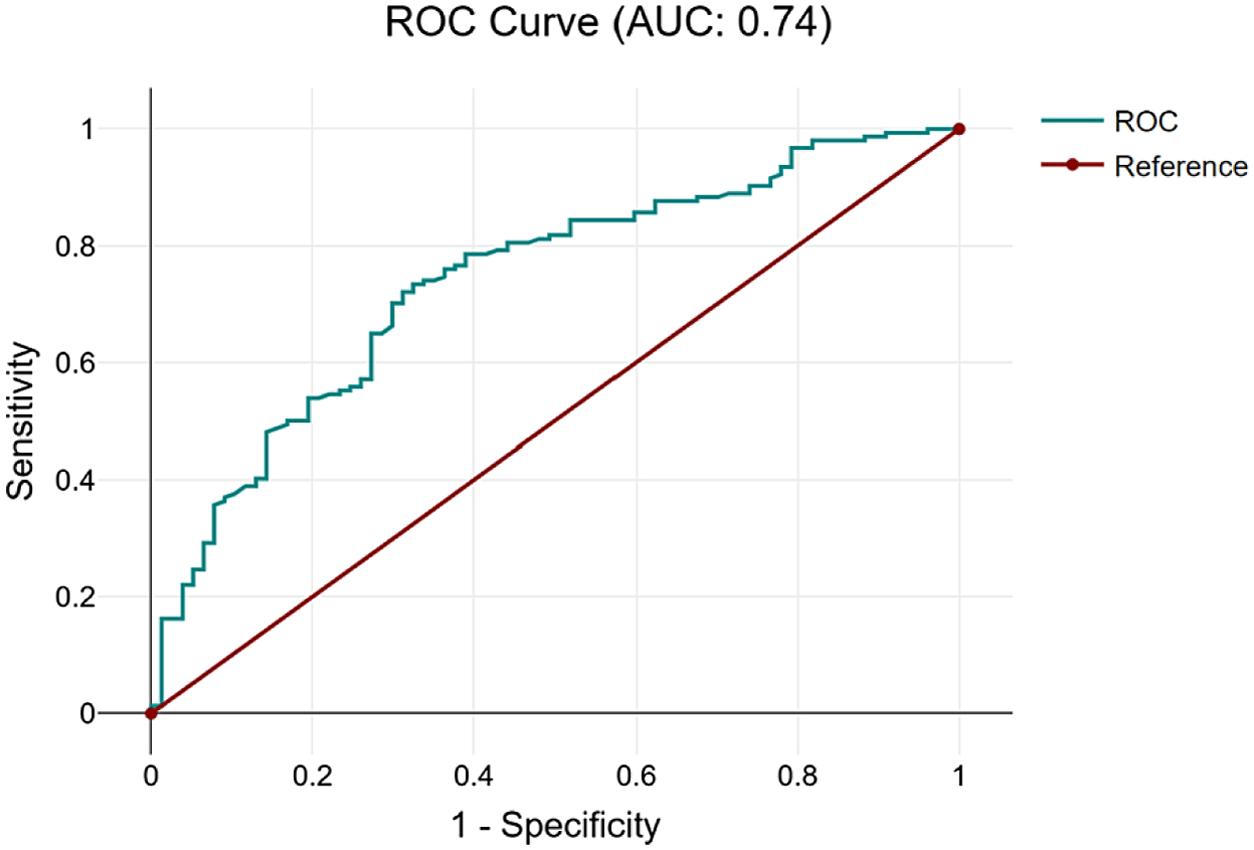
Figure4. Receiveroperatingcurvefortestcharacteristicsof neutrophil-to-lymphocyteratioinpredictingbacterialsourcein patientsmeeting ≥2SIRS*criteria.
ROC,receiveroperatorcurve;*SIRS,systemicinflammatory responsesyndrome.
patientsforwhomthephysicianis “onthefence” regarding antibioticadministration.
WhetherNLRwouldbeusefulinacutepresentationsof sepsiswithnegativeSIRSandqSOFAscreensisdifficultto assess.Wechosetoincludeonlypatientswithpositive clinicalexamfeaturesforsepsis,whichrepresentsworkup biaswithinourstudy.Thiswasdonesothatwecouldhavea standardizedprotocolbywhichtoenrollpatients,rather thansimplyenrollingeverypatientwhohadaCBCdrawn. Therearemanyclinicalpresentationsinwhichpatients “screennegative” forsepsisusingqSOFAandSIRScriteria, butthephysicianhasahighindexofsuspicionforother reasonsthatarelesseasilyquantified,orinwhomsepsisis stillonthedifferentialdiagnosis.These “screennegative” patientswithsepsisarebydefinitionthehardesttorecognize, andNLRmayhavethepotentialtorisk-stratifythem. FurtherstudymayhelptoidentifytherolethatNLRcould haveinscreeningpatients.
Itisimportanttoacknowledgetheperformanceof qSOFAandSIRSwithinthecontextofourstudy.Veryfew ofourenrolledpatientswhowentontohaveadiagnosesof sepsiswithbacterialsourceshadpositiveqSOFAscreens, whichisnotinkeepingwiththeexistingliteratureonqSOFA scores.Only11%ofourbacterialsepsispatientshadpositive qSOFAscores,and29%ofourpositiveqSOFAscreenswere notseptic.Becauseofthis,itisdifficulttospeaktoNLR’ s benefitinpatientswithpositiveqSOFAscreens,asthis representedtheminorityofourpatientpopulation,mostof whomwereenrolledonthebasisofvitalsignabnormalities consistentwithSIRS.Thiswouldbeanareafor furtherstudy.
Becausethiswasarelativelysmallstudyperformedata singleinstitutionandweenrolledpatientsasaconvenience sample,itsgeneralizabilityislimited.Theincidenceof diseasewasveryhighinourcohort,whichisimportantto
considerwheninterpretingourresults.Weenrolleda relativelyhigh-riskcohort,whichmeansthatourdatamay notbeapplicabletopatientswithnegativeqSOFA/SIRS screens.Toeffectivelymirrorreal-worldapplicationofthe NLRinpatients,weattemptedtoidentifypatientsina prospectivemannertoincludepatientswithphysiologic processesthatcausevitalsignabnormalitieswhereinfection mighthavebeenaconsiderationinthedifferentialdiagnosis, butultimatelythediagnosiswasnotsepsis.Further,this studyisalsolimitedbythestudyprotocolinclusioncriteria. Sincethiswasaprospectivestudywithwrittenconsentand patientswithalteredmentalstatuscouldnotconsent,and surrogateconsentwasnotalwaysavailable,thiscouldhave affectedtheyieldofNLRasascreeningtool,eitherpositively ornegatively.
SinceourstudyrequiredqSOFAandSIRSscreeningfor studyentry,itislimitedbytheaccuracywithwhichthose screenswereperformed.Atourinstitution,thesevaluesare inputbyatriagenurseandmaybesubjecttoindividual variabilityandskillset.Examplesofhowthiscouldhave affectedthestudyincludeinaccuraciesintemperature measurementsbasedonmethodorinaccuraciesincounting respiratoryrates.Additionally,ourqSOFAdatalikelywas affectedbythelackofemphasisonit;historically,and currently,ourinstitutionstressestheimportanceof considerationforSIRSwithsuspicionofsourceofinfection, withqSOFAofsecondaryimport.Itispossiblethatwemay nothaveemphasizedthedocumentationofitasmuchas SIRSgivensomewhatlessfamiliarity,resultinginmissed opportunitiesforenrollmentinpatientswhowereSIRS negativebutqSOFApositive.
Additionallimitationsincludethelackofinclusionof patientswhowereexcludedfromenrollmentbystudydesign. Non-Englishspeakerswereexcludedbecauseofinabilityto appropriatelytranslatetheinformedconsentforallcomers. Althoughthedrawingofbloodisofminimalrisktothefetus, pregnantpatientswereexcludedfromthecurrentstudy becauseduringpregnancytheneutrophilcountnaturally increasesduringthesecondandthirdtrimesters. Additionally,physiologicchangesofpregnancyincluding increasedheartrateandrespiratoryratemightmakethe patientSIRSpositive,despitetheabsenceofasevere infection.Patientstriagedtothetraumabaywereexcluded becauseofdifficultieswithconsentingpatientsanddictating diagnostictestingduringtheirtraumaevaluation.
ThisstudywasperformedinaperiodpriortotheCOVID19pandemic.Becauseofissueswithquarantiningpatients earlyinthepandemic,patientenrollmentwasstoppedatthe beginningofthepandemic.TheutilityofNLRasascreening testmaynotbeapplicableinapost-pandemicenvironment.
Theneutrophil-to-lymphocyteratioisasensitivetoolto helpidentifypatientswhomayhaveabacterialsourcefor
sepsis.Itisfasttouseandwithoutadditionalcosttothe patient.Inourstudy,acceptableperformancewas demonstratedwithacutoffof3.Furtherstudiesshouldfocus onvalidationofthese findingsinbroaderpopulations.
AddressforCorrespondence:RebeccaJeanmonod,MD,St.Luke’s UniversityHealthNetwork,businessaddress,801OstrumSt., Bethlehem,PA18015.Email: rebeccajeanmonod@yahoo.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Balakrishnanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CentersforDiseaseControlandPrevention.Whatissepsis?2023. Availableat: https://www.cdc.gov/sepsis/what-is-sepsis.html AccessedMay23,2023.
2.RuddKE,JohnsonSC,AgesaKM,etal.Global,regional,andnational sepsisincidenceandmortality,1990–2017:analysisfortheglobal burdenofdiseasestudy. Lancet. 2020;395(10219):200–11.
3.FrankCE,BuchmanTG,SimpsonSQ,etal.SepsisamongMedicare beneficiaries:4.Pre-coronavirusdisease2019updateJanuary 2012–February2020. CritCareMed. 2021;49(12):2058–69.
4.PaoliCJ,ReynoldsMA,SinhaM,etal.Epidemiologyandcostsofsepsis intheUnitedStates:ananalysisbasedontimingofdiagnosisand severitylevel. CritCareMed. 2018;46(12):1889–97.
5.Rangel-FraustoMS,PittetD,CostiganM,etal.Thenaturalhistory ofthesystemicinflammatoryresponsesyndrome(SIRS). JAMA. 1995;273(2):117–23.
6.RussellJA.Managementofsepsis. NEnglJMed. 2006;355(16):1699–713.
7.DellingerRP,LevyMM,CarletJM,etal.SurvivingSepsisCampaign: internationalguidelinesformanagementofseveresepsisandseptic shock:2008. CritCareMed. 2008;36(1):296–327.
8.SeymourCW,GestenF,PrescottHC,etal.Timetotreatmentand mortalityduringmandatedemergencycareforsepsis. NEnglJMed. 2017;376(23):2235–44.
9.WangHE,JonesAR,DonnellyJP.Revisednationalestimatesof emergencydepartmentvisitsforsepsisintheUnitedStates. CritCare Med. 2017;45(9):1443–9.
10.BarlamTF,CosgroveSE,AbboLM,etal.Implementinganantibiotic stewardshipprogram:guidelinesbytheInfectiousDiseasesSocietyof AmericaandtheSocietyforHealthcareEpidemiologyofAmerica. Clin InfectDis. 2016;62(10):e51–77.
11.GilbertBW,FairesL,MeisterA,etal.Comparisonofsepsis-3criteria versusSIRScriteriainscreeningpatientsforsepsisintheemergency department. AdvEmergNursJ. 2018;40(2):138–43.
12.UsmanOA,UsmanAA,WardM.ComparisonofSIRS,qSOFA,and NEWSfortheearlyidentificationofsepsisintheemergency department. AmJEmergMed. 2019;37(8):1490–7.
13.GauerR,ForbesD,BoyerN.Sepsis:diagnosisandmanagement. Am FamPhysician. 2020;101(7):409–18.
14.DykesLA,HeintzSJ,HeintzBH,etal.ContrastingqSOFAandSIRS criteriaforearlysepsisidentificationinaveteranpopulation. FedPract. 2019;36(Suppl2):S21–4.
15.WangC,XuR,ZengY,etal.AcomparisonofqSOFA,SIRSandNEWS inpredictingtheaccuracyofmortalityinpatientswithsuspectedsepsis: ameta-analysis. PLoSOne. 2022;17(4):e0266755.
16.TianH,ZhouJ,WengL,etal.AccuracyofqSOFAforthediagnosisof sepsis-3:asecondaryanalysisofapopulation-basedcohortstudy. J ThoracDis. 2019;11(5):2034–42.
17.TusgulS,CarronPN,YersinB,etal.LowsensitivityofqSOFA,SIRS criteriaandsepsisdefinitiontoidentifyinfectedpatientsatriskof complicationintheprehospitalsettingandattheemergencydepartment triage. ScandJTraumaResuscEmergMed. 2017;25(1):108.
18.PermanSM,MikkelsenME,GoyalM,etal.ThesensitivityofqSOFA calculatedattriageandduringemergencydepartmenttreatmentto rapidlyidentifysepsispatients. SciRep. 2020;10(1):20395.
19.Thomas-RueddelDO,PoidingerB,WeissM,etal.Hyperlactatemiais anindependentpredictorofmortalityanddenotesdistinctsubtypesof severesepsisandsepticshock. JCritCare. 2015;30(2):439.e1–6.
20.BorthwickHA,BruntLK,MitchemKL,etal.Doeslactatemeasurement performedonadmissionpredictclinicaloutcomeontheintensivecare
unit?Aconcisesystematicreview. AnnClinBiochem. 2012;49(Pt4):3391–4.
21.ZahorecR.Neutrophil-to-lymphocyteratiopast,presentandfuture perspectives. BratislLekListy. 2021;122(7):474–88.
22.HuangZ,FuZ,HuangW,etal.Prognosticvalueofneutrophil-tolymphocyteratioinsepsis:meta-analysis. AmJEmergMed. 2020;38(3):641–7.
23.DragoescuAN,PadureanuV,StanculescuAD,etal.Neutrophilto lymphocyteratio(NLR);ausefultoolfortheprognosisofsepsisinthe ICU. Biomedicines. 2021;10(1):75.
24.RussellCD,ParajuliA,GaleHJ,etal.Theutilityofperipheralblood leucocyteratiosasbiomarkersininfectiousdiseases:asystematic reviewandmeta-analysis. JInfect. 2019;78(5):339–48.
25.CheblRB,AssafM,KattoufN,etal.Theassociationbetweenthe neutrophiltolymphocyteratioandin-hospitalmortalityamong sepsispatients:Aprospectivestudy. Medicine(Baltimore). 2022;101(30):e29343.
26.LiT,DongG,ZhangM,etal.Associationofneutrophil-lymphocyteratio andthepresenceofneonatalsepsis. JImmunolRes. 2020;2020:7650713.
27.ZhangS,LuanX,ZhuangW,etal.Platelet-to-lymphocyteand neutrophil-to-lymphocyteratioaspredictivebiomarkersforearly-onset neonatalsepsis. JCollPhysiciansSurgPak. 2021;30(7):821–4.
28.OzdemirSA,OzerEA,IlhanO,etal.Canneutrophiltolymphocyte ratiopredictlate-onsetsepsisinpreterminfants? JClinLabAnal. 2018;32(4):e22338.
29.KaukonenKM,BaileyM,PilcherD,etal.Systemicinflammatory responsesyndromecriteriaindefiningseveresepsis. NEnglJMed. 2015;372(17):1629–38.
GuojunChen,MD*†∘
TianenZhou,PhD*†∘
JingtaoXu,MD*†
QiaohuaHu,MD*†
JunJiang,PhD*†
WeiganXu,MD*†
*FirstPeople’sHospitalofFoshan,DepartmentofEmergency,Foshan,Guangdong,China † FirstPeople’sHospitalofFoshan,ThePoisonTreatmentCentreofFoshan,Foshan, Guangdong,China
∘ GuojunChenandTianenZhouareco-firstauthorsandcontributedequallytothiswork
SectionEditor:QuincyK.Tran,MD,PhD
Submissionhistory:SubmittedNovember19,2023;RevisionreceivedApril24,2024;AcceptedApril26,2023
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18589
Background: Theprognosticvalueofbodytemperatureinsepsis-inducedcoagulopathy(SIC)remains unclear.Inthisstudyweaimedtoinvestigatetheassociationbetweentemperatureandmortalityamong SICpatients.
Methods: Weanalyzeddatafor9,860SICpatientsfromanintensivecaredatabase.Patientswere categorizedbymaximumtemperatureinthe first24hoursintothefollowing: ≤36.0°C;36.0–37.0°C; 37.0–38.0°C;38.0–39.0°C;and ≥39.0°C.Theprimaryoutcomewas28-daymortality.Weused multivariateregressiontoanalyzethetemperature-mortalityassociation.
Results: The37.0–38.0°C,38.0–39.0°Cand ≥39.0°Cgroupscorrelatedwithlower28-daymortality (adjustedHR0.70,0.76and0.72,respectively),whilethe <36.0°Cgroupcorrelatedwithhighermortality comparedtothe36.0–37.0°Cgroup(adjustedHR2.60).Anonlinearrelationshipwasobserved betweentemperatureandmortality.Subgroupanalysisfoundnoeffectmodificationexceptin cerebrovasculardisease.
Conclusion: Abodytemperatureintherangeof37.0–38.0°Cwasassociatedwithasignificantlylower mortalitycomparedtothenormaltemperature(36.0–37.0°C)group.Additionally,agradualbut statisticallyinsignificantincreaseinmortalityriskwasobservedwhenbodytemperatureexceeded 38.0°C.Furtherresearchshouldvalidatethese findingsandelucidateinvolvedmechanisms,especially incerebrovasculardiseasesubgroups.[WestJEmergMed.2024;25(5)697–707.]
Sepsis,definedaslife-threateningorgandysfunctiondue todysregulatedhostresponsetoinfection,1 frequentlyleads toderangementsincoagulationrangingfromsubtle activationtoovert,disseminatedintravascularcoagulation (DIC).2,3 Thisconditioninsepsisisassociatedwithmultiple organfailureandhighmortality.4,5 In2017theInternational SocietyonThrombosisandHaemostasis(ISTH)proposed “sepsis-inducedcoagulopathy” (SIC)criteriatoidentify
earlycoagulopathyinsepsis,definedbysepsisplus thrombocytopeniaandprolongedprothrombintime.4 SeveralstudieshavevalidatedSICasanearlyidentifierof impendingovertDICinsepsis.6,7 Sepsis-induced coagulopathycorrelateswithmortality,withratesexceeding 30%atascore ≥4.4 ComparedtoovertDICcriteria,SIC demonstratesgreatersensitivityinpredictingmortality.7
Insummary,SICrepresentsanearlyphaseofcoagulation dysfunctioninsepsisthatoftenprogressestoovertDIC.The
highmorbidityandmortalityassociatedwithSIChighlights theneedforearlyidentificationusingsimplecriteriasuchas theSICscore,allowingrapidinitiationofinterventionsthat mayimproveoutcomesinthishigh-riskpopulation. Monitoringbodytemperaturechangesisvitalinevaluating septicpatientprognosis,asfeverisacommonsymptom.8 Bothhypothermiaandhyperthermiainsepsisreflectimmune responsetoinfection.However,theirimplicationsfor prognosisremaindebated.9–13
Previousstudieshaveassociatedhypothermiawithpoor outcomes.14–19 Theprognosticvalueofhyperthermiaisless clear,withconflictingreports.11,13,20 Thishighlightstheneed toclarifytheroleofbodytemperatureinsepsis.
ConsideringthatSICsignificantlyinfluencessepsis prognosisbyalteringcoagulation,4,21,22 anexplorationofthe relationshipbetweentemperatureandSICwillenhanceour comprehensionofsepsispathophysiologyandfacilitatemore preciseprognosticationandmanagementstrategies. Nonetheless,theprognosticvalueofbodytemperature abnormalitiesspecificallywithinSIChasnotbeen comprehensivelyestablished.Therefore,weaimedto investigatetheassociationbetweenbodytemperatureand theshorttermmortalityofsepticpatientswithcoagulopathy. The findingsareexpectedtobridgeacriticalknowledgegap concerningtheintricateinterplaybetweentemperature regulationandcoagulationinsepsis.
MATERIALSANDMETHODS
DataSource
Thedatautilizedinthisstudywasextractedfromthe MedicalInformationMartforIntensiveCare-IV(MIMICIV)databasethroughtheemploymentofNavicatPremium 15software.MIMIC-IV,acollaborativeeffortbetweenBeth IsraelDeaconessMedicalCenter(BIDMC)and MassachusettsInstituteofTechnology(MIT),isa comprehensiverepositoryencompassingdatafromover 60,000adultintensivecareunit(ICU)admissionsatBeth IsraelDeaconessMedicalCenterspanningfrom2008to 2019.23 Thedata,collectedduringroutineclinicalcareat BIDMC,werede-identified,transformed,andmade accessibletoresearcherswhohavecompletedrequisite traininginhumanresearchethicsandenteredintoadatause agreement.Accesstothedatabasewassecuredbyour correspondingauthor,bearingcertificationNo.46450588. TheInstitutionalReviewBoardatBIDMCgrantedan exemptionfromobtaininginformedconsentandapproved thesharingoftheresearchresource.
Patientdataconformingtosepsis-inducedcoagulopathy criteriawereextractedfromtheMIMIC-IVdatabase’sICU records.Thepatientselectionprocessforthisstudyadhered tothefollowinginclusioncriteria:(1)hospitalstayduration of ≥24hours;(2)age ≥18years.Exclusioncriteria
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Bodytemperatureisacriticalvitalsign, butitsprognosticvalueinsepsis-induced coagulopathy(SIC)remainsunclear, withcon fl ictingevidenceonideal temperatureranges.
Whatwastheresearchquestion?
Weaimedtoinvestigatetheassociation betweenbodytemperatureand28-day mortalityamongSICpatients.
Whatwasthemajor findingofthestudy?
Comparedto36.0 – 37.0 ° C,37.0 – 38.0 ° Cwas associatedwithlowermortality(adjustedHR 0.70,95%CI0.62 – 0.79,P < 0.001).
Howdoesthisimprovepopulationhealth?
Identifyingtheoptimaltemperaturerange inSICcouldguidebetterthermoregulation management,potentiallyreducingmortality andimprovingoutcomesinthis high-riskpopulation.
encompassed:(1)presenceofgreaterthan10%missing individualdata;(2)outliers,indicatedbyvaluesexceeding themean ± 3StandardDeviation(SD).Incasesofmultiple ICUadmissions,solelydatafromthe firstICUadmissionof theinitialhospitalstaywereconsidered.
StructuredQueryLanguage(SQL)washarnessedto extractdatarecordedonthe firstdayofadmission.Extracted dataincludeddemographicdetails,fundamentalvitalsigns, comorbidities,basiclaboratoryparameters,andpretreatmentscoringsystems.Demographicdataencompassed race,gender,andage.Vitalsignsincorporatedheartrate, respiratoryrate,andbodytemperature.Bodytemperature wasroutinelymeasuredbynursesatbedside,primarily throughtheaxillaryandoralroute,at4–8hourintervals.For someICUpatients,occasionalcoretemperaturesfrom esophagealandrectalprobeswerealsoavailable.We extractedthemaximumtemperatureondayoneforeach patient.Comorbiditieswerecategorizedasmyocardial infarction,congestiveheartfailure,cerebrovasculardisease, chronicpulmonarydisease,renaldisease,anddiabetes. Laboratoryparametersencompassedhemoglobin,platelet count,whitebloodcellcount,bicarbonate,creatinine,urea nitrogen,glucose,ProthrombinTime(PT),Partial
ThromboplastinTime(PTT),andInternationalNormalized Ratio(INR).Additionally,theCharlsonComorbidityIndex (CMI),SequentialOrganFailureAssessment(SOFA)score, SimplifiedAcutePhysiologyScoreII(SAPSII),Renal ReplacementTherapy(RRT), first-dayventilationuse,and vasopressorusewereincluded.Variableswithmissingvalues ≥40%wereexcludedduringvariableselection.Forsomeof thecontinuousvariablesincludedwithmissingdata(seethe SupplementaryTableS1 formissingdata),weusethesimple substitutionmethodtodealwiththem.Missingvaluesare replacedwithmeansiftheyfollowanormalor approximatelynormaldistribution,andwithmediansifthey followaskeweddistribution.
Theprimaryoutcomemeasurewas28-daymortality, whilesecondaryoutcomesincluded90-daymortality, lengthofstay(LOS)inboththeIntensiveCareUnit(ICU), andhospital.
Allparticipantswerecategorizedinto fivegroupsbasedon theirmaximumbodytemperaturewithinthe first24hoursof hospitaladmission: ≤36.0°C,36.0–
C.Thereferencegroupwasdefinedas thetemperaturecategoryof36.0–37.0°C.Normallydistributed continuousvariableswerepresentedasmean ± standard deviation,whilenon-normallydistributeddataweredisplayed asmedian[interquartilerange(IQR)].Normalitydistribution wasassessedusingtheShapiro-Wilktest.Categoricaldata werepresentedascounts(percentages).Tocomparethe differencesacrossgroups,one-wayanalysesofvariance (normaldistribution),Kruskal–Wallistests(skewed distribution),andchi-squaretests(categoricalvariables) wereundertaken.
Univariatelogisticregressionanalyseswereperformedto exploretheassociationsbetweeneachvariableandtherisks of28-dayand90-daymortality,withtheresultspresentedin SupplementaryTablesS2andS3,respectively.
Theassociationbetweenbodytemperatureand28-day mortalitywasexaminedviaCoxproportionalhazard regression,withresultsexpressedasHazardRatios(HR) alongwith95%ConfidenceIntervals(CI).Foreach endpoint,fourmultivariateanalyticmodelsweredeveloped: Model1,unadjustedcovariates;Model2,covariates includinggender,age,race,heartrate,andrespiratoryrate; Model3,furtheradjustedforhemoglobin,plateletcount, INR,whitebloodcellcount,aniongap,bicarbonate,blood ureanitrogen,creatinine,glucose,PT,andPTT;and Model4,encompassingallcovariates.Lineartrendtests acrosstemperaturecategorieswereperformedusingthe mediantemperaturevalueineachgroup.
Wealsoexaminedthelinearityofthebodytemperaturemortalityassociationusingcurve fitting.Forthisanalysis,we
modeledtemperatureasacontinuousvariable,ratherthan usingthepre-definedtemperaturecategories.AtwopiecewiseCoxmodelwithsmoothingsplinewasusedto determinethethresholdrelationshipbetweenbody temperatureandmortality,withthethresholdpoint identifiedthroughlikelihoodratiotestingand bootstrapresampling.
Furthermore,potentialmodificationsoftherelationship betweenbodytemperatureandmortalitywereassessed, includingthefollowingvariables:age(<70vs. ≥70years), gender,SOFAscore(<4vs. ≥4),SAPSII(<42vs. ≥42), myocardialinfarct(yesvs.no),cerebrovasculardisease (yesvs.no),chronicpulmonarydisease(yesvs.no),diabetes mellitus(yesvs.no)andrenaldisease(yesvs.no).
Heterogeneityamongsubgroupswasassessedby multivariatecoxregression,andinteractionsbetween subgroupsandbodytemperaturewereexaminedby likelihoodratiotesting.Toadjustformultiplecomparisons inthesesubgroupanalyses,weappliedtheBonferroni correction.Specifically,wedividedthepredetermined significancelevelof α = 0.05bythenumberofsubgroup comparisons(9),resultinginaBonferroni-adjusted significancelevelof0.0056.Wethenevaluatedwhetherthe associationbetweentemperatureandSICmortalitydiffered significantlyineachsubgroup,usingthiscorrected significancethreshold.
Finally,Kaplan-Meiercurveswereconstructedtovisually examinetheassociationbetweentemperaturecategories andmortality.
AnalyseswereconductedusingRsoftware(http://www. R-project.org,TheRFoundation)andFreeStatistics software(version1.7),withtwo-sided p < 0.05considered statisticallysignificant.
WeusedClaudeAI,anartificialintelligencewriting assistantdevelopedbyAnthropic,toaidin finalpolishingof themanuscript.ClaudeAIprovidedsuggestivecontent whichwethenreviewed,edited,andapprovedbefore inclusion.Wetakefullresponsibilityforthecontentand conclusionsofthemanuscript.
Atotalof9,860patientsdiagnosedwithsepsis-induced coagulopathy(SIC)wereincludedinthiscomprehensivestudy (Figure1).Thedemographicdetails,vitalsigns,laboratory parameters,andcomorbiditiesofthesepatientsatbaselineare meticulouslypresentedin Table1.Notably,comparedto patientswithabodytemperaturebetween38.0–39.0°C,the mortalityratewasslightlyhigherinthegroupwithbody temperaturesabove39°C.However,thehighestmortalityrate wasobservedinthegroupwithbodytemperaturesbelow 36.0°C,suggestingabimodalrelationshipbetweenbody temperatureandmortalityinSICpatients.
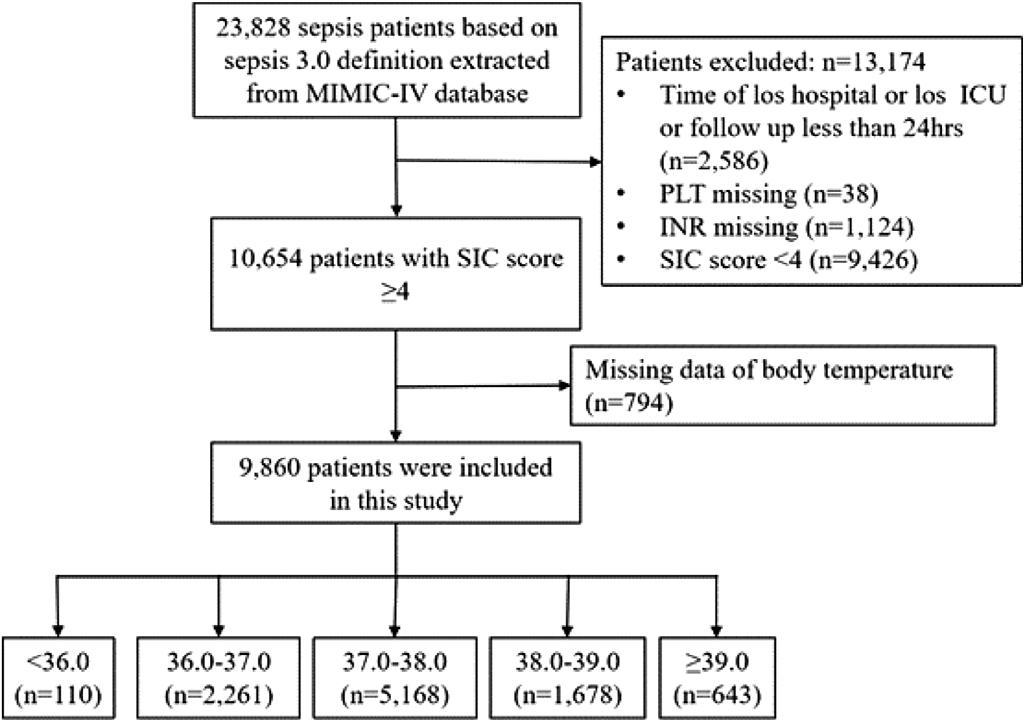
Figure1. Flowchartofthescreeningandenrollmentofstudy participants.MIMIC:MedicalInformationMartforIntensiveCare. ICU,IntensiveCareUnit; LOS,lengthofstay; PLT,platelet; INR, InternationalNormalizedRatio; SIC,sepsis-inducedcoagulopathy.
Table2 offersacomprehensiveoverviewoftheoutcomes’ associationwithvaryingbodytemperatures.Inthe unadjustedmodel(Model1),thehazardratios(HRs)and 95%confidenceintervals(CIs)for28-dayall-causemortality were2.82(2.17,3.66)fortemperatures <36.0;°C,0.62(0.56, 0.69)for37.0–38.0°C,0.63(0.55,0.72)for38.0–39.0°C,and 0.75(0.62,0.90)for ≥39.0°C,allcomparedtothereference groupof36.0–37.0°C.
InthefullyadjustedModel4,whichaccountedforgender, age,race,vitalsigns,laboratoryparameters,comorbidities, andseverityscores,theassociationbetweentemperatureand 28-daymortalityremainedstatisticallysignificant.This suggestsarobustinverserelationshipbetweenbody temperatureandshort-termmortalityriskinthis patientpopulation.
Theresultsfromtheadditionalregressionmodels(Models 2and3)wereprovidedin SupplementaryTableS4.These modelsshowedconsistent findings,withhighertemperatures beingassociatedwithlowermortalityrisk.
Whentemperaturewasexaminedasacontinuousvariable, thefullyadjustedModel4showedthatforevery1°Cincrease inbodytemperature,therewasan18%(HR0.82,95%CI 0.78–0.87)reductionintheriskof28-daymortality.
Thenon-linearrelationshipbetweentemperatureand 28-dayall-causemortalitywasfurtherdemonstratedbythe smoothcurve fittinganalysisdepictedin Figure2 (p for non-linearity <0.001).Asimilarprotectiveassociation wasalsoobservedfor90-dayall-causemortality (SupplementaryFigureS1).
Furthermore,ourmultivariatelinearregressionmodels revealedthatforevery1°Cincreaseinbodytemperature, therewasacorrespondingincreaseinICUlengthofstayby
0.40days(95%CI:0.24–0.55days)andtotalhospitallength ofstayby0.82days(95%CI:0.48–1.15days)inthefully adjustedanalysis.
Weconductedasmoothingfunctionanalysistoassessthe potentialnon-linearrelationshipbetweenbodytemperature and28-daymortalityinSICpatients.Afteradjustingfor potentialconfoundersincludingage,gender,laboratory resultsandcomorbidities,weobservedanon-linear associationbetweenbodytemperatureandriskof28-day mortality(Figure2).Thisnon-linearrelationshipwas alsoobservedwhenanalyzing90-daymortality (SupplementaryFigureS1).
Furthersplineanalysisrevealedathresholdeffect, withriskdecreasingasbodytemperatureincreasedupto 38.0°C(adjustedHR0.640;95%CI0.589–0.696),after whichriskslightlyincreasedbutwasnolonger statisticallysignificant(adjustedHR1.192;95%CI 0.984–1.444).(Table3)
Thethresholdeffectat38.0°Cisillustratedbythespline curvein Figure2,whichdepictstheestimatedadjusted hazardratios(solidline)andpointwise95%confidence intervals(shadedarea)fortherelationshipbetweenbody temperatureand28-daymortalityrisk.Ouranalysesindicate acomplexnon-linearassociationbetweenbodytemperature andmortalityriskinSICpatients,withhypothermia conferringthehighestrisk.
Toidentifyfactorsimpactingtheeffectofbody temperatureon28-daymortality,comprehensivesubgroup analyseswereconducted,asdepictedin Figure3.Interaction p -valueswerelargelynon-signi ficantacrossage,gender, severityscores,comorbidities,andothersubgroups. Notably,anexceptionwasobservedforthecerebrovascular diseasesubgroup(p < 0.001),wherepatientswithout cerebrovasculardiseaseexhibitedalower28-daymortality risk(adjustedHR:0.78,95%CI0.73~0.83).Analogous findingsarediscernibleinthe90-daysubgroupanalysis (SupplementaryFigureS2).
TheKaplan–Meiersurvivalanalysisin Figure4 highlights theimpactofvaryingbodytemperatureson 28-daysurvival.Mortalityrateswerenotablyhigherinthe <36.0groupandcomparativelylowerinthe37.0–38.0group whencontrastedwiththereferencegroup(36.0–37.0).This trendisreaffirmedwithadjustedHRsof2.6(95%CI1.99~ 3.42)and0.7(95%CI0.63~0.78),respectively(Table2). Consistentoutcomesareobservedinthe90-daysurvival analysis(SupplementaryFigureS3).
Table1. Baselineclinicalandlaboratorycharacteristicsofthestudypatients.
Characteristicn
Race,n(%)
White6,730(68.3)62(56.4)1,605(71)3,546(68.6)1,149(68.5)368(57.2)
Other3,130(31.7)48(43.6)656(29)1,622(31.4)529(31.5)275(42.8)
Gender,n(%)
Male6,049(61.3)66(60)1,291(57.1)3,192(61.8)1,089(64.9)411(63.9) Female3,811(38.7)44(40)970(42.9)1,976(38.2)589(35.1)232(36.1)
Vitalsign
Laboratorydata
HGB(g/dL),median(IQR)9.2(7.9,10.7)9.2(8.2,11.5)9.1(7.8,10.5)9.1(7.9,10.6)9.4(8.0,10.9)9.6(8.0,11.1)
PLT( × 10 9 /L),median(IQR)117.0(80.0,164.0)133.0(100.0,181.0)118.0(81.0,175.0)115.0(80.0,159.0)118.0(83.0,165.0)116.0(67.0,164.0)0.001 Glucose(mg/dL),median(IQR)143.0(117.0,190.0)203.0(141.0,323.8)142.0(115.0,188.0)141.0(116.0,187.0)147.5(120.0,194.0)154.0(122.0 ,199.0) < 0.001
BUN(mg/dL),median(IQR)24.0(16.0,41.0)29.5(19.2,55.2)29.0(18.0,51.0)24.0(16.0,39.0)22.0(15.0,35.0)22.0(14.5,37.0) < 0.001
Scr(mg/dL),median(IQR)1.2(0.9,2.0)1.6(1.1,3.4)1.3(0.9,2.2)1.2(0.8,1.8)1.2(0.9,1.8)1.2(0.9,2.0) < 0.001
INR,median(IQR)1.6(1.4,2.0)1.7(1.5,2.6)1.7(1.4,2.3)1.6(1.4,2.0)1.6(1.4,2.0)1.6(1.4,1.9) < 0.001
PT(s),median(IQR)17.5(15.5,22.1)18.9(16.1,27.6)18.1(15.8,24.3)17.3(15.4,21.7)17.2(15.3,21.1)17.5(15.6,20.9) < 0.001
PTT(s),median(IQR)36.7(31.1,49.9)47.8(36.8,85.4)38.7(32.1,54.5)36.2(30.9,48.8)36.0(30.9,47.4)35.9(30.8,48.0) < 0.001
Medicalhistory
Myocardialinfarct,n(%)1,712(17.4)31(28.2)456(20.2)865(16.7)274(16.3)86(13.4) < 0.001
Congestiveheartfailure,n(%)2,994(30.4)43(39.1)842(37.2)1,510(29.2)444(26.5)155(24.1) < 0.001
Cerebrovasculardisease,n(%)1,138(11.5)13(11.8)221(9.8)598(11.6)223(13.3)83(12.9)0.011
Chronicpulmonarydisease,n(%)2,379(24.1)30(27.3)578(25.6)1,269(24.6)373(22.2)129(20.1)0.012
Diabetes,n(%)2,901(29.4)22(20)705(31.2)1,533(29.7)469(27.9)172(26.7)0.016
Renaldisease,n(%)2,161(21.9)31(28.2)647(28.6)1,093(21.1)297(17.7)93(14.5) < 0.001
Diseaseseverityscore Charlsoncomorbidityindex,mean
Procedure
RRTuse,n(%)605(6.1)19(17.3)157(6.9)292(5.7)88(5.2)49(7.6) < 0.001
Table1. Continued.
Characteristicn = 9,860n =
Ventilatoruse,n(%)5,065(51.4)87(79.1)879(38.9)2,667(51.6)1,063(63.3)369(57.4) < 0.001
Vasopressoruse,n(%)5,341(54.2)78(70.9)1,193(52.8)2,796(54.1)917(54.6)357(55.5)0.005
Outcomes
< 0.001
< 0.001
< 0.001
< 0.001
Loshospital(days),median(IQR)days9.0(5.6,16.0)6.8(3.9,14.2)8.5(5.3,15.1)8.7(5.4,15.0)10.0(6.0,18.2)11.2(6.8,21.4)
LosICU(days),median(IQR)days3.1(1.8,6.2)4.4(2.6,7.4)2.9(1.7,5.3)2.9(1.7,5.6)3.8(2.0,7.7)4.8(2.5,9.3)
28-daymortality,n(%)2,062(20.9)61(55.5)622(27.5)938(18.2)305(18.2)136(21.2)
90-daymortality,n(%)2,754(27.9)68(61.8)811(35.9)1,292(25)408(24.3)175(27.2)
HR ,heartrate; RR ,respiratoryrate; WBC ,whitebloodcell; HGB ,hemoglobin; PLT ,platelets; AG ,aniongap; CO 2 , bicarbonate; BUN ,bloodureanitrogen; Scr ,serumcreatinine; INR ,InternationalNormalizedRatio; PT ,prothrombintime; PTT ,partialthromboplastintime; SOFA ,sequentialorganfailureassessment; SAPSII, simpli fi edacutephysiology scoreII; RRT, renalreplacementtherapy; LOS, lengthofstay.
Inourstudy,asignificantrevelationemergesfromthe analysis.Specifically,SICpatientswithinthe37.0–38°C temperaturerangeexhibitedthemostfavorableprognosis, characterizedbythelowestmortality.Conversely,lowbody temperature(<36.0°C)wasassociatedwithhighermortality intheSICpopulationsimilartothatobservedinotherseptic cohorts.Subgroupanalyses,asidefromcerebrovascular disease,demonstratednosubstantialeffectmodificationby age,gender,orcomorbidities.
Ourresultscontributenovelinsightsintotheimplications ofbodytemperatureinSIC,markingapioneeringattemptat investigatingthisassociation.Sepsis-inducedcoagulopathy holdsapivotalplaceinthespectrumofsepsis-related coagulationdisorders,intimatelyconnectedwith disseminatedintravascularcoagulation(DIC).24 Recognized foritsroleinthepathogenesisofsepsis, SICactsasabridgebetweenearlysystemicinflammationand full-blownDIC.Byhighlightingthepotential valueofSICasamarkerandapossibletherapeutictarget, ourstudyunderscoresitssignificanceinguidingclinical decisionsandfurtheringourunderstandingof sepsispathogenesis.
Theobserveddifferencesinmortalityandhospitalstay durationbasedontemperaturegroupsunderscorethe clinicalsignificanceoftemperaturemanagementinSIC. Patientsinthehypothermicgroup(<36.0°C)displayedthe highest28-daymortalityrisk,suggestiveofsevere physiologicaldistressandcompromisedorganfunction.25 Correspondingly,maintaininganormothermicrange (37.0–38.0°C)wasassociatedwithimprovedsurvival outcomes,highlightingthepotentialimportanceof normothermiainenhancingpatientprognosis.26 Ourstudy echoespreviousreportsassociatinglowertemperatureswith heightenedmortalityriskinsepticpatients.13,19 Notably,our definitionofhypothermia(<36.0°C)withintheSICcohort yieldeda2.6-foldincreaseinmortalityafteradjustingfor confoundingfactors,reaffirmingthesignificanceof thisobservation.
Theunderlyingmechanismslinkingtemperaturewith mortalityinsepsisaremultifaceted.Hypothermiacan contributetoimmunesuppression,impaired thermoregulation,anddisruptedcoagulationpathwaysby causingplateletdysfunctionandamilddecreaseinplatelet countorotherstepsinthecoagulationcascade,thereby exacerbatingmortalityrisk.27 Conversely,feverhasbeen linkedtoimprovedsurvivalduetoenhancedbacterial clearance,optimizedantibioticefficacy,andcontrolled inflammatoryresponses.11,28 Incontrasttoprior studiesinsepsispopulations,our findingsinthesepsisinducedcoagulopathy(SIC)cohortdidnotindicatethatan earlypeaktemperatureabove39.5°Cwasassociated withworseoutcomes.11,29 Infact,patientswith temperaturesinthe37.0–38.0°Crangeexhibitedthe
Table2. Resultsofmultivariateregressionanalysisbetweentemperatureandoutcomes.
Primaryoutcomes
28-daymortalitya
Temperature0.78(0.74~0.83)
Bodytemperature
<36.02.82(2.17~3.66)
<0.0010.82(0.78~0.87)0.001
<0.0012.6(1.99~3.42) <0.001
36.0–37.01(Ref)1(Ref)
37.0–38.00.62(0.56~0.69) <0.0010.7(0.63~0.78) <0.001
38.0~ 39.00.63(0.55~0.72) <0.0010.76(0.66~0.88)0.001
≥39.00.75(0.62~0.9)0.0020.72(0.59~0.87)0.001
Secondaryoutcomes
Bodytemperature
36.02.52(1.97~3.23)
36.0–37.01(Ref)1(Ref)
37.0–38.00.64(0.59~0.7) <0.0010.73(0.67~0.8) <0.001
38.0–39.00.63(0.56~0.71) <0.0010.79(0.69~0.89)
Note: ModelIadjustedfornothing.ModelIVadjustedforgender,age,race,HR,RR,hemoglobin,platelets,INR,WBC,aniongap, bicarbonate,bun,creatinine,glucose,PT,PTT,myocardialinfarction,congestiveheartfailure,cerebrovasculardisease,chronic pulmonarydisease,renaldisease,Charlsoncomorbidityindex,SOFAscore,SAPSII,RRT, firstdayventilationuseandvasopressoruse. aLogisticregressionanalysis. bLinearregressionanalysis.
*Regressioncoefficient(β). HR,hazardratio; CI,confidenceinterval; LOS,lengthofstay.
lowestmortality,similartothosewithtemperatures above39.0°C.
Wefoundthatnormothermia(37.0–38.0°C,definedasa mildfeverinsomecountries)wasassociatedwithreduced mortalitycomparedto36.0–37.0°C.Thisisconsistentwith previous findings.AmulticenterRCTbySchortgenetal. reportedexternalcoolingtoachievenormothermia (36.5–37.0°C)couldreduce14-daymortalitycomparedto externalheatingtoachievefevercontrol.8 However,aRCT byYoungetal.didnot findasignificantdifferencein90-day mortalitybetweenfevercontrolandnofevercontrol.30 Thediscrepancymaybeexplainedbythedifferenttarget temperatureranges.Overall,maintainingnormothermia ormildfeverappearstobebeneficialbasedon currentevidence.
Feveriscommoninsepsispatients.However,studieson theassociationbetweenhighfever(>39.0°C)andsepsis mortalityremaincontroversial.16,31 Ourstudyshowed slightlyincreasedmortalityinhighfeverpatientswithSIC thaninmildfeverpatients,butdidnotreachstatistically significanceFutureresearchiswarrantedtoclarifythis relationshipinSICpatients.
Moreover,ourresultsdemonstratedanonlinear relationshipbetweenbodytemperatureandboth28-dayand 90-dayall-causemortality.EachCelsiusdegreeincreasein temperaturecorrelatedwithan18%reductionin28-day mortality,underscoringthepotentialbenefitsofmaintaining normothermiaduringSICtreatment.However,the relationshipshiftedbeyondatemperaturethresholdof 38.0°C,whereconsistentlyincreasedtemperaturescorrelated
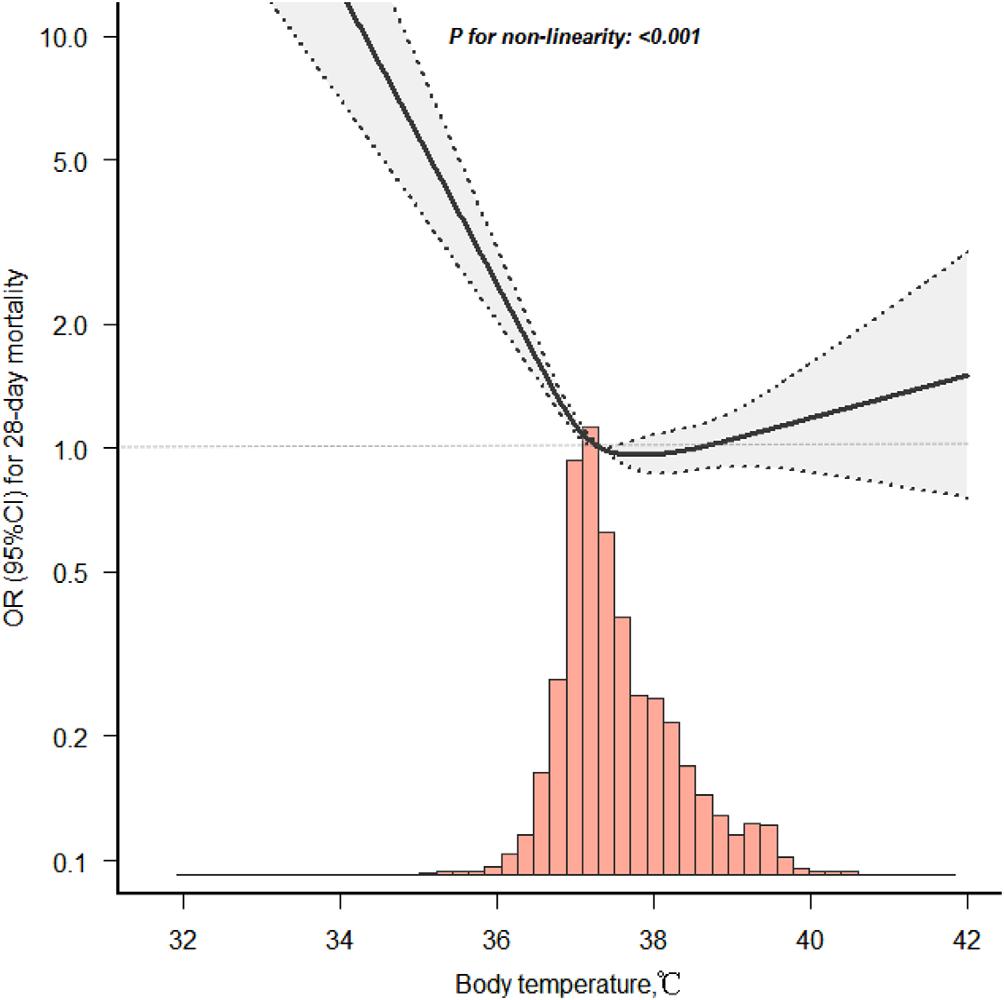
Figure2. Smoothcurve fittingfortemperatureand28-day mortalityinpatientswithsepsis-inducedcoagulopathy.
withgradual,albeitstatisticallyinsignificant,increases inmortality.
Notably,subgroupanalysisrevealednosignificant interactionon28-daymortalityinmostsubgroups, suggestingthatbodytemperaturemightindependently
Table3. Thresholdeffectanalysisoftheassociationbetweenthe bodytemperatureandthe28-daymortalityinSICpatients.
ThresholdofbodytemperatureHR(95%CI) <38.0950.640(0.589,0.696) ≥38.0951.192(0.984,1.444)
Note:Thedatahavebeenadjustedforallofthefactorsincludedin ModelIVin Table2 HR, hazardratio; CI, confidenceinterval; SIC, sepsisinducedcoagulopathy.
influencetheprognosisofSICpatientsregardlessoffactors likeage,gender,orothercomorbidities.However,a significantinteractionwasobservedincerebrovascular diseasepatients,indicatingthatthisspecificsubgroupmay haveuniquethermoregulationcharacteristicswarranting furtherinvestigation.32 Thephenomenonthatpatientswith sepsiscomplicatedbycerebrovasculardiseasedisplayed differentpatternsoffeverandoutcomeassociationsmerits closerinvestigation.Severalpossiblemechanismsmay underpinthisinteraction.First,thermoregulationin cerebrovasculardiseaseisimpaired.Central thermoregulationinvolvescomplexneuralcircuitrylikethe preopticanteriorhypothalamus.33 Ischemicorhemorrhagic strokecaninterrupttheinvolvedpathways,compromising thermoregulatorycapacity.34 Thismaycontributetoaltered feverresponsesinoursubgroupofpatients.Second,cerebral inflammationisexacerbatedbyfever.Animalstudiesshowed
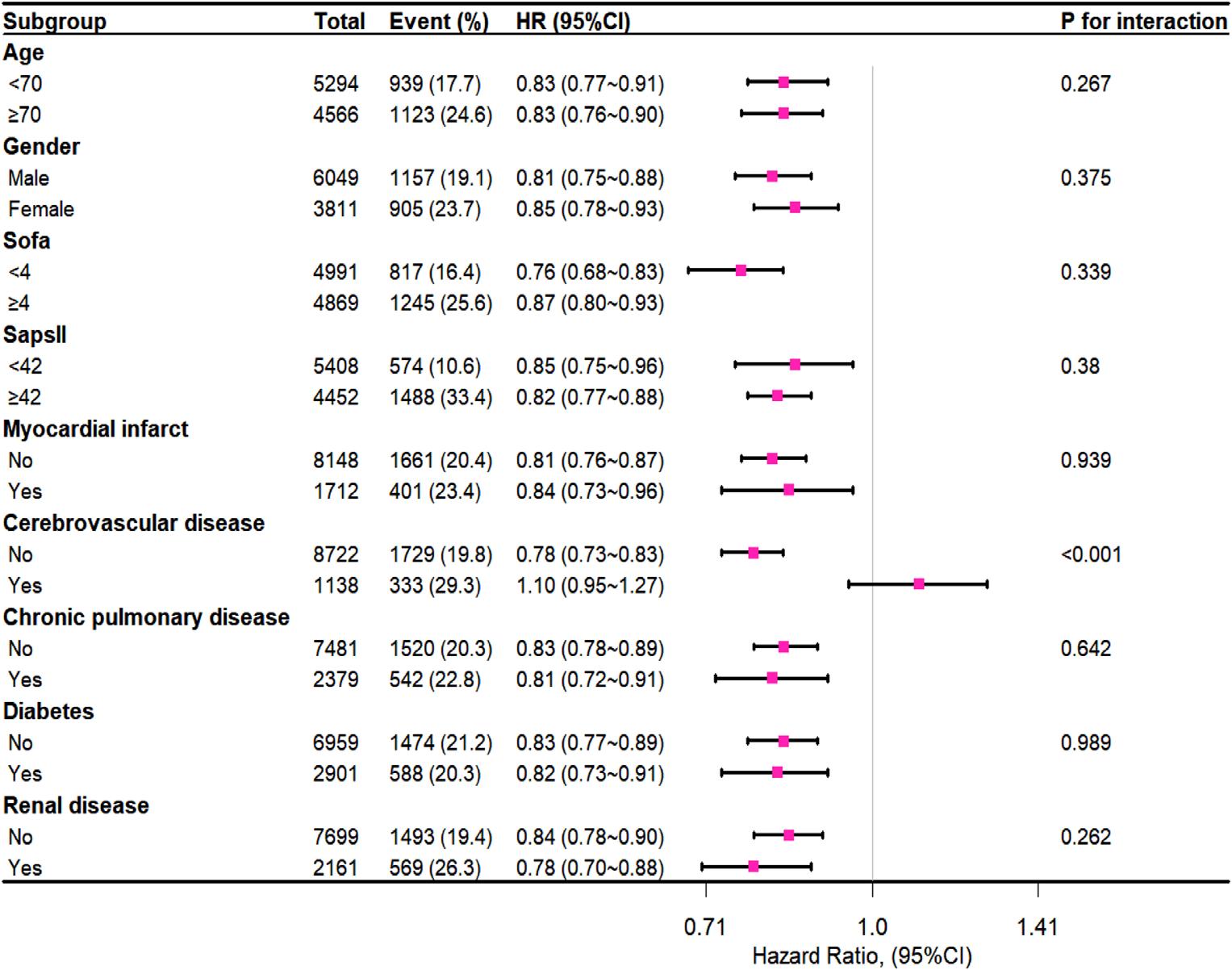
Figure3. Subgroupanalysisofassociationbetweentemperatureand28-daymortality.
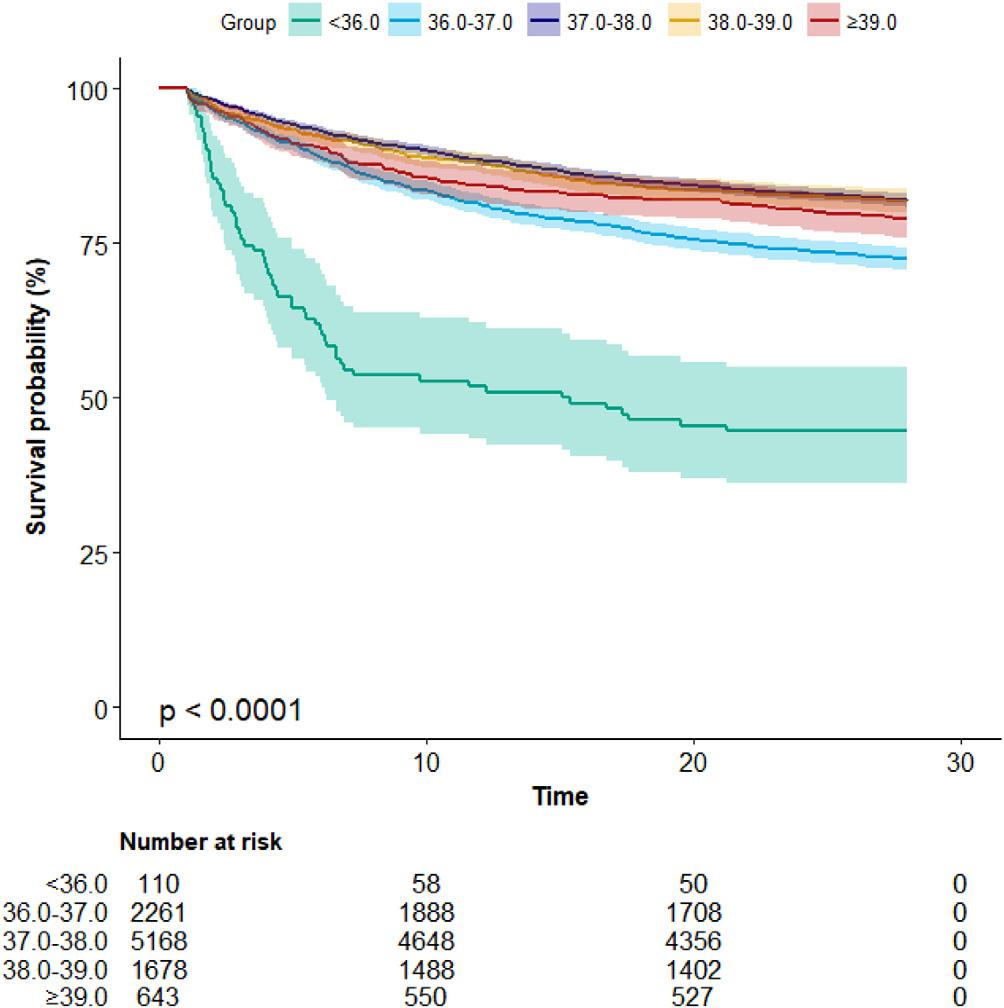
hyperthermiacanworsenischemicinjuriesviaincreased neutrophilinfiltration,blood-brainbarrierdysfunction, edemaformationandneuronalloss.35,36 Therefore,febrile responsesinsepsispatientswithpreexistingcerebrovascular lesionsmayworsensecondaryinsultsthrough neuroinflammation.Third,cerebralperfusionisimpairedby fever.Feverescalatesmetabolicdemandswhilesepticshock reducescerebralperfusion.37–39 Thecombinedeffectsmay createmismatchesinoxygensupplyanddemand,settingthe stageforischemicdamage.Strictfevercontrolmighthelp conserveneuronalviability.
Ourstudyholdsseveralnotablestrengths.Byexclusively focusingonSICpatients,weaddressacrucialgapinthe literature.Ourcomprehensiveanalysisbolstersthereliability andgeneralizabilityofour findings,whilealsouncovering novelcorrelationsandtheirimplications.Theobservednonlineartemperature-mortalityrelationshipaddsanewlayerof understandingtoSICmanagement,highlightingpotential harmatbothtemperatureextremes.
However,certainlimitationsshouldbeacknowledged. Ourstudy’sretrospectivenatureandrelianceondatafroma singlecenterintroducepotentialbiasesandlimitexternal validity.Inclusionofpatientsreceivingantipyreticsor temperaturemanagementcouldinfluenceobserved temperatures.Additionally,theuseofthehighestbody temperatureatICUadmissionmaynotcapturedynamic temperaturechanges.Itisalsoimportanttonotethatour analysiswaslimitedto9,860patientsoutoftheinitialcohort of23,828patientsduetothelackofavailableSICscores,
whichwasourprimaryindependentvariableofinterest.The exclusionofpatientswithoutSICscoresmayhave introducedpotentialselectionbias,asthesepatientscould havedifferedsystematicallyfromthoseincludedinthe analysis.However,thelargesamplesizeof9,860patients withcompletedatastillprovidesarobustbasisforour findings.Futurestudieswithmorecomprehensivedata collectionwouldbevaluabletofurthervalidateand generalizeourresults.
Inconclusion,ourstudyidentifiesanassociationthat meritsattentioninthecontextofSICpatientmanagementin ICUsettings.WefoundthatamongSICpatientsontheir first dayintheICU,abodytemperaturefrom37.0–38.0°Cwas associatedwithasignificantlyimprovedprognosis,marked bythelowestoverallmortalityrisk,whilethegroupwithlow bodytemperature(<36.0°C)exhibitedthehighestmortality risk.Additionally,agradualbutstatisticallynon-significant increaseinmortalityriskwasobservedwhenbody temperatureexceeded38.0°C.Futureresearchontheimpact ofrigoroustemperaturemanagementonSICpatient outcomes,andprospectivevalidationofourassociation betweentemperatureandsepsismortality,isneededto provideamorecomprehensiveunderstandingofthis complexrelationship.
AlldatainthearticlecanbeobtainedfromMIMIC-IV database(https://mimic.physionet.org/).
Theresearchprotocolforthisretrospectivestudyusinga de-identifieddatabasewasreviewedandapprovedbythe InstitutionalReviewBoard(IRB)oftheMassachusetts InstituteofTechnologyandBethIsraelDeaconessMedical Center.Therequirementforinformedconsentwaswaivedin accordancewiththeUSCodeofFederalRegulationsand institutionalguidelines.
AddressforCorrespondence:WeiganXu,MD,FirstPeople’s HospitalofFoshan,DepartmentofEmergency,No.81LingnanAve. North,ChanchengDistrict,Foshan,Guangdong,China.Email: 113101993@qq.com.JunJiang,PhD,FirstPeople’sHospitalof Foshan,DepartmentofEmergency,No.81LingnanAve.North, ChanchengDistrict,Foshan,Guangdong,China.
Email: jiangjungd2@163.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisworkwassupportedbythe
GuangdongMedicalScienceandTechnologyResearchFund Project(grantno.A2023178toZTE),theBasicandAppliedBasic ResearchFundofGuangdong(RegionalCooperationFundProject, 2022)(grantno.2022A1515140033toJJ),the14thFive-YearHighLevelMedicalKeySpecialtyProjectofFoshan,andtheFoshan ScienceandTechnologyInnovationProjects(2022)(grantno. 2220001004172toGJC).Thefundershadnoroleinstudydesign, datacollectionandanalysis,decisiontopublish,orpreparationofthe manuscript.Therearenootherconflictsofinterestorsourcesof fundingtodeclare.
Copyright:©2024Chenetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SingerM,DeutschmanCS,SeymourCW,etal.Thethirdinternational consensusdefinitionsforsepsisandsepticshock(Sepsis-3). JAMA. 2016;315(8):801.
2.IbaTandLevyJH.Derangementoftheendothelialglycocalyxinsepsis. JThrombHaemost. 2019;17(2):283–94.
3.LeviMandvanderPollT.Coagulationandsepsis. ThrombRes. 2017;149:38–44.
4.IbaT,NisioMD,LevyJH,etal.Newcriteriaforsepsis-induced coagulopathy(SIC)followingtherevisedsepsisdefinition:a retrospectiveanalysisofanationwidesurvey. BMJOpen. 2017;7(9):e017046.
5.GandoS,LeviM,TohCH.Disseminatedintravascularcoagulation. Nat RevDisPrimers. 2016;2:16037.
6.IbaT,ArakawaM,DiNisioM,etal.Newlyproposedsepsis-induced coagulopathyprecedesinternationalsocietyonthrombosisand haemostasisovert-disseminatedintravascularcoagulationandpredicts highmortality. JIntensiveCareMed. 2020;35(7):643–9.
7.YamakawaK,YoshimuraJ,ItoT,etal.Externalvalidationofthetwo newlyproposedcriteriaforassessingcoagulopathyinsepsis. ThrombHaemost. 2019;119(02):203–12.
8.SchortgenF,ClabaultK,KatsahianS,etal.Fevercontrolusingexternal coolinginsepticshock:arandomizedcontrolledtrial. AmJRespirCrit CareMed. 2012;185(10):1088–95.
9.PeresBotaD,LopesFerreiraF,MélotC,etal.Body temperaturealterationsinthecriticallyill. IntensiveCareMed. 2004;30(5):811–6.
10.DrewryAM,AblordeppeyEA,MurrayET,etal.Antipyretictherapyin criticallyillsepticpatients:asystematicreviewandmeta-analysis. CritCareMed. 2017;45(5):806–13.
11.YoungPJ,SaxenaM,BeasleyR,etal.Earlypeaktemperatureand mortalityincriticallyillpatientswithorwithoutinfection. IntensiveCare Med. 2012;38(3):437–44.
12.SchulmanCI,NamiasN,DohertyJ,etal.Theeffectofantipyretic therapyuponoutcomesincriticallyillpatients:arandomized, prospectivestudy. SurgInfect(Larchmt). 2005;6(4):369–75.
13.LeeB,InuiD,SuhG,etal.Associationofbodytemperatureand antipyretictreatmentswithmortalityofcriticallyillpatientswithand withoutsepsis:multi-centeredprospectiveobservationalstudy. Crit Care. 2012;16(1):R33.
14.LauplandKB,ZaharJR,AdrieC,etal.Severehypothermia increasestheriskforintensivecareunit-acquiredinfection. ClinInfectDis. 2012;54(8):1064–70.
15.RumbusZ,MaticsR,HegyiP,etal.Feverisassociatedwith reduced,hypothermiawithincreasedmortalityinsepticpatients: Ameta-analysisofclinicaltrials.LazzeriC,ed. PLoSONE. 2017;12(1):e0170152.
16.ShimazuiT,NakadaTaki,WalleyKR,etal.Significance ofbodytemperatureinelderlypatientswithsepsis. CritCare. 2020;24(1):387.
17.ItoY,KudoD,KushimotoS.Associationbetweenlowbodytemperature onadmissionandin-hospitalmortalityaccordingtobodymass indexcategoriesofpatientswithsepsis. Medicine. 2022;101(44):e31657.
18.KhodorkovskyB,YoussefE,AdamakosF,etal.Doesinitialtemperature intheemergencydepartmentpredictoutcomesinpatientsadmittedfor sepsis? JEmergMed. 2018;55(3):372–7.
19.KushimotoS,GandoS,SaitohD,etal.Theimpactofbodytemperature abnormalitiesonthediseaseseverityandoutcomeinpatientswith severesepsis:ananalysisfromamulticenter,prospectivesurveyof severesepsis. CritCare. 2013;17(6):R271.
20.BariePS,WilliamsMD,McCollamJS,etal.Benefit/riskprofileof drotrecoginalfa(activated)insurgicalpatientswithseveresepsis. AmJ Surg. 2004;188(3):212–20.
21.LeviM,TohCH,ThachilJ,etal.Guidelinesforthediagnosisand managementofdisseminatedintravascularcoagulation.British CommitteeforStandardsinHaematology. BrJHaematol. 2009;145(1):24–33.
22.GandoS,SaitohD,OguraH,etal.Amulticenter,prospectivevalidation studyoftheJapaneseassociationforacutemedicinedisseminated intravascularcoagulationscoringsysteminpatientswithseveresepsis. CritCare. 2013;17(3):R111.
23.JohnsonAEW,BulgarelliL,ShenL,etal.MIMIC-IV,afreelyaccessible electronichealthrecorddataset. SciData. 2023;10(1):1.
24.IbaTandLevyJH.Sepsis-inducedcoagulopathyanddisseminated intravascularcoagulation. Anesthesiology. 2020;132(5):1238–45.
25.RomanovskyAA.Thermoregulation:someconceptshavechanged. Functionalarchitectureofthethermoregulatorysystem. AmJPhysiol RegulCompPhysiol. 2007;292(1):R37–46.
26.YoungPJandSaxenaM.Fevermanagementinintensivecarepatients withinfections. CritCare. 2014;18(2):206.
27.PoldermanKH.Mechanismsofaction,physiologicaleffects, andcomplicationsofhypothermia. CritCareMed. 2009;37(7Suppl):S186–202.
28.SuffrediniAFandMunfordRS.Noveltherapiesforsepticshockoverthe past4decades. JAMA. 2011;306(2):194–9.
29.EgiMandMoritaK.Feverinnon-neurologicalcriticallyillpatients: asystematicreviewofobservationalstudies. JCritCare. 2012;27(5):428–33.
30.YoungP,SaxenaM,BellomoR,etal.Acetaminophenforfeverin criticallyillpatientswithsuspectedinfection. NEnglJMed. 2015;373(23):2215–24.
31.ShenY,LouY,ZhuS.Hyperthermiaisapredictorofhighmortalityin patientswithsepsis. CritCare. 2020;24(1):543.
32.GreerDM,FunkSE,ReavenNL,etal.Impactoffeveronoutcomein patientswithstrokeandneurologicinjury:acomprehensivemetaanalysis. Stroke. 2008;39(11):3029–35.
33.BoulantJA.Roleofthepreoptic-anteriorhypothalamusin thermoregulationandfever. ClinInfectDis. 2000;31(Suppl5):S157–61.
34.DebP,SharmaS,HassanKM.Pathophysiologicmechanismsofacute ischemicstroke:anoverviewwithemphasisontherapeuticsignificance beyondthrombolysis. Pathophysiology. 2010;17(3):197–218.
35.MaierCM,AhernKv,ChengML,etal.Optimaldepthanddurationof mildhypothermiainafocalmodeloftransientcerebralischemia:effects onneurologicoutcome,infarctsize,apoptosis,andinflammation. Stroke. 1998;29(10):2171–80.
36.LeeJE,YoonYJ,MoseleyME,etal.Reductioninlevelsofmatrix metalloproteinasesandincreasedexpressionoftissueinhibitorof metalloproteinase-2inresponsetomildhypothermiatherapyin experimentalstroke. JNeurosurg. 2005;103(2):289–97.
37.BurkhartCS,SiegemundM,SteinerLA.Cerebralperfusioninsepsis. CritCare. 2010;14(2):215.
38.SonnevilleR,deMontmollinE,PoujadeJ,etal.Potentiallymodifiable factorscontributingtosepsis-associatedencephalopathy. Intensive CareMed. 2017;43(8):1075–84.
39.MazeraudA,RighyC,BouchereauE,etal.Septic-associated encephalopathy:acomprehensivereview. Neurotherapeutics. 2020;17(2):392–403.
MichaelBerkenbush,MD,NRP
LaliSingh,DO
KellySessa,PharmD
RaghadSaadi,PharmD
SectionEditor:DavidPage,MD
MorristownMedicalCenter,SamethEmergencyDepartment, Morristown,NewJersey
Submissionhistory:SubmittedNovember16,2023;RevisionreceivedApril11,2024;AcceptedApril16,2024
ElectronicallypublishedJuly17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18584
Introduction: Theuseofpush-dosevasopressorstotreatanesthesia-inducedhypotensionisa commonevidence-basedpracticeamonganesthesiologists.Inmorerecentyears,theuseofpush-dose vasopressorshastransitionedtotheemergencydepartment(ED)andcriticalcaresetting.Thereis debateonthebestchoiceofapush-dosevasopressor,withpush-doseepinephrineorphenylephrine beingmorecommonlyused.Thisscopingreviewevaluatedpublicationsregardingtheclinicaluseof push-dosenorepinephrine.
Methods: WequeriedresearchstudiesinbothPubMedandGoogleScholarontheuseofpush-dose norepinephrineinhumansubjects,withnumerousrandomizedcontrolledtrialsthatcompare norepinephrinetoothervasopressorsincludingphenylephrine,ephedrine,andepinephrine.
Results: Alargemajorityofthestudieswereperformedinthesettingofspinalanesthesiapriorto cesareansection,whileseveralinvolvedtheadministrationofgeneralanesthesia,withlimited-to-no literatureintheemergencyandcriticalcaresetting.Ofthe27studiesthatweincludedinthereview, 17wererandomizedcontrolledtrials.Thesestudiesdemonstratedthatnorepinephrinewassafe andeffective.
Conclusion: Priorresearchhasdemonstratedthesuperiorityofnorepinephrineasapressorofchoice forvariousshockstates.Inthisreview,thesafetyandefficacyofpush-dosenorepinephrineis demonstrated,andfavorablehemodynamicmarkersareshownincomparisontootheragents.In addition,therearesomesafetyandef ficiencybenefitstousingpush-dosenorepinephrinefroman administrationstandpoint,aswellasclinicallyindecreasedneedforrepeatdoses.Furtherhigh-quality studiesintheemergencyandcriticalcarerealmwouldbebeneficialtoconfirmthese findings.[WestJ EmergMed.2024;25(5)708–714.]
Keywords: push-dosevasopressors;norepinephrine;anesthesia-inducedhypotension;criticalcare.
Theuseofpush-dosevasopressorstotreatanesthesia induced-hypotensionisacommon,evidence-basedpractice amonganesthesiologists,1 whichhastransitionedtothe emergencydepartment(ED)andcriticalcaresetting.Pushdosevasopressorsallowclinicianstourgentlystabilize patients’ hemodynamicsandprovideadditionaltimefor procedures(eg,intubations)andbridgingtocontinuous
infusions.Norepinephrine(NE)isthevasopressor ofchoiceinmostshockstatesdueinparttoadecreased incidenceofsideeffects,2 superiorhemodynamicprofile,3 andbettercontroloftheshockstate.4 Ourmainpurposein thisscopingreviewwastodeterminetheevidence forpush-doseNEcomparedtoothervasopressorswhile addressingthesafety,effectiveness,andefficiency ofthedrug.
Inthisstudyweevaluatedfull-textpublicationsinthe Englishlanguageregardingtheclinicaluseofpush-doseNE inhumansubjectsinaccordancewithPRISA-ScR guidelines.UsingPubMedandGoogleScholarinOctober 2022,literaturewasreviewedbasedonthefollowing keywords: “bolusnorepinephrine,”“push-dose norepinephrine,” andvariousformulationsof “norepinephrine/administrationanddosage” [Mesh]AND (pushbolusORbolusdose)Filters:English,Humans.Using ORincludingvariousothernamesfornorepinephrine includingDroxidop,Nordefrin,Normetanephrine, Levonorepinephrine,Noradrenaline,Levarterenol, Levonor,Levophed,LevophedBitartrate,orNoradrénaline tartraterenaudin.
Weidentified88articlesusingthesesearchterms(Figure). Thesearticleswerereviewedtodeterminewhetherthe administrationofNEwasstudiedasapushorbolusdose. WeexcludedthosewhichonlyincludedNEinfusions.One reviewerreviewedthestudiesforeligibility,whichwasthen confirmedindependentlybyasecondreviewer.Non-human studies,casereports,andletterstotheeditorswereexcluded. WealsoexcludedstudiesoncirculatingplasmalevelsofNE, aswellasarticleswhoseprimaryoutcomewasnot hemodynamics.OneexcludedarticlefocusedonNEuseto avoidpost-reperfusionsyndromeinlivertransplant,and anotherfocusedonumbilicalarterialpHinneonatesafter theirmothersreceivedNEduringtheircesareansection.Of theseincludedarticles,27studiesthatincludedpush-doseNE wereincludedinthefollowingreview.Thearticlesobtained werepublishedinorafter2015exceptforonestudy.5 Seventeenwererandomizedcontrolledtrials(RCT),and fourweredose-findingtrials.Therewerethreeprospective observationalstudiesandthreeliteraturereviews.
ThereweresevenRCTsthatcomparedNEwith phenylephrine,encompassingatotalof626patients,allin thesettingofmaternalpatientsreceivingspinalanesthesia forcesareansection.6–12 Norepinephrineshowedlessriskof bradycardiacomparedtophenylephrine.TheuseofNE requiredfewerbolusesthanphenylephrinetocorrect hypotensionandmaintainedhighercardiacoutputand strokevolumeincomparisontophenylephrine.Therewere nosafetyconcernswithNEusedperipherally.Therelative potencyratiousedonaveragewasnorepinephrine: phenylephrine1microgram(μg):12.5 μg.
Twodouble-blindedRCTscomparedNEwithboth phenylephrineandephedrine.13,14 Thesetwostudies involvedatotalof211patientsreceivingspinalanesthesiafor cesareansection.Norepinephrinehadfewerepisodesof bradycardiacomparedtophenylephrineandfewerepisodes oftachycardiacomparedtoephedrine.Inonestudy14 NE
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Push-dosevasopressorsarecommonlyusedin emergencyandcriticalcaresettings. Norepinephrineinfusionshavebeenshownto besuperiortoothervasopressors.
Whatwastheresearchquestion?
Wesoughttodeterminetheevidencefor push-dosenorepinephrinecomparedto othervasopressors.
Whatwasthemajor findingofthestudy?
Thesafetyandef fi cacyofpush-dose norepinephrineat4 – 16mcgisdemonstrated comparedtootheragents.
Howdoesthisimprovepopulationhealth?
Push-dosevasopressorsareacrucialpartof emergencyandcriticalcareandareusedfor hemodynamicstabilizationduringtimesensitivepatientemergencies.
maintainedahighermeanarterialpressure(MAP)compared totheothertwoagents.
Barakaetallookedatthehemodynamiceffectsin phenylephrine,NE,andepinephrineforintubatedpatients undergoingcoronaryarterybypassgrafting5.Phenylephrine andNEhadsimilarchangesinsystemicvascularresistance withoutsignificantchangeincardiacoutput.Allagents increasedMAPsimilarlyinthisstudy.Ofnote,thiswasthe onlystudywefoundthatcomparedpush-doseepinephrine withNE.
Threedouble-blindedRCTscomparedNEwithephedrine with276totalpatients.15–17 Ineachstudy,NEwasfoundto bemoreefficaciousthanephedrineinmaintainingMAPand wasalsoassociatedwithlesstachycardiaandfewertotal dosesgiven.Onestudyusedradialarterycathetersfor monitoringbothMAPandheartrate,whiletheothersused non-invasivemonitoringatstandardintervals.Thesestudies alsoincludedhypertensivepatientsundergoingspinal surgeryandpatientswithcoronaryarterydiseaseundergoing kneearthroscopy.
FourRCTscompareddifferentNEboluses/infusions,two ofwhichweredouble-blinded.18–21 Eachofthesestudieswas relatedtospinal-inducedhypotensionduringcesarean section,andprimarilyfocusedonpreventionofhypotension byadministrationofprophylacticNE.Infusionswere successfulinpreventinghypotension,andhigherboluses

(6 μgor0.10 μg/kg)performedbettercomparedtolower boluses(4mcgor0.05 μg/kg).
Therewerefourdose-findingtrialsincludingatotalof342 patientsundergoingspinalanesthesiaduringcesarean delivery.22–25 Differentmethodswereusedtodetermine efficacy,withtheprimarygoalofmaintainingsystolicblood pressureat80%oftheinitialreading.Foradouble-blind sequentialallocationstudywithbiasedcoinupanddown design,theED90 was5.8 μg.Usingrandomallocationgraded doseresponse,theED50 forNEwas10 μg.Anotherstudy comparingprophylacticversusrescuebolusofNEhasan ED90 of10.85 μgforprophylacticdoseand12.3 μgfor rescuedose.
Therewerethreeprospective,observationalstudies regardingpush-doseNE,oneduringgeneralanesthesiaand twoduringspinalanesthesiaforcesareansections.26–28 Two ofthesestudiescomparedNEagainstphenylephrine.27,29 Norepinephrineresultedinincreasedstrokevolume comparedtophenylephrine.Otherhemodynamiceffects weresimilarbetweenthetwoagents.Anotherstudyreviewed
theuseofNEcomparedtoephedrine,withNEshowing higherMAPsandlesstachycardiacomparedtoephedrine, alsolowernumberofbolusesneededfortreatmentof hypotension.28
Therewerethreepriorliteraturereviewsidentified.29–31 The firstperformedin2018identifiedninefull-textarticles regardingtheuseofnorepinephrine.30 Atthattime,itwas determinedthattheefficacyofNEissimilartophenylephrine withoutadverseoutcomes,showsimprovementincardiac outputanddecreasedriskofbradycardia.Asecondreview focusedonthepharmacologyofvariousvasopressorsand theirdiverseclinicalscenariosforuse(intraoperative, periprocedural,bridgetovasopressorinfusions,post-cardiac arrest,andanaphylaxis).31 Thisarticlealsocoveredthe safetyandcompoundingconcernswiththebedsidemixingof vasopressors.Dilutedconcentrationshavebeenshown tobesafeperipherally,althoughcentralaccessispreferred.A thirdreviewfocusedonanesthesiauseofvasopressors andaddressingthepharmacologyofcommonagents indetail.32
Push-doseepinephrineorphenylephrinearecommonly usedvasopressorsinthecriticalcaresettingforthetreatment ofhypotension.32 Epinephrinehasbothalphaandbeta effects,thusactingasaninopressor.Atlowerdoses(0.01to 0.1 μg/kg/min),epinephrinestimulatesbeta-1andbeta-2 receptorsandfunctionsasaninotrope,andathigherdoses (>0.1 μg/kg/min)italsostimulatesalpha-1causing vasoconstriction,thusincreasingbloodpressure. Phenylephrineisapurealpha-1agonistthatincreasesarterial andvenoustone,thusincreasingbloodpressure.Ephedrine hasbothalpha-1andbeta-1receptoractivity.Itisapopular choiceintheoperatingroomduetoitsrapidonset(one minute)andlongerdurationofaction(60minutes).
Norepinephrineisanalpha-1receptoragonistwith moderatebeta-1activityandminimalbeta-2activity.Itisan attractiveagentbecauseitshemodynamiceffectsare dominatedbyitsalpha-1activity,whileitsbeta-1activity providesjustenoughinotropytomaintaincardiacoutput. Thereareadvantagestousingpush-doseNEcomparedto othervasopressorsincludingsafety,effectiveness,efficiency, andcost.
Thepreparationofpush-dosevasopressorsisassociated withahighriskformedicationerrorsbecausethese medicationsareusuallymixedatthepatient’sbedsidefor immediateuseinstressfulsituations.33,34 Becauseofthishigh risk,itisrecommendedthatthesepreparationsbedouble checkedbyanotherhealthcareprofessionalpriorto administration.Immediatelyafterpreparation,allsyringes andbagsthatareusedintheprocessshouldbelabeledwith theappropriateconcentrationandmedicationnameto furtherpreventanymedicationerrors.
Comparedtocompoundingotherpush-dose vasopressors,anadvantagetopush-doseNEisthatitcan allowforlimitedpreparationdependingonpremixedbag availability.Ifusingapremixedbag4milligrams(mg)/250 milliliters(mL)tomakepush-doseNE,itwouldrequireno mixing,andtheoreticallylesschanceforcompounding errors.ForinstitutionsthatdonothavepremixNE4mg/ 250mL,thepreparationofpush-doseNEcanbemixedby withdrawingthe4mLofNEfromthe4mg/4mLvialand injectingitintoa250mLbagofnormalsaline.Fromthebag, withdraw10mLofNE-containing fluidintoa10mL syringe.The finalconcentrationwouldbe16 μg/mL ofnorepinephrine.
Allthedose-findingstudiesreviewedareinpregnant womenundergoingelectivecesareansectionsreceivingspinal anesthesia.However,thisdatacouldbeextrapolatedtothe criticalcaresettingwiththeunderstandingthatpatients mightrequirehigherempiricdoses.Basedonseveralstudies assessingpush-doseNE,dosesrangingfrom4–16 μgwere reportedtobesafeandeffectiveintreatingorpreventing
hypotensionduetospinalanesthesia.Aninitialpush-doseof NE4–16 μg(0.25–1mL)seemstobereasonableinthecritical caresetting.
Norepinephrineisthe first-linevasopressorforalmostall formsofshock,includingundifferentiatedshock, vasodilatory/septicshock,andcardiogenicshock.The2021 SurvivingSepsisCampaignrecommendsNEasthe first choiceinpatientswithsepticshock(Evans2021).35 Inthe CENSERtrial,patientswhoreceivedearlyNEhadbetter controloftheirshockstatebythesix-hourmark.4 Notonly doesNEimprovebloodpressure,butitalsoimproves cardiacoutput.36 ItwaspreviouslythoughtthatNEmight worsenorganhypoperfusioncomparedtoother vasopressors.However,ithassincebeenshownthatin patientswithseveresepticshock,thosewhoreceivedNEhad highersplanchniccirculationcomparedtothosewho receivedepinephrine.37
AstudydonebyMartinetalshowedthatpatientstreated withNEhadsignificantlylowerhospitalmortalitycompared tothosetreatedwithhigh-dosedopamineand/or epinephrine.38 Forcardiogenicshock,onestudyshowedthat NEhasalowerincidenceofrefractoryshockcomparedto epinephrine.39 Norepinephrinehasalsobeenshowntohavea decreasedriskofcausingarrhythmiascomparedto dopamine,whichmakesitpreferredoverothervasopressors, especiallyinacardiogenicshockstate.40 Inthesettingof hypovolemicorhemorrhageshock,thereisaconcernthat vasopressorsmaycompromisemicrocirculationandcause tissueischemiaduetoexcessivearteriolarvasoconstriction. However,arecentstudybyHarroisetalobservedthatNE preservedintestinalmicrocirculationduringhemorrhagic shockinmice.41 Additionally,therewasastudycompleted byPoloujadoffetalinrats,whichshowedthatwhenusing eitherahypotensiveornormotensivetargetfor fluid resuscitationinhemorrhagicshock,ratsthatreceivedNE infusionshadimprovedsurvivalcomparedtothosewho received fluidsonly.42
Theuseofpush-doseNEcanbeextendedtosettings beyondthatofshockstates,suchaspriortoorduring proceduresthatrequirehemodynamicoptimization,suchas endotrachealintubationortheinductionofgeneral anesthesia.BarakaetalcomparedtheeffectsofNE, phenylephrine,andepinephrineonpatientswhowere endotracheallyintubatedbeforeundergoingelective coronaryarterybypassgrafting.5 TheyfoundthattheNE grouphadthehighestincreaseinMAP(42.9%vs35%and 32.6%).Inaddition,thePrePAREtrialhasshownthata fluid bolusmaynotbeenoughtopreventcardiovascular collapse.43 Push-doseepinephrinehasgainedpopularityin theemergencyandcriticalcarerealmforthispurpose. However,randomizedtrialscomparingepinephrinetoNEin thissettinghavenotbeenperformed.
Usingasingleagentforbothpush-doseandcontinuous infusionrequiresoveralllessmedications/materialsthan compoundingtwodifferentagents,whichinturnimproves efficiencyincriticalcaresettingswhereeveryminutematters. Comparedtophenylephrine10mgvialsandepinephrine 1mgvials,theaveragewholesalepriceofNE4mgvialsis slightlymoreexpensivefortherequireddoseneededto preparepush-doseNE.44 However,incriticalcaresettings push-dosevasopressorsarecommonlyusedasabridgetoan infusion;therefore,theNEcostwouldbenegated,asthe samebagusedtomakeupthepush-doseNEcanbeusedfor theinfusion.
Thisreviewofpush-doseNEdemonstratedasignificant numberofdouble-blindedRCTs.However,nearlyallthe studieswereperformedintheoperatingtheater,withlimited dataintheEDorcriticalcaresetting.Patientsmaybeless optimized,andlikelywouldbeconsiderablyolderandhave morecomorbidities,thanthepopulationsofpregnant femalesprimarilystudiedinthisreviewundergoingspinal anesthesia.Inaddition,theoptimaldosingofNEmaynotbe accuratelyreflectedforthecriticalcaresetting.However,the lackofadverseeventsisreassuringforitssafetyprofile.Itis unclearwhethertheshorterhalf-lifeofNEwouldimpactits utilityforperiproceduraluse;however,theeffectofpushdoseNEremainedeitherequivalentorbetterthanother vasopressorsinthestudiesreviewed.Norepinephrine appearstobethevasopressorofchoicecomparedto phenylephrineandephedrine.Comparisonstopush-dose epinephrine,whichismorecommonlyusedinthecritical caresetting,arealsolacking.
Priorresearchhasdemonstratedthesuperiorityof norepinephrineasapressorofchoiceforvariousshock states,althoughitisrecognizedthattheclinicalsituationmay dictatewhichvasopressorisused.Inthisreview,thesafety andefficacyofpush-doseNEaredemonstrated,and favorablehemodynamicmarkersareshownincomparison tootheragents.Inaddition,therearesomesafetyand efficiencybenefitstousingpush-doseNE,frombothan administrationstandpointandclinicallyinadecreasedneed forrepeatdoses.Furtherhigh-qualitystudiesinthe emergencyandcriticalcarerealmwouldbebeneficialto confirmthese findings.
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Berkenbushetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.HoldenD,RamichJ,TimmE,etal.Safetyconsiderationsand guideline-basedsafeuserecommendationsfor “bolus-dose” vasopressorsintheemergencydepartment. AnnEmergMed. 2018;71(1):83–92.
2.DeBackerD,BistonP,DevriendtJ,etal.Comparisonofdopamine andnorepinephrineinthetreatmentofshock. NEnglJMed. 2010;362(9):779–89.
3.LuX,XuX,WuY.Norepinephrinewassuperiorindeathriskreducing andhemodynamicscomparedtodopamineintreatmentofpatientswith septicshock. Pteridines, 2021;32(1):5–10.
4.PermpikulC,TongyooS,ViarasilpaT,etal.Earlyuseofnorepinephrine insepticshockresuscitation(CENSER).Arandomizedtrial. AmJ RespirCritCareMed. 2019;199(9):1097–105.
5.BarakaA,HarounS,BaroodyMA,etal.Thehemodynamiceffectsof intravenousnorepinephrineversusepinephrineandphenylephrinein patientswithischemicheartdisease. MiddleEastJAnaesthesiol. 1991;11(1):53–62.
6.SharkeyAM,SiddiquiN,DowneyK,etal.Comparisonofintermittent intravenousbolusesofphenylephrineandnorepinephrinetoprevent andtreatspinal-inducedhypotensionincesareandeliveries: randomizedcontrolledtrial. AnesthAnalg. 2019;129(5):1312–8.
7.ChoWJ,ChoSY,LeeAR.Systemichemodynamiceffectsof norepinephrineversusphenylephrineinintermittentbolusdosesduring spinalanesthesiaforcesareandelivery. AnesthPainMed(Seoul). 2020;15(1):53–60.
8.WangX,MaoM,ZhangSS,etal.Bolusnorepinephrineand phenylephrineformaternalhypotensionduringelectivecesarean sectionwithspinalanesthesia:arandomized,double-blindedstudy. ChinMedJ(Engl). 2020;133(5):509–16.
9.MohtaM,DubeyM,MalhotraRK,etal.Comparisonofthepotencyof phenylephrineandnorepinephrinebolusdosesusedtotreatpost-spinal hypotensionduringelectivecaesareansection. IntJObstetAnesth. 2019;38:25–31.
AddressforCorrespondence:MichaelBerkenbush,MD,NRP, AtlanticHealth-MorristownMedicalCenter,Emergency Department,100MadisonAvenue,Morristown,NJ07960.Email: Michael.berkenbush@atlantichealth.org
10.PuthenveettilN,SivachalamSN,RajanS,etal.Comparisonof norepinephrineandphenylephrinebolusesforthetreatmentof hypotensionduringspinalanaesthesiaforcaesareansection: arandomisedcontrolledtrial. IndianJAnaesth. 2019;63(12):995–1000.
11.TiwariJP,VermaSJ,SinghAK.Aprospectiverandomizedstudy comparingthebolusdosesofnorepinephrineandphenylephrineforthe treatmentofspinalinducedhypotensionincesareansection. Cureus. 2022;14(7):e27166.
12.SundararajanC,SujathaC,AsokanA.Comparisonofnorepinephrine andphenylephrinebolusesduringspinalanesthesiaforcesarean delivery. AsianJMedSci. 2022;13(10):54–8.
13.WangX,MaoM,LiuS,etal.Acomparativestudyofbolus norepinephrine,phenylephrine,andephedrineforthetreatmentof maternalhypotensioninparturientswithpreeclampsiaduringcesarean deliveryunderspinalanesthesia. MedSciMonit. 2019;25:1093–101.
14.MahzadA,NikoubakhtN,FarahmandradR,etal.Evaluationofthe effectofnorepinephrine,ephedrineandphenylephrineonprophylaxis andtreatmentofhemodynamicchangesassociatedwithspinal anesthesiainelectivecesareansectionsurgeries. JPharmNegat. 2022;13(3):1310–7.
15.HassaniV,MovaseghiG,SafaeeyanR,etal.Comparisonofephedrine vs.norepinephrineintreatinganesthesia-inducedhypotensionin hypertensivepatients:randomizeddouble-blindedstudy. AnesthPain Med. 2018;8(4):e79626.
16.ElShafeiM,ElGendyH,ElFawyD.Norepinephrineversusephedrine forthepreventionofspinalanesthesia-inducedhypotensionincoronary arterydiseasepatientsundergoingkneearthroscopy. Ain-ShamsJ Anesthesiol. 2015;08:424–8.
17.ElagamyA,KamalyA,ShahinM,etal.Norepinephrineversus ephedrineforhypotensionprophylaxisduringcesareansectionunder spinalanesthesia. Ain-ShamsJAnesthesiol. 2021;13:3:1–6.
18.HassabelnabyYS,HasaninAM,AdlyN,etal.Comparisonoftwo norepinephrinerescuebolusformanagementofpost-spinal hypotensionduringcesareandelivery:arandomizedcontrolledtrial. BMCAnesthesiol. 2020;20(1):84.
19.LyuW,WeiP,TangW,etal.Preventingspinalhypotensionduring cesareanbirthwithtwoinitialbolusesofnorepinephrineinchinese parturients:arandomized,double-blind,controlledtrial. AnesthAnalg. 2023;136(1):94–100.
20.ElhalimMandMandourO.Comparativestudybetweennorepinephrine bolusandnorephinephrineinfusioninpreventionofpost-spinal hypotensionincesareansection. Al-AzharMed. 2018;47(2):329–36.
