Building
Stella












 Benedict
Natasha Loder Health editor The Economist October 11th-12th 2023 | London
Benedict
Natasha Loder Health editor The Economist October 11th-12th 2023 | London





Building
Stella












 Benedict
Natasha Loder Health editor The Economist October 11th-12th 2023 | London
Benedict
Natasha Loder Health editor The Economist October 11th-12th 2023 | London


I am excited to announce the much-awaited launch of the second edition of American Hospital & Healthcare Management Magazine 2023. I would like to thank my internal team of editors, dedicated advisory board members, and accomplished industry authors for their collaboration and timely inputs. Their unwavering commitment for excellence has played a pivotal role in creating top-quality content as always.
This second edition deep dives into top trending areas in global healthcare landscape, covering - Cardiovascular Medicine & Surgery, Telemedicine, Inpatient Lab Formularies & Applications of AI and Machine Learning in Patient Diagnosis & Care.
A collection of carefully blended noteworthy topics are mentioned below for your quick reference and introduction.
Samir Redzepagic, MD, Public Health Officer, Monash Public Health outlines how the Advancements in cardiovascular medicine and cardiac surgery have improved patient outcomes and healthcare. The role of minimally invasive techniques, digital health, and novel biomarkers have enhanced the efficiency and effectiveness of treating cardiovascular disease.
Shriya Sharma & Rohan Goswami from Mayo Clinic shares insight on how the emerging Telehealth domain uses electronic and telecommunications technologies to provide remote healthcare services, information, and education. They outline how telehealth complements in-person visits by utilizing virtual technologies, thus improving workflow efficiency, and enabling post-discharge monitoring.
Andrew Fletcher, Medical Director of Laboratory Stewardship, Accumen and Founder of Eutilogic Consulting speaks on Laboratory utilization & how it plays a crucial role in optimizing healthcare delivery and patient outcomes. He outlines how efficient and strategic utilization of laboratory services enhances diagnostic accuracy, facilitates timely treatment decisions, and promotes cost-effectiveness.
Benjamin W. Y. Lo, MD, Department of Neurological Surgery, Lenox Hill Hospital introduces the machine learning algorithms and the clinically robust computing models – Fuzzy Logic, Neural Networks and Bayesian Analysis that are heavily used in clinical outcome prediction model. These models complement classical approaches of regression analysis and decision tree analysis.
James Doulgeris, Chairman, Population Health Advisory Board, RSDSA elaborates on Artificial Intelligence and Digital Health. In an easy to follow Q&A he outlines how AI analyses extensive medical data for accurate diagnosis and personalized care. The data is getting constantly pumped from across a wide plethora of medical sensing devices resulting in the designing of a personal treatment plan and optimal patient care regime.
I hope you enjoy this latest edition of American Hospitals & Healthcare magazine as much as we did producing it. If you'd like to contribute an article or interview to be featured in our next issue, you can reach me via email: editorial@americanhhm.com
At the heart of our mission lies the invaluable input, ideas, and feedback from our cherished audience. We wholeheartedly welcome you to join us in this journey of growth and collaboration. Share your valuable thoughts and connect with us on social media to stay well-informed and actively engaged with the dynamic world of the Healthcare industry.
N D Vijaya Lakshmi EditorHEALTHCARE MANAGEMENT
06 Simplified Patient Scheduling Through Self-assessment Tools and Hospital System Integration
Piyanun Yenjit, Founder, Apuk Co., Ltd
14 Legal Implications of Medical Errors, Initiatives & Strategies for Patient SafetyThe Road Ahead
Shriya Sharma, MBBS, Division of Advanced Heart Failure and Transplant, Mayo Clinic
Rohan Goswami, MD, Director of Heart Transplant Innovation and Research, Mayo Clinic
20 How Managers Solve Healthcare’s Difficult Problem of Recruitment and Retention
Tom Atchison, President and Founder of Atchison Consulting
34 Cardiovascular Medicine & Surgery - Global Trends & Challenges
Samir Redzepagic, MD, Public Health Officer, Monash Public Health
44 Growth and Impact of Telemedicine in Improving Access to Healthcare


Shriya Sharma, MBBS, Division of Advanced Heart Failure and Transplant, Mayo Clinic
Rohan Goswami, MD, Director of Heart Transplant Innovation and Research, Mayo Clinic
57 Modern Thoracic Surgery – Bending the Borders
Dr. Paul Swatek, Head of the Thoracic Surgery, Department of thoracic surgery, Ingolstadt Clinic
62 Leveraging an Inpatient Reference Test Formulary to Reduce Costs
Andrew Fletcher, Medical Director of Laboratory Stewardship, Accumen and Founder of Eutilogic Consulting
78 Machine Learning & High Dimensional Data – Clinical Outcome
Prediction Using Bayesian Neural Networks with Fuzzy Logic Inferences
Benjamin W. Y. Lo, MD, Department of Neurological Surgery, Lenox Hill Hospital
49 Integration of AI and IoT: Transforming Healthcare through Innovation
Simon Waslander, Director of Collaboration, CureDAO
68 Artificial Intelligence and Digital Health
James Doulgeris, Chairman, Population Health Advisory Board, RSDSA
Andrey Andreevich Kapitonov

CEO
Oxygen Technologies LLC



Belarus
Aung Pyae Kyaw
Executive Director Asia
Royal Hospital
Myanmar
Eiman Shafa
Medical Director, Spine Surgery
Abbott Northwestern Hospital
USA
Gabe Rijpma CEO


Aceso Health
New Zealand
James Doulgeris
Chairman
Population Health Advisory Board, RSDSA
United States
Likaa Najuib
Medical Marketing Operational Officer, Alfa Cure Oncology Center
Egypt
Pinheiro Neto Joao
Chief Executive Officer

Meu Doutor
Angola
Piyanun Yenjit
Managing Director APUK Co.,Ltd

Thailand
Thitisak Kitthaweesin
Chief of Phramongkutklao Center of Academic and International Relations Administration, Thailand


Wanita Ramnath

CEO
International Pharmacy and Health Care Suriname
EDITOR
Vijaya Lakshmi N D

EDITORIAL TEAM
Sarah Richards
Debi Jones
Harry Callum
Supraja B R
ART DIRECTOR
M Abdul Hannan
PRODUCT MANAGER
Jeff Kenney
SENIOR PRODUCT ASSOCIATES
Sussane Vincent

John Milton
Peter Thomas
PRODUCT ASSOCIATE
Ethan Wade
CIRCULATION TEAM
Sam Smith
SUBSCRIPTIONS IN-CHARGE
Vijay Kumar Gaddam
HEAD-OPERATIONS
Sivala VNR
www.americanhhm.com
Ochre Digi Media
www.ochre-media.com
©Ochre Digi Media Private Limited. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, photocopying or otherwise, without prior permission of the publisher and copyright owner. Whilst every effort has been made to ensure the accuracy of the information in this publication, the publisher accepts no responsibility for errors or omissions. The products and services advertised are not endorsed by or connected with the publisher or its associates. The editorial opinions expressed in this publication are those of individual authors and not necessarily those of the publisher or of its associates.
Copies of American Hospital & Healthcare Managemen can be purchased at the indicated cover prices. For bulk order reprints minimum order required is 500 copies, POA.
Magazine Subscribe

A misleading first visit is a common cause of adverse treatment outcomes. When patients can access specialists directly, their judgment in selecting a provider may be flawed. The advanced self-assessment tool, integrated with the hospital system containing doctor information, can simplify patient-doctor scheduling and improve an appropriate specialty and experience.
Piyanun Yenjit Founder, Apuk Co., Ltd.Misleading initial visits are a common cause of adverse treatment outcomes. When patients have direct access to specialists, their judgment in selecting a provider may be flawed. The advanced self-assessment tool, integrated with the hospital system containing doctors’ information, can simplify patient-doctor scheduling and improve the appropriateness of specialty selection and patient experience.
Scheduling an appointment with a physician is an important step in maintaining patient health and well-being and preventing diagnosis. Several factors can guide individuals in determining the optimal time to seek medical assistance.
Availability: It is an important factor when finding a physician. For instance, it is essential to consider the alignment between physicians’ office hours and patients’ schedules, which may be limited or conflict with their availability.
Timeliness: It is important to consider how quickly the patient can receive medical treatment or further diagnosis in a timely manner. The physician should promptly conduct any necessary examinations, tests, and further investigations, which can help expedite any necessary treatments or interventions.
Readiness: Patients should have some basic knowledge about their symptoms or condition, not for self-diagnosis but to facilitate discussions with the physician.
Appropriateness: Several factors need to be taken into account, including:
Clinical appropriateness: It involves selecting a physician with the appropriate specialization that aligns with the patient’s condition. Some symptoms or conditions may be related to a specific area of expertise, such as general practice, EENT, internal medicine, pediatrics, etc. Choosing a physician with the right specialization ensures that you receive the most relevant and effective care for your condition.
Financial appropriateness: It pertains to the affordability of a patient’s financial situation under their insurance plan and coverage details. It is important to consider the possibilities of exclusions for certain medical conditions under the individual patient’s insurance policy.
Service and Location: It refers to the quality of care and level of service provided by each healthcare provider, such as a patientcentric approach, accessibility, staff service mindset, atmosphere, follow-up, aftercare service, etc.
Appropriate scheduling with a physician is crucial to ensure timely and effective healthcare. However, delays in diagnosis can occur, leading to poor treatment outcomes.
Accessibility is the first step in healthcare services. Delayed or inadequate access to healthcare services often results in unfavorable treatment outcomes. Particularly in cases of cancer, delayed diagnosis and treatment are the most common consequences of poor accessibility, significantly affecting prognosis, as early-stage detection leads to better outcomes.
For cancer patients, referring to the American Cancer Society (ACS) treatment outcomes are mostly related to cancer staging. The 5-year relative survival rate is an indicator for measuring cancer treatment outcomes. A relative survival rate compares people with the same type and stage of cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific stage of colon or rectal cancer is 80%, it means that people who have that cancer are, on average, about 80% as likely as people who do not have that cancer to live for at least 5 years after being diagnosed. The survival rate significantly depends on cancer staging.
• Localized: There is no sign that cancer has spread outside of the organ
• Regional: Cancer has spread outside the organ to nearby structures or lymph nodes
• Distant: Cancer has spread to distant parts of the body or distant lymph nodes (Table 1)
Patient factor:
Medical knowledge limitation: Each set of symptoms can be associated with various diseases that require different medical specialties. Some symptoms cannot be predicted based solely on their lesion location. For example, abdominal pain can indicate heart disease, and coughing, typically associated with respiratory tract issues, can also be a symptom of esophageal disease. Lack of awareness among patients and even inexperienced medical staff about the intricate relationship between symptoms and diseases can lead to the oversight of serious conditions. Here is an example table showcasing symptoms, possible causes, specialists, and severity levels: (Table 2)
Illness perception – Preferences and personality types can influence how individuals react to illness, and denial reactions commonly lead to delayed diagnosis and treatment. On the other hand, an over-concerned patient is most likely to see a more critical specialist
(e.g., an oncologist) with even less chance of cancer, which also leads to delayed treatment in the case of non-cancer patients.
Provider factor:
Proper doctor arrangement– Ensuring the adequate availability of specialists is a common challenge in healthcare. Healthcare providers need to allocate sufficient resources to ensure timely and appropriate treatment for patients' conditions while aligning with the expertise of the specialists. In certain areas, doctor practices may not be directly managed by the hospital, which can further complicate doctor scheduling.
Contact point– Convenience options for patients to select doctors and make appointments facilitate timely visits. However, due to technology constraints and privacy concerns, the contact portal may not be fully open for the patient in a secure way, so direct calling for an appointment is still the main channel in some areas.
Primary care based – Although assigning
a primary care physician as the first gate of evaluation, treatment, and management is the best approach for population-based healthcare management, it also has some risks especially delayed diagnosis, which may not be significant at the overall level but may be material for some individual cancer patients.
Other factors, e.g., geographic limitations.
Some of the above factors are uncontrollable from the patient and provider perspective, but there are opportunities for improvement in certain areas. For example, patient medical knowledge and perception, specialist arrangement, and appointment system can be optimized to enhance accessibility.
This article proposes a solution to improve accessibility in the context of healthcare systems that allow patients to directly access specialists through self-symptom assessment tools integrated with provider schedules.
In some countries, primary care systems serve as the initial point of contact for patients, with general practitioners, family physicians, or pediatricians providing a wide range of healthcare services, including health screening, diagnosis, and treatment before referring to
specialists when necessary. This approach helps manage healthcare costs and reduces the workload on specialty physicians. However, in certain situations, a “fast-track” approach to specialists may be necessary for patients with urgent concerns who require immediate consultation.
To effectively manage patient demand for healthcare services, it is essential to ensure an adequate supply of specialists appropriate for each patient's condition and to adopt responsive, just-in-time approaches to their needs.
Key concepts to consider include:
• Patients and physicians should aim to meet as soon as possible to ensure timely access to healthcare services.
• Performing self-assessment before consulting with physicians can help patients communicate effectively. It allows them to gather valuable information about their health, such as symptoms or conditions, medical history, family history, underlying
conditions, lifestyle factors, medication history, allergies, immunization history, etc. This information helps physicians understand patient health and provide appropriate care.
• Using patient input, technology, and medical data science, matching factors, can provide guidance such as:
o Patient’s likely differential diagnosis (DDX) or conditions that require further investigation or specialist consultation. The key objective is not to get the most precise diagnosis but to show a full list of possible diagnoses and their possibility scores.
o Utilizing technology, such as APIs, location tracking, or big data analysis, to match patient conditions with appropriate physicians and providers based on specialty, service, and location.
o Leveraging telemedicine and other technology-driven solutions to increase accessibility for patients, enabling them to access remote care services.
o Checking doctor availability and facilitating appointment requests, which are common features that patients need after receiving the assessment result. These features require connection technology such as API or simpler channels like email. However, ensuring a well-prepared doctor schedule in the hospital remains a key success factor, regardless of the connection channel.
Maintaining good health and well-being is
fundamental to life. Delayed diagnosis and treatment can have serious consequences on a patient’s health, leading to extensive treatment requirements, poorer outcomes, and increased health risks that may lead to long-term health issues, and higher healthcare costs. The primary cause of these issues is often the mismatched and untimely visits between patients and healthcare providers.
To mitigate the risks associated with delayed diagnosis and treatment, it is crucial to use appropriate self-assessment tools that help

patients choose the right provider and physician based on specialties as per their convenience. Additionally, healthcare providers must have well-organized doctor schedules to ensure good accessibility as this factor plays a major role. Lastly, integrating technology and medical data science can facilitate the connection and find the best match between a patient’s condition and an appropriate physician. This integration leads to simplified patient scheduling through self-assessment tools and hospital system integration.
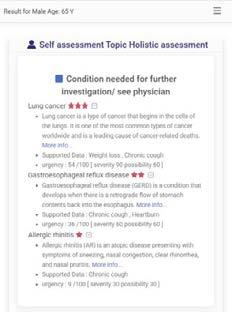
A patient [age 65, M] experiences chronic cough, heartburn, unintentional weight loss, and a history of smoking.
Utilizing medical data science technology, the patient receives a differential diagnosis or condition that requires further investigation or a visit to a physician. The system calculates the possibility and urgency score.
The condition shows likelihood in order from the most to the least: Lung Cancer, Gastroesophageal reflux disease, and Allergic rhinitis. The patient is provided with basic knowledge about each condition before seeing the physician.
The system also match patient conditions with appropriate physicians and providers based on specialty, service, and location.

A patient [age 45, F] experiences abdominal pain at epigastric, dyspnea, and weight loss.
Utilizing medical data science technology, the patient receives a differential diagnosis or condition that requires further investigation or a visit to a physician. The system calculates the possibility and urgency score.

The condition shows likelihood in order from the most to the least: Atrial fibrillation, coronary heart disease, Gallstone calculus, Gastric cancer, Acute gastritis, Peptic ulcer.

The patient is provided with basic knowledge about each condition before seeing the physician.
The system also matches patient conditions with appropriate physicians and providers based on specialty, service, and location.

Piyanun Yenjit is a country manager of HIMSS Thailand and founder of APUK, a healthcare digital transformation consultant and micro services provider, focusing on improvement in patient safety, process efficiency, and business growth. She is also experienced in electronic medical records with structured data implementation compatible with various quality assurance standards.




