The Ohio State University
Human oversight will be important to identify and address the sometimes unpredictable biases of AI


The Ohio State University
Human oversight will be important to identify and address the sometimes unpredictable biases of AI


We are delighted to announce the launch of our inaugural issue of European Hospitals and Healthcare Management magazine 2023, which brings us immense joy as a publishing house. This would not have been possible without the hard work and dedication of our team, the knowledgeable advisory board, and all the authors who believed in our vision of providing relevant and uncompromising quality content.
European Hospitals and Healthcare Management is the latest addition to our portfolio, following the success of AsianHHM and AmericanHHM. With a strategic focus on serving healthcare professionals across the European continent, we are committed to delivering timely and high-quality content that addresses the latest trends and topics relevant to the industry.
Our goal is to provide a delightful experience to our readers, leaving them in awe with the quality of our publication. We look forward to continuing to foster excellence in the healthcare industry through our magazine.
The healthcare industry is increasingly using technology and artificial intelligence (AI) to improve patient outcomes, increase efficiency, and reduce costs. AI in healthcare is the use of advanced algorithms and machine learning techniques to analyse complex medical data, automate tasks, and provide decision support for healthcare professionals.
One of the primary applications of AI in healthcare is in medical imaging. AI algorithms can analyze medical images such as X-rays, CT scans, and MRIs to help radiologists detect and diagnose diseases more accurately and quickly. AI can also help identify patterns and trends in medical data that may be difficult or impossible for humans to detect.
Despite the many benefits of AI in healthcare, there are also potential challenges and concerns. One concern is the potential for bias in AI algorithms, which may be based on historical data that reflects past discriminatory practices. Another challenge is ensuring the security and privacy of patient data, particularly in light of the increasing use of remote monitoring and telemedicine.
Overall, AI has the potential to revolutionize the healthcare industry, enabling more personalized and effective treatments, improving patient outcomes, and increasing efficiency and costeffectiveness. However, it is important to ensure that AI is developed and deployed in a responsible and ethical manner, with a focus on improving patient care and outcomes.
Our first issue contains a collection of articles and cover stories that aim to address the challenges posed by AI and advanced technology in healthcare, while also highlighting potential solutions. We are confident that this content will provide valuable insights and contribute to the ongoing discussion on how to navigate the complex intersection of healthcare and technology.
N D Vijaya Lakshmi EditorMai-Lan Ho
MD, Professor of Radiology The Ohio State University06 How Interdisciplinary Medicine helps to Reduce overall Healthcare Costs and How to Implement it
Willi Stappert, Founder & CEO, Verunion GmbH
Dr. Wulf-Peter Brockmann, Founder and Radiation Therapist, Institut OncoLight
13 The Impact of AI, ML, and Robots in European Healthcare Workforce
James Gillespie, Faculty, Saint Mary’s College
Brianna Geary, Junior Product Manager, Publicis Sapient
19 Employee Retention Strategy at Healthcare
Hassan Mostafa Mohammed, Chairman & Chief Executive Officer, ReyadaPro
34 The Evolution of Precision Medicine in Cardiology: Novel Biomarkers, Gene Expression Profiling, and Donor Heart Selection

Smruti Desai, MBBS, Division of Advanced Heart Failure and Transplant, Mayo Clinic
Smit Paghdar, MBBS Division of Advanced Heart Failure and Transplant, Mayo Clinic
Rohan M. Goswami, MD, Director of Heart Transplant Innovation and Research, Mayo Clinic
38 Artificial Intelligence for Brain MRI
Mai-Lan Ho, MD, Professor of Radiology, The Ohio State University

44 Technological Revolution in Healthcare –An Overview
Harshal A. Sanghvi, Research and Development Specialist, Advanced Research and a Doctoral Candidate, Florida Atlantic University
Gauri Parvathy, Medical Graduate, Tbilisi State Medical University
56 How to Maximize Personal Health Records (PHR) Data Utilization: Comprehensive Disease Screening Test Recommendation
Piyanun Yenjit, Founder and Managing Director, APUK Co Ltd.
62 Artificial Intelligence in Cancer Diagnosis
Shrey S Sukhadia, Assistant Director, Bioinformatics, Department of Pathology and Laboratory Medicine, Dartmouth-Hitchcock Medical Center
67 The Future of Telemedicine: Providing Accessible and Equitable Healthcare for All
Smruti Desai, MBBS, Division of Advanced Heart Failure and Transplant, Mayo Clinic
Smit Paghdar, MBBS Division of Advanced Heart Failure and Transplant, Mayo Clinic
Rohan M. Goswami, MD, Director of Heart Transplant Innovation and Research, Mayo Clinic
72 The Big Data Revolution in Healthcare
Simon Waslander, Director of Collaboration, Clinical Research, CureDAO
Andrey Andreevich Kapitonov
CEO, Oxygen Technologies Group, UK
Aung Pyae Kyaw
Executive Director, Asia Royal Hospital, Myanmar

David Anthony Pearce
Director, Business Alliance EMEA, Asensus Surgical, Germany


Eiman Shafa
Medical Director, Spine Surgery Abbott Northwestern Hospital, USA



Gabe Rijpma
CEO, Aceso Health, New Zealand

Guglielmo Brayda
CEO, Inframedica Sarl, Luxembourg


Hassan Mostafa Mohammed
Chairman & Chief Executive Officer, ReyadaPro, Saudi Arabia
Likaa Najuib
Medical Marketing Operational Officer, Alfacure Oncology Center, Egypt
Paola Antonini
Chief Scientific Officer, Meditrial Global CRO, Italy

Pinheiro Neto Joao
Chief Executive Officer, Meu Doutor, Angola

Piyanun Yenjit
Managing Director, APUK Co.,Ltd, Bangkok

Predrag Ristic

CEO, Pharmillennium Consulting L.L.C., Serbia

Simon Ferdinand Waslander
Director of Collaboration, CureDAO, Aruba
Thitisak Kitthaweesin
Chief of Phramongkutklao Center of Academic and International Relations Administration, Thailand

Vicknesh Krishnan
Associate Medical Director, Fresenius Medical Care
Malaysia Sdn. Bhd., Malaysia
EDITOR
Vijaya Lakshmi N D
EDITORIAL TEAM
Sarah Richards
Debi Jones
Harry Callum
Supraja B R
ART DIRECTOR
M Abdul Hannan
PRODUCT MANAGER
Jeff Kenney
SENIOR PRODUCT ASSOCIATES
Sussane Vincent
John Milton
Peter Thomas
PRODUCT ASSOCIATE
Ethan Wade
CIRCULATION TEAM
Sam Smith
SUBSCRIPTIONS IN-CHARGE
Vijay Kumar Gaddam
HEAD-OPERATIONS
Sivala VNR
www.europeanhhm.com
Ochre Media Group info@ochre-media.com www.ochre-media.com




©Ochre Media Private Limited. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, photocopying or otherwise, without prior permission of the publisher and copyright owner. Whilst every effort has been made to ensure the accuracy of the information in this publication, the publisher accepts no responsibility for errors or omissions.
The products and services advertised are not endorsed by or connected with the publisher or its associates. The editorial opinions expressed in this publication are those of individual authors and not necessarily those of the publisher or of its associates. Copies of European Hospital & Healthcare Managemen can be purchased at the indicated cover prices. For bulk order reprints minimum order required is 500 copies, POA.
Interdisciplinary medicine is an approach to healthcare that involves collaboration between different medical specialties. It has been shown to have several benefits, including improved patient outcomes, and reduced overall healthcare costs.
This article discusses how interdisciplinary medicine can help to reduce overall health costs and how interdisciplinary groups can be build based on formerly independent practices and clinics.
Willi Stappert Founder & CEO, Verunion GmbH Dr. Wulf-Peter Brockmann Founder and Radiation Therapist, Institut OncoLightTrends like ageing population on the one hand and rising public debt on the other put pressure on societies to reduce overall healthcare costs all over the world.
Governments in different countries try to keep costs under control by more or less the same measures even though with different weights on each of them. In general, these are:
• Encouraging preventative care
• Increasing price transparency
• Reducing administrative costs
• Encouraging the use of generic drugs
• Promoting telemedicine
• Value-based care
• Medicaid and Medicare reform
• Increasing competition among healthcare providers

As with any regulatory interference, all these efforts have their undeniable merits but exhibit destructive elements as well, if driven too far.
In the private sector different players promise to reduce costs by all sorts of new products and services in digitalization, hightech diagnostics, etc. Only time will tell, what of these “innovations” actually add value and what is pure marketing/hype.
Another, more organizational, concept to reduce costs and improve outcomes for patients that has been around for years is interdisciplinary medicine on which we focus in this article.
Interdisciplinary medicine, also known as teambased care, is a growing trend in healthcare that emphasizes collaboration between different medical specialties. This approach is designed to provide comprehensive, patient-centered care by addressing multiple aspects of a patient's health. Interdisciplinary medicine has been shown to have several benefits, including improved patient outcomes, increased patient satisfaction, and reduced overall healthcare costs.
In general, interdisciplinary medicine can help to reduce overall health costs by improving the coordination of care and reducing the need for duplicate or unnecessary tests and procedures. This is because interdisciplinary teams are able to share information and collaborate on treatment plans, which can lead to more efficient and effective care. Additionally, interdisciplinary teams are able to address multiple aspects of a patient's health, which can lead to better management of chronic conditions and fewer complications. Studies have shown that interdisciplinary teams can result in a reduction in hospitalizations and emergency department visits, as well as a decrease in overall healthcare costs.
It is important to integrate accompanying sociomedical activities and medical professions such as physiotherapy in order to shorten inpatient stays. This integration must be initiated directly by the hospital, i.e., by the hospital staff, in order to shorten, for example, orthopedic hospital stays, on the one hand through the exact timing of pre-operative diagnostics and sufficiently long physiotherapeutic exercises, and on the other hand, post-operatively through the scheduling of post-operative rehabilitative measures, as has worked so well in the Netherlands for years.
It is known that interdisciplinary care is associated with lower costs and fewer hospital readmissions for older adults with complex medical needs. Another primary way in which interdisciplinary medicine can help to reduce overall health costs is by preventing the development of chronic conditions. Chronic diseases, such as diabetes and heart disease, are responsible for a significant portion of healthcare costs in many modern societies. By addressing risk factors and promoting healthy behaviors, interdisciplinary teams can help to prevent the development of these conditions and reduce the need for expensive treatments. Also, interdisciplinary medicine is known to reduce overall health costs is by improving the coordination of care. In traditional healthcare systems, patients may see multiple healthcare professionals for different conditions, leading to a lack of coordination and communication. This
can result in duplicative tests and treatments, leading to increased costs. Interdisciplinary teams, on the other hand, work together to provide coordinated care and communicate effectively with one another, which can help to avoid these issues.
In the case of cancer treatment, interdisciplinary medicine can play an especially important role in reducing costs. Cancer treatment can be complex and costly, and often requires the expertise of multiple specialists. Interdisciplinary teams can help to ensure that patients receive the most appropriate and effective treatment, which can reduce the need for repeated or unnecessary treatments. Additionally, interdisciplinary teams can help to manage the side effects of treatment and provide supportive care, which can improve patient outcomes and reduce costs associated with complications or hospitalizations. It must be remembered that it is not always the most expensive oncological drugs that achieve the best effect, but possibly cytostatic drugs that have been used successfully for decades.
The same applies to oncological treatment with the aid of medical equipment. In each individual case, it is necessary to cost-critically examine when the most expensive maximum-dose radiation therapies come into question, and when series with radiofrequency treatments in combination with further, also chemotherapeutic treatments in low doses, can ultimately be used to achieve the same goal. A typical example from Germany would be:
Treatment with Cyberknife device (Accuray Computer-assisted robotic radiosurgery)

• Capital costs: approx. €10 million
• Individual therapy costs: approx. 10-20 k€
Treatment with radiofrequency hyperthermia device (Oncotherm EHY 3010)

• Capital costs: several hundred thousand €
• Costs for a comparable series of approx. 20 radiofrequency applications in combinations with further measures such as low-dose chemotherapies / methotrexate carrier therapies: approx. 7 k €
Interdisciplinary medicine can also help to reduce overall health costs in the case of cancer treatment. Cancer is one of the most costly diseases to treat and manage, and the cost of cancer care continues to rise. An interdisciplinary team can improve the coordination of care for cancer patients, which can help to reduce the costs of treatment and improve patient outcomes.
However, interdisciplinary teamwork using different therapeutic and diagnostic methods must not give physicians in an economically particularly lucrative area a financial advantage over other colleagues in their team.
Another practical example is integrative medicine, which combines conventional and complementary approaches to healthcare, can also contribute to cost savings in cancer treatment. For example, integrative medicine can include the use of complementary therapies such as acupuncture, massage, and mindbody practices. These therapies can help to reduce symptoms and improve quality of life for cancer patients, which can reduce the need for additional medical treatments and medications. Additionally, integrative medicine can include the use of dietary and lifestyle changes, which can help to prevent and manage chronic conditions and reduce overall healthcare costs.
The whole idea of interdisciplinary medicine has been there for decades now.
Its widespread implementation, however, faces several obstacles. These include a lack of communication and coordination among different healthcare professionals, a lack of training in interdisciplinary care, and a lack of reimbursement for interdisciplinary services. The latter may or may not be ever resolved, as it would require innovative thinking on behalf of politicians and their will to reconfigure regulation. The industry can, however, make steps to resolve other obstacles themselves. One strategy would be to build topic-specific groups for instance in the field of cancer treatments using a combination of mergers & acquisitions of clinics and practices as well as targeted greenfield investments. Such group can include practices / clinics in the field of:
• Diagnostics (radiology, laboratories, pathology)
• (Pharmaco-)Oncology
• Radio-oncology
• Nuclear medicine including diagnostics and therapies
• Treatments from alternative medicine by electromagnetic fields and hyperthermia
Such groups should then be led by one overall management and governance at the strategic level. This management should take the following steps to develop it into an effective specialized group:
Promote communication and collaboration among its healthcare professionals through the use of electronic medical records, interdisciplinary rounds, and regular meetings.
1. Provide training and education in
interdisciplinary care so that healthcare professionals develop the skills and knowledge necessary to effectively collaborate with their colleagues.
2. Develop “internal” reimbursement models that support interdisciplinary care. This would ensure that formerly independent practices/clinics are financially incentivized to work together to provide comprehensive care for patients.
3. Use telemedicine and other forms of remote communication so that healthcare professionals from geographic locations can collaborate and share information effectively.
4. Complement the often too generalists service portfolio of the formerly independent practices (e.g., radiology, laboratories) with more specialized expertise within the group’s strategic framework.
5. Support interdisciplinary research to improve understanding of disease and advance new treatment strategies that can be
shared within the group to improve patient outcomes and to enhance the group’s profile.
6. Annual compulsory periods for collaboration or on-site observation in the other specialties for their better understanding (e.g., PET-CT diagnostics, expansion of the use of laboratory tumor markers)
7. Preventing the intrusion of particular external interests into individual areas of expertise within a team.
8. Prevention of isolated special oncological diagnostic and therapy centers that create their own guidelines and pay so much attention to their own profitability that there is a danger that inexpensive but successful alternatives outside these centers will hardly be considered as off label use.
It is important to summarize that the obstacles to interdisciplinary medicine are not technological ones. They are partly regulatory but first and foremost organizational.
So far, strategic or private equity consolidators in the healthcare sector focused almost entirely on “mono-cultural” approaches: buying up smaller players (practices or clinics) in the same discipline as dentistry, radiology, ophthalmology and create big player. Most of the time, this buy & build projects are not followed by an appropriate integration. Also, true synergies between the acquired targets in such a mono-cultural groups are oftentimes rather limited. But almost never do these kinds of consolidations lead to any significant added value for patients. The consolidators love these projects because the value of a bigger group
Interdisciplinary medicine is a type of treatment that involves more than one specialty. Better patient outcomes and lower healthcare costs are the advantages of this approach
is disproportionately larger than the sum of the valuations of its separate elements. These groups can be then listed publicly or resold with handsome profits.
If the concept of interdisciplinary medicine is to be taken seriously, it seems worthwhile not only to concentrate on the above-mentioned specialist areas, but also to economically combine interdisciplinary oncological therapists together with their essential environment in the same way, so that the result is an overall oncological network that is as comprehensive as possible, in which no physician outperforms another of the same hierarchy financially and thus also does not allow overvaluation of individual areas.
The biggest problem of such cost containment, however, is the pharmaceutical industry, which up to now in Germany has been able to dictate its prices practically without resistance and even forces prices up to 50% higher when it discontinues common drugs under various arguments.
In Germany in recent years, a few consolidators started to acquire practices from different disciplines. However, if there is an actual strategy behind it, it is to get big fast for the same reasons as above and/or secure sales synergies (for instance between orthopedics and radiologists) which is a legal grey zone area. These approaches are not patient-centric either and are purely commercial.
Building a true interdisciplinary group and realizing all its intended benefits is beyond the comfort zones and not in line with incentive
structures of most consolidators who more often than not are led by ex-investment bankers or ex-management consultant. It is ultimately down to strong teams of charismatic entrepreneurs and medical professionals to put the idea into reality.
Dr. Wulf-Peter Brockmann is a specialist in radiology since 1984. From 1979 to 1994, he worked as a senior physician in the radiooncology department of a hospital. Since 1995, he has been working in private practice as a radiologist / radiation therapist. He has also been active in immunology and is a board member of the German Society for Hyperthermia.