21.ChoudharyS,DagarR,JeengerL,etal.Prophylacticco–administration oftwodifferentbolusdosesofnorepinephrineinspinal–induced hypotensionduringcaesareansection:aprospectiverandomized double–blindedstudy. JObstetAnaesthCritCare. 2020;10(2):111–7.
22.OnwocheiDN,NganKeeWD,FungL,etal.Norepinephrineintermittent intravenousbolusestopreventhypotensionduringspinalanesthesiafor cesareandelivery:asequentialallocationdose-findingstudy. Anesth Analg. 2017;125(1):212–8.
23.NganKeeWD.ARandom-allocationgradeddose-responsestudyof norepinephrineandphenylephrinefortreatinghypotension duringspinalanesthesiaforcesareandelivery. Anesthesiology. 2017;127(6):934–41.
24.XuT,ZhengJ,AnXH,etal.Norepinephrineintravenousprophylactic bolusversusrescuebolustopreventandtreatmaternalhypotension aftercombinedspinalandepiduralanesthesiaduringcesareandelivery: asequentialdose-findingstudy. AnnTranslMed. 2019;7(18):451.
25.WangT,HeQ,ZhangW,etal.DeterminationoftheED50 andED95 of intravenousbolusofnorepinephrineforthetreatmentofhypotension duringspinalanesthesiaforcesareandelivery. ExpTherMed. 2020;19(3):1763–70.
26.ValléeF,PassouantO,LeGallA,etal.Norepinephrinereducesarterial compliancelessthanphenylephrinewhentreatinggeneralanesthesiainducedarterialhypotension. ActaAnaesthesiolScand. 2017;61(6):590–600.
27.DesalegnM,ShitemawT,TamratH.Effectivenessofprophylacticbolus ephedrineversusnorepinephrineformanagementofpostspinal hypotensionduringelectivecaesareansectioninresourcelimited setting:aprospectivecohortstudy. AnesthesiolResPract. 2022;2022:7170301.
28.OsmaniS,AcharyaM,KamathS,etal.Comparisonofprophylactic phenylephrineversusnoradrenalinebolusesforhemodynamicstability duringelectivecesareandeliveryunderspinalanesthesia:an observationalstudy. AnaesthPain&IntensiveCare April;26(2):168–74.
29.WangX,ShenX,LiuS,etal.Theefficacyandsafetyofnorepinephrine anditsfeasibilityasareplacementforphenylephrinetomanage maternalhypotensionduringelectivecesareandeliveryunderspinal anesthesia. BiomedResInt. 2018;2018:1869189.
30.McPhersonKL,KovacicScherrerNL,HaysWB,etal.Areviewofpushdosevasopressorsintheperi-operativeandcriticalcaresetting. J PharmPract. 2023;36(4):925–32.
31.MetsB.Shouldnorepinephrine,ratherthanphenylephrine,be consideredtheprimaryvasopressorinanestheticpractice? Anesth Analg. 2016;122(5):1707–14.
32.JentzerJC,CoonsJC,LinkCB,etal.Pharmacotherapyupdateonthe useofvasopressorsandinotropesintheintensivecareunit. J CardiovascPharmacolTher. 2015;20(3):249–60.
33.ColeJB,KnackSK,KarlER,etal.Humanerrorsandadverse hemodynamiceventsrelatedto “pushdosepressors” intheemergency department. JMedToxicol. 2019;15(4):276–86.
34.TiltonLJandEgingerKH.Utilityofpush-dosevasopressorsfor temporarytreatmentofhypotensionintheemergencydepartment. JEmergNurs. 2016;42(3):279–81.
35.EvansL,RhodesA,AlhazzaniW,etal.SurvivingSepsisCampaign: internationalguidelinesformanagementofsepsisandsepticshock 2021. IntensiveCareMed. 2021;47(11):1181–247.
36.HamzaouiO,ScheerenTWL,TeboulJL.Norepinephrineinseptic shock:whenandhowmuch? CurrOpinCritCare. 2017;23(4):342–7.
37.DeBackerD,CreteurJ,SilvaE,etal.Effectsofdopamine, norepinephrine,andepinephrineonthesplanchniccirculationinseptic shock:Whichisbest? CritCareMed. 2003;31(6):1659–67.
38.MartinC,ViviandX,LeoneM,etal.Effectofnorepinephrineonthe outcomeofsepticshock. CritCareMed. 2000;28(8):2758–65.
IsPush-DoseNorepinephrineaBetterChoice?
39.LevyB,Clere-JehlR,LegrasA,etal.Epinephrineversus norepinephrineforcardiogenicshockafteracutemyocardialinfarction. JAmCollCardiol. 2018;72(2):173–82.
40.DeBackerD,BistonP,DevriendtJ,etal.Comparisonofdopamine andnorepinephrineinthetreatmentofshock. NEnglJMed. 2010;362(9):779–89.
41.HarroisA,BaudryN,HuetO,etal.Norepinephrinedecreases fluid requirementsandbloodlosswhilepreservingintestinalvilli microcirculationduring fluidresuscitationofuncontrolledhemorrhagic shockinmice. Anesthesiology. 2015;122(5):1093–102.
42.PoloujadoffMP,BorronSW,AmathieuR,etal.Improved survivalafterresuscitationwithnorepinephrineinamurine modelofuncontrolledhemorrhagicshock. Anesthesiology. 2007;107(4):591–6.
43.JanzDR,CaseyJD,SemlerMW,etal.Effectofa fluidboluson cardiovascularcollapseamongcriticallyilladultsundergoingtracheal intubation(PrePARE):arandomisedcontrolledtrial. LancetRespirMed. 2019;7(12):1039–47.
44.Medi-spanPriceRx.WoltersKluwer.2023.Availableat: https://www. uptodate.com/. AccessedFebruary20,2023.
AlexisE.Pelletier-Bui,MD*
TimothyFallon,MD†
LizaSmith,MD‡
TaniaStrout,PhD,MS†
MichelleFischer,MD,MPH§
MarkOlaf,DO∥
ErinMcDonough,MD¶
BrianBarbas,MD#
MichaelCirone,MD**
ElizabethBarrallWerley,MD§
*CooperUniversityHospital/CooperMedicalSchoolofRowanUniversity, DepartmentofEmergencyMedicine,Camden,NewJersey
† MaineMedicalCenter,TuftsUniversitySchoolofMedicine,Departmentof EmergencyMedicine,Portland,Maine
‡ UniversityofMassachusettsChanSchoolofMedicine,BaystateMedicalCenter, DepartmentofEmergencyMedicine,Springfield,Massachusetts
§ PennStateCollegeofMedicine/PennStateHealthMiltonS.HersheyMedical Center,DepartmentofEmergencyMedicine,Hershey,Pennsylvania
∥ GeisingerCommonwealthSchoolofMedicine,DepartmentofEmergency Medicine,Scranton,Pennsylvania
¶ UniversityofCincinnatiCollegeofMedicine,DepartmentofEmergencyMedicine, Cincinnati,Ohio
# LoyolaUniversityChicago,StritchSchoolofMedicine,LoyolaUniversityMedical Center,DepartmentofEmergencyMedicine,Maywood,Illinois
**UniversityofIllinois,DepartmentofEmergencyMedicine,Chicago,Illinois
SectionEditors:PaulLoganWeygandt,MD,andChrisMerritt,MD
Submissionhistory:SubmittedFebruary2,2024;RevisionreceivedApril22,2024;AcceptedJune3,2024
ElectronicallypublishedAugust27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.19392
Introduction: Programsignaling(PS),whichenablesresidencyapplicantstosignaltheirpreferencefora specificprogram,wasintroducedinemergencymedicine(EM)inthe2022–2023residencyapplicationcycle. InthisstudyweevaluatedEMprogramdirectors’ (PD)utilizationofPSinapplicationreviewandranking.This studyalsoexplorestherelationshipbetweenprogramcharacteristicsandnumberofsignalsreceivedaswell astherelativeimportanceandutilizationofsignalsrelatedtothenumberofsignalsreceived.
Methods: Thisisaninstitutionalreviewboard-approved,cross-sectionalstudyofPDsatAccreditation CouncilforGraduateMedicalEducation-accreditedEMresidencyprograms.Weuseddescriptive statisticstodescribethecharacteristicsofresidencyprogramsandpracticesaroundPS.Measuresof centraltendencyanddispersionsummarizedcontinuousvariables.Weusedchi-squareanalysisorthe Fisherexacttestforcomparisonsbetweengroupsforcategoricalvariables.Comparisonsforcontinuous variablesweremadeusingthe t-testforindependentsamplesoranalysisofvariance.
Results: Theresponseratewas41%(n = 113/277EMprograms).MostprogramsparticipatedinPS (n = 261/277EMprograms,94.2%).Meannumberofsignalsreceivedwas60(range2–203).Signals receivedvariedbasedonprogramcharacteristicsincludinggeographiclocationandprogramtype,duration, environment,andlongevity.MostusedPSinholisticreview(52.2%),butotherusesvariedbyproportionof applicationsthatweresignaled.TheimportanceofPSinapplicationreview(mean2.9;1–5scale,1 = not important,5 = extremelyimportant)andranklistpreparation(2.1)wasrelativelylowcomparedtoother applicationelementssuchasstandardizedlettersofevaluation(4.97forreview,4.90forranking).
Conclusion: ThestudyprovidesinsightsintoPSutilizationinEM’sinauguralyear.Wehaveidentified patternsofsignalusebasedonprogramcharacteristicsandnumberofsignalsreceivedthatcaninformsignal allocationandutilizationonanindividualapplicantandprogramlevel.Amorenuancedunderstandingof signalusecanprovidevaluableinsightasthespecialtyofEMgrappleswith fluctuationsinitsapplicant numbersandshiftingdemographicsofitsapplicantpool.[WestJEmergMed.2024;25(5)715–724.]
Programsignaling(PS)wasintroducedintotheresidency applicationprocessinresponsetotheincreasingnumberof applicationsreceivedbyprograms,exacerbatingthe challengeofcomprehensiveholisticreview.1 Subsequently, EMhasexperienceddrastic fluctuationsinthenumberof applicantspursuingEMandspecialtyMatchrates,aswellas unprecedentedchangestothedemographicsofits applicationpooloverthelastseveralyears.2 Evenwith variabilityinthenumberofapplicationstoemergency medicine(EM)inrecentyears,EMapplicationnumbers remainsignificantlyabovewhattheywere10yearsago.2,3 Programsignalingallowsapplicantstoassignsignalsto theirmostdesiredtrainingprograms,sothatprograms mayfocustheirholisticeffortstowardhigh-yieldinterview candidates,potentiallybenefitingbothapplicants andprograms.
ProgramsignalingwasimplementedinEMviathe ElectronicResidencyApplicationService(ERAS)inthe 2022–2023residencyapplicationcycle,allowingapplicants tosend fivesignalsatthetimeoftheirresidencyapplication submissionwithinstructiontonotsignaltheirhomeorawayrotationinstitutions.4 TheAssociationofAmericanMedical Colleges(AAMC)publishedgenericguidanceforprograms regardingtheuseofPSonlyduringtheinterview-offerphase andprogramsattestedtoacodeofconductregardingsignal usagewhenoptingintotheprocess,includingguidancenotto usePSinrankorderlist(ROL)decisions.5 Whiledatawas evaluatedbyERASacrossallparticipatingspecialties,and otherspecialtieshavereportedtheirownspecialty-specific data,opportunitiesremainedtofurtherinvestigatequestions specifictoPSwithinEM.6–18 Theuniquechallengesfacing EMcreatedanappetiteandunderscoredtheneedfor specialty-speci ficguidance.
Toprovideevidence-basedguidance,theERAS ApplicationWorkingGroup,asubsetoftheCouncilof ResidencyDirectorsinEM(CORDEM)Application ProcessImprovementCommittee,createdasurveyto addressmorenuancedEM-specificquestionsnotaskedor answeredbytheAAMCsurvey.Ourobjectiveinthisstudy wastodeterminehowEMprogramdirectors(PD)usedPSin theirapplicationreviewandrankingpracticesduringthe 2022–2023applicationcycle,particularlyinrelationtothe proportionofsignaledapplicationsreceived.Toour knowledge,nootherspecialtiesparticipatinginPShave reportedPSutilizationdatainthismanner.Wealsoexplored therelationshipbetweenprogramcharacteristicsandthe numberofsignalsreceived,includingcharacteristicsnot previouslystudiedbytheAAMCsuchasgeographic location,programlengthoftraining,programenvironment, andprogramlongevity.Lastly,weinvestigatedtherelative importanceandutilizationofsignalsincomparisontoother residencyapplicationelementsandinrelationtothenumber ofsignalsreceived.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Programsignaling(PS)wasintroducedinto theemergencymedicine(EM)residency applicationprocessin2022 – 2023viathe ElectronicResidencyApplicationService.
Whatwastheresearchquestion?
HowdidEMprogramdirectorsusePSin applicationreviewandranking?
Whatwasthemajor findingofthestudy?
52.2%ofprogramdirectorsusedPSin holisticreview.Otherusesvariedby proportionofsignaledapplications.
Howdoesthisimprovepopulationhealth? UnderstandingPSusagepatternshelps informPSallocationandusageonan individualapplicantandprogramlevel.
Weusedacross-sectionalstudydesign.Participantswere PDsinAccreditationCouncilforGraduationMedical Education(ACGME)-accreditedEMresidencyprograms participatinginthe2023NationalResidentMatching ProgramMatch.TheCORDmemberdirectory,crossreferencedwiththeACGMEAccreditationDataSystem publicsearchwebsite,wasusedtocompiletheemail distributionlist.WeeditedthelisttoreflectnewPDswhen possible(277).Thesurveywascreatedfollowingathorough literaturereviewandsynthesisofbackgroundinformation. QuestionswereiterativelyreviewedbyexpertsinEM medicaleducation.Thesurveywasfurtherrefinedafter conductingtwocognitiveinterviewswithEMresidency programleadersandthenpilotedbyseveralEMeducatorsto assessforclarityofthequestions.Datawasprimarily quantitative.Noidentifyinginformationwascollected.The studywasdesignedtotakeabout10minutestocomplete. Oursurveytoolisincludedin Appendix1.Thisstudywas approvedbytheinstitutionalreviewboardattheinstitution ofauthorsTFandTS.
Thesurveylinkwasdistributedviaemail.Wecollected datausingaconfidentialandsecureweb-based(Qualtrics, Provo,UT)surveyofEMresidencyPDsortheirdesignees. Anonymouslinkswerecreatedforeachpotentialrespondent anddistributedviaQualtrics.AsdescribedbyDillmanand
colleagues,oneweekpriortodistributionofthesurveylink, PDsreceivedabriefemailintroducingthestudyand informingthemthattheywouldreceivethestudylinkinthe comingweek.19 Participantsthenreceivedamessage containingthesurveylink.Non-respondersreceivedupto threeremindermessagesover fiveweeks.
DatawasdownloadedfromREDCap,hostedatMaine MedicalCenter,directlyintoSPSSforWindowsv27(IBM SPSSStatisticsforWindows,IBMCorp.,Armonk,NY) statisticalsoftwareforanalysis.Weuseddescriptivestatistics todescribethecharacteristicsofstudyparticipants’ residency trainingprograms.Programpracticesandexperiences aroundPSweredescribedusingnumbersandpercentagesfor eachcategoricalvariable.Wesummarizedcontinuous variablesusingmeasuresofcentraltendency(meanor median)anddispersion(standarddeviation,interquartile range[IQR]).Comparisonsbetweengroupsforcategorical variablesweremadeusingchi-squareanalysisortheFisher exacttest.Comparisonsforcontinuousvariablesweremade usingthe t -testforindependentsamplesoranalysisof variance.Weaccepteda P -valueof <0.05assignificant.We alsocomputeddifferencesbetweengroupsandtheir associated95%confidenceintervals(CI)andcreatedvisual datadisplaystoaidininterpretation.
ProgramCharacteristics
Wereceived113/277surveys(responserate41%). Participantsrepresenteddiversegeographicregions,withthe largestnumbersfromtheMiddleAtlantic,EastNorth CentralMidwest,andSouthAtlanticregions(Table1). Programsrepresentedweremostcommonlyurban, university-based,andthreeyearslengthofresidency training.Facultyatparticipatingprogramswerelargely universityorhospitalemployees,andmostprograms reportingbeingfoundedmorethan15years.
ProgramSignalingParticipationandApplicationsReceived
ThemajorityofrespondentsparticipatedinthePS componentoftheERASsupplementalapplicationduring the2022–2023residencyapplicationcycle(106,94%). Reasonsfornon-participationincludednotsigningupin time(three,2.7%),feelingthatitwouldnotcontributeto applicantrevieworinterviewofferdecisions(two,1.8%),and beinganewlyapprovedprogram(1,0.9%).Programs interviewedto fillameanandmedianof12postgraduate year(PGY)-1spots(range6–26spots,IQR8–15).The numberofsignalsreceivedbyparticipatingprogramsranged from2–203,withameanof60andmedianof50(IQR 23–86).Programsreportedreceiptofbetween283–1,400 applications(mean768,median772,IQR600–926).The proportionofapplicationsthatweresignaledranged
from0.7%to26.5%(mean7.3%,median6.5%, IQR3.9–10.1%).
Therewasamoderate,positivecorrelationbetweenthe numberofsignalsandthenumberofapplicationsreceived (r = 0.581, P < 0.001)andtheproportionofsignalsreceived increasedbaseduponthenumberofapplicationsreceived (P < 0.001)aswellastheproportionofapplicationsthat weresignaled(P < 0.001).Thenumberofsignalsreceived increasedasthenumberofPGY-1positionsincreased (P < 0.001).Fourquartilesweredeterminedforthenumber ofprogramsignalsreceived,thenumberofapplications received,andtheproportionofapplicationssignaled (SupplementalTable1)toallowforfurthercomparisonof dataassubsequentlydetailed.
Thenumberofsignalsreceiveddifferedsignificantlybased onseveralkeycharacteristics:geographiclocation,with greaternumbersofsignalsreceivedincoastalregions (P < 0.01);programduration,withfour-yearreceivingmore thanthree-yearprograms(P < 0.01);programtype,with urbanprogramsreceivingthemost(P < 0.01);program environment,withuniversity-basedprogramsreceivingthe most(P < 0.01);andlongevityofprogramswithprogramsin existence >15yearsreceivingthemost(P < 0.01). Additionaldetailisprovidedin Figures1 and 2 and SupplementalFigure1.
ProgramsmostcommonlyendorsedusingPSasone componentofholisticreview(59,52.2%).Additionalspecific waysthatsignalswereusedincludethefollowing:asa tiebreakerbetweentwoequallyqualifiedcandidates (45,39.8%);asascreeningtool(44,38.9%);tohelpprioritize theprogram’swaitlistorwaitlistorder(31,27.4%);andto sendaninterviewinvitationtoeveryapplicantwhosignaled theprogram(19,16.8%).Theproportionofapplicationsthat weresignaledappearedtoaffectthefrequencywithwhich programsendorsedusingsignalstoprioritizethewaitlist (P < 0.001),serveasatiebreaker(P < 0.001),andtosend interviewinvitationstoeverysignalingapplicant(P = 0.03) (Figure3).ParticipantsanticipatedusingPSinthe 2023–2024cyclesimilarlytotheirreporteduseinthe 2022–2023cycle,andsimilardifferenceswerealsonotedfor anticipatedusebasedontheproportionofapplicationsthat weresignaled.
Participantsratedtheimportanceofvariousapplication elementswhenconsideringinterviewinvitationsand preparingtheirprogram’srankorderlist(ROL)usinga 5-pointscale(1 = notimportantatall,5 = extremely important)(Table2).Participantsratedthestandardized letterofevaluation(SLOE)asthemostimportantelement
Table1. Characteristicsofparticipatingresidencyprogramsandsurveyrespondents.
Characteristic%(n)Comparisontoexistingprogramdata(percentageofprograms)
Professionalrole
*Programdirector100(113)
Geographicregion
MiddleAtlantic24.8(28)23.7a EastNorthCentralMidwest20.4(23)20.5a SouthAtlantic17.7(20)19.1a PacificWest11.5(13)10.6a WestSouthCentral11.5(13)9.9a NewEngland5.3(6)4.2a MountainWest4.4(5)3.9a WestNorthCentralMidwest2.7(3)3.9a EastSouthCentral1.8(2)4.2a Programlength
Threeyears77.0(87)80.6b
Fouryears23.0(26)19.4b Programenvironment
Urban63.7(72)Notavailable
Suburban30.1(34)Notavailable Rural6.2(7)Notavailable Programtype
University-based47.8(54)35.4a Community-based,university-affiliated36.3(41)46.2a Community-based15.9(18)18.4a Facultyemploymentmodel
Universityorhospital73.5(83)Notavailable Contractmanagementgroup18.6(21)Notavailable Democraticphysician-ledgroup8.0(9)Notavailable Programlongevity
<5years17.7(20)Notavailable 5–10years8.0(9)Notavailable 10–15years10.6(12)Notavailable >15years63.7(72)Notavailable *261/277EMprogramsparticipatedinPSfor2022–2023.All277programssurveyed. MiddleAtlantic = NJ,NY,PA;EastNorthCentralMidwest = IL,IN,MI,OH,WI;SouthAtlantic = DC,DE,GA,FL,MD,NC,SC,VA,WV,PR; PacificWest = AK,CA,HI,OR,WA;WestSouthCentral = AR,LA,OK,TX;NewEngland = CT,MA,ME,NH,RI,VT;MountainWest = AZ, CO,ID,MT,NM,NV,UT,WY;WestNorthCentralMidwest = IA,KS,MN,MO,ND,NE,SD;EastSouthCentral = AL,MS,KY,TN. aFellowshipandResidencyElectronicInteractiveDatabase(FREIDA), https://freida.ama-assn.org bEmergencyMedicineResidents’ Association(EMRA)MatchDatabase, https://match.emra.org/
whenreviewingapplications(mean4.97,95%CI4.93–5.00). TheSLOEs(mean4.90,95%CI4.83–4.97)andinterviewday performance(mean4.81,95%CI4.72–4.89)weremost importantwhenpreparingtheROL.Importanceofthe presenceorabsenceofaprogramsignalwhenreviewing applicationswasameanof2.9(95%CI2.67–3.13)and medianof3(2,4).Importanceofthepresenceorabsenceofa
programsignalwhenpreparingaROLwasameanof2.1 (95%CI1.87–2.32)andmedianof2(1–3).About30%of participants(28)endorsedthepresenceorabsence ofaprogramsignalasveryorextremelyimportant whenreviewingapplicationswhile11%(10)rated programsignalsasbeingequallyimportantto ROLdevelopment.
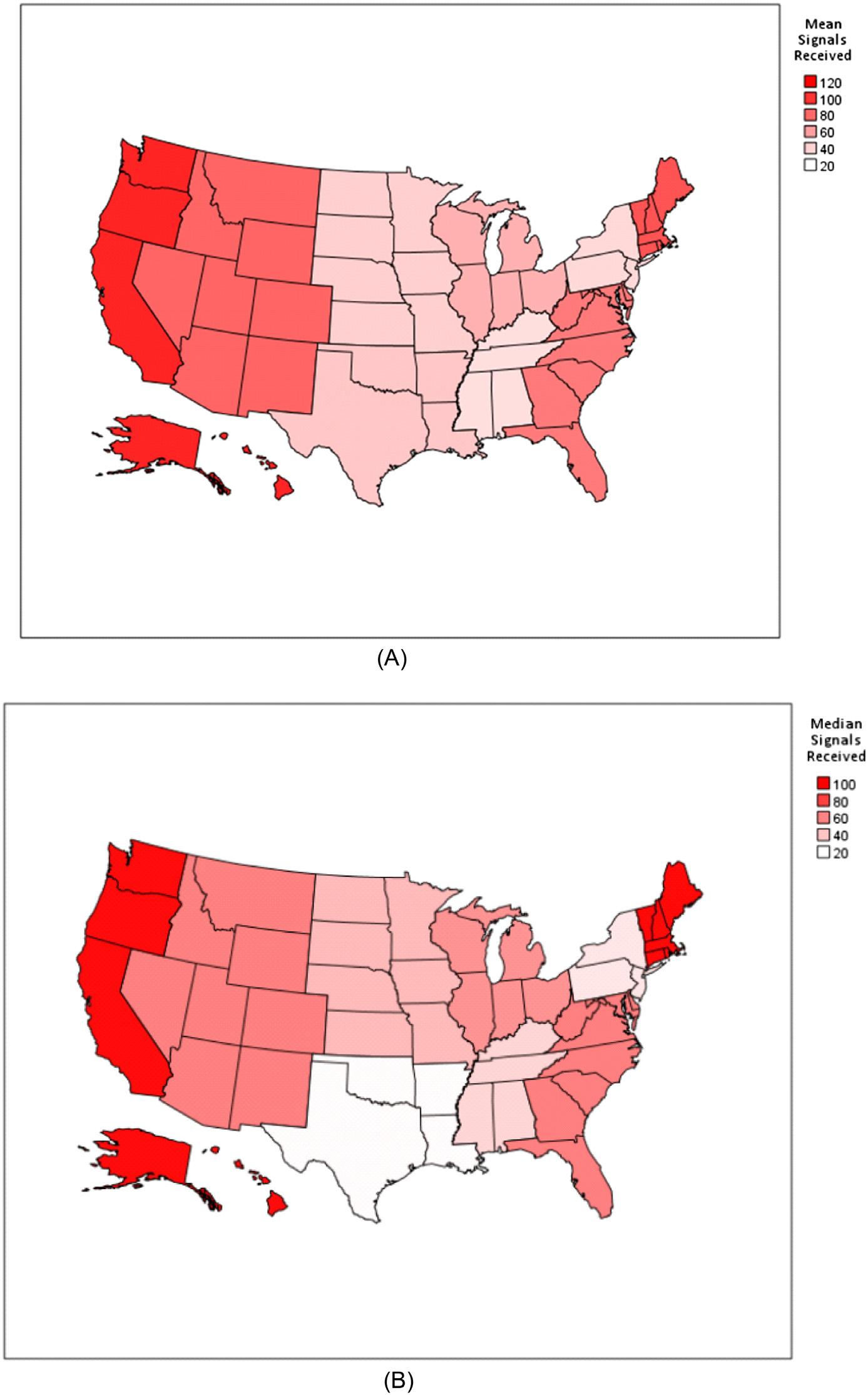
Figure1. (A)Meannumberofsignalsreceivedbygeographicregion.(B)Mediannumberofsignalsreceivedbygeographicregion. Geographicregionsinclude:EastNorthCentralMidwest(IL,IN,MI,OH,WI),EastSouthCentral(AL,MS,KY,TN),MiddleAtlantic(NJ,NY, PA),MountainWest(AZ,CO,ID,MT,NM,NV,UT,WY),NewEngland(CT,MA,ME,NH,RI,VT),Paci ficWest(AK,CA,HI,OR,WA),South Atlantic(DC,DE,GA,FL,MD,NC,SC,VA,WV,PR),WestNorthCentralMidwest(IA,KS,MN,MO,ND,NE,SD),andWestSouthCentral (AR,LA,OK,TX).
WeassessedfordifferencesinPDs’ relativeassessmentsof variousapplicationelementsbasedontheproportionof applicationsthatweresignaled(SupplementalFigure2).As theproportionofapplicationssignaledincreased,the
proportionofprogramsendorsingboardscoresas “extremelyimportant” decreased(P < 0.01).Asthe proportionofapplicationssignaledincreased,theproportion ofprogramsendorsingcommunicationbeforetheinterview
Volume25,No.5:September2024WesternJournal
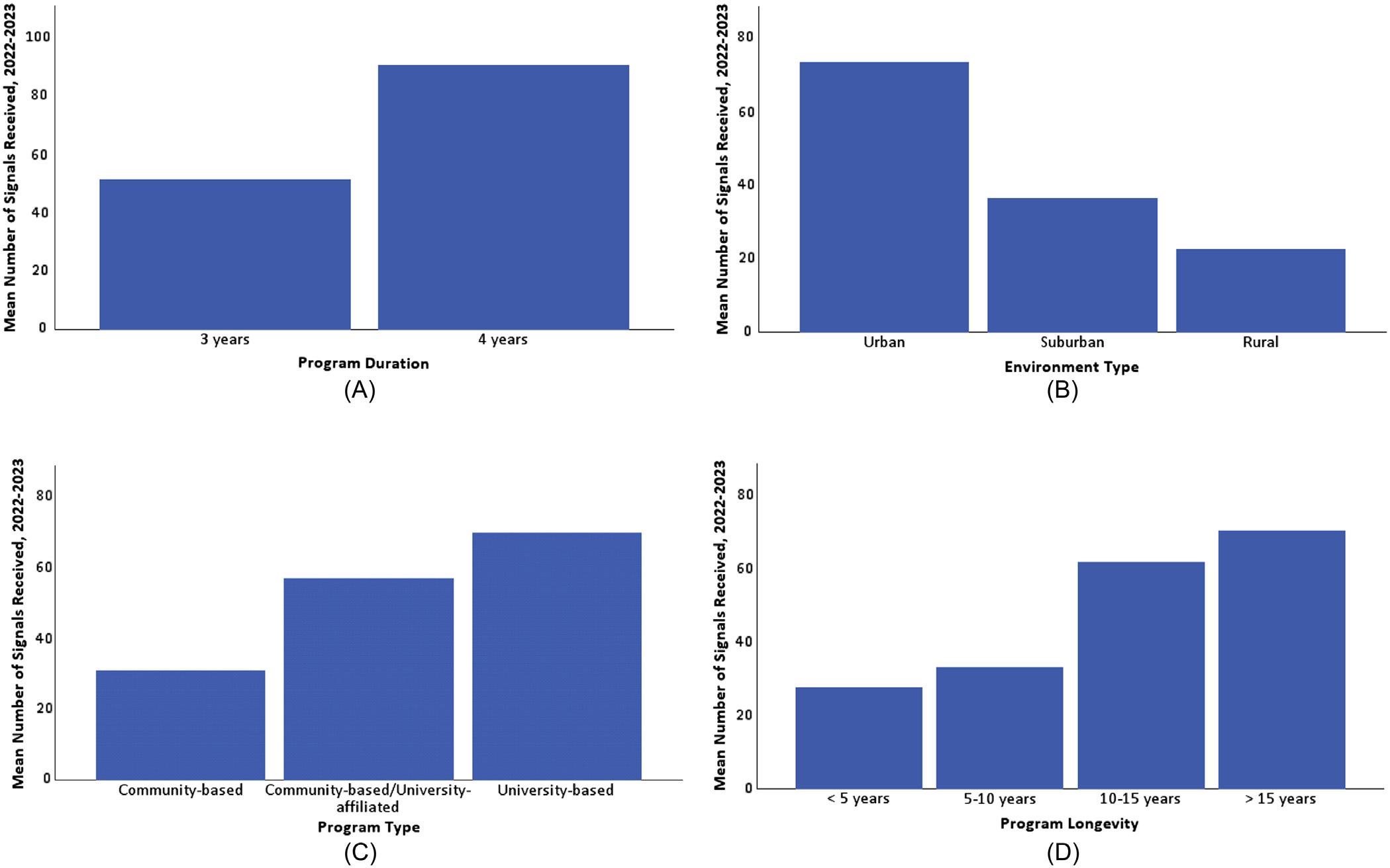
Figure2. Meannumberofsignalsreceivedbyprogramcharacteristics.(A)Meannumberofsignalsreceivedbyprogramduration.(B)Mean numberofsignalsreceivedbyenvironmenttype.(C)Meannumberofsignalsreceivedbyprogramtype.(D)Meannumberofsignalsreceived byprogramlongevity.
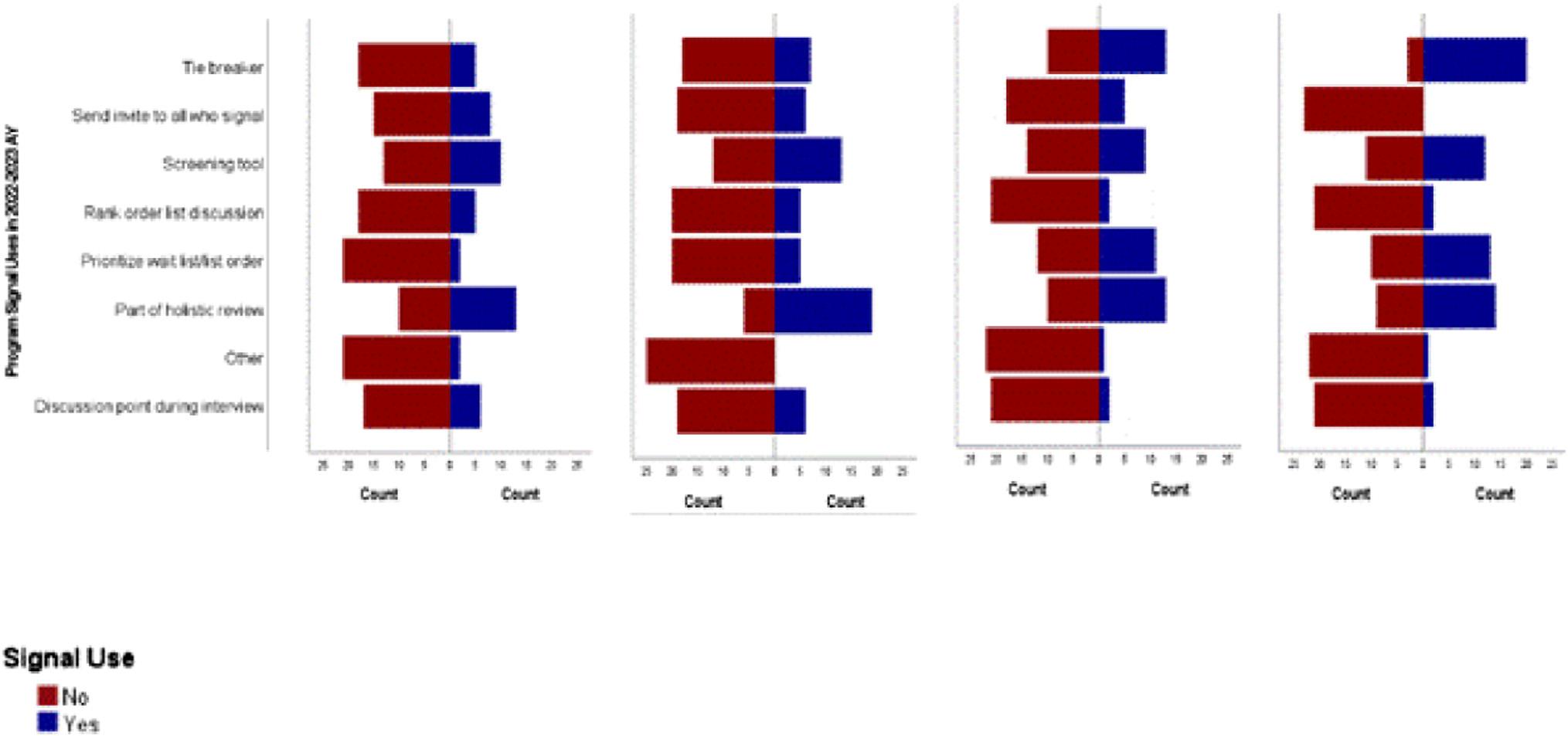
(A) Programs with 03.81% (Quartile 1) of applications signaled.
(B) Programs with 3.82-6.48% (Quartile 2) of applications signaled.
(C) Programs with 6.49-10.12% (Quartile 3) of applications signaled.
(D) Programs with 10.13-26.46% (Quartile 4) of applications signaled.
Figure3. Programsignaluseinthe2022–2023academicyearbytheproportionofapplicantssignaled.* *TheAAMCCodeofConduct,whichprogramsattesttowhensigninguptoparticipateinprogramsignaling(PS),specificallyprohibitstheuse ofPSinrank-orderlistdiscussionandpreparation.
Table2. Importanceofapplicationelements.
ApplicationelementImportancewhenreviewingapplicationsImportancewhenpreparingrankorderlist
Mean(95%CI)Mean(95%CI)
SLOEs4.97(4.93–5.00)4.90(4.83–4.97)
InterviewdayinteractionsN/A4.81(4.72–4.89)
Priorworkorlifeexperiences3.61(3.42–3.80)3.52(3.32–3.72)
Boardscores3.47(3.27–3.66)3.14(2.93–3.35)
MSPE3.44(3.24–3.65)3.32(3.12–3.53)
Extracurricularinvolvement3.36(3.17–3.54)3.25(3.05–3.45)
Presenceorabsenceofaprogramsignal2.90(2.67–3.13)2.10(1.87–2.32)
Communicationbeforeinterview2.64(2.42–2.87)2.89(2.65–3.13)
Researchexperience2.46(2.27–2.64)2.43(2.24–2.62)
Lettersofrecommendation2.40(2.22–2.58)2.33(2.15–2.52)
*5pointscalewhere5 = extremelyimportantand1 = notimportantatall. CI,confidenceinterval; SLOE,standardizedletterofevaluation; MSPE,medicalstudentperformanceevaluation.
as “notimportantatall” increasedwhiletheproportion ratingthisfactor “veryimportant” decreased(P < 0.01). Extracurricularinvolvementincreasedinimportanceasthe numberofapplicationssignaledincreased,withalarger proportionofparticipantsratingthisaspectofthe application “extremelyimportant” astheproportionof applicationssignaledincreased(P = 0.04).Programswith thelowestproportionofsignalingapplicantsweremore likelytorateresearchexperienceas “notimportantatall” thanthosewhohadalargerproportionofapplications signaled(P = 0.02).
Responsestooursurveyappeartobeappropriately representativeofprogramsnationwidewithregardto geographicdistribution,programlength,andprogramtype (Table1).20,21 Rangesandmediannumbersforapplications andPSdataaresimilartoERASdata,againdemonstrating thatoursurveyrespondentsreflectedarepresentativesample ofEMprogramsthatparticipatedinPSduringthestudied applicationcycle.6
Fordataanalysis,weusedquartilesbasedonthe percentageofsignalingapplicationsaprogramreceivedto correctforthedifferencesinrawnumbersbasedonprogram size.WiththenumberofsignalsallocatedtoeachEM applicantincreasingfrom fivetosevenforthe2023–2024 academicyear,itisreasonabletopresumethattheraw numberandpercentageofsignalingapplicantsprograms receivewillalsoproportionallyincrease.Thisdiscrepancy maymakeitmoredifficultforaprogramtoaccurately identifywithagivenquartilebasedonthisyear’sapplication data,butthesedatashouldstillserveasaroughguideby whichprogramscanassessthemselves.
Understandingtherelationshipbetweenprogram characteristicsandthenumberofreceivedprogramsignals canbehelpfulforbothprogramsandapplicants.Programs candeterminetheircompetitivenesswithinthecontextof similarprograms,whichcanbeparticularlyhelpfulinthe currentEMmatchenvironmentwithachangingapplicant demographicpoolandmanyprogramsgoingunmatched overthepastfewyears.2 Providingprogramswitha barometeragainstwhichtomeasuretheirowndemographics andproportionofsignaledapplicantsearlyintheapplication cyclecanhelpguidehowtheyincorporateprogramsignals intotheirapproachandmoreeffectivelyselectapplicants whowillbehighestyieldfortheirprograms.By understandingsignalingtrendsasrelatedtoprogram characteristics,advisorsandapplicantsmaybeableto strategicallydeterminethebestapproachforallocating signalstomaximizeeachsignal’simpact.
Inourstudy,wenotedthatthePaci fi cWestandNew Englandregionsdemonstratedthehighestmeanand mediansignalnumbers.Incontrast,programsintheEast SouthCentral,Mid-Atlantic,WestSouthCentral,and WestNorthCentralMidwestreceivedfewersignals.Itis reasonabletospeculatethatmanyofthesepatternsre fl ect overallpopulationdensitypatterns,suggestinglocal preferencesthatmirrortheUSpopulation.Thishypothesis alignswithourdata,whichshowedthatmoreurban(likely morepopulation-dense)programsreceivedahigher proportionofsignals.Theonlyregionthatdoesnot fi tthis hypothesisistheMid-Atlanticregion,whichisthemost denselypopulatedinthecountry,butwesuspectthevery highEMprogramdensityinthisregionlikelycontributed toprogramsignaldilution,leadingtolowersignals perprogram.
Onaverage,four-yearprogramsreceivedahigher proportionofsignalingapplicantsthanthree-yearprograms. Whileprogramlengthitselfmaybeadriverofthis,itmay alsobeduetootherconfoundingfeaturesmorecommonly associatedwithfour-yearprograms,includingurban location,universityaffiliation,andprogramdurationand stability.Ultimately,ourdatawasunabletodiscernthis difference.Programswiththelowestproportionofsignaling applicantsweremorelikelytobesmaller,rural,andnot academicallyaffiliated.Theseprogramsweremorelikelyto rateresearchexperienceas “notimportantatall.” We suspectthatthesesmaller,morecommunity-oriented programsmaybelessresearch-focusedintheir missionsand,therefore,emphasizeresearchlessintheir applicantselection.Applicantsmaybeabletousethis informationtotargettheirsignalsdependingon theirinterests.
Itseemsintuitivethattheproportionofsignaling applicantsaprogramreceiveswouldaffecthowthat programvaluesandusesthesignal,buttoourknowledge thisisthe firstdatatodemonstratethateffect.When examiningsignalinguseamongprogramsseparatedinto quartilesbasedontheproportionofsignalingapplicants, significantdifferencesemerged.Programsthatreceived lowerproportionsofsignalingapplicantsweremorelikely toreportofferinginterviewstoallsignalingapplicants whilethosewiththehighestproportionofsignaling applicantsweremorelikelytoincorporatesignalsasa screeningtoolortohelpprioritizetheprogram’swaitlistor wait-listorder.
Byaskingprogramstoratetheimportanceofvarious applicationelements,wehopedtogainanunderstandingof therelativeimportanceofPSinrelationtointerviewoffers andROLcreation.Receivingaprogramsignalin orthopedicswasrankedamongthemostimportantfactorsin residentselectionforinterview.13 WhileasuccessfulsubinternshipatthePD’sinstitutionandlettersof recommendationwerethehighest-rankedcriteriafor residentselectionforinterviewaturologyprograms,81%of urologyPDsreportedthatalackofasignalwouldnegatively impactinterviewofferchancesforanapplicant.18 Inour study,programsignalswerenotshowntoholdasmuch weightasinorthopedicsorurology.Programsignalswere onlyratedasmoreimportantthannarrativelettersof recommendation,pre-interviewcommunication,and researchexperience.
Howanapplicantperformsclinically(SLOEs,Medical StudentPerformanceEvaluation)isunderstandablymost important,withPSintendedtobeonlyonesmallpartofthe holisticapplicationreview.22 Studentscanbereassuredthat thetraditionallyvaluedportionsoftheEMapplication retaintheirimportancewellabovethevalueofaprogram signal,andprogramsacrossallquartilesareinterviewingand rankingstudentswhodidnotsendthemasignal.
Analyzingthisdatainamoregranularfashion,wedid observesomesignificantdifferencesintherelativeimportance ofresidencyapplicationelementsbetweenquartiles.Asthe proportionofsignalingapplicantsincreased,theproportionof participantsendorsingboardscoresas “extremelyimportant” decreased.Thisdiscrepancymayspeaktotheintendedability ofPStomitigatetheuseof filteringbehavior.Programswith smallerproportionsofsignalingapplicantsmaycontinueto seekoutstrategiestostratifytheirapplicantpooltobetter allocatetheirholisticreviewefforts,suchasusingboardscore filters.Programswithahigherproportionofsignaling applicants,ontheotherhand,maynotfeelthissamepressure. Alternatively,itispossiblethathavingbeenpromptedbythe introductionofPStoinvestigateprogramsbeforeapplying, applicantsmaystrategicallyhavechosentotargettheirsignals toprogramsthatadvertisedalackofboardscorecutoffs becausetheirscorefellbelowstatedcutoffsatotherprograms orbecausetheyvaluedprogramsthatdonotemphasize standardizedtestscores.
Ourdataalsodemonstratesthatastheproportionof signalingapplicantsincreased,theproportionofrespondents ratingpre-interviewcommunicationas “extremely important” decreasedandtheproportionofrespondents ratingpre-interviewcommunicationas “notimportantat all” increased.Thistrendsuggeststhatthesignalisserving itsintendedpurposeofallowingtheapplicantto meaningfullyexpressinterest,obviatingtheneedfor additional,extra-applicationcommunication,lesseningthe burdenforbothapplicantsandprograms.Italsosuggests thatPSreducestheimpactofothercommunication fromapplicants.
TheAAMCguidancewasconsistentinitsmessagingthat programsignalswereonlytobeusedduringtheapplication reviewandinterview-offerportionoftheapplicationcycle.It isworthnotingthatdespiteallprogramshavingattestedin thecodeofconductnottousePSintheconsiderationof ROLplacement,11%ofprogramsreportedprogramsignals tobeveryimportanttotheROLdevelopmentprocess.The 2022–23AAMCPDsurveyfoundsimilarresultsamongPD respondentsfromallspecialties.6 Programdirectorsmaybe extrapolatingthatastudentwhosignaledislikelytobea higherprobabilitymatchthanastudentwhodidnotsenda signal.Thisusepresumesthatstudentpreferencewillnotbe significantlyaffectedbytheirexperiencesengagingwith programsthroughouttheinterviewseasonandisatriskof being flawedlogic.However,itisimportantthatapplicants beawarethatsignalsmaybeusedbyPDsinthismannerand shouldtakethisintoconsiderationwhenchoosingwhere tosignal.
ParticipationofEMprogramsinPSremainedrobust forthe2023–2024cycle,with278of279programs participatingand97.5%ofapplicantsparticipating(email communicationfromAAMCERASPilotAdministration Director,JaymeBograd,January2024).24 Wehopethat
thisdatahelpsinformprogramsandapplicantsona morenuancedapproachtoPSintheEMresidency applicationprocess.
Respondents(113)comparedtothetotalnumberof ACGME-accreditedEMresidencyprograms(277)was limited.ThePDswhochosetorespondmaydifferfrom thosewhodidnotconcerningtheirPSexperience.Forty-six percentofEMprogramsdidnot fi llinthe2023Main ResidencyMatch. 25 Oursurveywasdistributedintheweeks thatfollowed.ThePDsexperiencingadif fi cultMatchcycle mayhavebeenmoreorlessinclinedto fi lloutasurvey regardingtheresidencyapplicationprocess.Universitybasedprogramswereover-represented.Community-based, university-af fi liatedprogramswereunder-represented. The11%ofprogramsthatreportedusingsignalsaspartof theirROLdiscussionsmaybeanunderestimateasother programsmaynothavebeencomfortabledisclosing behaviorthatwasknowinglyinviolationofthecode ofconduct.
Thisstudyprovidesdetaileddataandpatternsofsignaluse yieldinginsightsintoprogramsignalinginEM’sinaugural yearforbothprogramsandapplicants.Ourdataprovidesa morenuancedunderstandingofsignalutilizationacrossa spectrumofEMprogramsinawaythatallowsindividual programstogobeyondthegeneralAAMCrecommendations andcomparetheirapproachtothatofprogramswithsimilar characteristics.Identifyingpatternsofsignalusebasedon programcharacteristicscanalsoinformadvisingfor studentsdecidingonhowtobestallocatetheirsignals. AsEMcontinuestonavigate fluctuationsinitsapplicant numbersandshiftingdemographicsofitsapplicantpool, providinginsighttoguidesignaluseandutilization canhelppaveapathforwardforthespecialtytowardthegoal ofmoreefficiently findingtherightapplicantforthe rightprogram.
Copyright:©2024Pelletier-Buietal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.Pelletier-BuiAE,SchnappBH,SmithLG,etal.Makingourpreference known:preferencesignalingintheemergencymedicineresidency application. WestJEmergMed. 2021;23(1):72–5.
2.AssociationofAmericanMedicalColleges.ERASpreliminarydataasof January3eachseason.2024.Availableat: https://www.aamc.org/ media/6231/download?attachment.AccessedApril20,2024.
3.RamsayN.EMmatch2020bythenumbers.2020.Availableat: https:// www.emra.org/students/newsletter-articles/em-match-2020-bythe-numbers/.AccessedApril20,2024.
4.Pelletier-BuiA,WerleyE,CamejoM.EMRAhangouts-preference signaling101.2022.Availableat: https://www.emra.org/be-involved/ events–activities/emra-hangouts/20220721-preference-signaling AccessedApril20,2024.
5.AssociationofAmericanMedicalColleges.SupplementalERAS® application:guideforresidencyprograms.2022.Availableat: https://www.aamc.org/media/56451/download/ AccessedApril20,2024.
6.AssociationofAmericanMedicalColleges.SupplementalERAS® 2022–2023applicationcycle:evaluationofprogramsignaling.2023. Availableat: https://www.aamc.org/media/64591/download AccessedApril20,2024.
7.AssociationofAmericanMedicalColleges.SupplementalERAS® 2022–2023applicationcycle:resultsoftheprogramdirectorreaction survey.2023.Availableat: https://www.aamc.org/media/64996/ download.AccessedApril20,2024.
8.LaFeminaJ,RosmanIS,WallachSL,etal.Therelationshipbetween programandapplicantcharacteristicswithapplicantprogramsignalsin the2022residencyrecruitmentcycle: findingsfrom3specialties. AcadMed. 2024;99(4):430–6.
9.RosenblattAE,LaFeminaJ,SoodL,etal.Impactofpreferencesignals oninterviewselectionacrossmultipleresidencyspecialtiesand programs. JGradMedEduc. 2023;15(6):702–10.
10.BanksE,WinkelAF,MorganHK,etal.Programsignalinginobstetrics andgynecologyresidencyapplications. ObstetGynecol. 2024;143(2):281–3.
AddressforCorrespondence:AlexisPelletier-Bui,MD,Cooper MedicalSchoolofRowanUniversity/CooperUniversityHospital, DepartmentofEmergencyMedicine,401HaddonAve.,Education& ResearchBuilding,2ndFloor,CamdenNJ08103. Email: pelletier-bui-alexis@cooperhealth.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
11.BenjaminWJ,LenzeNR,BohmLA,etal.Impactofapplicants’ characteristicsandgeographicconnectionstoresidencyprogramson preferencesignalingoutcomesinthematch. AcadMed. 2024;99(4):437–44.
12.SergesketterAR,SongE,ShammasRL,etal.Preferencesignaling andtheintegratedplasticsurgerymatch:anationalsurveystudy. JSurgEduc. 2024;81(5):662–70.
13.SureshKV,CovarrubiasO,MunF,etal.Preferencesignalingsurvey ofprogramdirectors-afterthematch. JAmAcadOrthopSurg. 2024;32(5):220–7.
14.KotlierJL,MihalicAP,PetriglianoFA,etal.Understanding thematch:theeffectofsignaling,demographics,andapplicant characteristicsonmatchsuccessintheorthopaedic residencyapplicationprocess. JAmAcadOrthopSurg. 2024;32(5):e231–9.
15.CaiF,SouthworthE,SantiagoS,etal.Thegoldentickets:impactof preferencesignalingonobstetricsandgynecologyresidency applicants. AmJObstetGynecol. 2024;230(2):262.e1–9.
16.GrauerR,RantiD,GreeneK,etal.Characterizationofapplicant preferencesignals,invitationsforinterviews,andinclusiononmatch listsforresidencypositionsinurology[publishedcorrectionappears inJAMANetwOpen.2023;6(2):e233305]. JAMANetwOpen. 2023;6(1):e2250974.
17.ChangCWD,ThorneMC,MalekzadehS,etal.Two-yearinterviewand matchoutcomesofotolaryngologypreferencesignaling. Otolaryngol HeadNeckSurg. 2023;168(3):377–83.
18.Rodriguez-AlvarezJS,Munoz-LopezC,HarwoodSJr.,etal.Urology residencyapplicantselection:programdirectors’ newcriteria. Urology. 2024;S0090–4295(24):00141–9.
19.DillmanDA. MailandInternetusrveys:TheTailoredDesignMethod: 2007withNewInternet,VisualandMixed-ModeGuide.2nded. Hoboken,NJ:JohnWiley&Sons,2007.
20.AmericanMedicalAssociation.Fellowshipandresidencyelectronic interactivedatabase(FREIDA™).Availableat: https://freida.ama-assn. org.AccessedApril20,2024.
21.EmergencyMedicineResidents’ Association(EMRA).EMRAmatch database.Availableat: https://match.emra.org/ AccessedApril20,2024.
22.NationalResidentMatchingProgram.Resultsofthe2021NRMP programdirectorsurvey.2021.Availableat: https://www.nrmp.org/ wp-content/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf AccessedApril20,2024.
23.AssociationofAmericanMedicalColleges.Residencyprograms participatinginprogramsignaling.2023.Availableat: https:// students-residents.aamc.org/applying-residencies-eras/residencyprograms-participating-program-signaling.AccessedApril20,2024.
24.AssociationofAmericanMedicalColleges.Exploringtherelationship betweenprogramsignaling&interviewinvitationsacrossspecialties: 2024ERASpreliminaryanalysis.2024.Availableat: https://www.aamc. org/media/74811/download?attachment.AccessedApril20,2024.
25.NationalResidentMatchingProgram.Resultsanddata:2023main residencymatch.2023.Availableat: https://www.nrmp.org/wp-content/ uploads/2023/05/2023-Main-Match-Results-and-Data-Book-FINAL. pdf.AccessedApril20,2024.
SamaraHamou,BA*
ShayanGhiaee,MD,MS†
ChristineChung,MD‡
MaureenLloyd,MD‡
KellyKhem,MD§
XiaoChiZhang,MD,MS§
*SidneyKimmelMedicalCollege,Philadelphia,Pennsylvania † DepartmentofEmergencyMedicine,EmoryUniversity,Atlanta,Georgia ‡ DepartmentofOphthalmology,WillsEyeHospital,Philadelphia,Pennsylvania § DepartmentofEmergencyMedicine,ThomasJeffersonUniversity,Philadelphia, Pennsylvania
SectionEditors:JulesJung,MDandAndrewKetterer,MD
Submissionhistory:SubmittedOctober20,2023;RevisionreceivedMarch21,2024;AcceptedJune7,2024
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18514
Introduction: Eyeemergenciesmakeupnearly3%ofUSemergencydepartment(ED)visits.While emergencyphysicians(EP)shoulddiagnoseandtreattheseophthalmologicemergencies,many traineesreportlimitedocularexposureandinsufficienttrainingthroughouttheirresidencytoconfidently conductathoroughslit-lampexam.
Methods: Wecreatedaninterdisciplinary,simulation-basedmasterylearning(SBML)curriculumto teachemergencyattendingphysicianshowtooperatetheslitlampwithmultimodallearning methodologyatatertiaryacademiccenter.TheEPs firstdemonstratetheirinitialslit-lampcompetency witha20-itemchecklist,andtheythenreviewthenecessarycurricularcontenttopasstheirindependent readinesstestbeforecompletingtheirin-personteachinganddemonstrationsessionwithan ophthalmologyattendingtodemonstrateproceduralmastery(minimalpassingscore >90%).
Results: FifteenEPswereenrolled;allcompletedthe finalexamofthecurriculum.Thepre-andpostcurriculumchecklistscoresincreasedbyanaverageofsevenpoints(P = .002);86.7%ofEPsfelt confidentincompletingaslit-lampexamafterthecurriculum,comparedto20%atthebeginning.Fiveof 15reportedteachinglearnerswithinthetwo-monthpost-curricularperiod,rangingfrom5–30students. Thehands-onteachingwasthemostpositivelyreviewedelementofthecurriculum.
Conclusion: TheSBMLprogramsuccessfullytrainedEPsonperformingacomprehensiveslit-lamp examwithpromisingresultsofdownstreameducationtojuniorlearners.Weencourageotherinstitutions toleverageSBMLasateachingmodalityforprocedural-basedtrainingandadvocatecross-discipline educationinitiatives.[WestJEmergMed.2024;25(5)725–734.]
Theslit-lamp1 (Figure1A)isamicroscopethatallowsfor adetailedexaminationoftheanterioreyesegmentusinglight beammanipulation.Theslit-lampenablesphysiciansto diagnoseanteriorophthalmicpathologiessuchascorneal injuries,iritis,hyphema,hypopyon,andforeignbodies2; furthermore,itisessentialforperformingdetailed ophthalmologicexamtechniquessuchaslideversion, fluoresceinexamination,andforeignbodyremoval.3 The
Wood’slamp4 (Figure1B),incontrast,isahandhelddevice oftenusedtocharacterizeskinpigmentation,dermal infections,andmacroscopicinfectionswithabuilt-in magnifyinglensandultraviolet(UV)light.TheUV capabilitiescanhighlight fluoresceinstainingduringexternal ocularexamstoassesscornealpathologiesatlower magnification.WhiletheWood’slampoffersalessdetailed examinationthantheslitlamp,itisamoreportable diagnostictoolforlargerocularlesions,foreignbodies,or
specificreactionto fluoresceinstainingandmeetstheneedsof theemergencyphysician(EP)undercertainsituations.
Eyeemergenciesmakeupnearly3%ofUSemergency department(ED)visits,themostcommonofwhichare traumatic.5,6 Themostcommoneyeinjuryevaluatedinthe EDiscornealabrasion(superficialinjurytothecornea)and eyelidlaceration.Suchinjuriesarebestviewedunderhighfieldmagnifiedviewingusingtheslitlamptoassessfor concomitantinjuriesorco-infectionssuchascornealulcers, hypopyon/endophthalmitis,retainedforeignbody,full thicknesscorneallaceration,globeruptures,andseidel testing.7 Ocularemergenciessuchastraumaticgloberupture, ocularforeignbody,closed-angleglaucoma,and endophthalmitisarevisibleonlyusingtheslitlamp,andfall withintheEP’sscopeofpracticefordiagnosis,triaging,and management.8 Mismanagedophthalmicemergenciescan resultininappropriateconsultation,excessivetesting, financialburden,andevenirreversiblevisionloss.9 Despite thesignificanceandfrequencyofocularemergenciesacross theUS,manyEPsarenotconfidentperformingadetailed ophthalmicexam.10
PreviousliteraturehasfoundEPsreceivefewerthan10 hoursofophthalmiceducationduringresidencywithlow confidenceinperformingacomprehensiveophthalmicslitlampexam.11 Ophthalmiceducationthroughclerkshipsand didacticsinmedicalschoolisalsoindecline,leadingtothe unpreparednessofincomingresidentsbeforeanyformal residencytraining.11,12 However,itisimportantthatEPsbe confidentinusingtheslitlamptoappropriatelytriageand manageocularemergenciesaspartoftheAccreditation CouncilforGraduateMedicalEducation(ACGME) EmergencyMedicine(EM)MilestonesPatientCaredomain (PC8) – GeneralApproachtoProcedures,whichdesignatesa setofsequentialmilestonesforoverallprocedural competency,notfocusingonaspecificlistofprocedures.13
Theoptimallearningenvironmentforadultlearnersto performatechnicallychallengingprocedureshould incorporateelementsfromboththemasterylearningmodel andrapidcycledeliberatepractice(RCDP).Themastery
learningmodelensuresthatstudentscanmasteratopicif theyreceiveunlimitedtimeandsupportinlearningand reviewingmaterialuntilmasteryproficiencyisreached. Meanwhile,theRCDPmodelensureslearnerscanpractice skillsrepetitivelywhilereceivingbrief,interspersedfeedback toachieveadesignatedproficiencylevelbeforeproceedingto thenexttask.14,15–17 Withinmedicaleducation,simulationbasedmasterylearning(SBML)modelshavebeen successfullyimplementedacrossvariousspecialties,suchas emergencymedicine,generalsurgery,criticalcare,and gastroenterology.18,19,20 Inlightofsuccessful,smallerscaled studiesontheeffectivenessofslit-lamptrainingwithin undergraduatemedicaleducation,weproposeaSBML proceduraltrainingcurriculumthatcanenableadultlearners toconductdeliberateperformancesofintendedcognitiveor psychomotorskillsinsequentialorderwitharepetitiveskills assessment.15,21,22 Specific,informativefeedbackwillenable sustainedperformanceimprovementtoachieveslit-lamp mastery.23 Ourgoalwastodesignapilotinterdisciplinary coursethatcouldteachEPstocompleteacomprehensiveslitlampexamindiagnosingcommonanterioreyepathology.
Ourstudy,EmergencyDepartmentSlitLamp InterdisciplinaryTrainingviaLongitudinalAssessmentin MedicalPractice(EDSLITLAMP),isamulticentered, collaborativeprojectthatleveragestheconceptual frameworksofthemasterylearningmodelandRCDPto ensureproficiencyinconductingacomprehensiveslitlamp exam.Italsoservesasascaffoldfordeconstructingbarriers intraditionalsiloedmedicalpracticesandleadstoimproved patientcare,knowledgesynthesis,andresourceutilizationof ourconsultingservices.ThestudywasconductedatThomas JeffersonUniversity(TJUH)andtheWillsEyeHospital (WEH)from2021– 2023.Thehospitalswiththeirrespective EDs,are0.2milesapart,withstafffromeachinstitution workingasconsultantsattheother;WEHresidentsfunction asophthalmologyconsultationfortheTJUHED,while TJUHEPsfunctionasovernightmedicalemergency
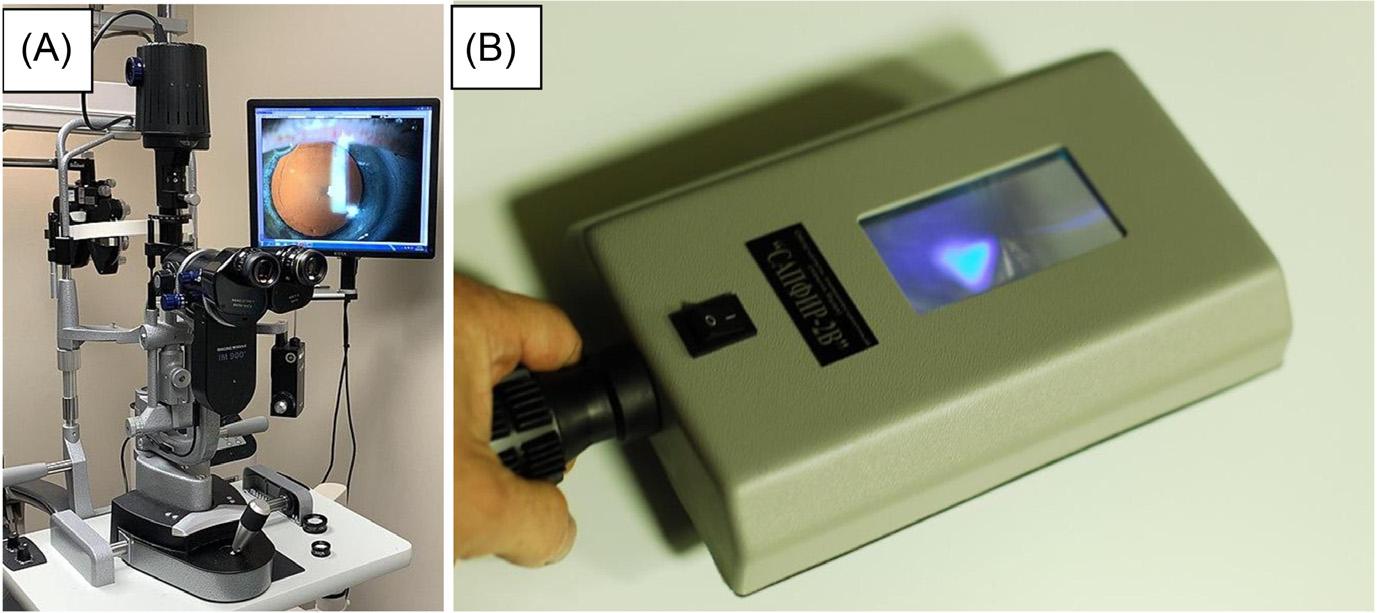
consultantsattheWEHED.Thegeographicand relationshipproximitycreatedidealconditionstodevelop andpilotaproceduralskillcompetenceSBMLcurriculum.
Emergencyphysicianswereselectedasideallearnersdue totheirleveloftraininganduniqueteachingresponsibilities. UsingtheTJUHEDlistservwerecruitedeligible participantsandofferedstaggered financialincentives.For thispilotstudy,werequiredaminimumof12participantsto meet5%type1errorand80%powerbasedonscore improvementfrombaselinetestingtopost-testing,as referencedbyMilleratal.24 TheEDSLITLAMPstudy leveragedtalentsfromcontentandeducationexpertsfrom bothinstitutionstocreateaninterdisciplinaryprocedural teachingcurriculum.ThesuccessofatraditionalSBML curriculumislinkedtothelearners’ skillacquisition.Our studyexpandsthismeasuretoincludeinterdisciplinary collaboration,demonstratingthesuccessfulalignment betweeneducationalandpatient-centeredgoalsthatbenefit bothdepartments.Toevaluatethecurriculum,weemployed allfourlevelsoftheKirkpatrickmodel.Usingpre-andposttestLikertscalequestionnaires,ourmeasurementofsuccess includedimprovedlearnerconfidence(level1),knowledge acquisition(level2),willingnessoflearnerstoincorporate theirskillsetinclinicalpractice(level3),anddisseminationof thisknowledgetojuniorlearners(level4).Anycurricular feedbackandimprovementswereextractedforfuture curriculariterations.
Aneeds-basedanalysisconductedatTJUHEDrevealed EPsdesiredhands-onslit-lampeducationandtrainingon identifyinganteriorsegmentophthalmiccomplaints.Since ophthalmologyisarecognizedcomponentoftheAmerican BoardofEmergencyMedicineexamcontent,weconstructed thepre-testclinicalcontentbasedoncriticalandcommon oculardiagnoses,themostcommonWEHED ophthalmologydischargediagnoses,andclinical identificationsdeemed “ can ’tmiss” bytheEDand ophthalmologydepartment.
Allcurricularcontents(lecturematerials,videorecording, pre-post-postassessments,studysurveys,masterylearning checklist)werecreatedbytheprincipalinvestigator[XCZ] withophthalmologyco-investigatorsconsultation[CC, MEL]basedontargetedneedsassessment.Thesematerials underwentsequentialreviewbyselectexpertsatWEHand weremodifiedsequentiallyuntilaconsensuswasreached. Theminimalpassingchecklistscorewasdeterminedtobe 90%,basedoncombineddeterminationfrom ophthalmologistexpertsatWEHandsimilarthreshold determinedbyMilleretal.24 Eachcurriculumassessment (AppendixA)wasconstructedtomirrorthenatural knowledge,skills,andattitudeprogressionfromthe ACGMEEMMilestonesPatientCareDomain(PC8).Due tothemultifacetednatureofEM,thereisnospecific proceduralmilestoneforperformingaslit-lampexam,as describedindetailintheACGMEOphthalmologyPC1:
DataAcquisition-BasicOphthalmologyExamandTesting (Level1).13 However,theEMPC8milestonesprovide structuredlanguageapplicabletomanyEDproceduresand advanceddevice-assistedmedicalexaminations(ie,slit-lamp exam).Pleasesee Table1 forthecorrelationbetweentheEM milestoneandEDSLITLAMPassessments.
Thelongitudinalcurriculumincludedfouruniquetime points(Time0–3)ofinterventionstaggeredoversixmonths (AppendixA, AppendixB).AtTime0,participants completedanin-personbaselineslit-lampexamthatwas video-recordedandreviewedbytwoindependent investigators[XCZ][MEL].AtTime1,theparticipants gainedaccesstoanasynchronouslearningpacketthat consistedofaPowerPointpresentationoncommonEDeye complaints,digitallibrarylinkstotheWEHManual,slitlampchecklist,andavideorecordingofacomprehensiveslitlampexamination.25 Theparticipantsalsogainedaccessto anindependentreadinessassessment(IRAT),whichwas requiredtobecompletedwithin30dayswithaminimum scoreof90%beforeproceedingtothenextin-personphaseof thestudy(AppendixA).
UponachievingthepassingIRATscore,theywereinvited toparticipateintheTime2(in-person)SBMLportionofthe studywheretheyweretocompleteanin-person demonstrationofacomprehensiveslit-lampexambya board-certifiedophthalmologist[CC]onastandardized patientvolunteer.Followingthedemonstration,participants weregivenunlimitedtimeforRCDPwithbrief,interspersed feedbackundertheobservationandteachingfromthe ophthalmologist.Participantswererequiredtocompletea minimum18of20checklistitemstoachievemastery (AppendixB).Uponcompletingthe finalchecklist,the participantswereaskedtocompleteacourseevaluationand learnerconfidencesurvey(AppendixC)withLikertscaling, subjectivecommentary,andavalidated5-itemCritical IncidenceQuestionnaire(CIQ)forcurricularimprovement. Giventheunpredictabilitynatureofthe “unlimited attempts” atTime2,allparticipantswerescheduledattwohourintervalstoallowfordevicepreparation,onetotworeattempts,debriefing,surveycompletion,andgeneral troubleshooting.AtTime3,participantscompleteda60-day post-examinationsurvey,assessingtheirocularknowledge, slit-lampconfidence,clinicalteachingopportunities,and relevantinterprofessionalrelationships.
WeusedaWilcoxonsigned-ranktesttodifferentiatethe checklistscoresbetweenthecurricularinterventionby incorporatingcollectedpaireddatabeforeandafterthe training,medianandinterquartilerangevaluesofsubtotal scoresattwo-timepoints.26 WeusedMcNemar’stestto comparingeachcategoricalsub-score(Yes/No)bytime pointsandcorresponding P -valuewithinthesame population.27 Thedescriptivesummariesofsurveyquestions atTime0,Time2,andthree-monthfollow-upwereanalyzed usingBonferroniadjusted P -values(multiplying P -value
Table1. Correspondingemergencydepartmentslit-lampassessmentstoACGMEEM*milestonegeneralapproachtoprocedures. ACGME
EMmilestonePC8BoldedPC8elementsrelatabletoperformingaslitlampexam CorrelatingEDSLITLAMP assessments
Level1 Identifies indicationsforaprocedureandpertinentanatomyand physiology.Performsbasictherapeuticprocedures (eg,suturing,splinting)
Level2Assessesindications,risks,benefits,andalternativesandobtains informedconsentinlow-tomoderate-risksituations.Performsand interpretsbasicprocedures,withassistance.Recognizes commoncomplications
Level3Assessesindications,risks,andbenefitsandweighsalternativesin high-risksituations.Performsandinterpretsadvancedprocedures, withguidance.Managescommoncomplications
Level4Actstomitigatemodifiableriskfactorsinhigh-risksituations. Independentlyperformsandinterpretsadvancedprocedures. Independentlyrecognizesandmanagescomplexand uncommoncomplications
Level5Teachesadvancedproceduresandindependentlyperformsrare, time-sensitiveprocedures. Performsproceduralpeerreview
AppendixA–Part II(clinical imageexamination)
AppendixB–Part I(slitlamp technical) AppendixB (final checklist)
AppendixA–Part III(ophthalmology exammix-n-match
AppendixB (final checklist)
AppendixC–ED SLITLAMP surveys
*ACGME EM,AccreditationCouncilforGraduateMedicalEducationEmergencyMedicine; PC,patientcare; EDSLITLAMP,Emergency DepartmentSlitLampInterdisciplinaryTraining.
fromWilcoxonsigned-ranktestbythenumberofmultiple tests,doublingthe P -values),whichwasdirectlycomparedto thepre-specified5%significancelevel.Allstatisticalanalyses wereperformedusingR4.1.2(RFoundationforStatistical Computing,Vienna,Austria).28
Thisstudywasapprovedbytheinstitutionalreviewboard atThomasJeffersonUniversityHospital(TJUH)in Philadelphia,PA.Informedconsentwasobtainedfrom participatingphysicians.Thisstudywasfundedbythe CenterforFacultyDevelopmentandNexusLearning PedagogyGrantatThomasJeffersonUniversity.
FifteenEPs(sixfemalesandninemales)wereenrolledin EDSLITLAMPduringthetwo-yearperiod;nonewerelost tofollow-up.Allparticipantswereboard-certifiedEPswith anaverageclinicalexperienceof7.8yearspost-residency graduation.AllEPscompletedthe finalexamofthe curriculuminoneattemptandallunder60minutes.
Table2 liststhe20stepsoftheslit-lampexamcurriculum checklist,comparingparticipantresultsfromrecordedslitlampattempts(Time0)tothe finalin-personassessment (Time2).Theintra-classcorrelationintestscoresbetween EPsandophthalmologistsatTime0(2raters)was0.98.We foundasignificantincreasebetweenthechecklist scoresbeforeandaftertheeducationinitiative, 12.0to19.0, P = 0.002.
Themostnotabledifferencesbetweenthepre-andpostcurricularinterventionwereasfollows:1)instructingthe patienttoclosetheireyeswhilepoweringupandpositioning
thepatientintheslitlampwiththeforeheadtouchingthe horizontalbarandchininthechinrest(P < 0.001); 2)adjustingthemicroscope90degreestofacialplanewith illuminationsetata45-degreeangle(P = 0.008); 3)performingananteriorchamberevaluation(P = 0.002); 4)lookingforcellsand flare(P = 0.021);and5)placing fluoresceinintheinferiorfornixoftheeye(P = 0.031).The mostmissedstepsatthebaselineexamwere:1)applyinga transparentfaceshield(26.7%);2)instructingpatientsto closetheireyeswhenthemachinewasturnedon(26.7%); 3)lookingforcellsand flare(26.7%).
Figures2 and 3 illustratelearners’ confidencein performingandteachingtheslit-lampexamatthebeginning ofthestudy(Time0),immediatelyafterachievingprocedural mastery(Time2),andtwomonthslater(Time3). Figure4 illustratesthelearners’ likelihoodinteachingtheslit-lamp examatTime0andTime2.Beforeparticipatingintheslitlampcurriculum,73%ofEPsalsoreportedrarelyornever performingaslit-lampexam,while80%ofEPsreported sometimesoroftenusingaWood’slampforocular complaints.Only20%ofEPsreportedfeelingconfidentin performingandteachingacomprehensiveslit-lampexam, while67%ofEPsreportedfeelingconfidentinusingand teachingWood’slampforocularexamination.
Aftercompletingtheslit-lampcurriculum(Time2),86.7% ofEPsreportedfeelingconfidentperforminga comprehensiveslit-lampexamforocularcomplaints,and 73.3%weremoreconfidentinteachingresidentshowto performaslit-lampexam.MostEPsstronglyagreedthatthe EDSLITLAMPcurriculumhelpedthemperforman
Table2. Descriptivesummaryofchecklistevaluationatpre-andpost-curricularandcomparisonbetweentimepoints.
ChecklistitemPerformed
1-Identifyslitlampanatomy.
2 -Applytransparentfaceshieldovertheslitlamp(COVID).
3-Sanitizeforeheadandchinrestforthepatient.
4-Applytopicaltetracaine/proparacaineonpatient’seyes.
5-Unlockinstrumentbaseandshiftbypullingtowardyou.
6-Adjusteyepiecesforyourinterpupillarydistanceand refractiveerror.
7-Adjusttableheightand/orchair(s)-neitherpatientnorexaminer shouldbehunchedover.
Time0,N(%) (N = 15)
Time2,N(%) (N = 15)
P-valuefrom exactMcNemar’s test
Yes13(86.7%)15(100%)0.50
Yes4(26.7%)15(100%) <0.001
Yes5(33.3%)14(93.3%)0.004
Yes8(53.3%)12(80.0%)0.22
Yes15(100%)15(100%) NA
Yes10(66.7%)14(93.3%)0.22
Yes12(80.0%)14(93.3%)0.50
8-Instructpatienttocloseeyeswhileyoupowerupbyturningon thelightsourceatlowvoltagesettingandfocusonrighteyelid. Positionpatientinslitlampwithforeheadtouchingthehorizontal barandchininthechinrest. Yes4(26.7%)15(100%) <0.001
9-Setmagnificationonlowestsettings(10xto12x),illuminationat largestapertureandwidestslitbeam.
Yes12(80.0%)15(100%)0.25
10-Adjustchinrestsothepatientissittingcomfortablywiththeir chinonthechinrestandtheirforeheadagainsttheheadrest. Yes12(80.0%)15(100%)0.25
11-Practicemacroandmicroadjustmentsoftheslidingbase withjoystick.
12-Adjustmicroscope90° tofacialplanewithilluminationset at45° angle(angleleftforpatient’srighteye,andrightfor lefteye).
13-Performouterstructureevaluation.
14-Performanteriorchamberevaluation.
15-Lookforcellsand flare.
16-Placeadropoftetracaine/proparacaineonasterile fluoresceinstrip.
17-Placethe fluoresceinintheinferiorfornixoftheeyebypulling downonthelowerlidandgentlytouchingthebulbar conjunctivawiththe fluoresceinstrip.
18-Adjustcobaltblue filterondiaphragmwheelatmaximumbeam heightandmediumwidthslitsettingfor fluoresceinevaluation.
19-Focustheslitbeamat9:00positiononlimbus.Moveacross thecorneatothe3:00positionbytiltingjoysticklaterally.
20-Pullinstrumentbasetowardyouwhen finishedandlockin position.Turnoff.
Yes14(93.3%)15(100%)1.00
Yes7(46.7%)15(100%)0.008
Yes14(93.3%)15(100%)1.00
Yes5(33.3%)15(100%)0.002
Yes4(26.7%)12(80.0%)0.02
Yes15(100%)15(100%) NA
Yes9(60.0%)15(100%)0.03
Yes14(93.3%)15(100%)1.00
Yes12(80.0%)15(100%)0.25
Yes4(26.7%)13(86.7%)0.004
Time0, median[IQR]
Time2, median[IQR] P-valuefrom Wilcoxonsigned ranktest
Subtotalscore 12.0[10,16]19.0[19,20]0.002
IQR, interquartilerange.
independentslit-lampexamandidentifycritical findingsfor commonocularcomplaints(80%),enhancingtheirlearning morethantraditionallecturesandreadingalone(86.7%).Of theasynchronousmaterials,thevideodemonstrationwasthe mostused(53%usedit “alot” ora “greatdeal”);the
PowerPointlectureandWEHManualweretheleastused.At twomonthspost-EDSLITLAMP(Time3),73%and67%of participantsexpressedextremeconfidenceinperformingand teachingaresidenthowtoperformaslit-lampexam.Fivetof 15EPsreportedteachinglearnerswithinthetwo-month
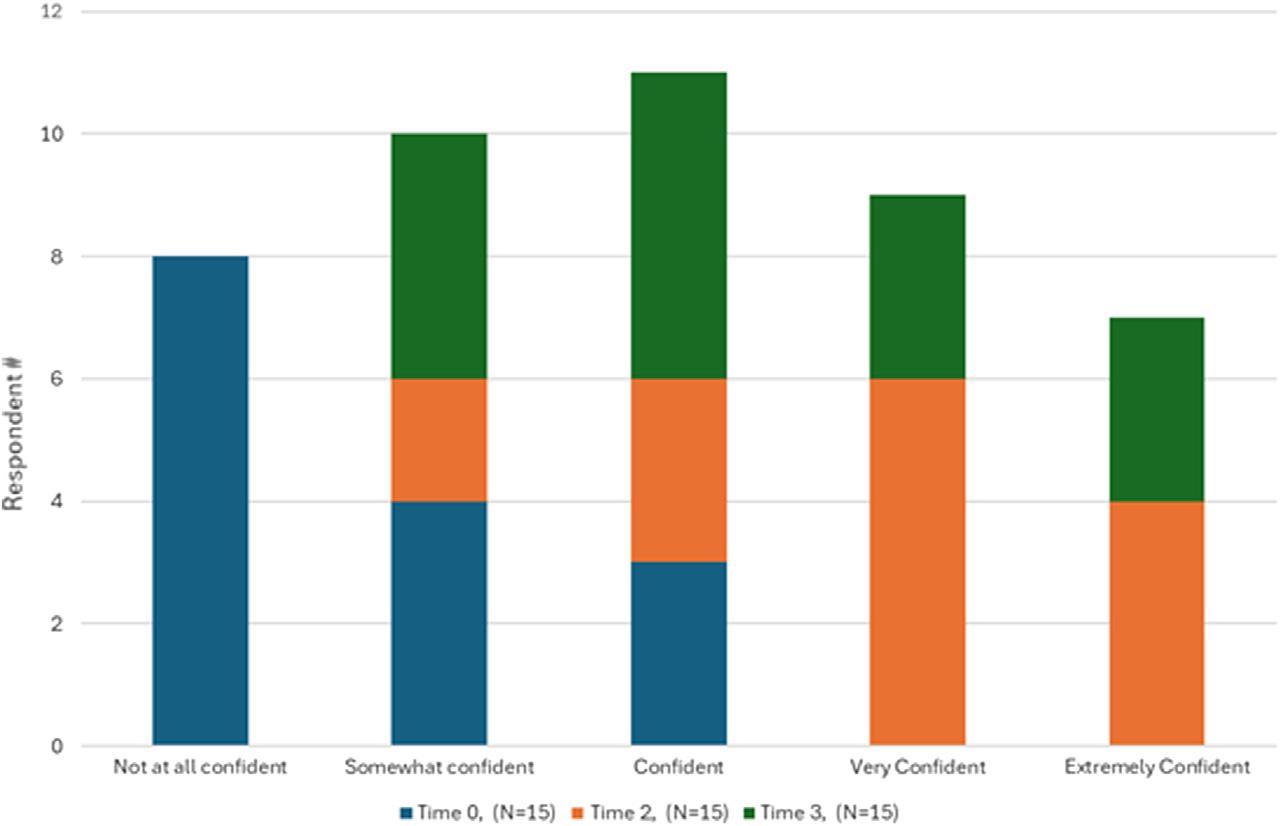
Figure2. Learnerconfidenceinperformingtheslit-lampexamatTime0(pre-curricular),Time2(immediatepost-SBMLcurriculum),and Time3(2-monthpost-SBMLcurriculum).
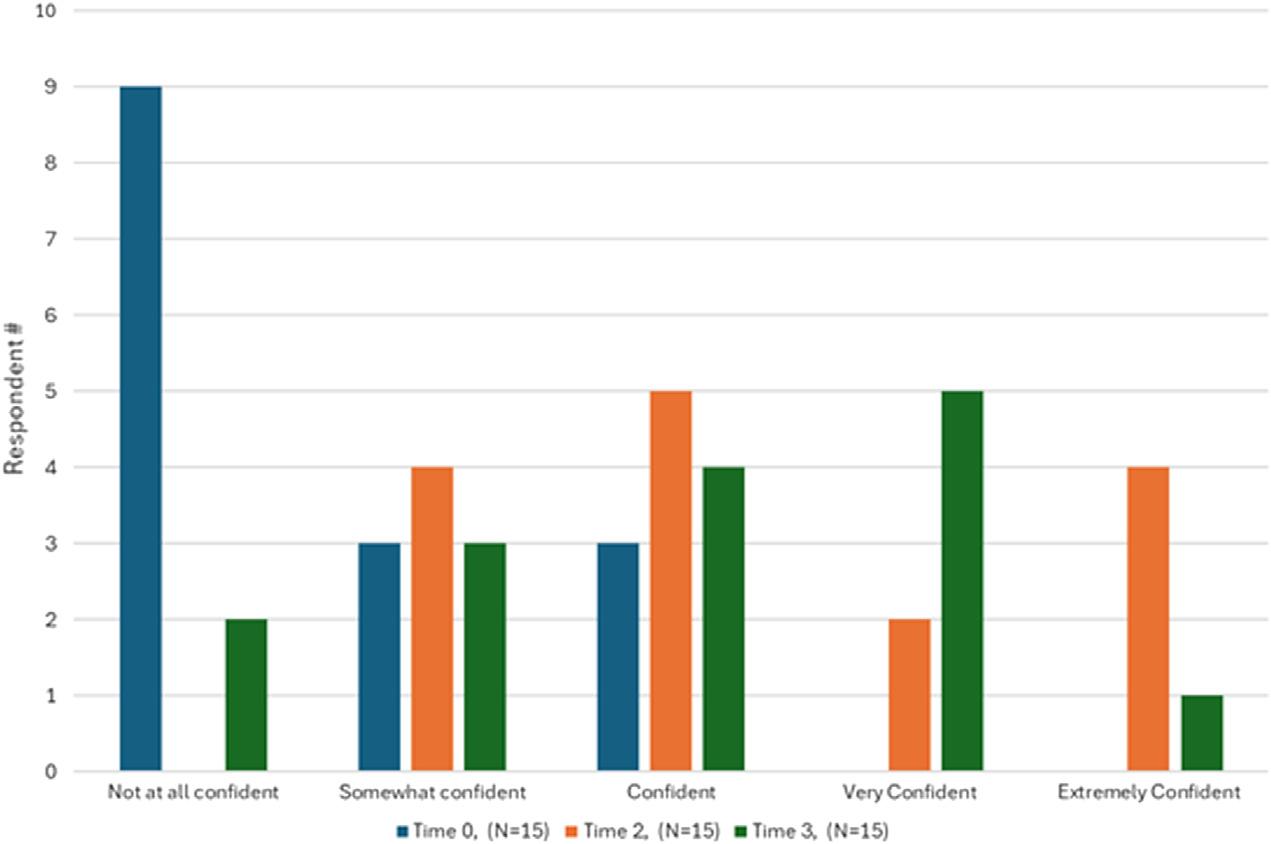
Figure3. Learnerconfidenceinteachingtheslit-lampexamatTime0(pre-curricular),Time2(immediatepost-SBMLcurriculum),Time3 (2-monthspost-SBMLcurriculum).
post-curricularperiod,rangingfrom5–30studentsper EPparticipant.
Table4summarizesthestatisticallysignificant findings fromthesurveyresponsesbasedonthethreetimeframes. Therewasastatisticallysignificantincreaseinself-reported confidencein1)performingacomprehensiveslitlampexam and2)teachingresidentstoperformthisexambetweenTime 0toTime2andTime0toTime3(P < 0.001).Therewasno differenceinrelianceonophthalmologyconsultationto modifyorreinforceatreatmentplanforocularcomplaints whencomparingTime0toTime3(P = 0.70, P = 0.814). Therewasalsonostatisticaldifferenceinthenumberof patientswithocularcomplaintsevaluatedbythestudy
participantsattheTJUHEDandWEHEDthroughoutthe study(P = 0.14, P = 1.00).
TheEDSLITLAMPcurriculumallowedEPstoincrease theiruseandconfidenceinperformingslit-lampexamsinthe ED.TheimpetusfortheprojectarosefromEPs’ intrinsic motivationtoprovidebetterpatientcare.Ourparticipant populationconsistedprimarilyofjuniorfacultywhowere initiallyuncomfortableperformingorteachingslit-lamp examsandpreferredusingtheWood’slamp.Upon completingthecurriculum,theEPsnotedasignificant increaseinself-reportedconfidenceinusingslit-lamps
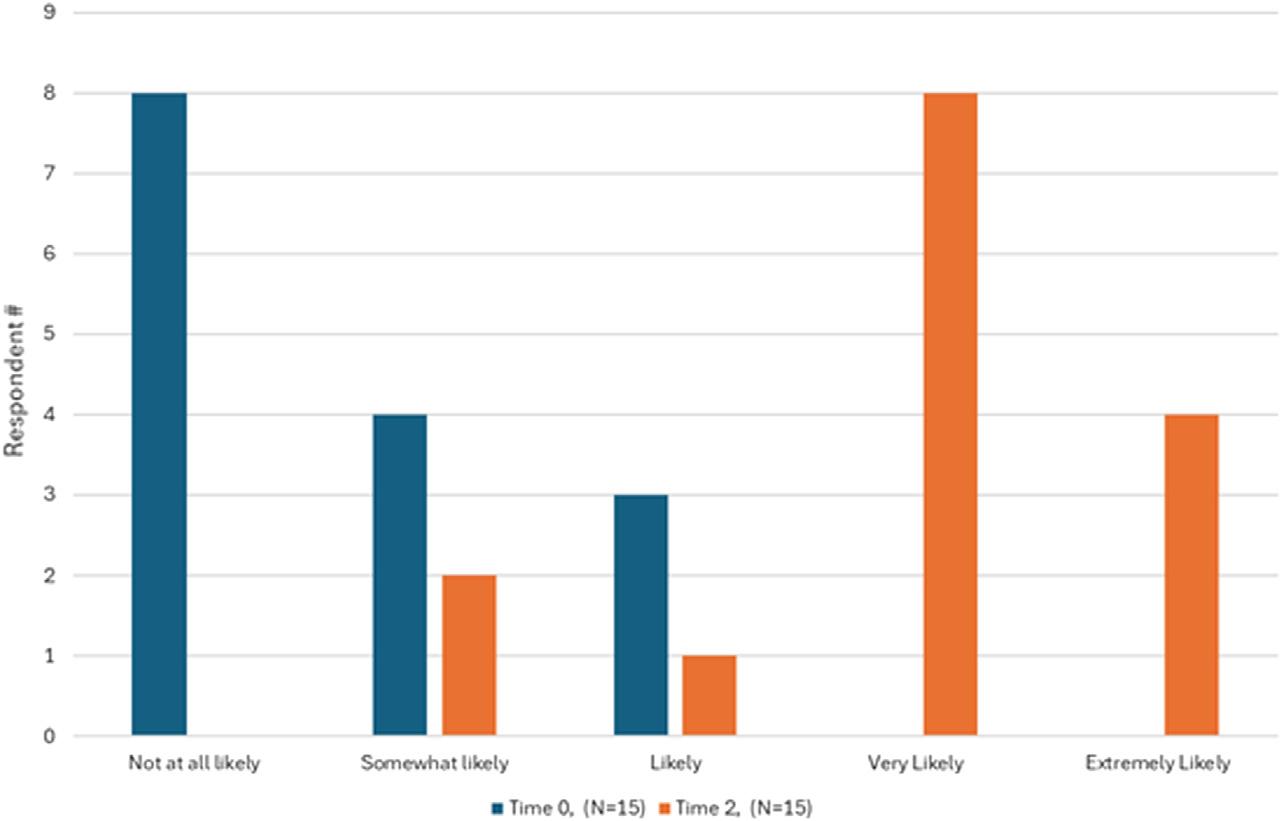
Learnerlikelihoodinteachingtheslit-lampexamatTime0(pre-curriculuar)andTime2(immediatepost-SBMLcurriculum).
andwereteachingmultiplejuniorlearnersduringtheir studyenrollment.
Theimprovementbetweenthepre-andpost-curricular proceduralcompetencyalsodemonstratestheimportanceof understandingthetechnicalnuancesoftheslit-lampexam andpracticingcriticaldevicemovement,suchascareful patientpositioning,adjustingofthechinstraps,changingthe microscopeangulation,andadjustingvaryingslit-lamp beamlengthsandwidthsfordiagnosingawiderangeof anteriorophthalmicpathologies.Theseskillsaredrastically differentthanthoserequiredtooperateaWood’slamp, whichactsprimarilyasamagnifyingglasswith UVcapabilities.
OurcurriculumachievedthreeofthefourKirkpatrick goals.Themajorityoftheparticipants(over80%)reported positivereactiontothecurriculum(thecurriculumhelped themperformaslit-lampexam,evaluateforcommon pathologies,andofferedmorethantraditionallectures) (Level1);alloftheparticipantsdemonstratedprocedural masteryatTime2(Level2);upwardsof50learnersreceived instructionsfromthestudyparticipantsonhowtousetheslit lampatTime3(Level3).Whiletherelianceon ophthalmologyconsultationdidnotrevealstatistically significantchanges,wepositthatimprovedprocedural acumenresultedinmoretargetedconsultationquestioning andimprovedrapportbetweenthemedicaldisciplines.
Sinceourparticipantswereboard-certifiedEPswith limitedavailabilities,themostvaluedcomponentofthe curriculumwasthein-personRCDPsessionwiththe ophthalmologist(Time2).Thiswasreflectedinalmostevery CIQitem,withspecificmentionofdirectguidancein positioningthebeamtolookforcellsand flare.Themost surprisingelementtomanyparticipantswashowmany oculardiagnosesrequiredtheslit-lampexamandthat learningtheprocedurewasnotascomplicatedastheyhad
initiallyanticipated.Incontrast,manyoftheparticipantsfelt mostdistancedorremovedfromthecurriculuminreviewing theasynchronouslearningmaterials.
Wewereunsurprisedtoseetheconfidencelevelsinusing Wood’slampunchangedbetweenthethreedifferenttime frames.Whiletheslitlampoffersasuperiorandin-depth evaluationoftheanteriorsegmentoftheeye,we acknowledgethatacomprehensiveslit-lampexamistimeandresource-consumingandmaynotaffecttheclinician’ s managementifthesuspectedpathologyinvolveslarger lesions,foreignbodies,orspecificreactionto fluorescein staining.TheWood’slampremainsaneasierand moreportablediagnostictoolforsomeocularpathologies, anditsuseintheclinicalarenaisstillacceptablein certainsituations.
Thisstudywasconductedatasingle,large,tertiary academiccenterwithanaffiliatedophthalmologyhospital andsupportedwithinternalgrantfunding.Whiletheresults werepositive,multiplefactorsciykdpreventthisstudyfrom beingreplicated,especiallyatcommunitysiteswithouta closerelationshipwithophthalmology.Oneofthemost significantchallengesisschedulingin-personevaluationsin thepre-curricularsession,aswellasthe finalin-person trainingandexamination.Weencounteredsignificant logisticalchallengesincreatingaschedulethatwasamenable totheophthalmologists,EPs(withunpredictableshift schedules),andresearchinvestigators,aswellas findinga consistentspaceintheWEHandWEHEDthathadaccess toanattached-observerscopetoensuretheparticipantswere focusingonthecorrectanatomicstructureduringtheir proceduraldemonstration.Thiswasfurtherexacerbated whenaccountingforthe “unlimitedattempts” forRCDP. Asthiswasourpilotstudywithadvancedlearners,we
Table3. Statisticalanalysisofsurveyquestionsbetweenthethreedifferentstudytimeframes.
Surveyquestion
Slitlamp
Based onyourcurrentpracticepatterns:how confidentareyouin:performingacomprehensiveslit lampexamforocularcomplaints?
Basedonyourcurrentpracticepatterns,how confidentareyouin:teachingresidentstoperforma comprehensiveslitlampexamforocularcomplaints
Howoftendoyou:performanindependentslit lampexamforocularcomplaints?