September 20th-21st 2023 | Brussels

More than: 350 in-person attendees | 90 speakers | 40 solution-focused sessions



The 9th annual summit will address cancer control for European citizens. Convening a wide range of critical stakeholders including policymakers, healthcare professionals and providers, regulators, payers, investors, industry and patient groups.



events.economist.com/world-cancer-series


Medicolegal issues are more recognized and prevalent in the field of medicine in recent years. They arise from incidents such as wrong-site surgery, limited physician oversight, and medication errors. Medical negligence can potentially risk the longevity of a physician’s career, and strategies to manage risk are key to improving patient outcomes.
Shriya Sharma MBBS, Division of Advanced Heart Failure and Transplant, Mayo Clinic Rohan Goswami MD, Director of Heart Transplant Innovation and Research, Mayo ClinicThe medical profession is widely recognized as one of the most honorable and esteemed occupations across the globe. Its primary purpose is to provide valuable and selfless assistance to humanity. Doctors can alter the course of a patient’s life if they are careful, sincere,
efficient, and skilled. However, nowadays, the relationship between providers and patients has become less personal and more formal. Providers are no longer seen as perfect and unquestionable. It is undeniable that humans are prone to making mistakes, and when such errors occur in the medical field, they can have serious and far-reaching consequences. In many instances, these mistakes stem from a combination of minor mishaps and various circumstances that converge – leading to potential catastrophe for the patient. At any point along this chain of events, there is a potential to intervene and prevent a catastrophe. However, if no intervention occurs, the situation may become disastrous. Providers involved in cases of medical negligence can potentially ruin their career and practice potential. The patient-provider relationship, if maintained, builds trust and allows for that trust to decrease the risk of litigation if such errors are maintained. Many patients after medical issues occur who feel connected, heard, and supported by their provider do not choose to consider legal action - given their feeling of good intention overpowering the complications that occurred from lack of oversight.
While most providers aim to establish a positive relationship with patients, it is concerning that nearly two-thirds of physicians aged 55 and older in the United States have faced at least
one lawsuit throughout their professional journey. Patients initiate lawsuits because they perceive that their concerns are ignored, their needs were neglected, and a lack of care was demonstrated, leading to unfavorable outcomes. When providers and patients have a solid relationship built on open communication, collaborative decision-making, and realistic expectations, both parties can have a positive healthcare experience.
Clinical negligence is a legal concept used to describe a situation in which a patient has experienced a medical mishap due to receiving inadequate care that falls below acceptable standards. In order to establish a case of clinical negligence, it is not sufficient to merely prove that a breach of duty occurred. It is also necessary to demonstrate causation, meaning that the harm suffered by the patient must directly result from that breach. Even if the quality of medical care provided was exceptionally low, if it did not lead to a substantial outcome or consequence, there is unlikely to be a viable legal case. Medicolegal issues that have gained significant attention involve incidents like performing surgery on the wrong body part, assigning procedures to non-physician operators (e.g. physician assistant, nurse practitioner, or medical trainee), and errors in the preparation of compounded medications.
What are some common errors made by medical professionals leading to medicolegal issues?

Clinical errors and malpractice claims are becoming increasingly significant in the field of medicine. One major concern is the potential risk of patients developing debilitating illnesses as a result of medical interventions while hospitalized. This risk not only contributes to the overall cost of healthcare but also adds to the burdens faced by patients. Some common errors are:
1. Avoidance: Physicians should not avoid interacting with patients and their relatives after a bad outcome. Comforting gestures and maintaining eye contact are important.
5. Failure to identify complications: Consent forms should accurately reflect known risks, and proper communication of complications is essential.
2. Defensive medicine: Unnecessary medical tests and procedures should be avoided to prevent complaints and potential malpractice.
3. Failure to communicate: Effective communication is crucial. Physicians should ensure that patients understand their diagnosis, treatment, and medications.
4. Failure to diagnose: Not diagnosing correctly is a leading cause of malpractice lawsuits. Patient information and communication play key roles in accurate diagnosis.
6. Inadequate follow-up: Physicians should ensure test results are received and reviewed and proper follow-up is conducted. Documentation is crucial.
7. Patient time: Allowing patients sufficient time to express concerns and show empathy can reduce the likelihood of a lawsuit.
8. Prescribing errors: Physicians should be aware of patients’ medications, reinforce proper usage, and encourage prompt reporting of any issues. Electronic prescribing and collaboration with pharmacists can help prevent errors.
Medical law is currently experiencing a significant transformation, but there is still much room for improvement in the legal framework regarding professional misconduct and negligence. There are measures that can be taken to reduce or prevent lawsuits related to medical negligence. To minimize legal disputes and create a safer healthcare environment, healthcare providers can implement the following strategies:
1. Prioritize patient satisfaction: Focus on meeting patient needs and ensuring their satisfaction with the care they receive.
2. Adhere to established policies and procedures: Strictly follow the prescribed
protocols and guidelines to ensure consistent, standardized care delivery.
3. Foster a patient-centered approach: Place the patient at the center of care by actively involving them in decision-making and considering their preferences and values.
4. Familiarize oneself with effective strategies for defending against malpractice claims: Stay informed about legal practices and strategies to effectively handle and defend against potential malpractice claims.
5. Utilize informed consent: Use informed consent as a tool for effective communication and decision-making, ensuring patients understand medical procedures' potential risks and outcomes.

6. Maintain thorough documentation: Record detailed information about clinical events, decision-making processes, and informed consent to promote transparency and provide a reliable reference for future assessments.
7. Be vigilant in recognizing and managing complications: Stay alert for potential complications and take prompt action to manage them, ensuring patient safety and well-being.
8. Communicate openly and with empathy: Engage in open and compassionate communication with patients and their families, particularly in
AUTHOR BIO

the event of complications. This fosters trust and reassurance.
9 Maintain regular contact during the post-complication period: Continuously engage with patients and their families, providing support and updates throughout the recovery process to enhance their trust and confidence.
By implementing these techniques, healthcare professionals can deliver optimal care, minimize legal disputes, and create a positive experience for patients.
References are available at www.americanhhm.com
Dr.Sharma, originally from Kathmandu, Nepal, is a Nepalese Army Institute of Health Sciences - College of Medicine graduate. She is currently a Research Fellow in the Division of Advanced Heart Failure and Transplant at the Mayo Clinic in Jacksonville, Florida. She is interested in staying current with the latest developments and contributing to the advancement of medicine with her clinical research in heart failure, artificial intelligence, and transplant medicine. Her aspirations are directed toward a future practicing cardiology, and she eagerly anticipates commencing her Residency training in internal medicine in 2024.
Dr.Goswami is a Transplant Cardiologist practicing at Mayo Clinic in Florida. He is a graduate of the American University of the Caribbean School of Medicine and completed his internal medicine residency at Columbia University College of Physicians and Surgeons – Stamford Hospital, a cardiology fellowship at The University of Tennessee Memphis, and a Transplant Fellowship in 2017 at Mayo Clinic in Florida. He has a keen interest in clinically focused artificial intelligence research to improve outcomes in patients with advanced heart failure. He has published articles in the field of both heart transplantation and artificial intelligence, as well as presented at Ai4 in 2020 on the future impact of AI in healthcare and invited lectures at the International Society of Heart and Lung Transplantation from 2021 to 2023. He looks forward to one day utilizing AI integration to prevent organ failure.



Talent management is a critical strategic challenge throughout healthcare today. Prior to 2020, there was a serious problem with shortages of physicians, nurses, and other care givers. The Covid pandemic moved this serious problem to a crisis level. Burn-out, quiet quitting and early retirement are some of the residual post-Covid phenomena. Most healthcare delivery systems have a need to identify, recruit, select and retain the most qualified professionals to serve their community. This very critical need to recruit and retain the best professionals is further hampered by another post-Covid factor of weak financials. Given these contemporary realities, this article will present some practical ways to recruit and retain high performers. The main thread throughout this discussion of the recruitment and retention is “Values Alignment.” Sustainable high performance is a function of the individual workers’ core values being aligned with the healthcare delivery system’s core values, which is often described as the organization’s Corporate Culture.
Tom Atchison President and Founder of Atchison ConsultingOrganizations are comprised of two very different, yet interdependent variables: tangibles and intangibles. Tangibles are those elements that can be observed and measured using standard quantitative techniques. Financials, productivity, quality outcomes, clinical processes are some of the more obvious tangibles. Employee engagement, trust, respect, pride, and perceived fairness are common intangibles. The most successful corporations use the corporate tangibles, personal intangibles and the corporate intangibles when designing the competencies needed for a job position. Less successful
companies focus mainly on tangibles such as academic credentials, history of employment, and salary requirements. Figure 1 shows the tangibles and intangibles which need to be considered in all recruitment, selection, and retention strategies. (Figure 1)
The most successful recruitment, selection and retention systems blend the tangibles and intangibles in all aspects—talent identification, selection, on-boarding, professional development, rewards, recognition, and, if necessary, de-selection.
The first step in creating a successful recruitment process is to identify the job competencies. This list of competencies must include the technical (tangible) and

the attitudinal (intangible) requirements for the job. The best way to decern the necessary competencies is by using “Trait Analysis.” Start with a blank poster board sheet and draw a line down the middle. On one side list the knowledge and skills a person must possess to be successful. And, on the other side, list the personal and attitudinal requirements the individual must display to fit into the corporate culture.
Once the two lists are created, then it is necessary to rank the items from “absolute requirements” to “nice to have requirements”.
This list should be used to draft “Help Wanted Ads” and to be used as a template for the interview and selection process. Too often individuals are hired for their technical expertise and then later fired for their lack of the necessary personal and attitudinal traits.
The main responsibility of all managers is to produce predictable results. This requires that valid and reliable performance data be produced daily. The challenge for managers is to balance the data collection so that the intangibles are measured with the same rigor and discipline as the tangibles. Too often departmental metrics are heavily weighted towards financial goals. While everyone agrees that financial goals are critical to corporate success, organizational metrics must also include data on the intangibles.
When profit trumps people, organizational culture can be significantly eroded. High performing healthcare organization view human capital and financial capital as equal variables that affect their sustainability. Both quantitative and qualitative metrics must be used. Quantitative metrics are the best way to measure the tangibles. Whereas qualitative metrics are designed to measure the intangibles. The most common qualitative measures are surveys that use a Likert scale, typically one through five. Likert based surveys are easy to use and the results are easy to calculate. However, they take a long time to distribute and complete. And surveys such as those measuring employee satisfaction may be conducted once a year, or in some cases once every two years. Human behavior is far too complicated, and changes are taking place too often for norm-based annual (or bi-annual)

Assuming the recruitment process has been successful and provided several candidates who possess the technical and personal traits to be successful, the task now is to select the “Best” among the “Good”. The job interview process must be designed to select the best candidate. One or both of two interview techniques need to be used. These techniques are “Value-based Interviews” and “Targeted Selection”. A detailed description of these techniques is beyond the scope of this article. However, a simple Google search will yield several good ideas on both techniques. The more successful interview processes include a team approach using the staff with whom the new hire will be working. The team, using the techniques mentioned above, can come to a consensus on the best person to hire.
The recruitment and selection process has been successful and now the new hire must learn about the organization into which they have joined. Historically, new
employee orientation has been a one-time presentation of JCAHO and human resources factors. Such presentations lasted a couple of hours, and then the new employees were sent to their jobs. This process was deficient in many ways. A better on-boarding process is heavily weighted with a discussion of the organization’s intangibles—mainly the Mission, Values and Vision, that is, Corporate Culture. This on-boarding process is led by the CEO and other members of the executive team. Today’s workforces are looking for a jobs that provide meaning, that give the individual some control over the decisions that affect their job, fair pay and benefits. Each of these areas need to be covered in an initial on-boarding process. And this acculturation process must be followed-up in departmental team meetings. Formal on-boarding is the first step of an individual’s acculturation, but it should not be the only time the worker hears about the organization’s mission (purpose), values (decision rules) and vision (the future).
employee satisfaction surveys to be of any use. An organization’s financial capital is examined daily, so should its human capital. Department managers working with human resources should do frequent, random, targeted, and short qualitative surveys. First, isolate
a critical human variable, such as: “Am I respected”; “Do I receive the information I need to do my job”; “I trust my manager”; “Do I feel part of a team” and “Do I have input into the decisions that affect my job.” Randomly select 25 staff to complete a 5-item survey
every day. After several days, patterns will begin to emerge that suggest an engaged or disengaged staff. This process can be done in several departments at once. Peter Drucker once stated that, “If you can’t measure it, you can’t manage it.” In today’s rapidly changing healthcare environment, human capital is too important not to measure every day.
by a personal vendetta. A better option is to interview staff on why they stay. The stay interview begins with the selection of the top 10% of the workforce defined by productivity and positive attitudes. Once these individuals are selected, HR personnel and departmental managers schedule one-on-one, 15-to-20minute interviews. The questions that these individuals are asked are simple and straight forward. Some sample questions are: Why do you continue to work here; What are the best features of your job; If you could change one aspect of your job, what would it be; and, What part of your job do you find most meaningful? The answers to these questions can be used to guide workplace improvements that increase the retention of high performers.
Finding, selecting, and on-boarding are the critical first steps to building a highperformance organization. However, all the financial and human costs in these early steps are wasted unless there is a strong process to retain the high performers. One of the best ways to retain high performers is by using “Stay Interviews.” A common HR practice is to use “exit interviews” to collect information on why people leave the organization. The exit interview process has some inherent weaknesses. For example, if the person is leaving because they are frustrated by their workload, or angry with their supervisor, the interview data will most likely be contaminated
Another critical component in the retention process is Employee Development. Even in an environment of limited financial capital, it is extremely important that staff are given the proper tools to accommodate the changes extant in today’s delivery systems. When staff feel depleted and frustrated with the rapid changes, they will reduce their productivity and will, very likely, begin “quiet quitting” or start to look for another job. Formal and informal (e.g., mentoring) staff development is a manager’s daily responsibility.
The role money plays in the recruitment and retention process is often misguided and counter-productive. Money must be perceived as fair. If it is perceived as unfair, staff will be
Alignment of core values drives sustainable high performance in healthcare, shaping the organization's corporate culture.
demotivated and may start looking for a job where compensation is perceived as fairer. However, there is an interesting inverse relationship between monetary perceived fairness and meaningful work. When an individual finds meaning in work, where they feel a purpose in doing and pride in the outcome, money is less important. But when work is devoid of meaning, purpose, and pride, then money is the only reason to do a job.
Two very important factors in retention are recognition and rewards. High performing cultures are generous with praise (recognition) for individual performance and money (rewards) for team/departmental achievement. Annual budgets should include a line item for rewarding performance.
A final caveat is de-selection, that is RIF, firing, or layoff. Sometimes managers need to remove one or more staff from the department. The reasons for this are typically due to financial limitations or poor performance. If the manager is using the metrics process described above of daily technical and attitudinal performance, then the separation process is a data-based, objective process. Without these data, the process can be perceived as subjective, which can destroy trust and weaken the culture.
Talent management is one of the biggest problems in today’s healthcare environment. Finding and selecting individuals with the right technical and attitudinal competencies for a
work setting is a daily challenge. The most effective recruitment and retention process is based on alignment of the individuals’ and corporate values. The goal, and the best metrics, of a successful recruitment and retention process include both tangible and intangible variables. The highest performing healthcare systems are productive, profitable and have very strong corporate cultures with measurably high employee engagement.
Tom Atchison is the President and Founder of Atchison Consulting LLC. Dr. Atchison consults with healthcare organizations on managed change programs, team building, conflict management and leadership development. Typically, he consults with senior executives, manager’s trustees and physician leaders. He has written several articles on organizational behavior. And has written six books. His 2022 book on Employee Engagement was awarded the James A. Hamilton book of the year award.

 Piyanun Yenjit Founder, Apuk Co., Ltd.
Piyanun Yenjit Founder, Apuk Co., Ltd.
1. How would you define valuebased care in the context of telemedicine, and what role does it play in improving patient outcomes?
Value-based care refers to the ratio of the quality of care to the cost of care. The familiarity between doctors and patients, the reduction of inequities, and the increased use of technology have all contributed to an improvement in the quality of telemedicine. As a result, the value of telemedicine is growing in terms of the variety of telemedicine modules that can serve consumer requirements, such as

improving accessibility to healthcare, quality, and population health.
Telemedicine plays a significant role in improving patient outcomes through accessibility improvements. It reduces the waiting time, allowing patients to receive treatment more quickly. Additionally, it brings the patient and the physician closer, reducing the need for frequent hospital or clinic visits and lowering transportation expenses.