Willi Stappert is an entrepreneur and a top-management consultant with 12+ years in strategy and corporate finance and cumulative transaction value of over € 2 bn. In his career, he worked for companies like EY and Stern Stewart in various client industries. In 2022, he co-founded a healthcare company which focuses on interdisciplinary medicine.


This article discusses the potential of artificial intelligence (AI), machine learning (ML), and the internet-of-things (IoT) in revolutionizing the European healthcare sector. The AI in Healthcare market is projected to grow substantially during the period from 2023 to 2028, prompted by increasing demand for improved healthcare services. The technology has the potential to enhance care outcomes, patient experience, and healthcare access while reducing workforce burnout. To harness AI's highest potential, European healthcare organizations and health systems must collaborate to introduce and scale AI in healthcare. They should assess their capabilities, develop regional or national AI strategies, set standards, redesign workforce planning and clinical education processes, provide incentives for collaboration, and address regulation and funding issues. By doing so, Europe can remain a leader in AI-driven healthcare, while improving access, affordability, quality, and safety for its citizens.
James Gillespie Faculty, Saint Mary’s College Brianna Geary Junior Product Manager, Publicis SapientArtificial intelligence (AI), machine learning (ML), internet-of-things (IoT), and robots in healthcare refers to the use of AI technologies such as image analysis, natural language processing and predictive analysis to improve access, affordability, quality, and safety.
These initiatives will cause positive disruption of existing processes, as well as the creation of entirely new processes, products, and services for providers and patients. The private, public, and NGO sectors in Europe all have increased interest in this likely positive impact. Specifically, this is reflected in the increased private equity and venture capital funding flowing to AI-related healthcare technology startups.
The AI in Healthcare market is expected to grow more than fivefold between 2023 to 2028, with a compound annual growth rate (CAGR) of 47.6% during the forecast period. The growth is driven by the increasing demand for improvised healthcare services due to the current imbalance between healthcare workforce and patients. This market for services will grow at a higher CAGR during the forecast period as compared to the software segment. Deep learning in the machine learning segment is projected to hold the majority of the market share in 2028, and the market for patients is expected to grow at the highest CAGR during the forecast period.
AI in healthcare is currently in its early stages, but there are already a growing number of use cases throughout Europe. These include software applications that allow patients to self-manage care, online symptom checkers, virtual agents to accomplish tasks in hospitals, and predictive analytics for early diagnoses. The impact of AI on healthcare in Europe and globally will be significant, but its full potential remains to be explored.
AI can offer effective tools for automating chores and supporting and educating clinicians, epidemiologists, and policymakers on the most effective ways to promote health at the population and individual levels
AI and robots can be used to address what is perhaps the most pressing long-term issue of European healthcare providers: Insufficient human capital. There are critical staffing shortages facing the European healthcare industry, especially nursing. The significant number of clinicians exiting the workforce due to retirement, burnout, and pandemicrelated stressors, combined with the increasing nurse turnover rates, indicate that there is a need for innovative solutions to address these challenges. These challenges will continue to increase as primary care physicians and nurses are expected to leave the industry in large numbers in the coming years.
On the non-clinical side, there are also hiring difficulties. Health IT hiring presents new challenges, including matching skillsets and cost, as competition in the market increases. The need for health IT professionals has grown with the move into digital health and the digitization of healthcare, leading
to a high demand for talent. Hospital cyberattacks have also increased the demand for cybersecurity talent. Moreover, many healthcare organizations are struggling under a vast pile of unfilled job postings.
AI and autonomous robot technology can be used to help healthcare staffing, including assisting with efficiency, productivity, and patient satisfaction. The specific benefits of AI, IoT, ML, and robots in healthcare include:
• Substantially lessen time spent on the rote, administrative tasks that can consume almost ¾ of a typical healthcare worker’s bandwidth. By automating rote tasks, AI can free up time for physicians, nurses, and other healthcare workers to focus on patient care and other more complex and specialized tasks, helping to reduce burnout.
• Improve diagnosis and treatment by implementing clinical decision-making software that can analyze large amounts of data.
• Automate nurse staffing and scheduling, decreasing manual work for nurse managers and increasing retention.
• Speed up job recruitment by automating over 90% of the hiring process for nursing vacancies.
• Leverage internet-of-things enabled badges to help collect data enterprisewide, gain real-time insights on equipment utilization, clinical workflows, and patient/ staff interactions to reduce operational bottlenecks, increase efficiency, and improve
patient experience.
• Run advanced workflow platforms to provide patients with proactive status updates, estimated wait times, and family text messaging. This proactive patient communications can provide peace of mind and keep patients and loved ones wellinformed throughout the care journey.
• Automated nurse call systems can reduce response times to patient needs, allowing healthcare staff to have more time to focus on patient care.
• Implement staff duress safety solutions that provide peace of mind to staff members, enabling them to request assistance to their exact location should it be needed. This reiterates that staff work in a safe environment where they are valued.
• Help implement automated asset tracking that allows clinical staff to locate within seconds and retrieve crucial equipment via IoT-enabled tags.
• Leverage real-time location technologies and digital wayfinding to improve the patient experience in 2023. Digital wayfinding can reduce stressors for patients and visitors by providing turn-by-turn directions to their destination. These solutions can also benefit healthcare facilities by reducing missed appointments and delayed patient care, making them a cost-effective and scalable option for improving the patient experience.
• Automate recruitment of unfilled or changed shifts to the right workforce based on skills competency, price point, and workload. It can direct prospective hires to new positions
and interview times with only a few items of screening information. This helps to reduce administrative tasks and eases the burden on HR staff, allowing them to focus on more nuanced connections with applicants during the interview process.
To encourage the introduction and scaling of AI in European health systems, there are several changes that need to happen. These include:
1. Working together to deliver quality
AI in healthcare: There needs to be more collaboration between healthcare professionals and AI developers to ensure that AI solutions are of high quality and fit seamlessly into the workflow of decision-makers. This means involving healthcare staff early in the design phase, focusing on user-centric design, emphasizing explainable, causal, and ethical AI, and building clinical evidence of quality and effectiveness.
2. Human-machine/robot collaboration: Institutions will have to develop teams with expertise in partnering with, procuring, and implementing AI products and services.
3. Overhauling education, learning, and skill-building: To increase digital literacy, as well as understanding the fundamentals of AI, ML, and genomics, healthcare systems should provide opportunities for continuous learning and technology training.
4.Improving data governance, interoperability, quality and security: This will require the private, public, and non-profit sectors to support efforts to generate, collect,
manage, govern, and analyze large volumes of high quality, anonymized data.
5. Managing cultural and organizational transformation: Effective leadership is key to introducing AI in healthcare. If the potential for patients and providers is to be maximized, the challenge is as much managerial as scientific or technological.
6. Developing new talent and creating new roles/positions. To achieve the successful introduction and utilization of AI/ML, new mission critical roles will need to be created such as data engineers, data scientists, statisticians, and technologists.
7. Scaling implementation and innovation: When it comes to the application of AI/ML to healthcare in Europe, scale does matter. This applies to biomedical research, digital health, translational research, and other fields. As part of this, large entities can collaborate on creating centers of excellence that facilitate regional and public-private partnerships to facilitate scaling AI in European healthcare.
8. Adoptions of new regulations, public policies and risk management: The European Health Organisation, the European Medicines Agency, the UK’s National Health Service, and other national and international regulatory agencies will need to clarify access to and utilization of data generated by AI, including issues related to ownership, privacy, and security.
9. Providing capital: To achieve scale, there will need to be utilization of both creative and traditional funding models to provide capital for startups and insure reimbursement of
AI applications. This includes encouraging the creation of centers of excellence and accelerators/incubators focused specifically on AI and healthcare.
10. Develop and promote responsible AI in healthcare, with a focus on ensuring that AI is implemented in a way that is ethical, transparent, and inclusive. This includes initiatives to support education and training programs for healthcare professionals, as well as efforts to establish guidelines and standards for the development and deployment of AI in healthcare. While some argue that AI can eliminate biases and improve efficiency, others have raised concerns about potential biases and discrimination. Since Ai can create substantial social stress, workers will need more insulation/ protection from algorithmic decision-making. The EU is working on legislation to regulate the use of AI in the workplace, but experts caution that workers need to be aware of the risks and advocate for their rights.
11. Address concerns about potential job displacement in the healthcare workforce. While it is unlikely that AI and ML will completely replace physicians and nurses, it is possible that certain tasks and responsibilities may be automated, leading to the need for job redeployment and retraining. For example, AI and ML may be used to perform repetitive and time-consuming tasks, such as analyzing medical images, enabling physicians and nurses to focus on more complex and specialized tasks, such as patient care and counseling. To address these concerns, there are ongoing efforts to develop strategies for job redeployment and retraining. This includes initiatives to support the development of new roles and responsibilities for healthcare workers, as well as education and training programs to help healthcare professionals acquire the skills needed to work alongside AI and ML technologies.
The use of artificial intelligence (AI) has the potential to transform healthcare delivery, including improvement in care outcomes, patient experience, and access to healthcare services. As demand for healthcare services continues to grow due to the aging European population, changing patient expectations, and lifestyle choices, AI can increase the effectiveness and efficiency of healthcare delivery for patients. Additionally, AI can help reduce burnout among health workers (e.g., physicians, nurses, physician assistants) by allowing them to spend more time working
By automating or enhancing the work of staff members and clinicians, AI can contribute value. We can use AI as a tool to help health workers perform better at their jobs and improve patient outcomes, and many repetitive tasks will eventually become completely automated
directly with patients. Ultimately, the goal is to ensure that the use of AI and ML in healthcare results in better patient outcomes and improved efficiency, while also supporting a sustainable and dynamic healthcare workforce.

In sum, healthcare organizations and health systems in Europe need to work together to introduce and scale AI in healthcare. Healthcare organizations need to assess their capabilities and define their ambition for AI, as health systems develop a regional or national AI strategy for healthcare, set standards, redesign workforce planning and clinical-education processes, provide incentives for collaboration, address regulation and funding issues, and ensure that funding and reimbursement mechanisms reflect the seriousness of innovation in healthcare. By working together, healthcare organizations and health systems can improve the quality and effectiveness of healthcare in Europe with the help of AI.
It is imperative for European healthcare organizations and health systems to assess their capabilities and willingness to commit resources for AI in healthcare. As part of this, there is certainly an opportunity to help grow an AI ecosystem via collaboration and joint solutions for patient populations. Health systems can develop a regional or national AI strategy for healthcare, set standards for digitization and data quality, redesign workforce planning and clinical-education processes, provide incentives for collaboration, and address regulation, liability, and funding issues. Overall, Europe is playing a growing role in the fast-moving market of AI in healthcare. In addition, its member countries have the potential to remain leaders in driving the future AI to benefit health systems, healthcare workers, caregivers, communities, and patients. AL, ML, and robots present a once-in-ageneration opportunity to improve access, affordability, quality, and safety in European healthcare.
James Gillespie is a faculty member in business administration and data analytics at Saint Mary’s College, Notre Dame Indiana. His education includes Northwestern University Kellogg School of Management, PhD, MS; Harvard University School of Law, JD; Princeton University School of Public Policy, MPA; and Massachusetts Institute of Technology, BS.

Healthcare enterprise management must thoroughly investigate the causes of employee(s) turnover, work to resolve and prevent high employee turnover, and implement employee(s) retention strategies as the foundation of business continuity and economic loss avoidance.
 Hassan Mostafa Mohammed Chairman & Chief Executive Officer, ReyadaPro
Hassan Mostafa Mohammed Chairman & Chief Executive Officer, ReyadaPro
Basically, employee turnover is not the responsibility of the HR department alone but also the responsibility of the organization's shareholders and senior management, who seek to achieve performance excellence. Employee turnover leads to a loss of profitability, productivity, knowledge,
and financial stability. To overcome employee turnover, management needs to show concern and care for all employees, pay attention to their affairs to the level of attaining their highest performance, try to solve their internal and external problems, and facilitate or eliminate their work obstacles to get the best out of work activities and ensure work runs smoothly and effectively.
Healthcare Professional Enterprise management needs to be clear & transparent in announcing the advancement opportunities for employees, revise and asses thoroughly actions and decisions affecting the workforce commitment, and applying strategic leadership in a wise manner.
“Healthcare Professional Enterprise Management needs to support employees' development through the creation of a career path, giving great concern to employee training to support their growth”.
There is no doubt that human beings are the most valuable fixed asset for any organization. To maintain an organization's progress and stability, it must retain competent personnel who are leading the organization toward its goals and maintaining its reputation. Top management at any organization needs to create comfortable and motivated employees, create an encouraging environment, and define programmes and services to improve employee retention strategies and ensure employees' happiness.
Considering the progress updates and changes, especially after the COVID-19 pandemic, in regulations, reimbursements, increased mergers and consolidations, and costcontainment initiatives that can severely affect organizational retention, employee retention becomes crucial in the healthcare industry, apart from the importance of employees’ satisfaction within the healthcare facility.
We need to understand the key components and the importance of measuring employee turnover, and learning how employee turnover affects patient care. We need to create a policy to retain quality employees. We need to seek out the real needs and expectations of the healthcare staff, especially physicians. Top management should consider adjusting their managerial perspectives when establishing new human resources policies or making decisions. The success of a healthcare organization depends on measuring employee turnover and the quality of care the organization delivers. Turnover of healthcare providers (physicians, nurses, etc.) is the primary cause of patient distrust and has a negative impact on hospital performance and progress.
When an employee leaves, duties may be shifted to the remaining personnel, adding an additional obligation and burden to them.
“Studies indicate the cost of turnover can average 150% of the employee's annual salary”.
Employee turnover affects the process of patient care. The majority of patients
prefer to be cared for by the same staff of a healthcare team each time because relationships are built between the patients and their respective healthcare teams. To develop an effective strategy, we need to determine the reasons for employees' leaving by conducting detailed exit interviews. Organizations need to focus on important issues to maintain a competent workforce in the long term, such as communication, decisionmaking, compensation, benefits, and career development; recruitment; appreciation and understanding; and management.
We need to create strategies for improving employee retention in healthcare. We need to learn how industry leaders put healthcare workers first and keep their employees. Satisfied employees are contributing to the delivery of high-quality care, reducing medication errors and malpractice claims, and
showing a good commitment to their patients and organization.
The reasons for the high turnover rate among healthcare workers include an ageing workforce, especially among nurses and physicians; a lack of educational opportunities for nurses, preventing them from entering the field; exhaustion; salary; career development; and work-life balance.
Healthcare employers can maintain employee satisfaction through strategies for improving employee retention such as:
(1) Improve recruiting and onboardingby attracting candidates using a combination of a good salary, good benefits, and a good work environment.

Employers must give people reasons to stay. We need to note that a good salary is only one factor in keeping employees. Good benefits, training, continuing education, and professional development are all important factors that must be addressed and handled carefully to ensure employee retention and happiness.
Employers need to announce their bonuses and rewards for the ideal employee who achieves the highest records.
“Employers should offer rewards, benefits, bonuses in a sound approach, to make and keep their employees’ happiness. Need to keep employees satisfactions all the times”.
(2) Training and developmentemployers need to give their employees room to be trained on administrative tasks and the latest technology related to their core function (such as phones, payroll and timesheet software, electronic health records, and other applications) that will breed the confidence to step comfortably into their new role.