Wood’slamp
Basedonyourcurrentpracticepatterns,how confidentareyouin:performingacomprehensive Wood’slampexamforocularcomplaints?
Basedonyourcurrentpracticepatterns,how confidentareyouin:teachingresidentstoperforma comprehensiveWood’slampexam(withaccesstoa slitlamp)forocularcomplaints?
Howoftendoyou:useawoodlamp(withaccess toaslitlamp)forocularcomplaints?
Ophthalmologyconsultationhabits
Howconfidentareyouinidentifyingcommon ocularpathologyseeninyourmainworksite(CC, MHD,UrgentCare)?
Onaverage,howmanyeyepathologiesdoyou seeatthemainworksite? 10[4,15]n/a*5[3,12.5]n/a*
Onaverage,howmanyeyepathologiesdoyou seeatotherfacilities?
Howoftendoyourelyonophthalmology consultationto:helpmodifyyourtreatmentplanfor ocularcomplaints? 3[3,3]n/a*3[2.5,3]
Howoftendoyourelyonophthalmology consultationto:reinforceyourtreatmentandplanfor ocularcomplaints? 3[2,3]n/a*3[2,3]
Howoftendoyourelyonophthalmology consultationto:provideadditionalinformationand guidancetoyourtreatmentandplanforocular complaints?
3[3,4]n/a*3[3,3.5] n/a* 1.00
Confidence levels:1 = Notatallconfident,5 = Extremelyconfident
Frequencylevels:1 = Never,5 = Always
aTime0 = pre-curricularevaluation.
bTime2 = immediatepostSBMLexam.FrequencyofslitlampandWood’slampusewereintentionallyomittedforTime2duetotheclose proximitybetweenTime0andTime2,thusresultingin ‘n/a’ forsomecalculations.
cTime3 = threemonthsafterSBMLexam.
CC,JeffersonHospitalinCenterCityPhiladelphia; MHD,JeffersonMethodistHospital; IQR,interquartilerange.
over-budgetedatwo-hourtemplateforeachlearner,which drasticallylimitedthenumberofparticipantswecould scheduleforthe finalin-personexam.
Duetothelongitudinalnatureofthisstudyandseveralinpersoncomponents,maintainingparticipantrecruitment andengagementwasalsodifficult.Ofthe50eligibleboardcertifiedTJUHEPs,only15EPsvolunteeredtoparticipate. Theprimarydeterrence,whendiscussedwithnonparticipants,wastimerestraintsandcommutingintothecity forin-personevaluationsandexaminations.Wesuggest implementingdedicatedteachingdays(ie,conferencedaysor facultymeetings)forlargerparticipantrecruitmentand subsequentfollow-upandexamination.
Thisstudywasfundedbyaninternalgrantthatprovided minor financialincentivesfortheparticipantsand standardizedpatientvolunteers.Whileourneeds-based analysisrevealedparticipantsweremorefocusedon promotingbetterpatientcare,manyoftheparticipants expressedappreciationforthestaggeredgiftcards,which alsoincentivizedthemtocompleteeachtimeline-specific survey.Allotherinvestigators’ efforts,incontrast,wereinkindandrequireddedicatednon-academicandnon-clinical timetoenrollparticipants,recordalltheinteractions,and provideunrestrictedtimeavailabilitiesforthe finalmastery assessment.Thisstudywasalsounanimouslysupportedby bothdepartmentalleadershipstopromoteabettercollegial relationshipandinterdisciplinaryeducationopportunity betweenorganizationswiththetwoprincipalinvestigators holdinguniqueleadershippositions,ophthalmology consultingdirector[CC]andEMclerkshipdirector[XCZ]. Wesuspectthatalsopositivelyaffectedourrecruitment processandthesuccessofthisinterdisciplinarytraining curriculum.Asthisstudywasconductedatanacademic hospitalinanurbansetting,ithasbeensuggestedthat academiccenterslikelyoverestimateEPcomfortand confidenceinthediagnosisandmanagementofophthalmic emergencies.9 Furthermore,theproximitybetweenbothEDs mayskewthedata,astheseEPsarelikelyexposedtofewer ophthalmicemergenciesthanhospitalswithoutanearbyeyefocusedED.
Ultimately,thebiggestlimitationtothispilotstudywas thelackofin-personskillassessmentatthe60-dayfollow-up duetolimitedstaffingandschedulingchallenges.Inlieuofan objectivecompetencyscore,weleveragedself-reported confidenceatthe60-daymarkasanapproximate measurementoftheskillretention.Werecognizethat learnersarepooratgaugingtheirownabilities,bothoverandunderestimatingtheirskillsbasedonavarietyoffactors. Itisnotablethat80%ofourlearnerswereinitially “not confident” incompletingacomprehensiveslit-lampexam priortotheSBMLcurriculumandscoredanaverage checklistscoreof60%.AtTime2,almost87%ofresponders were “ confident” incompletingacomprehensiveslit-lamp examafterreceivinganaveragechecklistscoreof95%.
Unfortunately,thereisnoassociationbetweenlearners’ confidenceandpassingrate(score >18)atTime0(Pearson chi-square3.46, P = 0.17)andTime2(Pearsonchi-square 0.833, P = 0.66),respectively.Whileweareunabletopredict howtheselearnerswouldhaveperformedontheirslit-lamp examtestatday60,weareencouragedtoseethenumberof studyparticipantswhocontinuedtoteachslit-lampexamfor juniorlearners.Weposittheseparticipantswilllikelyhave improvedsustainedcompetenceanddecreasedskilldecayby activelyteachingothers.Futurestudiesshouldbeconsidered toadda finalexamination(procedureormultiple-choice question)tovalidateourresults.
Emergencyphysiciansareexpectedtodiagnoseand manageocularcomplaintsaspartoftheirtrainingand clinicalpractice.Ourprimaryfocuswastocreatearigorous methodologictrainingcurriculum(slit-lampexam)fora specialty-focusedskillsetthatcouldresultindownstream teaching.Thisprojecthighlightedasignificantneedforslitlampexamtrainingwithinourinstitutionthatledtoa successfultransdisciplinarysimulation-basedmastery learningcurriculumandimprovedourEPs’ confidencein performingandteachingslit-lampexamstofutureclinicians. Furthermore,thisstudydemonstratesthatadultlearners, especiallyattendingphysicianvaluedirectinteractionwith clinicalinstructorswhenlearninganewskillsetandare intrinsicallymotivatedtohonetheirskillsetandteachitto futurelearnerswhentheyhaveachievedthismastery. WeencourageotherinstitutionstoleverageSBMLasa teachingmodalityforprocedural-basedtrainingand advocatecross-disciplineeducationinitiatives.Future investigationcouldincludecreatingamulticenterstudyto implementthiscurriculumatotheracademicinstitutionsand potentiallyincludeitinEMresidencytraining.
WewanttothanktheThomasJeffersonUniversityCenter forFacultyDevelopmentandNexusLearning(CFDNL)for theirgeneroussupportandgrantfundingincompleting thisstudy.
AddressforCorrespondence:XiaoChiZhang,MD,Thomas JeffersonUniversity,DepartmentofEmergencyMedicine,1020 SansomSt.,ThompsonBldg,Suite239,Philadelphia,PA19107. Email: Xiaochi.zhang@jefferson.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudyreceivedgrantfundingfrom theCenterforFacultyDevelopmentandNexusLearning(CFDNL) Pedagogy,ThomasJeffersonUniversity.Therearenoother conflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Hamouetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.User:OKJaguar.File:slitlampandbinocularmicroscope.2019. Availableat: https://commons.wikimedia.org/wiki/File: Slit_lamp_and_binocular_microscope.jpg.AccessedAugust26,2023.
2.KnoopK.Ophthalmologicproceduresintheemergencydepartment partIII:slitlampuseandforeignbodies. AcadEmergMed. 1995;2(3):224–30.
3.SeolSH,ChoJ,LeeWJ,ChoiSC.Useofaslit-lampmicroscopefor treatingimpactedfacialforeignbodiesintheemergencydepartment. ClinExpEmergMed. 2015;2(3):188–92.
4.User:Seawind60.File:Wood’sUVlamp.2013.Availableat: https:// commons.wikimedia.org/wiki/File:Wood%27s_UV_lamp.JPG AccessedAugust26,2023.
5.BabineauMandSanchezL.Ophthalmologicproceduresin theemergencydepartment. EmergMedClinNorthAm. 2008;26(1):17–34.
6.CheungCA,Rogers-MartelM,GolasL,etal.Hospital-basedocular emergencies:epidemiology,treatment,andvisualoutcomes. AmJ EmergMed. 2014;32(3):221–4.
7.OwensPLandMutterR.(2011).Statisticalbrief#112:Emergency departmentvisitsrelatedtoeyeinjuries,2008.In Healthcarecostand utilizationproject(HCUP)statisticalbriefs.Rockville,MD:Agencyfor HealthcareResearchandQuality.
8.TheWillsEyeEmergencyDepartment.Alleyes,allthetime. EyeLevel. 2021.Availableat: https://www.willseye.org/wp-content/uploads/2021/ 05/WEB_3009-Eye-Level-Spring-2021.pdf.AccessedOctober17, 2023.
9.UhrJH,GovernatoriNJ,ZhangQE,etal.Traininginandcomfortwith diagnosisandmanagementofophthalmicemergencies amongemergencymedicinephysiciansintheUnitedStates. Eye. 2020;34(9):1504–11.
10.DruckJ,ValleyMA,LowensteinSR.Proceduralskillstrainingduring emergencymedicineresidency:areweteachingtherightthings? WestJ EmergMed. 2009;10(3):152–6.
11.GelstonCDandPatnaikJL.Ophthalmologytrainingandcompetency levelsincareofpatientswithophthalmiccomplaintsinUnitedStates internalmedicine,emergencymedicineandfamilymedicineresidents. J EducEvalHealthProf. 2019;16:25.
12.GraubartEB,WaxmanEL,ForsterSH,etal.Ophthalmologyobjectives formedicalstudents:revisitingwhateverygraduatingmedicalstudent shouldknow. Ophthalmology. 2018;125(12):1842–3.
13.AccreditationCouncilforGraduateMedicalEducation(ACGME). Emergencymedicinemilestones.2023.Availableat: https://www. acgme-i.org/globalassets/acgme-international/milestones-2.0/ emergencymedicinemilestones2.0int.pdf.AccessedOctober17,2023.
14.Griswold-TheodorsonS,PonnuruS,DongC,etal.Beyondthe simulationlaboratory:arealistsynthesisreviewofclinical outcomesofsimulation-basedmasterylearning. AcadMed. 2015;90(11):1553–60.
15.ChanceyRJ,SampayoEM,LemkeDS,etal.Learners’ experiences duringrapidcycledeliberatepracticesimulations:aqualitativeanalysis. SimulHealthc. 2019;14(1):18–28.
16.LemkeDS,FielderEK,HsuDC,etal.Improvedteamperformance duringpediatricresuscitationsafterrapidcycledeliberatepractice comparedwithtraditionaldebriefing:apilotstudy. Pediatr EmergCare. 2019;35(7):480–6.
17.MavisSC,KreofskyBL,OukMY,etal.Trainingfellowsinneonatalteleresuscitationusingasimulation-basedmasterylearningmodel. ResuscitationPlus. 2021;8:100172.
18.ZendejasB,CookDA,BingenerJ,etal.Simulation-basedmastery learningimprovespatientoutcomesinlaparoscopicinguinalhernia repair:arandomizedcontrolledtrial. AnnSurg. 2011;254(3):502–9; discussion509–11.
19.FranklinBR,PlacekSB,GardnerAK,etal.PreparingfortheAmerican BoardofSurgery flexibleendoscopycurriculum:developmentofmultiinstitutionalproficiency-basedtrainingstandardsandpilottestingofa simulation-basedmasterylearningcurriculumfortheendoscopy trainingsystem. AmJSurg. 2018;216(1):167–73.
20.BarsukJH,McGaghieWC,CohenER,etal.Useofsimulation-based masterylearningtoimprovethequalityofcentralvenouscatheter placementinamedicalintensivecareunit. JHospMed. 2009;4(7):397–403.
21.QureshiN.InternationalperspectivefromSaudiArabiaon “procedural skillstrainingduringemergencymedicineresidency:areweteaching therightthings?” WestJEmergMed. 2009;10(3):157–8.
22.HoonpongsimanontW,NguyenK,DengW,etal.Effectivenessof a40-minuteophthalmologicexaminationteachingsessiononmedical studentlearning. WestJEmergMed. 2015;16(5):721–6.
23.Siddaiah-SubramanyaM,SmithS,LonieJ.Masterylearning: howisithelpful?Ananalyticalreview. AdvMedEducPract. 2017;8:269–75.
24.MillerDT,ZaidiHQ,SistaP,etal.Creationandimplementationofa masterylearningcurriculumforemergencydepartmentthoracotomy. WestJEmergMed. 2020;21(5):1258–65.
25.RutledgeBK.Thewillseyemanual:Officeandemergency roomdiagnosisandtreatmentofeyedisease. ArchOphthalmol. 1996;114(1):112.
26.McNemarQ.Noteonthesamplingerrorofthedifference betweencorrelatedproportionsorpercentages. Psychometrika. 1947;12(2):153–7.
27.ConoverWJ. PracticalNonparametricStatistics.Hoboken,NJ:John Wiley&Sons.1999.
28.R:TheRProjectforStatisticalComputing.June11,2023.Accessed August8,2023. https://www.r-project.org/
DianeL.Gorgas,MD*
KevinB.Joldersma,PhD†
FelixK.Ankel,MD‡
WallaceA.Carter,MD§
MelissaA.Barton,MD†
EarlJ.Reisdorff,MD†
*OhioStateUniversityWexnerMedicalCenter,DepartmentofEmergencyMedicine, Columbus,Ohio † AmericanBoardofEmergencyMedicine,EastLansing,Michigan ‡ RegionsHospital,DepartmentofEmergencyMedicine,St.Paul,Minnesota
§ WeillCornellMedicine,DepartmentofEmergencyMedicine,NewYork,NewYork
SectionEditors: KendraParekh,MD,andAbraFant,MD
Submissionhistory:SubmittedJanuary16,2024;RevisionreceivedJune14,2024;AcceptedJuly8,2024
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18703
Background: Theemergencymedicine(EM)milestonesareobjectivebehaviorsthatarecategorized intothematicdomainscalled “subcompetencies” (eg,emergencystabilization).Thescaleforrating milestonesispredicatedontheassumptionthatarating(level)of1.0correspondstoanincomingEM-1 residentandaratingof4.0isthe “targetrating” (albeitnotanexpectation)foragraduatingresident.Our aiminthisstudywastodeterminethefrequencywithwhichgraduatingresidentsreceivedthetarget milestoneratings.
Methods: Thisretrospective,cross-sectionalstudywasasecondaryanalysisofadatasetusedinaprior studybutwasnotreportedpreviously.WeanalyzedmilestonesubcompetencyratingsfromApril 25–June24,2022forcategoricalEMresidentsintheir finalyearoftraining.Ratingsweredichotomized asmeetingtheexpectedlevelatthetimeofprogramcompletion(ratingsof ≥3.5)andnotmeetingthe expectedlevelatthetimeofprogramcompletion(ratingsof ≤3.0).Wecalculatedthenumberofresidents whodidnotachievetargetratingsforeachofthesubcompetencies.
Results: InSpring2022,ofthe2,637residentsinthespringoftheirlastyearoftraining,1,613(61.2%) achievedaratingof ≥3.5oneverysubcompetencyand1,024(38.8%)failedtoachievethatratingonat leastonesubcompetency.Therewere250residents(9.5%)whofailedtoachievehalfoftheirexpected subcompetencyratingsand105(4.0%)whofailedtoachievetheexpectedrating(ie,ratingwas ≤3.0)on everysubcompetency.
Conclusion: WhenusinganEMmilestoneratingthresholdof3.5,only61.2%ofphysiciansachievedthe targetratingsforprogramgraduation;4.0%ofphysiciansfailedtoachievetargetratingsforany milestonesubcompetency;and9.5%ofphysiciansfailedtoachievethetargetratingsforgraduating residentsinhalfofthesubcompetencies.[WestJEmergMed.2024;25(5)735–738.]
WiththeadventoftheNextAccreditationSystem(NAS), theAccreditationCouncilforGraduateMedicalEducation (ACGME)introducedanewassessmentprocesscalledthe “milestones.”1 Themilestonesareobjectivebehaviorsthat reflectelementsofthemajorcompetencies(eg,patientcare, systems-basedpractice)inthematicdomainscalled “subcompetencies” (eg,emergencystabilization,patientandfamily-centeredcommunication).Themilestonescale
usesnineratingsfrom1.0,1.5,2.0,2.5,etc,to5.0.Thescaleis predicatedontheassumptionthatarating(level)of1.0 correspondstoanincomingemergencymedicine(EM)-1 residentandaratingof4.0isthegraduation “target,” albeit notagraduationexpectationorrequirement.Accordingto theACGME: “Level4isdesignedasagraduation goal but doesnot representagraduation requirement . ”2 TheEM milestoneshavebeenusedexclusivelyasaformative assessmentbytheACGME.Likewise,aphysician’sEM
milestoneratingsarenotconsideredwhendetermining theeligibilityofaphysiciantotaketheAmerican BoardofEmergencyMedicine(ABEM)written qualifyingexamination.
TheEMmilestoneswereintroducedin2012,andthe first ratingswerereportedin2013.3 TheEMmilestoneswere revisedin2021,resultingin22subcompetencies.Since2012, substantialvalidityevidencefortheEMmilestoneshasbeen accumulated.4–10 Aresident’smilestoneratingsareusually assignedbyclinicalcompetencycommittees(CCCs).Some subcompetencyratingsarebelowtargetlevels.Often,the subcompetencyratingsassignedbytheCCCsarelowerthan theratingsthatresidentsgivethemselves.11 Themilestones wereinitiallydesignedtohavearatingof4.0asthetargetfor aresidentcompletinganEMresidency.9 AggregateEM milestonesarereportedannuallybytheACGME.12 These dataandotherreportssuggestthatasubstantialnumberof graduatingresidentsarenotachievingalevel4ratingin manymilestonesubcompetencies.
Weundertookthisstudytodeterminethefrequency withwhichgraduatingresidentsreceivedthetarget milestonerating.
Thisretrospectivecross-sectionalstudywasasecondary analysisofanalreadyde-identifieddatasetusedinaprior study.13 Ourcurrentstudywasdeemedexemptfromhuman subjectresearchbytheWestern-CopernicusGroup InstitutionalReviewBoard.Thedatasetavailabletothe investigatorsdidnotincludephysicianorprogram characteristicsthatwouldallowamoredetailedanalysis.
Weanalyzedmilestonesubcompetencyratingsfrom Spring2022forcategoricalEMresidentsintheir finalyearof training.Thesemilestoneratingsweresubmittedbetween April25–June24.ThisratingsreportusedEMMilestones 2.0,whichincluded22subcompetencies.Thedatasethad beenprovidedearliertoABEMbytheACGMEaspartof theroutineEMmilestonessecuredata-sharingprocess.
Theprimarymeasurewasthenumberofsubcompetencies forwhichphysiciansfailedtoachieveatargetratingof3.5at thetimethattheSpringmilestoneratingsweresubmittedto theACGME.Becausetheratingsweresubmittedbetween AprilandJunepriortoresidencycompletion,andtheCCC couldhavedeterminedtheratingsevenearlierthanthat,an expectedratingforpurposesofthestudywasmodifiedtobe 3.5ratherthan4.0.Doingsoassumedthattheresidentwould achievearatingof4.0overtheremainingweekstomonthsof residencytraining.Wedeterminedthenumberofphysicians
whodidnotachievethetargetratingforthesubcompetencies (from0subcompetenciestoall22subcompetencies).
Ratingsweredichotomizedasmeetingthetargetlevelat thetimeofprogramcompletion(≥3.5)andnotmeetingthe targetlevelatthetimeofprogramcompletion(≤3.0).We calculatedthenumberofcompetenciesforwhichatarget ratingwasnotachieved.
InSpring2022,thereweremilestoneratingsfor2,637 residentsintheSpringoftheirlastyearoftrainingin279EM residencies.Therewere1,613residents(61.2%)whoachieved aratingof ≥3.5oneverysubcompetencyand1,024residents (38.8%)whofailedtoachievearatingof ≥ 3.5onatleastone subcompetency.Therewere250physicians(9.5%)whofailed tomeethalfoftheirtargetsubcompetencyratings.There were105residents(4.0%)whofailedtomeetthetargetrating (ie,ratingwas ≤3.0)oneverysubcompetency(Table).
Table. Thefrequencyofemergencymedicineresidentsreceiving targetmilestonesratingslowerthat3.5inSpring2022(n = 2,637).
First,theactuallevelofsubcompetencyachievementat graduationwasimpreciselyknown.Wechosearatingof ≥3.5torepresenttheperformancetarget,giventhatthe milestoneratingswereprovidedpriortothecompletionof theprogram.Usingaratingof4.0tobeassignedtwomonths priortograduationwouldlikelyunderestimate subcompetencyachievementandascoreof3.5attwo monthspriortoprogramcompletionwouldlikely overestimatesubcompetencyachievement.Anticipatingthat allresidentswitharatingof3.5wouldachievearatingof4.0 withinweekswasabenevolentassumption.Second, demographicdataonresidents(eg,gender)andprogram characteristics(eg,durationoftraining)wereunavailableto theinvestigators.Althoughthislackofadditional informationlimitedourabilitytodeterminefactors associatedwiththeratings,webelievethatthe findings aresufficientlysignificantontheirmeritandwarrant additionalinvestigation.
Third,wedidnotcorrelatepoorsubcompetencyratings withprogramextensionorremediation,thuslimitingthe opportunitytogatheranyevidenceofpredictiveor consequentialvalidity.Itispossiblethatnearlyevery physicianwhodidnotachievearatingof ≥3.5onnearlyhalf ofthemilestonesubcompetenciesunderwentremediation. Fourth,theratingsareassignedbyCCCs.Thestructuresof, andinformationusedbyCCCs,varybyEMresidency.14,15 Wedidnotattempttodeterminethereliabilityoraccuracyof theindividualratings.Moreover,wedidnotexaminethe potentialimpactofbiasintheratings.Priorstudiessuggested thatwomenwereassignedlowerperformanceratings.16,17 Sixth,theratingsusedforthisstudywerefromthe firstyear oftheEMMilestones2.0.Althoughtherewasadegreeof acclimationindevelopingfacilitywiththeEMMilestones 1.0,itislikelythatthesamedegreeofunfamiliaritywouldbe lesswiththemostrecentversion.Thedegreetowhichthe continueduseofEMMilestones2.0willchangeratingtrends isunknown.
Thisstudyisthe firstinEMtodemonstratethedegreeto whichphysicianscompletingEMresidenciesarenot achievingtargetsubcompetencyratings.Thesedatashowed thatofthe2,637residentsintheirlastyearoftraining,nearly oneintenfailedtomeettargetratingsforhalfoftheEM subcompetencies.Asimilar findingwasreportedfor physicianscompletingpediatricEMfellowships.18 However, thatreportusedatargetratingof4.0,not3.5asinourstudy. Consequently,67%ofpediatricEMfellowsdidnotattaina ratingofatleast4.0foratleastonesubcompetency.
Aphysicianshouldbeabletograduatefromresidency withoutscoring4.0onall22subcompetencies.Infact,all4.0 ratings(astraight-linescore)wouldbehighlyimprobable.19 Considerthehypotheticalsituationthatwouldresultfrom
themilestonesbeingusedinasummativemannerto determineABEMboardeligibility.Ifresidentswererequired tohavenomorethansixsubpar(ie, <3.5)milestoneratings (morethanone-fourthofthesubcompetencies),then353 residents(13.4%)intheir finalyearoftrainingwouldnotbe eligibletotaketheABEMwrittenqualifyingexamination. Giventheintentofthemilestonesasaformativeinstrument, ABEMmaintainsthepositionthatthemilestonesshouldnot beusedasasummativedeterminantofboardeligibility.
Therateofprogramextensionbyphysiciansbeyonda scheduledgraduationdatehasbeenreportedtobe approximately8.5%.13 Theseextensionsincludephysicians undergoingacademicremediation,aswellasprogram extensionsduetoapersonalleaveofabsence.Theprevalence ofphysiciansnotmeetinghalfofthetargetsubcompetency ratingswas9.5%.Basedonthese findings,therewere physicianswhofailedtomeetatleasthalfoftheEM milestonesubcompetenciesyetweredeemedcompetentto practiceautonomouslyasattestedbytheprogramdirector. Thislikelihooddoesnotchallengetheconstructvalidityof themilestones,nordoesitsuggestthatthetargetistoohigh. Inafact,apriorvaliditystudybyKorteetalusedprogram directorsurveydatatoverifytheappropriatenessofthe targetratings.9
Inthisstudywedidnotanalyzetheimpactoftraining length(EM1-3vsEM1-4).However,areviewofmeanscores wasundertakeninapriorinvestigationthatusedthesame studyperiod.13 ThescoressuggestthatresidentsinEM1-3 programstendedtohavehigherscoresthroughthe postgraduateyears(PGY)1–3.Forexample,inthePGY3year,residentsfromEM1-3programshadameanratingof 3.51(95%confidenceinterval[CI]3.50–3.53)andresidents fromEM1-4programshadameanratingof3.07(95%CI 3.05–3.09),whileEM4residentshadameanratingof3.67 (95%CI3.65–3.69).
Thisanalysisisaninitialexplorationintoamorethorough investigationofthe finalmilestonesratingthatanEM residentreceives.Thecurrentstudydoesnotidentifyvariable impactwithindemographicgroups,nordoesitprovideany indicesofpredictivevalidity.Giventhe findingsofthis analysis,amorethoroughanalysisofthemilestonesshould beundertakentodeterminetheirpsychometricqualitiesand subsequentutilityinthe field.Giventheuseofthemilestones asaformativeevaluationsystem,itshouldnotbeusedto makesummativedecisionssuchasthedeterminationof ABEMboardeligibility.Amorestructured,valid,and reliableprocessformakingthesummativedetermination thataphysicianhasdemonstratedthenecessary competenciestopracticesafelyandindependentlyis advisable.Moreover,suchadetailedsummativeprocess couldalsobeusedtomakeaconfidentdeterminationthata physicianiseligibleforboardcertification.Thisprocess wouldbeeasilyaccommodatedinamodelofcompetencybasedmedicaleducation.
ManyphysicianscompleteanEMresidencywithout meetingatargetratingforagraduatingresidentinuptohalf oftheEMmilestones.Someresidents(4%)didnotmeeta targetratinginanymilestone.These findingssupportthe continueduseofthemilestonesasaformativeinstrument, ratherthanatooltodetermineboardeligibility.
AddressforCorrespondence:DianeL.Gorgas,MD,American BoardofEmergencyMedicine,3000CoolidgeRoad,EastLansing, MI48823.Email: diane.gorgas@osumc.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Drs.Gorgas,Ankel,andCarterare membersoftheAmericanBoardofEmergencyMedicine(ABEM), BoardofDirectors.Drs.Joldersma,Barton,andReisdorffare employeesofABEM.ABEMreceivesnorevenuefromEmergency MedicineMilestonesreporting.Therearenootherconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Gorgasetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.NascaTJ,PhilibertI,BrighamT,etal.ThenextGMEaccreditation system–rationaleandbenefits. NEnglJMed. 2012;366(11):1051–6.
2.EmergencyMedicineMilestones.TheAccreditationCouncilfor GraduateMedicalEducation.2021.Availableat: https://www.acgme. org/globalassets/PDFs/milestones/emergencymedicinemilestones.pdf AccessedAugust4,2023.
3.BeesonMS,CarterWA,ChristopherTA,etal.Emergencymedicine milestones. JGradMedEduc. 2013;5(1Suppl1):5–13.
4.BeesonMS,CarterWA,ChristopherTA,etal.Thedevelopmentofthe emergencymedicinemilestones. AcadEmergMed. 2013;20(7):724–9.
5.BeesonMS,HolmboeES,KorteRC,etal.Initialvalidityanalysis oftheemergencymedicinemilestones. AcadEmergMed. 2015;22(7):838–44.
6.HamstraSJ,CuddyMM,JurichD,etal.Exploringtheassociation betweenUSMLEscoresandACGMEmilestoneratings:avalidity studyusingnationaldatafromemergencymedicine. AcadMed. 2021;96(9):1324–31.
7.HamstraSJ,YamazakiK,BartonMA,etal.Anationalstudyof longitudinalconsistencyinACGMEmilestoneratingsbyclinical competencycommittees:exploringanaspectofvalidityinthe assessmentofresidents’ competence. AcadMed. 2019;94(10):1522–31.
8.HolmboeES,YamazakiK,NascaTJ,etal.Usinglongitudinal milestonesdataandlearninganalyticstofacilitatetheprofessional developmentofresidents:earlylessonsfromthreespecialties. AcadMed. 2020;95(1):97–103.
9.KorteRC,BeesonMS,RussCM,etal.Theemergencymedicine milestones:avalidationstudy. AcadEmergMed. 2013;20(7):730–5.
10.PeckTC,DuboshN,RosenC,etal.Practicingemergencyphysicians reportperformingwellonmostemergencymedicinemilestones. JEmergMed. 2014;47(4):432–40.
11.GoldflamK,BodJ,Della-GiustinaD,etal.Emergencymedicine residentsconsistentlyratethemselveshigherthanattending assessmentsonACGMEmilestones. WestJEmergMed. 2015;16(6):931–5.
12.EdgarLaura,HoganSO,HolmboeES,etal.Milestones:National Report.2022. https://www.acgme.org/globalassets/pdfs/milestones/ 1160-ACGME-Milestones-Report-2022-R22.pdf AccessedAugust4,2023.
13.BeesonMS,BartonMA,ReisdorffEJ,etal.Comparisonofperformance databetweenemergencymedicine1–3and1–4programformats. JAmCollEmergPhysicians.Open 2023;4(3):e12991.
14.DotyCI,RoppoloLP,AsherS,etal.Howdoemergencymedicine residencyprogramsstructuretheirclinicalcompetencycommittees? Asurvey. AcadEmergMed. 2015;22(11):1351–4.
15.GoyalN,FoltJ,JaskulkaB,etal.Assessmentmethodsandresource requirementsformilestonereportingbyanemergencymedicineclinical competencycommittee. Med EducOnline. 2018;23(1):1538925.
16.SantenSA,YamazakiK,HolmboeES,etal.Comparisonofmaleand femaleresidentmilestoneassessmentsduringemergencymedicine residencytraining:Anationalstudy. AcadMed. 2020;95(2):263–8.
17.DayalA,O’ConnorDM,QadriU,etal.Comparisonofmalevsfemale residentmilestoneevaluationsbyfacultyduringemergencymedicine residencytraining. JAMAInternMed. 2017;177(5):651–7.
18.RoskindCG,LeonardK,BaghdassarianA,etal.Pediatricemergency medicinefellows’ milestoneevaluations:dotheyallmeetthetargetsfor graduation? AEMEducTrain. 2021;5(3):e10620.
19.BeesonMS,HamstraSJ,BartonMA,etal.Straightlinescoringby clinicalcompetencycommitteesusingemergencymedicinemilestones. JGradMedEduc. 2017;9(6):716–20.
NaomiP.Newton,MD* ChristopherFreeman,MD†
PatriciaPanakos,MD†
SectionEditor:PaulLoganWeygandt,MD
*EmoryUniversitySchoolofMedicine,DepartmentofEmergencyMedicine, Atlanta,Georgia
† JacksonHealthSystem,DepartmentofEmergencyMedicine,Miami,Florida
Submissionhistory:SubmittedOctober17,2023;RevisionreceivedApril28,2024;AcceptedMay30,2024
ElectronicallypublishedAugust16,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18509
Introduction: Socialmedicineseekstoincorporatepatients’ socialcontextsintotheirmedicalcare. Emergencyphysiciansareuniquelypositionedtoaddresssocialdeterminantsofhealth(SDoH)onthe frontlinesofthehealthcaresystem.Miami-DadeCounty(MDC)isadiverseandsociallyvulnerablearea. In2020,theUniversityofMiami-JacksonHealthSystem(UM-JHS)emergencymedicine(EM)residency programlaunchedamultimodal,resident-ledSocialEMprogramtoidentifyandaddressSDoHinthe emergencydepartment(ED).
Methods: Weuseafour-pillarapproachtoSDoHintheED:CurriculumIntegration;Community Outreach;AccesstoCare;andSocialJustice.ResidentsgraduatewithaknowledgeofSocialEM principlesthroughan18-monthcurriculum,anelective,andalongitudinaltrack.Wedeveloped sustainableinitiativesthroughinterdepartmentalandcommunity-basedpartnerships,includingaNarcan distributioninitiative,anED-basedprogramlinkinguninsuredpatientstofollow-upcare,ahuman traffickingeducationinitiative,andaqualityimprovementinitiativeforincarceratedpatients.
Results: Giventhatthe18-monthcurriculumwaslaunchedin2022,afullrotationofthecurriculumhad notbeencompletedasofthiswriting,anddatacollectionandanalysisisanongoingprocess.Theinitial pretestandpost-testsurveydatashowimprovementinknowledgeandconfidenceinmanagingSocial EMtopics.TheNarcaninitiativehasscreened1,188patients,ofwhom144havereceivedNarcan.The ED-basedpatientnavigationprogramhasenrolled31patientstodate,18ofwhomobtainedoutpatient care.Analysisoftheimpact/effectivenessoftheprogram’sotherinitiativesisongoing.
Conclusion: Toourknowledge,thisisoneofthemostrobustsocialEMprogramstodate,asmanyother programsprimarilyfocusonserviceopportunities.RootedintherevisedprinciplesofBloom’staxonomy ofcognitivelearning,thisprogrammovesbeyondunderstandingSocialEMtenetstogenerating solutionstoaddressSDoHinandoutsidetheED.[WestJEmergMed.2024;25(5)739–747.]
Socialmedicine,ortheincorporationofpatients’ social contextsintotheirmedicalcare,hasbecomeavibrant, interdisciplinarymovementthathasgainedtractionin medicalschools,residencies,andatthenationallevel.Social medicineemphasizestheimportanceofsocialdeterminants ofhealth(SDoH),or “theconditionsintheenvironments wherepeopleareborn,live,learn,work,play,worship,and agethataffectawiderangeofhealth,functioning,and
quality-of-lifeoutcomesandrisks.”1 TheUSDepartmentof HealthandHumanServiceslists fivecoreSDoHtoconsider duringpatientcare:economicstability;educationaccessand quality;healthcareaccessandquality;neighborhoodand builtenvironment;andsocialandcommunitycontext.1
AlthoughSDoHcanbeappliedtoallspecialties,theyare perhapsmostrelevanttoemergencymedicine(EM).Passage oftheEmergencyMedicalTreatmentandLaborAct (EMTALA)in19862 wasacknowledgmentthatemergency
physiciansareoftentheonlylinktothehealthcaresystemfor patientswith financiallimitations.Emergencyphysiciansare estimatedtoprovidetwo-thirdsofacutecareforall uninsuredpatientsandhalfofacutecareforallMedicaid patients.3 WhethertheyarerushingapatienttoCT,leading theirteamduringaresuscitation,orevaluatingpatientsina crowdedhallway,emergencyphysiciansareimmersedin longstanding,complexsocialissues:trauma;poverty; homelessness;mentalhealthdisorders;etc.Therefore, recognizingtheeffectsofSDoHonpatientcareiscriticalin theED.
JacksonMemorialHospital(JMH)istheprimarytraining sitefortheUniversityofMiami-JacksonHealthSystem (UM-JHS)EMresidencyprogram.Itisalsothethirdlargest publichospitalinthecountry.TheUM-JHSocialEM programwaslaunchedin2020toimprovetheincorporation ofpatients’ socialcontextsintotheircare.
WhendesigningaSocialEMprogram,keepingthe residency’slocationandpatientpopulationinmindis important.LikemostEDsacrossthenation,theJMHEDis aplaceofrefugeforpatientswhoseSDoHmaypreventthem fromobtainingcareelsewhere.Asasafety-nethospitalinthe seventhmostpopulouscountyinthenation,4 JMHservesa particularlydiversepatientpopulationwithstriking socioeconomicneeds.TheUMhealthsystemconducted formalneedsassessmentsofMiami-DadeCounty(MDC) from2019–2022,andtheUM-JHSSocialEMprogramwas designedtoreflecttheseneeds.4,5
TheUM-JHSSocialEMprogramwasdesignedtoensure thatallresidentsgraduatewiththeabilitytoincorporate theirpatients’ SDoHintoEDcareregardlessoftheir ultimatepracticelocations.However,certainaspectsofthis programweredesignedtoaddresstheuniqueneedsof MDC a “minority-majority” communitythatexperiences challengeswithEnglishproficiency,andinwhich20%ofthe populationlivesbelowthepovertylevel.4,5
Bloom’staxonomyofcognitivelearningobjectives outlinessixlevelsinthecognitivedomain:knowledge; comprehension;application;analysis;synthesis;and evaluation.6 Overtime,scholarshavesoughttorevisethis frameworkand,whentakenasawhole,theserevisionsplace lessemphasisonalinearprogressionthrougheachlevel.6 Instead,thereisanincreasedfocusongeneratingnew hypothesesanddevelopingprojectsthatuseandexpand upontheacquiredknowledge.6 Therefore,theUM-JHS SocialEMprogramseekstoshiftitsparticipantsfrompurely understandingSDoHastheypertaintoEM,togenerating effectivesolutionsforaddressingtheseSDoHinandoutside theED.TheSocialEMprogramoutlinessixgoalsforits residents,whoarethentaskedwithgeneratingeffective
solutionsanddesigningtheirownmeasurableoutcomesfor eachgoal.Uponsuccessfulcompletionofthisprogram, residentsshouldbeableto:
1.DefineandidentifySDoHintheEDandapplythese principlestobedsidecare.
2.EngagewithMDCoutsidetheEDandaddressits socialandmedicalneedsthroughlongitudinal involvementinlocaloutreachinitiatives.
3.Solidifyandshareacquiredknowledgethroughan 18-month,multimodalcurriculum.
4.Identifyandseektoaddressbarrierstomedicalcare experiencedbypatientswhousetheEDastheirmain sourceofhealthcare.
5.Identifyandseektoaddressrecurrentsocialjustice issuesencounteredintheED.
6.Enactpositivechangethroughadvocacyandquality improvementinitiativesathospital-wide,local,and/or nationallevels.
Sinceitslaunchin2020,theprogramhasbeendividedinto fourpillarsthataddresscoreareaswithinSocialEM: CurriculumIntegration;CommunityOutreach;Accessto Care;andSocialJustice(Figure1).Initiativeswithineach pillarwillbediscussedinaseparatesection.Anyone affiliatedwiththeUM-JHSEDcanparticipateininitiatives acrossallfourpillars.Manyoftheseinitiativesare longitudinal,allowingforvaryinglevelsofparticipation throughoutresidency.Additionally,thisprogramalsooffers leadership,peerteaching,andscholarlyopportunitiesthat maycounttowardexistingresidencyrequirements.
TheUM-JHShasathree-yearEMresidencyprogram, andeachofitsclasses(postgraduateyears[PGY]1–3)is comprisedof14–15residents.EMresidentsarenotrequired toparticipateintheSocialEMprogrambutareencouraged todoso.Theymaychoosetoserveasprogramleaders (Figure1),participateinthelongitudinaltrackand/ortwoweekelective(discussedindetailinsubsequentsections below),ortoparticipateinindividualinitiativesastheir schedulesallow.However,SocialEMprogramleadership developedaformalcurriculumtoensurethatallresidents graduatewithasolidunderstandingofcoreSocialEM principles,regardlessoftheirlevelofinvolvementwiththe program;thiswillbediscussedinaseparatesection.
Thisprogramwasdesignedtobeexecutedbyresidentsin collaborationwithfaculty,medicalstudents,andstaff.The programwasstructuredintoacoreleadershiphierarchyto appropriatelydividethelaborofdesigningandlaunching initiativesthatpertaintoeachpillar,whileensuringthat residentscompletetheirexistingclinicalandacademic




Figure1. Socialemergencymedicineprogramorganizationanddivisionoflabor.Programdirectorsconsistofonefacultydirectorand1–4 residentdirectors(EMresidentsselectedviaaformalapplicationprocess).Programdirectorsoverseeinitiativesacrossallfourpillarsbut spendadditionaltimeleadingCurriculumIntegrationinitiativestoensureaseamlessincorporationofSocialEMprinciplesintoresidency training.PillarleadersareEMresidentswhoareselectedbyprogramdirectorsviaaformalapplicationprocess;theydesignandoversee initiativesintheirassignedpillars.FacultymentorsaregenerallycorefacultyintheEMdepartmentwithexpertiseintheirassignedpillar. However,facultyinotherspecialtiesatUM-JHSmayalsoserveasmentorsiftheycurrentlyoverseeacommunityorhospital-basedinitiative thatcollaborateswiththeSocialEMprogram.(Forexample,afacultymentorfromthefamilymedicinedepartmentoverseestheIDEANeedle ExchangeClinic.)AnyoneaffiliatedwiththeEMdepartmentmayserveasateammember.Teammembersworkdirectlywiththeirassigned residentleadersanddividethetasksrequiredtolaunchandpublicizeinitiatives.
requirements(Figure1).Thisleadershiphierarchyorganizes, executes,andpublicizestheprogramanditsinitiatives.
Afacultydirectorandatleastoneresidentdirector overseetheprogramtogether(Figure1).Theoriginal directors,PatriciaPanakos,MD,andNaomiNewton,MD, authoredthispaperandconceptualizedtheprogram togetherinFall2020.ThecollaborationbetweenDrs. PanakosandNewtonwasbornefromasharedpassionfor socialmedicineandadesiretoimplementanEMresidencybasedprogramtoaddresstheSDoHofpatientsinMDC.Dr. PanakosistheassociateprogramdirectorfortheUM-JHS EMresidencyandhasundergoneformaltrainingin curriculumdevelopment.ShehasalsodevelopedED-based publichealthinitiativesatJHS,suchasauniversalscreening programforcommunicablediseases,includingHIV, hepatitisC,andsyphilis.Dr.Panakoscontinuesherroleas facultydirectorforthesocialEMprogram.Dr.Newtonisan alumnaoftheUM-JHSEMresidencyandservedaschief residentduringher finalyearoftraining.Sheassumedthe roleofthesocialEMprogram’sresidentdirectorasaPGY-1 andtransitionedherpositionuponhergraduationin2023. ShehasalsocollaboratedwithDr.Panakosonpublichealth
initiatives,includingauniversalHIVscreeninginitiativein JHS’spediatricED.Dr.Newtoniscurrentlypursuing atwo-yearfellowshipinhealthpolicyandadvocacyat EmoryUniversity.
Giventhattherewasnoprecedenceforsuchaprogramat UM-JHS,Drs.PanakosandNewtonworkedalmostdailyto createtheprogramandmaintainitssustainability,whilealso completingtheirexistingclinicalandacademic responsibilities.Drs.PanakosandNewtondesignedthe program ’soverallstructure,createdaformalselection processforpillarleaders,andidentifiedcommunitypartners andfacultymentorswithexpertiseinSocialEM.They presentedaformalproposalthatwasapprovedbyboththe chairoftheEDatJMHandtheUM-JHSEMresidency programdirectorinOctober2020.Theyalsodesignedand launchedthe18-monthcurriculum,two-weekelective,and longitudinaltrack,whicharedescribedinsubsequent sectionsofthispaper.Toaccountforcontinuedprogram growth,theoriginaldirectorsselectedfournewresident directorsforthe2023–2024academicyearviaaformal applicationprocess(Figure1).
Directorsapproveproposedinitiativesacrossallpillars andworkdirectlywithpillarleaderstotrackprogressand troubleshootchallenges.Theycheckinremotelywithpillar
leadersatleastbi-monthlytoensuretimelyproject completion.Theyalsopromotetheprogramata departmentalandhospital-widelevelandhelppillarleaders identifyfacultyandcommunitypartners(Figure1).Resident directorsarerecognizedwithaSocialEMleadershipaward upontheirgraduation.
AnaverageoftwoPGY-1orPGY-2EMresidentslead eachpillar.Interestedresidentsapplyforthispositionviaa briefelectronicapplication(GoogleSurvey)atthestartofthe academicyearandareselectedbythedirectors.Residents generallydonotserveasleadersofmorethanonepillar,as thispositionmustbebalancedwithexistingresidency obligations.Residentleadersreportdirectlytothedirectors anddedicateanaverageoftwotofourhoursperweekto theirroles.Asleadersprogressthroughtraining,theymay eitherremainintheirleadershiprolesortransitiontheirroles toincomingPGY-1sandPGY-2s.Allresidentleaderswho haveservedforatleastoneyeararerecognizedwithaspecial awardupongraduationfromresidency.
Leadersfocusondesigninginitiativesthatpertaintothe goalsoftheirassignedpillar.Theyidentifyappropriate partnerswithinJHSandMDCtoaidindevelopingand launchingtheseinitiatives(Figure1).PartnersincludeJHS faculty(includingthoseinnon-EMspecialties),local outreachorganizations(manyofwhichalreadyhad establishedrelationshipswithUM-JHSthroughmedical studentinvolvement),andotherJHS-affiliatedresidency programs(eg,pediatrics,internalmedicine,family medicine).Interdisciplinarycollaborationpreventsthe SocialEMprogramfrom “re-inventingthewheel” andhelps initiativesachievesuccesswithfewerfunding,resource,and logisticalrestrictions.Residentleadersdelegateday-to-day taskstoaninterdisciplinaryteamtodividethelaborof executingtheseinitiatives.Leadersarerequiredtocheckin remotelywiththeirteammembersatleastmonthlytodiscuss progressonpillarinitiatives.
Teammembersdividethetasksrequiredtolaunch initiativeswithintheirassignedpillar.Theyarerequiredto dedicateaminimumofonetotwohoursperweekonthese tasksandcheckinregularlywiththeirpillarleadersas previouslydiscussed.Thosewhodesiretodosomay participateinmorethanonepillarteam.Participationina pillarteamisopentoanyoneintheUM-JHSED.However, duringthe firstthreeyearsoftheprogram,teamswere primarilycomprisedofEM-boundUMmedicaland pharmacystudents,JHSclinicalpharmacyresidents,and hospitalstaff(eg,nursesandsocialworkers).
Inthefollowingsection,weprovideabroadoverviewof eachpillar’sobjectivesandhighlightseveralkeyinitiatives withineachpillar.Whenrelevant,pleaseseethe correspondingappendicesforadditionaldetails.
ThispillarincorporatesthetenetsofSocialEMinto residencytrainingtoempowerfuturegenerationsof emergencyphysicianstoapplySocialEMprinciplestotheir care.ThisistheonlypillarthatrequiresallEMresidentsto participatebecauseitsinitiativeshavebeenincorporatedinto theexistingresidencycurriculum.Doingsoensuresthatall EMresidentsgraduatewithanunderstandingofSDoHand theprinciplesofSocialEM,regardlessoftheirlevelof involvementinotherpillars.Ofnote,approvalfromthe institutionalreviewboardwasnotrequiredforthe developmentofthiscurriculum.
Wedevelopedandlaunchedamultimodal,18-month SocialEMcurriculumthathasbeenincorporatedintothe existing18-monthresidencydidacticschedule(AppendixA). Thecurriculumcovers18coresocialEMtopics(Table1)and includesjournalclubs,simulationcases,lectures,problembasedlearning,andinteractivegroupdiscussions.The curriculumisledbyfacultyandresidentswithexpertiseor
Table1. 18coreareasofstudywerechosentobecoveredmonthlyduringthe18-monthSocialEMcurriculum.Thiscurriculumisintegrated intostandardresidencydidacticschedule,whichrepeatsevery18months.Usingamultimodallearningformat,topicscanbepresentedas traditionallectures,case-baseddiscussionsandjournalclubs(“Cases”),orsimulations.Theinitialmodalitiesforeachtopicarelistedbelow; themodalitiesusedforeachtopicwillchangeevery18months(eg,thepediatrichealthlecturewouldbepresentedaseitheracaseor simulation18monthslater).Additionaldetailsregardinglogisticsandimplementationcanbefoundin AppendixA
1.Socialdeterminantsofhealth7.Implicitbias/racism13.Humantraffickinganddomesticviolence
2.Healthcarecoverageandaccess8.Homelessness14.Substanceabuseandharmreduction
3.Financialstability9.Healthliteracy15.Caringforincarceratedpatients
4.FrequentEDutilizers10.Immigration16.Highlycommunicablediseases/STIepidemics
5.Women’shealth11.Resourceinsecurity17.Languageandculturalbarrierstohealthcare
6.Pediatrichealth12.Trauma-informedcare18.Genderidentity
ED,emergencydepartment; STI,sexuallytransmittedinfection.
interestinthecoretopics.SocialEMleadershipassists presentersinidentifyinglearningobjectivesforeachsession, selectingtopics,anddevelopingcontent.Allconference attendeesparticipateinpre-andpost-surveystoassesstheir baselineknowledgeandtheeffectivenessofeachdidactic session.ResidentsarealsoaskedtoevaluatetheSocialEM curriculumduringtheannualresidencyprogramevaluation. SurveysandresultsarediscussedfurtherintheImpact/ Effectivenesssectionofthismanuscript.
In2022,welaunchedthetwo-weekSocialEMelectivefor residentswhodesireamorein-depthexperiencewiththe program(AppendixB).ThiselectiveisopentoPGY-2EM residentsduringtheirelectiveblockandiscomprisedof serviceopportunities,self-directedstudy,peerteaching,and initiativeparticipationacrossallpillars.ThePGY-2rotation scheduleisdesignedsothatonlyoneresidentcompletesan electiveinanygivenmonth.Therefore,theexperienceis personalizedforeachparticipatingresident.SocialEM directorsworkwiththeresidentaheadoftimetodesignan electiveschedulethatensuresparticipationacrossallpillars butallowsthemtoengagemoredeeplywithintheirpillar(s) ofinterest(AppendixB).
Wealsodesignedalongitudinaltrackthatwaslaunched the2023–2024academicyear.Trackparticipantsengageina
setnumberofoutreachevents,qualityimprovement initiatives,peerteaching,andself-directedstudyover18 months.Therequirementsarebasedonapointsystemthat ensuresengagementwithallpillarsbutallowsfordeeper explorationinareasofindividualinterest.Residentsmust reachaminimumof30pointstocompletethetrack (Figure2).Requirementsincludealongitudinalscholarly activitythatculminatesinapresentationatthelocal, regional,ornationallevels(eg,developingaprojectto addressfoodinsecurity).Theymustalsoparticipateinthe SocialEMdidacticcurriculumthroughpeerteaching, developingnewelementstothecurriculum,andmentoring medicalstudents.Participantslogtheirprogressviaanonline formandmustattendaminimumofninemonthlytrack meetingswiththeSocialEMdirectorsoveran18-month period.Upongraduation,residentswhocompletethetrack willreceiveaDistinctioninSocialEM.
Thispillarwasdesignedtoestablishameaningfulpresence inMDCbeyondbedsidecareandtoaddresssocialissues throughpartnershipswithlocalorganizations.Forexample, throughapartnershipwithMiamiStreetMedicine, participantsjoinaninterdisciplinaryteaminproviding
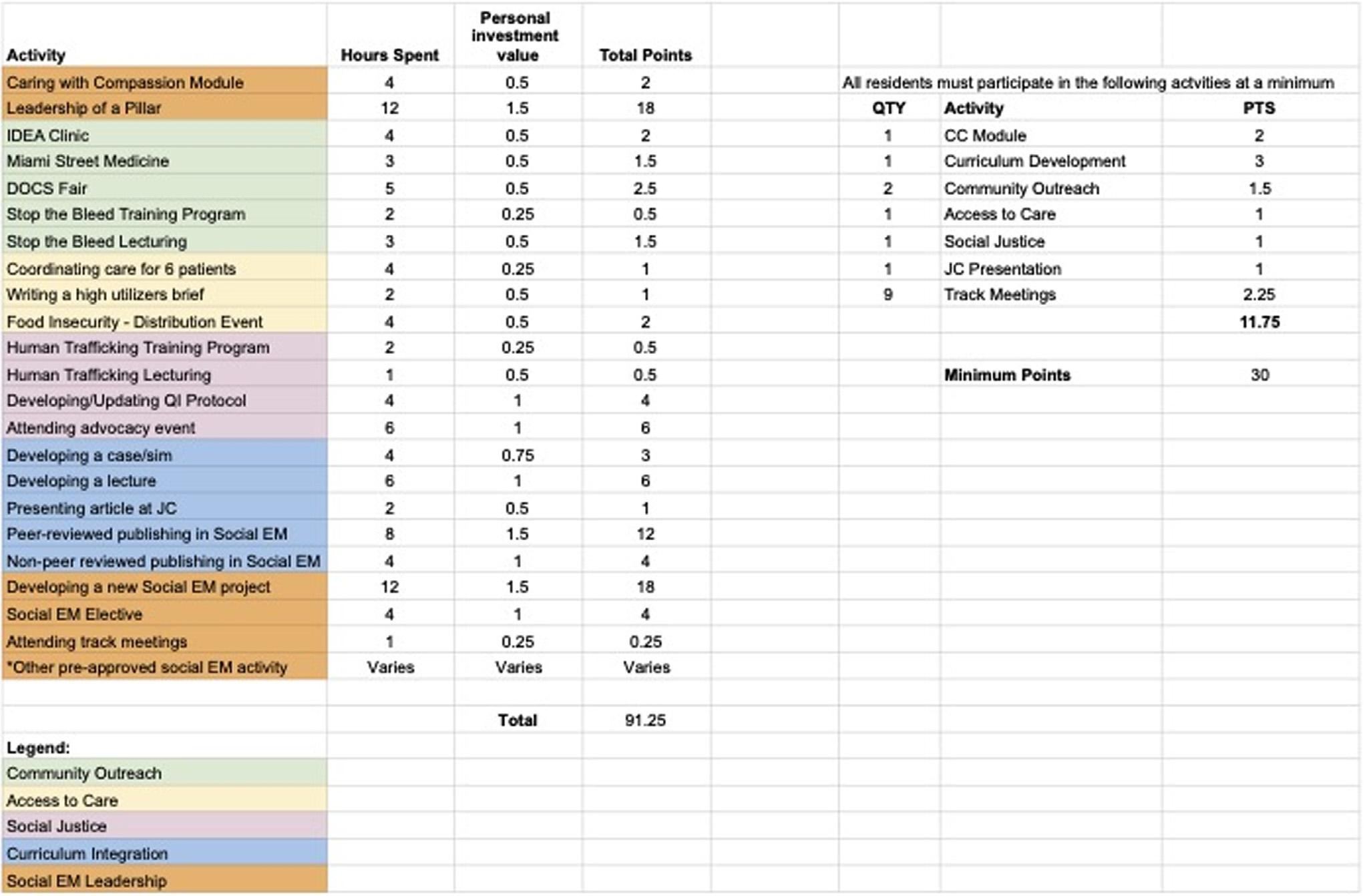
Figure2. Pointsystemforthe18-monthlongitudinaltrack.Notethatopportunitiesineachpillarmayvaryovertime.This figurelists opportunitiesfromthefallof2023.
regularmedicalcareatlocationscommonlyoccupiedby Miami’shomelesspopulation.Throughapartnershipwith theStoptheBleedCampaign,participantsundergoformal trainingtoserveaslocalinstructors.Participantsthenlead workshopsthatteachnon-medicalcommunitymembersto performbystandercardiopulmonaryresuscitationand stabilizevictimsofviolenceuntil firstrespondersarrive. ParticipantsmayserveasinstructorsforStoptheBleed eventsthroughoutMDC,astheirschedulesallow.
ThispillarlaunchedaNarcanprograminJuly2022,in partnershipwiththeUMIDEA(InfectiousDisease EliminationAct)NeedleExchangeClinicandtheUM MichaelWolfsonDepartmentofCommunityService (DOCS).ThisprogramseekstoaddressSouthFlorida’ s opioidepidemicandisinkeepingwiththestatewide EmergencyTreatmentforSuspectedOpioidOverdoseAct.7 Atcommunityhealthfairs,participantsprovidefreeopioid usedisorder(OUD)screening,basedonDiagnosticand StatisticalManualofMentalDisorders,5th ed,criteria.8 Narcanissubsequentlydistributedtothoseidentifiedtobeat highriskforlife-threateningoverdoses,andadditionalOUD counselingandtrainingonsafelyadministeringNarcan areprovided.9
AccesstoCare
Thispillarlinkschronicallyillpatients,highEDutilizers, andtheuninsuredtooutpatientcare.Italsoseeksto centralizeexistingsocialsupportresourceswithinUM-JHS andefficientlyaddressSDoHatthebedside.Througha partnershipwithDOCS,uninsuredpatientspresentingtothe EDwithchroniccomplaintsarepairedwithlong-term patientnavigators,whohelpthemsecureaffordable outpatientcareupondischarge.
TheHighUtilizersInitiativeaimstostreamlinethecareof patientswhofrequentlyvisittheED.Participantsconduct chartreviewsofindividuals flaggedasfrequentutilizersinthe electronichealthrecordandcreatepatientcarebriefsthat auto-populateintheircharts.Thesepatientsoftenpresentto theEDnumeroustimesaweekandreceivecarefrom differentclinicianseachtime.Byconsolidatingtheir pertinentmedicalinformation,thesebriefsallowforbetter, morestreamlinedpatientcarewithlessrepetitionoftestsand procedures.Thebriefsalsolessenthecognitiveloadofthe clinician,decreasingthetimespentonchartreviewsand helpingguidefuturecare.
ManypatientspresenttotheEDwithconditionsthatare exacerbatedbyalackofbasicresources.Itischallengingto addressthesecomplexSDoHamidstthetimeconstraintsof EDcare,andEDscannolongerrelyheavilyonsocial workersforassistance,duetothenationwidesocialworker shortage.10 ThispillarpartneredwithMiamiStreetMedicine andtheJMHPharmacyDepartmenttocreateresource guidesforpatientsandcliniciansinresponsetothisneed. Communityresourceguides(inEnglish,Spanish,and
HaitianCreole)provideinformationforaffordable outpatientclinics,prescriptions,mentalhealthservices, temporaryhousing,mealprograms,andsubstanceuse treatmentcenters,aswellasresourcesforpregnantpatients andvictimsofdomesticviolence.Clinicianresourcesinclude referralinformationforresident-runsubspecialtyclinics, instructionsforinitiatingbuprenorphineintheEDand referringpatientstomedication-assistedtreatmentclinics, andalgorithmsforhumantraffickingscreening.
Thispillartackleshealthinequityandinjusticeissues throughinterdisciplinaryeducationandquality improvementinitiatives.TheHumanTraffickingEducation Ambassadorprogram,inpartnershipwithJMH’sRape TreatmentCenter,teachesclinicianstoscreenforandtreat victimsofhumantrafficking.Floridahasthethirdhighest numberofhumantraffickingcasesinthenation,andMDC is,sadly,aknowntraffickinghub.11 Trainedresidentslead interactiveseminars,sharingHIPAA-complianttrafficking casesandteachingclinicianstoidentifyandaddressred flags fortrafficking.
Thispillaralsoseekstoimprovecareforincarcerated patientsintheED,particularlyconcerningpatientprivacy andexaminationsinthepresenceoflawenforcement. Initiativesincludearecentlypublishedreviewonthebarriers tocaringforthispopulationandrecommendationsto improvetheirdeliveryofcare.12 Wealsoimplementeda simulationsessiononcaringforincarceratedpatientsinto residencydidactics.
SocialEMleadershipisintheprocessofcompletinga formalimpactassessmentofthecurriculumintegrationpillar oftheprogramviaasingle-group,pretest-posttestdesign.6 Briefpre-andpost-didacticsessionsurveysaredesignedfor eachSocialEMtopicinthe18-monthcurriculum.Surveys aredesignedtoassessbaselineknowledgeofthetopicandthe changesinthisbaselineknowledgeafterthesession.Survey questionsalsoaddressrelevantepidemiologicalstatisticsand usefulcommunityresourcesforaddressingthetopicin MDC.Eachpost-surveyendswithablanksectionfor participantstowriteinanyadditionalfeedback,which SocialEMprogramleadershipusesforsubsequent didacticsessions.
Forconvenience,thesesurveysareadministeredvia electronicforms;conferenceattendeesscanQRcodestothe formsbeforeandafterthesession.Allresidents,faculty, students,andstaffinattendanceareeligibleforparticipation inthesurveys.However,thusfar,surveyparticipationhas generallybeenlimitedtoresidentattendees,asfaculty,staff, andstudentattendanceislessconsistent.Hospitalbadge
numbersareusedtocompareindividuals’ changesinpreandpost-sessionresponses.
Sincethe18-monthcurriculumwaslaunchedin2022,a fullrotationofthecurriculumhasnotbeencompletedasof thiswriting,anddatacollectionandanalysisisongoing. However,thusfar,thecurriculumtopicshavebeenwellreceived,withresidentsindicatinganimprovedconfidencein theirabilitytorecognizeandaddresstheseSocialEMissues atthebedside.Forexample, Figure3 showskeyresultsfrom thepre-andpost-surveysadministeredduringthe first sessionoftheformalcurriculumin2022 asimulation sessiononhighlycommunicablediseases/sexuallytransmittedinfection(STI)epidemics(Table1).Theseresults suggestefficacyinimprovingbaselineknowledgeand confidencewiththetopicofacuteHIVintheED,including epidemiology,communityresources,andinitiatingeither highlyactiveantiretroviraltherapyorpre-exposure prophylaxiswhenindicated.
Animpactassessmentofthetwo-weekelectiveispending, asonlyonePGY-2residenthadcompletedatthetimeofthis manuscript’sdevelopment.
Itischallengingtoconcretelyassesstheimpactofthe CommunityOutreachpillar,asitsservice-driveninitiatives aregenerallyqualitativeinnature.However,initialdata
fromtheNarcanInitiativehighlightsitsimpactonMDC.As ofMay2023,theprogramscreened1,188patientsacross MDC,ofwhom144receivedNarcan.Inrecognitionofthe NarcanInitiative’scurrentimpactandcontinuedgrowth, JMH’sDepartmentofEmergencyMedicinereceivedthe 2023UniversityofMiamiMitchellWolfsonSr.Department ofCommunityServiceaward.
Wearecurrentlyintheearlystagesofdatacollectionto analyzethesuccessoftheAccesstoCareinitiatives.Thusfar, thepatientnavigationprogramhasenrolled31EDpatients. Ofthesepatients,18wereabletosuccessfullycompletetheir navigationgoalsandobtainoutpatientcare.Thisprogram hasparticularlybenefittednon-English-speakingpatients, whoselanguagebarrierscanhindertheirabilitytonavigatea complexsystem.Forexample,navigatorswereable tolinkaSpanish-speakingpatienttooutpatientoncologic careforheruntreatedgynecologiccancer.Recently,a homeless,uninsuredpatientlivingattheMiamiRescue Mission(MRM)wastreatedforanacuteulcerative colitis flareintheED.Afterhewasdischarged,the navigatorsensuredthatheobtainedtimelyfollow-upatan MRM-affiliatedgastroenterologyclinic,astudent-runclinic staffedbyUMfaculty.Wearecontinuingtopublicize thisprogramandencourageemergencyclinicians
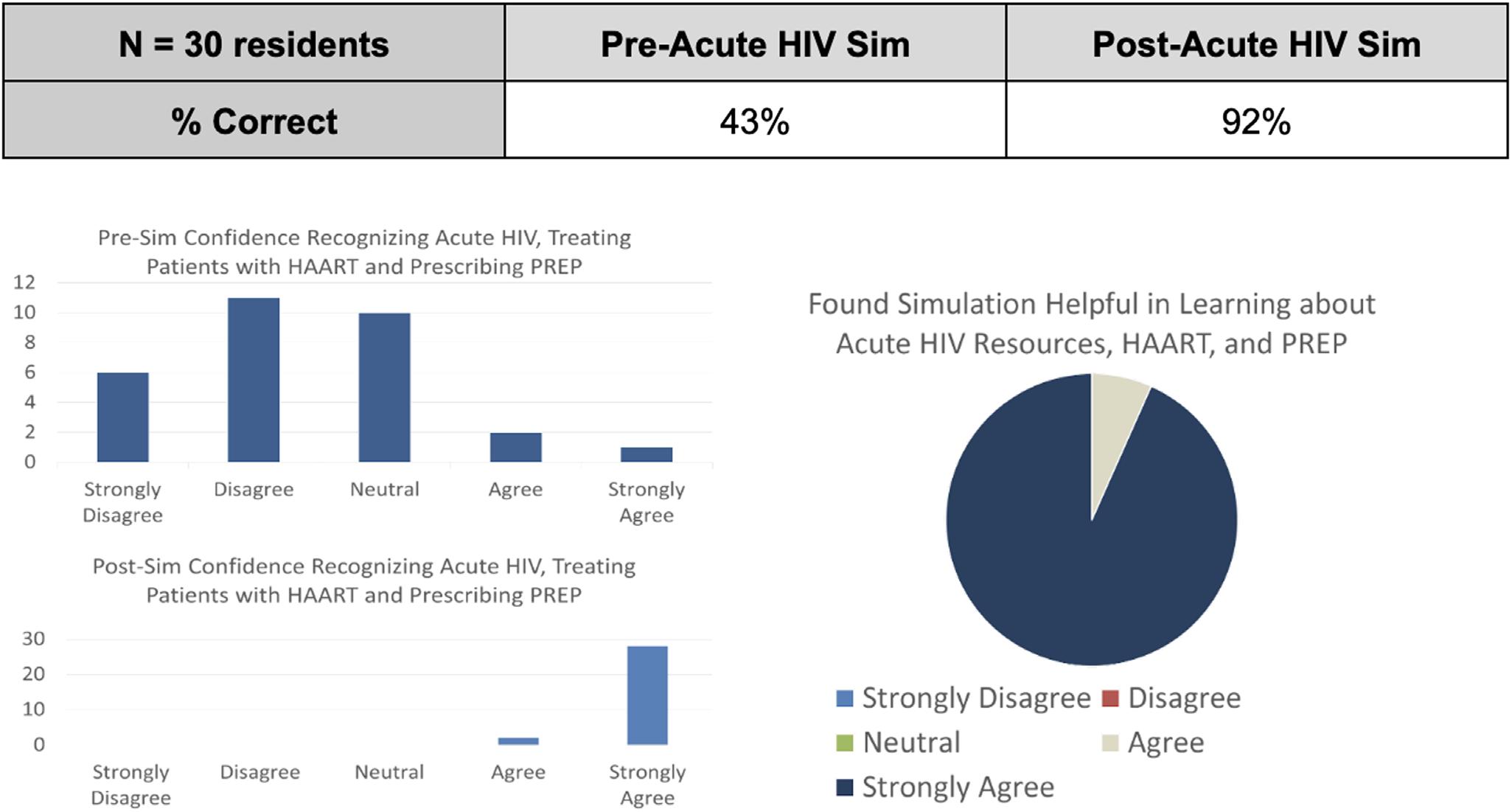
Figure3. Comparisonofkeypre-andpost-surveyresultsafterasimulationsessiononhighlycommunicablediseases/STIepidemics;30 residentscompletedthesurveys.Afterthesession,residentsindicatedanincreasedconfidenceintheirabilitytorecognizeacuteHIVand initiateHighlyActiveAntiretroviralTherapy(HAART)orPre-ExposureProphylaxis(PrEP)treatmentwhenindicated.Mostresidentsfound thesessionbeneficialinlearningaboutcommunityresourcesforEDpatientswithHIV,aswellasprescribingHAARTandPrEP.
toenrolltheirpatientsduringtheirshifts.Weare stillinthedatacollectionphaseoftheHigh Utilizersinitiative.
TheSocialJusticepillarinitiativesexperiencedseveral launchdelaysduetoCOVID-19pandemicrestrictionsand facultyturnover.Initiativeswereofficiallylaunched inthe2022–2023academicyear,anddataregardingtheir impactandeffectivenessispending.Thusfar,human traffickingeducationambassadorshavegiven well-receivedlecturestoJHS-affiliatedclinicsand toJMH’sfamilymedicine,pediatrics,andinternal medicineresidencies.
Sincetheprogramisunderthedirectguidanceofacurrent residencyassociateprogramdirector,thereiscontinual communicationbetweenSocialEMdirectorsandEM residencyleadership.Residencyleadershipactivelyengages withandprovidesinsightsintopillarinitiatives,leadingto timelychangestotheprogramwhendeemednecessary.For example,previousfeedbackledtothedevelopmentofthe electiveandlongitudinaltracks.ResidentsinthecoreSocial EMleadershipteamalsoobtainregularqualitativefeedback fromtheirpeersandsharethisfeedbackwiththeSocialEM directors.Thisprogramisalsoreviewedduringtheannual residencyprogramevaluationcommitteemeeting.This programhasfullEMdepartmentalsupport.
Overall,thisrobust,multimodal,resident-ledSocialEM programhasrapidlygrownoverthelastthreeyears,despite theCOVID-19pandemic.In2023,sixofthe14PGY-3 residentsgraduatedwithaSocialEMdistinction.The program ’sinterdisciplinarynatureensureditssuccess,as multipleinitiativeswerelaunchedwithoutsignificant fundingoradministrativerestrictions.Theprogramis receivingincreasingrecognition.Inadditiontothe previouslymentionedcommunityserviceawardforthe NarcanInitiative,theMDCchapteroftheStoptheBleed Campaignreceiveda2021awardfromthemayorforits educationinitiativesinlocalhighschools.In2023,wewere alsohonoredtoreceivethe2023ACEPSocialEMSection DistinguishedProgramAward.
Residents’ availabilityoftenlimitsconsistentparticipation inSocialEM.Residentshavemultipleclinicalandacademic responsibilities,andastheyprogressthroughtraining,their timeisfurtherlimitedbysearchingforjobsandapplyingfor fellowships.Inresponsetothislimitation,theelectiveand longitudinaltrackweredevelopedtoallowfor flexiblebut regularparticipation,asmanyrequirementscanbe
completedduringlighterrotations.Thedidacticcurriculum alsoensuresthatallresidentswillgraduatewiththesame baselineknowledgeofSocialEMtenets.Additionally,the SocialEMleadershipwilltransitioneverytwoyears, allowingjuniorresidentswithleadershiprolestopasson theirdutiestoincomingresidentsastheybecome seniorresidents.
Certainaspectsofthisprogramweredesignedtoaddress someofthesocialissuesthatareparticularlyprevalentin MDCandmaynotbegeneralizabletootherEMresidency programsintheUnitedStates.Otherresidencyprograms seekingtodeveloptheirownSocialEMinitiativesshould considertheuniqueneedsoftheirpatientpopulationswhen doingso.
Theprogram’ s firstthreeyearswerededicatedtooverall development,garneringparticipants, findingcommunity partners,andlaunchinginitiativesineachpillar.Therefore, datacollectiontoformallyassesstheprogram’simpactand effectivenessisstillinprocessandiscurrentlylimitedto initialdata(unblindedpre-andpost-testscompletedby residentparticipants)fromthelaunchofthe18-month didacticcurriculum.Thisdatamayalsobesubjectto selectionbias,asmostresidents,faculty,students,andstaff areexcitedabouttheSocialEMprogramandwant ittosucceed.
TheUniversityofMiami-JacksonHealthSystemSocial EMprogramwaslaunchedin2020toaddresstheSDoHof patientsinMiami-DadeCounty anareaofsigni fi cant medicalandsocialneed.Ittargetscriticalsocialissues throughfourpillars:CurriculumIntegration;Community Outreach;AccesstoCare;andSocialJustice.This multimodal,resident-runprogramachievedrapidsuccess inthreeyearsbydevelopingsustainableinitiativesin partnershipwithlocalorganizationsand otherUM-JHSdepartments.Ratherthanfocusing solelyonserviceopportunities,thisprogramenhances residents ’ knowledgeofSDoH,fostersthedevelopmentof qualityimprovementinitiatives,andprovides opportunitiestocreatemeaningfulchangeintheED andthecommunity.Thisprogramalsoprovidesresidents withleadershipandscholarlyopportunities.Wehope thatthisarticlewillinspireotherresidenciestodevelop similarprograms.
TheUniversityofMiami-JacksonHealthSystemSocial EmergencyMedicineprogramwouldnothavebeenpossible withouttheingenuity,dedication,andpassionofthe followingindividualsandorganizations.Thankyoufor everythingthatyouhavedoneandcontinuetodotocreate
positivechange:RachelArmstrong,MD;TatianaBarriga, MD;KelleyBenck;DanielBergholtz,MD;EmilyBrauer, MD;SandraCabrera,MD;DanielleCohen,MD;Emily Dawra,MD;LuisDeLaRosa,RN;ShaheenEmami; JoshuaGoldstein,MD;JamieHarris;Kristopher Hendershot,MD;ArmenHenderson,MD,MBA;Brooke Hensley,MD;SarahJabre,MD;JacksonHealthSystem ClinicalPharmacyResidency;JohnnatanMarin,MD;Julia Martinez,MD;ElizabethMay-Smith,MD;KellyMedwid, MD;MiamiStreetMedicine;VictoriaMcKee;Samantha Mosle;LienMorcate;KalebMorris;JudithOriental-Pierre, MD;RoxcyBoltonRapeTreatmentCenter;StoptheBleed; UniversityofMiamiIDEANeedleExchangeClinic; UniversityofMiami,MichaelWolfsonDepartmentof CommunityService;andMelissaVelasquez,MD.
AddressforCorrespondence:NaomiP.Newton,MD,Emory UniversityHospital,531AsburyCircle,AnnexSuiteN340,Atlanta,GA 30322.Email: naomi.newton@emory.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Newtonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.U.S.DepartmentofHealthandHumanServices.Healthypeople2030socialdeterminantsofhealth.Availableat: https://health.gov/ healthypeople/priority-areas/social-determinants-health AccessedMay2,2023.
2.ZibulewskyJ.TheEmergencyMedicalTreatmentandActiveLaborAct (EMTALA):whatitisandwhatitmeansforphysicians. Proc(BaylUniv MedCent). 2001;14(4):339–46.
3.AmericanCollegeofEmergencyPhysicians.UnderstandingEMTALA. Availableat: https://www.acep.org/life-as-a-physician/ethics–legal/ emtala/emtala-fact-sheet/.AccessedMay30,2023.
4.U-Health-UniversityofMiamiHealthSystem.Communityhealthneeds assessment2019–2021.Availableat: https://umiamihealth.org/-/media/ uhealth/chna/umhc-2019-community-health-needs-assessment.ashx AccessedMay15,2023.
5.FloridaDepartmentofHealthinMiami-DadeCounty.2022Community healthassessment.2022.Availableat: https://www.floridahealth.gov/ _media/miami-dade/community-reports/miamidade-cha.pdf AccessedMay15,2023.
6.ThomasPA,KernDE,HughesMT,etal.(Eds.),(2016).Goalsand objectives.In: CurriculumDevelopmentforMedicalEducation (53–56;130–133).3rded.Baltimore,MD:JohnsHopkinsUniversity Press,2016.
7.EmergencyTreatmentforSuspectedOpioidOverdose. Chapter381 Section887–2021FloridaStatutes,StateofFlorida2021Legislative Statutes,1Jan.2021.
8.AmericanPsychiatricAssociation.(2013). DiagnosticandStatistical ManualofMentalDisorders,5thed.(541–542).Washington,DC: AmericanPsychiatricAssociation.
9.BenkKN,GoldsteinJ,NewtonN,etal.Socialemergencymedicine: naloxoneoutoftheED&intothecommunity.2022.Availableat: https:// fcep.org/social-emergency-medicine-naloxone-out-of-the-ed-andinto-the-community/.AccessedFebruary3,2022.
10.LinVW,LinJ,ZhangX.USsocialworkerworkforcereportcard: forecastingnationwideshortages. SocWork. 2016;61(1):7–15.
11.Miami-DadeStateAttorney’sOffice.Floridafactsregardinghuman trafficking.Availableat: https://humantrafficking.miamisao.com/ human-trafficking.AccessedJune3,2023.
12.ArmstrongRE,HendershotKA,NewtonNP,etal.Addressing emergencydepartmentcareforpatientsexperiencingincarceration:a narrativereview. WestJEmergMed. 2023;24(4):654–61.
MarjorieA.Erdmann,MS,PhD*
IpeS.Paramel,MHA*
CariMarshall*
KarissaLeHew,BS†
AbigailKee,BS†
SarahSoliman,BS†
Authorscontinuedatendofpaper
SectionEditor:TehreemRehman,MD,MPH
*OklahomaStateUniversity,SpearsSchoolofBusiness,CenterforHealth SystemsInnovation,Stillwater,Oklahoma † OklahomaStateUniversityCenterforHealthSciences,Collegeof OsteopathicMedicine,Tulsa,Oklahoma
Submissionhistory:SubmittedDecember12,2023;RevisionreceivedMay22,2024;AcceptedMay24,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18626
Objective: Becauseadmittedemergencydepartment(ED)patientswaitingforaninpatientbed contributetodangerousEDcrowding,weconductedapatient flowinvestigationtodiscoverandsolve outflowdelays.Aftersolutionimplementation,wemeasuredwhetherthetimeadmittedEDpatients waitedtoleavetheEDwasreduced.
Methods: InJune2022,ateamusingLeanHealthcaremethodologiesidentified flowdelaysand underlyingbarriersinaMidwest,mid-sizedhospital.Wecalculatedbarriers’ magnitudesofburdenbythe frequencyofinvolvementindelays.DuringOctober–December2022,solutionstargetingbarrierswere implemented.InOctober2023,wetestedwhetherwaitingtime,definedasdailymediantimeinminutes fromadmissiondispositiontodeparture(ADtoD),declinedbyconductingindependentsample,singletailed t-testcomparingpre-topost-interventiontimeperiods,January1–September30,2022(273days) toJanuary1–September30,2023(273days).Additionally,weregressedADtoDontopre-/postperiod whilecontrollingforEDvolume(totaldailyadmissionsandEDdailyencounters)andhospitaloccupancy. ArunchartanalysisofmonthlymedianADtoDassessedimprovementsustainability.
Results: Processmappingrevealedthatthreedepartments(ED,environmentalservices[EVS],and transportservices)co-producedtheoutflowofadmittedEDpatientswherein18delayswereidentified. TheEVS-clinicalcarecollaborationfailuresexplained61%(11/18)ofdelays.Technologycontributedto 78%(14/18)ofdelaysprimarilybecausestaff’stechnologydidnotdisplayneededinformation,a conditionwecoined “digitalblindness.” Comparingpre-andpost-interventiondays(3,144patients admittedpre-interventionand3,256patientspost),themedianminutesapatientwaited(ADtoD) significantlydecreased(96.4to87.1minutes, P = 0.04),evenwhiledailyEDencountervolume significantlyincreased(110.7to117.3encountersperday, P < 0.001).Aftercontrollinginregressionfor otherfactorsassociatedwithwaiting,theinterventionreducedADtoDby12.7minutesperpatient (standarderror5.10, P = 0.01;95%confidenceinterval 22.7, 2.7).Weestimatethattheintervention translatedtoEDstaffavoiding689hoursofadmittedpatientboardingoverninemonths(ADtoD coefficient[ 12.7minutes]multipliedbypost-interventionEDadmissions[3,256]anddividedby60). Runchartanalysissubstantiatedtheintervention’ssustainabilityoverninemonths.
Conclusion: Aftersystemwidepatient flowinvestigation,solutionsresolvingdigitalblindnessand environmentalservices-clinicalcarecollaborationfailuressignificantlyreducedEDadmittedpatient boarding.[WestJEmergMed.2024;25(5)748–757.]
EmergencyphysiciansintheUnitedStateshaveraisedthe alarmaboutdangerousandworseningemergencydepartment (ED)crowding.1,2–4 Crowdingisassociatedwithpatient harm,2,5 increasedstaffstress,4,6 medicalerrors,7 andpatient mortality.5,8,9 Althoughthereisnotasinglecauseforcrowding, inlargepartitoccurswhenadmittedpatientsareboardedinthe EDbecauseaccesstoanappropriatebedisblocked.1,2–4,10,11 Accessblockstemsfromover-capacityunitsaswellasalarger, long-standingissue:inefficientpatient flowinUS hospitals.3,10,12–14 Inefficientpatient flownotonlybottlenecks patientsintheEDbutisalsoknowntodrivepatientoutcomes downandcostsup,12 twoproblemstheUSisurgentlyworking toresolve.15 Comparedtopeerhigh-incomecountries,theUS rankslastinhealthoutcomes16 and firstincosts.17
ConsideringthatreducingEDboardingtimeisassociated withreducedharmtopatientsandstaffandreducedcosts,11 policymakersresponsibleforcostandoutcometrendsand administratorsresponsibleforalleviatingcrowdingare acutelyinterestedinstrategiesthatimprovetheoutflowof admittedEDpatients.AmajorobstacletoimprovingED outflowisthatfewhospitalsareadeptatpatient flow investigationsandinterventions.Hospitalstendtoimprove patient flowonedepartmentatatime,assumingthatthese within-department flowefficienciesstackuptooverall gains.13 Expertswarnthatthisapproachcanbackfire.13,18 Well-intendeddepartmentimprovementprogramscan negativelyimpactpatient flowbecauseindividualsfocuson theirowndepartment’sefficiencyachievementsanddonot considertheeffectoftheiractionsonupstreamor downstreamdepartments.18 Moreover,becausehospital processesarecomplexanddeeplyinterlocked,19 itis unrealisticforstaffinonedepartmenttoaccuratelypredictor observeunintendedoutcomesinotherareas.
Administratorshavetriedtodecreaseboardingtimesby takingawithin-EDimprovementapproach;however,the interventionshavefailedandhaveevenworsened boarding.2,11 Forexample,Kelenetal’ s 2 literaturereview foundthat1)neitherincreasingthenumberofEDstaffnor improvingancillaryservices’ turnaroundtimehadany impactonboarding,and2)increasingthesizeoftheED madeturnaroundtimeworse.Whathasworkedtoimprove EDoutflowisdirectlyreducingaccessblocks.Onehospital reducedboardingbyblockingtheirsurgerydepartmentfrom usingacertainnumberofbedsbasedonapredictednumber ofEDadmissions.2 Anotherhospitaltookaprocessimprovementapproachandreducedaccessblocksbysimply dischargingpatientsearlierintheday,incrementally improvingaccessbyimprovingprocesses.14
Thepresentstudyistwo-pronged.InPhase1,wemoved awayfromsingle-departmentpatient flowinvestigationsand insteadconductedamulti-department,systemwide,patient flowstudytoidentifypotentialprocessimprovementsto reduceaccessdelays.InPhase2,weevaluatedtheeffectof
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
BoardingadmittedpatientsintheED threatenspatientandstaffhealth.Itisata crisislevelintheUS,butreducingithas provendif fi cult.
Whatwastheresearchquestion?
Canasystemwidepatient fl owinvestigation leadtosigni fi cantreductioninadmitted patientboardingtime?
Whatwasthemajor findingofthestudy?
Admittedpatientboardingwasreduced by12.7minutes/patient(P = 0.01;95% CI 22.7, 2.7).Technologywasthe primaryissue.
Howdoesthisimprovepopulationhealth?
These fi ndingswillhelpotherinstitutionsto reduceEDboardingandpreservecommunity accesstoemergentcarewithoutincreasingthe costofcare.
ourprocessimprovementsonadmittedEDpatientbed-wait timesmeasuredbydailymedianofadmissiondispositionto departure(ADtoD)minutescomparingpre-andpostprocessimprovementintervention.Wehypothesizedthata patient flowinvestigationwouldrevealdelaysandthatthe subsequentprocessimprovementwouldsignificantlyreduce thetimeadmittedEDpatientswaitedforabed.
In2022,amid-sized,urban-basedhospitalintheMidwest partneredwithauniversityhealthinnovationcenterthat specializesinworkflowdesigntohelpresolveadmittedED patientoutflowdelays,identifysolutions,andmeasurethe effectivenessofimplementedsolutions.Theinnovationteam chosetouseLeanHealthcaremethodologies.Lean Healthcarehasbeenappliedtoimprovepatientcare processesandmaterial flowsand,toalesserextent,patient flow.20,21 Leanisaproductionimprovementprocess developedbytheToyotaProductionSystem(ToyotaMotor Corp,Toyota,Aichi,Japan),whichhasbeenusedin healthcaretoincreaseefficiency,reducecosts,andimprove patientoutcomes.22 Leanprovidesapracticalapproachto understandingcomplexsystems.23
Theinnovationcentertrains first-andsecond-year medicalstudentsinLeanHealthcare,aprogramdesignedto teachsystemsthinkingearlierinmedicaleducation.24 In
2022,aLeanHealthcareexpertassembledateamofnine second-yearmedicalstudents,trainedtheminLean,and assignedthecurrentproblemtothemtoinvestigateandsolve collectively.Theinvestigationwasdeemednon-human subjectresearchbytheuniversityinstitutionalreviewboard.
ObservationalFieldInvestigation,ProcessMapping,and DelayIdentification
Theteam’ s fieldinvestigationwasconductedinJune2022. Hospitalexecutivesintroducedtheteamtoemployeesto ensurefrontlineworkercooperation.Theteamcollected proceduremanualsfromdepartmentsandcreatedan observationscheduletoinvestigatesegmentsofpatient flows fromEDadmissionthroughdischarge.Patientdelaysinthe EDwerethelongestbetween3 PM–8 PM;therefore,that periodwasprioritizedforobservation.
Thehospital’stechnologyincludedtheEpicelectronic healthrecordsystem(EHR)andtheEpicenvironmental servicessystem(EpicSystemsCorp,Verona,WI)withan Ascomphoneintegration(AscomHoldingAG,Baar, Switzerland).Over21days,theteamobservedandmapped patient flow,observedworkers,andfollowedpatients,noting workarounds,bottlenecks,andcoordinationpointswith otherdepartments.Teammembersdiscussedprocessesand patient flowwithover100staff,includingmanagers,ED staff,physicians,transfercoordinators,environmental services(EVS)staff,transporters,maintenancestaff,and receiving floornurses.Theteamidentifieddiscrepancies betweenprotocolsandactualwork,gatheredtime-stamped data,anddirectlytimedsomeprocesssteps.
Theteamintegratedtheprocessesandmappedthepatient journeyfromEDadmissionthroughdischargeandtheEVS processesusedtoturnabedbetweenpatientoccupancies.The teamused “swimlanes,” atechniquetomapprocessesoccurring simultaneouslyindifferentdepartments.Theteamcreatedalist ofdelays;delaysweredefinedaswhenpatient flowstalledfor anyreason.Theswimlanesidentifiedkeystaffrolesacross multipledepartmentsthatco-producedEDpatientoutflow.
Post-investigation,wegroupedcommonissues,named them,andbuiltaconceptualframeworkrepresentingsystemleveloutflowbarriers.Weassessedwhichbarrierscontributed toeachdelayandtalliedthefrequencywithwhicheachbarrier contributedtodelays.Wecomparedeachbarrier’smagnitude ofburdenbyfrequencyandpercentage(numberofdelays affectedbyabarrier/totalnumberofdelays);morethanone barriertypecouldbeassociatedwitheachdelay.
Wedesignedspecificsolutionsforadministrativeaction, organizedthembybarriertargeted,andsortedthemintoa 3 × 2matrixbythedegreetowhichthesolutionwasdeemed
controllable(controllable,probablycontrollable, uncontrollable)andtheestimatedassociatedcost(nocost, cost).Wereliedonthemagnitudeoftheburdentoprioritize solutionswithinthehighcontrollabilityandlow-cost categorytoprioritizeselectedsolutions.Inthefourthquarter of2022,solutionswereimplemented.
InOctober2023,weusedaquasi-experimentaldesignto evaluatewhetherinterventionsreducedthetimeadmitted patientswaitedtoleavetheED.Quasi-experimentaldesignsare appropriatetoassessinterventionswithoutrandom assignment.25 Wedefinedindividual-levelpatientwaitingtime asthetimefromwhenapatient’sdispositionbecame “admitted” intheEHRtowhenthatpatientdepartedtheED, ensuringthatweevaluatedonlyadmittedpatients.Fromthis data,theEHRprovidedadailymediantimeofpatients’ admissiondispositiontodepartureinminutes(ADtoD),andwe usedthedailymedianasaper-patientrepresentationtodetect waitingdifferencesbetweentwotimeperiods.Medianswere bothreadilyavailableintheEHRandpreferredinanalysisto avoidartificiallyhighorlowdailyvaluescausedbyoutliers.
Thetwotimeperiodswecomparedwerepre-intervention days(January1–September30,2022)andpost-intervention days(January1–September30,2023).Weexcludedthe periodfromOctober–December2022becauseitwasthe periodwhensolutionswerebeingimplemented.Matching months(January–September)forbothtimeperiods minimizesseasonaleffects,whichisaconcernwithED outcomeinvestigationsbecauseEDvolumesfollowseasonal trends.26 Thestrengthofusingday-levelmeasuresacrossthe twonine-monthtimeperiodsisthattheyprovideagood samplesize(totalnumberofdays546,273daysineach period)forstatisticalcomparisonvsmonthlyleveldata (18monthswith9ineachperiod).
Dayswerecategorizedasbelongingtoeitherthepre-or post-interventionperiodsamples.Becauseourhypothesiswas thattheADtoDwoulddecreaseinthesecondperiod,weused asingle-tailed t -testtocompareADtoDbetweenperiods.To describehowthetimeperiodsdifferedinEDvolumeand hospitalcapacity(factorsthatcouldtheoreticallyaffect ADtoD),wepulleddatabydayfor1)totalnumberof occupiedhospitalbeds,includingobservationbeds;2)total numberofpatientsadmittedfromtheED;and3)totalnumber ofEDencounters.Inadditiontodescriptiveanalytics,we conductedindependentsampletwo-tailed t -testsonthesethree variablestodetectperioddifferences.Finally,weused standardleastsquaresregressiontotestfortheeffectsofthe intervention(pre,post)onADtoD,whilecontrollingforED volumeandhospitaloccupancyvariables.
Weusedarunchartforavisual,temporalanalyticviewof improvementtoevaluatewhetherimprovementoccurred afterinterventionandtodeterminewhetherimprovements weresustainable.27
ObservationalFieldInvestigation,ProcessMapping,and BarrierIdentification
Thetotalpersonnelcostfortheinvestigationwas$16,000. Becausethehospitalpartneredwiththeuniversityinajoint efforttotrainmedicalstudentsinsystems-basedpractice,the investigationcameatnocosttothehospital.Theuniversity paideachoftheninemedicalstudents$12.50/hourfor0.5 full-timeequivalent(FTE)foraone-month(80hours) internship,whichtotaled$9,000.TheLeanconsultantwasa full-timeinnovationcenteremployeewhoweestimated dedicated0.75FTEforthemonth(90hours)atacostof $7,000,includingsalaryandbenefits.
TheteamidentifiedthatboardedEDpatientsprimarily waitedfortwosuppliesfromotherdepartments:cleanbeds providedbyEVS;andtransportservices.Thedepartments’ processeswereinterlocked;interlockingprocessesaredefined aswhenoneprocess flowisrelianton/triggeredbyanoutputof anotherprocess,suchasadigitalsignaloranaction.Mapping thesupplyprocessforeachandtheirintersectionwiththeED processgenerated Figure1.Wecalledthisthree-department processmap globalbedmanagement .Wecategorized flow throughbedmanagementintofourmulti-department collaborativesteps:1)processesusedtoprovideclean,ready beds;2)processesusedtoassignpatientstoopenbeds;3) processesusedtotransportapatientforbedoccupancy;and4) processesusedtoresupplybedsfreedfromdischarge.Across thesesteps,welogged18delays.Thelocationofthedelaysis depictedin Figure1.Asupplemental fileprovidesahigher qualityimage;anddetaileddescriptionsofdelaysarelistedin AppendixExhibitA
Acrosstheinterlockingdepartments,sixstaffrolescoproducedglobalbedmanagementwhomwenamed flow facilitators;fourwerepatientcare-based(transfer coordinator,transporters,EDnurses,and floornurses),and twowereEVS-based(supervisorandstaff).TheEVSand clinicalcarestaffdependedprimarilyontheEHRplatforms tosenddigitalsignalstoeachotherforcoordination,in
contrasttotransportservices,whichwerecoordinatedby phone.AnexampleofclinicalcaresendingEVSasignalwas when floornursesenteredapatient’sdischargeintotheEHR; thatentrytriggeredthepostingofthatpatient’sbedontothe EVScleaningqueue.Intotal,11ofthe18(61%)delayswere causedbyEVS-clinicalcarecollaborationfailurescausedby themnotperceivingthemselvesasacollaborativeteam. Becausetheylackedasharedgoaltoconnectpatientsas efficientlyaspossibletobeds,theylackedcommunication processestofacilitatethatprocess. AppendixExhibitA detailsEVSandclinicalcarestandardworkprocessesthat disregardedtheeffecttheyhadoneachother.TheEVSstaff hadnovisibilityintoclinicalinformationduetopatientdata protection.Therewasnoreasonthatclinicalcarestaff’ s visibilityintoEVSsystemswaslimited.
Weidentifiedfourcommon,system-levelcauses(barriers) forthe18delays.Twostemmedfromtechnologydesign (rigidsystemsettingsand “digitalblindness”)andtwo stemmedfrommanagementissues(workforceshortageand policyandprocedures).
Wefoundrigid systemsettings embeddedintechnology applicationspreventedstafffromchanginginaccurate informationsuchaswhenacleanbedwaslistedasdirty becauseEVSlackedaccesstochangebedstatusesnotassigned tothem. Digitalblindness, atermwecoinedtodescribethe commonconditionwhenstaffwereunabletoseepertinent informationduetopoortechnologydesign,suchasEVSnot seeingwhichbedshadwaitingpatients.Insum,usersreliedon inaccurateinformationormadedecisionswithoutcomplete information.Becausedigitalblindnesswaswidespreadacross clinicalcareandEVS,welabelledthreedistincttypes: true statusblindness (eg,beingshowntheinaccuratestatusofa bed), collaborationblindness (eg,assigningpatientstobeds withoutknowingorderofreadiness,causingpatientstoexit

theEDoutofadmissionorder),and sporadicoutput blindness (eg,nursedischargedataentrycreatingEVSdirtybednotificationin0–20minutes).