2.What are the main advantages or benefits of using telemedicine to deliver value-based care compared to traditional in-person care models?
The primary advantage of telemedicine lies in its capacity to enhance access to healthcare services, particularly for individuals who encounter obstacles to receiving traditional in-person care. Here are the main benefits of telemedicine:
Time-saving and convenience: Telemedicine eliminates the need for traveling, waiting in crowded waiting rooms, and taking time off work or school. This convenience saves time and reduces overall healthcare-related expenses for patients.
• Improved access to care: By eliminating geographical barriers, telemedicine enables patients to receive medical consultations regardless of their location. It is particularly beneficial for individuals in rural or remote areas where access to healthcare facilities may be limited. Telemedicine also benefits
patients with mobility issues or those who have difficulty traveling to a healthcare provider.
• Broadened specialist availability: Patients have the opportunity to consult with specialists located in various cities or even different countries, all without the requirement of extensive travel.
• Cost savings: Telemedicine eliminates transportation expenses, reduces the need for hospital visits, and minimizes the associated costs of in-person care. Additionally, telemedicine can reduce hospital readmissions and emergency department visits by enabling timely remote monitoring and intervention.
• Continuity of care: Telemedicine allows for ongoing monitoring and follow-up care, particularly for patients with chronic conditions. Healthcare professionals can remotely track patients' health status.
3.How do you ensure that telemedicine services maintain a high standard of quality and patient safety while focusing on valuebased care?
Quality monitoring is essential not only for telemedicine but also for in-person medical visits. Understanding the context of telemedicine is crucial to effective auditing and ensuring the maintenance of quality and patient safety in telemedicine services. International standards such as JCI and various HIMSS Analysis tools are beginning
to define the benchmarks for telemedicine. Additionally, the Telehealth Certification standards encompass relevant areas for telemedicine implementation and delivery.
4. What challenges or barriers exist in implementing value-based care through telemedicine, and how do you address them?
• Doctor competency: The doctor's lack of training in the telemedicine approach necessitates the acquisition of additional skills, including the ability to gather patient information and provide a summary without relying on a physical examination.
• Doctor concerns: The primary concern for doctors is the liability risk associated with telemedicine. In certain countries, regulatory frameworks may not adequately
support or address this liability risk for doctors.
• Customer perception: Many customers still prefer face-to-face visits over telemedicine services. Concerns about data privacy also contribute to their reluctance.

• Payor concerns on fraud: Payors may be concerned about the potential for fraud due to limitations in patient identification during telemedicine encounters. This can lead to hesitancy in promoting telemedicine services.
In summary, addressing the challenges and barriers in implementing value-based care through telemedicine requires a multi-faceted approach. This includes providing training to doctors, collaborating with regulators to establish clear guidelines, and educating customers about the benefits and data privacy

protections of telemedicine. By doing so, we can increase telemedicine utilization and promote its effective integration into value-based care.
5. What strategies or approaches can be used to measure and track the value delivered through telemedicine services, particularly in terms of patient satisfaction and outcomes?
• Define and track specific outcomes relevant to the telemedicine service, such as the percentage of offline visits after a telemedicine service and the percentage of revisit to telemedicine. High percentages of offline visits or revisit to telemedicine may indicate potential shortcomings or failures in the telemedicine service.
In addition, to gain a comprehensive understanding of the success or failure of telemedicine services, it is essential to consider a broader range of metrics and factors. These include patient satisfaction, clinical outcomes, cost-effectiveness, and care coordination. Furthermore, seeking feedback from patients and healthcare providers through surveys, qualitative interviews, or focus groups can provide invaluable perspectives on the effectiveness of telemedicine services. By analyzing these aspects, valuable insights can be gained into the challenges, barriers, and opportunities for improvement in telemedicine delivery.
6. How can we ensure that patients receive personalized and patientcentered care when utilizing telemedicine services within a valuebased care framework?
• Telemedicine protocols: Telemedicine programs need to ensure that they have appropriate protocols in place to deliver high-quality care remotely. This includes having mechanisms to accurately assess patients and provide appropriate treatment recommendations.
• Patient education: Patients should be educated about the nature of telemedicine services, including their limitations, potential risks, and benefits involved.
• Secure Data Transmission: Implementing secure data transmission protocols is crucial to protect patient information.
• Qualified healthcare providers: Healthcare providers should have qualified and competent staff for telemedicine services. This involves having healthcare professionals who are trained and experienced in providing remote care services.
• Outcome monitoring: Monitoring patient outcomes for continuous quality improvement.

7. Can you provide examples of specific telemedicine interventions or initiatives that have demonstrated significant value-based care outcomes for patients?
Mild diseases such as upper respiratory tract infections or diarrhea are scenarios that reflect the effectiveness of telemedicine.
These conditions often require only historytaking and do not necessitate advanced assessment skills or investigations. Early assessment through telemedicine can prevent further complications and reduce the cost of care by avoiding unnecessary admissions.
• Telemedicine for Chronic Disease: Telemedicine enables regular consultations for patients with chronic diseases like diabetes or heart disease. Patients can receive guidance on medication, self-care, and lifestyle adjustments from healthcare providers.
• Tele-rehabilitation: Virtual visits can deliver rehabilitation services and physical therapy, allowing patients to perform exercises and receive guidance from therapists. Telerehabilitation is particularly beneficial for patients with limited access to in-person rehabilitation services, improving their quality of life.

• Tele-triage: Tele-triage services provide initial assessments and guidance for non-emergency conditions remotely. This helps determine appropriate care pathways and reduces unnecessary visits to the emergency room.
• Telemonitoring for Home Health: Telemonitoring programs utilize connected devices to remotely monitor patients' vital signs, such as blood pressure, heart rate, and oxygen levels, in their home environment. These examples illustrate how telemedicine interventions have demonstrated significant
value-based care outcomes. Telemedicine services can be applied in various healthcare delivery areas and have shown efficiency in improving access, reducing costs, increasing patient satisfaction, and optimizing care coordination for a wide range of conditions and patient populations.
8. How can we engage patients and promote active participation in their care through telemedicine while maintaining a focus on value-based principles?
Reimbursement is the key to engagement. Moreover, highlighting the benefits of telemedicine, such as reduced waiting times for follow-up visits or offering discounts on medication costs or doctor’s fees, can further enhance patient engagement.
9. How can we incorporate the social determinants of health into
Telemedicine's transformative impact on value-based care sets a new standard for patient satisfaction and wellbeing.
a telemedicine-based value-based care approach to address health disparities and promote equitable outcomes?
Telemedicine can effectively address several health disparities, especially healthcare accessibility. Patients in remote areas can easily connect with healthcare professionals timely. This advantage is particularly significant for individuals with chronic diseases who require regular follow-up for improved clinical outcomes. However, it is important to ensure the availability of supporting staff and units, such as local public health technical officers and pharmacies, in these areas to support telemedicine services. Telemedicine can also facilitate virtual care teams to enable coordination and collaboration among multidisciplinary healthcare professionals, who can collectively develop and implement care plans. With the use of telemedicine, healthcare professionals can assess patients, including gathering information about social determinants of health, such as education, housing, social security, food security, and safety. Telemedicine also enables the use of data analytics to identify patients at a higher risk for health disparities based on social determinants. Healthcare providers can then provide patient education that is tailored to address specific social determinants as well.
telemedicine services and ensure effective value-based care delivery?
• Online self-assessment can help patients find the most suitable doctors for telemedicine consultations. Based on the responses provided by patients in the online self-assessment, an algorithm can consider the patient's condition factors using medical logic. Once the patient completes the selfassessment questionnaire, the matching algorithm can analyze the responses and identify doctors who are the best fit for the patient's needs. Factors such as specialty, experience, availability, and patient preferences can be taken into account. Recommended doctors or healthcare providers who are well-suited to the patient's specific health concerns can then be matched, followed by the implementation of a scheduling system that allows patients to easily book telemedicine consultations.
• Strong network connectivity with data security protection.
• Remote Patient Monitoring using connected devices enables the remote monitoring of patient vital signs and health. For example, patients with chronic conditions like diabetes or hypertension can use glucometers and blood pressure monitors at home, and the data can be transmitted to healthcare providers for real-time monitoring. This approach facilitates early detection of abnormal conditions, timely intervention, and improved patient outcomes.

• Technology to bridge telemedicine gaps, such as the use of face scanning to measure vital signs.
• Integration with personal health or social apps like WhatsApp or Line.
• System integration with related support services such as pharmacies or rehabilitation centers is crucial, and standardized data is a key factor for successful integration.
11. How do you collaborate with other healthcare providers, including specialists and primary care physicians, in the delivery of value-based care through telemedicine?
Telemedicine allows healthcare providers to collaborate and seek second opinions from specialists or other healthcare professionals located elsewhere. This collaboration is supported by checking doctor availability and facilitating appointment requests, which are common features that patients often require after receiving assessment results. These features can be implemented through connection technologies such as APIs or simpler channels like email. Regardless of the connection channel, ensuring a wellprepared doctor schedule in the hospital is essential for successful collaboration and accessibility. Healthcare providers must have well-organized doctor schedules to ensure timely availability. Integrating technology and utilizing medical data science can further enhance collaboration and help find the best
match between a patient's condition and an appropriate physician.
12. Looking ahead, what innovations or developments do you foresee in the field of valuebased care through telemedicine, and how do you plan to adapt and leverage them for the benefit of patients?
Pushing forward telemedicine into the doctor's curriculum will allow doctors to become more familiar with and specialize in telemedicine services.
Providing benefits such as reimbursement, discount medication, and other incentives. Key concepts and ideas include the following:
• Patients and physicians should aim to meet as soon as possible to ensure timely access to healthcare services.
• Performing online self-assessments before consulting with physicians can help patients communicate effectively. It allows them to gather valuable information about their health, such as symptoms or conditions, medical history, family history, underlying conditions, lifestyle factors, medication history, allergies, immunization history, etc. This information helps physicians understand patient health and provide appropriate care.

• Using patient input, technology, and medical data science, matching factors can provide guidance such as:
Patient's likely differential diagnosis (DDX)
or conditions that require further investigation or specialist consultation. The key objective is not to obtain the most precise diagnosis but to show a full list of possible diagnoses and their possibility score.
• Utilizing technology, such as APIs, location tracking, or big data analysis, to match patient conditions with appropriate physicians and providers based on specialty, service, and location.
• Leveraging telemedicine and other technology-driven solutions to increase accessibility for patients, enabling them to access remote care services.
• Checking doctor availability and facilitating appointment requests, which are common features that patients need after receiving the assessment result. These features require connection technology such as APIs or simpler channels like email. However, ensuring a well-prepared doctor schedule in the hospital remains a key success factor, regardless of the connection channel. Patients might process reimbursement via telemedicine, and they could even receive medication and supplies via tele-pharmacy, for instance. AUTHOR BIO Piyanun Yenjit is a country manager of HIMSS Thailand and founder of APUK, a healthcare digital transformation consultant and micro services provider, focusing on improvement in patient safety, process efficiency, and business growth. She is also experienced in electronic medical records with structured data implementation compatible with various quality assurance standards.

This article will explore the future directions in cardiac surgery, novel surgical techniques, and treatments, but also emerging diagnostic approaches such as microRNAs and epigenomics. It will also discuss the challenges and opportunities to improve cardiovascular health in developing countries, including the role of digital health and the need for sustainable financing. Specific regional issues were considered, with an emphasis on cultural sensitivity and prioritization. Overall, the essay will suggest a need for continued investment and innovation to address the global burden of cardiovascular disease.
Samir Redzepagic MD, Public Health Officer Monash Public HealthCardiac surgery is a rapidly advancing field that is constantly improving with new techniques, technologies, and approaches. In this essay, I will discuss some of the latest trends and advancements in cardiac surgery and the potential future directions for the field.

Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality worldwide. Timely and accurate diagnosis is critical for the effective management of CVD. In recent years, significant advances have been made in the development of new and emerging diagnostic approaches in cardiovascular medicine and cardiac surgery. These approaches range from the identification of novel blood biomarkers, such as microRNAs, to the use of epigenomics, gene detection, and DNA methylation. In this essay, we will explore these emerging diagnostic approaches and their potential applications in cardiovascular medicine and cardiac surgery.
However, there are several challenges associated with the use of these emerging diagnostic and treatment approaches in clinical practice. First, the use of these biomarkers requires specialized laboratory equipment and expertise, which may not be available in all healthcare settings. Second, the interpretation of these biomarkers can be complex, and there is a need for standardized protocols for their measurement and interpretation. Third, the cost of these biomarkers may be a barrier to their widespread use in clinical practice.
Despite these challenges, there is great enthusiasm for the use of these emerging diagnostic approaches in clinical practice. The development of point-of-care diagnostic tests that can be used in primary care settings could help overcome some of the challenges associated with the use of these biomarkers. Moreover, advances in machine learning and
artificial intelligence could help improve the interpretation of these biomarkers, leading to more accurate and reliable diagnoses.
The development of new and emerging diagnostic approaches in cardiovascular medicine and cardiac surgery has the potential to revolutionize the diagnosis and management of CVD. These diagnostic approaches hold great promise for the early and accurate diagnosis of CVD, allowing for early intervention and prevention. While there are several challenges associated with the use of these biomarkers and other diagnostic modalities in clinical practice, there is great enthusiasm for their use, and ongoing research is focused on overcoming these challenges.
Discussion:
Recent advances and future trends in cardiac surgery
Minimally Invasive Cardiac Surgery:
One of the biggest trends in cardiac surgery and cardiovascular medicine over the last two decades is the move towards minimally invasive procedures. This involves performing surgery through small incisions instead of the large incisions traditionally used in open-heart surgery. Minimally invasive surgery offers many benefits, including reduced blood loss, reduced pain, shorter hospital stays, and faster recovery times. Advances in technology and techniques have made it possible to perform many heart surgeries using minimally invasive techniques, including aortic valve replacement, mitral
valve repair, and bypass surgery. The future of cardiac surgery is likely to see even more minimally invasive procedures as technology continues to advance.
Another area of development in cardiac surgery is the use of robotic surgery. Robotic surgery involves the use of robotic arms controlled by a surgeon to perform the surgery. The robotic arms can make very precise movements and can access hard-to-reach areas, which can lead to better outcomes for patients. In addition, robotic surgery is less invasive than traditional open-heart surgery, which can lead to faster recovery times and less pain for patients. While robotic surgery is still in its early stages, it has the potential to revolutionize cardiac surgery in the future.
Tissue Engineering and Regenerative Medicine:
Tissue engineering and regenerative medicine are two areas of research that have the potential to transform cardiac surgery in the future. Tissue engineering involves growing new tissue in the laboratory and using it to replace damaged or diseased tissue in the body. This could be used to create new heart valves or even entire hearts. Regenerative medicine involves using the body's own cells to regenerate damaged or diseased tissue. This could be used to repair damaged heart tissue or to create new blood vessels. While tissue engineering and regenerative medicine are still
in the early stages of development, they have the potential to revolutionize the treatment of heart disease in the future.
Transcatheter aortic valve replacement (TAVR) is a minimally invasive procedure that is used to replace a diseased aortic valve. TAVR involves inserting a new valve through a small incision in the leg and guiding it up to the heart using a catheter. TAVR is less invasive than traditional open-heart surgery and has been shown to be just as effective in treating aortic valve disease. In the future, TAVR is likely to become even more common as the technology and techniques used in the procedure continue to improve.
It is a rapidly advancing technology that has the potential to transform many fields, including cardiac surgery and cardiovascular medicine in general. AI can be used to analyse large amounts of data and help surgeons make better decisions. For example, AI can be used to analyse imaging data and help surgeons identify the best approach for a particular patient. AI can also be used to help surgeons plan surgeries and simulate the outcome of different surgical approaches. While AI is still in its early stages in the field of cardiac surgery, it has the potential to improve outcomes for patients in the future.
With the advent of predictive, preventive, and personalised (3P) medicine that is increasingly becoming important to reduce cardiovascular events and increase life expectation worldwide we are moving into the new era of treating cardiovascular diseases. That involves tailoring medical treatment to an individual patient based on their unique characteristics, such as their genetics or their medical history. In cardiac surgery, personalized medicine could be used to identify patients who are at higher risk for complications during surgery and develop tailored treatment plans to minimize those risks. Personalized medicine could also be used to develop targeted therapies for specific types of heart disease. While personalized medicine is still in the early stages of development, it has the potential to improve outcomes for patients in the future.
In cardiovascular medicine they involve combining multiple procedures, such as open-
heart surgery and catheter-based interventions, into a single surgery (procedure). This can lead to faster recovery times and better outcomes for patients. Hybrid approaches are particularly useful for patients with complex heart conditions, such as those with both coronary artery disease and structural heart disease. Over the recent decade, hybrid coronary revascularisation has received considerable attention as being the most suitable revascularization strategy for patients with multi vessel coronary disease. In the future, hybrid approaches are likely to become even more common as the technology and techniques used in the procedures continue to improve.
Telemedicine:
Involves using technology to provide medical care remotely. In cardiac surgery, telemedicine can be used to provide follow-up care and monitor patients after surgery. This can be particularly useful for patients who live in rural areas or who have limited mobility. Telemedicine can also be used to provide virtual consultations with specialists, which can be helpful for patients who live far away from a specialized cardiac surgery centre. While telemedicine is still in its early stages in the field of cardiac surgery, it has the potential to improve access to care and reduce healthcare costs in the future.
Innovation and investment are the keys to conquering the global burden of cardiovascular disease, transforming lives and healthcare practices.
are efforts to improve the quality of care provided to patients. In cardiac surgery, quality improvement initiatives can involve tracking outcomes, identifying areas for improvement, and implementing changes to improve patient care. Quality improvement initiatives can also involve implementing best practices, such as using checklists during surgery to reduce errors. An example of such an initiative is EuroHeart which is an international collaboration that aims to improve the quality of cardiovascular care and facilitate observation and randomized research through continuous and longitudinal capture of individual patient data. By focusing on improving the quality of care provided to patients, quality improvement initiatives have the potential to improve outcomes and reduce complications in the future. It’s just one of the forgotten areas where we can make the current use of the emerging technologies being implemented to improve the quality of care.