The most critical issue in improving healthcare employee retention is for healthcare management to save adequate competent staffing and create appropriate scheduling. They directly affect the quality of care. especially at a time when patient loads are high, causing exhaustion and stress among nurses and leading to a turnover.
Healthcare providers who must schedule employees to effectively fulffulfillient needs employ a range of tactics, including:
• flexible schedules have the advantage of catering to the needs of nurses and other
healthcare workers who must balance work, family, and other obligations.
• Self-scheduling allows healthcare professionals, such as nurses, to decide when they work and how much overtime they accept.
• using data analytics, artificial intelligence, and machine learning to estimate demand and identify anticipated demand flows
Healthcare providers who need to schedule staff to adequately meet patient needs use a variety of strategies, such as:
• Flexible schedules have the advantage of meeting the needs of nurses and other health professionals who are balancing work and family or other demands.
• Self-scheduling gives nurses and other healthcare workers control over when they work and how much overtime they take on.
• Predicting demands using data analytics via artificial intelligence and machine learning to help identify likely flows in demand
(3) Prevent employee burnout - that results in a lack of motivation, poor job performance, and increased negativity. Burnout can lead to poor care quality, and overwork and exhaustion can lead to medical mistakes.
“According to the American Psychological Association, burnout is a physical, emotional, and mental condition caused by overwork and stress”.
Burnout Strategies: We can prevent that by applying the following approach: Adequate staffing and scheduling: Hiring temporary and permanent staff and using appropriate scheduling can help alleviate overwork.
Prepare employees for burnout risk: inform employees about the signs and symptoms of burnout and provide them with tools to help prevent it while they are students and juniors so that they are ready to face this critical issue and ensure their adaptability while performing their activities.
“A 2021 study by the Mayo Clinic found that one in five healthcare workers said they intended to reduce work hours or quit the profession in two years, due to burnout, fear of infection, anxiety, or a high workload”.
Concentrating on patient care without neglecting the necessary documentation [paperwork and/or software records]; reducing administrative tasks by hiring an assistant to keep the required records allows clinicians and
physicians to focus on caring for patients.Using the most recent technology means using the most recent applicable technology to ensure the best possible care for the patient in the shortest amount of time.
Treat burnout: Employers should ensure that employees receive the care and time they require to avoid the consequences of burning out, leaving work, and reducing the patient's care.
Hire the proper and sufficient staff as per the workload; inadequate staffing increases employee stress levels and accelerates burnout. A supportive organizational culture can help to reduce the stress and burnout that can cost your company quality employees by:
• Ask for and acknowledge employee input into quality care policies and procedures.
• Be responsive to employee issues and complaints.
• Be as flexible as possible with scheduling to accommodate individual needs, preferences, and emergencies.
• Establish or strengthen your organization’s employee support network.
(4) Employee engagement - is achieved by involving them in decision-making, showing care for their opinions, and giving them the room to take the right decision freely and smoothly as per the required task and patient case. This can be applied via:
Making coaching and mentoring programs: employers should invest in their staff’s career goals, helping some employees attain their responsibilities in the new task area
and encourage continuing education and certification via the presentation of continuing professional development (CPD), often referred to as continuing medical education (CME) credits or continuing education units (CEUs), as CPD has a positive impact on patient outcomes.
“According to the Journal of American Medicine, CPD programs in prescription drugs were associated with reduced healthcare costs for patients”.
Endorse values such as integrity, empowerment, perseverance, equality, discipline, and accountability in the organization. Support and develop employees via training and development plans; invest in employees. Celebrate successes and highlight individual achievements via a visual board and announcements. Present compensation and reward them at different intervals. Celebrate with them on their birthday and marriage day and give them a present. Show them care and support, even during family celebration events and in the case of family problems. Participate with employees and encourage them to make their own decisions about how the case should be handled. Encourage employees' creativity and use of the latest technology and data analytics in solving problems and getting the proper and right solutions in time without fear or blame for making any mistakes. Give employees thank-you cards for going to dinner and/or conferences. Take care with employee suggestions and ideas; show them you care with their input. Enhance, push, and
create opportunities for employees to become "leaders" at their jobs.
Save the necessary resources and more for them to perform their work freely and smoothly in order to achieve the best results. Encourage them to send their opinions and suggestions via clear, open, and simple channels. Make monthly meetings for them and celebrate with the best achiever to motivate others to be on track and support their retention in the organization. Ensure effective balancing between work and life; apply the "work-life balance" model.
Employee-led initiatives and autonomy: via encouraging employees to take their decisions in relevant cases without fear, which supports them and increases their confidence in their work process (such as free scheduling, using relevant and proper technology as required, etc.); In short, give employees the freedom to learn about their own needs and jobs.
“A report in the Journal of Healthcare Leadership showed that nurses who had autonomy and agency in their practice were more likely to stay in the profession, despite the pressures caused by the COVID-19 pandemic”.
(5) Identify and address work social barriers - such as transportation between the healthcare provider facility and the employee's home; working hours and staying late at night prevent the employee from leaving for his home, which is located in a rare area at late hours. Employers must support their employees
by showing concern for their personal and family matters as needed.
Improving employee retention in healthcare is crucial and requires great attention and care from healthcare leaders. A healthcare provider should have a business plan as part of their retention strategy. They should present in a clear and transparent way the proposal, progress measures, and management influences on the plan. When developing their business plan, they should think about and calculate the return on investment. They should have a value proposition for the organization's strengths and differentiate it from its competitors. They should measure progress towards meeting retention goals at regular intervals to keep their organization on track. They should hire competent personnel, ensuring the personnel has the required knowledge, experiences, skills, good attitude, and aptitude or innate qualities.
Employers should reward employees for their successes and take corrective action as required. Healthcare leaders should calculate and consider retention rate targets that achieve a competitive edge in the relevant market.
“Gering and Conner (2002), retaining a productive workforce is important for any organization because if the organization cannot retain its employees, it will not be able to exploit its human asset progress inside the organization”.
Healthcare employers need to support their employees and ensure their contribution to the progress and benefits of the organization.
They need to increase the contribution and engagement of their employees by motivating, encouraging, and acknowledging their efforts in the right way to ensure their retention. Create proper policies. Explain the organization's strategies and methodologies to keep personnel and avoid their leaving.
Maintaining competent personnel is much less expensive than hiring new ones. They should create and foster the proper environment, have plans and programmes for employee retention via compensation plan, reward, inform, and call them to be a part of the organization, and above all, be clear and transparent with them, willing and doing their best to ensure their comfort and happiness while doing their work, and giving their best and highest care for patients to achieve their satisfaction that elevated the organization's benefits, morale, and productivity.
“According to Gering and Conner (2002), retaining good workers is critical to any organization. If an organisation is not able to retain its employees, it will not be able to capitalize on the human assets developed within the organization”.
Healthcare employers should support the individual needs and circumstances of their employees. The lack of support, unsupportive relationships within employees’ working groups, and a health-care system that "puts business principles before care" are listed as factors resulting in job dissatisfaction and employee turnover.
Get creative. Be more creative about attracting and keeping quality employees. As workforce competition continues to heat up, unique benefit offerings such as these may be necessary to attract and retain qualified hospital and home healthcare employees. Prioritizing employees’ happiness: employees tend to stay with an employer who cares about their happiness and well-being. Implementing wellness initiatives and stress management strategies encourages employees to disconnect from work and care for their families and personnel issues after work. Apply the employee’s freedom criteria to design his own schedule, trusting him or her to get the work done. Be social; offer emotional support and resources to avoid employee burnout.
Dr. Hassan Mostafa Mohamed, Chairman & Chief Executive Officer at ReyadaPro is an entrepreneurial and growth-driven executive with more than 25 years of experience in pharmaceutical industries, including, Technical, sales & marketing, Production, Supply chain, Engineering/utilities, Quality, and regulatory issues. Mr Hassan is an expert in driving pharmaceutical facilities to accomplish corporate goals, building and leading technical & quality aspects with market consideration for rapid growth, and efficient operational excellence.


Digital health is a highly interdisciplinary field at the intersection of technology and medicine. Emerging applications include mobile health, telemedicine, and precision medicine. Stakeholders include patients, physicians, and researchers in academia, industry, and government. In this interview, a radiology physician-scientist reflects on the history and future of the specialty.
Mai-Lan Ho MD Professor of Radiology The Ohio State University
1. Can you briefly describe your background and the responsibilities of your current position fo our readers?
I am a radiology physician-scientist with engineering training and practice experience at multiple hospitals across the United States. In my current position, I balance clinical, research, and administrative responsibilities.
When on clinical service, I spend my time interpreting medical imaging examinations and consulting with physicians in various specialties to help them diagnose and manage patients. My research time is spent working alongside basic scientists and data scientists to improve the methods by which we acquire and analyze medical images. In my various leadership roles, I mentor other faculty and trainees, develop educational and diversity programs, build bridges between departments, and partner with other medical centers for global impact.
During COVID-19, the need for social distancing and quarantine greatly accelerated the adoption of digital health solutions. There was a powerful demand for mobile health, telemedicine, and precision medicine approaches. International collaborative teams were formed to facilitate big data sharing and analytics for real-time clinical tracking, multicenter research, and 3D printing/simulation. In the postpandemic era, these initiatives have continued to progress toward the ultimate vision of a holistic and patient-centered model of population health, in which digital technologies are used to deliver valuebased care and reduce socioeconomic disparities by predicting and preventing disease throughout the general community.
you think the future of the healthcare industry will hold for health and well-being, given the rapid advancement of technologies like AI and big data?
There is a looming crisis in healthcare related to the aging of our global population, overutilization of hospital resources, and medical staff burnout. Digital health could help move us toward general surveillance and preventative care before people ever reach the hospital, thus decreasing the overall burden on our healthcare system. Wearable monitoring devices, personalized assessment, and early interventions in lifestyle could help modify risk factors for subjects. For patients that do require medical care, we would be able to better diagnose and treat them using approaches tailored to their demographics and disease type. This is the grand vision of precision health: improved risk assessment and prognosis, earlier and more accurate disease diagnosis, and minimally invasive and targeted therapies to achieve best patient outcomes. However, this lofty goal will require international collaborations across multiple specialties to acquire the vast information required for “data-hungry” AI algorithms to derive complex patterns and accomplish large-scale predictions.

4. Many AI-based system developers ask themselves how to build their solutions so that they are “based on human values.” What ethical guidelines should apply to AI in healthcare?
The four principles of medical ethics are autonomy, non-maleficence, beneficence, and justice. When applied to AI, the key considerations include bias/discrimination, privacy/surveillance, and accountability/ responsibility. There are many potential sources of bias at the levels of problem selection, data collection, outcome definition, algorithm development, and postdeployment surveillance. The overwhelming majority of hospital admissions, clinical trials, and practice guidelines are derived from adult Caucasian males. Therefore, AI algorithms trained on these datasets will encode implicit bias and further exacerbate social inequities. Additional efforts must be made to train, validate, and test algorithms on underrepresented groups (gender, race, country) to ensure fair and robust results. Furthermore, with the standard “black box” approach providing limited access to inputs and operations, AI algorithms are not readily transparent or explainable. Thus, the use of AI may lead to medical mistakes or data breaches with devastating consequences for patients. Human oversight will be important to identify and address the sometimes unpredictable biases of AI, as exemplified by recent controversies around Watson, ChatGPT, and Bing.
5. The healthcare market has been dominated by a few digital trends, such as wearable technology, mobile applications, and digital therapeutics. Which of these strikes you as being overhyped?
Compared to conventional technology startups, the medical technology field is far more demanding and limited by regulatory considerations related to patient safety. The old Silicon Valley principle of “fake it till you make it” does not apply, as we have seen with companies like Theranos. Currently, the majority of MedTech ideas are overhyped, reflecting the persistent gap between commercial startups and clinical practice. In general, tech companies deal in “blue sky” thinking and are focused on a path to funding and acquisition. Industry vendors have limited understanding and appreciation for the logistics of routine clinical care. The few physicians employed in industry tend to be administrators and researchers who have moved away from traditional clinical care. On the flip side, clinicians are incredibly busy with patient responsibilities and are far more realistic about viable use cases. Furthermore, physicians do not have time to curate and annotate large amounts of data for AI training, unlike the general crowdsourcing of Mechanical Turk. Even some of the closest MedTech collaborations have failed due to the disconnect between vendors, who are primarily interested in acquiring patient data and finding quick routes to market; and hospitals, which want to protect their individual datasets and
develop clinically relevant solutions. To bridge this divide, we need to improve public-private partnerships and invest the time and resources necessary to solve truly challenging problems in medicine.
6. Digitalization must deal with a number of challenges, including interoperability, cyber security, ethics, and transparency of algorithms. Which do you think is the most significant for healthcare?

All of these are very important considerations for healthcare. Ultimately, digital health solutions need to be readily available to “anyone, anywhere, anytime.” Interoperability ensures that patients and various health systems can effectively exchange and utilize information. Cyber security is important to protect organizational applications, data, and infrastructure from attack. Ethical AI seeks to
provide inclusive, transparent, and explainable solutions for data analysis and management. As we learn more about AI and its pitfalls, we can begin to incentivize its positive and responsible use with public sector policies and formal legislation.
7. The gap between available healthcare capacity and the demand for health and wellness services is widening. Is it logical to believe that digitization would further this gap, or do you see it otherwise?
As I mentioned, there is a fundamental breakdown in communication between industry vendors and medical practitioners. Burnout is prevalent in healthcare, and the last thing people want to do is expend more effort to train a machine intended to “replace” or “perform better than” them. That has always been an unrealistic goal, and vendors are gradually coming to realize that they need to target more practical or narrow AI applications that encourage human-machine synergy. Ideally, digitization will bridge the gap between “healthy” and “diseased” populations by identifying at-risk individuals in the community, providing longitudinal counseling and feedback, and improving workflows for those admitted to the hospital. Modern machines are replacing many lower-level and mundane tasks that have comprised traditional human work. This could theoretically improve efficiency by freeing up individual time for more meaningful work, and reducing overall strain on the healthcare system.
8. The “first pandemic of the digital era” is COVID-19. Have we strengthened epidemiological monitoring through the best possible use of new technologies? What could be improved?
COVID-19 was a catalyst for open-source and real-time data sharing/tracking, both for epidemiological monitoring and other multicenter collaborations. In the postpandemic era, there is continued interest in digital technologies and accelerated innovation. We should sustain this momentum by building global informatics infrastructure and scalable public-private partnerships for data-driven and evidence-based medicine. Unfortunately, large-scale implementation will be hindered by corporate interests, political considerations, and socioeconomic disparities. From a logistical standpoint, many centers are moving toward training on-premise resources (edge
computing) on “small and wide” datasets that represent the local population, but are still diverse enough to provide viable AI solutions.
9. What changes in digital health solutions could we expect this year?
Several digital health technologies and tools are predicted for 2023. On the clinical side, we have increased consumerization with mobile options for preventative health, remote patient monitoring, and virtual doctor appointments. There is particular interest in elevating services for mental health, women’s health, and rural health. AI tools are improving physician workflow at multiple levels with clinic scheduling, patient prioritization, entering notes and orders, clinical decision support, and business analytics. In research, we are seeing the emergence of decentralized clinical trials to facilitate patient recruitment

Clinical and at-home healthcare will be enhanced by new tools. Digital tools will assist companies, payers, and providers in reaching underserved populations in ways that close care gaps
and access with digital tracking and reporting. Recent studies are utilizing digital biomarkers of disease (real-time tracking and radiologic data) and leveraging strategies to accelerate the drug development life cycle. Digital technologies can also provide feedback to assist patients with monitoring, rehabilitation, and behavioral therapies. Finally, bioinformatics tools are increasing our ability to mine large datasets for clinically relevant information and integrate disparate sources of information to guide patient diagnosis and management.
10. What is your key message to healthcare companies and device manufacturers regarding digital health solutions?
As I mentioned, most MedTech startups do not appreciate the challenges of real-world patient care and operationalization. I would exhort companies not to aim only for the low-hanging fruit, or seek to reinvent the wheel with variations on ideas that aren’t
truly helpful (and may actually do harm to patients). Don’t be afraid to invest in higherrisk and clinically meaningful questions, as long as you have robust clinical partners. Vendors need to engage actively practicing physicians who know the field and understand real-world problems. This can be accomplished by attending professional meetings, developing organic relationships, soliciting feedback, and respecting the input of expert consultants. Finally, clinicians are incredibly busy, and their first responsibility is to their patients. For any hospital collaboration, there will be wide-ranging legal and ethical considerations to be addressed with regard to training AI algorithms and sharing protected health information. Therefore, we need to target patient-centric models that provide optimal patient experience and value-based care.
11. What do you anticipate for your university operationally and tactically in 2023?
Like many universities, we have undergone major leadership transitions and challenges with finances and staffing shortages during the pandemic. Currently, the strategic focus is on building informatics infrastructure to streamline innovation and collaboration.
Robust information technology pipelines are central to advancing clinical excellence and research initiatives in neuroscience, oncology, and cardiovascular care. A major initiative aims to link our adult and pediatric electronic health records (EHRs), thus improving continuity
of care across the lifespan. Our university is also a world leader in digital pathology and genomics, which could be integrated with the EHR and other medical imaging databases (radiology, cardiology, gastroenterology) within a common vendor neutral archive (VNA) to enable precision health approaches.
12. Why does working in radiology continue to motivate you?
Radiology is an incredibly intellectual specialty—we touch almost every patient in the hospital, noninvasively image a wide range of pathologies, and serve as consultants to various physicians and scientists. As a result, we are constantly learning and adapting to new advances in imaging technology, clinical care, and data science. I truly enjoy working at the interface of multiple areas within science, engineering, and medicine. By participating on both the clinical and research sides, I can contribute to “bench-to-bedside” translation at multiple levels.
13. What kind of advice would you offer the next generation of female leaders? What do you believe is the most important factor they should consider if they want to progress in their careers?
Women have been held back professionally throughout history, but the outlook continues to improve. In light of recent social justice movements and elevated interest in workplace diversity, there is no time like the present to build on the advances of our forebears. To
quote Eleanor Roosevelt, “The world of the future is in our making. Tomorrow is now.” Self-knowledge is critical: reflect deeply on what you want out of life, and actively pursue your unique goals, rather than passively letting society decide your path for you. Seek out good role models, mentors, and sponsors early in your career—both supportive women and male allies—and commit to serving in that role for others. Finally, resilience is key; there is no success without failure. Over the course of your career, you will inevitably encounter both personal and professional setbacks, and how you respond to those makes you stronger.
Mai-Lan Ho is a Professor of Radiology and an international physician leader, scientist, and educator specializing in advanced imaging and precision health. She studied engineering at Stanford/MIT, medicine at Washington University, radiology at BIDMC/ Harvard, and neuroradiology at UCSF. Her books include Neuroradiology Signs, The AAWR Pocket Mentor, and Pediatric Neuroimaging: State-of-the-Art.