Delaysassociatedwithrigidsystemsettingsaredesignated as “S” in Figure1 and AppendixExhibitA.Alltypesof digitalblindnessaredesignatedas “D” in Figure1 and AppendixExhibitA
Transporters,clinicalcare,andEVSstaffsufferedfrom understaffingdueto workforceshortages, amanagement issueconstrainedbylocalresources.28–30 Policyand procedures contributedtodelaysintwoways.First,inall casesexceptonethedelaysassociatedwithworkforce shortagewerealsoassociatedwithpolicyandprocedure issues(AppendixExhibitA).Weconcludedthatpolicyand procedurescanreflectanassumptionofanoptimal workforcesupply,andadherencetothemduringshortages canbackfireandexacerbatedelays.ConsideroneEDpolicy thatrequiredEDnursestowait30minutesaftercalling transportservicesbeforeusingtheirowntechsfortransport. Adherencecreated30-minutedelayswhentransporterswere short-staffedandEDtechswereavailabletotransport.
Second,wediscoveredwithin-departmentproceduresthat causeddelaysinotherareas.Forexample,priorto intervention,EVSproceduresincludedallstaffchangingshift atthesametimeandconductingabriefmeetingatshift change.Toaccommodatebothshiftchangeandthemeeting, staffstoppedcleaningthequeuedbedsforonehoureveryday towinddowntheircleaningworkpre-shiftchange,toattend themeeting,andtorampituppost-shiftchange. Compoundingthisproblematicprocedure,itoccurredat3 PM, helpingtoexplainwhyEDpatientwaitingincreasedat3 PM eachday.TheEVSproceduresweren’ttheonlyproblematic ones;othersincludedallowingnursestodelaydischargeentry, thuseliminatingtimelysignalstoEVSofdirtybedsandno transportercancellationpolicycausingtransporterstowaste timelookingforalreadytransportedpatients.
Delaysassociatedwithworkforceshortagearedesignated witha “W” in Figure1 and AppendixExhibitA.Delays
causedbypolicyandproceduresaredesignatedwitha
Figure1 and AppendixExhibitA
Figure2 summarizesthesystem-levelbarriersand underlyingcauses.Ofthese,onlyworkforceshortagewasa recognizedcausefordelaysbeforeourinvestigation.
Usingthedelaydatacompiledandavailablein Appendix ExhibitA,wefoundthattechnology-basedbarriers(barriers associatedwithdigitalblindnessorsystemsettings)were twiceasprevalent(14/18;78%)comparedtomanagementbasedbarriers(barriersassociatedwithworkforceshortage orpolicyandprocedures)(7/18,39%).Digitalblindnesswas associatedwiththemostdelaysat61%(11/18),followedby systemsettings39%(7/18),policyandprocedures39%(7/18), andworkforceshortage33%(6/18)(see Figure3).
TheLeanteamgeneratedandevaluated25solutions (AppendixExhibitB).Overhalfoftheidentifiedsolutions (59%;13/22)wereconsideredcontrollableandestimatedto havenocostbasedoninformationtechnology(IT) capabilities.Solutionswithcostsreflectedtheneedtohire staff,whichmayormaynothavebeenviabledueto localshortages.28–30
Forsolutionselection,weturnedtothemagnitudeof burdencalculationpointingtodigitalblindness,system settings,andpolicyandprocedureissues,eachofwhichhada no-costsolution.Thefollowingsolutionswereimplementedin thefourthquarterof2022:1)theITdepartmentcorrectedthe systemsettingthatpreventedEVSstafffromupdatingdirty roomstobecleanedbyallowingEHRaccesstotheelectronic processesthatassignedEVSstafftorooms accessthat resolvedtransfercoordinatorblindnesstotruebedstatus;2) ITfurtherdecreasedtransfercoordinators’ digitalblindnessby creatingvisibilityintheEVScleaningqueue,therebyrevealing thelikelyorderofavailablebeds;and3)EVSmanagement changeddepartmentalpolicyandproceduresbystaggering EVSstaffshifts,toensurecontinuousprogressinreadybed supply,andeliminatingall-staffdailymeetings.Theeffectsof

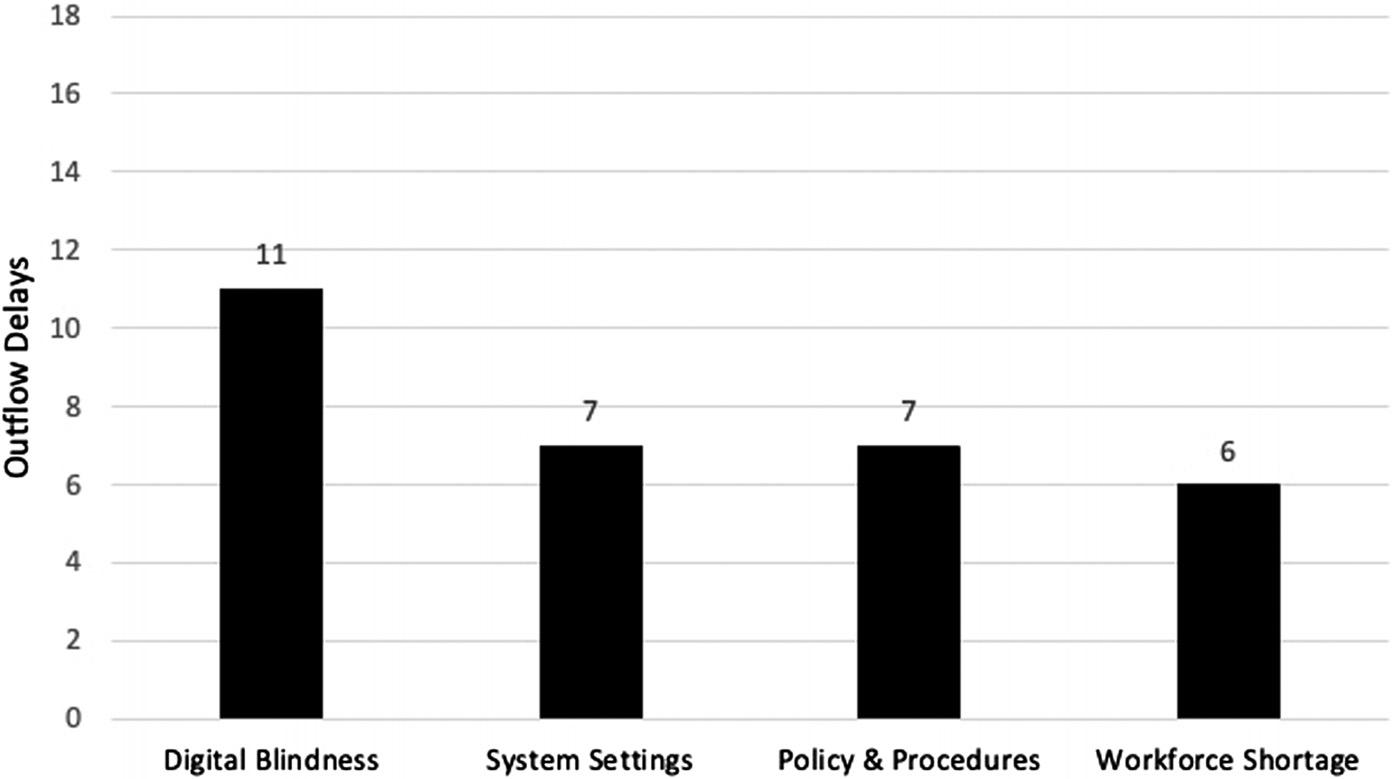
individualsolutionswerenotmeasured.Collectively,these solutionsweretheintervention.
WecompletedallstatisticalanalyseswithJMPPro16 software(SASInstitute,Cary,NC).Sample1(year2022preintervention)andSample2(2023post-intervention)eachhad thesamesamplesize(273).Descriptivestatisticsand independentsample t -testresultsarepresentedin Table1. ADtoD(themediannumberofminutesapatientwaited eachday)wassignificantlylowerinthepost-intervention period(P = 0.04),whiletheEDstaffmanagedsubstantially higheraveragedailyEDencounters(P < 0.001).Thenumber ofdailyadmitsdidnotsignificantlydiffer(P = 0.24),nordid thedailycensus(P = 0.51).Notably,aftertheintervention,a busierEDachievedlowerADtoDtimes.Regressionof ADtoDmediantimeontopre/postcategorizationwhile controllingforthreeotherindependentvariablesrevealsthat
Sample1: pre-intervention days
Jan–Sep2022 (n = 273)
theinterventionsignificantlyreducedADtoDtimesby12.7 minutes(P = 0.01). Table2 showstheintervention’seffectof admissiondispositiontodeparturemediantimes(ADtoD) whilecontrollingforbedoccupancybyday,totaladmitted EDpatientsbyday,andtotalEDencounterbyday.
Toestimatetheintervention’seffectonEDstaff’ s exposuretoadmittedpatientboarding,wemultipliedthe ADtoDcoefficient( 12.7minutes)representingeach patient’sreducedwaitingtimebythenumberofpostinterventionEDadmissions(3,256)anddividedby60to converttohours,resultinginanestimationthatEDstaff avoided689hoursofEDboardingoverthenine-month post-interventionperiod.
Inadditiontostatisticalsignificanceanalysessupporting theeffectivenessoftheintervention, Figure4 depictsa runchartsupportingthatimprovementoccurredafterthe interventionandtheinterventionachievedashift,arun ofatleastsixsub-baselinevalues.27 Baselineisthe
Sample2: post-intervention days
Jan–Sep2023 (n = 273)
ADtoD,admissiondispositiontodeparture; SE,standarderror; CI,confidenceinterval.
pre-interventionperiodmedianADtoD.Becauserundata mustbeinterpretedincontext,27 weinterpretedJanuary ADtoDincreasesasreflectingpeakhospitaloccupancy,the effectofwhichwasreducedinJanuary2023bythe interventionbutnoteliminated.ByFebruary2023the medianADtoDapproachedbaseline;afterward, improvementwassustained.
The findingsfromthisinvestigationindicatethat emergencyphysiciansandtheirpatientswereenduring unnecessaryoutflowdelaysdiscoverablethrougha systemwidepatient-flowinvestigation.Althoughovercapacityinpatientunitstendtodominatediscussionsabout EDboarding,2–4,11 wediscovereddelaysburiedin technologyandwithin-departmentprocedures.InPhase1, theuseofLeanmethodologiesrevealedtheoutflowprocess anditsdependenceonglobalbedmanagement(Figure1),
flowfacilitatorsandtheirrelianceontechnologyto collaborate,andthesystem-levelrootcausesdrivingdelays (Figure2).Theinvestigationledtodesigninglow-cost solutionsthatinPhase2achievedadministration’sgoalof reducingadmittedpatientboardingintheED.
Theinterventionconsistedofthreesolutionsgearedto improveEVS-clinicalcarecollaboration. T -testanalysisof pre-vspost-interventionperiodsshowedthatADtoDwas significantlydecreasedwhiletheEDwassignificantlybusier (Table1).Regressionanalysiscontrollingforeffectsfrom hospitalcapacityandEDvolumedemonstratedthatthe interventiondecreasedthemedianADtoDbynearly13 minutes(Table2).BecauseweestimatethattheEDstaff avoided689hoursofEDboardinginthepost-period,we contendthattheinterventionsubstantiallybenefitedstaff. Finally,chartingthemonthlymedianADtoDtrend substantiatedthatimprovementoccurredafterthe interventionperiodandwassustainable(Figure4).
Notsurprisingly,giventhewidespreadhealthcarestaffing shortagesof2022,28–30 workforceshortages affected outflow.Patientswaitedforunderstaffedtransportersto movethem,understaffednursestocompletedischarges,and understaffedEVStocleanrooms.However,ouranalysis showedthatthoseshortageshadthelowestmagnitudeof burdenonoutflowcomparedtoreadilysolvableissues: digitalblindness;systemsettings;andpolicyandprocedures (Figure3).Beforethepresentinvestigation,nooneatthe hospitalhadeverseentheinter-related,multi-department workflowsnecessarytomoveanadmittedpatientfromthe
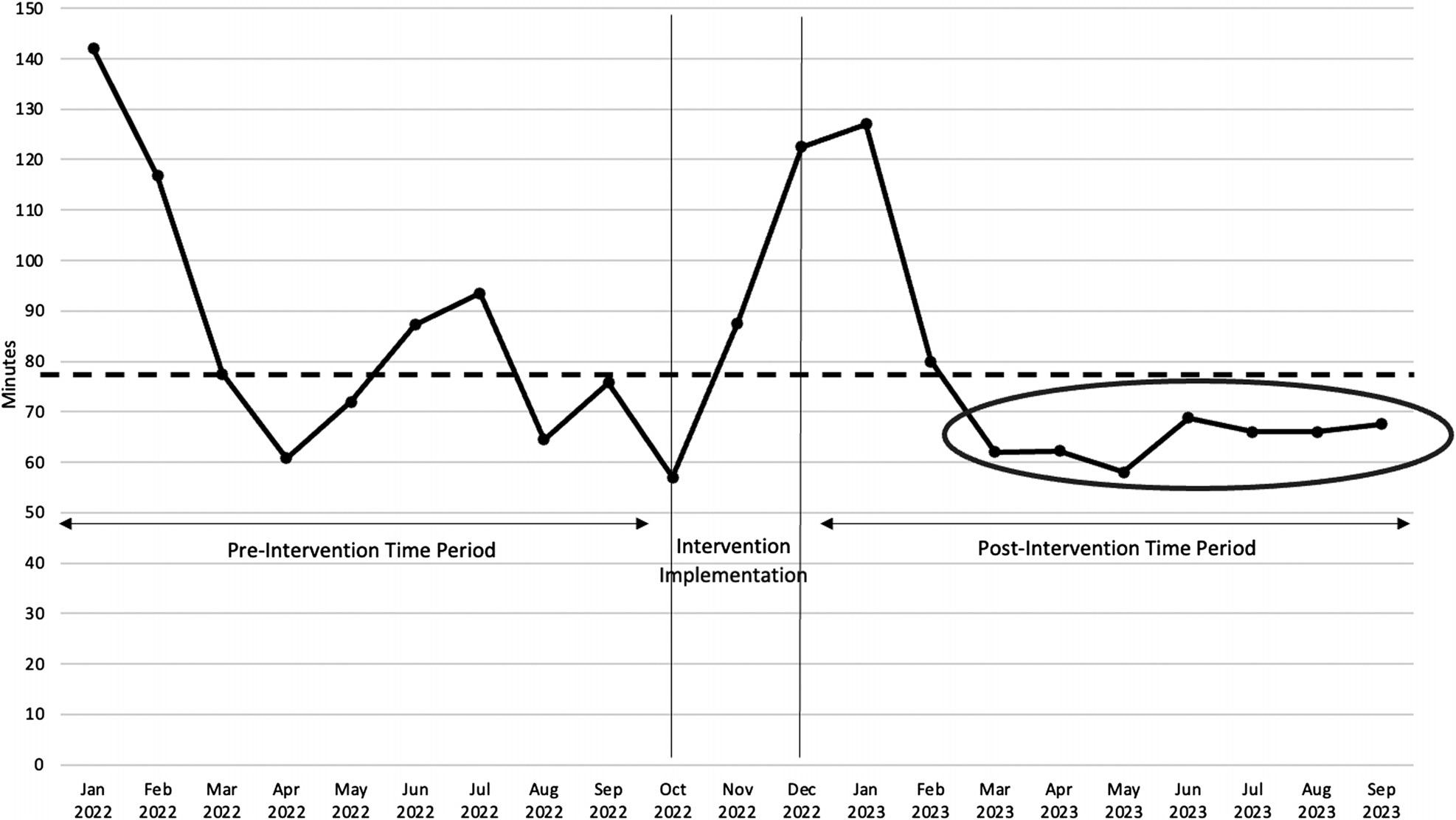
ArunchartdepictingtheadmittedpatientEDoutflowprocessimprovementwithsustainedmediantimeunder pre-interventionbaseline.
EDtoacleanbed.The flowmapandanalysisshifted administrationstrategiesforalleviatingboardingfrom saddlingfrontlineworkerstosolvetomakingtheseworkflow adjustmentsmanagementdecisions.
Thedegreetowhichtechnology hindered patient flowwas unexpected.Althoughresearchshowsthatnurseshavecalled fornew,effectivetechnologytoolstomanagethepatient flow foryears31 andsomeinitiativeshavebeencreated,18,32,33 our researchuncoveredshortcomingsofexistingtooldesign,an issuethathadgoneunnoticed.Theupsidetodiscovering problemswithexistingtechnologywastheavailabilityof low-andno-costsolutions.
AlthoughEHRsarethecomplexbackboneofhospital processes,theirembeddedprocesseswereunquestionedby staffanduntestedforoptimizationbyadministration. Althoughmultiplesystematicreviewshavereportedoncauses ofEDcrowding,2,3,11 nonesuggestedthattheefficiencyof technologyprocessesbetested.Therealityofhowmuchstaff reliedontechnologytocollaboratewithothersmade digital blindness thelargestbarrier.Digitalblindnessisanissuethat hasgoneunnamed;thus,themagnitudeofitseffectsonother processes,staff,andpatientshasgoneunmeasured.Defining digitalblindness openstheissueforpracticalexploration, futureresearch,andinnovationdesign.
Thepresentstudyresultsalsospotlighttheimportanceof EVS,whichhasbeenoverlookedincurrentresearch.Although EVSismentionedinafewpatient-flowimprovement studies,18,32 innocasewasEVS-clinicalcarecoordination centraloremphasized.Policymakersshouldtakenoticeof how,inthisstudy,within-hospitalintegrationlapseswere erodingcareandproductivity.Althoughtheintegrationof healthinformationsystemsbetweenhospitalsandclinicians monopolizesinitiativesacrossfederalagencies(ie,Agencyfor HealthcareResearchandQuality,34 CentersforDisease ControlandPrevention,35 CentersforMedicare&Medicaid Services36),wecallattentiontohowwithin-hospitalintegration issuesarethreateningpatientoutcomesandstressingstaff.
InsightsintoEDoutflowbarriersaretimelyforpractical application.TherearediscussionsthattheEDboardingtime standardwillbeloweredfromfourtotwohours,a50% reduction.2 Whenadministratorsseekstrategiestomeetthis aggressivereductioninboarding,werecommendanalyzing thebedmanagementcycleandprocesseswithLean methodologies.Ourprocessuncovereddelaysunnoticedby anysingledepartment,avoidedindividualpatient variabilitiesthatcanderail flowinvestigations,8 found problematicwithin-departmentefficiencysolutions,andwas appreciatedbyfrontlinestaff.Administrationreportedtothe innovationteamthattheybelievedtheinvestigation improvedmoraleandcreatedenthusiasmforthesubsequent solutionimplementationsbecausetheresultsexplained confusingworkplaceexperiences:whystaffdidnotknow whatwastakingsolongforEDpatientsto flowto floorbeds; whyEVSstaffwerenotcleaningadirtyroom;whyaclean
roomwouldgovacant;andwhysimilarEDpatientsexited outoforderofadmission.
Themainstrengthsofthisstudyareitscompletereviewof processesanddepartmentsaffectingEDpatientoutflowand thedurabilityoftheintervention’sgains.However,the generalizabilityofour findingsislimitedbecauseitisasinglesitestudyofamid-sizedhospitaloperatingoneEHRsystem duringaone-monthtimeframe.Datawasnottestedwith timeseriesmodeling,whichcouldprovideadditional temporalinsightsnotprovidedbypre/postdesign.A limitationtoreplicabilityisahospital’saccesstoLean Healthcaretraining,whichcoulddriveupthepriceofthe interventionbutmaybejustifiedgivenhowquicklytheteam couldpracticallyapplynewLeanskills.Moreover,the solutionsidentifieddonotaddressotherissuesdriving crowding,suchashighcommunitydemandforEDservices.
Asystemwidepatient-flowinvestigationatasinglehospital usedLeanmethods,whichprovedeffectiveinidentifyingthe barriersthatincreasedthetimeadmittedEDpatientswaited foraccesstobeds.Thebarriersweresystem-levelissues (technology,workforceshortage,andpolicyandprocedures); thegreatestwastechnology.Givenhealthcaresystems’ dependenceontechnologyandthecrisislevelofEDboarding, thisstudycallsformulticenterregionalandnationalresearch tounderstandtowhatextentwithin-hospitaltechnology integrationlapsesareblindingstaffanderodingcare. Meanwhile,administratorsshouldtesthowtheirtechnology supports(orhinders)environmentalservices-clinicalcare coordinationandbewaryoftheeffectof within-department efficiencygainsonpatient flow.Becausethecostofthe investigationwaslowandwewereabletogeneratesolutions for flowbarrierswithlittletonoassociatedcosts,weconclude thatthesetypesofinvestigationscanreduceEDcrowdingby movingadmittedpatientsoutoftheEDmorequicklywithout escalatingthecostofcare.
AUTHORSCONTINUED
AddressforCorrespondence:MarjorieA.Erdmann,MS,PhD, OklahomaStateUniversity,CenterforHealthSystemsInnovation, 1111W.17th St.,Tulsa,OK74107.Email: marjorie.erdmann@ okstate.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Erdmannetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.AmericanCollegeofEmergencyPhysicians.Boarding,crowdingand waittimes.Availableat: https://www.emergencyphysicians.org/article/ er101/boarding-crowding-and-wait-times.AccessedJuly21,2023.
2.KelenGD,WolfeR,D’OnofrioG,etal.Emergencydepartment crowding:thecanaryinthehealthcaresystem. NEJMCatalyst. 2021;2(5).
3.PearceS,MarchandT,ShannonT,etal.Emergencydepartment crowding:anoverviewofreviewsdescribingmeasurescauses,and harms. InternEmergMed. 2023;18(4):1137–58.
4.LokeDE,GreenKA,WesslingEG,etal.Clinicians’ insightson emergencydepartmentboarding:anexplanatorymixedmethodsstudy evaluatingpatientcareandclinicianwell-being. JtCommJQualPatient Saf. 2023;49(12):663–70.
5.RasouliHR,EsfahaniAA,NobakhtM,etal.Outcomesofcrowdingin emergencydepartments:asystematicreview. ArchAcadEmergMed. 2019;7(1):e52.
6.XuH,JohnstonANB,GreensladeJH,etal.Stressorsandcoping strategiesofemergencydepartmentnursesanddoctors:acrosssectionalstudy. AustralasianEmergCare. 2019;22(3):180–6.
7.EpsteinSK,HuckinsDS,LiuSW,etal.Emergencydepartment crowdingandriskofpreventablemedicalerrors. InternEmergMed. 2012;7(2):173–80.
8.GuttmannA,SchullMJ,VermeulenMJ,etal.Associationbetween waitingtimesandshort-termmortalityandhospitaladmissionafter departurefromemergencydepartment:populationbasedcohortstudy fromOntario,Canada. BMJ. 2011;342:d2983.
9.JoS,JeongT,JinYH,etal.EDcrowdingisassociatedwith inpatientmortalityamongcriticallyillpatientsadmittedviatheED: posthocanalysisfromaretrospectivestudy. AmJEmergMed. 2015;33(12):1725–31.
10.PalingS,LambertJ,CloutingJ,etal.Waitingtimesinemergency departments:exploringthefactorsassociatedwithlongerpatientwaits foremergencycareinEnglandusingroutinelycollecteddailydata. EmergMedJ. 2020;37(12):781–6.
11.AlsaifBK,AlotaibiAM,AlhammadWA,etal.Overcrowdinginthe emergencydepartment:abedmanagementstrategy. IntlJMedSciDen Res 2022;5(6):53–66.
12.HaradenCandResarR.Patient flowinhospitals:understandingand controllingitbetter. FrontHealthServManage. 2004;20(4):3–15.
13.ÅhlinP,AlmströmP,WänströmC.Whenpatientsgetstuck:a systematicliteraturereviewonthroughputbarriersinhospital-wide patientprocesses. HealthPolicy. 2022;126(2):87–98.
14.HammerC,DePrezB,WhiteJ,etal.Enhancinghospital-widepatient flowtoreduceemergencydepartmentcrowdingandboarding. JEmerg Nurs. 2022;48(5):603–9.
15.CentersforMedicareandMedicaidServices.CMSnationalquality strategy.2024.Availableat: https://www.cms.gov/medicare/quality/ meaningful-measures-initiative/cms-quality-strategy AccessedFebruary16,2024.
16.KuehnBM.U.S.healthsystemrankslastamonghigh-incomecountries. JAMA. 2021;326(11):999.
17.TheCommonwealthFund.Mirror,mirror2021:reflectingpoorly. Availableat: https://www.commonwealthfund.org/publications/ fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly. AccessedJuly11,2023.
18.TortorellaF,UkanowiczD,Douglas-NtaghaP,etal.Improving bedturnovertimewithabedmanagementsystem. JNursAdm. 2013;43(1):37–43.
19.GloubermanSandMintzbergH.Managingthecareofhealthandthe cureofdisease partI:differentiation. HealthCareManageRev. 2001;26(1):56–69.
20.BorgesGA,TortorellaG,RossiniM,etal.Leanimplementationin healthcaresupplychain:ascopingreview. JHealthOrganManag. 2019;33(3):304–22.
21.TlapaD,Zepeda-LugoCA,TortorellaGL,etal.EffectsofLean Healthcareonpatient flow:asystematicreview. ValueHealth. 2020;23(2):260–73.
22.AhnC,RundallTG,ShortellSM,etal.Leanmanagementand breakthroughperformanceimprovementinhealthcare. QualManag HealthCare. 2021;30(1):6–12.
23.D’AndreamatteoA,IanniL,LegaF,etal.Leaninhealthcare:a comprehensivereview. HealthPolicy. 2015;119(9):1197–209.
24.ErdmannMA,ParamelIS,MarshallCM.LeanHealthCareinternships:a novelsystems-basedpracticeeducationprogramforundergraduate medicalstudents. AcadMed. 2024;99(1):52–7.
25.PolitDF. NursingResearch:GeneratingandAssessingEvidencefor NursingPractice, 10thed.Philadelphia,PA:WoltersKluwerHealth, 2016.
26.TaylorRA,VenkateshA,ParwaniV,etal.Applyingadvancedanalytics toguideemergencydepartmentoperationaldecisions:aproof-ofconceptstudyexaminingtheeffectsofboarding. AmJEmergMed. 2018;36(9):1534–9.
27.PerlaRJ,ProvostLP,MurraySK.Therunchart:asimpleanalyticaltool forlearningfromvariationinhealthcareprocesses. BMJQuality& Safety. 2011;20(1):46–51.
28.AmericanHospitalAssociation.AHAsenatestatementonexamining healthcareworkforceshortages:wheredowegofromhere? Availableat: https://www.aha.org/testimony/2023-02-15-aha-senatestatement-examining-health-care-workforce-shortages-where-do-wego-here.AccessedFebruary16,2024.
29.SmileyRA,AllgeyerRL,ShoboY,etal.The2022National NursingWorkforcesurvey. JNursingRegul 2023;14(1,Supplement2):S1–90.
30.TheWorkforceTransformationTaskForce.ReportoftheWorkforce TransformationTaskForce.Availableat: https://oklahoma.gov/content/ dam/ok/en/governor/documents/WorkforceTransformationReportFinal.pdf. AccessedFebruary17,2024.
31.EvansB,PotvinC,JohnsonG,etal.Enhancingpatient flowinanacute carehospital:successfulstrategiesattheJuravinskiHospital. Healthc Q. 2011;14(3):66–74.
32.KhalifaM.Reducinglengthofstaybyenhancingpatients’ discharge:a practicalapproachtoimprovehospitalefficiency. StudHealthTechnol Inform. 2017;238:157–60.
33.KriegelJ,JehleF,MoserH,etal.Patientlogisticsmanagementof patient flowsinhospitals:acomparisonofBavarianandAustrian hospitals. IntJHealthcManag. 2016;9(4):257–68.
34.AgencyforHealthcareResearchandQuality.Healthinformation technologyintegration.Availableat: https://www.ahrq.gov/ncepcr/tools/ health-it/index.html.AccessedJuly12,2023.
35.CentersforDiseaseControlandPrevention.Healthinformation technology.Availableat: https://www.cdc.gov/opioids/pdf/ integration-framework.pdf.AccessedJuly12,2023.
36.CentersforMedicare&MedicaidServices.Promotinginteroperability programs.Availableat: https://www.cms.gov/regulations-andguidance/legislation/ehrincentiveprogram. AccessedJuly12,2023.
MichaelB.Henry,MD,MS*
EmilyFunsten,MS†a
MarisaA.Michealson,BA†a
DanielleAlbright,PhD‡
CameronS.Crandall,MD‡
DavidP.Sklar,MD‡§
NaomiGeorge,MD,MPH‡
MargaretGreenwood-Ericksen,MD,MSc‡
SectionEditor:ShiraSchlesinger,MD,MPH
*CreightonUniversityArizonaHealthEducationAlliance,Maricopa EmergencyMedicineResidency,Phoenix,Arizona
† UniversityofNewMexico,SchoolofMedicine,Albuquerque,NewMexico ‡ UniversityofNewMexico,SchoolofMedicine,DepartmentofEmergency Medicine,Albuquerque,NewMexico § ArizonaStateUniversity,CollegeofHealthSolutions,Phoenix,Arizona a Equalcontribution
Submissionhistory:SubmittedApril24,2024;RevisionreceivedAugust21,2024;AcceptedAugust23,2024
ElectronicallypublishedSeptember10,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20929
Introduction: TheUnitedStateslacksanationalinterfacilitypatienttransfercoordinationsystem.During thecoronavirus2019(COVID-19)pandemic,manyhospitalswereoverwhelmedandfaceddifficulties transferringsickpatients,leadingsomestatesandcitiestoformtransfercentersintendedtoassist sendingfacilities.Inthisstudyweaimedtoexploreclinicianexperienceswithnewlyimplemented transfercoordinationcenters.
Methods: Thismixed-methodsstudyusedabriefnationalsurveyalongwithin-depthinterviews.The AmericanCollegeofEmergencyPhysiciansEmergencyMedicinePracticeResearchNetwork(EMPRN) administeredthenationalsurveyinMarch2021.FromSeptember–December2021,semi-structured qualitativeinterviewswereconductedwithadministratorsandruralemergencycliniciansinArizonaand NewMexico,twostatesthatstartedtransfercentersduringCOVID-19.
Results: Among141respondents(of765,18.4%responserate)tothenationalEMPRNsurvey, only30%reportedimplementationorexpansionofatransfercoordinationcenterduringCOVID-19. ThosewithnewtransfercentersreportednochangeindifficultyofpatienttransfersduringCOVID-19 whilethosewithouthadincreaseddifficulty.The17qualitativeinterviewsexpandeduponthis,revealing fourmajorthemes:1)limitedresourcesforfacilitatingtransfersevenbeforeCOVID-19;2)increased numberofanddistancetotransferpartnersduringtheCOVID-19pandemic;3)generallypositive impactsoftransfercentersonworkflow,and4)thepotentialforcontinueduseofcentersto facilitatetransfers.
Conclusion: Transfercentersmayhaveoffsetpandemic-relatedtransferchallengesbroughtonbythe COVID-19pandemic.Clinicianswhofrequentlyneedtotransferpatientsmayparticularlybenefitfrom ongoingaccesstosuchtransfercoordinationservices.[WestJEmergMed.2024;25(5)758–766.]
Inearly2020,criticallyillpatientswithcoronavirus disease2019(COVID-19)overwhelmedmanyhospitalsand emergencydepartments(ED)acrosstheUnitedStates. Surgeswereunpredictable.Patientsoverransomehospitals, whileotherfacilitiesmadesignificantpreparationsfor COVID-19patientswhoneverarrived.1 Smallerhospitals neededtotransferpatientstofacilitieswithmorebeds, staffing,andspecialistservices.Theunpredictable distributionofpatientsandbedavailabilityplacedstrainon
somelargerregionalreceivinghospitals,leadingsomestates andhealthsystemstoidentifymechanismsto “load-level” patienttransfersamongreceivingfacilities.2
Historically,interfacilitypatienttransfersbetweensmall orruralhospitalsandlargerregionalhospitalshasoffered accesstocarethatmaynototherwisehavebeenavailable. HospitalsintheUStransferoveronemillionpatientsfor admissionannually,3 andnearlyeveryUShospital participatesinthetransferprocesseitherasareceiver,a sender,orboth.4 Thesetransfers,drivenbylimitedbed capacity,theneedforspecialtyservices,oralackof certaindiagnosticmodalities,arechallengingforreferring hospitalclinicians.5
Nationaleffortstotrackavailablehospitalcapacityand coordinatetransfersduringtheearlyCOVID-19pandemic wereseenaslargelydisorganizedandunreliable,leading manystates,cities,andhospitalstodeveloptheirown systems.6 TheArizonaDepartmentofHealthServices createdtheArizonaSurgeLine,acentralizedsystemstaffed bytransfercoordinatorswithaccesstoupdatedbedand ventilatorcapacitydataaroundthestate.2 NewMexico createdaCentralCommandCentertocoordinateplacement ofcriticalcarepatientsthrougha “hub-and-spoke” model.7 HospitalsinBoston,NewYorkCity,Chicago,Washington, andMinnesotamadesimilarefforts.1,8–12
Whileviewpointsandlaypressarticleshaveexplored transfercenterefficacy,researchdescribingthereachof transfercentersandtheirimpact,asperceivedbyclinicians, policymakers,andhospitalleadershiparelacking.Weuseda mixed-methodsapproach,includinganationalsurveyto describeaccesstotransfercentersbeforeandduringCOVID19,andsemi-structuredinterviewswithstakeholdersintwo statestogenerateanin-depthpictureofthefunctionandthe impactoftransfercenters.Wehypothesizedthat implementationofanewtransfercenterwouldleadtoeasier transferprocesses.
Weconductedanexplanatory,mixed-methodsstudywith anational,web-basedsurveytocapturethetransfer-center experiencesinavarietyofemergencycarepracticesettings followedbysemi-structuredqualitativeinterviewswith sendingfacilitycliniciansandadministratorsintwostates (ArizonaandNewMexico)toprovidedeeperinsightintothe experiencesofsendingfacilities.Bothstatesestablishednew interfacilitytransfercoordinationsystemsduringpeak COVID-19.The firstauthor’sinstitutionalreviewboard approvedthestudydesign.
AmultidisciplinaryteamofArizona-andNewMexicobasedresearchersfromamixofurbanandruralhospitals developedandrevisedthesurvey.Attendingphysicianswith clinical,administrative,andresearchexperiencewho
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Interfacilitypatienttransfersarechallenging forclinicianstoarrangeinruralandlimited resourcesettings.Thiswasexacerbatedbythe COVID-19pandemic.
Whatwastheresearchquestion?
Didtransfercoordinationcentersimprovethe clinicianexperienceofarrangingpatient transfersduringthepandemic?
Whatwasthemajor findingofthestudy?
Surveyresultsandinterviewssuggest transfercentersmayhaveoffsetpandemic transferchallenges.
Howdoesthisimprovepopulationhealth?
Clinicianswhofrequentlytransferpatients maybene fi tfromongoingaccesstotransfer coordinationservices.
practiceinreferringandreceivinghospitalsettings pilot-testedthesurveytoensurequestion-and-response relevanceandclarity.Publishedguidelinesinformed surveydevelopment.13,14
WeadministeredoursurveyusingtheAmericanCollege ofEmergencyPhysiciansEmergencyMedicinePractice ResearchNetwork(EMPRN),anationwidecohortof765 emergencyphysicianswhohavevolunteeredtoanswershort researchsurveysseveraltimesayear.Thesurveyincluded questionsonpracticesetting,transfercenterpresenceduring COVID-19,andtransferredpatients’ characteristics (AppendixA).Noincentiveswereofferedforparticipation. TheEMPRNsentsurveyinvitationsonMarch3,2021,with threeadditionalreminderemailsoverasix-weekwindow.
Wecalculatedsurveyresponseratebasedonthenumber ofEMPRNparticipantswhowereemailedthesurvey(765) andthenumberofsubmittedsurveyresponses.Nosurveys wereexcludedduetoitemnonresponse,sinceallbutoneof thequestionswererequiredforsurveysubmission.We collectedordinalresponsesforyearlyEDvolume,inpatient bedcapacity,andviewsonthefutureutilityoftransfer coordinationsystemsandLikert-scaledresponsesfor perceptionofCOVID-19impactandtransfermetrics.We defined sending facilitiesasthosethat always or mostly tendedtotransferpatientsoutcomparedtoreceiving patients.Wedefined receiving facilitiesasthosethat always
or mostly tendedtoreceivetransfers.Wedefinedatransfer centerasa “new/expandedcentralizedentity(suchasacall center)createdtocoordinateinterfacilitytransfers.” In additiontodescriptivecharacteristics,ourprimaryoutcome measureofinterestwasthetransfercentereffectonpatient transfersduringCOVID-19.Wecomparedsendingand receivingrespondents,facilitycharacteristics,effectsofthe COVID-19pandemic,andperceptionsoftransfercenters usingchi-square,Student t -test,Spearman’srho,Wilcoxon signed-ranktests,andMann-Whitneytests,asappropriate. Weusedatwo-tailedtypeIerrorrateof5%todetermine statisticalsignificance.WeusedJASP0.14.1.0(Universityof Amsterdam,Netherlands)forstatisticalanalyses.
Weconductedsemi-structuredinterviewstofurther exploreclinicianandpolicymakerperceptionsofinterfacility transfersbeforeandduringthepandemic,alongwiththe benefitsandchallengesofthenewtransfersystems. Researchersiterativelydevelopedtheinterviewguideswith inputfromphysiciansfrequentlyinvolvedinthetransfer process.Clinicianswhogaveinputonthedevelopmentofthe interviewtoolwerenotincludedamongthe finalinterviews. Theinterviewquestionsfocusedontheorganizationofand overallchallengesassociatedwithinterfacilitytransfersand ontheperceivedimpactsoftransfercentersonthetransfer processes(AppendixB).
Threeauthorsconductedtheinterviewsbetween September–December2021.Clinicianswhogaveinputonthe surveytoolhelpedidentifythe firstinterviewees.Wethenused snowballsamplingtorecruitcliniciansfromrural(sending) hospitalsthatfrequentlyneededtotransferpatientstoother facilitiesandadministratorstaskedwithimplementingand runningthetransfercentersduringCOVID-19.We interviewed fivecliniciansandthreeadministratorsfromNew Mexicoandsixcliniciansandthreeadministratorsfrom Arizonabeforethematicsaturationwasreachedandno furtherparticipantswererecruited.Interviewsgenerally rangedfrom30–60minutesinlength.Withpermission,we recordedtheinterviews,savedthemsecurely,andtranscribed themusingRevtranscriptionservices(Rev.ComInc,San Francisco,CA).Weassignedalphanumericidentifiersto transcriptsforconfidentiality.Eachofthethreeinterviewteammembersindependentlycodedthesameadministrator andclinicianinterviewtoensureconcordanceandtodevelopa codingstructurebeforeinductivelycodingandanalyzing themesontheremaininginterviews.Weusedaniterative processthroughouttheanalysistoensurereliabilityin thematiccategorydevelopment.
Atotalof141physicians(of765whoweresentthesurvey, 18.4%responserate)from39statesrespondedtothe
EMPRNsurvey.Respondentaverageagewas53,andmost wereWhiteandmale.Facilitiesthatprimarilytransferred patientstolargercenters(ie,sendingfacilities)tendedtohave loweryearlyEDvolumes(P < 0.001)andlessinpatientbed capacity(P < 0.001)comparedtofacilitiesthatprimarily receivedpatientsintransfer(ie,receivingfacilities)(Table1). Lackofspecialtyserviceswasthemostcommonreasonfor transferreportedamongbothsendersandreceivers;other reasonsincludedinadequatelocalinpatient-andintensive careunit(ICU)capacity(Figure1).
Mostrespondentsreportedmoderate-to-highperceived severityofCOVID-19impactintheirareas(mean3.9with1 beingthelowestseverityand5thehighestseverity). Physiciansatreceivingfacilitiesperceivedtheseverityofthe COVID-19pandemictobegreaterthansendingphysicians (P = 0.05),see Table1.Mostrespondentsalsoreported transfersovergreaterdistances(mean3.58)andincreased numberoftransferpartners(mean3.54)requiredto accomplishpatienttransfersduringtheCOVID-19 pandemiccomparedtoprior(mean3.00,indicatingno change).ReportedCOVID-19intensityappearedtobe correlatedtodistanceoftransfers(Spearman’srho0.141, P = 0.10)andnumberoftransferpartners(Spearman’srho 0.140, P = 0.10)althoughnotstatisticallysignificant.
Mostrespondentsreportednoaccesstoatransfercenter priortotheCOVID-19pandemic,orimplementationofa neworexpandedtransfercenterinresponsetoCOVID-19 (Table1).Atotalof37respondents(30%)reported implementationorexpansionofatransfercoordination centerinresponsetotheCOVID-19pandemic.Thosewho hadaneworexpandedcenterreportedsimilaramountsof overalleffort(mean2.91,whereamean = 3indicatesno change,Wilcoxonrank-sumtest, P = 0.55)andtimeto achievetransfers(mean3.17,Wilcoxon P = 0.32).In comparison,thosewhodidnothaveaneworexpanded centergenerallyreportedahigherdifficulty(mean3.89, Wilcoxonrank-sumtest P < 0.001)oftransferringpatients becauseoftheCOVID-19pandemic.
Ofthosewithaccesstoneworexpandedtransfercenters duringCOVID-19,mostsawutilityinhavingthesetransfer servicesavailableinthefuture.Among36respondentswith neworexpandedtransfercenters,15(42%)thoughtthey wouldbeusefulinthefuturebutonlyinemergency circumstancesand16(44%)thoughttheywouldbeusefulin allsituations.Incomparison,of83respondentswithout transfercenters,only17(20%)thoughttransfercenterscould helpinfutureemergencies,35(42%)thoughttheywouldbe usefulinallsituations,and31(37%)thoughtthesewouldnot behelpfulinthefuture.
Interviewswithadministratorsandsendingfacility cliniciansprovidedadditionalinsightontheutilityoftransfer centers.The17intervieweesincluded fivecliniciansandthree
*EMPRN,EmergencyMedicinePracticeResearchNetwork. Figure1. PerceivedreasonsnecessitatingpatienttransfersduringtheCOVID-19pandemic,receivingvssendingfacilities (%ofrespondents). COVID,coronavirus2019; ICU,intensivecareunit.
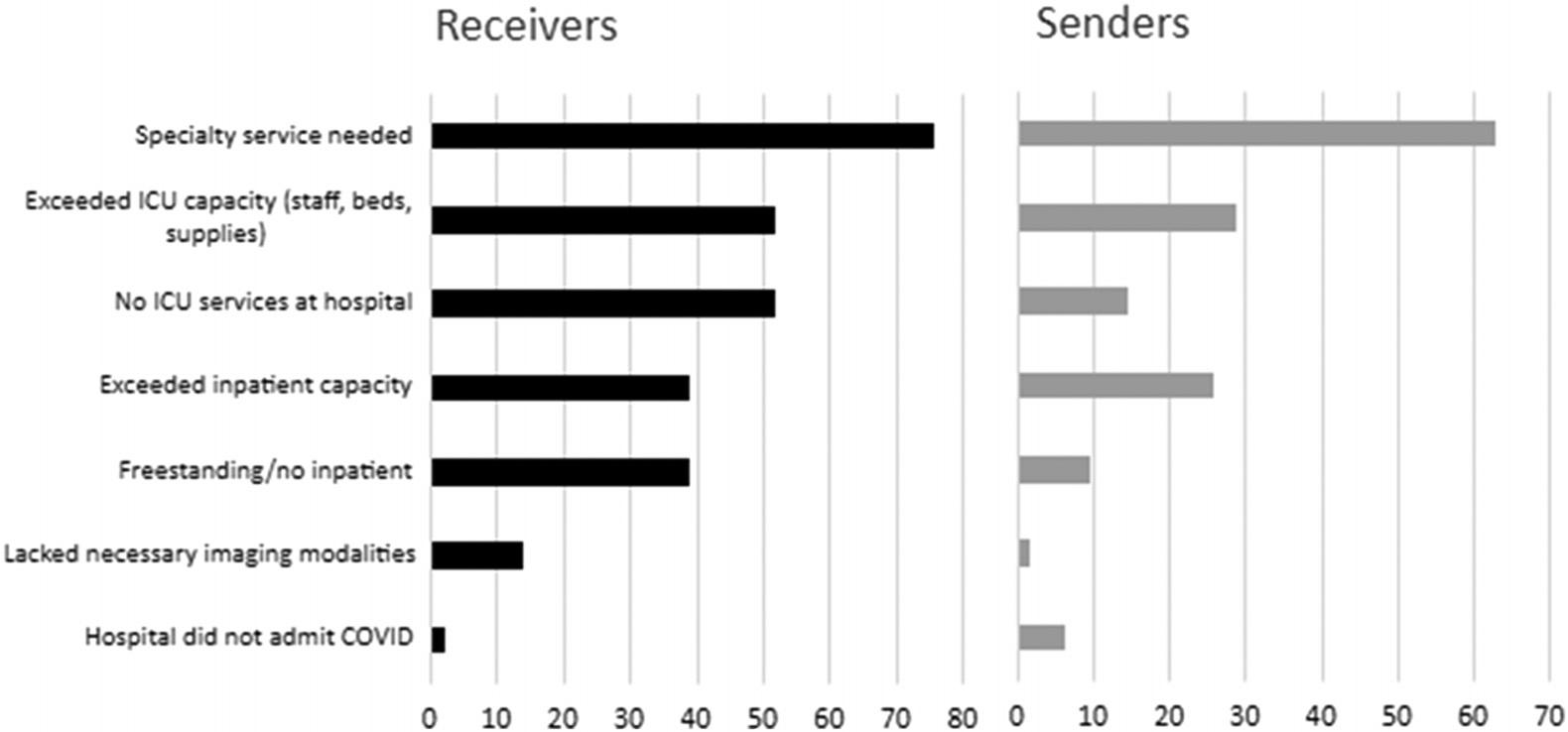
administratorsfromNewMexicoandsixcliniciansand threeadministratorsfromArizona.Theintervieweeswere mixedingenderandage.The11cliniciansincludedsix workingontribalhealthsitesofvaryingsizes(alargenumber ofruralfacilitiesintheregionserveNativeAmericantribes), oneatanon-tribalnonprofitcriticalaccesshospital,two atmid-sizedcommunitynonprofithospitals,oneat severalfreestandingEDs,andoneataruralcommunity teachinghospital.
Weidentifiedfourprimarythemesrelatedtothe functioningandutilityoftransfercenters,includingthe following:1)limitedresourcesforfacilitatingtransferseven beforeCOVID-19;2)increasednumberofanddistanceto transferpartnersduringtheCOVID-19pandemic;3) generallypositiveimpactsoftransfercentersonworkflow; and4)thepotentialforcontinueduseofcentersto facilitatetransfers.
Theme1:Limitedresourcestocoordinatetransfers
Intervieweesreportedthat,priortoandduringthe COVID-19pandemic,transfercoordinationplacedalarge burdenoncliniciansandstaffatsendingfacilities.One respondentnotedthattheyspent “ halfmyshiftonthe phone, ” andanothercalled “ asmanyas10to12facilities ” beforecompletingatransfer.Withoutcentralizedaccessto learnaboutwhichreceivingfacilitieshadneededbedsand specialtyservices, “ youhadnowayofknowingthatuntilyou actuallytalktosomebody. ”
Respondentsatsendingfacilitiesreportedavarietyof reasonsforpatienttransfer.Arespondentsummarizedthe relationshipbetweenresourcesanddecisionstotransfer:
Therearethree[reasons],oneislackofcapacity The otherreasoniscalled ‘serviceisnotavailable’ And thethirdreasonishigherlevelofcare thatthe patientistoosickforusandoursystem.
Beforetransfercenterimplementation,decisionswereoften basedonsendingclinicians’ personalrelationshipsand knowledgeofreceivingfacilities,totheextentthatone intervieweenotedtheir “ fi rst-namerelationships ” withthose atreceivingfacilities.
Theme2:IncreasedtransfercomplexityduringCOVID-19
Surveyrespondentsreportedincreasednumbersof transferpartnersandincreaseddistancesoftransfers, suggestingincreasingcomplexityofpatienttransferasan earlyresultofthepandemic.Interviewrespondents elaboratedonthecomplexitiesofthisexpandedtransfer area,withonenotingthat “ transferringpatientsmuch fartherdistances ” placesstrainon “ thepatientandontothe familyandtheirsupportnetwork. ” Anotherintervieweehad asimilarnumberoftransfersaspre-pandemicbut “ the complexityincreased,thenumberofphonecallsincreased. ”
Manyneededtoidentifynewreceivingfacilitiesbeyondtheir normaltransferpartnerstoaccesstheneededlevelofcare, specificallyICUbeds.Arespondentreported,
Beforethis[COVID-19pandemic],I’veneverhadto transferforbedavailability,butwedidstarthavingto dothatforICUbeds.[Forthesereasons] “lengthofstay intheemergencydepartmenthasgoneupdramatically.
Theme3:Thepositiveimpactoftransfercenters
Almostallrespondentsnotedthatthetransfercenters decreasedtheburdenofpatienttransfer,providingan importantresourceinmaintainingworkflow.Aprimary impactwasreductionintimespentonthephone,withone respondentlikingthatthey “ onlyhadtodialonenumber,give somebasicinfo youonlyhadtohaveoneconversation withonedoctor itdramaticallydecreasedadministrative work. ” Anotherintervieweenoted, “ better fl owthroughout ouremergencydepartmentsothatotherpatientscouldbe seenandcaredforaswell. ” Eventhosewhodidnotseeabig impactontheirtransferprocessacknowledgedthepossibility thatthecentershelpedsubtly:
Asthetransferringphysician,Ididnotseemuchchange Now,whatIcan’ttellyouiswhatitwouldbelike,giventhe ongoingsurges,iftherehadbeenanabsenceofthatcall center,thingscouldhavebeenmuchworse Maybeno changewasagoodthing,becausethealternativewas thatthingswould’vedeclinedinaverybadway.
Theme4:Transfercentersasapotentialpolicysolution
Thetransfercenterexperienceledintervieweestoconsider howthisarrangementmaycontributetoimprovedcare deliverybeyondthepandemic.Despitelowernumbersof COVID-19patientsatthetimeofinterview,oneclinician notedtransfersstill “ takingquiteabitoftime ::: transfer centerassistancecouldstillbeveryhelpful eventhough technicallytheCOVIDcrisishassubsided. ”
Onerespondentsuggestedastandingstatewidetransfer centercouldassistsendingfacilitiesandincreasepatient agency: “ Onephonenumberthatyoucallforanytransfers withinyourstate youcanputthatpatients ’ preferenceis transferredtoXhospitalortostaynearhome. ” Others statedtheywouldliketo “ expandthisouttootherdisease statesotherthanjustCOVID. ” Anotherwantedtosee “ a [phone]lineataminimumthatdealtwithallICUbeds withinaregion ::: abletoknowwhathospitalshadwhat servicesandputyouintouchwiththemratherthan [taking]awayfrompatientcare. ”
Meetingtheneedsofbothfacilitiesandcommunities requiressignificantplanningandcoordination.One respondentnoted,
Table2. Additionalqualitative findingsandextended-lengthquotes.
ThemeQuote
Limitedresourcesto coordinatetransfers
Youmakeallyourownphonecalls.SoI’vespentuptohalfmyshiftonthephone,randomly dialingphonenumbersfornon-COVIDpatientsbefore.
Therearetimeswhentheycallasmanyas10to12facilitiesbeforeyoucan findanacceptable bed sothemoretimespenttryingto findanappropriatefacilityforpatient,thefewerother patientsthatthatprovidercansee.
I’vespentmoretimeonthephone tryingtogetpeopletransferredduetoCOVIDthanIever thoughtwaspossible.
EvenifaplacesaidthattheyhavespecialtyservicescoveringspecialtyX,theymaynothaveit thatdayorthatweekandyouhadnowayofknowingthatuntilyouactuallytalktosomebody.You wouldn’tknowwhohadthetypeofbedavailablethatyouwerelookingfor.Soyou’d[make] multiplephonecallssayrequestinganICUbeduntilyoufoundsomebodywhohadanopenICU bed.Andsojustalotofredundancyofworkthattookawayfrompatientcaretime.
Therearethree[reasons],oneislackofcapacity,becausewecan’tadmitthatmanypatients becausewedon’thaveenoughnurses.Theotherreasoniscalled “serviceisnotavailable”,which meanswejustdon’thavetheservice,wedon’thavethespecialist,wedon’thavetheMRI,we don’thavetheCT,ourCTswentdown.There’salotofthingswedon’thave.Wedon’thave platelets,wedon’thavedialysis,don’thaveanyonetodoacardiaccheck.Eitherwedon’thavethe specialist,wedon’thavetheequipment,butwedon’thavetheservicethatserviceisnotavailable. Andthethirdreasonishigherlevelofcare.Andthat’sthatthepatientistoosickforusandour system,whichisdifferentthanserviceisnotavailable.Serviceisnotavailablewouldbeifwehad aneurologistandMRI,wecouldprobablykeepthepatient.Sothoseareonlythreereasonswe sendpeopleout.
Wehave firstnamerelationshipswithsomeoftheattendingphysicians,andthey’remorefamiliar withoursettingandourlimitations
Increasedtransfercomplexity duringCOVID
Wearenowtransferringpatientsmuchfartherdistances,whichisverysignificantontothepatient andontothefamilyandtheirsupportnetwork.Manypatientsarebeingtransferrednowtolocations wheretheydon’thavearidehome
Ithinktheproportionoftransferswasprobablysimilar.But,thecomplexityincreased,thenumber ofphonecallsincreased
Wedon’thavealotofspecialistsandsoitisnotinfrequentthatwehavetotransferforcertain specialistsbutbeforethis[COVIDpandemic],I’veneverhadtotransferforbedavailability,butwe didstarthavingtodothatforICUbeds
Ourlengthofstayintheemergencydepartmenthasgoneupdramatically,comparedfromevenin thelastmonth,wewereup109minutesonaverageforpatientsthatwerebeingadmitted
Thepositiveimpactof transfercenters
Transfercentersasapotential policysolution
Ithinkwhereitwasmostnotablewasjustthefactthatyouorasecretaryonlyhadtodialone number,givesomebasicinfo.Andthenoncetherewasanacceptinghospital,thenasaphysician, youonlyhadtohaveoneconversationwithonedoctor.Sometimesnoteventhat.Andsofromsort ofthatendoftheadministrativework,itdramaticallydecreasedadministrativework.
Sopatientshavingtowaitlesstimetogettoanappropriateinpatientfacilitywouldbebeneficial andthenwouldalsoallowustohavebetter flowthroughoutouremergencydepartmentsothat otherpatientscouldbeseenandcaredforaswell
Frommyend,asthetransferringphysician,Ididnotseemuchchange Now,whatIcan’ttell youiswhatitwouldbelike,giventheongoingsurges,iftherehadbeenanabsenceofthatcall center,thingscouldhavebeenmuchworse.Sointhebackofmymind,Ithinkaboutthat.Maybe nochangewasagoodthing,becausethealternativewasthatthingswould’vedeclinedinavery badway
We’restill findingthattheprocessto findanappropriatefacilityistakingquiteabitoftime.Andso thattransfercenterassistancecouldstillbeveryhelpfulevennowbecauseofthefactthatthe stateisjustseeinglimitedbedavailability,eventhoughtechnicallytheCOVIDcrisishassubsided. Onephonenumberthatyoucallforanytransferswithinyourstate.Andthatyoucanput thatpatients’ preferenceistransferredtoXhospitalortostaynearhomeorwhatever [theirpreference]is.
(Continuedonnextpage)
Table2. Continued.
ThemeQuote
Transfercentersasapotential policysolution
IthinkthatIwouldlovetoexpandthisouttootherdiseasestatesotherthanjustCOVID.Ithink havingthatcentralizedcommunicationsystemseemedtobeaveryeffectivemanner. HavingalineataminimumthatdealtwithsayallICUbedswithinaregion.Butideallyonelinethat wasabletoknowwhathospitalshadwhatservicesandputyouintouchwiththemratherthan havinghospitalstaffspendingmostoftheirtimedialingnumbersandawayfrompatientcare Iwouldbefullyinfavorofarobust,well-supportedtransfermechanism.Myimpressionisthat outsideofpandemictimesthereisnotawell-coordinatedtransferarchitectureforgettingpatients fromdeeplyruraltourbancentersandtertiarycarecenters veryhopefulthatwecanpull togetherawell-coordinatedtransferframework,whichrevolvesaroundtransfercenters Eveniftheycannotcovereverysingletransfer,especially,whenwe’reseeinghighervolumesand pressedfortimeandresourcesintheER,anythingthatcouldbedonetofacilitatepatients ultimatelygettingthecaretheyneedisahugebenefit.Ithinkthere’salsosortofasensethatifwe canoptimizetheresourceswithinthestatetoallowforcoordinationacrossthehospitalsystems, justhereforthesepatients,thatwouldbeidealaswell
Idon’tfeellikeIneeditduringnon-crisistimes,personally.Iusuallyhavebeenabletotransfer patientsprettyquick
We’resorural.There’snowhere Whenittakesussolongtogetabed,wealsostillhaveto arrangefor flightandfortheactualtransportation.So,ifittakes22hourstogetabed,andthenI don’thavea flightteamavailableforsixhours,that’s28hoursbeforethepatientleavesmy emergencydepartment,youknow?
CT,computedtomography; COVID,coronavirus2019; ICU,intensivecareunit; MRI,magneticresonanceimaging.
Outsideofpandemictimesthereisnotawell-coordinated transferarchitectureforgettingpatientsfromdeeplyrural tourbancentersandtertiarycarecenters ::: [Iam] hopefulthatwecanpulltogetherawell-coordinated transferframework.
Anothercommented,
Whenwe’reseeinghighervolumesandpressedfortime andresourcesintheER,anythingthatcouldbedoneto facilitatepatientsultimatelygettingthecaretheyneedis ahugebenefit ifwecanoptimizetheresourceswithin thestatetoallowforcoordinationacrossthehospital systems ::: thatwouldbeideal.
Asubsetofrespondentswaslessenthusiasticabout transfercentersoutsidethepandemiccontext.Onestated, “ Idon ’ tfeellikeIneeditduringnon-crisistimes,personally. Iusuallyhavebeenabletotransferpatientsprettyquick. ” Othersnotedinterrelatedchallengesthatwouldneedtobe overcomebeforefullyrealizingthebenefitsofatransfer center: “ We ’ resorural ::: wealsostillhavetoarrangefor fl ightandfortheactualtransportation. ” Additionaland expandedrespondentquotesareprovidedin Table2
Inthismixed-methodsstudy,wehypothesizedthat physiciansparticipatinginpatienttransfersduringCOVID19would findutilityinhavingaccesstotransfercoordination
centers.Inournationalsurvey,thosewithoutaccessto transfercentersreportedasignificantincreaseinthedifficulty ofexecutingtransfersduringCOVID-19surges,contrasting torespondentswithaccesstonewtransfercoordination servicesreportingnosignificantchangeineffortortimeto organizeapatienttransfer.Thissuggeststhattransfercenter implementationmayhaveoffsetpandemic-relatedtransfer challenges.Respondentswhohadexperiencewithtransfer centersalsoweremoresupportiveoftheirongoinguse, particularlyinfuturehealthcrises.
OurqualitativeinterviewsinArizonaandNewMexico, twostateswheretransfercenterswereimplemented,shed additionallightontheirbenefitswhileidentifyingareasfor futureimprovement.Withfewexceptions,theseclinicians foundthetransfercenterservicestobehelpful,specificallyin reducingtransferworkflowcomplexity.Sincethecompletion ofthisstudy,feedbackinArizonawassopositivethatthe stateevolveditstemporarytransfercenterintothefederal grant-funded “AZREACH” system,administeredbythe ArizonaPoisonandDrugInformationSystem.15
MostUShealthcarepractitionersdonotworkinareas servedbytransfercoordinationcenters,consistentwithour surveyresults.1,2,6–12 InthewakeoftheSeptember11,2001, terroristattacks,attemptsweremadetocreateanational centralizedsystembutwereneverwidelyimplemented.6 While someregionshavetransferpatternsforspecificconditions suchastraumaandacutemyocardialinfarction,16,17 transfers generallyoccurthroughinformal,looselycoordinated regionalnetworksthatsufferfromfragmentationandpoor
communication.4,5 Ourstudyconcurswithpriorresearch findingthatthelaborioustransferprocessrequiresthesending cliniciantoidentifyanacceptingfacilityusingtheirknowledge ofhistoricaltransferpatternsandinformalrelationships,and thecomplexcoordinationandmultiplephonecallscan distractfrompatientcare.5 Itispossiblethatexistingtransfer serviceswereavailabletosomeofourrespondentspriorto COVID-19butcliniciansonlybecameawareofthemdueto thestrainsofthepandemic.
Oursurveyfoundreceivingcentersreportedagreater perceivedimpactofCOVID-19.Receivinghospitalsare generallylocatedinurbanareas,whichexperiencedthe first wavesofCOVID-19duringatimeofintenseuncertaintyand fear.This,alongwithsubsequentsurgesofruraltransfersto urbanfacilities,mayhaveinfluencedtheperspectivesof receivinghospitalrespondents.18 Itisalsopossiblethat sendingfacilitiesandruralrespondentsfromthesurveymay havelivedinregionslessimpactedbyCOVID-19,orthat closerrelationshipsbetweenruralfacilitiesandtheirlocal communitiesmayyieldincreasedresilienceinrespondingto crises.19 However,thequalitativeinterviewsrevealedthat significantstressesfromCOVID-19,includingwithtransfers, alsoaffectcliniciansatsmallerfacilities.Thisislikely exacerbatedbythestrugglesofruralfacilitiestohire physicianswhooftenchoosetoworkinurbancenters,2 while inabilitytoretainstaffandrisingruralhospitalclosures21 placeanincreasedburdenamongthosewhoremain.Lackof specialistservicesandinpatient/ICUcapacitywerethetop reasonspromptingtransferspersendingandreceiving physicians,similartowhatwasreportedinpriorstudies.5
Smallandruralhospitalshavehadlongstanding challengestransferringpatientswithtime-sensitive conditions,whichwereamplifiedduringCOVID-19. Transfercentersseemtoholdgreatpromiseinmaking patienttransferlessonerous.AstheUShealthcaresystem continuestostrugglewithworseningstaffingissuesand patientcrowding,transfercentersmaybeonepartofthe largersolutiontogetpatientsneededcare.
Thelowresponserateinthenationalsurveypotentially limitsinterpretationandintroducesbias.Thestrict requirementtocompletenearlyallquestionsonthesurvey mayalsohaveledtounitnon-responseamongsome physicians.Whilewetriedtoimproveresponserateswith multipleemailremindersandashortersurvey,otherproven strategiescouldhavebeenconsidered,suchasreachingout viapostalmailorincludingincentives.22,23 Itdoesappear thatsurveyresponseratesmaybedecreasingovertimeand mayalsovarybymedicalspecialty,withsomehavinglow responseratesbelow30%.24,25
SinceEMPRNrequestssurveysbeasshortandsimpleas possibletoencourageparticipation,wefurtherexplored clinicians’ experiencesviakeyinformantinterviews.The
smallpoolofinterviewrespondentslimitedourqualitative data,whiletheuseofsnowballsamplingfromtwo neighboring,largelyruralstates(andmanytribalsites)may havelimitedthediversityofviewpointsandexternal generalizability.Futurestudiescouldincorporateexpanded interviewstogatherperspectivesfromcliniciansindifferent statesandpracticesettings.
ThewidespreadstrainontheUShealthcaresystemduring theCOVID-19pandemicmanifestedsignificantchallengesin interfacilitypatienttransfers.Cliniciansatsmall,rural facilitiesinArizonaandNewMexicofoundcentralized transfercoordinationcenterstobehelpful.Inthefuture, otherstatescouldconsidertrialingimplementationofsimilar services,bothincrisisandnon-crisistimes.
AddressforCorrespondence:MichaelB.Henry,MD,MS,Parker IndianHealthCenter,12033WAgencyAve.,ParkerAZ85344. Email: Mhenry12@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ThisworkwassupportedbyaResearch SeedGrantfromtheArizonaCollegeofEmergencyPhysicians (awardedonJanuary15,2021).Therearenootherconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Henryetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.DwyerJ.Onehospitalwasbesiegedbythevirus.Nearbywas ‘plentyof space.’ 2020.Availableat: https://www.nytimes.com/2020/05/14/ nyregion/coronavirus-ny-hospitals.html AccessedSeptember29,2020.
2.WhiteDB,VillarroelL,HickJL.Inequitableaccesstohospitalcare: protectingdisadvantagedpopulationsduringpublichealth emergencies. NewEngJMed. 2021;385(24):2211–4.
3.Hernandez-BoussardT,DaviesS,McDonaldK,etal.Interhospital facilitytransfersintheUnitedStates:anationwideoutcomesstudy. JPatientSaf. 2017;13(4):187–91.
4.IwashynaTJ,ChristieJD,MoodyJ,etal.Thestructureofcriticalcare transfernetworks. MedCare. 2009;47(7):787–93.
5.McNaughtonCD,BonnetK,SchlundtD,etal.Ruralinterfacility emergencydepartmenttransfers:frameworkandqualitativeanalysis. WestJEmergMed. 2020;21(4):857–64.
6.EvansMandBerzonA.Whyhospitalscan’thandleCOVIDsurges: They’re flyingblind.2020.Availableat: https://www.wsj.com/articles/ hospitals-covid-surge-data-11601478409?mod=hp_lead_pos10 AccessedOctober15,2020.
7.MedicalAdvisoryTeam.NewMexicoStatewideAcuteCareMedical SurgepPanforCOVID-19PandemicResponse.2020.Availableat: https://cv.nmhealth.org/wp-content/uploads/2020/04/NM-CSC-Plan-V. 4.17.20.pdf.AccessedNovember5,2023.
8.LeeAH,DunnPF,CooperS,etal.COVID-19level-loading: transferringemergencydepartmentpatientstoapartneracademic medicalcenterwithinahealthcaresystem. AmJMedQual. 2021;36(5):368–370.
9.IPAL(IllinoisProviderAccessLine)TransferCenter.Universityof IllinoisHospital&HealthSciencesSystem.2022.Availableat: https://hospital.uillinois.edu/referring-physicians/patient-transfer AccessedNovember5,2023.
10.SchorschK.TransferringpatientswithCOVID-19difficultinChicago. 2020. https://www.wbez.org/stories/one-chicago-hospital-called-for-8hours-to-transfer-covid-19-patients-thats-problematic-for-futureoutbreaks/1ecd60f3-f185-4deb-ae65-3e3ca25f0063 AccessedSeptember29,2020.
11.CityofChicago.ChicagoHospitalCapacityDashboard.2022.Available at: https://www.chicago.gov/city/en/sites/covid-19/home/ hospital-capacity-dashboard.html. AccessedNovember5,2023.
12.MitchellSH,RiglerJ,BaumK.Regionaltransfercoordinationand hospitalloadbalancingduringCOVID-19surges. JAMAHealthForum. 2022;3(2):e215048.
13.ArtinoAR,DurningSJ,SklarDP.Guidelinesforreportingsurveybasedresearchsubmittedtoacademicmedicine. AcadMed. 2018;93(3):337–40.
14.ArtinoAR,LaRochelleJS,DezeeKJ,etal.Developingquestionnaires foreducationalresearch:AMEEguideno.87. MedTeach. 2014;36(6):463–74.
15.UniversityofArizona.AZREACHFAQs.2023.Availableat: https:// az-reach.com/reach-faqs.AccessedNovember5,2023.
16.CommitteeonTraumaoftheAmericanCollegeofSurgeons.Regional traumasystems:optimalelements,integration,andassessment.
Systemsconsultationguide.2008.Availableat: https://www.facs. org/media/sgue1q5x/regionaltraumasystems.pdf. AccessedNovember5,2023.
17.JollisJG,GrangerCB,HenryTD,etal.SystemsofcareforST-segmentelevationmyocardialinfarction:areportfromtheAmericanHeart Association’smission:Lifeline. CircCardiovascQualOutcomes. 2012;5(4):423–8.
18.CDCNationalCenterforHealthStatistics.COVID-19hospital encountersbyurban-rurallocationofthehospitalbyweekfromselected hospitals.2022.Availableat: https://www.cdc.gov/nchs/covid19/nhcs/ hospital-encounters-by-urban-rural.htm.AccessedDecember7,2022.
19.AtkinsonMK,HickJL,SingerSJ,etal.Doruralhospitalshavean advantageduringapandemic?2022. https://www.healthaffairs.org/do/ 10.1377/forefront.20220321.42134/.AccessedDecember6,2022.
20.MohammadiaghdamN,DoshmangirL,BabaieJ,etal.Determining factorsintheretentionofphysiciansinruralandunderdevelopedareas: asystematicreview. BMCFamPract. 2020;21(1):216.
21.UnitedStatesGovernmentAccountabilityOffice.Ruralhospital closures:Affectedresidentshadreducedaccesstohealthcare services.2020. https://www.gao.gov/assets/gao-21-93.pdf AccessedSeptember21,2023.
22.PhillipsAW,ReddyS,DurningSJ.Improvingresponseratesand evaluatingnonresponsebiasinsurveys:AMEEguideno.102. MedTeach. 2016;38(3):217–28.
23.PhillipsAW,FriedmanBT,UtrankarA,etal.Surveysofhealth professionstrainees:prevalence,responserates,andpredictivefactors toguideresearchers. AcadMed. 2017;92(2):222–8.
24.CunninghamCT,QuanH,HemmelgarnB,etal.Exploringphysician specialistresponseratestoweb-basedsurveys. BMCMedRes Methodol. 2015;15:32.
25.CookJV,DickinsonHO,EcclesMP.Responseratesinpostalsurveysof healthcareprofessionalsbetween1996and2005:anobservational study. BMCHealthServRes. 2009;9:160.
JakeValentine,MD*
JonathanPoulson,DO†
JesusTamayo,BA‡
AmandaValentine,MEng,MSHI§
JacquelineLevesque,EdD*
ShaneJenks,MD,MEd†
SectionEditor:CaseyM.Clements,MD,PhD
*UniversityofHouston,TilmanJ.FertittaFamilyCollegeofMedicine, Houston,Texas † HCAHoustonHealthcare,Kingwood,Kingwood,Texas ‡ TheUniversityofNorthTexasHealthScienceCenter,FortWorth,Texas § UniversityofTexasHealthScienceCenteratHouston,Houston,Texas
Submissionhistory:SubmittedNovember13,2023;RevisionreceivedMarch8,2024;AcceptedMarch22,2024
ElectronicallypublishedJuly18,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18574
Introduction: Effectivemedicaleducationmustbalanceclinicalservicedemandsforinstitutionsand learningneedsoftrainees.Thequestionofwhetherthesearecompetingdemandsorcanserve complementaryroleshasprofoundimpactsongraduatemedicaleducation,rangingfromfunding decisionstothewillingnessofcommunity-basedhospitalsandphysicianstoincludelearnersattheir clinicalsites.Ourobjectiveinthisarticlewastosystematicallyreviewtheevidenceontheimpactof medicaltraineesonproductivityandefficiencyintheemergencydepartment(ED).
Methods: WequeriedPubMed,Embase,Scopus,andWebofSciencefromearliestavailabledatesto March2023.Weidentifiedallstudiesevaluatingtheimpactofmedicalstudentsand/orresidentsinthe EDoncommonlyusedproductivityandefficiencymetrics.OnlystudiesinEDsintheUnitedStateswere included.Noadditional filterswereused.WeassessedtheriskofbiasofincludedstudiesusingtheRisk ofBiasinNon-randomizedStudies – ofInterventions(ROBINS-I)tool.Certaintyofevidencewasrated usingtheGRADE(GradingofRecommendationsAssessment,DevelopmentandEvaluation)approach. Study findingswerecombinedinanarrativesynthesisandreportedaccordingtoPRISMAguidelines.
Results: Theliteraturesearchyielded3,390uniquearticlesforabstractscreening.Eighty-oneabstracts wereidentifiedasrelevanttoourPICOquestion(population,intervention,control,andoutcomes),76of whichhadretrievablefull-textarticlesandthethemesofwhichwerediscussedinanarrativesynthesis. Weselected13ofthefull-textarticlesfor finalinclusioninasystematicreview.Studieswereroughlysplit betweenobservational(6)andquasi-experimental(7)designs.Themajorityofstudies(11)weresinglesitestudies.OnlytwostudiescouldbegradedaslowriskofbiaspertheROBINS-Itool.
Conclusion: Low-GRADEevidencesuggeststhatstudentsandresidentsdecreaseEDefficiencybya statisticallysmalleffectsizeofdebatableclinicalimportance.ResidentsprovideamoderateboosttoED productivity.StudentsdonotproduceastatisticallyorclinicallysignificantimpactonEDproductivity. Residentsincreaseemergencydepartmentrelativevalueunitsrevenueby$26.30anhour,whilestudents havenoimpact.Bothtypesoflearnersdecreaseefficiency.[WestJEmergMed.2024;25(5)767–776.]
Therearecon fl ictingopinionsontheperceivedvalueof medicaltrainees,stemmingfromtheirdualrolesoflearning
andservice.Traineesde fi nevalueasmaximizinglearning opportunitiesandinteractionswithfaculty.Attending physiciansidentifyvalueastraineescompletingclerical
tasksandfreeinguptimeforpatientcare.Administrators seevaluethroughthelensofaddressingeconomic challengesofthehospital,withtraineesproviding potentialvalueviadocumentationandimprovementof organization-widemetrics bothofwhichareseenaslowvalueactivitiesbytrainees. 1 Itisnotpossibletosidestepthe con fl ictbetweentheseroles,astimespentonteaching activitiesduringanEMshiftisindependentlyassociated withresidentperceptionsontheeducationvalueof theshift.2
Thereareseveraladditionalstakeholderconsiderations pertinenttoourresearchquestion.Communitypreceptors areincreasinglyseekingcompensationforteachingtime.3 Currentpracticesregardingcompensationforteachingtime ofcommunitypreceptorsareinconsistent.3 Alogicmodel mightpositthattraineesdecreasecompensationtothe supervisingphysicianbydecreasingrelativevalueunits (RVU)orincreasingtheamountoftimespentpost-shiftvia teaching,feedback,ordeferringon-shiftactivitiesforthese purposes.Ifthisisthecase,thenthiswouldstrengthen argumentsforcompensatingphysiciansforaccommodating learnersonshift.Ofcourse,traineesalsoprovideservicesthat mightbevaluedbyattendingsphysicians,suchasdecreasing theirdocumentationburden,arrangingconsults,and gatheringpatienthistories.
Stakeholdersintheadministratorandhospitalleadership categorymightbemoreorlessinclinedtoenteranaffiliation agreementwithamedicalschoolorgraduatemedical education(GME)programdependingontheprojected impactonimportantefficiencymetrics.Lastly,andperhaps mostcontroversially,therearehigh-stakesdecisions regardingthecontinuationofindirectgraduatemedical education(IME)funding,whichrelyontheimplicit assumptionsthattraineesincreasethecostofcareatleast partlyduetoimpactsonattendingphysicianproductivity andefficiency.Thisisbasedondatafromtrainingsitesthat historicallyhaverepresentedlarge,urban,universityaffiliatedhospitals,withlimitedgeneralizabilitytothe majorityofEDsacrossthecountry.Medicarehas reimbursedhospitalsforIMEcostssince1983basedon theratioofresidentsperhospitalbedandthepremise thatthehighercostsofpatientcareatteachinghospitalsis duetothepresenceoftrainees.4 In2019,over$10billionin IMEpaymentsweredistributedtoteachinghospitals, supportingroughly90,000residentsatacostof$110,000 perresident.5
Despitethisclearlydemonstratedneedfordataonthe impactoftraineesonefficiencyandproductivityintheED, therearenorandomizedcontrolledtrials,systematicreviews, ormeta-analysesonthesubject.Inthisarticleweaimedto fill thatvoidbyexaminingexistingevidenceonthetopic, clarifyingcurrentgapsintheliterature,andmaking suggestionsforfutureresearch.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Learnerscanbebothanassetandaliabilityin termsofemergencydepartmentoperations.
Whatwastheresearchquestion?
Whatisthenetimpactoflearnerson ef fi ciencyandproductivityinthe emergencydepartment.
Whatwasthemajor findingofthestudy?
Residentsincreaseemergencydepartment relativevalueunitsrevenueby$26.30anhour, whilestudentshavenoimpact.Bothtypesof learnersdecreaseef fi ciency.
Howdoesthisimprovepopulationhealth?
This fi ndingmayguidestakeholders regardingdecisionsaboutreimbursementfor educationservicesorhavinglearnersin theirdepartment.
WequeriedPubMed,Embase,Scopus,andWebof SciencefromearliestavailabledatetoMarch9,2023.Search termsandsearchstrategyweredevelopedcollaborativelyby twocontentexpertsinmedicaleducation,onecontentexpert inhealthcareadministrationandpublicpolicy,andtwo researchlibrarians.OurPICOquestion(population, intervention,control,andoutcomes)was “Whatisthe impactoflearnersinthe(ED)onefficiencyandproductivity metrics?” Thepopulationforourquestionwaslearners.We includedbroadertermssuchas “trainee” and “learner” in oursearchstrategyincasetherewasliteratureonnontraditionalrotatorssuchasstudentsinundergraduate, scribe,oradvancedpracticepractitionerprograms.Wealso includedsynonymsusedtodescribemedicalstudentsand residentsuchas “clerk” and “intern” (AppendixA).
Theinterventionofinterestwaspresenceofalearner, comparedtoabsenceofalearner.Thelearnerhadtobe presentintheEDandunderthedirectsupervisionofan emergencymedicineattending.Ouroutcomewasefficiency andproductivity.Efficiencydescribedhowquicklypatients movedthroughthedepartmentandincludedsynonymssuch as “throughput.” Productivityreferredtohowmuchworkan attendingphysicianwasabletocomplete,mostcommonly measuredbypatientsseenorRVUsgeneratedperunitof time(AppendixA).ThesePICOcharacteristicswere capturedbythesearchtermsoutlinedin AppendixB.
The firstauthorreviewedtheinitial6,175resultstoensure thattheautomaticallydetectedduplicateswereappropriate andmanuallyexcludedundetectedduplicates.The remaining3,390abstractswerescreenedbytworeviewersto judgewhetherthearticlewouldsatisfyourPICOquestion, withdifferencesadjudicatedbyathirdreviewer.Reviewers workedindependentlyandwereblindedtotheresultofthe firstvoteforcasesinwhichtheyservedassecondreviewer. Adjudicationalsooccurredblindly,withoutaccesstothe individualreviewer’svotes.Ofthese81abstracts,76were availableforfull-textreview.Full-textreviewswere performedbythe firstauthorwithnotationsdescribing justificationforproposedinclusionorexclusion.Annotated fulltextswerethenputtoaconsensusvoteamongthefour reviewers.Weappliedanadditionalinclusioncriterionof studiesconductedintheUnitedStatesduringthisstep,owing todifferencesintrainingandsupervisionrequirementsfor medicaltraineesinothercountries.Recordswerecompiled usingCovidencesystematicreviewsoftware(VeritasHealth Innovation,Melbourne,Australia).
Thereferencessectionsofincludedstudieswerehandcheckedforadditionalcandidatesforinclusion,butthissearch didnotrevealanynewstudiestoaddtothe finalinclusionlist. Datawasextractedbythe firstauthorandorganizedby populationandoutcome.Theimpactofresidentsandstudents ontheoutcomecategoriesweredisplayedseparatelywhen possible.Weconstructedtablesand figuresaccordingtothe CochraneHandbookforSystematicReviewsof Interventions 6 Astandardizedeffectsize(Cohen d )with95% confidenceintervalswascalculatedforstudiesthatprovided thenecessarydata.Weratedcertaintyofevidenceusingthe GradingofRecommendation,Assessment,Developmentand Evaluation(GRADE)approach,adaptedforreviewsnot includingasingleestimateofeffect.7
WeassessedriskofbiaswasassessedusingtheRiskofBias inNon-randomizedStudies – ofInterventions(ROBINS-I) tool,8 withnotationsmadethroughCovidenceandconsensus assessmentvoteduponbythefourreviewers.Effectmeasures werepresentedasreportedbyeachincludedarticle.We presentedresultsofthesystematicreviewandnarrative synthesisaccordingtoPRISMAguidelines.9
AsearchofPubMed,Embase,Scopus,andWebof Scienceidentified6,175articleswith2,785duplicates,leaving 3,390articleabstractstobescreened.Weexcluded3,309 abstractsthatdidnotaddressourPICOquestions,yielding 81full-textarticlessoughtforretrieval, fiveofwhichwere unavailableastheywereabstract-onlypublications.Themes fromthese76articlesarediscussedinthenarrativesynthesis, witha final13selectedforinclusionforthesystematicreview (Figure1).Characteristicsofincludedstudiesare summarizedin AppendixC
ThemesofExcludedStudies
Commonreasonsforexclusionafterfull-textreviewwere wrongsettingorwrongoutcome.Somestudiesevaluated fellows10 ormoonlightingresidents11,12 whowerepracticing independentlyandnotbeingdirectlysupervisedbyanEM attending.AnEmory-basedstudyshowedEM-trained criticalcarefellowscaringforboardingintensivecareunit patientsgeneratedanadditional3.07RVUs/hourforthe department.10 NorthwesternUniversityevaluatedthe economicsofpayingresidentstoserveastriagephysiciansin amoonlightingroleintheirEDandfoundthatthereturnon investmentfrom “leftwithoutbeingseen” chargecapture was +54%.11 Svirskyetal(2013)showedasimilar moonlightingprogramreducedlengthofstay(LOS)by25 minutes.Thesestudieswerenotincludedinourreviewasthe residentsandfellowswereneitheractinginalearnerrolenor beingsupervisedbytheon-shiftEMattendingphysician.
SeveralexcludedstudiesinvolvedlearnersintheEDon non-EMserviceswhowerenotsupervisedbytheon-shiftEM attending.ReplacingasurgicalresidentwithanMLP (midlevelpractitioner)duringprotectededucationtime added67minutestoEDLOS.13 Residentpresenceona traumarotationdecreasedEDLOSforadmittedtrauma patients.14 Residentsonatraumaconsultservicedidnottake anylongerthanattendingsurgeonstocomplete consultations.15 Presenceofanin-housecardiologyfellow decreaseddoor-to-balloontimesforST-segmentelevation myocardialinfarction(STEMI).16
Somestudiesevaluatedtheimpactoflearnersonefficiency orthroughputmeasuresbutcomparedthemtoMLPsor simultaneouslyadjustedattendingphysicianstaffing. 16–18 McGarryetal(2010)usedapre-postdesignevaluatingLOS afteranewEMresidencyprogramwascreatedattheir hospital.Theyredistributed33%oftheattendingphysician coveragetowardthelow-acuity “urgent-care” areaoftheir department.TherewasaslightincreaseinLOSpostimplementationoftheresidencyprogram,butgreater differencesmayhavebeenmaskedbythefactthatthelowacuityarea theareamostlikelytobebottleneckedby clinicianefficiency hadmorecoverage.Frenchetal(2002) foundthatpatientswaitedanadditional20minutesfor dispositiondecisionswhenresidentswereabsenton conferencedays.However,conclusionsregardinglearner presencewouldbedifficulttomake,astheyreplacedthe roughly60hoursofresidentcoveragewith40hours ofMLPandfacultycoverage.Clearly,residentswereviewed asassetsrequiringincreasedstaffingtooffsettheirabsence, butthesestudiescomparetraineeperformancetoMLPor attendingphysicianperformanceratherthanstrictly presencevsabsenceoflearnersandwerethusomitted fromourreview.
Otherstudiestookplaceinapediatric-onlyED.These studiesgenerallydemonstratedanincreaseinLOSwith residentand/ormedicalstudentteams,likelymediated
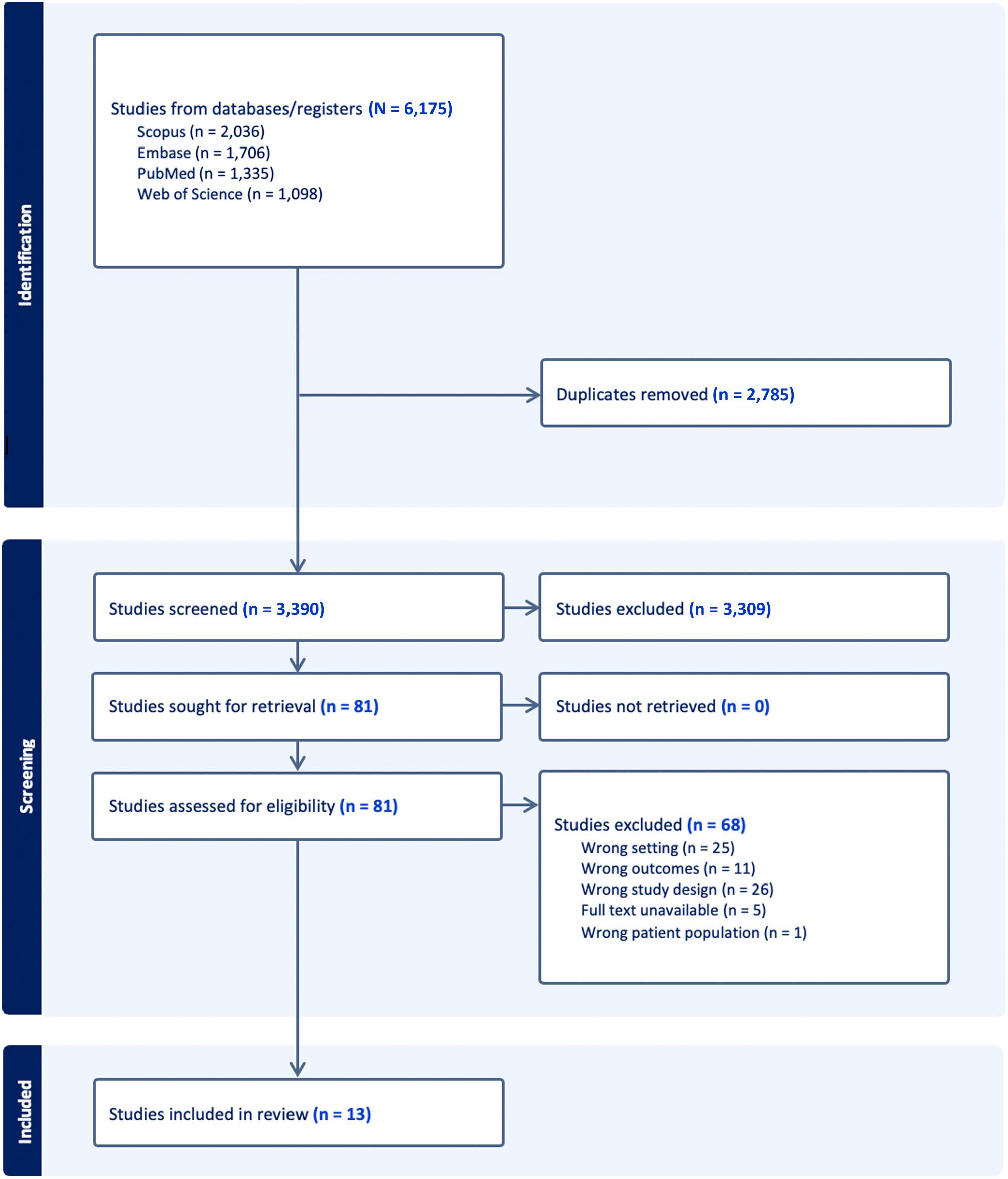
,PreferredReportingItemsforSystematicreviewsandMeta-Analyses.
throughincreasedlaboratoryandimagingutilization.19,20,21 Jadhavetal(2019)showedaclearassociationbetween residentinvolvementinacase,thenumberofstudiesordered, andtheLOSincreaseforthosecases.Coreyetal(2022) redemonstratedthese findingsandalsoshowedthatresident involvementwaslinkedwithanincreaseinRVUs/patient, againlikelymediatedbyincreasedtestutilization.Whilethis resultispotentiallypositivefromahospitaladministration perspectiveinthatitincreasesrevenue,italsolikely
representslow-valuecarethatinflatesthepatient’sbilland thecostofhealthcareasawhole.Wedidnotincludestudies frompediatricEDsastheyhaveverydifferentoperational characteristicsthanadultorcombinedEDs.
Thereweremultiplestudiesinothercountriesusinga naturalexperimentalconditionofferedbyjuniorphysicians goingonstrike,buttheapplicabilityofthesejuniordoctors toresidentphysiciansintheUSislimitedduetodifferencesin trainingandsupervisionrequirements.22,23,24,25 Studiesfrom
Korea,22 NewZealand,23 Spain,24 andAustralia25 all provideinterestingcasestudies,butthe “juniordoctor” terminologyisvariablydefined,sometimesreferringto independentlypracticingphysiciansandatothertimes referringtophysiciansintraining.
Studiesexcludedonthebasisofwrongoutcometendedto measurepatientsatisfactionorqualityofcaremetrics. Perhapsmostinterestingly,Michaeletal(2022)showedthat EMresidentsimprovedtime-limitedqualitymetricsfor stroke,sepsis,andSTEMI,whileoff-serviceresidentsinthe EDhadanegativeimpact.26
The13includedstudiesaddressedourPICOquestionby isolatingpresencevsabsenceoflearnerastheintervention andcomparisongroups,restrictingthepopulationto learnersintheEDunderthesupervisionoftheon-shift emergencymedicineattendingphysician,andincludeda measureofefficiencyorproductivity.
EfficiencymetricswereasdefinedbytheEmergency DepartmentBenchmarkingAllianceConsensusSummit (Figure2).27 Non-standardizeddefinitionsareexplainedin relationtothe figure.Otherabbreviationsencountered includeddLOS,whichstandsforlengthofstayfor dischargedpatients,andTT,whichistheintervalfrom treatmentspacetime “towhen[thepatient]iseither dischargedoradmittedtothehospital.”28 Itwasunclear whethertheendpointofthisintervalwasdispositionor departuretime,andtheauthorsdidnotrespondtoemail inquiriesrequestingclarification.
Sevenstudiesassessedtheimpactofresidentsonefficiency intheED(Table1).Most(6/7)ofthestudiesshowedasmall decreaseinefficiency.Themeasuredimpactsonefficiency wereallstatisticallysmall(Cohen d rangedfrom 0.15to 0.15),buttheclinicalsignificanceoftheimpactismore difficulttodetermine.Thenetdifferenceinefficiencyranged
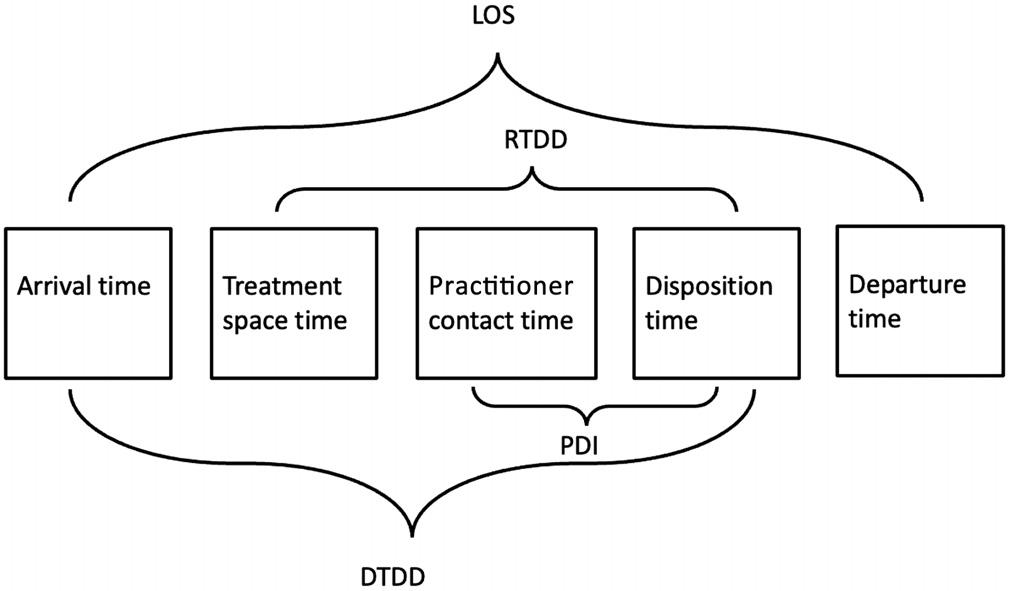
EmergencyDepartmentBenchmarkingAlliancetime stampsandintervals.
LOS,lengthofstay; DTDD,doortodispositiondecision; RTDD,room todispositiondecision; PDI,practitionerdispositioninterval.
from( 58)to73moreminutesspentintheED,withstudies clusteringreasonablywellaroundthemedianvalueof26 minutes.Atacademicdepartmentswithverylongaverage LOS,26minutesmaynotbeameaningfulincrease.These sevenstudies,withtheexceptionofthePittsetalstudy (2014),wereconductedatasingleacademicsite.32 Each study,withtheexceptionofLammersetal(2003),31 included anaveragetimemetricabovethreehours,helpingtoexplain thesmallstatisticaleffectsize.Weidentifiedthreeissueswith interpretationofclinicalmeaningfulnessoftheimpactof residentpresenceonEDefficiency.
Firstly,thevaryingmeasuresofefficiencymakesynthesis ofeffectsizeproblematic.Metricsthatincludetheinterval betweendispositionanddeparturetimeareinfluencedby boarding,whichisathroughputbottleneckthatislargely unaffectedbyresidentpresenceintheEDandservesto attenuateanydifferencesinefficiencybetweengroups.28,29,32 Theefficiencyoftheemergencyteamcaringforapatientwho spendsseveralhoursawaitinganinpatientbedispoorly reflectedinthesemetrics.
Secondly,someofthestudiesexcluded “fast-track” patients.28,33 Emergencydepartmentshaveseveralnamesfor thesesplit-flowmodels,whichallemphasizeidentifying patientswithlowerdepartmentalresourceneedswiththeaim ofexpeditingtheirworkupanddisposition.Thesearethe patientencountersinwhichefficiencyispotentiallymost subjecttothepresenceofatrainee,astheremaybeno competingthroughputbottleneckslikeimagingor laboratoryturnaroundtime.Exclusionoffast-trackpatients attenuatesmeasuredefficiencydifferences.