It involves focusing on the needs and preferences of the patient in the delivery of care. In cardiovascular medicine and surgery, patient centred care can involve providing information to patients about their condition and treatment options, involving patients in the decisionmaking process, and providing emotional support to patients and their families. By focusing on the needs and preferences of the patient, patient centred care has the potential to improve patient satisfaction and outcomes in the future. The most recent Covid-19 pandemic
has put into challenge this unique connection distancing the patient from the healthcare professionals and arising risks for the quality of patient care. The new reality has evolved into a revolutionary acceleration of adopting innovative and novel technologies in every domain of daily life from social interactions and entertainment to delivering medical services in broader context of the healthcare globally. The field of cardiovascular medicine and surgery is constantly evolving and improving with new techniques, technologies, and approaches. The future of cardiac surgery is likely to see even more minimally invasive procedures, robotic surgery, tissue engineering and regenerative medicine, transcatheter aortic valve replacement, artificial intelligence, personalized medicine, hybrid approaches, telemedicine, quality improvement initiatives, and patient centred care. By continuing to focus on improving patient outcomes and reducing
complications, the field of cardiac surgery has the potential to continue to improve and provide better care to patients in the future. The new and less invasive emerging treatments along personalised medical care are gaining more attention and acceptance and they will ultimately become the routine practice in medical care.
MicroRNAs:
mRNAs (miRNAs) are small non-coding RNA molecules that play an important role in the regulation of gene expression. miRNAs have been shown to be involved in the development and progression of CVD, and are thus promising biomarkers for the early diagnosis of CVD. Recent studies have demonstrated that the expression of specific miRNAs in the blood is altered in patients with CVD. For example, miR-208a and miR-499 are elevated in patients with acute myocardial infarction (AMI), while miR-1 and miR-133a are elevated in patients with heart failure. hese miRNAs have the potential to be used as diagnostic biomarkers for the early detection of CVD, as they are released within the body fluids (i.e., peripheral blood [PB], serum and plasma), they could be attractive as non-invasive biomarkers to monitor cardiovascular diseases and, as a future direction, possible therapeutic approaches for CVD treatments like heart failure (HR) and atrial fibrillation (AF).
It refers to the study of changes in gene expression that are not caused by changes in the DNA sequence. Epigenetic modifications, such as DNA methylation and histone modifications, have been shown to play a role in the development and progression of CVD. For example, DNA methylation of the ACE gene has been linked to the risk of hypertension and stroke. Similarly, histone modifications have been shown to be involved in the regulation of cardiac gene expression. Epigenetic modifications have the potential to be used as diagnostic biomarkers for CVD.
Genetic testing has been used for the diagnosis of inherited cardiac diseases, such as hypertrophic cardiomyopathy and long QT syndrome. Advances in next-generation sequencing (NGS) have made it possible to sequence multiple genes simultaneously, allowing for the rapid and cost-effective diagnosis of inherited cardiac diseases. In addition, genetic testing can be used to identify patients who are at increased risk of developing CVD, allowing for early intervention and prevention.
This potential diagnostic model is a type of epigenetic modification that involves the addition of a methyl group to the cytosine residue of DNA. DNA methylation has been shown to play a role in the development
and progression of CVD. For example, hypermethylation of the PPARα promoter has been linked to an increased risk of atherosclerosis. Similarly, hypomethylation of the KLF4 promoter has been shown to be involved in the development of atherosclerosis. DNA methylation has the potential to be used as a diagnostic biomarker for CVD.
Other emerging biomarkers for the diagnosis of CVD include high-sensitivity C-reactive protein (hs-CRP), growth differentiation factor-15 (GDF-15), and B-type natriuretic peptide (BNP). hs-CRP is a marker of systemic inflammation and has been shown to be associated with an increased risk of CVD. GDF-15 is a marker of cellular stress and has been shown to be associated with an increased risk of heart failure. BNP is a hormone that is released by the heart in response to stress and has been shown to be a marker of heart failure.
Advanced imaging techniques in cardiovascular medicine, such as MRI, CT, and PET, are becoming increasingly important in the diagnosis and treatment of CVD. These techniques enable non-invasive visualization of the heart and blood vessels, allowing for earlier diagnosis and more targeted treatment. Advances in imaging technology are also enabling the development of new minimally invasive surgical techniques.
Development of new and emerging diagnostic approaches in cardiovascular medicine and cardiac surgery holds great promise for the early and accurate diagnosis of CVD. Advances in the identification of novel blood biomarkers, such as microRNAs, epigenomics, gene detection, and DNA methylation, have the potential to revolutionize the diagnosis and management of CVD. These diagnostic approaches can help identify patients who are at high risk of developing CVD, allowing for early intervention and prevention. Moreover, these diagnostic approaches can help guide treatment decisions, allowing for more personalized and targeted therapy.
First, the use of these biomarkers requires specialized laboratory equipment and expertise, which may not be available in all healthcare settings. Second, the interpretation of these biomarkers can be complex, and there is a need for standardized protocols for their measurement and interpretation. Third, the cost of these biomarkers may be a barrier to their widespread use in clinical practice.
Despite these challenges, there is great enthusiasm for the use of these emerging
From micro RNAs to epigenomics, breakthroughs in diagnostics are paving the way for precision medicine in cardiac care.
The development of point-of-care diagnostic tests that can be used in primary care settings could help overcome some of the challenges associated with the use of these biomarkers. Moreover, advances in machine learning and artificial intelligence could help improve the interpretation of these biomarkers, leading to more accurate and reliable diagnoses.
There are several challenges and obstacles associated with the future directions in cardiovascular medicine and surgery that I would like to address in this review.
Many of the new technologies and approaches in cardiac surgery are expensive, which can limit their availability and impact. One potential solution is to focus on developing cost effective alternatives that can be used in resource limited settings. For example, pointof-care diagnostic tests can be developed that are affordable and easy to use, even in remote or underserved areas.
The cost of new technologies and approaches in cardiac surgery can be a major barrier to access, particularly in low- and middle-income countries. Patients in these settings may not be able to afford the latest treatments, which can lead to delays in diagnosis and treatment, and poorer outcomes. To address this challenge, it is important to focus on developing cost-effective
alternatives that can be used in resource limited settings, especially in developing countries.
Access to high-quality cardiac care can be a challenge for many patients, particularly those living in rural or remote areas. Telemedicine and remote monitoring technologies can help address this challenge, enabling patients to receive high-quality care without needing to travel long distances.
Many new technologies and approaches in cardiovascular medicine and surgery require regulatory approval before they can be used in clinical practice. This process can be slow and complex, which can delay the availability of new treatments. One solution is to streamline the regulatory process for these technologies, while ensuring that safety and efficacy are not compromised.
Cardiovascular medicine and surgery are highly specialized fields, and there is often a lack of interdisciplinary collaboration between different other related specialties. To address this challenge, it is important to foster greater collaboration and communication between different disciplines, including cardiology, radiology, genetics, and engineering. This can help drive innovation and improve patient outcomes.
As new technologies and approaches are developed, there are often ethical considerations that need to be taken into account. For example, the use of gene editing technologies raises questions about the potential risks and benefits, and how to ensure that these technologies are used in an ethical and responsible way. To address these challenges, it is important to engage in open and transparent discussions about the potential risks and benefits of new technologies, and to develop guidelines and regulations that ensure that they are used in an ethical and responsible way, not only on the local level but globally in particular.
Overall, while there are significant challenges associated with the future directions in cardiovascular medicine and surgery, there is also great promise for improving patient outcomes and quality of life. By focusing on developing cost-effective and accessible technologies, streamlining regulatory processes, fostering greater collaboration between different disciplines, and addressing ethical considerations, we can overcome these challenges and continue to drive innovation in the field of cardiac surgery. That can have a significant impact on patient care in developing countries and regions, particularly in areas with limited resources and infrastructure. By doing so, we can help ensure that all patients, regardless of where they live, have access to high-quality cardiac care.
In conclusion of this review, advancements in cardiovascular medicine and cardiac surgery have led to significant improvements in patient outcomes and overall healthcare. New and emerging technologies such as minimally invasive techniques, digital health, and the use of novel biomarkers have paved the way for more efficient and effective diagnosis and treatment of cardiovascular disease. However, these developments are not without their challenges, particularly in low-income and developing countries where limited resources and infrastructure often hinder the delivery of quality care.
Numerous obstacles faced by these countries can be addressed through a combination of strategies, including improved funding mechanisms, greater collaboration between governments and the private sector, and the deployment of innovative technologies and approaches that can deliver better care at lower cost. Efforts must also be made to address social and cultural barriers that may prevent individuals from seeking appropriate care or adhering to prescribed treatments.
Looking to the future, continued innovation in cardiovascular medicine and cardiac surgery will undoubtedly lead to further improvements in patient care and outcomes. The development of new technologies and techniques such as regenerative medicine, gene therapy, and tissue engineering hold great promise for the field. Digital health will continue to play an increasingly important role in the delivery of
cardiovascular care, particularly in remote and underserved areas.
Despite the many challenges that lie ahead, it is clear that the future of cardiovascular medicine and cardiac surgery is bright. By embracing new technologies and approaches, and working to overcome barriers to care, we can ensure that patients around the world receive the high-quality, effective care they need to live healthy, productive lives. However, it is important that these advancements are made accessible to everyone, regardless of income or location, to ensure that no one is left behind in the quest for improved cardiovascular health.
New generations of highly trained professionals are already changing the global landscape. It is reasonable to expect that they will address these issues better, as they will have access to improved education, training, and technological advancements. With the increasing emphasis on global health and equity, medical schools and training programs are placing greater emphasis on cultural competency, community engagement, and social determinants of health. As younger generations of healthcare professionals enter the field with a greater understanding of these issues, they will be better equipped to provide high-quality care that addresses the unique needs and challenges of patients in poor and developing countries.
The field of cardiovascular medicine and cardiac surgery is rapidly evolving, driven by new technologies, approaches, and research.
While there remain significant challenges to be addressed, particularly in low-income and developing countries, the future looks bright, with the promise of further improvements in patient care and outcomes. By continuing to invest in innovative technologies and approaches, and by working to overcome social, economic, and cultural barriers, we can ensure that everyone has access to the highquality cardiovascular care they need to live long and healthy lives. The unpredictability of the current global political and socioeconomic context will definitely shape the future of healthcare and well-being of every individual on our planet.
References are available at www.americanhhm.com
Dr Samir Redzepagic is an experienced cardiothoracic surgeon with over 25 years of experience in heart and lung transplant, on-pump and off-pump cardiac surgeries, and aortic surgical procedures. He completed his MD in Bosnia and his residency in Germany before moving to Australia, where he worked as a cardiac surgeon and held academic and clinicalappointments at various universities. He also completed a PhD in basic medical sciences onthe role of omega 3 fatty acids on transplanted cardiomyocytes. He is currently working in apublic health advisory role in Victoria, Australia, and is fluent in multiple languages.

Telehealth encompasses a wide range of electronic and telecommunications technologies, offering remote healthcare services, information, and education. While face-to-face encounters remain necessary in certain cases, telemedicine complements in-person visits by utilizing virtual technologies like video conferencing, reducing medical visits, improving workflow efficiency, and facilitating post-discharge monitoring.
Shriya Sharma MBBS, Division of Advanced Heart Failure and Transplant, Mayo ClinicRohan Goswami
MD, Director of Heart Transplant Innovation and Research, Mayo ClinicTelehealth — sometimes called telemedicine — allows healthcare providers to deliver care remotely without requiring an in-person visit. The terms telehealth and telemedicine are often used interchangeably, but they do

have some important distinctions. Telehealth is a broad collection of electronic and telecommunications technologies and has a wider range of remote healthcare services than telemedicine in healthcare delivery, information, and education. Both telehealth and telemedicine offer similar services, such as medical education, remote patient monitoring, videoconferencing consultations with patients, wireless health applications, and transmission of medical reports and images. However, while telemedicine focuses solely on remote clinical services, telehealth encompasses remote non-clinical services such as healthcare provider training, continuing medical education or public health education for providers, administrative meetings, provider-to-provider communication, and electronic information sharing to facilitate and support assessment, diagnosis, consultation, treatment, education, and care management.
Initially, the original concept of telehealth was to offer fundamental care to patients in remote and underserved areas. Wider acceptance and integration of telehealth into modern healthcare systems can be attributed to various factors. Notably, the transition of health care from fee-for-service models to models in which reimbursement is linked to patient and quality outcomes is one such factor. With increasing
Telemedicine revolutionizes healthcare through remote electronic and telecommunications technologies, using virtual tools like video conferencing to reduce in-person visits, streamline workflows, and facilitate postdischarge monitoring for enhanced patient care.
emphasis on providing quality patient care and cutting costs, telehealth has benefits and success being witnessed across various medical specialties and settings. Telehealth provides patients with a broad range of medical services, including lab tests or X-ray results, mental health treatment, prescription management, and follow-up appointments for chronic conditions like migraines, urinary tract infections, and skin conditions. Additionally, it offers physical therapy and occupational therapy, post-surgical follow-up, treatment and follow-up appointments, and urgent care issues such as colds, coughs, and stomach aches. With remote monitoring services, patients can manage their health goals and chronic conditions like diabetes, high blood pressure, and high cholesterol.
With the progress of mobile and electronic technologies, telemedicine has become increasingly accessible. As per the findings of a 2019 report published by the Pew Research Center, 90% of Americans utilize the Internet. Additionally, approximately 81% of Americans own a smartphone, almost 75% own desktop or laptop computers, and nearly 50% own tablet computers or e-readers. The increased availability of mobile technologies has played a vital role in the advancement of telemedicine.
The use of telemedicine has been experiencing a swift rise in the United States. According to reports, the percentage of US hospitals utilizing video and other technologies to connect with patients has increased from 35% to 76% between 2010 and 2017. Telemedicine in the United States experienced a significant peak in April 2020, during the initial surge of COVID-19 cases,