Precision medicine is the practice of tailoring medical management to each patient's unique traits - genetics, lifestyle, environment, and medical history.
Over the last decade, the field of precision medicine has grown in tandem with advances in genetic research, data analytics, and cognitive computing in the health information technology sector.

Smruti Desai, MBBS
Division of Advanced Heart Failure and Transplant, Mayo Clinic
Smit Paghdar
MBBS Division of Advanced Heart Failure and Transplant, Mayo Clinic
Rohan M. Goswami*
MD, Director of Heart Transplant Innovation and Research, Mayo Clinic
Precision medicine is a new method of preventing and treating disease that considers the individual characteristics of each patient, such as their genetics, lifestyle, environment, and medical history. As described by the President's Council of Advisors on Science and Technology: "[...] the tailoring of medical treatment to the individual characteristics of each patient, the ability to classify individuals into subpopulations that differ in their susceptibility to a particular disease or their response to a specific treatment […]". With this approach, medical professionals and researchers can predict more accurately which disease-specific treatments
and preventative measures will benefit specific populations, potentially sparing expenses and side effects.
Precision medicine comprises healthcare providers, patients, laboratories, and researchers. They collaborate to form a healthcare delivery model that strongly relies on a combination of patient data, specific analysis, and multifactorial research to prevent and treat diseases. Collections of genomic data from biospecimens create a strong ecosystem that may aid in disseminating information to other healthcare specialties.
Even though "precision medicine" is relatively new, the idea has long been present in healthcare, initially focusing on cancer and pharmacotherapy from its inception in the early 2000s to its explosion recently with the progression of data analytic techniques and
artificial intelligence. The use of precision medicine in day-to-day clinical practice is limited, but it will spread to a wide range of health and healthcare in the coming years.
Precision medicine has several uses that benefit patient care throughout their lifetime. Next-generation sequencing allows for rapid and accurate analysis of an individual's genetic code. This information can then be used to identify specific genetic mutations or variations that may influence a person's risk of developing certain diseases and their response to different treatments. In the current era, genetic screening is utilized before pregnancy to determine the likelihood of transferring congenital abnormalities to future generations. A pregnant woman can undergo whole genome sequencing of the baby or genetic testing to detect chromosomal abnormalities of the fetus between 8 and 12 weeks of pregnancy. Sequencing at birth can quickly identify severe diseases for which there may be treatable remedies that lower morbidity and death. Early concepts of precision medicine have also been applied with artificial intelligence to study pregnancy and its effect on the cardiovascular system, finding that AI-based electrocardiograms may help predict postpartum heart failure.
The evolution of advanced precision medicine in cardiology has led to the discovery of a broad range of novel biomarkers associated with the progression of cardiovascular disease. These biomarkers may improve risk assessment, decrease cardiovascular

morbidity and mortality, and are important diagnostic tools in clinical practice. For example, ST2 cardiac biomarker (also known as soluble interleukin 1 receptor-like 1 with transmembrane) has been suggested as a potential tool to assess for allograft rejection in heart transplant recipients. Soluble ST2 (sST2) is a biomarker of inflammation and fibrosis. Elevated sST2 levels (35 ng/mL) are linked to worse outcomes in heart failure patients. Troponin T and I molecules have amino acid sequences unique to cardiac tissue, making their assays extremely specific for detecting cardiac tissue injury. While troponin tests have improved in analytical sensitivity and precision over time, they offer a substantial advance in laboratory testing. They will help providers quickly diagnose patients with suspected acute coronary syndromes when appropriately applied.
In patients with advanced heart failure and more acute needs, the field of transplant medicine has grown to incorporate precision medicine to help patients survive longer, fuller lives. Gene expression profiling (GEP) is a key technology that has enabled the development of precision medicine in heart transplantation. GEP has evolved from tissue analysis to blood sample testing.
This information can help providers determine if the transplanted organ is at risk of rejection or if the patient is at risk of developing complications such as future coronary artery disease in the transplanted organ – a unique process that, once it begins, is difficult to control. Temporal monitoring of serial GEP
samples allows providers to optimize medical regimens and other aspects of care – such as diabetic status, lipid management, and optimization of cardiopulmonary rehabilitation. This pluripotent effect of GEP is an example of the broad-reaching implications of using precision medicine.
Precision medicine in heart transplantation is also being applied to selecting donor hearts. Donor hearts that are well-matched to the recipient regarding blood type and tissue compatibility are more likely to be successful. However, genetic differences between the donor and recipient can also play a role in the transplant's success. Gene expression profiling and other molecular techniques can help identify donor hearts that are a good match for the recipient at the genetic level, improving the likelihood of a successful transplant.
Using molecular imaging techniques in diagnostic imaging, such as strain pattern mapping in echocardiography, is a promising method that enables providers to assess the heart muscle's health precisely and repeatedly. Strain pattern mapping can thoroughly evaluate heart muscle function by measuring the strain, or distortion, as it contracts and relaxes. The method builds a map of the strain patterns in the heart muscle by analyzing the echocardiographic images using specialized software. Heart failure, ischemic heart disease, and valvular heart disease are just a few cardiovascular disorders that can be diagnosed and tracked using this data.
For instance, strain pattern mapping can detect early heart muscle alterations in
people more likely to experience adverse cardiovascular events, including heart attacks and heart failure. Providers can intervene with lifestyle changes, medications, or other treatments to avoid or delay the beginning of these events. In using this technique to identify patients with early indications of cardiovascular disease, with the ability to track them over time, both prevention and response are capable –with specificity to the individual patient. A plethora of technology is in the pipeline and continues to be innovated upon. Ultimately,
the future of healthcare is very promising because of advanced precision medicine. We can increase the accuracy of diagnoses, maximize treatment results, and ultimately improve our patients' overall health and well-being by customizing treatments to each patient's particular characteristics. We may anticipate even more fascinating developments in precision medicine as the industry develops innovative technology.
References are available at www.europeanhhm.com
Dr. Desai was born in Gujarat, India, and raised in Troy, Michigan. She is a graduate of the Surat Municipal Institute of Medical Education and Research. She is currently a Research Fellow at the Mayo Clinic in Jacksonville Florida’s Division of Advanced heart failure and Transplantation. She looks forward to a promising career as a cardiologist in the future as she hopes to begin her Residency training in internal medicine in 2023.

Dr. Goswami is a Transplant Cardiologist practicing at Mayo Clinic in Florida. He is a graduate of the American University of the Caribbean School of Medicine and completed his internal medicine residency at Columbia University College of Physicians and Surgeons – Stamford Hospital, a cardiology fellowship at The University of Tennessee Memphis, and a Transplant Fellowship in 2017 at Mayo Clinic in Florida. He has a keen interest in clinically focused artificial intelligence research to improve outcomes in patients with advanced heart failure. He has published articles in the field of both heart transplantation and artificial intelligence, as well as presented at Ai4 in 2020 on the future impact of AI in healthcare and invited lectures at the International Society of Heart and Lung Transplantation in both 2021 and 2022. He looks forward to one day utilizing AI integration to prevent organ failure.

Smit Paghdar, M.B.B.S. is an Advanced Heart Failure and Transplant Cardiology division Research Fellow at the Mayo Clinic in Jacksonville, Florida. Dr. Paghdar was born in Gujarat, India, and received his medical degree from the Surat Municipal Institute of Medical Education and Research (SMIMER). He looks forward to a promising career as a cardiologist in the future as he hopes to begin his Residency training in internal medicine in 2023.


AI is transforming health care, particularly in radiology given the large digital datasets. Neuroradiology applications such as brain MRI dominate the research arena, though clinical translation and validation have been limited. This article reviews the scope of neuroimaging use cases including normal variation, disease, safety, intervention, and workflow optimization.
Artificial intelligence (AI) is a broad and evolving field that develops computer systems to simulate human intelligence in areas such as visual perception, speech recognition, and decision-making. AI is currently transforming society and health care on multiple fronts including robotics, telemedicine, electronic health records, clinical decision support, and outcomes prediction.
A vast array of approaches can be utilized, including statistical machine learning and deep learning with neural networks. The Gartner hype cycle for AI illustrates the timing and trends for different subtypes of AI, from oldest (computer vision) to more recent technologies such as generative AI and neuromorphic computing. (Figure 1)
For each field of medicine, there are many opportunities as well as challenges. Radiology—which uses imaging technology to diagnose and treat disease—is a logical use case with large and diverse digital datasets.
Neuroradiology is one of the most challenging and interesting applications, with the complexities of brain structure and function serving as inspiration for the architecture of modern neural networks.

The workhorse of neuroradiology is magnetic resonance imaging (MRI), which utilizes magnetic fields to measure tissue properties in response to different magnetic pulse sequences. For a neuroradiologist
like me, learning to interpret a brain MRI requires years of training and practice to appreciate the complex variations related to technique, age, and disease. After reviewing each examination, I create a radiology report that contains the details of diagnosis and recommendations for management. In this fashion, radiologists play pivotal roles in the imaging care cycle of every patient. Upstream steps include examination ordering by the
referring clinician, patient scheduling, study protocoling, performance of the scan by a technologist, image generation, and addition to the radiologist worklist. Downstream steps can include image postprocessing to improve detection or diagnosis, secure data transfer to an approved site, and communication with the referring physician or patient.
Neuroimaging is a hot topic in AI radiology
research, accounting for nearly 25% of all publications. However, few ideas actually make it to market, of which the majority are vendor-funded with a paucity of peerreviewed evidence, demonstrable efficacy, and generalizability. Moreover, there is vast heterogeneity in deployment methods, pricing models, and regulatory classes. In other words, the very complexities that

make neuroradiology an attractive area for AI research have profoundly limited its clinical validation and translation. In this article, we will review the literature on potential AI use cases in neuroimaging, from normal age-related variation and disease processes through interventions and life cycle optimization. (Figure 2)
Lifespan: AI algorithms trained on global brain MRI repositories can provide standardized normative templates across the human lifespan with respect to age, sex, and race, corrected for site-specific technical parameters. These results can help quantify normal population variation and developmental stages, as well as improve identification of disease phenotypes with different treatment responses and outcomes.
Perinatal: AI can enhance fetal and neonatal image quality (accelerated scanning, motion correction, denoising); automate postprocessing and segmentation (biometry, volume reconstructions); perform image analysis (disease detection, classification); and provide decision support (outcomes prediction, need for intervention).
Congenital: AI can improve characterization and quantification of complex brain malformations such as callosal hypogenesis, cerebellar hypoplasia, malformations of cortical development, and holoprosencephaly.
Tumor: AI can perform standardized feature extraction (tumor mapping, atlas deformation, metastatic disease burden); enable precision diagnosis (integrated with

histology, grade, molecular information) and therapy (targeted biopsy, radiation, medical treatment); and facilitate decision support (tumor aggressiveness, response to therapy, quality of life, survival). (Figure 3)
White matter: AI can help classify and quantify lesion burden, assess temporal evolution, provide differential diagnosis, and predict functional outcome in white matter disorders.
Epilepsy: AI can provide multimodal correlation and quantitative feature extraction to improve lesion detection and classification; predict patient seizure burden and outcomes; and optimize medical and surgical treatment plans. (Figure 4)
Figure 4: Atlas-based radiomic approach for mapping of epileptogenic lesions in tuberous sclerosis. Red dots represent expert radiologistannotated lesions, while color heat maps represent overall radiomic deviation from normal age-matched controls in each atlas region.

Trauma: AI can evaluate clinical mechanism, grading, and risk scores; determine most appropriate imaging approach; identify acute hemorrhage and fractures; triage types of traumatic brain injury; and predict prognosis and utility of rehabilitation. (Figure 5)
Stroke: AI can assess risk factors and classify stroke subtypes (large vessel, small vessel, venous, perinatal, global hypoxiaischemia); map involved territories and predict progression; evaluate need for/benefits of intervention; and quantify complications (hemorrhage, herniation, hydrocephalus).
Hydrocephalus: AI can help in segmenting enlarged brain ventricles; determining pattern and etiology (obstructive versus communicating); quantifying shape and volume; and detecting temporal changes that require intervention (shunt failure or overshunting).
Safety: AI can aid with “better, faster, safer” imaging via safety modeling, scan
acceleration and denoising, contrast and radiation dose reduction/elimination, and image enhancement or synthesis.
Intervention: AI can assist with pre-procedural (patient selection, planning); peri-procedural (efficiency, quantification, navigation, equipment selection); and postprocedural (patient response, management) steps.
Workflow: AI can be applied to optimize the entire imaging life cycle including ordering, scheduling, protocoling, worklist triage, lesion detection, disease classification, image postprocessing, structured reporting, management recommendations, and communication with the referring clinician.
In conclusion, there is a broad spectrum of potential AI use cases in neuroradiology, each at a different stage of development with unique opportunities and challenges. Widespread adoption and implementation at AI will require global consortia and
public-private partnerships to facilitate big data sharing for training, testing, and validation. Because radiologic data is uniquely noninvasive, longitudinal, and quantifiable,
the use of AI could revolutionize precision medicine approaches when integrated with pathologic, genomic, and clinical information. We are on the cusp of a revolution in digital medicine, where radiologists can serve as technology/innovation drivers and central consultants for an integrated and interconnected model of global health.

References are available at www.europeanhhm.com
Mai-Lan Ho is Professor of Radiology and an international physician leader, scientist, and educator specializing in advanced imaging and precision health. She studied engineering at Stanford/MIT, medicine at Washington University, radiology at BIDMC/Harvard, and neuroradiology at UCSF. Her books include Neuroradiology Signs, The AAWR Pocket Mentor, and Pediatric Neuroimaging: State-of-the-Art.



Several health technology advancements have been made over the centuries, but few have had the broad impact of digital technology. Networking and computer technology have improved, expanding therapy options, and changing how doctors work. Computers in medicine were debated in the 1960s. As technology improved and prices fell, policies and data standards were created to encourage healthcare institutions to use new technologies for medical equipment like diagnostic imaging machines and routine record keeping. Artificial intelligence algorithms analyze medical images to diagnose and treat patients. Image segmentation, object detection, and image registration align multiple images of the same patient taken at different times or modalities.
Imaging for medical X-rays, such as CT, are the most common methods. Imaging technologies are used even more in drug development and imaging research. Focusing on such approaches helps researchers use
AI imaging aids in cancer and heart disease diagnosis, surgical planning, and image-guided procedures. imaging methods in research projects. A CT scan uses an X-ray beam to create a two-dimensional (2D) "slice" of the body. Repeating this process yields many stacked slices that form a complete organ image. Micro-CT imaging can be used in drug development studies to show how a drug affects organ structure. Many applications and research use biomedical signals to identify physiological processes. Common image processing methods improve medical imaging and biological processing. The electrocardiogram (ECG) example shows how bio signals from the heart are collected to display various heart states. ECGs can help doctors start treatment.
Technology advances have had a profound impact on the healthcare business, resulting in better patient outcomes, higher efficiency, and lower prices. Digital medical records, telehealth, smart wearables, machine learning, and blockchain have transformed the delivery of healthcare. Telemedicine has enabled distant utilization of medical facilities, particularly in rural places where access to healthcare is limited (Senbekov
et al., 2020). Wearable technology can track health parameters and remotely monitor patients, enabling early detection of potential health problems. AI has enhanced diagnosis accuracy and tailored possible treatments, while blockchain technology ensures secure and open record-keeping (Reddy et al., 2019). Technology advances have had a profound impact on the healthcare business, resulting in better patient outcomes, higher efficiency, and lower prices. Traditional paper records have been replaced with electronic health records, resulting in greater communication among healthcare practitioners and patient outcomes safety (Vassolo et al., 2021). Healthcare practitioners will keep embracing technology as it advances.