Thirdly,selectionandgroupallocationbiaseswere presentinvaryingdegreesoftheincludedstudies.Whenthe unitofanalysisistheindividualpatientencounter,30,32 there isahighriskofselectionbiasastheresidentsmaybe preferentiallyoptingforcomplexcases,whicharemorelikely tomeaningfullyaugmenttheirlearning.Thepresenceofa residentisthusbestviewedasaconfounder,tightly associatedwithcasecomplexity,whichisaknowndriverof LOS.41 Thislimitationisperhapsmoststronglypresentinthe Pittsetal(2014)study.32 Thisnationallyrepresentative sampleassessedLOSforpatientencountersthatincludeda residentcomparedtoencounterswithonlyanattending physician.Whiletheauthorsattemptedtolimitconfounding byadjustingforpatientfactorssuchasageandtriageacuity, thenuancesofpatientcomplexityarelikelytoescapethe simplificationofacontrolvariable.Theauthors’ suggestion that “residentsseevirtuallyallpatientsinmajorteaching EDs” appearsempiricallyuntruegiventhemultiplestudiesin ourreviewthatnotetheabsenceoflearnerinvolvementfor loweracuitypatientsinsplit-flowEDmodels.
Groupallocationbiasariseswhenthepropensityfor attendingphysicianstoworkwithresidentsislinkedto differencesinefficiencymetrics.Forexample,physiciansin educationleadership(corefaculty,assistantprogram
Table1. Studycharacteristicsgroupedbyparticipantandoutcomecategories.
Study(measure)
Efficiency – Residents
Andersonetal,201328 (TT)246visits7,689visits 58minutest 0.15[ 0.27, 0.02]K–S0.02
DeLaneyetal,201329 (LOS)
DeLaneyetal,201329 (DTDD)
153,703visits40,331visits26minutes*N/AN/AK–W <0.001
153,703visits40,331visits30minutes*N/AN/AK
Krautetal,202030 (RTDD)4,537visits3,421visits10minutes0.10[0.06,0.15]N/A0.01
Lammersetal,200331 (DTDD) N/AN/A40minutesN/AN/A t <0.001
Pittsetal,201432 (LOS)3,374visits25,808visits73minutes*N/AN/AN/A <0.05
Robinsonetal,202033 (PDI)103,871visits7,283visits18minutes0.15[0.13,0.17] t <0.001
Efficiency – Students
ChanandKass,199934 (dLOS)
DeLaneyetal,201329 (LOS)
DeLaneyetal,201329 (DTDD)
13,949visits40,331visits24minutes*N/AN/AK–W <0.001
13,949visits40,331visits15minutes*N/AN/AK–W <0.001
Ioannidesetal,201535 (LOS) 1,029,165
Smalleyetal,201436 (dLOS) 6,880visits2,188visits14minutes*N/AN/AWN/A
Efficiency – MixedTrainees
Dehonetal,201537 (LOS)377days18days2.4minutes0.07[ 0.41,0.54] t 0.28
Productivity – Residents
Bhatetal,201438 (PPH)1,935shifts2,199shifts0.12PPH0.34[0.28,0.41]
Clinkscalesetal,201639 (RVUs/patient)
Robinsonetal,202033 (PPH)
Productivity – Students
12,494visits11,560visits0.2RVUs/patient0.53[0.50,0.55]
103,871visits7,283visits0.4PPH0.21[0.19,0.24]
<0.001
Bhatetal,201438 (PPH)514shifts2,199shifts0.0PPH0.00[-0.10,0.10] t 0.99 Hilleretal,201440 (RVUs/shift) 101shifts101shifts0.13RVUs/shift0.01[ 0.27,0.28]
tDenotesdifferencesofmedians.Meanvaluesnotexplicitbutweredisplayedgraphicallyandacceptablyclosetostatedmedianvalues. *Denotesdifferencesofmedians.
TT,treatmenttime; LOS,lengthofstay; DTDD,doortodispositiontime; RTDD,roomtodispositiontime; dLOS,dischargelengthofstay; PDI,practitionerdispositioninterval; PPH,patientsperhour; RVU,relativevalueunit; t,two-tailedStudent t-test; K–S,Kolmogorov–Smirnovtest; K–W,Kruskal-Wallistest; W,Wilcoxonrank-sumtest.
directors,andprogramdirectors)wouldlikelybepulledto attendconference.Thesephysiciansasagroupmayexhibit differentpracticepatternsandefficiencytrendsthantheir colleagues.42 Thedirectionandmagnitudeofthisbiasis difficulttoguessowingtothepaucityofliteratureonthe topic.Robinsonetal(2020)didacommendablejobat controllingthisbiasbyonlyincludingdatafromattendings
with “balancedschedules” meaningthosewhoroutinely workshiftsbothwithandwithoutresidents.33 Therestofthe studiesthatusedshiftsastheunitofanalysisdonotmention orcontrolforthispossibleinteractionbetweenlearnerand attendingschedules.28,29,31
Fourstudiesassessedtheimpactofmedicalstudentson efficiencymetricsintheED.Most(4/5)showedthatstudent
Table2. Certaintyofevidenceofincludedstudies.
OutcomeEffect
Residentimpacton efficiency
Studentimpacton efficiency
Residentimpacton productivity
Studentimpacton productivity
Most(6/7)studiesshowedasmall tomoderatedecreaseinefficiency.
Most(4/5)studiesshowedasmall decreaseinefficiency.
All3studiesshowedanincreasein productivity,centeringaroundamedium effectsize.
Bothstudiesshowednoassociationwith productivity.
Numberof studiesCertaintyoftheevidence(GRADE)
7LOW 00 (duetoseriousriskofbiasandindirectness)
5LOW 00 (duetoseriousriskofbiasandindirectness)
3LOW 00 (duetoseriousriskofbiasandmoderate indirectness)
2LOW 00 (duetomoderateriskofbiasand severeindirectness)
GRADE,GradingofRecommendationsAssessment,DevelopmentandEvaluation.
presencehadastatisticallysmalldecreaseonEDefficiency, withimpactsrangingfrom( 5)to24minutesandamedian effectof14minutes.Similardifficultiesasmentionedabove precludedconclusionsontheclinicalsignificanceofthis impact.Theefficiencymeasuresgenerallyincludedboarding time,29,34–36 althoughexclusionoffast-trackpatientswasless ofathreatforthisgroup,asChanandKass(1999)and Smalleyetal(2014)focusedonlyondischargedpatients.34,36 SelectionbiaswaslikelypresentintheSmalleystudy,since themedicalstudentswerepartofaspeciallydesignated teachingservicethatonlysawpatientsinparticular treatmentrooms,presumablyinthehigher-acuityareasof theED.36
Groupallocationbiaswasrelativelywell-protected againstintheIoannidesetal(2015)studybyusinganatural experimentalblockdesignwithstudentsbeingpulled fromthedepartmenttoattendanesthesiatrainingforthelast weekofeachmonth-longrotation.35 Smalleyetaluseda similarconditionofstudentabsenceduringthelastFridayof eachrotation,duringwhichstudentstooktheirend-ofrotationexam.36 Therewouldbealessobviousconnection betweenattendingcharacteristics(ie,involvementin educationleadership)andlearnerpresenceunderthese conditionsthanwithonebasedonresidentconference timeascommonlyseeninthestudiesonresidentimpact ofEDefficiency.
Allthreestudiesthatmeasuredresidentimpacton productivityshowedamoderatetolargestatisticalincrease, withCohen d rangingfrom0.21–0.53.33,38,39 Theclinical significancecanperhapsbebestillustratedinthefollowing example,whichassumestheaverageoflevel4charting, reimbursedatthe2022rateof2.74RVUsperlevel4patient. ThePPHdifference(0.26)andRVUs/patientdifference(0.2) add0.76RVUs/hourtoanattendingphysician’ s
productivity.43 TheCentersforMedicareandMedicaid Servicesreimbursed$34.61/RVUin2022.43 Thus,a residentwouldbringanadditional$26.30/hourofrevenue fromworkRVUstotheED.Thetwostudiesonmedical studentimpactonproductivityshowednostatistically significantdifference.38,40
Lastly,Dehonetal(2015)offeredauniqueanalysis incorporatingthetotalnumberoflearnersintheED, inclusiveofbothstudentsandresidents.37 Thecorrelation approachtototalnumberoflearnersandefficiencyand productivitymetricsisinterestingbutpotentially flawedin thatthereisreasontothinkresidentandstudentpresencehas aninteractiveratherthancumulativeeffect.Thesuspicion thatresidentsmaymitigatestudentimpactsonefficiencyand productivityisreflectedinHilleretal’s(2014)observation that “residentsperformedthebulkofteachingandclinical supervision” ofmedicalstudents.40
Asummaryofthecertaintyofevidenceofincludedstudies isprovidedin Table2
Oursystematicreviewevaluated13studiesexaminingthe effectoflearnerpresenceonefficiencyandproductivityin EDs.Themajorityofthesestudies(10outof13)showed moderatetosevereriskofbias,leadingtolow-GRADE (GradingofRecommendationsAssessment,Development andEvaluation)evidenceforthefourinvestigatedoutcomes. Thisbiaswasprimarilyduetopotentialconfoundersand indirectnessofoutcomemeasures,factorswhichledusto downgradethereview’sevidencelevel.
Thelow-GRADEevidencesuggeststhatstudentsand residentscausestatisticallysmall-to-moderatedecreasesin EDefficiency,withdebatableclinicalmeaningfulness. ResidentsincreaseEDproductivitybyastatistically
andclinicallymoderateeffectsize.Studentsdonot produceastatisticallyorclinicallysignificantimpact onEDproductivity.
Wecanreviewtheimplicationsofthisreviewonthe multiplepartiesinvolvedinthedecisiontohostmedical studentsandresidentsatanemergencydepartment.
Hospitalanddepartmentaladministratorsmaycontinue tohaveconcernsaboutlearnerimpactonEDefficiency. Thisappearstobeatmostamodesteffectandcanbe reframedasanecessarycostforensuringaviable physicianpipeline.
Fromapublicpolicystandpoint,theroleoftraineesinthe inefficienciesofteachinghospitalsandincreasedcostofcare shouldcontinuetobeinvestigated.InEM,thereis24/7 bedsidesupervision,andmostresourceutilizationandall dispositiondecisionsarerunbyanattendingphysician.This mayexplainthenon-intuitivesuggestionthatEM postgraduateyear-(PGY)3residentsslowdowna departmentasmuchasinternsdo,31 possiblyduetogreater deferencetothePGY-3residentonmedicaldecisionmaking,whichincreaseslaboratoryandimaging utilization.19–21 Importantdifferenceslikelyexistbetween servicelinesintherelativecontributionoftraineesto inefficiencyanddecreasedproductivity.Whilecost-of-care differenceswerenotdirectlyaddressedbythisreview,it wouldnotappearthattraineesintheEDarealargesourceof varianceforefficiencyorproductivity.Forattending physicians,thisreviewshouldprovidereassurancethat havinglearnersonshiftwillnotnegativelyimpacttheir RVU-basedcompensation.
Medicalschoolswithoutsalariedclinicalfacultythathave built-inteachingexpectationswillneedtocontinuerecruiting communitypreceptors.Thedecisiontocompensatethese preceptorsremainscomplicated.3 Thereviewsuggeststhat attendingphysiciansbalanceteachingobligationswithout sacrificingproductivity.However,thisbalancemaybe achievedbydeferringlessurgentclinicalobligations,suchas charting,untilaftershiftend.Thiscouldcreateasignificant, unmeasuredtimecost.Futurestudiesmightinvestigatethe timespentaftershiftswhenaccommodatingtrainees,using timestampspulledfromelectronichealthrecords.
Thisreviewissubjecttocertainlimitations. Inconsistenciesinoutcomereportingprecludedmetaanalysis.Asanexample,therelativecontributionofastudy with1,935shiftsvsonewith103,871patientencountersis difficulttoreconcile,evenifstandardizedeffectsizesare available.Also,itwouldbechallengingtocombinean indirectefficiencymeasurelikeLOSwithamoredirect measurelikedoor-to-dispositiondecision.Thelearner populations’ varyingservicelinesandtraininglevelsadded anotherlayerofnuanceprecludingdirectcomparison betweenstudies.
Weidentifiedfourrepeatedthemesleadingtoanincreased riskofbias.First,themethodsofgroupallocationwereoften unclearinthestudies.Aphysician’stendencytoworkshifts withouttraineescouldrelatetotheirefficiencyor productivity.Onlytwostudiescontrolledforthis influence.33,41 Giventheethicalissuesthatwouldarisefroma randomizedexperimentaldesign,havinganatural experimentalsettingislikelythebestevidence-generating opportunitythatwillbeofferedonthetopicoftrainees’ impactonEDefficiencyandproductivity.Futureresearch shouldexplicitlyaddressorcontrolthispotentialbiasfrom groupallocation.
Second,cross-sectionaldesignsshouldcontinuetobe used.DatafromtheEmergencyDepartmentBenchmarking Alliancehaveshownaconsistent,gradualincreaseinED LOSfrom2010–2022,44 indicatingariskofmaturationbias inpre-/post-residencydesigns.31,39 Third,LOSisnota reliablemarkerofEDefficiencyasitisgreatlyinfluencedby externalfactorssuchasboardingtimes,whicharebeyondthe ED’scontrol.Futurestudiesshouldfocusonmetrics primarilyinfluencedbyEDoperations.
Fourth,theunitofanalysisshouldbeshifts,notindividual patientencounters.Thisapproachcanreducetheriskof reversecausation,whereresidentsarepreferentiallyassigned tomorecomplexpatients.Thepresenceofthisbiaswas highlightedinseveralstudies.29,30,32 Thiswouldalsocontrol forvaryingpracticesamongattendingphysiciansinwhich somemayindependentlyseelow-complexitycasesthatare felttobeunlikelytomeaningfullycontributetolearning.
The findingthatresidentsmaydecreaseEDefficiencyand onlymodestlyincreaseproductivitymaycontrastwiththe experienceofphysiciansat “resident-run” or “county” programs.Anecdotally,theseareunder-resourced departmentsthatrelyonresidentstoperformnecessary servicesthatwouldbeoffloadedtonon-physicianstaffat otherdepartments.Thesenon-RVU-generatingactivities suchasgatheringequipmentforprocedures,starting intravenouslines,andtransportingpatientswouldnotbe capturedinourstudy’sproductivitymetricsbutarecertainly necessaryandvalue-addedactivities.
ThelegalmandateofEHRimplementationaspartofthe 2009AmericanRecoveryandReinvestmentActmay challengeapplicabilityofearlierstudiessincepartofresident andstudentefficiencybenefitslikelyincludeoffloadingthe documentationburdenfromtheattendingphysician. However,thetimeincreasespentchartinganddocumenting post-EHRimplementationseemstobesmall,notwarranting theexclusionofpre-EHRstudies.45
Historically,thevastmajorityofmedicaltrainees havebeenlocatedatuniversity-associatedhospitalsthat representlarge,urban,tertiary-care,traumacenters. Thus,weexpectanysystematicreviewtobeskewedtoward thesecharacteristics.Ourreviewincluded11studies fromacademicsitesandonlyonefromacommunitysite,
whichlimitsgeneralizabilitytoEDsnotmatching thosecharacteristics.
Werecommendfutureresearchonthistopictofocuson communitytrainingsites,giventheirincreasingroleinGME training.46,47 Applying findingsfromacademicEDsto communityEDscanbemisleadingduetodifferencesin operationalcharacteristics.48 Theimpactoftraineeson efficiencyandproductivitycouldbemorepronouncedin smallercommunityEDsthatservealowerpercentageof complexpatientsanddonotemploythesplit-flowmodels commonlyusedinthestudiesincludedinourreview.
Oursystematicreviewprovideslow-GRADEevidence thatthepresenceoflearnersintheEDmaymodestly decreaseefficiency.However,thiseffectmaybeoffsetbya similarlymodestincreaseinattendingphysicianproductivity whensupervisingresidents.Medicalstudentsdonotimpact attendingphysicianproductivity.Thediscussionhighlights howtheseeffectsimpactthemultiplestakeholdersinmedical educationandoffersseveralconsiderationsforfuture researchonthistopic.
wp-content/uploads/imported-files/Recruiting-and-Maintaining-U.S. -Clinical-Training-Sites.pdf.AccessedJanuary26,2023.
4.NguyenNXandSheingoldSH.Indirectmedicaleducationand disproportionateshareadjustmentstoMedicareinpatientpayment rates. MedicareMedicaidResRev. 2011;1(4):001.04.a01.
5.MedPAC.ReporttoCongress:MedicareandtheHealthCareDelivery System.Chapter6:RevisingMedicare’sindirectmedicaleducation paymentstobetterreflectteachinghospitals’ costs.2021.Availableat: https://www.medpac.gov/wp-content/uploads/import_data/scrape_ files/docs/default-source/default-document-library/jun21_ch6_ medpac_report_to_congress_sec.pdf.AccessedApril10,2023.
6.SchünemannHJ,HigginsJP,VistGE,etal.Completing ‘summaryof findings’ tablesandgradingthecertaintyoftheevidence. In:Cochrane HandbookforSystematicReviewsofInterventions(375–402) Hoboken,NJ:JohnWiley&Sons,2019.
7.MuradMH,MustafaRA,SchünemannHJ,etal.Ratingthecertaintyin evidenceintheabsenceofasingleestimateofeffect. EvidBasedMed. 2017;22(3):85–7.
8.SterneJA,HernánMA,ReevesBC,etal.ROBINS-I:atoolforassessing riskofbiasinnon-randomisedstudiesofinterventions. BMJ. 2016;355:i4919.
9.PageMJ,McKenzieJE,BossuytPM,etal.ThePRISMA2020 statement:anupdatedguidelineforreportingsystematicreviews. BMJ. 2021;372:n71.
AddressforCorrespondence:JakeValentine,MD,Graduate MedicalEducation,22999USHwy59N,Kingwood,TX77339. Email: jvalent3@central.uh.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisresearchwassupported(inwhole orinpart)byHCAHealthcareand/oranHCAHealthcare-affiliated entity.Theviewsexpressedinthispublicationrepresentthoseofthe author(s)anddonotnecessarilyrepresenttheofficialviewsofHCA Healthcareoranyofitsaffiliatedentities.Therearenootherconflicts ofinterestorsourcesoffundingtodeclare.
Copyright:©2024Valentineetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.LundsgaardK,TolsgaardM,MortensenO,etal.Embracingmultiple stakeholderperspectivesindefiningtraineecompetence. AcadMed. 2019;94(6):838–46.
2.HexomB,TruegerNS,LeveneR,etal.Theeducationalvalueof emergencydepartmentteaching:Itisabouttime. InternEmergMed. 2017;12(2):207–12.
3.EriksonC,HamannR,LevitanT,etal.RecruitingandmaintainingU.S. clinicaltrainingjointreportofthe2013multi-disciplineclerkship/clinical trainingsitesurvey.2013.Availableat: https://paeaonline.org/
10.MaddenL,HocksteinM,FranczakM,etal.Assessmentofanovel emergencydepartment-basedcriticalcareconsultserviceinanurban Level-1traumacenter. AnnEmergMed. 2020;76(4):S81.
11.WestonV,JainSK,GottliebM,etal.Effectivenessofresident physiciansastriageliaisonprovidersinanacademicemergency department. WestJEmergMed. 2017;18(4):577–84.
12.SvirskyI,StonekingLR,GrallK,etal.Resident-initiatedadvancedtriage effectonemergencydepartmentpatient flow. JEmergMed. 2013;45(5):746–51.
13.MatsushimaK,DickinsonRM,SchaeferEW,etal.Academictimeata level1traumacenter:Noresident,noproblem? JSurgEduc. 2012;69(2):138–42.
14.OffnerP,HawkesA,MadayagR,etal.Generalsurgeryresidents improveefficiencybutnotoutcomeoftraumacare. JTrauma. 2003;55(1):14–7.
15.ZhangCS,WangL,SaxeJ.Emergencydepartmentdisposition: Dosurgicalresidentscontributetoinefficiency? AmJSurg. 2022;223(3):555–8.
16.KohanLC,NagarajanV,MillardMA,etal.Impactofaround-the-clockinhousecardiologyfellowcoverageondoor-to-balloontimeinan academicmedicalcenter. VascHealthRiskManag. 2017;13:139–42.
17.FrenchD,ZwemerFL,SchneiderS.Theeffectsoftheabsenceof emergencymedicineresidentsinanacademicemergencydepartment. AcadEmergMed. 2002;9(11):1205–10.
18.McGarryJ,KrallSP,McLaughlinT.Impactofresidentphysicianson emergencydepartmentthroughput. WestJEmergMed. 2010;11(4):333–5.
19.JadhavN,GramsK,AlweisR.CostofalearnerinpediatricED. JCommunityHospInternMedPerspect. 2019;9(2):80–5.
20.CoreyP,JadhavN,GramsK,etal.Thecostofalearnerinthepediatric emergencydepartment:acomparisonacrosstwopediatricemergency departments. PediatrEmergCare. 2022;38(12):e1688–91.
21.JamesC,HarperM,JohnstonP,etal.Effectoftraineesonlengthofstay inthepediatricemergencydepartment. AcadEmergMed. 2009;16(9):859–65.
22.SimJ,ChoiY,JeongJ.Changesinemergencydepartment performanceduringstrikeofjuniorphysiciansinKorea. EmergMedInt. 2021;2021:1786728.
23.HarveyM.Correlationofphysiciansenioritywithincreasedemergency departmentefficiencyduringaresidentdoctors’ strike. NZMedJ. 2008;121(1272):59–68.
24.SalazarA,CorbellaX,OnagaH,etal.Impactofaresidentstrikeon emergencydepartmentqualityindicatorsatanurbanteachinghospital. AcadEmergMed. 2001;8(8):804–8.
25.ThorntonVandHazellW.Juniordoctorstrikemodelofcare:reduced accessblockandpredominantfellowoftheAustralasianCollegefor EmergencyMedicinestaffingimproveemergencydepartment performance. EmergMedAustralas. 2008;20(5):425–30.
26.MichaelSS,ChurchRJ,MichaelSH,etal.Effectofresidentcomplement ontimelinessofstroketeamactivationinanacademicemergency department. JAmCollEmergPhysiciansOpen. 2022;3(1):e12643.
27.WilerJL,WelchS,PinesJ,etal.Emergencydepartmentperformance measuresupdates:Proceedingsofthe2014EmergencyDepartment BenchmarkingAllianceConsensusSummit. AcadEmergMed. 2015;22(5):542–53.
28.AndersonD,GoldenB,SilberholzJ,etal.Anempiricalanalysisofthe effectofresidentsonemergencydepartmenttreatmenttimes. IISE TransHealthcSystEng. 2013;3(3):171–80.
29.DeLaneyM,ZimmermanK,StroutT,etal.Theeffectofmedical studentsandresidentsonmeasuresofefficiencyandtimelinessinan academicmedicalcenteremergencydepartment. AcadMed. 2013;88(11):1723–31.
30.KrautAS,SheehyL,SchnappBH,etal.Effectofresidentphysiciansina supervisoryroleonefficiencyintheemergencydepartment. WestJ EmergMed. 2020;21(5):1266–9.
31.LammersRL,RoigerM,RiceL,etal.Theeffectofanewemergency medicineresidencyprogramonpatientlengthofstayinacommunity hospitalemergencydepartment. AcadEmergMed. 2003;10(7):725–30.
32.PittsSR,MorganSR,SchragerJD,etal.Emergencydepartment resourceusebysupervisedresidentsvsattendingphysiciansalone. JAMA. 2014;312(22):2394–400.
33.RobinsonRD,DibS,MclartyD,etal.Productivity,efficiency,andoverall performancecomparisonsbetweenattendingsworkingsoloversus attendingsworkingwithresidentsstaffingmodelsinanemergency department:alarge-scaleretrospectiveobservationalstudy. PLoS ONE. 2020;15(2):e0228719.
34.ChanLandKassLE.ImpactofmedicalstudentpreceptorshiponED patientthroughputtime. AmJEmergMed. 1999;17(1):41–3.
35.IoannidesKL,MamtaniM,ShoferFS,etal.Medicalstudentsinthe emergencydepartmentandpatientlengthofstay. JAMA. 2015;314(22):2411–3.
36.SmalleyCM,JacquetGA,SandeMK,etal.Impactofateachingservice onemergencydepartmentthroughput. WestJEmergMed. 2014;15(2):165–9.
37.DehonE,McLemoreG,McKenzieLK.Impactoftraineesonlengthof stayintheemergencydepartmentatanacademicmedicalcenter. South MedJ. 2015;108(5):245–8.
38.BhatR,DubinJ,MaloyK.Impactoflearnersonemergency medicineattendingphysicianproductivity. WestJEmergMed. 2014;15(1):41–4.
39.ClinkscalesJD,FesmireFM,HenningsJR,etal.Theeffectof emergencymedicineresidentsonclinicalefficiencyandstaffing requirements. AcadEmergMed. 2016;23(1):78–82.
40.HillerK,ViscusiC,BeskindD,etal.Costofanactingintern:clinical productivityintheacademicemergencydepartment. JEmergMed. 2014;47(2):216–22.
41.HockerMB,GerardoCJ,TheilingBJ,etal.NHAMCSvalidationof emergencyseverityindexasanindicatorofemergencydepartment resourceutilization. WestJEmergMed. 2018;19(5):855–62.
42.LiC,SyueY,TsaiT,etal.Theimpactofemergencyphysicianseniority onclinicalefficiency,emergencydepartmentresourceuse,patient outcomes,anddispositionaccuracy. Medicine(Baltimore). 2016;95(6):e2706.
43.DavisJ.CMSissuesthe2023physicianfeescheduleproposedreg. 2022.Availableat: https://www.acep.org/federal-advocacy/ federal-advocacy-overview/regs–eggs/regs–eggs-articles/ regs–eggs july–8–2022.AccessedNovember11,2023.
44.AugustineJ.A firstlookatemergencydepartmentdatafor2022.2023. Availableat: https://www.acepnow.com/article/a-first-look-atemergency-department-data-for-2022/.Accessed:May4,2023.
45.Calder-SprackmanS,ClaphamG,KandiahT,etal.Theimpactof adoptionofanelectronichealthrecordonemergencyphysicianwork:a timemotionstudy. JAmCollEmergPhysiciansOpen. 2021;2(1):e12362.
46.KadakiaKT,ZhengJ,BruchJD,etal.Comparisonofthe financialand operationalcharacteristicsoffor-profitandnonprofithospitalsreceiving federalgraduatemedicaleducationpayments,2011–2020. JAMA. 2023;329(2):173–5.
47.LassnerJW,AhnJ,SinghA,etal.Growthoffor-profitinvolvementin emergencymedicinegraduatemedicaleducationandassociation betweenfor-profitaffiliationandresidentsalary. AEMEducTrain. 2022;6(4):e10786.
48.ReznekMA,MichaelSS,HarbertsonCA,etal.Clinicaloperationsof academicversusnon-academicemergencydepartments:Adescriptive comparisonoftwolargeemergencydepartmentoperationssurveys. BMCEmergMed. 2019;19(1):72.
RameshKarra,MD*
AmberD.Rice,MD*†
AileenHardcastle,BS*
JustinV.Lara,BS*
AdrienneHollen,MS*
MelodyGlenn,MD*†
RachelMunn,DO*
PhilippHannan,MD*
BrittanyArcaris,MD*
DanielDerksen,MD*†
DanielW.Spaite,MD*†
JoshuaB.Gaither,MD*†
SectionEditor:ScottGoldstein,DO
*TheUniversityofArizona,CollegeofMedicine,DepartmentofEmergencyMedicine, Tucson,Arizona
† TheUniversityofArizona,CollegeofMedicine,DepartmentofEmergencyMedicine, Phoenix,Arizona
Submissionhistory:SubmittedAugust11,2023;RevisionreceivedApril23,2024;AcceptedJune17,2024
ElectronicallypublishedAugust27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18427
Background: Telemedicineremainsanunderusedtoolinruralemergencymedicalservces(EMS) systems.Ruralemergencymedicaltechnicians(EMT)andparamedicsciteconcernsthattelemedicine couldincreaseAdvancedLifeSupport(ALS)transports,extendon-scenetimes,andfacechallenges relatedtoconnectivityasbarrierstoimplementation.Ouraiminthisprojectwastoimplementa telemedicinesysteminaruralEMSsettingandassesstheimpactoftelemedicineonEMSmanagement ofpatientswithchestpainwhileevaluatingsomeoftheperceivedbarriers.
Methods: Thisstudywasamixed-methods,retrospectivereviewofqualityassurancedatacollected priortoandafterimplementationofatelemedicineprogramtargetingpatientswithchestpain.We comparedquantitativedatafromthe12-monthpre-implementationphasetodatafrom15monthspostimplementation.Patientswereincludediftheyhadachiefcomplaintofchestpainora12-lead electrocardiogramhadbeenobtained.TheprimaryoutcomewastherateofALStransportbeforeand afterprogramimplementation.SecondaryoutcomesincludedEMScallresponsetimesandEMSagency performanceonqualityimprovementbenchmarks.Qualitativedatawerealsocollectedaftereach telemedicineencountertoevaluateparamedic/EMTandEMSphysicianperceptionofcallquality.
Results: ThetelemedicinepilotprojectwasimplementedinSeptember2020.Overall,therewere58 successfulencounters.Forthisanalysis,weincluded38patientsinboththepre-implementationperiod (September9,2019–September10,2020)andthepost-implementationperiod(September11, 2020–December5,2021).Amongthispopulation,theALStransportratewas42%beforeand45%after implementation(oddsratio1.11;95%confidenceinterval0.45–2.76).TheEMSmedianout-of-service timeswere47minutesbefore,and33minutesafter(P = 0.07).Overall,64%ofparamedics/EMTsand 89%ofEMSphysiciansratedthetelemedicinecallqualityas “good.”
Conclusion: InthisruralEMSsystem,atelehealthplatformwassuccessfullyusedtoconnect paramedics/EMTstoboard-certifiedEMSphysiciansovera15-monthperiod.Telemedicineusedidnot alterratesofALStransportsanddidnotincreaseon-scenetime.Themajorityofparamedics/EMTs andEMSphysiciansratedthequalityofthetelemedicineconnectionas “good.” [WestJEmergMed. 2024;25(5)777–783.]
Telemedicinehasimprovedhealthcaredeliveryand outcomesforruralpopulations.1–5 Asruralcommunities acrosstheUnitedStates(US)struggletorecruit,train,and retainparamedicsandemergencymedicaltechnicians (EMT),thesecommuitiesareleftwithashortageofqualified individualstoprovidehealthcareandanincreasedcostto deliverthatcare.6–9 Telemedicineforemergencymedical services(EMS)maybeparticularlyusefulinrural communitiesthatfaceparamedicshortages.2–4
Withparamedicshortages,manyruralEMSagenciesoften dependonaloneparamedictoservetheircommunity.Inthis setting,whentwo911callsoverlap,theruralcommunityisleft withoutAdvancedLifeSupport(ALS)coverage.Thisgapin ALSserviceisparticularlyimportantinthecareofpatients withchestpain.Forexample,assumeanALStransportis neededinaruralcommunityandthesoleparamedicistaken outoftheserviceareaforhours.Thenassumethatduringthat sameperiod,asecond911callforchestpainoccurs.Forthat secondcall,thecommunityisleftwithonlyaBasicLife Support(BLS)responderwhocannotinterpret electrocardiograms(ECG).Inthisscenarioeitherahelicopter iscalled,increasingcostofservicedelivery,orthepatientis transportedemergentlybyBLSresponders,increasingriskto boththeEMTsandthepatient.Clearly,inthisscenariothere isthepotentialforatelemedicinephysiciantoreducesomeof theburdenplacedonresource-limitedcommunities.
However,wefoundthatsomeEMSsystemsarereluctant toimplementtheseprogramsforavarietyofreasons.
Paramedicssharedconcernsthataphysician’spolicyof mandatingALStransportforallpatientsmightlowerthe physician’sliabilityattheexpenseofincreasingthenumber ofALS-requiredtransports.Otherswereconcernedthat performingatelemedicinevisitwouldtakeasignificant amountoftime,thusfurtherreducingavailabilityofALS resources.Finally,therewerealsosomeconcernsaboutthe lackofaccesstocellulardataandwhetherthetelemedical solutionwouldbeavailablewhenneeded.
Thesepotentialbarriersareimportanttoevaluatepriorto widespreadimplementationofEMStelemedicinesolutions. Toevaluatethebenefitsandpotentialrisks,aruralEMS telemedicinepilotprojectwasimplementedtargetingpatients withchestpain.Throughoutthatpilotproject,program partnerscollectedqualityimprovement(QI)datatoensure thatthetelemedicineprogramwasfunctioningasdesigned anddidnotadverselyaffectsystemperformance.Ouraimin thisanalysiswastoevaluatequalitydatapointsandassessthe impactoftelemedicineonEMSmanagementofpatientswith chestpain;wealsoevaluatedperceivedbarriersbyEMSstaff.
Thisstudywasaretrospectivereviewofdatacollectedbya singleEMSagencythroughouttheproject.Wecollecteddata
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Telemedicineremainsunderusedinrural EMSsystems,withconcernsaboutincreasing ALStransports,extendingon-scenetimes, andconnectivityissues.
Whatwastheresearchquestion?
Howdoesimplementingtelemedicineinrural EMSaffectpatientmanagementandsystem performanceforchestpaincases?
Whatwasthemajor findingofthestudy?
TelemedicinedidnotchangeALStransport rates(42vs.45%,OR1.11,95%CI 0.45 – 2.76)orincreaseon-scenetimes(47vs. 33minutes,p = 0.07),and64%ofEMSstaff ratedcallqualitygood.
Howdoesthisimprovepopulationhealth?
TelemedicineallowsruralEMStomaintain ALSavailability,reducingstrainonlimited resourcesandpotentiallyimprovingoutcomes forchestpainpatients.
fortheprimarypurposeofQIandevaluationofthe telemedicineplatform.STROBEmethodologywasused.10 Weusedtwodatasetsforthisretrospectivereview.Firstly,we lookedatquantitativedatafromaprehospitalQIdatasetin whicha12-leadECGwasperformed.Secondly,weanalyzed theprimarychiefcomplaintofchestpain.CasesfromthatQI datasetwereincludedinthisanalysisiftheyoccurredduring the12-monthpre-implementationstudyperiodorthe 15-monthpost-implementationperiod.Wealsoevaluated qualitativedatafromasecondQIdatasetthatwascompleted byparamedics/EMTsandEMSphysiciansaftereach telemedicineplatformuse.Thatdatasetcontainedthe paramedic/EMTandEMSphysicians’ subjectiveevaluation ofthetelemedicinecallquality.
TheAzQualityprojectservedasapilotinitiativedesigned toestablishatelemedicineservice,enablingruralparamedics andEMTstoaccessurbanmedicalresourcesduring emergencycareforpatientsexperiencingchestpainwho dialed911.TheEMStelemedicinepilotwasimplementedat asingle,ruralEMSagency.Atthetimeofintroductionand duringnewemployeeorientation,bothEMTsand paramedicsweretaughthowtousethetelemedicinesystem viaabrieflectureandahands-onpracticesession.After
implementation,EMTsandparamedicswereinstructedto usetheTelemedicinetooltocontactboard-certifiedEMS physiciansforpatientsexperiencingchestpain24hoursa day,7daysaweek.Theycouldalsousethetoolforother encountersasneeded.Telemedicineserviceswereprovided byboard-certifiedEMSphysiciansfromasingle,largeEMS physiciangroup.
Thetelemedicinepilotprogramwasimplementedbythe Sonoita-ElginFireDistrict,aruralEMSagencyandsole911 respondingagencyforalarge,geographicallydiverseareain SoutheasternArizona.TheGD “e-Bridge” communication platform(GeneralDevicesLLC,Ridgefield,NJ)was selectedbytheprogramleadershipgroupasthetelemedicine platformforthispilotprogram.Thissoftwareallowed paramedics/EMTstoconductthetelemedicinevisitaswellas transmitphotosofECGsorotherclinicaldatatotheEMS physicians.Thee-Bridgesystemwasoperatedon commerciallyavailablesmartphones.
Priortoandduringthepilotproject,whenavailable, paramedicsrespondedtoall911calls.Whenunavailable, BLScrewswouldrespondalone.Bothparamedicsand EMTswereaskedtousethetelemedicinesystemanytime theyencounteredapatientwithchestpain.AfterEMTor paramedicpatientassessment,theEMSphysicianwas contactedviae-Bridgeandgivenabriefpatientpresentation. TheEMSphysicianhadaccesstothepatient’svitalsignsand 12-leadECGthroughthee-Bridgesoftware.Afterabrief interactionwiththepatient,thephysicianrisk-stratified patientsaslow,moderate,orhighriskforadverseevents duringtransporttodefinitivecare.Theparamedics/EMTs werethengivenonlinemedicaldirectionforground transportbyBLSforlow-riskpatients,ALSground transportformoderate-riskpatientsandhelicopterEMS transport(HEMS)ofpatientswhowerefelttobeathighrisk foradverseeventsduringtransport.
Theprimaryoutcomeofthisretrospectivereviewwasthe rateofBLS,ALS,andHEMStransport.Secondary outcomes(Table1)includedEMSsystemservicedelivery timesandsubjectiveevaluationofhowwelltheinteraction
went(good,fair,poor).TheEMSservicedeliverytimeswere collectedfromEMSagencycomputer-aideddispatch systems.Subjectivedataontheoverallsystemperformance andtelemedicineplatformcallqualitywerecollectedand managedusingResearchElectronicDataCapture (REDCap)toolshostedattheUniversityofArizona. REDCapisasecure,web-basedsoftwareplatform.11,12 Asurveywasalsolaunchedimmediatelyaftereach telemedicineencounter.Basiccalldata(dataandtime)was thenusedtolinkthesubjectivetelemedicineplatform evaluationtoEMScalldata.
TheEMSagencyanditsmedicaldirectorprovided deidentifiedQIdataforthepurposeofreviewforthis analysis.Simpledescriptivestatisticssummarizedtheresults. TheUniversityofArizonaInstitutionalReviewBoard approvedthereviewofthisproject’sQIdataanalysisand publication.TheRuralHealthEMSFlexSupplementgrant fromthefederalHealthResourcesandServices Administration(HRSA-19-095)fundedthisproject. Fundingwasusedforprojecttraining,implementationand QI,butnotforreportingontheproject.Thefundingagency wasnotinvolvedin1)designingorconductingthestudy; 2)collecting,managing,analyzing,orinterpretatingthe data;3)preparing,reviewing,orapprovingthemanuscript; or4)decidingtosubmitthemanuscriptforpublication.
Thetelemedicinepilotprogramwasinitiatedon September10,2020.Therewere58casesforwhichthe telemedicineplatformwasused.Qualityimprovementdata forpatientswithchestpainorforwhoma12-leadECGhad beenobtainedwereanalyzed12monthspriortotelemedicine implementation(September9,2019–September10,2020), and15monthsafterimplementation(September11,2020–December5,2021).Duringthepre-implementationperiod, theEMSagencyhadatotalof326medicalcalls.Duringthe post-implementationperiod,therewere411calls.Therewere
Table1. Secondaryoutcomesinstudyoftelemedicineuseby firstrespondersinruralArizona.
SecondaryoutcomeDefinition
Totalunitout-of-servicetimeTimefromdispatchtowhenthetransportingunitbecomesavailable. ResponsetimeTheintervalfromdispatchtoarrivalonscene.
On-scenetimeDurationfromarrivalonscenetoeithertheinitiationoftransportorthepointatwhichthepatient refusestransportortheunitbecomesavailablewithouttransport.
TransporttimeTimefromtheinitiationoftransporttowhentheunitisagainavailable. Responder/clinicianexperienceSubjectiveexperienceofparamedics/EMTsandEMSphysiciansusingthetelemedicinesystem ratesaspoor,fair,orgood.
EMT,emergencymedicaltechnician; EMS,emergencymedicalservices.
Table2. Demographicsandchestpaincallqualityimprovementbenchmarkperformance. Pre-implementationPost-implementation
Numberof911calls3838
P-value(p)oroddsratio(OR)with 95%confidenceinterval(95%CI)
Meanage7275 P = 0.34
Gender,female39%(n = 15)53%(n = 20)1.70(0.69–4.24)
Ethnicity
%White82%(n = 31)74%(n = 28)0.63(0.21–1.89)
%Non-White11%(n = 4)24%(n = 9)4.02(1.09–14.84)
%Unknown8%(n = 3)3%(n = 1)0.31(0.03–3.09)
Benchmarkperformance
3-leadacquired100%(n = 38)97%(n = 37)0.33(0.01–8.23)
12-leadacquired97%(n = 37)97%(n = 37)1.00(0.06–16.59)
Aspirinadministered45%(n = 17)42%(n = 16)1.11(0.45–2.76)
Nitroglycerinadministered21%(n = 11)18%(n = 7)1.80(0.61–5.30)
O2 administered37%(n = 14)37%(n = 14)1.00(0.40–2.48)
Primaryimpression
Chestpain76%(n = 29)79%(n = 30)0.91(0.29–2.82)
Palpitations11%(n= 4)13%(n = 5)1.29(0.32–5.22)
Difficultybreathing5%(n = 2)3%(n = 1)2.06(0.18–23.68)
Hypertension5%(n = 2)3%(n = 1)2.06(0.18–23.68)
Abdominalpain3%(n = 1)3%(n = 1)1.00(0.06–16.59)
O2,oxygen.
38chestpaincasesinthepre-implementationQIdatasetand 38casesduringthepost-implementationperiod.
Afterimplementationofthetelemedicineprogram,24 (63%)patientseligiblefortelemedicineconsultationreceived telemedicineservicesinrealtime,comparedtotwo(5%) patientsinthepre-implementationperiod.Preimplementationpatientsreceivedreal-timeonlinemedical directionbyeitherphoneorradio.Duringtheentire 15-monthproject,paramedics/EMTsusedthetelemedicine system58times.Outsidetheprimaryuseforpatientswith chestpain,otherusesincludedvariouscomplicatedmedical andmedicolegalsituationsinwhichtheparamedic/EMT wouldhavenormallycalledbyphoneorradioforonline medicaldirection.
Thedemographicandqualitybenchmarkdatacollected aspartofthepilotprogramisillustratedin Table2.The
pre-implementationchestpainpatientmeanagewasslightly lowerat72yearsold(interquartilerange[IQR]55–80)than thepost-implementationpatientsmeanof75(IQR55–80). Thepercentofnon-Whiteethnicity(identifiedbyparamedic) increasedfrom11%inthepre-implementaioncohortto24% inthepost-implementationcohort.TheEMSagency medicationadministrationratesandECGacquisitionrates wereessentiallythesame.
Overall,therewasaslightreductioninBLStransportsand slightincreaseinALStransports,althoughthesedidnot achievestatisticalsignificance(see Table3).Therewasalsoa non-significantincreaseinHEMStransportratesinthe implementationgroup.Lastly,therewasanon-significant reductioninpatientrefusal.
Table3. Dispositionofpatientsincludedinthechestpainqualityimprovementdataset.
,BasicLifeSupport; ALS,AdvancedLifeSupport; HEMS,helicopteremergencymedicalservice; CI,confidenceinterval.
TheEMSagencyresponseandtransporttimesdidnot changesignificantlyfollowingimplementation(see Table4). Medianout-of-servicetimewas127minutes(IQR49–172) beforeand95minutes(IQR52–159)afterimplementation. Thistotalout-of-serviceintervalincludedamedianresponse timeof11minutes(IRQ1–19)inthepre-implementation cohortand13minutes(IQR7–16)post-implementation. Medianon-scenetimewas27minutes(IQR21–61)inthe pre-implementationgroupand28minutes(IQR20–29) post-implementation.Amongthosepatientswhowere transported,mediantransporttimewas124minutes (IQR49–172)beforeand90minutes(IQR14–141) afterimplementation.
Followingimplementation,QIdatawerecollectedfrom thecaller/callrecipientsfor35of58(60%)calls.Inpost-call surveyscompletedbyparamedics/EMTs,thecallqualitywas notedtobe “good” or “fair” in86%ofthecalls.TheEMS physiciansjudged98%ofthecallstobe “good” or “fair.” Connectivityissueswereidentifiedasconcernsmoreoftenby paramedics/EMTsthanbyEMSphysicians(see Table5).
WhilelargerEMSagencieshaveadoptedtelemedicine servicestoimprovethebreadthofservicesprovidedtotheir communities(eg,MDAlly,ETHANproject),13–15 rural EMSagencieshavebeenslowertoadopttheseservicesdueto
Table5. Emergencymedicalservicesresponderandphysician subjectiveevaluationoftelemedicinecallquality.
Paramedics/EMTs, percent(number)
EMSphysicians, percent(number)
Completedsurveys62%(36)60%(35) Callquality
Good64%(23)89%(31)
Fair22%(8)9%(3)
Poor14%(5)3%(1)
Connectivityissue
Anyissue64%(23)14%(5)
Poorcellsignal6%(2)3%(1)
Laggingvideo6%(2)6%(2)
Poorsound3%(1)0%(0)
Missedcall6%(2)6%(2)
Other19%(7)0%(0)
EMS,emergencymedicalservice; EMT,emergency medicaltechnician.
limitedaccesstohigh-qualitytelecommunicationsystems andlowutilizationrates.16,17 Increasingly,platformssuchas AT&T’ s “FirstNet” andVerizon’ s “Frontline” havebecome moreaccessibletoruralEMSsystems.18,19 Thesesystems providehigh-speeddataservicesandprioritize firstrespondercommunicationsintimesofhighsystem usage.17,20,21 WiththesetoolsnowavailabletoruralEMS agencies,itisimportanttoevaluatetheimpactthat telemedicineprogramshaveonthesesystems.
Inthisretrospectivereview,aruralEMStelemedicine systemwasused58timesduringthe15-monthpilotproject forpatientswithavarietyofout-of-hospitalmedical emergencies.Overall,thetelemedicinesystemfunctioned wellwith89%ofEMSphysiciansand65%ofparamedics/ EMTsratingthetechnicalqualityofthetelemedicine encounteras “good.” Ofnote,theuseofanyformofonline medicaldirectionincreaseddramaticallyto63%inthepostimplementationphaseincomparisonto5%inthepreimplementationphase.
Ourprimarygoalinthisstudywastoevaluatetheimpact oftelemedicineserviceonthecareofpatientswithchestpain anddeterminewhethertelemedicinemightchangemodeof transport(BLSvsALSvsHEMS)totheclosesthospitalwith percutaneousinterventioncapabilities.Theultimategoal wastoallowALSresponderstostayinthecommunityand increasetheamountoftimeALSservicewasavailable.In thisretrospectiveanalysis,wefoundnostatistically significantdifferencedemonstratedintheBLS/ALS transportratesafterthetelemedicineprogramwas implementeddespiteagoalofincreasingBLStransports. Thereareseveralpossiblereasonsthatnochangeintransport rateswasobserved.Primarily,thesmallpatient-samplesize
bothbeforeandaftertheinterventionlimitstheabilityto detectachange.Moreover,theperiodfollowingthe interventioncoincidedwiththeonsetoftheCOVID-19 pandemic,aneventthatlikelyincreasedpatientacuitylevels aswellastheutilizationofHEMStransport,giventhe heightenedconcernovervirustransmission.Inthiscontext, groundambulancetransportforlongdistancesmayhave beenconsideredlesssafecomparedtoHEMS,duetothe perceivedincreasedriskofCOVID-19exposure,asground transporttimesaremuchlongerthanHEMStransporttimes.
Duringimplementation,paramedics/EMTsvoiced severalconcernsaboutusingtelemedicineintheruralEMS setting.Theseincludedtheconcernthatcontactinga physicianviathetelemedicineplatformwouldincreasetheir on-scenetimeandoverallout-of-servicetimes.Inthissmall cohort,theEMSsystemon-scenetimesandout-of-service timeswerenotincreasedbutrathertrendedtowardbeing shorter.Twofactorslikelycontributedtothis finding.First, withmultiplerespondersonsceneformost911responses, oneteammemberwasabletodiscussthecasewitha physicianwhiletherestoftheteamcontinuedtoprovide patientcare.Second,althoughnotmeasuredaspartofthis project,telemedicinecalldurationseemedtobeverybrief (1–2minutes)andlikelythisshortencounterdidnot significantlychangearelativelylongerEMSon-scenetime.
Thequalityoftelemedicinecommunicationwasaconcern forruralparamedics/EMTs.Inthisretrospectivereviewwe foundthatself-reportedtelemedicinesystemperformance wasmostlyreportedasgood.Paramedics/EMTsweremore likelytohaveconcernsaboutthetelemedicinesystemthan weretheEMSphysicians.Systemperformancecouldhave beenworseintheruralsettingduetolimiteddatatransfer;in otherwords,cellularservicewasmorelikelytobepoorinthe ruralthanurbansetting.However,ifthathadbeenthecase, onewouldexpectbothpartiestohavethesameissue.Itis alsopossiblethatwithalargeEMSusergroupandasmall EMSphysicianusergroup,theEMSphysiciansweresimply morecomfortableusingtheplatformandexperiencedfewer technicalissues.
Themajorityoftelemedicineconcernsexpressedby paramedics/EMTs,andEMSphysicianswerelaggingvideo andpoorcellsignal.Therewereseveninstancesinwhich paramedics/EMTslisted “other” issueswiththeplatform, butfurtherinformationwasnotavailable.Itwouldbe expectedthattherewouldbemoretelemedicinetechnical issuesontheparamedic/EMTsideinruralareasthanonthe EMSphysiciansidewherephysiciantookcallsinanurban, academiccenter.
Limitationsincludedthedatacollectionand implementationofthetelemedicinepilotprojectatasingle EMSagency.Additionally,thisanalysisreliedonretrospective reviewofdatacollectedforthepurposeofQI.Thesetwo
factorsintroduceboththestrongpossibilityofobserver biasandreportingbias.Also,thesmallnumberofencounters limitstatisticalanalysisandsignificance.Itispossible thatnotallchestpainpatientswereincludedintheQI datasetandmissingorincludedpatientscreatedan inclusionbias.
Thepost-interventionstudyperiodcoincidedwiththe COVID-19pandemic.Themassivepsycho-socialchangesthat occurredduringthisperiodalmostcertainlyimpactedthe communityinwhichthispilotprogramwasconducted. Unfortunately,theimpactofthepandemiconthisdatasetis unknown;however,theunfortunatetiminglikelyintroduceda confounderintoourresults.Finally,theEMSagency participatinginthisprojectwashighlyengagedandmotivated, asdemonstratedbyhighperformanceonEMSbenchmarks.It ispossiblethatitwasdifficulttodetectachangeinsystem performanceduetoboththelowcallvolumeandthehighqualitypatientcarealreadyprovidedbytheEMSagency.
InthisruralEMSsystem,atelehealthplatformwas successfullyusedtoconnectparamedics/EMTstoboardcertifiedEMSphysiciansovera15-monthperiodfor58 patients.Amongthosepatientswithchestpain,theuseof telemedicinedidnotresultinanychangeintherateofALS transportsorincreaseon-scenetimes.Overall,paramedics/ EMTsandEMSphysiciansratedthequalityofthe telemedicineconnectionasgood.Futurestudiescould expanduponthisworkbyexploringlargerpatient populationsanddiverseclinicalconditionstofurther establishtheefficacyoftelemedicineinruralEMSsettings. Additionally,examininglong-termpatientoutcomesand costeffectivenesscouldprovidemoreinsightintothe sustainedimpactoftelehealthinterventionsonrural emergencycare.
AddressforCorrespondence:RameshKarra,MD,TheUniversityof Arizona,1501NCampbellAve.Tucson,AZ,85724.Email: rkarra@ aemrc.arizona.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Portionsofthisworkweresupportedby theHealthResourcesandServiceAdministration(HRSA)Medicare RuralHospitalFlexibilityProgram – EmergencyMedicalServices Supplement;ArizonaRuralEMSAdvancedTelemedicine DemonstrationInitiative(AzREADI);HRSA-19-095.Thereareno otherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Karraetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.TsouC,RobinsonS,BoydJ,etal.Effectivenessoftelehealthinrural andremoteemergencydepartments:systematicreview. JMedInternet Res. 2021;23(11):e30632.
2.ButznerM.Telehealthinterventionsandoutcomesacrossrural communitiesintheUnitedStates:narrativereview. JMedInternetRes. 2021;23(8):e29575.
3.HaydenEM,DavisC,ClarkS,etal.Telehealthinemergencymedicine: aconsensusconferencetomaptheintersectionoftelehealthand emergencymedicine. AcadEmergMed. 2021;28(12):1452–74.
4.TottenAM,WomackDM,GriffinJC,etal.Telehealth-guidedprovider-toprovidercommunicationtoimproveruralhealth:asystematicreview. J TelemedTelecare. 2022:1357633x221139892.
5.TottenA,WomackDM,McDonaghMS,etal.Improvingruralhealth throughtelehealth-guidedprovider-to-providercommunication. NationalLibaryofMedicine. 2022.Availableat: https://doi.org/10. 23970/ahrqepccer254.AccessedFebruary5,2024.
6.ChapmanSA,CroweRP,BentleyMA.Recruitmentandretentionofnew emergencymedicaltechnician(EMT)-basicsandparamedics. Prehosp DisasterMed. 2016;31(S1):S70–86.
7.AmericanAmbulanceAssociationStaff.Congressionalletteronthe EMSworkforceshortage.2021.Availbleat: https://ambulance.org/ 2021/10/04/workforceshortage/.AccessedAugust11,2023.
8.SunnucksM.Searchingforanswers:shortageofparamedics,EMTs confrontsmalltowns,ruralareasacrossU.S. HeraldandNews. 2023. https://www.heraldandnews.com/news/searching-for-answersshortage-of-paramedics-emts-confront-small-towns-rural-areasacross-u-s/article_433c9c02-b3b7-11ed-a7b1-734cab17fa7f.html AccessedJuly14,2023.
9.ChuC,CramP,PangA,etal.Ruraltelemedicineusebeforeandduring theCOVID-19pandemic:repeatedcross-sectionalstudy. JMed InternetRes. 2021;23(4):e26960.
10.VonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. JClinEpidemiol. 2008;61(4):344–9.
11.HarrisPA,TaylorR,MinorBL,etal.TheREDCapconsortium:building aninternationalcommunityofsoftwareplatformpartners. JBiomed Inform. 2019;95:103208.
12.HarrisPA,TaylorR,ThielkeR,etal.Researchelectronicdatacapture (REDCap)–ametadata-drivenmethodologyandworkflowprocessfor providingtranslationalresearchinformaticssupport. JBiomedInform. 2009;42(2):377–81.
13.LangabeerJR2nd,GonzalezM,AlqusairiD,etal.Telehealth-enabled emergencymedicalservicesprogramreducesambulancetransportto urbanemergencydepartments. WestJEmergMed. 2016;17(6):713–20.
14.Champagne-LangabeerT,LangabeerJR,RobertsKE,etal.Telehealth impactonprimarycarerelatedambulancetransports. PrehospEmerg Care. 2019;23(5):712–7.
15.LangabeerJR2nd,Champagne-LangabeerT,AlqusairiD,etal.Costbenefitanalysisoftelehealthinpre-hospitalcare. JTelemedTelecare. 2017;23(8):747–51.
16.JacobsonCL,BasnetS,BhattA,etal.Emergencymedicaldispatcher trainingasastrategytoimprovepre-hospitalcareinlow-and middle-incomecountries:thecasestudyofNepal. IntJEmergMed. 2021;14(1):28.
17.PewResearchCenter.Internet/broadbandfactsheet.2021.Available at: https://www.pewresearch.org/internet/fact-sheet/internetbroadband/.AccessedJuly14,2023.
18.CarelessJ.HowFirstNetwillbroadencommunications.Thewireless broadbandnetworkwillconnectpolice, fireandEMSthroughmobile devices. EMSWorld. 2015;44(7):36–7.
19.WoodringM,WheelerD,SawyerME,etal.Apartnershipbetweenrural EMSandAT&TFirstNettoprovidetele-emergencycare. JHealthCare PoorUnderserved. 2022;33(4s):180–6.
20.HeZ,QinX,RengerR,etal.Usingspatialregressionmethodsto evaluateruralemergencymedicalservices(EMS). AmJEmergMed. 2019;37(9):1633–42.
21.MagantyA,ByrnesME,HammM,etal.Barrierstoruralhealthcarefrom theproviderperspective. RuralRemoteHealth. 2023;23(2):7769.
AndreaRoche,BS‡
EvanWatkins,BS,NRP*
AndrewPettit,BS*
JacobSlagle,BSME*
IsainZapata,PhD§
AndrewSeefeld,MD†
NenaLundgreenMason,PhD*
SectionEditor:ScottGoldstein,DO
*DartmouthCollege,GeiselSchoolofMedicine,DepartmentofMedicalEducation, Hanover,NewHampshire
† SpeareMemorialHospital,DepartmentofEmergencyMedicine,Plymouth, NewHampshire
‡ NewEnglandCollegeofOsteopathicMedicine,Biddeford,Maine § RockyVistaUniversity,CollegeofOsteopathicMedicine,Englewood,Colorado
Submissionhistory:SubmittedAugust21,2023;RevisionreceivedMarch8,2024;AcceptedMarch22,2024
ElectronicallypublishedJune28,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18439
Introduction: Whenusedappropriately,focusedlimited-scopeultrasoundexamscouldpotentially provideparamedicswithaccurateandactionablediagnosticinformationtoguideprehospitaldecisionmaking.Inthisstudyweaimedtoinvestigatetheimpactofa13-hourprehospitalultrasoundtraining courseonthesimulatedclinicaldecision-makingofparamedicsaswellastheirultrasoundskills, knowledge,andself-confidence.
Methods: Weevaluatedtheultrasoundcompetenceof31participantsusingpost-coursewrittenand practicalassessments.Writtenclinicaldecisionscenarioswereadministeredpre-andpost-training. Post-trainingscenariosincludedanuninterpretedultrasoundcliptoaiddecision-making.Scenarios includedextendedfocusedassessmentwithsonographyintrauma,pulmonaryexam,andfocused echocardiographycombinedwithcarotidpulsecheckexams.Correctanswerstoscenariosweredefined asthoseselectedbyaveteranemergencyphysician.Participantsalsoindicatedtheirconfidenceineach oftheirdecisionsusingaLikertscale.
Results: Trainingyieldedastatisticallysignificantincreaseinbothmeanscenarioscore(35.5% absoluteincrease)andmeanparticipantself-confidence(15.8%relativeincrease),acrossallexam/ decisiontypesassessed(P ≤ 0.001).Thefocusedpulmonaryexamyieldedthelargestincreaseinboth meanscoreimprovement(59.7%absoluteincrease)andparamedicconfidenceintheirdecisions (28.6%increase).
Conclusion: Trainedparamedicscanperformfocusedultrasoundexamsandaccuratelyinterpretand applyactionableexam findingsinthecontextofwrittenscenarios.Analysisthroughourmodel characterizedthetheoreticalclinicalyieldofeachprehospitalultrasoundexamanddemonstrated howeachexammayprovideimproveddecisionaccuracyinseveralspecificsimulatedclinical contexts.Theseresultsprovidesupportforgrowingevidencethatfocusedlimited-scopeultrasoundmay beaneffectiveprehospitaldiagnostictoolinthehandsoftrainedparamedics.[WestJEmergMed. 2024;25(5)784–792.]
Paramedicsmakecriticalprehospitaltreatmentand transportdecisionsthatoftengreatlyimpactpatient
outcomes.Appropriateprehospitaltreatmentandreceiving facilitychoices,aswellaseffectivepre-arrivalalerts,improve patientoutcomes,decreasetreatmentcost,andreduce
emergencydepartment(ED)crowding.1–3 Theprehospital environmentisinherentlycomplexanddynamicandcanbe resourcelimited,creatingsignificantbarrierstoobtaining accuratediagnosticinformationneededtomakeappropriate decisions.4–6 Whilestudiesindicatethatprehospitallung auscultationis54%accurate7 andpalpatedcarotidartery pulsecheckis55%accurate,8 prehospitalpredictionsof hospitalcareandclinicalcoursearegenerallyinaccurate.9,10 Diagnosticlimitationsrenderdecision-makinginthe field difficultandcannegativelyimpactpatientoutcomes.(For example,22%ofpatientstreatedwithprehospitalneedle decompressionfortensionpneumothoraxwerefound tonothaveapneumothoraxafterassessmentin theED.11)
Integrationofadvanceddiagnostictoolsintheprehospital settinghashistoricallybeensuccessfulinreducingdecision barriersandimprovingoutcomes.Useofelectrocardiograms improvedprehospitaldiagnosticpositivepredictivevaluefor acutemyocardialinfarctionfrom33%to93%.12 Point-ofcareultrasound(POCUS)isanadvanceddiagnostictoolthat hasimmensepotentialtoimprovetheaccuracyof prehospitaldecision-making.Limited-scopePOCUSisbeing implementedinemergencymedicalservices(EMS)agencies acrosstheUnitedStatesandinternationally.In2014,4.1%of respondingEMSmedicaldirectorsreporteduseofPOCUS bytheiragencies,and21.7%wereconsideringfuture implementation.13 Commonprehospitalultrasound(PHUS) examsincludetheextendedfocusedassessmentwith sonographyintrauma(eFAST),pulmonaryexam,and focusedechocardiographyduringcardiacarrest.Whenused appropriately,theseexamscanprovideparamedicswith accurateandactionablediagnosticinformationtoguide prehospitaldecisions.14
Forlimited-scopePHUStobesafelyimplemented,we needacomprehensiveunderstandingofthreecritical elements:paramedicperformance;paramedicinterpretation ofPOCUSexams;andtheappropriateapplicationofthose exam findingstosupportprehospitaldecisions.Previous studieshavedemonstratedsuccessfulexamacquisitionand interpretationbyparamedics,suchaseFAST,with100% interpretationaccuracyinamean2.6-minuteexamtime,15 lungultrasoundwithasensitivityof80%andspecificityof 72%fordetectingpulmonaryedema,16 and88%accurate imageinterpretationofechocardiographyduringcardiac arrest.17 Toourknowledge,nostudyhasexaminedhow POCUStrainingandeducationimpactaparamedic’sability toappropriatelyintegratePHUSexam findingsinto prehospitalcareinasimulatedenvironment.Training paramedicstoappropriatelyapply findingsisessentialtosafe implementationoftheseskillsinthe field.14 Athorough understandingofhowPHUS findingsimpactdecisionsabout prehospitaltreatment,receivingfacilitychoice,andprearrivalalertisneededpriortosafeandeffective implementationofPOCUSintheprehospitalsetting.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Appropriateprehospitaltreatmentimproves patientoutcomesandreducesEDcrowding.
Whatwastheresearchquestion?
Howdoesfocusedprehospitalultrasound trainingandknowledgeaffectparamedic clinicaldecisionsinasimulatedenvironment?
Whatwasthemajor findingofthestudy?
Therewasasigni fi cantincrease(p ≤ 0.001) inbothmeanscenarioscore(absolute35.5%, from55.1%to90.6%correct)andmean self-con fi dence(6.0%absolutefrom38to 44%,15.8%relative)acrossallexam/ decisiontypesassessed.
Howdoesthisimprovepopulationhealth?
Focused,limited-scopeultrasoundexams couldprovideparamedicswithaccurateand actionablediagnosticinformationtoguide prehospitaldecision-making.
Weexaminedhowahands-onPHUStrainingprogram impactedaccuracyofsimulatedparamedicdecision-making regardingprehospitaltreatment,receivingfacilitychoice, andpre-arrivalalertsusingwritten,clinicaldecision scenariosadministeredpre-andpost-training.Thescenarios includedeFAST,pulmonaryexam,andfocused echocardiographycombinedwithcarotidpulsecheckexams. InthisstudywealsoexaminedtheimpactofPHUStraining andimagingonparamedicself-confidenceintheirsimulated clinicaldecisions.Toaddcontextregardingtheeffectiveness oftheeducationprovidedbythePHUStraining administered,wealsoreporttheperformanceofthe participantsoncourseassessmentsincludingawritten knowledgeexamandscenario-basedpracticalexams.
Thiswasaprospectiveobservationalcohortstudy designedtoevaluatetheeffectivenessofasmall-scale,mixedmodality(containingasynchronousdigitalindependent prework,hands-onscanningpractice,andclinical applicationscenarios)trainingprogram.The13-hourcourse coveredlimited-scopePOCUSexamsthatwerefocused specificallyonaspectsandapplicationsoftheexamswith relevancetoprehospitalcare.Examsincludedwerethe eFAST,focusedpulmonaryexam,andfocused
echocardiographycombinedwithfocusedvascularexamfor Dopplerandvisualcarotidarterypulsatilityincardiacarrest. Thisstudywasapprovedandgivenanexemptdetermination bytheInstitutionalReviewBoardCommitteeforthe ProtectionofHumanSubjectsatDartmouthCollege (#00032581).Ultrasoundmachinesusedinthecourse sessionsincludedClariusHDportableultrasoundunits (ClariusMobileHealthCorp,Vancouver,BC,Canada),and ButterflyiQ+ (ButterflyNetworkInc,Burlington,MA).
NewHampshirehasapopulationof1.39millionwith >1,100licensedparamedicsworkinginthestate.18,19 New HampshireposesauniquechallengetoEMSsystems,given itsruralgeographywithoftenextendedtraveltimesto tertiarycarecenters.Participantsinthisstudywereprimarily full-timeparamedicslicensedinNewHampshire. Participantswererecruitedfortwoin-personPHUScourses deliveredontwodifferentdaysthroughadvertisementviathe NewHampshiteDivisionofFireStandardsandTraining andEmergencyMedicalServicesmailinglistandwebsite. Participantsweregivenanoverviewofthestudy,providedan optiontoopt-out,andsignedwrittenconsentforms.Thirtyoneparticipantswereenrolled.Wecollectedparticipant experience-level,demographic,andemploymentdataina post-trainingsurvey.
TheNewHampshireFireAcademy&EMShostedthe courseattheirtrainingfacilityin.Thewasnotinvolvedin planningorconductingthisstudyanddidnot financially supportanymembersofthestudyteamtoconductthisresearch project.Thecourseanditsmaterials(Appendix2)were assembled,created,overseen,anddeliveredbyaboard-certified emergencyphysicianandultrasoundexpertwhoalsoservesas anEMSmedicaldirectorinconjunctionwithparamedics.This physicianalsoselectedandtrainedasmallteamofinstructors withexpertiseinultrasoundimaging,paramedicine,and ultrasoundeducationtoassisthimindeliveringthecourse. Courseobjectivesincludedlearningappropriateindicationsfor PHUS,ultrasoundtransducermanipulation,comfortwiththe userinterface,abilitytointerpretresultsfromselectedPOCUS exams,andabilitytoapply findingstoclinicaldecision scenariosrelevanttoprehospitalcare.Specificdetailsregarding coursestructure,content,andstudent/instructorratioscanbe viewedin Appendix2
Priortothein-personcomponent,participantswere providedwiththreehoursofasynchronouseducation consistingofanintroductiontorelevantphysics,useof ultrasoundunits,integrationofultrasoundintoworkflow, selectedPOCUSexams,andcases.Thein-personcomponent ofthecourseconsistedofshortdidacticlectures,ampletime forhands-onpracticeusinglivemodels,groupdiscussionof
cases,andstandardizedscenarios.Lecturesreviewedselected POCUSexamsandexamplesofpathologyrelevantto prehospitalcare.Aninstructorprovidedguidanceandrealtimefeedbacktoparticipantsinsmallgroups.Contentwas reinforcedanddiscussedinalarge-groupsettingusing integrationquestionsandpollingsoftware.
Participantsendedthein-personcoursebytakinga writtenknowledgetestandcompletingsixscenario-based examscoveringcardiacarrest,respiratorydistress,and traumainEMScasesaspartofapracticalexam(Appendix 2).Forthepractical,participantsperformedselected POCUSexamsonlivemodelsinsmallgroupsandreceived predeterminedresultsviauninterpretedultrasoundvideo clipsaftersuccessfullycompletingtheexam.Scenario stationswereoperatedbycourseinstructors,and participantsreceived “ pass ” or “fail” gradesbasedonpreestablishedcriteriaforperformance,imageinterpretation, andtreatment/transportdecisions.Case-basedscenarios werecompletedasateamtosimulatetheprehospital environment,althougheachparticipanthadtoindividually acquireacardiac,lung,andeFASTexamonamodelwith normal findingsandsubsequentlyinterpretaunique ultrasoundimagewithpathologydisplayedonacomputer screenandthenapply findingstotheirtreatmentand transportplanwithoutinputfromotherteammembers.The post-coursewrittenexamconsistedof24multiple-choice questionsmappedtocourseobjectives(topicscoveredin writtenexamquestionscanbeviewedin Appendix2). Ascoreof ≥80%wassetasthepassingthresholdforthe writtenportionofthepost-courseexam.
Priortoreceivingeducationalcontent,participantswere givenwrittenclinicaldecisionscenarios(Table1 and Appendix1).Thisinstrumentwasdesignedtomeasurethe impactofPHUStrainingandavailabilityofuninterrupted ultrasoundimagesonparamedicclinicaldecisions.The instrumentconsistedof10vignettesthatwereintentionally ambiguous,reflectingtherealityofprehospitalemergency care.Scenariosprovidedanextensivedescriptionofthe scene,patientassessmentandhistoryofpresentillness/ injury,andwereeditedbymultipleinvestigators.
Editinginvestigatorsincludedanemergencyphysician andultrasoundexpertwhoalsoservesasanEMSmedical director;aparamedicwithover20yearsofexperiencein prehospitalEMSeducation;andseveralparamedics, advancedemergencymedicaltechnicians(EMT),andEMTBswith fieldexperience.Eachscenarioincludedoneormore questionsaboutprehospitaltreatment,receivingfacility choiceandtransportmodality,and/orpre-arrivalalert. Scenario-baseddecisionsweredesignedtospecifically
Table1. Clinicaldecisiontopicsandthetypeofprehospitalultrasoundexamincludedwithineachwritten,clinicaldecisionscenariolistedby scenarionumber.Eachscenarionumbercorrelateswiththenumberlistedin Appendix1,whichshowsthecompletetextofeachscenario.
ScenarionumberPHUSexamassessedScenariotypeClinicaldecisionquestions
Prehospitaltreatmentscenarios
2eFASTTraumaNeedledecompressionvsnoneedledecompressionin possiblepneumothorax
4eFASTTraumaTXAinfusionvsnoTXAwithanunclearbleedingsource
3FocusedpulmonaryRespiratoryTreatmentofCHFvsCOPD
5FocusedpulmonaryRespiratoryTreatmentofCHFvsCOPD
7Echo + carotidpulseCardiacarrestContinuationvsterminationofresuscitation
8Echo + carotidpulseCardiacarrestContinuationvsterminationofresuscitation Transportandpre-arrivalalertscenarios
1eFASTTraumaTraumacentervsclosestED,groundvsairtransport, pre-arrivaltraumaalertvsnoalert
6eFASTTraumaTraumacentervsclosestED,groundvsairtransport, pre-arrivaltraumaalertvsnoalert
9eFASTTraumaTraumacentervsclosestED,groundvsairtransport, pre-arrivaltraumaalertvsnoalert
10eFASTTraumaTraumacentervsclosestED,groundvsairtransport, pre-arrivaltraumaalertvsnoalert
PHUS, prehospitalultrasound; eFAST,extendedfocusedassessmentwithsonographyintrauma; TXA,tranexamicacid; CND,chestneedle decompression; CHF,congestiveheartfailure; COPD,chronicobstructivepulmonarydisease; ED,emergencydepartment; POCUS,pointof careultrasound.
maptoanassociatedelementoftheNewHampshire EMSprotocols.
Participantsalsoindicatedtheirconfidenceintheir decisionsusinga1–5Likertscale.Post-training,participants weregiventhesameinstrument,withtheadditionofan uninterpretedultrasoundclipthatcouldbefeasiblyacquired inthe fieldasadecisionaidineachscenario.Correctanswers weredefinedasthoseselectedbyaveteranemergency physicianwithexpertiseinbothPOCUSandEMS,who reviewedeachclinicaldecisionscenariowithandwithoutthe associatedultrasoundcliptoestablishthecorrectdecisions foreachscenarioregardlessofavailabilityofultrasound images.Forscenarioswheretransporttoatraumacenterwas indicatedascorrect,groundandairambulancetransporttoa traumacenterwerebothconsideredascorrectanswersto reducescenario-basederroraroundairambulance availability,weatherconditions,andspecificlocation,etc. (Appendix1).
Wecalculateddescriptivestatisticsforcategorical variablesasfrequencieswiththeirrespectivepercentages. Pre-vspost-scoreimprovementwasexpressedin percentages;however,allassessmentsforassociation performedontheprevspostwereperformedusingpaired t -testsontheactualscores.Weevaluatednormality assumptionsinapreliminaryevaluationofthedistributionof
thescoreandconfidencevariablesusinggraphicalmethods (boxplotsandhistograms);nomajorconcernswithmeeting thenormalityassumptionswereobserved.WeusednonparametricWilcoxonrank-sumtestsforprevspost confidence-assessmentsscores.Thiswastoaccommodatefor Likertscalesused.Confidenceassessmentsareexpressedas sumsandaredisplayedwiththeirrespectiveinterquartile ranges.Associationstopreviousexperienceswithultrasound wereassessedthroughlinearmodelswhereprevious experiencewascodedasacategoricalvariable.Preliminary poweranalysiswasnotperformedbecauseparticipantswere recruitedviaconveniencesampling.Weperformedall analysesusingSAS/STATv.9.4(SASInstituteInc,Cary, NC).Significantdifferencesweredeclaredat P ≤ 0.05, althoughexact P -valuesarepresented.
Ofthe31participantsinthisstudy,30completedthe demographicssurvey(Table2).Amajorityofthe participantscamefrom firedepartmentsorprivateEMS agenciesservingruralareasorsmalltowns.Amajorityof paramedicswerehighlyexperiencedwith >63%havingmore than16yearsinEMS.Nineofthe30paramedicsreported havingpriorultrasoundexperienceinsomecapacity,threeof whomdescribedtheirtrainingasspecifictoPHUS.Prior ultrasoundexperienceconsistedofvascularaccesstraining
Table2. Participantdemographicsandemploymentcontextsurvey. Participant-reporteddataregardingtheirpriorexperienceworkingin emergencymedicalservicesandwithultrasoundimaging.
Category Frequency(%) N = 30*
EMSagencytype
Firedepartment17(56.7)
Privateorganization4(13.3)
Hospital8(26.7)
Airmedical1(3.3)
Primaryserviceprovided
911withorw/otransportcapability21(70.0)
Interfacilitytransport1(3.3)
Equalmixof911andinterfacilitytransport6(20.0)
Clinicalservices1(3.3)
Mobileintegratedhealthcareand communityparamedicine 1(3.3)
YearsofEMSexperience
>21years16(53.3)
16–20years3(10.0)
11–15years5(16.7)
8–10years3(10.0)
5–7years3(10.0)
Sizeofcommunityserved
Rural(<2,500)5(16.7)
Smalltown(2,500–24,999)19(63.3)
Medium-sizetown(25,000–74,999)6(20.0)
Priorultrasoundexperience
Receivedpriortraining–anycapacity6(20.0)
Receivedpriortraining-specificallyfor EMSuse 3(10.0)
Nopriortraining21(70.0)
Priorultrasounduseonthejob
Prioruse–anycapacity4(13.3)
Prioruse–specificallyinEMSjob2(6.7)
Noprioruse24(80.0)
*30ofthe31studyparticipantsarerepresented,(Oneparticipantdid notcompletetheemploymentcontextsurvey.) EMS,emergencymedicalservices.
forallbuttwoparticipantswhoreportedmorein-depthprior training.Duringanalysisnosignificantassociationswere foundbetweenparticipants’ priorultrasoundorEMS experienceandperformanceoncourseassessmentorwritten clinicaldecisionscenarios.
Ofthe31(87.1%)participants,27obtainedapassing gradeonthewrittenpost-courseexam.Thecohortaverage
scorewas92.2%,witharangeof62.5–100%.Thescenariobasedpracticalexamhada100%passrate.
Datadepictingthecomparisonofthepre-andpost-course written,clinicaldecisionscenariosareshowninthe Figure TheadditionofPHUSimagingyieldedastatistically significantincreaseinbothmeanscoreandmeanparticipant self-confidenceacrossallPHUSexamtypesanddecision typesassessedbythisinstrument(P ≤ 0.001).Thepulmonary examyieldedthelargestincreaseinbothmeanscore improvement(59.7%)andparamedicconfidenceintheir decisions(28.6%).Thesmallestincreasesinimprovement wereobservedintheecho/carotidpulseexamcategoriesat 29%and12.5%,respectively.Whencomparingchangesin prehospitaltreatment,transport,andreceivingfacility decisions,thelargestincreaseinmeanscoreandconfidence wasseeninprehospitaltreatmentchoices.
Ofthe14scenarioquestionsansweredbyall31participants (434uniqueanswers),168answers(38.7%)were changedfromincorrecttocorrectwiththeaidof ultrasoundimages.
Participantpreviousexperienceswithultrasoundare presentedin Table2.Only9of30participantsreported havinganytypeofpreviousexperienceusingorbeingtrained withultrasoundimagingandonlytwoindividualsreported havingusedultrasoundonthejobbeforeparticipationinthis study.Weusedlinearmodelstolookforassociations betweenanytypeofpriorexperiencewithultrasoundthata participanthad,andtheirperformanceonstudyassessments; however,noassociationsweredetectedforanyofthe previousultrasoundexperience-typesreported.
Thepost-coursewrittentestevaluatedparticipantmastery ofthecourseobjectives;87.1%ofparticipantspassedthetest withanaveragescoreof92.2%,demonstratingthatthe courseeducatedparamedicsinbasictheory,knowledge,and interpretationofthethree,goal-directed,limitedwindow PHUSexams.Thisresultsupportsagrowingbodyof evidencethat1–2daysofinstructionacrossavarietyof instructionalmodalitiesandexamtypesislargelyadequate forparamedicstoachievecompetencywithlimitedscope PHUSexams.17,20–23
Thepracticaltestevaluatedparticipantpsychomotor skills,aswellastheabilitytointegratePHUSintoEMS workflow,accuratelyinterpretexams,andappropriately apply findingsinrealtime.Onehundredpercentof participantspassedthepractical,demonstratingthatthe coursesuccessfullytrainedparamedicstoacquire,interpret, andintegratePHUSintopracticalEMSscenarios.This
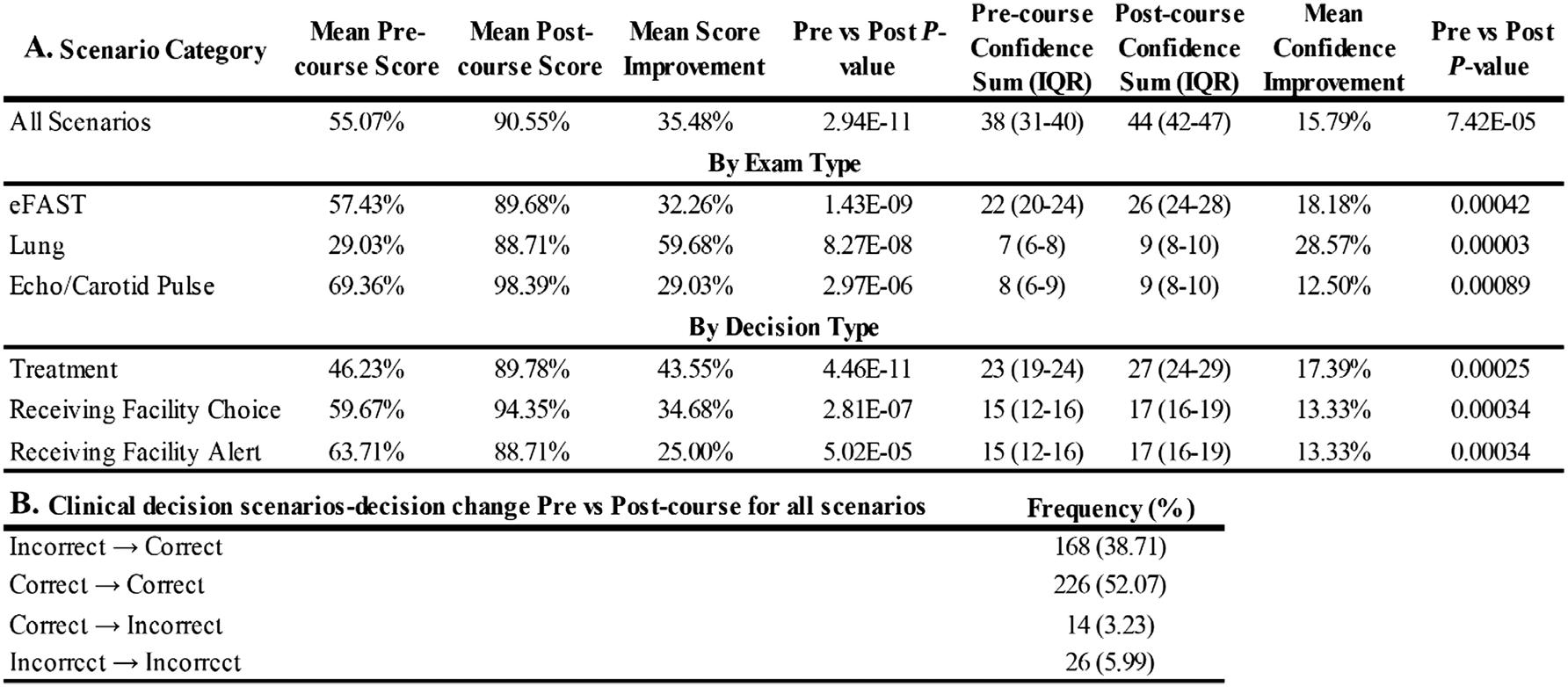
Figure. Changesinparamedics’ simulatedclinicaldecision-makingandself-con fidencefollowingtraining. PanelAdepictsthemeanimprovementinbothmeanscoreandparticipantself-confidenceassociatedwitheachwrittenclinicaldecision scenario(Table1 and Appendix1).Scoresaresortedbyspecificprehospitalultrasound(PHUS)examtypeandclinicaldecisiontype.Panel Breportshowaggregateparticipantresponsestoall10scenarioschangedwithregardtocorrectnesswhentheyhadaccesstouninterpreted PHUSimagesasadecisionaid.Allchangesarehighlysignificantat P ≤ 0.001. IQR,interquartilerange; eFast,extendedfocusedassessmentwithsonographyintrauma.
supportspreviousevidencethatparamedicscanacquireand interpretPHUSimagesinthe field.15–17,24
Thewrittenclinicaldecisionscenariosusedinthisstudy presentanovelwaytoevaluatetheimpactofPHUSon paramedicdecision-makinginarisk-freemanner.Theprecoursescenariosdidnotincludeultrasoundimagesand requiredtheparamedictomakedifficultandpotentially ambiguousdecisionsbasedonhistory,physicalexam,and conventionaldiagnosticsalone,accuratelymimickingthe difficultyofrealdecisionsmadeonshift.Manystudieshave showntheinaccuracyofconventionalprehospital diagnosticsandhighlightthedifficultyinpredictingpatient conditionanddispositionbasedonprehospitalhistoryand physicalexamalone.1,5–10 Accesstouninterpreted,raw ultrasoundclipsthattheparticipantsweretrainedtoacquire andcouldfeasiblyobtaininthe fieldyieldedastatistically significantincreaseincorrectdecisionmakinginevery categoryevaluated,includingtreatment,transport,andprearrivalalert.Meanscoresalsoincreasedsignificantlyinall typesofPHUSexamsevaluated(Figure).Despitepotential sourcesoferrordescribedabove,theseresultsprovidea compellingtheoreticalframeworktoanalyzehowPHUS mayimpactparamedicdecisions.
Accesstofocusedpulmonaryultrasoundacross respiratorydistressscenarios(3and5)improveddecision accuracyinprehospitaltreatmentby59.7%andconfidence by28.6%(Figure).Scenarios3and5requiredparticipantsto
determinewhethertofollowthecongestiveheartfailure (CHF)orchronicobstructivepulmonarydisease(COPD) treatmentprotocolsinapatientinrespiratorydistressof unclearetiologysuspectedtohaveCHFvsCOPD.Accessto uninterpretedPHUSsignificantlyimprovedthesedecisions. Thisresultsupportsexistingdatathatparamedicscan accuratelyinterpretlungultrasoundinthesettingof pulmonaryedema.16 Italsoindicatesthatintheunclear circumstanceofarespiratorydistresspatientwhereCHFvs COPDissuspected,focusedpulmonaryultrasoundmay provideimprovedaccuracyofparamedicworkingdiagnosis, increasedconfidence,andaccuracyofprehospitaltreatment inthisspecificclinicalsetting.Theabilityofparamedicsto appropriatelyapply findingstosupportsimulateddecisions indicatesthattheimproveddiagnosticaccuracyof pulmonaryultrasoundinundifferentiateddyspnea demonstratedoutsidetheUSmayalsobeapplicableinthe prehospitalcontextwithintheUS.25
ExtendedFocusedAssessmentwithSonographyinTrauma AccesstoeFASTimagesintrauma(scenarios1,2,4,6,9, 10)improvedoveralldecisionaccuracyby32.3%and confidenceby18.2%(Figure).Thisresulttheoretically supportspreviousstudiesthatparamedicscanaccurately interpretaneFASTexam.15,24 ItalsoindicatesthateFAST mayimproveparamedicaccuracyindeterminingthe appropriatetransportmethodandreceivingfacilitytypein complextraumapatients.Similarly,eFASTmayimprove theaccuracyofneedledecompressioninthisspecificclinical setting,whichmayhelptoreducethedemonstratedincidence ofunnecessaryprehospitalneedledecompression,aswellas
improvetheappropriateuseoftranexamicacidinfusionin unclearcircumstancessuchaswhenanintra-abdominal bleedingsourceisnotobviousonphysicalexam.11
FocusedEchocardiographyandPoint-of-careUltrasound (Carotid)PulseCheck
AccesstofocusedechocardiographyandPOCUS (carotid)pulsecheck(scenarios7and8)significantly improvedmeandecisionaccuracyby29%,andconfidenceby 12.5%.Scenariosrepresentedapulselesselectricalactivity (PEA)orasystolecardiacarrestcasewheretermination parametersweremetbyasmallmargin.Pseudo-PEAwasa feasiblepossibilityinscenario7.AccesstoPHUSimproved theaccuracyofappropriateterminationofresuscitationin theasystolescenario(8)aswellasappropriatecontinuation ofresuscitationinthePEAscenario,whichwasactually pseudo-PEAasidentifiedbyultrasoundexam.
Thisresultdemonstratesthatparamedicscanaccurately interprettheseexamsinthesettingofsimulatedcardiac arrest,supportingexistingdataonprehospital echocardiographyinterpretation.17,24 Additionally,focused echocardiographyandcarotidpulsecheckincardiacarrest mayimproveparamedicaccuracyindeterminingwhether andwhenterminationofresuscitationisappropriate.These resultsalsoprovideanoveltheoreticalrepresentationthat PHUSmaybeeffectiveinidentifyingandactingon prehospitalpseudo-PEAcardiacarrest.Lastly,theresult demonstratesthataccesstoPHUSincardiacarrestmay improveparamedicconfidenceinresuscitationdecisions, whichcanoftenbedifficultandstressful.17
Althoughsignificant,thesechangesinmeanscoreand confidencearethesmallestinmagnitudethatweobserved. Thismayhavebeenduetoincreasedcomplexityand difficultyinimageacquisitionandinterpretationofcardiac imagesascomparedtootherPHUSexams.Althoughresults demonstratethatparamedicscanperformandtheninterpret andapplysimulated findingsfromafocusedvascularexam forpresenceorabsenceofcarotidpulseasanadjunctto cardiacarrestechocardiography,thisisinthecontextofa purelysimulatedtheoreticalenvironmentanddoesnot provideanyinsightintotheclinicalvalidity,utility,orideal methodofcarotidpulsecheck,whichremainsanareaof activestudy.26,27
AsPHUSisimplemented,itssafetyandefficacywill dependonathoroughunderstandingofhowparamedics applyexam findingstoprehospitaltreatmentdecisions.The currentbodyofevidencehasnotyetestablishedtheclinical yield,benefits,andrisksregardingeachPHUSexamtype. Understandingwhichexamsresultinsignificantlyimproved accuracyofdecisionsthatleadtoanactionablechangein prehospitalmanagementisacrucialnextstep.Judiciousand preciseintegrationofexamsthatareproventohavegood
prehospitalyieldmayhavethepotentialtoimprovepatient carethroughimproveddiagnosticaccuracy.Conversely, inaccurateapplicationofPHUStestcharacteristics, incongruencewiththeoverallclinicalpicture,orimaging resultinginunactionableinformationmayresultinpoorly appliedexam findingswithriskssuchasovertriage,extended assessmenttime,ordeviationfromexistingstandardsofcare. AnalysisofPHUS,likethetheoreticalmodelinthisstudy, mayhelptoinformparamediceducationandprotocols neededtoensurethatPHUS findingsareappliedinamanner thatimprovesdecisionsandminimizesthesepotentialharms.
Thisstudyusedarelativelysmallsamplesizeof31 participants.Itexaminedparticipantdataacrosstwo repeatedPHUScourseswithidenticalcurricula,thesame coursedirector,andsimilarinstructors.Thereispotential variabilitybetweenthetwocoursesessionsdueto uncontrollablefactorssuchascoursedynamicsor participantinteractionorvaryingpriorexperiencewith ultrasoundimagingandEMS.Thethreehoursofcourse assignedpreworkwerecompletedonthehonorsystem,and thestudyteamcouldnotverifycompletionofthatprework. Thiscoursewaspubliclyadvertisedtoparamedics;thus,selfselectionbiascouldhaveinfluencedthosewhoparticipated byattractingparamedicswithmoreexperienceandadvanced training.Theclinicaldecisionscenarioswereatheoretical frameworktosimulatereal-worldprehospitalcare.Aswith anysuchinstrument,therearepotentialsourcesoferrorsuch asvariablesimulation fidelityandpotential misinterpretationofdepictedscenes.
Therepeateduseofthesamewrittenclinicaldecision scenariosbeforeandafterinterventionwithoutacontrol groupmayhaveintroducedpotentialconfounding.Because thepost-trainingscenarioscontainedadditionalinformation intheformofultrasoundimaging,itisdifficulttodetermine whetherchangesinparamedicaccuracywereinfluencedby repeatedassessment,theadditionalimaging,thetraining itself,oracombinationofthesefactors.Additionally,some oftheclinicaldecisionscenariosarewritteninamannerthat mayhave flaggedtheuninterpretedultrasoundimageas abnormal.However,theparticipantswerestillrequiredto identifythetypeofpositive findingsintheimageattachedto eachscenario,andcorrectlyapplythatinformationwithin theclinicalcontextofeachvignette.
Lastly,noneofthemodelspossessedpathology;therefore, studyparticipantswerenotabletoscanpathology themselvesduringthecourse.Rather,relevantpathological imageswerecoveredthoroughlyduringthedidacticsessions ofthecourse.Intermsofpreviousultrasoundexperience affectingparticipantscores,thecohortwaslimitedinits capacitytodetectsuchassociations.Thiscouldbebecauseof lowpowerduetoasmallportionoftheparticipanthaving
previousexperiencewithultrasoundingeneralorbecause thoseeffectsaresmallinthelargecontextofthis prehospitalapplication.
Furtherstudyinthe fieldisnecessarytoexpose paramedicstothetypicaldistractionsandsuboptimal imagingconditionstheywillexperienceinthe fieldto validatethesetheoretical,scenario-based findings,andto continueclassifyingtheclinicalyieldanddecisionsupportof PHUS,toguidethedevelopmentofPHUSprotocolsand bestpractices.Furtherstudyisalsoneededtocharacterize PHUSknowledgeandskillretentionovertime.
Thisstudyshowedthatwitha13-hourmixedmodality trainingprogram,paramedicscancompetentlyperform focusedeFAST,pulmonary,andcardiacarrestultrasound examsduringcourseassessments.Theycanalsoaccurately interpretexam findingsandapplytheseactionable findings withinascenariocontextresultinginatheoreticalsignificant increaseindecisionaccuracyandpotentialimprovementin prehospitalcare.Decisionanalysisthroughourclinical decisionscenariosmodelcharacterizedthetheoretical clinicalyieldofeachfocusedPHUSexamanddemonstrated howeachexammayprovideimproveddecisionaccuracyin severalspecificclinicalcontexts.Theseresultsprovide supportforgrowingevidencethatfocusedeFAST, pulmonary,andcardiacarrestultrasoundmaybesafeand effectiveprehospitaldiagnostictoolsinthehandsof trainedparamedics.
2.SmythMA,Brace-McDonnellSJ,PerkinsGD.Impactofprehospitalcare onoutcomesinsepsis:asystematicreview. WestJEmergMed. 2016;17(4):427–37.
3.HandolinLandJääskeläinenJ.Pre-notificationofarrivingtrauma patientattraumacentre:aretrospectiveanalysisoftheinformationin 700consecutivecases. ScandJTraumaResuscEmergMed. 2008;16(1):15.
4.O’HaraR,JohnsonM,SiriwardenaAN,etal.Aqualitativestudyof systemicinfluencesonparamedicdecisionmaking:caretransitionsand patientsafety. JHealthServResPolicy. 2014;20(1Suppl):45–53.
5.JonesCMC,CushmanJT,LernerEB,etal.Prehospitaltraumatriage decision-making:amodelofwhathappensbetweenthe9–1–1calland thehospital. PrehospEmergCare. 2015;20(1):6–14.
6.HuntRC,AllisonEJ,WhitleyTW,etal.ComparisonofEMTblood pressuremeasurementswithanautomatedbloodpressuremonitor:on scene,duringtransport,andintheemergencydepartment. AnnEmerg Med. 1985;14(9):871–5.
7.BrownLH,GoughJE,Bryan-BergDM,etal.Assessmentofbreath soundsduringambulancetransport. AnnEmergMed. 1997;29(2):228–31.