when it accounted for an impressive 69% of all doctor-patient visits.
Amidst the COVID pandemic, telemedicine has demonstrated immense potential in enhancing patients' access to quality and affordable healthcare while ensuring the safety of healthcare providers and patients by maintaining physical distancing measures. Telemedicine provides the convenience of avoiding the hassle of driving to a doctor's office or clinic, finding a parking spot, walking or waiting in a crowded room when you're unwell. Instead, you can consult with your doctor from the cozy comfort of your own bed or couch. Virtual visits also offer flexibility in scheduling, making finding a time that works for you easier. This flexibility can save you the trouble of taking time off from work or
arranging for childcare, depending on your schedule.
Issues like limited internet connectivity and the absence of Wi-Fi and video chat/webcam capabilities in both urban and rural regions can impede the full potential of telehealth, particularly among communities of color, the impoverished, and medically underserved populations. According to the Federal Communications Commission (FCC) and other sources, an estimated 21 to 42 million Americans lack access to high-speed internet. The digital divide has further aggravated the social and economic factors that hinder healthcare delivery and overall well-being. A study revealed that metropolitan areas had approximately 50 telemedicine visits per 10,000 individuals, while rural areas had around 31 visits per 10,000 individuals. Moreover, counties with low poverty levels had about 48 telehealth visits per 10,000 individuals, compared to only 15 visits per 10,000 individuals in high-poverty areas.
Telehealth plays a crucial role in promoting health equity by ensuring that all individuals, irrespective of their social or economic
background, have access to the healthcare they require and deserve. Achieving health equity in telehealth necessitates addressing issues related to digital literacy, technology, and analytics. Achieving health equity in telehealth involves addressing the needs of underserved communities, including low-income individuals, rural residents, people of color, immigrants, people with disabilities, older patients, and those with limited English proficiency or digital literacy. These communities often face barriers to healthcare access, resulting in higher mortality rates, increased disease burden, and limited treatment options. Limited access to technology, internet connectivity, suitable physical spaces for virtual visits, local telehealth providers, language barriers, and lack of adaptive equipment for disabilities are common obstacles to telehealth access. Overcoming these limitations requires interventions in digital literacy, technology, and analytics to ensure equitable healthcare delivery for all.
Telehealth has some drawbacks, including limitations with comprehensive physical examinations, possibilities for technical difficulties, security breaches, and regulatory barriers. When compared to in-person visits, telemedicine visits are more prone to privacy and security risks. While most telehealth systems follow strict encryption and abide
by the Health Insurance Portability and Accountability Act regulations, no platform is 100% safe from hackers or data breaches.
What are the current trends and future prospects for telehealth, considering its origin and historical trajectory?
Telehealth is a promising tool for public health, offering potential benefits like increasing access to care, improving patient-physician relationships, and saving healthcare costs. While face-to-face encounters remain necessary in some situations, telemedicine can supplement in-person visits by reducing
medical visits through virtual technologies like video conferencing. Its efficiency also streamlines workflows, making managing recovery and monitoring discharged patients easier. At the end of the day, the utilization of technology is more integrated now than ever before. Furthermore, innovations in remote sensing technologies, patient education and improvement in health literacy, and practice adoption will continue to shape this growing trend. All in all, telemedicine offers a mutually beneficial situation for patients and healthcare providers.
References are available at www.americanhhm.com
AUTHOR BIO
Dr.Sharma, originally from Kathmandu, Nepal, is a Nepalese Army Institute of Health Sciences - College of Medicine graduate. She is currently a Research Fellow in the Division of Advanced Heart Failure and Transplant at the Mayo Clinic in Jacksonville, Florida. She is interested in staying current with the latest developments and contributing to the advancement of medicine with her clinical research in heart failure, artificial intelligence, and transplant medicine. Her aspirations are directed toward a future practicing cardiology, and she eagerly anticipates commencing her Residency training in internal medicine in 2024.
Dr.Goswami is a Transplant Cardiologist practicing at Mayo Clinic in Florida. He is a graduate of the American University of the Caribbean School of Medicine and completed his internal medicine residency at Columbia University College of Physicians and Surgeons – Stamford Hospital, a cardiology fellowship at The University of Tennessee Memphis, and a Transplant Fellowship in 2017 at Mayo Clinic in Florida. He has a keen interest in clinically focused artificial intelligence research to improve outcomes in patients with advanced heart failure. He has published articles in the field of both heart transplantation and artificial intelligence, as well as presented at Ai4 in 2020 on the future impact of AI in healthcare and invited lectures at the International Society of Heart and Lung Transplantation from 2021 to 2023. He looks forward to one day utilizing AI integration to prevent organ failure.

AI and IoT integration in the healthcare industry offers exciting possibilities for transforming patient care and the healthcare industry as a whole. As these technologies continue to evolve, it is crucial to address challenges and ethical considerations to ensure a positive and equitable impact.
Simon Director of Collaboration CureDAO
1: What are some of the key challenges in deploying AI algorithms on resource-constrained IoT devices, and how can these challenges be addressed?
Before we go into the details of the Internet of Things and Artificial Intelligence. We should cover some basic points that illustrate the enormous challenges and opportunities facing global healthcare systems.
On the challenges side, United Nations projections indicate that the over 65 years of age is projected to rise to over 1.6 billion by 2050. Placing unprecedented strain on already overstretched healthcare systems.
On the opportunities side we are seeing tremendous innovation on the level of individual sensors in terms of precision, continuity and comfort. Also the total amount of IoT sensors is estimated to grow nearly 1.5 billion by 2030.
The current generation of sensors available in non-hospital consumer devices such as smart watches or smart bracelets lacks safety and accuracy with a host of reliability and security issues. An example by Smith et al. 2023 take
sleep measurement by consumer devices as an example of this.. Smart watches are too unreliable and inconsistent to create valid Artificial Intelligence-based learning models while using smart bracelets results in the loss of large amounts of data.
The solutions to this come from both the inherent sensor technology and the AI-based algorithms. A review by Vaghasiya et al. 2023, outlines the new-generation of hospital-grade sensors. The following graphic is from that review. (Figure 1)
On the AI-algorithm side Smith et al. 2023, notes that algorithms need to be tailored to the general characteristics of specific disease categories in order to reduce false positives.

Then using support vector machines such as LASVM, ISVM, and K-prototypes clustering, algorithms can be generated which reduce false signals but that is also accurate.
Smith et al. 2023 notes the example of a wearable sensor for knee osteoarthritis patients that calculates optimal exercise intensity.
2: Healthcare generates vast amounts of data from various sources. How can federated learning be leveraged in AI and IoT-integrated healthcare systems to perform collaborative analysis while ensuring data privacy?
A review by Chen et al. 2023, provides a short overview of issues regarding the security and privacy of IoT wearable sensors. The issues of security and privacy are very real and pose an even greater threat to vulnerable patient populations such as the elderly.
According to a review by Dayan et al 2021, “Federated Learning is a method used to train AI models on disparate data sources, without the data being transported or exposed outside their original location.”
Also, in the Dayan et al. 2021 review a client-server technique is discussed.
“The client-server sends an ‘untrained’ model to other servers (‘nodes’) that conduct partial training tasks, in turn sending the results back to be merged in the central (‘federated’) server. This is conducted as an iterative process until training is complete.”
In these cases, only the model weights and gradients are communicated between client sites and federated servers.
3: Are there any ongoing efforts to establish industry-wide standards for AI and IoT integration in healthcare, and how do they impact innovation and adoption in the field?
Looking at the sector we can note two types of regulation. On one side efforts from industry participants and academia themselves and on the other side regulation by government bodies.
With regard to efforts from the industry, we can note the EQUATOR Network’s efforts in the realm of creating reporting guidelines for prediction models and algorithms.
This checklist is called TRIPOD and can be found openly via the following link: www. tripod-statement.org/resources/
With this industry tries to create a more homogenous playing field with regard to algorithms including AI and deep learning.
Regulation of AI, algorithms, and hospitalgrade medical devices are regulated by the European Union by the European Medical Agency. In the European Union all medical devices if they are to be used legally must have a so-called CE (Conformité Européenne) mark on the device or algorithm to note that it has passed certain conformity tasks.
In the United States, the FDA also regulates AI algorithms and hospital-grade IoT wearable’s under their medical device regulations.
That regulation is necessary is something everyone agrees on to maintain standards and levels because of the unique nature of medical algorithms and devices.
The following infographic from “Medical Futurist” shows that despite regulation there are now hundreds of algorithms available for medical professionals in nearly all specialties. (Figure 2)

4: Beyond diagnostics and treatment, how can AI and IoT technologies contribute to disease prevention and population health management?
The greatest opportunities for AI and IoT lies in the continuous and longitudinal assessment of real-time patient data. Combined with instantaneous alarms when
an emergency such as a heart attack or stroke does arise.
The opportunities are vast, from predicting disease events before they occur through predictive algorithms, potentially preventing an entire disease event such as a heart attack and saving enormous amounts of human suffering and monetary resources. Also, remote care for underprivileged rural area inhabitants.
In the review by Chen et al. 2023 the concept of a complete “Smart Home” for geriatric patients was discussed. The following graphic is from that review. (Figure 3)

The resulting smart home will continuously monitor the patient's health, activities, and
wellbeing, combined with alert systems to inform caregivers remotely about any emergencies or abnormalities that may occur. Lastly, the algorithms will be tailored to the specific disease cases of the patient.
This is an enormously complex topic where the industry and regulators are still seeking to catch up with the large progress enabled by technology.
5: What ethical considerations should be considered as AI and IoT technologies continue to grow, particularly when dealing with sensitive patient data and life-critical decisions?
The World Health Organization has recently published a guideline for the healthcare sector entitled “Ethics & Governance of Artificial Intelligence for Health” (www.who.int/ publications/i/item/9789240029200)
Key points discussed in this extensive guidance report are:
- Human Rights to Health
- Data protection laws and policies
- Principles for use of AI in healthcare

- Bioethics laws and policies
- Regulatory considerations
With regard to ethics, key considerations are standards for human supervision, human
warranty, and the evaluation of models by humans and clinicians. Also, the informed consent process has to be rigorously followed.
Looking at regulations many organizations are currently in the process of drafting updated guidance for these technologies in the coming years. As an industry key points will be data privacy adherence, security, and especially good clinical validation of AI models before they enter healthcare sphere.
In general we have to state that the healthcare sector as a whole is the sector which will see the most demand for jobs in the United States according to a recent McKinsey report. (Figure 4)
This report estimates that the sector will see a shortage of 3.5 million jobs in the near future mainly due to aging population demographics.
That being said the topic of AI and automated IoT sensor technology does raise the very valid point with regards to the job security of individual jobs. Especially if in the future it becomes the case that an AI-algorithm might be better suited at specific scenarios than human practitioners. In this case it might even become unethical to have humans doing certain tasks.
What is especially crucial to understand that physicians take more than a decade
of intense education to be trained for their roles? As a result this group might be much more difficult to re-task and retrain these professionals to take over novel roles that will be simultaneously created by the AI&IoT revolution.
Those most at risk for displacement longterm are both on the extreme specialization end. Such as specialist radiologists, pathologists, and ophthalmologists. Mostly the image-based diagnosis specialties. On the other end, much simpler healthcare professions such as those doing routine patient controls, data-entry professions and costumer services will also most certainly be automated.
What best to do in this complex case of job displacement, is to have active lifelong learning trajectories and to use these professionals as educators for future medical physicians in a university role.
7: What novel applications or emerging technologies hold the most promise for further advancing AI and IoT integration in healthcare?
With regards to IoT sensors, novel two-dimensional materials with improved flexibility, enhanced mechanical stability, high sensitivity, and excellent accuracy are already being developed and are now ready to enter the clinics.
Looking at security & privacy, blockchain cryptography, and a later stage Quantum Computing based encryption offer tantalizing
potential albeit Quantum computing is still some ways off from being deployable for these purposes. But blockchain and smart contract technology is already being deployed by various parties within the healthcare sector.

Lastly, artificial intelligence the development of enhanced computing technology either through specialized semiconductor chips, novel techniques to decrease LLM-based computing needs, and the ever-increasing total global cloud computing infrastructure makes the future of AI in general and especially in the ultracomplex healthcare sector very bright indeed. References are available at www.americanhhm.com
Simon Ferdinand Waslander is the Director of Collaboration at CureDAO, where he leverages his BSc. in Medicine from the University of Groningen and MSc. in Healthcare Innovation from Maastricht University. With a profound interest in the biomedical aspects of human longevity, Simon has made significant contributions during his tenures at BioViva, Ageless Partner, and AGI Laboratory. Currently, he specializes in fostering synergies with a diverse network of academic, private, and government contacts at CureDAO. He is also an Expert Coach for start-ups in North Netherlands through the VentureLab North start-up community.


The development of modern minimal invasive surgery began 1991 with the first minimal invasive anatomic resection in Milan. Since then, VATS has more and more become the standard for major resections of the lung. Improvement in instruments, cameras and powered devices also made more complex surgery like broncho- and angioplastic operations possible. The evolution of VATS now leads to uniportal VATS also combined with robotic devices, which makes also complex procedures in thoracic surgery doable with just a uniportal approach to the chest cavity. Also, artificial intelligence has begun to have an impact in medicine, especially in the diagnostics of diseases. This will mark a new area of possibilities.
Dr. Paul Swatek Head of the Thoracic Surgery Department of thoracic surgery Ingolstadt ClinicAt the beginning of the 20th century the german surgent Werner Körte successfully performed a lobectomy. Up to the 1980s this procedure was the standard in the treatment of not only lung cancer, but also for the management of infections and other diseases of the lung and mediastinum. Due to the development of more modern surgical instruments and the rise of laparoscopic surgery there were several surgeons seeking
for a less traumatic approach for anatomical lung resections. Improvement of technical possibilities, esp. the development of good quality cameras for laparoscopy made surgeons think outside the box. As a result, in the year 1991 Giancarlo Roviaro of Milano completed a lobectomy only using minimal invasive access to the pleural cavity. After that and due to the significant reduction of perioperative pain more and more techniques evolved. Another side effect was the reduction of the hospitalization of patients and the less morbidity associated with these techniques. So, it was no surprise that this new kind of treatment spread quickly around the world.
Pioneers in the field of minimal invasive surgery like Dr. Diego Gonzales Rivas have
always wanted to get the maximum out of this approach to the lung and mediastinum. Complex resections with reconstruction of bronchus and anastomosis of the pulmonary artery were first considered to be impossible by VATS. With the development of more specialized instruments even those complex resections became possible and also, the size of the incisions could be further reduced and the so called “needle-VATS” evolved. Reduction of the number of ports led to even more reduction of pain, leading to the first lobectomy performed via uniportal VATS in the year 2010 by Dr. Rivas. Patients leaving the hospital on the 2nd or 3rd day with hardly any pain were the result of such procedures. Since then, many thoracic surgeons adopted this uniportal techniques and it spread all over the world. Dr. Rivas and his team

revolutionized the approach not only for small tumors, but also complex resections, which has been showed by publishing the first uniportal sleeve resection in 2013. Soon, there were not only sleeve resections performed by uniportal VATS, but also other complex resections like sulcus superior tumors or resections of the chest wall as well as reconstructions of the pulmonary artery. Also new approaches to the mediastinum like the uniportal subxiphoid approach were developed, and there was not only the resection of mediastinal mass but also the treatment of lung cancer possible through this incision which is entirely avoiding the intercostal bundle and so the pain is avoided even more.
As these techniques improved and the median age of patients is rising, not only the surgeons were looking for improvement, but also the anesthesiologists were seeking to improve the outcome for the patients, so “minimal invasive anaesthesia” in form of non-intubated VATS was re-invented, after several decades of pneumologists having a similar approach, though they were limited by instruments and lack of high-definition cameras. It has been showed, that under spontaneous breathing thorascopic procedures are safely done with less complications like pneumonia and even less systemic inflammatory reaction of the body. Therefore, it is especially suitable for the elderly patient or patients with fibrosis of the lung.
From Milan's inception to a global impact: VATS becomes the gold standard for lung resections, revolutionizing thoracic surgery worldwide.
The first robotic assisted surgery on a human being took part in the year 1985 using a PUMA 200 robot arm. Since then, in the 1990ies scientists developed more specialized robotic units to fit the purpose of surgery with surgeon-controlled manipulators. This led to the approval of the DaVinci® robotic system, which is in newer Versions still in broad use today. The usage of robotic devices in thoracic surgery begun around 2008, when the first publications were done.
There are several advantages in using a robotic device in surgery, especially if there is a tight space to work within. Especially urologic procedures as the surgery of the prostate, the robotic approach is proven to have advantages. Zahid et all showed in a recent publication advantages like shorter length of stay and less complications when operative procedures are done by robotic systems. Based on this, robotic platforms became also used in thoracic surgery. By using robotic systems, the limitations of minimal invasive procedures have changed,
and so has the number of operations increased. Usually, the access to the chest cavity in robotic surgery is achieved with one utilityincision, one camera-port and two further access points for instruments.