The purpose of this literature review is to provide an overview of the current state of technology in healthcare and its impact on patient care. It aims to identify the various technologies that have been implemented in healthcare and their benefits and limitations, as well as the challenges associated with the integration of technology. It also seeks to identify gaps in existing research and identify areas for further investigation. For example, the review may examine the effectiveness of telemedicine in improving access to healthcare in rural areas and identify areas where further research is needed. It may also explore the potential of artificial intelligence to improve diagnostic accuracy and personalized treatment options.
A literature review on the integration of technology in healthcare is broad, examining the implementation of electronic health records, telemedicine, wearable technology, artificial intelligence, and blockchain. It also explores the benefits and limitations of these technologies in areas such as patient care, healthcare provider communication, data privacy and security, and cost reduction. However, the review has limitations, such as limited availability and quality of the literature, biased toward studies published in English or specific geographic regions, and not capturing the most recent developments in technology in healthcare. Additionally, it may not address the cultural, social, and economic factors that impact the implementation of technology.
Definition:
Health technology, according to the World Health Organization, is the application of scientific knowledge and skill to the development of medical tools, methods, systems, vaccines, and drugs that may improve people's quality of life and solve health issues.
Artificial intelligence (AI), big data, telemedicine, blockchain, and smart devices, among other digital medical technologies, may help make healthcare more affordable, adaptable, and accessible for all, particularly in low-income nations. These technologies have the potential to improve therapeutic treatments, and diagnostics methods, and automate physically demanding occupations. Yet, in the fields of biomedical research and healthcare, AI cannot totally replace humans (Mitchell & Kan, 2019). Finally, there is hope that these technologies will aid in the resolution of crucial issues in healthcare and medical education.
Technology in healthcare has the potential to improve patient outcomes by enhancing diagnosis accuracy, reducing medical errors, and enabling better monitoring of chronic conditions. A study found that telehealth interventions led to improved outcomes in patients with heart failure, reduced hospital readmissions, and improved quality of life (Wake et al., 2020). Technology can also streamline workflows, reduce administrative burdens, and enable better resource allocation, leading to increased efficiency and productivity among healthcare providers. A study conducted in 2017 found that the implementation of electronic health records (EHRs) resulted in increased efficiency and productivity among healthcare providers (Adler-Milstein & Jha, 2017). Additionally, the integration of technology in healthcare has been shown to reduce costs and improve patient satisfaction.
Challenges of implementing technology in healthcare:
Numerous studies have noted difficulties in deploying technology in healthcare, such as the high cost of installing electronic health records (EHRs) and technical knowledge. Adler-Milstein et al. (2017) discovered, for example, that the high cost of deploying electronic health records (EHRs) was a substantial obstacle for many healthcare institutions (Adler-Milstein & Jha, 2017). According to a systematic study and metaanalysis, one of the most significant challenges connected with the introduction of telemedicine in healthcare is resistance to change. To boost patient acceptance, healthcare organizations must engage in solid security protocols for data and include patients in the creation and execution of mHealth technology (Wake et al., 2020). Furthermore, patients, particularly those who were unfamiliar with or had limited access to technology, were frequently apprehensive to employ mHealth devices.

By providing more efficient, precise, and individualized care, technology can greatly improve healthcare quality. EHRs and other digital health tools can let doctors share patient information in real-time, reducing errors and enhancing care coordination. O'Malley et al. (2017) discovered that the adoption of EHRs was associated with greater care quality, including better adherence to clinical standards and better outcomes for patients with chronic conditions. Another technology that can improve healthcare quality is telemedicine, which allows for more accessible and timely care, and personalized medicine, which allows for more precise and individualized treatment programs.
Technology has the potential to enhance the patient experience in healthcare by providing patients with more convenient and accessible care, improving communication and education, and increasing patient engagement and satisfaction. One way this can be done is using patient portals and mobile health (mHealth) applications, which enable patients to access their health information, communicate with providers, and manage their health from anywhere. A study by Gualtieri et al. (2018) found that the use of patient portals and mHealth applications was associated with
Healthcare technology has given medical professionals cuttingedge tools to enhance patient treatment. Doctors can see a full patient history using EHRs and make informed decisions
improved patient engagement and satisfaction (Winter & Davidson, 2022). Virtual reality (VR) and augmented reality (AR) have the potential to provide immersive and interactive educational experiences, and AI can identify patterns and insights that enable providers to deliver more targeted and effective care. A study found that the use of VR and AR was associated with improved patient education and engagement, particularly in the context of surgical procedures and rehabilitation (Dhar et al., 2021).
The use of technology in healthcare has the potential to increase the efficiency of healthcare delivery by streamlining processes, reducing administrative burden, and improving communication and collaboration between providers. Electronic health records (EHRs), telemedicine and AI are prime examples of technology that have been shown to improve
efficiency in healthcare delivery.
A study by Adler-Milstein et al. found that the use of EHRs was associated with increased efficiency in ambulatory care settings (AdlerMilstein & Jha, 2017). A study found that the use of telemedicine was associated with reduced wait times and travel for patients, as well as increased efficiency in primary care practices (Ashwood et al., 2017). Chen et al found that an AI system was able to diagnose skin cancer with a level of accuracy comparable to dermatologists, suggesting the potential for AI to improve the efficiency and accuracy of diagnosis (Chen et al., 2020).
The use of technology in healthcare has the potential to generate cost savings by reducing administrative and operational costs, increasing efficiency, and improving patient outcomes. The use of EHRs, telemedicine, AI, and machine learning are examples of technologies that have been shown to generate cost savings and have the potential to transform the way healthcare is delivered.
Adler-Milstein et al. found that the use of EHRs was associated with lower Medicare spending, suggesting that the implementation of EHRs could lead to significant cost savings in healthcare delivery (Adler-Milstein & Jha, 2017). A study found that the use of telemedicine was associated with reduced healthcare spending and increased costeffectiveness, particularly in rural and underserved areas (Jacob et al., 2020). Lu et
al. (2019) found that the use of an AI system for chest radiograph interpretation resulted in significant cost savings by reducing the need for radiologist interpretation and follow-up tests (Lu et al., 2020).
Resistance to change is a significant challenge in the implementation of technology in healthcare due to a variety of reasons, such as fear of job loss, lack of training, and perceived disruption to workflow. A study found that healthcare providers may resist adopting new technologies due to a lack of awareness and training, perceived disruption, and concerns about job security (Houwink et al., 2020). EHRs are a prime example of technology implementation in healthcare that has faced resistance from healthcare providers and staff due to concerns over loss of productivity and workflow disruption, as well as a lack of training and support (Mitchell & Kan, 2019). To overcome this resistance, healthcare organizations must provide training and support, address job security, and ensure that new technologies are integrated smoothly into existing workflows.
Privacy and security concerns are major challenges with implementing technology in healthcare, as healthcare organizations
increasingly rely on digital technologies to store and exchange sensitive patient data. One area of concern is the use of electronic health records (EHRs) and mobile health (mHealth) technologies, which can pose privacy risks. A study found that healthcare providers expressed concerns about the security of EHRs and the potential for breaches of patient data (Sieck et al., 2018).

To address these concerns, healthcare organizations must implement appropriate safeguards to protect patient privacy and ensure that sensitive patient data remains secure, such as encryption and secure data storage protocols, as well as the implementation of strict access controls and authentication mechanisms to prevent unauthorized data access.
The implementation of technology in healthcare raises several ethical and legal considerations, which can present significant challenges for healthcare organizations. These considerations include issues related to data privacy, informed consent, and the appropriate use of patient data. A study found that healthcare providers and patients may have differing opinions on the use of patient data for research purposes, highlighting the need for clear guidelines and informed consent procedures (Houwink et al., 2020). Additionally, the use of AI and ML in healthcare may be hampered by concerns over data privacy and bias (Senbekov et al., 2020). Healthcare organizations must take appropriate steps to address these concerns,
including the implementation of clear guidelines and informed consent procedures, as well as compliance with relevant regulatory frameworks.
The integration of new technology into existing healthcare systems can present significant challenges for healthcare organizations. A study found that the successful implementation of new technology requires careful planning and coordination across different departments and stakeholders (Nambisan & Nambisan, 2017). Additionally, the need for interoperability between different systems is critical for providing high-quality, coordinated care. Finally, new technology must be aligned with the broader strategic goals of the healthcare
organization. Healthcare organizations must take a holistic approach to technology implementation, considering the needs of all stakeholders and ensuring that the new technology is able to seamlessly integrate with existing systems (Johnson et al., 2021).
Artificial intelligence (AI) is an emerging trend in healthcare technology that has the potential to transform healthcare delivery. AI systems can be used for a wide range of applications, including medical imaging analysis, clinical decision-making, and personalized medicine. A study found that AI-based algorithms were able to accurately diagnose lung cancer from CT scans with a higher accuracy than human radiologists (Gore, 2020). Another area where AI has shown promise is clinical decisionmaking. A study found that an AI-based system was able to accurately predict patient mortality rates and length of hospital stay, providing clinicians with valuable insights for making treatment decisions (Reddy et al., 2019). By analyzing large amounts of patient data AI systems also have the potential to improve personalized medicine by enabling more targeted and precise treatment approaches. However, there are also challenges that must be addressed to ensure the safe and effective use of AI in healthcare. Continued investment in research and development, as well as robust
regulatory frameworks, will be critical for realizing the full potential of AI.
Telemedicine and virtual care are being integrated into healthcare systems to increase efficiency and promote social distancing measures. These solutions can help manage prolonged waiting times and reduce the risk of disease progression, as well as minimize in-person visits and faceto-face contact to reduce the transmission of the virus and protect medical practitioners from infection (Bokolo Anthony Jnr, 2020). However, there are challenges to effective implementation, such as patient privacy, quality of images and video, and difficulty in performing some diagnoses. To implement telemedicine into outpatient practices, steps are recommended, such as using existing systems and platforms, identifying high-risk or urgent patients, deferring nonessential visits until a later time, establishing a pathway for contact and evaluation for urgent patients, and making sure patients are aware of a clear line of communication to minimize emergency department overuse for noncritical issues (Senbekov et al., 2020).
Wearable devices in healthcare are portable electronic devices that can be worn on the body to perceive, record, analyze, regulate, and intervene to maintain health and treat
diseases. They integrate mechanical functions with microelectronics and computing power to achieve real-time, online, accurate, and intelligent detection and analysis of human physiological and pathological information. Wearable devices are characterized by wireless mobility, interactivity, sustainability, simple operation, and wearability (Pevnick et al., 2018). They follow the 4P medical model of preventive, predictive, personalized, and participatory medicine and can play a significant role in advancing precision medicine by enabling the measurement of clinically relevant parameters showing the health status of individuals. Wrist-worn heart rate monitors are commonly used by consumers and can measure heart rates with less than 10% error compared to reference standard devices (Chiang et al., 2021). However, automatic transmission of patient-initiated data to smartphones and remote servers may present challenges as massive volumes of data have not been shown to beneficially inform clinical care.
Blockchain technology is an emerging trend in healthcare technology that has the potential to transform healthcare data management. It is a decentralized and secure ledger system that can be used to store and share healthcare data in a secure and transparent manner. One area where blockchain has shown promise is in healthcare data management, where it can securely store and share patient data with other
healthcare providers. It can also ensure data privacy and security by enabling patients to control their own data and grant permission to healthcare providers to access it. A study found that blockchain-based systems could improve the accuracy and completeness of patient records while ensuring data privacy and security (He et al., 2019). Another area where blockchain has shown promise is in clinical trials. By using blockchain to record clinical trial data securely and transparently, researchers can ensure that trial data is accurate and complete, reducing the risk of errors and fraud (Maslove et al., 2018). Additionally, blockchain can help streamline the clinical trial process by enabling more efficient and transparent data sharing between researchers, sponsors, and regulatory bodies.
A study found that blockchain-based systems could improve the efficiency and transparency of the clinical trial process while reducing the risk of errors and fraud (Mettler, 2016).
Technology and data integration will provide a proactive strategy to preventive health instead of just a reactive treatment approach
3D printing is an emerging technology that has the potential to transform the healthcare industry by enabling the creation of patientspecific implants, prosthetics, and other medical devices. It involves the layer-bylayer printing of materials such as plastic, metal, and even living cells to create complex structures with high precision. 3D printing has shown promise in creating customized implants and prosthetics that are tailored to the unique needs and anatomy of individual patients, leading to better patient outcomes (Chae et al., 2020). It has also shown promise in the creation of complex anatomical models for surgical planning and education, which can help improve surgical outcomes, reduce surgical time, and enhance patient safety. A study found that 3D-printed models could improve surgical outcomes by providing better visualization and understanding of complex anatomical structures (Chae et al., 2020).
The rapid pace of technological advancements in healthcare is paving the way for a future of healthcare delivery that is more efficient, effective, and patient-centered. There are several emerging technologies that have the potential to revolutionize healthcare delivery, such as telemedicine, wearables and sensors, and AI. Telemedicine can help improve access to healthcare, reduce healthcare costs, and enhance patient satisfaction (Senbekov et al., 2020). Wearables and sensors can track patient health data, and AI can help healthcare providers make more accurate diagnoses, develop personalized treatment plans, and improve care coordination. A study found that wearables and sensors could improve patient outcomes and reduce healthcare costs by enabling early intervention and proactive care management (Winter & Davidson, 2022). A study found that AI could improve healthcare delivery by reducing diagnostic errors, enhancing efficiency, and improving patient outcomes (Hosny et al., 2018). However, there are also challenges that must be addressed, such as data privacy and security concerns, regulatory frameworks, and workforce training.
The future of healthcare technology presents both challenges and opportunities. To ensure that these emerging technologies

are accessible and affordable for all patients, reimbursement policies, regulatory frameworks, and infrastructure development must be addressed. To reduce healthcare costs and improve efficiency, healthcare providers can use AI, telemedicine, and wearables to streamline processes, reduce administrative burdens, and improve care coordination (Cappon et al., 2019). A study found that the adoption of telemedicine could result in significant cost savings for healthcare organizations (Li et al., 2020). To improve patient engagement and empowerment, these technologies can help improve patient outcomes and satisfaction.
To address these challenges and leverage these opportunities, continued investment in research and development, a collaboration between stakeholders, and a commitment to ensuring that these technologies are accessible, affordable, and secure for all patients.
As healthcare technology continues to evolve, policymakers will play a critical role in shaping its future. One key policy implication is the need to develop regulations and guidelines to ensure that these technologies are safe, effective, and accessible for all patients. A study highlights the need for a comprehensive regulatory framework that balances innovation with patient safety and data privacy (Vassolo et al., 2021). To address the digital divide, policymakers can promote initiatives to expand broadband access, improve digital
literacy, and increase access to telemedicine and other remote monitoring technologies. Additionally, policymakers must address the ethical and legal implications of these emerging technologies, such as data privacy, informed consent, and liability. A study highlights the need for clear guidelines on the use of AI in healthcare, particularly with respect to issues such as bias, transparency, and accountability (Davenport & Kalakota, 2019).
Healthcare technology has come a long way in the past decade, with medical devices becoming more advanced and sophisticated, telemedicine enabling remote medical care, and electronic health records improving patient safety. However, there are still challenges to address, such as interoperability, data security and privacy, and the need to integrate technology seamlessly into clinical workflows. To address these challenges, a research agenda is proposed to develop standards for interoperability, ensure data security, develop reliable AI algorithms, and engage patients in their care. Interoperability is a top priority, as it enables different systems to exchange data seamlessly, resulting in better-coordinated care and improved patient outcomes. Data security and privacy is another critical area for future research, as healthcare technology must ensure that patient data is protected, and patient privacy is respected.
AI algorithms are essential for improving diagnostic accuracy and predicting patient
outcomes. Telemedicine has the potential to reduce healthcare costs and improve access to care, and patient engagement is critical for improving patient outcomes. Future research should focus on developing technologies that can engage patients in care and improve their health literacy.
In conclusion, healthcare technology has come a long way in the past decade and has the potential to revolutionize the way healthcare is provided. Medical devices, telemedicine, electronic health records, health information exchange, and artificial intelligence have all contributed to improving patient outcomes and enhancing the quality of care provided. However, challenges remain, such as interoperability, data security and privacy, and integrating technology seamlessly into clinical workflows.
To address these challenges and advance the field further, a research agenda is proposed. This agenda includes developing standards for interoperability, ensuring data security and privacy, developing reliable AI algorithms, enhancing telemedicine, and engaging patients in their care. By focusing on these areas, healthcare technology can continue to improve patient outcomes and enhance the quality of care provided.
References are available at www.europeanhhm.com
Harshal A. Sanghvi is currently a Research and Development Specialist at Advanced Research and a Doctoral Candidate at Florida Atlantic University, USA. Harshal also serves as a Program Chair for Institute for Certified Computing Professionals (ICCP), USA. He currently has NSF I Corps and Seed Grants and he is leading them. He has a Masters in IT-IMS, a PG Diploma in Finance Management, and a Bachelors in Electronics. His research includes Augmented and Mixed Reality, Medical Imaging and Interventions, Internet of Things, Artificial Intelligence, Embedded System Design. He is also a Startup India Board Member at several universities across India and has delivered over 150 sessions on Technology and Entrepreneurship.

