Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE
Health Equity
654 Addressing Emergency Department Care for Patients Experiencing Incarceration: A Narrative Review
Rachel E. Armstrong, Kristopher A. Hendershot, Naomi P. Newton, Patricia D. Panakos
662 A Virtual National Diversity Mentoring Initiative to Promote Inclusion in Emergency Medicine




Tatiana Carrillo, Lorena Martinez Rodriguez, Adaira Landry, Al’ai Alvarez, Alyssa Ceniza, Riane Gay, Andrea Green, Jessica Faiz
668 Skin Tone and Gender of High-Fidelity Simulation Manikins in Emergency Medicine Residency Training and their Use in Cultural Humility Training
Marie Anderson Wofford, Cortlyn Brown, Bernard Walston, Heidi Whiteside, Joseph Rigdon, Phil Turk
675 Social Determinants of Health Screening at an Urban Emergency Department Urgent Care During COVID-19

Haeyeon Hong, Kalpana Narayan Shankar, Andrew Thompson, Pablo Buitron De La Vega, Rashmi Koul, Emily C. Cleveland Manchanda, Sorraya Jaiprasert, Samantha Roberts, Tyler Pina, Emily Anderson, Jessica Lin, Gabrielle A. Jacquet
680 A National Snapshot of Social Determinants of Health Documentation in Emergency Departments
Caitlin R. Ryus, Alexander T. Janke, Rachel L. Granovsky, Michael A. Granovsky
ED Operations
685 A Real-World Experience: Retrospective Review of Point-of-Care Ultrasound Utilization and Quality in Community Emergency Departments
Courtney M. Smalley, Erin L. Simon, McKinsey R. Muir, Baruch S. Fertel
693 Applying a Smartwatch to Predict Work-related Fatigue for Emergency Healthcare Professionals: Machine Learning Method
Sot Shih-Hung Liu, Cheng-Jiun Ma, Fan-Ya Chou, Michelle Yuan-Chiao Cheng, Chih-Hung Wang, Chu-Lin Tsai, Wei-Jou Duh, Chien-Hua Huang, Feipei Lai, Tsung-Chien Lu
Contents continued on page iii
Volume 24, Number 4, July 2023 Open Access at WestJEM.com ISSN 1936-900X A Peer-Reviewed, International Professional Journal Western Journal of Emergency Medicine VOLUME 24, NUMBER 4, July 2023 PAGES 654-872
West
Andrew W. Phillips, MD, Associate Editor DHR Health-Edinburg, Texas
Edward Michelson, MD, Associate Editor Texas Tech University- El Paso, Texas
Dan Mayer, MD, Associate Editor Retired from Albany Medical College- Niskayuna, New York
Wendy Macias-Konstantopoulos, MD, MPH, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Gayle Galletta, MD, Associate Editor University of Massachusetts Medical SchoolWorcester, Massachusetts
Yanina Purim-Shem-Tov, MD, MS, Associate Editor Rush University Medical Center-Chicago, Illinois
Resident Editors
AAEM/RSA
John J. Campo, MD Harbor-University of California, Los Angeles Medical Center
Tehreem Rehman, MD
Advocate Christ Medical Center
ACOEP
Justina Truong, DO
Kingman Regional Medical Center
Section Editors
Behavioral Emergencies
Leslie Zun, MD, MBA Chicago Medical School
Marc L. Martel, MD
Hennepin County Medical Center
Cardiac Care
Fred A. Severyn, MD
University of Colorado School of Medicine
Sam S. Torbati, MD
Cedars-Sinai Medical Center
Clinical Practice
Cortlyn W. Brown, MD Carolinas Medical Center
Casey Clements, MD, PhD Mayo Clinic
Patrick Meloy, MD
Emory University
Nicholas Pettit, DO, PhD
Indiana University
David Thompson, MD University of California, San Francisco
Kenneth S. Whitlow, DO
Kaweah Delta Medical Center
Critical Care
Christopher “Kit” Tainter, MD
University of California, San Diego
Gabriel Wardi, MD
University of California, San Diego
Joseph Shiber, MD
University of Florida-College of Medicine
Matt Prekker MD, MPH
Hennepin County Medical Center
David Page, MD
University of Alabama
Erik Melnychuk, MD
Geisinger Health
Quincy Tran, MD, PhD
University of Maryland
Mark I. Langdorf, MD, MHPE, Editor-in-Chief University of California, Irvine School of MedicineIrvine, California
Shahram Lotfipour, MD, MPH, Managing Editor University of California, Irvine School of MedicineIrvine, California
Michael Gottlieb, MD, Associate Editor Rush Medical Center-Chicago, Illinois
Niels K. Rathlev, MD, Associate Editor Tufts University School of Medicine-Boston, Massachusetts
Rick A. McPheeters, DO, Associate Editor Kern Medical- Bakersfield, California
Gentry Wilkerson, MD, Associate Editor University of Maryland
Disaster Medicine
John Broach, MD, MPH, MBA, FACEP
University of Massachusetts Medical School UMass Memorial Medical Center
Christopher Kang, MD Madigan Army Medical Center
Education
Danya Khoujah, MBBS
University of Maryland School of Medicine
Jeffrey Druck, MD University of Colorado
John Burkhardt, MD, MA University of Michigan Medical School
Michael Epter, DO Maricopa Medical Center
ED Administration, Quality, Safety
David C. Lee, MD Northshore University Hospital
Gary Johnson, MD Upstate Medical University
Brian J. Yun, MD, MBA, MPH
Harvard Medical School
Laura Walker, MD Mayo Clinic
León D. Sánchez, MD, MPH Beth Israel Deaconess Medical Center
William Fernandez, MD, MPH
University of Texas Health-San Antonio
Robert Derlet, MD
Founding Editor, California Journal of Emergency Medicine
University of California, Davis
Emergency Medical Services
Daniel Joseph, MD
Yale University
Joshua B. Gaither, MD
University of Arizona, Tuscon
Julian Mapp
University of Texas, San Antonio
Shira A. Schlesinger, MD, MPH
Harbor-UCLA Medical Center
Geriatrics
Cameron Gettel, MD Yale School of Medicine
Stephen Meldon, MD Cleveland Clinic
Luna Ragsdale, MD, MPH
Duke University
Health Equity
Emily C. Manchanda, MD, MPH
Boston University School of Medicine
Shadi Lahham, MD, MS, Deputy Editor Kaiser Permanente- Irvine, California
Susan R. Wilcox, MD, Associate Editor Massachusetts General Hospital- Boston, Massachusetts
Elizabeth Burner, MD, MPH, Associate Editor University of Southern California- Los Angeles, California
Patrick Joseph Maher, MD, MS, Associate Editor Ichan School of Medicine at Mount Sinai- New York, New York
Donna Mendez, MD, EdD, Associate Editor University of Texas-Houston/McGovern Medical School- Houston Texas
Danya Khoujah, MBBS, Associate Editor
University of Maryland School of Medicine- Baltimore, Maryland
Faith Quenzer Temecula Valley Hospital
San Ysidro Health Center
Mandy J. Hill, DrPH, MPH
UT Health McGovern Medical School
Payal Modi, MD MScPH
University of Massachusetts Medical
Infectious Disease
Elissa Schechter-Perkins, MD, MPH
Boston University School of Medicine
Ioannis Koutroulis, MD, MBA, PhD
George Washington University School of Medicine and Health Sciences
Kevin Lunney, MD, MHS, PhD
University of Maryland School of Medicine
Stephen Liang, MD, MPHS
Washington University School of Medicine
Victor Cisneros, MD, MPH
Eisenhower Medical Center
Injury Prevention
Mark Faul, PhD, MA
Centers for Disease Control and Prevention
Wirachin Hoonpongsimanont, MD, MSBATS
Eisenhower Medical Center
International Medicine
Heather A.. Brown, MD, MPH
Prisma Health Richland
Taylor Burkholder, MD, MPH
Keck School of Medicine of USC
Christopher Greene, MD, MPH
University of Alabama
Chris Mills, MD, MPH
Santa Clara Valley Medical Center
Shada Rouhani, MD
Brigham and Women’s Hospital
Legal Medicine
Melanie S. Heniff, MD, JD
Indiana University School of Medicine
Greg P. Moore, MD, JD
Madigan Army Medical Center
Statistics and Methodology
Shu B. Chan MD, MS Resurrection Medical Center
Stormy M. Morales Monks, PhD, MPH Texas Tech Health Science University
Soheil Saadat, MD, MPH, PhD University of California, Irvine
James A. Meltzer, MD, MS
Albert Einstein College of Medicine
Musculoskeletal
Juan F. Acosta DO, MS Pacific Northwest University
Rick Lucarelli, MD
Medical City Dallas Hospital
William D. Whetstone, MD
University of California, San Francisco
Neurosciences
Antonio Siniscalchi, MD
Annunziata Hospital, Cosenza, Italy
Pediatric Emergency Medicine
Paul Walsh, MD, MSc
University of California, Davis
Muhammad Waseem, MD
Lincoln Medical & Mental Health Center
Cristina M. Zeretzke-Bien, MD University of Florida
Public Health
Jacob Manteuffel, MD
Henry Ford Hospital
John Ashurst, DO
Lehigh Valley Health Network

Tony Zitek, MD
Kendall Regional Medical Center
Trevor Mills, MD, MPH
Northern California VA Health Care
Erik S. Anderson, MD
Alameda Health System-Highland Hospital
Technology in Emergency Medicine
Nikhil Goyal, MD
Henry Ford Hospital
Phillips Perera, MD
Stanford University Medical Center
Trauma
Pierre Borczuk, MD
Massachusetts General Hospital/Havard Medical School
Toxicology
Brandon Wills, DO, MS
Virginia Commonwealth University
Jeffrey R. Suchard, MD University of California, Irvine
Ultrasound
J. Matthew Fields, MD
Thomas Jefferson University
Shane Summers, MD
Brooke Army Medical Center
Robert R. Ehrman
Wayne State University
Ryan C. Gibbons, MD
Temple Health
Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine



Volume 24, No. 4: July 2023 i Western Journal of Emergency Medicine Available in MEDLINE, PubMed, PubMed Central, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org
Medicine
Emergency
Population Health Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Western Journal of Emergency
: Integrating
Care with
Western
Amin A. Kazzi, MD, MAAEM The American University of Beirut, Beirut, Lebanon
Anwar Al-Awadhi, MD
Mubarak Al-Kabeer Hospital, Jabriya, Kuwait
Arif A. Cevik, MD United Arab Emirates University College of Medicine and Health Sciences, Al Ain, United Arab Emirates
Abhinandan A.Desai, MD University of Bombay Grant Medical College, Bombay, India
Bandr Mzahim, MD King Fahad Medical City, Riyadh, Saudi Arabia
Brent King, MD, MMM University of Texas, Houston
Christopher E. San Miguel, MD Ohio State University Wexner Medical Center
Daniel J. Dire, MD University of Texas Health Sciences Center San Antonio
David F.M. Brown, MD Massachusetts General Hospital/ Harvard Medical School
Douglas Ander, MD Emory University
Editorial Board
Edward Michelson, MD Texas Tech University
Edward Panacek, MD, MPH University of South Alabama
Francesco Della Corte, MD
Azienda Ospedaliera Universitaria
“Maggiore della Carità,” Novara, Italy
Francis Counselman, MD Eastern Virginia Medical School
Gayle Galleta, MD
Sørlandet Sykehus HF, Akershus Universitetssykehus, Lorenskog, Norway
Hjalti Björnsson, MD Icelandic Society of Emergency Medicine
Jacob (Kobi) Peleg, PhD, MPH Tel-Aviv University, Tel-Aviv, Israel
Jaqueline Le, MD Desert Regional Medical Center
Jeffrey Love, MD The George Washington University School of Medicine and Health Sciences
Jonathan Olshaker, MD Boston University
Katsuhiro Kanemaru, MD University of Miyazaki Hospital, Miyazaki, Japan
Kenneth V. Iserson, MD, MBA University of Arizona, Tucson
Khrongwong Musikatavorn, MD King Chulalongkorn Memorial Hospital, Chulalongkorn University, Bangkok, Thailand
Leslie Zun, MD, MBA Chicago Medical School
Linda S. Murphy, MLIS University of California, Irvine School of Medicine Librarian
Nadeem Qureshi, MD St. Louis University, USA Emirates Society of Emergency Medicine, United Arab Emirates
Niels K. Rathlev, MD Tufts University School of Medicine
Pablo Aguilera Fuenzalida, MD Pontificia Universidad Catolica de Chile, Región Metropolitana, Chile
Peter A. Bell, DO, MBA Baptist Health Sciences University
Peter Sokolove, MD University of California, San Francisco
Rachel A. Lindor, MD, JD Mayo Clinic
Robert M. Rodriguez, MD University of California, San Francisco
Robert Suter, DO, MHA UT Southwestern Medical Center
Robert W. Derlet, MD University of California, Davis
Rosidah Ibrahim, MD Hospital Serdang, Selangor, Malaysia
Samuel J. Stratton, MD, MPH Orange County, CA, EMS Agency
Scott Rudkin, MD, MBA University of California, Irvine

Scott Zeller, MD University of California, Riverside
Steven H. Lim, MD Changi General Hospital, Simei, Singapore
Terry Mulligan, DO, MPH, FIFEM
ACEP Ambassador to the Netherlands Society of Emergency Physicians
Vijay Gautam, MBBS University of London, London, England
Wirachin Hoonpongsimanont, MD, MSBATS
Siriraj Hospital, Mahidol University, Bangkok, Thailand
Editorial Staff Advisory Board
Elena Lopez-Gusman, JD California ACEP American College of Emergency Physicians

Jennifer Kanapicki Comer, MD FAAEM California Chapter Division of AAEM Stanford University School of Medicine
DeAnna McNett, CAE American College of Osteopathic Emergency Physicians

Kimberly Ang, MBA UC Irvine Health School of Medicine
Randall J. Young, MD, MMM, FACEP California ACEP American College of Emergency Physicians Kaiser Permanente
Mark I. Langdorf, MD, MHPE, MAAEM, FACEP UC Irvine Health School of Medicine
Robert Suter, DO, MHA American College of Osteopathic Emergency Physicians UT Southwestern Medical Center

Shahram Lotfipour, MD, MPH FAAEM, FACEP UC Irvine Health School of Medicine
Jorge Fernandez, MD, FACEP UC San Diego Health School of Medicine
Isabelle Nepomuceno, BS Executive Editorial Director
Visha Bajaria, BS WestJEM Editorial Director
Emily Kane, MA WestJEM Editorial Director
Stephanie Burmeister, MLIS WestJEM Staff Liaison
Cassandra Saucedo, MS Executive Publishing Director
Nicole Valenzi, BA WestJEM Publishing Director
June Casey, BA Copy Editor
Western Journal of Emergency Medicine ii Volume 24, No. 4: July 2023 Available in MEDLINE, PubMed, PubMed Central, Europe PubMed Central, PubMed Central Canada, CINAHL, SCOPUS, Google Scholar, eScholarship, Melvyl, DOAJ, EBSCO, EMBASE, Medscape, HINARI, and MDLinx Emergency Med. Members of OASPA. Editorial and Publishing Office: WestJEM/Depatment of Emergency Medicine, UC Irvine Health, 3800 W. Chapman Ave. Suite 3200, Orange, CA 92868, USA Office: 1-714-456-6389; Email: Editor@westjem.org Official Journal of the California Chapter of the American College of Emergency Physicians, the America College of Osteopathic Emergency Physicians, and the California Chapter of the American Academy of Emergency Medicine
Integrating Emergency Care with Population Health Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Journal of Emergency Medicine:
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
JOURNAL FOCUS
Emergency medicine is a specialty which closely reflects societal challenges and consequences of public policy decisions. The emergency department specifically deals with social injustice, health and economic disparities, violence, substance abuse, and disaster preparedness and response. This journal focuses on how emergency care affects the health of the community and population, and conversely, how these societal challenges affect the composition of the patient population who seek care in the emergency department. The development of better systems to provide emergency care, including technology solutions, is critical to enhancing population health.
Table of Contents
703 Impact of Care Initiation Model on Emergency Department Orders and Operational Metrics: Cohort Study
Andy Hung-Yi Lee, Rebecca E. Cash, Alice Bukhman, Dana Im, Damarcus Baymon, Leon D Sanchez, Paul C. Chen
Behavioral Health
710 Disparities in Emergency Department Naloxone and Buprenorphine Initiation
Joan Papp, Charles Louis Emerman
717 Flow through the Emergency Department for Patients Presenting with Substance Use Disorder in Alberta, Canada
Jonah Edmundson, Kevin Skoblenick, Rhonda J. Rosychuk
Education
728 Perception of Quiet Students in Emergency Medicine: An Exploration of Narratives in the Standardized Letter of Evaluation
John K. Quinn, Jillian Mongelluzzo, Alyssa Nip, Joe Graterol, Esther H. Chen
732 Impact of Faculty Incentivization on Resident Evaluations
Viral Patel, Alexandra Nordberg, Richard Church, Jennifer L. Carey
Health Outcomes
737 Single-step Optimization in Triaging Large Vessel Occlusion Strokes: Identifying Factors to Improve Door-to-groin Time for Endovascular Therapy
Joshua Rawson, Ashley Petrone, Amelia Adcock
743
Violence and Abuse: A Pandemic Within a Pandemic
Paula J. Whiteman, Wendy L. Macias-Konstantopoulos, Pryanka Relan, Anita Knopov, Megan L. Ranney, Ralph J. Riviello
Critical Care
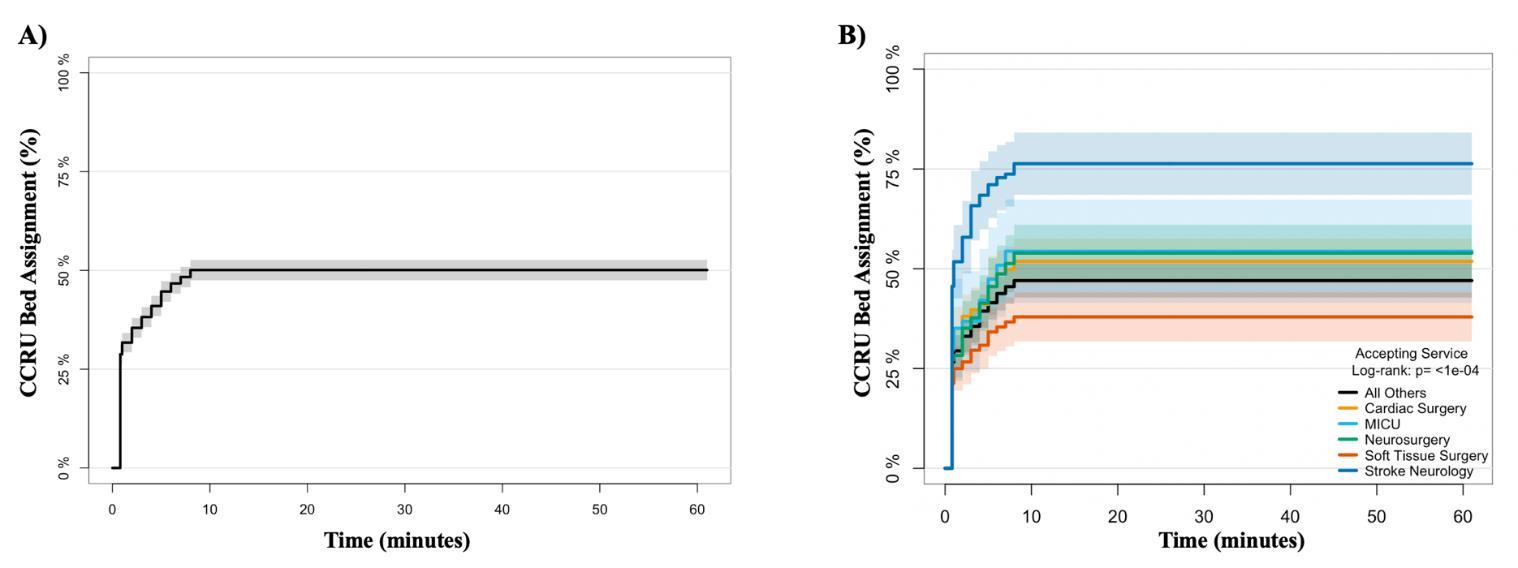
751 Examining Predictors of Early Admission and Transfer to the Critical Care Resuscitation Unit
Quincy K. Tran, Daniel Najafali, Tiffany Cao, Megan Najafali, Nelson Chen, Iana Sahadzic, Ikram Afridi, Ann Matta, William Teeter, Daniel J. Haase
763 Arterial Monitoring in Hypertensive Emergencies: Significance for the Critical Care Resuscitation Unit
Quincy K. Tran, Dominique Gelmann, Manahel Zahid, Jamie Palmer, Grace Hollis, Emily Engelbrecht-Wiggans, Zain Alam, Ann Elizabeth Matta, Emily Hart, Daniel J. Haase
Technology
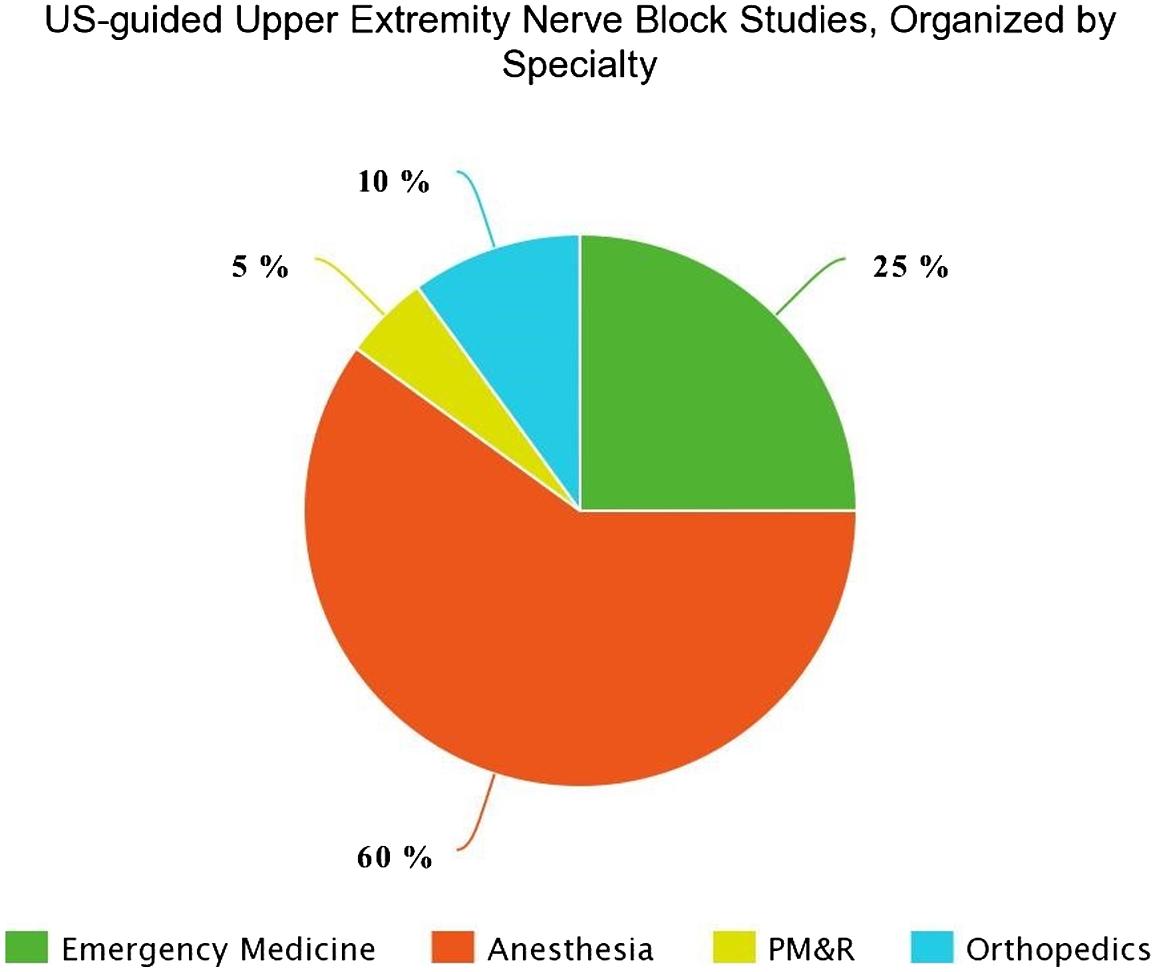
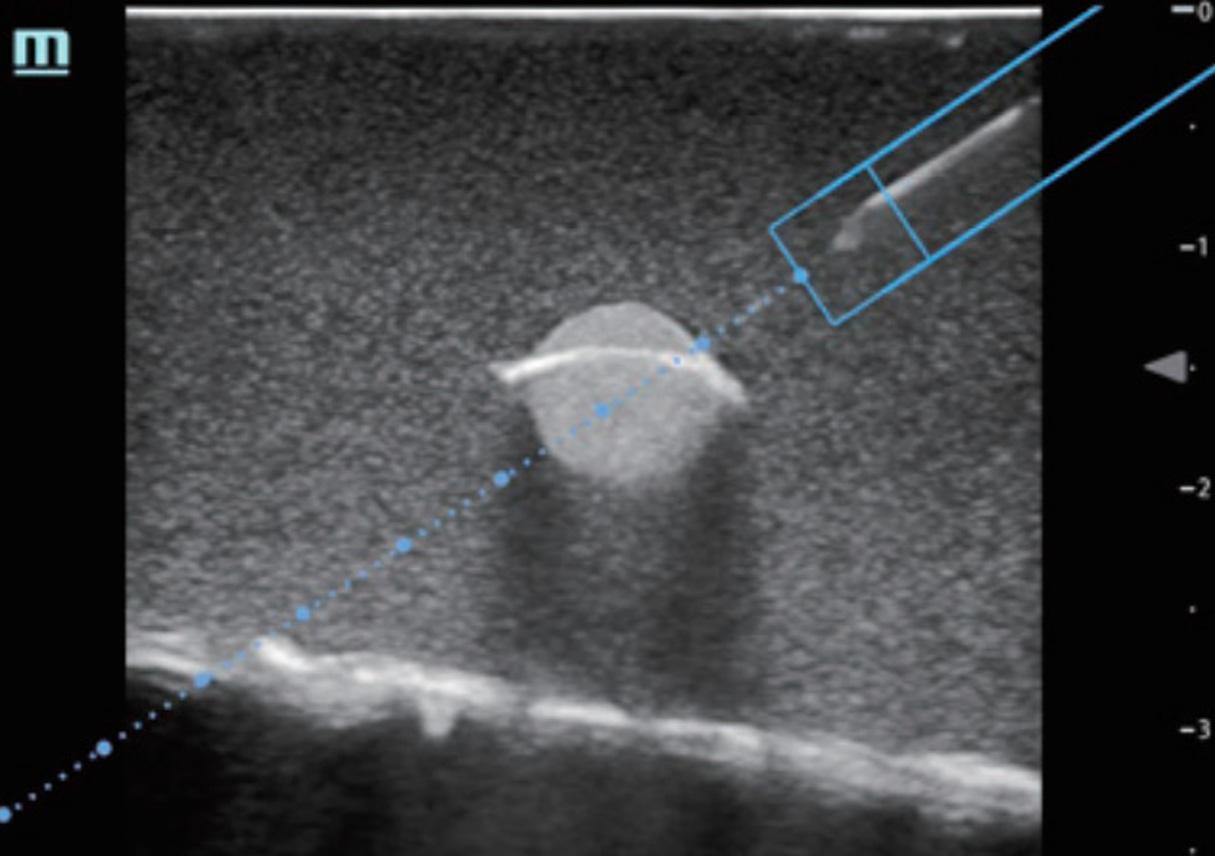
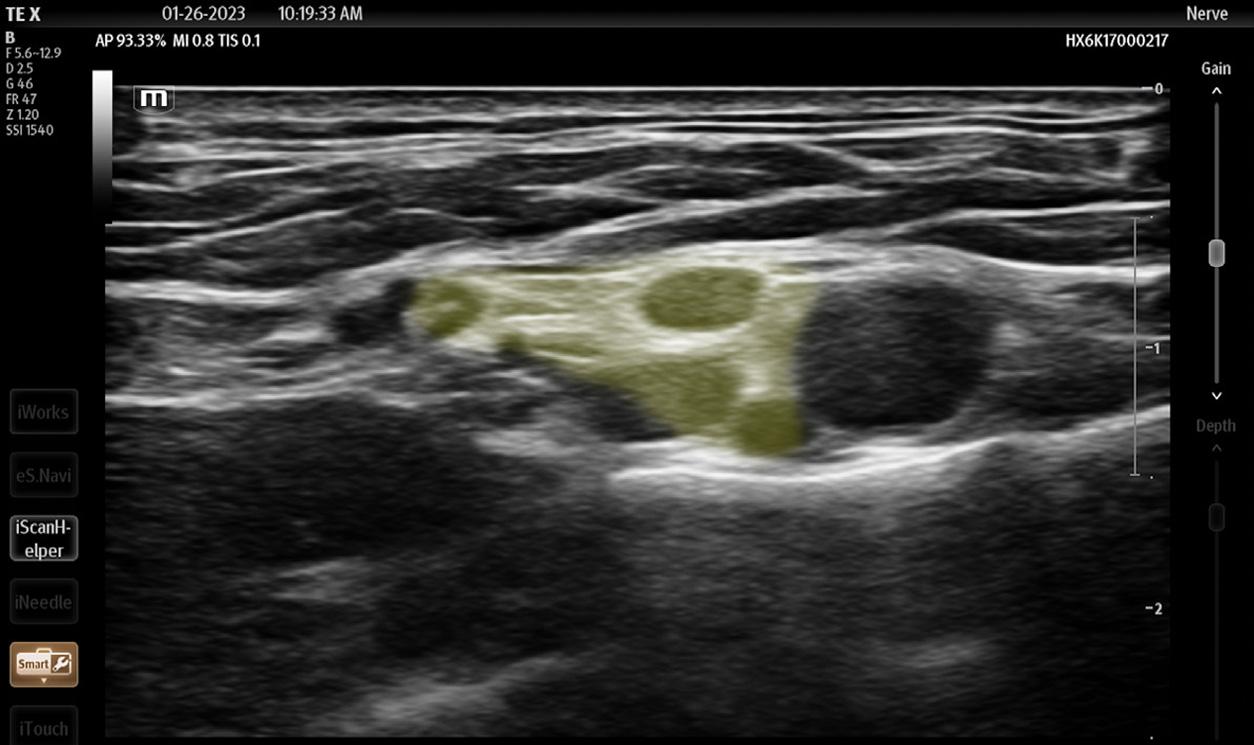
774 Block Time: A Multispecialty Systematic Review of Efficacy and Safety of Ultrasound-guided Upper Extremity Nerve Blocks
Campbell Belisle Haley, Andrew R. Beauchesne, John Christian Fox, Ariana M. Nelson
Policies for peer review, author instructions, conflicts of interest and human and animal subjects protections can be found online at www.westjem.com.
Emergency
Volume 24, No. 4: July 2023 iii Western Journal of
Medicine
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate Web of Science, Science Citation Index Expanded
Table of Contents continued
Prehospital Care
786 Community Paramedicine Intervention Reduces Hospital Readmission and Emergency Department Utilization for Patients with Cardiopulmonary Conditions
Aaron Burnett, Sandi Wewerka, Paula Miller, Ann Majerus, John Clark, Landon Crippes, Tia Radant
Clinical Practice
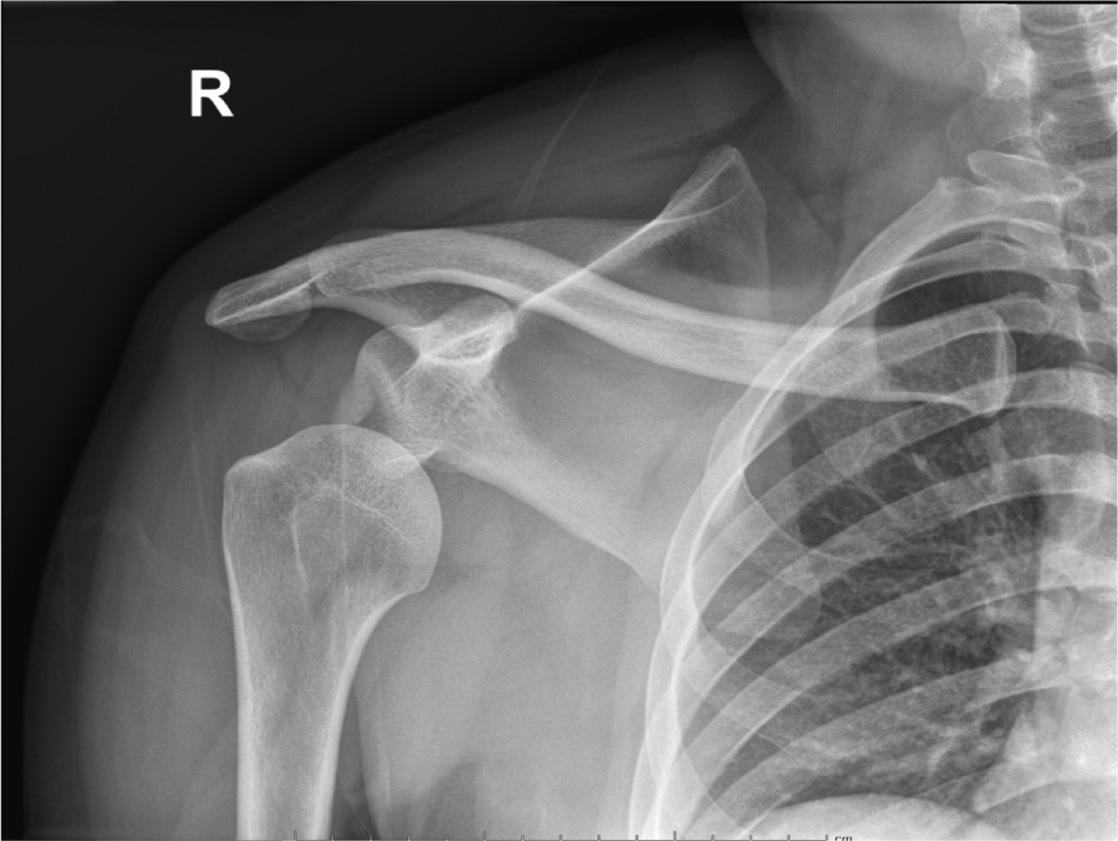
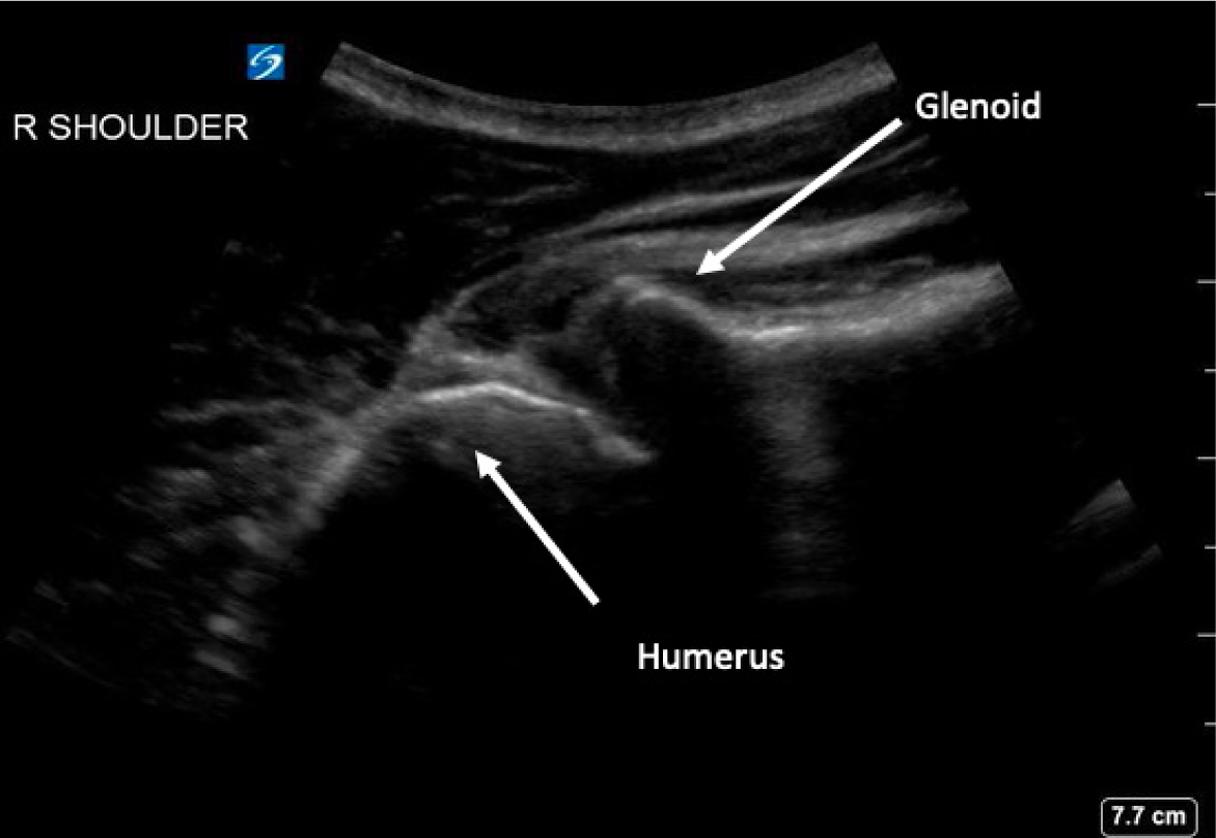
793 Utility of Supraclavicular Brachial Plexus Block for Anterior Shoulder Dislocation: Could It Be Useful?
Michael Shalaby, Melissa Smith, Lam Tran, Robert Farrow
Trauma
798 Haboob Dust Storms and Motor Vehicle Collision-related Trauma in Phoenix, Arizona
Michael B. Henry, Michael Mozer, Jerome J. Rogich, Kyle Farrell, Jonathan W. Sachs, Jordan Selzer, Vatsal Chikani, Gail Bradley, Geoff Comp
Emergency Medical Services
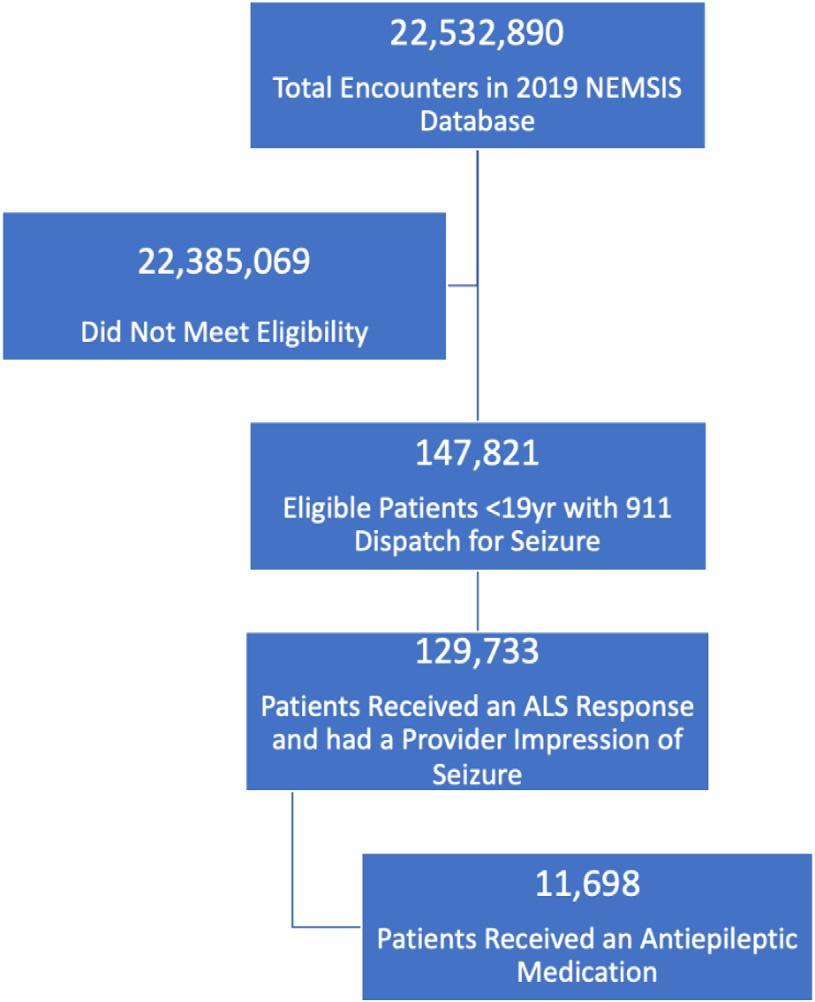
805 National Variation in EMS Response and Antiepileptic Medication Administration for Children with Seizures in the Prehospital Setting
Maytal T. Firnberg, E. Brooke Lerner, Nan Nan, Chang-Xing Ma, Manish I. Shah, N.Clay Mann, Peter S. Dayan
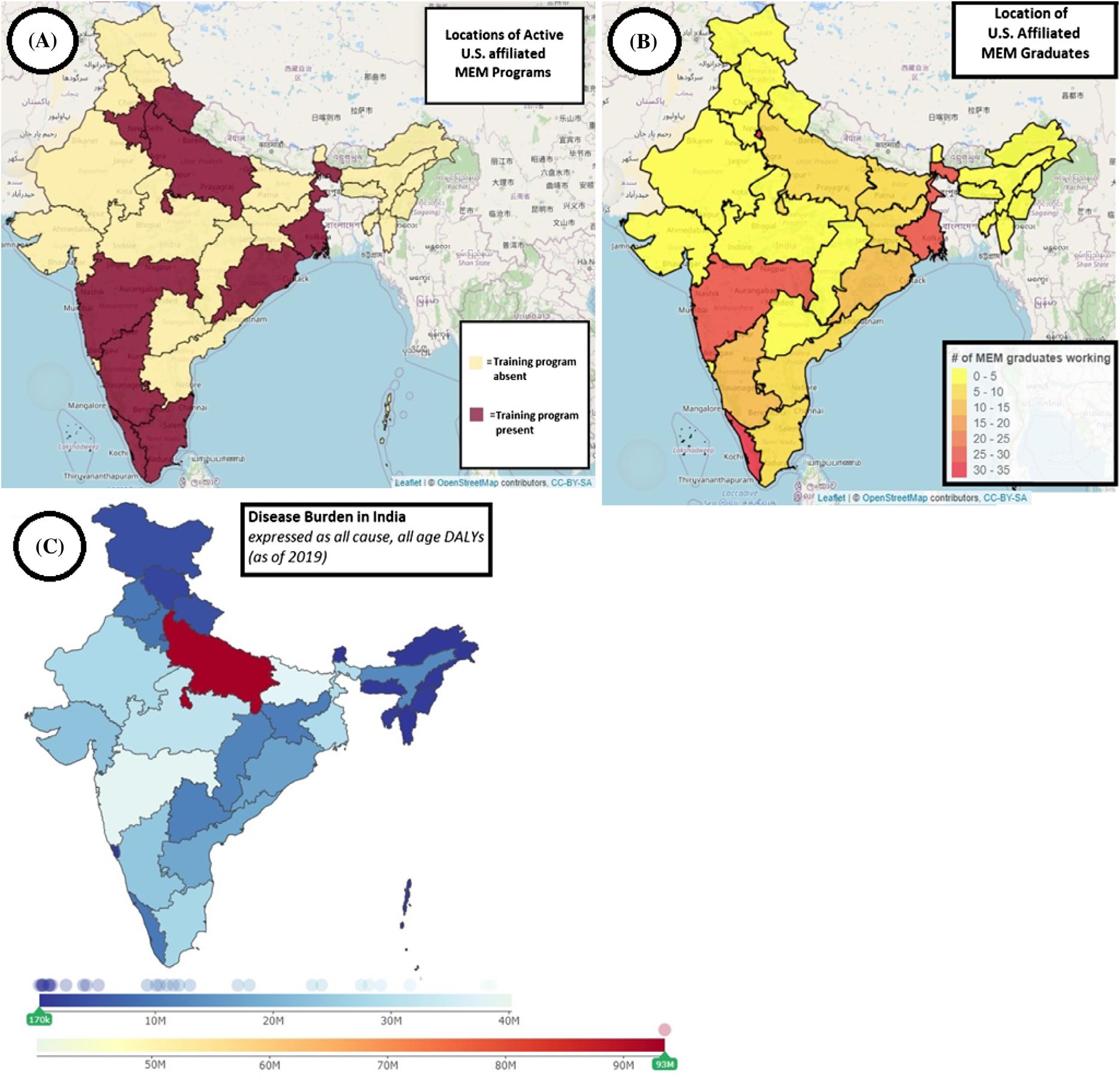
International Emergency Medicine
814 Contribution of 15 Years (2007–2022) of Indo-US Training Partnerships to the Emergency Physician Workforce Capacity in India
Joseph D. Ciano, Katherine Douglass, Kevin J. Davey, Shweta Gidwani, Ankur Verma, Sanjay Jaiswal, John Acerra
Western Journal of Emergency Medicine iv Volume 24, No. 4: July 2023
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
Indexed in MEDLINE, PubMed, and Clarivate
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber
Albany Medical College
Albany, NY
Allegheny Health Network
Pittsburgh, PA
American University of Beirut
Beirut, Lebanon
AMITA Health Resurrection Medical Center
Chicago, IL
Arrowhead Regional Medical Center
Colton, CA
Baylor College of Medicine
Houston, TX
Baystate Medical Center Springfield, MA
Bellevue Hospital Center New York, NY
Beth Israel Deaconess Medical Center
Boston, MA
Boston Medical Center
Boston, MA
Brigham and Women’s Hospital
Boston, MA
Brown University Providence, RI
Carl R. Darnall Army Medical Center Fort Hood, TX
Cleveland Clinic Cleveland, OH
Columbia University Vagelos New York, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
Conemaugh Memorial Medical Center Johnstown, PA
Crozer-Chester Medical Center Upland, PA
Desert Regional Medical Center Palm Springs, CA
Detroit Medical Center/ Wayne State University Detroit, MI
Eastern Virginia Medical School Norfolk, VA
Einstein Healthcare Network Philadelphia, PA
Eisenhower Medical Center Rancho Mirage, CA
Emory University Atlanta, GA
Franciscan Health Carmel, IN
Geisinger Medical Center Danville, PA
Grand State Medical Center Allendale, MI
Healthpartners Institute/ Regions Hospital Minneapolis, MN
Hennepin County Medical Center Minneapolis, MN
Henry Ford Medical Center Detroit, MI
Henry Ford Wyandotte Hospital Wyandotte, MI
California Chapter Division of American Academy of Emergency Medicine
Mediterranean Academy of Emergency Medicine
INTEGRIS Health
Oklahoma City, OK
Kaiser Permenante Medical Center
San Diego, CA
Kaweah Delta Health Care District
Visalia, CA
Kennedy University Hospitals
Turnersville, NJ
Kent Hospital
Warwick, RI
Kern Medical
Bakersfield, CA
Lakeland HealthCare
St. Joseph, MI
Lehigh Valley Hospital and Health Network
Allentown, PA
Loma Linda University Medical Center
Loma Linda, CA
Louisiana State University Health Sciences Center
New Orleans, LA
Louisiana State University Shreveport
Shereveport, LA
Madigan Army Medical Center
Tacoma, WA
Maimonides Medical Center
Brooklyn, NY
Maine Medical Center
Portland, ME
Massachusetts General Hospital/Brigham and Women’s Hospital/ Harvard Medical
Boston, MA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine
Sociedad Argentina de Emergencias
Mayo Clinic
Jacksonville, FL
Mayo Clinic College of Medicine
Rochester, MN
Mercy Health - Hackley Campus
Muskegon, MI
Merit Health Wesley
Hattiesburg, MS
Midwestern University
Glendale, AZ
Mount Sinai School of Medicine New York, NY
New York University Langone Health
New York, NY
North Shore University Hospital
Manhasset, NY
Northwestern Medical Group
Chicago, IL
NYC Health and Hospitals/ Jacobi New York, NY
Ohio State University Medical Center
Columbus, OH
Ohio Valley Medical Center
Wheeling, WV
Oregon Health and Science University
Portland, OR
Penn State Milton S. Hershey Medical Center
Hershey, PA
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
Sociedad Chileno Medicina Urgencia
Thai Association for Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Volume 24, No. 4: July 2023 v Western Journal of
Medicine
Emergency
Web
Index
of Science, Science Citation
Expanded
Indexed
Western Journal of Emergency Medicine:
Integrating Emergency Care with Population Health
This open access publication would not be possible without the generous and continual financial support of our society sponsors, department and chapter subscribers.
Professional Society Sponsors
American College of Osteopathic Emergency Physicians
California American College of Emergency Physicians
Academic Department of Emergency Medicine Subscriber
Prisma Health/ University of South Carolina SOM Greenville Greenville, SC
Regions Hospital Emergency Medicine Residency Program
St. Paul, MN
Rhode Island Hospital
Providence, RI
Robert Wood Johnson University Hospital
New Brunswick, NJ
Rush University Medical Center
Chicago, IL
St. Luke’s University Health Network
Bethlehem, PA
Spectrum Health Lakeland
St. Joseph, MI
Stanford Stanford, CA
SUNY Upstate Medical University
Syracuse, NY
Temple University
Philadelphia, PA
Texas Tech University Health Sciences Center
El Paso, TX
The MetroHealth System/ Case Western Reserve University
Cleveland, OH
UMass Chan Medical School
Worcester, MA
University at Buffalo Program Buffalo, NY
State Chapter Subscriber
Arizona Chapter Division of the American Academy of Emergency Medicine
California Chapter Division of the American Academy of Emergency Medicine
Florida Chapter Division of the American Academy of Emergency Medicine
International Society Partners
Emergency Medicine Association of Turkey
Lebanese Academy of Emergency Medicine
University of Alabama Medical Center Northport, AL
University of Alabama, Birmingham
Birmingham, AL
University of Arizona College of Medicine-Tucson
Tucson, AZ
University of California, Davis Medical Center
Sacramento, CA
University of California, Irvine
Orange, CA
University of California, Los Angeles Los Angeles, CA
University of California, San Diego
La Jolla, CA
University of California, San Francisco San Francisco, CA
UCSF Fresno Center
Fresno, CA
University of Chicago Chicago, IL
University of Cincinnati Medical Center/ College of Medicine Cincinnati, OH
University of Colorado Denver Denver, CO
University of Florida
Gainesville, FL
University of Florida, Jacksonville Jacksonville, FL
California Chapter Division of American Academy of Emergency Medicine
University of Illinois at Chicago
Chicago, IL
University of Iowa
Iowa City, IA
University of Louisville
Louisville, KY
University of Maryland
Baltimore, MD
University of Massachusetts
Amherst, MA
University of Michigan
Ann Arbor, MI
University of Missouri, Columbia
Columbia, MO
University of North Dakota School of Medicine and Health Sciences
Grand Forks, ND
University of Nebraska Medical Center
Omaha, NE
University of Nevada, Las Vegas
Las Vegas, NV
University of Southern Alabama
Mobile, AL
University of Southern California
Los Angeles, CA
University of Tennessee, Memphis Memphis, TN
University of Texas, Houston Houston, TX
University of Washington
Seattle, WA
Great Lakes Chapter Division of the American Academy of Emergency Medicine
Tennessee Chapter Division of the American Academy of Emergency Medicine
Norwegian Society for Emergency Medicine
Sociedad Argentina de Emergencias
University of WashingtonHarborview Medical Center
Seattle, WA
University of Wisconsin Hospitals and Clinics
Madison, WI
UT Southwestern Dallas, TX
Valleywise Health Medical Center
Phoenix, AZ
Virginia Commonwealth University Medical Center Richmond, VA
Wake Forest University
Winston-Salem, NC
Wake Technical Community College
Raleigh, NC
Wayne State
Detroit, MI
Wright State University
Dayton, OH
Yale School of Medicine
New Haven, CT
Uniformed Services Chapter Division of the American Academy of Emergency Medicine
Virginia Chapter Division of the American Academy of Emergency Medicine
Sociedad Chileno Medicina Urgencia
Thai Association for Emergency Medicine
Mediterranean Academy of Emergency Medicine
To become a WestJEM departmental sponsor, waive article processing fee, receive electronic copies for all faculty and residents, and free CME and faculty/fellow position advertisement space, please go to http://westjem.com/subscribe or contact:
Stephanie Burmeister
WestJEM Staff Liaison
Phone: 1-800-884-2236
Email: sales@westjem.org
Western Journal of Emergency Medicine vi Volume 24, No. 4: July 2023
in MEDLINE,
and Clarivate Web of Science, Science Citation Index Expanded
PubMed,
AddressingEmergencyDepartmentCareforPatients ExperiencingIncarceration:ANarrativeReview
RachelE.Armstrong,MD*
KristopherA.Hendershot,MD*
NaomiP.Newton,MD*
PatriciaD.Panakos,MD†
SectionEditor:TrevorMills,MD,MPH
*UniversityofMiami,Miami,Florida
† JacksonHealthSystem,Miami,Florida
Submissionhistory:SubmittedSeptember30,2022;RevisionreceivedMarch22,2023;AcceptedMarch23,2023
ElectronicallypublishedJune28,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59057
Patientsexperiencingincarcerationfaceamultitudeofhealthcaredisparities.Thesepatientsare disproportionatelyaffectedbyavarietyofchronicmedicalconditions.Patientswhoareincarcerated oftenremainshackledthroughouttheirhospitalcourse,experiencebiasfrommembersofthehealthcare team,andhavemanybarrierstoprivacygiventheomnipresenceofcorrectionsofficers.Despitethis, manyphysiciansreportlittleformaltrainingoncaringforthisuniquepatientpopulation.Inthisnarrative review,weexaminethecurrentliteratureonpatientswhoareincarcerated,especiallyasitpertainsto theircareintheemergencydepartment(ED).Wealsoproposesolutionstoaddressthesebarrierstocare intheEDsetting.[WestJEmergMed.2023;24(4)654–661.]
INTRODUCTION
TheUnitedStateshasover1.6millionincarcerated people.1 Thispopulationhasbeenhistoricallymedically underservedandfacesavarietyofhealthcaredisparities. Individualswhoareincarceratedaremorelikelythanthe generalpopulationtohavemedicalconditionssuchas diabetes,hypertension,HIV,hepatitisC,andtuberculosis.2,3 Theoftensubstandardlivingconditionsinjailsandprisons alsonegativelyimpactincarceratedpatients’ health.For example,themorbidityandmortalityfromCOVID-19was significantlyhigherinprisonsthaninthegeneralpublic.4,5 Whileincarcerationsometimesconnectsindividualswho havenothadpreviousaccesstocarewithcontinuityofcare andmedicationforchronicconditions,manyindividualsare stillunabletoaccessadequatetreatmentwhile incarcerated.6,7 Forexample,cancerpatientsreport inadequateaccesstopainmedications,patientsfacebarriers toacutesurgicalcare,andpregnantpatientsreport inadequateprenatalcare.8,9,10 Evenwhenpatientsareableto accesscarewhileincarcerated,theyoftenfaceimmense barrierstohealthcareoncereleased.2,3
Inadditiontothedisparitiesnotedabove,incarcerationis associatedwithmentalillnessandearlymortality.When comparedtonon-incarceratedpeople,thosewhoare incarceratedhavehigherratesofmajordepression,bipolar
disorder,andschizophrenia.11
16 Furthermore, incarcerationitselfmaypredisposeindividualstomental illness,asexperiencingincarcerationisariskfactorfor developinga firstpsychoticepisode.17 Substanceuse disorders(SUD)aremoreprevalentintheincarcerated populationthanthegeneralpopulation.18 Manycorrectional facilitiesdonotprovideadequatetreatmentforSUD,which canleadtosituationsoflife-threateningwithdrawalin individualswithbenzodiazepineandalcoholuse disorder.19,20 Individualswithopioidusedisorderhavea markedlyincreasedriskofopioidoverdoseafterrelease, especiallyiftheyarenotstartedonmedication-assisted treatmentwhileincarcerated.21
24 Withregardtomortality, studieshaveshownthatpeoplewhohavebeenincarcerated haveanincreasedriskofdeathatayoungeragewhen comparedtothegeneralpopulation.25,26 Thisriskof prematuredeathinincarceratedpeopledisproportionately affectsBlackpopulationswhencomparedtoother demographicgroups.27,28
Itisimpossibletodiscussthedisparitiesfacedby incarceratedpatientswithoutrecognizingthatthecriminal justicesystemisonebasedonracialoppression.29 Black Americansareincarcerated,wrongfullyconvicted,and stoppedandsearchedbypoliceatdisproportionatelyhigher ratesthanWhiteAmericans.30
33 Thehistoryofpolicingis
–
–
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 654
SOCIAL EMERGENCY
POPULATION HEALTHAND
MEDICINE
alsorootedinsystemicracism.Inthe18th and19th centuries, groupscalled “slavepatrols” wouldsearchforanddetain enslavedpeoplewhoescaped;thesegroupsareconsidered thebasisof “modern-daypolicing.”34,35 Whenformalpolice departmentswereestablishedintheearly20th century,these organizationsservedalargeroleinenforcingJimCrowlaws (lawsintheSouththatinstitutionalizedracialsegregation, suchasrequiringseparatewaterfountainsforBlackand Whitepeople).34 Inthelate20th century,thesystemic criminalizationofrecreationaldrugusefromPresident RonaldReagan’ s “WaronDrugs” andPresidentBill Clinton’sViolentCrimeControlandLawEnforcementAct disproportionatelytargetedBlackandLatino Americans.36,37 Thesearesomeexamples,butbynomeans anexhaustivelist,ofhowsystemicracismislinkedtothe criminaljusticesystemintheUS.
Whilethisreviewfocusesonpatientswhoare incarcerated,patientspresenttotheemergencydepartment (ED)invarioustypesofcustody.Oftenpatientsarebrought totheEDaftertheyarearrestedbutbeforetheyare convictedofacrimesothatemergentmedicalconcernscan beaddressedpriortobooking.Somepatientsarebroughtin whiledetainedbyUSImmigrationandCustoms
Enforcementofficers.PatientsmayalsopresenttotheED duringthepre-trialperiodorpost-convictionfromjailor prison.Patientsfrombothjailsandprisonsexperience barrierstohealthcare,buttherearegreatdiscrepanciesinthe careprovidedatjails,basedonthevariationinajail’ssize andresourcesandgiventhatpeopletypicallyspendlesstime injailsthaninprisons.6,38,39 Additionally,smallerjailsmay contractoutmostoftheirmedicalservices,andjailsare subjecttolessregulatoryhealthcareoversightthanprisons.39 Whilewewillfocusonthecareofindividualswhoare incarcerated,manyoftheprinciplesoutlinedinthisarticle areapplicabletopatientsinvarioustypesofcustody.
Physiciansemployedbyjailsandprisonsfaceanethical dilemmatermed “dualloyalty,” meaningtheconflictin interestbetweencaringfortheirpatientandcateringto thedemandsoftheprisonadministration.40 Sometimes, physiciansareaskedtoperformtasksthatgoagainsttheir roleashealers,ie,toperformdrugtestswithoutapatient’ s consent,towithholdanexpensivemedicaltreatmentdespite itbeingthestandardofcare,andtoperformmedicalexams forthepurposeof “certify[ing]thatprisonersare fitfor imprisonment.”40 Similarly,emergencyphysiciansmustbe awareoftheconflictsofinterestthatarisewhencaringfor patientswhoareincarcerated,suchascaseswhentheyare askedto “medicallyclear” apatientpriortobookingor performtestsorexamsthatarenotclinicallyindicated.
Penalharmreferstoany “plannedgovernmentalact wherebyacitizenisharmed” forpunitivereasons;theharmis considered “justifiablepreciselybecauseitisanoffenderwho issuffering.”41,42 AlthoughtheEighthAmendmentofthe USConstitutionbroadly “prohibitscruelandunusual
punishment,” itwasnotuntilthe1976SupremeCourt rulinginthecaseof EstellevGamble thatpenalharm inthecontextofmedicalcarewasexplicitlydeemed unconstitutional.43 The EstellevGamble ruling,which centeredon “thedeliberateindifferenceofthemedicalneeds ofprisoners,” setaclearprecedentfortherightsof incarceratedpatientstoaccessiblemedicalcare(including inpatientandspecialistcare).43,44 Failuretoprovide incarceratedpatientswiththesame “standardofcare” as non-incarceratedpatientshashenceforthbeenconsidereda violationoftheEighthAmendment.44 However,inpractice, upholdingthehealthcarerightsofincarceratedpatientsis morechallengingtoenforce.45
Inthisnarrativereview,wewillidentifyseveralbarriersto maintainingthestandardofcareforincarceratedpatientsin theED.Wehopetoincreaseawarenessofthesedisparities andproposesolutionstobetteraddresstheminclinical practice.34,46
BARRIERSTOCARE
Throughourreviewoftheexistingliterature,weidentified multiplebarrierstotreatingincarceratedpatientsintheED: biasedcarefromphysicians;presenceoflawenforcement; anduseofphysicalrestraints.
Bias
Membersofthehealthcareteam,includingphysiciansand nurses,oftenhavetheirownpreconceivednotionsabout incarceratedpatientsthatultimatelyaffectpatientcare.A surveystudyofformerlyincarceratedindividualsfoundthat manypatientshaveexperienceddiscriminationbasedon theircriminalrecord.47 Manypatientsalsoreported discriminationinthehealthcaresettingduetotheirraceand ethnicity.47 Thissurveystudyalsofoundthatformerly incarceratedindividualswithincreasedEDutilization reportedahigherrateofdiscriminationfromhealthcare professionals.47
However,manyphysiciansalreadyrecognizethe disparitiesinthecareofpatientswhoareincarcerated.One recentqualitativestudybyDouglasetalacknowledgesthe needtooptimizequalityofcareforincarceratedpatients.48 Inthispaper,surgicalresidentsweresurveyedabouttheir encounterswithlawenforcementwhilecaringforpatients experiencingincarceration.Thesurgicalresidentsnoted manychallengeswhencaringforthesepatients,including barrierstoadequatefollow-upcareandthedesignated holdingareasforincarceratedpatientsthatmaycontribute to “substandardcare” ordecreasedmonitoringofcritically illpatients.48
Biashasbeenreportedamongmanymembersofthe healthcareteam.Thestudy “CaringforHospitalized IncarceratedPatients:PhysicianandNurseExperience” by Brooksetalexaminedphysicianandnurseexperienceswhen caringforhospitalizedincarceratedpatientsusingopenand
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 655 Armstrongetal. AddressingEDCareforPatientsExperiencingIncarceration
closed-endedsurveyquestions.49 Amajorityofphysicians believedpatientswhowereincarceratedreceivedless frequentnon-medicalinterventions(definedas “socialwork support,physicaltherapyvisits,nutritionconsults”)during hospitalizationthanotherpatients.49 Over30%ofphysicians believedthatthesepatientsreceived “fewerdiagnostictests” and “fewermedicalinterventions” thanotherpatients.49
PatientPrivacy
Therearealsomanylimitstopatientprivacywhencaring forpatientswhoareincarceratedintheED.Thepresenceof correctionsofficerswhoaccompanythesepatientstotheED oftenleadstoprotectedhealthinformation(PHI)being sharedifmembersofthehealthcareteamdonotaskofficers tostepawayduringthehistoryandphysical.43,50
InthesurveystudybyBrooksetal,ahigherpercentageof nurseswhencomparedtophysiciansreportedthattheykept lawenforcementintheexamroomswhenperformingtheir historiesandphysicals.49 Still,35%ofphysiciansreported notaskingcorrectionsofficerstoleaveduringpatient encounters,andover50%ofthephysiciansreportednot askingforshacklestoberemovedduringtheirhistoriesand physicals.49 Inthesurvey,physiciansalsoidentifiedalackof formaltrainingintheirmedicaleducationwhencaringfor thisgroupofpatients.49
ManysurgicalresidentsintheDouglasetalstudy recognizedincarceratedpatients’ barrierstoprivacy.The majorityofresidentsinthisstudyreportedwitnessing incidentswhenlawenforcementofficerswouldquestion patientsduringtraumaassessments,attimesdisruptingthe primaryandsecondarysurveyandimpingingonpatient privacy.48 Inaddition,manyresidentsreportedinstances whenan “armedguardwaspresentintheoperatingroom” duringasurgicalprocedure.48 Oneresidentreportedan instancewhenanofficerrequestedanethanollevelona patient,eventhoughthistestwasnotpertinenttothe patient’scareatthattime.48
Theliteraturealsodescribesinstanceswhenlaw enforcement,namelypoliceofficers,haverequestedinvasive bodysearchesandtestsonpatients,althoughthesetestswere notclinicallyindicated.51,52 Inasurveystudy,emergency physiciansreportedbreachesofpatientprivacyinthe presenceoflawenforcement,includinginstanceswhen officerssolicitedPHI.53 Physiciansreportedbeinguncertain oftheexactroleandlimitationsoflawenforcementintheir workplace.53
Whilephysiciansshouldalwaysstrivetomaintainpatient privacy,therearecircumstancesinwhichaspectsofpatient caremayneedtobedisclosedtolawenforcement.For example,PHImayneedtobedisclosedifapatientrequires specifictreatmentorfollow-upcareintheoutpatientsetting. Giventhedelaysthatcanoccurinthecareofincarcerated patients,instructionsmayneedtobeexplicitlywrittenor discussedwithlawenforcementtoensureappropriatecare
occursafterdischargefromtheED.54 However,physicians shouldalwaysattempttoobtainapprovalfrompatientsprior tosharingtheirPHI.Therearealsoinstanceswhere incarceratedpatientsmayexhibitviolentbehaviorthatposes asafetythreattothemselvesortoEDstaff.Inthese instances,itisappropriatetointerviewpatientsinthe presenceoflawenforcement.
PhysicalRestraints
Physiciansaretaughttousephysicalrestraintswithcaution andonlywhenabsolutelynecessary.Physicalhospital restraints,whichareoftenappliedtoprotectpatientsafety,are associatedwithnumerouscomplications.Forexample,there isastatisticallysignificantincreasedincidenceofpulmonary embolismanddeepveinthrombosisinpatientswhoare physicallyrestrained.55,56 Furthermore,restraintsare associatedwithdelirium,emotionaldistress,rhabdomyolysis, injury,andevendeathwhenimproperlyused.57–59 Indeed, boththeAmericanCollegeofEmergencyPhysicians(ACEP) andTheJointCommissionhavepublishedstandardsonthe criterianecessarytojustifyrestraintuseandminimizeharm associatedwithrestraints.59–61
Despitethecautionadvisedwhenusingphysicalrestraints, patientswhoareincarceratedoftenarrivetotheEDin shacklesandremaininshacklesthroughoutthecourseoftheir EDstay.Somesurgeryresidentshaveevenreportedcaringfor patientswhoareshackledtothebedwhileintubatedand sedated.48 Therearesomepoliciesinplacetolimittheuseof shacklesinclinicalsettings.Recognizingtherisksofphysical restraintsinpregnancy,manystateshavemandatedagainst physicalrestraintsforpatientswhoareincarceratedinthe perinatalperiod.62 Federalpolicieshavealsobeenenactedto restrictuseofphysicalrestraintsinpregnancy,exceptwhen considerednecessaryforsafetyreasons.62
Thereisadearthofprotectionsforpatientswhoarenot pregnant.Non-pregnant,incarceratedpatientsoftenremain shackledthroughouttheirhospitalstay;thisincludesthose whoareterminallyillandthosewhoareintubatedand sedated.63–65 Thereislittledatatosupportthemedical rationaleforshacklingand,indeed,itsuseismainly determinedbyfederalandlocalpolicytobearequirement duringtransport.63,64,66–68 Adiscussiononwaystoaddress shacklingintheEDisincludedbelow.
STRATEGIESTOIMPROVECARE
Inthissection,weproposeseveralstrategiestoimprove thequalityofEDcareforpatientswhoareincarcerated. Thesesuggestionsarenotexhaustive;muchmoreresearchis requiredtofurtherinvestigatethemanydisparitiesthese patientsface.
Bias
HofmeisterandSoprychdiscusstheimportanceof includingformalteachingontreatingincarceratedpatientsin
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 656 AddressingEDCareforPatientsExperiencingIncarceration Armstrongetal.
medicalcurricula.69 Theauthorsdiscusshowtheuseof workshopsonimplicitbiasescanbeincorporatedinto residentmedicaleducation.Theworkshoptheyperformed allowedresidentphysicianstoself-reflectontheirbiases andbetterrecognizethedisparitiesthatspecificallyaffect incarceratedpatients.69 Thereshouldbeincreased curriculumdevelopmentinmedicaleducationthat focusesonaddressingthebiasesfacedbypatientswho areincarcerated.
Privacy
TheUSDepartmentofHealthandHumanServices outlinesPHIprotectionsforpatientswhoareincarcerated. SharingofPHIisonlypermittedinafewdistinct circumstances,suchaswhenhealthcarecliniciansare respondingtoarequestfor “PHI[that]isneededtoprovide healthcare” tothepatient,orwhenthePHIisnecessaryto protectthehealth/safetyoftheindividualorpeoplearound them.70 Asonecanimagine,informationmaybe inadvertentlydivulgedtocorrectionsofficersiftheemergency physician(EP),nursepractitioner(NP),orphysicianassistant (PA)conductsthehistoryandphysicalwithcorrections officersintheroom.43 Atoolkitforprotectingpatientprivacy createdbytheWorkingGrouponPolicingandPatientRights oftheGeorgetownUniversityHealthJusticeAlliance recommendsthatEPs,NPs,andPAsaskofficerstostepoutof “earshot” toprotectPHIand “preventaccidental disclosures.”50 EPs,NPs,andPAsshouldalsoobtainpatient consentpriortolabtestsandprocedures.50 The “Medical ProviderToolkit” andACEPalsonotethatwhilelaw enforcementpersonnelmayevenprovidewarrantsforspecific testsandexamssuchasbodycavitysearches,EPs,NPs,and PAscanrefuseiftheyarenotclinicallyindicatedorarenotin thepatient’sbestinterest.50,71
PhysicalRestraints
Justascertainfederalandstatepoliciesadvocatefor limitingshackleuseinpregnantpatients,sotooshouldthere beagreateremphasisplacedontheremovalofshackleson patientswhoarenotpregnant.Wheninterviewed,many physiciansandnursesreportednotrequestingthatshackles beremoved.49 Asmentionedabove,thereislittledatato supporttheuseofshackles,andmanyoftherulesand regulationsregardingshackleusefocusontransportation. Barrierstoshackleremovalareoftenduetoknowledge deficitsandunclearinstitutionalguidelinessurrounding shackling.EPs,NPs,andPAsshouldrecognizetheharms associatedwithshacklesandrequesttheirremovalwhenever possible,astheseareoftennotmedicallynecessary.50,64
Indeed,theInternationalAssociationforHealthcare Security&Safetystatesthatitistheresponsibilityofthe physicianandothermembersofthehealthcareteamto “assessthesafetyofcontinueduseofrestraint.”72 In addition,itisthedutyofthecorrectionsofficers,andnotthe
medicalteam,toensurethepatient’ssecurity.64 Giventhat thereareoftenunclearguidelinessurroundingshacklesand non-medicalrestraints,hospitalsshouldalsosetforththeir ownguidelinestoupholdtheprincipleofmedicalnonmaleficenceinalltreatmentareasincludingtheED.64
Tominimizeharm,physiciansshouldavoidandadvocate againsttheshacklingofpatientsintheproneposition.This typeofrestraintconfersanevengreaterriskofcomplications andhasbeenlinkedtocardiopulmonaryarrest,especiallyin agitatedpatients.73 Controversyremainsastowhetherthisis secondarytopositionalasphyxia;Steinbergprovideda reviewofthecurrentliteraturedetailinghowthecauseof suddendeathinpronerestraintis “multifactorial,” resulting from “reducedcardiacoutput,” metabolicacidosis,and impairedventilation.73 WhiletheJointCommissiondoesnot explicitlyprohibitpronerestraint,hospitalsarerequiredto reportanydeathsthatoccurwhileapatientisrestrained.74,75 Sincepronerestrainthasbeenidentifiedasacontributorto deathinsubjectswhoareagitated,manyinstitutionshave createdpoliciesagainstitsuse.76,77
Advocacy
WeencourageEPstoadvocateforchangeinthecarceral systemandintheirowninstitutionstoimprovethe healthcareofpatientswhoareincarcerated.Issuesof inadequatelivingconditionsinprisons,prisoncrowding,and discriminationoutsidethehospitalhavebeenwell documented.78–81 Giventhehealthimplicationsofthese issues,physiciansshouldrecognizeandadvocateforbetter livingsituationsforthesevulnerablepatients.82 Conditions forpatientswhoareincarceratedaresometimesinadequate inthehospital.SomehospitalEDshaveseparateholding areasforpatientswhoareincarcerated.Thequalityofcarein theseEDholdingareascouldbeimprovedbyincreasingthe staffing,resources,andattentiontothesesections.48 Physiciansshouldadvocateforbetterconditionsfor incarceratedpatients,bothwithintheEDandwithout.
ContinuityofCare
Inadditiontothereportedsubstandardcarethat incarceratedpatientsreceivewhileinthehospitalsetting, therearemanybarrierstoappropriatemedicalcarein correctionalfacilities.Thearticle “EmergencyMedicalCare ofIncarceratedPatients:OpportunitiesforImprovement andCostSavings” byMartinetalisachartreviewof incarceratedpatients’ EDvisitsatasingleinstitution.54 Patientsreportedbarrierstocare,suchasdifficultyaccessing prescriptionmedicationsforchronicconditions.54 Inlightof this,EPs,NPs,andPAsshouldaskpatientswhoare incarceratedabouttheiraccesstomedicationsforchronic conditionsandrefillappropriateprescriptionspriorto discharge.Inaddition,therearemanydocumentedcasesof patientseventuallypresentingtothemedicalsystemwith late-stageillnessesthatcouldhavebeentreatedearlierifthey
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 657 Armstrongetal. AddressingEDCareforPatientsExperiencingIncarceration
hadbeenpreviouslyidentified.79 WeencourageEPs,NPs, andPAstoreferpatientstospecialistsandrecommendclinic visitswhenappropriate.79
Education
Thereisalackofformaleducationsurroundingcarefor incarceratedpatients.Inadditiontobiasworkshops, theimplementationoflectures,case-baseddiscussions,and simulationcasescanprovideresidents,attendingphysicians, NPs,andPAswiththetoolsnecessarytocareforthisunique patientpopulation.Wedevelopedandsuccessfully implementedasimulationcaseforresidentlearnersinvolving thepresentationofapatientexperiencingincarceration. Thissimulationaimedtoexposelearnerstotheissuesunique toincarceratedpatientsaswellaspromotediscussiononthe removalofshacklesduringEDcare,implicitbiases,and protectingPHI.Weareintheprocessofanalyzingsurveydata fromthissimulationsession,andresultsareforthcoming.
CONCLUSION
Incarceratedpatientsarepartofavulnerablepopulation thatcurrentlyreceivessubstandardcareinmanyhealthcare settings,includingEDs.Thebiasesheldbymembersofthe healthcareteam,thepresenceofcorrectionsofficers,and pervasiveuseofrestraintscontributetothenumerous healthcareinequities.Wehaveproposedstrategiesto improvethequalityofcareforthisgroupofpatients, recognizingthatchangesmustbemadeonthephysician level,throughoutmedicaleducation,andinstitutionally.
“ Medicineshouldbeviewedassocialjusticeworkinaworld thatissosickandsorivenbyinequities. ” 83 – Dr.PaulFarmer.
AddressforCorrespondence:RachelE.Armstrong,MD,University ofMiami,DepartmentofEmergencyMedicine,1611NW12thAve# ECC1135Miami,FL33136.Email: rxa1022@miami.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Armstrongetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.Highesttolowest-prisonpopulationtotal[Internet].HighesttoLowestPrisonPopulationTotal|WorldPrisonBrief.Availableat: https://www. prisonstudies.org/highest-to-lowest/prison-population-total AccessedMarch22,2023.
2.DumontDM,BrockmannB,DickmanS,etal.Publichealthand theepidemicofincarceration. AnnuRevPublicHealth 2012;33:325–39.
3.RichJD,BeckwithCG,MacmaduA,etal.Clinicalcareofincarcerated peoplewithHIV,viralhepatitis,ortuberculosis. Lancet 2016;388(10049):1103–14.
4.MarquezN,WardJA,ParishK,etal.COVID-19incidenceandmortality infederalandstateprisonscomparedwiththeUSpopulation,April5, 2020,toApril3,2021. JAMA. 2021;326(18):1865–7.
5.SalonerB,ParishK,WardJA,etal.COVID-19casesanddeathsin federalandstateprisons. JAMA.2020;324(6):602–603.
6.PuglisiLB,WangEA.Healthcareforpeoplewhoareincarcerated. Nat RevDisPrimers.2021;7(1):1–2.
7.CommitteeonCausesandConsequencesofHighRatesof Incarceration;CommitteeonLawandJustice;DivisionofBehavioral andSocialSciencesandEducation;NationalResearchCouncil;Board ontheHealthofSelectPopulations;InstituteofMedicine. Healthand Incarceration:AWorkshopSummary.Washington(DC):National AcademiesPress(US);2013Aug8.1,ImpactofIncarcerationon Health.Availableat: https://www.ncbi.nlm.nih.gov/books/NBK201966/
8.LinJT,MathewP.Cancerpainmanagementinprisons:asurveyof primarycarepractitionersandinmates. JPainSymptomManag 2005;29(5):466–73.
9.BuskoA,Soe-LinH,BarberC,etal.Postmortemincidenceofacute surgical-andtrauma-associatedpathologicconditionsinprisoninmates inMiamiDadeCounty,Florida. JAMASurg.2019;154(1):87
8.
10.WangL.ChronicPunishment:Theunmethealthneedsofpeopleinstate prisons.PrisonPolicyInitiative.PublishedJune2022.Availableat: https://www.prisonpolicy.org/reports/chronicpunishment.html AccessedSeptember30,2022.
11.HirschtrittME,BinderRL.Interruptingthementalillness–incarcerationrecidivismcycle. JAMA.2017;317(7):695–696.
12.BaillargeonJ,BinswangerIA,PennJV,etal.Psychiatricdisordersand repeatincarcerations:therevolvingprisondoor. AmJPsychiatry 2009;166(1):103–9.
13.FovetT,GeoffroyPA,VaivaG,etal.Individualswithbipolardisorder andtheirrelationshipwiththecriminaljusticesystem:acriticalreview. PsychiatrServ.2015;66(4):348–53.
14.MulveyEP,SchubertCA.Mentallyillindividualsinjailsandprisons. CrimeandJustice.2017;46(1):231–77.
15.BronsonJ,BerzofskyM.Indicatorsofmentalhealthproblemsreported byprisonersandjailinmates,2011–12. BurJusticeStatSpecRep. 2017(SpecialIssue):1–6.
16.Mentalillness,humanrights,andUSprisons.HumanRights Watch.Published2020.Availableat: https://www.hrw.org/news/ 2009/09/22/mental-illness-human-rights-and-us-prisons AccessedMarch24,2023.
17.RamsayCE,GouldingSM,BroussardB,etal.Prevalenceand psychosocialcorrelatesofpriorincarcerationsinanurban, predominantlyAfrican-Americansampleofhospitalizedpatientswith first-episodepsychosis. JAmAcadPsychiatryLaw.2011;39(1):57–64.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 658 AddressingEDCareforPatientsExperiencingIncarceration Armstrongetal.
18.FazelS,YoonIA,HayesAJ.Substanceusedisordersinprisoners:an updatedsystematicreviewandmeta-regressionanalysis inrecentlyincarceratedmenandwomen. Addiction 2017;112(10):1725–39.
19.FiscellaK,PlessN,MeldrumS,etal.Alcoholandopiatewithdrawalin USjails. AmJPublicHealth.2004;94(9):1522–4.
20.FiscellaK,NoonanM,LeonardSH,etal.Drug-andalcohol-associated deathsinUSJails. JCorrectHealthCare.2020;26(2):183–93.
21.MerrallEL,KariminiaA,BinswangerIA,etal.Meta-analysisof drug-relateddeathssoonafterreleasefromprison. Addiction 2010;105(9):1545
54.
22.MaltaM,VaratharajanT,RussellC,etal.Opioid-relatedtreatment, interventions,andoutcomesamongincarceratedpersons:asystematic review. PLoSmedicine.2019;16(12):e1003002.
23.Overdosedeathsandjailincarceration-nationaltrendsandracial VeraInstituteofJustice.Availableat: https://www.vera.org/publications/ overdose-deaths-and-jail-incarceration/national-trends-and-racialdisparities.AccessedMarch17,2023.
24.Howisopioidusedisordertreatedinthecriminaljusticesystem? NationalInstituteonDrugAbusewebsite.2021.Availableat: https:// nida.nih.gov/publications/research-reports/medications-to-treat-opioidaddiction/how-opioid-use-disorder-treated-in-criminal-justice-system AccessedMarch21,2023.
25.WitteveenD.Prematuredeathriskfromyoungadulthoodincarceration. SociolQ.2021:1–28.
26.RuchDA,SteelesmithDL,BrockG,etal.Mortalityandcauseofdeath amongyouthspreviouslyincarceratedinthejuvenilelegalsystem. JAMANetwOpen.2021;4(12):e2140352.
27.SykesBL,ChavezE,StrongJ.Massincarcerationandinmatemortality intheUnitedStates deathbydesign? JAMANetwOpen. 2021;4(12):e2140349.
28.Bovell-AmmonBJ,XuanZ,Paasche-OrlowMK,etal.Associationof incarcerationwithmortalitybyracefromanationallongitudinalcohort study. JAMANetwOpen.2021;4(12):e2133083.
29.BrewerRM,HeitzegNA.Theracializationofcrimeandpunishment: criminaljustice,color-blindracism,andthepoliticaleconomyofthe prisonindustrialcomplex. AmBehavSci.2008;51(5):625–44.
30.GelbartC.Studyshowsraceissubstantialfactorin wrongfulconvictions.EqualJusticeInitiative.2022.Availableat: https:// eji.org/news/study-shows-race-is-substantial-factor-in-wrongfulconvictions/.AccessedMarch17,2023.
31.Racialandethnicdisparitiesinthecriminaljusticesystem.National ConferenceofStateLegislatures.UpdatedMay2022.Availableat: https://www.ncsl.org/civil-and-criminal-justice/racial-and-ethnicdisparities-in-the-criminal-justice-system.AccessedMarch17,2023.
32.PiersonE,SimoiuC,OvergoorJ,etal.Alarge-scaleanalysisofracial disparitiesinpolicestopsacrosstheUnitedStates. NatHumBehav 2020;4(7):736–45.
33.LofstromM,HayesJ,MartinB,etal.Racialdisparitiesinlaw enforcementstops.PublicPolicyInstituteofCalifornia.2021.
Availableat: https://www.ppic.org/publication/racial-disparitiesin-law-enforcement-stops/.AccessedMarch21,2023.
34.Theoriginsofmoderndaypolicing.NAACP.Availableat: https://naacp. org/find-resources/history-explained/origins-modern-day-policing AccessedMarch17,2023.
35.BrucatoB.Policingraceandracingpolice:theoriginofUSPolicein slavepatrols. SocialJustice. 2020;47(3/4(161/162)), 115–136.
36.CummingsAD,RamirezSA.Theracistrootsofthewarondrugs andthemythofequalprotectionforpeopleofcolor. UALRLRev 2021;44:453.
37.LevinsH.TheWaronDrugsasstructuralracism.Universityof PennsylvaniaLeonardDavisInstituteofHealthEconomics.2021. Availableat: https://ldi.upenn.edu/our-work/research-updates/the-waron-drugs-as-structural-racism/.AccessedMarch21,2023.
38.GatesA,ArtigaS,RudowitzR.Healthcoverageandcarefortheadult criminaljustice-involvedpopulation.KFF.2014.Availableat: https:// www.kff.org/uninsured/issue-brief/health-coverage-and-care-for-theadult-criminal-justice-involved-population/.AccessedMarch19,2023.
39.DumontDM,GjelsvikA,RedmondN,etal.Jailsaspublichealth partners:incarcerationanddisparitiesamongmedicallyunderserved men. IntJMensHealth.2013;12(3):213–227.
40.PontJ,StöverH,WolffH.Dualloyaltyinprisonhealthcare. AmJPublic Health.2012;102(3):475–80.
41.ClearTR. HarminAmericanPenology.StateUniversityofNewYork Press;1994:3–4.
42.CullenFT.Assessingthepenalharmmovement. JRCD 1995;32(3):338–358.
43.HaberLA,EricksonHP,RanjiSR,etal.Acutecareforpatients whoareincarcerated:areview. JAMAInternMed 2019;179(11):1561–1567.
44.RoldWJ.ThirtyyearsafterEstellev.Gamble:alegalretrospective. JCorrectHealthCare.2008;14(1):11–20.
45.SonntagH.Medicinebehindbars:Regulatingandlitigatingprison healthcareunderstatelawfortyyearsafterEstellev.Gamble. CaseW ResLRev.2017;68:603.
46.RecognizingtheNeedsofincarceratedpatientsintheemergency department.ACEP.2006.Availableat: https://www.acep.org/ administration/resources/recognizing-the-needs-of-incarceratedpatients-in-the-emergency-department/ AccessedSeptember29,2022.
47.FrankJW,WangEA,Nunez-SmithM,etal.Discriminationbasedon criminalrecordandhealthcareutilizationamongmenrecently releasedfromprison:adescriptivestudy. HealthJustice 2014;2:6.
48.DouglasAD,ZaidiMY,MaatmanTK,etal.Caringforincarcerated patients:Caniteverbeequal? JSurgEduc.2021;78(6):e154–60.
49.BrooksKC,MakamAN,HaberLA.Caringforhospitalizedincarcerated patients:physicianandnurseexperience[publishedonlineaheadof print,2021Jan6]. JGenInternMed.2021;1–3.
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 659 Armstrongetal. AddressingEDCareforPatientsExperiencingIncarceration
50.WorkingGrouponPolicingandPatientRightsoftheGeorgetown UniversityHealthJusticeAlliance.PoliceintheEmergencyDepartment: AMedicalProviderToolkitforProtectingPatienPrivacy. EMRA.2021. Availableat: https://www.law.georgetown.edu/health-justicealliance/wp-content/uploads/sites/16/2021/05/Police-in-the-EDMedical-Provider-Toolkit.pdf.AccessedMarch21,2023.
51.SongJS.Policingtheemergencyroom. HarvLRev 2020;134:2647–2720.
52.TessierW,KeeganW.Mandatorybloodtesting:Whencanpolice compelahealthprovidertodrawapatient’sbloodtodetermine bloodlevelsofalcoholorotherintoxicants? MoMed. 2019;116(4):274–277.
53.HaradaMY,Lara-MillánA,ChalwellLE.Policedpatients:Howthe presenceoflawenforcementintheemergencydepartmentimpacts medicalcare. AnnEmergMed.2021;78(6):738–48.
54.MartinRA,CoutureR,TaskerN,etal.Emergencymedicalcareof incarceratedpatients:opportunitiesforimprovementandcostsavings. PloSOne.2020;15(4):e023224
55.HiroseN,MoritaK,NakamuraM,etal.Associationbetweentheduration ofphysicalrestraintandpulmonaryembolisminpsychiatricpatients: Anestedcase–controlstudyusingaJapanesenationwidedatabase. ArchPsychiatrNurs.2021;35(5):534–40.
56.IshidaT,KatagiriT,UchidaH,etal.Incidenceofdeepveinthrombosis inrestrainedpsychiatricpatients. Psychosomatics. 2014;55(1):69–75.
57.PanY,JiangZ,YuanC,etal.Influenceofphysicalrestraintondelirium ofadultpatientsinICU:anestedcase-controlstudy. JClinNurs 2018;27(9–10):1950–1957.
58.VanRompaeyB,ElseviersMM,SchuurmansMJ,etal.Riskfactorsfor deliriuminintensivecarepatients:aprospectivecohortstudy. CritCare 2009;13(3):R77.Epub2009May20.
59.GuerreroP,MycykMB.Physicalandchemicalrestraints(anupdate). EmergMedClinNorthAm.2020;38(2):437–451.
60.Useofpatientrestraints[Internet]. ACEP.UpdatedApril2014.Available at: https://www.acep.org/patient-care/policy-statements/use-ofpatient-restraints/.AccessedSeptember29,2022.
61.JointCommissionStandardsonRestraintandSeclusion/Nonviolent CrisisInterventionTrainingProgram.CrisisPrevention.Updated2010. Availableat: https://www.crisisprevention.com/CPI/media/Media/ Resources/alignments/Joint-Commission-RestraintSeclusion-Alignment-2011.pdf.AccessedSeptember29,2022.
62.DignamB,AdashiEY.Healthrightsinthebalance:thecaseagainst perinatalshacklingofwomenbehindbars. HealthHumRights 2014;16:13.
63.DiTomasM,BickJ,WilliamsB.Shackledattheendoflife:Wecando better. AmJBioeth.2019;19(7):61–3.
64.HaberLA,PrattLA,EricksonHP,WilliamsBA.Shacklinginthehospital. JGenInternMed.2022;37(5):1258–60.
65.ScarletS,DreesenE.Surgeryinshackles:Whataresurgeons’ obligationstoincarceratedpatientsintheoperatingroom? AMAJ Ethics.2017;19(9):939
46.
66.UnitedStatesCode,2006Edition,Supplement3,Title42-thePublic HealthandWelfare.Title42-ThePublicHealthandWelfareChapter 136-ViolentCrimeControlandLawEnforcement.SubchapterI –PrisonsPartB-MiscellaneousProvisions.Sec.13726b-Federal regulationofprisonertransportcompanies.Published2009.Lawin effectasofFebruary1,2010.Availableat: https://www.govinfo.gov/app/ details/USCODE-2009-title42/USCODE-2009-title42-chap136subchapI-partB-sec13726b.AccessedSeptember29,2020.
67.Useofforceandapplicationofrestraints.USDepartmentofJustice: FederalBureauofPrisons.Updated2014.Availableat: https://www. bop.gov/policy/progstat/5566_006.pdf.AccessedSeptember29,2022.
68.UseofRestraints.DeschutesCountySherriff’sOffice.Published 2020.Availableat: https://sheriff.deschutes.org/CD-8-5%20Use %20of%20Restraints%20030220_Redacted.pdf
AccessedSeptember29,2022.
69.HofmeisterS,SoprychA.Teachingresidentphysiciansthepowerof implicitbiasandhowitimpactspatientcareutilizingpatientswhohave experiencedincarcerationasamodel. IntJPsychiatryMed 2017;52(4–6):345–54.
70.Whendoestheprivacyruleallowcoveredentitiestodiscloseprotected healthinformationtolawenforcementofficials?USDepartmentof Health&HumanServices.Updated2022.Availableat: https://www.hhs. gov/hipaa/for-professionals/faq/505/what-does-the-privacy-rule-allowcovered-entities-to-disclose-to-law-enforcement-officials/index.html AccessedSeptember26,2022.
71.LawEnforcementInformationGatheringintheEmergency Department.ACEP.Updated2017.Availableat: https://www. acep.org/patient-care/policy-statements/law-enforcementinformation-gathering-in-the-emergency-department/ AccessedSeptember26,2022.
72.HenkelS.ViolenceinHealthcareandtheUseofHandcuffs.IAHSS Foundation.2018Oct2;IAHSS-FRS-18-03.Availableat: https://iahssf. org/assets/IAHSS-Foundation-Violence-in-Healthcare-and-the-Useof-Handcuffs.pdf.AccessedSeptember26,2022.
73.SteinbergA.Pronerestraintcardiacarrest:Acomprehensivereviewof thescientificliteratureandanexplanationofthephysiology. MedSci Law.2021;61(3):215–226.
74.JointCommissionStandardsonRestraintandSeclusion/Nonviolent CrisisInterventionTrainingProgram.CrisisPrevention.Updated2010. Availableat: https://www.crisisprevention.com/CPI/media/Media/ Resources/alignments/Joint-Commission-Restraint-SeclusionAlignment-2011.pdf.AccessedSeptember29,2022.
75.LevinsonDR,GeneralI.Hospitalreportingofdeathsrelatedtorestraint andseclusion.DepartmentofHealthandHumanServices.Published 2006.Availableat: https://oig.hhs.gov/oei/reports/oei-09-04-00350.pdf AccessedMarch19,2023.
76.GuarinoC.HolyCrossHealth:RestraintandPhysicalHold.Date Approved:October1,2018.Availableat: https://www.trinity-health.org/ assets/documents/credentialing/hcmdss-restraintand-physical-hold-policy.pdf.AccessedMarch21,2023.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 660 AddressingEDCareforPatientsExperiencingIncarceration Armstrongetal.
77.RestraintandSeclusion.TheUniversityofToledo.EffectiveDate: August1,2019.Availableat: https://www.utoledo.edu/policies/utmc/ nursing/unit/senior-behavioral-health/pdfs/3364-120-98.pdf AccessedMarch21,2023.
78.JonesA.Cruelandunusualpunishment:whenstatesdon’tprovideair conditioninginprison.PrisonPolicyInitiative.Published2019.Available at: https://www.prisonpolicy.org/blog/2019/06/18/air-conditioning/ AccessedSeptember29,2022.
79.ScarletS,DreesenEB.Surgicalcareofincarceratedpatients:doing therightthing,explicitbias,andethics. Surgery.2021;170(3):983–5.
80.MillerA.OvercrowdinginNebraska’sprisonsiscausingamedicaland mentalhealthcarecrisis.Published2017.Availableat: https://www. aclu.org/news/prisoners-rights/overcrowding-nebraskasprisons-causing.AccessedSeptember29,2022.
81.WidraE.Sinceyouasked:Justhowovercrowdedwereprisonsbefore thepandemic,andatthistimeofsocialdistancing,howovercrowdedare theynow?PrisonPolicyInitiative.Published2020.Availableat: https:// www.prisonpolicy.org/blog/2020/12/21/overcrowding/ AccessedSeptember29,2022.
82.AllenSA,WakemanSE,CohenRL,etal.PhysiciansinUSprisons intheeraofmassincarceration. IntJPrisonHealth 2010;6(3):100–106.
83.PaulFarmerMarquardB.Dr.,whotirelesslybroughthealthcare totheworld’sneediest,diesat62-TheBostonGlobe[Internet]. BostonGlobe.com TheBostonGlobe;2022.Availableat: https://www. bostonglobe.com/2022/02/21/metro/dr-paul-farmer-whotirelessly-brought-health-care-worlds-neediest-dies-62/ AccessedSeptember29,2022.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 661 Armstrongetal. AddressingEDCareforPatientsExperiencingIncarceration
BRIEF EDUCATIONAL ADVANCES
AVirtualNationalDiversityMentoringInitiativetoPromote InclusioninEmergencyMedicine
TatianaCarrillo,DO*
LorenaMartinezRodriguez,DO†
AdairaLandry,MD,MEd‡
Al’aiAlvarez,MD§
AlyssaCeniza,BSW∥
RianeGay,MPA∥
AndreaGreen,MD¶
JessicaFaiz,MD,MSHPM#
SectionEditor:TehreemRehman,MD
*UniversityofPennsylvania,DepartmentofEmergencyMedicine,Philadelphia, Pennsylvania
† UniversityofSouthFlorida,DepartmentofEmergencyMedicine,Tampa,Florida
‡ HarvardMedicalSchool,DepartmentofEmergencyMedicine,Boston, Massachusetts
§ StanfordUniversity,DepartmentofEmergencyMedicine,Stanford,California
∥ AmericanCollegeofEmergencyPhysicians,Dallas,Texas
¶ TexasTechUniversityHealthSciencesCenter/UniversityMedicalCenterof ElPaso,ElPaso,Texas
# NationalClinicianScholarsProgram,VAGreaterLosAngelesHealthcare SystemandUCLA,LosAngeles,California
Submissionhistory:SubmittedDecember21,2022;RevisionreceivedMarch30,2023;AcceptedMarch27,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59666
Introduction: Traineesunderrepresentedinmedicine(URiM)faceadditionalchallengesseeking communityinpredominantlywhiteacademicspaces,astheyjuggletheeffectsofinstitutional,interpersonal, andinternalizedracismwhileundergoingmedicaltraining.Tooffersupportandaspacetosharethese uniqueexperiences,mentorshipforURiMtraineesisessential.However,URiMtraineeshavelimitedaccess tomentorshipfromURiMfaculty.Toaddressthisgap,wedevelopedanationalvirtualmentoringprogram thatpairedURiMtraineesinterestedinemergencymedicine(EM)withexperiencedmentors.
Methods: WedescribetheimplementationofavirtualDiversityMentoringInitiative(DMI)gearedtoward supportingURiMtraineesinterestedinEM.Theprogramdevelopmentinvolved1)partneringofnational EMorganizationstoobtainfunding;(2)identifyingacomprehensiveplatformtofacilitateparticipant communication,artificialintelligence-enabledmatching,andongoingdatacollection;3)focusingon targetedrecruitmentofURiMtrainees;and(4)fosteringregularleadershipmeetingcadenceto customizetheplatformandoptimizethementorshipexperience.
Conclusion: Wefoundthatbyusingavirtualplatform,theDMIenhancedtheef ficiencyofmentormenteepairing,tailoredmatchesbasedonparticipants’ interestsandthebandwidthofmentors,and successfullyestablishedcross-institutionalconnectionstosupportthementorshipneedsofURiM trainees.[WestJEmergMed.2023;24(4)662–667.]
BACKGROUND
Traineesunderrepresentedinmedicine(URiM)* face challengesseekingcommunityinpredominantlyWhite
academicspaces,astheyjuggletheeffectsofinstitutional, interpersonal,andinternalizedracismthroughoutmedical training.1–12 Theseeffectscancontributetoincreased
*TheAssociationofAmericanMedicalColleges(AAMC)definedthetermunderrepresentedminority(URM)toreflecttheracialgroupsofBlack,MexicanAmerican,mainlandPuertoRican,andNativeAmerican(AmericanIndianandnativesofAlaskaandHawaii).In2003,toencompasstheracialandethnic populationswithinmedicinewhoareunderrepresentedwhencomparedtotheirrespectivenumbersinthecontextofthegreaterpopulation,thiswasfurther clarifiedto “underrepresentedinmedicine” (URiMorUIM).AlthoughwerecognizetheuseofURiMorUIMinterchangeably,forconsistency,wehaveused thetermURiMthroughoutthispaper.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 662
experiencesoftheimposterphenomenonamongURiM trainees,whichcannegativelyaffectperformance.13–20 Lack ofsocialnetworkswithinmedicineandinformalknowledge duetodifferencesinparentaleducationandresources contributetobarrierstoinclusionandcareersuccess.21–25 To offersupportandaspacetosharetheseuniqueexperiences, mentorshipforURiMtraineesisessentialinacademic medicine,inadditiontoitsbenefitsofpromotinggreater careersatisfaction,productivity,andphysicianwellness.26–36
However,thereisascarcityofmentorshipforURiM trainees,whoespeciallybenefitfromfacultyofdiversegender identitiesandracialandethnicbackgrounds.37,38 URiM facultyareinstrumentalinpromotinginclusivetraining environmentsandhavebeenshowntoincreaseresidency programs ’ abilitytorecruitBlack,Latinx,andNative Americanresidentsandincreasegraduationratesamong URiMstudents.39–43 Unfortunately,thismentorshipis limitedbythesmallnumberofURiMfaculty,whoalready takeonadisproportionateburdenofmentorship.44–47 This minoritytaxcontributestoincreasedburnout,decreased productivity,anddecreasedcareerpromotion.48–51
Toaddressthisgap,wedevelopedanationalvirtual mentoringprogramthatstrategicallypairsURiMtrainees interestedinEMwithmentorsfamiliarwithmedical educationandcareerdevelopment.Wedescribehowto implementamodeltoexpandmentorshipaccessforURiM traineesandadvancerepresentation,inclusion,and belonginginEM.
OBJECTIVES
ThevirtualDiversityMentoringInitiative(DMI)aimed to(1)provideanaccessibleandsafeenvironmentforURiM participantstoshareexperiences;(2)connectwithother URiMtraineesandmentorsinEM;and(3)providepractical strategiestothrivepersonallyandprofessionallyasfuture emergencyphysicians.WemeasuredtheseobjectivesbyselfreportedsurveysregardingsatisfactionwiththeDMIand mentees’ abilitytoachievementorshipgoals.Thisstudywas deemedexemptfrominstitutionalreviewboard(IRB)review bytheStanfordIRB.
INNOVATIONDESIGN
TheAmericanCollegeofEmergencyPhysicians(ACEP) andtheEmergencyMedicineResidents’ Association(EMRA) partneredtoformtheDMIinSeptember2019.Facultyand traineesbeta-testedseveralvirtualmentoringplatforms.The primaryneedforavirtualformatwastheabilitytoscalethe DMIforlargecohortsbyenhancingtheefficiencyofmatching mentor-menteepairs,asopposedtomanualpairing.Other importantfeaturesincludedauser-friendlyinterface,asinglesign-onfeatureusingexistingACEPlogins,andtheabilityto collectdataonparticipantinteractionsandmentor-mentee pairsforreportableoutcomes.
WechosetheChronussoftware(ChronusLLC,Bellevue, WA)foritscomprehensiveplatformwiththeabilityto performartificialintelligence-enabledmatchingofmentormenteepairs,enrollparticipants,facilitateparticipant communication,andcollectlongitudinaldata.52 Chronus includedanaccountmanagerthatgeneratedreports, orientedusers,andtroubleshootedissues,beyondthe informationtechnologysupportthatmostotherplatforms offered.
Uponprograminitiation,mentorsandmenteescompleted aquestionnaireintheChronusplatformindicatingtheir goals,areasofexpertiseand,formentorstheirnumberof desiredmentees.Chronusthensuggestedpairingsbasedon responses.Menteeshadthe finalchoicetoselecttheirmentor fromashortlist.
Threementorshipcycleswerecompleted:August 2020–February2021,March2021–September2021,and October2021–June2022.WeadvertisedthroughTwitter, EMmedicaleducationnetworks(e.g.,CouncilofResidency DirectorsinEM),theEMRADiversityandInclusion committee,andtargetedoutreachtoHistoricallyBlack CollegesandUniversities’ EMinterestgroupstorecruit participants.
Tosupplementindividualmentor-menteerelationships, nine60-minuteeducationalandnetworkingeventsfor programparticipants,called “#MixMatchMingle,” were heldthroughoutthethreecyclestocreateacommunalspace toshareexperiences.Theformatofthe#MixMatchMingle eventsrangedfrominvitedguestspeakerstofacilitator-led discussionsonatopic.Eventthemesarelistedin Table1 and werechosenbytheleadershipteam,whohadvariouslevels oftrainingandfacultyexperience,diverseracialandethnic backgrounds,memberswhowere first-generationin medicine,andfacultyspecializinginmedicaleducation.By strategicallypairingmentorsandURiMmenteesbasedon theirgoalsandinterestsandfosteringawidercommunity withthe#MixMatchMinglecurriculum,DMIuses mentorshipasapedagogicalapproachtoEMcareer guidance.Italsoleveragesstrategiesgroundedinsocial capitalandsocialnetworktheorytoaddresspotential disparitiesininformalnetworksandknowledgein academia.53,54
Monthlyquantitativeandqualitativedatawerecollected viaChronusthroughouteachcycletomeasureprogram efficacyandinformsubsequentiterations(fullsurveyin SupplementalMaterial).Incrementaliterationsofworkflow andcustomizationoftheplatformwerenecessaryas unexpectedchallengesarose.Forexample,whenthenumber ofenrolleesdidnotmatchthenumberofparticipantspaired, wefoundthatitwaslargelyduetolackofparticipantprofile completion.Thus,weadjustedautomatede-mailreminders andmoreexplicitlycommunicatedtheimportanceofprofile completiontoparticipants.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 663 Carrilloetal. AVirtualNationalDiversityMentoringInitiativetoPromoteInclusioninEM
“
CohortIntroduction(orientationtoChronus,TheWhy’sand How’sofEffectiveMentorship)
AddressingImpostorPhenomenon
ResidencyApplicationPreparationandTips
COVID-19PandemicReflectionsandPracticing
Self-Compassion
ThrivingProfessionallyandFinancially:BuildingyourWealthin theStockMarket
LifeHacks” andTimeManagement
TransitionsinMedicineandtheRoleofMentorship
Mentor/Mentee-shipatDifferentCareerLevels
PathwaystoLeadershipinEM
COVID-19,coronavirusdisease2019; EM,emergencymedicine.
IMPACT/EFFECTIVENESS
Atotalof87mentorsand270menteesparticipatedinthe DMI.Theaveragementortomenteeratiowas1to1.6. Anonymoussurveysweredistributedtoparticipants.Ofthe 270mentees,215(79.6%)respondedtotheend-of-cohort survey.SuccessfulimplementationoftheDMIrequired fundingandstaffsupport,platformtroubleshooting,and earlyschedulingofeventsforparticipants.Weleveragedan existingpartnershipbetweenACEPandanacutecare staffingcompanyVituity(CEPAmerica,Inc,Emeryville, CA)tofundChronus.Administrativeandphysician programleadersmetbiweeklytodiscussdatageneratedby theplatform,troubleshootissueswithmentor-mentee pairing,anddesignthe#MixMatchMinglecurriculum. Thevirtualmentoringformatsuccessfullyprovidedaccess tomentorsdedicatedtoincreasingrepresentationin
RaceorEthnicity
MiddleEastern14(3.9)4(4.6)10(3.7)
*Participantswholisted “other” forleveloftrainingcitedrolessuchasMD-PhD,MBBS,osteopathicmedicalstudent,andchiefresident. MS,medicalstudent; PGY,postgraduateyear.
Table1. Topicsof#MixMatchMingleevents.
TotalN(%)MentorsMentees N(%)35787(24.4)270(75.6) Gender Men96(26.9)41(47.1)55(20.4) Women251(70.3)42(48.3)209(77.4) Non-Binary6(1.7)1(1.2)5(1.9) Transgender3(0.8)2(2.3)1(0.4) Undisclosed1(0.3)1(1.2)0 LevelofTraining MSYear1or292(25.8)092(34.1) MSYear3or4135(37.8)0135(50.0) PGY136(10.1)15(17.2)21(7.8) PGY210(2.8)3(3.4)7(2.6) PGY315(4.2)7(8.0)8(3.0) PGY46(1.7)5(5.7)1(0.4) Fellow19(5.3)18(20.7)1(0.4) Attending(1–5yearspost-residency)14(3.9)13(14.9)1(0.4)
yearspost-residency)6(1.7)6(6.9)0
Table2. CharacteristicsofuniqueparticipantsofthevirtualDiversityMentoringInitiativeacrossthreecohorts(August2020–June2022).
Attending(5+
Other*24(6.7)20(23.0)4(1.5)
Asian63(17.6)11(12.6)52(19.3) Black121(33.9)24(27.6)97(35.9) Latino/a74(20.7)13(14.9)61(22.6)
NativeAmerican5(1.4)05(1.9) NativeHawaiianorPacificIslander2(0.6)1(1.2)1(0.4) White60(16.8)33(37.9)27(10) Other18(5.0)1(1.2)17(6.3)
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 664 AVirtualNationalDiversityMentoringInitiativetoPromoteInclusioninEM Carrilloetal.
medicine.Travellimitationsduringthepandemicespecially impactedmedicalstudentsenrolledatinstitutionswithout associatedEMprograms.55
57 Oneparticipantnoted, “ I reallyappreciatedthevirtualformat,especiallysincemy mentorisacrossthecountry.Itmadeforaunique opportunitythatwouldn ’ thavebeenpossibleotherwise. ” Thevirtualformatlentitselftoparticipant flexibility,with anothermenteenoting, “ Theonlineformatmadeit convenientformetoparticipatedespitemyhecticand unsureschedule. ”
Inthesurveydistributeduponcohortcompletion,105of 117(89.7%)menteerespondentsratedthattheywere “satisfied” or “stronglysatisfied” withtheirmentorship,and 107of117(91.5%)menteerespondentsstatedthatthey achievedthegoalssetfortheirmentorshiprelationship. Menteesdescribedtheimpactoftheirmentoring relationshipsonbothpersonalandprofessionallevels,with onesharing, “ [Mentorname]reallychangedthegamefor me.IwasnotsureifIwantedtocontinuewithmedical school.NowIknowthatInotonlywanttobecomeadoctor, butIwanttobeinemergencymedicineforsure. ” Another participantnoted, “ [Mentorname]isamazingandnotonly doIfeellikeIhaveamentorforlife,butI ’ vealsogaineda goodfriend. ”
The fluidityofthementorshipstructurehadmixed feedback.Whilesomeparticipantsenjoyedorganically buildingrelationshipswiththeirmentorsthroughmore casualinteractions,otherssuggestedbenefitingfromamore structuredcurriculumandconcretegoalsetting.Wefound thatengagementwiththe#MixMatchMingleeventswaned asthepandemiccontinued,whichmayinparthavebeendue to “Zoomfatigue.”58,59 Giventhatparticipantscitedpositive experiencesduringone-on-onementor-menteemeetings,we reallocatedeffortsbydecreasingthenumberofprogramwideevents.
WewereencouragedthattheproportionofURiM mentorswasdisproportionatelyhigherthantheir representationinEM.Balancingthebenefitsofhaving raciallyconcordantmentorswithmitigatingtheminoritytax onthesementorswaschallenging.60,61 However, compensationandacademicincentivesformentor participationcouldbeeffective.62–64
LIMITATIONS
Thisstudyhadlimitations.First,physicianleadersdidnot haveprotectedtimeforthispilotinitiative,limitingtheir availabilityformeetingsandrecruitmentefforts.Dedicated administrativestaffandprotectedtimeforphysicianleadersis criticalforprogramsustainability.Furthermore,amentorship platformwithautomatedmatchingmaybecost-prohibitive formanyinstitutions,atacostof$42,000annually. Becauseparticipantswereonlyabletoselectoneraceor ethnicity,wewereunabletocapturetheperspectivesof multiracialparticipants.Finally,thedatadidnotinclude
intersectionalidentitiessuchassexualorientation,religion, disabilitystatus,andbeing first-generation,whichmayhave contributedtoparticipants’ experiences.65 Withadded support,targetedrecruitmentcouldhavebeenexpandedto Hispanic-servinginstitutionsandothernationalstudent organizations.
CONCLUSION
ThenationalvirtualDiversityMentoringInitiative successfullyprovidedaccesstocross-institutional connectionsandsupportedthespecificmentorshipneedsof URiMtrainees.Usingavirtualplatformenhancedthe efficiencyofmentor-menteepairingandallowedfortailored matchesbasedonparticipants’ interestandbandwidthof mentors.Themajorityofmenteesreportedsatisfactionwith theirmentorrelationships,highlightingsupportfortheir personalandprofessionalgrowth.Supportfromnational organizationstofundvirtualDMIforEMinterestgroups andresidencyprogramscanbridgegeographicalgapsin mentorshipandsponsorship.Wehopethatthismodelis translatedbeyondEMandinspiresthelaunchof personalizedmentorshipresourcesforURiMtraineesto furtherinclusionandasenseofbelonging,whilebroadly advancingrepresentationinmedicine.
ACKNOWLEDGMENTS
InmemoriamofDr.Adetolu “Tolu” Odufuye,a dedicatedmentoroftheDMIandadvocateforequityin emergencymedicine.Dr.JessicaFaizwassupportedbythe VAOfficeofAcademicAffiliationsthroughtheNational ClinicianScholarsProgram.Theviewsexpressedinthis articlearethoseoftheauthorsanddonotnecessarilyreflect thepositionorpolicyoftheDepartmentofVeteransAffairs, theUSgovernment,orotheraffiliatedinstitutions.
AddressforCorrespondence:JessicaFaiz,MD,MSHPM,National ClinicianScholarsProgram,VAGreaterLosAngelesHealthcare SystemandUCLA,1100GlendonAve.,Ste.900,LosAngeles, CA90024.Email: jfaiz@mednet.ucla.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.FundingforChronuswasprovidedby Vituity,aphysician-ledpartnershipthatworkswithhospitalsinacute carestaffing,practicemanagement,andinnovation.Vituityprovided supporttoassistinunderwritingtheadministrativeanddevelopment coststostartandmaintaintheDMIprogram.Therearenoconflictsof interesttodeclare.
Copyright:©2023Carrilloetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 665 Carrilloetal. AVirtualNationalDiversityMentoringInitiativetoPromoteInclusioninEM
REFERENCES
1.TiakoMJN,RayV,SouthEC.Medicalschoolsasracialized organizations:howrace-neutralstructuressustainracialinequality inmedicaleducation anarrativereview. JGenInternMed 2022;37:2259–66.
2.LeveyRE.Sourcesofstressforresidentsandrecommendationsfor programstoassistthem. AcadMed.2001;76(2):142–50.
3.CarrPL,PalepuA,SzalachaL,etal. “Flyingbelowtheradar”: aqualitativestudyofminorityexperienceandmanagementof discriminationinacademicmedicine. MedEduc.2007;41:601–9.
4.McDadeW.DiversityandInclusioningraduatemedicaleducation. ACGME.2019.Availableat: https://southernhospitalmedicine.org/ wp-content/uploads/2019/10/McDade-ACGME-SHM-PresentationMcDade-Final.pdf.AccessedFebruary3,2023.
5.LallMD,BilimoriaKY,LuDW,etal.Prevalenceofdiscrimination,abuse, andharassmentinemergencymedicineresidencytrainingintheUS. JAMANetwOpen.2021;4(8):1–15.
6.Osseo-AsareA,BalasuriyaL,HuotSJ,etal.Minorityresident physicians’ viewsontheroleofrace/ethnicityintheirtraining experiencesintheworkplace. JAMANetwOpen.2018;1(5):e182723.
7.McFarlingUL. ‘Itwasstolenfromme’:Blackdoctorsareforced outoftrainingprogramsatfarhigherratesthanwhiteresidents.
STATNews.Availableat: https://www.statnews.com/2022/06/20/ black-doctors-forced-out-of-training-programs-at-far-higherrates-than-white-residents/.PublishedJune20,2022.
AccessedJune21,2022.
8.TiakoMJN,SouthEC,RayV.Medicalschoolsasracialized organizations:Aprimer. AnnInternMed.2021;174(8):1143–4.
9.JonesCP.Levelsofracism:atheoreticframeworkandagardener’stale. AmJPublicHealth.2020;90(8):1212–5.
10.Heard-GarrisN,BoydR,KanK,etal.Structuringpoverty:howracism shapeschildpovertyandchildandadolescenthealth. AcadPediatr 2021;21(8):S108
16.
11.ChenC,GoldG,CannessonM,etal.Callingoutaversiveracismin academicmedicine. NEnglJMed.2021;385(27):2499–501.
12.GrubbsV.Perspective:racisminacademicmedicineishindering progresstowardhealthequity.2023.Availableat: https://www.chcf.org/ publication/perspective-racism-academic-medicinehinderingprogress-toward-health-equity/.AccessedFebruary17,2023.
13.ClancePR,ImesSA.Theimposterphenomenoninhighachieving women:dynamicsandtherapeuticintervention. PsychotherTheory, ResPract.1978;15(3):2044–8.
14.MullangiS,JagsiR.Impostersyndrome:Treatthecause,notthe symptom. JAMA.2019;322(5):403–4.
15.BravataD,MadhusudhanD,BoroffM,CokleyK.Commentary: prevalence,predictors,andtreatmentofimpostersyndrome: asystematicreview. JMentHealClinPsychol.2020;4(3):12–6.
16.EwingKM,RichardsonTQ,James-MyersL,etal.Therelationship betweenracialidentityattitudes,worldview,andafricanamerican graduatestudents’ experienceoftheimposterphenomenon. JBlack Psychol.1996;22(1):53–66.
17.CokleyK,McClainS,EncisoA,etal.Anexaminationoftheimpactof minoritystatusstressandimpostorfeelingsonthementalhealthof diverseethnicminoritycollegestudents. JMulticultCounsDevel 2013;41(2):82–95.
18.BernardDL,LigeQM,WillisHA,SosooEE,NeblettEW.Impostor phenomenonandmentalhealth:theinfluenceofracialdiscrimination andgender. JCounsPsychol.2017;64(2):155–66.
19.BernardDL,HoggardLS,NeblettEW.Racialdiscrimination,racial identity,andimpostorphenomenon:aprofileapproach. CultDiversEthn MinorPsychol.2018;24(1):51–61.
20.JamisonL.Whyeveryonefeelslikethey’refakingit. NewYorker.2023. Availableat: https://www.newyorker.com/magazine/2023/02/13/ the-dubious-rise-of-impostor-syndrome.AccessedFebruary6,2023.
21.MargolisE.(2001). TheHiddenCurriculuminHigherEducation.1sted. Oxfordshire,England:Routledge.
22.CavendishW,PerezD,Ocasio-StoutenburgL.Liftingasyouclimb: socialcapitaldevelopmentthroughaspirationalpeermentoring. Educ UrbanSoc. 2022;(7).
23.PernaLW,TitusMA.Therelationshipbetweenparentalinvolvementas socialcapitalandcollegeenrollment:anexaminationofracial/ethnic groupdifferences. JHigherEduc.2005;76(5):485–518.
24.JollyP. AnalysisinBrief-January2008:DiversityofU.S.Medical StudentsbyParentalIncome. 2008;8.
25.HillLD,BregmanA,AndradeF.Socialcapitalforcollege:network compositionandaccesstoselectiveinstitutionsamongurbanhigh schoolstudents. UrbanEduc.2015;50(3):316–45.
26.AhnJ.TheRoleofSocialNetworkLocationsintheCollegeAccess MentoringofUrbanYouth. EducUrbanSoc.2010;42(7):839–59.
27.SambunjakD,StrausSE,Maruši´cA.Mentoringinacademicmedicine:a systematicreview. JAMA.2006;296(9):1103–15.
28.PalamaraK,McKinleySK,ChuJT,etal.Impactofavirtualprofessional developmentcoachingprogramontheprofessionalfulfillmentandwellbeingofwomensurgeryresidents. AnnSurg.2023;277(2):188–95.
29.PalepuA,FriedmanRH,BarnettRC,etal.Juniorfacultymembers’ mentoringrelationshipsandtheirprofessionaldevelopmentinU.S. medicalschools. AcadMed.1998;73(3):318–23.
30.HitchcockMA,BlandCJ,HekelmanFP,etal.Professionalnetworks:the influenceofcolleaguesontheacademicsuccessoffaculty. AcadMed 1995;70(12):1108–16.
31.CoatesWC,HobgoodCD,BirnbaumA,etal.FacultyDevelopment: academicopportunitiesforemergencymedicinefacultyoneducation careertracks. AcadEmergMed.2003;10(10):1113–7.
32.PrendergastHM,HeinertSW,EricksonTB,etal.Evaluationofan enhancedpeermentoringprogramonscholarlyproductivityand promotioninacademicemergencymedicine:a five-yearreview. JNatl MedAssoc.2019;111(6):600–5.
33.KoopmanRJ,ThiedkeCC.Viewsoffamilymedicinedepartmentchairs aboutmentoringjuniorfaculty. MedTeach.2005;27(8):734–7.
34.FlintJH,JahangirA,BrownerBD,etal.Thevalueofmentorshipin orthopaedicsurgeryresidenteducation:theresidents’ perspective. JBoneJtSurgery,Inc.2009;91(4):1017–22.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 666 AVirtualNationalDiversityMentoringInitiativetoPromoteInclusioninEM Carrilloetal.
35.DonovanA.Viewsofradiologyprogramdirectorsontheroleof mentorshipinthetrainingofradiologyresidents. AmJRoentgenol 2010;194(3):704–8.
36.CastiglioniA,BelliniLM,SheaJA.Programdirectors ’ viewsofthe importanceandprevalenceofmentoringininternalmedicine residencies. JGenInternMed.2004;19(7):779–82.
37.PenalozaNG,ZailaArdinesKE,DoesS,etal.Educationsomeonelike me:anexaminationoftheimportanceofrace-concordantmentorshipin urology. Urology.2023;171:41
8.
38.YehiaBR,CronholmPF,WilsonN,etal.Mentorshipandpursuitof academicmedicinecareers:Amixedmethodsstudyofresidentsfrom diversebackgrounds. BMCMedEduc.2014;14(1).
39.AgawuA,FahlC,AlexisD,etal.Theinfluenceofgenderand underrepresentedminoritystatusonmedicalstudentrankingof residencyprograms. JNatlMedAssoc.2019;111(6):665–73.
40.PhitayakornR,MacklinEA,GoldsmithJ,etal.Applicants’ self-reported prioritiesinselectingaresidencyprogram. JGradMedEduc.2015; 7(1):21–6.
41.South-PaulJE,CampbellKM,Poll-HunterN,etal.Mentoringasabuffer forthesyndemicimpactofracismandCOVID-19amongdiversefaculty withinacademicmedicine. IntJEnvironResPublicHealth 2021;18(9):4920–1.
42.StoutR,ArchieC,CrossD,etal.Therelationshipbetweenfaculty diversityandgraduationratesinhighereducation. IntercultEduc 2018;29(3):399–417.
43.KuMC,LiYE,ProberC,etal.Decisions,decisions:howprogram diversityinfluencesresidencyprogramchoice. JAmCollSurg 2011;213(2):294–305.
44.BonifacinoE,UfomataEO,FarkasAH,etal.Mentorshipof underrepresentedphysiciansandtraineesinacademicmedicine: asystematicreview. JGenInternMed.2021;36(4):1023–34.
45.MensahMO.MarketingMedicine’sDiversity:IssuingPromissoryNotes forHealthCareEquity. JAMA.2021;326(16):1581–2.
46.RodriguezJE,CampbellKM,FogartyJP,etal.Underrepresented minorityfacultyinacademicmedicine:asystematicreviewofURM facultydevelopment. FamMed.2014;46(2):100–4.
47.TrejoJ.Theburdenofserviceforfacultyofcolortoachievediversityand inclusion:theminoritytax. MolBiolCell.2020;31(25):2752–4.
48.WilliamsonT,GoodwinR,UbelP.Minoritytaxreform avoiding overtaxingminoritieswhenweneedthemmost. NEnglJMed 2021;384:1877–9.
49.FangD,MoyE,ColburnL,etal.Racialandethnicdisparitiesinfaculty promotioninacademicmedicine. JAMA.2000;284(9):1085–92.
50.CampbellKM.TheDiversityeffortsdisparityinacademicmedicine. IntJ EnvironResPublicHealth.2021;18(9):4529.
51.GuevaraJP,AdangaE,AvakameE,etal.Minorityfacultydevelopment programsandunderrepresentedminorityfacultyrepresentationatUS medicalschools. JAMA.2013;310(21):2297–304.
52.ChronusMentoringSoftware.Availableat: https://chronus.com/ ps-chronus-mentoring-software-easy-efficient-and-measurable?
utm_source=google&utm_medium=cpc&utm_campaign=Brand%7C Exact&utm_content=AG_92950350383_PT__CR_452153865819_ DV_c&utm_term=KW_chronusmentoringplatform_MT_e&gclid= Cj0KCQjw0PW.AccessedJuly1,2019.
53.ArnessonK,AlbinssonG.Mentorship–apedagogicalmethodfor integrationoftheoryandpracticeinhighereducation. NordJStudEduc Policy.2017;3(3):202–17.
54.NationalAcademiesofSciences,Engineering,andMedicine2019. The ScienceofEffectiveMentorshipinSTEMM.Washington,DC:The NationalAcademiesPress.
55.AkersA,BloughC,IyerMS.COVID-19implicationsonclinical clerkshipsandtheresidencyapplicationprocessformedicalstudents. Cureus.2020;12(4):e7800.
56.LangilleAndrew,Hornack,etal.Applyingemergencymedicineduringa pandemic – advicefororphanprogrammedicalStudents.Resident StudentOrganization.2020.Availableat: https://acoep-rso.org/ the-fast-track/applying-emergency-medicine-during-a-pandemic advice-for-orphan-program-medical-students/.AccessedJune1,2022.
57.CORDAdvisingStudentsCommitteeinEM(ASC-EM). Orphan ApplicantEmergencyMedicineApplyingGuide.2021.Availableat: https://www.cordem.org/globalassets/files/student-resources/ applying-guide orphan.pdf.AccessedJune1,2022.
58.BailensonJN.Nonverbaloverload:atheoreticalargumentforthe causesofZoomfatigue. AmPsycholAssoc.2021;2(1):1–6.
59.WalkerT.How “Zoomfatigue” impactscommunicationwithstudents. NationalEducationAssociation.2020.Availableat: https://www.nea. org/advocating-for-change/new-from-nea/how-zoom-fatigue-impactscommunication-students.AccessedJune1,2022.
60.ClevelandManchandaEC,LingAY,BottcherJL,etal.Threedecadesof demographictrendsamongacademicemergencyphysicians. JAmColl EmergPhysiciansOpen.2022;3(4).
61.CampbellKM,RodríguezJE.Addressingtheminoritytax:perspectives fromtwodiversityleadersonbuildingminorityfacultysuccessin academicmedicine. AcadMed.2019;94(12):1854–7.
62.RodríguezJE,CampbellKM,PololiLH.Addressingdisparitiesin academicmedicine:whatoftheminoritytax? BMCMedEduc.2015; 15(1):1–5.
63.FaucettEA,BrennerMJ,ThompsonDM,etal.Tacklingtheminoritytax: aroadmaptoredistributingengagementindiversity,equity,and inclusioninitiatives. Otolaryngol-HeadNeckSurg.2022; 166(6):1174–81.
64.brownim.diversityMatters:Tippingthescalesontheminoritytax. EmergMedNews.2021;43(7):9.
65.CrenshawK.Demarginalizingtheintersectionofraceandsex:ablack feministcritiqueofantidiscriminationdoctrine,feministtheory,and antiracistpolitics. LivingWithContradictControvFemSocEthics 2018;1989(1):39–52.
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 667 Carrilloetal. AVirtualNationalDiversityMentoringInitiativetoPromoteInclusioninEM
SkinToneandGenderofHigh-FidelitySimulationManikins inEmergencyMedicineResidencyTrainingandtheirUse inCulturalHumilityTraining
MarieAndersonWofford,MD,MPH* CortlynBrown,MD*
BernardWalston,MD†
HeidiWhiteside,MS‡
JosephRigdon,PhD‡
PhilipTurk,MS,PhD§
*AtriumHealth,DepartmentofEmergencyMedicine,Charlotte, NorthCarolina
† UniversityofNorthCarolinaChapelHillSchoolofMedicine,ChapelHill, NorthCarolina
‡ WakeForestUniversitySchoolofMedicine,DepartmentofBiostatisticsand DataScience,Winston-Salem,NorthCarolina
§ UniversityofMississippiMedicalCenter,DepartmentofDataScience, Jackson,Mississippi
SectionEditors:MandyJ.Hill,DrPH,MPH;MichaelGottlieb,MD
Submissionhistory:SubmittedNovember17,2022;RevisionreceivedMarch14,2023;AcceptedApril13,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.59459
Introduction: Itisimportantforphysicianstolearnhowtoprovideculturallysensitivecare.Cultural humilityisdefinedasalifelongprocesswithagoalof fixingpowerimbalancesandcreatinginstitutional accountabilitythroughlearningaboutanother’scultureaswellasperformingself-explorationaboutone’s ownbeliefs,identities,andbiases.Onewaytoteachculturalhumilityinmedicineissimulation.However, therearenopeer-reviewedpublishedstudiesthatexaminewhethertheskintoneorgenderofthehighfidelitysimulationmanikins(HFSM)usedbyemergencymedicine(EM)residencyprogramsreflectsthe USpopulationnorwhetherhigh-fidelitysimulationisusedtoteachculturalhumility.Weaimedtoaddress thatgapintheliterature.OurprimaryobjectivewastoevaluatewhatproportionofEMresidency programsuseHFStoteachculturalhumility.Oursecondaryobjectivewastoevaluatewhethertheskin toneandgenderbreakdownoftheEMresidencyprogramHFSMisrepresentativeoftheUSpopulation.
Methods: Weconductedasimplerandomsampleof80EMresidencyprogramstocharacterizeHFSMand culturalhumilitytraining.Selectedprogramswere emailedaquestionnaire.KeyoutcomesincludedHFSM skintoneandgenderandwhetherculturalhumilitywas taughtviaHFSM.Wecalculatedpointandinterval estimatesfortheproportionofdark-,medium-,andlight-tonedskinandtheproportionoffemaleandmale manikins.Confidenceintervalswereemployedtotestthenullhypothesisthatdark/medium/lightskintonewas 20/20/60andthatthefemale/maleratiowas50/50.BothratioswereextrapolatedfromtheUSCensusdata.
Results: Ourresponseratewas74%(59/80).Fifty-fiveof59EMresidencyprogramsthathadmanikins (0.93,95%confidenceinterval[CI]0.88–0.99)reporteddataonatotalof348manikins.Thirty-nineofthe 55programswithmanikinsreportedusingHFStoteachculturalhumility(0.71,95%CI0.60–0.82). Proportionsoflight-,medium-,anddark-tonedmanikinswere0.52(0.43–0.62),0.38(0.29–0.47),and 0.10(0.07–0.14),respectively.ProportionsofmaleandfemaleHFSMwere0.69(0.64–0.76)and0.31 (0.24–0.36),respectively.Thenullhypothesesthatskintonefollowsa60/20/20splitandgenderfollowsa 50/50splitwererejected,asnotallconfidenceintervalscontainedthesehypothesizedvalues.
Conclusion: WhilemostEMresidencyprogramssurveyedusehigh-fidelitysimulationtoteachcultural humility,themanikinsdonotreflecteithertheskintoneorgenderoftheUSpopulation.[WestJEmerg Med.2023;24(4)668–674.]
WesternJournal of EmergencyMedicine Volume24,No.4:July2023 668 ORIGINAL RESEARCH
INTRODUCTION
ThecurrentUnitedStatespoliticalclimateandrecent, raciallychargedevents,coupledwithevidencethatminority groupsoftenfacehigherratesofchronicdiseasesandworse medicaloutcomes,havehighlightedtheimportanceof diversity,equity,andinclusion(DEI)effortswithinthe medical field.1 Culturalhumilityisdefinedasalifelong processwithagoalof fixingpowerimbalancesandcreating institutionalaccountabilitythroughlearningaboutanother’ s cultureaswellasperformingself-explorationaboutone’ s ownbeliefs,identities,andbiases.TheAccreditationCouncil forGraduateMedicalEducation(ACGME)requires culturalhumilitytraininginmedicalresidencycurricula. Manyemergencymedicine(EM)residencyprograms, however,havenoformalDEIcurricula.2,3 Whilelectures aretheprimarymethodofcomplyingwithACGME teachingrequirements,high-fidelitysimulation(HFS) isusedaswell.
AlthoughthereisdebateaboutthedefinitionofHFSand high-fidelitysimulationmanikins(HFSM),4 forthisstudywe usedthedefinitionprovidedbythesimulationresource websiteHealthySimulation.com,whichstatesthat “high fidelitysimulationisahealthcareeducationmethodology thatinvolvestheuseofsophisticatedlife-likemanikins (sometimescalledmannequins)inrealisticpatient environments.”5 StudieshaveshownthatHFSresultsin improvedclinicalperformanceandprovidesasafe spacetopracticehigh-riskclinicalscenariosand procedures.6,7 Despitethisutility,thereisadearthof literatureonwhetherHFSMsareusedtoteach culturalhumility.
Farondaetalconductedanintegrativereviewof simulationlearningthemesandfoundthatwhilecultural sensitivityandcompetence,insightandunderstanding, communication,andconfidenceandcomfortwere mentioned,therewerenostudiesthatmentionedcultural humility.8,9 Inaddition,thereislimitedpublishedresearchon theskincolorandgenderofsimulationmanikins.Thisisof particularimportanceinestablishingarealisticenvironment inwhichthemanikinsreflectthepatientpopulation encounteredbythetrainee.Inonestudy,94%ofmanikins andsimulationbodypartsinanadvertisementbrochurewere whitewhileonly6%wereblack.10 Anotherstudyreported that68.75%ofthesimulationcentersthatrespondedtoa surveydistributedvialistservesandGoogleGroupshad manikinsofcolorand65.63%hadbodyparts/tasktrainers ofcolor.11 Ofnote,noneofthesestudiesfocusedontheuseof HFSMinEMresidencyprograms.
Oursearchfoundonlyonestudydemonstratingtheuseof simulationtoteachculturalhumilityinEMtraining.WardGainesetalusedmasssimulationtoteachEMresidentskey conceptsinhealthcaredisparitiessuchasrace/ethnicity, genderbias,stereotyping,andprivilege.Theseresidents
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Culturalhumilitytrainingisarequiredaspect ofEMresidenttraining.High- fi delity simulationmanikins(HFSM)areauseful modalityforresidenteducation.
Whatwastheresearchquestion?
DotheHFSMskincolorandgender proportionsre fl ecttheUSpopulation?Do EMresidencyprogramsuseHFSMtoteach culturalhumility?
Whatwasthemajor findingofthestudy?
Light-,medium-,anddark-coloredHFSM were0.52(95%CI:0.43,0.62),0.38(0.29, 0.47),and0.10(0.07,0.14),respectively. MaleandfemaleHFSMwere0.69(0.64, 0.76)and0.31(0.24,0.36),respectively.The HFSMdonotre fl ecttheUSpopulation gendernorskincolor.
Howdoesthisimprovepopulationhealth?
HFSMisameanstoteachculturalhumilityin EM.HavingHFSMsrepresentativeoftheUS populationcanpotentiallyhelptraineesbetter carefordiversepopulations.
reportedincreasedperceivedconfidenceoftheseconcepts afterthesimulation.2 Thisstudy,however,wasfocusedon standardizedpatientsanddidnotincludeHFSM.Norare thereanypeer-reviewed,publishedstudiesthatexplorethe skintoneorgenderdiversityofHFSMatEMresidency programsorwhethertheseprogramsuseHFSMstoteach culturalhumility.
Our fi rstobjectiveinthisstudywastoevaluatewhat proportionofEMresidencyprogramswithHFSuse HFSMstoteachculturalhumility.Oursecondobjective wastoevaluatewhethertheskintoneandgender breakdownoftheHFSMsusedbytheseprogramsrefl ects thatoftheUSpopulationand,therefore,thepotential patientpopulation.Wehypothesizedthattherewouldbea smallpercentageofEMprogramsthatuseHFSMsfor culturalhumilitytrainingandthatthegenderandskin-tone breakdownofmanikinswoulddifferfromthatofthe overallUSpopulation.
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 669 Woffordetal. DiversityofHigh-FidelitySimulationManikins
METHODS StudyDesignandSetting
WeadministeredaquestionnairetoasubsetofEM residencyprogramsacrossthecountrydeterminedbysimple randomsampling(see Appendix2 fordetailsonsampling methods)fromApril2021
September2021.Thestudywas deemedexemptbytheAtriumHealthCarolinasInstitutional ReviewBoardandwasdesignedtocomplywithquality standardsforsurveyreportinginmedicalliterature.12
SurveyDesign
Astherewerenoquestionnairesthataddressedourstudy objectives,wecollaboratedwithanexpertsurvey methodologistonthecreationofthesurvey,whichwepiloted toourintendedaudiencewith25responses.Several improvementsweremadethroughthisprocess,including clarifyingthatsurveyquestionswerespecifictoHFSM. Inaddition,toreflectpurchasingoptions,skincolorwas changedfromethnicitydefined(eg,BlackorAfrican American)toskintonedefined(light,medium,anddark), andgenderwassimplifiedtomalevsfemale.Response burdenwasdecreasedthroughskippatternsandbreaks.The finalquestionnaire(see Appendix1)consistedof10questions groupedinto1)EMresidencyprogramdemographics, 2)HFSMskintoneandgenderbreakdown,and3)utilization ofsimulationmanikinstoteachculturalhumility. Participantsgenerallycompletedthequestionnairewithin fiveminutes.Thequestionnairedidnotincludeany identifyinginformationrequiringblinding.
DataAnalysis
Weconductedasimplerandomsampleof80ofthetotal (220)EMresidencyprogramsintheUS.Oursurveywas distributedviaemailtoprogramdirectorswithtwofollowupphonecallsfornon-respondents.Severalprogramsuseda simulationcenterthatwasnotaffiliatedwiththeprogram institution.Inthosecases,wedistributedoursurveyviathe methodsabovetotherespectivesimulationcenterdirectors. Notwoprogramsfromthesimplerandomsample,however, usedthesamesimulationcenter.
Thesamplesizewaschosentoyieldconfidenceintervals (CI)withacceptableaprioriprecisionforestimation(see Appendix2).Consentwasobtainedelectronically.We estimatedproportionsofEMresidencyprogramsoffering scenarioswithculturalhumilityasaprimaryorsecondary learninggoal,usingsurveysamplingmethodologydescribed inThompson.13
Aswewereunabletoidentifyaccuratedataonthe variationsinskintonesintheUSpopulation,we extrapolatedskintonefromthe2020USCensusraceand ethnicitydata.14 Theproportionof “Whitealone(not Hispanic)” wasclassifiedaslightskin,andtheproportionof peoplewhoidentifiedas “Asianalone,”“AmericanIndian,” “PacificIslander,”“twoormoreraces,”“Hispanicor
Latino,” and “Blackalone” wassplitintoapproximately evenlyproportionedgroupsofmedium-anddark-skin-toned manikins(20%eachofthepopulation).
Asmanikinskintone(light,medium,dark)andgender (female,male)aremultinomialdataclusteredbysimulation center,thedataislikelycorrelated.15 Toestimatethe proportionsofinterest,we fitageneralizedlinearmixedmodel withaninterceptasa fixedeffectandsimulationcenterrandom effects.Weconductedlikelihoodratiotestsontherandom effectsvariancecomponent(s)ofsimulationcentertotestfor significantcenter-to-centervariabilitywithrespecttothe multinomialdata.Wethenmarginalizedandrefitthemodel andinvertedthelinkfunctiontorecoverestimatesofthe proportions.Weusedstratifiedblockbootstrappingtoobtain asetof98.30%bootstrappercentileCIswhere,importantly, resamplingwasdonebysimulationcentertopreservethe correlationstructureamongthedata.16 Weemployed98.3% CIstopreservefamilywisealpha at0.05.Wetestedhypotheses aboutrepresentation(50/50male/femaleand60/20/20 light/medium/dark)byexaminingwhetherornotthenull hypothesizedvalueswerecontainedbythebootstrapCIs.
RESULTS
Surveyresponseratewas74%(59/80).Demographicsof therespondingEMresidencyprogramsarereportedin Table1.Respondingprogramsmostfrequentlywereinthe Northeast(37%),followedbytheSouth(27%),Midwest (19%),andWest(17%)andweremostfrequentlythree-year programs(71%).
Ofthe59EMresidencyprogramsthatrespondedtothe survey,55reportedusingHFSMasapartoftheirresidency curricula(0.93,95%CI0.88–0.99)(Table2);and39ofthose 55programswithmanikinsreportedhavingHFScases whereculturalhumilitywasaprimaryorsecondarylearning
–
Demographicinformation ofrespondentprogramRespondents(n = 59) Region South 16(27%) Northeast 22(37%) Midwest 11(19%) West 10(17%) TypeofProgram 3-yearEM 42(71%) 4-yearEM 16(27%) Other 1(2%) 3–5-yearEM/IM 0(0%) 3–5-yearEM/Peds 0(0%) EM, emergencymedicine; IM,internalmedicine; Peds,pediatrics. WesternJournal of EmergencyMedicine Volume24,No.4:July2023 670 DiversityofHigh-FidelitySimulationManikins Woffordetal.
Table1. Descriptivesummaryof59surveyrespondents.
objective(0.71,95%CI0.60–0.82).Ofthose39programs,35 respondedwiththepercentage(0–100)oftotalHFScases usingculturalhumilityasaprimaryorsecondary learningobjective,andthemeanresponsewas 15.9(95%CI11.4–20.4).
The59respondingEMprogramsreporteddataona totalof348manikins.Therewere5.9manikinsperEM residencyprogram,witharangeof0–23.Thegeneralized, linearmixedmodelrejectedthenullhypothesisofnocenterto-centervariabilityforskintone(P =<0.000)andgender
(P =<0.0001).Therefore,weproceededwithbootstrapping asdescribedpreviouslytoestimateproportionsandobtain appropriateCIs.
Proportionsofmanikinswithlight,medium,anddark skintoneswere0.52(0.43–0.62),0.38(0.29–0.47),and0.10 (0.07–0.14),respectively.Proportionsofmaleandfemale HFSMwere0.69(0.64–0.76)and0.31(0.24–0.36), respectively.Thenullhypothesesthatskintonefollowsa 60/20/20splitandgenderfollowsa50/50splitwererejected, asnotallCIscontainedthesehypothesizedvalues.Results aregraphicallysummarizedin Figure1.
Whenrespondentswereaskedwhytheirprogramsdidnot havediversityintermsofHFSMskintone(Table3),20% (11/55)reportedthehighcostofHFSM,22%(12/55) reportednotknowingthatdifferentskincolorswere available,16%(9/55)saidthatatthetimeofpurchaseonly oneskintonewasavailable,and7%(4/55)statedtheydidnot thinkthathavingdifferentskincolorsmattered.Whenasked forpotentialreasonsforthelackofdiversityintermsof HFSMgender(Table3),20%ofrespondents(11/55) reportedthehighcostofHFSM,13%(7/55)statedtheydid notthinkthathavingdifferentgendersmattered,and11% (6/55)reportedthatfemalemanikinswerenotavailableatthe timeofpurchase.Inaddition,22%(12/55)ofrespondents reportedthatsomemanikingenitaliacanbealteredto representdifferentgenders;so,purchasersdidnotthinkit wasnecessarytobuymanikinsthat,genitaliaaside, representedspecificgenders.
DISCUSSION
AlthoughHFSisusedinmanyaspectsofgraduate medicaleducation,thisisthe firstpublishedstudytoour knowledgereportingtheuseofHFSMtoteachcultural humility.Additionally,thisisthe firstpublishedstudythat reportsontheskincolorandgenderdiversityofHFSMused
Gender Proporti on 0 .00.2 0 .40.60.81.0 Representative Observed MaleFemale Skin Color P r o por t ion 0.00.20.40 60.81.0 Representative Observed LightMediumDark
Figure1. Representativenessofhigh-fidelitysimulationmanikingenderandskintone.Errorbarsrepresent95%confidenceintervals.
PhenotypicappearanceofHFSM usedbyrespondentprograms TotalManikins (n = 348) Manikingender Male 242(70%) Female 106(30%) Manikinskintone Light 183(53%) Medium 130(37%) Dark 35(10%) Culturalhumilityasalearningobjectivefor HFScases(n = 55) Yes 39(71%) No 16(29%) PercentofHFScaseswithculturalhumility asaprimaryorsecondarylearningobjective (mean ± standarderroramong35 responders) 15.9(SE: ± 2.2) HFSM,
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 671 Woffordetal. DiversityofHigh-FidelitySimulationManikins
Table2. Quantitativeanalysisofhigh-fidelitysimulationmanikins (HFSM)usedbyemergencymedicineresidencyprogramswith regardtotheskintoneandgenderdiversityoftheHFSMsandtheir useinculturalhumilitytraining.
high-fidelity simulationmanikins.
Ifyounoticedthatyouhaveveryfewhighfidelity simulationmanikinswithoneskin color,whydoyoubelievethatisthecase?
extrapolationofUSCensusdata.Lastly,wefoundthatthere weresignificantlymoremale-thanfemale-genderedHFSM. ThisalsodiffersfromtheUSCensusdataofan estimated50%ofthepopulationwhoidentifyasmaleand female,respectively.14
Therearenumerouspotentialbenefitstoprogramshaving diverseHFSM.First,oneofthemainbenefitsofHFSisthe realisticnatureofthemanikins.Asimulation-basedlearning environmentshouldnotoverwhelmthelearnerwith extraneouspropsanditemsthatmaycreateaneffectof realismattheexpenseofcognitiveburden.4 Fromourown experiences,itisveryhardtostay “incharacter” whena phenotypicallymalemanikinhasapinkdressontosignify thatitisactuallyfemale.Tosimplifythelearning environmentwhileensuringrealism,itismoreappropriateto usetheactualgenderandskincolorofmanikinsratherthan addingpropssuchasadress.15
Ifyounoticedthatyouhaveveryfewhighfidelitysimulationmanikinsfromonegender, whydoyoubelievethatisthecase?
Second,asthephysicianworkforcebecomesmore diverse,soistheimportanceofinclusivity.Farondaetal foundthatdiversityinsimulationcanleadtofeelingsof inclusivityintraineesandaidsinthecreationofamore inclusivelearningenvironment. 11 Inaddition,using HFSMstoteachculturalhumilitycanpotentiallyactasa bridgetotheexplorationoftopicsrelatedtodisparitiesin carethatarerelated,amongotherthings,toreligious backgrounds,spiritualbeliefs,andtheimpactofone ’ s cultureonhealthcaredelivery.Forexample,havingdiverse HFSMmayleadtoaresidentbecomingawareofanethnic orgenderbiasthattheypossess.Perhapsaresidentmay realizethattheyassumedthatalight-skinmannequinhas highhealthliteracy.
1Freeresponsethatdidnot fitotherthemes. 2Noresponse.
byEMresidencyprograms.The findingsofthisstudy addvaluetotheadvancementofDEIinitiativesin EMtraining.
WeinvestigatedtheproportionofEMresidencyprograms thatuseHFSMstoteachculturalhumilityaswellaswhether theHFSMusedreflectedtheskincolorandgenderoftheUS population.WehypothesizedthatmostEMRPswouldnot useHFSMstoteachCHandthattheskincolorandgender breakdownoftheHFSMswouldnotberepresentativeofthe USpopulation.
OurstudyfoundthatwhilethemajorityofEMresidency programsusedHFSMtoteachculturalhumility,theskin toneandgenderbreakdownofthemanikinsuseddidnot reflecttheUSpopulation.Morespecifically,significantly, moremanikinswerefoundtobemedium-colored(38%)in comparisontoextrapolationofUSCensusdata(20%).In addition,only10%oftheHFSMhaddarkskintone comparedtothe20%oftheUSpopulationfromthe
Ultimately,webelievethatteachingculturalhumilitywith HFSMsthatreflecttheactualpatientpopulationservedisan importantsupplementtoclassroomlecturesandwillhelp EMtraineeslearnhowtointeractwithdiversepatientsand providequalityhealthcarethroughaculturallenstopatients fromdifferentvalues,beliefs,andbehaviors.
Commonthemesamongoursurveyrespondentsto explaintheskintoneandgenderdisparitybetweenHFSM andtheUSpopulationwerethattheydidnotbelievethat “havingHFSMofdifferentskincolorsorgendersmattered,” “itcoststoomuchtopurchaseHFSM” andthat “atthetime ofpurchase,diverseoptionswerenotavailable.” Atpresent, manycompaniessuchasLaerdalMedical,CAEHealth,and GaumardScientificmakemale-andfemale-genderedHFSM withvariousskin-coloroptions.These,however,haveonly recentlybeenofferedorareoflimitedavailability.11 For example,althoughsimulationmanikinshavebeenavailable formanyyears,onemajormanufacturingcompany introducedasimulationmannequinavailableinmediumand darkskintonesin2018.Inasimilarvein,anAfrican-descent upgradekitwasalsomadeavailableformanikinsin2020 throughthiscompany.Intermsofcost,theaveragepricecan rangefrom$10,000–$100,000dependingonthemodel,type,
Surveyquestion Respondents (n = 55)
Table3. Qualitativeanalysisofthemesregardingwhyhigh-fidelity simulationmanikinsdonotmatchtheUSpopulationintermsofskin toneandgender.
Coststoomuch 11(20%) Didnotknowthereweredifferentskin colorsavailable 12(22%) Didnotthinkthathavingdifferentskin colorsmattered 4(7%) Otherskincolorsnotavailableattimeof purchase 9(16%) Other1 14(25%) Missing2 5(9%)
Coststoomuch11(20%) Didnotknowthereweredifferentgenders available 2(4%) Didnotthinkthathavingdifferentgenders mattered 7(13%) Genderisinterchangeable12(22%) Femalemanikinsnotavailableattimeof purchase 6(11%) Other1 11(20%) Missing2 6(11%)
WesternJournal of EmergencyMedicine Volume24,No.4:July2023 672 DiversityofHigh-FidelitySimulationManikins Woffordetal.
andfunctionality.17 Itisimportanttonote,however,thatfor companiesthatofferdiverseHFSM,thecostisgenerallythe sameregardlessofskincolororgender.
Otherprogramstalkedaboutthecommonuseofprops, accessories,andvernaculartosimulatethefemalegender andethnicitieswithdarkskintones.Forexample,survey respondentsalsonotedusinginterchangeablegenitaliaona stereotypicallymasculineHFSMtoportrayafemale patient.Throughoutourtraining,wehavepersonallyseen theuseofAfrowigsonmanikinswithlightskintonesto portrayaBlackpatientandtheuseofpinkshirtsor “stick on ” femalegenitaliaonaHFSMwithastereotypically masculinebodytoportrayafemalepatient,thelatterof whichwerecommonlyreportedbyoursurveyrespondents. Whiletheseareacost-effectivewayto “ change ” thegender orethnicityofaHFSM,theymaypromoteharmful stereotypes.Inaddition,thesepracticesdecreasethe realismofthescenario,whichunderminesoneof themainbene fi tsofHFS:theabilitytopracticeina realisticenvironment.