New companies like Avateramedical, the Versius robotic system by CMS and many more systems are now entering the market for robotic surgery. This will hopefully lower the prices of such systems, making them more accessible for lower volume centers and also for developing countries. Advantages of such systems are the nearly perfect 3-dimensional view, the reduction of tremor as well as the precision in working with them. Especially the training with such devices will be different and challenging in the future, as there are many different interfaces to be dealt with.
In recent years, the group of Diego Gonzales Rivas together with Dr. Mugurel Bosînceanu combined the uniportal approach with the usage of robotic surgery. After the first successful uniportal RATS in September 2021 there were several more performed by this team as they published in 2023. Due to the experience and the setup even more complex cases have been performed, such like sleeveresections an also angioplastic procedures by just gaining accsess to the chest by a single 3 to 4 centimeter small incision. The big advantage of this method is the excellent view of structures through the 3 dimensional device which is
presenting perfect view to the surgeon’s eye. Another advantage of using the robot is to improve the possibilities of movement of the used devices.
This allows a much more precise way of performing the operation compared to the stable instruments for conventional uVATS, though they might be bend for better usage.
Some centers, like the Shanghai Pulmonary Hospital, also use a Bi-portal approach for thoracic robotic surgery (B-RATS). It has been too short of a time to compare the oncological outcomes of these two methods, but first results in short term follow up show equal results in both techniques. Long term comparison of course is missing, but it is a promising way to go.
In 2023, Dr. Rivas and Dr. Zardo of the Hannover Medical School successfully performed the first ever non-intubated uniportal RATS, which is a great achievement in combining these two very modern techniques. But there is the need for new protocols in thoracic surgery to be able to implant these pioneer steps in the daily use of surgeons around the world.
Current improvement in the systems, more surgeons taking part in advanced robotic or VATS surgery will develop these techniques even more. Nowadays there are new robotic platforms available and existing ones are further developed an are currently entering the market such as the DaVinci SP®, which provides kind of a uniportal design with even more flexible arms. It is to be expected that with the increase of robotic surgeries performed the limits will be further bent. Also, other robotic systems like the vicarioussurgical-system® will enter the market, with smaller access to the bodies cavities and more degrees of freedom of movement.
With the development of artificial intelligence nowadays there is a lot of room for improvement in the treatment of a patient. There are several publications that already show the capability of AI in diagnostics. But not only in diagnostic is the AI of advantage. Also, during operations, the monitoring of the patient could be improved, and therefore the safety of anesthesiology during the procedure. By using AI in the analyzation of surgical procedures it is also to be expected to further improve the safety of the patient and the capabilities of the surgeons. As in any field, a thorough analysis of errors will lead to better quality.
The use of modern technologies like robot platforms as well as the ability of minimal invasive surgeons will definitely improve the
way patients will be treated in the future. Artificial intelligence as well as machine learning will have a huge impact in medicine as well. First steps of implementing AI in diagnostic pathways have already been set with promising outcome. Therefore, it is to be expected, that the early diagnostics of not only lung cancer, but also other entities will significantly improve over the next decade. There will be a shift in diagnostics towards early-stage cancer and more people will be suitable for surgery.
Dr. Paul Swatek is currently working as a Head of the Thoracic Surgery, Department of thoracic surgery, Ingolstadt Clinic, he has completed his studies at the Medical University of Graz, where he focused on thoracic surgery and obtained his degree. Following his academic journey, he gained extensive experience as a consultant in the field. Eventually, he took over the leadership of the Department of Thoracic Surgery at the Ingolstadt Clinic in Germany. His expertise lies in performing oncological resections and employing a minimally invasive approach to thoracic surgery, utilizing the uniportal approach.


As most inpatient revenue is dependent on Diagnosis Related Group payment, cost reduction is necessary to protect margins. This study examines the impact on inpatient reference test order spend when an efficient formulary, including reference test identification, relative cost, and turnaround time is embedded within an electronic order entry system.
Andrew Fletcher Medical Director of Laboratory Stewardship, Accumen and Founder of Eutilogic ConsultingOver the past few decades there has been enormous growth in healthcare expenditure in the United States. Furthermore, healthcare spending is projected to grow at an average rate of 5.8% per year and by 2024 will comprise 20.1% of gross domestic product. Due to the overwhelming costs attributable to healthcare delivery, payers ranging from Medicare and Medicaid to private health insurance companies are rapidly moving to
pay for performance reimbursement strategies such as the Medicare Shared Savings Plan, Medicare Access & CHIP Reauthorization Act (MACRA), and other value-based payment models. Given these challenges, it is essential for healthcare systems to reduce unnecessary expenditures and maximize quality and value. Within this context, effective laboratory utilization is critical as laboratory testing is the single highest-volume medical activity. An estimated 13 billion tests are performed in the United States each year. In addition, approximately 70% of downstream medical decisions are based on laboratory results.
Laboratory testing is not typically associated with adverse events, but significant patient harm can occur if errors are made. The three most common causes of patient harm are ordering the wrong test, failure to retrieve test results, and misinterpreting a test result. Studies have also shown that 10-30% of laboratory tests are unnecessary or inappropriate and 5% of genetic tests are frank medical errors. For these reasons, there is a great deal of interest in developing techniques and strategies to ensure appropriate laboratory utilization.
Several articles describe examples of successful laboratory utilization strategies, including the creation of multidisciplinary formulary committees and implementation of electronic laboratory utilization management systems. The move toward creation of laboratory formularies is logical given exponential growth in diagnostic test
development. By one estimate approximately 8-10 new genetic tests enter the healthcare market daily. With the expanding list of available tests, laboratory formularies provide guidance in appropriate test selection ensuring quality and value.
While creating a laboratory formulary via a multidisciplinary utilization committee and integrating utilization management into an electronic order entry system serves as a strong basis for laboratory utilization efforts, little has been published on the impact when information such as identification of reference tests (versus testing performed in house), approximate cost, and estimated turn-around time (TAT) are provided to clinicians within a provider order entry (POE) system.
This paper examines the financial impact of a laboratory formulary created at a regional tertiary hospital with 400-500 beds. The test formulary was embedded as a test menu –including identification of reference tests, approximate cost, and TAT estimates – in the inpatient physician order entry system. The focus of this paper is to examine the impact on test ordering patterns when identification of reference tests, approximate cost and TAT is embedded into the test names within a formulary in an inpatient POE system.
The hospital in this study is a non-profit, 400-500 bed, level 1 trauma center on the
east coast of the United States, serving multiple surrounding rural counties. In addition, this hospital serves as a teaching hospital affiliated with a nearby university. During the one-year timeframe of this study, the hospital had approximately 24,600 inpatient discharges, approximately 265,000 outpatient visits, and the laboratory performed approximately 1,430,000 billable tests (combined in house and reference tests).
Prior to this study, the Medical Executive Committee of the study facility established a multidisciplinary Laboratory Utilization Committee chaired by a Pathologist with ad hoc members including department chairs of internal medicine and various subspecialties (oncology, infectious diseases, pediatrics, and gastroenterology). Key activities included consolidation of reference testing from multiple reference labs to a primary reference laboratory and reduction of redundant in-house tests.
In several instances, it was determined that the recent electronic medical record implementation had contributed to poor test utilization. For example, some tests were routed to the incorrect performing reference laboratory due to mismatched test codes, test naming conventions were non-standardized leading to ordering confusion, and to rapidly deploy order sets within the new order entry system not all order sets were reviewed by the laboratory to ensure appropriateness. Physicians were also encouraged to save preferential orders
within the order entry system as “Physician Favorites” or “Preference Items” without secondary review.
Within the first-year, significant cost savings were achieved by laboratory utilization efforts – primarily through consolidation of reference testing to a single primary reference lab where possible, addressing the need for laboratory order-set review, and monitoring of physician favorites. Over this period of initial improvement, the actual volume of reference testing had not been reduced and volumes were still higher than prior to the transition to the order entry system. For these reasons, the committee decided to next attempt the creation of an inpatient reference test formulary.
When originally implemented, the inpatient order entry system laboratory menu was populated with 847 reference tests. Many were built as orderable for no other reason as they had been previously built in the laboratory information system. As a starting point for the draft formulary, the volume of reference testing over the preceding 12-month period was reviewed and reference tests with fewer than four tests ordered were excluded from the menu (approximately 400 unique tests). Select problematic tests ordered more than four times per year (Folate Red Blood Cell, Methylenetetrahydrofolate Reductase, 1, 25-Dihydoxy Vitamin D, etc.) and other tests
determined by the committee members as likely being non-contributory to inpatient care were also excluded. Upon completion, the revised test menu in the order entry system decreased
from 847 reference tests to 176 tests. Of note, while 671 tests had been eliminated, clinicians were still able to order “non-formulary” tests by free texting a special lab request to the laboratory with a brief explanation justifying the request.
During the process of creating the formulary, members of the multidisciplinary committee voiced concern over the inability of ordering physicians to readily determine which tests represented reference tests versus in-house tests, lack of knowledge regarding cost, and absence of TAT information. By adding TAT data it was proposed that inpatient test ordering decisions might be impacted by whether results would be available during a patient’s hospital admission versus postdischarge. While the physicians voiced interest in knowing this information, there was also great concern about the possible impact of including additional clinical decision support
in the order entry system that may contribute to “pop-up” fatigue.
Based on these recommendations, the utilization committee elected to embed reference test identification, relative cost, and approximate TAT directly into the test name within the order entry system for all reference tests on the formulary. For example, “Homocysteine” became “Homocysteine (REF, $$, 3d)” wherein “REF” identified the test as a reference test, each “$” sign represented $50 cost increments based on institutional costing tool data, and “3d” represented an approximate three-day TAT.
Much discussion centered on the appropriate format of cost data within the test menu. Initial consideration was given to providing exact reference laboratory cost or patient charge but maintaining accurate pricing presented challenges given fluctuations in test cost over time. Also, secondary to wide variation in payer reimbursement (Medicare vs private insurance vs self-pay) determining potential out of pocket expense for patients was not feasible. Instead, by using “$” signs in $50 increments based on data from the institutional costing tool, a practical sense of relative cost scale was imparted rather than contending with possible pitfalls associated with providing the precise reimbursement or cost.
In summary, the formulary consisting of 176 reference tests (instead of 847) with embedded reference test identification and TAT became the list of orderable reference tests in the inpatient order entry system.
Critical cost reduction measures are vital to safeguarding inpatient revenue and maintaining sustainable margins within the healthcare system.
Reference test invoices from the primary reference laboratory were reviewed for the 12-month period prior to the revised formulary incorporation within the order entry system as were invoices from the 12-month period following implementation. Specifically, invoices were reviewed by hospital financial analysts to identify inpatient test cost, specifically excluding outpatient cost (not impacted by the changes made within the inpatient order entry system).
As demonstrated in Table 1, during the 12 months following the implementation of the lab formulary with reference test identification, relative cost, and TAT on all 176 reference tests, average inpatient reference costs per month decreased by 35% as compared to the average monthly cost calculated from the 12 months prior to implementation. This represents an average monthly savings of $11,026 with a projected yearly cost saving of $132,309. (Table 1)
While implementation of the inpatient reference test formulary reduced the average monthly inpatient reference spend by 35%
during the study timeframe, average monthly inpatient admissions decreased by 5.1% and the case mix index (CMI) increased from 1.42 to 1.47 (3.5% increase). The precise impact of the small decline in admissions on inpatient reference test ordering is uncertain in the face of slightly increasing CMI, but the net result is unlikely to fully account for the overall 35% reduction in average monthly inpatient reference spend.
During the study timeframe, no other educational activities were employed to address misordered reference tests and the number of active medical staff at the study hospital remained relatively static. Therefore, the cost reduction does not appear related to a decrease in medical staff or possible turnover of high-volume ordering physicians.
In summary, the 35% decrease in monthly average reference lab cost appears to be the result of the formulary based upon removing tests ordered less than four times per year, elimination of tests not likely to contribute to inpatient care, and embedding identification of reference test, relative cost, and TAT in the order entry system.
No formal process was employed to assess medical staff response to implementation of the formulary but inquiries at various
medical staff functions and committees were unanimously positive. Members of the medical staff voiced greater satisfaction due to streamlining of previously lengthy menus presenting numerous similar and generally unneeded tests. Staff comments also centered on appreciation for the identification of reference tests as most had little to no awareness of tests performed in house versus reference testing. Several providers voiced specific examples where test selection for specific patients was guided by comparing TAT to identify optimal inpatient diagnostic strategy. One factor that may have contributed to the overall level of physician support was the creation of the formulary based on the input of various members of the medical staff on the utilization committee and inclusion of their suggestions. In this regard, the formulary was more an example of physician engagement than strictly a cost-cutting tool.
The results demonstrate the benefit of creating an efficient inpatient reference test formulary that includes reference test identification, relative cost, and TAT data. Developing a laboratory formulary with an emphasis on removing infrequently ordered tests, deleting commonly misordered tests, and embedding reference test identification, cost, and TAT, decreases inpatient reference test spend. With more efficient test ordering, the downstream impact on medical decisions,
while difficult to measure directly, likely generates exponential savings beyond that achieved for the laboratory budget alone. As healthcare systems face the challenge of transitioning to value-based payment models, optimal laboratory utilization strategies are critical to delivering high quality care while containing the growing costs attributable to healthcare in the United States.
expenses.

Artificial Intelligence is rapidly transforming healthcare. From tentative footholds in radiology and clinical laboratories, it is blossoming from a diagnostic tool to a generative prodigy that will soon surpass human expertise leading to better control and management of chronic disease, the root cause of all acute diseases, to their cure.
James Doulgeris Chairman, Population Health Advisory Board, RSDSA
1. How would you describe the role of artificial intelligence (AI) in the field of digital health, and what potential benefits does it offer to patients and healthcare providers?
Artificial Intelligence (AI) is rapidly transforming the practice of healthcare. From tentative footholds in radiology and clinical laboratories, it is blossoming into an essential diagnostic tool that is tireless, flawless in its detailed examinations and performs it all with impressive speed and fidelity.
For now, it is also only as good as its programmers, relying on humans for insight, performing the routine work and leaving the thinking to people. As AI evolves and learns, it will soon surpass human expertise leading to better control of chronic disease, the number one cost and killer to earlier diagnoses and cures for everything from viruses like COVID to cancers.
Here are the key areas where AI has made significant contributions in today’s healthcare landscape:
1. Disease Detection and Diagnosis: AI algorithms can process and interpret medical imaging at a speed and accuracy level that exceeds human capability leading to earlier and more accurate diagnosis of conditions ranging from cancers to cardiovascular diseases. With virtually every disease state, early diagnosis is the key to a successful cure.
2. Predictive Analytics: AI can analyze numerous data points from a patient's medical history, genetic information, and lifestyle habits, called social determinants of health, to predict the risk of chronic disease leading to acute events and allow for early intervention. This capability impacts a range of areas to improve health status from long term chronic conditions to avoiding hospital readmissions.
3. Treatment Personalization: AI has become an essential tool to develop personalized treatment plans in an area called pharmacogenomics, which is the study of how genetic makeup can affect one’s response to drugs by considering a patient’s medical history, genetics, and
lifestyle. Also called precision medicine, pharmacogenomics can dramatically improve the efficacy of treatments and reduce sideeffects tailored to each individual.
4. Drug Discovery: AI can expedite the process of drug discovery and clinical testing by predicting how different chemical compounds interact. As AI moves into generative stages (self-learning), the development of new treatments for a multitude of conditions can be accelerated by years.
5. Population Health: AI has made managing health status and trends from an individual to a population basis possible. By gathering patient data in electronic medical records to create single page patient overviews for primary care physicians, AI has moved the physician relationship from the exam room laptop to the patient by summarizing everything from diagnostic testing to vital sign trends. On a population health basis, by managing big data, AI provides tools to manage chronic disease on large scales to identify comorbidities associated with primary disease states from rare diseases to diabetes, kidney disease and cancer to name a few.
6. Risk Identification and Management: As a general rule, fifty percent of the cost of healthcare is created by five percent of the patients. All of these patients are in an acute stage of illness. It is also true that under the age of 65, over 75% of the cost is caused by chronic disease and over 65 the cost raises to over 95%. There are three stages of health status – episodic, chronic, and acute. Episodic conditions are
events like injuries that will heal with little or no lasting effect. Chronic diseases need to be managed to be slowed, stopped, or reversed so that they do not progress to an acute stage. Using AI to assess risk to identify patients in the 75th to 95th percentile, or those who will move to the 95th to 100th percentile that consumes 50% of our costs is the key to population health management. While we are putting things in terms of cost, we are really talking in terms of managing the health status of people – meaning their quality of life, their life span, their time with their families. Integrating new information datasets such as social determinants of health (like socioeconomic status, education level, physical
environment) in their risk predictions and treatment recommendations can enhance the effectiveness of chronic disease management while leading to more holistic and equitable healthcare.
7. Administrative Tasks and Data Accuracy: AI can do more than assist with administrative and clinical record-keeping tasks such as scheduling appointments, billing, and patient records management, it can perform them virtually autonomously allowing healthcare staff to focus on patient care while minimizing human error. Taking human error out of practice and hospital operations is not just an administrative matter of efficiency, it is a critical component to ensuring the quality of data entering population