8.EberleB,DickW,SchneiderT,etal.Checkingthecarotidpulsecheck: diagnosticaccuracyof firstrespondersinpatientswithandwithouta pulse. Resuscitation. 1996;33(2):107–16.
9.LevineSV,ColwellCB,PonsPT,etal.Howwelldoparamedicspredict admissiontothehospital?Aprospectivestudy. JEmergMed. 2006;31(1):1–5.
10.Fraess-PhillipsA.Canparamedicssafelyrefusetransportofnon-urgent patients? PrehopsDisasterMed. 2016;31(6):667–74.
11.BlaivasM.Inadequateneedlethoracostomyrateintheprehospital settingforpresumedpneumothorax. JUltrasoundMed. 2010;29(9):1285–9.
AddressforCorrespondence:NenaLundgreenMason,PhD, DartmouthCollege,GeiselSchoolofMedicine,Departmentof MedicalEducation,1RopeFerryRd.,Hanover,NH03755. Email: nenalundgreen@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Theauthorsreceived financialsupport fromtheCarmenPettapieceStudentResearchFellowshipandthe UniversityofNewEnglandCollegeofOsteopathicMedicine.There arenootherconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Rocheetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.KoivulahtiO,TommilaM,HaavistoE.Theaccuracyofpreliminary diagnosesmadebyparamedics – Across-sectionalcomparativestudy. ScandJTraumaResuscEmergMed. 2020;28(1):70.
12.AufderheideT,HendleyG,ThakurR,etal.Thediagnosticimpactof prehospital12-leadelectrocardiography. AnnEmergMed. 1989;18(4):440.
13.TaylorJA,McLaughlinK,McRaeA,etal.Useofprehospitalultrasound inNorthAmerica:asurveyofemergencymedicalservicesmedical directors. BMCEmergMed. 2014;14:6.
14.BrookeM,WaltonJ,ScuttD.Paramedicapplicationofultrasoundinthe managementofpatientsintheprehospitalsetting:areviewofthe literature. EmergMedJ. 2010;27(9):702–7.
15.HeegaardWG,HildebrandtD,SpearDS,etal.Prehospital ultrasoundbyparamedics:resultsof fieldtrial. AcadEmergMed. 2010;17(6):624–30.
16.SchoeneckJH,CoughlinR,BaloescuC,etal.Paramedic-performed prehospitalpoint-of-careultrasoundforpatientswithundifferentiated dyspnea:apilotstudy. WestJEmergMed. 2021;22(3):750–5.
17.KreiserMA,HillB,KarkiD,etal.Point-of-careultrasoundusebyEMS providersinout-of-hospitalcardiacarrest. PrehospDisasterMed. 2022;37(1):39–44.
18.UnitedStatesCensusBureau.QuickFacts.Availableat: https://www. census.gov/quickfacts/fact/table/US/PST045222.AccessedApril5,2023.
19.FireandEmergencyMedicalServicesAd-HocCommittee.Recruitment &retention:Reportandrecommendations.2022.Availableat: https://www.nh.gov/safety/divisions/fstems/documents/ 2022RecruitmentandRetentionReportFINAL.pdf AccessedMarch16,2023.
20.GuyA,BrysonA,WheelerS,etal.Ablendedprehospitalultrasound curriculumforcriticalcareparamedics. AirMedJ. 2019;38(6):426–30.
21.McCallumJ,VuE,SweetD,etal.Assessmentofparamedicultrasound curricula:asystematicreview. AirMedJ. 2015;34(6):360–8.
22.ChinEJ,ChanCH,MortazaviR,etal.Apilotstudyexaminingthe viabilityofaprehospitalassessmentwithultrasoundforemergencies (PAUSE)protocol. JEmergMed. 2013;44(1):142–9.
23.BrookeM,WaltonJ,ScuttD,etal.Acquisitionandinterpretationof focuseddiagnosticultrasoundimagesbyultrasound-naiveadvanced
paramedics:triallingaPHUSeducationprogramme. EmergMedJ. 2011;29(4):322–6.
24.HeegaardWG,PlummerD,DriesDJ,etal.Ultrasoundfortheair medicalclinician. AirMedJ. 2004;23(2):20–3.
25.ZanattaM,BenatoP,DeBattistiS,etal.Pre-hospitallungultrasoundfor cardiacheartfailureandCOPD:Isitworthwhile? CritUltrasoundJ. 2018;10(1):22.
26.KangSY,JoIJ,LeeGT,etal.Point-of-careultrasoundcompressionof thecarotidarteryforpulsedeterminationincardiopulmonary resuscitation. Resuscitation. 2022;179:206–13.
27.BadraK,CoutinA,SimardR,etal.ThePOCUSpulsecheck:a randomizedcontrolledcrossoverstudycomparingpulsedetectionby palpationversusbypoint-of-careultrasound. Resuscitation. 2019;139:17–23.
AmberD.Rice,MD,MS*§
PhilippL.Hannan,MD*§
Memu-iyeKamara,DO**
JoshuaB.Gaither,MD*†
RobynBlust,MPH*∥
VatsalChikani,MD∥
FrancoCastro-Marin,MD‡
GailBradley,MD*∥
BentleyJ.Bobrow,MD#**
RachelMunn,DO*§
MaryKnotts,MD*§
JustinLara,BS*†
SectionEditor:ScottGoldstein,DO
*CollegeofMedicine,DepartmentofEmergencyMedicine,TheUniversityofArizona, Tucson,Arizona
† CollegeofMedicine,DepartmentofEmergencyMedicine,TheUniversityofArizona, Phoenix,Arizona
‡ HonorHealthScottsdaleOsbornMedicalCenter,EmergencyDepartment, Scottsdale,Arizona
§ UniversityofArizona,ArizonaEmergencyMedicineResearchCenter, CollegeofMedicine,Tucson,Arizona
∥ ADHSBureauofEMSandTrauma,ArizonaDepartmentofHealthServices, Phoenix,Arizona
¶ McGovernMedicalSchool,TexasEmergencyMedicineResearchCenter, Houston,Texas
Affiliationscontinuedatendofpaper
Submissionhistory:SubmittedJune2,2023;RevisionreceivedApril9,2024;AcceptedMay16,2024
ElectronicallypublishedAugust27,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18342
Introduction: Historically,prehospitalcareoftraumapatientshasincludednearlyuniversaluseofa cervicalcollar(C-collar)andlongspineboard(LSB).Duetorecentevidencedemonstratingharmin usingLSBs,implementationofnewspinalmotionrestriction(SMR)protocolsintheprehospitalsetting shouldreduceLSBuse,evenamongpatientswithspinalcordinjury.Ourgoalinthisstudywasto evaluatetheratesofandreasonsforLSBuseinhigh-riskpatients thosewithhospital-diagnosedspinal cordinjury(SCI) afterstatewideimplementationofSMRprotocols.
Methods: Applyingdatafromastateemergencymedicalservices(EMS)registrytoastatehospital dischargedatabase,weidentifiedcasesinwhichaparticipatingEMSagencyprovidedcareforapatient laterdiagnosedinthehospitalwithaSCI.Caseswerethenretrospectivelyreviewedtodeterminethe prevalenceofbothLSBandC-collarusebeforeandafteragencyadoptionofaSMRprotocol.We reviewedcaseswithLSBuseafterSMRprotocolimplementationtodeterminethemotivationsdriving continuedLSBuse.Weusedsimpledescriptivestatistics,oddsratios(OR)with95%confidence intervals(CI)todescribetheresults.
Results: Weidentified52EMSagenciesinthestateofArizonawith417,979encounters.Therewere 225patientswithSCI,ofwhom74wereexcluded.TheLSBswereusedin52pre-SMR(81%)and49 post-SMR(56%)cases.TheoddsofLSBuseafterSMRprotocolimplementationwas70%lowerthanit hadbeenbeforeimplementation(OR0.297,95%CI0.139–0.643; P = 0.002).UseofaC-collarafter SMRimplementationwasnotsignificantlychanged(OR0.51,95%CI0.23–1.143; P = 0.10).Inthe49 casesofLSBuseafteragencySMRimplementation,themostcommonreasonsforLSBplacementwere easeoflifting(63%),placementbynon-transportingagency(18%),andextrication(16.3%).High suspicionofSCIwasdeterminedastheprimaryorsecondaryreasonfornotremovingLSBafter assessmentin63%ofthosewithLSBplacement,followedbymultipletransfersrequired(20%),and criticalillness(10%).
Conclusion: Implementationofselectivespinalmotionrestrictionprotocolswasassociatedwitha statisticallysignificantdecreaseintheutilizationoflongspineboardsamongprehospitalpatientswith acutetraumaticspinalcordinjury.[WestJEmergMed.2024;25(5)793–799.]
PrehospitalcareoftraumapatientsintheUnitedStateshas historicallyincludedthenearuniversaluseofspinal immobilization(SI)byprehospitalprofessionals.1 Traditional SIincludescervicalcollar(C-collar)application,alongrigid spineboard(LSB),securingstraps,andheadblocksorother rotationalsupport.1 Thehistoricalrationaletomaintainthis practiceassumessafetyandefficacyoftraditionalSIandaims tominimizemedicolegalconcerns,highmorbidity,andcost associatedwithspinalcordinjuries(SCI).2 Assumptionshave beenmadethroughouttheyearsthatSIperformedinthis mannerisprotectivebyreducingmovementofpotentialspinal fracturesandthattheriskofsecondarySCIandassociated morbidityismitigatedwithuseofLSB.2
Prehospitalevidencetosupporttheseassumptionsis sparse,leavingopentoquestionthesupposedbenefits.3–6 Hauswaldetalperformedalarge,retrospectivereview comparingimmobilizedandnon-immobilizedtrauma patientsanddemonstratedlowerratesofneurologicinjuryin patientswhowerenotimmobilizedonLSBs.7 Further complicatingtheuseofLSBsisthedifficultyinquantifying theactualrisksandbenefitsofSIduetothecomplexnature ofSCI.8–10 Numerousstudiesdescribetherealandpotential harmsofusingrigidLSBsandothertraditionalpracticesof SIequipmentduringthecareofacutelyinjuredpatients. WhileLSBusemayfacilitateextricationsinthetrauma setting,theiruseincreasesmorbiditybycausingpainand injury,includingpressurenecrosis,especiallyinpatients requiringlongtransporttimes.11 Furthermore,LSB usehasbeencorrelatedwithanincreasednumberof radiologystudiesorderedandsubsequentradiation exposuretopatients,increasedhospitalcost, inhibitionofrespiratoryfunction,andincreased intracranialpressure.11–18
In2018,apositionstatementonspinalmotionrestriction (SMR)waspublishedbytheAmericanCollegeof EmergencyPhysicians,theNationalAssociationofEMS Physicians,andtheAmericanCollegeofSurgeons CommitteeonTrauma.Thispositionstatementhighlighted theneedforSMRasthepreferredmethodofreducingspinal motionafteraninjuryandthatcompleteSIisnotpossible. Thispositionstatementhelpedprovideastandardofcarefor prehospitalpatientswithpossibleSCI,includinglanguage statingthatLSBs “shouldnotbeusedasatherapeutic interventionorprecautionarymeasure.”19 Toaddressthis recommendation,thestateofArizonaimplementeda statewideSMRprotocolwiththegoalofdecreasingLSBuse inhigh-risktraumapatients.Thisprotocol(IMAGE)deemphasizedLSBsbyrecommendingthatpatienttimeon LSBsbeminimized.
InthisstudyweaimedtoevaluateratesofLSBuseafter statewideimplementationofthisSMRprotocolinhigh-risk traumapatients,whomwedefinedashavingadischarge diagnosisofSCI.Thisstudywillinformfutureresearchon
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Longspineboards(LSB)havebeenshownto causeharm.Spinalmotionrestriction(SMR) protocolsaimtoreduceLSBuseinpatients withsuspectedspinalinjurytominimize negativeeffects.
Whatwastheresearchquestion?
Wesoughttoevaluatetheratesofandreasons forLSBuseinhigh-riskpatientsafter statewideimplementationofaSMRprotocol.
Whatwasthemajor findingofthestudy?
StatewideSMRprotocolimplementationwas associatedwitha70%lowerrateinLSBuse (OR0.297,95%CI0.139 – 0.643;P = 0.002).
Howdoesthisimprovepopulationhealth?
ImplementationofSMRprotocolsdecreases LSBuseand,thus,thepotentialharms resultingusingthem.
theeffectivenessofSMRprotocolimplementationand hopefullyresultinthereductionofsecondaryinjuryin patientswithSCI.Additionally,weaimedtoclarify clinicalreasoningusedbycliniciansintheirdecisionto applyandnotlaterremoveaLSB,incontrasttoSMR protocolguidance.
Thiswasaretrospective,observational,multiagency, prehospitalstudyincludingcasesfromJanuary1,2013–December31,2015intheArizonaPrehospitalInformation andEmergencyMedicalServicesRegistrySystem (AZ-PIERS)andtheHospitalDischargeDatabase(HDD). BothdatasourcesaremaintainedbytheArizona DepartmentofHealthServices.TheAZ-PIERSdataset, whichismanagedbythedepartment’sBureauofEmergency MedicalServicesandTraumaSystem,isavoluntarypatient registrythatallowsEMSagenciestocollectandtransmit electronicpatientcaredatatotheState.Thedatabase includesbothrequiredandoptionalreportingelementsin NationalEMSInformationSystemformat.TheAZ-PIERS capturesagencyinformation,patientdemographics, responsetimes,incidentlocation,andtreatment.TheHDD collectsinpatientandemergencydepartmentvisitsfromall Arizonalicensedhospitalsexceptfederalhealthcarefacilities
suchastheVeteran’sAdministration,Departmentof Defense,ortribalhospitals.
TheEMStransportsinAZ-PIERSwerelinkedtothestate dischargedatabaseusingastepwisedeterministiclinkage algorithmwithdirectidentifiers(firstname,lastname,date ofbirth,SocialSecuritynumber,gender,dateofincident/ hospitaladmission,hospitalname).Pre-andpost-SMR protocolimplementationcohortswereidentifiedbasedon agencyprotocolimplementationdate,excludingathreemonthrun-inperiod.Foragenciesthatimplementedan SMRprotocolduringthestudyperiod,wereviewedthe protocoltoverifythatcriticalcomponentsofSMRwere present.Thesecomponentsincludedthefollowing:protocol applicationtopatientswithtraumaticinjury;identification ofasubgroupofpatientsveryunlikelytohaveaspinalinjury whoweresubsequentlyexcluded;andrestrictionofspinal motionwithoutrequiringLSBuse,meaningthataC-collar, scoopstretcher,vacuumsplint,orambulancestretcherwas used.Ofnote,SMRprotocolsdidrequiretheuseofa C-collarandmostallowedforthepatienttobepositioned withtheheadofthegurneyelevatedto30° ifthepatientdid nothavepainwithelevationfortheheadofthebed.
OfthecaseswithmatchedEMSandhospitaldata,this studyincludedonlypatientswithahospital-diagnosedSCI. Thesepatientswereincludedbecauseofthehigherrisk natureofinjuryandriskforsubsequentsecondarySCI. Thesepatientswereidentifiedasthosewithaprincipal diagnosisoftraumaticinjury(InternationalClassificationof Diseases,9th and10th Revisions,ClinicalModification [ICD-9]code800–959or[ICD-10]codeS00–T34orT79) mappingintotheUSCentersforDiseaseControland Prevention’sICD-9-CM(Barellmatrix)andtheproposed frameworkforICD-10-CMdiagnosiscodesforadiagnosisof SCI.20 Forthosecasesidentified,prehospitaldocumentation wasreviewedtodetermineC-collarandLSBuse.Caseswere excludedifagencySMRimplementationdatewasunknown; encounterswerenotedtobeinduplicate;patientshadno traumaintheprior24hours;reviewersdeemedinsufficient documentationtodeterminemethodofimmobilization;or managementinvolvedinterfacilitytransport.Theprevalence ofbothLSBandC-collarusewasdeterminedamongpatients withSCIandcomparedbetweenthepre-andpost-SMR cohortsusingsimpledescriptivestatisticsincludingoddsratios (OR)with95%confidenceintervals(CI).
ThecasesofSCIpost-SMRimplementationthathadLSB placedbyprehospitalcrewweresecondarilyreviewedbytwo independentphysicianreviewersusingaqualitative methodologytodeterminethelikelyreasonsforLSBuse. Theycategorizedcasesbasedonwhattheydeterminedtobe themostlikelyreasonforapplyingaLSBandfornot removingitpriortotransport.Weusedsimpledescriptive statisticstoanalyzethisqualitativeanalysis,withcalculation ofkappastatistictoevaluatethereliabilityofthe tworaters’ determination.
Thefollowingpossiblereasonsforinitialandcontinued LSBuseweredefinedapriori:
• Toimprovetheeaseofliftingduetothelocationofthe injuredpatientrelativetotheambulancegurneyorsize ofthepatient.
• LSBwasplacedbyanon-transportingagencyonscene.
• LSBwasrequiredforextricationofthepatientfroma difficult-to-accesslocation.
• Casesinwhichthereviewerswereunabletodetermine thereasonforplacingthepatientonaLSB.
ThefollowingpossiblereasonsfornotremovingtheLSB onceinthetransportvehicleweredefinedapriori:
• Documentedneurologicsymptomsorother documented findingmakingthepatienthigh probabilityofhavingSCI.
• PatientrequiredLSBformultipletransfersfromone agencytoanotherfortransportpurposes.
• Documentedmedicallycomplicatedpatientwith criticalillness,whohadalteredlevelofconsciousnessor wasintubated.
• Casesinwhichthereviewerswereunabletodeterminea clearreasonformaintainingLSBimmobilization throughouttransport.
ThisstudywasreviewedbytheArizonaDepartmentof HealthServicesHumanSubjectsReviewBoardand approvedforpublicationonMarch17,2016.
Therewere1,123,178EMStransportsenteredintothe AZ-PIERSdatasetduringthestudyperiod,andatotalof 1,005,978(89.6%)weresuccessfullylinkedtoHDDcases. Weincluded63EMSagencieswithaknownSMR implementationstatusintheanalysis.Ofthese,52 transitionedtoanSMRprotocol,resultinginidentification of417,979EMSencountersinthefullstudypopulation. Fromthose,weidentifiedacohortofpatientswithany diagnosisofspinaltrauma,totaling5,178encounters.Within thispopulation,225uniqueSCIcaseswereidentified. Narrativereportsofthoserecordswereexaminedbytwo independentreviewerstodeterminethemethodof immobilization.Seventy-fourcaseswereexcludedfromthe analysisforbeingSCIofnontraumaticcause(21), interfacilitytransfers(11),andthosethatdidnotcontain enoughinformationtodeterminethemethodof immobilization(42).Thestudygroupincluded151cases, whichweredividedintopre-(64cases)andpostimplementation(87cases)cohorts.(Figure1)
63EMS Agencies implementing SMR 52EMS Agencies Transitioned toSMR
87Cases Post-SMR 49with LSBuse Post-SMR
74casesExcluded (42)NotenoughInformation (11)InterfacilityTransport (21)non-traumatic
Figure1. Flowchartofspinalcordinjurycasesandlongspinal boardusebeforeandafterimplementionofaspinalmotion restrictionprotocol.
EMS,emergencymedicalservices; SMR,spinalmotionrestriction.
Thedistributionofdemographic,mechanism/intentof injury,andoutcomeinformationweresimilarbetweenthe pre-andpost-SMRcohortsasillustratedin Table1.The
Table1. Demographics.
resultsoftheprimaryanalysiscanbeseenin Table2.Ofthe 151SCIcasesincluded,LSBswereusedin52pre-SMR (81%)and49post-SMR(56%)cases.TheoddsofLSBuse afterSMRimplementationwere70%lowerthanitwas beforeimplementation(OR0.297,95%CI0.139–0.643; P = 0.002).C-collaruseafterSMRimplementation wasnotsignificantlychanged(OR = 0.51,95%CI: 0.23–1.143; P = 0.10).
ThesecondaryanalysisidentifyingreasonsforLSBuse afterSMRprotocolimplementationareillustratedin Table3.Ofthe49cases,themostcommonreasonsforLSB placementwereasfollows:easeoflifting(63%);placement bynon-transportingagency(18%);andextrication(16.3%). HighsuspicionofSCIwasthoughttobetheprimaryor secondaryreasonfornotremovingLSBafterassessmentin themajority(53%)ofcases,followedbymultiple transfersrequired(10%),andcriticalillness(10%).In26%of cases,therewasnotaclearreasonformaintainingfull
Medianage(Q1,Q3)70(48,83)70(50,84)0.09 ISS,n(%)
<151,631(84.4%)2,715(83.6%)0.46 >= 15301(15.6%)531(16.4%)
Missing0(0.0%)0(0.0%)
Gender,n(%)
Female1,072(55.5%)1,811(55.8%)0.83
Male860(44.5%)1,435(44.2%)
Missing0(0.0%)0(0.0%)
Race/ethnicity,n(%)
White1,557(80.6%)2,680(82.6%) <0.001
Black28(1.4%)72(2.2%)
Hispanic/Latino232(12.0%)373(11.5%)
AsianorPacificIslander22(1.1%)46(1.4%)
NativeAmericanorAlaskanNative57(3.0%)44(1.4%)
Refused/unknown36(1.9%)31(1.0%)
Mechanismofinjury,n(%)
Fall1,015(52.5%)1,715(52.8%)0.25
Motorvehicletraffic523(27.1%)874(26.9%)
Struckby/against42(2.2%)67(2.1%)
Cut/pierce1(0.1%)2(0.1%)
Overexertion48(2.5%)49(1.5%)
Other224(11.6%)351(10.8%)
Missing79(4.1%)188(5.8%)
Intentofinjury,n(%)
(Continuedonnextpage)
Table1. Continued.
Pre-SMRPost-SMR P-value (N = 1,932)(N = 3,246)
Unintentional1,855(96.0%)3,076(94.8%)0.91
Suicide6(0.3%)10(0.3%)
Homicide31(1.6%)49(1.5%)
Other4(0.2%)4(0.1%)
Undetermined36(1.9%)107(3.3%)
Hospitaldischargestatus,n(%)
Home1,028(53.2%)1,609(49.6%) <0.001
SNF/ALF/rehab/longterm673(34.8%)1,312(40.4%)
Expired/hospice68(3.5%)142(4.4%)
Other163(8.4%)183(5.6%)
ISS,InjurySeverityScore; SNF,skillednursingfacility; ALF,assistedlivingfacility; rehab,rehabilitationfacility.
Table2. Ratesoflongspinalboardandcervical-collarusepre-andpost-implementationofaspinalmotionrestrictionprotocol. Pre-SMRimplementation (n = 64) Post-SMRimplementation (n = 87)
PatientswithLSBplacedfortransport(%)52(81.25)49(56.32)0.297(0.139–0.643)
PatientswithC-collarplacedfortransport(%)53(82.81)62(71.26)0.51(0.23–1.143)
LSB,longspinalboard; SMR,spinalmotionrestriction; CI,confidenceinterval; C-collar,cervicalcollar.
Table3. Reasonsforlongspinalboarduseinpatientswithdiagnosedspinalcordinjury.
ReasonforLSBinitialplacement(n = 49)
PrimaryreasonLSBwasnotremoved priortotransport(n = 49)
Extrication(%)8(16.33)Highsuspicionofspinalcordinjury(%)26(53.06)
Easeofliftingnon-ambulatorypatientfrom theground(%) 31(63.27)Requiredtransferbetweenagencies(%)5(10.20)
Placedbynon-transportingagency(%)9(18.37)Criticalillness(ie,unconscious,intubated)(%)5(10.20)
Other(%)1(2.04)Otherorunclearreasoning(%)13(26.53)
LSB,longspinalboard.
spinalprecautionsthroughouttransport.Therewasastrong levelofagreementbetweentheraters’ determinationsofthe reasonsforLSBplacementandreasonsforno discontinuation(kappa,0.8209and0.8108,respectively).
Resultsofthisstudysuggestthatimplementationofa selectiveSMRprotocol,whichfocusedonreducingLSBuse, wasassociatedwithastatisticallysignificantdecreaseinbut noteliminationofLSBuseamongprehospitalpatientswith
acutetraumaticSCI.Itisnotablethattherewassucha significantdecreaseinLSBuseevenintheveryhighestrisk cohortoftraumapatientsstudiedhere thosewithhospitaldiagnosedSCI.Asexpected,therateofC-collarusewasnot affectedbytheseprotocolchangesastheprotocol implementeddidnotmakethemoptional.Thisdatasupports thattheadoptionofSMRprotocolsbyprehospitalagencies doesleadtodecreasedratesofLSBuse,eveninpatientswith high-riskinjuries,andmaysubsequentlyreducethe secondarycomorbidityassociatedwiththesedevices.
TheuseofC-collarsdidnotdeclinesignificantlyasaresult oftheprotocolchanges,asEMSprofessionalswererequired tousethedeviceforpatientsmeetinghigh-riskcriteria.This findingwasexpectedgiventhattheSMRprotocolrequires continueduseofthesetoolstolimitspinalmotion.The observationthatratesofC-collarusedidnotdecreaselends additionalsupporttotheconclusionthattheSMRprotocol resultedinadecreaseinLSBuseratherthanothersystemrelatedchangesorconfoundersresultinginthischange.
ThemostpracticalandleastcontroversialuseofLSBin traumacareisforextrication.Itdoesseemthatthiswasa factorinasmallnumberofcases.Similarly,themost commonreasonforLSBuseafterSMRprotocol implementation(63%ofcaseswhereLSBswereused)was thatEMSprofessionalsappearedtousetheLSBtoliftanonambulatorypatientfromthegroundtothegurney. PerhapsmorecontroversialislimitingtheuseofLSBfor patientswithexam findingssuggestiveofSCI.Inthisstudy, inmorethanhalfofcaseswithLSBplacement,clinicians documentedaconcerningorabnormalneurologicalexam findinganddocumentedthataLSBhadbeenusedduetoa possibleSCI.Inthesecases,perhapsimprovededucational outreachwouldlimitLSBusetothepracticalneedto liftapatientandencourageLSBremovalprior totransportation.
InpatientswhohadaLSBplacedfortheirmovementtoa gurney,frequentlynoreasonwascitedastowhythe patientwasnotrolledoffthespineboardpriorto transportation.Insomecases,thepatient’scarerequired multipletransfersbetweenagencies,orthepatientwas intubatedorhadothersignsofcriticalillnessorairway compromise,whichmayhavemaderemovingthespine boardchallengingorsimplywasnotapriorityintreatmentat thetime.
Limitationsofthisstudyincludetheretrospectivecollection ofthedatafromprehospitalEMSdocumentation. Additionally,theAZ-PIERSdatabaselacksdata fieldsthat wouldhaveprovidedspecificreasonsEMSusedaLSB,and limitedinformationwasavailablefromthenarrativesto qualitativelyassesswhytheychosetouseaLSB.As mentionedabove,thereasonsforLSBusewerenotclearin someofthenarratives,andwhileprovidinginsightintothe thoughtprocessoftheEMSprofessionals,thenarrativesmay notrepresenttheactualprimarymotivationfor placingandnotremovingpatientsfromLSBs.Neitherwere weabletoguaranteethateachEMSagencyimplementedtheir SMRprotocolinthesamemanner.WhilemanyoftheEMS agencies’ selectiveSMRprotocolswerereviewedforthe presenceofcertaincriticalelements,theywerenotidentical; andalthoughstandardizededucationalmaterialwas available,theuniformityoftheeducationgiventothethe EMSprofessionalscouldnotbeevaluated.
Prehospitaluseofalongspinalboardinhigh-riskpatients andthosewithahospital-diagnosedspinalcordinjury, significantlydecreasedafterimplementationofspinal motionrestrictionprotocols.Continueduseofthelong spinalboardafterSMRprotocolimplementationappeared tobemostcommonwhenEMSprofessionalsperceiveda practicaldifficultyoruneasewithbeingabletolift,move, andcarryinjuredpatientswithouttheuseofaLSB.Aswith allparadigmsshiftsinpolicy,itdoestaketimeforcomplete adherencetonewpracticesandprocedures.Thisiswhere visualfeedbackandqualityimprovementprogramsplaya largerole,highlightingtheneedtoprovideguidance regardingwhenaLSBshouldbeusedandtheoptimaltiming ofremovingpatientsfromaLSBtominimizecomplications.
#McGovernMedicalSchoolatTheUniversityofTexasHealth ScienceCenteratHouston,Houston,Texas
** TowerHealth-ReadingHospital,PhiladelphiaCollegeof OsteopathicMedicine,Reading,Pennsylvania
AddressforCorrespondence:AmberD.Rice,MD,TheUniversityof Arizona,DepartmentofEmergencyMedicine,P.O.Box245057, Tucson,AZ5057.Email: arice@aemrc.arizona.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Riceetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.NationalAssociationofEmergencyMedicalTechnicians,American CollegeofSurgeons,TheCommitteeonTrauma. PHTLS: Pre-HospitalTraumaLifeSupport.Burlington,MA:Jones&Bartlett Learning;1986.
2.TenBrinkeJG,GroenSR,DehnadM,etal.Prehospitalcareofspinal injuries:ahistoricalquestforreasoningandevidence. EurSpineJ. 2018;27(12):2999–3006.
3.KornhallDK,JorgensenJJ,BrommelandT,etal.TheNorwegian guidelinesfortheprehospitalmanagementofadulttraumapatientswith potentialspinalinjury. ScandJTraumaResuscEmergMed. 2017;25(1):2.
4.TheodoreN,HadleyMN,AarabiB,etal.Prehospitalcervical spinalimmobilizationaftertrauma. Neurosurgery. 2013;72(Suppl2):22–34.
5.HoodNandConsidineJ.Spinalimmobilisatoninpre-hospitaland emergencycare:asystematicreviewoftheliterature. AustralasEmerg NursJ. 2015;18(3):118–37.
6.KwanI,BunnF,RobertsI.Spinalimmobilisationfortraumapatients. CochraneDatabaseSystRev. 2001;2001(2):CD002803.
7.HauswaldM,OngG,TandbergD,etal.Out-of-hospitalspinal immobilization:itseffectonneurologicinjury. AcadEmergMed. 1998;5(3):214–9.
8.BramlettHMandDietrichWD.Progressivedamageafterbrainand spinalcordinjury:pathomechanismsandtreatmentstrategies. Prog BrainRes. 2007;161:125–41.
9.TatorCHandRowedDW.Currentconceptsintheimmediate managementofacutespinalcordinjuries. CanMedAssocJ. 1979;121(11):1453–64.
10.MarshallLF,KnowltonS,GarfinSR,etal.Deteriorationfollowingspinal cordinjury.Amulticenterstudy. JNeurosurg. 1987;66(3):400–4.
11.LinaresHA,MawsonAR,SuarezE,etal.Associationbetweenpressure soresandimmobilizationintheimmediatepost-injuryperiod. Orthopedics. 1987;10(4):571–3.
12.RaphaelJHandChotaiR.Effectsofthecervicalcollaroncerebrospinal fluidpressure. Anaesthesia. 1994;49(5):437–9.
13.SchafermeyerRW,RibbeckBM,GaskinsJ,etal.Respiratory effectsofspinalimmobilizationinchildren. AnnEmergMed. 1991;20(9):1017–9.
14.PodolskySM,HoffmanJR,PietrafesaCA.Neurologic complicationsfollowingimmobilizationofcervicalspinefractureina patientwithankylosingspondylitis. AnnEmergMed. 1983;12(9):578–80.
15.ChanD,GoldbergR,TasconeA,etal.Theeffectofspinal immobilizationonhealthyvolunteers. AnnEmergMed. 1994;23(1):48–51.
16.ChanD,GoldbergRM,MasonJ,etal.Backboardversusmattresssplint immobilization:acomparisonofsymptomsgenerated. JEmergMed. 1996;14(3):293–8.
17.CordellWH,HollingsworthJC,OlingerML,etal.Painandtissueinterfacepressuresduringspine-boardimmobilization. AnnEmergMed. 1995;26(1):31–6.
18.BauerDandKowalskiR.Effectofspinalimmobilizationdeviceson pulmonaryfunctioninthehealthy,nonsmokingman. AnnEmergMed. 1988;17(9):915–8.
19.FischerPE,PerinaDG,DelbridgeTR,etal.Spinalmotionrestrictionin thetraumapatient.Ajointpositionstatement. PrehospEmergCare. 2018;22(6):659–61.
20.UniversityofArizonaEMSProgram.Spinalmotionrestriction procedure.2022.Availableat: https://emergencymed.arizona.edu/ sites/default/files/ems-public/uag_2022_spinal_motion_restriction.pdf AccessedMarch1,2023.
FionaE.Gallahue,MD*
LouisJ.Ling,MD†
LeoQuigley,PhD,MPH‡
DianDowlingEvans,PhD,ENP-C§
EdwardSalsberg,MPA‡
RobertE.Suter,DO,MHA∥¶
CatherineA.Marco,MD#
SectionEditor:MarkI.Langdorf,MD,MHPE
*TheUniversityofWashington,DepartmentofEmergencyMedicine, Seattle,Washington
† UniversityofMinnesota,DepartmentofEmergencyMedicine, Minneapolis,Minnesota
‡ GeorgeWashingtonUniversityFitzhughMullanInstituteforHealthWorkforce Equity,Washington,DC
§ EmoryUniversityNellHodgsonWoodruffSchoolofNursing,Atlanta,Georgia
∥ SamHoustonStateUniversityCollegeofOsteopathicMedicine,Offi ceofthe Dean,Conroe,Texas
¶ UniformedServicesUniversityoftheHealthSciences,DepartmentofMilitary Medicine,Bethesda,Maryland
# PennStateHealthMiltonS.HersheyMedicalCenter,Departmentof EmergencyMedicine,Hershey,Pennsylvania
Submissionhistory:SubmittedAugust13,2024;RevisionreceivedAugust22,2024;AcceptedAugust23,2024
ElectronicallypublishedSeptember9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.33606
Objective: Themedicalliteraturehasdemonstrateddisparitiesandvariabilityinphysiciansalariesand, specifically,emergencyphysician(EP)salaries.Wesoughttoinvestigateindividualphysician characteristics,includingsexandeducationalbackground,togetherwithindividualpreferencesof graduatingEPs,andtheirassociationwiththesalaryoftheir firstjob.
Methods: TheAmericanCollegeofEmergencyPhysiciansandtheGeorgeWashingtonUniversity MullanInstitutesurveyed2019graduatingEPs.Thesurveyincludedrespondents’ demographicand educationalbackground,post-trainingjobcharacteristicsandlocation,hospitalcharacteristics, importanceofdifferentpersonalpriorities,andstartingsalaries.Weperformedamultivariableregression analysistodeterminehowsalarieswereassociatedwithjobtypesandindividuals’ characteristics.
Results: Wesentsurveysto2,192graduatingresidentsin2019.Ofthese,487(22.2%)responded,and 270(55.4%)accepted first-timeclinicaljobsandincludedsalarydata(12.3%ofallsurveyssent).Male sex,osteopathictraining,andfull-timeworkweresignificantlyassociatedwithhighersalary.Menand womenprioritizeddifferentfactorsintheirjobsearch.Womenweremorelikelytoconsidersuchfactors asparentalleavepolicy,proximitytofamily,desiredpracticesetting,typeofhospital,anddesired locationasimportant.Salary/compensationwasconsideredveryimportantby51.8%ofmenand29.6% ofwomen.Men’smediansalarywas$30,000morethanwomen’s(p = 0.01,95%CI +$6,929 +$53,071),asignificantpaydifferential.
Conclusion: Salariesofgraduatingemergencymedicineresidentsareassociatedwiththeresident’s sexanddegreetype:doctorofosteopathicmedicineordoctorofallopathicmedicine.Multiplefactors maycontributetomenhavinghighersalariesthanwomen,andsomeofthisdifferencereflectsdifferent prioritiesintheirjobsearch.Womenweremorelikelytoconsiderjobconditionsandsettingtobe moreimportant,whilemenconsideredsalaryandcompensationmoreimportant.[WestJEmergMed. 2024;25(5)800–808.]
Background
Previousreportshavedemonstrateddisparitiesand variabilityinphysiciansalariesand,specifically,emergency physician(EP)salariesbyavarietyoffactors.1–7 Disparities bysexwithmenearningmorethanwomeniswell documented,3,5–7 butthepossiblecausesofthisdisparity alongwiththeassociationofotherfactorswithsalary differencesisnotaswelldescribed.Wereviewpossible associationswiththisvariabilityinstartingsalariesofnew EPresidencygraduatesin2019.
Graduatingemergencymedicineresidentphysicianshave personalcharacteristicsthatmayinfluencetheselectionof theirvery firstjob.Theseincludepersonalpreferencesthat influencetheirjob-selectiondecisionsandmayimpactthe finalsalaryofthejobtheyultimatelyselect.Individualsmay havepreferencesinselectingtheirjob.Thechoicesmadeby womenandmenmaybedifferent.Unfortunately,verylittle isknownaboutthesefactorstoguideyoungEPsastheygo throughtheprocessofjobselection.
WepresenttheresultsofananalysisofasurveyofEPs completingtheirresidencytrainingthatincludedawide rangeofquestionsaboutthetypeofjobstheyconsidered, theirpersonalandprofessionaldemographics,factorsthat impactedtheirjobselectiondecisionand, finally,thejobthat waschosenandresultingsalary.Ourgoalwastodescribethe associationofpersonaltraitsandjobcharacteristicswiththe salaryofthe firstjob,includingtheimpactofthegraduate’ s sex.Wecomparedandcontrastedtheprioritiesofwomen andmenintheirjobhunt.Weperformedasecondary regressionanalysistoinvestigatetheimpactofsexaloneon salary,independentofthesepreferences.Byfocusingon individualsobtainingtheirvery firstjobposttraining,we eliminatedtheimpactofmid-careerjobchangesorjob changesforcareeradvancementinassessingtheimpactof suchfactorsastheEP’ ssex.
SurveyInstrument
Aspartofalargerinitiativetostudytheworkforceneeds forEPsinthenearfuture,theAmericanCollegeof EmergencyPhysicians(ACEP)andtheGeorgeWashington UniversityMullanInstitute fieldedasurveytoall2019 graduatingEMresidents,approximately4–8weekspriorto graduation.8 ThisstudyreviewedasubsetofgraduatingEM residents’ personalcharacteristics,educationalbackground, andcharacteristicsoftheirjobchoices.Weuseda multivariablequantileregressionanalysistoestimatethe possibleimpactofsomeofthesefactorsonthesalariesof their firstpost-residencyclinicaljob.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Physiciansalarieshavedemonstrated disparitiesandvariability.Multiplefactors maybeassociatedwithsalarydifferences.
Whatwastheresearchquestion?
Whatfactorsimpactsalariesofemergency medicinegraduates?
Whatwasthemajor findingofthestudy?
Men ’ smediansalarywas$30,000more thanwomen ’ s(p = 0.01,95% CI + $6,929 + $53,071).
Howdoesthisimprovepopulationhealth?
Thisstudysuggeststhatthesalariesofnew EMgraduatesareimpactedbymultiple factorsincludinggender.
Theresearchdesignandsurveywereapprovedbythe GeorgeWashingtonUniversityInstitutionalReviewBoard. Weadaptedthesurveytoolfromsimilarsurveysusedbythe MullanInstituteforstudiesofotherphysicianspecialty graduatesandfurtheradjusteditbasedonfeedbackfrom subjectexpertsandpilot-testingamongEPs.Thesurvey questionsofferedafour-pointLikertscale(veryimportant, important,oflittleimportance,notimportantatall),witha not-applicableoption,forpriorityfactorsinajob.(See SupplementaryMaterial.)
ThesurveywasdistributedviaemailinMayandJune 2019,approximately4–8weekspriortotheirgraduation,to 2,192residentswithintheACEPdatabasewhoreportedthey wouldcompletetheirtrainingprogramin2019.The2,192 residentsrepresentedapproximately97.3%ofthe2,253 residentsintheir finalyearoftrainingonDecember31,2018, asreportedbytheAmericanBoardofEmergencyMedicine.9 Anoriginalemailwasfollowedbyuptothreeremindersfor non-respondents.Asanincentive,10giftcardswithavalue of$150weredistributedrandomlytorespondents.The onlinesurveyusedREDCap(ResearchElectronicData Capture)software,hostedatGeorgeWashingtonUniversity MullanInstitute.10
Wecollecteddataincludingrespondents’ demographic andeducationalbackground,educationaldebt,post-training jobs,jobmarketexperiences,andfactorsinfluencingpost-
trainingjobplans.Welookedatthesefactorsandtheir associationwiththesalariesofthe firstjobselectedbythe270 graduatesofEMresidencieswhohadacceptedaclinical positionpost-residencyandsuppliedtheirbasesalary.
Physicianincomeisassociatedwithfactorssuchas specialty,sex,race,ethnicity,academicpractice,boardcertificationstatus,andworkintensity.2–6 Theprimary statisticalanalysisinvolvedanoverviewofthesefactors.11 In asecondaryanalysisweusedquantileregressionina multivariableanalysisestimatingtheremainingsalary differencesbysexwhenmultiplefactorswerecontrolledfor. Selectionofvariablesforthemodelwasguidedbyasimilar regressionanalysisinasurveyofallUS-basedACEP membersinwhichthevariablesusedwerechosento representincome-associatedfactorsincludingspecialty,sex, race,ethnicity,academicpractice,board-certificationstatus, andworkintensity.1–7 Thevariablesincludedinthemodel wereasfollows:age;workingfullvsparttime;racial minoritystatus(Black,AmericanIndianorAlaskanNative vsWhiteorAsian);ethnicity(Hispanicvsnon-Hispanic); urbanvsruralorsemi-ruralpractice(where “urban” means beinglocatedinacityof50,000ormoreresidents, “semirural” refersto “urbanclusters” of2,500to49,999residents asdefinedforthe2010census,and “rural” referstoareas withfewerthan2,500residents);employmentinanacademic medicalcenter;countryofmedicalschool(international medicalgraduatevsgraduateofUSandCanadianmedical school);medicaldegreetype(doctorofallopathicmedicine vsdoctorofosteopathicmedicine[MDvsDO]);whether workingasecondaryjob;andworkingforafor-profitvsa non-profitorganization.
Allrespondentswereaskedtoself-definetheirsituation accordingtothestatedcriteria.Fortheregressionmodelwe treatedthecategoricalincomevariableasapointvariableby definingannualincomeasthemid-pointofthe$10,000 rangesusedinthesurveyquestionaire,whileagewastreated asacontinuous(wholenumberofyears)variable.Allother variablesweredichotomouswithvaluesderivedfromyes/no surveyresponses,withtheexceptionofwhetherworkingfor for-profitornon-profitorganizationswheretheresponse optionswereyes/no/don’tknow.Toavertthelossof51 respondentswhostatedthattheydidnotknowthefor-profit ornon-profitstatusoftheiremployingorganization,the valueofthisvariablefor “don’tknow” respondentswas imputedasthemeanoftheyes/noresponsevalueacross respondentswhodidrespondyesorno;itwasassumedthat notknowingfor-profitornon-profitorganizationalstatus wasrandomlydistributedacrossbothsexes.
Quantileregressionistypicallyusedwhentheassumptions ofnormaldistributiondonothold,asisoftenthecasein salarydistributions.12 Thismethodenabledustogenerate resultsatthelower(25%)andhigher(75%)incomequartiles
oftheincomedistributionaswellasatthedistribution’ s center(median).Theresultsofthelowerandhigherquantile regressionanalysisarenotseparatelyreportedastheyclosely resembledtheresultatthemedian.Theyareavailablefrom theauthors.
Owingtomissingdataamongthe270respondents,the finalregressionanalysisincluded258observations.The13 independentvariablesusedinthemodeland258 observationsallowedtheregressionmodeltoadheretothe generaloverfittingguidelineofapproximately20 observationsperoutcomevariable.11 Wecarriedoutatest foroverfittingoutusingtheStata “ overfit” command,which reportsbothin-sampleandout-of-sampleshrinkage statistics,foreachregressionresult.13 Datawereanalyzed usingStata1614 (StataCorp,LLC,CollegeStation,TX).
Atotalof487graduatingresidentsreturnedthesurvey.Of these,the270respondentswhoaccepted first-timeclinicaljobs andincludedsalarydatacomprisedthegroupthatwas analyzed.Threeofthe270respondentswhodidnotidentifya binarygenderwereexcludedfromthesex-specificanalysis.Of the270respondents,258hadcompletedatathatcouldbe analyzedfortheregression.Ofthe270,169(62.6%)selfidentifiedasmen,98(36.3%)aswomen,andthree(1.1%) preferredtoself-describeornotanswer.Of262whogavetheir age,234(89.3%)wereunder36yearsold.Of268respondents, 211(78.7%)wereWhite,35(13.1%)wereAsian, five(1.9%) wereBlack,and17(6.4%)were “other” ormorethanonerace. Ofthe270graduates,171(63.3%)hadthreeyearsoftraining, 94(34.8%)hadfouryearsand five(1.9%)had ≥5years.
ComparedtoABEMdata,theproportionofrespondents whoreportedcompletingthree-yearprogramswaslessthan thepercentageofthosecompletingthree-yearprograms nationallyattheendofcalendaryear2018(63.6%vs70.2%) andskewedmoreWhitethanEMresidentsnationally(78.7% vs63%),andlessBlack(1.9%vs4%)thanresidentsin trainingduring2018–2019.9 Of264respondentswithdata, 93(35.2%)hadeducationaldebtexceeding$300,000,while themedianeducationaldebtwas$237,500.Almostthree quarters(72.4%)reported “quiteabit” or “agreatdeal” of salaryvariabilityintheirjobsearch(Table1).
Table1. Perceivedvariabilityofphysicians’ salaries.*
Howmuchsalaryvariability(intermsof totalannualincome)wasthere?NumberPercent Quiteabit13851.5% Agreatdeal5620.9% Verylittleornone5119.0% Onlygotoneoffersocan’tsay238.6% Total268100
*268ofthe270respondedtothisquestion.
Toassessthemultiplefactorsthatappearedlinkedtothe salariesearnedbynewlygraduatingresidentsweuseda quantileregressionanalysistocontrolformanyofthese factorstogetheratdifferentquantilesoftheincome distribution.Theassessmentaccountedforbothpart-time andfull-timework.Themoststatisticallysignificantfactor wasgendergap,withmenmakingamedian$30,000more thanwomen($244,200vs$214,200),followedbyDO graduateswhomadeamedian$30,000morethantheirMD counterparts(median$274,200formenvs$244,200for womenwhoareDOgraduates),andfull-timeworkers makingamedianof$43,000morethanthoseworkingparttime($287,349formenvs$257,349forwomenwhoare full-timeworkers)(Table3).
Otherfactorsthatwerenotsignificantbuttrendedtoward apositiveimpactonsalarywerenon-academiccenter employmentcomparedtoacademicandsemi-rural/rural comparedtourbanjobs.Twothirdsofgraduatesaccepted jobsatsitesincitiesdespitelowersalaries.Menwere morelikelytoacceptjobsassociatedwithhigherpay insmallercommunities,non-academicsettings,and smallerhospitals.
Sensitivityanalysisincludedrunningthemodelwithand withoutthefor-profitvariable.Withandwithoutimputation ofthevaluesofthefor-profitvariabledidnotsignificantly altertheresults,whichappearedtoberobusttominor variationsinthemodel.Similarly,theresultsdidnotchange substantiallybetweenlinearregressionandquantile regression,likelybecausetheincomedistributioninthis sampleappearedtocloselyfollowanormaldistribution basedonShapiro-WilkandShapiro-Franciatestsof normalityandStata’ s “sktest” forskewnessandkurtosis.
Respondentsratedfactorstheyconsideredinselectinga jobwithresponseoptionsrangingfrom “veryimportant” to “notimportantatall.” Wefocusedonfactorsratedas “ very important” comparedtootherresponses(excluding “not applicable”),reportedin Table2A,and “veryimportant” and “important” togethercomparedtoof “littleimportance” and “notimportant,” reportedin Table2B.Therationale behindthisisthat “veryimportant” factorscouldbe consideredcriticalinthejobselectiondecisionandtheir absencecouldeliminateapossiblejob,while “important” factorscouldbeconsiderednicetohaveand,therefore,only aswingfactorinjobselectionifthe “veryimportant” criteria weremet.Thefactorsarelistedinorderofthepercent differenceofpreferencesofwomenovermen.Factorsatthe topof Tables2A and 2B havethegreatestdifferenceinwhat womenconsideredimportantcomparedtomen;factorsat thebottomarethosethatmenconsideredmoreimportant thanwomen.
Generally,womenconsideredlifestyleandwork-life balancefactorsintheirjob-seekingchoicesmorethanmen. Parentalleavepolicy,proximitytofamily,thepractice setting,thetypeofhospital,andlocationofthehospital werestatisticallymoreoftencitedbywomenas “ very important ” factors,whilesalary/compensationwas statisticallymorefrequentlynotedformen.Whenadding “nicetohave”“important ” factorstothe “veryimportant ” factors,adifferentlistofprioritieswasstatisticallydifferent forwomenandmen.Forwomen,theparentalleavepolicy, meetingvisarequirements,thepatientpopulation, employmentoptionsforthespouse,stayinginthesame regionasthetrainingprogram,availabilityofmentors, supportiveacademicenvironment,andurbanvsrural settingcouldbeconsidered “nicetohave ”.Salary/ compensationwastheonlyfactorstatisticallymore importantformenthanforwomen.
Therearemanyfactorsassociatedwiththesalariesthat graduatesreceive.1–6 Threefactorsarestatistically significant.Themostsignificantfactorresultingingreater payisthegendergap,followedbyaDOdegreeand,not surprising,thatfull-timeemploymentpaysmorethanparttimeemployment.15 Incomparison,asimilarrecentsurveyof allACEPmembersfoundsexwassignificantlyassociated withbasesalarybuttypeofdegreewasnot.1 New osteopathicgraduatesarereportedinotherstudiestobe moreinclinedtochoosepositionsinnon-academicsettingsin smallercommunities,bothofwhichappearassociatedwith highersalaries.16,17 Apredominanceofallgraduates acceptedjobsatsitesincitiesdespitethelowersalaries.This isnotsurprisingwhenconsideringthe “veryimportant” preferencesthataresummarizedin Table2A
Thereareannualsurveysofemployersthatcollectdataon averagesalaryandcompensationbyspecialtysuchasthe ModernHealthcarePhysicianCompensationDatabaseand theMedicalGroupManagementAssociation.18,19 Most surveysincludealljobsfornewandexperiencedphysciansin differentphasesoftheircareersandusuallydonot differentiatebetweentypeofhospital,hospitalsite,andother factorsthatareinherenttotheirlocalcommunity.Thejobs mayhavedifferentproportionsofclinicalandadministrative orleadershipresponsibilities,whichmaymakeitdifficutto comparebetweenjobs.ThisACEP-MullenInstitutesurveyis uniqueinthatitfocusedspecificallyonstartingsalariesof graduatestakingtheirvery firstentry-leveljob.Evenforthis well-definedtypeofposition,therewas “quiteabit” or “ a greatdeal” ofvarianceinthejobstheywereoffered,(Table1) asnotedbygraduates.
Apersistentgendergaphasbeenidentifiedinnumerous studies,despitemanyyearsofattentioninmanyprofessions, manyotherspecialties;EMappearstobeno different.5,6,7,15,20,21,22 Wefoundagapattributabletosex
Parentalleavepolicy207925.361424.221.121.7520 <
Proximitytofamily419344.14216425.618.59.26530.002*
Jobs/practiceindesired practicesetting 529853.16816840.512.63.95910.05*
Typeofhospital229822.4161649.812.67.97000.01*
Jobs/practiceindesiredlocation769877.611016765.911.74.030.05*
Employmentforspouse/partner267534.73314223.211.53.23730.07
Patientpopulationtobeserved249724.72216213.611.15.17530.02* Weather259626.03116618.77.31.96430.16
Availabilityofmentors169317.21716310.46.82.42040.12
Supportiveacademicenvironment139214.1121607.56.62.87360.09
Frequencyofweekendduties239823.53216719.24.30.69680.40
Sortedinorderofthedifferenceinpercentageofwomenrespondingas “veryimportant” comparedtomen(column7).
*P < .05significance.
**Sincenoteveryrespondentansweredeveryquestion,Nisthetotalnumberofwomenandmenrespondingtothequestion. EM,emergencymedicine; NP,nursepractitioner; PA,physicianassistant.
aloneof$30,000atthemedian,whichwasconsistentacross theincomedistribution.Reisdorffetalfoundasignificant gendergapof$43,565forasampleofallACEPmembers, andMadsenetalfoundasmallerbutstillsignificant differenceof$19,418foracademicEMfaculty.1,22 The impactofsexinphysicianpayseemspersistentthroughouta careerandcouldtranslatetoanover$2millionnetincome
differenceovera40-yearcareer.23 Ourresultsondifferencein jobpreferencesbysexsuggestthatthereasonsforthegap maynotbeentirelysystemicbutmaybeatleastpartly associatedwiththedifferentlocationsandtypeofjobsthat menandwomenselect.
Graduatingresidentshavemanyfactorstoconsiderand eachindividualwillhavedifferentpersonalprioritiesaswell
Table2B. “Veryimportant” and “important” vsof “littleimportance” and “notimportantatall”:factorsinfluencingjobselectionformenand womensortedbydifferenceinpercent.*
Factoris
Parentalleavepolicy517964.6%3114221.842.8%39.7066 <
Job/practicemeets visarequirements
92634.6%75413%21.6%5.14250.02*
Patientpopulationtobeserved729774.2%9116256.2%18.0%8.47760.004* Employmentforspouse/partner537570.7%7514252.817.9%6.46360.01*
Availabilityofpart-timeposition327642.1%3413724.8%17.3%6.83170.01*
Stayinginsamecity/region asEMtraining
Availabilityofmentors619365.6%8216350.3%15.3%5.61060.02*
Supportiveacademicenvironment419244.6%5016031.2%13.4%4.48890.03*
Ruralvsurban719773.2%10016560.6%12.6%4.27130.04*
Frequencyofweekendduties699870.4%9816758.7%11.7%3.64340.06
Typeofhospital709871.4%9816459.8%11.6%3.63300.06
Proximitytofamily689373.1%10216462.2%10.9%3.16220.08
Opportunitiesforteaching389440.4%5316232.7%7.7%1.54310.21
Frequencyofovernightshifts739874.5%11716570.5%4.5%0.39310.53
Opportunitiesforresearch7907.8%61603.75%4.05%1.89560.17
Jobsindesiredpracticesetting869887.8%14616886.9%0.9%0.04010.84 Costofliving639764.9%10516464%0.9%0.02270.88 Partnershipopportunity378245.1%6614944.3%0.8%0,01460.90
Jobs/Practiceindesiredlocation949895.9%15916795.2%0.7%0.07180.79
7.6%6.05950.01*
Sortedinorderofthedifferenceinpercentageofwomenrespondingas “veryimportantorimportant” comparedtomen(column7). *P < .05significance.
**Sincenoteveryrespondentansweredeveryquestion,Nisthetotalnumberofwomenandmenrespondingtothequestion. EM,emergencymedicine; NP,nursepractitioner; PA,physicianassistant.
asdifferentcareergoals.Womenarestatisticallylesslikely thanmentoconsiderhighsalaryasveryimportantandmore likelytoconsidermorenon-salaryfactors,aslistedin Tables2A and 2B,asmoreimportantthanmen.The long-term financialimpactofthesedecisionsareunknown andwerenotconsideredintheanalysis,butthesepersonal prioritiesmaycontributetotheunexplainedandpersistent salarydifferencesbysex.
Weconfirmedthatsalarymaybeimpacted,butlessso, basedonlocationofpractice,sizeofthecityandthesetting, withacademicandlargehospitalspayinglessthansmaller, ruralandcommunityhospitals.Menweremorelikelyto acceptjobsassociatedwithhigherpayinsmaller communities,non-academicsettings,smallerhospitals,or exclusivelyEMpracticeconsistentwithatleastoneother study.24 AsananticipatedsurplusofEPsisprojected,its
Table3. Quantileregressionresults(median). CategoryCharacteristicVariable
Non-minority255(98.8%)reference
Non-Hispanic246(95.3%)reference
AgeIncreasingageMean$ 1,246( 4,535 + 2,044) 0.46242,954212,954
TrainingTraining location3 International medical graduate 10(3.9%)$+48,096( 9,067 + 105,529) 0.10292,296262,296 USorCanadian graduate 248(96.1%)reference
Non-academic190(73.6%)reference
0.62237,936207,936
Nosecondary job 188(72.9%)reference
1Basesalaryonly.
2Under-representedminorityofBlack,NativeAmerican,andAlaskancomparedtoallothers.
3InternationalmedicalgraduatecomparedtoCanadianandAmericanschoolsaccreditedbytheLiaisonCommitteeonMedicalEducation andAmericanOsteopathicAssociation.
4DO,osteopathicphysicians,comparedto MD,allopathicphysicians.
*P > |t|: P-valueinregressiontable: P < .05significance.
**Thisisthemediansalaryformales/femaleswithallothervariablessettotheirnullvalue,includingthecontinuousvariableforage.
†Thistableshowsresultsfor258respondents.
impactwillbefeltmostdirectlybygraduatingresidentswho arenewtothejobmarketandmostcloselyinvestedinthe supplyanddemand.25 Ofnote,thissurveywascompleted priortotheCOVID-19pandemic.
Therewereseverallimitationstothestudy.Thesampleof 270residentsanalyzedandthe258whohadcomplete(or imputed)datafortheregressionanalysisrepresents
approximately12%ofallgraduatingresidentsin2019;thus, whileitcannotbeconsideredarepresentativesample,itdoes provideinsightintosomeofthefactorsconsideredby graduatingresidentsthatmaybeassociatedwiththeir salaries.Understandingsalarywasnottheprimarypurpose ofthelargerinitiative,buttheresultingdatasetincluded salarydataforrespondentswhohadacceptedapostresidencyjob.Theanalysiscomparedrespondents’ base salarieswithoutconsiderationofadditionalincomesources suchasincentivepaymentsandmaynotrepresentall anticipatedincome.Likeallsurveysrelyingonself-reported data,thepotentialexistsforinaccuraciesorrecallbias. Surveyrespondentswereaskedtoreporttheirsalarieswithin $10,000ranges;so,thepointvaluesusedintheanalysis presumethatactualsalarieswereevenlydistributedwithin eachsalaryrange,whichcouldhaveresultedinsome inaccuracyinsalaryreporting.
Althoughthereisvariabilityinsupplyanddemandof emergencyphysiciansbystate,ourintentwasanational scope;thus,analysisofthesalariesandjobopportunities withinspecificregionsorstateswasnotperformed.Whilethe originalsurveytoolhasbeenusedwidelywithgraduatesof otherspecialties,validationofthissurveytoolwaslimitedto content-expertcomments,pilot-testingwithinEM,and modificationbasedonfeedbackreceived.1 Wedidnot exploreanynumericalmeasuresoffactorloadingor surveyconsistency.
Theregressionmodelwaslimitedto13variablestoaddress overfitting,necessitatingdifficultchoicesastowhichvariables toincludeandhowbesttoconstructdummyvariablesfrom categoricalones.Nevertheless,theresultsofasensitivity analysisthatfoundonlyminorchangesintheresultswhen alternativevariablelistingswereexploredsuggestthatthe regressionmodelwasnotsensitivetochangesinmodel specification.Finally,theregressionanalysisusedasample thatwasslightlysmallerthanthemainsample(258vs270) owingtomissingdataonsomevariables.Itisassumedthatthe 258werecloselyrepresentativeofthelargersample,giventhe smalldifferenceinnumbersbetweenthetwosamples.
Asampleof2019graduatingEMresidentsreported varianceinsalariesthatdependedonseveralvariables.Men andosteopathicphysicianswerepaidsignificantlymorein their firstjobsthanwomenandallopathicphysicians.In exploringpossiblereasonsforthegapinpaybetweenmen andwomen,womenarestatisticallymorelikelythanmento considerlifestylefactorssuchasparentalleavepolicy, proximitytofamily,joblocation,practicesetting,andtypeof hospitalaspriorities.Menarestatisticallymorelikelyto considersalaryandcompensationmoreimportantthan women.Nevertheless,thegapinpaybetweenmenand womenEMgraduatesisnotfullyexplainedbythefactors
wewereabletoincludeinouranalysis,andother explanationsmustbesoughtfortheportionofthegendergap thatremainsunexplained.
AddressforCorrespondence:FionaE.Gallahue,MD,TheUniversity ofWashington,DepartmentofEmergencyMedicine,3259th Ave., Box359702,Seattle,WA,206-744-2556.Email: fiogal@uw.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsourcesand financialormanagementrelationshipsthatcouldbeperceivedas potentialsourcesofbias.Financialsupportwasprovidedbythe AmericanCollegeofEmergencyPhysicians(ACEP),AmericanBoard ofEmergencyMedicine(ABEM),AmericanCollegeofOsteopathic EmergencyPhysicians(ACOEP),AmericanOsteopathicBoardof EmergencyMedicine(AOBEM),CouncilofEmergencyMedicine ResidencyDirectors(CORD),EmergencyMedicineResidents’ Association(EMRA),andSocietyforAcademicEmergencyMedicine (SAEM).ESandLQreceivedfundingfromtheAmericanCollegeof EmergencyPhysicians(ACEP),AmericanBoardofEmergency Medicine(ABEM),AmericanCollegeofOsteopathicEmergency Physicians(ACOEP),AmericanOsteopathicBoardofEmergency Medicine(AOBEM),CouncilofEmergencyMedicineResidency Directors(CORD),EmergencyMedicineResidents’ Association (EMRA),andSocietyforAcademicEmergencyMedicine(SAEM)for thedataacquisitionandanalysis.Therearenootherconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Gallahueetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.ReisdorffEJ,MasselinkLE,GallahueFE,etal.Factorsassociatedwith emergencyphysicianincome. JAmCollEmergPhysiciansOpen. 2023;4(2):e12949.
2.ChenYW,WestfalML,ChangDC,etal.Contributionofunequalnew patientreferralstofemalesurgeonunder-employment. AmJSurg. 2021;222(4):746–50.
3.LeighJP,TancrediD,JerantA,etal.Physicianwagesacross specialties:informingthephysicianreimbursementdebate. ArchInternMed. 2010;170(19):1728–34.
4.NassehKandVujicicM.Earningsofemployedandself-employed UShealthcareprofessionals,2001to2015. JAMANetwOpen. 2018;1(2):e180431.
5.LyDP,SeaburySA,JenaAB.Differencesinincomesofphysiciansin theUnitedStatesbyraceandsex:observationalstudy. BMJ. 2016;353:i2923.
6.JagsiR,GriffithKA,StewartA,etal.Genderdifferencesinthesalariesof physicianresearchers. JAMA. 2012;307(22):2410–7.
7.AsgariMM,CarrPL,BatesCK.Closingthegenderwagegap andachievingprofessionalequityinmedicine. JAMA. 2019;321(17):1665–6.
8.MarcoCA,CourtneyDM,LingLJ,etal.Theemergencymedicine physicianworkforce:projectionsfor2030. AnnEmergMed. 2021;78(6):726–37.
9.NelsonLS,KeimSM,BeesonMS,etal.AmericanBoardofEmergency Medicinereportonresidencyandfellowshiptraininginformation (2018–2019). AnnEmergMed. 2019;73(5):524–41.
10.HarrisPA,TaylorR,ThielkeR,etal.Researchelectronicdatacapture (REDCap)–Ametadata-drivenmethodologyandworkflowprocessfor providingtranslationalresearchinformaticssupport. JBiomedInform. 2009;42(2):377–81.
11.WearsRLandLewisRJ.StatisticalmodelsandOccam’srazor. Acad EmergMed. 1999;6(2):93–4.
12.LeCookBandManningWG.Thinkingbeyondthemean:apractical guideforusingquantileregressionmethodsforhealthservices research. ShanghaiArchPsychiatry. 2013;25(1):55–9.
13.BilgerMandManningWG.Measuringoverfittinginnonlinearmodels:a newmethodandanapplicationtohealthexpenditures. HealthEcon. 2015;24(1):75–85.
14.StataCorpLLC.StataStatisticalSoftware.2019.
15.FreundKM,RajA,KaplanSE,etal.Inequitiesinacademic compensationbygender:afollow-uptotheNationalFacultySurvey cohortstudy. AcadMed. 2016;91(8):1068–73.
16.RanasinghePD.InternationalmedicalgraduatesintheUSphysician workforce. JAmOsteopathAssoc. 2015;115(4):236–41.
17.FordyceMA,DoescherMP,ChenFM,etal.Osteopathicphysiciansand internationalmedicalgraduatesintheruralprimarycarephysician workforce. FamMed. 2012;44(6):396–403.
18.KatzB.2019–2020emergencyphysiciancompensationreport. Availableat: https://www.acepnow.com/article/2019-2020emergency-physician-compensation-report/#comments AccessedAugust20,2024.
19.ChristG.Modernhealthcare’sannualphysiciancompensationsurvey. Availableat: https://www.modernhealthcare.com/businessdata/sf1079/ physician-compensation:-2021.AccessedMay30,2022.
20.WilerJL,RoundsK,McGowanB,etal.Continuationofgender disparitiesinpayamongacademicemergencymedicinephysicians. AcadEmergMed. 2019;26(3):286–92.
21.CatenaccioE,RochlinJM,SimonHK.Addressinggender-based disparitiesinearningpotentialinacademicmedicine. JAMANetwOpen. 2022;5(2):e220067.
22.MadsenTE,LindenJA,RoundsK,etal.Currentstatusofgenderand racial/ethnicdisparitiesamongacademicemergencymedicine physicians. AcadEmergMed. 2017;24(10):1182–92.
23.WhaleyCM,KooT,AroraVM,etal.Femalephysiciansearnan estimated$2millionlessthanmalephysiciansoverasimulated40-year career. HealthAff(Millwood). 2021;40(12):1856–64.
24.BaughJJ,LaiS,WilliamsonK,etal.Emergencymedicineresidents withhigherlevelsofdebtarelesslikelytochooseacademic jobs,butthereisadifferencebygender. AEMEducTrain. 2021;5(1):63–9.
25.ClayCE,SullivanAF,BennettCL,etal.Supplyanddemandof emergencymedicineboard-certifiedemergencyphysiciansbyU.S. state,2017. AcadEmergMed. 2021;28(1):98–106.
DietrichJehle,MD*
KrishnaK.Paul,BS* StanleyTroung,BA*
JacksonM.Rogers,BS*
BlakeMireles,MBS*
JohnJ.Straub,BS* GeorgiyGolovko,PhD†
MatthewM.Talbott,DO* RonaldW.Lindsey,MD‡
CharlesP.Mouton,MS,MBA,MD§
SectionEditor:DavidThompson,MD
*UniversityofTexasMedicalBranch,DepartmentofEmergencyMedicine, Galveston,Texas
† UniversityofTexasMedicalBranch,DepartmentofPharmacologyand Toxicology,Galveston,Texas
‡ UniversityofTexasMedicalBranch,DepartmentofOrthopaedicSurgeryand Rehabilitation,Galveston,Texas
§ UniversityofTexasMedicalBranch,DepartmentofFamilyMedicine, Galveston,Texas
Submissionhistory:SubmittedOctober27,2023;RevisionreceivedApril19,2024;AcceptedApril26,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18531
Introduction: Patientswithlongbonefracturesoftenpresenttotheemergencydepartment(ED)with severepainandaretypicallytreatedwithopioidandnon-opioidanalgesics.Historicaldatarevealsracial disparitiesinanalgesicadministration,withWhitepatientsmorelikelytoreceiveanalgesics.Withthe diversifyingUSpopulation,healthequityisincreasinglycrucial.Inthisstudyweaimedtoevaluatethe earlyadministrationofopioidandnon-opioidanalgesiaamongBlackandWhitepatientswithlongbone andfemurfracturesinEDsoverdifferenttimeframesusingasubstantialdatabase.
Methods: WeretrospectivelyextractedInformationfrom57UShealthcareorganizationswithinthe TriNetXdatabase,encompassing95millionpatients.TheEDrecordsfrom2003–2023weresubjectedto propensityscorematchingforageandgender.Wefocusedonfourcohorts:twocomprisingBlackand Whitepatientsdiagnosedwithlongbonefractures,andanothertwowithBlackandWhitepatients diagnosedsolelywithfemurfractures.Weexaminedanalgesicadministrationratesover20years (2003–2023)at five-yearintervals(2003–2008;2008–2013;2013–2018;2018–2023),andfurther analyzedtheratesforthemostrecenttwo-yearperiod(2021–2023).
Results: Disparitiesinanalgesicadministrationsignificantlydiminishedoverthestudyperiod.For patientswithlongbonefractures(1,095,052),theopioidadministrationgapnarrowedfrom6.3%to1.1%, whilenon-opioidadministrationdisparitiesreducedfrom4.4%to0.3%.Similartrendswerenotedfor femurfractures(265,181).By2021–2023,nosignificantdifferencesinanalgesicadministrationwere observedbetweenracialgroups.
Conclusion: Overthepast20years,thegapinearlyadministrationofopioidandnon-opioidanalgesics forBlackandWhitepatientspresentingwithlongbonefracturesorfemurfractureshasbeen disappearing.[WestJEmergMed.2024;25(5)809–816.]
Patientswithlongbonefracturesroutinelypresenttothe emergencydepartment(ED)withseverepain,requiring effectivepainmanagementstrategies.Over178millionnew fractureswererecordedworldwidein2019,and approximately60%ofthosewerelongbonefractures.1,2 Standardmanagementprinciplesusenon-opioidandopioid analgesicstotreattheseverepainoftenassociatedwithlong bonefractures.3 Therehavebeen findingssuggestingthatnot allpatients’ painwasbeingtreatedequitably.Anational studypublishedin2008thatcovereda13-yearperiodshowed thatnon-HispanicWhitepatientswere8%(31%vs23%) morelikelythanBlackpatientstoreceiveopioidsforpainrelatedconditionsincludingnephrolithiasisandlongbone fractures.4 Severalsubsequentstudieshaveshownthesame trend,showingthatnon-HispanicWhitepatientsweremore likelytobetreatedwithpainmedicationsthanotherracesfor longbonefractures.4–10
Incontrast,somerecentsmallerstudieshavereportedno statisticallysignificantracialdifferencesinanalgesic prescribingforpatientswithlongbonefractures.11–14 Forexample,astudypublishedin2021with6,441pediatric visitsshowedtherewasnosignificantdifferenceinthe rateofopioidsprescribedtochildrenwhowereBlack, Hispanic,orotherracevsnon-HispanicWhitechildrenwho weretreatedforlongbonefracturesatmultiplehospitals from2012–2019.15
AsthepopulationoftheUnitedStatesgrows,itsdiversity isexpectedtoincreaseaswell.Minoritygroupsareprojected toexceedover50%oftheUSpopulationby2044.16 Thus,healthequityandawarenessofdifferentialtreatment basedonraceorethnicitybecomesmoresignificant. Thefundamentalidealinmedicineistoensureahealthcare systemthatdoesnotproduceinequitablehealth treatmentandoutcomesbasedonanindividual’ s demographiccharacteristics.
Ourprimaryobjectivewastoinvestigatepotentialracial inequalitiesintheadministrationofopioidandnon-opioid analgesicsforpatientswithlongboneandfemurfracturesin theED.
StudyDesignandSetting
Thisstudyemployedapropensity-matched,retrospective designtoevaluatealargenationaldatabase,TriNetX,over varioustimeperiods.Usingthe “UnitedStatesCollaborative Network” withintheplatform,containingde-identified electronichealthrecordsofapproximately95million patientsfrom57healthcareorganizations,wecreatedtwo setsofcohortsonDecember27,2022.Theseorganizations arelargelytertiaryacademiccentersandtheirsatellite
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Effectivepainmanagementforlongbone fracturesiscrucial.Disparitiesinanalgesic prescribingbasedonracehighlighttheneed forhealthequity.
Whatwastheresearchquestion?
Arethereinequitiesinadministrationof analgesiaforlongbonefracturesofBlackvs Whitepatients?
Whatwasthemajor findingofthestudy?
From2003to2023,theopioidadministration gapnarrowedfrom6.3%(P < 0.001,CI 0.65 – 0.75)to0.2%(P = 0.78,CI0.98 – 1.03).
Howdoesthisimprovepopulationhealth?
Racialdisparitiesareasigni fi cantbarrierto equitabletreatment,andthisstudyhelpsshed lightonthecurrentstateofhealthcare.
facilities.Thereisrepresentationfromallgeographicregions oftheUnitedStates.
Weselectedpatientsfromallagegroups.Toprotect patientprivacy,thosewhowere ≥90yearsofagewere groupedas90withintheTrinetXdatabase.Inthe firstsetof cohortsstudied,Cohort1.1containedBlackpatientswith longbonefractures,whileCohort1.2containedWhite patientswithlongbonefractures.Longbonefracturesare definedusingtheInternationalClassificationofDiseases, 10th Rev,procedurecodingsystem(ICD-10)fordiagnosisof fracturesoftheshaftofthetibiaandfemur,lowerendof ulna,upperendofradius,shaftofulnaand fibula,lowerend ofradius,forearm,andshoulderandupperarm.TheICD-10 codesarelistedin Table1.Ofnote,multiplefracture diagnosesmaybepresentinonevisit.Inthesecondsetof cohorts,Cohort2.1hadBlackpatientswithonlyfemur fracturesandCohort2.2hadWhitepatientswithonlyfemur fractures.Inthesecohorts,patientshadcomethrough emergencydepartmentservices(CPT:1013711)withinthe prior20years.
Wefurtherexploredthecohortsbylookingatasubgroup analysisover five-yearintervalsrangingfrom2003–2008, 2008–2013,2013–2018,and2018–2023.Theserounded cutoffswerechosenforeaseofinterpretation.Weanalyzed eachintervalfromJanuaryofthestartingyeartoJanuary1 ofthe finalyear.Bothlongboneandfemurfracturecohorts
Table1. InternationalClassificationofDiseases,10th Rev,for fracturediagnosisindatabase.
FracturediagnosisICD-10-CM
No.offractures indatabase
ShoulderandupperarmS421,073,481
ForearmS521,072,733
LowerradiusS52.5679,479
FemurS72597,633
LowerulnaS52.6346,093
ShaftoftibiaS82.2290,731
UpperradiusS52.1259,067
ShaftofulnaS52.2228,245
Unspecifiedshaftof fibula, initialencounter,closed S82.409A57,426
ICD-10-CM,InternationalClassificationofDiseases,10th Rev, ClinicalModification.
werechoseninparttocontrolforconfoundersincaseswith multiplefractures,butalsobecausefemurfracturescomprise amorehomogeneousgroupthatmoreconsistentlyneeds analgesia.Institutionalreviewboardapprovalwasnot requiredforthisstudy,asTriNetXprovidesdatathathas beende-identified,whichrestrictsaccesstoprotectedhealth information(forusersofthedatabase).17
Demographicsincludedself-reportedgenderrace, ethnicity,andmaritalstatus,whichmaptoHealthLevel7 administrativestandards.Genderwascodedasmaleor female.RaceandethnicitywererecodedintoHispanic,nonHispanicWhite,andnon-HispanicBlack.
Fromeachcohort,twodifferentoutcomeswereevaluated: treatmentwithopioidanalgesics(VA:CN101)andtreatment withnon-opioidanalgesics(VA:CN103).Theadministration datapresentedwasbinary:whetherthepatienthadreceived
anyamountofanalgesiaornot.Thetimewindowwas adjustedfortheoutcometooccuronthesamedayorupto onedayfromtheindexeventforeachcohort.Patientswere excludedfromthecohortiftheyreceivedtheoutcomeprior tothevisit,suchasthosewhomayhavehadadocumented acuteorchronicopioid/non-opioidprescriptionprior toarrival.
UsingtheTriNetXdatabase,a1:1propensityscorematch wasproducedwithlinearandlogisticregression.Weused greedynearestneighbormatchingwithtoleranceof0.1and differencebetweenpropensity ≤0.1.18 Balanceoncovariates wasassessedusingstandardizedmeandifference,and absolutevaluesof >0.1wereconsideredpositiveforresidual imbalance.TheTriNetXplatformusesinputmatricesof user-identifiedcovariatesandconductslinearandlogistic regressionanalysistoobtainpropensityscoresforindividual subjects.TriNetXrandomizestheorderofrowstoeliminate biasresultingfromthenearestneighboralgorithms.This studymethodologyhasbeenpreviouslyvalidated.17
Wecomparedcohortsbeforeandafterpropensity matching.Propensitymatchingwasdonethroughthe “BalanceCohorts” toolinTriNetXtocontrolforageatthe diagnosisofthefractureandgender.Therewerestatistically significantdifferencesinthedemographicsforallcompared cohortspriortopropensitymatching.Demographicsbefore andafterpropensitymatchingforthecohortswithlongbone fracturesorfemurfracturesinthelast20yearsareshownin Table2.Duetorecentincreasesinsocietalawarenessfor differentialtreatmentbasedonracialdisparities,asecond subgroupanalysiswasalsocompletedonJanuary1,2023,to analyzethesameoutcomes(opioidanalgesicsandnonopioidanalgesicsonthesamedaytoonedayafteremergency care)forBlackcomparedtoWhitepatientsoverthemost recenttwoyears(2021–2023).
Weusedthemeasure-of-associationtoolinTriNetXto performunivariateanalysiswhereriskratio(RR),95% confidenceinterval(CI),andprobabilityvalues(P )were
Table2. DemographicsforBlackpatientsvsWhitepatientsfrom2003–2023beforeandafterpropensityscorematching.
LongbonefracturesBlackpatientsbeforeWhitepatientsbeforeBlackpatientsafterWhitepatientsafter Totalpatients172,411901,998172,411172,411
FemurfracturesBlackpatientsbeforeWhitepatientsbeforeBlackpatientsafterWhitepatientsafter
Male22,441(57%)91,567(41.5%)22,441(57%)22,441(57%)
calculatedtoshowcomparisonsofoutcomesforthetime intervalscorrespondingtoeachcohortstudied.Thedatawas reportedasRRswith95%CIfromthe finalanalysis,which wascompletedonDecember29,2022.Statisticalsignificance wassetatatwo-sidedalpha <0.05.
Inthisstudyweanalyzed94,990,854patientsfrom57 healthcareorganizationsintheUnitedStatesCollaborative NetworkdatabaseinTriNetX.Therewere2,477,404 patientsidentifiedwithlongbonefractures(272,690Black and1,716,194White)and597,833patientswithonlyfemur fractures(67,905Blackand431,613White)beforerestricting toEDvisits.AfterrestrictingthestudytotheED,175,354 Blackand919,698Whitepatientswerefoundwithlongbone fractures.Usingthe five-yearintervalsfromthesubgroup analysisoflongbonefractures,thenumberofBlackpatients foundwere9,917(2003–2008);27,294(2008–13);67,767 (2013–18);and82,008(2018–23)whilethenumberofWhite patientsfoundwere44,864(2003–2008);147,130(2008–13); 340,320(2013–18);and459,479(2018–23),respectively.
ForpatientswhocamethroughtheEDintheprior 20yearswithfemurfractures,therewere40,084Blackand 225,097Whitepatients.Lookingatthesame five-year intervalsforthesubgroupanalysisoffemurfractures,there were2,092(2003–2008)5,827(2008–13);15,521(2013–18); and19,677(2018–23)Blackpatients,whiletherewere9,301 (2003–2008);33,098(2008–13);82,390(2013–18);and 117,103(2018–23)Whitepatients,respectively.Wedefined raceas “unknown” in19%ofthepatientpopulation.The geographicdistributionofpatientsinthecohortsofED patientswithlongbonefractureswas25%fromthe
Northeast,20%fromtheMidwest,39%fromtheSouth,and 13%fromtheWesternUS.
Opioidanalgesiaforpatientswithlongbonefractures increasedforbothcohorts,shiftingfrom14.4%ofBlackand 20.7%(RR0.697,95%CI0.647–0.751)ofWhitepatients between2003–2008to45.8%ofBlackand46.9%(RR0.978, 95%CI0.964–0.992)ofWhitepatientsbetween2018–2023. Similarincreasesareseenwithnon-opioidanalgesia,going from13.1%ofBlackand17.5%ofWhitepatients(RR0.751, 95%CI0.692–0.815)between2003–2008to42.0%forBlack and41.7%ofWhitepatients(RR1.007,95%CI0.991–1.024) between2018-2023.Additionaldatacanbefoundin Table3 and Table4.Thedifferencebetweenopioidanalgesics prescribedforBlackvsWhitepatientswithlongbone fractureshasoveralldecreasedfromasignificant6.3%gapto 1.1%gapfromthetimeintervalsof2003–2008to2018–2023, asseenin Figure1.Forpatientswithlongbonefracturesin theEDintheprior20years(80%arefromthemostrecent 10years),37.7%ofBlackpatientsreceivedopioidanalgesia comparedto39.8%ofWhitepatients(RR0.947,95%CI 0.937–0.957),while34%ofBlackpatientsreceivednonopioidanalgesiacomparedto35.6%ofWhitepatients(RR 0.955,95%CI0.944–0.967).
Opioidanalgesiaforpatientswithfemurfractureshas beenincreasingforbothcohorts,goingfrom17.8%ofBlack and22.6%ofWhitepatients(RR0.786,95%CI0.667–0.926) between2003–2008to68.1%ofBlackand69.4%ofWhite patients(RR0.982,95%CI0.961–1.003)between 2018–2023.Thisincreaseisalsoseeninnon-opioidanalgesia, increasingfrom16.3%ofBlackand18.7%ofWhitepatients (RR0.876,95%CI0.732–1.047)between2003–2008to
Table3. OpioidanalgesicadministrationforBlackpatientsvsWhitepatientsfrom2003–2023afterpropensityscorematching.
LongbonefracturesBlackpatients%(n)Whitepatients%(n)RR(95%CI)
2003–200814.4%(997)20.7%(1,346)0.697(0.647,0.751)
2008–201319.5%(3,318)24.6%(4,210)0.792(0.761,0.824)
2013–201838.8%(14,250)40.1%(15,392)0.969(0.952,0.986)
2018–202345.8%(19,178)46.9%(21,168)0.978(0.964,0.992)
2021–202345.0%(7,223)44.8%(7,643)1.003(0.981,1.028)
2003–202337.7%(37,412)39.8%(41,408)0.947(0.937,0.957)
FemurfracturesBlackpatients%(n)Whitepatients%(n)RR(95%CI)
2003–200817.8%(213)22.6%(248)0.786(0.667,0.926)
2008–201329.9%(839)29.7%(806)1.006(0.928,1.091)
2013–201854.1%(3,495)53.0%(3,401)1.021(0.989,1.055)
2018–202368.1%(5,196)69.4%(5,511)0.982(0.961,1.003)
2021–202369.6%(2,186)70.1%(2,228)0.993(0.962,1.026)
2003–202354.8%(9,726)54.4%(9,777)1.008(0.989,1.027)
RR,relativerisk; CI,confidenceinterval;timeintervalsfrominitialJan1to finalJan1.
Table4. Non-opioidanalgesicadministrationforBlackpatientsvsWhitepatientsfrom2003–2023afterpropensityscorematching. LongbonefracturesBlackpatients%(n)Whitepatients%(n)RR(95%CI)
2003–200813.1%(886)17.5%(1,072)0.751(0.692,0.815)
2008–201319.0%(3,109)23.6%(3,985)0.807(0.774,0.841)
2013–201834.8%(12,004)36.3%(13,774)0.957(0.939,0.976)
2018–202342.0%(15,044)41.7%(17,582)1.007(0.991,1.024)
2021–202341.0%(5,473)40.0%(6,270)1.025(0.996,1.054)
2003–202334.0%(30,735)35.6%(35,604)0.955(0.944,0.967) FemurfracturesBlackpatients%(n)Whitepatients%(n)RR(95%CI)
2003–200816.3%(196)18.7%(199)0.876(0.732,1.047)
2008–201325.4%(695)25.5%(722)0.995(0.910,1.089)
2013–201845.1%(2,817)45.0%(2,966)1.004(0.966,1.043)
2018–202358.6%(4,034)59.0%(4,464)0.994(0.967,1.021)
2021–202358.5%(1,668)59.1%(1,798)0.990(0.948,1.033)
2003–202346.3%(7,712)45.3%(8,120)1.023(0.999,1.046) RR,relativerisk; CI,confidenceinterval;timeintervalsfrominitialJan1to finalJan1.
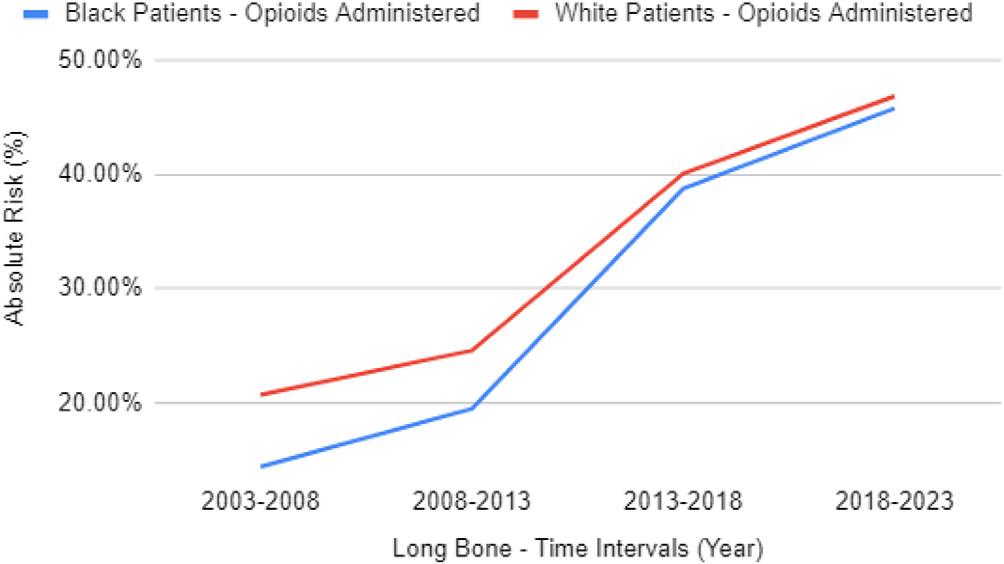
RateofopioidadministrationforBlackpatientsvsWhite patientswithlongbonefracturesafterpropensitymatching.
58.6%ofBlackand59%ofWhitepatients(RR0.994,95% CI0.967–1.021)between2018–2023.Additionaldatacanbe foundin Table3 and Table4.Thedifferencebetweenopioid analgesicsprescribedforBlackvsWhitepatientswithfemur fractureshasoveralldecreasedfroma4.8%gapto1.3%gap fromthetimeintervalsof2003–2008to2018–2023,asseenin Figure2.ForpatientswithfemurfracturesintheEDinthe prior20years(80%arefromthemostrecent10years),opioid analgesiawasgivento54.8%ofBlackvs54.4%ofWhite patients(RR1.008,95%CI0.989–1.027)whilenon-opioid analgesiawasgivento46.3%ofBlackvs45.3%ofWhite patients(RR1.023,95%CI0.999–1.046).
InthesubgroupanalysisperformedJanuary5,2023, administrationofopioidanalgesicsandnon-opioid analgesicsforBlackpatientswascomparedtoWhitepatients
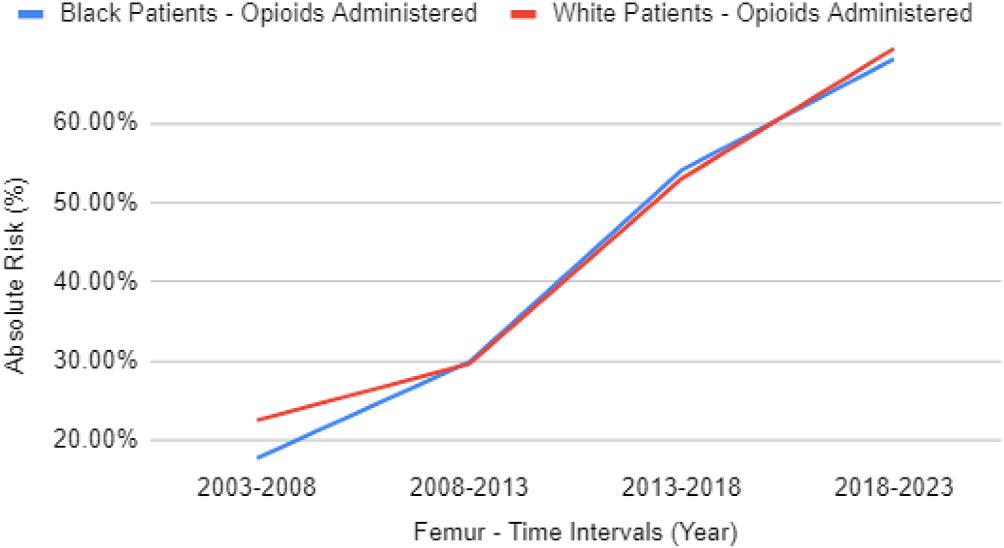
RateofopioidadministrationforBlackpatientsvsWhite patientswithfemurfracturesafterpropensitymatching.
forlongboneandonlyfemurfracturesduringEDvisitsfrom 2021–2023.Beforepropensitymatchingwasperformed,a totalof229,395patientswereidentifiedwithlongbone fracturesand62,761patientswithonlyfemurfractures duringthisperiod.Afterpropensitymatching,therewerea totalof69,668patientswithlongbonefracturesand18,992 patientswithonlyfemurfracturesduringthisperiod.The analysisafterpropensitymatchingshowedthatBlackand Whitepatientswerebothgivencomparableopioidanalgesics (45.0%vs44.8%,RR1.00,95%CI0.980–1.028)andnonopioidanalgesics(41.0%vs.40.0%,RR1.025,95%CI 0.996–1.054)forlongbonefracturesduringthistime interval.Whenevaluatingforonlyfemurfractures,the findingswerealsocomparable.BlackandWhitepatients weregivenequivalentopioidanalgesics(69.6%vs70.1%,RR 0.993,95%CI0.962–1.026)andnon-opioidanalgesics (58.5%vs59.1%,RR0.990,95%CI0.948–1.033).
Theoutcomesforprescribingofopioidanalgesicsand non-opioidanalgesicsforBlackvsWhitepatientspresenting totheEDinalltimeintervalsandsubgroupswereall collectedonthesamedayorwithin24hoursaftertheindex event.Duringtheperiod2003–2008,Whitepatientswere prescribedsignificantlymoreopioidanalgesicsthanBlack patients;however,thegaphasbeendecreasing,andbetween theyears2021–2023,wefoundnosignificantdifferenceinthe numberofopioidanalgesicsprescribedforeitherthelong bonefractureorfemurfracturecohorts.
Theobjectiveofthisstudywastoinvestigatethe relationshipbetweenracialdisparitiesandtheadministration ofbothopioidandnon-opioidanalgesicsfollowingvarious longboneandfemurfractures,andthetrendovera20-year timespantodeterminewhetherdisparitieshavediminished. Thesampleincludedover2.4millionpatientsacrosstheUS whowereevaluatedforpainassociatedwithlongbone fractures.Previousstudieshaveconcludedthatthepainfor thesefracturesisundermanagedfornon-Whitepatients.6 In the2003–2008cohort,the findingsofpreviousstudieswere confirmed,thatWhitenon-Hispanicpatientswerepreviously administeredanalgesiasignificantlymoreoftenthanother demographics.4–8,10 Theresultsofthisstudysuggestthatthe gapbetweenanalgesiaadministrationrateshasdiminished. Infact,therewasnostatisticalsignificanceinopioidsgivento BlackpatientswithlongbonefracturesoverWhitepatients overthemostrecentyears(2021–2023).Resultsweresimilar withandwithoutpropensitymatchingofthegiven populations.Thecohortsoffemurfracturesshowedsimilar findings;however,thegapinadministrationofopioids appearstohavenarrowedin2008andhasremained insignificantupto2023.
Employingpropensitymatchingbyageandgenderis importantinthisdatabase,giventhemarkeddifferencesinthe epidemiologyoflongboneandfemurfracturesacrossraces. Notably,racialdisparitiesinfractureincidenceareevident acrossvariousagegroups,frompreschoolto60yearsofage. Blackmalesshowasignificantlyhigherincidenceoffractures uptotheageof62,whileBlackfemalesexperienceamodestly elevatedrateoffracturesuntiltheageof40.Furthermore, fracturesattributedtoviolencearetenfoldhigheramong Blackindividualscomparedtootherracialgroups. Interestingly,despitepossessinggreaterbonedensity,Black individuals,includingbothchildrenandadults,exhibitan increasedsusceptibilitytofracturesacrossmostnon-fallrelatedinjurymechanisms.Thishighlightsthecomplexityof thefactorsinfluencingfracturerisksandthesignificanceof consideringage,gender,andraceintheanalysis.19
Thisstudydemonstratesthat,overall,opioid administrationhasincreasedoverthepast20years.Several factorscontributedtothistrend,includingrecent
misrepresentationsbydrugcompaniesabouttherisks associatedwithopioids,20 aswellaspolicyinitiativesfrom theJointCommissiononAccreditationofHealthcare Organizationswhichincentivizedhospitalsandphysicians formoreaggressivepainmanagement.Theresultsare consistentwitha2008studythatshowedanincreasein opioiduseduringtimesshortlyafterthelaunchofJoint Commissioninitiatives.4 In1997,painstandardswere developedthroughpoliciesdevelopedbytheJoint Commissionduetoaneedfororganizedpainassessment. Thepoliciesemphasizedpainasthe “5thvitalsign,” which resultedinanupwardtrendforadministrationand prescriptionofopioidmedicationsastreatment.21
Timetopainmanagementbecameacorequalitymetricby whichEDsweremeasuredformultipleyearsandwaslinked toMedicareCMSreimbursement.Physiciansandhospitals wereevaluatedbasedontheirpaintreatmentpractices,and financialincentiveswereprovidedformeetingcertain criteria.This,inconjunctionwithincreasedsocietal awarenessregardingdisparitiesinhealthcare,mayhave playedaroleinnarrowingthegapinanalgesia administrationbetweenBlackandWhitepatients.The combinationofperformance-basedassessmentsand incentives,alongwithheightenedpublicconsciousness,likely contributedtochangesinpainmanagementpracticesthat addressedpreviouslyexistingdisparities.Therehasbeena morerecenttrendasaresultoftheopiatepandemicthat showsoverallopioidprescriptionsarenowdecreasingto allpatients.14
Theresultsofthisstudyhaveimportantimplicationsfor theacutemanagementofpatientswithlongbonefracturesin theUS.Inadequatelytreatedpainhasbeenfoundtobea majorpublichealthchallengeintheUS,andracialand ethnicminoritygroupshavehistoricallyappearedtobeata highriskofreceivinginadequatepaintreatmentintheED.4 Whilestudiesasrecentas2020haveconcludedthatracial andethnicminoritiesarelesslikelytoreceiveanalgesiafor acutetrauma,10 theresultsofthisstudyshowthatthe differentialintreatmenthasdisappeared.Weincorporateda largersamplesizethatisapproximately10timeslargerthan anypreviousstudyonthistopic,andthroughpropensity matchingsomeoftheconfoundingvariableswereeliminated thatmayhaveskewedpreviousdata.Futurestudiesshould aimtoaddressothervariablescontributingtothisdecreasein disparityandincorporatemorestratificationofraceand ethnicitytodeterminewhetherotherdisparitiesarepresent. Otherpossiblerelationships,suchasratesofanalgesicrefusal byrace,prehospitaladministrationofanalgesia,disparities inassessmentofpainscorebyemergencyclinicians,and languagebarriersshouldalsobeanalyzed.