Whileweacknowledgethebarriers,particularlycostand availability,toobtainingdiverseHFSM,westilladvocatefor theinvestmentindiverseHFSM.Weencourageregionaland nationalEMandsimulationsocietiestocreategrantsto provideindividualinstitutionswiththefundstoincreasethe diversityoftheirsimulationproducts.Inaddition,programs shouldbudgetandsetasidefundswithagoaltoincrease diversitywithinsimulation.Whenfundsarenotavailable,we recommendprogramsconsiderthepurchaseof interchangeable “headskins,” suchasthosebyLaerdal Medical,whichcanserveasrealisticmaskstochangetheage orskintoneoftheHFSM.18 Whilenotideal,thesearea reasonablyaffordableoptionforprogramsinterestedin acquiringmorediversesimulationmodelsatalowercost. Wheneventheseoptionsarenotavailable,programsshould considersharingresourceswithotherinstitutionswith diversesimulationproducts.
Wealsoadvocateformanufacturerstoincreasethe diversityoftheirproductofferingsbycreatingHFSMthat trulyreflectvariousgendersandethnicities(inadditionto differingbodysizes/shapesandages)ratherthanjust “merely changingthepigmentoftheskin” asonerespondentnoted.It isnotenough,however,toincreaseproductofferings.Itis
importantthatadvertisingbeconductedthroughalensof equityaswell.
Inadditiontoensuringdiversityofsimulationproducts,it isimportanttouseHFSMtoteachculturalhumility.We wereunableto findanyopen-accessHFSMscenarioswith culturalhumilityasalearninggoal.Therefore,inadditionto increasingdiversityofproducts,wealsoadvocateforthe creationofanopen-accessdatabaseofHFSMscenarios focusedonculturalhumilitythatcanbeusedbyEM residencyprograms.Onesurveyrespondentsuggestedthe useof “scenariosthatareconductedusingourtranslatorline, ifneeded,anddiscusslanguageandsocial/culturalnormsin thedebrief.”
LIMITATIONS
Thereareseverallimitationsofourstudy.First,the photographsusedinoursurveyasexamplesoflight-, medium-,anddarkskintonemanikinswereonlyfromone company(Figure2),althoughinourreviewtheywere consistentwithproductofferingsfromothercompanies.An additionallimitationwasournecessaryextrapolationofthe USCensusdataonethnicitytoskincolor.Thisinherentlycan leadtobiasbut,unfortunately,wastheonlymethodto statisticallycategorizedata.Inaddition,therewere21EM residencyprogramsthatdidnotrespondtooursurvey.There aremanypossibleexplanationsfornotresponding.TheseEM programsmaynothavehadHFSM(whichcouldimposea biasontheestimateoftheproportionofallEMprogramsthat haveHFSM),theymayhaveunfortunatelysufferedfrom “diversityfatigue,”19 ormayhavejustnothadtimeto completethesurvey.Inaddition,severalrespondentsnoted havingmanikinswithinterchangeablegenitalia.Tolimit confusion,however,weclarifiedthatsurveyresponsesshould bebasedontheoverallappearanceofthemanikin.Lastly,we alsowanttoacknowledgethatgenderwasreducedtoabinary onlytoreflectthelimitedpurchasingoptionsforHFSMs.
CONCLUSION
OurstudyfoundthatwhilemostEMresidencyprograms usedhigh-fidelitysimulationmanikinstoteachcultural humility,themanikinsuseddidnotreflecteithertheskin colororgenderproportionsoftheUSpopulation.Further studieswillexplorethevarioususesofHFStoteachcultural
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 673
Figure2. LaerdalSimMan3Ginlight,medium,anddarkskintones.
Woffordetal. DiversityofHigh-FidelitySimulationManikins
humilityandcomprehensivelyevaluatetheeffectivenessof culturalhumilitytraininginEMresidencyprograms.
AddressforCorrespondence:CortlynBrown,MD,AtriumHealth, DepartmentofEmergencyMedicine,1000BlytheBlvd,Charlotte, NC28203.Email: Cortlyn.brown@atriumhealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Woffordetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.WilsonV.PeopleofcolorwillbeamajorityoftheAmericanworkingclass in2032:Whatthismeansfortheefforttogrowwagesandreduce inequality.TheEconomicPolicyInstitute.2016.Availableat: https:// www.epi.org/publication/the-changing-demographics-of-americasworking-class/.Accessed:June30,2023.
2.Ward-GainesJ,BuchananJA,AngerhoferC,etal.Teachingemergency medicineresidentshealthequitythroughsimulationimmersion. AEM EducTrain. 2021;29(5)(Suppl1):S102–7.
3.CorsinoL,FullerAT.Educatingfordiversity,equity,andinclusion:A reviewofcommonlyusededucationalapproaches. JClinTranslSci. 2021Aug9;5(1):e169.
4.MeurlingL,HedmanL.,LidefeltK.-J.,etal.Comparisonofhigh-andlow equipment fidelityduringpaediatricsimulationteamtraining:acase controlstudy. BMCMedEduc. 2014;14:221.
5.BolingB.,Hardin-PierceM.Theeffectofhigh-fidelitysimulationon knowledgeandconfidenceincriticalcaretraining:Anintegrativereview. NurseEducPract 2016;16(1):287
93.
6.ForondaC.L.,BaptisteD.-L.,ReinholdtM.M.,etal.CulturalHumility:A ConceptAnalysis. JTranscultNurs. 2016;27(3):210–7.
7.ForondaC.L.,BaptisteD.-L.,PfaffT.,etal.CulturalCompetencyand CulturalHumilityinSimulation-BasedEducation:AnIntegrativeReview. ClinicalSimulationinNursing 2018;15:42–60.
8.ForondaC.L.,BaptisteD.-L.,OckimeyJ.AsSimpleasBlackandWhite: ThePresenceofRacialDiversityinSimulationProductAdvertisements. ClinicalSimulationinNursing 2017;13:24.
9.ForondaC.,PratherS.L.,BaptisteD.,etal.Underrepresentationof RacialDiversityinSimulation:AnInternationalStudy. NursEduc Perspect. 2020;41(3):152–6.
10.BennettC.,KhanguraS.,BrehautJ.C.,etal.ReportingGuidelinesfor SurveyResearch:AnAnalysisofPublishedGuidanceandReporting Practices. PLoSMed. 2010;8(8):e1001069.
11.ThompsonS.K.(2012).Sampling.Hoboken,NewJersey,USA:Wiley.
12.JensenE.,JonesN.,RabeM.,etal.2020U.S.PopulationMoreRacially andEthnicallyDiverseThanMeasuredin2010.2021.Availableat: https://www.census.gov/library/stories/2021/08/2020-united-statespopulation-more-racially-ethnically-diverse-than-2010.html Accesseddate:June30,2023.
13.KussO.,McLerranD.Anoteontheestimationofthemultinomiallogistic modelwithcorrelatedresponsesinSAS. CompMethsandPrgmsin Biomedicine. 2007;87(3):262–9.
14.ShermanM.,CessieS.le.Acomparisonbetweenbootstrapmethods andgeneralizedestimatingequationsforcorrelatedoutcomesin generalizedlinearmodels. CommsinStats-SimandComp. 1997;26:901–925.
15.CostiucN.HowMuchDoesaHumanPatientSimulatorCost?2021. Availableat: https://www.healthysimulation.com/30911/humanpatient-simulator-cost/.Accesseddate:June30,2023.
16.CrownoverJ.G.,HenrichsK.,OjaK.J.Mask-Ed™:Let’sGetRealWith Simulation. NurseEducator. 2022;47(2):96–101.
17.WaldonV.DiversityFatigue:Whatitisandwhyitmatters.Diversity Fatigue:Whatitisandwhyitmatters.Availableat: https://www. employerscouncil.org/resources/diversity-fatigue-what-it-is-and-whyit-matters/.Accesseddate:June30,2023.
18.MooreD.S.,McCabeG.P.,CraigB.A.(2017). Introductiontothe practiceofstatistics.USA:W.H.Freeman,MacmillanLearning.
–
WesternJournal of EmergencyMedicine Volume24,No.4:July2023 674 DiversityofHigh-FidelitySimulationManikins Woffordetal.
SocialDeterminantsofHealthScreeningatanUrbanEmergency DepartmentUrgentCareDuringCOVID-19
HaeyeonHong,MD*†
KalpanaNarayanShankar,MD,MSc,MS*†‡
AndrewThompson,MD*
PabloBuitronDeLaVega,MD§
RashmiKoul,MD*
EmilyC.ClevelandManchanda,MD,MPH*†∥
SorrayaJaiprasert,MPH*
SamanthaRoberts,MPH*
TylerPina*
EmilyAnderson¶
JessicaLin¶
GabrielleA.Jacquet,MD,MPH*†
SectionEditor:MandyHill,DrPH,MPH
*BostonMedicalCenter,DepartmentofEmergencyMedicine, Boston,Massachusetts
† BostonUniversitySchoolofMedicine,DepartmentofEmergency Medicine,Boston,Massachusetts
‡ BrighamandWomen’sHospital,DepartmentofEmergency Medicine,Boston,Massachusetts
§ BostonUniversitySchoolofMedicine,DepartmentofInternal Medicine,Boston,Massachusetts
∥ AmericanMedicalAssociation,CenterforHealthEquity,Boston, Massachusetts
¶ BostonUniversitySchoolofMedicine,Boston,Massachusetts
Submissionhistory:SubmittedSeptember30,2022;RevisionreceivedApril12,2023;AcceptedApril21,2023
ElectronicallypublishedJuly17,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59068
Introduction: Socialdeterminantsofhealth(SDoH)impactpatients’ healthoutcomes,yetscreening methodsinemergencydepartments(ED)arenotconsistentorstandardized.TheSDoH-relatedhealth disparitiesmayhavewidenedduringthecoronavirus2019(COVID-19)pandemic,especiallyamong patientswhoprimarilyreceivetheirmedicalcareinEDs.WesoughttoidentifySDoHamongEDurgent carepatientsduringtheCOVID-19pandemicatanurbansafety-nethospital,assesstheimpactofthe pandemicontheirSDoH,studythefeasibilityofSDoHscreeningandresourcereferrals,andidentify preferredmethodsofresourcereferralsandbarrierstoaccessingresources.
Methods: ResearchassistantsscreenedEDurgentcarepatientsusingavalidatedSDoHscreener, inquiringabouttheimpactofCOVID-19ontheirSDoH.Aprintedresourceguidewasprovided.Two weekslater,afollow-uptelephonesurveyassessedforbarrierstoresourceconnectionandpatients’ preferredmethodsforresourcereferrals.Thisstudywasdeemedexemptbyourinstitutional reviewboard.
Results: Ofthe418patientspresentedwithascreener,414(99.0%)patientscompletedthescreening.Of thosescreened,296(71.5%)reportedatleastoneadverseSDoH,mostcommonlyeducation(38.7%), foodinsecurity(35.3%),andemployment(31.0%).Housinginsecuritywasreportedby21.0%.Overhalfof patients(57.0%)endorsedCOVID-19affectingtheirSDoH.Duringfollow-up,156of234(67%)attempted callsweresuccessfuland36/156(23.1%)reportedattemptingtoconnectwitharesource,withmost attemptsmadeforstablehousing(11.0%)andfood(7.7%).Reasonsfornotcontactingtheprovided resourcesincludedlackoftime(37.8%)andforgettingtodoso(26.3%).Patientspreferredresourceguides tobeprinted(34.0%)andsentviatextmessagetotheirmobiledevices(25.6%).
Conclusion: ManyurgentcarepatientsofthisurbanEDreportedatleastoneadverseSDoH,the majorityofwhichwereexacerbatedbytheCOVID-19pandemic.This findingfurtheremphasizesthe needtoallocatemoreresourcestostandardizeandexpandSDoHscreeninginEDs.Additionally, hospitalsshouldincreaseavailabilityofprintedorelectronicSDoHresourceguides,resourcenavigators, andinterpretersbothduringandafterEDvisits.[WestJEmergMed.2023;24(4)675–679.]
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 675 BRIEF RESEARCH REPORT
INTRODUCTION
Background
Socialdeterminantsofhealth(SDoH)impactpatients’ healthoutcomes,1,2 yetattemptstocapturethisinformation intheemergencydepartment(ED)havenotbeenconsistent orstandardized.3
5 PriorresearchconfirmsthattheED servesaparticularlyvulnerablepopulationwithhighratesof socialneeds.6 Bylaw,emergencyphysiciansaremandatedto careforeverypatientwhoseekscarefromtheED,whether formedicalorsocialneeds,furthernecessitatingbetter understandingofpatients’ SDoH.7,8 However,mostEDs currentlyscreenforSDoHatamuchlowerratethanfor othersocialrisksincludingviolence,substanceuse,ormental health.4 In2017,anelectronichealthrecord(EHR)-based SDoHscreeningandreferralprogramwasdevelopedatour urban,safety-nethospitalfortheadultambulatorycare clinics.9 Thisprogramvalidatedascreenerassessingeight SDoHdomains:housing;food;transportation;utilities; employment;medication;dependentcare;andeducation. ApartialSDoHscreeningimplementedin2019intheadult EDatourinstitutionwaslimitedtopatientscoveredby Medicaidandthosewhowereuninsured.Withthesecriteria onlyasmallfractionoftotalEDpatientswasscreenedfor SDOH,therebymissingmanysafety-nethospitalpatients facingtenuoussocialcircumstances.
Importance
AlthoughtheEDcaresformanypatientswithsignificant socialneedsnegativelyaffectingtheirhealthoutcomes,little isknownabouttheprevalenceofunmetsocialneedsofthis patientpopulation.Additionally,thecoronavirusdisease 2019(COVID-19)pandemichaspenetratedeveryaspectof dailylifeandmaydisproportionatelyaffecttheSDoHofthe patientscaredforatsafety-nethospitals.10
GoalsofthisInvestigation
InthisstudyweaimedtounderstandtheburdenofSDoH amongEDurgentcarepatientsduringthepandemicand evaluatethefeasibilityofimplementingaSDoHscreening andastandardreferralguideprovisionintheEDurgent caresetting.
METHODS StudyDesignandSetting
Thisobservationalstudyassessedthenumberofpatients whoscreenedpositiveforadverseSDoH.Forpatientswho endorsedatleastoneadverseSDoH,thestudyassessedthe impactofCOVID-19onSDoH.Weevaluatedthefeasibility ofscreeningforSDO0HinEDurgentcarebydetermining theproportionofpatientswhoagreedtoparticipateand completedthescreeningprocess.Thedemographicsofthe participatingurgentcarepatientswerecomparedtothoseof thegeneraladultEDpatients.Thisstudywasdeemedexempt bytheourinstitutionalreviewboard.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Socialdeterminantsofhealth(SDoH) impactpatients ’ healthoutcomes,especially withthewideneddisparitiesduringthe COVID-19pandemic.
Whatwastheresearchquestion?
Weidenti fi edSDoHamongacohortof patientsinasafety-neturgentcareandthe feasibilityofSDoHscreeningandreferrals.
Whatwasthemajor findingofthestudy? Screeningfeasibilitywas99%,and71.5% reportedatleastoneSDoH,mostcommonly education(38.7%)andfood(35.3%).
Howdoesthisimprovepopulationhealth? Moreresourcesneedtobeallocatedto standardizeandexpandSDoHscreeningin theEDandtofurtheroptimizethesocial resourceprovisionprocess.
SelectionofParticipants
Aconveniencesamplewastakenbytrainedresearch assistants(RA)whoapproachedallpatients ≥18yearsoldin theEDurgentcarefor3–4hoursbetweenthepeakhoursof 8 AM–4 PM onweekdays.Participantswereexcludedifthey wereexperiencingalteredmentalstatus,hadbeenscreened withinthelastsixmonths,orifscreeningwouldinterferewith necessarymedicalcare.PatientswithlimitedEnglish proficiencywerescreenedusingaprofessional telephoneinterpreter.
Screening,Referral,andAssessments
Patientswhoagreedtoparticipatewerescreenedforeight SDoHdomains:housing;food;transportation;utilities; employment;medication;dependentcare;andeducation. Forclarificationofterminology,apositivescreeningfora SDoHdomain(ie, “ yes ” forhousinginsecurity)inthisstudy isreferredtoasanadverseSDoH.11 Patientswhoreportedat leastoneadverseSDoHwereprovidedwithaprintedreferral guidecomprisedofalistofcommunityresourcesfrequently usedbytheEDsocialworkteam.Wethenassessedpatients’ perceivedimpactofCOVID-19ontheirSDoH.Allscreening datawererecordedbothinREDCapelectronicdatacapture toolshostedatBostonUniversityMedicalCenterandinthe electronichealthrecord.Twotothreeweeksafterthe
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 676
Hongetal.
SDoHScreeningatanUrbanEDUrgentCareDuringCOVID-19
screening,RAscompletedfollow-upsurveysbytelephoneto identifypatients’ preferredmethodsofresourcereferraland anybarrierstoresourceconnectionandutilization. Amaximumof fiveattemptsforcontact(phonecallortext) weremadebeforeapatientwasdeemedlosttofollow-up.
Outcomes
Theprimaryoutcomefeaturedtheprevalenceand distributionofeightSDoHofEDurgentcarepatientsduring theCOVID-19pandemic.Thesecondaryoutcomesincluded feasibilityofSDoHscreeningandreferralinEDurgentcare, assessmentofpatient-perceivedimpactoftheCOVID-19 pandemiconSDoH,andthepreferredmethodsof resourcereferral.
Analysis
DescriptivestatisticswereobtainedusingSASv9.4(SAS InstituteInc,Cary,NC)softwareforpatientage,gender, race,ethnicity,preferredlanguage,andZIPcode.Wethen analyzedprevalenceofeachSDoHwasbydemographic usingchi-squareandFisherexacttests,andweanalyzedthe impactofCOVID-19onreportingoneadverseSDoHusing logisticregression.
RESULTS
CharacteristicsofStudySubjects
Ofthetotalestimated2018EDurgentcarepatientsduring thetimesofscreeningoverthecourseof13weeks,418 patients(20.7%)werepresentedwithascreenerviathe conveniencesamplemethod.Ofthosepresentedwitha screener,414(99.0%)patientscompletedthescreening.The participantswerepredominantlymale(229,55.3%), averaging43yearsold.Theparticipantsself-identifiedas Blacknon-Hispanic(58.7%),Hispanic(19.8%),White (16.2%),andother(Table1).Preferredlanguagesofthe participantsincludedEnglish(89.1%),Spanish(6.0%), HaitianCreole(2.2%),andother.Thepopulationcaptured inthisstudy,whencomparedtothatofthegeneralpatient populationseenintheadultEDofthishospital,wasfoundto havedifferencesincludingmoreBlacknon-Hispanic(this study58.7%vsadultED41.0%),lessHispanic(19.8%vs 26.4%),aswellasmoreEnglish-speaking(89.1vs71%), amongothers.
MainResults
Ofthosescreened,themajority(71.5%)reportedatleast oneadverseSDoH.ThemostcommonlyreportedSDoHwas interestinfurthereducation(38.7%),followedbyfood insecurity(35.3%),andunemployment(31.0%).Housing insecuritywasreportedby21.0%.Ofthosewhoreportedat leastoneadverseSDoH,83.5%requestedhelpandfurther resourcesduringthevisit.
AsfortheCOVID-19-relatedresults,atotalof236 (57.0%)patientsreportedthattheirSDoHwerenegatively
patientswhoparticipatedinsocialdeterminantsofhealthscreening.
Unknown8(2.7)2(1.69)
Asian4(1.35)4(3.39)
Other3(1.01)1(0.85)
PreferredLanguage English268(90.54)101(85.59)
Spanish16(5.41)9(7.63)
HaitianCreole7(2.36)2(1.69)
Portuguese2(0.68)0(0)
Other2(0.68)3(2.54)
CapeVerdeanCreole1(0.34)3(2.54) SDoH,socialdeterminantsofhealth.
impactedbythepandemic.WithineachcategoryofSDoH, caregivingfortheelderlyandchildrenwasmostlikelyto havebeennegativelyimpactedbythepandemic(86%), followedbyemployment(84%)andpayingformedication (84%)(Table2).
AsforthefeasibilityoftheSDoHscreening,thereported timetakenfromrecruitingapatienttocompletingthe screeningrangedfrom5–10minutes.Almostallpatients (414/418,99%)completedthescreeningwhenapproachedby trainedRAs.Ofthe234attemptedfollow-upcalls,156(67%) patientsweresuccessfullyreachedduringfollow-upphone calls.Ofthose,36(23.1%)reportedattemptingtoconnect witharesource,withmostattemptsmadeforhousing (11.0%)andfood(7.7%).Reasonsfornotcontactingthe providedresourcesincludedlackoftime(37.8%)and forgettingtodoso(26.3%).Patientspreferredresource guidestobeprinted(34.0%),sentviatextmessagetotheir mobiledevices(25.6%),andexplainedinpersonbya resourcenavigator(23.1%).
Demographic Information AdverseSDoH, n(%) NoAdverse SDoH,n(%) Agen = 296n = 118 18–
–
Male167(56.4)62(52.4)
Table1. Demographicsoftheemergencydepartmenturgentcare
35106(35.81)39(33.05) 36–5097(32.77)36(30.51) 51–6580(27.03)37(31.36) 66
7512(4.05)5(4.24) 75–801(0.34)1(0.85) Gender
Female129(43.6)56(47.5)
Raceandethnicity BlackNon-Hispanic174(58.78)69(58.47) Hispanic/Latino56(18.92)26(22.03) WhiteNon-Hispanic51(17.23)16(13.56)
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 677 Hongetal. SDoHScreeningatanUrbanEDUrgentCareDuringCOVID-19
DISCUSSION
Thisstudysupportsthehypothesisthatmanypatientsof thisurban,safety-nethospital’sEDurgentcarehavenotable adverseSDoH,therebysignifyingamuch-neededcontinued effortinimplementinguniversalSDoHscreeninginED urgentcaresettings.MorethanhalfofallscreenedEDurgent carepatientsendorsedCOVID-19’simpactontheirSDoH, sheddinglightonthetangibletollthepandemichastakenon thispatientpopulation.Whenadedicated,trainedstaff memberapproachespatients,theSDoHscreeningprocess wasshowntobefeasible.However,thefollow-upsurvey revealsacleardiscrepancybetweenreferralguideprovision andpatients’ likelihoodtoconnectwitharesource. Toaddressthisgap,departmentsshouldincrease availabilityofprintedorelectronicSDoHresourceguides andconsiderengagingresourcenavigatorswithinterpreter servicesbothduringandafterEDvisits.Nextstepsinthis endeavorincludeoptimizingthetimepointofscreening (triage,waitingroom,patientroom),moretrainingofRAsto minimizebiasandimproverapport,anddecidingwho
shouldperformthescreeningforpracticalityandefficiencyin theED.Anothernextstepistoconsiderdigitalscreening tools(tablet,computerkiosk),aspriorstudieshaveshown feasibilityandacceptabilityofdigitalscreeningfor socialrisk.12,13
LIMITATIONS
Limitationsofthisstudyincludethelackof randomizationandpotentialbiasintheselectionof conveniencesamplesinEDurgentcarebetweenthehoursof 8 AM–4 PM.Giventhatpatientswhofrequentlyvisitthe generaladultEDofthissafety-nethospitalduringevening hoursanecdotallyhavehigherratesofhousingandfood insecurity,anddifferentillnessacuity,thefactthattheywere notincludedintheurgentcarestudymeanswemayhave underestimatedtheprevalenceofcertainSDoH;itmayalso explainthedifferenceinrace,ethnicityandpreferred languagesseeninthiscohortwhencomparedtothegeneral adultEDpopulation.Thislimitstheapplicabilityofour
findingstothegeneralpopulation.
SocialDeterminantofHealthDomain(SDoH)AdverseSDoH,n(%)NoAdverseSDoH,n(%) P-value Educationn = 160n = 254 COVID-19Impacted 111(69.38)125(49.21) <.0001 COVID-19notimpacted 49(30.63)129(50.79) Foodn = 146n = 268 COVID-19impacted 117(80.14)119(44.40) <.0001 COVID-19notimpacted 29(19.86)149(55.60) Employmentn = 128n = 286 COVID-19impacted 107(83.59)129(45.10) <.0001 COVID-19notimpacted 21(16.41)157(54.90) Utilitiesn = 96n = 318 COVID-19impacted 77(80.21)159(50.00) <.0001 COVID-19notimpacted 19(19.79)159(50.00) LivingSituationn = 85n = 329 COVID-19impacted 69(81.18)167(50.76) <.0001 COVID-19notimpacted 16(18.82)162(49.24) Transportationn = 83n = 331 COVID-19impacted 65(78.31)171(51.66) <.0001 COVID-19notimpacted 18(21.69)160(48.34) Medicinesn = 74n = 340 COVID-19impacted 62(83.78)174(51.18) <.0001 COVID-19notimpacted 12(16.22)166(48.82) Caregivingn = 37n = 377 COVID-19impacted 32(86.49)204(54.11) <.0001 COVID-19notImpacted 5(13.51)173(45.89) COVID-19,coronavirus2019. WesternJournal of EmergencyMedicineVolume24,No.4:July2023 678 SDoHScreeningatanUrbanEDUrgentCareDuringCOVID-19 Hongetal.
Table2. EffectofCOVID-19pandemiconeachsocialdeterminantofhealthdomain.
CONCLUSION
ManyEDurgentcarepatientsinthisstudyreportedat leastoneadversesocialdeterminantofhealth,themajorityof whichwereexacerbatedbytheCOVID-19pandemic. Hospitalsshouldfactorinthe findingsofthisstudyasthey prepareforthenegativesocialimpactsfromtheCOVID-19 pandemic,highlightingtheneedtoallocatemoreresourcesto standardizeandexpandSDoHscreeninginEDsandto increaseavailabilityofprintedorelectronicSDoHresource guides,resourcenavigators,andinterpretersbothduringand afterEDvisits.
AddressforCorrespondence:HaeyeonHong,MD,BostonMedical Center,DepartmentofEmergencyMedicine,800HarrisonAvenue, BCDbuilding,Boston,MA02118.Email: haeyeon.hong@bmc.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Hongetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.BravemanP,GottliebL.Thesocialdeterminantsofhealth: It’stimetoconsiderthecausesofthecauses. PublicHealthRep 2014;129(1_suppl2):19–31.
2.GaleaS,TracyM,HoggattKJ,etal.Estimateddeathsattributableto socialfactorsintheUnitedStates. AmJPublicHealth 2011;101(8):1456–65.
3.WallaceAS,LutherB,GuoJW,etal.Implementingasocial determinantsscreeningandreferralinfrastructureduringroutine emergencydepartmentvisits,Utah,2017–2018. PrevChronicDis 2020;17:190339.
4.Samuels-KalowME,BoggsKM,CashRE,etal.Screeningforhealthrelatedsocialneedsofemergencydepartmentpatients. AnnEmerg Med.2021;77(1):62–8.
5.CullenD,WoodfordA,FeinJ.Foodforthought:arandomizedtrialof foodinsecurityscreeningintheemergencydepartment. AcadPediatr 2019;19(6):646–51.
6.MalechaPW,WilliamsJH,KunzlerNM,etal.Materialneedsof emergencydepartmentpatients:asystematicreview.AsherSL,ed. AcadEmergMed. 2018;25(3):330–59.
7.GordonJA.Thehospitalemergencydepartmentasasocialwelfare institution. AnnEmergMed.1999;33(3):321–5.
8.AndersonE,LippertS,NewberryJ,etal.Addressingsocial determinantsofhealthfromtheemergencydepartmentthroughsocial emergencymedicine. WestJEmergMed.2016;17(4):487–9.
9.BuitrondelaVegaP,LosiS,SpragueMartinezL,etal.Implementing anEHR-basedscreeningandreferralsystemtoaddresssocial determinantsofhealthinprimarycare. MedCare. 2019;57Suppl6Suppl2:S133–9.
10.MurrayE,RooseveltGE,VogelJA.Screeningforhealth-relatedsocial needsintheemergencydepartment:adaptabilityand fidelityduringthe COVID-19pandemic. AmJEmergMed. 2022;54:323.e1–4.
11.Samuels-KalowME,CiccoloGE,LinMP,etal.Theterminologyof socialemergencymedicine:measuringsocialdeterminantsofhealth, socialrisk,andsocialneed. JAmCollEmergPhysiciansOpen 2020;1(5):852–6.
12.KocielnikR,AgapieE,ArgyleA,etal.HarborBot:achatbot forsocialneedsscreening. AMIAAnnuSympProc 2019;552–61.
13.HassanA,SchererEA,PikcilingisA,etal.Improvingsocial determinantsofhealth. AmJPrevMed.2015;49(6):822–31.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 679 Hongetal. SDoHScreeningatanUrbanEDUrgentCareDuringCOVID-19
POPULATION HEALTHAND SOCIAL EMERGENCY MEDICINE
ANationalSnapshotofSocialDeterminantsofHealth DocumentationinEmergencyDepartments
CaitlinR.Ryus,MD,MPH* AlexanderT.Janke,MD*§ RachelL.Granovsky,MSc† MichaelA.Granovsky,MD‡
*YaleSchoolofMedicine,DepartmentofEmergencyMedicine,NewHaven, Connecticut
† UniversityofCaliforniaSanFrancisco,InstituteforHealthandAging,SanFrancisco, California
‡ LogixHealth,Bedford,Massachusetts
§ VAHSR&DCenterfortheStudyofHealthcareInnovation,Implementation, &Policy/InstituteforHealthcarePolicyandInnovation,UniversityofMichigan, AnnArbor,Michigan
SectionEditor: EmilyClevelandManchanda,MD,MPH
Submissionhistory:SubmittedJuly26,2022;RevisionreceivedApril17,2023;AcceptedApril28,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58149
Introduction: Documentationandmeasurementofsocialdeterminantsofhealth(SDoH)arecriticalto clinicalcareandtohealthcaredeliverysystemreformstargetinghealthequity.TheSDoHarecodifiedin the InternationalClassificationofDisease10th Rev (ICD-10)Zcodes.However,Zcodesarelistedinonly 1-2%ofinpatientcharts.LittleisknownaboutthefrequencyofZcodeutilizationspecificallyamong emergencydepartment(ED)patientpopulationsnationally.
Methods: Thiswasarepeatedcross-sectionalanalysisofEDvisitdataintheUnitedStatesfromthe NationwideEmergencyDepartmentSamplefrom2016–2019.WecharacterizedtheuseofZcodesand describedassociationsbetweenZcodeuseandpatient-andhospital-levelfactorsincludingthefollowing: age;gender;race;insurancestatus;EDdisposition;EDsize;hospitalurban-ruralstatus;ownership;and clinicalconditions.WecalculatedunadjustedoddsratiosforlikelihoodofZcodereportingforeachEDvisit.
Results: Ofapproximately140millionEDvisitsperyear,0.65%hadanassociatedZcodein2016,rising to1.17%by2019.VisitsweremorelikelytohaveanassociatedZcodeforadultsage <65,male,Black, Medicaidorself-paypatients,andpatientsadmittedtothehospital.LargerEDs,thoseinmetropolitan areas,academiccenters,andgovernment-runhospitalsweremorelikelytoreportZcodes.Themost commonlyassociatedclinicalconditionswereasfollows:schizophreniaspectrumandotherpsychotic disorders;depressivedisorder;andalcohol-relateddisorders.
Conclusion: ThereisapaucityofZcodedocumentationinthehealthrecordsofEDpatients,although useisuptrending.Furtherresearchiswarrantedtobetterunderstandthedriversofclinicians’ useof Zcodesandtoimproveontheirutility.[WestJEmergMed.2023;24(4)680–684.]
INTRODUCTION
Documentationandmeasurementofsocialdeterminantsof health(SDoH)arecriticaltohigh-qualityclinicalcare, populationhealthresearch,andtohealthcaredeliverysystem reformstargetinghealthequity.In2014,theInstituteof Medicinerecommendedthatsocialandbehavioraldomainsbe incorporatedintopatients’ electronichealthrecords.In2015,
thesedomainswerecodifiedinthe InternationalClassi fi cation ofDisease,TenthRev (ICD-10)Zcodes,designating “health hazardsrelatedtosocioeconomicandpsychosocial circumstance” inclusiveofinadequatehousing,unemployment, educationandliteracy,socialenvironment,and financial instability.TheICD-10,whichisusedbyallmembernationsof theWorldHealthOrganization,istranslatedinto43languages
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 680
andservesasthebasisforreportinghealthstatus,mortality,and medicalreimbursements.1 TheubiquitoususeofICD-10codes makestheZcodesalogicalmechanismfordocumentationand datacollectiononSDoH.2
DocumentationofZcodeshasincreasedsincetheir introductioninOctober2015.3 However,despitethisincrease, priorstudieshaveshownthatZcodesarelistedinonly1–2%of inpatientcharts identifyingamuchsmallerpopulationthan incorrespondingpopulation-levelstatisticsforhomelessness, unemployment,andloweducationalattainment.3
Ahighprevalenceofsocialvulnerabilityamongemergency department(ED)patients4 demandsaccuratedocumentation ofSDoH.Theexistingliteraturehasfocusedprimarilyon inpatientsamples,singlehealthcaresystems,orstates.The frequencyofZcodeusespecificallyamongEDpatient populationsinanationalsamplehasnotbeenexamined. Inthiswork,wedescribethefrequencyofICD-10Zcode documentationinEDchartsusingtheNationwideEmergency DepartmentSample(NEDS).5 Weexaminepatient-and hospital-levelcharacteristicsassociatedwithdocumentation ofZcodesinEDsintheUnitedStatesfrom2016
2019.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Zcodesforsocialdeterminantsofhealth (SDoH)aredocumentedinonly1–2%of charts identifyingamuchsmaller populationthanincorrespondingpopulationlevelstatistics.
Whatwastheresearchquestion?
HowfrequentlyareZcodesdocumentedin EDvisits?Whatcharacteristicsareassociated withtheiruse?
Whatwasthemajor fi ndingofthestudy?
WhiledocumentationofZcodesforEDvisits isinfrequent,ithasincreasedfrom0.65%of EDvisitsin2016to1.17%by2019.
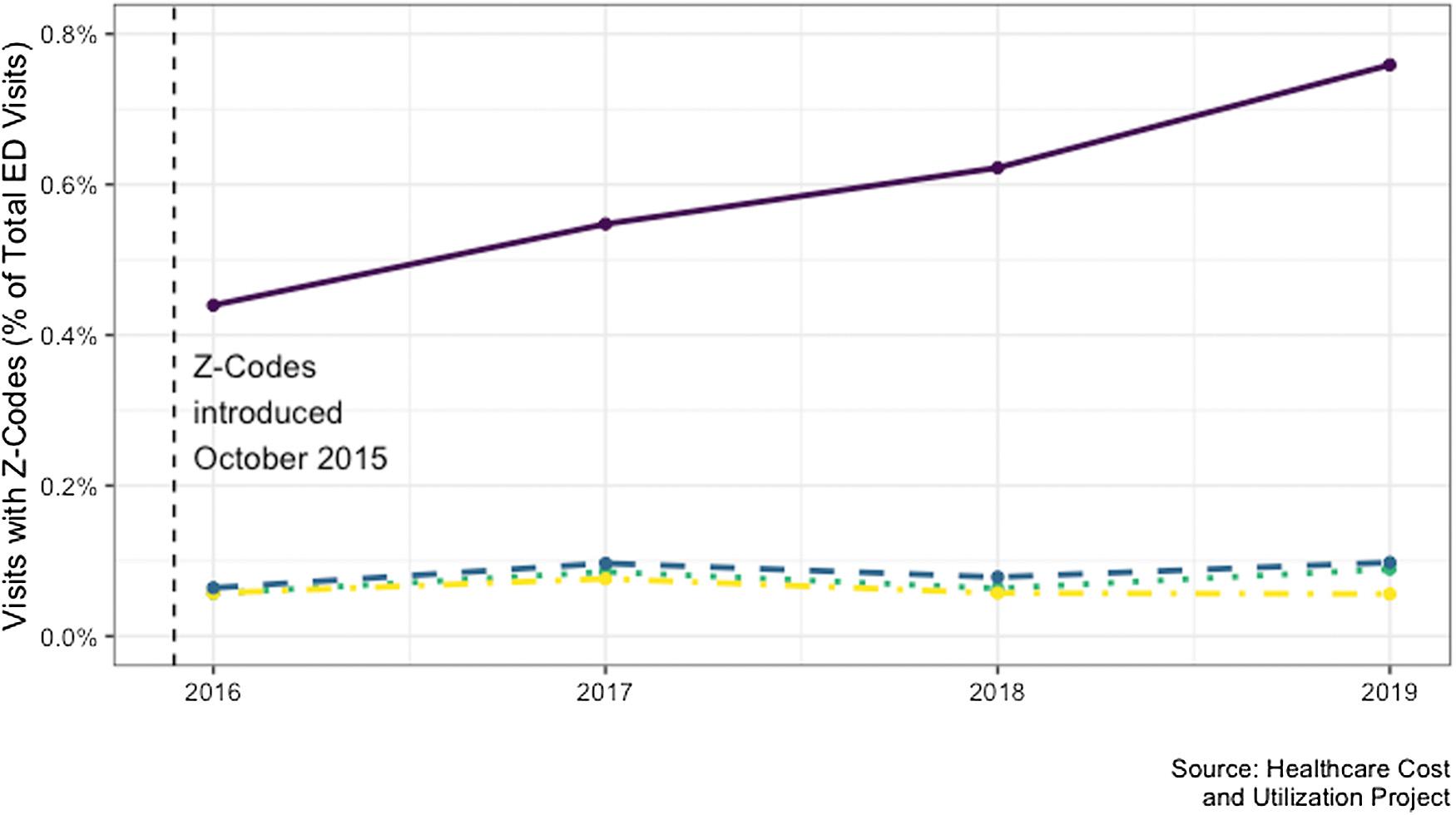
Howdoesthisimprovepopulationhealth?
METHODS
Thiswasarepeatedcross-sectionalanalysisofEDvisit dataintheUSfromNEDSfrom2016
2019.5 TheNEDS, whichisthelargestall-payersclaimsdatasetrepresenting 900+ EDsacrosstheUS,employscomplexsurveyweights designedtoprovidereliableestimatesfornationwideED visittrends.WecharacterizedZcodeuseanddescribed associationsbetweentheuseofZcodesandpatient-and hospital-levelfactors.Variablesincludedwereage,gender, race,insurancestatus,EDdisposition,EDsize,hospital urban-ruralstatus,ownership,andUSCensusRegion.We calculatedunadjustedoddsratiosforlikelihoodofZcode reportingforeachEDvisit.Additionally,weexaminedthe
Thehighprevalenceofsocialvulnerability amongEDpatientsdemandsaccurate documentationofSDoHtoaddressdriversof healthinequity.
mostcommonclinicalconditions,accordingtoClinical ClassificationsSoftwareRefined(CCSR)codes,associated withpatientencountersthathadatleastoneZcode documented.TheCCSRaggregatesICD-10diagnosiscodes into530categoriesforclinicalconditions.Surveyweights wereimplementedfornationallyrepresentativeestimates,
–
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 681 Ryusetal. SocialDeterminantsofHealthDocumentationinEDs
Figure1. Documentationofsocialdeterminantsofhealthamongemergencydepartmentvisitsnationwide.
andstandarderrorswereadjustedforcomplexsampling design.AllanalyseswereperformedinR4.0.2 (RFoundationforStatisticalComputing,Vienna,Austria).
RESULTS
Oftheapproximately140millionEDvisitsineachyear, 0.65%hadanassociatedZcodein2016,risingto1.17%by 2019.Themostreportedcategorywas “problemswith housingandeconomiccircumstances,” anduseofthiscode grewprecipitouslyfrom2016to2019(from0.44%to0.78%) (Figure1).
VisitsweremorelikelytohaveanassociatedZcodefor adultsaged41–64comparedtoaged19–25,malecompared tofemalepatients,thosewhoidentifiedtheirraceasBlackor NativeAmericancomparedtothosewhoidentifiedWhite, thosewithMedicaidorself-paycomparedtoprivate insurance,andthosewhowereadmittedtothehospital (Table1).Examinationofhospital-levelcharacteristics showedtheZcodesweremorelikelytobeusedatlargerEDs withmorethan80,000annualvisitscomparedtosmaller EDswithfewerthan20,000visits,andacademiccompared tonon-teachinghospitals.Zcodeswerelesslikelytobeused athospitalsinmicropolitanandsmallmetropolitanareas comparedtolargemetropolitanareas,andnot-for-profitand investor-ownedhospitalscomparedtogovernment-run hospitals(Table1).Themostcommonlyassociatedclinical conditionswereasfollows:schizophreniaspectrumand otherpsychoticdisorders(3,747;7.4%);depressivedisorder (3,521;6.9%);andalcohol-relateddisorders(,479,6.9%) (Table2).
DISCUSSION
Our findingsdemonstratethepaucityofZcode documentation3 specificallyamongEDpatients,although theuseofZcodesisgenerallyuptrending.Nearlyallthe growthinZcodeuseisattributableto “issuesrelatedto housingandeconomiccircumstances.” Zcodesaremore likelytobeusedinEDsatlarger,urban,teachinghospitals andamongadultsage <65,male,Black,Medicaidrecipient, oruninsured.Previousstudiesoninpatientsampleshave similarlyfoundthathospitalsthatuseZcodesaremorelikely tobelarger,private,not-forprofit,urban,teachinghospitals andthatpatientsaremorelikelytobemale,Medicaid recipients,oruninsured.6,7 Theclinicalconditionsmost associatedwithZcodeuseinEDswerepsychiatric-and substanceuse-relatedcodes.Thisissimilartopreviouswork oninpatientsamplesthatshowedadmissionsformental healthandsubstanceusedisordersaremorelikelytoinclude Zcodes.3,6,7 Despitetheuniquelyhighprevalenceofsocial vulnerabilityamongEDpatients,thedocumentationofZ codesintheEDappearstofollowapatternsimilarto inpatientZcodedocumentation.
Visit-levelcharacteristics Primarypayer(insurancestatus) Privateinsurance(ref) Medicaid4.23[3.79–4.72] Medicare2.53[2.28–2.81] Self-pay3.83[3.38–4.34] Other3.86[2.49–5.99] Gender Female(ref) Male2.21[2.09–2.33] Race White(ref) Black1.26[1.11–1.44] Hispanic0.72[0.63–0.82] NativeAmerican1.53[1.11–2.10] Asian/PacificIslander0.60[0.50–0.72] Other0.98[0.78–1.23] Age 0–180.39[0.34–0.45] 19–25(ref) 26–321.55[1.47–1.64] 33–401.91[1.79–2.03] 41–642.20[2.05–2.37] 65-0.69[0.62–0.76] Admission 3.89[3.48–4.35] Hospital-levelcharacteristics Region Northeast1.17[0.87–1.59] Midwest(ref) South1.03[0.75–1.41] West2.29[1.72–3.04] Urban/RuralDesignation Largemetropolitan(ref) Smallmetropolitan0.79[0.64–0.98] Micropolitan0.33[0.26–0.42] Hospitalcontrol Government* –Private,not-for-profit0.56[0.41–0.78] Private,investor-owned0.57[0.38–0.85] Teachingstatus Metropolitanteaching1.69[1.39–2.06] Metropolitannon-teaching(ref) (Continuedonnextpage) WesternJournal of EmergencyMedicineVolume24,No.4:July2023 682 SocialDeterminantsofHealthDocumentationinEDs Ryusetal.
Table1. FactorsassociatedwithuseofZcodes.
UnadjustedORs
UnadjustedORs
LIMITATIONS
Binarylogisticregressionmodelswereestimatedusingthe NationwideEmergencyDepartmentSample2019datawith adjustmentforweightingandcomplexsampledesignandwith standarderrorsclusteredbyhospital. ORs,oddsratios; ref,referencecategory; ED,emergencydepartment.
Thisrepeatedcross-sectionalanalysisofNEDShas multiplelimitations.First,theabsenceofadocumented Zcodeforapatientencounterdoesnotnecessarilymean therewasnodocumentationofSDoHelsewhereinthe patient’shealthrecord.However,suchgranulardatawas unavailable.Furthermore,inthisanalysiswewereunableto characterizehowstronglythemedicaldecision-makingfor theclinicalencounterwasrelatedtotheSDoHdocumented intheZcodes.Finally,astherewerenoclinicalorpatientorientedoutcomes,wewereunabletocommentofthe associationsamongdocumentingSDoH,clinicalcare, andoutcomes.
CONCLUSION
TheEDshouldplayacriticalroleinmonitoringand respondingtoevolvinghealthdisparitiesbyservingasa bellwetherforshiftsinlocalsocioeconomiclandscapes, analogoustosyndromicsurveillancesystemswhereED documentationisusedtotrackshiftinginfectiousdisease burden.10 InthisstudywefoundthatdocumentationofZ codesforEDvisitsisinfrequentbuthasincreasedfrom 0.65%ofEDvisitsin2016to1.17%by2019.Further researchiswarrantedtobetterunderstandthedriversof clinicians’ useofZcodesandtoimproveontheirutility. Emergencydepartmentsareuniquelypositionedwithinthe houseofmedicineandthesocialsafetynettoidentifyand addresssocialdeterminantsofhealth.Onlybyimproved measurementcanwebegintocraftpolicysolutionsto addresstheseimportantdriversofhealthinequity.
AddressforCorrespondence:CaitlinR.Ryus,MD,MPH,Yale SchoolofMedicine,464CongressAveSuite260,NewHaven,CT, 06519.Email: Caitlin.Ryus@yale.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
PriorstudieshaveproposedthatlowratesofZcodeuse arerelatedtoclinicianuncertaintyonZcoderelevancetoa givenmedicalencounter,ambiguityinZcodesthemselves, andalackofsystematizedconnectionstoclinicalscreening instrumentsandactivities.8 ConnectingSDoHtobilling structuresandpaymentmodelsmayaddresssomeofthese barrierstodocumentationandmoresubstantivelyaddress theneedsofpatientswithhighsocialacuity.8 Future implementationmustalsobesensitivetotheriskof incorporatingstigmatizinglanguageorcodifyingstereotypes withinthemedicalrecord.9
Copyright:©2023Ryusetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.WorldHealthOrganization.FrequentlyAskedQuestionsforICD-11. Availableat: https://www.who.int/standards/classifications/ frequently-asked-questions.AccessedApril11,2023.
2.JacobsZG.Codifyingsocialdeterminantsofhealth:agapinthe ICD-10-CM. JGenInternMed.2021;36(10):3205–07.
CountPercentCumulative Schizophreniaspectrumand otherpsychoticdisorders 3,7477.4%7.4% Depressivedisorders3,5216.9%14.3% Alcohol-userelateddisorders3,4796.9%21.2% Suicidalideation/attempt/ intentionalself-harm 1,9443.8%25.0% Bipolarandrelateddisorders1,5383.0%28.0% Musculoskeletalpain,notlow backpain 1,4772.9%30.9% Skinandsubcutaneoustissue infections 1,4622.9%33.8% Septicemia1,3182.6%36.4% Nonspecificchestpain1,2122.4%38.8% Diabetesmellituswith complication 1,0482.1%40.9% Trauma-andstressor-related disorders 9751.9%42.8% Stimulant-userelateddisorders9721.9%44.7%
Table2. MostcommonlyassociatedprimaryClinicalClassifications SoftwareRefinedcodesamongpatientswithanycodeforsocial determinantsofhealth.
Table1.
Continued.
TotalEDvisits <20,000(ref) 20–40,0001.44[0.92–2.24] 40–60,0001.72[1.09–2.72] 60–80,0001.75[1.10–2.77] 80,000+ 2.06[1.30–3.24]
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 683 Ryusetal. SocialDeterminantsofHealthDocumentationinEDs
3.GuoY,ChenZ,XuK,etal.InternationalClassificationofDiseases, TenthRevision,ClinicalModificationsocialdeterminantsofhealth codesarepoorlyusedinelectronichealthrecords. WestJEmergMed 2020;99(52).
4.MolinaMF,LiCN,ManchandaEC,etal.Prevalenceofemergency departmentsocialriskandsocialneeds. WJEmergMed 2020;21(6):152.
5.HCUPNationwideEmergencyDepartmentSample(NEDS).Healthcare CostandUtilizationProject(HCUP).2017,2018,2019.In.Agencyfor HealthcareResearchandQuality,Rockville,MD.
6.TruongHP,LukeAA,HammondG,etal.Utilizationofsocial determinantsofhealthICD-10Z-codesamonghospitalizedpatientsin theUnitedStates,2016-2017. Medcare.2020;58(12):1037.
7.WeeksWB,CaoSY,LesterCM,etal.UseofZ-codestorecordsocial determinantsofhealthamongfee-for-serviceMedicarebeneficiariesin 2017. JGenInternMed.2020;35(3):952–5.
8.GottliebL,TobeyR,CantorJ,etal.Integratingsocialandmedicaldata toimprovepopulationhealth:opportunitiesandbarriers. HealthAffairs 2016;35(11):2116–23.
9.ParkJ,SahaS,CheeB,etal.Physicianuseofstigmatizing languageinpatientmedicalrecords. JAMANetworkOpen 2021;4(7):e2117052–e2117052.
10.HughesHE,EdeghereO,O’BrienSJ,etal.Emergencydepartment syndromicsurveillancesystems:asystematicreview. BMCPublic Health.2020;20(1):1–15.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 684 SocialDeterminantsofHealthDocumentationinEDs Ryusetal.
AReal-WorldExperience:RetrospectiveReviewofPoint-of-Care
UltrasoundUtilizationandQualityinCommunity EmergencyDepartments
CourtneyM.Smalley,MD*†
*ClevelandClinicHealthSystem,EmergencyServicesInstitute,Cleveland,Ohio
ErinL.Simon,DO
ठMcKinseyR.Muir,MHSA*
BaruchS.Fertel,MD,MPA∥
SectionEditor
† ClevelandClinicLernerCollegeofMedicineofCaseWesternReserveUniversity, Cleveland,Ohio
‡ ClevelandClinicAkronGeneral,DepartmentofEmergencyMedicine,Akron,Ohio
§ NortheastOhioMedicalUniversity,Rootstown,Ohio
∥ ColumbiaUniversityVagelosCollegeofPhysiciansandSurgeons,Departmentof EmergencyMedicine,NewYork,NewYork
:MarkI.Langdorf,MD,MHPE
Submissionhistory:SubmittedSeptember22,2022;RevisionreceivedFebruary24,2023;AcceptedFebruary24,2023
ElectronicallypublishedJune30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58965
Introduction: Point-of-careultrasound(POCUS)iscommonlyusedintheemergencydepartment(ED) asarapiddiagnostictool.Emergencymedicine(EM)hasbeenanearlyadopterofPOCUSwith indicationsexpandingoverthelast10years.Whiletheliteraturedescribeswidespreaduseamong academicsites,thereislittledataonclinicalPOCUSutilizationatnon-academicEDs.Wesoughtto describecommunityemergencyphysician(EP)useofPOCUSbyquantifyingthenumberandtypeof studiesperformed,characteristicsoftheperformingphysician,andqualitymetrics.
Methods: Priortothestudyperiod,allEPsunderwentastandardizedtrainingandcredentialingprogram. AretrospectivereviewofallPOCUSstudiesacross11non-academicEDsfromOctober1, 2018–September30,2020wasperformedbyfellowship-trainedphysicians,whoidentifiedphysician, examtype,andresidencygraduationyear.Thestudieswerethencross-referencedwithqualityreview reportsthatassessedimageacquisition,imageinterpretation,andimagelabeling.Weperformed descriptivestatistics.
Results: Duringthestudyperiod,5,099POCUSstudieswereperformedby170EPs.Examsmost frequentlyperformedwerecardiac(24%),focusedassessmentofsonographyintrauma(21.7%),and pregnancy(16.2%).RecentEMresidencygraduates(<10years)werehigherutilizersofPOCUSwitha groupmeanof1.3examsper100patients.Ofthestudiesdone,86%hadnoqualityissues.
Conclusion: CommunityPOCUSdemonstratesaheavyfocusoncoreexamsperformedbyrecentEM residencygraduateswithminimalqualityissuesafterastandardizedtrainingprogram.Thisstudyisthe firsttoquantifyactualcommunityPOCUSuseinmultipleEDsandmayimpactcredentialingandskills maintenancerequirements.[WestJEmergMed.2023;24(4)685–692.]
INTRODUCTION
Point-of-careultrasound(POCUS)useinbedsidepatient careisgrowingexponentiallyamongmultiplemedical specialtiesandisacommonmodalityusedbyemergency physicians(EP).1–4 Inemergencymedicine(EM),POCUS
hasbeenconsideredavaluabletoolatthebedsidesincewell before2009,whentheAmericanCollegeofEmergency Physicians(ACEP)adoptedguidelinesrecommending formalresidencytraininginPOCUS.1,5,6 TraineesinEMare thusgraduatingwithextensiveexperienceinPOCUS,
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 685 ORIGINAL RESEARCH
andthefrequencyofuseinclinicalpracticehas grown.
Whiletheliteraturedescribesthewidespreaduseof POCUSamongacademicemergencydepartments(ED)and anexpandingrepertoireofnovelindications,thereislittle dataonclinicaluseamongcommunityEPsinlocations withoutresidency-orfellowship-trainingprograms.Ina 2011studyinwhichEMprogramdirectorsweresurveyed, researchersfoundthatgreaterthanhalfofgraduating residents(57.1%)pursuedcareersdirectlyinthecommunity aftergraduation.7 Anotherstudyin2019confirmedthis finding,reportingthat63%ofresidencygraduatesfroma 10-yearcohortacceptednon-academic,communityEM positions.8 Academicphysiciansareeagertoexpand POCUS.Asitbecomesmorefrequentlyused,itisessentialto examinetheuseofthismodalityincommunityEMsettings. Inaddition,itisimportanttodeterminecurrentuseof POCUS,thefactorsthataffectitsuse,andpotentialquality issuessincemostEPsworkinnon-academicsettings.This mayhelpguidetheimplementationoftrainingandquality programsforcommunityPOCUSandidentifyfuture trainingneeds,credentialing,skillsmaintenance, infrastructure,andresourcesasPOCUSexpandsacross multiplespecialtiesandamongpractitionersofvarious traininglevels.
ForavarietyofreasonsPOCUShasbeenenthusiastically adoptedinacademicsettings,includingtheembracingofa noveltechnique,thepresenceoftrainees,EDcrowding, limitedavailabilityofradiology-basedultrasoundorother imaging,andtheabilitytomakearapidbedsidediagnosis.It isunclearwhetheracommunitysettingwithitsassociated demandsontheclinicians,aswellaspotentiallymore resources,wouldengenderwidespreadadoptionofPOCUS.
Inourhealthcaresystem,multiplecommunityEDshave POCUSreadilyavailabletoEPs.TostandardizethePOCUS programacrossmultiplesitesinthecommunityandestablish areliablequalityassurance(QA)program,asystemwide POCUScredentialingprogramwasdevelopedtoassessthe privilegesofEPsbetweenJanuary1,2017–July1,2018. Duringthisperiod,allacademic,urban,suburban,and freestandingEDswerestandardizedininformation technologyworkflow,machinepurchasing,privileges, credentialing,coding/billing,andQAreview.9 Thisallowed ourphysicianstomovefromEDtoEDwithoutany significantworkfloworprivilegingchangesandensuredthe samelevelofqualityacrossmultipledepartments(high reliability).AformalQAprogramwasestablishedattheend ofthisperiod.
InthisstudyourobjectivewastoreviewactualPOCUS useamongcommunityEPsinalargehealthcaresystemafter implementingastandardizedcredentialingprogram.We assessedthetypesofstudiesperformed,demographicdataof physicians,numberofyearssinceresidencygraduation, numberofstudiesperformedper100patients,andquality
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Point-of-careultrasound(POCUS)is commonlyusedinacademicEDsasa diagnostictool.
Whatwastheresearchquestion?
WhatisthescopeofPOCUSuseby communityemergencyphysicians,bythe quanti fi ednumberandexamtypes,physician characteristics,andqualitymetrics?
Whatwasthemajor findingofthestudy?
Mostcommonexamsperformedwere cardiac,FAST,andpregnancy.Recent residencycompletionwasassociatedwith higherPOCUSuse;86%ofstudieshadno qualityissues.
Howdoesthisimprovepopulationhealth?
Thisstudymayhelpguideimplementationof trainingandqualityprogramsforcommunity POCUSandidentifyfuturetrainingneeds, credentialing,andinfrastructure.
metricsofPOCUSstudies.Inaddition,weaimedto determinethefrequencyofstudies,themost-usedexams,the effectofresidencygraduationyearonuse,andwhether qualityissuesexistinthecommunity,non-academicsetting.
METHODS StudyDesign
Thisretrospective,multicenterstudyinvolved11EDs acrossalarge,integratedhealthcaresysteminwhichall hospitalsarelocatedwithinonestate.Thisstudywas implementedaspartofaPOCUSqualityimprovement projectforthehealthcaresystemandwasinstitutionalreview boardapprovedasexempt.
DescriptionofCredentialingProgramPriortoIntervention Period
Toobtainhighqualitydataoncommunityusageand qualitymeasures,weperformedthestudyaftera standardizedPOCUSprogramwasimplementedacrossEDs inthesystem,asdescribedinapreviouspaper.9 Briefly,this POCUScredentialinginitiativewasimplementedfrom January1,201–July1,2018across fiveurbancommunity EDs,threesuburbancommunityEDs,andthree freestandingEDswithacombinedtotalof >500,000patient encountersperyear.Priortothebeginningofthisprogram,
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 686
RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs Smalleyetal.
Smalleyetal.
RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs
allhospitalshaddifferentguidelinesforPOCUSprivileges. TostandardizePOCUSprivilegesacrossthehospitals,a centralizedcredentialingprocesswascreatedinwhich privilegesweremadeidenticalacrossallhospitals.Uniform POCUSprivilegingwasinstitutedbasedoncurrentACEP guidelines6 (Table1).Eachhospital’smedicalexecutive committeeapprovedprivileges,therebycreating standardizationacrossthehealthcaresystem.Additionally, discreteelectronichealthrecord(EHR)orders,image archivalworkflow,templateddocumentationforstudy interpretation,andrequirementsforbillingwereidentical acrossthehospitals.Allhospitalswerestandardizedtothe sameultrasoundmachine,theMindrayTE-7(Mindray NorthAmerica,Mahwah,NJ)andthesameEHR(Epic SystemsCorporation,Verona,WI).
Withregardtophysiciantraining,duetothelargenumber ofphysiciansatier-basedultrasoundcredentialingsystem wasemployedsuchthatphysicianshadtodemonstrate competencyinallexamswithinthetiertobecome credentialedforthosestudies.Thiswasdonetosimplifythe trackingof >150EPsat11hospitals.Todetermineinitial privilegegroups,physicianswereclassifiedintotwogroups basedonthedateofresidencygraduationtodeterminea residency-basedpathwaygroupandapractice-based pathwaygroup.Perpreviouspublication,asrecommended bytheresidency-basedpathwayoftheACEPpolicy statement,ifaphysiciangraduatedduringorafter2008,the physicianwasgrantedintermediatePOCUSprivileges.9
Physicianswhograduatedpriorto2008wereaskedto
providealetterfromtheirresidencydirector,theirresidency programultrasounddirector,orasupervisorataprevious jobdocumentingpreviousPOCUStrainingthatmetACEP requirements.
Theremainderofthephysicianswhodidnotmeetthe abovecriteriawererequiredtoattendaninternal departmentalPOCUScourseandundergoapractice-based pathwaytoobtainbasicand/orintermediatecredentialing. Thispractice-basedPOCUScredentialingpathwaywas supervisedbythedirectorofemergencyultrasound.Thiswas ahighlymonitoredprogramwithdetailsdescribedinaprior paper. 9 Additionally,todeterminecompetency,physicians wereallowedtoscheduleone-on-onescanningsessionswith thedirectorofemergencyultrasoundiftheyhadbeen activelyscanningbeforetheupgrades,andstandardization madeitpossibleforultrasoundleadershiptotrackscans.
ParticipantsforStudy
AnycommunityEPworkingatanurban,suburban,or freestandingEDwithinthehealthcaresystemwhocompleted theultrasoundcredentialingprogramdescribedabovewas includedinthestudy.Weexcludedphysicianswhoprimarily practicedatthemainacademicquaternarycarehospital whereanEMresidencyprogramwasbasedandthatalsohad POCUSfellowship-trainedphysiciansonthefaculty.Ifan EPworkedattheacademicsiteandacommunitysiteduring thestudyperiod,thephysicianwasincludedinthestudyand onlytheirPOCUSstudiesfromthecommunitysiteswere includedinthedataset.Inaddition,anyEPwhojoinedthe
CredentialingtierApplicationsNumberofexamsrequired
Basicultrasound (allexamtypesrequired forcompletion)
Intermediateultrasound (allexamtypesrequired forcompletion)
Advancedultrasound (abilitytocredentialfor individualexamtypesin thiscategory)
Generalapplications: focusedassessmentwithsonographyin trauma(FAST);ultrasound-guidedvenousaccessplacement; abdominalaortaaneurysm
Generalapplications: pregnancy;echo;biliary;urinarytract;DVT; thoracic;softtissue/musculoskeletal;ocular;and proceduralguidance
Adnexalpathology
Advancedecho Appendicitis
Bowel(includingintussception)
Diverticulitis
Pyloricstenosis
Smallbowelobstruction
Testicular
TranscranialDoppler
Transesophagealecho
Requirementsforpoint-of-careultrasoundstudy
Adequateimageacquisition
Adequateimageinterpretation
Appropriatelabelingofeachimage
AAA,abdominalaorticaneurysm; DVT,deepveinthrombosis; POCUS,point-of-careultrasound.
FAST:25exams
AAA:25exams
CentralLine:10exams
150totalexams
(90examsifcompletedBasic CredentialingTier)
25examsperexamtype
Table1. Point-of-careultrasoundprivileges.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 687
EMgrouppracticeaftercompletionoftheultrasound credentialingprogramin2018wasrequiredtotakethe internaldepartmentalPOCUScourse(thesamecourse requiredfornewphysicianswhounderwentthepracticebasedcredentialingpathway).ThiscoursewastaughtbyEM POCUSleadershipandreviewedtherecommendedimage acquisitionrequirementsforeachPOCUSexam:EHR orders,imagearchival,documentation,andchart requirementsforbilling.
POCUSWorkflow
Astandardworkflowwasimplementedacrossthesystem. PhysiciansplacedanorderintheEHRforthespecific POCUSexamsubtypedesired:focusedassessmentof sonographyintrauma(FAST);rightupperquadrantfor gallbladderpathology;pelvicforearlypregnancy,etc.The orderthengeneratedapatientworklistonthePOCUS machinewithinthatindividualED.ThoseEDswithmultiple machinesusedasharedworklist.TheperformingEP accessedthepatientmedicalrecordfortheexamand attheendoftheexam,theimageswerepusheddirectlyto thepicturearchivingandcommunicatingsystemandtothe EHR.Nomiddlewarewasused.Thisimagewasimmediately viewableandavailableforqualityreviewtoallEHRusers acrossthesystem.IntheEHR,theordercreatedareminder tointerprettheimageusinganexam-speci ficandfocused templaterecommendedbytheACEPstandardizedreporting guidelines.
Eachweek,anautomatedreportofallPOCUSorderswas generatedandexportedtoasecureserver.Information extractedincludepatientname,medicalrecordnumber,date andtimeofstudy,typeofstudysubtypeasdefinedbythe orderplacedintheEHR,andimageinterpretationofstudy. ThisdatabasewasusedforQAbyEDPOCUSleadership.
Concurrently,arecommendedPOCUSimage compendiumwasdistributedtoallEPs(Appendix1).The compendiumidentifiesstandardviewstobeobtainedaswell aslabelingnomenclaturetobeusedwhenscanning. Additionally,eachmachineatallhospitalswasloadedwith standardized,presetdescriptorlabelstoaffixontheimages.
Intervention,DataCollection,andQualityAssurance Process
AllPOCUSstudiesperformedbycredentialedEPsfrom October1,2018–September30,2020wereincludedinthe analysis.Weexcludedstudiesthatwereperformedfor educationalpurposes,performedbynon-EPs(consultant), ornon-credentialedEPs’ ultrasoundexams.Weconducted statisticalanalysisusingSASsoftware(SASInstitute,Inc., Cary,NC).Wecomputeddescriptivestatisticsaswellas mediansandmeans.
DataextractedincludedthedateofthePOCUSexam, location,POCUSexamtype,attendingphysician,physician interpretation,andQA findings.Additionally,each
physician’sdateofhireandresidencygraduationdatewas identified.ThePOCUSexamtypewascategorizedbythe EHRentryorder.ThePOCUSexamwasassignedtothe attendingphysicianwhoorderedthestudythroughtheEHR. Forthisstudy,weexaminedthenumberofresidencycohort groupsin five-yearincrementstodeterminehowPOCUS usagehaschangedoversmallincrementsoftime.
TheEDPOCUSQAprogramrequiredanultrasound fellowship-trainedEPtoreviewallstudies.Allstudieswere reviewedwithinfourweeksofacquisition.Eachwas reviewedforthreefocusareas:1)imageacquisition,defined asthe “abilitytoacquiretherequiredimagesforaparticular POCUSstudyasdefinedbytheimagecompendium” ; 2)imageinterpretation,definedas “theabilityforthe physiciantomakethecorrectinterpretationtoanswerthe definedclinicalquestion”;and3)labelingofimages,defined as “labelingofimagessuchthatindependentreviewersof POCUSimagescandeterminetheanatomicallocationofthe study.” Whenareviewerdoubtedoneofthequalitative qualitymeasures,anadditionalPOCUSreviewerwas consulted.
AmonthlyQAreportsummarizingallexamsand pertinentteachingpointswassenttoallEPs.Asneeded, specificfeedbackwassenttotheperformingphysician,and casesweresenttopeerreviewifasignificantqualityissuewas identified.
RESULTS
Duringthetwo-yearstudyperiod,atotalof5,099POCUS studieswereperformedacross11communityEDswithinthe healthcaresystem.Atotalof170EPsmetinclusioncriteria; 29wereexcludedastheyworkedexclusivelyattheacademic center. Table2 demonstratesthenumberandpercentageof themostcommonexamsperformed.Inthecommunity, limitedcardiac,FAST,andlimitedpregnancyexamswere themostcommonexams,accountingfor61.9%oftotal studies.Themostinfrequentlyperformedexamsinthe communityweredeepvenousthrombosis(DVT),appendix, andtesticularultrasound.
Ofthe170communityEPsperformingPOCUS,yearsof residencygraduationwererecordedasadeterminantof exposuretoPOCUS.Asdemonstratedin Table3,more recentEMresidencygraduateswerehigherutilizersof POCUSwithagroupmeanof1.3examsper100patients. ResidencygraduatesinEMfrom2005-2009and2010-2014 had0.83examsper100patientsand0.80examsper100 patients,respectively.Therewasasignificantdecreasein examsper100patientsforthe2000-2004graduates.Inthe pre-2000residencygroup,themeannumberofPOCUS examsper100patientswas0.78.However,whenexamining thisphysiciangroup,twophysicianswhoworkedattrauma hospitalsperformed85%(900/1,062)ofexamsinthis category,whichskewedtheresults.Whenweexcludedthese twophysiciansfromthedataset,astheywerethoughttobe
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 688 RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs Smalleyetal.
Smalleyetal.
RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs
ExamcategoryPOCUSexams%ofTotal
inappropriately.Lessthan4%(166/5,099)didnothaveany interpretationassociatedwiththestudy.Therefore,these couldnotbeassessedforimageinterpretation.Lessthan 0.01%hadmorethanonequalityconcern(32/5,099).
DISCUSSION
Wepresentthe firstobjectivestudytoquantifyPOCUS studiesperformedbycommunityEPs.Wefoundthatcore studiesareperformedmostoften,andthereisahigher propensityforthesestudiestobeperformedbyrecent residencygraduates.
Abdomenother1102.2%
Other591.2% Joint450.9%
POCUS,point-of-careultrasound; OB,obstetrics; FAST,focused assessmentwithsonographyintrauma;E-FAST,extended focusedassessmentwithsonographyintrauma; DVT,deepvein thrombosis.
outliers,themeannumberofPOCUSexamper100patients was0.26.
WhenreviewingtheQAdata,wefoundthat4,395/5,099 (86%)ofPOCUSstudieshadnoqualityissues(86%) (Table4).Withregardtothespecificqualityconcern, 245/5,099(4.8%)hadinadequateimageacquisition,51/5,099 (1.0%)hadinadequateimageinterpretation,and210/5,099 (4.1%)hadimagesthatwereeithernotlabeledorlabeled
Manystudieshaveusedsurveymethodstoassessexam typewithoutretrospectivedatatodemonstrateactual utilization.Forexample,arecentCanadianstudysurveyed EPsandfoundthatFAST,cardiacarrest,andpregnancy werethemostcommonlyreportedapplicationsused.In addition,thephysician’sagewasnegativelyassociatedwith POCUSuse.10 Astudyfrom2006foundthatrespondents whoworkedincommunitysettingsreportedusingPOCUS primarilyforFAST,cardiacarrest,andpericardial effusion.11 Lastly,arecentsurveystudyassessingnonacademicEDsinArizonafoundthatthemostcommon studiesperformedatcommunitysitesweretrauma,cardiac, andlineplacement.12 Ourstudy,usingretrospective methods,objectivelyconfirmsprevioussurveydatathat communityEPsperformcoreexamsforlife-threatening concernsincommunityEDs.Additionally,FAST,cardiac, andobstetricalexamswerethemostcommonscans performedinourcommunityEDhealthcaresystem,which alignswithpreviousstudies.
Ourstudyalsofoundthatlesscommonlyperformed exams,suchasbiliary,joint,DVT,appendix,andtesticular ultrasound,wererarelydone.Therecouldbemanyreasons forthis,whichincludeanEP’slackofconfidencein performingtheexam,difficultyinacquiringcorrectimages, riskofincorrectinterpretation,andtheamountoftime neededtoperformabedsideexam.Someoftheseexamsmay notroutinelybedoneinEMresidencytrainingand,thus, thereislimitedexperience.Additionally,itcouldbethata
POCUS,point-of-careultrasound; Yr,year.
Residency group(Yr) Physician count(N)Patients(N) POCUS exams(N) POCUSexamsper100patients GrouprateGroupmeanGroupmedian Pre-20003696,5561,0621.100.780.11 2000–20042158,9131270.220.210.03 2005–20092768,6749061.320.830.19 2010–201436120,0981,0190.850.800.33 2015–201943147,2021,9411.321.300.74 2020+ 72,776441.592.030.77 Grandtotal170494,2195,0991.030.910.31
Table3. Physicianresidencygraduationyearinrelationtopoint-of-careultrasoundexamsperformedper100patients.
Table2. Frequencyofpoint-of-careultrasoundexamtypesin communityhospitalemergencydepartments.
Cardiac1,22224.0% FAST1,10921.7% Ob82616.2% Skin4919.6% Lung3567.0% Aorta1813.5%
Ocular1793.5% Kidney1272.5% Bladder1232.4% Biliary1182.3% E-FAST1132.2%
DVT250.5% Appendix70.1%
Proceduralultrasound70.1% Scrotum10.0% GRANDTOTAL5,099100.0%
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 689
physician’slackofconfidencewithmorecomplexexamsled tooptingtoobtainradiology-basedultrasoundstudies. Lastly,itmaybethattheseexamsrequiremoretimeatthe bedside,whichmaypreventcommunityEPsfrom performingthemroutinely.
Previoussurveystudiesdescribelineplacementasamore commonexamtypereported.Giventhatitisstrongly recommendedinoursystemthatultrasoundbeusedfor centrallineplacement,wedosuspectthatthereislikely undercountingofitsuseforlineplacement.Thismaybe becausemanyofthecommunityEDsdonothavethe personnelorresourcestoassistphysicianswithsavingthe imagesduringsterileproceduresorthatitmaynothavebeen seenasofcriticalimportanceduringtheprocedureandwas thusneglected.Therefore,ournumbersarelikelylowas imageacquisitionintotheEHRmaylimitourabilitytotruly assesstheincidenceofPOCUSforlineplacement.However, POCUSforlineplacementisnotadiagnosticmodalitybut ratheraproceduralaid,andourdatadoesreflecttheuseof POCUSasadiagnosticmodalityinthecommunity.
Althoughwedidnotperformanystatisticalcomparison analysestodeterminestatisticallysignificantdifferences acrossresidencygroupsinthiscohort,thedatafromour studypointstoapossibletrendsuggestingthatthegreaterthe numberofyearsfromresidencygraduation,thelesslikelythe EPwastoperformPOCUSper100patients.Wesuspect physicianswhograduatedwithoutformalPOCUStraining duringresidencyarenotaslikelytopickupthisnewskilland useitatthebedside.WhilethereissparsedatalinkingEM residencygraduationwiththeutilizationofPOCUSin practice,therearesmallerstudiesthatdemonstratePOCUS trainingduringresidencypositivelyimpactsclinical utilizationwithinoneyearafteradedicatedcourse.13,14
OurstudyattemptedtoexamineallcommunityEPsinour healthcaresystemandtheirPOCUSutilization.Objective studynumbersperformedper100patientssuggestatrend towardanoveralldecreaseinPOCUSutilizationwith greaternumberofyearsfromresidencygraduation.Thedata
maybeusefultoinstitutionsdevelopingPOCUScurricula, training,andcredentialingprogramsforpracticingEPsas thedatasuggeststhatthispopulationwilllikelynotuse POCUSasfrequentlyasEMresidencygraduateswhowere trainedinPOCUS.
Oneareathatdeservesdiscussionfromourdatasetwasthe pre-2000residencygraduategroup.Ourdatafoundan uptickinthegroupwhograduatedpriorto2000.Tobetter understandthisoutlierinthedataset,weperformeda detailedanalysis,whichrevealedthattwoEPsinthisgroup performed85%ofthePOCUSexams.Thesetwophysicians workatLevel2traumacenters,whichmayexplaintheirhigh utilizationofPOCUS.Whenthesetwophysicianswere excludedfromthepre-2000cohort,thetotalnumberof examsperformeddroppedfrom1,072to172withagroup meanof0.26POCUSexamsper100patients.Thislikelyis morerepresentativeofthisEPgroupwhograduatedpriorto 2000andisconsistentwiththe2000-2004cohort.However,it raisesthequestionofwhetherolderresidencygraduatesmay developanaffinityforPOCUSintheproperclinicalsetting andwhetheruniversalPOCUScredentialingofEPsis beneficial.Additionally,anotherquestionthatoccursis whetheritisbeneficialtotrainmodalitiesmostusedinthe clinicalenvironmentinwhichthephysicianpracticesor whethertrainingshouldconsistofallACEP-recommended studies.
Finally,qualityisametricthatisofutmostimportance whenperformingPOCUSexams.Ourstudydemonstrates thatPOCUSinthecommunityEDproduceshigh-quality, reliablePOCUSstudies.Afteracomprehensivecredentialing programwithimagingcompendiumrecommendationsanda standardizedreportingsystem,mostexamsperformed metbasicqualitymetricsforimageacquisition,image interpretation,andlabeling.Thisdemonstratesthatquality studieswithcompliancecanbeachievedinthecommunity EDwhenacomprehensivecredentialingprogramwith standardizationofPOCUSisimplemented.Thisprogram couldbehelpfulforotherspecialtiesorforcommunity hospitalswithnewornovicescannerstryingto implementguidelinesandbestpracticeswithregard toPOCUS.
Overall,the findingsfromourcommunityassessmentare thatcorePOCUSexamsaremostcommonlyperformedwith fewqualityissues.HospitalsystemsornewPOCUS programsmaybenefitfromfocusingoncoretraining,solid competencyassessmentprograms,bestpracticesfor privilegingandcredentialing,andstandardizingworkflowto ensurehigh-qualityoutcomes.Furtherstudieswillneedto continuetoassesstheuseofPOCUSincommunityEDs tofurtherexaminepatientoutcomes.
LIMITATIONS
Onepotentiallimitationsofourstudyisthatthedata includesonlystudiesorderedthroughtheEHRwithimages
Numberof studies(N) Noqualityissues 4,395 Qualityissue Imageacquisition(IA)245 Imageinterpretation(II)51 Imagelabeling210 Nointerpretation166 >1Qualityissue IA + nolabel16 II + nolabel7 IA,II,andnolabel9 Total 5,099 WesternJournal of EmergencyMedicineVolume24,No.4:July2023 690
Table4. Qualitymetricsforpoint-of-careultrasoundperformed.
RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs Smalleyetal.
Smalleyetal.
RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs
thatweresavedanddocumentedwithinthesystemandhad billingnotescompleted.Itispossiblethatotherstudies, knownas “phantomscans,” couldhavebeenperformedat thebedsidewithoutimageacquisitionintotheEHRwith appropriatedocumentation.Wehadnowayofassessingthe numberof “phantomscans” usingourcurrentEHR,butwe acknowledgethatthiscouldbeapotentialconfoundertoour study.Alongthistheme,webelievethatmostofour communityEPsdidnotsaveimagesforcentralline placementand,thus,thereisnodataontheirperformance. However,thehealthcaresystemrecommendsPOCUSasbest practiceforcentrallineplacement.
AnotherlimitationwasthatasmallgroupofEPs practicedatbothacademicandcommunitysiteswithinour system.Whilethestudyonlyincludedtheircommunity POCUSexams,thesephysiciansmaybemoreapttouse POCUSduetotheirexposureattheacademicsitewhere residentstraininPOCUSandperformfrequentexams.This mayskewthisphysiciangroup’sPOCUSnumbersinthe community,andwecouldnotaccountforthesefew physiciansinourstudygroup.Intermsofadditional limitationsrelatedtothephysiciangroup,wewereunableto obtainretrospectiveinformationabouthowmanystudiesor howfrequentlythephysiciangroupwasscanningfromthe timeoftheirresidencygraduationtothebeginningofthe studyorcontinuedcompetency.
Lastly,anothervariablethatcouldhaveaffectedtheuseof POCUSincommunityEDswastheavailabilityof24-hour, radiology-performedandinterpretedultrasoundstudies. Manyofoursiteshada24-houron-siteradiology ultrasound,whileothershadsomelimitedon-callaccess duringovernighthours.Unfortunately,therewasnoreliable waytotellwhenradiology-basedultrasoundwas unavailable.PossiblereasonsforcommunityEPs’ limiteduse ofPOCUSmaybetheheavierworkload,absenceof trainees,andeaseofaccesstoradiology-basedultrasound exams,especiallywhenrequestedbyconsulting services.
CONCLUSION
Theuseofpoint-of-careultrasoundincommunityEDs demonstratesaheavyfocusonthecoreexamsinEMpractice withincreasedutilizationbyrecentresidencygraduates. Moststudieshadnoqualityissueswithimageinterpretation, imageacquisition,orlabelingasdefinedbytheguidelines withinourprivilegingprogram.Ourstudydemonstratesthat POCUScanbereliablyperformedincommunityEDsand thatasourworkforcecontinuestoshifttowardmore recentresidencygraduates,theuseofPOCUSinthe communityEDswillcontinuetogrow.Building standardizedinfrastructureincommunitysitestoallowfor furtheruseofPOCUSmaybeadvantageousforhealthcare systems.
AddressforCorrespondence:CourtneyM.Smalley,MD,Cleveland ClinicHealthSystem,EmergencyServicesInstitute,9500Euclid Avenue,E19,Cleveland,Ohio44195.Email: courtney.smalley@ gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Smalleyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.AmericanCollegeofEmergencyPhysicians.AmericanCollegeof EmergencyPhysicians.ACEPEmergencyUltrasoundGuidelines2001. AnnEmergMed. 2001;38(4):470–81.
2.SoniNJ,SchnobrichD,MathewsBK,etal.Point-of-careultrasoundfor hospitalists:apositionstatementoftheSocietyofHospitalMedicine. JHospMed. 2019;14:E1–E6.
3.AmericanAcademyofFamilyPhysicians.recommendedcurriculum guidelinesforfamilymedicineresidents:point-of-careultrasound guidelines.Availableat: https://www.aafp.org/dam/AAFP/documents/ medical_education_residency/program_directors/ Reprint290D_POCUS.pdf.AccessedJuly1,2021.
4.MooreCL,CopelJA.Point-of-careultrasonography. NEnglJMed. 2011;364(8):749–57.
5.AmericanCollegeofEmergencyPhysicians.Emergencyultrasound guidelines. AnnEmergMed. 2009;53(4):550–70.
6.UltrasoundGuidelines:Emergency,Point-of-careandclinical ultrasoundguidelinesinmedicine. AnnEmergMed. 2017;69(5):e27–e54.
7.BurkhardtJ,KowalenkoT,MeurerW.Academiccareerselectionin Americanemergencymedicineresidents. AcadEmergMed. 2011;18Suppl2:S48–S53.
8.SinghaprichaT,MinkhorstO,MoranT,etal.Predictorsofaninitial academicpositioninemergencymedicine. WestJEmergMed. 2019;20(1):127–31.
9.SmalleyCM,FertelBS,BroderickE.Standardizingpoint-of-care ultrasoundcredentialingacrossalargehealthcaresystem. JtCommJ QualPatientSaf. 2020;46(8):471–6.
10.LeschynaM,HatamE,BrittonS,etal.Currentstateofpoint-of-care ultrasoundusageinCanadianemergencydepartments. Cureus 2019;11(3):e4246.
11.MooreCL,MolinaAA,LinH.Ultrasonographyincommunity emergencydepartmentsintheUnitedStates:accessto ultrasonographyperformedbyconsultantsandstatusofemergency physician-performedultrasonography. AnnEmergMed 2006;47(2):147–53.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 691
12.AminiR,WymanMT,HernandezNC,etal.Useofemergency ultrasoundinArizonacommunityemergencydepartments. JUltrasound Med.2017;36(5):913–21.
13.ChenWL,HsuCP,WuPH,etal.Comprehensiveresidency-based point-of-careultrasoundtrainingprogramincreasesultrasound
utilizationintheemergencydepartment. Medicine(Baltimore) 2021;100(5):e24644.
14.SmalleyCM,SimonEL,MuirMR,etal.Point-of-careultrasoundtraining andcredentialingformid-latecareeremergencyphysicians:Isitworth it? POCUSJ. 2021;6(2):56–7.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 692 RetrospectiveReviewofPOCUltrasoundUtilizationandQualityinCommunityEDs Smalleyetal.
ApplyingaSmartwatchtoPredictWork-relatedFatigue forEmergencyHealthcareProfessionals: MachineLearningMethod
SotShih-HungLiu,MD,MSc*†
Cheng-JiunMa,PhD‡
Fan-YaChou,BSc*§
MichelleYuan-ChiaoCheng,BS,MBA‡
Chih-HungWang,MD,PhD*§
Chu-LinTsai,MD,ScD*§
Wei-JouDuh,PhD‡
Chien-HuaHuang,MD,PhD*§
FeipeiLai,PhD†∥
Tsung-ChienLu,MD,PhD*§
SectionEditor: PhilipsPerera,Jr,MD
*NationalTaiwanUniversityHospital,DepartmentofEmergency Medicine,Taipei,Taiwan
† NationalTaiwanUniversity,GraduateInstituteofBiomedicalElectronics andBioinformatics,Taipei,Taiwan
‡ MOSTJointResearchCenterforAITechnologyandAllVISTA Healthcare(AINTU),Taipei,Taiwan
§ NationalTaiwanUniversity,DepartmentofEmergencyMedicine, CollegeofMedicine,Taipei,Taiwan
∥ NationalTaiwanUniversity,DepartmentofComputerScienceand InformationEngineering,Taipei,Taiwan
Submissionhistory:SubmittedJuly23,2022;RevisionreceivedApril3,2023;AcceptedMay1,2023
ElectronicallypublishedJuly7,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58139
Introduction: Healthcareprofessionalsfrequentlyexperiencework-relatedfatigue,whichmay jeopardizetheirhealthandputpatientsafetyatrisk.Inthisstudy,weappliedamachinelearning(ML) approachbasedondatacollectedfromasmartwatchtoconstructpredictionmodelsofwork-related fatigueforemergencyclinicians.
Methods: Weconductedthisprospectivestudyattheemergencydepartment(ED)ofatertiaryteaching hospitalfromMarch10–June20,2021,wherewerecruitedphysicians,nurses,andnursepractitioners. Allparticipantsworeacommerciallyavailablesmartwatchcapableofmeasuringvariousphysiological dataduringtheexperiment.ParticipantscompletedtheMultidimensionalFatigueInventory(MFI)web formbeforeandaftereachoftheirworkshifts.Wecalculatedandlabeledthebefore-and-after-shiftscore differencesbetweeneachpairofscores.Usingseveraltree-basedalgorithms,weconstructedthe predictionmodelsbasedonfeaturescollectedfromthesmartwatch.Recordsweresplitintotraining/ validationandtestingsetsata70∶30ratio,andweevaluatedtheperformancesusingtheareaunderthe curve(AUC)measureofreceiveroperatingcharacteristiconthetestset.
Results: Intotal,110participantswereincludedinthisstudy,contributingtoasetof1,542effective records.Oftheserecords,85(5.5%)werelabeledashavingwork-relatedfatiguewhensettingtheMFI differencebetweentwostandarddeviationsasthethreshold.Themeanageoftheparticipantswas29.6. Mostoftherecordswerecollectedfromnurses(87.7%)andfemales(77.5%).Weselectedaunionof31 featurestoconstructthemodels.Fortotalparticipants,CatBoostclassifierachievedthebest performancesofAUC(0.838,95%confidenceinterval[CI]0.742–0.918)toidentifywork-relatedfatigue. Byfocusingonasubgroupofnurses <35yearsinage,XGBoostclassifierobtainedexcellent performanceofAUC(0.928,95%CI0.839–0.991)onthetestset.
Conclusion: Byusingfeaturesderivedfromasmartwatch,wesuccessfullybuiltMLmodelscapableof classifyingtheriskofwork-relatedfatigueintheED.Bycollectingmoredatatooptimizethemodels,it shouldbepossibletousesmartwatch-basedMLmodelsinthefuturetopredictwork-relatedfatigueand adoptpreventivemeasuresforemergencyclinicians.[WestJEmergMed.2023;24(4)693–702.]
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 693
ORIGINAL RESEARCH
INTRODUCTION
Work-relatedfatigueisamajorconcernintheworkplace. Work-relatedfatigueamongmedicalpersonnelcanaffectthe healthandwell-beingofemergencyhealthcareprofessionals (EHP)andputpatientsafetyatrisk.1–6 Causesoffatiguein theworkplacemaybeduetoeitherphysiologicalfactors, suchaslongworkshiftsorheavyworkload,orpsychological aspectssuchasstress.2,7 Researchersfoundthatifemployees workedmorethan55hoursperweek,thechancesofgettinga strokeorcoronaryheartdiseasewouldincreaseby33%and 13%,respectively,comparedtoemployeeswhoseworking hoursmetthe55-hourstandard.8 Anotherstudyshowedthat doctorsinTaiwanmighthavegreateroccupationalpressure andahigherdepressionrate(13.3%)thanthatfoundinthe generalpopulation(3.7%).9 Toreducehealthcareworkload andpreventhumanerrorsduringclinicalpracticeby determininghowtodetectwork-relatedfatigueearlierand adoptpreventivemeasuresisworthyofcarefulstudy.
Numerousstudieshavefocusedonwork-relatedfatigue; however,mostwereconductedsubjectivelybyusingselfreportmeasuressuchasquestionnaires,surveys,orrating scalescompletedafterwork.10–12 Untilnow,fewstudieshave lookedatobjectivewaysofcollectingreal-timedatafrom EPsandotherhealthcareworkerswhileonshift.Withthe advancementofinformationtechnologyandtheadventof wearabledevicescapableofunobtrusivelycollecting real-timebiosensordatawithoutaffectingtheworkflowof medicalstaff,itispossibletodevelopasmartwatch-based predictionmodelofwork-relatedfatigueforEHPs.Inthe past,wearabledevicesfocusedmoreonhealthmonitoring fortheelderlyorfalldetectioninpatientswithmovement disorders.13 Now,wearabledevicesareusedwithmachine learning(ML)todeterminewhetherapatienthasdepression ortofacilitatethedeliveryofhigh-qualitycardiopulmonary resuscitation.14,15
ArecentreviewarticlebyMartinsetalfocusedonfatigue monitoringthroughwearables.Theyretrievedatotalof612 articlesintheirliteraturesearchandincluded60articlesfor analysis.Oftheincludedresearch,themostcommonstudies wererelatedtodrowsinessdetectionfordrivers(33),followed bythedetectionofphysicalfatigue,mentalfatigue,muscle fatigueand,lastly,vigilancedetection.Althoughfourstudies focusedonthehealthcaredomain,nonelookedathealthcare professionals.Threeofthosestudieswererelatedtofatigue detectionforrehabilitationpatients,andoneexaminedmental fatiguedetectioninahealthypopulation.Ofthe60studies includedinthereviewbyMartinsetal,only fivereportedonthe useofasmartwatchasthesignalsourceforfatiguedetection.16
Apartfromthatreview,onestudydescribedtheuseofa wearablephotoplethysmography(PPG)biosensorto evaluatethefeasibilityofcollectingandanalyzingPPGdata forburnoutinEPswhiletheywork.Sincethisstudyshowed nosignificantchangesinpulserateandpulseratevariability overthecourseofanEP’sacademicyear,itsuggestedthat
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Emergencyhealthcareprofessionals frequentlyexperiencework-relatedfatigue, whichcanimpacttheirhealthandputpatients atrisk.
Whatwastheresearchquestion?
Canmachinelearningbasedonsmartwatch datapredictwork-relatedfatiguein emergencyhealthcareprofessionals?
Whatwasthemajor findingofthestudy?
CatBoostclassi fi erachievedanareaunderthe curveof0.838(95%CI0.742 – 0.918)for identifyingwork-relatedfatigueinstudy participants.
Howdoesthisimprovepopulationhealth?
Byusingsmartwatchdataandmachine learning,work-relatedfatiguecanpotentially beidenti fi edandprevented,improvingpatient safetyandhealthcareprofessionals ’ health.
alternativemethodswouldhavetobeexploredtomeasure stressamongEPsatwork.17
Asmartwatchisawearabledevicewiththefunctionof bothtellingtimeandactingasasourceforcollecting physiologicdataderiveddirectlyfromthewearer’sbody becauseofitsproximitytotheskin.Todaymostofthe commerciallyavailablesmartwatchesclaimtohavethe abilitytotrackthewearer’shealthbyprovidingdata,suchas numberoffootsteps,heartrate,bloodpressure,andoximetry viatheembeddedbiosensors.Althoughtheaccuracyofthe measureddataderivedfromsmartwatchesvariesdepending onthedevicemanufacturer,mostmainstreamdevicescan reliablymeasureheartrate,steps,andotherhealth evaluationindicators.18
Itisreasonabletoconcludethatwecancollectreal-time physiologicdatatransmittedfromthesmartwatchwornby healthcareworkerstobuildawork-relatedfatigueprediction model.Bycombiningobjectivedatacollectedfroma wearabledevicewiththesubjectiveresultsofthewellvalidatedMultidimensionalFatigueInventory(MFI)(filled outbytheparticipantsasatoolforfatiguelabeling),19 we soughttoapplyMLapproachestoconstructawork-related fatiguepredictionmodelforemergencyhealthcare professionals.Wehypothesizedthatasmartwatch-basedML modelcouldserveasareliablemethodtodetectfatiguefor EHPsworkingintheemergencydepartment(ED).
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 694 ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod Liuetal.
METHODS StudySettings
Thisprospectiveobservationalstudywasconducted March10–June20,2021attheEDofNationalTaiwan UniversityHospital(NTUH),a2,400-bed,universityaffiliated,tertiaryteachinghospitalwithadailycensusof ≈300emergencyvisits.Werecruitedemergencycare professionals,includingEPs,nurses,andnursepractitioners >20yearsofage,excludinganyonewhocouldnottolerate wearingasmartwatch.Eachparticipantwasprovidedwith anASUSVivoWatchSP(ASUSTeKInc,Taipei,Taiwan),a commerciallyavailablesmartwatchcapableofmeasuring heartrate,bloodpressure,oxygensaturation,andfootsteps usingtheembeddedsensors.Thesmartwatchalsofeatures calorieconsumption,heartratevariability(HRV),andstress indexbasedonproprietaryalgorithmsnotshowntothe public.Participantswerenotallowedtoremovethe smartwatchwhiletheywereatwork.Ninesmartphones (ASUSZenfone7)weresetupintheED,actingasgateways tosynchronizeandtransmitdatawithaprivatecloudvia Bluetoothprotocol(BluetoothSIG,Inc,KirklandWA). Eachphonewaspairedwith50smartwatchesoverthecourse ofthestudy.
TheMultidimensionalFatigueInventory
TheMachine-LearningMethod
Inadditiontoparticipants’ demographicdataandthe timeseriesdataofbloodpressure,heartrate,HRV, footsteps,andcalorieconsumption,weretrievedthestress indextransmittedfromthesmartwatchestotheprivatecloud asthemainfeaturesforconstructingMLmodels.Weuseda setoftimewindows(first,second,andfourthhours)and statisticalfunctions(eg,minimum,maximum,mean,slope, SD,etc)tocreatemorefeaturesastheinputvariables.Inthe featurespacewealsoincludedtheone-hot-encoded(awayto convertvariablesforuseinMLalgorithms)demographicsof thestudyparticipants.Missingdatawereautomatically imputedwithdummyvariablesbytheMLmodels.Initially, 696featureswereincludedastheinputvariablesforthe subsequentMLtask.
Weusedseveraltree-basedalgorithms including randomforest(RF),gradientboosting(GB),eXtreme gradientboosting(XGBoost)(anopensourcesoftware library),lightgradientboostingmachine(LightGBM)(an opensourceforadistributedgradient-boostingframework forMLdevelopedbyMicrosoftCorp,Redmond,WA),and categoricalboosting(CatBoost)classifiers toconstructthe predictionmodelsofwork-relatedfatigueforclinicalstaffin theED.WedefinedthebetweenMFIscoredifferencesof morethantwoSDsineachpairofworkshiftsasworkrelatedfatigueandusedthemasthebinaryclassification labelforthisstudy.Wedividedallrecordsintotwosets chronologically,70%ofwhichwereassignedtothetraining andvalidationsetand30%tothetestset.Weusedk-fold cross-validationduringthemodeltrainingprocessbysetting kfrom7to10toobtainthebestperformances.
21
TheMFIisa20-itemself-reportscaledesignedto evaluate fi vedimensionsoffatigue:generalfatigue;physical fatigue;reducedmotivation;reducedactivity;andmental fatigue.Thisinstrumentwasoriginallydevelopedinthe Netherlandsforpatientswithcancerandchronicfatigue andhasbeentranslatedandvalidatedinseveralother languages(includingMandarin)fordifferent populations. 19
Eachdimensioncontainsfouritems(two itemsinapositiveandtwoinanegativedirection)tobe scoredona fi ve-pointLikertscalerangingfrom1(yes,that istrue)to5(no,thatisnottrue).Thenegativeitems(items2, 5,9,10,13,14,16,17,18,19)mustberecordedbeforethe scoresareaddedup.Thesummationoftheobtainablescore rangesfrom20(absenceoffatigue)to100(maximum fatigue).
Forthisstudy,theoriginalMFIscalewastranslated intoaTraditionalChineseversionbasedonprevious publications19,20 (SupplementaryTable1).Participantswere askedtocompleteanMFIwebformbeforeandaftereachof theirworkshifts.Wecalculatedthedifferencesbetweeneach pairofwork-shiftscoresforthesubsequentMLtaskof labelingwork-relatedfatigue.Wesetthebetween-score differenceofMFIwithmorethan10,morethanoneSD,or morethantwoSDsaspositivelabelsofwork-relatedfatigue. Theresearchmethodwasapprovedbytheinstitutional reviewboard(NTUH-RECNo.:202011024RIND)of NTUH.Allparticipantssignedaninformedconsentform beforeparticipatinginthestudy.
Weadoptedatwo-stepmethodasourfeatureselection strategy.First,wedeselectedthosefeatureswithhigh correlation.Second,werankedtheselectedfeaturesbyusing entropymeasuresbasedoninformationgaintheory.22 Iteratively,webuiltourmodelsbytryingfromthetop fifth importantfeaturesandaddedonemoreuntilthelastselected features,and finallyfoundasetoffeaturestoconstructthe bestmodelsintermsoftheperformanceofareaunderthe curve(AUC)measureofreceiveroperatingcharacteristic (ROC).Featuresofcontinuousdatawereexpressedasmean andSD(ormodeandinterquartilerangedependingonthe normalitytest),whereascategoricaldatawereexpressedas countsandproportions.Wealsopresentedunivariate descriptivestatisticstoevaluatedifferencesbetweenclasses byusingStudent t -test,chi-squaredtest,Fisherexacttest,or Mann-WhitneyUtestdependingonthedistribution.
Toresolvetheclassimbalanceproblemforwork-related fatigueprediction,weusedthesyntheticminority oversamplingtechniquemethod(SMOTE),which oversampledtheminorityclassduringthetrainingprocess.23 TheselectionofthemodelswasbasedontheAUC performanceinthetestset,whichwassetastheprimary evaluationmetricofthestudy.Foreachmodelwealso
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 695
Liuetal. ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod
reportedotherperformancemeasures,includingareaunder theprecision-recallcurve(AUPRC),accuracy,negative predictivevalue(NPV),precision(orpositivepredictive value[PPV]),recall(orsensitivity,ortruepositiverate), specificity(truenegativerate),kappa,andF-1score,The entropymeasuresforfeaturerankingwereperformedusing Weka3.8,acollectionofMLalgorithmsfordata-mining tasks(UniversityofWaikato,Hamilton,NewZealand).24 OtherMLanalyseswereperformedusingPython3.8with thepackagescikit-learn0.23.1installed(PythonSoftware Foundation,Fredericksburg,VA).25
RESULTS
Weincluded110participantsinthisstudy,withaset of1,542effectiverecordscollected.Eachparticipant contributedtoatleastonerecord,rangingfrom1–23records. Ofthem,85(5.5%)werelabeledashavingwork-related fatigue(twoSDsasthethreshold)basedonourstudy definition.Themeanageoftheparticipantswas29.6years (SD6.3),and77.5%oftherecordswereforfemales.Mostof thecollectedrecordswerefromnurses(87.7%),followedby nursepractitioners(7.7%)andEPs(4.5%)(P < 0.001).Upto 47.7%ofthecollectedrecordswereontheeveningshift, 44.5%onthedayshift,and7.8%onthenightshift(P < .001). Thecharacteristicsofthedemographicfeaturesinthestudy populationareshownin Table1.
Thecharacteristicsandunivariateanalysesoftheselected featuresbetweenparticipantswithorwithoutwork-related fatiguearesummarizedin Supplementary Table2,shown respectivelyforthetrainingandtestingsets.Basedonour featureselectionstrategy, finallytherewasaunionof31 featuresselectedtoconstructthemodels.Ofthem,thework starttimewastheonlydemographicfeatureselected.The other30featureswerederivedfromthesmartwatch,ofwhich 11wererelatedtoheartrate,seventobloodpressure, fiveto stressindex,threetoHRV,threetocalorieassumption,and onerelatedtofootsteps.
Theentropymeasuresfortherankingofthe31selected featuresareshownin Figure1.Theinitiallyincluded696 featuresandthepercentagesofdatamissingareshownin Supplementary Table3.Thedescriptionofthethreetypesof thecandidatefeatures(demographics,sensordatafromthe smartwatch,andstatisticaldataderivedfromthesensor data)areshownin Supplementary Table4
Fortotalparticipants,theclassificationresults(basedon thebestAUCintermsofthedifferentthresholdsfor labeling),includingAUC,AUPRC,appa,accuracy,F1score,precision(PPV),specificity,andNPVonthetraining andtestingsetsarepresentedin Table2.Byadjustingthe thresholdofwork-relatedfatiguelabelingfromtwoSDsto oneSDor20pointsofthebetweendifferencesoftheMFI score,hereweshowmerelythetopclassifierintermsofAUC. ByusingtheCatBoostclassifier,thebestperformancesof AUCandAUPRCinthetestsetwere0.838(95%confidence
interval[CI]0.742–0.918)and0.527(95%CI0.344–0.699), respectively(Figure2).Conductingfurthersubgroup analysiswhenfocusedonnurses <35yearsofage,XGBoost classifierachievedthebestperformanceintermsofAUCof 0.928(95%CI0.839–0.991)whensettingthethresholdfor work-relatedfatigueastwoSDs.Meanwhile,other performancemeasuresforthissubgrouparepresentedin Table3.Inthismodel,AUPRCwas0.781(95%CI 0.617–0.0.919)(Figure2).
DISCUSSION
InthisstudyweappliedMLtechniquestopredictworkrelatedfatigueforclinicalstaffwhoworkedattheEDina tertiaryhospitalinTaiwan.Using31selectedfeatures derivedfromawearabledevice,wesuccessfullybuiltML modelscapableofclassifyingtheriskofwork-relatedfatigue intheEDenvironment.Insteadofusingbasemodelslike decisiontreelearning,weusedseveraltree-basedalgorithms toconstructthepredictionmodels.Wechosethese algorithmsfortheirabilitytomanagethenon-linearrelation withbetterperformanceincopingwithasmallamountof data.Thesealgorithmswerealsolessaffectedbymissing valuesandwereindependenttofeaturescaleand normalizationaswell.26 Whilesettingthework-related fatiguethresholdastwoSDsdifferencebetweenthe before-and-after-workMFIscores,weobtainedgood discriminatoryperformancetopredictwork-relatedfatigue takingAUCastheperformanceindicator.Ofthealgorithms weused,CatBoost(AUC0.838)outperformedRF,GB, XGBoost,andLightGBMclassifierswhenappliedtothe testingsetforthewholecohortofparticipants.Sinceyounger participantsmayhavebeenmorelikelytohavework-related fatigue27 andnursesmadeupthemajorityoftheresearch group(andtheirworkcontentmightbedifferentfromEPs andnursepractitioners),weperformedasubgroupanalysis byfocusingonnurses <35.Inthissubgroupanalysis,the XGBoostclassifier(AUC0.928)outperformedtheotherson thetestingsetinthissubgroup(Figure2).
FeatureSelectionUsingEntropyandInformationGain Entropyisameasureoftheuncertaintyorrandomnessin thedata.Itiscalculatedasthesumofthenegativeofthe probabilityofeachclassmultipliedbythelogarithmofthe probabilityofeachclass.Indecisiontreealgorithms,entropy isusedtodeterminehowmuchinformationafeaturecan provideuswithinreducingtheuncertaintyofthetarget variable.24 Theentropyiszerowhenalltheinstancesinaset belongtothesameclassandismaximumwhentheinstances areequallydividedamongallclasses.Informationgainisa measureofhowmuchaparticularfeaturehelpsinreducing theuncertaintyofthetargetvariable.Inotherwords,ittells ushowusefulaparticularfeatureisinclassifyingthetarget variable.Informationgainiscalculatedbysubtractingthe weightedaverageentropyofthetargetvariableafterthe
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 696 ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod Liuetal.
Liuetal. ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod
§WeusedtheStudent t-testasthestatisticalmethodtocomparethevariableageandchi-squaredtestforremainingvariables. ϕSenioritymeansyearsofworkingasahealthcareprofessional.
featureisusedforclassificationfromtheentropyofthetarget variablebeforethefeatureisused.Thefeaturewiththe highestinformationgainischosenastherootnodeofthe decisiontree.
Weusedentropyandinformationgainasamethodof featureselection(insteadofthecommonlyusedunivariate analysis),givenitsabilitytorankthefeaturesintheorderof theirrespectiveinformationgains,sothatwecouldselect featuresbasedonthethresholdintheMLalgorithms.As shownin Figure1,wecanseetherelativelylowinformation gainof0.00525givenbythefeature “maximumofheartrate
forthelast1-hourtimeinterval” andtherelativelyhigher informationgainof0.036543givenbythefeature “minimum ofsystolicpressuredividedbydiastolicpressureforthe first 4-hourtimeinterval.” Insummary,entropyandinformation gaincouldbeusedtodeterminethebestfeaturetousefor classification,withthegoalofreducingtheuncertaintyofthe targetvariableandmaximizingtheinformationgain.
ComparisonwithPreviousStudies
Work-relatedfatiguemighthavebothphysicaland psychologicaladverseeffectsonEDclinicalstaff,which
Variables(features) Total (N = 1,542) Trainingcohort (n = 1,079) Testingcohort (n = 463) P value Gender .07 Female 1,195(77.5)850(78.8)345(74.5) Male 347(22.5)229(21.2)118(25.5) Age,mean(SD) 29.6(6.3)29.6(6.4)30.5(3.5).84§ Role <.001 Doctor 70(4.5)38(3.5)32(6.9) Nursepractitioner 119(7.7)104(9.6)15(3.2) Nurse 1353(87.7)937(86.8)416(89.8) Worktype <.001 Nightshift 121(7.8)34(3.2)87(18.8) Eveningshift 735(47.7)519(48.1)216(46.7) Dayshift 686(44.5)526(48.7)160(34.6) Workhours,mean(SD) 8.3(0.8)8.2(0.7)8.4(1.0) <.001 Seniorityϕ,mean(SD) 6.3(5.1)6.4(5.1)5.3(6.7).76 Dayofweek .012 Monday 222(14.4)171(15.8)51(11.0) Tuesday 232(15.0)170(15.8)62(13.4) Wednesday 249(16.1)153(14.2)96(20.7) Thursday 222(14.4)153(14.2)69(14.9) Friday 213(13.8)155(14.4)58(12.5) Saturday 198(12.8)135(12.5)63(13.6) Sunday 206(13.4)142(13.2)64(13.8) Workstarttime <.001 7:00 AM 60(3.9)53(4.9)7(1.5) 7:30 AM 569(36.9)437(40.5)132(28.5) 8:00 AM 44(2.9)29(2.7)15(3.2) 9:00 AM 13(0.8)7(0.6)6(1.3) 2:30 PM 57(3.7)49(4.5)8(1.7) 3:30 PM 678(44.0)470(43.6)208(44.9) 8:00 PM 26(1.7)9(0.8)17(3.7) 11:30 PM 95(6.2)25(2.3)70(15.1)
Table1. Characteristicsofthedemographicfeaturesinthestudypopulation.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 697
Figure1. Featureimportancerankedbytheinformationgain(entropy).Arrangedinanascendingorder(fromtoptobottom),therelativelylow informationgainof0.00525wasgivenbythefeatureof “maximumofheartrateforthelast1-hourtimeinterval” andtherelativelyhigher informationgainof0.036543wasgivenbythefeature “minimumofsystolicpressuredividedbydiastolicpressureforthe first4-hourtime interval.”
AUC,areaunderthereceiveroperatingcharacteristiccurve; AUPRC:areaundertheprecisionrecallcurve; PPV,positivepredictivevalue; NPV, negativepredictivevalue.
 Table2. Performancemeasuresforthetotalparticipants.
Table2. Performancemeasuresforthetotalparticipants.
TrainingTesting Threshold 2SDs (=35.8) 1SD (=17.9) 202SDs (=35.8) 1SD (=17.9) 20 Model CatBoostGradientBoostingXGBoostCatBoostGradientBoostingXGBoost Positivecount 57163277284696 AUC 110.9960.8380.7590.647 AUPRC 0.9910.9980.9890.5270.430.354 F1 0.8370.9790.9530.50.3720.352 Kappa 0.8290.9750.9370.4770.2880.182 Sensitivity 0.7190.9820.960.3930.4570.354 Specificity 10.9960.9810.9890.890.828 PPV 10.9760.9470.6880.3130.351 NPV 0.9850.9970.9860.9620.9370.831 Accuracy 0.9850.9940.9760.9520.8470.73
Totalparticipants
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 698 ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod Liuetal.
Liuetal. ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod
<35yearsinage.(A)AUConthetrainingcohort(B)AUConthetestingcohort(C)AUPRConthetrainingcohort(D)AUPRConthetesting cohort. AUC,areaunderthereceiveroperatingcharacteristic(ROC)curves; AUPRC,areaundertheprecisionrecallcurve.
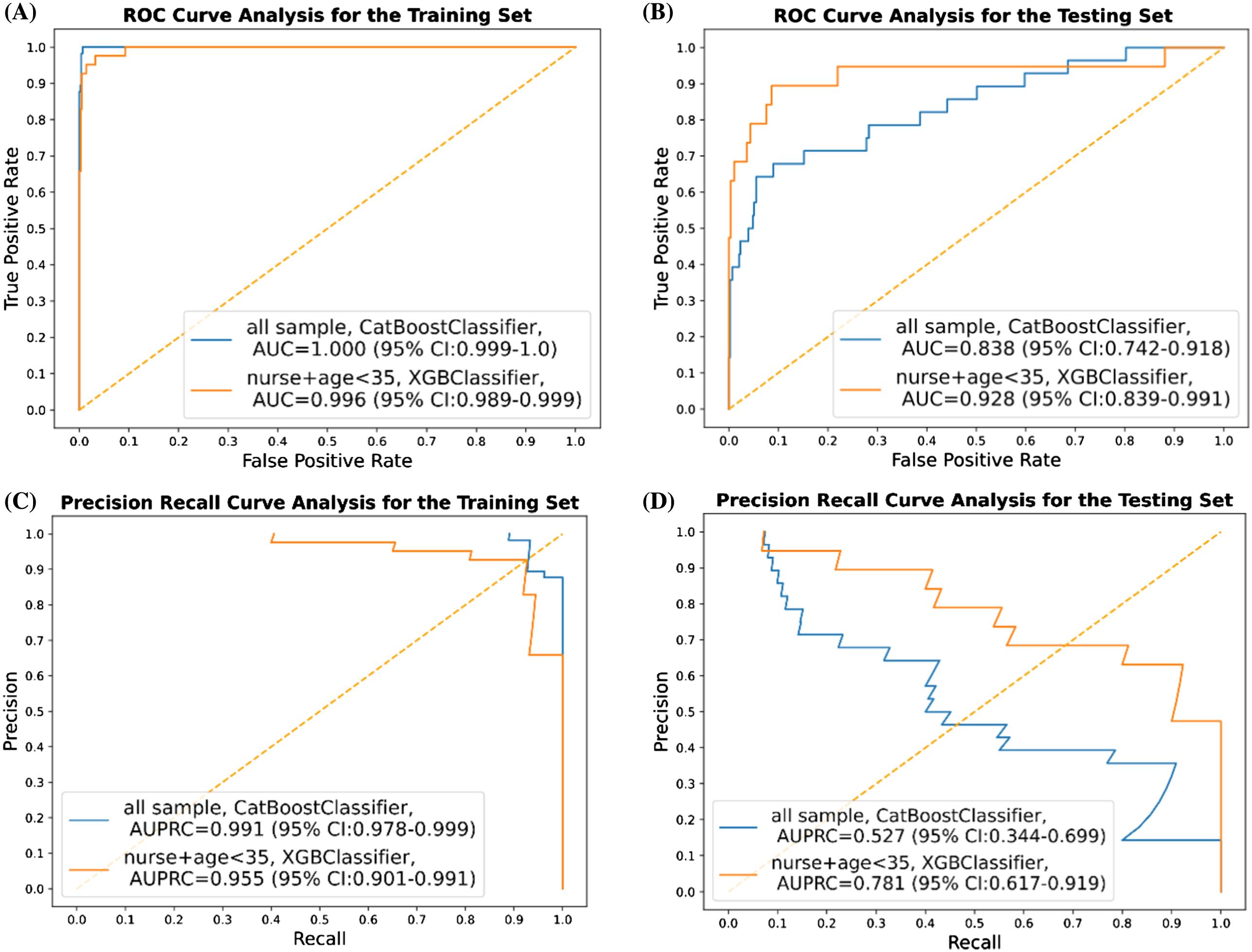
couldleadtoharmfuleventsbothforthemandtheirpatients. Untilnow,previousresearchstudiesforwork-relatedfatigue inhealthcarepractitionersweremostlyconductedinthe formofaquestionnairesurveyratherthanreal-time monitoring.10–12 Withtheadvancementofwearabledevices andthedevelopmentofartificialintelligenceinmedicine, noveltechnologymayfacilitatereal-timeidentificationof work-relatedfatigueinthehealthcaredomain.However, previousstudiesusingwearablemonitoringmethods havefocusedmoreondrowsinessdetectionfordrivers’ occupationalhealth,orfatiguedetectionforrehabilitation patientsratherthanforhealthcareprofessionals.16 Withthe combinationofwearabletechnologyandMLalgorithms, thesemodelswereconsideredtoperformbetterthan traditionalmethodsofdetectingfatigue.However,littlewas knownaboutthedataqualityduringthephaseofmodel development.16 Inthisstudy,wesuccessfullyconstructedML modelsbasedonasmartwatchtoidentifywork-related
fatigue,whichcanserveasabasistoimplementaworkrelatedfatiguepredictionmodelforemergencyhealthcare professionals.
InterpretationofCurrentStudy
Inadditiontoself-reportedsymptoms,theautonomic nervoussystem,especiallyHRV,wasthoughttobean indicatorrelatedtowork-relatedfatigue.28 Inourstudy, of31featuresselectedtoconstructtheMLmodels,three featureswererelatedtoHRV,11toheartrate,seventoblood pressure, fivetostressindex,threetocalorieassumption,and onewasrelatedtofootsteps.
Ourstudyincluded1,542before-and-afterMFIscales completedbyparticipantswhoworeasmartwatchwhileon shiftfromMarch10–June20,2021.Oftheparticipants,85 (5.5%)showedwork-relatedfatigueandwerejudgedtohave work-relatedfatiguebyourstudydefinition.Thetraining/ validationandtestingsetsweredividedchronologicallybya
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 699
Figure2. PerformancemeasuresofthebestmachinelearningmodelintermsofAUCandAUPRCforallsamplesandforsubgroupofnurses
ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod
Nurses <35yearsold
AUC,areaunderthereceiveroperatingcharacteristiccurve; AUPRC,areaundertheprecisionrecallcurve; PPV,positivepredictivevalue; NPV,negativepredictivevalue.
ratioof70∶30tosimulateaprospective,randomized controlledtrial.OurstudyachievedgoodAUCresultsforall populationsandobtainedexcellentperformanceinthe subgroupanalysisfornurses <35yearsold.
Therateofwork-relatedfatigueinourpopulationwaslow (5.5%),whichdoesnotcoincidewithpreviouslyreportedrates ofburnoutforEPs.Asaddressedintworeviewarticles,EPs’ burnoutrateswereestimatedtobe25–60%dependingonthe study.29,30 However,mostofthereviewedstudiesfocusedon researchpapersthatusedtheMaslachBurnoutInventory (MBI)toassesstheprevalenceofburnout.Althoughthe MBIisawell-validatedtoolandaddressesthreescales (emotionalexhaustion,depersonalization,andpersonal accomplishment),itmainlyfocusesonthepsychological aspectofburnoutratherthanthe fivedimensionsoffatigueper theMFI,whichweusedinourstudy.
InadditiontoAUC,weevaluatedaseriesofperformance measuresinourconstructedmodels,includingaccuracy, NPV,PPV(precision),sensitivity(recall),specificity,kappa, andF1score(Tables2 and 3).Precisionreferstohowoften thepredictionsforpositiveclassaretrue,whilerecallrefersto howaccuratelyourmodelcanretrievetherelevantrecords. Theclassimbalanceproblemexistsinthisstudy.The incidenceofwork-relatedfatigueisonly5.5%inourstudy. Althoughweobtainedanextremelyhighspecificityvalue (0.828to0.989)andNPV(0.831to0.962)intheconstructed MLmodelsforallpopulations,ourresultsshowedthatthe sensitivityvalues(0.354to0.457),precision(0.313to0.688), andAUPRC(0.354to0.527)wererelativelylow(Table2). Thisimpliesthatwemustpaymoreattentiontotheclinical staffwithpredicatedwork-relatedfatigue,ratherthanthose without.
DuetotheexcellentperformancesinspecificityandNPV, ourMLmodelsmayalsobeusedasatoolforidentifying clinicalstaffwhoarenotatriskforwork-relatedfatigue. Whensuchahighspecificitytoolyieldsapositiveprediction, wecanconfidentlyruleintheriskofwork-relatedfatiguefor thisEPornurse.Whenwefocusedonnurses <35yearsold, ourpredictionmodelsshowedsomedegreeofimprovement dependingonthemodelsweused,whichmeansthatdifferent healthcareprofessionalsmayhavedifferentpatternsof work-relatedfatigue(Table3).
FeasibilityforClinicalApplication
Work-relatedfatiguewouldexertbothphysicaland psychologicalstressonclinicalstaff,whichcouldfurtherlead toharmfuleventstohealthcareprofessionalsandpatientsas well.Fromthepreviousresearch,work-relatedfatiguewas mainlyreportedinaformofaquestionnairesurveyrather thandetectioninatimelyfashion.10–12 Withourconstructed MLmodel,work-relatedfatiguecouldbemonitoredand documentedinrealtime,andevenintheearlyperiodofthe workshiftbecausemanyofthe31selectedfeatureswere extractedinthe firstone-hourorfour-hourtimeinterval (Figure1).Whenclinicalstaffarethoughttohaveworkrelatedfatiguepredictedbyourmodel,weshouldtryto understandtheirphysicalandpsychologicalhealthand initiateriskassessmentandpreventivemeasures.
Moreover,wecanevenadjustandsystemizethedemandof theworkforceaccordingtothefrequencyofthepositive outputofwork-relatedfatigue.Work-relatedfatiguemay resultinaworkforceshortagebecauseofsickleaveor resignations.31 Aninsufficientworkforcecouldleadto increasingwork-relatedfatigueduetoadditionalstressfrom
Table3. Performancemeasuresforthesubgroupofnursesyoungerthan35yearsold.
TrainingTesting Threshold 2SDs (=38.2) 1SD (=19.1) 202SDs (=38.2) 1SD (=19.1) 20 Model XGBoostRandomForestXGBoostXGBoostRandomForestXGBoost Positivecount 4197174193466 AUC 0.9960.9980.9280.9280.8130.738 AUPRC 0.9550.9890.8810.7810.6090.577 F1 0.9050.9260.750.5560.4290.462 Kappa 0.8990.9130.6850.5150.3280.357 Sensitivity 0.9270.9690.6380.7890.6180.364 Specificity 0.9920.980.9790.9280.8370.939 PPV 0.8840.8870.910.4290.3280.632 NPV 0.9950.9950.8890.9850.9440.838 Accuracy 0.9880.9780.8930.9190.8110.811
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 700
Liuetal.
havingtoshareagreaterworkloadorunfamiliaritywiththe worktobedone.Toescapetheviciouscircle,detectingclinical staffwhohavework-relatedfatigueandthenadjusting workforcedemand flexiblyisofparamountimportanceforthe medicalpersonnelintheEDandtheirpatients.
LIMITATIONS
Therearelimitationstothisstudy.First,welabeledworkrelatedfatiguebyusingaself-assessmentscale,theMFI, whichcouldbesubjectivetoreportingbias.However,the biasmayhavebeenminimalsinceMFIisawell-validated toolworldwide.20
21 Second,thisstudywasconductedinan EDofasingle,tertiaryteachinghospitalwithasmallsample sizethatincludedonlyafewovernightworkers(7.8%),and focusedmostlyonnurseswhowere <35yearsinage(the predominantnursegroupworkinginourED).Selectionbias mayhavebeenintroducedsinceparticipantswereenrolled voluntarilyandnotalltypesofclinicalstaffintheEDwere enrolled.Forthegeneralizabilityofthemodels,furtherstudy mayberequiredtocollectmoredatafromdiversemedical staffnotincludedinthisstudy.
Third,becauseofthelowpositivityrateofwork-related fatigueinourpopulation,ourconstructedMLmodels encounteredtheproblemofimbalancedclassificationand falsenegatives.32
Toobtainbetterperformances,weusedthe SMOTEmethodduringthemodeltrainingprocessto balancethedataset.Inaddition,weevaluatedtheprediction performancesofourmodelswithmostoftheavailable performancemeasures,includingAUC,AUPRC,precision, andrecall,therebyavoidingover-interpretationbyanyofthe results.Fourth,ourmodelsachievedperfectperformance (AUCnearone)inthetrainingsetbutobtainedonly excellentperformanceinthetestingset,andthatraisedthe concernofoverfitting.Suchoverfittingconcerncanalsobe seenintheresultsofhighvariance(largeconfidenceinterval) inthepredictionmodelwebuilt.Inournextstep,weplanto collectmoredataandadoptmorerobustalgorithmsbefore ourmodelcanbegeneralizabletothetargetpopulation.
Fifth,weevaluatedonlytheshort-term,work-related fatigueforashiftgiventhatwelabeleditbyusingthe betweenMFIdifferenceasthelabelingmethod.Further studyisneededtoinvestigatethemethodthatcouldmeasure thelongitudinalfatigue,stress,orburnouteffectsofworking intheED.Finally,duetothepolicyofintellectualproperty protectionintheconsumerelectronicsindustry,theproduct manufacturerwouldnotdiscloseanydetailrelatedtothe dataquality.Webelievethateventhoughtheaccuracyofthe signalderivedfromthesensorofthesmartwatchisuncertain, thetrendandchangesofthesignalcanstillserveasthe featuresforbuildingafatigue-detectionmodel.
CONCLUSION
Wesuccessfullyconstructedsmartwatch-based,machine learningmodelstopredictwork-relatedfatiguewithgreat
discriminationabilitybasedonthefeaturesmonitoredbya smartwatch.Implementationofthistoolmaybeusefulto identifyEDclinicalstaffatriskofwork-relatedfatigue. Giventhesmallsamplesizeinthisstudy,moredata collectionandfurtherprospectivevalidationtodetermine theeffectivenessofusageofthispredictionmodelwillbe necessarybeforeitcanbeappliedindailyclinicalpractice.
AddressforCorrespondence:Tsung-ChienLu,MD,PhD,National TaiwanUniversityHospital,DepartmentofEmergencyMedicine, No.7,ZhongshanS.Rd.,ZhongzhengDist.,TaipeiCity100, Taiwan.Email: jonathanlu@ntu.edu.tw
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Liuetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/ by/4.0/
REFERENCES
1.SwaenGM,VanAmelsvoortLG,BültmannU,etal.Fatigueasarisk factorforbeinginjuredinanoccupationalaccident:resultsfromthe MaastrichtCohortStudy. OccupEnvironMed. 2003;60Suppl1 (Suppl1):i88–92.
2.BargerLK,CadeBE,AyasNT,etal.Extendedworkshiftsandtheriskof motorvehiclecrashesamonginterns. NEnglJMed 2005;352(2):125–34.
3.AyasNT,BargerLK,CadeBE,etal.Extendedworkdurationand theriskofself-reportedpercutaneousinjuriesininterns. JAMA 2006;296(9):1055–62.
4.BargerLK,AyasNT,CadeBE,etal.Impactofextended-durationshifts onmedicalerrors,adverseevents,andattentionalfailures. PLoSMed 2006;3(12):e487.
5.WestCP,TanAD,HabermannTM,etal.Associationofresidentfatigue anddistresswithperceivedmedicalerrors. JAMA 2009;302(12):1294–300.
6.KellerSM.Effectsofextendedworkshiftsandshiftworkonpatient safety,productivity,andemployeehealth. AAOHNJ 2009;57(12):497–502;quiz503-504.
7.AkerstedtT,WrightKPJr.Sleeplossandfatigueinshiftworkandshift workdisorder. SleepMedClin.2009;4(2):257–71.
8.KivimäkiM,JokelaM,NybergST,etal.Longworkinghoursandriskof coronaryheartdiseaseandstroke:asystematicreviewandmetaanalysisofpublishedandunpublisheddatafor603,838individuals. Lancet.2015;386(10005):1739–46.
9.WangLJ,ChenCK,HsuSC,etal.Activejob,healthyjob?Occupational stressanddepressionamonghospitalphysiciansinTaiwan. IndHealth 2011;49(2):173–84.
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 701 Liuetal. ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod
10.WinwoodPC,WinefieldAH,DawsonD,etal.Developmentand validationofascaletomeasurework-relatedfatigueandrecovery:the OccupationalFatigueExhaustion/RecoveryScale(OFER). JOccup EnvironMed.2005;47(6):594–606.
11.DeVriesJ,MichielsenHJ,VanHeckGL.Assessmentoffatigueamong workingpeople:acomparisonofsixquestionnaires. OccupEnviron Med. 2003;60Suppl1(Suppl1):i10
5.
12.JasonLA,EvansM,BrownM,etal.Fatiguescalesandchronicfatigue syndrome:issuesofsensitivityandspecificity. DisabilStudQ 2011;31(1):1375.
13.LuTC,FuCM,MaMH,etal.Healthcareapplicationsofsmartwatches.a systematicreview. ApplClinInform.2016;7(3):850–69.
14.KumarP,ChauhanR,StephanT,etal. “AMachineLearning ImplementationforMentalHealthCare.Application:SmartWatchfor DepressionDetection,” 202111thInternationalConferenceonCloud Computing,DataScience&Engineering(Confluence), 2021,pp.568–74.
15.LuTC,ChenY,HoTW,etal.Anoveldepthestimationalgorithmofchest compressionforfeedbackofhigh-qualitycardiopulmonaryresuscitation basedonasmartwatch. JBiomedInform.2018;87:60–5.
16.AdãoMartinsNR,AnnaheimS,SpenglerCM,etal.Fatiguemonitoring throughwearables:astate-of-the-artreview. FrontPhysiol 2021;12:790292.
17.PetersGA,WongML,JosephJW,etal.Pulseratevariabilityin emergencyphysiciansduringshifts:pilotcross-sectionalstudy. JMIR MhealthUhealth.2019;7(10):e13909.
18.XieJ,WenD,LiangL,etal.Evaluatingthevalidityofcurrentmainstream wearabledevicesin fitnesstrackingundervariousphysicalactivities: comparativestudy. JMIRMhealthUhealth.2018;6(4):e94.
19.SmetsEM,GarssenB,BonkeB,etal.Themultidimensionalfatigue inventory(MFI)psychometricqualitiesofaninstrumenttoassess fatigue. JPsychosomRes.1995;39(3):315–25.
20.ChuangLL,ChuangYF,HsuMJ,etal.Validityandreliabilityofthe TraditionalChineseversionoftheMultidimensionalFatigueInventoryin generalpopulation. PLoSOne.2018;13(5):e0189850.
21.Ba ¸ sogluF,ÖncüJ,KuranB,etal.Thereliabilityandvalidityofthe TurkishversionofMultidimensionalFatigueInventory-20forthe evaluationofdifferentdimensionsoffatigueinpatientswith fibromyalgia. TurkJPhysMedRehabil.2020;66(4):436–43.
22.ShannonCE.Amathematicaltheoryofcommunication. BellSystTech J.1948;27(3):379–423.
23.ChawlaNV,BowyerKW,HallLO,etal.SMOTE:syntheticminorityoversamplingtechnique. JArtIntellRes.2002;16:321–57.
24.FrankE,HallMA,WittenIH.TheWEKAWorkbench.OnlineAppendix. In: DataMining:PracticalMachineLearningToolsandTechniques, Burlington,MA:MorganKaufmann.4thEd,2016.
25.PedregosaF,VaroquauxG,GramfortA,etal.Scikit-learn:machine learninginPython. JMLR.2011;12:2825–30.
26.SinghA,ThakurN,SharmaA.Areviewofsupervisedmachinelearning algorithms. 20163rdInternationalConferenceonComputingfor SustainableGlobalDevelopment(INDIACom);2016;pp.1310–15, IEEE,2016.
27.HoJC,LeeMB,ChenRY,etal.Work-relatedfatigueamongmedical personnelinTaiwan. JFormosMedAssoc.2013;112(10):608–15.
28.TranY,WijesuriyaN,TarvainenM,etal.Therelationshipbetween spectralchangesinheartratevariabilityandfatigue. JPsychophysiol 2009;23(3):143–51.
29.AroraM,AshaS,ChinnappaJ,etal.Reviewarticle:burnoutin emergencymedicinephysicians. EmergMedAustralas 2013;25(6):491–5.
30.ZhangQ,MuMC,HeY,etal.Burnoutinemergencymedicine physicians:ameta-analysisandsystematicreview. Medicine (Baltimore).2020;99(32):e21462.
31.LiuY,WuLM,ChouPL,etal.Theinfluenceofwork-relatedfatigue,work conditions,andpersonalcharacteristicsonintenttoleaveamongnew nurses. JNursScholarsh.2016;48(1):66–73.
32.HoensTR,ChawlaNV.Imbalanceddatasets:fromsamplingto classifiersIn: ImbalancedLearning,Hoboken,NJ:JohnWiley&Sons, Ltd,2013:pp.43–59.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 702 ApplyingaSmartwatchtoPredictWork-relatedFatigueforEHPs:MachineLearningMethod Liuetal.
ImpactofCareInitiationModelonEmergencyDepartment OrdersandOperationalMetrics:CohortStudy
AndyHung-YiLee,MD,MBA*†‡
RebeccaE.Cash,MD†‡
AliceBukhman,MD*†§
DanaIm,MD*†
DamarcusBaymon,MD*†§
LeonD.Sanchez,MD*†§
PaulC.Chen,MD*†
SectionEditor:GaryJohnson,MD
*BrighamandWomen’sHospital,DepartmentofEmergencyMedicine,Boston, Massachusetts,USA
† HarvardMedicalSchool,Boston,Massachusetts,USA
‡ MassachusettsGeneralHospital,DepartmentofEmergencyMedicine,Boston, Massachusetts,USA
§ BrighamandWomen’sFaulkner’sHospital,DepartmentofEmergencyMedicine, JamaicaPlain,Massachusetts,USA
Submissionhistory:SubmittedNovember2,2022;RevisionreceivedMarch21,2023;AcceptedApril3,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59340
Introduction: Emergencydepartments(ED)employmanystrategiestoaddresscrowdingandprolonged waittimes.Theyincludefront-endCareInitiationandclinician-in-triagemodelsthatstartthediagnosticand therapeuticprocesswhilethepatientwaitsforacarespaceintheED.Theobjectiveofthisstudywasto quantifytheimpactofaCareInitiationmodelonresourceutilizationandoperationalmetricsintheED.
Methods: WeperformedaretrospectiveanalysisofEDvisitsatourinstitutionduringOctober2021. BaselinecharacteristicswerecomparedwithChi-squareandquantileregression.Weused t-teststo calculateunadjusteddifferenceinoutcomemeasures,includingnumberoflaboratorytestsorderedand averagetimepatientsspentinthewaitingroomandtheEDtreatmentroom,andthetimefromarrivaluntil EDdisposition.Weperformedpropensityscoreanalysisusingmatchingandinverseprobability weightingtoquantifythedirectimpactofCareInitiationonoutcomemeasures.
Results: Therewere2,407EDpatientencounters,1,191(49%)ofwhomarrivedduringthehourswhen CareInitiationwasactive.Atotalof811(68%)ofthesepatientsunderwentCareInitiation,whilethe remainderproceededdirectlytothemaintreatmentarea.PatientsweremorelikelytoundergoCare Initiationiftheyhadloweracuityandlowerriskofadmission,andiftheEDwasbusierasmeasuredbythe numberofrecentarrivalsandpercentageofoccupiedEDbeds.Afteradjustingforpatient-specificand department-levelcovariates,CareInitiationdidnotincreasethenumberofdiagnosticlaboratorytests ordered.CareInitiationwasassociatedwithincreasedwaitingroomtimeby1.8hoursandlongertime fromarrivaluntildispositionby1.3hours,butwithdecreasedtimeinthemaintreatmentareaby0.6hours, whichrepresentsa15%reduction.
Conclusion: CareInitiationwasassociatedwitha15%reductionintimespentinthemainEDtreatmentarea butlongerwaitingroomtimeandlongertimeuntilEDdispositionwithoutsignificantlyincreasingthenumberof laboratorystudiesordered.WhilepreviousstudiesproducedsimilarresultswithCareInitiationmodels accessingalldiagnosticmodalitiesincludingimaging,ourstudydemonstratesthatamorelimitedCare InitiationmodelcanstillresultinoperationalbenefitsforEDs.[WestJEmergMed.2023;24(4)703–709.]
INTRODUCTION
Emergencydepartments(ED)oftenexperiencesignificant crowding,whichcanleadtoprolongedpatientwaittimes
andworseoutcomes.1,2 Thishasbeenexacerbatedby increasingnumbersofadmittedpatientsboardingintheED whilewaitingforaninpatientbed.Theseinpatientboarders
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 703
ORIGINAL RESEARCH
consumeEDresourcesincludingbedsandstaffandslowthe department’sabilitytomanagenewlyarrivingpatients.3,4 MultiplestrategieshavebeenemployedbyEDsacrossthe countrytopreventdelaysincare,includingtheuseofCare Initiationandclinician-in-triagemodels.5,6
CareInitiationandclinician-in-triagemodelsinvolve placinganemergencyphysicianorphysicianassistant(PA) atthepointoftriagewhocanrapidlyscreenpatientsand determineinitialplansofcare.7 Theclinicianisoften empoweredtotreatanddirectlydischargepatientswith straightforwardcomplaintsandinitiateevaluationand treatmentforpatientswithmorecomplexcomplaints.8
Multiplestudiesintheliteraturedescribesingle-site implementationofthesemodelsindifferentEDsettings,9–11 buttheirimpactmaydependoncapabilitiesandresources dedicatedtothesefront-endmodelsandmayalsodependon specificcharacteristicsoftheindividualsites,suchaspatient populations,staffinglevels,andbottlenecksincare.7
Moreover,theirprimaryfocushasbeenonoperational metricssuchasleftwithoutbeingseen(LWBS)rates, door-to-cliniciantime,andEDlengthofstay,12 andfewof thesestudiesattemptedtoquantifytheeffectofCare InitiationmodelsonutilizationofEDresources.
TheCareInitiationsystematourinstitutiondiffersfrom manyothersinthatitisrestrictedtolaboratorydiagnostic testingandisdeployedatanacademicmedicalcenterwitha highlycomplextransplantandoncologicpopulation.Our objectiveinthisstudywastoassesstheimpactofCare Initiationatourinstitutionbycomparingthenumberof diagnostictestsorderedandtoassesswhetherthis strategyoffersthesameoperationalimprovementsseen inotherstudies.
METHODS
StudyDesignandSetting
Weperformedaretrospectivecohortstudyofpatients presentingtoouracademicEDintheNortheasternUnited StatesinthemonthofOctober2021.TheEDisaLevelI traumacenter,comprehensivestrokecenter;itisaffiliated withacomprehensiveoncologictreatmentcenterandhadan annualcensusof ≈65,000EDvisitsin2021.Thestudywas approvedbytheinstitutionalreviewboard(Protocol 2022P000264)andperformedaccordingto STROBEguidelines.13
TheCareInitiationprogramintheEDwasimplemented inJanuary2021andwasdesignedtostartlaboratory work-upincludingbloodandurinestudiesonwaitingroom patients.Theprogramoperatedfromnoontomidnighton weekdaysandwasstaffedbyaPAwithatleasttwoyearsof experienceworkingintheED.ThePAwouldscreenall triagedpatientsinthewaitingroomandbasedontheir clinicalevaluationwouldorderlabstudiesbasedonwhat theydeterminedwouldbeneededaspartoftheEDwork-up. Therequiredbloodandurinesampleswouldbeobtainedand
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Manyemergencydepartments(ED)have implementedCareInitiationtostartthe diagnosticwork-upofpatientswhiletheyare stillinthewaitingroom.
Whatwastheresearchquestion?
WeanalyzedhowCareInitiationimpactsthe numberoflabordersandEDoperational metrics.
Whatwasthemajor findingofthestudy?
CareInitiationdidnotincreaselaborder numbersandwasassociatedwith0.6fewer hoursinanEDbed.
Howdoesthisimprovepopulationhealth?
CareInitiationcanhelpaddressEDcapacity constraintswithoutsigni fi cantlyincreasing thecostofcare.
thepatientreturnedtothewaitingroom,wherethepatient continuedtowaitforacarespaceintheED(Figure1).The CareInitiationPAwasnotauthorizedtoorderradiologic studiesinthisprogram.WhenCareInitiationwasnotactive, patientswouldwaitinthewaitingroomuntilanopencare spacewasavailableintheEDasperusualcare.
OutcomeMeasuresandDataCollection
Weobtaineddatawereobtainedfromtheelectronic healthrecord(EpicSystemsCorporation,Verona,WI)for allEDencountersatourinstitutioninOctober2021.TheED encounterswerecategorizedbasedonwhetherCare Initiationwasactiveandwhethertheencounterproceeded throughtheCareInitiationprogram.WeexcludedED encountersinwhichpatientsarrivedviaemergencymedical services(groundorair)ornolabworkwasorderedasthey werenotconsideredforCareInitiationattriage.Individual patientvariablesincludedpatientage,gender,race/ethnicity, andEmergencySeverityIndex(ESI).Operation-level variablesincludednumberofEDarrivalsinthepriorfour hoursattimeofpatientpresentationandpercentageofED bedoccupancyattimeofEDpresentation.Timestampswere obtainedforeachpatientencounter,whichincludedED arrival,EDrooming,andEDdisposition.Primaryoutcome variablesincludedthenumberofdiagnosticlabtestsordered priortoEDdispositionandthelengthoftimethepatient spentinthemainED.Thelabtestsincludedwerecompiled fromalistofthe25mostfrequentlyorderedlabtestsinthe
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 704 ImpactofCareInitiationModelonEDOrdersandOperationalMetrics Leeetal.
EDatourinstitution(Supplement1).Secondaryoutcome variablesincludedEDwaitingtimeandtimefromEDarrival toEDdisposition.
DataandStatisticalAnalysis
Weanalyzeddataattheencounterlevelandperformed statisticalanalysesinStata15(StataCorp,CollegeStation, TX).Comparisonsbetweencontinuousvariableswere calculatedfordemographicvariablesusingmediansand quantileregressionsandforoutcomevariablesusingStudent t -tests.Wecalculatedcomparisonsbetweencategorical variablesusingchi-squaretests,andweusedlogistic regressiontocalculatetheunadjustedandadjustedtreatment effectofCareInitiation.Becauseoftheobservationalnature ofthedataandunequalprobabilityofselectionforCare Initiation,whichcanintroducebias,weperformedseveral sensitivityanalyses.Propensityscorematchingwas performedbasedonpatientage,gender,ESI,numberofED arrivalswithinthepriorfourhours,andpercentage occupancyofEDbedsascovariatesinalogisticmodelto quantifythematchedeffectofCareInitiationonoutcome measures.Additionalsensitivityanalysisoftheoutcome measureswasperformedusinginverseprobabilityweighting.
RESULTS
ExcludingpatientswhoarrivedviaEMS,therewere2,407 EDpatientencountersatourinstitutionwherelabtesting wasordered(Table1).Ofthose2,407encounters,1,191 occurredwhentheCareInitiationprogramwasactive,and 811(68%)underwentCareInitiationwhiletheother380 encounters(32%)proceededdirectlytotheED.Among patientswhoarrivedduringCareInitiationhours,patients
whounderwentCareInitiationweremorelikelytobefemale (65%vs54%),hadloweracuitybyESI(median3vs2),and werelesslikelytobeadmittedtothehospital(37%vs45%) (P < 0.05forallcomparisons).Patientswerealsomorelikely tobypassCareInitiationwhentherewerefewerEDarrivals inthepriorfourhours(medians61vs64)andwhenthe percentageofoccupiedEDbedswaslower(median85%vs 86%)(P < 0.05forallcomparisons).Moreover,patientswho arrivedduringCareInitiationhoursweremorelikelytobe WhitethanBlackandtendedtohavehigheracuitybyESI andrateofadmissioncomparedtopatientswhoarrived outsideCareInitiationhours.OutsideCareInitiationhours, therealsotendedtobefewerarrivalsinthepriorfourhours andasmallerpercentageofoccupiedEDbeds.
PatientswhoproceededthroughCareInitiationhadfewer labtestsorderedpriortoEDdispositionthanpatientswho proceededdirectlytothemaintreatmentarea(6.8vs7.3lab orders, P < 0.01).Thisdifferencewasnotstatistically significantafteraccountingforpatient-specificvariablesof age,gender,andESIacuity(Table2).Patientswhoarrived duringCareInitiationhourshadmorelabtestsordered thanthosewhoarrivedoutsideofCareInitiationhours (7.0vs6.5, P < 0.01).
PatientswhoexperiencedCareInitiationhadasignificantly longertimeinthewaitingroom(3.2vs1.2hours, P < 0.01) andlongertimefromEDarrivaltoEDdisposition(6.7vs5.1 hours, P < 0.01)comparedtopatientswhodidnotproceed throughCareInitiation(Table3).Thesedifferencesdecreased inmagnitudebutpersistedevenafteradjustingforpatientspecificvariablesofage,gender,andESIacuity.However, theyhadashorterlengthoftimespentinthemainED treatmentarea(3.6vs3.9hours,
< 0.01),andthispersisted
ED Arrival Pa ent evaluated at Triage Direct to main ED Pa ent stable and appropriate for Care Ini a on? No Yes Care Ini a on Ac ve? No Yes Available bed in main ED? Yes No PA performs screening evalua on and orders diagnos c labs
P
Pa ent to wai ng room. Move to main ED when bed available. Expedite movement for cri cal lab result or clinical deteriora on
RN performs lab draw
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 705 Leeetal. ImpactofCareInitiationModelonEDOrdersandOperationalMetrics
Figure1. CareInitiationmodel.
PatientsarrivingduringCareInitiationhours
PatientsarrivingoutsideCare Initiationhours Patientsproceedingthrough CareInitiation Patientsproceeding directlytomainEDAllpatients
Numberofpatients(N)8113801,216
Age:median(IQR)49(32,66)53(34,69)51(33,66)
*P < 0.05.
afteraccountingforpatient-specificvariablesofage,gender, andESIacuity.DuringhourswhenCareInitiationwasnot active,patientsexperiencedshorterlengthoftimeinthe waitingroom(1.2vs2.5hours, P < 0.01)andlesstimefrom arrivaltoEDdisposition(5.4vs6.2hours)butlongertimein themaintreatmentarea(4.2vs3.7hours,p < 0.01).
Givenintrinsicdifferencesbetweenpatientgroupsbasedon timeofarrivalandwhethertheyproceedthroughCare Initiation,weperformedpropensityscoreanalysiswith matchingandinverseprobabilityweightingtoevaluatethe directimpactofCareInitiationonoutcomemeasures.After matchingpatientsbasedonindividualpatientfactorsofage,
gender,andESIandbasedonED-leveloperationalvariables ofnumberofEDarrivalsinpriorfourhoursandpercentage occupancyofEDbeds,wefoundthatCareInitiationdidnot significantlyaffectthenumberoflabstudiesordered. However,CareInitiationdidsignificantlyimpacttimemetrics forpatientsbyonaverageshorteningtimeinthemain treatmentareaforpatientsby0.6hours(P < 0.01)and lengtheningtimeinthewaitingroomby1.8hours(P < 0.01) andtimefromarrivaltoEDdispositionby1.3hours (P < 0.01).Thisoverallshortenedthelengthoftimethat patientsoccupiedabedintheEDby15%.Covariatebalance wasacceptablebasedonstandardizeddifferencesandvariance
Table1. Patientdemographics.
Gender:N(%) Female530(65)*206(54)*746(61) Male281(35)*174(46)*470(39) Race:N(%) Asian34(4)12(3)48(4) Black138(17)63(17)280(23) White473(58)238(63)646(53) Other/multiple166(20)67(18)242(20) Ethnicity:N(%) Hispanic157(19)75(20)256(21) Non-Hispanic654(81)305(80)960(79) ESIAcuity:N(%) 10(0)*4(1)*0(0) 2303(37)*233(61)*509(42) 3496(61)*128(34)*660(54) 412(1)*14(4)*45(4) 50(0)*1(0)*0(0) NumberofEDarrivalsintheprior4 hours:median(IQR) 64(59,71)*61(52,69)*38(24,53) PercentageEDbedoccupancy atEDarrival: medianpercentage(IQR) 86(83,89)*85(81,89)*69(59,76) EDdisposition:N(%) Admission301(37)*170(45)*384(32) EDobservation5(1)*12(3)*23(2) Discharge505(62)*198(52)*809(67)
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 706 ImpactofCareInitiationModelonEDOrdersandOperationalMetrics Leeetal.
ED,emergencydepartment; IQR,interquartilerange; ESI,EmergencySeverityIndex.
**p < 0.05.
ED,emergencydepartment; ATE,averagetreatmenteffect; CI,confidenceinterval.
ratio(Supplement2).Repeatingthisanalysisusinginverse probabilityweightingproducedsimilarresults(Table3).
DISCUSSION
Emergencydepartmentsconsideringtheimplementation ofCareInitiationandclinicianintriageoftenhaveconcerns thattheseprocesseswillincreasetheoverallnumberoflab testsorderedforapatient.Thisconcernisunderstandable,as emergencyclinicianstrytoanticipatethelikelydiagnostic work-upafterperformingonlyabriefassessmentofthe patient.Inourstudy,CareInitiationdidnotsignificantly increasethenumberoflabordersbeforeEDdisposition, evenafterpropensityscorematchingofpatientcohorts.We foundnobroadconsensusinpreviousliteratureonthistopic. WhenCareInitiationisappliedtoabroadpopulation,some studiessuggestthatitisassociatedwithmorediagnostic
testingincludingradiologyimaging.11,14 Otherstudies focusingspecificallyonpatientswithabdominalpainhave foundeithernodifferenceorhigheruseofdiagnostic imaging.15,16 Theremayalsobesubstantialdifferences dependingonthetypeofclinician(emergencyphysicianvs advancedpracticepractitioner[APP]vstriagenurse) performingthisCareInitiationrole.Twostudiesfoundthat triagenursesordermoreteststhanphysicians,17,18 while anothershowednodifferencesintotalnumberoftests betweenAPPscomparedtophysicians.19 Ourstudy, althoughlimitedtoafront-endmodelthatinvolvesaPA orderingonlylabtests,didnotshowanincreasedutilization oflaboratorydiagnostictestingforpatientswhoproceed throughCareInitiationevenafteraccountingforpatientspecificfactorsthroughpropensityscorematching.Our resultssupporttheroleofAPPsinCareInitiationand
PatientsarrivingduringCare Initiationhours Patientsarriving outsideCare Initiationhours Patients proceedingthrough CareInitiation: average(SD) Patients proceedingdirectly tomainED: average(SD) Allpatients: average(SD) CareInitiation unadjustedaverage treatmenteffect: unadjustedATE (95%CI) CareInitiation adjustedaverage treatmenteffect: adjustedATE (95%CI) Numberofpatients(N)811380121611911182 Numberoflaborders priortoEDdisposition 6.8(2.8)*7.3(3.8)*6.5(3.2) 0.6 ( 1.0to 0.1) 0.3 ( 0.8to0.1) Waitingroomtimein hours 3.2(1.6)*1.2(1.6)*1.2(1.4)2.0 (1.8to2.2) 1.7 (1.5to1.9) TimeinmainEDin hours 3.6(2.0)*3.9(2.1)*4.2(2.1) 0.4 ( 0.6to 0.1) 0.5 ( 0.8to0.2) Totaltimefromarrival todispositioninhours 6.7(2.6)*5.1(2.6)*5.5(2.5)1.6 (1.0to1.9) 1.2 (0.8to1.5)
Table2. Studyoutcomemeasureswithoutcohortmatching.
PropensityscorematchingInverseprobabilityweighting Averagetreatmenteffectof CareInitiation(95%CI) P-value Averagetreatmenteffectof CareInitiation(95%CI) P-value NumberoflaborderspriortoED disposition:average(SD) 0.2( 0.7to0.3)0.39 0.4( 0.9to0.1)0.11 Waitingroomtimeinhours:average(SD)1.8(1.3to2.0) <0.011.6(1.4to1.9) <0.01 TimeinmainEDinhours:average(SD) 0.6( 0.9to 0.3) <0.01 0.5( 0.8to 0.2) <0.01 Totaltimefromarrivaltodispositionin hours:average(SD) 1.3(0.9to1.6) <0.011.1(0.8to1.5) <0.01
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 707 Leeetal. ImpactofCareInitiationModelonEDOrdersandOperationalMetrics
Table3. Propensityscoreandinverseprobabilityweightinganalysis.
ED,emergencydepartment; CI,confidenceinterval.
providereassuranceagainstoverutilizationofdiagnostic resources,althoughfurthermonitoringparticularlywith regardtoradiologyiswarrantedbasedontheliterature.
WewereabletoshowthatCareInitiationshortenedthe lengthoftimepatientsspendinanEDbedby0.6hours, whichissigni ficantgiventhisrepresentsa15%reduction. However,thiscameatthecostofincreasingapatient’ stotal timeintheEDuntildisposition,mostlyduetolongertime inthewaitingroom.Thisisconsistentwithprevious literaturethatshowedshorterlengthoftimeinanEDbed butalongertimeuntildisposition20 whencliniciansintriage initiateEDwork-up.ThisisdesirableformostEDsasthey areabletousetimeinthewaitingroomtoadvancecare whileminimizingtimeinanEDbed,whichisascarcer resource.Furthermore,itissigni fi cantthatwhilemost previousstudiesobservedthisreductionoftimeinanED bedwhenthetriageclinicianhadfullaccesstoalllab andimagingtestsincludingcomputedtomography,we wereabletodemonstrateasimilareffectthroughlab ordersalone.
comparingpre-andpost-implementationoutcomes. Moreover,propensityscorematchingcanintroduce additionalbiasintothedataset,butthisismostlikely amelioratedbyreproducingthesameresultswithinverse probabilityweightingmethodology.Finally,ourresultsare likelynotapplicabletoveryhigh-acuityorlow-acuity patientsduetotheirdeliberateexclusionfromCareInitiation models,whichisacommonpracticeinEDsacross thecountry.
CONCLUSION
Overall,CareInitiationatourinstitutiondidnot significantlyincreasethenumberoflabdiagnostictests orderedandresultedinshorteningtheaveragelengthoftime spentinanEDbedby0.6hours,whichis15%oftheaverage timetoEDdisposition.AlthougheveryEDfacesunique challengesinthroughputandefficiency,implementationof CareInitiationandotherclinician-in-triageprogramsmay offersomereliefespeciallyinEDswithprolongedwaittimes andsignificantcrowding.
AddressforCorrespondence:AndyHung-YiLee,MD,MBA,Harvard MedicalSchool,DepartmentofEmergencyMedicine,5Emerson Place,Suite101Boston,MA02114.Email: alee85@partners.org
23
Thisisnotablebecausewaitingfordiagnosticimaging resourcesisoftenanoperationalbottleneckthatispartofthe “criticalpath” formanypatients,7 andtheremayalsobe logisticchallengesforpatientsinthewaitingroomtojointhe queuefordiagnosticimaging.TheseadvantagesofCare Initiationareinadditiontoimprovingothercommon EDmetricssuchasreducingdoor-to-cliniciantimeand LWBSrates,whichhavebeenextensivelystudiedin theliterature.21
CareInitiationmayalsohaveadditionalbenefitsfor patientswhodonotgothroughtheprocessitself.Ourdata suggeststhateventhepatientcohortwhobypassedCare InitiationexperiencedshortertimeinanEDbedbefore dispositioncomparedtowhenCareInitiationwasnotactive. ThismaybebecausefasterthroughputofCareInitiation patientsthroughEDbedsallowsresourcestobefocusedon higheracuitypatients.Moreover,havingaclinicianintriage mayallowmorefrequentreassessmentofwaitingroom patientsandidentificationofthosewhomaydecompensate afterspendingseveralhourswaitingwithrelatively infrequentmonitoring.
LIMITATIONS
Thereareseverallimitationstoourstudy.First,thiswasa single-center,retrospectivecohortstudythatexaminedED encountersoccurringoverthespanofamonthandusedan institutional-specificformofCareInitiation.Ourdata, therefore,maynotbeapplicabletoallEDsdespitesharing manysimilaritieswithothermodels.Wehavesince transitionedtowardaCareInitiationmodeldesignedto dischargepatientsdirectlyfromtheCareInitiationarea, whichwillbethesubjectoffurtherstudy.Wewerealso limitedinthescopeofourdatatoafterdeploymentofCare Initiation;additionalanalysescouldbeperformedwhen
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financialrelationshipswithanycompaniesthatarerelevanttothis study.Therearenoconflictsofinterestorsourcesoffunding todeclare.
Copyright:©2023Leeetal.Thisisanopenaccessarticledistributed inaccordancewiththetermsoftheCreativeCommonsAttribution (CCBY4.0)License.See: http://creativecommons.org/licenses/by/ 4.0/
REFERENCES
1.MorleyC,UnwinM,PetersonGM,etal.Emergencydepartment crowding:asystematicreviewofcauses,consequencesandsolutions. PLoSOne.2018;13(8):e0203316.
2.BadrS,NyceA,AwanT,etal.Measuresofemergencydepartment crowding,asystematicreview.Howtomakesenseofalonglist. Open AccessEmergMed.2022;14:5–14.
3.SmalleyCM,SimonEL,MeldonSW,etal.Theimpactofhospital boardingontheemergencydepartmentwaitingroom. JAmCollEmerg PhysiciansOpen.2020;1(5):1052–9.
4.TrzeciakS,RiversEP.Emergencydepartmentovercrowdinginthe UnitedStates:anemergingthreattopatientsafetyandpublichealth. EmergMedJ.2003;20(5):402–5.
5.DerletRW,RichardsJR.Tensolutionsforemergencydepartment crowding. WestJEmergMed.2008;9(1):24–7.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 708 ImpactofCareInitiationModelonEDOrdersandOperationalMetrics Leeetal.
6.BenabbasR,ShahR,ZonnoorB,etal.Impactoftriageliaisonprovider onemergencydepartmentthroughput:asystematicreviewandmetaanalysis. AmJEmergMed.2020;38(8):1662–70.
7.FranklinBJ,LiKY,SomandDM,etal.Emergencydepartmentprovider intriage:assessingsite-specificrationale,operationalfeasibility,and financialimpact. JAmCollEmergPhysiciansOpen.2021;2(3):e12450.
8.RoweBH,GuoX,Villa-RoelC,etal.Theroleoftriageliaisonphysicians onmitigatingovercrowdinginemergencydepartments:asystematic review. AcadEmergMed.2011;18(2):111–20.
9.BurstromL,EngstromML,CastrenM,etal.Improvedqualityand efficiencyaftertheintroductionofphysician-ledteamtriageinan emergencydepartment. UpsJMedSci.2016;121(1):38–44.
10.NestlerDM,FratzkeAR,ChurchCJ,etal.Effectofaphysicianassistant astriageliaisonprovideronpatientthroughputinanacademic emergencydepartment. AcadEmergMed.2012;19(11):1235–41.
11.LauksJ,MramorB,BaumgartlK,etal.Medicalteamevaluation:effect onemergencydepartmentwaitingtimeandlengthofstay. PLoSOne 2016;11(4):e0154372.
12.SpencerS,StephensK,Swanson-BiearmanB,etal.Healthcareprovider intriagetoimproveoutcomes. JEmergNurs.2019;45(5):561–6.
13.vonElmE,AltmanDG,EggerM,etal.STROBEInitiative.The StrengtheningtheReportingofObservationalStudiesinEpidemiology (STROBE)Statement:GuidelinesforReportingObservationalStudies. AnnInternMed.2007;147(8):573
7.
14.MarshallA,ColeskaA,WardM,etal.116Theeffectofaphysicianin triageonnumberofordersplaced. AnnEmergMed.2019;74(4):S47.
15.BegazT,ElashoffD,GroganTR,etal.Initiatingdiagnosticstudieson patientswithabdominalpaininthewaitingroomdecreasestimespentin anemergencydepartmentbed:arandomizedcontrolledtrial. Ann EmergMed.2017;69(3):298–307.
16.MatzK,BrittT,LaBondV.CTorderingpatternsforabdominalpainby physicianintriage. AmJEmergMed.2017;35(7):974–7.
17.GottliebM,FarcyDA,MorenoLA,etal.Triagenurse-orderedtestingin theemergencydepartmentsetting:areviewoftheliteratureforthe clinician. JEmergMed.2021;60(4):570–5.
18.SeabergDC,MacLeodBA.Correlationbetweentriagenurse andphysicianorderingofEDtests. AmJEmergMed.1998;16(1):8–11.
19.BegazT,ElashoffD,GroganTR,etal.Differencesintestordering betweennursepractitionersandattendingemergencyphysicians whenactingasproviderintriage. AmJEmergMed 2017;35(10):1426–9.
20.RussS,JonesI,AronskyD,etal.Placingphysicianordersattriage:the effectonlengthofstay. AnnEmergMed.2010;56(1):27–33.
21.LoveRA,MurphyJA,LietzTE,etal.Theeffectivenessofaproviderin triageintheemergencydepartment:aqualityimprovementinitiativeto improvepatient flow. AdvEmergNursJ.2012;34(1):65–74.
22.ShahR,LenoR,SinertR.Impactofprovider-in-triageinasafety-net hospital. JEmergMed.2020;59(3):459–65.
23.SemberM,DonleyC,EgglestonM.Implementationofaproviderin triageanditseffectonleftwithoutbeingseenrateatacommunity traumacenter. OpenAccessEmergMed.2021;13:137–41.
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 709 Leeetal. ImpactofCareInitiationModelonEDOrdersandOperationalMetrics
DisparitiesinEmergencyDepartmentNaloxone andBuprenorphineInitiation
JoanPapp,MD CharlesEmerman,MD
MetroHealthCampusofCaseWesternReserveUniversity,DepartmentofEmergency Medicine,Cleveland,Ohio
SectionEditor: YaninaPurim-Shem-Tov,MD,MS
Submissionhistory:SubmittedAugust27,2022;RevisionreceivedJanuary30,2023;AcceptedFebruary8,2023
ElectronicallypublishedJune30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58636
Introduction: Prescribingofbuprenorphineandnaloxoneintheemergencydepartment(ED)hasbeen showntobeaneffectiveintervention.Thepurposeofthisstudywastodeterminethefrequency ofprescribingofnaloxoneandbuprenorphineandthesub-groupsthatmaybemoreorlesslikelyto receivetreatment.
Methods: Weusedanationalelectronichealthrecorddatabasetoidentifypatientswithopioidpoisoning oroverdosepresentingbetweenJanuary2019–December2021.Patientswhowereprescribed naloxoneorbuprenorphinewereidentifiedinthisdatasetandthenfurthersegmentedbasedonselfidentifiedgender,age,racialandethnicidentity,incomecategories,andsocialvulnerabilityindexinorder toidentifysub-groupsthatmaybelesslikelytobeprescribedtreatment.
Results: Wefound74,004patientsinthedatabasewhomweidentifiedaspresentingtotheEDwithan opioidpoisoningoroverdose.Overall,22.8%weredischargedwithaprescriptionfornaloxone,while 0.9%ofpatientsweredischargedwithbuprenorphineproducts.Patientswerelesslikelytoreceive naloxoneprescriptionsiftheywerefemale,WhiteorPacificIslander,non-Hispanic,notbetweentheages of18–65,andnon-Englishspeaking.Wefoundthesamepatternforbuprenorphineprescriptionsexcept thattheresultswerenotsignificantforethnicityandEnglish-speaking.
Conclusion: Despiteevidencesupportingitsuse,buprenorphineisnotprescribedfromtheEDina substantialproportionofpatients.Naloxoneisprescribedtoahigherpercentage,althoughstillaminorityof patientsreceiveit.Somesub-groupsaredisadvantagedintheprescribingoftheseproducts.Furtherstudy mayassistinimprovingtheprescribingofthesetherapies.[WestJEmergMed.2023;24(4)710–716.]
INTRODUCTION
SincetheonsetoftheCOVID-19pandemicin2020,the opioidoverdosecrisishasworsenedwithover100,000deaths intheUnitedStatesbetweenMay2020–April2021,agrim 28.5%increasefromtheprioryear.1,2,3 Theemergency department(ED)isavitalentrypointintothehealthcare systemforpatientsseekingcareforopioidusedisorder (OUD)anditsassociatedcomplicationsandoffersacritical opportunitytoprovidelifesavinginterventionssuchas medicationtotreatopioidusedisorder(MOUD)andtakehomenaloxone.
HighlyeffectivemedicationsapprovedbytheUSFood andDrugAdministrationtotreatandreducetheharmful effectsofOUDandillicitopioiduseareavailablebut underused,andtheyareofteninaccessibletopeoplewhouse opioids.TheMOUDwithbuprenorphineormethadoneis evidence-based,welltolerated,retainspeopleintreatment, reducesillicitopioiduseathighdoses,andreduces mortality.4,5,6,7 TreatmentforOUDinitiatedintheEDis feasible,leadstodecreasedillicitdruguseandincreasedlongtermretentionandengagementwhenpairedwithfollow-up addictiontreatmentservices.8,9
Despiteanabundanceof
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 710 ORIGINAL RESEARCH
evidence,lessthan35%ofadultswithOUDreceivedMOUD treatmentin2019acrossalltreatmentsettings.10
Take-homenaloxoneisanothercriticaltooltoreduce overdosemortalityandrequiresminimaltrainingtobeused effectively.11,12 Despitesupportingevidence,studiesindicate thattake-homenaloxoneaccessispoor,withfewerthanhalf ofoverdosepatientsreceivingaprescriptionforthe medicationwithinonehealthcaresystemandonlyoneof13 patientsreceivingaprescriptionnationally.13,14 Someofthe reportedbarriersincludecost,patientreceptiveness, regulatorybarriers,andhealthcarestafftime.15
Arecentpriorstudyhasindicatedthatnationally, followingnon-fataloverdoseintheED,onlyoneof12 patientsareinitiatedonbuprenorphine.14 Thatstudyfound differencesinprescribingbasedongender,age,geographic location,andinsurancestatus.Thedatabaseusedinthat studyunder-representedtheuninsuredandMedicaid patients,andtherewerelimitationsintheabilitytostudy somesubsetsofpatients.Ourpurposeinthisstudywasto evaluatewhetherdisparitiesexistforracialandethnic minoritiesinnaloxoneandbuprenorphineprescribingfor patientspresentingtotheEDwithanopioidoverdose.
METHODS
TheAzureCosmosdatabase(MicrosoftCorporation, RedmondWA)iscomposedofsubmissionsfrom organizationsthatparticipateintheEpicelectronichealth recordsystem(EpicSystemsCorporation,Verona,WA).
ParticipatingorganizationscontributeaHIPAA-defined, limiteddatasetforallpatientsintothedatabase.Individuals fromparticipatingorganizationscanobtainauserlicenseto querythedatabase.Atthetimeofthisstudy,therewere approximately130,000,000uniquepatientsintheCosmos dataset.Thestateswiththehighestpopulationsinclude California,Texas,Illinois,Ohio,andNewYork.The databasedoesnotallowtheidentificationofthespecific organizations,orthecharacteristicsoftheorganizations, associatedwithindividualpatients.
Weusedtheencounterdatamodeltoquerythedatabase. PatientswithanencountertypethatincludedanEDvisit withoutahospitaladmissionwereselected.Patientswho expiredduringtheEDencounterwereeliminated.We furthercategorizedencounterstoselectthosewitha SystematizedNomenclatureofMedicine(SNOMED) diagnosisofheroin,methadone,morphine,andfentanylor opioidpoisoningoroverdose.TheSNOMEDisthecoding terminologyplatformmaintainedbytheInternational HealthTerminologyStandardsOrganization.These diagnoseswerechosenbasedonananalysisofdiagnoses associatedwithEDnaloxoneadministration.Weidentified theprescribingofMOUDfornaloxoneorbuprenorphine usingtheprescribing fieldwithinthedatabase.
TheCosmosdatasetincludesself-identifiedgender,selfdeclaredracialandethnicidentities,andageamongother
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Buprenorphineiseffectiveatreducingillicit opioiduseandincreasestreatmentretention wheninitiatedintheemergencydepartment.
Whatwastheresearchquestion?
Amongpatientswhopresenttotheemergency department(ED)withanopioidoverdose,do racialandethnicdisparitiesexistfor prescribingnaloxoneandbuprenorphine?
Whatwasthemajor findingofthestudy?
Thesetreatmentsarenotoftenprescribedin theED.Prescribingdisparitiesaresmall, likelyduetogreateraccesstoDEA-waivered cliniciansinraciallydiverseZIPcodes.
Howdoesthisimprovepopulationhealth?
Disparitiesinbuprenorphineandnaloxone prescribingmaybereducedwithgreater overallaccesstothesetreatmentsintheED.
demographicparameters.Inthisdatabaseyoucannot determinetheexactpatientage;therefore,weusedvarious ageranges.Thedatabasecontainsasocialvulnerability index(SVI)basedoncensustractdatawithahigherindex indicatinggreatervulnerability.16 TheSVIincludes componentsofestimatedincome,age,disability,household composition,minoritystatus,language,housing,and transportation.Wehavereportedourdataastheabsolute numbersandfrequency.Becausethedatabasemaintains HIPPAcomplianceanynumberslessthan10arereportedas 10.Statisticalcomparisonsweremadeusingthechi-square testusinga P <0.05toindicatesignificance.Thedatais reportedwiththe P- value.Ourinstitutionalreviewboard (IRB)determinedthatthestudydidnotrequireIRB approvalasitusesaHIPPA-compliantlimiteddatasetfor analysis.
RESULTS
Therewereapproximately53millionEDvisitscontained withintheCosmosdatabaseduringthestudyperiod.Of these,74,004mettheentrycriteriabasedontheSNOMED criteria.Patientswereclassifiedasfollows:67%weremale, 76%White,and18%Black;95%werebetweentheagesof1865;and96%reportedthemselvestobeEnglishspeakers.
Theproportionofpatientsprescribednaloxonebyselfreportedgender,age,race,ethnicityandsocialvulnerability
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 711 Pappetal.
DisparitiesinEmergencyDepartmentNaloxoneandBuprenorphineInitiation
index(SVI)arereportedin Table1.Wefoundthatthat 22.8%ofpatientsreceivedaprescriptionfornaloxone followinganEDvisitforopioidpoisoningoroverdose. Femalepatientswerelesslikelytoreceiveaprescription comparedtomales.PatientsclassifiedasWhiteandPacific Islanderwereleastlikelytoreceivenaloxoneprescriptions. Patientsclassifiedasnon-Hispanicwereleastlikelytoreceive prescriptionsaswerepatientsbelowtheageof18andabove theageof65,alongwithnon-Englishspeakers.Although thereweredifferencesinprescribingbasedontheSVIitdid notfollowaconsistentpattern.
Buprenorphineprescribingbysubgroupisreportedin Table2.Wefoundverylowprescribingratesfor buprenorphineoverallatonly0.9%.Likeour findingsfor naloxone,thegroupsleastlikelytoreceivebuprenorphine werewomenandWhitepatients;however,unlikenaloxone prescribing,patients <18and >65wereslightlymorelikelyto receiveaprescriptionforbuprenorphine.Thenumbersfor patients <18,however,werelowandestimatedduetothe constraintsofthedatabase.Therewereinconsistentresults basedontheSVI.
DISCUSSION
Theopioidoverdoseepidemicthatstartedinthemid1990swithprescriptionmedicationshasprogressively becomemorelethalasillicitsubstanceshavereplaced pharmaceuticals.Thefaceofatypicalopioiduserhasalso changedwiththisshifttoimpactamoreraciallydiverse population.IntheyearsprecedingtheCOVID-19pandemic, mortalitywashighestamongWhitemales;however,new datasuggeststhisischanging.Therewasa48.8%increasein overdosefatalitiesamongBlackscomparedtoa26.3% increaseforWhitesbetween2019–2020.17 Connecticutwas the firststatetoreportthattheoverdosefatalityratefor BlackshadoutpacedtherateforWhitesin2019;andin2020 forthe firsttimeinovertwodecadestheUSsawanoverdose deathrateinBlacksthatoutpacedWhitesby16.3%asthe COVID-19pandemicpummeledtheUS.17,18
All-causemortalityinthe12monthsafteranonfatal opioidoverdoseis4.7deathsper100-personyears.7
FollowinganEDoverdose,amongpatientsonanyMOUD theoddsofasubsequentoverdosedeathisreducedby30%, andlengthofstayissignificantlyreduced.19 Buprenorphine
NaloxoneNoNaloxone NumberPercentNumberPercent P-value Female5,15221.9%18,39878.1% P = .000 Male11,71623.3%38,66276.7% Other2127.6%5572.4% White12,14521.7%43,80678.3% P < .000 Black3,53027.0%9,52273.0% AmericanIndian22726.8%62073.2% Asian9525.4%27974.6% Other1,89524.3%5,89075.7% NativeHawaiian4620.5%17879.5% Hispanic1,30423.3%4,28276.7% P = 0.02 NotHispanic14,71822.7%50,17377.3% Other86724.6%2,66075.4% <18years8210.2%72089.8% P < .000 18–30years4,63123.5%15,11776.5% 30–65years11,54523.0%38,72477.0% >65years63119.8%2,55480.2% SVI <25th3,00622.9%10,09777.1% P = 0.04 SVI25th–50th4,53222.3%15,77777.7% SVI50th–75th6,09221.7%21,92178.3% SVI>75th11,34922.4%39,36777.6% English-speaking16,32823.0%54,79077.0% P = .000 Non-Englishspeaking55119.6%2,26780.4% SVI,socialvulnerabilityindex. WesternJournal of EmergencyMedicineVolume24,No.4:July2023 712
Table1. Prescribingofnaloxonebysub-groups.
DisparitiesinEmergencyDepartmentNaloxoneandBuprenorphineInitiation Pappetal.
DisparitiesinEmergencyDepartmentNaloxoneandBuprenorphineInitiation
isassociatedwithadecreaseinall-causemortalityand opioid-relatedmortality.7 ProvidingMOUDintheED environmentisfeasible,althoughbothrealandperceived implementationbarriersexistincludingstateprescribing laws,stigmarelatedtotreatingpatientswithaddiction, insurancerestrictionsandreimbursement,timeconstraints forbusyclinicians,andtimelyfollow-up.20,21 TheUSDrug EnforcementAdministration(DEA)DATA-2000waiver requirementandbuprenorphine-prescribinglimitsposeda significantbarriertotreatmentaccessduringthe studyperiod.Thatchangedin2023whenthisrequirement waseliminatedbytheUSCongress,pavigtheway forimprovedaccesstobuprenorphinetreatment forOUD.
TheabsenceofopioidwithdrawalintheEDshouldnotbe abarriertoprescribingbuprenorphine,althoughitisoften perceivedassuch.Buprenorphinemaybeadministeredto patientsintheEDwhoareinopioidwithdrawaland prescribedtoanypatientwithmoderateorsevereOUD alongwithdetailedinstructionsforhomeinductionwhen opioidwithdrawalbegins.22 Opioidwithdrawalmaybe
delayedinpatientswhoaredependentonlong-actingopioids likemethadone;however,fentanylanditsanaloguesarethe mostprevalentillicitopioidsleadingtooverdosefatalitywith half-livesrangingbetweenof0.15–7.7hourswhen injected.14,23
Formanywholiveinareaswithpooraccess,theEDmay betheonlyopportunitytoinitiateMOUD.A2020reportby theOfficeoftheInspectorGeneral(OIG)foundthat40%of UScountiesdidnothaveasinglecliniciancapableof providingMOUDwithbuprenorphineand56%ofcounties withgreatestneedforMOUDhadinadequatecapacityto providethiscare.21 Whentheproportionofwaivered cliniciansisexaminedbyZIPcodeandraceandethnicity composition,theraciallydiverseZIPcodeshaveagreater proportionofclinicianscapableofprovidingMOUD, suggestingthatavailabilityofawaiveredclinicianislessofa barrierforraciallydiversepopulations.24 Onceinitiated, treatmentretentionforpatientsonMOUDissimilarforall genders,races,andethnicities.25
OurstudyshowedthatWhitepatientswerelesslikelyto receiveaprescriptionforMOUDintheED.Thisiscounter
BuprenorphineNoBuprenorphine NumberPercentNumberPercent P -value Female1710.3%49,876 P < 00001 Male5022.1%23,37997.9% Other1011.6%7688.4% White4440.8%55,50799.2% P < 00001 Black1681.3%12,88498.7% AmericanIndian101.2%84298.8% Asian102.6%36997.4% NativeHawaiian104.3%22195.7% Other931.2%7,69298.8% Hispanic631.1%5,52398.9% P = .012 NotHispanic5730.9%64,31899.1% Other371.0%3,49099.0% <18years101.2%80298.8% P < 0.02 18–30years1470.7%19,60199.3% 30–65years4921.0%49,77799.0% >65years341.1%3,15198.9% SVI <25th1491.1%12,95498.9% P = .00001 SVI25th–50th2531.2%20,05698.8% SVI50th–75th2791.0%27,73499.0% SVI>75th6761.3%50,04098.7% English-speaking6560.9%70,46299.1% P = 0.09 Non-Englishspeaking170.6%2,80199.4% SVI,socialvulnerabilityindex. Volume24,No.4:July2023WesternJournal of EmergencyMedicine 713
Table2. Prescribingofbuprenorphinebysub-groups.
Pappetal.
toanumberofotherstudiesthathavefoundthatBlacksor otherminoritypatientsarelesslikelytoreceiveMOUD acrossthespectrumoftreatmentsettings.26 Priorresearch alsoindicatedthatdisparitiesexistamongracialgroups’ receiptofharmreductionservicesandmedicationstotreat addiction,withWhiteshavinggreateraccesstoalltreatment modalities.MedicationsforOUDarealsolesslikelytobe offeredtoBlacksandHispanicsinshort-termresidential treatment,andtheyarealsolesslikelytocompleteaninitial treatmentepisodethanWhites.27–28 WhentheCOVID-19 pandemichit,accesstoMOUDandharmreductionservices weredisruptedamongracialorethnicminoritieswhoselfreportedthattheywere8–10timeslesslikelytohaveaccessto cleansyringesandnaloxonethannon-HispanicWhites.29
Whileourresultsarediscrepantfromotherstudiesthat reportontreatmentacrossthespectrumoftreatment settings,oursisthe firsttoexamineprescribingdisparitiesin theEDsetting.ThedifferencesinMOUDprescribingare smallandmayreflecttheoverallincreaseinopioiduseand overdoserateamongminorities,whoaremore geographicallyconcentratedinareaswithhigheraccessto DATA-waiveredclinicians.24
Asintwoearliersingle-centerstudies,wealsofoundan increaseinnaloxoneprescribingforHispanicpatients.In thosepreviousstudies,Hispanicpatientsweremorelikely thannon-HispanicBlacksandnon-HispanicWhitesto receiveaprescriptionfornaloxoneafteropioidoverdose. Anotherstudydidnot findadifferenceinthereceiptof naloxoneamongtheHispanicpopulation.30
Inourstudy,wefoundinconsistentdifferencesin treatmentbasedontheSVI.Inpriorwork,CABridge,a programoftheCaliforniaPublicInstituteofHealth,found thatlow-incomepatientsandthosewithunstablehousing weremorelikelytoacceptandreceivetreatment.31,32 By contrast,patientswithnon-Medicaidinsurance,stable housing,andolderpatientswerelesslikelytoreceive treatment.TheCABridgeprogramattributedthistoasocial cognitivetheoryperspective;however,furtherstudyis neededtoevaluatethereasonsthatpatientswithfewer resourcesareseeminglymorelikelytoacceptandreceive treatment.32
Weareunabletodefinitivelydeterminethereasonforthe discrepantresultsbetweenourstudyandpriorwork; however,thepreviousstudiesevaluatedMOUDand naloxoneaccessinavarietyofEDandnon-EDsettingsusing differentmethodologies.
LIMITATIONS
Thisstudywasdependentontheaccuracyofdiagnosis codingthatmapstoSNOMEDconcepts.Theremaybeother patientswithopioidoverdosewhowerecodedinadifferent manner,suchashavingalteredmentalstatuswithout specifyinganoverdose.Further,patientsmayhavepresented withanoverdosealthoughtheywerethencodedwitha
relatedmedicalproblemsuchasaspirationpneumoniaor anyoftheothercomplicationsofopioidoverdose.We lookedattheprescribingofMOUDco-incidentwithanED encounter.Additionalpatientsmayhavehadcounseling duringtheEDencounterthatledtoafollow-upvisit wheretheywereprovidedwithMOUD.Thisstudywas focusedontheprescribingbasedonanEDvisit,andwe excludedpatientswhowereadmittedandwhomayhave subsequentlyreceivednaloxoneorbuprenorphine prescriptions.
Ourdatasearchedprescribedmedicationsanddidnot includepatientswhomayhavebeengivennaloxonekits ratherthanhavingthemprescribed.Ourstudywasnot designedtoevaluatethatpossibility.Nordiditexamine prescription fillrates,whichwouldhaveprovidedadditional informationregardingaccesstothesetreatmentsandmaybe adverselyimpactedbythepatient’shealthcarecoverageand SVI.NotallpatientswhoareeligibletoreceiveMOUDare willingtoacceptit.Inthisdatabasestudywecouldnot determinethereasonthatpatientswerenotprescribed medicationastheymayhavebeenofferedthemedication andrefusedit.Wedidnotexcludepatientsbeingsentto residentialorlong-termtreatmentfacilities.Itispossiblethat theemergencyphysiciansmayhavedeferredstarting MOUDtothephysiciansinthosesettings,althoughwehave nowaytodeterminethis.
Further,thenatureoftheCosmosdatabasedidnot allowustodeterminecharacteristicsofthetreating hospitalsnorwhethertheyhaveaddictionconsultservices. Asapartofourreviewofthedataweevaluatedthe diagnosesforallpatientswhoreceivedbuprenorphine prescriptionsfromtheEDandfoundthatthevastmajority wereforinitiationorcontinuationofOUDtreatment.Itis possiblethatsomeofthepatientscodedforopioidabuse alsohadanoverdose,althoughwewereunableto determinethis.Thenatureofthisdatabasedidnotallowus toperformmultipleregressionanalysistolookat relationshipsbetween,for example,gender,race,orage. TheCosmosdatabaseslightlyover-representsbothWhite andBlackpatientsandunder-representstheHispanic populationcomparedtotheoverallUSpopulation. Finally,noinformationregardingpatients’ insurance statuswasavailabletoanalyze.
CONCLUSION
Despitesupportingevidencefortheiruse,naloxoneand buprenorphineareinfrequentlyprescribedfollowinganED opioidoverdose.Whitesandfemalesareleastlikelytoreceive aprescriptionforbuprenorphineintheEDwhileWhites, femalesandPacificIslandersareleastlikelytoreceivea naloxoneprescription.DisparitiesexistinEDprescribing patternsforbothbuprenorphineandnaloxone,butthe disparitiesweresmallinthisstudyandmayreflectgreater accesstotreatmentinraciallydiverseZIPcodesandagreater
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 714 DisparitiesinEmergencyDepartmentNaloxoneandBuprenorphineInitiation Pappetal.
willingnesstoaccepttreatmentamonglow-incomepatients withunstablehousing.Furtherstudyisneededtodetermine whatfactorscontributetothesedisparities,whatinterventions canbeimplementedtoreducethem,andwhetheradditional disparitiespreventpatientsfrom fillinganEDprescription. TheeliminationoftheDEADATA-2000waiverin2023may impactthesedisparitiesandwillrequirefuturestudy.
AddressforCorrespondence:JoanPapp,MD,MetroHealthMedical CenterCampusofCaseWesternReserveUniversity,Departmentof EmergencyMedicine,2500MetroHealthDrive,Cleveland,Ohio 44019.Email: jpapp@metrohealth.org
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Pappetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.MorelandB,LeeR.Emergencydepartmentvisitsandhospitalizations forselectednonfatalinjuriesamongadultsaged ≥65yearsUnitedStates,2018. MMWRMorbMortalWklyRep 2021;70(18):661–6.
2.CDC.Provisionaldrugoverdosedeathcounts.2023.Availableat: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm AccessedMarch2,2023.
3.LuoF,LiM,FlorenceC.State-leveleconomiccostsofopioiduse disorderandfatalopioidoverdose-UnitedStates,2017. MMWRMorb MortalWklyRep.2021;70(15):541–6.
4.MattickRP,BreenC,KimberJ,etal.Buprenorphinemaintenance versusplaceboormethadonemaintenanceforopioiddependence. CochraneDatabaseSystRev.2014;(2):CD002207.
5.HerringAA,VosooghiAA,LuftigJ,etal.High-dosebuprenorphine inductionintheemergencydepartmentfortreatmentofopioiduse disorder. JAMANetwOpen.2021;4(7):e2117128.
6.MaJ,BaoYP,WangRJ,etal.Effectsofmedication-assistedtreatment onmortalityamongopioidsusers:asystematicreviewandmetaanalysis. MolPsychiatry.2019;24(12):1868–83.
7.LarochelleMR,BernsonD,LandT,etal.Medicationforopioiduse disorderafternonfatalopioidoverdoseandassociationwithmortality:a cohortstudy. AnnInternMed.2018;169(3):137–45.
8.ReuterQR,SantosAD,McKinnonJ,etal.Long-termtreatmentretention ofanemergencydepartmentinitiatedmedicationforopioidusedisorder program. AmJEmergMed.2022;55:98–102.
9.D’OnofrioG,ChawarskiMC,O’ConnorPG,etal.Emergency department-initiatedbuprenorphineforopioiddependencewith
continuationinprimarycare:outcomesduringandafterintervention. JGenInternMed.2017;32(6):660–6.
10.JonesCM,McCance-KatzEF.Co-occurringsubstanceuseandmental disordersamongadultswithopioidusedisorder. DrugAlcoholDepend 2019;197:78–82.
11.WalleyAY,XuanZ,HackmanHH,etal.Opioidoverdoseratesand implementationofoverdoseeducationandnasalnaloxonedistributionin Massachusetts:interruptedtimeseriesanalysis. BMJ.2013;346:f174.
12.Doe-SimkinsM,QuinnE,XuanZ,etalOverdoserescuesbytrained anduntrainedparticipantsandchangeinopioiduseamongsubstanceusingparticipantsinoverdoseeducationandnaloxonedistribution programs:aretrospectivecohortstudy. BMCPublicHealth.2014;14:297.
13.WeinerSG,CarrollAD,BrisbonNM,etal.Evaluatingdisparitiesin prescribingofnaloxoneafteremergencydepartmenttreatmentofopioid overdose. JSubstAbuseTreat.2022:108785.
14.ChuaKP,DahlemCHY,NguyenTD,etal.Naloxoneandbuprenorphine prescribingfollowingusemergencydepartmentvisitsforsuspected opioidoverdose:August2019toApril2021. AnnEmergMed. 2022;79(3):225–36.
15.SalvadorJG,SussmanAL,TakedaMY,etal.Barrierstoand recommendationsfortake-homenaloxonedistribution:perspectives fromopioidtreatmentprogramsinNewMexico. HarmReductJ. 2020;17(1):31.
16.HeitgerdJL,DentAL,ElmoreKA,etal.Communityhealthstatus indicators:addingageospatialcomponent. PrevChronicDis 2008;5(3):A96.
17.FriedmanJ,HansenH.Blackandnativeoverdosemortalityovertook thatofWhiteIndividualsduringtheCOVID-19pandemic. medRxiv 2021.2021.11.02.21265668.
18.WuZH,YongQ,WalkerJM,etal.Fentanyl,heroin,andcocaine overdosefatalitiesareshiftingtotheBlackcommunity:ananalysisofthe StateofConnecticut. JRacialEthnHealthDisparities 2022;9(2):722–30.
19.ShastryS,NobelI,AllenLR,etal.Prioruseofmedicationsforopioiduse disorderinEDpatientswithopioidoverdose:prevalence,misuseand overdoseseverity. AmJEmergMed.2022;51:114–8.
20.ThompsonRA,JohnsonD,KizewskiAL,etal.Assessingwaiveredand non-waiveredphysicianbarrierstotreatingpatientswithsubstanceuse disorders:across-sectionalKentuckypilot. JAddictDis.2022:1–9.
21.USDepartmentofHealthandHumanServices.Geographicdisparities affectaccesstobuprenorphineservicesforopioidusedisorder.2020. Availableat: https://oig.hhs.gov/oei/reports/oei-12-17-00240.asp AccessedMarch25,2023.
22.CunninghamCO,GiovannielloA,LiX,etal.Acomparisonof buprenorphineinductionstrategies:patient-centeredhome-based inductionsversusstandard-of-careoffice-basedinductions. JSubst AbuseTreat.2011;40(4):349–56.
23.O’DonnellJ,TanzLJ,GladdenRM,etal.Trendsinandcharacteristics ofdrugoverdosedeathsinvolvingillicitlymanufacturedfentanylsUnitedStates,2019-2020. MMWRMorbMortalWklyRep 2021;70(50):1740–6.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 715 Pappetal. DisparitiesinEmergencyDepartmentNaloxoneandBuprenorphineInitiation
24.HirchakKA,AmiriS,KordasG,etal.Variationsinnationalavailabilityof waiveredbuprenorphineprescribersbyracialandethniccompositionof zipcodes. SubstAbuseTreatPrevPolicy.2022;17(1):41.
25.HochheimerM,UnickGJ.Systematicreviewandmeta-analysisof retentionintreatmentusingmedicationsforopioidusedisorderby medication,race/ethnicity,andgenderintheUnitedStates. Addict Behav.2022;124:107113.
26.RobbinsM,HarozR,MazzarelliA,etal.Buprenorphineuseand disparitiesinaccessamongemergencydepartmentpatientswithopioid usedisorder:across-sectionalstudy. JSubstAbuseTreat 2021;130:108405.
27.StahlerGJ,MennisJ,BaronDA.Racial/ethnicdisparitiesintheuseof medicationsforopioidusedisorder(MOUD)andtheireffectson residentialdrugtreatmentoutcomesintheUS. DrugAlcoholDepend 2021;226:108849.
28.StahlerGJ,MennisJ.Treatmentoutcomedisparitiesforopioidusers: Arethereracialandethnicdifferencesintreatmentcompletion
acrosslargeUSmetropolitanareas? DrugAlcoholDepend 2018;190:170–8.
29.RosalesR,JanssenT,YermashJ,etal.Personsfromracialandethnic minoritygroupsreceivingmedicationforopioidusedisorder experiencedincreaseddifficultyaccessingharmreductionservices duringCOVID-19. JSubstAbuseTreat.2022;132:108648.
30.ReddyNG,JackaB,ZiobrowskiHN,etal.Race,ethnicity,and emergencydepartmentpost-overdosecare. JSubstAbuseTreat 2021;131:108588.
31.KalminMM,Goodman-MezaD,AndersonE,etal.Votingwiththeirfeet: socialfactorslinkedwithtreatmentforopioidusedisorderusingsamedaybuprenorphinedeliveredinCaliforniahospitals. DrugAlcohol Depend.2021;222:108673.
32.SnyderH,KalminMM,MoulinA,etal.Rapidadoptionoflow-threshold buprenorphinetreatmentatCaliforniaemergencydepartments participatingintheCABridgeProgram. AnnEmergMed 2021;78(6):759–72.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 716 DisparitiesinEmergencyDepartmentNaloxoneandBuprenorphineInitiation Pappetal.
FlowthroughtheEmergencyDepartmentforPatientsPresenting withSubstanceUseDisorderinAlberta,Canada
JonahEdmundson* KevinSkoblenick,PhD†‡§ RhondaJ.Rosychuk,PhD∥¶
*TheKing’sUniversity,DepartmentofBiology,Edmonton,Canada
† UniversityofAlberta,DepartmentofEmergencyMedicine,Edmonton,Canada
‡ RoyalAlexandraHospital,Edmonton,Canada
§ UniversityofAlberta,NeuroscienceandMentalHealthInstitute,Edmonton,Canada
∥ UniversityofAlberta,DepartmentofPediatrics,Edmonton,Canada
¶ Women&Children’sHealthResearchInstitute,Edmonton,Canada
SectionEditor:Le´onD.Sánchez,MD,MPH
Submissionhistory:SubmittedMarch6,2023;RevisionreceivedApril4,2023;AcceptedApril18,2023
ElectronicallypublishedJuly7,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.60350
Introduction: Since2016theprovinceofAlberta,Canada,hasseenasignificantincreaseinsubstance usedisorder(SUD)presentationstotheemergencydepartment(ED)withalargesurgeduringthe COVID-19pandemic.Inthisretrospectivestudywedeconstructthetotallengthofstay(LOS)intheED intostagesforpatientspresentingwithSUDandestimatetheeffectsofcovariatesonthetimeto transitionbetweenstages.
Methods: UsingtheCanadianCodingStandardsforInternationalClassificationofDiseases,10th Modification,codesF10.0-F19.9andT36.0-T50.9,weextracteddatafromtheNationalAmbulatoryCare ReportingSystembetweenApril1,2019–March31,2020onallEDpresentationsforSUDbyAlberta residents.WeusedamultistatemodeltodeconstructtheEDLOSintoeightmutuallyexclusivestatesand determinewhichfactorsaffectedthetimespentineachstate.
Results: Weanalyzed66,880presentations(37,530patients).Themeanagewas37.2years,and 61%weremale.ThemediantotalLOSintheEDwas6hours13minutes.Patientspresentingwith methamphetamines(METH)intoxicationandpatientsfromlow-incomeneighborhoodshadsignificantly increasedtransitiontimesbetweenallstates.Oppositethis,opiateusewasassociatedwithfaster transitiontimesbetweenalmostallstates.MetroEDsexperiencedslowertransitionswhenattemptingto dischargeoradmitpatientswhencomparedtourbanorruralEDs.Emergencydepartmentcrowdingalso hadadramaticeffectonphysicianinitialassessmenttimes,whiledischargeandadmissiontimesin patientspresentingwithSUDwerealsosignificantlyaffected.
Conclusion: PatientswithSUDexperienceavarietyofdelaysduringtheirEDstay.ThosewithMETH intoxicationandthosefromthelowestincomeneighborhoodsweremostlikelytoexperienceslower transitionsfromstatetostateintheEDandmaybenefitfromafocusedapproachtoimproveED flow. [WestJEmergMed.2023;24(4)717–727.]
INTRODUCTION
Emergencydepartments(ED)areseeingasteadyincrease inpresentationsrelatedtosubstanceusedisorder(SUD).1 Since2016theprovinceofAlberta,Canada,hasseena significantincreaseofSUDpresentationstotheEDwitha largesurgeduringtheCOVID-19pandemic.2 These
presentationsareassociatedwithincreasedresource utilizationwhencomparedtonon-SUDpresentationsand increasedhealthcareexpenditurecosts,particularlyin stimulantusedisorder,suchasmethamphetamine(METH) use. 3 MethamphetamineuseandsubsequentED-related presentationsarerapidlyincreasingintheUS4
6 and
–
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 717 BRIEF RESEARCH REPORT
Canada,7
9 accompaniedbyanincreasedEDlengthofstay (LOS)whencomparedtonon-METH-relateddiagnoses.10 Similarly,alcoholusehasseenasignificantincreaseinED presentations11 creatingfurtherissuesduetoitswellestablishedprolongingeffectonapatient’sEDLOS.12 Ithas beenpreviouslyestablishedthatEDcrowdingcontributesto poorerpatientoutcomesinallmeasureddomains.13 With thisincreasingEDburdenduetoSUD,moreresearchis requiredtoimproveED flowfortheSUDpatient.By identifyingbottlenecksintheirtransitiontoadmissionor discharge,optimaltargetsmaybeidentifiedthatwould producethemostimpactfulchangeontheiroverallEDLOS andEDcrowding.
Theprimaryobjectivesofthisretrospectivestudywereto deconstructthetotalLOSintheEDintostages(alsoknown asstates)throughtheuseofamultistatemodelandto estimatetheeffectsofcovariatesonthetimetotransition betweenstates.Asecondaryobjectivewastodeterminehow EDcrowdingmaybeassociatedwiththetimespentin eachstate.
METHODS StudyDesign
Inthispopulation-based,retrospectivecohortstudywe useddataextractedfromtheNationalAmbulatoryCare ReportingSystem(NACRS).14 TheHealthResearchEthics BoardoftheUniversityofAlberta(Pro00098444)approved thisstudy.AlbertaHealthServices,thedatacustodians, providedoperationalandadministrativeapproval.Adatasharingagreementgoverneddatause.Informedconsentwas notobtainedfromindividualpatients,andonlyde-identified datawereshared.Nofundingorganizationhadanyrolein theconductandreportingofthisstudy.
StudySettingandPopulation
WeextracteddataforallpresentationstoallEDsin Alberta,CanadafromApril1,2019–March31,2020. AlbertaisaprovinceinwesternCanadawith109EDsthat serveapopulationof4.5millionpeople.15 Patients presentingwithsubstanceusedisorderformedthestudy population.Presentationswereclassifiedassubstanceuseif anyoneofthe10diagnostic fieldshadInternational StatisticalClassificationofDiseasesandRelatedHealth Problems(ICD-10-CA)16 codesofmentalandbehavioral disordersduetopsychoactivesubstanceuse(F10.0toF19.9) orpoisoningbydrugs,medicaments,andbiological substances(T36.0toT50.9).Thesewerethesamecodesused byDiRicoetal.17
StudyProtocol
TheNACRSdatasetincludedbasicdemographic informationsuchasage,gender,andgeography(postalcode andhealthzoneofresidence).Dates/timesofkeypointsof theEDpresentation(eg,start;physicianinitialassessment
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Substanceusedisordersareanincreasingly commoncomponentofemergencydepartment patientpresentationswithexcessiveresource utilizationfortheirmanagement.
Whatwastheresearchquestion?
Howdoesadiagnosisofsubstanceuse disorderaffectapatient ’ s fl owthroughthe emergencydepartment?
Whatwasthemajor findingofthestudy? Whencomparedtoothersubstances, methamphetamineusespeci fi callycauseda prolongedtransitiontimefromstatetostate.
Howdoesthisimprovepopulationhealth?
Emergencydepartment fl owmaybeimproved bytargetinginterventionsthatexpeditethe careofpatientswithmethamphetamineuse disorder.
[PIA];dispositiondecision),andEDfacilityarereported. Arrivalmode(eg,ambulance),severityofapatient’ s conditionuponarrivalbasedontheCanadianTriageand AcuityScale(CTAS:1 = resuscitation,2 = emergent, 3 = urgent,4 = lessurgent,5 = non-urgent),18 andupto10 diagnosis fieldsusingICD-10-CAcodesareprovided. Presentationswerecategorizedbysubstancetypeifanyofthe diagnosis fieldsincludedalcohol(anyF10[alcohol-related disorders]),METuse;anyF15[otherstimulant-related disorders]orT43.6[poisoningby,adverseeffectofand underdosingofpsychostimulants]),opioids(anyF11[opioidrelateddisorders]orT40[poisoningby;adverseeffectof; andunderdosingofnarcoticsandpsychodysleptics [hallucinogens]]),andother.Dispositionincluded16 categoriesthatweregroupedintodischarged,admitted, transferred,leftwithoutbeingseen(LWBS),leftagainst medicaladvice(LAMA),anddied.Therewerefew individualswhodiedintheED,andtheywereexcluded fromtheanalyses.
WedeterminedanindicatorofEDcrowdingby calculatingthemediantimefromarrivaltoPIAforall presentationsforanyconditionineachhourforeachED. Timesoveronehourwereconsideredtobecrowdedin agreementwithpublishedguidelines.19
LinkagesweremadebyAlbertaHealthServicestoother AlbertaHealthdatabasestoobtainadditionalvariables.The
–
WesternJournal of EmergencyMedicine Volume24,No.4:July2023 718 FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder Edmundsonetal.
CharlsonComorbidityIndex20 basedonatwo-year lookbackusingNACRSandDischargeAbstractDatabase21 recordswasdichotomizedintothosewithoutcomorbidities (ie,0)andthosewithatleastonecomorbidity(ie, ≥1). UsingthePampalonIndex,22 wecollapsedtheaverage incomeofpeopleaged >15yearsintocategories <$25,000, $25,000
$50,000,and >$50,000.Andanurbanstatus variablewithfourcategoriesthatwerecollapsedinto metropolitan,urban,rural,andruralremotewereprovided basedonlocalgeographicboundariesofthepatient’ s residence.
KeyOutcomeMeasures
Allpatientsbegininthestartstate.Wedeterminedthe timeassociatedwiththisastheminimumofthetriagetime andthetimethepatientpresentedtotheED.Ifapatient decidestoleavepriortobeingseenbyaphysician,theyare consideredLWBS,inwhichcasethetimefortransitionisthe timeassociatedwithpatientdeparturefromtheED.Oncea patientisseenbyaphysician,theymovetothePIAstate,for whichanexacttimeisrecorded.FromthePIAstate,patients maymovetothedischargedispositionstate,orthephysician maydecidetoadmitortransferthepatientinstead,inwhich casetheymovetotheadmit/transferdispositiondecision state.Thetimeforboththesetransitionsisgivenbythetime todisposition.ForpatientswhoseEDpresentationendsin LAMA,thetimeisgivenbythetimeassociatedwithpatient departurefromtheED.Ifthedecisionismadetoadmit ortransferthepatient,patientsmustwaitagainbefore transitioningintotheadmittedortransferredstates.Ineither case,thetimeforthistransitionisgivenbythetimeofpatient departurefromtheED.
DataAnalysis
Summarystatisticssuchascounts,percentages,medians, andinterquartileranges(IQR)representedas25th percentile,
75th percentile)describethecharacteristicsofED presentations.Weusedamultistatemodellingframeworkto modelthe flowthroughtheEDbyconsideringeightmutually exclusivestatesasdepictedin Figure1:start;PIA;discharge dispositiondecision;admit/transferdispositiondecision; admitted;transferred;LWBS;andLAMA.Initialmodels consideredonecovariateatatimetoprovideunadjusted hazardratios(HR).Fullmodelsusedallcovariates,and thesemodelsweresubsequentlyreducedviabackwards selectionuntilmaximumparsimonywasachieved(asper Akaike’sinformationcriterion23).Foralltransitions,the covariatesconsideredweregender,age,comorbidity,income category,weekendindicator(SaturdayandSundaywere groupedas “weekend”),shift(day:0800-1559,evening:16002359,night:0000-0759),arrivalbyambulance,urbanstatus, CTAS,indicatorsforalcohol,MET,andopioiduse diagnoses,andthePIAcrowdingindicator.
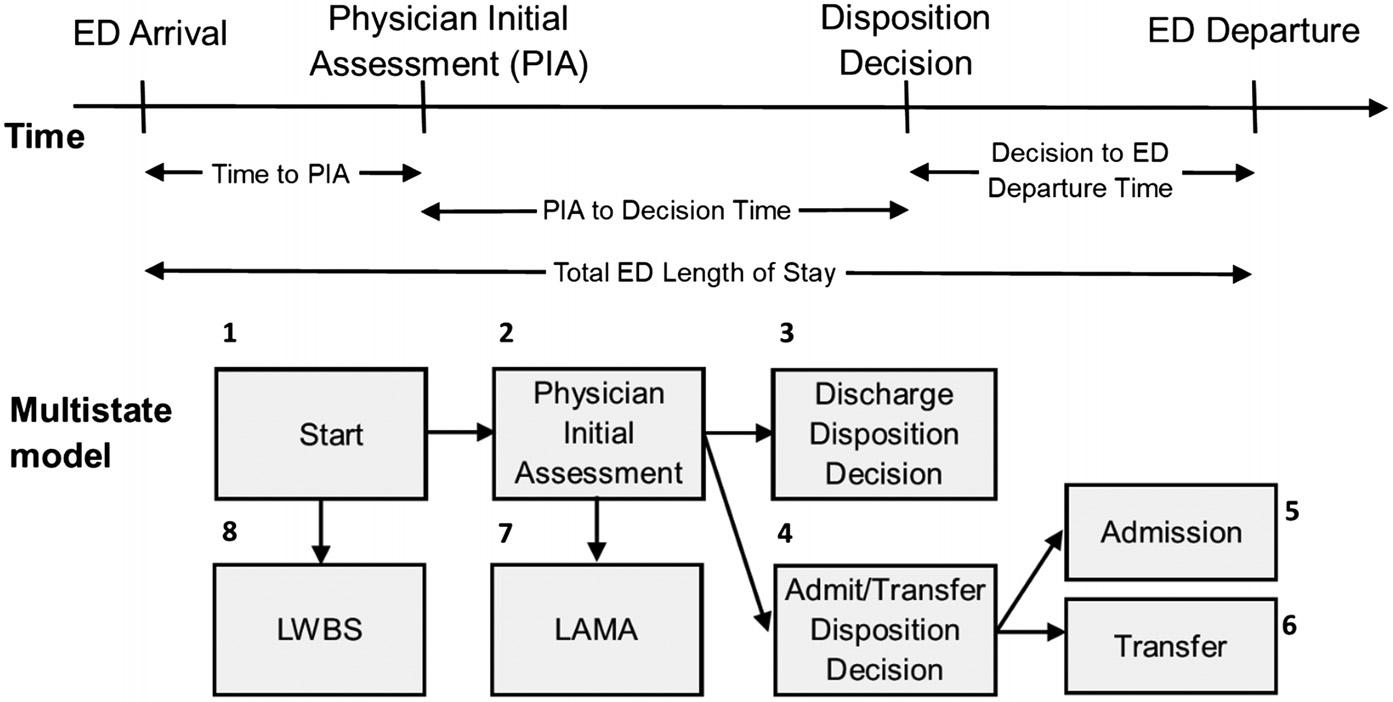
WecompletedanalysesinthestatisticalsoftwareR(R FoundationforStatisticalComputing,Vienna,Austria).24 Themsmpackage25 wasusedto fitallmodels,andtheforest plotpackage26 displaysHRsalongwith95%confidence intervals.AHR >1indicatesthatthetimetotransitionis shorterforindividualsofthatgroupcomparedtothe referencegroup,andaHR <1indicatesthatthetimeto transitionislongerforindividualsofthatgroupcomparedto thereferencegroup.
RESULTS
CharacteristicsofEDPresentations
Duringthestudyperiod,therewere2,302,147 presentationstoAlbertaEDs,and66,880presentationswere forsubstanceuse(37,530patients)andavailableforanalysis (FigureS1).Themajorityofpatientshadrepeated presentations(78%),whileonly22%presentedtotheED once.Themajorityofpresentationswerebymales(61.2%, Table1),fromthemetropolitanareas(61.5%)inthehealth
–
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 719 Edmundsonetal. FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder
Figure1. Multistatemodeloftransitionsthroughtheemergencydepartment. LWBS,leftwithoutbeingseen; LAMA,leftagainstmedicaladvice.
zonesofEdmonton(36.1%)andCalgary(32.6%),andfrom neighborhoodswheretheaverageincomewasatleast $25,000(41.9%with$25,000–$50,000,43.4%with
>$50,000).Weekendswerepopulardaysforpresentations (69.3%),andpresentationsweremostlyconsideredurgent (CTAS342.9%)oremergency(CTAS237.5%).Based onthepriortwoyearsofEDandhospitalizationdata, comorbiditieswerenotpresentforthevastmajorityof presentations(73.5%),andalcoholwasthemostcommon substanceatthepresentation(49.0%).Almost65%of presentationsendedindischarge,19.3%endedinadmission, and7.4%endedintransfer.
Overall,themediantimespentintheEDwas6hours(h) 13minutes(min)(IQR3h20min,11h36min, Table2, Figure2).Patientswereseenbyaphysicianinamedian timeof1h13min(IQR32min,2h29min),andonceseen, dischargedpatientshadamediantimetodischargeof3h 36min(IQR1h32min,7h20min)andadmittedpatientstook longerwithamediantimetoadmissionof5h39min(IQR3h 8min,9h31min).Wenotethatbecausemostofthe4,204 patientswhoweretransferred(State6)hadaninstantaneous transitionfromthedispositiondecisionstate(State4), thekeysummarystatisticsare0h.
MultistateModelling
Wefocusedonafewtransitionsusingthemultivariable modelandhaveprovidedallresultsforunadjustedHRsand adjustedHRsin TablesS1andS2,respectively,withforest plotsforadjustedHRsin FiguresS2–S4
ForthestarttoPIAtransition(State1toState2),patients residinginurban(HR1.27),rural(HR1.44),andrural remote(HR1.44)municipalitiessawthephysicianquicker
n(%) Ageinyears,mean(SD) 37.215.1 Gender Male 40,91361.2 Female 25,96138.8 Missing 60.0 HealthZoneofResidence North 7,47411.2 Edmonton 24,15936.1 Central 6,5109.7 Calgary 21,79232.6 South 5,7058.5 Missing 1,2401.9 PopulationCentreTypeofResidence Metro 41,11961.5 Urban 7,25610.8 Rural 12,37918.5 Remote 1,8162.7 Missing 4,3106.4 AverageNeighborhoodIncome < $25,000 5,5508.3 $25,000–$50,000 28,02041.9 > $50,000 29,00043.4 Missing 4,3106.4 NumberofComorbiditiespertheCharlson ComorbidityIndex 0 49,15873.5 ≥1 17,72226.5 ArrivalMode Ambulance 32,73148.9 DayofWeek Weekday 46,31969.3 Weekend 20,56130.7 TimeofDay Day(0800–1559) 21,19431.7 Evening(1600–2359) 28,16242.1 Night(0000–0759) 17,52426.2 TriageLevel 1 = Resuscitation 2,2223.3 2 = Emergent 25,06337.5 3 = Urgent 28,67142.9 4 = LessUrgent 9,13113.7 5 = Non-urgent 1,2361.8 Missing 5570.8 (Continued onnextcolumn)
Table1. Characteristicsof67,416emergenydepartment presentationsforsubstanceuse.
n(%) DiagnosticCategory Alcohol 32,78049.0 Methamphetamines 10,75916.1 Opioids 9,72014.5 Noneoftheabove 16,83725.2 Disposition Discharged 43,19064.6 Admitted 12,92119.3 Transferred 4,9187.4 Leftbeforebeingseen 3,6525.5 Leftagainstmedicaladvice 2,1993.3 CrowdingLevel Crowded(mediantimeto physicianinitialassessment >1 hour) 48,14972.0 ED, emergencydepartment. WesternJournal of EmergencyMedicine Volume24,No.4:July2023 720 FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder Edmundsonetal.
Table1. Continued.
Figure2. Summaries(25th percentile,median,75th percentile)ofthetotallengthofstay(A)andthetimespentineachstatebasedonstarting state:(B)start,(C)physicianinitialassessment(PIA),and(D)dispositiondecision. ED,emergencydepartment.
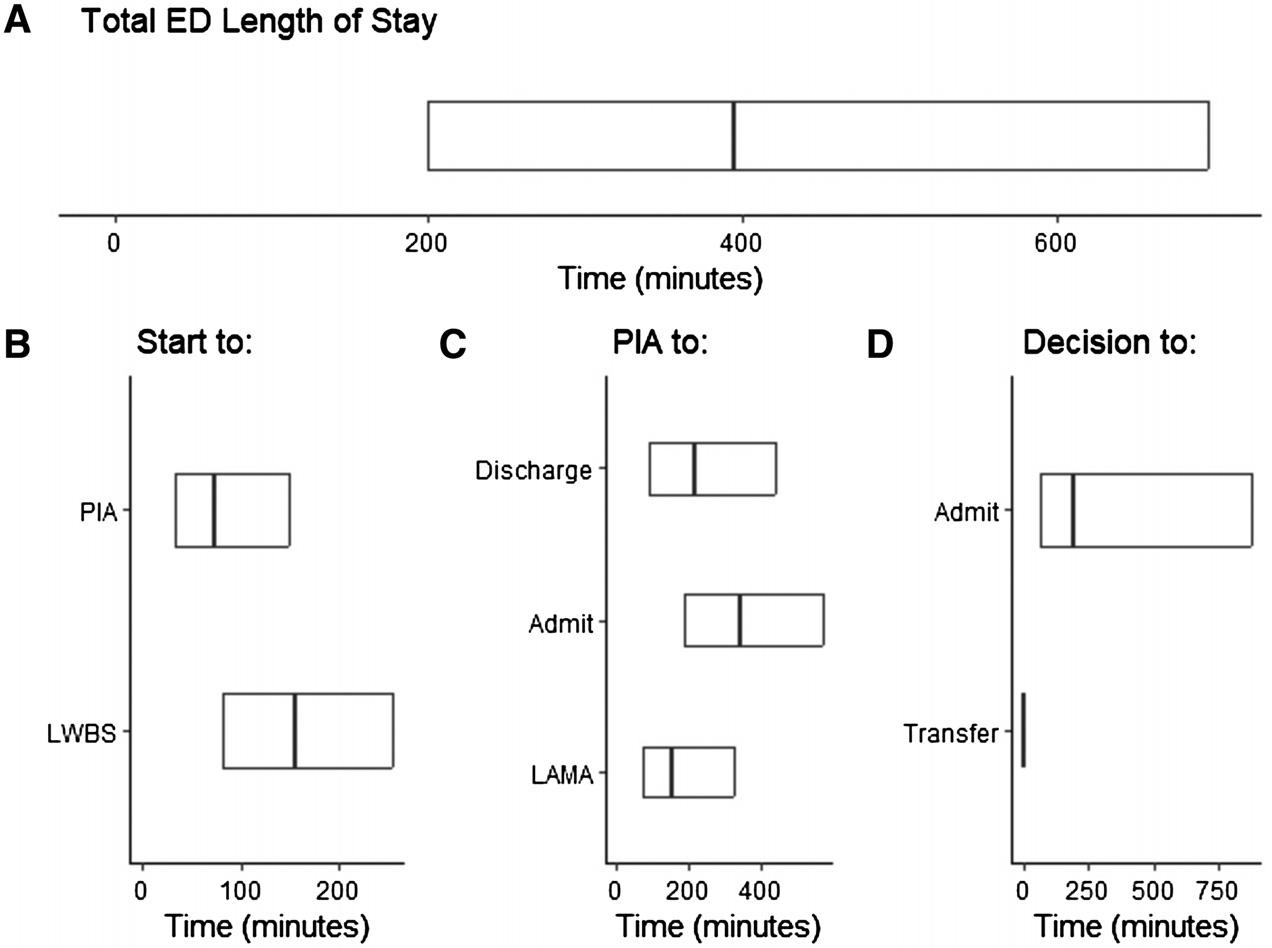
thanpatientsfrommetropolitanmunicipalities.Patientswith SUDweresignificantlyaffectedbycrowding.aspatientsin crowdedEDshadlongertimestowaittoseeaphysicianthan patientspresentingtouncrowdedEDs(HR0.35, Figure3). PatientspresentingwithMETHusealsohadlongertimes thanthosewithoutMETHuse(HR0.89).Lastly,patients fromthelowestincomeneighborhoodshadalonger transitiontimetoPIAthanthosefromneighborhoodswith averageincomes >$50,000(HR0.82).
Onceseenbyaphysician,loweracuity(CTAS4:HR1.56, CTAS5:HR2.44)andopioid-relatedconcerns(HR1.30) hadshortertimesfromPIAtodischargedispositiondecision (State2to3, Figure4).Longertimeswereassociatedwith arrivingbyambulance(HR0.80),presentingwithMETH
use(HR0.79),withatleastonecomorbidity(HR0.85), beingfemale(HR0.90),andolderage(HR0.92per 10years).
Forpatientswhosedispositiondecisionwasadmissionor transfer(State2to4),higheracuity(CTAS1:HR1.39; CTAS2:HR1.11),livinginanon-metropolitan municipality(urban:HR1.36;rural:HR1.29;remote:HR 1.53),havingatleastonecomorbidity(HR1.18),andolder age(HR1.11per10years)hadshortertransitiontimes (Figure5).Livinginaneighborhoodwithlowaverage income(<$25,000,HR0.73),arrivingafter4 PM (evening shift:HR0.7;nightshift:HR0.72),arrivingonaweekend (HR0.91),arrivingbyambulance(HR0.91),andpresenting withalcohol(HR0.94)orMETHuse(HR0.89)was
PeriodnMedian(25th percentile,75th percentile) TotalLengthofStay 66,8806h13min 3h20min,11h36min Start toPhysicianInitialAssessment(PIA)(State1to2)61,1671h13min 0h32min,2h29min PIAtoDischargeDisposition(State2to3) 43,1893h36min 1h32min,7h20min PIAtoAdmitorTransferDisposition(State2to4) 15,7635h39min 3h8min,9h31min AdmitorTransferDispositiontoAdmission(State4to5)12,9063h16min 1h4min,14h32min AdmitorTransferDispositiontoTransfer(State4to6) 4,2040h0min 0h0min,0h0min StarttoLeftWithoutBeingSeen(State1to8) 3,6522h34min 1h21min,4h14min PIAtoLeftAgainstMedicalAdvice(State2to7) 1,4172h35min 1h10min,5h25min h, hours; min,minutes. Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 721 Edmundsonetal. FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder
Table2. Summariesofthetimespentineachstate.
associatedwithlongertransitiontimes.Therewasno evidenceofEDcrowdingaffectingthistransition.
Thefactorsassociatedwithashortertimeforpatientsto beadmittedoutoftheED(State4to5, Figure6)included livinginanon-metropolitanmunicipality(urban:HR1.76; rural:H2.00;remote:HR3.13),presentingwithopioid-(HR 1.25)oralcohol-relatedconcerns(HR1.28),andbeing female(HR1.17).Conversely,livinginaneighborhoodwith alowaverageincome(<$25,000:HR0.79),presentingwith METH-relatedconcerns(HR0.71),andpresentingtoa crowdedED(HR0.79)wereassociatedwithlongertimesto admission.
DISCUSSION
Inthispopulation-basedstudyweusedover37,000 patientswithover66,000EDpresentationstoexaminethe flowthroughtheEDforthosepresentingwithSUD.The medianLOSofpatientsincludedinourstudy(6h13m)is comparabletothemedianLOSforall-causepatients presentingtomajorEDsinAlbertaasreportedbythe provincialvisualanalyticsplatformTableau(TableauLLC, Seattle,WA)duringthesametimeperiod(6h18min).27 The totalLOSwasdeconstructedintoaneight-statemultistate
model,andthereweredifferenttransition-specificeffectsfor theexplanatoryvariables.ThetransitiontoPIAtimeisone oftenusedasabenchmarktoawellfunctioningED.19 WithinthisdetailedlookatSUDpresentationstotheED,it isapparentthatcrowdingparticularlyaffectstheSUD patient’sPIAtime.Additionally,patientsfrom neighborhoodswiththelowestmedianincomehavelonger transitiontimestotheirPIA,aresultthatechoesaprior studyexaminingwaittimesintheunhousedpopulation.28 Apreviousstudy29 identifiedthatyoungadultsexperiencing homelessnesshavelongertotalEDstays,andthedata presentedheremayhighlightonefactorforthisinaSUD population.Athemethatbecameapparentwiththis firststate transitionwasthatMETHusewasassociatedwithprolonged timeintheED.The firststatetransitiontoPIAshoweda modestincreaseintransitiontimeforMETHuse.When compoundedacrossallstatetransitionshowever,this particularSUDpresentationcreatessignificantdelaysin ED flow.
Thedecisiontodischargeapatientwasthesecondstate transitionanalyzedandshowedapredictableeffectamong thoseSUDpatientswithlowacuity.OfallSUDpatients, thosewithopiateusepresentationwereabletotransition