health systems is accurate. Poor data leads to poor information. Poor information leads to improper actionable information, which can and does have a negative impact on patient care and outcomes.
8. Telemedicine: AI literally makes telemedicine possible because of the shortage of clinical personnel and the preference of the younger generation to interact virtually whenever possible. Chatbots and virtual health assistants can provide 24/7 support, answering patient inquiries, and accurate and essential triage ensuring available clinical personnel are treating cases best managed by human intervention. Again, with generative AI, as these systems learn, they will be able to manage more and more satisfying the needs and wants of the emerging patient base as it ages into the system.
9. Mental Health: AI tools like chatbots already offer psychological support and interventions, supplementing traditional mental health care services and serving to triage acute cases to human intervention.
10. Remote Monitoring and Wearables: AI is used in devices that monitor vital signs, physical activity, fall monitoring and emergency alerts, sleep patterns, glucose levels, oxygen levels and much more are commonplace. Many of us use them without even thinking about their function in the form of smart watches. Wearables and remote monitoring devices already play an important role in alerting emergency services of acute events from heart attacks to falls. If a patient does not cancel the
alarm, help will be on the way, an essential when time is literally a matter of life and death.
2. What are some key applications of AI in digital health that have improved healthcare outcomes?
Here are some specific examples where AI has been employed to make a significant improvement in healthcare:
1. Medical Imaging and Diagnosis: Google's DeepMind is an AI system that can diagnose eye diseases as precisely as the best ophthalmologists. Zebra Medical Vision reads medical imaging such as X-rays, CT scans and MRI scans to detect a range of conditions autonomously efficiently, accurately and rapidly.
2. Predictive Analytics: AI systems can examine patient data from everything from wearables to hospital monitors in real-time to predict potential health crises before they happen. For instance, Google's DeepMind can predict an acute kidney event up to 48 hours before it happens, providing doctors with a valuable window to intervene and save lives.
3. Precision Medicine: Tempus uses AI to treat cancer using pharmacogenetics and by analyzing clinical and molecular data. This allows physicians to make real-time, datadriven decisions, improving outcomes.
4. Drug Discovery: Atomwise uses AI to predict molecular combinations that are most likely to have a desirable therapeutic effect for specific disease states, significantly speeding up the process of drug discovery, speeding
the research and development stage for new drugs substantially.
5. Mental Health Support: AI chatbots like Woebot provide psychological support helping patients to manage their mental health. While not a replacement for professional help, these tools support traditional therapy by providing immediate help whenever it is needed.
6.Remote Patient Monitoring: The IWatch continues to make impressive strides by measuring oxygen levels, detecting atrial fibrillation, sleep disorders, falls with automatic calls for emergency help and soon, glucose levels for diabetics in real time. It also provides a wide range of other health and fitness metrics when paired with the iPhone health app.
New applications are coming online, particularly those using generative AI in a disease, diagnostic and individualized class basis quickly becoming more effective the more they are used, promise to revolutionize healthcare in ways that we have yet to appreciate.
3. How do you ensure the ethical use of AI in digital health, particularly in terms of patient privacy, data security, and algorithm transparency?
Ensuring the ethical use of AI in digital health is crucial to maintain trust and protect the interests of patients. This has always been a dilemma with healthcare analytics and using healthcare data, particularly big data. The more data there is available, the better the
systems work. Deidentification is not hard to accomplish. On the other hand, deidentifying patients denies them the benefits of early diagnosis of diseases that could be life altering or threating. Finding a balance is challenging. Nonetheless, here are some measures that can help:
1. Patient Privacy and Consent: Patient privacy laws like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. or the General Data Protection Regulation (GDPR) in the EU provide protection at the expense of a massive, and expensive bureaucracy. Deidentification and informed consent combined with what the data will be used for provides the belt and suspenders underpinning patient privacy.
2. Data Security: High level cybersecurity is essential. Regular security audits, vulnerability assessments, and the use of encryption can help ensure data is kept safe.
3. Algorithmic Transparency: To mitigate issues related to equity, bias and fairness, there should be reasonable transparency about how algorithms work and make decisions.
4. Validation and Testing: AI systems should undergo rigorous testing and validation before they are deployed and be continuously monitored post-deployment as well.
5. Accountability: It is essential that a chain of accountability within each organization be in place so that when things go wrong, they can be addressed promptly and by qualified personnel.
6. Inclusivity and Fairness: The data used to
Intelligence
Digital Health
the future of healthcare, unleashing a new era of precision medicine and patient-centric care.
train AI systems should be obtained from a standardized data set to ensure they are representative of diverse populations to avoid bias in predictions and recommendations.
4. Can you share specific examples of AI-driven technologies or solutions that have had a significant impact on patient care and health management?
AI has had its greatest impact in diagnostics, particularly for radiology and ophthalmology:
1. Aidoc analyzes CT scans to identify acute abnormalities such as strokes, pulmonary embolisms, and cervical spine fractures.
2. Zebra Medical Vision reads and analyzes X-rays, CT scans, and MRI scans serving to detect a wide range of cancers, cardiovascular conditions, liver diseases, and related conditions earlier than traditional radiology substantially improving outcomes.
3. Google's DeepMind worked with Moorfield’s Eye Hospital to develop an AI system that can diagnose eye diseases with a rate of accuracy equal to or exceeding the best ophthalmologists leading to earlier diagnosis and improved outcomes.
4.AliveCor's KardiaMobile, pairs with a smartphone to detect atrial fibrillation, a common heart rhythm disorder that if left untreated, can lead to serious health issues like stroke. iPhone pairs with iWatch to perform the same function.
5. Butterfly Network's Butterfly iQ is a handheld ultrasound device connected to a smartphone to capture and analyze ultrasound images enabling point-of-care ultrasound imaging, making medical imaging more accessible and convenient.
6. Tempus analyzes clinical and molecular data to help physicians make real-time, data-driven cancer care decisions. Their work in genomics and precision medicine has been transformative in providing personalized treatment plans for cancer patients.
7. IBM Watson Health for Oncology uses AI to analyze a patient’s medical information and offers evidence-based treatment options. It helps doctors make more informed decisions about patient care.
5. What challenges or barriers exist in the integration of AI into digital health systems, and how do you address them to ensure successful implementation?
The dynamic duo of Artificial
and
is reshaping
AI in healthcare has a set of challenges that must be overcome. Here are my top six areas that give me the most concern:

1.Data Privacy and Security: Stringent privacy laws hurt as much as they help. A lot of work must be done for laws to catch up with technology to make the two work effectively together. This is a big ask because the knowledge gap between legislators and technology companies is broad and widening by the day.
2. Data Quality and Interoperability: Inconsistent or incomplete data can reduce the accuracy of AI systems. The human factor is a systemic and continuing concern, and it is not going away anytime soon. The newer generations moving into the workforce do not have the same work ethic and training to maintain consistency and accuracy as the generation leaving the workforce. This is a societal issue that, ironically, AI must be used to
overcome. Moreover, different healthcare systems and vendors often use different formats or standards for their data, making interoperability a significant challenge. This is where legislation lags behind reality. Requirements for standardization have been put in place but are not enforced. It is time for the public and private sectors to get on the same page for the public good.
3. Lack of Understanding and Trust: Many healthcare providers may not understand AI well enough to trust its use in patient care, and their concerns are not unfounded. If AI makes a mistake, it could potentially lead to patient harm. Healthcare providers are data driven and cost benefit studies are required to illustrate the overall benefits of AI usage versus delaying usage. Delaying progress to achieve perfection is a very expensive undertaking.
4. Regulatory Challenges: Particularly in the United States, federal regulation and
state regulation are at odds with voids and considerable inconsistencies. Again, everyone must get on the same page for the public good.
5. Ethical and Bias Issues: Using broad databases representing a true public model without political or assumed bias in a standardized model for all AI training will ensure that everyone is working from reality instead of a politicized construct. This is easier said than done. It will take considerable leadership and political will to get this right.
6. Technical Infrastructure: Healthcare providers need a strong technical infrastructure to implement AI. Not all healthcare systems may have the necessary hardware, software, and technical expertise. Using the cloud as a common system is an obvious solution, however, it also has a glaring vulnerability because it represents a singular, very large target.
6. How do you strike a balance between the use of AI and the human touch in healthcare delivery, and how does this impact patient experiences and outcomes?
There is no reason to strike a balance between using AI and the human touch in healthcare delivery because AI is a tool to enhance the quality, efficiency, and effectiveness of patient care, not a replacement for it.
When I was at Osler Health, we did a study comparing over 10,000 patients who received only physical therapy for chronic back pain and an equal number of patients who received
only chiropractic care. Surprisingly for us, the patients receiving chiropractic care cost over $2,000 per year each less than those receiving traditional physical therapy at a savings of over $20 million dollars per year.
Upon further investigation, the patients were happier, healthier and reported lower pain levels. What made the difference according to patients? Physical therapy, while it delivered results, was work, it was painful, it was demanding. Chiropractic on the other hand did not necessarily deliver the same clinical results, but it was nurturing, caring and made them feel better overall.
Similarly, AI while can provide extraordinary efficiency, precision, and access to new forms of treatment it cannot replace the empathy, understanding, and human touch and connection that a human healthcare provider can offer.
Simply, good news or bad news, it is also all about faith in the caregiver, not the machine assisting the caregiver regardless of how smart, advanced or competent it is. AI cannot hold a patient’s hand, reassure them or give them a hug.
7. What are the most promising areas or domains within digital health where AI can make a transformative impact in the near future?
Artificial intelligence has a singular advantage over human intelligence – the ability to process massive amounts of data and transform it
into understandable and often actionable information.
The advent of generative AI, or artificial intelligence that improves itself autonomously, is going to be the game changer going forward.
This is a generation beyond machine learning and a step into cognitive intelligence where decisions cease to be made by algorithms and begin to be made using applied experience, intuitive pattern recognition and sentient intuition. The most important aspect of this newfound capability would be curiosity and independently taking the initiative to satisfy it.
A good example would be taking a large dataset of emergency room visits and wondering why some areas are higher than others. Then taking the initiative to regionalize the higher areas, match them to physician practices and having the intuition to visit practice websites to determine if the practices closed for lunch, were available for off hours call and comparing them statistically to practices where emergency room visits were lower.
This would be a daunting task for an analytic staff, if the staff were available for a weekslong study despite the millions of dollars that could be saved and pressure removed from hospital emergency rooms, a reward of tens of thousands of dollars for every dollar spent on the study.
For an advanced AI system, the study would happen automatically with a full report and detailed actionable plan distributed to management in the time it would take for
management to pose the question.
And, this one simple intuitive spark, one of so many they would have to be prioritized by the level of impact to avoid overwhelming the human side of the system, would materially improve patient safety, services, efficiency, effectiveness, and cost in both hospitals and practices alike.
The same impact on the clinical side of healthcare benefiting hand in hand with infrastructure improvements would not just be transformative, it would be revolutionary.
The inherent bias of politics, special interests, unions, medical specialties, local, state and federal governments and bureaucracies and all other stakeholders must agree to stand aside and allow a complete dataset representing the entire population as it is be the baseline dataset.
These facts will be our friends and a robust AI system will be the tool to provide actionable information and a plan to improve upon them.
9. How does AI contribute to personalized medicine and
treatment plans in the context of digital health, and what challenges do you face in implementing this approach?
Presently, AI is a great tool for physicians and
8. How do you ensure that AI algorithms and models used in digital health are accurate, reliable, and free from bias, to prevent potential harm to patients?
individualized
other healthcare professionals. In the near future, it will be a brilliant collaborator that provides unparalleled insight while physicians interpret and communicate on a human to human basis.
10. How do you involve healthcare professionals and patients in the development and evaluation of AI-based digital health solutions to ensure user-centered design and usability?
I have a hard and fast rule before implementing new systemic programs: collaborate twice with three separate groups then program once. Field test, adjust. Repeat. Repeat then repeat again until every group in every region is reasonably satisfied.
I also have one other rule – never let perfection stand in the way of progress. Set a reasonable timeline and stick to it.
11. Can you discuss the role of AI in predictive analytics and early detection of diseases in digital health, and how it can contribute to preventive healthcare?
Predictive analytics are all about preventative care, whether they are employed for risk management or used in a diagnostic setting to detect disease in a lab or imaging study. The smarter AI becomes, the more accurate and complete the instructions, information and directions will be to the healthcare provider.
12. Looking ahead, what future trends or advancements do you anticipate in the intersection of AI and digital health, and how do you plan to stay at the forefront of these developments?
Staying at the forefront of any technology is a matter of planning, prioritizing and deployable resources.
The field is racing forward so quickly in so many ways and areas, it is not so much what to keep up with but what is most needed and what providers can most afford.
Other considerations are hardware, how to pay for it and where to put it if systems are not cloud based and, if they are, how to securely move all those masses of data securely in limited bandwidth. Then there are added operating costs from energy to debt service.
Analytic systems can and should make up their cost with savings, but in a hospital system, for example, cannibalizing revenues to share savings can and usually is a losing proposition, and a big one if it is done in a big way. The hospital world is still a fee for service world.
Since medically retiring after 35 years in CEO roles in hospitals and value-based care providers, James Doulgeris stays active by advising healthcare companies and systems in the AI and analytics spaces, and as a healthcare journalist and novelist. He also volunteers to develop analytic tools to create actionable information to improve care and treatments for the rare disease community.

Advances in biostatistics and computing have led to the creation of novel types of machine learning algorithms for clinical outcome prediction models. Three clinically and statistically robust models include artificial neural networks, fuzzy logic and bayesian analysis. These techniques complement classical approaches of regression analysis and decision tree analysis. This editorial explains the novel outcome prediction system using Bayesian neural networks with fuzzy logic. This novel approach can be practically applied to both clinical and non-clinical settings.
Benjamin W. Y. Lo MD, Department of Neurological Surgery, Lenox Hill HospitalBayesian analysis enables incorporation of new data with existing knowledge. Based on this knowledge, the researcher expresses the
degree of belief about a certain parameter in the form of a prior probability distribution. The normal bell-shaped distribution is an example of a probability distribution. This prior probability distribution is then combined with its likelihood of occurrence, forming a posterior probability distribution (posterior probability = prior probability X likelihood).

The end result of Bayesian analysis is the formation of a posterior probability distribution (Figure 1). It represents a revised or updated belief after taking new data into account. If there is lack of existing knowledge on the subject of interest, the researcher can still use Bayesian techniques. Here, the researcher is encouraged to use vague or uninformed prior probabilities.
Artificial neural networks mimic biological neural systems. In biological systems, incoming dendrites collect signals which

feed to the neuron (Figure 2). An electrical signal propagates along the axon with neurotransmitter discharge at the synapse. Examples of biological neural networks include the human brain and retina.
In artificial neural networks,input variables converge on a number of nodes. Nodes are grouped into layers. Layers are linked to each other via interconnection links. Between input and output layers, there can exist one or two hidden layers (Figure 3). Latent variables make up the hidden layer(s). In order to advance from one layer to the next, signals are processed via activation functions.
Artificial neural networks assume all or none logic. In the case of clinical outcome prediction, subjects are classified as having good or bad
prognosis. Within each layer, nodes in the artificial neural network are connected with each other via connection links. Activation functions and associated weights are applied to these connection links. Artificial neural networks are intelligent systems that can learn and change behaviour by themselves as they gain experience. They also take into account latent variables or unobserved variables. These variables are not directly measured or accounted for during the design of the artificial neural network.

Fuzzy logic allows for uncertainty in disease diagnosis and prognosis. Fuzzy logic functions can carry any value from 0 to 1 (Figure 4). It, therefore, recognizes grey zones in diagnosis and prognosis, and registers diseases along a severity spectrum from mild to severe. One of the advantages

of fuzzy logic is its explicit knowledge representation. The individual using fuzzy logic can:
1. specify inputs, control actions and outputs, and
2. clarify, or defuzzify, the entire process by adding crisp control actions, such as cutoff levels for diagnoses and prognoses, as well as trigger threshold levels for treatment.
By doing do, all actions in fuzzy logic can be accounted for (process of verification). Optimization is also achievable to create efficient fuzzy logic systems. Unlike artificial neural networks where learning is done by the networks themselves as they gain experience from datasets, fuzzy logic systems cannot train themselves. The designer derives all action commands manually in the form of “if-then” rules. The final fuzzy logic system can be represented in various ways, including equation or conceptual diagram formats.
A multilayer perceptron artificial neural networks model is illustrated in Figure 5, where the output as follows:

In the Bayesian approach to artificial neural networks, the goal is to find the predictive distribution for target values in the new test case/model, given inputs for that case and inputs/targets in training cases. Here, the probability of data according to a particular model is an integral, representing the summation of all possible parameter values weighted by the strength of belief (as assigned by the researcher) in these parameter values. In a Bayesian neural network, the posterior probability density is proportional to the product of prior probability density and its associated likelihood, where the likelihood is the product of probabilities of data given parameters (weights and biases).