Becausethiswasaretrospectivestudy,causationbetween racialdisparitiesandopioidadministrationcouldnotbe
established.However,thesizeofthisstudy – 2.4millionvs 157,000-inconjunctionwithpropensitymatching,gaveus greaterpowertoidentifydifferencesinoutcomesbetween groupscomparedtopreviousstudies.3,11–15
Inthispropensity-matchedretrospectivestudyoutofthis nationaldatabase,itbecomesdifficulttoevaluateclinical detailsabouteachpatientencountersuchaspainscores, amountofanalgesia,compliancetomedicationsgiven, EmergencySeverityIndexacuitylevel,multitrauma,and informationabouttheprescriber.Thisleadstolackof objectivelymeasuringtheeffectivenessoftheanalgesia, whetheradditionaltreatmentwasneededaftertheinitial analgesia,and,overall,alimitationinjudgingthe effectivenessofthetreatmentitself.Thisstudy,however,was dedicatedtoamoreshort-termapproachregardingtheuseof medicationsintheED,notnecessarilytheeffectivenessof post-encounterormedicationsprescribedupondischarge.
Theremaybeanissuewithgranularityofthevisittypeand dateindatacollectedfromICD9/10-basedsystems.This differenceshouldnotbesignificantbetweenthegroupsor leadtoconfounding.Approximately80%ofthepatient populationisfromthepast10yearsasmanyadditional healthcareorganizationshaverecentlyjoinedtheTriNetX database.Asaresult,thedatasetthatincludesall20yearsis skewedtowardmorerecentpatients.Thiseffectisminimized bylookingattwo-and five-yearperiods.
Additionally,theinabilitytoobtaininsuranceinformation foreachpatientmayhaveposedaparticularchallengeasthis canaccountforcertainbiasesthataffect financialaccessto treatmentandmaynotbemeasurableonthisscale.7 Ouraim wastoeliminateconfoundingvariablessuchasthis,and furtherinformationoninsuranceperpatientmayprovidedata allowingustobetterunderstandthedifferencesbeing measuredinthesesetsafterpropensitymatching.Although propensitymatchingwasperformedfordemographic information,theremaybepre-existingmedicalconditionsthat impactpainseverityandadministrationofanalgesiaforwhich thestudydidnotcontrol.Inaddition,racewasnotknownfor approximatelyone-fifthofthepatientpopulation.
IntheTriNetXdatabase,theidentitiesordesignationsof thehealthcareorganizationsandtheirrespectivesitesarenot disclosedsincethedataisde-identified.Consequently,we couldnotconsideranyclusteringbyhospital.Thislimitation issignificantastheremaybeinherentdifferencesinthe populationcharacteristicsacrossvarioushospitalsystemsor sites,whichcouldinfluencetheadministrationpatternsof analgesiaandpotentiallyintroducebiasintotheresults. Moreover,ourdatabasedoesnotprovideinformationthat allowedustodiscernwhetheranalgesicswereadministered toindividualpatientsintheprehospitalsetting,whichmay haveservedasanadditionalconfoundingfactor.Thereis evidenceindicatingthatpriorto2020,disparitiesexistedin theadministrationofpainmedicationintheprehospital setting.Thiswasobservedincasesinvolvingbothnon-
traumaticandtraumaticpainfulconditions,wherethe probabilityofBlackpatientsreceivingpainmedicationwas lowerwhencomparedtoWhitepatients.22
Thisretrospectiveanalysisprovidesevidencefrom healthcarecentersacrosstheUSthatthereisnolongera significantdifferenceintheadministrationofopioidand non-opioidanalgesicsbetweenBlackandWhitepatients diagnosedwithlongboneandfemurfractures.
AddressforCorrespondence:DietrichJehle,MD,Universityof TexasMedicalBranch,EmergencyBuilding,Room3.124H,301 UniversityBlvd.,Galveston,Texas77555.Email: dijehle@utmb.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudywasconductedwiththe supportoftheInstituteforTranslationalSciencesattheUniversityof TexasMedicalBranch,supportedinpartbyaClinicaland TranslationalScienceAward(UL1TR001439)fromtheNational CenterforAdvancingTranslationalSciences,NationalInstitutesof Health.Thecontentissolelytheresponsibilityoftheauthorsand doesnotnecessarilyrepresenttheofficialviewsoftheNational InstitutesofHealth.Therearenootherconflictsofinterestorsources offundingtodeclare.
Copyright:©2024Jehleetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.GBD2019FractureCollaborators.Global,regional,andnationalburden ofbonefracturesin204countriesandterritories,1990–2019:a systematicanalysisfromtheGlobalBurdenofDiseaseStudy2019. LancetHealthyLongev. 2021;2(9):e580–92.
2.BerghC,WennergrenD,MöllerM,etal.Fractureincidenceinadultsin relationtoageandgender:astudyof27,169fracturesintheSwedish FractureRegisterinawell-definedcatchmentarea. PLoSOne. 2020;15(12):e0244291.
3.AmbossIcon.Generalprinciplesoffractures.2022.Availableat: https:// www.amboss.com/us/knowledge/General_principles_of_fractures/ AccessedFebruary17,2023.
4.PletcherMJ,KerteszSG,KohnMA,etal.Trendsinopioidprescribingby race/ethnicityforpatientsseekingcareinUSemergencydepartments. JAMA. 2008;299(1):70–8.
5.MeghaniSH,ByunE,GallagherRM.Timetotakestock:ameta-analysis andsystematicreviewofanalgesictreatmentdisparitiesforpaininthe UnitedStates. PainMed. 2012;13(2):150–74.
6.MinickP,ClarkPC,DaltonJA,etal.Long-bonefracturepain managementintheemergencydepartment. JEmergNurs. 2012;38(3):211–7.
7.YoungMF,HernHG,AlterHJ,etal.Racialdifferencesinreceiving morphineamongprehospitalpatientswithblunttrauma. JEmergMed. 2013;45(1):46–52.
8.LeeP,LeSauxM,SiegelR,etal.Racialandethnicdisparitiesinthe managementofacutepaininUSemergencydepartments:metaanalysisandsystematicreview. AmJEmergMed. 2019;37(9):1770–7.
9.KennelJ,WithersE,ParsonsN,etal.Racial/ethnicdisparitiesinpain treatment:evidencefromOregonemergencymedicalservices agencies. MedCare. 2019;57(12):924–9.
10.BenzingAC,BellC,DerazinM,etal.Disparitiesinopioidpain managementforlongbonefractures. JRacialEthnHealthDisparities. 2020;7(4):740–5.
11.YenK,KimM,StremskiES,etal.Effectofethnicityandraceontheuse ofpainmedicationsinchildrenwithlongbonefracturesinthe emergencydepartment. AnnEmergMed. 2003;42(1):41–7.
12.DickasonRM,ChauhanV,MorA,etal.Racialdifferencesinopiate administrationforpainreliefatanacademicemergencydepartment. WestJEmergMed. 2015;16(3):372–80.
13.SinghalA,TienYY,HsiaRY.Racial-ethnicdisparitiesinopioid prescriptionsatemergencydepartmentvisitsforconditionscommonly associatedwithprescriptiondrugabuse. PLoSOne. 2016;11(8):e0159224.
14.RomanelliRJ,ShenZ,SzwerinskiN,etal.Racialandethnicdisparities inopioidprescribingforlongbonefracturesatdischargefromthe emergencydepartment:across-sectionalanalysisof22centersfroma healthcaredeliverysysteminNorthernCalifornia. AnnEmergMed. 2019;74(5):622–31.
15.GoyalMK,DrendelAL,ChamberlainJM,etal.Racial/ethnicdifferences inedopioidprescriptionsforlongbonefractures:trendsovertime. Pediatrics. 2021;148(5):e2021052481.
16.ColbySLandOrtmanJM.Projectionsofthesizeandcompositionofthe U.S.population:2014to2060.2021.Availableat: https://www.census. gov/library/publications/2015/demo/p25-1143.html AccessedFebruary17,2023.
17.MurphyLR,HillTP,PaulK,etal.Tenecteplaseversusalteplasefor acutestroke:mortalityandbleedingcomplications. AnnEmergMed. 2023;82(6):720–8.
18.HarrisonSL,Fazio-EynullayevaE,LaneDA,etal.Atrial fibrillationand theriskof30-dayincidentthromboembolicevents,andmortalityin adults ≥ 50yearswithCOVID-19. JArrhythm. 2020;37(1):231–7.
19.PressleyJC,KendigTD,FrencherSK,etal.Epidemiologyofbone fractureacrosstheagespaninBlacksandWhites. JTrauma. 2011;71(5Suppl2):S541–8.
20.HaffajeeRLandMelloMM.Drugcompanies’ liabilityfortheopioid epidemic. NEnglJMed. 2017;377(24):2301–5.
21.BakerDW.TheJointCommission’spainstandards:originsand evolution.2017.Availableat: https://www.jointcommission.org/-/media/ tjc/documents/resources/pain-management/pain_std_history_web_ version_05122017pdf.pdf?db=web&hash=E7D12A5C3BE9DF031F3 D8FE0D8509580&hash=E7D12A5C3BE9DF031F3D8FE0D8509580 AccessedFebruary17,2023.
22.AcevesA,CroweRP,ZaidiHQ,etal.Disparitiesinprehospitalnontraumaticpainmanagement. PrehospEmergCare.2023(6):794–9.
JacquelineJ.Mahal,MD,MBA*† FernandoGonzalez,MD†
DeirdreKokasko,BS* AhavaMuskat,MD†
*JacobiMedicalCenter,DepartmentofEmergencyMedicine,Bronx,NewYork † AlbertEinsteinCollegeofMedicine,Bronx,NewYork
SectionEditor:IoannisKoutroulis,MD,MBA,PhD
Submissionhistory:SubmittedApril17,2023;RevisionreceivedApril24,2024;AcceptedMay3,2024
ElectronicallypublishedAugust1,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18067
Introduction: Emergencydepartment(ED)patientsrequiringimmediatetreatmentoftenbypassatriage processthatincludesHIVscreening.Inthisstudyweaimedtoinvestigatethepotentialmissed opportunitytoscreenthesepatientsforHIV.
Methods: Weconductedthiscross-sectionalstudyinamunicipalEDoverasix-weekperiodbetween June–August2019.ThepatientpopulationinthisstudyarrivedintheEDasapre-notificationfrom prehospitalservicesordesignatedbytheambulanceorwalk-intriagenurseasrequiringimmediate medicalattention.Medicalstudentresearcherscollecteddemographicdataandcategorizedpatients intothreeclinicalgroups(trauma,medical,psychiatric).Theydocumentedthepatient’seligibilityforHIV screeningasdeterminedbyaphysicianandconfirmedthatthepatientmetcriteriaofclearmentalstatus, controlledpain,stablevitalsigns,andabilitytocontributetoamedicalhistoryandphysicalexamination. Thestudentresearchersdidthisatinitialpresentationandthenagainduringthepatient’sEDstayofupto eighthours.Thestudyoutcomesmeasuredthepercentageoftotalpatientswithineachclinicalgroup (trauma,medical,psychiatric)abletoengageintheHIVscreeningprocessuponarrivalandduringan eight-hourEDstay.
Results: Onaverage,700patientspermonthareannouncedonarrivalviaoverheadpage,indicating thattheyrequireimmediatemedicalattention.Duringthesix-weekstudy,205patients(approximately 20%oftotal)wereenrolled:114trauma;56medical;and35psychiatricpresentations.Theaverage patientagewas53;60%ofpatientsweremale.Niney-eight(48%)patientswereeligibleforHIV screeningwithinaneight-hourEDstay;63(31%)wereabletobescreeneduponinitialpresentationand 35(17%)inthe firsteighthoursoftheirEDvisit.Withinmedicalandtraumasubgroups,therewasno significantdifferenceintheproportion(36%)ofpatientsthatcouldbescreeneduponpresentation. Amongthepsychiatricpresentations,only five(14%)wereabletobescreenedduringtheirhospitalstay.
Conclusion: Triageprotocolsforhigh-acuitymedico-surgicalpatientsresultedinamissedopportunity toscreen48%ofpatientsforHIV.Acutepsychiatricpatientsrepresentedaparticularmissedopportunity. WeadvocateforuniversalHIVscreening,facilitatedthroughelectronicbestpracticeadvisoriesanda modifiedtriagetailoredtohigheracuitypatients.ImplementingthesechangeswouldensurethatHIV screeningisnotoverlookedinhigh-acuityEDpatients,leadingtoearlydetectionandtimely interventions.[WestJEmergMed.2024;25(5)817–822.]
TheUSCentersforDiseaseControlandPrevention (CDC)reported131.3millionvisitstoUnitedStates emergencydepartments(ED)in2020.1 In2014,7%of patientswhovisitedtheEDreportedalackofaccessto cliniciansratherthanseriousnessoftheirmedicalcondition asthereasonfortheirlastEDvisit.2 Approximately1.2 millionpeoplelivewithHIVintheUS,and13%areunaware ofthediagnosis.3 ThisincidenceofHIVinfections,coupled withsignificantEDvolumeanduseoftheEDforprimary care,continuestomaketheEDacriticalpointof engagementwiththemedicalsystemand,thus,an opportunitytoprovideHIVscreening.4–7
SincetheCDC’s2006recommendationforopt-outHIV screeningforpatientsinallhealthcaresettings,therehasbeen ampleliteratureonuniversalHIVscreeningintheED; however,acutelyillpatientsareoftenexcludedfromdata collection.8–10 OnestudyfocusingonHIVscreeningof acutelyillmedicalpatientsintheEDfoundthatthemajority ofthepatientsdiagnosedwithHIVwereadmittedwithAIDS andhadanaverageofthreeprevioushealthcarevisitspriorto HIVscreening.11 Whenconsideringtraumapatientsinthe ED,theliteraturereportsHIVscreeningratesthatrange from25.2–64.1%.12–14 Arecentpapercomparingscreening intraumatomedicinepatientsfoundthatscreeningin traumapatientswaslowerthaninmedicalpatients,yetHIV rateswerehigherintraumavsmedicalpatients.14 Both studiesdemonstratethatitisfeasibletotestthesehigher acuitypatientsandsuggestthathigh-acuitypatientsmaybe anothermissedopportunityintheEDtoidentifypreviously undiagnosedHIV.
Inoursetting,ifapatientisacutelyillorinjuredrequiring immediatemedicalattention,thepatientisannouncedviaan overheadintercomandismovedtoaresuscitationbay, bypassingthetriageprocessthatincludesrequiredHIV screening.PerNewYorkStatePublicHealthLaw(PHL),15 therearethreeexceptionstotherequiredHIVtestingoffer: life-threateningillness;recenttestingandnorecentrisk behaviors;andadeterminationbytheattendingthatthe patientdoesnothavementalcapacity.Wehypothesizethat ourtriageprocessofautomaticallyexcludingpatients identifiedviaoverheadpagepresentsmissedopportunitiesto screenotherwiseeligiblepatients.
Thiswasasingle-site,cross-sectionalstudy.Ourobjective wastomeasurewhatpercentageofpatientsdeemedacute, andwhothusbypassedthetriageprocessthatincludesHIV screeninginordertoreceiveimmediatemedicalevaluation, wereabletobescreenedforHIVduringtheirEDstay.The protocolwasapprovedbytheAlbertEinsteinCollegeof MedicineandtheNewYorkCityHealth&Hospitals institutionalreviewboardsandwasdeemedexemptfrom
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
WhileuniversalHIVscreeningintheEDisa well-knownandreviewedclinicalactivity, acutelyinjuredandmedicallyillpatientsare oftenexcluded.
Whatwastheresearchquestion?
Dopatientswhopresentemergentlytoan urbanEDpresentamissedopportunityfor HIVscreening?
Whatwasthemajor findingofthestudy?
Ofthe205acutelyill,injuredorpsychiatric patientsinthisstudywhobypassedtypical HIVscreeningintriage,98(48%)were screenedforHIVduringtheireight-hour EDstay,with63(31%)screenedupon initialpresentation.
Howdoesthisimprovepopulationhealth?
ThisstudyhighlightsagapinHIVscreening andamissedopportunityfortestingHIVin EDpatients.
requiringconsent.Thisstudyisreportedusingthe StrengtheningtheReportingofObservationalStudiesin Epidemiology(STROBE)guidelines.16
Thisstudywasconductedinamunicipal,adultED withLevel1traumadesignationinNewYorkCitywithan annualcensusofapproximately73,000andapproximately 15%ofpatientsarrivingbyambulance.Enrollmentoccurred overasix-weekperiodfromJune–August2019.Three medicalstudentresearchers(SR)werepresentinthe EDforapproximately13hoursperday,5–7days perweek.
ThepatientpopulationinthisstudyarrivedintheEDasa pre-notificationfromprehospitalservicesorwasdesignated bytheambulanceorwalk-intriagenurseasrequiring immediatemedicalattention.Thesepatientswereeither EmergencySeverityIndex(ESI)1or2,wereannouncedvia anoverheadintercomsystem,andmovedtoaresuscitation bay.Inrealtime,SRsreportedtotheresuscitationbayto recorddemographicdataincludingage,gender,chief complaint,date,andtimeofpresentation.Theyassigned patientstooneofthreeclinicalgroups:trauma;medical;
orpsychiatric.Psychiatricpatientsincludedthosewith agitationsecondarytosubstanceuse,primarypsychiatric presentation,oradualdiagnosis.Theattendingorresident physiciandeterminedwhetherthepatientcouldengageinthe HIVscreeningprocess,andtheSRscheckedthatthepatient metcriteriaofclearmentalstatus,controlledpain,stable vitalsigns,andabilitytocontributetomedicalhistoryand physicalexamination.
IfapatientcouldnotengageintheHIVscreeningprocess, butanappropriatehealthcareproxy(HCP)waspresentto provideconsent,thepatientwasconsideredscreenable. Verbalconsentofthepatientorthepatientproxyisrequired priortoorderingtheHIVtestinaccordancewithNewYork StatePHL2781/2781a17;however,askingtheHCPfor consentforHIVtestingisnottypicallydoneinourED. Patientswhowerenotimmediatelyabletoparticipateinthe HIVscreeningprocesswerereassessedatfourandeight hoursafterpresentation.Eighthourswaschosensincethe averagelengthofstayinthisEDisapproximately sevenhours.
WewereunabletoreceiveHIVtestresultsforpatients whowerebotheligibleandoptedinfortesting.Thestudy periodstraddledahospital-widetransitiontoanew electronichealthrecordsystem(EHR),whichincludeda changeintheHIVtestingprotocol,leadingtolostand canceledbloodtests.
Theprimarystudyoutcomeswerethepercentagesof patientsineachoftheclinicalgroups(trauma,medical, psychiatric)whowereabletoengageintheHIVtest screeningprocessatarrivalandbyorbeforeeighthours. Meanagewithstandarddeviationwerereportedforeach clinicalgroupandcomparedtothemeanoftheentirecohort. SinceconsentviaHCPisatypicalinpractice,wereport thenumberofpatientsandtheaverageageofthis patientsubgroup.
Wecomparedtheproportionofpatientsineachclinical groupandtheproportionthatcouldengageintheHIV screeningatarrivalandbyorbeforeeighthoursusingthe
traumagroupasthereferencegroup.Weused χ 2 tocompare proportionsandtheStudent t -testtocomparemeanswiththe α at.05orlessfortwo-tailedtestsofsignificance.Analysis wascompletedinExcel2019(MicrosoftCorporation, Redmond,WA).
InourED,approximately700patientspermonthare calledoverheadonarrivalandmovedtotheresuscitation bay.Duringthesix-weekstudyperiod,205patientswere enrolled,capturingapproximately20%ofoverhead notifications.TheaveragetimeofdaytheSRrespondedto theoverheadpagewas3:40 PM with23%ofpatientsbeing seenafter8 PM ontheovernightshift.Ameanmaleageof 44.7vsameanfemaleageof66.6wasstatisticallysignificant inthetraumagrouponly(P < .001, Table1).Themedical andpsychiatricclinicalsubgroupshadnostatistically significantdifferenceinagebygender.Theproportionof patientsinthemedicalclinicalsubgroupdidnotdiffer statisticallyfromthetraumareferencegroup(Table1).Eight (4%)patientswereincludedasscreenablebecauseaHCP providedconsent;averageageoftheseeightpatientswas65 witharangeof23–91.
Ofthe205patients,98(48%)wereabletoengageinHIV screeningduringtheireight-hourEDstay.Ofthese98 patients,63(31%)wereabletobescreeneduponinitial presentationandanadditional35(17%)inthe firsteight hoursoftheirEDvisit.Whencategorizedbypresentation type,61(54%)of114traumapatients,32(57%)of56medical patients,and five(14%)of35psychiatricpatientswereableto engageinHIVscreeningduringtheireight-hourEDstay. Therewasnostatisticaldifferencebetweenabilityto participateinscreeningbetweentraumaandmedicalclinical presentations(Table2).Comparedtotraumaandmedical patients,psychiatricnotificationshadasignificantlylower abilitytobescreenedbytheeight-hourmark(P < .03).The patient’slevelofpsychiatricacuity,beinginpolicecustody, orleavinguponsobrietywerereasonsthat30(86%)ofthe35 psychiatricpatientswerenotabletobescreenedwithineight hoursintheED.
1Medicalandpsychiatricclinicalsubtypewerecomparedtothetraumagroupasareference. 2Meanagebygenderwerecomparedwithineachclinicalsub-type.
Table2. PercentageofpatientsbypresentationtypeandtimewhowereabletobescreenedforHIV.
Presentationsub-type Patients (totalN = 205) Screenedatpresentation (t = 0hours) P-valueScreened ≤ 8hours P-value Trauma11441(36%)20(18%) Medical5620(36%)0.9712(21%)0.52 Psychiatric352(6%) <0.0013(8%)0.03
Thissingle-site,cross-sectionalstudydemonstratedthat 36%ofpatientswhopresentedwithemergentmedicalor traumaclinicalpresentations,thusbypassingHIVscreening intriage,wereabletobescreenedatinitialpresentation.An additional21%whopresentedformedicaland18%for traumapresentationswereabletobescreenedbyeighthours intotheirEDstay.Theresultswerestatisticallyconsistent betweenpatientsinthemedicalortraumaclinical presentationgroupsandstatisticallylesslikelyforpsychiatric patients.Notably,86%ofpsychiatricpatientswereunableto bescreenedwithineighthoursintheED.
With1in7people,ornearly165,000intheUnited States,18 unawareoftheirHIVstatus,universal,nontargetedHIVscreeninginhigh-volumesettingslikeEDs remainsaneffectivestrategy.StudiesfrombothOaklandand Chicagoreportthatapproximately50%ofnewHIV diagnoseswouldhavebeenmissedhadtheyusedatargeted, symptom-andrisk-basedscreeningmethodology.19–23 Ina randomizedclinicalstudycomparingatargetedvsanontargetedscreeningapproach,Haukoosetalconcludedthat targetedscreeningwasnotsuperior,althoughitwasmore efficientwithfewertestscompleted.24
Inadditiontothescreeningmethodology,thelocationof HIVscreeningmayinfluencethecompletionoftesting. ScreeningforHIVcanoccurduringtriage,registration,inthe waitingroomwithkiosksanddedicatedstaff,oratthebedside drivenbyaclinician.InTanetal,theauthorsreviewed20HIV testingprotocols.25 Theyfoundthatofferratesarehighest duringregistrationandattriage,attributedtosystematic questioning,reaching100%insomestudies.Theofferof testingdoesnot,however,equatetoacceptanceoftesting.The highestacceptancerateswerefoundatthebedsideandinthe waitingroom,oftenbecausethepersondoingthescreening wouldalsobeconductingthetest.25 Screeningandtesting protocolsdifferbysiteandresourcesavailable,making generalizabilityacrossallEDsettingsdifficult.
TriageisoneofthemostimportantprocessesintheED. Toguideclinicianswiththistask,triagescoresareusedto provideanobjectivemeasureofpatientacuitytofocusonthe sickestpatients.TheEmergencySeverityIndex(ESI)triage scoreisthemostusedintheUS26 andistheoneusedinour institution.Studiesreportgreatvariabilitywithpoorto moderateaccuracy,27,28 especiallyinhigh-acuitypatients. TheAmericanCollegeofSurgeonsCommitteeonTrauma recommendsanover-triagerateof25–50%onactivationof
traumateamsattraumacenters,andtheliteraturereportsa rangeof18–91%.29–32 Thisvariabilitymaybenecessaryto ensureprompttreatmentoflife-threateninginjuriesand illnesses,whilealsoreducingthenumberofacutepatients treatedatnon-traumacenters.29
Over-triageandanemphasisonimmediateintervention presumesineligibilityforHIVscreeninginourtriage processthatwouldtypicallyincludeuniversal,nontargetedHIVscreening.Patientswithhighacuity(ESI1 and2)werenotinformedofHIVscreeninginourstudy,as wasthecaseinotherstudies. 15 , 33 Thefocusonidentifying, stabilizing,andtreatingacuteinjuryorillnesssensibly supersedestheHIVscreeningprocess.Atrueuniversal HIVscreeningprotocolshouldincludeallpatients regardlessofESIandincludeanindividualassessmentto determineabilitytoconsent,ratherthanpresumed ineligibility.Whileweha dthemanpowertoreassess patientsperiodically,thisresource-heavymodelisnot likelytobebroadlyreplicable.
Evenwiththeabilitytoreassessperiodically,wefoundthat 86%ofacutepsychiatricpatientswerenotabletobescreened forHIVatinitialpresentationorwithineighthoursintheED. InallstagesoftheHIVcarecascade,thepatientpopulation thatstruggleswithmentalhealthismetwithchallenges. MentalhealthdisordersincreasetheriskofHIVacquisitionby 4–10times34,35 and,atthesametime,interferewithHIV testingandlearningone’sHIVstatus.36 Thestrugglewith depression,anxiety,trauma,andsubstanceuseisasubstantial barriertoHIVpreventionmethods(ie,condoms,pre-exposure prophylaxis),andadultswithmentalhealthdisorderswere morelikelytobeinvolvedinbehaviorsassociatedwithHIV acquisitionortransmissionthanadultswithoutmental disorders.37,38 Struggleswithmentalhealthcontributetopoor retentionincareandanti-retroviraladherence.38,39 Without thebenefitofviralsuppressionachievedwithanti-retroviral treatment,acute-carehospitalizationsforpatientswithHIV andmentalhealthdisordersarehigherthanforHIVpatients withoutmentalhealthdisorders.39,40 Oftheacutepatients presentingtotheED,our findingssuggestthatpatientswith mentalhealthpresentationsand,inparticular,acutemental healthcrisesmayrequireanalternativeoradditionalapproach toHIVscreeningandtesting.
TheEDisoneplacetostartthecarecascadewithuniversal testing.However,weseethattheacutepatient,andespecially thepatientwithacutementalhealthpresentations,may requireanalternativeapproach,otherthanduringinitial
triage,toensurethatscreeningoccurs.UsingtheEHRhas beenshowntooptimizescreeningandtestingandtoincrease identificationofnewHIVinfections.41,42 BuildinganESI1 and2ordersetthatincludesanHIVtestcouldbeonemeansto addressHIVscreeningintothecareofacutelyillpatients.The HIVtestintheordersetwouldrequiretheclinicianto acknowledgescreeningeligibilityandverbalconsentpriorto finalizingtheorder.Abestpracticeadvisorywithscriptsfor clinicianstouseopt-outlanguagecouldbeprogrammedto fire ifpatientshaven’tyetbeenscreenedduringthecurrentED encounterandhaven’treceivedHIVtestingina predeterminedlook-backperiod.Thisstrategycouldaddress anypatientwhomayhavemissedHIVscreeningortestingin theED,notjustouracutepatientswhomissourtriage screening.Anynewapproachorcombinationofapproaches wouldrequireimplementationplansandprocessesandfuture investigationbeforebeingacceptedassolutions.
Thiswasnotacompletesampleofallacutepatients presentingtotheEDduringthestudyperiodsincewedidnot haveSRs24hoursaday.Thiswasasingle-sitestudyina LevelItraumacenterwithhighvolume,whichcontributesto problemswithgeneralizabilitymainlyfornon-urban hospitalsettings.TheapproachtoHIVscreeningislikelyto bevariableinotherEDsandmaynotoccuraspartofthe triageprocess.Differencesinlawsandregulationsfortesting andconsentmayalsocontributetothelackof generalizabilityofthese findings.Thedeterminationofbeing abletobescreenedisclinician-dependent,withpossiblebias towardHIVscreeningandtestingintheEDandwhether peopleshouldbeasked.Wearenotabletoreportthedisease prevalenceinthissmalldataset.TheHIVtestresultswerenot reportedduetoinconsistenttestingandlabprotocolsfor HIVtestingasthehospitalmigratedtoanewEHRsystem duringthetestingperiod.Whilenotthefocusofthestudy,we acknowledgethatthisdataandcollectionofHIVriskfactors forpatientswouldhavebeenavaluableadditiontothestudy.
ThisstudyhighlightsagapinHIVscreeninginEDsanda missedopportunityfortestingforHIVinEDpatients.We foundthatcloseto48%ofpatientswhopresentforemergent careandmissedtheHIVuniversalscreeningthatoccurs duringtriageinourinstitutioncouldengageinthescreening processeitheratpresentationorduringtheirEDstay.And weidentifiedanalreadyvulnerablegroup psychiatric patients thatappearstobeineligibleforscreeningwithin anEDstay,leavingustoconsiderwhetherthesepatientswill determinetheirHIVstatus.Futureresearchisneededto assesstheeffectivenessofelectronicbestpracticeadvisories andbuilt-inHIVscreeningandtestingordersetsinhigher acuitypatients,aswellasapproachestomeetingtheneedsof theacuteandvulnerablepsychiatricpatient.
AddressforCorrespondence:Dr.JacquelineJ.Mahal,Directorof EmergencyHIVServices,JacobiMedicalCenter,Departmentof EmergencyMedicine,1400PelhamParkwaySouth,Bronx,NY 10461.Email: mahalj@nychhc.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Mahaletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CairnsCandKangK.NationalHospitalAmbulatoryMedicalCare Survey:2020emergencydepartmentsummarytables.2022.Available at: https://dx.doi.org/10.15620/cdc:121911.AccessedJanuary10, 2024.
2.GindiRM,BlackLI,CohenRA.Reasonsforemergencyroomuse amongU.S.adultsaged18–64:NationalHealthInterviewSurvey,2013 and2014. NatlHealthStatReport. 2016;90:1–16.
3.HIV.gov.U.S.statistics.2022.Availableat: https://www.hiv.gov/hivbasics/overview/data-and-trends/statistics.AccessedMay31,2023.
4.USPreventiveServicesTaskForce,OwensDK,DavisonKW,etal. ScreeningforHIVinfection:USPreventiveServicesTaskForce recommendationstatement. JAMA. 2019;321(23):2326–36.
5.KecojevicA,LindsellCJ,LyonsMS,etal.Publichealthandclinical impactofincreasingemergencydepartment-basedHIVtesting: perspectivesfromthe2007conferenceoftheNationalEmergency DepartmentHIVTestingConsortium. AnnEmergMed. 2011;58(1Suppl1):S151–9.e1.
6.WhiteDAE,GiordanoTP,PasalarS,etal.AcuteHIVdiscovered duringroutineHIVscreeningwithHIVantigen-antibodycombination testsin9USemergencydepartments. AnnEmergMed. 2018;72(1):29–40.e2.
7.BransonB,HandsfieldH,LampeM,etal.Revisedrecommendationsfor HIVtestingofadults,adolescents,andpregnantwomeninhealth-care settings.2006.Availableat: https://www.cdc.gov/mmwr/preview/ mmwrhtml/rr5514a1.htm.AccessedFebruary13,2023.
8.WhiteD,ScribnerA,VahidniaF,etal.HIVscreeninginanurban emergencydepartment:comparisonofscreeningusinganopt-inversus anopt-outapproach. AnnEmergMed. 2011;58(1):S89–95.
9.HaukoosJS,HopkinsE,ByynyRL,etal.Patientacceptanceofrapid HIVtestingpracticesinanurbanemergencydepartment:assessmentof the2006CDCrecommendationsforHIVscreeninginhealthcare settings. AnnEmergMed. 2008Mar;51(3):303–9,309.e1.
10.PisculliML,ReichmannWM,LosinaE,etal.Factorsassociatedwith refusalofrapidHIVtestinginanemergencydepartment. AIDSBehav. 2011;15(4):734–42.
11.LubelchekRJ,KrocsKA,LevineDL,etal.Routine,rapidHIVtestingof medicineserviceadmissionsintheemergencydepartment. AnnEmerg Med. 2011;58(1):S65–70.
12.PickettML,TaverasLR,Turner-WenttT,etal.HIVscreeningandearly referralinthetraumapopulation:theexperienceofalargesafetynet hospital. JSurgRes. 2020;245:360–6.
13.PrivetteAR,WhiteB,FergusonPL,etal.Adifferentformofinjury prevention:successfulscreeningandreferralforhuman immunodeficiencyvirusandhepatitisCvirusinatraumapopulation. J TraumaAcuteCareSurg. 2018;85(5):977–83.
14.StanfordKA,EllerD,SchmittJ,etal.HighrateofHIVamongtrauma patientsparticipatinginroutineemergencydepartmentscreening. AIDS Behav. 2023;27(11):3669–77.
15.NewYorkStateSenate,signedintolawonAugust31,2010.NewYork StateconfidentialitylawandHIV:PublicHealthLaw,27-F.Availableat: https://www.health.ny.gov/publications/9192.pdf AccessedJanuary10,2024.
16.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. JClinEpidemiol. 2008;61(4):344–9.
17.NewYorkPublicHealthLawSection2781 – HIVrelatedtesting.2016. Availableat: https://www.nysenate.gov/legislation/laws/PBH/2781 AccessedJanuary10,2024.
18.HIV.gov.ToomanypeoplelivingwithHIVintheU.S.don’tknowit.2019. Availableat: https://www.hiv.gov/blog/too-many-people-living-hivus-don-t-know-it.AccessedJanuary10,2024.
19.LyonsMS,LindsellCJ,RuffnerAH,etal.Randomizedcomparisonof universalandtargetedHIVscreeningintheemergencydepartment. JAcquirImmuneDeficSyndr. 2013;64(3):315–23.
20.WhiteDA,ScribnerAN,SchuldenJD,etal.ResultsofarapidHIV screeninganddiagnostictestingprograminanurbanemergency department. AnnEmergMed. 2009;54(1):56–64.
21.LyssSB,BransonBM,KrocKA,etal.DetectingunsuspectedHIV infectionwitharapidwhole-bloodHIVtestinanurbanemergency department. JAcquirImmuneDeficSyndr. 2007;44(4):435–42.
22.EscuderoDJ,BahamonM,PanakosP,etal.Howtobestconduct universalHIVscreeninginemergencydepartmentsisfarfromsettled. JAmCollEmergPhysiciansOpen. 2021;2(1):e12352.
23.BlumbergSJandDickeyWC.PrevalenceofHIVriskbehaviors,risk perceptions,andtestingamongUSadultswithmentaldisorders. JAcquirImmunedeficSyndr. 2003;32(1):77–9.
24.HaukoosJS,LyonsMS,RothmanRE,etal.ComparisonofHIV screeningstrategiesintheemergencydepartment:arandomized clinicaltrial. JAMANetwOpen. 2021;4(7):e2117763.
25.TanR,HugliO,CavassiniM,etal.Non-targetedHIVtestinginthe emergencydepartment:notjust how but where ExpertRevAntiInfect Ther. 2018;16(12):893–905.
26.McHughM,TanabeP,McClellandM,etal.Morepatientsaretriaged usingtheemergencyseverityindexthananyothertriageacuitysystem intheUnitedStates. AcadEmergMed. 2012;19(1):106–9.
27.MistryB,StewartDeRamirezS,KelenG,etal.Accuracyandreliability ofemergencydepartmenttriageusingtheemergencyseverity index:aninternationalmulticenterassessment. AnnEmergMed. 2018;71(5):581–7.e3.
28.ZachariasseJM,vanderHagenV,SeigerN,etal.Performanceoftriage systemsinemergencycare:asystematicreviewandmeta-analysis. BMJOpen. 2019;9(5):e026471.
29.DavisJW,DirksRC,SueLP,etal.Attemptingtovalidatetheovertriage/ undertriagematrixataLevelItraumacenter. JTraumaAcuteCareSurg. 2017;83(6):1173–8.
30.HoffJJ,CarrollG,HongR.Presenceofundertriageandovertriage insimpletriageandrapidtreatment. AmJDisasterMed. 2017;12(3):147–54.m.
31.NewgardCD,StaudenmayerK,HsiaRY,etal.Thecostofovertriage: morethanone-thirdoflow-riskinjuredpatientsweretakentomajor traumacenters. HealthAff(Millwood). 2013;32(9):1591–9.
32.LernerEB,ShahMN,CushmanJT,etal.Doesmechanismof injurypredicttraumacenterneed? PrehospEmergCare. 2011;15(4):518–25.
33.LinJ,BaghikarS,Mauntel-MediciC,etal.Patientandsystemfactors relatedtomissedopportunitiesforscreeninginanelectronicmedical record-driven,opt-outHIVscreeningprogramintheemergency department. AcadEmergMed. 2017;24(11):1358–68.
34.CentersforDiseaseControlandPrevention(CDC).HIVpreventionin theUnitedStates:newopportunities,newexpectations.2015.Available at: https://stacks.cdc.gov/view/cdc/39420.AccessedMay31,2023.
35.HobkirkAL,ToweSL,LionR,etal.PrimaryandsecondaryHIV preventionamongpersonswithseverementalillness:recent findings. CurrHIVAIDSRep. 2015;12(4):406–12.
36.RemienRH,StirrattMJ,NguyenN,etal.MentalhealthandHIV/AIDS: theneedforanintegratedresponse. AIDS. 2019;33(9):1411–20.
37.CollinsPY,VellozaJ,ConcepcionT,etal.InterveningforHIVprevention andmentalhealth:areviewofgloballiterature. JIntAIDSSoc. 2021;24Suppl2(Suppl2):e25710.
38.JoskaJA,KaliskiSZ,BenatarSR.Patientswithseverementalillness:a newapproachtotestingforHIV. SAfrMedJ. 2008;98(3):213–7.
39.St-JeanM,TafessuH,ClossonK,etal.ThesyndemiceffectofHIV/HCV co-infectionandmentalhealthdisordersonacutecarehospitalization rateamongpeoplelivingwithHIV/AIDS:apopulation-based retrospectivecohortstudy. CanJPublicHealth. 2019;110(6):779–91.
40.MijchA,BurgessP,JuddF,etal.Increasedhealthcareutilizationand increasedantiretroviraluseinHIV-infectedindividualswithmental healthdisorders. HIVMedicine. 2006;7(4):205–12.
41.ShaBE,KniukstaR,ExnerK,etal.Evolutionofanelectronichealth recordbased-humanimmunodeficiencyvirus(HIV)screeningprogram inanurbanemergencydepartmentfordiagnosingacuteandchronic HIVinfection. JEmergMed. 2019;57(5):732–9.
42.KershawC,TaylorJL,HorowitzG,etal.Useofanelectronicmedical recordreminderimprovesHIVscreening. BMCHealthServRes. 2018;18(1):14.
ChristopherL.Bennett,MD,MSc,MA*
M.KitDelgado,MD,MS†
MelissaPasao,BS*
JaniceA.Espinola,MPH‡
KrislynM.Boggs,MPH‡
CarlosA.CamargoJr.,MD,DrPH‡§
*StanfordUniversitySchoolofMedicine,DepartmentofEmergency Medicine,Stanford,California
† UniversityofPennsylvania,DepartmentofEmergencyMedicine, Philadelphia,Pennsylvania
‡ MassachusettsGeneralHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts
§ HarvardT.H.ChanSchoolofPublicHealth,DepartmentofEpidemiology, Boston,Massachusetts
SectionEditor:FaithQuenzer,DO,MPH
Submissionhistory:SubmittedSeptember28,2023;RevisionreceivedFebruary23,2024;AcceptedApril5,2024
ElectronicallypublishedJuly17,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18488
Introduction: IntheUnitedStates,morechronicandpreventivehealthcareisbeingdeliveredinthe emergencydepartment(ED)setting.Understandingtheavailabilityofpreventivehealthservicesinthe EDsettingiscrucial.Ourgoalwastounderstandtheavailabilityofasubsetofpreventivehealthservices inUSEDsandexplorehowthathaschangedovertime.
Methods: In2022–2023,usingtheNationalEmergencyDepartmentInventory(NEDI)-USA,we surveyedarandom20%(1,064)samplingofall5,613USEDs.WeaskeddirectorsoftheseEDsabout theavailabilityofandpreferencefor12preventivehealthservices,socialworkeravailability,selfreportedpercentageofuninsuredEDpatients,andmeasuresofEDcrowding.Wealsoaskedabout perceptionsofbarrierstoimplementingpreventivehealthservicesintheED.Weusedunadjustedand multivariablelogisticregressionmodelstocompareservicefrequencyin2022–2023toprior findings from2008–2009thatrepresenteda5.7%randomsamplingofallEDs.
Results: Among302responderstothe2022–2023survey(5.4%randomsampling,28.4%response rate),94%reportedofferingatleastonepreventivehealthservice,withamedianof fiveservices.The mostcommonserviceofferedwasintimatepartnerviolencescreening(83%),whiletheleastcommon wasroutineHIVscreening(19%).Sevenservices(eg,intimatepartnerviolence,alcoholrisk,and smokingcessationscreening)hadahigheroddsofbeingofferedin2022–2023thanin2008–2009; findingswereunchangedinsensitivityanalyses.Asmallproportionofdirectorsopposedoffering preventivehealthservices.However,manyexpressedconcernsthatpreventivehealthservicesinthe EDwouldleadtolongerlengthsofstay(56%),increasedcoststotheirED(58%),adiversionofstafftime fromprovidingacutecare(50%),orthattheirpatientswouldnothaveaccesstoadequatefollowup(49%).
Conclusion: NearlyallEDsofferatleastonepreventivehealthservice.Manyoffermultipleservices; rateswerehigherthanthoseidentifiedin2008–2009,inbothunadjustedandmultivariablemodels. Althoughlimitedbytheresponserate,thisworkprovidesthemostrecentandcomprehensivesnapshot ofthetypeandfrequencyofasubsetofpreventivehealthservicescurrentlyofferedinUSEDs.[WestJ EmergMed.2024;25(5)823–827.]
AlargeproportionofUShealthcareisdeliveredinthe emergencydepartment(ED)setting.1 Asanentrypointinto thehealthcaresystem,EDsareprovidinganincreasing proportionofbothemergentandnon-emergent(ie,chronic andpreventive)care,1,2 inpartduetoinsufficientaccessto primarycare,populationgrowth,andanagingpopulation withincreasinglycomplexmedicalneeds.Therecentendof thePublicHealthEmergencyforCOVID-19andsubsequent unwindingoftheMedicaidcontinuousenrollmentprovision likelyentailsgreaterEDutilizationforbothchronicand preventivehealthcareneeds.3 However,itremainsunclear whatpreventivehealthservicesarecurrentlybeingofferedin theEDsettingandhowthishaschangedovertime.Findings fromthisstudycouldhelpframethechanginglandscape aroundEDreimbursementsandincentivestructures.
Astudyconductedin2008–2009engagedEDdirectors, determinedtheavailabilityofasubsetofpreventivehealth servicesofferedinarandomsamplingofUSEDs,and characterizedperceivedbarrierstoimplementingthese services.4 Ourobjectivewastoprovideanupdated assessmentoftheavailabilityofasubsetofpreventivehealth servicesfollowingtheonsetofCOVID-19inEDs,giventhe expectationthatresourcesareincreasinglyallocatedto preventivecare.Theunderlyinggoalwastoofferinsightinto andcontributetotheknowledgebasesupportingeffortsto improveandoptimizehealthcaredeliverywithinthe EDsetting.
WeusedtheNationalEmergencyDepartmentInventory (NEDI)-USAasasamplingframeworkforthisstudy.The NEDI-USAisacomprehensivedatabaseofallnon-federal, non-specialtyUSEDs;informationavailableattheED-level (eg,teachinghospitalaffiliationandannualvisitvolume)is updatedannually.5 FromNEDI-USA,wegenerateda randomlistof1,064EDs(≈20%ofallUSEDs).5 Onthe basisofthisrandomlist,directorswerecontacteduptothree times(fromWinter2022toSpring2023)viae-mailormail. Non-responderswerecontactedbytrainedresearch assistantsviatelephone.4
Theinstrumentwasapreviouslyimplementedsurvey (2008–2009)thatcharacterizedtheavailabilityof(and preferencefor)11preventivehealthservices,ED-levelsocial workeravailability,self-reportedpercentageofEDpatients whowereuninsured,andmeasuresofEDcrowdingina5.7% randomsamplingofUSEDs(Appendix).4 Ifaservicewas notoffered,thesurveyaskedwhetheritcouldbeoffered givenexistingresources.Directorswerealsoaskedabout perceptionsofbarrierstoimplementingpreventivehealth servicesintheED.InlinewithupdatedUSCentersfor DiseaseControlandPrevention(CDC)recommendations encouraginghepatitisCscreening,the2022–2023surveyalso inquiredaboutavailabilityofroutinehepatitisscreening.6
PopulationHealthResearchCapsule
Whatdowealreadyknow?
AlargeproportionofallUnitedStates(US) healthcareisdeliveredintheemergency department(ED);thisincludesagrowing amountofpreventivecare.
Whatwastheresearchquestion?
Tounderstandhowtheprovisionofasubsetof preventivehealthservicesinUSEDshas changedovertime.
Whatwasthemajor findingofthestudy?
NearlyallEDsstudied(94%)reported offeringatleastonepreventivehealthservice, withamedianof fi veservices.
Howdoesthisimprovepopulationhealth?
Thisworkprovidesthemostrecentsnapshot ofthetypeandfrequencyofasubsetof preventivehealthservicescurrentlyofferedin USEDs.
Otherwiseallotherdataelements,includingthedefinitionof crowding(ie,atleastoneofthreeCDCcriteria:average waitingtimeofonehourorgreater;leftwithoutbeingseen rateof3%ormore;oranytimeonambulancediversion) wereunchanged.4
Ininitialanalyses,wesummarizeddatawithdescriptive statistics(eg,counts,proportions,andmedianswith interquartileranges[IQR]),andcomparisonswere conductedusingstatisticaltests(eg, χ2andKruskal-Wallis tests).Logisticregressionwasthenemployedtoassessthe oddsofpreventivehealthservicesbeingofferedmore frequentlyin2022–2023thanin2008–2009.Wealso conductedsensitivityanalyseswithmultivariablemodels adjustingforcriticalaccesshospitalstatus.Thesedatawere summarizedwithoddsratios(OR)and95%confidence intervals(CI).Atwo-tailed P < 0.05wasconsidered statisticallysignificant.AnalyseswerecompletedinStata 15.1(StataCorp,CollegeStation,TX)andRStudio(https:// www.R-project.org),and figureswerecreatedinRand Datawrapperrelease0.4.6(https://app.datawrapper.de/). ThisstudywasapprovedbytheStanfordUniversity InstitutionalReviewBoardandfollowedthe StrengtheningtheReportingofObservationalstudiesin Epidemiology(STROBE)guidelinesfor observationalstudies.7
Table. Characteristicsofresponders,non-responders,andtheNationalEmergencyDepartmentInventory-USA. NEDI-USA, N = 5,613%
*Responders, n = 302%(95%CI)
Non-responders, n = 762%(95%CI) P-value
Medianannualvisitvolume(IQR)20,000(7,300–42,350)14,216(5,000–37,000)16,572(7,300–38,000)0.07
Hospitaltype
Teachinghospital56(4–9)5(3–6)0.36
Traumacenter 0.85
No8385(80–88)84(81–86)
Basic87(5–11)7(6–9)
Advanced98(5–12)9(7–11)
Criticalaccesshospital2441(36–47)32(29–36) <0.01
Urbaninfluencecode <0.01
Urban6651(45–57)57(53–60)
Largerural1413(10–17)17(15–20)
Smallrural2036(31–42)26(23–29)
USregion
Northeast1112(9–16)14(11–16)
Midwest2734(29–40)36(32–39)
South4334(29–39)37(34–41)
West1920(16–25)14(11–16)
*ConfidenceintervalsnotcalculatedforNEDI-USAbecauseentireUSpopulationofEDsisincluded;valuesdonotrelyonanestimate.The 302responders(28.4%responserate)reflecta5.4%randomsamplingofall5,613EDsintheUS;NEDI-USAreflectsED-levelinformation fromthe2019NEDI-USA.
CI,confidenceinterval; ED,emergencydepartment;IQR,interquartilerange; NEDI-USA,NationalEmergencyDepartmentInventory-USA.
Characteristicsofresponders,non-responders,and NEDI-USAoverallarepresentedinthe Table.The302 responders(28.4%responserate)reflecta5.4%random samplingofall5,613USEDs.Withtheexceptionofahigher proportionofrespondersrepresentingsmall,rural,critical accesshospitalEDs(comparedtoNEDI-USAandnonresponders),EDcharacteristicswereotherwisesimilar.For context,characteristicsofrespondersin2008–2009and 2022–2023arepresentedin SupplementalTable1;therewere asimilarnumberoftotalrespondersin2008–2009(277,5.7% randomsampleofallEDs).In2022–2023,responderswere similarlymoreoftenfromcriticalaccesshospitalsthanin 2008–2009;theyalsoreportedlessEDsocialworker availabilityand inthecontextofthepreviouspassageof theAffordableCareAct werelesslikelytoreporthaving morethan35%oftheirpatientsbeinguninsured.8
Nearlyall(94%)directorsreportedthattheirEDs routinelyofferatleastoneofthe12preventivehealth services,withamedian(IQR)of5(3–7)servicesoffered.The mostcommonserviceofferedwasintimatepartnerviolence screening,whiletheleastcommonwasroutineHIV screening.Nearlyallthepreventivehealthservices,except HIVandhypertensionscreening,weremorefrequently offeredin2022–2023thanin2008–2009(Figure1).Sevenof
theserviceshadhigheroddsofbeingofferedin2022–2023 thanin2008–2009; findingswereunchangedafter adjustmentforcriticalaccesshospitalstatus (SupplementalTable2).
Further,amongdirectorswhoreportedthattheirEDdid notofferaparticularpreventivehealthservice,manystill reportedthatresourceswereavailabletooffersuchservices (Figure2).Whenaskedabouttheir “firstchoice” ofservice theywouldmostliketooffer,alcoholriskscreening, counseling,andreferralwasmostcommon,whileroutine HIVandhepatitisscreeningwereleastcommon.Onlya smallproportionofEDdirectorsthoughtthatpreventive healthservicesshouldnotbeofferedintheED.However,as highlightedinthe SupplementalFigure,manyexpressed concern(ie,stronglyagreedoragreed)thatoffering preventivehealthservicesintheEDwouldleadtoeither longerlengthsofstay(56%)orincreasedcoststotheirED (58%),orwouldrequireadiversionofstafftimefrom providingacutecare(50%),orthattheirpatientswouldnot haveaccesstoadequatefollow-up(49%).
AmongarandomsamplingofUSEDs,nearlyalloffered atleastonepreventivehealthservice,manycurrentlyhave theresourcestooffermore,andonlyaminorityofdirectors
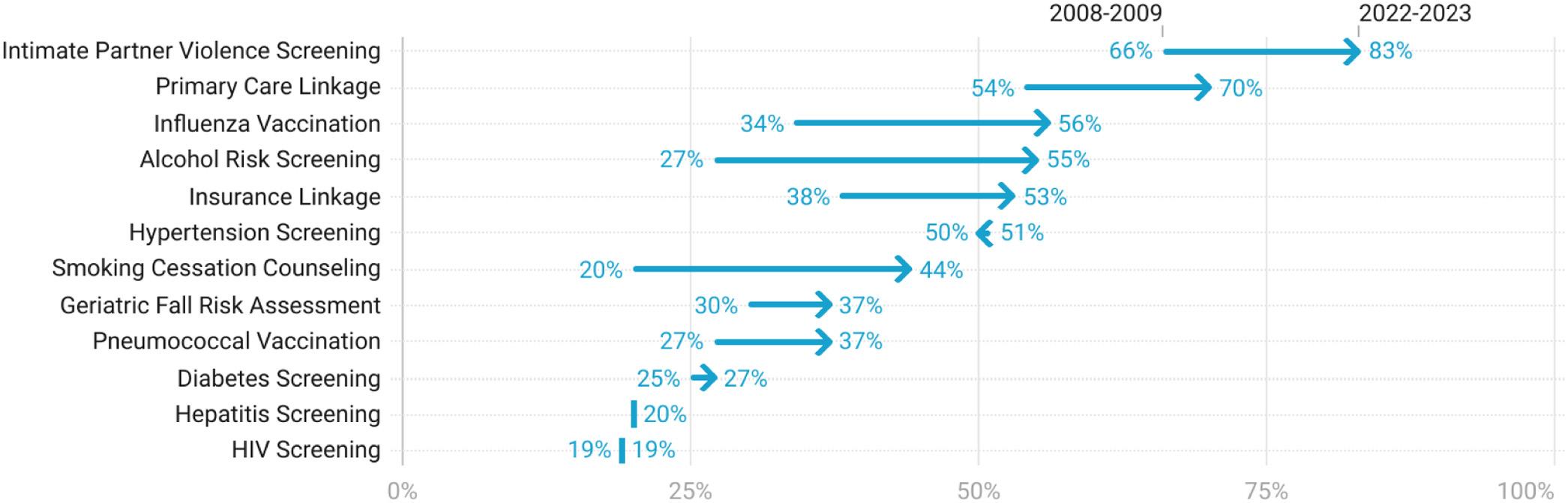
Figure1. Availabilityofpreventivehealthservices,2008–2009and2022–2023. Theindividualpreventivehealthservicesaresortedbymostfrequenttoleastfrequent.Hepatitisscreeningwasnotincludedinthe 2008–2009study;valuesreflect2022–2023data.Nearlyallthepreventivehealthservicesweremorefrequentlyofferedin2022–2023than in2008–2009.
expressedthebeliefthatpreventivehealthservicesshouldnot beofferedintheEDsetting.Theresultsrepresentanincrease inboththeoverallproportionofEDsofferingatleastone preventivehealthserviceandthemediannumberofservices offeredperEDsince2008–2009.4 This findingisconsistent withrecentworkdemonstratingthatEDsareprovidinga growingamountofchronicandpreventivecareintheUS.1,2 Acomponentoftheresultsmightbeexplainedbythehigh proportionofrespondersfromcriticalaccesshospitalsand theuniquemissiontheseEDshavewithintheirlocal communities.Reassuringly,adjustmentforcritical accesshospitalsdidnotmateriallyaltertheobserved temporaldifference.
Althoughweareunabletocommentontheunderlying reasonswhy(orwhynot)aparticularEDoffersaparticular preventivehealthservice,thereasonsarelikely
multifactorial.Servicesthataremandatedorstrongly encouraged,comparedtoservicesthatareneither,arelikely moreoftenoffered.Further,servicesthatarelesstime-and resource-intensive(eg,aseriesofscreeningquestions comparedtocheckingahemoglobinA1corperforminga HIVantigen/antibodytest)arealsomorelikelytobeoffered. AcomponentlikelyalsodependsonboththeEDandits availableresources,andtheuniqueneedsofthepatient populationsservedintheseEDs.
Theobservedchangesoccurredinthesettingoftherecent unwindingofMedicaid’scontinuousenrollmentprovision, withtheprospectthatmillionsofAmericanswilllose or havealreadylost Medicaidcoverage.3 Thislosswilllikely translateintoincreasedratesofEDutilizationforboth emergentandnon-emergent(eg,chronicandpreventive)care acrossthecountry.Giventhestaffing,crowding,and
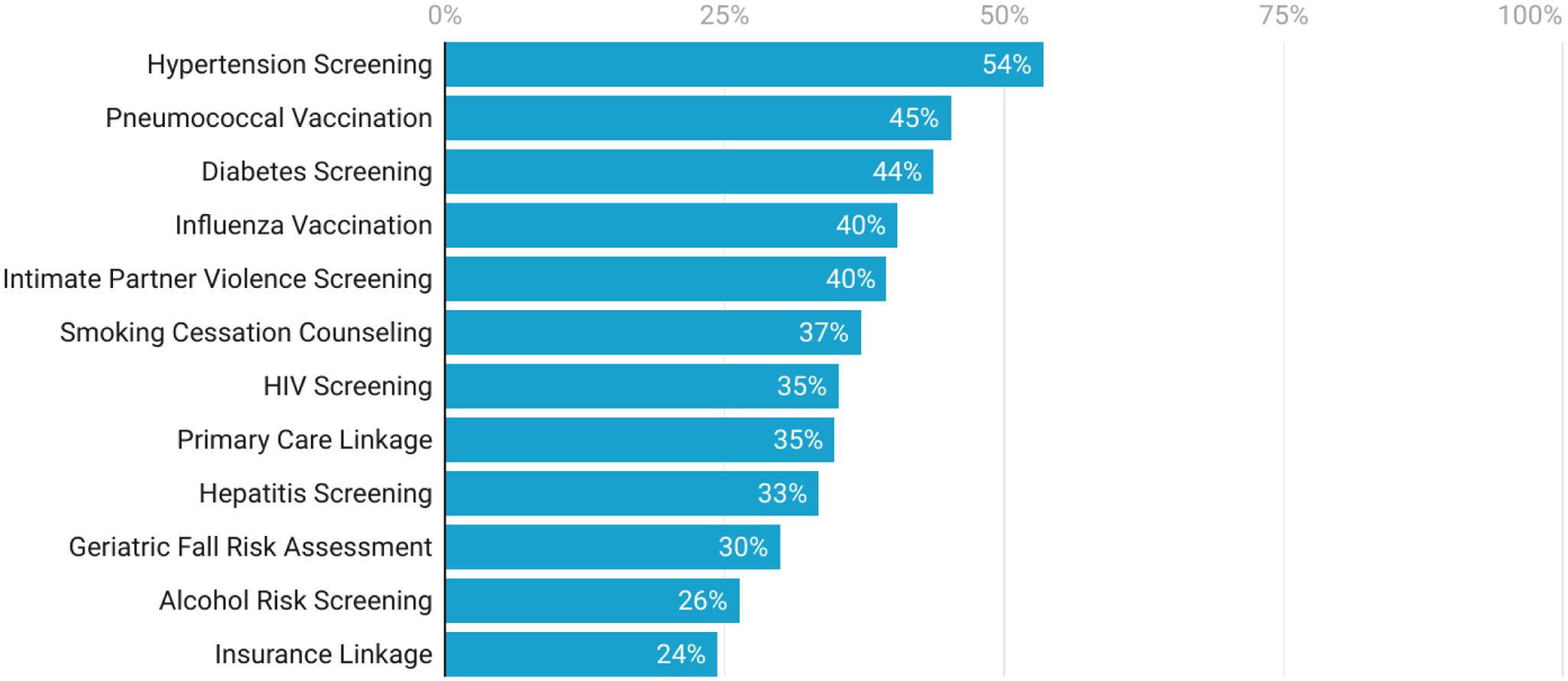
Figure2. Abilitytoofferpreventivehealthserviceswithexistingstaffandfundingin2022–2023. Emergencydepartmentdirectorswereaskedwhethertheyhadasysteminplacetoroutinelyprovideaparticularpreventivehealthservice. Thosewhoreported “no” (ie,didnotofferaparticularservice)werefurtheraskedwhethertheycouldalreadyofferthatserviceroutinelygiven existingstaffandfunding.Theindividualpreventivehealthservicesaresortedbymosttoleastfrequentlyreportedasbeingpossibletooffer.
boardingcrisesinEDs,whichwereexacerbatedbythe COVID-19pandemic,EDresourcesareexpectedtobe furtherstrained.9
Ourworkhasseveralimportantlimitations,amongthem oursurvey-basedapproachandresponserate.Asurveyisthe onlyfeasiblemeanstostudythistopic;theseservicesarenot typicallybilledforortrackableinanysystematicnational sampleofUSEDs.Reassuringly,ourgoalofobtaininga similarlysizedrandomsamplingofEDsasin2008–2009was met,andourresponserateisconsistentwithrecentwork demonstratingsurvey-fatigueamonghealthcareworkers duringCOVID-19andlowersurveyresponserates.10 For context,weprovidedetailedcomparisonsofhowresponders comparetonon-responders,NEDI-USA,andto2008–2009 responders.Giventhislimitation,andthatbothtimepoints reflectdistinctrandomsamplings,weintentionallyavoided formalpairwisecomparisonsbetween2008–2009and 2022–2023responders.Instead,weincorporateda conservativeapproachusingdescriptivestatisticsand conductedregressiontodemonstratethatadjustmentfor criticalaccesshospitalstatusdidnotmateriallychange our findings.
Second,wecanonlycommentonavailabilityforthe preventivehealthservicesweconsidered;neithercouldwe commentonthe fidelity,comprehensiveness,oreffectiveness ofanyofthepreventivehealthservicesstudied.Ourobjective wastoprovideanupdatedassessmentoftheavailabilityofa subsetofpreventivehealthservicesintheEDsetting,withthe goalofhighlightingtheincreasingamountofnon-emergent carebeingprovided.Third,givenourgoalofusingthesame surveyvehicletofacilitatecomparisonsagainstpriorwork wecannotcommentontheextentof,orED-leveldifferences in,theseservices.Theseissuesareimportantandmeritfuture investigationbutarebeyondthescopeofthecurrentwork. Theseissues,andworkfocusedoncosteffectiveness, reimbursements,and financialincentivesofpreventivehealth servicesofferedinEDsettings,arethefocusofcurrentand futureeffortsbyourgroup.Despitetheselimitations,our findingsrepresentthemostcurrentandcomprehensive snapshotoftheavailabilityandfrequencyofpreventive healthservicescurrentlyofferedinUSEDs.
Nearlyall.EDsintheUnitedStatesofferatleastone preventivehealthservice.ManyEDsoffermultipleservices, andrateswerehigherthanthoseidentifiedin2008–2009in bothunadjustedandmultivariablemodels.Althoughlimited bythelowresponserate,thisworkprovidesthemostrecent snapshotofthetypeandfrequencyofasubsetofpreventive healthservicescurrentlyofferedinUSEDs.
AddressforCorrespondence:ChristopherBennett,MD,MSc,MA, StanfordUniversitySchoolofMedicine, DepartmentofEmergency Medicine,3145PorterDr.,WingB-2ndFloor,PaloAlto,CA94304. Email: cleebennett@stanford.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Bennettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.MarcozziD,CarrB,LiferidgeA,etal.Trendsinthecontributionof emergencydepartmentstotheprovisionofhospital-associatedhealth careintheUSA. IntJHealthServ. 2018;48(2):267–88.
2.ChouSC,VenkateshAK,TruegerNS,etal.Primarycareofficevisitsfor acutecaredroppedsharplyin2002–15,whileEDvisitsincreased modestly. HealthAff. 2019;38(2):268–75.
3.TolbertJandAmmulaM.10thingstoknowabouttheunwindingofthe Medicaidcontinuousenrollmentprovision.2023.Availableat: https:// www.kff.org/medicaid/issue-brief/10-things-to-know-about-theunwinding-of-the-medicaid-continuous-enrollment-provision/ AccessedSeptember28,2023.
4.DelgadoMK,AcostaCD,GindeAA,etal.Nationalsurveyofpreventive healthservicesinUSemergencydepartments. AnnEmergMed. 2011;57(2):104–8.e2.
5.SullivanAF,RichmanIB,AhnCJ,etal.AprofileofUS emergencydepartmentsin2001. AnnEmergMed. 2006;48(6):694–701.
6.CentersforDiseaseControlandPrevention.Testingrecommendations forhepatitisCvirusinfection.2023.Availableat: https://www.cdc.gov/ hepatitis/hcv/guidelinesc.htm.AccessedSeptember28,2023.
7.vonElmE,AltmanDG,EggerM,etal.TheStrengtheningtheReporting ofObservationalStudiesinEpidemiology(STROBE)statement: guidelinesforreportingobservationalstudies. Lancet. 2007;370(9596):1453–7.
8.BlumenthalD,AbramsM,NuzumR.TheAffordableCareActat5years. NEnglJMed. 2015;372(25):2451–8.
9.KelenGD,WolfeR,D’OnofrioG,etal.Emergencydepartment crowding:thecanaryinthehealthcaresystem.2021.Availableat: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0217 AccessedFebruary23,2024.
10.deKoningR,EgizA,KotechaJ,etal.SurveyfatigueduringtheCOVID19pandemic:ananalysisofneurosurgerysurveyresponserates. Front Surg. 2021;8:690680.
GiselleAppel,BA*
AhmedT.Shahzad,BA*
KestrelReopelle,MD†
StephenDiDonato,PhD‡
FrancesRusnack,DO§
DimitriosPapanagnou,MD,EdD,MPH∥
*ThomasJeffersonUniversity,SidneyKimmelMedicalCollege, Philadelphia,Pennsylvania
† IcahnSchoolofMedicine,DepartmentofEmergencyMedicine, NewYork,NewYork
‡ ThomasJeffersonUniversity,CollegeofNursing,Philadelphia,Pennsylvania
§ NewYorkUniversityGrossmanLongIslandSchoolofMedicine, DepartmentofEmergencyMedicine,NewYork,NewYork
∥ ThomasJeffersonUniversity,SidneyKimmelMedicalCollege, DepartmentofEmergencyMedicine,Philadelphia,Pennsylvania
SectionEditor:AndrewPhillips,MD,MEd
Submissionhistory:SubmittedOctober6,2023;RevisionreceivedMarch20,2024;AcceptedMarch25,2024
ElectronicallypublishedJune28,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.18498
Purpose: Duringthethird-yearemergencymedicine(EM)clerkship,medicalstudentsareimmersedin traumaticincidentswiththeirpatientsandclinicalteams.Trauma-informedmedicaleducation(TIME) appliestrauma-informedcare(TIC)principlestohelpstudentsmanagetrauma.Weaimedtoqualitatively describetheextenttowhichstudentsperceivedthesixTIMEdomainsastheynavigatedcriticalincidents duringtheirEMclerkship.
Methods: Weemployedaconstructivist,modifiedgroundedtheoryapproachtoexploremedical students’ experiences.Weusedthecriticalincidenttechniquetoelicitnarrativestobetterunderstandthe sixTIMEdomainsastheynaturallyappearintheclerkship.Participantswereaskedtodescribea traumaticincidenttheyexperiencedduringtheclerkship,followedbytheclerkship’sroleinhelpingthem managetheincident.Usingtheframeworkmethod,transcriptswereanalyzed1)deductivelybymatching transcriptexcerptstorelevantTIMEdomainsand2)inductivelybygeneratingdenovothemestocapture factorsthataffectedstudents’ handlingoftraumaduringcriticalincidents.
Results: TwelveparticipantswereenrolledandinterviewedinJuly2022. “Safety” wasthemost frequentlydescribedTIMEdomain,whereas “Gender,Cultural,andHistoricalissues” and “Peer Support” werediscussedleast.Inductiveanalysisrevealedthemesthathinderedorsupportedtheir abilitytomanagetraumaticexperiences,whichweregroupedintothreecategories:1)student interactionswiththelearningenvironment:complexsocialdeterminantsofhealth,inequalitiesincare, andovertdiscrimination;2)studentinteractionswithpatients:ethicallyambiguouscare,witnessing acutepatientpresentations,andreactivationofpasttrauma;and3)studentinteractionswithsupervisors: powerdynamics,invalidationofcontributions,role-modeling,andstudentempowerment.
Conclusion: ThesixTIMEdomainsarerepresentedinstudents’ perceptionsofimmediate,stressful criticalincidentsduringtheirEMclerkship,with “Safety” beingthemostcommonlydescribed;however, thedegreetowhichthesedomainsaresupportedinstudents’ experiencesoftheEMclerkshipdiffer,and instancesofinadequatelyexperienceddomainsmaycontributetostudentdistress.Understandingthe EMclerkshipthroughthespecificlensofstudents’ experiencesoftraumamaybeaneffectivestrategyto guidecurricularchangesthatpromoteasupportivelearningenvironmentforstudentsintheemergency department.[WestJEmergMed.2024;25(5)828–837.]
Overrecentyears,emergencydepartments(ED)across theUnitedStateshaveservedaspointsofcareforvictimsof wideninghealthdisparities,increasingsociopoliticalunrest, theCOVID-19virus,andincreasingnumbersofmass shootings.TheEDworkplacealsoservesasaclinical learningenvironmentforlearnersacrossmultiplehealth professions,routinelyexposingthemtotraumathatis intrinsictoemergencymedicine(EM)practiceandcare deliveryintheUS.Medicalstudentsareathighriskfor sustainingpsychologicalandemotionaltraumafromtheir encounterswithpatientsandinteractionswithmembersof theirEDcareteams oftenforthe firsttimeintheir professionalcareers.1–3
Studentshaveprevious lyreportedthattheir undergraduatemedicaleducation(UME)traininghasnot adequatelypreparedthemtocopewithsuchstressful events. 2 Aninabilitytopositivelycopewithstresscan negativelyimpactstudents ’ health,contributetoanxiety, depression,and/ordetachment. 4 – 6 Notonlycanthis stresshaveapsychologicalimpactonwell-being,but itcanalsoimpactstudents ’ abilitytoadvocatefor themselves,theirpeers,andtheirpatientsoverthecourse oftheirtraining.
Researchsuggeststhattheimpactofstressfuleventson studentscanbelessenedoramplifiedbystructuralsupport embeddedinformalcurriculum.Frameworks,suchas trauma-informedmedicaleducation(TIME),haveoutlined whatstructuralsupportmaylooklikeinUME.Traumainformedmedicaleducationrepresentsanapproach thatappliestrauma-informedcare(TIC)principlestoUME tohelpstudentsrecognizeandaddresstraumainreal time.7 Itaimstocreatealearningcultureguidedbysix
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Medicalstudentsareimmersedintraumatic incidentswhentheyrotatethroughthe EDduringtheemergencymedicine (EM)clerkship.
Whatwastheresearchquestion?
Towhatextentdomedicalstudentsperceive thedomainsoftrauma-informedmedical education(TIME)astheynavigatetheED clinicalenvironment?
Whatwasthemajor findingofthestudy?
ThedegreetowhichTIMEdomainsare supportedinstudents ’ experiencesoftrauma differ,andinstancesofinadequately experienceddomainsmaycontributeto studentdistress.
Howdoesthisimprovepopulationhealth?
BetteridentifyingopportunitiesfortraumainformededucationintheEMclerkshipcan supportstudentsandtheirwell-being.
trauma-informeddomains:safety;trustandtransparency; peersupport;collaborationandmutuality;empowerment, voice,andchoice;andcultural,historic,andgender considerations(Table1).8
SafetyCouldthestudentexpresstheirthoughtsaboutthesituationopenly?Didthestudentwonderifthey wouldbenegativelyimpactediftheyvoicedtheiropinion?
TrustandtransparencyWasthestudentbriefedaboutthesituationbeforetheyexperiencedit?
PeersupportWereanyofthestudent’speersinthesituation,too?Howdidthestudentinteractwith thesepeers?
CollaborationandmutualityWasthestudentabletointeractwiththeirfaculty?
Didthestudentwitnessalackofprofessionalism?Whathappened?Howwasthislackof professionalismrespondedto?
Empowerment,voice,and choice
Cultural,historic,andgender considerations
Ifthestudenthadfeedbackforyourclerkshipand/orotherpeople,howdidtheydeliverthis feedback?
Ifthestudentneededtotaketimeawayfromthesituationorclerkship,wasthereroomintheir scheduletodoso?Howcouldtheyrequestthistimeiftheyneededit?
Werethereothersinthissituationwhohadasimilarracial,ethnic,orgenderidentityas thestudent?
Werethereotherswhoseracial,ethnic,orgenderidentitiesweredifferentfromthestudent’s?
WhilesomemedicalcollegeshaveincorporatedTIME domainsintotheircurriculum,9 theextenttowhichTIME domainsinformthethird-yearEMclerkshipcurriculum remainsunclearandunexplored.Bybetterunderstandingthe studentexperienceofthethird-yearEMclerkship,educators couldtakepracticalstepstoadequatelypreparelearnersfor thechallengesposedbytheEDclinicallearning environment.Inthisqualitativestudy,weaimedtodescribe specificTIMEdomainsstudentsexperienceastheyare naturallyimmersedintheclinicalenvironment.Specifically, weaimedtoidentifytowhatextentstudentsperceivedTIME domainstobepresentwithinthethird-yearEMclerkship curriculumtosupporttheirabilitytonavigatehigh-stress criticalincidentsintheED.
Wetookamodifiedconstructivistgroundedtheory approachtocollect,describe,andanalyzethird-yearmedical students’ perceivedstressfulincidentsduringtheirEM clerkshipintheirthird-yearofmedicaltraining.We employedthecriticalincidenttechnique(CIT),adata collectionmethodthatguidesparticipantstodisclosevivid descriptionsofa “criticalincident.” Formally,perCITa criticalincidentisdefinedas “anyobservablehumanactivity thatissufficientlycompleteinitselftopermitinferencesand predictionstobemadeaboutthepersonperformingthe act.”10 AspartofourCITmethod,participantswereaskedto recountanddescribeaspecific,stressfulcriticalincidentthat theyexperiencedduringtheirEMclerkship.Itisimportant tonotethattwostudyinvestigatorshaveconsiderable experiencewithqualitativeresearchmethods(SD,DP),and onestudyinvestigatorhasextensiveexperiencewiththeCIT method(DP).Also,oneresearchteammember(SD)isa trainedtraumacounselorwithanextensiveTICbackground. Thestudyprotocolwasapprovedbytheinstitutionalreview boardofThomasJeffersonUniversity,anddatawas collectedinJuly2022.
Becausewesoughttounderstandtheexperiencesof medicalstudentsintheEMclerkship,weintentionallyand exclusivelysampledthird-yearmedicalstudents.We recruitedthird-yearmedicalstudentswhohadcompleted theirEMclerkshipatanurban,academic,tertiary-care medicalcenteratThomasJeffersonUniversityHospitalin Philadelphia,Pennsylvania.Twostudyinvestigators(KR, DP)arefacultyinthisdepartmentandarefamiliarwiththe practiceenvironment.
Studentparticipantswereidentifiedthroughpurposive conveniencesampling.InJuly2022,thestudyteamsent recruitmentemailstostudentlistservsatourrespective medicalschools.Criteriaforinclusionwerethatthe participantwasathird-yearmedicalstudentandhad successfullycompletedtherequiredEMclerkshipduringthe
studyperiod.Participantswereenrolledthroughtargeted emailsdescribingthestudyandassurancethatparticipation wasvoluntary.Studyparticipantsandtheirrespective narrativeswerede-identifiedusinganinternallydeveloped codingscheme.
Thestudyconsistedofaseriesofcriticalincident interviewswiththird-yearmedicalstudents,each30–45 minuteslong,thatwereconductedinAugust2022.Informed consentwasobtainedfromrecruitedstudents.Afterabrief demographicelectronicquestionnairewascompleted, interviewswerescheduledwithparticipants.Eachinterview wasconductedvirtuallyusingvideoconferencingsoftware (ZoomVideoCommunications,Inc,SanJose,CA)withtwo membersoftheresearchteamwhoweretrainedineliciting criticalincidentsthroughinterviews.Participantswere compensated$75fortheirparticipationinthestudy.
Interviewswereconductedusingadetailedinterview protocolwithquestionsthatwereinformedbytheTIME framework(Appendix).Theinterviewprotocolwas developedbythestudyinvestigatorsandwaspilotedwith twomedicalstudentstooptimizeinterviewquestions.Pilot interviewdatawereincludedintheanalysis.Student participantswereaskedtodescribeakeyincidentduring theirEMclerkshipwhentheyexperiencedasignificant trauma.AnaudiorecordingfromeachZoominterviewwas transcribedusingautomatedtranscriptionsoftware,which wasthenmanuallyreviewedbymembersofthestudyteam fortranscriptionaccuracy.Transcriptswerede-identified.
Dataforeachparticipant’stranscriptwasreducedto captureacriticalstory.Foreachtranscript,theparticipant’ s narrativewasre-organizedchronologicallyintoacoherent, re-storiednarrative.Bytakingaconstructivistandmodified groundedtheoryapproach,weinductivelyanalyzedrestoriedcriticalincidents.Throughaseriesofseveraliterative conversations,andperCITbestpractices,wemanually developedassertions(organizedinExcel[MicrosoftCorp, RedmondWA])aboutthemeaningofeachincidentasit relatedtotheresearchquestion.Toorganizeoverarching themesfromassertions,weconductedaseriesofvirtualcardsortingactivitiesthatwerefacilitatedthroughseveralvirtual GoogleJamboardactivities.Iterativecross-incidentanalyses withthestudyteaminformedconnections,associations,and relationshipsforthemesthatemergedfromtheassertions. Thisallowedourteamtogenerateanoverarchingframework ofobservedthemesandrelationships.
Togroundourinductive findingsandmoredirectlyassess thedegreetowhichstudents’ perceivedTIMEdomains duringtheirclerkship,weundertookadeductiveapproachin whichexcerptsfromeachparticipant’snarrativewere matchedwiththemostrelevantTIMEdomaindiscussed
(ie,avividdescriptionoftheimpacttheEDlearning environmenthadonastudent’sabilitytoopenlyexpresstheir opinionswasmatchedtotheTIMEdomainof “Safety”). ForcriticalincidentswheremultipleTIMEdomainswere identified,weselectedthemostdominantTIMEdomain. Toensureinternalvalidityofdatainterpretation,theentire teamofinvestigatorsmettoreviewallinductiveassertions anddeductivecategorizations.Discrepancieswereresolved throughiterativeconversationsoverthe10-month studyperiod.
Weidentifiedandinterviewed12studentparticipants. Studysizewasinformedbydatasaturation,information power,andanalyticalanddatasufficiency.11 Theaverageage ofparticipantswas25.5yearsold;50%identifiedasmaleand 50%asfemale.Themajorityofparticipantsidentifiedas White(8of12participants)(Table2).Participants’ critical incidentsalignedwithdeductivecodesborrowedfromthe TIMEframework(Table3).Participantsdescribedelements of “Safety,” whetherpsychologicalorphysical,most frequentlyacrossall50interviews,whereas “Gender, Cultural,andHistoricalissues” and “PeerSupport” were discussedtheleast(13each).
Analysisofcriticalincidentswithcross-casecomparisons revealedthatthemeswereclassifiedintothreecategories:1) studentinteractionswiththeEDclinicallearning environment;2)studentinteractionswiththeirsupervisors; and3)studentinteractionswiththeirpatients(Table4).
StudentInteractionswiththeEDClinical LearningEnvironment
NavigatingSocialDeterminantsofHealth Studentsstruggledwithhavingtonavigateandreconcile thecomplexsocialdeterminantsofhealth(SDoH)for patientsseekingcareintheED.Thiswasoftenaccompanied byintenseemotionandstressinstudents.
So,Iobviouslywasalittlestressedoutbecause patientscryingobviouslyisnotsomethingIhave experienced ::: That’sjustsomethingthatIhadn’tdone onmyownyet.Andsobeinginthepatient’ srooms withthemcryingandmejusttryingtobelike, “What doIdo?DoIwantto fixitrightaway?” SoIwaslike, “MaybeIshouldgogetsomeone.Maybehewantsto talkaboutwhyhe’sfeelingthisway.” Iwasn’treally toldhowtodealwiththat.
Studentsexperienceduncertaintywhennavigatingovert patientsuffering,psychosocialfactorsthatfurther complicatedcareplans,andhavingconversationswiththeir patients.Consequently,studentsdesiredmoresupport duringtheseencountersintheformofgreaterpreparationfor thepatientencounter,emotionalsupport,andeffectiverole-
Table2. Demographicsofparticipants.
CharacteristicN = 12
Age
21–244(33%)
25–275(42%)
27+ 3(25%)
Gender Man6(50%)
Woman6(50%)
Race
Asian/NativeHawaiian/PacificIslander3(25%) White8(67%) Hispanic1(8%)
modelingfromtheirsupervisors.Theyalsoexpressedan interestinopportunitiestodebriefandmakesenseofthese challengingencounters.
Studentsexperiencedhesitationanddistresswhen navigatinginstancesofperceivedcareinequitieswiththeir treatmentteams(eg,whenthereasonwhytwopatients withsimilarpresentationsreceivingdifferenttreatments wasunclear).
Andthispatientlooksexactlythesame. AndIwassort oflike,What’sthedifference?Theywerelike, “Youcould tellthisone’s[thepatient’s]uncomfortable.” Ithoughtthe otheronelookeduncomfortable,butwhatever.Weended updoingjustalotmoreforher,andIcouldn’treally identifyanydifferencebetweenthetwocases.Ithought theywereboththesame ::: “Hey,didthatjusthappen, though?” Ithoughtithappened.Orlike, “AmI hallucinating?”
Inequityincareisaconceptrepeatedlyintroducedinthe preclinicalyears;however,studentsfeltunpreparedto navigatediscussionswiththeircolleagueswhenthey recognizedinequitydirectlyinfluencingthecaretheywere delivering.Moreover,athird-yearmedicalstudent’srelative lackofexperienceintheclinicalrealmandunfamiliaritywith theuniqueenvironmentoftheirrotation(eg,teamdynamics, patientpopulation,location),addedfurtherambiguitytothe situation.Studentsfeltunabletocommunicatetheirconcern andadvocatefortheirpatients.
NavigatingRace,Gender,andSocioeconomic Discrimination
Discrimination(ie,racial,cultural,and/orgender-based) intheworkplacehinderedthepsychologicalsafetyof studentsbelongingtominoritygroupsthatwere
Table3. Frequencyofdeductivethemes.
TIMEdomainRepresentativequote(s)
Safety “Imadeanappointmentwithschoolcounselingservices.Ifelt fine. IkindofthoughtIwasgoingtohave,like,weirddreamsorfeel weird.AndIwastotallyunaffected,butIdon’tknow.Younever know.Idon’tthinkI’veeverseensomeone beentherewhen theypronouncesomeonedead.Itwaskindofmy firstexperience andeventhen,Iwasstillperiphery.[Counseling]waslike, ‘Iwas goingtoreachouttoyouanyway.Wemadealistofthosepeople whocameupattheschoolcounselingcenter’smeeting.’ Iwas feeling fine,soitwasn’tlike, ‘Wow,that’sgreat!’;butitwaskindof niceforsomeonetobe, ‘It’sokaythatyoufeel fine.Youshouldn’t feelbadthatyou’renot,like,hauntedbythis,’ ifthatmakessense.”
Empowerment, voice,choice
Collaborationand mutuality
Transparencyand trustworthiness
Frequencytable (asnumberof instancesacrossall transcripts) Percentageof allinstances (%)
“SoIreadtheattendingalittlebitonedge,listeningtowhatthey’re saying,andthentheysay, ‘Yeah,likeyoudidn’tevenlookintotheir mouth.Andyeah,itjustwasnot,notorganized.’ AndIwaslikein myhead,likethinking, “Wait,what?LikeI100%didaneuroexam, andIhadhimopenuphismouthandsay,checkfornineandten. AndthenIhadhimpointhistongueoutto,totherightandleft.” AndthenIwaslike, ‘Okay,whatdoIdonow?DoIcontradictmy attending?Orjustsay, ‘Sure?’” 3020
“Thephysicianbroughttheeventupquickly.Oncehewasonthe phone,consultedsurgeryandthenhungupandhesaid, ‘It’sreally importantthatwetakeownershipofwhathappenedhere.Instead oflyingand/ormakingexcuses,wetakeownershipandsaywhat happened.’ Butthenhestillhadtogodootherthings,andthenI wastheonewhoinitiated[moreconversationabouttheevent], whichIthinkwasappropriatefrommysenseandfromthe attendingsense,aconversationabouttheevent,mostlyfora learningexperienceformetotalkaboutwhathappened.”
“Ithinkitwouldhavebeennicetohavesomeacknowledgment becauselike,partofthefrustrationisfeelinglikeyou’retheonly personwhoseesitthisway,youknow?Andit’slike,itwouldhave beenniceifmyattendingturnedtomeandwaslike, ‘Hey,likethat waskindofproblematic.Ihopeyoudon’tthinkthatweallthinkthat waybecausewedon’tlikethatkindofthing.’ Ithinkitwouldhave counteractedalittlebitofthedisillusionmentIfeeltowards medicineingeneral.”
2517
1812
Gender,cultural,and historicalissues
“Ithinkthere’salwaysthatfeeling,especiallylikeasayoung femaletrainee,IfeellikeIkindofhavetoputonabravefaceand notshowthatmuchemotion.Idon’tknow.Likeit’sgoodtoappear investedinyourpatients,butit’snotgoodtobelike, ‘Oh,likethisis theworstthingthat’severhappened,blah,blah,blah.’ Because obviouslyallthesepeoplehaveseenworse.So,no,Idon’tthink thatanyonewouldhavewrittenmeabadreviewifIwasshowing thatIwasupset.ButIdothinkitsubconsciouslyimpactswhat peoplethinkofyou.Like,youknow,maybeshe’snotcutoutfor this fieldorsomething.”
Peersupport “Andso,IthinkthatmademefeellikeIhadtobetheone responsibleforensuringthatthiswomanwasabletogethomeand avoidfurtherintimatepartnerviolence.IreallyfeltlikeIwastheone whodecided,like,whethershewouldbeundergoingmoreviolence thatnight.”
TIME,trauma-informedmedicaleducation.
138.7
138.7
OverarchinggroupingIndividualthemes
Students’ interactionswithpatientsReactivationofpasttrauma
Emotionaldiscomfortassociatedwithnavigatingethicsanduncertainty
Emotionaldiscomfortwhenwitnessinghighacutepatientcareforthe firsttime
Students’ interactionswithsupervisorsPowerdynamicsdiminishingstudentclinicalautonomy
Novalidationforstudentclinicalcontributions
Role-modelingasameanstosupportstudents
Empowermentandfeedbackasameanstocreatepsychologicalsafety
Students’ interactionwiththeEDclinical learningenvironment
ED,emergencydepartment.
Navigatingsocialdeterminantsofhealth
Respondingtoobservedinequitiesincare
Navigatingrace,gender,andsocioeconomicdiscrimination
discriminatedagainst evenwhentheseactswerenot directedtostudents(eg,atstafforpatientsbelongingtothe student’sminoritygroup).
It’salsodisappointingbecauseIfeltlikemyattending didn’treallysayanythingtogoagainstthat.Hewasn’t agreeingwithher,buthewaslike, “Ohyeah.” Hekind ofjustdismisseditanddidn’tengagetoomuch.
Adiscriminatoryexperiencecoupledwithsilent complacency(ie,alackofacknowledgmentofsuchevents fromclinicalteammembers,particularlyfacultyand supervisorswhoweretaskedwithadvocating,teaching,and protectingstudents)complicatedstudents’ responsestosuch eventsandmarginalizedtheirroleintheclinicalworkplace. Importantly,studentsofcolor(asintheabovecase)feltless empoweredontheteam,especiallywhenbeingtheirteam’ s onlymemberofcolor.
PowerDynamicsDiminishingStudentClinicalAutonomy Powerdynamicsinterferedwithstudents’ abilityto advocatefortheirpatientsandcontributedtotheirstress whenimmersedintheclinicalenvironment.Thesepower dynamicshinderedtheirabilitytoclarifycomplexmedical andsocialcasesbecausetheyfearedbeingperceivedas unknowledgeable.Furthermore,theywerelesslikelytoask foradiscussionand/ordebriefingtoresolvetheirfeelings surroundingpatientencountersastheydidnotwanttobe perceivedasemotionalor “weak” :
Ifeltsadandkindofdisappointedthatotherphysicians weren ’ttakingitseriously,thatweneededtogetherout ofthereandwecouldatleastprovideresources,orwe coulddomoretoacknowledgethatshe’sherefor
intimatepartnerviolence-relatedconcernsandthatno onereallycaredaboutwhathappenedaftersheleft.
Studentsoftenfoundthemselvestornbetweenthedesireto investmoretimeincaringforandadvocatingonbehalfof theirpatientsandtheneedtomaintainefficiency, subordination,andastrongperformanceforevaluatorswho assessedtheirclinicalskills,oftenoverlookingunassessedyet equallyvitalinterpersonalskills(ie,demonstratingempathy, advocatingforpatients).
AndIdidn’treallyfeellikeIcouldexplaintothe physician, “Hey,thisissomethingthatisreally importanttomethatIthinkshouldbehandled differently.” Ijustdidn’tfeelthatwasmyplacewith someonewhohadalotofcontrolovermygrade.Itwas thiswarbetweenwhatIfeelwasbestformyfuture gradesandwhatIfeltwasmorallyright.
Alackofacknowledgmentofstudents’ contributionsto thecareteam,eitherinrealtimeorontheirevaluation, causedstudentstoexperiencedistress.Incomplexclinical situationswherestudentsfelttheyhadmeaningfully contributedtopatientcare,alackofvalidationofthe student’scomposure,adaptability,and/orjudgment hinderedtheirabilitytoassimilatetothecareteamand triggereddissociationfromanddisillusionmenttowardthe clerkshipexperience.
Yougetanevaluationforeverysinglestuffyouworkon. MyEMevaluationdidn’tsayanythingabout[themass shootingevent].Itwasn’tlikeIneededanyonetobe “Wow,shedidn’tfreakout” or “Shewascalm.” It didn’thavetobethat.Andmyevaluationwasn’tbad,
itwasfair Justtome,that’skindofalargeeventthat happened.Itjustfeltkindofweirdthatthatcontext wasmissing.
Modelingofintegrity,professionalism(ie, accountability),anddebriefingbysupervisorshelped studentsprocesspoorclinicalperformanceandgainclosure duringiatrogeniccomplications.
Thephysicianbroughttheeventupquickly.Once[he[ hungupaftertalkingwithsurgery,hesaid, “It’sreally importantthatwetakeownershipofwhathappened here.Insteadoflyingandormakingexcuses,wetake ownership.” Thenhepersonallyaddressedmyfeelings andmypotentialblamingofmyselfforthesituation andreassuredthatitwasn’tmyfault.Andthesethings hesaid,whichisadmirable,andhowyoutakefull,full ownershipforthecomplication.
Participantnarrativessuggestedthattakingownership overastressfulortraumaticincidentofferedasenseof agencyandopenedopportunitiesforpositiveclinical learning,insteadofleavingthestudentfeelingpowerlessto speakoractontheevent.Thenegativeimpactofperforming aclinicalerrorwasmitigatedbasedonhownextactionsteps wereframed.
Asstudentsworkedthroughavarietyofclinical encountersduringtheirrotation,onefactorthatwasoften describedassupportingstudents’ psychologicalsafetywas feelingempoweredbytheirteamandreceivingtimely feedbackbefore,during,and/orafteraclinicalsituation.
Themputtingthattrustinme mademewanttotryto dothebestthatIcouldinthissituationwithalimited numberofexperiences.
Inthisparticularincident,thestudentfoundthemselvesin anemergentencounterwithapatientincardiacarrestand wastaskedwithintubatingthepatient.Althoughthestudent feltuncertain,theteam’strustandempowermenttoperform acriticalroleimprovedtheirsenseofagencyandsecurityand helpedmotivatethemtoperformthetask.
Clinicalsituationsinvolvingpatientswhowerevictims ofdomesticviolencereactivatedtraumainstudentswith similarexperiences.
[Listeningtoherdisclosure]wasdefinitelyhardbecause I’vehadnotasextremebutsimilarexperiences.I resonatedwithher,andIthinkthatmadeitalotmore challenging.Wecouldatleastprovideresourcesordo moretoacknowledgethatshe’shereforintimate partnerviolence-relatedconcerns.Noonereallycared aboutwhathappenedaftersheleft,orpeoplewerenot eventotallyawareofit.
Theclerkshipcurriculumdidnotpreparethisstudentto managetheguiltassociatedwithtreatingdomesticabuse victims(orasenseof “notdoingenough”).Thestudentfelt disappointedthatothermembersoftheclinicalteamwere notacknowledgingconcernsforfuturedomesticviolence risk.Consequently,thestudentdidnotfeeltheycouldopenly expressthemselveswiththeirsuperiorswhohadcontrolover theirsummativeassessment(ie,grade).
EmotionalDiscomfortAssociatedwithNavigatingEthics andUncertainty
Ethicallyambiguoussituationsaboundinmedicine. However,theseethicallychallengingsituations suchas instancesinwhichpatientswerephysically/chemically restrained,proceduresthatwereperformedonpatientswith alteredmentalstates,orcriticalmedicaldecisionsthatwere madebypatientsurrogates causedstudentstoexperience emotionaldiscomfortthatmadeitdifficulttonavigatethese situationsinrealtime.