WesternJournal of EmergencyMedicine Volume24,No.4:July2023 722 FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder Edmundsonetal.
Figure3. Forestplotofadjustedhazardratiosandassociated95%confidenceintervalsbycovariatesforthestart(State1)tophysicianinitial assessment(State2)transitionforthemultivariablemodel. HR,hazardratio; CI,confidenceinterval.
tothisstatethefastest(HR1.30).Withtheavailabilityofa rapidreversalagentforopiates(naloxone),themedical managementofopiateintoxicationcanpotentiallybe completedwithinminutes30 andthepatientcanpotentially bedischargedwithin1–2hours.Subsequentmonitoringand addressingtheunderlyingopiateusedisorderoftenmakeup thebulkofthispatient’sEDLOS.31 Theeffectofgender,age, andmodeofarrivalhavepreviouslybeenidentifiedto increaseapatient’sEDLOS,32 butthedatapresentedhere showthatthisdifferencemaybeprimarilyinfluencedbythe timetophysician’sdecisiontodischarge.
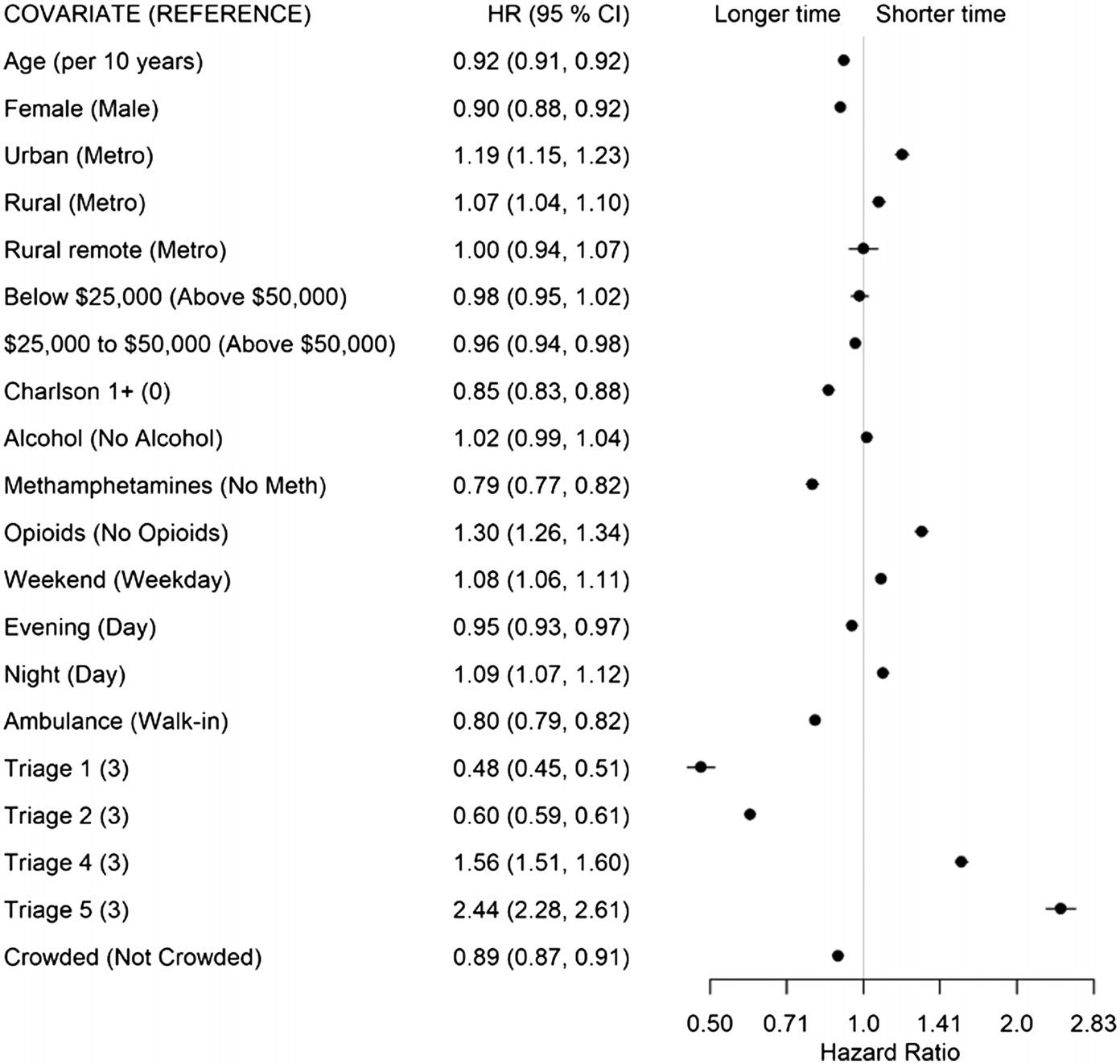
TheeffectoftheCharlsonComorbidityIndexon prolongingthisspecifictransitionbetweenstatesisnovelto ourstudy.PreviousstudiesaddressingEDLOShavefound nosignificanteffectofapatient’sdiseaseburdenontheir LOS;however,thesestudieswereperformedincountries outsideofNorthAmerica,wherenon-emergencyphysicians maybethe firsttreatingphysicianandtheanalyseswere insteadfocusedonfactorsthatextendedthetotalED LOS.33,34 Liketheprevioustransitionanalysis,METHuse wasassociatedwithaprolongeddecisiontodischarge.This couldpotentiallybeduetotheclinicalcourseofMETH intoxication,wherechemicalrestraintsaremoreoften
required,35 andthephysiologicaleffectsofMETHcanlast morethan12hours.36
Theemergencyphysician’sdecisiontoconsultan admittingserviceforthepatientwasthethirdtransitionstate analyzed.InEDswithoutanappropriateadmittingservice, thisinsteadreflectedthedecisiontotransferthepatientoutof theEDtoalargercenterthatcouldaccommodatethe patient’sadmission.Unsurprisingly,allthosepatientswho hadahigheracuity,additionalcomorbidities,orwereolder hadthistransitioncompletedmorequickly.AllnonmetropolitanEDswerealsoabletomakethistransition morequickly.Thiscouldbeduetothephysician’sfaster recognitionofapatientwhocannotbemanagedattheir smallercenterandrequirestransfer,orabetterrelationship betweentheEDandinpatientunits,whichfacilitates improvedunderstandingofpatientswhowouldbenefitfrom admission.
Thosefactorsprolongingadecisiontoadmitapatient includepatientpresentationduringtheeveningorweekend hoursandpatientswhoarrivebyambulance.Qualitative studieshavepreviouslytouchedonsomeoftheseitems37,38 thathighlighthealthcaresystemimpactsonpatient disposition.Ourstudyprovidesquantitativeevidencethat
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 723 Edmundsonetal. FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder
Figure4. Forestplotofadjustedhazardratiosandassociated95%confidenceintervalsbycovariatesforthephysicianinitialassessment (State2)todischargedispositiondecision(State3)transitionforthemultivariablemodel. HR,hazardratio; CI,confidenceinterval.
supportsthese findingsintheSUDpatientpopulation.Like thetransitiontimesforadecisiontodischarge,thosepatients withalcoholorMETHusedisorderalsoexhibitedprolonged time-to-admissiondecisions.Thisislikelyduetotheperiod ofobservationcommontobothpresentationstodetermine whethertheirsymptomswillrequireadditionalsupportinthe formofinpatientalcoholwithdrawaltreatments39 orfurther psychiatricassessmentoftheMETH-usepatient.40 Lastly, thosepatientsfromthelowestincomebracket(which encompassespatientsexperiencinghomelessness) experiencedsignificantlylongertransitiontimesbetween thesestates.
The finalstatetransition thatofadecisiontoadmit/ transferthepatientandtheirdeparturefromtheED showedadramaticallyfastertransitiontimeinthenon-metro EDs.Thisislikelyduetosimilarfactorsthatinfluencedthe previousstatechange,namelythesmallerEDs’ relationship withtheiradmittingservicesortheabilitytotransferthe patienttoanothersiteforfurthermanagement.Additionally, thosepatientspresentingwitheitheralcoholoropiateuse wereadmittedmuchmorequickly.Bothpresentationshave welldefined,nearlyalgorithmicmanagementstrategies consistingofalcoholwithdrawalmanagementintheformof