Dr. Gauri Parvathy is a medical graduate from Tbilisi State Medical University. She is very passionate about investigating the intersection of healthcare and technology and is very eager to learn about the latest updates and trends related to the use of technology in healthcare systems. Her research interests include the intersection of healthcare and technology.

Periodic health examinations (PHE) are a critical step in disease screening and prevention. However, most people and non-primary care professionals can only list some appropriate investigations. Selfassessment with common information in the Personal Health Records (PHR) application plus advanced medical logic is one solution to getting a comprehensive PHE item.
Piyanun Yenjit Founder and Managing Director APUK Co Ltd.Disease screening is the process of identifying high-risk patients with specific diseases from the general population. This process for an asymptomatic population differs from early diagnosis, which is suitable for patients with symptoms. Cancer represents a good example to show the several benefits of screening. Here are some examples:
• Reduction in the incidence and mortality of colorectal cancer.
• Less aggressive treatment, e.g., chemotherapy for breast cancer.
• Early-stage treatment also reduces overall healthcare budget spending, according to the health economic perspective. However, the disease screening programme is not without risk. The most common adverse events resulting from inappropriate screening are false positive and false negative results, over diagnosis, and overtreatment.
• False-positive screening results often lead to unnecessary additional investigation and complication. Aside from that, psychological
effects such as depression and anxiety may be discovered. In the healthcare system's management view, this unnecessary intervention may impact other patients' waiting times.
• False negative screening results also lead to delayed diagnosis and treatment. This error may bring liability and reputational risk to the healthcare provider.
• Overdiagnosis and overtreatment: true positive results may not benefit. There are some diseases in which early and late detection make no difference in treatment outcomes. For example, a disease with slow progress.
A Recommends, net benefit is substantial
B Recommends, net benefit is moderate
To avoid the above events, selecting screening tests for patients based on evidencebased medicine is essential. Among standard references, the U.S. Preventive Services Task Force (USPSTF) is a reliable and easy-to-use resource for primary care physicians and nurses.
The USPSTF is an independent volunteer panel of national experts in preventive and evidence-based medicine. The Task Force works to improve the health of people nationwide by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications. Task Force members come
C Selective offering this service to individual patients

D Recommends against the service
I Current evidence is insufficient
from the fields of preventive medicine and primary care. The Task Force assigns each recommendation a letter grade based on the strength of the evidence and the balance of benefits and harms of a preven tive service.
(Table 1)
Although disease screening references are already in place, according to the author's survey of doctors and nurses from one of Newsweek's top 250 world's best hospitals in 2022 with more than ten years of experience in the primary care setting and a screening package that was conducted in February 2023, it shows that all patients were suggested to take at least one unnecessary screening test. Electrocardiograms and tumor markers are the most common unnecessary screening tests.
• Ovarian cancer: The guideline recommends against screening for ovarian cancer in asymptomatic women. This recommendation applies to asymptomatic women who are not known to have a high-risk hereditary cancer syndrome. (Grade D)
• Cardiovascular disease: recommends against screening with resting or exercise electrocardiography (ECG) to prevent cardiovascular disease (CVD) events in asymptomatic adults at low risk of CVD events. (Grade D)
Moreover, the majority of them didn't receive complete guidance on the best screening tests or appropriate screening tests. The five investigations listed below are prioritized in the 55-year-old population based on disease severity and frequency of neglect.
• Osteoporosis: recommends screening for osteoporosis with bone measurement testing to prevent osteoporotic fractures in postmenopausal women younger than 65 years who are at increased risk of osteoporosis, as determined by a formal clinical risk assessment tool. (Grade B)
• Colorectal cancer screening is recommended for all adults aged 50 to 75 (Grade A).
• Breast cancer screening mammography every two years for women aged 50 to 74 years (Grade B).
• Cervical cancer screening is recommended every 3 years for women aged 30 to 65 years, every 5 years for high-risk human papillomavirus (hrHPV) testing alone, or every 5 years for hrHPV testing in combination with cytology (co-testing) (Grade A).
• Lung cancer: The CDC recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 50 to 80 years who have a 20-pack-year smoking history and who currently smoke or have quit within the past 15 years. (Grade B)
Attitude: Most screening staff suggest screening tests based on age and gender. Only a small portion of the information from the assessment form—which asks about the underlying disease, family history, and lifestyle risk—is used in the analysis. These data are also used to evaluate in some cases. Still, it depends on the screening staff’s experience. Patients
usually focus on non-invasive off-label cancer screening investigations, e.g., carcinoembryonic antigen (CEA), alpha-fetoprotein (AFP), etc. Osteoporosis is also overlooked because of the low level of concern in the general population.

History-taking limitation: As screening is a general health approach, it requires a multidimensional history, including a sexual and some health risk history, e.g., illicit drug use. This data is confidential and will take some time to gather and consolidate. The short period of assessment time and taking the assessment
in a non-private area are the key barriers to getting a complete history.
Complexity and variation of screening standards: an indication for some screening tests is not straightforward. Also, there are several steps in the analysis required to get the recommendation. For example, the number of cigarettes smoked per year is required for lung cancer screening recommendations.
Financial concern: Although colon cancer screening is clearly recommended for adults aged 50–75, some populations may still be prevented from getting the necessary screenings because they lack full financial coverage.
Test preparation: Some tests require more preparation and more time. For example, a half-day is required for bowel preparation before a colonoscopy.
Solutions: Giving the patient more time to fill out the data in a suitable format in a private area with a standard medical analysis by an experienced assessor appears to be the best approach to obtaining a screening test list. Unfortunately, this ideal solution requires a lot of resources, especially investments in healthcare staff allocation and training.
Currently, there are many personal health records (PHR) applications or other applications that a user can use to enter necessary personal and medical data for screening test analysis. For example, in health insurance-related applications the required data standard, completeness, and input method
are the key challenges for data input. Moreover, there is still room for improvement in terms of analytics features and healthcare provider connectivity. After reviewing 5 personal health record apps with ratings higher than 4 stars in the App Store as of February 23, it was discovered that in all apps, a user is able to input the majority of the necessary data to analyze a personalized screening test. Therefore, comprehensive data input in a comfortable environment (without rushing and in private) is no longer a concerning issue.
The medical standard microservice is one solution that can be used to analyze screening tests and connect to healthcare providers. Although free-text input is also more useful via the Natural Language Processing (NLP) microservice, Simplemedlogic (SML) is a sample of self-assessment that includes effective medical analysis. Also, even though SML has not yet been connected to any PHR
or healthcare provider, it has demonstrated the ability to connect via API, as shown in Figure 1.

Screening tests provide strong benefits to the general population and the healthcare system. A medical guideline is already in place to prevent adverse events like false negatives and overdiagnosis, but there are some implementation barriers, such as healthcare workers' attitudes, the complexity of the guidelines, and the limitations of a historytaking environment. To achieve excellent disease screening, a complete history review and advanced medical analysis are the key actions. While PHR is used for data input, medical microservice plug-ins can also be the solution for better analysis. This combination will make health screening more complete and affordable.
Hosting Promotions Lead Generation
Engage people to your business Gain Market Confidence Be an Authority
Use
Grow your audience with increased reach, impact and user-friendliness
Rise above geographical boundaries
Generate new business
Gain the strong web presence differentiating yourself from competitors
Connect and engage with your target audience

Give more exposure to industry specific people
Increase your brand profile and share your capabilities with leading industry professionals

Over the past several decades, pathologists and clinicians have evaluated tumors using several data modalities such as Radiology/Imaging, Pathology, Genomics and Drug Discovery. These have been correlated with each other either manually or using sophisticated statistical approaches. Artificially Intelligent (AI) models trained on radiographic or histopathologybased images have been known to predict status of tumors (i.e., whether it’s benign or cancerous). AI models have also been trained on radiographic image features to predict gene expressions in cancer. Further, all the aforementioned modalities (or features from them) could be stitched together into an AI model to predict patient outcomes in cancer.
Shrey S Sukhadia Assistant Director, Bioinformatics, Department of Pathology and Laboratory Medicine, Dartmouth-Hitchcock Medical CenterThe screening of cancer patients in the clinic encompasses various data modalities, including imaging using radiological techniques that include computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography followed by a surgical biopsy of the tumor region of interest (ROI) as segmented by radiologists on these images using software such as 3dSlicer, ITK-SNAP and Myrian Studio. The biopsied tumor material, also termed as “specimen” is examined by a pathologist for its shape, size and other physical features. The specimen is then cut into thin slices, i.e., “histological sections” that are fixed on a glass slide using paraffin-formalin, followed by their staining using hematoxylin that aids visualization of several components of the underlying cells, such as cell nuclei and ribosomes, under a microscope. This setup allows pathologists to analyze and mark several cellular or protein markers present in the specimen. Further, these slides are sent to a genomics laboratory to scrape off the tumor material that is processed further to extract and purify Deoxyribonucleic acid (DNA) and Ribonucleic acid (RNA). The DNA and RNA undergo several procedures in the laboratory to ultimately prepare high quality libraries that undergo sequencing using either short or long read sequencers such as Illumina’s Novaseq or Pacbio’s Sequel II, respectively that allude DNA-mutations and RNA-expression in the specimen using sophisticated bioinformatics techniques. These DNA-mutations and
RNA-expression are interpreted further by genomic experts and reported to the clinician who ordered genomic test for the tumor specimen of the respective patient.
Based on the results from Radiology, Histopathology and genomics, a treatment regime is determined for the patient at a tumor board, where all clinicians and pathologists discuss patient cases and arrive at a consensus for their treatment plan. This may include one or several therapies such as Radiation, Chemotherapy, Drugs targeted to specific genes/proteins or an Immunotherapy. Post the completion of these therapies, a patient’s tumor

Cancer detection algorithms are a great way to spot mutations and abnormal cell division at the very beginning of cancer. Early cancer detection plays a crucial role in the battle against cancer and saves lives
is re-examined at either radiology/imaging or histopathology or both, to deem whether the tumor had undergone a size-reduction or remained unaffected by the therapy.
AI models could encompass results from each of the aforementioned techniques (or tests) and help predict one result from a set of others, or predict the therapy outcomes or chances of disease recurrence in patients from all of their test-results stitched together into a well-validated model. AI could be categorized mainly into two techniques: a) Machine Learning (ML), and b) Deep Learning (DL). Machine learning works well with the quantitative features/results extracted from the aforementioned techniques, while deep learning could intake high dimensional images from Radiology or Microscopic-scanning of specimen slides from histopathology to identify several image patterns in an automated way
and inform diagnosis. ML enables analysis of feature-associations across multiple datamodalities more granularly as compared to DL. ML models encompass the regression- or classification-based supervised models that could be trained and validated to predict either gene or protein expression in tumors from their radiological image-features, or predict therapy-response or disease-recurrence in patients using a combination of features (or results) from radiological, pathological and genomic examination of their tumors and the respective treatments administered. Whereas DL models include the unsupervised neural networks that self-learn the patterns from radiological or pathological images or genomic result-matrix to predict the status of tumors (i.e., whether its cancerous or benign) or a response to their treatment for the respective patients.

The application of AI models requires adoption of robust software, one of which recently released and named “ImaGene” (Figure 1) (https://doi.org/10.1093/bioadv/ vbac079). Such software allows researchers to train models on tumor specific features/results from aforementioned techniques/tests using a variety of ML model-types such as MultiTask Linear Regression/LASSO, Decision Trees, Random Forest, Support Vector Classifier and Multi-Layer Perceptron Classifier (aka supervised neural networks) to predict gene expressions (or any omics outcomes) from radiology image features.

Deep learning algorithms primarily include four types: a) Feed-Forward, where every neuron of layer “j” connects with the neuron of
layer “j+1” with the information-flow direction set to be “forward”,
b) Convolutional Neural Network (CNN) where weighted sums are calculated at each neuron for the data positions,
c) Recurrent Neural Network (RNN), used for processing of sequential or time-series data and
d) Autoencoder, which conducts non-linear dimensionality reduction.
Breast tumor MRIs had been recently tested through deep learning algorithms to predict whether the tumors were benign, which would ultimately help reduce unnecessary and painful biopsies in patients to deem the status of tumor, i.e. cancerous or benign (https:// www.science.org/doi/10.1126/scitranslmed. abo4802 ). Deep Learning approaches have also been applied in histopathology domain to
train for instance hematoxylin-eosin-stained breast cancer microscopy images to predict whether the respective tissue is benign or cancerous (https://doi.org/10.1038/s41598022-19278-2).
The Cancer Imaging Archive (TCIA) portal hosts radiology imaging and omic datasets from multiple studies in cancer conducted either at The Cancer Genome Atlas (TCGA) or by a specific research group such as Non-Small Cell Lung Cancer (NSCLC) Radiogenomics

(Figure 2). TCIA also hosts the supporting clinical data for the specimens enabling the AI-based imaging-omic research. TCIA hosts data from several groups such as: a) Cancer Moonshot Biobank (CMB), b) Applied proteogenomics Organizational Learning and
Outcomes (APOLLO) and c) Clinical Proteomic Tumor Analysis Consortium (CPTAC). All these groups together provide terabytes of data that could be trained through AI models to predict patient outcomes in cancer near future.
In a nutshell, AI aids clinicians and pathologists with the prediction of the status of tumors in patients using either their radiographic or histopathological images or both together. AI-based models pave the way for researchers to predict omic-based features for tumors from their imaging features. Further, AI-based techniques enable stitching of features from imaging and omic modalities to predict therapy-outcome or disease-recurrence in cancer patients. Publicly available software such as “ImaGene” and data sources such as TCIA and TCGA enable the build and validation of AI models in imagingomic domain. Cross-validation of AI models on patient-data across various hospitals or research organizations would boost their accuracy in predicting patient outcomes in cancer and contribute to advance the field of cancer-diagnosis and research. AUTHOR
Shrey Sukhadia has been leading Bioinformatics efforts since 12 years at clinical laboratories in top tier hospitals in United States, such as Dartmouth-Health, Phoenix Children’s Hospital and Hospital of the University of Pennsylvania. Through his PhD at Queensland University of Technology in Australia, he has developed a robust AI-based software platform “ImaGene” that facilitates the build and validation of several AI models for the prediction of omics data such as genomic, proteomic, patient/therapy outcomes or disease recurrences from the imaging or multi-omics (i.e., imaging features mixed with any omics feature) datasets.