[Thefaciallaceration]neededtoberepaired.Butthe patient,understandably,whowasconfusedreallydidn’t wantustouchingheranddidn’twantitdone ::: What weendedupdoingisholdingthepatientdownwhile theresidentrepairedthefaciallaceration.Andduring theentiretime,shewasobviouslyveryunhappy,kept ontellingustostop,andtoldtheresidentthatshe wouldgether fired.Wewereabletosuccessfully completetheprocedure,whichwasourgoal.
TheeducationalexperienceoftheEMclerkshipis primarilybasedonclinicalencounters.However,witnessing acutemanifestationsofpatients’ conditions,suchasphysical disfigurementorinabilitytocommunicate,overwhelmed studentsandimpededtheirabilitytoeffectivelymanagethe concernsoftheirpatients.Intheexamplebelow,while physicaldisfigurementwasexpected,thestudentfeltstunted byalackofpreparationonhowtonavigateanencounter withapatientwithalternativemethodsofcommunication andwasoverallunpreparedfortheeffectthatthepatient’ s physicaldisfigurementwouldhaveontheirowncomposure.
Ihaveneverseensomeonedisabledforawhile;Ifeellike wedohavepropertrainingonthat.ButthenwhenIsee, “Oh,myGod,hewasn’tlikethisatinybitago,andnowhe isbecauseofdisease.Theyusedtobefullyableandnow they’renot.” Iwastryingtowalkalineofthebestwayto communicate,whichwasadifferentexperiencethanIever hadbefore.Itwasreallyhardtoseeapersoninthatstate, especiallywhenyou’renotexpectingit.I’llremember whathewaslikeforever.
Studentexperiencesexploredinthisstudyreinforceprior literature’sunderstandingsoftheEDasastressful environmentandtheEMclerkshipasaneducationalsetting thatmayexposestudentstotraumathatexceedstheir existingcopingabilities.Thedeductiveandinductive analysesundertakeninthisstudyrevealinsightsaboutthe natureofthesestressorsthroughthelensofstudents’ experiencesduringtheirthird-yearEMclerkship.The deductiveapproachmatchedincidentssharedwithin12 students’ narrativestothesixTIMEdomains,whereasthe inductiveapproachofthisqualitativedatageneratedanovel groupof10overarchingthemes.
Overall,thedeductiveanalysisdemonstratedthatTIME domainswererepresentedinstudents’ perceptionsofEM clerkshipeducationalstructures(eg,mentors,policies,types ofpatientinteraction)astheynavigatedcriticalincidents. However,therearedifferencesinthefrequencyofandways inwhichcertaindomainsarerepresentedandsupportedin thestudents’ perceptionofexistingcurricularstructures. “Safety” wasbyfarthemostfrequentlymatchedTIME domaintoexcerptswithinstudents’ narratives(34%ofall identifiedinstances),followedby “Empowerment,Voice, andChoice” and “CollaborationandMutuality” (20%and 17%ofinstances,respectively).
Incontrast,theTIMEdomainsof “Transparencyand Trustworthiness,”“GenderCultural,andHistoricalIssues,” and “PeerSupport” werelesscommonlyidentifiedas dominantdomainsacrossstudents’ criticalincidents(12%, 8.7%,and8.7%ofinstances,respectively).Excerptsthatwere matchedtotheseTIMEdomainsoftendescribedinstancesin whichthesedomainswerediscussedbutnotpositively reinforcedinthecurrentclerkshipcurriculum(Table3).For example,anexcerptmatchedto “Safety” mayhaveexpressed anexperienceinwhichastudentfeltunabletovoicetheir opinionsopenlyduetoperceivednegativeconsequences.In contrast,otherexcerptsinstudentnarrativesreflected instancesinwhichaparticularTIMEdomainmayhavebeen wellrepresentedandsupportedbytheirclerkshipexperience. Forinstance,asdescribedin Table3,anexcerptthatwas matchedto “CollaborationandMutuality” demonstrated howthisdomainwassupportedbyasupervisor’srolemodelingofprofessionalism.
Often,instanceswhereTIMEdomainswerepositively reinforcedresultedinstrongerstudentresilienceand handlingofcriticalincidents,whereasthelackof positivereinforcementofTIMEdomainsresultedin studentdistress.Theprevalenceof “Safety” asadomain identifiedacrossincidents(oftenasadomainthatwasnot wellsupported)mayindicatethatstudentsexperience “Safety” asoneofthemostsalientdomainsthataffects theirabilitytomanagestressfulsituationscomparedto otherdomains.
Theinductiveapproachgenerated10denovothemesthat describestudents’ perceptionsoftraumaduringtheEM clerkshipandcanbebroadlyorganizedandunderstoodas emergingfromthreetypesofstudentinteractions:withthe clinicalenvironment;withsupervisors;andwithpatients (Table4). “Students’ interactionwiththeclinicallearning environment” describetheimmutablecontextual environmentoftheclerkshipexperience(eg,social,racial, and/orculturalfactors)thatinfluencestudents’ interactions withothersandincludesnavigatingSDoH,actingon perceivedinequities,andhandlingdiscriminationintheED. Incontrast, “Students’ interactionswithsupervisors” capturesthethemesofpowerdynamics,distressfrom invalidatedcontributionstotheteam,role-modeling, feedback,andempowerment.
Finally,thethirdcategory, “Students’ interactionswith patients,” encompassesthemesofemotionaldiscomfortwith ethicalambiguity,emotionaldistressfromacutepatientcare conditions,andreactivationofpreviouspersonaltrauma. Overall,thesethreefamiliesofthemespaintapictureofthe third-yearEMclerkshipinwhichstudentsperceive themselvestobeatthecenterofthecomplexlearning environmentoftheED,continuouslyinterfacingwith patientsandsupervisorsinapre-existing, fixed, socioeconomic,political,andculturalcontextthatshapesthe learningexperience.The10themesthatdescribethis complexsettinghavepotentialtoeither “enable” or “disable” effectivestudentmanagementoftheir criticalincidents.
Whencomparingtheinductivelygeneratedframework withtheTIMEframeworkinhowtheycapturestudents’ experiencesofthethird-yearEMclerkship,bothframeworks demonstrateaconsiderabledegreeofoverlapbutdifferin howtheycategorizestudents’ responsestocriticalincidents. Bothframeworksdescribetheinfluenceofpowerstructures, debriefs,transparencyofexpectations,genderandcultural issuesonstudents’ experiences.However,wheretheTIME frameworkcategorizestheseideasbasedonthetypeof stressor,theinductiveframeworkcategorizesthesameideas basedonwhomthestudentwasinteractingwith.Thus,one ofthelargestdifferencestoemergebetweenthedeductive andinductiveanalysiswasnotthecontentofthemesbutthe overallprinciplesbywhichtheapproachesorganizedand understoodthecontentofstudentnarratives.
WefeltthattheTIMEframeworkyieldedabroader,less specificpictureofstudents’ experienceswithcriticalincidents thatwerenotaseffectiveatcapturingthenuancesand complexitiesofstudents’ experiencesandspecificstressors (eg,SDoH,patientdisfigurement,inequitiesinpatientcare, ethicaldilemmas,lackofautonomyandvalidation)asthe inductiveframework.Thisdiscrepancymaystemfromthe factthattheTIMEdomainsarenotbasedspecificallyonthe third-yearEMclerkshipbutinsteadongeneralideasfound throughoutUME.Inaddition,theTIMEdomainsas envisionedbyBrownetaldrawonstructures,suchas institutionalpolicies,counselingservices,andself-care techniques,thatextendbeyondthestructures(ie,mentors, patients)thatstudentsactivelyinteractwithwhencritical incidentsoccur.7
Bycomparison,becauseour findingsoriginateentirely fromstudentexperiencesduringtheseincidents,this frameworkmaybebetterabletocaptureamoredetailedand student-informedunderstandingofthetrauma-informed structuresinthethird-yearEMclerkshipthatmost significantlyimpacttheirabilitytonavigateacutestress. Accordingly,ourobservedthemesmayofferamorerelevant lenstoassessforeducationalandenvironmentalstructures specifictothethird-yearEMclerkshipthathinderor promotestudents’ responsestocriticalincidents,while TIMEdomainsmayoffernon-specificrelevanceincapturing experiencesoftraumaacrossvariousclerkships.
Severallimitationsofthisstudyareworthnoting.Asthis studywasconductedasaninterviewseriesusingconvenience samplingatoneinstitution,the findingsmaynotbefully generalizable.However,the findingsofourstudymayserve asafoundationforfuturestudies,whichmaybeableto betterassessthegeneralizabilityoftheir findingsinthe contextofthisstudy’s.Ourlimitedsamplesizeraises concernsabouttheextenttowhichour findingsare generalizableacrossEMclerkshipsintheUSortoa broaderpopulationofmedicalstudentsacrossvarious geographiclocations.
Somedegreeofrecallbiasalsolikelyaffectedourstudyas participantsweremorelikelytorememberthemostsalient elements,positiveornegative,oftheirexperiencesintheED whileomittingdescriptionsofotherfactorsthataidedor impededtheirabilitytomanagethesituation.Weattempted tolimittheeffectofrecallbiasbyusingacriticalincident technique-guidedquestionnairethataskedparticipantsto activelyrecallasmanyelementsofthesituationas possible(eg,location,timeofday,surroundings,involved people,etc)toavoidomission.Also,thedegreeofsafetythat participantsfeltindisclosingtheirtruefeelingstothe interviewermayhaveaffecteddisclosureoftraumatic incidentsacrossourparticipantpool,whichmight havebeenreducedbyaneutral,third-partyinterviewernot
affiliatedwithouracademicinstitution.Futurestudiesmight employacross-sectionalqualitativeapproachin whichrepresentativesitesacrossthecountrycan besampled.
Atpresent,studentsexperienceallsixTIMEdomains duringtheirthird-yearEMclerkship,withsomedomains experiencedmorethanothers.Thedomainsof “Safety,” “Empowerment,Voice,andChoice,” and “Collaboration andMutuality” arefrequentlydescribedinstudentaccounts ofrespondingtoimmediate,stressfulcriticalincidentsduring theclerkship.TheinadequateperceptionofcertainTIME domainsinEMundergraduatemedicaleducationduring criticalincidentsmaycontributetostudentdistressand hinderstudents’ abilitytorespondtotheirperceivedtrauma. Consideringthe findingslaidforthbythisstudy,thespecific natureofstudents’ experiencesoftraumaduringtheEM clerkshipmaybeaneffectivetooltoguidecurricularchanges thatimprovestudents’ abilitytomanageimmediatestressors intheclinicalenvironment.
AddressforCorrespondence:DimitriosPapanagnou,MD,EdD, MPH,ThomasJeffersonUniversity,SidneyKimmelMedical College,DepartmentofEmergencyMedicine,1025WalnutSt., CollegeBuilding,Suite100,Room101,Philadelphia,PA19107. Email: Dimitrios.Papanagnou@jefferson.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Fundingforthisstudywasprovided throughtheSocietyforAcademicEmergencyMedicine(SAEM) FoundationthroughtheSAEMF/RAMSMedicalStudentResearch Grant,whichwasawardedtoMs.GiselleAppel(mentor,D. Papanagnou).Therearenootherconflictsofinterestorsourcesof fundingtodeclare.
Copyright:©2024Appeletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.PessagnoR,FooteCE,AponteR.Dealingwithdeath:medical students’ experienceswithpatientloss. Omega-JDeathDying. 2014;68(3):207–28.
2.Al-MateenCS,LinkerJA,DamleN,etal.Vicarioustraumatization andcopinginmedicalstudents:apilotstudy. AcadPsychiatr. 2014;39(1):90–3.
3.Rhodes-KropfJ,CarmodySS,SeltzerD,etal. “Thisisjusttoo awful;Ijustcan’tbelieveIexperiencedthat ”:medicalstudents’ reactionstotheir “mostmemorable” patientdeath. AcadMed. 2005;80(7):634–40.
4.BatleyNJ,BakhtiR,ChamiA,etal.Theeffectofpatientdeathon medicalstudentsintheemergencydepartment. BMCMedEduc. 2017;17(1):110.
5.CookAF,AroraVM,RasinskiKA,etal.Theprevalenceofmedical studentmistreatmentanditsassociationwithburnout. AcadMed. 2014;89(5):749–54.
6.ScaerRC. TheBodyBearstheBurden:Trauma,dissociation,and Disease.London,UK:Taylor&FrancisGroup,2014.
7.BrownT,BermanS,McDanielK,etal.Trauma-informedmedical education(TIME):advancingcurricularcontentandeducational context. AcadMed. 2021;96(5):661–7.
8.SubstanceAbuseandMentalHealthServicesAdministration. SAMHSA’sconceptoftraumaandguidancefortraumainformed approach.2014.Availableat: https://ncsacw.acf.hhs.gov/userfiles/files/ SAMHSA_Trauma.pdf.AccessedAugust11,2022.
9.McClintonAandLaurencinCT.JustinTIME:Trauma-informedmedical education. JRacialEthnHealthDisparities. 2020;7(6):1046–52.
10.ButterfieldLD,BorgenWA,AmundsonNE,etal.Fiftyyearsofthe criticalincidenttechnique:1954–2004andbeyond. QualRes. 2005;5(4):475–97.
11.GuestG,MacQueenKM,NameyEE. AppliedThematicAnalysis ThousandOaks,CA:SAGEPublications,Inc,2012.
PhyllisF.Agran,MD,MPH*†‡
DianeG.Winn,RN,MPH†
SoheilSaadat,MD,MPH,PhD‡ JayaR.Bhalla,BS†
VanNguyenGreco,MD*† NakiaC.Best,PhD,RN§ ShahramLot fipour,MD,MPH‡
SectionEditor:CristinaM.Zeretzke,MD
*UniversityofCaliforniaIrvineSchoolofMedicine,DepartmentofPediatrics, Irvine,California
† AmericanAcademyofPediatricsOrangeCounty,NewportBeach,California ‡ UniversityofCaliforniaIrvineSchoolofMedicine,DepartmentofEmergency Medicine,Irvine,California
§ UniversityofCaliforniaIrvine,SueandBillGrossSchoolofNursing, Irvine,California
Submissionhistory:SubmittedMarch17,2024;RevisionreceivedJuly8,2024;AcceptedAugust23,2024
ElectronicallypublishedSeptember9,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.20356
BackgroundandObjectives: Drowning,theleadingcauseofunintentionalinjurydeathamong Californiachildrenlessthan fiveyearsofage,averaged49annualfatalitiesfortheyears2010–2021.The CaliforniaPoolSafetyActaimstoreducefatalitiesbyrequiringsafetymeasuresaroundresidentialpools. ThisstudywasdesignedtoanalyzeannualfatalityratesanddrowningincidentsinCaliforniaamong children1–4yearsofagefrom2017–2021.
Methods: Weidentifiedfatalities,injuryhospitalizations,andemergencydepartment(ED)visitsfrom CaliforniastatevitalstatisticsdeathdataandstatehospitalandEDdischargedatausingtheEpiCenter CaliforniaInjuryDataOnlinewebsite.
Results: Overthe five-yearstudyperiod,4,166drowningincidentswereidentified:234werefatalities, 846werehospitalizations,and3,086wereEDvisits.Theobserveddifferenceinfatalityratesfrom2017 to2021failedtoachievestatisticalsignificance(P = 0.88).Location-basedanalysisofthe234fatal drowningincidentsrevealedthatpoolswerethemostcommoninjurysite,accountingfor65%of thecases.
Conclusion: Drowningremainstheleadingcauseofunintentional,injury-relateddeathamong Californiachildren1–4yearsofage,astheannualrateoffatalityoverthe five-yearstudyperioddidnot decline.WhiletheEpiCenterCaliforniaInjuryDataOnlinewebsiteisexcellentforanalyzingannual ratesofdrowningincidentsamongCaliforniaresidentsovertime,itislimitedinprovidinginsightinto modifiableriskfactorsandeventcircumstancesthatcanfurtherinformprevention.Thedevelopmentof robustintegratedfatalandnon-fatallocal,state,andnationalsystematicdatacollectionsystemscould aidinmovingtheneedleindecreasingpoolfatalitiesamongyoungchildren.[WestJEmergMed. 2024;25(5)838–844.]
Drowningistheleadingcauseofunintentional,injuryrelateddeathamongchildren1–4yearsofageintheUSand California,andthesecondleadingcauseofunintentional, injury-relateddeathamongchildren5–9yearsofage.1,2,3 For theyears2010–2021,therewasanaverageof49child
fatalitiesamongthoselessthan fiveyearsold.California’ s populationisnearly40millionlivingin58counties.4 The CaliforniaDepartmentofPublicHealth(CDPH)EpiCenter onlinedatabaserevealsthatdrowninghasbeentheleading causeofinjurydeathamongCaliforniaresidents1–4yearsof agefornearly25years.4 Amongchildrenwhosurvive
drowning,alargenumberexperiencelifelongdisabilitiesthat rangefromminortosevere.TheCaliforniaDepartmentof DevelopmentalServices2022ClientDevelopmentand EvaluationReportdocumentsacaseloadofmorethan 700personswhorequirelifelongservicesasaresultof nonfataldrowning.5
Californiaisoneoffourstatesthataddresstheprevention ofresidentialpooldrowningthroughstatelegislation.The firstCaliforniaPoolSafetyActwentintoeffectonJanuary1, 1997,andwasupdatedin2017.Inpart,theCaliforniaPool SafetyLawincreasedthenumberofrequiredsafetyfeatures aroundresidentialpoolsfromonetotwo,expanded allowablesafetydevices,andexpandedtheinspection process. 6 Thelawcoverspoolsandspasatprivate,singlefamilyresidencesatthetimeofsale,transferofproperty, orremodel.
Thepurposeofthisdataanalysiswastoexaminethe annualfatalityratesandcharacterizedrowningincidents amongCaliforniachildren1–4yearsofage(Universityof CaliforniaIrvineIRB#1735.)
WeobtainedthedataforthisstudyfromtheEpiCenter CaliforniaInjuryDataOnlinewebsite.Thisisa comprehensivesourceofinjurydatalimitedtoCalifornia residents.EpiCenterdataincludesfatalities,injury hospitalizations,andemergencydepartment(ED)visits.4 DrowningfatalitieswereidentifiedfromtheCDPHusing InternationalClassificationofDiseases,10th Rev,Clinical Modification(ICD-10-CM)cause-of-deathcodesappearing intheunderlyingcause-of-death fieldasfollows:W65–W74; X71;X92;Y21;W65–W74;X71;X92;andY21.We calculatedfatalityratesfromtheCaliforniaDepartmentof FinanceReportP-3:CompleteStateandCountyProjections Dataset(Baseline2019PopulationProjections;Vintage 2020Release).4
InjuryhospitalizationsandEDvisitswereidenti fied fromtheCaliforniaDepartmentofHealthCareAccessand Information(HCAI)PatientDischargeDataset(PDD)and theEDdataset,respectively.ThePDDincludesrecordsof inpatientdischargesfromCalifornia-licensedhospitals, includinggeneralacutecare,acutepsychiatric,chemical dependencyrecovery,andpsychiatrichealthfacilities.The EDdataincludesrecordsofpatientface-to-faceencounters withcliniciansathospitalslicensedtoprovideemergency medicalcare.IfanEDencounterresultedinasamehospitaladmission,theEDencounterwouldbecombined withthePDDrecordandonlyappearasahospitalization. Weidenti fi eddrowninghospitalizationsandEDvisits usingICD-10-CMcodesappearinginanyof25diagnosis fi eldsand12externalcause-of-morbidity fi elds. 7 On theEpiCenterinteractivewebsite,weselected
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Drowningistheleadingcauseof unintentional,injury-relateddeathamong children1 – 4yearsofageintheUS andCalifornia.
Whatwastheresearchquestion?
Weexaminedrecentfatalityratesand characterizeddrowningincidentsamong Californiachildren1 – 4-yearsofage.
Whatwasthemajor findingofthestudy?
Annualdrowningfatalityrates(2017 – 2021) didnotdecline(P = 0.88),and65%of fatalitiesoccurredinpools.
Howdoesthisimprovepopulationhealth?
Thisstudyoffersanewperspectiveontheneed forrobustdatacollectionsystemsthataidin movingtheneedleindecreasingpoolfatalities amongyoungchildren.
“drowning/submersion” undertheInjuryMechanism drop-downmenufordeaths,hospitalizations,andED visits.Thisincludedunintentional,intentional,and undeterminedintentdrownings.
ConsistentwithCaliforniaHealthandHumanServices De-IdentificationGuidelines,EpiCenterdoesnotprovide dataforresultswithfewerthan11cases.Becauseofthedeidentificationguidelines,wewereonlyabletodeterminethat lessthan4%offatalcaseswereintentunknownor intentional.Lessthan1%ofhospitalizedand~0.3%ofED caseswereclassifiedasintentional.
Welookedattheoverallincidenceofcasesamong Californiachildren1–4yearsofagefortheyears2017–2021 andtheratesoffatalities,hospitalizations,andEDvisits. Dataelementsreviewedincludedageinyears,sexofchild, race/ethnicity,locationofincident,outcome(fatal, hospitalization,EDvisit),disposition,andlengthofstay. Incidentlocationisdefinedasthebodyofwater,basedon ICD-10/ICD-10-CMcodedescriptions(eg,pool,bathtub,or openbodyofwater).Race/ethnicityiscategorizedasfollows: Hispanic;White;Asian;Black;multiracial;andPacific Islander.Wecalculatedincidenceratesand95%confidence intervalsassumingaPoissondistributionofdrowningdata. P -valueswerecalculatedbasedonthechi-squaretestby exactcalculationmethod.WeusedStata17.0SE(StataCorp LLC,CollegeStationTX)forstatisticalanalysis.
Duringthestudyperiod,2017–2021,atotalof4,166 drowningincidentsweredocumented. Table1 showsthe annualincidenceofdrowningbyfatality,hospitalization, andEDvisit. Table2 showstheincidencerate(IR)of drowningbyageandsex.Theincidenceofdrowningwas highestamongthe2-year-oldagegroup(P < 0.01). Table3 showstheIRofdrowningpermonthanddayoftheweek during2017–2021.DrowningwasmostprevalentinJune andJulyandleastprevalentinDecemberandJanuary (P < 0.001).Similarly,drowningwasmoreprevalenton weekendscomparedtoweekdays(P < 0.001).
Drowningincidentsamong234(5.62%)caseswerefatal. Ofthenonfatalcases,2,438(58.52%)patientsweretreated andreleasedfromtheED;628(15.07%)required hospitalizationforlessthanadayorovernight;136(3.26%) stayedinthehospitalfor2–4days;82(1.97%)hadhospital staysexceedingfourdays;and648(15.55%)wereeither transferredfromtheEDorhadunknowndispositions.
Thefatalityratesvariedfrom2.2per100,000population in2017to2.5per100,000in2021,buttheobserveddifference failedtoattainstatisticalsignificance(P = 0.88).Thisis contrarytothedecreaseinEDvisitsandhospitalization
duringthesameperiod.Thecasefatalityratioforthe1-yearoldagegroupstoodat7.86%(6.32–9.64%),whichwashigher thanforotheragegroups(P < 0.001).Similarly,thecase fatalityratioformaleswas6.48%(5.52–7.54%),exceeding thefatalityratioforfemales,whichwas4.47%(3.56–5.53%) (P = 0.005).Theanalysisoffataldrowningincidentsamong 234childrenaged1–4years,basedonthelocation,showed thatpoolswerethemostcommonsite,accountingfor65% (152cases).Bathtubsfollowedat14%(32cases),natural bodiesofwaterat11%(27cases),and10%(23cases) occurredatotherorunspecifiedwatersources.
Fataldrowningratesbyrace/ethnicitywerehighest amongBlackandmultiracialchildren(3.3/100,000), followedbyWhitechildren(3.0/100,000),Hispanic children(2.1/100,000),andthelowestratewasamongAsian children(1.8/100,000).
Drowningremainstheleadingcauseofdeathamong Californiachildren1–4yearsofage.Theannualrateof fatalityoverthe five-yearstudyperioddidnotdecline.
Overthe five-yearstudyperiod(2017–2021),4,166 drowningincidentswerereportedamongCaliforniachildren 1–4yearsofage,anannualaverageof833incidents.Of
Table1. AnnualdrowningratesofCaliforniachildren1–4yearsofage:2017–2021.
= 234)Hospitalizations(N = 846)EDvisits(N = 3,086)Total(N = 4,166)
*Rate:Incidencerateper100,000person-year. ED,emergencydepartment.
Table2. DemographicsofthedrowningincidenceofCaliforniachildren1–4yearsofage:2017–2021.
*Rate:Incidencerateper100,000person-year. ED,emergencydepartment.
Table3. TimingofthedrowningincidenceinCaliforniachildren1–4yearsofage:2017–2021.
Fatalities (N = 234)
Hospitalizations (N = 846)
EDvisits (N = 3,086)
Total (N = 4,166)
Month17.75*9.1%2023.6%5764.8%88 21311.5%2824.8%7263.7%113 37.75*5.4%3121.6%10571.4%147 4247.5%7022.0%22470.4%318 5286.8%9723.6%28669.6%411 6384.3%17219.7%66476.0%874 7434.5%16817.4%75478.1%965 8294.9%11819.8%44875.3%595 9175.4%5718.0%24276.6%316 107.75*4.6%3923.0%12371.1%173 117.75*7.7%2524.8%6865.4%104 121114.7%2128.0%4357.3%75
DayofweekSunday374.2%18320.6%66975.3%889 Monday244.8%10521.1%36874.0%497 Tuesday347.6%9821.9%31670.5%448 Wednesday306.7%7917.7%33875.6%447 Thursday327.4%8720.1%31372.5%432 Friday387.8%10120.8%34671.3%485 Saturday394.0%19319.9%73676.0%968
*Thenumberofincidentswasrecordedas “<11,” andwearbitrarilyreplacedthemwith7.75,contributingtothegrandtotalof4,166. ED,emergencydepartment.
these,nearly6%werefataland94%werenonfatal drownings.ThehighestIRwasamongchildrentwoyearsof age.Incidentsinthesummermonths(JuneandJuly)andon weekendsweremostprevalent.Racial/ethnicratesareonly availableforfatalitiesdueto2019modificationstoraceand ethnicitycodingintheHCAIhospitaldischargeandEDvisit data.FatalityrateswerehighestamongBlackand multiracialchildren.ThehighestratesamongBlackchildren havebeendocumentedinotherstudiesaswell,indicatingthe needtoaddressdisparities.3,8,9,10,11,12
Apreviousanalysisfoundthatannualratesof unintentionalfataldrowningsfrom1999–2020among Californiachildren1–4yearsofageatalllocationsandat swimmingpoolsdidnotdeclinesignificantly.13 Fortheyears 2017–2021,ofthe234fatalitiesamongchildren1–4yearsof age,65%occurredatpools,similartothe findingsinother studies.Thecodingdoesnotdifferentiatethelocationof pools(eg,residentialorcommunity),whicharegovernedby differentregulations.However,itiswelldocumentedthat fatalincidentsamongyoungchildrenaremostcommonat residentialpools.TheNationalCenterforFatalityReview
andPrevention(NCFRP)reportedthat52%offatal drowningsoccurredinahomeorresidentialpool.The ConsumerProductSafetyCommissionPoolorSpa Submersion2023Reportalsorevealedthatamongthe fatalities,84%wereataresidentialpool.2,3,11,12,14 Thisdata highlightstheneedtoprioritizepreventioneffortsthattarget pooldrownings.Fornonfatalcases,wecouldnotdetermine whetherthelocationwasapoolorotherbodyofwater becauseofthelargeproportionofT75.1ICD-10-CMcodes correspondingto “Unspecifiedeffectsofdrowningand nonfatalsubmersion.”
Foreveryfatalityamongthe1–4-yearagegroupinthis study,therewere18nonfatalincidents.This finding highlightstheneedtoincludeandcomparefatalandnonfatal incidentstobetterunderstandthecircumstancesand modifiableriskfactors,suchassubmersiontimebefore rescueandinitiationofcardiopulmonaryresuscitationatthe site.15,16,17,18 ThecurrentCaliforniapoolsafetylawisSB-442 PublicHealth:Pools:Drownings2017.6 Basedonits provisions,coverage,andinspectionrequirements,wewould notexpecttoseeareductioninadrowningfatalitybecause
1)fatalityisarareevent;2)wehavenodocumentation ofthedegreetowhichpoolownersremaincompliantafter theone-timeinspection;and3)althoughtwo “safety features” arerequired,onlyoneoftheoptionsisabest practice anenclosurethatisolatesthepoolfromaccess tothehomemeetingCaliforniaBuildingStandards Codespecifications.
Basedonthese findings,robustintegratedfataland nonfatallocal,state,andnationalsystematicdatacollection systemsthatenhanceourunderstandingoftheepidemiology andmodifiableriskfactorsincludingregionaldifferencesare necessarytomovetheneedleindecreasingpoolfatalities amongyoungchildren.Comprehensivesurveillancesystems wouldalsoincludeallportalsofdataentry,beginningwith firstresponderssuchaslifeguards,emergencymedical services,andlawenforcement.Standarddefinitionsand codingusingICD-10andIC1-10-CM,datasourcelinkages, real-timeelectronicdataentry,timelyanalysisandreporting, andstate-of-the-arttechnologytoimprovedatavariable capturewillincreaseourknowledgeand filldatagaps.19,20,21 PreliminaryresultsfromtheDrowningDeathScene InvestigationandtheChildDeathReview(CDR)Projectof theNCFRPalsoindicatethatthewidespreaduseofa standardizedtoolwill fillasignificantdatagapinknowledge toinformprevention.22
LocalCDR,aprocessthatallowsforamultidisciplinary comprehensivereviewofchildfatalitiesusingdatacollected frommultiplesources,hasbeenusedeffectivelyforboth surveillanceandtoinformprevention.23,24,25 TheHaddon Matrixmodelasappliedtodrowningcapturesthemultiple layersofprotectionandinterventionstointerruptthe progressiontoadeathbydrowningandcanbeintegrated intocasefatalityreview.9,26 TheInjuryEquityFramework theoreticmodelprovidesfurtherguidanceonsystematicdata collectionandanalysisthatcanbeconsideredinthelocal childdeathreviewprocess.27
Inadditiontopediatricians(childabuse,intensivists, primarycare),localCDRteamsideallyinclude representativesfromthecountychildprotectivesocial services,lawenforcement,publichealthandschoolnursing, andthecoroner’sormedicalexaminer’soffices.The coroner ’soffice(andoftenlawenforcement)conducts detailedinvestigationsincasesofunexpectedchilddeath, especiallythosewhodiewithoutbeingtransportedto hospitals.Otherteammembersmayalsohaveadditional interactionwiththechildorfamily.28 Theavailabilityof guidelinesonthetypeofinformationtogatherinfatal drowningcasesshouldimprovedatacapturebyCDR teammembers.
Physicianinvolvementinimprovingthequalityand quantityofdatainhealthrecorddocumentationandthe subsequentCDRprocessfurtherdetailsthecircumstances
andprovidesinsightintofutureprevention recommendations.Further,reportingtocountychild protectiveservicesifthereareconcernsforlackof appropriatesupervisionorsafeguardscanresultin additionalresourcesorservicesforthefamilytoprevent futureincidents.Childdeathreviewasasurveillancetool withactionrecommendationsiseffective.23,24,25 Pediatricianscanadvocateforintegratingnon-fatal drowningintothefatalityreview.
TheAmericanAcademyofPediatrics(AAP)strongly recommendsthatstatesestablishsystematicreportingonthe circumstancesofdrowning.9 Arobuststatewidedata collectionandanalysissystemprovidesinformationto developbestpractices,communityinterventions,and relevantpublicpolicies.TheCaliforniaLegislaturefounda solutiontothestatewidedrowningdatacollectiongapin reportingfatalandnonfatalincidentswhenCalifornia SenateBill855(Newman,Ch.817,Stat.2022:Child DrowningDataCollectionPilotProgram)waschaptered intolaw.Implementationofadatacollectionsystembythe CDPHmovesusclosertotheAAPrecommendationthat statesestablishsystematicreporting.Strengtheningour countyCDRteamsinreviewingdrowningcasesand includingnonfatalcasesforanalysisshouldcontributetoa robuststatewidesurveillancesystemandcanbeamodelfor otherstates.9,10,29
Thereareseverallimitationstothisstudy.TheCDPH EpiCenteronlinepubliclyavailabledatabase,basedonvital statisticsandhospital/emergencydischargedata,enablesan analysisofannualratesofdrowningincidentsonlyamong Californiaresidentsovertime.ChildrenwhovisitCalifornia andourpopulartouristattractionsarenotcountedifthey sustainafatalornonfataldrowning.Moreover,thedatabase islimitedinidentifyingmodifiableriskfactorsandevent circumstancesthatcanfurtherinformdata-driven preventionstrategiesandpolicies.
TheratiosoffataltohospitalizationtoEDvisitsmay includedoublecountsassomeEDencountersmayalsobe includedinthehospitaldata.Wedonothaveexposuredata. Additionally,wecouldnotdeterminetheextentof unreportedincidents.AsKoonpointedout,theCDPH publiclyaccessibledatarelatedtodrowningwasnotdesigned forresearch.14 Finally,asignificantdatagaprelatesto thelocationofthepoolforhospitalandEDvisitsdueto ICD-10-CMcodingvariability.
Drowningremainstheleadingcauseofunintentional, injury-relateddeathamongCaliforniachildren1–4yearsof age,astheannualrateoffatalityoverthe five-yearstudy perioddidnotdecline.WhiletheEpiCenterCaliforniaInjury DataOnlinewebsiteisexcellentforanalyzingannualratesof
drowningincidentsamongCaliforniaresidentsovertime,it islimitedinprovidinginsightintomodifiableriskfactorsand eventcircumstancesthatcanfurtherinformprevention. Currently,inconsistentandincompletedatahamperthe identificationandmonitoringoftrends,riskfactors,and preventionrecommendations.Incorporatingdataelements inthecontextoftheinjuryequityframeworkwillfurther guideinterventions.27 Systematicchilddeathreview, combinedwithallchilddrowningincidentinvestigationscan informevidence-basedbestpractices,community interventionsandtheimplementatonofeffectiveand impactfulpublicpolicies.
ThankyoutoOrionStewart,PhD,researchscientist, CaliforniaDepartmentofHealth,InjuryandViolence PreventionBranchforreviewingandcontributingtothis study.WealsothanktheCaliforniaKids’ PlatesProgram, CaliforniaDepartmentofPublicHealthInjuryandViolence PreventionBranchforsupportingthisprojectwith partialfunding.
AddressforCorrespondence:PhyllisAgran,MD,MPH,Universityof CaliforniaIrvineSchoolofMedicine,DepartmentofEmergency Medicine,3800W.ChapmanAve.,Suite3200,Orange,CA92868. Email: pagran@hs.uci.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Thisstudywassupportedbypartial fundingfromtheCaliforniaKids’ PlatesProgram,California DepartmentofPublicHealthInjuryandViolencePreventionBranch. TheCaliforniaKids’ PlatesProgram,CaliforniaDepartmentofPublic HealthInjuryandViolencePreventionBranchhadnoroleinthe designandconductofthestudy.Therearenootherconflictsof interestorsourcesoffundingtodeclare.
Copyright:©2024Agranetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.CentersforDiseaseControlandPrevention.WISQARS(Web-based InjuryStatisticsQueryandReportingSystem).2019.Availableat: https://www.cdc.gov/injury/wisqars/index.html AccessedMarch2,2024.
2.CunninghamRM,WaltonMA,CarterPM.Themajorcausesofdeath inchildrenandadolescentsintheUnitedStates. NEnglJMed. 2018;379(25):2468–75.
3.SpencerM,HedegaardH,WarnerM.Unintentionaldrowningdeaths amongchildrenaged0–17years:UnitedStates,1999–2019. NCHS DataBrief. 2021;(413).
4.CaliforniaDepartmentofPublicHealth.EpiCenter:Californiainjurydata online.2021.Availableat: https://skylab4.cdph.ca.gov/epicenter/ AccessedMarch2,2024.
5.CaliforniaDepartmentofDevelopmentalServices.Drowning prevention.Availableat: https://www.dds.ca.gov/initiatives/ drowning-prevention.AccessedMarch2,2024.
6.NewmanJ.CaliforniaStateSenate.SenatebillSB-442PublicHealth: Pools:Drownings.(2017–2018).2017.Availableat: https://leginfo. legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201720180 SB442&search_keywords=pool+safety.AccessedMarch2,2024.
7.HedegaardH,JohnsonRL,GarnettMF,etal.TheInternational ClassificationofDiseases,10thRevision,ClinicalModification (ICD–10–CM)externalcause-of-injuryframeworkforcategorizing mechanismandintentofinjury.2019.Availableat: https://www.cdc.gov/ nchs/data/injury/nhsr136-508.pdf.AccessedMarch2,2024.
8.ClemensT,MorelandB,LeeR.Persistentracial/ethnicdisparities infatalunintentionaldrowningratesamongpersonsaged ≤29years UnitedStates,1999–2019. MorbMortalWklyRep. 2021;70(24):869–74.
9.DennySA,QuanL,GilchristJ,etal.Preventionofdrowning.Policy Statement. Pediatrics. 2019;143(5):e20190850.
10.DennySA,QuanL,GilchristJ,etal.Preventionofdrowning.Techincal Report. Pediatrics. 2021;148(2):e2021052227.
11.NationalCenterforFatalityReviewandPrevention.Drowningcase registry.Availableat: https://ncfrp.org/cdr/drowning-case-registry/ AccessedMarch2,2024.
12.YangT.Poolorspasubmersion:Estimatednonfataldrowninginjuries andreporteddrownings,2023report.2023.Availableat: https://www. cpsc.gov/s3fs-public/Pool-or-Spa-Submersion-Estimated-NonfatalDrowning-Injuries-and-Reported-Drownings-2023-Report.pdf? VersionId=aKdoue0fOpavlEc1E6FBLzYzIAKO8lyW AccessedMarch2,2024.
13.AgranP,WinnD,NguyenGrecoV,etal.Californiachilddrowning: anewperspective.2023.Availableat: https://www.aap-oc.org/ wp-content/uploads/2023/10/CA-Child-Drowning-AbstractPosterNCE-AAP-2023_QR-Code.pdf.AccessedOctober23,2023.
14.KoonW,StewartO,BranderR,etal.Burdenoffataldrowningin California,2005–2019. InjPrev. 2023;29(5):371–7.
15.PeriF,LauraDeNardi,CanutoA,etal.Drowninginchildrenand predictiveparameters. PediatrEmergCare. 2023;39(7):516–23.
16.RaessL,DarmsA,Meyer-HeimA.Drowninginchildren:retrospective analysisofincidentcharacteristics,predictingparameters,andlongtermoutcome. Children. 2020;7(7):70.
17.QuanL,BierensJJLM,LisR,etal.Predictingoutcomeofdrowningat thescene:asystematicreviewandmeta-analyses. Resuscitation. 2016;104:63–75.
18.LouxT,MansuriF,BrooksSE,etal.Factorsassociatedwithpediatric drowningadmissionsandoutcomesatatraumacenter,2010–2017. AmJEmergMed. 2021;39:86–91.
19.AgranP,WinnD,BhallaJ.PartnersforChildhoodDrowningPrevention: 2023–2024.2023.Availableat: https://www.aap-oc.org/wp-content/
uploads/2023/09/Partners-For-Childhood-Drowning-Prevention2023-2024-92023.pdf.AccessedMarch2,2024.
20.MeddingsDR,ScarrJP,LarsonK,etal.Drowningprevention: turningthetideonaleadingkiller. LancetPublicHealth. 2021;6(9):e692–5.
21.PedenAE,SarramiP,DinhM,etal.Descriptionandpredictionof outcomeofdrowningpatientsinNewSouthWales,Australia:protocol foradatalinkagestudy. BMJOpen. 2021;11(1):e042489.
22.CollierA,JoyS,FraleyG.P2A002:Usingenhanceddeathscene investigationandchilddeathreviewtobetterunderstandandprevention drowningamongchildrenandyouth.2023.Availableat: https:// aapexperience23.eventscribe.net/fsPopup.asp?PosterID=620497& mode=posterInfo.AccessedOctober23,2023.
23.QuanL,PilkeyD,GomezA,etal.Analysisofpaediatricdrowningdeaths inWashingtonstateusingthechilddeathreview(CDR)forsurveillance: whatCDRdoesanddoesnottellusaboutlethaldrowninginjury. Inj Prev. 2011;17Suppl1:i28–33.
24.WirtzSJ,FosterV,LenartGA.Assessingandimprovingchilddeath reviewteamrecommendations. InjPrev. 2011;17Suppl1:i64–70.
25.DesapriyaE,SonesM,RamanzinT,etal.Injuryprevention inchilddeathreview:childpedestrianfatalities. InjPrev. 2011;17Suppl1:i4–9.
26.HaddonW.Thechangingapproachtotheepidemiology,prevention, andameliorationoftrauma:thetransitiontoapproachesetiologically ratherthandescriptivelybased. AmJPublicHealthNationsHealth. 1968;58(8):1431–8.
27.KendiSandMacyML.Theinjuryequityframework establishing aunifiedapproachforaddressinginequities. NEnglJMed. 2023;388(9):774–6.
28.AgranP,WinnD,AndersonC,etal.(2010).Drowningof1–4-year-old childreninswimmingpoolsandspassurveillancehandbook.2010. Availableat: https://www.aap-oc.org/wp-content/uploads/2022/10/ Drowning-Surveillance-Handbook-Final-2011.pdf AccessedMarch2,2024.
29.NewmanJ.CaliforniaStateSenate.SB-855ChildhoodDrowningData CollectionPilotProgram.(2021–2022).2022.Availableat: https:// leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id= 202120220SB855.AccessedMarch2,2024.
FarisF.Halaseh,BS*
JustinS.Yang,BA*
CliffordN.Danza,BS*
RamiHalaseh,MD†
LindseySpiegelman,MD,MBA‡
SectionEditor:ChrisBaker,MD
*UniversityofCalifornia,Irvine,SchoolofMedicine,Irvine,California † KaiserPermanenteSanFrancisco,DepartmentofInternalMedicine, SanFrancisco,California ‡ UniversityofCalifornia,Irvine,DepartmentofEmergencyMedicine, Irvine,California
Submissionhistory:SubmittedDecember21,2023;RevisionreceivedJune21,2024;AcceptedJune21,2024
ElectronicallypublishedAugust13,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18650
Providingappropriatepatienteducationduringamedicalencounterremainsanimportantareafor improvementacrosshealthcaresettings.Personalizedresourcescanofferanimpactfulwaytoimprove patientunderstandingandsatisfactionduringorafterahealthcarevisit.ChatGPTisanovelchatbot computerprogramdesignedtosimulateconversationwithhumans thathasthepotentialtoassistwith care-relatedquestions,clarifydischargeinstructions,helptriagemedicalproblemurgency,andcould potentiallybeusedtoimprovepatient-cliniciancommunication.However,duetoitstraining methodology,ChatGPThasinherentlimitations,includingtechnicalrestrictions,riskofmisinformation, lackofinputstandardization,andprivacyconcerns.Medicolegalliabilityalsoremainsanopenquestion forphysiciansinteractingwiththistechnology.Nonetheless,carefulutilizationofChatGPTinclinical medicinehasthepotentialtosupplementpatienteducationinimportantways.[WestJEmergMed. 2024;25(5)845–855.]
Effectivecommunicationandcounselingbetween cliniciansandpatientsiscrucialforhigh-qualityhealthcare, particularlyintheemergencydepartment(ED)wheretime constraintsandevolvingdiagnosticscancomplicate discussionsaboutcurrentandpost-hospitalcare.Thismakes patienteducationanimportantgaptoaddress.Theurgency andcomplexityofemergencycasesoftenhinder comprehensiveinformationdelivery,leavingpatients’ questionsunanswered.Inquiriesabouttheircondition, treatmentoptions,andprognosisarevitalforpatient understandingandengagementindecision-making.A systematicreviewexaminingthefactorsthatinfluencethe patientexperienceintheEDhighlightedphysician-patient communicationasthemostcommonfactoraffecting patientsatisfaction.1 Addressingtheseconcernsnotonly boostssatisfactionbutalsoempowerspatients,improving healthoutcomes.
Effectivedischargeinstructionsareessentialforapatient’ s post-emergencycare,asambiguityorinadequate explanationcanresultinconfusion,noncompliance,and
subsequentreadmission.2,3 Arecentstudyrevealedthat24% ofpatientsdonotfullyunderstandtheirfollow-upplan,64% struggletocomprehendtheirreturn-to-EDinstructions,and 42%donotreceivecompletedischargeinstructions.3 Improvingdischargecommunicationcanenhancetransition tofollow-upcare,therebyimprovingpatientcareoutcomes andreducingavoidablereadmission.Inadditionto communicationchallenges,patientsmaystruggletoidentify themostappropriatetypeofcarefortheirconditions.The EDoftenseescasesthatcouldbemoreeffectivelymanaged inprimarycareorurgentcaresettings.About13–27%ofall EDvisitsareconsiderednon-urgentinnature,resultingin approximately$4.4billionannualcost.4 Identifyingfactors thatcontributetounnecessaryemergencycareutilizationcan aidthedevelopmentoftargetedinterventionsand educationalinitiativesaimedatredirectingpatientstomore appropriateavenuesoftreatment.
Furthermore,increasinglydiversepatientpopulations bringlanguagebarrierstotheforefrontofcareintheED. PatientswithlimitedEnglishproficiencyoftenfaceobstacles inunderstandingtheirdiagnosesandtreatmentplans.One
studiedshowedonly52%ofnon-Englishspeakerswere satisfiedwiththeirEDvisit,comparedto71%ofEnglish speakers.5 Strategiestoreducetheinequitableimpactof languagebarriershasobviousbenefitsforpatientsafetyand outcomesintheED.
Onemethodtoaddresstheselimitationscouldbeclinical applicationofamachinelearning(ML)largelanguage model(LLM),suchasChatGPT(OpenAI,LP,San Francisco,CA).AnML-basedchatbotcanlearnfromavast arrayoftrainingdataanduserinteractionstoimprove performanceandefficacyofitsdeliveredcommunication.In recentperformanceevaluations,ChatGPTscoredabovethe nationalaverageonpubliclyavailablerenditionsofStep1, Step2-ClinicalKnowledge,andStep3oftheUnitedStates MedicalLicensingExam(USMLE).6 Themodel’sUSMLE performancecontinuestoimprovewithnewupdates,suchas GPT-4,whichadditionallyoffersimage-analysis capabilities.7 Modelsarealsobeingusedtotrainmedical studentsandpreparethemforclerkships.8–10 These benchmarksdemonstrateChatGPT’ s fluencywithbasic medicalinformationattheknowledgelevelofamedical schoolgraduate.
Patientsoftenundertakeaninternetsearchofmedical topicsbeforeorafterspeakingwithaphysician.However, withavastarrayofinformationandmisinformation availableontheinternet,physiciansandotherhealthcare professionalsremainanimportantinterfacetosource reliablemedicalknowledge.Here,weevaluatethepotential rolethatLLMslikeChatGPTcouldhaveasapersonalized educationalresourceforpatientsseekingemergency medicaltreatment.
ChatGPTisatext-basedchatbotthatfacilitatesuser interactionthroughnaturallanguage.TheMLmodelforthe publiclyavailableversions,GPT-3.5andGPT-4,were trainedonwrittentextdrawnfromavastspectrumofonline databases.Pretrainingenablesthemodelstoconstructa robustlinguisticframework.Furtherconditioningincludes assignment-specificadjustments,humanfeedbackthatcan bolsteritsconversationalabilities,andrigoroustestingto ensureresilienceagainstchallenginguserqueries.This processiscriticalforaligningthemodel’soutputwith nuancedhumandialogue,enhancingitscapacitytoprovide preciseandcontextuallyappropriateresponses.10
GPT-4isthelatestiterationofthisLLM,withan enhancedarchitecturethatnotonlyunderstandsand generatestextualcontentbutalsointerpretsandrespondsto visualinput.11 Furthermore,whileexperimentalfeaturesin GPT-4includethepotentialforcurrentinternetdata,such capabilitieshavenotbeenbroadlyreleasedtousers.The broaderimplicationsofthislimitation,includingthebalance betweenmodelautonomyandthenecessityforhuman oversight,areexaminedfurtherinthesectionontechnical
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
CurrentpatienteducationintheEDis inadequate,oftenleadingto misunderstandingandnoncompliancewith post-careinstructions.
Whatwastheresearchquestion?
HowcanthechatbotChatGPTimprove patienteducationintheEDsetting?
Whatwasthemajor findingofthestudy?
ChatGPThelpstriage,clarifydischarge,and providecareinstructions.
Howdoesthisimprovepopulationhealth?
ChatGPTcanenhancepatienteducation, improvingcomprehensionandadherenceto follow-upcare,reducingunnecessaryED visitsandenhancingoveralloutcomes.
restrictions.Nevertheless,thecurrentcapabilitiesof ChatGPTareanimportantleaptowardacollaborativerole thathumansandAIsystemswillshareinnavigatingcomplex real-worldapplications.12
TheEDisasettingwithaparticularlyhighdemandfor efficientandclearpatienteducationatdischargegiventhe potentialreappearanceorsequelaeofconditionsrequiring emergentevaluation.However,theEDalsooftenimposesa highdegreeofconstraintonpatient-clinicianinteraction time.Eveninthesettingoflow-acuityconditions,an observationalstudyshowedthecombinedamountoftime physicians,nurses,andtechniciansspentwithpatientsonce theyareassignedtoabedwasabout25%oftotalpatient lengthofstay.13 Thefactorsunderlyinglimitedinteraction timearemultifactorial,butoften-citedcontributingreasons includepatientvolumeandhighloadofdocumentation requirements.Offeringaresourcethatisadaptiveand responsivetopatientconcernsrelevanttotheirspecific situationisanimportantgapintheED.ChatGPTcan provideaninteractivemodalitythatispersonalizedtomeet thisgapforthehealthcareeducationneedsofpatientsand theirclinicians.
ChatGPTmayoffermultiplebenefitsforpatientsinthe ED.Itcanquicklygivepersonalizedresponsestoqueriesona widerangeofhealthcaretopics.Forexample,thesoftware
canprovidepurpose-andrisk-basedinformationabout proceduresapatientortheirfamilymembermayundergo duringanEDencounter(Figure1A).ChatGPToffers
backgroundinformationabouttheprocedureandrefersto thecareteamforfurtherencounter-basedquestionsand concerns.Theinformationprovidedaboutaprocedure,such
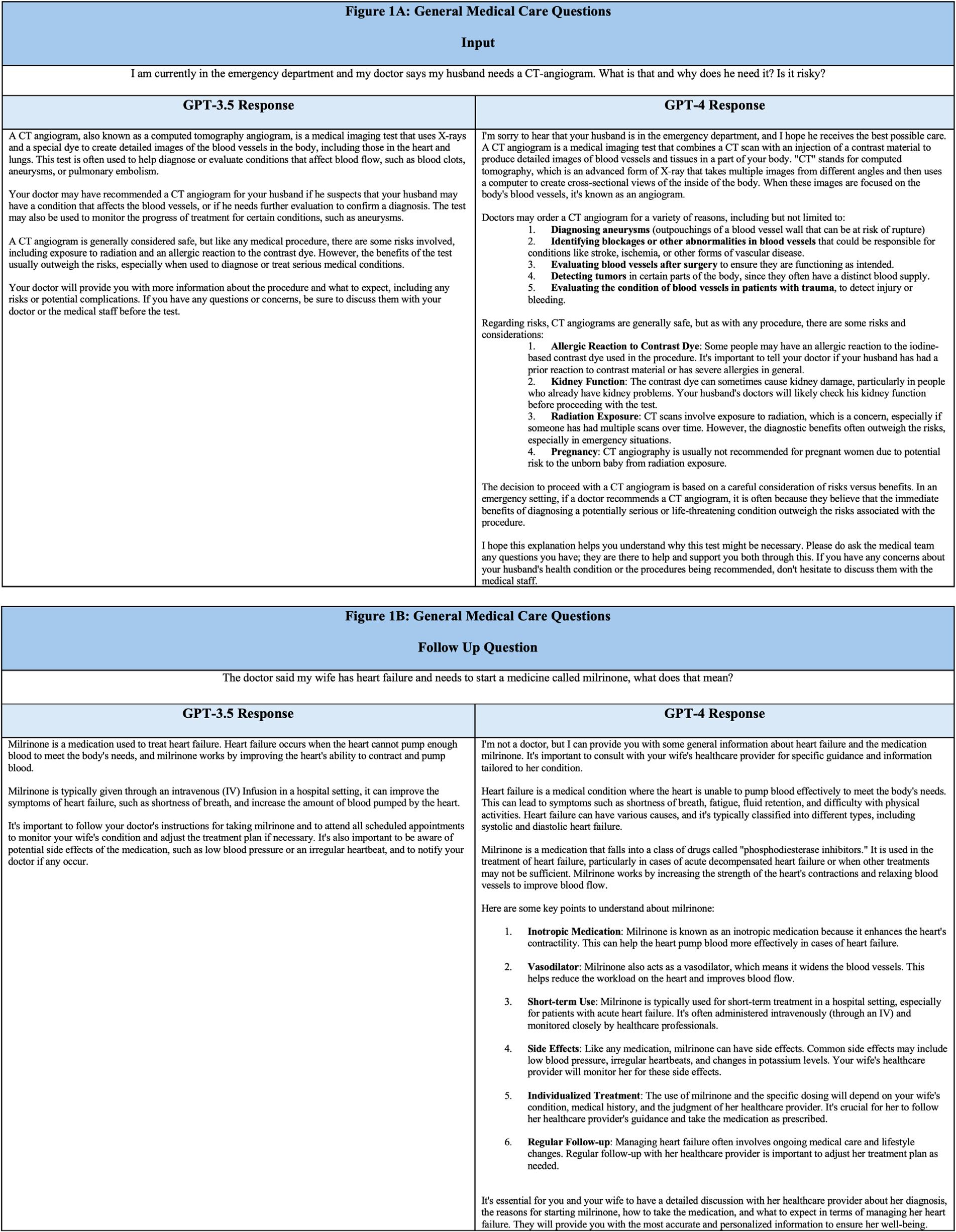
Figure1. (A–B)SelectedQ&Arelatingtomedicalcare.InputsarehumanquestionsandoutputsweregeneratedbyChatGPT.
ascomputedtomographyangiographyinthisexample, describesaninitialdepthofresponsethatislikelyadequate foralayperson’sintroduction.Incontrasttoconductinga generalinternetsearchforthepurposesandrisksofthis procedure,ChatGPTsummarizesthepertinentinformation inaconversationalformatthatiseasilyaccessibletotheuser.
AnotherexampledemonstratesChatGPT’ssensitivityto slightalterationsofmeaningwhenaskedaboutmedical conditionsandmedications.Theuser firstasksaquestion aboutthepurposeofthemedicationmilrinoneforastated conditionofheartfailure(Figure1B).Thesoftware’ s responseexplainsashortsummaryforboththecondition andthemedication.
Giventhesamesetofprompts,thereareseveral differencesbetweenGPT-3.5andGPT-4outputs.GPT-4 outputsarelengthier,withclearerstructuretotheanswer approach.Intheseexamples,thereappearstobeatendency towarditemizinglists.Thereisalsoanobservedempathetic bentwithapparentself-anthropomorphizationbystarting sentenceswith “I.” Whilefurtherstudyontheend-user impactofthismodeliterationiswarranted,GPT-4appears tooffermorecomprehensiveinformationthanGPT-3.5for selecthealthcare-associatedqueries(Figure1).
DischargeinstructionsforpatientsleavingtheEDare importantforpatientsafetyandsatisfaction.However, studiesshowthatpatientsoftendonotfullyunderstandthe after-careinstructionsprovidedtothem.2,14,15 Poor adherencetomedicaladviceorfollow-upmaybe attributableinparttoagapinmedicalunderstanding. Personalizedeffortstoincreasepatientadherenceto dischargeinstructionshavefocusedonstafffollow-upvia phonecallorSMSmessaging,buttheseinterventionsbear relativelyhightimeandmonetaryrequirements,anddonot alwaysprovidepositiveresults.16–18 ChatGPTcanbeusedto improvepatientunderstandingofinstructionsgivenbya clinician.Itsnatural-languageinterfaceallowspatientstoask questionsasiftheywereconversingwithahuman (Figure2A, 2B).Similartendenciesareobservedcomparing theGPT-4modeltoGPT-3.5,withlongeranswers,increased listcreation,andgreateruseof first-orsecond-person writingstyle.
NavigatingtheUShealthcaresystemtodeterminethe appropriateentityfromwhichtoseekcareisoftena significantchallengeforpatients.TheEDremainsoneofthe onlysettingsinwhichrelativelytimelyevaluationandcareis availableandisoftenusedasasafetynetforpatientswithno healthinsurance.However,evenpatientswithinsuranceand adesignatedprimarycarephysiciansometimesoptforan EDvisitduetobarriersaccessingtheirphysician.Benefitsof comprehensiveevaluationandservices,withimaging,labs,
andpharmacyprovidedinonelocationisacompetitive convenienceforpatients.19,20 Dueinparttothesefactors, annualEDutilizationratescontinuetorisedisproportionate todemographicfactors,increasingburdenonEDresources forconditionsthatarebetteraddressedinpreventivecaresettings.21
ChatGPTcanprovideguidanceinseekingurgentvs emergentcare.Inoneexample,apatientwithsymptoms typicalofaurinarytractinfectionasksifavisittothe emergencyroomisadvisable( Figure3A ).Theresponse indicatesthatcareshouldbesoughtbutsuggestsurgent careorprimarycaresettingsfor fi rst-lineevaluation,given thestatedsymptoms.Theresponsealsoprovidesexamples ofmoreserioussymptomsthatindicateneedforemergent evaluation.Guidingapatient ’ sdecisionmatrixina personalized,interactivemannermaybeanimpactfulway toencouragethemtoseekanappropriatelevelof care.ReducinginstancesofEDutilizationforlow-acuity healthconcernsassistseffortstoreduceEDcrowding, whichcanhavewide-rangingbene fi tsforhealthcare systemsbyimprovingpatientoutcomes.22 Futurestudy couldexaminetheusefulnessofChatGPTintriage scenarios,comparedtocurrentmodalitiessuchasnurse advicephonelines.
ChatGPTcanalsoofferguidanceduringprehospital emergencies,detailingstep-by-stepinstructionsto respondersandadvisinghowtoseekanappropriatelevelof care.Forexample,ChatGPTdescribesrecommended actionsuponencounteringasyncopalpatient(Figure3B). Prehospital-interventioneducationgearedtoward laypersonshasbeenakeyfocusinpublichealth,particularly forconditionssuchascardiacarrest,stroke,andmajor hemorrhage.Whilecertainpracticesarebesttaughtina hands-ondemonstrationsetting,ChatGPTmaybea valuablereferenceresourceforlaypersonsactinginthe capacityofanemergencyresponder.23
ChatGPTcanofferreal-timetranslationforlanguages includingEnglish,Spanish,French,German,Italian, Portuguese,Chinese,Japanese,Korean,Arabic,Dutch, Polish,Russian,andmore.Whilereal-timetranslationisof crucialimportanceforEDhistory-taking,translatorservices arebecomingubiquitousduetothegrowingpopularityof tele-healthconsultationdevices.Thebenefitsofusing softwarewithtranslationcapabilitytoaddresspatient questionsisapparentinprehospitalandpost-disposition settings.Forexample,ChatGPToffersthesameresponsefor aquestionasked firstinEnglish,andtheninSpanish (Figure4).ComparedtoGPT-3.5,GPT-4’sEnglishresponse takesamorecautiousapproachtoprovidingmedical guidance.However,GPT-4’sSpanishresponseappearsmore likeGPT-3.5intheunhedgedencouragementforfurther medicalcare.Thisdifferencemaybeduetoavarietyof

factors:modellanguagetraining;translation filters;or underlyingdifferencesintrainingdataitself.Further discussionoftechnicallimitationsisdiscussedinthesection ontechnicalrestrictions.Futurestudiesshouldinvestigate
Figure2. (A–B).SelectedquestionsrelatingtodischargeinstructionsandChatGPToutput. Volume25,No.5:September2024WesternJournal
theaccuracyofChatGPTtranslationsandcomparethe resultstoalternativemodalitieslikecertifiedmedical translators,orothertext-onlymodalitieslikeGoogle Translate,inaclinicalhealthcareenvironment.24,25
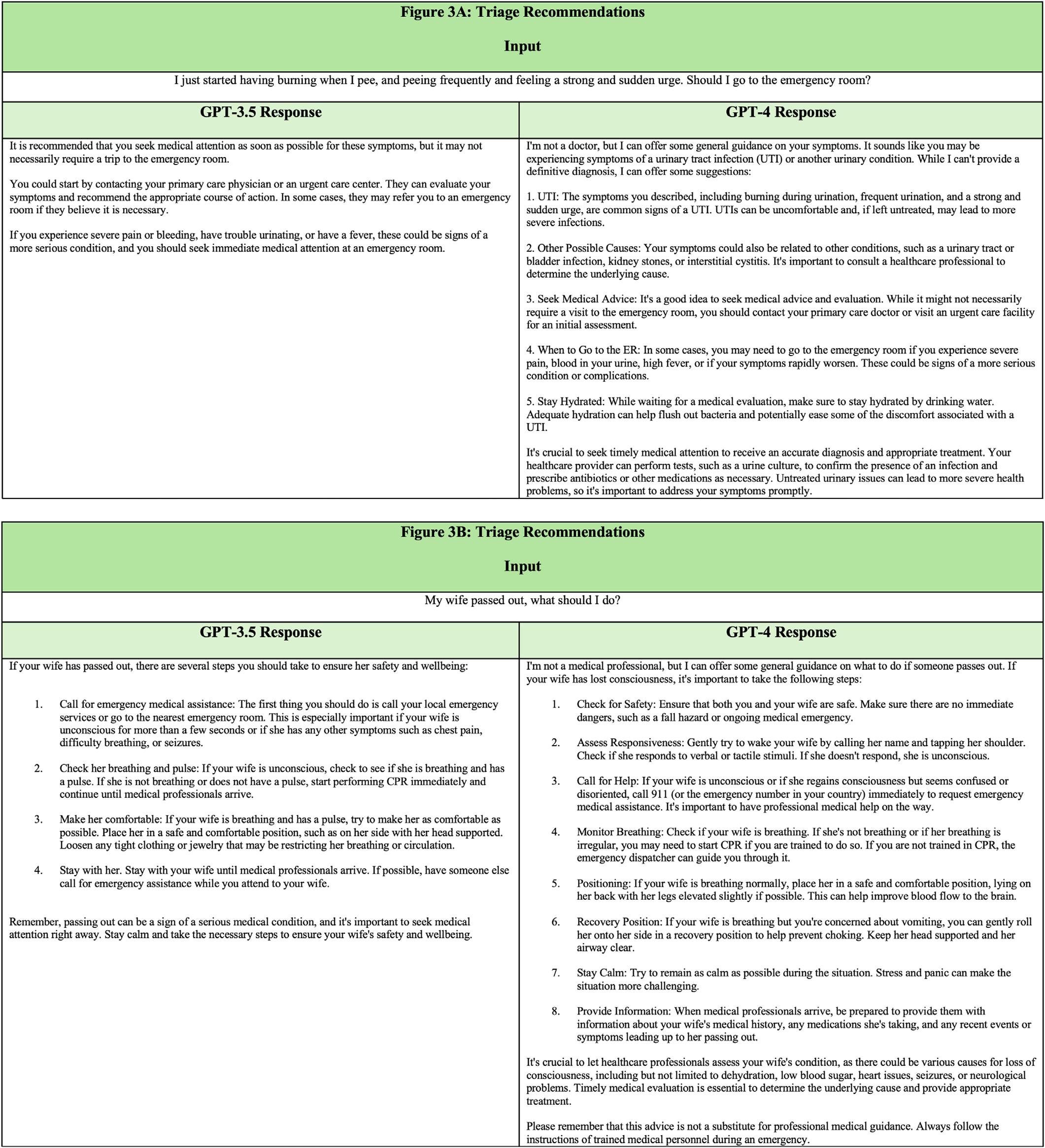
Figure3. (A–B).ChatGPTinputandoutput.TopoutputdemonstratesChatGPTtriagerecommendationsandbottomoutputsignifiesurgent responseinstructions.
ChatGPTiscurrentlyeasilyaccessibleandoffersano-cost useraccountforthepublic.Asubscription-basedupgradeis alsooffered,whichprovidesquickerresponsetimesandearly accesstonewfeatures.7 UtilizationofChatGPTtoassist
patienteducationforvariousaspectsofcare,including understandinghealthconditions,dischargeinstructions,and whentoseekemergencymedicalcaremaysavehospitaltime, money,andresources.Emergencydepartmemtspendingisa growing financialconcernonanationallevelbutmaybe
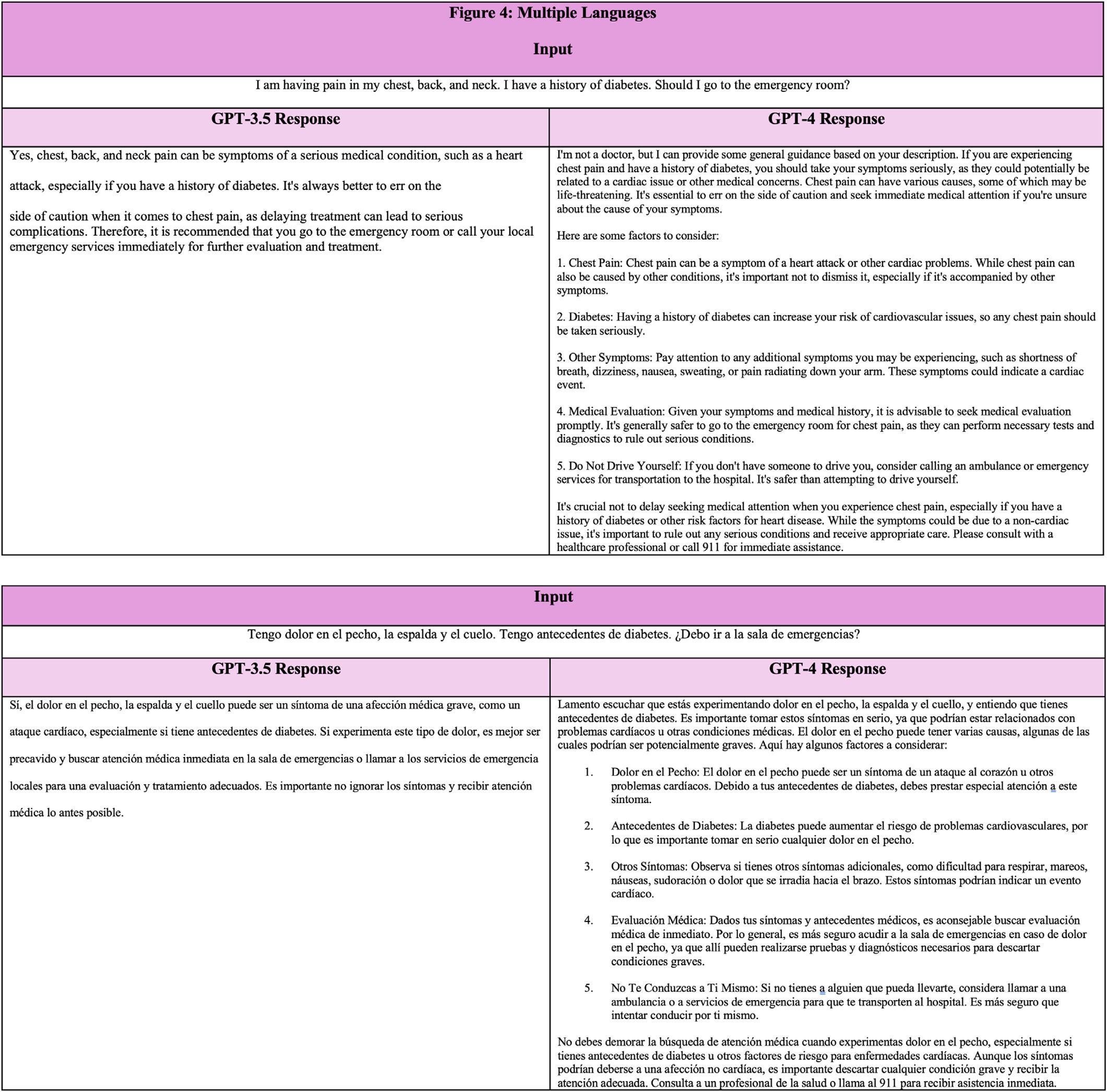
alleviatedbyreducingthefrequencyofpresentationsfor preventablecausesandavoidablevisits.26 Byproviding personalguidanceonwhentoseekemergencycare, ChatGPThasthepotentialtomakeimportantcontributions toloweringhospitalburden.
TechnicalRestrictions
UsingChatGPTinemergencymedicinecarriescertain risks.Onemajorconcernisthatthemodelcanprovide
differentresponsestothesameorsimilarquestions,which affectsitsreliabilityandusefulness.BecauseChatGPTis basedonaMLalgorithm,itmaygeneratedifferentresponses tosimilarquestionsdependingonavarietyoffactors,suchas theorderorcontextofwordsusedasinput.Inarecentstudy onChatGPT’sresponses,identicalquestionsregarding cirrhosisandhepatocellularcarcinomaweresubmittedtwice andindependentlygraded.ChatGPTwasabletoproduce twosimilarresponses90.48%ofthetime.Althoughthis numbermayberegardedashighreproducibility,itraises
concernsoverthepotentialconsistencyofofferingmedical advicetolaypersons.Althoughmostinstanceswillprovide theuserwiththesameinformation,ChatGPT’ sresponsesare basedonprobability.27 Futurestudiesshouldanalyzethis variabilitytodeterminetheimpactonresponse appropriatenessfortheuser.
Inadditiontooutputvariability,thereisalsoapotential fordifferencesinusercomprehension.Thisunderscores anotherrisk:thepotentialfordifferencesincomprehension andinterpretationoftheinformationprovidedtolaypersons. Althoughthislimitationiscommonamongmanydifferent technologies,thesedifferencesincomprehensioncanleadto potentiallyadverseoutcomesforpatients.Giventhese considerations,itiscrucialtoexercisecautionandapply criticalthinkingwhenusingChatGPTasasourceof informationinhealthcareinteractions.Itisessentialtobe awareofthepotentialfordevelopingoverconfidencein ChatGPT’srecommendations,andtheriskforanchoring onaspecificdiagnosisorimpressionforbothpatients andclinicians.
Responsevariabilityandinterpretationofresponsescan impacttheconsistencyandreliabilityofthismodel.Itis importantforcliniciansandpatientstobeawareofthese risks,andtouseChatGPTasasupplementarytoolrather thanaprimarysourceofinformation.Therefore,ongoing improvementsinthetechnologyandcontinuedtrainingof thealgorithmshouldbepursued.Effortstoincorporate currentmedicalliteratureintothetrainingdatacould enhancethereliabilityandrelevanceofChatGPT’ s responses.However,itremainsessentialtorecognizethe dynamicnatureofclinicalpracticeandtheimportanceof relyingonevidence-basedguidelinestoensurepatientsafety andwell-being.
Ensuringaccurateandtruthfulinformationiscrucial whenusingChatGPT,asmisinformationcanhaveserious consequencesforpatientcare.ChatGPT’strainingdatais limitedtoinformationavailablebefore2021.Medical knowledgeandpracticeshaveevolvedsincethisknowledge cutoffpoint,andChatGPTmayreferenceinformationthatis outdatedornolongerapplicabletocurrentmedical practices.AccordingtotheChatGPTstudyforcirrhosisand hepatocellularcarcinoma,ChatGPT’sanswerscontaineda mixofcorrectandincorrectinformation.Thepercentageof responsesthatwereclassifiedashavingbothcorrectand incorrectoroutdatedanswerswas22%inbasicknowledge, 33%indiagnosis,25%intreatment,18%inlifestyle,and50% inpreventivemedicine.28 However,whilethisstudy highlightspotentiallimitationsofChatGPT’saccuracyin respondingtoquestionsabouthepatocellularcarcinoma,itis importanttorecognizethatfurtherresearchisneededto comprehensivelyevaluatetheaccuracyofChatGPT’ s responsesacrossallmedicaldomains.Physiciansand
patientsmustremaincautiouswhenusingChatGPTand seekconfirmationfromotherreliablesourcesbeforemaking decisionsbasedontheinformationprovided.
Anotherconcernisthemodel’sopaquealgorithm,which cangenerateplausiblesoundingbutinaccurateor nonsensicalanswers,aphenomenonknownas “hallucinations” 29 Evidenceofthiscanbeseeninfabricated sourceswhenChatGPTisaskedtoprovidereferencesfora givenresponse.30 ChatGPT’strainingmayhaveincluded scientificliteraturecitationdatasets,butitsgenerative algorithmdoesnotallowforone-to-onedatasource matching,resultinginaresponsethatprovidescompletely fabricatedsources.Patientsmaybelesslikelytoquestionthe accuracyofChatGPT’sresponsesiftheyarepresentedwitha sourceandsimplyassumethattheinformationhasbeen verified.Thiscanultimatelyleadtopatientsmaking decisionsthatarenotintheirbestinterestandmayeven resultinharm.
Thereiscurrentlyunavoidableriskofmisinformation whenusingChatGPTforpatienteducationinemergency medicine.Tomitigatethisrisk,itisimportanttomanage expectationsandriskthresholds.Physiciansandpatients shouldbeadvisedoftherisksandbenefitsofthistechnology. Additionally,regularevaluationandimprovementof themodelwillhelpminimizetheriskofinaccuracies andmisunderstandings.
Ensuringpatientprivacyandsecurityisanotherconcern whenusingChatGPTforpatientencounters.Unauthorized accesstoprotectedhealthinformation(PHI)canleadto identitytheft,insurancefraud,andothertypesofharmtothe patient.Forphysicians,unauthorizeddisclosuresviolatethe HealthInsurancePortabilityandAccountabilityAct (HIPAA)andcanleadtodisciplinaryaction,lossof licensure,andlegalliability.OpenAI,thecreatorsof ChatGPT,havestatedthatdatausedwithChatGPTwill remainsecuredbydefault,withanopt-outoptiontoshare dataforresearchandqualityimprovement.Nevertheless, majorcorporationssuchasVerizonandJPMorgan&Co. haverestrictedemployeesfromaccessingChatGPTdueto concernsoverpossibledatabreaches.31 Sensitivehealthcare informationcouldbeatasimilarrisk.
WhilethepublicavailabilityoftheChatGPTapplication programminginterfacemakesiteasytointegrateinto websitesandapplications,italsoraisesconcernsaboutthe securityandprivacyofpatientinformation.Astheuseof artificialintelligence(AI)chatbotsbecomemorewidespread, itisincreasinglyimportanttoensurethatthesetechnologies areusedinawaythatprotectspatientprivacyandcomplies withregulationssuchasHIPAA.IntegratingChatGPTinto aHIPAA-compliantframeworkmayhelpaddressthese concerns.Healthcaretechnologyleadersmusttakenecessary measurestoprotectPHI.
IntegrationofChatGPTintoemergencymedicine presentsacomplexlandscapeofmedicolegalandethical implications.32 Wehavepreviouslydiscussedlimitations withthesoftware:potentialformisdiagnosisanddelayed treatmentisasignificantconcern.Artificialintelligence systems,whileadvanced,maynotalwaysaccurately interpretpatientsymptoms,whichisdependentuponthe qualityofuserinputandthesoftware’sunderstanding.This haspotentialtoinfluencepatientoutcomes,andthereare numeroussituationsthatcoulddothesame.
Considerthefollowinghypothetical,ethicalscenarios:
• ChatGPTrecommendsagainstseekingcare,which resultsinaharmfulorlife-threateningpatientoutcome.
• ChatGPTprovidesfalseinformationtoapatient.
• Patientsinadequatelyadvisedontherisks/benefitsof ChatGPTmisinterpretitsanalysis.
• PatientPHIisaccessedduringadatabreachorduring theperformanceimprovementprocess.
• ChatGPTprovidesinformationthatisnotuptodateor conflictswithcurrentguidelines.
Intheunfortunatecircumstancewhereoneormoreofthese eventsoccurandlegalactionistaken,whoshouldbeheld responsible OpenAI,clinicians,orboth?Thisisacurrent challengethatnecessitatesfurtherinterdisciplinarydiscussion betweenstakeholders.33 Nonetheless,therearestepsthatmust betakentohelpminimizeriskforallpartiesinvolved.For example,thereshouldberestrictionsplacedonLLMspriorto officialimplementationinthe field.Whetherthrough legislationoranindependentbody,ChatGPTmustadhereto regulatorystandardsthatensureHIPAA-complianceand informedconsent.34 PhysiciansandOpenAImustalsowork towardeducationonpotentialrisksofthesoftware.Physicians andotherhealthcareprofessionalsshouldalsoimplement legalformsandliabilitywaiversintothecareprocesstoensure protectionininstanceswheretheseregulationsfail.
Thenextmajorstepthatmustbetakenistovalidate ChatGPT’sefficacyandsafetyinclinicalsettings.32 Oneofthe majorbarriersthatresearchersmayfaceistheever-changing updatestothesoftware,whichisalsoalimitationofthispaper. NotonlyisChatGPTcontinuallybeingupdated,butthe protocolsbywhich fine-tuning,updates,andfurthertraining occurareconfidential.10 ThisinherentlymakesChatGPT difficulttostudy.However,potentialfuturestudieswith ChatGPTaremanyandshouldassesstheaccuracy,safety, readability,andsemanticanalysisofthesoftware.Onesuch futurestudycouldconsidertheefficacyofpatienttriagefor ChatGPTandtriagenursephonecalls.Futurestudiesshould alsoinvestigatethecostbenefitofimplementingsuchasystem intoEDworkflow,eitherfortriage,dischargeinstructions,or
both.Thisshouldbecorroboratedbyexaminingpotential algorithmbiasintherealworld.32,34,35
Asstatedpreviously,ChatGPTcannotreplaceaphysician. AlthoughOpenAIhasmadesignificantstridesindevelopinga softwarethatcommunicatesina morehuman-like,empathetic mannercomparedtopreviouschatbots,currenttechnology stilllackstheoversightandnuanceofferedbyahuman.This technologycannotreplaceanin-depthhistory,physicalexam, orclinicalreasoning.However,giventhecurrentrateof progressonthesetechnologies,itwouldbenaivetoconsidera futureindependentoftechnology-assistedpatientencounters. Forthisreason,physiciansandhealthcareprofessionalsmust beinvolvedinresearchanddevelopmentoversighttoensure accuratedataisavailableontheseplatforms,andthatthese technologiesarebeingdevelopedwiththerightintentions. PhysiciansshouldalsocontinuetobeinformedonAI developments,sothattheycanplayaproactiverolein educatingpatientsonthebenefits,limitations,andliabilityof thesoftware.Furtherstudiesmustalsoexaminethelegal implicationsforphysicians,patients,andOpenAI,as ChatGPTandhealthcarecontinuetointersect.
ThispaperdescribestheuseofChatGPTasan educationalresourceforpatientsseekingemergencymedical treatment.Althoughlimitationssuchastechnicalissues, misinformationrisk,lackofinputstandardization,and privacyconcernsexist,thissoftwareofferscompelling benefitsforpatienteducation.Thesoftwarecananswer questionsspecifictopatientsandtheirpresentations, allowingforapersonalizededucationalresource.ChatGPT canalsoclarifydischargeinstructions,helptriageurgentvs emergentconditions,anditcanrespondinmultiple languages.Physiciansmustunderstandthesebenefitsand limitationstobestguidepatientsandconductfurther researchinnewAItechnologies.
AddressforCorrespondence:FarisF.Halaseh,BS,Universityof California,IrvineSchoolofMedicine,1001HealthSciencesRd., Irvine,CA92617.Email: fhalaseh@hs.uci.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Halasehetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SonisJD,AaronsonEL,LeeRY,etal.Emergencydepartmentpatient experience:asystematicreviewoftheliterature. JPatientExp. 2018;5(2):101–6.
2.DeSaiC,JanowiakK,SecheliB,etal.Empoweringpatients:simplifying dischargeinstructions. BMJOpenQual. 2021;10(3):e001419.
3.SheikhH,BrezarA,DzwonekA,etal.Patientunderstandingof dischargeinstructionsintheemergencydepartment:dodifferent patientsneeddifferentapproaches? IntJEmergMed. 2018;11(1):5.
4.WeinickRM,BurnsRM,MehrotraA.Manyemergencydepartmentvisits couldbemanagedaturgentcarecentersandretailclinics. HealthAff (Millwood). 2010;29(9):1630–6.
5.CarrasquilloO,OravEJ,BrennanTA,etal.Impactoflanguagebarriers onpatientsatisfactioninanemergencydepartment. JGenInternMed. 1999;14(2):82–7.
6.KungTH,CheathamM,MedenillaA,etal.PerformanceofChatGPTon USMLE:potentialforAI-assistedmedicaleducationusinglarge languagemodels. PLOSDigitHealth. 2023;2(2):e0000198.
7.OpenAI.GPT-4isOpenAI’smostadvancedsystem,producingsafer andmoreusefulresponses.Availableat: https://openai.com/product/ gpt-4.AccessedonMay5,2023.
8.SallamM.ChatGPTutilityinhealthcareeducation,research,and practice:systematicreviewonthepromisingperspectivesandvalid concerns. Healthcare(Basel). 2023;11(6):887.
9.ScherrR,HalasehFF,SpinaA,etal.ChatGPTinteractivemedical simulationsforearlyclinicaleducation:casestudy. JMIRMedEduc. 2023;9:e49877.
10.ThirunavukarasuAJ,TingDSJ,ElangovanK,etal.Largelanguage modelsinmedicine. NatMed. 2023;29(8):1930–40.
11.KunitsuY.ThepotentialofGPT-4asasupporttoolforpharmacists: analyticalstudyusingtheJapanesenationalexaminationfor pharmacists. JMIRMedEduc. 2023;9:e48452.
12.HoriuchiD,TatekawaH,ShimonoT,etal.AccuracyofChatGPT generateddiagnosisfrompatient’smedicalhistoryandimaging findings inneuroradiologycases. Neuroradiology. 2024;66(1):73–9.
13.McCarthyDM,EngelKG,BuckleyBA,etal.Talk-timeinthe emergencydepartment:durationofpatient-providerconversations duringanemergencydepartmentvisit. JEmergMed. 2014;47(5):513–9.
14.EngelKG,BuckleyBA,ForthVE,etal.Patientunderstandingof emergencydepartmentdischargeinstructions:whereareknowledge deficitsgreatest? AcadEmergMed. 2012;19(9):e1035–44.
15.ZavalaSandShafferC.Dopatientsunderstanddischargeinstructions? JEmergNurs. 2011;37(2):138–40.
16.SuffolettoB,CalabriaJ,RossA,etal.Amobilephonetextmessage programtomeasureoralantibioticuseandprovidefeedbackon adherencetopatientsdischargedfromtheemergencydepartment. AcadEmergMed. 2012;19(8):949–58.
17.SuffolettoBandYealyDM.Thetroublewithmedicationadherenceafter emergencycare. AnnEmergMed. 2013;62(3):235–6.
18.vanLoon-vanGaalenM,vanderLindenMC,GusseklooJ,etal. Telephonefollow-uptoreduceunplannedhospitalreturnsforolder emergencydepartmentpatients:arandomizedtrial. JAmGeriatrSoc. 2021;69(11):3157–66.
19.CosterJE,TurnerJK,BradburyD,etal.Whydopeoplechoose emergencyandurgentcareservices?Arapidreviewutilizinga systematicliteraturesearchandnarrativesynthesis. AcadEmergMed. 2017;24(9):1137–49.
20.VogelJA,RisingKL,JonesJ,etal.Reasonspatientschoosethe emergencydepartmentoverprimarycare:aqualitativemetasynthesis. JGenInternMed. 2019;34(11):2610–9.
21.LaneBH,MallowPJ,HookerMB,etal.TrendsinUnitedStates emergencydepartmentvisitsandassociatedchargesfrom2010to 2016. AmJEmergMed. 2020;38(8):1576–81.
22.MorleyC,UnwinM,PetersonGM,etal.Emergencydepartment crowding:asystematicreviewofcauses,consequencesandsolutions. PLoSOne. 2018;13(8):e0203316.
23.AhnC.ExploringChatGPTforinformationofcardiopulmonary resuscitation. Resuscitation. 2023;185:109729.
24.KhoongEC,SteinbrookE,BrownC,etal.AssessingtheuseofGoogle TranslateforSpanishandChinesetranslationsofemergency departmentdischargeinstructions. JAMAInternMed. 2019;179(4):580–2.
25.TairaBR,KregerV,OrueA,etal.ApragmaticassessmentofGoogle Translateforemergencydepartmentinstructions. JGenInternMed. 2021;36(11):3361–5.
26.ScottKW,LiuA,ChenC,etal.HealthcarespendinginU.S.emergency departmentsbyhealthcondition,2006–2016. PLoSOne. 2021;16(10):e0258182.
27.TaecharungrojV. “WhatcanChatGPTdo?” Analyzingearlyreactionsto theinnovativeAIchatbotonTwitter. BigDataCognComput. 2023;7(1):35.
28.YeoYH,SamaanJS,NgWH,etal.Assessingtheperformanceof ChatGPTinansweringquestionsregardingcirrhosisandhepatocellular carcinoma. ClinMolHepatol. 2023;29(3):721–32.
29.AlkaissiHandMcFarlaneSI.ArtificialhallucinationsinChatGPT: implicationsinscientificwriting. Cureus. 2023;15(2):e35179.
30.GravelJ,D’Amours-GravelM,OsmanlliuE.Learningtofakeit:limited responsesandfabricatedreferencesprovidedbyChatGPTfor medicalquestions. MayoClinicProceedings:DigitalHealth. 2023;1(3):226–34.
31.LukpatA.JPMorganrestrictsemployeesfromusingChatGPTVerizon andotherorganizationshavealsoblockedaccesstothepopularAI chatbot.2023.Availableat: https://www.wsj.com/articles/jpmorganrestricts-employees-from-using-chatgpt-2da5dc34?mod= Searchresults_pos3&page=1.AccessedonMay5,2023.
32.ChenaisG,LagardeE,Gil-JardineC.Artificialintelligencein emergencymedicine:viewpointofcurrentapplicationsandforeseeable opportunitiesandchallenges. JMedInternetRes. 2023;25:e40031.
33.BakdashL,AbidA,GourisankarA,etal.ChattingbeyondChatGPT: advancingequitythroughAI-drivenlanguageinterpretation. JGenInternMed. 2024;39(3):492–5.
34.WangC,LiuS,YangH,etal.EthicalconsiderationsofusingChatGPTin healthcare. JMedInternetRes. 2023;25:e48009.
35.VenturaCAIandDentonEE.Artificialintelligencechatbotsand emergencymedicalservices:perspectivesontheimplicationsof generativeAIinprehospitalcare. OpenAccessEmergMed. 2023;15:289–92.
GillianCooper,BS§
VainaviGambhir‡
ZoeGasparotti,BSN∥
SamanthaCamp,BA§
WilliamGum,BS§ RobinsonOkolo,BS§ RiyaRaikar‡
ChadSchrier,MSN,RN¶ JessicaDowning,MD*†‡
QuincyK.Tran,MD,PhD*†‡
*UniversityofMarylandSchoolofMedicine,DepartmentofEmergencyMedicine, Baltimore,Maryland
† UniversityofMarylandSchoolofMedicine,TheRAdamsCowleyShockTrauma Center,Baltimore,Maryland
‡ UniversityofMarylandSchoolofMedicine,DepartmentofEmergencyMedicine, TheResearchAssociatePrograminEmergencyMedicineandCriticalCare, Baltimore,Maryland
§ UniversityofMarylandSchoolofMedicine,Baltimore,Maryland
∥ UniversityofMarylandMedicalCenter,TheCriticalCareResuscitationUnit, Baltimore,Maryland
¶ UniversityofMarylandMedicalCenter,DepartmentofStrokeNeurology, Baltimore,Maryland
SectionEditor:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedJanuary3,2024;RevisionreceivedMarch21,2024;AcceptedMarch25,2024 ElectronicallypublishedJune28,2024
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.18668
DearEditors:
Wereadwithgreatinterest, “AShorterDoor-in-Door-out TimeIsAssociatedwithImprovedOutcomeinLargeVessel OcclusionStroke,” bySigaletal.1 Firstly,wewouldliketo congratulatetheauthorsontheir WestJEM publicationthat highlightsimportantconceptsformanagementofpatients withischemicstrokefromlargevesselocclusion(LVOS)in theemergencydepartment(ED).However,wehadafew commentsregardingtheirconclusionsaboutdoor-in-doorout(DIDO)timeandstrokeoutcomes.Notably,thetitle statesthatshorterDIDOtimecorrelatestoimprovedstroke outcomes,buttheirmultivariablelogisticregressionanalysis demonstratedthatDIDOwasnotstatisticallysignificant (Table4,OR1.13,95%CI0.99–1.30).Whiletheunivariate analysissuggestedthatEDpatientswithgoodoutcomehad shortenedDIDO,thisconclusionshouldnotbemadewhen theirmultivariateregressionsuggestedotherwise.
Theauthors’ findingsanddiscussionalsosuggestthatED DIDOtimesarenotrelevanttostrokeoutcomes.Thisis controversialbecausetherewerealsoconflictingreportsfrom previousstudies.2,3 Inthispresentpaper,theauthorslooked atspecifictimeintervalsforDIDOthresholds(≤60minutes, >60minutes, ≤90minutes, >90minutes, ≤120minutes, >120minutes),whichtheyincludedintheirunivariate analysisbutnottheirmultivariablelogisticregression analysis.Bycategorizingcontinuousvariables,the authorsriskedlosingthegranularityofthevariablesand perhapsstatisticalpower;however,itisunknownwhether theseintervalswouldhaveshownsignificanceon multivariablelogisticregressionanalysis,asopposedto
assessingDIDOsolelyasacontinuousvariableinthe logisticregression.
Ontheotherhand,theauthorsreportedthatthey calculated90-daymodifiedRankinScale(mRS)viaelectronic healthrecords(EHR)andalsoretrospectivelycalculated 90-daymRSvaluesfor77(18%)oftheirpatients.However, retrospectivecalculationsofmRSareinherentlybiased,as clinicianstendtoscoreapatient’sdisabilityashigherthan whatwasexperiencedbythepatient,andtheirqualityoflife lower.4,5 Therefore,itispossiblethatoutcomemeasureswere moresubjectiveandcouldaffecttheauthors’ analyses.
Additionally,datafromourcomprehensivestrokecenter (CSC),forwhichpatientswithLVOSandthrombectomy undergoprospective90-daymRSassessmentaspartofthe clinicalcareforallstrokepatients,reportedthatdifferenttime intervalsareassociatedwithimprovedoutcomeforpatients withLVOS.Weanalyzedthedataof203patientswithLVOS whopresentedtoourCSCviaourcriticalcareresuscitationunit (CCRU)betweenJanuary2019–May2021forthrombectomy, usingamachinelearningalgorithm(classificationand regressiontree[CART]).TheCARTalgorithmusesrecursive partitioningtoidentifyimportantpredictorsandassignthese predictorswithrelativevariableimportance(RVI).Themost importantpredictorswouldbegivenaRVIof100%;other predictorswouldsubsequentlybeassignedRVIvaluesas percentageofthemostimportantfactor.
SimilarlytoSigaletal’sstudy,ouranalysisfoundthatwhile NationalInstitutesofHealthStrokeScaleandagewere significantfactorsassociatedwithpatientoutcomes (Appendix1),theEDDIDOtimewasalsoasignificantfactor
withaRVIof27.6%(Appendix1).Furthermore,theDIDO timeatourCSC’sresuscitationunitwasalsoanimportant factorwithaRVIof62.7%.Allthetimeintervalsinour analysiswereenteredintheCARTascontinuousvariables. Nevertheless,wehypothesizethatthelackofsignificancein theauthors’ multivariablelogisticregressionmaybebecause theirpatients’ 90-daymRSvalueswereobtainedviaEHR,in contrasttoourdata,whichresultedfromprospectively collected90-daymRSvalues.However,theresultthatthe CCRU’sDIDOwasasignificantfactorwithhigherRVI valuesthanEDDIDOforpatients’ outcomecouldalso provideanotherpossibleexplanationforthe findingsinSigal etalandSchevingetalthatEDDIDOmightnotbea significantfactor.ItcouldbethatwhatwasdelayedinED DIDOtimewaslatermadeupbytheteamsattheCSConce patientsweretransferredfromtheEDs.However,further studiesarenecessarytoconfirmorrefuteourobservation. Despiteourconcerns,wewholeheartedlyagreewiththe authorsthatcliniciansneedtoexpeditepatientswhohave LVOStoundergothrombectomy,regardlessofwherethey areduringthecriticaltimeperiod.
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2024Cooperetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
1.SigalA,IsenbergD,KraussC,etal.Ashorterdoor-in-door-outtimeis associatedwithimprovedoutcomeinlargevesselocclusionstroke. WestJEmergMed. 2023;24(5):931–938.
2.McTaggartRA,MoldovanK,OliverLA,etal.Door-in-door-outtimeat primarystrokecentersmaypredictoutcomeforemergentlargevessel occlusionpatients. Stroke. 2018;49(12):2969–74.
3.SchevingWL,FroehlerM,HartK,etal.Inter-facilitytransferforpatients withacutelargevesselocclusionstrokereceivingmechanical thrombectomy. AmJEmergMed. 2021;39:132–6.
AddressforCorrespondence:QuincyK.Tran,MD,PhD,University ofMarylandSchoolofMedicine,DepartmentofEmergency Medicine,22SouthGreeneSt.,SuiteT3N45,Baltimore,MD21201. Email: qtran@som.umaryland.edu
4.SucharewH,KleindorferD,KhouryJC,etal.Derivingplaceof residence,modifiedRankinscale,andEuroQol-5Dscoresfromthe medicalrecordforstrokesurvivors. CerebrovascDis. 2021;50(5):567–73.
5.QuinnTJ,RayG,AtulaS,etal.DerivingmodifiedRankinscoresfrom medicalcase-records. Stroke. 2008;39(12):3421–3.