benzodiazepines,41 andopiateintoxicationmanagement withnaloxone.TheassociationofMETHusewithalonger timetoadmissionmaybeduetothemanagement uncertaintysurroundingit.42 PatientswithMETHuse disordercanbebehaviorallydifficult,43 exhibitaggressiveor bizarrebehaviors,andmaybeaccompaniedbymore trauma44 whencomparedtootherSUDpresentations. Emergencydepartmentcrowdingalsonegativelyimpacteda SUDpatient’stransitiontotheadmittedstate,a findingthat hasbeenechoedovernumerousstudiesofEDcrowding.45,46 Lastly,patientsfromareaswiththelowestmedianincome onceagainspentmoretimeinthistransitorystate.This patientcohorthasbeenidentifiedtobemostatriskforpoor clinicaloutcomes47,48 followinganEDpresentationand athighestriskforleavingAMA.49 Theextendeddelays betweennumerousstatetransitionsservetohighlightsomeof theshortcomingsofboththeEDandadmittingteamsin theircare.
LIMITATIONS
Ourstudyhaslimitationsincludingthosetypicalofdata collectedforadministrativepurposes.Weusedthetimes providedforeachstatetransitionandthosetimesmayhave
WesternJournal of EmergencyMedicine Volume24,No.4:July2023 724 FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder Edmundsonetal.
Figure5. Forestplotofadjustedhazardratiosandassociated95%confidenceintervalsbycovariatesforthephysicianinitialassessment (State2)toadmit/transferdispositiondecision(State4)transitionforthemultivariablemodel. HR,hazardratio; CI,confidenceinterval.
beenreportedinerrorormayhavebeenmissing.Theremay beotherimportantvariablesthatcontributedtothetimes spentineachstatethatwewereunabletoaccountforinour analysis.Thesemayincludecharacteristicsofthepatientor characteristicsoftheED,suchasstaffing,thatarenot availableinthedatasources.
CONCLUSION
Takentogether,thisstudydemonstratedtwopervasive themesacrossallstatetransitions.Patientswhopresented withmethamphetaminesusedisorderhaddelayed transitionsbetweenallstatesanalyzedduringtheirEDvisit. Similarly,patientsfromlow-incomeneighborhoodsalsohad delaysinalmostalltransitionsanalyzed.Withthedata presentedhere,theemergencymedicinecommunitymay benefitfromimprovedED flowbyfocusingonimproving transitiontimesforthelowsocioeconomicstatuspatientwith METHusedisorder.Duetothechallengeswithmanaging METHintoxication,furtherresearchtoimprovetreatment pathwaysforthesepatientswillultimatelyhelpED flowas well.Additionalresourcesmayberequiredtoassistthe urbanEDwithmanagingtheinfluxofthesepatientswith
substanceusedisorderandtheiroveralleffectonED crowding.
AddressforCorrespondence:RhondaJ.Rosychuk,PhD,University ofAlberta,DepartmentofPediatrics,1140587AvenueNW, Edmonton,Alberta,CanadaT6G1C9.Email: rhonda.rosychuk@ ualberta.ca
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Edmundsonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.BeckerlegW,HudginsJ.Substanceuse-relatedemergencydepartment visitsandresourceutilization. WestJEmergMed. 2022;23(2):166–73.
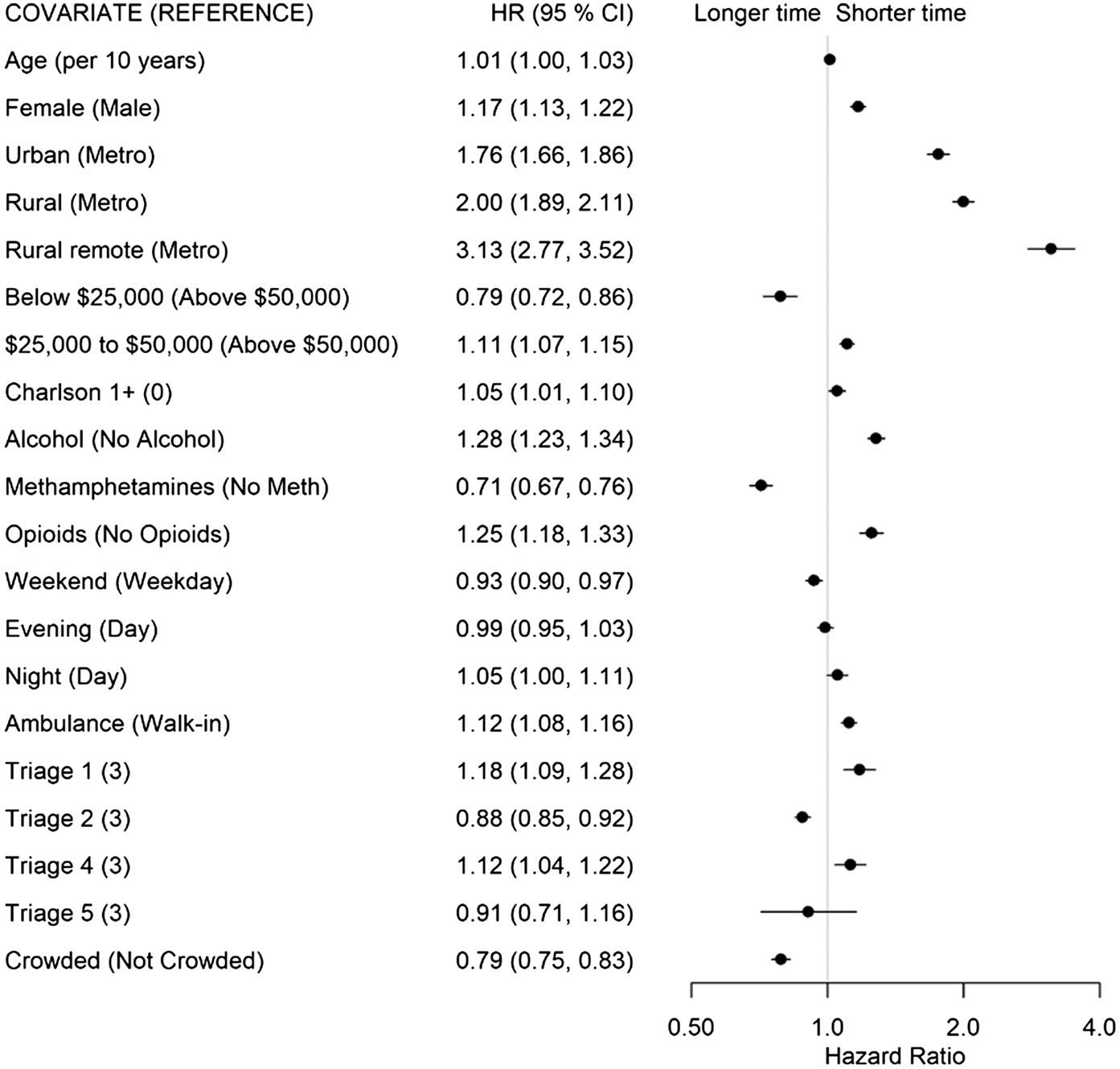
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 725 Edmundsonetal. FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder
Figure6. Forestplotofadjustedhazardratiosandassociated95%confidenceintervalsbycovariatesfortheadmit/transferdisposition decision(State4)toadmission(State5)transitionforthemultivariablemodel. HR,hazardratio; CI,confidenceinterval.
2.GovernmentofAlberta.Albertasubstanceusesurveillancesystem, updatedFebruary,2023.2023.Availableat: https://healthanalytics. alberta.ca/SASVisualAnalytics/?reportUri=%2Freports%2Freports% 2F1bbb695d-14b1-4346-b66e-d401a40f53e6§ionIndex=0&sso_ guest=true&reportViewOnly=true&reportContextBar=false&saswelcome=false.AccessedFebruary15,2023.
3.PetersonC,LiM,XuL,etal.Assessmentofannualcostofsubstance usedisorderinUShospitals. JAMANetwOpen.2021;4(3): e210242
e210242.
4.HanB,ComptonWM,JonesCM,etal.Methamphetamineuse, methamphetamineusedisorder,andassociatedoverdosedeaths amongUSadults. JAMAPsychiatry.2021;78(12):1329–42.
5.HootsB,Vivolo-KantorA,SethP.Theriseinnon-fatalandfatal overdosesinvolvingstimulantswithandwithoutopioidsintheUnited States. Addiction.2020;115(5):946–58.
6.Vivolo-KantorAM,HootsBE,SethP,etal.Recenttrendsand associatedfactorsofamphetamine-typestimulantoverdosesin emergencydepartments. DrugAlcoholDepend.2020;216:108323.
7.BachP,HayashiK,MilloyMJ,etal.Characterisingtheincreasing prevalenceofcrystalmethamphetamineuseinVancouver,Canada, from2006-2017:Agender-basedanalysis. DrugAlcoholRev. 2020; 39(7):932–40.
8.TardelliVS,JohnstoneS,XuB,etal.Markedincreaseinamphetaminerelatedemergencydepartmentvisitsandinpatientadmissionsin Toronto,Canada,2014-2021. CanJPsychiatry.2023;68(4):249–56.
9.CanadianCentreonSubstanceUseandAddiction.Methamphetamine (Canadiandrugsummary).Ottawa,ON2018.Availableat: https://www. ccsa.ca/sites/default/files/2019-04/CCSA-Canadian-Drug-SummaryMethamphetamine-2018-en.pdf.AccessedJune1,2023.
10.TolesM,JiangCS,GoebertD,etal.Methamphetamineinemergency psychiatry. AddictDisordTheirTreat.2006;5(4):191–9.
11.MyranDT,HsuAT,SmithG,etal.Ratesofemergencydepartmentvisits attributabletoalcoholuseinOntariofrom2003to2016:aretrospective population-levelstudy. CMAJ.2019;191(29):E804–E810.
12.KleinLR,DriverBE,MinerJR,etal.Emergencydepartmentlength ofstayforethanolintoxicationencounters. AmJEmergMed.2018; 36(7):1209–14.
13.MorleyC,UnwinM,PetersonGM,etal.Emergencydepartment crowding:asystematicreviewofcauses,consequencesandsolutions. PLoSOne.2018;13(8):e0203316.
14.CanadianInstituteforHealthInformation. NationalAmbulatoryCare ReportingSystem(NACRS)metadata.Ottawa,ON:CanadianInstitute forHealthInformation;2020.Availableat: https://www.cihi.ca/en/ types-of-care/hospital-care/emergency-and-ambulatory-care/nacrsmetadata.AccessedJune1,2023.
15.Alberta.GovernmentofAlberta.Populationstatistics.2022.Availableat: https://www.alberta.ca/population-statistics.aspx AccessedJuly13,2022.
16.CanadianInstituteforHealthInformation.TheCanadianEnhancement ofICD-10(InternationalStatisticalClassificationofDiseasesand RelatedHealthProblems,TenthRevision).Ottawa,ON:Canadian
InstituteforHealthInformation;2001.Availableat: http://assets.ibc.ca/ Documents/Auto%20Insurance/ICD-10-CA%202015.pdf.Accessed June1,2023.
17.DiRicoR,NambiarD,StoovéM,etal.DrugoverdoseintheED:arecord linkagestudyexaminingemergencydepartmentICD-10coding practicesinacohortofpeoplewhoinjectdrugs. BMCHealthServRes 2018;18(1):945.
18.BullardMJ,UngerB,SpenceJ,etal.RevisionstotheCanadian EmergencyDepartmentTriageandAcuityScale(CTAS)adult guidelines. CJEM.2008;10(2):136–51.
19.AffleckA,ParksP,DrummondA,etal.Emergencydepartment overcrowdingandaccessblock. CJEM.2013;15(6):359–70.
20.CharlsonME,PompeiP,AlesKL,etal.Anewmethodofclassifying prognosticcomorbidityinlongitudinalstudies:Developmentand validation. JChronicDis.1987;40(5):373–83.
21.CanadianInstituteforHealthInformation.Dischargeabstractdatabase (DAD).Availableat: https://www.cihi.ca/en/types-of-care/hospital-care/ acute-care/dad-metadata.AccessedMarch1,2022.
22.PampalonR,HamelD,GamacheP,etal.Adeprivationindexforhealth planninginCanada. ChronicDisCanada.2009;29(4):178–91.
23.AkaikeH.(2011).Akaike’sinformationcriterion.In:LovricM. InternationalEncyclopediaofStatisticalScience. Berlin,Heidelberg: SpringerBerlinHeidelberg.
24.R:Alanguageandenvironmentforstatisticalcomputing [computerprogram]2021.Vienna,Austria:RFoundationforStatistical Computing.Availableat: http://www.r-project.org/ AccessedJune1,2023.
25.JacksonCH.Multi-statemodelsforpaneldata:themsmpackageforR. JStatSoftw.2011;38(8):1–29.
26.Forestplot:Advancedforestplotusing ‘grid’ graphics.Rpackage version2.0.1.[computerprogram]2021.Availableat: https://www. rdocumentation.org/packages/forestplot/versions/3.1.1/topics/ forestplot.AccessedJune1,2023.
27.AlbertaHealthServicesAnalytics.ProvincialELOSvsALOS dashboard.[dashboardshowingmonthlyandquarterlyresultsforthe ratioofacutelengthofstayversusexpectedlengthofstay(fortypical inpatientcases),byfacility].AHSTableauReportingPlatform2018. AccessedFebruary15,2023.
28.AyalaA,TegtmeyerK,AtassiG,etal.Theeffectofhomelessnesson patientwaittimesintheemergencydepartment. JEmergMed.2021;60 (5):661–8.
29.NamE,PalmerAN,PatelM.Characteristicsofemergencydepartment visitsbyhomelessyoungadultsintheUS. JAdolescHealth.2021;69(2): 302–7.
30.ParthviR,AgrawalA,KhanijoS,etal.Acuteopiateoverdose:anupdate onmanagementstrategiesinemergencydepartmentandcriticalcare unit. AmJTher.2019;26(3):e380
e387.
31. StrayerRJ,HawkK,HayesBD,etal.Managementofopioiduse disorderintheemergencydepartment:awhitepaperpreparedforthe AmericanAcademyofEmergencyMedicine. JEmergMed.2020; 58(3):522–46.
–
–
WesternJournal of EmergencyMedicine Volume24,No.4:July2023 726 FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder Edmundsonetal.
32.SarıyerG,AtamanMG,Kızıloglu I.Analyzingmainandinteraction effectsoflengthofstaydeterminantsinemergencydepartments. IntJ HealthPolicyManag.2020;9(5):198–205.
33.SirÖ,HesselinkG,VanDenBogaertM,etal.Riskfactorsforprolonged lengthofstayofolderpatientsinanacademicemergencydepartment:a retrospectivecohortstudy. EmergMedInt.2019;2019:4937827.
34.vanderVeenD,RemeijerC,FogtelooAJ,etal.Independent determinantsofprolongedemergencydepartmentlengthofstayina tertiarycarecentre:aprospectivecohortstudy. ScandJTraumaResusc EmergMed.2018;26(1):81.
35.MurphyCEI,WangRC,CoralicZ,etal.Associationbetween methamphetamineuseandpsychiatrichospitalization,chemical restraint,andemergencydepartmentlengthofstay. AcadEmergMed 2020;27(11):1116
25.
36.JonesR,WoodsC,UsherK.Ratesandfeaturesofmethamphetaminerelatedpresentationstoemergencydepartments:anintegrative literaturereview. JClinNurs.2018;27(13-14):2569–82.
37.CalderLA,ForsterAJ,StiellIG,etal.Mappingouttheemergency departmentdispositiondecisionforhigh-acuitypatients. AnnEmerg Med.2012;60(5):567–76.
38.PopeI,BurnH,IsmailSA,etal.Aqualitativestudyexploringthefactors influencingadmissiontohospitalfromtheemergencydepartment. BMJ Open.2017;7(8):e011543.
39.MorganMY.Acutealcoholtoxicityandwithdrawalintheemergency roomandmedicaladmissionsunit. ClinMed(Lond).2015;15(5):486–9.
40.SibandaNC,KornhaberR,HuntGE,etal.Prevalenceandriskfactorsof emergencydepartmentpresentationswithmethamphetamine intoxicationordependence:asystematicreviewandmeta-analysis.
IssuesMentHealthNurs.2019;40(7):567–78.
41.WolfC,CurryA,NachtJ,etal.Managementofalcoholwithdrawalinthe emergencydepartment:currentperspectives. OpenAccessEmerg Med.2020;12:53–65.
42.IsoardiKZ,AylesSF,HarrisK,etal.Methamphetaminepresentationsto anemergencydepartment:managementandcomplications. Emerg MedAustralas.2019;31(4):593–9.
43.Glasner-EdwardsS,MooneyLJ.Methamphetaminepsychosis: epidemiologyandmanagement. CNSDrugs.2014;28(12):1115–26.
44.SchermerCR,WisnerDH.Methamphetamineuseintrauma patients:apopulation-basedstudy. JAmCollSurg 1999;189(5):442–9.
45.BullardMJ,Villa-RoelC,BondK,etal.Trackingemergencydepartment overcrowdinginatertiarycareacademicinstitution. HealthcQ.2009; 12(3):99–106.
46. OlshakerJS,RathlevNK.Emergencydepartmentovercrowdingand ambulancediversion:theimpactandpotentialsolutionsofextended boardingofadmittedpatientsintheemergencydepartment. JEmerg Med.2006;30(3):351–6.
47.YamamotoA,NeedlemanJ,GelbergL,etal.Associationbetween homelessnessandopioidoverdoseandopioid-relatedhospital admissions/emergencydepartmentvisits. SocSciMed 2019;242:112585.
48.BaggettTP,HwangSW,O’ConnellJJ,etal.Mortalityamonghomeless adultsinBoston:shiftsincausesofdeathovera15-yearperiod. JAMA InternMed.2013;173(3):189–95.
49.KuBS,ScottKC,KerteszSG,etal.Factorsassociatedwithuseofurban emergencydepartmentsbytheUShomelesspopulation. PublicHealth Rep.2010;125(3):398–405.
–
Volume24,No.4:July2023 WesternJournal of EmergencyMedicine 727 Edmundsonetal. FlowThroughtheEDforPatientsPresentingwithSubstanceUseDisorder
PerceptionofQuietStudentsinEmergencyMedicine:An ExplorationofNarrativesintheStandardizedLetterofEvaluation
JohnK.Quinn,MD
JillianMongelluzzo,MD,MAEd
AlyssaNip,MD
JosephGraterol,MD
EstherH.Chen,MD
UniversityofCalifornia,SanFrancisco,DepartmentofEmergencyMedicine, SanFrancisco,California
SectionEditor:JeffreyLove,MD,MHPE,andDanielleHart,MD,MACM
Submissionhistory:SubmittedJune15,2022;RevisionreceivedMarch16,2023;AcceptedMarch17,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.57756
Introduction: TheStandardizedLetterofEvaluation(SLOE)isdesignedtoassistemergencymedicine (EM)residencyprogramsindifferentiatingapplicantsandinselectingthosetointerview.TheSLOE narrativecomponentsummarizesthestudent’sclinicalskillsaswellastheirnon-cognitiveattributes.The purposeofthisqualitativeinvestigationwastoexplorehowstudentsdescribedintheSLOEasquietare perceivedbyfacultyandtobetterunderstandhowthismayimpacttheirresidencycandidacy.
Methods: ThisretrospectivecohortstudyincludedallSLOEssubmittedtooneEMresidencyprogram duringoneapplicationcycle.WeanalyzedsentencesintheSLOEnarrativedescribingstudentsas “quiet,”“shy,” and/or “reserved.” Usinggroundedtheory,thematiccontentanalysiswithaconstructivist approach,weidentified fivemutuallyexclusivethemesthatbestcharacterizedtheusageofthese targetwords.
Results: Weidentified fivethemes:1)quiettraitsportrayedasimplied-negativeattributes(62.4%); 2)quietstudentsportrayedasovershadowedbymoreextravertedpeers(10.3%);3)quietstudents portrayedasunfitforfast-pacedclinicalsettings(3.4%);4) “quiet” portrayedasapositiveattribute (10.3%);and5) “quiet” commentsdeemeddifficulttoassessduetolackofcontext(15.6%).
Conclusion: Wefoundthatquietpersonalitytraitswereoftenportrayedasnegativeattributes.Further, commentsoftenlackedclinicalcontext,leavingthemvulnerabletomisunderstandingorbias.More researchisneededtodeterminehowquietstudentsperformcomparedtotheirnon-quietpeersandto determinewhatchangestoinstructionalpracticesmaysupportthequietstudentandhelpcreateamore inclusivelearningenvironment.[WestJEmergMed.2023;24(4)728–731.]
INTRODUCTION
Theemergencymedicine(EM)StandardizedLetterof Evaluation(SLOE)isahigh-stakesassessmentdesignedto assistresidencyprogramsindifferentiatingapplicantsandis consideredimportantinthedecisiontointerview.1,2 The narrativecomponentsummarizesthestudent’sknowledge, clinicalskills,andnon-cognitiveattributesshowntobe predictorsofperformance.3–5 However,thenarrativemaybe difficulttointerpretduetotheuseofoverlygenerallanguage andhiddencode,bothcommoninwrittenassessment.6–9
Further,commentsaboutpersonalityoftenlackclinical context,whichreducestheirusefulnessandmakesthem vulnerabletomisinterpretationorbias.6–8
WebecameinterestedinSLOEnarrativesreferencing quietstudentsduringapplicantreviewwhenweobservedless enthusiasmforstudentsdescribedasquiet,evenforthose withstrongobjectiveapplicationdata.Whilenon-cognitive attributesareimportantcomponentsofholisticassessment, personalitytraitsshouldnotnecessarilyhinderastrong application.3–5 Nostudiesshowthatquietindividualsare
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 728 BRIEF RESEARCH REPORT
unsuitedforEMorarelesssuccessfulinEMcareers. However,inaninternalmedicinesetting, “quiet” was interpretedbyattendingsasa “red flag ” inclerkshipwritten evaluations, 9,10 andstudentsdescribedasquietintheir SLOEscoredloweronbothglobalassessmentand anticipatedranklist.11 Wefoundnootherresearch examininghowquietindividualsperformorhowthey wereperceivedinEM.Thepurposeofthisqualitative investigationwastoexplorehowquietstudentsaredescribed intheSLOEnarrativeandhowthislanguagemay impactcandidacy.
METHODS
StudyDesignandPopulation
Weconductedasubgroupanalysisofaretrospective cohortstudyofallcoreEMrotationSLOEssubmitted throughtheElectronicResidencyApplicationService (ERAS)tooneEMresidencyprogramduringthe2016–2017 applicationcycle.WeexcludedSLOEsfromnon-Liaison CommitteeonMedicalEducationaccreditedschoolsand applicantswhograduatedfrommedicalschoolbeforeor duringtheapplicationcycle.Thestudywasapprovedbythe institutionalreviewboardandtheAssociationofAmerican MedicalColleges.
StudyProtocolandDataAnalysis
AuthorJMdownloadedSLOEsfromERASinto REDCap(ResearchElectronicDataCapturetoolshostedat UCSanFrancisco).andde-identifiedthempriortoanalysis. AnalysiswasperformedbyJKQ,EHC,andJM,allwith traininginmedicaleducationresearchmethodologyand educationleadershipexperience(chiefresident,associate residencydirector,andassistantresidencydirector).JKQ andEHCbrainstormedwordstypicallyusedtodescribe quietindividualsandchosethetarget-descriptorsquiet,shy, andreserved(collectivelytermed “quiet”)becausepassive, introverted,andtimidwereuncommon(3,2,and1, respectively)andalwaysco-occurredwithtarget-descriptors. Weanalyzedonlythesentencecontainingthetargetdescriptorswithoutexploringtheentirenarrative.We analyzeddatausinggroundedtheorythematiccontent analysiswithaconstructivistapproach.12 Therewasnopreexistingtheoryaboutthedatathatweaimedtoproveor disprove;instead,thegoalwastoexploreSLOEnarrativecommentsandconstructmeaningfromthemtoprovide perspectiveonhowquietstudentsareperceived.
Withoutapresetideaofhowdatawouldbesorted,JKQ andEHCindependentlybegantheinitialcodingbyreading eachcommentandconsideringhowitwasusedtodescribe thestudent.Asusagepatternsemergedtheywerecodedas like-comments.JMreadasubsetofthedata.Toestablish thatthedatasetwassufficientforthepurposeofthe investigation,wecodedthe firsthalfofthedatasetandthen determinedthatnonewpatternsemergedinthesecondhalf.
Weprogressedtoexplainingourcodingschemes,comparing them,andlookingforsimilaritiesanddifferences.Through aniterativeprocessofconstantcomparisonwecombined, deleted,andrefinedcodes,mergingthemintooverarching themes.Weusedaspreadsheettovisuallyorganizecodesand finalthemes.
RESULTS
Wereviewed1,582SLOEsfrom696applicants.Ofthese, 117SLOEsreferencedquietapplicantsandwereanalyzed. Theadjective “quiet” occurredin102SLOEs. “Reserved” occurredin28SLOEsandco-occurred14timeswith “quiet.” “Shy” occurredin11SLOEsandco-occurred fivetimes with “quiet.”
Initialcodingrevealedusagerelatedtointerpersonal skills,initiative,disposition,patientinteractions,leadership, medicalknowledge,responsetofeedback,workhabits,and fitnessforEM.Furtheranalysisrevealedthatmanytarget sentencesdidnot fitintothesecategories,lackedclinical context,andweredifficulttointerpret.Weeventually reachedaconsensusonaframeworkof fivemutually exclusiveoverarchingthemesthatincludedallcomments, bestrepresentedthescopeofusagepatterns,andwouldbe mostmeaningfulinaddressingourstudypurpose(Table1).
Theme1comments,62.4%describequiettraits asimplied-negativeattributes.Commentsarelabeled “implied” becausequietisnotexplicitlycallednegativebut istypicallycoupledwithacontrastingpositivetraitthat appearstobeanefforttomitigatethenegativityofthequiet comment(eg, “Quietbuthardworking”).Thestructureofthe sentencemakesitclearthatquietisnegative,butitisnot evidentinwhatwayortowhatdegreeitisnegative.Asmaller numberofcommentslinkedthequiettraitwith anotherseeminglynegativeattribute(eg, “Quietandtimidat times”).Theimpliednegativityofthesecomments coupledwiththelackofcontextmayadverselyaffectthe applicant’scandidacy.
Theme2comments(10.3%)describequietstudentsas beingovershadowedbymoreextravertedpeersandthus moredifficulttoassess.Thesecommentsalsodidnotexplain howperformancewasimpactedbythequiettrait,onlythat thestudentwasnotabletodemonstratevalueasacandidate orperformattheleveloftheirpeers,whichpresumably hindersapplicantcandidacy.
Theme3comments3.4%)questionthe fitnessofquiet studentsforfast-pacedclinicalsettings.However,these commentsdidnotdetailhow,ortowhatdegree,thestudent’ s quietnessspecificallyaffectedperformance,makingthem vulnerabletomisinterpretation.Thesecommentswould likelyalsohindercandidacy,astheabilitytoperformwellin allclinicalsettingsispresumablyseenasnecessaryina successfulEMresident.
Theme4comments(10.3%) “quiet” isportrayedas apositiveattributeandtendstodescribeleadershipstyle,
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 729 Quinnetal. QuietStudentsinEM:ExplorationoftheStandardizedLOE
Table1. Thematicanalysisof117sentencescontainingthewords “quiet” , “shy” or “reserved”
ThemeSubthemesExamples
Theme1)Impliednegative (n = 73)
1A)Quietnatureismitigatedby associatingwithapositiveinterpersonal skill.
1B)Quietnatureismitigatedby associatingwithapositiveattribute unrelatedtoquietpersonality.
“Quietbutwasalwaysabletocommunicateeffectively.” “Somewhatreservedbutcanbeassertivewhen necessary.”
“Quietbuthardworking.”“Canbereservedattimesbut isincrediblyintelligent.”
Theme2)Quietstudentsmay beovershadowedbyothers (n = 12)
2A)Quietstudentsovershadowedby moreextravertedstudents.
2B)Quietstudents’ clinicalskillsdif ficult toassessduetotheirquietpersonality.
“Quietdemeanorandpresenceof flashierstudents preventedahigherranking.”“Overshadowed,quieter thanpeers,disappearedintobackgroundmostofthe month.”
“Truncatedpresentationsandquietdemeanormakeit dif ficulttoevaluatetruepotential.”“SoquietIcouldnot judgelevelofengagement.”
Theme3)Quietstudentsmay belesssuitedforcertainclinical settings(n = 4)
3A)Quietstudentsperceivedastoo passive,slow,orunassertiveforabusy clinicalsetting.
3B)Quietstudentsperceivedasless adaptabletothedemandsofabusy clinicalsetting.
“Quiet,passivenaturemaynotbesuitedforhighpaced inner-cityED.”“Quietandunassumingpersonality, somenotedthistobeaconcern,particularlyinabusy countyED,othersdidn’t.”
“Calm,quiet,reserveddemeanor-somestaffquestion adaptabilitytochaoticED.”
Theme4)Positivetrait(n = 12)
Theme5)Equivocal(n = 16)
ED,emergencydepartment; EM,emergencymedicine.
patientinteractions,orabilitytoperformunderpressure, ratherthandescribingstudentpersonality.Thisadditional contextmayhavecontributedtotheoverallperceptionof “quiet” asapositiveattribute.Theme5comments(15.6%) wereconsideredequivocalinthattheinvestigatorseitherdid notagreeonthepositivityornegativityoftheir interpretation,orthecommentslackedsufficientcontextto interprettheintendedmeaning(eg, “Studentwas initiallyquiet”).
DISCUSSION
Wefoundthatquiettraitswereusuallyportrayedas negativeattributesand,therefore,hadthepotentialto adverselyaffectthecandidacyofaconsiderablenumberof applicants.Theanalysisalsorevealedthatacrossthemes thequiettraitwasrarelydescribedintermsofclinical competency.Thisisconcerningbecauseanegativecomment thatlackscontextrequiresthereadertorelyoninferences orassumptionsthatmayresultinunfairlyjudgingthe applicant.Providingexamplesthatdescribeobserved behaviorandclinicalskill,ratherthanreferencing personality,willimprovethequalityandfairnessof theassessment.6,7
“Soothingdemeanorandquietconfidencewillsuitquite wellthroughouttheircareer.”“Quietdemeanor,kind bedsidemannerwhichisanassetwithpatients.”
“Alittlequiet,wedonotthinkthiswillhinderabilitytobe averycapableEMresident.”“Quiet”
Our findingsthatquietstudentsaredescribedasbeing overshadowedbymoreextravertedpeers,moredifficultto assess,andless fitforfast-pacedclinicalsettingssuggestthe possibilitythatcurrentinstructionalpracticesfavormore outgoingstudents.Inaclinicalsettingwherebeingassertive isviewedfavorably,quietstudentsmaybejudgedunfairlyas beinglessknowledgeableorprepared.3,13 Changesto instructionalpracticesthatmaybetterservequietstudents includethefollowing:providingadditionalstudent observations6;usingstandardizedassessment-tools14,15; expandingassessmentcriteriatoincludestrengthsofthe introvert13;providingfacultydevelopmenttoimprove qualityofwrittenassessment7;usinggroup-writtenSLOEs thatmayreducebias1,2;andprovidingstudentmentorship.3
LIMITATIONS
ThisstudywaslimitedtoSLOEsfromapplicantstoa singleinstitutionduringoneapplicationcycle.Weanalyzed onlythesentencecontainingthetarget-descriptors;reading theentirenarrativemayhaveprovidedadditionalcontext. Target-descriptorsmaybedefineddifferentlybydifferent evaluatorsandreadersandmayormaynotbeused interchangeably.Further,readersmayinterpretthe
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 730 QuietStudentsinEM:ExplorationoftheStandardizedLOE Quinnetal.
positivityornegativityoftheusagedifferentlythanthe investigators.Thetarget-descriptorsmaynotreflectstudent personalitybutratherhowtheywereperceivedbytheir evaluatorintheclinicalsetting.Applicantsdidnotreceivea personalityinventorynordidtheyself-reporttheir personalitytype.Wedidnotidentifythegenderofapplicant ortheSLOEwriter,whichpreventedusfromdetermining whetherour findingswereaffectedbygender.Nordidwe identifythepositionorexperienceofthewriter,orwhether individualorgroupprocesswasused.Wedidnotattemptto associatequietvsnon-quietstatuswithaninvitation tointerview.
CONCLUSION
Wefoundthatquietpersonalitytraitswereoftenportrayed asnegativeattributesintheStandardizedLetterof Evaluation.Additionally,clinicalcontextwasrarely provided,leavingcommentsopentovariableinterpretation andpossiblemisunderstandingofstudentcompetency.
These findingsaddtoourunderstandingaboutquietstudents inEM,butmoreresearchisneededtodeterminehow quiet-labeledstudentsperformcomparedtotheirnon-quiet peersandtodeterminewhatchangestoinstructionalpractices maysupportthequietstudentandhelpcreateamoreinclusive learningenvironmentwhereallstudentscanthrive.
AddressforCorrespondence:JohnK.Quinn,MD,Universityof California:SanFrancisco,DepartmentofEmergencyMedicine,505 ParnassusAve,SanFrancisco,CA94143.Email: john.quinn@ucsf. edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Quinnetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.LoveJN,DotyCI,SmithJL,etal.Theemergencymedicinegroup StandardizedLetterofEvaluationasaworkplace-basedassessment: ThevalidityIsinthedetail. WestJEmergMed.2020;21(3):600–9.
2.NegaardM,AssimacopoulosE,HarlandK,etal.Emergencymedicine residencyselectioncriteria:anupdateandcomparison. AEMEduc Train.2018;2(2):146–53.
3.KhanMA,MalviyaM,EnglishK,etal.Medicalstudentpersonalitytraits andclinicalgradesintheinternalmedicineclerkship. MedSciEduc 2021;31(2):637–45.
4.PinesJM,AlfarajS,BatraS,etal.FactorsImportanttotop clinicalperformanceinemergencymedicineresidency:results ofanideationsurveyandDelphipanel. AEMEducTrain 2018;2(4):269–76.
5.SobowaleK,HamSA,CurlinFA,etal.Personalitytraitsareassociated withacademicachievementinmedicalschool:anationally representativestudy. AcadPsychiatry.2018;42(3):338–45.
6.JacksonJL,KayC,JacksonWC,etal.Thequalityofwrittenfeedbackby attendingsofinternalmedicineresidents. JGenInternMed 2015;30(7):973–8.
7.LedfordR,BurgerA,LaRochelleJ,etal.Exploringperspectivesfrom internalmedicineclerkshipdirectorsintheUSAoneffectivenarrative evaluation:resultsfromtheCDIMnationalsurvey. MedSciEduc 2020;30(1):155–61.
8.LyePS,BiernatKA,BraggDS,etal.Apleasuretoworkwith–ananalysis ofwrittencommentsonstudentevaluations. AmbulPediatr 2001;1(3):128–31.
9.GinsburgS,KoganJR,GingerichA,etal.Takenoutofcontext:hazards intheinterpretationofwrittenassessmentcomments. AcadMed 2020;95(7):1082–8.
10.GinsburgS,McIlroyJ,OulanovaO,etal.Towardauthenticclinical evaluation:pitfallsinthepursuitofcompetency. AcadMed 2010;85(5):780–6.
11.QuinnJK,MongelluzzoJ,AddoN,etal.TheStandardizedLetterof Evaluation:howweperceivethequietstudent. WestJEmergMed 2023;24(2):259–63.
12.CoatesWC,JordanJ,ClarkeSO.Apracticalguideforconducting qualitativeresearchinmedicaleducation:Part2-Codingandthematic analysis. AEMEducTrain.2021;5(4):e10645.
13.DavidsonB,GilliesRA,PelletierAL.Introversionandmedicalstudent education:challengesforbothstudentsandeducators. TeachLearn Med.2015;27(1):99–104.
14.DavisKR,BankenJA.Personalitytypeandclinicalevaluationsinan obstetrics/gynecologymedicalstudentclerkship. AmJObstetGynecol 2005;193(5):1807
10.
15.SchellRM,DilorenzoAN,LiHF,etal.Anesthesiologyresident personalitytypecorrelateswithfacultyassessmentofresident performance. JClinAnesth.2012;24(7):566–72.
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 731 Quinnetal. QuietStudentsinEM:ExplorationoftheStandardizedLOE
ImpactofFacultyIncentivizationonResidentEvaluations
ViralPatel,MD
AlexandraNordberg,MD
RichardChurch,MD
JenniferL.Carey,MD
SectionEditor: JeffreyDruck,MD
UniversityofMassachusettsChanMedicalSchool,DepartmentofEmergencyMedicine, Worcester,Massachusetts
Submissionhistory:SubmittedOctober24,2022;RevisionreceivedMarch14,2023;AcceptedMarch29,2023
ElectronicallypublishedJuly12,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59267
Introduction: IntheProgramRequirementsforGraduateMedicalEducationinEmergencyMedicine, theAccreditationCouncilforGraduateMedicalEducationrequiresfrequentandroutinefeedback.Itisa commonchallengeforprogramleadershiptoobtainadequateandeffectivesummativeevaluations.
Methods: Thisisaretrospective,case-crossover,interventionalstudyconductedinanacademic medicalcenter.Thisstudyoccurredoveratwo-yearperiod,withaninterventionbetweenyearsoneand two.Throughoutyeartwoofthestudy,facultyincentivecompensationwaslinkedtocompletionofend-ofshiftevaluations.Wecomparedpre-anpost-implementationdatausingpairedsample t-testswiththe significancelevel P < .05applied.
Results: Afterimplementationoftheincentivemetrictherewasanincreaseinthenumberoftotal evaluationsby42%(P = .001).Themeannumberofevaluationssubmittedbyeachfacultypershift increasedfrom0.45to0.86(SD0.56, P < .001).Overall,32ofthe38facultymembers(84.2%)hadan increaseinthenumberofevaluationssubmittedpershiftduringtheinterventionperiodwithanaverage increaseof0.5evaluationspershift(range0.01–1.54).
Conclusion: Incentivizingfacultytosubmitresidentevaluationsthroughuseofbonuscompensation increasedthenumberofevaluationsatourinstitution.Thisinformationmaybeappliedbyotherprograms toincreaseresidentevaluations.[WestJEmergMed.2023;24(4)732–736.]
INTRODUCTION
TheAccreditationCouncilforGraduateMedical Education(ACGME)requiresemergencymedicine(EM) residencyprogramstoobtainfrequentfeedbackforresident physiciansthatisbothsummativeandformative.1 To accomplishthis,manyprogramsemployanevaluationform thatistobecompletedbyfacultyattheconclusionofeach residentshift.2,3 Thisformativefeedbackiscompiledby clinicalcompetencycommitteestocreatesummative feedbackforresidents,comparingeachresidentagainst milestonesandtheirpeers.Thisassiststheprogramdirector inmakingevaluativedecisionsregardingtheperformance andabilitiesoftrainees.
Consistentlyobtainingend-of-shiftfeedbackfromfaculty hasbeenatargetedareaofimprovementwithinmedical
training.2,4–7 Differentstrategieshavebeenexecuted,with digitalcollectionbeingshowntoimprovefacultyresponse ratescomparedtopapersystems.8,9 Yetevenwithsuch implementationthereisstillalackofsufficientfeedback collectiontoconstructaglobal,summativeevaluationof residentsinallmilestones.2,10 Strategieshavebeen implementedtoimprovefacultyengagementand participationineducationalcampaignsattheundergraduate medicaleducationandgraduatemedicaleducation(GME) levels.2,4–7 Thereisevidencethat financiallybased incentivizationhasledtoimprovedfacultyparticipationin learnerevaluation,notablyonamonthlyorend-of-rotation basis.7 Therefore,wehypothesizedthatemployingsuchan incentivizationprocesswouldincreasetheoverallquantityof residentend-of-shiftevaluationscompletedbyfaculty.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 732 BRIEF RESEARCH REPORT
OurstudyaddressestheACGMErequirementfor increasedfrequencyofevaluation,effectivelyonanear-daily basis,andshowsthat financialstrategiescanmotivatefaculty toengageinthislevelofparticipation.Ourstudyappearsto bethe firstofitskindindirectingattentiontothe requirementsnecessaryfortheprovisionofextensive,timely feedbacktoourlearners.
METHODS
Thiswasaretrospective,case-crossoverinterventional studyconductedatanacademicEMresidencytrainingsite. Thisstudywasreviewedanddeemedexemptbythe institutionalreviewboard.Atourinstitution,end-of-shift evaluationscontainthecompetenciesfromtheACGME milestone-basedratingscaleandspaceforfree-text comments.Evaluationscaneitherberequestedbythe residentorself-initiatedbythefacultymember.
Thisstudyoccurredoveratwo-yearperiodformOctober 1,2019
September30,2021,coincidingwiththe fiscalyear (FY)calendarsfor2020(FY20)and2021(FY2021).During the firstyearofthestudy(FY20),facultyincentive compensationwasnotconnectedtoresidentevaluations.At themidpointofthestudyperiodanincentivecompensation planwasintroducedlinkingthecompletionofend-of-shift evaluationstotheyear-endbonusforFY21.Faculty bonuses,whichareawardedannually,areapercentageof basesalarybrokendownbyclinicalandacademicmetrics. Pointsareearnedtoachievetheacademicbonus;completion of40end-of-shiftevaluationsearns25%ofthepointsneeded forthefullacademicbonus.Forafacultymemberatthe assistantprofessorlevelreceivingthefullacademicbonus, meetingthisfulfilmenttranslatestoapproximately$4,875.
Wereviewedthenumberofend-of-shiftevaluations completedinthepre-implementationtothepostimplementationperiodandcomparedbytheoverallnumber ofcompletedevaluationsandthenumberofcompleted evaluationspershiftbyeachattendingphysician.We determinedtheoverallnumberofcompletedevaluations,as wellasthenumberofcompletedevaluationspershiftper attendingandcomparedthenumberofend-of-shift evaluationscompletedinthepre-implementationperiodto thepost-implementationperiod.
Allfacultywhoworkedattheprimaryteachingsiteand wereeligiblefortheannualincentivecompensationbonus metstudycriteria.Allresident-supervisionshiftswere includedinthestudy.Exclusioncriteriaincludedfacultynot employedduringthedurationofthestudyperiodandfaculty whodidnotworkwithresidentsduringthestudyperiod. Onlyevaluationsthatwerecompletedandsubmittedwere includedinthisstudy.Weperformedsubgroupanalysisto comparefordifferencesbetweenmaleandfemalephysicians, andjuniorfaculty(definedforthisstudyaswithinthe first 10yearsofaninitialfacultyappointmentatthecompletion ofthestudyperiod)andseniorfaculty.Weusedour
institution’sresidencymanagementsystem,Medhub (Minneapolis,MN),whichreportedend-of-shiftevaluations conductedbyfacultyofresidentsduringthestudyperiod.
Wecomparedthetotalnumberofevaluationscompleted byeachfacultymemberduringthepre-andpostimplementationperiodsbasedontheMedhubdata.Multiple residentsmaybeworkingduringafacultyshift;therefore, eachfacultymembermaysubmitmultipleevaluationsper shift.Wecalculatedthenumberofevaluationspershiftbased onthetotalnumberofevaluationsperattendingandtotal numberofqualifyingshifts.Wecomparedeachattending physicianpre-implementationtopost-implementationto determineanychangeinthetotalnumberofevaluationsand thenumberofevaluationspershiftperattending.Forthis initialanalysis,thefocuswasintentionallylimitedto quantitativedataevaluation.Weanalyzeddatausing GraphPadPrismversion9(GraphpadSoftware,SanDiego, CA).Pre-andpost-implementationdataandsubgroup analysiswerecomparedusing t -testswiththesignificance level P < 0.05applied.
RESULTS
Duringthestudyperiod,65physicianssubmittedresident evaluations.Amongthem,27didnotmeetinclusioncriteria forthestudyandwereexcluded.Reasonsforexclusionof facultywereasfollows:notemployedduringtheentirestudy period(14);employedasfellows(10);ordidnotworkatthe teachinghospitalforthedurationofthestudy(3).Therewere 38attendingseligibleforthestudy;39.5%werefemaleand 60.5%werejuniorfaculty.Amongthejuniorfaculty,47.8% werefemale;26.7%oftheseniorfacultywerefemale.We included2,778residentevaluationsinthestudy.Thetotal numberofevaluationssubmittedpre-implementationofthe incentivemetric(FY20)was1,149.Afterimplementation, thetotalnumbersubmitted(FY21)was1,629,anincreasein 42%increaseforyeartwo(P = 0.001).
Eachindividualattendingshiftwasreviewed,andthe averagenumberofevaluationssubmittedpershift(forany shiftworkedwithresidents)isreportedin Figure1b.The meannumberofevaluationssubmittedpershiftpreimplementationoftheincentivemetricwas0.45(SD0.47). Afterimplementationoftheincentivemetric,themean numberofevaluationssubmittedpershiftincreasedto0.86 (SD0.56),astatisticallysignificantincrease(P < .001).
Overall,84.2%offacultymembershadanincreaseinthe numberofevaluationssubmittedpershift.Thebreakdown byfemale,male,junior,andseniorfacultyaredetailed in Table1
Acrossallattendingswhohadanincreasednumberof evaluationsduringthepost-implementationperiod,the averageincreasewas0.5evaluationspershift(range 0.01–1.54).Amongthefourwhosubmittedfewerevaluations pershiftduringtheinterventionperiod,theaveragedecrease was0.19evaluationspershift(range0.01–0.55). Figure2
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 733
Pateletal.
ImpactofFacultyIncentivizationonResidentEvaluations
comparestheaveragenumberofevaluationspershiftfor femalesvsmalesinthepre-andpost-implementationperiod andjuniorvsseniorfaculty.Bothfemalefacultyandmale facultyhadasignificantincreaseinthenumberof evaluationspre-andpost-implementation(P = .027, P < .0001,respectively)(Figure2a).However,malefaculty hadagreateroverallincreaseintheaveragenumberof evaluationspershift(P = .049). Figure2b showstheincrease pre-andpost-implementationforjuniorandsenior faculty,whichwassignificantwithinbothgroups (P < 1, P < .001,respectively).Seniorfacultycompletion ratehadaslightlyhigherincreasethanforjuniorfaculty; however,thisdidnotreachstatisticalsignificance.
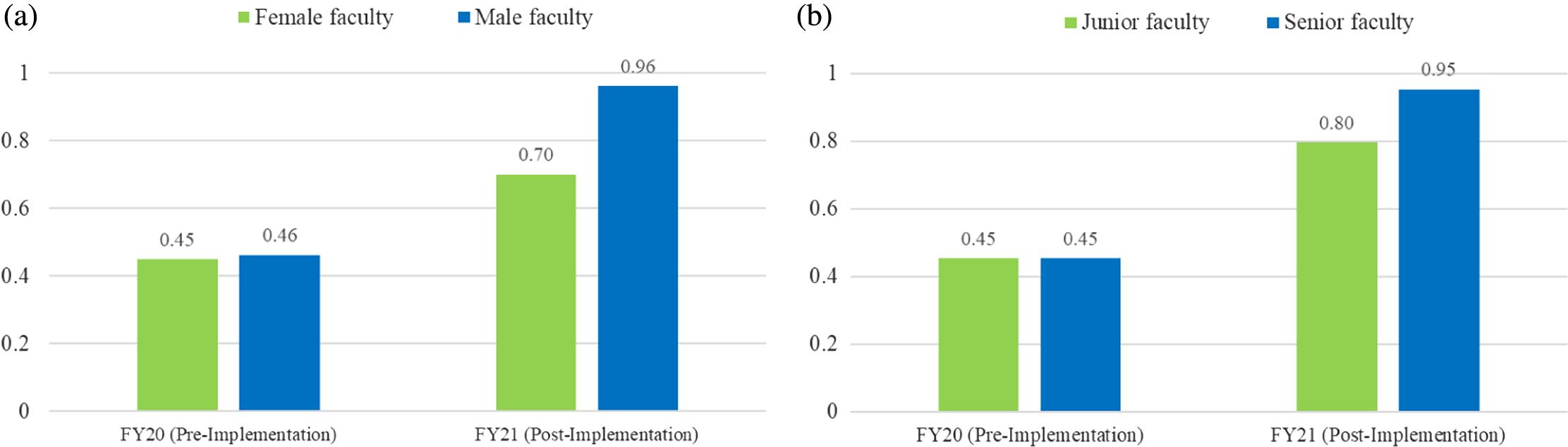
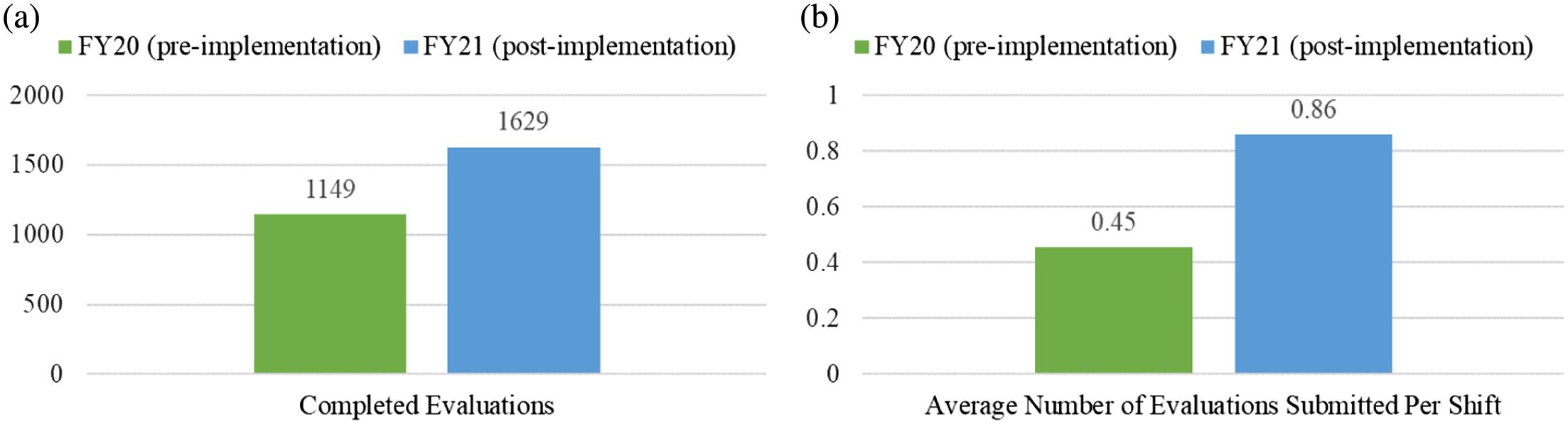
DISCUSSION
financial-incentivemetric(statisticallysignificant,
ficant,
Inthisstudyweidentifyastrategyforimprovingthe collectionofresidentevaluationsfromfacultymembersata primaryacademicEMresidencyteachingsite.Specifically, thestudydemonstratesthatthemajorityofattending physiciansexhibitedanincreaseinthenumberofevaluations theysubmittedpershift,resultinginasignificantincreasein thetotalnumbersubmittedbytheentirestudygroupafter implementationofafacultyincentivizationstrategy.This incentivizationstrategyassistedourprogramtomeetthe ACGMErequirementsforfrequentresidentfeedback. Comparisonofsubgroupsshowsthatwhilebothfemaleand malefacultyhadasignificantincreaseinthenumberof evaluationspost-implementation,theaverageincreasein evaluationspershiftformalefacultywasgreaterthanin femalefaculty.Thismayreflectthetrendoffemalefaculty beinglessabletobeacademicallyproductiveduringthe COVID-19pandemic.11–13
Avarietyofwaystoincreasefacultycontributionstothe myriadofinstructionalneedsintheGMErealmhavebeen investigated.Suchendeavorsincludeassigning “valueunits” toscholasticcontributions,sometimestermed “educational valueunits” (EVU)or “academicrelativevalueunits” (aRVU)tobeusedinadiversemannerbasedon
Figure1a. Completionofresidentevaluationsbyfacultypre-andpost-implementationofa
P = .001). 1b. Averagenumberofevaluationssubmittedpershiftpre-andpost-implementationoftheincentivemetric(statisticallysigni
P < .001).
IncreaseDecreaseNochange Allfaculty(N = 38)84.2%10.5%5.3% Femalefaculty(n = 15)73.3%13.3%13.3% Malefaculty(n = 23)91.3%8.7%0% Juniorfaculty(n = 23)82.6%8.7%8.7% Seniorfaculty(n = 15)86.6%13.3%0%
Table1. Percentagechangeinnumberofevaluationssubmittedper shiftafterimplementationof financialincentive.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 734 ImpactofFacultyIncentivizationonResidentEvaluations
Figure2a. Averagenumberofevaluationscompletedpershiftbyfemaleandmalefacultypre-andpost-implementationoftheincentive metric. 2b. Averagenumberofevaluationscompletedpershiftbyjuniorandseniorfacultypre-andpost-implementationofthe financialincentivemetric.
Pateletal.
departmentalneeds.OneacademicEMgroupconcerned withthemarginalizationofeducationalpursuitsdevelopeda “mission-basedbudget” inwhichanEVUsystemassigns activitiestofacultywithalignedfunding,whichledtoa significantimprovementinthecompletionofobligations.14 Maetalhasshownthatacademicproductivityofafaculty couldbemeasuredand,thus, fiscallyrewardedbasedonthe accruingof “academicpoints” visavisaRVUsandusingan associatedbonussystem.15
AFacultyIncentiveTaskForcewithinanothergroupof emergencyphysicianscreatededucationalactivity categories,assignedstandardizedtimevaluescorrelatingto EVUsforeachactivity,andthensetathresholdoftotal EVUstobemetinordertoreceivecompensation,which resultedinincreasedfacultycompletionofresidentand fellowmonthlyevaluationsaswellasattendanceatdidactic conferences.16 Similarly,Pughetaldemonstratedthatthe implementationofquarterlybonusesincreasedfaculty participationinconferencesandresidentevaluations.7
Evaluationofresidentsmustbewelldocumentedand trendedtoallowforpropersummativeassessment,teaching, andidentificationofpossibleinterventions.Consideringthis, programleadershipneedstocuratefrequentfeedbackto createasufficientvolumefromdiversefacultyacrosstime. Thus,thefocusofthisinvestigationwasintentionallylimited tothequantitativeanalysisregardingnumbersof evaluations.Thiswasdonefromtheperspectiveofprogram administrationandtheACGMErequirementforfrequency/ amountoffeedbackusingthemilestonescales.
LIMITATIONS
Limitationsofthisstudyincludethefactthatitwas conductedatasinglesiteandonlyforthedurationofasingle fiscalyear.Inthisstudywecomparedthenumberof evaluations,nottheiroverallquality.Itisimportanttonote thattheCOVID-19pandemicoccurredduringthestudy period,causingdisruptionstophysicianstaffingandsalaries nationally.Withinourinstitution,emergencyphysician workhoursandsalarieswerenotreducedduetothe pandemicanddidnotaffectthefaculty’sabilityto submitevaluations.
CONCLUSION
Incentivizingfacultythroughuseofabonus compensationstructureincreasedthenumberofevaluations ofresidentssubmittedatourinstitution.Thisinformation maybeappliedbyotherprogramstoincreasethenumber andfrequencyofresidentevaluations.
AddressforCorrespondence:JenniferCarey,MD,ChanMedical School,UniversityofMassachusetts,DepartmentofEmergency Medicine,55LakeAvenueNorth.Worcester,MA01655.Email: Jennifer.Carey@umassmemorial.org
ImpactofFacultyIncentivizationonResidentEvaluations
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Pateletal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.AccreditationCouncilforGraduateMedicalEducation(ACGME).(2021, July).ACGMEProgramRequirementsforGraduateMedicalEducation inEmergencyMedicine.Availableat: https://www.acgme.org/ globalassets/PFAssets/ProgramRequirements/110_ EmergencyMedicine_2020.pdf?ver=2020-06-26-125701-320&ver= 2020-06-26-125701-320.AccessedJune6,2022.
2.DehonE,JonesJ,PuskarichM,etal.Useofemergencymedicine milestonesasitemsonend-of-shiftevaluationsresultsin overestimatesofresidents’ proficiencylevel. JGradMedEduc 2015;7:192–6.
3.DayalA,O’ConnorDM,QadriU,etal.Comparisonofmalevsfemale residentmilestoneevaluationsbyfacultyduringemergencymedicine residencytraining. JAMAIntern.Med.2017;177:651–7.
4.TewsMC,TreatRW,NanesM.IncreasingcompletionrateofanM4 Emergencymedicinestudentend-of-shiftevaluationusingamobile electronicplatformandreal-timecompletion. WestJEmergMed 2016;17:478–83.
5.ChiuDT,SolanoJJ,UllmanE,etal.Theintegrationofelectronicmedical studentevaluationsintoanemergencydepartmenttrackingsystemis associatedwithincreasedqualityandquantityofevaluations. JEmerg Med.2016;51:432–9.
6.TobiasA,SobehartR,DoshiAA,SuffolettoB.Implementationofawebbasedtoolwithtextmessagepromptstoimproveend-of-shift assessmentsforemergencymedicineresidents. JGradMedEduc 2020;12:753–8.
7.PughA,FordT,MadsenT,etal.Impactofa financialincentive onthecompletionofeducationalmetrics. IntJEmergMed.2020;13:60.
8.TheAnesthesiologyAnnualMeetingAmericanSocietyof Anesthesiologists.ImprovingFacultyParticipationinResident Evaluation:ApplyingNewTechnologytoanOldProblem.2001. Availableat: http://www.asaabstracts.com/strands/asaabstracts/ abstract.htm?year=2001&index=14&absnum=1125 AccessedJune6,2022.
9.NableJV,BhatR,IssermanJ,etal.Learnerperceptionsofelectronic end-of-shiftevaluationsonanemergencymedicineclerkship. AEM EducTrain.2021;5:75–8.
10.MenchettiI,EaglesD,GhanemD,etal.Genderdifferencesin emergencymedicineresidentassessment:ascopingreview. AEM EducTrain.2022;6:e10808.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 735
Pateletal.
11.IpeTS,GoelR,HowesL,etal.TheimpactofCOVID-19onacademic productivitybyfemalephysiciansandresearchersintransfusion medicine. Transfusion 2021;61:1690–3.
12.SharpEA,PelletierJH,FriehlingE,etal.Gender,parentingstatus,and theacademicproductivityofpediatriciansduringtheCOVID-19 Pandemic. HospPediatr.2022;12:e379–88.
13.EllinasEH,ArkTK,KaljoK,etal.Winnersandlosersinacademic productivityduringtheCOVID-19pandemic:Isthegendergapwidening forfaculty? JWomensHealth(Larchmt) 2022;31:487–94.
14.ReganL,JungJ,KelenGD.Educationalvalueunits:amission-based approachtoassigningandmonitoringfacultyteachingactivitiesinan academicmedicaldepartment. AcadMed.2016;91:1642–6.
15.MaOJ,HedgesJR,NewgardCD.TheacademicRVU:tenyears developingametricforand financiallyincentingacademicproductivityat OregonHealth&ScienceUniversity. AcadMed.2017;92:1138–44.
16.HouseJ,SantenSA,CarneyM,etal.Implementationofaneducation valueunit(EVU)systemtorecognizefacultycontributions. WestJ EmergMed.2015;16:952–6.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 736
ImpactofFacultyIncentivizationonResidentEvaluations Pateletal.
Single-stepOptimizationinTriagingLargeVesselOcclusion Strokes:IdentifyingFactorstoImproveDoor-to-groinTime forEndovascularTherapy
JoshuaRawson,MD*
AshleyPetrone,PhD†
‡
AmeliaAdcock,MD
*WestVirginiaUniversitySchoolofMedicine,Morgantown,WestVirginia † WestVirginiaUniversity,DepartmentofPathology,Morgantown,WestVirginia ‡ WestVirginiaUniversity,DepartmentofNeurology;CerebrovascularDivision,Morgantown, WestVirginia
SectionEditor:KennethS.Whitlow,DO,FAAEM
Submissionhistory:SubmittedJanuary19,2023;RevisionreceivedMarch24,2023;AcceptedMarch27,2023
ElectronicallypublishedJune30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59770
Introduction: Althoughacutestrokeendovasculartherapy(EVT)hasdramaticallyimprovedoutcomes inacuteischemicstroke(AIS)patientswithlargevesselocclusions(LVO),accesstoEVT-capable centersremainslimited,particularlyinruralareas.Therefore,itisessentialtooptimizetriagesystemsfor EVT-eligiblepatients.Onestrategymaybetheuseofatelestrokenetworkthattypicallyconsistsof multiplespokesitesthatreceiveaconsultationtodetermineappropriatenessofpatienttransfertoan EVT-capablehubsite.StandardizationofAISprotocolsmaybenecessarytoachievetargetdoor-togroin(DTG)timesoflessthan60minutesinEVT-eligiblepatientsuponhubarrival.Specifically,the decisiontoobtainvascularimagingatthetransferringhubsitevsdelayinguntilarrivalatthehubis controversial.ThepurposeofthisstudywastoidentifyfactorsassociatedwithreducedDTGtimein LVO-AISpatients.
Methods: Weperformedaretrospectivechartreviewforallpatientstreatedovera3.5-yearperiodatour homehubinstitution.Patientswereclassifiedastelestroketransfers,non-telestroketransfers,and direct-to-hubpresentations.Werecordeddemographicinformation,DTGtime,reperfusionstatus,length ofstay(LOS),functionalstatusatdischarge,seven-daymortality,andthesitewherevascularimaging computedtomographyangiography(CTA) wasobtained.Weperformedbinarylogisticregressionto identifyfactorsassociatedwithDTG <60minutes.
Results: InthesampleofEVT-eligiblepatients(n = 383),CTAwasperformedatthespokesitepriorto transfertothehubinstitutionin53%ofcases.Further,59%oftelestroketransfercasesreceivedaCTA priortotransfercomparedtoonly40%ofnon-telestroketransfers(59vs40%, P = 0.01).ADoor-to-groin time <60minuteswasachievedin67%oftransferpatientswhoreceivedpre-transferCTAcomparedto only22%oftransferpatientswhoreceivedCTAuponhubarrivaland17%ofpatientswhopresented directlytothehub.Ultimately,transferpatientswhoreceivedCTApriortotransferwere7.2timesmore likelytohaveaDTG <60minutescomparedtothosewhodidnot(OR7.2,95%confidenceinterval 3.5–14.7; P < 0.001).
Conclusion: Pre-transfercomputedtomographyangiographywastheonlysignificantpredictorof achievingtargetdoor-to-grointimesoflessthan60minutes.BecauseDTGtimehasbeenwell establishedasapredictorofclinicaloutcomes,includingpre-transferCTAinastandardizedacute ischemicstrokeprotocolmayprovebeneficial.Our findingsalsoillustratetheneedtooptimizedirect-tohubstrokealertsandtelestrokerelationshipstominimizeworkflowdisruptions,whichbecamemore apparentduringthepandemic.[WestJEmergMed.2023;24(4)737–742.]
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 737
ORIGINAL RESEARCH
INTRODUCTION
Endovasculartherapy(EVT)forlargevesselocclusion acuteischemicstroke(LVO-AIS)isnowthestandardofcare foreligiblepatients.1 However,roughlyhalfofall Americans,predominantlythoseresidinginruralareas,lack timely(<60minutes[min])accesstocenterscapableof performingEVT.2 Therefore,optimaltriagesystemsfor LVO-AISpatientsareessentialforemergencydepartments (ED)andhealthsystemsinruralregionsthatmaybelocated hoursfromanEVT-capablecenter.Telestrokenetworksare apotenttoolthatimprovesclinicaloutcomesinresourcelimitedruralareas.3,4
Door-to-groin(DTG)timehasbeenshowntobean independentpredictoroffavorableoutcomesinAISpatients undergoingEVT.5,6 However,itremainsunclearwhether spoke-siteparticipationinahub’stelestrokenetworkdirectly contributestoshorterDTGtimes.Thetimingofthevascular imagingrequiredpriortoapatientundergoingEVTmust alsobeconsideredwithrespecttoDTGtime.Theresultsof previousstudiesevaluatingtheeffectofpre-transfervascular imagingonDTGtimehavebeeninconsistent,withsome studiesindicatingeitherprolongedorimprovedDTG.7–9 Therefore,itremainscontroversialastowhethercomputed tomographyangiography(CTA)shouldbeperformedprior totransferinpatientswithsuspectedLVO-AIS.
TheCOVID-19pandemichighlightedinefficienciesinthe triagingofAISpatients,particularlyduetoresource limitationsandstaffingissues.Althoughalarge,singlecenterstudydetailedadeclineofnearly32%instrokecode activationsatthebeginningofthepandemicinApril2020, therateofEVTremainedconsistentcomparedtothelast severalyears.10
AsCOVID-19continuestorequiretherapid reallocationofresourcesandstaff,withfurtherlong-term effectsonstaffing,itiscriticalthatEDsandstroketeams efficientlytriagepatientswhomaybecandidatesforEVT. Decreasingthenumberoffutiletransfersisalsoakey componentofreducingtheburdenonhubcenters.We previouslyreportedanavertedtransferrateof65%usingour telestrokenetworkinWestVirginia,11 astateinwhich34of its55countiesaredesignatedaseitherruralorsuper-rural. Considerationoffactorsthatimpactthetriageprocess,such aspre-transferCTAoraccesstotelestrokeconsultation, servestomaximizetheefficiencywithwhichhubEDsand comprehensivestrokecenterscanprovidecare.
Inthisstudy,wesoughttodeterminetheprimaryfactors contributingtotargethub-DTGtimesinLVO-AISpatients undergoingEVT.Ouroverarchinggoalwastoidentify factorsthatmayimpacttheefficiencyofthetriageprocessfor strokepatientswithLVOsinEDsandstrokecenters.
METHODS
WeconductedthisstudyatWestVirginiaUniversity Hospital,atertiary-carefacilitywithacomprehensivestroke centerthatservesasthetelestrokehubof29spokehospitals.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Endovasculartherapy(EVT)isatimesensitivetreatmentforacuteischemicstroke (AIS)thathasdramaticallyimprovedpatient outcomes.ItcanonlybeperformedatEVTcapableinstitutions.
Whatwastheresearchquestion?
Wesought to identifyfactorsassociatedwith reduceddoor-to-groin(DTG)timesinAIS patientswithlargevesselocclusion.
Whatwasthemajor findingofthestudy?
Transferpatientswhoreceivedcomputed tomographyangiographypriortotransfer were7.2timesmorelikelytohaveaDTG < 60mincomparedtothosewhodidnot.
Howdoesthisimprovepopulationhealth?
Triagesystemsmustbeoptimizedtoprovide timelyEVT.Thisisofparticularimportance topatientsinresource-limitedruralareas.
Thisorganizationalframeworkwaspreviouslydescribedin moredetail.11 Thisstudyreceivedinstitutionalreviewboard approval,andtherequirementforpatient-informedconsent requirementwaswaivedbasedonretrospectivechartreview. BetweenJanuary2016–September2021,weperformeda retrospectivechartreviewofallLVO-AISpatientswho receivedEVTatourhubinstitution.Thisincludeddirect-tohubEDpresentations,aswellastransferpatientsfrom spokesites.
Thehub-and-spokemodelarrangesservice-deliveryassets intoanetworkconsistingofananchorestablishment(hub), whichoffersafullarrayofservices,complementedby secondaryestablishments(spokes),whichoffermorelimitedservicearrays,routingpatientsneedingmoreintensive servicestothehubfortreatment.Ournetworkhad29spokes rangingfromcriticalaccesshospitalstolargecommunityacademiccentersacrossfourstates(WestVirginia, Maryland,Ohio,andPennsylvania).Furthermore,transfers werecategorizedastelestrokevsnon-telestroketransfers.
Variablescollectedfromeachpatient’schartincludedthe following:siteofinitialpresentation(direct-to-hubvs transfer);telestrokespoke-sitetransfer;ornon-telestrokesite transfer.OthervariablescollectedincludedNational InstitutesofHealthStrokeScale(NIHSS)scoresupon arrivalandatdischarge,recanalizationstatus(thrombolysis incerebralinfarction)afterEVT,andhublengthofstay.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 738
Rawsonetal.
Single-stepOptimizationinTriagingLargeVesselOcclusionStrokes
FunctionaloutcomewasassessedusingthemodifiedRankin scale(mRS)atorwithin90daysofdischarge;patientswith mRS >2wereconsideredtohavepoorfunctionaloutcome. Mortalityratewithin90daysofdischargewasalso determined.WecalculatedDTGtimeforallpatients,defined astheelapsedtimebetweenhubarrivaltimetogroin punctureatthestartofEVT.
WeperformedstatisticalanalysisusingSPSSStatistics 27.0(IBMCorporation,Armonk,NY).Allstudyvariables wereassessedfornormalityusingShapiro-Wilktestingto determineappropriateparametricornon-parametrictests forunadjustedcomparisonsbetweenindependentvariables. Wecomparedfrequenciesandproportionsofstudyvariables usingachi-square(x2)test.Weusedbinarylogistic regressiontodeterminewhethertherewasanassociation betweenstudyvariables,includingNIHSSscore,telestroke vsnon-telestroke,orpre-transferCTAwithaDTG <60min. Weverifiedthatthedatadidnotviolatetheassumptionsof logisticregression,includingperformingaBox-Tidwelltest tocheckforlinearitybetweenthepredictorsandthelogit.We performedabackwardstepwiseregressionmodelwhereby eachvariablewasenteredinthe firststepofthemodel,and variablesthatremainedinthelaststepofthemodelwere consideredsignificantpredictorsofDTG <60min.
RESULTS
Atotalof383patientsmetinclusioncriteriaforthisstudy; 189(49%)presenteddirectlytoourhubinstitution(direct-tohub);and194(51%)arrivedasatransfer.MedianDTGtime wassignificantlyshorterintransferpatientscomparedto direct-to-hubpatients(62vs83min, P < 0.001).Similarly, DTG <60minwasachievedinasignificantlyhigher proportionoftransferpatientscomparedtodirect-to-hub(47 vs17%, P < 0.001).
Ofthetransfers,71%receivedatelestrokeconsultpriorto transfer.MedianDTGtimewassignificantlyshorterin telestroketransfertodirect-to-hubpatients(61vs83min, P < 0.0001),andDTG <60minwasachievedina significantlyhigherproportionoftelestroketransferpatients
comparedtodirect-to-hub(50vs17%, P < 0.001)(Table1). TherewasnodifferenceinmedianDTGtimeintelestroke comparedtonon-telestroketransfers(61vs78min, P = 0.30),norwasthereadifferenceinDTG <60minin telestrokecomparedtonon-telestroketransfers(50vs38%, P = 0.13).Whiletherewasnosignificantdifferenceinmedian DTGtimebetweendirect-to-hubpatientsandnon-telestroke transfers(83vs78min, P = 0.75),DTG <60minwas achievedinasignificantlyhigherproportionofnontelestroketransferpatientscomparedtodirect-to-hub(38vs 17%, P = 0.003)(Table1).
In53%ofcases,CTAwasperformedatthespokesiteprior totransfertothehubinstitution.Further,59%oftelestroke transfercasesreceivedaCTApriortotransfercomparedto only40%ofnon-telestroketransfers(59vs40%, P = 0.011) (Table2).Inallofthetransferpatientswhodidnotreceivea CTAatthespoke,CTAwasobtaineduponarrivaltothehub. Asexpected,medianDTGtimewasshorterintransfer patientswhoreceivedpre-transferCTAcomparedtotransfer patientswhoreceivedCTAuponhubarrival(45vs83min, P < 0.001)(Table2).Further,therewasnodifferencein medianDTGtimebetweentransferpatientswhoreceived CTAuponhubarrivalandpatientswhopresenteddirectlyto thehubinstitution(direct-to-hub)(83vs83min, P = 0.92). Similarly,DTG <60minwasachievedin67%oftransfer patientswhoreceivedpre-transferCTAcomparedtoonly 22%oftransferpatientswhoreceivedCTAuponhubarrival and17%ofpatientswhopresenteddirect-to-hub(Table2). ArepeatCTAwasobtaineduponarrivalin67%of transferpatientsdespitealsohavingreceivedaCTAatthe spoke.Therewasnosignificantdifferenceinthefrequencyof repeatCTAintelestrokecomparedtonon-telestroke transfers(63vs86%, P = 0.09).Asexpected,intransfer patientswhoreceivedpre-transferCTA,medianDTGwas significantlyshorterinpatientswhodidnotreceiverepeat CTAuponarrivalatthehubcomparedtothosewithrepeat CTA(26vs59min, P < 0.001).Similarly,DTG <60minwas achievedin100%oftransferpatientswhoreceivedpretransferCTAbutdidnotrequirerepeatCTAuponarrivalat
± SD)14 ± 614 ± 715 ± 80.478
Door-to-grointime(DTG)(median[IQR]minutes)83[37]61[47]78[50] <0.0001
DTGtime <60min(%)175038 <0.0001 EVTrecanalization(%)3742300.329
Lengthofstay(median[IQR]days)5[4]7[7]7[10]0.108
Dischargemortality(%)1719190.832
90-daymRS0-2(%)3624320.081
Variable Directtohub (n = 189) Telestroke Transfer(n = 134) Non-telestroke Transfer(n = 60) P-value BaselineNIHSS(mean
Table1. Unadjustedcomparisonofdirect-to-hub,telestroketransfer,andnon-telestroketransferpatients.
of EmergencyMedicine 739 Rawsonetal.
NIHSS, NationalInstitutesofHealthStrokeScale;EVT,endovasculartherapy; IQR,interquartilerange; mRS,modifiedRankinScale.
Volume24,No.4:July2023WesternJournal
Single-stepOptimizationinTriagingLargeVesselOcclusionStrokes
thehubcomparedto53%whoreceivedpre-transferCTA plusrepeatatthehub(100vs53%, P < 0.001).
Interestingly,medianDTGwasshorterinpatientswho receivedpre-transferCTAandsubsequentlyreceiveda repeatCTAuponhubarrivalcomparedtotransferpatients whoonlyreceivedaCTAuponarrivaltothehub(59vs83, P = 0.02).Similarly,DTG <60minwasachievedin53%of patientswhoreceivedpre-transferCTAandsubsequently receivedarepeatCTAuponhubarrivalcomparedtoonly 22%oftransferpatientswhoonlyreceivedaCTAupon arrivaltohub(53vs22%, P < 0.001).
Weusedbinarylogisticregressionanalysistodetermine whichstudyvariablescouldpredictaDTG <60minin transferpatients,controllingforthefollowingvariables enteredinthe firststep:baselineNIHSSscore;telestrokevs non-telestroke;CTApriortotransfer;andrepeatCTAatthe hub.TheonlyvariablethatremainedinthemodelwasCTA priortotransfer,astransferpatientswhoreceivedCTAprior totransferwere7.2timesmorelikelytohaveaDTG in < 60mincomparedtothosewhodidnot(oddsratio[OR] 7.2,95%confidenceinterval[CI]3.5-14.7; P < 0.001).
DespitethereducedDTGtimesamongthosewithpretransferCTA,weobservednodifferenceinpatientoutcomes onthebasisofsuccessfulrecanalizationrate,lengthofstay, functionalstatus(mRS),ormortality.
DISCUSSION
Withinourstudypopulation,pre-transferCTAwasthe onlysignificantpredictorofachievingbenchmarkDTG metrics.Additionally,patientswhoreceivedtelestroke consultationweremorelikelytohavereceivedCTApriorto arrival.GiventhatasignificantproportionofLVO-AIS patientswilloccuramongpatientsfarfromEVT-capable centers, flexiblesolutionsandinnovationinpracticeare necessarytoexpeditetreatment.Onekeycomponenttothe triageandtransferprocessisCTAacquisition.
Debatepersistsregardingwhetherpre-transferCTA optimizestreatmentorsimplyprolongstransfertoanEVTcapablecenterwhereimageacquisitionmaybemore operational.Intheiranalysisoftwotelestrokenetworks,Al KasabetaldeterminedthatAISpatientswithLVOwho receivedpre-transferCTAhadlongerDTGtimesthanthose whoreceivedCTAatthehubhospital.7 Thiswasattributed
totheinterventionalteambeingactivatedatthehubhospital onlyafterCTAwasrepeatedbythedirect-to-hubteam; however,frequencyofrepeatCTAwasnotreported.In contrast,ourstudydemonstratedthatpatientswere7.2times morelikelytohaveaDTGtime <60miniftheyunderwent pre-transferCTA.
RepeatCTheadisobtainedinpatientswithprolonged transfertime(>2hours),andrepeatCTAistypically performedincaseswithlowerAlbertaStrokeProgramEarly CTScores(ASPECTS),implyinglargerinfarctioncore. Amongourpopulation,interfacilitytransportisvulnerable toavarietyoffactorsincludingruralgeography,astatewide lackofemergencymedicalservicesresourcesviagroundor air,aswellasweatherpatternsimpedinghelicoptertransfer approximately50%ofthetime.Giventhesefactors,most transferredpatientshaveprolongedtransfertimes,as demonstratedwitha67%rateofrepeatimaging.ADTG <60minwasachievedin100%oftransferpatientswho receivedpre-transferCTAbutdidnotrequirerepeatCTA uponarrivalatthehub,comparedto53%ofpatientswho receivedpre-transferCTAplusrepeatatthehub(100vs. 53%, P < 0.001).However,DTG <60minwasachievedin 53%ofpatientswhoreceivedpre-transferCTAand subsequentlyreceivedarepeatCTAuponhubarrival comparedtoonly22%oftransferpatientswhoonlyreceived aCTAuponarrivaltohub(53vs22%, P < 0.001).Therefore, evenincaseswhereCTAmustberepeatedatthehub,thereis stillareductioninDTGtime,andevenincludingpatients withrepeatCTA,patientswhoreceivedCTApriorto transferwere7.2timesmorelikelytohaveaDTGtime <60mincomparedtothosewhodidnot(OR7.2,95%CI3.514.7; P < 0.001).Therefore,theobservedimprovementin DTGtimeintransferpatientscannotbesolelyattributedto simplytimesavedbyobtainingCTApriortotransfer;rather, itislikelyrelatedtoadvancedpre-notificationandactivation oftheneurointerventionalteam,leadingtomoreefficient triageandexpeditedEDcourse.
These findingsunderscorethevalueofenhancedprenotificationofincomingLVOpatients.Pre-notification systemsareestablishedaseffectivewaystoexpedite treatmentintime-criticalconditionssuchasstroke.12
14 Telestrokefacilitatesstreamliningofcommunicationfrom spoketohub,especiallyduringthetransferprocess,and
–
Variable CTAobtainedpriorto transfer(n = 102) CTAuponhubarrival only(n = 92) P-value Receivedtelestrokeconsultation(%)5940 0.011 Door-to-grointime(DTG)(median[IQR]minutes)45[46]83[47] <0.001 DTG <60min(%)6722 <0.001 RepeatCTAathub(%)67- -
Table2. Unadjustedcomparisonoftransferpatientsbycomputedtomographyangiographystatus.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 740
Rawsonetal.
CTA,computedtomographyangiography; IQR,interquartilerange.
Single-stepOptimizationinTriagingLargeVesselOcclusionStrokes
Single-stepOptimizationinTriagingLargeVesselOcclusionStrokes
involvementofallstakeholders(receivingemergency medicine,neurology,andneuro-interventionalteams) priortopatienttransfermaximizesefficiency.Although implementationandmaintenanceoftelestrokesystems requiresignificantresourcesandcommitmentfromall networkpartners,15,16 thebenefitsfromapatientandpayor perspectivearewell-established.17–21 Wehaveshownhere thattransferpatientsfromtelestrokespokesitesweremore likelytoreceivepre-transferCTAthantransferpatientsfrom non-telestrokesites,withpre-transferleadingtoimproved DTGtimes.SunetaldemonstratedthatDTGtime,along withunmodifiablefactorssuchaspatientage,NIHSSscore, andreperfusionstatus,wasmoststronglyassociatedwith favorablepatientoutcomesfollowingAIS.5
Whileestablishingorparticipatinginatelestrokenetwork maynotbefeasibleinsomeareas,standardizingimaging protocolsforallpotentialAIS-LVOpatientsshouldbea priority.Theimportanceofanefficienttriageprocesshas beenfurtherhighlightedbytheCOVID-19pandemic.
DisruptionsinEVT-workflowbecamemorecommonduring thepandemicduetoreallocationofstaff.10 Amoreuniform triageprocesswouldlimitdelaysinfacilitatingtime-critical acutestroketherapy.Althoughtelestrokeconsultationdid notindependentlypredictashorterDTGtime,pre-transfer CTAwasobtainedinasignificantlyhigherproportionof telestrokecomparedtonon-telestroketransfers,whichmay indirectlycontributetodecreasedDTGtime.
Our findingsdemonstratethatpatientswhoreceivepretransferCTAaremorelikelytoachieveDTGtime ≤60minutes.Includingpre-transferCTAaspartofa standardizedprotocolforAISpatientscouldpotentially decreasethetimeandresourceburdenontheover-populated andunderstaffedhubhospitals.NotonlycanCTAconfirm thatapatienthasatargetlesionamenabletoEVT,butit equallyservestoidentifypatientswhoarenotcandidatesfor intervention,therebyreducingfutiletransfersoravoiding resource-heavyhelicopter flights.Althoughwedidnot observeimprovedoutcomesamongcaseswithshortened DTGtimes,itiswellestablishedthatDTGtimeisapowerful predictorofclinicaloutcome.5,6,22
LIMITATIONS
Ourstudyhasseverallimitations.First,theelapsedtime fromarrivaltospoketotransferfromspoke doorin/door outtime couldnotbereliablyobtainedforalltransfer patients.Therefore,wewereunabletodeterminethenet effectofpre-transferCTAondoorin/dooroutandDTG time.Futurestudiesarenecessarytoevaluatedoorin/door outtimesatthetransfersite,withandwithoutCTA,to confirmthatpre-transferCTAdoesnotdelaytimeoftransfer thatexceedstheimprovementofDTGtimeatthehub. Furthermore,whilethisstudyonlyevaluatedDTGtimeata singlehubsite,thediversityofgeography(spanningfour states)andvolume(rangingfromcriticalaccesshospitalsto
primarystrokecenters)amongparticipatingspokesitesis alsoanotablestrength.ThisdatademonstratesthatpretransferCTAcanbereasonablyacquiredacrossavarietyof practiceenvironments.
Webelievethe findingsofthisstudyaregeneralizableto bothruralandnon-ruralareas.Ourruralacademiccenter, whichservesmuchofthe1.8-million-personpopulationof WestVirginia,istheonlycenterwithEVT-capabilitiesinthe region.Whilemanyofourpatientsmaybeaffectedby factorsthataremoreuniquetothisarea,suchasprolonged transportationtimesduetogeography,nearly50%ofUS residentsliveinareaswithsimilarhealthcaredensities,2 indicatingthatthisisasignificantproblemthroughoutthe country.Thus,theassociationbetweenobtainingpretransfervascularimagingandreducedDTGtimeis generalizabletobothruralandnon-ruralareas.
Lastly,weobservednosignificantassociationbetween reducedDTGtimeandimprovedpatientoutcomesonthe basisofsuccessfulrecanalizationrate,lengthofstay, functionalstatus(mRS),ormortality.Theabsenceofaclear outcomecorrelateinourdatamaybeduetotherelatively smallsamplesize,aswellastoourinabilitytocontrolforall confoundingfactors,includingindividualsiteoperating procedures,telestrokeutilizationrates,transfermodalities, anddistancetraveledtoarriveatthehub.
CONCLUSION
Reductionindoor-to-grointimeremainsanimportant benchmarktoadvancethetreatmentofacuteischemicstroke patientswithlargevesselocclusions.Althoughseveral multitier,leanqualityimprovementinitiativeshavebeen developedtooptimizeworkflow, 23–27 ourstudyprovides evidencethatfocusingeffortsonpre-transfervascular imagingaloneyieldspowerfulresults.Furthermore,our findingsunderscoreanimportantimplementation opportunityforemergencymedicineleadersthatalso facilitatescollaborationacrossdisciplinesandhealth systems.
AddressforCorrespondence:AmeliaAdcock,MD,WestVirginia University,DepartmentofNeurology,1MedicalCenterDriveSuite 9180,Morgantown,WV26506.Email: akadcock@hsc.wvu.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.ThisworkwassupportedbytheUS DepartmentofHumanandHealthResources[6H2ARH39982-0202,2020]
Copyright:©2023Rawsonetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 741
Rawsonetal.
REFERENCES
1.ChenCJ,DingD,StarkeRM,etal.Endovascularvsmedical managementofacuteischemicstroke. Neurology.2015;85(22): 1980–90.
2.SarrajA,SavitzS,PujaraD,etal.Endovascularthrombectomyforacute ischemicstrokes:currentUSaccessparadigmsandoptimization methodology. Stroke.2020;51(4):1207–17.
3.LazarusG,PermanaAP,NugrohoSW,etal.Telestrokestrategiesto enhanceacutestrokemanagementinruralsettings:Asystematic reviewandmeta-analysis. BrainBehav.2020;10(10):e01787.
4.SimpsonAN,HarveyJB,DiLemboSM,etal.Populationhealth indicatorsassociatedwithastatewidetelestrokeprogram. TelemedJE Health.2020;26(9):1126–33.
5.SunCH,RiboM,GoyalM,etal.Door-to-puncture:apracticalmetricfor capturingandenhancingsystemprocessesassociatedwith endovascularstrokecare,preliminaryresultsfromtherapidreperfusion registry. JAmHeartAssoc.2014;3(2):e000859.
6.GoyalM,JadhavAP,BonafeA,etal.Analysisofworkflowandtimeto treatmentandtheeffectsonoutcomeinendovasculartreatmentof acuteischemicstroke:resultsfromtheSWIFTPRIMERandomized ControlledTrial. Radiology.2016;279(3):888–97.
7.AlKasabS,AlmallouhiE,HarveyJ,etal.Doorindooroutand transportationtimesin2telestrokenetworks. NeurolClinPract 2019;9(1):41–7.
8.KansagraAP,WallaceAN,CurfmanDR,etal.Streamlinedtriageand transferprotocolsimprovedoor-to-puncturetimeforendovascular thrombectomyinacuteischemicstroke. ClinNeurolNeurosurg 2018;166:71–5.
9.AghaebrahimA,SauvageauE,Aguilar-SalinasP,etal.Referralfacility CTperfusionpriortointer-facilitytransferinpatientsundergoing mechanicalthrombectomy. JNeurointervSurg.2018;10(9):818–22.
10.DowlatshahiD,StottsG,BourgoinA,etal.Decreasedstroke presentationratesatacomprehensivestrokecenterduringCOVID-19. CanJNeurolSci.2021;48(1):118–21.
11.AdcockAK,ChoiJ,AlviM,etal.Expandingacutestrokecareinrural America:amodelforstatewidesuccess. TelemedJEHealth. 2019.
12.SavageML,PoonKK,JohnstonEM,etal.Pre-hospitalambulance notificationandinitiationoftreatmentofSTelevationmyocardial infarctionisassociatedwithsignificantreductionindoor-to-balloontime forprimaryPCI. HeartLungCirc.2014;23(5):435–43.
13.AghaebrahimA,StreibC,RangarajuS,etal.Streamliningdoorto recanalizationprocessesinendovascularstroketherapy. JNeurointerv Surg.2017;9(4):340–5.
14.KimDH,KimB,JungC,etal.ConsensusstatementsbyKoreanSociety ofInterventionalNeuroradiologyandKoreanStrokeSociety: HyperacuteEndovascularTreatmentWorkflowtoReduceDoor-toReperfusionTime. JKoreanMedSci.2018;33(19):e143.
15.TummaA,BerzouS,JaquesK,etal.Considerationsforthe implementationofatelestrokenetwork:asystematicreview. JStroke CerebrovascDis.2021;31(1):106171.
16.BustiC,GamboniA,CalabròG,etal.Telestroke:barrierstothe transition. FrontNeurol.2021;12:689191.
17.JohanssonT,WildC.Telemedicineinacutestrokemanagement: systematicreview. IntJTechnolAssessHealthCare.2010;26(2): 149–55.
18.MorenoA,SchwammLH,SiddiquiKA,etal.Frequenthub-spoke contactisassociatedwithimprovedspokehospitalperformance:results fromtheMassachusettsGeneralHospitalTelestrokeNetwork. Telemed JEHealth.2018;24(9):678–83.
19.MalikP,AnwarA,PatelR,etal.Expansionofthedimensionsinthe currentmanagementofacuteischemicstroke. JNeurol.2021;268(9): 3185–202.
20.DumitrascuOM,DemaerschalkBM.Telestroke. CurrCardiolRep 2017;19(9):85.
21.WallutL,PeyronC,Hervieu-BegueM,etal.Efficiencyoftelemedicine foracutestroke:acost-effectivenessanalysisfromaFrenchpilotstudy. IntJTechnolAssessHealthCare.2020;36(2):126–32.
22.SaverJL,GoyalM,vanderLugtA,etal.Timetotreatmentwith endovascularthrombectomyandoutcomesfromischemicstroke:a meta-analysis. JAMA.2016;316(12):1279–88.
23.RaiAT,SmithMS,BooS,etal.The ‘pit-crew’ modelforimprovingdoorto-needletimesinendovascularstroketherapy:aSix-Sigmaproject. JNeurointervSurg.2016;8(5):447–52.
24.CheungVJ,WaliAR,Santiago-DieppaDR,etal.Improvingdoortogroin puncturetimeformechanicalthrombectomyviaiterativequalityprotocol interventions. Cureus.2018;10(3):e2300.
25.WangH,ThevathasanA,DowlingR,etal.Streamliningworkflow forendovascularmechanicalthrombectomy:lessonslearned fromacomprehensivestrokecenter. JStrokeCerebrovascDis 2017;26(8):1655–62.
26.DhandS,O’ConnorP,HughesC,etal.Acuteischemicstroke:acute managementandselectionforendovasculartherapy. SeminIntervent Radiol.2020;37(2):109–18.
27.FordAL,WilliamsJA,SpencerM,etal.Reducingdoor-to-needletimes usingToyota’sleanmanufacturingprinciplesandvaluestreamanalysis. Stroke.2012;43(12):3395–8.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 742 Single-stepOptimizationinTriagingLargeVesselOcclusionStrokes Rawsonetal.
EXPERT COMMENTARY
ViolenceandAbuse:APandemicWithinaPandemic
PaulaJ.Whiteman,MD
SectionEditor: ShahramLotfipour,MD,MPH
Submissionhistory:SubmittedAugust15,2022;RevisionreceivedApril21,2023;AcceptedJune26,2023
ElectronicallypublishedJuly17,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58405
Introduction: DuringtheCOVID-19pandemic,associetystruggledwithincreasingdiseaseburden, economichardships,andwithdiseasemorbidityandmortality,governmentsandinstitutionsbegan implementingstay-at-homeorshelter-in-placeorderstohelpstopthespreadofthevirus.Althoughwellintentioned,oneunintendedadverseconsequencewasanincreaseinviolence,abuse,andneglect.
Methods: Wereviewedtheliteratureontheeffectthepandemichadondomesticviolence,childand elderabuseandneglect,humantrafficking,andgunviolence.Inthispaperweexplorecommonthemes andcausesofthisviolenceandoffersuggestionstohelpmitigateriskduringongoingandfuture pandemics.Justastheseformsofviolenceprimarilytargetat-risk,vulnerablepopulations,sodid pandemic-relatedviolencetargetmarginalizedpopulationsincludingwomen,children,Blacks,andthose withlowersocioeconomicstatus.Thisbecame,andremains,apublichealthcrisiswithinacrisis.Inearly 2021,theAmericanCollegeofEmergencyPhysicians(ACEP)PublicHealthandInjuryCommitteewas taskedwithreviewingtheimpactthepandemichadonviolenceandabuseastheresultofaresolution passedatthe2020ACEPCouncilmeeting.
Conclusion: MeasuresmeanttohelpcontrolthespreadoftheCOVID-19pandemichadmany unintendedconsequencesandplacedpeopleatriskforviolence.Emergencydepartments(ED), althoughstressedandstrainedduringthepandemic,remainasafetynetforsurvivorsofviolence.Aswe moveoutofthispandemic,hospitalsandEDsneedtofocusonstepsthatcanbetakentoensurethey preserveandexpandtheirabilitytoassistvictimsshouldanotherpandemicorglobalhealthcrisis develop.[WestJEmergMed.2023;24(4)743–750.]
Keywords: pandemic;elderabuse;humantrafficking;COVID-19;gunviolence;intimatepartner violence;childabuse;fear.
1
2
3
4
6
7
8
9 RalphJ.Riviello,MD,MS10 1 Cedars-SinaiMedicalCenter,LosAngeles,California 2 CenterforSocialJusticeandHealthEquity,Boston,Massachusetts 3 MGHFreedomClinic,Boston,Massachusetts 4 HarvardMedicalSchool,DepartmentofEmergencyMedicine,Boston, Massachusetts 5 MassachusettsGeneralHospital,DepartmentofEmergencyMedicine, Boston,Massachusetts 6 EmoryHealthcareNetwork,Atlanta,Georgia 7 WorldHealthOrganization,Emergency,TraumaandAcuteCare Programme,Geneva,Switzerland 8 BrownUniversity,WarrenAlpertMedicalSchool,Providence,RhodeIsland 9 YaleSchoolofPublicHealth,YaleUniversity,NewHaven,Connecticutt 10 UniversityofTexasHealthSanAntonio,LozanoLongSchoolofMedicine, DepartmentofEmergencyMedicine,SanAntonio,Texas
WendyL.Macias-Konstantopoulos, MD,MPH,MBA
,
,
,5 PryankaRelan,MD,MPH
,
AnitaKnopov,MD
MeganL.Ranney,MD,MPH
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 743
INTRODUCTION
Inearly2020,astheworldwasthrustintotheCOVID-19 pandemic,countriesstruggledwithincreasingdisease burden,economichardships,anddiseasemorbidityand mortality,whichledtotheimplementationofstay-at-home orderstohelpstopviralspread.Thisledtoincreasedstress, anxiety,andwork/schoolabsence.1 Unintendedadverse consequencesincludedincreasesinviolence,domestic violence(DV),childandelderabuseandneglect,human trafficking,andgunviolence.Inthisarticlewelookatthe impactoftheCOVID-19pandemiconviolenceandits relationshiptoDV,childandelderabuseandneglect,human trafficking,andgunviolence,andweoffersuggestionsto helpmitigateviolenceandbettermanageourresponseinthe faceofthisuncertainty.
METHODS
AgroupofexpertsinthetopicsofDV,childabuseand neglect,humantrafficking,elderabuseandneglect,andgun violencecametogethertosummarizetheliteratureavailable regardingtheCOVID-19pandemicanditsimpacton thesetopics.
DOMESTICVIOLENCE
Soonaftertheimplementationofpandemicmitigation measures,reportsofDVsurgedglobally.ThisledtoUnited NationsSecretaryGuterres’ ominouswarning: “Weknow lockdownsandquarantinesareessentialtosuppressing COVID-19,buttheycantrapwomenwithabusive partners Overthepastweeks,astheeconomicandsocial pressureshavegrown,wehaveseenahorrifyingsurgein domesticviolence.”2 Mediareportsquicklycalledattention tolinksbetweenpandemiclockdownordersandworldwide increasesinintimatepartnerviolence.3 Whileanyonecanbe avictimofDV,womenaredisproportionatelyaffected;thus, forthispaperwerefertofemalevictims.
ResearchersinNewZealandpreviouslyshowedthatall formsoffamilyviolence(DV,childabuse,andelderabuse) increaseduringandafterlarge-scalecrises.4 Examplesofthe widespreadimpactofpandemiclockdownsareabundant.In 2020the Guardian reportedaglobalsurgeinreportsofDV.5 Brazilexperienceda40–50%increaseinDV,andSpainhada 20%increaseinthenumberofhelplinecallsinthe firstfew daysoflockdown.5 InCyprus,thenumberofhotlinecalls rose30%withinoneweekofits firstCOVID-19case.6 Inthe UnitedKingdom(UK),Refuge oneoftheleading domesticabuseorganizations reporteda25%increasein helplinecallsinthesevendaysfollowingUKlockdown measures. 6 Duringthesameperiod,Refugenoteda150% increaseinwebsitevisits.7 InChina’sHubeiprovince,DV tripledwhencomparingFebruary2020toFebruary2019.6 InFrancereportsofDVincreased30%andin Argentina25%.6
InMarch2020reportsofDVwithintheUnitedSates followedasimilartrajectory:thePortland[Oregon]Police Bureaurecordeda22%increaseinfamilyviolencecalls 8 ; theSanAntonio[Texas]PoliceDepartmentsawan18% increase 9 ;inAlabamatheJeffersonCountySheriff ’ sOf fi ce reporteda27%increaseinMarch2020comparedtoMarch 2019 11 ;andtheNewYorkCityPoliceDepartment respondedtoa10%increaseinDVcallsinMarch2020 comparedtoMarch2019. 11 InFebruary2021,the NationalCommissiononCOVID-19andCriminalJustice (NCCCJ)reportedthatDVincidentsintheUSincreased by8.1%afterlockdownorderswereissued. 12 TheNCCCJ reportincludedpolicecalllogs,DVcrimereports, emergencylineregistries,andhealthrecords.Despitethese increasesinreportsandhotlinecalls,USemergency departments(ED)sawasigni fi cantdecreaseinvisits relatedtointimatepartnerviolence(442vs484)and suspectedchildabuseandneglect(884vs.1,038)during March15-October10,2020,comparedtothesameperiod in2019. 13
HotlineandhelplinecallssurgedintheUS,withthe NationalDVHotlinereportingacontactvolumeincreaseof 9%and ≈10%ofcallerscitingCOVID-19asafactor.15
BetweenMarch-May2020,90%ofcallersreported experiencingemotional/verbalabuse,61%physicalabuse, 16%digitalabuse(useoftechnologytobully,harass,stalk,or intimidate),and11%sexualabuse.15 Somehotlinesnoted decreasedcallvolumesassurvivorswereunabletoaccess hotlinesduetoisolationandabusercontact.
HomicidesrelatedtoDVincreased.In2020morethan 2,000peoplewerekilledintheUSinDV-relatedshootings, anincreaseof4%from2019,withdisproportionateincreases inTexas(69%),Maryland(93%),Missouri(67%),andUtah (160%).16 Inasurveyoflawenforcementpersonnelfocused onDVresponse,33%reportedanincreaseinDVhomicides intheircommunitiesandhalfreportedabusersthreateningto shootsurvivors.17 Spain’ s firstDVfatalityoccurred
fivedaysafterlockdown.TheUKaswellsawanincrease inDV-relatedhomicides.18
CasesofDVroseduringthepandemicaslockdownplaced thosevulnerablepopulationsincloseproximitytotheir abusers.19–22 Socialisolationofsurvivorsmadethemmore susceptibletoabusewithfewresourcesforhelp.
Unemployment,economic/financialstrain,diseasefears, childcarestressandhomeschooling,depression,anddrug andalcoholuseallincreasedDVriskinthehome,resultingin anincreaseinallformsofviolence.ThosevictimsinpreexistingviolentrelationshipsaswellasinpreviouslynonviolentrelationshipshaddifficultyreachingouttoDV hotlines;whilesomehotlineshaddramaticincreasesincall volume,othersexperiencedfewercalls.Withoutin-person accesstofamily,friends,andco-workers,visibleinjuriesgo unnoticedandsubtlecluesmayhavebeenmissedwithface maskshidingvisiblefacialtrauma.Video-conferencing
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 744 ViolenceandAbuse:APandemicWithinaPandemic Whitemanetal.
platformsallowcamerastobeofforadjusted,blocking physicalsignsoftheabuseortheabuseroff-screen.
Aidfromsocialserviceagencies,DVagencies,shelters, andrapecrisiscenterswaslimitedwithsomeorganizations deemednon-essential.Infrastructure,technology,and financiallimitationscurtailedthetransitiontoremote response.Remotelystaffedhotlinesandhelplinesstayed open.Sheltersfacedlossesofvolunteersandworkersand difficultyimplementingsocialdistancingandpersonal protectiveequipment(PPE)protocolsandcleaning/ disinfectingmeasuresinthefaceofsupplyshortages.
ManyEDsandhospitalsseverelyrestrictedvisitors, includingDVandsexualassaultadvocates,crisisworkers, andshelterstaff,leavingvictimswithoutadequatesupport whilebeingevaluatedforinjuriesorfollowingsexualassault. WhenallowedintotheEDorhospital,agencieswere requiredtoprovidetheirownPPE,despitesupplyshortages. Goingforward,hospitalsshouldestablishpoliciesallowing socialserviceagenciesaccesstosurvivorsandtoprovide thoseworkerswithappropriatePPEduringapandemic. EmergencydepartmentsneedtoensuretheyscreenALL patientsforviolenceatthetimeofthevisit/hospitalization andprovideappropriateagencyreferrals.Giventhe unprecedentedaccessabusershavetovictims,resourcesneed tobecompact,easilyconcealable,andnon-discoverable. Hospitalsshouldworkwithlocalagenciestoensureaccessto services,personnel,andresources.Stategovernmentsneedto re-classifysocialserviceagenciesasessential,allowingthem tocontinuetheirimportantwork.
Agenciesneedtodothefollowing:1)developprotocols andpoliciesthatallowforeasytransitiontoworkfrom home;2)enhanceinformationtechnologyinfrastructurein anticipationoffuturepandemicsorlockdownswithstaff education;and3)instituteroutine,camera-onemployee checkstoensuretheirwell-being.
CHILDABUSEANDNEGLECT
TheWorldHealthOrganization,UnitedNations Women,andUNICEFreleasedajointstatementcallingfor theprotectionofchildrenfromviolenceincluding maltreatment,gender-basedviolence,andsexual exploitation.23 AreportfromtheUSCentersforDisease ControlandPreventionfoundthatdespiteadramatic decreaseintotalpediatricEDvisitsduringlockdown,the numberofhospitalizationsfromchildabuseandneglect remainedstable,representingadramaticincreaseinthe yearlypercentageofEDvisitsrelatedtochildabuseand neglectamongallagegroups.24 TheNationalChildAbuse Hotlineallowsanyone,includingchildren,tocallinor report.In2018and2019thehotlinereceived93,000and 90,000calls,respectively.25,26 Bycontrast,in fiscalyear2020 therewereover112,000calls,representinga23%increase.27
ThesameCOVID-19lockdownmeasuresaffectingDV survivorsaffectedchildrenaswell.Thisincludessocial
isolation,virtualeducation,and financialandhousing insecurities.Thepresenceofchildrenathomecontinuously insteadofawayatschoolordaycareledtoaddedstress,with parentsandcaregiversdeniedrespitefromdirectchildcare duties.Homelifebecameprivate.Withoutvisitorstothe homeandchildrenbarredfromattendingschooland extracurricularactivities,therewasnodirectinteractionwith potential,mandatedreportersorconcernedcitizens.
Childrenhadlessopportunitytoprivatelyconfideinorask forhelpfromteachers,counselors,friends,andhealthcare personnelwhowouldotherwiserecognizesignsofabuse.
Ifanindividualdoesn’talreadyliveinasafeenvironment, thenlockdownbecomesmoredangeroustothem.Sheltering inplacemayleadtochildneglectassupervisingadults engageinothernecessarytasks.Abusershavingunlimited accesstonewhouseholdmembers,bothrelatedandnonrelated,insharedlivingspace,potentiallyplacedchildrenat furtherrisk.
Withoutthein-personsupervisionofteachersorother school-basedmandatedreporters,virtuallearninglimits assessmentofchildrenforabuseorneglect,especiallyas virtuallearningviacamerasonlyshowspartofthechildor theirenvironment.Theactualhouseholdenvironmentwas potentiallyobscuredwithpreloadedbackgroundsorchildren beingoutsidethehometoaccessbetterWi-Fi.
Similarly,caseworkersconductingvirtualvisitswerenot abletofullyassesshome-lifesituations.Foodinsecuritymay havebeenmissed.Childrenwhoreliedonschoolbreakfast andlunchprogramsastheirsourceofhealthynutritious mealslackedadequatenutritiousfoodduringlockdown, negativelyaffectinghealthandlearning.Mandatedreporters didnothavethesamelevelofpre-pandemiccontactwith children,giventheimplementationofvirtuallearningand telemedicinevisits.Abusershadgreaterabilitytocoverupor limitvisualizationoftelltalesignsofabuse.Officialreportsto childprotectiveservicesdecreasedsignificantlybyabout2070%,possiblyattributabletofewerin-personcontactswith mandatedreporters.27
Childabuseandneglectispreventable.Pandemicand disastersrequireheightenedmethodsofsurveillance, reporting,andinvestigationofcases.Preventionstrategies includethefollowing:offeringeconomicsupport;allowing parents flexibleworkschedulestobalancechildcareand workresponsibilities;andimplementingmechanismstoget childrensafelybackinschoolfortheirmentalhealthand physicalwell-being.Schoolsneed flexibilityforin-person servicesforchildren,includingaccesstonutritiousmeals withcommunitysupporttohelpwiththeseefforts.
AvisittotheEDmaybeachild’sonlyaccesstohelp. Emergencyphysiciansshouldconductthoroughhistoryand physicalexamsofchildren,payingattentiontoemotional well-being,signsofphysicalinjury,neglect,andotherred flagsofchildabuse.Consultstosocialservicesandchild protectiveservices(CPS)shouldnotberestrictedduetoa
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 745 Whitemanetal. ViolenceandAbuse:APandemicWithinaPandemic
pandemicorlimitedaccesstoPPE.TheCPSagencies musthavemechanismstocontinuetoconductin-person andin-hospitalevaluationsandhaveprocessesfor virtualhomevisitswiththeabilitytoprovideother neededservices.
EXPLOITATIONANDHUMANTRAFFICKING
Societalsafetymeasuresmeanttoprotectagainst COVID-19transmissionfurtherisolatedat-risk,exploited, andtraffickedindividuals,posingaddedbarrierstopotential victimidentificationandassistance.Vulnerabilityto exploitationandtraffickinghasbeenexacerbatedbyboththe riseinfamilyviolenceandhousehold financialinsecurity. WidespreadschoolclosuresuniquetotheCOVID-19 pandemicresultedinchildrenspendingmoretimeonline, possiblyunsupervised,asparentsorlegalguardianswho wereessentialworkershadtojuggleworkandhomelife.
TheremotedigitalerausheredinbytheCOVID-19 pandemicledtoexponentialgrowthinpredatorycyber activityincludingthetargetedsolicitationofminorsthrough socialmedia,chatrooms,andgamingplatforms.Asearlyas the firstquarterof2020,cybersecuritygroupsbegantodetect chatterwithinchildsexualabusematerial(CSAM) subscriptionforumsandotherpartsofthedarknetdescribing thepandemicasauniqueopportunitytoenticechildren onlineandincludinginstructionsonhowtoaccesschildrento produceandshareCSAM.28
30 TheNationalCenterfor MissingandExploitedChildren(NCMEC)experienced “ an explosioninreporting” totheir CyberTipline earlyon.28,29 In May2020,duringthe firstwaveofshutdowns,reportstothe NCMECtiplinenumberedalmost1.7million,ascompared to ≈745,000reportsinMay2019.29
AccordingtoNCMEC,reportsinvolvingat-riskchildren fromacrossthecountryincreasedby28%fromanaverageof ≈326,680perweekin2019toaweeklyaverageof ≈418,290 reportsduring2020.28 Reportsofonlineenticements experiencedanexponentialgrowthof97.5%from19,174 totalreportsin2019to37,872in2020.28 Thedramaticrisein criminalcyberactivityandtheconcomitantrisktochildren arethoughttoberelatedtoincreasedtimeonlinewhile sociallydistancing,adultboredom,andpreoccupationwith sexualthoughts,andadoublinginthenumberofchatterson CSAMforumssincethestartoftheCOVID-19pandemic.30
Survivorsoftraffickinginrecovery,alreadystrugglingto establishthemselvessociallyand financially,havehadto endurefoodandhousinginsecurityandlackofemployment opportunitiesduringthegeneraleconomicdownturn.While somebenefitedfromevictionmoratoriums,manyothers werelefthomelessduetojoblossandinabilitytopayrent. Socioeconomicstressorsassociatedwiththepandemic increasedtheriskofsurvivorsbeingre-traffickedandof at-riskindividualsbeingnewlytrafficked.Thepressuresfor moneytopayforfood,housing,andothernecessitiesmay leadindividualstoacceptexploitativework,engagein
commercialsexwork,andcommerciallysexually exploitchildren.
Tocompoundtheproblem,frontlinehealthandsocial serviceorganizations andtheprecariouslocalmechanisms forreferral experiencedseveredisruptionsoftheir everydayoutreachandserviceactivities.Anylegalor immigrationproceedingsinprogresspriortothestartofthe pandemiclikelywereunexpectedlysuspendedresultingin prolongedstatesofabeyance,uncertainty,andnon-closure forvictimsandsurvivors.Consequently,theCOVID-19 pandemicmayhaveexactedaheaviertollonthephysical, mental,emotional,and financialhealthofvictimsand survivorsthaniscurrentlyunderstood.
ELDERABUSEANDNEGLECT
Elderabuseandneglectis “anintentionalact,orfailureto act,byacaregiveroranotherpersoninarelationship involvinganexpectationoftrustthatcausesorcreatesarisk ofharmtoanolderadult.”31 Typesofabuseincludephysical, sexual,emotionalorpsychological,aswellas financialabuse, andneglect.BeforeCOVID-19,anestimatedoneinsixolder personsweresubjecttoabusegloballywithonein10US residents ≥60yearssubjecttoabuse.Post-COVID-19 increasesinelderabusewerereportedworldwide.32
Previouslymentionedriskfactorsmaybeexacerbatedin elderlypopulations.
Thereareassociatedriskfactorsofelderabusethatcanbe assessedandmanagedbymedicalandpublichealth professionalssuchasdiagnosesofmentalillness,alcoholuse disorder,andgreaterdegreesof financialandemotional dependenceexperiencedbyavulnerableelder.Riskfactors varyamongindividuals,relationships,communities,and cultures.Identifiedprotectivefactorsincludehighlevelsof communitycohesionandcoordinationofresourcesand servicesforolderpeople.Withearlyrecognitionofrisk factorsandimplementationofprotectivestrategies,elder abusecanbeprevented.
Therewasanincreaseinmentalhealthissuesforpersons ofallagesinpartduetoimplementationofmandatorypublic healthandsocialmeasuressuchasphysicaldistancing, isolation,andrestrictionsonmovement.Onestudyreported thatelderabuseincreasedtoonein fiveolderpeopleinthe USduringtheCOVID-19pandemic.33 Reportsincludethose livinginlong-termcarefacilitiesorothercommunity settings,aswellasthoselivingwithcaregivers.
Thoselivingawayfromcaregiverswerefurtherisolated, withlessdirectaccesstoservicesandadecreaseinavailable communicationmethods.Olderpeopleoftenhaveless technologicaccessandliteracy,makingitdifficultto navigatewithoutin-personsupport.Giventheirsocial isolation,olderadultshavebecomemoredependenton caregivers,riskingabuserexploitation.Caregivershadtheir ownhealthandsafetytoworryabout,aswellasconcerns about financialandotherresourcesneededtocareforthe
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 746 ViolenceandAbuse:APandemicWithinaPandemic Whitemanetal.
olderpersonsintheirlife,leadingtoincreasedstressand burdenonallinvolved,andfurtherriskofexploitationof resourcessuchasSocialSecuritybenefitsdesignatedforolder people.Increasedstigmawasplacedonolderpeople,asthose mostseverelyaffectedbyCOVID-19weresometimesgiven prioritymedicalresourcesoveryoungerpeoplewithagreater chanceofsurvival.
Governmentsandpublichealthprofessionalsmust acknowledgethatelderabuseexists.Emergencyclinicians shouldscreenallolderpeopleforpossibleabuseandconsider riskfactorsandprotectivefactorsduringeveryencounter. EspeciallyontheEDfrontlineandprimarycareoffices, healthcareprofessionalsmustbeawareoflocal/state reportingmandates.Anysuspectedmistreatmentshouldbe reportedaccordingtolocal/statemandates(usuallyviaAdult ProtectiveServices).
Animpactfulwaytopreventmistreatmentistoincrease socialconnectednesswitholderpeopleandtheircaregiversin ourcommunities.Withpersistentphysicaldistancing,we needtotryhardertostayclosesocially viaphoneandvideo calls,messaging,oroutsidemeeting tostayconnectedand checkinwithotherstoreduceisolation.
GUNVIOLENCE
Thepandemichasbeenassociatedwithincreased firearms purchasingbothbyexperiencedownersand first-timebuyers. Withthestartofthepandemic,asurgeinUSgunsaleswas tiedtostay-at-homeordersandthe firstwaveofpandemicrelatedunemployment.35,36 Astheyearprogressedand politicalpolarizationincreased,peoplecontinuedtoarm themselves;40millionbackgroundchecksforgunpurchases wererecordedin2020.35,36 Almostone-quarterofthose seekinggunshadnotpreviouslyowneda firearm.Woman andBlacksshowedthegreatestincreasesin firearm purchasing.Historically,increasesin firearmpurchaseshave beenlinkedwithelectionsorrestrictivepolicyworries.But theCOVID-19pandemicdivergedfromthistrendandwas linkedtofearassociatedwiththepandemic,lockdown, racism,elections,andthepolice.
Both firearmassaultandDVincidentsintheUSincreased by8.1%inthe firstmonthsfollowingtheimpositionofstayat-homeorders.18 PeopleatriskofDVareathighriskof beingkilledbya firearmwithoveronehalfofallintimate partnerhomicidescommittedwithguns.37 Inastudy conductedatLevelItraumacentersacrossPhiladelphia, Abdallahetalfoundthatintentionalorviolenttrauma,such as firearmviolence,stabbings,andassaults,significantly increasedwhencomparingsixweekspriortoand10weeks afterimplementationofstay-at-homeorders;otherstudies reportedgreaterincreasesinshootingsafterlockdownwas lifted.38 Recognizingthesynergisticepidemic,orsyndemic, ofracism,COVID-19,and firearminjuryisimportant. PreliminarydatashowedBlacksweretwiceaslikelyas WhitestodiefromCOVID-19.38 Blacksarealsoeighttimes
morelikelytobekilledbya firearmthanWhites.34
Preliminarystatisticsfrom2020suggestthattheCOVID-19 pandemiccompoundedracialinequitiesin firearmviolence. InastudyconductedusingthePhiladelphiaPolice Departmentdataregistryofshootingvictims,researchers notedthataspikeinthenumberofpeopleshotperweek dependedonatemporalrelationshiptoPhiladelphia’ s first COVID-19lockdown.40
Finally,morethanhalfofdeathsfrom firearmsoccurfrom suicide.Althoughpreliminarydatasuggestssuicidedeaths droppedin2020comparedwith2019,itisanticipatedthatthe mentalhealthburdenofthepandemicwillpeaklaterthanthe actualpandemic.The1918SpanishFlupandemic,for example,wasassociatedwithanincreaseindeathbysuicide, suggestingthesocialisolationlink.41 Firearmswereshownto reducethetimeperiodof firstsuicidalthoughtsandattempts, aswellastosignificantlyincreasethelethalityofthose attempts.42 Withincreasedaccessto firearms,numbersof firsttimebuyers,andfeelingsofsocialisolation,thereisahighrisk offutureincreasesinsuicidesrelatedto firearminjury.
WhilethesummativeeffectoftheCOVID-10pandemicand thegunviolencepandemic,andtheirrelationshiptoeachother, hasnotyetbeenstudied,thereiscauseforconcern. Recognitionofriskisthe firststeptowardimprovedprevention of firearminjury.Emergencycliniciansareuniquelypositioned tointerveneaswecareforvulnerablepatientswhomaybe facingDV,racialviolence,ordepressivesymptoms.Screening of all EDpatientsmaymakeadifference.
COVID-19FEARANDNEGLECT
Duringthepandemic,therewasadocumenteddecreasein EDvisitsformedicalandtraumaticconditions,myocardial infarctions,stroke,andhyperglycemiccrises.43–46 Forty percentofadultsdeferredcareforfearofcatchingCOVID-19, leadingtoseriousmorbidityandmortality.47 AnACEPstudy foundthat80%ofthosesurveyedwereconcernedabout contractingCOVID-19fromotherEDpatientsorvisitors, and29%activelydelayedoravoidedseekingmedicalcaredue totheseconcerns.48 Anothersurveyregardingnon-COVID19-relatedcomplaintsfound59%wereunlikelytousetheED andanother20% “didn’tknow.”49
Emergencyphysicianshavecountlessstoriesofpatients delayingmedicalcareduetofearofcontractingdisease. Manyofthesepatientspresentedverylateintothecourseof theirdisease,sufferingunnecessarycomplicationsand potentiallypermanentconsequences.Suchinstancesraisethe questionofwhendoesfearofdiseaseturnintoactualneglect, andcomplicatetheassessmentofabuseandneglect, particularlyofdependentpopulations.
Patientsexercisetheirautonomywhendecidingwhether toseekcareduetofearofCOVID-19.Whatifthatdecision weremadeforthepatientbysomeoneelse?Areparents neglectfulwhenchoosingnottotaketheirchildtothedoctor orEDforcarebecauseoffearssurroundingCOVID-19?Isit
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 747 Whitemanetal. ViolenceandAbuse:APandemicWithinaPandemic
childneglectifparentsdelayseekingcarefortheir9-year-old withrightlowerquadrantabdominalpainforaweek resultinginperforatedappendicitisrequiringpercutaneous drainage,prolongedparenteralantibiotics,anddelayed appendectomy?IsthisreportabletoCPS?
Conversely,thereistheexampleofanelderlywomanwho fallswithimmediatehippainandinabilitytowalkandwhose refusaloffamilymembers’ offertotakehertotheEDleaves herbedboundforaweek.Familyboughtdiapersfortoileting andgavehermealsinbed.Finally,whenthepainescalated, sheagreedtopresenttotheEDwhereshewasdiagnosedwith anintertrochanterichipfracturewithassociateddeepvein thrombosis.Isthisself-neglectorelderneglect?Nursing homestaffassumearesidentwithfever,bodyaches, abdominalpain,andnausea/vomiting/diarrheahasCOVID19duringanoutbreakintheirfacilityanddon’tsendherto theEDforthreedaysdespiteanegativeCOVID-19test.She wasfoundtohaveincarceratedbowelwithsepsis.Wasthe nursinghomeneglectfulforanchoringonCOVID-19 becauseoftheirfacility’sconcomitantoutbreak?Arethese eventsreportabletoAdultProtectiveServices?
Childneglectisdefinedasthefailureofaparentorother personwithresponsibilityforthechildtoprovideneeded food,clothing,shelter,medicalcare,orsupervisiontothe degreethatthechild’shealth,safety,andwell-beingare threatenedwithharm.50 Similarly,elderneglectisdefinedas failurebyacaregiverorotherpersoninatrustrelationshipto protectanelderfromharmorthefailuretomeetneedsfor essentialmedicalcare,nutrition,hydration,hygiene, clothing,andbasicactivitiesofdailyneedsorshelter,which resultsinaseriousriskofcompromisedhealthand/orsafety relativetoage,healthstatus,andculturalnorms.31 Selfneglectisthebehaviorofanelderlypersonthatthreatenshis/ herownhealthandsafety.31
Duringnon-pandemictimes,mostclinicianswouldbelieve thatthesequestionsposedabovewereproofofneglect. However,pandemicfears,especiallyduringsurges,madethis judgmentdifficult.Inassessingsituations,severalfactorsmust beconsidered,includingintent,expectationoftrust,risk,and harm.Thekeyquestiontoconsideris “whatwastheintentor intentionalityofthedecision?” Wasdelayingcaremaliciousor honoringthepatient’swishes?Incasesofself-neglect,the competenceanddecision-makingcapacityofthepatientmust beconsidered.Itisnotself-neglectifthepatienthas competenceanddecision-makingcapacity.31
Classifyingactionsasneglectrequiresthought.Onedoes notwanttowrongfullyaccuseor,conversely,missred flags andpossiblysubjectthepatienttomoreseriousabuse. EmergencyphysiciansshouldemployEDsocialworkersto helpwithdifficultcases.WithregardtoCOVID-19fear, localandnationalorganizationsneededtoeducatethepublic aboutseekingappropriatemedicalcareandthetrueriskof diseasetransmissioninhealthcaresettings.Patienteducation iskeytoensuretimelyandappropriatemedicalcare.
Withtheadventofvaccination,hopefullythesefears werelessened.
LIMITATIONS
Theauthorswhoperformedtheliteraturesearchand reviewwerenotblinded.Thetrueextentofpandemic-related violenceremains,andwilllikelyremain,incompletely reportedandunderstood.Asaresult,theavailable quantitativedataislimited.Anecdotalevidencesuggeststhat pandemicsrequireincreasedvigilanceforsignsof interpersonalabuseandviolence.Moreover,andperhaps morepressing,athoroughrisk-benefitanalysisofuniversal lockdownsasamitigationstrategymustbeconductedto furtherourunderstandingandensureadequateemergency preparednessduringfuturerespiratorypandemics,givena muchearlierpredictionthatlockdownswouldbeoflittlehelp andwouldincreaseviolence.Finally,wedidnotfocuson specificpreventiontechniquesrelatedtoCOVID-19,as researchonthissubjectwassparse.
CONCLUSION
Itisevidentthatmeasuresmeanttohelpcontrolthe spreadoftheCOVID-19pandemichadmanyunintended consequencesandplacedpeopleatriskforviolence.The pandemicleftabuseandviolencevictimsfeelingisolatedwith feweroptionsforhelpanddecreasedopportunitiesfor recognition.Hospitalsandviolencepreventionprograms needtostartplanningforthenextpandemicwitha focusonpreservingorexpandingaccesstoservices, strengtheningsocialserviceagencypartnerships,and ensuringtheseagencieshaveaccesstotheEDwith properPPE.
AddressforCorrespondence:RalphJ.Riviello,MD,MS,University ofTexasHealthSanAntonio,LozanoLongSchoolofMedicine, DepartmentofEmergencyMedicine,7703FloydCurlDrive, MC7736,SanAntonio,TX78229.Email: riviellor@uthscsa.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Whitemanetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.COVID-19MentalDisordersCollaborators.Globalprevalenceand burdenofdepressiveandanxietydisordersin204countriesand territoriesin2020duetotheCOVID-19pandemic. Lancet.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 748 ViolenceandAbuse:APandemicWithinaPandemic Whitemanetal.
2021;398(10312):1700–1712. https://doi.org/10.1016/S0140-6736(21)
02143-7
2.TogohI.UNChiefurgesgovernments: “Prioritisewomen’ssafety” as domesticabusesurgesduringcoronaviruslockdowns. Forbes.2020.
Availableat: https://www.forbes.com/sites/isabeltogoh/2020/04/06/ un-chief-urges-governments-prioritise-womens-safety-as-domesticabuse-surges-during-coronavirus-lockdowns/?sh=6b460626172f
AccessedMay15,2022.
3.TaubA.AnewCOVID-19crisis:domesticabuserisesworldwide. NY Times.2020.Availableat: Coronavirus-domestic-violence.html
AccessedMay15,2022.
4.NewZealandFamilyViolenceClearinghouse(NZFVC).Preventingand respondingtofamily,whanauandsexualviolenceduringCOVID-19. 2020.Availableat: https://nzfvc.org.nz/covid-19/preventingresponding-violence-covid-19.AccessedMay15,2022.
5. TheGuardian.Lockdownsaroundtheworldbringriseindomestic violence.2020.Availableat: https://www.theguardian.com/society/ 2020/mar/28/lockdowns-world-rise-domestic-violence
AccessedMay15,2022.
6.UNWomen.COVID-19andendingviolenceagainstwomenandgirls. 2020.Availableat: https://www.unwomen.org/-/media/headquarters/ attachments/sections/library/publications/2020/issue-brief-covid-19and-ending-violence-against-women-and-girls-en.pdf?la=en&vs= 5006.AccessedMay15,2022.
7.KellyK,MorganT.Coronavirus:domesticabusecallsup25%since lockdown,charitysays.BBC,2020.Availableat: https://www.bbc.co.uk/ news/uk-52157620.AccessedMay15,2022.
8.PortlandPoliceBureau.Trendsanalysis:preandpostschoolclosures. 2020.Availableat: https://www.portland.gov/police/chiefs-office/ documents/2020-police-annual-report/download
AccessedMay15,2022.
9.ManagementCoSAOoE.Socialdistancingdoesn’tmeansafety distancing.DepartmentofGovernmentandPublicAffairs;2020. Availableat: https://www.sanantonio.gov/gpa/News/ArtMID/24373/ ArticleID/18724/Social-distancing-doesn.AccessedMay15,2022.
10.MoneyJ.JeffersonCountyexperiencingincreaseindomestic violencecrimesduringCovid-19pandemic.JeffersonCounty Sheriff’sOffice;2020.Availableat: https://jeffcosheriffal.com
AccessedMay15,2022.
11.NewYorkCityPoliceDepartment.Domesticviolencereports.NewYork CityPoliceDepartment;2020.Availableat: https://www1.nyc.gov/site/ nypd/stats/reports-analysis/domestic-violence.page
AccessedMay15,2022.
12.NationalCommissiononCOVID-19andCriminalJustice(NCCCJ). Impactreport:COVID-19anddomesticviolencetrends.Feb23,2021.
Availableat: https://covid19.counciloncj.org/2021/02/23/impact-reportcovid-19-and-domestic-violence-trends/.AccessedMay15,2022.
13.HollandKM,JonesC,Vivolo-KantorAM,etal.TrendsinUSemergency departmentvisitsformentalhealth,overdose,andviolenceoutcomes beforeandduringtheCOVID-19pandemic. JAMAPsychiatry.
2021;78(4):372
9.doi: 10.1001/jamapsychiatry.2020.4402
14.NationalDomesticViolenceHotline.Asnapshotofdomesticviolence duringCOVID-19.2020.Availableat: https://www.thehotline.org/ resources/a-snapshot-of-domestic-violence-during-covid-19/ AccessedMay15,2021.
15.NationalDomesticViolenceHotline.COVID-19specialreport.2020. Availableat: https://www.thehotline.org/wp-content/uploads/media/ 2020/09/The-Hotline-COVID-19-60-Day-Report.pdf AccessedMay16,2021.
16.GlaunD.Ahandfulofstatesfueledanationalincreaseindomestic violenceshootingdeathsasCOVID-19spread. Frontline 2021. Availableat: https://www.pbs.org/wgbh/frontline/article/nationalincrease-domestic-violence-shooting-deaths-during-covid-19/. AccessedMay15,2021.
17.LynchK,LoganTK.Assessingchallenges,needs,andinnovationsin gender-basedviolenceservicesduringtheCOVID-19pandemic:results summaryreport.SanAntonio,TX:UniversityofTexasatSanAntonio, CollegeforHealth,CommunityandPolicy.2021.Availableat: https:// assets.speakcdn.com/assets/2497/covid__gender_based_violence_ final_report.pdf.AccessedMay16,2021.
18.Ingala-SmithKCountingdeadwomen.2020.Availableat: https:// kareningalasmith.com/.AccessedMay16,2021.
19.PiqueroAR,JenningsWG,JemisonE,KaukinenC,KnaulFM. DomesticviolenceduringtheCOVID-19pandemic-evidencefroma systematicreviewandmeta-analysis. JCrimJust.74(2021)101806, https://doi.org/10.1016/j.crimjus.2021.101806
20.EvansML,LindauerM,FarrellM.ApandemicwithinapandemicintimatepartnerviolenceduringCOVID-19. NEnglJMed. 2020;338:2302–4.doi: 10.1056/NEJMp2024046
21.Bradbury-JonesC,IshamL.Thepandemicparadox:theconsequences ofCOVID-19ondomesticviolence. JClinNurs. 2020;29:2047–9, doi: 10.1111/jocn.15296
22.WorldHealthOrganization.Jointleaders’ statement–violenceagainst children:ahiddencrisisoftheCOVID-19pandemic.2020.Availableat: https://www.who.int/news/item/08-04-2020-joint-leader-s-statement violence-against-children-a-hidden-crisis-of-the-covid-19-pandemic AccessedMay20,2021.
23.SwedoE,IdaikkadarN,LeemisR,DiasT,etal.TrendsinU.S. emergencydepartmentvisitsrelatedtosuspectedorconfirmedchild abuseandneglectamongchildrenandadolescentsaged < 18years beforeandduringtheCOVID-19pandemic–UnitedStates, January2019-September2020. MMWRMorbMortalWklyRep. 2020;69(49):1841–7.
24.ChildHelp.HotlineimpactreportFY2018.Availableat: https://www. childhelp.org/wp-content/uploads/2019/03/Hotline-Impact-ReportFY18.pdf.AccessedMay20,2021.
25.ChildHelp.Hotlineimpactreport,FY2019.Availableat: https://www. childhelp.org/wp-content/uploads/2020/02/Hotline-Impact-ReportFY19v2.pdf.AccessedMay20,2021.
26.ChildHelp.Hotlineimpactreport,FY2020.Availableat: https://www. childhelp.org/wp-content/uploads/2020/10/Hotline-Impact-ReportFY20.pdf.AccessedMay20,2021.
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 749 Whitemanetal. ViolenceandAbuse:APandemicWithinaPandemic
27.WelchM,HaskinsR.WhatCOVID-19meansforAmerica’schildwelfare system.Washington,DC:BrookingsInstitution;2020.Availableat: https://www.brookings.edu/research/what-covid-19-means-foramericas-child-welfare-system/.AccessedMay20,2021.
28.O’DonnellB. “COVID-19andMissing&ExploitedChildren:Datafrom Jan1,2020 – Dec31,2020.” NationalCenterforMissing&Exploited Children,Blog,04-30-2021.Availableat: https://www.missingkids.org/ blog/2020/covid-19-and-missing-and-exploited-children
AccessedJuly9,2023.
29.ScottMacFarlaneRickYarborough,JonesSteve. “OnlinePredator ComplaintsSpikeDuringthePandemic.” NBC4Washington,2020. Availableat: https://www.nbcwashington.com/news/onlinepredator-complaints-spike-during-pandemic/2377394/
AccessedJuly7,2023.
30.ParksA,SparreC,SöderquistE,ArverS,AnderssonG,KaldoV,etal. IllegalonlinesexualbehaviorduringtheCOVID-19pandemic:acallfor actionbasedonexperiencedfromtheongoingPreventItresearchstudy.
ArchSexBehav. 2020;48(5):1433–5.doi: 10.1007/s10508-020-01750-7
31.HallJ,KarchDC,CrosbyA.Elderabusesurveillance:uniform definitionsandrecommendedcoredataelements.Atlanta,GA:The CentersforDiseaseControlandPrevention;2016.Availableat: https:// www.cdc.gov/violenceprevention/pdf/EA_Book_Revised_2016.pdf
AccessedJune3,2022.
32.YunusRM,AbdullahNN,FirdausMAM.Elderabuseandneglectinthe midstofCOVID-19. JGlobHealth. 2021;11:03122.doi: 10.7189/jogh. 11.03122.PMID:doi:34912545.
33.ChangES,LevyBR.HighprevalenceofelderabuseduringtheCOVID19pandemic:riskandresiliencefactors. AmJGeriPsych.2021. https:// doi.org/10.1016/j.jagp.2021.01.007
34.CentersforDiseaseControlandPrevention(CDC).Web-basedInjury StatisticsQueryandReportingSystems:FatalInjuryReports.2019. Availableat: http://www.cdc.gov/injury/wisqars/fatal_injury_reports. html.AccessedJune1,2021.
35.ArthurRob,AsherJeff. “Whatdrovethehistoricallylargemurderspikein 2020?” TheIntercept,2021.Availableat: theintercept.com/2021/02/21/ 2020-murder-homicide-rate-causes/.AccessedJune1,2021.
36.SutherlandM,McKenneyM,ElkubiliA.GunviolenceduringCOVID-19 pandemic:paradoxicaltrendsinNewYorkCity,Chicago, LosAngelesandBaltimore. AmJEmergMed. 2021;39:225-6.
37.DomesticViolenceandFirearms.TheEducationalFundtoStopGun Violence,2020.Availableat: efsgv.org/learn/type-of-gun-violence/ domestic-violence-and-firearms/.AccessedJune1,2021.
38.AbdallahH,ZhaoC,KaufmanE,etal.IncreasedFirearmInjury DuringtheCOVID-19Pandemic:AHiddenUrbanBurden. JAmCollSurg. 2021;232(2):159–68.e3.
39.NeumanScott. “COVID-19deathrateforBlackAmericanstwice thatforWhites,newreportsays.” NPR,NPR,2020.Availableat: www.npr.org/sections/coronavirus-live-updates/2020/08/13/ 902261618/covid-19-death-rate-for-black-americans-twice-that-forwhites-new-report-says.AccessedJune1,2021.
40.BeardJ,JacobyS,MaherZ,etal.Changesinshootingincidencein Philadelphia,Pennsylvania,betweenMarchandNovember2020. JAMA. 2021;325(13):1327–28.
41.EghigianGreg,PhD. “TheSpanishFlupandemicandmentalhealth: ahistoricalperspective.” PsychiatricTimes.2020.Availableat: www. psychiatrictimes.com/view/spanish-flu-pandemic-and-mental-healthhistorical-perspective.AccessedJune1,2021.
42.ShanessaE,CaitlinS,BurkaS.Lethalityof firearmsrelativetoother suicidemethods:apopulationbasedstudy. JEpidemiolCommun Health. 2003;57:120–4.
43.MasroorS.CollateraldamageofCOVID-19pandemic:delayedmedical care. JCardSurg. 2020;35(6):1345–7.
44.MessacL,KnopovA,HortonM.Delayedcare-seekingfornon-COVID illnessesinRhodeIsland. RIMedJ. 2020;103(4):10–11.
45.AsarpotaDM,WyssKJ,MarcoCA.Casereport:fearofCOVID-19 leadstogangrene. ACEPNow.2021.Availableat: https://www. acepnow.com/article/case-report-fear-of-covid-19-leads-togangrene/?singlepage=1&theme=print-friendly
AccessedJune15,2021.
46.LangeSJ,RitcheyMD,GoodmanAB,etal.Potentialindirecteffectsof theCOVID-19pandemiconuseofemergencydepartmentsforacute life-threateningconditions UnitedStates,January–May2020. Morb MortalWklyRep. 2020;69(25):795–800.
47.CzeislerMÉ,MarynakK,ClarkeKEN,etal.Delayoravoidance ofmedicalcarebecauseofCOVID-19–relatedconcerns UnitedStates,June2020. MMWRMorbMortalWklyRep. 2020;69(36):1250–7.
48.Publicpoll:emergencycareconcernsamidstCOVID-19.ACEP website.Availableat: https://www.emergencyphysicians.org/ globalassets/emphysicians/all-pdfs/acep-mc-covid19-april-pollanalysis.pdf.AccessedMay29,2020.
49.Nationaltrackingpoll#2004100April29–30,2020.MorningConsult website.Availableat: https://morningconsult.com/wp-content/uploads/ 2020/05/2004100_crosstabs_CONTENT_CORONAVIRUS_RVs_v2_ JB.pdf.AccessedMay22,2020.
50.ChildWelfareInformationGateway.Definitionsofchildabuseand neglect.Washington,DC:USDepartmentofHealthandHuman Services,2019.Availableat: https://www.childwelfare.gov/pubPDFs/ define.pdf.AccessedJune15,2021.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 750 ViolenceandAbuse:APandemicWithinaPandemic Whitemanetal.
Examining Predictors of Early Admission and Transfer to the Critical Care Resuscitation Unit
Quincy K. Tran, MD, PhD*†#
Daniel Najafali, BS||
Tiffany Cao, BS‡§
Megan Najafali, MHS‡
Nelson Chen, BS§
Iana Sahadzic, BS‡
Ikram Afridi, BS‡
Ann Matta, CRNP#
William Teeter, MD*†#
Daniel J. Haase, MD*†#
Section Editor: Christopher Tainter, MD
University of Maryland School of Medicine, Department of Emergency Medicine, Baltimore, Maryland
University of Maryland School of Medicine, The R Adams Cowley Shock Trauma Center, Baltimore, Maryland
University of Maryland School of Medicine, The Research Associate Program in Emergency Medicine and Critical Care, Department of Emergency Medicine, Baltimore, Maryland
University of Maryland School of Medicine, Baltimore, Maryland
University of Illinois Urbana-Champaign, Carle Illinois College of Medicine, Champaign, Illinois
University of Maryland Medical Center, The Critical Care Resuscitation Unit, Baltimore, Maryland
Submission history: Submitted September 8, 2023; Revision received March 15, 2023; Accepted March 7, 2023
Electronically published: June 28, 2023
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.58356
Introduction: Previous studies have demonstrated that rapid transfer to definitive care improves the outcomes for many time-sensitive conditions. The critical care resuscitation unit (CCRU) improves the operations of the University of Maryland Medical Center (UMMC) by expediting the transfers and resuscitations for critically ill patients who exceed the resources at other facilities. In this study we investigated CCRU transfer patterns to determine patient characteristics and logistical factors that influence bed assignments and transfer to the CCRU. We hypothesized that CCRU physicians prioritize transfer for critically ill patients. Therefore, those patients would be transferred faster.
Methods: We performed a retrospective review of all non-traumatic adult patients transferred to the CCRU from other hospitals between January 1–December 31, 2018. The primary outcome was the interval from transfer request to CCRU bed assignment. The secondary outcome was the interval from transfer request to CCRU arrival. We used multivariate logistic regressions to determine associations with the outcomes of interest.
Results: A total of 1,741 patients were admitted to the CCRU during the 2018 calendar year. Of those patients, 1,422 were transferred from other facilities and were included in the final analysis. Patients’ mean age was 57 ± 17 years with a median Sequential Organ Failure Assessment (SOFA) score of 3 [interquartile range 1-6]. Median time from transfer request to CCRU bed assignment was 8 (0-70) minutes. A total of 776 (55%) patients underwent surgical intervention after arrival. Using the median transfer request to bed assignment time, we found that patients requiring stroke neurology (odds ratio [OR] 5.49, 95% confidence interval [CI] 2.85-10.86), having higher SOFA score (OR 1.04, 95% CI 1.0011.07), and needing an immediate operation (OR 2.85, 95% CI 1.98-4.13) were associated with immediate bed assignment time (≤8 minutes). Patients who were operated on (OR 0.74, 95% CI 0.55-0.99) were significantly less likely to have an immediate bed assignment time.
Conclusion: The CCRU expedited the transfer of critically ill patients who needed urgent interventions from outside facilities. Higher SOFA scores and the need for urgent neurological or surgical intervention were associated with near-immediate CCRU bed assignment. Other institutions with similar models to the CCRU should perform studies to confirm our observations. [West J Emerg Med. 2023;24(4)751–762.]
olume 24, o. 4: July 20 23 751 Western Journal of Emergency Medicine Original Research
* † ‡ § || #
INTRODUCTION
When caring for a patient exceeds the initial hospital’s resources, patients are usually transferred to tertiary or quaternary medical centers for higher levels of care. The transfer of patients from either the emergency department (ED) or intensive care unit (ICU) to regional referral centers, interhospital transfer (IHT), is becoming more common.1,2 However, the system for medical IHT is not robust and most of the highvolume referral medical centers do not have immediate ICU bed availability.3,4 As a result, the IHT of critically ill patients is often delayed, leading to worse patient outcomes.5
Furthermore, certain patients are found to have time-sensitive disease and will need transfer to tertiary or quaternary care centers for immediate diagnostic or therapeutic interventions. Early intervention or early arrival at referral centers have been associated with improved outcomes for patients who had Type A aortic dissection, ruptured abdominal aortic aneurysm, intracranial hypertension, or ischemic stroke from large vessel occlusion.6-9
To expedite IHT and optimize outcomes for patients with critical illness or time-sensitive conditions, the critical care resuscitation unit (CCRU) at the University of Maryland Medical Center (UMMC) was created in July 2013. The CCRU streamlines the IHT process by providing timely and effective resuscitation for patients who need further interventions from a quaternary care medical center. The CCRU has been found to outpace traditional ICUs by providing care for a higher number of patients with critical illnesses or time-sensitive diseases, while also leading to improved outcomes.4,10 However, details about how the CCRU physicians triage and prioritize transfer requests while optimizing patient volume has not been described. In this study we aimed to investigate and describe factors that contribute to early bed assignment and early transfer to the CCRU. Determining these factors can provide further information for administrators at other facilities that might be interested in setting up a similar unit.
METHODS
Study Design and Clinical Setting
We performed a retrospective analysis of data from all adult patients who were transferred from other hospitals to the CCRU between January 1-December 31, 2018 (the latest year that this data became available). All nontraumatic adult patients who were admitted from other hospitals to the CCRU during this period were eligible. We excluded patients who were admitted to the CCRU from within our medical center (intrahospital transfer), either from our institution’s ED or another inpatient unit. This study was exempt from formal consent by our institutional review board (HP-00084554).
The CCRU is a six-bed, ICU-based resuscitation unit that is staffed around the clock by one attending physician,
Population Health Research Capsule
What do we already know about this issue? Interhospital transfers of critically ill patients are often delayed as there is no immediate ICU bed availability.
What was the research question? What are the transfer patterns and patient characteristics that lead to immediate bed assignment at the critical care resuscitation unit (CCRU)?
What was the major finding of the study? Patients admitted to stroke neurology, with higher SOFA score, and needing immediate surgery, were associated with immediate bed assignment time (≤8 minutes).
How does this improve population health? A CCRU expedites the transfer of critically ill patients from outside facilities who are in need of urgent intervention.
one advanced practice provider (APP), and three to four nurses who are required to have at least two years of prior ICU experience. The operational costs to staff the CCRU, represented in full-time equivalents (FTE), are 5.0 FTE for APPs, 5.0 FTE for attending physicians, and 32.0 FTE for nurses. When a referring clinician needs to transfer a patient with critical illness or time-sensitive disease to our quaternary medical center, the referring clinician first contacts the Maryland ExpressCare (MEC) Center, which handles all transfer logistics for our institution. The MEC personnel then contact the on-call specialty physician and the appropriate ICU physician for possible transfer. When no ICU bed is available, the CCRU attending physician is involved with the transfer request for an available CCRU bed.
Once the patient is considered appropriate for transfer by the specialist and the CCRU attending physician, the CCRU attending assigns an available bed to the patient, as appropriate. This assigned bed is now reserved until this patient arrives. Once a bed is assigned to the patient, the CCRU team and the accepting physicians at UMMC leave the decision of transport to the referring clinicians. The sending facility will arrange for the most appropriate mode of transport (eg, ground vs air transport, private vs academic-affiliated transport teams) for the patient, according to the transport team’s availability and the patient’s acuity.
Western Journal of Emergency Medicine 752 Predictors of Early Admission and Transfer to the CCRU Tran et al.
olume 24, o. 4: July 20 23
The CCRU is a fluid and dynamic unit. Regarding the capacity of the CCRU, “empty” beds may already be promised to a patient in transit; thus, even though a patient is not physically occupying the bed, it is technically not empty. The CCRU attendings triage patients’ acuity levels and the demands of the unit for appropriate bed assignment. There is an agreement within the medical center that when the CCRU is reaching its capacity that any available bed in the medical center will be given to a CCRU patient. Typically, when the CCRU is reaching its capacity, such as a situation where five of the six beds are occupied, the CCRU calls the appropriate inpatient unit(s) to alert them, so that the CCRU can get their first available bed when it becomes available.
Once a patient arrives at the CCRU, the patient will receive resuscitation from the CCRU team as indicated and timely diagnostics or therapeutic intervention(s) from specialists, such as a thrombectomy for ischemic stroke from large vessel occlusion, or cannulation for extracorporeal membrane oxygenation (ECMO), etc. In addition, patients may be taken to the operating room (OR) for emergent surgery, which was defined as within 12 hours of CCRU arrival.4 Once a patient undergoes adequate resuscitation and treatment by the multidisciplinary clinical teams, the patient will be moved to another appropriate inpatient unit at our medical center for further longitudinal care.
Data Collection
We extracted the following data from the CCRU records and our institution’s electronic health records: the date and time that the referring clinicians contacted MEC for a transfer request; the date and time that the CCRU attending physicians assigned a bed to each patient; and the date and time that patients arrived at the CCRU. We also extracted other clinical data, such as components of the Sequential Organ Failure Assessment (SOFA) score upon a patient’s arrival at the CCRU. The SOFA score served as a surrogate for a patient’s disease severity at the sending facility, prior to arrival at the CCRU. We also collected other laboratory values that were not part of the SOFA score, such as serum lactate concentrations, white blood cell count, and hemoglobin concentrations. We collected the types of continuous infusions prior to CCRU arrival, such as insulin and anti-hypertensive infusions, as a marker of care intensity at the referring facilities.
The UMMC is a quaternary medical center with a capacity of approximately 800 beds. There are five adult nontrauma ICUs: the cardiac surgical ICU; coronary care unit; neurocritical care unit; medical ICU (MICU); and surgical ICU. UMMC has a system in place to handle transfer requests from another hospital via MEC. MEC works to connect the transferring clinicians with the relevant ICU for possible admission. If patients are deemed appropriate for admission but the corresponding ICU does not have available beds, the CCRU will be included in the consultation. The transfer records of patients coming from another hospital to UMMC are
maintained by MEC as part of their operations, which manages all incoming IHT.
We extracted the data used from non-CCRU units in this study from the MEC database. Prior to commencement of data extraction, investigators who were blinded to the study’s hypothesis were trained by the principal investigator with sets of 10 patients until data accuracy reached at least 90% agreement. Data was extracted into a standardized Excel spreadsheet (Microsoft Corporation, Redmond, WA). Up to 5% of data was double-checked by an independent investigator to maintain inter-rater agreement of ≥90%. The data abstracters were blinded to the study hypothesis and objectives. Our study adhered to the reporting practices outlined by Worster et al.11 Our study also met the minimum requirements outlined by Lowenstein’s editorial regarding medical records review in emergency medicine.12 If a component of the SOFA score was missing, we imputed a normal value.
Outcome Measures
The primary outcome was the percentage of patients who were immediately assigned a bed at the CCRU (≤8 minutes) from time of transfer request. Our secondary outcome was the percentage of patients who arrived early to the CCRU, which was defined by the median time interval from transfer request to CCRU arrival (<180 minutes). An additional outcome investigated was mortality of patients transferred to the CCRU.
Statistical Analysis
We did not perform a sample-size calculation for this descriptive study, presuming that we would obtain an adequate sample size for our analysis by using a full calendar year of CCRU admissions. Based on a previous study, it was estimated that we would have approximately 1,400 patients using a full calendar year of CCRU admissions.10 By using the median time from transfer request to bed assignment or CCRU arrival as cut-off points to dichotomize our primary and secondary outcomes, we estimated that we would have approximately 700 patients for each of our outcomes. This would provide enough of a sample size to accommodate multivariable logistic regressions with at least 70 independent variables, according to the previous recommendation of 10 counts of outcome events per each independent variable.13
We used descriptive analyses to present patients’ demographic and clinical information with mean (±SD or median (interquartile range [IQR]), or frequency (percentage) as appropriate. Continuous variables between groups were compared with the Student t-test or the Mann-Whitney U test, while categorical variables were compared with the Pearson chi-squared test or Fisher exact test, as indicated. We performed multivariate logistic regressions with dichotomous outcomes as immediate CCRU bed assignment
53 Western Journal of Emergency Medicine Tran et al.
Predictors of Early Admission and Transfer to the CCRU
olume 24, o. 4: July 20 23
Predictors of Early Admission and Transfer to the CCRU Tran et al. (vs normal CCRU bed assignment), early CCRU arrival (vs normal CCRU arrival), or deceased (vs living). All relevant independent variables were determined a priori and were used in the regression models.
Prior to data analysis, we performed preliminary analyses and defined immediate CCRU bed assignment as the median of the time interval from transfer request to CCRU bed assignment as the cut-off time for our dichotomous outcome (immediate vs normal CCRU bed assignment). Similarly, the median time interval from transfer request to CCRU arrival was the cut-off point for the dichotomous outcome of early CCRU arrival vs normal CCRU arrival. We assessed multicollinearity of the models using variance inflation factor (VIF). A threshold of VIF ≥5 was used to deem any factor as having multicollinearity. Any independent variable with VIF ≥5 would meet the threshold for having high collinearity and would be excluded from the multivariable logistic regression. No independent variable met this threshold in any of our models. All models were assessed for goodness of fit using the Hosmer–Lemeshow test. A P > 0.05 was the threshold indicating that the model was an appropriate fit.
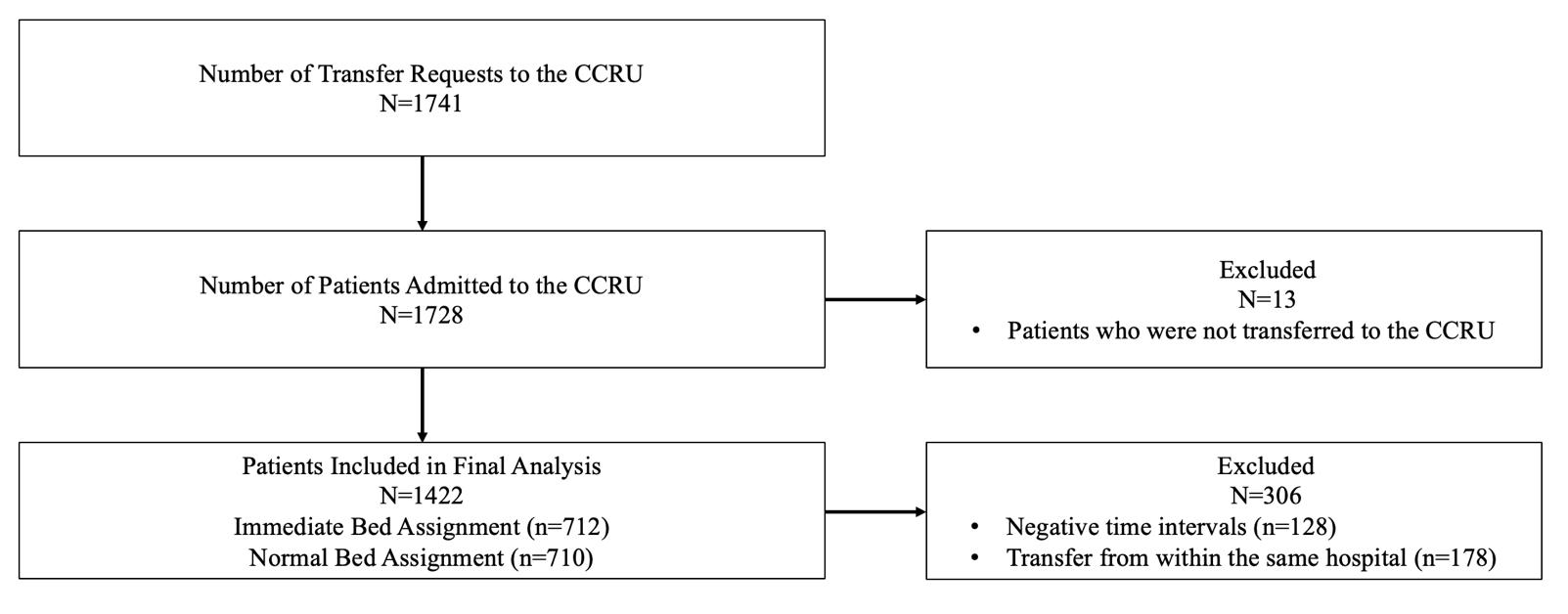
We performed all statistical analyses with Minitab version 19.0 (Minitab, LLC, State College, PA) or using R version 4.1.0 (R Project for Statistical Computing, Vienna, Austria) and RStudio version 1.4.1717 software (RStudio PBC, Boston, MA). All two-sided P-values < 0.05 were considered statistically significant.
RESULTS
Patient Demographics of All UMMC Facilities and Patients Triaged to the CCRU
We identified 1,741 patients who were admitted to the CCRU during the study period, and 1,422 patients who were transferred from other hospitals with sufficient data included in our final analysis (Figure 1). There were 712 (50%) patients who had immediate bed assignment to the CCRU,
defined as within eight minutes. There were 750 (53%) patients who arrived at the CCRU within 180 minutes from the time of transfer request, while the majority of patients (1,168, 82%) arrived at the CCRU within 360 minutes from the time of transfer request.
Demographic data are reported in Table 1A for the 5,717 patients from all UMMC units comprised of the following: CCRU; any adult, non-trauma ICU; ED; and other inpatient units (intermediate care unit or surgical or medical wards). Patients who were transferred to the CCRU had the shortest time interval from transfer request to bed assignment, with a median (IQR) of 8 [0-70] minutes (P < 0.001), when compared to patients who were transferred to other inpatient units at our medical center. When stratifying patients by admission location (CCRU vs ICU vs ED vs other inpatient units), the CCRU had statistically significant higher rates of air transport compared to other units (17% CCRU vs 10% ICU vs 1% ED, vs 4% other inpatient units, P < 0.001).
The CCRU patients’ demographic data are reported in Table 1B stratified by bed assignment time (immediate vs normal). Patients who were immediately assigned a CCRU bed also arrived at the CCRU faster than those who received a normal bed assignment time (Table 1C). Patients with normal bed assignment time had a statistically lower rate of initiation of mechanical ventilation (37% immediate vs 29% normal, P = 0.002) and lower proportion receiving anti-hypertensive infusion, when compared with patients who had immediate bed assignment time (15% immediate vs 10% normal, P = 0.005). Among all patients who underwent surgical interventions, a greater number of patients with normal bed assignment time underwent surgery during hospitalization at UMMC (58% normal vs 51% immediate, P = 0.009), but a significantly higher proportion of patients with immediate bed assignment were taken to the OR within 12 hours compared to those patients who had normal bed assignment (27% immediate vs 20% normal, P = 0.002). More patients with normal bed assignment were discharged home and survived
Western Journal of Emergency Medicine 54
olume 24, o. 4: July 20 23
Figure 1. Patient selection diagram outlining patients included in the final analysis. CCRU, critical care resuscitation unit.
Tran et al.
Predictors of Early Admission and Transfer to the CCRU
*All UMMC does not include pediatric or trauma patients.
**ICU patients are separate from CCRU.
^Indicates that the top group of P-values was calculated excluding the unknown or other/unknown group and that the bottom group of P-values was calculated with the unknown or other/unknown groups with either Pearson chi-square test or Fisher exact test as appropriate.
†Bold cells indicate statistically significant findings (P < 0.05).
P-values written as P1, P2, P3 where: P1 = CCRU vs. ICU; P2 = CCRU vs. ED; P3 = CCRU vs. Other Inpatient Units CCRU, critical care resuscitation unit; ED, emergency department; ICU, intensive care unit; IQR, interquartile range; min, minutes; km, kilometers; NA, not applicable; UMMC, University of Maryland Medical Center.
compared to patients with immediate bed assignment time (44% normal vs 38% immediate, P = 0.014).
Primary Outcome: Transfer Request to Bed Assignment
The Kaplan–Meier curves presented in Figure 2A and Figure 2B depict each time interval from transfer request
to CCRU bed assignment. The top five accepting services based on volume for the CCRU during the 2018 calendar year were as follows: 1) cardiac surgery (297, 21%); 2) soft tissue surgery (240, 16%); 3) neurosurgery (191, 13%); 4) acute care emergency services (147, 10%); and 5) vascular surgery (134, 9%). Appendix 1 provides a complete list of accepting
55 Western Journal of Emergency Medicine
Variables All UMMC* UMMC CCRU UMMC ICU** UMMC ED UMMC other inpatient units P† Total patients, N 5,717 1,422 1,046 817 2,432 NA Age (years), mean (SD) 56 (18) 57 (17) 59 (16) 48 (18) 54 (17) < 0.001, < 0.001, < 0.001 Type of transport, N (%)^ Air 443 (8) 240 (17) 103 (10) 10 (1) 90 (4) < 0.001, < 0.001, < 0.001 Ground 5134 (90) 1182 (83) 941 (90) 716 (88) 2295 (94) < 0.001, < 0.001, < 0.001 Unknown 140 (2) 0 (0) 2 (0) 91 (11) 47 (2) Ground distance (km), median [IQR] 44 [11-75] 44 [13-75] 44 [13-74] 21 [8-64] 44 [13-92] 0.035, < 0.001, 0.68 Type of referring hospital, N (%)^ Teaching 1,837 (32) 460 (32) 379 (36) 233 (28) 765 (31) 0.037, 0.041, 0.72 Community 3,663 (64) 962 (68) 663 (63.5) 397 (49) 1641 (68) Other/unknown 217 (4) 0 (0) 4 (0.5) 187 (23) 26 (1) 0.005, < 0.001, < 0.001 Transfer request to placement (min), median [IQR] 88 [15-410] 8 [0-70] 243 [77-660] 20 [10-53] 221 [50-1055] < 0.001, < 0.001, < 0.001 Admission day of the week, N (%) Weekday (Monday-Friday) 4,323 (76) 1,046 (74) 806 (77) 538 (66) 1933 (79) 0.047, < 0.001, < 0.001 Weekend (Saturday-Sunday) 1394 (24) 376 (26) 240 (23) 279 (34) 499 (21) Admission time of the day, N (%) Day time (7:00 AM-7:00 PM) 3,881 (68) 679 (48) 801 (77) 496 (61) 1905 (78) < 0.001, < 0.001, < 0.001 Evening time (7:01 PM-06:59 AM) 1,836 (32) 743 (52) 245 (23) 321 (39) 527 (22) Accepting service, N (%)^ Emergency general surgery 223 (4) 147 (10) 1 (0) 0 (0) 75 (3) Cardiac surgery 732 (13) 297 (21) 106 (10) 0 (0) 329 (14) Cardiology 906 (16) 12 (1) 373 (36) 0 (0) 521 (21) Neurology 317 (6) 114 (8) 145 (14) 0 (0) 58 (2) Neurosurgery 392 (7) 191 (13) 164 (16) 0 (0) 37 (2) < 0.001, NA, < 0.001 Oncology 208 (4) 2 (1) 0 (0) 0 (0) 206 (8) Pulmonary and critical care 311 (5) 57 (4) 252 (14) 0 (0) 2 (0) < 0.001, < 0.001, < 0.001 Thoracic surgery 99 (2) 25 (2) 0 (0) 0 (0) 74 (3) Transplant 334 (6) 38 (3) 3 (0) 0 (0) 293 (12) Vascular surgery 224 (4) 134 (9) 1 (0) 0 (0) 89 (4) Other accepting services 1,971 (34) 405 (28) 1 (0) 817 (100) 748 (31)
Table 1A. Demographics and clinical features of patients from all University of Maryland Medical Center units in 2018.
olume 24, o. 4: July 20 23
Predictors of Early Admission and Transfer to the CCRU Tran et
Table
critical care resuscitation unit; dL, deciliter; DM, diabetes mellitus; Fri, Friday; g, gram; HTN, hypertension; IQR, interquartile range; km, kilometer; µL, microliter; mmol, millimole; Mon, Monday; ng, nanogram; NA, not applicable; Sat, Saturday; SOFA, Sequential Organ Failure Assessment; SD, standard deviation; Sun, Sunday; WBC, white blood cell.
services for patients being transferred to the CCRU. Figure 2B illustrates the CCRU bed assignment at each time interval from transfer requests for respective accepting services.
Figure 3A demonstrates the time from transfer request and that ~50% of patients arrive at the CCRU within three hours. The time interval that patients arrive at the CCRU stratified by accepting service is represented in Figure 3B.
The covariates that were significantly associated with our primary outcome of interest—transfer request to bed assignment ≤8 minutes—are reported in Table 2. The full multivariate model is reported in Appendix 2. Patients requiring stroke neurology (odds ratio [OR] 5.49, 95% confidence interval [CI] 2.85-10.86, P < 0.001), with an increased SOFA score (OR 1.04, 95% CI 1.00-1.07, P =
0.047), and receiving surgical operation within 12 hours (OR 2.85, 95% CI 1.98-4.13, P < 0.001) were associated with immediate bed assignment time. However, patients who would receive any surgical intervention during hospitalization (OR 0.74, 95% CI 0.55-0.99, P = 0.044) were significantly less likely to have an immediate bed assignment time.
Secondary Outcome: Transfer Request to Arrival at the Critical Care Resuscitation Unit
We reported the statistically significant findings from our multivariate analysis of our secondary outcomes in Table 2 and the full multivariate models are available in Appendix 3. Factors significantly associated with increased likelihood of transfer request to CCRU arrival time <180 minutes were
Western Journal of Emergency Medicine 56
al.
Variables All patients Immediate bed assignment (≤ 8Minutes) Normal bed assignment (>8 Minutes) P† Total patients, N 1,422 712 710 NA Age (years), mean (SD) 57 (17) 58 (17) 57 (16) 0.72 Gender, N (%) Male 783 (55) 378 (53) 405 (57) 0.13 Female 639 (46) 334 (47) 305 (43) Past medical history, N (%) HTN 644 (45) 326 (46) 318 (45) 0.71 DM 347 (24) 165 (23) 182 (26) 0.28 Any liver disease 99 (7) 45 (6) 54 (8) 0.34 Any kidney disease 238 (17) 114 (16) 124 (17) 0.46 Any heart disease 315 (22) 157 (22) 158 (22) 0.93 Type of referring hospital, N (%) Teaching hospital 460 (32) 237 (33) 223 (31) 0.45 Non-teaching hospital 962 (68) 475 (67) 487 (69) Ground distance (km), mean (SD) 55 (56) 56 (58) 54 (54) 0.45 Transport by air, N (%) 240 (17) 157 (22) 83 (12) < 0.001 Transfer request details, N (%) Transfer request weekdays (Mon-Fri) 1046 (74) 517 (73) 529 (75) 0.42 Transfer request weekend (Sat-Sun) 376 (26) 195 (27) 181 (25) Transfer request at night 743 (52) 313 (44) 430 (61) < 0.001 Transfer request weekend night 208 (15) 103 (14) 105 (15) 0.86 Laboratory values WBC count (counts/µL), mean (SD) 14.28 (15.51) 14.60 (19.70) 13.96 (9.78) 0.44 Hemoglobin (g/dL), mean (SD) 11.5 (4.3) 11.7 (3.5) 11.4 (5.0) 0.13 Serum lactate (mmol/dL), mean (SD) 2.30 (2.32) 2.49 (2.59) 2.11 (2.00) 0.002 First troponin level (ng/L), median [IQR] 0.020 [0.010-0.110] 0.020 [0.010-0.120] 0.020 [0.010-0.100] 0.47 SOFA score, median [IQR] 3 [1-6] 3 [1-7] 2 [1-6] 0.001 †Bold cells indicate statistically significant findings (P < 0.05). CCRU,
1B. Demographics of accepted patients triaged to the critical care resuscitation unit.
olume 24, o. 4: July 20 23
Tran et al.
Predictors of Early Admission and Transfer to the CCRU