Telemedicine has the potential to provide accessible and equitable healthcare. The use of telemedicine has accelerated after the COVID19 pandemic, especially in the field of cardiology. Our article explores the applications of telemedicine for patients with heart failure, including remote monitoring and consultation, and the benefits and limitations of telemedicine.
Smruti Desai
MBBS,
Division of Advanced Heart Failure and Transplant, Mayo ClinicSmit Paghdar
MBBS Division of Advanced Heart Failure and Transplant, Mayo Clinic
Rohan M. Goswami* MD, Director of Heart Transplant Innovation and Research, Mayo ClinicRemote healthcare and telemedicine utilize various information technology to provide healthcare services remotely between a patient and provider when both parties are distant. These services expanded rapidly during the beginning of the COVID–19 pandemic and remain a crucial part of healthcare delivery today. Before March 2020, telemedicine was used periodically, with approximately 76% of the United States hospital healthcare systems employing
remote healthcare delivery on a case-by-case basis. Although numerous specialties utilize these modalities, Cardiology, Radiology, and Psychiatry use remote healthcare and telemedicine most frequently.
The COVID-19 pandemic has highlighted the need for alternative approaches to care delivery for patients with advanced heart failure, including telemedicine. Heart failure is a chronic condition characterized by the inability of the heart to pump enough blood to meet the body's needs, leading to symptoms such as shortness of breath, fatigue, and leg swelling. This condition affects millions and often leads to recurrent exacerbations and hospitalizations. Traditional management of heart failure involves regular visits to a healthcare provider, medication management, and lifestyle modifications. However, patient non-compliance with guideline-directed medical therapy (Figure 1) and failure to optimize hemodynamics can lead to poor patient outcomes.
Telemedicine can also facilitate communication between patients and healthcare providers, exchanging important information and allowing for adjustments to treatment plans as needed. As a result, providers have been increasingly using telehealth services to care for patients with cardiovascular disorders. Remote monitoring of heart failure patients can improve diagnosis and treatment accuracy and timeliness.
In managing heart failure, telemedicine has several applications. Remote monitoring
involves using wearable devices or homebased monitoring systems to collect realtime data on a patient's vital signs (e.g., blood pressure, heart rate, heart rhythm) and other physiological parameters. This information is then transmitted to a healthcare provider, which allows healthcare providers to monitor patients remotely and collect data without requiring them to visit a physical medicine facility. For example, CardioMEMS (Abbott, GA) is a wireless monitoring system implanted in a patient's pulmonary artery to measure pulmonary artery pressure in patients with heart failure. Healthcare professionals can remotely monitor the readings and modify treatment plans, with published data showing decreased hospital readmission rates. Similarly, implantable cardioverterdefibrillators (ICD) can remotely monitor the device's function and detect abnormal heart rhythms, sending reports to monitoring providers to intervene. Remote EKG monitoring devices (e.g., LivCor, AliveCor, etc.) are another example of telehealth and telemedicine. This technology allows patients to record ECG (electrocardiogram) tests from their homes using a wearable device connected to their smartphone. Data collected by the device is sent to healthcare providers, who can use it to diagnose abnormalities.
Tele-education involves using technology to provide educational resources to patients with various cardiac conditions, including videos or webinars for self-care strategies. Tele-consultation allows patients to receive
care remotely from a healthcare provider, nutritionist, physical therapist, or nurse coordinator without an in-person visit. In patients with advanced heart failure and many other ailments, remote technologies have aided in connecting with other patients using virtual 'rooms' to discuss their conditions and treatment plans to help support each other through their journey.
Increased utility of remote healthcare services during COVID–19 revealed numerous advantages: controlling the spread of infective illnesses, pre-screening patients before in-person visits, reducing physician burnout, diversifying practice patterns, preventing germ exposure to vulnerable populations (e.g., chronically ill, pregnant, elderly, or immunocompromised), maintenance in the continuity of care, and enhanced the protocolization for data collection and interpretation). Despite the numerous potential advantages, telemedicine does have its limitations. Some significant challenges include patient familiarity with technology, reliability of remote technology, healthcare data breaches, and absence of physical

examination. Furthermore, lacking human touch limits the patient-provider connection, which could be a potential cause for unearthing mental health issues and a greater need for future counseling.
Currently, there is a lack of standardization across telemedicine platforms, making it difficult for healthcare providers to use multiple systems and for patients' participation.
Regional variations in telemedicine regulations make them challenging to understand and may increase providers' complexity in adhering to telemedicine regulations. Furthermore, some telemedicine solutions could be insecure, and providers may be concerned that patient privacy cannot be maintained. Telemedicine use can also be made more difficult by a lack of compatibility with electronic health record systems. Telemedicine technology and equipment rely entirely on hardware and software, requiring extra support and training for employees or caregivers. To tackle some of these hurdles, low cost of equipment setup, redundant patient safety features, and
standardization of electronic health records may increase the utilization of telehealth and telemedicine.
The outlook for telemedicine in healthcare is positive. With the proliferation of wearable technologies and the increasing adoption of electronic medical records, telemedicine will continue to play a significant role in managing cardiovascular conditions. As more providers utilize remote healthcare technologies, increasing adoption into other specialties may offer a new method for delivering equitable healthcare to patients in need.
References are available at www.europeanhhm.com
Dr.Desai was born in Gujarat, India, and raised in Troy, Michigan. She is a graduate of the Surat Municipal Institute of Medical Education and Research. She is currently a Research Fellow at the Mayo Clinic in Jacksonville Florida’s Division of Advanced heart failure and Transplantation. She looks forward to a promising career as a cardiologist in the future as she hopes to begin her Residency training in internal medicine in 2023.

Dr.Goswami is a Transplant Cardiologist practicing at Mayo Clinic in Florida. He is a graduate of the American University of the Caribbean School of Medicine and completed his internal medicine residency at Columbia University College of Physicians and Surgeons – Stamford Hospital, a cardiology fellowship at The University of Tennessee Memphis, and a Transplant Fellowship in 2017 at Mayo Clinic in Florida. He has a keen interest in clinically focused artificial intelligence research to improve outcomes in patients with advanced heart failure. He has published articles in the field of both heart transplantation and artificial intelligence, as well as presented at Ai4 in 2020 on the future impact of AI in healthcare and invited lectures at the International Society of Heart and Lung Transplantation in both 2021 and 2022. He looks forward to one day utilizing AI integration to prevent organ failure.

Smit Paghdar, M.B.B.S. is an Advanced Heart Failure and Transplant Cardiology division Research Fellow at the Mayo Clinic in Jacksonville, Florida. Dr. Paghdar was born in Gujarat, India, and received his medical degree from the Surat Municipal Institute of Medical Education and Research (SMIMER). He looks forward to a promising career as a cardiologist in the future as he hopes to begin his Residency training in internal medicine in 2023.




The healthcare sector has seen a massive explosion in the amount of data, healthcare applications, and algorithms. In this introduction article we will discuss how the Big Data revolution can benefit the healthcare sector.

The global healthcare sector is facing various challenges, fueled by the worldwide demographic trend of aging populations. In 2050, over 2.1 billion people will be over the age of 60, and by 2100, this number will rise to over 3.1 billion.
Simon Waslander Director of Collaboration, Clinical Research, CureDAOSource: United Nations.
These trends are putting enormous strain on global healthcare systems, especially in socialized universal coverage systems such as those seen in Europe. OECD data show that healthcare spending has been rising faster than economic growth as measured by GDP for decades.

Source: Healthcare spending as a percentage of GDP in 31 OECD countries.
Note: Source: OECD health data, 2010.
This trend of ever-rising costs and an aging demographic tsunami can be seen as an existential threat to universal healthcare systems.
The field of "Big Data" is one of the most exciting prospects for global healthcare stakeholders to implement, therefore there is light at the end of the tunnel in the shape of technical advancement.
The global healthcare sector produces truly staggering amounts of data. In 2013, the global healthcare sector produced 153 exabytes of data; by 2020 this number would have soared to over 2.314 exabytes.
This data can come from all stakeholders in the healthcare industry and from the patients themselves, including smartphones and wearable sensors all the way to detailed patient records and pharmaceutical company research, among many other sources.
The sheer volume of these data sets is mindboggling, to say the least. But what is "Big Data"?
Source: Micron, International Data Corporation, “Harnessing the Power of Data in Health,” Stanford Medicine 2017. Health Trends report, June 2017


Various academic authors (ref 1) have sought to define big data according to their attributes within the industry, better known as the 7 V’s:
• Quantity (which refers to the amount of data)
• Rapidity (the speed with which new data is generated)
Variety of (heterogeneity of data; many different types of healthcare data)
• Flexibility (inconsistency of data)
Veracity (the reliability and calibre of the data); Visualization (ability to interpret data and resulting insights)
• Value (the goal of big data analytics is to find hidden knowledge in massive amounts of data).
Overall, Big Data cannot be analyzed through standard methods; for the analysis and value extraction of such data sets, technically advanced software applications that can utilize fast and cost-efficient high-end computational power are often needed. Also, tools such as deep learning and artificial intelligence can play a crucial facilitative role in this regard.
(Ref 2)
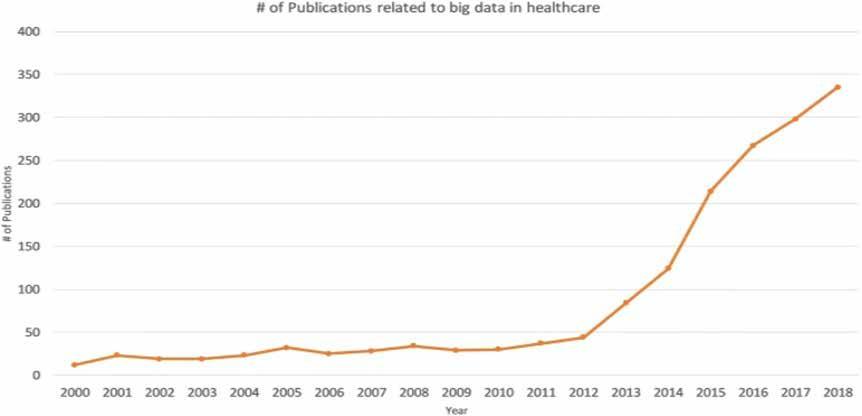
For good reason, there has been an astounding
explosion in academic research on big data. (ref 2)
But what are the potential advantages for the entire healthcare ecosystem arising from big data? A scientific review article by Dash et al. 2019 (ref 2) provides a thorough overview, identifying four key areas where big data will add the most value for healthcare sector stakeholders.
1. Improving the quality of healthcare services
2. Supporting the work of medical personnel
3. Supporting scientific and research activity.
4. Business and management
Improving the quality of healthcare services.
• Medical professionals can receive access to clinical decision support tools that use
Source: Reference 2.
this massive amount of data to help them make better treatment choices.
• Data analysis can elucidate more costeffective personalized treatment modalities.
• Predicting disease occurrence both individually and within large cohorts
Supporting the work of medical personnel.
• use of the "Internet of Things" (IoT) and other sensor technology for live monitoring of a patient
• Risk stratification involves identifying patients most at risk for complications or disease.
• Health management on a societal level
• Personalized medicine, which also uses more advanced IoT sensors and novel “omics” and aging-based clocks, can usher in a period of extremely personalized medicine.
• Predictive analytics involves being able to forecast a potential health event before it occurs.
• Supporting work and research in the creation of novel pharmaceutical agents.
• Personalized clinical trials
• Being able to predict the severity of a novel agent's side effects before it is administered to a person
• Use Predictive Analytics for better drug design.
Business and management.
• Creating overviews and monitoring dashboards for managers
• Detection of organizational inefficiencies.
• Predictive analytics for an organization such as future workflows, occupancy rates, and use of certain pharmaceuticals
At the moment massive amounts of personal health data are being created and stored. This includes data from classic sources such as medical health records, pharmacy documents and clinical trial data. But a huge amount of data is also being created from novel applications such as trackers of diet, exercise, sleep and many more factors.
Sadly, this massive aggregate amount of data is being stored in individual highly private siloes.
To truly revolutionize the healthcare sector, data from various different sources including:
• Pharmaceutical companies
• Individuals
• Web Development/App companies
• Disease Advocacy Groups
• Digital Health Businesses
• Governments Should be anonymized and aggregated in a global digital healthcare data marketplace. In this respect blockchain technology and unique NFT creation are key enablers of this possibility to create a global open marketplace for medical data.
The advantages for the healthcare sector in aggregate but especially per user are massive indeed. Here we name a few benefits for key stakeholders:
• Pharmaceutical companies can reduce their development costs and clinical trial expenses. Also novel off-label uses for existing pharmaceuticals can be discovered at little to no extra development cost.
• Individuals will gain royalties for the data they share, creating tradable value for their data.
• Web developers can reduce their development costs for various applications, making contributing development companies more innovative and competitive.
• Governments can see reductions in aggregate societal-level healthcare costs through novel discoveries facilitated by this data sharing marketplace.
With global healthcare systems under increasing strain, novel, cost-effective solutions are in high demand. The revolution in medical big data and all the innovation surrounding it present large, relatively low-cost solutions that can be implemented by healthcare organizations and professionals.
In the future, for this innovation to become truly radical, data owners such as hospitals, pharmaceutical companies, and individual patients should cooperate to share their data
in an open fashion. Combining various siloed datasets holds unimaginable promise to further accelerate the Big Data revolution.

References are available at www.europeanhhm.com
Simon Waslander is currently part of CureDAO as the Director of Collaboration. Simon specializes in creating multiplicative synergies with a network of academic, private, and government contacts. He has a BSc. in Medicine from the University of Groningen and a MSc. Healthcare Innovation from Maastricht University. He has a deep and keen interest in the biomedical aspects of human longevity. In his professional career, Simon has had tenures at BioViva, Ageless Partner, and AGI Laboratory. He is also an Expert Coach for start-ups in North Netherlands via the VentureLab North start-up community.
The upcoming 10th edition of MEDICAL FAIR THAILAND 2023 will feature a physical trade show from September 13–15 at BITEC, Bangkok, as well as a 7-day online extension from September 16–22.
Messe Düsseldorf Asia (MDA) is the organization behind the 2023 edition of Medical Fair Thailand. With a long history dating back to 2003, the exhibition has become the most reputable international medical and healthcare event and information hub in Southeast Asia.
Medical Fair Thailand 2023 gives you the best business opportunities to navigate the Thai and Southeast Asian markets, with a focus on tools and supplies for the hospital, diagnostic, pharmaceutical, medical, and rehabilitation sectors.
Join us at MEDICAL FAIR ASIA, the leading healthcare event in the region that connects you to a global audience both physically and virtually.

Start making plans for your participation today for the newest in medical technology, innovation, supplies, and solutions!
MEDICAL FAIR THAILAND 2023
Date: Live-in-person – September 13–15, 2023
Online – September 16–22, 2023
Location: BITEC, Bangkok
Website: https://www.medicalfair-thailand.com/



















The healthcare ecosystem consists of those who pay, those who benefit and those who are responsible. New Care Models are helping to align these interests and share capacity across the ecosystem, all enabled by a modern digital infrastructure.
Varian is a Siemens Healthineers company driving progress in cancer care. It is using software and automated processes to help oncology professionals collaborate and develop more precise and holistic cancer treatments, making cancer care easier to manage and deliver.
Kenneth Daniel Tan from Varian explains the importance of network care in Oncology care space which would guarantee standardised clinical decision making protocols like centralised telediagnostic radiology and centralised treatment planning. It also renders the capability to streamline workflows with the treatment providers that would reduce the need for human effort.
The benefits of network care among many are standardised high-quality care, shared knowledge base optimised infrastructure and decreased reliance on human intervention. He further goes into the various network care models and gives insights on their pros and cons.
Designation: President, Asia Pacific & Japan
Organization: Varian Medical Systems
Kenneth Tan is the President of Asia Pacific and Japan at Varian Medical Systems. He joined Varian in January 2017. Varian is a global leader in solutions for advancing cancer treatment; specialising in radiotherapy, radiosurgery, proton therapy, brachytherapy and oncology informatics software.
Kenneth has 20 years of experience in healthcare; having held Commercial leadership roles in Varian, Medtronic, Covidien, Boston Scientific and Novartis. More than 14 years are in the implantable, disposable medical devices, capital equipment and managed services; covering various Global markets and regions in Asia Pacific. He has deep experience in developing and executing strategic growth plans in China, Japan, India, and South-East Asia.
Kenneth has held various leadership roles in Sales, Marketing, Strategy and P&L Management. In recent years, he has built his success around driving complex strategic shifts through organisations; in areas of business strategy and organisational transformation. The hallmarks of his tenure are growth acceleration, businessmodel innovation and a strong leadership team.
Get direct access by scanning the QR Code
Kenneth obtained his BBA from the University of South Australia and a diploma in Biotechnology (Medical Technology) from Singapore Polytechnic.

April 17-21, 2023
Chicago, USA
https://www.himss.org/events/himss23-nordicdelegation
HIMSS offers a unique depth and breadth of expertise in health innovation, public policy, workforce development, research and digital health transformation to advise leaders, stakeholders and influencers across the global health ecosystem on best practices.

Listed Under: Information Technology
International Conference on Surgery & Anesthesia |
France
https://phronesisonline.com/cardiology-congress/ WCCD 2023 will provide the opportunity for a comprehensive overview of the new information on risk factors for different cardiac diseases and breakthrough emerging therapies and technologies.
Listed Under: Medical Sciences
April 24-25, 2023
Zurich, Switzerland
https://heart.euroscicon.com/
Heart 2023 Conferences will be an examination of the newest successions in heart disease recovery and prevention and on new analysis of innovation within the field of cardiac specialty.