Principles of fuzzy logic, as discussed above, can then be applied to Bayesian neural networks. Here, all actions (verification) in fuzzy logic are accounted for, and optimization is achievable. Bayesian neural networks with fuzzy logic inferences can be represented as follows:
Expected outcome of function (fuzzyBayesian neural network)
= defuzzification technique applied to a Bayesian neural network where defuzz can be max-min, centroid, left of mean, right of mean, or another defuzzification crisp control action rule.
Bayesian neural networks with fuzzy logic inferences can be applied to both clinical and non-clinical systems. In clinical outcome prediction using high dimensional data, Bayesian neural networks can be conceptually summarized as follows: Based on one’s own experience, one can specify (fuzzy logic) where along a spectrum of probabilities (provided by the Bayesian neural networks) the outcome lies. If the outcome falls outside the spectrum in real case scenario, the researcher is then encouraged to investigate unknown elements (latent variables) influencing the outcome variable in question.
Bayesian neural networks with fuzzy logic can be applied to both clinical and non-clinical settings. In clinical outcome prediction, it makes use
of existing knowledge, recognizes unknown areas, incorporates one’s clinical reasoning and experience, as well as compensates for uncertainty in prognostication.
Illustrations are provided by medical illustrator, Aurora W.M. Lo, B.Com (Toronto) CPA (Illinois).
and
His
focus is cerebrovascular disorders. His research focus characterizes brainbody interactions in Neurocritical care patients with cerebrovascular disorders. Dr. Lo’s qualifications include FRCSC certification in Neurosurgery (2009), FRCSC certification in critical care medicine (2011), and MSc and PhD degrees in clinical epidemiology and biostatistics from McMaster University, Canada. His clinical experience includes working as a neurosurgeon and neuroICU specialist at St. Michael’s Hospital, University of Toronto; Montreal Neurological Institute & Hospital, McGill University; and Northwell Health Lenox Hill Hospital, Manhattan, New York.


August 11-12th, 2023
New York City, New York
About Event: MLHC is an annual research meeting that exists to bring together two usually insular disciplines: computer scientists with artificial intelligence, machine learning, and big data expertise, and clinicians/medical researchers.
https://www.mlforhc.org/
Listed Under: Information Technology
4th Edition of International Precision Medicine Conference
August 17-19, 2023
Online Event
About Event: Precision medicine is a brand-new approach to illness treatment and prevention. Precision medicine strives to establish a personalized and unique treatment and preventative regimen for each patient based on their entire medical profile, including genetic data, medical history, environmental factors, and even lifestyle. The design of a one-of-a-kind treatment necessitates access to almost all of an individual's specific medical data.
https://precision-medicine.magnusconferences. com/index.php
Listed Under: Medical Sciences
August 25-28, 2023
Amsterdam - Netherlands
About Event: SC Congress you will have the opportunity to connect, gain new perspectives, and create synergies with the global cardiology community. It really is four days that matter. Wherever you are in the world, whatever your role in supporting patients that face cardiovascular disease, we hope you will join forces with us in Amsterdam, or online. Together we can make a difference.
https://www.escardio.org/Congresses-Events/ESCCongress

Listed Under: Medical Sciences
September 04, 2023
Dusseldorf, Germany
About Event: International Conference on Advanced General Surgery and Oncology Is a platform with all the field's leading scientists, outstanding researchers, academic people, and industrialists from national and international locations.
https://www.sciencecite.com/event/index. php?id=2093912
Listed Under: Surgical Specialty

September 05, 2023
Hamburg, Germany
About Event: International Conference on Neurology and Health Care ICNHC. This phenomenal event will see some of the biggest names in the world of technology and engineering uniting together on the same platform for one goal - accelerating technological development through improved learning, research propagation, skill development and networking.
https://iiter.org/conf/index.php?id=2085891#
Listed Under: Medical Sciences
September 25th-26th, 2023
Hamburg, Germany
About Event: International Congress on Neuromuscular Diseases (ICNEDI-23), will welcome leading scientists, practitioners, and academicians from the field or concerning the field on one platform. https://www.wrfconference.com/event/index. php?id=2035532
Listed Under: Medical Sciences
October 03, 2023
Hamburg, Germany
About Event: International Conference on Health Information Technology and Healthcare Efficiency is a platform with all the field's leading scientists, outstanding researchers, academic people, and industrialists from national and international locations. https://www.sciencecite.com/event/index. php?id=2094233
Listed Under: Technology, Equipment’s & Devices

13-14 September, 2023
Basel, Switzerland
About Event: Intelligent Health is THE only largescale, global summit that purely focuses on AI in healthcare and brings together the world’s brightest AI health brains from pharmaceutical, biotech, medtech, health provisions, clinicians, tech companies, startups, investment, and science to advance discussions on how to apply AI and drive technological collaboration in healthcare.
https://intelligenthealth.ai/
Listed Under: Information Technology
October 19 -21, 2023
Boston, Massachusetts, USA
About Event: The conference will enlighten the theme “BRAIN: Bolstering & Renovating Advanced techniques In Neurology” and will focus on its agenda to bring together distinguished scientists, researchers, academicians, notable neurologist, healthcare professionals, surgeons, nurses, caregivers, pharmacists, industry icons and government representatives to discuss the latest innovations, trends, and problems in the field.
https://neurologycongress.com/
Listed Under: Medical Sciences
Stryker has introduced the Ortho Q Guidance system, a cutting-edge solution that empowers surgeons to achieve advanced surgical planning and guidance during hip and knee procedures.

With convenient control accessible from the sterile field, the system integrates a redesigned, state-of-theart camera for enhanced optical tracking, coupled with sophisticated algorithms provided by the newly launched Ortho Guidance software.
This powerful combination equips surgeons with additional capabilities for surgical planning and guidance.
When utilized alongside Ortho Q, the Ortho Guidance software (specifically designed for Express Knee, Precision Knee, and Versatile Hip) acts as a comprehensive planning and intraoperative guidance system, optimizing procedural efficiency and speed through an intelligent and streamlined workflow.
The Ortho Q Guidance system encompasses notable features:

• The Implant agnostic software is compatible with various implants, enabling surgeons to utilize their preferred choice and granting facilities the flexibility to cater to diverse service line requirements within a single platform.
• Dedicated software for Triathlon implants provides surgeons with valuable clinical feedback, further enhancing their surgical experience.
• The system's compact design allows for seamless integration both in the operating room and the ambulatory surgical center (ASC) setting.

Shimadzu Medical Systems USA, a Shimadzu Corporation subsidiary, has introduced new V series Glass-Free Flat Panel Detectors (FPD) that are now compatible with its general radiography systems.
With the introduction of the Glass-Free FPDs, the company’s V series lineup is now complete, providing comprehensive support for diverse imaging needs.
Featuring an ultra-fine 99-micron small pixel pitch, these detectors excel at capturing intricate details in X-ray images.
Furthermore, their lightweight design not only reduces the physical strain on radiology technologists but also enhances durability, offering increased resilience against accidental drops. To address the healthcare worker shortage and meet the demands of medical facilities, Shimadzu is proud to introduce the V series Glass-Free Flat Panel Detectors (FPDs).
Available in three sizes (17"x17", 14"x17",and 10"x12"), these state-of-the-art detectors are compatible with its RADspeed Pro style edition V series and MobileDaRt Evolution MX8 V type systems.
By continuously enhancing our digital radiography system lineup, the company aims to provide comprehensive solutions that cater to the diverse needs of clinical environments.
Read the complete post
Read the complete post






Abbott has achieved a groundbreaking milestone with the launch of AVEIR™, the world's first dual-chamber leadless pacemaker system designed to address abnormal or slow heart rhythms.
This breakthrough device has received approval from the U.S. Food and Drug Administration, paving the way for expanded access to leadless pacing for millions of individuals across the United States. With over 80% of pacemaker recipients requiring pacing in both the right atrium and right ventricle, this innovative system revolutionizes treatment options.
The AVEIR DR pacemaker system incorporates Abbott's proprietary i2i™ communication technology, enabling synchronized or coordinated cardiac pacing between two leadless pacemakers based on each person's clinical needs.
Through the utilization of high-frequency pulses transmitted via the body's naturally conductive blood characteristics, i2i technology facilitates seamless communication between the paired, co-implanted devices.
This conductive communication is vital, as it consumes significantly less battery power compared to inductive, radio frequency, or Bluetooth® communication methods commonly used in traditional pacemakers or implantable medical devices.
With a compact size of approximately one-tenth that of a traditional pacemaker, the AVEIR DR leadless pacing system consists of two devices: the previouslyapproved AVEIR VR single chamber device for pacing the right ventricle, and the newly-approved AVEIR AR single chamber device for pacing the right atrium.
The AVEIR DR system incorporates Abbott's novel i2i technology, overcoming engineering challenges by enabling beat-to-beat communication between the two leadless pacemakers.
Clarius Mobile Health, a renowned provider of highdefinition handheld ultrasound systems, and Usono, an innovative developer of ultrasound accessories, have joined forces at the ECSS Paris 2023 congress to introduce an unprecedented wireless and wearable ultrasound imaging solution.
This groundbreaking technology caters to researchers studying human anatomy in motion.

The wearable ultrasound solution combines the Clarius HD3 high-definition wireless ultrasound scanner with research software and Usono's ProbeFix Dynamic, enabling hands-free, stable, and reproducible ultrasound imaging during exercise and other activities that involve crucial motion and continuous scanning.
This innovation marks the first wireless dynamic ultrasound imaging solution designed specifically for researchers in the fields of sports medicine, rehabilitation, and related areas.

Clarius ultrasound tools for research provide researchers with access to internally collect raw data, gyroscope collection, a programmable interface, and custom software for real-time analysis anywhere, ensuring a comprehensive and flexible research experience.
In contrast to traditional pacemakers, leadless devices are implanted directly into the heart using minimally invasive procedures, eliminating the need for cardiac leads. As a result, leadless pacemakers minimize Read the complete post
Read the complete post

potential complications associated with leads and infections, while also offering a shorter and less restrictive recovery period following implantation.

In a significant development, Dexcom, Inc. has officially announced that the next-generation Dexcom G7 Continuous Glucose Monitoring System has received approval from Health Canada.
This groundbreaking system is now available for individuals of all ages, starting from two years old, who are managing diabetes.
With over 3 million Canadians affected by the complex and burdensome condition of diabetes, the importance of managing glucose levels and making daily treatment decisions cannot be overstated.
However, the recent approval of Dexcom G7 by Health Canada brings a game-changing technology that promises to ease the management of diabetes for Canadians.
This revolutionary system has demonstrated its potential to reduce hospitalizations and emergency room visits related to hypoglycemia by an impressive 42 percent*.
By granting access to Dexcom G7, Health Canada empowers individuals with a tool that enhances their diabetes management and potentially improves their overall well-being.
Dexcom G7 revolutionizes diabetes management by offering users a powerful yet simple solution that empowers them to gain better control over their condition.
This innovative system features a low-profile, all-inone sensor and transmitter that warms up in record time, surpassing any other CGM available on the market†,5. With Dexcom G7, users can effortlessly access realtime glucose readings, which are automatically transmitted to their compatible smart device‡ or receiver, eliminating the need for routine scanning or finger pricking.
The system includes a range of customizable alerts, including predictive urgent low alerts that help prevent potentially dangerous hypoglycemic events and enable users to spend more time within their target glucose range**,2,3,4.
Dexcom G7 also facilitates seamless information sharing with family, loved ones, and healthcare teams through cutting-edge remote monitoring and reporting capabilities††, ensuring support and collaboration anytime and anywhere.

Dexcom G7 introduces a range of new features and enhancements that take diabetes management to the next level:
• Unprecedented Size: The Dexcom G7 sensor is the smallest ever, being 60% smaller than the Dexcom G6. It offers multiple approved wear locations, ensuring a comfortable and discreet experience‡‡.
• Streamlined Design: With the all-in-one sensor and transmitter, Dexcom G7 simplifies the entire CGM system, making it more user-friendly and convenient.
• Swift Sensor Warm-Up: Dexcom G7 boasts a remarkable 30-minute warm-up time, which is twice as fast as any other CGM available. This quick start allows for a seamless and hassle-free experience.
• Extended Grace Period: Users now have a generous 12-hour grace period to replace finished sensors, providing greater flexibility and convenience during transitions between sensor sessions.
• Enhanced Alert Customization: Dexcom G7 offers improved alert customization, catering to individual user needs and preferences. This allows for a more personalized and tailored experience.
• Redesigned Mobile App: The mobile app accompanying Dexcom G7 has been redesigned and simplified, providing a user-friendly interface. Integration with Dexcom Clarity§§ ensures seamless data analysis and reporting for users.
These new features and enhancements with Dexcom G7 redefine diabetes management, offering users unmatched comfort, flexibility, and control over their condition.
Read the complete post


Baxter International Inc has introduced advanced ICU bed, Hillrom Progressa+ in the United States. This new bed incorporates advanced technology and features that aim to facilitate patient care and aid in their recovery process.
The Progressa+ bed offers a range of technologies specifically designed to address pulmonary needs, ensure skin protection, and support early mobility protocols.
US Medical Innovations, LLC (USMI) has unveiled the Canady Flex RoboWrist™, a cutting-edge robotic surgery device designed for both open and laparoscopic procedures in the United States.
With its existing approval and successful utilization in the Middle East, Europe, and Asia, this innovative device has already made a significant impact worldwide.
The Canady Flex RoboWrist is a handheld surgical instrument with full articulation and motorization, featuring a range of end effectors such as a hook, scissors, needle driver, and dissector.
It offers three degrees of freedom and an impressive 360 degrees of rotation. The device is compatible with the USMI XL-1000 electrosurgical generator, providing the option of utilizing the mono scissors or hook for electrosurgery.
To support pulmonary health, the bed provides in-bed percussion, vibration, and continual lateral rotation therapies. These therapies are intended to reduce complications associated with immobility and promote better respiratory outcomes. Additionally, the improved bed frame allows for easier access to the head of the bed, facilitating procedures like intubation.
In terms of skin protection, the Progressa+ bed is equipped with enhanced support surfaces that promote optimal skin health and wound healing. The inclusion of a new top cover makes cleaning easier, enhancing hygiene and infection control measures.
Another notable feature of the Progressa+ bed is its support for early patient mobility. By integrating an advanced lift system, the bed enables the care team to facilitate patient mobility protocols while minimizing the risk of injury for clinicians. The one-button FullChair function, along with sit-to-stand Chair Egress, assists clinicians in safely and easily moving patients.
The Progressa+ bed is currently available in the United States, and Baxter has plans to launch it in additional markets worldwide over the next 18 months. It is part of Baxter's comprehensive portfolio of beds and surfaces tailored to meet the diverse needs of care environments.
Read the complete post
The primary purpose of the Flex RoboWrist is to facilitate tissue dissection, transection, and suturing during various surgical procedures. It excels in open, endoscopic, and minimally invasive surgeries, including laparoscopic, urologic, gynecologic, general, and thoracic procedures.
This remarkable device boasts exceptional precision, enabling surgeons to perform intricate procedures with unparalleled accuracy. By employing advanced robotic technology, the Flex RoboWrist ensures precise movements, thereby reducing the risk of human error and enhancing overall surgical outcomes.
With state-of-the-art automation and intelligent control systems, the device optimizes surgical workflows, saving valuable time in the operating room. Surgeons can now focus more on critical decisionmaking, while the Flex RoboWrist handles repetitive tasks, ultimately improving efficiency.
In addition to its impressive functionality, the Canady Flex RoboWrist is a cost-effective solution. It can be autoclaved up to 50 times, eliminating the need for disposables and providing significant savings. This feature, coupled with its exceptional durability, contributes to its overall cost-effectiveness and sustainability.
Read the complete post


Grow your audience with increased reach, impact and user-friendliness
Rise above geographical boundaries
Generate new business
Gain the strong web presence differentiating yourself from competitors
Connect and engage with your target audience

Give more exposure to industry specific people
Increase your brand profile and share your capabilities with leading industry professionals