Table 1C. Clinical characteristics of accepted patients triaged to the critical care resuscitation unit.
†Bold cells indicate statistically significant findings (P < 0.05).
CCRU, critical care resuscitation unit; ECMO, extracorporeal membrane oxygenation; IQR, interquartile range; IR, interventional radiology; LOS, length of stay; min, minutes; NA, not applicable; OR, operating room.
CCRU,
757 Western Journal of Emergency Medicine
Variables All patients Immediate bed assignment (≤ 8Minutes) Normal bed assignment (>8 Minutes) P† Total patients, N 1,422 712 710 NA Transfer request to bed assignment (min), median [IQR] 8 [0-70] 0 [0-3] 70 [22-254] < 0.001 Transfer request to arrival (min), median [IQR] 174 [115-290] 131 [93-183] 253 [163-447] < 0.001 CCRU LOS (hours), median [IQR] 7 [4-18] 6 [3-15] 8 [4-19] < 0.001 Continuous infusion, N (%) Any anti-hypertensive 184 (13) 110 (15) 74 (10) 0.005 Insulin 189 (13) 92 (13) 97 (14) 0.68 Invasive mechanical ventilation on arrival 471 (33) 264 (37) 207 (29) 0.002 Any blood transfusion on arrival 146 (10) 80 (11) 66 (9) 0.23 Type of procedure, N (%) Cannulation for ECMO 25 (2) 15 (2) 10 (1) 0.32 Intra-aortic balloon pump 15 (1) 4 (1) 11 (2) 0.07 IR 29 (2) 18 (3) 11 (2) 0.19 Other procedure 30 (2) 20 (3) 10 (1) 0.07 Any surgical intervention 776 (55) 364 (51) 412 (58) 0.009 To OR within 12 hours 324 (23) 192 (27) 142 (20) 0.002 Patients’ dispositions, N (%) Discharge home 580 (41) 269 (38) 311 (44) Acute rehab 327 (23) 182 (26) 145 (20) Skilled nursing home 253 (18) 116 (16) 137 (19) 0.014 Dead or hospice 218 (15) 123 (17) 95 (13) Other 44 (3) 22 (3) 22 (3)
Figure 2. Kaplan-Meier curve for bed assignment to the CCRU (A) Time intervals for bed assignment to the CCRU for all patients. (B) Comparison of time intervals for bed assignment to the CCRU based on accepting service.
* The 50% mark indicates the censored time.
olume 24, o. 4: July 20 23
critical care resuscitation unit; MICU, medical intensive care unit.
patients being accepted by stroke neurology (OR 12.81, 95% CI 6.09-28.51, P < 0.001) and being taken to the OR for emergent surgical intervention (OR 3.15, 95% CI 2.12-4.71, P < 0.001). Higher SOFA score (OR 0.96, 95% CI 0.92-0.99, P = 0.033) was associated with decreased likelihood of arrival within 180 minutes.
Other Outcome: Predictors for Mortality Among Patients Transferred to the CCRU
The statistically significant covariates are presented in Table 2 for the outcome of mortality and the result of the complete multivariate logistic regression is available in Appendix 3. Accepting services associated with a significant likelihood of mortality were neurosurgery (OR 4.14, 95% CI 1.87-9.37, P < 0.001) and stroke neurology (OR 3.00, 95% CI 1.20-7.52, P = 0.019). Each gram per deciliter increase in hemoglobin was protective and associated with 12% decreased risk of death (OR 0.88, 95% CI 0.80-0.95, P = 0.002).
All of the model’s Hosmer–Lemeshow goodness of fit tests returned P > 0.05, indicating the data fit the models well, and all VIF values for each covariate were <5 indicating that multicollinearity was not present.
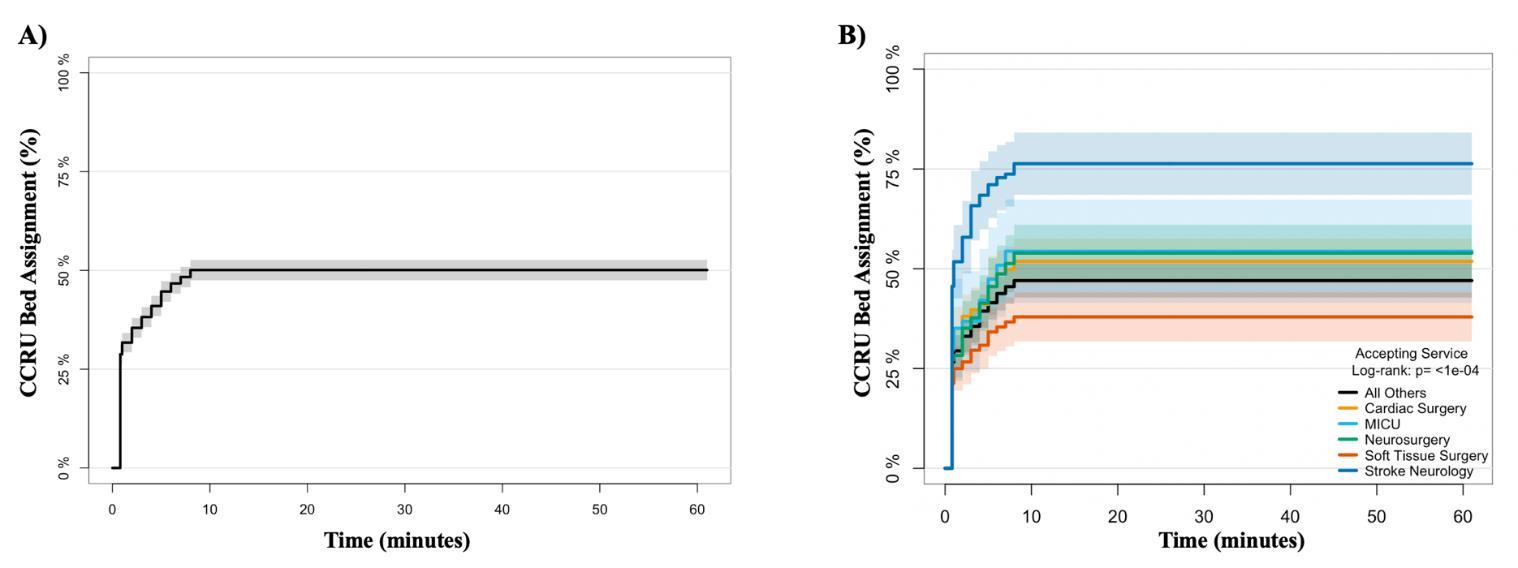
DISCUSSION
When originally conceptualized, the purpose of the CCRU similar to the model of trauma transfer was to provide “immediate ICU access to accommodate IHT with time-sensitive surgical critical illness,” while “decreasing lost admissions, minimizing transfer times, and improving outcomes of known trauma critical care transfers.”4 Having demonstrated a significant increase in the volume of transfers, decreased transfer times, and decreased time to operative intervention, the CCRU expanded its patient population, including other critical care emergencies requiring intervention, such as acute ischemic stroke caused by large
vessel occlusion and coronary interventions.4,9,10 While formalized systems exist for patients transferred between hospitals with traumatic etiologies, ST-segment elevation myocardial infarction and stroke, there are no formal systems to ensure timely transfer for other highly morbid, highly fatal, and time-sensitive conditions, including acute aortic diseases, toxicologic, obstetric, septic, respiratory, and other vascular emergencies. The CCRU demonstrates that such a regionalized ICU is feasible, although further studies are necessary to elucidate how units like the CCRU could affect the operations of referring hospitals.
In general, the literature supports the conclusion that patients with critical illness or time-sensitive diseases should be referred to large-volume centers with multiple advanced modalities and therapeutic options that are not available at most acute care hospitals.14 However, bed availability is usually a prime factor in the delay of care for these patients as ICU bed utilization in most hospitals is not oriented toward the acceptance of outside transfers. Furthermore, there is no formal system to triage and prioritize the transfer of these patients. Therefore, immediate acceptance to an ICU bed is difficult for most units, and a significant amount of time and uncertainty is lost in the interim between initial consult and eventual bed assignment. A traditional ICU may need to decide whether to leave a bed open, while other critically ill patients wait in the ED or other part of the hospital. On the other hand, a traditional ICU may fill all the available beds and then waitlist patients from other hospitals.
The CCRU offers solutions to avoid many problems that traditional ICUs face when they are confronted with an emergent bed request. One of our guiding principles is to maintain bed availability continuously for emergent transfer requests for patients with all disease states. The CCRU has been largely successful in being able to accommodate appropriate requests for emergent transfer by maintaining
Western Journal of Emergency Medicine 758 Predictors of Early Admission and Transfer to the CCRU Tran et al.
Figure 3. Kaplan-Meier curve for arrival at the CCRU: (A) Time intervals for all patients arriving to the CCRU. (B) Comparison of time intervals from arrival to the CCRU based on accepting service. CCRU, critical care resuscitation unit; MICU, medical intensive care unit.
olume 24, o. 4: July 20 23
Tran et al.
Predictors of Early Admission and Transfer to the CCRU
Table 2. Multivariate logistic regression measuring association of demographic and clinical factors with the primary outcome of transfer request to bed assignment ≤8 minutes and the secondary outcomes of transfer request to CCRU* arrival < 180 minutes and mortality
Multivariate regression results
*Only variables with significant association with the outcome of interest are reported (P < 0.05).
CI, confidence interval; CCRU, critical care resuscitation unit; g/dL, grams per deciliter; LL, lower limit 95% CI; mmol/dL, millimole per deciliter; ng, nanogram; OR, odds ratio; OR, operating room; SOFA, Sequential Organ Failure Assessment; UMMC, University of Maryland Medical Center; UL, upper limit 95% CI.
effective flow management through the entire system with institutional support.
In this study we investigated the triage process and the prioritization of patients who needed to be transferred for higher levels of care. We evaluated patient characteristics and logistical factors associated with rapid acceptance and transfer to the CCRU by comparing those patients with immediate assignment vs those who waited a more standard time for
bed assignment after initial consult. Not surprisingly, those patients with immediate bed assignment were more likely to have a more rapid arrival, arrive by air, and undergo surgical interventions within 12 hours of arrival. These patients also had higher SOFA scores and were more likely to be mechanically ventilated or receiving continuous infusions. All these characteristics are arguably markers found in those illnesses requiring more time-sensitive intervention,
59 Western Journal of Emergency Medicine
Variables OR 95% CI LL 95% CI UL P Primary Outcome: Transfer Request to Bed Assignment ≤ 8minutes Accepting service – Stroke neurology 5.487 2.852 10.858 < 0.001 Need for OR within 12 hours 2.847 1.977 4.125 < 0.001 CCRU transfer request – Day 2.351 1.759 3.153 < 0.001 CCRU transfer request – Weekend night 2.248 1.279 3.958 0.005 Arrival SOFA score – each increment 1.036 1.001 1.073 0.047 Any OR 0.738 0.549 0.991 0.044 Accepting service – Soft tissue surgery 0.593 0.352 0.997 0.049 Secondary Outcome: Transfer Request to CCRU Arrival < 180 minutes Accepting service – Stroke neurology 12.814 6.092 28.510 < 0.001 Need for OR within 12 hours 3.146 2.120 4.711 < 0.001 Accepting service – Neurosurgery 2.813 1.575 5.075 < 0.001 Accepting service – Pulmonary critical care 2.415 1.098 5.411 0.029 Accepting service – Vascular surgery 1.897 1.053 3.442 0.033 Accepting service – Cardiac surgery 1.865 1.126 3.115 0.016 Any infusion on arrival 1.712 1.292 2.274 < 0.001 CCRU transfer request – Day 1.428 1.048 1.949 0.024 Serum lactate – each mmol/dL 1.080 1.011 1.156 0.025 Distance from UMMC – each kilometer 0.991 0.988 0.995 < 0.001 Arrival SOFA score – each increment 0.960 0.924 0.996 0.033 Transport type – ground 0.195 0.126 0.296 < 0.001 Any OR 0.712 0.520 0.974 0.033 Secondary Outcome: Mortality Accepting service – Neurosurgery 4.137 1.870 9.365 < 0.001 Accepting service – Stroke neurology 3.002 1.196 7.523 0.019 Arrival SOFA score – each increment 1.265 1.202 1.333 < 0.001 Serum lactate – each mmol/dL 1.153 1.068 1.251 < 0.001 Age – each year 1.037 1.023 1.052 < 0.001 Arrival troponin – each ng/L 1.010 1.003 1.020 0.016 Hemoglobin – each g/dL 0.875 0.804 0.950 0.002
olume 24, o. 4: July 20 23
Predictors of Early Admission and Transfer to the CCRU Tran et al. resuscitation, or higher care intensity and, therefore, highest priority for immediate bed assignment. Furthermore, the time-sensitive nature for those patients who require timely intervention and resuscitation is likely the main driver of early transfer and would seemingly affect their outcomes.
The triage and prioritization process for early CCRU bed assignment and transfer may have explained previous observations regarding critically ill patients’ outcomes. Previously, we have shown that patients requiring higher critical care intensity who were transferred from other hospitals’ EDs to the CCRU were associated with lower likelihood of mortality when compared with those admitted to other traditional adult non-trauma ICUs in our own medical center. 10 Similarly, patients who received early intervention at an ED-based resuscitation unit were also associated with lower 30-day mortality. 15 Thus, our triage process eliminated lost time and uncertainty for the referring clinicians, while potentially optimizing patients’ outcomes.
In this study, the severity and characteristics of patients requiring immediate bed assignment were largely supported by the primary and secondary outcome analyses. Criteria such as the severity of illness, as indicated by high SOFA scores, needing operative intervention within 12 hours, and admission of these patients to the stroke neurology service at a comprehensive stroke center, are plausible factors to necessitate immediate bed assignment. Similarly, when predicting which patients would be associated with a higher burden of morbidity and mortality, those with emergent need for neurosurgical and stroke intervention seem natural candidates and an intuitive choice. Patients with strokes have a time-sensitive disease if the patient is a candidate for mechanical thrombectomy (eg, occlusion in a large vessel such as the middle cerebral artery or internal carotid artery); thus, they would be prioritized by the CCRU team during triage.
Minimizing the time from symptom onset to reperfusion for candidates of mechanical thrombectomy is known to impact patient outcomes; thus, the CCRU is designed to expedite transfer for these patients in conjunction with our comprehensive stroke center.16 Hemorrhagic stroke would also be another reason patients are prioritized if they require interventions to prevent increased intracranial pressure. Furthermore, severity of illness is directly linked to mortality; therefore, it is not surprising that arrival SOFA score, high serum lactate, age, and troponin would be the multivariate factors predictive for mortality, as each can reasonably be associated with mortality itself in undifferentiated critical illness.
The time intervals from transfer request to CCRU arrival for the early arrival group is multifactorial. As our institution is a comprehensive stroke center, it is not surprising that the strongest factor for a patient arriving rapidly to our medical center is for emergent intervention by the stroke neurology team. Similarly, those patients needing emergent evaluations and interventions by neurosurgery, vascular surgery, and cardiac surgery, as well as other patients requiring
any medication infusion and those resulting in operative intervention within 12 hours would be priorities for transfer in most situations. On the other hand, those patients who were requested for transfer during daylight hours would theoretically undergo early surgical interventions upon arrival, and these patients would also benefit from the higher nursing staffing and resources available when compared to nighttime levels at most institutions.17
Given the complexity and myriad of factors that play a role in the transport of patients to our center, distance and ground transport negatively affecting the intervals between transfer request and arrival time are appropriate. Similarly, patients who would need to be transferred for non-urgent but complex surgical interventions that are only available at a quaternary medical center may not need to be transferred immediately, thereby explaining how those patients undergoing any operative intervention during their hospitalization at our medical center did not arrive at the CCRU within 180 minutes. However, patients having higher arrival SOFA score, but not an elevated serum lactate, did not arrive to the CCRU early. This was a curious and counterintuitive finding that warrants further study. It is probable that patients who were critically ill with high SOFA scores were associated with prolonged stabilization before patients could be stable for transfer; thus, it could have taken them longer to be transferred, although a bed was already ready for them.18,19
Single elevation of lactate could be multifactorial from several conditions, including but not limited to status epilepticus or hypovolemia. Therefore, those patients can be evaluated along the way with resuscitation at the referring center. Typically, lactate can be cleared with prompt and effective treatment. Upon evaluation of a patient for transfer to the CCRU, a CCRU attending asks about factors such as ventilator mode, arterial blood gas(es), resulted laboratory values, and vasopressor requirements, among other factors, so that a mental picture can be created of the patient’s SOFA score prior to arrival. The SOFA score is a composite metric that involves a patient’s neurologic, cardiac, renal, hematologic, and hepatic status. All components of the SOFA score will be asked at the time of transfer request and then an idea will be formed of how critically ill the patient is. This will then become more objective when a SOFA score is calculated when the patient arrives. Based on the clinical picture of the patient, the CCRU attendings will prioritize how soon a patient will come to the CCRU and their bed assignment time. Lactate does play a role in prioritization but only if lactate is elevated and caused by a condition that requires intervention at a quaternary care center such as elevation caused by an ischemic limb, ischemic bowel, or severe acute respiratory distress syndrome requiring ECMO, among other conditions.
One peculiarity throughout the modeling is the negative association with any operative intervention or acceptance by our soft tissue surgery service. This potential inconsistency is likely a result of our policy for the admission and management of patients with soft tissue infection. The R Adams Cowley
Western Journal of Emergency Medicine 6
olume 24, o. 4: July 20 23
Shock Trauma Center at the University of Maryland is a regional referral center for soft tissue infections and surgery. During the day between 7 am and 5 pm, all surgical operations and transfer requests are handled by the regular soft tissue surgery team, which is staffed by our trauma surgeons who specialize in soft tissue infection. The service is covered during overnight hours by the on-call trauma service.
To avoid taking the attention of trauma surgeons away from the critically ill trauma patients, our clinical practice is to admit all patients with soft tissue infections to the CCRU first, thus allowing our critical care staff to evaluate and manage these complex patients. Unless these patients need urgent surgical intervention, which the trauma surgeons will carry out, these patients will otherwise undergo scheduled operations, as clinically indicated, at a later day with the regular soft tissue surgeons. Therefore, while the acuity of those patients who have necrotizing fasciitis would be high and would require urgent interventions and immediate bed assignment, most patients with soft tissue infections do not require immediate surgical intervention at arrival, either because they have received an initial debridement at the referring hospital or they have an intermediate acuity disease state (eg, cellulitis, abscess, etc) that warrants longer wait times for transport and subsequent surgical interventions at a later time. Nevertheless, the patients with soft tissue infections, which represent approximately 13% of our population, could partly explain these observations. Future studies specifically involving patients with soft tissue infection are needed to further investigate this phenomenon.
LIMITATIONS
Our study has several strengths, as well as some limitations that should be highlighted. We only focused on the patients who were accepted to the CCRU; we did not have data regarding patients who were not accepted to the CCRU. When the CCRU reaches its capacity and immediate bed assignment is not possible, referring clinicians may opt to contact other tertiary facilities to transfer their patients. Our study involved a large and heterogenous patient population; therefore, we had to categorize patients according to the accepting services and could not identify the individual disease states that would necessitate immediate bed assignment. For example, all patients who were admitted to our medical intensive care unit were categorized as being accepted by the pulmonary and critical care service. These patients could span a variety of conditions, such as respiratory failure, gastrointestinal bleeding, septic shock, etc. Finally, we used the SOFA score as a surrogate marker for disease severity, but it does not apply to all disease states, such as patients with stroke or spontaneous intracerebral hemorrhage.
CONCLUSION
Our study showed that patients who had high acuity or required urgent surgical intervention, such as patients
with ischemic stroke, were given highest priority to have immediate bed assignments at the CCRU. However, patients who had high SOFA scores or were referred during overnight hours were associated with longer intervals between transfer request to arrival at the CCRU. Further studies are necessary to confirm our observations and to investigate the relationship between this group of patients and their outcomes.
Address for Correspondence: Quincy K. Tran, MD, PhD, University of Maryland School of Medicine, Department of Emergency Medicine, 22 South Greene Street, Suite T3N45, Baltimore, MD 21201. Email: qtran@som.umaryland.edu.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
Copyright: © 2023 Tran et al. This is an open access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) License. See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1. Iwashyna TJ, Christie JD, Moody J, et al. The structure of critical care transfer networks. Med Care. 2009;47(7):787-93.
2. Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Crit Care Med. 2012;40(8):2470-8.
3. Barnato AE, Kahn JM, Rubenfeld GD, et al. Prioritizing the organization and management of intensive care services in the United States: the PrOMIS Conference. Crit Care Med. 2007;35(4):1003-11.
4. Scalea TM, Rubinson L, Tran Q, et al. Critical care resuscitation unit: an innovative solution to expedite transfer of patients with time-sensitive critical illness. J Am Coll Surg. 2016;222(4):614-21.
5. Rincon F, Mayer SA, Rivolta J, et al. Impact of delayed transfer of critically ill stroke patients from the emergency department to the neuro-ICU. Neurocrit Care. 2010;13(1):75-81.
6. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897-903.
7. Zdanowski Z, Danielsson G, Jonung T, et al. Outcome of treatment of ruptured abdominal aortic aneurysms depending on the type of hospital. Eur J Surg. 2002;168(2):96-100.
8. Tran QK, Dave S, Haase DJ, et al. Transfer of patients with spontaneous intracranial hemorrhage who need external ventricular drain: Does admission location matter? West J Emerg Med 2021;22(2):379-88.
9. Tran QK, Yarbrough KL, Capobianco P, et al. Comparison of outcomes after treatment of large vessel occlusion in a critical care resuscitation unit or a neurocritical care unit. Neurocrit Care
61 Western Journal of Emergency Medicine
et al.
Tran
Predictors of Early Admission and Transfer to the CCRU
olume 24, o. 4: July 20 23
Predictors of Early Admission and Transfer to the CCRU Tran et al.
2020;32(3):725-33.
10. Tran QK, O’Connor J, Vesselinov R, et al. The critical care resuscitation unit transfers more patients from emergency departments faster and is associated with improved outcomes. J Emerg Med 2020;58(2):280-289.
11. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448-51.
12. Lowenstein SR. Medical record reviews in emergency medicine: the blessing and the curse. Ann Emerg Med. 2005;45(4):452-5.
13. van Smeden M, de Groot JA, Moons KG, et al. No rationale for 1 variable per 10 events criterion for binary logistic regression analysis. BMC Med Res Methodol. 2016;16(1):163.
14. Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med 2003;349(22):2117-27.
15. Gunnerson KJ, Bassin BS, Havey RA, et al. Association of an
emergency department-based intensive care unit with survival and inpatient intensive care unit admissions. JAMA Netw Open 2019;2(7):e197584.
16. Jahan R, Saver JL, Schwamm LH, et al. Association between time to treatment with endovascular reperfusion therapy and outcomes in patients with acute ischemic stroke treated in clinical practice. JAMA 2019;322(3):252-63.
17. Dhaini SR, Simon M, Ausserhofer D, et al. Trends and variability of implicit rationing of care across time and shifts in an acute care hospital: a longitudinal study. J Nurs Manag. 2020;28(8):1861-72.
18. Strauch U, Bergmans DC, Winkens B, et al. Short-term outcomes and mortality after interhospital intensive care transportation: an observational prospective cohort study of 368 consecutive transports with a mobile intensive care unit. BMJ Open. 2015;5(4):e006801.
19. Loftus TJ, Wu Q, Wang Z, et al. Delayed interhospital transfer of critically ill patients with surgical sepsis. J Trauma Acute Care Surg 2020;88(1):169-75.
Western Journal of Emergency Medicine 62
olume 24, o. 4: July 20 23
ArterialMonitoringinHypertensiveEmergencies: SignificancefortheCriticalCareResuscitationUnit
QuincyK.Tran,MD,PhD†‡§
DominiqueGelmann,MD*
ManahelZahid,BS§
JamiePalmer,BS*
GraceHollis,BS§
EmilyEngelbrecht-Wiggans,MS*
ZainAlam,BS§
AnnElizabethMatta,CRNP†
EmilyHart,CRNP†
DanielJ.Haase,MD†‡
SectionEditor: DavidPage,MD
*UniversityofMarylandSchoolofMedicine,Baltimore,Maryland
† UniversityofMarylandSchoolofMedicine,PrograminTrauma, TheRAdamsCowleyShockTraumaCenter,Baltimore,Maryland
‡ DepartmentofEmergencyMedicine,UniversityofMarylandSchoolof Medicine,Baltimore,Maryland
§ UniversityofMarylandSchoolofMedicine,DepartmentofEmergency Medicine,TheResearchAssociatePrograminEmergencyMedicineand CriticalCare,Baltimore,Maryland
Submissionhistory:SubmittedNovember8,2023;RevisionreceivedApril11,2023;AcceptedApril21,2023
ElectronicallypublishedJuly17,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59373
Introduction: Bloodpressuremeasurementisimportantfortreatingpatients.Itisknownthatthereisa discrepancybetweencuffbloodpressurevsarterialbloodpressuremeasurement.Howeverfewstudies haveexploredtheclinicalsignificanceofdiscrepanciesbetweencuff(CPB)vsarterialbloodpressure (ABP).OurstudyinvestigatedwhetherdifferencesinCBPandABPledtochangeinmanagementfor patientswithhypertensiveemergenciesandfactorsassociatedwiththischange.
Methods: ThisprospectiveobservationalstudyincludedadultpatientsadmittedbetweenJanuary 2019–May2021toaresuscitationunitwithhypertensiveemergencies.Wedefinedclinicalsignificance ofdiscrepanciesasadiscrepancybetweenCBPandABPthatresultedinchangeofclinical management.Weusedstepwisemultivariablelogisticregressiontomeasureassociationsbetween clinicalfactorsandoutcomes.
Results: Of212patientsweanalyzed,88(42%)hadchangeinmanagement.Meandifferencebetween CBPandABPwas17milligramsofmercury(SD14).Increasingtheexistingrateofantihypertensive infusionoccurredin38(44%)patients.Higherbodymassindex(oddsratio[OR]1.04,95%confidence Interval[CI]1.0001–1.08, P-value <0.05)andhistoryofperipheralarterialdisease(OR0.16,95%CI 0.03–0.97, P-value <0.05)werefactorsassociatedwithclinicalsignificanceofdiscrepancies.
Conclusion: Approximately40%ofhypertensiveemergencieshadaclinicalsigni fi canceof discrepancywarrantingmanagementchangewhenarterialbloodpressurewasinitiated.Further studiesarenecessarytocon fi rmourobservationsandtoinvestigatethebene fi t-riskratioofABP monitoring.[WestJEmergMed.2023;24(4)763 –773.]
INTRODUCTION
Bloodpressure(BP)monitoringisanessentialcomponent ofmanaginghypertensivediseaseprocesses,manyofwhich requiremaintenanceofspecificBPwindows.Intra-arterial bloodpressure(ABP)monitoringiswidelyconsideredthe
goldstandardofBPmeasurementincriticalcaresettings; however,itsinvasivenaturealsopresentssomerarebut seriousrisksincludingbleeding,thrombosis,infection, embolism,andnervedamage.1,2
Additionally,littleresearch hasbeendonetodemonstratewhetheritsuseisassociated
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 763
ORIGINAL RESEARCH
withchangesinclinicalmanagementwhencomparedto noninvasivecuffbloodpressure(CBP)monitoring,suchas oscillometricCBPmeasurement.Therefore,thenecessityof ABPmonitoringhasbeenquestioned.3,4
Previousstudieshaveshown,however,thatdiscrepancies existbetweennoninvasiveCBPandinvasiveABP measurement.5–12
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Discrepancybetweenarterial(ABP)vscuff bloodpressure(CBP)monitoringexists. CBPiscommonlyusedalthoughABP monitoringisconsideredthegoldstandard.
Whatwastheresearchquestion?
Doesadiscrepancybetweenthetwoblood pressuremonitoringmodalitiesresultin changeofclinicalmanagement?
25
AccuracyofCBPmeasurementmaybe affectedbyobesity,cufflocation,age,andarterial stiffness.13–16 AccuratemeasurementofBPisimportant,as briefepisodesofeitherhypotensionorhypertensionare associatedwithhigherratesofmortalityandother unfavorableoutcomesinvariouscriticalillnesses.17–22 Useof CBPgenerallyunderestimatesintra-arterialsystolic(SBP)in hypertensivediseases,whichmayleadtomismanagementof patientswithconditionsrequiringadherencetospecificBP guidelines.6,10,23
Additionally,ABPmonitoringoffersthe benefitofreal-timecontinuousmonitoring,whilecuff measurementsaretypicallyperformedintermittently.
Guidelinesestablishedbyseveralprofessionalsocieties recommendspecificBPgoalsforvarioushypertensivedisease states.Forexample,currentguidelinesformanagementof acuteaorticdiseasessuggestaSBPgoalof <120millimetersof mercury(mmHg)inTypeAdissectionandSBPgoalof <140mmHginTypeBdissection.26 Additionalguidelines existforischemicstroke,27 spontaneousintracerebral hemorrhage,28 andpreeclampsia,29 amongothers.As previouslydiscussed,operatingwithinasafeBPmarginhas importantclinicalimplications.Forexample,inpatientswith acuteaorticpathology,bothhypotensionandhypertensionare associatedwithincreasedmortalityrisk.18,21,22 Thishighlights theimportanceofaccuratecontinuousBPmeasurement tomaintainpressureswithinspecificparameters.
Afewpreviousstudiesprovideevidencefortheutilityof ABPmonitoringinhypertensivecriticallyillpatients. ManiosetalfoundthatCBPmeasurementsunderestimate ABPinpatientswithischemicstroke,mostmarkedlyinthose withcriticallyhighSBP.11
AretrospectivestudybyRaffman etaldemonstratedthatnearlyoneinthreepatientswith hypertensivediseaseadmittedtoaresuscitationunithada differencebetweenABPandCBPthatwouldresultina changeinclinicalmanagement.6 However,thesestudieswere limitedbysmallsamplesizeortheuseofhypothetical definitionsofchangeinmanagement,respectively.
Ourprospectivestudysoughttoinvestigatetheclinical significanceofthedifferencebetweenABPmonitoringvs CBPmonitoring,inrealtime,amongpatientswith hypertensivecriticalillnesses.Wespecificallyaimedto determinewhetherthedifferenceinmonitoringbetweenCBP andABPwouldresultinchangeinclinicalmanagementfor patientswithhypertensiveemergenciesandtoidentify clinicalfactorspredictingchangeinmanagementbetween thetwomeasurementmodalities.Wehypothesizedthatthe differencebetweenmonitoringofABPandCBPvalues
Whatwasthemajor findingofthestudy? 88patients(42%)hadachangeof managementinrealtimeresultingin increasingdosesofantihypertensive medication.
Howdoesthisimprovepopulationhealth?
Inapatientwithhypertensiveemergency whosebloodpressureisatborderlineof recommendedguidelines,ABPshouldbe considered.
wouldleadtoachangeinBPmanagementinatleast30%of ourpatientswithhypertensiveemergencies.
METHODS StudySetting
Thisprospectiveobservationalstudytookplaceinthe criticalcareresuscitationunit(CCRU),anintensivecareunit (ICU)-basedresuscitationunitthatwascreatedatour quaternary-careinstitutionwiththegoalofexpediting transferofpatientswithtime-sensitivecriticalillnessesfrom otherhospitalswhentherearenoavailablebedsatoneofour traditionalICUs.30,31 Thesepatients’ criticalillnessesusually exceedthecapabilityofthesendinghospitals;so,upontheir arrivalattheCRRU,theyreceiveimmediateresuscitation andtimelyICU-levelcare.Oncepatientsarestabilized,they aremovedtoappropriateinpatientbeds.PerCCRUclinical policy,allpatientsreceivingantihypertensivemedication infusionorrequiringhemodynamicmonitoringwillneed ABPmonitoring,andanarterialcatheterisplacedupon arrivaltotheunit.TheCCRUclinicianswouldplacea majorityofarterialcannulations,incompliancewithour institutionalprotocolsformaximumsterility.Thestudywas approvedbyourinstitutionalreviewboard(HP-00079864) andwasexemptedfromformalconsent.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 764 ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU Tranetal.
PatientSelection
Weincludedconsecutiveadultpatientswithany hypertensiveemergencydiagnosis(ischemicstroke, spontaneousintracerebralh emorrhage,acuteaortic diseases)whorequiredABPmonitoringuponadmissionto theCCRUbetweenJanuary2019 – May2021.Patientswho hadCBPandABPmeasurementswithin60minutesofeach otherwereeligible.Exclusioncriteriaincludedthe following:arterialcatheterinplacepriortoarrival; arterialcatheterandBPcuffplacementonoppositesideof body(ie,cuffpressureonleftarmwhilearterialcatheterin rightradialartery);unrelia blearterialmeasurements accordingtotheclinicians;useofvasopressorspriortoor startingatthetimeofarterialcatheterplacement.We additionallyexcludedpatientswithnon-hypertensive diagnoses(eg,sepsis,organischemia,pancreatitis, anybleeding,respiratoryfailure).Weexcludedthese patientsbecausetheirBPsa remanageddifferently. Patientswhorequirevasopressorsorhavenonhypertensivediagnosesaremanagedinaccordance withtheirmeanarterialpressure,insteadofSBP,as recommendedbypreviousmanagementguidelinesfor hypertensiveemergencies.
ProspectiveDataCollection
Priortothestudyrecruitmentperiod,wecreateda standardizedformandeducatedtheCCRUclinicians (nursingstaff,advancedpracticepractitioners,residents, fellowphysicians)ontheuseoftheformforallpatients requiringarterialcatheterplacement.MostoftheCCRU nursingstaffwereblindedtothestudyhypothesisandwere notinvolvedinpreparationofthemanuscript.Theform containedsectionsforclinicianstorecordpatient demographicinformation(age,gender,medicalrecord number,diagnosis,goalofBP),CBPvalues,ABPvalues, arterialcathetersite(right/leftradialorfemoral),cuffsite (right/leftarmorleg),andmanagementdecisionsasguided byeachBPvalue.
Beforeplacingthearterialcatheter,theCCRUnurseor theclinicianprospectively filledouttheforminrealtimeto indicateCBPvaluesimmediatelyandtheassociated managementaccordingtotheCBPmonitoringvalues (eg,decreasenicardipineinfusionfrom7.5milligramsper hour[mg/hr]to5mg/hr).Afterarterialcatheterplacement, thecliniciansadditionallyrecordedtheABPmonitoring valuesandthemanagementdecisionguidedbthosevalues (eg,increasenicardipineinfusionfrom7.5mg/hourto 10mg/hour,etc).AnAPPandtheprincipalinvestigator adjudicatedthemissingdataontheprospectivedata collectionform,usingpatients’ electronichealthrecords (EHR).Weidentifiedapproximately23patients(11%)who didnothaveadiagnosisthatrequiredABPmonitoringinthe CCRU.Theseincluded14patientswithaorticaneurysms andnineotherdiagnoses.
RetrospectiveDataCollection
Membersoftheresearchteamretrospectivelycollected additionalpatientdatafromourinstitution’sEHR. Extracteddemographicinformationincludedage,gender, bodymassindex(BMI),andpastmedicalhistory.Theyalso collectedclinicaldataduringhospitalization,includinglab values(serumcreatinineandlactate),echocardiography results(ejectionfraction,presenceofleftventricular hypertrophy),medicationsusedatthetimeofarterial cannulation,andpatientoutcomes(deceased,dischargedto home,dischargedtoacuterehabilitationfacility,etc). Additionally,theycollectedinformationregarding complicationsassociatedwitharterialcathetercannulations andtotaldurationofarterialcatheterinsertion.Wedefined arterialcathetercomplicationsasbleeding,aneurysm, extremitynecrosis,localnervedamage,ordefinitivesource oflocalorsystemicinfectionorembolism.32 Wehadplanned toimputeanymissingretrospectivedatawiththe population’smean;however,nodatawasmissingasallthe recordeddatawaspartoftheclinicalstandardofcare.
Weobtainedallretrospectivedataincompliancewith methodologicstandardsformedicalrecordreview.33
Membersoftheresearchteamwerenotblindedtothestudy hypothesis.Eachinvestigatorreceivedtrainingindata extractionfrompatientrecordsandinputdataintoa standardizedExcelspreadsheet(MicrosoftCorporation, Redmond,WA).Toreducebias,investigatorscollected specificsubsetsofdataonly;forexample,thosewhorecorded hospitaloutcomesdidnotcollectBPmeasurementsorlab valuesandviceversa.Theseniorinvestigatorreviewedthe accuracyofdataduringthetrainingphasetoensuregreater than90%agreementbeforeteammembersstarteddata collection.Additionally,theseniorinvestigatorrandomly recheckedupto20%ofthecollecteddatatoensureaccuracy throughouttheprocess.
OutcomeMeasures
Ourprimaryoutcomewastheprevalenceofclinically significantdifferencebetweenmeasurementsofABPand CBPmonitoring.Wedefinedthisasadifferenceinclinical managementbasedonthevaluesobtainedfromABPvsCBP monitoring,asdeterminedinrealtimebythecliniciansupon placementofthearterialcatheters.Forexample,the AmericanHeartAssociationTaskForceonPractice GuidelinesrecommendsaSBPof ≤120mmHgfortypeA aorticdissection.26 Weidentifiedclinicallysignificant differenceasadifferencebetweenABPandCBPthat resultedinachangeinBPmanagementtoadhereto theseguidelines.
IfapatientwithTypeAaorticdissectionhadCBPof 115mmHgandABPof125mmHg,thedifferenceinBP measurementsnecessitatedachangeinmanagementbetween thetwomodalities.Inthiscase,theCBPvalueindicatedthe SBPwasatgoalandnofurtheractionwasneeded.In
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 765 Tranetal. ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU
contrast,theABPsuggestedthatincreasingthedoseofthe currentantihypertensiveinfusionwaswarranted. Alternatively,ifthepatienthadCBPof135mmHgandABP of145mmHg,theclinicianindicatedthatbothvalues requiredincreasingthedoseofcurrentantihypertensive infusion,inaccordancewiththeguidelinestolowerSBPto ≤120mmHg.Thus,thisactionindicatedthatnoclinically significantdifferenceexisted.
Oursecondaryoutcomesincludedmeandifference betweenCBPmonitoringandABPmonitoringandthe percentageofpatientswithdifferenceof ≥20mmHg betweenthetwomodalities.Giventhatpreviousguidelines suggestedthatpatientswithadifferenceof ≥20mmHg maybeatriskforworseoutcomesthanthosewitha difference ≤20mmHg,34 wedeterminedthiscutoffto beasigni fi cantdifferenceinthisstudy.Weadditionally reportedfactorsassociatedwitheithertheprimaryor secondaryoutcomes.