April 20-21, 2023
France
https://www.phronesisonline.com/surgeryanesthesia-conference/
ICSA-2023 provide a unique platform to bring together worldwide distinguished academicians in the field of Various Surgeons, Anaesthesiologists, Doctors, Medical Professionals, Surgical tool technicians, Pharmaceutical Industrialists, business professionals, scientists, industry researchers and scholars to exchange about growing research and technologies.
Listed Under: Surgical Speciality
April 20-21, 2023
Listed Under: Medical Sciences
April 27-29, 2023
India
https://www.medicalfair-india.com/
Medical Fair India is to Explore how the latest digital technologies and new approaches shaping healthcare.
Listed Under: Technology, Equipment & Devices
May 16-17, 2023
San Diego, California
https://events.reutersevents.com/healthcare/digitalhealth-usa
Digital Health hosts 300+ digital leaders over two intensive days of learning, idea sharing, collaborating, and networking to help accelerate the transformation that our consumers desire and our care teams deserve.
Topics Covered: Interoperability and Health Data, Automation in healthcare, Change Management, Cybersecurity, Virtual and Remote Care.
Listed Under: Information Technology
Hybrid Event | May 25-26, 2023
Dubai, UAE
https://www.neuralscience.scientexconference. com/
The International Conference on Neuroscience and Neurology welcomes all the ingenious neurologists, neuroscientists, neurosurgeons, psychologists, psychiatrists, and Allied health professionals for developing consensus in contentious areas in Neuroscience and Neurology
Listed Under: Medical Sciences
Hybrid Event | May 25-26, 2023
Dubai, UAE
https://www.neurology.scientexconference.com/ Neurology 2023 is up with an excellent opportunity for Neurological experts in the field of Medicine, Industry, Pharma, Surgery, Teaching, and Learning Practices
Listed Under: Medical Sciences
May 25-26, 2023
Dubai, UAE
https://www.nursingcare.scientexconference.com/
About Event: The conference theme is "Exploring advanced technology practices in Nursing care and Patient safety" with the goal of educating attendees on the most recent challenges in nursing care, illuminating the most recent trends, and analyzing the future of Patient safety and Healthcare science.
Listed Under: Medical Sciences
Hybrid Event | May 18-19, 2023
Dubai, UAE
https://www.cardiology.scientexconference.com/ Cardiology 2023 conference features more compelling presentations in 27 scientific session categories that point up basic, clinical, and translational sciences as they progress toward a better understanding of stroke pathophysiology with the aim of developing more effective remedies
Listed Under: Medical Sciences

July 17-18, 2023
Osaka, Japan
https://www.meetingsint.com/conferences/ cardiology
Cardiololgy 2023 is all about “Exploring New Advanced Researches and Frontiers in Cardiology". The primary point of this gathering is to discover all aspects in the fields of Cardiology like Cardiovascular infections, Pediatric Cardiology, Heart Transplantation, and Interventional cardiology research and in addition to other various subjects.
Listed Under: Medical Sciences


Hybrid Event | May 18-19, 2023
Dubai, UAE
https://www.heartcongress.scientexconference. com/
The Cardiology 2023 Conference provides a stimulating chance for the developing generations engaged in numerous cardiac research projects to advance their expertise in the field of cardiovascular diseases. It will also share scientific knowledge and experience, giving people the chance to learn about various cardiac disorders and cardiovascular treatments.
Listed Under: Medical Sciences
June 21-22, 2023
Paris, France
https://nursingworldcongress.com/
Nursing World 2023 aims to foster and conduct collaborative interdisciplinary research in stateof-the-art methodologies and technologies within Nursing & Advanced Healthcare. It provide invaluable opportunities to extend and strengthen the Nursing and Healthcare community
Listed Under: Healthcare Management
July 20-21, 2023
Florida, USA
https://internalmedicine.euroscicon.com/
The theme of this meeting is “Current Research and Advances in Internal Medicine “where you can get a platform to share your ideas and research work to the world
Listed Under: Medical Sciences
August 16-18, 2023
Bangkok
https://www.medlabasia.com/en/home.html
Medlab Asia and Asia Health, stemming from seven years of success in Singapore, the exhibition now moves to Bangkok, Thailand enabling access to a larger Asian market with new key medical and trade profiles.

Listed Under: Technology, Equipment & Devices
August 23-25, 2023
Philippines
https://www.philmedical.com/
Philippines Medical Technology Expo 2023, is the only specialized medical, dental, pharmaceutical, and laboratory event in the Philippines that brings together an international congregation of Medical & Healthcare, Dental, Pharmaceutical and Laboratory equipment, services, supplies and technology gathered in Manila to showcase the latest developments in the industries.
Listed Under: Technology, Equipment & Devices
September 7-8, 2023
Pennsylvania, America
https://www.terrapinn.com/conference/diseaseprevention-control-summit-america/
The Disease Prevention & Control Summit is more than just an event, it is a chance to partner, learn, connect, and make great strides towards preventing and combating infectious disease outbreaks of today and tomorrow.
Listed Under: Medical Sciences
September 18 -20, 2023
Valencia, Spain
https://cardiologyworldconference.com/
The global colloquium will highlight the theme “Revealing Innovations in Cardiology for a Healthier Heart” and it aims to accelerate scientific discoveries and major milestones in the current situation, trials, and advances in cardiology research and related fields.
Listed Under: Medical Sciences

Varian and Nova Scotia Health have launched a partnership to drive the digital transformation of the health system's comprehensive oncology service line.
A unified, interconnected network of multidisciplinary oncology software and services supporting patient care across eight centres, including regional centres located all across the province, will be established as part of the five year Oncology Transformation Project (OTP), which will build upon and integrate Nova Scotia Health's current Varian software capabilities.
Together with Varian, Nova Scotia Health will focus on resolving the haphazard interactions and manual procedures that affect patient treatment. The OTP will also go beyond cancer treatment in an effort to enhance health system coordination.
According to the terms of the agreement, Varian will provide Nova Scotia Health with a range of multi-disciplinary oncology solutions designed to improve patient care throughout the entire cancer care continuum, from screening to survivorship, and to facilitate communication between cancer patients and their healthcare professionals.
The agreement also covers the addition of InSightive™ Gen2, Varian's comprehensive analytics tool that enables clinic professionals to transform raw data into useful insights in order to make decisions more quickly and efficiently.


Farrer Park Hospital announced the launch of a clinical collaboration with Allegiant Regional Care (ARC) Hospitals to promote continuing medical education among specialists and physicians.

The collaboration was officially launched at a joint surgical conference held at Cebu, Philippines on 11 February.
The conference marked the start of the two healthcare providers’ plans to cooperate on improving patient care and promoting clinical innovation.
In Lapu-Lapu City, Cebu, ARC Healthcare manages a 100-bed medical facility. Dr. Alex. E. Alegrado, the provider's medical director, explained that holding the conference would advance the medical education of the affiliated physicians of ARC Hospitals by allowing them to hear from eminent and reputable specialists from FPH.
Dr. Melissa Teo, a surgical oncologist from FPH, discussed advancements in melanoma, sarcoma, cytoreductive surgery, and hyperthermic intraperitoneal chemotherapy (HIPEC) during the conference.
According to Anavasi Diagnostics, the FDA has now granted the AscencioDx® COVID-19 Test and The AscencioDx® Molecular Analyzer an Emergency Use Permit (EUA).
The AscencioDx® COVID-19 test yields findings for the detection of SARS-CoV-2 RNA. The AscencioDx system's portability and affordability make it possible to perform high-quality point-of-care molecular testing in a variety of healthcare settings, including facilities like urgent care facilities, mobile testing locations, assisted living facilities, and more.
The test reduces the possibility of missing a novel strain by targeting numerous areas of the viral genome using proprietary assay chemistry. The AscencioDx proprietary platform will also facilitate quick product development for new viral and bacterial targets, such as strains linked to sexual health, RSV, influenza, and more.
Contrary to more expensive and complex PCR testing, the AscencioDx Molecular Detector's proprietary compact design uses RT-LAMP (reverse transcription loop-mediated isothermal amplification) technology and doesn't require sending a sample to a different location or waiting days for results.
The AscencioDx Molecular Detector and COVID-19 Test generate less biowaste because the detector can be used for at least 3,000 test rounds. It doesn't require batteries or other electrical components to be discarded after use, unlike the majority of single-use molecular tests.
Compared to other molecular POC tests, the AscencioDx system comes with less packing and disposable parts.



Agilon Health Inc. and Lexington Clinic have


Read the complete post
announced their new partnership in order to change the primary care delivery system at Lexington Clinic to a full-risk, value-based care approach.
This transformation will improve the results and standard of treatment for Medicare patients in Central Kentucky beginning in 2024.
This new collaboration with Lexington Clinic highlights the increasing desire among primary care doctors to switch to a model of care for their Medicare patients that puts an emphasis on quality and outcomes.
As a new partner group for 2024, Lexington Clinic will be a part of Agilon's growing network of physician partners. Agilon's aligned alliances, purpose-built platform, and peer network of like-minded physicians are accelerating at scale the shift to a value-based, Total Care Model for senior patients.
Read the complete post
Read the complete post
A combined epigenetic-genetic blood test for the early detection of coronary heart disease, PrecisionCHD™, has been launched by Cardio Diagnostics Holdings.
The second clinical test created by Cardio Diagnostics' in-house AI-driven Combined Epigenetic-Genetic Engine is the PrecisionCHD.
PrecisionCHD uses genetic (single nucleotide polymorphism) and epigenetic (DNA methylation) biomarkers as well as a proprietary machine-learning model developed by analyzing billions of genomic and epigenomic data points to detect coronary heart disease with better than 75% sensitivity in both men and women.
The Actionable Clinical Intelligence tool that comes with PrecisionCHD maps a patient's individual biomarker profile onto modifiable risk factors like smoking, diabetes, hypertension, and hypercholesterolemia, which are considered to be major drivers to coronary heart disease.
The non-invasive, simple test gives medical professionals an alternative to conventional CHD diagnostic methods and offers a detailed, personalized patient report on the state of their CHD.
Read the complete post


Asensus Surgical has disclosed a multi-year partnership with Google Cloud to incorporate the latter's secure cloud data architecture and machine learning (ML) technologies and to further develop the PerformanceGuided Surgery™ (PGS) framework, which is made possible by the Intelligent Surgical Unit™ (ISUTM) of Asensus Surgical.
Performance-Guided Surgery can assist surgeons in carrying out operations more precisely and quickly, eventually assisting surgeons in avoiding complications and enhancing patient outcomes.
The ISU is a platform for real-time intraoperative surgical image analytics that uses augmented intelligence to help lower surgical variability and offers tools to lessen a surgeon's cognitive fatigue while gathering clinical information about the surgical process. For doctors and hospitals, Asensus will allow patient access portals and performance dashboards, and Google Cloud's secure cloud data architecture will collect this information.
Asensus will use Google Cloud's machine learning technologies to analyze the data and derive clinical intelligence that can be used by hospitals and surgeons along with constantly enhancing the software in the ISU to provide better intra-operative clinical insight.
Olympus Corporation has agreed to purchase Taewoong Medical, a medical device business with its headquarters in Korea for a total of about US $370 million in cash.
Taewoong produces medical devices like gastrointestinal (GI) metallic stents, which aid in removing obstructions or strictures brought on by cancer or other illnesses.
The Korean medical device manufacturer will receive up to US $114.5 million in potential future milestone payments in addition to US $255.5 million at closing under the terms of the deal.
The deal is anticipated to close by June 30, 2023, subject to certain customary closing conditions.
The biliary system, oesophagus, colon, and duodenum can all be treated with the help of Taewoong's assortment of medical devices, which also includes metallic GI stents.
Strong radial force and high flexibility are said to be combined in its metallic stents, allowing them to adapt to the curve of anatomical structures like biliary tracts and the oesophagus.
Taewoong provides a wide selection of premium stents with distinctive design and technological capabilities to help medical professionals using minimally invasive procedures.
With the acquisition, the company expands its product line to include Taewoong's medical devices, making it a complete market supplier of several GI solutions.

Through its collaboration with Tribun Health, Canon
Medical Informatics has expanded the Enterprise Imaging (EI) suite of products to include pathology.


As part of their precision informatics roadmaps, this gives healthcare companies new capability to effectively integrate pathology into their enterprise imaging plans.
Canon Medical offers healthcare companies an allin-one suite of choices and a single comprehensive partnership for their most imaging-intensive departments, including radiology, cardiology, endoscopy, and now pathology.
Canon Medical’s EI suite combines disease-centric solutions to promote sub-specialty collaboration. Tribun Health’s KLAS-leading CaloPix solution was the perfect intelligent extension with same cultural fit to Canon Medical and its solutions and services.
Some of the biggest, most complicated, and dynamic companies in the world are powered by Canon Medical solutions.
Read the complete post
A revolutionary test that can measure the progression and durability of Chimeric Antigen Receptor T-Cell (CAR-T) treatment in patients with pre-B cell acute lymphoblastic leukaemia and B cell lymphomas has been made available, according to Eurofins Viracor LLC.
The test is made to make it easier for clinicians to comprehend how CAR-T therapy is working for their patients.
CAR-T therapy is a cutting-edge type of immunotherapy that uses genetically modified T-cells to target cancer cells and has demonstrated promising outcomes in the treatment of a number of cancers.
The test is intended to give clinicians a precise and thorough evaluation of the CAR-T cell population in the patient's body and may provide information about the efficacy of the therapy
The launch of this test represents a significant advancement in the assessment and administration of CAR-T treatment for cancer patients.
It is anticipated to be a useful tool for assisting clinicians in selecting the most appropriate course of therapy for their patients.
Read the complete post


Memora Health and Moffitt Cancer Center have announced a partnership to scale data-driven cancer care.
The groundbreaking collaboration will combine Moffitt's oncology expertise with Memora's clinical intelligence care platform to enhance the patient experience and give Moffitt's clinicians and provider’s direct access to the platform in order to meet urgent patient requirements.
Clinicians all over the world frequently use Moffitt's clinical insights to inform treatment choices for patients getting oncology care. However, these clinical insights have not been used to directly engage with patients in a manner that would allow them to be educated, adhere to their treatment regimens, and be monitored for symptoms specific to their diagnosis.
By automating care journeys, Memora's platform makes complicated care delivery for patients and their providers simpler. The programme offers patients constant two-way contact about their care and intelligently assigns patient questions and clinical concerns to the best members of the care team.
Eko has announced the launch of the SENSORA™ Cardiac Disease Monitoring Platform.


The current version of SENSORA™ includes both AI and Care Pathway Analytics software, which objectively identifies structural murmurs, a sign of valvular heart disease, and provides downstream visibility and metrics of the patient journey through the healthcare system.
The stethoscope, one of the most widely used medical instruments in the world, is combined with the most recent developments in applied machine learning to create the cardiovascular disease detection tool known as SENSORA™.
Eko has invented a detection tool that will grow as the company develops apps for more cardiac conditions by using its digital stethoscopes to record and analyze electrical signals and heart sounds.
During a routine visit with their primary care physician, patients with valvular heart disease (VHD) can be more reliably and accurately diagnosed with valvular heart disease (VHD) with the SENSORA™ FDA-cleared structural murmur detection.
The company's current portfolio includes five FDA 510(k) cleared digital solutions in addition to two machine learning algorithms, named ELEFT and EKO, being developed to detect pulmonary hypertension in addition to its software that detects a weak heart pump.
A multiscale X-ray microscope built on nanoCT (computed tomography) for commercial and academic research was unveiled by Bruker as the SKYSCAN™ 2214 CMOS Edition.
The highly effective and proven SKYSCAN 2214 platform now includes the most recent scientific CMOS (sCMOS) detector technology, taking highresolution X-ray imaging to a new level.
The cutting-edge modular design of the SKYSCAN 2214 CMOS accommodates up to four detectors for your samples and uses. It's new 6MP flat screen and three enhanced 15/16MP sCMOS detectors have the largest field of vision for true 3D resolution down to the 500n range.
Due to their extensive dynamic range and exceptionally low noise, the new sCMOS detectors also shine at imaging high- and low-density features in the same object.
The SKYSCAN 2214 CMOS Edition is enhanced by the user-friendly 3D.SUITE software, which allows for simple data gathering, sophisticated image analysis, and potent visualization. Advanced features like spiral scanning and variable rotation step tomography are part of this potent software package.
Furthermore, features that would normally be hidden when using only absorption contrast imaging can be seen when using phase retrieval algorithms for propagation-based phase contrast X-ray imaging.
The minimal maintenance requirements of SKYSCAN 2214 CMOS Edition increase system uptime and lower total cost of ownership.