SampleSizeCalculation
Wecalculatedoursamplesizeaccordingtoapriorstudy fromRuszala.10 Basedonthisstudy,whichreportedthat ABPmonitoringwasassociatedwithapproximately20% higherprevalenceofpatientswhoreceivedmorefrequent interventionsduringtransport,wecalculatedthatwewould need97patientsineachgroup(total194patients)todetecta differenceof20%ofprevalenceofclinicalmanagement betweenCBPandABPmonitoring,witha = 0.05andpower of80%.
DataAnalysis
Weuseddescriptiveanalysistopresentpatientdata. Categoricalvariablesarepresentedaspercentages,and continuousvariablesarereportedasmean(+/-SD)ormedian (interquartilerange),asapplicable.Weanalyzeddifferences
betweengroupsofcontinuousvariablesusingtheStudent t -testorMannWhitneyUtest,whilethechi-squaretestwas usedforcategoricalvariables.
TographicallyrepresentthedistributionsofABPand CBPmonitoringdifferences,weusedtheBland-Altman analysis.TheY-axisoftheBland-Altmangraphsdepicted thevaluesof[ABP-CBP]differences.IfABPvaluesare >CBPvalues,therewouldbemoredotsinthepositiveregion oftheY-axis.TheX-axisrepresentedtherangesof patients’ CBPmonitoringvalues.Adisperseddistribution alongtheX-axiswouldsuggestthatthedifferences between[ABP-CBP]occurredatallrangesofCBP monitoringvalues.
Weusedforwardstepwisemultivariablebinarylogistic regressionstoidentifyassociationsbetweenindependent variablesandtheoutcomes(clinicallysignificantdifference, ABP-CBPdifference >20mmHg).Weaprioridetermined theindependentvariablesincludedinregressionanalysis, whicharelistedin Appendix1.Goodness-of-fit, multicollinearity,anddiscriminatorycapabilityofthe multivariablelogisticregressionmodelswerealsoassessed.A Hosmer-Lemeshowtestwith P -value > 0.05indicatesa modelwithagood fitofindependentvariables.Wereported thevarianceinflationfactors(VIF)forassessmentofthe multicollinearityofindependentvariables,andfactorswith VIF ≥5wereconsideredtohavehighmulticollinearityand thuswereremovedfromthelogisticregression.The discriminatorycapabilityoftheregressionswasassessedvia theareaunderthereceiveroperatingcurve(AUROC). ModelswithAUROCapproaching 1or +1were consideredhavingperfectdiscriminatorycapabilitybetween dichotomousoutcomes.
WeperformedallstatisticaltestsusingMinitabversion 19.0(MinitabCorp,StateCollege,PA).A P -valueofless than0.05wasconsideredstatisticallysignificant.
Figure1. Patientselectiondiagram.Atotalof212patientswithhypertensivediseaseandarterialcathetercannulationwereincludedin analysis.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 766 ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU Tranetal.
CCRU,criticalcareresuscitationunit; BP,bloodpressure.
RESULTS
PatientCharacteristics
Weidentifiedatotalof350patientswithhypertensive diagnosesandarterialcathetercannulationforABP
monitoringbetweenJanuary2019–May2021(Figure1). Amongthesepatients,212metourinclusioncriteriaand wereincludedinanalysis.Atotalof88patients(42%)hada changeofmanagementinrealtime(Table1).Therewasonly
Table1. Characteristicsofhypertensivepatientswithchangeinmanagementvspatientswithoutchangeinmanagementbetweenintraarterialandnoninvasivebloodpressuremonitoring.
IntracerebralhemorrhagewithIVH28(13)14(11)14(16)0.3
IntracerebralhemorrhagewithoutIVH19(9)8(7)11(13)0.1
TypeAaorticdissection42(20)27(22)15(17)0.4
TypeBaorticdissection33(16)21(17)12(14)0.5
Other3 9(4)5(4)4(5)0.9
1Transthoracicechocardiogramwasavailableforallpatientsintheanalysis.
2Wedidnotperformastatisticalanalysisduetothepresenceofzerocountsinthissubgroup.
3Otherdiagnosesincludedpatientswiththreeiliacaneurysms,tworenalarteryaneurysms,twononspecifichypertensiveemergencies, pre-eclampsia,andonenon-ST-elevationmyocardialinfarction.
BMI,bodymassindex; EF,ejectionfraction; IABP,intra-arterialbloodpressure; IVH,intraventricularhemorrhage; LVEF,leftventricular ejectionfraction; LVH,leftventricularhypertrophy; NIBP,noninvasivebloodpressure; TPA,tissueplasminogenactivator.
Demographic Allpatients N = 212 Nochangeinmanagement N = 124(58.5%) Changeinmanagement N = 88(41.5%) P-value Age,mean(SD)63(14)62(13)62(15)0.9 Gender,N(%) Male130(61)77(62)53(60)0.8 Female82(39)47(38)35(40)0.8 BMI,mean(SD)29.0(6.7)28.2(6.0)30.1(7.4)0.4 Clinicaldata Serumlactate,mean(SD)2.1(1.6)2.1(1.7)2.1(1.3)0.8 LeftventricularEF,mean(SD)1 0.60(0.12)0.60(0.12)0.60(0.12)0.9 Leftventricularhypertrophy,N(%)128(60)74(60)54(62)0.7 Arterialcatheterlocation,N(%) Right126(59)75(60)51(58)0.7 Left86(41)49(40)37(42)0.7 Radial209(99)121(98)88(100)N/A2 Other(brachial,femoral)3(1)3(2)0(0)N/A2 TimebetweenIABPandNIBP measurementinminutes,mean(SD) 1.2(2.3)1.0(2.0)1.4(2.7)0.7 Pre-existingconditions,N(%) Diabetesmellitus51(24)28(23)23(26)0.6 Hypertension177(84)101(82)76(86)0.3 Coronaryarterydisease25(12)16(13)9(10)0.6 Peripheralarterialdisease6(3)2(2)4(5)0.2 Kidneydisease37(18)23(19)14(16)0.6 Obesity83(39)44(36)39(44)0.2 Diagnosis,N(%) Aorticaneurysm14(7)11(9)3(3)0.09 StrokewithoutTPA19(9)10(8)9(10)0.6 StrokewithTPA18(9)10(8)8(9)0.8 Subarachnoidhemorrhage30(14)18(15)12(14)0.9
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 767 Tranetal. ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU
one(0.5%)complicationfromarterialcatheteruseamong theentiregroupofpatients(Table2).Otherhospital outcomesweresimilarbetweenthegroups.
Oftheincludedpatients,themostfrequenthypertensive diagnosesincludedspontaneousintraparenchymal hemorrhage(22%),typeAdissection(20%),typeB dissection(16%),andsubarachnoidhemorrhage(14%) (Table1).Baselineclinicalcharacteristics(age,BMI,serum lactate,leftventricularejectionfraction,presenceof ventricularhypertrophy)weresimilarbetweenpatientswith changeinmanagementandthosewithout.Additionally,
therewerenostatisticallysignificantdifferencesbetweenthe twogroupswithrespecttopre-existingmedicalconditions, arterialcatheterlocation,ortimeinminutesbetweenABP andCBPmeasurement.
DifferenceBetweenArterialBloodPressure-Cuff BloodPressure
ThemeandifferencebetweenABPandCBPintheoverall studypopulationwas17mmHg(SD14),withamean differenceof11mmHg(SD10)inthegroupwithout clinicallysignificantBPdifferenceand26mmHg(SD14)in
Table2. Bloodpressurevalues,interventions,andclinicaloutcomesamongpatientsadmittedtothecriticalcareresuscitationunitwith hypertensivedisease.Higherarterialbloodpressure(ABP)valueswereassociatedwithchangeinmanagementbetweenABPandcuffblood pressuremonitoring.
1Wedidnotperformastatisticalanalysisduetothepresenceofzerocountsinthissubgroup.
ABP,arterialbloodpressure; ABPM,arterialbloodpressuremonitoring; CBP,cuffbloodpressure; CBPM,cuffbloodpressuremonitoring; ICU,intensivecareunit; mmHg,millimetersofmercury; SBP,systolicbloodpressure;IQR,interquarttilerange.
Allpatients N = 212 Nochangeinmanagement N = 124(58.5%) Changeinmanagement N = 88(41.5%) P-value Bloodpressurevalues ABPSBP(mmHg), mean(SD) 145(23)145(27)162(34) <0.001 CBPSBP(mmHg), mean(SD) 138(24)139(28)145(28)0.2 ABP-CBPdfference(mmHg), mean(SD) 17(14)11(10)26(14) <0.001 PatientswithABP-CBPdifference ≥20mmHg, N(%) 78(37)24(19)54(61) <0.001 Clinicalinterventions Mechanicalventilation, N(%) 57(27)32(26)25(28)0.7 Medication, N(%) Betablocker62(29)37(29)25(28)0.8 Calciumchannelblocker134(63)75(60)59(67)0.3 Bothbetaandcalciumchannelblocker49(23)29(23)20(23)0.9 >1Betablocker2(1)1(1)1(1)0.8 >1Calciumchannelblocker8(4)5(4)3(3)0.8 Propofol38(18)25(20)13(15)0.3 Fentanyl60(28)38(31)22(25)0.4 Patientswitharteriallinecomplication, N(%) 1(0.5)0(1.1)1(0)N/A1 Hospitalcourse(days), median[IQR] Lengthofarterialcatheterplacement2[1–4]2[1–3]2[1–4]0.1 Hospitallengthofstay10[5–18.25]10[5–19.25]9.5[5–17]0.96 ICUlengthofstay6[3–12.25]6[3–13]6[3–11]0.9 Dischargedestination, N(%) Home,self-care38(18)20(16)18(20)0.4 Homehealthcare,acutecare,or rehabilitationcenter 133(63)82(66)51(58)0.2 Skillednursingfacility11(5)6(5)5(6)0.98 Deceased/Hospice31(15)16(13)15(17)0.4
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 768 ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU Tranetal.
Figure2. (A)Bland-Altmangraphdepictingthedifferencebetweeninitialarterialbloodpressureandcuffbloodpressuremonitoringvaluesfor allhypertensivepatients.(B
D)Bland-Altmangraphcomparinginitialvaluesofarterialbloodpressureandcuffbloodpressuremonitoring valuesforhypertensivepatientswhoreceivedordidnotreceive(B)betablockerantihypertensivemedicationaloneforantihypertensive therapy;(C)calciumchannelblockerantihypertensivemedicationaloneforantihypertensivetherapy;and(D)bothbetablockerandcalcium channelblockerantihypertensivemedication.ABPM,arterialbloodpressuremonitoring;CBPM,cuffbloodpressuremonitoring;mmHg, millimetersofmercury.
ABPM,arterialbloodpressuremonitoring; CBPM,cuffbloodpressuremonitoring; mmHg,millimetersofmercury.
thegroupwithclinicallysignificantdifference(Table2). Seventy-eightpatients(37%)hadadifferenceinBPof ≥20mmHgbetweenthetwomodalities.
TheBland-Altmangraphillustrating[ABP-CBP] differencesamongtheincludedpatientsdemonstratedthat themeandifferencebetweenthetwoBPmeasurementswas 10.6mmHg(Figure2A).Thegraphalsoshowedthatalarge percentageofpatientshadABPmonitoringvalues >CBP monitoringvalues.Thesetrendswereobservedamong patientswhoreceivedbeta-blockerinfusions(Figure2B), calciumchannelblockerinfusions(Figure2C),orbothbetablockerandcalciumchannelblockerinfusions(Figure2D). Similarly,amongthesepatientswithhypertensive

emergencies,alargepercentagehad[ABP-CBP]differences ≥20mmHg,comparedtothenumberofpatientswhohad [ABP-CBP]differences ≥−20mmHg.
ClinicallySignificantDifference
Withinourstudypopulation,88of212patients(42%)had aclinicallysignificantdifferencebetweenCBPandABP monitoringasdemonstratedbyachangeinmanagement betweenthetwomeasurementmodalities(Table2).Of patientswithachangeinmanagementasguidedby ABPvsCBPmonitoring,44%requiredanincreasein antihypertensivemedicationdoseperABPbutnotper CBPvalues,and40%warrantedanewantihypertensive
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 769 Tranetal. ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU
Table3. Managementdecisionsforhypertensivecriticallyillpatients withandwithoutclinicallysignificantdifferencebetweenarterial bloodpressureandcuffbloodpressuremeasurement.
TypeofBPmanagementintervention
Patientswithchangeinclinicalmanagement accordingtoABPvsCBPmeasurement, N = 88
Increaseexistingmedicationdose38(44)
Decreaseexistingmedicationdose7(6)
Addnewantihypertensivemedication35(40)
Maintaininfusionversusdiscontinuing8(9)
Patientswithoutchangeinclinical managementbetweenABPvsCBP measurement,N = 124
Continueexistingregimen(nochanges)79(64)
Table4. Stepwisemultivariablelogisticregressionforidentification ofclinicalfactorsassociatedwithclinicallysignificantdifference betweenarterialbloodpressureandcuffbloodpressure measurements.Predeterminedfactorswereenteredintomodels andonlyfactorswithasignificantassociationwerereported.Models foreachoutcomemeasureshowedbothfood fitofindependent variablesandgooddiscriminatorycapability(higherAUROC).
Primaryoutcome:clinically significantdifference betweenABPandCBP1
Secondaryoutcome: differencebetweenABPand CBP ≥20mmHg2
1Hosmer-LemeshowDF = 8;chi-square = 14.12, P-value = 0.079. AUROC = 0.64.
2Hosmer-LemeshowDF = 8;chi-square = 7.04, P-value = 0.532. AUROC = 0.67.
ABP,arterialbloodpressure; BP,bloodpressure; CBP
medicationaccordingtoABPbutnotCBPmonitoring.
Another6%requiredadecreaseddoseofantihypertensive infusionperABPbutnotperCBPmonitoring,and9% requiredmaintenanceofanantihypertensiveinfusionper ABPmonitoringwhenCBPmonitoringindicated discontinuationoftheinfusion(Table3).
Ofpatientswhodidnothaveachangeinmanagement betweenABPandCBPmonitoring,64%required continuationofthecurrentregimen,23%requiredan increaseddoseofcurrentantihypertensiveinfusionoran additionofanewmedicationperbothvalues,and2% warrantedadecreaseddoseperbothCBPandABP monitoring(Table3).In11%ofpatients,bothCBP-and ABP-monitoredmeasurementswarrantedinitiationofanew antihypertensivemedication.
PredictorsofChangeinManagement
Ourmultivariableregressionsidentifiedthateachunit increaseofBMIwasassociatedwith4%higherlikelihoodof havingachangeinmanagementamongpatientswith hypertensiveemergencies(oddsratio[OR1.04,95% confidenceinterval[CI]1.00–1.08, P -value <0.05).Patients whohadhistoryofperipheralarterialdisease(OR0.16,95% CI0.03–0.97, P -value <0.05)werealsoassociatedwithhaving lowerlikelihoodofaclinicallysignificantdifferencebetween ABPandCBPmonitoring(Table4).Thismodelhadan acceptablediscriminatorycapabilitywithAUROCof0.64.
ABP,arterialbloodpressure; AUROC,areaunderthereceiver operatingcharacteristiccurve; CBP,cuffbloodpressure; CI, ConfidenceInterval; mmHg,millimetermercury; OR,oddsratio.
Additionally,amultivariablelogisticregressionidentifiedthat right-sidedarterialcatheterswereassociatedwithsignificantly loweroddsfor[ABP-CBPmonitoring]difference ≥20mmHg (OR0.46,95%CI0.25–0.85, P -value <0.05)(Table4).The modelalsohadacceptableAUROCof0.67.
DISCUSSION
Whiletworetrospectivestudieshavedemonstrated clinicallyrelevantdifferencesinCBPandABP measurements,6,12 toourknowledgethisisthe first prospectivestudyinvestigatingtheclinicalrelevanceof differencesbetweenCBPandABPmonitoringamong patientswithdifferentdiagnosesofhypertensive emergencies.Theresultsofthisobservationalstudysupport ourhypothesisthatthediscrepancybetweenABPandCBP measurementsleadstoachangeinBPmanagementinalarge percentageofpatientswithhypertensiveemergencies.
Inthisstudy,CBPmonitoringunderestimatedABP monitoring(by17mmHgonaverage),andmeasurementof thelatterwarrantedincreasesinantihypertensive medication.ThissuggeststhattheuseofCBPmonitoring alonetoguidemanagementofpatientswithhypertensive emergenciesmayresultinunrecognizedanduntreatedlevels ofhypertension.Bartonetalsuggestedthatpatientswith spontaneousintracerebralhemorrhagewhosustained hypertensionduringtheacutephaseintheemergency department(ED)wereassociatedwithpoorneurological
Numberof patients(%)
BothABPandCBPwarrantedan increasedantihypertensivedose 29(23) BothABPandCBPwarranteda decreasedantihypertensivedose 3(2) BothABPandCBPwarrantedinitiationof newantihypertensivemedication 13(11)
,cuffblood pressure.
OR95%CI P-value
PeripheralarterialDisease0.16(0.03–0.97)0.046
Bodymassindex1.04(1.001,1.084)0.045
Right-sidedarterial catheterlocation 0.46(0.25,0.85)0.013
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 770 ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU Tranetal.
outcomeatone-monthand12-monthfollow-ups.35 Similarly,patientswithacuteuncomplicatedtypeBaortic dissectionbutwhocontinuetohavehypertensionwere associatedwithhigherin-hospitalmortality,comparedto thosewhohavecontrolledBP.36
Althoughpatientoutcomes(whichwerenotthe outcomesinthisobservationalandexploratorystudy)in univariateanalyseswerenotdifferentbetweengroupswith orwithoutclinicallyrelevantdifferences,cliniciansshould thusconsidertheuseofABPmonitoringinhypertensive patientsforwhomadherencetospeci fi cBPgoalsis important.Additionally,whenapatientishavingBPatthe borderlinerecommendedbycurrentguidelines,coupled withprolongedboardingtimeintheED,theadditionof ABPmonitoringwouldprovidehelpfulinformationfor furthermedicaldecision-making,asithasbeenshownthat CBPmonitoringisnotasreliable.37 Futurestudiesshould furtherinvestigateourobservationtobettercharacterize theassociationbetweenCBPandABPmonitoring differencesandpatientoutcomes.
TheuseofinvasiveABPmonitoringisnotentirelywithout riskandexpense.RisksofABPmonitoringincludebleeding, thrombosis,infection,embolism,andnervedamage; however,theincidenceofcomplicationsislowwithmajor complicationsoccurringinlessthan1%ofcases.3,4,33 We foundonereportedcomplicationofsofthematomawithin ourstudysampleof212patients,producinganoverall complicationrateof0.5%.Ontheotherhand,wefounda changeinmanagementrateof42%inpatientswiththeuseof ABPmonitoring.Thus,thepotentialbenefitofABP monitoringinguidingclinicalmanagementappearedto outweightherisksofharminourpatients.
TheuseofABPmonitoringdoesincuradditionalcostof care.Atourinstitution,theone-time,per-patientsupplycost forinitiationofABPmonitoringisapproximately$55US dollars(USD).Withachangeinmanagementrateof42% amongourpatientsuponinsertionofanarterialcatheter,ABP monitoringwasabletodetectonechangeinmanagementfor approximatelyeverythreepatients.Thetotalcosttodetect oneclinicallysignificantBPdifferenceforeverythreepatients withhypertensivecriticalillnessis,therefore,$165USD.This observationalandexploratorystudywasnotdesignedto detectdifferencesinpatientoutcomessuchasmortality,ICU orhospitallengthofstay,anddidnotdemonstrateadirect benefitforABPmonitoringinthestudypatientpopulation. Furtherstudiesshouldinvestigatethebenefits-riskratio betweenpotentialbenefitsvs financialcostandcomplications betweenABPandCBPmonitoring.
Withinourpatientpopulation,patientswithclinically significantdifferencebetweenCBPandABPmonitoringhad higherBMIthanthosewithoutaclinicallysignificant difference(30.1vs28.2,respectively),althoughthedifference wasnotstatisticallysignificant.Previousstudieshave identifiedanassociationbetweenobesityandgreater
differencesbetweenABPandCBPmonitoring,withCBP measurementstypicallyunderestimatingdirectintra-arterial SBP.13,14 Thisisthoughttobeduetothearmcircumference ofobesepatientspreventingproper fitofBPcuffs,althougha definitivecausehasnotbeenidentified.13,14
Our findingthatpatientswithperipheralarterydisease wereassociatedwithloweroddsofchangeinclinical managementappearedcounterintuitiveat first.However,a studybyIidaetalsuggestedthatpatientswitharterial stiffnesswouldhavehigherBPthanthosewhodidnot.16 Therefore,itwouldbeprobablethat both ABPandCBP monitoringvaluesfrompatientswithperipheralartery disease,andtheirresultingarterialstiffness,wouldbehigher thantherecommendedgoalofSBPbyguidelines.Thus,both ABPandCBPmonitoringvalueswouldrecommendan increaseofcurrentantihypertensiveinfusion,whichisnot consideredachangeinclinicalmanagementbyour definition.However,ourpatientpopulationincludedonlysix (3%)patientswithperipheralarterydisease;furtherstudies withhigherpercentagesofpatientswithperipheralartery diseasearenecessarytoconfirmourobservations.Theresult fromourmultivariablelogisticregressionalsoshowedthat ABPmonitoringontherightsidewasassociatedwithlower likelihoodofgreaterdifferencesbetweenCBPandABP. Whileourstudycouldnotexplainthese findings,itcouldbea confounding findingoritcouldbeduetothenumberof patientswithacuteaorticdissectionwithinourpatient population.Patientswithacuteaorticdissectionhavebeen showntohavegreaterdifferencesbetweenbotharms,with BPontheleftarmbeingaffectedmore.38 Thisphenomenon wouldhavecausedbiggerdifferencesbetweenCBPandABP ontheleftside.However,furtherstudiesincludingonly patientswithacuteaorticdiseasesareneededtoconfirmor refuteourobservation.
Althoughidentificationofspecificsubsetsofpatientswho wouldmostbenefitfromABPmonitoringmaybehelpfulin directingtheplacementofarterialcathetersintheacute stagesofillness,ourstudyrevealedveryfewpredictorsof such.ThehighincidenceofclinicallyrelevantABP-CBP discrepancyandlackofcleardistinctionastowhichpatients aremorelikelytorequiredifferentBPmanagementafter placementofanarterialcathetersuggestthatclinicians shouldconsiderinvasiveABPmonitoringmoreoftenin patientswithhypertensiveemergenciesrequiringa continuousantihypertensiveinfusions,atleastduringthe acuteresuscitationphase.
LIMITATIONS
Ourstudyhasseverallimitations,the firsthavingtodo withtheclinicalsettingandthepatientpopulation.Although mostofthesediseasestatesareencounteredintheEDsetting, theresultsinoursettingmaynotbeapplicabletomanyEDs. Thus,ourstudymaylackexternalvalidity.Additionally,we didnotaddressanydownstreamconsequences,suchas
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 771 Tranetal. ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU
clinicaloutcomesandthroughputsthatcouldhavebeen derivedfromthechangeofclinicalmanagementofthese patients,asthistopicwasbeyondthescopeofthisstudy.The heterogeneityofourpatientpopulationwithrespectto hypertensiveemergencydiagnosislimitsourabilitytodraw conclusionsaboutspecificsubsetsofhypertensivedisease. Becauseintra-arterialBPmonitoringisconsideredthegold standard,wedidnotrandomizepatientstomanagement guidedbyABPvsCBPmonitoringtodetermineassociations betweeneachmeasurementmodalityandpatientoutcomes. Finally,ourlimitedsamplesizemayhavepreventedaccurate depictionoftheincidenceofarterialcathetercomplications orpatient-relatedoutcomes.Despitetheselimitations,our studydoesprovidefurtherevidencetosupporttheuseof invasivearterialcathetersforBPmonitoringinpatientswith hypertensiveemergenciesandrequiringcontinuous antihypertensiveinfusions.
CONCLUSION
Approximately4in10patientswithhypertensive emergencieshadachangeinmanagementbetween monitoringofcuffbloodpressurevsarterialbloodpressure monitoring,indicatingclinicalrelevanceofthediscrepancy inBPvaluesobtainedbythesetwomeasurementmodalities. PatientswithhighBMIwereassociatedwithhigher likelihoodofrequiringchangeofmanagementduetothe discrepanciesbetweenABPandCBPmonitoring.Additional studiesandlessheterogenouspatientpathologiesare recommendedtofurtherexplorepatientoutcomesassociated withthese findings.Furtherstudiesarenecessarytoconfirm ourobservationsandtoinvestigatethebenefit-riskratioof arterialbloodpressuremonitoring.
AddressforCorrespondence:QuincyKTran,MD,PhD,Universityof MarylandSchoolofMedicine,TheRAdamsCowleyShockTrauma Center,22SouthGreeneStreet,SuiteT3N45,Baltimore,MD21201.
Email: Qtran@som.umaryland.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Tranetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.NuttallG,BurckhardtJ,HadleyA,etal.Surgicalandpatientriskfactors forseverearteriallinecomplicationsinadults. Anesthesiology 2016;124(3):590–597.
2.WeinerR,RyanE,Yohannes-TomicichJ.Arteriallinemonitoringand placement.In:OropelloJM,PastoresSM,KvetanV.eds. CriticalCare McGrawHill;Availableat: https://accessmedicine.mhmedical.com/ content.aspx?bookid=1944§ionid=143522170 AccessedMarch4,2023.
3.HsuDJ,FengM,KothariR,etal.Theassociationbetweenindwelling arterialcathetersandmortalityinhemodynamicallystablepatients withrespiratoryfailure:apropensityscoreanalysis. Chest 2015;148(6):1470–1476.
4.GarlandA.ArteriallinesintheICU:acallforrigorouscontrolledtrials. Chest.2014;146(5):1155–1158.
5.FujiiT,NishiwakiK.Comparingoscillometricnoninvasiveand invasiveintra-arterialbloodpressuremonitoringintermneonates undergeneralanesthesia:aretrospectivestudy. PaediatrAnaesth 2020;30(12):1396–1401.
6.RaffmanA,ShahU,BarrJF,etal.Predictorsofclinicallyrelevant differencesbetweennoninvasiveversusarterialbloodpressure. AmJ EmergMed.2021;43:170–174.
7.DionneJM,BremnerSA,BayganiSK,etal.Methodofbloodpressure measurementinneonatesandinfants:asystematicreviewand analysis. JPediatr.2020;221:23–31.e5.
8.BurA,HerknerH,VlcekM,etal.Factorsinfluencingtheaccuracy ofoscillometricbloodpressuremeasurementincriticallyillpatients. CritCareMed.2003;31(3):793–799.
9.KimSH,LilotM,SidhuKS,etal.Accuracyandprecisionofcontinuous noninvasivearterialpressuremonitoringcomparedwithinvasivearterial pressure:asystematicreviewandmeta-analysis. Anesthesiology 2014;120(5):1080–1097.
10.RuszalaMW,ReimerAP,HickmanRL,etal.Useofarterialcatheters inthemanagementofacuteaorticdissection. AirMedJ 2014;33(6):326–330.
11.ManiosE,VemmosK,TsivgoulisG,etal.Comparisonofnoninvasive oscillometricandintra-arterialbloodpressuremeasurementsin hyperacutestroke. BloodPressMonit.2007;12(3):149–156.[published correctionappearsin BloodPressMonit. 2007Oct;12(5):349.Eleni, Koroboki[correctedtoKoroboki,Eleni].
12.KevilleMP,GelmannD,HollisG,etal.Arterialorcuffpressure:clinical predictorsamongpatientsinshockinacriticalcareresuscitationunit. AmJEmergMed.2021;46:109–115.
13.AnastN,OlejniczakM,IngrandeJ,etal.Theimpactofbloodpressure cufflocationontheaccuracyofnoninvasivebloodpressure measurementsinobesepatients:anobservationalstudy. CanJ Anaesth.2016;63(3):298–306.
14.AraghiA,BanderJJ,GuzmanJA.Arterialbloodpressuremonitoringin overweightcriticallyillpatients:invasiveornoninvasive? CritCare 2006;10(2):R64.
15.PiconeDS,SchultzMG,OtahalP,etal.Influenceofageonupperarm cuffbloodpressuremeasurement. Hypertension.2020;75(3):844–850.
16.IidaM,IshiguroY,UedaN,etal.Inter-armdifferenceofsystolicblood pressuremeasuredbyautomateddouble-cuffdeviceisassociatedwith
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 772 ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU Tranetal.
arterialstiffnessinpatientswithhypertension. BloodPressMonit 2020;25(1):26
33.
17.SpaiteDW,HuC,BobrowBJ,etal.Mortalityandprehospitalblood pressureinpatientswithmajortraumaticbraininjury:implicationsforthe hypotensionthreshold. JAMASurg.2017;152(4):360–368.
18.KauvarDS,SarfatiMR,KraissLW.Intraoperativebloodproduct resuscitationandmortalityinrupturedabdominalaorticaneurysm. JVascSurg.2012;55(3):688–692.
19.VincentJL,NielsenND,ShapiroNI,etal.Meanarterialpressureand mortalityinpatientswithdistributiveshock:aretrospectiveanalysisof theMIMIC-IIIdatabase. AnnIntensiveCare.2018Nov8;8(1):107.
20.SeamonMJ,FeatherC,SmithBP,etal.Justonedrop:thesignificance ofasinglehypotensivebloodpressurereadingduringtrauma resuscitations. JTrauma.2010;68(6):1289
1295.
21.BossoneE,GorlaR,LaBountyTM,etal.Presentingsystolicblood pressureandoutcomesinpatientswithacuteaorticdissection. JAm CollCardiol.2018;71(13):1432–1440.
22.IMPROVEtrialinvestigators,PowellJT,HinchliffeRJ,etal. ObservationsfromtheIMPROVEtrialconcerningtheclinicalcareof patientswithrupturedabdominalaorticaneurysm. BrJSurg 2014;101(3):216–224.
23.PiconeDS,SchultzMG,OtahalP,etal.Accuracyofcuff-measured bloodpressure:systematicreviewsandmeta-analyses. JAmColl Cardiol.2017;70(5):572
586.
24.SeidlerováJ,T mováP,RokytaR,etal.Factorsinfluencingthe accuracyofnon-invasivebloodpressuremeasurementsinpatients admittedforcardiogenicshock. BMCCardiovascDisord 2019;19(1):150.
25.RebescoMR,PinkstonMC,SmyrniosNA,etal.Acomparisonofnoninvasivebloodpressuremeasurementstrategieswithintra-arterial measurement. PrehospDisasterMed.2020;35(5):516–523.
26.HiratzkaLF,BakrisGL,BeckmanJA,etal.2010ACCF/AHA/AATS/ ACR/ASA/SCA/SCAI/SIR/STS/SVMGuidelinesforthediagnosisand managementofpatientswiththoracicaorticdisease.AReportofthe AmericanCollegeofCardiologyFoundation/AmericanHeart AssociationTaskForceonPracticeGuidelines,AmericanAssociation forThoracicSurgery,AmericanCollegeofRadiology,AmericanStroke Association,SocietyofCardiovascularAnesthesiologists,Societyfor CardiovascularAngiographyandInterventions,Societyof InterventionalRadiology,SocietyofThoracicSurgeons,andSociety forVascularMedicine[publishedcorrectionappearsin JAmColl Cardiol. 2013Sep10;62(11):1039-40]. JAmCollCardiol.
2010;55(14):e27
e129.
27.PowersWJ,RabinsteinAA,AckersonT,etal.GuidelinesfortheEarly ManagementofPatientswithAcuteIschemicStroke:2019Updateto
the2018GuidelinesfortheEarlyManagementofAcuteIschemic Stroke:AGuidelineforHealthcareProfessionalsfromtheAmerican HeartAssociation/AmericanStrokeAssociation[publishedcorrection appearsinStroke.2019Dec;50(12):e440-e441]. Stroke 2019;50(12):e344–e418.
28.HemphillJC3rd,GreenbergSM,AndersonCS,etal.Guidelinesforthe ManagementofSpontaneousIntracerebralHemorrhage:AGuideline forHealthcareProfessionalsfromtheAmericanHeartAssociation/ AmericanStrokeAssociation. Stroke.2015;46(7):2032–2060.
29.WebsterK,FishburnS,MareshM,etal.Diagnosisandmanagementof hypertensioninpregnancy:summaryofupdatedNICEguidance. BMJ 2019;366:l5119.
30.ScaleaTM,RubinsonL,TranQ,etal.Criticalcareresuscitationunit:an innovativesolutiontoexpeditetransferofpatientswithtime-sensitive criticalillness. JAmCollSurg.2016;222(4):614–621.
31.TranQK,O’ConnorJ,VesselinovR,etal.Thecriticalcareresuscitation unittransfersmorepatientsfromemergencydepartmentsfaster andisassociatedwithimprovedoutcomes. JEmergMed 2020;58(2):280–289.
32.ScheerB,PerelA,PfeifferUJ.Clinicalreview:complicationsandrisk factorsofperipheralarterialcathetersusedforhaemodynamic monitoringinanaesthesiaandintensivecaremedicine. CritCare 2002;6(3):199–204.
33.WorsterA,BledsoeRD,CleveP,etal.Reassessingthemethodsof medicalrecordreviewstudiesinemergencymedicineresearch. Ann EmergMed.2005;45(4):448–451.
34.ClarkCE,PowellRJ.Thedifferentialbloodpressuresignin generalpractice:prevalenceandprognosticvalue. FamPract 2002;19(5):439–441.
35.BartonCW,HemphillJC3rd.Cumulativedoseofhypertension predictsoutcomeinintracranialhemorrhagebetterthanAmerican HeartAssociationguidelines. AcadEmergMed 2007;14(8):695–701.
36.TrimarchiS,EagleKA,NienaberCA,etal.Importanceofrefractory painandhypertensioninacutetypeBaorticdissection:insightsfromthe InternationalRegistryofAcuteAorticDissection(IRAD). Circulation 2010;122(13):1283–1289.
37.RibezzoS,SpinaE,DiBartolomeoS,etal.Noninvasivetechniquesfor bloodpressuremeasurementarenotareliablealternativetodirect measurement:arandomizedcrossovertrialinICU. ScientificWorld Journal.2014:353628.
38.UmSW,OhleR,PerryJJ.Bilateralbloodpressuredifferentialasa clinicalmarkerforacuteaorticdissectionintheemergencydepartment. EmergMedJ.2018;35(9):556–558.
–
–
–
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 773 Tranetal. ArterialMonitoringinHypertensiveEmergencies:SignificancefortheCCRU
BlockTime:AMultispecialtySystematicReviewofEfficacyand
SafetyofUltrasound-guidedUpperExtremityNerveBlocks
CampbellBelisleHaley,MD*
AndrewR.Beauchesne,MD†
JohnChristianFox,MD*
ArianaM.Nelson,MD‡
SectionEditor: RobertEhrman
ElectronicallypublishedJune30,2023
*UniversityofCalifornia,IrvineMedicalCenter,DepartmentofEmergencyMedicine, Orange,California
† BethIsraelDeaconessMedicalCenter,DepartmentofRadiology,Boston, Massachusetts
‡ UniversityofCalifornia,IrvineMedicalCenter,DepartmentofAnesthesiology, Orange,California
Submissionhistory:SubmittedJanuary10,2022;RevisionreceivedSeptember22,2022;AcceptedOctober5,2022
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.56058
Introduction: Ultrasound-guidedperipheralnerveblockadeisacommonpainmanagementstrategyto decreaseperioperativepainandopioid/generalanestheticuse.Inthisarticleourgoalwasto systematicallyreviewpublicationssupportingupperextremitynerveblocksdistaltothebrachialplexus. Weassessedtheefficacyandsafetyofmedian,ulnar,radial,suprascapular,andaxillarynerveblocksby reviewingpreviousstudies.
Methods: WesearchedMEDLINEandEmbasedatabasestocapturestudiesinvestigatingthesenerve blocksacrossallspecialties.Wescreenedtitlesandabstractsaccordingtoagreed-uponinclusion/ exclusioncriteria.Wethenconductedahandsearchofreferencestoidentifystudiesnotfoundinthe initialsearchstrategy.
Results: Weincluded20studieswith1,273enrolledpatientsinqualitativeanalysis.Bothanesthesiology (12,60%)andemergencymedicine(5,25%)specialtieshaveevidenceofsafeandeffectiveuseofradial, ulnar,median,suprascapular,andaxillaryblocksfornumerousclinicalapplications.Recently,multiple randomizedcontrolledtrialsshowsuprascapularnerveblocksmayresultinlowerpainscoresinpatients withshoulderdislocationsandrotatorcuffinjuries,aswellasinpatientsundergoinganesthesiafor shouldersurgery.
Conclusion: Distalupperextremitynerveblocksunderultrasoundguidancemaybesafe,practical strategiesforbothacuteandchronicpaininperioperative,emergent,andoutpatientsettings.Theseblocks provideaccessible,opioid-sparingpainmanagement,andtheiruseacrossmultiplespecialtiesmaybe expandedwithincreasedproceduraleducationoftrainees.[WestJEmergMed.2023;24(4)774–785.]
INTRODUCTION
blocks.2,3 Upperextremitynerveblocksarealsousedin outpatientsettingsbysportsmedicine,physicalmedicineand rehabilitation,andneurology.4-6 Despitethis,mostupper extremitynerveblocksareperformedbyanesthesiology perioperatively.ItislesscommonforEPstobetrainedin distalupperextremityblockssuchassuprascapular,median, ulnar,andradialnerveblocks.7,8 Ourgoalinthisreviewwas toassessthecurrentstateofevidencebehindUS-guided upperextremitynerveblocksacrossallspecialties. REVIEW ARTICLE
Overthreemillionupperextremitytraumas,38.4%of whicharedigitalinjuries,presenttoemergencydepartments (ED)intheUnitedStatesannually.1 Manyoftheseinjuries aretreatedwithoralorintravenousanalgesia,whilemore complicatedcasesoftenresultinconsultationwithacutepain service.However,thereisevidencethatemergency physicians(EP)canprovidesafeandefficaciouspainrelief usingultrasound(US)-guided(upperextremitynerve WesternJournal of EmergencyMedicineVolume24,No.4:July2023 774
Despitetheirwidespreaduseindifferentspecialties,there arenopriormultidisciplinarysystematicreviewsofthese blocks.7,9-11 Incontrast,therearemanypublishedsystematic reviewsofbrachialplexusblocks,whicharestandardofcare formostupperextremitysurgeries.12,13 Proximalbrachial plexusblocksarerarelyperformedbyEPsduetothe perceivedriskofpneumothoraxanddiaphragmatic paralysis,whiledistalblocksrequireskillsalreadyfamiliarto EPs,suchasUS-guidedvascularaccess,fasciailiacusnerve block,andmusculoskeletalultrasound.14-17 These ultrasoundapplicationsarecurrentlystandardofpracticefor EPs.18
Nerveblockadehasthepotentialtoprovidesafe, opioid-sparinganalgesiaintheEDinvulnerablepopulations suchaselderlypatients,thosesufferingfromsubstanceuse disorders,andchildren.Additionally,arecentsurveyof expertsinemergencymedicine(EM)supportedthenotion thatUS-guidedregionalanesthesiashouldbeadeveloped curriculuminallEMresidencies.19
Ourobjectiveinthisreviewwastosystematicallyevaluate theevidencesupportingUS-guideddistalupperextremity nerveblocksacrossallspecialtiesanddeterminetheirefficacy andsafety.Wehopetoinformfutureeducationalinitiatives inEMandencourageEPstogaincompetenceinUS-guided nerveblockstotreatpainoptimally.20
METHODS
WesearchedMEDLINEandEmbasedatabasesto capturestudiesfromtheinceptionofeachdatabasetoMarch 7,2021.Wedevelopedasearchstrategywithguidancefrom sentinelarticlesusingkeywordsfromthesearticlesasMeSH termsandconsultedamedicallibrarianforareviewofour searchstrategy(Appendix1).Duplicatereferenceswere removedusingEndNote.Titlesandabstractswerescreened bytwoindependentinvestigatorsusingtheRayyanscreening app(RayyanSystemsInc,Cambridge,MA)accordingto specificinclusionsandexclusioncriteria(Appendix2).21 We includedrandomizedcontrolledtrials,case-controlled studies,cross-sectionalstudies,andcohortstudiesassessing theefficacyofUS-guidedupperextremitynerveblocks comparedtootherformsofanalgesiaortechniquesofnerve block(Appendix1).
Outcomesincludedthosestudiesrelatedtopainand safety.Studiestakingplaceperioperatively,emergent settings,andoutpatientclinicalenvironmentswereall considered.Twoauthors(CBHandAB)wereresponsiblefor screeningarticlesbasedoninclusioncriteria,usingthetitle, abstractand,ifneeded,thefull-textarticle.Disagreementsin articleinclusion(6/85studies)werereconciledthrough consensusdevelopmentbyfurtherdiscussionofmethodsand outcomesusingthedefinedinclusion/exclusioncriteria.A handsearchwasalsoconductedbyusingthereferencesofall full-textscreenedstudiestoidentifystudiesthatmayhave beenmissedfromthesearchstrategy.Ourstudywas reviewedbylocalinstitutionalreviewboard(IRB),which
determinedthisdoesnotconstitutehumansubjectresearch andwas,therefore,exemptfromIRBreview.
Wecreatedstandardizedformstoextractindividualstudy dataregardingstudydetailsanddesign,population characteristics,andresultsforoutcomesofinterest.Wealso completedriskofbiasonallincludedstudiesusingthe revisedCochranerisk-of-biastool(RoB2).22
RESULTS
Ourliteraturesearchandstudyselectionprocessidentified 936abstractsbysearchofMEDLINEandEmbase databases(Figure1).Abstractscreeningidentifiedatotalof 85referencesforfull-textscreening.Handsearchof referencesinallfull-textscreenedarticlesidentifiedtwo additionalstudiesforinclusion.Atotalof20studieswere deemedeligibleforinclusion(Appendix2).Theseincluded studiesfromthespecialtiesofanesthesia(60%),EM(25%), orthopedics(measuredwithmultipleoutcomesincluding reductioninscoresonthevisualanalogscale(VAS), comparisontolandmark-guidedblocks,andcomparisonto pharmacologicpaincontrol(Table1).Studiesthathad overallpositiveoutcomesbythesemeasureswereconsidered “effective” blocksforthepurposesofthissystematicreview. Ofthe20totalincludedstudies,fourstudiedblock effectivenessforchronicpain.
MixedForearmBlocks
Fivepublicationsstudiedtheefficacyofcombined forearmnerveblocks(median,ulnar,andradialnerves) (Table1A).Onerandomizedcontrolledtrial(RCT) indicatedmedian/radial/ulnarcombinedblockwas successfulasprimaryanesthesiaforhandsurgery97%ofthe time,whiletwosingle-arm,interventionalstudiesintheED indicatedtheeffectivenessofcombinedblocksforhand injuriesrequiringproceduralinterventions.7,9,10 A retrospectivecohortstudyanalyzingallforearmblocks completedbytheanesthesiologydepartmentatanacademic center(536)showednoneurologiccomplications.23 One RCTofcombinedmedial/ulnarblocksinpatients undergoingcarpaltunnelreleasesurgeryshowed93% effectiveness(Table1B).2
IndividualForearmBlocks
TwostudiesassessedtheeffectivenessofUS-guidedulnar nerveblockandshoweda100%successrateinblocking pinpricksensation(Table1C).24,25 Threestudiesassessed mediannerveblock(Table1D).26
28 Onedeterminedthere wasnodifferenceinsuccesswhenusinghydrodissectionwith amediannerveblockandreported100%successofUSguidedblockofindex finger/thenareminencesensation.26 Anotherstatedcircumferentialspreadofthenerveblock visualizedonUSincreasedsuccessfrom81
100%(P < 0.05).28 Finally,astudyofpediatricpatientsundergoing triggerthumbsurgeryfound50(100%)successfulmedian
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 775
–
–
BelisleHaleyetal.
ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks
Articles identified through Ovid MEDLINE (n = 492)
AdditionalArticles identified through Embase (n = 598)
6 articles were located by hand search, 2 were included in analysis
nerveblocksintheUS-guidedgroupvs50(64%)using landmarksalone.27 Twoprospectivestudiesofradialnerve blocksdemonstratedimprovementsinpainscores.Inone, patientswithCollesfractureundergoingreductionhadVAS decreasefrom8.2(7.6–8.8)to3.53(2.7–4.3)withUS-guided radialnerveblock.29 Thesecondstudydemonstrated improvementinhandosteoarthritispainover2–4weeks.30
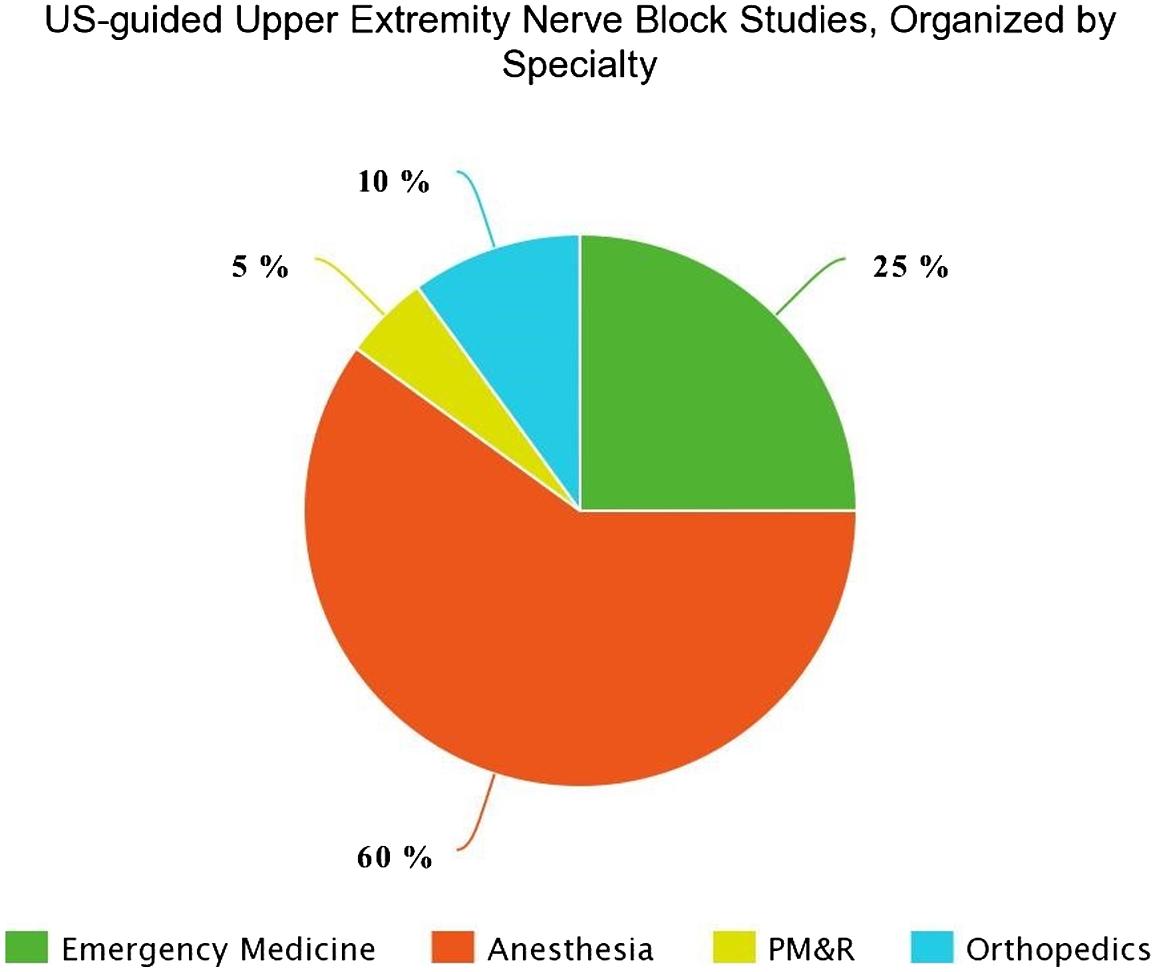
AxillaryandSuprascapularShoulderBlocks
ThereweretwoRCTsofcombinedsuprascapularand axillaryblocksintheperioperativesetting.Oneshowedthat inrotatorcuffsurgerythecombinationblockwassuperiorto suprascapularblockalone,andtheotherfoundtheseblocks providedsignificantlylessanalgesiathantheinterscalene brachialplexusblockforarthroscopicshouldersurgery (Table2A).31,32
FiveRCTsassessedtheUS-guidedsuprascapularnerve block(Table2B).OneEDstudyfoundthisblockdecreased painofshoulderdislocationreductionfrommeanVAS85 (70
withadhesivecapsulitis.34,35 Inoneanesthesiastudy18of83 patients(21.7%)experiencedhemidiaphragmaticparalysis withUS-guidedsuprascapularnerveblock,whileanother foundsuprascapularblockshavelessrespiratoryeffectthan brachialplexusblocks.36,37
98)to45(33
45)anddecreasedtimetodischarge comparedtosedationanalgesia.33 Twostudiesin orthopedicsstudiedtheUS-guidedsuprascapularblock.One demonstratedimprovementinConstant-Murleyscores12 weekspost-blockforpatientswithrotatorcufftears comparedtopatientsreceivingsubacromialinjection; anotherfoundanonsignificantchangeinVASforpatients
–
–
Screening Included Eligibility Identification
(n
in full text screen (n =
abstract screen (n =
Full-text articles
for eligibility (n =
Full-text
Articles after duplicates removed
= 936) Articles included
85) Records excluded by
851)
assessed
24)
articles excluded, with reasons (n = 60) Studies included in qualitative synthesis (n = 20)
Figure1. FlowdiagramofsearchstrategyforUS-guidedupperextremityblocksusingPRISMAprotocol. US,ultrasound; PRISMA,PreferredReportingItemsforSystematicReviewsandMeta-Analysis.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 776 ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks BelisleHaleyetal.
Figure2. Totalproportionofstudiesincludedinqualitativeanalysis byspecialty. US,ultrasound; PM&R,physicalmedicineandrehabilitation.
Table1. Summaryofpublishedstudiesinvestigatingtheef fi cacyandsafetyofultrasound-guidedperipheralforearmnerveblocks.
NAVASTenof11
ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks
patientshada clinically meaningful reductionin VASpainscore ( > 13mm reduction); median reductionin VASscorewas 5.0cm(IQR3.0, 8.0; P = .003)
NAVASMeanVAS decreasedfrom 5.8to0.8 ( P = .04);seven of10with complete resolutionof pain
Nodifferencein thenumberof blocksableto beusedasa primary anesthetic betweenthetwo groups(97%vs 93%forforearm andbrachial groups, respectively)
Blockas primary anesthetic
Ultrasound- guidedbrachial plexusblock
Ultrasound- guidedforearm blockswere signi fi cantly morelikelyto
Pinprick sensation
Landmark-based wristblockwith anultrasound- guidedsaline forearmblock
(
(Year)
A.Mixedforearmblockperformed(i.e.,median,ulnar,and/orradial)
ED(EM)AcuteUltrasound- guidedblockof theradial, median,and/or ulnarnerves
Patientswith hand pathology requiring procedural intervention
2239* [21 –60]
Single-arm interventional; N = 11
Liebmann etal. (2006)
ED(EM)AcuteUltrasound- guidedblocks ofulnar, median,and radialnerves combined
Pediatric patientswith handinjuries requiring procedural intervention
3011* [9 –17]
Single-arm interventional; N = 10
Frenkel etal. (2015)
AcuteUltrasound- guided median,ulnar, orradialnerve blocks
Perioperative (Anesthesia)
Patients undergoing hand surgery
RCT;N = 603049* [36 –58]
Soberon etal. (2015)
ED(EM)AcuteUltrasound- guidedforearm blockwitha salineplacebo wristblock
> 18Healthy volunteers
RCT;N = 1218
Sohoni etal. (2016)
Mean
(SD) [Range] Health Status Setting (Specialty) Acuteor Chronic Pain Intervention orExposureControlOutcome Key Findings Complications (n);type
Authors
Study Design:N enrolled No.of Blocks Performed
Agein Years
0
0
0
0
Continuedonnextpage ) Volume24,No.4:July2023WesternJournal of EmergencyMedicine 777 BelisleHaleyetal.
Table1. Continued.
topinprick comparedto anatomic wristblocks (78%vs56%, respectively; P = 0.032)
complications Only complications reported
1;Transient mechanical paresthesia
0 ( ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks BelisleHaleyetal.
Nodifferencein VASscores duringpost- block venipuncture (30vs30, P = 0.26).Success ratewas93%in bothgroups.
VAS;success rateofblock
Nervestimulation guidednerve blockofmedian andulnarnerve
0
Complete sensoryblockin allpatientswas achievedinboth groups.
Ultrasound- guidedulnar nerveblock withadded dexmedetomidine Successrate ofblock
6.87(5.78 –7.93)
VASto pinprick
Ultrasound- guidedulnar nerveblockwith added dexamethasone
guidedwrist blocks
AcuteUltrasound- guidedmedian andulnar nerveblocksat thewrist
AcuteUltrasound- guidedulnar nerveblock
AcuteUltrasound- guidedulnar nerveblock
Regional anesthesia (Anesthesia)
Perioperative (Anesthesia)
Research ward (anesthesia)
RCT;N = 2412NRHealthy volunteers
C.Ulnar Marhofer etal. (2013)
Research ward (anesthesia)
7230* [22 –55] Healthy volunteers
Crossover study;N = 24
Marhofer etal. (2019)
hourduration, 6.0(4.5 –10.0) minuteonsetof ropivacaine block,no relevanteffectof dexamethasone onsensory block Continuedonnextpage ) WesternJournal of EmergencyMedicineVolume24,No.4:July2023 778
Authors (Year) Study Design:N enrolled No.of Blocks Performed Mean Agein Years (SD) [Range] Health Status Setting (Specialty) Acuteor Chronic Pain Intervention orExposureControlOutcome Key Findings Complications (n);type blocksensation
AcuteUltrasound-
Sites etal. (2012) NAPostoperative neurologic
Cohort53655Patients receiving US-guided nerveblock 2003-2011 0
B.Median,UlnarCombinedstudies Macaire etal. (2008)
RCT;N = 603048(12)Patients undergoing carpal tunnel release
BelisleHaleyetal.
2ingroup withoutD5 hydrodissection; Intraneural injections
Nodifferencein thepercentage ofpatientswith completecold andlighttouch blocksatindex fi nger(100%vs 98.1%and 95.2%vs 96.2%)and thenar eminence(100 v98.1and97.5 vs88.2) betweengroups
Coldandlight touchblockto index fi nger andthenar eminence
Ultrasound- guidedmedian nerveblockwith priordextrose5% hydrodissection
AcuteUltrasound- guidedmedian nerveblock
Perioperative (Anesthesia)
Healthy volunteers
Table1. Continued.
D.Median
RCT;N = 100NRI:40.5 (15.6); C:41.0 (18.2)
Dufour etal. (2012)
0
0
Theintended circumferential spreadgroup hadahigher successrate compared tonon- circumferential spreadgroup (100%v81%, P < 0.05).
Successrate ofsensory block
Ultrasound- guidedmedian nerveblock withnon- circumferential spread
AcuteUltrasound- guidedmedian nerveblock with circumferential spread
Research ward (anesthesia)
Healthy volunteers
42NR [18 –45]
Crossover study;N = 21
Marhofer etal. (2014)
m-CHEOPS*50/50 successful mediannerve blocksinUS group,37/50of landmarkgroup
Landmark-guided mediannerve block
AcuteUltrasound- guidedmedian nerveblock
Perioperative (Anesthesia)
Pediatric patients undergoing trigger thumb surgery
RCT5026 months [NR]
Liuetal. (2018)
0 (
NRVASfor fracture reduction
ED(EM)AcuteUltrasound- guidedradial nerveblock
15NRPatientswith
Colles fracture
E.Radial
Singlearm interventional
Unluer etal. (2008)
Authors (Year) Study Design:N enrolled No.of Blocks Performed Mean Agein Years (SD) [Range] Health Status Setting (Specialty) Acuteor Chronic Pain Intervention orExposureControlOutcome Key Findings Complications (n);type
Continuedonnextpage ) Volume24,No.4:July2023WesternJournal of EmergencyMedicine 779
VASdecreased from8.2 (7.6 –8.8) preprocedureto 3.53(2.73 –4.34) postprocedure ASystematicReviewofEffi
cacyandSafetyofUltrasound-guidedUENerveBlocks
Continued.
VASdecreased from8(6 –9)to 1(0 –6)after fourweeksfor nerveblock group, signi fi cant differencefrom exercisegroup
ExercisealoneVASafter2,4 weeks
ChronicUltrasound- guidedblock super fi cial branchof radialnerve + exercise
Patientswith osteoarthritis Research ward(PM&R)
RCT2550 [46 –64]
Okmen etal. (2018)
NA ,notavailable; PM&R ,physicalmedicineandrehabilitation; VAS ,visualanalogscore; EM ,emergencymedicine; ED ,emergencydepartment; m-CHEOPS ,modi
ed Children ’ sHospitalofEasternOntarioPainScale; NR ,notreported; RCT ,randomizedcontrolledtrial.
*Indicatesmedianage.
Health
Acuteor
Intervention orExposureControlOutcome
Table1.
Authors (Year) Study Design:N enrolled No.of Blocks Performed Mean Agein Years (SD) [Range]
Status Setting (Specialty)
Chronic Pain
Key Findings Complications (n);type
NR
fi
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 780 ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks BelisleHaleyetal.
BelisleHaleyetal. ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks
Complications(n); type
13/21;Rebound pain.No
paresthesiaorlong- termcomplications
0
0
NR
18/83; Hemidiaphragmatic paralysisofany kind
Table2. Summaryofpublishedstudiesinvestigatingtheef fi cacyofultrasound-guidedshouldernerveblocks.
Status Interventionor ExposureControlOutcomeKeyFindings
Mean Agein Years (SD) [Range] Acuteor Chronic Pain
fi cantreductionin VASwith suprascapular block + axillaryblock comparedto suprascapularalone
VASSigni
Ultrasound- guided suprascapular nerveblock alone
ChronicUltrasound- guided suprascapular + axillarynerve blockwith ropivacaine
Perioperative (Anesthesia)
NRSscoreStaticNRSscoreof
5.45inPACU,4.006 hourspost-operatively forsuprascapular + axillary.Signi fi cantly lessanalgesiathan interscalenebrachial plexusblock6hr
VASVASdecreasedfrom mean85(70 –98)to mean45(33 –55). Meantimeto dischargesigni fi cantly lowerinnerveblock groupcomparedto sedationgroup
Suprascapularnerve blockoutperformed Subacromialinjection, improvedCMscore from35.3(SD12.8)to 57.6(SD10)in12 weeks
Constant- MurleyScore at12weeks post-injection
41%ofanterior(17/42) and2%ofposterior(1/ 41)hadsome hemidiaphragmatic paralysis
Diaphragmatic excursionon US
0 (
Ultrasound- guided interscalene blockof brachial plexus
AcuteUltrasound- guided suprascapular + axillarynerve blockpriorto general anesthesia
Perioperative (Anesthesia)
Sedation analgesiawith 1 –2mg/kgof ketamine
ED(EM)AcuteUltrasound- guided suprascapular nerveblock
Patientswith shoulder dislocation
Subacromial injection
ChronicUltrasound- guided suprascapular nerveblock
Outpatient (orthopedics)
Patientswith rotatorcuff tears
Ultrasound- guided posterior suprascapular block
AcuteUltrasound- guidedanterior suprascapular block
Perioperative (Anesthesia)
Patients undergoing shoulder surgery
VASatweek 12
Distal approachto ultrasound-
ChronicProximal approachto ultrasound-
Outpatient (orthopedics)
Patientswith adhesive capsulitis
Authors (Year)
2155.8 (39 –72)
RCT; N = 42
A.SuprascapularandAxillary Lee etal. (2014)
3046.5 (SD 14.5)
RCT; N = 60
Dhir etal. (2016)
2124 (21 –73)
B.Suprascapular
Tezel etal. (2014)
RCT; N = 42
Coory etal. (2019)
RCT; N = 83
Ferre etal. (2020)
4755.3 [39 –76]
RCT; N = 47
Bae etal. (2020)
Strati fi edbyproximal vs.distalapproach: proximalhadVAS Continuedonnextpage ) Volume24,No.4:July2023WesternJournal of EmergencyMedicine 781
Study Design: N enrolled Health
No.of Blocks Performed Setting (Specialty)
Patientswith tornrotator cuffs
Patients undergoing arthroscopic shoulder surgery
RCT; N = 41
2170 (43 –85)
8356.6 (11.6)
Table2. Continued.
ComparedSSBto brachialplexus block,less respiratoryeffect withSSB
Interventionor
ExposureControlOutcomeKeyFindings
Acuteor Chronic Pain
Setting (Specialty)
Health Status
Mean Agein Years (SD) [Range]
No.of Blocks Performed
Study Design: N enrolled
Authors (Year)
decreasefrom6.8 + / 1.5baselineto3.7 + / 1.3at12weeks.Distal VASpainscore improvedfrom6.2 + / 1.6to3.6 + / 2.0at12 weeks.
PainScore, FVCreduction Bothanterior suprascapular(19/20) andposterior suprascapular(19/20) hadhighlyeffective blockadeat30 minutes,lessreduction ofFVCcomparedto interscaleneblock
guided suprascapular nerveblock
Complications(n); type guided suprascapular nerveblock
Ultrasound- guided interscalene blockof brachial plexus
AcuteUltrasound- guidedanterior andposterior suprascapular nerveblock
Perioperative (Anesthesia)
4041.8Patients undergoing arthroscopic shoulder surgery
RCT; N = 40
Limetal. (2020)
NRSscale:0 = nopainto10 = worstpainimaginable.ConstantMurleyScore:combinedfunctionalandpainscoreforshoulderinjury(0 –100) US ,ultrasound; mg/kg ,milligram/kilogram; PACU ,post-anesthesiacareunit; FVC ,forcedexpiratoryvolume; SSB ,suprascapular-axillarynerveblock,VAS,visualanalog score; EM ,emergencymedicine; ED ,emergencydepartment; NR ,notreported; RCT ,randomizedcontrolledtrial.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 782 ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks BelisleHaleyetal.
BelisleHaleyetal. ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks
Median, Ulnar, Radial
-Hand injuries*
-Pediatric hand injuries*
-Hand surgery
Median, Ulnar
-Carpal tunnel surgery
Suprascapular and Axillary
-Torn rotator cuff
-Arthroscopic shoulder surgery
Median
-Trigger thumb surgery
Radial
-Colles’fracture reduction*
-Osteoarthritis
Suprascapular
-Shoulder dislocation reduction*
-Torn rotator cuff
-Shoulder surgery
-Adhesive capsulitis
Risk-of-biasAssessment
WeassessedRoBfor17outcomesin16studies,including twocross-overstudies(Appendix4).Briefly,14outcomes (82%)hadlowRoBduetotherandomizationprocess,and12 outcomes(71%)hadlowRoBduetodeviationsfromthe intendedinterventions.Additionally,allassessedoutcomes (100%)hadlowRoBduetomissingoutcomedata,and13 (76%)hadlowRoBduetomeasurementoftheoutcome. Notably,12outcomes(71%)hadsomeRoBduetothe selectionofthereportedresults,withtheotherstudieshaving lowRoB.
DISCUSSION
WeevaluatedthemultispecialtyevidencebehindUSguidedupperextremitynerveblockstosupportfuture educationalinterventionsinEM.Ourreviewsupportsusing upperextremityblocksformultipleindicationsintheED (Figure3).7,23,32,36 Morebroadly,thissuggestshighefficacy andfewcomplicationswhenperformingupperextremity peripheralnerveblocksperioperativelyandintheED. Despitethisevidence,therearenospecificrecommendations fromtheAccreditationCouncilforGraduateMedical EducationortheAmericanCollegeofEmergencyPhysicians aboutwhichnerveblockswouldbebeneficialtopatients presentingtoEDs.18,20 However,arecentsurveyfound significantsupportforanUS-guidedregionalanesthesia curriculumforEMresidents.19
Our findingsalsopredictabenefitfrommorestandardized EPeducationinUS-guidedregionalanesthesia,whichhas thepotentialtodecreasetheneedforproceduralsedationand opioiduseintheEDwhileprovidingsafe,adequateanalgesia forhandandforearminjuries.36 Populationssuchaspatients withsubstanceusedisorderandolderpatientsmaybenefit fromregionalpainmanagementratherthancentralnervous system-activepharmaceuticals.
LIMITATIONS
Thisstudyhasseverallimitations,includingourinability tomakeinferencesbetweenthespecialtiesofanesthesiaand EM.Regionalanesthesiaisayear-longfellowshipin
anesthesia,andanesthesiaresidentshaveformaltrainingin regionalnerveblocksthroughouttheirresidency.Inmany EDs,US-guidedregionalanesthesiahasbecomestandard, butthisremainsinstitution-dependent.Sinceweare comparingheterogeneousdata(intermsoftrainingand proceduralskill),ourstudyislimitedtoasystematicreview ratherthanameta-analysis.
Tomaketrulyquantitativestatements,wewouldneedthe statisticalanalysisthatonlyameta-analysiswouldprovide. ThisfactoralsolimitedourabilitytofullyfollowPRISMA checklistguidelines.Wealsodefinedeffectivenessbroadlyas apositivestudyresult,butthisspecificwasquitevaried betweenthestudies.Despitethis,the findingthatthese proceduresarelowriskwasconsistentthroughoutourreview ofstudies.Furtherresearchshouldbemultifacetedand interventional.Themosteffectiveapproachmaybea multicenterRCTthatincludesbothaneducationalinitiative onUS-guidednerveblocksforEMresidentsandastudy determiningeffectivenessoftheseblockscomparedto pharmacologicpaincontrol.
CONCLUSION
Thereisevidencethatultrasound-guidedupperextremity nerveblocksaresafeandeffectivebasedonmultiplepositive outcomesfromdifferentspecialties.Improvedtrainingin US-guidednerveblocksinemergencymedicinehasthe potentialtoprovideasafealternativetopharmacologicpain managementorproceduralsedation.Inaddition,giventhe significantintersectionbetweenthe fieldsofanesthesiaand EMinUS-guidedprocedures,moreformaleducational collaborationmayimprovethetechniqueandtrainingof traineesbycombiningtheconsiderabletalentsofboth fields inperformingtheseprocedures.
AddressforCorrespondence:CampbellBelisleHaley,MD,UC Irvine,DepartmentofEmergencyMedicine,3800ChapmanAve, Suite3200,Orange,CA92868.Email: belisleh@hs.uci.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 783
Figure3. Clinicalapplicationsofultrasound-guideddistalupperextremitiesfoundonsystematicreview. *Studyperformedintheemergencydepartment.
and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023BelisleHaleyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.OotesD,LambersK,RingD.Theepidemiologyofupperextremity injuriespresentingtotheemergencydepartmentintheUnitedStates. Hand(NY).2012;7(1):18–22.
2.SohoniA,NagdevA,TakharS,etal.Forearmultrasound-guidednerve blocksvslandmark-basedwristblocksforhandanesthesiainhealthy volunteers. AmJEmergMed. 2016;34(4):730–4.
3.AminiR,KartchnerJZ,NagdevA,etal.Ultrasound-guidednerveblocks inemergencymedicinepractice. JUltrasoundMed. 2016;35(4):731–6.
4.YurgilJL,HulsoppleCD,LeggitJC.Nerveblocks:PartI.Upper extremity. AmFamPhysician. 2020;101(11):654–64.
5.GlomsetJL,KimE,TokishJM,etal.Reductionofpostoperativehip arthroscopypainwithanultrasound-guidedfasciailiacablock:a prospectiverandomizedcontrolledtrial. AmJSportsMed. 2020;48(3): 682–8.
6.PalamarD,UluduzD,SaipS,etal.Ultrasound-guidedgreateroccipital nerveblock:anefficienttechniqueinchronicrefractorymigrainewithout aura? PainPhysician. 2015;18(2):153–62.
7.FrenkelO,LiebmannO,FischerJW.Ultrasound-guidedforearmnerve blocksinkids:anovelmethodforpaincontrolinthetreatmentofhandinjuredpediatricpatientsintheemergencydepartment. PediatrEmerg Care. 2015;31(4):255–9.
8.NealJM.Ultrasound-guidedregionalanesthesiaandpatientsafety:an evidence-basedanalysis. RegAnesthPainMed. 2010;35(2Suppl): S59–67.
9.Sober´onJR,CrookshankJW,NossamanBD,etal.Distalperipheral nerveblocksintheforearmasanalternativetoproximalbrachialplexus blockadeinpatientsundergoinghandsurgery:aprospectiveand randomizedpilotstudy. JHandSurgAm. 2016;41(10):969–77.
10.LiebmannO,PriceD,MillsC,etal.Feasibilityofforearm ultrasonography-guidednerveblocksoftheradial,ulnar,andmedian nervesforhandproceduresintheemergencydepartment. AnnEmerg Med. 2006;48(5):558–62.
11.ChellyJE,GregerJ,GebhardR.Distalnerveblocksatthewristfor outpatientcarpal. AnesthAnalg. 2002;95:351–5.
12.VermeylenK,EngelenS,SermeusL,etal.Supraclavicularbrachial plexusblocks:reviewandcurrentpractice. ActaAnaesthesiol. 2012; 63(1):15–21.
13.GuoCW,MaJX,MaXL,etal.Supraclavicularblockversusinterscalene brachialplexusblockforshouldersurgery:ameta-analysisofclinical controltrials. InternationalJSurg. 2017;45:85–91.
14.ChenKC,LinACM,ChongCF,etal.Anoverviewofpoint-of-care ultrasoundforsofttissueandmusculoskeletalapplicationsinthe emergencydepartment. JIntensiveCare. 2016;4(1).
15.Situ-LaCasseAe.Utilityofpoint-of-caremusculoskeletalultrasoundin theevaluationofemergencydepartmentmusculoskeletalpathology. WorldJofEmergMed. 2018;9(4):262.
16.WernerHC,VieiraRL,RempellRG,etal.AnEducationalinterventionto improveultrasoundcompetencyinultrasound-guidedcentralvenous access. PediatrEmergCare. 2016;32(1):1–5.
17.FalyarC,TolaD.Ultrasound-guidedfasciailiacablocksinthe emergencydepartment. GeriatrNurs(NewYork,NY). 2019;40(4):441–4.
18.LewissRE,PearlM,NomuraJT,etal.CORD-AEUS:Consensus DocumentfortheEmergencyUltrasoundMilestoneProject.BurtonJ, ed. AcadEmergMed. 2013;20(7):740–5.
19.TuckerRV,PetersonWJ,MinkJT,etal.Defininganultrasound-guided regionalanesthesiacurriculumforemergencymedicine. AEMEduc Train. 2020;5(3):e10557.
20.Acgme.ACGMEProgramRequirementsforGraduateMedical EducationinEmergencyMedicine.2019.Availableat: https://www. acgme.org/globalassets/PFAssets/ProgramRequirements/110_ EmergencyMedicine_2020.pdf?ver=2020-06-26-125701-320&ver= 2020-06-26-125701-320.AccessedSeptember9,2021.
21.OuzzaniM,HammadyH,FedorowiczZ,etal.Rayyan aweband mobileappforsystematicreviews. SystRev. 2016;5(1):210.
22.HigginsJ,SavovicJ,PageM.RevisedCochranerisk-of-biastoolfor randomizedtrials(RoB2).Availableat: https://methods.cochrane.org/ bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomizedtrials.AccessedApril22,2021.
23.SitesBD,TaenzerAH,HerrickMD,etal.Incidenceoflocalanesthetic systemictoxicityandpostoperativeneurologicsymptomsassociated with12,668ultrasound-guidednerveblocks:ananalysisfroma prospectiveclinicalregistry. RegAnesthPainMed. 2012;37(5):478–82.
24.MarhoferD,KettnerSC,MarhoferP,etal.Dexmedetomidineasan adjuvanttoropivacaineprolongsperipheralnerveblock:avolunteer study. BrJAnaesth. 2013;110(3):438–42.
25.MarhoferP,ColumbM,HopkinsPM,etal.Dexamethasoneasan adjuvantforperipheralnerveblockade:arandomised,triple-blinded crossoverstudyinvolunteers. BrJAnaesth. 2019;122(4):525–31.
26.DufourE,DonatN,JaziriS,etal.Ultrasound-guidedperineural circumferentialmediannerveblockwithandwithoutpriordextrose5% hydrodissection:aprospectiverandomizeddouble-blinded noninferioritytrial. AnesthAnalg. 2012;115(3):728–33.
27.LiuW,LiuJ,TanX,etal.Ultrasound-guidedlowerforearmmediannerve blockinopensurgeryfortriggerthumbin1-to3-year-oldchildren:a randomizedtrial. PaediatrAnaesth. 2018;28(2):134–41.
28.MarhoferD,KarmakarMK,MarhoferP,etal.Doescircumferential spreadoflocalanaestheticimprovethesuccessofperipheralnerve block? BrJAnaesth. 2014;113(1):177–85.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 784 ASystematicReviewofEf
BelisleHaleyetal.
ficacyandSafetyofUltrasound-guidedUENerveBlocks
29.UnluerEE,KaragozA,UnluerS,etal.Ultrasound-guidedsupracondylar radialnerveblockforCollesFracturesintheED. AmJEmergMed. 2016;34(8):1718–20.
30.MetinÖkmenB,ÖkmenK,AltanL.Effectivenessofsuperficialradial nerveblockonpain,function,andqualityoflifeinpatientswithhand osteoarthritis:aprospective,randomizedandcontrolledsingle-blind study. ArchRheumatol. 2018;33(4):464–72.
31.LeeJJ,KimD-Y,HwangJ-T,etal.Effectofultrasonographicallyguided axillarynerveblockcombinedwithsuprascapularnerveblockin arthroscopicrotatorcuffrepair:arandomizedcontrolledtrial. Arthroscopy. 2014;30(8):906–14.
32.DhirS,SondekoppamRV,SharmaR,etal.Acomparisonofcombined suprascapularandaxillarynerveblockstointerscalenenerveblock foranalgesiainarthroscopicshouldersurgery:anequivalencestudy. RegAnesthPainMed. 2016;41(5):564–71.
33.TezelO,KaldirimU,BilgicS,etal.Acomparisonofsuprascapularnerve blockandproceduralsedationanalgesiainshoulderdislocation reduction. AmJEmergMed. 2014;32(6):549–52.
34.CooryJA,ParrAF,WilkinsonMP,etal.Efficacyofsuprascapularnerve blockcomparedwithsubacromialinjection:arandomizedcontrolledtrial inpatientswithrotatorcufftears. JShoulderElbowSurg.
2019;28(3):430–6.
35.BaeKH,ParkKC,JeongGM,etal.Proximalvsdistalapproachof ultrasound-guidedsuprascapularnerveblockforpatientswithadhesive capsulitisoftheshoulder:prospectiverandomizedcontrolledtrial. ArchPhysMedRehab. 2020;102(5):819–27.
36.FerréF,PommierM,LaumonerieP,etal.Hemidiaphragmaticparalysis followingultrasound-guidedanteriorvs.posteriorsuprascapularnerve block:adouble-blind,randomisedcontroltrial. Anaesthesia.
2020;75(4):499–508.
37.LimYC,KooZK,HoVW,etal.Randomized,controlledtrialcomparing respiratoryandanalgesiceffectsofinterscalene,anterior suprascapular,andposteriorsuprascapularnerveblocksfor arthroscopicshouldersurgery. KoreanJAnesthesiol.
2020;73(5):408–16.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 785 BelisleHaleyetal. ASystematicReviewofEfficacyandSafetyofUltrasound-guidedUENerveBlocks
CommunityParamedicineInterventionReducesHospital ReadmissionandEmergencyDepartmentUtilization forPatientswithCardiopulmonaryConditions
AaronBurnett,MD*
SandiWewerka,MPH†
PaulaMiller,MPH†
AnnMajerus,NRP,CP*‡
JohnClark,BS*
LandonCrippes†
TiaRadant,MS,NRP*
*RegionsHospital,St.Paul,Minnesota
† CriticalCareResearchCenter,RegionsHospital,St.Paul,Minnesota
‡ St.PaulFireDepartment,St.Paul,Minnesota
SectionEditor: ShiraSchlesinger,MD,MPH
Submissionhistory:SubmittedJune24,2022;RevisionreceivedMarch14,2023;AcceptedMay1,2023
ElectronicallypublishedJuly10,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.57862
Objective: Patientsdischargedfromthehospitalwithdiagnosesofmyocardialinfarction,congestive heartfailureoracuteexacerbationofchronicobstructivepulmonarydisease(COPD)havehighratesof readmission.Wesoughttoquantifytheimpactofacommunityparamedicine(CP)interventionon hospitalreadmissionandemergencydepartment(ED)andclinicutilizationforpatientsdischargedwith theseconditionsandtocalculatethedifferenceinhealthcarecosts.
Methods: Thiswasaprospective,observationalcohortstudywithamatchedhistoricalcontrol.The groupswerematchedforqualifyingdiagnosis,age,gender,andZIPcode.Theinterventiongroup received1–2homevisitsperweekbyacommunityparamedicfor30days.Wecalculatedthenumberof all-causehospitalreadmissionsandEDandclinicvisits,anduseddescriptivestatisticstocompare cohorts.
Results: Includedinthestudywere78interventionpatientsand78controls.Comparedtocontrols,fewer subjectsintheCPcohorthadexperiencedareadmissionat120days(34.6%vs64.1%, P < 0.001)and 210days(43.6%vs75.6%, P < 0.001)afterdischarge.At210daystheCPcohorthad40.9%fewertotal hospitaladmissions,saving218beddaysand$410,428inhealthcarecosts.TheCPcohorthad40.7% fewertotalEDvisits.
Conclusion: Patientswhoreceivedapost-hospitalcommunityparamedicinterventionhadfewer hospitalreadmissionsandEDvisits,whichresultedinsaving218beddaysanddecreasinghealthcare costsby$410,428.IncorporationofahomeCPinterventionof30daysinthispatientpopulationhasthe potentialtobenefitpayors,hospitals,andpatients.[WestJEmergMed.2023;24(4)786–792.]
INTRODUCTION Problem
Wedesignedthisinvestigationtoquantifytheimpactofa one-monthcommunityparamedic(CP)interventiononallcausehospitalreadmissionsandvisitstoemergency departments(ED)andclinicsat30,120and210dayspost-
hospitaldischargeforpatientswithcongestiveheartfailure (CHF),acutemyocardialinfarction(AMI)andchronic obstructivepulmonarydisease(COPD)ascomparedtoa matchedcontrolgroup.Wealsoquantifiedthedifferencein totalcostofcarebetweencohortsoverthedatacollection period.OurhypothesiswasthataCPinterventionwould
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 786
ORIGINAL RESEARCH
decreasethenumberofall-causereadmissions,EDvisits,and totalcostofcare,andincreaseclinicutilization.
Background
Patientsreadmittedtothehospitaloftenhavepoor outcomesandincurhighhealthcarecosts.1 Inaddition, patientsatisfactionscoresaresignificantlyandnegatively correlatedwiththehospital’s30-dayreadmissionratesfor AMI,CHF,andpneumonia(PNA).2 PatientswithCHF haveuptoa25%chanceofbeingreadmittedtothehospital within30days,3,4 whilethoseoddsarenearly20%inpatients withAMI5 and15%inpatientswithexacerbationsof COPD.6 Moreover,themajorityofreadmissionsforpatients withAMI,CHF,orPNAoccurwithinthe firsttwoweeksof hospitaldischarge.7 Reducinghospitalreadmissionsand repeatEDvisitsforpatientswithcommonchronic conditionsisakeyfeatureofhealthcarereformeffortsfor bothcliniciansandpayors.
AspartoftheHospitalReadmissionsReduction Program,Medicarepaymentshavebeenreducedupto3%to hospitalswithexcessreadmissionsforsixconditions, includingCHF,AMI,andCOPD,since2012.8 Predictive modelinghasbeenusedtoidentifyfactors(eg,age, socioeconomicstatus,primarylanguage,multiple medications,andplaceofresidence)thatputpatientswith CHF,AMIandCOPDathighestriskforreadmission.9 Studiesthathavelookedattheabilityofpredictivemodeling toidentifypatientswithacutecardiopulmonarydiagnoses whoareathighestriskof30-dayreadmissionvarygreatlyin theirconclusions.Noconsensushasbeenreachedon interventionstotargetthehighestriskgroup.10
Withvaryingratesofsuccess,hospitalshaveimplemented numerousapproachestoreducereadmissionsincluding singleandbundledstrategies,improvedcarecoordination, betterhospitaldischargeeducation,medication reconciliation,schedulingoffollow-upvisitsbefore discharge,andstandardizationofcommunicationtoolsat discharge.11–19 Identificationofaminimumthresholdbundle ofinterventionsproventoreducereadmissionsremains elusive.Patientsreportfeelingunpreparedfordischarge;the primaryreasonsforreadmissionincludehavingdifficulty performingactivitiesofdailyliving,havingproblems adheringtooraccessingmedications,andlackofsocial support.20
Oneinterventionthathasbeenproposedtodecrease hospitalreadmissionsistheinclusionofacommunity paramedicintheoutpatientcareplan.Community paramedicsareadvanced,subspecializedparamedicswho haveundergoneadditionaltrainingdesignedtotransitionthe applicationoftheirAdvancedLifeSupportskillsetfromthe emergencysettingtotheprimarycaresetting.Community paramedicinetakesadvantageoftheknowledgebaseand mobilecapabilitiesofparamedicsandleveragesstheirability toconductin-homeassessments.PriorworkwithCPshas
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Patientsdischargedfromthehospitalwith diagnosesofmyocardialinfarction, congestiveheartfailure,orchronic obstructivepulmonarydiseasehave highratesofreadmission.
Whatwastheresearchquestion?
Canacommunityparamedicintervention reducehospitalandemergencydepartment (ED)readmissioninthispatientpopulation?
Whatwasthemajor findingofthestudy?
Communityparamedic(CP)intervention reducedreadmissionsat120(34.6%vs 64.1%,P < 0.001)and210days(43.6%vs 75.6%,P < 0.001)
Howdoesthisimprovepopulationhealth?
ImplementationofaCPprogramdecreases theneedforre-hospitalizationanddecreases healthcarecostsinthispatientpopulation.
beenreported,however,publishedresearchontheimpactof CPsonEDutilizationandhospitalreadmissionsforpatients withAMI,COPDorCHFisscarce.Priorpublishedstudies oncommunityparamedicinehavedemonstratedgenerally positiveresultsbuthavemainlyfocusedonreducing911calls andEDusage.
Purpose
ThemainlimitationtotheintegrationofCPsintothe currenthealthcaremodelasarecognizeddisciplineisthe paucityofsafety,ef fi cacy,andlong-termoutcomesdatato demonstratetheirimpactonpatientcare.Ourgoalinthis studywastocontributetothisdialoguebydescribingthe impactofaCPinterventionon210-dayhospital readmissionandEDandclinicutilizationinpatients dischargedfromanacutehospitalizationwithAMI,CHF, oranacuteexacerbationofCOPDascomparedtoa matchedcontrolgroup.Ourprojectisthe firsttoexamine theimpactofaCPinterventionbyusingaprospective, observationalcohortwithamatchedhistoricalcontrol.We followedpatientsfor210daysafterdischarge(180days aftercompletionoftheCPintervention)inanattemptto betterexploretheimpactoftheinterventiononthepatient’ s longertermhealth.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 787 Burnettetal. CPReducesHospitalReadmissionforPatientswithCardiopulmonaryConditions
METHODS DesignandSetting
Thisprojectwasreviewedbyourorganization’sResearch SubjectsProtectionProgramofficeandwasgrantedawaiver fromongoingoversightfromtheinstitutionalreviewboard. Thelocalurban fire/emergencymedicalservices(EMS) agency,incollaborationwiththelocalLevelItraumacenter, createdaCPprogramin2014staffedbycertifiedcommunity paramedics.The firedepartmentemployedthecommunity paramedics,andmedicaldirectionwasprovidedbyanEMS board-certifiedphysicianfromthetraumacenter.
SelectionofParticipants
InJanuary2015,webegantoprospectivelyidentify patientsadmittedtothehospitalforAMI,COPDorCHF. Participantsmetthefollowinginclusioncriteria:1) ≥18years old;2)livedinthesamecitywherethehospitalislocated; 3)dischargedfromanacuteadmissionwithadiagnosisof CHF,AMI,orCOPD;4)wasnoteligiblefortraditional homehealthcare;and5)wasreferredbyanin-patient treatmentteam.Exclusioncriteriawereasfollows:
1)non–English-speaking;2)planningamoveoutsidecity limitsinthe60daysafterenrollment;and3)beingaprisoner. Participantswereapproachedbytheresearchteamand offeredparticipationafteritwasdeterminedtheymetthe inclusioncriteriaandtheirtreatingclinicianhadplaceda referralfortheintervention.
Ahistoricalcontrolcohortwasmatchedonage,gender, qualifyingdiagnosis,andZIPcodeofresidence.We retrospectivelyobtaineddataregardingcontrolpatients fromagroupofpatientsadmittedtothehospitalduringthe samedatacollectionperiodwhometeligibilitycriteriabut didnotparticipateintheintervention.Controlgroup patientswerenotofferedtheinterventionnorwerethey referredfortheintervention;however,theymetallother enrollmentcriteria.Ifacontrolpatienthadmultiplehospital visitsduringthesearchperiod,oneofthevisitswaschosen atrandom.
Interventions
PatientswereenrolledintheCPinterventionpriorto hospitaldischarge.Whenpossible,andwithfewexceptions, thepatientandtheCPmetduringenrollmentwhilethe patientwasstillhospitalized.UpondischargetheCPvisited thepatientintheirhomewithin48hoursandsubsequently 1
2timesperweekfor30days.Whilethehomevisit containedstandardizedelements(Figure1),theCPswere allowedtoindividualizehowtheyprioritizedthespecific requiredelementsbasedontheirneedsassessmentforeach patient.
TheCPsweregrantedaccesstothehospitalelectronic healthrecord(EHR)forreviewofpatientmedicalhistory, buttheycompleteddocumentationofeachvisitin theambulanceserviceelectronicpatientcarereport
INTERVENTIONS
Physical Exam
Performauscultation of lung sounds, heart sounds, assessment of wounds, Assess for edema, skin condition, level of consciousness/memory, general vision, hearing and mobility.
Measurement of Vital Signs
Measureblood pressure, pulse, respiratory rate, pulse oximetry, blood glucose, temperature, weight.
Medication Reconciliation
Reconcile medications from all sources. Identify missing or duplicate medications, pillbox set-up.Confirm adequate supply of current medications, refills as needed. Assist with transfer to a more convenient pharmacy.
Medication Education
Confirm timing of doses, why medications are needed, potential side effects or adverse reactions.
Disease Specific Education
CHF: Reinforce importance of low-sodium diet and daily weights, including instruction on how to measure weight;provide scales when needed.
AMI: Teach appropriate use of nitroglycerin, reinforcing cardiac rehabilitation principles.
COPD: Educate the patient on proper use of steroid vs bronchodilator inhalers for rescue care;proper use and home maintenance of home oxygen equipment .
Nutrition Education
Explain elements of a low-sodium diet, diabetes-specific diet education as needed.
Evaluation of Social Needs
Determinetransportation, housing, food access, health insurance, social support system. Refer to community resources such as social work or community health worker as appropriate.
Communication with Primary/Specialty Physician
Provideassistance with making and keeping all medical appointments; titration of medications. Identifyadditional durable medical equipment or inhome medication needs.
Safety Evaluation
Conduct home safety assessments, including fall and fire hazards. Evaluate for evidence of acute illness or injury requiring prompt physician intervention.
(HealthEMS,StrykerCorp,Redmond,WA).Physician supervisionoftheCPinterventionwasprovidedbythe ambulanceservice’sEMSmedicaldirectorinpartnership withthepatient’sprimarycareteam.Communicationwith theprimarycarephysiciantypicallyoccurredviaatelephone calltotheregisterednurseattheclinicwhowouldrelay informationtothephysician.Patientsatisfactionsurveys wereadministeredbyaresearchstaffmemberatthe final homevisit.
Measurements
WeusedmanualreviewoftheEHRtoquantifyhealthcare utilizationforthisproject.UsingtheCareEverywhere functionoftheEHR,staffwereabletoidentifyhealthcare visitswithinourintegratedcaredeliverysystemandwithin mostoftheotherlocalhealthcaresystems.
Patientdemographicsaresummarizedusingdescriptive statisticsin Table1.Wecalculatedhealthcareutilization (admissions,EDvisits,andclinicvisits)bycohortat30days (attheconclusionoftheCPintervention),120days,and210 dayspost-hospitaldischargeforbothgroups(Figure2).We comparedthepercentageofsubjectsbytypeandtimepoint ofutilizationusingchi-squaretests(Table2).
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 788 CPReducesHospitalReadmissionforPatientswithCardiopulmonaryConditions Burnettetal.
Figure1. Standardizedelementsofcommunityparamedicvisits. AMI,acutemyocardialinfarction; COPD,chronicobstructive pulmonarydisease;CHF,congestiveheartfailure.
Wecomputedthemedianutilizationcountpersubjectand generatedanincidencerateratio(IRR)usingPoisson regression(Table3).Totalutilizationcountbytypeandtime pointforeachcohortwasalsocomputed(Table4).We calculatedhealthcaresavingsbycomparingactualcoststo thehealthcaresystemfortheCPgroupandthecontrol group.AveragecosttotheprogramperCPhomevisitwas $100inclusiveofCPsalary,vehicleuse,fuelandsupply expenses,andphysicianmedicaldirection.Patientsreceived anaverageof fiveCPvisits.Averagecostperhospital admissionwas$6,413.00foranaveragelengthofstayoffour daysbasedonthehospital’saverageforthediagnoses includedintheintervention.

RESULTS
Findings
Theinterventionandcontrolcohortseachconsistedof78 patients.Therewerenosignificantdemographicdifferences betweentheCPandcontrolgroups(Table1).Comparedto controls,fewersubjectsintheCPcohorthadexperienceda readmissionat120daysand210daysafterdischarge (Table2).AsignificantlyhigherpercentageofCPsubjects hadatleastoneclinicvisitinthe first30days,althoughthis differencewasnotobservedat120or210days.Regression resultsforhospitalreadmissionsindicatedalowerlikelihood ofreadmissionsforCPsubjectsthroughoutthefollow-up periodcomparedtocontrols(30daysIRR0.53;120days
CPcohort(N = 78)Controlcohort(N = 78) P-value Age -Median(IQR)63.5(17.0)64(17.0)0.81 Gender- N(%) 0.87 Male44(56.41%)43(55.13%) Female34(43.59%)35(44.87%) Race- N(%) 0.80 AmericanIndianorAlaskaNative0(0%)1(1.28%) Asian1(1.28%)1(1.28%) BlackorAfrican-American23(29.49%)24(30.77%) HispanicorLatino1(1.28%)1(1.28%) NativeHawaiianorother0(0%)1(1.28%) White52(66.67%)50(64.10%) Other1(1.28%)0(0%)
Congestiveheartfailure Chronicobstructivepulmonarydisease Acutemyocardialinfarction IQR,interquartilerange.
Table1. Subjectcharacteristicsatbaseline.
Qualifyingdiagnosis
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 789 Burnettetal. CPReducesHospitalReadmissionforPatientswithCardiopulmonaryConditions
Figure2. Programtimeline. CP,communityparamedicine.
Table2. Cumulativepercentageofpatientsineachcohortwhohad atleastonehospitalreadmission,emergencydepartmentvisit,or clinicvisitateachstudytimepoint.
*Boldindicatesstatisticalsignificanceat α = 0.05. CP,communityparamedicine; ED,emergencydepartment.
IRR0.52;and210daysIRR0.59).Similarly,regression resultsforEDvisitsalsoindicatedlowerlikelihoodofED utilizationforCPsubjectscomparedtocontrols(30days IRR0.50;120daysIRR0.54;and210daysIRR0.59) (Table3).At210daysafterdischargetherewere56(40.9%) fewerhospitaladmissionsintheCPcohort(81vs137),which resultedinsaving218beddaysand$410,428inhealthcare costs(Table4).PatientsintheCPcohorthad70(40.7%) fewerEDvisits(102vs172).Ofthe78patientsintheCP cohort,78(100%)recommendedthisprogramtootherson theexitsurvey.
DISCUSSION
Ashealthcaresystemsevolve,newcaredeliverymodels areneededtocontrolcosts,improveoutcomes,andincrease patientsatisfaction.OurdatasuggestthatCPscanbepartof thesolutionbydecreasinghospitalreadmissionsandED visitsforapopulationthathasbeenshowntohavehighrates ofreadmission.Traditionally,post-dischargereadmission studieshavetargetedaperiodof30days.Ourproject quantifieddifferencesinhealthcareutilizationbetween cohortsat30,120,and210daysafterhospitaldischargeinan attempttobetterexploretheimpactoftheone-monthCP interventiononthepatient’slongertermhealth.Duringthis periodthebenefitsoftheCPinterventionweremaintained, thepatientsremainedoutofboththehospitalandtheED, andthetotalcostofcarewasdecreased.Therewereno identifiedincreasedadverseeventsintheinterventiongroup. Patientsurveysadministeredatthe finalparamedicvisit indicatedthatpatientsoverwhelminglyrecommendedthis
*Boldindicatesstatisticalsignificanceat α = 0.05. CP, communityparamedicine; ED,emergencydepartment; IQR,interquartilerange.
intervention,demonstratingthatitimprovedthepatient experience.
EstablishingapermanentroleforCPsinahospital system’sreadmission-avoidanceprocessesrequiresthatthe CPprogramdevelopsmechanismstoensure financial
Dayspost discharge CPcohort (N =
Controlcohort (N =
P-value* Hospital readmissions 3020.5%32.1%0.10 12034.6%64.1% <0.001* 21043.6%75.6% <0.001* EDvisits 3024.4%37.2%0.08 12042.3%65.4% <0.01* 21052.6%79.5% <0.001* Clinicvisits 3092.3%70.5% <0.001* 12093.6%85.9%0.11 21094.9%88.5%0.15
78)
78)
Dayspost discharge CPcohort (N = 78) Controlcohort (N = 78) Hospitalreadmissions 301834 1204994 21081137 EDvisits 302346 12062115 210102172 Clinicvisits 30175145 120389363 210536492
Table4. Healthcareutilizationeventtotalcountbycohortandtime fromdischarge.
Dayspost discharge CP cohort (N = 78) Control cohort (N = 78) Incidence rateratio 95% confidence interval Hospital readmissions Median(IQR) 300(0)0(1)0.53 0.30–0.94 1200(1)1(2)0.52 0.37–0.74 2100(1)1(1)0.59 0.45–0.78 EDvisits Median(IQR) 300(0)0(1)0.50 0.30–0.82 1200(1)1(2)0.54 0.40–0.73 2101(2)1(2)0.59 0.46–0.76 Clinicvisits Median(IQR) 302(2)1(3)1.210.97–1.50 1204(5)3(7)1.070.93–1.24 2106(7)4.5(7)1.090.96–1.23
Table3. Medianhealthcareutilizationcountperpatientbycohort andtimefromdischarge.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 790 CPReducesHospitalReadmissionforPatientswithCardiopulmonaryConditions Burnettetal.
sustainability.Ourdatademonstratethecostsavingsthat werepossiblewithaCPintervention.Inourcase,thesavings werenotrelateddirectlytothehospitalbutinsteadwere reflectedinthedecreasedtotalcostofcarefortheinsurers coveringthepatient’smedicalcosts.Toobtainaccesstothese costsavingstofundaCPprogram,insurersmustbe persuadedtocoverCPvisits.Ourdatashouldmakethese conversationsmoreempiricalandevidencedbased.
Whiletheprimarycostsavingsdemonstratedbyour interventionwastothebenefitofthepayors,theincreased availabilityofhospitalbeddayswasadirectbenefittoour hospital.Likemanytertiarycarecenters,ourhospitalis routinelyoperatingat95%capacitywithmultipleepisodesof >100%capacitypermonth.ThisinturnresultsinED boardingandthepotentialforambulancediversions,which havebeenshowntohaveanegative financialimpactona hospital.21 InthiswayourCPinterventionofferedadirect benefittothereceivinghospital;however,the financial impacttothehospitalwasdifficulttoquantify,whichcould leadtochallengesinadvocatingforahospital-financedCP program.
Ourprojectisthe firsttoexaminetheimpactofaCP interventionbyusingaprospective,observationalcohort withamatchedhistoricalcontrolstudydesign.Byfocusing onacutecardiopulmonaryprocesseswewereabletonarrow ourCPs’ medicalassessmentonthemostcommon componentsofthispopulation’soutpatientmanagement includingmedications,comorbidities,andsigns/symptoms ofdecompensation.Conductingtheassessmentinthe patients’ homes,asopposedtotheclinic,allowedourCPsan opportunitytovisualizethepatients’ livingconditionsand foodresourcesandtohaveconversationsabout transportation,addiction,andmentalhealthtobetter evaluatethesocialdeterminantsoftreatmentfailure.Many ofthesecontributingfactorswereincompletelyunderstood whenthepatientvisitedtheprimarycareclinic,askeydata thatcouldbefoundonlyinthehomewereunavailable.
LIMITATIONS
Therewerelimitationstothestudy.Community paramedicshavevariededucationandclinicalexperiencein providingpost-acutecare.Wewereunabletoidentifywhat specificCPintervention(s)ledtothedecreasesinobserved healthcareutilization.Whileourprojectfollowedpatients for210daysafterhospitalizationand180daysafter completionoftheCPintervention,wewerenotableto extrapolateourdatapastthispoint.Additionally,although ourEHRcaptureshealthcareutilizationatmanylocal healthcaresystems,itispossiblethatpatientsincludedinthe CPorcontrolgroupshadadditionalvisitsorhospitalizations thatwerenotincludedinthisanalysis.However,becauseit wasunlikelythatitdifferedbetweentheCPandcontrol groups,itisunlikelythatitintroducedbiasintotheprimary analysis.Whilewewereabletodescribecostsavingstothe
healthcaresystemforthisintervention,wewerenotableto describethecostsassociatedwithprogramstart-upor ongoingprogramming.
CONCLUSION
Ourprojectdemonstratedthatanin-homecommunity paramedicinterventionconductedfor30dayswithpatients dischargedfromthehospitalforCHF,AMIorCOPD resultedindecreasedhospitalreadmissionsanddecreased EDvisitsat30,120and210daysafterhospitaldischarge.In addition,asavingsof$410,428forpayorsandanincreaseof 218availablehospitalbeddayswasrealizedinthe interventioncohort.IncorporationofahomeCP interventionof30daysinthispatientpopulationhasthe potentialtobenefitpayors,hospitalsand,mostimportantly, patients.Theimplicationsofour findingsareimportant.As healthcaresystemsseekinnovativeapproachestoreduce cost,improvequalityofcare,andenhancepatient experience,newcaremodelsmustbeimplemented.This projectdemonstratesthata30-day,communityparamedic interventioninthehomeforpatientsdischargedfroman acutehospitalizationforCHF,AMIorCOPDresultsin decreasedhospitalandEDreadmissionswhiledecreasingthe totalcostofcareandimprovinghospitalbedavailability.
AddressforCorrespondence:TiaRadant,MS,NRP,Regions Hospital,MS13801B,640JacksonStreet,SaintPaul,Minnesota 55101.Email: Tia.M.Radant@HealthPartners.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Burnettetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.JencksSF,WilliamsMV,ColemanEA.Rehospitalizationsamong patientsintheMedicarefee-for-serviceprogram. NEnglJMed 2009;360(14):1418–28.
2.BouldingW,GlickmanSW,ManaryMP,etal.Relationshipbetween patientsatisfactionwithinpatientcareandhospitalreadmissionwithin 30days. AmJManagCare.2011;17(1):41–8.
3.BernheimSM,GradyJN,LinZ,etal.Nationalpatternsofriskstandardizedmortalityandreadmissionforacutemyocardialinfarction andheartfailure:updateonpubliclyreportedoutcomesmeasures basedonthe2020release. CircCardiovascQualOutcomes 2010;3:459–67.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 791 Burnettetal. CPReducesHospitalReadmissionforPatientswithCardiopulmonaryConditions
4.RossJS,ChenJ,LinZ,etal.Recentnationaltrendsinreadmissionrates afterheartfailurehospitalization. CircHeartFail.2010;3:97–103.
5.KheraR,JainS,PandeyA,etal.Comparisonofreadmissionratesafter acutemyocardialinfarctionin3patientagegroups(18-44,45to64,and ≥65years)intheUnitedStates. AmJCardiol.2017;120(10):1761–7.
6.SimmeringJE,PolgreenLA,ComellasAP,etal.Identifyingpatients withCOPDathighestriskofreadmission. ChronicObstrPulmDis 2016;3(4):729–38.
7.DharmarajanK,HsiehAF,LinZ,etal.Diagnosesandtimingof30-day readmissionsafterhospitalizationforheartfailure,acutemyocardial infarction,orpneumonia. JAMA.2013;309(4):355–63.
8.CentersforMedicare&MedicaidServices.NewStratifiedMethodology Hospital-LevelImpactFileUserGuide.Availableat: https://www.cms. gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/ Downloads/HRRP_StratMethod_ImpctFile_UG.PDF
AccessedAugust14,2018.
9.ZhouH,DellaPR,RobertsP,etal.Utilityofmodelstopredict28-dayor 30-dayunplannedhospitalreadmissions:anupdatedsystematic review. BMJOpen.2016;6(6):e011060.
10.ShamsI,AjorlouS,YangK.Apredictiveanalyticsapproachtoreducing 30-dayavoidablereadmissionsamongpatientswithheartfailure,acute myocardialinfarction,pneumonia,orCOPD. HealthCareManageSci 2015;18(1):19–34.
11.GallagherRA,PorterS,MonuteauxMC,etal.Unscheduledreturnvisits totheemergencydepartment:theimpactoflanguage. PediatrEmerg Care.2013;29(5):579–83.
12.BradleyEH,YakushevaO,HorwitzLI,etal.Identifyingpatientsat increasedriskforunplannedreadmission. MedCare.2013;51(9):761–6.
13.OkoniewskaBM,SantanaMJ,Holroyd-LeducJ,etal.Theseamless transfer-of-careprotocol:arandomizedcontrolledtrialassessingthe
efficacyofanelectronictransfer-of-carecommunicationtool. BMC HealthServRes.2012;12:414.
14.StewartS,CarringtonMJ,MarwickTH,etal.Impactofhomeversus clinic-basedmanagementofchronicheartfailure:theWHICH?(Which HeartFailureInterventionIsMostCost-Effective&ConsumerFriendlyin ReducingHospitalCare)multicenter,randomizedtrial. JAmColl Cardiol.2012;60(14):1239–48.
15.ThomasR,HuntleyA,MannM,etal.Specialistclinicsforreducing emergencyadmissionsinpatientswithheartfailure:asystematicreview andmeta-analysisofrandomisedcontrolledtrials. Heart 2013;99(4):233–9.
16.WongFK,ChauJ,SoC,etal.Cost-effectivenessofahealth-social partnershiptransitionalprogramforpost-dischargemedicalpatients. BMCHealthServRes.2012;12:479.
17.PhillipsCO,WrightSM,KernDE,etal.Comprehensivedischarge planningwithpostdischargesupportforolderpatientswithcongestive heartfailure:ameta-analysis. JAMA.2004;291:1358–67.
18.RichMW,BeckhamV,WittenbergC,etal.Amultidisciplinary interventiontopreventthereadmissionofelderlypatientswith congestiveheartfailure. NEnglJMed.1995;333:1190–5.
19.SchmidtS,SheikzadehS,BeilB,etal.Acceptanceoftelemonitoringto enhancemedicationcomplianceinpatientswithchronicheartfailure. TelemedJEHealth.2008;14:426–33.
20.KangoviS,GrandeD,MeehanP,etal.Perceptionsofreadmitted patientsonthetransitionfromhospitaltohome. JHospMed 2012;7(9):709–12.
21.FalvoT,GroveL,StachuraR,etal.The financialimpactofambulance diversionsandpatientelopements. AcadEmergMed. 2007;14(1):58–62.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 792 CPReducesHospitalReadmissionforPatientswithCardiopulmonaryConditions Burnettetal.
UtilityofSupraclavicularBrachialPlexusBlockforAnterior ShoulderDislocation:CouldItBeUseful?
MichaelShalaby,MD
MelissaSmith,MD
LamTran,MD
RobertFarrow,MD
SectionEditor: JuanAcosta,MD
MountSinaiMedicalCenterMiamiBeach,MiamiBeach,Florida
Submissionhistory:SubmittedOctober10,2022;RevisionreceivedMarch27,2023;AcceptedMarch27,2023
ElectronicallypublishedJune30,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59272
Anteriorshoulderdislocations(ASD)representa commonandpainfulorthopedicinjuryintheemergency department(ED).ThemanagementofASDvariesbroadly frommanualreductionsviascapularmanipulationwithor withoutpainmedicationtoproceduralsedationand anesthesia(PSA),andvariousregionalanesthesia(RA) techniques.Thereductionapproachoftendependsonthe patient’ssubjectivepainresponse,theexpecteddifficultyof reduction,andthephysician’sexperiencewitheachmethod. Oftheanestheticoptionsfordifficultshoulderreductions,we generallyfavorRAtechniquesoverPSA.WhileseveralRA techniqueshavebeendiscussedintheliterature,one techniquethathasyettobeanalyzedisthesupraclavicular brachialplexusnerveblock(SBP).Webelievethereis evidencetosuggestthattheSBPwouldserveasanexcellent anestheticoptionforpatientswithASDandsignificantpain oranexpecteddifficultreduction.
ANTERIORSHOULDERDISLOCATION–DIAGNOSIS ANDMANAGEMENT
Anteriorshoulderdislocations(ASD)arefairlycommon intheemergencydepartment(ED);theyaccountfor45%of alljointdislocationsandcarrya2%prevalenceinthegeneral population.1 Becauseofthesignificantpainpatientsoften endure,timelymanagementisimperative.DiagnosingASD istraditionallyviaradiograph(Figure1),butemergency physiciansareadeptatidentifyingitwithpoint-of-care ultrasound(POCUS)alonewithnearly100%sensitivityand specificity2 (Figure2).Unfortunately,95%ofpatientswith ASDexperiencerecurrenceofthisagonizingcondition.3
Adequateanalgesiacanbecriticaltothemanagementof ASD,andfailuretoobtain first-passsuccessportendslower ratesofclosedreduction.4 Approachestoreductioninclude analgesiawithintravenousandperosmedications, proceduralsedationandanesthesia(PSA),andregional anesthesia(RA).The firstoption,though,generallyonly bluntspainandthusportendsa16%failureinreduction;5 so, weseldomemployitexceptforpatientswhoareinonlymild
distress,suchasthosewithrecurrentASD.Forthe managementofmostASDintheED,thefundamental choiceliesbetweenPSAandRA.
Toitsmerit,PSAisanalgesic,anxiolytic,anesthetic,and importantly,amnestic;withappropriatedosagespatients achieveadequate(althoughtemporary)paincontrolanddo notrecallthereduction.Furthermore,PSAallowsphysicians withlittleornoexperienceinRAorotheranesthetic procedures(suchasintra-articularinjection)toreduceASD successfully.However,PSAistime-andlabor-intensive, mandatingthepresenceofanurseintheroomduringthe entireprocedure.UseofPSAalsonecessitatesclosepatient airwayandcardiacmonitoringduetotherisksofrespiratory depression,hypotension,andvomiting.6 Itgenerally lengthensEDvisits,aspatientsmustreachclinicalsobriety beforebeingdischarged.Dependingonthedosesof anestheticsused,patientsmaytakehourstometabolizethe inductionagentssufficiently.6 Emergencyphysiciansalso shouldnotoverlookthesocialaspectofPSA,asintoxicated patientsoftenbecomedisinhibitedandmayfeelembarrassed afterward.Lastly,PSAexposespatientstoopioids,and80% ofheroinaddictionbeginswithmedicallydispensedopioids.7
REGIONALANESTHESIA CURRENTUSESAND NEWTECHNOLOGIES
Regionalanesthesia,ontheotherhand,circumventsmost ofthedrawbacksofPSA.Regionalanesthesiarequiresonly thattheperformingphysicianbepresentintheroomwiththe patientonthecardiacandairwaymonitor.Patientscan remainawake,alert,andoriented,andifperformedproperly RAcancompletelyanesthetizetheaffectedarea,asisthecase inbrachialplexus(BP)blockadeforupperextremityinjuries.8 Furthermore,dependingontheanestheticused,patientscan bedischargedhomewithinhourstodaysofanesthesiapostreduction,anespeciallydesirableoutcomeforpatientswith fracture-dislocations.UseofRAcanalsodecreasethelength ofstay9 andincreasepatientsatisfaction.10
Shouldanattemptednerveblockeitherprovidesubpar anesthesiaorfailcompletely,theadministrationoflocal
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 793 EDITORIAL
anestheticsdoesnotprecludethesubsequentuseofPSA. However,likemostinvasiveinterventionsRAposesitsown perils,includingriskofnervedamage,vascularpuncture, pneumothorax(dependingonanatomiclocation)and,most importantly,localanestheticsystemictoxicity,thus necessitatingcardiacandairwaymonitoring.11 Yetunlike withPSA,stepscanbetakentoavertsuchcomplications, whicharemostoftenminimizedwithincreasingphysician skillandarenottheresultofpatientphysiologyalone.There aremanyRAoptionsforemergencyphysicianstoreduce ASD:interscaleneandinfraclavicularBPblockade, suprascapularnerveblock,andintra-articularinjectionof localanestheticintotheglenohumeraljoint.6 Mostrecently, Yuetalpublishedacaseseriesonthesuccessfuluseofthe retroclavicularapproachtotheinfraclavicularregion (RAPTIR),aninfraclavicularBPblock,foranterior shoulderreduction.6
TheuseofRAintheEDisendorsedbytheAmerican CollegeofEmergencyPhysicians(ACEP),whichina2021 policystatementemphasizedthatultrasound-guidednerve blocksare “notonlywithinthescopeofthepracticeof emergencyphysicians,butrepresentacorecomponentofa multimodalpathwaytocontrolpainforpatientsinthe emergencydepartment.”12 Academicemergencymedicine leadersareonboardwithACEP’sstatement:Inasurvey studyofprogramdirectorsandultrasounddepartment directors,nearlyallagreedthatRAisanintegralpartof residenteducation.13 CurriculaforteachingRAarebeing activelydevelopedacrossresidencyprograms,14 and residentscontinuetoshowaneagernesstolearnandthe capacitytoperformRAtechniques.15 Whenitisclinically appropriate,wefavorRAintheEDforthereductionof fracturesanddislocations.
SupraclavicularBrachialPlexusBlock WhyItWillWork forAnteriorShoulderDislocation

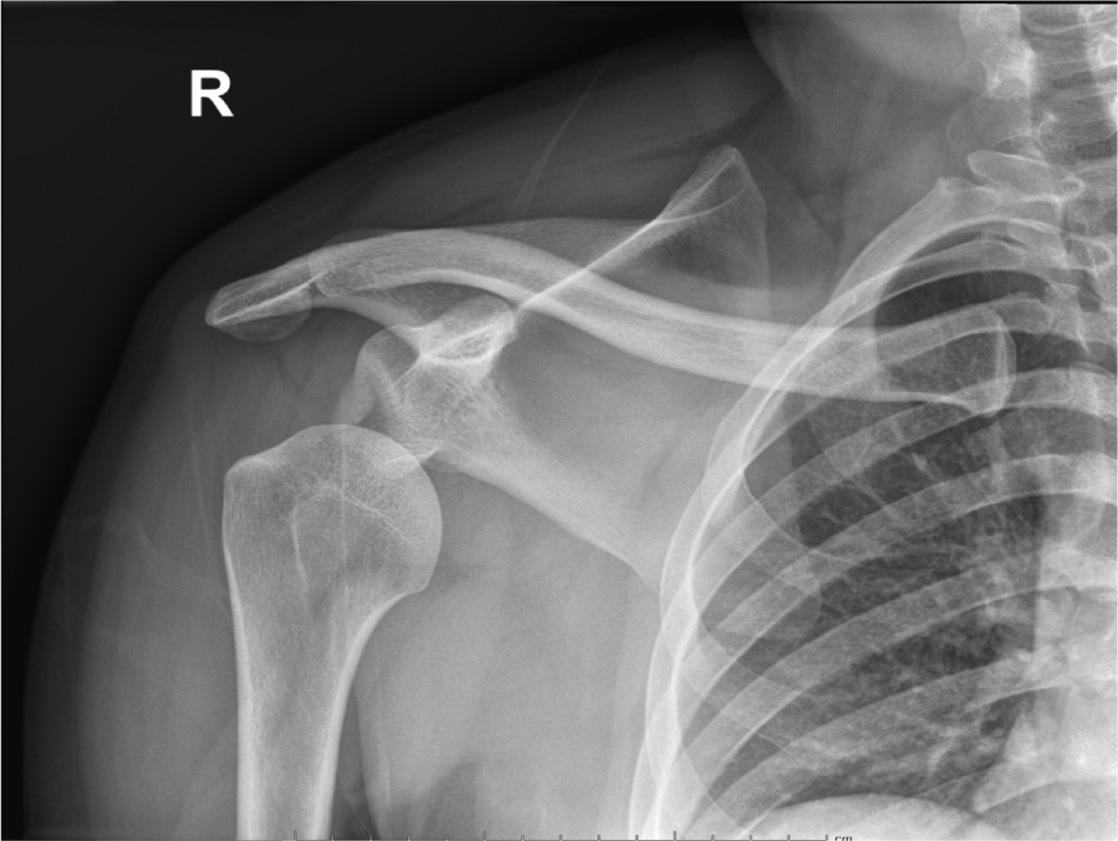
TheSBPblockanesthetizestheupperlimbandshoulder bytargetingalltrunksanddivisionsoftheBP16 (Figure3). TheSBPblockcanbeperformedinanypositioninwhichthe patientiscomfortable,aslongasthepatient’sheadisturned tothecontralateralside.Afterplacingahigh-frequency (10 5megahertz)linearprobeimmediatelysuperiortothe clavicle,theSBPisvisualizedwiththesubclavianartery medial,the firstribcaudal,andthepleuradeeptotherib16 (Figure4).ManyfeaturesoftheSBPblockmakeits applicationintheEDfavorableforbothphysicianand patient.First,theSBPisveryshallow(usually1
2 centimetersdeeptotheskin)andeasilyidentifiedwhenall othernecessarystructures(subclavianartery, firstrib,pleura)
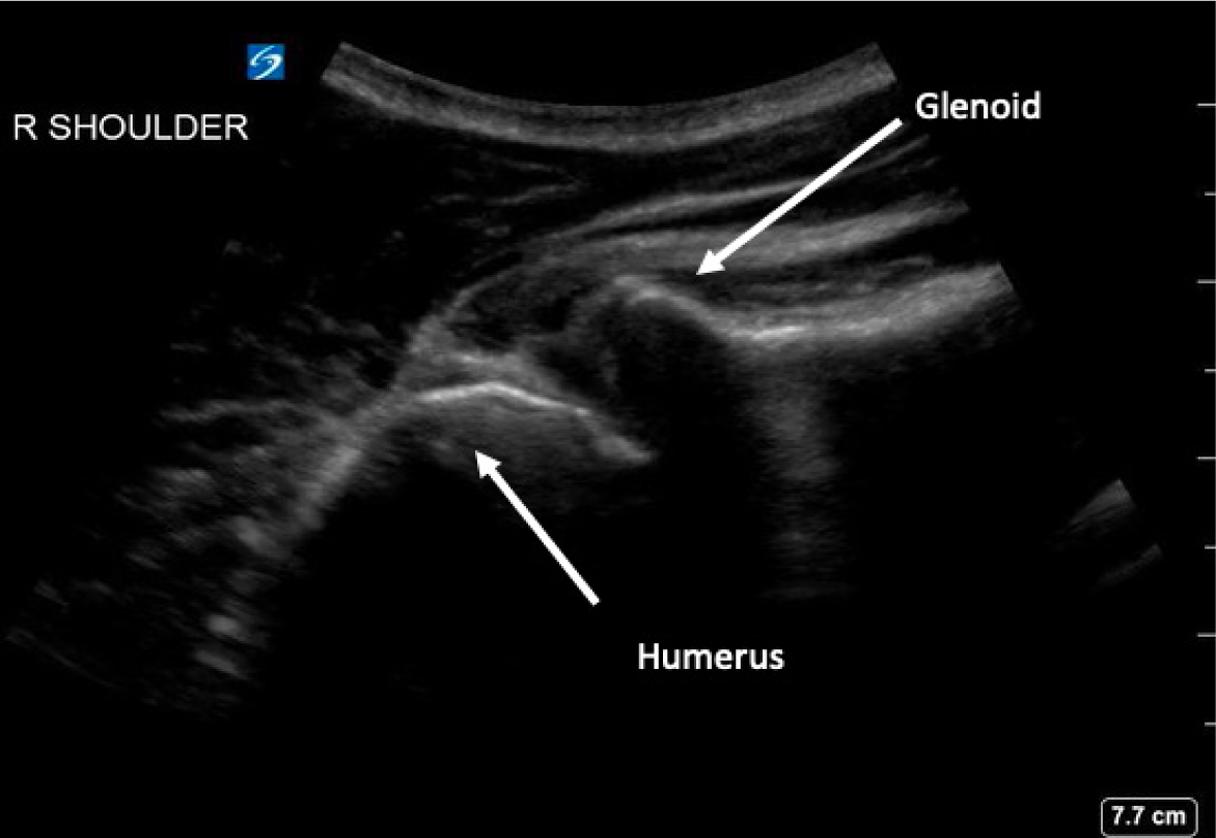
–
Figure1. Radiographofanteriorshoulderdislocation,courtesyof NiravJoshi,MD,MountSinaiMedicalCenter,MiamiBeach.
Figure2. Posteriorshoulderultrasounddemonstratinganteriorly dislocatedhumeralhead,courtesyofMichaelRosselli,DO, MountSinaiMedicalCenter,MiamiBeach.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 794
Figure3. Thebrachialplexus.ImagecourtesyofAnthony Casazza.
UtilityofSupraclavicularBrachialPlexusBlockforAnteriorShoulderDislocation Shalabyetal.
Shalabyetal.
UtilityofSupraclavicularBrachialPlexusBlockforAnteriorShoulderDislocation
arealsovisiblewithinthe fieldofviewonPOCUS. Moreover,the firstribactsasabackstop,sothatshouldthe physicianovershoottheSBPwiththeblockneedle,a resultingpneumothoraxmaybeavoided.
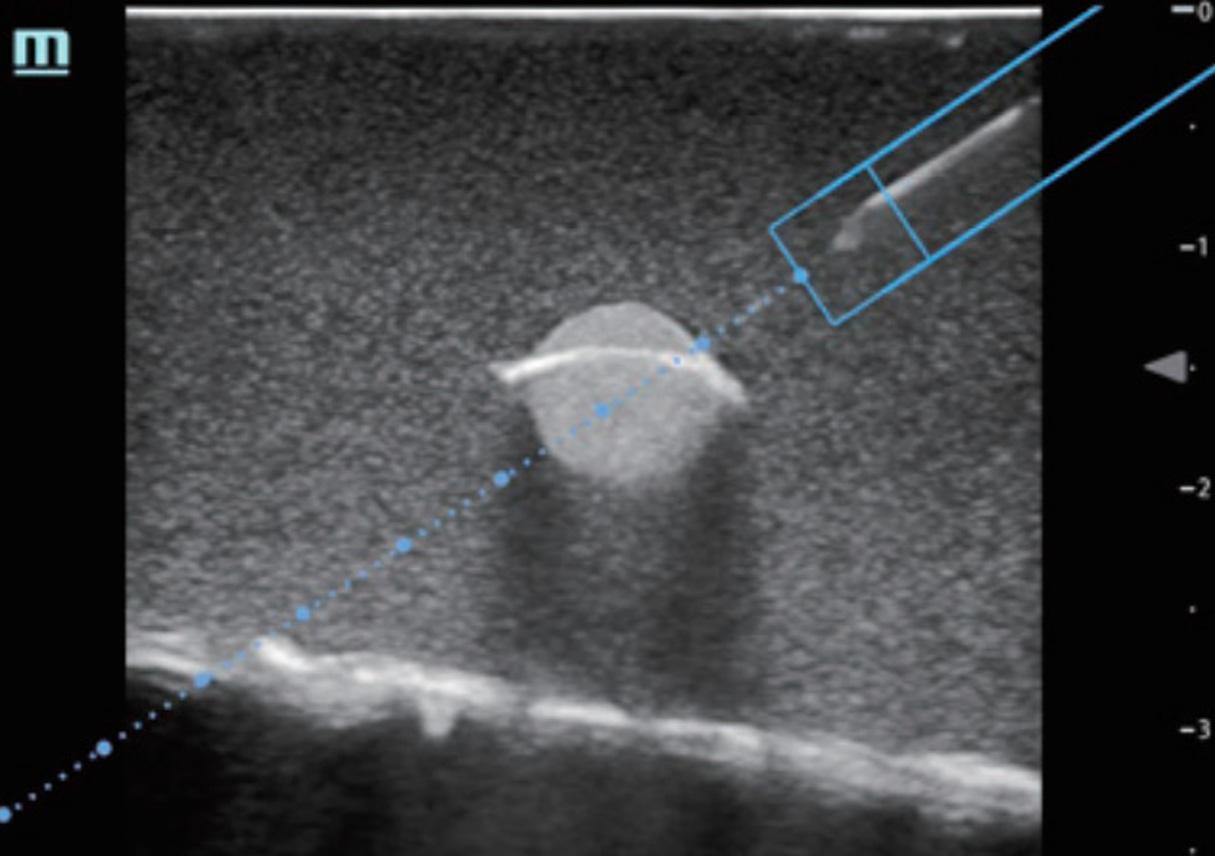
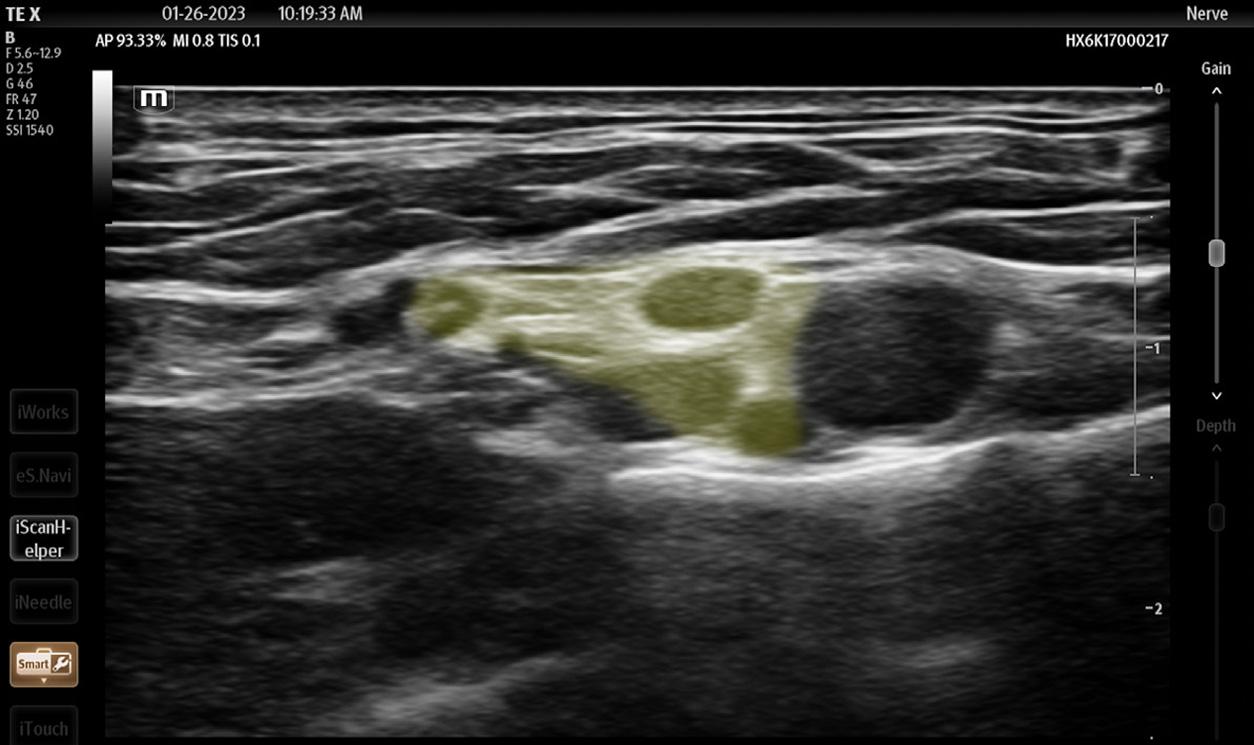
Additionally,thesetupissimple:dependingonthe patient’sbodyhabitustheSBPblockonlyrequiresa 22gaugeneedleandusuallynotaspinalneedle,aswellasa shortlinearprobeeasilyheldandmanipulatedinonehand. Ifthephysicianisskilledenough,sheorhecandirectly aspirateandinjectwithasyringeinsteadofhavingan assistantcontrolaspirationandinjectionwithasyringe connectedtotheneedleviatubing.WeprefertheMiller weight-baseddosingforlocalanesthetic,basedonthe patient’scalculatedidealbodyweight.17 However,inour experience,usually15millilitersoflocalanestheticinjected directlyintotheplexussheathisadequateforanesthesiaof theupperlimb,whichfrequentlyentailslessthanthe maximumamountoflocalanestheticforanadultpatient.
AlthoughtheSBPblockhasclassicallybeenusedformore distalprocedures,16 thespreadofanestheticwithintheBP sheathafteranSBPblocksupportsitsuseforthereductionof ASD.Theglenohumeraljointandintrinsicshouldermuscles derivetheirsensoryinnervationfromthesuprascapular, lateralpectoral,axillary,andlowersubscapularnerves.18
Byanesthetizingthesesensorynerves,theSBPblock anesthetizestheglenohumeraljointcapsuleandalleviates paininducedbyanASD.Additionally,disruptionofthe othercordsoftheBPweakensorparalyzesmusclesofthe upperextremitythatactivelyresistreduction,evenin patientswhoareundertheinfluenceofPSA.6 Forpatients whosufferfromassociatedHill-Sachsdeformity,which induceslingeringdiscomfortpost-reduction,longeracting anestheticssuchasbupivacaineorropivacaineprovidehours ordaysofrelief.19 AndwhiletheSBPisalreadyeasyto perform,newercart-basedPOCUSsystemsareequipped withsettingsthathighlighttheBPandprovideneedle trajectoryguidance(TEX,MindrayNorthAmerica,

Mahwah,NJ)(Figures5, 6).TheSBPblockiscomfortable forpatient;blockperformanceallowspatientstoremainin theirpreferredpositiononthestretcher.
Ofnote,althoughtheSBPblockcarriesalow complicationrate,someexpertsarewaryofintracluster injection.Gadsenetalarguethatbasedoncadavericstudies, theinadvertent,sub-perineuralspreadofanestheticmay resultinaxonaldamage.20 Othercomplicationsinclude pneumothorax,hemidiaphragmaticparalysis,and subclavianarterypuncture,duetotheproximityofboth thesestructurestotheSBP.Clinically,however,the SBPissafe.UltrasoundusefortheSBPblockhasbeen demonstratedtonearlyeliminatetheriskofpneumothorax andneuronalinjury.21–24 Furthermore,inouropinion ifthetreatingphysicianmaintainsappropriateneedle visualizationthroughouttheprocedure whichshouldbe feasiblegiventheshallownatureoftheSBPblock boththe lungsandthesubclavianarterywillremainwelloutofthe needletrajectory.Andwhilemostoftentheperformanceof
Figure4. Supraclavicularbrachialplexus(SBP)(yellow), subclavianartery(red), firstrib(beige),andpleura(pink).The needle(upperrightcorneroftheimage)approachestheSBPfrom lateraltomedial.ImagecourtesyofAnthonyCasazza.
Figure5. Ultrasoundimageofsupraclavicularbrachialplexus highlightedinyellow(SmartNerve),MindrayTEX,MindrayNorth America,ImagecourtesyofAndrewParrish.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 795
Figure6. Magnetizedneedletrajectoryguidance(ESpacial Navi),MindrayTE7,MindrayNorthAmerica.
anSBPblockwillrequiretwooperators(onetoinjectand onetoguidetheneedle),possiblylimitingitsuseinsettings withlimitedstaffing,askilledphysiciancanperformthe entireprocedurewithasingleneedleandsyringe.Overall,the SBPblockissafe,convenient,comfortable,andsuitable forASD.
Theinterscaleneblock,commonlyusedforshoulder pathologyintheED,alsoprovidesexcellentanesthesia fortheshoulderbytargetingtheC5toC7nerveroots.25 However,inouropinion,itismoredifficulttoperform:The targetnervesaresmaller,hardertovisualizeonPOCUS,and probemanipulationismoretechnicallychallengingbecause theBPattheleveloftheanteriorandmiddlescalenemuscles isfartheruptheneckandrequiresasteadiergriponthe probe,asopposedtothemorefavorablepositionoftheprobe restingontheclavicleintheSBPblock.Inapatientinsevere distresswhohastroublelyingstill,theperformanceofthis blockmayrepresentadifficulttask.Lastly,theinterscalene blockisknowntocarryaslightlyhigherriskofpermanent nervedamage.26 Intra-articularinjection,ontheotherhand, anesthetizestheglenohumeraljointcapsulebutdoesnot paralyzespasticmusclesand,therefore,itdoesnotmake ASDreductioneasierforthepatientorthephysician.
DISCUSSION
Anteriorshoulderdislocationisprevalent,painful,and tendstorecurinpatientswithpreviousepisodes.Reduction withoutsufficientanalgesiamaybeintolerableforpatients,5 andfailedinitialattemptsleadtomoreopenreductions.4
Thus,alleffortsshouldbemadetomakepatients comfortablepriortoreduction.Althoughmostphysicians arefamiliarwithPSA,itistime-consuming,labor-intensive, increasesthelengthofstayforpatientsintheED,risks airwaycompromise,exposespatientstoopioids,anddoes notimpartlastinganalgesia.Ontheotherhand,RAis learnable,involvesfewerpersonnel,andgenerallydoesnot poseairwayriskoroversedation.Fromourexperience, patientsleavetheEDsatisfied,inatimelymanner,andwith potentiallylastingpainrelief.
Itshouldalsobenotedthatwepracticeinacommunityacademicsettingandoftenworkshiftswithoutresident physicianstoassistwithperformingRA.Newerultrasound systemsmakeRAmoreuser-friendlyandlessintimidating forphysicians.TheSBPblockprovidesreliableanesthesia,is easytoperform,safe,andallowspatientstoremainina comfortableposition.Moreover,theuseoftheSBPblockis alreadycommonplacepriortoshouldersurgery.27 Whilethe interscaleneblockisalsoeffective,inthesettingofanASDit maybemuchmoretechnicallydifficultfortheoperator. Intra-articularinjectionisalsohelpfulforpainbutdoesnot paralyzemuscles.Therefore,weproposethatanoninferioritytrialbeundertakentoinvestigatethefeasibility andeffectivenessoftheSBPblockcomparedtothe
interscaleneblockorintra-articularinjectionforthe reductionofASDintheED.
CONCLUSION
Thesupraclavicularbrachialplexusnerveblockshould provideanesthesiaforpatientswithananteriorshoulder dislocationbytargetingallsensorynervesresponsiblefor nociceptionassociatedwithanASD,aswellasweakening/ paralyzingmusclesthatactivelyresistreductiondueto spasms.IfaninfraclavicularBPblockprovidesanesthesia forASD,6 whyshouldaSBPblocknotaswell?
AddressforCorrespondence:MichaelShalaby,MD,MountSinai MedicalCenterMiamiBeach,4300AltonRoad,MiamiBeach, FL33140.Email: michaelshalaby89@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Shalabyetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.KhiamiF,GéromettaA,LoriautP.Managementofrecent first-time anteriorshoulderdislocations. OrthopTraumatolSurgRes. 2015;101(1Suppl):S51–7.
2.GottliebM,PatelD,MarksA,PeksaGD.Ultrasoundforthediagnosisof shoulderdislocationandreduction:asystematicreviewandmetaanalysis. AcadEmergMed. 2022;29(8):999–1007.
3.HayesK,CallananM,WaltonJ,etal.Shoulderinstability:management andrehabilitation. JOrthopSportsPhysTher. 2002;32(10):497–509.
4.KanjiA,AtkinsonP,FraserJ,etal.Delaystoinitialreductionattemptare associatedwithhigherfailureratesinanteriorshoulderdislocation:a retrospectiveanalysisoffactorsaffectingreductionfailure. EmergMed J. 2016;33(2):130–3.
5.FuruhataR,KamataY,MatsumuraN,etal.Riskfactorsforfailure ofreductionofanteriorglenohumeraldislocationwithoutsedation. JShoulderElbowSurg. 2021;30(2):306–11.
6.YuM,ShalabyM,LuftigJ,etal.Ultrasound-guidedretroclavicular approachtotheinfraclavicularregion(RAPTIR)brachialplexusblockfor anteriorshoulderreduction. JEmergMed. 2022;63(1):83–7.
7.NationalAcademiesofSciences,Engineering,andMedicine,Health andMedicineDivision,BoardonHealthSciencesPolicy,etal. Trendsin OpioidUse,Harms,andTreatment.NationalAcademiesPress(US), 2017.Availableat: https://www.ncbi.nlm.nih.gov/books/NBK458661/ AccessedOctober16,2022.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 796
Shalabyetal.
UtilityofSupraclavicularBrachialPlexusBlockforAnteriorShoulderDislocation
8.GelberJ,LuftigJ,MantuaniD.Ultrasound-guidedretroclavicular approachtotheinfraclavicularregion(RAPTIR)anesthesiafor challengingupperextremityreductions. JEmergMed. 2021;60(6):772–6.
9.BlaivasM,AdhikariS,LanderL.Aprospectivecomparisonofprocedural sedationandultrasound-guidedinterscalenenerveblockforshoulder reductionintheemergencydepartment. AcadEmergMed. 2011;18(9):922–7.
10.MalikA,ThomS,HaberB,etal.Regionalanesthesiaintheemergency department:anoverviewofcommonnerveblocktechniquesandrecent literature. CurrEmergHospMedRep. 2022;10(3):54–66.
11.GreensmithJ,MurrayW.Complicationsofregionalanesthesia. Curr OpinAnaesthesiol. 2006;19(5):531–7.
12. Ultrasound-GuidedNerveBlocks.Availableat https://www.acep.org/ patient-care/policy-statements/ultrasound-guided-ne.rve-blocks/ Accessed8Oct.2022.
13.WilsonCL,ChungK,FongT.Challengesandvariationsinemergency medicineresidencytrainingofultrasound-guidedregionalanesthesia techniques. AEMEducTrain. 2017;1(2):158–64.
14.TuckerRV,PetersonWJ,MinkJT,etal.Defininganultrasound-guided regionalanesthesiacurriculumforemergencymedicine. AEMEduc Train. 2021;5(3).
15.AkhtarS,HwangU,DickmanE.Abriefeducationalinterventionis effectiveinteachingthefemoralnerveblockprocedureto first-yearemergencymedicineresidents. JEmergMed. 2013;45(5):726–30.
16. NYSORA.Ultrasound-guidedsupraclavicularbrachialplexusnerve block.2018.Availableat: https://www.nysora.com/topics/ regional-anesthesia-for-specific-surgical-procedures/ upper-extremity-regional-anesthesia-for-specific-surgical-procedures/ anesthesia-and-analgesia-for-elbow-and-forearm-procedures/ ultrasound-guided-supraclavicular-brachial-plexus-block/ AccessedOctober16,2022.
17.BerdeCB,StrichartzGR.Miller’sanesthesia.In: LocalAnesthetics, 4thed.ElsevierAcademicPress.2015:1028–1054.
18.LaumonerieP,DalmasY,TibboME,etal.Sensoryinnervationofthe humanshoulderjoint:thethreebridgestobreak.” ShoulderElbowSurg. 2020;29(12):e499–507.
19.ProvencherMT,FrankRM,LeclereLE,etal.TheHill-Sachslesion: diagnosis,classification,andmanagement. JAmAcadOrthopSurg. 2012;20(4):242–52.
20.GadsdenJ,OrebaughS.Targetedintraclustersupraclavicularbrachial plexusblock:toocloseforcomfort. BrJAnaesth. 2019;122(6):713–5.
21.PerlasA,LoboG,LoN,etal.Ultrasound-guidedsupraclavicularblock: outcomeof510consecutivecases.” RegAnesthPainMed.
2009;32(2):171–6.
22.WilliamsSR,ChouinardP,ArcandG,Ultrasoundguidancespeeds executionandimprovesthequalityofsupraclavicularblock. Anesth Analg. 2003;97(5):1518–23.
23.KapralS,KrafftP,EibenbergerK,etal.Ultrasound-guided supraclavicularapproachforregionalanesthesiaofthebrachialplexus. AnesthAnalg. 1994;78(3):507–13.
24.FrancoCD,GlossFJ,VoronovG,etal.Supraclavicularblockinthe obesepopulation:ananalysisof2020blocks. AnesthAnalg.
2006;102(4):1252–4.
25.KimE,ChoiCH,KimJH.EffectsofC8nerverootblockduring interscalenebrachialplexusblockonanesthesiaoftheposterior shoulderinpatientsundergoingarthroscopicshouldersurgery:study protocolforaprospectiverandomizedparallel-groupcontrolledtrial. Trials. 2019;20(1):533.
26.HussainN,GoldarG,RaginaN,etal.Suprascapularandinterscalene nerveblockforshouldersurgery:asystematicreviewandmetaanalysis. Anesthesiology. 2017;127(6):998–1013.
27.GuoCW,MaJX,MaXL,etal.Supraclavicularblockversusinterscalene brachialplexusblockforshouldersurgery:ameta-analysisofclinical controltrials. IntJSurg. 2017;45:85–91.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 797 Shalabyetal. UtilityofSupraclavicularBrachialPlexusBlockforAnteriorShoulderDislocation
HaboobDustStormsandMotorVehicleCollision-related TraumainPhoenix,Arizona
MichaelBHenry,MD,MS*
MichaelMozer,DO*
JeromeJRogich,MD,MS*†
KyleFarrell,MD‡
JonathanWSachs,MD,MPH§
JordanSelzer,MD,MPH*∥
VatsalChikani,MPH¶
GailBradley,MD¶
GeoffComp,DO*
SectionEditor: MarkI.Langdorf,MD,MHPE
*ValleywiseHealthMedicalCenter,CreightonUniversityArizonaHealthEducation Alliance,DepartmentofEmergencyMedicine,Phoenix,Arizona
† StanfordSchoolofMedicine,DepartmentofEmergencyMedicine,PaloAlto, California
‡ CreightonUniversitySchoolofMedicine-PhoenixCampus,Phoenix,Arizona § PhoenixChildren’sHospital,DepartmentofPediatrics,Phoenix,Arizona
∥ GeorgeWashingtonUniversitySchoolofMedicine,DepartmentofEmergency Medicine,Washington,D.C.
¶ BureauofEMSandTraumaSystem,ArizonaDepartmentofHealthServices, Tuscon,Arizona
Submissionhistory:SubmittedNovember7,2022;RevisionreceivedApril6,2023;AcceptedApril20,2023
ElectronicallypublishedJuly17,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.59381
Background: TheSonoranDesertregion,encompassingmostofsouthernArizona,hasanextreme climatethatisfamousforduststormsknownashaboobs.Thesestormsleadtodecreasedvisibility andpotentiallyhazardousdrivingconditions.Inthisstudyweevaluatetherelationshipbetween haboobeventsandemergencydepartment(ED)visitsduetomotorvehiclecollisions(MVCs)in Phoenix,Arizona.
Methods: ThisstudyisaretrospectiveanalysisofMVC-relatedtraumapresentationstoPhoenix,AZ, hospitalsbeforeandfollowinghaboobduststorms.Theseeventswereidentifiedfrom2009–2017 primarilyusingPhoenixInternationalAirportweatherdata.De-identifiedtraumadatawereobtainedfrom theArizonaDepartmentofHealthServices(ADHS)ArizonaStateTraumaRegistry(ASTR)fromseven traumacenterswithina10-mileradiusoftheairport.WecomparedMVC-relatedtraumausingsix-and 24-hourwindowsbeforeandfollowingtheonsetofhaboobevents.
Results: Therewere31,133MVC-relatedtraumaencountersincludedfrom2009–2017and111haboob eventsmeetingmeteorologicalcriteriaduringthatperiod.Therewasa17%decreaseinMVC-relatedED encountersinthesixhoursfollowinghaboobonsetcomparedtobeforeonset(235vs283, P = 0.04),with proportionallymoreinjuriesamongmales(P < 0.001)andhighermortality(P = 0.02).Therewasno differenceinfrequencyofpresentations(P = 0.82),demographics,oroutcomesamongthe24-hourpreandpost-haboobgroups.
Conclusion: HaboobduststormsinPhoenix,Arizona,areassociatedwithadecreaseinMVC-related injuriesduringthesix-hourperiodfollowingstormonset,likelyindicatingthesuccessofpublicsafety messagingefforts.Malesmadeupahigherproportionofthoseinjuredduringthestorms,suggestinga targetforfutureinterventions.Futurepublic-targetedweather-safetyinitiativesshouldbeaccompanied morecloselybymonitoringandevaluationeffortstoassessforeffectiveness.[WestJEmergMed. 2023;24(4)798–804.]
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 798 ORIGINAL RESEARCH
HaboobDustStormsandMVCollision-relatedTraumainPhoenix,AZ
INTRODUCTION
Weathereventsareknowntohaveaprofoundeffecton humanhealth.TheSonoranDesertregion,encompassing mostofsouthernArizona,hasanextremeclimatethatis famousforameteorologicalphenomenonknownasa “haboob.” Theword,ofArabicorigin,originallydescribed stormsintheMiddleEastandNorthAfricaandwas first usedtodescribesimilareventsinthesouthwesternUnited Statesina1972paperbyIdsoetal.1 Thehaboobisaunique duststormoccurringwhendesertsedimentissentairborne bytheconvectivedowndraftsofthunderstorms.The advancingwallsofdusttypicallydevelopsoutheastof TucsonandtravelnortheasttowardPhoenix.Theycanreach overakilometerinheightandareaccompaniedbyhigh winds,rapiddecreasesinvisibilityandtemperature,and increasesinairborneparticulatematter.2–4
Duststormsexertnegativehealtheffectsindifferentways. Forexample,studiesinavarietyofcontextssuggestthat particlesunder10micrometersindiameter(PM10)fromdust stormsmaybeassociatedwithincreasedhospitalvisitsand emergencydepartment(ED)visits,especiallyfrom cardiopulmonarydisease.5–11 Locally,Dimitrovaetal showedacorrelationbetweenparticulatematterand childhoodasthmaattacksinPhoenix,whileTongetal suggestthatincreasedduststormactivitymaybelinked toanuptickinfungal Coccidioides infections.12,13 The increaseinparticulatematteralsoleadstodecreased visibility,whichmayleadtohazardousdriving conditions.
Over fivemillionmotorvehiclecollisions(MVCs)resultin thedeathsofaround40,000U.S.residentseveryyear.14,15
Anestimated16–25%oftrafficfatalitiesmayberelatedto adverseweather,particularlyduetorainandwetconditions, costingtensofbillionsofdollarsandthousandsoflives yearly.15,16 Whilelow-visibilityconditionshavebeen associatedwithMVCsandfatalities,15 thereislimited researchspecificallyregardingtheimpactofhaboobsonthe frequencyofMVC-relatedtraumasecondarytoadverse drivingconditions.
Duststormsarethethirdleadingcauseofweather-related fatalitiesbehindextremeheat/coldand flash floodingin Arizona.3 Duststormmodelinghasidentifiedtwoduststorm hotspotsforMVCs:attheintersectionofInterstate8and Interstate10nearCasaGrande,aswellasattheintersection ofI-10andI-17inPhoenix.17 AccordingtotheNational OceanicandAtmosphericAdministration,1,521dustrelatedMVCsoccurredinArizonabetween1955–2011 resultingin157deathsand1,324injuries.18
Withrapidpopulationgrowthinthestateandevidencefor climatechangecausingincreasingseverityofhaboobs, understandingtheeffectsofsevereweatherondriving conditionsandMVC-relatedhealthoutcomesiscrucial.2–4 Elucidatingthisrelationshipcanhelpimprovedriversafety aswellaspreparednessofEDsandemergencymedical
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Manymotorvehiclecollisions(MVC)and associatedinjuriesareduetoadverseweather conditions.
Whatwastheresearchquestion?
Thisstudyexplorestherelationshipbetween MVCtraumaandduststorms( “ haboobs ” )in thePhoenix,Arizona,area.
Whatwasthemajor findingofthestudy?
Therewasa17%decrease(P = 0.04)in MVCinjuriesduringthesix-hourperiod followinghaboobonset.
Howdoesthisimprovepopulationhealth?
Publicsafetymessagingregardingadverse weatherconditionsmayhelpdriversavoid dangerousconditions.
services(EMS)personnel.Theprimaryoutcomeofthisstudy wasthechangeinfrequencyofEDvisitsforMVC-related traumafollowingonsetofahaboob.Secondaryoutcomes assessedwerechangesingroupcharacteristicsof demographics,transportmethods,andclinicaloutcome measuresamongthosewithMVC-relatedtraumafollowing ahaboob.
METHODS
ThiswasaretrospectiveanalysisofMVC-relatedtrauma presentationstoPhoenix,Arizona,hospitalsbeforeandafter haboobduststormeventsfrom2009–2017.Thisstudywas approvedbytheArizonaDepartmentofHealthServices (ADHS)HumanSubjectReviewBoardandtheValleywise HealthInstitutionalReviewBoard.
IdentificationofHaboobEvents
Haboobeventsarecharacterizedbyauniquearrayof meteorologicalpatternsthatarerelativelyrapidandintense comparedtoothertypesofstorms.Mostdistinguishingisthe significantdecreaseinvisibility,alongwithanacuterisein theamountofdustandhighwinds,andarapiddropin temperature.Thesechangesareobservedfromthebaseline meteorologyoveraperiodofhours.Thereisnoestablished strictmeteorologicaldefinitionofhaboob,noristherea quantifiablemethodofdistinguishingonefromotherdust storms.Forthepurposesofthisstudy,wedevelopedasetof criteriatodefinehaboobeventsbasedonpreviously
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 799
Henryetal.
publishedattemptsatidentificationandsimulationof haboobsintheregion.1,4,18
Haboobeventcriteriaconsistofanacutedropinvisibility tolessthanorequaltosevenmilesatPhoenixSkyHarbor InternationalAirportweatherstation(KPHX)withintwo hoursofeither
1.AnacuteriseinPM10togreaterthanorequalto 200 μg/m3 indiameter,or
2.AnacuteriseinPM10togreaterthanorequalto 100 μg/m3 andwindgustsgreaterthan38milesperhour.
Haboobeventswereidentifiedfrompubliclyavailable historicalclimateandairqualitydatafortheperiodof January1,2009
December31,2017.Weatherdatafor visibilityandwindwereobtainedfromtheNationalClimate DataCenterasaLocalClimatologicalDatasetsourcedfrom theKPHXweatherstation.19 Thesedatarepresentthe pointconditionsatKPHXincentralPhoenix,themost comprehensiveandwidelyreferencedweatherstationin themetropolitanarea.Particulatematterdatasetswere requestedfromtheEnvironmentalProtectionAgencyAir QualitySystem,anddailymaximumPM10wasobtained fromthenearbyairmonitoringsitesatCentralPhoenix (site04-013-3002),Tempe(site04-013-4005,)andSouth Scottsdale(site04-013-3003,)20 Ofnote,theTempeand SouthScottsdaleairmonitoringsitesdidnotgoonlineuntil 2012.Oneoftheauthors(JWSachs)requestedandprocessed datafromtheabovesources.Particulateandweatherdata werecombinedandcleanedinExcel2019(Microsoft Corporation,Redmond,WA)andvisualizedusingPowerBI 2019(Microsoft)andTimeSeries2019(ZoomCharts, Riga,Latvia).
Theidentificationprocessinvolvedthemanualreviewof plottedclimatologicaldata.Whilehaboobsareknowntobe associatedwithrapiddropsintemperature,theutilityofthis variablewaspoor.Classificationwasmadechallengingdue toqualityproblemswiththeclimateandairqualitydatasets. Forexample,dailyPM10andwindgustvalueswere frequentlymissing.Whensevereinconsistenciesarose,we attemptedtocorrelateasuspectedeventwithanonline eyewitnessaccountorarchivednewsreport.
Identi
ficationofMotorVehicleCollision-relatedTrauma
De-identifiedtraumadatawereobtainedfromtheADHS ArizonaStateTraumaRegistry(ASTR)from2009–2017. IncludedpatientencounterswereallinvolvedinMVC-related traumaasdefinedby “DataElementI2_14a:CDC Mechanism/CauseCategoryforPrimaryICD-10External CauseCode.” Allageswereincluded.Data fieldscollected includeddemographics(age,gender,state,andcountryof residence),accidentdetails(dateandtimeofinjury,ZIPcode andcountyofinjury),methodoftransportation,andoutcome measures(EDdisposition,totallengthofEDplusinpatient stay,totalhospitalcharges,andmortalityoutcome).
LiteratureonthesizeofhaboobsinArizonaislimitedand widelyvariable,withstormsizes10–20milesinlength describedatWilliamsAirForceBaseranginguptowitnessed stormwallsover100mileslongoutsidePhoenix.1,18,21 To includeencountersfromareasmostlikelytobeaffectedby haboobconditions,presentationswereincludedfromthe sevenLevelI-designatedtraumacenterswithin10linear milesoftheKPHXweatherstation.Injuriesthatoccurred outsideMaricopaCountywereexcludedastheseMVCswere deemedlesslikelytobelinkedtothehaboobeventmeasured atKPHX.Alsoexcludedwererecordswherethetimeand dateofinjurywerenotexplicitlyrecorded.
DataAnalysis
DataanalysiswasconductedusingJASPversion0.14.1 (Jeffrey’sAmazingStatisticsProgram,Universityof Amsterdam,TheNetherlands,2021).Basicdescriptive statisticswereperformedontheentiredatasetofallMVCrelatedencountersfrom2009–2017.
Aswithdataregardingthesizeofhaboobs,dataontheir durationinArizonaislimitedandvariable,andsome commonlycitedsourcesusedatafromothercountries.22,23 Brazeldescribeddust-relatedvisibilityreductionsinArizona occurring78minutespriortoand229minutes(SD220)after thestormfront,whileIdsoreportedanaverageofonehourbut uptothreehours.1,24
Eagarfoundthathighparticulatesare founduptoonetotwohoursduringhaboobs,whilesome milderduststormshadconditionslastingupto12hours.4 Crooksreportedthatwhilehalfofhaboobslastedlessthanone hour,asignificantnumberlastedlongerthansevenhours.11
Basedonthesestudies,tocreateaninclusivetimewindow capturingthemajorityofMVCinjuriespotentiallylinkedtoa haboobeventwedefined “post-haboob” MVCtraumaas occurringuptosixhoursaftertheonsetofhaboobconditions. Thecontrolgroupof “pre-haboob” MVCtraumaincludes injuriesoccurringinthesixhoursleadinguptohaboobonset. Additionally,werepeatedtheanalysisusinga24-hour windowbeforeandafterhaboobonsettoassesswhether lingeringweatherconditionswerelinkedtochangesinMVC frequency.ThefrequencyofMVC-relatedtraumainthe pre-haboob(control)andpost-haboob(exposure)groups werecomparedusingbinomialanalysis.Additionally, pre-andpost-haboobMVCtraumawascomparedwith subgroupanalysesfordemographics,transportmethods, andoutcomemeasuresusingtheStudent t -testfor continuousvariablesandchi-squaredtestfor categoricalvariables.
Occasionally,severalhaboobsoccurredinrapid succession,forexample,withapatientsimultaneously qualifyingas “post-” (theearlierhaboob)and “ pre” (thesubsequenthaboob).Inthesecases,weconsideredthe patienttobeinthe “post-haboob” groupofthe first eventanddiscardedsubsequentencounterslinked tolateroverlappinghaboobs.
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 800 HaboobDustStormsandMVCollision-relatedTraumainPhoenix,AZ Henryetal.
RESULTS
FromJanuary1,2009–December31,2017,therewere 31,133patientencountersmeetingcriteria(MVC-related traumapresentingtooneofthesevenincludedhospitals within10milesofKPHX).Themeanageofallencounterswas 35.8years(SD19.6,range0
101),and58.9%ofthepatients weremale.TheEDdispositionof67.3%ofthepatientswas admissionfromtheED;29.6%weredischarged,2.0%diedin theED,0.6%requiredtransfertoanotherhospital,and0.4% bypassedtheEDasadirectadmission.Arizonastateresidents included97.0%ofthepatients.Groundambulance transported88.5%and6.7%viahelicopter,while4.5%were EDwalk-ins.Themeantotallengthofstayforallpatients(ED plusinpatient)was3.3days(SD6.7days,range0
309days). Themortalityratewas4.1%.
HaboobEvents
From2009–2017,therewere111haboobeventsmeeting ourinclusioncriteria.Themaximumnumberofhaboobsina singleyearwas23(in2011)andtheminimumwasthree (in2010),withameanof12haboobsperyear(SD6.6).
Thegreatestnumberofhaboobsduringtheseyearshappened inthemonthsofJuly(33),followedbyAugustand September,respectively(29and21).See Figures1 and 2
Haboob-relatedMVCPatientPresentations
Analysisusing24-hourpre-andpost-haboobperiods revealedthat815patientswereinjuredpre-haboobcompared to825inapost-haboobperiod(P = 0.82).Therewasno demographicdifferencebetweenthesegroupsregardingage, gender,orArizonaresidence(P = 0.10,0.21,and0.53, respectively).Asimilarnumberofpatientsinthe24-hourpreandpost-haboobperiodsweretransportedbyhelicopter comparedtogroundambulanceinbothgroups(P = 0.07). Outcomesoftotallengthofstay,hospitalcharges,and mortalitywerealsosimilarinbothgroups(P = 0.25,0.88,and 0.80,respectively).Weexcluded143patientencounters(8.0% ofMVCinjurieswithin24hoursofahaboobonset)dueto overlappinghaboobtimeframes.
Analysisusingsix-hourpre-andpost-haboobperiods demonstratedaroughly17%decreaseinMVCinjuriesinthe six-hourperiodfollowinghaboobonset(235vs283, P = 0.04).Thesix-hourpost-haboobperiodhada proportionallyhighernumberofinjuredmales(P < 0.001), whiletherewasnodifferenceinageorArizonaresidence (P = 0.23and0.50,respectively).Nosignificantdifferencewas notedinhelicoptervsgroundambulancetransport(P = 0.06). WhileLOSandtotalhospitalchargesweresimilarinsix-hour pre-andpost-haboobpatients(P = 0.52and0.82),therewasa highermortalitynotedinthepost-haboobperiod(P = 0.02). Fourpatientencounters(0.008%ofthosewithinsixhoursofa haboobonset)wereexcludedfromtwooccasionsof overlappinghaboobtimeframes.Pleasesee Table1
DISCUSSION
Thisstudyevaluatedtherelationshipbetweenhaboob duststormeventsandMVC-relatedEDvisitsinPhoenix, AZ.Priorstudieshavedemonstratedthegeneralrelationship betweenbadweatherandpoorvisibilityandMVC fatalities,15,16 andquantifiedhaboob-relatedMVCsand associatedmorbidityandmortalityinArizona.3,17 However, wearenotawareofanystudycomparingthenumberof MVC-relatedinjuriesfollowinghaboobonsetcompared withbaseline,oranystudydescribingchangesinthenumbers ofMVC-relatedinjurycasespresentingtolocalEDsaround thetimeofahaboobevent.
Interestingly,thefrequencyofMVC-relatedinjuries decreasedduringthesix-hourperiodfollowinghaboobonset byapproximately17%.Nosignificantdecreasewasseen whenconsideringpresentationsduringa24-hourperiod followinghaboobonset;thismaybebecausethedurationof mosthaboobsisonlyseveralhours 1,4,11,24 and,therefore,a 24-hourperiodincludesmanynon-haboob-relatedincidents, withthemisclassificationbiasingourresultstowardthenull. Thisdropininjuryfrequencynotedduringthesix-hourposthaboobperiodmaybeduetochangesindriverbehavior secondarytopublicsafetymessagingsystems.Alarge haboob-linkedmulticarcollisionin2011ledto collaborationsbetweentheArizonaDepartmentof
–
–
0 5 10 15 20 25 200920102011201220132014201520162017
Number of yearly haboobs, 2009-2017
0 5 10 15 20 25 30 35 JanFebMarAprMayJunJulAugSepOctNovDec
Figure1. Numberofhaboobsperyearfrom2009–2017.
Number of haboobs by month, 2009-2017
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 801 Henryetal. HaboobDustStormsandMVCollision-relatedTraumainPhoenix,AZ
Figure2. Numberofhaboobsbymonth,averagedfrom 2009–2017.
Transportation,theNationalWeatherService,Arizona DepartmentofPublicSafety,andtheGovernor’sOffice ofHighwaySafetyinrollingoutthe “PullAside,Stay Alive” campaign.Thecampaignhasincludedradioalerts, televisionmessaging,andincreasedroadsidesignage,even encouragingpublicparticipationviawhimsicalaspects suchasthe “HaboobHaikuChallenge.”25
Currentrobust,publichealthmessaginginArizonamay besuccessfulinkeepingdriversofftheroadandsafeduring haboobs,similarlytowhatwasnotedwithadecreasein MVCsinVirginiafollowingarolloutofwirelessalerts regarding flash floods26 andinsouthernCaliforniawiththe useofchangeablemessagesigns.27 ACanadianstudyin2010 similarlyshowedthatriskofMVCsassociatedwithrainfall significantlydecreasedovertwodecades,whichcould partiallybeattributedtodriverbehaviors,inadditiontoroad andvehicularimprovements.28 AlthoughMVCinjuries decreasedduringthesixhoursfollowinghaboobonset,there wasahigherproportionoffatalitiesamongcasespresenting totheincludedEDs,suggestingthatthosewhodidnot stayofftheroadswereinvolvedinmoreseriouscollisions; however,otheroutcomemetricsoflengthofstay andhospitalchargesdidnotsuggestadifference.
Whilemaleswereoverallmorelikelytosufferfroman MVCinjury,consistentwithpriortrendssecondarytorisky behaviorsandnumberofmilesdriven,29 males werealsodisproportionatelyrepresentedamonginjuries occurringduringthesix-hourwindowfollowinghaboobs. Onestudyfoundthatfemalesmaybesuperiortomalesat keepingwithintheirlanesduringfoggyweatherconditions,30 andeveninnon-UScontextssurveyssuggestthatmale drivingbehaviorsmayexacerbateriskssecondaryto inclementweather.31
Itwashypothesizedthatnon-Arizonaresidentsmayhave representedalargernumberofMVCsduringhaboobsdueto unfamiliaritywiththeseweatherevents,buttherewasno
differenceinresidencyamongthoseinjuredinhaboobs. Therewasanapparentdifferenceinboththesix-and24-hour groups,althoughultimatelystatisticallyinsignificant,in transportmodewithproportionallyfewerhelicopter EMSfollowinghaboobs,unsurprisinggiventheassociation withbadweatherandanincreasednumberof fatalcrashes.
LIMITATIONS
Thisstudyhadseverallimitations.Whileweconducted theanalysisunderthepresumptionthatMVCinjuries occurringinthehoursfollowinghaboobonsetcouldbe linkedtoweather,thedatasetsweuseddidnotexplicitlysay whethertheweatherwasacausativefactorintheMVCs. Weatherdatawasnotavailableontheexactspatiotemporal patternsofthestorms,andtraumadataincludedZIPcodes asopposedtospecificintersections;thus,beyondincluding casespresentingtohospitalswithintheradiusandexcluding injuriessustainedoutsideMaricopaCounty,therewasno moreclearwaytomorepreciselylinkweatherandthe MVCs.WhileweattributedchangesinMVCfrequency followinghaboobonsettoweatherconditionsandvisibility, thereareconfoundersthatcouldnotbeassessedinthisstudy (suchassubstanceorcellphoneuseorvehiclemechanical issues),butwerelikelycontrolledinouranalysis.
Additionally,becausepre-/post-classificationofMVCs occurringduringperiodswhenmultiplehaboobshappened inrapidsuccessionwasimpossible,theseeventswere removed.Theyrepresentedonlyasmallproportionof encounters,andtheirremovaldidnotbiastheresults.
Selectionofthecontrolsforcomparisontopost-haboob injurieswaschallenging,sincemanychangingtraffic conditionscouldaffectMVCandinjuryfrequency(for example,decreasedMVCnumbersfollowingeveningstorms mayhavebeenmorerelatedtonatural fluctuationsin commuternumbers).However,wedecidedthatdespite
All24-hourhaboobperiod6-hourhaboobperiod pre-post- P-valuepre-post- P-value MVCinjuries(#patients)31,1338158250.82283235 0.04 Age(meanyears)35.834.636.20.1033.836.00.23 Gender(%male)58.958.261.20.2151.265.5 <0.001 Placeofresidence(%Arizona)96.496.996.40.596.194.80.50 Transport(%helivsgroundambo)7.07.45.10.077.03.20.06 TotalED + admitLOS(days)3.33.53.10.253.53.00.52 Totalhospitalcharges(mean$)65,76063,91363,1040.8860,63163,0560.82 Finaloutcome(%mortality)4.12.83.00.801.14.3 0.02 Excluded(#patients)1434
Table1. Demographicsandoutcomesofpatientspresentingwithin24-andsix-hourwindowsfollowinghaboobeventonset.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 802
MVC, motorvehiclecollision; ED, emergencydepartment; LOS,lengthofstay; heli,helicopter; ambo,ambulance.
HaboobDustStormsandMVCollision-relatedTraumainPhoenix,AZ Henryetal.
time-of-dayvariationsintraffic,thehourspreceding haboobseventswereotherwisethebestcontrols,andwith enoughincludedhaboobeventsthedailytrafficvariations betweenpre-andpost-haboobtimeperiodswere negligible.
Anotherlimitationwasduetodatasetcompletion;for example,whilemany fieldswereconsistently filledoutonthe ASTR,othersliketotalhospitalchargeswerenotavailable formanycases.Additionalinformationforinjury characterizationwasalsounavailable;therefore,mortality, lengthofstay,andhospitalchargeswereusedasproxiesfor injuryseverity.Theavailabledatalikelyunderestimated traumabecausenotallMVC-relatedinjuriesledto activationofhospitaltraumateams(andtherewaslikely variationintraumateamactivationbetweeninstitutions unaccountedforhere);thus,theremayhavebeenanumber ofminorinjuriesnotincluded,whileincidentsofMVCrelatedmortalitiesthatwerenottransportedfromthescene alsowouldnothavebeenincluded.
CONCLUSION
HaboobduststormsinPhoenix,Arizona,maybe followedbyadecreaseinmotorvehiclecollision-related injuriesduringthesix-hourperiodfollowingstormonset, perhapsduetothesuccessofpublicsafetymessagingefforts. Malesmadeupahigherproportionofthoseinjuredduring thestorms,suggestingatargetforfutureinterventions. Futurepublic-targetedweathersafetyinitiativesshouldbe accompaniedmorecloselybymonitoringandevaluation effortstoassessforeffectiveness.
AddressforCorrespondence:MichaelBHenry,MD,MS,Valleywise Health,DepartmentofEmergencyMedicine,2601ERooseveltSt., Phoenix,AZ85008,USA.Email: Mhenry12@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Henryetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.IdsoSB,IngramRS,PritchardJM.AnAmericanhaboob. BullAm MeteorolSoc.1972;53(10):930
935.
2.RamanA,ArellanoAF,BrostJJ.Revisitinghaboobsinthesouthwestern UnitedStates:anobservationalcasestudyofthe5July2011Phoenix duststorm. AtmosEnviron.2014;89:179
188.
3.LaderG,RamanA,DavisJT,WatersK. NOAATechnicalMemorandum NWS-WR290.BlowingDustandDustStorms:OneofArizona’sMost UnderratedWeatherHazards;2016.
4.EagarJD,HerckesP,HartnettHE.Thecharacterizationofhaboobsand thedepositionofdustinTempe,AZfrom2005to2014. AeolianRes 2017;24:81–91.
5.EbrahimiSJA,EbrahimzadehL,EslamiA,BidarpoorF.Effectsofdust stormeventsonemergencyadmissionsforcardiovascularand respiratorydiseasesinSanandaj,Iran. JEnvironHealthSciEng 2014;12(1):110.
6.MerrifieldA,SchindelerS,JalaludinB,SmithW.Healtheffectsofthe September2009duststorminSydney,Australia:Didemergency departmentvisitsandhospitaladmissionsincrease? EnvironHealth 2013;12:32.
7.GeravandiS,SicardP,KhaniabadiYO,etal.Acomparativestudyof hospitaladmissionsforrespiratorydiseasesduringnormalanddusty daysinIran. EnvironSciPollRes.2017;24:18152–18159.
8.BarnettAG,FraserJF,MunckL.Theeffectsofthe2009duststormon emergencyadmissionstoahospitalinBrisbane,Australia. IntJ Biometeorol.2012;56:719–726.
9.CastillejosM,Borja-AburtoVH,DockeryDW,GoldDR,LoomisD. Airbornecoarseparticlesandmortality. InhalToxicol 2000;12(Sup1):61–72.
10.HefflinBJ,JalaludinB,McClureE,etal.Surveillanceforduststormsand respiratorydiseasesinWashingtonstate,1991. ArchEnvironHealth 1994;49(3):170–174.
11.CrooksJL,CascioWE,PercyMS,ReyesJ,NeasLM,HilbornED. Theassociationbetweenduststormsanddailynon-accidental mortalityintheUnitedStates,1993-2005. EnvironHealthPerspect 2016;124(11):1735–1743.
12.DimitrovaR,LurponglukanaN,FernandoH,etal.Relationshipbetween particulatematterandchildhoodasthma:basisofafuturewarning systemforcentralPhoenix. AtmosChemPhys.2012;12:2479–2490.
13.TongDQ,WangJXL,GillTE,LeiH,WangB.Intensifiedduststorm activityandValleyfeverinfectioninthesouthwesternUnitedStates. GeophysResLett.2017;44:4304–4312.
14.USDOT.MotorVehicleSafetyData.USDepartmentofTransportation NationalTransportationStatistics.Published2022.Availableat: https://www.bts.gov/content/motor-vehicle-safety-data AccessedSeptember4,2022.
15.AshleyWS,StraderS,DziublaDC,HaberlieA.Drivingblind: weather-relatedvisionhazardsandfatalmotorvehiclecrashes. BullAmMeteorolSoc.2015;96(5):755–778.
16.SahaS,SchrammP,NolanA,HessJ.Adverseweatherconditionsand fatalmotorvehiclecrashesintheUnitedStates,1994-2012. Environ Health.2016;15(1):104.
17.MohebbiA,GreenGT,AkbariyehS,YuF,RussoBJ,SmaglikEJ. Developmentofduststormmodelingforuseinfreewaysafetyand operationsmanagement:anArizonacasestudy. TranspResRec 2019;2673(5):175–187.
–
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 803 Henryetal. HaboobDustStormsandMVCollision-relatedTraumainPhoenix,AZ
18.VukovicA,VujadinovicM,PejanovicG,etal.Numericalsimulationof “anAmericanhaboob.” AtmosChemPhys.2014;14(7):3211–3230.
19.NOAANationalCentersforEnvironmentalInformation.ClimateData
Online.Published2019.Availableat: https://www.ncei.noaa.gov/cdoweb/.AccessedDecember31,2018.
20.EnvironmentalProtectionAgency.AirQualitySystem(AQS)API.
Published2019.Availableat: https://aqs.epa.gov/aqsweb/documents/ data_api.html.AccessedDecember31,2018.
21.HugenholtzPG.ClimateandCoccidioidomycosis.In: Proceedingsof SymposiumonCoccidioidomycosis.PublicHealthHealthService,Bureau ofStateServices,CommunicableDiseaseCenter;1957:136–143.
22.SuttonLJ.NoteonHaboobs. JRMeteorolSoc.1931;54:72–73.
23.FreemanMH.DuststormsoftheAnglo-EgyptianSudan. MeteorolRep 1952;2(11).
24.BrazelAJ,NicklingWG,LeeJ.Effectofantecedentmoistureconditions onduststormgenerationinArizona.In:NicklingWG,ed. Aeolian Geomorphology:BinghamtomGeomorphologySymposium17.Vol2. Routledge;1986.
25.DouglasL,KrugelD. “PullAside,StayAlive” ArizonaDOT’s effortstocommunicateabouttheweather.ArizonaDepartmentof TransportationPublicInformationOffice.Published2013.
Availableat: http://www.3cma.org/DocumentCenter/View/2362/
Raising-Arizona---L-Douglas-and-D-Krugel?bidId= AccessedSeptember4,2022.
26.FerrisJS,NewburnDA.Wirelessalertsfor flash floodwarningsand theimpactoncaraccidents. SSRN.2016. https://papers.ssrn.com/sol3/ papers.cfm?abstract_id=2828710
27.KopitchL,SaphoresJDM.AssessingEffectivenessofChangeable MessageSignsonSecondaryCrashes.In: TransportationResearch Board90thAnnualMeeting;2011.
28.AndreyJ.Long-termtrendsinweather-relatedcrashrisks. JTransp Geogr.2010;18(2):247–258.
29.IIHS.FatalityFacts2020:Malesandfemales.InsuranceInstitutefor HighwaySafety.Published2022.Availableat: https://www.iihs.org/ topics/fatality-statistics/detail/males-and-females AccessedSeptember4,2022.
30.AhmedMM,DasA,KhanMN,HammitB,AliE. DriverPerformanceand BehaviorinAdverseWeatherConditions:MicrosimulationandVariable SpeedLimitImplementationoftheSHRP2NaturalisticDrivingStudy Results-Phase3.Laramie:DepartmentofCivilandEngineering, UniversityofWyoming;2021.
31.BakhshiV,AghabaykK,ParishadN,etal.Evaluatingrainyweather effectsondrivingbehaviourDimensionsofDrivingBehaviour Questionnaire. JAdvTransp.2022;2022(4):1–10.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 804 HaboobDustStormsandMVCollision-relatedTraumainPhoenix,AZ Henryetal.
NationalVariationinEMSResponseandAntiepileptic MedicationAdministrationforChildrenwithSeizures inthePrehospitalSetting
MaytalT.Firnberg,MD*
E.BrookeLerner,PhD,MS,EMT-P†
NanNan,MA†
Chang-XingMa,PhD†
ManishI.Shah,MD,MS‡
N.ClayMann,PhD,MS,MBA§
PeterS.Dayan,MD,MSc*
SectionEditor: MuhammadWaseem,MD
*ColumbiaUniversityIrvingMedicalCenter,NewYork,NY
† StateUniversityofNewYorkatBuffalo,Buffalo,NY
‡ BaylorCollegeofMedicineandTexasChildren’sHospital,Houston,Texas
§ UniversityofUtah,SaltLakeCity,Utah
Submissionhistory:SubmittedNovember10,2022;RevisionreceivedMarch6,2023;AcceptedApril21,2023
ElectronicallypublishedJuly17,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59396
BackgroundandObjectives: PrehospitalAdvancedLifeSupport(ALS)isimportanttoimprovepatient outcomesinchildrenwithseizures,yetdataislimitedregardingnationalprehospitalvariationinALS responseforthesechildren.WeaimedtodeterminethevariationinALSresponseandprehospital administrationofantiepilepticmedicationforchildrenwithseizuresacrosstheUnitedStates.
Methods: Weanalyzedchildren <19yearswith9-1-1dispatchcodesforseizureinthe2019National EmergencyMedicalServicesInformationSystemdataset.WedefinedALSresponseasALSparamedic,ALS-AdvancedEmergencyMedicalTechnician,orALS-intermediateresponses.We conductedregressionanalysestoidentifyassociationsbetweenALSresponse(primaryoutcome), antiepilepticadministration(secondaryoutcome)andage,gender,location,andUScensusregions.
Results: Of147,821pediatriccallsforseizures,88%receivedALSresponses.ReceiptofALSresponse wasassociatedwithurbanicity,withwilderness(adjustedoddsratio[aOR]0.44,0.39-0.49)andrural (aOR0.80,0.75-0.84)locationslesslikelytohaveALSresponsesthanurbanareas.Of129,733 emergencymedicalservice(EMS)activationswithanALSresponder’simpressionofseizure, antiepilepticmedicationswereadministeredin9%.Medicationadministrationwasindependently associatedwithage(aOR1.008,95%confidenceinterval[CI]1.005-1.010)andgender(aOR1.22,95% CI1.18-1.27),withfemalesreceivingmedicationsmorethanmales.Ofthe11,698childrenwhoreceived antiepilepticmedications,midazolamwasthemostcommonlyused(83%).
Conclusion: ThemajorityofchildrenintheUSreceiveALSresponsesforseizures.Although medicationsareinfrequentlyadministered,themajoritywhoreceivedmedicationshadmidazolamgiven, whichisthecurrentstandardofcare.Furtherresearchshoulddeterminetheproportionofchildrenwho arecontinuingtoseizeuponEMSarrivalandwouldmostbenefitfromimmediatetreatment.[WestJ EmergMed.2023;24(4)805–813.]
INTRODUCTION
Emergencymedicalservices(EMS)personneltransport approximatelythreemillionchildrenannuallyintheUnited
States,representing10%ofallEMStransports.1 Seizures accountfor10%ofthesepediatricEMSencounters.2 While manyseizuresresolvespontaneouslyandquicklywithout
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 805 ORIGINAL RESEARCH
NationalVariationinEMSResponseandAntiepilepticMedicationAdministration
intervention,rapidadvanced-levelcarecanbecriticalfor improvingoutcomesinthosewhodonot.Thelikelihoodof seizurecessation,eitherspontaneouslyorwithantiepileptic treatment,decreaseswithlongerseizureduration.3,4 Prolongedseizuredurationisassociatedwithboth increasedmorbidity,suchaschronicneurologicaldeficit, andmortality.5
Seizuredurationisonepotentiallymodifiablefactorthat canaffectoutcomes,andmostcurrenttreatmentprotocols recommendthatthe firstantiepilepticmedicationbe administeredwithin fiveminutesofseizureonsetwitha secondmedicationgivenby10minutes.6 Seizuretreatment requiresAdvancedLifeSupport(ALS)trainingand skill,duetothepotentialnecessityforadministering controlledantiepilepticmedicationsortheneedforairwayor circulatorysystemsupport,neitherofwhichcanbe providedbyaBasicLifeSupport(BLS)response.TheEMS personnelcertifiedinBLSdonotcarryantiepileptic medications.Apriorstudyevaluatingprehospital treatmentofstatusepilepticusshowedthattimely ALSprehospitaltreatmentimproved patientoutcomes.7
Studiesregardingtheprehospitalmanagementof childrenwithseizureshavebeenprimarilyatthepatient levelanddescribelocalorregionalcare.Thosestudies havenotreportednationalleveldata. 8-10 Thereisno publishednationaldatathatdescribesthevariationin prehospitallevelofcareandmanagementusedfor childrenwithseizures.Nationwide,BLSpersonnel outnumberALSandIntermediateLifeSupport personnelcombinedbyafactorofapproximately threetoone.11 ThedistributionoftheseEMSpersonnel mayintroducevariabilityinEMSresponsetype andmanagement.
TheNationalEMSInformationSystem(NEMSIS) providesanopportunitytounderstandthevariationin responseacrossthecountryforchildrenwithhighacuity complaints.12 IdentifyingthevariationinEMSresponseand understandingcurrentpracticesinprehospitalmanagement areimportantatboththepatientandsystemlevel.Atthe patientlevel,thedatamayidentifypotentialareaswherethe careissuboptimal,suchasreceivingmedicationsthatarenot thestandardofcareorprolongedtimetoadministrationof medications.Atthesystemlevel,thisdatamayreveal opportunitiesforsystem-andregional–levelimprovements inprotocolsandpolicies.Inthisstudy,weaimedto determinethevariationintypesofEMSresponseto9-1-1 callsforpediatricseizuresacrosstheUS,basedonpatient demographicsandgeographiclocation.Secondarily,we aimedtodeterminethefrequencywithwhich childrenreceivedanantiepilepticmedicationand whetherthisdifferedbasedonpatientdemographics andlocation.
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue? Timelypediatricseizuretreatmentiscrucial topreventmorbidityandmortality.Variation inEMSseizurecareunderscorestheneedfor systemsimprovement.
Whatwastheresearchquestion?
IstherevariationinEMSresponseand medicationadministrationforpediatric seizuresintheUnitedStates?
Whatwasthemajor findingofthestudy? AdvancedLifeSupportresponsewas88%: lowerinruralareascomparedtourban(aOR 0.80).Antiepilepticswereadministeredin 9%,slightlyhigherinolderpatients.
Howdoesthisimprovepopulationhealth? Thisdataenhancesourunderstandingof nationalEMSresponsesandmanagementfor childrenwithseizuresbasedonpatient geographyanddemographics.
METHODS StudyDesign
Weconductedaretrospective,cross-sectionalanalysisof theNEMSISpublicresearchdataset.12 Ourinstitutional reviewboardgrantedthisstudyexemptstatus.
DataSource
TheNEMSISprojectisanationalefforttostandardize EMSdatacollectedbyEMSpersonnel.Thedatabaseforthe projectismanagedbytheNEMSISTechnicalAssistance Center(currentlylocatedattheUniversityofUtahSchoolof Medicine,SaltLakeCity,UT)andsupportedbytheOfficeof EmergencyMedicalServicesoftheNationalHighway TrafficSafetyAdministration.LocalEMSagenciessubmit datatotheirstatedatabase,ofwhichasubsetisthenexported tothenationaldatabase.13 Forthisstudy,weusedthe2019 NEMSISPublicReleaseDataset(version3),whichincludes 22,532,890EMSactivationssubmittedby9,599EMS agenciesserving43USstatesandterritoriesduringthe2019 calendaryear.
Participants:SelectionofEMSResponses
Weincludedchildren <19yearsinagewhoaccessed9-1-1 EMSforcomplaintsofseizuresorconvulsionsduringthe 2019calendaryear.Weexcludedinterfacilitytransfers.To
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 806
Firnbergetal.
identifyrelevantcasesofEMSactivationsforthecareof pediatricseizures,weusedcodesfromtheNEMSISdataset thatrelatedtoreasonfordispatchasconvulsionorseizures (eDispatch.01-2301025).Toassessthepotentialdifferences betweendispatchreasonandtheEMSresponder’ s impression(eSituation.11andeSituation.12),wealso identifiedchildrenforwhomtheprimaryorsecondary responderimpressionwasdocumentedasseizureor convulsion.Theseimpressionsweredocumentedas InternationalClassificationofDiseases,10th Rev,Clinical Modification(ICD-10-CM)codesthatwererecordedby EMSpersonnel.WeincludedallICD-10-CMcodesthat refertoseizure,whichincludeICD-10-CMcodeswiththe prefixesofR56,G40,andP90.
Outcomes
TheprimaryoutcomeofourstudywasreceiptofALS responseforpatientswithdispatchcomplaintsofseizures, asBLSpersonnelareunabletoadministerantiepileptic medications.WedefinedALSresponseasanyofthe following:ALS-paramedic,ALS
AdvancedEmergency MedicalTechnician(AEMT),orALS-intermediate(as describedwithinNEMSISelementeResponse.15).We definedBLSresponseasanyofthefollowing:BLS–Basic/ EMT,BLS-AEMT,BLS-FirstResponder, BLS–Intermediate(asdescribedwithineResponse.15).
ThesecondaryoutcomewasreceiptofanEMSadministeredantiepilepticmedicationamongpatientswith anALSresponseandtheEMSresponder’simpressionof seizure.Weincludedallformulationsofthefollowingseizure abortivemedicationsasdocumentedineMedication.03: midazolam,lorazepam,diazepam,levetiracetam,phenytoin, phenobarbital,andclonazepam.Weassessedthetimingof medicationadministrationintwoways:a)calculatedasthe timefromthetimeofdispatch(eTimes.03)tothetimeof medicationadministration(eMedication.01);andb) calculatedasthetimefromEMSarrivalonscene(eTimes.06) tothetimeofmedicationadministration(eMedication.01). Wecalculatedthesetwotimesastheformerincludesthetime toarriveonthescene,whilethesecondexcludesthisperiod.
CovariatesandDefinitions
FromtheNEMSISdatabase,wecollectedthefollowing covariates:patientdemographics(age,gender,race,and ethnicity);insurancestatus(privateinsurance,Medicaid, self-pay,noinsuranceidentified,other,ormissing);census region(Midwest,Northeast,South,andWest);and urbanicitybasedontheU.SDepartmentofAgriculture
UrbanInfluenceCodes(urban,suburban,rural, andwilderness).
StatisticalAnalysis
Wesummarizedourdatausingstandarddescriptive statistics.Forourprimaryoutcome(receiptofALS
response),weconductedamultivariablelogisticregression analysistodetermineitsrelationshiptothefollowing covariates:patientdemographics(age,gender);census region;andurbanicity.Weexcludedanyvariablesthatwere missing >20%.
Foroursecondaryoutcome(receiptofantiepileptic medication),weanalyzedonlythosepatientsforwhomALS carewasdispatchedandhadanEMSresponder’simpression ofseizure.Weconductedalogisticregressionanalysisto determinetherelationshipbetweenreceiptofanantiepileptic medicationandage,gender,censusregion,andurbanicity. Forallregressionmodeling,weassessedformulticollinearity usingvarianceinflationfactorsanddeterminedmodel goodness-of-fit.Forvariablesthatwerecollinear,wechose onlyoneofthevariablestofurtheranalyze.
Lastly,wecalculatedthenumberwithEMSresponder impressionofseizure(eSituation.11and.12)dividedby numberwithEMSdispatchforseizure(eDispatch.01)to understandhowfrequentlytheseimpressionsmatched.
RESULTS
Weidentified147,821eligibleEMSactivationsfor pediatricpatients <19yearsofagewith9-1-1dispatchfor seizureorconvulsion. Figure1 and Table1 notethatthe majorityofchildrenreceivedanALSresponse(88%),which wasevenlydistributedbyageandgender.Mostencounters overalloccurredinurbanareas(84%).Mostpatientshad missingorunknowndataforrace,ethnicity,andinsurance status;therefore,thisdatawasnotanalyzedfurther.Inthe
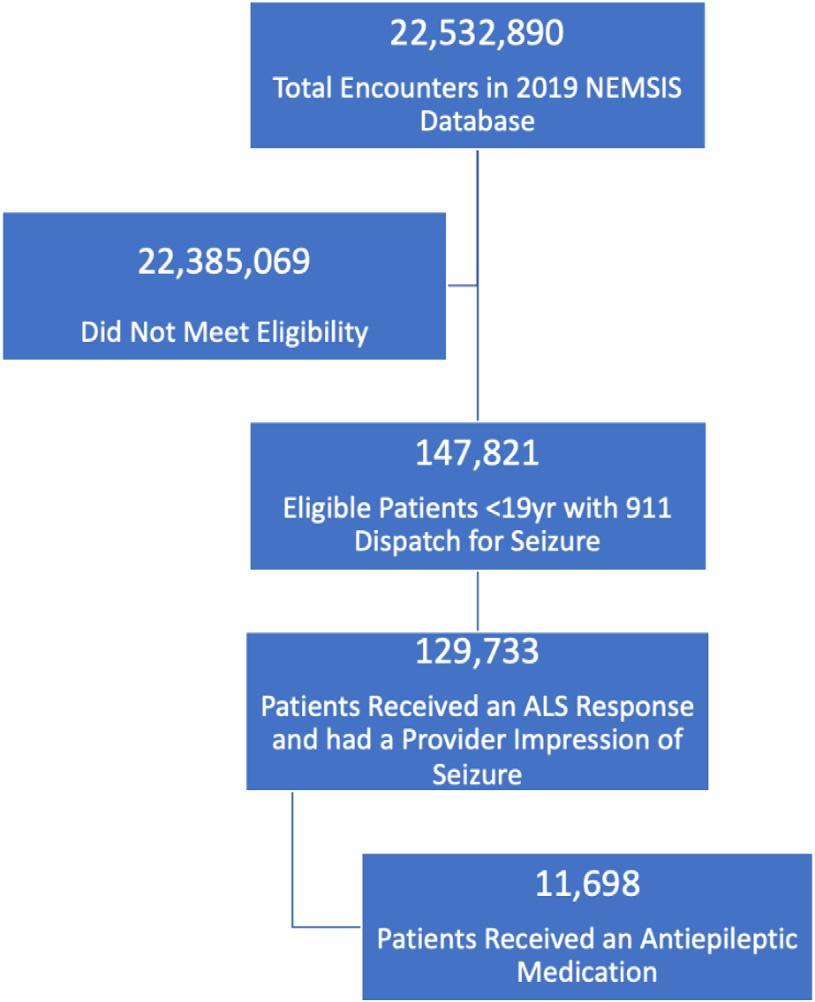
–
Figure1. Patient flowdiagram.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 807 Firnbergetal. NationalVariationinEMSResponseandAntiepilepticMedicationAdministration
NEMSIS,NationalEmergencyMedicalServicesInformation System; ALS,AdvancedLifeSupport.
multivariableanalysis(Table2),receiptofALSresponse increasedmarginallyforeveryyearincreaseinageand decreasedforthoselivinginruralorwildernesslocations.
Weidentified11,698EMSactivationsforwhichpatients receivedanantiepilepticmedication,representing9%of encountersthatreceivedanALSresponseandhadanEMS responder’simpressionofseizure.Theadministrationofan antiepilepticmedicationwasevenlydistributedacrossallage groups,regions,andurbanicity(Table3).Inthe multivariableanalysis(Table4),receiptofanantiepileptic
medicationwassignificantlyhigherinfemalescompared tomales.
Ofthe147,821EMSactivationsthathadadispatch indicationofseizure,109,684(74%)alsohadanEMS responder’sprimaryorsecondaryimpressionofseizure. Midazolamwasthemostcommonlyadministered medication,comprising83%ofallantiepilepticmedications administered(Supplement2).Themediandocumentedtime fromdispatchtomedicationadministrationforall encounterswas16.75minutes(Table5).Urbanareashadthe
ResponseUnitLevelofCare AllPatientsAdvancedLevelResponseBasicLevelResponse N = 147,821n(%),N = 129,695n(%),N = 18,126 P-values Agegroup,years 0.55 <17,6186,670(88)948(12)
5-920,99218,367(87)2,625(13)
Gender 0.66
Male77,71468,278(88)9,436(12) Missing1,285899(70)386(30) Region <0.001 Northeast15,98611,784(73)4,238(27) South68,38761,750(90)6,637(10) Midwest25,02922,243(89)2,786(11) West38,32633,920(89)4,406(11) Missing9334(37)59(63) Urbanicity <0.001 Urban123,909109,516(88)14,393(12) Suburban7,8136,921(89)892(11) Rural9,2807,975(86)1,305(14) Wilderness1,9421,499(77)443(23) Missing4,8773,784(78)1,093(22)
Table1. Levelofemergencymedicalservicescareforchildrenwithdispatchseizurecode.
1-451,67645,303(88)6,373(12)
10-1426,88523,624(88)3,261(12) 15-1840,65035,731(88)4,919(12)
Female68,82260,518(88)8,304(12)
AdjustedOddsRatio 95%WaldConfidence Limits P-values Ageinyears1.0021.0001.0050.07 Gender:femalevsmale1.0060.971.040.72 Urbanicity: Wildernessvsurban0.440.390.49 <0.001 Ruralvsurban0.790.750.84 <0.001 Suburbanvsurban1.010.941.090.80 WesternJournal of EmergencyMedicineVolume24,No.4:July2023 808 NationalVariationinEMSResponseandAntiepilepticMedicationAdministration Firnbergetal.
Table2. Regressionmodel:independentassociationswithreceiptofAdvancedLifeSupport-levelcare.
1-449,9924,064(8)45,928(92)
5-919,0162,093(11)16,923(89)
10-1422,5661,869(8)20,697(92)
15-1831,2663,027(10)28,239(90)
Female58,9605,879(10)53,081(90)
fastesttimestomedicationadministration(median16.44 minutes[min])andwildernesstheslowest(median 21.00min).Themediantimetoadministrationof antiepilepticmedicationfromdispatchwasmostrapidfor childreninthe1–4yearsagegroup(median15.82min)and slowestinthose15
18yearsofage(median18.00min).
ThemediandocumentedtimefromEMSarrivalonscene tomedicationadministrationwas9.63min(Table6).From EMSarrivalonscenetomedicationadministration,children inthe1
4yearsagegrouphadthefastestmedication
administrationtime(median8.68min),whilechildreninthe 10–14yearsagegrouphadtheslowest(median10.53min). Uponregressionanalysis,(Table7),timetomedication administrationwassignificantlyfasterinurbanareasand sloweraspatientageincreased.
DISCUSSION
InthisretrospectiveanalysisoftheNEMSISdatabase, mostchildrenwithadispatchcodeforseizurereceivedan ALSresponse.AlthoughALSresponseswerestatistically
–
–
AllPatientsAntiepilepticMedication Administered AntiepilepticMedication NotAdministered, No.(%)No.(%) N = 129,733N = 11,698N = 118,035 P-values Agegroup,years <0.001 <
Table3. Antiepilepticmedicationadministrationbypatientdemographicsandgeographiclocations.
16,893645(9)6,248(91)
Gender <0.001
Male70,2185,793(8)64,425(92) Missing55526(5)529(95) Region <0.001 Northeast10,943859(8)10,084(92) South61,7525,948(10)55,804(90) Midwest20,8891,914(9)18,975(91) West36,1172,974(8)33,143(92) Missing323(9)29(91) Urbanicity 0.66 Urban110,97710,005(9)100,972(91) Suburban6,347589(9)5,758(91) Rural7,301656(9)6,645(91) Wilderness1,408116(8)1,292(92) Missing3,700332(9)3,368(91)
EffectAdjustedOddsRatio 95%WaldConfidence Limits P-values Age(inyears)1.0081.0051.01 <0.001 Gender:femalevsmale1.221.181.27 <0.001 Urbanicity:wildernessvsurban0.990.911.080.27 Urbanicity:ruralvsurban1.010.931.110.78 Urbanicity:suburbanvsurban0.900.741.090.77 Volume24,No.4:July2023WesternJournal of EmergencyMedicine 809 Firnbergetal. NationalVariationinEMSResponseandAntiepilepticMedicationAdministration
Table4. Regressionmodel:independentassociationswithmedicationbeingadministered.
NationalVariationinEMSResponseandAntiepilepticMedicationAdministration
Table6. Timefromemergencymedicalservicesarrivalonsceneto medicationadministration(inminutes).
N Lower QuartileMedian Upper Quartile P-values
N Lower QuartileMedian Upper Quartile P-value
Allpatients*11,3825.439.6316.00
Age(years) <.001
<16265.009.0015.00
1–43,9405.008.6814.72
5–92,0235.589.8816.00
10–141,8216.0010.5318.27
15–182,9725.9110.3117.50
Gender0.72
Female5,7345.409.4516.10
Male5,6235.459.8716.00
Missing255.009.4516.92
Region <.001
Northeast8365.9110.8317.00
South5,8145.8810.0017.00
Midwest1,8405.288.8214.30
*Filteredtoremovetimes <0minutesand >180minutes.
lessfrequentinruralandwildernesssettings,itisnotablethat eveninwildernesssettings,morethanthree-quartersofEMS activationsforchildrenreceivedALSresponses.Thisis reassuringasBLSpersonnelareunabletoadminister antiepilepticmedications,andatthetimeofanEMScallfor seizureitisunknownwhethertheseizurewillself-resolve, continue,orrecur.Asexpected,seizureabortivemedications wereadministeredtoarelativelysmallfraction(~9%)of childrenreceivinganALSresponseforseizures,consistent withpreviouslyreportedratesofactivepediatricseizuresin theprehospitalsetting.14 Despitetherelativelysmall proportionofseizuresthatreceivemedications,thosethatdo notself-resolvequicklymayprogresstoresultinsignificant morbidityandmortalitywithoutintervention.3-6
Midazolamwasthemostcommonlyadministered medicationacrossallregionsandurbanicities,possiblydue totheabilitytodeliveritbymanyroutesanditsheat-stability relativetootherbenzodiazepines.15 Whiletherewasmodest
variationinmediantimesfromdispatchtomedication administrationbasedonage,region,andurbanicity,median timesacrosslocationswerebeyondtypicalseizure durationsforwhichabortiveantiepilepticmedicationsare consideredoptimal.5 Thetimestomedicationadministration werenotunexpectedgiventhattheyincluderesponse timetothescene,timetoaccessthepatient,andinitial evaluation.Similarly,therewasmodestvariationinmedian timesfromEMSarrivalonscenetomedication administrationbasedonage,region,andurbanicity.The mediantimeof9.63minforallpatientsmaybean opportunityforfurtherresearchintocausesofpossible medicationadministrationdelays.
PriordataonALSresponseaswellasthereceiptand timingofseizuremedicationadministrationinthe prehospitalsettinghasbeenlimitedduetothelackof nationaldata-aggregationefforts.However,smallerscale studiesnotedasimilarmediantimetointervention.This includesonestudyofthreeurbanEMSsystemsthatreported
West2,8895.008.8815.58 Missing36.009.0021.00 Urbanicity <.001 Urban9,7515.409.5016.00 Suburban5656.0010.6317.00 Rural6385.179.8416.00 Wilderness1085.2712.0019.02 Missing3205.8310.2116.93
*Filteredtoremovetimes <0minutesand >180minutes.
Table5. Timefromdispatchtomedicationadministration (inminutes).
Allpatients*11,50911.7716.7524.00 Age(years) <.001 <163111.4215.8223.43 1–43,99711.0515.6722.12 5–92,04711.8217.0023.58 10–141,83712.6717.8826.03 15–182,99712.0818.0025.22 Gender0.82 Female5,87911.7216.7224.00 Male5,79311.8516.8024.00 Missing2612.0015.3224.43 Region <.001 Northeast84212.0018.0025.17 South5,86512.4817.8525.00 Midwest1,86211.0515.5121.47 West2,93710.6715.3322.53 Missing318.0019.0030.00 Urbanicity <.001 Urban9,86211.6316.4423.57 Suburban57413.0018.9927.22 Rural63812.0317.4326.00 Wilderness11014.0021.0034.30
Missing32512.5718.5525.00
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 810
Firnbergetal.
a14-minmediantimetointerventionafterarrivalonscene.14 Anotherstudyofninechildren’shospitalsfounda30-minute mediantimefromonsetofseizurestoadministrationof antiepilepticdrugsintheoutpatientsetting.8 Ourdata providesalargerperspectiveofseizuremanagement nationallyandreflectsboththetimetoreachapatientafter dispatchandthetimeEMSarrivesonscenetomedication administration.Giventhatthetimetomedication administrationexceedstheoptimaltimeatwhich medicationisexpectedtohaveeffect,ourdatastrongly suggeststheneedforabortivemedicationstobereadily availableinthehomesofchildrenwithseizuredisorders, includingnewerproductssuchasintranasalmidazolam anddiazepam.Priorstudieshavedemonstratedreduction inmorbidityandcostsassociatedwithhospitalvisits whenseizureabortivemedicationisavailablefor at-homeadministration.16
Thehighfrequencyofmidazolamuseacrosspatient demographicsandgeographysuggestsadoptionofbest clinicalpracticeandrecommendations.9 Among benzodiazepines,midazolamcanbeadministeredbymultiple routes,includingintramuscularandintranasal,which bypassesthepotentiallytime-intensivestepofobtaining peripheralintravenous(IV)access.In2012,publicationofthe resultsoftheRapidAnticonvulsantMedicationPriorto ArrivalTrial(RAMPART),alarge,multicenter,randomized clinicaltrialofprehospitalpatientswithseizures, demonstratedthatintramuscularmidazolamwassuperiorto IVlorazepamatterminatingconvulsionspriortoarrivaltothe emergencydepartment.17,18 AnationalstudyusingNEMSIS demonstratedsubstantialincreaseinmidazolamuseafterthe publicationofRAMPART.19 AnotherstudyofthreeEMS agenciesinanurbansettingsimilarlyfoundhighratesof midazolamuse.14 Ourdatadidnotethaturbansettingshad thehighestproportionateuseofmidazolam,whichcould reflectthecontributionsofmedicaldirectorswithboardcertificationinEMSaturbanacademicinstitutions
ormorepracticalissuesrelatedtoavailability orstorage.
ThedevelopmentandgrowthofNEMSISallowsfora robustassessmentofnationalprehospitaldata.Inthisstudy, NEMSIScontributedtoourunderstandingofnationalEMS responsesforhigheracuitypediatriccomplaintsbasedon patientgeographyanddemographics.TheAmerican AcademyofPediatricsandotherprofessionalorganizations haverecommendedthatEMSsystemsandagencies contributetothedatabase.20 AsNEMSISexpandsandthe dataavailablebecomesmoregranular,otherstudies regardingresourceuseandthequalityofcarewillbecome increasinglypossibletobetterunderstandtrendsand opportunitiesforimprovementinpediatricprehospitalcare. Forexample,wewereunabletoanalyzeinsurancestatusor raceandethnicityduetolargeamountsofmissingdata.As EMSdocumentationadvancesandNEMSISbecomesmore complete,futureresearchwillbeabletodetermineequityof accesstohighlevelpediatriccare.
LIMITATIONS
Ourstudyhaslimitationsinherenttoretrospectivelarge databasestudies.Identificationofthetargetpopulationcan bechallenging,astheaccuracyofdocumentationcollected andcataloguedwithinNEMSIScouldnotbeverified. However,bycapturingbothreasonfordispatchandEMS responderimpression,wewereabletobestestimatethe degreetowhichourtargetpopulationmayhaverepresented thosewhohadseizures.Althoughitwasimpossibleto identifythosewhoactuallyseizedduringEMScareorthe etiologyoftheirseizure,ourdataisconsistentwithsmaller researchstudiesonthistopic.Regardlessofetiologyofthe seizure,priordatasuggeststhatseizuresoflongerduration arehardertoabortandareassociatedwithhighermorbidity andmortalitywithrecommendationstoadministerabortive medicationswithin fiveminutes.
ThelackofstandardizationacrossEMSelectronichealth recordsystemsanddocumentationaffectsdataconsistency. Weattemptedtoovercomethepotentialvariationin identifyingchildrenwithseizuresbyusinganinclusivelistof ICD-10-CMcodes.However,differentagenciesmayhave useddifferentcodeswhenmappingtheirlocallycollected dataintotheEMSdatabase.Additionally,werecognizethat thedatabasedidnotallowustoascertainwhetherchildren whoreceivedanantiepilepticmedicationrequiredoneand whetherchildrenwhodidnotreceiveanantiepileptic medicationdidnotrequireone.However,thesimilar proportionofchildrenreceivingabortivetherapyacross geographiclocationsisreassuring.
Finally,animportantpotentiallimitationisthatALS andBLSmaybede fi neddifferentlyacrossEMSagencies andgeographysuchthattruncatingmultiplecategoriesof EMSprofessionalsintoALSandBLSmaynotre fl ectthe
Effect Estimated Mean Difference Standard Error P-values Age(years)0.160.02 <.001 Gender(male referent) 0.030.230.14 Urbanicity: -Wildernessvsurban (referent) 6.841.17 <.001 -Ruralvsurban (referent) 2.200.50 <.001 -Suburbanvsurban (referent) 2.430.52 <.001 Volume24,No.4:July2023WesternJournal of EmergencyMedicine 811 Firnbergetal. NationalVariationinEMSResponseandAntiepilepticMedicationAdministration
Table7. Regressionmodel:independentassociationswithtimingto medicationadministration.
differencesincapabilitiesacrossresponders(e.g.ability toprovidemedications)acrosssettings.Further,from ourdata,wewereunabletodifferentiatebetween patientsservedinatwo-tieredEMSsystemandthose whowerenot.
CONCLUSION
ThemajorityofpediatricpatientsacrosstheUSreceived anAdvancedLifeSupportresponseforseizures;however, thoseinruralorwildernesssettingsweresomewhatlesslikely toreceiveanALSresponse.Althoughmedicationsare infrequentlyadministered,themajorityofthosewhowere administeredamedicationreceivedmidazolam,whichisthe currentstandardofcare.Furtherresearchisrequiredto determinetheproportionofchildrenwhoarecontinuingto seizeuponEMSarrivalandwouldmostbenefitfrom immediateandappropriatetreatment.
AddressforCorrespondence:MaytalFirnberg,MD,MountSinai IcahnSchoolofMedicine,DepartmentofEmergencyMedicine,1 GustaveLLevyPlace,Fl12,NewYork,NY10029.Email: maytal. firnberg@gmail.com
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Firnbergetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.FoltinGL,DayanP,TunikM,etal.PrehospitalWorkingGroup ofthePediatricEmergencyCareAppliedResearchNetwork. Prioritiesforpediatricprehospitalresearch. PediatrEmergCare. 2010;26(10):773–7.
2.ShahMN,DavisCO,BauerC,etal.PreferencesforEMStransport andpediatricemergencydepartmentcare. PrehospEmergCare. 2008;12(2):169–75.
3.GurcharranK,GrinspanZM.Theburdenofpediatricstatus epilepticus:epidemiology,morbidity,mortality,andcosts. Seizure. 2019;68:3–8.
4.SilvermanEC,SporerKA,LemieuxJM,etal.Prehospitalcareforthe adultandpediatricseizurepatient:currentevidence-based recommendations. WestJEmergMed. 2017;18(3):419–436.
5.WhelessJW.Treatmentofstatusepilepticusinchildren. PediatrAnn. 2004;33(6):376–83.
6.SánchezFernándezI,AbendNS,AgadiS,etal.PediatricStatus EpilepticusResearchGroup(pSERG).Timefromconvulsivestatus
epilepticusonsettoanticonvulsantadministrationinchildren. Neurology. 2015;84(23):2304–11.
7.SilbergleitR,DurkalskiV,LowensteinD,etal;Intramuscularversus Intravenoustherapyforprehospitalstatusepilepticus. NEnglJMed. 2012;366(7):591–600.
8.SánchezFernándezI,AbendNS,AgadiS,etal.Timefromconvulsive statusepilepticusonsettoanticonvulsantadministrationinchildren. Neurology. 2015;84(23):2304–11.
9.ShahMI,MaciasCG,DayanPS,etal.Anevidence-basedguidelinefor pediatricprehospitalseizuremanagementusinggrademethodology. PrehospEmergCare. 2014;18Suppl1:15–24.
10.ShahMI,CareyJM,RappSE,etal.Impactofhigh-fidelitypediatric simulationonparamedicseizuremanagement. PrehospEmergCare. 2016;20(4):499–507.
11.DavisCS,SouthwellJ,NiehausV,etal.Emergencymedicalservice naloxoneaccess:anationalsystematiclegalreview. AcadEmergMed. 2014.
12.NationalEMSInformationSystemTechnicalResources.Dataset Dictionaries.Availableat: https://nemsis.org/media/nemsis_v3/ release-3.4.0/DataDictionary/PDFHTML/EMSDEMSTATE_National/ NEMSISDataDictionary.pdf.AccessedJuly24,2020.
13.MannNC,KaneL,DaiM,etal.Descriptionofthe2012NEMSIS public-releaseresearchdataset. PrehospEmergCare. 2015;19(2):232–40.
14.ShahMI,OstermayerDG,BrowneLR,etal.Multicenterevaluationof prehospitalseizuremanagementinchildren. PrehospEmergCare. 2020:1–12.
15.McMullanJasonT,etal.Degradationofbenzodiazepinesafter 120daysofEMSdeployment. PrehosplEmerCare 18(3)2014:368–74.
16.O’DellC,ShinnarS,Ballaban-GilKR,etal.Rectaldiazepamgel inthehomemanagementofseizuresinchildren. PediatrNeurol. 2005;33(3):166–72.
17.SilbergleitR,LowensteinD,DurkalskiV,etal.NeurologicalEmergency TreatmentTrials(NETT)investigators.RAMPART(Rapid AnticonvulsantMedicationPriortoArrivalTrial):adouble-blind randomizedclinicaltrialoftheefficacyofintramuscularmidazolam versusintravenouslorazepamintheprehospitaltreatmentofstatus epilepticusbyparamedics. Epilepsia. 2011;52Suppl8(Suppl8): 45–7.
18.SilbergleitR,DurkalskiV,LowensteinD,etal.NETTinvestigators. Intramuscularversusintravenoustherapyforprehospitalstatus epilepticus. NEnglJMed. 2012;366(7):591–600.
19.Shtull-LeberE,SilbergleitR,MeurerWJ.Pre-hospitalmidazolamfor benzodiazepine-treatedseizuresbeforeandaftertheRapid AnticonvulsantMedicationPriortoArrivalTrial:anationalobservational cohortstudy. PLoSOne. 2017;12(3):e0173539.
20.MooreB,ShahMI,Owusu-AnsahS,etal.AmericanAcademyof Pediatrics,CommitteeonPediatricEmergencyMedicineandSectionon EmergencyMedicineEMSSubcommittee;AmericanCollegeof EmergencyPhysicians,EmergencyMedicalServicesCommittee; EmergencyNursesAssociation,PediatricCommittee;National
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 812 NationalVariationinEMSResponseandAntiepilepticMedicationAdministration Firnbergetal.
AssociationofEmergencyMedicalServicesPhysicians,Standardsand ClinicalPracticeCommittee;NationalAssociationofEmergency MedicalTechnicians,EmergencyPediatricCareCommittee;Pediatric ReadinessinEmergencyMedicalServicesSystems;PolicyStatement; OrganizationalPrinciplestoGuideandDefinetheChildHealth CareSystemand/orImprovetheHealthofAllChildren.Pediatric readinessinemergencymedicalservicessystems. AnnEmergMed. 2020;75(1):e1–e6.AccessedJune28,2021.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 813 Firnbergetal. NationalVariationinEMSResponseandAntiepilepticMedicationAdministration
Contributionof15Years(2007–2022)ofIndo-USTraining PartnershipstotheEmergencyPhysicianWorkforce CapacityinIndia
JosephD.Ciano,DO,MPH*
KatherineDouglass,MD,MPH†
KevinJ.Davey,MD†
ShwetaGidwani,MD,FRCEM†‡
AnkurVerma,MEM,MBBS§
SanjayJaiswal,MEM,MBBS§
JohnAcerra,MD,MPH*
SectionEditor: ShadaRouhani,MD
*NorthwellLongIslandJewishMedicalCenter,DepartmentofEmergency Medicine,GlenOaks,NewYork
† GeorgeWashingtonUniversitySchoolofMedicine&HealthSciences, DepartmentofEmergencyMedicine,WashingtonDC
‡ Chelsea&WestminsterNHSTrust,London,UnitedKingdom
§ MaxSuperSpecialtyHospital,Patparganj,DepartmentofEmergencyMedicine, NewDelhi,India
Submissionhistory:SubmittedJanuary16,2023;RevisionreceivedMarch30,2023;AcceptedMarch23,2023
ElectronicallypublishedJuly17,2023
Fulltextavailablethroughopenaccessat http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.59912
Background: Indo-USMastersinEmergencyMedicine(MEM)certificationcoursesarerigorousthreeyearemergencymedicine(EM)trainingcoursesthatoperateasapartnershipbetweenaffiliatehospitals oruniversitiesintheUnitedStateswithestablishedEMtrainingprogramsandlocalpartnersitesinIndia. Throughouttheir15yearsofoperation,theseglobaltrainingpartnershipshavecontributedtotheEM workforceinIndia.OurobjectiveinthisstudywastodescribeIndo-USMEMprogramgraduates,their workenvironments,andtheircontributiontothegrowthofacademicEMandtothecoronavirusdisease 2019(COVID-19)response.
Methods: AnelectronicsurveywascreatedbyUSandIndianMEMcoursestakeholdersanddistributed to714US-affiliatedMEMprogramgraduates.Thesurveyquestionsinvestigatedwheregraduateswere working,theirworkenvironmentsandinvolvementinteachingandresearch,andtheirinvolvementinthe COVID-19response.Weconsolidatedtheresultsintothreedomains:workenvironmentandclinical contribution;academiccontribution;andcontributiontotheCOVID-19response.
Results: Thesurveyresponseratewas46.9%(335responses).Mostgraduatesreportedworkingwithin India(210,62.7%)andinanemergencydepartment(ED)setting(304,91.0%).Themostcommon reasonforpracticingoutsideofIndiawasdifficultywithformalMEMcertificaterecognitionwithinIndia (97,79.5%).Overhalfofgraduatesreporteddedicatingover25%oftheirworkhourstoteachingothers aboutEM(223,66.6%),abouthalfreportedpresentingresearchprojectsatconferencesontheregional, national,orinternationallevel(168,50.5%),andalmostallgraduateswereengagedintreatingCOVID19patientsduringthepandemic(333,99.4%).Mostgraduatesagreedorstronglyagreedthattheywere satisfiedwiththeiroverallMEMtraining(296,88.4%)andconfidentintheirabilitytopracticeEM (306,91.6%).
Conclusion: Indo-USMEMgraduateshavemadeanotablecontributiontoEMinIndiathroughclinical servicedelivery,teaching,andresearch,evenmoreessentialinthecontextoftheCOVID-19pandemic. TherolesofthesegraduatesshouldbeacknowledgedandcancontributefurthertoexpandEMspecialty andsystemsdevelopmentacrossIndia.[WestJEmergMed.2023;24(4)814–822.]
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 814 ORIGINAL RESEARCH
Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce
INTRODUCTION
Emergencymedicine(EM)inIndiahasreachedmany developmentalmilestonessinceitsformalrecognitionin 2009bytheMedicalCouncilofIndia.PostgraduateEM trainingprogramshavegrowninnumberinrecentyears; however,thenumberofavailabletrainingpositionsremains vastlyinadequateforacountryof1.32billionpeople.1,2 Roadtrafficinjuriesandnon-communicablediseases,such asischemicheartdiseaseandstroke,areamongstthetop causesofmorbidityandmortalityacrossIndiawitha growingprevalenceacrossallstates.1,2 Theseconditions requiretime-sensitiveinterventionsanddiagnosticsthat emergencyphysicians(EP)aretrainedtorecognize andprovide.
AccreditationofEMtrainingprogramsinIndiais overseenbytheNationalMedicalCommission(NMC, formerlytheMedicalCouncilofIndia)andtheNational BoardofExaminations(NBE).3 – 6 Asof2018,theMedical CouncilofIndiahadfullyapprovedonly73training positionsforEMwithingovernment-fundedpublic hospitals,offeredin29of460medicalcollegesinIndia coveringjusteightstatesandtwounionterritories.Asof March2022,thesehadincreasedto187trainingpositions. 4 In2014theNBE,whichoverseesresidencytrainingin privatehospitals,alsorecog nizedEMasaspecialtyandset outitsEMcurriculumandexaminationprocess. By2018,theNBEwasofferinganadditional121training positions,although52oftheseremainedvacantasof July2017. 7
Evenifallthetrainingpositionswere filled,Indiahasthe capacitytotrainonly308EPsannually.Bycomparison,the UnitedStateshas2,278EMtrainingseatsperyear,and 58,000activeboard-certifiedEPsforapopulationlessthan onequarterthesizeofthatofIndia.8,9 TheUnited Kingdom’s(UK)publiclyfundedNationalHealthService hasoneEPforevery10,000people.Indiawouldneedabout 132,000EPs today toreachsimilardoctor-population ratios.10 Thisgapinclinicianratioshasbeenfeltby hospitalskeentoprovideemergencyandurgentcare servicesinIndia.InresponsetotheEMtraininggap, awidearrayofEMeducationalprograms,courses,and conferenceshavebeendevelopedinIndiaoverthelast twodecades.3,10
SimilarpartnershipstodevelopEMexistinother countriesintheearlystagesofspecialtydevelopment.11 US-MEMprogramsoperateasapartnershipbetween affiliatehospitalsoruniversitiesintheUSthathave establishedEMtrainingprogramsandlocalpartnersitesin India.10–13 TheMEMprogramsarerigorousthree-year programsthatemulatethestructureofUStraining programs,includingsupervisedclinicalexperienceinEM, clinicalrotationsthroughoutrelevantspecialties, didactics,traineeassessment,andexaminationsto measurecompetence.14 SimilartomanyWestern
PopulationHealthResearchCapsule
Whatdowealreadyknowaboutthisissue?
Emergencymedicinetrainingpositionsin Indiahaveincreasedbutremaininsuf fi cient. Indo-USMastersinEM(MEM)programs buildemergencyphysiciancapacityinIndia.
Whatwastheresearchquestion?
HowhaveIndo-USMEMgraduates contributedtophysicianworkforcecapacity inIndiaoverthelast15years?
Whatwasthemajor findingofthestudy?
MostMEMgraduatesworkwithinIndia (210,62.7%)inanEDsetting(304,91.0%).
Howdoesthisimprovepopulationhealth?
Developingemergencyphysicianworkforce capacitywillcontributetoimproved populationhealththroughclinicalservice deliveryandEMspecialtydevelopment.
residencytrainingprograms,mostIndo-USMEMcourses followa36-monthmodularcurriculumwithrequired readingsfromEMtexts(eg, Tintinalli ’ sEmergency Medicine )andassignedquestionsfrompurchased questionbanks.15
InstitutionalfacultyaffiliatesfromtheUSvisitIndia throughouttheyeartoassistlocalfacultyinbedside teaching,didactics,residentassessments,andexams.15 Most coursesitesofferresidentstheopportunitytoparticipateina rotationatthepartneringUSinstitution,althoughmost residentscompletetheirMEMcourseentirelyinIndia.Since theinceptionofthe firstMEMprogramin2007,MEM programshavetrainedover700graduatesthroughoutIndia. Giventhedurationofoperationofthesetrainingprograms, wesoughttodescribethecontributionsofIndo-USMEM graduatesaspartofthepostgraduateEMtraininglandscape inIndia.
WebelievethatunderstandingtheseIndo-USmodelsisof particularimportanceandrelevancenow,bothbecauseof thevast,unmetcliniciangapandtheevolvingpoliticaland regulatorylandscapeinIndia,whichisedgingtowardsmore internationaluniversity-partnershipmodelsofeducationand training.Ofnote,on5January2023,theUniversityGrants Commissionunveiledadraftseekingpublicfeedbackon theproposaltofacilitateentryandoperationofforeign universitiesinIndia.16 Inthispaper,wefocusondescribing detailsof15years(2007–2022)ofIndo-UStraining
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 815 Cianoetal.
partnershipsandtheirimpactonEPworkforcecapacity inIndiawithrespecttothegraduates’ workenvironments andtheircontributiontothegrowthofacademicEM andmorerecentcontributiontothecoronavirus2019 (COVID-19)response.
METHODS
Anelectronicsurveywascreatedanddistributedto714 US-affiliatedIndianMEMprogramgraduates.Survey questionswerewrittenbyUSinstitutionalstakeholders involvedinIndianMEMprogramdevelopmentand operations,namelyNorthwellHealthinNewYorkand GeorgeWashingtonUniversity(GW)inWashington,DC. KeyprogramfacultymembersinIndia,allofwhomare MEMalumni,wereaskedtoreviewthesurveyquestionsand providefeedbackduringthesurveydevelopmentphase. Somechangesweremadebasedontheserecommendations priortoitsdistribution.ThesurveywaswritteninEnglish, asaworkingproficiencyinEnglishisarequirementofMEM courseadmission.Noidentifyinginformationwascollected, andtheprojectwasdeemedexemptbytheNorthwellHealth InstitutionalReviewBoard.
domainsforanalysis.REDCap(ResearchElectronic DataCapture)isasecure,web-basedsoftware platformdesignedtosupportdatacapturefor researchstudies.
RESULTS
Thetotalsurveyresponseratewas46.9%(335 responses).Thesurveyresponserateforeachinstitutional af filiatewasasfollows:GW,46%(300responses); NorthwellHealth70%(32responses);SUNYUpstate15% (tworesponses);andUMD,5%(oneresponse).Results werecategorizedintothreemajordomains.Thesedomains includedtheclinicalcontributiontoEM,academic contributiontoEM,andinvolvementintheCOVID-19 response.Keyresultsaredescribedbelowwithmore detailedresultsdepictedin Tables1– 5.Theresponsesto eachquestionareexpressedinthetablesinorderof decreasingprevalence.Demographicinformationis summarizedin Table1.
Thesurveyconsistedof32
40items,dependentontheuse ofbranchinglogictocreatea flowofrelevantquestions. Responseoptionswereacombinationofmultiple-choice;a “checkallthatapply” clickbox;short-answerquestionswith freetext;andquestionswitha five-pointLikertscale.The purposeofthequestionswastodeterminewheregraduates wereworking(insideoroutsideIndia),theirwork environments(clinical,non-clinical,research,withinan emergencydepartment[ED]vsanothersetting,etc), involvementinteachingandresearch,confidenceintheirEM practice,satisfactionwiththeirMEMtraining,and involvementintheCOVID-19response.Thesurvey instrumentisincludedin AppendixA
SurveyrecipientsincludedonlyMEMprograms af fi liatedwithUSinstitutions.Programdirectorswere contactedtocollectcontactinformationforprogram graduates.TheMEMtrainingsitesthatwecontacted includethosethatworkwiththefollowingaf fi liates intheUS:GW;NorthwellHealth;StateUniversityof NewYork(SUNY)Upstate(Syracuse,NY);andthe UniversityofMaryland(UMD)(Baltimore,MD).Atthe timeofourproject,thetotalnumberofMEMgraduatesfor eachsitewasasfollows:647(GW);46(NorthwellHealth); 13(SUNYUpstate);and20(UMD).Ofthe726MEM graduates,contactinformationwasobtainedfor714 graduates(98.3%).Surveysweredistributedviaemailtoall 714MEMprogramgraduatesfromDecember 2021–February2022with2–3reminderemailssentto increaseresponserates.Surveyresultswerecollected electronicallywithREDCapresearchsoftware hostedatNorthwellHealthandconsolidatedinto
ThemajorityofMEMgraduatesreportedworking withinIndia(210,62.7%)andwithinanEDwork environment(304,91.0%).TheUK(54,19.4%)and UnitedArabEmirates(17,5.1%)werethemostcommon locationsforworkoutsideIndia.Themostcommonreason forchoosingtopracticeoutsideIndiawasduetodif fi culty withformalrecognitionoftheMEMcerti fi catewithinIndia (97,79.5%),followedbydifferencesinsalary(71,58.2%) andstandardofliving(58,47.5%).Mostgraduates practicingoutsideIndiareportedthedecisiontoleave IndiawasmadeaftercompletingtheMEMprogram(96, 80.0%).GraduatesreportedworkingmainlyintheDelhi NationalCapitalRegion(NCR)(35,16.8%),Maharashtra (28,13.5%),andKerala(31,14.9%);however, graduates’ practicelocationswerebroadlylocated throughoutIndia.
Morethanhalfofgraduatesreporteddedicatingover25% oftheirworkhourstoteachingothersaboutEM,withnurses (218,66.5%),otherphysicians(191,58.2%),paramedics (191,58.2%),andcommunitymembers(129,39.3%)listedas commonrecipientsofeducationalactivities.Abouthalfofall graduatesreportedpresentingresearchprojectsatacademic conferences(168,50.5%)andendorsedmembershipin nationalEMprofessionalorganizations,suchastheSociety forEmergencyMedicineIndia(SEMI)andINDUS-EM (170,50.7%).Almostallgraduateswereengagedintreating COVID-19patientsduringthepandemic(333,99.4%)with morethan70%ofgraduatesdedicatingoverhalfoftheir workhourstoCOVID-19patientcare.Mostgraduates agreedorstronglyagreedthattheyweresatisfiedwiththeir overallMEMtraining(296,88.4%),wellpreparedtoworkin theED(311,92.8%),andconfidentintheirabilitytopractice EM(306,91.6%).
–
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 816 Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce Cianoetal.
Table1. Demographicsofsurveyparticipants. (#ofrespondents,%ofrespondents)
WhatyeardidyougraduatefromyourMEMprogram?
2020(60,17.9%)
2019(46,13.7%)
2018(42,12.5%)
2017(42,12.5%)
2016(40,11.9%)
2015(32,9.6%)
2021(27,8.1%)
2014(18,5.4%)
WhichUnitedStates-affiliateisassociated withyourMEMprogram?
GeorgeWashingtonUniversity(300,89.6%)
NorthwellHealth(formerlyNorthShore
LIJHealthSystem)(32,9.6%)
StateUniversityofNewYorkUpstate(2,0.6%)
UniversityofMaryland(1,0.3%)
WithinwhichhospitaldidyoucompleteyourMEMtraining?
KokilabenDhirubhaiAmbaniHospital(KDAH)(49,14.6%)
Peerless(48,14.3%)
AsterMIMSCalicut(36,10.7%)
MissionHospital-Durgapur(32,9.6%)
MAXSAKET(25,7.5%)
Moolchand(18,5.4%)
BabyMemorialHospital(16,4.8%)
MAXPPG(14,4.2%)
AsterMedcityKochi(14,4.2%)
MeenakshiMissionHospital&ResearchCenter(12,3.6%)
AMRI-Bhubaneswar(12,3.6%)
GlobalHospital-Bangalore(12,3.6%)
DISCUSSION
Datafromthecurrentstudydescribesthecontributionof Indo-USMEMgraduatestoEMspecialtydevelopmentin Indiaoverthelast15years.
WorkEnvironmentandClinicalContribution
Themajorityofgraduatesreportedthattheycontinueto practicewithinIndia(62.7%)andinanEDsetting(91%).Of thosethatdidleave,themainreasonscitedincludelackof recognitionoftheirMEMcertificateinIndia(79.5%),better salaries(58.2%),andgreateropportunitiesforprofessional growth(56.6%).Sincetheirinceptionin2007,Indo-US MEMcourseshavetrainedover700EPs,andamajorityare stillworkinginEDsinIndia.Thenumberofpostgraduate DiplomateofNationalBoard(DNB)andMDseatsoffered inEMarestillfarfewerthanthoseofferedinothercountries, suchastheUSorUK,despiteIndiahavingasubstantially largerpopulation.5,13,17 TheMEMseatsmaycontinueto fill thegapinIndia’sEMclinicalworkforceuntilDNBandMD seatsinEMhavesignificantlyincreased.GraduatesofMEM programsworkinginIndiashouldbelookedatasaresource
2013(13,3.9%)
2012(7,2.1%)
2011(5,1.5%)
2010(3,0.9%)
2009(0,0.0%)
2008(0,0.0%)
2007(0,0.0%)
MAXShalimarBagh(11,3.3%)
Believer’sChurch(8,2.4%)
AsterCMIBangalore(6,1.8%)
MAXSmart(6,1.8%)
Other(4,1.2%)
MAXDehradun(3,0.9%)
GlobalHospital-Chennai(2,0.6%)
MAXVaishali(2,0.6%)
KIMS-Trivandrum(2,0.6%)
MAXMohali(1,0.3%)
DMAcademyWayanad(1,0.3%)
ApolloGlennEaglesHospital-Kolkata(1,0.3%)
forspecialtydevelopmentinIndia.Manyserveinleadership rolesintheirhospitalsandtakepartineducatingmedical studentsandfutureEPs.
StepsshouldbetakentorecognizeMEMgraduatesasEM specialiststoimproveretentionofphysicianswhoreceive additionalEMtrainingaftertheirMBBS[Bachelorof MedicineandBachelorofSurgery,whichisequivalentto MDdegreeintheUS].Thismayleadtomoreprofessional opportunitiesthroughouttheprivateandpublicsector, improvedjobsecurity,andmorecompetitivesalaries.
GeographicalDistributionofSkilledEmergencyWorkforce Ourdataindicatesthatmanygraduateschoosetoworkin morewell-resourcedurbanareas,suchasDelhiNCR, Kerala,andMaharashtra,acommontrendseenacross differenttypesofhealthcareworkersthroughoutIndia.18 Thesesamestateshavedoctordensitiesabovethenational averageof79.7doctorsper100,000population.18 Whilethis isnotsurprising,itisalsonoteworthythat10.6%ofMEM graduatesarepracticinginlower-income-per-capitastates, suchasUttarPradesh(eight,3.8%),Jharkhand(seven,
–
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 817 Cianoetal. Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce
MEM, MastersinEmergencyMedicine.
(#ofrespondents,
%ofrespondents)
Wheredograduateswork?
WithinIndia(210,62.7%)
UnitedKingdom(65,19.4%)
UnitedArabEmirates (17,5.1%)
Other(10,3.0%)
UnitedStates(9,2.7%)
SaudiArabia(8,2.4%)
WithinwhichIndianstatesare graduatesworking?
DelhiNCR(35,16.8%)
Kerala(31,14.9%)
Maharashtra(28,13.5%)
WestBengal(27,13.0%)
Karnataka(12,5.8%)
Odisha(12,5.8%)
TamilNadu(10,4.8%)
UttarPradesh(8,3.8%)
Jharkhand(7,3.4%)
Bihar(6,2.9%)
AndhraPradesh(6,2.9%)
Gujarat(4,1.9%)
Haryana(4,1.9%)
Punjab(4,1.9%)
Rajasthan(3,1.4%)
Whyaresomegraduates practicingoutsideofIndia?
Difficultieswithformal recognitionofyourMEM certificateinIndia(97,79.5%)
Differenceinsalary (71,58.2%)
Differenceinstandardofliving (58,47.5%)
WorkingenvironmentinIndia (46,37.7%)
Lackofjobopportunitiesin EMinIndia(15,12.3%)
Relocatetobenearfamily (5,4.1%)
Opportunityforprofessional growth(69,56.6%)
Other(4,3.3%)
Qatar(8,2.4%)
Kuwait(5,1.5%)
Bahrain(2,0.6%)
Australia(1,0.3%)
NewZealand(0,0.0%)
Table3.
graduates. (#ofrespondents, %ofrespondents)
Howmuchtimedograduates reportteachingemergency medicinetoothers?
26–50%(129,38.5%)
0–25%(112,33.4%)
51–75%(83,24.8%)
76–100%(11,3.3%)
Havegraduatesattended facultydevelopmentor teachingcourses?
Whattypesofeducationand trainingaregraduatesengaged in?
Educationandtrainingfor nurses(218,66.5%)
Educationandtrainingforother physicians(191,58.2%)
Educationandtrainingfor paramedics(191,58.2%)
Uttarakhand(3,1.4%)
Assam(3,1.4%)
Chhattisgarh(3,1.4%)
Nagaland(1,0.5%)
Meghalaya(1,0.5%)
Manipur(1,0.5%)
Telangana(1,0.5%)
MadhyaPradesh(1,0.5%)
ArunachalPradesh(0,0.0%)
Goa(0,0.0%)
HimachalPradesh(0,0.0%)
Mizoram(0,0.0%)
Sikkim(0,0.0%)
Tripura(0,0.0%)
Whendidgraduateswhoare practicingoutsideofIndia decidetoleaveIndia?
After finishingtheMEM program(96,80.0%)
WhileIwasenrolledinthe MEMprogram(14,11.7%)
BeforeenrollingintheMEM program(10,8.3%)
No(203,60.6%)
Yes(132,39.4%)
Community/laypersoneducation (129,39.3%)
Prehospitalcaredevelopment (113,34.5%)
Educationandtrainingfor ayurvedichealers(34,10.4%) Other(18,5.5%)
Havegraduatespresented researchprojectsorabstracts ataregional,national,or internationalconferenceor meeting?
Yes(168,50.5%) No(165,49.5%)
Aregraduatesmembersof emergencymedicine professionalorganizations withinIndia? (eg,SEMI,INDUS)? Yes(170,50.7%) No(165,49.3%)
Havegraduatesattendedor completedtrainingindiversity andinclusionorhealth equity? No(227,68.0%) Yes(107,32.0%)
Havegraduatespublishedan abstract,textbookchapter,or researcharticleinapeerreviewedmedicaljournal? No(215,64.2%)
Yes(120,35.8%)
Havegraduatesbeenapartof organizinganemergency medicineconference(national orinternational)? No(209,62.4%)
Yes(126,37.6%)
3.4%),Bihar(six,2.9%),andMadhyaPradesh(one,0.5%).
Thesestateshavesomeofthelowestphysiciandensitieswith Biharstatebeingoneofthelowestat52.6physiciansper 100,000population.9 Lower-income-per-capitastatesin Indiahavebeentransitioning,albeitataslowerratethanthe wealthierstates,towardsapredominantnon-communicable diseaseburden,similartothepatternsofdiseaseseenaround
theworld.19 Since2000,lowerincomestateshaveattributed morethan50%oftheirtotaldeathstonon-communicable diseases.1 ThisisrelevanttoEMworkforcedistributionas theacutemanagementofnon-communicabledisease complications,suchasmyocardialinfarctions,strokes,and diabeticemergencies,isanareaofEMexpertise.Although MEMgraduatenumbersfromthecurrentstudyinlowincomestatesaresmall,theircontributionisnotableinthe contextoflowspecialist-physiciandensitiesandpoor funding.Tohighlightthisconcept,wecreatedgeographical heatmapsofIndiadescribingthelocationsofactive US-MEMprograms(Figure1A)andthelocations
Table2. WorkenvironmentandclinicalcontributionofMastersin EmergencyMedicinegraduates.
MEM, MastersinEmergencyMedicine, NCR,NationalCapital Region.
AcademiccontributionofMastersinEmergencyMedicine
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 818 Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce Cianoetal.
MEM, MastersinEmergencyMedicine; SEMI, SocietyofEmergency MedicineIndia.
Table4. InvolvementintheCOVID-19response. (#ofrespondents, %ofrespondents)
DidgraduatestreatCOVID-19 patientsduringtheCOVID-19 pandemic?
Yes(333,99.4%)
No(2,0.6%)
Howmuchtimedidgraduates reportspendingcaringfor COVID-19patientsduringthe pandemic?
76–100%(131,39.1%)
51–75%(114,34.0%)
26–50%(76,22.7%)
0–25%(14,4.2%)
FoundationofIndia,andInstituteforHealth MetricsandEvaluation.21
Didgraduatesparticipatein COVID-19response planning?
Yes,withinmydepartment (i.e.,emergencydepartment, ICU,etc)(178,53.1%)
Yes,withinmyhospital (105,31.3%)
No(30,9.0%)
Yes,withinmycityorregion (12,3.6%)
Yes,withinmystate (10,3.0%)
(#ofrespondents, %ofrespondents)
MyMEMtraininghasmademe confidentinmyabilitytopractice emergencymedicine.
Stronglyagree(264,79.0%)
Agree(42,12.6%)
Neutral(9,2.7%)
Disagree(3,0.9%)
Stronglydisagree(16,4.8%)
Iamsatisfiedoverallwithmy MEMtraining.
Stronglyagree(218,65.1%)
Agree(78,23.3%)
Neutral(12,3.6%)
Disagree(9,2.7%)
Stronglydisagree(18,5.4%)
MyMEMtraininghas preparedmewellforworking intheemergency department.
Stronglyagree(267,79.7%)
Agree(44,13.1%)
Neutral(5,1.5%)
Disagree(3,0.9%)
Stronglydisagree(16,4.8%)
Locationsofactivetrainingprograms(Figure1A)and stateswheregraduateschoosetowork(Figure1B)overlap withIndianstateswithmid-rangetohighdiseaseburdens (Figure1C)asexpressedbystateswithlightblue-whiteand marooncolors.Someexamplesin Figure1C areUttar Pradesh,Bihar,Maharashtra,andWestBengal.Although thehighdiseaseburdenofthesestatesmayinpartbedueto thesebeingsomeofthemostpopulousstatesofIndia,the highDALYsoftheselocationscannotbedenied.Manyof thesestatesalsohouseUS-affiliatedMEMprogramsto promotetheclinicalandacademicdevelopmentofEM.
InadditiontotheneedtogrowEPtrainingopportunities, emigrationofskilledphysiciansfromIndiaisanotherbarrier tocreatingandmaintainingarobustworkforce.Wefound that37.3%ofMEMgraduatesreportpracticingmedicine outsideIndiaaftergraduation.High-incomecountries,such astheUK,Canada,theUS,Gulfcountries,andAustralia, havehistoricallyfunctionedascommonemigrationsitesfor trainedmedicalspecialistsfromIndia.22,23 TheOrganization forEconomicCooperationandDevelopmentestimatedthat over90,000physicianswhotrainedinIndianowwork outsideIndiawiththeUSandUKasthemostcommon receivingcountries.22 ThismigrationofMEMgraduatesis notuniquetoEM,tothispartnershipprogram,ortoIndia. Thenetmigrationofhealthcareworkersfromlow-and middle-incomecountriestohigherincomecountriesisa causeforgrowingconcernglobally,resultinginafewarticles onamoremanagedformofcircularmigration.24,25 This considerationcouldpromptactioninhigherrecognitionof MEMtrainingandtheneedformoreopportunitiesfor professionalgrowth.
AcademicContributions
MEM, MastersinEmergencyMedicine.
ofworkingUSMEMgraduates(Figure1B)usinga web-enabledheatgeo-mappingtool.20 AheatmapofIndia demonstratingdifferencesindiseaseburdenasall-cause disability-adjustedlifeyears(DALYs)[yearsoflifelostdue toprematuremortality](Figure1C)wascreatedusingthe GlobalBurdenofDiseaseIndiaComparetoolfromthe IndianCouncilofMedicalResearch,PublicHealth
Manygraduatesreportinvolvementinacademicteaching andresearchactivities.Whilemorethanhalfofgraduates citeinvolvementintheeducationandtrainingofother physicians,nurses,paramedics,laypeople,andayurvedic healersarealsotaughtbyMEMgraduates.Thisillustrates thebroadreachacrossdisciplinesand fieldsbywhich graduate-lededucationcanoccur.Italsohighlightsan importantconceptinglobalEMcapacity-buildingasthe trainingofoneEPcanimpacttheknowledgeandexperience ofmultipleothermembersofthehealthcareteamand surroundingcommunity.GraduatesimpartingtheirEM knowledgetoothersreachesfarbeyondtheircontributionto thecountry’sspecializedclinicalworkforce;itexpandsthe competencyandspecializedclinicalknowledgeofthe hospital-basedhealthcareteam,nurses,prehospital personnel,andcommunitymembers.Educationmayalso empowerotherstocontinuetogrowtheirknowledgeand participateinotherEM-basedinitiativesandtraining.
Table5. SatisfactionandconfidenceinMastersinEmergency Medicinetraining.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 819 Cianoetal. Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce
MEM, MastersinEmergencyMedicine; ICU,intensivecareunit.
locationsofUS-MEMgraduates(1B),anddifferencesindiseaseburdenasall-causedisability-adjustedlifeyears(1C)depictedusingthe GBDIndiaComparetoolfromtheIndianCouncilofMedicalResearch.
Otheracademicpursuitsreportedbygraduatesinclude presentingresearchabstractsorprojectsatconferences, membershipinnationalEMorganizations,andpublishing abstracts,textbookchapters,orresearcharticles.Publishing researchandeducationalmaterialscreatesconcrete deliverablesthatcanenhancetheknowledgeofothers. Publicationscanbeusedtosupportcontext-specificEM policies,suchasnewemergencymedicalservicesprotocols, andtheycanassistinlocaladvocacy.Publicationof scholarlyworkalsoconnectsIndiatoaglobalacademic communityandestablishestheroleofMEMgraduatesasan emergingexpertresourceinthe fieldofEM.
AcademicEMorganizationsinIndia,suchasSEMI, INDUS-EM,andtheAcademicCollegeofEmergency
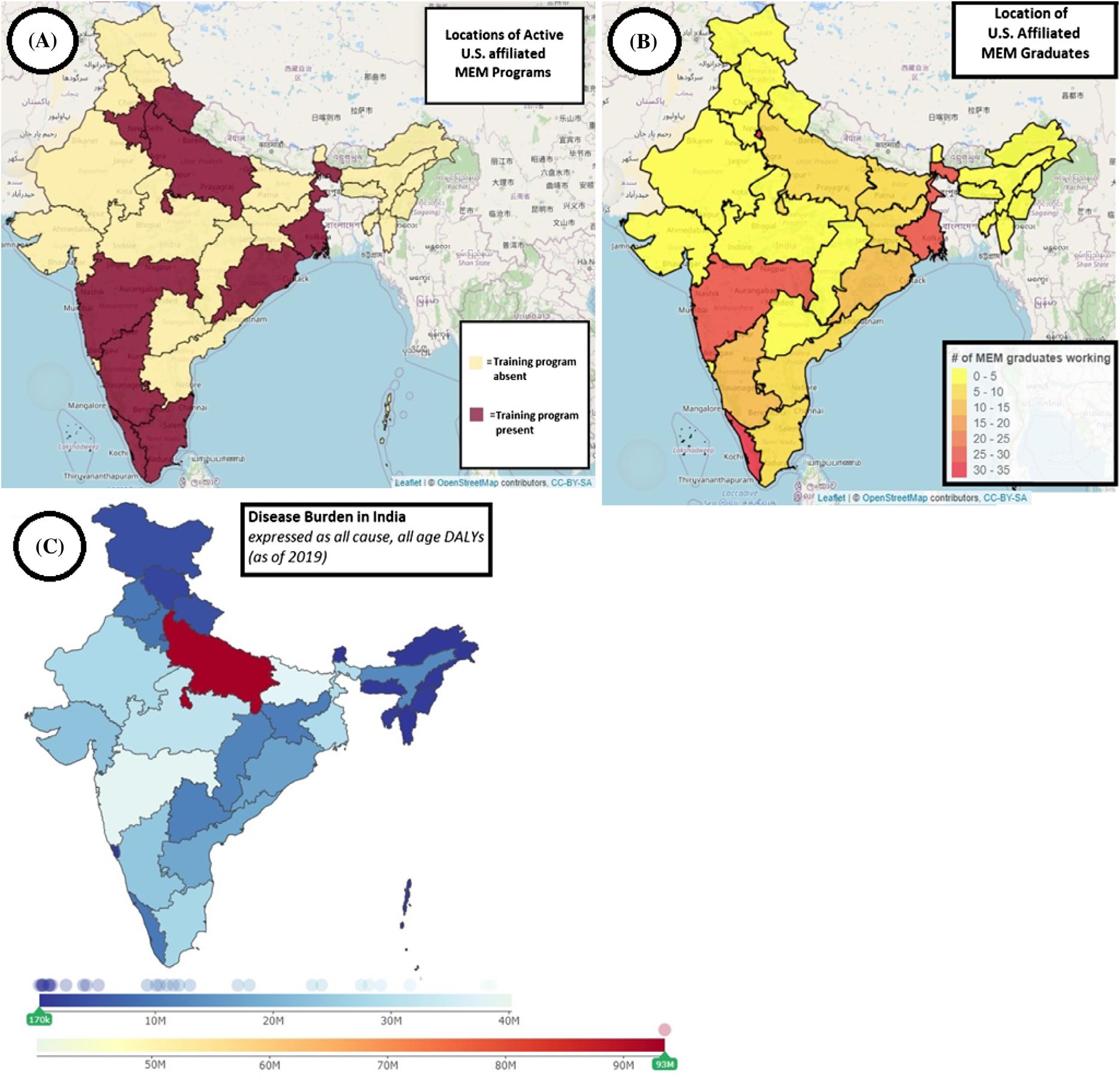
ExpertsinIndia,shouldfocusonexpandingopportunities forprofessionalgrowth.Offeringmorecourseson professionaldevelopment,expandingteachingandresearch skills,andincreasingthenumberofeducationalconferences andprofessionalnetworkingeventsaresomeactionsthat couldhelpcreateanenvironmentwheregreaterprofessional growthispossible.
ContributiontoCOVID-19Response
TheCOVID-19pandemicdevastatedmanyhealth systemsglobally.Whiletheavailabilityofvaccinationsand enforcementofbasicpublichealthprecautionsarecrucially importantinreducingmorbidityandmortality,havinga well-equippedEMworkforceonthefrontlineisanother
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 820 Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce Cianoetal.
Figure1. GeographicalheatmapsofIndiadepictingthelocationsofactiveU.S.MastersinEmergencyMedicine(US-MEM)(1A),the
importantaspectofpandemicmanagementandplanning.Of theUS-affiliatedMEMgraduateswhoparticipatedinthis study,99.4%reportedbeinginvolvedincaringfor COVID-19patientsduringthepandemic.Almost40% reportedthat76-100%oftheirworktimewasspentcaringfor COVID-19patients.Morethanhalfofgraduateswere involvedinhigherlevelCOVID-19responseplanningwithin theirclinicaldepartmentorhospital.Theimportanceofthese contributionscannotbeunderstated,particularly consideringthedevastatingimpactoftheCOVID-19 pandemicinIndia,andthecontributionsofMEMgraduates totheCOVID-19response.Furthermore,our findings highlightthechallengesfacedbytheseEPsandexemplify theneedforchangestobeinstitutedaroundtheformal recognitionofUS-affiliatedMEMgraduatestoretain moreEM-traineddoctorsinIndia.
LIMITATIONS
ThisdescriptivestudyfocusedonthecontributionsofUSaffiliatedMEMtrainingprogramgraduates.Therefore,the dataisnotinclusiveofalltypesofMEMprogramsinIndia. AlongsidetheUS-affiliatedMEMprogramsdescribedinthis study,otherMEMprogramshaveemergedfrequently affiliatedwithlocalIndianprofessionalsocieties.Weopted tonotincludenon-USaffiliatedMEMprogramsinour study.Thiswasachoicewemadeduringthedevelopment phaseofourprojectasUS-affiliatedprogramshaveamore comparablestructure,design,andassessmentofresidents thannon-US-affiliatedMEMprograms.
Thesurveyresponserateforthisstudywas46.9%andmay notrepresentthemajorityofUS-affiliatedMEMgraduates. Themajorityofsurveyrespondentsalsoreportedgraduating withinthelast fiveyears;thus,oldergraduateswhomaybe workinginothergeographicorclinicalsettingsmaybe under-represented.Nevertheless,ourresultsreportthe feedbackofalmosthalfofallgraduates.Giventhesurvey format,thisstudymayhavebeensubjecttoselectionbias,as residentswhohadamorenegativeormorepositive experiencewiththeirMEMeducationmayhavefeltmoreor lesscompelledtocompletethesurvey.Thesurveywas designedanddistributedbykeyUSinstitutional stakeholdersinMEMprograms,andalthoughnoidentifying informationwascollectedfromrespondents,thismayhave ledtobiasintheresponses.Themajorityofrespondents camefromtheGW-affiliatedMEMprograms.Thiswas expectedasGW-affiliatedMEMprogramspossessthe majorityoftheIndo-USprogramsitesandseatscomparedto otherUSinstitutions.Asaresult,thisstudymayoverly representthesegraduates.GraduatesfromNorthwell Health-affiliatedprogramshadthehighestsurveyresponse ratecomparedtootherprograms,althoughtheyonly contributedto9.6%ofallsurveyrespondents.Contact informationwasunavailablefor22ofthe736(1.7%)MEM graduates;thus,theywerenotincludedinthestudy.This
smallpercentageislikelynegligible,andwedonotbelieveit significantlyinfluencedthe findingsofourstudy.
CONCLUSION
TheresultsofthisreportdescribethecontributionsofUSaffiliatedMastersinEmergencyMedicinegraduatesonEM specialtydevelopmentinIndia.Oursurvey-basedreport highlightstheimportantroleofMEMgraduatesoverthelast 15years.Theroleofthesegraduatesshouldbeconsideredas ameanstoexpediteEMspecialtydevelopment,systems development,andclinicalcareacrossIndia.AsIndiaworks todevelopmoreformaltrainingpathways,MEMgraduates willcontinuetocontributetothedeliveryofpatientcareand thegrowthoftheemergencycaresystem.
AddressforCorrespondence:JosephD.Ciano,DO,MPH,Northwell LongIslandJewishMedicalCenter,DepartmentofEmergency Medicine270-0576thAve,Queens,NY11040.Email: jciano@ northwell.edu
ConflictsofInterest:Bythe WestJEMarticlesubmissionagreement, allauthorsarerequiredtodiscloseallaffiliations,fundingsources and financialormanagementrelationshipsthatcouldbeperceived aspotentialsourcesofbias.Noauthorhasprofessionalor financial relationshipswithanycompaniesthatarerelevanttothisstudy. Therearenoconflictsofinterestorsourcesoffundingtodeclare.
Copyright:©2023Cianoetal.Thisisanopenaccessarticle distributedinaccordancewiththetermsoftheCreativeCommons Attribution(CCBY4.0)License.See: http://creativecommons.org/ licenses/by/4.0/
REFERENCES
1.Indiastate-leveldiseaseburdeninitiativecollaboration.Nationswithina nation:variationsinepidemiologicaltransitionacrossthestatesofIndia, 1990-2016intheGlobalBurdenofDiseaseStudy. TheLancet 2017;390(10111):2437–60.
2.GidwaniS,JenaNN.Perspectivearticlefor EuropeanJournalof EmergencyMedicine:emergencymedicineinIndia. EurJEmergMed 2020;27(5):317–8.
3.SriramV,BaruR,BennettS.Regulatingrecognitionandtrainingfornew medicalspecialtiesinIndia:thecaseofemergencymedicine. Health PolicyPlan.2018;33:840–52.
4.NationalMedicalCommission.Collegeandcoursesearch. MD-EmergencyMedicineseats.Availableat: https://www. nmc.org.in/information-desk/college-and-course-search/ AccessedMarch28,2022.
5.NationalBoardofExaminations:DepartmentofAccreditation.NBE accreditedseats.22February2022.Availableat: https://accr.natboard. edu.in/online_user/frontpage.php?v=4.AccessedMarch28,2022.
6.SriramV,BaruR,HyderAA,BennettS.Bureaucraciesandpower: examiningtheMedicalCouncilofIndiaandthedevelopmentof emergencymedicineinIndia. SocSciMed.2020;256:113038.
Volume24,No.4:July2023WesternJournal of EmergencyMedicine 821 Cianoetal. Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce
7.DiplomateofNationalBoard.Indicativeseatmatrix:DNBPDCET(Post Diploma)CentralizedCounselingJanuary2018AdmissionSession. 2018.Availableat: https://www.natboard.edu.in/pdoof/pbnotice2018/ cns/DNB%20PDCET%20Indicative%20Seat%20Matrix%20Jan% 202018%20-%2028.03.2018.pdf?h88233erhx90wsd0q2wk2s2ks2.
AccessedMarch28,2022.
8.NationalResidentMatchingProgram.Resultsanddata:2018main residencymatch®.2018.Availableat: http://www.nrmp.org/wp-content/ uploads/2018/04/Main-Match-Result-and-Data-2018.pdf
AccessedMarch23,2023.
9.MichasF.NumberofspecialistdoctorsinUSby field, Statista.2022. Availableat: www.statista.com/statistics/209424/us-number-ofactive-physicians-by-specialty-area/.AccessedMarch23,2023.
10.SriramV,HyderA,BennettS.Themakingofanewspecialty:apolicy analysisofthedevelopmentofemergencymedicineinIndia. IntJHealth PolicyManag.2018;7(11):993–1006.
11.RybarcxykMM,LudmerN,BroccoliMC,etal.Emergencymedicine trainingprogramsinlow-andmiddle-incomecountries:asystemic review. AnnGlobHealth.2020;86(1):60.
12.DouglassK,PoussonA,GidwaniS,etal.Postgraduateemergency medicinetraininginIndia:aneducationalpartnershipwiththeprivate sector. JEmergMed.2015;49(5):746–54.
13.SriramV,GeorgeA,BaruR,etal.Socialization,legitimationandthe transferofbiomedicalknowledgetolow-andmiddle-incomecountries: analyzingthecaseofemergencymedicineinIndia. IntJEquityHealth 2018;17:142.
14.DouglassK,GidwaniS,MehtaS,etal.Whitepaperonemergency medicineandtraininginIndia:Wherearewenowandwhereshouldwe gonext?Emergencymedicineeducationandtraininginindia:aneeds analysis.2018.Availableat: https://reaganinstitute.smhs.gwu.edu/ sites/g/ files/zaskib1031/files/2022-06/White%20paper-Emergency% 20Medicine%20Education%20and%20Training%20in%20India.pdf AccessedMarch23,2023.
15.CianoJD,AcerraJ,TangA.Developmentofaremotelearning educationalmodelforinternationalemergencymedicinetraineesinthe eraofCOVID-19. IntJEmergMed.2022;15(1):2.
16.UniversityGrantsCommission.SettingupandOperationofCampuses ofForeignHigherEducationalInstitutionsinIndia.2023.Availableat:
https://www.ugc.ac.in/pdfnews/9214094_Draft-Setting-up-andOperation-of-Campuses-of-Foreign-Higher-EducationalInstitutions-in-India-Regulations-2023.pdf.AccessedMarch23,2023. 17NationalResidentMatchingProgram.AdvanceDataTables:2022Main ResidencyMatch.2022.Availableat: https://www.nrmp.org/wp-content/ uploads/2022/03/Advance-Data-Tables-2022-FINAL.pdf AccessedMarch23,2023.
18.AnandS,FanV.ThehealthworkforceinIndia.TheWorldHealth Organization.2016.Availableat: https://apps.who.int/iris/bitstream/ handle/10665/250369/9789241510523-eng.pdf? sequence=1&isAllowed=y.AccessedMarch23,2023.
19.WorldHealthOrganization.Thetop10causesofdeath.2020.Available at: https://www.who.int/news-room/fact-sheets/detail/the-top-10causes-of-death.AccessedMarch23,2023.
20.BabickiS,ArndtD,MarcuA,etal.Heatmapper:web-enabledheat mappingforall. NucleicAcidsRes.2016;44:W147–53.
21.IndianCouncilofMedicalResearch,PublicHealthFoundationofIndia, andInstituteforHealthMetricsandEvaluation.GBDIndiaCompare Data Visualization.NewDelhi:ICMR,PHFI,andIHME.2020. Availableat: http://vizhub.healthdata.org/gbd-compare/india AccessedMay2,2022.
22.PotnuruB.AggregateavailabilityofdoctorsinIndia:2014–2030. Indian JPublicHealth.2017;61(3):182–7.
23.MullanF.Themetricsofphysicianbraindrain. NEnglJMed 2005;353(17):1810–8.
24.WorldHealthOrganizationInternationalLabourOrganization,and OrganizationforEconomicCo-operationandDevelopment.The InternationalPlatformOnHealthWorkerMobility:ElevatingDialogue, KnowledgeandInternationalCooperation.2017.Availableat: https:// www.who.int/publications/m/item/the-international-platform-onhealthworker-mobility.AccessedMarch23,2023.
25.WorldHealthOrganization.WHOGlobalCodeofPracticeonthe InternationalRecruitmentOfHealthPersonnel:ReportoftheWHO ExpertAdvisoryGroupontheRelevanceandEffectivenessoftheWHO GlobalCodeofPracticeontheInternationalRecruitmentofHealth Personnel.2020.Availableat: https://apps.who.int/gb/ebwha/pdf_files/ WHA73/A73_9-en.pdf.AccessedMarch23,2023.
WesternJournal of EmergencyMedicineVolume24,No.4:July2023 822 Contributionof15yrsofIndo-USTrainingPartnershipstotheEPWorkforce Cianoetal.












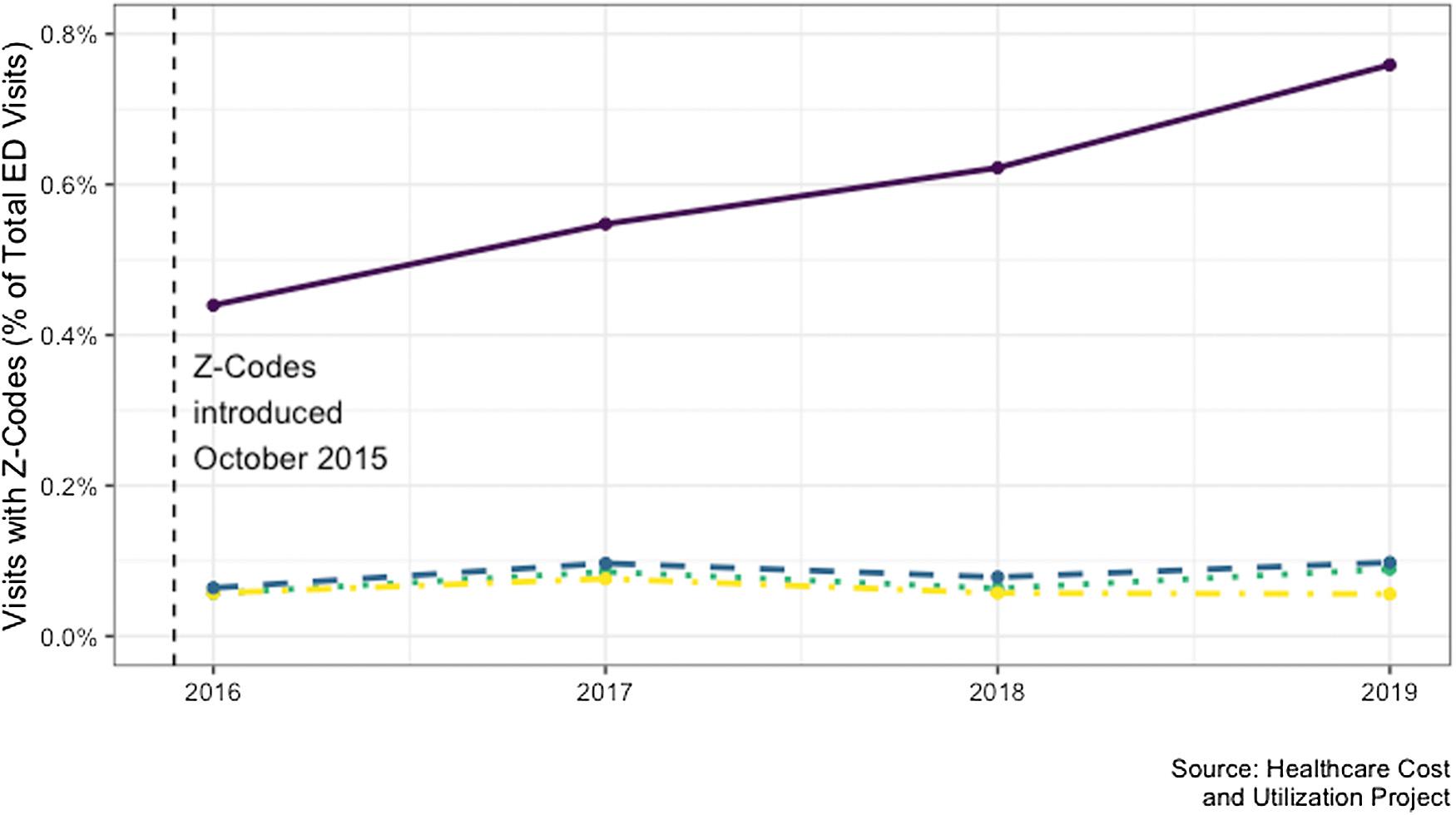
 Table2. Performancemeasuresforthetotalparticipants.
Table2. Performancemeasuresforthetotalparticipants.